User login
Long-term behavioral follow-up of children exposed to mood stabilizers and antidepressants: A look forward
Much of the focus of reproductive psychiatry over the last 1 to 2 decades has been on issues regarding risk of fetal exposure to psychiatric medications in the context of the specific risk for teratogenesis or organ malformation. Concerns and questions are mostly focused on exposure to any number of medications that women take during the first trimester, as it is during that period that the major organs are formed.
More recently, there has been appropriate interest in the effect of fetal exposure to psychiatric medications with respect to risk for obstetrical and neonatal complications. This particularly has been the case with respect to antidepressants where fetal exposure to these medications, which while associated with symptoms of transient jitteriness and irritability about 20% of the time, have not been associated with symptoms requiring frank clinical intervention.
Concerning mood stabilizers, the risk for organ dysgenesis following fetal exposure to sodium valproate has been very well established, and we’ve known for over a decade about the adverse effects of fetal exposure to sodium valproate on behavioral outcomes (Lancet Neurol. 2013 Mar;12[3]:244-52). We also now have ample data on lamotrigine, one of the most widely used medicines by reproductive-age women for treatment of bipolar disorder that supports the absence of a risk of organ malformation in first-trimester exposure.
Most recently, in a study of 292 children of women with epilepsy, an evaluation of women being treated with more modern anticonvulsants such as lamotrigine and levetiracetam alone or as polytherapy was performed. The results showed no difference in language, motor, cognitive, social, emotional, and general adaptive functioning in children exposed to either lamotrigine or levetiracetam relative to unexposed children of women with epilepsy. However, the researchers found an increase in anti-epileptic drug plasma level appeared to be associated with decreased motor and sensory function. These are reassuring data that really confirm earlier work, which failed to reveal a signal of concern for lamotrigine and now provide some of the first data on levetiracetam, which is widely used by reproductive-age women with epilepsy (JAMA Neurol. 2021 Aug 1;78[8]:927-936). While one caveat of the study is a short follow-up of 2 years, the absence of a signal of concern is reassuring. With more and more data demonstrating bipolar disorder is an illness that requires chronic treatment for many people, and that discontinuation is associated with high risk for relapse, it is an advance in the field to have data on risk for teratogenesis and data on longer-term neurobehavioral outcomes.
There is vast information regarding reproductive safety, organ malformation, and acute neonatal outcomes for antidepressants. The last decade has brought interest in and analysis of specific reports of increased risk of both autism spectrum disorder (ASD) and attention-deficit/hyperactivity disorder (ADHD) following fetal exposure to antidepressants. What can be said based on reviews of pooled meta-analyses is that the risk for ASD and ADHD has been put to rest for most clinicians and patients (J Clin Psychiatry. 2020 May 26;81[3]:20f13463). With other neurodevelopmental disorders, results have been somewhat inconclusive. Over the last 5-10 years, there have been sporadic reports of concerns about problems in a specific domain of neurodevelopment in offspring of women who have used antidepressants during pregnancy, whether it be speech, language, or motor functioning, but no signal of concern has been consistent.
In a previous column, I addressed a Danish study that showed no increased risk of longer-term sequelae after fetal exposure to antidepressants. Now, a new study has examined 1.93 million pregnancies in the Medicaid Analytic eXtract and 1.25 million pregnancies in the IBM MarketScan Research Database with follow-up up to 14 years of age where the specific interval for fetal exposure was from gestational age of 19 weeks to delivery, as that is the period that corresponds most to synaptogenesis in the brain. The researchers examined a spectrum of neurodevelopmental disorders such as developmental speech issues, ADHD, ASD, dyslexia, and learning disorders, among others. They found a twofold increased risk for neurodevelopmental disorders in the unadjusted models that flattened to no finding when factoring in environmental and genetic risk variables, highlighting the importance of dealing appropriately with confounders when performing these analyses. Those confounders examined include the mother’s use of alcohol and tobacco, and her body mass index and overall general health (JAMA Intern Med. 2022;182[11]:1149-60).
Given the consistency of these results with earlier data, patients can be increasingly comfortable as they weigh the benefits and risks of antidepressant use during pregnancy, factoring in the risk of fetal exposure with added data on long-term neurobehavioral sequelae. With that said, we need to remember the importance of initiatives to address alcohol consumption, poor nutrition, tobacco use, elevated BMI, and general health during pregnancy. These are modifiable risks that we as clinicians should focus on in order to optimize outcomes during pregnancy.
We have come so far in knowledge about fetal exposure to antidepressants relative to other classes of medications women take during pregnancy, about which, frankly, we are still starved for data. As use of psychiatric medications during pregnancy continues to grow, we can rest a bit more comfortably. But we should also address some of the other behaviors that have adverse effects on maternal and child well-being.
Dr. Cohen is the director of the Ammon-Pinizzotto Center for Women’s Mental Health at Massachusetts General Hospital (MGH) in Boston, which provides information resources and conducts clinical care and research in reproductive mental health. He has been a consultant to manufacturers of psychiatric medications. Email Dr. Cohen at [email protected].
Much of the focus of reproductive psychiatry over the last 1 to 2 decades has been on issues regarding risk of fetal exposure to psychiatric medications in the context of the specific risk for teratogenesis or organ malformation. Concerns and questions are mostly focused on exposure to any number of medications that women take during the first trimester, as it is during that period that the major organs are formed.
More recently, there has been appropriate interest in the effect of fetal exposure to psychiatric medications with respect to risk for obstetrical and neonatal complications. This particularly has been the case with respect to antidepressants where fetal exposure to these medications, which while associated with symptoms of transient jitteriness and irritability about 20% of the time, have not been associated with symptoms requiring frank clinical intervention.
Concerning mood stabilizers, the risk for organ dysgenesis following fetal exposure to sodium valproate has been very well established, and we’ve known for over a decade about the adverse effects of fetal exposure to sodium valproate on behavioral outcomes (Lancet Neurol. 2013 Mar;12[3]:244-52). We also now have ample data on lamotrigine, one of the most widely used medicines by reproductive-age women for treatment of bipolar disorder that supports the absence of a risk of organ malformation in first-trimester exposure.
Most recently, in a study of 292 children of women with epilepsy, an evaluation of women being treated with more modern anticonvulsants such as lamotrigine and levetiracetam alone or as polytherapy was performed. The results showed no difference in language, motor, cognitive, social, emotional, and general adaptive functioning in children exposed to either lamotrigine or levetiracetam relative to unexposed children of women with epilepsy. However, the researchers found an increase in anti-epileptic drug plasma level appeared to be associated with decreased motor and sensory function. These are reassuring data that really confirm earlier work, which failed to reveal a signal of concern for lamotrigine and now provide some of the first data on levetiracetam, which is widely used by reproductive-age women with epilepsy (JAMA Neurol. 2021 Aug 1;78[8]:927-936). While one caveat of the study is a short follow-up of 2 years, the absence of a signal of concern is reassuring. With more and more data demonstrating bipolar disorder is an illness that requires chronic treatment for many people, and that discontinuation is associated with high risk for relapse, it is an advance in the field to have data on risk for teratogenesis and data on longer-term neurobehavioral outcomes.
There is vast information regarding reproductive safety, organ malformation, and acute neonatal outcomes for antidepressants. The last decade has brought interest in and analysis of specific reports of increased risk of both autism spectrum disorder (ASD) and attention-deficit/hyperactivity disorder (ADHD) following fetal exposure to antidepressants. What can be said based on reviews of pooled meta-analyses is that the risk for ASD and ADHD has been put to rest for most clinicians and patients (J Clin Psychiatry. 2020 May 26;81[3]:20f13463). With other neurodevelopmental disorders, results have been somewhat inconclusive. Over the last 5-10 years, there have been sporadic reports of concerns about problems in a specific domain of neurodevelopment in offspring of women who have used antidepressants during pregnancy, whether it be speech, language, or motor functioning, but no signal of concern has been consistent.
In a previous column, I addressed a Danish study that showed no increased risk of longer-term sequelae after fetal exposure to antidepressants. Now, a new study has examined 1.93 million pregnancies in the Medicaid Analytic eXtract and 1.25 million pregnancies in the IBM MarketScan Research Database with follow-up up to 14 years of age where the specific interval for fetal exposure was from gestational age of 19 weeks to delivery, as that is the period that corresponds most to synaptogenesis in the brain. The researchers examined a spectrum of neurodevelopmental disorders such as developmental speech issues, ADHD, ASD, dyslexia, and learning disorders, among others. They found a twofold increased risk for neurodevelopmental disorders in the unadjusted models that flattened to no finding when factoring in environmental and genetic risk variables, highlighting the importance of dealing appropriately with confounders when performing these analyses. Those confounders examined include the mother’s use of alcohol and tobacco, and her body mass index and overall general health (JAMA Intern Med. 2022;182[11]:1149-60).
Given the consistency of these results with earlier data, patients can be increasingly comfortable as they weigh the benefits and risks of antidepressant use during pregnancy, factoring in the risk of fetal exposure with added data on long-term neurobehavioral sequelae. With that said, we need to remember the importance of initiatives to address alcohol consumption, poor nutrition, tobacco use, elevated BMI, and general health during pregnancy. These are modifiable risks that we as clinicians should focus on in order to optimize outcomes during pregnancy.
We have come so far in knowledge about fetal exposure to antidepressants relative to other classes of medications women take during pregnancy, about which, frankly, we are still starved for data. As use of psychiatric medications during pregnancy continues to grow, we can rest a bit more comfortably. But we should also address some of the other behaviors that have adverse effects on maternal and child well-being.
Dr. Cohen is the director of the Ammon-Pinizzotto Center for Women’s Mental Health at Massachusetts General Hospital (MGH) in Boston, which provides information resources and conducts clinical care and research in reproductive mental health. He has been a consultant to manufacturers of psychiatric medications. Email Dr. Cohen at [email protected].
Much of the focus of reproductive psychiatry over the last 1 to 2 decades has been on issues regarding risk of fetal exposure to psychiatric medications in the context of the specific risk for teratogenesis or organ malformation. Concerns and questions are mostly focused on exposure to any number of medications that women take during the first trimester, as it is during that period that the major organs are formed.
More recently, there has been appropriate interest in the effect of fetal exposure to psychiatric medications with respect to risk for obstetrical and neonatal complications. This particularly has been the case with respect to antidepressants where fetal exposure to these medications, which while associated with symptoms of transient jitteriness and irritability about 20% of the time, have not been associated with symptoms requiring frank clinical intervention.
Concerning mood stabilizers, the risk for organ dysgenesis following fetal exposure to sodium valproate has been very well established, and we’ve known for over a decade about the adverse effects of fetal exposure to sodium valproate on behavioral outcomes (Lancet Neurol. 2013 Mar;12[3]:244-52). We also now have ample data on lamotrigine, one of the most widely used medicines by reproductive-age women for treatment of bipolar disorder that supports the absence of a risk of organ malformation in first-trimester exposure.
Most recently, in a study of 292 children of women with epilepsy, an evaluation of women being treated with more modern anticonvulsants such as lamotrigine and levetiracetam alone or as polytherapy was performed. The results showed no difference in language, motor, cognitive, social, emotional, and general adaptive functioning in children exposed to either lamotrigine or levetiracetam relative to unexposed children of women with epilepsy. However, the researchers found an increase in anti-epileptic drug plasma level appeared to be associated with decreased motor and sensory function. These are reassuring data that really confirm earlier work, which failed to reveal a signal of concern for lamotrigine and now provide some of the first data on levetiracetam, which is widely used by reproductive-age women with epilepsy (JAMA Neurol. 2021 Aug 1;78[8]:927-936). While one caveat of the study is a short follow-up of 2 years, the absence of a signal of concern is reassuring. With more and more data demonstrating bipolar disorder is an illness that requires chronic treatment for many people, and that discontinuation is associated with high risk for relapse, it is an advance in the field to have data on risk for teratogenesis and data on longer-term neurobehavioral outcomes.
There is vast information regarding reproductive safety, organ malformation, and acute neonatal outcomes for antidepressants. The last decade has brought interest in and analysis of specific reports of increased risk of both autism spectrum disorder (ASD) and attention-deficit/hyperactivity disorder (ADHD) following fetal exposure to antidepressants. What can be said based on reviews of pooled meta-analyses is that the risk for ASD and ADHD has been put to rest for most clinicians and patients (J Clin Psychiatry. 2020 May 26;81[3]:20f13463). With other neurodevelopmental disorders, results have been somewhat inconclusive. Over the last 5-10 years, there have been sporadic reports of concerns about problems in a specific domain of neurodevelopment in offspring of women who have used antidepressants during pregnancy, whether it be speech, language, or motor functioning, but no signal of concern has been consistent.
In a previous column, I addressed a Danish study that showed no increased risk of longer-term sequelae after fetal exposure to antidepressants. Now, a new study has examined 1.93 million pregnancies in the Medicaid Analytic eXtract and 1.25 million pregnancies in the IBM MarketScan Research Database with follow-up up to 14 years of age where the specific interval for fetal exposure was from gestational age of 19 weeks to delivery, as that is the period that corresponds most to synaptogenesis in the brain. The researchers examined a spectrum of neurodevelopmental disorders such as developmental speech issues, ADHD, ASD, dyslexia, and learning disorders, among others. They found a twofold increased risk for neurodevelopmental disorders in the unadjusted models that flattened to no finding when factoring in environmental and genetic risk variables, highlighting the importance of dealing appropriately with confounders when performing these analyses. Those confounders examined include the mother’s use of alcohol and tobacco, and her body mass index and overall general health (JAMA Intern Med. 2022;182[11]:1149-60).
Given the consistency of these results with earlier data, patients can be increasingly comfortable as they weigh the benefits and risks of antidepressant use during pregnancy, factoring in the risk of fetal exposure with added data on long-term neurobehavioral sequelae. With that said, we need to remember the importance of initiatives to address alcohol consumption, poor nutrition, tobacco use, elevated BMI, and general health during pregnancy. These are modifiable risks that we as clinicians should focus on in order to optimize outcomes during pregnancy.
We have come so far in knowledge about fetal exposure to antidepressants relative to other classes of medications women take during pregnancy, about which, frankly, we are still starved for data. As use of psychiatric medications during pregnancy continues to grow, we can rest a bit more comfortably. But we should also address some of the other behaviors that have adverse effects on maternal and child well-being.
Dr. Cohen is the director of the Ammon-Pinizzotto Center for Women’s Mental Health at Massachusetts General Hospital (MGH) in Boston, which provides information resources and conducts clinical care and research in reproductive mental health. He has been a consultant to manufacturers of psychiatric medications. Email Dr. Cohen at [email protected].
Staving off holiday weight gain
Five pounds of weight gain during the holidays is a disproven myth that pops up annually like holiday lights. But before you do a happy dance and pile that extra whipped cream on your pie, you should know two things. One, people do gain weight during the holidays. Two, the extra pounds tend to stick around because most people never lose their holiday weight. Over time, these extra pounds can lead to obesity and weight-related conditions such as diabetes and hypertension.
Let’s be clear. Your weight is one of many markers of your wellness and metabolic health. However, weight changes can indicate that your health is off balance. Holiday weight gain often comes from indulging in increased rich foods, less physical activity, higher stress levels, and sleep disruption.
Optimizing lifestyle factors and trying to lose weight is challenging any time of the year. However, the holiday bustle makes losing weight during this time even more challenging for most people. But maintaining your weight and overall wellness is manageable with three simple shifts in mindset, mindful eating, and meal strategy. Let’s discuss each.
Mindset
From personal and professional experience, I see two primary attitudes regarding holiday eating. They are either “I’ll wait till January to go on a diet” or “I’m on a diet, so I can’t eat anything I like during the holidays.” Both attitude extremes prevent enjoyable and healthy eating during the holidays because they place the focus on food. With both mindsets, food is in control, which leaves you feeling out of control. Rather than having an “all or none” mindset during the holidays, I encourage you to ask yourself:
- “What matters most to me during the holidays?” In a recent survey, 72% of Americans said they look forward to during the holidays. Although food often accompanies family celebrations, it’s the time with family that matters most. Choose to savor sweet time spent with loved ones instead of stuffing yourself with excess sugary sweets.
- “How can I enjoy myself without food or alcoholic beverages?” So often, we eat or drink certain foods out of habit. Shift your mindset from “we always do this” to “what could we do instead?” Asking this question may be the doorway to creating new, non–food-centered traditions.
- “How can I have the foods I love during the holidays and still meet my weight and wellness goals?” This question helps you create opportunities instead of depriving yourself. Rather than depriving yourself, you could cut back on snacking or reduce your sugar intake elsewhere. Or add an extra workout session or stress reduction practice during the holidays.
Mindful eating
The purpose of mindful eating isn’t weight loss. Some studies suggest it may help maintain weight. More importantly, mindfulness can improve your relationship with food and promote wellness. Traditional tips for mindful eating include doing the following as you eat: Being present in the moment, not judging your food, slowing down, and savoring the taste of your food. During the holidays, asking additional questions may enhance mindful eating. For instance:
- “Am I eating to avoid uncomfortable emotions?” The holidays can trigger emotions such as grief, sadness, and anxiety. Also, preexisting can worsen. Decadent foods become a quick fix leading to more emotional eating during this season. Addressing these emotions can help you avoid overeating during the holidays. For mental health resources, visit the
- “What food or drink do I most enjoy during the holidays?” Trying to resist your favorite holiday treats can be an exhausting test of “willpower.” Eventually, and psychological reasons, and you “cheat” on your plan to not eat holiday treats. To prevent this painful battle of treat versus cheat, plan to eat your “indulgence food” in moderation. Savor the foods you enjoy. Then cut out the rest of the food you don’t like or feel you must eat because “Aunty Sarah will feel bad.”
Meal strategy
Many holiday treats and parties are unavoidable unless you plan to hide in a cave for the next few weeks. Rather than torturing yourself nibbling on celery and sipping on sparkling water during your holiday event, create a strategy. For 8 years, I’ve been on my weight loss and wellness journey. I have a holiday strategy that helps my patients, clients, and me maintain our weight and wellness during the holidays. One critical part of the strategy is to anticipate indulgence events. Specifically, look at all the planned holiday events and choose three indulgence events. The rest of the time, do your best to stay on your plan. Knowing your indulgence events to look forward to gives you a sense of control over when you indulge. On non-indulgent days, think, “I can eat it but choose not to” instead of the limiting thought, “I can’t eat that.” Choice is a powerful tool. Once at an indulgence event, I focus on mindful eating and enjoying people around me, which cuts down on overeating just because “I can.”
This holiday season is a reunion time for many people, after enduring long separations from family and friends due to the pandemic. Relishing time with loved ones should be your focus during the holidays – not eating yourself into worse health or worrying about dieting. Even if you choose not to make all the shifts in mindset, mindful eating, and meal strategy mentioned, choosing even one change to focus on can help you both enjoy the holidays and have increased control over your weight and wellness. Whatever you do, may you and your loved ones have a safe, healthy, and enjoyable holiday season.
Sylvia Gonsahn-Bollie, MD, DipABOM, is an integrative obesity specialist who specializes in individualized solutions for emotional and biological overeating. She is CEO and lead physician at Embrace You Weight and Wellness, Telehealth & Virtual Counseling. She has disclosed having no relevant financial relationships. A version of this article first appeared on Medscape.com.
Five pounds of weight gain during the holidays is a disproven myth that pops up annually like holiday lights. But before you do a happy dance and pile that extra whipped cream on your pie, you should know two things. One, people do gain weight during the holidays. Two, the extra pounds tend to stick around because most people never lose their holiday weight. Over time, these extra pounds can lead to obesity and weight-related conditions such as diabetes and hypertension.
Let’s be clear. Your weight is one of many markers of your wellness and metabolic health. However, weight changes can indicate that your health is off balance. Holiday weight gain often comes from indulging in increased rich foods, less physical activity, higher stress levels, and sleep disruption.
Optimizing lifestyle factors and trying to lose weight is challenging any time of the year. However, the holiday bustle makes losing weight during this time even more challenging for most people. But maintaining your weight and overall wellness is manageable with three simple shifts in mindset, mindful eating, and meal strategy. Let’s discuss each.
Mindset
From personal and professional experience, I see two primary attitudes regarding holiday eating. They are either “I’ll wait till January to go on a diet” or “I’m on a diet, so I can’t eat anything I like during the holidays.” Both attitude extremes prevent enjoyable and healthy eating during the holidays because they place the focus on food. With both mindsets, food is in control, which leaves you feeling out of control. Rather than having an “all or none” mindset during the holidays, I encourage you to ask yourself:
- “What matters most to me during the holidays?” In a recent survey, 72% of Americans said they look forward to during the holidays. Although food often accompanies family celebrations, it’s the time with family that matters most. Choose to savor sweet time spent with loved ones instead of stuffing yourself with excess sugary sweets.
- “How can I enjoy myself without food or alcoholic beverages?” So often, we eat or drink certain foods out of habit. Shift your mindset from “we always do this” to “what could we do instead?” Asking this question may be the doorway to creating new, non–food-centered traditions.
- “How can I have the foods I love during the holidays and still meet my weight and wellness goals?” This question helps you create opportunities instead of depriving yourself. Rather than depriving yourself, you could cut back on snacking or reduce your sugar intake elsewhere. Or add an extra workout session or stress reduction practice during the holidays.
Mindful eating
The purpose of mindful eating isn’t weight loss. Some studies suggest it may help maintain weight. More importantly, mindfulness can improve your relationship with food and promote wellness. Traditional tips for mindful eating include doing the following as you eat: Being present in the moment, not judging your food, slowing down, and savoring the taste of your food. During the holidays, asking additional questions may enhance mindful eating. For instance:
- “Am I eating to avoid uncomfortable emotions?” The holidays can trigger emotions such as grief, sadness, and anxiety. Also, preexisting can worsen. Decadent foods become a quick fix leading to more emotional eating during this season. Addressing these emotions can help you avoid overeating during the holidays. For mental health resources, visit the
- “What food or drink do I most enjoy during the holidays?” Trying to resist your favorite holiday treats can be an exhausting test of “willpower.” Eventually, and psychological reasons, and you “cheat” on your plan to not eat holiday treats. To prevent this painful battle of treat versus cheat, plan to eat your “indulgence food” in moderation. Savor the foods you enjoy. Then cut out the rest of the food you don’t like or feel you must eat because “Aunty Sarah will feel bad.”
Meal strategy
Many holiday treats and parties are unavoidable unless you plan to hide in a cave for the next few weeks. Rather than torturing yourself nibbling on celery and sipping on sparkling water during your holiday event, create a strategy. For 8 years, I’ve been on my weight loss and wellness journey. I have a holiday strategy that helps my patients, clients, and me maintain our weight and wellness during the holidays. One critical part of the strategy is to anticipate indulgence events. Specifically, look at all the planned holiday events and choose three indulgence events. The rest of the time, do your best to stay on your plan. Knowing your indulgence events to look forward to gives you a sense of control over when you indulge. On non-indulgent days, think, “I can eat it but choose not to” instead of the limiting thought, “I can’t eat that.” Choice is a powerful tool. Once at an indulgence event, I focus on mindful eating and enjoying people around me, which cuts down on overeating just because “I can.”
This holiday season is a reunion time for many people, after enduring long separations from family and friends due to the pandemic. Relishing time with loved ones should be your focus during the holidays – not eating yourself into worse health or worrying about dieting. Even if you choose not to make all the shifts in mindset, mindful eating, and meal strategy mentioned, choosing even one change to focus on can help you both enjoy the holidays and have increased control over your weight and wellness. Whatever you do, may you and your loved ones have a safe, healthy, and enjoyable holiday season.
Sylvia Gonsahn-Bollie, MD, DipABOM, is an integrative obesity specialist who specializes in individualized solutions for emotional and biological overeating. She is CEO and lead physician at Embrace You Weight and Wellness, Telehealth & Virtual Counseling. She has disclosed having no relevant financial relationships. A version of this article first appeared on Medscape.com.
Five pounds of weight gain during the holidays is a disproven myth that pops up annually like holiday lights. But before you do a happy dance and pile that extra whipped cream on your pie, you should know two things. One, people do gain weight during the holidays. Two, the extra pounds tend to stick around because most people never lose their holiday weight. Over time, these extra pounds can lead to obesity and weight-related conditions such as diabetes and hypertension.
Let’s be clear. Your weight is one of many markers of your wellness and metabolic health. However, weight changes can indicate that your health is off balance. Holiday weight gain often comes from indulging in increased rich foods, less physical activity, higher stress levels, and sleep disruption.
Optimizing lifestyle factors and trying to lose weight is challenging any time of the year. However, the holiday bustle makes losing weight during this time even more challenging for most people. But maintaining your weight and overall wellness is manageable with three simple shifts in mindset, mindful eating, and meal strategy. Let’s discuss each.
Mindset
From personal and professional experience, I see two primary attitudes regarding holiday eating. They are either “I’ll wait till January to go on a diet” or “I’m on a diet, so I can’t eat anything I like during the holidays.” Both attitude extremes prevent enjoyable and healthy eating during the holidays because they place the focus on food. With both mindsets, food is in control, which leaves you feeling out of control. Rather than having an “all or none” mindset during the holidays, I encourage you to ask yourself:
- “What matters most to me during the holidays?” In a recent survey, 72% of Americans said they look forward to during the holidays. Although food often accompanies family celebrations, it’s the time with family that matters most. Choose to savor sweet time spent with loved ones instead of stuffing yourself with excess sugary sweets.
- “How can I enjoy myself without food or alcoholic beverages?” So often, we eat or drink certain foods out of habit. Shift your mindset from “we always do this” to “what could we do instead?” Asking this question may be the doorway to creating new, non–food-centered traditions.
- “How can I have the foods I love during the holidays and still meet my weight and wellness goals?” This question helps you create opportunities instead of depriving yourself. Rather than depriving yourself, you could cut back on snacking or reduce your sugar intake elsewhere. Or add an extra workout session or stress reduction practice during the holidays.
Mindful eating
The purpose of mindful eating isn’t weight loss. Some studies suggest it may help maintain weight. More importantly, mindfulness can improve your relationship with food and promote wellness. Traditional tips for mindful eating include doing the following as you eat: Being present in the moment, not judging your food, slowing down, and savoring the taste of your food. During the holidays, asking additional questions may enhance mindful eating. For instance:
- “Am I eating to avoid uncomfortable emotions?” The holidays can trigger emotions such as grief, sadness, and anxiety. Also, preexisting can worsen. Decadent foods become a quick fix leading to more emotional eating during this season. Addressing these emotions can help you avoid overeating during the holidays. For mental health resources, visit the
- “What food or drink do I most enjoy during the holidays?” Trying to resist your favorite holiday treats can be an exhausting test of “willpower.” Eventually, and psychological reasons, and you “cheat” on your plan to not eat holiday treats. To prevent this painful battle of treat versus cheat, plan to eat your “indulgence food” in moderation. Savor the foods you enjoy. Then cut out the rest of the food you don’t like or feel you must eat because “Aunty Sarah will feel bad.”
Meal strategy
Many holiday treats and parties are unavoidable unless you plan to hide in a cave for the next few weeks. Rather than torturing yourself nibbling on celery and sipping on sparkling water during your holiday event, create a strategy. For 8 years, I’ve been on my weight loss and wellness journey. I have a holiday strategy that helps my patients, clients, and me maintain our weight and wellness during the holidays. One critical part of the strategy is to anticipate indulgence events. Specifically, look at all the planned holiday events and choose three indulgence events. The rest of the time, do your best to stay on your plan. Knowing your indulgence events to look forward to gives you a sense of control over when you indulge. On non-indulgent days, think, “I can eat it but choose not to” instead of the limiting thought, “I can’t eat that.” Choice is a powerful tool. Once at an indulgence event, I focus on mindful eating and enjoying people around me, which cuts down on overeating just because “I can.”
This holiday season is a reunion time for many people, after enduring long separations from family and friends due to the pandemic. Relishing time with loved ones should be your focus during the holidays – not eating yourself into worse health or worrying about dieting. Even if you choose not to make all the shifts in mindset, mindful eating, and meal strategy mentioned, choosing even one change to focus on can help you both enjoy the holidays and have increased control over your weight and wellness. Whatever you do, may you and your loved ones have a safe, healthy, and enjoyable holiday season.
Sylvia Gonsahn-Bollie, MD, DipABOM, is an integrative obesity specialist who specializes in individualized solutions for emotional and biological overeating. She is CEO and lead physician at Embrace You Weight and Wellness, Telehealth & Virtual Counseling. She has disclosed having no relevant financial relationships. A version of this article first appeared on Medscape.com.
Update on high-grade vulvar interepithelial neoplasia
Vulvar squamous cell carcinomas (VSCC) comprise approximately 90% of all vulvar malignancies. Unlike cervical SCC, which are predominantly human papilloma virus (HPV) positive, only a minority of VSCC are HPV positive – on the order of 15%-25% of cases. Most cases occur in the setting of lichen sclerosus and are HPV negative.
Lichen sclerosus is a chronic inflammatory dermatitis typically involving the anogenital area, which in some cases can become seriously distorted (e.g. atrophy of the labia minora, clitoral phimosis, and introital stenosis). Although most cases are diagnosed in postmenopausal women, LS can affect women of any age. The true prevalence of lichen sclerosus is unknown. Recent studies have shown a prevalence of 1 in 60; among older women, it can even be as high as 1 in 30. While lichen sclerosus is a pruriginous condition, it is often asymptomatic. It is not considered a premalignant condition. The diagnosis is clinical; however, suspicious lesions (erosions/ulcerations, hyperkeratosis, pigmented areas, ecchymosis, warty or papular lesions), particularly when recalcitrant to adequate first-line therapy, should be biopsied.
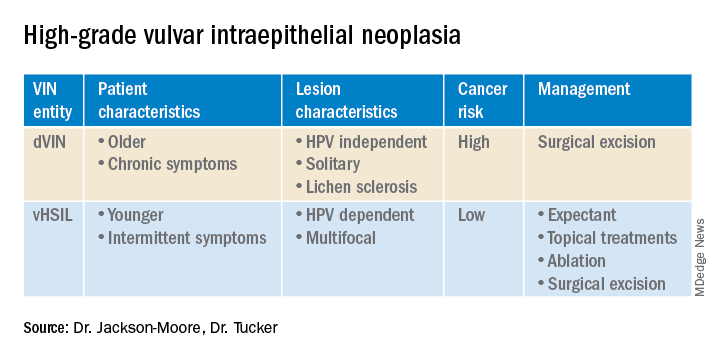
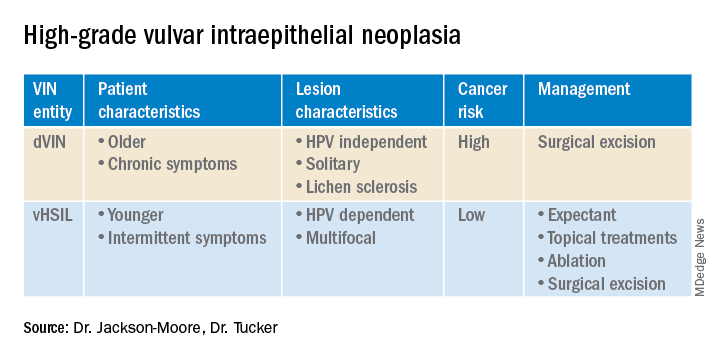
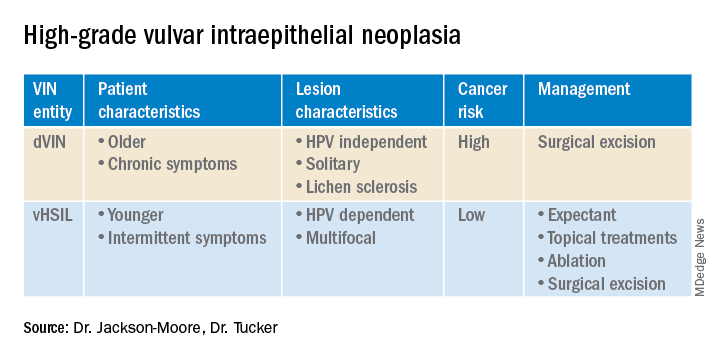
VSCC arises from precursor lesions or high-grade vulvar intraepithelial neoplasia (VIN). The 2015 International Society for the Study of Vulvovaginal Disease nomenclature classifies high-grade VIN into high-grade squamous intraepithelial lesion (HSIL) and differentiated VIN (dVIN). Most patients with high-grade VIN are diagnosed with HSIL or usual type VIN. A preponderance of these lesions (75%-85%) are HPV positive, predominantly HPV 16. Vulvar HSIL (vHSIL) lesions affect younger women. The lesions tend to be multifocal and extensive. On the other hand, dVIN typically affects older women and commonly develops as a solitary lesion. While dVIN accounts for only a small subset of patients with high-grade VIN, these lesions are HPV negative and associated with lichen sclerosus.
Both disease entities, vHSIL and dVIN, are increasing in incidence. There is a higher risk and shortened period of progression to cancer in patients with dVIN compared to HSIL. The cancer risk of vHSIL is relatively low. The 10-year cumulative VSCC risk reported in the literature is 10.3%; 9.7% for vHSIL and 50% for dVIN. Patients with vHSIL could benefit from less aggressive treatment modalities.
Patients present with a constellation of signs such as itching, pain, burning, bleeding, and discharge. Chronic symptoms portend HPV-independent lesions associated with lichen sclerosus while episodic signs are suggestive of HPV-positive lesions.
The recurrence risk of high-grade VIN is 46%-70%. Risk factors for recurrence include age greater than 50, immunosuppression, metasynchronous HSIL, and multifocal lesions. Recurrences occur in up to 50% of women who have undergone surgery. For those who undergo surgical treatment for high-grade VIN, recurrence is more common in the setting of positive margins, underlying lichen sclerosis, persistent HPV infection, and immunosuppression.
Management of high-grade VIN is determined by the lesion characteristics, patient characteristics, and medical expertise. Given the risk of progression of high-grade VIN to cancer and risk of underlying cancer, surgical therapy is typically recommended. The treatment of choice is surgical excision in cases of dVIN. Surgical treatments include CO2 laser ablation, wide local excision, and vulvectomy. Women who undergo surgical treatment for vHSIL have about a 50% chance of the condition recurring 1 year later, irrespective of whether treatment is by surgical excision or laser vaporization.
Since surgery can be associated with disfigurement and sexual dysfunction, alternatives to surgery should be considered in cases of vHSIL. The potential for effect on sexual function should be part of preoperative counseling and treatment. Women treated for VIN often experience increased inhibition of sexual excitement and increased inhibition of orgasm. One study found that in women undergoing vulvar excision for VIN, the impairment was found to be psychological in nature. Overall, the studies of sexual effect from treatment of VIN have found that women do not return to their pretreatment sexual function. However, the optimal management of vHSIL has not been determined. Nonsurgical options include topical therapies (imiquimod, 5-fluorouracil, cidofovir, and interferon) and nonpharmacologic treatments, such as photodynamic therapy.
Imiquimod, a topical immune modulator, is the most studied pharmacologic treatment of vHSIL. The drug induces secretion of cytokines, creating an immune response that clears the HPV infection. Imiquimod is safe and well tolerated. The clinical response rate varies between 35% and 81%. A recent study demonstrated the efficacy of imiquimod and the treatment was found to be noninferior to surgery. Adverse events differed, with local pain following surgical treatment and local pruritus and erythema associated with imiquimod use. Some patients did not respond to imiquimod; it was thought by the authors of the study that specific immunological factors affect the clinical response.
In conclusion, high-grade VIN is a heterogeneous disease made up of two distinct disease entities with rising incidence. In contrast to dVIN, the cancer risk is low for patients with vHSIL. Treatment should be driven by the clinical characteristics of the vulvar lesions, patients’ preferences, sexual activity, and compliance. Future directions include risk stratification of patients with vHSIL who are most likely to benefit from topical treatments, thus reducing overtreatment. Molecular biomarkers that could identify dVIN at an early stage are needed.
Dr. Jackson-Moore is associate professor in gynecologic oncology at the University of North Carolina at Chapel Hill. Dr. Tucker is assistant professor of gynecologic oncology at the university.
References
Cendejas BR et al. Am J Obstet Gynecol. 2015 Mar;212(3):291-7.
Lebreton M et al. J Gynecol Obstet Hum Reprod. 2020 Nov;49(9):101801.
Thuijs NB et al. Int J Cancer. 2021 Jan 1;148(1):90-8. doi: 10.1002/ijc.33198. .
Trutnovsky G et al. Lancet. 2022 May 7;399(10337):1790-8. Erratum in: Lancet. 2022 Oct 8;400(10359):1194.
Vulvar squamous cell carcinomas (VSCC) comprise approximately 90% of all vulvar malignancies. Unlike cervical SCC, which are predominantly human papilloma virus (HPV) positive, only a minority of VSCC are HPV positive – on the order of 15%-25% of cases. Most cases occur in the setting of lichen sclerosus and are HPV negative.
Lichen sclerosus is a chronic inflammatory dermatitis typically involving the anogenital area, which in some cases can become seriously distorted (e.g. atrophy of the labia minora, clitoral phimosis, and introital stenosis). Although most cases are diagnosed in postmenopausal women, LS can affect women of any age. The true prevalence of lichen sclerosus is unknown. Recent studies have shown a prevalence of 1 in 60; among older women, it can even be as high as 1 in 30. While lichen sclerosus is a pruriginous condition, it is often asymptomatic. It is not considered a premalignant condition. The diagnosis is clinical; however, suspicious lesions (erosions/ulcerations, hyperkeratosis, pigmented areas, ecchymosis, warty or papular lesions), particularly when recalcitrant to adequate first-line therapy, should be biopsied.
VSCC arises from precursor lesions or high-grade vulvar intraepithelial neoplasia (VIN). The 2015 International Society for the Study of Vulvovaginal Disease nomenclature classifies high-grade VIN into high-grade squamous intraepithelial lesion (HSIL) and differentiated VIN (dVIN). Most patients with high-grade VIN are diagnosed with HSIL or usual type VIN. A preponderance of these lesions (75%-85%) are HPV positive, predominantly HPV 16. Vulvar HSIL (vHSIL) lesions affect younger women. The lesions tend to be multifocal and extensive. On the other hand, dVIN typically affects older women and commonly develops as a solitary lesion. While dVIN accounts for only a small subset of patients with high-grade VIN, these lesions are HPV negative and associated with lichen sclerosus.
Both disease entities, vHSIL and dVIN, are increasing in incidence. There is a higher risk and shortened period of progression to cancer in patients with dVIN compared to HSIL. The cancer risk of vHSIL is relatively low. The 10-year cumulative VSCC risk reported in the literature is 10.3%; 9.7% for vHSIL and 50% for dVIN. Patients with vHSIL could benefit from less aggressive treatment modalities.
Patients present with a constellation of signs such as itching, pain, burning, bleeding, and discharge. Chronic symptoms portend HPV-independent lesions associated with lichen sclerosus while episodic signs are suggestive of HPV-positive lesions.
The recurrence risk of high-grade VIN is 46%-70%. Risk factors for recurrence include age greater than 50, immunosuppression, metasynchronous HSIL, and multifocal lesions. Recurrences occur in up to 50% of women who have undergone surgery. For those who undergo surgical treatment for high-grade VIN, recurrence is more common in the setting of positive margins, underlying lichen sclerosis, persistent HPV infection, and immunosuppression.
Management of high-grade VIN is determined by the lesion characteristics, patient characteristics, and medical expertise. Given the risk of progression of high-grade VIN to cancer and risk of underlying cancer, surgical therapy is typically recommended. The treatment of choice is surgical excision in cases of dVIN. Surgical treatments include CO2 laser ablation, wide local excision, and vulvectomy. Women who undergo surgical treatment for vHSIL have about a 50% chance of the condition recurring 1 year later, irrespective of whether treatment is by surgical excision or laser vaporization.
Since surgery can be associated with disfigurement and sexual dysfunction, alternatives to surgery should be considered in cases of vHSIL. The potential for effect on sexual function should be part of preoperative counseling and treatment. Women treated for VIN often experience increased inhibition of sexual excitement and increased inhibition of orgasm. One study found that in women undergoing vulvar excision for VIN, the impairment was found to be psychological in nature. Overall, the studies of sexual effect from treatment of VIN have found that women do not return to their pretreatment sexual function. However, the optimal management of vHSIL has not been determined. Nonsurgical options include topical therapies (imiquimod, 5-fluorouracil, cidofovir, and interferon) and nonpharmacologic treatments, such as photodynamic therapy.
Imiquimod, a topical immune modulator, is the most studied pharmacologic treatment of vHSIL. The drug induces secretion of cytokines, creating an immune response that clears the HPV infection. Imiquimod is safe and well tolerated. The clinical response rate varies between 35% and 81%. A recent study demonstrated the efficacy of imiquimod and the treatment was found to be noninferior to surgery. Adverse events differed, with local pain following surgical treatment and local pruritus and erythema associated with imiquimod use. Some patients did not respond to imiquimod; it was thought by the authors of the study that specific immunological factors affect the clinical response.
In conclusion, high-grade VIN is a heterogeneous disease made up of two distinct disease entities with rising incidence. In contrast to dVIN, the cancer risk is low for patients with vHSIL. Treatment should be driven by the clinical characteristics of the vulvar lesions, patients’ preferences, sexual activity, and compliance. Future directions include risk stratification of patients with vHSIL who are most likely to benefit from topical treatments, thus reducing overtreatment. Molecular biomarkers that could identify dVIN at an early stage are needed.
Dr. Jackson-Moore is associate professor in gynecologic oncology at the University of North Carolina at Chapel Hill. Dr. Tucker is assistant professor of gynecologic oncology at the university.
References
Cendejas BR et al. Am J Obstet Gynecol. 2015 Mar;212(3):291-7.
Lebreton M et al. J Gynecol Obstet Hum Reprod. 2020 Nov;49(9):101801.
Thuijs NB et al. Int J Cancer. 2021 Jan 1;148(1):90-8. doi: 10.1002/ijc.33198. .
Trutnovsky G et al. Lancet. 2022 May 7;399(10337):1790-8. Erratum in: Lancet. 2022 Oct 8;400(10359):1194.
Vulvar squamous cell carcinomas (VSCC) comprise approximately 90% of all vulvar malignancies. Unlike cervical SCC, which are predominantly human papilloma virus (HPV) positive, only a minority of VSCC are HPV positive – on the order of 15%-25% of cases. Most cases occur in the setting of lichen sclerosus and are HPV negative.
Lichen sclerosus is a chronic inflammatory dermatitis typically involving the anogenital area, which in some cases can become seriously distorted (e.g. atrophy of the labia minora, clitoral phimosis, and introital stenosis). Although most cases are diagnosed in postmenopausal women, LS can affect women of any age. The true prevalence of lichen sclerosus is unknown. Recent studies have shown a prevalence of 1 in 60; among older women, it can even be as high as 1 in 30. While lichen sclerosus is a pruriginous condition, it is often asymptomatic. It is not considered a premalignant condition. The diagnosis is clinical; however, suspicious lesions (erosions/ulcerations, hyperkeratosis, pigmented areas, ecchymosis, warty or papular lesions), particularly when recalcitrant to adequate first-line therapy, should be biopsied.
VSCC arises from precursor lesions or high-grade vulvar intraepithelial neoplasia (VIN). The 2015 International Society for the Study of Vulvovaginal Disease nomenclature classifies high-grade VIN into high-grade squamous intraepithelial lesion (HSIL) and differentiated VIN (dVIN). Most patients with high-grade VIN are diagnosed with HSIL or usual type VIN. A preponderance of these lesions (75%-85%) are HPV positive, predominantly HPV 16. Vulvar HSIL (vHSIL) lesions affect younger women. The lesions tend to be multifocal and extensive. On the other hand, dVIN typically affects older women and commonly develops as a solitary lesion. While dVIN accounts for only a small subset of patients with high-grade VIN, these lesions are HPV negative and associated with lichen sclerosus.
Both disease entities, vHSIL and dVIN, are increasing in incidence. There is a higher risk and shortened period of progression to cancer in patients with dVIN compared to HSIL. The cancer risk of vHSIL is relatively low. The 10-year cumulative VSCC risk reported in the literature is 10.3%; 9.7% for vHSIL and 50% for dVIN. Patients with vHSIL could benefit from less aggressive treatment modalities.
Patients present with a constellation of signs such as itching, pain, burning, bleeding, and discharge. Chronic symptoms portend HPV-independent lesions associated with lichen sclerosus while episodic signs are suggestive of HPV-positive lesions.
The recurrence risk of high-grade VIN is 46%-70%. Risk factors for recurrence include age greater than 50, immunosuppression, metasynchronous HSIL, and multifocal lesions. Recurrences occur in up to 50% of women who have undergone surgery. For those who undergo surgical treatment for high-grade VIN, recurrence is more common in the setting of positive margins, underlying lichen sclerosis, persistent HPV infection, and immunosuppression.
Management of high-grade VIN is determined by the lesion characteristics, patient characteristics, and medical expertise. Given the risk of progression of high-grade VIN to cancer and risk of underlying cancer, surgical therapy is typically recommended. The treatment of choice is surgical excision in cases of dVIN. Surgical treatments include CO2 laser ablation, wide local excision, and vulvectomy. Women who undergo surgical treatment for vHSIL have about a 50% chance of the condition recurring 1 year later, irrespective of whether treatment is by surgical excision or laser vaporization.
Since surgery can be associated with disfigurement and sexual dysfunction, alternatives to surgery should be considered in cases of vHSIL. The potential for effect on sexual function should be part of preoperative counseling and treatment. Women treated for VIN often experience increased inhibition of sexual excitement and increased inhibition of orgasm. One study found that in women undergoing vulvar excision for VIN, the impairment was found to be psychological in nature. Overall, the studies of sexual effect from treatment of VIN have found that women do not return to their pretreatment sexual function. However, the optimal management of vHSIL has not been determined. Nonsurgical options include topical therapies (imiquimod, 5-fluorouracil, cidofovir, and interferon) and nonpharmacologic treatments, such as photodynamic therapy.
Imiquimod, a topical immune modulator, is the most studied pharmacologic treatment of vHSIL. The drug induces secretion of cytokines, creating an immune response that clears the HPV infection. Imiquimod is safe and well tolerated. The clinical response rate varies between 35% and 81%. A recent study demonstrated the efficacy of imiquimod and the treatment was found to be noninferior to surgery. Adverse events differed, with local pain following surgical treatment and local pruritus and erythema associated with imiquimod use. Some patients did not respond to imiquimod; it was thought by the authors of the study that specific immunological factors affect the clinical response.
In conclusion, high-grade VIN is a heterogeneous disease made up of two distinct disease entities with rising incidence. In contrast to dVIN, the cancer risk is low for patients with vHSIL. Treatment should be driven by the clinical characteristics of the vulvar lesions, patients’ preferences, sexual activity, and compliance. Future directions include risk stratification of patients with vHSIL who are most likely to benefit from topical treatments, thus reducing overtreatment. Molecular biomarkers that could identify dVIN at an early stage are needed.
Dr. Jackson-Moore is associate professor in gynecologic oncology at the University of North Carolina at Chapel Hill. Dr. Tucker is assistant professor of gynecologic oncology at the university.
References
Cendejas BR et al. Am J Obstet Gynecol. 2015 Mar;212(3):291-7.
Lebreton M et al. J Gynecol Obstet Hum Reprod. 2020 Nov;49(9):101801.
Thuijs NB et al. Int J Cancer. 2021 Jan 1;148(1):90-8. doi: 10.1002/ijc.33198. .
Trutnovsky G et al. Lancet. 2022 May 7;399(10337):1790-8. Erratum in: Lancet. 2022 Oct 8;400(10359):1194.
The importance of connection and community
You only are free when you realize you belong no place – you belong every place – no place at all. The price is high. The reward is great. ~ Maya Angelou
At 8 o’clock, every weekday morning, for years and years now, two friends appear in my kitchen for coffee, and so one identity I carry includes being part of the “coffee ladies.” While this is one of the smaller and more intimate groups to which I belong, I am also a member (“distinguished,” no less) of a slightly larger group: the American Psychiatric Association, and being part of both groups is meaningful to me in more ways than I can describe.
When I think back over the years, I – like most people – have belonged to many people and places, either officially or unofficially. It is these connections that define us, fill our time, give us meaning and purpose, and anchor us. We belong to our families and friends, but we also belong to our professional and community groups, our institutions – whether they are hospitals, schools, religious centers, country clubs, or charitable organizations – as well as interest and advocacy groups. And finally, we belong to our coworkers and to our patients, and they to us, especially if we see the same people over time. Being a psychiatrist can be a solitary career, and it can take a little effort to be a part of larger worlds, especially for those who find solace in more individual activities.
As I’ve gotten older, I’ve noticed that I belong to fewer of these groups. I’m no longer a little league or field hockey mom, nor a member of the neighborhood babysitting co-op, and I’ve exhausted the gamut of council and leadership positions in my APA district branch. I’ve joined organizations only to pay the membership fee, and then never gone to their meetings or events. The pandemic has accounted for some of this: I still belong to my book club, but I often read the book and don’t go to the Zoom meetings as I miss the real-life aspect of getting together. Being boxed on a screen is not the same as the one-on-one conversations before the formal book discussion. And while I still carry a host of identities, I imagine it is not unusual to belong to fewer organizations as time passes. It’s not all bad, there is something good to be said for living life at a less frenetic pace as fewer entities lay claim to my time.
In psychiatry, our patients span the range of human experience: Some are very engaged with their worlds, while others struggle to make even the most basic of connections. Their lives may seem disconnected – empty, even – and I find myself encouraging people to reach out, to find activities that will ease their loneliness and integrate a feeling of belonging in a way that adds meaning and purpose. For some people, this may be as simple as asking a friend to have lunch, but even that can be an overwhelming obstacle for someone who is depressed, or for someone who has no friends.
Patients may counter my suggestions with a host of reasons as to why they can’t connect. Perhaps their friend is too busy with work or his family, the lunch would cost too much, there’s no transportation, or no restaurant that could meet their dietary needs. Or perhaps they are just too fearful of being rejected.
Psychiatric disorders, by their nature, can be very isolating. Depressed and anxious people often find it a struggle just to get through their days, adding new people and activities is not something that brings joy. For people suffering with psychosis, their internal realities are often all-consuming and there may be no room for accommodating others. And finally, what I hear over and over, is that people are afraid of what others might think of them, and this fear is paralyzing. I try to suggest that we never really know or control what others think of us, but obviously, this does not reassure most patients as they are also bewildered by their irrational fear. To go to an event unaccompanied, or even to a party to which they have been invited, is a hurdle they won’t (or can’t) attempt.
The pandemic, with its initial months of shutdown, and then with years of fear of illness, has created new ways of connecting. Our “Zoom” world can be very convenient – in many ways it has opened up aspects of learning and connection for people who are short on time,or struggle with transportation. In the comfort of our living rooms, in pajamas and slippers, we can take classes, join clubs, attend Alcoholics Anonymous meetings, go to conferences or religious services, and be part of any number of organizations without flying or searching for parking. I love that, with 1 hour and a single click, I can now attend my department’s weekly Grand Rounds. But for many who struggle with using technology, or who don’t feel the same benefits from online encounters, the pandemic has been an isolating and lonely time.
It should not be assumed that isolation has been a negative experience for everyone. For many who struggle with interpersonal relationships, for children who are bullied or teased at school or who feel self-conscious sitting alone at lunch, there may not be the presumed “fear of missing out.” As one adult patient told me: “You know, I do ‘alone’ well.” For some, it has been a relief to be relieved of the pressure to socialize, attend parties, or pursue online dating – a process I think of as “people-shopping” which looks so different from the old days of organic interactions that led to romantic interactions over time. Many have found relief without the pressures of social interactions.
Community, connection, and belonging are not inconsequential things, however. They are part of what adds to life’s richness, and they are associated with good health and longevity. The Harvard Study of Adult Development, begun in 1938, has been tracking two groups of Boston teenagers – and now their wives and children – for 84 years. Tracking one group of Harvard students and another group of teens from poorer areas in Boston, the project is now on its 4th director.
George Vaillant, MD, author of “Aging Well: Surprising Guideposts to a Happier Life from the Landmark Harvard Study of Adult Development” (New York: Little, Brown Spark, 2002) was the program’s director from 1972 to 2004. “When the study began, nobody cared about empathy or attachment. But the key to healthy aging is relationships, relationships, relationships,” Dr. Vaillant said in an interview in the Harvard Gazette.
Susan Pinker is a social psychologist and author of “The Village Effect: How Face-to-Face Contact Can Make Us Healthier and Happier” (Toronto: Random House Canada, 2014). In her 2017 TED talk, she notes that in all developed countries, women live 6-8 years longer than men, and are half as likely to die at any age. She is underwhelmed by digital relationships, and says that real life relationships affect our physiological states differently and in more beneficial ways. “Building your village and sustaining it is a matter of life and death,” she states at the end of her TED talk.
I spoke with Ms. Pinker about her thoughts on how our personal villages change over time. She was quick to tell me that she is not against digital communities. “I’m not a Luddite. As a writer, I probably spend as much time facing a screen as anyone else. But it’s important to remember that digital communities can amplify existing relationships, and don’t replace in-person social contact. A lot of people have drunk the Kool-Aid about virtual experiences, even though they are not the same as real life interactions.
“Loneliness takes on a U-shaped function across adulthood,” she explained with regard to how age impacts our social connections. “People are lonely when they first leave home or when they finish college and go out into the world. Then they settle into new situations; they can make friends at work, through their children, in their neighborhood, or by belonging to organizations. As people settle into their adult lives, there are increased opportunities to connect in person. But loneliness increases again in late middle age.” She explained that everyone loses people as their children move away, friends move, and couples may divorce or a spouse dies.
“Attrition of our social face-to-face networks is an ugly feature of aging,” Ms. Pinker said. “Some people are good at replacing the vacant spots; they sense that it is important to invest in different relationships as you age. It’s like a garden that you need to tend by replacing the perennials that die off in the winter.” The United States, she pointed out, has a culture that is particularly difficult for people in their later years.
My world is a little quieter than it once was, but collecting and holding on to people is important to me. The organizations and affiliations change over time, as does the brand of coffee. So I try to inspire some of my more isolated patients to prioritize their relationships, to let go of their grudges, to tolerate the discomfort of moving from their places of comfort to the temporary discomfort of reaching out in the service of achieving a less solitary, more purposeful, and healthier life. When it doesn’t come naturally, it can be hard work.
Dr. Miller is a coauthor of “Committed: The Battle Over Involuntary Psychiatric Care” (Johns Hopkins University Press, 2016). She has a private practice and is assistant professor of psychiatry and behavioral sciences at Johns Hopkins University, Baltimore. She has disclosed no relevant financial relationships.
You only are free when you realize you belong no place – you belong every place – no place at all. The price is high. The reward is great. ~ Maya Angelou
At 8 o’clock, every weekday morning, for years and years now, two friends appear in my kitchen for coffee, and so one identity I carry includes being part of the “coffee ladies.” While this is one of the smaller and more intimate groups to which I belong, I am also a member (“distinguished,” no less) of a slightly larger group: the American Psychiatric Association, and being part of both groups is meaningful to me in more ways than I can describe.
When I think back over the years, I – like most people – have belonged to many people and places, either officially or unofficially. It is these connections that define us, fill our time, give us meaning and purpose, and anchor us. We belong to our families and friends, but we also belong to our professional and community groups, our institutions – whether they are hospitals, schools, religious centers, country clubs, or charitable organizations – as well as interest and advocacy groups. And finally, we belong to our coworkers and to our patients, and they to us, especially if we see the same people over time. Being a psychiatrist can be a solitary career, and it can take a little effort to be a part of larger worlds, especially for those who find solace in more individual activities.
As I’ve gotten older, I’ve noticed that I belong to fewer of these groups. I’m no longer a little league or field hockey mom, nor a member of the neighborhood babysitting co-op, and I’ve exhausted the gamut of council and leadership positions in my APA district branch. I’ve joined organizations only to pay the membership fee, and then never gone to their meetings or events. The pandemic has accounted for some of this: I still belong to my book club, but I often read the book and don’t go to the Zoom meetings as I miss the real-life aspect of getting together. Being boxed on a screen is not the same as the one-on-one conversations before the formal book discussion. And while I still carry a host of identities, I imagine it is not unusual to belong to fewer organizations as time passes. It’s not all bad, there is something good to be said for living life at a less frenetic pace as fewer entities lay claim to my time.
In psychiatry, our patients span the range of human experience: Some are very engaged with their worlds, while others struggle to make even the most basic of connections. Their lives may seem disconnected – empty, even – and I find myself encouraging people to reach out, to find activities that will ease their loneliness and integrate a feeling of belonging in a way that adds meaning and purpose. For some people, this may be as simple as asking a friend to have lunch, but even that can be an overwhelming obstacle for someone who is depressed, or for someone who has no friends.
Patients may counter my suggestions with a host of reasons as to why they can’t connect. Perhaps their friend is too busy with work or his family, the lunch would cost too much, there’s no transportation, or no restaurant that could meet their dietary needs. Or perhaps they are just too fearful of being rejected.
Psychiatric disorders, by their nature, can be very isolating. Depressed and anxious people often find it a struggle just to get through their days, adding new people and activities is not something that brings joy. For people suffering with psychosis, their internal realities are often all-consuming and there may be no room for accommodating others. And finally, what I hear over and over, is that people are afraid of what others might think of them, and this fear is paralyzing. I try to suggest that we never really know or control what others think of us, but obviously, this does not reassure most patients as they are also bewildered by their irrational fear. To go to an event unaccompanied, or even to a party to which they have been invited, is a hurdle they won’t (or can’t) attempt.
The pandemic, with its initial months of shutdown, and then with years of fear of illness, has created new ways of connecting. Our “Zoom” world can be very convenient – in many ways it has opened up aspects of learning and connection for people who are short on time,or struggle with transportation. In the comfort of our living rooms, in pajamas and slippers, we can take classes, join clubs, attend Alcoholics Anonymous meetings, go to conferences or religious services, and be part of any number of organizations without flying or searching for parking. I love that, with 1 hour and a single click, I can now attend my department’s weekly Grand Rounds. But for many who struggle with using technology, or who don’t feel the same benefits from online encounters, the pandemic has been an isolating and lonely time.
It should not be assumed that isolation has been a negative experience for everyone. For many who struggle with interpersonal relationships, for children who are bullied or teased at school or who feel self-conscious sitting alone at lunch, there may not be the presumed “fear of missing out.” As one adult patient told me: “You know, I do ‘alone’ well.” For some, it has been a relief to be relieved of the pressure to socialize, attend parties, or pursue online dating – a process I think of as “people-shopping” which looks so different from the old days of organic interactions that led to romantic interactions over time. Many have found relief without the pressures of social interactions.
Community, connection, and belonging are not inconsequential things, however. They are part of what adds to life’s richness, and they are associated with good health and longevity. The Harvard Study of Adult Development, begun in 1938, has been tracking two groups of Boston teenagers – and now their wives and children – for 84 years. Tracking one group of Harvard students and another group of teens from poorer areas in Boston, the project is now on its 4th director.
George Vaillant, MD, author of “Aging Well: Surprising Guideposts to a Happier Life from the Landmark Harvard Study of Adult Development” (New York: Little, Brown Spark, 2002) was the program’s director from 1972 to 2004. “When the study began, nobody cared about empathy or attachment. But the key to healthy aging is relationships, relationships, relationships,” Dr. Vaillant said in an interview in the Harvard Gazette.
Susan Pinker is a social psychologist and author of “The Village Effect: How Face-to-Face Contact Can Make Us Healthier and Happier” (Toronto: Random House Canada, 2014). In her 2017 TED talk, she notes that in all developed countries, women live 6-8 years longer than men, and are half as likely to die at any age. She is underwhelmed by digital relationships, and says that real life relationships affect our physiological states differently and in more beneficial ways. “Building your village and sustaining it is a matter of life and death,” she states at the end of her TED talk.
I spoke with Ms. Pinker about her thoughts on how our personal villages change over time. She was quick to tell me that she is not against digital communities. “I’m not a Luddite. As a writer, I probably spend as much time facing a screen as anyone else. But it’s important to remember that digital communities can amplify existing relationships, and don’t replace in-person social contact. A lot of people have drunk the Kool-Aid about virtual experiences, even though they are not the same as real life interactions.
“Loneliness takes on a U-shaped function across adulthood,” she explained with regard to how age impacts our social connections. “People are lonely when they first leave home or when they finish college and go out into the world. Then they settle into new situations; they can make friends at work, through their children, in their neighborhood, or by belonging to organizations. As people settle into their adult lives, there are increased opportunities to connect in person. But loneliness increases again in late middle age.” She explained that everyone loses people as their children move away, friends move, and couples may divorce or a spouse dies.
“Attrition of our social face-to-face networks is an ugly feature of aging,” Ms. Pinker said. “Some people are good at replacing the vacant spots; they sense that it is important to invest in different relationships as you age. It’s like a garden that you need to tend by replacing the perennials that die off in the winter.” The United States, she pointed out, has a culture that is particularly difficult for people in their later years.
My world is a little quieter than it once was, but collecting and holding on to people is important to me. The organizations and affiliations change over time, as does the brand of coffee. So I try to inspire some of my more isolated patients to prioritize their relationships, to let go of their grudges, to tolerate the discomfort of moving from their places of comfort to the temporary discomfort of reaching out in the service of achieving a less solitary, more purposeful, and healthier life. When it doesn’t come naturally, it can be hard work.
Dr. Miller is a coauthor of “Committed: The Battle Over Involuntary Psychiatric Care” (Johns Hopkins University Press, 2016). She has a private practice and is assistant professor of psychiatry and behavioral sciences at Johns Hopkins University, Baltimore. She has disclosed no relevant financial relationships.
You only are free when you realize you belong no place – you belong every place – no place at all. The price is high. The reward is great. ~ Maya Angelou
At 8 o’clock, every weekday morning, for years and years now, two friends appear in my kitchen for coffee, and so one identity I carry includes being part of the “coffee ladies.” While this is one of the smaller and more intimate groups to which I belong, I am also a member (“distinguished,” no less) of a slightly larger group: the American Psychiatric Association, and being part of both groups is meaningful to me in more ways than I can describe.
When I think back over the years, I – like most people – have belonged to many people and places, either officially or unofficially. It is these connections that define us, fill our time, give us meaning and purpose, and anchor us. We belong to our families and friends, but we also belong to our professional and community groups, our institutions – whether they are hospitals, schools, religious centers, country clubs, or charitable organizations – as well as interest and advocacy groups. And finally, we belong to our coworkers and to our patients, and they to us, especially if we see the same people over time. Being a psychiatrist can be a solitary career, and it can take a little effort to be a part of larger worlds, especially for those who find solace in more individual activities.
As I’ve gotten older, I’ve noticed that I belong to fewer of these groups. I’m no longer a little league or field hockey mom, nor a member of the neighborhood babysitting co-op, and I’ve exhausted the gamut of council and leadership positions in my APA district branch. I’ve joined organizations only to pay the membership fee, and then never gone to their meetings or events. The pandemic has accounted for some of this: I still belong to my book club, but I often read the book and don’t go to the Zoom meetings as I miss the real-life aspect of getting together. Being boxed on a screen is not the same as the one-on-one conversations before the formal book discussion. And while I still carry a host of identities, I imagine it is not unusual to belong to fewer organizations as time passes. It’s not all bad, there is something good to be said for living life at a less frenetic pace as fewer entities lay claim to my time.
In psychiatry, our patients span the range of human experience: Some are very engaged with their worlds, while others struggle to make even the most basic of connections. Their lives may seem disconnected – empty, even – and I find myself encouraging people to reach out, to find activities that will ease their loneliness and integrate a feeling of belonging in a way that adds meaning and purpose. For some people, this may be as simple as asking a friend to have lunch, but even that can be an overwhelming obstacle for someone who is depressed, or for someone who has no friends.
Patients may counter my suggestions with a host of reasons as to why they can’t connect. Perhaps their friend is too busy with work or his family, the lunch would cost too much, there’s no transportation, or no restaurant that could meet their dietary needs. Or perhaps they are just too fearful of being rejected.
Psychiatric disorders, by their nature, can be very isolating. Depressed and anxious people often find it a struggle just to get through their days, adding new people and activities is not something that brings joy. For people suffering with psychosis, their internal realities are often all-consuming and there may be no room for accommodating others. And finally, what I hear over and over, is that people are afraid of what others might think of them, and this fear is paralyzing. I try to suggest that we never really know or control what others think of us, but obviously, this does not reassure most patients as they are also bewildered by their irrational fear. To go to an event unaccompanied, or even to a party to which they have been invited, is a hurdle they won’t (or can’t) attempt.
The pandemic, with its initial months of shutdown, and then with years of fear of illness, has created new ways of connecting. Our “Zoom” world can be very convenient – in many ways it has opened up aspects of learning and connection for people who are short on time,or struggle with transportation. In the comfort of our living rooms, in pajamas and slippers, we can take classes, join clubs, attend Alcoholics Anonymous meetings, go to conferences or religious services, and be part of any number of organizations without flying or searching for parking. I love that, with 1 hour and a single click, I can now attend my department’s weekly Grand Rounds. But for many who struggle with using technology, or who don’t feel the same benefits from online encounters, the pandemic has been an isolating and lonely time.
It should not be assumed that isolation has been a negative experience for everyone. For many who struggle with interpersonal relationships, for children who are bullied or teased at school or who feel self-conscious sitting alone at lunch, there may not be the presumed “fear of missing out.” As one adult patient told me: “You know, I do ‘alone’ well.” For some, it has been a relief to be relieved of the pressure to socialize, attend parties, or pursue online dating – a process I think of as “people-shopping” which looks so different from the old days of organic interactions that led to romantic interactions over time. Many have found relief without the pressures of social interactions.
Community, connection, and belonging are not inconsequential things, however. They are part of what adds to life’s richness, and they are associated with good health and longevity. The Harvard Study of Adult Development, begun in 1938, has been tracking two groups of Boston teenagers – and now their wives and children – for 84 years. Tracking one group of Harvard students and another group of teens from poorer areas in Boston, the project is now on its 4th director.
George Vaillant, MD, author of “Aging Well: Surprising Guideposts to a Happier Life from the Landmark Harvard Study of Adult Development” (New York: Little, Brown Spark, 2002) was the program’s director from 1972 to 2004. “When the study began, nobody cared about empathy or attachment. But the key to healthy aging is relationships, relationships, relationships,” Dr. Vaillant said in an interview in the Harvard Gazette.
Susan Pinker is a social psychologist and author of “The Village Effect: How Face-to-Face Contact Can Make Us Healthier and Happier” (Toronto: Random House Canada, 2014). In her 2017 TED talk, she notes that in all developed countries, women live 6-8 years longer than men, and are half as likely to die at any age. She is underwhelmed by digital relationships, and says that real life relationships affect our physiological states differently and in more beneficial ways. “Building your village and sustaining it is a matter of life and death,” she states at the end of her TED talk.
I spoke with Ms. Pinker about her thoughts on how our personal villages change over time. She was quick to tell me that she is not against digital communities. “I’m not a Luddite. As a writer, I probably spend as much time facing a screen as anyone else. But it’s important to remember that digital communities can amplify existing relationships, and don’t replace in-person social contact. A lot of people have drunk the Kool-Aid about virtual experiences, even though they are not the same as real life interactions.
“Loneliness takes on a U-shaped function across adulthood,” she explained with regard to how age impacts our social connections. “People are lonely when they first leave home or when they finish college and go out into the world. Then they settle into new situations; they can make friends at work, through their children, in their neighborhood, or by belonging to organizations. As people settle into their adult lives, there are increased opportunities to connect in person. But loneliness increases again in late middle age.” She explained that everyone loses people as their children move away, friends move, and couples may divorce or a spouse dies.
“Attrition of our social face-to-face networks is an ugly feature of aging,” Ms. Pinker said. “Some people are good at replacing the vacant spots; they sense that it is important to invest in different relationships as you age. It’s like a garden that you need to tend by replacing the perennials that die off in the winter.” The United States, she pointed out, has a culture that is particularly difficult for people in their later years.
My world is a little quieter than it once was, but collecting and holding on to people is important to me. The organizations and affiliations change over time, as does the brand of coffee. So I try to inspire some of my more isolated patients to prioritize their relationships, to let go of their grudges, to tolerate the discomfort of moving from their places of comfort to the temporary discomfort of reaching out in the service of achieving a less solitary, more purposeful, and healthier life. When it doesn’t come naturally, it can be hard work.
Dr. Miller is a coauthor of “Committed: The Battle Over Involuntary Psychiatric Care” (Johns Hopkins University Press, 2016). She has a private practice and is assistant professor of psychiatry and behavioral sciences at Johns Hopkins University, Baltimore. She has disclosed no relevant financial relationships.
A plane crash interrupts a doctor’s vacation
Emergencies happen anywhere, anytime – and sometimes physicians find themselves in situations where they are the only ones who can help. “Is There a Doctor in the House?” is a new series telling these stories.
When the plane crashed, I was asleep. I had arrived the evening before with my wife and three sons at a house on Kezar Lake on the Maine–New Hampshire border. I jumped out of bed and ran downstairs. My kids had been watching a float plane circling and gliding along the lake. It had crashed into the water and flipped upside down. My oldest brother-in-law jumped into his ski boat and we sped out to the scene.
All we can see are the plane’s pontoons. The rest is underwater. A woman has already surfaced, screaming. I dive in.
I find the woman’s husband and 3-year-old son struggling to get free from the plane through the smashed windshield. They manage to get to the surface. The pilot is dead, impaled through the chest by the left wing strut.
The big problem: A little girl, whom I would learn later is named Lauren, remained trapped. The water is murky but I can see her, a 5- or 6-year-old girl with this long hair, strapped in upside down and unconscious.
The mom and I dive down over and over, pulling and ripping at the door. We cannot get it open. Finally, I’m able to bend the door open enough where I can reach in, but I can’t undo the seatbelt. In my mind, I’m debating, should I try and go through the front windshield? I’m getting really tired, I can tell there’s fuel in the water, and I don’t want to drown in the plane. So I pop up to the surface and yell, “Does anyone have a knife?”
My brother-in-law shoots back to shore in the boat, screaming, “Get a knife!” My niece gets in the boat with one. I’m standing on the pontoon, and my niece is in the front of the boat calling, “Uncle Todd! Uncle Todd!” and she throws the knife. It goes way over my head. I can’t even jump for it, it’s so high.
I have to get the knife. So, I dive into the water to try and find it. Somehow, the black knife has landed on the white wing, 4 or 5 feet under the water. Pure luck. It could have sunk down a hundred feet into the lake. I grab the knife and hand it to the mom, Beth. She’s able to cut the seatbelt, and we both pull Lauren to the surface.
I lay her out on the pontoon. She has no pulse and her pupils are fixed and dilated. Her mom is yelling, “She’s dead, isn’t she?” I start CPR. My skin and eyes are burning from the airplane fuel in the water. I get her breathing, and her heart comes back very quickly. Lauren starts to vomit and I’m trying to keep her airway clear. She’s breathing spontaneously and she has a pulse, so I decide it’s time to move her to shore.
We pull the boat up to the dock and Lauren’s now having anoxic seizures. Her brain has been without oxygen, and now she’s getting perfused again. We get her to shore and lay her on the lawn. I’m still doing mouth-to-mouth, but she’s seizing like crazy, and I don’t have any way to control that. Beth is crying and wants to hold her daughter gently while I’m working.
Someone had called 911, and finally this dude shows up with an ambulance, and it’s like something out of World War II. All he has is an oxygen tank, but the mask is old and cracked. It’s too big for Lauren, but it sort of fits me, so I’m sucking in oxygen and blowing it into the girl’s mouth. I’m doing whatever I can, but I don’t have an IV to start. I have no fluids. I got nothing.
As it happens, I’d done my emergency medicine training at Maine Medical Center, so I tell someone to call them and get a Life Flight chopper. We have to drive somewhere where the chopper can land, so we take the ambulance to the parking lot of the closest store called the Wicked Good Store. That’s a common thing in Maine. Everything is “wicked good.”
The whole town is there by that point. The chopper arrives. The ambulance doors pop open and a woman says, “Todd?” And I say, “Heather?”
Heather is an emergency flight nurse whom I’d trained with many years ago. There’s immediate trust. She has all the right equipment. We put in breathing tubes and IVs. We stop Lauren from seizing. The kid is soon stable.
There is only one extra seat in the chopper, so I tell Beth to go. They take off.
Suddenly, I begin to doubt my decision. Lauren had been underwater for 15 minutes at minimum. I know how long that is. Did I do the right thing? Did I resuscitate a brain-dead child? I didn’t think about it at the time, but if that patient had come to me in the emergency department, I’m honestly not sure what I would have done.
So, I go home. And I don’t get a call. The FAA and sheriff arrive to take statements from us. I don’t hear from anyone.
The next day I start calling. No one will tell me anything, so I finally get to one of the pediatric ICU attendings who had trained me. He says Lauren literally woke up and said, “I have to go pee.” And that was it. She was 100% normal. I couldn’t believe it.
Here’s a theory: In kids, there’s something called the glottic reflex. I think her glottic reflex went off as soon as she hit the water, which basically closed her airway. So when she passed out, she could never get enough water in her lungs and still had enough air in there to keep her alive. Later, I got a call from her uncle. He could barely get the words out because he was in tears. He said Lauren was doing beautifully.
Three days later, I drove to Lauren’s house with my wife and kids. I had her read to me. I watched her play on the jungle gym for motor function. All sorts of stuff. She was totally normal.
Beth told us that the night before the accident, her mother had given the women in her family what she called a “miracle bracelet,” a bracelet that is supposed to give you one miracle in your life. Beth said she had the bracelet on her wrist the day of the accident, and now it’s gone. “Saving Lauren’s life was my miracle,” she said.
Funny thing: For 20 years, I ran all the EMS, police, fire, ambulance, in Boulder, Colo., where I live. I wrote all the protocols, and I would never advise any of my paramedics to dive into jet fuel to save someone. That was risky. But at the time, it was totally automatic. I think it taught me not to give up in certain situations, because you really don’t know.
Dr. Dorfman is an emergency medicine physician in Boulder, Colo., and medical director at Cedalion Health.
A version of this article first appeared on Medscape.com.
Emergencies happen anywhere, anytime – and sometimes physicians find themselves in situations where they are the only ones who can help. “Is There a Doctor in the House?” is a new series telling these stories.
When the plane crashed, I was asleep. I had arrived the evening before with my wife and three sons at a house on Kezar Lake on the Maine–New Hampshire border. I jumped out of bed and ran downstairs. My kids had been watching a float plane circling and gliding along the lake. It had crashed into the water and flipped upside down. My oldest brother-in-law jumped into his ski boat and we sped out to the scene.
All we can see are the plane’s pontoons. The rest is underwater. A woman has already surfaced, screaming. I dive in.
I find the woman’s husband and 3-year-old son struggling to get free from the plane through the smashed windshield. They manage to get to the surface. The pilot is dead, impaled through the chest by the left wing strut.
The big problem: A little girl, whom I would learn later is named Lauren, remained trapped. The water is murky but I can see her, a 5- or 6-year-old girl with this long hair, strapped in upside down and unconscious.
The mom and I dive down over and over, pulling and ripping at the door. We cannot get it open. Finally, I’m able to bend the door open enough where I can reach in, but I can’t undo the seatbelt. In my mind, I’m debating, should I try and go through the front windshield? I’m getting really tired, I can tell there’s fuel in the water, and I don’t want to drown in the plane. So I pop up to the surface and yell, “Does anyone have a knife?”
My brother-in-law shoots back to shore in the boat, screaming, “Get a knife!” My niece gets in the boat with one. I’m standing on the pontoon, and my niece is in the front of the boat calling, “Uncle Todd! Uncle Todd!” and she throws the knife. It goes way over my head. I can’t even jump for it, it’s so high.
I have to get the knife. So, I dive into the water to try and find it. Somehow, the black knife has landed on the white wing, 4 or 5 feet under the water. Pure luck. It could have sunk down a hundred feet into the lake. I grab the knife and hand it to the mom, Beth. She’s able to cut the seatbelt, and we both pull Lauren to the surface.
I lay her out on the pontoon. She has no pulse and her pupils are fixed and dilated. Her mom is yelling, “She’s dead, isn’t she?” I start CPR. My skin and eyes are burning from the airplane fuel in the water. I get her breathing, and her heart comes back very quickly. Lauren starts to vomit and I’m trying to keep her airway clear. She’s breathing spontaneously and she has a pulse, so I decide it’s time to move her to shore.
We pull the boat up to the dock and Lauren’s now having anoxic seizures. Her brain has been without oxygen, and now she’s getting perfused again. We get her to shore and lay her on the lawn. I’m still doing mouth-to-mouth, but she’s seizing like crazy, and I don’t have any way to control that. Beth is crying and wants to hold her daughter gently while I’m working.
Someone had called 911, and finally this dude shows up with an ambulance, and it’s like something out of World War II. All he has is an oxygen tank, but the mask is old and cracked. It’s too big for Lauren, but it sort of fits me, so I’m sucking in oxygen and blowing it into the girl’s mouth. I’m doing whatever I can, but I don’t have an IV to start. I have no fluids. I got nothing.
As it happens, I’d done my emergency medicine training at Maine Medical Center, so I tell someone to call them and get a Life Flight chopper. We have to drive somewhere where the chopper can land, so we take the ambulance to the parking lot of the closest store called the Wicked Good Store. That’s a common thing in Maine. Everything is “wicked good.”
The whole town is there by that point. The chopper arrives. The ambulance doors pop open and a woman says, “Todd?” And I say, “Heather?”
Heather is an emergency flight nurse whom I’d trained with many years ago. There’s immediate trust. She has all the right equipment. We put in breathing tubes and IVs. We stop Lauren from seizing. The kid is soon stable.
There is only one extra seat in the chopper, so I tell Beth to go. They take off.
Suddenly, I begin to doubt my decision. Lauren had been underwater for 15 minutes at minimum. I know how long that is. Did I do the right thing? Did I resuscitate a brain-dead child? I didn’t think about it at the time, but if that patient had come to me in the emergency department, I’m honestly not sure what I would have done.
So, I go home. And I don’t get a call. The FAA and sheriff arrive to take statements from us. I don’t hear from anyone.
The next day I start calling. No one will tell me anything, so I finally get to one of the pediatric ICU attendings who had trained me. He says Lauren literally woke up and said, “I have to go pee.” And that was it. She was 100% normal. I couldn’t believe it.
Here’s a theory: In kids, there’s something called the glottic reflex. I think her glottic reflex went off as soon as she hit the water, which basically closed her airway. So when she passed out, she could never get enough water in her lungs and still had enough air in there to keep her alive. Later, I got a call from her uncle. He could barely get the words out because he was in tears. He said Lauren was doing beautifully.
Three days later, I drove to Lauren’s house with my wife and kids. I had her read to me. I watched her play on the jungle gym for motor function. All sorts of stuff. She was totally normal.
Beth told us that the night before the accident, her mother had given the women in her family what she called a “miracle bracelet,” a bracelet that is supposed to give you one miracle in your life. Beth said she had the bracelet on her wrist the day of the accident, and now it’s gone. “Saving Lauren’s life was my miracle,” she said.
Funny thing: For 20 years, I ran all the EMS, police, fire, ambulance, in Boulder, Colo., where I live. I wrote all the protocols, and I would never advise any of my paramedics to dive into jet fuel to save someone. That was risky. But at the time, it was totally automatic. I think it taught me not to give up in certain situations, because you really don’t know.
Dr. Dorfman is an emergency medicine physician in Boulder, Colo., and medical director at Cedalion Health.
A version of this article first appeared on Medscape.com.
Emergencies happen anywhere, anytime – and sometimes physicians find themselves in situations where they are the only ones who can help. “Is There a Doctor in the House?” is a new series telling these stories.
When the plane crashed, I was asleep. I had arrived the evening before with my wife and three sons at a house on Kezar Lake on the Maine–New Hampshire border. I jumped out of bed and ran downstairs. My kids had been watching a float plane circling and gliding along the lake. It had crashed into the water and flipped upside down. My oldest brother-in-law jumped into his ski boat and we sped out to the scene.
All we can see are the plane’s pontoons. The rest is underwater. A woman has already surfaced, screaming. I dive in.
I find the woman’s husband and 3-year-old son struggling to get free from the plane through the smashed windshield. They manage to get to the surface. The pilot is dead, impaled through the chest by the left wing strut.
The big problem: A little girl, whom I would learn later is named Lauren, remained trapped. The water is murky but I can see her, a 5- or 6-year-old girl with this long hair, strapped in upside down and unconscious.
The mom and I dive down over and over, pulling and ripping at the door. We cannot get it open. Finally, I’m able to bend the door open enough where I can reach in, but I can’t undo the seatbelt. In my mind, I’m debating, should I try and go through the front windshield? I’m getting really tired, I can tell there’s fuel in the water, and I don’t want to drown in the plane. So I pop up to the surface and yell, “Does anyone have a knife?”
My brother-in-law shoots back to shore in the boat, screaming, “Get a knife!” My niece gets in the boat with one. I’m standing on the pontoon, and my niece is in the front of the boat calling, “Uncle Todd! Uncle Todd!” and she throws the knife. It goes way over my head. I can’t even jump for it, it’s so high.
I have to get the knife. So, I dive into the water to try and find it. Somehow, the black knife has landed on the white wing, 4 or 5 feet under the water. Pure luck. It could have sunk down a hundred feet into the lake. I grab the knife and hand it to the mom, Beth. She’s able to cut the seatbelt, and we both pull Lauren to the surface.
I lay her out on the pontoon. She has no pulse and her pupils are fixed and dilated. Her mom is yelling, “She’s dead, isn’t she?” I start CPR. My skin and eyes are burning from the airplane fuel in the water. I get her breathing, and her heart comes back very quickly. Lauren starts to vomit and I’m trying to keep her airway clear. She’s breathing spontaneously and she has a pulse, so I decide it’s time to move her to shore.
We pull the boat up to the dock and Lauren’s now having anoxic seizures. Her brain has been without oxygen, and now she’s getting perfused again. We get her to shore and lay her on the lawn. I’m still doing mouth-to-mouth, but she’s seizing like crazy, and I don’t have any way to control that. Beth is crying and wants to hold her daughter gently while I’m working.
Someone had called 911, and finally this dude shows up with an ambulance, and it’s like something out of World War II. All he has is an oxygen tank, but the mask is old and cracked. It’s too big for Lauren, but it sort of fits me, so I’m sucking in oxygen and blowing it into the girl’s mouth. I’m doing whatever I can, but I don’t have an IV to start. I have no fluids. I got nothing.
As it happens, I’d done my emergency medicine training at Maine Medical Center, so I tell someone to call them and get a Life Flight chopper. We have to drive somewhere where the chopper can land, so we take the ambulance to the parking lot of the closest store called the Wicked Good Store. That’s a common thing in Maine. Everything is “wicked good.”
The whole town is there by that point. The chopper arrives. The ambulance doors pop open and a woman says, “Todd?” And I say, “Heather?”
Heather is an emergency flight nurse whom I’d trained with many years ago. There’s immediate trust. She has all the right equipment. We put in breathing tubes and IVs. We stop Lauren from seizing. The kid is soon stable.
There is only one extra seat in the chopper, so I tell Beth to go. They take off.
Suddenly, I begin to doubt my decision. Lauren had been underwater for 15 minutes at minimum. I know how long that is. Did I do the right thing? Did I resuscitate a brain-dead child? I didn’t think about it at the time, but if that patient had come to me in the emergency department, I’m honestly not sure what I would have done.
So, I go home. And I don’t get a call. The FAA and sheriff arrive to take statements from us. I don’t hear from anyone.
The next day I start calling. No one will tell me anything, so I finally get to one of the pediatric ICU attendings who had trained me. He says Lauren literally woke up and said, “I have to go pee.” And that was it. She was 100% normal. I couldn’t believe it.
Here’s a theory: In kids, there’s something called the glottic reflex. I think her glottic reflex went off as soon as she hit the water, which basically closed her airway. So when she passed out, she could never get enough water in her lungs and still had enough air in there to keep her alive. Later, I got a call from her uncle. He could barely get the words out because he was in tears. He said Lauren was doing beautifully.
Three days later, I drove to Lauren’s house with my wife and kids. I had her read to me. I watched her play on the jungle gym for motor function. All sorts of stuff. She was totally normal.
Beth told us that the night before the accident, her mother had given the women in her family what she called a “miracle bracelet,” a bracelet that is supposed to give you one miracle in your life. Beth said she had the bracelet on her wrist the day of the accident, and now it’s gone. “Saving Lauren’s life was my miracle,” she said.
Funny thing: For 20 years, I ran all the EMS, police, fire, ambulance, in Boulder, Colo., where I live. I wrote all the protocols, and I would never advise any of my paramedics to dive into jet fuel to save someone. That was risky. But at the time, it was totally automatic. I think it taught me not to give up in certain situations, because you really don’t know.
Dr. Dorfman is an emergency medicine physician in Boulder, Colo., and medical director at Cedalion Health.
A version of this article first appeared on Medscape.com.
Sick call
They call me and I go.
– William Carlos Williams
I never get sick. I’ve never had the flu. When everyone’s got a cold, I’m somehow immune. The last time I threw up was June 29th, 1980. You see, I work out almost daily, eat vegan, and sleep plenty. I drink gallons of pressed juice and throw down a few high-quality supplements. Yes, I’m that guy: The one who never gets sick. Well, I was anyway.
I am no longer that guy since our little girl became a supersocial little toddler. My undefeated welterweight “never-sick” title has been obliterated by multiple knockouts. One was a wicked adenovirus that broke the no-vomit streak. At one point, I lay on the luxury gray tile bathroom floor hoping to go unconscious to make the nausea stop. I actually called out sick that day. Then with a nasty COVID-despite-vaccine infection. I called out again. Later with a hacking lower respiratory – RSV?! – bug. Called out. All of which our 2-year-old blonde, curly-haired vector transmitted to me with remarkable efficiency.
In fact, That’s saying a lot. Our docs, like most, don’t call out sick.
We physicians have legendary stamina. Compared with other professionals, we are no less likely to become ill but a whopping 80% less likely to call out sick.
Presenteeism is our physician version of Omerta, a code of honor to never give in even at the expense of our, or our family’s, health and well-being. Every medical student is regaled with stories of physicians getting an IV before rounds or finishing clinic after their water broke. Why? In part it’s an indoctrination into this thing of ours we call Medicine: An elitist club that admits only those able to pass O-chem and hold diarrhea. But it is also because our medical system is so brittle that the slightest bend causes it to shatter. When I cancel a clinic, patients who have waited weeks for their spot have to be sent home. And for critical cases or those patients who don’t get the message, my already slammed colleagues have to cram the unlucky ones in between already-scheduled appointments. The guilt induced by inconveniencing our colleagues and our patients is more potent than dry heaves. And so we go. Suck it up. Sip ginger ale. Load up on acetaminophen. Carry on. This harms not only us, but also patients whom we put in the path of transmission. We become terrible 2-year-olds.
Of course, it’s not always easy to tell if you’re sick enough to stay home. But the stigma of calling out is so great that we often show up no matter what symptoms. A recent Medscape survey of physicians found that 85% said they had come to work sick in 2022.
We can do better. Perhaps creating sick-leave protocols could help? For example, if you have a fever above 100.4, have contact with someone positive for influenza, are unable to take POs, etc. then stay home. So might building rolling slack into schedules to accommodate the inevitable physician illness, parenting emergency, or death of an beloved uncle. And if there is one thing artificial intelligence could help us with, it would be smart scheduling. Can’t we build algorithms for anticipating and absorbing these predictable events? I’d take that over an AI skin cancer detector any day. Yet this year we’ll struggle through the cold and flu (and COVID) season again and nothing will have changed.
Our daughter hasn’t had hand, foot, and mouth disease yet. It’s not a question of if, but rather when she, and her mom and I, will get it. I hope it happens on a Friday so that my Monday clinic will be bearable when I show up.
Dr. Benabio is director of Healthcare Transformation and chief of dermatology at Kaiser Permanente San Diego. The opinions expressed in this column are his own and do not represent those of Kaiser Permanente. Dr. Benabio is @Dermdoc on Twitter. Write to him at [email protected]
They call me and I go.
– William Carlos Williams
I never get sick. I’ve never had the flu. When everyone’s got a cold, I’m somehow immune. The last time I threw up was June 29th, 1980. You see, I work out almost daily, eat vegan, and sleep plenty. I drink gallons of pressed juice and throw down a few high-quality supplements. Yes, I’m that guy: The one who never gets sick. Well, I was anyway.
I am no longer that guy since our little girl became a supersocial little toddler. My undefeated welterweight “never-sick” title has been obliterated by multiple knockouts. One was a wicked adenovirus that broke the no-vomit streak. At one point, I lay on the luxury gray tile bathroom floor hoping to go unconscious to make the nausea stop. I actually called out sick that day. Then with a nasty COVID-despite-vaccine infection. I called out again. Later with a hacking lower respiratory – RSV?! – bug. Called out. All of which our 2-year-old blonde, curly-haired vector transmitted to me with remarkable efficiency.
In fact, That’s saying a lot. Our docs, like most, don’t call out sick.
We physicians have legendary stamina. Compared with other professionals, we are no less likely to become ill but a whopping 80% less likely to call out sick.
Presenteeism is our physician version of Omerta, a code of honor to never give in even at the expense of our, or our family’s, health and well-being. Every medical student is regaled with stories of physicians getting an IV before rounds or finishing clinic after their water broke. Why? In part it’s an indoctrination into this thing of ours we call Medicine: An elitist club that admits only those able to pass O-chem and hold diarrhea. But it is also because our medical system is so brittle that the slightest bend causes it to shatter. When I cancel a clinic, patients who have waited weeks for their spot have to be sent home. And for critical cases or those patients who don’t get the message, my already slammed colleagues have to cram the unlucky ones in between already-scheduled appointments. The guilt induced by inconveniencing our colleagues and our patients is more potent than dry heaves. And so we go. Suck it up. Sip ginger ale. Load up on acetaminophen. Carry on. This harms not only us, but also patients whom we put in the path of transmission. We become terrible 2-year-olds.
Of course, it’s not always easy to tell if you’re sick enough to stay home. But the stigma of calling out is so great that we often show up no matter what symptoms. A recent Medscape survey of physicians found that 85% said they had come to work sick in 2022.
We can do better. Perhaps creating sick-leave protocols could help? For example, if you have a fever above 100.4, have contact with someone positive for influenza, are unable to take POs, etc. then stay home. So might building rolling slack into schedules to accommodate the inevitable physician illness, parenting emergency, or death of an beloved uncle. And if there is one thing artificial intelligence could help us with, it would be smart scheduling. Can’t we build algorithms for anticipating and absorbing these predictable events? I’d take that over an AI skin cancer detector any day. Yet this year we’ll struggle through the cold and flu (and COVID) season again and nothing will have changed.
Our daughter hasn’t had hand, foot, and mouth disease yet. It’s not a question of if, but rather when she, and her mom and I, will get it. I hope it happens on a Friday so that my Monday clinic will be bearable when I show up.
Dr. Benabio is director of Healthcare Transformation and chief of dermatology at Kaiser Permanente San Diego. The opinions expressed in this column are his own and do not represent those of Kaiser Permanente. Dr. Benabio is @Dermdoc on Twitter. Write to him at [email protected]
They call me and I go.
– William Carlos Williams
I never get sick. I’ve never had the flu. When everyone’s got a cold, I’m somehow immune. The last time I threw up was June 29th, 1980. You see, I work out almost daily, eat vegan, and sleep plenty. I drink gallons of pressed juice and throw down a few high-quality supplements. Yes, I’m that guy: The one who never gets sick. Well, I was anyway.
I am no longer that guy since our little girl became a supersocial little toddler. My undefeated welterweight “never-sick” title has been obliterated by multiple knockouts. One was a wicked adenovirus that broke the no-vomit streak. At one point, I lay on the luxury gray tile bathroom floor hoping to go unconscious to make the nausea stop. I actually called out sick that day. Then with a nasty COVID-despite-vaccine infection. I called out again. Later with a hacking lower respiratory – RSV?! – bug. Called out. All of which our 2-year-old blonde, curly-haired vector transmitted to me with remarkable efficiency.
In fact, That’s saying a lot. Our docs, like most, don’t call out sick.
We physicians have legendary stamina. Compared with other professionals, we are no less likely to become ill but a whopping 80% less likely to call out sick.
Presenteeism is our physician version of Omerta, a code of honor to never give in even at the expense of our, or our family’s, health and well-being. Every medical student is regaled with stories of physicians getting an IV before rounds or finishing clinic after their water broke. Why? In part it’s an indoctrination into this thing of ours we call Medicine: An elitist club that admits only those able to pass O-chem and hold diarrhea. But it is also because our medical system is so brittle that the slightest bend causes it to shatter. When I cancel a clinic, patients who have waited weeks for their spot have to be sent home. And for critical cases or those patients who don’t get the message, my already slammed colleagues have to cram the unlucky ones in between already-scheduled appointments. The guilt induced by inconveniencing our colleagues and our patients is more potent than dry heaves. And so we go. Suck it up. Sip ginger ale. Load up on acetaminophen. Carry on. This harms not only us, but also patients whom we put in the path of transmission. We become terrible 2-year-olds.
Of course, it’s not always easy to tell if you’re sick enough to stay home. But the stigma of calling out is so great that we often show up no matter what symptoms. A recent Medscape survey of physicians found that 85% said they had come to work sick in 2022.
We can do better. Perhaps creating sick-leave protocols could help? For example, if you have a fever above 100.4, have contact with someone positive for influenza, are unable to take POs, etc. then stay home. So might building rolling slack into schedules to accommodate the inevitable physician illness, parenting emergency, or death of an beloved uncle. And if there is one thing artificial intelligence could help us with, it would be smart scheduling. Can’t we build algorithms for anticipating and absorbing these predictable events? I’d take that over an AI skin cancer detector any day. Yet this year we’ll struggle through the cold and flu (and COVID) season again and nothing will have changed.
Our daughter hasn’t had hand, foot, and mouth disease yet. It’s not a question of if, but rather when she, and her mom and I, will get it. I hope it happens on a Friday so that my Monday clinic will be bearable when I show up.
Dr. Benabio is director of Healthcare Transformation and chief of dermatology at Kaiser Permanente San Diego. The opinions expressed in this column are his own and do not represent those of Kaiser Permanente. Dr. Benabio is @Dermdoc on Twitter. Write to him at [email protected]
Keeping up with the evidence (and the residents)
I work with medical students nearly every day that I see patients. I recently mentioned to a student that I have a limited working knowledge of the brand names of diabetes medications released in the past 10 years. Just like the M3s, I need the full generic name to know whether a medication is a GLP-1 inhibitor or a DPP-4 inhibitor, because I know that “flozins” are SGLT-2 inhibitors and “glutides” are GLP-1 agonists. The combined efforts of an ambulatory care pharmacist and some flashcards have helped me to better understand how they work and which ones to prescribe when. Meanwhile, the residents are capably counseling on the adverse effects of the latest diabetes agent, while I am googling its generic name.
The premise of science is continuous discovery. In the first 10 months of 2022, the US Food & Drug Administration approved more than 2 dozen new medications, almost 100 new generics, and new indications for dozens more.1,2 The US Preventive Services Task Force (USPSTF) issued 13 new or reaffirmed recommendations in the first 10 months of 2022, and it is just one of dozens of bodies that issue guidelines relevant to primary care.3 PubMed indexes more than a million new articles each year. Learning new information and changing practice are crucial to being an effective clinician.
In this edition of JFP, Covey and Cagle4 write about updates to the USPSTF’s lung cancer screening guidelines. The authors reference changing evidence that led to the revised recommendations. When the original guideline was released in 2013, it drew on the best available evidence at the time.5 The National Lung Screening Trial, which looked at CT scanning compared with chest x-rays as screening tests for lung cancer, was groundbreaking in its methods and results.6 However, it was not without its flaws. It enrolled < 5% Black patients, and so the recommendations for age cutoffs and pack-year cutoffs were made based on the majority White population from the trial.
Black patients experience a higher mortality from lung cancer and are diagnosed at an earlier age and a lower cumulative pack-year exposure than White patients.7 Other studies have explored the social and political factors that lead to these disparities, which range from access to care to racial segregation of neighborhoods and tobacco marketing practices.7 When the USPSTF performed its periodic update of the guideline, it had access to additional research. The updates reflect the new information.
Every physician has a responsibility to find a way to adapt to important new information in medicine. Not using SGLT-2 inhibitors in the management of diabetes would be substandard care, and my patients would suffer for it. Not adopting the new lung cancer screening recommendations would exclude patients most at risk of lung cancer and allow disparities in lung cancer morbidity and mortality to grow.7,8Understanding the evidence behind the recommendations also reminds me that the guidelines will change again. These recommendations are no more static than the first guidelines were. I’ll be ready when the next update comes, and I’ll have the medical students and residents to keep me sharp.
1. US Food & Drug Administration. Novel drug approvals for 2022. Accessed October 27. 2022. www.fda.gov/drugs/new-drugs-fda-cders-new-molecular-entities-and-new-therapeutic-biological-products/novel-drug-approvals-2022
2. US Food & Drug Administration. First generic drug approvals. Accessed October 27. 2022. www.fda.gov/drugs/drug-and-biologic-approval-and-ind-activity-reports/first-generic-drug-approvals
3. US Preventive Services Task Force. Recommendations. Accessed October 27, 2022. www.uspreventiveservicestaskforce.org/uspstf/topic_search_results?topic_status=P
4. Covey CL, Cagle SD. Lung cancer screening: New evidence, updated guidance. J Fam Pract. 2022;71:398-402;415.
5. US Preventive Services Task Force. Lung cancer: screening. December 31, 2013. Accessed October 27, 2022. www.uspreventiveservicestaskforce.org/uspstf/recommendation/lung-cancer-screening-december-2013
6. National Lung Screening Trial Research Team. Reduced lung-cancer mortality with low-dose computed tomographic screening. N Engl J Med. 2011;365:395-409. doi: 10.1056/NEJMoa1102873
7. Pinheiro LC, Groner L, Soroka O, et al. Analysis of eligibility for lung cancer screening by race after 2021 changes to US Preventive Services Task Force screening guidelines. JAMA network open. 2022;5:e2229741. doi: 10.1001/jamanetworkopen.2022.29741
8. US Preventive Services Task Force. Screening for lung cancer: US Preventive Services Task Force Recommendation Statement. JAMA. 2021;325:962-970. doi: 10.1001/jama.2021.1117
I work with medical students nearly every day that I see patients. I recently mentioned to a student that I have a limited working knowledge of the brand names of diabetes medications released in the past 10 years. Just like the M3s, I need the full generic name to know whether a medication is a GLP-1 inhibitor or a DPP-4 inhibitor, because I know that “flozins” are SGLT-2 inhibitors and “glutides” are GLP-1 agonists. The combined efforts of an ambulatory care pharmacist and some flashcards have helped me to better understand how they work and which ones to prescribe when. Meanwhile, the residents are capably counseling on the adverse effects of the latest diabetes agent, while I am googling its generic name.
The premise of science is continuous discovery. In the first 10 months of 2022, the US Food & Drug Administration approved more than 2 dozen new medications, almost 100 new generics, and new indications for dozens more.1,2 The US Preventive Services Task Force (USPSTF) issued 13 new or reaffirmed recommendations in the first 10 months of 2022, and it is just one of dozens of bodies that issue guidelines relevant to primary care.3 PubMed indexes more than a million new articles each year. Learning new information and changing practice are crucial to being an effective clinician.
In this edition of JFP, Covey and Cagle4 write about updates to the USPSTF’s lung cancer screening guidelines. The authors reference changing evidence that led to the revised recommendations. When the original guideline was released in 2013, it drew on the best available evidence at the time.5 The National Lung Screening Trial, which looked at CT scanning compared with chest x-rays as screening tests for lung cancer, was groundbreaking in its methods and results.6 However, it was not without its flaws. It enrolled < 5% Black patients, and so the recommendations for age cutoffs and pack-year cutoffs were made based on the majority White population from the trial.
Black patients experience a higher mortality from lung cancer and are diagnosed at an earlier age and a lower cumulative pack-year exposure than White patients.7 Other studies have explored the social and political factors that lead to these disparities, which range from access to care to racial segregation of neighborhoods and tobacco marketing practices.7 When the USPSTF performed its periodic update of the guideline, it had access to additional research. The updates reflect the new information.
Every physician has a responsibility to find a way to adapt to important new information in medicine. Not using SGLT-2 inhibitors in the management of diabetes would be substandard care, and my patients would suffer for it. Not adopting the new lung cancer screening recommendations would exclude patients most at risk of lung cancer and allow disparities in lung cancer morbidity and mortality to grow.7,8Understanding the evidence behind the recommendations also reminds me that the guidelines will change again. These recommendations are no more static than the first guidelines were. I’ll be ready when the next update comes, and I’ll have the medical students and residents to keep me sharp.
I work with medical students nearly every day that I see patients. I recently mentioned to a student that I have a limited working knowledge of the brand names of diabetes medications released in the past 10 years. Just like the M3s, I need the full generic name to know whether a medication is a GLP-1 inhibitor or a DPP-4 inhibitor, because I know that “flozins” are SGLT-2 inhibitors and “glutides” are GLP-1 agonists. The combined efforts of an ambulatory care pharmacist and some flashcards have helped me to better understand how they work and which ones to prescribe when. Meanwhile, the residents are capably counseling on the adverse effects of the latest diabetes agent, while I am googling its generic name.
The premise of science is continuous discovery. In the first 10 months of 2022, the US Food & Drug Administration approved more than 2 dozen new medications, almost 100 new generics, and new indications for dozens more.1,2 The US Preventive Services Task Force (USPSTF) issued 13 new or reaffirmed recommendations in the first 10 months of 2022, and it is just one of dozens of bodies that issue guidelines relevant to primary care.3 PubMed indexes more than a million new articles each year. Learning new information and changing practice are crucial to being an effective clinician.
In this edition of JFP, Covey and Cagle4 write about updates to the USPSTF’s lung cancer screening guidelines. The authors reference changing evidence that led to the revised recommendations. When the original guideline was released in 2013, it drew on the best available evidence at the time.5 The National Lung Screening Trial, which looked at CT scanning compared with chest x-rays as screening tests for lung cancer, was groundbreaking in its methods and results.6 However, it was not without its flaws. It enrolled < 5% Black patients, and so the recommendations for age cutoffs and pack-year cutoffs were made based on the majority White population from the trial.
Black patients experience a higher mortality from lung cancer and are diagnosed at an earlier age and a lower cumulative pack-year exposure than White patients.7 Other studies have explored the social and political factors that lead to these disparities, which range from access to care to racial segregation of neighborhoods and tobacco marketing practices.7 When the USPSTF performed its periodic update of the guideline, it had access to additional research. The updates reflect the new information.
Every physician has a responsibility to find a way to adapt to important new information in medicine. Not using SGLT-2 inhibitors in the management of diabetes would be substandard care, and my patients would suffer for it. Not adopting the new lung cancer screening recommendations would exclude patients most at risk of lung cancer and allow disparities in lung cancer morbidity and mortality to grow.7,8Understanding the evidence behind the recommendations also reminds me that the guidelines will change again. These recommendations are no more static than the first guidelines were. I’ll be ready when the next update comes, and I’ll have the medical students and residents to keep me sharp.
1. US Food & Drug Administration. Novel drug approvals for 2022. Accessed October 27. 2022. www.fda.gov/drugs/new-drugs-fda-cders-new-molecular-entities-and-new-therapeutic-biological-products/novel-drug-approvals-2022
2. US Food & Drug Administration. First generic drug approvals. Accessed October 27. 2022. www.fda.gov/drugs/drug-and-biologic-approval-and-ind-activity-reports/first-generic-drug-approvals
3. US Preventive Services Task Force. Recommendations. Accessed October 27, 2022. www.uspreventiveservicestaskforce.org/uspstf/topic_search_results?topic_status=P
4. Covey CL, Cagle SD. Lung cancer screening: New evidence, updated guidance. J Fam Pract. 2022;71:398-402;415.
5. US Preventive Services Task Force. Lung cancer: screening. December 31, 2013. Accessed October 27, 2022. www.uspreventiveservicestaskforce.org/uspstf/recommendation/lung-cancer-screening-december-2013
6. National Lung Screening Trial Research Team. Reduced lung-cancer mortality with low-dose computed tomographic screening. N Engl J Med. 2011;365:395-409. doi: 10.1056/NEJMoa1102873
7. Pinheiro LC, Groner L, Soroka O, et al. Analysis of eligibility for lung cancer screening by race after 2021 changes to US Preventive Services Task Force screening guidelines. JAMA network open. 2022;5:e2229741. doi: 10.1001/jamanetworkopen.2022.29741
8. US Preventive Services Task Force. Screening for lung cancer: US Preventive Services Task Force Recommendation Statement. JAMA. 2021;325:962-970. doi: 10.1001/jama.2021.1117
1. US Food & Drug Administration. Novel drug approvals for 2022. Accessed October 27. 2022. www.fda.gov/drugs/new-drugs-fda-cders-new-molecular-entities-and-new-therapeutic-biological-products/novel-drug-approvals-2022
2. US Food & Drug Administration. First generic drug approvals. Accessed October 27. 2022. www.fda.gov/drugs/drug-and-biologic-approval-and-ind-activity-reports/first-generic-drug-approvals
3. US Preventive Services Task Force. Recommendations. Accessed October 27, 2022. www.uspreventiveservicestaskforce.org/uspstf/topic_search_results?topic_status=P
4. Covey CL, Cagle SD. Lung cancer screening: New evidence, updated guidance. J Fam Pract. 2022;71:398-402;415.
5. US Preventive Services Task Force. Lung cancer: screening. December 31, 2013. Accessed October 27, 2022. www.uspreventiveservicestaskforce.org/uspstf/recommendation/lung-cancer-screening-december-2013
6. National Lung Screening Trial Research Team. Reduced lung-cancer mortality with low-dose computed tomographic screening. N Engl J Med. 2011;365:395-409. doi: 10.1056/NEJMoa1102873
7. Pinheiro LC, Groner L, Soroka O, et al. Analysis of eligibility for lung cancer screening by race after 2021 changes to US Preventive Services Task Force screening guidelines. JAMA network open. 2022;5:e2229741. doi: 10.1001/jamanetworkopen.2022.29741
8. US Preventive Services Task Force. Screening for lung cancer: US Preventive Services Task Force Recommendation Statement. JAMA. 2021;325:962-970. doi: 10.1001/jama.2021.1117
New recommendations for hyperglycemia management
This transcript has been edited for clarity.
I’m Dr. Neil Skolnik. Today we’re going to talk about the consensus report by the American Diabetes Association and the European Association for the Study of Diabetes on the management of hyperglycemia.
After lifestyle modifications, metformin is no longer the go-to drug for every patient in the management of hyperglycemia. It is recommended that we assess each patient’s personal characteristics in deciding what medication to prescribe. For patients at high cardiorenal risk, refer to the left side of the algorithm and to the right side for all other patients.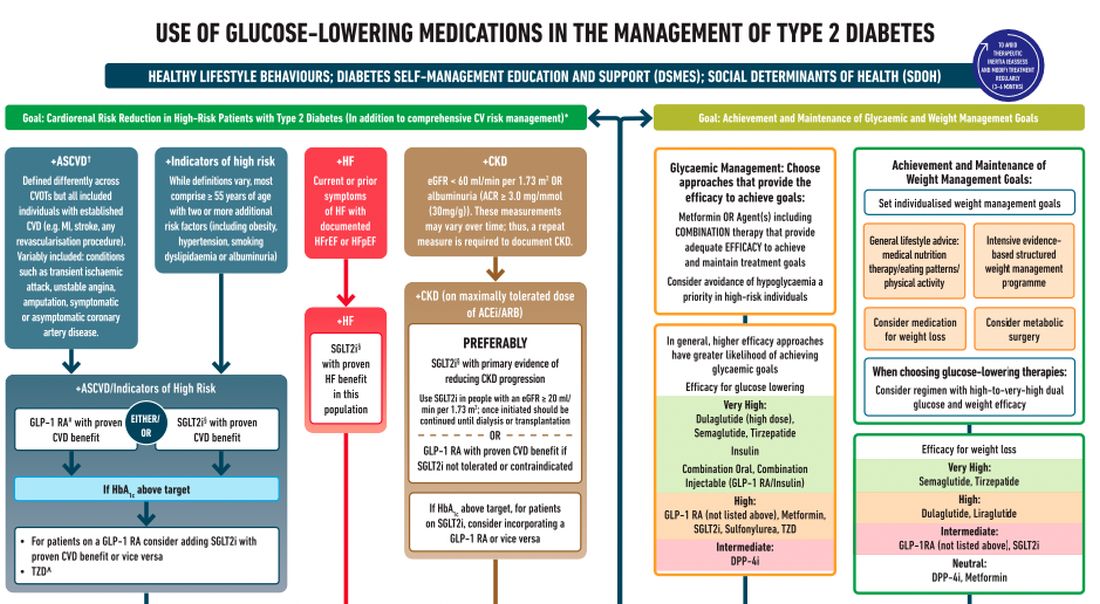
Cardiovascular disease. First, assess whether the patient is at high risk for atherosclerotic cardiovascular disease (ASCVD) or already has ASCVD. How is ASCVD defined? Either coronary artery disease (a history of a myocardial infarction [MI] or coronary disease), peripheral vascular disease, stroke, or transient ischemic attack.
What is high risk for ASCVD? Diabetes in someone older than 55 years with two or more additional risk factors. If the patient is at high risk for or has existing ASCVD then it is recommended to prescribe a glucagon-like peptide 1 (GLP-1) agonist with proven CVD benefit or an sodium-glucose cotransporter 2 (SGLT-2) inhibitor with proven CVD benefit.
For patients at very high risk for ASCVD, it might be reasonable to combine both agents. The recommendation to use these agents holds true whether the patients are at their A1c goals or not. The patient doesn’t need to be on metformin to benefit from these agents. The patient with reduced or preserved ejection fraction heart failure should be taking an SGLT-2 inhibitor.
Chronic kidney disease. Next up, chronic kidney disease (CKD). CKD is defined by an estimated glomerular filtration rate < 60 mL/min/1.73 m2 or a urine albumin to creatinine ratio > 30. In that case, the patient should be preferentially on an SGLT-2 inhibitor. Patients not able to take an SGLT-2 for some reason should be prescribed a GLP-1 receptor agonist.
If someone doesn’t fit into that high cardiorenal risk category, then we go to the right side of the algorithm. The goal then is achievement and maintenance of glycemic and weight management goals.
Glycemic management. In choosing medicine for glycemic management, metformin is a reasonable choice. You may need to add another agent to metformin to reach the patient’s glycemic goal. If the patient is far away from goal, then a medication with higher efficacy at lowering glucose might be chosen.
Efficacy is listed as:
- Very high efficacy for glucose lowering: dulaglutide at a high dose, semaglutide, tirzepatide, insulin, or combination injectable agents (GLP-1 receptor agonist/insulin combinations).
- High glucose-lowering efficacy: a GLP-1 receptor agonist not already mentioned, metformin, SGLT-2 inhibitors, sulfonylureas, thiazolidinediones.
- Intermediate glucose lowering efficacy: dipeptidyl peptidase 4 (DPP-4) inhibitors.
Weight management. For weight management, lifestyle modification (diet and exercise) is important. If lifestyle modification alone is insufficient, consider either a medication that specifically helps with weight management or metabolic surgery.
We particularly want to focus on weight management in patients who have complications from obesity. What would those complications be? Sleep apnea, hip or knee pain from arthritis, back pain – that is, biomechanical complications of obesity or nonalcoholic fatty liver disease. Medications for weight loss are listed by degree of efficacy:
- Very high efficacy for weight loss: semaglutide, tirzepatide.
- High efficacy for weight loss: dulaglutide and liraglutide.
- Intermediate for weight loss: GLP-1 receptor agonist (not listed above), SGLT-2 inhibitor.
- Neutral for weight loss: DPP-4 inhibitors and metformin.
Where does insulin fit in? If patients present with a very high A1c, if they are on other medications and their A1c is still not to goal, or if they are catabolic and losing weight because of their diabetes, then insulin has an important place in management.
These are incredibly important guidelines that provide a clear algorithm for a personalized approach to diabetes management.
Dr. Skolnik is professor, department of family medicine, Sidney Kimmel Medical College, Philadelphia, and associate director, department of family medicine, Abington (Pa.) Jefferson Health. He reported conflicts of interest with AstraZeneca, Teva, Eli Lilly, Boehringer Ingelheim, Sanofi, Sanofi Pasteur, GlaxoSmithKline, Merck, and Bayer. A version of this article first appeared on Medscape.com.
This transcript has been edited for clarity.
I’m Dr. Neil Skolnik. Today we’re going to talk about the consensus report by the American Diabetes Association and the European Association for the Study of Diabetes on the management of hyperglycemia.
After lifestyle modifications, metformin is no longer the go-to drug for every patient in the management of hyperglycemia. It is recommended that we assess each patient’s personal characteristics in deciding what medication to prescribe. For patients at high cardiorenal risk, refer to the left side of the algorithm and to the right side for all other patients.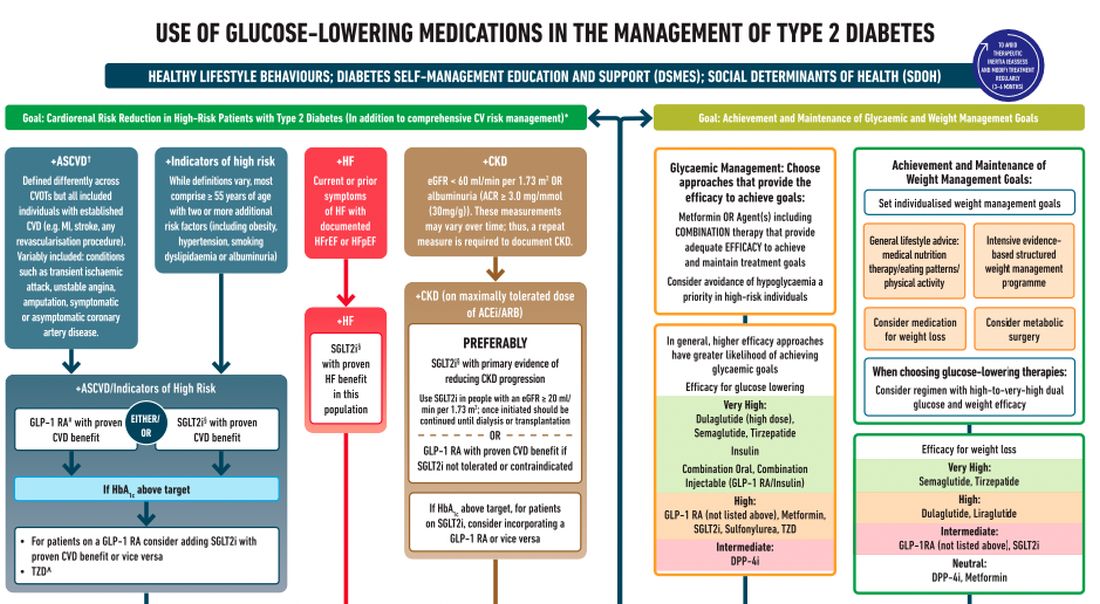
Cardiovascular disease. First, assess whether the patient is at high risk for atherosclerotic cardiovascular disease (ASCVD) or already has ASCVD. How is ASCVD defined? Either coronary artery disease (a history of a myocardial infarction [MI] or coronary disease), peripheral vascular disease, stroke, or transient ischemic attack.
What is high risk for ASCVD? Diabetes in someone older than 55 years with two or more additional risk factors. If the patient is at high risk for or has existing ASCVD then it is recommended to prescribe a glucagon-like peptide 1 (GLP-1) agonist with proven CVD benefit or an sodium-glucose cotransporter 2 (SGLT-2) inhibitor with proven CVD benefit.
For patients at very high risk for ASCVD, it might be reasonable to combine both agents. The recommendation to use these agents holds true whether the patients are at their A1c goals or not. The patient doesn’t need to be on metformin to benefit from these agents. The patient with reduced or preserved ejection fraction heart failure should be taking an SGLT-2 inhibitor.
Chronic kidney disease. Next up, chronic kidney disease (CKD). CKD is defined by an estimated glomerular filtration rate < 60 mL/min/1.73 m2 or a urine albumin to creatinine ratio > 30. In that case, the patient should be preferentially on an SGLT-2 inhibitor. Patients not able to take an SGLT-2 for some reason should be prescribed a GLP-1 receptor agonist.
If someone doesn’t fit into that high cardiorenal risk category, then we go to the right side of the algorithm. The goal then is achievement and maintenance of glycemic and weight management goals.
Glycemic management. In choosing medicine for glycemic management, metformin is a reasonable choice. You may need to add another agent to metformin to reach the patient’s glycemic goal. If the patient is far away from goal, then a medication with higher efficacy at lowering glucose might be chosen.
Efficacy is listed as:
- Very high efficacy for glucose lowering: dulaglutide at a high dose, semaglutide, tirzepatide, insulin, or combination injectable agents (GLP-1 receptor agonist/insulin combinations).
- High glucose-lowering efficacy: a GLP-1 receptor agonist not already mentioned, metformin, SGLT-2 inhibitors, sulfonylureas, thiazolidinediones.
- Intermediate glucose lowering efficacy: dipeptidyl peptidase 4 (DPP-4) inhibitors.
Weight management. For weight management, lifestyle modification (diet and exercise) is important. If lifestyle modification alone is insufficient, consider either a medication that specifically helps with weight management or metabolic surgery.
We particularly want to focus on weight management in patients who have complications from obesity. What would those complications be? Sleep apnea, hip or knee pain from arthritis, back pain – that is, biomechanical complications of obesity or nonalcoholic fatty liver disease. Medications for weight loss are listed by degree of efficacy:
- Very high efficacy for weight loss: semaglutide, tirzepatide.
- High efficacy for weight loss: dulaglutide and liraglutide.
- Intermediate for weight loss: GLP-1 receptor agonist (not listed above), SGLT-2 inhibitor.
- Neutral for weight loss: DPP-4 inhibitors and metformin.
Where does insulin fit in? If patients present with a very high A1c, if they are on other medications and their A1c is still not to goal, or if they are catabolic and losing weight because of their diabetes, then insulin has an important place in management.
These are incredibly important guidelines that provide a clear algorithm for a personalized approach to diabetes management.
Dr. Skolnik is professor, department of family medicine, Sidney Kimmel Medical College, Philadelphia, and associate director, department of family medicine, Abington (Pa.) Jefferson Health. He reported conflicts of interest with AstraZeneca, Teva, Eli Lilly, Boehringer Ingelheim, Sanofi, Sanofi Pasteur, GlaxoSmithKline, Merck, and Bayer. A version of this article first appeared on Medscape.com.
This transcript has been edited for clarity.
I’m Dr. Neil Skolnik. Today we’re going to talk about the consensus report by the American Diabetes Association and the European Association for the Study of Diabetes on the management of hyperglycemia.
After lifestyle modifications, metformin is no longer the go-to drug for every patient in the management of hyperglycemia. It is recommended that we assess each patient’s personal characteristics in deciding what medication to prescribe. For patients at high cardiorenal risk, refer to the left side of the algorithm and to the right side for all other patients.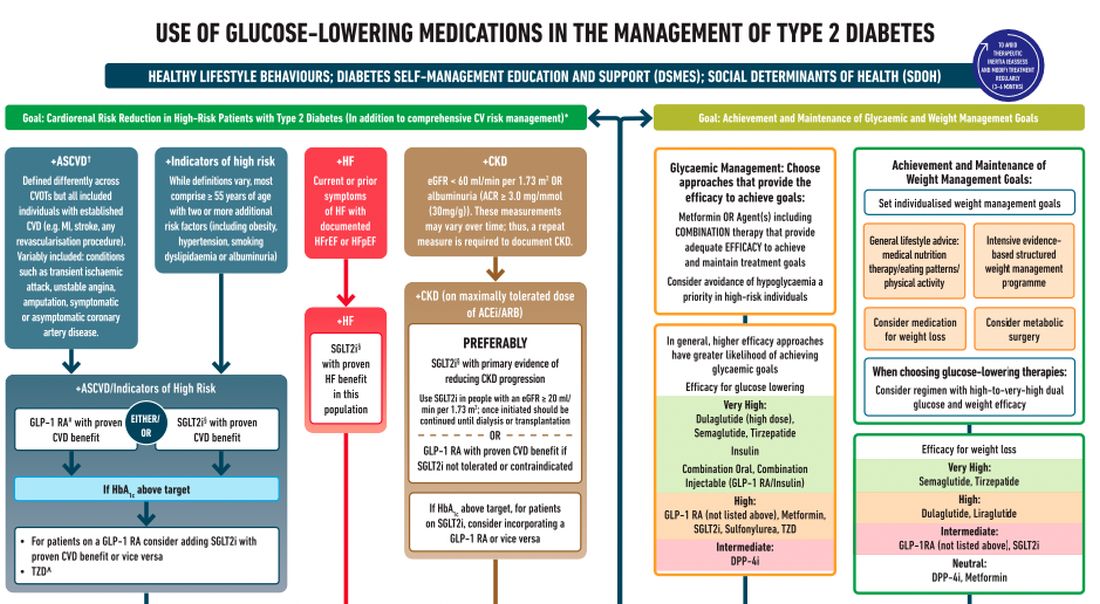
Cardiovascular disease. First, assess whether the patient is at high risk for atherosclerotic cardiovascular disease (ASCVD) or already has ASCVD. How is ASCVD defined? Either coronary artery disease (a history of a myocardial infarction [MI] or coronary disease), peripheral vascular disease, stroke, or transient ischemic attack.
What is high risk for ASCVD? Diabetes in someone older than 55 years with two or more additional risk factors. If the patient is at high risk for or has existing ASCVD then it is recommended to prescribe a glucagon-like peptide 1 (GLP-1) agonist with proven CVD benefit or an sodium-glucose cotransporter 2 (SGLT-2) inhibitor with proven CVD benefit.
For patients at very high risk for ASCVD, it might be reasonable to combine both agents. The recommendation to use these agents holds true whether the patients are at their A1c goals or not. The patient doesn’t need to be on metformin to benefit from these agents. The patient with reduced or preserved ejection fraction heart failure should be taking an SGLT-2 inhibitor.
Chronic kidney disease. Next up, chronic kidney disease (CKD). CKD is defined by an estimated glomerular filtration rate < 60 mL/min/1.73 m2 or a urine albumin to creatinine ratio > 30. In that case, the patient should be preferentially on an SGLT-2 inhibitor. Patients not able to take an SGLT-2 for some reason should be prescribed a GLP-1 receptor agonist.
If someone doesn’t fit into that high cardiorenal risk category, then we go to the right side of the algorithm. The goal then is achievement and maintenance of glycemic and weight management goals.
Glycemic management. In choosing medicine for glycemic management, metformin is a reasonable choice. You may need to add another agent to metformin to reach the patient’s glycemic goal. If the patient is far away from goal, then a medication with higher efficacy at lowering glucose might be chosen.
Efficacy is listed as:
- Very high efficacy for glucose lowering: dulaglutide at a high dose, semaglutide, tirzepatide, insulin, or combination injectable agents (GLP-1 receptor agonist/insulin combinations).
- High glucose-lowering efficacy: a GLP-1 receptor agonist not already mentioned, metformin, SGLT-2 inhibitors, sulfonylureas, thiazolidinediones.
- Intermediate glucose lowering efficacy: dipeptidyl peptidase 4 (DPP-4) inhibitors.
Weight management. For weight management, lifestyle modification (diet and exercise) is important. If lifestyle modification alone is insufficient, consider either a medication that specifically helps with weight management or metabolic surgery.
We particularly want to focus on weight management in patients who have complications from obesity. What would those complications be? Sleep apnea, hip or knee pain from arthritis, back pain – that is, biomechanical complications of obesity or nonalcoholic fatty liver disease. Medications for weight loss are listed by degree of efficacy:
- Very high efficacy for weight loss: semaglutide, tirzepatide.
- High efficacy for weight loss: dulaglutide and liraglutide.
- Intermediate for weight loss: GLP-1 receptor agonist (not listed above), SGLT-2 inhibitor.
- Neutral for weight loss: DPP-4 inhibitors and metformin.
Where does insulin fit in? If patients present with a very high A1c, if they are on other medications and their A1c is still not to goal, or if they are catabolic and losing weight because of their diabetes, then insulin has an important place in management.
These are incredibly important guidelines that provide a clear algorithm for a personalized approach to diabetes management.
Dr. Skolnik is professor, department of family medicine, Sidney Kimmel Medical College, Philadelphia, and associate director, department of family medicine, Abington (Pa.) Jefferson Health. He reported conflicts of interest with AstraZeneca, Teva, Eli Lilly, Boehringer Ingelheim, Sanofi, Sanofi Pasteur, GlaxoSmithKline, Merck, and Bayer. A version of this article first appeared on Medscape.com.
Microtox and Mesotox
The terms when they mention one of these terms.
Let’s settle the nomenclature confusion. In this column, I define and outline suggested terminology based on studies and my 15 years of experience using neuromodulators. If any readers or colleagues disagree, please write to me and we can discuss the alternatives in a subsequent article; if you agree, please also write to me so we can collaboratively correct the discrepancies in the literature accordingly.
The term mesotherapy, originating from the Greek “mesos” referring to the early embryonic mesoderm, was identified in the 1950’s by Dr. Michel Pistor, a French physician who administered drugs intradermally. The term was defined as a minimally invasive technique by which drugs or bioactive substances are given in small quantities through dermal micropunctures. Drugs administered intradermally diffuse very slowly and therefore, stay in the tissue longer than those administered intramuscularly.
Thus, Mesotox is defined not by the concentration of the neuromodulator or location, but by the depth of injection in the superficial dermis. It can be delivered through individual injections or through a microneedling pen.
Microtox refers to the dilution of the neuromodulator at concentrations below the proposed dilution guidelines of the manufacturer: Less than 2.5 U per 0.1 mL for onabotulinumtoxinA (OBA), incobotulinumtoxinA (IBA), and prabotulinumtoxinA (PBA); and less than 10 U per 0.1 mL for abobotulinumtoxinA (ABO), This method allows for the injection of superficial cutaneous muscles softening the dynamic rhytids without complete paralysis.
Mesotox is widely used off label for facial lifting, reduction in skin laxity or crepiness, flushing of rosacea, acne, hyperhidrosis of the face, keloids, seborrhea, neck rejuvenation, contouring of the mandibular border, and scalp oiliness. Based on a review of articles using this technique, dilution methods were less than 2.5 U per 1 mL (OBA, IBA) and less than 10 U per 0.1 mL (ABO) depth of injection was the superficial to mid-dermis with injection points 0.5 cm to 1 cm apart.
In a study by Atwa and colleagues, 25 patients with mild facial skin laxity received intradermal Botox-A on one side and saline on the other. This split face study showed a highly significant difference with facial lifting on the treated side. Mesotox injection points vary based on the clinical indication and area being treated.
The treatment of dynamic muscles using standard neuromodulator dosing protocols include the treatment of the glabella, crow’s feet, forehead lines, masseter hypertrophy, bunny lines, gummy smile, perioral lines, mentalis hypertonia, platysmal bands, and marionette lines.
However, hyperdilute neuromodulators or Microtox can effectively be used alone or in combination with standard dosing for the following off-label uses. Used in combination with standard dosing of the forehead lines, I use Microtox in the lateral brow to soften the frontalis muscle without dropping the brow in patients with a low-set brow or lid laxity. I also use it for the jelly roll of the eyes and to open the aperture of the eyes. Along the nose, Microtox can also be used to treat a sagging nasal tip, decrease the width of the ala, and treat overactive facial muscles adjacent to the nose resulting in an overactive nasolabial fold.
Similarly, Microtox can be used to treat lateral smile lines and downward extensions of the crow’s feet. In all of the aforementioned treatment areas, I recommend approximately 0.5-1 U of toxin in each area divided at 1-cm intervals.Mesotox and Microtox are both highly effective strategies to treat the aging face. However, the nomenclature is not interchangeable. I propose that the term Mesotox be used only to articulate or define the superficial injection of a neuromodulator for the improvement of the skin that does not involve the injection into or paralysis of a cutaneous muscle (“tox” being used generically for all neuromodulators). I also propose that the term Microtox should be used to define the dilution of a neuromodulator beyond the manufacturer-recommended dilution protocols – used for the paralysis of a cutaneous muscle. In addition, I recommend that the terms MicroBotox and MesoBotox no longer be used. These procedures all have risks, and adverse events associated with Microtox and Mesotox are similar to those of any neuromodulator injection at FDA-recommended maximum doses, and dilution and storage protocols and proper injection techniques need to be followed. Expertise and training is crucial and treatment by a board-certified dermatologist or plastic surgeon is imperative.
Dr. Talakoub and Naissan O. Wesley, MD, are cocontributors to this column. Dr. Talakoub is in private practice in McLean, Va. Dr. Wesley practices dermatology in Beverly Hills, Calif. This month’s column is by Dr. Talakoub. Write to her at [email protected]. Dr. Talakoub had no relevant disclosures.
References
Awaida CJ et al. Plast Reconstr Surg. 2018 Sep;142(3):640-9.
Calvani F et al. Plast Surg (Oakv). 2019 May;27(2):156-61.
Iranmanesh B et al. J Cosmet Dermatol. 2022 Oct;21(10):4160-70.
Kandhari R et al. J Cutan Aesthet Surg. 2022 Apr-Jun;15(2):101-7.
Lewandowski M et al. Molecules. 2022 May 13;27(10):3143.
Mammucari M et al. Eur Rev Med Pharmacol Sci. 2011 Jun;15(6):682-94.
Park KY et al. Ann Dermatol. 2018 Dec;30(6):688-93.
Pistor M. Chir Dent Fr. 1976;46:59-60.
Rho NK, Gil YC. Toxins (Basel). 2021 Nov 19;13(11):817.
Wu WTL. Plast Reconstr Surg. 2015 Nov;136(5 Suppl):92S-100S.
Zhang H et al. Clin Cosmet Investig Dermatol. 2021 Apr 30;14:407-17.
The terms when they mention one of these terms.
Let’s settle the nomenclature confusion. In this column, I define and outline suggested terminology based on studies and my 15 years of experience using neuromodulators. If any readers or colleagues disagree, please write to me and we can discuss the alternatives in a subsequent article; if you agree, please also write to me so we can collaboratively correct the discrepancies in the literature accordingly.
The term mesotherapy, originating from the Greek “mesos” referring to the early embryonic mesoderm, was identified in the 1950’s by Dr. Michel Pistor, a French physician who administered drugs intradermally. The term was defined as a minimally invasive technique by which drugs or bioactive substances are given in small quantities through dermal micropunctures. Drugs administered intradermally diffuse very slowly and therefore, stay in the tissue longer than those administered intramuscularly.
Thus, Mesotox is defined not by the concentration of the neuromodulator or location, but by the depth of injection in the superficial dermis. It can be delivered through individual injections or through a microneedling pen.
Microtox refers to the dilution of the neuromodulator at concentrations below the proposed dilution guidelines of the manufacturer: Less than 2.5 U per 0.1 mL for onabotulinumtoxinA (OBA), incobotulinumtoxinA (IBA), and prabotulinumtoxinA (PBA); and less than 10 U per 0.1 mL for abobotulinumtoxinA (ABO), This method allows for the injection of superficial cutaneous muscles softening the dynamic rhytids without complete paralysis.
Mesotox is widely used off label for facial lifting, reduction in skin laxity or crepiness, flushing of rosacea, acne, hyperhidrosis of the face, keloids, seborrhea, neck rejuvenation, contouring of the mandibular border, and scalp oiliness. Based on a review of articles using this technique, dilution methods were less than 2.5 U per 1 mL (OBA, IBA) and less than 10 U per 0.1 mL (ABO) depth of injection was the superficial to mid-dermis with injection points 0.5 cm to 1 cm apart.
In a study by Atwa and colleagues, 25 patients with mild facial skin laxity received intradermal Botox-A on one side and saline on the other. This split face study showed a highly significant difference with facial lifting on the treated side. Mesotox injection points vary based on the clinical indication and area being treated.
The treatment of dynamic muscles using standard neuromodulator dosing protocols include the treatment of the glabella, crow’s feet, forehead lines, masseter hypertrophy, bunny lines, gummy smile, perioral lines, mentalis hypertonia, platysmal bands, and marionette lines.
However, hyperdilute neuromodulators or Microtox can effectively be used alone or in combination with standard dosing for the following off-label uses. Used in combination with standard dosing of the forehead lines, I use Microtox in the lateral brow to soften the frontalis muscle without dropping the brow in patients with a low-set brow or lid laxity. I also use it for the jelly roll of the eyes and to open the aperture of the eyes. Along the nose, Microtox can also be used to treat a sagging nasal tip, decrease the width of the ala, and treat overactive facial muscles adjacent to the nose resulting in an overactive nasolabial fold.
Similarly, Microtox can be used to treat lateral smile lines and downward extensions of the crow’s feet. In all of the aforementioned treatment areas, I recommend approximately 0.5-1 U of toxin in each area divided at 1-cm intervals.Mesotox and Microtox are both highly effective strategies to treat the aging face. However, the nomenclature is not interchangeable. I propose that the term Mesotox be used only to articulate or define the superficial injection of a neuromodulator for the improvement of the skin that does not involve the injection into or paralysis of a cutaneous muscle (“tox” being used generically for all neuromodulators). I also propose that the term Microtox should be used to define the dilution of a neuromodulator beyond the manufacturer-recommended dilution protocols – used for the paralysis of a cutaneous muscle. In addition, I recommend that the terms MicroBotox and MesoBotox no longer be used. These procedures all have risks, and adverse events associated with Microtox and Mesotox are similar to those of any neuromodulator injection at FDA-recommended maximum doses, and dilution and storage protocols and proper injection techniques need to be followed. Expertise and training is crucial and treatment by a board-certified dermatologist or plastic surgeon is imperative.
Dr. Talakoub and Naissan O. Wesley, MD, are cocontributors to this column. Dr. Talakoub is in private practice in McLean, Va. Dr. Wesley practices dermatology in Beverly Hills, Calif. This month’s column is by Dr. Talakoub. Write to her at [email protected]. Dr. Talakoub had no relevant disclosures.
References
Awaida CJ et al. Plast Reconstr Surg. 2018 Sep;142(3):640-9.
Calvani F et al. Plast Surg (Oakv). 2019 May;27(2):156-61.
Iranmanesh B et al. J Cosmet Dermatol. 2022 Oct;21(10):4160-70.
Kandhari R et al. J Cutan Aesthet Surg. 2022 Apr-Jun;15(2):101-7.
Lewandowski M et al. Molecules. 2022 May 13;27(10):3143.
Mammucari M et al. Eur Rev Med Pharmacol Sci. 2011 Jun;15(6):682-94.
Park KY et al. Ann Dermatol. 2018 Dec;30(6):688-93.
Pistor M. Chir Dent Fr. 1976;46:59-60.
Rho NK, Gil YC. Toxins (Basel). 2021 Nov 19;13(11):817.
Wu WTL. Plast Reconstr Surg. 2015 Nov;136(5 Suppl):92S-100S.
Zhang H et al. Clin Cosmet Investig Dermatol. 2021 Apr 30;14:407-17.
The terms when they mention one of these terms.
Let’s settle the nomenclature confusion. In this column, I define and outline suggested terminology based on studies and my 15 years of experience using neuromodulators. If any readers or colleagues disagree, please write to me and we can discuss the alternatives in a subsequent article; if you agree, please also write to me so we can collaboratively correct the discrepancies in the literature accordingly.
The term mesotherapy, originating from the Greek “mesos” referring to the early embryonic mesoderm, was identified in the 1950’s by Dr. Michel Pistor, a French physician who administered drugs intradermally. The term was defined as a minimally invasive technique by which drugs or bioactive substances are given in small quantities through dermal micropunctures. Drugs administered intradermally diffuse very slowly and therefore, stay in the tissue longer than those administered intramuscularly.
Thus, Mesotox is defined not by the concentration of the neuromodulator or location, but by the depth of injection in the superficial dermis. It can be delivered through individual injections or through a microneedling pen.
Microtox refers to the dilution of the neuromodulator at concentrations below the proposed dilution guidelines of the manufacturer: Less than 2.5 U per 0.1 mL for onabotulinumtoxinA (OBA), incobotulinumtoxinA (IBA), and prabotulinumtoxinA (PBA); and less than 10 U per 0.1 mL for abobotulinumtoxinA (ABO), This method allows for the injection of superficial cutaneous muscles softening the dynamic rhytids without complete paralysis.
Mesotox is widely used off label for facial lifting, reduction in skin laxity or crepiness, flushing of rosacea, acne, hyperhidrosis of the face, keloids, seborrhea, neck rejuvenation, contouring of the mandibular border, and scalp oiliness. Based on a review of articles using this technique, dilution methods were less than 2.5 U per 1 mL (OBA, IBA) and less than 10 U per 0.1 mL (ABO) depth of injection was the superficial to mid-dermis with injection points 0.5 cm to 1 cm apart.
In a study by Atwa and colleagues, 25 patients with mild facial skin laxity received intradermal Botox-A on one side and saline on the other. This split face study showed a highly significant difference with facial lifting on the treated side. Mesotox injection points vary based on the clinical indication and area being treated.
The treatment of dynamic muscles using standard neuromodulator dosing protocols include the treatment of the glabella, crow’s feet, forehead lines, masseter hypertrophy, bunny lines, gummy smile, perioral lines, mentalis hypertonia, platysmal bands, and marionette lines.
However, hyperdilute neuromodulators or Microtox can effectively be used alone or in combination with standard dosing for the following off-label uses. Used in combination with standard dosing of the forehead lines, I use Microtox in the lateral brow to soften the frontalis muscle without dropping the brow in patients with a low-set brow or lid laxity. I also use it for the jelly roll of the eyes and to open the aperture of the eyes. Along the nose, Microtox can also be used to treat a sagging nasal tip, decrease the width of the ala, and treat overactive facial muscles adjacent to the nose resulting in an overactive nasolabial fold.
Similarly, Microtox can be used to treat lateral smile lines and downward extensions of the crow’s feet. In all of the aforementioned treatment areas, I recommend approximately 0.5-1 U of toxin in each area divided at 1-cm intervals.Mesotox and Microtox are both highly effective strategies to treat the aging face. However, the nomenclature is not interchangeable. I propose that the term Mesotox be used only to articulate or define the superficial injection of a neuromodulator for the improvement of the skin that does not involve the injection into or paralysis of a cutaneous muscle (“tox” being used generically for all neuromodulators). I also propose that the term Microtox should be used to define the dilution of a neuromodulator beyond the manufacturer-recommended dilution protocols – used for the paralysis of a cutaneous muscle. In addition, I recommend that the terms MicroBotox and MesoBotox no longer be used. These procedures all have risks, and adverse events associated with Microtox and Mesotox are similar to those of any neuromodulator injection at FDA-recommended maximum doses, and dilution and storage protocols and proper injection techniques need to be followed. Expertise and training is crucial and treatment by a board-certified dermatologist or plastic surgeon is imperative.
Dr. Talakoub and Naissan O. Wesley, MD, are cocontributors to this column. Dr. Talakoub is in private practice in McLean, Va. Dr. Wesley practices dermatology in Beverly Hills, Calif. This month’s column is by Dr. Talakoub. Write to her at [email protected]. Dr. Talakoub had no relevant disclosures.
References
Awaida CJ et al. Plast Reconstr Surg. 2018 Sep;142(3):640-9.
Calvani F et al. Plast Surg (Oakv). 2019 May;27(2):156-61.
Iranmanesh B et al. J Cosmet Dermatol. 2022 Oct;21(10):4160-70.
Kandhari R et al. J Cutan Aesthet Surg. 2022 Apr-Jun;15(2):101-7.
Lewandowski M et al. Molecules. 2022 May 13;27(10):3143.
Mammucari M et al. Eur Rev Med Pharmacol Sci. 2011 Jun;15(6):682-94.
Park KY et al. Ann Dermatol. 2018 Dec;30(6):688-93.
Pistor M. Chir Dent Fr. 1976;46:59-60.
Rho NK, Gil YC. Toxins (Basel). 2021 Nov 19;13(11):817.
Wu WTL. Plast Reconstr Surg. 2015 Nov;136(5 Suppl):92S-100S.
Zhang H et al. Clin Cosmet Investig Dermatol. 2021 Apr 30;14:407-17.











