User login
Bringing you the latest news, research and reviews, exclusive interviews, podcasts, quizzes, and more.
div[contains(@class, 'read-next-article')]
div[contains(@class, 'nav-primary')]
nav[contains(@class, 'nav-primary')]
section[contains(@class, 'footer-nav-section-wrapper')]
nav[contains(@class, 'nav-ce-stack nav-ce-stack__large-screen')]
header[@id='header']
div[contains(@class, 'header__large-screen')]
div[contains(@class, 'read-next-article')]
div[contains(@class, 'main-prefix')]
div[contains(@class, 'nav-primary')]
nav[contains(@class, 'nav-primary')]
section[contains(@class, 'footer-nav-section-wrapper')]
footer[@id='footer']
section[contains(@class, 'nav-hidden')]
div[contains(@class, 'ce-card-content')]
nav[contains(@class, 'nav-ce-stack')]
div[contains(@class, 'view-medstat-quiz-listing-panes')]
div[contains(@class, 'pane-article-sidebar-latest-news')]
The VA, California, and NYC requiring employee vaccinations
-- or, in the case of California and New York City, undergo regular testing.
The VA becomes the first federal agency to mandate COVID vaccinations for workers. In a news release, VA Secretary Denis McDonough said the mandate is “the best way to keep Veterans safe, especially as the Delta variant spreads across the country.”
VA health care personnel -- including doctors, dentists, podiatrists, optometrists, registered nurses, physician assistants, and chiropractors -- have 8 weeks to become fully vaccinated, the news release said. The New York Times reported that about 115,000 workers will be affected.
The trifecta of federal-state-municipal vaccine requirements arrived as the nation searches for ways to get more people vaccinated to tamp down the Delta variant.
Some organizations, including the military, have already said vaccinations will be required as soon as the Food and Drug Administration formally approves the vaccines, which are now given under emergency use authorizations. The FDA has said the Pfizer vaccine could receive full approval within months.
California Gov. Gavin Newsom said the requirements he announced July 27 were the first in the nation on the state level.
“As the state’s largest employer, we are leading by example and requiring all state and health care workers to show proof of vaccination or be tested regularly, and we are encouraging local governments and businesses to do the same,” he said in a news release.
California employees must provide proof of vaccination or get tested at least once a week. The policy starts Aug. 2 for state employees and Aug. 9 for state health care workers and employees of congregate facilities, such as jails or homeless shelters.
California, especially the southern part of the state, is grappling with a COVID-19 surge. The state’s daily case rate more than quadrupled, from a low of 1.9 cases per 100,000 in May to at least 9.5 cases per 100,000 today, the release said.
In New York City, Mayor Bill de Blasio had previously announced that city health and hospital employees and those working in Department of Health and Mental Hygiene clinical settings would be required to provide proof of vaccination or have regular testing.
On July 27 he expanded the rule to cover all city employees, with a Sept. 13 deadline for most of them, according to a news release.
“This is what it takes to continue our recovery for all of us while fighting back the Delta variant,” Mayor de Blasio said. “It’s going to take all of us to finally end the fight against COVID-19.”
“We have a moral responsibility to take every precaution possible to ensure we keep ourselves, our colleagues and loved ones safe,” NYC Health + Hospitals President and CEO Mitchell Katz, MD, said in the release. “Our city’s new testing requirement for city workers provides more [peace] of mind until more people get their safe and effective COVID-19 vaccine.”
NBC News reported the plan would affect about 340,000 employees.
A version of this article first appeared on WebMD.com.
-- or, in the case of California and New York City, undergo regular testing.
The VA becomes the first federal agency to mandate COVID vaccinations for workers. In a news release, VA Secretary Denis McDonough said the mandate is “the best way to keep Veterans safe, especially as the Delta variant spreads across the country.”
VA health care personnel -- including doctors, dentists, podiatrists, optometrists, registered nurses, physician assistants, and chiropractors -- have 8 weeks to become fully vaccinated, the news release said. The New York Times reported that about 115,000 workers will be affected.
The trifecta of federal-state-municipal vaccine requirements arrived as the nation searches for ways to get more people vaccinated to tamp down the Delta variant.
Some organizations, including the military, have already said vaccinations will be required as soon as the Food and Drug Administration formally approves the vaccines, which are now given under emergency use authorizations. The FDA has said the Pfizer vaccine could receive full approval within months.
California Gov. Gavin Newsom said the requirements he announced July 27 were the first in the nation on the state level.
“As the state’s largest employer, we are leading by example and requiring all state and health care workers to show proof of vaccination or be tested regularly, and we are encouraging local governments and businesses to do the same,” he said in a news release.
California employees must provide proof of vaccination or get tested at least once a week. The policy starts Aug. 2 for state employees and Aug. 9 for state health care workers and employees of congregate facilities, such as jails or homeless shelters.
California, especially the southern part of the state, is grappling with a COVID-19 surge. The state’s daily case rate more than quadrupled, from a low of 1.9 cases per 100,000 in May to at least 9.5 cases per 100,000 today, the release said.
In New York City, Mayor Bill de Blasio had previously announced that city health and hospital employees and those working in Department of Health and Mental Hygiene clinical settings would be required to provide proof of vaccination or have regular testing.
On July 27 he expanded the rule to cover all city employees, with a Sept. 13 deadline for most of them, according to a news release.
“This is what it takes to continue our recovery for all of us while fighting back the Delta variant,” Mayor de Blasio said. “It’s going to take all of us to finally end the fight against COVID-19.”
“We have a moral responsibility to take every precaution possible to ensure we keep ourselves, our colleagues and loved ones safe,” NYC Health + Hospitals President and CEO Mitchell Katz, MD, said in the release. “Our city’s new testing requirement for city workers provides more [peace] of mind until more people get their safe and effective COVID-19 vaccine.”
NBC News reported the plan would affect about 340,000 employees.
A version of this article first appeared on WebMD.com.
-- or, in the case of California and New York City, undergo regular testing.
The VA becomes the first federal agency to mandate COVID vaccinations for workers. In a news release, VA Secretary Denis McDonough said the mandate is “the best way to keep Veterans safe, especially as the Delta variant spreads across the country.”
VA health care personnel -- including doctors, dentists, podiatrists, optometrists, registered nurses, physician assistants, and chiropractors -- have 8 weeks to become fully vaccinated, the news release said. The New York Times reported that about 115,000 workers will be affected.
The trifecta of federal-state-municipal vaccine requirements arrived as the nation searches for ways to get more people vaccinated to tamp down the Delta variant.
Some organizations, including the military, have already said vaccinations will be required as soon as the Food and Drug Administration formally approves the vaccines, which are now given under emergency use authorizations. The FDA has said the Pfizer vaccine could receive full approval within months.
California Gov. Gavin Newsom said the requirements he announced July 27 were the first in the nation on the state level.
“As the state’s largest employer, we are leading by example and requiring all state and health care workers to show proof of vaccination or be tested regularly, and we are encouraging local governments and businesses to do the same,” he said in a news release.
California employees must provide proof of vaccination or get tested at least once a week. The policy starts Aug. 2 for state employees and Aug. 9 for state health care workers and employees of congregate facilities, such as jails or homeless shelters.
California, especially the southern part of the state, is grappling with a COVID-19 surge. The state’s daily case rate more than quadrupled, from a low of 1.9 cases per 100,000 in May to at least 9.5 cases per 100,000 today, the release said.
In New York City, Mayor Bill de Blasio had previously announced that city health and hospital employees and those working in Department of Health and Mental Hygiene clinical settings would be required to provide proof of vaccination or have regular testing.
On July 27 he expanded the rule to cover all city employees, with a Sept. 13 deadline for most of them, according to a news release.
“This is what it takes to continue our recovery for all of us while fighting back the Delta variant,” Mayor de Blasio said. “It’s going to take all of us to finally end the fight against COVID-19.”
“We have a moral responsibility to take every precaution possible to ensure we keep ourselves, our colleagues and loved ones safe,” NYC Health + Hospitals President and CEO Mitchell Katz, MD, said in the release. “Our city’s new testing requirement for city workers provides more [peace] of mind until more people get their safe and effective COVID-19 vaccine.”
NBC News reported the plan would affect about 340,000 employees.
A version of this article first appeared on WebMD.com.
Mayo, Cleveland Clinics top latest U.S. News & World Report hospital rankings
This year’s expanded report debuts new ratings for seven “important procedures and conditions to help patients, in consultation with their doctors, narrow down their choice of hospital based on the specific type of care they need,” Ben Harder, managing editor and chief of health analysis, said in a news release.
With new ratings for myocardial infarction, stroke, hip fracture, and back surgery (spinal fusion), the report now ranks 17 procedures and conditions.
Also new to the 2021 report, which marks the 32nd edition, is a look at racial disparities in health care and the inclusion of health equity measures alongside the hospital rankings.
The new measures examine whether the patients each hospital has treated reflect the racial and ethnic diversity of the surrounding community, among other aspects of health equity.
“At roughly four out of five hospitals, we found that the community’s minority residents were underrepresented among patients receiving services such as joint replacement, cancer surgery and common heart procedures,” Mr. Harder said.
“Against this backdrop, however, we found important exceptions – hospitals that provide care to a disproportionate share of their community’s minority residents. These metrics are just a beginning; we aim to expand on our measurement of health equity in the future,” Mr. Harder added.
Mayo and Cleveland Clinic remain tops
Following the Mayo Clinic, the Cleveland Clinic once again takes the No. 2 spot in the magazine’s latest annual honor roll of best hospitals, which highlights hospitals that deliver exceptional treatment across multiple areas of care.
UCLA Medical Center, Los Angeles, holds the No. 3 spot in 2021. In 2020, UCLA Medical Center and New York–Presbyterian Hospital–Columbia and Cornell, New York, sat in a tie at No. 4.
In 2021, Johns Hopkins Hospital, Baltimore, which held the No. 3 spot in 2020, drops to No. 4, while Massachusetts General Hospital in Boston takes the No. 5 spot, up from No. 6 in 2020.
Rounding out the top 10 (in order) are Cedars-Sinai Medical Center, Los Angeles; New York–Presbyterian Hospital–Columbia and Cornell, New York; NYU Langone Hospitals, New York; UCSF Medical Center, San Francisco; and Northwestern Memorial Hospital, Chicago.
2021-2022 Best Hospitals honor roll
1. Mayo Clinic, Rochester, Minn.
2. Cleveland Clinic, Cleveland
3. UCLA Medical Center, Los Angeles
4. Johns Hopkins Hospital, Baltimore
5. Massachusetts General Hospital, Boston
6. Cedars-Sinai Medical Center, San Francisco
7. New York–Presbyterian Hospital–Columbia and Cornell, New York
8. NYU Langone Hospitals, New York
9. UCSF Medical Center, San Francisco
10. Northwestern Memorial Hospital, Chicago
11. University of Michigan Hospitals–Michigan Medicine, Ann Arbor.
12. Stanford Health Care–Stanford Hospital, Palo Alto, Calif.
13. Hospitals of the University of Pennsylvania–Penn Presbyterian, Philadelphia
14. Brigham and Women’s Hospital, Boston
15. Mayo Clinic–Phoenix, Phoenix
16. Houston Methodist Hospital, Houston
17. (tie) Barnes-Jewish Hospital, St. Louis
17. (tie) Mount Sinai Hospital, New York Rush University Medical Center, Chicago
19. Rush University Medical Center, Chicago
20. Vanderbilt University Medical Center, Nashville, Tenn.
For the 2021-2022 rankings and ratings, the magazine compared more than 4,750 hospitals nationwide in 15 specialties and 17 procedures and conditions.
At least 2,039 hospitals received a high performance rating in at least one of the services rated; 11 hospitals received high performance in all 17. A total of 175 hospitals were nationally ranked in at least one specialty
For specialty rankings, the University of Texas MD Anderson Cancer Center continues to hold the No. 1 spot in cancer care, the Hospital for Special Surgery continues to be No. 1 in orthopedics, and the Cleveland Clinic continues to be No. 1 in cardiology and heart surgery.
Top five for cancer
1. University of Texas MD Anderson Cancer Center, Houston
2. Memorial Sloan Kettering Cancer Center, New York
3. Mayo Clinic, Rochester, Minn.
4. Dana-Farber/Brigham & Women’s Cancer Center, Boston
5. Cleveland Clinic, Cleveland
Top five for cardiology and heart surgery
1. Cleveland Clinic, Cleveland
2. Mayo Clinic, Rochester, Minn.
3. Cedars-Sinai Medical Center, Los Angeles
4. New York–Presbyterian Hospital–Columbia and Cornell, New York
5. NYU Langone Hospitals, New York
Top five for orthopedics
1. Hospital for Special Surgery, New York
2. Mayo Clinic, Rochester, Minn.
3. Cedars-Sinai Medical Center, Los Angeles
4. NYU Langone Orthopedic Hospital, New York
5. UCLA Medical Center, Los Angeles
The magazine noted that data for the 2021-2022 Best Hospitals rankings and ratings were not affected by the COVID-19 pandemic, which began after the end of the data collection period.
The methodologies used in determining the rankings are based largely on objective measures, such as risk-adjusted survival, discharge-to-home rates, volume, and quality of nursing, among other care-related indicators.
The full report is available online.
A version of this article first appeared on Medscape.com.
This year’s expanded report debuts new ratings for seven “important procedures and conditions to help patients, in consultation with their doctors, narrow down their choice of hospital based on the specific type of care they need,” Ben Harder, managing editor and chief of health analysis, said in a news release.
With new ratings for myocardial infarction, stroke, hip fracture, and back surgery (spinal fusion), the report now ranks 17 procedures and conditions.
Also new to the 2021 report, which marks the 32nd edition, is a look at racial disparities in health care and the inclusion of health equity measures alongside the hospital rankings.
The new measures examine whether the patients each hospital has treated reflect the racial and ethnic diversity of the surrounding community, among other aspects of health equity.
“At roughly four out of five hospitals, we found that the community’s minority residents were underrepresented among patients receiving services such as joint replacement, cancer surgery and common heart procedures,” Mr. Harder said.
“Against this backdrop, however, we found important exceptions – hospitals that provide care to a disproportionate share of their community’s minority residents. These metrics are just a beginning; we aim to expand on our measurement of health equity in the future,” Mr. Harder added.
Mayo and Cleveland Clinic remain tops
Following the Mayo Clinic, the Cleveland Clinic once again takes the No. 2 spot in the magazine’s latest annual honor roll of best hospitals, which highlights hospitals that deliver exceptional treatment across multiple areas of care.
UCLA Medical Center, Los Angeles, holds the No. 3 spot in 2021. In 2020, UCLA Medical Center and New York–Presbyterian Hospital–Columbia and Cornell, New York, sat in a tie at No. 4.
In 2021, Johns Hopkins Hospital, Baltimore, which held the No. 3 spot in 2020, drops to No. 4, while Massachusetts General Hospital in Boston takes the No. 5 spot, up from No. 6 in 2020.
Rounding out the top 10 (in order) are Cedars-Sinai Medical Center, Los Angeles; New York–Presbyterian Hospital–Columbia and Cornell, New York; NYU Langone Hospitals, New York; UCSF Medical Center, San Francisco; and Northwestern Memorial Hospital, Chicago.
2021-2022 Best Hospitals honor roll
1. Mayo Clinic, Rochester, Minn.
2. Cleveland Clinic, Cleveland
3. UCLA Medical Center, Los Angeles
4. Johns Hopkins Hospital, Baltimore
5. Massachusetts General Hospital, Boston
6. Cedars-Sinai Medical Center, San Francisco
7. New York–Presbyterian Hospital–Columbia and Cornell, New York
8. NYU Langone Hospitals, New York
9. UCSF Medical Center, San Francisco
10. Northwestern Memorial Hospital, Chicago
11. University of Michigan Hospitals–Michigan Medicine, Ann Arbor.
12. Stanford Health Care–Stanford Hospital, Palo Alto, Calif.
13. Hospitals of the University of Pennsylvania–Penn Presbyterian, Philadelphia
14. Brigham and Women’s Hospital, Boston
15. Mayo Clinic–Phoenix, Phoenix
16. Houston Methodist Hospital, Houston
17. (tie) Barnes-Jewish Hospital, St. Louis
17. (tie) Mount Sinai Hospital, New York Rush University Medical Center, Chicago
19. Rush University Medical Center, Chicago
20. Vanderbilt University Medical Center, Nashville, Tenn.
For the 2021-2022 rankings and ratings, the magazine compared more than 4,750 hospitals nationwide in 15 specialties and 17 procedures and conditions.
At least 2,039 hospitals received a high performance rating in at least one of the services rated; 11 hospitals received high performance in all 17. A total of 175 hospitals were nationally ranked in at least one specialty
For specialty rankings, the University of Texas MD Anderson Cancer Center continues to hold the No. 1 spot in cancer care, the Hospital for Special Surgery continues to be No. 1 in orthopedics, and the Cleveland Clinic continues to be No. 1 in cardiology and heart surgery.
Top five for cancer
1. University of Texas MD Anderson Cancer Center, Houston
2. Memorial Sloan Kettering Cancer Center, New York
3. Mayo Clinic, Rochester, Minn.
4. Dana-Farber/Brigham & Women’s Cancer Center, Boston
5. Cleveland Clinic, Cleveland
Top five for cardiology and heart surgery
1. Cleveland Clinic, Cleveland
2. Mayo Clinic, Rochester, Minn.
3. Cedars-Sinai Medical Center, Los Angeles
4. New York–Presbyterian Hospital–Columbia and Cornell, New York
5. NYU Langone Hospitals, New York
Top five for orthopedics
1. Hospital for Special Surgery, New York
2. Mayo Clinic, Rochester, Minn.
3. Cedars-Sinai Medical Center, Los Angeles
4. NYU Langone Orthopedic Hospital, New York
5. UCLA Medical Center, Los Angeles
The magazine noted that data for the 2021-2022 Best Hospitals rankings and ratings were not affected by the COVID-19 pandemic, which began after the end of the data collection period.
The methodologies used in determining the rankings are based largely on objective measures, such as risk-adjusted survival, discharge-to-home rates, volume, and quality of nursing, among other care-related indicators.
The full report is available online.
A version of this article first appeared on Medscape.com.
This year’s expanded report debuts new ratings for seven “important procedures and conditions to help patients, in consultation with their doctors, narrow down their choice of hospital based on the specific type of care they need,” Ben Harder, managing editor and chief of health analysis, said in a news release.
With new ratings for myocardial infarction, stroke, hip fracture, and back surgery (spinal fusion), the report now ranks 17 procedures and conditions.
Also new to the 2021 report, which marks the 32nd edition, is a look at racial disparities in health care and the inclusion of health equity measures alongside the hospital rankings.
The new measures examine whether the patients each hospital has treated reflect the racial and ethnic diversity of the surrounding community, among other aspects of health equity.
“At roughly four out of five hospitals, we found that the community’s minority residents were underrepresented among patients receiving services such as joint replacement, cancer surgery and common heart procedures,” Mr. Harder said.
“Against this backdrop, however, we found important exceptions – hospitals that provide care to a disproportionate share of their community’s minority residents. These metrics are just a beginning; we aim to expand on our measurement of health equity in the future,” Mr. Harder added.
Mayo and Cleveland Clinic remain tops
Following the Mayo Clinic, the Cleveland Clinic once again takes the No. 2 spot in the magazine’s latest annual honor roll of best hospitals, which highlights hospitals that deliver exceptional treatment across multiple areas of care.
UCLA Medical Center, Los Angeles, holds the No. 3 spot in 2021. In 2020, UCLA Medical Center and New York–Presbyterian Hospital–Columbia and Cornell, New York, sat in a tie at No. 4.
In 2021, Johns Hopkins Hospital, Baltimore, which held the No. 3 spot in 2020, drops to No. 4, while Massachusetts General Hospital in Boston takes the No. 5 spot, up from No. 6 in 2020.
Rounding out the top 10 (in order) are Cedars-Sinai Medical Center, Los Angeles; New York–Presbyterian Hospital–Columbia and Cornell, New York; NYU Langone Hospitals, New York; UCSF Medical Center, San Francisco; and Northwestern Memorial Hospital, Chicago.
2021-2022 Best Hospitals honor roll
1. Mayo Clinic, Rochester, Minn.
2. Cleveland Clinic, Cleveland
3. UCLA Medical Center, Los Angeles
4. Johns Hopkins Hospital, Baltimore
5. Massachusetts General Hospital, Boston
6. Cedars-Sinai Medical Center, San Francisco
7. New York–Presbyterian Hospital–Columbia and Cornell, New York
8. NYU Langone Hospitals, New York
9. UCSF Medical Center, San Francisco
10. Northwestern Memorial Hospital, Chicago
11. University of Michigan Hospitals–Michigan Medicine, Ann Arbor.
12. Stanford Health Care–Stanford Hospital, Palo Alto, Calif.
13. Hospitals of the University of Pennsylvania–Penn Presbyterian, Philadelphia
14. Brigham and Women’s Hospital, Boston
15. Mayo Clinic–Phoenix, Phoenix
16. Houston Methodist Hospital, Houston
17. (tie) Barnes-Jewish Hospital, St. Louis
17. (tie) Mount Sinai Hospital, New York Rush University Medical Center, Chicago
19. Rush University Medical Center, Chicago
20. Vanderbilt University Medical Center, Nashville, Tenn.
For the 2021-2022 rankings and ratings, the magazine compared more than 4,750 hospitals nationwide in 15 specialties and 17 procedures and conditions.
At least 2,039 hospitals received a high performance rating in at least one of the services rated; 11 hospitals received high performance in all 17. A total of 175 hospitals were nationally ranked in at least one specialty
For specialty rankings, the University of Texas MD Anderson Cancer Center continues to hold the No. 1 spot in cancer care, the Hospital for Special Surgery continues to be No. 1 in orthopedics, and the Cleveland Clinic continues to be No. 1 in cardiology and heart surgery.
Top five for cancer
1. University of Texas MD Anderson Cancer Center, Houston
2. Memorial Sloan Kettering Cancer Center, New York
3. Mayo Clinic, Rochester, Minn.
4. Dana-Farber/Brigham & Women’s Cancer Center, Boston
5. Cleveland Clinic, Cleveland
Top five for cardiology and heart surgery
1. Cleveland Clinic, Cleveland
2. Mayo Clinic, Rochester, Minn.
3. Cedars-Sinai Medical Center, Los Angeles
4. New York–Presbyterian Hospital–Columbia and Cornell, New York
5. NYU Langone Hospitals, New York
Top five for orthopedics
1. Hospital for Special Surgery, New York
2. Mayo Clinic, Rochester, Minn.
3. Cedars-Sinai Medical Center, Los Angeles
4. NYU Langone Orthopedic Hospital, New York
5. UCLA Medical Center, Los Angeles
The magazine noted that data for the 2021-2022 Best Hospitals rankings and ratings were not affected by the COVID-19 pandemic, which began after the end of the data collection period.
The methodologies used in determining the rankings are based largely on objective measures, such as risk-adjusted survival, discharge-to-home rates, volume, and quality of nursing, among other care-related indicators.
The full report is available online.
A version of this article first appeared on Medscape.com.
AMA, 55 other groups urge health care vax mandate
As COVID-19 cases, hospitalizations, and deaths mount again across the country, the American Medical Association (AMA), the American Nursing Association, and 54 other
This injunction, issued July 26, covers everyone in healthcare, Emanuel Ezekiel, MD, PhD, chair of the department of medical ethics and health policy at the University of Pennsylvania, Philadelphia, and the organizer of the joint statement, said in an interview.
That includes not only hospitals, but also physician offices, ambulatory surgery centers, home care agencies, skilled nursing facilities, pharmacies, laboratories, and imaging centers, he said.
The exhortation to get vaccinated also extends to federal and state healthcare facilities, including those of the military health system — TRICARE and the Department of Veterans Affairs — which instituted a mandate the same day.
The American Hospital Association (AHA) and other hospital groups recently said they supported hospitals and health systems that required their personnel to get vaccinated. Several dozen healthcare organizations have already done so, including some of the nation’s largest health systems.
A substantial fraction of U.S. healthcare workers have not yet gotten vaccinated, although how many are unvaccinated is unclear. An analysis by WebMD and Medscape Medical News estimated that 25% of hospital workers who had contact with patients were unvaccinated at the end of May.
More than 38% of nursing workers were not fully vaccinated by July 11, according to an analysis of Centers for Medicare & Medicaid Services data by LeadingAge, which was cited by the Washington Post. And more than 40% of nursing home employees have not been fully vaccinated, according to the Centers for Disease Control and Prevention.
The joint statement did not give any indication of how many employees of physician practices have failed to get COVID shots. However, a recent AMA survey shows that 96% of physicians have been fully vaccinated.
Ethical commitment
The main reason for vaccine mandates, according to the healthcare associations’ statement, is “the ethical commitment to put patients as well as residents of long-term care facilities first and take all steps necessary to ensure their health and well-being.”
In addition, the statement noted, vaccination can protect healthcare workers and their families from getting COVID-19.
The statement also pointed out that many healthcare and long-term care organizations already require vaccinations for influenza, hepatitis B, and pertussis.
Workers who have certain medical conditions should be exempt from the vaccination mandates, the statement added.
While recognizing the “historical mistrust of health care institutions” among some healthcare workers, the statement said, “We must continue to address workers’ concerns, engage with marginalized populations, and work with trusted messengers to improve vaccine acceptance.”
There has been some skepticism about the legality of requiring healthcare workers to get vaccinated as a condition of employment, partly because the U.S. Food and Drug Administration has not yet fully authorized any of the COVID-19 vaccines.
But in June, a federal judge turned down a legal challenge to Houston Methodist’s vaccination mandate.
“It is critical that all people in the health care workforce get vaccinated against COVID-19 for the safety of our patients and our colleagues. With more than 300 million doses administered in the United States and nearly 4 billion doses administered worldwide, we know the vaccines are safe and highly effective at preventing severe illness and death from COVID-19.
“Increased vaccinations among health care personnel will not only reduce the spread of COVID-19 but also reduce the harmful toll this virus is taking within the health care workforce and those we are striving to serve,” Susan Bailey, MD, immediate past president of the AMA, said in a news release.
A version of this article first appeared on Medscape.com.
As COVID-19 cases, hospitalizations, and deaths mount again across the country, the American Medical Association (AMA), the American Nursing Association, and 54 other
This injunction, issued July 26, covers everyone in healthcare, Emanuel Ezekiel, MD, PhD, chair of the department of medical ethics and health policy at the University of Pennsylvania, Philadelphia, and the organizer of the joint statement, said in an interview.
That includes not only hospitals, but also physician offices, ambulatory surgery centers, home care agencies, skilled nursing facilities, pharmacies, laboratories, and imaging centers, he said.
The exhortation to get vaccinated also extends to federal and state healthcare facilities, including those of the military health system — TRICARE and the Department of Veterans Affairs — which instituted a mandate the same day.
The American Hospital Association (AHA) and other hospital groups recently said they supported hospitals and health systems that required their personnel to get vaccinated. Several dozen healthcare organizations have already done so, including some of the nation’s largest health systems.
A substantial fraction of U.S. healthcare workers have not yet gotten vaccinated, although how many are unvaccinated is unclear. An analysis by WebMD and Medscape Medical News estimated that 25% of hospital workers who had contact with patients were unvaccinated at the end of May.
More than 38% of nursing workers were not fully vaccinated by July 11, according to an analysis of Centers for Medicare & Medicaid Services data by LeadingAge, which was cited by the Washington Post. And more than 40% of nursing home employees have not been fully vaccinated, according to the Centers for Disease Control and Prevention.
The joint statement did not give any indication of how many employees of physician practices have failed to get COVID shots. However, a recent AMA survey shows that 96% of physicians have been fully vaccinated.
Ethical commitment
The main reason for vaccine mandates, according to the healthcare associations’ statement, is “the ethical commitment to put patients as well as residents of long-term care facilities first and take all steps necessary to ensure their health and well-being.”
In addition, the statement noted, vaccination can protect healthcare workers and their families from getting COVID-19.
The statement also pointed out that many healthcare and long-term care organizations already require vaccinations for influenza, hepatitis B, and pertussis.
Workers who have certain medical conditions should be exempt from the vaccination mandates, the statement added.
While recognizing the “historical mistrust of health care institutions” among some healthcare workers, the statement said, “We must continue to address workers’ concerns, engage with marginalized populations, and work with trusted messengers to improve vaccine acceptance.”
There has been some skepticism about the legality of requiring healthcare workers to get vaccinated as a condition of employment, partly because the U.S. Food and Drug Administration has not yet fully authorized any of the COVID-19 vaccines.
But in June, a federal judge turned down a legal challenge to Houston Methodist’s vaccination mandate.
“It is critical that all people in the health care workforce get vaccinated against COVID-19 for the safety of our patients and our colleagues. With more than 300 million doses administered in the United States and nearly 4 billion doses administered worldwide, we know the vaccines are safe and highly effective at preventing severe illness and death from COVID-19.
“Increased vaccinations among health care personnel will not only reduce the spread of COVID-19 but also reduce the harmful toll this virus is taking within the health care workforce and those we are striving to serve,” Susan Bailey, MD, immediate past president of the AMA, said in a news release.
A version of this article first appeared on Medscape.com.
As COVID-19 cases, hospitalizations, and deaths mount again across the country, the American Medical Association (AMA), the American Nursing Association, and 54 other
This injunction, issued July 26, covers everyone in healthcare, Emanuel Ezekiel, MD, PhD, chair of the department of medical ethics and health policy at the University of Pennsylvania, Philadelphia, and the organizer of the joint statement, said in an interview.
That includes not only hospitals, but also physician offices, ambulatory surgery centers, home care agencies, skilled nursing facilities, pharmacies, laboratories, and imaging centers, he said.
The exhortation to get vaccinated also extends to federal and state healthcare facilities, including those of the military health system — TRICARE and the Department of Veterans Affairs — which instituted a mandate the same day.
The American Hospital Association (AHA) and other hospital groups recently said they supported hospitals and health systems that required their personnel to get vaccinated. Several dozen healthcare organizations have already done so, including some of the nation’s largest health systems.
A substantial fraction of U.S. healthcare workers have not yet gotten vaccinated, although how many are unvaccinated is unclear. An analysis by WebMD and Medscape Medical News estimated that 25% of hospital workers who had contact with patients were unvaccinated at the end of May.
More than 38% of nursing workers were not fully vaccinated by July 11, according to an analysis of Centers for Medicare & Medicaid Services data by LeadingAge, which was cited by the Washington Post. And more than 40% of nursing home employees have not been fully vaccinated, according to the Centers for Disease Control and Prevention.
The joint statement did not give any indication of how many employees of physician practices have failed to get COVID shots. However, a recent AMA survey shows that 96% of physicians have been fully vaccinated.
Ethical commitment
The main reason for vaccine mandates, according to the healthcare associations’ statement, is “the ethical commitment to put patients as well as residents of long-term care facilities first and take all steps necessary to ensure their health and well-being.”
In addition, the statement noted, vaccination can protect healthcare workers and their families from getting COVID-19.
The statement also pointed out that many healthcare and long-term care organizations already require vaccinations for influenza, hepatitis B, and pertussis.
Workers who have certain medical conditions should be exempt from the vaccination mandates, the statement added.
While recognizing the “historical mistrust of health care institutions” among some healthcare workers, the statement said, “We must continue to address workers’ concerns, engage with marginalized populations, and work with trusted messengers to improve vaccine acceptance.”
There has been some skepticism about the legality of requiring healthcare workers to get vaccinated as a condition of employment, partly because the U.S. Food and Drug Administration has not yet fully authorized any of the COVID-19 vaccines.
But in June, a federal judge turned down a legal challenge to Houston Methodist’s vaccination mandate.
“It is critical that all people in the health care workforce get vaccinated against COVID-19 for the safety of our patients and our colleagues. With more than 300 million doses administered in the United States and nearly 4 billion doses administered worldwide, we know the vaccines are safe and highly effective at preventing severe illness and death from COVID-19.
“Increased vaccinations among health care personnel will not only reduce the spread of COVID-19 but also reduce the harmful toll this virus is taking within the health care workforce and those we are striving to serve,” Susan Bailey, MD, immediate past president of the AMA, said in a news release.
A version of this article first appeared on Medscape.com.
When it comes to young women, regular check-ins support ongoing PrEP use
The secret, said Gonasagrie Nair, MBChB, faculty of medicine and health sciences at Stellenbosch University, Zimbabwe, is offering intensive wraparound services to support teenagers – a lesson that may be useful as adolescent and family medicine professionals in the United States begin to roll out HIV prevention in their clinics.
This is important in the United States because cisgender Black women make up 60% of all new HIV cases in the United States while accounting for just 14% of the overall U.S. population. The Centers for Disease Control and Prevention has found that only about 1% of Black Americans who could benefit from PrEP have access to it.
“Younger women and adolescent girls in particular face a number of cultural and social challenges that impact their ability to make decisions related to their own health,” said Dr. Nair, who presented the data at the International AIDS Society (IAS) Conference 2021. “The adherence support provided by this study empowered them to make choices and stick to these choices,” she said.
In total, 247 women and girls aged 16 to 21 who were without HIV were enrolled in the Reversing the Epidemic in Africa with Choices in HIV Prevention (REACH) trial in two sites in South Africa and one each in Uganda and Zimbabwe beginning in February 2019. One-third of the participants were minors; the average age was 18.2 years.
The women were good candidates for PrEP. More than 1 in 3 of the women started the study with a sexually transmitted infection (STI), the most prevalent of which was chlamydia. This is often a good marker for condomless sex. Of the participants, 89% had a primary sex partner; a quarter of those thought their partner was having sex with other people. Only 7% of participants reported being very worried about acquiring HIV. More than 1 in 3 (39%) weren’t worried about HIV at all. This conforms to previous data suggesting that those who could most benefit from PrEP often don’t perceive their own vulnerability.
In the study, the women were randomly assigned two groups. In one group, the participants used the dapivirine ring for 6 months; in the other, participants used oral PrEP for 6 months. The participants then swapped prevention methods and used the alternative method for 6 more months. After a year of trying both methods, the women will be asked to choose one of the two prevention method or to stop PrEP altogether. At the IAS conference, the researchers reported interim data from the first year of the study, before the girls had the opportunity to choose for themselves.
During that first year, girls received intensive adherence support, including daily or weekly text check-ins, phone check-ins, peer buddy support, additional onsite counseling visits, access to adherence support groups, participation in online support groups via apps such as WhatsApp, and in-person social events designed to empower young women and to teach them skills. Support included discussion of adherence, contraceptives, and STIs. In addition, when girls came in for study visits, staff provided feedback on how adherent the girls had been, as determined on the basis of residual levels of dapivirine in the rings or, with regard to oral pills, drug levels as determined with blood spots.
Girls were considered to have had high adherence if they were found to have oral PrEP concentrations equivalent to four or more doses per week or if residual levels of dapivirine in their rings were 0.1071 mg/d. Moderate adherence was the equivalent of one to three doses of oral PrEP a week or dapivirine levels between 0.0321 mg/d and 0.1071 mg/d.
In total, 95.6% of ring users showed some adherence to the ring. Of those, adherence was high for 50.2%; 49.8% used the ring perfectly. For oral PrEP, 98.5% showed some level of PrEP use; for 58.6%, lab results suggested adherence high enough to provide protection from HIV, and 22% took their pills at least six times a week. Between the two arms, 54.3% of all participants used the medication sufficiently to be protected from HIV.
One person acquired HIV during the study. Dr. Nair did not say which study arm that participant was in or how adherent that person has been to their prevention method.
That level of adherence is on par with studies in the United States, which have found 56% adherence to PrEP among adolescent and young men who have sex with men. But the level of adherence is far higher than has been found in other studies that tested oral PrEP among women who did not have a partner with HIV. In particular, the VOICE and FEM-PrEP trials were both stopped early for lack of adherence. In those placebo-controlled oral-PrEP trials, fewer than 25% of participants used the oral prevention pills. Although adherence to the vaginal ring was estimated to be 61% for women older than 25 in the ASPIRE trial, it was effectively zero among women aged 18 to 21 years. Adherence has been the “bugaboo of efficacy for PrEP in young women,” said Judith Auerbach, PhD, independent science and policy consultant and professor of medicine at the University of California, San Francisco. But health care professionals have a long way to go to support young people in general in using PrEP.
“Yes, this shows improvement compared to previous studies,” Dr. Auerbach told this news organization. “But is it sufficient to have an epidemiological impact at the population level?”
Medical Advocacy and Outreach (MAO) is an HIV clinic and services program in Montgomery, Alabama, that offers a clinic specifically for some of their 144 clients to receive oral PrEP. In addition to in-person testing, MAO offers home HIV testing and lab work and televisits to support the college students they serve in taking PrEP whether they’re at school or at home on break. Currently, MAO provides a series of support groups and other social support programs for their clients living with HIV, but there are none for those receiving PrEP. The organization is in the process of hiring a social worker for the PrEP side of the clinic.
Until that person is on board, “I’m their support system in an unofficial capacity,” Shericka Williams, MPH, told this news organization. She runs education programs at MAO and handles all the phone calls from PrEP clients. “My title changes a lot, but the one I like to go with most often is the PrEP navigator,” she said.
She said she was intrigued by the dapivirine ring and oral PrEP data but said that currently, the women they serve are still learning that PrEP is for them, too. The women report that all the ads and all the information they receive is aimed at gay or bisexual men or transgender women. It takes a while for them to recognize that they could benefit, so a lot of the work that Ms. Williams does is focused on explaining the benefit of PrEP.
In MAO, the number of women receiving PrEP fluctuates more than for men. Mostly, women start PrEP because of they are in a relationship with someone who receives HIV care from MAO’s other wing – women who potentially would experience less vulnerability to HIV if their partners had undetectable viral loads. The other reason women take it is because they suspect that their partner is cheating or because they are in abusive relationships in which they want their partner to use a condom but the partner won’t. As in the PrEP trials, they often see women discontinue PrEP when they leave those relationships. In part, her job is to educate women regarding all the ways PrEP could serve them.
“Most of the time, they’re just no longer in that relationship, and they’re just taking some time for themselves,” she said in an interview. “We definitely try to bring up other reasons to stay on PrEP, but we don’t want to seem like we’re bullying someone to stay on it.”
Dr. Nair, Dr. Auerbach, and Ms. Williams report no relevant financial relationships.
A version of this article first appeared on Medscape.com.
The secret, said Gonasagrie Nair, MBChB, faculty of medicine and health sciences at Stellenbosch University, Zimbabwe, is offering intensive wraparound services to support teenagers – a lesson that may be useful as adolescent and family medicine professionals in the United States begin to roll out HIV prevention in their clinics.
This is important in the United States because cisgender Black women make up 60% of all new HIV cases in the United States while accounting for just 14% of the overall U.S. population. The Centers for Disease Control and Prevention has found that only about 1% of Black Americans who could benefit from PrEP have access to it.
“Younger women and adolescent girls in particular face a number of cultural and social challenges that impact their ability to make decisions related to their own health,” said Dr. Nair, who presented the data at the International AIDS Society (IAS) Conference 2021. “The adherence support provided by this study empowered them to make choices and stick to these choices,” she said.
In total, 247 women and girls aged 16 to 21 who were without HIV were enrolled in the Reversing the Epidemic in Africa with Choices in HIV Prevention (REACH) trial in two sites in South Africa and one each in Uganda and Zimbabwe beginning in February 2019. One-third of the participants were minors; the average age was 18.2 years.
The women were good candidates for PrEP. More than 1 in 3 of the women started the study with a sexually transmitted infection (STI), the most prevalent of which was chlamydia. This is often a good marker for condomless sex. Of the participants, 89% had a primary sex partner; a quarter of those thought their partner was having sex with other people. Only 7% of participants reported being very worried about acquiring HIV. More than 1 in 3 (39%) weren’t worried about HIV at all. This conforms to previous data suggesting that those who could most benefit from PrEP often don’t perceive their own vulnerability.
In the study, the women were randomly assigned two groups. In one group, the participants used the dapivirine ring for 6 months; in the other, participants used oral PrEP for 6 months. The participants then swapped prevention methods and used the alternative method for 6 more months. After a year of trying both methods, the women will be asked to choose one of the two prevention method or to stop PrEP altogether. At the IAS conference, the researchers reported interim data from the first year of the study, before the girls had the opportunity to choose for themselves.
During that first year, girls received intensive adherence support, including daily or weekly text check-ins, phone check-ins, peer buddy support, additional onsite counseling visits, access to adherence support groups, participation in online support groups via apps such as WhatsApp, and in-person social events designed to empower young women and to teach them skills. Support included discussion of adherence, contraceptives, and STIs. In addition, when girls came in for study visits, staff provided feedback on how adherent the girls had been, as determined on the basis of residual levels of dapivirine in the rings or, with regard to oral pills, drug levels as determined with blood spots.
Girls were considered to have had high adherence if they were found to have oral PrEP concentrations equivalent to four or more doses per week or if residual levels of dapivirine in their rings were 0.1071 mg/d. Moderate adherence was the equivalent of one to three doses of oral PrEP a week or dapivirine levels between 0.0321 mg/d and 0.1071 mg/d.
In total, 95.6% of ring users showed some adherence to the ring. Of those, adherence was high for 50.2%; 49.8% used the ring perfectly. For oral PrEP, 98.5% showed some level of PrEP use; for 58.6%, lab results suggested adherence high enough to provide protection from HIV, and 22% took their pills at least six times a week. Between the two arms, 54.3% of all participants used the medication sufficiently to be protected from HIV.
One person acquired HIV during the study. Dr. Nair did not say which study arm that participant was in or how adherent that person has been to their prevention method.
That level of adherence is on par with studies in the United States, which have found 56% adherence to PrEP among adolescent and young men who have sex with men. But the level of adherence is far higher than has been found in other studies that tested oral PrEP among women who did not have a partner with HIV. In particular, the VOICE and FEM-PrEP trials were both stopped early for lack of adherence. In those placebo-controlled oral-PrEP trials, fewer than 25% of participants used the oral prevention pills. Although adherence to the vaginal ring was estimated to be 61% for women older than 25 in the ASPIRE trial, it was effectively zero among women aged 18 to 21 years. Adherence has been the “bugaboo of efficacy for PrEP in young women,” said Judith Auerbach, PhD, independent science and policy consultant and professor of medicine at the University of California, San Francisco. But health care professionals have a long way to go to support young people in general in using PrEP.
“Yes, this shows improvement compared to previous studies,” Dr. Auerbach told this news organization. “But is it sufficient to have an epidemiological impact at the population level?”
Medical Advocacy and Outreach (MAO) is an HIV clinic and services program in Montgomery, Alabama, that offers a clinic specifically for some of their 144 clients to receive oral PrEP. In addition to in-person testing, MAO offers home HIV testing and lab work and televisits to support the college students they serve in taking PrEP whether they’re at school or at home on break. Currently, MAO provides a series of support groups and other social support programs for their clients living with HIV, but there are none for those receiving PrEP. The organization is in the process of hiring a social worker for the PrEP side of the clinic.
Until that person is on board, “I’m their support system in an unofficial capacity,” Shericka Williams, MPH, told this news organization. She runs education programs at MAO and handles all the phone calls from PrEP clients. “My title changes a lot, but the one I like to go with most often is the PrEP navigator,” she said.
She said she was intrigued by the dapivirine ring and oral PrEP data but said that currently, the women they serve are still learning that PrEP is for them, too. The women report that all the ads and all the information they receive is aimed at gay or bisexual men or transgender women. It takes a while for them to recognize that they could benefit, so a lot of the work that Ms. Williams does is focused on explaining the benefit of PrEP.
In MAO, the number of women receiving PrEP fluctuates more than for men. Mostly, women start PrEP because of they are in a relationship with someone who receives HIV care from MAO’s other wing – women who potentially would experience less vulnerability to HIV if their partners had undetectable viral loads. The other reason women take it is because they suspect that their partner is cheating or because they are in abusive relationships in which they want their partner to use a condom but the partner won’t. As in the PrEP trials, they often see women discontinue PrEP when they leave those relationships. In part, her job is to educate women regarding all the ways PrEP could serve them.
“Most of the time, they’re just no longer in that relationship, and they’re just taking some time for themselves,” she said in an interview. “We definitely try to bring up other reasons to stay on PrEP, but we don’t want to seem like we’re bullying someone to stay on it.”
Dr. Nair, Dr. Auerbach, and Ms. Williams report no relevant financial relationships.
A version of this article first appeared on Medscape.com.
The secret, said Gonasagrie Nair, MBChB, faculty of medicine and health sciences at Stellenbosch University, Zimbabwe, is offering intensive wraparound services to support teenagers – a lesson that may be useful as adolescent and family medicine professionals in the United States begin to roll out HIV prevention in their clinics.
This is important in the United States because cisgender Black women make up 60% of all new HIV cases in the United States while accounting for just 14% of the overall U.S. population. The Centers for Disease Control and Prevention has found that only about 1% of Black Americans who could benefit from PrEP have access to it.
“Younger women and adolescent girls in particular face a number of cultural and social challenges that impact their ability to make decisions related to their own health,” said Dr. Nair, who presented the data at the International AIDS Society (IAS) Conference 2021. “The adherence support provided by this study empowered them to make choices and stick to these choices,” she said.
In total, 247 women and girls aged 16 to 21 who were without HIV were enrolled in the Reversing the Epidemic in Africa with Choices in HIV Prevention (REACH) trial in two sites in South Africa and one each in Uganda and Zimbabwe beginning in February 2019. One-third of the participants were minors; the average age was 18.2 years.
The women were good candidates for PrEP. More than 1 in 3 of the women started the study with a sexually transmitted infection (STI), the most prevalent of which was chlamydia. This is often a good marker for condomless sex. Of the participants, 89% had a primary sex partner; a quarter of those thought their partner was having sex with other people. Only 7% of participants reported being very worried about acquiring HIV. More than 1 in 3 (39%) weren’t worried about HIV at all. This conforms to previous data suggesting that those who could most benefit from PrEP often don’t perceive their own vulnerability.
In the study, the women were randomly assigned two groups. In one group, the participants used the dapivirine ring for 6 months; in the other, participants used oral PrEP for 6 months. The participants then swapped prevention methods and used the alternative method for 6 more months. After a year of trying both methods, the women will be asked to choose one of the two prevention method or to stop PrEP altogether. At the IAS conference, the researchers reported interim data from the first year of the study, before the girls had the opportunity to choose for themselves.
During that first year, girls received intensive adherence support, including daily or weekly text check-ins, phone check-ins, peer buddy support, additional onsite counseling visits, access to adherence support groups, participation in online support groups via apps such as WhatsApp, and in-person social events designed to empower young women and to teach them skills. Support included discussion of adherence, contraceptives, and STIs. In addition, when girls came in for study visits, staff provided feedback on how adherent the girls had been, as determined on the basis of residual levels of dapivirine in the rings or, with regard to oral pills, drug levels as determined with blood spots.
Girls were considered to have had high adherence if they were found to have oral PrEP concentrations equivalent to four or more doses per week or if residual levels of dapivirine in their rings were 0.1071 mg/d. Moderate adherence was the equivalent of one to three doses of oral PrEP a week or dapivirine levels between 0.0321 mg/d and 0.1071 mg/d.
In total, 95.6% of ring users showed some adherence to the ring. Of those, adherence was high for 50.2%; 49.8% used the ring perfectly. For oral PrEP, 98.5% showed some level of PrEP use; for 58.6%, lab results suggested adherence high enough to provide protection from HIV, and 22% took their pills at least six times a week. Between the two arms, 54.3% of all participants used the medication sufficiently to be protected from HIV.
One person acquired HIV during the study. Dr. Nair did not say which study arm that participant was in or how adherent that person has been to their prevention method.
That level of adherence is on par with studies in the United States, which have found 56% adherence to PrEP among adolescent and young men who have sex with men. But the level of adherence is far higher than has been found in other studies that tested oral PrEP among women who did not have a partner with HIV. In particular, the VOICE and FEM-PrEP trials were both stopped early for lack of adherence. In those placebo-controlled oral-PrEP trials, fewer than 25% of participants used the oral prevention pills. Although adherence to the vaginal ring was estimated to be 61% for women older than 25 in the ASPIRE trial, it was effectively zero among women aged 18 to 21 years. Adherence has been the “bugaboo of efficacy for PrEP in young women,” said Judith Auerbach, PhD, independent science and policy consultant and professor of medicine at the University of California, San Francisco. But health care professionals have a long way to go to support young people in general in using PrEP.
“Yes, this shows improvement compared to previous studies,” Dr. Auerbach told this news organization. “But is it sufficient to have an epidemiological impact at the population level?”
Medical Advocacy and Outreach (MAO) is an HIV clinic and services program in Montgomery, Alabama, that offers a clinic specifically for some of their 144 clients to receive oral PrEP. In addition to in-person testing, MAO offers home HIV testing and lab work and televisits to support the college students they serve in taking PrEP whether they’re at school or at home on break. Currently, MAO provides a series of support groups and other social support programs for their clients living with HIV, but there are none for those receiving PrEP. The organization is in the process of hiring a social worker for the PrEP side of the clinic.
Until that person is on board, “I’m their support system in an unofficial capacity,” Shericka Williams, MPH, told this news organization. She runs education programs at MAO and handles all the phone calls from PrEP clients. “My title changes a lot, but the one I like to go with most often is the PrEP navigator,” she said.
She said she was intrigued by the dapivirine ring and oral PrEP data but said that currently, the women they serve are still learning that PrEP is for them, too. The women report that all the ads and all the information they receive is aimed at gay or bisexual men or transgender women. It takes a while for them to recognize that they could benefit, so a lot of the work that Ms. Williams does is focused on explaining the benefit of PrEP.
In MAO, the number of women receiving PrEP fluctuates more than for men. Mostly, women start PrEP because of they are in a relationship with someone who receives HIV care from MAO’s other wing – women who potentially would experience less vulnerability to HIV if their partners had undetectable viral loads. The other reason women take it is because they suspect that their partner is cheating or because they are in abusive relationships in which they want their partner to use a condom but the partner won’t. As in the PrEP trials, they often see women discontinue PrEP when they leave those relationships. In part, her job is to educate women regarding all the ways PrEP could serve them.
“Most of the time, they’re just no longer in that relationship, and they’re just taking some time for themselves,” she said in an interview. “We definitely try to bring up other reasons to stay on PrEP, but we don’t want to seem like we’re bullying someone to stay on it.”
Dr. Nair, Dr. Auerbach, and Ms. Williams report no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Vaccine breakthrough cases rising with Delta: Here’s what that means
At a recent town hall meeting in Cincinnati, President Joe Biden was asked about COVID-19 cases, hospitalizations, and deaths rising in response to the Delta variant.
Touting the importance of vaccination, “We have a pandemic for those who haven’t gotten a vaccination. It’s that basic, that simple,” President Biden said at the event, which was broadcast live on CNN.
“If you’re vaccinated, you’re not going to be hospitalized, not going to the ICU unit, and not going to die,” he said, adding “you’re not going to get COVID if you have these vaccinations.”
Unfortunately, it’s not so simple. Fully vaccinated people continue to be well protected against severe disease and death, even with Delta, Because of that, many experts continue to advise caution, even if fully vaccinated.
“I was disappointed,” Leana Wen, MD, MSc, an emergency physician and visiting professor of health policy and management at George Washington University’s Milken School of Public Health in Washington, told CNN in response to the president’s statement.
“I actually thought he was answering questions as if it were a month ago. He’s not really meeting the realities of what’s happening on the ground,” she said. “I think he may have led people astray.”
Vaccines still work
Recent cases support Dr. Wen’s claim. Fully vaccinated Olympic athletes, wedding guests, healthcare workers, and even White House staff have recently tested positive. So what gives?
The vast majority of these illnesses are mild, and public health officials say they are to be expected.
“The vaccines were designed to keep us out of the hospital and to keep us from dying. That was the whole purpose of the vaccine and they’re even more successful than we anticipated,” says William Schaffner, MD, an infectious disease expert at Vanderbilt University in Nashville.
As good as they are, these shots aren’t perfect. Their protection differs from person to person depending on age and underlying health. People with immune function that’s weakened because of age or a health condition can still become seriously ill, and, in very rare cases, die after vaccination.
When people are infected with Delta, they carry approximately 1,000 times more virus compared with previous versions of the virus, according to a recent study. All that virus can overwhelm even the strong protection from the vaccines.
“Three months ago, breakthroughs didn’t occur nearly at this rate because there was just so much less virus exposure in the community,” said Michael Osterholm, PhD, director of the Center for Infectious Disease Research and Policy at the University of Minnesota in Minneapolis.
Breakthroughs by the numbers
In Los Angeles County, where 69% of residents over age 12 have been fully vaccinated, COVID-19 cases are rising, and so, too, are cases that break through the protection of the vaccine.
In June, fully vaccinated people accounted for 20%, or 1 in 5, COVID cases in the county, which is the most populous in the United States. The increase mirrors Delta’s rise. The proportion of breakthrough cases is up from 11% in May, 5% in April, and 2% in March, according to the Los Angeles County Department of Public Health.
In the United Kingdom, which is collecting the best information on infections caused by variants, the estimated effectiveness of the vaccines to prevent an illness that causes symptoms dropped by about 10 points against Delta compared with Alpha (or B.1.1.7).
After two doses, vaccines prevent symptomatic infection about 79% of the time against Delta, according to data compiled by Public Health England. They are still highly effective at preventing hospitalization, 96% after two doses.
Out of 229,218 COVID infections in the United Kingdom between February and July 19, 28,773 — or 12.5% — were in fully vaccinated people. Of those breakthrough infections, 1,101, or 3.8%, required a visit to an emergency room, according to Public Health England. Just 474, or 2.9%, of fully vaccinated people required hospital admission, and 229, or less than 1%, died.
Unanswered questions
One of the biggest questions about breakthrough cases is how often people who have it may pass the virus to others.
“We know the vaccine reduces the likelihood of carrying the virus and the amount of virus you would carry,” Dr. Wen told CNN. But we don’t yet know whether a vaccinated person with a breakthrough infection may still be contagious to others.
For that reason, the Centers for Disease Control and Prevention says that fully vaccinated people still need to be tested if they have symptoms and shouldn’t be out in public for at least 10 days after a positive test.
How should fully vaccinated people behave? That depends a lot on their underlying health and whether or not they have vulnerable people around them.
If you’re older or immunocompromised, Dr. Schaffner recommends what he calls the “belt-and-suspenders approach,” in other words, do everything you can to stay safe.
“Get vaccinated for sure, but since we can’t be absolutely certain that the vaccines are going to be optimally protective and you are particularly susceptible to serious disease, you would be well advised to adopt at least one and perhaps more of the other mitigation measures,” he said.
These include wearing a mask, social distancing, making sure your spaces are well ventilated, and not spending prolonged periods of time indoors in crowded places.
Taking young children to visit vaccinated, elderly grandparents demands extra caution, again, with Delta circulating, particularly as they go back to school and start mixing with other kids.
Dr. Schaffner recommends explaining the ground rules before the visit: Hugs around the waist. No kissing. Wearing a mask while indoors with them.
Other important unanswered questions are whether breakthrough infections can lead to prolonged symptoms, or “long covid.” Most experts think that’s less likely in vaccinated people.
And Dr. Osterholm said it will be important to see whether there’s anything unusual about the breakthrough cases happening in the community.
“I think some of us have been challenged by the number of clusters that we’ve seen,” he said. “I think that really needs to be examined more.”
A version of this article first appeared on Medscape.com.
At a recent town hall meeting in Cincinnati, President Joe Biden was asked about COVID-19 cases, hospitalizations, and deaths rising in response to the Delta variant.
Touting the importance of vaccination, “We have a pandemic for those who haven’t gotten a vaccination. It’s that basic, that simple,” President Biden said at the event, which was broadcast live on CNN.
“If you’re vaccinated, you’re not going to be hospitalized, not going to the ICU unit, and not going to die,” he said, adding “you’re not going to get COVID if you have these vaccinations.”
Unfortunately, it’s not so simple. Fully vaccinated people continue to be well protected against severe disease and death, even with Delta, Because of that, many experts continue to advise caution, even if fully vaccinated.
“I was disappointed,” Leana Wen, MD, MSc, an emergency physician and visiting professor of health policy and management at George Washington University’s Milken School of Public Health in Washington, told CNN in response to the president’s statement.
“I actually thought he was answering questions as if it were a month ago. He’s not really meeting the realities of what’s happening on the ground,” she said. “I think he may have led people astray.”
Vaccines still work
Recent cases support Dr. Wen’s claim. Fully vaccinated Olympic athletes, wedding guests, healthcare workers, and even White House staff have recently tested positive. So what gives?
The vast majority of these illnesses are mild, and public health officials say they are to be expected.
“The vaccines were designed to keep us out of the hospital and to keep us from dying. That was the whole purpose of the vaccine and they’re even more successful than we anticipated,” says William Schaffner, MD, an infectious disease expert at Vanderbilt University in Nashville.
As good as they are, these shots aren’t perfect. Their protection differs from person to person depending on age and underlying health. People with immune function that’s weakened because of age or a health condition can still become seriously ill, and, in very rare cases, die after vaccination.
When people are infected with Delta, they carry approximately 1,000 times more virus compared with previous versions of the virus, according to a recent study. All that virus can overwhelm even the strong protection from the vaccines.
“Three months ago, breakthroughs didn’t occur nearly at this rate because there was just so much less virus exposure in the community,” said Michael Osterholm, PhD, director of the Center for Infectious Disease Research and Policy at the University of Minnesota in Minneapolis.
Breakthroughs by the numbers
In Los Angeles County, where 69% of residents over age 12 have been fully vaccinated, COVID-19 cases are rising, and so, too, are cases that break through the protection of the vaccine.
In June, fully vaccinated people accounted for 20%, or 1 in 5, COVID cases in the county, which is the most populous in the United States. The increase mirrors Delta’s rise. The proportion of breakthrough cases is up from 11% in May, 5% in April, and 2% in March, according to the Los Angeles County Department of Public Health.
In the United Kingdom, which is collecting the best information on infections caused by variants, the estimated effectiveness of the vaccines to prevent an illness that causes symptoms dropped by about 10 points against Delta compared with Alpha (or B.1.1.7).
After two doses, vaccines prevent symptomatic infection about 79% of the time against Delta, according to data compiled by Public Health England. They are still highly effective at preventing hospitalization, 96% after two doses.
Out of 229,218 COVID infections in the United Kingdom between February and July 19, 28,773 — or 12.5% — were in fully vaccinated people. Of those breakthrough infections, 1,101, or 3.8%, required a visit to an emergency room, according to Public Health England. Just 474, or 2.9%, of fully vaccinated people required hospital admission, and 229, or less than 1%, died.
Unanswered questions
One of the biggest questions about breakthrough cases is how often people who have it may pass the virus to others.
“We know the vaccine reduces the likelihood of carrying the virus and the amount of virus you would carry,” Dr. Wen told CNN. But we don’t yet know whether a vaccinated person with a breakthrough infection may still be contagious to others.
For that reason, the Centers for Disease Control and Prevention says that fully vaccinated people still need to be tested if they have symptoms and shouldn’t be out in public for at least 10 days after a positive test.
How should fully vaccinated people behave? That depends a lot on their underlying health and whether or not they have vulnerable people around them.
If you’re older or immunocompromised, Dr. Schaffner recommends what he calls the “belt-and-suspenders approach,” in other words, do everything you can to stay safe.
“Get vaccinated for sure, but since we can’t be absolutely certain that the vaccines are going to be optimally protective and you are particularly susceptible to serious disease, you would be well advised to adopt at least one and perhaps more of the other mitigation measures,” he said.
These include wearing a mask, social distancing, making sure your spaces are well ventilated, and not spending prolonged periods of time indoors in crowded places.
Taking young children to visit vaccinated, elderly grandparents demands extra caution, again, with Delta circulating, particularly as they go back to school and start mixing with other kids.
Dr. Schaffner recommends explaining the ground rules before the visit: Hugs around the waist. No kissing. Wearing a mask while indoors with them.
Other important unanswered questions are whether breakthrough infections can lead to prolonged symptoms, or “long covid.” Most experts think that’s less likely in vaccinated people.
And Dr. Osterholm said it will be important to see whether there’s anything unusual about the breakthrough cases happening in the community.
“I think some of us have been challenged by the number of clusters that we’ve seen,” he said. “I think that really needs to be examined more.”
A version of this article first appeared on Medscape.com.
At a recent town hall meeting in Cincinnati, President Joe Biden was asked about COVID-19 cases, hospitalizations, and deaths rising in response to the Delta variant.
Touting the importance of vaccination, “We have a pandemic for those who haven’t gotten a vaccination. It’s that basic, that simple,” President Biden said at the event, which was broadcast live on CNN.
“If you’re vaccinated, you’re not going to be hospitalized, not going to the ICU unit, and not going to die,” he said, adding “you’re not going to get COVID if you have these vaccinations.”
Unfortunately, it’s not so simple. Fully vaccinated people continue to be well protected against severe disease and death, even with Delta, Because of that, many experts continue to advise caution, even if fully vaccinated.
“I was disappointed,” Leana Wen, MD, MSc, an emergency physician and visiting professor of health policy and management at George Washington University’s Milken School of Public Health in Washington, told CNN in response to the president’s statement.
“I actually thought he was answering questions as if it were a month ago. He’s not really meeting the realities of what’s happening on the ground,” she said. “I think he may have led people astray.”
Vaccines still work
Recent cases support Dr. Wen’s claim. Fully vaccinated Olympic athletes, wedding guests, healthcare workers, and even White House staff have recently tested positive. So what gives?
The vast majority of these illnesses are mild, and public health officials say they are to be expected.
“The vaccines were designed to keep us out of the hospital and to keep us from dying. That was the whole purpose of the vaccine and they’re even more successful than we anticipated,” says William Schaffner, MD, an infectious disease expert at Vanderbilt University in Nashville.
As good as they are, these shots aren’t perfect. Their protection differs from person to person depending on age and underlying health. People with immune function that’s weakened because of age or a health condition can still become seriously ill, and, in very rare cases, die after vaccination.
When people are infected with Delta, they carry approximately 1,000 times more virus compared with previous versions of the virus, according to a recent study. All that virus can overwhelm even the strong protection from the vaccines.
“Three months ago, breakthroughs didn’t occur nearly at this rate because there was just so much less virus exposure in the community,” said Michael Osterholm, PhD, director of the Center for Infectious Disease Research and Policy at the University of Minnesota in Minneapolis.
Breakthroughs by the numbers
In Los Angeles County, where 69% of residents over age 12 have been fully vaccinated, COVID-19 cases are rising, and so, too, are cases that break through the protection of the vaccine.
In June, fully vaccinated people accounted for 20%, or 1 in 5, COVID cases in the county, which is the most populous in the United States. The increase mirrors Delta’s rise. The proportion of breakthrough cases is up from 11% in May, 5% in April, and 2% in March, according to the Los Angeles County Department of Public Health.
In the United Kingdom, which is collecting the best information on infections caused by variants, the estimated effectiveness of the vaccines to prevent an illness that causes symptoms dropped by about 10 points against Delta compared with Alpha (or B.1.1.7).
After two doses, vaccines prevent symptomatic infection about 79% of the time against Delta, according to data compiled by Public Health England. They are still highly effective at preventing hospitalization, 96% after two doses.
Out of 229,218 COVID infections in the United Kingdom between February and July 19, 28,773 — or 12.5% — were in fully vaccinated people. Of those breakthrough infections, 1,101, or 3.8%, required a visit to an emergency room, according to Public Health England. Just 474, or 2.9%, of fully vaccinated people required hospital admission, and 229, or less than 1%, died.
Unanswered questions
One of the biggest questions about breakthrough cases is how often people who have it may pass the virus to others.
“We know the vaccine reduces the likelihood of carrying the virus and the amount of virus you would carry,” Dr. Wen told CNN. But we don’t yet know whether a vaccinated person with a breakthrough infection may still be contagious to others.
For that reason, the Centers for Disease Control and Prevention says that fully vaccinated people still need to be tested if they have symptoms and shouldn’t be out in public for at least 10 days after a positive test.
How should fully vaccinated people behave? That depends a lot on their underlying health and whether or not they have vulnerable people around them.
If you’re older or immunocompromised, Dr. Schaffner recommends what he calls the “belt-and-suspenders approach,” in other words, do everything you can to stay safe.
“Get vaccinated for sure, but since we can’t be absolutely certain that the vaccines are going to be optimally protective and you are particularly susceptible to serious disease, you would be well advised to adopt at least one and perhaps more of the other mitigation measures,” he said.
These include wearing a mask, social distancing, making sure your spaces are well ventilated, and not spending prolonged periods of time indoors in crowded places.
Taking young children to visit vaccinated, elderly grandparents demands extra caution, again, with Delta circulating, particularly as they go back to school and start mixing with other kids.
Dr. Schaffner recommends explaining the ground rules before the visit: Hugs around the waist. No kissing. Wearing a mask while indoors with them.
Other important unanswered questions are whether breakthrough infections can lead to prolonged symptoms, or “long covid.” Most experts think that’s less likely in vaccinated people.
And Dr. Osterholm said it will be important to see whether there’s anything unusual about the breakthrough cases happening in the community.
“I think some of us have been challenged by the number of clusters that we’ve seen,” he said. “I think that really needs to be examined more.”
A version of this article first appeared on Medscape.com.
Electrosurgical hysteroscopy: Principles and expert techniques for optimizing the resectoscope loop
Hysteroscopic mechanical morcellators have gained popularity given their ease of use. Consequently, the resectoscope loop is being used less frequently, which has resulted in less familiarity with this device. The resectoscope loop, however, not only is cost effective but also allows for multiple distinct advantages, such as cold loop dissection of myomas and the ability to obtain electrosurgical hemostasis during operative hysteroscopy.
In this article, we review the basics of electrosurgical principles, compare outcomes associated with monopolar and bipolar resectoscopes, and discuss tips and tricks for optimizing surgical techniques when using the resectoscope loop for hysteroscopic myomectomy.
Evolution of hysteroscopy
The term hysteroscopy comes from the Greek words hystera, for uterus, and skopeo, meaning “to see.” The idea to investigate the uterus dates back to the year 1000 when physicians used a mirror with light to peer into the vaginal vault.
The first known successful hysteroscopy occurred in 1869 when Pantaleoni used an endoscope with a light source to identify uterine polyps in a 60-year-old woman with abnormal uterine bleeding. In 1898, Simon Duplay and Spiro Clado published the first textbook on hysteroscopy in which they described several models of hysteroscopic instruments and techniques.
In the 1950s, Harold Horace Hopkins and Karl Storz modified the shape and length of lenses within the endoscope by substituting longer cylindrical lenses for the old spherical lenses; this permitted improved image brightness and sharpness as well as a smaller diameter of the hysteroscope. Between the 1970s and 1980s, technological improvements allowed for the creation of practical and usable hysteroscopic instruments such as the resectoscope. The resectoscope, originally used in urology for transurethral resection of the prostate, was modified for hysteroscopy by incorporating the use of electrosurgical currents to aid in procedures.
Over the past few decades, continued refinements in technology have improved visualization and surgical techniques. For example, image clarity has been markedly improved, and narrow hysteroscope diameters, as small as 3 to 5 mm, require minimal to no cervical dilation.
Monopolar and bipolar resectoscopes
Electrosurgery is the application of an alternating electrical current to tissue to achieve the clinical effects of surgical cutting or hemostasis via cell vaporization or coagulation. Current runs from the electrosurgical unit (ESU) to the active electrode of the surgical instrument, then goes from the active electrode through the patient’s tissue to the return electrode, and then travels back to the ESU. This flow of current creates an electrical circuit (FIGURE).
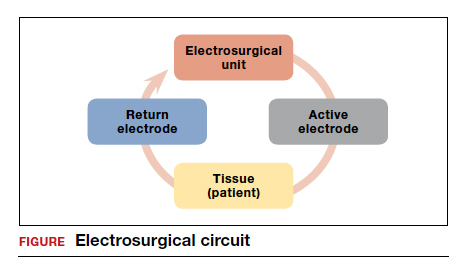
All electrosurgical devices have an active and a return electrode. The difference between monopolar and bipolar resectoscope devices lies in how the resectoscope loop is constructed. Bipolar resectoscope loops house the active and return electrodes on the same tip of the surgical device, which limits how much of the current flows through the patient. Alternatively, monopolar resectoscopes have only the active electrode on the tip of the device and the return electrode is off the surgical field, so the current flows through more of the patient. On monopolar electrosurgical devices, the current runs from the ESU to the active electrode (monopolar loop), which is then applied to tissue to produce the desired tissue effect. The current then travels via a path of least resistance from the surgical field through the patient to the return electrode, which is usually placed on the patient’s thigh, and then back to the ESU. The return electrode is often referred to as the grounding pad.
Continue to: How monopolar energy works...
How monopolar energy works
When first developed, all resectoscopes used monopolar energy. As such, throughout the 1990s, the monopolar resectoscope was the gold standard for performing electrosurgical hysteroscopy. Because the current travels a long distance between the active and the return electrode in a monopolar setup, a hypotonic, nonelectrolyte-rich medium (a poor conductor), such as glycine 1.5%, mannitol 5%, or sorbitol 3%, must be used. If an electrolyte-rich medium, such as normal saline, is used with a monopolar device, the current would be dispersed throughout the medium outside the operative field, causing unwanted tissue effects.
Although nonelectrolyte distension media improve visibility when encountering bleeding, they can be associated with hyponatremia, hyperglycemia, and even lifethreatening cerebral edema. Furthermore, glycine use is contraindicated in patients with renal or hepatic failure since oxidative deamination may cause hyperammonemia. Because of these numerous risk factors, the fluid deficit for hypotonic, nonelectrolyte distension media is limited to 1,000 mL, with a suggested maximum fluid deficit of 750 mL for elderly or fragile patients. Additionally, because the return electrode is off the surgical field in monopolar surgery, there is a risk of current diversion to the cervix, vagina, or vulva because the current travels between the active electrode on the surgical field to the return electrode on the patient’s thigh. The risk of current diversion is greater if there is damage to electrode insulation, loss of contact between the external sheath and the cervix, or direct coupling between the electrode and the surrounding tissue.
Advantages of the bipolar resectoscope
Because of the potential risks associated with the monopolar resectoscope, over the past 25 years the bipolar resectoscope emerged as an alternative due to its numerous benefits (TABLE 1).
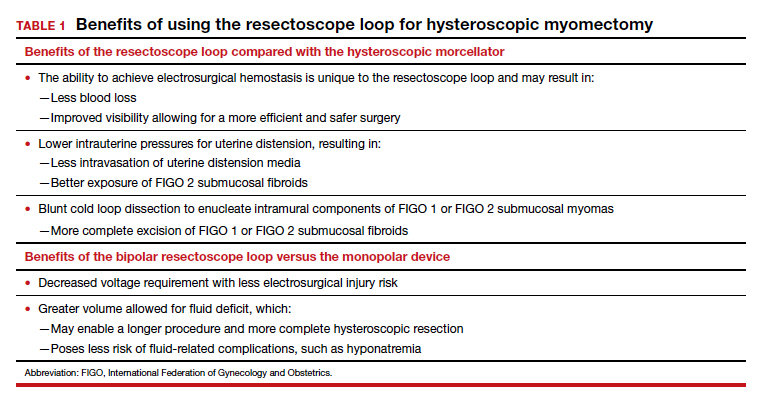
Unlike monopolar resectoscopes, bipolar resectoscopes require an electrolyte-rich distension medium such as 0.9% normal saline or lactated Ringer’s. These isotonic distension media allow a much higher fluid deficit (2,500 mL for healthy patients, 1,500 mL for elderly patients or patients with comorbidities) as the isotonic solution is safer to use. Furthermore, it allows for lower voltage settings and decreased electrical spread compared to the monopolar resectoscope since the current stays between the 2 electrodes. Because isotonic media are miscible with blood, however, a potential drawback is that in cases with bleeding, visibility may be more limited compared to hypotonic distension media.
Evidence on fertility outcomes
Several studies have compared operative and fertility outcomes with the use of monopolar versus bipolar hysteroscopy.
In a randomized controlled trial (RCT) comparing outcomes after hysteroscopy with a monopolar (glycine 1.5%) versus bipolar (0.9% normal saline) 26 French resectoscope loop, Berg and colleagues found that the only significant difference between the 2 groups was that the change in serum sodium pre and postoperatively was greater in the monopolar group despite having a smaller mean fluid deficit (765 mL vs 1,227 mL).1
Similarly, in a study of fertility outcomes after monopolar versus bipolar hysteroscopic myomectomy with use of a 26 French resectoscope Collins knife, Roy and colleagues found no significant differences in postoperative pregnancy rates or successful pregnancy outcomes, operative time, fluid deficit, or improvement in menstrual symptoms.2 However, the monopolar group had a much higher incidence of postoperative hyponatremia (30% vs 0%) that required additional days of hospitalization despite similar fluid deficits of between 600 and 700 mL.2
Similar findings were noted in another RCT that compared operative outcomes between monopolar and bipolar resectoscope usage during metroplasty for infertility, with a postoperative hyponatremia incidence of 17.1% in the monopolar group versus 0% in the bipolar group despite similar fluid deficits.3 Energy type had no effect on reproductive outcomes in either group.3
Continue to: How does the resectoscope compare with mechanical tissue removal systems?...
How does the resectoscope compare with mechanical tissue removal systems?
In 2005, the first hysteroscopic mechanical tissue removal system was introduced in the United States, providing an additional treatment method for such intrauterine masses as fibroids and polyps.
Advantages. Rather than using an electrical current, these tissue removal systems use a rotating blade with suction that is introduced through a specially designed rigid hysteroscopic sheath. As the instrument incises the pathology, the tissue is removed from the intrauterine cavity and collected in a specimen bag inside the fluid management system. This immediate removal of tissue allows for insertion of the device only once during initial entry, decreasing both the risk of perforation and operative times. Furthermore, mechanical tissue removal systems can be used with isotonic media, negating the risks associated with hypotonic media. Currently, the 2 mechanical tissue removal systems available in the United States are the TruClear and the MyoSure hysteroscopic tissue removal systems.
Studies comparing mechanical tissue removal of polyps and myomas with conventional resectoscope resection have found that mechanical tissue removal is associated with reduced operative time, fluid deficit, and number of instrument insertions.4-8 However, studies have found no significant difference in postoperative patient satisfaction.7,9
Additionally, hysteroscopic tissue removal systems have an easier learning curve. Van Dongen and colleagues conducted an RCT to compare resident-in-training comfort levels when learning to use both a mechanical tissue removal system and a traditional resectoscope; they found increased comfort with the hysteroscopic tissue removal system, suggesting greater ease of use.10
Drawbacks. Despite their many benefits, mechanical tissue removal systems have some disadvantages when compared with the resectoscope. First, mechanical tissue removal systems are associated with higher instrument costs. In addition, they have extremely limited ability to achieve hemostasis when encountering blood vessels during resection, resulting in poor visibility especially when resecting large myomas with feeding vessels.
Hysteroscopic mechanical tissue removal systems typically use higher intrauterine pressures for uterine distension compared with the resectoscope, especially when trying to improve visibility in a bloody surgical field. Increasing the intrauterine pressure with the distension media allows for compression of the blood vessels. As a result, however, submucosal fibroids classified as FIGO 2 (International Federation of Gynecology and Obstetrics) may be less visible since the higher intrauterine pressure can compress both blood vessels and submucosal fibroids
Additionally, mechanical tissue removal systems have limited ability to resect the intramural component of FIGO 1 or FIGO 2 submucosal fibroids since the intramural portion is embedded in the myometrium. Use of the resectoscope loop instead allows for a technique called the cold loop dissection, which uses the resectoscope loop to bluntly dissect and enucleate the intramural component of FIGO 1 and FIGO 2 submucosal myomas from the surrounding myometrium without activating the current. This blunt cold loop dissection technique allows for a deeper and more thorough resection. Often, if the pseudocapsule plane is identified, even the intramural component of FIGO 1 or FIGO 2 submucosal fibroids can be resected, enabling complete removal.
Lastly, mechanical tissue removal systems are not always faster than resectoscopes for all pathology. We prefer using the resectoscope for larger myomas (>3 cm) as the resectoscope allows for resection and removal of larger myoma chips, helping to decrease operative times. Given the many benefits of the resectoscope, we argue that the resectoscope loop remains a crucial instrument in operative gynecology and that learners should continue to hone their hysteroscopic skills with both the resectoscope and mechanical tissue removal systems.
Tips and tricks for hysteroscopic myomectomy with the resectoscope loop
In the video below, "Bipolar resectoscope: Optimizing safe myomectomy," we review specific surgical techniques for optimizing outcomes and safety with the resectoscope loop. These include:
- bow-and-arrow technique
- identification of the fibroid anatomy (pseudocapsule plane)
- blunt cold loop dissection
- the push-and-tuck method
- efficient electrosurgical hemostasis (TABLE 2).
Although we use bipolar energy during this resection, the resection technique using the monopolar loop is the same.
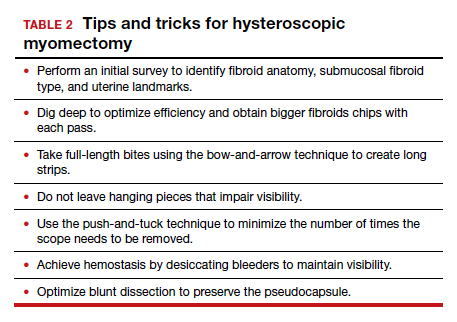
The takeaway
The resectoscope loop is a valuable tool that offers gynecologic surgeons a wider range of techniques for myomectomy. It also offers several surgical and clinical advantages. It is important to train residents in the use of both hysteroscopic mechanical tissue removal systems and resectoscope loops. ●
- Berg A, Sandvik L, Langebrekke A, et al. A randomized trial comparing monopolar electrodes using glycine 1.5% with two different types of bipolar electrodes (TCRis, Versapoint) using saline, in hysteroscopic surgery. Fertil Steril. 2009;91:1273- 1278.
- Roy KK, Metta S, Kansal Y, et al. A prospective randomized study comparing unipolar versus bipolar hysteroscopic myomectomy in infertile women. J Hum Reprod Sci. 2017;10:185-193.
- Roy KK, Kansal Y, Subbaiah M, et al. Hysteroscopic septal resection using unipolar resectoscope versus bipolar resectoscope: prospective, randomized study. J Obstet Gynaecol Res. 2015;41:952-956.
- Borg MH, Shehata A. Uterine morcellator versus resectoscopy in the management of heavy menstrual flow in reproductiveage women. J Gyn Res. 2016;2:1-8.
- Emanuel MH, Wamsteker K. The intra uterine morcellator: a new hysteroscopic operating technique to remove intrauterine polyps and myomas. J Minim Invasive Gynecol. 2005;12:62-66.
- Smith PP, Middleton LJ, Connor M, et al. Hysteroscopic morcellation compared with electrical resection of endometrial polyps: a randomized controlled trial. Obstet Gynecol. 2014;123:745-751.
- Vitale SG, Sapia F, Rapisarda AMC, et al. Hysteroscopic morcellation of submucous myomas: a systematic review. Biomed Res Int. 2017;2017:6848250.
- Stoll F, Lecointre L, Meyer N, et al. Randomized study comparing a reusable morcellator with a resectoscope in the hysteroscopic treatment of uterine polyps: the RESMO study. J Minimal Invasive Gyn. 2021;28:801-810.
- Lee MM, Matsuzono T. Hysteroscopic intrauterine morcellation of submucosal fibroids: preliminary results in Hong Kong and comparisons with conventional hysteroscopic monopolar loop resection. Hong Kong Med J. 2016;22:56-61.
- van Dongen H, Emanuel MH, Wolterbeek R, et al. Hysteroscopic morcellator for removal of intrauterine polyps and myomas: a randomized controlled pilot study among residents in training. J Minim Invasive Gynecol. 2008;15:466-471.
Hysteroscopic mechanical morcellators have gained popularity given their ease of use. Consequently, the resectoscope loop is being used less frequently, which has resulted in less familiarity with this device. The resectoscope loop, however, not only is cost effective but also allows for multiple distinct advantages, such as cold loop dissection of myomas and the ability to obtain electrosurgical hemostasis during operative hysteroscopy.
In this article, we review the basics of electrosurgical principles, compare outcomes associated with monopolar and bipolar resectoscopes, and discuss tips and tricks for optimizing surgical techniques when using the resectoscope loop for hysteroscopic myomectomy.
Evolution of hysteroscopy
The term hysteroscopy comes from the Greek words hystera, for uterus, and skopeo, meaning “to see.” The idea to investigate the uterus dates back to the year 1000 when physicians used a mirror with light to peer into the vaginal vault.
The first known successful hysteroscopy occurred in 1869 when Pantaleoni used an endoscope with a light source to identify uterine polyps in a 60-year-old woman with abnormal uterine bleeding. In 1898, Simon Duplay and Spiro Clado published the first textbook on hysteroscopy in which they described several models of hysteroscopic instruments and techniques.
In the 1950s, Harold Horace Hopkins and Karl Storz modified the shape and length of lenses within the endoscope by substituting longer cylindrical lenses for the old spherical lenses; this permitted improved image brightness and sharpness as well as a smaller diameter of the hysteroscope. Between the 1970s and 1980s, technological improvements allowed for the creation of practical and usable hysteroscopic instruments such as the resectoscope. The resectoscope, originally used in urology for transurethral resection of the prostate, was modified for hysteroscopy by incorporating the use of electrosurgical currents to aid in procedures.
Over the past few decades, continued refinements in technology have improved visualization and surgical techniques. For example, image clarity has been markedly improved, and narrow hysteroscope diameters, as small as 3 to 5 mm, require minimal to no cervical dilation.
Monopolar and bipolar resectoscopes
Electrosurgery is the application of an alternating electrical current to tissue to achieve the clinical effects of surgical cutting or hemostasis via cell vaporization or coagulation. Current runs from the electrosurgical unit (ESU) to the active electrode of the surgical instrument, then goes from the active electrode through the patient’s tissue to the return electrode, and then travels back to the ESU. This flow of current creates an electrical circuit (FIGURE).
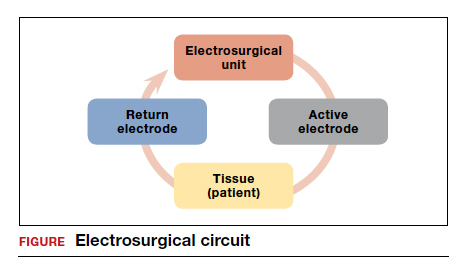
All electrosurgical devices have an active and a return electrode. The difference between monopolar and bipolar resectoscope devices lies in how the resectoscope loop is constructed. Bipolar resectoscope loops house the active and return electrodes on the same tip of the surgical device, which limits how much of the current flows through the patient. Alternatively, monopolar resectoscopes have only the active electrode on the tip of the device and the return electrode is off the surgical field, so the current flows through more of the patient. On monopolar electrosurgical devices, the current runs from the ESU to the active electrode (monopolar loop), which is then applied to tissue to produce the desired tissue effect. The current then travels via a path of least resistance from the surgical field through the patient to the return electrode, which is usually placed on the patient’s thigh, and then back to the ESU. The return electrode is often referred to as the grounding pad.
Continue to: How monopolar energy works...
How monopolar energy works
When first developed, all resectoscopes used monopolar energy. As such, throughout the 1990s, the monopolar resectoscope was the gold standard for performing electrosurgical hysteroscopy. Because the current travels a long distance between the active and the return electrode in a monopolar setup, a hypotonic, nonelectrolyte-rich medium (a poor conductor), such as glycine 1.5%, mannitol 5%, or sorbitol 3%, must be used. If an electrolyte-rich medium, such as normal saline, is used with a monopolar device, the current would be dispersed throughout the medium outside the operative field, causing unwanted tissue effects.
Although nonelectrolyte distension media improve visibility when encountering bleeding, they can be associated with hyponatremia, hyperglycemia, and even lifethreatening cerebral edema. Furthermore, glycine use is contraindicated in patients with renal or hepatic failure since oxidative deamination may cause hyperammonemia. Because of these numerous risk factors, the fluid deficit for hypotonic, nonelectrolyte distension media is limited to 1,000 mL, with a suggested maximum fluid deficit of 750 mL for elderly or fragile patients. Additionally, because the return electrode is off the surgical field in monopolar surgery, there is a risk of current diversion to the cervix, vagina, or vulva because the current travels between the active electrode on the surgical field to the return electrode on the patient’s thigh. The risk of current diversion is greater if there is damage to electrode insulation, loss of contact between the external sheath and the cervix, or direct coupling between the electrode and the surrounding tissue.
Advantages of the bipolar resectoscope
Because of the potential risks associated with the monopolar resectoscope, over the past 25 years the bipolar resectoscope emerged as an alternative due to its numerous benefits (TABLE 1).
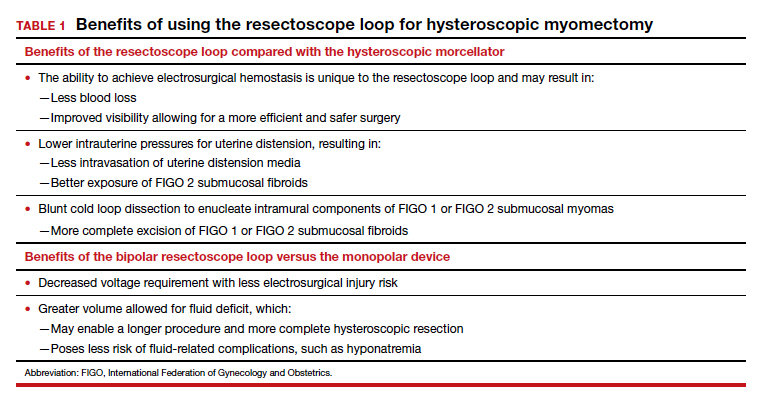
Unlike monopolar resectoscopes, bipolar resectoscopes require an electrolyte-rich distension medium such as 0.9% normal saline or lactated Ringer’s. These isotonic distension media allow a much higher fluid deficit (2,500 mL for healthy patients, 1,500 mL for elderly patients or patients with comorbidities) as the isotonic solution is safer to use. Furthermore, it allows for lower voltage settings and decreased electrical spread compared to the monopolar resectoscope since the current stays between the 2 electrodes. Because isotonic media are miscible with blood, however, a potential drawback is that in cases with bleeding, visibility may be more limited compared to hypotonic distension media.
Evidence on fertility outcomes
Several studies have compared operative and fertility outcomes with the use of monopolar versus bipolar hysteroscopy.
In a randomized controlled trial (RCT) comparing outcomes after hysteroscopy with a monopolar (glycine 1.5%) versus bipolar (0.9% normal saline) 26 French resectoscope loop, Berg and colleagues found that the only significant difference between the 2 groups was that the change in serum sodium pre and postoperatively was greater in the monopolar group despite having a smaller mean fluid deficit (765 mL vs 1,227 mL).1
Similarly, in a study of fertility outcomes after monopolar versus bipolar hysteroscopic myomectomy with use of a 26 French resectoscope Collins knife, Roy and colleagues found no significant differences in postoperative pregnancy rates or successful pregnancy outcomes, operative time, fluid deficit, or improvement in menstrual symptoms.2 However, the monopolar group had a much higher incidence of postoperative hyponatremia (30% vs 0%) that required additional days of hospitalization despite similar fluid deficits of between 600 and 700 mL.2
Similar findings were noted in another RCT that compared operative outcomes between monopolar and bipolar resectoscope usage during metroplasty for infertility, with a postoperative hyponatremia incidence of 17.1% in the monopolar group versus 0% in the bipolar group despite similar fluid deficits.3 Energy type had no effect on reproductive outcomes in either group.3
Continue to: How does the resectoscope compare with mechanical tissue removal systems?...
How does the resectoscope compare with mechanical tissue removal systems?
In 2005, the first hysteroscopic mechanical tissue removal system was introduced in the United States, providing an additional treatment method for such intrauterine masses as fibroids and polyps.
Advantages. Rather than using an electrical current, these tissue removal systems use a rotating blade with suction that is introduced through a specially designed rigid hysteroscopic sheath. As the instrument incises the pathology, the tissue is removed from the intrauterine cavity and collected in a specimen bag inside the fluid management system. This immediate removal of tissue allows for insertion of the device only once during initial entry, decreasing both the risk of perforation and operative times. Furthermore, mechanical tissue removal systems can be used with isotonic media, negating the risks associated with hypotonic media. Currently, the 2 mechanical tissue removal systems available in the United States are the TruClear and the MyoSure hysteroscopic tissue removal systems.
Studies comparing mechanical tissue removal of polyps and myomas with conventional resectoscope resection have found that mechanical tissue removal is associated with reduced operative time, fluid deficit, and number of instrument insertions.4-8 However, studies have found no significant difference in postoperative patient satisfaction.7,9
Additionally, hysteroscopic tissue removal systems have an easier learning curve. Van Dongen and colleagues conducted an RCT to compare resident-in-training comfort levels when learning to use both a mechanical tissue removal system and a traditional resectoscope; they found increased comfort with the hysteroscopic tissue removal system, suggesting greater ease of use.10
Drawbacks. Despite their many benefits, mechanical tissue removal systems have some disadvantages when compared with the resectoscope. First, mechanical tissue removal systems are associated with higher instrument costs. In addition, they have extremely limited ability to achieve hemostasis when encountering blood vessels during resection, resulting in poor visibility especially when resecting large myomas with feeding vessels.
Hysteroscopic mechanical tissue removal systems typically use higher intrauterine pressures for uterine distension compared with the resectoscope, especially when trying to improve visibility in a bloody surgical field. Increasing the intrauterine pressure with the distension media allows for compression of the blood vessels. As a result, however, submucosal fibroids classified as FIGO 2 (International Federation of Gynecology and Obstetrics) may be less visible since the higher intrauterine pressure can compress both blood vessels and submucosal fibroids
Additionally, mechanical tissue removal systems have limited ability to resect the intramural component of FIGO 1 or FIGO 2 submucosal fibroids since the intramural portion is embedded in the myometrium. Use of the resectoscope loop instead allows for a technique called the cold loop dissection, which uses the resectoscope loop to bluntly dissect and enucleate the intramural component of FIGO 1 and FIGO 2 submucosal myomas from the surrounding myometrium without activating the current. This blunt cold loop dissection technique allows for a deeper and more thorough resection. Often, if the pseudocapsule plane is identified, even the intramural component of FIGO 1 or FIGO 2 submucosal fibroids can be resected, enabling complete removal.
Lastly, mechanical tissue removal systems are not always faster than resectoscopes for all pathology. We prefer using the resectoscope for larger myomas (>3 cm) as the resectoscope allows for resection and removal of larger myoma chips, helping to decrease operative times. Given the many benefits of the resectoscope, we argue that the resectoscope loop remains a crucial instrument in operative gynecology and that learners should continue to hone their hysteroscopic skills with both the resectoscope and mechanical tissue removal systems.
Tips and tricks for hysteroscopic myomectomy with the resectoscope loop
In the video below, "Bipolar resectoscope: Optimizing safe myomectomy," we review specific surgical techniques for optimizing outcomes and safety with the resectoscope loop. These include:
- bow-and-arrow technique
- identification of the fibroid anatomy (pseudocapsule plane)
- blunt cold loop dissection
- the push-and-tuck method
- efficient electrosurgical hemostasis (TABLE 2).
Although we use bipolar energy during this resection, the resection technique using the monopolar loop is the same.
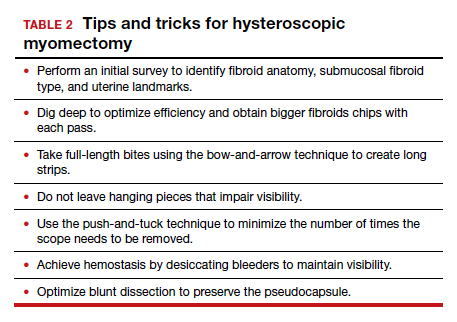
The takeaway
The resectoscope loop is a valuable tool that offers gynecologic surgeons a wider range of techniques for myomectomy. It also offers several surgical and clinical advantages. It is important to train residents in the use of both hysteroscopic mechanical tissue removal systems and resectoscope loops. ●
Hysteroscopic mechanical morcellators have gained popularity given their ease of use. Consequently, the resectoscope loop is being used less frequently, which has resulted in less familiarity with this device. The resectoscope loop, however, not only is cost effective but also allows for multiple distinct advantages, such as cold loop dissection of myomas and the ability to obtain electrosurgical hemostasis during operative hysteroscopy.
In this article, we review the basics of electrosurgical principles, compare outcomes associated with monopolar and bipolar resectoscopes, and discuss tips and tricks for optimizing surgical techniques when using the resectoscope loop for hysteroscopic myomectomy.
Evolution of hysteroscopy
The term hysteroscopy comes from the Greek words hystera, for uterus, and skopeo, meaning “to see.” The idea to investigate the uterus dates back to the year 1000 when physicians used a mirror with light to peer into the vaginal vault.
The first known successful hysteroscopy occurred in 1869 when Pantaleoni used an endoscope with a light source to identify uterine polyps in a 60-year-old woman with abnormal uterine bleeding. In 1898, Simon Duplay and Spiro Clado published the first textbook on hysteroscopy in which they described several models of hysteroscopic instruments and techniques.
In the 1950s, Harold Horace Hopkins and Karl Storz modified the shape and length of lenses within the endoscope by substituting longer cylindrical lenses for the old spherical lenses; this permitted improved image brightness and sharpness as well as a smaller diameter of the hysteroscope. Between the 1970s and 1980s, technological improvements allowed for the creation of practical and usable hysteroscopic instruments such as the resectoscope. The resectoscope, originally used in urology for transurethral resection of the prostate, was modified for hysteroscopy by incorporating the use of electrosurgical currents to aid in procedures.
Over the past few decades, continued refinements in technology have improved visualization and surgical techniques. For example, image clarity has been markedly improved, and narrow hysteroscope diameters, as small as 3 to 5 mm, require minimal to no cervical dilation.
Monopolar and bipolar resectoscopes
Electrosurgery is the application of an alternating electrical current to tissue to achieve the clinical effects of surgical cutting or hemostasis via cell vaporization or coagulation. Current runs from the electrosurgical unit (ESU) to the active electrode of the surgical instrument, then goes from the active electrode through the patient’s tissue to the return electrode, and then travels back to the ESU. This flow of current creates an electrical circuit (FIGURE).
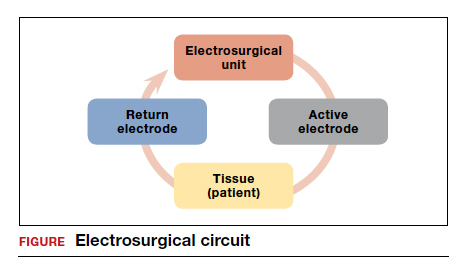
All electrosurgical devices have an active and a return electrode. The difference between monopolar and bipolar resectoscope devices lies in how the resectoscope loop is constructed. Bipolar resectoscope loops house the active and return electrodes on the same tip of the surgical device, which limits how much of the current flows through the patient. Alternatively, monopolar resectoscopes have only the active electrode on the tip of the device and the return electrode is off the surgical field, so the current flows through more of the patient. On monopolar electrosurgical devices, the current runs from the ESU to the active electrode (monopolar loop), which is then applied to tissue to produce the desired tissue effect. The current then travels via a path of least resistance from the surgical field through the patient to the return electrode, which is usually placed on the patient’s thigh, and then back to the ESU. The return electrode is often referred to as the grounding pad.
Continue to: How monopolar energy works...
How monopolar energy works
When first developed, all resectoscopes used monopolar energy. As such, throughout the 1990s, the monopolar resectoscope was the gold standard for performing electrosurgical hysteroscopy. Because the current travels a long distance between the active and the return electrode in a monopolar setup, a hypotonic, nonelectrolyte-rich medium (a poor conductor), such as glycine 1.5%, mannitol 5%, or sorbitol 3%, must be used. If an electrolyte-rich medium, such as normal saline, is used with a monopolar device, the current would be dispersed throughout the medium outside the operative field, causing unwanted tissue effects.
Although nonelectrolyte distension media improve visibility when encountering bleeding, they can be associated with hyponatremia, hyperglycemia, and even lifethreatening cerebral edema. Furthermore, glycine use is contraindicated in patients with renal or hepatic failure since oxidative deamination may cause hyperammonemia. Because of these numerous risk factors, the fluid deficit for hypotonic, nonelectrolyte distension media is limited to 1,000 mL, with a suggested maximum fluid deficit of 750 mL for elderly or fragile patients. Additionally, because the return electrode is off the surgical field in monopolar surgery, there is a risk of current diversion to the cervix, vagina, or vulva because the current travels between the active electrode on the surgical field to the return electrode on the patient’s thigh. The risk of current diversion is greater if there is damage to electrode insulation, loss of contact between the external sheath and the cervix, or direct coupling between the electrode and the surrounding tissue.
Advantages of the bipolar resectoscope
Because of the potential risks associated with the monopolar resectoscope, over the past 25 years the bipolar resectoscope emerged as an alternative due to its numerous benefits (TABLE 1).
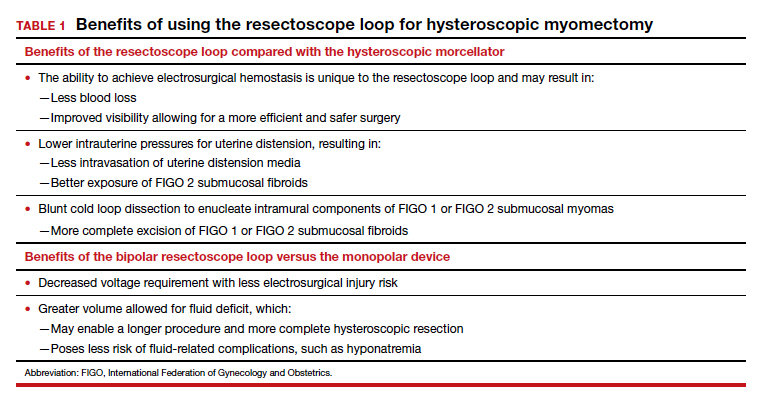
Unlike monopolar resectoscopes, bipolar resectoscopes require an electrolyte-rich distension medium such as 0.9% normal saline or lactated Ringer’s. These isotonic distension media allow a much higher fluid deficit (2,500 mL for healthy patients, 1,500 mL for elderly patients or patients with comorbidities) as the isotonic solution is safer to use. Furthermore, it allows for lower voltage settings and decreased electrical spread compared to the monopolar resectoscope since the current stays between the 2 electrodes. Because isotonic media are miscible with blood, however, a potential drawback is that in cases with bleeding, visibility may be more limited compared to hypotonic distension media.
Evidence on fertility outcomes
Several studies have compared operative and fertility outcomes with the use of monopolar versus bipolar hysteroscopy.
In a randomized controlled trial (RCT) comparing outcomes after hysteroscopy with a monopolar (glycine 1.5%) versus bipolar (0.9% normal saline) 26 French resectoscope loop, Berg and colleagues found that the only significant difference between the 2 groups was that the change in serum sodium pre and postoperatively was greater in the monopolar group despite having a smaller mean fluid deficit (765 mL vs 1,227 mL).1
Similarly, in a study of fertility outcomes after monopolar versus bipolar hysteroscopic myomectomy with use of a 26 French resectoscope Collins knife, Roy and colleagues found no significant differences in postoperative pregnancy rates or successful pregnancy outcomes, operative time, fluid deficit, or improvement in menstrual symptoms.2 However, the monopolar group had a much higher incidence of postoperative hyponatremia (30% vs 0%) that required additional days of hospitalization despite similar fluid deficits of between 600 and 700 mL.2
Similar findings were noted in another RCT that compared operative outcomes between monopolar and bipolar resectoscope usage during metroplasty for infertility, with a postoperative hyponatremia incidence of 17.1% in the monopolar group versus 0% in the bipolar group despite similar fluid deficits.3 Energy type had no effect on reproductive outcomes in either group.3
Continue to: How does the resectoscope compare with mechanical tissue removal systems?...
How does the resectoscope compare with mechanical tissue removal systems?
In 2005, the first hysteroscopic mechanical tissue removal system was introduced in the United States, providing an additional treatment method for such intrauterine masses as fibroids and polyps.
Advantages. Rather than using an electrical current, these tissue removal systems use a rotating blade with suction that is introduced through a specially designed rigid hysteroscopic sheath. As the instrument incises the pathology, the tissue is removed from the intrauterine cavity and collected in a specimen bag inside the fluid management system. This immediate removal of tissue allows for insertion of the device only once during initial entry, decreasing both the risk of perforation and operative times. Furthermore, mechanical tissue removal systems can be used with isotonic media, negating the risks associated with hypotonic media. Currently, the 2 mechanical tissue removal systems available in the United States are the TruClear and the MyoSure hysteroscopic tissue removal systems.
Studies comparing mechanical tissue removal of polyps and myomas with conventional resectoscope resection have found that mechanical tissue removal is associated with reduced operative time, fluid deficit, and number of instrument insertions.4-8 However, studies have found no significant difference in postoperative patient satisfaction.7,9
Additionally, hysteroscopic tissue removal systems have an easier learning curve. Van Dongen and colleagues conducted an RCT to compare resident-in-training comfort levels when learning to use both a mechanical tissue removal system and a traditional resectoscope; they found increased comfort with the hysteroscopic tissue removal system, suggesting greater ease of use.10
Drawbacks. Despite their many benefits, mechanical tissue removal systems have some disadvantages when compared with the resectoscope. First, mechanical tissue removal systems are associated with higher instrument costs. In addition, they have extremely limited ability to achieve hemostasis when encountering blood vessels during resection, resulting in poor visibility especially when resecting large myomas with feeding vessels.
Hysteroscopic mechanical tissue removal systems typically use higher intrauterine pressures for uterine distension compared with the resectoscope, especially when trying to improve visibility in a bloody surgical field. Increasing the intrauterine pressure with the distension media allows for compression of the blood vessels. As a result, however, submucosal fibroids classified as FIGO 2 (International Federation of Gynecology and Obstetrics) may be less visible since the higher intrauterine pressure can compress both blood vessels and submucosal fibroids
Additionally, mechanical tissue removal systems have limited ability to resect the intramural component of FIGO 1 or FIGO 2 submucosal fibroids since the intramural portion is embedded in the myometrium. Use of the resectoscope loop instead allows for a technique called the cold loop dissection, which uses the resectoscope loop to bluntly dissect and enucleate the intramural component of FIGO 1 and FIGO 2 submucosal myomas from the surrounding myometrium without activating the current. This blunt cold loop dissection technique allows for a deeper and more thorough resection. Often, if the pseudocapsule plane is identified, even the intramural component of FIGO 1 or FIGO 2 submucosal fibroids can be resected, enabling complete removal.
Lastly, mechanical tissue removal systems are not always faster than resectoscopes for all pathology. We prefer using the resectoscope for larger myomas (>3 cm) as the resectoscope allows for resection and removal of larger myoma chips, helping to decrease operative times. Given the many benefits of the resectoscope, we argue that the resectoscope loop remains a crucial instrument in operative gynecology and that learners should continue to hone their hysteroscopic skills with both the resectoscope and mechanical tissue removal systems.
Tips and tricks for hysteroscopic myomectomy with the resectoscope loop
In the video below, "Bipolar resectoscope: Optimizing safe myomectomy," we review specific surgical techniques for optimizing outcomes and safety with the resectoscope loop. These include:
- bow-and-arrow technique
- identification of the fibroid anatomy (pseudocapsule plane)
- blunt cold loop dissection
- the push-and-tuck method
- efficient electrosurgical hemostasis (TABLE 2).
Although we use bipolar energy during this resection, the resection technique using the monopolar loop is the same.
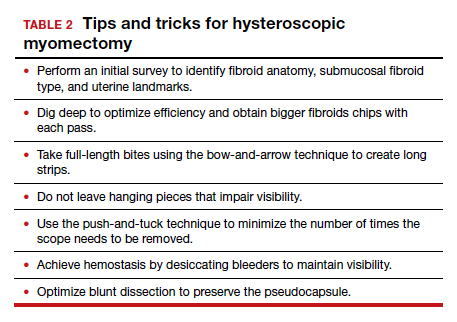
The takeaway
The resectoscope loop is a valuable tool that offers gynecologic surgeons a wider range of techniques for myomectomy. It also offers several surgical and clinical advantages. It is important to train residents in the use of both hysteroscopic mechanical tissue removal systems and resectoscope loops. ●
- Berg A, Sandvik L, Langebrekke A, et al. A randomized trial comparing monopolar electrodes using glycine 1.5% with two different types of bipolar electrodes (TCRis, Versapoint) using saline, in hysteroscopic surgery. Fertil Steril. 2009;91:1273- 1278.
- Roy KK, Metta S, Kansal Y, et al. A prospective randomized study comparing unipolar versus bipolar hysteroscopic myomectomy in infertile women. J Hum Reprod Sci. 2017;10:185-193.
- Roy KK, Kansal Y, Subbaiah M, et al. Hysteroscopic septal resection using unipolar resectoscope versus bipolar resectoscope: prospective, randomized study. J Obstet Gynaecol Res. 2015;41:952-956.
- Borg MH, Shehata A. Uterine morcellator versus resectoscopy in the management of heavy menstrual flow in reproductiveage women. J Gyn Res. 2016;2:1-8.
- Emanuel MH, Wamsteker K. The intra uterine morcellator: a new hysteroscopic operating technique to remove intrauterine polyps and myomas. J Minim Invasive Gynecol. 2005;12:62-66.
- Smith PP, Middleton LJ, Connor M, et al. Hysteroscopic morcellation compared with electrical resection of endometrial polyps: a randomized controlled trial. Obstet Gynecol. 2014;123:745-751.
- Vitale SG, Sapia F, Rapisarda AMC, et al. Hysteroscopic morcellation of submucous myomas: a systematic review. Biomed Res Int. 2017;2017:6848250.
- Stoll F, Lecointre L, Meyer N, et al. Randomized study comparing a reusable morcellator with a resectoscope in the hysteroscopic treatment of uterine polyps: the RESMO study. J Minimal Invasive Gyn. 2021;28:801-810.
- Lee MM, Matsuzono T. Hysteroscopic intrauterine morcellation of submucosal fibroids: preliminary results in Hong Kong and comparisons with conventional hysteroscopic monopolar loop resection. Hong Kong Med J. 2016;22:56-61.
- van Dongen H, Emanuel MH, Wolterbeek R, et al. Hysteroscopic morcellator for removal of intrauterine polyps and myomas: a randomized controlled pilot study among residents in training. J Minim Invasive Gynecol. 2008;15:466-471.
- Berg A, Sandvik L, Langebrekke A, et al. A randomized trial comparing monopolar electrodes using glycine 1.5% with two different types of bipolar electrodes (TCRis, Versapoint) using saline, in hysteroscopic surgery. Fertil Steril. 2009;91:1273- 1278.
- Roy KK, Metta S, Kansal Y, et al. A prospective randomized study comparing unipolar versus bipolar hysteroscopic myomectomy in infertile women. J Hum Reprod Sci. 2017;10:185-193.
- Roy KK, Kansal Y, Subbaiah M, et al. Hysteroscopic septal resection using unipolar resectoscope versus bipolar resectoscope: prospective, randomized study. J Obstet Gynaecol Res. 2015;41:952-956.
- Borg MH, Shehata A. Uterine morcellator versus resectoscopy in the management of heavy menstrual flow in reproductiveage women. J Gyn Res. 2016;2:1-8.
- Emanuel MH, Wamsteker K. The intra uterine morcellator: a new hysteroscopic operating technique to remove intrauterine polyps and myomas. J Minim Invasive Gynecol. 2005;12:62-66.
- Smith PP, Middleton LJ, Connor M, et al. Hysteroscopic morcellation compared with electrical resection of endometrial polyps: a randomized controlled trial. Obstet Gynecol. 2014;123:745-751.
- Vitale SG, Sapia F, Rapisarda AMC, et al. Hysteroscopic morcellation of submucous myomas: a systematic review. Biomed Res Int. 2017;2017:6848250.
- Stoll F, Lecointre L, Meyer N, et al. Randomized study comparing a reusable morcellator with a resectoscope in the hysteroscopic treatment of uterine polyps: the RESMO study. J Minimal Invasive Gyn. 2021;28:801-810.
- Lee MM, Matsuzono T. Hysteroscopic intrauterine morcellation of submucosal fibroids: preliminary results in Hong Kong and comparisons with conventional hysteroscopic monopolar loop resection. Hong Kong Med J. 2016;22:56-61.
- van Dongen H, Emanuel MH, Wolterbeek R, et al. Hysteroscopic morcellator for removal of intrauterine polyps and myomas: a randomized controlled pilot study among residents in training. J Minim Invasive Gynecol. 2008;15:466-471.
CDC panel updates info on rare side effect after J&J vaccine
Despite recent reports of Guillain-Barré Syndrome (GBS) after the Johnson & Johnson vaccine,
The company also presented new data suggesting that the shots generate strong immune responses against circulating variants and that antibodies generated by the vaccine stay elevated for at least 8 months.
Members of the Advisory Committee on Immunization Practices (ACIP) did not vote, but discussed and affirmed their support for recent decisions by the Food and Drug Administration and CDC to update patient information about the very low risk of GBS that appears to be associated with the vaccine, but to continue offering the vaccine to people in the United States.
The Johnson & Johnson shot has been a minor player in the U.S. vaccination campaign, accounting for less than 4% of all vaccine doses given in this country. Still, the single-dose inoculation, which doesn’t require ultra-cold storage, has been important for reaching people in rural areas, through mobile clinics, at colleges and primary care offices, and in vulnerable populations – those who are incarcerated or homeless.
The FDA says it has received reports of 100 cases of GBS after the Johnson & Johnson vaccine in its Vaccine Adverse Event Reporting System database through the end of June. The cases are still under investigation.
To date, more than 12 million doses of the vaccine have been administered, making the rate of GBS 8.1 cases for every million doses administered.
Although it is still extremely rare, that’s above the expected background rate of GBS of 1.6 cases for every million people, said Grace Lee, MD, a Stanford, Calif., pediatrician who chairs the ACIP’s Vaccine Safety Technical Work Group.
So far, most GBS cases (61%) have been among men. The midpoint age of the cases was 57 years. The average time to onset was 14 days, and 98% of cases occurred within 42 days of the shot. Facial paralysis has been associated with an estimated 30%-50% of cases. One person, who had heart failure, high blood pressure, and diabetes, has died.
Still, the benefits of the vaccine far outweigh its risks. For every million doses given to people over age 50, the vaccine prevents nearly 7,500 COVID-19 hospitalizations and nearly 100 deaths in women, and more than 13,000 COVID-19 hospitalizations and more than 2,400 deaths in men.
Rates of GBS after the mRNA vaccines made by Pfizer and Moderna were around 1 case for every 1 million doses given, which is not above the rate that would be expected without vaccination.
The link to the Johnson & Johnson vaccine prompted the FDA to add a warning to the vaccine’s patient safety information on July 12.
Also in July, the European Medicines Agency recommended a similar warning for the product information of the AstraZeneca vaccine Vaxzevria, which relies on similar technology.
Good against variants
Johnson & Johnson also presented new information showing its vaccine maintained high levels of neutralizing antibodies against four of the so-called “variants of concern” – Alpha, Gamma, Beta, and Delta. The protection generated by the vaccine lasted for at least 8 months after the shot, the company said.
“We’re still learning about the duration of protection and the breadth of coverage against this evolving variant landscape for each of the authorized vaccines,” said Mathai Mammen, MD, PhD, global head of research and development at Janssen, the company that makes the vaccine for J&J.
The company also said that its vaccine generated very strong T-cell responses. T cells destroy infected cells and, along with antibodies, are an important part of the body’s immune response.
Antibody levels and T-cell responses are markers for immunity. Measuring these levels isn’t the same as proving that shots can fend off an infection.
It’s still unclear exactly which component of the immune response is most important for fighting off COVID-19.
Dr. Mammen said the companies are still gathering that clinical data, and would present it soon.
“We will have a better view of the clinical efficacy in the coming weeks,” he said.
A version of this article first appeared on Medscape.com.
Despite recent reports of Guillain-Barré Syndrome (GBS) after the Johnson & Johnson vaccine,
The company also presented new data suggesting that the shots generate strong immune responses against circulating variants and that antibodies generated by the vaccine stay elevated for at least 8 months.
Members of the Advisory Committee on Immunization Practices (ACIP) did not vote, but discussed and affirmed their support for recent decisions by the Food and Drug Administration and CDC to update patient information about the very low risk of GBS that appears to be associated with the vaccine, but to continue offering the vaccine to people in the United States.
The Johnson & Johnson shot has been a minor player in the U.S. vaccination campaign, accounting for less than 4% of all vaccine doses given in this country. Still, the single-dose inoculation, which doesn’t require ultra-cold storage, has been important for reaching people in rural areas, through mobile clinics, at colleges and primary care offices, and in vulnerable populations – those who are incarcerated or homeless.
The FDA says it has received reports of 100 cases of GBS after the Johnson & Johnson vaccine in its Vaccine Adverse Event Reporting System database through the end of June. The cases are still under investigation.
To date, more than 12 million doses of the vaccine have been administered, making the rate of GBS 8.1 cases for every million doses administered.
Although it is still extremely rare, that’s above the expected background rate of GBS of 1.6 cases for every million people, said Grace Lee, MD, a Stanford, Calif., pediatrician who chairs the ACIP’s Vaccine Safety Technical Work Group.
So far, most GBS cases (61%) have been among men. The midpoint age of the cases was 57 years. The average time to onset was 14 days, and 98% of cases occurred within 42 days of the shot. Facial paralysis has been associated with an estimated 30%-50% of cases. One person, who had heart failure, high blood pressure, and diabetes, has died.
Still, the benefits of the vaccine far outweigh its risks. For every million doses given to people over age 50, the vaccine prevents nearly 7,500 COVID-19 hospitalizations and nearly 100 deaths in women, and more than 13,000 COVID-19 hospitalizations and more than 2,400 deaths in men.
Rates of GBS after the mRNA vaccines made by Pfizer and Moderna were around 1 case for every 1 million doses given, which is not above the rate that would be expected without vaccination.
The link to the Johnson & Johnson vaccine prompted the FDA to add a warning to the vaccine’s patient safety information on July 12.
Also in July, the European Medicines Agency recommended a similar warning for the product information of the AstraZeneca vaccine Vaxzevria, which relies on similar technology.
Good against variants
Johnson & Johnson also presented new information showing its vaccine maintained high levels of neutralizing antibodies against four of the so-called “variants of concern” – Alpha, Gamma, Beta, and Delta. The protection generated by the vaccine lasted for at least 8 months after the shot, the company said.
“We’re still learning about the duration of protection and the breadth of coverage against this evolving variant landscape for each of the authorized vaccines,” said Mathai Mammen, MD, PhD, global head of research and development at Janssen, the company that makes the vaccine for J&J.
The company also said that its vaccine generated very strong T-cell responses. T cells destroy infected cells and, along with antibodies, are an important part of the body’s immune response.
Antibody levels and T-cell responses are markers for immunity. Measuring these levels isn’t the same as proving that shots can fend off an infection.
It’s still unclear exactly which component of the immune response is most important for fighting off COVID-19.
Dr. Mammen said the companies are still gathering that clinical data, and would present it soon.
“We will have a better view of the clinical efficacy in the coming weeks,” he said.
A version of this article first appeared on Medscape.com.
Despite recent reports of Guillain-Barré Syndrome (GBS) after the Johnson & Johnson vaccine,
The company also presented new data suggesting that the shots generate strong immune responses against circulating variants and that antibodies generated by the vaccine stay elevated for at least 8 months.
Members of the Advisory Committee on Immunization Practices (ACIP) did not vote, but discussed and affirmed their support for recent decisions by the Food and Drug Administration and CDC to update patient information about the very low risk of GBS that appears to be associated with the vaccine, but to continue offering the vaccine to people in the United States.
The Johnson & Johnson shot has been a minor player in the U.S. vaccination campaign, accounting for less than 4% of all vaccine doses given in this country. Still, the single-dose inoculation, which doesn’t require ultra-cold storage, has been important for reaching people in rural areas, through mobile clinics, at colleges and primary care offices, and in vulnerable populations – those who are incarcerated or homeless.
The FDA says it has received reports of 100 cases of GBS after the Johnson & Johnson vaccine in its Vaccine Adverse Event Reporting System database through the end of June. The cases are still under investigation.
To date, more than 12 million doses of the vaccine have been administered, making the rate of GBS 8.1 cases for every million doses administered.
Although it is still extremely rare, that’s above the expected background rate of GBS of 1.6 cases for every million people, said Grace Lee, MD, a Stanford, Calif., pediatrician who chairs the ACIP’s Vaccine Safety Technical Work Group.
So far, most GBS cases (61%) have been among men. The midpoint age of the cases was 57 years. The average time to onset was 14 days, and 98% of cases occurred within 42 days of the shot. Facial paralysis has been associated with an estimated 30%-50% of cases. One person, who had heart failure, high blood pressure, and diabetes, has died.
Still, the benefits of the vaccine far outweigh its risks. For every million doses given to people over age 50, the vaccine prevents nearly 7,500 COVID-19 hospitalizations and nearly 100 deaths in women, and more than 13,000 COVID-19 hospitalizations and more than 2,400 deaths in men.
Rates of GBS after the mRNA vaccines made by Pfizer and Moderna were around 1 case for every 1 million doses given, which is not above the rate that would be expected without vaccination.
The link to the Johnson & Johnson vaccine prompted the FDA to add a warning to the vaccine’s patient safety information on July 12.
Also in July, the European Medicines Agency recommended a similar warning for the product information of the AstraZeneca vaccine Vaxzevria, which relies on similar technology.
Good against variants
Johnson & Johnson also presented new information showing its vaccine maintained high levels of neutralizing antibodies against four of the so-called “variants of concern” – Alpha, Gamma, Beta, and Delta. The protection generated by the vaccine lasted for at least 8 months after the shot, the company said.
“We’re still learning about the duration of protection and the breadth of coverage against this evolving variant landscape for each of the authorized vaccines,” said Mathai Mammen, MD, PhD, global head of research and development at Janssen, the company that makes the vaccine for J&J.
The company also said that its vaccine generated very strong T-cell responses. T cells destroy infected cells and, along with antibodies, are an important part of the body’s immune response.
Antibody levels and T-cell responses are markers for immunity. Measuring these levels isn’t the same as proving that shots can fend off an infection.
It’s still unclear exactly which component of the immune response is most important for fighting off COVID-19.
Dr. Mammen said the companies are still gathering that clinical data, and would present it soon.
“We will have a better view of the clinical efficacy in the coming weeks,” he said.
A version of this article first appeared on Medscape.com.
Advice on biopsies, workups, and referrals
Over the next 2 months we will dedicate this column to some general tips and pearls from the perspective of a gynecologic oncologist to guide general obstetrician gynecologists in the workup and management of preinvasive or invasive gynecologic diseases. The goal of these recommendations is to minimize misdiagnosis or delayed diagnosis and avoid unnecessary or untimely referrals.
Perform biopsy, not Pap smears, on visible cervical and vaginal lesions
The purpose of the Pap smear is to screen asymptomatic patients for cervical dysplasia or microscopic invasive disease. Cytology is an unreliable diagnostic tool for visible, symptomatic lesions in large part because of sampling errors, and the lack of architectural information in cytologic versus histopathologic specimens. Invasive lesions can be mischaracterized as preinvasive on a Pap smear. This can result in delayed diagnosis and unnecessary diagnostic procedures. For example, if a visible, abnormal-appearing, cervical lesion is seen during a routine visit and a Pap smear is performed (rather than a biopsy of the mass), the patient may receive an incorrect preliminary diagnosis of “high-grade dysplasia, carcinoma in situ” as it can be difficult to distinguish invasive carcinoma from carcinoma in situ on cytology. If the patient and provider do not understand the limitations of Pap smears in diagnosing invasive cancers, they may be falsely reassured and possibly delay or abstain from follow-up for an excisional procedure. If she does return for the loop electrosurgical excision procedure (LEEP), there might still be unnecessary delays in making referrals and definitive treatment while waiting for results. Radical hysterectomy may not promptly follow because, if performed within 6 weeks of an excisional procedure, it is associated with a significantly higher risk for perioperative complication, and therefore, if the excisional procedure was unnecessary to begin with, there may be additional time lost that need not be.1
Some clinicians avoid biopsy of visible lesions because they are concerned about bleeding complications that might arise in the office. Straightforward strategies to control bleeding are readily available in most gynecology offices, especially those already equipped for procedures such as LEEP and colposcopy. Prior to performing the biopsy, clinicians should ensure that they have supplies such as gauze sponges and ring forceps or packing forceps, silver nitrate, and ferric subsulfate solution (“Monsel’s solution”) close at hand. In the vast majority of cases, direct pressure for 5 minutes with gauze sponges and ferric subsulfate is highly effective at resolving most bleeding from a cervical or vaginal biopsy site. If this does not bring hemostasis, cautery devices or suture can be employed. If all else fails, be prepared to place vaginal packing (always with the insertion of a urinary Foley catheter to prevent urinary retention). In my experience, this is rarely needed.
Wherever possible, visible cervical or vaginal (or vulvar, see below) lesions should be biopsied for histopathology, sampling representative areas of the most concerning portion, in order to minimize misdiagnosis and expedite referral and definitive treatment. For necrotic-appearing lesions I recommend taking multiple samples of the tumor, as necrotic, nonviable tissue can prevent accurate diagnosis of a cancer. In general, Pap smears should be reserved as screening tests for asymptomatic women without visible pathology.
Don’t treat or refer low-grade dysplasia, even if persistent
Increasingly we are understanding that low-grade dysplasia of the lower genital tract (CIN I, VAIN I, VIN I) is less a precursor for cancer, and more a phenomenon of benign HPV-associated changes.2 This HPV change may be chronically persistent, may require years of observation and serial Pap smears, and may be a general nuisance for the patient. However, current guidelines do not recommend intervention for low-grade dysplasia of the lower genital tract.2 Interventions to resect these lesions can result in morbidity, including perineal pain, vaginal scarring, and cervical stenosis or insufficiency. Given the extremely low risk for progression to cancer, these morbidities do not outweigh any small potential benefit.
When I am conferring with patients who have chronic low-grade dysplasia I spend a great deal of time exploring their understanding of the diagnosis and its pathophysiology, their fears, and their expectation regarding “success” of treatment. I spend the time educating them that this is a sequela of chronic viral infection that will not be eradicated with local surgical excisions, that their cancer risk and need for surveillance would persist even if surgical intervention were offered, and that the side effects of treatment would outweigh any benefit from the small risk of cancer or high-grade dysplasia.
In summary, the treatment of choice for persistent low-grade dysplasia of the lower genital tract is comprehensive patient education, not surgical resection or referral to gynecologic oncology.
Repeat sampling if there’s a discordance between imaging and biopsy results
Delay in cancer diagnosis is one of the greatest concerns for front-line gynecology providers. One of the more modifiable strategies to avoid missed or delayed diagnosis is to ensure that there is concordance between clinical findings and testing results. Otherwise said: The results and findings should make sense in aggregate. An example was cited above in which a visible cervical mass demonstrated CIN III on cytologic testing. Another common example is a biopsy result of “scant benign endometrium” in a patient with postmenopausal bleeding and thickened endometrial stripe on ultrasound. In both of these cases there is clear discordance between physical findings and the results of pathology sampling. A pathology report, in all of its black and white certitude, seems like the most reliable source of information. However, always trust your clinical judgment. If the clinical picture is suggesting something far worse than these limited, often random or blind samplings, I recommend repeated or more extensive sampling (for example, dilation and curettage). At the very least, schedule close follow-up with repeated sampling if the symptom or finding persists. The emphasis here is on scheduled follow-up, rather than “p.r.n.,” because a patient who was given a “normal” pathology result to explain her abnormal symptoms may not volunteer that those symptoms are persistent as she may feel that anything sinister was already ruled out. Make certain that you explain the potential for misdiagnosis as the reason for why you would like to see her back shortly to ensure the issue has resolved.
Biopsy vulvar lesions, minimize empiric treatment
Vulvar cancer is notoriously associated with delayed diagnosis. Unfortunately, it is commonplace for gynecologic oncologists to see women who have vulvar cancers that have been empirically treated, sometimes for months or years, with steroids or other topical agents. If a lesion on the vulva is characteristically benign in appearance (such as condyloma or lichen sclerosis), it may be reasonable to start empiric treatment. However, all patients who are treated without biopsy should be rescheduled for a planned follow-up appointment in 2-3 months. If the lesion/area remains unchanged, or worse, the lesion should be biopsied before proceeding with a change in therapy or continued therapy. Once again, don’t rely on patients to return for evaluation if the lesion doesn’t improve. Many patients assume that our first empiric diagnosis is “gospel,” and therefore may not return if the treatment doesn’t work. Meanwhile, providers may assume that patients will know that there is uncertainty in our interpretation and that they will know to report if the initial treatment didn’t work. These assumptions are the recipe for delayed diagnosis. If there is too great a burden on the patient to schedule a return visit because of social or financial reasons then the patient should have a biopsy prior to initiation of treatment. As a rule, empiric treatment is not a good strategy for patients without good access to follow-up.
Dr. Rossi is assistant professor in the division of gynecologic oncology at the University of North Carolina at Chapel Hill. She has no relevant financial disclosures. Email her at [email protected].
References
1. Sullivan S. et al Gynecol Oncol. 2017 Feb;144(2):294-8.
2. Perkins R .et al J Low Genit Tract Dis. 2020 Apr;24(2):102-31.
Over the next 2 months we will dedicate this column to some general tips and pearls from the perspective of a gynecologic oncologist to guide general obstetrician gynecologists in the workup and management of preinvasive or invasive gynecologic diseases. The goal of these recommendations is to minimize misdiagnosis or delayed diagnosis and avoid unnecessary or untimely referrals.
Perform biopsy, not Pap smears, on visible cervical and vaginal lesions
The purpose of the Pap smear is to screen asymptomatic patients for cervical dysplasia or microscopic invasive disease. Cytology is an unreliable diagnostic tool for visible, symptomatic lesions in large part because of sampling errors, and the lack of architectural information in cytologic versus histopathologic specimens. Invasive lesions can be mischaracterized as preinvasive on a Pap smear. This can result in delayed diagnosis and unnecessary diagnostic procedures. For example, if a visible, abnormal-appearing, cervical lesion is seen during a routine visit and a Pap smear is performed (rather than a biopsy of the mass), the patient may receive an incorrect preliminary diagnosis of “high-grade dysplasia, carcinoma in situ” as it can be difficult to distinguish invasive carcinoma from carcinoma in situ on cytology. If the patient and provider do not understand the limitations of Pap smears in diagnosing invasive cancers, they may be falsely reassured and possibly delay or abstain from follow-up for an excisional procedure. If she does return for the loop electrosurgical excision procedure (LEEP), there might still be unnecessary delays in making referrals and definitive treatment while waiting for results. Radical hysterectomy may not promptly follow because, if performed within 6 weeks of an excisional procedure, it is associated with a significantly higher risk for perioperative complication, and therefore, if the excisional procedure was unnecessary to begin with, there may be additional time lost that need not be.1
Some clinicians avoid biopsy of visible lesions because they are concerned about bleeding complications that might arise in the office. Straightforward strategies to control bleeding are readily available in most gynecology offices, especially those already equipped for procedures such as LEEP and colposcopy. Prior to performing the biopsy, clinicians should ensure that they have supplies such as gauze sponges and ring forceps or packing forceps, silver nitrate, and ferric subsulfate solution (“Monsel’s solution”) close at hand. In the vast majority of cases, direct pressure for 5 minutes with gauze sponges and ferric subsulfate is highly effective at resolving most bleeding from a cervical or vaginal biopsy site. If this does not bring hemostasis, cautery devices or suture can be employed. If all else fails, be prepared to place vaginal packing (always with the insertion of a urinary Foley catheter to prevent urinary retention). In my experience, this is rarely needed.
Wherever possible, visible cervical or vaginal (or vulvar, see below) lesions should be biopsied for histopathology, sampling representative areas of the most concerning portion, in order to minimize misdiagnosis and expedite referral and definitive treatment. For necrotic-appearing lesions I recommend taking multiple samples of the tumor, as necrotic, nonviable tissue can prevent accurate diagnosis of a cancer. In general, Pap smears should be reserved as screening tests for asymptomatic women without visible pathology.
Don’t treat or refer low-grade dysplasia, even if persistent
Increasingly we are understanding that low-grade dysplasia of the lower genital tract (CIN I, VAIN I, VIN I) is less a precursor for cancer, and more a phenomenon of benign HPV-associated changes.2 This HPV change may be chronically persistent, may require years of observation and serial Pap smears, and may be a general nuisance for the patient. However, current guidelines do not recommend intervention for low-grade dysplasia of the lower genital tract.2 Interventions to resect these lesions can result in morbidity, including perineal pain, vaginal scarring, and cervical stenosis or insufficiency. Given the extremely low risk for progression to cancer, these morbidities do not outweigh any small potential benefit.
When I am conferring with patients who have chronic low-grade dysplasia I spend a great deal of time exploring their understanding of the diagnosis and its pathophysiology, their fears, and their expectation regarding “success” of treatment. I spend the time educating them that this is a sequela of chronic viral infection that will not be eradicated with local surgical excisions, that their cancer risk and need for surveillance would persist even if surgical intervention were offered, and that the side effects of treatment would outweigh any benefit from the small risk of cancer or high-grade dysplasia.
In summary, the treatment of choice for persistent low-grade dysplasia of the lower genital tract is comprehensive patient education, not surgical resection or referral to gynecologic oncology.
Repeat sampling if there’s a discordance between imaging and biopsy results
Delay in cancer diagnosis is one of the greatest concerns for front-line gynecology providers. One of the more modifiable strategies to avoid missed or delayed diagnosis is to ensure that there is concordance between clinical findings and testing results. Otherwise said: The results and findings should make sense in aggregate. An example was cited above in which a visible cervical mass demonstrated CIN III on cytologic testing. Another common example is a biopsy result of “scant benign endometrium” in a patient with postmenopausal bleeding and thickened endometrial stripe on ultrasound. In both of these cases there is clear discordance between physical findings and the results of pathology sampling. A pathology report, in all of its black and white certitude, seems like the most reliable source of information. However, always trust your clinical judgment. If the clinical picture is suggesting something far worse than these limited, often random or blind samplings, I recommend repeated or more extensive sampling (for example, dilation and curettage). At the very least, schedule close follow-up with repeated sampling if the symptom or finding persists. The emphasis here is on scheduled follow-up, rather than “p.r.n.,” because a patient who was given a “normal” pathology result to explain her abnormal symptoms may not volunteer that those symptoms are persistent as she may feel that anything sinister was already ruled out. Make certain that you explain the potential for misdiagnosis as the reason for why you would like to see her back shortly to ensure the issue has resolved.
Biopsy vulvar lesions, minimize empiric treatment
Vulvar cancer is notoriously associated with delayed diagnosis. Unfortunately, it is commonplace for gynecologic oncologists to see women who have vulvar cancers that have been empirically treated, sometimes for months or years, with steroids or other topical agents. If a lesion on the vulva is characteristically benign in appearance (such as condyloma or lichen sclerosis), it may be reasonable to start empiric treatment. However, all patients who are treated without biopsy should be rescheduled for a planned follow-up appointment in 2-3 months. If the lesion/area remains unchanged, or worse, the lesion should be biopsied before proceeding with a change in therapy or continued therapy. Once again, don’t rely on patients to return for evaluation if the lesion doesn’t improve. Many patients assume that our first empiric diagnosis is “gospel,” and therefore may not return if the treatment doesn’t work. Meanwhile, providers may assume that patients will know that there is uncertainty in our interpretation and that they will know to report if the initial treatment didn’t work. These assumptions are the recipe for delayed diagnosis. If there is too great a burden on the patient to schedule a return visit because of social or financial reasons then the patient should have a biopsy prior to initiation of treatment. As a rule, empiric treatment is not a good strategy for patients without good access to follow-up.
Dr. Rossi is assistant professor in the division of gynecologic oncology at the University of North Carolina at Chapel Hill. She has no relevant financial disclosures. Email her at [email protected].
References
1. Sullivan S. et al Gynecol Oncol. 2017 Feb;144(2):294-8.
2. Perkins R .et al J Low Genit Tract Dis. 2020 Apr;24(2):102-31.
Over the next 2 months we will dedicate this column to some general tips and pearls from the perspective of a gynecologic oncologist to guide general obstetrician gynecologists in the workup and management of preinvasive or invasive gynecologic diseases. The goal of these recommendations is to minimize misdiagnosis or delayed diagnosis and avoid unnecessary or untimely referrals.
Perform biopsy, not Pap smears, on visible cervical and vaginal lesions
The purpose of the Pap smear is to screen asymptomatic patients for cervical dysplasia or microscopic invasive disease. Cytology is an unreliable diagnostic tool for visible, symptomatic lesions in large part because of sampling errors, and the lack of architectural information in cytologic versus histopathologic specimens. Invasive lesions can be mischaracterized as preinvasive on a Pap smear. This can result in delayed diagnosis and unnecessary diagnostic procedures. For example, if a visible, abnormal-appearing, cervical lesion is seen during a routine visit and a Pap smear is performed (rather than a biopsy of the mass), the patient may receive an incorrect preliminary diagnosis of “high-grade dysplasia, carcinoma in situ” as it can be difficult to distinguish invasive carcinoma from carcinoma in situ on cytology. If the patient and provider do not understand the limitations of Pap smears in diagnosing invasive cancers, they may be falsely reassured and possibly delay or abstain from follow-up for an excisional procedure. If she does return for the loop electrosurgical excision procedure (LEEP), there might still be unnecessary delays in making referrals and definitive treatment while waiting for results. Radical hysterectomy may not promptly follow because, if performed within 6 weeks of an excisional procedure, it is associated with a significantly higher risk for perioperative complication, and therefore, if the excisional procedure was unnecessary to begin with, there may be additional time lost that need not be.1
Some clinicians avoid biopsy of visible lesions because they are concerned about bleeding complications that might arise in the office. Straightforward strategies to control bleeding are readily available in most gynecology offices, especially those already equipped for procedures such as LEEP and colposcopy. Prior to performing the biopsy, clinicians should ensure that they have supplies such as gauze sponges and ring forceps or packing forceps, silver nitrate, and ferric subsulfate solution (“Monsel’s solution”) close at hand. In the vast majority of cases, direct pressure for 5 minutes with gauze sponges and ferric subsulfate is highly effective at resolving most bleeding from a cervical or vaginal biopsy site. If this does not bring hemostasis, cautery devices or suture can be employed. If all else fails, be prepared to place vaginal packing (always with the insertion of a urinary Foley catheter to prevent urinary retention). In my experience, this is rarely needed.
Wherever possible, visible cervical or vaginal (or vulvar, see below) lesions should be biopsied for histopathology, sampling representative areas of the most concerning portion, in order to minimize misdiagnosis and expedite referral and definitive treatment. For necrotic-appearing lesions I recommend taking multiple samples of the tumor, as necrotic, nonviable tissue can prevent accurate diagnosis of a cancer. In general, Pap smears should be reserved as screening tests for asymptomatic women without visible pathology.
Don’t treat or refer low-grade dysplasia, even if persistent
Increasingly we are understanding that low-grade dysplasia of the lower genital tract (CIN I, VAIN I, VIN I) is less a precursor for cancer, and more a phenomenon of benign HPV-associated changes.2 This HPV change may be chronically persistent, may require years of observation and serial Pap smears, and may be a general nuisance for the patient. However, current guidelines do not recommend intervention for low-grade dysplasia of the lower genital tract.2 Interventions to resect these lesions can result in morbidity, including perineal pain, vaginal scarring, and cervical stenosis or insufficiency. Given the extremely low risk for progression to cancer, these morbidities do not outweigh any small potential benefit.
When I am conferring with patients who have chronic low-grade dysplasia I spend a great deal of time exploring their understanding of the diagnosis and its pathophysiology, their fears, and their expectation regarding “success” of treatment. I spend the time educating them that this is a sequela of chronic viral infection that will not be eradicated with local surgical excisions, that their cancer risk and need for surveillance would persist even if surgical intervention were offered, and that the side effects of treatment would outweigh any benefit from the small risk of cancer or high-grade dysplasia.
In summary, the treatment of choice for persistent low-grade dysplasia of the lower genital tract is comprehensive patient education, not surgical resection or referral to gynecologic oncology.
Repeat sampling if there’s a discordance between imaging and biopsy results
Delay in cancer diagnosis is one of the greatest concerns for front-line gynecology providers. One of the more modifiable strategies to avoid missed or delayed diagnosis is to ensure that there is concordance between clinical findings and testing results. Otherwise said: The results and findings should make sense in aggregate. An example was cited above in which a visible cervical mass demonstrated CIN III on cytologic testing. Another common example is a biopsy result of “scant benign endometrium” in a patient with postmenopausal bleeding and thickened endometrial stripe on ultrasound. In both of these cases there is clear discordance between physical findings and the results of pathology sampling. A pathology report, in all of its black and white certitude, seems like the most reliable source of information. However, always trust your clinical judgment. If the clinical picture is suggesting something far worse than these limited, often random or blind samplings, I recommend repeated or more extensive sampling (for example, dilation and curettage). At the very least, schedule close follow-up with repeated sampling if the symptom or finding persists. The emphasis here is on scheduled follow-up, rather than “p.r.n.,” because a patient who was given a “normal” pathology result to explain her abnormal symptoms may not volunteer that those symptoms are persistent as she may feel that anything sinister was already ruled out. Make certain that you explain the potential for misdiagnosis as the reason for why you would like to see her back shortly to ensure the issue has resolved.
Biopsy vulvar lesions, minimize empiric treatment
Vulvar cancer is notoriously associated with delayed diagnosis. Unfortunately, it is commonplace for gynecologic oncologists to see women who have vulvar cancers that have been empirically treated, sometimes for months or years, with steroids or other topical agents. If a lesion on the vulva is characteristically benign in appearance (such as condyloma or lichen sclerosis), it may be reasonable to start empiric treatment. However, all patients who are treated without biopsy should be rescheduled for a planned follow-up appointment in 2-3 months. If the lesion/area remains unchanged, or worse, the lesion should be biopsied before proceeding with a change in therapy or continued therapy. Once again, don’t rely on patients to return for evaluation if the lesion doesn’t improve. Many patients assume that our first empiric diagnosis is “gospel,” and therefore may not return if the treatment doesn’t work. Meanwhile, providers may assume that patients will know that there is uncertainty in our interpretation and that they will know to report if the initial treatment didn’t work. These assumptions are the recipe for delayed diagnosis. If there is too great a burden on the patient to schedule a return visit because of social or financial reasons then the patient should have a biopsy prior to initiation of treatment. As a rule, empiric treatment is not a good strategy for patients without good access to follow-up.
Dr. Rossi is assistant professor in the division of gynecologic oncology at the University of North Carolina at Chapel Hill. She has no relevant financial disclosures. Email her at [email protected].
References
1. Sullivan S. et al Gynecol Oncol. 2017 Feb;144(2):294-8.
2. Perkins R .et al J Low Genit Tract Dis. 2020 Apr;24(2):102-31.
CDC revamps STI treatment guidelines
On July 22, the Centers for Disease Control and Prevention released updated sexually transmitted infection treatment guidelines to reflect current screening, testing, and treatment recommendations. The guidelines were last updated in 2015.
The new recommendations come at a pivotal moment in the field’s history, Kimberly Workowski, MD, a medical officer at the CDC’s Division of STD Prevention, told this news organization in an email. “The COVID-19 pandemic has caused decreased clinic capacity and drug and diagnostic test kit shortages,” she says. Many of these shortages have been resolved, she added, and it is important that health care professionals use the most current evidence-based recommendations for screening and management of STIs.
Updates to these guidelines were necessary to reflect “continued advances in research in the prevention of STIs, new interventions in terms of STI prevention, and thirdly, changing epidemiology,” Jeffrey Klausner, MD, MPH, an STI specialist with the Keck School of Medicine at the University of Southern California, Los Angeles, said in an interview. “There’s been increased concern about antimicrobial resistance, and that’s really driven some of the key changes in these new STI treatment guidelines.”
Notable updates to the guidelines include the following:
- Updated treatment recommendations for gonorrhea, chlamydia, , and
- Two-step testing for diagnosing genital virus
- Expanded risk factors for testing in pregnant women
- Information on FDA-cleared rectal and oral tests to diagnose chlamydia and gonorrhea
- A recommendation that universal screening be conducted at least once in a lifetime for adults aged 18 years and older
Dr. Workowski emphasized updates to gonorrhea treatment that built on the recommendation published in December 2020 in Morbidity and Mortality Weekly Report. The CDC now recommends that gonorrhea be treated with a single 500-mg injection of ceftriaxone, and if chlamydial infection is not ruled out, treating with a regimen of 100 mg of oral doxycycline taken twice daily for 7 days. Other gonorrhea treatment recommendations include retesting patients 3 months after treatment and that a test of cure be conducted for people with pharyngeal gonorrhea 1 to 2 weeks after treatment, using either culture or nucleic-acid amplification tests.
“Effectively treating gonorrhea remains a public health priority,” Dr. Workowski said. “Gonorrhea can rapidly develop antibiotic resistance and is the second most commonly reported bacterial STI in the U.S., increasing 56% from 2015 to 2019.”
The updates to syphilis screening for pregnant women are also important, added Dr. Klausner. “We’ve seen a dramatic and shameful rise in congenital syphilis,” he said. In addition to screening all pregnant women at the first prenatal visit, the CDC recommends retesting for syphilis at 28 weeks’ gestation and at delivery if the mother lives in an area where the prevalence of syphilis is high or if she is at risk of acquiring syphilis during pregnancy. An expectant mother is at higher risk if she has multiple sex partners, has an STI during pregnancy, has a partner with an STI, has a new sex partner, or misuses drugs, the recommendations state.
Dr. Klausner also noted that the updates provide more robust guidelines for treating transgender individuals and incarcerated people.
The treatment guidelines are available online along with a wall chart and a pocket guide that summarizes these updates. The mobile app with the 2015 guidelines will be retired at the end of July 2021, Dr. Workowski said. An app with these updated treatment recommendations is in development and will be available later this year.
A version of this article first appeared on Medscape.com.
On July 22, the Centers for Disease Control and Prevention released updated sexually transmitted infection treatment guidelines to reflect current screening, testing, and treatment recommendations. The guidelines were last updated in 2015.
The new recommendations come at a pivotal moment in the field’s history, Kimberly Workowski, MD, a medical officer at the CDC’s Division of STD Prevention, told this news organization in an email. “The COVID-19 pandemic has caused decreased clinic capacity and drug and diagnostic test kit shortages,” she says. Many of these shortages have been resolved, she added, and it is important that health care professionals use the most current evidence-based recommendations for screening and management of STIs.
Updates to these guidelines were necessary to reflect “continued advances in research in the prevention of STIs, new interventions in terms of STI prevention, and thirdly, changing epidemiology,” Jeffrey Klausner, MD, MPH, an STI specialist with the Keck School of Medicine at the University of Southern California, Los Angeles, said in an interview. “There’s been increased concern about antimicrobial resistance, and that’s really driven some of the key changes in these new STI treatment guidelines.”
Notable updates to the guidelines include the following:
- Updated treatment recommendations for gonorrhea, chlamydia, , and
- Two-step testing for diagnosing genital virus
- Expanded risk factors for testing in pregnant women
- Information on FDA-cleared rectal and oral tests to diagnose chlamydia and gonorrhea
- A recommendation that universal screening be conducted at least once in a lifetime for adults aged 18 years and older
Dr. Workowski emphasized updates to gonorrhea treatment that built on the recommendation published in December 2020 in Morbidity and Mortality Weekly Report. The CDC now recommends that gonorrhea be treated with a single 500-mg injection of ceftriaxone, and if chlamydial infection is not ruled out, treating with a regimen of 100 mg of oral doxycycline taken twice daily for 7 days. Other gonorrhea treatment recommendations include retesting patients 3 months after treatment and that a test of cure be conducted for people with pharyngeal gonorrhea 1 to 2 weeks after treatment, using either culture or nucleic-acid amplification tests.
“Effectively treating gonorrhea remains a public health priority,” Dr. Workowski said. “Gonorrhea can rapidly develop antibiotic resistance and is the second most commonly reported bacterial STI in the U.S., increasing 56% from 2015 to 2019.”
The updates to syphilis screening for pregnant women are also important, added Dr. Klausner. “We’ve seen a dramatic and shameful rise in congenital syphilis,” he said. In addition to screening all pregnant women at the first prenatal visit, the CDC recommends retesting for syphilis at 28 weeks’ gestation and at delivery if the mother lives in an area where the prevalence of syphilis is high or if she is at risk of acquiring syphilis during pregnancy. An expectant mother is at higher risk if she has multiple sex partners, has an STI during pregnancy, has a partner with an STI, has a new sex partner, or misuses drugs, the recommendations state.
Dr. Klausner also noted that the updates provide more robust guidelines for treating transgender individuals and incarcerated people.
The treatment guidelines are available online along with a wall chart and a pocket guide that summarizes these updates. The mobile app with the 2015 guidelines will be retired at the end of July 2021, Dr. Workowski said. An app with these updated treatment recommendations is in development and will be available later this year.
A version of this article first appeared on Medscape.com.
On July 22, the Centers for Disease Control and Prevention released updated sexually transmitted infection treatment guidelines to reflect current screening, testing, and treatment recommendations. The guidelines were last updated in 2015.
The new recommendations come at a pivotal moment in the field’s history, Kimberly Workowski, MD, a medical officer at the CDC’s Division of STD Prevention, told this news organization in an email. “The COVID-19 pandemic has caused decreased clinic capacity and drug and diagnostic test kit shortages,” she says. Many of these shortages have been resolved, she added, and it is important that health care professionals use the most current evidence-based recommendations for screening and management of STIs.
Updates to these guidelines were necessary to reflect “continued advances in research in the prevention of STIs, new interventions in terms of STI prevention, and thirdly, changing epidemiology,” Jeffrey Klausner, MD, MPH, an STI specialist with the Keck School of Medicine at the University of Southern California, Los Angeles, said in an interview. “There’s been increased concern about antimicrobial resistance, and that’s really driven some of the key changes in these new STI treatment guidelines.”
Notable updates to the guidelines include the following:
- Updated treatment recommendations for gonorrhea, chlamydia, , and
- Two-step testing for diagnosing genital virus
- Expanded risk factors for testing in pregnant women
- Information on FDA-cleared rectal and oral tests to diagnose chlamydia and gonorrhea
- A recommendation that universal screening be conducted at least once in a lifetime for adults aged 18 years and older
Dr. Workowski emphasized updates to gonorrhea treatment that built on the recommendation published in December 2020 in Morbidity and Mortality Weekly Report. The CDC now recommends that gonorrhea be treated with a single 500-mg injection of ceftriaxone, and if chlamydial infection is not ruled out, treating with a regimen of 100 mg of oral doxycycline taken twice daily for 7 days. Other gonorrhea treatment recommendations include retesting patients 3 months after treatment and that a test of cure be conducted for people with pharyngeal gonorrhea 1 to 2 weeks after treatment, using either culture or nucleic-acid amplification tests.
“Effectively treating gonorrhea remains a public health priority,” Dr. Workowski said. “Gonorrhea can rapidly develop antibiotic resistance and is the second most commonly reported bacterial STI in the U.S., increasing 56% from 2015 to 2019.”
The updates to syphilis screening for pregnant women are also important, added Dr. Klausner. “We’ve seen a dramatic and shameful rise in congenital syphilis,” he said. In addition to screening all pregnant women at the first prenatal visit, the CDC recommends retesting for syphilis at 28 weeks’ gestation and at delivery if the mother lives in an area where the prevalence of syphilis is high or if she is at risk of acquiring syphilis during pregnancy. An expectant mother is at higher risk if she has multiple sex partners, has an STI during pregnancy, has a partner with an STI, has a new sex partner, or misuses drugs, the recommendations state.
Dr. Klausner also noted that the updates provide more robust guidelines for treating transgender individuals and incarcerated people.
The treatment guidelines are available online along with a wall chart and a pocket guide that summarizes these updates. The mobile app with the 2015 guidelines will be retired at the end of July 2021, Dr. Workowski said. An app with these updated treatment recommendations is in development and will be available later this year.
A version of this article first appeared on Medscape.com.
Necessary or not, COVID booster shots are probably on the horizon
The drug maker Pfizer recently announced that vaccinated people are likely to need a booster shot to be effectively protected against new variants of COVID-19 and that the company would apply for Food and Drug Administration emergency use authorization for the shot. Top government health officials immediately and emphatically announced that the booster isn’t needed right now – and held firm to that position even after Pfizer’s top scientist made his case and shared preliminary data with them on July 12.
This has led to confusion. Is the protection that has allowed them to see loved ones and go out to dinner fading?
Ultimately, the question of whether a booster is needed is unlikely to determine the FDA’s decision. If recent history is predictive, booster shots will be here before long. That’s because of the outdated, 60-year-old basic standard the FDA uses to authorize medicines for sale: Is a new drug “safe and effective?”
The FDA, using that standard, will very likely have to authorize Pfizer’s booster for emergency use, as it did the company’s prior COVID shot. The booster is likely to be safe – hundreds of millions have taken the earlier shots – and Pfizer reported that it dramatically increases a vaccinated person’s antibodies against SARS-CoV-2. From that perspective, it may also be considered very effective.
But does that kind of efficacy matter? Is a higher level of antibodies needed to protect vaccinated Americans? Though antibody levels may wane some over time, the current vaccines deliver perfectly good immunity so far.
What if a booster is safe and effective in one sense but simply not needed – at least for now?
Reliance on the simple “safe and effective” standard – which certainly sounds reasonable – is a relic of a time when there were far fewer and simpler medicines available to treat diseases and before pharmaceutical manufacturing became one of the world’s biggest businesses.
The FDA’s 1938 landmark legislation focused primarily on safety after more than 100 Americans died from a raspberry-flavored liquid form of an early antibiotic because one of its ingredients was used as antifreeze. The 1962 Kefauver-Harris Amendments to the Federal Food, Drug, and Cosmetic Act set out more specific requirements for drug approval: Companies must scientifically prove a drug’s effectiveness through “adequate and well-controlled studies.”
In today’s pharmaceutical universe, a simple “safe and effective” determination is not always an adequate bar, and it can be manipulated to sell drugs of questionable value. There’s also big money involved: Pfizer is already projecting $26 billion in COVID revenue in 2021.
The United States’ continued use of this standard to let drugs into the market has led to the approval of expensive, not necessarily very effective drugs. In 2014, for example, the FDA approved a toenail fungus drug that can cost up to $1,500 a month and that studies showed cured fewer than 10% of patients after a year of treatment. That’s more effective than doing nothing but less effective and more costly than a number of other treatments for this bothersome malady.
It has also led to a plethora of high-priced drugs to treat diseases like cancers, multiple sclerosis and type 2 diabetes that are all more effective than a placebo but have often not been tested very much against one another to determine which are most effective.
In today’s complex world, clarification is needed to determine just what kind of effectiveness the FDA should demand. And should that be the job of the FDA alone?
For example, should drugmakers prove a drug is significantly more effective than products already on the market? Or demonstrate cost-effectiveness – the health value of a product relative to its price – a metric used by Britain’s health system? And in which cases is effectiveness against a surrogate marker – like an antibody level – a good enough stand-in for whether a drug will have a significant impact on a patient’s health?
In most industrialized countries, broad access to the national market is a two-step process, said Aaron Kesselheim, a professor of medicine at Harvard Medical School, Boston, who studies drug development, marketing and law and recently served on an FDA advisory committee. The first part certifies that a drug is sufficiently safe and effective. That is immediately followed by an independent health technology assessment to see where it fits in the treatment armamentarium, including, in some countries, whether it is useful enough to be sold at all at the stated price. But there’s no such automatic process in the United States.
When Pfizer applies for authorization, the FDA may well clear a booster for the U.S. market. The Centers for Disease Control and Prevention, likely with advice from National Institutes of Health experts, will then have to decide whether to recommend it and for whom. This judgment call usually determines whether insurers will cover it. Pfizer is likely to profit handsomely from a government authorization, and the company will gain some revenue even if only the worried well, who can pay out of pocket, decide to get the shot.
To make any recommendation on a booster, government experts say they need more data. They could, for example, as Anthony S. Fauci, MD, has suggested, eventually green-light the additional vaccine shot only for a small group of patients at high risk for a deadly infection, such as the very old or transplant recipients who take immunosuppressant drugs, as some other countries have done.
But until the United States refines the FDA’s “safe and effective” standard or adds a second layer of vetting, when new products hit the market and manufacturers promote them, Americans will be left to decipher whose version of effective and necessary matters to them.
KHN (Kaiser Health News) is a national newsroom that produces in-depth journalism about health issues. Together with Policy Analysis and Polling, KHN is one of the three major operating programs at KFF (Kaiser Family Foundation). KFF is an endowed nonprofit organization providing information on health issues to the nation.
The drug maker Pfizer recently announced that vaccinated people are likely to need a booster shot to be effectively protected against new variants of COVID-19 and that the company would apply for Food and Drug Administration emergency use authorization for the shot. Top government health officials immediately and emphatically announced that the booster isn’t needed right now – and held firm to that position even after Pfizer’s top scientist made his case and shared preliminary data with them on July 12.
This has led to confusion. Is the protection that has allowed them to see loved ones and go out to dinner fading?
Ultimately, the question of whether a booster is needed is unlikely to determine the FDA’s decision. If recent history is predictive, booster shots will be here before long. That’s because of the outdated, 60-year-old basic standard the FDA uses to authorize medicines for sale: Is a new drug “safe and effective?”
The FDA, using that standard, will very likely have to authorize Pfizer’s booster for emergency use, as it did the company’s prior COVID shot. The booster is likely to be safe – hundreds of millions have taken the earlier shots – and Pfizer reported that it dramatically increases a vaccinated person’s antibodies against SARS-CoV-2. From that perspective, it may also be considered very effective.
But does that kind of efficacy matter? Is a higher level of antibodies needed to protect vaccinated Americans? Though antibody levels may wane some over time, the current vaccines deliver perfectly good immunity so far.
What if a booster is safe and effective in one sense but simply not needed – at least for now?
Reliance on the simple “safe and effective” standard – which certainly sounds reasonable – is a relic of a time when there were far fewer and simpler medicines available to treat diseases and before pharmaceutical manufacturing became one of the world’s biggest businesses.
The FDA’s 1938 landmark legislation focused primarily on safety after more than 100 Americans died from a raspberry-flavored liquid form of an early antibiotic because one of its ingredients was used as antifreeze. The 1962 Kefauver-Harris Amendments to the Federal Food, Drug, and Cosmetic Act set out more specific requirements for drug approval: Companies must scientifically prove a drug’s effectiveness through “adequate and well-controlled studies.”
In today’s pharmaceutical universe, a simple “safe and effective” determination is not always an adequate bar, and it can be manipulated to sell drugs of questionable value. There’s also big money involved: Pfizer is already projecting $26 billion in COVID revenue in 2021.
The United States’ continued use of this standard to let drugs into the market has led to the approval of expensive, not necessarily very effective drugs. In 2014, for example, the FDA approved a toenail fungus drug that can cost up to $1,500 a month and that studies showed cured fewer than 10% of patients after a year of treatment. That’s more effective than doing nothing but less effective and more costly than a number of other treatments for this bothersome malady.
It has also led to a plethora of high-priced drugs to treat diseases like cancers, multiple sclerosis and type 2 diabetes that are all more effective than a placebo but have often not been tested very much against one another to determine which are most effective.
In today’s complex world, clarification is needed to determine just what kind of effectiveness the FDA should demand. And should that be the job of the FDA alone?
For example, should drugmakers prove a drug is significantly more effective than products already on the market? Or demonstrate cost-effectiveness – the health value of a product relative to its price – a metric used by Britain’s health system? And in which cases is effectiveness against a surrogate marker – like an antibody level – a good enough stand-in for whether a drug will have a significant impact on a patient’s health?
In most industrialized countries, broad access to the national market is a two-step process, said Aaron Kesselheim, a professor of medicine at Harvard Medical School, Boston, who studies drug development, marketing and law and recently served on an FDA advisory committee. The first part certifies that a drug is sufficiently safe and effective. That is immediately followed by an independent health technology assessment to see where it fits in the treatment armamentarium, including, in some countries, whether it is useful enough to be sold at all at the stated price. But there’s no such automatic process in the United States.
When Pfizer applies for authorization, the FDA may well clear a booster for the U.S. market. The Centers for Disease Control and Prevention, likely with advice from National Institutes of Health experts, will then have to decide whether to recommend it and for whom. This judgment call usually determines whether insurers will cover it. Pfizer is likely to profit handsomely from a government authorization, and the company will gain some revenue even if only the worried well, who can pay out of pocket, decide to get the shot.
To make any recommendation on a booster, government experts say they need more data. They could, for example, as Anthony S. Fauci, MD, has suggested, eventually green-light the additional vaccine shot only for a small group of patients at high risk for a deadly infection, such as the very old or transplant recipients who take immunosuppressant drugs, as some other countries have done.
But until the United States refines the FDA’s “safe and effective” standard or adds a second layer of vetting, when new products hit the market and manufacturers promote them, Americans will be left to decipher whose version of effective and necessary matters to them.
KHN (Kaiser Health News) is a national newsroom that produces in-depth journalism about health issues. Together with Policy Analysis and Polling, KHN is one of the three major operating programs at KFF (Kaiser Family Foundation). KFF is an endowed nonprofit organization providing information on health issues to the nation.
The drug maker Pfizer recently announced that vaccinated people are likely to need a booster shot to be effectively protected against new variants of COVID-19 and that the company would apply for Food and Drug Administration emergency use authorization for the shot. Top government health officials immediately and emphatically announced that the booster isn’t needed right now – and held firm to that position even after Pfizer’s top scientist made his case and shared preliminary data with them on July 12.
This has led to confusion. Is the protection that has allowed them to see loved ones and go out to dinner fading?
Ultimately, the question of whether a booster is needed is unlikely to determine the FDA’s decision. If recent history is predictive, booster shots will be here before long. That’s because of the outdated, 60-year-old basic standard the FDA uses to authorize medicines for sale: Is a new drug “safe and effective?”
The FDA, using that standard, will very likely have to authorize Pfizer’s booster for emergency use, as it did the company’s prior COVID shot. The booster is likely to be safe – hundreds of millions have taken the earlier shots – and Pfizer reported that it dramatically increases a vaccinated person’s antibodies against SARS-CoV-2. From that perspective, it may also be considered very effective.
But does that kind of efficacy matter? Is a higher level of antibodies needed to protect vaccinated Americans? Though antibody levels may wane some over time, the current vaccines deliver perfectly good immunity so far.
What if a booster is safe and effective in one sense but simply not needed – at least for now?
Reliance on the simple “safe and effective” standard – which certainly sounds reasonable – is a relic of a time when there were far fewer and simpler medicines available to treat diseases and before pharmaceutical manufacturing became one of the world’s biggest businesses.
The FDA’s 1938 landmark legislation focused primarily on safety after more than 100 Americans died from a raspberry-flavored liquid form of an early antibiotic because one of its ingredients was used as antifreeze. The 1962 Kefauver-Harris Amendments to the Federal Food, Drug, and Cosmetic Act set out more specific requirements for drug approval: Companies must scientifically prove a drug’s effectiveness through “adequate and well-controlled studies.”
In today’s pharmaceutical universe, a simple “safe and effective” determination is not always an adequate bar, and it can be manipulated to sell drugs of questionable value. There’s also big money involved: Pfizer is already projecting $26 billion in COVID revenue in 2021.
The United States’ continued use of this standard to let drugs into the market has led to the approval of expensive, not necessarily very effective drugs. In 2014, for example, the FDA approved a toenail fungus drug that can cost up to $1,500 a month and that studies showed cured fewer than 10% of patients after a year of treatment. That’s more effective than doing nothing but less effective and more costly than a number of other treatments for this bothersome malady.
It has also led to a plethora of high-priced drugs to treat diseases like cancers, multiple sclerosis and type 2 diabetes that are all more effective than a placebo but have often not been tested very much against one another to determine which are most effective.
In today’s complex world, clarification is needed to determine just what kind of effectiveness the FDA should demand. And should that be the job of the FDA alone?
For example, should drugmakers prove a drug is significantly more effective than products already on the market? Or demonstrate cost-effectiveness – the health value of a product relative to its price – a metric used by Britain’s health system? And in which cases is effectiveness against a surrogate marker – like an antibody level – a good enough stand-in for whether a drug will have a significant impact on a patient’s health?
In most industrialized countries, broad access to the national market is a two-step process, said Aaron Kesselheim, a professor of medicine at Harvard Medical School, Boston, who studies drug development, marketing and law and recently served on an FDA advisory committee. The first part certifies that a drug is sufficiently safe and effective. That is immediately followed by an independent health technology assessment to see where it fits in the treatment armamentarium, including, in some countries, whether it is useful enough to be sold at all at the stated price. But there’s no such automatic process in the United States.
When Pfizer applies for authorization, the FDA may well clear a booster for the U.S. market. The Centers for Disease Control and Prevention, likely with advice from National Institutes of Health experts, will then have to decide whether to recommend it and for whom. This judgment call usually determines whether insurers will cover it. Pfizer is likely to profit handsomely from a government authorization, and the company will gain some revenue even if only the worried well, who can pay out of pocket, decide to get the shot.
To make any recommendation on a booster, government experts say they need more data. They could, for example, as Anthony S. Fauci, MD, has suggested, eventually green-light the additional vaccine shot only for a small group of patients at high risk for a deadly infection, such as the very old or transplant recipients who take immunosuppressant drugs, as some other countries have done.
But until the United States refines the FDA’s “safe and effective” standard or adds a second layer of vetting, when new products hit the market and manufacturers promote them, Americans will be left to decipher whose version of effective and necessary matters to them.
KHN (Kaiser Health News) is a national newsroom that produces in-depth journalism about health issues. Together with Policy Analysis and Polling, KHN is one of the three major operating programs at KFF (Kaiser Family Foundation). KFF is an endowed nonprofit organization providing information on health issues to the nation.