User login
Bringing you the latest news, research and reviews, exclusive interviews, podcasts, quizzes, and more.
div[contains(@class, 'read-next-article')]
div[contains(@class, 'nav-primary')]
nav[contains(@class, 'nav-primary')]
section[contains(@class, 'footer-nav-section-wrapper')]
nav[contains(@class, 'nav-ce-stack nav-ce-stack__large-screen')]
header[@id='header']
div[contains(@class, 'header__large-screen')]
div[contains(@class, 'read-next-article')]
div[contains(@class, 'main-prefix')]
div[contains(@class, 'nav-primary')]
nav[contains(@class, 'nav-primary')]
section[contains(@class, 'footer-nav-section-wrapper')]
footer[@id='footer']
section[contains(@class, 'nav-hidden')]
div[contains(@class, 'ce-card-content')]
nav[contains(@class, 'nav-ce-stack')]
div[contains(@class, 'view-medstat-quiz-listing-panes')]
div[contains(@class, 'pane-article-sidebar-latest-news')]
Complying with the Americans With Disabilities Act
. And 7 years ago, the government raised the penalties for failing to do so. So it might be time to re-educate yourself on what the ADA requires.
ADA compliance is not an issue that we talk about or provide training for in medical schools or with our professional organizations. Since fines for small businesses are now $75,000 for a first offense and $150,000 for each subsequent violation, this could be an expensive oversight that malpractice and other liability policies will not cover.
A 2019 study in Boston examined physicians’ knowledge of legal obligations when caring for patients with disabilities. Researchers concluded that most physicians interviewed “exhibited a superficial or incorrect understanding of their legal responsibilities to patients with a disability.” If you feel you’re in that boat, you might want to consult federal guidance with information and common questions physicians ask about their ADA obligations.
The ADA defines a person with a disability as someone with “a physical or mental impairment that substantially limits one or more life activities”; someone with a record of such an impairment; or someone who is “regarded as having such an impairment.” Among the ADA standards required for accessible exam rooms, according to the guidance:
- The entry door to the exam room should be a minimum width of 32 inches when the door is opened at a 90-degree angle.
- There should be a minimum of 30 by 48 inches of clear floor space next to the exam table.
- An accessible exam table should be able to be lowered to the height of the patient’s wheelchair seat, 17 to 19 inches from the floor.
This does not mean that all of your exam rooms must meet these standards, of course; but if you see any patients with disabilities – and who doesn’t? – you need at least one room that meets the criteria.
Federal guidance also includes requirements on removal of architectural barriers, accessible parking, and entrance and maneuvering spaces – which apply to both for-profit and nonprofit organizations. Among them:
- Designated accessible parking spaces must be included among any parking the business provides for the public “if doing so is readily achievable.” Those parking spaces should be the closest to the accessible entrance, on level ground. The spaces should be at least eight feet wide, with an access aisle on either side.
- For accessible spaces for cars, the adjacent access aisle must be at least five feet wide; for van spaces, eight feet wide.
- “If achievable,” an accessible service counter must have a maximum height of 36 inches, with a clear floor space of 30 by 48 inches to permit the use of a wheelchair.
A common misconception is that only new construction and alterations need to be accessible, and that older facilities are “grandfathered,” but that’s not true. Because the ADA is a civil rights law and not a building code, ADA rules apply equally to all facilities, young and old. This is particularly important to remember in light of the long-standing cottage industry of attorneys who sue small businesses for alleged ADA violations.
Another common mistake made by physicians who lease their office space is to assume that their landlord is responsible for meeting all ADA obligations. In fact, The ADA places the legal obligation on both the landlord and the tenant. The landlord and the tenant may decide among themselves who will actually make the changes and provide the aids and services, but both remain legally responsible.
Another aspect that you might not have thought of is access to your website. While ADA applicability to online services remains vague, lawsuits have been filed, and are likely to increase. Online accessibility issues that have been identified include:
- Ability to find and process information on a website (e.g., providing audio descriptions for video content, for the sight-impaired).
- Ability to navigate and use a website (e.g., ensuring that all site functions are easily accessible with only a keyboard).
- Ability to comprehend all information (including clearly understandable error messages).
Hearing-impaired patients present their own considerations for delivering adequate care, which I will discuss in my next column.
Dr. Eastern practices dermatology and dermatologic surgery in Belleville, N.J. He is the author of numerous articles and textbook chapters, and is a longtime monthly columnist for Dermatology News. Write to him at [email protected].
. And 7 years ago, the government raised the penalties for failing to do so. So it might be time to re-educate yourself on what the ADA requires.
ADA compliance is not an issue that we talk about or provide training for in medical schools or with our professional organizations. Since fines for small businesses are now $75,000 for a first offense and $150,000 for each subsequent violation, this could be an expensive oversight that malpractice and other liability policies will not cover.
A 2019 study in Boston examined physicians’ knowledge of legal obligations when caring for patients with disabilities. Researchers concluded that most physicians interviewed “exhibited a superficial or incorrect understanding of their legal responsibilities to patients with a disability.” If you feel you’re in that boat, you might want to consult federal guidance with information and common questions physicians ask about their ADA obligations.
The ADA defines a person with a disability as someone with “a physical or mental impairment that substantially limits one or more life activities”; someone with a record of such an impairment; or someone who is “regarded as having such an impairment.” Among the ADA standards required for accessible exam rooms, according to the guidance:
- The entry door to the exam room should be a minimum width of 32 inches when the door is opened at a 90-degree angle.
- There should be a minimum of 30 by 48 inches of clear floor space next to the exam table.
- An accessible exam table should be able to be lowered to the height of the patient’s wheelchair seat, 17 to 19 inches from the floor.
This does not mean that all of your exam rooms must meet these standards, of course; but if you see any patients with disabilities – and who doesn’t? – you need at least one room that meets the criteria.
Federal guidance also includes requirements on removal of architectural barriers, accessible parking, and entrance and maneuvering spaces – which apply to both for-profit and nonprofit organizations. Among them:
- Designated accessible parking spaces must be included among any parking the business provides for the public “if doing so is readily achievable.” Those parking spaces should be the closest to the accessible entrance, on level ground. The spaces should be at least eight feet wide, with an access aisle on either side.
- For accessible spaces for cars, the adjacent access aisle must be at least five feet wide; for van spaces, eight feet wide.
- “If achievable,” an accessible service counter must have a maximum height of 36 inches, with a clear floor space of 30 by 48 inches to permit the use of a wheelchair.
A common misconception is that only new construction and alterations need to be accessible, and that older facilities are “grandfathered,” but that’s not true. Because the ADA is a civil rights law and not a building code, ADA rules apply equally to all facilities, young and old. This is particularly important to remember in light of the long-standing cottage industry of attorneys who sue small businesses for alleged ADA violations.
Another common mistake made by physicians who lease their office space is to assume that their landlord is responsible for meeting all ADA obligations. In fact, The ADA places the legal obligation on both the landlord and the tenant. The landlord and the tenant may decide among themselves who will actually make the changes and provide the aids and services, but both remain legally responsible.
Another aspect that you might not have thought of is access to your website. While ADA applicability to online services remains vague, lawsuits have been filed, and are likely to increase. Online accessibility issues that have been identified include:
- Ability to find and process information on a website (e.g., providing audio descriptions for video content, for the sight-impaired).
- Ability to navigate and use a website (e.g., ensuring that all site functions are easily accessible with only a keyboard).
- Ability to comprehend all information (including clearly understandable error messages).
Hearing-impaired patients present their own considerations for delivering adequate care, which I will discuss in my next column.
Dr. Eastern practices dermatology and dermatologic surgery in Belleville, N.J. He is the author of numerous articles and textbook chapters, and is a longtime monthly columnist for Dermatology News. Write to him at [email protected].
. And 7 years ago, the government raised the penalties for failing to do so. So it might be time to re-educate yourself on what the ADA requires.
ADA compliance is not an issue that we talk about or provide training for in medical schools or with our professional organizations. Since fines for small businesses are now $75,000 for a first offense and $150,000 for each subsequent violation, this could be an expensive oversight that malpractice and other liability policies will not cover.
A 2019 study in Boston examined physicians’ knowledge of legal obligations when caring for patients with disabilities. Researchers concluded that most physicians interviewed “exhibited a superficial or incorrect understanding of their legal responsibilities to patients with a disability.” If you feel you’re in that boat, you might want to consult federal guidance with information and common questions physicians ask about their ADA obligations.
The ADA defines a person with a disability as someone with “a physical or mental impairment that substantially limits one or more life activities”; someone with a record of such an impairment; or someone who is “regarded as having such an impairment.” Among the ADA standards required for accessible exam rooms, according to the guidance:
- The entry door to the exam room should be a minimum width of 32 inches when the door is opened at a 90-degree angle.
- There should be a minimum of 30 by 48 inches of clear floor space next to the exam table.
- An accessible exam table should be able to be lowered to the height of the patient’s wheelchair seat, 17 to 19 inches from the floor.
This does not mean that all of your exam rooms must meet these standards, of course; but if you see any patients with disabilities – and who doesn’t? – you need at least one room that meets the criteria.
Federal guidance also includes requirements on removal of architectural barriers, accessible parking, and entrance and maneuvering spaces – which apply to both for-profit and nonprofit organizations. Among them:
- Designated accessible parking spaces must be included among any parking the business provides for the public “if doing so is readily achievable.” Those parking spaces should be the closest to the accessible entrance, on level ground. The spaces should be at least eight feet wide, with an access aisle on either side.
- For accessible spaces for cars, the adjacent access aisle must be at least five feet wide; for van spaces, eight feet wide.
- “If achievable,” an accessible service counter must have a maximum height of 36 inches, with a clear floor space of 30 by 48 inches to permit the use of a wheelchair.
A common misconception is that only new construction and alterations need to be accessible, and that older facilities are “grandfathered,” but that’s not true. Because the ADA is a civil rights law and not a building code, ADA rules apply equally to all facilities, young and old. This is particularly important to remember in light of the long-standing cottage industry of attorneys who sue small businesses for alleged ADA violations.
Another common mistake made by physicians who lease their office space is to assume that their landlord is responsible for meeting all ADA obligations. In fact, The ADA places the legal obligation on both the landlord and the tenant. The landlord and the tenant may decide among themselves who will actually make the changes and provide the aids and services, but both remain legally responsible.
Another aspect that you might not have thought of is access to your website. While ADA applicability to online services remains vague, lawsuits have been filed, and are likely to increase. Online accessibility issues that have been identified include:
- Ability to find and process information on a website (e.g., providing audio descriptions for video content, for the sight-impaired).
- Ability to navigate and use a website (e.g., ensuring that all site functions are easily accessible with only a keyboard).
- Ability to comprehend all information (including clearly understandable error messages).
Hearing-impaired patients present their own considerations for delivering adequate care, which I will discuss in my next column.
Dr. Eastern practices dermatology and dermatologic surgery in Belleville, N.J. He is the author of numerous articles and textbook chapters, and is a longtime monthly columnist for Dermatology News. Write to him at [email protected].
New AMA president discusses pandemic during inaugural address
He has encountered “all manner of unexpected situations” and feels “more than prepared” to serve as president of the American Medical Association, he said.
At the same time, “I still find myself a little nervous about it,” Dr. Harmon said in an interview the day after he was sworn in as president. “I would be less than candid if I didn’t tell you that. I don’t mean intimidated. ... It’s almost like before an athletic event.”
Dr. Harmon was sworn in June 15 as the 176th president of the AMA during the virtual Special Meeting of the AMA House of Delegates. He follows Susan R. Bailey, MD, an allergist from Fort Worth, Tex., in leading the organization, which has more than 270,000 members.
Advancing health equity
During his inaugural address, Dr. Harmon discussed the pandemic and the AMA’s plan to advance health equity.
COVID-19 “has revealed enormous gaps in how we care for people and communities in America, demonstrated in the disproportionate impact of this pandemic on communities of color and in the weaknesses of our underfunded and underresourced public health infrastructure,” Dr. Harmon said.
He described medical professionals as being “at war against seemingly formidable adversaries,” including the pandemic, the effects of prolonged isolation on emotional and behavioral health, and political and racial tension. There is an “immense battle to rid our health system – and society – of health disparities and racism,” he said. “As we face these battles, we must remember that our actions as physicians and as leaders will have far-reaching consequences.”
Other challenges before the AMA include vaccinating patients, recovering from the ongoing pandemic, removing unnecessary obstacles to care, ending an epidemic of drug overdoses, improving outcomes for patients with chronic disease, incorporating technology in ways that benefit doctors and patients, and preparing future physicians, Dr. Harmon noted.
“We are going to embed the principles of equity and racial justice within the AMA and throughout our health system,” added Dr. Harmon, who has been an AMA board member since 2013 and served as board chair from 2017 to 2018. He highlighted the AMA’s strategic plan, released in May 2021, to advance health equity and justice and improve the quality of care for people who have been marginalized.
“Meaningful progress won’t happen until we, as doctors, recognize how profoundly systemic racism influences the health of our patients, and until we commit to taking action within our own spheres of influence,” Dr. Harmon said. “As a family doctor in a very diverse state, I have treated people from all backgrounds, and have seen inequities up close, inequities that understandably lead to distrust.”
Commenting in an interview on JAMA’s controversial tweet and podcast related to structural racism from earlier this year that have been deleted and removed from JAMA’s website, Dr. Harmon said, JAMA maintains editorial independence from the AMA, but that direction from a journal oversight committee could lead to changes at the journal that could help prevent similar incidents.
“We’ll support whatever the journal oversight committee suggests,” Dr. Harmon said.
“We had public statements about [the podcast]. I do think that we’ll be able to move very quickly in a stronger direction to address the issue of systemic racism,” Dr. Harmon said. “The AMA has acknowledged that it is a public health threat. We have acknowledged that it is ... a political description versus a biologic construct. So, I would anticipate that you’ll find changes.”
The AMA began developing its strategic plan to advance equity several years ago, Dr. Harmon noted. “I think we are very well poised to move forward and attack this enemy of health disparity.”
AAFP president supporting Dr. Harmon’s inauguration
Among those congratulating Dr. Harmon on his inauguration was Ada Stewart, MD, a fellow family physician and South Carolina resident who is the president of the American Academy of Family Physicians.
“We are very excited that family physician Dr. Gerald Harmon will serve as president of the AMA this coming year,” Dr. Stewart said. “Family medicine encompasses the very essence of medicine – treating the whole person, in the context of family, community, and each individual’s unique circumstances. As a family physician, Dr. Harmon brings important perspectives from the front lines of primary care. His commitment to health equity and evidence-based care, as well as his concern for practice sustainability and physician well-being, will serve him well as he leads the house of medicine into the future.”
Dr. Harmon has practiced as a family medicine specialist in Georgetown, S.C., for more than 30 years. He is a member of the clinical faculty for the Tidelands Health Medical University of South Carolina family medicine residency program, advises a community health system, and is vice president of a multispecialty physician practice. In addition, Dr. Harmon is the medical director of a nonprofit hospice and volunteers as medical supervisor for his local school district.
Dr. Harmon received his undergraduate degree in physics and mathematics from the University of South Carolina, Columbia, and received his medical degree from the Medical University of South Carolina, Charleston. He completed a residency training program in family medicine with the U.S. Air Force at Eglin (Fla.) AFB, Florida.
During a 35-year military career, Dr. Harmon served as chief surgeon for the National Guard Bureau and assistant surgeon general for the U.S. Air Force. He retired from the military as a major general.
Dr. Harmon and his wife, Linda, have three married children and eight grandchildren.
Every now and then, a bucket of tomatoes or even a half bushel of corn shows up in the back of Dr. Harmon’s pickup truck, with a note on the window thanking him. “That really touches you deeply,” Dr. Harmon said. “I practice that type of medicine and I’m honored to be able to do that every day.”
He has encountered “all manner of unexpected situations” and feels “more than prepared” to serve as president of the American Medical Association, he said.
At the same time, “I still find myself a little nervous about it,” Dr. Harmon said in an interview the day after he was sworn in as president. “I would be less than candid if I didn’t tell you that. I don’t mean intimidated. ... It’s almost like before an athletic event.”
Dr. Harmon was sworn in June 15 as the 176th president of the AMA during the virtual Special Meeting of the AMA House of Delegates. He follows Susan R. Bailey, MD, an allergist from Fort Worth, Tex., in leading the organization, which has more than 270,000 members.
Advancing health equity
During his inaugural address, Dr. Harmon discussed the pandemic and the AMA’s plan to advance health equity.
COVID-19 “has revealed enormous gaps in how we care for people and communities in America, demonstrated in the disproportionate impact of this pandemic on communities of color and in the weaknesses of our underfunded and underresourced public health infrastructure,” Dr. Harmon said.
He described medical professionals as being “at war against seemingly formidable adversaries,” including the pandemic, the effects of prolonged isolation on emotional and behavioral health, and political and racial tension. There is an “immense battle to rid our health system – and society – of health disparities and racism,” he said. “As we face these battles, we must remember that our actions as physicians and as leaders will have far-reaching consequences.”
Other challenges before the AMA include vaccinating patients, recovering from the ongoing pandemic, removing unnecessary obstacles to care, ending an epidemic of drug overdoses, improving outcomes for patients with chronic disease, incorporating technology in ways that benefit doctors and patients, and preparing future physicians, Dr. Harmon noted.
“We are going to embed the principles of equity and racial justice within the AMA and throughout our health system,” added Dr. Harmon, who has been an AMA board member since 2013 and served as board chair from 2017 to 2018. He highlighted the AMA’s strategic plan, released in May 2021, to advance health equity and justice and improve the quality of care for people who have been marginalized.
“Meaningful progress won’t happen until we, as doctors, recognize how profoundly systemic racism influences the health of our patients, and until we commit to taking action within our own spheres of influence,” Dr. Harmon said. “As a family doctor in a very diverse state, I have treated people from all backgrounds, and have seen inequities up close, inequities that understandably lead to distrust.”
Commenting in an interview on JAMA’s controversial tweet and podcast related to structural racism from earlier this year that have been deleted and removed from JAMA’s website, Dr. Harmon said, JAMA maintains editorial independence from the AMA, but that direction from a journal oversight committee could lead to changes at the journal that could help prevent similar incidents.
“We’ll support whatever the journal oversight committee suggests,” Dr. Harmon said.
“We had public statements about [the podcast]. I do think that we’ll be able to move very quickly in a stronger direction to address the issue of systemic racism,” Dr. Harmon said. “The AMA has acknowledged that it is a public health threat. We have acknowledged that it is ... a political description versus a biologic construct. So, I would anticipate that you’ll find changes.”
The AMA began developing its strategic plan to advance equity several years ago, Dr. Harmon noted. “I think we are very well poised to move forward and attack this enemy of health disparity.”
AAFP president supporting Dr. Harmon’s inauguration
Among those congratulating Dr. Harmon on his inauguration was Ada Stewart, MD, a fellow family physician and South Carolina resident who is the president of the American Academy of Family Physicians.
“We are very excited that family physician Dr. Gerald Harmon will serve as president of the AMA this coming year,” Dr. Stewart said. “Family medicine encompasses the very essence of medicine – treating the whole person, in the context of family, community, and each individual’s unique circumstances. As a family physician, Dr. Harmon brings important perspectives from the front lines of primary care. His commitment to health equity and evidence-based care, as well as his concern for practice sustainability and physician well-being, will serve him well as he leads the house of medicine into the future.”
Dr. Harmon has practiced as a family medicine specialist in Georgetown, S.C., for more than 30 years. He is a member of the clinical faculty for the Tidelands Health Medical University of South Carolina family medicine residency program, advises a community health system, and is vice president of a multispecialty physician practice. In addition, Dr. Harmon is the medical director of a nonprofit hospice and volunteers as medical supervisor for his local school district.
Dr. Harmon received his undergraduate degree in physics and mathematics from the University of South Carolina, Columbia, and received his medical degree from the Medical University of South Carolina, Charleston. He completed a residency training program in family medicine with the U.S. Air Force at Eglin (Fla.) AFB, Florida.
During a 35-year military career, Dr. Harmon served as chief surgeon for the National Guard Bureau and assistant surgeon general for the U.S. Air Force. He retired from the military as a major general.
Dr. Harmon and his wife, Linda, have three married children and eight grandchildren.
Every now and then, a bucket of tomatoes or even a half bushel of corn shows up in the back of Dr. Harmon’s pickup truck, with a note on the window thanking him. “That really touches you deeply,” Dr. Harmon said. “I practice that type of medicine and I’m honored to be able to do that every day.”
He has encountered “all manner of unexpected situations” and feels “more than prepared” to serve as president of the American Medical Association, he said.
At the same time, “I still find myself a little nervous about it,” Dr. Harmon said in an interview the day after he was sworn in as president. “I would be less than candid if I didn’t tell you that. I don’t mean intimidated. ... It’s almost like before an athletic event.”
Dr. Harmon was sworn in June 15 as the 176th president of the AMA during the virtual Special Meeting of the AMA House of Delegates. He follows Susan R. Bailey, MD, an allergist from Fort Worth, Tex., in leading the organization, which has more than 270,000 members.
Advancing health equity
During his inaugural address, Dr. Harmon discussed the pandemic and the AMA’s plan to advance health equity.
COVID-19 “has revealed enormous gaps in how we care for people and communities in America, demonstrated in the disproportionate impact of this pandemic on communities of color and in the weaknesses of our underfunded and underresourced public health infrastructure,” Dr. Harmon said.
He described medical professionals as being “at war against seemingly formidable adversaries,” including the pandemic, the effects of prolonged isolation on emotional and behavioral health, and political and racial tension. There is an “immense battle to rid our health system – and society – of health disparities and racism,” he said. “As we face these battles, we must remember that our actions as physicians and as leaders will have far-reaching consequences.”
Other challenges before the AMA include vaccinating patients, recovering from the ongoing pandemic, removing unnecessary obstacles to care, ending an epidemic of drug overdoses, improving outcomes for patients with chronic disease, incorporating technology in ways that benefit doctors and patients, and preparing future physicians, Dr. Harmon noted.
“We are going to embed the principles of equity and racial justice within the AMA and throughout our health system,” added Dr. Harmon, who has been an AMA board member since 2013 and served as board chair from 2017 to 2018. He highlighted the AMA’s strategic plan, released in May 2021, to advance health equity and justice and improve the quality of care for people who have been marginalized.
“Meaningful progress won’t happen until we, as doctors, recognize how profoundly systemic racism influences the health of our patients, and until we commit to taking action within our own spheres of influence,” Dr. Harmon said. “As a family doctor in a very diverse state, I have treated people from all backgrounds, and have seen inequities up close, inequities that understandably lead to distrust.”
Commenting in an interview on JAMA’s controversial tweet and podcast related to structural racism from earlier this year that have been deleted and removed from JAMA’s website, Dr. Harmon said, JAMA maintains editorial independence from the AMA, but that direction from a journal oversight committee could lead to changes at the journal that could help prevent similar incidents.
“We’ll support whatever the journal oversight committee suggests,” Dr. Harmon said.
“We had public statements about [the podcast]. I do think that we’ll be able to move very quickly in a stronger direction to address the issue of systemic racism,” Dr. Harmon said. “The AMA has acknowledged that it is a public health threat. We have acknowledged that it is ... a political description versus a biologic construct. So, I would anticipate that you’ll find changes.”
The AMA began developing its strategic plan to advance equity several years ago, Dr. Harmon noted. “I think we are very well poised to move forward and attack this enemy of health disparity.”
AAFP president supporting Dr. Harmon’s inauguration
Among those congratulating Dr. Harmon on his inauguration was Ada Stewart, MD, a fellow family physician and South Carolina resident who is the president of the American Academy of Family Physicians.
“We are very excited that family physician Dr. Gerald Harmon will serve as president of the AMA this coming year,” Dr. Stewart said. “Family medicine encompasses the very essence of medicine – treating the whole person, in the context of family, community, and each individual’s unique circumstances. As a family physician, Dr. Harmon brings important perspectives from the front lines of primary care. His commitment to health equity and evidence-based care, as well as his concern for practice sustainability and physician well-being, will serve him well as he leads the house of medicine into the future.”
Dr. Harmon has practiced as a family medicine specialist in Georgetown, S.C., for more than 30 years. He is a member of the clinical faculty for the Tidelands Health Medical University of South Carolina family medicine residency program, advises a community health system, and is vice president of a multispecialty physician practice. In addition, Dr. Harmon is the medical director of a nonprofit hospice and volunteers as medical supervisor for his local school district.
Dr. Harmon received his undergraduate degree in physics and mathematics from the University of South Carolina, Columbia, and received his medical degree from the Medical University of South Carolina, Charleston. He completed a residency training program in family medicine with the U.S. Air Force at Eglin (Fla.) AFB, Florida.
During a 35-year military career, Dr. Harmon served as chief surgeon for the National Guard Bureau and assistant surgeon general for the U.S. Air Force. He retired from the military as a major general.
Dr. Harmon and his wife, Linda, have three married children and eight grandchildren.
Every now and then, a bucket of tomatoes or even a half bushel of corn shows up in the back of Dr. Harmon’s pickup truck, with a note on the window thanking him. “That really touches you deeply,” Dr. Harmon said. “I practice that type of medicine and I’m honored to be able to do that every day.”
Supreme Court upholds Affordable Care Act
The challengers were comprised of 18 GOP-dominated states, led by Texas, that took issue with the ACA’s individual mandate – which required most Americans to have health insurance or pay a tax penalty.
But Congress reduced the penalty to zero in 2017. Challengers argued that without the mandate, the rest of the law should be scrapped, too. The court ruled that eliminated the harm the states were claiming.
“To have standing, a plaintiff must ‘allege personal injury fairly traceable to the defendant’s allegedly unlawful conduct and likely to be redressed by the requested relief,’” the majority wrote. “No plaintiff has shown such an injury ‘fairly traceable’ to the ‘allegedly unlawful conduct’ challenged here.”
Justice Stephen Breyer authored the opinion. Justices Samuel Alito and Neil Gorsuch dissented.
The decision said that the mandate in question did not require the 18 states that brought the complaint to pay anything, and therefore they had no standing.
President Joe Biden has said he plans to build on the ACA – which was enacted while he was vice president – to offer coverage to more Americans.
This marks the third time the Supreme Court spared the Obama-era law from GOP attacks. The mandate was also upheld in 2012 in a 5 to 4 ruling.
American Medical Association president Gerald Harmon, MD, also called for building on the ruling to expand the law.
“With yet another court decision upholding the ACA now behind us, we remain committed to strengthening the current law and look forward to policymakers advancing solutions to improve the ACA,” Dr. Harmon said in a statement. “The AMA will continue working to expand access to health care and ensure that all Americans have meaningful, comprehensive, and affordable health coverage to improve the health of the nation.”
House Speaker Nancy Pelosi (D-Calif.), a longtime advocate for the ACA, called the decision a “landmark victory for Democrats.”
“Thanks to the tireless advocacy of Americans across the country and Democrats in Congress, the Affordable Care Act endures as a pillar of American health and economic security alongside Medicare, Medicaid and Social Security,” she said in a statement.
Senate Majority Leader Chuck Schumer (D-N.Y.) also celebrated the ruling.
“The Affordable Care Act has won. The Supreme Court has just ruled: the ACA is here to stay and now we’re going to try to make it bigger and better,” he said, according to CNN. “For more than a decade, the assault on our health care law was relentless from Republicans in Congress, from the executive branch itself and from Republican attorneys general in the courts. Each time in each arena, the ACA has prevailed.”
This article was updated June 17, 2021.
A version of this article first appeared on WebMD.com.
The challengers were comprised of 18 GOP-dominated states, led by Texas, that took issue with the ACA’s individual mandate – which required most Americans to have health insurance or pay a tax penalty.
But Congress reduced the penalty to zero in 2017. Challengers argued that without the mandate, the rest of the law should be scrapped, too. The court ruled that eliminated the harm the states were claiming.
“To have standing, a plaintiff must ‘allege personal injury fairly traceable to the defendant’s allegedly unlawful conduct and likely to be redressed by the requested relief,’” the majority wrote. “No plaintiff has shown such an injury ‘fairly traceable’ to the ‘allegedly unlawful conduct’ challenged here.”
Justice Stephen Breyer authored the opinion. Justices Samuel Alito and Neil Gorsuch dissented.
The decision said that the mandate in question did not require the 18 states that brought the complaint to pay anything, and therefore they had no standing.
President Joe Biden has said he plans to build on the ACA – which was enacted while he was vice president – to offer coverage to more Americans.
This marks the third time the Supreme Court spared the Obama-era law from GOP attacks. The mandate was also upheld in 2012 in a 5 to 4 ruling.
American Medical Association president Gerald Harmon, MD, also called for building on the ruling to expand the law.
“With yet another court decision upholding the ACA now behind us, we remain committed to strengthening the current law and look forward to policymakers advancing solutions to improve the ACA,” Dr. Harmon said in a statement. “The AMA will continue working to expand access to health care and ensure that all Americans have meaningful, comprehensive, and affordable health coverage to improve the health of the nation.”
House Speaker Nancy Pelosi (D-Calif.), a longtime advocate for the ACA, called the decision a “landmark victory for Democrats.”
“Thanks to the tireless advocacy of Americans across the country and Democrats in Congress, the Affordable Care Act endures as a pillar of American health and economic security alongside Medicare, Medicaid and Social Security,” she said in a statement.
Senate Majority Leader Chuck Schumer (D-N.Y.) also celebrated the ruling.
“The Affordable Care Act has won. The Supreme Court has just ruled: the ACA is here to stay and now we’re going to try to make it bigger and better,” he said, according to CNN. “For more than a decade, the assault on our health care law was relentless from Republicans in Congress, from the executive branch itself and from Republican attorneys general in the courts. Each time in each arena, the ACA has prevailed.”
This article was updated June 17, 2021.
A version of this article first appeared on WebMD.com.
The challengers were comprised of 18 GOP-dominated states, led by Texas, that took issue with the ACA’s individual mandate – which required most Americans to have health insurance or pay a tax penalty.
But Congress reduced the penalty to zero in 2017. Challengers argued that without the mandate, the rest of the law should be scrapped, too. The court ruled that eliminated the harm the states were claiming.
“To have standing, a plaintiff must ‘allege personal injury fairly traceable to the defendant’s allegedly unlawful conduct and likely to be redressed by the requested relief,’” the majority wrote. “No plaintiff has shown such an injury ‘fairly traceable’ to the ‘allegedly unlawful conduct’ challenged here.”
Justice Stephen Breyer authored the opinion. Justices Samuel Alito and Neil Gorsuch dissented.
The decision said that the mandate in question did not require the 18 states that brought the complaint to pay anything, and therefore they had no standing.
President Joe Biden has said he plans to build on the ACA – which was enacted while he was vice president – to offer coverage to more Americans.
This marks the third time the Supreme Court spared the Obama-era law from GOP attacks. The mandate was also upheld in 2012 in a 5 to 4 ruling.
American Medical Association president Gerald Harmon, MD, also called for building on the ruling to expand the law.
“With yet another court decision upholding the ACA now behind us, we remain committed to strengthening the current law and look forward to policymakers advancing solutions to improve the ACA,” Dr. Harmon said in a statement. “The AMA will continue working to expand access to health care and ensure that all Americans have meaningful, comprehensive, and affordable health coverage to improve the health of the nation.”
House Speaker Nancy Pelosi (D-Calif.), a longtime advocate for the ACA, called the decision a “landmark victory for Democrats.”
“Thanks to the tireless advocacy of Americans across the country and Democrats in Congress, the Affordable Care Act endures as a pillar of American health and economic security alongside Medicare, Medicaid and Social Security,” she said in a statement.
Senate Majority Leader Chuck Schumer (D-N.Y.) also celebrated the ruling.
“The Affordable Care Act has won. The Supreme Court has just ruled: the ACA is here to stay and now we’re going to try to make it bigger and better,” he said, according to CNN. “For more than a decade, the assault on our health care law was relentless from Republicans in Congress, from the executive branch itself and from Republican attorneys general in the courts. Each time in each arena, the ACA has prevailed.”
This article was updated June 17, 2021.
A version of this article first appeared on WebMD.com.
AHA: Don’t delay COVID shot while CDC reviews myocarditis cases
While the investigation into cases of myocarditis possibly associated with COVID vaccines proceeds, the American Heart Association/American Stroke Association (ASA) continue to urge everyone who is eligible for the vaccine to get it without delay.
“We remain confident that the benefits of vaccination far exceed the very unusual risks,” the leadership of the AHA/ASA said in a statement issued June 12.
“The risks of COVID-19 infection include its potentially fatal consequences and the potential long-term health effects that are still revealing themselves, including lingering consequences affecting the heart, brain, vascular system, and other organs after infection,” they point out.
Late last week, the Centers for Disease Control and Prevention alerted health care providers that the COVID-19 Vaccine Safety Technical Work Group (VaST) of the Advisory Committee on Immunization Practices (ACIP) will meet June 18 to review cases of myocarditis reported in adolescents and young adults after they received a COVID-19 vaccine manufactured by Pfizer-BioNTech or Moderna.
The CDC is monitoring the Vaccine Adverse Events Reporting System (VAERS) and the Vaccine Safety Datalink (VSD) for cases of myocarditis that have been associated with the mRNA vaccines against SARS-CoV-2 from Pfizer and Moderna.
These cases may occur more often in males than females and more frequently after the second dose than the first dose of either mRNA vaccine. Symptoms typically occur in the 3 days after administration.
“The CDC’s ongoing investigation into cases of suspected myocarditis reflects a strong and steadfast commitment to transparency and the importance of scientific rigor on all fronts. We applaud the CDC’s unwavering efforts to lead our nation’s scientific and public health efforts, including ensuring the continued safety of the COVID-19 vaccines,” the AHA/ASA states.
They emphasize that vaccinations should continue, and say it’s important to consider the details of the suspected myocarditis cases being investigated by the CDC.
As of June 11, more than 306 million doses of COVID-19 vaccines have been administered in the United States (since Dec. 14, 2020) and nearly 43% of Americans – more than 142 million people – are now fully vaccinated.
According to the June 10 CDC VAERS report detailing adverse events through May 31:
- 789 cases of suspected myocarditis have been reported, with 475 involving people younger than 30 years; 79 cases reported were in patients 16 or 17 years old.
- The vast majority (81%) of the 270 patients younger than 30 years who were discharged from care after suspected myocarditis related to COVID-19 vaccination have recovered fully; the remaining 19% of patients report ongoing symptoms or complete data are missing.
- 196 cases of suspected myocarditis after a COVID-19 vaccine were reported in young adults 18 to 24 years of age, which is higher than expected for this age group.
As of May 31, only about 9% of the COVID-19 vaccine doses administered were to people 16 to 24 years of age, which is why this “higher-than-normal rate of possible myocarditis cases” warrants investigation, the AHA/ASA says.
They note that these suspected myocarditis cases were reported to VAERS because of their proximity to COVID-19 vaccine administration.
It remains to be determined which cases meet the clinical criteria for a diagnosis of myocarditis and whether they have any direct connection to the COVID-19 vaccine, the AHA/ASA says.
They urge all health care professionals to be aware of “very rare” adverse events that could be related to a COVID-19 vaccine, including myocarditis, blood clots, low platelets, and symptoms of severe inflammation.
They advise asking patients who present with symptoms related to these conditions about the timing of recent COVID vaccinations, as needed, to confirm the diagnosis and provide appropriate treatment quickly.
The AHA will be at the CDC’s June 18 meeting to review the latest evidence on cases of suspected myocarditis after the COVID-19 vaccine, the statement adds.
The statement notes that it reflects the views of the AHA/ASA and its scientific leadership, including current president Mitchel S.V. Elkind, MD, PhD; immediate past-president Robert A. Harrington, MD; president-elect Donald M. Lloyd-Jones, MD; AHA/ASA chief science and medical officer Mariell Jessup, MD; and chief medical officer for prevention Eduardo Sanchez, MD, MPH.
A version of this article first appeared on Medscape.com.
While the investigation into cases of myocarditis possibly associated with COVID vaccines proceeds, the American Heart Association/American Stroke Association (ASA) continue to urge everyone who is eligible for the vaccine to get it without delay.
“We remain confident that the benefits of vaccination far exceed the very unusual risks,” the leadership of the AHA/ASA said in a statement issued June 12.
“The risks of COVID-19 infection include its potentially fatal consequences and the potential long-term health effects that are still revealing themselves, including lingering consequences affecting the heart, brain, vascular system, and other organs after infection,” they point out.
Late last week, the Centers for Disease Control and Prevention alerted health care providers that the COVID-19 Vaccine Safety Technical Work Group (VaST) of the Advisory Committee on Immunization Practices (ACIP) will meet June 18 to review cases of myocarditis reported in adolescents and young adults after they received a COVID-19 vaccine manufactured by Pfizer-BioNTech or Moderna.
The CDC is monitoring the Vaccine Adverse Events Reporting System (VAERS) and the Vaccine Safety Datalink (VSD) for cases of myocarditis that have been associated with the mRNA vaccines against SARS-CoV-2 from Pfizer and Moderna.
These cases may occur more often in males than females and more frequently after the second dose than the first dose of either mRNA vaccine. Symptoms typically occur in the 3 days after administration.
“The CDC’s ongoing investigation into cases of suspected myocarditis reflects a strong and steadfast commitment to transparency and the importance of scientific rigor on all fronts. We applaud the CDC’s unwavering efforts to lead our nation’s scientific and public health efforts, including ensuring the continued safety of the COVID-19 vaccines,” the AHA/ASA states.
They emphasize that vaccinations should continue, and say it’s important to consider the details of the suspected myocarditis cases being investigated by the CDC.
As of June 11, more than 306 million doses of COVID-19 vaccines have been administered in the United States (since Dec. 14, 2020) and nearly 43% of Americans – more than 142 million people – are now fully vaccinated.
According to the June 10 CDC VAERS report detailing adverse events through May 31:
- 789 cases of suspected myocarditis have been reported, with 475 involving people younger than 30 years; 79 cases reported were in patients 16 or 17 years old.
- The vast majority (81%) of the 270 patients younger than 30 years who were discharged from care after suspected myocarditis related to COVID-19 vaccination have recovered fully; the remaining 19% of patients report ongoing symptoms or complete data are missing.
- 196 cases of suspected myocarditis after a COVID-19 vaccine were reported in young adults 18 to 24 years of age, which is higher than expected for this age group.
As of May 31, only about 9% of the COVID-19 vaccine doses administered were to people 16 to 24 years of age, which is why this “higher-than-normal rate of possible myocarditis cases” warrants investigation, the AHA/ASA says.
They note that these suspected myocarditis cases were reported to VAERS because of their proximity to COVID-19 vaccine administration.
It remains to be determined which cases meet the clinical criteria for a diagnosis of myocarditis and whether they have any direct connection to the COVID-19 vaccine, the AHA/ASA says.
They urge all health care professionals to be aware of “very rare” adverse events that could be related to a COVID-19 vaccine, including myocarditis, blood clots, low platelets, and symptoms of severe inflammation.
They advise asking patients who present with symptoms related to these conditions about the timing of recent COVID vaccinations, as needed, to confirm the diagnosis and provide appropriate treatment quickly.
The AHA will be at the CDC’s June 18 meeting to review the latest evidence on cases of suspected myocarditis after the COVID-19 vaccine, the statement adds.
The statement notes that it reflects the views of the AHA/ASA and its scientific leadership, including current president Mitchel S.V. Elkind, MD, PhD; immediate past-president Robert A. Harrington, MD; president-elect Donald M. Lloyd-Jones, MD; AHA/ASA chief science and medical officer Mariell Jessup, MD; and chief medical officer for prevention Eduardo Sanchez, MD, MPH.
A version of this article first appeared on Medscape.com.
While the investigation into cases of myocarditis possibly associated with COVID vaccines proceeds, the American Heart Association/American Stroke Association (ASA) continue to urge everyone who is eligible for the vaccine to get it without delay.
“We remain confident that the benefits of vaccination far exceed the very unusual risks,” the leadership of the AHA/ASA said in a statement issued June 12.
“The risks of COVID-19 infection include its potentially fatal consequences and the potential long-term health effects that are still revealing themselves, including lingering consequences affecting the heart, brain, vascular system, and other organs after infection,” they point out.
Late last week, the Centers for Disease Control and Prevention alerted health care providers that the COVID-19 Vaccine Safety Technical Work Group (VaST) of the Advisory Committee on Immunization Practices (ACIP) will meet June 18 to review cases of myocarditis reported in adolescents and young adults after they received a COVID-19 vaccine manufactured by Pfizer-BioNTech or Moderna.
The CDC is monitoring the Vaccine Adverse Events Reporting System (VAERS) and the Vaccine Safety Datalink (VSD) for cases of myocarditis that have been associated with the mRNA vaccines against SARS-CoV-2 from Pfizer and Moderna.
These cases may occur more often in males than females and more frequently after the second dose than the first dose of either mRNA vaccine. Symptoms typically occur in the 3 days after administration.
“The CDC’s ongoing investigation into cases of suspected myocarditis reflects a strong and steadfast commitment to transparency and the importance of scientific rigor on all fronts. We applaud the CDC’s unwavering efforts to lead our nation’s scientific and public health efforts, including ensuring the continued safety of the COVID-19 vaccines,” the AHA/ASA states.
They emphasize that vaccinations should continue, and say it’s important to consider the details of the suspected myocarditis cases being investigated by the CDC.
As of June 11, more than 306 million doses of COVID-19 vaccines have been administered in the United States (since Dec. 14, 2020) and nearly 43% of Americans – more than 142 million people – are now fully vaccinated.
According to the June 10 CDC VAERS report detailing adverse events through May 31:
- 789 cases of suspected myocarditis have been reported, with 475 involving people younger than 30 years; 79 cases reported were in patients 16 or 17 years old.
- The vast majority (81%) of the 270 patients younger than 30 years who were discharged from care after suspected myocarditis related to COVID-19 vaccination have recovered fully; the remaining 19% of patients report ongoing symptoms or complete data are missing.
- 196 cases of suspected myocarditis after a COVID-19 vaccine were reported in young adults 18 to 24 years of age, which is higher than expected for this age group.
As of May 31, only about 9% of the COVID-19 vaccine doses administered were to people 16 to 24 years of age, which is why this “higher-than-normal rate of possible myocarditis cases” warrants investigation, the AHA/ASA says.
They note that these suspected myocarditis cases were reported to VAERS because of their proximity to COVID-19 vaccine administration.
It remains to be determined which cases meet the clinical criteria for a diagnosis of myocarditis and whether they have any direct connection to the COVID-19 vaccine, the AHA/ASA says.
They urge all health care professionals to be aware of “very rare” adverse events that could be related to a COVID-19 vaccine, including myocarditis, blood clots, low platelets, and symptoms of severe inflammation.
They advise asking patients who present with symptoms related to these conditions about the timing of recent COVID vaccinations, as needed, to confirm the diagnosis and provide appropriate treatment quickly.
The AHA will be at the CDC’s June 18 meeting to review the latest evidence on cases of suspected myocarditis after the COVID-19 vaccine, the statement adds.
The statement notes that it reflects the views of the AHA/ASA and its scientific leadership, including current president Mitchel S.V. Elkind, MD, PhD; immediate past-president Robert A. Harrington, MD; president-elect Donald M. Lloyd-Jones, MD; AHA/ASA chief science and medical officer Mariell Jessup, MD; and chief medical officer for prevention Eduardo Sanchez, MD, MPH.
A version of this article first appeared on Medscape.com.
The most important meal of the day, with extra zinc
Busting the myth of skipping breakfast
Your mother told you that breakfast was the most important meal of the day. Cereal marketing teams banked on that, selling breakfast to millions of people based on a common turn of phrase like “an apple a day keeps the doctor away.” Well, what if the notion of breakfast’s importance isn’t just marketing BS?
A new study suggests that adults who don’t eat breakfast are setting themselves up for a nutritional gap. Common breakfast foods pack a ton of calcium, fiber, and vitamin C from milk, cereals, and fruit. Christopher Taylor, PhD, senior author of the study and professor of dietetics at the Ohio State University, Columbus, said that if you’re not getting those nutrients from foods at breakfast, there’s a tendency to skip them throughout the rest of your day.
Data from a sample of the National Health and Nutrition Examination Survey – 30,889 adults aged 19 and older who participated between 2005 and 2016 – showed that 15.2% of participants reported skipping breakfast.
The research team then estimated nutrient consumption using federal dietary studies and guidelines and compared it to Food and Nutrition Board of National Academies nutrient recommendations. The breakfast skippers, they determined, were missing out on pronounced levels of fiber, magnesium, iron, calcium, and vitamins A, B1, B2, B3, C, and D and were more likely to fall prey to lower-quality snacking. Cue those Oreos at 3 pm.
You may get more total calories within the day by eating breakfast, but your lunch, dinner, and snacks are much larger when you skip it. So the case of breakfast being the most important meal of the day checks out. Who knew that Tony the Tiger – and Mom – were actually on to something?
The bitter taste of a healthy liver
Alcohol and liver disease. They go together like, well, alcohol and liver disease. But alcohol isn’t the only reason people get liver disease, and now there’s a potential new treatment for people with hepatic steatosis on the way to becoming nonalcoholic fatty liver disease: beer.
Okay, not literally beer, but a pair of compounds derived from hops, the plant that gives beer its color and bitter flavor. In a study published in eLife, researchers from Oregon State University fed mice either a low-fat diet or a high-fat diet to induce hepatic steatosis, with some on the high-fat diet receiving either xanthohumol, a prenylated flavonoid from the hop plant, or tetrahydroxanthohumol, a hydrogenated derivative of xanthohumol.
Mice that received tetrahydroxanthohumol not only gained weight at a far slower rate than that of mice on the normal high-fat diet, their blood sugar remained stable; xanthohumol was similarly effective if the dosage was higher. The researchers noted that the two chemicals were effective because they acted as antagonists for the PPAR-gamma protein, which controls glucose metabolism and fatty cell activation. The chemicals bind to the protein but don’t activate it, meaning fat is unable to build up in the cells. No fat means no hepatic steatosis, which means no liver disease.
The researchers caution that more research is needed to determine the chemicals’ effectiveness in humans, but the classic line from a great animated philosopher still holds true: Alcohol may really be the source of, and solution to, all of life’s problems.
Life’s great mysteries, from A to zinc
Thanks to science, we now have answers to what were once unanswerable questions: Is Jello a solid or a liquid? If someone leads but no one follows, are they just out for a walk? Does zinc inhibit or promote the growth of kidney stones? How many licks does it take to get to the center of a Tootsie Pop? (Turns out science really did answer this one.)
If you’re anything like us, then you’ve been following the big debate on the two competing theories involving the role of zinc in kidney stone formation for years. One theory says that zinc stops the growth of calcium oxalate crystals that make up stones. The other says that zinc alters the surfaces of crystals, which encourages growth.
We can’t stand the suspense any longer, so here goes: The answer to “does zinc inhibit or promote the growth of kidney stones?” is … yes.
“What we see with zinc is something we haven’t seen before. It does slow down calcium oxalate crystal growth and at the same time it changes the surface of the crystals, causing defects in the form of intergrowths. These abnormalities create centers for new crystals to nucleate and grow,” said senior author Jeffrey Rimer, PhD, of the University of Houston.
In vitro experimentation, computational modeling, and atomic force microscopy don’t lie: Zinc ions have a unique ability “to alter the termination of crystal surfaces.” They tried alternative ions found in urine, including magnesium, and there was no effect on crystal formation.
With this one great mystery now solved, we contacted Dr. Rimer to ask him about the whole “sound of one hand clapping” business. He hasn’t cracked that one yet, but he did want to speak to our supervisor. So many of life’s unanswered questions, so little time. Oh well.
Babies’ ‘gut instinct’ to cry
At some point or another, you’ve probably been told not to “be such a baby” when you were scared of something. If you’ve been called a crybaby, it may be an indicator that you had a different gut microbiome as an infant.
Investigators from Michigan State University and the University of North Carolina say that babies who react more strongly to scary situations have different gut microbiomes compared with babies who don’t have such a strong reaction. The way babies react to scary situations can say a lot about their future, and there is even some evidence that gut microbiomes may have something to do with mental health.
Physicians who support neurologic development may one day be able to use this research on gut microbiomes to help monitor people’s neurological health. “This early developmental period is a time of tremendous opportunity for promoting healthy brain development. The microbiome is an exciting new target that can be potentially used for that,” said Rebecca Knickmeyer of MSU, leader of the study, which was published in Nature Communications. And loyal LOTME followers already know about the OpenBiome Microbiome Library, aka the “Amazon of bacteria.”
So the next time someone tells you not to be such a baby when you’re scared of something, tell them it’s not your fault. Blame it on your gut microbiome!
Busting the myth of skipping breakfast
Your mother told you that breakfast was the most important meal of the day. Cereal marketing teams banked on that, selling breakfast to millions of people based on a common turn of phrase like “an apple a day keeps the doctor away.” Well, what if the notion of breakfast’s importance isn’t just marketing BS?
A new study suggests that adults who don’t eat breakfast are setting themselves up for a nutritional gap. Common breakfast foods pack a ton of calcium, fiber, and vitamin C from milk, cereals, and fruit. Christopher Taylor, PhD, senior author of the study and professor of dietetics at the Ohio State University, Columbus, said that if you’re not getting those nutrients from foods at breakfast, there’s a tendency to skip them throughout the rest of your day.
Data from a sample of the National Health and Nutrition Examination Survey – 30,889 adults aged 19 and older who participated between 2005 and 2016 – showed that 15.2% of participants reported skipping breakfast.
The research team then estimated nutrient consumption using federal dietary studies and guidelines and compared it to Food and Nutrition Board of National Academies nutrient recommendations. The breakfast skippers, they determined, were missing out on pronounced levels of fiber, magnesium, iron, calcium, and vitamins A, B1, B2, B3, C, and D and were more likely to fall prey to lower-quality snacking. Cue those Oreos at 3 pm.
You may get more total calories within the day by eating breakfast, but your lunch, dinner, and snacks are much larger when you skip it. So the case of breakfast being the most important meal of the day checks out. Who knew that Tony the Tiger – and Mom – were actually on to something?
The bitter taste of a healthy liver
Alcohol and liver disease. They go together like, well, alcohol and liver disease. But alcohol isn’t the only reason people get liver disease, and now there’s a potential new treatment for people with hepatic steatosis on the way to becoming nonalcoholic fatty liver disease: beer.
Okay, not literally beer, but a pair of compounds derived from hops, the plant that gives beer its color and bitter flavor. In a study published in eLife, researchers from Oregon State University fed mice either a low-fat diet or a high-fat diet to induce hepatic steatosis, with some on the high-fat diet receiving either xanthohumol, a prenylated flavonoid from the hop plant, or tetrahydroxanthohumol, a hydrogenated derivative of xanthohumol.
Mice that received tetrahydroxanthohumol not only gained weight at a far slower rate than that of mice on the normal high-fat diet, their blood sugar remained stable; xanthohumol was similarly effective if the dosage was higher. The researchers noted that the two chemicals were effective because they acted as antagonists for the PPAR-gamma protein, which controls glucose metabolism and fatty cell activation. The chemicals bind to the protein but don’t activate it, meaning fat is unable to build up in the cells. No fat means no hepatic steatosis, which means no liver disease.
The researchers caution that more research is needed to determine the chemicals’ effectiveness in humans, but the classic line from a great animated philosopher still holds true: Alcohol may really be the source of, and solution to, all of life’s problems.
Life’s great mysteries, from A to zinc
Thanks to science, we now have answers to what were once unanswerable questions: Is Jello a solid or a liquid? If someone leads but no one follows, are they just out for a walk? Does zinc inhibit or promote the growth of kidney stones? How many licks does it take to get to the center of a Tootsie Pop? (Turns out science really did answer this one.)
If you’re anything like us, then you’ve been following the big debate on the two competing theories involving the role of zinc in kidney stone formation for years. One theory says that zinc stops the growth of calcium oxalate crystals that make up stones. The other says that zinc alters the surfaces of crystals, which encourages growth.
We can’t stand the suspense any longer, so here goes: The answer to “does zinc inhibit or promote the growth of kidney stones?” is … yes.
“What we see with zinc is something we haven’t seen before. It does slow down calcium oxalate crystal growth and at the same time it changes the surface of the crystals, causing defects in the form of intergrowths. These abnormalities create centers for new crystals to nucleate and grow,” said senior author Jeffrey Rimer, PhD, of the University of Houston.
In vitro experimentation, computational modeling, and atomic force microscopy don’t lie: Zinc ions have a unique ability “to alter the termination of crystal surfaces.” They tried alternative ions found in urine, including magnesium, and there was no effect on crystal formation.
With this one great mystery now solved, we contacted Dr. Rimer to ask him about the whole “sound of one hand clapping” business. He hasn’t cracked that one yet, but he did want to speak to our supervisor. So many of life’s unanswered questions, so little time. Oh well.
Babies’ ‘gut instinct’ to cry
At some point or another, you’ve probably been told not to “be such a baby” when you were scared of something. If you’ve been called a crybaby, it may be an indicator that you had a different gut microbiome as an infant.
Investigators from Michigan State University and the University of North Carolina say that babies who react more strongly to scary situations have different gut microbiomes compared with babies who don’t have such a strong reaction. The way babies react to scary situations can say a lot about their future, and there is even some evidence that gut microbiomes may have something to do with mental health.
Physicians who support neurologic development may one day be able to use this research on gut microbiomes to help monitor people’s neurological health. “This early developmental period is a time of tremendous opportunity for promoting healthy brain development. The microbiome is an exciting new target that can be potentially used for that,” said Rebecca Knickmeyer of MSU, leader of the study, which was published in Nature Communications. And loyal LOTME followers already know about the OpenBiome Microbiome Library, aka the “Amazon of bacteria.”
So the next time someone tells you not to be such a baby when you’re scared of something, tell them it’s not your fault. Blame it on your gut microbiome!
Busting the myth of skipping breakfast
Your mother told you that breakfast was the most important meal of the day. Cereal marketing teams banked on that, selling breakfast to millions of people based on a common turn of phrase like “an apple a day keeps the doctor away.” Well, what if the notion of breakfast’s importance isn’t just marketing BS?
A new study suggests that adults who don’t eat breakfast are setting themselves up for a nutritional gap. Common breakfast foods pack a ton of calcium, fiber, and vitamin C from milk, cereals, and fruit. Christopher Taylor, PhD, senior author of the study and professor of dietetics at the Ohio State University, Columbus, said that if you’re not getting those nutrients from foods at breakfast, there’s a tendency to skip them throughout the rest of your day.
Data from a sample of the National Health and Nutrition Examination Survey – 30,889 adults aged 19 and older who participated between 2005 and 2016 – showed that 15.2% of participants reported skipping breakfast.
The research team then estimated nutrient consumption using federal dietary studies and guidelines and compared it to Food and Nutrition Board of National Academies nutrient recommendations. The breakfast skippers, they determined, were missing out on pronounced levels of fiber, magnesium, iron, calcium, and vitamins A, B1, B2, B3, C, and D and were more likely to fall prey to lower-quality snacking. Cue those Oreos at 3 pm.
You may get more total calories within the day by eating breakfast, but your lunch, dinner, and snacks are much larger when you skip it. So the case of breakfast being the most important meal of the day checks out. Who knew that Tony the Tiger – and Mom – were actually on to something?
The bitter taste of a healthy liver
Alcohol and liver disease. They go together like, well, alcohol and liver disease. But alcohol isn’t the only reason people get liver disease, and now there’s a potential new treatment for people with hepatic steatosis on the way to becoming nonalcoholic fatty liver disease: beer.
Okay, not literally beer, but a pair of compounds derived from hops, the plant that gives beer its color and bitter flavor. In a study published in eLife, researchers from Oregon State University fed mice either a low-fat diet or a high-fat diet to induce hepatic steatosis, with some on the high-fat diet receiving either xanthohumol, a prenylated flavonoid from the hop plant, or tetrahydroxanthohumol, a hydrogenated derivative of xanthohumol.
Mice that received tetrahydroxanthohumol not only gained weight at a far slower rate than that of mice on the normal high-fat diet, their blood sugar remained stable; xanthohumol was similarly effective if the dosage was higher. The researchers noted that the two chemicals were effective because they acted as antagonists for the PPAR-gamma protein, which controls glucose metabolism and fatty cell activation. The chemicals bind to the protein but don’t activate it, meaning fat is unable to build up in the cells. No fat means no hepatic steatosis, which means no liver disease.
The researchers caution that more research is needed to determine the chemicals’ effectiveness in humans, but the classic line from a great animated philosopher still holds true: Alcohol may really be the source of, and solution to, all of life’s problems.
Life’s great mysteries, from A to zinc
Thanks to science, we now have answers to what were once unanswerable questions: Is Jello a solid or a liquid? If someone leads but no one follows, are they just out for a walk? Does zinc inhibit or promote the growth of kidney stones? How many licks does it take to get to the center of a Tootsie Pop? (Turns out science really did answer this one.)
If you’re anything like us, then you’ve been following the big debate on the two competing theories involving the role of zinc in kidney stone formation for years. One theory says that zinc stops the growth of calcium oxalate crystals that make up stones. The other says that zinc alters the surfaces of crystals, which encourages growth.
We can’t stand the suspense any longer, so here goes: The answer to “does zinc inhibit or promote the growth of kidney stones?” is … yes.
“What we see with zinc is something we haven’t seen before. It does slow down calcium oxalate crystal growth and at the same time it changes the surface of the crystals, causing defects in the form of intergrowths. These abnormalities create centers for new crystals to nucleate and grow,” said senior author Jeffrey Rimer, PhD, of the University of Houston.
In vitro experimentation, computational modeling, and atomic force microscopy don’t lie: Zinc ions have a unique ability “to alter the termination of crystal surfaces.” They tried alternative ions found in urine, including magnesium, and there was no effect on crystal formation.
With this one great mystery now solved, we contacted Dr. Rimer to ask him about the whole “sound of one hand clapping” business. He hasn’t cracked that one yet, but he did want to speak to our supervisor. So many of life’s unanswered questions, so little time. Oh well.
Babies’ ‘gut instinct’ to cry
At some point or another, you’ve probably been told not to “be such a baby” when you were scared of something. If you’ve been called a crybaby, it may be an indicator that you had a different gut microbiome as an infant.
Investigators from Michigan State University and the University of North Carolina say that babies who react more strongly to scary situations have different gut microbiomes compared with babies who don’t have such a strong reaction. The way babies react to scary situations can say a lot about their future, and there is even some evidence that gut microbiomes may have something to do with mental health.
Physicians who support neurologic development may one day be able to use this research on gut microbiomes to help monitor people’s neurological health. “This early developmental period is a time of tremendous opportunity for promoting healthy brain development. The microbiome is an exciting new target that can be potentially used for that,” said Rebecca Knickmeyer of MSU, leader of the study, which was published in Nature Communications. And loyal LOTME followers already know about the OpenBiome Microbiome Library, aka the “Amazon of bacteria.”
So the next time someone tells you not to be such a baby when you’re scared of something, tell them it’s not your fault. Blame it on your gut microbiome!
The good old days
“It’s good to be in something from the ground floor. I came too late for that. ... But lately, I’m getting the feeling that I came in at the end. The best is over.” –Tony Soprano
For me, I’m unsure. Sometimes it feels like our best days are behind us. When I was a kid, we explored life in pond water, watching water fleas and hydra swim under our Child World toy microscopes. Today, kids learn to eat Tide Pods from TikTok. Back when I was young, a doctor’s appointment was a special occasion! My brothers and I had a bath and got dressed in our Sunday best for our appointment with Dr. Bellin, a genteel, gray-haired pediatrician who worked out of his Victorian office with wooden floors and crystal door handles. Contrast that with the appointment I had with a patient the other day, done by telephone while she was in line ordering at Starbucks. I waited patiently for her to give her order.
This ache I feel for the past is called nostalgia. At one time, it was a diagnosable condition. It was first used by Dr. Johannes Hofer in the 17th century to describe Swiss soldiers fighting in foreign lands. From the Greek, it means “homecoming pain.” Although over time nostalgia has lost its clinical meaning, the feeling of yearning for the past has dramatically gained in prevalence. The word “nostalgia” appears more in print now than at any point since 1800. We are most nostalgic during times of duress, it seems. This, no doubt, is because it’s comforting to think we’d be better off back in pastoral, idyll times, back when work ended at 5 p.m. and cotton balls were soaked in alcohol and office visits ended with a lollipop on a loop.
Of course, the good old days weren’t really better. We have a selective view of history – as many things were contemptible or bad then as now. Yes, Dr. Bellin was the consummate professional, but thank goodness, I didn’t have acute lymphocytic leukemia or Haemophilus influenzae type B or even suffocate under a pile of blankets while sleeping on my stomach. Without doubt, clinically we’re much better today. Also back then, there was hardly a consideration for atrocious racial disparities in care. We’ve not come far, but we are at least better off today than a few decades ago. And what about medicine as a profession? Although he had loads of autonomy and respect, Dr. Bellin also started every day of his 50-year career at 6 a.m. rounding in the newborn nursery before seeing patients in the office 6 days a week. Not many of us would trade our practice for his.
Yet, there’s reasons to be nostalgic. Chart notes might have been barely legible, but at least they served a purpose. The problem-oriented medical record was intended to logically capture and organize data. SOAP notes were invented to help us think better, to get diagnoses correct, to succinctly see progress. Today, notes are written for administrators and payers and patients. As a result, they’re often useless to us.
And although it may have been inconvenient to sit in the waiting room reading Highlights magazine, I’m unsure it was a worse user experience, compared with a chain pharmacy “virtual” doctor visit. (Particularly because you could always drop pennies down the large hot-air iron floor grate in the corner).
The thrumming undercurrent of progress promises artificial intelligence and genomics and wearable diagnostics in our future. But the assumption is the new things will be better suited to our needs than the old. Sometimes, they are not. Sometimes technology diminishes us instead of enhancing us.
I cannot count how many times I’ve hit my head or whacked my shin because our Tesla Model X doors open by magic and of their own accord. Back when I was young, we opened car doors by pulling on the door handle. I sometimes miss those days.
Dr. Benabio is director of Healthcare Transformation and chief of dermatology at Kaiser Permanente San Diego. The opinions expressed in this column are his own and do not represent those of Kaiser Permanente. Dr. Benabio is @Dermdoc on Twitter. Write to him at [email protected].
“It’s good to be in something from the ground floor. I came too late for that. ... But lately, I’m getting the feeling that I came in at the end. The best is over.” –Tony Soprano
For me, I’m unsure. Sometimes it feels like our best days are behind us. When I was a kid, we explored life in pond water, watching water fleas and hydra swim under our Child World toy microscopes. Today, kids learn to eat Tide Pods from TikTok. Back when I was young, a doctor’s appointment was a special occasion! My brothers and I had a bath and got dressed in our Sunday best for our appointment with Dr. Bellin, a genteel, gray-haired pediatrician who worked out of his Victorian office with wooden floors and crystal door handles. Contrast that with the appointment I had with a patient the other day, done by telephone while she was in line ordering at Starbucks. I waited patiently for her to give her order.
This ache I feel for the past is called nostalgia. At one time, it was a diagnosable condition. It was first used by Dr. Johannes Hofer in the 17th century to describe Swiss soldiers fighting in foreign lands. From the Greek, it means “homecoming pain.” Although over time nostalgia has lost its clinical meaning, the feeling of yearning for the past has dramatically gained in prevalence. The word “nostalgia” appears more in print now than at any point since 1800. We are most nostalgic during times of duress, it seems. This, no doubt, is because it’s comforting to think we’d be better off back in pastoral, idyll times, back when work ended at 5 p.m. and cotton balls were soaked in alcohol and office visits ended with a lollipop on a loop.
Of course, the good old days weren’t really better. We have a selective view of history – as many things were contemptible or bad then as now. Yes, Dr. Bellin was the consummate professional, but thank goodness, I didn’t have acute lymphocytic leukemia or Haemophilus influenzae type B or even suffocate under a pile of blankets while sleeping on my stomach. Without doubt, clinically we’re much better today. Also back then, there was hardly a consideration for atrocious racial disparities in care. We’ve not come far, but we are at least better off today than a few decades ago. And what about medicine as a profession? Although he had loads of autonomy and respect, Dr. Bellin also started every day of his 50-year career at 6 a.m. rounding in the newborn nursery before seeing patients in the office 6 days a week. Not many of us would trade our practice for his.
Yet, there’s reasons to be nostalgic. Chart notes might have been barely legible, but at least they served a purpose. The problem-oriented medical record was intended to logically capture and organize data. SOAP notes were invented to help us think better, to get diagnoses correct, to succinctly see progress. Today, notes are written for administrators and payers and patients. As a result, they’re often useless to us.
And although it may have been inconvenient to sit in the waiting room reading Highlights magazine, I’m unsure it was a worse user experience, compared with a chain pharmacy “virtual” doctor visit. (Particularly because you could always drop pennies down the large hot-air iron floor grate in the corner).
The thrumming undercurrent of progress promises artificial intelligence and genomics and wearable diagnostics in our future. But the assumption is the new things will be better suited to our needs than the old. Sometimes, they are not. Sometimes technology diminishes us instead of enhancing us.
I cannot count how many times I’ve hit my head or whacked my shin because our Tesla Model X doors open by magic and of their own accord. Back when I was young, we opened car doors by pulling on the door handle. I sometimes miss those days.
Dr. Benabio is director of Healthcare Transformation and chief of dermatology at Kaiser Permanente San Diego. The opinions expressed in this column are his own and do not represent those of Kaiser Permanente. Dr. Benabio is @Dermdoc on Twitter. Write to him at [email protected].
“It’s good to be in something from the ground floor. I came too late for that. ... But lately, I’m getting the feeling that I came in at the end. The best is over.” –Tony Soprano
For me, I’m unsure. Sometimes it feels like our best days are behind us. When I was a kid, we explored life in pond water, watching water fleas and hydra swim under our Child World toy microscopes. Today, kids learn to eat Tide Pods from TikTok. Back when I was young, a doctor’s appointment was a special occasion! My brothers and I had a bath and got dressed in our Sunday best for our appointment with Dr. Bellin, a genteel, gray-haired pediatrician who worked out of his Victorian office with wooden floors and crystal door handles. Contrast that with the appointment I had with a patient the other day, done by telephone while she was in line ordering at Starbucks. I waited patiently for her to give her order.
This ache I feel for the past is called nostalgia. At one time, it was a diagnosable condition. It was first used by Dr. Johannes Hofer in the 17th century to describe Swiss soldiers fighting in foreign lands. From the Greek, it means “homecoming pain.” Although over time nostalgia has lost its clinical meaning, the feeling of yearning for the past has dramatically gained in prevalence. The word “nostalgia” appears more in print now than at any point since 1800. We are most nostalgic during times of duress, it seems. This, no doubt, is because it’s comforting to think we’d be better off back in pastoral, idyll times, back when work ended at 5 p.m. and cotton balls were soaked in alcohol and office visits ended with a lollipop on a loop.
Of course, the good old days weren’t really better. We have a selective view of history – as many things were contemptible or bad then as now. Yes, Dr. Bellin was the consummate professional, but thank goodness, I didn’t have acute lymphocytic leukemia or Haemophilus influenzae type B or even suffocate under a pile of blankets while sleeping on my stomach. Without doubt, clinically we’re much better today. Also back then, there was hardly a consideration for atrocious racial disparities in care. We’ve not come far, but we are at least better off today than a few decades ago. And what about medicine as a profession? Although he had loads of autonomy and respect, Dr. Bellin also started every day of his 50-year career at 6 a.m. rounding in the newborn nursery before seeing patients in the office 6 days a week. Not many of us would trade our practice for his.
Yet, there’s reasons to be nostalgic. Chart notes might have been barely legible, but at least they served a purpose. The problem-oriented medical record was intended to logically capture and organize data. SOAP notes were invented to help us think better, to get diagnoses correct, to succinctly see progress. Today, notes are written for administrators and payers and patients. As a result, they’re often useless to us.
And although it may have been inconvenient to sit in the waiting room reading Highlights magazine, I’m unsure it was a worse user experience, compared with a chain pharmacy “virtual” doctor visit. (Particularly because you could always drop pennies down the large hot-air iron floor grate in the corner).
The thrumming undercurrent of progress promises artificial intelligence and genomics and wearable diagnostics in our future. But the assumption is the new things will be better suited to our needs than the old. Sometimes, they are not. Sometimes technology diminishes us instead of enhancing us.
I cannot count how many times I’ve hit my head or whacked my shin because our Tesla Model X doors open by magic and of their own accord. Back when I was young, we opened car doors by pulling on the door handle. I sometimes miss those days.
Dr. Benabio is director of Healthcare Transformation and chief of dermatology at Kaiser Permanente San Diego. The opinions expressed in this column are his own and do not represent those of Kaiser Permanente. Dr. Benabio is @Dermdoc on Twitter. Write to him at [email protected].
Remove sex designation from public part of birth certificates, AMA advises
Requiring the designation can lead to discrimination and unnecessary burden on individuals whose current gender identity does not align with their designation at birth when they register for school or sports, adopt, get married, or request personal records.
A person’s sex designation at birth would still be submitted to the U.S. Standard Certificate of Live Birth for medical, public health, and statistical use only, report authors note.
Willie Underwood III, MD, MSc, author of Board Report 15, explained in reference committee testimony that a standard certificate of live birth is critical for uniformly collecting and processing data, but birth certificates are issued by the government to individuals.
Ten states allow gender-neutral designation
According to the report, 48 states (Tennessee and Ohio are the exceptions) and the District of Columbia allow people to amend their sex designation on their birth certificate to reflect their gender identities, but only 10 states allow for a gender-neutral designation, usually “X,” on birth certificates. The U.S. Department of State does not currently offer an option for a gender-neutral designation on U.S. passports.
“Assigning sex using binary variables in the public portion of the birth certificate fails to recognize the medical spectrum of gender identity,” Dr. Underwood said, and it can be used to discriminate.
Jeremy Toler, MD, a delegate from GLMA: Health Professionals Advancing LGBTQ Equality, testified that there is precedent for information to be removed from the public portion of the birth certificates. And much data is collected for each live birth that doesn’t show up on individuals’ birth certificates, he noted.
Dr. Toler said transgender, gender nonbinary, and individuals with differences in sex development can be placed at a disadvantage by the sex label on the birth certificate.
“We unfortunately still live in a world where it is unsafe in many cases for one’s gender to vary from the sex assigned at birth,” Dr. Toler said.
Not having this data on the widely used form will reduce unnecessary reliance on sex as a stand-in for gender, he said, and would “serve as an equalizer” since policies differ by state.
Robert Jackson, MD, an alternate delegate from the American Academy of Cosmetic Surgery, spoke against the measure.
“We as physicians need to report things accurately,” Dr. Jackson said. “All through medical school, residency, and specialty training we were supposed to delegate all of the physical findings of the patient we’re taking care of. I think when the child is born, they do have physical characteristics either male or female, and I think that probably should be on the public record. That’s just my personal opinion.”
Sarah Mae Smith, MD, delegate from California, speaking on behalf of the Women Physicians Section, said removing the sex designation is important for moving toward gender equity.
“We need to recognize [that] gender is not a binary but a spectrum,” she said. “Obligating our patients to jump through numerous administrative hoops to identify as who they are based on a sex assigned at birth primarily on genitalia is not only unnecessary but actively deleterious to their health.”
Race was once public on birth certificates
She noted that the report mentions that previously, information on the race of a person’s parents was included on the public portion of the birth certificate and that information was recognized to facilitate discrimination.
“Thankfully, a change was made to obviate at least that avenue for discriminatory practices,” she said. “Now, likewise, the information on sex assigned at birth is being used to undermine the rights of our transgender, intersex, and nonbinary patients.”
Arlene Seid, MD, MPH, an alternate delegate from the American Association of Public Health Physicians, said the resolution protects the aggregate data “without the discrimination associated with the individual data.”
Sex no longer has a role to play in the jobs people do, she noted, and the designation shouldn’t have to be evaluated for something like a job interview.
“Our society doesn’t need it on an individual basis for most of what occurs in public life,” Dr. Seid said.
Dr. Underwood, Dr. Toler, Dr. Jackson, Dr. Smith, and Dr. Seid declared no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Requiring the designation can lead to discrimination and unnecessary burden on individuals whose current gender identity does not align with their designation at birth when they register for school or sports, adopt, get married, or request personal records.
A person’s sex designation at birth would still be submitted to the U.S. Standard Certificate of Live Birth for medical, public health, and statistical use only, report authors note.
Willie Underwood III, MD, MSc, author of Board Report 15, explained in reference committee testimony that a standard certificate of live birth is critical for uniformly collecting and processing data, but birth certificates are issued by the government to individuals.
Ten states allow gender-neutral designation
According to the report, 48 states (Tennessee and Ohio are the exceptions) and the District of Columbia allow people to amend their sex designation on their birth certificate to reflect their gender identities, but only 10 states allow for a gender-neutral designation, usually “X,” on birth certificates. The U.S. Department of State does not currently offer an option for a gender-neutral designation on U.S. passports.
“Assigning sex using binary variables in the public portion of the birth certificate fails to recognize the medical spectrum of gender identity,” Dr. Underwood said, and it can be used to discriminate.
Jeremy Toler, MD, a delegate from GLMA: Health Professionals Advancing LGBTQ Equality, testified that there is precedent for information to be removed from the public portion of the birth certificates. And much data is collected for each live birth that doesn’t show up on individuals’ birth certificates, he noted.
Dr. Toler said transgender, gender nonbinary, and individuals with differences in sex development can be placed at a disadvantage by the sex label on the birth certificate.
“We unfortunately still live in a world where it is unsafe in many cases for one’s gender to vary from the sex assigned at birth,” Dr. Toler said.
Not having this data on the widely used form will reduce unnecessary reliance on sex as a stand-in for gender, he said, and would “serve as an equalizer” since policies differ by state.
Robert Jackson, MD, an alternate delegate from the American Academy of Cosmetic Surgery, spoke against the measure.
“We as physicians need to report things accurately,” Dr. Jackson said. “All through medical school, residency, and specialty training we were supposed to delegate all of the physical findings of the patient we’re taking care of. I think when the child is born, they do have physical characteristics either male or female, and I think that probably should be on the public record. That’s just my personal opinion.”
Sarah Mae Smith, MD, delegate from California, speaking on behalf of the Women Physicians Section, said removing the sex designation is important for moving toward gender equity.
“We need to recognize [that] gender is not a binary but a spectrum,” she said. “Obligating our patients to jump through numerous administrative hoops to identify as who they are based on a sex assigned at birth primarily on genitalia is not only unnecessary but actively deleterious to their health.”
Race was once public on birth certificates
She noted that the report mentions that previously, information on the race of a person’s parents was included on the public portion of the birth certificate and that information was recognized to facilitate discrimination.
“Thankfully, a change was made to obviate at least that avenue for discriminatory practices,” she said. “Now, likewise, the information on sex assigned at birth is being used to undermine the rights of our transgender, intersex, and nonbinary patients.”
Arlene Seid, MD, MPH, an alternate delegate from the American Association of Public Health Physicians, said the resolution protects the aggregate data “without the discrimination associated with the individual data.”
Sex no longer has a role to play in the jobs people do, she noted, and the designation shouldn’t have to be evaluated for something like a job interview.
“Our society doesn’t need it on an individual basis for most of what occurs in public life,” Dr. Seid said.
Dr. Underwood, Dr. Toler, Dr. Jackson, Dr. Smith, and Dr. Seid declared no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Requiring the designation can lead to discrimination and unnecessary burden on individuals whose current gender identity does not align with their designation at birth when they register for school or sports, adopt, get married, or request personal records.
A person’s sex designation at birth would still be submitted to the U.S. Standard Certificate of Live Birth for medical, public health, and statistical use only, report authors note.
Willie Underwood III, MD, MSc, author of Board Report 15, explained in reference committee testimony that a standard certificate of live birth is critical for uniformly collecting and processing data, but birth certificates are issued by the government to individuals.
Ten states allow gender-neutral designation
According to the report, 48 states (Tennessee and Ohio are the exceptions) and the District of Columbia allow people to amend their sex designation on their birth certificate to reflect their gender identities, but only 10 states allow for a gender-neutral designation, usually “X,” on birth certificates. The U.S. Department of State does not currently offer an option for a gender-neutral designation on U.S. passports.
“Assigning sex using binary variables in the public portion of the birth certificate fails to recognize the medical spectrum of gender identity,” Dr. Underwood said, and it can be used to discriminate.
Jeremy Toler, MD, a delegate from GLMA: Health Professionals Advancing LGBTQ Equality, testified that there is precedent for information to be removed from the public portion of the birth certificates. And much data is collected for each live birth that doesn’t show up on individuals’ birth certificates, he noted.
Dr. Toler said transgender, gender nonbinary, and individuals with differences in sex development can be placed at a disadvantage by the sex label on the birth certificate.
“We unfortunately still live in a world where it is unsafe in many cases for one’s gender to vary from the sex assigned at birth,” Dr. Toler said.
Not having this data on the widely used form will reduce unnecessary reliance on sex as a stand-in for gender, he said, and would “serve as an equalizer” since policies differ by state.
Robert Jackson, MD, an alternate delegate from the American Academy of Cosmetic Surgery, spoke against the measure.
“We as physicians need to report things accurately,” Dr. Jackson said. “All through medical school, residency, and specialty training we were supposed to delegate all of the physical findings of the patient we’re taking care of. I think when the child is born, they do have physical characteristics either male or female, and I think that probably should be on the public record. That’s just my personal opinion.”
Sarah Mae Smith, MD, delegate from California, speaking on behalf of the Women Physicians Section, said removing the sex designation is important for moving toward gender equity.
“We need to recognize [that] gender is not a binary but a spectrum,” she said. “Obligating our patients to jump through numerous administrative hoops to identify as who they are based on a sex assigned at birth primarily on genitalia is not only unnecessary but actively deleterious to their health.”
Race was once public on birth certificates
She noted that the report mentions that previously, information on the race of a person’s parents was included on the public portion of the birth certificate and that information was recognized to facilitate discrimination.
“Thankfully, a change was made to obviate at least that avenue for discriminatory practices,” she said. “Now, likewise, the information on sex assigned at birth is being used to undermine the rights of our transgender, intersex, and nonbinary patients.”
Arlene Seid, MD, MPH, an alternate delegate from the American Association of Public Health Physicians, said the resolution protects the aggregate data “without the discrimination associated with the individual data.”
Sex no longer has a role to play in the jobs people do, she noted, and the designation shouldn’t have to be evaluated for something like a job interview.
“Our society doesn’t need it on an individual basis for most of what occurs in public life,” Dr. Seid said.
Dr. Underwood, Dr. Toler, Dr. Jackson, Dr. Smith, and Dr. Seid declared no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Toxic chemicals found in many cosmetics
People may be absorbing and ingesting potentially toxic chemicals from their cosmetic products, a new study suggests.
– per- and polyfluoroalkyl substances. Many of these chemicals were not included on the product labels, making it difficult for consumers to consciously avoid them.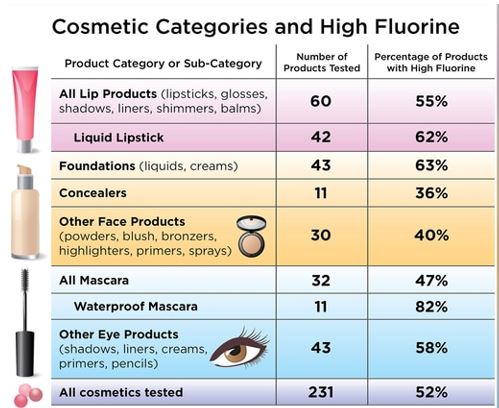
“This study is very helpful for elucidating the PFAS content of different types of cosmetics in the U.S. and Canadian markets,” said Elsie Sunderland, PhD, an environmental scientist who was not involved with the study.
“Previously, all the data had been collected in Europe, and this study shows we are dealing with similar problems in the North American marketplace,” said Dr. Sunderland, a professor of environmental chemistry at the Harvard School of Public Health, Boston.
PFAS are a class of chemicals used in a variety of consumer products, such as nonstick cookware, stain-resistant carpeting, and water-repellent clothing, according to the Centers for Disease Control and Prevention. They are added to cosmetics to make the products more durable and spreadable, researchers said in the study.
“[PFAS] are added to change the properties of surfaces, to make them nonstick or resistant to stay in water or oils,” said study coauthor Tom Bruton, PhD, senior scientist at the Green Science Policy Institute in Berkeley, Calif. “The concerning thing about cosmetics is that these are products that you’re applying to your skin and face every day, so there’s the skin absorption route that’s of concern, but also incidental ingestion of cosmetics is also a concern as well.”
The CDC says some of the potential health effects of PFAS exposure includes increased cholesterol levels, increased risk of kidney and testicular cancer, changes in liver enzymes, decreased vaccine response in children, and a higher risk of high blood pressure or preeclampsia in pregnant women.
“PFAS are a large class of chemicals. In humans, exposure to some of these chemicals has been associated with impaired immune function, certain cancers, increased risks of diabetes, obesity and endocrine disruption,” Dr. Sunderland said. “They appear to be harmful to every major organ system in the human body.”
For the current study, published online in Environmental Science & Technology Letters, Dr. Bruton and colleagues purchased 231 cosmetic products in the United States and Canada from retailers such as Ulta Beauty, Sephora, Target, and Bed Bath & Beyond. They then screened them for fluorine.Three-quarters of waterproof mascara samples contained high fluorine concentrations, as did nearly two-thirds of foundations and liquid lipsticks, and more than half of the eye and lip products tested.
The authors found that different categories of makeup tended to have higher or lower fluorine concentrations. “High fluorine levels were found in products commonly advertised as ‘wear-resistant’ to water and oils or ‘long-lasting,’ including foundations, liquid lipsticks, and waterproof mascaras,” Dr. Bruton and colleagues wrote.
When they further analyzed a subset of 29 products to determine what types of chemicals were present, they found that each cosmetic product contained at least 4 PFAS, with one product containing 13.The PFAS substances found included some that break down into other chemicals that are known to be highly toxic and environmentally harmful.
“It’s concerning that some of the products we tested appear to be intentionally using PFAS, but not listing those ingredients on the label,” Dr. Bruton said. “I do think that it is helpful for consumers to read labels, but beyond that, there’s not a lot of ways that consumers themselves can solve this problem. ... We think that the industry needs to be more proactive about moving away from this group of chemicals.”
Dr. Sunderland said a resource people can use when trying to avoid PFAS is the Environmental Working Group, a nonprofit organization that maintains an extensive database of cosmetics and personal care products.
“At this point, there is very little regulatory activity related to PFAS in cosmetics,” Dr. Sunderland said. “The best thing to happen now would be for consumers to indicate that they prefer products without PFAS and to demand better transparency in product ingredient lists.”
A similar study done in 2018 by the Danish Environmental Protection Agency found high levels of PFAS in nearly one-third of the cosmetics products it tested.
People can also be exposed to PFAS by eating or drinking contaminated food or water and through food packaging. Dr. Sunderland said some wild foods like seafood are known to accumulate these compounds in the environment.
“There are examples of contaminated biosolids leading to accumulation of PFAS in vegetables and milk,” Dr. Sunderland explained. “Food packaging is another concern because it can also result in PFAS accumulation in the foods we eat.”
Although it’s difficult to avoid PFAS altogether, the CDC suggests lowering exposure rates by avoiding contaminated water and food. If you’re not sure if your water is contaminated, you should ask your local or state health and environmental quality departments for fish or water advisories in your area.
A version of this article first appeared on WebMD.com.
People may be absorbing and ingesting potentially toxic chemicals from their cosmetic products, a new study suggests.
– per- and polyfluoroalkyl substances. Many of these chemicals were not included on the product labels, making it difficult for consumers to consciously avoid them.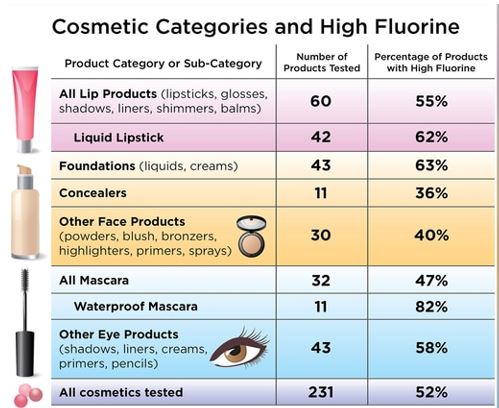
“This study is very helpful for elucidating the PFAS content of different types of cosmetics in the U.S. and Canadian markets,” said Elsie Sunderland, PhD, an environmental scientist who was not involved with the study.
“Previously, all the data had been collected in Europe, and this study shows we are dealing with similar problems in the North American marketplace,” said Dr. Sunderland, a professor of environmental chemistry at the Harvard School of Public Health, Boston.
PFAS are a class of chemicals used in a variety of consumer products, such as nonstick cookware, stain-resistant carpeting, and water-repellent clothing, according to the Centers for Disease Control and Prevention. They are added to cosmetics to make the products more durable and spreadable, researchers said in the study.
“[PFAS] are added to change the properties of surfaces, to make them nonstick or resistant to stay in water or oils,” said study coauthor Tom Bruton, PhD, senior scientist at the Green Science Policy Institute in Berkeley, Calif. “The concerning thing about cosmetics is that these are products that you’re applying to your skin and face every day, so there’s the skin absorption route that’s of concern, but also incidental ingestion of cosmetics is also a concern as well.”
The CDC says some of the potential health effects of PFAS exposure includes increased cholesterol levels, increased risk of kidney and testicular cancer, changes in liver enzymes, decreased vaccine response in children, and a higher risk of high blood pressure or preeclampsia in pregnant women.
“PFAS are a large class of chemicals. In humans, exposure to some of these chemicals has been associated with impaired immune function, certain cancers, increased risks of diabetes, obesity and endocrine disruption,” Dr. Sunderland said. “They appear to be harmful to every major organ system in the human body.”
For the current study, published online in Environmental Science & Technology Letters, Dr. Bruton and colleagues purchased 231 cosmetic products in the United States and Canada from retailers such as Ulta Beauty, Sephora, Target, and Bed Bath & Beyond. They then screened them for fluorine.Three-quarters of waterproof mascara samples contained high fluorine concentrations, as did nearly two-thirds of foundations and liquid lipsticks, and more than half of the eye and lip products tested.
The authors found that different categories of makeup tended to have higher or lower fluorine concentrations. “High fluorine levels were found in products commonly advertised as ‘wear-resistant’ to water and oils or ‘long-lasting,’ including foundations, liquid lipsticks, and waterproof mascaras,” Dr. Bruton and colleagues wrote.
When they further analyzed a subset of 29 products to determine what types of chemicals were present, they found that each cosmetic product contained at least 4 PFAS, with one product containing 13.The PFAS substances found included some that break down into other chemicals that are known to be highly toxic and environmentally harmful.
“It’s concerning that some of the products we tested appear to be intentionally using PFAS, but not listing those ingredients on the label,” Dr. Bruton said. “I do think that it is helpful for consumers to read labels, but beyond that, there’s not a lot of ways that consumers themselves can solve this problem. ... We think that the industry needs to be more proactive about moving away from this group of chemicals.”
Dr. Sunderland said a resource people can use when trying to avoid PFAS is the Environmental Working Group, a nonprofit organization that maintains an extensive database of cosmetics and personal care products.
“At this point, there is very little regulatory activity related to PFAS in cosmetics,” Dr. Sunderland said. “The best thing to happen now would be for consumers to indicate that they prefer products without PFAS and to demand better transparency in product ingredient lists.”
A similar study done in 2018 by the Danish Environmental Protection Agency found high levels of PFAS in nearly one-third of the cosmetics products it tested.
People can also be exposed to PFAS by eating or drinking contaminated food or water and through food packaging. Dr. Sunderland said some wild foods like seafood are known to accumulate these compounds in the environment.
“There are examples of contaminated biosolids leading to accumulation of PFAS in vegetables and milk,” Dr. Sunderland explained. “Food packaging is another concern because it can also result in PFAS accumulation in the foods we eat.”
Although it’s difficult to avoid PFAS altogether, the CDC suggests lowering exposure rates by avoiding contaminated water and food. If you’re not sure if your water is contaminated, you should ask your local or state health and environmental quality departments for fish or water advisories in your area.
A version of this article first appeared on WebMD.com.
People may be absorbing and ingesting potentially toxic chemicals from their cosmetic products, a new study suggests.
– per- and polyfluoroalkyl substances. Many of these chemicals were not included on the product labels, making it difficult for consumers to consciously avoid them.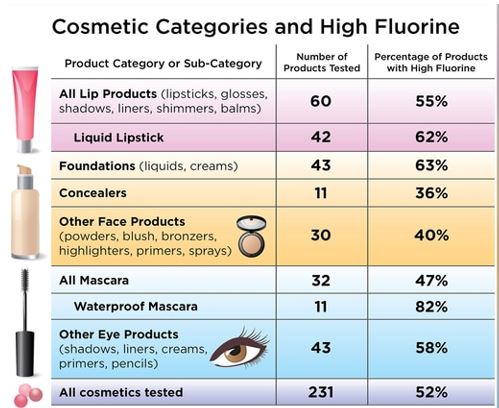
“This study is very helpful for elucidating the PFAS content of different types of cosmetics in the U.S. and Canadian markets,” said Elsie Sunderland, PhD, an environmental scientist who was not involved with the study.
“Previously, all the data had been collected in Europe, and this study shows we are dealing with similar problems in the North American marketplace,” said Dr. Sunderland, a professor of environmental chemistry at the Harvard School of Public Health, Boston.
PFAS are a class of chemicals used in a variety of consumer products, such as nonstick cookware, stain-resistant carpeting, and water-repellent clothing, according to the Centers for Disease Control and Prevention. They are added to cosmetics to make the products more durable and spreadable, researchers said in the study.
“[PFAS] are added to change the properties of surfaces, to make them nonstick or resistant to stay in water or oils,” said study coauthor Tom Bruton, PhD, senior scientist at the Green Science Policy Institute in Berkeley, Calif. “The concerning thing about cosmetics is that these are products that you’re applying to your skin and face every day, so there’s the skin absorption route that’s of concern, but also incidental ingestion of cosmetics is also a concern as well.”
The CDC says some of the potential health effects of PFAS exposure includes increased cholesterol levels, increased risk of kidney and testicular cancer, changes in liver enzymes, decreased vaccine response in children, and a higher risk of high blood pressure or preeclampsia in pregnant women.
“PFAS are a large class of chemicals. In humans, exposure to some of these chemicals has been associated with impaired immune function, certain cancers, increased risks of diabetes, obesity and endocrine disruption,” Dr. Sunderland said. “They appear to be harmful to every major organ system in the human body.”
For the current study, published online in Environmental Science & Technology Letters, Dr. Bruton and colleagues purchased 231 cosmetic products in the United States and Canada from retailers such as Ulta Beauty, Sephora, Target, and Bed Bath & Beyond. They then screened them for fluorine.Three-quarters of waterproof mascara samples contained high fluorine concentrations, as did nearly two-thirds of foundations and liquid lipsticks, and more than half of the eye and lip products tested.
The authors found that different categories of makeup tended to have higher or lower fluorine concentrations. “High fluorine levels were found in products commonly advertised as ‘wear-resistant’ to water and oils or ‘long-lasting,’ including foundations, liquid lipsticks, and waterproof mascaras,” Dr. Bruton and colleagues wrote.
When they further analyzed a subset of 29 products to determine what types of chemicals were present, they found that each cosmetic product contained at least 4 PFAS, with one product containing 13.The PFAS substances found included some that break down into other chemicals that are known to be highly toxic and environmentally harmful.
“It’s concerning that some of the products we tested appear to be intentionally using PFAS, but not listing those ingredients on the label,” Dr. Bruton said. “I do think that it is helpful for consumers to read labels, but beyond that, there’s not a lot of ways that consumers themselves can solve this problem. ... We think that the industry needs to be more proactive about moving away from this group of chemicals.”
Dr. Sunderland said a resource people can use when trying to avoid PFAS is the Environmental Working Group, a nonprofit organization that maintains an extensive database of cosmetics and personal care products.
“At this point, there is very little regulatory activity related to PFAS in cosmetics,” Dr. Sunderland said. “The best thing to happen now would be for consumers to indicate that they prefer products without PFAS and to demand better transparency in product ingredient lists.”
A similar study done in 2018 by the Danish Environmental Protection Agency found high levels of PFAS in nearly one-third of the cosmetics products it tested.
People can also be exposed to PFAS by eating or drinking contaminated food or water and through food packaging. Dr. Sunderland said some wild foods like seafood are known to accumulate these compounds in the environment.
“There are examples of contaminated biosolids leading to accumulation of PFAS in vegetables and milk,” Dr. Sunderland explained. “Food packaging is another concern because it can also result in PFAS accumulation in the foods we eat.”
Although it’s difficult to avoid PFAS altogether, the CDC suggests lowering exposure rates by avoiding contaminated water and food. If you’re not sure if your water is contaminated, you should ask your local or state health and environmental quality departments for fish or water advisories in your area.
A version of this article first appeared on WebMD.com.
AMA acknowledges medical education racism of past, vows better future
The report received overwhelming support at the House of Delegates, the AMA’s legislative policy making body, during an online meeting held June 13.
The Council on Medical Education’s report recommends that the AMA acknowledge the harm caused by the Flexner Report, which was issued in 1910 and has since shaped medical education. The Flexner Report caused harm not only to historically Black medical schools, but also to physician workforce diversity and to the clinical outcomes of minority and marginalized patients, according to the medical education advisory body.
The council also recommended conducting a study on medical education with a focus on health equity and racial justice, improving diversity among healthcare workers, and fixing inequitable outcomes from minorities and marginalized patient populations.
The report comes on the heels of the resignation of JAMA editor-in-chief Howard Bauchner, MD, and another high-ranking editor following a February podcast on systemic racism in medicine. The AMA has since released a strategic plan addressing racism and health inequity that has divided membership.
Flexner Report’s effect on physician diversity
The Council on Medical Education’s report observed that as a result of the Flexner Report’s recommendations, 89 medical schools, including 5 of the 7 existing medical schools training Black physicians, were closed because they didn’t meet the report’s standards. In addition, the report created a limited role for Black physicians while “hint[ing] that Black physicians possessed less potential and ability than their White counterparts,” read the Council’s report.
In addition to consigning the role of the Black physician to “educating the [Black] race to know and to practice fundamental hygienic principles,” the Flexner Report also observed that “a well-taught negro sanitarian will be immensely useful,” per the Council’s report.
The impact of the closure of medical schools training Black physicians was dramatic. According to the Council’s report, in 1964, 93% of medical students in the United States were men and 97% of those students were non-Hispanic White.
Today, 56% of physicians identify as White, 17% as Asian, 6% as Hispanic, and 5% as Black or African American, per the Association of American Medical Colleges; nearly 14% of active physicians didn’t report their race in the survey. By means of contrast, the U.S. population in 2019 was 60% White, 19% Latino/Hispanic, 13% Black or African American, and 6% Asian American, according to the Brookings Institute.
Abraham Flexner, who wrote the Flexner Report, is often referred to as the “father of modern medical education,” according to the AAMC. In November, the AAMC observed that the Flexner Report contained racist and sexist ideas and that his work contributed to the closure of historically Black medical schools. Both statements were included in AAMC’s announcement about the removal of Flexner’s name from its most prestigious award. As of January, the award is now called the AAMC Award for Excellence in Medical Education.
Pathway programs can increase diversity
Pathway programs, which leverage targeted milestones along the journey to becoming a physician in order to increase diversity, were an area of focus in the council’s report. These programs “can exert a meaningful, positive effect on student outcomes and increase diversity across various levels of educational settings,” according to its report.
Centers of Excellence, which provides grants for mentorship and training programs, is one of many pathway programs. During the 2018-2019 academic year, Centers of Excellence supported more than 1,300 trainees – 99% of them were underrepresented minorities and 64% came from financially or educationally disadvantaged backgrounds. In 2006, federal funding was cut to these programs and the number of Centers of Excellence fell.
Still, the report cites the passage of federal funding in 2020 of $50 million for public institutions of higher education that train physicians; educational institutions in states with a projected primary care shortage in 2025 are given priority in the grant-funding process.
AMA council’s report garners support from delegates
Delegates voiced overwhelming support of the council’s report during the June 13 meeting. Lou Edje, MD, a Perrysburgh, Ohio–based family physician, voiced strong support for the council’s report, in particular its recommendations that recognize the harm caused by the Flexner Report. Dr. Edje observed that the Flexner Report, with its elimination of five of seven Black medical schools, “[set] back admissions of Black students into medicine by 50 years.”
“Empathy is what we are called to have as physicians. I implore you to simply substitute your ethnicity into these quotes to help understand the historic need for health equity in medicine today. This CME report is part of the antidote to Flexner. We support [it] fully,” concluded Dr. Edje, who spoke for the Great Lakes States Coalition of the AMA.
Rohan Khazanchi, a medical student at the University of Nebraska, Omaha, and a member of the council, said, “Our broad attempt with this report was twofold: to fill gaps in AMA policy with evidence-based recommendations which could improve diversity in our health workforce and, second, to enhance our organization’s vision for truth, reconciliation, and healing to redress the historic marginalization of minoritized physicians in medicine.”
According to an AMA spokesperson, the House of Delegates will vote on this and other policies this week, after which the policies are considered final.
A version of this article first appeared on Medscape.com.
The report received overwhelming support at the House of Delegates, the AMA’s legislative policy making body, during an online meeting held June 13.
The Council on Medical Education’s report recommends that the AMA acknowledge the harm caused by the Flexner Report, which was issued in 1910 and has since shaped medical education. The Flexner Report caused harm not only to historically Black medical schools, but also to physician workforce diversity and to the clinical outcomes of minority and marginalized patients, according to the medical education advisory body.
The council also recommended conducting a study on medical education with a focus on health equity and racial justice, improving diversity among healthcare workers, and fixing inequitable outcomes from minorities and marginalized patient populations.
The report comes on the heels of the resignation of JAMA editor-in-chief Howard Bauchner, MD, and another high-ranking editor following a February podcast on systemic racism in medicine. The AMA has since released a strategic plan addressing racism and health inequity that has divided membership.
Flexner Report’s effect on physician diversity
The Council on Medical Education’s report observed that as a result of the Flexner Report’s recommendations, 89 medical schools, including 5 of the 7 existing medical schools training Black physicians, were closed because they didn’t meet the report’s standards. In addition, the report created a limited role for Black physicians while “hint[ing] that Black physicians possessed less potential and ability than their White counterparts,” read the Council’s report.
In addition to consigning the role of the Black physician to “educating the [Black] race to know and to practice fundamental hygienic principles,” the Flexner Report also observed that “a well-taught negro sanitarian will be immensely useful,” per the Council’s report.
The impact of the closure of medical schools training Black physicians was dramatic. According to the Council’s report, in 1964, 93% of medical students in the United States were men and 97% of those students were non-Hispanic White.
Today, 56% of physicians identify as White, 17% as Asian, 6% as Hispanic, and 5% as Black or African American, per the Association of American Medical Colleges; nearly 14% of active physicians didn’t report their race in the survey. By means of contrast, the U.S. population in 2019 was 60% White, 19% Latino/Hispanic, 13% Black or African American, and 6% Asian American, according to the Brookings Institute.
Abraham Flexner, who wrote the Flexner Report, is often referred to as the “father of modern medical education,” according to the AAMC. In November, the AAMC observed that the Flexner Report contained racist and sexist ideas and that his work contributed to the closure of historically Black medical schools. Both statements were included in AAMC’s announcement about the removal of Flexner’s name from its most prestigious award. As of January, the award is now called the AAMC Award for Excellence in Medical Education.
Pathway programs can increase diversity
Pathway programs, which leverage targeted milestones along the journey to becoming a physician in order to increase diversity, were an area of focus in the council’s report. These programs “can exert a meaningful, positive effect on student outcomes and increase diversity across various levels of educational settings,” according to its report.
Centers of Excellence, which provides grants for mentorship and training programs, is one of many pathway programs. During the 2018-2019 academic year, Centers of Excellence supported more than 1,300 trainees – 99% of them were underrepresented minorities and 64% came from financially or educationally disadvantaged backgrounds. In 2006, federal funding was cut to these programs and the number of Centers of Excellence fell.
Still, the report cites the passage of federal funding in 2020 of $50 million for public institutions of higher education that train physicians; educational institutions in states with a projected primary care shortage in 2025 are given priority in the grant-funding process.
AMA council’s report garners support from delegates
Delegates voiced overwhelming support of the council’s report during the June 13 meeting. Lou Edje, MD, a Perrysburgh, Ohio–based family physician, voiced strong support for the council’s report, in particular its recommendations that recognize the harm caused by the Flexner Report. Dr. Edje observed that the Flexner Report, with its elimination of five of seven Black medical schools, “[set] back admissions of Black students into medicine by 50 years.”
“Empathy is what we are called to have as physicians. I implore you to simply substitute your ethnicity into these quotes to help understand the historic need for health equity in medicine today. This CME report is part of the antidote to Flexner. We support [it] fully,” concluded Dr. Edje, who spoke for the Great Lakes States Coalition of the AMA.
Rohan Khazanchi, a medical student at the University of Nebraska, Omaha, and a member of the council, said, “Our broad attempt with this report was twofold: to fill gaps in AMA policy with evidence-based recommendations which could improve diversity in our health workforce and, second, to enhance our organization’s vision for truth, reconciliation, and healing to redress the historic marginalization of minoritized physicians in medicine.”
According to an AMA spokesperson, the House of Delegates will vote on this and other policies this week, after which the policies are considered final.
A version of this article first appeared on Medscape.com.
The report received overwhelming support at the House of Delegates, the AMA’s legislative policy making body, during an online meeting held June 13.
The Council on Medical Education’s report recommends that the AMA acknowledge the harm caused by the Flexner Report, which was issued in 1910 and has since shaped medical education. The Flexner Report caused harm not only to historically Black medical schools, but also to physician workforce diversity and to the clinical outcomes of minority and marginalized patients, according to the medical education advisory body.
The council also recommended conducting a study on medical education with a focus on health equity and racial justice, improving diversity among healthcare workers, and fixing inequitable outcomes from minorities and marginalized patient populations.
The report comes on the heels of the resignation of JAMA editor-in-chief Howard Bauchner, MD, and another high-ranking editor following a February podcast on systemic racism in medicine. The AMA has since released a strategic plan addressing racism and health inequity that has divided membership.
Flexner Report’s effect on physician diversity
The Council on Medical Education’s report observed that as a result of the Flexner Report’s recommendations, 89 medical schools, including 5 of the 7 existing medical schools training Black physicians, were closed because they didn’t meet the report’s standards. In addition, the report created a limited role for Black physicians while “hint[ing] that Black physicians possessed less potential and ability than their White counterparts,” read the Council’s report.
In addition to consigning the role of the Black physician to “educating the [Black] race to know and to practice fundamental hygienic principles,” the Flexner Report also observed that “a well-taught negro sanitarian will be immensely useful,” per the Council’s report.
The impact of the closure of medical schools training Black physicians was dramatic. According to the Council’s report, in 1964, 93% of medical students in the United States were men and 97% of those students were non-Hispanic White.
Today, 56% of physicians identify as White, 17% as Asian, 6% as Hispanic, and 5% as Black or African American, per the Association of American Medical Colleges; nearly 14% of active physicians didn’t report their race in the survey. By means of contrast, the U.S. population in 2019 was 60% White, 19% Latino/Hispanic, 13% Black or African American, and 6% Asian American, according to the Brookings Institute.
Abraham Flexner, who wrote the Flexner Report, is often referred to as the “father of modern medical education,” according to the AAMC. In November, the AAMC observed that the Flexner Report contained racist and sexist ideas and that his work contributed to the closure of historically Black medical schools. Both statements were included in AAMC’s announcement about the removal of Flexner’s name from its most prestigious award. As of January, the award is now called the AAMC Award for Excellence in Medical Education.
Pathway programs can increase diversity
Pathway programs, which leverage targeted milestones along the journey to becoming a physician in order to increase diversity, were an area of focus in the council’s report. These programs “can exert a meaningful, positive effect on student outcomes and increase diversity across various levels of educational settings,” according to its report.
Centers of Excellence, which provides grants for mentorship and training programs, is one of many pathway programs. During the 2018-2019 academic year, Centers of Excellence supported more than 1,300 trainees – 99% of them were underrepresented minorities and 64% came from financially or educationally disadvantaged backgrounds. In 2006, federal funding was cut to these programs and the number of Centers of Excellence fell.
Still, the report cites the passage of federal funding in 2020 of $50 million for public institutions of higher education that train physicians; educational institutions in states with a projected primary care shortage in 2025 are given priority in the grant-funding process.
AMA council’s report garners support from delegates
Delegates voiced overwhelming support of the council’s report during the June 13 meeting. Lou Edje, MD, a Perrysburgh, Ohio–based family physician, voiced strong support for the council’s report, in particular its recommendations that recognize the harm caused by the Flexner Report. Dr. Edje observed that the Flexner Report, with its elimination of five of seven Black medical schools, “[set] back admissions of Black students into medicine by 50 years.”
“Empathy is what we are called to have as physicians. I implore you to simply substitute your ethnicity into these quotes to help understand the historic need for health equity in medicine today. This CME report is part of the antidote to Flexner. We support [it] fully,” concluded Dr. Edje, who spoke for the Great Lakes States Coalition of the AMA.
Rohan Khazanchi, a medical student at the University of Nebraska, Omaha, and a member of the council, said, “Our broad attempt with this report was twofold: to fill gaps in AMA policy with evidence-based recommendations which could improve diversity in our health workforce and, second, to enhance our organization’s vision for truth, reconciliation, and healing to redress the historic marginalization of minoritized physicians in medicine.”
According to an AMA spokesperson, the House of Delegates will vote on this and other policies this week, after which the policies are considered final.
A version of this article first appeared on Medscape.com.
Focus on cardiovascular disease
Cardiovascular disease is the leading cause of women’s death in the United States, accounting for 1 in every 5 female deaths per year according to the Centers for Disease Control and Prevention. Most risk factors for cardiovascular disease are modifiable. With a disease so prevalent in women’s health, obstetricians and gynecologists can assist patients in modifying these risk factors. This, however, is easier said than done.
One of the rate-limiting steps in assisting patients is the process of identifying an individual’s risk factors. This can be a time-consuming task in a women’s health appointment that is already busy with ObGyn-specific concerns, but technology can assist us.
Cardiovascular health app considerations
Many smartphone applications and websites are available that can alleviate the time constraints for identifying these individual modifiable risk factors. When evaluating cardiovascular risk factor apps for patients, keep these qualities (as outlined in the ACOG-recommended rubric) in mind: design, functionality, usefulness, and accuracy.
The patient-centered resources that assist women in identifying cardiovascular risk factors and that provide tools to positively impact these risk factors through lifestyle changes can help women achieve improved cardiovascular health. Recommendations include 1) manage blood pressure, 2) control cholesterol, 3) reduce blood sugar, 4) get active, 5) eat better, 6) lose weight, and 7) stop smoking.
National organizations’ smartphone apps guide the patient through a handful of questions about their current lifestyle, gender, age, and basic laboratory values. Their individual “heart health” results of these questions distribute the 7 risk factors to 3 categories based on the need to focus, improve, or celebrate. Through nonthreatening videos, patients can improve their scores themselves and bring the areas they need to focus, or improve, to their ObGyn’s attention for further assistance.
While adding one more task to an already busy practice can seem daunting, there are great technology resources that can be leveraged to successfully address this important health metric. By using the ACOG-recommended rubric and focusing on the app characteristics identified above, you can find one that works best for you and your patients and incorporate it into your practice today. ●
Cardiovascular disease is the leading cause of women’s death in the United States, accounting for 1 in every 5 female deaths per year according to the Centers for Disease Control and Prevention. Most risk factors for cardiovascular disease are modifiable. With a disease so prevalent in women’s health, obstetricians and gynecologists can assist patients in modifying these risk factors. This, however, is easier said than done.
One of the rate-limiting steps in assisting patients is the process of identifying an individual’s risk factors. This can be a time-consuming task in a women’s health appointment that is already busy with ObGyn-specific concerns, but technology can assist us.
Cardiovascular health app considerations
Many smartphone applications and websites are available that can alleviate the time constraints for identifying these individual modifiable risk factors. When evaluating cardiovascular risk factor apps for patients, keep these qualities (as outlined in the ACOG-recommended rubric) in mind: design, functionality, usefulness, and accuracy.
The patient-centered resources that assist women in identifying cardiovascular risk factors and that provide tools to positively impact these risk factors through lifestyle changes can help women achieve improved cardiovascular health. Recommendations include 1) manage blood pressure, 2) control cholesterol, 3) reduce blood sugar, 4) get active, 5) eat better, 6) lose weight, and 7) stop smoking.
National organizations’ smartphone apps guide the patient through a handful of questions about their current lifestyle, gender, age, and basic laboratory values. Their individual “heart health” results of these questions distribute the 7 risk factors to 3 categories based on the need to focus, improve, or celebrate. Through nonthreatening videos, patients can improve their scores themselves and bring the areas they need to focus, or improve, to their ObGyn’s attention for further assistance.
While adding one more task to an already busy practice can seem daunting, there are great technology resources that can be leveraged to successfully address this important health metric. By using the ACOG-recommended rubric and focusing on the app characteristics identified above, you can find one that works best for you and your patients and incorporate it into your practice today. ●
Cardiovascular disease is the leading cause of women’s death in the United States, accounting for 1 in every 5 female deaths per year according to the Centers for Disease Control and Prevention. Most risk factors for cardiovascular disease are modifiable. With a disease so prevalent in women’s health, obstetricians and gynecologists can assist patients in modifying these risk factors. This, however, is easier said than done.
One of the rate-limiting steps in assisting patients is the process of identifying an individual’s risk factors. This can be a time-consuming task in a women’s health appointment that is already busy with ObGyn-specific concerns, but technology can assist us.
Cardiovascular health app considerations
Many smartphone applications and websites are available that can alleviate the time constraints for identifying these individual modifiable risk factors. When evaluating cardiovascular risk factor apps for patients, keep these qualities (as outlined in the ACOG-recommended rubric) in mind: design, functionality, usefulness, and accuracy.
The patient-centered resources that assist women in identifying cardiovascular risk factors and that provide tools to positively impact these risk factors through lifestyle changes can help women achieve improved cardiovascular health. Recommendations include 1) manage blood pressure, 2) control cholesterol, 3) reduce blood sugar, 4) get active, 5) eat better, 6) lose weight, and 7) stop smoking.
National organizations’ smartphone apps guide the patient through a handful of questions about their current lifestyle, gender, age, and basic laboratory values. Their individual “heart health” results of these questions distribute the 7 risk factors to 3 categories based on the need to focus, improve, or celebrate. Through nonthreatening videos, patients can improve their scores themselves and bring the areas they need to focus, or improve, to their ObGyn’s attention for further assistance.
While adding one more task to an already busy practice can seem daunting, there are great technology resources that can be leveraged to successfully address this important health metric. By using the ACOG-recommended rubric and focusing on the app characteristics identified above, you can find one that works best for you and your patients and incorporate it into your practice today. ●