User login
Lamotrigine interactions with oral contraceptives
Ms. A, age 20, presents to the clinic after experiencing difficulty sleeping, depressed mood, fatigue, and difficulty concentrating. Her psychiatric history includes bipolar II disorder (BD II), predominantly with depressive episodes. Ms. A’s current medications include a combination of lamotrigine 200 mg/d and bupropion extended-release 450 mg/d, and her symptoms were well maintained until 2 weeks ago. When her psychiatrist performs a medication reconciliation at her medication management appointment, Ms. A indicates she started taking an oral contraceptive, ethinyl estradiol and norgestimate, approximately 1 month ago for management of endometriosis symptoms. She is not currently taking any other medications or supplements.
Lamotrigine is indicated for epilepsy and as maintenance treatment for BD I. It is also used off-label to treat other mood disorders. After oral administration, lamotrigine is rapidly and fully absorbed with a high bioavailability (98%). The principal metabolic pathway is via glucuronic acid conjugation, leading to the major inactive metabolite 2-N-glucuronide. Minor metabolites include 5-N-glucuronide and a 2-N-glucuronide metabolite.1
Combined oral contraceptives contain an estrogen component, typically ethinyl estradiol, and a progestin component, which varies based on the specific formulation. The metabolism of ethinyl estradiol occurs through cytochrome P450 (CYP)3A4, CYP2C9, sulfation, and glucuronidation. For progestin—the second component of combined oral contraceptives and the lone component of progestin-only oral contraceptives—metabolism occurs via CYP3A4 and conjugation reactions.2 This article focuses on lamotrigine interactions specifically with oral contraceptives, but it is important to note that other formulations of combined hormonal contraceptives, such as the combined contraceptive patch (Ortho Evra) and vaginal ring (NuvaRing), would be expected to interact in the same way as oral formulations.3
Bidirectional interaction
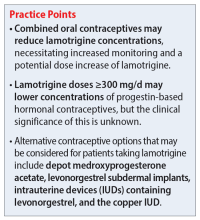
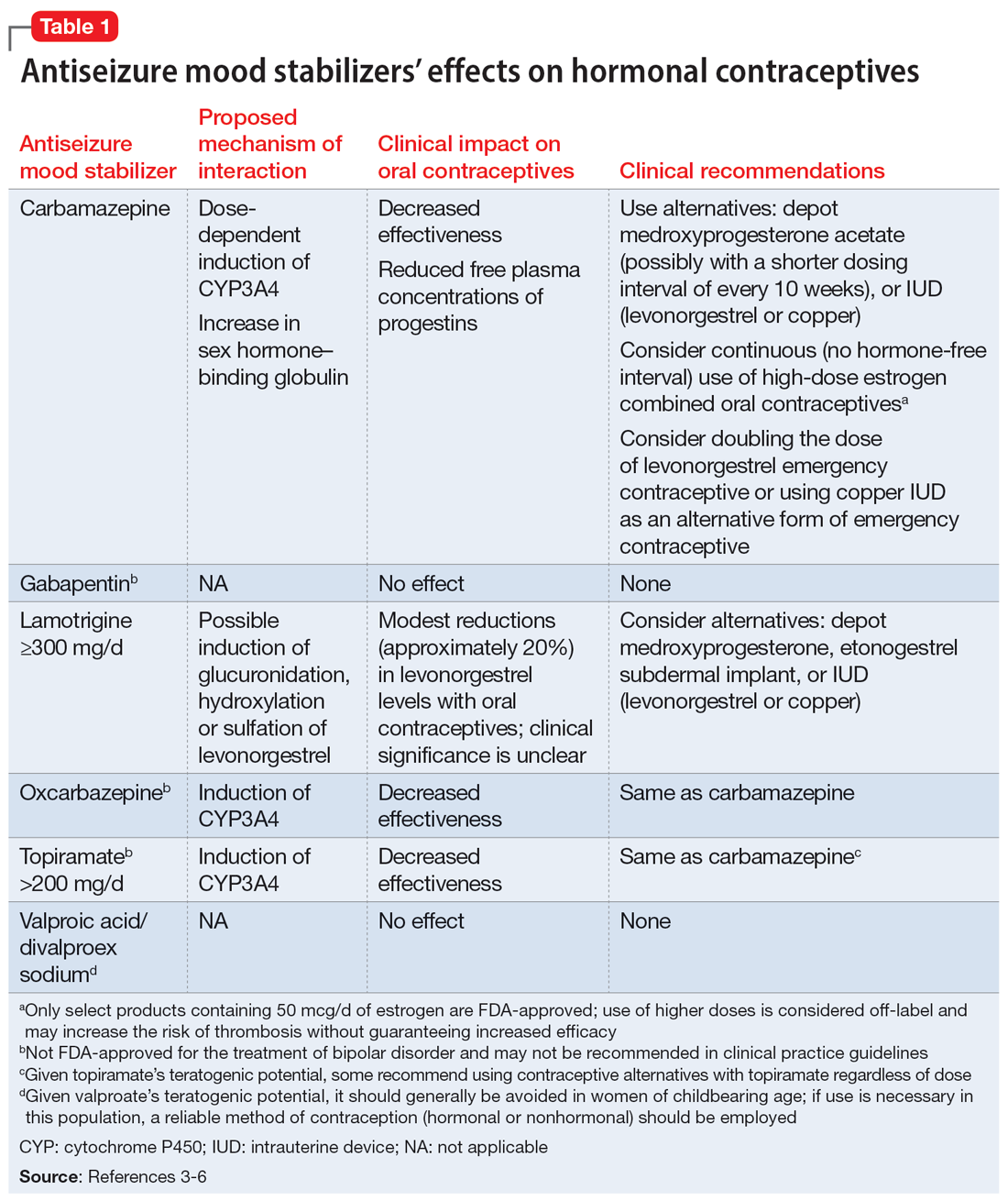
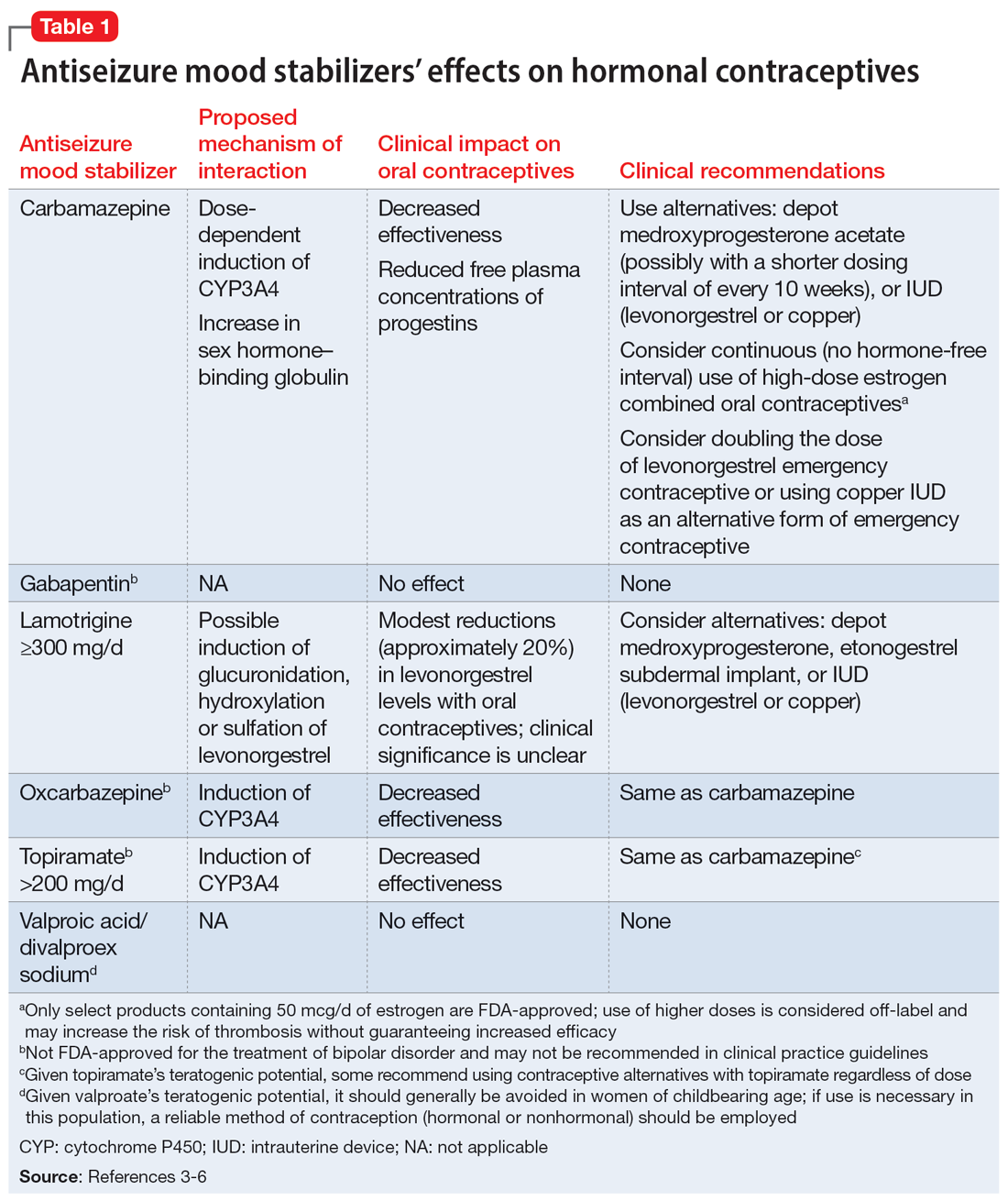
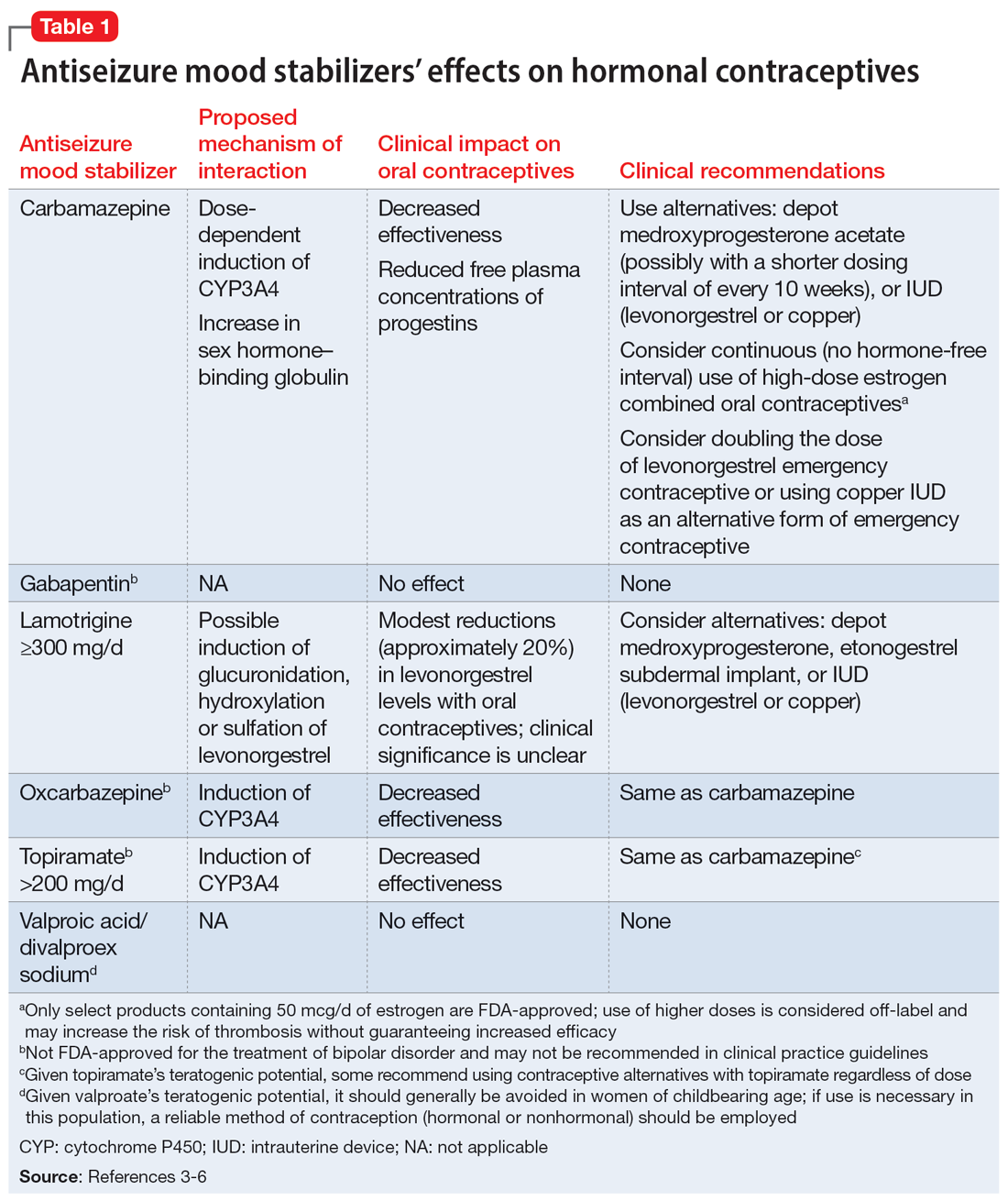
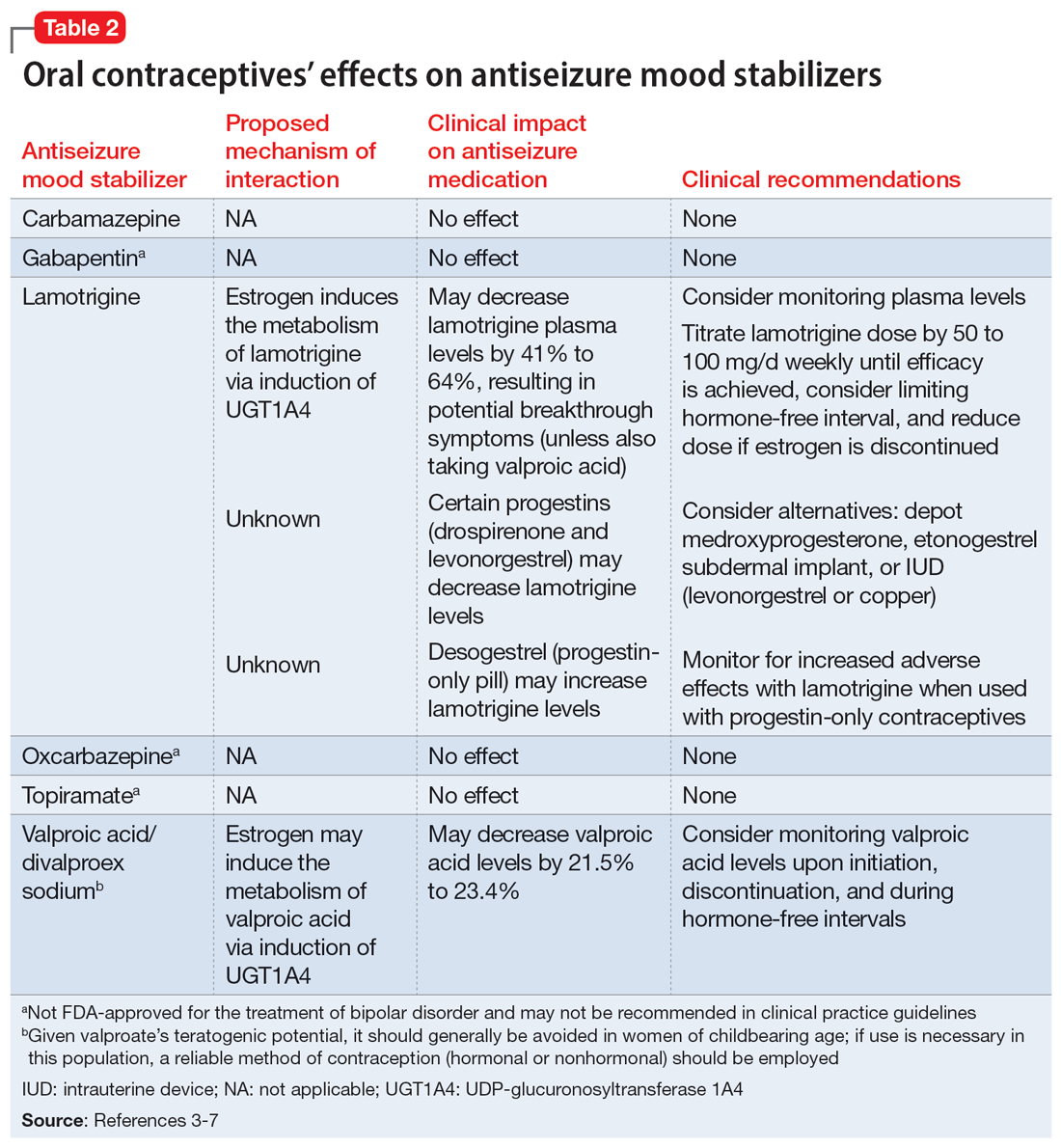
While many antiseizure medications are known to interact with and potentially decrease the efficacy of oral contraceptives (Table 13-6), the interactions between lamotrigine and oral contraceptives is uniquely bidirectional. Combined oral contraceptives are thought to interact with lamotrigine primarily via the estrogen component, which causes increased metabolism of lamotrigine through induction of glucuronidation. This drug interaction decreases the plasma concentrations of lamotrigine in the body by up to 2-fold, resulting in an increased risk of seizures or inadequate mood stabilization.1 This effect on metabolism is very rapid, resulting in decreases in lamotrigine concentrations within 1 week.4,7 A recent study suggested that certain progestins may also contribute to decreased plasma levels of lamotrigine, but the mechanism for this is unknown (Table 23-7).8
Clinicians should consider increasing the lamotrigine dose (potentially as much as 2-fold) in a patient who initiates treatment with a combined hormonal contraceptive. Dose increases should not be >50 to 100 mg/d every week.1 Collect lamotrigine blood levels before starting a hormonal contraceptive and during dose titration. While there is not a well-established therapeutic range for lamotrigine in BD, expert consensus recommends a range of 1 to 6 mcg/mL.8
The lamotrigine dose should be decreased if combined hormonal contraceptives are discontinued. Dose decreases should not exceed 25% of the total daily dose per week.1 Desogestrel, a progestin-only medication, may increase exposure to lamotrigine, but this has not been observed in research with other progestins.5,9 When starting a progestin-only pill, monitor patients for signs of lamotrigine toxicity (ataxia, diplopia, dizziness) and consider monitoring their blood levels.
An important consideration to note with combined oral contraceptives is the hormone-free interval, also known as the pill-free week. Due to the rapid effect of estrogens, the lamotrigine concentrations have been shown to rise, even double, during this hormone-free interval, so patients should be closely monitored for adverse effects.3 Some recommend use of an extended cycle regimen (with a limited hormone-free interval), or continuous cycle regimen (with no hormone-free interval) to avoid fluctuations in lamotrigine levels.3,5 Additionally, data suggest that in patients taking lamotrigine and valproate, which inhibits glucuronidation, oral contraceptives do not cause reductions in lamotrigine concentrations.2,5 In these instances, dose increases of lamotrigine are not needed.
Continue to: The metabolism of ethinyl estradiol...
The metabolism of ethinyl estradiol and progestin are susceptible to CYP3A4 induction and increased glucuronidation. Serum concentrations may be reduced by ≥50% when used concomitantly with CYP enzyme–inducing medications, which could possibly result in subtherapeutic levels and unplanned pregnancy.3 CYP3A4 induction occurs for up to 4 weeks after discontinuation of an enzyme-inducing agent, pointing to the need for alternative or backup contraception during this time.3 Lamotrigine is not a CYP enzyme–inducing medication; it is unlikely to affect the efficacy of oral contraceptives in the same manner as other antiseizure medications. However, a study of lamotrigine and the combined hormonal contraceptive ethinyl estradiol and levonorgestrel demonstrated reduced exposure to levonorgestrel, resulting in breakthrough bleeding.5
In a study on the coadministration of lamotrigine and combined oral contraceptives, Sidhu et al4 observed a small mean reduction (20%) in progestin concentrations when lamotrigine was used at a dose of 300 mg/d. Although there is no research suggesting decreased effectiveness in preventing pregnancy when lamotrigine is used with combined oral contraceptives, progestin-only oral contraceptives, or progestin implants, additional or alternative contraceptive methods may be considered based on this pharmacokinetic data, particularly in patients who require lamotrigine doses ≥300 mg/d.5
CASE CONTINUED
Given when Ms. A started the oral contraceptive, the treatment team determines it is likely that an interaction with lamotrigine is causing her resurgence of depressive symptoms. Her care team decides to titrate the lamotrigine gradually to 300 mg/d, then 400 mg/d if needed, while carefully monitoring for signs of a serious rash. This dosage increase may help Ms. A achieve symptom remission. Monitoring plasma levels may be considered, although it is unknown what plasma level was effective for Ms. A before she started the oral contraceptive. Ms. A would need to be counseled regarding the effect of higher doses of lamotrigine on the effectiveness of the oral contraceptive.
Although it does not appear Ms. A is using the oral contraceptive specifically to prevent pregnancy, the team informs her about the possibility of unintended pregnancy with this medication combination. If Ms. A was also using the medication for this indication, alternative contraceptive options would include medroxyprogesterone acetate, levonorgestrel implants, or an intrauterine device (levonorgestrel or copper, though copper would not be effective for endometriosis symptom management). Ms. A should consult with her gynecologist regarding the most appropriate option for her endometriosis. If the decision is made to discontinue her oral contraceptive in the future, the lamotrigine dose should be decreased to her previously effective dose of 200 mg/d.
Related Resources
- Makino KK, Hatters Friedman S, Amin J. Emergency contraception for psychiatric patients. Current Psychiatry. 2022;21(11):34-39,44-45. doi:10.12788/cp.0300
- MGH Center for Women’s Mental Health. You asked: is there an interaction between lamotrigine and oral contraceptives? September 29, 2015. https://womensmentalhealth.org/posts/you-asked-is-there-an-interaction-between-lamotrigine-andoral-contraceptives/
Drug Brand Names
Bupropion extended-release • Wellbutrin XL
Carbamazepine • Equetro, Tegretol
Desogestrel • Cerazette
Divalproex sodium • Depakote
Ethinyl estradiol and etonogestrel • NuvaRing
Ethinyl estradiol and norelgestromin • Ortho Evra
Ethinyl estradiol and norgestimate • Ortho Tri-Cyclen, TriNessa, others
Etonogestrel • Implanon, Nexplanon
Gabapentin • Neurontin
Lamotrigine • Lamictal
Levonorgestrel emergency contraceptive pill • AfterPill, Plan B
Levonorgestrel intrauterine device • Mirena, Skyla
Medroxyprogesterone acetate • Depo-Provera
Oxcarbazepine • Trileptal
Topiramate • Topamax
Valproic acid • Depakene
1. Lamictal [package insert]. Research Triangle Park, NC: GlaxoSmithKline; 2020.
2. Lee CR. Drug interactions and hormonal contraception. Trends in Urology Gynaecology & Sexual Health. 2009;14(3):23-26.
3. Williams D. Antiepileptic drugs and contraception. US Pharm. 2014;39(1):39-42.
4. Sidhu J, Job S, Singh S, et al. The pharmacokinetic and pharmacodynamic consequences of the co-administration of lamotrigine and a combined oral contraceptive in healthy female subjects. Br J Clin Pharmacol. 2006;61(2):191-199. doi:10.1111/j.1365-2125.2005.02539.x
5. Faculty of Sexual & Reproductive Healthcare. Clinical guidance: drug interactions with hormonal contraception. Published May 9, 2022. Accessed September 28, 2022. https://www.fsrh.org/documents/ceu-clinical-guidance-drug-interactions-with-hormonal/
6. Johnston CA, Crawford PM. Anti-epileptic drugs and hormonal treatments. Curr Treat Options Neurol. 2014;16(5):288. doi:10.1007/s11940-014-0288-3
7. Christensen J, Petrenaite V, Atterman J, et al. Oral contraceptives induce lamotrigine metabolism: evidence from a double-blind, placebo-controlled trial. Epilepsia. 2007;48(3):484-489. doi:10.1111/j.1528-1167.2007.00997.x
8. Hiemke C, Bergemann N, Clement HW, et al. Consensus guidelines for therapeutic drug monitoring in neuropsychopharmacology: update 2017. Pharmacopsychiatry. 2018;51(1-02):9-62. doi:10.1055/s-0043-116492
9. Rauchenzauner M, Deichmann S, Pittschieler, et al. Bidirectional interaction between oral contraception and lamotrigine in women with epilepsy – role of progestins. Seizure. 2020;74:89-92. doi:10.1016/j.seizure.2019.11.011
Ms. A, age 20, presents to the clinic after experiencing difficulty sleeping, depressed mood, fatigue, and difficulty concentrating. Her psychiatric history includes bipolar II disorder (BD II), predominantly with depressive episodes. Ms. A’s current medications include a combination of lamotrigine 200 mg/d and bupropion extended-release 450 mg/d, and her symptoms were well maintained until 2 weeks ago. When her psychiatrist performs a medication reconciliation at her medication management appointment, Ms. A indicates she started taking an oral contraceptive, ethinyl estradiol and norgestimate, approximately 1 month ago for management of endometriosis symptoms. She is not currently taking any other medications or supplements.
Lamotrigine is indicated for epilepsy and as maintenance treatment for BD I. It is also used off-label to treat other mood disorders. After oral administration, lamotrigine is rapidly and fully absorbed with a high bioavailability (98%). The principal metabolic pathway is via glucuronic acid conjugation, leading to the major inactive metabolite 2-N-glucuronide. Minor metabolites include 5-N-glucuronide and a 2-N-glucuronide metabolite.1
Combined oral contraceptives contain an estrogen component, typically ethinyl estradiol, and a progestin component, which varies based on the specific formulation. The metabolism of ethinyl estradiol occurs through cytochrome P450 (CYP)3A4, CYP2C9, sulfation, and glucuronidation. For progestin—the second component of combined oral contraceptives and the lone component of progestin-only oral contraceptives—metabolism occurs via CYP3A4 and conjugation reactions.2 This article focuses on lamotrigine interactions specifically with oral contraceptives, but it is important to note that other formulations of combined hormonal contraceptives, such as the combined contraceptive patch (Ortho Evra) and vaginal ring (NuvaRing), would be expected to interact in the same way as oral formulations.3
Bidirectional interaction
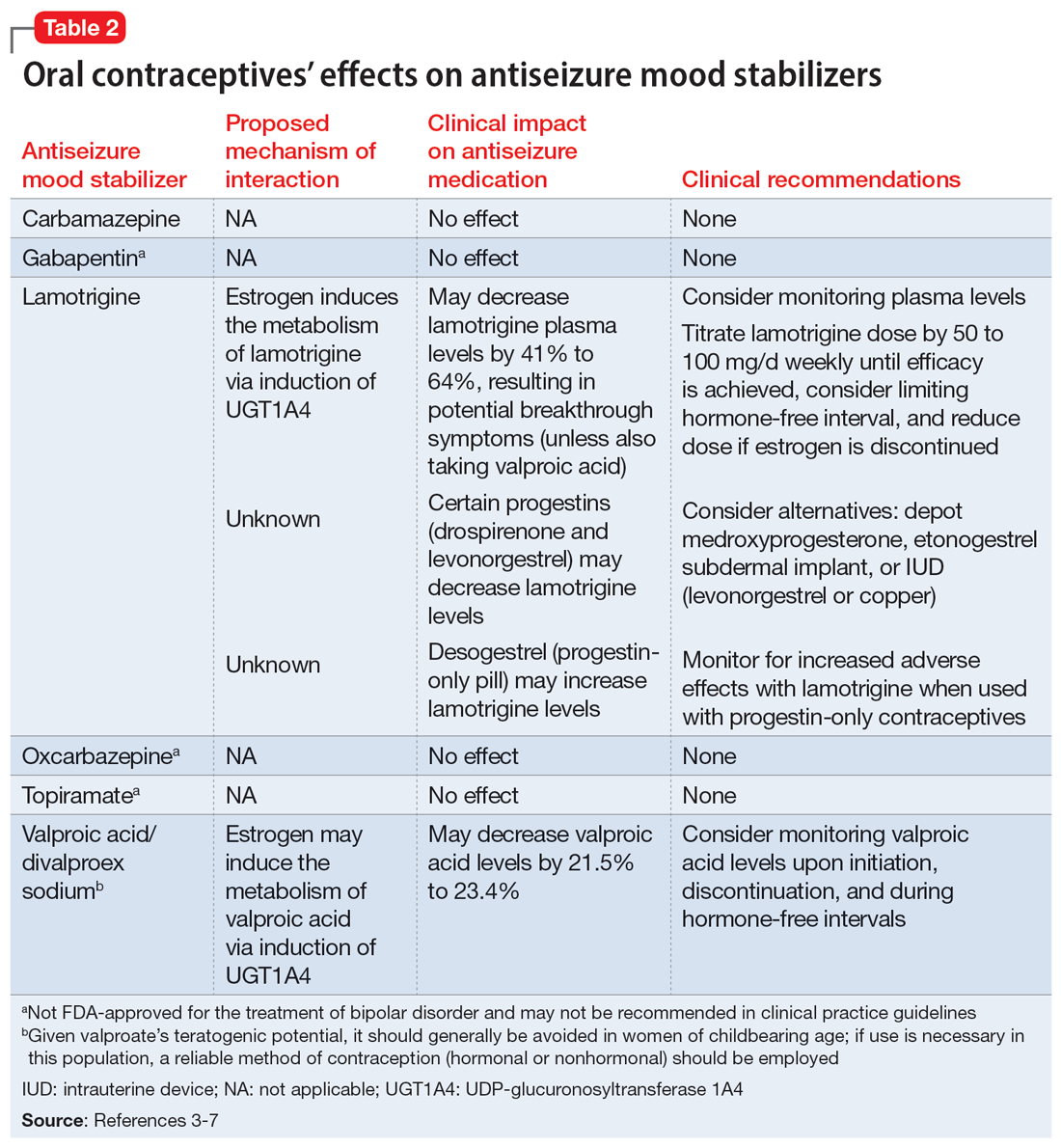
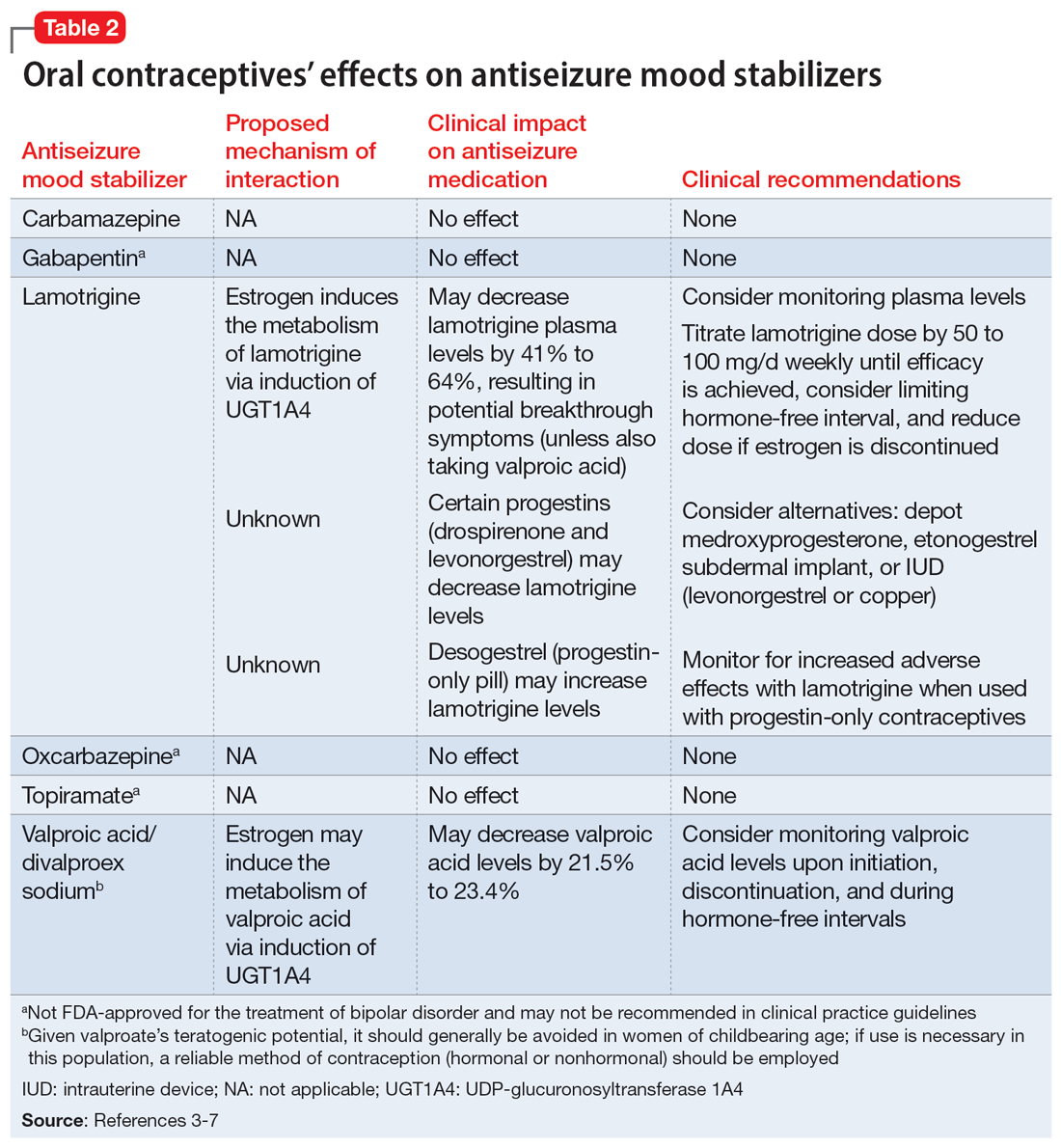
While many antiseizure medications are known to interact with and potentially decrease the efficacy of oral contraceptives (Table 13-6), the interactions between lamotrigine and oral contraceptives is uniquely bidirectional. Combined oral contraceptives are thought to interact with lamotrigine primarily via the estrogen component, which causes increased metabolism of lamotrigine through induction of glucuronidation. This drug interaction decreases the plasma concentrations of lamotrigine in the body by up to 2-fold, resulting in an increased risk of seizures or inadequate mood stabilization.1 This effect on metabolism is very rapid, resulting in decreases in lamotrigine concentrations within 1 week.4,7 A recent study suggested that certain progestins may also contribute to decreased plasma levels of lamotrigine, but the mechanism for this is unknown (Table 23-7).8
Clinicians should consider increasing the lamotrigine dose (potentially as much as 2-fold) in a patient who initiates treatment with a combined hormonal contraceptive. Dose increases should not be >50 to 100 mg/d every week.1 Collect lamotrigine blood levels before starting a hormonal contraceptive and during dose titration. While there is not a well-established therapeutic range for lamotrigine in BD, expert consensus recommends a range of 1 to 6 mcg/mL.8
The lamotrigine dose should be decreased if combined hormonal contraceptives are discontinued. Dose decreases should not exceed 25% of the total daily dose per week.1 Desogestrel, a progestin-only medication, may increase exposure to lamotrigine, but this has not been observed in research with other progestins.5,9 When starting a progestin-only pill, monitor patients for signs of lamotrigine toxicity (ataxia, diplopia, dizziness) and consider monitoring their blood levels.
An important consideration to note with combined oral contraceptives is the hormone-free interval, also known as the pill-free week. Due to the rapid effect of estrogens, the lamotrigine concentrations have been shown to rise, even double, during this hormone-free interval, so patients should be closely monitored for adverse effects.3 Some recommend use of an extended cycle regimen (with a limited hormone-free interval), or continuous cycle regimen (with no hormone-free interval) to avoid fluctuations in lamotrigine levels.3,5 Additionally, data suggest that in patients taking lamotrigine and valproate, which inhibits glucuronidation, oral contraceptives do not cause reductions in lamotrigine concentrations.2,5 In these instances, dose increases of lamotrigine are not needed.
Continue to: The metabolism of ethinyl estradiol...
The metabolism of ethinyl estradiol and progestin are susceptible to CYP3A4 induction and increased glucuronidation. Serum concentrations may be reduced by ≥50% when used concomitantly with CYP enzyme–inducing medications, which could possibly result in subtherapeutic levels and unplanned pregnancy.3 CYP3A4 induction occurs for up to 4 weeks after discontinuation of an enzyme-inducing agent, pointing to the need for alternative or backup contraception during this time.3 Lamotrigine is not a CYP enzyme–inducing medication; it is unlikely to affect the efficacy of oral contraceptives in the same manner as other antiseizure medications. However, a study of lamotrigine and the combined hormonal contraceptive ethinyl estradiol and levonorgestrel demonstrated reduced exposure to levonorgestrel, resulting in breakthrough bleeding.5
In a study on the coadministration of lamotrigine and combined oral contraceptives, Sidhu et al4 observed a small mean reduction (20%) in progestin concentrations when lamotrigine was used at a dose of 300 mg/d. Although there is no research suggesting decreased effectiveness in preventing pregnancy when lamotrigine is used with combined oral contraceptives, progestin-only oral contraceptives, or progestin implants, additional or alternative contraceptive methods may be considered based on this pharmacokinetic data, particularly in patients who require lamotrigine doses ≥300 mg/d.5
CASE CONTINUED
Given when Ms. A started the oral contraceptive, the treatment team determines it is likely that an interaction with lamotrigine is causing her resurgence of depressive symptoms. Her care team decides to titrate the lamotrigine gradually to 300 mg/d, then 400 mg/d if needed, while carefully monitoring for signs of a serious rash. This dosage increase may help Ms. A achieve symptom remission. Monitoring plasma levels may be considered, although it is unknown what plasma level was effective for Ms. A before she started the oral contraceptive. Ms. A would need to be counseled regarding the effect of higher doses of lamotrigine on the effectiveness of the oral contraceptive.
Although it does not appear Ms. A is using the oral contraceptive specifically to prevent pregnancy, the team informs her about the possibility of unintended pregnancy with this medication combination. If Ms. A was also using the medication for this indication, alternative contraceptive options would include medroxyprogesterone acetate, levonorgestrel implants, or an intrauterine device (levonorgestrel or copper, though copper would not be effective for endometriosis symptom management). Ms. A should consult with her gynecologist regarding the most appropriate option for her endometriosis. If the decision is made to discontinue her oral contraceptive in the future, the lamotrigine dose should be decreased to her previously effective dose of 200 mg/d.
Related Resources
- Makino KK, Hatters Friedman S, Amin J. Emergency contraception for psychiatric patients. Current Psychiatry. 2022;21(11):34-39,44-45. doi:10.12788/cp.0300
- MGH Center for Women’s Mental Health. You asked: is there an interaction between lamotrigine and oral contraceptives? September 29, 2015. https://womensmentalhealth.org/posts/you-asked-is-there-an-interaction-between-lamotrigine-andoral-contraceptives/
Drug Brand Names
Bupropion extended-release • Wellbutrin XL
Carbamazepine • Equetro, Tegretol
Desogestrel • Cerazette
Divalproex sodium • Depakote
Ethinyl estradiol and etonogestrel • NuvaRing
Ethinyl estradiol and norelgestromin • Ortho Evra
Ethinyl estradiol and norgestimate • Ortho Tri-Cyclen, TriNessa, others
Etonogestrel • Implanon, Nexplanon
Gabapentin • Neurontin
Lamotrigine • Lamictal
Levonorgestrel emergency contraceptive pill • AfterPill, Plan B
Levonorgestrel intrauterine device • Mirena, Skyla
Medroxyprogesterone acetate • Depo-Provera
Oxcarbazepine • Trileptal
Topiramate • Topamax
Valproic acid • Depakene
Ms. A, age 20, presents to the clinic after experiencing difficulty sleeping, depressed mood, fatigue, and difficulty concentrating. Her psychiatric history includes bipolar II disorder (BD II), predominantly with depressive episodes. Ms. A’s current medications include a combination of lamotrigine 200 mg/d and bupropion extended-release 450 mg/d, and her symptoms were well maintained until 2 weeks ago. When her psychiatrist performs a medication reconciliation at her medication management appointment, Ms. A indicates she started taking an oral contraceptive, ethinyl estradiol and norgestimate, approximately 1 month ago for management of endometriosis symptoms. She is not currently taking any other medications or supplements.
Lamotrigine is indicated for epilepsy and as maintenance treatment for BD I. It is also used off-label to treat other mood disorders. After oral administration, lamotrigine is rapidly and fully absorbed with a high bioavailability (98%). The principal metabolic pathway is via glucuronic acid conjugation, leading to the major inactive metabolite 2-N-glucuronide. Minor metabolites include 5-N-glucuronide and a 2-N-glucuronide metabolite.1
Combined oral contraceptives contain an estrogen component, typically ethinyl estradiol, and a progestin component, which varies based on the specific formulation. The metabolism of ethinyl estradiol occurs through cytochrome P450 (CYP)3A4, CYP2C9, sulfation, and glucuronidation. For progestin—the second component of combined oral contraceptives and the lone component of progestin-only oral contraceptives—metabolism occurs via CYP3A4 and conjugation reactions.2 This article focuses on lamotrigine interactions specifically with oral contraceptives, but it is important to note that other formulations of combined hormonal contraceptives, such as the combined contraceptive patch (Ortho Evra) and vaginal ring (NuvaRing), would be expected to interact in the same way as oral formulations.3
Bidirectional interaction
While many antiseizure medications are known to interact with and potentially decrease the efficacy of oral contraceptives (Table 13-6), the interactions between lamotrigine and oral contraceptives is uniquely bidirectional. Combined oral contraceptives are thought to interact with lamotrigine primarily via the estrogen component, which causes increased metabolism of lamotrigine through induction of glucuronidation. This drug interaction decreases the plasma concentrations of lamotrigine in the body by up to 2-fold, resulting in an increased risk of seizures or inadequate mood stabilization.1 This effect on metabolism is very rapid, resulting in decreases in lamotrigine concentrations within 1 week.4,7 A recent study suggested that certain progestins may also contribute to decreased plasma levels of lamotrigine, but the mechanism for this is unknown (Table 23-7).8
Clinicians should consider increasing the lamotrigine dose (potentially as much as 2-fold) in a patient who initiates treatment with a combined hormonal contraceptive. Dose increases should not be >50 to 100 mg/d every week.1 Collect lamotrigine blood levels before starting a hormonal contraceptive and during dose titration. While there is not a well-established therapeutic range for lamotrigine in BD, expert consensus recommends a range of 1 to 6 mcg/mL.8
The lamotrigine dose should be decreased if combined hormonal contraceptives are discontinued. Dose decreases should not exceed 25% of the total daily dose per week.1 Desogestrel, a progestin-only medication, may increase exposure to lamotrigine, but this has not been observed in research with other progestins.5,9 When starting a progestin-only pill, monitor patients for signs of lamotrigine toxicity (ataxia, diplopia, dizziness) and consider monitoring their blood levels.
An important consideration to note with combined oral contraceptives is the hormone-free interval, also known as the pill-free week. Due to the rapid effect of estrogens, the lamotrigine concentrations have been shown to rise, even double, during this hormone-free interval, so patients should be closely monitored for adverse effects.3 Some recommend use of an extended cycle regimen (with a limited hormone-free interval), or continuous cycle regimen (with no hormone-free interval) to avoid fluctuations in lamotrigine levels.3,5 Additionally, data suggest that in patients taking lamotrigine and valproate, which inhibits glucuronidation, oral contraceptives do not cause reductions in lamotrigine concentrations.2,5 In these instances, dose increases of lamotrigine are not needed.
Continue to: The metabolism of ethinyl estradiol...
The metabolism of ethinyl estradiol and progestin are susceptible to CYP3A4 induction and increased glucuronidation. Serum concentrations may be reduced by ≥50% when used concomitantly with CYP enzyme–inducing medications, which could possibly result in subtherapeutic levels and unplanned pregnancy.3 CYP3A4 induction occurs for up to 4 weeks after discontinuation of an enzyme-inducing agent, pointing to the need for alternative or backup contraception during this time.3 Lamotrigine is not a CYP enzyme–inducing medication; it is unlikely to affect the efficacy of oral contraceptives in the same manner as other antiseizure medications. However, a study of lamotrigine and the combined hormonal contraceptive ethinyl estradiol and levonorgestrel demonstrated reduced exposure to levonorgestrel, resulting in breakthrough bleeding.5
In a study on the coadministration of lamotrigine and combined oral contraceptives, Sidhu et al4 observed a small mean reduction (20%) in progestin concentrations when lamotrigine was used at a dose of 300 mg/d. Although there is no research suggesting decreased effectiveness in preventing pregnancy when lamotrigine is used with combined oral contraceptives, progestin-only oral contraceptives, or progestin implants, additional or alternative contraceptive methods may be considered based on this pharmacokinetic data, particularly in patients who require lamotrigine doses ≥300 mg/d.5
CASE CONTINUED
Given when Ms. A started the oral contraceptive, the treatment team determines it is likely that an interaction with lamotrigine is causing her resurgence of depressive symptoms. Her care team decides to titrate the lamotrigine gradually to 300 mg/d, then 400 mg/d if needed, while carefully monitoring for signs of a serious rash. This dosage increase may help Ms. A achieve symptom remission. Monitoring plasma levels may be considered, although it is unknown what plasma level was effective for Ms. A before she started the oral contraceptive. Ms. A would need to be counseled regarding the effect of higher doses of lamotrigine on the effectiveness of the oral contraceptive.
Although it does not appear Ms. A is using the oral contraceptive specifically to prevent pregnancy, the team informs her about the possibility of unintended pregnancy with this medication combination. If Ms. A was also using the medication for this indication, alternative contraceptive options would include medroxyprogesterone acetate, levonorgestrel implants, or an intrauterine device (levonorgestrel or copper, though copper would not be effective for endometriosis symptom management). Ms. A should consult with her gynecologist regarding the most appropriate option for her endometriosis. If the decision is made to discontinue her oral contraceptive in the future, the lamotrigine dose should be decreased to her previously effective dose of 200 mg/d.
Related Resources
- Makino KK, Hatters Friedman S, Amin J. Emergency contraception for psychiatric patients. Current Psychiatry. 2022;21(11):34-39,44-45. doi:10.12788/cp.0300
- MGH Center for Women’s Mental Health. You asked: is there an interaction between lamotrigine and oral contraceptives? September 29, 2015. https://womensmentalhealth.org/posts/you-asked-is-there-an-interaction-between-lamotrigine-andoral-contraceptives/
Drug Brand Names
Bupropion extended-release • Wellbutrin XL
Carbamazepine • Equetro, Tegretol
Desogestrel • Cerazette
Divalproex sodium • Depakote
Ethinyl estradiol and etonogestrel • NuvaRing
Ethinyl estradiol and norelgestromin • Ortho Evra
Ethinyl estradiol and norgestimate • Ortho Tri-Cyclen, TriNessa, others
Etonogestrel • Implanon, Nexplanon
Gabapentin • Neurontin
Lamotrigine • Lamictal
Levonorgestrel emergency contraceptive pill • AfterPill, Plan B
Levonorgestrel intrauterine device • Mirena, Skyla
Medroxyprogesterone acetate • Depo-Provera
Oxcarbazepine • Trileptal
Topiramate • Topamax
Valproic acid • Depakene
1. Lamictal [package insert]. Research Triangle Park, NC: GlaxoSmithKline; 2020.
2. Lee CR. Drug interactions and hormonal contraception. Trends in Urology Gynaecology & Sexual Health. 2009;14(3):23-26.
3. Williams D. Antiepileptic drugs and contraception. US Pharm. 2014;39(1):39-42.
4. Sidhu J, Job S, Singh S, et al. The pharmacokinetic and pharmacodynamic consequences of the co-administration of lamotrigine and a combined oral contraceptive in healthy female subjects. Br J Clin Pharmacol. 2006;61(2):191-199. doi:10.1111/j.1365-2125.2005.02539.x
5. Faculty of Sexual & Reproductive Healthcare. Clinical guidance: drug interactions with hormonal contraception. Published May 9, 2022. Accessed September 28, 2022. https://www.fsrh.org/documents/ceu-clinical-guidance-drug-interactions-with-hormonal/
6. Johnston CA, Crawford PM. Anti-epileptic drugs and hormonal treatments. Curr Treat Options Neurol. 2014;16(5):288. doi:10.1007/s11940-014-0288-3
7. Christensen J, Petrenaite V, Atterman J, et al. Oral contraceptives induce lamotrigine metabolism: evidence from a double-blind, placebo-controlled trial. Epilepsia. 2007;48(3):484-489. doi:10.1111/j.1528-1167.2007.00997.x
8. Hiemke C, Bergemann N, Clement HW, et al. Consensus guidelines for therapeutic drug monitoring in neuropsychopharmacology: update 2017. Pharmacopsychiatry. 2018;51(1-02):9-62. doi:10.1055/s-0043-116492
9. Rauchenzauner M, Deichmann S, Pittschieler, et al. Bidirectional interaction between oral contraception and lamotrigine in women with epilepsy – role of progestins. Seizure. 2020;74:89-92. doi:10.1016/j.seizure.2019.11.011
1. Lamictal [package insert]. Research Triangle Park, NC: GlaxoSmithKline; 2020.
2. Lee CR. Drug interactions and hormonal contraception. Trends in Urology Gynaecology & Sexual Health. 2009;14(3):23-26.
3. Williams D. Antiepileptic drugs and contraception. US Pharm. 2014;39(1):39-42.
4. Sidhu J, Job S, Singh S, et al. The pharmacokinetic and pharmacodynamic consequences of the co-administration of lamotrigine and a combined oral contraceptive in healthy female subjects. Br J Clin Pharmacol. 2006;61(2):191-199. doi:10.1111/j.1365-2125.2005.02539.x
5. Faculty of Sexual & Reproductive Healthcare. Clinical guidance: drug interactions with hormonal contraception. Published May 9, 2022. Accessed September 28, 2022. https://www.fsrh.org/documents/ceu-clinical-guidance-drug-interactions-with-hormonal/
6. Johnston CA, Crawford PM. Anti-epileptic drugs and hormonal treatments. Curr Treat Options Neurol. 2014;16(5):288. doi:10.1007/s11940-014-0288-3
7. Christensen J, Petrenaite V, Atterman J, et al. Oral contraceptives induce lamotrigine metabolism: evidence from a double-blind, placebo-controlled trial. Epilepsia. 2007;48(3):484-489. doi:10.1111/j.1528-1167.2007.00997.x
8. Hiemke C, Bergemann N, Clement HW, et al. Consensus guidelines for therapeutic drug monitoring in neuropsychopharmacology: update 2017. Pharmacopsychiatry. 2018;51(1-02):9-62. doi:10.1055/s-0043-116492
9. Rauchenzauner M, Deichmann S, Pittschieler, et al. Bidirectional interaction between oral contraception and lamotrigine in women with epilepsy – role of progestins. Seizure. 2020;74:89-92. doi:10.1016/j.seizure.2019.11.011
From smiling to smizing: Assessing the affect of a patient wearing a mask
Although the guidelines for masking in hospitals and other health care settings have been revised and face masks are no longer mandatory, it is important to note that some patients and clinicians will choose to continue wearing masks for various personal or clinical reasons. While effective in reducing transmission of the coronavirus, masks have created challenges in assessing patients’ affective states, which impacts the accuracy of diagnosis and treatment. This article discusses strategies for assessing affect in patients wearing face masks.
How masks complicate assessing affect
One obvious challenge masks present is they prevent clinicians from seeing their patients’ facial expressions. Face masks cover the mouth, nose, and cheeks, all of which are involved in communicating emotions. As a result, clinicians may miss important cues that could inform their assessment of a patient’s affect. For example, when a masked patient is smiling, it is difficult to determine whether their smile is genuine or forced. A study that evaluated the interpretation of 6 emotions (angry, disgusted, fearful, happy, neutral, and sad) in masked patients found that emotion recognition was significantly reduced for all emotions except for fearful and neutral faces.1
Another challenge is the potential for misinterpretation. Health care professionals may rely more heavily on nonverbal cues, such as body language, to interpret a patient’s affect. However, these cues can be influenced by other factors, such as cultural differences and individual variations in communication style. Culture is a key component in assessing nonverbal emotion reading cues.2
Strategies to overcome these challenges
There are several strategies clinicians can use to overcome the difficulties of assessing affect while a patient is wearing a mask:
Focus on other nonverbal cues, such as a patient’s posture and hand gestures. Verbal cues—such as tone of voice, choice of words, and voice inflection—can also provide valuable insights. For example, a patient who speaks in a hesitant or monotone voice may be experiencing anxiety or depression. Clinicians can ask open-ended questions, encouraging patients to expand on their emotions and provide further information about their affect.
Maintain eye contact. Eye contact is an essential component of nonverbal communication. The eyes are “the window of the soul” and can convey various emotions including happiness, sadness, fear, anger, surprise, trust, interest, and empathy. Maintaining eye contact is crucial for building positive relationships with patients, and learning to smile with your eyes (smize) can help build rapport.
Take advantage of technology. Clinicians can leverage telemedicine to assess affect. Telemedicine platforms, which have become increasingly popular during the COVID-19 pandemic, allow clinicians to monitor patients remotely and observe nonverbal cues. Virtual reality technology can also help by documenting physiological responses such as heart rate and skin conductance.
Use standardized assessment tools, as these instruments can aid in assessing affect. For example, the Patient Health Questionnaire-9 and Generalized Anxiety Disorder 7-item scale are standardized questionnaires assessing depression and anxiety, respectively. Administering these tools to patients wearing a face mask can provide information about their affective state.
1. Carbon CC. Wearing face masks strongly confuses counterparts in reading emotions. Front Psychol. 2020;11:566886. doi:10.3389/fpsyg.2020.566886
2. Yuki M, Maddux WW, Masuda T. Are the windows to the soul the same in the East and West? Cultural differences in using the eyes and mouth as cues to recognize emotions in Japan and the United States. J Exp Soc Psychol. 2007;43(2):303-311.
Although the guidelines for masking in hospitals and other health care settings have been revised and face masks are no longer mandatory, it is important to note that some patients and clinicians will choose to continue wearing masks for various personal or clinical reasons. While effective in reducing transmission of the coronavirus, masks have created challenges in assessing patients’ affective states, which impacts the accuracy of diagnosis and treatment. This article discusses strategies for assessing affect in patients wearing face masks.
How masks complicate assessing affect
One obvious challenge masks present is they prevent clinicians from seeing their patients’ facial expressions. Face masks cover the mouth, nose, and cheeks, all of which are involved in communicating emotions. As a result, clinicians may miss important cues that could inform their assessment of a patient’s affect. For example, when a masked patient is smiling, it is difficult to determine whether their smile is genuine or forced. A study that evaluated the interpretation of 6 emotions (angry, disgusted, fearful, happy, neutral, and sad) in masked patients found that emotion recognition was significantly reduced for all emotions except for fearful and neutral faces.1
Another challenge is the potential for misinterpretation. Health care professionals may rely more heavily on nonverbal cues, such as body language, to interpret a patient’s affect. However, these cues can be influenced by other factors, such as cultural differences and individual variations in communication style. Culture is a key component in assessing nonverbal emotion reading cues.2
Strategies to overcome these challenges
There are several strategies clinicians can use to overcome the difficulties of assessing affect while a patient is wearing a mask:
Focus on other nonverbal cues, such as a patient’s posture and hand gestures. Verbal cues—such as tone of voice, choice of words, and voice inflection—can also provide valuable insights. For example, a patient who speaks in a hesitant or monotone voice may be experiencing anxiety or depression. Clinicians can ask open-ended questions, encouraging patients to expand on their emotions and provide further information about their affect.
Maintain eye contact. Eye contact is an essential component of nonverbal communication. The eyes are “the window of the soul” and can convey various emotions including happiness, sadness, fear, anger, surprise, trust, interest, and empathy. Maintaining eye contact is crucial for building positive relationships with patients, and learning to smile with your eyes (smize) can help build rapport.
Take advantage of technology. Clinicians can leverage telemedicine to assess affect. Telemedicine platforms, which have become increasingly popular during the COVID-19 pandemic, allow clinicians to monitor patients remotely and observe nonverbal cues. Virtual reality technology can also help by documenting physiological responses such as heart rate and skin conductance.
Use standardized assessment tools, as these instruments can aid in assessing affect. For example, the Patient Health Questionnaire-9 and Generalized Anxiety Disorder 7-item scale are standardized questionnaires assessing depression and anxiety, respectively. Administering these tools to patients wearing a face mask can provide information about their affective state.
Although the guidelines for masking in hospitals and other health care settings have been revised and face masks are no longer mandatory, it is important to note that some patients and clinicians will choose to continue wearing masks for various personal or clinical reasons. While effective in reducing transmission of the coronavirus, masks have created challenges in assessing patients’ affective states, which impacts the accuracy of diagnosis and treatment. This article discusses strategies for assessing affect in patients wearing face masks.
How masks complicate assessing affect
One obvious challenge masks present is they prevent clinicians from seeing their patients’ facial expressions. Face masks cover the mouth, nose, and cheeks, all of which are involved in communicating emotions. As a result, clinicians may miss important cues that could inform their assessment of a patient’s affect. For example, when a masked patient is smiling, it is difficult to determine whether their smile is genuine or forced. A study that evaluated the interpretation of 6 emotions (angry, disgusted, fearful, happy, neutral, and sad) in masked patients found that emotion recognition was significantly reduced for all emotions except for fearful and neutral faces.1
Another challenge is the potential for misinterpretation. Health care professionals may rely more heavily on nonverbal cues, such as body language, to interpret a patient’s affect. However, these cues can be influenced by other factors, such as cultural differences and individual variations in communication style. Culture is a key component in assessing nonverbal emotion reading cues.2
Strategies to overcome these challenges
There are several strategies clinicians can use to overcome the difficulties of assessing affect while a patient is wearing a mask:
Focus on other nonverbal cues, such as a patient’s posture and hand gestures. Verbal cues—such as tone of voice, choice of words, and voice inflection—can also provide valuable insights. For example, a patient who speaks in a hesitant or monotone voice may be experiencing anxiety or depression. Clinicians can ask open-ended questions, encouraging patients to expand on their emotions and provide further information about their affect.
Maintain eye contact. Eye contact is an essential component of nonverbal communication. The eyes are “the window of the soul” and can convey various emotions including happiness, sadness, fear, anger, surprise, trust, interest, and empathy. Maintaining eye contact is crucial for building positive relationships with patients, and learning to smile with your eyes (smize) can help build rapport.
Take advantage of technology. Clinicians can leverage telemedicine to assess affect. Telemedicine platforms, which have become increasingly popular during the COVID-19 pandemic, allow clinicians to monitor patients remotely and observe nonverbal cues. Virtual reality technology can also help by documenting physiological responses such as heart rate and skin conductance.
Use standardized assessment tools, as these instruments can aid in assessing affect. For example, the Patient Health Questionnaire-9 and Generalized Anxiety Disorder 7-item scale are standardized questionnaires assessing depression and anxiety, respectively. Administering these tools to patients wearing a face mask can provide information about their affective state.
1. Carbon CC. Wearing face masks strongly confuses counterparts in reading emotions. Front Psychol. 2020;11:566886. doi:10.3389/fpsyg.2020.566886
2. Yuki M, Maddux WW, Masuda T. Are the windows to the soul the same in the East and West? Cultural differences in using the eyes and mouth as cues to recognize emotions in Japan and the United States. J Exp Soc Psychol. 2007;43(2):303-311.
1. Carbon CC. Wearing face masks strongly confuses counterparts in reading emotions. Front Psychol. 2020;11:566886. doi:10.3389/fpsyg.2020.566886
2. Yuki M, Maddux WW, Masuda T. Are the windows to the soul the same in the East and West? Cultural differences in using the eyes and mouth as cues to recognize emotions in Japan and the United States. J Exp Soc Psychol. 2007;43(2):303-311.
Homelessness in urban areas: The role of mental illness and need for collaboration
Editor’s note: Readers’ Forum is a department for correspondence from readers that is not in response to articles published in
As an emergency department (ED) psychiatrist with 25 years of experience working in a large city, I am growing increasingly concerned about the escalating number of individuals experiencing homelessness in urban areas.
Homelessness remains a critical issue across the United States. The news reports from major urban areas are startling. In my own practice, I encounter approximately 10,000 patients annually, and at least one-half of them are homeless. Additionally, 75% of these patients who are homeless experience addiction, and many have lost all social support. Due to overcrowding at our area’s shelters, they resort to using the ED as a shelter because most of our shelters are overcrowded. This situation has caused an overwhelming overload in the ED and left staff disheartened and difficult to retain.
The relationship between mental illness and homelessness is complex and multifaceted. Research suggests that up to one-third of individuals who are homeless have serious mental illness.1 Mental illness can contribute to homelessness by impeding individuals’ ability to maintain employment, housing, and social relationships. Conversely, homelessness can worsen mental illness (especially in younger individuals, who are most vulnerable) by exposing individuals to traumatic experiences, substance abuse, and other stressors.2
One approach to effectively address homelessness in urban areas is provide supportive housing that incorporates access to mental health services. Research has demonstrated that offering stable housing and mental health services to individuals experiencing homelessness can significantly improve their mental and physical health and reduce their reliance on costly emergency services.3,4
Collaboration between the health care system and government is also essential. By working together, the health care system and government can develop comprehensive strategies, allocate resources, and implement interventions that address the physical and mental health needs of individuals who are homeless and provide them with the necessary support and services. This collaboration is essential to create sustainable solutions and make a meaningful impact in combating homelessness.5
Addressing homelessness in urban areas requires a comprehensive approach that recognizes the critical role of mental illness and necessity for collaborative solutions. While our ED has implemented certain measures, such as allowing patients to remain on 23-hour holds to prevent immediate re-admission, additional interventions are needed. These include expanding shelters and transitional housing programs, which are currently in short supply, and developing street medicine programs to meet individuals where they are and improve compliance with medications. By implementing these strategies, we can help minimize the impact of homelessness on individuals with mental illness and enhance the health and well-being of individuals experiencing homelessness.
1. Folsom DP, Hawthorne W, Lindamer L, et al. Prevalence and risk factors for homelessness and utilization of mental health services among 10,340 patients with serious mental illness in a large public mental health system. Am J Psychiatry. 2005;162(2):370-376. doi:10.1176/appi.ajp.162.2.370
2. Davis JP, Diguiseppi G, De Leon J, et al. Understanding pathways between PTSD, homelessness, and substance use among adolescents. Psychol Addict Behav. 2019;33(5):467-476. doi:10.1037/adb0000488
3. Larimer ME, Malone DK, Garner MD, et al. Health care and public service use and costs before and after provision of housing for chronically homeless persons with severe alcohol problems. JAMA. 2009;301(13):1349-1357. doi:10.1001/jama.2009.414
4. Wolitski RJ, Kidder DP, Pals SL, et al; Housing and Health Study Team. Randomized trial of the effects of housing assistance on the health and risk behaviors of homeless and unstably housed people living with HIV. AIDS Behav. 2010;14(3):493-503. doi:10.1007/s10461-009-9643-x
5. Sleet DA, Francescutti LH. Homelessness and public health: a focus on strategies and solutions. Int J Environ Res Public Health. 2021;18(21):11660. doi:10.3390/ijerph182111660
Editor’s note: Readers’ Forum is a department for correspondence from readers that is not in response to articles published in
As an emergency department (ED) psychiatrist with 25 years of experience working in a large city, I am growing increasingly concerned about the escalating number of individuals experiencing homelessness in urban areas.
Homelessness remains a critical issue across the United States. The news reports from major urban areas are startling. In my own practice, I encounter approximately 10,000 patients annually, and at least one-half of them are homeless. Additionally, 75% of these patients who are homeless experience addiction, and many have lost all social support. Due to overcrowding at our area’s shelters, they resort to using the ED as a shelter because most of our shelters are overcrowded. This situation has caused an overwhelming overload in the ED and left staff disheartened and difficult to retain.
The relationship between mental illness and homelessness is complex and multifaceted. Research suggests that up to one-third of individuals who are homeless have serious mental illness.1 Mental illness can contribute to homelessness by impeding individuals’ ability to maintain employment, housing, and social relationships. Conversely, homelessness can worsen mental illness (especially in younger individuals, who are most vulnerable) by exposing individuals to traumatic experiences, substance abuse, and other stressors.2
One approach to effectively address homelessness in urban areas is provide supportive housing that incorporates access to mental health services. Research has demonstrated that offering stable housing and mental health services to individuals experiencing homelessness can significantly improve their mental and physical health and reduce their reliance on costly emergency services.3,4
Collaboration between the health care system and government is also essential. By working together, the health care system and government can develop comprehensive strategies, allocate resources, and implement interventions that address the physical and mental health needs of individuals who are homeless and provide them with the necessary support and services. This collaboration is essential to create sustainable solutions and make a meaningful impact in combating homelessness.5
Addressing homelessness in urban areas requires a comprehensive approach that recognizes the critical role of mental illness and necessity for collaborative solutions. While our ED has implemented certain measures, such as allowing patients to remain on 23-hour holds to prevent immediate re-admission, additional interventions are needed. These include expanding shelters and transitional housing programs, which are currently in short supply, and developing street medicine programs to meet individuals where they are and improve compliance with medications. By implementing these strategies, we can help minimize the impact of homelessness on individuals with mental illness and enhance the health and well-being of individuals experiencing homelessness.
Editor’s note: Readers’ Forum is a department for correspondence from readers that is not in response to articles published in
As an emergency department (ED) psychiatrist with 25 years of experience working in a large city, I am growing increasingly concerned about the escalating number of individuals experiencing homelessness in urban areas.
Homelessness remains a critical issue across the United States. The news reports from major urban areas are startling. In my own practice, I encounter approximately 10,000 patients annually, and at least one-half of them are homeless. Additionally, 75% of these patients who are homeless experience addiction, and many have lost all social support. Due to overcrowding at our area’s shelters, they resort to using the ED as a shelter because most of our shelters are overcrowded. This situation has caused an overwhelming overload in the ED and left staff disheartened and difficult to retain.
The relationship between mental illness and homelessness is complex and multifaceted. Research suggests that up to one-third of individuals who are homeless have serious mental illness.1 Mental illness can contribute to homelessness by impeding individuals’ ability to maintain employment, housing, and social relationships. Conversely, homelessness can worsen mental illness (especially in younger individuals, who are most vulnerable) by exposing individuals to traumatic experiences, substance abuse, and other stressors.2
One approach to effectively address homelessness in urban areas is provide supportive housing that incorporates access to mental health services. Research has demonstrated that offering stable housing and mental health services to individuals experiencing homelessness can significantly improve their mental and physical health and reduce their reliance on costly emergency services.3,4
Collaboration between the health care system and government is also essential. By working together, the health care system and government can develop comprehensive strategies, allocate resources, and implement interventions that address the physical and mental health needs of individuals who are homeless and provide them with the necessary support and services. This collaboration is essential to create sustainable solutions and make a meaningful impact in combating homelessness.5
Addressing homelessness in urban areas requires a comprehensive approach that recognizes the critical role of mental illness and necessity for collaborative solutions. While our ED has implemented certain measures, such as allowing patients to remain on 23-hour holds to prevent immediate re-admission, additional interventions are needed. These include expanding shelters and transitional housing programs, which are currently in short supply, and developing street medicine programs to meet individuals where they are and improve compliance with medications. By implementing these strategies, we can help minimize the impact of homelessness on individuals with mental illness and enhance the health and well-being of individuals experiencing homelessness.
1. Folsom DP, Hawthorne W, Lindamer L, et al. Prevalence and risk factors for homelessness and utilization of mental health services among 10,340 patients with serious mental illness in a large public mental health system. Am J Psychiatry. 2005;162(2):370-376. doi:10.1176/appi.ajp.162.2.370
2. Davis JP, Diguiseppi G, De Leon J, et al. Understanding pathways between PTSD, homelessness, and substance use among adolescents. Psychol Addict Behav. 2019;33(5):467-476. doi:10.1037/adb0000488
3. Larimer ME, Malone DK, Garner MD, et al. Health care and public service use and costs before and after provision of housing for chronically homeless persons with severe alcohol problems. JAMA. 2009;301(13):1349-1357. doi:10.1001/jama.2009.414
4. Wolitski RJ, Kidder DP, Pals SL, et al; Housing and Health Study Team. Randomized trial of the effects of housing assistance on the health and risk behaviors of homeless and unstably housed people living with HIV. AIDS Behav. 2010;14(3):493-503. doi:10.1007/s10461-009-9643-x
5. Sleet DA, Francescutti LH. Homelessness and public health: a focus on strategies and solutions. Int J Environ Res Public Health. 2021;18(21):11660. doi:10.3390/ijerph182111660
1. Folsom DP, Hawthorne W, Lindamer L, et al. Prevalence and risk factors for homelessness and utilization of mental health services among 10,340 patients with serious mental illness in a large public mental health system. Am J Psychiatry. 2005;162(2):370-376. doi:10.1176/appi.ajp.162.2.370
2. Davis JP, Diguiseppi G, De Leon J, et al. Understanding pathways between PTSD, homelessness, and substance use among adolescents. Psychol Addict Behav. 2019;33(5):467-476. doi:10.1037/adb0000488
3. Larimer ME, Malone DK, Garner MD, et al. Health care and public service use and costs before and after provision of housing for chronically homeless persons with severe alcohol problems. JAMA. 2009;301(13):1349-1357. doi:10.1001/jama.2009.414
4. Wolitski RJ, Kidder DP, Pals SL, et al; Housing and Health Study Team. Randomized trial of the effects of housing assistance on the health and risk behaviors of homeless and unstably housed people living with HIV. AIDS Behav. 2010;14(3):493-503. doi:10.1007/s10461-009-9643-x
5. Sleet DA, Francescutti LH. Homelessness and public health: a focus on strategies and solutions. Int J Environ Res Public Health. 2021;18(21):11660. doi:10.3390/ijerph182111660
More on an asymmetric life, transient global amnesia
More on an asymmetric life
I enjoy receiving
Too often, families bear the burden of an individual’s hyperfocused pursuits. I hope your wife has been able to pursue her occupation with the same zeal and commitment. We have all read biographies of driven individuals and, unfortunately, someone pays the price for another’s success. For every Steve Jobs, there is a Lisa Jobs.
If we were surgeons, I would applaud your essay. However, we are psychiatrists. If anything, we balance out the reductionist forces in medicine. When every other physician claims a cure with medications or procedures, we look at all aspects of the patient’s life to find the appropriate treatment. At least that’s what we should be doing.
I was part of the first class of residents to work under the 80-hours-per-week restrictions. I was grateful for the extra time to rest, exercise, and spend time with my wife. The 80-hour restrictions improved resident wellness and had no impact on patient care. There are intangible benefits of diverting the mind from a chosen pursuit (such as creativity).
There is no doubt that becoming number 1 in any field requires a tremendous amount of determination, sacrifice, and effort. But not everyone gets to be first. Our society’s single-minded focus on being the best has had a major impact on mental health, especially for children. I hope you can address that in a future editorial.
Sudhir Nagaraja, DO, MS
Fredericksburg, Virginia
Dr. Nasrallah responds
Thank you for your letter about my editorial. You obviously believe in leading a balanced life, and that’s fine if you so choose. I described why I decided at an early age to lead an intensive, “purpose-driven life,” which requires investing much more time than others do, to achieve my lofty goals and excel in my area of expertise (academic psychiatry). It is really a “calling,” and those who score an extraordinary achievement (a moonshot) in their life, including Olympic gold medalists, entrepreneurs, inventors, or Nobel laureates, must do exactly what I do. I am not urging anyone to do what I have chosen to do in my life. Everyone defines for themselves what constitutes the pursuit of happiness.
You mentioned my wife. Let me assert that she is highly successful as a mother and as a research psychologist. She is my extremely valuable life partner and very supportive of what I do. I am fortunate to have chosen well!
Continue to: More on transient global amnesia
More on transient global amnesia
Your recent article on transient global amnesia (TGA) (“Transient global amnesia: Psychiatric precipitants, features, and comorbidities,”
I witnessed TGA, experienced by my brother, while on a surf trip. After bodyboarding for about an hour in cold water, wearing a full wet suit and hood, he met me on the beach. He recognized me and knew my name but had no idea where we were, how we got there, or other events from earlier that morning. There was no stressor, just the usual surfing excitement. We went to a local emergency department, where the physical examination, usual laboratory tests, and neuroimaging were normal. After approximately 5 hours, he began to fully recall recent events. Ten years later, there has been no recurrence. The only change in his surfing habits has been to avoid using a hood with neck coverage.
In 2022, Papadis et al1 described a case of concurrent Takotsubo cardiomyopathy and TGA, noting that cardiovascular dysfunction and neurologic dysfunction may be provoked by an emotional or stressful situation. The interesting observations of capture myopathy from animal literature appear similar to human reactions to trauma.1-3
Case reports of scopolamine intoxication have been linked to TGA. Severe memory disturbances, characteristics of dry mouth, blurred vision, and tachycardia were evident. Certain South American plant extracts popularly known as “Burundanga” have anticholinergic effects. Severe anterograde amnesia and submissiveness represent the 2 most notorious clinical signs of Burundanga intoxication.4
As one reviews single and groups of case studies, several things stand out. The hallmark of TGA is the sudden inability to make new memories, which resolves in a few hours. The brief and isolated dysfunction is what distinguishes this condition from most episodic disorders, but a clinician should not prognosticate too much without screening for ischemic or metabolic disturbance. Common associated precursors include Valsalva-associated activities, emotional stress with anxiety, acute pain, cold water immersion, static neck posture, and age older than 55.5,6
Neuropsychiatric disorders involve the neuron and its connections. Major reflexes automate the processes of the “neurocardiac” axis. The vasovagal reflex (Barcroft/Edholm reflex), diving reflex, baroreceptor reflex, Cushing reflex, and others depend upon the conversion of a mechanical stimulus to neurotransmission. The reflexes have sensors, afferent paths, a central processing, and efferent paths that lead to events or experiences. CNS processing is complex but the brainstem, amygdala, prefrontal cortex, and some cortical regions are involved. Neurocardiac reactions can come from pathologic events, including ischemia, metabolic disturbance, pain signals, or emotional effects within the axis.7-11
Understanding neurocardiac reflexes may help our progress with challenging clinical conditions, such as chronic pain, trauma, and cognitive impairment. The broad use of vagus nerve stimulation is one indicator of the power of this focus.12-19 Lewis20 suggested increased susceptibility to retrograde jugular venous flow could cause regional brain ischemia, resulting in TGA. The competency of jugular venous valves during the Valsalva maneuver could be assessed with Doppler ultrasound. Abnormalities could be managed, and results assessed.20,21 Vascular shunting from memory regions in the brain to essential neurocardiac control areas should be considered.
Cholinergic processes are active in the parasympathetic nervous system, sustained attention, working memory, executive functions, and mood. Increased central cholinergic activity may lead to depression. Scopolamine, in its therapeutic range, has antidepressant effects but in toxic doses is a dissociative agent.22,23 While cholinesterase inhibitors are used in Alzheimer disease, cholinergic agonists have yet to play a large role in general psychiatry or functional neurology.
TGA continues to provide a window into memory, functional disorders, psychological defenses, and adaptive neurocardiac processes. Continued clinical care and research might include gradual adaptation to cold water immersion, caution with the Valsalva maneuver, cholinergic support, managing the trapped response, avoiding interference with normal jugular flow, and evaluation for jugular venous insufficiency.
Because a variety of medical procedures can trigger TGA, health care professionals in many fields need to understand this symptom complex.24-27 Thanks to the authors for raising the awareness of TGA for psychiatrists.
Mark Chandler, MD
Durham, North Carolina
References
1. Papadis A, Svab S, Brugger N, et al. “Broken heart” and “broken brain”: which connection? Cardiol Res. 2022;13(1):65-70. doi:10.14740/cr1336
2. Blumstein DT, Buckner J, Shah S, et al. The evolution of capture myopathy in hooved mammals: a model for human stress cardiomyopathy? Evol Med Public Health. 2015;2015(1):195-203. doi:10.1093/emph/eov015
3. Seguel M, Paredes E, Pavés H, et al. Capture-induced stress cardiomyopathy in South American fur seal pups (Arctophoca australis gracilis). Marine Mammal Science. 2014;30(3): 1149-1157. https://doi.org/10.1111/mms.12079
4. Ardila A, Moreno C. Scopolamine intoxication as a model of transient global amnesia. Brain Cogn. 1991;15(2):236-245. doi:10.1016/0278-2626(91)90028-7
5. Bartsch T, Deuschl G. Transient global amnesia: functional anatomy and clinical implications. Lancet Neurol. 2010;9(2):205-214. doi:10.1016/S1474-4422(09)70344-8
6. Spiegel DR, Smith J, Wade RR, et al. Transient global amnesia: current perspectives. Neuropsychiatr Dis Treat. 2017;13:2691-2703. doi:10.2147/NDT.S130710
7. Yartsev A. Cardiac reflexes. August 15, 2020. Updated May 19, 2023. Accessed June 12, 2023. https://derangedphysiology.com/main/cicm-primary-exam/required-reading/cardiovascular-system/Chapter%20491/cardiac-reflexes
8. Lemaitre F, Chowdhury T, Schaller B. The trigeminocardiac reflex - a comparison with the diving reflex in humans. Arch Med Sci. 2015;11(2):419-426. doi:10.5114/aoms.2015.50974
9. Lindholm P, Lundgren CE. The physiology and pathophysiology of human breath-hold diving. J Appl Physiol (1985). 2009;106(1):284-292. doi:10.1152/japplphysiol.90991.2008
10. Tansey EA, Johnson CD. Recent advances in thermoregulation. Adv Physiol Educ. 2015;39(3):139-148. doi:10.1152/advan.00126.2014
11. Alboni P, Alboni M. Vasovagal syncope as a manifestation of an evolutionary selected trait. J Atr Fibrillation. 2014;7(2):1035. doi:10.4022/jafib.1035
12. Badran BW, Austelle CW. The future is noninvasive: a brief review of the evolution and clinical utility of vagus nerve stimulation. Focus (Am Psychiatr Publ). 2022;20(1):3-7. doi:10.1176/appi.focus.20210023
13. Suarez-Roca H, Mamoun N, Sigurdson MI, et al. Baroreceptor modulation of the cardiovascular system, pain, consciousness, and cognition. Compr Physiol. 2021;11(2):1373-1423. doi:10.1002/cphy.c190038
14. Pinna T, Edwards DJ. A systematic review of associations between interoception, vagal tone, and emotional regulation: potential applications for mental health, wellbeing, psychological flexibility, and chronic conditions. Front Psychol. 2020;11:1792. doi:10.3389/fpsyg.2020.01792
15. Howland RH. Vagus nerve stimulation. Curr Behav Neurosci Rep. 2014 Jun;1(2):64-73. doi:10.1007/s40473-014-0010-5
16. Panneton WM, Gan Q. The mammalian diving response: inroads to its neural control. Front Neurosci. 2020;14:524. doi:10.3389/fnins.2020.00524
17. Khurana RK, Wu R. The cold face test: a non-baroreflex mediated test of cardiac vagal function. Clin Auton Res. 2006;16(3):202-207. doi:10.1007/s10286-006-0332-9
18. Montirosso R, Provenzi L, Tronick E, et al. Vagal tone as a biomarker of long-term memory for a stressful social event at 4 months. Dev Psychobiol. 2014;56(7):1564-1574. doi:10.1002/dev.21251
19. Hansen AL, Johnsen BH, Thayer JF. Vagal influence on working memory and attention. Int J Psychophysiol. 2003;48(3):263-274. doi:10.1016/s0167-8760(03)00073-4
20. Lewis SL. Aetiology of transient global amnesia. Lancet. 1998;352(9125):397-399. doi:10.1016/S0140-6736(98)01442-1
21. Han K, Chao AC, Chang FC, et al. Obstruction of venous drainage linked to transient global amnesia. PLoS One. 2015;10(7):e0132893. doi:10.1371/journal.pone.0132893
22. Picciotto MR, Higley MJ, Mineur YS. Acetylcholine as a neuromodulator: cholinergic signaling shapes nervous system function and behavior. Neuron. 2012;76(1):116-129. doi:10.1016/j.neuron.2012.08.036
23. Dulawa SC, Janowsky DS. Cholinergic regulation of mood: from basic and clinical studies to emerging therapeutics. Mol Psychiatry. 2019;24(5):694-709. doi:10.1038/s41380-018-0219-x
24. Grande LA, Loeser JD, Samii A. Recurrent transient global amnesia with intrathecal baclofen. Anesth Analg. 2008;106(4):1284-1287. doi:10.1213/ane.0b013e318165e1c6
25. Carrard J, Lambert AC, Genné D. Transient global amnesia following a whole-body cryotherapy session. BMJ Case Rep. 2017;2017:bcr2017221431. doi:10.1136/bcr-2017-221431
26. Jeong M, Kim WS, Kim AR, et al. Medical procedure-related transient global amnesia. Eur Neurol. 2018;80(1-2):42-49. doi:10.1159/000493163
27. Shah B, Hussain MW. Concussion causing transient global amnesia: further insights into pathophysiology? Neurology. 2020;95(20 Suppl 1):S16. doi:10.1212/01.wnl.0000720020.86134.9d
More on an asymmetric life
I enjoy receiving
Too often, families bear the burden of an individual’s hyperfocused pursuits. I hope your wife has been able to pursue her occupation with the same zeal and commitment. We have all read biographies of driven individuals and, unfortunately, someone pays the price for another’s success. For every Steve Jobs, there is a Lisa Jobs.
If we were surgeons, I would applaud your essay. However, we are psychiatrists. If anything, we balance out the reductionist forces in medicine. When every other physician claims a cure with medications or procedures, we look at all aspects of the patient’s life to find the appropriate treatment. At least that’s what we should be doing.
I was part of the first class of residents to work under the 80-hours-per-week restrictions. I was grateful for the extra time to rest, exercise, and spend time with my wife. The 80-hour restrictions improved resident wellness and had no impact on patient care. There are intangible benefits of diverting the mind from a chosen pursuit (such as creativity).
There is no doubt that becoming number 1 in any field requires a tremendous amount of determination, sacrifice, and effort. But not everyone gets to be first. Our society’s single-minded focus on being the best has had a major impact on mental health, especially for children. I hope you can address that in a future editorial.
Sudhir Nagaraja, DO, MS
Fredericksburg, Virginia
Dr. Nasrallah responds
Thank you for your letter about my editorial. You obviously believe in leading a balanced life, and that’s fine if you so choose. I described why I decided at an early age to lead an intensive, “purpose-driven life,” which requires investing much more time than others do, to achieve my lofty goals and excel in my area of expertise (academic psychiatry). It is really a “calling,” and those who score an extraordinary achievement (a moonshot) in their life, including Olympic gold medalists, entrepreneurs, inventors, or Nobel laureates, must do exactly what I do. I am not urging anyone to do what I have chosen to do in my life. Everyone defines for themselves what constitutes the pursuit of happiness.
You mentioned my wife. Let me assert that she is highly successful as a mother and as a research psychologist. She is my extremely valuable life partner and very supportive of what I do. I am fortunate to have chosen well!
Continue to: More on transient global amnesia
More on transient global amnesia
Your recent article on transient global amnesia (TGA) (“Transient global amnesia: Psychiatric precipitants, features, and comorbidities,”
I witnessed TGA, experienced by my brother, while on a surf trip. After bodyboarding for about an hour in cold water, wearing a full wet suit and hood, he met me on the beach. He recognized me and knew my name but had no idea where we were, how we got there, or other events from earlier that morning. There was no stressor, just the usual surfing excitement. We went to a local emergency department, where the physical examination, usual laboratory tests, and neuroimaging were normal. After approximately 5 hours, he began to fully recall recent events. Ten years later, there has been no recurrence. The only change in his surfing habits has been to avoid using a hood with neck coverage.
In 2022, Papadis et al1 described a case of concurrent Takotsubo cardiomyopathy and TGA, noting that cardiovascular dysfunction and neurologic dysfunction may be provoked by an emotional or stressful situation. The interesting observations of capture myopathy from animal literature appear similar to human reactions to trauma.1-3
Case reports of scopolamine intoxication have been linked to TGA. Severe memory disturbances, characteristics of dry mouth, blurred vision, and tachycardia were evident. Certain South American plant extracts popularly known as “Burundanga” have anticholinergic effects. Severe anterograde amnesia and submissiveness represent the 2 most notorious clinical signs of Burundanga intoxication.4
As one reviews single and groups of case studies, several things stand out. The hallmark of TGA is the sudden inability to make new memories, which resolves in a few hours. The brief and isolated dysfunction is what distinguishes this condition from most episodic disorders, but a clinician should not prognosticate too much without screening for ischemic or metabolic disturbance. Common associated precursors include Valsalva-associated activities, emotional stress with anxiety, acute pain, cold water immersion, static neck posture, and age older than 55.5,6
Neuropsychiatric disorders involve the neuron and its connections. Major reflexes automate the processes of the “neurocardiac” axis. The vasovagal reflex (Barcroft/Edholm reflex), diving reflex, baroreceptor reflex, Cushing reflex, and others depend upon the conversion of a mechanical stimulus to neurotransmission. The reflexes have sensors, afferent paths, a central processing, and efferent paths that lead to events or experiences. CNS processing is complex but the brainstem, amygdala, prefrontal cortex, and some cortical regions are involved. Neurocardiac reactions can come from pathologic events, including ischemia, metabolic disturbance, pain signals, or emotional effects within the axis.7-11
Understanding neurocardiac reflexes may help our progress with challenging clinical conditions, such as chronic pain, trauma, and cognitive impairment. The broad use of vagus nerve stimulation is one indicator of the power of this focus.12-19 Lewis20 suggested increased susceptibility to retrograde jugular venous flow could cause regional brain ischemia, resulting in TGA. The competency of jugular venous valves during the Valsalva maneuver could be assessed with Doppler ultrasound. Abnormalities could be managed, and results assessed.20,21 Vascular shunting from memory regions in the brain to essential neurocardiac control areas should be considered.
Cholinergic processes are active in the parasympathetic nervous system, sustained attention, working memory, executive functions, and mood. Increased central cholinergic activity may lead to depression. Scopolamine, in its therapeutic range, has antidepressant effects but in toxic doses is a dissociative agent.22,23 While cholinesterase inhibitors are used in Alzheimer disease, cholinergic agonists have yet to play a large role in general psychiatry or functional neurology.
TGA continues to provide a window into memory, functional disorders, psychological defenses, and adaptive neurocardiac processes. Continued clinical care and research might include gradual adaptation to cold water immersion, caution with the Valsalva maneuver, cholinergic support, managing the trapped response, avoiding interference with normal jugular flow, and evaluation for jugular venous insufficiency.
Because a variety of medical procedures can trigger TGA, health care professionals in many fields need to understand this symptom complex.24-27 Thanks to the authors for raising the awareness of TGA for psychiatrists.
Mark Chandler, MD
Durham, North Carolina
References
1. Papadis A, Svab S, Brugger N, et al. “Broken heart” and “broken brain”: which connection? Cardiol Res. 2022;13(1):65-70. doi:10.14740/cr1336
2. Blumstein DT, Buckner J, Shah S, et al. The evolution of capture myopathy in hooved mammals: a model for human stress cardiomyopathy? Evol Med Public Health. 2015;2015(1):195-203. doi:10.1093/emph/eov015
3. Seguel M, Paredes E, Pavés H, et al. Capture-induced stress cardiomyopathy in South American fur seal pups (Arctophoca australis gracilis). Marine Mammal Science. 2014;30(3): 1149-1157. https://doi.org/10.1111/mms.12079
4. Ardila A, Moreno C. Scopolamine intoxication as a model of transient global amnesia. Brain Cogn. 1991;15(2):236-245. doi:10.1016/0278-2626(91)90028-7
5. Bartsch T, Deuschl G. Transient global amnesia: functional anatomy and clinical implications. Lancet Neurol. 2010;9(2):205-214. doi:10.1016/S1474-4422(09)70344-8
6. Spiegel DR, Smith J, Wade RR, et al. Transient global amnesia: current perspectives. Neuropsychiatr Dis Treat. 2017;13:2691-2703. doi:10.2147/NDT.S130710
7. Yartsev A. Cardiac reflexes. August 15, 2020. Updated May 19, 2023. Accessed June 12, 2023. https://derangedphysiology.com/main/cicm-primary-exam/required-reading/cardiovascular-system/Chapter%20491/cardiac-reflexes
8. Lemaitre F, Chowdhury T, Schaller B. The trigeminocardiac reflex - a comparison with the diving reflex in humans. Arch Med Sci. 2015;11(2):419-426. doi:10.5114/aoms.2015.50974
9. Lindholm P, Lundgren CE. The physiology and pathophysiology of human breath-hold diving. J Appl Physiol (1985). 2009;106(1):284-292. doi:10.1152/japplphysiol.90991.2008
10. Tansey EA, Johnson CD. Recent advances in thermoregulation. Adv Physiol Educ. 2015;39(3):139-148. doi:10.1152/advan.00126.2014
11. Alboni P, Alboni M. Vasovagal syncope as a manifestation of an evolutionary selected trait. J Atr Fibrillation. 2014;7(2):1035. doi:10.4022/jafib.1035
12. Badran BW, Austelle CW. The future is noninvasive: a brief review of the evolution and clinical utility of vagus nerve stimulation. Focus (Am Psychiatr Publ). 2022;20(1):3-7. doi:10.1176/appi.focus.20210023
13. Suarez-Roca H, Mamoun N, Sigurdson MI, et al. Baroreceptor modulation of the cardiovascular system, pain, consciousness, and cognition. Compr Physiol. 2021;11(2):1373-1423. doi:10.1002/cphy.c190038
14. Pinna T, Edwards DJ. A systematic review of associations between interoception, vagal tone, and emotional regulation: potential applications for mental health, wellbeing, psychological flexibility, and chronic conditions. Front Psychol. 2020;11:1792. doi:10.3389/fpsyg.2020.01792
15. Howland RH. Vagus nerve stimulation. Curr Behav Neurosci Rep. 2014 Jun;1(2):64-73. doi:10.1007/s40473-014-0010-5
16. Panneton WM, Gan Q. The mammalian diving response: inroads to its neural control. Front Neurosci. 2020;14:524. doi:10.3389/fnins.2020.00524
17. Khurana RK, Wu R. The cold face test: a non-baroreflex mediated test of cardiac vagal function. Clin Auton Res. 2006;16(3):202-207. doi:10.1007/s10286-006-0332-9
18. Montirosso R, Provenzi L, Tronick E, et al. Vagal tone as a biomarker of long-term memory for a stressful social event at 4 months. Dev Psychobiol. 2014;56(7):1564-1574. doi:10.1002/dev.21251
19. Hansen AL, Johnsen BH, Thayer JF. Vagal influence on working memory and attention. Int J Psychophysiol. 2003;48(3):263-274. doi:10.1016/s0167-8760(03)00073-4
20. Lewis SL. Aetiology of transient global amnesia. Lancet. 1998;352(9125):397-399. doi:10.1016/S0140-6736(98)01442-1
21. Han K, Chao AC, Chang FC, et al. Obstruction of venous drainage linked to transient global amnesia. PLoS One. 2015;10(7):e0132893. doi:10.1371/journal.pone.0132893
22. Picciotto MR, Higley MJ, Mineur YS. Acetylcholine as a neuromodulator: cholinergic signaling shapes nervous system function and behavior. Neuron. 2012;76(1):116-129. doi:10.1016/j.neuron.2012.08.036
23. Dulawa SC, Janowsky DS. Cholinergic regulation of mood: from basic and clinical studies to emerging therapeutics. Mol Psychiatry. 2019;24(5):694-709. doi:10.1038/s41380-018-0219-x
24. Grande LA, Loeser JD, Samii A. Recurrent transient global amnesia with intrathecal baclofen. Anesth Analg. 2008;106(4):1284-1287. doi:10.1213/ane.0b013e318165e1c6
25. Carrard J, Lambert AC, Genné D. Transient global amnesia following a whole-body cryotherapy session. BMJ Case Rep. 2017;2017:bcr2017221431. doi:10.1136/bcr-2017-221431
26. Jeong M, Kim WS, Kim AR, et al. Medical procedure-related transient global amnesia. Eur Neurol. 2018;80(1-2):42-49. doi:10.1159/000493163
27. Shah B, Hussain MW. Concussion causing transient global amnesia: further insights into pathophysiology? Neurology. 2020;95(20 Suppl 1):S16. doi:10.1212/01.wnl.0000720020.86134.9d
More on an asymmetric life
I enjoy receiving
Too often, families bear the burden of an individual’s hyperfocused pursuits. I hope your wife has been able to pursue her occupation with the same zeal and commitment. We have all read biographies of driven individuals and, unfortunately, someone pays the price for another’s success. For every Steve Jobs, there is a Lisa Jobs.
If we were surgeons, I would applaud your essay. However, we are psychiatrists. If anything, we balance out the reductionist forces in medicine. When every other physician claims a cure with medications or procedures, we look at all aspects of the patient’s life to find the appropriate treatment. At least that’s what we should be doing.
I was part of the first class of residents to work under the 80-hours-per-week restrictions. I was grateful for the extra time to rest, exercise, and spend time with my wife. The 80-hour restrictions improved resident wellness and had no impact on patient care. There are intangible benefits of diverting the mind from a chosen pursuit (such as creativity).
There is no doubt that becoming number 1 in any field requires a tremendous amount of determination, sacrifice, and effort. But not everyone gets to be first. Our society’s single-minded focus on being the best has had a major impact on mental health, especially for children. I hope you can address that in a future editorial.
Sudhir Nagaraja, DO, MS
Fredericksburg, Virginia
Dr. Nasrallah responds
Thank you for your letter about my editorial. You obviously believe in leading a balanced life, and that’s fine if you so choose. I described why I decided at an early age to lead an intensive, “purpose-driven life,” which requires investing much more time than others do, to achieve my lofty goals and excel in my area of expertise (academic psychiatry). It is really a “calling,” and those who score an extraordinary achievement (a moonshot) in their life, including Olympic gold medalists, entrepreneurs, inventors, or Nobel laureates, must do exactly what I do. I am not urging anyone to do what I have chosen to do in my life. Everyone defines for themselves what constitutes the pursuit of happiness.
You mentioned my wife. Let me assert that she is highly successful as a mother and as a research psychologist. She is my extremely valuable life partner and very supportive of what I do. I am fortunate to have chosen well!
Continue to: More on transient global amnesia
More on transient global amnesia
Your recent article on transient global amnesia (TGA) (“Transient global amnesia: Psychiatric precipitants, features, and comorbidities,”
I witnessed TGA, experienced by my brother, while on a surf trip. After bodyboarding for about an hour in cold water, wearing a full wet suit and hood, he met me on the beach. He recognized me and knew my name but had no idea where we were, how we got there, or other events from earlier that morning. There was no stressor, just the usual surfing excitement. We went to a local emergency department, where the physical examination, usual laboratory tests, and neuroimaging were normal. After approximately 5 hours, he began to fully recall recent events. Ten years later, there has been no recurrence. The only change in his surfing habits has been to avoid using a hood with neck coverage.
In 2022, Papadis et al1 described a case of concurrent Takotsubo cardiomyopathy and TGA, noting that cardiovascular dysfunction and neurologic dysfunction may be provoked by an emotional or stressful situation. The interesting observations of capture myopathy from animal literature appear similar to human reactions to trauma.1-3
Case reports of scopolamine intoxication have been linked to TGA. Severe memory disturbances, characteristics of dry mouth, blurred vision, and tachycardia were evident. Certain South American plant extracts popularly known as “Burundanga” have anticholinergic effects. Severe anterograde amnesia and submissiveness represent the 2 most notorious clinical signs of Burundanga intoxication.4
As one reviews single and groups of case studies, several things stand out. The hallmark of TGA is the sudden inability to make new memories, which resolves in a few hours. The brief and isolated dysfunction is what distinguishes this condition from most episodic disorders, but a clinician should not prognosticate too much without screening for ischemic or metabolic disturbance. Common associated precursors include Valsalva-associated activities, emotional stress with anxiety, acute pain, cold water immersion, static neck posture, and age older than 55.5,6
Neuropsychiatric disorders involve the neuron and its connections. Major reflexes automate the processes of the “neurocardiac” axis. The vasovagal reflex (Barcroft/Edholm reflex), diving reflex, baroreceptor reflex, Cushing reflex, and others depend upon the conversion of a mechanical stimulus to neurotransmission. The reflexes have sensors, afferent paths, a central processing, and efferent paths that lead to events or experiences. CNS processing is complex but the brainstem, amygdala, prefrontal cortex, and some cortical regions are involved. Neurocardiac reactions can come from pathologic events, including ischemia, metabolic disturbance, pain signals, or emotional effects within the axis.7-11
Understanding neurocardiac reflexes may help our progress with challenging clinical conditions, such as chronic pain, trauma, and cognitive impairment. The broad use of vagus nerve stimulation is one indicator of the power of this focus.12-19 Lewis20 suggested increased susceptibility to retrograde jugular venous flow could cause regional brain ischemia, resulting in TGA. The competency of jugular venous valves during the Valsalva maneuver could be assessed with Doppler ultrasound. Abnormalities could be managed, and results assessed.20,21 Vascular shunting from memory regions in the brain to essential neurocardiac control areas should be considered.
Cholinergic processes are active in the parasympathetic nervous system, sustained attention, working memory, executive functions, and mood. Increased central cholinergic activity may lead to depression. Scopolamine, in its therapeutic range, has antidepressant effects but in toxic doses is a dissociative agent.22,23 While cholinesterase inhibitors are used in Alzheimer disease, cholinergic agonists have yet to play a large role in general psychiatry or functional neurology.
TGA continues to provide a window into memory, functional disorders, psychological defenses, and adaptive neurocardiac processes. Continued clinical care and research might include gradual adaptation to cold water immersion, caution with the Valsalva maneuver, cholinergic support, managing the trapped response, avoiding interference with normal jugular flow, and evaluation for jugular venous insufficiency.
Because a variety of medical procedures can trigger TGA, health care professionals in many fields need to understand this symptom complex.24-27 Thanks to the authors for raising the awareness of TGA for psychiatrists.
Mark Chandler, MD
Durham, North Carolina
References
1. Papadis A, Svab S, Brugger N, et al. “Broken heart” and “broken brain”: which connection? Cardiol Res. 2022;13(1):65-70. doi:10.14740/cr1336
2. Blumstein DT, Buckner J, Shah S, et al. The evolution of capture myopathy in hooved mammals: a model for human stress cardiomyopathy? Evol Med Public Health. 2015;2015(1):195-203. doi:10.1093/emph/eov015
3. Seguel M, Paredes E, Pavés H, et al. Capture-induced stress cardiomyopathy in South American fur seal pups (Arctophoca australis gracilis). Marine Mammal Science. 2014;30(3): 1149-1157. https://doi.org/10.1111/mms.12079
4. Ardila A, Moreno C. Scopolamine intoxication as a model of transient global amnesia. Brain Cogn. 1991;15(2):236-245. doi:10.1016/0278-2626(91)90028-7
5. Bartsch T, Deuschl G. Transient global amnesia: functional anatomy and clinical implications. Lancet Neurol. 2010;9(2):205-214. doi:10.1016/S1474-4422(09)70344-8
6. Spiegel DR, Smith J, Wade RR, et al. Transient global amnesia: current perspectives. Neuropsychiatr Dis Treat. 2017;13:2691-2703. doi:10.2147/NDT.S130710
7. Yartsev A. Cardiac reflexes. August 15, 2020. Updated May 19, 2023. Accessed June 12, 2023. https://derangedphysiology.com/main/cicm-primary-exam/required-reading/cardiovascular-system/Chapter%20491/cardiac-reflexes
8. Lemaitre F, Chowdhury T, Schaller B. The trigeminocardiac reflex - a comparison with the diving reflex in humans. Arch Med Sci. 2015;11(2):419-426. doi:10.5114/aoms.2015.50974
9. Lindholm P, Lundgren CE. The physiology and pathophysiology of human breath-hold diving. J Appl Physiol (1985). 2009;106(1):284-292. doi:10.1152/japplphysiol.90991.2008
10. Tansey EA, Johnson CD. Recent advances in thermoregulation. Adv Physiol Educ. 2015;39(3):139-148. doi:10.1152/advan.00126.2014
11. Alboni P, Alboni M. Vasovagal syncope as a manifestation of an evolutionary selected trait. J Atr Fibrillation. 2014;7(2):1035. doi:10.4022/jafib.1035
12. Badran BW, Austelle CW. The future is noninvasive: a brief review of the evolution and clinical utility of vagus nerve stimulation. Focus (Am Psychiatr Publ). 2022;20(1):3-7. doi:10.1176/appi.focus.20210023
13. Suarez-Roca H, Mamoun N, Sigurdson MI, et al. Baroreceptor modulation of the cardiovascular system, pain, consciousness, and cognition. Compr Physiol. 2021;11(2):1373-1423. doi:10.1002/cphy.c190038
14. Pinna T, Edwards DJ. A systematic review of associations between interoception, vagal tone, and emotional regulation: potential applications for mental health, wellbeing, psychological flexibility, and chronic conditions. Front Psychol. 2020;11:1792. doi:10.3389/fpsyg.2020.01792
15. Howland RH. Vagus nerve stimulation. Curr Behav Neurosci Rep. 2014 Jun;1(2):64-73. doi:10.1007/s40473-014-0010-5
16. Panneton WM, Gan Q. The mammalian diving response: inroads to its neural control. Front Neurosci. 2020;14:524. doi:10.3389/fnins.2020.00524
17. Khurana RK, Wu R. The cold face test: a non-baroreflex mediated test of cardiac vagal function. Clin Auton Res. 2006;16(3):202-207. doi:10.1007/s10286-006-0332-9
18. Montirosso R, Provenzi L, Tronick E, et al. Vagal tone as a biomarker of long-term memory for a stressful social event at 4 months. Dev Psychobiol. 2014;56(7):1564-1574. doi:10.1002/dev.21251
19. Hansen AL, Johnsen BH, Thayer JF. Vagal influence on working memory and attention. Int J Psychophysiol. 2003;48(3):263-274. doi:10.1016/s0167-8760(03)00073-4
20. Lewis SL. Aetiology of transient global amnesia. Lancet. 1998;352(9125):397-399. doi:10.1016/S0140-6736(98)01442-1
21. Han K, Chao AC, Chang FC, et al. Obstruction of venous drainage linked to transient global amnesia. PLoS One. 2015;10(7):e0132893. doi:10.1371/journal.pone.0132893
22. Picciotto MR, Higley MJ, Mineur YS. Acetylcholine as a neuromodulator: cholinergic signaling shapes nervous system function and behavior. Neuron. 2012;76(1):116-129. doi:10.1016/j.neuron.2012.08.036
23. Dulawa SC, Janowsky DS. Cholinergic regulation of mood: from basic and clinical studies to emerging therapeutics. Mol Psychiatry. 2019;24(5):694-709. doi:10.1038/s41380-018-0219-x
24. Grande LA, Loeser JD, Samii A. Recurrent transient global amnesia with intrathecal baclofen. Anesth Analg. 2008;106(4):1284-1287. doi:10.1213/ane.0b013e318165e1c6
25. Carrard J, Lambert AC, Genné D. Transient global amnesia following a whole-body cryotherapy session. BMJ Case Rep. 2017;2017:bcr2017221431. doi:10.1136/bcr-2017-221431
26. Jeong M, Kim WS, Kim AR, et al. Medical procedure-related transient global amnesia. Eur Neurol. 2018;80(1-2):42-49. doi:10.1159/000493163
27. Shah B, Hussain MW. Concussion causing transient global amnesia: further insights into pathophysiology? Neurology. 2020;95(20 Suppl 1):S16. doi:10.1212/01.wnl.0000720020.86134.9d
Discontinuing Disease-Modifying Therapies in Nonactive Secondary Progressive MS:Review of the Evidence
Multiple sclerosis (MS) is an immune-mediated demyelinating disorder. There are 2 broad categories of MS: relapsing, also called active MS; and progressive MS. Unfortunately, there is no cure for MS, but disease-modifying therapies (DMTs) can help prevent relapses and new central nervous system lesions in people living with active MS. For patients with the most common type of MS, relapsing-remitting MS (RRMS), DMTs are typically continued for decades while the patient has active disease. RRMS will usually transition to secondary progressive MS (SPMS), which can present as active SPMS or nonactive SPMS. The latter is the type of MS most people with RRMS eventually experience.
A 2019 study estimated that nearly 1 million people in the United States were living with MS.1 This population estimate indicated the peak age-specific prevalence of MS was 55 to 64 years. Population data demonstrate improved mortality rates for people diagnosed with MS from 1997 to 2012 compared with prior years.2 Therefore, the management of nonactive SPMS is an increasingly significant area of need. There are currently no DMTs on the market approved for nonactive SPMS, and lifelong DMTs in these patients are neither indicated nor supported by evidence. Nevertheless, the discontinuation of DMTs in nonactive SPMS has been a long-debated topic with varied opinions on how and when to discontinue.
The 2018 American Academy of Neurology (AAN) guideline recommends that clinicians advise patients with SPMS to discontinue DMT use if they do not have ongoing relapses (or gadolinium-enhanced lesions on magnetic resonance imaging activity) or have not been ambulatory (Expanded Disability Status Scale [EDSS] ≥ 7) for ≥ 2 years.3 In recent years, there has been increased research on nonactive SPMS, specifically on discontinuation of DMTs. This clinical review assesses the recent evidence from a variety of standpoints, including the effect of discontinuing DMTs on the MS disease course and quality of life (QOL) and the perspectives of patients living with MS. Based on this evidence, a conversation guide will be presented as a framework to aid with the clinician-patient discussion on discontinuing MS DMTs.
Disease Modifying Therapies
Roos and colleagues used data from 2 large MS cohorts: MSBase and Observatoire Français de la Sclérose en Plaques (OFSEP) to compare high-efficacy vs low-efficacy DMT in both active and nonactive SPMS.4 In the active SPMS group, the strength of DMTs did not change disability progression, but high-efficacy DMTs reduced relapses better than the low-efficacy DMTs. On the other hand, the nonactive SPMS group saw no difference between DMTs in both relapse risk and disability progression. Another observational study of 221 patients with RRMS who discontinued DMTs noted that there were 2 independent predictors for the absence of relapse following DMT discontinuation: being aged > 45 years and the lack of relapse for ≥ 4 years prior to DMT discontinuation.5 Though these patients still may have been classified as RRMS, both these independent predictors for stability postdiscontinuation of DMTs are the typical characteristics of a nonactive SPMS patient.
Pathophysiology may help explain why DMT discontinuation seems to produce no adverse clinical outcomes in people with nonactive SPMS. Nonactive SPMS, which follows after RRMS, is largely correlated with age. In nonactive SPMS, there is less B and T lymphocyte migration across the blood-brain barrier. Furthermore, a lifetime of low-grade inflammation during the RRMS phase results in axonal damage and declined repair capacity, which produces the predominance of neurodegeneration in the nonactive SPMS disease process.6 This pathophysiologic difference between active and nonactive disease not only explains the different symptomatology of these MS subtypes, but also could explain why drugs that target the inflammatory processes more characteristic of active disease are not effective in nonactive SPMS.
Other recent studies explored the impact of age on DMT efficacy for patients with nonactive SPMS. A meta-analysis by Weidman and colleagues pooled trial data across multiple DMT classes in > 28,000 patients.7 The resulting regression model predicted zero efficacy of any DMT in patients who are aged > 53 years. High-efficacy DMTs only outperformed low-efficacy DMTs in people aged < 40.5 years. Another observational study by Hua and colleagues saw a similar result.8 This study included patients who discontinued DMT who were aged ≥ 60 years. The median follow-up time was 5.3 years. Of the 178 patients who discontinued DMTs, only 1 patient had a relapse. In this study, the age for participation provided a higher likelihood that patients included were in nonactive SPMS. Furthermore, the outcome reflects the typical presentation of nonactive SPMS where, despite the continuation or discontinuation of DMT, there was a lack of relapses. When comparing patients who discontinued DMTs with those who continued use, there was no significant difference in their 25-foot walk times, which is an objective marker for a more progressive symptom seen in nonactive MS.
The DISCOMS trial (NCT03073603) has been completed, but full results are not yet published. In this noninferiority trial, > 250 patients aged ≥ 55 years were assessed on a variety of outcomes, including relapses, EDSS score, and QOL. MS subtypes were considered at baseline, and subgroup analysis looking particularly at the SPMS population could provide further insight into its effect on MS course.
Quality of Life
Whether discontinuation of DMTs is worth considering in nonactive SPMS, it is also important to consider the risks and burdens associated with continuation. Medication administration burdens come with all MS DMTs whether there is the need to inject oneself, increased pill burden, or travel to an infusion clinic. The ever-rising costs of DMTs also can be a financial burden to the patient.9 All MS DMTs carry risks of adverse effects (AEs). These can range from a mild injection site reaction to severe infection, depending on the DMT used. Many of these severe AEs, such as opportunistic infections and cancer, have been associated with either an increased risk of occurrence and/or worsened outcomes in older adults who remain on DMTs, particularly moderate- to high-efficacy DMTs, such as sphingosine-1- phosphate receptor modulators, fumarates, natalizumab, alemtuzumab, cladribine, and anti-CD20 antibodies.10 In a 2019 survey of 377 patients with MS, 63.8% of respondents ranked safety as the most important reason they would consider discontinuing their DMTs.11 In addition, a real-world study comparing people with nonactive SPMS who continued DMTs vs those who discontinued found that discontinuers reported better QOL.8
Conversation Guide for Discontinuing Therapies
The 2019 survey that assessed reasons for discontinuation also asked people with nonactive SPMS whether they thought they were in a nonactive disease stage, and what was their likelihood they would stop DMTs.11 Interestingly, only 59.4% of respondents self-assessed their MS as nonactive, and just 11.9% of respondents were willing to discontinue DMTs.11 These results suggest that there may be a need for patient education about nonactive SPMS and the rationale to continue or discontinue DMTs. Thus, before broaching the topic of discontinuation, explaining the nonactive SPMS subtype is important.
Even with a good understanding of nonactive SPMS, patients may be hesitant to stop using DMTs that they previously relied on to keep their MS stable. The 2019 survey ranked physician recommendation as the third highest reason to discontinue DMTs.11 Taking the time to explain the clinical evidence for DMT discontinuation may help patients better understand a clinician’s recommendation and inspire more confidence.
Another important aspect of DMT discontinuation decision making is creating a plan for how the patient will be monitored to provide assurance if they experience a relapse. The 2019 survey asked patients what would be most important to them for their management plan after discontinuing DMT; magnetic resonance imaging and neurologic examination monitoring ranked the highest.11 The plan should include timing for follow-up appointments and imaging, providing the patient comfort in knowing their MS will be monitored and verified for the relapse stability that is expected from nonactive SPMS. In the rare case a relapse does occur, having a contingency plan and noting the possibility of restarting DMTs is an integral part of reassuring the patient that their decision to discontinue DMTs will be treated with the utmost caution and individualized to their needs.
Lastly, highlighting which aspects of MS treatment will continue to be a priority in nonactive SPMS, such as symptomatic medication management and nonpharmacologic therapy, is important for the patient to recognize that there are still opportunities to manage this phase of MS. There are many lifestyle modifications that can be considered complementary to medical management of MS at any stage of the disease. Vascular comorbidities, such as hypertension, hyperlipidemia, and diabetes, have been associated with more rapid disability progression in MS.12 Optimized management of these diseases may slow disability progression, in addition to the benefit of improved outcomes of the vascular comorbidity. Various formats of exercise have been studied in the MS population. A meta-analysis of aerobic, resistance, and combined exercise found benefits in these formats on health-related QOL.13
Many dietary strategies have been studied in MS. A recent network meta-analysis reviewed some of the more commonly studied diets, including low-fat, modified Mediterranean, ketogenic, anti-inflammatory, Paleolithic, intermittent fasting, and calorie restriction vs a usual diet.14 Although the overall quality of evidence was low, the Paleolithic and modified Mediterranean showed greater reductions in fatigue, as well as increased physical and
As with any health care decision, it is important to involve the patient in a joint decision regarding their care. This may mean giving the patient time to think about the information presented, do their own research, talk to family members or other clinicians, etc. The decision to discontinue DMT may not happen at the same appointment it is initially brought up at. It may even be reasonable to revisit the conversation later if discontinuation is not something the patient is amenable to at the time.
Conclusions
There is high-quality evidence that discontinuing DMTs in nonactive SPMS is not a major detriment to the MS disease course. Current literature also suggests that there may be benefits to discontinuation in this MS subtype in terms of QOL and meeting patient values. Additional research particularly in the nonactive SPMS population will continue to improve the knowledge and awareness of this aspect of MS DMT management. The growing evidence in this area may make discontinuation of DMT in nonactive SPMS a less-debatable topic, but it is still a major treatment decision that clinicians must thoroughly discuss with the patient to provide high-quality, patient-centered care.
1. Wallin MT, Culpepper WJ, Campbell JD, et al. The prevalence of MS in the United States: a population-based estimate using health claims data. Neurology. 2019;92(10):e1029-e1040. doi:10.1212/WNL.0000000000007035
2. Lunde HMB, Assmus J, Myhr KM, Bø L, Grytten N. Survival and cause of death in multiple sclerosis: a 60-year longitudinal population study. J Neurol Neurosurg Psychiatry. 2017;88(8):621-625. doi:10.1136/jnnp-2016-315238
3. Rae-Grant A, Day GS, Marrie RA, et al. Practice guideline recommendations summary: disease-modifying therapies for adults with multiple sclerosis: report of the Guideline Development, Dissemination, and Implementation Subcommittee of the American Academy of Neurology. Neurology. 2018;90(17):777-788. doi:10.1212/WNL.0000000000005347
4. Roos I, Leray E, Casey R, et al. Effects of high- and low-efficacy therapy in secondary progressive multiple sclerosis. Neurology. 2021;97(9):e869-e880. doi:10.1212/WNL.0000000000012354
5. Bsteh G, Feige J, Ehling R, et al. Discontinuation of disease-modifying therapies in multiple sclerosis - clinical outcome and prognostic factors. Mult Scler. 2017;23(9):1241-1248. doi:10.1177/1352458516675751
6. Musella A, Gentile A, Rizzo FR, et al. Interplay between age and neuroinflammation in multiple sclerosis: effects on motor and cognitive functions. Front Aging Neurosci. 2018;10:238. Published 2018 Aug 8. doi:10.3389/fnagi.2018.00238
7. Weideman AM, Tapia-Maltos MA, Johnson K, Greenwood M, Bielekova B. Meta-analysis of the age-dependent efficacy of multiple sclerosis treatments. Front Neurol. 2017;8:577. Published 2017 Nov 10. doi:10.3389/fneur.2017.00577
8. Hua LH, Harris H, Conway D, Thompson NR. Changes in patient-reported outcomes between continuers and discontinuers of disease modifying therapy in patients with multiple sclerosis over age 60. Mult Scler Relat Disord. 2019;30:252-256. doi:10.1016/j.msard.2019.02.028
9. San-Juan-Rodriguez A, Good CB, Heyman RA, Parekh N, Shrank WH, Hernandez I. Trends in prices, market share, and spending on self-administered disease-modifying therapies for multiple sclerosis in Medicare part D. JAMA Neurol. 2019;76(11):1386-1390. doi:10.1001/jamaneurol.2019.2711
10. Schweitzer F, Laurent S, Fink GR, et al. Age and the risks of high-efficacy disease modifying drugs in multiple sclerosis. Curr Opin Neurol. 2019;32(3):305-312. doi:10.1097/WCO.0000000000000701
11. McGinley MP, Cola PA, Fox RJ, Cohen JA, Corboy JJ, Miller D. Perspectives of individuals with multiple sclerosis on discontinuation of disease-modifying therapies. Mult Scler. 2020;26(12):1581-1589. doi:10.1177/1352458519867314
12. Marrie RA, Rudick R, Horwitz R, et al. Vascular comorbidity is associated with more rapid disability progression in multiple sclerosis. Neurology. 2010;74(13):1041-1047. doi:10.1212/WNL.0b013e3181d6b125
13. Flores VA, Šilic´ P, DuBose NG, Zheng P, Jeng B, Motl RW. Effects of aerobic, resistance, and combined exercise training on health-related quality of life in multiple sclerosis: Systematic review and meta-analysis. Mult Scler Relat Disord. 2023;75:104746. doi:10.1016/j.msard.2023.104746
14. Snetselaar LG, Cheek JJ, Fox SS, et al. Efficacy of diet on fatigue and quality of life in multiple sclerosis: a systematic review and network meta-analysis of randomized trials. Neurology. 2023;100(4):e357-e366. doi:10.1212/WNL.0000000000201371
Multiple sclerosis (MS) is an immune-mediated demyelinating disorder. There are 2 broad categories of MS: relapsing, also called active MS; and progressive MS. Unfortunately, there is no cure for MS, but disease-modifying therapies (DMTs) can help prevent relapses and new central nervous system lesions in people living with active MS. For patients with the most common type of MS, relapsing-remitting MS (RRMS), DMTs are typically continued for decades while the patient has active disease. RRMS will usually transition to secondary progressive MS (SPMS), which can present as active SPMS or nonactive SPMS. The latter is the type of MS most people with RRMS eventually experience.
A 2019 study estimated that nearly 1 million people in the United States were living with MS.1 This population estimate indicated the peak age-specific prevalence of MS was 55 to 64 years. Population data demonstrate improved mortality rates for people diagnosed with MS from 1997 to 2012 compared with prior years.2 Therefore, the management of nonactive SPMS is an increasingly significant area of need. There are currently no DMTs on the market approved for nonactive SPMS, and lifelong DMTs in these patients are neither indicated nor supported by evidence. Nevertheless, the discontinuation of DMTs in nonactive SPMS has been a long-debated topic with varied opinions on how and when to discontinue.
The 2018 American Academy of Neurology (AAN) guideline recommends that clinicians advise patients with SPMS to discontinue DMT use if they do not have ongoing relapses (or gadolinium-enhanced lesions on magnetic resonance imaging activity) or have not been ambulatory (Expanded Disability Status Scale [EDSS] ≥ 7) for ≥ 2 years.3 In recent years, there has been increased research on nonactive SPMS, specifically on discontinuation of DMTs. This clinical review assesses the recent evidence from a variety of standpoints, including the effect of discontinuing DMTs on the MS disease course and quality of life (QOL) and the perspectives of patients living with MS. Based on this evidence, a conversation guide will be presented as a framework to aid with the clinician-patient discussion on discontinuing MS DMTs.
Disease Modifying Therapies
Roos and colleagues used data from 2 large MS cohorts: MSBase and Observatoire Français de la Sclérose en Plaques (OFSEP) to compare high-efficacy vs low-efficacy DMT in both active and nonactive SPMS.4 In the active SPMS group, the strength of DMTs did not change disability progression, but high-efficacy DMTs reduced relapses better than the low-efficacy DMTs. On the other hand, the nonactive SPMS group saw no difference between DMTs in both relapse risk and disability progression. Another observational study of 221 patients with RRMS who discontinued DMTs noted that there were 2 independent predictors for the absence of relapse following DMT discontinuation: being aged > 45 years and the lack of relapse for ≥ 4 years prior to DMT discontinuation.5 Though these patients still may have been classified as RRMS, both these independent predictors for stability postdiscontinuation of DMTs are the typical characteristics of a nonactive SPMS patient.
Pathophysiology may help explain why DMT discontinuation seems to produce no adverse clinical outcomes in people with nonactive SPMS. Nonactive SPMS, which follows after RRMS, is largely correlated with age. In nonactive SPMS, there is less B and T lymphocyte migration across the blood-brain barrier. Furthermore, a lifetime of low-grade inflammation during the RRMS phase results in axonal damage and declined repair capacity, which produces the predominance of neurodegeneration in the nonactive SPMS disease process.6 This pathophysiologic difference between active and nonactive disease not only explains the different symptomatology of these MS subtypes, but also could explain why drugs that target the inflammatory processes more characteristic of active disease are not effective in nonactive SPMS.
Other recent studies explored the impact of age on DMT efficacy for patients with nonactive SPMS. A meta-analysis by Weidman and colleagues pooled trial data across multiple DMT classes in > 28,000 patients.7 The resulting regression model predicted zero efficacy of any DMT in patients who are aged > 53 years. High-efficacy DMTs only outperformed low-efficacy DMTs in people aged < 40.5 years. Another observational study by Hua and colleagues saw a similar result.8 This study included patients who discontinued DMT who were aged ≥ 60 years. The median follow-up time was 5.3 years. Of the 178 patients who discontinued DMTs, only 1 patient had a relapse. In this study, the age for participation provided a higher likelihood that patients included were in nonactive SPMS. Furthermore, the outcome reflects the typical presentation of nonactive SPMS where, despite the continuation or discontinuation of DMT, there was a lack of relapses. When comparing patients who discontinued DMTs with those who continued use, there was no significant difference in their 25-foot walk times, which is an objective marker for a more progressive symptom seen in nonactive MS.
The DISCOMS trial (NCT03073603) has been completed, but full results are not yet published. In this noninferiority trial, > 250 patients aged ≥ 55 years were assessed on a variety of outcomes, including relapses, EDSS score, and QOL. MS subtypes were considered at baseline, and subgroup analysis looking particularly at the SPMS population could provide further insight into its effect on MS course.
Quality of Life
Whether discontinuation of DMTs is worth considering in nonactive SPMS, it is also important to consider the risks and burdens associated with continuation. Medication administration burdens come with all MS DMTs whether there is the need to inject oneself, increased pill burden, or travel to an infusion clinic. The ever-rising costs of DMTs also can be a financial burden to the patient.9 All MS DMTs carry risks of adverse effects (AEs). These can range from a mild injection site reaction to severe infection, depending on the DMT used. Many of these severe AEs, such as opportunistic infections and cancer, have been associated with either an increased risk of occurrence and/or worsened outcomes in older adults who remain on DMTs, particularly moderate- to high-efficacy DMTs, such as sphingosine-1- phosphate receptor modulators, fumarates, natalizumab, alemtuzumab, cladribine, and anti-CD20 antibodies.10 In a 2019 survey of 377 patients with MS, 63.8% of respondents ranked safety as the most important reason they would consider discontinuing their DMTs.11 In addition, a real-world study comparing people with nonactive SPMS who continued DMTs vs those who discontinued found that discontinuers reported better QOL.8
Conversation Guide for Discontinuing Therapies
The 2019 survey that assessed reasons for discontinuation also asked people with nonactive SPMS whether they thought they were in a nonactive disease stage, and what was their likelihood they would stop DMTs.11 Interestingly, only 59.4% of respondents self-assessed their MS as nonactive, and just 11.9% of respondents were willing to discontinue DMTs.11 These results suggest that there may be a need for patient education about nonactive SPMS and the rationale to continue or discontinue DMTs. Thus, before broaching the topic of discontinuation, explaining the nonactive SPMS subtype is important.
Even with a good understanding of nonactive SPMS, patients may be hesitant to stop using DMTs that they previously relied on to keep their MS stable. The 2019 survey ranked physician recommendation as the third highest reason to discontinue DMTs.11 Taking the time to explain the clinical evidence for DMT discontinuation may help patients better understand a clinician’s recommendation and inspire more confidence.
Another important aspect of DMT discontinuation decision making is creating a plan for how the patient will be monitored to provide assurance if they experience a relapse. The 2019 survey asked patients what would be most important to them for their management plan after discontinuing DMT; magnetic resonance imaging and neurologic examination monitoring ranked the highest.11 The plan should include timing for follow-up appointments and imaging, providing the patient comfort in knowing their MS will be monitored and verified for the relapse stability that is expected from nonactive SPMS. In the rare case a relapse does occur, having a contingency plan and noting the possibility of restarting DMTs is an integral part of reassuring the patient that their decision to discontinue DMTs will be treated with the utmost caution and individualized to their needs.
Lastly, highlighting which aspects of MS treatment will continue to be a priority in nonactive SPMS, such as symptomatic medication management and nonpharmacologic therapy, is important for the patient to recognize that there are still opportunities to manage this phase of MS. There are many lifestyle modifications that can be considered complementary to medical management of MS at any stage of the disease. Vascular comorbidities, such as hypertension, hyperlipidemia, and diabetes, have been associated with more rapid disability progression in MS.12 Optimized management of these diseases may slow disability progression, in addition to the benefit of improved outcomes of the vascular comorbidity. Various formats of exercise have been studied in the MS population. A meta-analysis of aerobic, resistance, and combined exercise found benefits in these formats on health-related QOL.13
Many dietary strategies have been studied in MS. A recent network meta-analysis reviewed some of the more commonly studied diets, including low-fat, modified Mediterranean, ketogenic, anti-inflammatory, Paleolithic, intermittent fasting, and calorie restriction vs a usual diet.14 Although the overall quality of evidence was low, the Paleolithic and modified Mediterranean showed greater reductions in fatigue, as well as increased physical and
As with any health care decision, it is important to involve the patient in a joint decision regarding their care. This may mean giving the patient time to think about the information presented, do their own research, talk to family members or other clinicians, etc. The decision to discontinue DMT may not happen at the same appointment it is initially brought up at. It may even be reasonable to revisit the conversation later if discontinuation is not something the patient is amenable to at the time.
Conclusions
There is high-quality evidence that discontinuing DMTs in nonactive SPMS is not a major detriment to the MS disease course. Current literature also suggests that there may be benefits to discontinuation in this MS subtype in terms of QOL and meeting patient values. Additional research particularly in the nonactive SPMS population will continue to improve the knowledge and awareness of this aspect of MS DMT management. The growing evidence in this area may make discontinuation of DMT in nonactive SPMS a less-debatable topic, but it is still a major treatment decision that clinicians must thoroughly discuss with the patient to provide high-quality, patient-centered care.
Multiple sclerosis (MS) is an immune-mediated demyelinating disorder. There are 2 broad categories of MS: relapsing, also called active MS; and progressive MS. Unfortunately, there is no cure for MS, but disease-modifying therapies (DMTs) can help prevent relapses and new central nervous system lesions in people living with active MS. For patients with the most common type of MS, relapsing-remitting MS (RRMS), DMTs are typically continued for decades while the patient has active disease. RRMS will usually transition to secondary progressive MS (SPMS), which can present as active SPMS or nonactive SPMS. The latter is the type of MS most people with RRMS eventually experience.
A 2019 study estimated that nearly 1 million people in the United States were living with MS.1 This population estimate indicated the peak age-specific prevalence of MS was 55 to 64 years. Population data demonstrate improved mortality rates for people diagnosed with MS from 1997 to 2012 compared with prior years.2 Therefore, the management of nonactive SPMS is an increasingly significant area of need. There are currently no DMTs on the market approved for nonactive SPMS, and lifelong DMTs in these patients are neither indicated nor supported by evidence. Nevertheless, the discontinuation of DMTs in nonactive SPMS has been a long-debated topic with varied opinions on how and when to discontinue.
The 2018 American Academy of Neurology (AAN) guideline recommends that clinicians advise patients with SPMS to discontinue DMT use if they do not have ongoing relapses (or gadolinium-enhanced lesions on magnetic resonance imaging activity) or have not been ambulatory (Expanded Disability Status Scale [EDSS] ≥ 7) for ≥ 2 years.3 In recent years, there has been increased research on nonactive SPMS, specifically on discontinuation of DMTs. This clinical review assesses the recent evidence from a variety of standpoints, including the effect of discontinuing DMTs on the MS disease course and quality of life (QOL) and the perspectives of patients living with MS. Based on this evidence, a conversation guide will be presented as a framework to aid with the clinician-patient discussion on discontinuing MS DMTs.
Disease Modifying Therapies
Roos and colleagues used data from 2 large MS cohorts: MSBase and Observatoire Français de la Sclérose en Plaques (OFSEP) to compare high-efficacy vs low-efficacy DMT in both active and nonactive SPMS.4 In the active SPMS group, the strength of DMTs did not change disability progression, but high-efficacy DMTs reduced relapses better than the low-efficacy DMTs. On the other hand, the nonactive SPMS group saw no difference between DMTs in both relapse risk and disability progression. Another observational study of 221 patients with RRMS who discontinued DMTs noted that there were 2 independent predictors for the absence of relapse following DMT discontinuation: being aged > 45 years and the lack of relapse for ≥ 4 years prior to DMT discontinuation.5 Though these patients still may have been classified as RRMS, both these independent predictors for stability postdiscontinuation of DMTs are the typical characteristics of a nonactive SPMS patient.
Pathophysiology may help explain why DMT discontinuation seems to produce no adverse clinical outcomes in people with nonactive SPMS. Nonactive SPMS, which follows after RRMS, is largely correlated with age. In nonactive SPMS, there is less B and T lymphocyte migration across the blood-brain barrier. Furthermore, a lifetime of low-grade inflammation during the RRMS phase results in axonal damage and declined repair capacity, which produces the predominance of neurodegeneration in the nonactive SPMS disease process.6 This pathophysiologic difference between active and nonactive disease not only explains the different symptomatology of these MS subtypes, but also could explain why drugs that target the inflammatory processes more characteristic of active disease are not effective in nonactive SPMS.
Other recent studies explored the impact of age on DMT efficacy for patients with nonactive SPMS. A meta-analysis by Weidman and colleagues pooled trial data across multiple DMT classes in > 28,000 patients.7 The resulting regression model predicted zero efficacy of any DMT in patients who are aged > 53 years. High-efficacy DMTs only outperformed low-efficacy DMTs in people aged < 40.5 years. Another observational study by Hua and colleagues saw a similar result.8 This study included patients who discontinued DMT who were aged ≥ 60 years. The median follow-up time was 5.3 years. Of the 178 patients who discontinued DMTs, only 1 patient had a relapse. In this study, the age for participation provided a higher likelihood that patients included were in nonactive SPMS. Furthermore, the outcome reflects the typical presentation of nonactive SPMS where, despite the continuation or discontinuation of DMT, there was a lack of relapses. When comparing patients who discontinued DMTs with those who continued use, there was no significant difference in their 25-foot walk times, which is an objective marker for a more progressive symptom seen in nonactive MS.
The DISCOMS trial (NCT03073603) has been completed, but full results are not yet published. In this noninferiority trial, > 250 patients aged ≥ 55 years were assessed on a variety of outcomes, including relapses, EDSS score, and QOL. MS subtypes were considered at baseline, and subgroup analysis looking particularly at the SPMS population could provide further insight into its effect on MS course.
Quality of Life
Whether discontinuation of DMTs is worth considering in nonactive SPMS, it is also important to consider the risks and burdens associated with continuation. Medication administration burdens come with all MS DMTs whether there is the need to inject oneself, increased pill burden, or travel to an infusion clinic. The ever-rising costs of DMTs also can be a financial burden to the patient.9 All MS DMTs carry risks of adverse effects (AEs). These can range from a mild injection site reaction to severe infection, depending on the DMT used. Many of these severe AEs, such as opportunistic infections and cancer, have been associated with either an increased risk of occurrence and/or worsened outcomes in older adults who remain on DMTs, particularly moderate- to high-efficacy DMTs, such as sphingosine-1- phosphate receptor modulators, fumarates, natalizumab, alemtuzumab, cladribine, and anti-CD20 antibodies.10 In a 2019 survey of 377 patients with MS, 63.8% of respondents ranked safety as the most important reason they would consider discontinuing their DMTs.11 In addition, a real-world study comparing people with nonactive SPMS who continued DMTs vs those who discontinued found that discontinuers reported better QOL.8
Conversation Guide for Discontinuing Therapies
The 2019 survey that assessed reasons for discontinuation also asked people with nonactive SPMS whether they thought they were in a nonactive disease stage, and what was their likelihood they would stop DMTs.11 Interestingly, only 59.4% of respondents self-assessed their MS as nonactive, and just 11.9% of respondents were willing to discontinue DMTs.11 These results suggest that there may be a need for patient education about nonactive SPMS and the rationale to continue or discontinue DMTs. Thus, before broaching the topic of discontinuation, explaining the nonactive SPMS subtype is important.
Even with a good understanding of nonactive SPMS, patients may be hesitant to stop using DMTs that they previously relied on to keep their MS stable. The 2019 survey ranked physician recommendation as the third highest reason to discontinue DMTs.11 Taking the time to explain the clinical evidence for DMT discontinuation may help patients better understand a clinician’s recommendation and inspire more confidence.
Another important aspect of DMT discontinuation decision making is creating a plan for how the patient will be monitored to provide assurance if they experience a relapse. The 2019 survey asked patients what would be most important to them for their management plan after discontinuing DMT; magnetic resonance imaging and neurologic examination monitoring ranked the highest.11 The plan should include timing for follow-up appointments and imaging, providing the patient comfort in knowing their MS will be monitored and verified for the relapse stability that is expected from nonactive SPMS. In the rare case a relapse does occur, having a contingency plan and noting the possibility of restarting DMTs is an integral part of reassuring the patient that their decision to discontinue DMTs will be treated with the utmost caution and individualized to their needs.
Lastly, highlighting which aspects of MS treatment will continue to be a priority in nonactive SPMS, such as symptomatic medication management and nonpharmacologic therapy, is important for the patient to recognize that there are still opportunities to manage this phase of MS. There are many lifestyle modifications that can be considered complementary to medical management of MS at any stage of the disease. Vascular comorbidities, such as hypertension, hyperlipidemia, and diabetes, have been associated with more rapid disability progression in MS.12 Optimized management of these diseases may slow disability progression, in addition to the benefit of improved outcomes of the vascular comorbidity. Various formats of exercise have been studied in the MS population. A meta-analysis of aerobic, resistance, and combined exercise found benefits in these formats on health-related QOL.13
Many dietary strategies have been studied in MS. A recent network meta-analysis reviewed some of the more commonly studied diets, including low-fat, modified Mediterranean, ketogenic, anti-inflammatory, Paleolithic, intermittent fasting, and calorie restriction vs a usual diet.14 Although the overall quality of evidence was low, the Paleolithic and modified Mediterranean showed greater reductions in fatigue, as well as increased physical and
As with any health care decision, it is important to involve the patient in a joint decision regarding their care. This may mean giving the patient time to think about the information presented, do their own research, talk to family members or other clinicians, etc. The decision to discontinue DMT may not happen at the same appointment it is initially brought up at. It may even be reasonable to revisit the conversation later if discontinuation is not something the patient is amenable to at the time.
Conclusions
There is high-quality evidence that discontinuing DMTs in nonactive SPMS is not a major detriment to the MS disease course. Current literature also suggests that there may be benefits to discontinuation in this MS subtype in terms of QOL and meeting patient values. Additional research particularly in the nonactive SPMS population will continue to improve the knowledge and awareness of this aspect of MS DMT management. The growing evidence in this area may make discontinuation of DMT in nonactive SPMS a less-debatable topic, but it is still a major treatment decision that clinicians must thoroughly discuss with the patient to provide high-quality, patient-centered care.
1. Wallin MT, Culpepper WJ, Campbell JD, et al. The prevalence of MS in the United States: a population-based estimate using health claims data. Neurology. 2019;92(10):e1029-e1040. doi:10.1212/WNL.0000000000007035
2. Lunde HMB, Assmus J, Myhr KM, Bø L, Grytten N. Survival and cause of death in multiple sclerosis: a 60-year longitudinal population study. J Neurol Neurosurg Psychiatry. 2017;88(8):621-625. doi:10.1136/jnnp-2016-315238
3. Rae-Grant A, Day GS, Marrie RA, et al. Practice guideline recommendations summary: disease-modifying therapies for adults with multiple sclerosis: report of the Guideline Development, Dissemination, and Implementation Subcommittee of the American Academy of Neurology. Neurology. 2018;90(17):777-788. doi:10.1212/WNL.0000000000005347
4. Roos I, Leray E, Casey R, et al. Effects of high- and low-efficacy therapy in secondary progressive multiple sclerosis. Neurology. 2021;97(9):e869-e880. doi:10.1212/WNL.0000000000012354
5. Bsteh G, Feige J, Ehling R, et al. Discontinuation of disease-modifying therapies in multiple sclerosis - clinical outcome and prognostic factors. Mult Scler. 2017;23(9):1241-1248. doi:10.1177/1352458516675751
6. Musella A, Gentile A, Rizzo FR, et al. Interplay between age and neuroinflammation in multiple sclerosis: effects on motor and cognitive functions. Front Aging Neurosci. 2018;10:238. Published 2018 Aug 8. doi:10.3389/fnagi.2018.00238
7. Weideman AM, Tapia-Maltos MA, Johnson K, Greenwood M, Bielekova B. Meta-analysis of the age-dependent efficacy of multiple sclerosis treatments. Front Neurol. 2017;8:577. Published 2017 Nov 10. doi:10.3389/fneur.2017.00577
8. Hua LH, Harris H, Conway D, Thompson NR. Changes in patient-reported outcomes between continuers and discontinuers of disease modifying therapy in patients with multiple sclerosis over age 60. Mult Scler Relat Disord. 2019;30:252-256. doi:10.1016/j.msard.2019.02.028
9. San-Juan-Rodriguez A, Good CB, Heyman RA, Parekh N, Shrank WH, Hernandez I. Trends in prices, market share, and spending on self-administered disease-modifying therapies for multiple sclerosis in Medicare part D. JAMA Neurol. 2019;76(11):1386-1390. doi:10.1001/jamaneurol.2019.2711
10. Schweitzer F, Laurent S, Fink GR, et al. Age and the risks of high-efficacy disease modifying drugs in multiple sclerosis. Curr Opin Neurol. 2019;32(3):305-312. doi:10.1097/WCO.0000000000000701
11. McGinley MP, Cola PA, Fox RJ, Cohen JA, Corboy JJ, Miller D. Perspectives of individuals with multiple sclerosis on discontinuation of disease-modifying therapies. Mult Scler. 2020;26(12):1581-1589. doi:10.1177/1352458519867314
12. Marrie RA, Rudick R, Horwitz R, et al. Vascular comorbidity is associated with more rapid disability progression in multiple sclerosis. Neurology. 2010;74(13):1041-1047. doi:10.1212/WNL.0b013e3181d6b125
13. Flores VA, Šilic´ P, DuBose NG, Zheng P, Jeng B, Motl RW. Effects of aerobic, resistance, and combined exercise training on health-related quality of life in multiple sclerosis: Systematic review and meta-analysis. Mult Scler Relat Disord. 2023;75:104746. doi:10.1016/j.msard.2023.104746
14. Snetselaar LG, Cheek JJ, Fox SS, et al. Efficacy of diet on fatigue and quality of life in multiple sclerosis: a systematic review and network meta-analysis of randomized trials. Neurology. 2023;100(4):e357-e366. doi:10.1212/WNL.0000000000201371
1. Wallin MT, Culpepper WJ, Campbell JD, et al. The prevalence of MS in the United States: a population-based estimate using health claims data. Neurology. 2019;92(10):e1029-e1040. doi:10.1212/WNL.0000000000007035
2. Lunde HMB, Assmus J, Myhr KM, Bø L, Grytten N. Survival and cause of death in multiple sclerosis: a 60-year longitudinal population study. J Neurol Neurosurg Psychiatry. 2017;88(8):621-625. doi:10.1136/jnnp-2016-315238
3. Rae-Grant A, Day GS, Marrie RA, et al. Practice guideline recommendations summary: disease-modifying therapies for adults with multiple sclerosis: report of the Guideline Development, Dissemination, and Implementation Subcommittee of the American Academy of Neurology. Neurology. 2018;90(17):777-788. doi:10.1212/WNL.0000000000005347
4. Roos I, Leray E, Casey R, et al. Effects of high- and low-efficacy therapy in secondary progressive multiple sclerosis. Neurology. 2021;97(9):e869-e880. doi:10.1212/WNL.0000000000012354
5. Bsteh G, Feige J, Ehling R, et al. Discontinuation of disease-modifying therapies in multiple sclerosis - clinical outcome and prognostic factors. Mult Scler. 2017;23(9):1241-1248. doi:10.1177/1352458516675751
6. Musella A, Gentile A, Rizzo FR, et al. Interplay between age and neuroinflammation in multiple sclerosis: effects on motor and cognitive functions. Front Aging Neurosci. 2018;10:238. Published 2018 Aug 8. doi:10.3389/fnagi.2018.00238
7. Weideman AM, Tapia-Maltos MA, Johnson K, Greenwood M, Bielekova B. Meta-analysis of the age-dependent efficacy of multiple sclerosis treatments. Front Neurol. 2017;8:577. Published 2017 Nov 10. doi:10.3389/fneur.2017.00577
8. Hua LH, Harris H, Conway D, Thompson NR. Changes in patient-reported outcomes between continuers and discontinuers of disease modifying therapy in patients with multiple sclerosis over age 60. Mult Scler Relat Disord. 2019;30:252-256. doi:10.1016/j.msard.2019.02.028
9. San-Juan-Rodriguez A, Good CB, Heyman RA, Parekh N, Shrank WH, Hernandez I. Trends in prices, market share, and spending on self-administered disease-modifying therapies for multiple sclerosis in Medicare part D. JAMA Neurol. 2019;76(11):1386-1390. doi:10.1001/jamaneurol.2019.2711
10. Schweitzer F, Laurent S, Fink GR, et al. Age and the risks of high-efficacy disease modifying drugs in multiple sclerosis. Curr Opin Neurol. 2019;32(3):305-312. doi:10.1097/WCO.0000000000000701
11. McGinley MP, Cola PA, Fox RJ, Cohen JA, Corboy JJ, Miller D. Perspectives of individuals with multiple sclerosis on discontinuation of disease-modifying therapies. Mult Scler. 2020;26(12):1581-1589. doi:10.1177/1352458519867314
12. Marrie RA, Rudick R, Horwitz R, et al. Vascular comorbidity is associated with more rapid disability progression in multiple sclerosis. Neurology. 2010;74(13):1041-1047. doi:10.1212/WNL.0b013e3181d6b125
13. Flores VA, Šilic´ P, DuBose NG, Zheng P, Jeng B, Motl RW. Effects of aerobic, resistance, and combined exercise training on health-related quality of life in multiple sclerosis: Systematic review and meta-analysis. Mult Scler Relat Disord. 2023;75:104746. doi:10.1016/j.msard.2023.104746
14. Snetselaar LG, Cheek JJ, Fox SS, et al. Efficacy of diet on fatigue and quality of life in multiple sclerosis: a systematic review and network meta-analysis of randomized trials. Neurology. 2023;100(4):e357-e366. doi:10.1212/WNL.0000000000201371
A Case of Duodenocaval Fistula in the Setting of Respiratory Failure Initially Confused for Transfusion-Related Acute Lung Injury
A duodenocaval fistula (DCF) is seen when a connection exists between the duodenum and the inferior vena cava. It is a rare entity that is commonly missed and presents a diagnostic challenge due to its nonspecific presenting symptoms.1,2 Patients commonly present with gastrointestinal (GI) bleeding or sepsis. Here we present a case of a 37-year-old man who presented to the hospital for a workup related to melena but went into cardiac arrest prior to an esophagogastroduodenoscopy. Unfortunately, on autopsy, the patient was found to have a DCF. We highlight the diagnostic challenge associated with DCF and how in this case the presentation was confused by a diagnosis of possible transfusion-related acute lung injury (TRALI). To the best of our knowledge, this is also the first description of a case of DCF associated with food embolism to the lungs causing respiratory failure.
Case Presentation
A 37-year-old man with a history significant for bulimia presented to the hospital with a 3-day history of melena and reports of dizziness. The patient did not report being on any prescribed medications but noted that he took 4 aspirin daily to “calm his nerves.” The rest of the patient’s history was unremarkable aside from a reported history of induced emesis 3 to 4 times per week for an extended period up until 2 weeks before admission.
On admission, his vital signs demonstrated tachycardia and orthostatic hypotension. Pertinent findings on physical examination were skin pallor, a normal lung examination, mild epigastric tenderness, and guaiac-positive stools. He was alert and oriented to person, place, and time with no focal deficits. His admission laboratory tests were notable for a hemoglobin (Hb) level of 4.6 g/dL (reference range, 14-17.9), a white blood cell count of 13.5 K/cm (reference range, 4.5-11), an international normalized ratio of 1.21, a blood urea nitrogen of 61 mg/dL (reference range, 10-20), and a creatinine of 2.3 mg/dL (reference range, 0.8-1.4). The patient was placed on 2 L of oxygen via nasal cannula for comfort rather than true hypoxia. A chest X-ray on admission was negative with no signs of infiltrate, edema, or widened mediastinum. An abdominal X-ray was significant for a dilated stomach consistent with bulimia with no abdominal free air or signs of obstruction. The case was discussed with the gastroenterology service who felt that the patient needed to be more hemodynamically stable before pursuing endoscopic evaluation.
He was admitted to the intensive care unit and give a transfusion of 4 units of fresh frozen plasma and 2 packed red blood cells (PRBCs) without any issues. During the infusion of a third PRBC, he developed chills, tachycardia, and hypertension with accompanying respiratory distress characterized by wheezing, decreased breath sounds bilaterally, and a decrease in oxygen saturation to 70% on 2 L supplemental oxygen. He responded to treatment with meperidine, methylprednisolone sodium succinate, albuterol nebulizer, and acetaminophen. A new chest X-ray was read as “development of pulmonary edema vs bilateral pneumonitis.” A transfusion reaction was reported to the blood bank and a diagnosis of TRALI was considered. That evening, he completed a dose of platelets and another PRBC without difficulty after he was premedicated with meperidine, methylprednisolone sodium succinate, and acetaminophen. During the night, the patient spiked a temperature of 40.3 °C that was successfully treated with a cooling blanket and acetaminophen.
The following morning the patient was found to be tachypneic and tachycardic with his face mask off. His symptoms were corrected by replacing his face mask. He claimed he felt anxious about getting more transfusions and that he had breathing problems like this at home in the recent past. The patient requested an aspirin to calm his nerves. Over the course of the day, his Hb level dropped from 6.6 g/dL to 5.9 g/dL, and 2 washed leukopoor PRBCs were ordered.
The first unit was infused uneventfully, but after 125 cc of the second unit, the patient developed respiratory distress, rigors, and hypotension to 70/58 mm Hg despite premedication. He again was treated successfully with increased face mask support. A few rales were noted, but his fluid balance was even. A second transfusion reaction was filed with the blood bank and based on the 2 transfusion-associated events with no other clear explanation for his symptoms, the clinical team favored the TRALI diagnosis. However, the blood bank was suspicious this might not be TRALI as the previous night the patient had 2 episodes of respiratory distress with drops in oxygen saturation unassociated with transfusions. The patient was clinically stable for the remainder of the night.
Early the following morning the patient was scheduled for an esophagogastroduodenoscopy to evaluate for a source of his bleeding. At the beginning of the procedure, a unit of washed leukoreduced PRBCs was hung for a Hb level of 6.9 g/dL. No bleeding source was noted in the stomach, but as the endoscope was passed into the duodenum, and after an infusion of only 25 cc of RBCs, the patient became cyanotic and went into cardiac arrest. Despite advanced resuscitation efforts over 90 minutes, the patient could not be successfully resuscitated and died while in the endoscopy suite. A transfusion reaction workup was initiated but was unremarkable. The transfusion medicine staff was suspicious that something other than TRALI was the cause of the patient’s respiratory distress as he had respiratory distress remote to the transfusions and the unit was prepared correctly before administration. The patient’s family agreed to an autopsy.
Pathology
A full autopsy was performed 22 hours after the patient died. The lungs were congested and of increased weight: The right lung was 800 g, and the left was 750 g. The right lower lobe had a wedge-shaped infarction measuring 6 cm × 5 cm fed by a thrombosed vessel. Multiple small hemorrhagic wedge-shaped areas were noted in the left lung. An ulcer measuring 6 cm × 5 cm was noted just distal to the pylorus. At the base of this ulcer was a 1.5 cm × 0.5 cm tract that communicated with the inferior vena cava (Figure 1).
A postmortem blood culture was positive for Clostridium perfringens (C perfringens) and Candida albicans (C Albicans). Interestingly, one of the collected blood culture vials exploded en route to the laboratory, presumably due to the presence of many gas-forming C perfringens bacteria.
On microscopic examination of the autopsy samples, gram-positive rods were observed in the tissue of multiple organs, including the heart, lungs, liver, and kidneys (Figure 2).
Serology
Fourteen days after the patient’s death, both PRBC units infused during transfusion reactions were positive for granulocyte antibodies by immunofluorescence and agglutination techniques. Human leukocyte antigen antibody testing was also sent but was not found in either the donor or patient.
Discussion
Our case illustrates the unique and challenging diagnosis of DCF given the rarity of presentation and how quickly patients may clinically decompensate. After an extensive search of the medical literature, we were only able to identify about 40 previous cases of DCF, of which 37 were described in one review.1 DCF, although rare, should be considered at risk for forming in the following settings: migrating inferior vena cava filter, right nephrectomy and radiotherapy, duodenal peptic ulcer, abdominal trauma, and oncologic settings involving metastatic malignancy requiring radiation and/or surgical grafting of the inferior vena cava.1-4 When the diagnosis is considered, computed tomography (CT) is the best initial imaging modality as it allows for noninvasive evaluation of both the inferior vena cava and nonadjacent structures. A commonality of our case and those described in the literature is the diagnostic mystery and nonspecific symptoms patients present with, thus making CT an appropriate diagnostic modality. Endoscopy is useful for the further workup of GI bleeding and the diagnosis of peptic ulcer disease.5 In our case, given the patient’s autopsy findings and history of extensive nonsteroidal anti-inflammatory drug use, the duodenal peptic ulcer was likely the precipitating factor for his DCF.
The most challenging aspect in diagnosing DCF is that many times patients present with nonspecific symptoms, and given its rarity it is not something that is usually at the forefront of most differentials.2 This diagnostic difficulty may elucidate why there is such a relatively high mortality rate—nearly 40%—associated with DCF and why many times accurate diagnosis is not made until autopsy.1,3 The most common presenting manifestations are sepsis and/or GI bleeding; in less than half the cases described in the literature patients had both sepsis and GI bleeding. In our case, the patient had signs of melena but was not felt to be septic as his presenting signs were felt to be in the setting of blood loss and dehydration (given his history of bulimia), not an acute infectious source.
In retrospect, one of the more confounding aspects of this case is the clinical picture concerning for TRALI. The patient required supplemental oxygen throughout his hospitalization and decompensated while or after receiving a transfusion, thus having TRALI on the differential was not felt inappropriate at that time. However, this case also illustrates the power of an anchoring bias, and perhaps the clinical team anchored on the diagnosis of TRALI too quickly before considering other possible etiologies for the patient’s respiratory distress. TRALI can be one of the most challenging diagnoses to make in the field of transfusion medicine as there are no definitive diagnostic criteria.6 It is felt to be a clinical diagnosis of exclusion as there is no pathognomonic sign or diagnostic test to confirm it as the cause of the patient’s respiratory distress, though anti–human leukocyte antigen antibodies commonly are present.6,7 Considering how quickly the patient decompensated on day 2 of hospitalization and the presence of C perfringens bacteremia, which
Conclusions
Our investigation reports a case of a DCF in the setting of significant duodenal peptic ulcer disease. We highlight the diagnostic challenge that this commonly lethal etiology presents. We believe ours is the first case in which it was confused for TRALI and associated with food embolism to the lungs causing hypoxic respiratory failure. We want to highlight that DCF, though rare, should be considered for patients who present with GI bleeding and hypoxic respiratory failure.
1. Guillem PG, Binot D, Dupuy-Cuny J, et al. Duodenocaval fistula: a life-threatening condition of various origins. J Vasc Surg. 2001;33(3):643-645. doi:10.1067/mva.2001.111741
2. Ippolito D, Querques G, Drago SG, Bonaffini PA, Sironi S. Duodenocaval fistula in a patient with inferior vena cava leiomyosarcoma treated by surgical resection and caval polytetrafluoroethylene prosthesis. Case Rep Radiol. 2015;2015:1-5. doi:10.1155/2015/575961
3. Guo Y, Zhang YQ, Lin W. Radiological diagnosis of duodenocaval fistula: a case report and literature review. World J Gastroenterol. 2010;16(18):2314-2316. doi:10.3748/wjg.v16.i18.2314
4. Perera GB, Wilson SE, Barie PS, Butler JA. Duodenocaval fistula: A late complication of retroperitoneal irradiation and vena cava replacement. Ann Vasc Surg. 2004;18(1):52-58. doi:10.1007/s10016-003-0097-8
5. Addeo P, Rosso E, Oussoultzoglou E, Jaeck D, Pessaux P, Bachellier P. Inferior vena cava graft-enteric fistula after extended hepatectomy with caval replacement. J Vasc Surg. 2012;55(1):226-229. doi:10.1016/j.jvs.2011.05.118
6. Chapman CE, Stainsby D, Jones H, et al. Ten years of hemovigilance reports of transfusion-related acute lung injury in the United Kingdom and the impact of preferential use of male donor plasma. Transfusion. 2009;49(3):440-452. doi:10.1111/j.1537-2995.2008.01948.x
7. Fontaine MJ, Malone J, Mullins FM, Grumet FC. Diagnosis of transfusion-related acute lung injury: TRALI or not TRALI? Ann Clin Lab Sci. 2006;36(1):53-58.
8. Yang C-C, Hsu P-C, Chang H-J, Cheng C-W, Lee M-H. Clinical significance and outcomes of clostridium perfringens bacteremia—a 10-year experience at a tertiary care hospital. Int J Infect Dis. 2013;17(11):e9of55-e960. doi:10.1016/j.ijid.2013.03.001
A duodenocaval fistula (DCF) is seen when a connection exists between the duodenum and the inferior vena cava. It is a rare entity that is commonly missed and presents a diagnostic challenge due to its nonspecific presenting symptoms.1,2 Patients commonly present with gastrointestinal (GI) bleeding or sepsis. Here we present a case of a 37-year-old man who presented to the hospital for a workup related to melena but went into cardiac arrest prior to an esophagogastroduodenoscopy. Unfortunately, on autopsy, the patient was found to have a DCF. We highlight the diagnostic challenge associated with DCF and how in this case the presentation was confused by a diagnosis of possible transfusion-related acute lung injury (TRALI). To the best of our knowledge, this is also the first description of a case of DCF associated with food embolism to the lungs causing respiratory failure.
Case Presentation
A 37-year-old man with a history significant for bulimia presented to the hospital with a 3-day history of melena and reports of dizziness. The patient did not report being on any prescribed medications but noted that he took 4 aspirin daily to “calm his nerves.” The rest of the patient’s history was unremarkable aside from a reported history of induced emesis 3 to 4 times per week for an extended period up until 2 weeks before admission.
On admission, his vital signs demonstrated tachycardia and orthostatic hypotension. Pertinent findings on physical examination were skin pallor, a normal lung examination, mild epigastric tenderness, and guaiac-positive stools. He was alert and oriented to person, place, and time with no focal deficits. His admission laboratory tests were notable for a hemoglobin (Hb) level of 4.6 g/dL (reference range, 14-17.9), a white blood cell count of 13.5 K/cm (reference range, 4.5-11), an international normalized ratio of 1.21, a blood urea nitrogen of 61 mg/dL (reference range, 10-20), and a creatinine of 2.3 mg/dL (reference range, 0.8-1.4). The patient was placed on 2 L of oxygen via nasal cannula for comfort rather than true hypoxia. A chest X-ray on admission was negative with no signs of infiltrate, edema, or widened mediastinum. An abdominal X-ray was significant for a dilated stomach consistent with bulimia with no abdominal free air or signs of obstruction. The case was discussed with the gastroenterology service who felt that the patient needed to be more hemodynamically stable before pursuing endoscopic evaluation.
He was admitted to the intensive care unit and give a transfusion of 4 units of fresh frozen plasma and 2 packed red blood cells (PRBCs) without any issues. During the infusion of a third PRBC, he developed chills, tachycardia, and hypertension with accompanying respiratory distress characterized by wheezing, decreased breath sounds bilaterally, and a decrease in oxygen saturation to 70% on 2 L supplemental oxygen. He responded to treatment with meperidine, methylprednisolone sodium succinate, albuterol nebulizer, and acetaminophen. A new chest X-ray was read as “development of pulmonary edema vs bilateral pneumonitis.” A transfusion reaction was reported to the blood bank and a diagnosis of TRALI was considered. That evening, he completed a dose of platelets and another PRBC without difficulty after he was premedicated with meperidine, methylprednisolone sodium succinate, and acetaminophen. During the night, the patient spiked a temperature of 40.3 °C that was successfully treated with a cooling blanket and acetaminophen.
The following morning the patient was found to be tachypneic and tachycardic with his face mask off. His symptoms were corrected by replacing his face mask. He claimed he felt anxious about getting more transfusions and that he had breathing problems like this at home in the recent past. The patient requested an aspirin to calm his nerves. Over the course of the day, his Hb level dropped from 6.6 g/dL to 5.9 g/dL, and 2 washed leukopoor PRBCs were ordered.
The first unit was infused uneventfully, but after 125 cc of the second unit, the patient developed respiratory distress, rigors, and hypotension to 70/58 mm Hg despite premedication. He again was treated successfully with increased face mask support. A few rales were noted, but his fluid balance was even. A second transfusion reaction was filed with the blood bank and based on the 2 transfusion-associated events with no other clear explanation for his symptoms, the clinical team favored the TRALI diagnosis. However, the blood bank was suspicious this might not be TRALI as the previous night the patient had 2 episodes of respiratory distress with drops in oxygen saturation unassociated with transfusions. The patient was clinically stable for the remainder of the night.
Early the following morning the patient was scheduled for an esophagogastroduodenoscopy to evaluate for a source of his bleeding. At the beginning of the procedure, a unit of washed leukoreduced PRBCs was hung for a Hb level of 6.9 g/dL. No bleeding source was noted in the stomach, but as the endoscope was passed into the duodenum, and after an infusion of only 25 cc of RBCs, the patient became cyanotic and went into cardiac arrest. Despite advanced resuscitation efforts over 90 minutes, the patient could not be successfully resuscitated and died while in the endoscopy suite. A transfusion reaction workup was initiated but was unremarkable. The transfusion medicine staff was suspicious that something other than TRALI was the cause of the patient’s respiratory distress as he had respiratory distress remote to the transfusions and the unit was prepared correctly before administration. The patient’s family agreed to an autopsy.
Pathology
A full autopsy was performed 22 hours after the patient died. The lungs were congested and of increased weight: The right lung was 800 g, and the left was 750 g. The right lower lobe had a wedge-shaped infarction measuring 6 cm × 5 cm fed by a thrombosed vessel. Multiple small hemorrhagic wedge-shaped areas were noted in the left lung. An ulcer measuring 6 cm × 5 cm was noted just distal to the pylorus. At the base of this ulcer was a 1.5 cm × 0.5 cm tract that communicated with the inferior vena cava (Figure 1).
A postmortem blood culture was positive for Clostridium perfringens (C perfringens) and Candida albicans (C Albicans). Interestingly, one of the collected blood culture vials exploded en route to the laboratory, presumably due to the presence of many gas-forming C perfringens bacteria.
On microscopic examination of the autopsy samples, gram-positive rods were observed in the tissue of multiple organs, including the heart, lungs, liver, and kidneys (Figure 2).
Serology
Fourteen days after the patient’s death, both PRBC units infused during transfusion reactions were positive for granulocyte antibodies by immunofluorescence and agglutination techniques. Human leukocyte antigen antibody testing was also sent but was not found in either the donor or patient.
Discussion
Our case illustrates the unique and challenging diagnosis of DCF given the rarity of presentation and how quickly patients may clinically decompensate. After an extensive search of the medical literature, we were only able to identify about 40 previous cases of DCF, of which 37 were described in one review.1 DCF, although rare, should be considered at risk for forming in the following settings: migrating inferior vena cava filter, right nephrectomy and radiotherapy, duodenal peptic ulcer, abdominal trauma, and oncologic settings involving metastatic malignancy requiring radiation and/or surgical grafting of the inferior vena cava.1-4 When the diagnosis is considered, computed tomography (CT) is the best initial imaging modality as it allows for noninvasive evaluation of both the inferior vena cava and nonadjacent structures. A commonality of our case and those described in the literature is the diagnostic mystery and nonspecific symptoms patients present with, thus making CT an appropriate diagnostic modality. Endoscopy is useful for the further workup of GI bleeding and the diagnosis of peptic ulcer disease.5 In our case, given the patient’s autopsy findings and history of extensive nonsteroidal anti-inflammatory drug use, the duodenal peptic ulcer was likely the precipitating factor for his DCF.
The most challenging aspect in diagnosing DCF is that many times patients present with nonspecific symptoms, and given its rarity it is not something that is usually at the forefront of most differentials.2 This diagnostic difficulty may elucidate why there is such a relatively high mortality rate—nearly 40%—associated with DCF and why many times accurate diagnosis is not made until autopsy.1,3 The most common presenting manifestations are sepsis and/or GI bleeding; in less than half the cases described in the literature patients had both sepsis and GI bleeding. In our case, the patient had signs of melena but was not felt to be septic as his presenting signs were felt to be in the setting of blood loss and dehydration (given his history of bulimia), not an acute infectious source.
In retrospect, one of the more confounding aspects of this case is the clinical picture concerning for TRALI. The patient required supplemental oxygen throughout his hospitalization and decompensated while or after receiving a transfusion, thus having TRALI on the differential was not felt inappropriate at that time. However, this case also illustrates the power of an anchoring bias, and perhaps the clinical team anchored on the diagnosis of TRALI too quickly before considering other possible etiologies for the patient’s respiratory distress. TRALI can be one of the most challenging diagnoses to make in the field of transfusion medicine as there are no definitive diagnostic criteria.6 It is felt to be a clinical diagnosis of exclusion as there is no pathognomonic sign or diagnostic test to confirm it as the cause of the patient’s respiratory distress, though anti–human leukocyte antigen antibodies commonly are present.6,7 Considering how quickly the patient decompensated on day 2 of hospitalization and the presence of C perfringens bacteremia, which
Conclusions
Our investigation reports a case of a DCF in the setting of significant duodenal peptic ulcer disease. We highlight the diagnostic challenge that this commonly lethal etiology presents. We believe ours is the first case in which it was confused for TRALI and associated with food embolism to the lungs causing hypoxic respiratory failure. We want to highlight that DCF, though rare, should be considered for patients who present with GI bleeding and hypoxic respiratory failure.
A duodenocaval fistula (DCF) is seen when a connection exists between the duodenum and the inferior vena cava. It is a rare entity that is commonly missed and presents a diagnostic challenge due to its nonspecific presenting symptoms.1,2 Patients commonly present with gastrointestinal (GI) bleeding or sepsis. Here we present a case of a 37-year-old man who presented to the hospital for a workup related to melena but went into cardiac arrest prior to an esophagogastroduodenoscopy. Unfortunately, on autopsy, the patient was found to have a DCF. We highlight the diagnostic challenge associated with DCF and how in this case the presentation was confused by a diagnosis of possible transfusion-related acute lung injury (TRALI). To the best of our knowledge, this is also the first description of a case of DCF associated with food embolism to the lungs causing respiratory failure.
Case Presentation
A 37-year-old man with a history significant for bulimia presented to the hospital with a 3-day history of melena and reports of dizziness. The patient did not report being on any prescribed medications but noted that he took 4 aspirin daily to “calm his nerves.” The rest of the patient’s history was unremarkable aside from a reported history of induced emesis 3 to 4 times per week for an extended period up until 2 weeks before admission.
On admission, his vital signs demonstrated tachycardia and orthostatic hypotension. Pertinent findings on physical examination were skin pallor, a normal lung examination, mild epigastric tenderness, and guaiac-positive stools. He was alert and oriented to person, place, and time with no focal deficits. His admission laboratory tests were notable for a hemoglobin (Hb) level of 4.6 g/dL (reference range, 14-17.9), a white blood cell count of 13.5 K/cm (reference range, 4.5-11), an international normalized ratio of 1.21, a blood urea nitrogen of 61 mg/dL (reference range, 10-20), and a creatinine of 2.3 mg/dL (reference range, 0.8-1.4). The patient was placed on 2 L of oxygen via nasal cannula for comfort rather than true hypoxia. A chest X-ray on admission was negative with no signs of infiltrate, edema, or widened mediastinum. An abdominal X-ray was significant for a dilated stomach consistent with bulimia with no abdominal free air or signs of obstruction. The case was discussed with the gastroenterology service who felt that the patient needed to be more hemodynamically stable before pursuing endoscopic evaluation.
He was admitted to the intensive care unit and give a transfusion of 4 units of fresh frozen plasma and 2 packed red blood cells (PRBCs) without any issues. During the infusion of a third PRBC, he developed chills, tachycardia, and hypertension with accompanying respiratory distress characterized by wheezing, decreased breath sounds bilaterally, and a decrease in oxygen saturation to 70% on 2 L supplemental oxygen. He responded to treatment with meperidine, methylprednisolone sodium succinate, albuterol nebulizer, and acetaminophen. A new chest X-ray was read as “development of pulmonary edema vs bilateral pneumonitis.” A transfusion reaction was reported to the blood bank and a diagnosis of TRALI was considered. That evening, he completed a dose of platelets and another PRBC without difficulty after he was premedicated with meperidine, methylprednisolone sodium succinate, and acetaminophen. During the night, the patient spiked a temperature of 40.3 °C that was successfully treated with a cooling blanket and acetaminophen.
The following morning the patient was found to be tachypneic and tachycardic with his face mask off. His symptoms were corrected by replacing his face mask. He claimed he felt anxious about getting more transfusions and that he had breathing problems like this at home in the recent past. The patient requested an aspirin to calm his nerves. Over the course of the day, his Hb level dropped from 6.6 g/dL to 5.9 g/dL, and 2 washed leukopoor PRBCs were ordered.
The first unit was infused uneventfully, but after 125 cc of the second unit, the patient developed respiratory distress, rigors, and hypotension to 70/58 mm Hg despite premedication. He again was treated successfully with increased face mask support. A few rales were noted, but his fluid balance was even. A second transfusion reaction was filed with the blood bank and based on the 2 transfusion-associated events with no other clear explanation for his symptoms, the clinical team favored the TRALI diagnosis. However, the blood bank was suspicious this might not be TRALI as the previous night the patient had 2 episodes of respiratory distress with drops in oxygen saturation unassociated with transfusions. The patient was clinically stable for the remainder of the night.
Early the following morning the patient was scheduled for an esophagogastroduodenoscopy to evaluate for a source of his bleeding. At the beginning of the procedure, a unit of washed leukoreduced PRBCs was hung for a Hb level of 6.9 g/dL. No bleeding source was noted in the stomach, but as the endoscope was passed into the duodenum, and after an infusion of only 25 cc of RBCs, the patient became cyanotic and went into cardiac arrest. Despite advanced resuscitation efforts over 90 minutes, the patient could not be successfully resuscitated and died while in the endoscopy suite. A transfusion reaction workup was initiated but was unremarkable. The transfusion medicine staff was suspicious that something other than TRALI was the cause of the patient’s respiratory distress as he had respiratory distress remote to the transfusions and the unit was prepared correctly before administration. The patient’s family agreed to an autopsy.
Pathology
A full autopsy was performed 22 hours after the patient died. The lungs were congested and of increased weight: The right lung was 800 g, and the left was 750 g. The right lower lobe had a wedge-shaped infarction measuring 6 cm × 5 cm fed by a thrombosed vessel. Multiple small hemorrhagic wedge-shaped areas were noted in the left lung. An ulcer measuring 6 cm × 5 cm was noted just distal to the pylorus. At the base of this ulcer was a 1.5 cm × 0.5 cm tract that communicated with the inferior vena cava (Figure 1).
A postmortem blood culture was positive for Clostridium perfringens (C perfringens) and Candida albicans (C Albicans). Interestingly, one of the collected blood culture vials exploded en route to the laboratory, presumably due to the presence of many gas-forming C perfringens bacteria.
On microscopic examination of the autopsy samples, gram-positive rods were observed in the tissue of multiple organs, including the heart, lungs, liver, and kidneys (Figure 2).
Serology
Fourteen days after the patient’s death, both PRBC units infused during transfusion reactions were positive for granulocyte antibodies by immunofluorescence and agglutination techniques. Human leukocyte antigen antibody testing was also sent but was not found in either the donor or patient.
Discussion
Our case illustrates the unique and challenging diagnosis of DCF given the rarity of presentation and how quickly patients may clinically decompensate. After an extensive search of the medical literature, we were only able to identify about 40 previous cases of DCF, of which 37 were described in one review.1 DCF, although rare, should be considered at risk for forming in the following settings: migrating inferior vena cava filter, right nephrectomy and radiotherapy, duodenal peptic ulcer, abdominal trauma, and oncologic settings involving metastatic malignancy requiring radiation and/or surgical grafting of the inferior vena cava.1-4 When the diagnosis is considered, computed tomography (CT) is the best initial imaging modality as it allows for noninvasive evaluation of both the inferior vena cava and nonadjacent structures. A commonality of our case and those described in the literature is the diagnostic mystery and nonspecific symptoms patients present with, thus making CT an appropriate diagnostic modality. Endoscopy is useful for the further workup of GI bleeding and the diagnosis of peptic ulcer disease.5 In our case, given the patient’s autopsy findings and history of extensive nonsteroidal anti-inflammatory drug use, the duodenal peptic ulcer was likely the precipitating factor for his DCF.
The most challenging aspect in diagnosing DCF is that many times patients present with nonspecific symptoms, and given its rarity it is not something that is usually at the forefront of most differentials.2 This diagnostic difficulty may elucidate why there is such a relatively high mortality rate—nearly 40%—associated with DCF and why many times accurate diagnosis is not made until autopsy.1,3 The most common presenting manifestations are sepsis and/or GI bleeding; in less than half the cases described in the literature patients had both sepsis and GI bleeding. In our case, the patient had signs of melena but was not felt to be septic as his presenting signs were felt to be in the setting of blood loss and dehydration (given his history of bulimia), not an acute infectious source.
In retrospect, one of the more confounding aspects of this case is the clinical picture concerning for TRALI. The patient required supplemental oxygen throughout his hospitalization and decompensated while or after receiving a transfusion, thus having TRALI on the differential was not felt inappropriate at that time. However, this case also illustrates the power of an anchoring bias, and perhaps the clinical team anchored on the diagnosis of TRALI too quickly before considering other possible etiologies for the patient’s respiratory distress. TRALI can be one of the most challenging diagnoses to make in the field of transfusion medicine as there are no definitive diagnostic criteria.6 It is felt to be a clinical diagnosis of exclusion as there is no pathognomonic sign or diagnostic test to confirm it as the cause of the patient’s respiratory distress, though anti–human leukocyte antigen antibodies commonly are present.6,7 Considering how quickly the patient decompensated on day 2 of hospitalization and the presence of C perfringens bacteremia, which
Conclusions
Our investigation reports a case of a DCF in the setting of significant duodenal peptic ulcer disease. We highlight the diagnostic challenge that this commonly lethal etiology presents. We believe ours is the first case in which it was confused for TRALI and associated with food embolism to the lungs causing hypoxic respiratory failure. We want to highlight that DCF, though rare, should be considered for patients who present with GI bleeding and hypoxic respiratory failure.
1. Guillem PG, Binot D, Dupuy-Cuny J, et al. Duodenocaval fistula: a life-threatening condition of various origins. J Vasc Surg. 2001;33(3):643-645. doi:10.1067/mva.2001.111741
2. Ippolito D, Querques G, Drago SG, Bonaffini PA, Sironi S. Duodenocaval fistula in a patient with inferior vena cava leiomyosarcoma treated by surgical resection and caval polytetrafluoroethylene prosthesis. Case Rep Radiol. 2015;2015:1-5. doi:10.1155/2015/575961
3. Guo Y, Zhang YQ, Lin W. Radiological diagnosis of duodenocaval fistula: a case report and literature review. World J Gastroenterol. 2010;16(18):2314-2316. doi:10.3748/wjg.v16.i18.2314
4. Perera GB, Wilson SE, Barie PS, Butler JA. Duodenocaval fistula: A late complication of retroperitoneal irradiation and vena cava replacement. Ann Vasc Surg. 2004;18(1):52-58. doi:10.1007/s10016-003-0097-8
5. Addeo P, Rosso E, Oussoultzoglou E, Jaeck D, Pessaux P, Bachellier P. Inferior vena cava graft-enteric fistula after extended hepatectomy with caval replacement. J Vasc Surg. 2012;55(1):226-229. doi:10.1016/j.jvs.2011.05.118
6. Chapman CE, Stainsby D, Jones H, et al. Ten years of hemovigilance reports of transfusion-related acute lung injury in the United Kingdom and the impact of preferential use of male donor plasma. Transfusion. 2009;49(3):440-452. doi:10.1111/j.1537-2995.2008.01948.x
7. Fontaine MJ, Malone J, Mullins FM, Grumet FC. Diagnosis of transfusion-related acute lung injury: TRALI or not TRALI? Ann Clin Lab Sci. 2006;36(1):53-58.
8. Yang C-C, Hsu P-C, Chang H-J, Cheng C-W, Lee M-H. Clinical significance and outcomes of clostridium perfringens bacteremia—a 10-year experience at a tertiary care hospital. Int J Infect Dis. 2013;17(11):e9of55-e960. doi:10.1016/j.ijid.2013.03.001
1. Guillem PG, Binot D, Dupuy-Cuny J, et al. Duodenocaval fistula: a life-threatening condition of various origins. J Vasc Surg. 2001;33(3):643-645. doi:10.1067/mva.2001.111741
2. Ippolito D, Querques G, Drago SG, Bonaffini PA, Sironi S. Duodenocaval fistula in a patient with inferior vena cava leiomyosarcoma treated by surgical resection and caval polytetrafluoroethylene prosthesis. Case Rep Radiol. 2015;2015:1-5. doi:10.1155/2015/575961
3. Guo Y, Zhang YQ, Lin W. Radiological diagnosis of duodenocaval fistula: a case report and literature review. World J Gastroenterol. 2010;16(18):2314-2316. doi:10.3748/wjg.v16.i18.2314
4. Perera GB, Wilson SE, Barie PS, Butler JA. Duodenocaval fistula: A late complication of retroperitoneal irradiation and vena cava replacement. Ann Vasc Surg. 2004;18(1):52-58. doi:10.1007/s10016-003-0097-8
5. Addeo P, Rosso E, Oussoultzoglou E, Jaeck D, Pessaux P, Bachellier P. Inferior vena cava graft-enteric fistula after extended hepatectomy with caval replacement. J Vasc Surg. 2012;55(1):226-229. doi:10.1016/j.jvs.2011.05.118
6. Chapman CE, Stainsby D, Jones H, et al. Ten years of hemovigilance reports of transfusion-related acute lung injury in the United Kingdom and the impact of preferential use of male donor plasma. Transfusion. 2009;49(3):440-452. doi:10.1111/j.1537-2995.2008.01948.x
7. Fontaine MJ, Malone J, Mullins FM, Grumet FC. Diagnosis of transfusion-related acute lung injury: TRALI or not TRALI? Ann Clin Lab Sci. 2006;36(1):53-58.
8. Yang C-C, Hsu P-C, Chang H-J, Cheng C-W, Lee M-H. Clinical significance and outcomes of clostridium perfringens bacteremia—a 10-year experience at a tertiary care hospital. Int J Infect Dis. 2013;17(11):e9of55-e960. doi:10.1016/j.ijid.2013.03.001
COVID-19 Incidence After Emergency Department Visit
At the onset of the COVID-19 pandemic, patient encounters with the health care system plummeted.1-3 The perceived increased risk of contracting COVID-19 while obtaining care was thought to be a contributing factor. In outpatient settings, one study noted a 63% decrease in visits to otolaryngology visits in Massachusetts, and another noted a 33% decrease in dental office visits at the onset of the pandemic in 2020 compared with the same time frame in 2019.2,4 Along with mask mandates and stay-at-home orders, various institutions sought to mitigate the spread of COVID-19 through different protocols, including the use of social distancing, limitation of visitors, and telehealth. Despite some of these measures, nosocomial infections were not uncommon. For example, one hospital in the United Kingdom reported that 15% of COVID-19 inpatient cases in a 6-week period in 2020 were probably or definitely hospital acquired. These patients had a 36% case fatality rate.5
Unlike outpatient treatment centers, however, the emergency department (ED) is mandated by the Emergency Medical Treatment and Labor Act to provide a medical screening examination and to stabilize emergency medical conditions to all patients presenting to the ED. Thus, high numbers of undifferentiated and symptomatic patients are forced to congregate in EDs, increasing the risk of transmission of COVID-19. This perception of increased risk led to a 42% decrease in ED visits during March and April 2020 at the onset of the COVID-19 pandemic.1 Correspondingly, there was a 20% decrease in code stroke activations at a hospital in Canada and a 38% decrease in ST-elevation myocardial infarction activations across 9 United States hospital systems.6,7
Limited studies have been conducted to date to determine whether contracting COVID-19 while in the ED is a risk. One retrospective case-control study evaluating 39 EDs in the US showed that ED colocation with known patients with COVID-19 was not associated with an increased risk of COVID-19 transmission.5 However, this study also recognized that infection control strategies widely varied by location and date.
In this study, we report the incidence of COVID-19 infections within 21 days after the initial visit for symptoms not associated with COVID-19 infection to the Veterans Affairs Greater Los Angeles Healthcare System (VAGLAHS) ED and compared it with that of COVID-19 infections for tests performed within the VAGLAHS.
Program Description
As a quality improvement measure, the
Patients with specific symptoms noted during triage, such as those associated with COVID-19 diagnosis, respiratory infections, fever, and/or myalgias, were isolated in their own patient room. Electronic tablets were used for persons under investigation and patients with COVID-19 to communicate with family and/or medical staff who did not need to enter the patient’s room. Two-hour disinfection protocols were instituted for high-risk patients who were moved during the course of their treatment (ie, transfer to another bed for admission or discharge). All staff was specifically trained in personal protective equipment (PPE) donning and doffing, and 2-physician airway teams were implemented to ensure proper PPE use and safe COVID-19 intubations.
COVID-19 Infections
Electronic health records of patients who visited the VAGLAHS ED for symptoms not related to COVID-19 were reviewed from
A total of 8708 patients who came to the ED with symptoms not associated with COVID-19 infection and had a COVID-19 test within 21 days of the ED visit met the inclusion criteria. The overall average positivity rate at the VAGLAHS ED for symptoms not associated with COVID-19 infection was 1.1% from June 1, 2020, to June 30, 2021. The positivity rate by month ranged from 0% to 6.7% for this period (Figure).
Discussion
Implementing COVID-19 mitigation measures in the VAGLAHS ED helped minimize exposure and subsequent infection of COVID-19 for veterans who visited the VAGLAHS ED with symptoms not associated with COVID-19 infection. Contextualizing this with the overall average monthly positivity rate of veterans in the VAGLAHS catchment area (10.9%) or Los Angeles County (7.9%) between June 1, 2020, to June 30, 2021, veterans who visited the VAGLAHS ED for symptoms not associated with COVID-19 infection were less likely to test positive for COVID-19 within 21 days (1.1%), suggesting that the extensive measures taken at the VAGLAHS ED were effective.8
Many health care systems in the US and abroad have experimented with different transmission mitigation strategies in the ED. These tactics have included careful resource allocation when PPE shortages occur, incorporation of airway teams with appropriate safety measures to reduce nosocomial spread to health care workers, and use of a cohorting plan to separate persons under investigation and patients with COVID-19 from other patients.9-15 Additionally, forward screening areas were incorporated similar to the COVID-19 tent that was instituted at the VAGLAHS ED to manage patients who were referred to the ED for COVID-19 testing during the beginning of the pandemic, which prevented symptomatic patients from congregating with asymptomatic patients.14,15
Encouragingly, some of these studies reported no cases of nosocomial transmission in the ED.11,13 In a separate study, 14 clusters of COVID-19 cases were identified at one VA health care system in which nosocomial transmission was suspected, including one in the ED.16 Using contact tracing, no patients and 9 employees were found to have contracted COVID-19 in that cluster. Overall, among all clusters examined within the health care system, either by contact tracing or by whole-genome sequencing, the authors found that transmission from health care personnel to patients was rare. Despite different methodologies, we also similarly found that ED patients in our VA facility were unlikely to become infected with COVID-19.
While the low incidence of positive COVID-19 tests cannot be attributed to any one method, our data provide a working blueprint for enhanced ED precautions in future surges of COVID-19 or other airborne diseases, including that of future pandemics.
Limitations
Notably, although the VA is the largest health care system in the US, a considerable number of veterans may present to non-VA EDs to seek care, and thus their data are not included here; these veterans may live farther from a VA facility or experience higher barriers to care than veterans who exclusively or almost exclusively seek care within the VA. As a result, we are unable to account for COVID-19 tests completed outside the VA. Moreover, the wild type SARS-CoV-2 virus was dominant during the time frame chosen for this assessment, and data may not be generalizable to other variants (eg, omicron) that are known to be more highly transmissible.17 Lastly, although our observation was performed at a single VA ED and may not apply to other facilities, especially in light of different mitigation strategies, our findings still provide support for approaches to minimizing patient and staff exposure to COVID-19 in ED settings.
Conclusions
Implementation of COVID-19 mitigation measures in the VAGLAHS ED may have minimized exposure to COVID-19 for veterans who visited the VAGLAHS ED for symptoms not associated with COVID-19 and did not put one at higher risk of contracting COVID-19. Taken together, our data suggest that patients should not avoid seeking emergency care out of fear of contracting COVID-19 if EDs have adequately instituted mitigation techniques.
1. Hartnett KP, Kite-Powell A, DeVies J, et al; National Syndromic Surveillance Program Community of Practice. Impact of the COVID-19 pandemic on emergency department visits—United States, January 1, 2019-May 30, 2020. MMWR Morb Mortal Wkly Rep. 2020;69(23):699-704. doi:10.15585/mmwr.mm6923e1
2. Fan T, Workman AD, Miller LE, et al. The impact of COVID-19 on otolaryngology community practice in Massachusetts. Otolaryngol Head Neck Surg. 2021;165(3):424-430. doi:10.1177/0194599820983732
3. Baum A, Kaboli PJ, Schwartz MD. Reduced in-person and increased telehealth outpatient visits during the COVID-19 pandemic. Ann Intern Med. 2021;174(1):129-131. doi:10.7326/M20-3026
4. Kranz AM, Chen A, Gahlon G, Stein BD. 2020 trends in dental office visits during the COVID-19 pandemic. J Am Dent Assoc. 2021;152(7):535-541,e1. doi:10.1016/j.adaj.2021.02.01
5. Ridgway JP, Robicsek AA. Risk of coronavirus disease 2019 (COVID-19) acquisition among emergency department patients: a retrospective case control study. Infect Control Hosp Epidemiol. 2021;42(1):105-107. doi:10.1017/ice.2020.1224
6. Bres Bullrich M, Fridman S, Mandzia JL, et al. COVID-19: stroke admissions, emergency department visits, and prevention clinic referrals. Can J Neurol Sci. 2020;47(5):693-696. doi:10.1017/cjn.2020.101
7. Garcia S, Albaghdadi MS, Meraj PM, et al. Reduction in ST-segment elevation cardiac catheterization laboratory activations in the United States during COVID-19 pandemic. J Am Coll Cardiol. 2020;75(22):2871-2872. doi:10.1016/j.jacc.2020.04.011
8. LA County COVID-19 Surveillance Dashboard. Accessed July 25, 2022. https://covid19.lacounty.gov/dashboards
9. Wallace DW, Burleson SL, Heimann MA, et al. An adapted emergency department triage algorithm for the COVID-19 pandemic. J Am Coll Emerg Physicians Open. 2020;1:1374-1379. doi:10.1002/emp2.12210
10. Montrief T, Ramzy M, Long B, Gottlieb M, Hercz D. COVID-19 respiratory support in the emergency department setting. Am Journal Emerg Med. 2020;38(10):2160-2168. doi:10.1016/j.ajem.2020.08.001
11. Alqahtani F, Alanazi M, Alassaf W, et al. Preventing SARS-CoV-2 transmission in the emergency department by implementing a separate pathway for patients with respiratory conditions. J Complement Integr Med. 2022;19(2):383-388. doi:10.1515/jcim-2020-0422
12. Odorizzi S, Clark E, Nemnom MJ, et al. Flow impacts of hot/cold zone infection control procedures during the COVID-19 pandemic in the emergency department. CJEM. 2022;24(4):390-396. doi:10.1007/s43678-022-00278-0
13. Wee LE, Fua TP, Chua YY, et al. Containing COVID-19 in the emergency department: the role of improved case detection and segregation of suspect cases. Acad Emerg Med. 2020;27(5):379-387. doi:10.1111/acem.13984
14. Tan RMR, Ong GYK, Chong SL, Ganapathy S, Tyebally A, Lee KP. Dynamic adaptation to COVID-19 in a Singapore paediatric emergency department. Emerg Med J. 2020;37(5):252-254. doi:10.1136/emermed-2020-20963
15. Quah LJJ, Tan BKK, Fua TP, et al. Reorganising the emergency department to manage the COVID-19 outbreak. Int J Emerg Med. 2020;13(1):32. doi:10.1186/s12245-020-00294-w
16. Jinadatha C, Jones LD, Choi H, et al. Transmission of SARS-CoV-2 in inpatient and outpatient settings in a Veterans Affairs health care system. Open Forum Infect Dis. 2021;8(8):ofab328. doi:10.1093/ofid/ofab328
17. Riediker M, Briceno-Ayala L, Ichihara G, et al. Higher viral load and infectivity increase risk of aerosol transmission for Delta and Omicron variants of SARS-CoV-2. Swiss Med Wkly. 2022;152:w30133. doi:10.4414/smw.2022.w30133
At the onset of the COVID-19 pandemic, patient encounters with the health care system plummeted.1-3 The perceived increased risk of contracting COVID-19 while obtaining care was thought to be a contributing factor. In outpatient settings, one study noted a 63% decrease in visits to otolaryngology visits in Massachusetts, and another noted a 33% decrease in dental office visits at the onset of the pandemic in 2020 compared with the same time frame in 2019.2,4 Along with mask mandates and stay-at-home orders, various institutions sought to mitigate the spread of COVID-19 through different protocols, including the use of social distancing, limitation of visitors, and telehealth. Despite some of these measures, nosocomial infections were not uncommon. For example, one hospital in the United Kingdom reported that 15% of COVID-19 inpatient cases in a 6-week period in 2020 were probably or definitely hospital acquired. These patients had a 36% case fatality rate.5
Unlike outpatient treatment centers, however, the emergency department (ED) is mandated by the Emergency Medical Treatment and Labor Act to provide a medical screening examination and to stabilize emergency medical conditions to all patients presenting to the ED. Thus, high numbers of undifferentiated and symptomatic patients are forced to congregate in EDs, increasing the risk of transmission of COVID-19. This perception of increased risk led to a 42% decrease in ED visits during March and April 2020 at the onset of the COVID-19 pandemic.1 Correspondingly, there was a 20% decrease in code stroke activations at a hospital in Canada and a 38% decrease in ST-elevation myocardial infarction activations across 9 United States hospital systems.6,7
Limited studies have been conducted to date to determine whether contracting COVID-19 while in the ED is a risk. One retrospective case-control study evaluating 39 EDs in the US showed that ED colocation with known patients with COVID-19 was not associated with an increased risk of COVID-19 transmission.5 However, this study also recognized that infection control strategies widely varied by location and date.
In this study, we report the incidence of COVID-19 infections within 21 days after the initial visit for symptoms not associated with COVID-19 infection to the Veterans Affairs Greater Los Angeles Healthcare System (VAGLAHS) ED and compared it with that of COVID-19 infections for tests performed within the VAGLAHS.
Program Description
As a quality improvement measure, the
Patients with specific symptoms noted during triage, such as those associated with COVID-19 diagnosis, respiratory infections, fever, and/or myalgias, were isolated in their own patient room. Electronic tablets were used for persons under investigation and patients with COVID-19 to communicate with family and/or medical staff who did not need to enter the patient’s room. Two-hour disinfection protocols were instituted for high-risk patients who were moved during the course of their treatment (ie, transfer to another bed for admission or discharge). All staff was specifically trained in personal protective equipment (PPE) donning and doffing, and 2-physician airway teams were implemented to ensure proper PPE use and safe COVID-19 intubations.
COVID-19 Infections
Electronic health records of patients who visited the VAGLAHS ED for symptoms not related to COVID-19 were reviewed from
A total of 8708 patients who came to the ED with symptoms not associated with COVID-19 infection and had a COVID-19 test within 21 days of the ED visit met the inclusion criteria. The overall average positivity rate at the VAGLAHS ED for symptoms not associated with COVID-19 infection was 1.1% from June 1, 2020, to June 30, 2021. The positivity rate by month ranged from 0% to 6.7% for this period (Figure).
Discussion
Implementing COVID-19 mitigation measures in the VAGLAHS ED helped minimize exposure and subsequent infection of COVID-19 for veterans who visited the VAGLAHS ED with symptoms not associated with COVID-19 infection. Contextualizing this with the overall average monthly positivity rate of veterans in the VAGLAHS catchment area (10.9%) or Los Angeles County (7.9%) between June 1, 2020, to June 30, 2021, veterans who visited the VAGLAHS ED for symptoms not associated with COVID-19 infection were less likely to test positive for COVID-19 within 21 days (1.1%), suggesting that the extensive measures taken at the VAGLAHS ED were effective.8
Many health care systems in the US and abroad have experimented with different transmission mitigation strategies in the ED. These tactics have included careful resource allocation when PPE shortages occur, incorporation of airway teams with appropriate safety measures to reduce nosocomial spread to health care workers, and use of a cohorting plan to separate persons under investigation and patients with COVID-19 from other patients.9-15 Additionally, forward screening areas were incorporated similar to the COVID-19 tent that was instituted at the VAGLAHS ED to manage patients who were referred to the ED for COVID-19 testing during the beginning of the pandemic, which prevented symptomatic patients from congregating with asymptomatic patients.14,15
Encouragingly, some of these studies reported no cases of nosocomial transmission in the ED.11,13 In a separate study, 14 clusters of COVID-19 cases were identified at one VA health care system in which nosocomial transmission was suspected, including one in the ED.16 Using contact tracing, no patients and 9 employees were found to have contracted COVID-19 in that cluster. Overall, among all clusters examined within the health care system, either by contact tracing or by whole-genome sequencing, the authors found that transmission from health care personnel to patients was rare. Despite different methodologies, we also similarly found that ED patients in our VA facility were unlikely to become infected with COVID-19.
While the low incidence of positive COVID-19 tests cannot be attributed to any one method, our data provide a working blueprint for enhanced ED precautions in future surges of COVID-19 or other airborne diseases, including that of future pandemics.
Limitations
Notably, although the VA is the largest health care system in the US, a considerable number of veterans may present to non-VA EDs to seek care, and thus their data are not included here; these veterans may live farther from a VA facility or experience higher barriers to care than veterans who exclusively or almost exclusively seek care within the VA. As a result, we are unable to account for COVID-19 tests completed outside the VA. Moreover, the wild type SARS-CoV-2 virus was dominant during the time frame chosen for this assessment, and data may not be generalizable to other variants (eg, omicron) that are known to be more highly transmissible.17 Lastly, although our observation was performed at a single VA ED and may not apply to other facilities, especially in light of different mitigation strategies, our findings still provide support for approaches to minimizing patient and staff exposure to COVID-19 in ED settings.
Conclusions
Implementation of COVID-19 mitigation measures in the VAGLAHS ED may have minimized exposure to COVID-19 for veterans who visited the VAGLAHS ED for symptoms not associated with COVID-19 and did not put one at higher risk of contracting COVID-19. Taken together, our data suggest that patients should not avoid seeking emergency care out of fear of contracting COVID-19 if EDs have adequately instituted mitigation techniques.
At the onset of the COVID-19 pandemic, patient encounters with the health care system plummeted.1-3 The perceived increased risk of contracting COVID-19 while obtaining care was thought to be a contributing factor. In outpatient settings, one study noted a 63% decrease in visits to otolaryngology visits in Massachusetts, and another noted a 33% decrease in dental office visits at the onset of the pandemic in 2020 compared with the same time frame in 2019.2,4 Along with mask mandates and stay-at-home orders, various institutions sought to mitigate the spread of COVID-19 through different protocols, including the use of social distancing, limitation of visitors, and telehealth. Despite some of these measures, nosocomial infections were not uncommon. For example, one hospital in the United Kingdom reported that 15% of COVID-19 inpatient cases in a 6-week period in 2020 were probably or definitely hospital acquired. These patients had a 36% case fatality rate.5
Unlike outpatient treatment centers, however, the emergency department (ED) is mandated by the Emergency Medical Treatment and Labor Act to provide a medical screening examination and to stabilize emergency medical conditions to all patients presenting to the ED. Thus, high numbers of undifferentiated and symptomatic patients are forced to congregate in EDs, increasing the risk of transmission of COVID-19. This perception of increased risk led to a 42% decrease in ED visits during March and April 2020 at the onset of the COVID-19 pandemic.1 Correspondingly, there was a 20% decrease in code stroke activations at a hospital in Canada and a 38% decrease in ST-elevation myocardial infarction activations across 9 United States hospital systems.6,7
Limited studies have been conducted to date to determine whether contracting COVID-19 while in the ED is a risk. One retrospective case-control study evaluating 39 EDs in the US showed that ED colocation with known patients with COVID-19 was not associated with an increased risk of COVID-19 transmission.5 However, this study also recognized that infection control strategies widely varied by location and date.
In this study, we report the incidence of COVID-19 infections within 21 days after the initial visit for symptoms not associated with COVID-19 infection to the Veterans Affairs Greater Los Angeles Healthcare System (VAGLAHS) ED and compared it with that of COVID-19 infections for tests performed within the VAGLAHS.
Program Description
As a quality improvement measure, the
Patients with specific symptoms noted during triage, such as those associated with COVID-19 diagnosis, respiratory infections, fever, and/or myalgias, were isolated in their own patient room. Electronic tablets were used for persons under investigation and patients with COVID-19 to communicate with family and/or medical staff who did not need to enter the patient’s room. Two-hour disinfection protocols were instituted for high-risk patients who were moved during the course of their treatment (ie, transfer to another bed for admission or discharge). All staff was specifically trained in personal protective equipment (PPE) donning and doffing, and 2-physician airway teams were implemented to ensure proper PPE use and safe COVID-19 intubations.
COVID-19 Infections
Electronic health records of patients who visited the VAGLAHS ED for symptoms not related to COVID-19 were reviewed from
A total of 8708 patients who came to the ED with symptoms not associated with COVID-19 infection and had a COVID-19 test within 21 days of the ED visit met the inclusion criteria. The overall average positivity rate at the VAGLAHS ED for symptoms not associated with COVID-19 infection was 1.1% from June 1, 2020, to June 30, 2021. The positivity rate by month ranged from 0% to 6.7% for this period (Figure).
Discussion
Implementing COVID-19 mitigation measures in the VAGLAHS ED helped minimize exposure and subsequent infection of COVID-19 for veterans who visited the VAGLAHS ED with symptoms not associated with COVID-19 infection. Contextualizing this with the overall average monthly positivity rate of veterans in the VAGLAHS catchment area (10.9%) or Los Angeles County (7.9%) between June 1, 2020, to June 30, 2021, veterans who visited the VAGLAHS ED for symptoms not associated with COVID-19 infection were less likely to test positive for COVID-19 within 21 days (1.1%), suggesting that the extensive measures taken at the VAGLAHS ED were effective.8
Many health care systems in the US and abroad have experimented with different transmission mitigation strategies in the ED. These tactics have included careful resource allocation when PPE shortages occur, incorporation of airway teams with appropriate safety measures to reduce nosocomial spread to health care workers, and use of a cohorting plan to separate persons under investigation and patients with COVID-19 from other patients.9-15 Additionally, forward screening areas were incorporated similar to the COVID-19 tent that was instituted at the VAGLAHS ED to manage patients who were referred to the ED for COVID-19 testing during the beginning of the pandemic, which prevented symptomatic patients from congregating with asymptomatic patients.14,15
Encouragingly, some of these studies reported no cases of nosocomial transmission in the ED.11,13 In a separate study, 14 clusters of COVID-19 cases were identified at one VA health care system in which nosocomial transmission was suspected, including one in the ED.16 Using contact tracing, no patients and 9 employees were found to have contracted COVID-19 in that cluster. Overall, among all clusters examined within the health care system, either by contact tracing or by whole-genome sequencing, the authors found that transmission from health care personnel to patients was rare. Despite different methodologies, we also similarly found that ED patients in our VA facility were unlikely to become infected with COVID-19.
While the low incidence of positive COVID-19 tests cannot be attributed to any one method, our data provide a working blueprint for enhanced ED precautions in future surges of COVID-19 or other airborne diseases, including that of future pandemics.
Limitations
Notably, although the VA is the largest health care system in the US, a considerable number of veterans may present to non-VA EDs to seek care, and thus their data are not included here; these veterans may live farther from a VA facility or experience higher barriers to care than veterans who exclusively or almost exclusively seek care within the VA. As a result, we are unable to account for COVID-19 tests completed outside the VA. Moreover, the wild type SARS-CoV-2 virus was dominant during the time frame chosen for this assessment, and data may not be generalizable to other variants (eg, omicron) that are known to be more highly transmissible.17 Lastly, although our observation was performed at a single VA ED and may not apply to other facilities, especially in light of different mitigation strategies, our findings still provide support for approaches to minimizing patient and staff exposure to COVID-19 in ED settings.
Conclusions
Implementation of COVID-19 mitigation measures in the VAGLAHS ED may have minimized exposure to COVID-19 for veterans who visited the VAGLAHS ED for symptoms not associated with COVID-19 and did not put one at higher risk of contracting COVID-19. Taken together, our data suggest that patients should not avoid seeking emergency care out of fear of contracting COVID-19 if EDs have adequately instituted mitigation techniques.
1. Hartnett KP, Kite-Powell A, DeVies J, et al; National Syndromic Surveillance Program Community of Practice. Impact of the COVID-19 pandemic on emergency department visits—United States, January 1, 2019-May 30, 2020. MMWR Morb Mortal Wkly Rep. 2020;69(23):699-704. doi:10.15585/mmwr.mm6923e1
2. Fan T, Workman AD, Miller LE, et al. The impact of COVID-19 on otolaryngology community practice in Massachusetts. Otolaryngol Head Neck Surg. 2021;165(3):424-430. doi:10.1177/0194599820983732
3. Baum A, Kaboli PJ, Schwartz MD. Reduced in-person and increased telehealth outpatient visits during the COVID-19 pandemic. Ann Intern Med. 2021;174(1):129-131. doi:10.7326/M20-3026
4. Kranz AM, Chen A, Gahlon G, Stein BD. 2020 trends in dental office visits during the COVID-19 pandemic. J Am Dent Assoc. 2021;152(7):535-541,e1. doi:10.1016/j.adaj.2021.02.01
5. Ridgway JP, Robicsek AA. Risk of coronavirus disease 2019 (COVID-19) acquisition among emergency department patients: a retrospective case control study. Infect Control Hosp Epidemiol. 2021;42(1):105-107. doi:10.1017/ice.2020.1224
6. Bres Bullrich M, Fridman S, Mandzia JL, et al. COVID-19: stroke admissions, emergency department visits, and prevention clinic referrals. Can J Neurol Sci. 2020;47(5):693-696. doi:10.1017/cjn.2020.101
7. Garcia S, Albaghdadi MS, Meraj PM, et al. Reduction in ST-segment elevation cardiac catheterization laboratory activations in the United States during COVID-19 pandemic. J Am Coll Cardiol. 2020;75(22):2871-2872. doi:10.1016/j.jacc.2020.04.011
8. LA County COVID-19 Surveillance Dashboard. Accessed July 25, 2022. https://covid19.lacounty.gov/dashboards
9. Wallace DW, Burleson SL, Heimann MA, et al. An adapted emergency department triage algorithm for the COVID-19 pandemic. J Am Coll Emerg Physicians Open. 2020;1:1374-1379. doi:10.1002/emp2.12210
10. Montrief T, Ramzy M, Long B, Gottlieb M, Hercz D. COVID-19 respiratory support in the emergency department setting. Am Journal Emerg Med. 2020;38(10):2160-2168. doi:10.1016/j.ajem.2020.08.001
11. Alqahtani F, Alanazi M, Alassaf W, et al. Preventing SARS-CoV-2 transmission in the emergency department by implementing a separate pathway for patients with respiratory conditions. J Complement Integr Med. 2022;19(2):383-388. doi:10.1515/jcim-2020-0422
12. Odorizzi S, Clark E, Nemnom MJ, et al. Flow impacts of hot/cold zone infection control procedures during the COVID-19 pandemic in the emergency department. CJEM. 2022;24(4):390-396. doi:10.1007/s43678-022-00278-0
13. Wee LE, Fua TP, Chua YY, et al. Containing COVID-19 in the emergency department: the role of improved case detection and segregation of suspect cases. Acad Emerg Med. 2020;27(5):379-387. doi:10.1111/acem.13984
14. Tan RMR, Ong GYK, Chong SL, Ganapathy S, Tyebally A, Lee KP. Dynamic adaptation to COVID-19 in a Singapore paediatric emergency department. Emerg Med J. 2020;37(5):252-254. doi:10.1136/emermed-2020-20963
15. Quah LJJ, Tan BKK, Fua TP, et al. Reorganising the emergency department to manage the COVID-19 outbreak. Int J Emerg Med. 2020;13(1):32. doi:10.1186/s12245-020-00294-w
16. Jinadatha C, Jones LD, Choi H, et al. Transmission of SARS-CoV-2 in inpatient and outpatient settings in a Veterans Affairs health care system. Open Forum Infect Dis. 2021;8(8):ofab328. doi:10.1093/ofid/ofab328
17. Riediker M, Briceno-Ayala L, Ichihara G, et al. Higher viral load and infectivity increase risk of aerosol transmission for Delta and Omicron variants of SARS-CoV-2. Swiss Med Wkly. 2022;152:w30133. doi:10.4414/smw.2022.w30133
1. Hartnett KP, Kite-Powell A, DeVies J, et al; National Syndromic Surveillance Program Community of Practice. Impact of the COVID-19 pandemic on emergency department visits—United States, January 1, 2019-May 30, 2020. MMWR Morb Mortal Wkly Rep. 2020;69(23):699-704. doi:10.15585/mmwr.mm6923e1
2. Fan T, Workman AD, Miller LE, et al. The impact of COVID-19 on otolaryngology community practice in Massachusetts. Otolaryngol Head Neck Surg. 2021;165(3):424-430. doi:10.1177/0194599820983732
3. Baum A, Kaboli PJ, Schwartz MD. Reduced in-person and increased telehealth outpatient visits during the COVID-19 pandemic. Ann Intern Med. 2021;174(1):129-131. doi:10.7326/M20-3026
4. Kranz AM, Chen A, Gahlon G, Stein BD. 2020 trends in dental office visits during the COVID-19 pandemic. J Am Dent Assoc. 2021;152(7):535-541,e1. doi:10.1016/j.adaj.2021.02.01
5. Ridgway JP, Robicsek AA. Risk of coronavirus disease 2019 (COVID-19) acquisition among emergency department patients: a retrospective case control study. Infect Control Hosp Epidemiol. 2021;42(1):105-107. doi:10.1017/ice.2020.1224
6. Bres Bullrich M, Fridman S, Mandzia JL, et al. COVID-19: stroke admissions, emergency department visits, and prevention clinic referrals. Can J Neurol Sci. 2020;47(5):693-696. doi:10.1017/cjn.2020.101
7. Garcia S, Albaghdadi MS, Meraj PM, et al. Reduction in ST-segment elevation cardiac catheterization laboratory activations in the United States during COVID-19 pandemic. J Am Coll Cardiol. 2020;75(22):2871-2872. doi:10.1016/j.jacc.2020.04.011
8. LA County COVID-19 Surveillance Dashboard. Accessed July 25, 2022. https://covid19.lacounty.gov/dashboards
9. Wallace DW, Burleson SL, Heimann MA, et al. An adapted emergency department triage algorithm for the COVID-19 pandemic. J Am Coll Emerg Physicians Open. 2020;1:1374-1379. doi:10.1002/emp2.12210
10. Montrief T, Ramzy M, Long B, Gottlieb M, Hercz D. COVID-19 respiratory support in the emergency department setting. Am Journal Emerg Med. 2020;38(10):2160-2168. doi:10.1016/j.ajem.2020.08.001
11. Alqahtani F, Alanazi M, Alassaf W, et al. Preventing SARS-CoV-2 transmission in the emergency department by implementing a separate pathway for patients with respiratory conditions. J Complement Integr Med. 2022;19(2):383-388. doi:10.1515/jcim-2020-0422
12. Odorizzi S, Clark E, Nemnom MJ, et al. Flow impacts of hot/cold zone infection control procedures during the COVID-19 pandemic in the emergency department. CJEM. 2022;24(4):390-396. doi:10.1007/s43678-022-00278-0
13. Wee LE, Fua TP, Chua YY, et al. Containing COVID-19 in the emergency department: the role of improved case detection and segregation of suspect cases. Acad Emerg Med. 2020;27(5):379-387. doi:10.1111/acem.13984
14. Tan RMR, Ong GYK, Chong SL, Ganapathy S, Tyebally A, Lee KP. Dynamic adaptation to COVID-19 in a Singapore paediatric emergency department. Emerg Med J. 2020;37(5):252-254. doi:10.1136/emermed-2020-20963
15. Quah LJJ, Tan BKK, Fua TP, et al. Reorganising the emergency department to manage the COVID-19 outbreak. Int J Emerg Med. 2020;13(1):32. doi:10.1186/s12245-020-00294-w
16. Jinadatha C, Jones LD, Choi H, et al. Transmission of SARS-CoV-2 in inpatient and outpatient settings in a Veterans Affairs health care system. Open Forum Infect Dis. 2021;8(8):ofab328. doi:10.1093/ofid/ofab328
17. Riediker M, Briceno-Ayala L, Ichihara G, et al. Higher viral load and infectivity increase risk of aerosol transmission for Delta and Omicron variants of SARS-CoV-2. Swiss Med Wkly. 2022;152:w30133. doi:10.4414/smw.2022.w30133
Barriers to Implementation of Telehealth Pre-anesthesia Evaluation Visits in the Department of Veterans Affairs
Days or weeks before a scheduled surgical or invasive procedure involving anesthesia, evaluations are conducted to assess a patient’s condition and risk, optimize their status, and prepare them for their procedure. A comprehensive pre-anesthesia evaluation visit includes a history of present illness, the evaluation of comorbidities and medication use, the assessment of health habits such as alcohol and tobacco use, functional capacity and nutritional assessments, and the identification of social support deficiencies that may influence recovery. It also includes a focused physical examination and laboratory and other ancillary testing as needed and may include optimization interventions such as anemia management or prehabilitation. Conducting pre-anesthesia evaluations before surgery has been shown to reduce delays and cancellations, unnecessary preprocedure testing, hospital length of stay, and in-hospital mortality.1-4
The pre-anesthesia evaluation is usually conducted in person, although other modalities have been in use for several years and have accelerated since the advent of the COVID-19 pandemic. Specifically, audio-only telephone visits are used in many settings to conduct abbreviated forms of a pre-anesthesia evaluation, typically for less-invasive procedures. When patients are evaluated over the telephone, the physical examination and testing are deferred until the day of the procedure. Another modality is the use of synchronous video telehealth. Emerging evidence for the use of video-based care in anesthesiology provides encouraging results. Several institutions have proven the technological feasibility of performing preoperative evaluations via video.5,6 Compared with in-person evaluations, these visits seem to have similar surgery cancellation rates, improved patient satisfaction, and reduced wait times and costs.7-9
As part of a quality improvement project, we studied the use of telehealth for pre-anesthesia evaluations within the US Department of Veterans Affairs (VA). An internal review found overall low utilization of these modalities before the COVID-19 pandemic that accelerated toward telehealth during the pandemic: The largest uptake was with telephone visits. Given the increasing adoption of telehealth for pre-anesthesia evaluations and the marked preference for telephone over video modalities among VA practitioners during the COVID-19 pandemic, we sought to understand the barriers and facilitators to the adoption of telephone- and video-based pre-anesthesia evaluation visits within the VA.
Methods
Our objective was to assess health care practitioners’ (HCPs) preferences regarding pre-anesthesia evaluation modalities (in-person, telephone, or video), and the perceived advantages and barriers to adoption for each modality. We followed the Strengthening the Reporting of Observational studies in Epidemiology (STROBE) guideline and Checklist for statistical Assessment of Medical Papers (CHAMP) statement.10,11 The survey was deemed a quality improvement activity that was exempt from institutional review board oversight by the VA National Anesthesia Program Office and the VA Office of Connected Care.
A survey was distributed to all VA anesthesiology service chiefs via email between April 27, 2022, and May 3, 2022. Three emails were sent to each participant (initial invitation and 2 reminders). The respondents were asked to identify themselves by facility and role and to indicate whether their anesthesiology service performed any pre-anesthesia evaluations, including any telephone- or video-based evaluations; and whether their service has a dedicated pre-anesthesia evaluation clinic.
A second set of questions referred to the use of telephone- and video-based preprocedure evaluations. The questions were based on branch logic and depended on the respondent’s answers concerning their use of telephone- and video-based evaluations. Questions included statements about perceived barriers to the adoption of these pre-anesthesia evaluation modalities. Each item was rated on a 5-point Likert scale, (completely disagree [1] to completely agree [5]). A third section measured acceptability and feasibility of video using the validated Acceptability of Intervention Measure (AIM) and Feasibility of Intervention Measure (FIM) questionnaires.12 These instruments are 4-item measures of implementation outcomes that are often considered indicators of implementation success.13 Acceptability is the perception among implementation stakeholders that a given treatment, service, practice, or innovation is agreeable, palatable, or satisfactory. Feasibility is defined as the extent to which a new treatment or an innovation can be successfully used or carried out within a given agency or setting.13 The criterion for acceptability is personal, meaning that different HCPs may have differing needs, preferences, and expectations regarding the same intervention. The criterion for feasibility is practical. An intervention may be considered to be feasible if the required tasks can be performed easily or conveniently. Finally, 2 open-ended questions allowed respondents to identify the most important factor that allowed the implementation of telehealth for pre-anesthesia evaluations in their service, and provide comments about the use of telehealth for pre-anesthesia evaluations at the VA. All questions were developed by the authors except for the 2 implementation measure instruments.
The survey was administered using an electronic survey platform (Qualtrics, version April 2022) and sent by email alongside a brief introductory video. Participation was voluntary and anonymous, as no personal information was collected. Responses were attributed to each facility, using the self-declared affiliation. When an affiliation was not provided, we deduced it using the latitude/longitude of the respondent, a feature included in the survey software. No incentives were provided. Data were stored and maintained in a secure VA server. All completed surveys were included. Some facilities had > 1 complete response, and all were included. Facilities that provided > 1 response and where responses were discordant, we clarified with the facility service chief. Incomplete responses were excluded from the analysis.
Statistics
For this analysis, the 2 positive sentiment responses (agree and completely agree) and the 2 negative sentiment responses (disagree and completely disagree) in the Likert scale were collapsed into single categories (good and poor, respectively). The neither agree nor disagree responses were coded as neutral. Our analysis began with a visual exploration of all variables to evaluate the frequency, percentage, and near-zero variance for categorical variables.14 Near-zero variance occurs when a categorical variable has a low frequency of unique values over the sample size (ie, the variable is almost constant), and we addressed it by combining different variable categorizations. We handled missing values through imputation algorithms followed by sensitivity analyses to verify whether our results were stable with and without imputation. We performed comparisons for the exploratory analysis using P values for one-way analysis of variance tests for numeric variables and χ2 tests for categorical variables. We considered P values < .05 to be statistically significant. We also used correlation matrices and plots as exploratory analysis tools to better understand all items’ correlations. We used Pearson, polychoric, and polyserial correlation tests as appropriate for numeric, ordinal, and logical items.
Our modeling strategy involved a series of generalized linear models (GLMs) with a Gaussian family, ie, multiple linear regression models, to assess the association between (1) facilities’ preferences regarding pre-anesthesia evaluation modalities; (2) advantages between modalities; and (3) barriers to the adoption of telehealth and the ability to perform different pre-anesthesia evaluation-related tasks. In addition, we used backward deletion to reach the most parsimonious model based on a series of likelihood-ratio tests comparing nested models. Results are reported as predicted means with 95% confidence intervals, with results being interpreted as significant when any 2 predicted means do not overlap between different estimates along with P for trends < .001. We performed all analyses using the R language.15
Results
Of 109 surveyed facilities, 50 (46%) responded to the survey. The final study sample included 67 responses, and 55 were included in the analysis. Twelve responses were excluded from the analysis as they were either incomplete or test responses. Three facilities had > 1 complete response (2 facilities had 2 responses and 1 facility had 4 responses), and these were all included in the analysis.
Thirty-six locations were complex inpatient facilities, and 32 (89%) had pre-anesthesia evaluation clinics (Table 1).
The ability to obtain a history of present illness was rated good/very good via telephone for 34 respondents (92%) and 25 for video (86%). Assessing comorbidities and health habits was rated good/very good via telephone for 32 respondents (89%) and 31 respondents (86%), respectively, and via video for 24 respondents (83%) and 23 respondents (79%), respectively (Figure 1).
To compare differences between the 2 remote pre-anesthesia evaluation modalities, we created GLMs evaluating the association between each modality and the perceived ability to perform the tasks. For GLMs, we transformed the values of the categories into numerical (ie, 1, poor; 2, neutral; 3, good). Compared with telephone, video was rated more favorably regarding the assessment of nutritional status (mean, 2.1; 95% CI, 1.8-2.3 vs mean, 2.4; 95% CI, 2.2-2.7; P = .04) (eAppendix 1, available at doi:10.12788/fp.0387). No other significant differences in ratings existed between the 2 remote pre-anesthesia evaluation modalities.
The most significant barriers (cited as significant or very significant in the survey) included the inability to perform a physical examination, which was noted by 13 respondents (72%) and 15 respondents (60%) for telephone and video, respectively. The inability to obtain vital signs was rated as a significant barrier for telephone by 12 respondents (67%) and for video by 15 respondents (60%)(Figure 2).
The average FIM score was 3.7, with the highest score among respondents who used both phone and video (Table 2). The average AIM score was 3.4, with the highest score among respondents who used both telehealth modalities. The internal consistency of the implementation measures was excellent (Cronbach’s α 0.95 and 0.975 for FIM and AIM, respectively).
Discussion
We surveyed 109 anesthesiology services across the VA regarding barriers to implementing telephone- and video-based pre-anesthesia evaluation visits. We found that 12 (23%) of the 50 anesthesiology services responding to this survey still conduct the totality of their pre-anesthesia evaluations in person. This represents an opportunity to further disseminate the appropriate use of telehealth and potentially reduce travel time, costs, and low-value testing, as it is well established that remote pre-anesthesia evaluations for low-risk procedures are safe and effective.6
We also found no difference between telephone and video regarding users’ perceived ability to perform any of the basic pre-anesthesia evaluation tasks except for assessing patients’ nutritional status, which was rated as easier using video than telephone. According to those not using telephone and/or video, the biggest barriers to implementation of telehealth visits were the inability to obtain vital signs and to perform a physical examination. This finding was unexpected, as facilities that conduct remote evaluations typically defer these tasks to the day of surgery, a practice that has been well established and shown to be safe and efficient. Respondents also identified patient-level factors (eg, patient preference, lack of telephone or computer) as significant barriers. Finally, feasibility ratings were higher than acceptability ratings with regards to the implementation of telehealth.
In 2004, the first use of telehealth for pre-anesthesia evaluations was reported by Wong and colleagues.16 Since then, several case series and a literature review have documented the efficacy, safety, and patient and HCP satisfaction with the use of telehealth for pre-anesthesia evaluations. A study by Mullen-Fortino and colleagues showed reduced visit times when telehealth was used for pre-anesthesia evaluation.8 Another study at VA hospitals showed that 88% of veterans reported that telemedicine saved them time and money.17 A report of 35 patients in rural Australia reported 98% satisfaction with the video quality of the visit, 95% perceived efficacy, and 87% preference for telehealth compared with driving to be seen in person.18 These reports conflict with the perceptions of the respondents of our survey, who identified patient preference as an important barrier to adoption of telehealth. Given these findings, research is needed on veterans’ perceptions on the use of telehealth modalities for pre-anesthesia evaluations; if their perceptions are similarly favorable, it will be important to communicate this information to HCPs and leadership, which may help increase subsequent telehealth adoption.
Despite the reported safety, efficacy, and high satisfaction of video visits among anesthesiology teams conducting pre-anesthesia evaluations, its use remains low at VA. We have found that most facilities in the VA system chose telephone platforms during the COVID-19 pandemic. One possibility is that the adoption of video modalities among pre-anesthesia evaluation clinics in the VA system is resource intensive or difficult from the HCP’s perspective. When combined with the lack of perceived advantages over telephone as we found in our survey, most practitioners resort to the technologically less demanding and more familiar telephone platform. The results from FIM and AIM support this. While both telephone and video have high feasibility scores, acceptability scores are lower for video, even among those currently using this technology. Our findings do not rule out the utility of video-based care in perioperative medicine. Rather than a yes/no proposition, future studies need to establish the precise indications for video for pre-anesthesia evaluations; that is, situations where video visits offer an advantage over telephone. For example, video could be used to deliver preoperative optimization therapies, such as supervised exercise or mental health interventions or to guide the achievement of certain milestones before surgery in patients with chronic conditions, such as target glucose values or the treatment of anemia. Future studies should explore the perceived benefits of video over telephone among centers offering these more advanced optimization interventions.
Limitations
We received responses from a subset of VA anesthesiology services; therefore, they may not be representative of the entire VA system. Facilities designated by the VA as inpatient complex were overrepresented (72% of our sample vs 50% of the total facilities nationally), and ambulatory centers (those designed by the VA as ambulatory procedural center with basic or advanced capabilities) were underrepresented (2% of our sample vs 22% nationally). Despite this, the response rate was high, and no geographic area appeared to be underrepresented. In addition, we surveyed pre-anesthesia evaluation facilities led by anesthesiologists, and the results may not be representative of the preferences of HCPs working in nonanesthesiology led pre-anesthesia evaluation clinics. Finally, just 11 facilities used both telephone and video; therefore, a true direct comparison between these 2 platforms was limited. The VA serves a unique patient population, and the findings may not be completely applicable to the non-VA population.
Conclusions
We found no significant perceived advantages of video over telephone in the ability to conduct routine pre-anesthesia evaluations among a sample of anesthesiology HCPs in the VA except for the perceived ability to assess nutritional status. HCPs with no telehealth experience cited the inability to perform a physical examination and obtain vital signs as the most significant barriers to implementation. Respondents not using telephone cited concerns about safety. Video visits in this clinical setting had additional perceived barriers to implementation, such as lack of information technology and staff support and patient-level barriers. Video had lower acceptability by HCPs. Given findings that pre-anesthesia evaluations can be conducted effectively via telehealth and have high levels of patient satisfaction, future work should focus on increasing uptake of these remote modalities. Additionally, research on the most appropriate uses of video visits within perioperative care is also needed.
1. Starsnic MA, Guarnieri DM, Norris MC. Efficacy and financial benefit of an anesthesiologist-directed university preadmission evaluation center. J Clin Anesth. 1997;9(4):299-305. doi:10.1016/s0952-8180(97)00007-x
2. Kristoffersen EW, Opsal A, Tveit TO, Berg RC, Fossum M. Effectiveness of pre-anaesthetic assessment clinic: a systematic review of randomised and non-randomised prospective controlled studies. BMJ Open. 2022;12(5):e054206. doi:10.1136/bmjopen-2021-054206
3. Ferschl MB, Tung A, Sweitzer B, Huo D, Glick DB. Preoperative clinic visits reduce operating room cancellations and delays. Anesthesiology. 2005;103(4):855-9. doi:10.1097/00000542-200510000-00025
4. Blitz JD, Kendale SM, Jain SK, Cuff GE, Kim JT, Rosenberg AD. preoperative evaluation clinic visit is associated with decreased risk of in-hospital postoperative mortality. Anesthesiology. 2016;125(2):280-294. doi:10.1097/ALN.0000000000001193
5. Dilisio RP, Dilisio AJ, Weiner MM. Preoperative virtual screening examination of the airway. J Clin Anesth. 2014;26(4):315-317. doi:10.1016/j.jclinane.2013.12.010
6. Kamdar NV, Huverserian A, Jalilian L, et al. Development, implementation, and evaluation of a telemedicine preoperative evaluation initiative at a major academic medical center. Anesth Analg. 2020;131(6):1647-1656. doi:10.1213/ANE.0000000000005208
7. Azizad O, Joshi GP. Telemedicine for preanesthesia evaluation: review of current literature and recommendations for future implementation. Curr Opin Anaesthesiol. 2021;34(6):672-677. doi:10.1097/ACO.0000000000001064
8. Mullen-Fortino M, Rising KL, Duckworth J, Gwynn V, Sites FD, Hollander JE. Presurgical assessment using telemedicine technology: impact on efficiency, effectiveness, and patient experience of care. Telemed J E Health. 2019;25(2):137-142. doi:10.1089/tmj.2017.0133
9. Zhang K, Rashid-Kolvear M, Waseem R, Englesakis M, Chung F. Virtual preoperative assessment in surgical patients: a systematic review and meta-analysis. J Clin Anesth. 2021;75:110540. doi:10.1016/j.jclinane.2021.110540
10. Mansournia MA, Collins GS, Nielsen RO, et al. A CHecklist for statistical Assessment of Medical Papers (the CHAMP statement): explanation and elaboration. Br J Sports Med. 2021;55(18):1009-1017. doi:10.1136/bjsports-2020-103652
11. von Elm E, Altman DG, Egger M, et al. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) Statement: guidelines for reporting observational studies. Int J Surg. 2014;12(12):1495-1499. doi:10.1016/j.ijsu.2014.07.013
12. Weiner BJ, Lewis CC, Stanick C, et al. Psychometric assessment of three newly developed implementation outcome measures. Implement Sci. 2017;12(1):108. doi:10.1186/s13012-017-0635-3
13. Proctor E, Silmere H, Raghavan R, et al. Outcomes for implementation research: conceptual distinctions, measurement challenges, and research agenda. Adm Policy Ment Health. 2011;38(2):65-76. doi:10.1007/s10488-010-0319-7
14. Kuhn M, Johnson K. Applied Predictive Modeling. Springer; 2013.
15. Team RC. A language and environment for statistical computing. 2018. Accessed December 16, 2022. https://www.R-project.org
16. Wong DT, Kamming D, Salenieks ME, Go K, Kohm C, Chung F. Preadmission anesthesia consultation using telemedicine technology: a pilot study. Anesthesiology. 2004;100(6):1605-1607. doi:10.1097/00000542-200406000-00038
17. Zetterman CV, Sweitzer BJ, Webb B, Barak-Bernhagen MA, Boedeker BH. Validation of a virtual preoperative evaluation clinic: a pilot study. Stud Health Technol Inform. 2011;163:737-739. doi: 10.3233/978-1-60750-706-2-737
18. Roberts S, Spain B, Hicks C, London J, Tay S. Telemedicine in the Northern Territory: an assessment of patient perceptions in the preoperative anaesthetic clinic. Aust J Rural Health. 2015;23(3):136-141. doi:10.1111/ajr.12140
Days or weeks before a scheduled surgical or invasive procedure involving anesthesia, evaluations are conducted to assess a patient’s condition and risk, optimize their status, and prepare them for their procedure. A comprehensive pre-anesthesia evaluation visit includes a history of present illness, the evaluation of comorbidities and medication use, the assessment of health habits such as alcohol and tobacco use, functional capacity and nutritional assessments, and the identification of social support deficiencies that may influence recovery. It also includes a focused physical examination and laboratory and other ancillary testing as needed and may include optimization interventions such as anemia management or prehabilitation. Conducting pre-anesthesia evaluations before surgery has been shown to reduce delays and cancellations, unnecessary preprocedure testing, hospital length of stay, and in-hospital mortality.1-4
The pre-anesthesia evaluation is usually conducted in person, although other modalities have been in use for several years and have accelerated since the advent of the COVID-19 pandemic. Specifically, audio-only telephone visits are used in many settings to conduct abbreviated forms of a pre-anesthesia evaluation, typically for less-invasive procedures. When patients are evaluated over the telephone, the physical examination and testing are deferred until the day of the procedure. Another modality is the use of synchronous video telehealth. Emerging evidence for the use of video-based care in anesthesiology provides encouraging results. Several institutions have proven the technological feasibility of performing preoperative evaluations via video.5,6 Compared with in-person evaluations, these visits seem to have similar surgery cancellation rates, improved patient satisfaction, and reduced wait times and costs.7-9
As part of a quality improvement project, we studied the use of telehealth for pre-anesthesia evaluations within the US Department of Veterans Affairs (VA). An internal review found overall low utilization of these modalities before the COVID-19 pandemic that accelerated toward telehealth during the pandemic: The largest uptake was with telephone visits. Given the increasing adoption of telehealth for pre-anesthesia evaluations and the marked preference for telephone over video modalities among VA practitioners during the COVID-19 pandemic, we sought to understand the barriers and facilitators to the adoption of telephone- and video-based pre-anesthesia evaluation visits within the VA.
Methods
Our objective was to assess health care practitioners’ (HCPs) preferences regarding pre-anesthesia evaluation modalities (in-person, telephone, or video), and the perceived advantages and barriers to adoption for each modality. We followed the Strengthening the Reporting of Observational studies in Epidemiology (STROBE) guideline and Checklist for statistical Assessment of Medical Papers (CHAMP) statement.10,11 The survey was deemed a quality improvement activity that was exempt from institutional review board oversight by the VA National Anesthesia Program Office and the VA Office of Connected Care.
A survey was distributed to all VA anesthesiology service chiefs via email between April 27, 2022, and May 3, 2022. Three emails were sent to each participant (initial invitation and 2 reminders). The respondents were asked to identify themselves by facility and role and to indicate whether their anesthesiology service performed any pre-anesthesia evaluations, including any telephone- or video-based evaluations; and whether their service has a dedicated pre-anesthesia evaluation clinic.
A second set of questions referred to the use of telephone- and video-based preprocedure evaluations. The questions were based on branch logic and depended on the respondent’s answers concerning their use of telephone- and video-based evaluations. Questions included statements about perceived barriers to the adoption of these pre-anesthesia evaluation modalities. Each item was rated on a 5-point Likert scale, (completely disagree [1] to completely agree [5]). A third section measured acceptability and feasibility of video using the validated Acceptability of Intervention Measure (AIM) and Feasibility of Intervention Measure (FIM) questionnaires.12 These instruments are 4-item measures of implementation outcomes that are often considered indicators of implementation success.13 Acceptability is the perception among implementation stakeholders that a given treatment, service, practice, or innovation is agreeable, palatable, or satisfactory. Feasibility is defined as the extent to which a new treatment or an innovation can be successfully used or carried out within a given agency or setting.13 The criterion for acceptability is personal, meaning that different HCPs may have differing needs, preferences, and expectations regarding the same intervention. The criterion for feasibility is practical. An intervention may be considered to be feasible if the required tasks can be performed easily or conveniently. Finally, 2 open-ended questions allowed respondents to identify the most important factor that allowed the implementation of telehealth for pre-anesthesia evaluations in their service, and provide comments about the use of telehealth for pre-anesthesia evaluations at the VA. All questions were developed by the authors except for the 2 implementation measure instruments.
The survey was administered using an electronic survey platform (Qualtrics, version April 2022) and sent by email alongside a brief introductory video. Participation was voluntary and anonymous, as no personal information was collected. Responses were attributed to each facility, using the self-declared affiliation. When an affiliation was not provided, we deduced it using the latitude/longitude of the respondent, a feature included in the survey software. No incentives were provided. Data were stored and maintained in a secure VA server. All completed surveys were included. Some facilities had > 1 complete response, and all were included. Facilities that provided > 1 response and where responses were discordant, we clarified with the facility service chief. Incomplete responses were excluded from the analysis.
Statistics
For this analysis, the 2 positive sentiment responses (agree and completely agree) and the 2 negative sentiment responses (disagree and completely disagree) in the Likert scale were collapsed into single categories (good and poor, respectively). The neither agree nor disagree responses were coded as neutral. Our analysis began with a visual exploration of all variables to evaluate the frequency, percentage, and near-zero variance for categorical variables.14 Near-zero variance occurs when a categorical variable has a low frequency of unique values over the sample size (ie, the variable is almost constant), and we addressed it by combining different variable categorizations. We handled missing values through imputation algorithms followed by sensitivity analyses to verify whether our results were stable with and without imputation. We performed comparisons for the exploratory analysis using P values for one-way analysis of variance tests for numeric variables and χ2 tests for categorical variables. We considered P values < .05 to be statistically significant. We also used correlation matrices and plots as exploratory analysis tools to better understand all items’ correlations. We used Pearson, polychoric, and polyserial correlation tests as appropriate for numeric, ordinal, and logical items.
Our modeling strategy involved a series of generalized linear models (GLMs) with a Gaussian family, ie, multiple linear regression models, to assess the association between (1) facilities’ preferences regarding pre-anesthesia evaluation modalities; (2) advantages between modalities; and (3) barriers to the adoption of telehealth and the ability to perform different pre-anesthesia evaluation-related tasks. In addition, we used backward deletion to reach the most parsimonious model based on a series of likelihood-ratio tests comparing nested models. Results are reported as predicted means with 95% confidence intervals, with results being interpreted as significant when any 2 predicted means do not overlap between different estimates along with P for trends < .001. We performed all analyses using the R language.15
Results
Of 109 surveyed facilities, 50 (46%) responded to the survey. The final study sample included 67 responses, and 55 were included in the analysis. Twelve responses were excluded from the analysis as they were either incomplete or test responses. Three facilities had > 1 complete response (2 facilities had 2 responses and 1 facility had 4 responses), and these were all included in the analysis.
Thirty-six locations were complex inpatient facilities, and 32 (89%) had pre-anesthesia evaluation clinics (Table 1).
The ability to obtain a history of present illness was rated good/very good via telephone for 34 respondents (92%) and 25 for video (86%). Assessing comorbidities and health habits was rated good/very good via telephone for 32 respondents (89%) and 31 respondents (86%), respectively, and via video for 24 respondents (83%) and 23 respondents (79%), respectively (Figure 1).
To compare differences between the 2 remote pre-anesthesia evaluation modalities, we created GLMs evaluating the association between each modality and the perceived ability to perform the tasks. For GLMs, we transformed the values of the categories into numerical (ie, 1, poor; 2, neutral; 3, good). Compared with telephone, video was rated more favorably regarding the assessment of nutritional status (mean, 2.1; 95% CI, 1.8-2.3 vs mean, 2.4; 95% CI, 2.2-2.7; P = .04) (eAppendix 1, available at doi:10.12788/fp.0387). No other significant differences in ratings existed between the 2 remote pre-anesthesia evaluation modalities.
The most significant barriers (cited as significant or very significant in the survey) included the inability to perform a physical examination, which was noted by 13 respondents (72%) and 15 respondents (60%) for telephone and video, respectively. The inability to obtain vital signs was rated as a significant barrier for telephone by 12 respondents (67%) and for video by 15 respondents (60%)(Figure 2).
The average FIM score was 3.7, with the highest score among respondents who used both phone and video (Table 2). The average AIM score was 3.4, with the highest score among respondents who used both telehealth modalities. The internal consistency of the implementation measures was excellent (Cronbach’s α 0.95 and 0.975 for FIM and AIM, respectively).
Discussion
We surveyed 109 anesthesiology services across the VA regarding barriers to implementing telephone- and video-based pre-anesthesia evaluation visits. We found that 12 (23%) of the 50 anesthesiology services responding to this survey still conduct the totality of their pre-anesthesia evaluations in person. This represents an opportunity to further disseminate the appropriate use of telehealth and potentially reduce travel time, costs, and low-value testing, as it is well established that remote pre-anesthesia evaluations for low-risk procedures are safe and effective.6
We also found no difference between telephone and video regarding users’ perceived ability to perform any of the basic pre-anesthesia evaluation tasks except for assessing patients’ nutritional status, which was rated as easier using video than telephone. According to those not using telephone and/or video, the biggest barriers to implementation of telehealth visits were the inability to obtain vital signs and to perform a physical examination. This finding was unexpected, as facilities that conduct remote evaluations typically defer these tasks to the day of surgery, a practice that has been well established and shown to be safe and efficient. Respondents also identified patient-level factors (eg, patient preference, lack of telephone or computer) as significant barriers. Finally, feasibility ratings were higher than acceptability ratings with regards to the implementation of telehealth.
In 2004, the first use of telehealth for pre-anesthesia evaluations was reported by Wong and colleagues.16 Since then, several case series and a literature review have documented the efficacy, safety, and patient and HCP satisfaction with the use of telehealth for pre-anesthesia evaluations. A study by Mullen-Fortino and colleagues showed reduced visit times when telehealth was used for pre-anesthesia evaluation.8 Another study at VA hospitals showed that 88% of veterans reported that telemedicine saved them time and money.17 A report of 35 patients in rural Australia reported 98% satisfaction with the video quality of the visit, 95% perceived efficacy, and 87% preference for telehealth compared with driving to be seen in person.18 These reports conflict with the perceptions of the respondents of our survey, who identified patient preference as an important barrier to adoption of telehealth. Given these findings, research is needed on veterans’ perceptions on the use of telehealth modalities for pre-anesthesia evaluations; if their perceptions are similarly favorable, it will be important to communicate this information to HCPs and leadership, which may help increase subsequent telehealth adoption.
Despite the reported safety, efficacy, and high satisfaction of video visits among anesthesiology teams conducting pre-anesthesia evaluations, its use remains low at VA. We have found that most facilities in the VA system chose telephone platforms during the COVID-19 pandemic. One possibility is that the adoption of video modalities among pre-anesthesia evaluation clinics in the VA system is resource intensive or difficult from the HCP’s perspective. When combined with the lack of perceived advantages over telephone as we found in our survey, most practitioners resort to the technologically less demanding and more familiar telephone platform. The results from FIM and AIM support this. While both telephone and video have high feasibility scores, acceptability scores are lower for video, even among those currently using this technology. Our findings do not rule out the utility of video-based care in perioperative medicine. Rather than a yes/no proposition, future studies need to establish the precise indications for video for pre-anesthesia evaluations; that is, situations where video visits offer an advantage over telephone. For example, video could be used to deliver preoperative optimization therapies, such as supervised exercise or mental health interventions or to guide the achievement of certain milestones before surgery in patients with chronic conditions, such as target glucose values or the treatment of anemia. Future studies should explore the perceived benefits of video over telephone among centers offering these more advanced optimization interventions.
Limitations
We received responses from a subset of VA anesthesiology services; therefore, they may not be representative of the entire VA system. Facilities designated by the VA as inpatient complex were overrepresented (72% of our sample vs 50% of the total facilities nationally), and ambulatory centers (those designed by the VA as ambulatory procedural center with basic or advanced capabilities) were underrepresented (2% of our sample vs 22% nationally). Despite this, the response rate was high, and no geographic area appeared to be underrepresented. In addition, we surveyed pre-anesthesia evaluation facilities led by anesthesiologists, and the results may not be representative of the preferences of HCPs working in nonanesthesiology led pre-anesthesia evaluation clinics. Finally, just 11 facilities used both telephone and video; therefore, a true direct comparison between these 2 platforms was limited. The VA serves a unique patient population, and the findings may not be completely applicable to the non-VA population.
Conclusions
We found no significant perceived advantages of video over telephone in the ability to conduct routine pre-anesthesia evaluations among a sample of anesthesiology HCPs in the VA except for the perceived ability to assess nutritional status. HCPs with no telehealth experience cited the inability to perform a physical examination and obtain vital signs as the most significant barriers to implementation. Respondents not using telephone cited concerns about safety. Video visits in this clinical setting had additional perceived barriers to implementation, such as lack of information technology and staff support and patient-level barriers. Video had lower acceptability by HCPs. Given findings that pre-anesthesia evaluations can be conducted effectively via telehealth and have high levels of patient satisfaction, future work should focus on increasing uptake of these remote modalities. Additionally, research on the most appropriate uses of video visits within perioperative care is also needed.
Days or weeks before a scheduled surgical or invasive procedure involving anesthesia, evaluations are conducted to assess a patient’s condition and risk, optimize their status, and prepare them for their procedure. A comprehensive pre-anesthesia evaluation visit includes a history of present illness, the evaluation of comorbidities and medication use, the assessment of health habits such as alcohol and tobacco use, functional capacity and nutritional assessments, and the identification of social support deficiencies that may influence recovery. It also includes a focused physical examination and laboratory and other ancillary testing as needed and may include optimization interventions such as anemia management or prehabilitation. Conducting pre-anesthesia evaluations before surgery has been shown to reduce delays and cancellations, unnecessary preprocedure testing, hospital length of stay, and in-hospital mortality.1-4
The pre-anesthesia evaluation is usually conducted in person, although other modalities have been in use for several years and have accelerated since the advent of the COVID-19 pandemic. Specifically, audio-only telephone visits are used in many settings to conduct abbreviated forms of a pre-anesthesia evaluation, typically for less-invasive procedures. When patients are evaluated over the telephone, the physical examination and testing are deferred until the day of the procedure. Another modality is the use of synchronous video telehealth. Emerging evidence for the use of video-based care in anesthesiology provides encouraging results. Several institutions have proven the technological feasibility of performing preoperative evaluations via video.5,6 Compared with in-person evaluations, these visits seem to have similar surgery cancellation rates, improved patient satisfaction, and reduced wait times and costs.7-9
As part of a quality improvement project, we studied the use of telehealth for pre-anesthesia evaluations within the US Department of Veterans Affairs (VA). An internal review found overall low utilization of these modalities before the COVID-19 pandemic that accelerated toward telehealth during the pandemic: The largest uptake was with telephone visits. Given the increasing adoption of telehealth for pre-anesthesia evaluations and the marked preference for telephone over video modalities among VA practitioners during the COVID-19 pandemic, we sought to understand the barriers and facilitators to the adoption of telephone- and video-based pre-anesthesia evaluation visits within the VA.
Methods
Our objective was to assess health care practitioners’ (HCPs) preferences regarding pre-anesthesia evaluation modalities (in-person, telephone, or video), and the perceived advantages and barriers to adoption for each modality. We followed the Strengthening the Reporting of Observational studies in Epidemiology (STROBE) guideline and Checklist for statistical Assessment of Medical Papers (CHAMP) statement.10,11 The survey was deemed a quality improvement activity that was exempt from institutional review board oversight by the VA National Anesthesia Program Office and the VA Office of Connected Care.
A survey was distributed to all VA anesthesiology service chiefs via email between April 27, 2022, and May 3, 2022. Three emails were sent to each participant (initial invitation and 2 reminders). The respondents were asked to identify themselves by facility and role and to indicate whether their anesthesiology service performed any pre-anesthesia evaluations, including any telephone- or video-based evaluations; and whether their service has a dedicated pre-anesthesia evaluation clinic.
A second set of questions referred to the use of telephone- and video-based preprocedure evaluations. The questions were based on branch logic and depended on the respondent’s answers concerning their use of telephone- and video-based evaluations. Questions included statements about perceived barriers to the adoption of these pre-anesthesia evaluation modalities. Each item was rated on a 5-point Likert scale, (completely disagree [1] to completely agree [5]). A third section measured acceptability and feasibility of video using the validated Acceptability of Intervention Measure (AIM) and Feasibility of Intervention Measure (FIM) questionnaires.12 These instruments are 4-item measures of implementation outcomes that are often considered indicators of implementation success.13 Acceptability is the perception among implementation stakeholders that a given treatment, service, practice, or innovation is agreeable, palatable, or satisfactory. Feasibility is defined as the extent to which a new treatment or an innovation can be successfully used or carried out within a given agency or setting.13 The criterion for acceptability is personal, meaning that different HCPs may have differing needs, preferences, and expectations regarding the same intervention. The criterion for feasibility is practical. An intervention may be considered to be feasible if the required tasks can be performed easily or conveniently. Finally, 2 open-ended questions allowed respondents to identify the most important factor that allowed the implementation of telehealth for pre-anesthesia evaluations in their service, and provide comments about the use of telehealth for pre-anesthesia evaluations at the VA. All questions were developed by the authors except for the 2 implementation measure instruments.
The survey was administered using an electronic survey platform (Qualtrics, version April 2022) and sent by email alongside a brief introductory video. Participation was voluntary and anonymous, as no personal information was collected. Responses were attributed to each facility, using the self-declared affiliation. When an affiliation was not provided, we deduced it using the latitude/longitude of the respondent, a feature included in the survey software. No incentives were provided. Data were stored and maintained in a secure VA server. All completed surveys were included. Some facilities had > 1 complete response, and all were included. Facilities that provided > 1 response and where responses were discordant, we clarified with the facility service chief. Incomplete responses were excluded from the analysis.
Statistics
For this analysis, the 2 positive sentiment responses (agree and completely agree) and the 2 negative sentiment responses (disagree and completely disagree) in the Likert scale were collapsed into single categories (good and poor, respectively). The neither agree nor disagree responses were coded as neutral. Our analysis began with a visual exploration of all variables to evaluate the frequency, percentage, and near-zero variance for categorical variables.14 Near-zero variance occurs when a categorical variable has a low frequency of unique values over the sample size (ie, the variable is almost constant), and we addressed it by combining different variable categorizations. We handled missing values through imputation algorithms followed by sensitivity analyses to verify whether our results were stable with and without imputation. We performed comparisons for the exploratory analysis using P values for one-way analysis of variance tests for numeric variables and χ2 tests for categorical variables. We considered P values < .05 to be statistically significant. We also used correlation matrices and plots as exploratory analysis tools to better understand all items’ correlations. We used Pearson, polychoric, and polyserial correlation tests as appropriate for numeric, ordinal, and logical items.
Our modeling strategy involved a series of generalized linear models (GLMs) with a Gaussian family, ie, multiple linear regression models, to assess the association between (1) facilities’ preferences regarding pre-anesthesia evaluation modalities; (2) advantages between modalities; and (3) barriers to the adoption of telehealth and the ability to perform different pre-anesthesia evaluation-related tasks. In addition, we used backward deletion to reach the most parsimonious model based on a series of likelihood-ratio tests comparing nested models. Results are reported as predicted means with 95% confidence intervals, with results being interpreted as significant when any 2 predicted means do not overlap between different estimates along with P for trends < .001. We performed all analyses using the R language.15
Results
Of 109 surveyed facilities, 50 (46%) responded to the survey. The final study sample included 67 responses, and 55 were included in the analysis. Twelve responses were excluded from the analysis as they were either incomplete or test responses. Three facilities had > 1 complete response (2 facilities had 2 responses and 1 facility had 4 responses), and these were all included in the analysis.
Thirty-six locations were complex inpatient facilities, and 32 (89%) had pre-anesthesia evaluation clinics (Table 1).
The ability to obtain a history of present illness was rated good/very good via telephone for 34 respondents (92%) and 25 for video (86%). Assessing comorbidities and health habits was rated good/very good via telephone for 32 respondents (89%) and 31 respondents (86%), respectively, and via video for 24 respondents (83%) and 23 respondents (79%), respectively (Figure 1).
To compare differences between the 2 remote pre-anesthesia evaluation modalities, we created GLMs evaluating the association between each modality and the perceived ability to perform the tasks. For GLMs, we transformed the values of the categories into numerical (ie, 1, poor; 2, neutral; 3, good). Compared with telephone, video was rated more favorably regarding the assessment of nutritional status (mean, 2.1; 95% CI, 1.8-2.3 vs mean, 2.4; 95% CI, 2.2-2.7; P = .04) (eAppendix 1, available at doi:10.12788/fp.0387). No other significant differences in ratings existed between the 2 remote pre-anesthesia evaluation modalities.
The most significant barriers (cited as significant or very significant in the survey) included the inability to perform a physical examination, which was noted by 13 respondents (72%) and 15 respondents (60%) for telephone and video, respectively. The inability to obtain vital signs was rated as a significant barrier for telephone by 12 respondents (67%) and for video by 15 respondents (60%)(Figure 2).
The average FIM score was 3.7, with the highest score among respondents who used both phone and video (Table 2). The average AIM score was 3.4, with the highest score among respondents who used both telehealth modalities. The internal consistency of the implementation measures was excellent (Cronbach’s α 0.95 and 0.975 for FIM and AIM, respectively).
Discussion
We surveyed 109 anesthesiology services across the VA regarding barriers to implementing telephone- and video-based pre-anesthesia evaluation visits. We found that 12 (23%) of the 50 anesthesiology services responding to this survey still conduct the totality of their pre-anesthesia evaluations in person. This represents an opportunity to further disseminate the appropriate use of telehealth and potentially reduce travel time, costs, and low-value testing, as it is well established that remote pre-anesthesia evaluations for low-risk procedures are safe and effective.6
We also found no difference between telephone and video regarding users’ perceived ability to perform any of the basic pre-anesthesia evaluation tasks except for assessing patients’ nutritional status, which was rated as easier using video than telephone. According to those not using telephone and/or video, the biggest barriers to implementation of telehealth visits were the inability to obtain vital signs and to perform a physical examination. This finding was unexpected, as facilities that conduct remote evaluations typically defer these tasks to the day of surgery, a practice that has been well established and shown to be safe and efficient. Respondents also identified patient-level factors (eg, patient preference, lack of telephone or computer) as significant barriers. Finally, feasibility ratings were higher than acceptability ratings with regards to the implementation of telehealth.
In 2004, the first use of telehealth for pre-anesthesia evaluations was reported by Wong and colleagues.16 Since then, several case series and a literature review have documented the efficacy, safety, and patient and HCP satisfaction with the use of telehealth for pre-anesthesia evaluations. A study by Mullen-Fortino and colleagues showed reduced visit times when telehealth was used for pre-anesthesia evaluation.8 Another study at VA hospitals showed that 88% of veterans reported that telemedicine saved them time and money.17 A report of 35 patients in rural Australia reported 98% satisfaction with the video quality of the visit, 95% perceived efficacy, and 87% preference for telehealth compared with driving to be seen in person.18 These reports conflict with the perceptions of the respondents of our survey, who identified patient preference as an important barrier to adoption of telehealth. Given these findings, research is needed on veterans’ perceptions on the use of telehealth modalities for pre-anesthesia evaluations; if their perceptions are similarly favorable, it will be important to communicate this information to HCPs and leadership, which may help increase subsequent telehealth adoption.
Despite the reported safety, efficacy, and high satisfaction of video visits among anesthesiology teams conducting pre-anesthesia evaluations, its use remains low at VA. We have found that most facilities in the VA system chose telephone platforms during the COVID-19 pandemic. One possibility is that the adoption of video modalities among pre-anesthesia evaluation clinics in the VA system is resource intensive or difficult from the HCP’s perspective. When combined with the lack of perceived advantages over telephone as we found in our survey, most practitioners resort to the technologically less demanding and more familiar telephone platform. The results from FIM and AIM support this. While both telephone and video have high feasibility scores, acceptability scores are lower for video, even among those currently using this technology. Our findings do not rule out the utility of video-based care in perioperative medicine. Rather than a yes/no proposition, future studies need to establish the precise indications for video for pre-anesthesia evaluations; that is, situations where video visits offer an advantage over telephone. For example, video could be used to deliver preoperative optimization therapies, such as supervised exercise or mental health interventions or to guide the achievement of certain milestones before surgery in patients with chronic conditions, such as target glucose values or the treatment of anemia. Future studies should explore the perceived benefits of video over telephone among centers offering these more advanced optimization interventions.
Limitations
We received responses from a subset of VA anesthesiology services; therefore, they may not be representative of the entire VA system. Facilities designated by the VA as inpatient complex were overrepresented (72% of our sample vs 50% of the total facilities nationally), and ambulatory centers (those designed by the VA as ambulatory procedural center with basic or advanced capabilities) were underrepresented (2% of our sample vs 22% nationally). Despite this, the response rate was high, and no geographic area appeared to be underrepresented. In addition, we surveyed pre-anesthesia evaluation facilities led by anesthesiologists, and the results may not be representative of the preferences of HCPs working in nonanesthesiology led pre-anesthesia evaluation clinics. Finally, just 11 facilities used both telephone and video; therefore, a true direct comparison between these 2 platforms was limited. The VA serves a unique patient population, and the findings may not be completely applicable to the non-VA population.
Conclusions
We found no significant perceived advantages of video over telephone in the ability to conduct routine pre-anesthesia evaluations among a sample of anesthesiology HCPs in the VA except for the perceived ability to assess nutritional status. HCPs with no telehealth experience cited the inability to perform a physical examination and obtain vital signs as the most significant barriers to implementation. Respondents not using telephone cited concerns about safety. Video visits in this clinical setting had additional perceived barriers to implementation, such as lack of information technology and staff support and patient-level barriers. Video had lower acceptability by HCPs. Given findings that pre-anesthesia evaluations can be conducted effectively via telehealth and have high levels of patient satisfaction, future work should focus on increasing uptake of these remote modalities. Additionally, research on the most appropriate uses of video visits within perioperative care is also needed.
1. Starsnic MA, Guarnieri DM, Norris MC. Efficacy and financial benefit of an anesthesiologist-directed university preadmission evaluation center. J Clin Anesth. 1997;9(4):299-305. doi:10.1016/s0952-8180(97)00007-x
2. Kristoffersen EW, Opsal A, Tveit TO, Berg RC, Fossum M. Effectiveness of pre-anaesthetic assessment clinic: a systematic review of randomised and non-randomised prospective controlled studies. BMJ Open. 2022;12(5):e054206. doi:10.1136/bmjopen-2021-054206
3. Ferschl MB, Tung A, Sweitzer B, Huo D, Glick DB. Preoperative clinic visits reduce operating room cancellations and delays. Anesthesiology. 2005;103(4):855-9. doi:10.1097/00000542-200510000-00025
4. Blitz JD, Kendale SM, Jain SK, Cuff GE, Kim JT, Rosenberg AD. preoperative evaluation clinic visit is associated with decreased risk of in-hospital postoperative mortality. Anesthesiology. 2016;125(2):280-294. doi:10.1097/ALN.0000000000001193
5. Dilisio RP, Dilisio AJ, Weiner MM. Preoperative virtual screening examination of the airway. J Clin Anesth. 2014;26(4):315-317. doi:10.1016/j.jclinane.2013.12.010
6. Kamdar NV, Huverserian A, Jalilian L, et al. Development, implementation, and evaluation of a telemedicine preoperative evaluation initiative at a major academic medical center. Anesth Analg. 2020;131(6):1647-1656. doi:10.1213/ANE.0000000000005208
7. Azizad O, Joshi GP. Telemedicine for preanesthesia evaluation: review of current literature and recommendations for future implementation. Curr Opin Anaesthesiol. 2021;34(6):672-677. doi:10.1097/ACO.0000000000001064
8. Mullen-Fortino M, Rising KL, Duckworth J, Gwynn V, Sites FD, Hollander JE. Presurgical assessment using telemedicine technology: impact on efficiency, effectiveness, and patient experience of care. Telemed J E Health. 2019;25(2):137-142. doi:10.1089/tmj.2017.0133
9. Zhang K, Rashid-Kolvear M, Waseem R, Englesakis M, Chung F. Virtual preoperative assessment in surgical patients: a systematic review and meta-analysis. J Clin Anesth. 2021;75:110540. doi:10.1016/j.jclinane.2021.110540
10. Mansournia MA, Collins GS, Nielsen RO, et al. A CHecklist for statistical Assessment of Medical Papers (the CHAMP statement): explanation and elaboration. Br J Sports Med. 2021;55(18):1009-1017. doi:10.1136/bjsports-2020-103652
11. von Elm E, Altman DG, Egger M, et al. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) Statement: guidelines for reporting observational studies. Int J Surg. 2014;12(12):1495-1499. doi:10.1016/j.ijsu.2014.07.013
12. Weiner BJ, Lewis CC, Stanick C, et al. Psychometric assessment of three newly developed implementation outcome measures. Implement Sci. 2017;12(1):108. doi:10.1186/s13012-017-0635-3
13. Proctor E, Silmere H, Raghavan R, et al. Outcomes for implementation research: conceptual distinctions, measurement challenges, and research agenda. Adm Policy Ment Health. 2011;38(2):65-76. doi:10.1007/s10488-010-0319-7
14. Kuhn M, Johnson K. Applied Predictive Modeling. Springer; 2013.
15. Team RC. A language and environment for statistical computing. 2018. Accessed December 16, 2022. https://www.R-project.org
16. Wong DT, Kamming D, Salenieks ME, Go K, Kohm C, Chung F. Preadmission anesthesia consultation using telemedicine technology: a pilot study. Anesthesiology. 2004;100(6):1605-1607. doi:10.1097/00000542-200406000-00038
17. Zetterman CV, Sweitzer BJ, Webb B, Barak-Bernhagen MA, Boedeker BH. Validation of a virtual preoperative evaluation clinic: a pilot study. Stud Health Technol Inform. 2011;163:737-739. doi: 10.3233/978-1-60750-706-2-737
18. Roberts S, Spain B, Hicks C, London J, Tay S. Telemedicine in the Northern Territory: an assessment of patient perceptions in the preoperative anaesthetic clinic. Aust J Rural Health. 2015;23(3):136-141. doi:10.1111/ajr.12140
1. Starsnic MA, Guarnieri DM, Norris MC. Efficacy and financial benefit of an anesthesiologist-directed university preadmission evaluation center. J Clin Anesth. 1997;9(4):299-305. doi:10.1016/s0952-8180(97)00007-x
2. Kristoffersen EW, Opsal A, Tveit TO, Berg RC, Fossum M. Effectiveness of pre-anaesthetic assessment clinic: a systematic review of randomised and non-randomised prospective controlled studies. BMJ Open. 2022;12(5):e054206. doi:10.1136/bmjopen-2021-054206
3. Ferschl MB, Tung A, Sweitzer B, Huo D, Glick DB. Preoperative clinic visits reduce operating room cancellations and delays. Anesthesiology. 2005;103(4):855-9. doi:10.1097/00000542-200510000-00025
4. Blitz JD, Kendale SM, Jain SK, Cuff GE, Kim JT, Rosenberg AD. preoperative evaluation clinic visit is associated with decreased risk of in-hospital postoperative mortality. Anesthesiology. 2016;125(2):280-294. doi:10.1097/ALN.0000000000001193
5. Dilisio RP, Dilisio AJ, Weiner MM. Preoperative virtual screening examination of the airway. J Clin Anesth. 2014;26(4):315-317. doi:10.1016/j.jclinane.2013.12.010
6. Kamdar NV, Huverserian A, Jalilian L, et al. Development, implementation, and evaluation of a telemedicine preoperative evaluation initiative at a major academic medical center. Anesth Analg. 2020;131(6):1647-1656. doi:10.1213/ANE.0000000000005208
7. Azizad O, Joshi GP. Telemedicine for preanesthesia evaluation: review of current literature and recommendations for future implementation. Curr Opin Anaesthesiol. 2021;34(6):672-677. doi:10.1097/ACO.0000000000001064
8. Mullen-Fortino M, Rising KL, Duckworth J, Gwynn V, Sites FD, Hollander JE. Presurgical assessment using telemedicine technology: impact on efficiency, effectiveness, and patient experience of care. Telemed J E Health. 2019;25(2):137-142. doi:10.1089/tmj.2017.0133
9. Zhang K, Rashid-Kolvear M, Waseem R, Englesakis M, Chung F. Virtual preoperative assessment in surgical patients: a systematic review and meta-analysis. J Clin Anesth. 2021;75:110540. doi:10.1016/j.jclinane.2021.110540
10. Mansournia MA, Collins GS, Nielsen RO, et al. A CHecklist for statistical Assessment of Medical Papers (the CHAMP statement): explanation and elaboration. Br J Sports Med. 2021;55(18):1009-1017. doi:10.1136/bjsports-2020-103652
11. von Elm E, Altman DG, Egger M, et al. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) Statement: guidelines for reporting observational studies. Int J Surg. 2014;12(12):1495-1499. doi:10.1016/j.ijsu.2014.07.013
12. Weiner BJ, Lewis CC, Stanick C, et al. Psychometric assessment of three newly developed implementation outcome measures. Implement Sci. 2017;12(1):108. doi:10.1186/s13012-017-0635-3
13. Proctor E, Silmere H, Raghavan R, et al. Outcomes for implementation research: conceptual distinctions, measurement challenges, and research agenda. Adm Policy Ment Health. 2011;38(2):65-76. doi:10.1007/s10488-010-0319-7
14. Kuhn M, Johnson K. Applied Predictive Modeling. Springer; 2013.
15. Team RC. A language and environment for statistical computing. 2018. Accessed December 16, 2022. https://www.R-project.org
16. Wong DT, Kamming D, Salenieks ME, Go K, Kohm C, Chung F. Preadmission anesthesia consultation using telemedicine technology: a pilot study. Anesthesiology. 2004;100(6):1605-1607. doi:10.1097/00000542-200406000-00038
17. Zetterman CV, Sweitzer BJ, Webb B, Barak-Bernhagen MA, Boedeker BH. Validation of a virtual preoperative evaluation clinic: a pilot study. Stud Health Technol Inform. 2011;163:737-739. doi: 10.3233/978-1-60750-706-2-737
18. Roberts S, Spain B, Hicks C, London J, Tay S. Telemedicine in the Northern Territory: an assessment of patient perceptions in the preoperative anaesthetic clinic. Aust J Rural Health. 2015;23(3):136-141. doi:10.1111/ajr.12140
Fireworks, Veterans, and PTSD: The Ironies of the Fourth of July
My first wish is to see this plague to Mankind, war, banished from the Earth; & the Sons and daughters of this World employed in more pleasing & innocent amusements than in preparing implements, & exercising them for the destruction of the human race.
General George Washington1
When I was a child, every Fourth of July holiday my father would take me to the military fireworks display at Fort Sam Houston in Texas. We would take our place in the long cascade of cars parked at the huge parade ground in front of Brooke Army Medical Center. It was the most spectacular display of the year not to be found anywhere else in the city. Army fire engines and medics were always on site in case anything went wrong, which rarely occurred thanks to the pyrotechnic experts who ran the display.
Later, when I began my psychiatric residency at the US Department of Veterans Affairs (VA) New Mexico Healthcare System, I quickly learned a darker truth about fireworks. What seemed to me and many other civilians in General Washington’s words, a “pleasing and innocent amusement,” instead was a distressing and terrifying revisiting of trauma for many service members and veterans, likely including my father, who was a World War II combat veteran.
Fireworks are so closely linked to the birth of our young nation that we often forget they were invented in China a millennia ago. Fireworks were first associated with the fledgling nation in the middle of the War of Independence. On July 4, 1776, representatives of the 13 colonies signed the Declaration of Independence. In one of several ironies of history, what was used at the initial commemorations was not fireworks but the very “implements of destruction,” to use Washington’s phrase—guns and cannons. The demonstrations of firepower were meant to be morale boosters. After the war, the dangers of the detonations were recognized, and firearms were replaced with the fireworks we still launch today.2
The country celebrates the holiday with cookouts, parades, brass band concerts, and of course fireworks. Added to the organized shows are the millions of citizens who demonstrate private patriotism by shooting off fireworks in their neighborhoods. In 2021, Americans spent $1.5 billion on fireworks, and 33% said they planned to attend a public display.3
However, people are increasingly recognizing the negative side of fireworks for wild and companion animals and the environment. Most of us who have dogs and I am sure cats, horses, and other animals dread the impending darkness of the Fourth as it signals the coming loud noise and the cringing, pacing animals who want to run yet have nowhere to go to be safe from the sound.4
Sitting in the clinic with veterans, I realized it was not only pets and wildlife that feared the ultimate American holiday but also the very individuals who fought to preserve the freedom those fireworks celebrate. The VA’s National Center for Posttraumatic Stress Disorder (PTSD) estimates that about 7% of veterans will meet the diagnostic criteria for PTSD in their lifetimes. The prevalence of PTSD differs, depending on the methodology used, era and type of services, and demographics. Some studies have found higher rates of PTSD in women, young veterans, and those who served in Vietnam. Among the veterans who receive health care at the VA, like those I saw in the clinic, 23 in 1000 may have PTSD.5
We, after all, are remarkably similar in physiology to other mammals, and not surprisingly, veterans with PTSD exhibit many of the same reactions to fireworks. The sights, sounds, and odor of fireworks, as well as the vocal responses of the crowd at large displays evoke memories that trigger fear and anxiety. Many veterans experience flashbacks in which they relive combat and training accidents and have nightmares of those events, interrupting sleep. The instinct of many veterans is to avoid the holiday altogether: Many patients I knew sought refuge in remote mountain campsites often to find that even there they were not safe from revelers.
Avoidance being a cardinal symptom and coping mechanism of PTSD, therapists advise other methods of managing the Fourth of July, such as distractions that are calming and people who are reassuring. Therapists often rehearse self-talk scripts and teach breathing exercises targeted to break the behavioral conditioning that links present innocuous sensory overstimulation with a past life-threatening danger. The heat of summer worsens the stress, cooling down literally and figuratively can help.6
Many VA medical centers send announcements to the media or have their experts do interviews to educate the public about the potentially traumatizing effects of fireworks. They also encourage veterans who are apprehensive about the holiday to seek additional mental health help, including the Veterans Crisis Line. With my patients, we started early and developed a preventive plan to manage the anticipatory apprehension and arrange a means of enduring the ordeal. I do not have data to prove it, but anecdotally I know from my years on-call that visits to VA emergency departments and admissions to our inpatient psychiatry unit always increased around Independence Day in part because some veterans used drugs and/or alcohol to dampen their stress response.
VA experts also have advice for the families and friends of veterans who want to reduce the impact of fireworks and other holiday activities on them. Many veterans will feel at once intensely present to the disturbing aspects like fireworks and crowds and at the same time, distant and separated from the more positive parts of celebrations like being with loved ones in the outdoors. We can simply ask the veterans in our lives and neighborhoods how the festivities affect them and how we can help them get through the long hot night.7 Yet it would not be America without some controversy, and opinions are divided even among veterans about whether yard signs that say, “Combat Veteran Lives Here Please Be Courteous With Fireworks” enhance or impede the effort to increase awareness of the connection between fireworks, veterans, and PTSD.8
This editorial began with my own story of enjoying fireworks to emphasize that my aim is not to ruin the fun but to ask us to think before we shoot and consider the veterans near us for whom our recreation may cause unnecessary distress. Fourth of July would not have been possible without the soldiers who fought and died in the American Revolution and all the conflicts since. We owe it to all who have worn the uniform for the United States of America to remember the extraordinary toll it has taken on their ability to live ordinary lives. Like General Washington, we should vow to end the wars that wounded them so future generations will be able to join in celebrating Independence Day.
1. From George Washington to David Humphreys, 25 July 1785. Accessed June 19, 2023. https://founders.archives.gov/documents/Washington/04-03-02-0142
2. Waxman OB. How fireworks became a Fourth of July tradition. TIME. Accessed June 19, 2023. https://time.com/4828701/first-fireworks-history-july-4th
3. Velasquez F. Here’s how much Americans are spending on food, alcohol, and fireworks this Fourth of July. Accessed June 19, 2023. https://www.cnbc.com/2021/07/04/how-much-americans-are-spending-on-fourth-of-july.html
4. Fireworks: growing evidence they distress animals builds case to restrict use. The Conversation. Accessed June 19, 2023. https://theconversation.com/fireworks-growing-evidence-they-distress-animals-builds-case-to-restrict-use-191472
5. US Department of Veterans Affairs. Epidemiology and impact of PTSD. Accessed June 17, 2023. https://www.ptsd.va.gov/professional/treat/essentials/epidemiology.asp#two,
6. US Department of Veterans Affairs. Independence Day celebrations can trigger PTSD in veterans. Press release. Accessed June 19, 2023. https://www.va.gov/new-jersey-health-care/news-releases/independence-day-celebrations-can-trigger-ptsd-in-veterans
7. Tips for veterans celebrating Independence Day. VA News. https://news.va.gov/62393/some-helpful-tips-to-remember-for-this-4th-of-july
8. Faith S. Veterans, July 4, and fireworks: don’t be courteous, just be American. Military.com. Accessed June 19, 2023. https://www.military.com/july-4th/veterans-july-4-and-fireworks-dont-be-courteous-just-be-american.html
My first wish is to see this plague to Mankind, war, banished from the Earth; & the Sons and daughters of this World employed in more pleasing & innocent amusements than in preparing implements, & exercising them for the destruction of the human race.
General George Washington1
When I was a child, every Fourth of July holiday my father would take me to the military fireworks display at Fort Sam Houston in Texas. We would take our place in the long cascade of cars parked at the huge parade ground in front of Brooke Army Medical Center. It was the most spectacular display of the year not to be found anywhere else in the city. Army fire engines and medics were always on site in case anything went wrong, which rarely occurred thanks to the pyrotechnic experts who ran the display.
Later, when I began my psychiatric residency at the US Department of Veterans Affairs (VA) New Mexico Healthcare System, I quickly learned a darker truth about fireworks. What seemed to me and many other civilians in General Washington’s words, a “pleasing and innocent amusement,” instead was a distressing and terrifying revisiting of trauma for many service members and veterans, likely including my father, who was a World War II combat veteran.
Fireworks are so closely linked to the birth of our young nation that we often forget they were invented in China a millennia ago. Fireworks were first associated with the fledgling nation in the middle of the War of Independence. On July 4, 1776, representatives of the 13 colonies signed the Declaration of Independence. In one of several ironies of history, what was used at the initial commemorations was not fireworks but the very “implements of destruction,” to use Washington’s phrase—guns and cannons. The demonstrations of firepower were meant to be morale boosters. After the war, the dangers of the detonations were recognized, and firearms were replaced with the fireworks we still launch today.2
The country celebrates the holiday with cookouts, parades, brass band concerts, and of course fireworks. Added to the organized shows are the millions of citizens who demonstrate private patriotism by shooting off fireworks in their neighborhoods. In 2021, Americans spent $1.5 billion on fireworks, and 33% said they planned to attend a public display.3
However, people are increasingly recognizing the negative side of fireworks for wild and companion animals and the environment. Most of us who have dogs and I am sure cats, horses, and other animals dread the impending darkness of the Fourth as it signals the coming loud noise and the cringing, pacing animals who want to run yet have nowhere to go to be safe from the sound.4
Sitting in the clinic with veterans, I realized it was not only pets and wildlife that feared the ultimate American holiday but also the very individuals who fought to preserve the freedom those fireworks celebrate. The VA’s National Center for Posttraumatic Stress Disorder (PTSD) estimates that about 7% of veterans will meet the diagnostic criteria for PTSD in their lifetimes. The prevalence of PTSD differs, depending on the methodology used, era and type of services, and demographics. Some studies have found higher rates of PTSD in women, young veterans, and those who served in Vietnam. Among the veterans who receive health care at the VA, like those I saw in the clinic, 23 in 1000 may have PTSD.5
We, after all, are remarkably similar in physiology to other mammals, and not surprisingly, veterans with PTSD exhibit many of the same reactions to fireworks. The sights, sounds, and odor of fireworks, as well as the vocal responses of the crowd at large displays evoke memories that trigger fear and anxiety. Many veterans experience flashbacks in which they relive combat and training accidents and have nightmares of those events, interrupting sleep. The instinct of many veterans is to avoid the holiday altogether: Many patients I knew sought refuge in remote mountain campsites often to find that even there they were not safe from revelers.
Avoidance being a cardinal symptom and coping mechanism of PTSD, therapists advise other methods of managing the Fourth of July, such as distractions that are calming and people who are reassuring. Therapists often rehearse self-talk scripts and teach breathing exercises targeted to break the behavioral conditioning that links present innocuous sensory overstimulation with a past life-threatening danger. The heat of summer worsens the stress, cooling down literally and figuratively can help.6
Many VA medical centers send announcements to the media or have their experts do interviews to educate the public about the potentially traumatizing effects of fireworks. They also encourage veterans who are apprehensive about the holiday to seek additional mental health help, including the Veterans Crisis Line. With my patients, we started early and developed a preventive plan to manage the anticipatory apprehension and arrange a means of enduring the ordeal. I do not have data to prove it, but anecdotally I know from my years on-call that visits to VA emergency departments and admissions to our inpatient psychiatry unit always increased around Independence Day in part because some veterans used drugs and/or alcohol to dampen their stress response.
VA experts also have advice for the families and friends of veterans who want to reduce the impact of fireworks and other holiday activities on them. Many veterans will feel at once intensely present to the disturbing aspects like fireworks and crowds and at the same time, distant and separated from the more positive parts of celebrations like being with loved ones in the outdoors. We can simply ask the veterans in our lives and neighborhoods how the festivities affect them and how we can help them get through the long hot night.7 Yet it would not be America without some controversy, and opinions are divided even among veterans about whether yard signs that say, “Combat Veteran Lives Here Please Be Courteous With Fireworks” enhance or impede the effort to increase awareness of the connection between fireworks, veterans, and PTSD.8
This editorial began with my own story of enjoying fireworks to emphasize that my aim is not to ruin the fun but to ask us to think before we shoot and consider the veterans near us for whom our recreation may cause unnecessary distress. Fourth of July would not have been possible without the soldiers who fought and died in the American Revolution and all the conflicts since. We owe it to all who have worn the uniform for the United States of America to remember the extraordinary toll it has taken on their ability to live ordinary lives. Like General Washington, we should vow to end the wars that wounded them so future generations will be able to join in celebrating Independence Day.
My first wish is to see this plague to Mankind, war, banished from the Earth; & the Sons and daughters of this World employed in more pleasing & innocent amusements than in preparing implements, & exercising them for the destruction of the human race.
General George Washington1
When I was a child, every Fourth of July holiday my father would take me to the military fireworks display at Fort Sam Houston in Texas. We would take our place in the long cascade of cars parked at the huge parade ground in front of Brooke Army Medical Center. It was the most spectacular display of the year not to be found anywhere else in the city. Army fire engines and medics were always on site in case anything went wrong, which rarely occurred thanks to the pyrotechnic experts who ran the display.
Later, when I began my psychiatric residency at the US Department of Veterans Affairs (VA) New Mexico Healthcare System, I quickly learned a darker truth about fireworks. What seemed to me and many other civilians in General Washington’s words, a “pleasing and innocent amusement,” instead was a distressing and terrifying revisiting of trauma for many service members and veterans, likely including my father, who was a World War II combat veteran.
Fireworks are so closely linked to the birth of our young nation that we often forget they were invented in China a millennia ago. Fireworks were first associated with the fledgling nation in the middle of the War of Independence. On July 4, 1776, representatives of the 13 colonies signed the Declaration of Independence. In one of several ironies of history, what was used at the initial commemorations was not fireworks but the very “implements of destruction,” to use Washington’s phrase—guns and cannons. The demonstrations of firepower were meant to be morale boosters. After the war, the dangers of the detonations were recognized, and firearms were replaced with the fireworks we still launch today.2
The country celebrates the holiday with cookouts, parades, brass band concerts, and of course fireworks. Added to the organized shows are the millions of citizens who demonstrate private patriotism by shooting off fireworks in their neighborhoods. In 2021, Americans spent $1.5 billion on fireworks, and 33% said they planned to attend a public display.3
However, people are increasingly recognizing the negative side of fireworks for wild and companion animals and the environment. Most of us who have dogs and I am sure cats, horses, and other animals dread the impending darkness of the Fourth as it signals the coming loud noise and the cringing, pacing animals who want to run yet have nowhere to go to be safe from the sound.4
Sitting in the clinic with veterans, I realized it was not only pets and wildlife that feared the ultimate American holiday but also the very individuals who fought to preserve the freedom those fireworks celebrate. The VA’s National Center for Posttraumatic Stress Disorder (PTSD) estimates that about 7% of veterans will meet the diagnostic criteria for PTSD in their lifetimes. The prevalence of PTSD differs, depending on the methodology used, era and type of services, and demographics. Some studies have found higher rates of PTSD in women, young veterans, and those who served in Vietnam. Among the veterans who receive health care at the VA, like those I saw in the clinic, 23 in 1000 may have PTSD.5
We, after all, are remarkably similar in physiology to other mammals, and not surprisingly, veterans with PTSD exhibit many of the same reactions to fireworks. The sights, sounds, and odor of fireworks, as well as the vocal responses of the crowd at large displays evoke memories that trigger fear and anxiety. Many veterans experience flashbacks in which they relive combat and training accidents and have nightmares of those events, interrupting sleep. The instinct of many veterans is to avoid the holiday altogether: Many patients I knew sought refuge in remote mountain campsites often to find that even there they were not safe from revelers.
Avoidance being a cardinal symptom and coping mechanism of PTSD, therapists advise other methods of managing the Fourth of July, such as distractions that are calming and people who are reassuring. Therapists often rehearse self-talk scripts and teach breathing exercises targeted to break the behavioral conditioning that links present innocuous sensory overstimulation with a past life-threatening danger. The heat of summer worsens the stress, cooling down literally and figuratively can help.6
Many VA medical centers send announcements to the media or have their experts do interviews to educate the public about the potentially traumatizing effects of fireworks. They also encourage veterans who are apprehensive about the holiday to seek additional mental health help, including the Veterans Crisis Line. With my patients, we started early and developed a preventive plan to manage the anticipatory apprehension and arrange a means of enduring the ordeal. I do not have data to prove it, but anecdotally I know from my years on-call that visits to VA emergency departments and admissions to our inpatient psychiatry unit always increased around Independence Day in part because some veterans used drugs and/or alcohol to dampen their stress response.
VA experts also have advice for the families and friends of veterans who want to reduce the impact of fireworks and other holiday activities on them. Many veterans will feel at once intensely present to the disturbing aspects like fireworks and crowds and at the same time, distant and separated from the more positive parts of celebrations like being with loved ones in the outdoors. We can simply ask the veterans in our lives and neighborhoods how the festivities affect them and how we can help them get through the long hot night.7 Yet it would not be America without some controversy, and opinions are divided even among veterans about whether yard signs that say, “Combat Veteran Lives Here Please Be Courteous With Fireworks” enhance or impede the effort to increase awareness of the connection between fireworks, veterans, and PTSD.8
This editorial began with my own story of enjoying fireworks to emphasize that my aim is not to ruin the fun but to ask us to think before we shoot and consider the veterans near us for whom our recreation may cause unnecessary distress. Fourth of July would not have been possible without the soldiers who fought and died in the American Revolution and all the conflicts since. We owe it to all who have worn the uniform for the United States of America to remember the extraordinary toll it has taken on their ability to live ordinary lives. Like General Washington, we should vow to end the wars that wounded them so future generations will be able to join in celebrating Independence Day.
1. From George Washington to David Humphreys, 25 July 1785. Accessed June 19, 2023. https://founders.archives.gov/documents/Washington/04-03-02-0142
2. Waxman OB. How fireworks became a Fourth of July tradition. TIME. Accessed June 19, 2023. https://time.com/4828701/first-fireworks-history-july-4th
3. Velasquez F. Here’s how much Americans are spending on food, alcohol, and fireworks this Fourth of July. Accessed June 19, 2023. https://www.cnbc.com/2021/07/04/how-much-americans-are-spending-on-fourth-of-july.html
4. Fireworks: growing evidence they distress animals builds case to restrict use. The Conversation. Accessed June 19, 2023. https://theconversation.com/fireworks-growing-evidence-they-distress-animals-builds-case-to-restrict-use-191472
5. US Department of Veterans Affairs. Epidemiology and impact of PTSD. Accessed June 17, 2023. https://www.ptsd.va.gov/professional/treat/essentials/epidemiology.asp#two,
6. US Department of Veterans Affairs. Independence Day celebrations can trigger PTSD in veterans. Press release. Accessed June 19, 2023. https://www.va.gov/new-jersey-health-care/news-releases/independence-day-celebrations-can-trigger-ptsd-in-veterans
7. Tips for veterans celebrating Independence Day. VA News. https://news.va.gov/62393/some-helpful-tips-to-remember-for-this-4th-of-july
8. Faith S. Veterans, July 4, and fireworks: don’t be courteous, just be American. Military.com. Accessed June 19, 2023. https://www.military.com/july-4th/veterans-july-4-and-fireworks-dont-be-courteous-just-be-american.html
1. From George Washington to David Humphreys, 25 July 1785. Accessed June 19, 2023. https://founders.archives.gov/documents/Washington/04-03-02-0142
2. Waxman OB. How fireworks became a Fourth of July tradition. TIME. Accessed June 19, 2023. https://time.com/4828701/first-fireworks-history-july-4th
3. Velasquez F. Here’s how much Americans are spending on food, alcohol, and fireworks this Fourth of July. Accessed June 19, 2023. https://www.cnbc.com/2021/07/04/how-much-americans-are-spending-on-fourth-of-july.html
4. Fireworks: growing evidence they distress animals builds case to restrict use. The Conversation. Accessed June 19, 2023. https://theconversation.com/fireworks-growing-evidence-they-distress-animals-builds-case-to-restrict-use-191472
5. US Department of Veterans Affairs. Epidemiology and impact of PTSD. Accessed June 17, 2023. https://www.ptsd.va.gov/professional/treat/essentials/epidemiology.asp#two,
6. US Department of Veterans Affairs. Independence Day celebrations can trigger PTSD in veterans. Press release. Accessed June 19, 2023. https://www.va.gov/new-jersey-health-care/news-releases/independence-day-celebrations-can-trigger-ptsd-in-veterans
7. Tips for veterans celebrating Independence Day. VA News. https://news.va.gov/62393/some-helpful-tips-to-remember-for-this-4th-of-july
8. Faith S. Veterans, July 4, and fireworks: don’t be courteous, just be American. Military.com. Accessed June 19, 2023. https://www.military.com/july-4th/veterans-july-4-and-fireworks-dont-be-courteous-just-be-american.html
Commentary: New treatments for mantle cell lymphoma and B-cell lymphoma, July 2023
Mantle cell lymphoma (MCL) is a rare and often heterogenous subtype of non-Hodgkin lymphoma (NHL). Though patients can experience prolonged remissions after frontline therapy, most patients ultimately relapse. Treatment of relapsed/refractory disease can be challenging, but there have recently been a growing number of therapeutic options in this setting. Covalent Bruton tyrosine kinase (BTK) inhibitors, for example, have demonstrated activity in patients with MCL and are approved by the US Food and Drug Administration (FDA) for relapsed/refractory disease. Chimeric antigen receptor (CAR) T-cell therapy is also an effective option for relapsed/refractory disease, though this is typically available only at select centers and is associated with toxicities, such as cytokine release syndrome and neurologic toxicity.
Recently, a novel BTK inhibitor, pirtobrutinib, has also been studied across NHL, including MCL (Wang et al) Pirtobrutinib is a selective, noncovalent BTK inhibitor with the ability to bind both the C481S-mutant and wild-type BTK. The multicenter, phase 1/2 BRUIN study included 90 patients with MCL who were previously treated with a covalent BTK inhibitor. Patients in the phase 1 portion of the study were treated with oral pirtobrutinib at a dose of 25-300 mg once daily, and patients in the phase 2 study were treated at the recommended dose of 200 mg once daily. The overall response rate was 57.8% (95% CI 46.9%-68.1%), with the complete response rate being 20.0%. At a median follow-up of 12 months, the median duration of response was 21.6 (95% CI 7.5 to not reached) months. Treatment-related adverse events that were grade 3 or higher were not frequent, with neutropenia (8.5%) being the most common. Of note, grade 3 or higher hemorrhage and atrial fibrillation, which can be seen with BTK inhibitors, were rare, occurring in 3.7% and 1.2% of patients, respectively. Based on the results of this study, pirtobrutinib has been approved by the FDA for patients with relapsed/refractory MCL after at least two prior lines of therapy, including a BTK inhibitor. This is an appealing oral option for patients with relapsed disease.
Options for patients with relapsed/refractory large B-cell lymphoma (LBCL) have also significantly increased in recent years. One of the most important advances in this disease has been the use of anti-CD19 CAR T-cell therapy. There are currently three FDA-approved options for patients with relapsed/refractory LBCL who have received at least two prior lines of therapy.1-3 More recently, axicabtagene ciloleucel (axi-cel) and lisocabtagene maraleucel (liso-cel) have also been approved for the second line based on the results of the ZUMA-7 and TRANSFORM studies, respectively.4,5
Longer follow-up of the ZUMA-7 trial continues to confirm the advantage of axi-cel over standard-care therapy for patients with primary refractory or early relapse of disease, now with evidence of an overall survival advantage (Westin et al). The ZUMA-7 trial included 359 adults with LBCL (refractory to or relapsed within 12 months of first-line treatment) who were randomly assigned to receive axi-cel (n = 180) or standard care (n = 179). At a median follow-up of 47.2 mo, patients receiving axi-cel vs standard care had a significantly longer median overall survival (not reached vs 31.1 mo; hazard ratio [HR] 0.73; P = .03) and an absolute improvement in overall survival (8.6 percentage points at 4 years). No new treatment-related deaths were reported since the primary event-free survival analysis. These data confirm that early use of axi-cel is preferred over standard-care therapy with high-dose chemotherapy and autologous stem cell transplantation.
Another important study that was recently published looked at the role of mental health on outcomes in patients with diffuse large B-cell lymphoma (DLBCL) (Kuczmarski et al). Though it is known that mental health disorders can decrease the quality of life of patients with cancer, there is limited information on the survival implications of these issues. A recent retrospective cohort study analyzed the data of 13,244 patients aged 67 years or older with DLBCL from the Surveillance, Epidemiology, and End Results (SEER)–Medicare registry, of which, 2094 patients had depression, anxiety, or both at the time of their DLBCL diagnosis. At a median follow-up of 2.0 years, patients with depression, anxiety, or both vs without any mental disorder had significantly lower 5-year overall survival rates (27.0% vs 37.4%; HR 1.37; 95% CI 1.29-1.44). They also found that those patients with preexisting depression vs without any mental disorder have the worst survival (23.4% vs 38.0%; HR 1.37; P < .0001). Though the mechanism accounting for decreased survival is not clear, the authors postulate that mental health disorders may lead to delays or interruptions in lymphoma-directed therapy. They also note the potential for increased barriers to care in patients with mental health disorders, which may result in nonadherence in this patient population. Regardless, these results highlight the importance of mental health screening and interventions in patients with DLBCL.
Additional References
- Neelapu SS, Locke FL, Bartlett NL, et al. Axicabtagene ciloleucel CAR T-Cell therapy in refractory large B-cell lymphoma. N Engl J Med. 2017;377:2531-2544. doi: 10.1056/NEJMoa1707447
- Schuster SJ, Bishop MR, Tam CS, et al; JULIET Investigators. Tisagenlecleucel in adult relapsed or refractory diffuse large B-cell lymphoma. N Engl J Med. 2019;380:45-56. doi: 10.1056/NEJMoa1804980
- Abramson JS, Palomba ML, Gordon LI, et al. Lisocabtagene maraleucel for patients with relapsed or refractory large B-cell lymphomas (TRANSCEND NHL 001): A multicentre seamless design study. Lancet. 2020;396:839-852. doi: 10.1016/S0140-6736(20)31366-0
- Locke FL, Miklos DB, Jacobson CA, et al; All ZUMA-7 Investigators and Contributing Kite Members. Axicabtagene ciloleucel as second-line therapy for large B-cell lymphoma. N Engl J Med. 2022;386:640-654. doi: 10.1056/NEJMoa2116133
- Kamdar M, Solomon SR, Arnason J, et al; TRANSFORM Investigators. Lisocabtagene maraleucel versus standard of care with salvage chemotherapy followed by autologous stem cell transplantation as second-line treatment in patients with relapsed or refractory large B-cell lymphoma (TRANSFORM): Results from an interim analysis of an open-label, randomised, phase 3 trial. Lancet. 2022;399:2294-2308. doi: 10.1016/S0140-6736(22)00662-6
Mantle cell lymphoma (MCL) is a rare and often heterogenous subtype of non-Hodgkin lymphoma (NHL). Though patients can experience prolonged remissions after frontline therapy, most patients ultimately relapse. Treatment of relapsed/refractory disease can be challenging, but there have recently been a growing number of therapeutic options in this setting. Covalent Bruton tyrosine kinase (BTK) inhibitors, for example, have demonstrated activity in patients with MCL and are approved by the US Food and Drug Administration (FDA) for relapsed/refractory disease. Chimeric antigen receptor (CAR) T-cell therapy is also an effective option for relapsed/refractory disease, though this is typically available only at select centers and is associated with toxicities, such as cytokine release syndrome and neurologic toxicity.
Recently, a novel BTK inhibitor, pirtobrutinib, has also been studied across NHL, including MCL (Wang et al) Pirtobrutinib is a selective, noncovalent BTK inhibitor with the ability to bind both the C481S-mutant and wild-type BTK. The multicenter, phase 1/2 BRUIN study included 90 patients with MCL who were previously treated with a covalent BTK inhibitor. Patients in the phase 1 portion of the study were treated with oral pirtobrutinib at a dose of 25-300 mg once daily, and patients in the phase 2 study were treated at the recommended dose of 200 mg once daily. The overall response rate was 57.8% (95% CI 46.9%-68.1%), with the complete response rate being 20.0%. At a median follow-up of 12 months, the median duration of response was 21.6 (95% CI 7.5 to not reached) months. Treatment-related adverse events that were grade 3 or higher were not frequent, with neutropenia (8.5%) being the most common. Of note, grade 3 or higher hemorrhage and atrial fibrillation, which can be seen with BTK inhibitors, were rare, occurring in 3.7% and 1.2% of patients, respectively. Based on the results of this study, pirtobrutinib has been approved by the FDA for patients with relapsed/refractory MCL after at least two prior lines of therapy, including a BTK inhibitor. This is an appealing oral option for patients with relapsed disease.
Options for patients with relapsed/refractory large B-cell lymphoma (LBCL) have also significantly increased in recent years. One of the most important advances in this disease has been the use of anti-CD19 CAR T-cell therapy. There are currently three FDA-approved options for patients with relapsed/refractory LBCL who have received at least two prior lines of therapy.1-3 More recently, axicabtagene ciloleucel (axi-cel) and lisocabtagene maraleucel (liso-cel) have also been approved for the second line based on the results of the ZUMA-7 and TRANSFORM studies, respectively.4,5
Longer follow-up of the ZUMA-7 trial continues to confirm the advantage of axi-cel over standard-care therapy for patients with primary refractory or early relapse of disease, now with evidence of an overall survival advantage (Westin et al). The ZUMA-7 trial included 359 adults with LBCL (refractory to or relapsed within 12 months of first-line treatment) who were randomly assigned to receive axi-cel (n = 180) or standard care (n = 179). At a median follow-up of 47.2 mo, patients receiving axi-cel vs standard care had a significantly longer median overall survival (not reached vs 31.1 mo; hazard ratio [HR] 0.73; P = .03) and an absolute improvement in overall survival (8.6 percentage points at 4 years). No new treatment-related deaths were reported since the primary event-free survival analysis. These data confirm that early use of axi-cel is preferred over standard-care therapy with high-dose chemotherapy and autologous stem cell transplantation.
Another important study that was recently published looked at the role of mental health on outcomes in patients with diffuse large B-cell lymphoma (DLBCL) (Kuczmarski et al). Though it is known that mental health disorders can decrease the quality of life of patients with cancer, there is limited information on the survival implications of these issues. A recent retrospective cohort study analyzed the data of 13,244 patients aged 67 years or older with DLBCL from the Surveillance, Epidemiology, and End Results (SEER)–Medicare registry, of which, 2094 patients had depression, anxiety, or both at the time of their DLBCL diagnosis. At a median follow-up of 2.0 years, patients with depression, anxiety, or both vs without any mental disorder had significantly lower 5-year overall survival rates (27.0% vs 37.4%; HR 1.37; 95% CI 1.29-1.44). They also found that those patients with preexisting depression vs without any mental disorder have the worst survival (23.4% vs 38.0%; HR 1.37; P < .0001). Though the mechanism accounting for decreased survival is not clear, the authors postulate that mental health disorders may lead to delays or interruptions in lymphoma-directed therapy. They also note the potential for increased barriers to care in patients with mental health disorders, which may result in nonadherence in this patient population. Regardless, these results highlight the importance of mental health screening and interventions in patients with DLBCL.
Additional References
- Neelapu SS, Locke FL, Bartlett NL, et al. Axicabtagene ciloleucel CAR T-Cell therapy in refractory large B-cell lymphoma. N Engl J Med. 2017;377:2531-2544. doi: 10.1056/NEJMoa1707447
- Schuster SJ, Bishop MR, Tam CS, et al; JULIET Investigators. Tisagenlecleucel in adult relapsed or refractory diffuse large B-cell lymphoma. N Engl J Med. 2019;380:45-56. doi: 10.1056/NEJMoa1804980
- Abramson JS, Palomba ML, Gordon LI, et al. Lisocabtagene maraleucel for patients with relapsed or refractory large B-cell lymphomas (TRANSCEND NHL 001): A multicentre seamless design study. Lancet. 2020;396:839-852. doi: 10.1016/S0140-6736(20)31366-0
- Locke FL, Miklos DB, Jacobson CA, et al; All ZUMA-7 Investigators and Contributing Kite Members. Axicabtagene ciloleucel as second-line therapy for large B-cell lymphoma. N Engl J Med. 2022;386:640-654. doi: 10.1056/NEJMoa2116133
- Kamdar M, Solomon SR, Arnason J, et al; TRANSFORM Investigators. Lisocabtagene maraleucel versus standard of care with salvage chemotherapy followed by autologous stem cell transplantation as second-line treatment in patients with relapsed or refractory large B-cell lymphoma (TRANSFORM): Results from an interim analysis of an open-label, randomised, phase 3 trial. Lancet. 2022;399:2294-2308. doi: 10.1016/S0140-6736(22)00662-6
Mantle cell lymphoma (MCL) is a rare and often heterogenous subtype of non-Hodgkin lymphoma (NHL). Though patients can experience prolonged remissions after frontline therapy, most patients ultimately relapse. Treatment of relapsed/refractory disease can be challenging, but there have recently been a growing number of therapeutic options in this setting. Covalent Bruton tyrosine kinase (BTK) inhibitors, for example, have demonstrated activity in patients with MCL and are approved by the US Food and Drug Administration (FDA) for relapsed/refractory disease. Chimeric antigen receptor (CAR) T-cell therapy is also an effective option for relapsed/refractory disease, though this is typically available only at select centers and is associated with toxicities, such as cytokine release syndrome and neurologic toxicity.
Recently, a novel BTK inhibitor, pirtobrutinib, has also been studied across NHL, including MCL (Wang et al) Pirtobrutinib is a selective, noncovalent BTK inhibitor with the ability to bind both the C481S-mutant and wild-type BTK. The multicenter, phase 1/2 BRUIN study included 90 patients with MCL who were previously treated with a covalent BTK inhibitor. Patients in the phase 1 portion of the study were treated with oral pirtobrutinib at a dose of 25-300 mg once daily, and patients in the phase 2 study were treated at the recommended dose of 200 mg once daily. The overall response rate was 57.8% (95% CI 46.9%-68.1%), with the complete response rate being 20.0%. At a median follow-up of 12 months, the median duration of response was 21.6 (95% CI 7.5 to not reached) months. Treatment-related adverse events that were grade 3 or higher were not frequent, with neutropenia (8.5%) being the most common. Of note, grade 3 or higher hemorrhage and atrial fibrillation, which can be seen with BTK inhibitors, were rare, occurring in 3.7% and 1.2% of patients, respectively. Based on the results of this study, pirtobrutinib has been approved by the FDA for patients with relapsed/refractory MCL after at least two prior lines of therapy, including a BTK inhibitor. This is an appealing oral option for patients with relapsed disease.
Options for patients with relapsed/refractory large B-cell lymphoma (LBCL) have also significantly increased in recent years. One of the most important advances in this disease has been the use of anti-CD19 CAR T-cell therapy. There are currently three FDA-approved options for patients with relapsed/refractory LBCL who have received at least two prior lines of therapy.1-3 More recently, axicabtagene ciloleucel (axi-cel) and lisocabtagene maraleucel (liso-cel) have also been approved for the second line based on the results of the ZUMA-7 and TRANSFORM studies, respectively.4,5
Longer follow-up of the ZUMA-7 trial continues to confirm the advantage of axi-cel over standard-care therapy for patients with primary refractory or early relapse of disease, now with evidence of an overall survival advantage (Westin et al). The ZUMA-7 trial included 359 adults with LBCL (refractory to or relapsed within 12 months of first-line treatment) who were randomly assigned to receive axi-cel (n = 180) or standard care (n = 179). At a median follow-up of 47.2 mo, patients receiving axi-cel vs standard care had a significantly longer median overall survival (not reached vs 31.1 mo; hazard ratio [HR] 0.73; P = .03) and an absolute improvement in overall survival (8.6 percentage points at 4 years). No new treatment-related deaths were reported since the primary event-free survival analysis. These data confirm that early use of axi-cel is preferred over standard-care therapy with high-dose chemotherapy and autologous stem cell transplantation.
Another important study that was recently published looked at the role of mental health on outcomes in patients with diffuse large B-cell lymphoma (DLBCL) (Kuczmarski et al). Though it is known that mental health disorders can decrease the quality of life of patients with cancer, there is limited information on the survival implications of these issues. A recent retrospective cohort study analyzed the data of 13,244 patients aged 67 years or older with DLBCL from the Surveillance, Epidemiology, and End Results (SEER)–Medicare registry, of which, 2094 patients had depression, anxiety, or both at the time of their DLBCL diagnosis. At a median follow-up of 2.0 years, patients with depression, anxiety, or both vs without any mental disorder had significantly lower 5-year overall survival rates (27.0% vs 37.4%; HR 1.37; 95% CI 1.29-1.44). They also found that those patients with preexisting depression vs without any mental disorder have the worst survival (23.4% vs 38.0%; HR 1.37; P < .0001). Though the mechanism accounting for decreased survival is not clear, the authors postulate that mental health disorders may lead to delays or interruptions in lymphoma-directed therapy. They also note the potential for increased barriers to care in patients with mental health disorders, which may result in nonadherence in this patient population. Regardless, these results highlight the importance of mental health screening and interventions in patients with DLBCL.
Additional References
- Neelapu SS, Locke FL, Bartlett NL, et al. Axicabtagene ciloleucel CAR T-Cell therapy in refractory large B-cell lymphoma. N Engl J Med. 2017;377:2531-2544. doi: 10.1056/NEJMoa1707447
- Schuster SJ, Bishop MR, Tam CS, et al; JULIET Investigators. Tisagenlecleucel in adult relapsed or refractory diffuse large B-cell lymphoma. N Engl J Med. 2019;380:45-56. doi: 10.1056/NEJMoa1804980
- Abramson JS, Palomba ML, Gordon LI, et al. Lisocabtagene maraleucel for patients with relapsed or refractory large B-cell lymphomas (TRANSCEND NHL 001): A multicentre seamless design study. Lancet. 2020;396:839-852. doi: 10.1016/S0140-6736(20)31366-0
- Locke FL, Miklos DB, Jacobson CA, et al; All ZUMA-7 Investigators and Contributing Kite Members. Axicabtagene ciloleucel as second-line therapy for large B-cell lymphoma. N Engl J Med. 2022;386:640-654. doi: 10.1056/NEJMoa2116133
- Kamdar M, Solomon SR, Arnason J, et al; TRANSFORM Investigators. Lisocabtagene maraleucel versus standard of care with salvage chemotherapy followed by autologous stem cell transplantation as second-line treatment in patients with relapsed or refractory large B-cell lymphoma (TRANSFORM): Results from an interim analysis of an open-label, randomised, phase 3 trial. Lancet. 2022;399:2294-2308. doi: 10.1016/S0140-6736(22)00662-6