User login
Confirmed: Growth in overdose deaths is exponential
Overdose death rates for individual drugs show no particular patterns since the turn of the century, but the exponential growth of overall drug mortality actually started before the opioid epidemic, according to an analysis of almost 600,000 unintentional overdose deaths since 1979.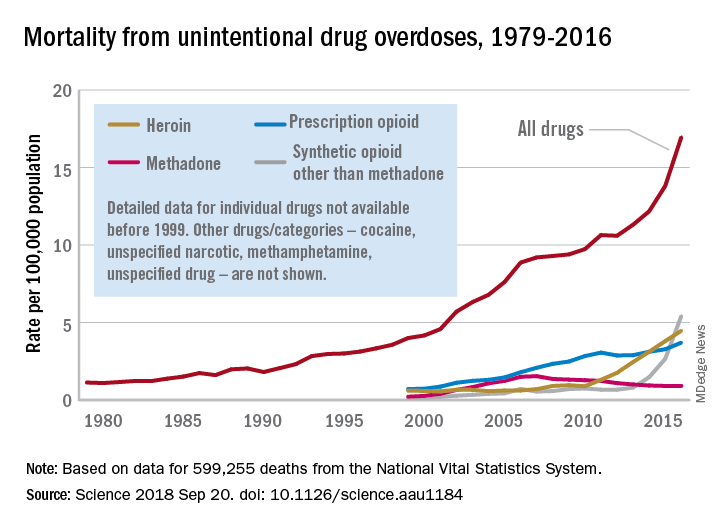
“The current epidemic of overdose deaths due to prescription opioids, heroin, and fentanyl appears to be the most recent manifestation of a more fundamental, longer-term process,” senior author Donald S. Burke, MD, of the University of Pittsburgh, said in a written statement.
Overdose mortality from all types of drugs rose from 1.13 per 100,000 population in 1979 to 16.96 per 100,000 in 2016, based on data for 599,255 deaths from unintentional drug overdoses in the National Vital Statistics System, they reported in Science.
When the investigators plotted annual drug overdose mortality over that 38-year period, they saw a smooth upward exponential curve with a doubling time of about 9 years. “This remarkably smooth, long-term epidemic growth pattern really caught our attention,” Dr. Burke said. “If we can figure it out, we should be able to bend that curve downward.”
The individual drug types that make up the whole, however, are a different story. “There is no regular or predictable pattern to the overdose rates for any of these drugs. Cocaine overdose death rates curved down and up and down and back up over the past 20 years. Methadone deaths have been on a downturn since the mid-2000s. Prescription opioids have been on a fairly steady, steep climb. Heroin deaths shot up in 2010, followed in 2013 by synthetic opioids, such as fentanyl,” lead author Hawre Jalal, MD, PhD, also of the university, said in the statement.
Geographic and demographic analyses produced the same absence of patterns. the researchers wrote.
The study was supported by grants from the Centers for Disease Control and Prevention and the Robert Wood Johnson Foundation. The investigators said they have no competing interests.
SOURCE: Jalal H et al. Science 2018 Sep 20. doi: 10.1126/science.aau1184.
Overdose death rates for individual drugs show no particular patterns since the turn of the century, but the exponential growth of overall drug mortality actually started before the opioid epidemic, according to an analysis of almost 600,000 unintentional overdose deaths since 1979.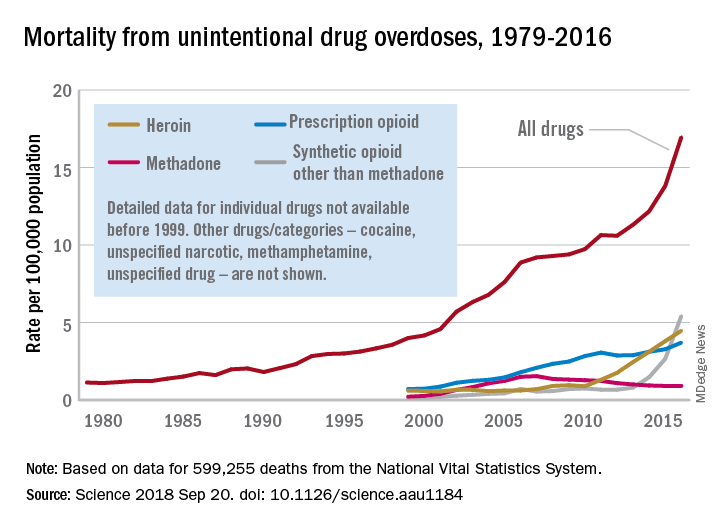
“The current epidemic of overdose deaths due to prescription opioids, heroin, and fentanyl appears to be the most recent manifestation of a more fundamental, longer-term process,” senior author Donald S. Burke, MD, of the University of Pittsburgh, said in a written statement.
Overdose mortality from all types of drugs rose from 1.13 per 100,000 population in 1979 to 16.96 per 100,000 in 2016, based on data for 599,255 deaths from unintentional drug overdoses in the National Vital Statistics System, they reported in Science.
When the investigators plotted annual drug overdose mortality over that 38-year period, they saw a smooth upward exponential curve with a doubling time of about 9 years. “This remarkably smooth, long-term epidemic growth pattern really caught our attention,” Dr. Burke said. “If we can figure it out, we should be able to bend that curve downward.”
The individual drug types that make up the whole, however, are a different story. “There is no regular or predictable pattern to the overdose rates for any of these drugs. Cocaine overdose death rates curved down and up and down and back up over the past 20 years. Methadone deaths have been on a downturn since the mid-2000s. Prescription opioids have been on a fairly steady, steep climb. Heroin deaths shot up in 2010, followed in 2013 by synthetic opioids, such as fentanyl,” lead author Hawre Jalal, MD, PhD, also of the university, said in the statement.
Geographic and demographic analyses produced the same absence of patterns. the researchers wrote.
The study was supported by grants from the Centers for Disease Control and Prevention and the Robert Wood Johnson Foundation. The investigators said they have no competing interests.
SOURCE: Jalal H et al. Science 2018 Sep 20. doi: 10.1126/science.aau1184.
Overdose death rates for individual drugs show no particular patterns since the turn of the century, but the exponential growth of overall drug mortality actually started before the opioid epidemic, according to an analysis of almost 600,000 unintentional overdose deaths since 1979.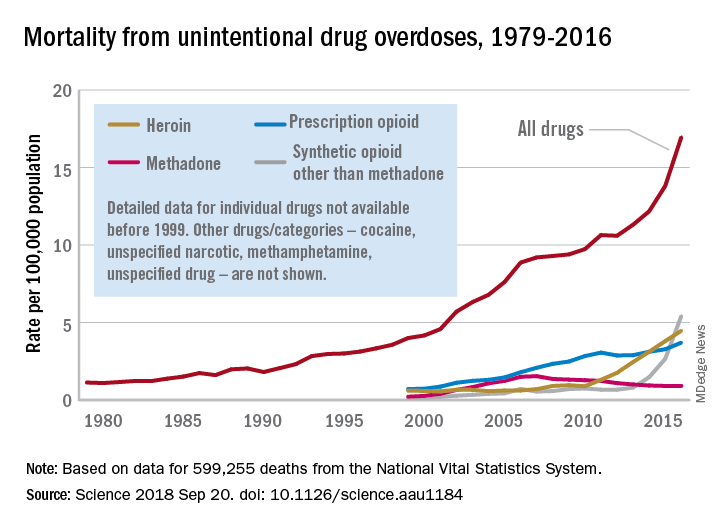
“The current epidemic of overdose deaths due to prescription opioids, heroin, and fentanyl appears to be the most recent manifestation of a more fundamental, longer-term process,” senior author Donald S. Burke, MD, of the University of Pittsburgh, said in a written statement.
Overdose mortality from all types of drugs rose from 1.13 per 100,000 population in 1979 to 16.96 per 100,000 in 2016, based on data for 599,255 deaths from unintentional drug overdoses in the National Vital Statistics System, they reported in Science.
When the investigators plotted annual drug overdose mortality over that 38-year period, they saw a smooth upward exponential curve with a doubling time of about 9 years. “This remarkably smooth, long-term epidemic growth pattern really caught our attention,” Dr. Burke said. “If we can figure it out, we should be able to bend that curve downward.”
The individual drug types that make up the whole, however, are a different story. “There is no regular or predictable pattern to the overdose rates for any of these drugs. Cocaine overdose death rates curved down and up and down and back up over the past 20 years. Methadone deaths have been on a downturn since the mid-2000s. Prescription opioids have been on a fairly steady, steep climb. Heroin deaths shot up in 2010, followed in 2013 by synthetic opioids, such as fentanyl,” lead author Hawre Jalal, MD, PhD, also of the university, said in the statement.
Geographic and demographic analyses produced the same absence of patterns. the researchers wrote.
The study was supported by grants from the Centers for Disease Control and Prevention and the Robert Wood Johnson Foundation. The investigators said they have no competing interests.
SOURCE: Jalal H et al. Science 2018 Sep 20. doi: 10.1126/science.aau1184.
FROM SCIENCE
New perspectives keep SHM relevant
Atashi Mandal, MD, finds committee work illuminating and gratifying
Editor’s note: SHM occasionally puts the spotlight on some of our most active members who are making substantial contributions to hospital medicine. Visit www.hospitalmedicine.org for more information on how you can lend your expertise to help improve the care of hospitalized patients.
This month, The Hospitalist spotlights Atashi Mandal, MD , a Med-Peds hospitalist in Huntington Beach, Calif. Dr. Mandal has been a member of SHM since for more than a decade, has served on the Public Policy Committee, and is currently serving on the Patient Experience Committee.
How did you initially hear about SHM, and why did you become a member?
I was a newly minted hospitalist and eagerly searching for a way to use my CME allowance, when I discovered SHM’s annual conference, which happened to be nearby in San Diego that year. I also was intrigued by, and excited to learn more about, an organization that dedicated itself only to hospital medicine. After attending the conference, I was hooked!
As a member of more than a decade, what aspects of your membership have you found to be most valuable?
I’ve always been very impressed by the quality and variety of the educational offerings. As a Med-Peds hospitalist, I can happily attest to greater inclusion of pediatric-specific content and a more robust presence of pediatric hospitalists over the years. Moreover, I am very appreciative of SHM’s progressive attitude as demonstrated by incorporating topics such as gender disparities, LGBTQ health, and the opioid crisis into our curriculum. I also have greatly enjoyed the networking opportunities with fellow hospitalists, some of whom I am happy to say have also become good friends over the years. More recently over the past few years, I’ve participated on committees, which has been an illuminating and gratifying way to help shape SHM’s current and future directives.
Describe your role on the Public Policy Committee. What did the committee accomplish during your term?
I was very honored to serve as a member of this committee for three terms. The staff is truly superhuman and amazing, considering how well they stay abreast of the swiftly changing administrative and legislative currents in health care. Just during my tenure as an SHM member, we’ve witnessed paramount shifts in our practice and culture, from the passage of MACRA, [the Medicare Access and CHIP Reauthorization Act] to the opioid epidemic. The Public Policy Committee identifies issues that affect our practice as hospitalists and advocates on our behalf through various means, from submitting comments and letters as well as personally meeting with our regulatory agencies such as CMS [Centers for Medicare & Medicaid Services], and our federal legislators. Some major victories were the acquisition of our specialty billing code and approval of an advanced care billing code. Additionally, the committee has been tirelessly advocating for reform with observation status. We have submitted comments to legislative committees regarding the opioid crisis and continue to work with MACRA as it affects our membership. While I served, I took a special interest in mental health and pediatric issues, including CHIP [Children’s Health Insurance Program] reauthorization and the 21st Century Cures Act.
What is Hill Day, and what can Hospital Medicine 2019 attendees expect to gain from participating?
Hill Day is a truly educational, exciting – and most important – fun opportunity to hone our advocacy skills and gain some real-world experience interacting with legislators and their staffs. On the last day of the annual conference attendees can travel to D.C., where we will spend about a half-day meeting with our respective state’s legislators or their staff. We typically discuss two or three preselected bills that can directly impact our practice as hospitalists. The legislators and their staffers generally are not aware of how certain legislative items can greatly benefit or adversely affect our patients, and they therefore rely on front-line clinicians like us to provide this narrative, much to their gratitude. I learn a lot and have even more fun each time I go to Capitol Hill, so I strongly encourage everyone to participate in this unique opportunity.
Do you have any advice for early-career hospitalists looking to gain experience and get involved with SHM?
I would encourage you to find your voice and participate! Whether by joining a committee or a Special Interest Group or just chatting on one of the many stimulating forums, we each have something to bring to the table, irrespective of our tenure as hospitalists. The new perspectives mingling with those that are well established is what keeps our organization relevant, so I look forward to new ideas and fresh faces!
Ms. Steele is a marketing communications specialist at the Society of Hospital Medicine.
Atashi Mandal, MD, finds committee work illuminating and gratifying
Atashi Mandal, MD, finds committee work illuminating and gratifying
Editor’s note: SHM occasionally puts the spotlight on some of our most active members who are making substantial contributions to hospital medicine. Visit www.hospitalmedicine.org for more information on how you can lend your expertise to help improve the care of hospitalized patients.
This month, The Hospitalist spotlights Atashi Mandal, MD , a Med-Peds hospitalist in Huntington Beach, Calif. Dr. Mandal has been a member of SHM since for more than a decade, has served on the Public Policy Committee, and is currently serving on the Patient Experience Committee.
How did you initially hear about SHM, and why did you become a member?
I was a newly minted hospitalist and eagerly searching for a way to use my CME allowance, when I discovered SHM’s annual conference, which happened to be nearby in San Diego that year. I also was intrigued by, and excited to learn more about, an organization that dedicated itself only to hospital medicine. After attending the conference, I was hooked!
As a member of more than a decade, what aspects of your membership have you found to be most valuable?
I’ve always been very impressed by the quality and variety of the educational offerings. As a Med-Peds hospitalist, I can happily attest to greater inclusion of pediatric-specific content and a more robust presence of pediatric hospitalists over the years. Moreover, I am very appreciative of SHM’s progressive attitude as demonstrated by incorporating topics such as gender disparities, LGBTQ health, and the opioid crisis into our curriculum. I also have greatly enjoyed the networking opportunities with fellow hospitalists, some of whom I am happy to say have also become good friends over the years. More recently over the past few years, I’ve participated on committees, which has been an illuminating and gratifying way to help shape SHM’s current and future directives.
Describe your role on the Public Policy Committee. What did the committee accomplish during your term?
I was very honored to serve as a member of this committee for three terms. The staff is truly superhuman and amazing, considering how well they stay abreast of the swiftly changing administrative and legislative currents in health care. Just during my tenure as an SHM member, we’ve witnessed paramount shifts in our practice and culture, from the passage of MACRA, [the Medicare Access and CHIP Reauthorization Act] to the opioid epidemic. The Public Policy Committee identifies issues that affect our practice as hospitalists and advocates on our behalf through various means, from submitting comments and letters as well as personally meeting with our regulatory agencies such as CMS [Centers for Medicare & Medicaid Services], and our federal legislators. Some major victories were the acquisition of our specialty billing code and approval of an advanced care billing code. Additionally, the committee has been tirelessly advocating for reform with observation status. We have submitted comments to legislative committees regarding the opioid crisis and continue to work with MACRA as it affects our membership. While I served, I took a special interest in mental health and pediatric issues, including CHIP [Children’s Health Insurance Program] reauthorization and the 21st Century Cures Act.
What is Hill Day, and what can Hospital Medicine 2019 attendees expect to gain from participating?
Hill Day is a truly educational, exciting – and most important – fun opportunity to hone our advocacy skills and gain some real-world experience interacting with legislators and their staffs. On the last day of the annual conference attendees can travel to D.C., where we will spend about a half-day meeting with our respective state’s legislators or their staff. We typically discuss two or three preselected bills that can directly impact our practice as hospitalists. The legislators and their staffers generally are not aware of how certain legislative items can greatly benefit or adversely affect our patients, and they therefore rely on front-line clinicians like us to provide this narrative, much to their gratitude. I learn a lot and have even more fun each time I go to Capitol Hill, so I strongly encourage everyone to participate in this unique opportunity.
Do you have any advice for early-career hospitalists looking to gain experience and get involved with SHM?
I would encourage you to find your voice and participate! Whether by joining a committee or a Special Interest Group or just chatting on one of the many stimulating forums, we each have something to bring to the table, irrespective of our tenure as hospitalists. The new perspectives mingling with those that are well established is what keeps our organization relevant, so I look forward to new ideas and fresh faces!
Ms. Steele is a marketing communications specialist at the Society of Hospital Medicine.
Editor’s note: SHM occasionally puts the spotlight on some of our most active members who are making substantial contributions to hospital medicine. Visit www.hospitalmedicine.org for more information on how you can lend your expertise to help improve the care of hospitalized patients.
This month, The Hospitalist spotlights Atashi Mandal, MD , a Med-Peds hospitalist in Huntington Beach, Calif. Dr. Mandal has been a member of SHM since for more than a decade, has served on the Public Policy Committee, and is currently serving on the Patient Experience Committee.
How did you initially hear about SHM, and why did you become a member?
I was a newly minted hospitalist and eagerly searching for a way to use my CME allowance, when I discovered SHM’s annual conference, which happened to be nearby in San Diego that year. I also was intrigued by, and excited to learn more about, an organization that dedicated itself only to hospital medicine. After attending the conference, I was hooked!
As a member of more than a decade, what aspects of your membership have you found to be most valuable?
I’ve always been very impressed by the quality and variety of the educational offerings. As a Med-Peds hospitalist, I can happily attest to greater inclusion of pediatric-specific content and a more robust presence of pediatric hospitalists over the years. Moreover, I am very appreciative of SHM’s progressive attitude as demonstrated by incorporating topics such as gender disparities, LGBTQ health, and the opioid crisis into our curriculum. I also have greatly enjoyed the networking opportunities with fellow hospitalists, some of whom I am happy to say have also become good friends over the years. More recently over the past few years, I’ve participated on committees, which has been an illuminating and gratifying way to help shape SHM’s current and future directives.
Describe your role on the Public Policy Committee. What did the committee accomplish during your term?
I was very honored to serve as a member of this committee for three terms. The staff is truly superhuman and amazing, considering how well they stay abreast of the swiftly changing administrative and legislative currents in health care. Just during my tenure as an SHM member, we’ve witnessed paramount shifts in our practice and culture, from the passage of MACRA, [the Medicare Access and CHIP Reauthorization Act] to the opioid epidemic. The Public Policy Committee identifies issues that affect our practice as hospitalists and advocates on our behalf through various means, from submitting comments and letters as well as personally meeting with our regulatory agencies such as CMS [Centers for Medicare & Medicaid Services], and our federal legislators. Some major victories were the acquisition of our specialty billing code and approval of an advanced care billing code. Additionally, the committee has been tirelessly advocating for reform with observation status. We have submitted comments to legislative committees regarding the opioid crisis and continue to work with MACRA as it affects our membership. While I served, I took a special interest in mental health and pediatric issues, including CHIP [Children’s Health Insurance Program] reauthorization and the 21st Century Cures Act.
What is Hill Day, and what can Hospital Medicine 2019 attendees expect to gain from participating?
Hill Day is a truly educational, exciting – and most important – fun opportunity to hone our advocacy skills and gain some real-world experience interacting with legislators and their staffs. On the last day of the annual conference attendees can travel to D.C., where we will spend about a half-day meeting with our respective state’s legislators or their staff. We typically discuss two or three preselected bills that can directly impact our practice as hospitalists. The legislators and their staffers generally are not aware of how certain legislative items can greatly benefit or adversely affect our patients, and they therefore rely on front-line clinicians like us to provide this narrative, much to their gratitude. I learn a lot and have even more fun each time I go to Capitol Hill, so I strongly encourage everyone to participate in this unique opportunity.
Do you have any advice for early-career hospitalists looking to gain experience and get involved with SHM?
I would encourage you to find your voice and participate! Whether by joining a committee or a Special Interest Group or just chatting on one of the many stimulating forums, we each have something to bring to the table, irrespective of our tenure as hospitalists. The new perspectives mingling with those that are well established is what keeps our organization relevant, so I look forward to new ideas and fresh faces!
Ms. Steele is a marketing communications specialist at the Society of Hospital Medicine.
Is CMS becoming more open to PTAC recommendations?
Recommendations on potential physician-focused alternative payment models so far have gained little traction with officials at the Centers for Medicare & Medicaid Services, but that could be changing.
At a recent meeting of the Physician-Focused Payment Model Technical Advisory Committee (PTAC), Alex Azar, secretary of the Department of Health & Human Services, and Seema Verma, administrator of the Centers for Medicare & Medicaid Services, attended briefly, according to officials at the American College of Emergency Physicians. ACEP was having its proposal evaluated by PTAC.
Physician organizations have been puzzled as to why federal health officials have yet to approve a physician-developed alternative payment model (APM) under the Quality Payment Program, despite several being recommended by PTAC. In fact, no physician-developed APM has even been sent to the Center for Medicare and Medicaid Innovation for further testing and refinement.
ACEP’s model, the Acute Unscheduled Care Model, “provides incentives to safely discharge Medicare beneficiaries from the ED by facilitating and rewarding postdischarge care coordination,” the organizations notes in the model description submitted to PTAC. “The model ensures that emergency physicians who make the decision to provide safe, efficient outpatient care have the necessary tools to support this transformation and are rewarded for their decision making.”
Going into the meeting, the preliminary evaluation report had the PTAC reviewers agreeing unanimously that the model met 7 of the secretary’s 10 criteria for a physician-focused APM, that the majority agreed on the 8th criterion, and a majority agreed that the model did not meet criteria on the remaining two items.
PTAC reviewers “thought that we met all 10 criteria for models that the secretary put forth for evaluating physician-focused payment models,” Jeffrey Davis, ACEP Director of Regulatory Affairs, said in an interview, adding that the attendance of Mr. Azar and Ms. Verma at the meeting was a positive development.
“I think we were especially inspired by the fact that Secretary Azar, Administrator Verma, and Adam Boehler, the new head of [Center for Medicare and Medicaid Innovation], spoke at the beginning of the PTAC meeting,” he said, adding that while no models have been formally implemented or even designated for testing, they said that ideas are being incorporated into model development going on at the CMS.
Ms. Verma went so far as to tweet that “this group of leading experts volunteer their time to improve our healthcare system, and we greatly value their input.”
“We still think [PTAC] is a great avenue to get our model into the public arena,” Mr. Davis said. “We are optimistic.”
Recommendations on potential physician-focused alternative payment models so far have gained little traction with officials at the Centers for Medicare & Medicaid Services, but that could be changing.
At a recent meeting of the Physician-Focused Payment Model Technical Advisory Committee (PTAC), Alex Azar, secretary of the Department of Health & Human Services, and Seema Verma, administrator of the Centers for Medicare & Medicaid Services, attended briefly, according to officials at the American College of Emergency Physicians. ACEP was having its proposal evaluated by PTAC.
Physician organizations have been puzzled as to why federal health officials have yet to approve a physician-developed alternative payment model (APM) under the Quality Payment Program, despite several being recommended by PTAC. In fact, no physician-developed APM has even been sent to the Center for Medicare and Medicaid Innovation for further testing and refinement.
ACEP’s model, the Acute Unscheduled Care Model, “provides incentives to safely discharge Medicare beneficiaries from the ED by facilitating and rewarding postdischarge care coordination,” the organizations notes in the model description submitted to PTAC. “The model ensures that emergency physicians who make the decision to provide safe, efficient outpatient care have the necessary tools to support this transformation and are rewarded for their decision making.”
Going into the meeting, the preliminary evaluation report had the PTAC reviewers agreeing unanimously that the model met 7 of the secretary’s 10 criteria for a physician-focused APM, that the majority agreed on the 8th criterion, and a majority agreed that the model did not meet criteria on the remaining two items.
PTAC reviewers “thought that we met all 10 criteria for models that the secretary put forth for evaluating physician-focused payment models,” Jeffrey Davis, ACEP Director of Regulatory Affairs, said in an interview, adding that the attendance of Mr. Azar and Ms. Verma at the meeting was a positive development.
“I think we were especially inspired by the fact that Secretary Azar, Administrator Verma, and Adam Boehler, the new head of [Center for Medicare and Medicaid Innovation], spoke at the beginning of the PTAC meeting,” he said, adding that while no models have been formally implemented or even designated for testing, they said that ideas are being incorporated into model development going on at the CMS.
Ms. Verma went so far as to tweet that “this group of leading experts volunteer their time to improve our healthcare system, and we greatly value their input.”
“We still think [PTAC] is a great avenue to get our model into the public arena,” Mr. Davis said. “We are optimistic.”
Recommendations on potential physician-focused alternative payment models so far have gained little traction with officials at the Centers for Medicare & Medicaid Services, but that could be changing.
At a recent meeting of the Physician-Focused Payment Model Technical Advisory Committee (PTAC), Alex Azar, secretary of the Department of Health & Human Services, and Seema Verma, administrator of the Centers for Medicare & Medicaid Services, attended briefly, according to officials at the American College of Emergency Physicians. ACEP was having its proposal evaluated by PTAC.
Physician organizations have been puzzled as to why federal health officials have yet to approve a physician-developed alternative payment model (APM) under the Quality Payment Program, despite several being recommended by PTAC. In fact, no physician-developed APM has even been sent to the Center for Medicare and Medicaid Innovation for further testing and refinement.
ACEP’s model, the Acute Unscheduled Care Model, “provides incentives to safely discharge Medicare beneficiaries from the ED by facilitating and rewarding postdischarge care coordination,” the organizations notes in the model description submitted to PTAC. “The model ensures that emergency physicians who make the decision to provide safe, efficient outpatient care have the necessary tools to support this transformation and are rewarded for their decision making.”
Going into the meeting, the preliminary evaluation report had the PTAC reviewers agreeing unanimously that the model met 7 of the secretary’s 10 criteria for a physician-focused APM, that the majority agreed on the 8th criterion, and a majority agreed that the model did not meet criteria on the remaining two items.
PTAC reviewers “thought that we met all 10 criteria for models that the secretary put forth for evaluating physician-focused payment models,” Jeffrey Davis, ACEP Director of Regulatory Affairs, said in an interview, adding that the attendance of Mr. Azar and Ms. Verma at the meeting was a positive development.
“I think we were especially inspired by the fact that Secretary Azar, Administrator Verma, and Adam Boehler, the new head of [Center for Medicare and Medicaid Innovation], spoke at the beginning of the PTAC meeting,” he said, adding that while no models have been formally implemented or even designated for testing, they said that ideas are being incorporated into model development going on at the CMS.
Ms. Verma went so far as to tweet that “this group of leading experts volunteer their time to improve our healthcare system, and we greatly value their input.”
“We still think [PTAC] is a great avenue to get our model into the public arena,” Mr. Davis said. “We are optimistic.”
Guideline offers comprehensive approach for ICU clinicians
A new (PADIS).
The guideline builds upon the 2013 Clinical Practice Guidelines for the Management of Pain, Agitation, and Delirium (PAD) in Adult Patients in the ICU. Given the comprehensive nature of the PADIS guideline, an accompanying commentary was published simultaneously to help with implementation and interpretation. Both papers are the result of a large-scale, multicenter collaboration and were published in Critical Care Medicine.
A panel of 32 international experts, four methodologists, and four survivors of critical illness used the Grading of Recommendations Assessment, Development and Evaluation approach to develop the PADIS guideline.
“Thousands of hours were invested by these guidelines’ authors, who were in turn were supported by formal and informal collaborators, over the 3.5 years it took to produce this effort,” reported lead author John W. Devlin, PharmD, of the department of pharmacy and health systems sciences, Bouvé College of Health Sciences at Northeastern University, Boston, and his colleagues.
Compared with the 2013 PAD guideline, the PADIS guideline includes new sections regarding rehabilitation/mobility and sleep. “We sought to clarify conceptual definitions within these relatively new critical care research domains,” the panel wrote. “The recommendation rationales, fueled by debate and discussion, circled back to the bedside experience – and the perspective of what was best for patients – held by all panelists and methodology experts.”
The result is extensive and comprehensive, consisting of both broad and specific descriptions of current ICU practices and associated evidence; the guideline includes 37 recommendations, 32 ungraded, nonactionable statements, and two good practice statements. Of note, conditional recommendations far outnumber strong recommendations (34 vs. 3). Reasons for conditional rather than strong recommendations are discussed in rationale sections within the guideline and in the accompanying paper.
“Although our goal was to provide specific recommendations for each question, we suspect some guideline readers may be discouraged by the conditional nature of many recommendations and daunted by the breadth of topics discussed,” wrote Michele C. Balas, PhD, of the Ohio State University College of Nursing in Columbus, and her colleagues. Dr. Balas was on the guideline panel and is the lead author of the accompanying article intended to facilitate implementation and interpretation.
One of the more challenging recommendations surrounds the use of antipsychotics for delirious patients. Although this intervention has become relatively common, the guideline stands against it.
“It should be emphasized that there are few supportive data on ICU antipsychotic use and that the initiation of psychoactive medications during critical illness often results in their inappropriate continuation after ICU discharge,” wrote Dr. Balas and her coauthors.
Along with a hard look at existing practices, the panel actively sought to expand upon the 2013 guideline with new interventions. Discussions ranged from the less conventional, such as aromatherapy, to the more established, such as polypharmacy. Questions, recommendations, and rationale are clearly described for each topic, with clear supporting evidence. Where evidence is missing, the panel recommends future research possibilities.
“One example is the consideration of multiple pharmacologic and nonpharmacologic coanalgesic approaches to the ICU patient,” wrote Dr. Devlin and his coauthors. “When the published evidence was insufficient, limited to a narrow population or specific intervention (e.g., for procedural analgesia), or outright absent to answer the questions we posed, we structured evidence gap descriptors to inform clinicians where the uncertainty lay, and intended to provide sufficient information to apprise and invite researchers to address these gaps.”
The authors disclosed funding from AstraZeneca, Baxter, Covidien, and others.
SOURCE: Devlin JW et al. Crit Care Med. 2018 Sep 1. doi: 10.1097/CCM.0000000000003299; Balas MC et al. Crit Care Med. 2018 Sep 1. doi: 10.1097/CCM.0000000000003307.
A new (PADIS).
The guideline builds upon the 2013 Clinical Practice Guidelines for the Management of Pain, Agitation, and Delirium (PAD) in Adult Patients in the ICU. Given the comprehensive nature of the PADIS guideline, an accompanying commentary was published simultaneously to help with implementation and interpretation. Both papers are the result of a large-scale, multicenter collaboration and were published in Critical Care Medicine.
A panel of 32 international experts, four methodologists, and four survivors of critical illness used the Grading of Recommendations Assessment, Development and Evaluation approach to develop the PADIS guideline.
“Thousands of hours were invested by these guidelines’ authors, who were in turn were supported by formal and informal collaborators, over the 3.5 years it took to produce this effort,” reported lead author John W. Devlin, PharmD, of the department of pharmacy and health systems sciences, Bouvé College of Health Sciences at Northeastern University, Boston, and his colleagues.
Compared with the 2013 PAD guideline, the PADIS guideline includes new sections regarding rehabilitation/mobility and sleep. “We sought to clarify conceptual definitions within these relatively new critical care research domains,” the panel wrote. “The recommendation rationales, fueled by debate and discussion, circled back to the bedside experience – and the perspective of what was best for patients – held by all panelists and methodology experts.”
The result is extensive and comprehensive, consisting of both broad and specific descriptions of current ICU practices and associated evidence; the guideline includes 37 recommendations, 32 ungraded, nonactionable statements, and two good practice statements. Of note, conditional recommendations far outnumber strong recommendations (34 vs. 3). Reasons for conditional rather than strong recommendations are discussed in rationale sections within the guideline and in the accompanying paper.
“Although our goal was to provide specific recommendations for each question, we suspect some guideline readers may be discouraged by the conditional nature of many recommendations and daunted by the breadth of topics discussed,” wrote Michele C. Balas, PhD, of the Ohio State University College of Nursing in Columbus, and her colleagues. Dr. Balas was on the guideline panel and is the lead author of the accompanying article intended to facilitate implementation and interpretation.
One of the more challenging recommendations surrounds the use of antipsychotics for delirious patients. Although this intervention has become relatively common, the guideline stands against it.
“It should be emphasized that there are few supportive data on ICU antipsychotic use and that the initiation of psychoactive medications during critical illness often results in their inappropriate continuation after ICU discharge,” wrote Dr. Balas and her coauthors.
Along with a hard look at existing practices, the panel actively sought to expand upon the 2013 guideline with new interventions. Discussions ranged from the less conventional, such as aromatherapy, to the more established, such as polypharmacy. Questions, recommendations, and rationale are clearly described for each topic, with clear supporting evidence. Where evidence is missing, the panel recommends future research possibilities.
“One example is the consideration of multiple pharmacologic and nonpharmacologic coanalgesic approaches to the ICU patient,” wrote Dr. Devlin and his coauthors. “When the published evidence was insufficient, limited to a narrow population or specific intervention (e.g., for procedural analgesia), or outright absent to answer the questions we posed, we structured evidence gap descriptors to inform clinicians where the uncertainty lay, and intended to provide sufficient information to apprise and invite researchers to address these gaps.”
The authors disclosed funding from AstraZeneca, Baxter, Covidien, and others.
SOURCE: Devlin JW et al. Crit Care Med. 2018 Sep 1. doi: 10.1097/CCM.0000000000003299; Balas MC et al. Crit Care Med. 2018 Sep 1. doi: 10.1097/CCM.0000000000003307.
A new (PADIS).
The guideline builds upon the 2013 Clinical Practice Guidelines for the Management of Pain, Agitation, and Delirium (PAD) in Adult Patients in the ICU. Given the comprehensive nature of the PADIS guideline, an accompanying commentary was published simultaneously to help with implementation and interpretation. Both papers are the result of a large-scale, multicenter collaboration and were published in Critical Care Medicine.
A panel of 32 international experts, four methodologists, and four survivors of critical illness used the Grading of Recommendations Assessment, Development and Evaluation approach to develop the PADIS guideline.
“Thousands of hours were invested by these guidelines’ authors, who were in turn were supported by formal and informal collaborators, over the 3.5 years it took to produce this effort,” reported lead author John W. Devlin, PharmD, of the department of pharmacy and health systems sciences, Bouvé College of Health Sciences at Northeastern University, Boston, and his colleagues.
Compared with the 2013 PAD guideline, the PADIS guideline includes new sections regarding rehabilitation/mobility and sleep. “We sought to clarify conceptual definitions within these relatively new critical care research domains,” the panel wrote. “The recommendation rationales, fueled by debate and discussion, circled back to the bedside experience – and the perspective of what was best for patients – held by all panelists and methodology experts.”
The result is extensive and comprehensive, consisting of both broad and specific descriptions of current ICU practices and associated evidence; the guideline includes 37 recommendations, 32 ungraded, nonactionable statements, and two good practice statements. Of note, conditional recommendations far outnumber strong recommendations (34 vs. 3). Reasons for conditional rather than strong recommendations are discussed in rationale sections within the guideline and in the accompanying paper.
“Although our goal was to provide specific recommendations for each question, we suspect some guideline readers may be discouraged by the conditional nature of many recommendations and daunted by the breadth of topics discussed,” wrote Michele C. Balas, PhD, of the Ohio State University College of Nursing in Columbus, and her colleagues. Dr. Balas was on the guideline panel and is the lead author of the accompanying article intended to facilitate implementation and interpretation.
One of the more challenging recommendations surrounds the use of antipsychotics for delirious patients. Although this intervention has become relatively common, the guideline stands against it.
“It should be emphasized that there are few supportive data on ICU antipsychotic use and that the initiation of psychoactive medications during critical illness often results in their inappropriate continuation after ICU discharge,” wrote Dr. Balas and her coauthors.
Along with a hard look at existing practices, the panel actively sought to expand upon the 2013 guideline with new interventions. Discussions ranged from the less conventional, such as aromatherapy, to the more established, such as polypharmacy. Questions, recommendations, and rationale are clearly described for each topic, with clear supporting evidence. Where evidence is missing, the panel recommends future research possibilities.
“One example is the consideration of multiple pharmacologic and nonpharmacologic coanalgesic approaches to the ICU patient,” wrote Dr. Devlin and his coauthors. “When the published evidence was insufficient, limited to a narrow population or specific intervention (e.g., for procedural analgesia), or outright absent to answer the questions we posed, we structured evidence gap descriptors to inform clinicians where the uncertainty lay, and intended to provide sufficient information to apprise and invite researchers to address these gaps.”
The authors disclosed funding from AstraZeneca, Baxter, Covidien, and others.
SOURCE: Devlin JW et al. Crit Care Med. 2018 Sep 1. doi: 10.1097/CCM.0000000000003299; Balas MC et al. Crit Care Med. 2018 Sep 1. doi: 10.1097/CCM.0000000000003307.
FROM CRITICAL CARE MEDICINE
Key clinical point: The 2018 PADIS guideline recommends intervention strategies for adult ICU patients with pain, agitation/sedation, delirium, immobility, and sleep disruption.
Major finding: The guideline includes 37 recommendations; 32 ungraded, nonactionable statements; and two good practice statements.
Study details: A clinical practice guideline was created by 32 international experts, four methodologists, and four survivors of critical illness.
Disclosures: The authors declared funding from AstraZeneca, Baxter, Covidien, and others.
Sources: Devlin JW et al. Crit Care Med. 2018 Sep 1. doi: 10.1097/CCM.0000000000003299; Balas MC et al. Crit Care Med. 2018 Sep 1. doi: 10.1097/CCM.0000000000003307.
FDA issues new REMS for immediate-release opioids
Opioid prescribers will need to be mindful of a new, expanded Risk Evaluation and Mitigation Strategy issued Sept. 18 by the Food and Drug Administration, covering immediate-release opioid analgesics used in the outpatient setting. The strategy also applies to extended-release and long-acting opioids, which have been subject to REMS since 2012.
The new REMS program requires for the first time that training be made available to health care providers who are involved in pain management. For the purposes of this REMS program, the training is not limited to just the prescriber, but includes nurses and pharmacists.
, including alternatives to opioids for pain management.
The FDA said it is in the process of approving a new label for opioids that will contain information about health care provider education that is now a part of the REMS.
“Our new effort is aimed at arming providers with the most current and comprehensive information on the appropriate management of pain,” FDA Commissioner Scott Gottlieb, MD, said in a statement. “Appropriate prescribing practices and education are important steps that we are prioritizing to help address the human and financial toll of this crisis.”
Dr. Gottlieb added that the goal of the new REMS is to help prescribers with the latest evidence on the appropriate amount of doses that should be prescribed for a given condition and that the “aim is to reduce overall dispensing as a way to further reduce exposure to these drugs. Our goal is to help prevent patients from becoming addicted by decreasing unnecessary or inappropriate exposure to opioids and fostering rational prescribing to enable appropriate access to those patients who have legitimate medical need for these medicines.”
The FDA also approved a new guidance document that includes updated educational content.
Opioid prescribers will need to be mindful of a new, expanded Risk Evaluation and Mitigation Strategy issued Sept. 18 by the Food and Drug Administration, covering immediate-release opioid analgesics used in the outpatient setting. The strategy also applies to extended-release and long-acting opioids, which have been subject to REMS since 2012.
The new REMS program requires for the first time that training be made available to health care providers who are involved in pain management. For the purposes of this REMS program, the training is not limited to just the prescriber, but includes nurses and pharmacists.
, including alternatives to opioids for pain management.
The FDA said it is in the process of approving a new label for opioids that will contain information about health care provider education that is now a part of the REMS.
“Our new effort is aimed at arming providers with the most current and comprehensive information on the appropriate management of pain,” FDA Commissioner Scott Gottlieb, MD, said in a statement. “Appropriate prescribing practices and education are important steps that we are prioritizing to help address the human and financial toll of this crisis.”
Dr. Gottlieb added that the goal of the new REMS is to help prescribers with the latest evidence on the appropriate amount of doses that should be prescribed for a given condition and that the “aim is to reduce overall dispensing as a way to further reduce exposure to these drugs. Our goal is to help prevent patients from becoming addicted by decreasing unnecessary or inappropriate exposure to opioids and fostering rational prescribing to enable appropriate access to those patients who have legitimate medical need for these medicines.”
The FDA also approved a new guidance document that includes updated educational content.
Opioid prescribers will need to be mindful of a new, expanded Risk Evaluation and Mitigation Strategy issued Sept. 18 by the Food and Drug Administration, covering immediate-release opioid analgesics used in the outpatient setting. The strategy also applies to extended-release and long-acting opioids, which have been subject to REMS since 2012.
The new REMS program requires for the first time that training be made available to health care providers who are involved in pain management. For the purposes of this REMS program, the training is not limited to just the prescriber, but includes nurses and pharmacists.
, including alternatives to opioids for pain management.
The FDA said it is in the process of approving a new label for opioids that will contain information about health care provider education that is now a part of the REMS.
“Our new effort is aimed at arming providers with the most current and comprehensive information on the appropriate management of pain,” FDA Commissioner Scott Gottlieb, MD, said in a statement. “Appropriate prescribing practices and education are important steps that we are prioritizing to help address the human and financial toll of this crisis.”
Dr. Gottlieb added that the goal of the new REMS is to help prescribers with the latest evidence on the appropriate amount of doses that should be prescribed for a given condition and that the “aim is to reduce overall dispensing as a way to further reduce exposure to these drugs. Our goal is to help prevent patients from becoming addicted by decreasing unnecessary or inappropriate exposure to opioids and fostering rational prescribing to enable appropriate access to those patients who have legitimate medical need for these medicines.”
The FDA also approved a new guidance document that includes updated educational content.
Expert panel updates guidelines on antithrombotic therapy for AF
For patients with , experts said in a comprehensive, updated guideline.
The 113-page guideline, published in the journal CHEST®, provides antithrombotic treatment recommendations for atrial fibrillation based on different levels of risk for stroke and in a variety of clinical presentations.
Altogether, the new guidelines highlight 60 key recommendations from the 12-person expert panel, chaired by Gregory Y.H. Lip, MD, of the Institute of Cardiovascular Sciences, University of Birmingham (England).
To develop the guidelines, the panel conducted a systematic literature review of relevant articles released since the 2012 publication of Thrombolytic Therapy: American College of Chest Physicians (ACCP) Evidence-Based Clinical Practice Guidelines (9th Edition).
Since that time, “there have been substantial developments in atrial fibrillation thromboprophylaxis, whether with regard to risk assessment, antithrombotic drugs, or non-drug approaches,” panelists said in their report.
The panel graded the quality of the new evidence found in the literature review, and then undertook a consensus development process. Each recommendation and statement required at least 80% consensus to pass.
Their treatment recommendations in the report are focused on three topic areas: stroke and bleeding risk assessment, antithrombotic therapy in general, and antithrombotic therapy in special situations, such as acute coronary syndrome and stenting, chronic atrial flutter, pregnancy, and chronic kidney disease.
Stroke prevention is the main priority in a “holistic approach” to management of atrial fibrillation, the panelists said in the report.
“Many of the risk factors leading to incident AF are also risk factors for ischemic stroke, and the promotion of an integrated or holistic approach to AF management is needed, incorporating stroke prevention, addressing symptoms and risk factor management,” they said.
No antithrombotic therapy is needed for patients who have atrial fibrillation without valvular heart disease, the panelists concluded.
For patients with at least one nongender CHA2DS2-VASc stroke risk factor, oral anticoagulation is recommended over aspirin, aspirin and clopidogrel, or no therapy, they said.
In high-risk patients, including males with two or more CHA2DS2-VASc risk factors and females with three or more, novel oral anticoagulants are recommended over adjusted-dose warfarin, they added.
At each patient contact, patients with atrial fibrillation should receive bleeding risk assessment starting with potentially modifiable risk factors such as uncontrolled blood pressure or excessive alcohol intake, according to the expert panel.
High-risk patients, as indicated by a HAS-BLED score of 3 or greater, should have more frequent and regular follow-up, they said.
The expert panel report concludes with a discussion on practical and patient-centered issues.
“Patient education is essential to provide patients with sufficient information to enable them to make an informed decision about whether or not they wish to take oral anticoagulants, and if they do, which oral anticoagulant they would prefer,” Dr. Lip and his colleagues said in their report.
Dr. Lip disclosed a potential conflict of interest with Boehringer Ingelheim. Expert panel members reported disclosures related to Boston Scientific, Medtronic, St. Jude Medical, Biotronik, MSD, Novartis, Pfizer, Bayer, Servier, Gilead, Bristol-Myers Squibb, AstraZeneca, and others.
SOURCE: Lip GYH et al. CHEST. 2018 Aug 21. pii: S0012-3692(18)32244-X.
For patients with , experts said in a comprehensive, updated guideline.
The 113-page guideline, published in the journal CHEST®, provides antithrombotic treatment recommendations for atrial fibrillation based on different levels of risk for stroke and in a variety of clinical presentations.
Altogether, the new guidelines highlight 60 key recommendations from the 12-person expert panel, chaired by Gregory Y.H. Lip, MD, of the Institute of Cardiovascular Sciences, University of Birmingham (England).
To develop the guidelines, the panel conducted a systematic literature review of relevant articles released since the 2012 publication of Thrombolytic Therapy: American College of Chest Physicians (ACCP) Evidence-Based Clinical Practice Guidelines (9th Edition).
Since that time, “there have been substantial developments in atrial fibrillation thromboprophylaxis, whether with regard to risk assessment, antithrombotic drugs, or non-drug approaches,” panelists said in their report.
The panel graded the quality of the new evidence found in the literature review, and then undertook a consensus development process. Each recommendation and statement required at least 80% consensus to pass.
Their treatment recommendations in the report are focused on three topic areas: stroke and bleeding risk assessment, antithrombotic therapy in general, and antithrombotic therapy in special situations, such as acute coronary syndrome and stenting, chronic atrial flutter, pregnancy, and chronic kidney disease.
Stroke prevention is the main priority in a “holistic approach” to management of atrial fibrillation, the panelists said in the report.
“Many of the risk factors leading to incident AF are also risk factors for ischemic stroke, and the promotion of an integrated or holistic approach to AF management is needed, incorporating stroke prevention, addressing symptoms and risk factor management,” they said.
No antithrombotic therapy is needed for patients who have atrial fibrillation without valvular heart disease, the panelists concluded.
For patients with at least one nongender CHA2DS2-VASc stroke risk factor, oral anticoagulation is recommended over aspirin, aspirin and clopidogrel, or no therapy, they said.
In high-risk patients, including males with two or more CHA2DS2-VASc risk factors and females with three or more, novel oral anticoagulants are recommended over adjusted-dose warfarin, they added.
At each patient contact, patients with atrial fibrillation should receive bleeding risk assessment starting with potentially modifiable risk factors such as uncontrolled blood pressure or excessive alcohol intake, according to the expert panel.
High-risk patients, as indicated by a HAS-BLED score of 3 or greater, should have more frequent and regular follow-up, they said.
The expert panel report concludes with a discussion on practical and patient-centered issues.
“Patient education is essential to provide patients with sufficient information to enable them to make an informed decision about whether or not they wish to take oral anticoagulants, and if they do, which oral anticoagulant they would prefer,” Dr. Lip and his colleagues said in their report.
Dr. Lip disclosed a potential conflict of interest with Boehringer Ingelheim. Expert panel members reported disclosures related to Boston Scientific, Medtronic, St. Jude Medical, Biotronik, MSD, Novartis, Pfizer, Bayer, Servier, Gilead, Bristol-Myers Squibb, AstraZeneca, and others.
SOURCE: Lip GYH et al. CHEST. 2018 Aug 21. pii: S0012-3692(18)32244-X.
For patients with , experts said in a comprehensive, updated guideline.
The 113-page guideline, published in the journal CHEST®, provides antithrombotic treatment recommendations for atrial fibrillation based on different levels of risk for stroke and in a variety of clinical presentations.
Altogether, the new guidelines highlight 60 key recommendations from the 12-person expert panel, chaired by Gregory Y.H. Lip, MD, of the Institute of Cardiovascular Sciences, University of Birmingham (England).
To develop the guidelines, the panel conducted a systematic literature review of relevant articles released since the 2012 publication of Thrombolytic Therapy: American College of Chest Physicians (ACCP) Evidence-Based Clinical Practice Guidelines (9th Edition).
Since that time, “there have been substantial developments in atrial fibrillation thromboprophylaxis, whether with regard to risk assessment, antithrombotic drugs, or non-drug approaches,” panelists said in their report.
The panel graded the quality of the new evidence found in the literature review, and then undertook a consensus development process. Each recommendation and statement required at least 80% consensus to pass.
Their treatment recommendations in the report are focused on three topic areas: stroke and bleeding risk assessment, antithrombotic therapy in general, and antithrombotic therapy in special situations, such as acute coronary syndrome and stenting, chronic atrial flutter, pregnancy, and chronic kidney disease.
Stroke prevention is the main priority in a “holistic approach” to management of atrial fibrillation, the panelists said in the report.
“Many of the risk factors leading to incident AF are also risk factors for ischemic stroke, and the promotion of an integrated or holistic approach to AF management is needed, incorporating stroke prevention, addressing symptoms and risk factor management,” they said.
No antithrombotic therapy is needed for patients who have atrial fibrillation without valvular heart disease, the panelists concluded.
For patients with at least one nongender CHA2DS2-VASc stroke risk factor, oral anticoagulation is recommended over aspirin, aspirin and clopidogrel, or no therapy, they said.
In high-risk patients, including males with two or more CHA2DS2-VASc risk factors and females with three or more, novel oral anticoagulants are recommended over adjusted-dose warfarin, they added.
At each patient contact, patients with atrial fibrillation should receive bleeding risk assessment starting with potentially modifiable risk factors such as uncontrolled blood pressure or excessive alcohol intake, according to the expert panel.
High-risk patients, as indicated by a HAS-BLED score of 3 or greater, should have more frequent and regular follow-up, they said.
The expert panel report concludes with a discussion on practical and patient-centered issues.
“Patient education is essential to provide patients with sufficient information to enable them to make an informed decision about whether or not they wish to take oral anticoagulants, and if they do, which oral anticoagulant they would prefer,” Dr. Lip and his colleagues said in their report.
Dr. Lip disclosed a potential conflict of interest with Boehringer Ingelheim. Expert panel members reported disclosures related to Boston Scientific, Medtronic, St. Jude Medical, Biotronik, MSD, Novartis, Pfizer, Bayer, Servier, Gilead, Bristol-Myers Squibb, AstraZeneca, and others.
SOURCE: Lip GYH et al. CHEST. 2018 Aug 21. pii: S0012-3692(18)32244-X.
FROM CHEST
White coats and provider attire: Does it matter to patients?
What is appropriate “ward garb”?
The question of appropriate ward garb is a problem for the ages. Compared with photo stills and films from the 1960s, the doctors of today appear like vagabonds. No ties, no lab coats, and scrub tops have become the norm for a number (a majority?) of hospital-based docs – and even more so on the surgical wards and in the ER.
Past studies have addressed patient preferences for provider dress, but none like the results of a recent survey.
From the University of Michigan, Ann Arbor, comes a physician attire survey of a convenience sample of 4,000 patients at 10 U.S. academic medical centers. It included both inpatients and outpatients, and used the design of many previous studies, showing patients the same doctor dressed seven different ways. After viewing the photographs, the patients received surveys as to their preference of physician based on attire, as well as being asked to rate the physician in the areas of knowledge, trust, care, approachability, and comfort.
You can see the domains: casual, scrubs, and formal, each with and without a lab coat. The seventh category is business attire (future C-suite wannabes – you know who you are).
Over half of the participants indicated that how a physician dresses was important to them, with more than one in three stating that this influenced how happy they were with care received. Overall, respondents indicated that formal attire with white coats was the most preferred form of physician dress.
I found the discussion in the study worthwhile, along with the strengths and weaknesses of the author’s outline. They went to great lengths to design a nonbiased questionnaire and used a consistent approach to shooting their photos. They also discussed lab coats, long sleeves, and hygiene.
But what to draw from the findings? Does patient satisfaction matter or just clinical outcomes? Is patient happiness a means to an end or an end unto itself? Can I even get you exercised about a score of 6 versus 8 (a 25% difference)? For instance, imagine the worst-dressed doc – say shorts and flip-flops. Is that a 5.8 or a 2.3? The anchor matters, and it helps to put the ratings in context.
Read the full post at hospitalleader.org.
Dr. Flansbaum works for Geisinger Health System in Danville, Pa., in both the divisions of hospital medicine and population health. He is a founding member of the Society of Hospital Medicine and served as a board member and officer.
Also in The Hospital Leader
•Hospitalists Can Improve Patient Trust…in Their Colleagues by Chris Moriates, MD, SFHM
•Treatment of Type II MIs by Brad Flansbaum, MD, MPH, MHM
•The $64,000 Question: How Can Hospitalists Improve Their HCAHPS Scores? by Leslie Flores, MHA, SFHM
What is appropriate “ward garb”?
What is appropriate “ward garb”?
The question of appropriate ward garb is a problem for the ages. Compared with photo stills and films from the 1960s, the doctors of today appear like vagabonds. No ties, no lab coats, and scrub tops have become the norm for a number (a majority?) of hospital-based docs – and even more so on the surgical wards and in the ER.
Past studies have addressed patient preferences for provider dress, but none like the results of a recent survey.
From the University of Michigan, Ann Arbor, comes a physician attire survey of a convenience sample of 4,000 patients at 10 U.S. academic medical centers. It included both inpatients and outpatients, and used the design of many previous studies, showing patients the same doctor dressed seven different ways. After viewing the photographs, the patients received surveys as to their preference of physician based on attire, as well as being asked to rate the physician in the areas of knowledge, trust, care, approachability, and comfort.
You can see the domains: casual, scrubs, and formal, each with and without a lab coat. The seventh category is business attire (future C-suite wannabes – you know who you are).
Over half of the participants indicated that how a physician dresses was important to them, with more than one in three stating that this influenced how happy they were with care received. Overall, respondents indicated that formal attire with white coats was the most preferred form of physician dress.
I found the discussion in the study worthwhile, along with the strengths and weaknesses of the author’s outline. They went to great lengths to design a nonbiased questionnaire and used a consistent approach to shooting their photos. They also discussed lab coats, long sleeves, and hygiene.
But what to draw from the findings? Does patient satisfaction matter or just clinical outcomes? Is patient happiness a means to an end or an end unto itself? Can I even get you exercised about a score of 6 versus 8 (a 25% difference)? For instance, imagine the worst-dressed doc – say shorts and flip-flops. Is that a 5.8 or a 2.3? The anchor matters, and it helps to put the ratings in context.
Read the full post at hospitalleader.org.
Dr. Flansbaum works for Geisinger Health System in Danville, Pa., in both the divisions of hospital medicine and population health. He is a founding member of the Society of Hospital Medicine and served as a board member and officer.
Also in The Hospital Leader
•Hospitalists Can Improve Patient Trust…in Their Colleagues by Chris Moriates, MD, SFHM
•Treatment of Type II MIs by Brad Flansbaum, MD, MPH, MHM
•The $64,000 Question: How Can Hospitalists Improve Their HCAHPS Scores? by Leslie Flores, MHA, SFHM
The question of appropriate ward garb is a problem for the ages. Compared with photo stills and films from the 1960s, the doctors of today appear like vagabonds. No ties, no lab coats, and scrub tops have become the norm for a number (a majority?) of hospital-based docs – and even more so on the surgical wards and in the ER.
Past studies have addressed patient preferences for provider dress, but none like the results of a recent survey.
From the University of Michigan, Ann Arbor, comes a physician attire survey of a convenience sample of 4,000 patients at 10 U.S. academic medical centers. It included both inpatients and outpatients, and used the design of many previous studies, showing patients the same doctor dressed seven different ways. After viewing the photographs, the patients received surveys as to their preference of physician based on attire, as well as being asked to rate the physician in the areas of knowledge, trust, care, approachability, and comfort.
You can see the domains: casual, scrubs, and formal, each with and without a lab coat. The seventh category is business attire (future C-suite wannabes – you know who you are).
Over half of the participants indicated that how a physician dresses was important to them, with more than one in three stating that this influenced how happy they were with care received. Overall, respondents indicated that formal attire with white coats was the most preferred form of physician dress.
I found the discussion in the study worthwhile, along with the strengths and weaknesses of the author’s outline. They went to great lengths to design a nonbiased questionnaire and used a consistent approach to shooting their photos. They also discussed lab coats, long sleeves, and hygiene.
But what to draw from the findings? Does patient satisfaction matter or just clinical outcomes? Is patient happiness a means to an end or an end unto itself? Can I even get you exercised about a score of 6 versus 8 (a 25% difference)? For instance, imagine the worst-dressed doc – say shorts and flip-flops. Is that a 5.8 or a 2.3? The anchor matters, and it helps to put the ratings in context.
Read the full post at hospitalleader.org.
Dr. Flansbaum works for Geisinger Health System in Danville, Pa., in both the divisions of hospital medicine and population health. He is a founding member of the Society of Hospital Medicine and served as a board member and officer.
Also in The Hospital Leader
•Hospitalists Can Improve Patient Trust…in Their Colleagues by Chris Moriates, MD, SFHM
•Treatment of Type II MIs by Brad Flansbaum, MD, MPH, MHM
•The $64,000 Question: How Can Hospitalists Improve Their HCAHPS Scores? by Leslie Flores, MHA, SFHM
Hospitalist movers and shakers – Sept. 2018
Modern Healthcare recently announced its list of the 50 Most Influential Physician Executives and Leaders, and hospital medicine was well represented among the honorees. The honored physicians were selected by a panel of experts and peers for their leadership and impact on the profession.
Topping the list was Scott Gottlieb, MD, the commissioner of the Food and Drug Administration. Dr. Gottlieb was confirmed to his position in May 2017 and, in his first year, has focused on price transparency and the approval of generic medications.
Dr. Gottlieb was deputy commissioner of the FDA from 2005-2007, and he has worked as an advisor and analyst for GlaxoSmithKline, the American Enterprise Institute, Vertex Pharmaceuticals, and Avilene Health.
Dr. Gottlieb earned his medical degree from the Icahn School of Medicine at Mount Sinai, New York, and completed his residency at Mount Sinai Hospital. He has worked as a hospitalist at New York University’s Tisch Hospital, the Hospital for Joint Diseases, and Stamford (Conn.) Hospital.
Patrick Conway, MD, was listed at number 23 on Modern Healthcare’s 50 Most Influential Physician Executives and Leaders. Formerly the deputy administrator for innovation and quality at the Centers for Medicare & Medicaid Services, Dr. Conway recently became president and chief executive officer of Blue Cross and Blue Shield of North Carolina.
Dr. Conway is known for his ability to develop and promote alternative payment models. He was elected to the National Academy of Medicine’s Institute of Medicine in 2014 and was selected as a Master of Hospital Medicine by the Society of Hospital Medicine.
Lynn Massingale, MD, the cofounder and chairman of TeamHealth, was named one of the 50 Most Influential Physician Executives and Leaders for a third year running, coming in at number 27 on the list. Dr. Massingale, who also recently was named to the Tennessee Healthcare Hall of Fame, founded TeamHealth in 1979 and was its chief executive officer for 30 years before assuming the role of chairman in 2008.
TeamHealth provides outsourced emergency medicine, hospitalist, critical care, anesthesiology, and acute care surgery services, among other specialties, at more than 3,200 facilities and physician groups across the United States.
Veeravat Taecharvongphairoj, MD, a veteran internist and hospitalist at Hemet Valley Medical Center in Hemet, Calif., has been honored by the International Association of Healthcare Professionals in its Leading Physicians of the World publication.
Dr. Taecharvongphairoj completed his residency at the University of Hawaii, Honolulu, before accepting a fellowship in hospital and palliative care at Cedars-Sinai Medical Center, Los Angeles. He is a member of the American Academy of Hospice and Palliative Medicine.
Sean Bain, MD, has been selected to the Glen Falls (N.Y.) Hospital Foundation Board of Trustees for 2018. Dr. Bain works as a hospitalist/internist at Glen Falls Hospital, where he is the president of medical staff. He manages the credentialing, continuing education, and policies and practices for the staff’s providers.
Dr. Bain received his medical degree at Albany (N.Y.) Medical College and served his residency at Wake Forest Baptist Medical Center, Winston-Salem, N.C.
George Harrison, MD, has been tabbed the new chief medical officer at Fairview Park Hospital in Dublin, Ga. Dr. Harrison will be charged with managing clinical quality and patient safety, staff relations, and clinical integration strategies at the hospital.
Prior to his appointment, Dr. Harrison was the codirector of the hospitalist program at Fairview Park. The Georgia native previously worked in management roles at urgent care centers, family practice centers, and hospitalist programs in North Carolina, South Carolina, and Georgia. He is a member of the American Academy of Family Physicians, the Society of Hospital Medicine, and the American Academy of Physician Leaders.
Dr. Harrison taught high school geometry and chemistry before earning his medical degree at the Morehouse School of Medicine, Atlanta. He did his residency at Duke University Medical Center, Durham, N.C.
BUSINESS MOVES
U.S. Acute Care Solutions (Canton, Ohio), a physician-owned, national provider of emergency medicine and hospitalist services, has extended its relationship with Central Health of Colorado and western Kansas. USACS has acquired the physicians of Front Range Emergency Specialists (Colorado Springs, Colo.), Southwest Emergency Physicians (Durango, Colo.), and Southern Colorado Emergency Specialists (Pueblo, Colo.).
USACS’s acquisition of these three physician groups adds care to more than 175,000 patients each year in central and southwest Colorado. USACS cares for more than 6 million patients per year at more than 200 locations across the United States.
VEP Healthcare (Concord, Calif.), an emergency medicine and hospitalist staffing company, has signed on to manage hospitalist and ED services at City Hospital at White Rock in Dallas. Its goals are to increase patient satisfaction, decrease wait times in seeing providers, raise recommendation rates, and lower malpractice claims.
White Rock is a 218-bed, community hospital providing care to East Texas since 1959.
Modern Healthcare recently announced its list of the 50 Most Influential Physician Executives and Leaders, and hospital medicine was well represented among the honorees. The honored physicians were selected by a panel of experts and peers for their leadership and impact on the profession.
Topping the list was Scott Gottlieb, MD, the commissioner of the Food and Drug Administration. Dr. Gottlieb was confirmed to his position in May 2017 and, in his first year, has focused on price transparency and the approval of generic medications.
Dr. Gottlieb was deputy commissioner of the FDA from 2005-2007, and he has worked as an advisor and analyst for GlaxoSmithKline, the American Enterprise Institute, Vertex Pharmaceuticals, and Avilene Health.
Dr. Gottlieb earned his medical degree from the Icahn School of Medicine at Mount Sinai, New York, and completed his residency at Mount Sinai Hospital. He has worked as a hospitalist at New York University’s Tisch Hospital, the Hospital for Joint Diseases, and Stamford (Conn.) Hospital.
Patrick Conway, MD, was listed at number 23 on Modern Healthcare’s 50 Most Influential Physician Executives and Leaders. Formerly the deputy administrator for innovation and quality at the Centers for Medicare & Medicaid Services, Dr. Conway recently became president and chief executive officer of Blue Cross and Blue Shield of North Carolina.
Dr. Conway is known for his ability to develop and promote alternative payment models. He was elected to the National Academy of Medicine’s Institute of Medicine in 2014 and was selected as a Master of Hospital Medicine by the Society of Hospital Medicine.
Lynn Massingale, MD, the cofounder and chairman of TeamHealth, was named one of the 50 Most Influential Physician Executives and Leaders for a third year running, coming in at number 27 on the list. Dr. Massingale, who also recently was named to the Tennessee Healthcare Hall of Fame, founded TeamHealth in 1979 and was its chief executive officer for 30 years before assuming the role of chairman in 2008.
TeamHealth provides outsourced emergency medicine, hospitalist, critical care, anesthesiology, and acute care surgery services, among other specialties, at more than 3,200 facilities and physician groups across the United States.
Veeravat Taecharvongphairoj, MD, a veteran internist and hospitalist at Hemet Valley Medical Center in Hemet, Calif., has been honored by the International Association of Healthcare Professionals in its Leading Physicians of the World publication.
Dr. Taecharvongphairoj completed his residency at the University of Hawaii, Honolulu, before accepting a fellowship in hospital and palliative care at Cedars-Sinai Medical Center, Los Angeles. He is a member of the American Academy of Hospice and Palliative Medicine.
Sean Bain, MD, has been selected to the Glen Falls (N.Y.) Hospital Foundation Board of Trustees for 2018. Dr. Bain works as a hospitalist/internist at Glen Falls Hospital, where he is the president of medical staff. He manages the credentialing, continuing education, and policies and practices for the staff’s providers.
Dr. Bain received his medical degree at Albany (N.Y.) Medical College and served his residency at Wake Forest Baptist Medical Center, Winston-Salem, N.C.
George Harrison, MD, has been tabbed the new chief medical officer at Fairview Park Hospital in Dublin, Ga. Dr. Harrison will be charged with managing clinical quality and patient safety, staff relations, and clinical integration strategies at the hospital.
Prior to his appointment, Dr. Harrison was the codirector of the hospitalist program at Fairview Park. The Georgia native previously worked in management roles at urgent care centers, family practice centers, and hospitalist programs in North Carolina, South Carolina, and Georgia. He is a member of the American Academy of Family Physicians, the Society of Hospital Medicine, and the American Academy of Physician Leaders.
Dr. Harrison taught high school geometry and chemistry before earning his medical degree at the Morehouse School of Medicine, Atlanta. He did his residency at Duke University Medical Center, Durham, N.C.
BUSINESS MOVES
U.S. Acute Care Solutions (Canton, Ohio), a physician-owned, national provider of emergency medicine and hospitalist services, has extended its relationship with Central Health of Colorado and western Kansas. USACS has acquired the physicians of Front Range Emergency Specialists (Colorado Springs, Colo.), Southwest Emergency Physicians (Durango, Colo.), and Southern Colorado Emergency Specialists (Pueblo, Colo.).
USACS’s acquisition of these three physician groups adds care to more than 175,000 patients each year in central and southwest Colorado. USACS cares for more than 6 million patients per year at more than 200 locations across the United States.
VEP Healthcare (Concord, Calif.), an emergency medicine and hospitalist staffing company, has signed on to manage hospitalist and ED services at City Hospital at White Rock in Dallas. Its goals are to increase patient satisfaction, decrease wait times in seeing providers, raise recommendation rates, and lower malpractice claims.
White Rock is a 218-bed, community hospital providing care to East Texas since 1959.
Modern Healthcare recently announced its list of the 50 Most Influential Physician Executives and Leaders, and hospital medicine was well represented among the honorees. The honored physicians were selected by a panel of experts and peers for their leadership and impact on the profession.
Topping the list was Scott Gottlieb, MD, the commissioner of the Food and Drug Administration. Dr. Gottlieb was confirmed to his position in May 2017 and, in his first year, has focused on price transparency and the approval of generic medications.
Dr. Gottlieb was deputy commissioner of the FDA from 2005-2007, and he has worked as an advisor and analyst for GlaxoSmithKline, the American Enterprise Institute, Vertex Pharmaceuticals, and Avilene Health.
Dr. Gottlieb earned his medical degree from the Icahn School of Medicine at Mount Sinai, New York, and completed his residency at Mount Sinai Hospital. He has worked as a hospitalist at New York University’s Tisch Hospital, the Hospital for Joint Diseases, and Stamford (Conn.) Hospital.
Patrick Conway, MD, was listed at number 23 on Modern Healthcare’s 50 Most Influential Physician Executives and Leaders. Formerly the deputy administrator for innovation and quality at the Centers for Medicare & Medicaid Services, Dr. Conway recently became president and chief executive officer of Blue Cross and Blue Shield of North Carolina.
Dr. Conway is known for his ability to develop and promote alternative payment models. He was elected to the National Academy of Medicine’s Institute of Medicine in 2014 and was selected as a Master of Hospital Medicine by the Society of Hospital Medicine.
Lynn Massingale, MD, the cofounder and chairman of TeamHealth, was named one of the 50 Most Influential Physician Executives and Leaders for a third year running, coming in at number 27 on the list. Dr. Massingale, who also recently was named to the Tennessee Healthcare Hall of Fame, founded TeamHealth in 1979 and was its chief executive officer for 30 years before assuming the role of chairman in 2008.
TeamHealth provides outsourced emergency medicine, hospitalist, critical care, anesthesiology, and acute care surgery services, among other specialties, at more than 3,200 facilities and physician groups across the United States.
Veeravat Taecharvongphairoj, MD, a veteran internist and hospitalist at Hemet Valley Medical Center in Hemet, Calif., has been honored by the International Association of Healthcare Professionals in its Leading Physicians of the World publication.
Dr. Taecharvongphairoj completed his residency at the University of Hawaii, Honolulu, before accepting a fellowship in hospital and palliative care at Cedars-Sinai Medical Center, Los Angeles. He is a member of the American Academy of Hospice and Palliative Medicine.
Sean Bain, MD, has been selected to the Glen Falls (N.Y.) Hospital Foundation Board of Trustees for 2018. Dr. Bain works as a hospitalist/internist at Glen Falls Hospital, where he is the president of medical staff. He manages the credentialing, continuing education, and policies and practices for the staff’s providers.
Dr. Bain received his medical degree at Albany (N.Y.) Medical College and served his residency at Wake Forest Baptist Medical Center, Winston-Salem, N.C.
George Harrison, MD, has been tabbed the new chief medical officer at Fairview Park Hospital in Dublin, Ga. Dr. Harrison will be charged with managing clinical quality and patient safety, staff relations, and clinical integration strategies at the hospital.
Prior to his appointment, Dr. Harrison was the codirector of the hospitalist program at Fairview Park. The Georgia native previously worked in management roles at urgent care centers, family practice centers, and hospitalist programs in North Carolina, South Carolina, and Georgia. He is a member of the American Academy of Family Physicians, the Society of Hospital Medicine, and the American Academy of Physician Leaders.
Dr. Harrison taught high school geometry and chemistry before earning his medical degree at the Morehouse School of Medicine, Atlanta. He did his residency at Duke University Medical Center, Durham, N.C.
BUSINESS MOVES
U.S. Acute Care Solutions (Canton, Ohio), a physician-owned, national provider of emergency medicine and hospitalist services, has extended its relationship with Central Health of Colorado and western Kansas. USACS has acquired the physicians of Front Range Emergency Specialists (Colorado Springs, Colo.), Southwest Emergency Physicians (Durango, Colo.), and Southern Colorado Emergency Specialists (Pueblo, Colo.).
USACS’s acquisition of these three physician groups adds care to more than 175,000 patients each year in central and southwest Colorado. USACS cares for more than 6 million patients per year at more than 200 locations across the United States.
VEP Healthcare (Concord, Calif.), an emergency medicine and hospitalist staffing company, has signed on to manage hospitalist and ED services at City Hospital at White Rock in Dallas. Its goals are to increase patient satisfaction, decrease wait times in seeing providers, raise recommendation rates, and lower malpractice claims.
White Rock is a 218-bed, community hospital providing care to East Texas since 1959.
Azithromycin for COPD exacerbations may reduce treatment failure
PARIS – In patients with a chronic obstructive pulmonary disease (provided improvement in a variety of outcomes at 90 days, including risk of death, according to a placebo-controlled trial presented as a late-breaker at the annual congress of the European Respiratory Society.
In patients with COPD, “azithromycin initiated in the acute setting and continued for 3 months appears to be safe and potentially effective,” reported Wim Janssens, MD, PhD, division of respiratory medicine, University Hospital, Leuven, Belgium.
The phrase “potentially effective” was used because the primary endpoint, which was time to treatment failure, fell just short of statistical significance (P = .053), but the rate of treatment failures, which was a coprimary endpoint (P = .04), and all of the secondary endpoints, including mortality at 90 days (P = .027), need for treatment intensification (P = .02) and need for an intensive care unit (ICU) admission (P = .003), were significantly lower in the group receiving azithromycin rather than placebo.
In a previous trial, chronic azithromycin therapy on top of usual care in patients frequently hospitalized for COPD was associated with a reduction in the risk of exacerbations and an improvement in quality of life (N Engl J Med. 2011;365:689-98). However, Dr. Janssens explained that this strategy is not commonly used because it was associated with a variety of adverse events, not least of which was QTc prolongation.
The study at the meeting, called the BACE trial, was designed to test whether azithromycin could be employed in a more targeted approach to control exacerbations. In the study, 301 COPD patients hospitalized with an acute exacerbation were randomized within 48 hours of admission to azithromycin or placebo. For the first 3 days, azithromycin was administered in a 500-mg dose. Thereafter, the dose was 250 mg every second day. Treatment was stopped at 90 days.
The primary outcome was time to treatment failure, a novel composite endpoint of any of three events: the need for treatment intensification, the need for step-up hospital care (either ICU admission or hospital readmission), or death by any cause. The two treatment arms were also compared for safety, including QTc prolongation.
The treatment failure rates were 49% in the azithromycin arm and 60% in the placebo arm, producing a hazard ratio (HR) of 0.73. Although this outcome fell short of significance, Dr. Janssens suggested that benefits over the 90 days of treatment are supported by the secondary outcomes. However, he also cautioned that most relative advantages for azithromycin over placebo were found to dissipate over time.
“The maximum separation between the azithromycin and placebo arms [for the primary outcome] occurred at 120 days or 30 days after the medication was stopped,” Dr. Janssens reported. After this point, the two arms converged and eventually overlapped.
However, the acute benefits appeared to be substantial. For example, average hospital stay over the 90-day treatment period was reduced from 40 to 10 days (P = .0061), and the ICU days fell from 11 days to 3 days in the azithromycin relative to the placebo group. According to Dr. Janssens, the difference in hospital stay carries “important health economic potential that deserves further attention.”
Of the three QTc events that occurred during the course of the study, one was observed in the placebo group. There was no significant difference in this or other adverse events, according to Dr. Janssens.
It is notable that the design for the BACE trial called for 500 patients. When enrollment was slow, the design was changed on the basis of power calculations indicating that 300 patients would be sufficient to demonstrate a difference. It is unclear whether a larger study would have permitted the difference in the primary endpoint to advance from a trend.
Dr. Janssens reports no conflicts of interest relevant to this study.
PARIS – In patients with a chronic obstructive pulmonary disease (provided improvement in a variety of outcomes at 90 days, including risk of death, according to a placebo-controlled trial presented as a late-breaker at the annual congress of the European Respiratory Society.
In patients with COPD, “azithromycin initiated in the acute setting and continued for 3 months appears to be safe and potentially effective,” reported Wim Janssens, MD, PhD, division of respiratory medicine, University Hospital, Leuven, Belgium.
The phrase “potentially effective” was used because the primary endpoint, which was time to treatment failure, fell just short of statistical significance (P = .053), but the rate of treatment failures, which was a coprimary endpoint (P = .04), and all of the secondary endpoints, including mortality at 90 days (P = .027), need for treatment intensification (P = .02) and need for an intensive care unit (ICU) admission (P = .003), were significantly lower in the group receiving azithromycin rather than placebo.
In a previous trial, chronic azithromycin therapy on top of usual care in patients frequently hospitalized for COPD was associated with a reduction in the risk of exacerbations and an improvement in quality of life (N Engl J Med. 2011;365:689-98). However, Dr. Janssens explained that this strategy is not commonly used because it was associated with a variety of adverse events, not least of which was QTc prolongation.
The study at the meeting, called the BACE trial, was designed to test whether azithromycin could be employed in a more targeted approach to control exacerbations. In the study, 301 COPD patients hospitalized with an acute exacerbation were randomized within 48 hours of admission to azithromycin or placebo. For the first 3 days, azithromycin was administered in a 500-mg dose. Thereafter, the dose was 250 mg every second day. Treatment was stopped at 90 days.
The primary outcome was time to treatment failure, a novel composite endpoint of any of three events: the need for treatment intensification, the need for step-up hospital care (either ICU admission or hospital readmission), or death by any cause. The two treatment arms were also compared for safety, including QTc prolongation.
The treatment failure rates were 49% in the azithromycin arm and 60% in the placebo arm, producing a hazard ratio (HR) of 0.73. Although this outcome fell short of significance, Dr. Janssens suggested that benefits over the 90 days of treatment are supported by the secondary outcomes. However, he also cautioned that most relative advantages for azithromycin over placebo were found to dissipate over time.
“The maximum separation between the azithromycin and placebo arms [for the primary outcome] occurred at 120 days or 30 days after the medication was stopped,” Dr. Janssens reported. After this point, the two arms converged and eventually overlapped.
However, the acute benefits appeared to be substantial. For example, average hospital stay over the 90-day treatment period was reduced from 40 to 10 days (P = .0061), and the ICU days fell from 11 days to 3 days in the azithromycin relative to the placebo group. According to Dr. Janssens, the difference in hospital stay carries “important health economic potential that deserves further attention.”
Of the three QTc events that occurred during the course of the study, one was observed in the placebo group. There was no significant difference in this or other adverse events, according to Dr. Janssens.
It is notable that the design for the BACE trial called for 500 patients. When enrollment was slow, the design was changed on the basis of power calculations indicating that 300 patients would be sufficient to demonstrate a difference. It is unclear whether a larger study would have permitted the difference in the primary endpoint to advance from a trend.
Dr. Janssens reports no conflicts of interest relevant to this study.
PARIS – In patients with a chronic obstructive pulmonary disease (provided improvement in a variety of outcomes at 90 days, including risk of death, according to a placebo-controlled trial presented as a late-breaker at the annual congress of the European Respiratory Society.
In patients with COPD, “azithromycin initiated in the acute setting and continued for 3 months appears to be safe and potentially effective,” reported Wim Janssens, MD, PhD, division of respiratory medicine, University Hospital, Leuven, Belgium.
The phrase “potentially effective” was used because the primary endpoint, which was time to treatment failure, fell just short of statistical significance (P = .053), but the rate of treatment failures, which was a coprimary endpoint (P = .04), and all of the secondary endpoints, including mortality at 90 days (P = .027), need for treatment intensification (P = .02) and need for an intensive care unit (ICU) admission (P = .003), were significantly lower in the group receiving azithromycin rather than placebo.
In a previous trial, chronic azithromycin therapy on top of usual care in patients frequently hospitalized for COPD was associated with a reduction in the risk of exacerbations and an improvement in quality of life (N Engl J Med. 2011;365:689-98). However, Dr. Janssens explained that this strategy is not commonly used because it was associated with a variety of adverse events, not least of which was QTc prolongation.
The study at the meeting, called the BACE trial, was designed to test whether azithromycin could be employed in a more targeted approach to control exacerbations. In the study, 301 COPD patients hospitalized with an acute exacerbation were randomized within 48 hours of admission to azithromycin or placebo. For the first 3 days, azithromycin was administered in a 500-mg dose. Thereafter, the dose was 250 mg every second day. Treatment was stopped at 90 days.
The primary outcome was time to treatment failure, a novel composite endpoint of any of three events: the need for treatment intensification, the need for step-up hospital care (either ICU admission or hospital readmission), or death by any cause. The two treatment arms were also compared for safety, including QTc prolongation.
The treatment failure rates were 49% in the azithromycin arm and 60% in the placebo arm, producing a hazard ratio (HR) of 0.73. Although this outcome fell short of significance, Dr. Janssens suggested that benefits over the 90 days of treatment are supported by the secondary outcomes. However, he also cautioned that most relative advantages for azithromycin over placebo were found to dissipate over time.
“The maximum separation between the azithromycin and placebo arms [for the primary outcome] occurred at 120 days or 30 days after the medication was stopped,” Dr. Janssens reported. After this point, the two arms converged and eventually overlapped.
However, the acute benefits appeared to be substantial. For example, average hospital stay over the 90-day treatment period was reduced from 40 to 10 days (P = .0061), and the ICU days fell from 11 days to 3 days in the azithromycin relative to the placebo group. According to Dr. Janssens, the difference in hospital stay carries “important health economic potential that deserves further attention.”
Of the three QTc events that occurred during the course of the study, one was observed in the placebo group. There was no significant difference in this or other adverse events, according to Dr. Janssens.
It is notable that the design for the BACE trial called for 500 patients. When enrollment was slow, the design was changed on the basis of power calculations indicating that 300 patients would be sufficient to demonstrate a difference. It is unclear whether a larger study would have permitted the difference in the primary endpoint to advance from a trend.
Dr. Janssens reports no conflicts of interest relevant to this study.
REPORTING FROM THE ERS CONGRESS 2018
Key clinical point: Initiating azithromycin in patients with COPD exacerbation at the time of hospitalization improves short-term outcomes.
Major finding: Relative to placebo, azithromycin provided a borderline reduction in treatment failure (P = .053) while reducing mortality (P = .027).
Study details: Multicenter, placebo-controlled trial.
Disclosures: Dr. Janssens reports no conflicts of interest relevant to this study.
AAP guidelines emphasize gender-affirmative care
according to an American Academy of Pediatrics policy statement published in Pediatrics.
The policy statement defines the gender-affirmative care model as one that provide “developmentally appropriate care that is oriented toward understanding and appreciating the youth’s gender experience,” wrote Jason Rafferty, MD, of the department of pediatrics at Hasbro Children’s Hospital in Providence, R.I., and the department of child psychiatryf at Emma Pendleton Bradley Hospital, East Providence, R.I. Dr. Rafferty serves on the AAP Committee on Psychosocial Aspects of Child and Family Health. The AAP Committee on Adolescence, Section on Lesbian, Gay, Bisexual, and Transgender Health and Wellness also participated in writing this policy statement.
The model emphasizes four main points, according to the statement:
- Transgender and gender-diverse identities are not mental disorders.
- Variations in gender identity are “normal aspects of human diversity.”
- Gender identity “evolves as a result of the interaction between biology, development, socialization, and culture.”
- Any mental health issue “most often stems from stigma and negative experiences” rather than being “intrinsic” to the child.
In the gender-affirmative approach, a supportive, nonjudgmental partnership between you, the patient, and the patient’s family is encouraged to “facilitate exploration of complicated emotions and gender-diverse expressions while allowing questions and concerns to be raised,” Dr. Rafferty said. This contrasts with “reparative” or “conversion” treatment, which seeks to change rather than accept the patient’s gender identity.
The AAP statement also recommends accessibility of family therapy, addressing the emotional and mental health needs not only of the patient, but also the parents, caregivers, and siblings.
The policy statement provides definitions for common terminology and distinguishes between “sex” as assigned at birth, based on anatomy, and “gender identity,” described as one’s internal sense of self. It also emphasizes that gender identity is not synonymous with sexual orientation, although the two may be interrelated. “The Gender Book” website is a resource that explains these terms and concepts.
A 2015 study revealed that 25% of transgender adults avoided a necessary doctor appointment because they feared mistreatment. Creating an environment at your office where TGD patients feel safe is key. This can be done by displaying posters or having flyers about lesbian, gay, bisexual, transgender, and questioning (LGBTQ) issues and having a gender-neutral bathroom. Educate staff by having diversity training that makes them sensitive to the needs of LGBTQ youth and their families. Patient-asserted names and pronouns should be used by staff and reflected in the EHR. “Explaining and maintaining confidentiality procedures promotes openness and trust, particularly with youth who identify as LGBTQ,” according to the statement. “Maintaining a safe clinical space can provide at least one consistent, protective refuge for patients and families, allowing authentic gender expression and exploration that builds resiliency.”
Barriers to care cited in the report include fear of discrimination by providers, lack of access to physical and sexual health services, inadequate mental health resources, and lack of provider continuity. The AAP recommends that EHRs respect the gender identity of the patient. Further research into health disparities, as well as establishment of standards of care, also are needed, the author notes.
The stigma and discrimination often experienced by TGD youth lead to feelings of rejection and isolation. Prior research has shown that transgender adolescents and adults have high rates of depression, anxiety, eating disorders, self-harm, and suicide, the report noted. One retrospective study found that 56% of transgender youth reported previous suicidal ideation, compared with 20% of those who identified as cisgender, and 31% reported a prior suicide attempt, compared with 11% cisgender youth. TGD youth also experience high rates of homelessness, violence, substance abuse, and high-risk sexual behaviors, studies have shown.
The statement also addresses issues such as medical interventions for pubertal suppression, surgical affirmation, difficulties with obtaining insurance coverage because of being transgender, family acceptance, safety in schools and communities, and medical education.
No disclosures or funding sources were reported.
SOURCE: Rafferty J et al. Pediatrics. 2018;142(4):e20182162.
The AAP policy offers a more detailed overview of the health care needs of transgender and gender-diverse (TGD) youth than was previously available, with data to support these recommendations.
Future efforts should focus on expanding the definition and components of gender-affirmative care, as well as training providers to be more competent in providing this care by introducing these concepts earlier in medical training so that pediatricians feel comfortable with implementation.
The new guidelines “emphasize that care for TGD youth is a rapidly evolving field,” and that “continued support is needed for research, education, and advocacy in this arena so we can provide the best level of evidence-based care to TGD youth.”
Gayathri Chelvakumar, MD, is an attending physician in the division of adolescent medicine at Nationwide Children’s Hospital and an assistant professor of clinical pediatrics at Ohio State University, both in Columbus. She was asked to comment on the AAP guidelines.
The AAP policy offers a more detailed overview of the health care needs of transgender and gender-diverse (TGD) youth than was previously available, with data to support these recommendations.
Future efforts should focus on expanding the definition and components of gender-affirmative care, as well as training providers to be more competent in providing this care by introducing these concepts earlier in medical training so that pediatricians feel comfortable with implementation.
The new guidelines “emphasize that care for TGD youth is a rapidly evolving field,” and that “continued support is needed for research, education, and advocacy in this arena so we can provide the best level of evidence-based care to TGD youth.”
Gayathri Chelvakumar, MD, is an attending physician in the division of adolescent medicine at Nationwide Children’s Hospital and an assistant professor of clinical pediatrics at Ohio State University, both in Columbus. She was asked to comment on the AAP guidelines.
The AAP policy offers a more detailed overview of the health care needs of transgender and gender-diverse (TGD) youth than was previously available, with data to support these recommendations.
Future efforts should focus on expanding the definition and components of gender-affirmative care, as well as training providers to be more competent in providing this care by introducing these concepts earlier in medical training so that pediatricians feel comfortable with implementation.
The new guidelines “emphasize that care for TGD youth is a rapidly evolving field,” and that “continued support is needed for research, education, and advocacy in this arena so we can provide the best level of evidence-based care to TGD youth.”
Gayathri Chelvakumar, MD, is an attending physician in the division of adolescent medicine at Nationwide Children’s Hospital and an assistant professor of clinical pediatrics at Ohio State University, both in Columbus. She was asked to comment on the AAP guidelines.
according to an American Academy of Pediatrics policy statement published in Pediatrics.
The policy statement defines the gender-affirmative care model as one that provide “developmentally appropriate care that is oriented toward understanding and appreciating the youth’s gender experience,” wrote Jason Rafferty, MD, of the department of pediatrics at Hasbro Children’s Hospital in Providence, R.I., and the department of child psychiatryf at Emma Pendleton Bradley Hospital, East Providence, R.I. Dr. Rafferty serves on the AAP Committee on Psychosocial Aspects of Child and Family Health. The AAP Committee on Adolescence, Section on Lesbian, Gay, Bisexual, and Transgender Health and Wellness also participated in writing this policy statement.
The model emphasizes four main points, according to the statement:
- Transgender and gender-diverse identities are not mental disorders.
- Variations in gender identity are “normal aspects of human diversity.”
- Gender identity “evolves as a result of the interaction between biology, development, socialization, and culture.”
- Any mental health issue “most often stems from stigma and negative experiences” rather than being “intrinsic” to the child.
In the gender-affirmative approach, a supportive, nonjudgmental partnership between you, the patient, and the patient’s family is encouraged to “facilitate exploration of complicated emotions and gender-diverse expressions while allowing questions and concerns to be raised,” Dr. Rafferty said. This contrasts with “reparative” or “conversion” treatment, which seeks to change rather than accept the patient’s gender identity.
The AAP statement also recommends accessibility of family therapy, addressing the emotional and mental health needs not only of the patient, but also the parents, caregivers, and siblings.
The policy statement provides definitions for common terminology and distinguishes between “sex” as assigned at birth, based on anatomy, and “gender identity,” described as one’s internal sense of self. It also emphasizes that gender identity is not synonymous with sexual orientation, although the two may be interrelated. “The Gender Book” website is a resource that explains these terms and concepts.
A 2015 study revealed that 25% of transgender adults avoided a necessary doctor appointment because they feared mistreatment. Creating an environment at your office where TGD patients feel safe is key. This can be done by displaying posters or having flyers about lesbian, gay, bisexual, transgender, and questioning (LGBTQ) issues and having a gender-neutral bathroom. Educate staff by having diversity training that makes them sensitive to the needs of LGBTQ youth and their families. Patient-asserted names and pronouns should be used by staff and reflected in the EHR. “Explaining and maintaining confidentiality procedures promotes openness and trust, particularly with youth who identify as LGBTQ,” according to the statement. “Maintaining a safe clinical space can provide at least one consistent, protective refuge for patients and families, allowing authentic gender expression and exploration that builds resiliency.”
Barriers to care cited in the report include fear of discrimination by providers, lack of access to physical and sexual health services, inadequate mental health resources, and lack of provider continuity. The AAP recommends that EHRs respect the gender identity of the patient. Further research into health disparities, as well as establishment of standards of care, also are needed, the author notes.
The stigma and discrimination often experienced by TGD youth lead to feelings of rejection and isolation. Prior research has shown that transgender adolescents and adults have high rates of depression, anxiety, eating disorders, self-harm, and suicide, the report noted. One retrospective study found that 56% of transgender youth reported previous suicidal ideation, compared with 20% of those who identified as cisgender, and 31% reported a prior suicide attempt, compared with 11% cisgender youth. TGD youth also experience high rates of homelessness, violence, substance abuse, and high-risk sexual behaviors, studies have shown.
The statement also addresses issues such as medical interventions for pubertal suppression, surgical affirmation, difficulties with obtaining insurance coverage because of being transgender, family acceptance, safety in schools and communities, and medical education.
No disclosures or funding sources were reported.
SOURCE: Rafferty J et al. Pediatrics. 2018;142(4):e20182162.
according to an American Academy of Pediatrics policy statement published in Pediatrics.
The policy statement defines the gender-affirmative care model as one that provide “developmentally appropriate care that is oriented toward understanding and appreciating the youth’s gender experience,” wrote Jason Rafferty, MD, of the department of pediatrics at Hasbro Children’s Hospital in Providence, R.I., and the department of child psychiatryf at Emma Pendleton Bradley Hospital, East Providence, R.I. Dr. Rafferty serves on the AAP Committee on Psychosocial Aspects of Child and Family Health. The AAP Committee on Adolescence, Section on Lesbian, Gay, Bisexual, and Transgender Health and Wellness also participated in writing this policy statement.
The model emphasizes four main points, according to the statement:
- Transgender and gender-diverse identities are not mental disorders.
- Variations in gender identity are “normal aspects of human diversity.”
- Gender identity “evolves as a result of the interaction between biology, development, socialization, and culture.”
- Any mental health issue “most often stems from stigma and negative experiences” rather than being “intrinsic” to the child.
In the gender-affirmative approach, a supportive, nonjudgmental partnership between you, the patient, and the patient’s family is encouraged to “facilitate exploration of complicated emotions and gender-diverse expressions while allowing questions and concerns to be raised,” Dr. Rafferty said. This contrasts with “reparative” or “conversion” treatment, which seeks to change rather than accept the patient’s gender identity.
The AAP statement also recommends accessibility of family therapy, addressing the emotional and mental health needs not only of the patient, but also the parents, caregivers, and siblings.
The policy statement provides definitions for common terminology and distinguishes between “sex” as assigned at birth, based on anatomy, and “gender identity,” described as one’s internal sense of self. It also emphasizes that gender identity is not synonymous with sexual orientation, although the two may be interrelated. “The Gender Book” website is a resource that explains these terms and concepts.
A 2015 study revealed that 25% of transgender adults avoided a necessary doctor appointment because they feared mistreatment. Creating an environment at your office where TGD patients feel safe is key. This can be done by displaying posters or having flyers about lesbian, gay, bisexual, transgender, and questioning (LGBTQ) issues and having a gender-neutral bathroom. Educate staff by having diversity training that makes them sensitive to the needs of LGBTQ youth and their families. Patient-asserted names and pronouns should be used by staff and reflected in the EHR. “Explaining and maintaining confidentiality procedures promotes openness and trust, particularly with youth who identify as LGBTQ,” according to the statement. “Maintaining a safe clinical space can provide at least one consistent, protective refuge for patients and families, allowing authentic gender expression and exploration that builds resiliency.”
Barriers to care cited in the report include fear of discrimination by providers, lack of access to physical and sexual health services, inadequate mental health resources, and lack of provider continuity. The AAP recommends that EHRs respect the gender identity of the patient. Further research into health disparities, as well as establishment of standards of care, also are needed, the author notes.
The stigma and discrimination often experienced by TGD youth lead to feelings of rejection and isolation. Prior research has shown that transgender adolescents and adults have high rates of depression, anxiety, eating disorders, self-harm, and suicide, the report noted. One retrospective study found that 56% of transgender youth reported previous suicidal ideation, compared with 20% of those who identified as cisgender, and 31% reported a prior suicide attempt, compared with 11% cisgender youth. TGD youth also experience high rates of homelessness, violence, substance abuse, and high-risk sexual behaviors, studies have shown.
The statement also addresses issues such as medical interventions for pubertal suppression, surgical affirmation, difficulties with obtaining insurance coverage because of being transgender, family acceptance, safety in schools and communities, and medical education.
No disclosures or funding sources were reported.
SOURCE: Rafferty J et al. Pediatrics. 2018;142(4):e20182162.
FROM PEDATRICS


















