User login
Is nedocromil effective in preventing asthmatic attacks in patients with asthma?
Nedocromil (Tilade) is effective for the treatment of mild persistent asthma. It has not been shown to be effective in more severe forms of asthma for both children and adults. Although no studies looked specifically at exacerbation rates, multiple clinical and biologic outcomes (symptom scores, quality of life measures, bronchodilator use, forced expiratory flow in 1 second [FEV1], and peak expiratory flow rate [PEFR]) improved with nedocromil use compared with placebo.
The most effective dose for preventing exacerbations appears to be 4 mg (2 puffs) 4 times a day (SOR: A, multiple randomized controlled trials [RCTs] and meta-analyses). More severe forms of asthma respond better to inhaled steroids than to nedocromil (SOR: A, multiple RCTs). Nedocromil may allow some patients with severe asthma to use lower doses of inhaled steroids (SOR: C, conflicting RCTs). Nedocromil is also effective for the treatment of exercise-induced asthma (SOR: A, multiple RCTs and meta-analyses).
In general, about 50% to 70% of patients respond to nedocromil (SOR: A, multiple RCTs and meta-analyses). Unfortunately, which patients respond is not predictable from clinical parameters.1 Nedocromil is worth trying in mild persistent asthma, particularly for children where the parents are worried about the growth issues associated with inhaled steroids. Side effects (sore throat, nausea, and headache) are mild and infrequent. Maximal efficacy is usually seen after 6 to 8 weeks.
Evidence summary
A systematic review encompassing 127 trial centers and 4723 patients concluded that inhaled nedocromil was effective for a variety of patients with asthma. Significant improvements were noted in FEV1, PEFR, use of bronchodilators, symptom scores, and quality of life scores. The reviewers found nedocromil to be most effective for patients with moderate disease already taking bronchodilators,2 corresponding to the “mild persistent asthma” category ( Table ).
A contemporaneous European RCT, not included in the review, compared 4 mg of inhaled nedocromil 4 times daily with inhaled placebo among 209 asthmatic children for 12 weeks.3 After 8 weeks, they found a statistically significant reduction in total daily asthma symptom scores (50% nedocromil vs 9% placebo; P<.01). The proportion of parents and children rating treatment as moderately or very effective was 78% in the treatment group and 59% in the placebo group (number needed to treat [NNT]=5.2; P<.01); clinicians’ ratings were 73% for nedocromil and 50% for placebo (NNT=4.3; P<.01). The frequency of side effects—including nausea, headache, and sleepiness—did not reach statistical significance; however, the nedocromil group reported up to a 20% incidence of sore throat. Most of the studies reported no dropouts due to side effects.
When patients are already using inhaled steroids, the evidence is less clear whether nedocromil confers additional benefits, such as fewer exacerbations or lower inhaled steroid doses. Two small studies of patients either already on inhaled steroids4 or considered to be steroid-resistant5 found nonsignificant trends towards reductions in bronchodilator use, increased PEFR, increased FEV1, and improved quality of life. Although both studies were underpowered, the study on steroid-resistant asthma did find a statistically significant 20% improvement in PEFR and decreased bronchodilator use for 50% of patients at 8 and 12 weeks.
The inherent waxing and waning nature of asthma makes demonstrating benefits difficult. Furthermore, nedocromil tends to have an all-ornothing effect rather than a dose-response gradient. Unfortunately, none of these trials found useful predictors to help clinicians determine which patients respond.1,5
In a Cochrane Review, 20 RCTs involving 280 participants showed that 4 mg (2 puffs) of nedocromil inhaled 15 to 60 minutes prior to exercise significantly reduced the severity and duration of exercise-induced asthma for both adults and children. The maximum percentage fall in FEV1 improved significantly compared with placebo, with a weighted mean difference of 15.5% (95% confidence interval, 13.2–18.1). In addition, the time to complete recovery was shortened from 30 minutes with placebo to 10 minutes with nedocromil.6
TABLE
Classification of asthma
| Classification | Symptom frequency | Spirometry findings |
|---|---|---|
| Severe persistent | Continual symptoms | PEFR <60% Variability >30% |
| Moderate persistent | Daily symptoms, more than 1 night per week | PEFR >60% but <80% Variability >30% |
| Mild persistent | More than twice per week but less than daily; more than 2 nights per month | PEFR >80% Variability 20%–30% |
| Mild intermittent | Less than once per week; less than or equal to 2 nights per month | PEFR >80% Variability <20% |
| Source: Global Initiative for Asthma, National Heart, Lung and Blood Institute 2003.7 | ||
Recommendations from others
The Global Initiative for Asthma and the National Heart, Lung and Blood Institute Expert Panel Report list nedocromil as an option for the treatment of exercise-induced asthma and mild persistent asthma for adults and children. However, it is listed as a second choice to the use of inhaled steroids in the case of mild persistent asthma. It is not recommended for moderate or severe persistent asthma, or for mild intermittent asthma.7
Nedocromil and cromolyn sodium are safe but many patients do not respond
Ron Baldwin, MD
University of Wyoming Family Practice Residency at Casper
Inhaled nedocromil and cromolyn sodium have long been recognized as agents with an excellent safety profile. Unfortunately, as pointed about above, many patients do not respond to these agents. In addition, 4-times-daily dosing makes compliance difficult. Clinicians and parents must weigh the theoretical risk of inhaled corticosteroid-induced growth retardation with this potential differential in effectiveness.
1. Parish RC, Miller LJ. Nedocromil sodium. Ann Pharmacother 1993;27:599-606.
2. Edwards AM, Stevens MT. The clinical efficacy of inhaled nedocromil sodium (Tilade) in the treatment of asthma. Eur Respir J 1993;6:35-41.
3. Armenio L, Baldini G, Baldare M, et al. Double blind, placebo controlled study of nedocromil sodium in asthma. Arch Dis Child 1993;68:193-197.
4. O’Hickey SP, Rees PJ. High dose nedocromil sodium as an addition to inhaled corticosteroids in the treatment of asthma. Respir Med 1994;88:499-502.
5. Marin JM, Carrizo SJ, Garcia R, Ejea MV. Effects of nedocromil sodium in steroid-resistant asthma: a randomized controlled trial. J Allergy Clin Immunol 1996;97:602-610.
6. Spooner CH, Saunders LD, Rowe BH. Nedocromil sodium for preventing exercise-induced bronchoconstriction (Cochrane Review). The Cochrane Library, Issue 4, 2003. Chichester, UK: John Wiley & Sons, Ltd.
7. Global Strategy for Asthma Management and Prevention. Bethesda, Md: Global Initiative for Asthma, National Heart, Lung and Blood Institute; 2003.
Nedocromil (Tilade) is effective for the treatment of mild persistent asthma. It has not been shown to be effective in more severe forms of asthma for both children and adults. Although no studies looked specifically at exacerbation rates, multiple clinical and biologic outcomes (symptom scores, quality of life measures, bronchodilator use, forced expiratory flow in 1 second [FEV1], and peak expiratory flow rate [PEFR]) improved with nedocromil use compared with placebo.
The most effective dose for preventing exacerbations appears to be 4 mg (2 puffs) 4 times a day (SOR: A, multiple randomized controlled trials [RCTs] and meta-analyses). More severe forms of asthma respond better to inhaled steroids than to nedocromil (SOR: A, multiple RCTs). Nedocromil may allow some patients with severe asthma to use lower doses of inhaled steroids (SOR: C, conflicting RCTs). Nedocromil is also effective for the treatment of exercise-induced asthma (SOR: A, multiple RCTs and meta-analyses).
In general, about 50% to 70% of patients respond to nedocromil (SOR: A, multiple RCTs and meta-analyses). Unfortunately, which patients respond is not predictable from clinical parameters.1 Nedocromil is worth trying in mild persistent asthma, particularly for children where the parents are worried about the growth issues associated with inhaled steroids. Side effects (sore throat, nausea, and headache) are mild and infrequent. Maximal efficacy is usually seen after 6 to 8 weeks.
Evidence summary
A systematic review encompassing 127 trial centers and 4723 patients concluded that inhaled nedocromil was effective for a variety of patients with asthma. Significant improvements were noted in FEV1, PEFR, use of bronchodilators, symptom scores, and quality of life scores. The reviewers found nedocromil to be most effective for patients with moderate disease already taking bronchodilators,2 corresponding to the “mild persistent asthma” category ( Table ).
A contemporaneous European RCT, not included in the review, compared 4 mg of inhaled nedocromil 4 times daily with inhaled placebo among 209 asthmatic children for 12 weeks.3 After 8 weeks, they found a statistically significant reduction in total daily asthma symptom scores (50% nedocromil vs 9% placebo; P<.01). The proportion of parents and children rating treatment as moderately or very effective was 78% in the treatment group and 59% in the placebo group (number needed to treat [NNT]=5.2; P<.01); clinicians’ ratings were 73% for nedocromil and 50% for placebo (NNT=4.3; P<.01). The frequency of side effects—including nausea, headache, and sleepiness—did not reach statistical significance; however, the nedocromil group reported up to a 20% incidence of sore throat. Most of the studies reported no dropouts due to side effects.
When patients are already using inhaled steroids, the evidence is less clear whether nedocromil confers additional benefits, such as fewer exacerbations or lower inhaled steroid doses. Two small studies of patients either already on inhaled steroids4 or considered to be steroid-resistant5 found nonsignificant trends towards reductions in bronchodilator use, increased PEFR, increased FEV1, and improved quality of life. Although both studies were underpowered, the study on steroid-resistant asthma did find a statistically significant 20% improvement in PEFR and decreased bronchodilator use for 50% of patients at 8 and 12 weeks.
The inherent waxing and waning nature of asthma makes demonstrating benefits difficult. Furthermore, nedocromil tends to have an all-ornothing effect rather than a dose-response gradient. Unfortunately, none of these trials found useful predictors to help clinicians determine which patients respond.1,5
In a Cochrane Review, 20 RCTs involving 280 participants showed that 4 mg (2 puffs) of nedocromil inhaled 15 to 60 minutes prior to exercise significantly reduced the severity and duration of exercise-induced asthma for both adults and children. The maximum percentage fall in FEV1 improved significantly compared with placebo, with a weighted mean difference of 15.5% (95% confidence interval, 13.2–18.1). In addition, the time to complete recovery was shortened from 30 minutes with placebo to 10 minutes with nedocromil.6
TABLE
Classification of asthma
| Classification | Symptom frequency | Spirometry findings |
|---|---|---|
| Severe persistent | Continual symptoms | PEFR <60% Variability >30% |
| Moderate persistent | Daily symptoms, more than 1 night per week | PEFR >60% but <80% Variability >30% |
| Mild persistent | More than twice per week but less than daily; more than 2 nights per month | PEFR >80% Variability 20%–30% |
| Mild intermittent | Less than once per week; less than or equal to 2 nights per month | PEFR >80% Variability <20% |
| Source: Global Initiative for Asthma, National Heart, Lung and Blood Institute 2003.7 | ||
Recommendations from others
The Global Initiative for Asthma and the National Heart, Lung and Blood Institute Expert Panel Report list nedocromil as an option for the treatment of exercise-induced asthma and mild persistent asthma for adults and children. However, it is listed as a second choice to the use of inhaled steroids in the case of mild persistent asthma. It is not recommended for moderate or severe persistent asthma, or for mild intermittent asthma.7
Nedocromil and cromolyn sodium are safe but many patients do not respond
Ron Baldwin, MD
University of Wyoming Family Practice Residency at Casper
Inhaled nedocromil and cromolyn sodium have long been recognized as agents with an excellent safety profile. Unfortunately, as pointed about above, many patients do not respond to these agents. In addition, 4-times-daily dosing makes compliance difficult. Clinicians and parents must weigh the theoretical risk of inhaled corticosteroid-induced growth retardation with this potential differential in effectiveness.
Nedocromil (Tilade) is effective for the treatment of mild persistent asthma. It has not been shown to be effective in more severe forms of asthma for both children and adults. Although no studies looked specifically at exacerbation rates, multiple clinical and biologic outcomes (symptom scores, quality of life measures, bronchodilator use, forced expiratory flow in 1 second [FEV1], and peak expiratory flow rate [PEFR]) improved with nedocromil use compared with placebo.
The most effective dose for preventing exacerbations appears to be 4 mg (2 puffs) 4 times a day (SOR: A, multiple randomized controlled trials [RCTs] and meta-analyses). More severe forms of asthma respond better to inhaled steroids than to nedocromil (SOR: A, multiple RCTs). Nedocromil may allow some patients with severe asthma to use lower doses of inhaled steroids (SOR: C, conflicting RCTs). Nedocromil is also effective for the treatment of exercise-induced asthma (SOR: A, multiple RCTs and meta-analyses).
In general, about 50% to 70% of patients respond to nedocromil (SOR: A, multiple RCTs and meta-analyses). Unfortunately, which patients respond is not predictable from clinical parameters.1 Nedocromil is worth trying in mild persistent asthma, particularly for children where the parents are worried about the growth issues associated with inhaled steroids. Side effects (sore throat, nausea, and headache) are mild and infrequent. Maximal efficacy is usually seen after 6 to 8 weeks.
Evidence summary
A systematic review encompassing 127 trial centers and 4723 patients concluded that inhaled nedocromil was effective for a variety of patients with asthma. Significant improvements were noted in FEV1, PEFR, use of bronchodilators, symptom scores, and quality of life scores. The reviewers found nedocromil to be most effective for patients with moderate disease already taking bronchodilators,2 corresponding to the “mild persistent asthma” category ( Table ).
A contemporaneous European RCT, not included in the review, compared 4 mg of inhaled nedocromil 4 times daily with inhaled placebo among 209 asthmatic children for 12 weeks.3 After 8 weeks, they found a statistically significant reduction in total daily asthma symptom scores (50% nedocromil vs 9% placebo; P<.01). The proportion of parents and children rating treatment as moderately or very effective was 78% in the treatment group and 59% in the placebo group (number needed to treat [NNT]=5.2; P<.01); clinicians’ ratings were 73% for nedocromil and 50% for placebo (NNT=4.3; P<.01). The frequency of side effects—including nausea, headache, and sleepiness—did not reach statistical significance; however, the nedocromil group reported up to a 20% incidence of sore throat. Most of the studies reported no dropouts due to side effects.
When patients are already using inhaled steroids, the evidence is less clear whether nedocromil confers additional benefits, such as fewer exacerbations or lower inhaled steroid doses. Two small studies of patients either already on inhaled steroids4 or considered to be steroid-resistant5 found nonsignificant trends towards reductions in bronchodilator use, increased PEFR, increased FEV1, and improved quality of life. Although both studies were underpowered, the study on steroid-resistant asthma did find a statistically significant 20% improvement in PEFR and decreased bronchodilator use for 50% of patients at 8 and 12 weeks.
The inherent waxing and waning nature of asthma makes demonstrating benefits difficult. Furthermore, nedocromil tends to have an all-ornothing effect rather than a dose-response gradient. Unfortunately, none of these trials found useful predictors to help clinicians determine which patients respond.1,5
In a Cochrane Review, 20 RCTs involving 280 participants showed that 4 mg (2 puffs) of nedocromil inhaled 15 to 60 minutes prior to exercise significantly reduced the severity and duration of exercise-induced asthma for both adults and children. The maximum percentage fall in FEV1 improved significantly compared with placebo, with a weighted mean difference of 15.5% (95% confidence interval, 13.2–18.1). In addition, the time to complete recovery was shortened from 30 minutes with placebo to 10 minutes with nedocromil.6
TABLE
Classification of asthma
| Classification | Symptom frequency | Spirometry findings |
|---|---|---|
| Severe persistent | Continual symptoms | PEFR <60% Variability >30% |
| Moderate persistent | Daily symptoms, more than 1 night per week | PEFR >60% but <80% Variability >30% |
| Mild persistent | More than twice per week but less than daily; more than 2 nights per month | PEFR >80% Variability 20%–30% |
| Mild intermittent | Less than once per week; less than or equal to 2 nights per month | PEFR >80% Variability <20% |
| Source: Global Initiative for Asthma, National Heart, Lung and Blood Institute 2003.7 | ||
Recommendations from others
The Global Initiative for Asthma and the National Heart, Lung and Blood Institute Expert Panel Report list nedocromil as an option for the treatment of exercise-induced asthma and mild persistent asthma for adults and children. However, it is listed as a second choice to the use of inhaled steroids in the case of mild persistent asthma. It is not recommended for moderate or severe persistent asthma, or for mild intermittent asthma.7
Nedocromil and cromolyn sodium are safe but many patients do not respond
Ron Baldwin, MD
University of Wyoming Family Practice Residency at Casper
Inhaled nedocromil and cromolyn sodium have long been recognized as agents with an excellent safety profile. Unfortunately, as pointed about above, many patients do not respond to these agents. In addition, 4-times-daily dosing makes compliance difficult. Clinicians and parents must weigh the theoretical risk of inhaled corticosteroid-induced growth retardation with this potential differential in effectiveness.
1. Parish RC, Miller LJ. Nedocromil sodium. Ann Pharmacother 1993;27:599-606.
2. Edwards AM, Stevens MT. The clinical efficacy of inhaled nedocromil sodium (Tilade) in the treatment of asthma. Eur Respir J 1993;6:35-41.
3. Armenio L, Baldini G, Baldare M, et al. Double blind, placebo controlled study of nedocromil sodium in asthma. Arch Dis Child 1993;68:193-197.
4. O’Hickey SP, Rees PJ. High dose nedocromil sodium as an addition to inhaled corticosteroids in the treatment of asthma. Respir Med 1994;88:499-502.
5. Marin JM, Carrizo SJ, Garcia R, Ejea MV. Effects of nedocromil sodium in steroid-resistant asthma: a randomized controlled trial. J Allergy Clin Immunol 1996;97:602-610.
6. Spooner CH, Saunders LD, Rowe BH. Nedocromil sodium for preventing exercise-induced bronchoconstriction (Cochrane Review). The Cochrane Library, Issue 4, 2003. Chichester, UK: John Wiley & Sons, Ltd.
7. Global Strategy for Asthma Management and Prevention. Bethesda, Md: Global Initiative for Asthma, National Heart, Lung and Blood Institute; 2003.
1. Parish RC, Miller LJ. Nedocromil sodium. Ann Pharmacother 1993;27:599-606.
2. Edwards AM, Stevens MT. The clinical efficacy of inhaled nedocromil sodium (Tilade) in the treatment of asthma. Eur Respir J 1993;6:35-41.
3. Armenio L, Baldini G, Baldare M, et al. Double blind, placebo controlled study of nedocromil sodium in asthma. Arch Dis Child 1993;68:193-197.
4. O’Hickey SP, Rees PJ. High dose nedocromil sodium as an addition to inhaled corticosteroids in the treatment of asthma. Respir Med 1994;88:499-502.
5. Marin JM, Carrizo SJ, Garcia R, Ejea MV. Effects of nedocromil sodium in steroid-resistant asthma: a randomized controlled trial. J Allergy Clin Immunol 1996;97:602-610.
6. Spooner CH, Saunders LD, Rowe BH. Nedocromil sodium for preventing exercise-induced bronchoconstriction (Cochrane Review). The Cochrane Library, Issue 4, 2003. Chichester, UK: John Wiley & Sons, Ltd.
7. Global Strategy for Asthma Management and Prevention. Bethesda, Md: Global Initiative for Asthma, National Heart, Lung and Blood Institute; 2003.
Evidence-based answers from the Family Physicians Inquiries Network
Blocking the ‘munchies’ receptor: A novel approach to obesity
Marijuana has long been known to stimulate appetite, particularly for sweet foods.1 The naughty boys in my fraternity called it “the munchies;” the professionals call it hyperphagia. Cannabinoid receptor (CB1) stimulation by marijuana’s main active component—9-THC—is believed to induce this behavior. Clinicians have successfully used this effect to treat AIDS-related wasting syndrome and other anorexic conditions.2
CB1 is widely expressed throughout the brain and seems to inhibit release of various neurotransmitters.3 How this effect leads to increased appetite is unclear, but it may result from a decrease in the appetite-suppressing effects of hormones such as leptin. In other words, tweaking the CB1 receptor may take the “brakes” off appetite.
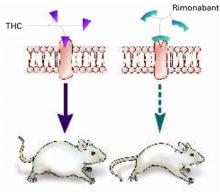
Some researchers have speculated that if stimulating CB1 triggers appetite, blocking the receptor might inhibit it (Figure 1).
THE ‘MUNCHIES’ IN MICE
Rimonabant (SR141716), an experimental agent, is a potent and selective CB1 antagonist.
Ravinet Trillou et al fed mice a high-fat diet known to induce obesity.4 The mice were randomized to receive rimonabant or placebo while maintained on the highly palatable diet. The authors asked: Would rimonabant help the mice lose weight even when they could eat as much delicious fatty food as they wanted?
Figure 1 Blocking CB1 may prevent weight gain
Δ9-THC activates the cannabinoid receptor (CB1), stimulating appetite and leading to weight gain in mice (left). When the same receptor is blocked, appetite is controlled (right).
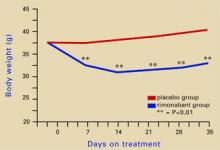
Source: Illustration for CURRENT PSYCHIATRY by Marcia HartsockRimonabant induced a sustained body weight reduction of approximately 20% in the treatment group compared with the placebo group across 5 weeks (Figure 2). Estimated fat stores among the treatment group were depleted by slightly more than 50%.
The authors noted that the mice in the treatment group had decreased their food intake, but the decrease was not sufficient to explain the weight loss. They speculate that rimonabant could activate metabolic processes and decrease intake.
RIMONABANT’S ROLE IN PSYCHIATRY
Phase III human trials of rimonabant are under way for obesity as well as smoking cessation.5 In uncontrolled studies, rimonabant has been shown to help people avoid weight gain while quitting smoking.5
If rimonabant shows effectiveness in controlled trials and is safe in humans, it could be most valuable. Obesity in industrial countries is epidemic and causes serious secondary morbidity, including diabetes, arthritis, and hypertension. Rimonabant, if approved by the FDA, could reach the market by early 2006.6
It is unknown whether rimonabant’s metabolic effects could offset those of many psychotropics. As psychiatrists, we often must stop an effective antipsychotic or antidepressant because it is causing significant weight gain. A treatment that would prevent medication-induced weight gain could improve patient compliance and, ultimately, outcomes.
MANAGING SCHIZOPHRENIA
Some evidence also suggests that rimonabant may offer additional benefits for patients with schizophrenia beyond weight reduction or smoking cessation.
Figure 2 Rimonabant’s effects on weight in mice on a high-fat diet
Source: Adapted from reference 4.Leweke et al found increased endogenous cannabinoids in the CSF of patients with schizophrenia, suggesting that a cannabinoid signaling imbalance may contribute to the disorder’s pathogenesis.7 However, 72 patients with schizophrenia or schizoaffective disorder who took rimonabant for 6 weeks showed no improvement compared with a placebo group.8
1. Abel EL. Cannabis: effects on hunger and thirst. Behav Biol 1975;15:255-81.
2. Beal JE, Olson R, Laubenstein L, et al. Dronabinol as a treatment for anorexia associated with weight loss in patients with AIDS. J Pain Symptom Manage 1995;10:89-97.
3. Iversen L. Cannabis and the brain. Brain 2003;126:1252-70.
4. Ravinet Trillou C, Arnone M, Delgorge C, et al. Anti-obesity effect of SR141716, a CB1 receptor antagonist, in diet-induced obese mice. Am J Physiol Regul Integr Comp Physiol 2003;284:R345-53.
5. Fernandez JR, Allison DB. Rimonabant Sanofi-Synthelabo. Curr Opin Investig Drugs 2004;5:430-5.
6. The Website for the Drug Development Industry. Acomplia (rimonabant)—investigational agent for the management of obesity. London: SPGMedia. Available at: http://www. drugdevelopment-technology.com/projects/rimonabant/. Accessed Oct. 14, 2004.
7. Leweke FM, Giuffrida A, Wurster U, et al. Elevated endogenous cannabinoids in schizophrenia. Neuroreport 1999;10:1665-9.
8. Meltzer HY, Arvanitis L, Bauer D, et al. Placebo-controlled evaluation of four novel compounds for the treatment of schizophrenia and schizoaffective disorder. Am J Psychiatry 2004;161:975-84.
Marijuana has long been known to stimulate appetite, particularly for sweet foods.1 The naughty boys in my fraternity called it “the munchies;” the professionals call it hyperphagia. Cannabinoid receptor (CB1) stimulation by marijuana’s main active component—9-THC—is believed to induce this behavior. Clinicians have successfully used this effect to treat AIDS-related wasting syndrome and other anorexic conditions.2
CB1 is widely expressed throughout the brain and seems to inhibit release of various neurotransmitters.3 How this effect leads to increased appetite is unclear, but it may result from a decrease in the appetite-suppressing effects of hormones such as leptin. In other words, tweaking the CB1 receptor may take the “brakes” off appetite.
Some researchers have speculated that if stimulating CB1 triggers appetite, blocking the receptor might inhibit it (Figure 1).
THE ‘MUNCHIES’ IN MICE
Rimonabant (SR141716), an experimental agent, is a potent and selective CB1 antagonist.
Ravinet Trillou et al fed mice a high-fat diet known to induce obesity.4 The mice were randomized to receive rimonabant or placebo while maintained on the highly palatable diet. The authors asked: Would rimonabant help the mice lose weight even when they could eat as much delicious fatty food as they wanted?
Figure 1 Blocking CB1 may prevent weight gain
Δ9-THC activates the cannabinoid receptor (CB1), stimulating appetite and leading to weight gain in mice (left). When the same receptor is blocked, appetite is controlled (right).
Source: Illustration for CURRENT PSYCHIATRY by Marcia HartsockRimonabant induced a sustained body weight reduction of approximately 20% in the treatment group compared with the placebo group across 5 weeks (Figure 2). Estimated fat stores among the treatment group were depleted by slightly more than 50%.
The authors noted that the mice in the treatment group had decreased their food intake, but the decrease was not sufficient to explain the weight loss. They speculate that rimonabant could activate metabolic processes and decrease intake.
RIMONABANT’S ROLE IN PSYCHIATRY
Phase III human trials of rimonabant are under way for obesity as well as smoking cessation.5 In uncontrolled studies, rimonabant has been shown to help people avoid weight gain while quitting smoking.5
If rimonabant shows effectiveness in controlled trials and is safe in humans, it could be most valuable. Obesity in industrial countries is epidemic and causes serious secondary morbidity, including diabetes, arthritis, and hypertension. Rimonabant, if approved by the FDA, could reach the market by early 2006.6
It is unknown whether rimonabant’s metabolic effects could offset those of many psychotropics. As psychiatrists, we often must stop an effective antipsychotic or antidepressant because it is causing significant weight gain. A treatment that would prevent medication-induced weight gain could improve patient compliance and, ultimately, outcomes.
MANAGING SCHIZOPHRENIA
Some evidence also suggests that rimonabant may offer additional benefits for patients with schizophrenia beyond weight reduction or smoking cessation.
Figure 2 Rimonabant’s effects on weight in mice on a high-fat diet
Source: Adapted from reference 4.Leweke et al found increased endogenous cannabinoids in the CSF of patients with schizophrenia, suggesting that a cannabinoid signaling imbalance may contribute to the disorder’s pathogenesis.7 However, 72 patients with schizophrenia or schizoaffective disorder who took rimonabant for 6 weeks showed no improvement compared with a placebo group.8
Marijuana has long been known to stimulate appetite, particularly for sweet foods.1 The naughty boys in my fraternity called it “the munchies;” the professionals call it hyperphagia. Cannabinoid receptor (CB1) stimulation by marijuana’s main active component—9-THC—is believed to induce this behavior. Clinicians have successfully used this effect to treat AIDS-related wasting syndrome and other anorexic conditions.2
CB1 is widely expressed throughout the brain and seems to inhibit release of various neurotransmitters.3 How this effect leads to increased appetite is unclear, but it may result from a decrease in the appetite-suppressing effects of hormones such as leptin. In other words, tweaking the CB1 receptor may take the “brakes” off appetite.
Some researchers have speculated that if stimulating CB1 triggers appetite, blocking the receptor might inhibit it (Figure 1).
THE ‘MUNCHIES’ IN MICE
Rimonabant (SR141716), an experimental agent, is a potent and selective CB1 antagonist.
Ravinet Trillou et al fed mice a high-fat diet known to induce obesity.4 The mice were randomized to receive rimonabant or placebo while maintained on the highly palatable diet. The authors asked: Would rimonabant help the mice lose weight even when they could eat as much delicious fatty food as they wanted?
Figure 1 Blocking CB1 may prevent weight gain
Δ9-THC activates the cannabinoid receptor (CB1), stimulating appetite and leading to weight gain in mice (left). When the same receptor is blocked, appetite is controlled (right).
Source: Illustration for CURRENT PSYCHIATRY by Marcia HartsockRimonabant induced a sustained body weight reduction of approximately 20% in the treatment group compared with the placebo group across 5 weeks (Figure 2). Estimated fat stores among the treatment group were depleted by slightly more than 50%.
The authors noted that the mice in the treatment group had decreased their food intake, but the decrease was not sufficient to explain the weight loss. They speculate that rimonabant could activate metabolic processes and decrease intake.
RIMONABANT’S ROLE IN PSYCHIATRY
Phase III human trials of rimonabant are under way for obesity as well as smoking cessation.5 In uncontrolled studies, rimonabant has been shown to help people avoid weight gain while quitting smoking.5
If rimonabant shows effectiveness in controlled trials and is safe in humans, it could be most valuable. Obesity in industrial countries is epidemic and causes serious secondary morbidity, including diabetes, arthritis, and hypertension. Rimonabant, if approved by the FDA, could reach the market by early 2006.6
It is unknown whether rimonabant’s metabolic effects could offset those of many psychotropics. As psychiatrists, we often must stop an effective antipsychotic or antidepressant because it is causing significant weight gain. A treatment that would prevent medication-induced weight gain could improve patient compliance and, ultimately, outcomes.
MANAGING SCHIZOPHRENIA
Some evidence also suggests that rimonabant may offer additional benefits for patients with schizophrenia beyond weight reduction or smoking cessation.
Figure 2 Rimonabant’s effects on weight in mice on a high-fat diet
Source: Adapted from reference 4.Leweke et al found increased endogenous cannabinoids in the CSF of patients with schizophrenia, suggesting that a cannabinoid signaling imbalance may contribute to the disorder’s pathogenesis.7 However, 72 patients with schizophrenia or schizoaffective disorder who took rimonabant for 6 weeks showed no improvement compared with a placebo group.8
1. Abel EL. Cannabis: effects on hunger and thirst. Behav Biol 1975;15:255-81.
2. Beal JE, Olson R, Laubenstein L, et al. Dronabinol as a treatment for anorexia associated with weight loss in patients with AIDS. J Pain Symptom Manage 1995;10:89-97.
3. Iversen L. Cannabis and the brain. Brain 2003;126:1252-70.
4. Ravinet Trillou C, Arnone M, Delgorge C, et al. Anti-obesity effect of SR141716, a CB1 receptor antagonist, in diet-induced obese mice. Am J Physiol Regul Integr Comp Physiol 2003;284:R345-53.
5. Fernandez JR, Allison DB. Rimonabant Sanofi-Synthelabo. Curr Opin Investig Drugs 2004;5:430-5.
6. The Website for the Drug Development Industry. Acomplia (rimonabant)—investigational agent for the management of obesity. London: SPGMedia. Available at: http://www. drugdevelopment-technology.com/projects/rimonabant/. Accessed Oct. 14, 2004.
7. Leweke FM, Giuffrida A, Wurster U, et al. Elevated endogenous cannabinoids in schizophrenia. Neuroreport 1999;10:1665-9.
8. Meltzer HY, Arvanitis L, Bauer D, et al. Placebo-controlled evaluation of four novel compounds for the treatment of schizophrenia and schizoaffective disorder. Am J Psychiatry 2004;161:975-84.
1. Abel EL. Cannabis: effects on hunger and thirst. Behav Biol 1975;15:255-81.
2. Beal JE, Olson R, Laubenstein L, et al. Dronabinol as a treatment for anorexia associated with weight loss in patients with AIDS. J Pain Symptom Manage 1995;10:89-97.
3. Iversen L. Cannabis and the brain. Brain 2003;126:1252-70.
4. Ravinet Trillou C, Arnone M, Delgorge C, et al. Anti-obesity effect of SR141716, a CB1 receptor antagonist, in diet-induced obese mice. Am J Physiol Regul Integr Comp Physiol 2003;284:R345-53.
5. Fernandez JR, Allison DB. Rimonabant Sanofi-Synthelabo. Curr Opin Investig Drugs 2004;5:430-5.
6. The Website for the Drug Development Industry. Acomplia (rimonabant)—investigational agent for the management of obesity. London: SPGMedia. Available at: http://www. drugdevelopment-technology.com/projects/rimonabant/. Accessed Oct. 14, 2004.
7. Leweke FM, Giuffrida A, Wurster U, et al. Elevated endogenous cannabinoids in schizophrenia. Neuroreport 1999;10:1665-9.
8. Meltzer HY, Arvanitis L, Bauer D, et al. Placebo-controlled evaluation of four novel compounds for the treatment of schizophrenia and schizoaffective disorder. Am J Psychiatry 2004;161:975-84.
A ‘FRESH’ way to manage trauma
Ameliorating emotional trauma is key to avoiding long-term functional impairment. Consider a FRESH approach that involves families/friends, reassurance/retelling, education, addressing substance abuse, sleeplessness, and suicide risk, and taking a careful history.
Family and friends can be valuable to treatment but clinicians often overlook their importance. Overwhelmed or traumatized family members who are not counseled about the patient’s symptoms can undermine treatment by dismissing symptoms and withdrawing support. Involve them by emphasizing their supportive role. Alert them to normal and problematic trauma responses and stress disorder symptoms.
Reassurance/retelling. Explain that emotional pain is normal but usually fades with time. Consider effects of survivor guilt: Encourage the patient to retell the experience, but do not demand this. Help patients identify and correct thought distortions that foster avoidance. Though controversial,1 critical incident debriefing and cognitive-behavioral therapy can help the patient recount the trauma and ultimately restore a sense of self, enjoyment of life, and expectations of safety, control, and trust.2
Educate patients about normal variable stress responses. Warn traumatized patients against engaging in high-risk behaviors, through which they may try to deny their vulnerability, fear, and loss of control. Explain symptoms and risk factors for depression, posttraumatic stress disorder (PTSD), and other anxiety disorders.
Substance abuse, sleeplessness, and suicide are possible outcomes of trauma. Prescribe a non-narcotic sleep-promoting medication if insomnia is problematic. Alternately, consider a selective serotonin or serotonin-norepinephrine reuptake inhibitor3,4 at normal or low starting dosages if presenting symptoms suggest an emerging anxiety or mood disorder or PTSD. Watch for signs of survivor guilt—such as an unrealistic sense of responsibility for the trauma—that can lead to depression with suicide risk after a significant loss.
History. Watch for factors that predict PTSD and comorbid disorders (trauma severity and chronicity, involvement of interpersonal violence, fear of death). Previous trauma, PTSD, depression, anxiety, personality disorder, childhood victimization, substance abuse, and poor social support increase the risk. Avoidance, numbing, dissociation, high guilt, and low acknowledged anger correlate with increased PTSD risk. Follow up with patients who exhibit these risk factors every 1 to 2 weeks with medication and/or psychotherapy.
1. Cloak NL, Edwards P. Psychological first aid: Emergency care for terrorism and disaster survivors. Current Psychiatry 2004;3(5):12-23.
2. Bisson JI. Early interventions following traumatic events. Psychiatr Ann 2003;1:37-44.
3. Davidson JR, Rothbaum BO, van der Kolk BA, et al. Multicenter, double-blind comparison of sertraline and placebo in the treatment of posttraumatic stress disorder. Arch Gen Psychiatry 2001;58:485-92.
4. Marshall RD, Beebe KL, Oldham M, et al. Efficacy and safety of paroxetine treatment for chronic PTSD: a fixed-dose, placebo-controlled study. Am J Psychiatry 2001;158:1982-8.
Dr. Sobel is a clinical instructor, University of California-San Diego School of Medicine, and consulting psychiatrist, University of San Diego Counseling Center.
Ameliorating emotional trauma is key to avoiding long-term functional impairment. Consider a FRESH approach that involves families/friends, reassurance/retelling, education, addressing substance abuse, sleeplessness, and suicide risk, and taking a careful history.
Family and friends can be valuable to treatment but clinicians often overlook their importance. Overwhelmed or traumatized family members who are not counseled about the patient’s symptoms can undermine treatment by dismissing symptoms and withdrawing support. Involve them by emphasizing their supportive role. Alert them to normal and problematic trauma responses and stress disorder symptoms.
Reassurance/retelling. Explain that emotional pain is normal but usually fades with time. Consider effects of survivor guilt: Encourage the patient to retell the experience, but do not demand this. Help patients identify and correct thought distortions that foster avoidance. Though controversial,1 critical incident debriefing and cognitive-behavioral therapy can help the patient recount the trauma and ultimately restore a sense of self, enjoyment of life, and expectations of safety, control, and trust.2
Educate patients about normal variable stress responses. Warn traumatized patients against engaging in high-risk behaviors, through which they may try to deny their vulnerability, fear, and loss of control. Explain symptoms and risk factors for depression, posttraumatic stress disorder (PTSD), and other anxiety disorders.
Substance abuse, sleeplessness, and suicide are possible outcomes of trauma. Prescribe a non-narcotic sleep-promoting medication if insomnia is problematic. Alternately, consider a selective serotonin or serotonin-norepinephrine reuptake inhibitor3,4 at normal or low starting dosages if presenting symptoms suggest an emerging anxiety or mood disorder or PTSD. Watch for signs of survivor guilt—such as an unrealistic sense of responsibility for the trauma—that can lead to depression with suicide risk after a significant loss.
History. Watch for factors that predict PTSD and comorbid disorders (trauma severity and chronicity, involvement of interpersonal violence, fear of death). Previous trauma, PTSD, depression, anxiety, personality disorder, childhood victimization, substance abuse, and poor social support increase the risk. Avoidance, numbing, dissociation, high guilt, and low acknowledged anger correlate with increased PTSD risk. Follow up with patients who exhibit these risk factors every 1 to 2 weeks with medication and/or psychotherapy.
Ameliorating emotional trauma is key to avoiding long-term functional impairment. Consider a FRESH approach that involves families/friends, reassurance/retelling, education, addressing substance abuse, sleeplessness, and suicide risk, and taking a careful history.
Family and friends can be valuable to treatment but clinicians often overlook their importance. Overwhelmed or traumatized family members who are not counseled about the patient’s symptoms can undermine treatment by dismissing symptoms and withdrawing support. Involve them by emphasizing their supportive role. Alert them to normal and problematic trauma responses and stress disorder symptoms.
Reassurance/retelling. Explain that emotional pain is normal but usually fades with time. Consider effects of survivor guilt: Encourage the patient to retell the experience, but do not demand this. Help patients identify and correct thought distortions that foster avoidance. Though controversial,1 critical incident debriefing and cognitive-behavioral therapy can help the patient recount the trauma and ultimately restore a sense of self, enjoyment of life, and expectations of safety, control, and trust.2
Educate patients about normal variable stress responses. Warn traumatized patients against engaging in high-risk behaviors, through which they may try to deny their vulnerability, fear, and loss of control. Explain symptoms and risk factors for depression, posttraumatic stress disorder (PTSD), and other anxiety disorders.
Substance abuse, sleeplessness, and suicide are possible outcomes of trauma. Prescribe a non-narcotic sleep-promoting medication if insomnia is problematic. Alternately, consider a selective serotonin or serotonin-norepinephrine reuptake inhibitor3,4 at normal or low starting dosages if presenting symptoms suggest an emerging anxiety or mood disorder or PTSD. Watch for signs of survivor guilt—such as an unrealistic sense of responsibility for the trauma—that can lead to depression with suicide risk after a significant loss.
History. Watch for factors that predict PTSD and comorbid disorders (trauma severity and chronicity, involvement of interpersonal violence, fear of death). Previous trauma, PTSD, depression, anxiety, personality disorder, childhood victimization, substance abuse, and poor social support increase the risk. Avoidance, numbing, dissociation, high guilt, and low acknowledged anger correlate with increased PTSD risk. Follow up with patients who exhibit these risk factors every 1 to 2 weeks with medication and/or psychotherapy.
1. Cloak NL, Edwards P. Psychological first aid: Emergency care for terrorism and disaster survivors. Current Psychiatry 2004;3(5):12-23.
2. Bisson JI. Early interventions following traumatic events. Psychiatr Ann 2003;1:37-44.
3. Davidson JR, Rothbaum BO, van der Kolk BA, et al. Multicenter, double-blind comparison of sertraline and placebo in the treatment of posttraumatic stress disorder. Arch Gen Psychiatry 2001;58:485-92.
4. Marshall RD, Beebe KL, Oldham M, et al. Efficacy and safety of paroxetine treatment for chronic PTSD: a fixed-dose, placebo-controlled study. Am J Psychiatry 2001;158:1982-8.
Dr. Sobel is a clinical instructor, University of California-San Diego School of Medicine, and consulting psychiatrist, University of San Diego Counseling Center.
1. Cloak NL, Edwards P. Psychological first aid: Emergency care for terrorism and disaster survivors. Current Psychiatry 2004;3(5):12-23.
2. Bisson JI. Early interventions following traumatic events. Psychiatr Ann 2003;1:37-44.
3. Davidson JR, Rothbaum BO, van der Kolk BA, et al. Multicenter, double-blind comparison of sertraline and placebo in the treatment of posttraumatic stress disorder. Arch Gen Psychiatry 2001;58:485-92.
4. Marshall RD, Beebe KL, Oldham M, et al. Efficacy and safety of paroxetine treatment for chronic PTSD: a fixed-dose, placebo-controlled study. Am J Psychiatry 2001;158:1982-8.
Dr. Sobel is a clinical instructor, University of California-San Diego School of Medicine, and consulting psychiatrist, University of San Diego Counseling Center.
Liability in patient suicide
Clinical psychiatrists often find it hard to evaluate suicide risk and understand their potential legal liability. Prevalence of suicidality compounds this challenge: Up to one-third of the general population in the United States have suicidal thoughts at some point.1 Although most people who consider suicide do not act on those thoughts, 51% of psychiatrists report having had a patient who committed suicide.2
Because patient suicide risk is real, psychiatrists often worry about malpractice claims. Although post-suicide lawsuits account for the largest number of malpractice suits against psychiatrists,3,4 a psychiatrist’s risk of being sued for malpractice is still quite low.3 Even when sued, clinicians win up to 80% of cases.3
Still, with malpractice claims increasing overall, clinicians should understand their potential liability in preventing suicide and the basic principles behind a malpractice claim.
Patient jumps from window after suicide watch is called off
Los Angeles County (CA) superior court
A 24-year-old man was hospitalized after attempting suicide by ingesting prescription pills and alcohol. He was admitted to the general medical floor with a 24-hour sitter to guard against additional suicide attempts. When the psychiatrist tried to evaluate him, he found the patient unresponsive because of the pills’ effects.
The next day, the psychiatrist evaluated the patient and recommended that the patient be transferred to the psychiatric unit and that the sitter be continued. Four hours later, without a further evaluation, the psychiatrist recommended moving the patient to another room and canceling the sitter.
The next day, the patient jumped from his sixth-floor hospital room window. He sustained traumatic brain injury.
The patient’s guardian ad litem argued that discontinuing the sitter was negligent. The defendant argued that discontinuation was within the parameters of proper care.
- The jury found for the defense.
Patient commits suicide hours after ER discharge
Lake County (IL) circuit court
A 36-year-old man was being treated by a psychiatrist for major depressive disorder. The patient owned several guns for hunting and target shooting and had a state-issued firearm owner’s identification card.
In October 2003, the patient presented to the emergency room and was examined by a mental health assessment staff. The psychiatrist recommended voluntary admission to the psychiatric unit for 23 hours.
The patient’s father discouraged the admission and stated that the patient could lose his gun owner’s card as a result. The patient was subsequently discharged. Within 24 hours after discharge, the patient shot himself in the chest and died.
The deceased’s estate argued that the psychiatrist should have admitted the patient involuntarily. The psychiatrist claimed no obligation to involuntary admission and argued that the patient did not meet criteria typically used for such admission.
- The jury found for the defense.
Doctor’s hanging attempt in hospital causes permanent brain damage
Morris County (NJ) district court
A cardiologist was admitted to the hospital’s psychiatric unit after decompensating. While hospitalized, he attempted suicide by hanging in a clinic bathroom. He suffered permanent brain injury as a result of the hanging. Because the injury left him in a childlike state, he required constant care.
The patient’s attorney argued that hospital personnel knew he was suicidal yet did not adequately supervise him. The attorney also argued that the injury cost his client $5 million in lost income.
The defense reported that the hospital had placed the patient on suicide watch and that staff checked him every 5 minutes. The defense also argued that the bathroom where the suicide was attempted was impossible to monitor.
- The jury found for the defense.
Dr. Grant’s observations
To win a malpractice claim, the injured party must show four things:
Duty to care for the patient existed based on the provider’s relationship with the patient. Whether on a hospital floor or in the emergency room, once a doctor-patient relationship has been established, the provider agrees to provide non-negligent care.
Negligence. The physician or hospital personnel acted negligently and violated the duty of care. This concept is based upon a “standard of care” —ie, what other psychiatrists would do in this situation.
Harm. Even if someone has acted negligently, a malpractice case cannot go forward if no harm has been suffered.
Causation. The negligent act caused the harm.
The defendants most likely won the cases cited above because the injured parties could not establish negligence. Clinicians are not negligent for merely failing to predict suicide, as the inability to predict suicide has been demonstrated.5,6 Clinicians, however, must follow the profession’s standard of care, assess the relative degree of risk, and form a treatment and safety plan consistent with that risk.4
Based on relevant case law, the following actions can decrease the risk of patient suicide—and a resultant malpractice claim:
- Conduct a comprehensive evaluation of the patient and his or her suicide risk. Ask about:
- Consider hospitalizing at-risk patients. If you decide against hospitalization, provide a comprehensive safety plan. In the gun owner’s case, such a plan would include arranging with the family to remove firearms. Implement additional anti-suicide precautions, such as more-intensive outpatient therapy or involving family members in treatment.
- Document suicide risk assessment and the reasons for your treatment decisions. Juries may interpret lack of documented information in the patient’s favor.
- Design a treatment plan for hospitalized patients to reduce suicide risk. Consider the patient’s reaction to constant surveillance. For example, checking a paranoid patient every 5 minutes may be more therapeutic than a constant watch while providing adequate safety. Thoroughly document your reasons behind the plan.
1. Hirschfeld RMA, Russell JM. Assessment and treatment of suicidal patients. N Engl J Med 1997;337:910-5.
2. Chemtob CM, Hamada RS, Bauer GB, et al. Patient suicide: frequency and impact on psychiatrists. Am J Psychiatry 1988;145:224-8.
3. Baerger DR. Risk management with the suicidal patient: lessons from case law. Prof Psychol Res Pract 2001;32:359-66.
4. Packman WL, O’Connor Pennuto T, Bongar B, Orthwein J. Legal issues of professional negligence in suicide cases. Behav Sci Law 2004;22:697-713.
5. Pokorny AD. Prediction of suicide in psychiatric patients. Arch Gen Psychiatry 1983;40:249-57.
6. Pokorny AD. Suicide prediction revisited. Suicide Life Threat Behav 1993;23:1-10.
7. Bell v. New York City Health and Hospitals Corp., 456 NYS 2d 787 (App. Div. 1982).
8. Simon RI. The suicidal patient. In: Lifson LE, Simon SI (eds). The mental health practitioner and the law: A comprehensive handbook. Cambridge, MA: Harvard University Press, 1998;166-86.
Clinical psychiatrists often find it hard to evaluate suicide risk and understand their potential legal liability. Prevalence of suicidality compounds this challenge: Up to one-third of the general population in the United States have suicidal thoughts at some point.1 Although most people who consider suicide do not act on those thoughts, 51% of psychiatrists report having had a patient who committed suicide.2
Because patient suicide risk is real, psychiatrists often worry about malpractice claims. Although post-suicide lawsuits account for the largest number of malpractice suits against psychiatrists,3,4 a psychiatrist’s risk of being sued for malpractice is still quite low.3 Even when sued, clinicians win up to 80% of cases.3
Still, with malpractice claims increasing overall, clinicians should understand their potential liability in preventing suicide and the basic principles behind a malpractice claim.
Patient jumps from window after suicide watch is called off
Los Angeles County (CA) superior court
A 24-year-old man was hospitalized after attempting suicide by ingesting prescription pills and alcohol. He was admitted to the general medical floor with a 24-hour sitter to guard against additional suicide attempts. When the psychiatrist tried to evaluate him, he found the patient unresponsive because of the pills’ effects.
The next day, the psychiatrist evaluated the patient and recommended that the patient be transferred to the psychiatric unit and that the sitter be continued. Four hours later, without a further evaluation, the psychiatrist recommended moving the patient to another room and canceling the sitter.
The next day, the patient jumped from his sixth-floor hospital room window. He sustained traumatic brain injury.
The patient’s guardian ad litem argued that discontinuing the sitter was negligent. The defendant argued that discontinuation was within the parameters of proper care.
- The jury found for the defense.
Patient commits suicide hours after ER discharge
Lake County (IL) circuit court
A 36-year-old man was being treated by a psychiatrist for major depressive disorder. The patient owned several guns for hunting and target shooting and had a state-issued firearm owner’s identification card.
In October 2003, the patient presented to the emergency room and was examined by a mental health assessment staff. The psychiatrist recommended voluntary admission to the psychiatric unit for 23 hours.
The patient’s father discouraged the admission and stated that the patient could lose his gun owner’s card as a result. The patient was subsequently discharged. Within 24 hours after discharge, the patient shot himself in the chest and died.
The deceased’s estate argued that the psychiatrist should have admitted the patient involuntarily. The psychiatrist claimed no obligation to involuntary admission and argued that the patient did not meet criteria typically used for such admission.
- The jury found for the defense.
Doctor’s hanging attempt in hospital causes permanent brain damage
Morris County (NJ) district court
A cardiologist was admitted to the hospital’s psychiatric unit after decompensating. While hospitalized, he attempted suicide by hanging in a clinic bathroom. He suffered permanent brain injury as a result of the hanging. Because the injury left him in a childlike state, he required constant care.
The patient’s attorney argued that hospital personnel knew he was suicidal yet did not adequately supervise him. The attorney also argued that the injury cost his client $5 million in lost income.
The defense reported that the hospital had placed the patient on suicide watch and that staff checked him every 5 minutes. The defense also argued that the bathroom where the suicide was attempted was impossible to monitor.
- The jury found for the defense.
Dr. Grant’s observations
To win a malpractice claim, the injured party must show four things:
Duty to care for the patient existed based on the provider’s relationship with the patient. Whether on a hospital floor or in the emergency room, once a doctor-patient relationship has been established, the provider agrees to provide non-negligent care.
Negligence. The physician or hospital personnel acted negligently and violated the duty of care. This concept is based upon a “standard of care” —ie, what other psychiatrists would do in this situation.
Harm. Even if someone has acted negligently, a malpractice case cannot go forward if no harm has been suffered.
Causation. The negligent act caused the harm.
The defendants most likely won the cases cited above because the injured parties could not establish negligence. Clinicians are not negligent for merely failing to predict suicide, as the inability to predict suicide has been demonstrated.5,6 Clinicians, however, must follow the profession’s standard of care, assess the relative degree of risk, and form a treatment and safety plan consistent with that risk.4
Based on relevant case law, the following actions can decrease the risk of patient suicide—and a resultant malpractice claim:
- Conduct a comprehensive evaluation of the patient and his or her suicide risk. Ask about:
- Consider hospitalizing at-risk patients. If you decide against hospitalization, provide a comprehensive safety plan. In the gun owner’s case, such a plan would include arranging with the family to remove firearms. Implement additional anti-suicide precautions, such as more-intensive outpatient therapy or involving family members in treatment.
- Document suicide risk assessment and the reasons for your treatment decisions. Juries may interpret lack of documented information in the patient’s favor.
- Design a treatment plan for hospitalized patients to reduce suicide risk. Consider the patient’s reaction to constant surveillance. For example, checking a paranoid patient every 5 minutes may be more therapeutic than a constant watch while providing adequate safety. Thoroughly document your reasons behind the plan.
Clinical psychiatrists often find it hard to evaluate suicide risk and understand their potential legal liability. Prevalence of suicidality compounds this challenge: Up to one-third of the general population in the United States have suicidal thoughts at some point.1 Although most people who consider suicide do not act on those thoughts, 51% of psychiatrists report having had a patient who committed suicide.2
Because patient suicide risk is real, psychiatrists often worry about malpractice claims. Although post-suicide lawsuits account for the largest number of malpractice suits against psychiatrists,3,4 a psychiatrist’s risk of being sued for malpractice is still quite low.3 Even when sued, clinicians win up to 80% of cases.3
Still, with malpractice claims increasing overall, clinicians should understand their potential liability in preventing suicide and the basic principles behind a malpractice claim.
Patient jumps from window after suicide watch is called off
Los Angeles County (CA) superior court
A 24-year-old man was hospitalized after attempting suicide by ingesting prescription pills and alcohol. He was admitted to the general medical floor with a 24-hour sitter to guard against additional suicide attempts. When the psychiatrist tried to evaluate him, he found the patient unresponsive because of the pills’ effects.
The next day, the psychiatrist evaluated the patient and recommended that the patient be transferred to the psychiatric unit and that the sitter be continued. Four hours later, without a further evaluation, the psychiatrist recommended moving the patient to another room and canceling the sitter.
The next day, the patient jumped from his sixth-floor hospital room window. He sustained traumatic brain injury.
The patient’s guardian ad litem argued that discontinuing the sitter was negligent. The defendant argued that discontinuation was within the parameters of proper care.
- The jury found for the defense.
Patient commits suicide hours after ER discharge
Lake County (IL) circuit court
A 36-year-old man was being treated by a psychiatrist for major depressive disorder. The patient owned several guns for hunting and target shooting and had a state-issued firearm owner’s identification card.
In October 2003, the patient presented to the emergency room and was examined by a mental health assessment staff. The psychiatrist recommended voluntary admission to the psychiatric unit for 23 hours.
The patient’s father discouraged the admission and stated that the patient could lose his gun owner’s card as a result. The patient was subsequently discharged. Within 24 hours after discharge, the patient shot himself in the chest and died.
The deceased’s estate argued that the psychiatrist should have admitted the patient involuntarily. The psychiatrist claimed no obligation to involuntary admission and argued that the patient did not meet criteria typically used for such admission.
- The jury found for the defense.
Doctor’s hanging attempt in hospital causes permanent brain damage
Morris County (NJ) district court
A cardiologist was admitted to the hospital’s psychiatric unit after decompensating. While hospitalized, he attempted suicide by hanging in a clinic bathroom. He suffered permanent brain injury as a result of the hanging. Because the injury left him in a childlike state, he required constant care.
The patient’s attorney argued that hospital personnel knew he was suicidal yet did not adequately supervise him. The attorney also argued that the injury cost his client $5 million in lost income.
The defense reported that the hospital had placed the patient on suicide watch and that staff checked him every 5 minutes. The defense also argued that the bathroom where the suicide was attempted was impossible to monitor.
- The jury found for the defense.
Dr. Grant’s observations
To win a malpractice claim, the injured party must show four things:
Duty to care for the patient existed based on the provider’s relationship with the patient. Whether on a hospital floor or in the emergency room, once a doctor-patient relationship has been established, the provider agrees to provide non-negligent care.
Negligence. The physician or hospital personnel acted negligently and violated the duty of care. This concept is based upon a “standard of care” —ie, what other psychiatrists would do in this situation.
Harm. Even if someone has acted negligently, a malpractice case cannot go forward if no harm has been suffered.
Causation. The negligent act caused the harm.
The defendants most likely won the cases cited above because the injured parties could not establish negligence. Clinicians are not negligent for merely failing to predict suicide, as the inability to predict suicide has been demonstrated.5,6 Clinicians, however, must follow the profession’s standard of care, assess the relative degree of risk, and form a treatment and safety plan consistent with that risk.4
Based on relevant case law, the following actions can decrease the risk of patient suicide—and a resultant malpractice claim:
- Conduct a comprehensive evaluation of the patient and his or her suicide risk. Ask about:
- Consider hospitalizing at-risk patients. If you decide against hospitalization, provide a comprehensive safety plan. In the gun owner’s case, such a plan would include arranging with the family to remove firearms. Implement additional anti-suicide precautions, such as more-intensive outpatient therapy or involving family members in treatment.
- Document suicide risk assessment and the reasons for your treatment decisions. Juries may interpret lack of documented information in the patient’s favor.
- Design a treatment plan for hospitalized patients to reduce suicide risk. Consider the patient’s reaction to constant surveillance. For example, checking a paranoid patient every 5 minutes may be more therapeutic than a constant watch while providing adequate safety. Thoroughly document your reasons behind the plan.
1. Hirschfeld RMA, Russell JM. Assessment and treatment of suicidal patients. N Engl J Med 1997;337:910-5.
2. Chemtob CM, Hamada RS, Bauer GB, et al. Patient suicide: frequency and impact on psychiatrists. Am J Psychiatry 1988;145:224-8.
3. Baerger DR. Risk management with the suicidal patient: lessons from case law. Prof Psychol Res Pract 2001;32:359-66.
4. Packman WL, O’Connor Pennuto T, Bongar B, Orthwein J. Legal issues of professional negligence in suicide cases. Behav Sci Law 2004;22:697-713.
5. Pokorny AD. Prediction of suicide in psychiatric patients. Arch Gen Psychiatry 1983;40:249-57.
6. Pokorny AD. Suicide prediction revisited. Suicide Life Threat Behav 1993;23:1-10.
7. Bell v. New York City Health and Hospitals Corp., 456 NYS 2d 787 (App. Div. 1982).
8. Simon RI. The suicidal patient. In: Lifson LE, Simon SI (eds). The mental health practitioner and the law: A comprehensive handbook. Cambridge, MA: Harvard University Press, 1998;166-86.
1. Hirschfeld RMA, Russell JM. Assessment and treatment of suicidal patients. N Engl J Med 1997;337:910-5.
2. Chemtob CM, Hamada RS, Bauer GB, et al. Patient suicide: frequency and impact on psychiatrists. Am J Psychiatry 1988;145:224-8.
3. Baerger DR. Risk management with the suicidal patient: lessons from case law. Prof Psychol Res Pract 2001;32:359-66.
4. Packman WL, O’Connor Pennuto T, Bongar B, Orthwein J. Legal issues of professional negligence in suicide cases. Behav Sci Law 2004;22:697-713.
5. Pokorny AD. Prediction of suicide in psychiatric patients. Arch Gen Psychiatry 1983;40:249-57.
6. Pokorny AD. Suicide prediction revisited. Suicide Life Threat Behav 1993;23:1-10.
7. Bell v. New York City Health and Hospitals Corp., 456 NYS 2d 787 (App. Div. 1982).
8. Simon RI. The suicidal patient. In: Lifson LE, Simon SI (eds). The mental health practitioner and the law: A comprehensive handbook. Cambridge, MA: Harvard University Press, 1998;166-86.
Treating osteoporosis in post-menopausal women: A case approach
Asymptomatic Pituitary Metastases
A DASH-like diet can decrease cardiovascular risk, but barriers to implementation exist
Ten tips to help you control your high blood pressure
The DASH diet for high blood pressure: From clinical trial to dinner table
Changes in recommended treatments for mild and moderate asthma
- Every patient with persistent asthma, regardless of disease severity, should use a daily controller medication.
- Consider an inhaled corticosteroid (ICS) first when choosing controller medications for long-term treatment of mild, moderate, and severe persistent asthma in adults and children. Leukotriene modifiers, cromolyn, and nedocromil may be considered as alternative, not preferred, controller medications for patients with persistent asthma.
- Long-acting β2-adrenergic agonists should not be used as monotherapy.
- Long-term use of ICSs within labeled doses is safe for children in terms of growth, bone mineral density, and adrenal function; nonetheless, asthma should be monitored and ICS therapy stepped down to the lowest effective dose.
- Low-to medium-dose ICSs are not associated with the development of cataracts or glaucoma in children, but high cumulative lifetime doses may slightly increase the prevalence of cataracts in adults and elderly patients.
- ICSs are recommended for use in pregnant women with asthma; budesonide is the only ICS rated Pregnancy Category B.
Consider an adult with the following characteristics. To which disease severity would you assign this patient’s asthma?
- Forced expiratory volume in 1 second (FEV1) or peak expiratory flow (PEF) ≥80%
- PEF variability 20%–30%
- Daytime symptoms less than once a day
- Nighttime symptoms more than 1 night a week.
This patient is said to have moderate persistent asthma based on nighttime symptoms. An accurate classification of a patient’s asthma is the foundation for selecting an appropriate treatment strategy.
In 2002 the National Asthma Education and Prevention Program (NAEPP) updated select topics1from its 1997 Guidelines for the Diagnosis and Management of Asthma.2 These evidence-based revisions to the stepwise approach to asthma management were made following a systematic review of the literature (see Search function).
A comprehensive search of Medline and EMBASE databases was performed to identify controlled clinical studies relevant to each topic that were published (in English or foreign languages with English abstracts) from 1980 through August 2000. The search included studies published before 1980 if referenced in the post-1980 literature. Studies that did not include control groups were excluded, except for those reporting adverse effects of ICSs. Studies that met the study selection criteria established for each topic were included in a systematic review of the evidence. An expert panel reviewed the evidence, along with additional literature published since August 2000, and reached a consensus on whether the evidence supported 1997 guideline recommendations or indicated a need for revision. Writing committees were then assigned to developed position statements for each topic. The level of evidence for included studies was rated based on the system of Jadad and colleagues,3 where A = randomized controlled trials, rich body of data; B = randomized controlled trials, limited data; C = nonrandomized trials and observational studies; D = panel consensus judgment.
This article reviews the 2002 NAEPP recommendations for the use of controller medications for asthma, including:
- Relative effectiveness of inhaled corticosteroids (ICSs) versus other controller medications
- Safety of long-term ICS use in children
- Potential benefits of early ICS treatment.
We emphasize mild and moderate persistent asthma because the recommended treatments for these levels of severity have been most affected by the recent guideline changes. We also discuss a recent change by the US Food and Drug Administration (FDA) in its pregnancy category rating for an ICS.
2002 Stepwise approach to asthma management
New criteria for classifying asthma severity
The NAEPP classifies asthma severity according to symptoms and lung function in adults and children older than 5 years, and symptoms in children 5 years and younger.1 Persistent asthma is classified as mild, moderate, or severe according to the feature of greatest severity.
Asthma severity should be assigned according to symptoms before treatment.1 Because it is difficult to predict which infants and young children who wheeze with acute viral upper respiratory infection will go on to develop persistent asthma, new criteria have been detailed to help distinguish these children from those with transient wheeze (Table 1).1,4
TABLE 1
Criteria for children with intermittent wheeze
Infants and young children meeting these criteria should receive controller therapy for asthma:
|
AND presence of risk factors for development of persistent asthma:
|
Choosing pharmacologic treatment according to asthma classification
Quick-relief medications, which include the short-acting β2-agonists (SABAs), are taken as needed to promptly reverse acute airflow obstruction and relieve accompanying symptoms.2
Asthma controller medications (ie, ICSs, cromolyn sodium, long-acting β2-adrenergic-agonists [LABAs], leukotriene modifiers, nedocromil, and theophylline) are used daily to achieve and maintain long-term control of persistent asthma. All patients with persistent asthma, regardless of disease severity, should use a daily controller. Criteria for determining asthma severity and updated recommendations for the use of controller treatment in mild and moderate persistent asthma are presented in the Figure.3,5 Levels of evidence justifying NAEPP treatment recommendations are shown in Table 2.
For use in children. Asthma controller medications approved for use in children younger than 5 years include the fluticasone dry-powder inhalers (Flovent, Rotadisk, and Flovent Diskus), which are approved for children as young as 4 years (Flovent Diskus is not yet commercially available), and nebulized budesonide inhalation suspension (Pulmicort Respules), which is approved for children as young as 12 months.
The LABAs formoterol (Foradil) and salmeterol (Serevent Diskus) are approved for children as young as 5 and 4 years, respectively. Cromolyn sodium nebulizer solution is approved for children as young as 2 years, and theophylline is available for use at any age.
Based on safety and extrapolation of efficacy data in older patients, the oral granule formulation of the leukotriene receptor antagonist (LTRA) montelukast (Singulair) is approved for children as young as 1 year, and the chewable tablets are approved for children 2 to 5 years of age. Zafirlukast (Accolate) is approved for use in children 5 years and older.
New recommendations for mild persistent asthma. Recommendations for the treatment of mild and moderate persistent asthma have changed considerably from the 1997 guidelines. ICSs are now the preferred controller medications, based on greater efficacy. The updated guidelines no longer recommend an initial trial of cromolyn or nedocromil for the treatment of mild persistent asthma; these agents, along with the leukotriene modifiers and slow-release theophylline, are now considered alternatives to low-dose ICSs for adults and children older than 5 years with mild persistent disease (Figure).
According to the NAEPP update, daily low-dose ICS treatment also is preferred for the control of mild persistent asthma in preschool children. As in older children, cromolyn and nedocromil are no longer considered appropriate initial treatments for infants and children 5 years and younger. Cromolyn is considered an alternative controller, whereas nedocromil is no longer recommended for use.
New recommendations for moderate persistent asthma. For adults and children older than 5 years with moderate persistent asthma, revision to the guidelines involved recommendation of a low- to medium-dose ICS plus a LABA as the preferred controller treatment (Figure). Comparative low, medium, and high daily doses for ICSs are shown in Table 3 .1
For preschool children, preferred controller treatments for moderate persistent asthma include low-dose ICSs plus a LABA, or increasing ICSs within the medium-dose range (Figure). Recommendations for the use of LABAs as add-on therapy in this age group are based on extrapolation of data from older patients, since therapy with an ICS/LABA combination has not been adequately studied in children younger than 5 years. Four studies included in the NAEPP evaluation showed clear benefit of medium-dose ICSs in this age group, supporting the use of medium-dose ICSs as a preferred option.6-9 LABAs are not recommended for use without an ICS, and the only ICS/LABA combination product currently available has been FDA approved only for patients aged 12 years and older.
TABLE 2
Levels of evidence for NAEPP assessments*
| Medication | NAEPP assessment | SOR* |
|---|---|---|
| ICS | Preferred treatment for children of all ages with persistent asthma | A (A) |
| SABA | ICSs improve asthma control compared with as-needed SABAs | A (A) |
| Cromolyn/nedocromil | For use as alternative, not preferred, treatment of mild persistent asthma in children of all ages (cromolyn) or children >5 years of age (nedocromil) | A (A) |
| LABA | For use with ICSs as the preferred combination treatment for moderate and severe persistent asthma in children >5 years of age | A (A) |
| For use as a preferred option for combination treatment in children 5 years of age | B (B) | |
| Leukotriene modifier | For use as alternative, not preferred, treatment of mild persistent asthma and as ICS adjunct in moderate persistent asthma | B (B) |
| Theophylline | For use as an alternative ICS add-on in moderate or severe persistent asthma if serum concentrations are monitored | D (D) |
| Not considered an alternative controller for young children with mild persistent asthma due to potential adverse effects in infants with frequent febrile illnesses | ||
| *Highest level of evidence available is reported. Strengths of recommendation are based on the method of Jadad et al.3 Strength of evidence based on the Oxford Center for Evidence-Based Medicine5 is in parentheses. SOR, strength of recommendation; NAEPP, National Asthma Education and Prevention Program; ICS, inhaled corticosteroid; SABA, short-acting β2-adrenergic agonist; LABA, long-acting β2-adrenergic agonist. | ||
TABLE 3
Estimated comparative daily doses for inhaled corticosteroids*
| Drug | Low daily dose | Medium daily dose | High daily dose | |||
|---|---|---|---|---|---|---|
| Adult | Child† | Adult | Child† | Adult | Child† | |
| Beclomethasone CFC 42 or 84 μg/puff | 168–504 μg | 84–336 μg | 504–840 μg | 336–672 μg | >840 μg | >672 μg |
| Beclomethasone HFA 40 or 80 μg/puff | 80–240 μg | 80–160 μg | 240–480 μg | 160–320 μg | >480 μg | >320 μg |
| Budesonide DPI 200 μg/inhalation | 200–600 μg | 200–400 μg | 600–1200 μg | 400–800 μg | >1200 μg | >800 μg |
| Budesonide inhalation suspension for nebulization (child dose) | 0.5mg | 1.0 mg | 2.0 mg | |||
| Fluticasone MDI 44, 110, or 220 μg/puff | 88–264 μg | 88–176 μg | 264–660 μg | 176–440 μg | >660 μg | >440 μg |
| Fluticasone DPI 50, 100, or 250 μg/inhalation | 100–300 μg | 100–200 μg | 300–600 μg | 200–400 μg | >600 μg | >400 μg |
| Triamcinolone acetonide 100 μg/puff | 400–1000 μg | 400–800 μg | 1000–2000 μg | 800–1200 μg | >2000 μg | >1200 μg |
| *The most important determinant of appropriate dosing is the clinician’s judgment of the patient’s response to therapy. This updated comparative dose chart is based on review of recently published clinical trials involving more than 5000 patients and published reviews. Some doses may be outside package labeling, especially in the high-dose range. | ||||||
| †Children 12 years of age. | ||||||
| CFC, chlorofluorocarbon; HFA, hydrofluoroalkane; DPI, dry-powder inhaler; MDI, metered-dose inhaler. | ||||||
FIGURE
Updated National Asthma Education and Prevention Program recommendations for long-term controller treatment in mild and moderate persistent asthma
Topics in the management of asthma in children
Recognizing the need for continual appraisal of the benefits and risks of asthma medications in children, the NAEPP Expert Panel considered new studies comparing the effectiveness of ICS monotherapy with that of as-needed SABAs and other controllers used as monotherapy in children with mild or moderate persistent asthma. In addition, the safety of long-term ICS use in children was evaluated based on vertical growth, bone mineral density, ocular toxicity, and adrenal suppression.
Effectiveness of ICSs compared with other asthma medications
Short-acting β2-adrenergic agonists. Eight studies met the eligibility criteria for evaluating the effectiveness of ICSs versus as-needed SABAs.6,10-16 Six studies (4 involving budesonide) in children 5 years and older showed that ICSs improve lung function and symptoms and reduce the need for emergency intervention compared with as-needed SABAs.1 Among all studies included in the NAEPP update, the Childhood Asthma Management Program (CAMP) Research Group Study,9 a placebo-controlled study of inhaled budesonide and nedocromil, contributed the most evidence. Studies with children 5 years and younger are limited to 2 small studies enrolling a total of 69 children.6,15 Consistent with studies of older children, these studies indicate that ICSs improve asthma control compared with as-needed SABAs.1
Cromolyn and nedocromil. Despite well-established safety profiles, cromolyn and nedocromil are no longer recommended as first-line therapy for children, even those with mild disease. New recommendations reflect the greater effectiveness of inhaled budesonide compared with nedocromil demonstrated in the CAMP study,10 and the lack of apparent benefit of cromolyn as maintenance treatment in childhood asthma reported by Tasche and colleagues in a systematic review of the literature.17
In the CAMP study, children 5 to 12 years of age receiving inhaled budesonide showed greater reductions in symptoms and albuterol use, lower rates of hospitalization and urgent care visits, and less need for additional asthma therapy and oral prednisone compared with placebo over 4 to 6 years of treatment.10 The marginal effectiveness of nedocromil demonstrated in the CAMP study mirrored that of cromolyn reported in the review of 24 randomized placebo-controlled studies by Tasche and colleagues.1,17
For children 5 years and younger, the NAEPP Expert Panel took into account 1 randomized placebo-controlled study conducted with children 2 to 5 years of age; it showed improvements in lung function, symptoms, and bronchial hyperre-activity with inhaled budesonide.9 Support for the new NAEPP recommendations preferring ICSs for preschool children is found in a more recent open-label study18 that showed greater symptom improvement and significantly lower rates of asthma exacerbations, urgent care visits, and oral prednisone use with budesonide inhalation suspension, compared with cromolyn sodium nebulizer solution (Intal Nebulizer Solution) in children 2 to 6 years of age with persistent asthma.
Leukotriene modifiers. The LTRAs zafir-lukast and montelukast are approved for use in children. According to the NAEPP Expert Panel, studies have shown only modest improvements in lung function and other asthma control outcomes with LTRA monotherapy in children as young as 6 and 2 years, respectively.1 Because studies comparing ICSs with LTRAs in children are lacking, findings of greater overall efficacy of ICSs in adults with persistent asthma have been extrapolated for use with children; clear superiority of ICSs versus LTRAs in most outcomes has resulted in the recommendation for ICSs as the preferred treatment for mild persistent asthma in children.
Long-acting β2-adrenergic agonists. There is no role for LABAs as monotherapy in asthma. No studies have compared the effectiveness of ICS versus LABA monotherapy in children younger than 5 years, and studies in older children have shown greater effectiveness of inhaled beclomethasone versus salmeterol.14,19 In the study by Verberne and colleagues, salmeterol monotherapy was associated with deterioration in FEV1.19 In a more recent study that included patients as young as 16 years, a switch from ICS to LABA treatment was associated with a significant increase in treatment failures and exacerbations.20
Theophylline. Only 1 study has compared outcomes with low-dose ICSs versus theophylline in adults and children.21 Although limited, the data support greater effectiveness of ICSs based on symptoms, bronchial hyperresponsiveness, and the need for β2-adrenergic agonists and oral corticosteroids.1
Safety of long-term ICS use in children
Systemic corticosteroids have the potential to suppress growth over the long term.2 Short-term growth studies with ICSs show an average reduction in growth velocity of 1 cm per year during the first year of treatment, but the CAMP study showed that initial reductions in growth velocity with inhaled budesonide were not maintained over a 4- to 6-year treatment period.1,10
Although catch-up growth was not observed in the CAMP study, Agertoft and Pedersen reported no effect of long-term treatment with inhaled budesonide (mean 9.2 years) on final adult height.22 Based on these long-term prospective studies of budesonide, showing only a transient reduction in growth velocity and attainment of expected final adult height, and retrospective studies including inhaled beclomethasone, the Expert Panel concluded that the ICS class is safe regarding growth effects.
According to the NAEPP Expert Panel, clinical study data for children monitored for up to 6 years strongly suggest that ICSs are safe when used at recommended doses (strength of recommendation: A).1 The panel could not rule out a potential cumulative effect of ICS use on some conditions, (eg, osteoporosis, cataracts, glaucoma) in adulthood, as sufficient long-term data are not available.
The panel did conclude that low- to medium-dose ICSs (Table 3) appear to have no serious adverse effects on bone mineral density in children.
Likewise, low- to medium-dose ICS use was not associated with the development of cataracts or glaucoma in children, although the potential for high cumulative lifetime doses of ICSs to slightly increase the prevalence of cataracts in adults and elderly patients was noted.
Strong evidence also indicates that ICS effects on adrenal function are usually clinically insignificant at low to medium doses; however, certain individuals may be at higher risk for hypothalam-ic pituitary adrenal axis effects while using conventional ICS doses.1
Although ICSs are safe when used within labeled dosing, it is still preferable to maintain doses at the lowest effective dose. In general, treatment should be reviewed every 1 to 6 months and doses reduced in a stepwise fashion when possible.1 For children showing a favorable response to treatment, a step down in dose should be considered, but not more frequently than every 3 months. If children show no clear response to treatment within 4 to 6 weeks, consider an alternative treatment or diagnosis.1
Safety of long-term ICS use in pregnant women
Uncontrolled asthma during pregnancy is associated with an increased risk of perinatal complications. 23 Since the consequences of not using asthma controllers during pregnancy can be worse than those with using them, daily controller treatment is recommended for all pregnant women with persistent asthma. 23
The American College of Obstetricians and Gynecologists and the American College of Allergy, Asthma and Immunology previously recommended cromolyn as the treatment of choice for pregnant women with mild persistent asthma. ICSs were recommended for patients whose asthma was inadequately controlled with cromolyn. 24 Beclomethasone and budesonide were the ICSs of choice for pregnant women and those who might become pregnant, with a preference for budesonide when high-dose therapy was indicated.24
These recommendations predate the 2002 NAEPP recommendations for ICSs as preferred therapy in mild persistent asthma and the 2004 NAEPP recommendations for ICSs as the first-choice controller therapy for mild persistent asthma during pregnancy. 25 Among ICSs, one (inhaled budesonide) has an FDA Pregnancy Category B rating based on studies showing no risk in pregnant women. 26,27 All other ICSs are rated Pregnancy Category C.
Based on current evidence, it seems reasonable to consider whether budesonide should now be the preferred therapy for mild persistent asthma during pregnancy.
Effects of early treatment on asthma progression
The potential for early ICS intervention to prevent progression of mild or moderate persistent asthma was evaluated solely with data from children enrolled in the CAMP study. 10 The NAEPP Expert Panel concluded that CAMP study data do not support a progressive decline in lung function in children aged 5 to 12 years with mild or moderate persistent asthma, but do suggest that lung function decline is influenced by age of asthma onset.
According to the panel, CAMP data suggest that most deficits in lung function growth due to childhood asthma occur during the first 3 years of life. Preliminary results of the recent START study (Inhaled Steroid Treatment As Regular Therapy in Early Asthma), 28 conducted with 7165 corticosteroidnaïve patients 5 to 66 years of age with recent onset mild persistent asthma, did show a decline in lung function in patients with mild persistent disease.
Although improvements in prebronchodilator and postbronchodilator FEV1 were significant after 3 years of treatment with inhaled budes-onide, differences from placebo in both outcomes were greatest after the first year. When patients with mild persistent disease inhaled budesonide once daily in addition to normal treatment within 2 years of asthma onset,28 they enjoyed considerable protection from severe and life-threatening asthma exacerbations and overall greater asthma control.
- Budesonide • Pulmicort
- Rhinocort Cromolyn • Intal
- Fluticasone • Flovent
- Formoterol • Foradil
- Montelukast • Singulair
- Nedocromil • Tilade
- Salmeterol • Servent
- Triamcinolone acetonide • Azmacort
- Zafirlukast • Accolate
Corresponding author
Gregory J. Redding, MD, Children’s Hospital and Regional Medical Center, 4800 Sand Point Way, NE, Seattle, WA 98105-0371. E-mail: [email protected].
1. National Asthma Education and Prevention Program. Expert panel report: guidelines for the diagnosis and management of asthma. Update on selected topics–2002. J Allergy Clin Immunol 2002;110(5 suppl):S141-S219.
2. National Asthma Education and Prevention Program Expert Panel Report 2: Guidelines for the Diagnosis and Management of Asthma. Bethesda, Md: National Heart, Lung, and Blood Institute; National Institutes of Health; 1997. Publication 97;4051.-
3. Jadad AR, Moher M, Browman GP, Booker L, Sigouin C, Fuentes M, et al. Systematic reviews and meta-analyses on treatment of asthma: critical evaluation. BMJ 2000;320:537-540.
4. Castro-Rodríguez JA, Holberg CJ, Wright AL, Martinez FD. A clinical index to define risk of asthma in young children with recurrent wheezing. Am J Respir Crit Care Med 2000;162:1403-1406.
5. Oxford Centre for Evidence-based Medicine Levels of Evidence Available atwww.cebm.net/levels_faq.asp . Accessed January 8, 2004.
6. Connett GJ, Warde C, Wooler E, Lenney W. Use of budes-onide in severe asthmatics aged 1–3 years. Arch Dis Child 1993;69:351-355.
7. de Blic J, Delacourt C, Le Bourgeois M, Mahut B, Ostinelli J, Caswell C, et al. Efficacy of nebulized budesonide in treatment of severe infantile asthma: a double-blind study. J Allergy Clin Immunol 1996;98:14-20.
8. Bisgaard H, Gillies J, Groenewald M, Maden C, . for an International Study Group The effect of inhaled fluticas-one propionate in the treatment of young asthmatic children: a dose comparison study. Am J Respir Crit Care Med 1999;160:126-131.
9. Nielsen KG, Bisgaard H. The effect of inhaled budesonide on symptoms, lung function, and cold air and metha-choline responsiveness in 2- to 5-year–old asthmatic children. Am J Respir Crit Care Med 2000;162:1500-1506.
10. Childhood Asthma Management Program Research Group. Long-term effects of budesonide or nedocromil in children with asthma. N Engl J Med 2000;343:1054-1063.
11. Agertoft L, Pedersen S. Effects of long-term treatment with an inhaled corticosteroid on growth and pulmonary function in asthmatic children. Respir Med 1994;88:373-381.
12. Hoekstra MO, Grol MH, Bouman K, Stijnen T, Koëter GH, Kauffman HF, et al. Fluticasone propionate in children with moderate asthma. Am J Respir Crit Care Med 1996;154:1039-1044.
13. Jónasson G, Carlsen K-H, Blomqvist P. Clinical efficacy of low-dose inhaled budesonide once or twice daily in children with mild asthma not previously treated with steroids. Eur Respir J 1998;12:1099-1104.
14. Simons FER and the Canadian Beclomethasone Dipropionate-Salmeterol Xinafoate Study Group. A comparison of beclomethasone, salmeterol, and placebo in children with asthma. N Engl J Med 1997;337:1659-1665.
15. Storr J, Lenney CA, Lenney W. Nebulized beclomethasone dipropionate in preschool asthma. Arch Dis Child 1986;61:270-273.
16. Van Essen-Zandvliet EE, Hughes MD, Waalkens HJ, Duiverman EJ, Pocock SJ, Kerrebijn KF. and the Dutch Chronic Non-Specific Lung Disease Study Group Effects of 22 months of treatment with inhaled corticosteroids and/or beta-2-agonists on lung function, airway responsiveness, and symptoms in children with asthma. Am Rev Respir Dis 1992;146:547-554.
17. Tasche MJA, Uijen JHJM, Bernsen RMD, de Jongste JC, van der Wouden JC. Inhaled disodium cromoglycate (DSCG) as maintenance therapy in children with asthma: a systematic review. Thorax 2000;55:913-920.
18. Leflein JG, Szefler SJ, Murphy KR, Fitzpatrick S, Cruz-Rivera M, Miller CJ, et al. Nebulized budesonide inhalation suspension compared with cromolyn sodium nebulizer solution for asthma in young children: results of a randomized outcomes trial. Pediatrics 2002;109:866-872.
19. Verberne AAPH, Frost C, Duiverman EJ, Grol MH, Kerrebijn KF. and the Dutch Paediatric Asthma Study Group Addition of salmeterol versus doubling the dose of beclomethasone in children with asthma. Am J Respir Crit Care Med 1998;158:213-219.
20. Lazarus SC, Boushey HA, Fahy JV, Chinchilli VM, Lemanske RF Jr, Sorkness CA, , et al. for the Asthma Clinical Research Network of the National Heart Lung and Blood Institute. Long-acting 2-agonist monotherapy vs continued therapy with inhaled corticosteroids in patients with persistent asthma: a randomized controlled trial. JAMA 2001;285:2583-2593.
21. Reed CE, Offord KP, Nelson HS, Li JT, Tinkelman DG. and the American Academy of Allergy, Asthma and Immunology Beclomethasone Dipropionate-Theophylline Study Group. Aerosol beclomethasone dipropionate spray compared with theophylline as primary treatment for chronic mild or moderate persistent asthma. J Allergy Clin Immunol 1998;101:14-23.
22. Agertoft L, Pedersen S. Effect of long-term treatment with inhaled budesonide on adult height in children with asthma. N Engl J Med 2000;343:1064-1069.
23. National Asthma Education Program (NAEP). Report of the Working Group on Asthma and Pregnancy: Management of Asthma during Pregnancy. Bethesda, Md: National Heart, Lung, and Blood Institute; National Institutes of Health, 1993. NIH Publication No. 96-141593.
24. American College of Obstetricians and Gynecologists (ACOG) and the American College of Allergy, Asthmaand Immunology (ACAAI). The use of newer asthma and allergy medications during pregnancy. Ann Allergy Asthma Immunol 2000;84:475-480.
25. National Asthma Education and Prevention Program. NAEPP Expert Panel Report. Managing Asthma During Pregnancy: Recommendations for Pharmacologic Treatment—Update 2004. Bethesda, Md: National Heart, Lung, and Blood Institute; National Institutes of Health. NIH Publication No. 04-5246. March 2004.
26. Källén B, Rydhstroem H, Äberg A. Congenital malformations after the use of inhaled budesonide in early pregnancy. Obstet Gynecol 1999;93:392-395.
27. Ericson A, Källén B. Use of drugs during pregnancy—unique Swedish registration method that can be improved. Information From the Swedish Medical Products Agency 1999;1:8-11.
28. Pauwels RA, Pedersen S, Busse WW, Tan WC, Chen Y-Z, Ohlsson SV, et al. for the START Investigators Group. Early intervention with budesonide in mild persistent asthma. Lancet 2003;361:1071-1076.
- Every patient with persistent asthma, regardless of disease severity, should use a daily controller medication.
- Consider an inhaled corticosteroid (ICS) first when choosing controller medications for long-term treatment of mild, moderate, and severe persistent asthma in adults and children. Leukotriene modifiers, cromolyn, and nedocromil may be considered as alternative, not preferred, controller medications for patients with persistent asthma.
- Long-acting β2-adrenergic agonists should not be used as monotherapy.
- Long-term use of ICSs within labeled doses is safe for children in terms of growth, bone mineral density, and adrenal function; nonetheless, asthma should be monitored and ICS therapy stepped down to the lowest effective dose.
- Low-to medium-dose ICSs are not associated with the development of cataracts or glaucoma in children, but high cumulative lifetime doses may slightly increase the prevalence of cataracts in adults and elderly patients.
- ICSs are recommended for use in pregnant women with asthma; budesonide is the only ICS rated Pregnancy Category B.
Consider an adult with the following characteristics. To which disease severity would you assign this patient’s asthma?
- Forced expiratory volume in 1 second (FEV1) or peak expiratory flow (PEF) ≥80%
- PEF variability 20%–30%
- Daytime symptoms less than once a day
- Nighttime symptoms more than 1 night a week.
This patient is said to have moderate persistent asthma based on nighttime symptoms. An accurate classification of a patient’s asthma is the foundation for selecting an appropriate treatment strategy.
In 2002 the National Asthma Education and Prevention Program (NAEPP) updated select topics1from its 1997 Guidelines for the Diagnosis and Management of Asthma.2 These evidence-based revisions to the stepwise approach to asthma management were made following a systematic review of the literature (see Search function).
A comprehensive search of Medline and EMBASE databases was performed to identify controlled clinical studies relevant to each topic that were published (in English or foreign languages with English abstracts) from 1980 through August 2000. The search included studies published before 1980 if referenced in the post-1980 literature. Studies that did not include control groups were excluded, except for those reporting adverse effects of ICSs. Studies that met the study selection criteria established for each topic were included in a systematic review of the evidence. An expert panel reviewed the evidence, along with additional literature published since August 2000, and reached a consensus on whether the evidence supported 1997 guideline recommendations or indicated a need for revision. Writing committees were then assigned to developed position statements for each topic. The level of evidence for included studies was rated based on the system of Jadad and colleagues,3 where A = randomized controlled trials, rich body of data; B = randomized controlled trials, limited data; C = nonrandomized trials and observational studies; D = panel consensus judgment.
This article reviews the 2002 NAEPP recommendations for the use of controller medications for asthma, including:
- Relative effectiveness of inhaled corticosteroids (ICSs) versus other controller medications
- Safety of long-term ICS use in children
- Potential benefits of early ICS treatment.
We emphasize mild and moderate persistent asthma because the recommended treatments for these levels of severity have been most affected by the recent guideline changes. We also discuss a recent change by the US Food and Drug Administration (FDA) in its pregnancy category rating for an ICS.
2002 Stepwise approach to asthma management
New criteria for classifying asthma severity
The NAEPP classifies asthma severity according to symptoms and lung function in adults and children older than 5 years, and symptoms in children 5 years and younger.1 Persistent asthma is classified as mild, moderate, or severe according to the feature of greatest severity.
Asthma severity should be assigned according to symptoms before treatment.1 Because it is difficult to predict which infants and young children who wheeze with acute viral upper respiratory infection will go on to develop persistent asthma, new criteria have been detailed to help distinguish these children from those with transient wheeze (Table 1).1,4
TABLE 1
Criteria for children with intermittent wheeze
Infants and young children meeting these criteria should receive controller therapy for asthma:
|
AND presence of risk factors for development of persistent asthma:
|
Choosing pharmacologic treatment according to asthma classification
Quick-relief medications, which include the short-acting β2-agonists (SABAs), are taken as needed to promptly reverse acute airflow obstruction and relieve accompanying symptoms.2
Asthma controller medications (ie, ICSs, cromolyn sodium, long-acting β2-adrenergic-agonists [LABAs], leukotriene modifiers, nedocromil, and theophylline) are used daily to achieve and maintain long-term control of persistent asthma. All patients with persistent asthma, regardless of disease severity, should use a daily controller. Criteria for determining asthma severity and updated recommendations for the use of controller treatment in mild and moderate persistent asthma are presented in the Figure.3,5 Levels of evidence justifying NAEPP treatment recommendations are shown in Table 2.
For use in children. Asthma controller medications approved for use in children younger than 5 years include the fluticasone dry-powder inhalers (Flovent, Rotadisk, and Flovent Diskus), which are approved for children as young as 4 years (Flovent Diskus is not yet commercially available), and nebulized budesonide inhalation suspension (Pulmicort Respules), which is approved for children as young as 12 months.
The LABAs formoterol (Foradil) and salmeterol (Serevent Diskus) are approved for children as young as 5 and 4 years, respectively. Cromolyn sodium nebulizer solution is approved for children as young as 2 years, and theophylline is available for use at any age.
Based on safety and extrapolation of efficacy data in older patients, the oral granule formulation of the leukotriene receptor antagonist (LTRA) montelukast (Singulair) is approved for children as young as 1 year, and the chewable tablets are approved for children 2 to 5 years of age. Zafirlukast (Accolate) is approved for use in children 5 years and older.
New recommendations for mild persistent asthma. Recommendations for the treatment of mild and moderate persistent asthma have changed considerably from the 1997 guidelines. ICSs are now the preferred controller medications, based on greater efficacy. The updated guidelines no longer recommend an initial trial of cromolyn or nedocromil for the treatment of mild persistent asthma; these agents, along with the leukotriene modifiers and slow-release theophylline, are now considered alternatives to low-dose ICSs for adults and children older than 5 years with mild persistent disease (Figure).
According to the NAEPP update, daily low-dose ICS treatment also is preferred for the control of mild persistent asthma in preschool children. As in older children, cromolyn and nedocromil are no longer considered appropriate initial treatments for infants and children 5 years and younger. Cromolyn is considered an alternative controller, whereas nedocromil is no longer recommended for use.
New recommendations for moderate persistent asthma. For adults and children older than 5 years with moderate persistent asthma, revision to the guidelines involved recommendation of a low- to medium-dose ICS plus a LABA as the preferred controller treatment (Figure). Comparative low, medium, and high daily doses for ICSs are shown in Table 3 .1
For preschool children, preferred controller treatments for moderate persistent asthma include low-dose ICSs plus a LABA, or increasing ICSs within the medium-dose range (Figure). Recommendations for the use of LABAs as add-on therapy in this age group are based on extrapolation of data from older patients, since therapy with an ICS/LABA combination has not been adequately studied in children younger than 5 years. Four studies included in the NAEPP evaluation showed clear benefit of medium-dose ICSs in this age group, supporting the use of medium-dose ICSs as a preferred option.6-9 LABAs are not recommended for use without an ICS, and the only ICS/LABA combination product currently available has been FDA approved only for patients aged 12 years and older.
TABLE 2
Levels of evidence for NAEPP assessments*
| Medication | NAEPP assessment | SOR* |
|---|---|---|
| ICS | Preferred treatment for children of all ages with persistent asthma | A (A) |
| SABA | ICSs improve asthma control compared with as-needed SABAs | A (A) |
| Cromolyn/nedocromil | For use as alternative, not preferred, treatment of mild persistent asthma in children of all ages (cromolyn) or children >5 years of age (nedocromil) | A (A) |
| LABA | For use with ICSs as the preferred combination treatment for moderate and severe persistent asthma in children >5 years of age | A (A) |
| For use as a preferred option for combination treatment in children 5 years of age | B (B) | |
| Leukotriene modifier | For use as alternative, not preferred, treatment of mild persistent asthma and as ICS adjunct in moderate persistent asthma | B (B) |
| Theophylline | For use as an alternative ICS add-on in moderate or severe persistent asthma if serum concentrations are monitored | D (D) |
| Not considered an alternative controller for young children with mild persistent asthma due to potential adverse effects in infants with frequent febrile illnesses | ||
| *Highest level of evidence available is reported. Strengths of recommendation are based on the method of Jadad et al.3 Strength of evidence based on the Oxford Center for Evidence-Based Medicine5 is in parentheses. SOR, strength of recommendation; NAEPP, National Asthma Education and Prevention Program; ICS, inhaled corticosteroid; SABA, short-acting β2-adrenergic agonist; LABA, long-acting β2-adrenergic agonist. | ||
TABLE 3
Estimated comparative daily doses for inhaled corticosteroids*
| Drug | Low daily dose | Medium daily dose | High daily dose | |||
|---|---|---|---|---|---|---|
| Adult | Child† | Adult | Child† | Adult | Child† | |
| Beclomethasone CFC 42 or 84 μg/puff | 168–504 μg | 84–336 μg | 504–840 μg | 336–672 μg | >840 μg | >672 μg |
| Beclomethasone HFA 40 or 80 μg/puff | 80–240 μg | 80–160 μg | 240–480 μg | 160–320 μg | >480 μg | >320 μg |
| Budesonide DPI 200 μg/inhalation | 200–600 μg | 200–400 μg | 600–1200 μg | 400–800 μg | >1200 μg | >800 μg |
| Budesonide inhalation suspension for nebulization (child dose) | 0.5mg | 1.0 mg | 2.0 mg | |||
| Fluticasone MDI 44, 110, or 220 μg/puff | 88–264 μg | 88–176 μg | 264–660 μg | 176–440 μg | >660 μg | >440 μg |
| Fluticasone DPI 50, 100, or 250 μg/inhalation | 100–300 μg | 100–200 μg | 300–600 μg | 200–400 μg | >600 μg | >400 μg |
| Triamcinolone acetonide 100 μg/puff | 400–1000 μg | 400–800 μg | 1000–2000 μg | 800–1200 μg | >2000 μg | >1200 μg |
| *The most important determinant of appropriate dosing is the clinician’s judgment of the patient’s response to therapy. This updated comparative dose chart is based on review of recently published clinical trials involving more than 5000 patients and published reviews. Some doses may be outside package labeling, especially in the high-dose range. | ||||||
| †Children 12 years of age. | ||||||
| CFC, chlorofluorocarbon; HFA, hydrofluoroalkane; DPI, dry-powder inhaler; MDI, metered-dose inhaler. | ||||||
FIGURE
Updated National Asthma Education and Prevention Program recommendations for long-term controller treatment in mild and moderate persistent asthma
Topics in the management of asthma in children
Recognizing the need for continual appraisal of the benefits and risks of asthma medications in children, the NAEPP Expert Panel considered new studies comparing the effectiveness of ICS monotherapy with that of as-needed SABAs and other controllers used as monotherapy in children with mild or moderate persistent asthma. In addition, the safety of long-term ICS use in children was evaluated based on vertical growth, bone mineral density, ocular toxicity, and adrenal suppression.
Effectiveness of ICSs compared with other asthma medications
Short-acting β2-adrenergic agonists. Eight studies met the eligibility criteria for evaluating the effectiveness of ICSs versus as-needed SABAs.6,10-16 Six studies (4 involving budesonide) in children 5 years and older showed that ICSs improve lung function and symptoms and reduce the need for emergency intervention compared with as-needed SABAs.1 Among all studies included in the NAEPP update, the Childhood Asthma Management Program (CAMP) Research Group Study,9 a placebo-controlled study of inhaled budesonide and nedocromil, contributed the most evidence. Studies with children 5 years and younger are limited to 2 small studies enrolling a total of 69 children.6,15 Consistent with studies of older children, these studies indicate that ICSs improve asthma control compared with as-needed SABAs.1
Cromolyn and nedocromil. Despite well-established safety profiles, cromolyn and nedocromil are no longer recommended as first-line therapy for children, even those with mild disease. New recommendations reflect the greater effectiveness of inhaled budesonide compared with nedocromil demonstrated in the CAMP study,10 and the lack of apparent benefit of cromolyn as maintenance treatment in childhood asthma reported by Tasche and colleagues in a systematic review of the literature.17
In the CAMP study, children 5 to 12 years of age receiving inhaled budesonide showed greater reductions in symptoms and albuterol use, lower rates of hospitalization and urgent care visits, and less need for additional asthma therapy and oral prednisone compared with placebo over 4 to 6 years of treatment.10 The marginal effectiveness of nedocromil demonstrated in the CAMP study mirrored that of cromolyn reported in the review of 24 randomized placebo-controlled studies by Tasche and colleagues.1,17
For children 5 years and younger, the NAEPP Expert Panel took into account 1 randomized placebo-controlled study conducted with children 2 to 5 years of age; it showed improvements in lung function, symptoms, and bronchial hyperre-activity with inhaled budesonide.9 Support for the new NAEPP recommendations preferring ICSs for preschool children is found in a more recent open-label study18 that showed greater symptom improvement and significantly lower rates of asthma exacerbations, urgent care visits, and oral prednisone use with budesonide inhalation suspension, compared with cromolyn sodium nebulizer solution (Intal Nebulizer Solution) in children 2 to 6 years of age with persistent asthma.
Leukotriene modifiers. The LTRAs zafir-lukast and montelukast are approved for use in children. According to the NAEPP Expert Panel, studies have shown only modest improvements in lung function and other asthma control outcomes with LTRA monotherapy in children as young as 6 and 2 years, respectively.1 Because studies comparing ICSs with LTRAs in children are lacking, findings of greater overall efficacy of ICSs in adults with persistent asthma have been extrapolated for use with children; clear superiority of ICSs versus LTRAs in most outcomes has resulted in the recommendation for ICSs as the preferred treatment for mild persistent asthma in children.
Long-acting β2-adrenergic agonists. There is no role for LABAs as monotherapy in asthma. No studies have compared the effectiveness of ICS versus LABA monotherapy in children younger than 5 years, and studies in older children have shown greater effectiveness of inhaled beclomethasone versus salmeterol.14,19 In the study by Verberne and colleagues, salmeterol monotherapy was associated with deterioration in FEV1.19 In a more recent study that included patients as young as 16 years, a switch from ICS to LABA treatment was associated with a significant increase in treatment failures and exacerbations.20
Theophylline. Only 1 study has compared outcomes with low-dose ICSs versus theophylline in adults and children.21 Although limited, the data support greater effectiveness of ICSs based on symptoms, bronchial hyperresponsiveness, and the need for β2-adrenergic agonists and oral corticosteroids.1
Safety of long-term ICS use in children
Systemic corticosteroids have the potential to suppress growth over the long term.2 Short-term growth studies with ICSs show an average reduction in growth velocity of 1 cm per year during the first year of treatment, but the CAMP study showed that initial reductions in growth velocity with inhaled budesonide were not maintained over a 4- to 6-year treatment period.1,10
Although catch-up growth was not observed in the CAMP study, Agertoft and Pedersen reported no effect of long-term treatment with inhaled budesonide (mean 9.2 years) on final adult height.22 Based on these long-term prospective studies of budesonide, showing only a transient reduction in growth velocity and attainment of expected final adult height, and retrospective studies including inhaled beclomethasone, the Expert Panel concluded that the ICS class is safe regarding growth effects.
According to the NAEPP Expert Panel, clinical study data for children monitored for up to 6 years strongly suggest that ICSs are safe when used at recommended doses (strength of recommendation: A).1 The panel could not rule out a potential cumulative effect of ICS use on some conditions, (eg, osteoporosis, cataracts, glaucoma) in adulthood, as sufficient long-term data are not available.
The panel did conclude that low- to medium-dose ICSs (Table 3) appear to have no serious adverse effects on bone mineral density in children.
Likewise, low- to medium-dose ICS use was not associated with the development of cataracts or glaucoma in children, although the potential for high cumulative lifetime doses of ICSs to slightly increase the prevalence of cataracts in adults and elderly patients was noted.
Strong evidence also indicates that ICS effects on adrenal function are usually clinically insignificant at low to medium doses; however, certain individuals may be at higher risk for hypothalam-ic pituitary adrenal axis effects while using conventional ICS doses.1
Although ICSs are safe when used within labeled dosing, it is still preferable to maintain doses at the lowest effective dose. In general, treatment should be reviewed every 1 to 6 months and doses reduced in a stepwise fashion when possible.1 For children showing a favorable response to treatment, a step down in dose should be considered, but not more frequently than every 3 months. If children show no clear response to treatment within 4 to 6 weeks, consider an alternative treatment or diagnosis.1
Safety of long-term ICS use in pregnant women
Uncontrolled asthma during pregnancy is associated with an increased risk of perinatal complications. 23 Since the consequences of not using asthma controllers during pregnancy can be worse than those with using them, daily controller treatment is recommended for all pregnant women with persistent asthma. 23
The American College of Obstetricians and Gynecologists and the American College of Allergy, Asthma and Immunology previously recommended cromolyn as the treatment of choice for pregnant women with mild persistent asthma. ICSs were recommended for patients whose asthma was inadequately controlled with cromolyn. 24 Beclomethasone and budesonide were the ICSs of choice for pregnant women and those who might become pregnant, with a preference for budesonide when high-dose therapy was indicated.24
These recommendations predate the 2002 NAEPP recommendations for ICSs as preferred therapy in mild persistent asthma and the 2004 NAEPP recommendations for ICSs as the first-choice controller therapy for mild persistent asthma during pregnancy. 25 Among ICSs, one (inhaled budesonide) has an FDA Pregnancy Category B rating based on studies showing no risk in pregnant women. 26,27 All other ICSs are rated Pregnancy Category C.
Based on current evidence, it seems reasonable to consider whether budesonide should now be the preferred therapy for mild persistent asthma during pregnancy.
Effects of early treatment on asthma progression
The potential for early ICS intervention to prevent progression of mild or moderate persistent asthma was evaluated solely with data from children enrolled in the CAMP study. 10 The NAEPP Expert Panel concluded that CAMP study data do not support a progressive decline in lung function in children aged 5 to 12 years with mild or moderate persistent asthma, but do suggest that lung function decline is influenced by age of asthma onset.
According to the panel, CAMP data suggest that most deficits in lung function growth due to childhood asthma occur during the first 3 years of life. Preliminary results of the recent START study (Inhaled Steroid Treatment As Regular Therapy in Early Asthma), 28 conducted with 7165 corticosteroidnaïve patients 5 to 66 years of age with recent onset mild persistent asthma, did show a decline in lung function in patients with mild persistent disease.
Although improvements in prebronchodilator and postbronchodilator FEV1 were significant after 3 years of treatment with inhaled budes-onide, differences from placebo in both outcomes were greatest after the first year. When patients with mild persistent disease inhaled budesonide once daily in addition to normal treatment within 2 years of asthma onset,28 they enjoyed considerable protection from severe and life-threatening asthma exacerbations and overall greater asthma control.
- Budesonide • Pulmicort
- Rhinocort Cromolyn • Intal
- Fluticasone • Flovent
- Formoterol • Foradil
- Montelukast • Singulair
- Nedocromil • Tilade
- Salmeterol • Servent
- Triamcinolone acetonide • Azmacort
- Zafirlukast • Accolate
Corresponding author
Gregory J. Redding, MD, Children’s Hospital and Regional Medical Center, 4800 Sand Point Way, NE, Seattle, WA 98105-0371. E-mail: [email protected].
- Every patient with persistent asthma, regardless of disease severity, should use a daily controller medication.
- Consider an inhaled corticosteroid (ICS) first when choosing controller medications for long-term treatment of mild, moderate, and severe persistent asthma in adults and children. Leukotriene modifiers, cromolyn, and nedocromil may be considered as alternative, not preferred, controller medications for patients with persistent asthma.
- Long-acting β2-adrenergic agonists should not be used as monotherapy.
- Long-term use of ICSs within labeled doses is safe for children in terms of growth, bone mineral density, and adrenal function; nonetheless, asthma should be monitored and ICS therapy stepped down to the lowest effective dose.
- Low-to medium-dose ICSs are not associated with the development of cataracts or glaucoma in children, but high cumulative lifetime doses may slightly increase the prevalence of cataracts in adults and elderly patients.
- ICSs are recommended for use in pregnant women with asthma; budesonide is the only ICS rated Pregnancy Category B.
Consider an adult with the following characteristics. To which disease severity would you assign this patient’s asthma?
- Forced expiratory volume in 1 second (FEV1) or peak expiratory flow (PEF) ≥80%
- PEF variability 20%–30%
- Daytime symptoms less than once a day
- Nighttime symptoms more than 1 night a week.
This patient is said to have moderate persistent asthma based on nighttime symptoms. An accurate classification of a patient’s asthma is the foundation for selecting an appropriate treatment strategy.
In 2002 the National Asthma Education and Prevention Program (NAEPP) updated select topics1from its 1997 Guidelines for the Diagnosis and Management of Asthma.2 These evidence-based revisions to the stepwise approach to asthma management were made following a systematic review of the literature (see Search function).
A comprehensive search of Medline and EMBASE databases was performed to identify controlled clinical studies relevant to each topic that were published (in English or foreign languages with English abstracts) from 1980 through August 2000. The search included studies published before 1980 if referenced in the post-1980 literature. Studies that did not include control groups were excluded, except for those reporting adverse effects of ICSs. Studies that met the study selection criteria established for each topic were included in a systematic review of the evidence. An expert panel reviewed the evidence, along with additional literature published since August 2000, and reached a consensus on whether the evidence supported 1997 guideline recommendations or indicated a need for revision. Writing committees were then assigned to developed position statements for each topic. The level of evidence for included studies was rated based on the system of Jadad and colleagues,3 where A = randomized controlled trials, rich body of data; B = randomized controlled trials, limited data; C = nonrandomized trials and observational studies; D = panel consensus judgment.
This article reviews the 2002 NAEPP recommendations for the use of controller medications for asthma, including:
- Relative effectiveness of inhaled corticosteroids (ICSs) versus other controller medications
- Safety of long-term ICS use in children
- Potential benefits of early ICS treatment.
We emphasize mild and moderate persistent asthma because the recommended treatments for these levels of severity have been most affected by the recent guideline changes. We also discuss a recent change by the US Food and Drug Administration (FDA) in its pregnancy category rating for an ICS.
2002 Stepwise approach to asthma management
New criteria for classifying asthma severity
The NAEPP classifies asthma severity according to symptoms and lung function in adults and children older than 5 years, and symptoms in children 5 years and younger.1 Persistent asthma is classified as mild, moderate, or severe according to the feature of greatest severity.
Asthma severity should be assigned according to symptoms before treatment.1 Because it is difficult to predict which infants and young children who wheeze with acute viral upper respiratory infection will go on to develop persistent asthma, new criteria have been detailed to help distinguish these children from those with transient wheeze (Table 1).1,4
TABLE 1
Criteria for children with intermittent wheeze
Infants and young children meeting these criteria should receive controller therapy for asthma:
|
AND presence of risk factors for development of persistent asthma:
|
Choosing pharmacologic treatment according to asthma classification
Quick-relief medications, which include the short-acting β2-agonists (SABAs), are taken as needed to promptly reverse acute airflow obstruction and relieve accompanying symptoms.2
Asthma controller medications (ie, ICSs, cromolyn sodium, long-acting β2-adrenergic-agonists [LABAs], leukotriene modifiers, nedocromil, and theophylline) are used daily to achieve and maintain long-term control of persistent asthma. All patients with persistent asthma, regardless of disease severity, should use a daily controller. Criteria for determining asthma severity and updated recommendations for the use of controller treatment in mild and moderate persistent asthma are presented in the Figure.3,5 Levels of evidence justifying NAEPP treatment recommendations are shown in Table 2.
For use in children. Asthma controller medications approved for use in children younger than 5 years include the fluticasone dry-powder inhalers (Flovent, Rotadisk, and Flovent Diskus), which are approved for children as young as 4 years (Flovent Diskus is not yet commercially available), and nebulized budesonide inhalation suspension (Pulmicort Respules), which is approved for children as young as 12 months.
The LABAs formoterol (Foradil) and salmeterol (Serevent Diskus) are approved for children as young as 5 and 4 years, respectively. Cromolyn sodium nebulizer solution is approved for children as young as 2 years, and theophylline is available for use at any age.
Based on safety and extrapolation of efficacy data in older patients, the oral granule formulation of the leukotriene receptor antagonist (LTRA) montelukast (Singulair) is approved for children as young as 1 year, and the chewable tablets are approved for children 2 to 5 years of age. Zafirlukast (Accolate) is approved for use in children 5 years and older.
New recommendations for mild persistent asthma. Recommendations for the treatment of mild and moderate persistent asthma have changed considerably from the 1997 guidelines. ICSs are now the preferred controller medications, based on greater efficacy. The updated guidelines no longer recommend an initial trial of cromolyn or nedocromil for the treatment of mild persistent asthma; these agents, along with the leukotriene modifiers and slow-release theophylline, are now considered alternatives to low-dose ICSs for adults and children older than 5 years with mild persistent disease (Figure).
According to the NAEPP update, daily low-dose ICS treatment also is preferred for the control of mild persistent asthma in preschool children. As in older children, cromolyn and nedocromil are no longer considered appropriate initial treatments for infants and children 5 years and younger. Cromolyn is considered an alternative controller, whereas nedocromil is no longer recommended for use.
New recommendations for moderate persistent asthma. For adults and children older than 5 years with moderate persistent asthma, revision to the guidelines involved recommendation of a low- to medium-dose ICS plus a LABA as the preferred controller treatment (Figure). Comparative low, medium, and high daily doses for ICSs are shown in Table 3 .1
For preschool children, preferred controller treatments for moderate persistent asthma include low-dose ICSs plus a LABA, or increasing ICSs within the medium-dose range (Figure). Recommendations for the use of LABAs as add-on therapy in this age group are based on extrapolation of data from older patients, since therapy with an ICS/LABA combination has not been adequately studied in children younger than 5 years. Four studies included in the NAEPP evaluation showed clear benefit of medium-dose ICSs in this age group, supporting the use of medium-dose ICSs as a preferred option.6-9 LABAs are not recommended for use without an ICS, and the only ICS/LABA combination product currently available has been FDA approved only for patients aged 12 years and older.
TABLE 2
Levels of evidence for NAEPP assessments*
| Medication | NAEPP assessment | SOR* |
|---|---|---|
| ICS | Preferred treatment for children of all ages with persistent asthma | A (A) |
| SABA | ICSs improve asthma control compared with as-needed SABAs | A (A) |
| Cromolyn/nedocromil | For use as alternative, not preferred, treatment of mild persistent asthma in children of all ages (cromolyn) or children >5 years of age (nedocromil) | A (A) |
| LABA | For use with ICSs as the preferred combination treatment for moderate and severe persistent asthma in children >5 years of age | A (A) |
| For use as a preferred option for combination treatment in children 5 years of age | B (B) | |
| Leukotriene modifier | For use as alternative, not preferred, treatment of mild persistent asthma and as ICS adjunct in moderate persistent asthma | B (B) |
| Theophylline | For use as an alternative ICS add-on in moderate or severe persistent asthma if serum concentrations are monitored | D (D) |
| Not considered an alternative controller for young children with mild persistent asthma due to potential adverse effects in infants with frequent febrile illnesses | ||
| *Highest level of evidence available is reported. Strengths of recommendation are based on the method of Jadad et al.3 Strength of evidence based on the Oxford Center for Evidence-Based Medicine5 is in parentheses. SOR, strength of recommendation; NAEPP, National Asthma Education and Prevention Program; ICS, inhaled corticosteroid; SABA, short-acting β2-adrenergic agonist; LABA, long-acting β2-adrenergic agonist. | ||
TABLE 3
Estimated comparative daily doses for inhaled corticosteroids*
| Drug | Low daily dose | Medium daily dose | High daily dose | |||
|---|---|---|---|---|---|---|
| Adult | Child† | Adult | Child† | Adult | Child† | |
| Beclomethasone CFC 42 or 84 μg/puff | 168–504 μg | 84–336 μg | 504–840 μg | 336–672 μg | >840 μg | >672 μg |
| Beclomethasone HFA 40 or 80 μg/puff | 80–240 μg | 80–160 μg | 240–480 μg | 160–320 μg | >480 μg | >320 μg |
| Budesonide DPI 200 μg/inhalation | 200–600 μg | 200–400 μg | 600–1200 μg | 400–800 μg | >1200 μg | >800 μg |
| Budesonide inhalation suspension for nebulization (child dose) | 0.5mg | 1.0 mg | 2.0 mg | |||
| Fluticasone MDI 44, 110, or 220 μg/puff | 88–264 μg | 88–176 μg | 264–660 μg | 176–440 μg | >660 μg | >440 μg |
| Fluticasone DPI 50, 100, or 250 μg/inhalation | 100–300 μg | 100–200 μg | 300–600 μg | 200–400 μg | >600 μg | >400 μg |
| Triamcinolone acetonide 100 μg/puff | 400–1000 μg | 400–800 μg | 1000–2000 μg | 800–1200 μg | >2000 μg | >1200 μg |
| *The most important determinant of appropriate dosing is the clinician’s judgment of the patient’s response to therapy. This updated comparative dose chart is based on review of recently published clinical trials involving more than 5000 patients and published reviews. Some doses may be outside package labeling, especially in the high-dose range. | ||||||
| †Children 12 years of age. | ||||||
| CFC, chlorofluorocarbon; HFA, hydrofluoroalkane; DPI, dry-powder inhaler; MDI, metered-dose inhaler. | ||||||
FIGURE
Updated National Asthma Education and Prevention Program recommendations for long-term controller treatment in mild and moderate persistent asthma
Topics in the management of asthma in children
Recognizing the need for continual appraisal of the benefits and risks of asthma medications in children, the NAEPP Expert Panel considered new studies comparing the effectiveness of ICS monotherapy with that of as-needed SABAs and other controllers used as monotherapy in children with mild or moderate persistent asthma. In addition, the safety of long-term ICS use in children was evaluated based on vertical growth, bone mineral density, ocular toxicity, and adrenal suppression.
Effectiveness of ICSs compared with other asthma medications
Short-acting β2-adrenergic agonists. Eight studies met the eligibility criteria for evaluating the effectiveness of ICSs versus as-needed SABAs.6,10-16 Six studies (4 involving budesonide) in children 5 years and older showed that ICSs improve lung function and symptoms and reduce the need for emergency intervention compared with as-needed SABAs.1 Among all studies included in the NAEPP update, the Childhood Asthma Management Program (CAMP) Research Group Study,9 a placebo-controlled study of inhaled budesonide and nedocromil, contributed the most evidence. Studies with children 5 years and younger are limited to 2 small studies enrolling a total of 69 children.6,15 Consistent with studies of older children, these studies indicate that ICSs improve asthma control compared with as-needed SABAs.1
Cromolyn and nedocromil. Despite well-established safety profiles, cromolyn and nedocromil are no longer recommended as first-line therapy for children, even those with mild disease. New recommendations reflect the greater effectiveness of inhaled budesonide compared with nedocromil demonstrated in the CAMP study,10 and the lack of apparent benefit of cromolyn as maintenance treatment in childhood asthma reported by Tasche and colleagues in a systematic review of the literature.17
In the CAMP study, children 5 to 12 years of age receiving inhaled budesonide showed greater reductions in symptoms and albuterol use, lower rates of hospitalization and urgent care visits, and less need for additional asthma therapy and oral prednisone compared with placebo over 4 to 6 years of treatment.10 The marginal effectiveness of nedocromil demonstrated in the CAMP study mirrored that of cromolyn reported in the review of 24 randomized placebo-controlled studies by Tasche and colleagues.1,17
For children 5 years and younger, the NAEPP Expert Panel took into account 1 randomized placebo-controlled study conducted with children 2 to 5 years of age; it showed improvements in lung function, symptoms, and bronchial hyperre-activity with inhaled budesonide.9 Support for the new NAEPP recommendations preferring ICSs for preschool children is found in a more recent open-label study18 that showed greater symptom improvement and significantly lower rates of asthma exacerbations, urgent care visits, and oral prednisone use with budesonide inhalation suspension, compared with cromolyn sodium nebulizer solution (Intal Nebulizer Solution) in children 2 to 6 years of age with persistent asthma.
Leukotriene modifiers. The LTRAs zafir-lukast and montelukast are approved for use in children. According to the NAEPP Expert Panel, studies have shown only modest improvements in lung function and other asthma control outcomes with LTRA monotherapy in children as young as 6 and 2 years, respectively.1 Because studies comparing ICSs with LTRAs in children are lacking, findings of greater overall efficacy of ICSs in adults with persistent asthma have been extrapolated for use with children; clear superiority of ICSs versus LTRAs in most outcomes has resulted in the recommendation for ICSs as the preferred treatment for mild persistent asthma in children.
Long-acting β2-adrenergic agonists. There is no role for LABAs as monotherapy in asthma. No studies have compared the effectiveness of ICS versus LABA monotherapy in children younger than 5 years, and studies in older children have shown greater effectiveness of inhaled beclomethasone versus salmeterol.14,19 In the study by Verberne and colleagues, salmeterol monotherapy was associated with deterioration in FEV1.19 In a more recent study that included patients as young as 16 years, a switch from ICS to LABA treatment was associated with a significant increase in treatment failures and exacerbations.20
Theophylline. Only 1 study has compared outcomes with low-dose ICSs versus theophylline in adults and children.21 Although limited, the data support greater effectiveness of ICSs based on symptoms, bronchial hyperresponsiveness, and the need for β2-adrenergic agonists and oral corticosteroids.1
Safety of long-term ICS use in children
Systemic corticosteroids have the potential to suppress growth over the long term.2 Short-term growth studies with ICSs show an average reduction in growth velocity of 1 cm per year during the first year of treatment, but the CAMP study showed that initial reductions in growth velocity with inhaled budesonide were not maintained over a 4- to 6-year treatment period.1,10
Although catch-up growth was not observed in the CAMP study, Agertoft and Pedersen reported no effect of long-term treatment with inhaled budesonide (mean 9.2 years) on final adult height.22 Based on these long-term prospective studies of budesonide, showing only a transient reduction in growth velocity and attainment of expected final adult height, and retrospective studies including inhaled beclomethasone, the Expert Panel concluded that the ICS class is safe regarding growth effects.
According to the NAEPP Expert Panel, clinical study data for children monitored for up to 6 years strongly suggest that ICSs are safe when used at recommended doses (strength of recommendation: A).1 The panel could not rule out a potential cumulative effect of ICS use on some conditions, (eg, osteoporosis, cataracts, glaucoma) in adulthood, as sufficient long-term data are not available.
The panel did conclude that low- to medium-dose ICSs (Table 3) appear to have no serious adverse effects on bone mineral density in children.
Likewise, low- to medium-dose ICS use was not associated with the development of cataracts or glaucoma in children, although the potential for high cumulative lifetime doses of ICSs to slightly increase the prevalence of cataracts in adults and elderly patients was noted.
Strong evidence also indicates that ICS effects on adrenal function are usually clinically insignificant at low to medium doses; however, certain individuals may be at higher risk for hypothalam-ic pituitary adrenal axis effects while using conventional ICS doses.1
Although ICSs are safe when used within labeled dosing, it is still preferable to maintain doses at the lowest effective dose. In general, treatment should be reviewed every 1 to 6 months and doses reduced in a stepwise fashion when possible.1 For children showing a favorable response to treatment, a step down in dose should be considered, but not more frequently than every 3 months. If children show no clear response to treatment within 4 to 6 weeks, consider an alternative treatment or diagnosis.1
Safety of long-term ICS use in pregnant women
Uncontrolled asthma during pregnancy is associated with an increased risk of perinatal complications. 23 Since the consequences of not using asthma controllers during pregnancy can be worse than those with using them, daily controller treatment is recommended for all pregnant women with persistent asthma. 23
The American College of Obstetricians and Gynecologists and the American College of Allergy, Asthma and Immunology previously recommended cromolyn as the treatment of choice for pregnant women with mild persistent asthma. ICSs were recommended for patients whose asthma was inadequately controlled with cromolyn. 24 Beclomethasone and budesonide were the ICSs of choice for pregnant women and those who might become pregnant, with a preference for budesonide when high-dose therapy was indicated.24
These recommendations predate the 2002 NAEPP recommendations for ICSs as preferred therapy in mild persistent asthma and the 2004 NAEPP recommendations for ICSs as the first-choice controller therapy for mild persistent asthma during pregnancy. 25 Among ICSs, one (inhaled budesonide) has an FDA Pregnancy Category B rating based on studies showing no risk in pregnant women. 26,27 All other ICSs are rated Pregnancy Category C.
Based on current evidence, it seems reasonable to consider whether budesonide should now be the preferred therapy for mild persistent asthma during pregnancy.
Effects of early treatment on asthma progression
The potential for early ICS intervention to prevent progression of mild or moderate persistent asthma was evaluated solely with data from children enrolled in the CAMP study. 10 The NAEPP Expert Panel concluded that CAMP study data do not support a progressive decline in lung function in children aged 5 to 12 years with mild or moderate persistent asthma, but do suggest that lung function decline is influenced by age of asthma onset.
According to the panel, CAMP data suggest that most deficits in lung function growth due to childhood asthma occur during the first 3 years of life. Preliminary results of the recent START study (Inhaled Steroid Treatment As Regular Therapy in Early Asthma), 28 conducted with 7165 corticosteroidnaïve patients 5 to 66 years of age with recent onset mild persistent asthma, did show a decline in lung function in patients with mild persistent disease.
Although improvements in prebronchodilator and postbronchodilator FEV1 were significant after 3 years of treatment with inhaled budes-onide, differences from placebo in both outcomes were greatest after the first year. When patients with mild persistent disease inhaled budesonide once daily in addition to normal treatment within 2 years of asthma onset,28 they enjoyed considerable protection from severe and life-threatening asthma exacerbations and overall greater asthma control.
- Budesonide • Pulmicort
- Rhinocort Cromolyn • Intal
- Fluticasone • Flovent
- Formoterol • Foradil
- Montelukast • Singulair
- Nedocromil • Tilade
- Salmeterol • Servent
- Triamcinolone acetonide • Azmacort
- Zafirlukast • Accolate
Corresponding author
Gregory J. Redding, MD, Children’s Hospital and Regional Medical Center, 4800 Sand Point Way, NE, Seattle, WA 98105-0371. E-mail: [email protected].
1. National Asthma Education and Prevention Program. Expert panel report: guidelines for the diagnosis and management of asthma. Update on selected topics–2002. J Allergy Clin Immunol 2002;110(5 suppl):S141-S219.
2. National Asthma Education and Prevention Program Expert Panel Report 2: Guidelines for the Diagnosis and Management of Asthma. Bethesda, Md: National Heart, Lung, and Blood Institute; National Institutes of Health; 1997. Publication 97;4051.-
3. Jadad AR, Moher M, Browman GP, Booker L, Sigouin C, Fuentes M, et al. Systematic reviews and meta-analyses on treatment of asthma: critical evaluation. BMJ 2000;320:537-540.
4. Castro-Rodríguez JA, Holberg CJ, Wright AL, Martinez FD. A clinical index to define risk of asthma in young children with recurrent wheezing. Am J Respir Crit Care Med 2000;162:1403-1406.
5. Oxford Centre for Evidence-based Medicine Levels of Evidence Available atwww.cebm.net/levels_faq.asp . Accessed January 8, 2004.
6. Connett GJ, Warde C, Wooler E, Lenney W. Use of budes-onide in severe asthmatics aged 1–3 years. Arch Dis Child 1993;69:351-355.
7. de Blic J, Delacourt C, Le Bourgeois M, Mahut B, Ostinelli J, Caswell C, et al. Efficacy of nebulized budesonide in treatment of severe infantile asthma: a double-blind study. J Allergy Clin Immunol 1996;98:14-20.
8. Bisgaard H, Gillies J, Groenewald M, Maden C, . for an International Study Group The effect of inhaled fluticas-one propionate in the treatment of young asthmatic children: a dose comparison study. Am J Respir Crit Care Med 1999;160:126-131.
9. Nielsen KG, Bisgaard H. The effect of inhaled budesonide on symptoms, lung function, and cold air and metha-choline responsiveness in 2- to 5-year–old asthmatic children. Am J Respir Crit Care Med 2000;162:1500-1506.
10. Childhood Asthma Management Program Research Group. Long-term effects of budesonide or nedocromil in children with asthma. N Engl J Med 2000;343:1054-1063.
11. Agertoft L, Pedersen S. Effects of long-term treatment with an inhaled corticosteroid on growth and pulmonary function in asthmatic children. Respir Med 1994;88:373-381.
12. Hoekstra MO, Grol MH, Bouman K, Stijnen T, Koëter GH, Kauffman HF, et al. Fluticasone propionate in children with moderate asthma. Am J Respir Crit Care Med 1996;154:1039-1044.
13. Jónasson G, Carlsen K-H, Blomqvist P. Clinical efficacy of low-dose inhaled budesonide once or twice daily in children with mild asthma not previously treated with steroids. Eur Respir J 1998;12:1099-1104.
14. Simons FER and the Canadian Beclomethasone Dipropionate-Salmeterol Xinafoate Study Group. A comparison of beclomethasone, salmeterol, and placebo in children with asthma. N Engl J Med 1997;337:1659-1665.
15. Storr J, Lenney CA, Lenney W. Nebulized beclomethasone dipropionate in preschool asthma. Arch Dis Child 1986;61:270-273.
16. Van Essen-Zandvliet EE, Hughes MD, Waalkens HJ, Duiverman EJ, Pocock SJ, Kerrebijn KF. and the Dutch Chronic Non-Specific Lung Disease Study Group Effects of 22 months of treatment with inhaled corticosteroids and/or beta-2-agonists on lung function, airway responsiveness, and symptoms in children with asthma. Am Rev Respir Dis 1992;146:547-554.
17. Tasche MJA, Uijen JHJM, Bernsen RMD, de Jongste JC, van der Wouden JC. Inhaled disodium cromoglycate (DSCG) as maintenance therapy in children with asthma: a systematic review. Thorax 2000;55:913-920.
18. Leflein JG, Szefler SJ, Murphy KR, Fitzpatrick S, Cruz-Rivera M, Miller CJ, et al. Nebulized budesonide inhalation suspension compared with cromolyn sodium nebulizer solution for asthma in young children: results of a randomized outcomes trial. Pediatrics 2002;109:866-872.
19. Verberne AAPH, Frost C, Duiverman EJ, Grol MH, Kerrebijn KF. and the Dutch Paediatric Asthma Study Group Addition of salmeterol versus doubling the dose of beclomethasone in children with asthma. Am J Respir Crit Care Med 1998;158:213-219.
20. Lazarus SC, Boushey HA, Fahy JV, Chinchilli VM, Lemanske RF Jr, Sorkness CA, , et al. for the Asthma Clinical Research Network of the National Heart Lung and Blood Institute. Long-acting 2-agonist monotherapy vs continued therapy with inhaled corticosteroids in patients with persistent asthma: a randomized controlled trial. JAMA 2001;285:2583-2593.
21. Reed CE, Offord KP, Nelson HS, Li JT, Tinkelman DG. and the American Academy of Allergy, Asthma and Immunology Beclomethasone Dipropionate-Theophylline Study Group. Aerosol beclomethasone dipropionate spray compared with theophylline as primary treatment for chronic mild or moderate persistent asthma. J Allergy Clin Immunol 1998;101:14-23.
22. Agertoft L, Pedersen S. Effect of long-term treatment with inhaled budesonide on adult height in children with asthma. N Engl J Med 2000;343:1064-1069.
23. National Asthma Education Program (NAEP). Report of the Working Group on Asthma and Pregnancy: Management of Asthma during Pregnancy. Bethesda, Md: National Heart, Lung, and Blood Institute; National Institutes of Health, 1993. NIH Publication No. 96-141593.
24. American College of Obstetricians and Gynecologists (ACOG) and the American College of Allergy, Asthmaand Immunology (ACAAI). The use of newer asthma and allergy medications during pregnancy. Ann Allergy Asthma Immunol 2000;84:475-480.
25. National Asthma Education and Prevention Program. NAEPP Expert Panel Report. Managing Asthma During Pregnancy: Recommendations for Pharmacologic Treatment—Update 2004. Bethesda, Md: National Heart, Lung, and Blood Institute; National Institutes of Health. NIH Publication No. 04-5246. March 2004.
26. Källén B, Rydhstroem H, Äberg A. Congenital malformations after the use of inhaled budesonide in early pregnancy. Obstet Gynecol 1999;93:392-395.
27. Ericson A, Källén B. Use of drugs during pregnancy—unique Swedish registration method that can be improved. Information From the Swedish Medical Products Agency 1999;1:8-11.
28. Pauwels RA, Pedersen S, Busse WW, Tan WC, Chen Y-Z, Ohlsson SV, et al. for the START Investigators Group. Early intervention with budesonide in mild persistent asthma. Lancet 2003;361:1071-1076.
1. National Asthma Education and Prevention Program. Expert panel report: guidelines for the diagnosis and management of asthma. Update on selected topics–2002. J Allergy Clin Immunol 2002;110(5 suppl):S141-S219.
2. National Asthma Education and Prevention Program Expert Panel Report 2: Guidelines for the Diagnosis and Management of Asthma. Bethesda, Md: National Heart, Lung, and Blood Institute; National Institutes of Health; 1997. Publication 97;4051.-
3. Jadad AR, Moher M, Browman GP, Booker L, Sigouin C, Fuentes M, et al. Systematic reviews and meta-analyses on treatment of asthma: critical evaluation. BMJ 2000;320:537-540.
4. Castro-Rodríguez JA, Holberg CJ, Wright AL, Martinez FD. A clinical index to define risk of asthma in young children with recurrent wheezing. Am J Respir Crit Care Med 2000;162:1403-1406.
5. Oxford Centre for Evidence-based Medicine Levels of Evidence Available atwww.cebm.net/levels_faq.asp . Accessed January 8, 2004.
6. Connett GJ, Warde C, Wooler E, Lenney W. Use of budes-onide in severe asthmatics aged 1–3 years. Arch Dis Child 1993;69:351-355.
7. de Blic J, Delacourt C, Le Bourgeois M, Mahut B, Ostinelli J, Caswell C, et al. Efficacy of nebulized budesonide in treatment of severe infantile asthma: a double-blind study. J Allergy Clin Immunol 1996;98:14-20.
8. Bisgaard H, Gillies J, Groenewald M, Maden C, . for an International Study Group The effect of inhaled fluticas-one propionate in the treatment of young asthmatic children: a dose comparison study. Am J Respir Crit Care Med 1999;160:126-131.
9. Nielsen KG, Bisgaard H. The effect of inhaled budesonide on symptoms, lung function, and cold air and metha-choline responsiveness in 2- to 5-year–old asthmatic children. Am J Respir Crit Care Med 2000;162:1500-1506.
10. Childhood Asthma Management Program Research Group. Long-term effects of budesonide or nedocromil in children with asthma. N Engl J Med 2000;343:1054-1063.
11. Agertoft L, Pedersen S. Effects of long-term treatment with an inhaled corticosteroid on growth and pulmonary function in asthmatic children. Respir Med 1994;88:373-381.
12. Hoekstra MO, Grol MH, Bouman K, Stijnen T, Koëter GH, Kauffman HF, et al. Fluticasone propionate in children with moderate asthma. Am J Respir Crit Care Med 1996;154:1039-1044.
13. Jónasson G, Carlsen K-H, Blomqvist P. Clinical efficacy of low-dose inhaled budesonide once or twice daily in children with mild asthma not previously treated with steroids. Eur Respir J 1998;12:1099-1104.
14. Simons FER and the Canadian Beclomethasone Dipropionate-Salmeterol Xinafoate Study Group. A comparison of beclomethasone, salmeterol, and placebo in children with asthma. N Engl J Med 1997;337:1659-1665.
15. Storr J, Lenney CA, Lenney W. Nebulized beclomethasone dipropionate in preschool asthma. Arch Dis Child 1986;61:270-273.
16. Van Essen-Zandvliet EE, Hughes MD, Waalkens HJ, Duiverman EJ, Pocock SJ, Kerrebijn KF. and the Dutch Chronic Non-Specific Lung Disease Study Group Effects of 22 months of treatment with inhaled corticosteroids and/or beta-2-agonists on lung function, airway responsiveness, and symptoms in children with asthma. Am Rev Respir Dis 1992;146:547-554.
17. Tasche MJA, Uijen JHJM, Bernsen RMD, de Jongste JC, van der Wouden JC. Inhaled disodium cromoglycate (DSCG) as maintenance therapy in children with asthma: a systematic review. Thorax 2000;55:913-920.
18. Leflein JG, Szefler SJ, Murphy KR, Fitzpatrick S, Cruz-Rivera M, Miller CJ, et al. Nebulized budesonide inhalation suspension compared with cromolyn sodium nebulizer solution for asthma in young children: results of a randomized outcomes trial. Pediatrics 2002;109:866-872.
19. Verberne AAPH, Frost C, Duiverman EJ, Grol MH, Kerrebijn KF. and the Dutch Paediatric Asthma Study Group Addition of salmeterol versus doubling the dose of beclomethasone in children with asthma. Am J Respir Crit Care Med 1998;158:213-219.
20. Lazarus SC, Boushey HA, Fahy JV, Chinchilli VM, Lemanske RF Jr, Sorkness CA, , et al. for the Asthma Clinical Research Network of the National Heart Lung and Blood Institute. Long-acting 2-agonist monotherapy vs continued therapy with inhaled corticosteroids in patients with persistent asthma: a randomized controlled trial. JAMA 2001;285:2583-2593.
21. Reed CE, Offord KP, Nelson HS, Li JT, Tinkelman DG. and the American Academy of Allergy, Asthma and Immunology Beclomethasone Dipropionate-Theophylline Study Group. Aerosol beclomethasone dipropionate spray compared with theophylline as primary treatment for chronic mild or moderate persistent asthma. J Allergy Clin Immunol 1998;101:14-23.
22. Agertoft L, Pedersen S. Effect of long-term treatment with inhaled budesonide on adult height in children with asthma. N Engl J Med 2000;343:1064-1069.
23. National Asthma Education Program (NAEP). Report of the Working Group on Asthma and Pregnancy: Management of Asthma during Pregnancy. Bethesda, Md: National Heart, Lung, and Blood Institute; National Institutes of Health, 1993. NIH Publication No. 96-141593.
24. American College of Obstetricians and Gynecologists (ACOG) and the American College of Allergy, Asthmaand Immunology (ACAAI). The use of newer asthma and allergy medications during pregnancy. Ann Allergy Asthma Immunol 2000;84:475-480.
25. National Asthma Education and Prevention Program. NAEPP Expert Panel Report. Managing Asthma During Pregnancy: Recommendations for Pharmacologic Treatment—Update 2004. Bethesda, Md: National Heart, Lung, and Blood Institute; National Institutes of Health. NIH Publication No. 04-5246. March 2004.
26. Källén B, Rydhstroem H, Äberg A. Congenital malformations after the use of inhaled budesonide in early pregnancy. Obstet Gynecol 1999;93:392-395.
27. Ericson A, Källén B. Use of drugs during pregnancy—unique Swedish registration method that can be improved. Information From the Swedish Medical Products Agency 1999;1:8-11.
28. Pauwels RA, Pedersen S, Busse WW, Tan WC, Chen Y-Z, Ohlsson SV, et al. for the START Investigators Group. Early intervention with budesonide in mild persistent asthma. Lancet 2003;361:1071-1076.