User login
Could a vaccine (and more) fix the fentanyl crisis?
This discussion was recorded on Aug. 31, 2022. This transcript has been edited for clarity.
Robert Glatter, MD: Welcome. I’m Dr. Robert Glatter, medical advisor for Medscape Emergency Medicine. Today we have Dr. Paul Christo, a pain specialist in the Division of Pain Medicine at Johns Hopkins University School of Medicine in Baltimore, Maryland, and host of the national radio show Aches and Gains on SiriusXM Radio, joining us to discuss the ongoing and worsening fentanyl crisis in the U.S.
Welcome, Dr Christo.
Paul J. Christo, MD, MBA: Thanks so much for having me.
Dr. Glatter: I want to begin with a sobering statistic regarding overdoses. , based on recent data from the CDC.
Let’s start by having you explain how deadly fentanyl is in terms of its potency compared with morphine and heroin.
Dr. Christo: Fentanyl is considered a synthetic opioid. It’s not a naturally occurring opioid like morphine, for example, or codeine. We use this drug, fentanyl, often in the anesthesia well. We’ve used it for many years as an anesthetic for surgery very safely. In the chronic pain world, we’ve used it to help reduce chronic pain in the form of a patch.
What we’re seeing now, though, is something entirely different, which is the use of synthetic fentanyl as a mind- and mood-altering substance for those who don’t have pain, and essentially those who are buying this off the street. Fentanyl is about 80-100 times more potent than morphine, so you can put that in perspective in terms of its danger.
Dr. Glatter: Let me have you take us through an evolution of the opioid crisis from the 1990s, from long-acting opioid OxyContin, which was approved in 1995, to where we are now. There are different phases. If you could, educate our audience on how we got to where fentanyl is now the most common opiate involved in drug overdoses.
Dr. Christo: It really stems from the epidemic related to chronic pain. We have over 100 million people in the United States alone who suffer from chronic pain. Most chronic pain, sadly, is undertreated or untreated. In the ‘90s, in the quest to reduce chronic pain to a better extent, we saw more and more literature and studies related to the use of opioids for noncancer pain (e.g., for lower back pain).
There were many primary care doctors and pain specialists who started using opioids, probably for patients who didn’t really need it. I think it was done out of good conscience in the sense that they were trying to reduce pain. We have other methods of pain relief, but we needed more. At that time, in the ‘90s, we had a greater use of opioids to treat noncancer pain.
Then from that point, we transitioned to the use of heroin. Again, this isn’t among the chronic pain population, but it was the nonchronic pain population that starting using heroin. Today we see synthetic fentanyl.
Addressing the synthetic opioid crisis
Dr. Glatter: With fentanyl being the most common opiate we’re seeing, we’re having problems trying to save patients. We’re trying to use naloxone, but obviously in increasing amounts, and sometimes it’s not adequate and we have to intubate patients.
In terms of addressing this issue of supply, the fentanyl is coming from Mexico, China, and it’s manufactured here in the United States. How do we address this crisis? What are the steps that you would recommend we take?
Dr. Christo: I think that we need to better support law enforcement to crack down on those who are manufacturing fentanyl in the United States, and also to crack down on those who are transporting it from, say, Mexico – I think it’s primarily coming from Mexico – but from outside the United States to the United States. I feel like that’s important to do.
Two, we need to better educate those who are using these mind- and mood-altering substances. We’re seeing more and more that it’s the young-adult population, those between the ages of 13 and 25, who are starting to use these substances, and they’re very dangerous.
Dr. Glatter: Are these teens seeking out heroin and it happens to be laced with fentanyl, or are they actually seeking pure fentanyl? Are they trying to buy the colorful pills that we know about? What’s your experience in terms of the population you’re treating and what you could tell us?
Dr. Christo: I think it’s both. We’re seeing young adults who are interested in the use of fentanyl as a mind- and mood-altering substance. We’re also seeing young and older adults use other drugs, like cocaine and heroin, that are laced with fentanyl, and they don’t know it. That’s exponentially more dangerous.
Fentanyl test strips
Dr. Glatter: People are unaware that there is fentanyl in what they’re using, and it is certainly leading to overdoses and deaths. I think that parents really need to be aware of this.
Dr. Christo: Yes, for sure. I think we need better educational methods in the schools to educate that population that we’re talking about (between the ages of 13 and 25). Let them know the dangers, because I don’t think they’re aware of the danger, and how potent fentanyl is in terms of its lethality, and that you don’t need very much to take in a form of a pill or to inhale or to inject intravenously to kill yourself. That is key – education at that level – and to let those who are going to use these substances (specifically, synthetic fentanyl) know that they should consider the use of fentanyl test strips.
Fentanyl test strips would be primarily used for those who are thinking that they’re using heroin but there may be fentanyl in there, or methamphetamine and there may be fentanyl, and they don’t know. The test strip gives them that knowledge.
The other harm reduction strategies would be the use of naloxone, known as Narcan. That’s a lifesaver. You just have to spritz it into the nostril. You don’t do it yourself if you’re using the substance, but you’ve got others who can do it for you. No question, that’s a lifesaver. We need to make sure that there’s greater availability of that throughout the entire country, and we’re seeing some of that in certain states. In certain states, you don’t need a prescription to get naloxone from the pharmacy.
Dr. Glatter: I think it’s so important that it should be widely available. Certainly, the COVID-19 pandemic exacerbated the number of overdoses we saw. Are overdoses coming down or are we still at a level that’s close to 2020?
Dr. Christo: Unfortunately, we’re still seeing the same level, if not seeing it escalate. Certainly, the pandemic, because of the economic cost associated with the pandemic – loss of employment, underemployment – as well as the emotional stress of the pandemic led many people to use substances on the street in order to cope. They’re coping mechanisms, and we really haven’t seen it abate quite yet.
Dr. Glatter: Do you have a message for the lawmakers on Capitol Hill as to what we can do regarding the illegal manufacturing and distribution, how we can really crack down? Are there other approaches that we could implement that might be more tangible?
Dr. Christo: Yes. No. 1 would be to support law enforcement. No. 2 would be to create and make available more overdose prevention centers. The first was in New York City. If you look at the data on overdose prevention centers, in Canada, for example, they’ve seen a 35% reduction in overdose deaths. These are places where people who are using can go to get clean needles and clean syringes. This is where people basically oversee the use of the drug and intervene if necessary.
It seems sort of antithetical. It seems like, “Boy, why would you fund a center for people to use drugs?” The data from Canada and outside Canada are such that it can be very helpful. That would be one of my messages to lawmakers as well.
Vaccines to combat the synthetic opioid crisis
Dr. Glatter: Do you think that the legislators could approach some of these factories as a way to crack down, and have law enforcement be more aggressive? Is that another possible solution?
Dr. Christo: It is. Law enforcement needs to be supported by the government, by the Biden administration, so that we can prevent the influx of fentanyl and other drugs into the United States, and also to crack down on those in the United States who are manufacturing these drugs – synthetic fentanyl, first and foremost – because we’re seeing a lot of deaths related to synthetic fentanyl.
Also, we’re seeing — and this is pretty intriguing and interesting – the use of vaccines to help prevent overdose. The first human trial is underway right now for a vaccine against oxycodone. Not only that, but there are other vaccines that are in animal trials now against heroin, cocaine, or fentanyl. There’s hope there that we can use vaccines to also help reduce deaths related to overdose from fentanyl and other opioids.
Dr. Glatter: Do you think this would be given widely to the population or only to those at higher risk?
Dr. Christo: It would probably be targeting those who are at higher risk and have a history of drug abuse. I don’t think it would be something that would be given to the entire population, but it certainly could be effective, and we’re seeing encouraging results from the human trial right now.
Dr. Glatter: That’s very intriguing. That’s something that certainly could be quite helpful in the future.
One thing I did want to address is law enforcement and first responders who have been exposed to dust, or inhaled dust possibly, or had fentanyl on their skin. There has been lots of controversy. The recent literature has dispelled the controversy that people who had supposedly passed out and required Narcan after exposure to intact skin, or even compromised skin, had an overdose of fentanyl. Maybe you could speak to that and dispel that myth.
Dr. Christo: Yes, I’ve been asked this question a couple of times in the past. It’s not sufficient just to have contact with fentanyl on the skin to lead to an overdose. You really need to ingest it. That is, take it by mouth in the form of a pill, inhale it, or inject it intravenously. Skin contact is very unlikely going to lead to an overdose and death.
Dr. Glatter: I want to thank you for a very informative interview. Do you have one or two pearls you’d like to give our audience as a takeaway?
Dr. Christo: I would say two things. One is, don’t give up if you have chronic pain because there is hope. We have nonopioid treatments that can be effective. Two, don’t give up if you have a substance use disorder. Talk to your primary care doctor or talk to emergency room physicians if you’re in the emergency room. The Substance Abuse and Mental Health Services Administration is a good resource, too. SAMHSA has an 800 number for support and a website. Take the opportunity to use the resources that are available.
Dr. Glatter is assistant professor of emergency medicine at Lenox Hill Hospital in New York City and at Hofstra University, Hempstead, N.Y. He is an editorial advisor and hosts the Hot Topics in EM series on Medscape. He is also a medical contributor for Forbes.
Dr. Christo is an associate professor and a pain specialist in the department of anesthesiology and critical care medicine at Johns Hopkins University, Baltimore. He also serves as director of the multidisciplinary pain fellowship program at Johns Hopkins Hospital. Christo is the author of Aches and Gains, A Comprehensive Guide to Overcoming Your Pain, and hosts an award-winning, nationally syndicated SiriusXM radio talk show on overcoming pain, called Aches and Gains.
A version of this article first appeared on Medscape.com.
This discussion was recorded on Aug. 31, 2022. This transcript has been edited for clarity.
Robert Glatter, MD: Welcome. I’m Dr. Robert Glatter, medical advisor for Medscape Emergency Medicine. Today we have Dr. Paul Christo, a pain specialist in the Division of Pain Medicine at Johns Hopkins University School of Medicine in Baltimore, Maryland, and host of the national radio show Aches and Gains on SiriusXM Radio, joining us to discuss the ongoing and worsening fentanyl crisis in the U.S.
Welcome, Dr Christo.
Paul J. Christo, MD, MBA: Thanks so much for having me.
Dr. Glatter: I want to begin with a sobering statistic regarding overdoses. , based on recent data from the CDC.
Let’s start by having you explain how deadly fentanyl is in terms of its potency compared with morphine and heroin.
Dr. Christo: Fentanyl is considered a synthetic opioid. It’s not a naturally occurring opioid like morphine, for example, or codeine. We use this drug, fentanyl, often in the anesthesia well. We’ve used it for many years as an anesthetic for surgery very safely. In the chronic pain world, we’ve used it to help reduce chronic pain in the form of a patch.
What we’re seeing now, though, is something entirely different, which is the use of synthetic fentanyl as a mind- and mood-altering substance for those who don’t have pain, and essentially those who are buying this off the street. Fentanyl is about 80-100 times more potent than morphine, so you can put that in perspective in terms of its danger.
Dr. Glatter: Let me have you take us through an evolution of the opioid crisis from the 1990s, from long-acting opioid OxyContin, which was approved in 1995, to where we are now. There are different phases. If you could, educate our audience on how we got to where fentanyl is now the most common opiate involved in drug overdoses.
Dr. Christo: It really stems from the epidemic related to chronic pain. We have over 100 million people in the United States alone who suffer from chronic pain. Most chronic pain, sadly, is undertreated or untreated. In the ‘90s, in the quest to reduce chronic pain to a better extent, we saw more and more literature and studies related to the use of opioids for noncancer pain (e.g., for lower back pain).
There were many primary care doctors and pain specialists who started using opioids, probably for patients who didn’t really need it. I think it was done out of good conscience in the sense that they were trying to reduce pain. We have other methods of pain relief, but we needed more. At that time, in the ‘90s, we had a greater use of opioids to treat noncancer pain.
Then from that point, we transitioned to the use of heroin. Again, this isn’t among the chronic pain population, but it was the nonchronic pain population that starting using heroin. Today we see synthetic fentanyl.
Addressing the synthetic opioid crisis
Dr. Glatter: With fentanyl being the most common opiate we’re seeing, we’re having problems trying to save patients. We’re trying to use naloxone, but obviously in increasing amounts, and sometimes it’s not adequate and we have to intubate patients.
In terms of addressing this issue of supply, the fentanyl is coming from Mexico, China, and it’s manufactured here in the United States. How do we address this crisis? What are the steps that you would recommend we take?
Dr. Christo: I think that we need to better support law enforcement to crack down on those who are manufacturing fentanyl in the United States, and also to crack down on those who are transporting it from, say, Mexico – I think it’s primarily coming from Mexico – but from outside the United States to the United States. I feel like that’s important to do.
Two, we need to better educate those who are using these mind- and mood-altering substances. We’re seeing more and more that it’s the young-adult population, those between the ages of 13 and 25, who are starting to use these substances, and they’re very dangerous.
Dr. Glatter: Are these teens seeking out heroin and it happens to be laced with fentanyl, or are they actually seeking pure fentanyl? Are they trying to buy the colorful pills that we know about? What’s your experience in terms of the population you’re treating and what you could tell us?
Dr. Christo: I think it’s both. We’re seeing young adults who are interested in the use of fentanyl as a mind- and mood-altering substance. We’re also seeing young and older adults use other drugs, like cocaine and heroin, that are laced with fentanyl, and they don’t know it. That’s exponentially more dangerous.
Fentanyl test strips
Dr. Glatter: People are unaware that there is fentanyl in what they’re using, and it is certainly leading to overdoses and deaths. I think that parents really need to be aware of this.
Dr. Christo: Yes, for sure. I think we need better educational methods in the schools to educate that population that we’re talking about (between the ages of 13 and 25). Let them know the dangers, because I don’t think they’re aware of the danger, and how potent fentanyl is in terms of its lethality, and that you don’t need very much to take in a form of a pill or to inhale or to inject intravenously to kill yourself. That is key – education at that level – and to let those who are going to use these substances (specifically, synthetic fentanyl) know that they should consider the use of fentanyl test strips.
Fentanyl test strips would be primarily used for those who are thinking that they’re using heroin but there may be fentanyl in there, or methamphetamine and there may be fentanyl, and they don’t know. The test strip gives them that knowledge.
The other harm reduction strategies would be the use of naloxone, known as Narcan. That’s a lifesaver. You just have to spritz it into the nostril. You don’t do it yourself if you’re using the substance, but you’ve got others who can do it for you. No question, that’s a lifesaver. We need to make sure that there’s greater availability of that throughout the entire country, and we’re seeing some of that in certain states. In certain states, you don’t need a prescription to get naloxone from the pharmacy.
Dr. Glatter: I think it’s so important that it should be widely available. Certainly, the COVID-19 pandemic exacerbated the number of overdoses we saw. Are overdoses coming down or are we still at a level that’s close to 2020?
Dr. Christo: Unfortunately, we’re still seeing the same level, if not seeing it escalate. Certainly, the pandemic, because of the economic cost associated with the pandemic – loss of employment, underemployment – as well as the emotional stress of the pandemic led many people to use substances on the street in order to cope. They’re coping mechanisms, and we really haven’t seen it abate quite yet.
Dr. Glatter: Do you have a message for the lawmakers on Capitol Hill as to what we can do regarding the illegal manufacturing and distribution, how we can really crack down? Are there other approaches that we could implement that might be more tangible?
Dr. Christo: Yes. No. 1 would be to support law enforcement. No. 2 would be to create and make available more overdose prevention centers. The first was in New York City. If you look at the data on overdose prevention centers, in Canada, for example, they’ve seen a 35% reduction in overdose deaths. These are places where people who are using can go to get clean needles and clean syringes. This is where people basically oversee the use of the drug and intervene if necessary.
It seems sort of antithetical. It seems like, “Boy, why would you fund a center for people to use drugs?” The data from Canada and outside Canada are such that it can be very helpful. That would be one of my messages to lawmakers as well.
Vaccines to combat the synthetic opioid crisis
Dr. Glatter: Do you think that the legislators could approach some of these factories as a way to crack down, and have law enforcement be more aggressive? Is that another possible solution?
Dr. Christo: It is. Law enforcement needs to be supported by the government, by the Biden administration, so that we can prevent the influx of fentanyl and other drugs into the United States, and also to crack down on those in the United States who are manufacturing these drugs – synthetic fentanyl, first and foremost – because we’re seeing a lot of deaths related to synthetic fentanyl.
Also, we’re seeing — and this is pretty intriguing and interesting – the use of vaccines to help prevent overdose. The first human trial is underway right now for a vaccine against oxycodone. Not only that, but there are other vaccines that are in animal trials now against heroin, cocaine, or fentanyl. There’s hope there that we can use vaccines to also help reduce deaths related to overdose from fentanyl and other opioids.
Dr. Glatter: Do you think this would be given widely to the population or only to those at higher risk?
Dr. Christo: It would probably be targeting those who are at higher risk and have a history of drug abuse. I don’t think it would be something that would be given to the entire population, but it certainly could be effective, and we’re seeing encouraging results from the human trial right now.
Dr. Glatter: That’s very intriguing. That’s something that certainly could be quite helpful in the future.
One thing I did want to address is law enforcement and first responders who have been exposed to dust, or inhaled dust possibly, or had fentanyl on their skin. There has been lots of controversy. The recent literature has dispelled the controversy that people who had supposedly passed out and required Narcan after exposure to intact skin, or even compromised skin, had an overdose of fentanyl. Maybe you could speak to that and dispel that myth.
Dr. Christo: Yes, I’ve been asked this question a couple of times in the past. It’s not sufficient just to have contact with fentanyl on the skin to lead to an overdose. You really need to ingest it. That is, take it by mouth in the form of a pill, inhale it, or inject it intravenously. Skin contact is very unlikely going to lead to an overdose and death.
Dr. Glatter: I want to thank you for a very informative interview. Do you have one or two pearls you’d like to give our audience as a takeaway?
Dr. Christo: I would say two things. One is, don’t give up if you have chronic pain because there is hope. We have nonopioid treatments that can be effective. Two, don’t give up if you have a substance use disorder. Talk to your primary care doctor or talk to emergency room physicians if you’re in the emergency room. The Substance Abuse and Mental Health Services Administration is a good resource, too. SAMHSA has an 800 number for support and a website. Take the opportunity to use the resources that are available.
Dr. Glatter is assistant professor of emergency medicine at Lenox Hill Hospital in New York City and at Hofstra University, Hempstead, N.Y. He is an editorial advisor and hosts the Hot Topics in EM series on Medscape. He is also a medical contributor for Forbes.
Dr. Christo is an associate professor and a pain specialist in the department of anesthesiology and critical care medicine at Johns Hopkins University, Baltimore. He also serves as director of the multidisciplinary pain fellowship program at Johns Hopkins Hospital. Christo is the author of Aches and Gains, A Comprehensive Guide to Overcoming Your Pain, and hosts an award-winning, nationally syndicated SiriusXM radio talk show on overcoming pain, called Aches and Gains.
A version of this article first appeared on Medscape.com.
This discussion was recorded on Aug. 31, 2022. This transcript has been edited for clarity.
Robert Glatter, MD: Welcome. I’m Dr. Robert Glatter, medical advisor for Medscape Emergency Medicine. Today we have Dr. Paul Christo, a pain specialist in the Division of Pain Medicine at Johns Hopkins University School of Medicine in Baltimore, Maryland, and host of the national radio show Aches and Gains on SiriusXM Radio, joining us to discuss the ongoing and worsening fentanyl crisis in the U.S.
Welcome, Dr Christo.
Paul J. Christo, MD, MBA: Thanks so much for having me.
Dr. Glatter: I want to begin with a sobering statistic regarding overdoses. , based on recent data from the CDC.
Let’s start by having you explain how deadly fentanyl is in terms of its potency compared with morphine and heroin.
Dr. Christo: Fentanyl is considered a synthetic opioid. It’s not a naturally occurring opioid like morphine, for example, or codeine. We use this drug, fentanyl, often in the anesthesia well. We’ve used it for many years as an anesthetic for surgery very safely. In the chronic pain world, we’ve used it to help reduce chronic pain in the form of a patch.
What we’re seeing now, though, is something entirely different, which is the use of synthetic fentanyl as a mind- and mood-altering substance for those who don’t have pain, and essentially those who are buying this off the street. Fentanyl is about 80-100 times more potent than morphine, so you can put that in perspective in terms of its danger.
Dr. Glatter: Let me have you take us through an evolution of the opioid crisis from the 1990s, from long-acting opioid OxyContin, which was approved in 1995, to where we are now. There are different phases. If you could, educate our audience on how we got to where fentanyl is now the most common opiate involved in drug overdoses.
Dr. Christo: It really stems from the epidemic related to chronic pain. We have over 100 million people in the United States alone who suffer from chronic pain. Most chronic pain, sadly, is undertreated or untreated. In the ‘90s, in the quest to reduce chronic pain to a better extent, we saw more and more literature and studies related to the use of opioids for noncancer pain (e.g., for lower back pain).
There were many primary care doctors and pain specialists who started using opioids, probably for patients who didn’t really need it. I think it was done out of good conscience in the sense that they were trying to reduce pain. We have other methods of pain relief, but we needed more. At that time, in the ‘90s, we had a greater use of opioids to treat noncancer pain.
Then from that point, we transitioned to the use of heroin. Again, this isn’t among the chronic pain population, but it was the nonchronic pain population that starting using heroin. Today we see synthetic fentanyl.
Addressing the synthetic opioid crisis
Dr. Glatter: With fentanyl being the most common opiate we’re seeing, we’re having problems trying to save patients. We’re trying to use naloxone, but obviously in increasing amounts, and sometimes it’s not adequate and we have to intubate patients.
In terms of addressing this issue of supply, the fentanyl is coming from Mexico, China, and it’s manufactured here in the United States. How do we address this crisis? What are the steps that you would recommend we take?
Dr. Christo: I think that we need to better support law enforcement to crack down on those who are manufacturing fentanyl in the United States, and also to crack down on those who are transporting it from, say, Mexico – I think it’s primarily coming from Mexico – but from outside the United States to the United States. I feel like that’s important to do.
Two, we need to better educate those who are using these mind- and mood-altering substances. We’re seeing more and more that it’s the young-adult population, those between the ages of 13 and 25, who are starting to use these substances, and they’re very dangerous.
Dr. Glatter: Are these teens seeking out heroin and it happens to be laced with fentanyl, or are they actually seeking pure fentanyl? Are they trying to buy the colorful pills that we know about? What’s your experience in terms of the population you’re treating and what you could tell us?
Dr. Christo: I think it’s both. We’re seeing young adults who are interested in the use of fentanyl as a mind- and mood-altering substance. We’re also seeing young and older adults use other drugs, like cocaine and heroin, that are laced with fentanyl, and they don’t know it. That’s exponentially more dangerous.
Fentanyl test strips
Dr. Glatter: People are unaware that there is fentanyl in what they’re using, and it is certainly leading to overdoses and deaths. I think that parents really need to be aware of this.
Dr. Christo: Yes, for sure. I think we need better educational methods in the schools to educate that population that we’re talking about (between the ages of 13 and 25). Let them know the dangers, because I don’t think they’re aware of the danger, and how potent fentanyl is in terms of its lethality, and that you don’t need very much to take in a form of a pill or to inhale or to inject intravenously to kill yourself. That is key – education at that level – and to let those who are going to use these substances (specifically, synthetic fentanyl) know that they should consider the use of fentanyl test strips.
Fentanyl test strips would be primarily used for those who are thinking that they’re using heroin but there may be fentanyl in there, or methamphetamine and there may be fentanyl, and they don’t know. The test strip gives them that knowledge.
The other harm reduction strategies would be the use of naloxone, known as Narcan. That’s a lifesaver. You just have to spritz it into the nostril. You don’t do it yourself if you’re using the substance, but you’ve got others who can do it for you. No question, that’s a lifesaver. We need to make sure that there’s greater availability of that throughout the entire country, and we’re seeing some of that in certain states. In certain states, you don’t need a prescription to get naloxone from the pharmacy.
Dr. Glatter: I think it’s so important that it should be widely available. Certainly, the COVID-19 pandemic exacerbated the number of overdoses we saw. Are overdoses coming down or are we still at a level that’s close to 2020?
Dr. Christo: Unfortunately, we’re still seeing the same level, if not seeing it escalate. Certainly, the pandemic, because of the economic cost associated with the pandemic – loss of employment, underemployment – as well as the emotional stress of the pandemic led many people to use substances on the street in order to cope. They’re coping mechanisms, and we really haven’t seen it abate quite yet.
Dr. Glatter: Do you have a message for the lawmakers on Capitol Hill as to what we can do regarding the illegal manufacturing and distribution, how we can really crack down? Are there other approaches that we could implement that might be more tangible?
Dr. Christo: Yes. No. 1 would be to support law enforcement. No. 2 would be to create and make available more overdose prevention centers. The first was in New York City. If you look at the data on overdose prevention centers, in Canada, for example, they’ve seen a 35% reduction in overdose deaths. These are places where people who are using can go to get clean needles and clean syringes. This is where people basically oversee the use of the drug and intervene if necessary.
It seems sort of antithetical. It seems like, “Boy, why would you fund a center for people to use drugs?” The data from Canada and outside Canada are such that it can be very helpful. That would be one of my messages to lawmakers as well.
Vaccines to combat the synthetic opioid crisis
Dr. Glatter: Do you think that the legislators could approach some of these factories as a way to crack down, and have law enforcement be more aggressive? Is that another possible solution?
Dr. Christo: It is. Law enforcement needs to be supported by the government, by the Biden administration, so that we can prevent the influx of fentanyl and other drugs into the United States, and also to crack down on those in the United States who are manufacturing these drugs – synthetic fentanyl, first and foremost – because we’re seeing a lot of deaths related to synthetic fentanyl.
Also, we’re seeing — and this is pretty intriguing and interesting – the use of vaccines to help prevent overdose. The first human trial is underway right now for a vaccine against oxycodone. Not only that, but there are other vaccines that are in animal trials now against heroin, cocaine, or fentanyl. There’s hope there that we can use vaccines to also help reduce deaths related to overdose from fentanyl and other opioids.
Dr. Glatter: Do you think this would be given widely to the population or only to those at higher risk?
Dr. Christo: It would probably be targeting those who are at higher risk and have a history of drug abuse. I don’t think it would be something that would be given to the entire population, but it certainly could be effective, and we’re seeing encouraging results from the human trial right now.
Dr. Glatter: That’s very intriguing. That’s something that certainly could be quite helpful in the future.
One thing I did want to address is law enforcement and first responders who have been exposed to dust, or inhaled dust possibly, or had fentanyl on their skin. There has been lots of controversy. The recent literature has dispelled the controversy that people who had supposedly passed out and required Narcan after exposure to intact skin, or even compromised skin, had an overdose of fentanyl. Maybe you could speak to that and dispel that myth.
Dr. Christo: Yes, I’ve been asked this question a couple of times in the past. It’s not sufficient just to have contact with fentanyl on the skin to lead to an overdose. You really need to ingest it. That is, take it by mouth in the form of a pill, inhale it, or inject it intravenously. Skin contact is very unlikely going to lead to an overdose and death.
Dr. Glatter: I want to thank you for a very informative interview. Do you have one or two pearls you’d like to give our audience as a takeaway?
Dr. Christo: I would say two things. One is, don’t give up if you have chronic pain because there is hope. We have nonopioid treatments that can be effective. Two, don’t give up if you have a substance use disorder. Talk to your primary care doctor or talk to emergency room physicians if you’re in the emergency room. The Substance Abuse and Mental Health Services Administration is a good resource, too. SAMHSA has an 800 number for support and a website. Take the opportunity to use the resources that are available.
Dr. Glatter is assistant professor of emergency medicine at Lenox Hill Hospital in New York City and at Hofstra University, Hempstead, N.Y. He is an editorial advisor and hosts the Hot Topics in EM series on Medscape. He is also a medical contributor for Forbes.
Dr. Christo is an associate professor and a pain specialist in the department of anesthesiology and critical care medicine at Johns Hopkins University, Baltimore. He also serves as director of the multidisciplinary pain fellowship program at Johns Hopkins Hospital. Christo is the author of Aches and Gains, A Comprehensive Guide to Overcoming Your Pain, and hosts an award-winning, nationally syndicated SiriusXM radio talk show on overcoming pain, called Aches and Gains.
A version of this article first appeared on Medscape.com.
Is exercise effective for constipation?
I recently presented a clinical scenario about a patient of mine named Brenda. This 35-year-old woman came to me with symptoms that had been going on for a year already. I asked for readers’ comments about my management of Brenda.
I appreciate the comments I received regarding this case. The most common suggestion was to encourage Brenda to exercise, and a systematic review of randomized clinical trials published in 2019 supports this recommendation. This review included nine studies with a total of 680 participants, and the overall effect of exercise was a twofold improvement in symptoms associated with constipation. Walking was the most common exercise intervention, and along with qigong (which combines body position, breathing, and meditation), these two modes of exercise were effective in improving constipation. However, the one study evaluating resistance training failed to demonstrate a significant effect. Importantly, the reviewers considered the collective research to be at a high risk of bias.
Exercise will probably help Brenda, although some brainstorming might be necessary to help her fit exercise into her busy schedule. Another suggestion focused on her risk for colorectal cancer, and Dr. Cooke and Dr. Boboc both astutely noted that colorectal cancer is increasingly common among adults at early middle age. This stands in contrast to a steady decline in the prevalence of colorectal cancer among U.S. adults at age 65 years or older. Whereas colorectal cancer declined by 3.3% annually among U.S. older adults from 2011 to 2016, there was a reversal of this favorable trend among individuals between 50 and 64 years of age, with rates increasing by 1% annually.
The increase in the incidence of colorectal cancer among adults 50-64 years of age has been outpaced by the increase among adults younger than 50 years, who have experienced a 2.2% increase in the incidence of colorectal cancer annually between 2012 and 2016. Previously, the increase in colorectal cancer among early middle-aged adults was driven by higher rates of rectal cancer, but more recently this trend has included higher rates of proximal and distal colon tumors. In 2020, 12% of new cases of colorectal cancer were expected to be among individuals younger than 50 years.
So how do we act on this context in the case of Brenda? Her history suggests no overt warning signs for cancer. The history did not address a family history of gastrointestinal symptoms or colorectal cancer, which is an important omission.
Although the number of cases of cancer among persons younger than 50 years may be rising, the overall prevalence of colorectal cancer among younger adults is well under 1%. At 35 years of age, it is not necessary to evaluate Brenda for colorectal cancer. However, persistent or worsening symptoms could prompt a referral for colonoscopy at a later time.
Finally, let’s address how to practically manage Brenda’s case, because many options are available. I would begin with recommendations regarding her lifestyle, including regular exercise, adequate sleep, and whatever she can achieve in the FODMAP diet. I would also recommend psyllium as a soluble fiber and expect that these changes would help her constipation. But they might be less effective for abdominal cramping, so I would also recommend peppermint oil at this time.
If Brenda commits to these recommendations, she will very likely improve. If she does not, I will be more concerned regarding anxiety and depression complicating her illness. Treating those disorders can make a big difference.
In addition, if there is an inadequate response to initial therapy, I will initiate linaclotide or lubiprostone. Plecanatide is another reasonable option. At this point, I will also consider referral to a gastroenterologist for a recalcitrant case and will certainly refer if one of these specific treatments fails in Brenda. Conditions such as pelvic floor dysfunction can mimic irritable bowel syndrome with constipation and merit consideration.
However, I really believe that Brenda will feel better. Thanks for all of the insightful and interesting comments. It is easy to see how we are all invested in improving patients’ lives.
Dr. Vega is a clinical professor of family medicine at the University of California, Irvine. He reported disclosures with McNeil Pharmaceuticals. A version of this article first appeared on Medscape.com.
I recently presented a clinical scenario about a patient of mine named Brenda. This 35-year-old woman came to me with symptoms that had been going on for a year already. I asked for readers’ comments about my management of Brenda.
I appreciate the comments I received regarding this case. The most common suggestion was to encourage Brenda to exercise, and a systematic review of randomized clinical trials published in 2019 supports this recommendation. This review included nine studies with a total of 680 participants, and the overall effect of exercise was a twofold improvement in symptoms associated with constipation. Walking was the most common exercise intervention, and along with qigong (which combines body position, breathing, and meditation), these two modes of exercise were effective in improving constipation. However, the one study evaluating resistance training failed to demonstrate a significant effect. Importantly, the reviewers considered the collective research to be at a high risk of bias.
Exercise will probably help Brenda, although some brainstorming might be necessary to help her fit exercise into her busy schedule. Another suggestion focused on her risk for colorectal cancer, and Dr. Cooke and Dr. Boboc both astutely noted that colorectal cancer is increasingly common among adults at early middle age. This stands in contrast to a steady decline in the prevalence of colorectal cancer among U.S. adults at age 65 years or older. Whereas colorectal cancer declined by 3.3% annually among U.S. older adults from 2011 to 2016, there was a reversal of this favorable trend among individuals between 50 and 64 years of age, with rates increasing by 1% annually.
The increase in the incidence of colorectal cancer among adults 50-64 years of age has been outpaced by the increase among adults younger than 50 years, who have experienced a 2.2% increase in the incidence of colorectal cancer annually between 2012 and 2016. Previously, the increase in colorectal cancer among early middle-aged adults was driven by higher rates of rectal cancer, but more recently this trend has included higher rates of proximal and distal colon tumors. In 2020, 12% of new cases of colorectal cancer were expected to be among individuals younger than 50 years.
So how do we act on this context in the case of Brenda? Her history suggests no overt warning signs for cancer. The history did not address a family history of gastrointestinal symptoms or colorectal cancer, which is an important omission.
Although the number of cases of cancer among persons younger than 50 years may be rising, the overall prevalence of colorectal cancer among younger adults is well under 1%. At 35 years of age, it is not necessary to evaluate Brenda for colorectal cancer. However, persistent or worsening symptoms could prompt a referral for colonoscopy at a later time.
Finally, let’s address how to practically manage Brenda’s case, because many options are available. I would begin with recommendations regarding her lifestyle, including regular exercise, adequate sleep, and whatever she can achieve in the FODMAP diet. I would also recommend psyllium as a soluble fiber and expect that these changes would help her constipation. But they might be less effective for abdominal cramping, so I would also recommend peppermint oil at this time.
If Brenda commits to these recommendations, she will very likely improve. If she does not, I will be more concerned regarding anxiety and depression complicating her illness. Treating those disorders can make a big difference.
In addition, if there is an inadequate response to initial therapy, I will initiate linaclotide or lubiprostone. Plecanatide is another reasonable option. At this point, I will also consider referral to a gastroenterologist for a recalcitrant case and will certainly refer if one of these specific treatments fails in Brenda. Conditions such as pelvic floor dysfunction can mimic irritable bowel syndrome with constipation and merit consideration.
However, I really believe that Brenda will feel better. Thanks for all of the insightful and interesting comments. It is easy to see how we are all invested in improving patients’ lives.
Dr. Vega is a clinical professor of family medicine at the University of California, Irvine. He reported disclosures with McNeil Pharmaceuticals. A version of this article first appeared on Medscape.com.
I recently presented a clinical scenario about a patient of mine named Brenda. This 35-year-old woman came to me with symptoms that had been going on for a year already. I asked for readers’ comments about my management of Brenda.
I appreciate the comments I received regarding this case. The most common suggestion was to encourage Brenda to exercise, and a systematic review of randomized clinical trials published in 2019 supports this recommendation. This review included nine studies with a total of 680 participants, and the overall effect of exercise was a twofold improvement in symptoms associated with constipation. Walking was the most common exercise intervention, and along with qigong (which combines body position, breathing, and meditation), these two modes of exercise were effective in improving constipation. However, the one study evaluating resistance training failed to demonstrate a significant effect. Importantly, the reviewers considered the collective research to be at a high risk of bias.
Exercise will probably help Brenda, although some brainstorming might be necessary to help her fit exercise into her busy schedule. Another suggestion focused on her risk for colorectal cancer, and Dr. Cooke and Dr. Boboc both astutely noted that colorectal cancer is increasingly common among adults at early middle age. This stands in contrast to a steady decline in the prevalence of colorectal cancer among U.S. adults at age 65 years or older. Whereas colorectal cancer declined by 3.3% annually among U.S. older adults from 2011 to 2016, there was a reversal of this favorable trend among individuals between 50 and 64 years of age, with rates increasing by 1% annually.
The increase in the incidence of colorectal cancer among adults 50-64 years of age has been outpaced by the increase among adults younger than 50 years, who have experienced a 2.2% increase in the incidence of colorectal cancer annually between 2012 and 2016. Previously, the increase in colorectal cancer among early middle-aged adults was driven by higher rates of rectal cancer, but more recently this trend has included higher rates of proximal and distal colon tumors. In 2020, 12% of new cases of colorectal cancer were expected to be among individuals younger than 50 years.
So how do we act on this context in the case of Brenda? Her history suggests no overt warning signs for cancer. The history did not address a family history of gastrointestinal symptoms or colorectal cancer, which is an important omission.
Although the number of cases of cancer among persons younger than 50 years may be rising, the overall prevalence of colorectal cancer among younger adults is well under 1%. At 35 years of age, it is not necessary to evaluate Brenda for colorectal cancer. However, persistent or worsening symptoms could prompt a referral for colonoscopy at a later time.
Finally, let’s address how to practically manage Brenda’s case, because many options are available. I would begin with recommendations regarding her lifestyle, including regular exercise, adequate sleep, and whatever she can achieve in the FODMAP diet. I would also recommend psyllium as a soluble fiber and expect that these changes would help her constipation. But they might be less effective for abdominal cramping, so I would also recommend peppermint oil at this time.
If Brenda commits to these recommendations, she will very likely improve. If she does not, I will be more concerned regarding anxiety and depression complicating her illness. Treating those disorders can make a big difference.
In addition, if there is an inadequate response to initial therapy, I will initiate linaclotide or lubiprostone. Plecanatide is another reasonable option. At this point, I will also consider referral to a gastroenterologist for a recalcitrant case and will certainly refer if one of these specific treatments fails in Brenda. Conditions such as pelvic floor dysfunction can mimic irritable bowel syndrome with constipation and merit consideration.
However, I really believe that Brenda will feel better. Thanks for all of the insightful and interesting comments. It is easy to see how we are all invested in improving patients’ lives.
Dr. Vega is a clinical professor of family medicine at the University of California, Irvine. He reported disclosures with McNeil Pharmaceuticals. A version of this article first appeared on Medscape.com.
The role of repeat uterine curettage in postmolar gestational trophoblastic neoplasia
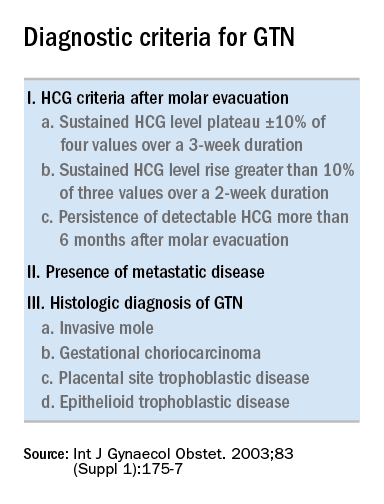
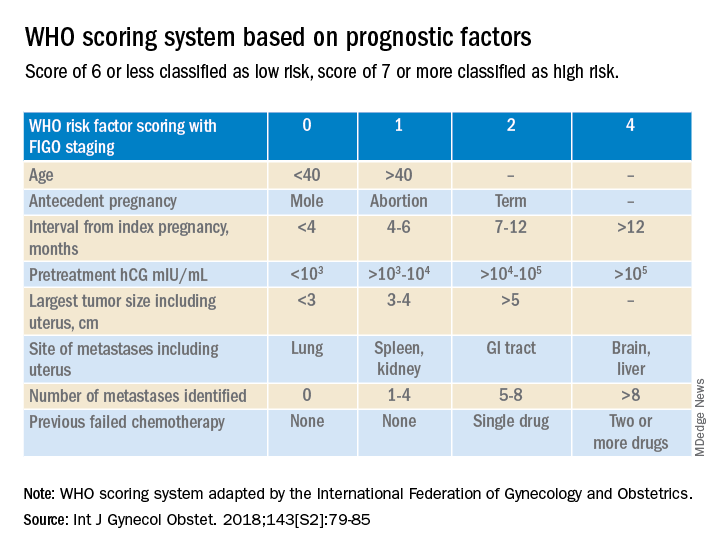
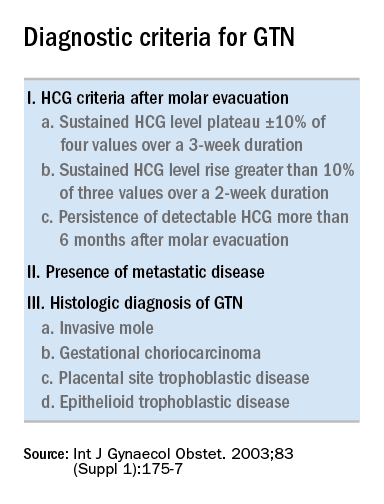
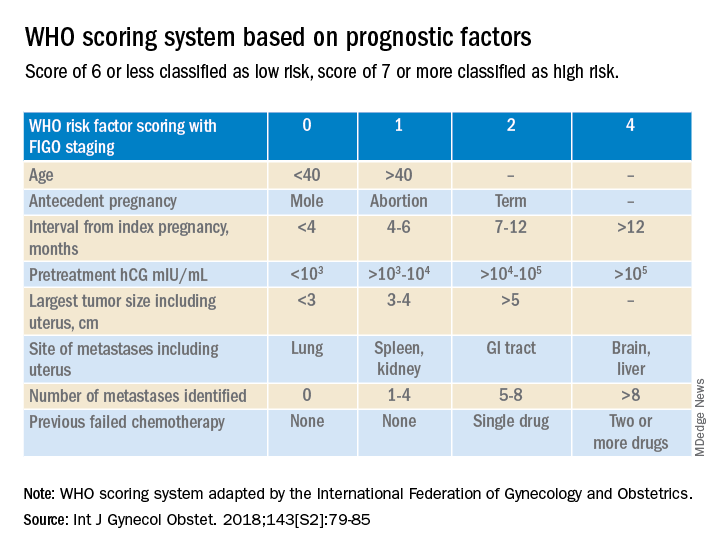
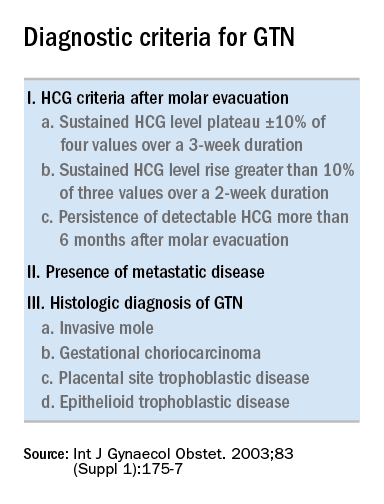
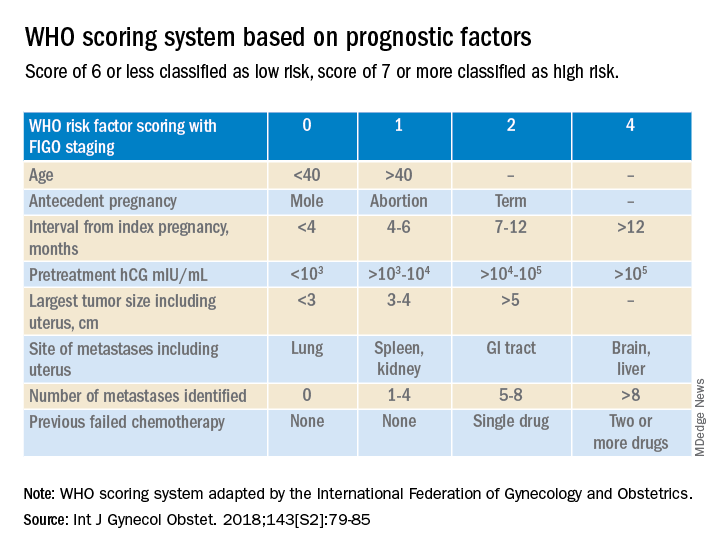
Trophoblastic tissue is responsible for formation of the placenta during pregnancy. Gestational trophoblastic disease (GTD), a group comprising benign (hydatidiform moles) and malignant tumors, occurs when gestational trophoblastic tissue behaves in an abnormal manner. Hydatidiform moles, which are thought to be caused by errors in fertilization, occur in approximately 1 in 1,200 pregnancies in the United States. Gestational trophoblastic neoplasia (GTN) refers to the subgroup of these trophoblastic or placental tumors with malignant behavior and includes postmolar GTN, invasive mole, gestational choriocarcinoma, placental-site trophoblastic tumor (PSTT), and epithelioid trophoblastic tumor. Postmolar GTN arises after evacuation of a molar pregnancy and is most frequently diagnosed by a plateau or increase in human chorionic gonadotropin (hCG).1 The risk of postmolar GTN is much higher after a complete mole (7%-30%) compared with a partial mole (2.5%-7.5%).2 Once postmolar GTN is diagnosed, a World Health Organization score is assigned to determine if patients have low- or high-risk disease.3 The primary treatment for most GTN is chemotherapy. A patient’s WHO score helps determine whether they would benefit from single-agent or multiagent chemotherapy. The standard of care for low-risk disease is single-agent chemotherapy with either methotrexate or actinomycin D.
The role of a second uterine curettage, after the diagnosis of low-risk postmolar GTN, has been controversial because of the limited data and disparate outcomes reported. In older retrospective series, a second curettage affected treatment or produced remission in only 9%-20% of patients and caused uterine perforation or major hemorrhage in 5%-8% of patients.4,5 Given relatively high rates of major complications compared with surgical cure or decreased chemotherapy cycles needed, only a limited number of patients seemed to benefit from a second procedure. On the other hand, an observational study of 544 patients who underwent second uterine evacuation after a presumed diagnosis of persistent GTD found that up to 60% of patients did not require chemotherapy afterward.6 Those with hCG levels greater than 1,500 IU/L or histologic evidence of GTD were less likely to have a surgical cure after second curettage. The indications for uterine evacuations were varied across these studies and make it nearly impossible to compare their results.
More recently, there have been two prospective trials that have tackled the question of the utility of second uterine evacuation in low-risk, nonmetastatic GTN. The Gynecologic Oncology Group performed a single-arm prospective study in the United States that enrolled patients with postmolar GTN to undergo second curettage as initial treatment of their disease.7 Of 60 eligible patients, 40% had a surgical cure (defined as normalization of hCG followed by at least 6 months of subsequent normal hCG values). Overall, 47% of patients were able to avoid chemotherapy. All surgical cures were seen in patients with WHO scores between 0 and 4. Importantly, three women were diagnosed with PSTT, which tends to be resistant to methotrexate and actinomycin D (treatment for nonmetastatic PSTT is definitive surgery with hysterectomy). The study found that hCG was a poor discriminator for achieving surgical cure. While age appeared to have an association with surgical cure (cure less likely for younger and older ages, younger than 19 and older than 40), patient numbers were too small to make a statistical conclusion. There were no uterine perforations and one patient had a grade 3 hemorrhage (requiring transfusion).
In the second prospective trial, performed in Iran, 62 patients were randomized to either second uterine evacuation or standard treatment after diagnosis of postmolar GTN.8 All patients in the surgical arm received a cervical ripening agent prior to their procedure, had their procedure under ultrasound guidance, and received misoprostol afterward to prevent uterine bleeding. Among those undergoing second uterine evacuation, 50% were cured (no need for chemotherapy). Among those needing chemotherapy after surgery, the mean number of cycles of chemotherapy needed (3.07 vs. 6.69) and the time it took to achieve negative hCG (3.23 vs. 9.19 weeks) were significantly less compared with patients who did not undergo surgery. hCG prior to second uterine evacuation could distinguish response to surgery compared with those needing chemotherapy (hCG of 1,983 IU/L or less was the level determined to best predict response). No complications related to surgery were reported.
Given prospective data available, second uterine evacuation for treatment of nonmetastatic, low-risk postmolar GTN is a reasonable treatment option and one that should be considered and discussed with patients given the potential to avoid chemotherapy or decrease the number of cycles needed. It may be prudent to limit the procedure to patients with an hCG less than 1,500-2,000 IU/L and to those between the ages of 20 and 40. While uterine hemorrhage and perforation have been reported in the literature, more recent data suggest low rates of these complications. Unfortunately, given the rarity of the disease and the historically controversial use of second curettage, little is known about the effects on future fertility that this procedure may have, including the development of uterine synechiae.
Dr. Tucker is assistant professor of gynecologic oncology at the University of North Carolina at Chapel Hill.
References
1. Ngan HY et al, FIGO Committee on Gynecologic Oncology. Int J Gynaecol Obstet. 2003 Oct;83 Suppl 1:175-7. Erratum in: Int J Gynaecol Obstet. 2021 Dec;155(3):563.
2. Soper JT. Obstet Gynecol. 2021 Feb.;137(2):355-70.
3. Ngan HY et al. Int J Gynecol Obstet. 2018;143:79-85.
4. Schlaerth JB et al. Am J Obstet Gynecol. 1990 Jun;162(6):1465-70.
5. van Trommel NE et al. Gynecol Oncol. 2005 Oct;99(1):6-13.
6. Pezeshki M et al. Gynecol Oncol. 2004 Dec;95(3):423-9.
7. Osborne RJ et al. Obstet Gynecol. 2016 Sep;128(3):535-42.
8. Ayatollahi H et al. Int J Womens Health. 2017 Sep 21;9:665-71.
Trophoblastic tissue is responsible for formation of the placenta during pregnancy. Gestational trophoblastic disease (GTD), a group comprising benign (hydatidiform moles) and malignant tumors, occurs when gestational trophoblastic tissue behaves in an abnormal manner. Hydatidiform moles, which are thought to be caused by errors in fertilization, occur in approximately 1 in 1,200 pregnancies in the United States. Gestational trophoblastic neoplasia (GTN) refers to the subgroup of these trophoblastic or placental tumors with malignant behavior and includes postmolar GTN, invasive mole, gestational choriocarcinoma, placental-site trophoblastic tumor (PSTT), and epithelioid trophoblastic tumor. Postmolar GTN arises after evacuation of a molar pregnancy and is most frequently diagnosed by a plateau or increase in human chorionic gonadotropin (hCG).1 The risk of postmolar GTN is much higher after a complete mole (7%-30%) compared with a partial mole (2.5%-7.5%).2 Once postmolar GTN is diagnosed, a World Health Organization score is assigned to determine if patients have low- or high-risk disease.3 The primary treatment for most GTN is chemotherapy. A patient’s WHO score helps determine whether they would benefit from single-agent or multiagent chemotherapy. The standard of care for low-risk disease is single-agent chemotherapy with either methotrexate or actinomycin D.
The role of a second uterine curettage, after the diagnosis of low-risk postmolar GTN, has been controversial because of the limited data and disparate outcomes reported. In older retrospective series, a second curettage affected treatment or produced remission in only 9%-20% of patients and caused uterine perforation or major hemorrhage in 5%-8% of patients.4,5 Given relatively high rates of major complications compared with surgical cure or decreased chemotherapy cycles needed, only a limited number of patients seemed to benefit from a second procedure. On the other hand, an observational study of 544 patients who underwent second uterine evacuation after a presumed diagnosis of persistent GTD found that up to 60% of patients did not require chemotherapy afterward.6 Those with hCG levels greater than 1,500 IU/L or histologic evidence of GTD were less likely to have a surgical cure after second curettage. The indications for uterine evacuations were varied across these studies and make it nearly impossible to compare their results.
More recently, there have been two prospective trials that have tackled the question of the utility of second uterine evacuation in low-risk, nonmetastatic GTN. The Gynecologic Oncology Group performed a single-arm prospective study in the United States that enrolled patients with postmolar GTN to undergo second curettage as initial treatment of their disease.7 Of 60 eligible patients, 40% had a surgical cure (defined as normalization of hCG followed by at least 6 months of subsequent normal hCG values). Overall, 47% of patients were able to avoid chemotherapy. All surgical cures were seen in patients with WHO scores between 0 and 4. Importantly, three women were diagnosed with PSTT, which tends to be resistant to methotrexate and actinomycin D (treatment for nonmetastatic PSTT is definitive surgery with hysterectomy). The study found that hCG was a poor discriminator for achieving surgical cure. While age appeared to have an association with surgical cure (cure less likely for younger and older ages, younger than 19 and older than 40), patient numbers were too small to make a statistical conclusion. There were no uterine perforations and one patient had a grade 3 hemorrhage (requiring transfusion).
In the second prospective trial, performed in Iran, 62 patients were randomized to either second uterine evacuation or standard treatment after diagnosis of postmolar GTN.8 All patients in the surgical arm received a cervical ripening agent prior to their procedure, had their procedure under ultrasound guidance, and received misoprostol afterward to prevent uterine bleeding. Among those undergoing second uterine evacuation, 50% were cured (no need for chemotherapy). Among those needing chemotherapy after surgery, the mean number of cycles of chemotherapy needed (3.07 vs. 6.69) and the time it took to achieve negative hCG (3.23 vs. 9.19 weeks) were significantly less compared with patients who did not undergo surgery. hCG prior to second uterine evacuation could distinguish response to surgery compared with those needing chemotherapy (hCG of 1,983 IU/L or less was the level determined to best predict response). No complications related to surgery were reported.
Given prospective data available, second uterine evacuation for treatment of nonmetastatic, low-risk postmolar GTN is a reasonable treatment option and one that should be considered and discussed with patients given the potential to avoid chemotherapy or decrease the number of cycles needed. It may be prudent to limit the procedure to patients with an hCG less than 1,500-2,000 IU/L and to those between the ages of 20 and 40. While uterine hemorrhage and perforation have been reported in the literature, more recent data suggest low rates of these complications. Unfortunately, given the rarity of the disease and the historically controversial use of second curettage, little is known about the effects on future fertility that this procedure may have, including the development of uterine synechiae.
Dr. Tucker is assistant professor of gynecologic oncology at the University of North Carolina at Chapel Hill.
References
1. Ngan HY et al, FIGO Committee on Gynecologic Oncology. Int J Gynaecol Obstet. 2003 Oct;83 Suppl 1:175-7. Erratum in: Int J Gynaecol Obstet. 2021 Dec;155(3):563.
2. Soper JT. Obstet Gynecol. 2021 Feb.;137(2):355-70.
3. Ngan HY et al. Int J Gynecol Obstet. 2018;143:79-85.
4. Schlaerth JB et al. Am J Obstet Gynecol. 1990 Jun;162(6):1465-70.
5. van Trommel NE et al. Gynecol Oncol. 2005 Oct;99(1):6-13.
6. Pezeshki M et al. Gynecol Oncol. 2004 Dec;95(3):423-9.
7. Osborne RJ et al. Obstet Gynecol. 2016 Sep;128(3):535-42.
8. Ayatollahi H et al. Int J Womens Health. 2017 Sep 21;9:665-71.
Trophoblastic tissue is responsible for formation of the placenta during pregnancy. Gestational trophoblastic disease (GTD), a group comprising benign (hydatidiform moles) and malignant tumors, occurs when gestational trophoblastic tissue behaves in an abnormal manner. Hydatidiform moles, which are thought to be caused by errors in fertilization, occur in approximately 1 in 1,200 pregnancies in the United States. Gestational trophoblastic neoplasia (GTN) refers to the subgroup of these trophoblastic or placental tumors with malignant behavior and includes postmolar GTN, invasive mole, gestational choriocarcinoma, placental-site trophoblastic tumor (PSTT), and epithelioid trophoblastic tumor. Postmolar GTN arises after evacuation of a molar pregnancy and is most frequently diagnosed by a plateau or increase in human chorionic gonadotropin (hCG).1 The risk of postmolar GTN is much higher after a complete mole (7%-30%) compared with a partial mole (2.5%-7.5%).2 Once postmolar GTN is diagnosed, a World Health Organization score is assigned to determine if patients have low- or high-risk disease.3 The primary treatment for most GTN is chemotherapy. A patient’s WHO score helps determine whether they would benefit from single-agent or multiagent chemotherapy. The standard of care for low-risk disease is single-agent chemotherapy with either methotrexate or actinomycin D.
The role of a second uterine curettage, after the diagnosis of low-risk postmolar GTN, has been controversial because of the limited data and disparate outcomes reported. In older retrospective series, a second curettage affected treatment or produced remission in only 9%-20% of patients and caused uterine perforation or major hemorrhage in 5%-8% of patients.4,5 Given relatively high rates of major complications compared with surgical cure or decreased chemotherapy cycles needed, only a limited number of patients seemed to benefit from a second procedure. On the other hand, an observational study of 544 patients who underwent second uterine evacuation after a presumed diagnosis of persistent GTD found that up to 60% of patients did not require chemotherapy afterward.6 Those with hCG levels greater than 1,500 IU/L or histologic evidence of GTD were less likely to have a surgical cure after second curettage. The indications for uterine evacuations were varied across these studies and make it nearly impossible to compare their results.
More recently, there have been two prospective trials that have tackled the question of the utility of second uterine evacuation in low-risk, nonmetastatic GTN. The Gynecologic Oncology Group performed a single-arm prospective study in the United States that enrolled patients with postmolar GTN to undergo second curettage as initial treatment of their disease.7 Of 60 eligible patients, 40% had a surgical cure (defined as normalization of hCG followed by at least 6 months of subsequent normal hCG values). Overall, 47% of patients were able to avoid chemotherapy. All surgical cures were seen in patients with WHO scores between 0 and 4. Importantly, three women were diagnosed with PSTT, which tends to be resistant to methotrexate and actinomycin D (treatment for nonmetastatic PSTT is definitive surgery with hysterectomy). The study found that hCG was a poor discriminator for achieving surgical cure. While age appeared to have an association with surgical cure (cure less likely for younger and older ages, younger than 19 and older than 40), patient numbers were too small to make a statistical conclusion. There were no uterine perforations and one patient had a grade 3 hemorrhage (requiring transfusion).
In the second prospective trial, performed in Iran, 62 patients were randomized to either second uterine evacuation or standard treatment after diagnosis of postmolar GTN.8 All patients in the surgical arm received a cervical ripening agent prior to their procedure, had their procedure under ultrasound guidance, and received misoprostol afterward to prevent uterine bleeding. Among those undergoing second uterine evacuation, 50% were cured (no need for chemotherapy). Among those needing chemotherapy after surgery, the mean number of cycles of chemotherapy needed (3.07 vs. 6.69) and the time it took to achieve negative hCG (3.23 vs. 9.19 weeks) were significantly less compared with patients who did not undergo surgery. hCG prior to second uterine evacuation could distinguish response to surgery compared with those needing chemotherapy (hCG of 1,983 IU/L or less was the level determined to best predict response). No complications related to surgery were reported.
Given prospective data available, second uterine evacuation for treatment of nonmetastatic, low-risk postmolar GTN is a reasonable treatment option and one that should be considered and discussed with patients given the potential to avoid chemotherapy or decrease the number of cycles needed. It may be prudent to limit the procedure to patients with an hCG less than 1,500-2,000 IU/L and to those between the ages of 20 and 40. While uterine hemorrhage and perforation have been reported in the literature, more recent data suggest low rates of these complications. Unfortunately, given the rarity of the disease and the historically controversial use of second curettage, little is known about the effects on future fertility that this procedure may have, including the development of uterine synechiae.
Dr. Tucker is assistant professor of gynecologic oncology at the University of North Carolina at Chapel Hill.
References
1. Ngan HY et al, FIGO Committee on Gynecologic Oncology. Int J Gynaecol Obstet. 2003 Oct;83 Suppl 1:175-7. Erratum in: Int J Gynaecol Obstet. 2021 Dec;155(3):563.
2. Soper JT. Obstet Gynecol. 2021 Feb.;137(2):355-70.
3. Ngan HY et al. Int J Gynecol Obstet. 2018;143:79-85.
4. Schlaerth JB et al. Am J Obstet Gynecol. 1990 Jun;162(6):1465-70.
5. van Trommel NE et al. Gynecol Oncol. 2005 Oct;99(1):6-13.
6. Pezeshki M et al. Gynecol Oncol. 2004 Dec;95(3):423-9.
7. Osborne RJ et al. Obstet Gynecol. 2016 Sep;128(3):535-42.
8. Ayatollahi H et al. Int J Womens Health. 2017 Sep 21;9:665-71.
Yes, we should talk politics and religion with patients
From our first days as medical students, we are told that politics and religion are topics to be avoided with patients, but I disagree. Knowing more about our patients allows us to deliver better care.
Politics and religion: New risk factors
The importance of politics and religion in the health of patients was clearly demonstrated during the COVID-19 pandemic. Lives were needlessly lost because of stands taken based on religious beliefs or a political ideology. Families, friends, and the community at large were impacted.
Over my years of practice, I have found that while these are difficult topics to address, they should not be avoided. Studies have shown that open acknowledgement of religious beliefs can affect both clinical outcomes and well-being. Religion and spirituality are as much a part of our patient’s lives as the physical parameters that we measure. To neglect these significant aspects is to miss the very essence of the individual.
I made it a practice to ask patients about their religious beliefs, the extent to which religion shaped their life, and whether they were part of a church community. Knowing this allowed me to separate deep personal belief from stances based on personal freedom, misinformation, conspiracies, and politics.
I found that information about political leanings flowed naturally in discussions with patients as we trusted and respected each other over time. If I approached politics objectively and nonjudgmentally, it generally led to meaningful conversation. This helped me to understand the patient as an individual and informed my diagnosis and treatment plan.
Politics as stress
For example, on more than one occasion, a patient with atrial fibrillation presented with persistent elevated blood pressure and pulse rate despite adherence to the medical regimen that I had prescribed. After a few minutes of discussion, it was clear that excessive attention to political commentary on TV and social media raised their anxiety and anger level, putting them at greater risk for adverse outcomes. I advised that they refocus their leisure activities rather than change or increase medication.
It is disappointing to see how one of the great scientific advances of our lifetime, vaccination science, has been tarnished because of political or religious ideology and to see the extent to which these beliefs influenced COVID-19 vaccination compliance. As health care providers, we must promote information based on the scientific method. If patients challenge us and point out that recommendations based on science seem to change over time, we must explain that science evolves on the basis of new information objectively gathered. We need to find out what information the patient has gotten from the Internet, TV, or conspiracy theories and counter this with scientific facts. If we do not discuss religion and politics with our patients along with other risk factors, we may compromise our ability to give them the best advice and treatment.
Our patients have a right to their own spiritual and political ideology. If it differs dramatically from our own, this should not influence our commitment to care for them. But we have an obligation to challenge unfounded beliefs about medicine and counter with scientific facts. There are times when individual freedoms must be secondary to public health. Ultimately, it is up to the patient to choose, but they should not be given a “free pass” on the basis of religion or politics. If I know something is true and I would do it myself or recommend it for my family, I have an obligation to provide this recommendation to my patients.
Religious preference is included in medical records. It is not appropriate to add political preference, but the patient benefits if a long-term caregiver knows this information.
During the pandemic, for the first time in my 40+ years of practice, some patients questioned my recommendations and placed equal or greater weight on religion, politics, or conspiracy theories. This continues to be a very real struggle.
Knowing and understanding our patients as individuals is critical to providing optimum care and that means tackling these formally taboo topics. If having a potentially uncomfortable conversation with patients allows us to save one life, it is worth it.
Dr. Francis is a cardiologist at Inova Heart and Vascular Institute, McLean, Va. He disclosed no relevant conflict of interest. A version of this article first appeared on Medscape.com.
From our first days as medical students, we are told that politics and religion are topics to be avoided with patients, but I disagree. Knowing more about our patients allows us to deliver better care.
Politics and religion: New risk factors
The importance of politics and religion in the health of patients was clearly demonstrated during the COVID-19 pandemic. Lives were needlessly lost because of stands taken based on religious beliefs or a political ideology. Families, friends, and the community at large were impacted.
Over my years of practice, I have found that while these are difficult topics to address, they should not be avoided. Studies have shown that open acknowledgement of religious beliefs can affect both clinical outcomes and well-being. Religion and spirituality are as much a part of our patient’s lives as the physical parameters that we measure. To neglect these significant aspects is to miss the very essence of the individual.
I made it a practice to ask patients about their religious beliefs, the extent to which religion shaped their life, and whether they were part of a church community. Knowing this allowed me to separate deep personal belief from stances based on personal freedom, misinformation, conspiracies, and politics.
I found that information about political leanings flowed naturally in discussions with patients as we trusted and respected each other over time. If I approached politics objectively and nonjudgmentally, it generally led to meaningful conversation. This helped me to understand the patient as an individual and informed my diagnosis and treatment plan.
Politics as stress
For example, on more than one occasion, a patient with atrial fibrillation presented with persistent elevated blood pressure and pulse rate despite adherence to the medical regimen that I had prescribed. After a few minutes of discussion, it was clear that excessive attention to political commentary on TV and social media raised their anxiety and anger level, putting them at greater risk for adverse outcomes. I advised that they refocus their leisure activities rather than change or increase medication.
It is disappointing to see how one of the great scientific advances of our lifetime, vaccination science, has been tarnished because of political or religious ideology and to see the extent to which these beliefs influenced COVID-19 vaccination compliance. As health care providers, we must promote information based on the scientific method. If patients challenge us and point out that recommendations based on science seem to change over time, we must explain that science evolves on the basis of new information objectively gathered. We need to find out what information the patient has gotten from the Internet, TV, or conspiracy theories and counter this with scientific facts. If we do not discuss religion and politics with our patients along with other risk factors, we may compromise our ability to give them the best advice and treatment.
Our patients have a right to their own spiritual and political ideology. If it differs dramatically from our own, this should not influence our commitment to care for them. But we have an obligation to challenge unfounded beliefs about medicine and counter with scientific facts. There are times when individual freedoms must be secondary to public health. Ultimately, it is up to the patient to choose, but they should not be given a “free pass” on the basis of religion or politics. If I know something is true and I would do it myself or recommend it for my family, I have an obligation to provide this recommendation to my patients.
Religious preference is included in medical records. It is not appropriate to add political preference, but the patient benefits if a long-term caregiver knows this information.
During the pandemic, for the first time in my 40+ years of practice, some patients questioned my recommendations and placed equal or greater weight on religion, politics, or conspiracy theories. This continues to be a very real struggle.
Knowing and understanding our patients as individuals is critical to providing optimum care and that means tackling these formally taboo topics. If having a potentially uncomfortable conversation with patients allows us to save one life, it is worth it.
Dr. Francis is a cardiologist at Inova Heart and Vascular Institute, McLean, Va. He disclosed no relevant conflict of interest. A version of this article first appeared on Medscape.com.
From our first days as medical students, we are told that politics and religion are topics to be avoided with patients, but I disagree. Knowing more about our patients allows us to deliver better care.
Politics and religion: New risk factors
The importance of politics and religion in the health of patients was clearly demonstrated during the COVID-19 pandemic. Lives were needlessly lost because of stands taken based on religious beliefs or a political ideology. Families, friends, and the community at large were impacted.
Over my years of practice, I have found that while these are difficult topics to address, they should not be avoided. Studies have shown that open acknowledgement of religious beliefs can affect both clinical outcomes and well-being. Religion and spirituality are as much a part of our patient’s lives as the physical parameters that we measure. To neglect these significant aspects is to miss the very essence of the individual.
I made it a practice to ask patients about their religious beliefs, the extent to which religion shaped their life, and whether they were part of a church community. Knowing this allowed me to separate deep personal belief from stances based on personal freedom, misinformation, conspiracies, and politics.
I found that information about political leanings flowed naturally in discussions with patients as we trusted and respected each other over time. If I approached politics objectively and nonjudgmentally, it generally led to meaningful conversation. This helped me to understand the patient as an individual and informed my diagnosis and treatment plan.
Politics as stress
For example, on more than one occasion, a patient with atrial fibrillation presented with persistent elevated blood pressure and pulse rate despite adherence to the medical regimen that I had prescribed. After a few minutes of discussion, it was clear that excessive attention to political commentary on TV and social media raised their anxiety and anger level, putting them at greater risk for adverse outcomes. I advised that they refocus their leisure activities rather than change or increase medication.
It is disappointing to see how one of the great scientific advances of our lifetime, vaccination science, has been tarnished because of political or religious ideology and to see the extent to which these beliefs influenced COVID-19 vaccination compliance. As health care providers, we must promote information based on the scientific method. If patients challenge us and point out that recommendations based on science seem to change over time, we must explain that science evolves on the basis of new information objectively gathered. We need to find out what information the patient has gotten from the Internet, TV, or conspiracy theories and counter this with scientific facts. If we do not discuss religion and politics with our patients along with other risk factors, we may compromise our ability to give them the best advice and treatment.
Our patients have a right to their own spiritual and political ideology. If it differs dramatically from our own, this should not influence our commitment to care for them. But we have an obligation to challenge unfounded beliefs about medicine and counter with scientific facts. There are times when individual freedoms must be secondary to public health. Ultimately, it is up to the patient to choose, but they should not be given a “free pass” on the basis of religion or politics. If I know something is true and I would do it myself or recommend it for my family, I have an obligation to provide this recommendation to my patients.
Religious preference is included in medical records. It is not appropriate to add political preference, but the patient benefits if a long-term caregiver knows this information.
During the pandemic, for the first time in my 40+ years of practice, some patients questioned my recommendations and placed equal or greater weight on religion, politics, or conspiracy theories. This continues to be a very real struggle.
Knowing and understanding our patients as individuals is critical to providing optimum care and that means tackling these formally taboo topics. If having a potentially uncomfortable conversation with patients allows us to save one life, it is worth it.
Dr. Francis is a cardiologist at Inova Heart and Vascular Institute, McLean, Va. He disclosed no relevant conflict of interest. A version of this article first appeared on Medscape.com.
COMMENT & CONTROVERSY
CAN WE RETURN TO THE ABCS OF CRAFTING A MEDICAL RECORD NOTE?
ROBERT L. BARBIERI, MD (OCTOBER 2021)
Physicians can help provide EMR fixes
I appreciate Dr. Barbieri’s editorials and insight on many issues facing our profession. I would like to offer my comments on a recent article.
If you want your brakes fixed, don’t go to a shoe maker. Physicians seem to have lost our sense of who is most competent in determining the best way to practice and communicate medical care. Somehow we have turned this over to the bureaucrats, who seem to find ways to complicate the lives of both providers and patients. Maybe we are too busy caring for patients and trying to find ways to alleviate the burden placed on our time by the electronic medical record (EMR) system, which was touted as an improvement in medical care and increasing provider efficiency. Most of the time I hear my colleagues describing ways to “work around” an EMR system that has immense deficiencies in providing accurate information in a way that is easily digested by whomever is viewing the record. The universal ability to transfer information is simply not true. One colleague had the same office version of Cerner as was used in the hospital setting but was unable to send information back and forth due to the danger of the potential to corrupt the system.
Dr. Barbieri mentioned his work around to make the record easier for the patient to read. I ask, what about the coding descriptions, which most systems are now requiring physicians to put in at the time of the encounter? In the past this was done by certified coders, who undergo a 1- to 2-year training program, and is now being performed by physicians who have minimal to no training in coding. (And who, by the way, can be fined for both under- and over coding.) The example Dr. Barbieri put forth for obesity comes to mind and is part of the medical record in all cases. The terminology used by ICD10 is not so kind and requires some imagination when trying to find the right code for many diagnoses.
When will we stop allowing others, who know little about medicine and caring for patients, to tell us how to provide the care that we have trained for 7-12 years on how best to deliver?
William Sutton, MD
Muncie, Indiana
Dr. Barbieri responds
I thank Dr. Sutton for providing his experience with the electronic medical record. I agree with him that bureaucrats often create health care rules that do more to hinder than help patients. With regard to coding and billing, I use ICD-10 codes and usually bill based on time, which includes both face-to-face time with the patient and time spent reviewing the patient’s medical records. Now that federal regulations require medical notes to be shared with patients, I craft my history, assessment, and plan with language that is easy for a patient to accept and understand, avoiding medical terms that patients might misinterpret.
Should microscopy be replaced?
I agree with many points Dr. Barbieri made in his editorial. However, I do not agree that the microscopic examination of the vaginal discharge should be replaced. NAAT offers some advantages, but it does not offer a complete assessment of the vaginal ecosystem and microbiome. I believe that NAAT should be used in conjunction with the pelvic examination and microscopic examination of the vaginal discharge.
Microscopic examination of the vaginal discharge can reveal:
- whether or not the squamous epithelial cells are estrogenized. The absence of estrogen will, along with physical findings, indicate the possibility that the patient is experiencing atrophic vaginitis.
- the presence of estrogenized squamous epithelial cells. Plus, a finding of erythema of the vaginal epithelium indicates that the patient has an inflammatory condition and vaginitis, suggesting a possible infection in addition to vaginitis.
- the presence of white blood cells >5/40X magnification, which indicates the possible presence of infection in addition to vaginitis (eg, BV).
I agree that NAAT can confirm an initial diagnosis or refute it. In the latter case, the physician can change treatment accordingly. In the absence or in conjunction with the presence of a sexually transmitted infection, the composition of the vaginal microbiome is significant (ie, determining if vaginal dysbiosis is present). Performing a comprehensive evaluation, determining if the most common pathogens are present in aerobic vaginitis and/or BV, plus completing a Lactobacillus panel can be expensive. If insurance companies do not pay for such testing, patients will be reluctant to pay out of pocket for these tests.
My final comment addresses the administration of NAAT for aerobic vaginitis, and for BV, it is probably an ineffective treatment. Vaginal dysbiosis is based on whether the appropriate species of Lactobacillus is present, and the concentration. Treatment most likely will be based on replenishing or restoring the appropriate species of Lactobacillus to dominance.
Sebastian Faro, MD, PhD
Houston, Texas
Dr. Barbieri responds
I agree with Dr. Faro; when used by highly trained clinicians, microscopy is an excellent tool for evaluating vaginal specimens. Expert clinicians, such as Dr. Faro, with a focus on infectious diseases do not need to rely on NAAT testing except for identifying cases of T vaginalis infection. However, in standard clinical practice, microscopy performs poorly, resulting in misdiagnosis.1 In the average clinical practice, NAAT testing may help improve patient outcomes.
1. Gaydos CA, Beqaj S, Schwebke JR, et al. Clinical validation of a test for the diagnosis of vaginitis. Obstet Gynecol. 2017;130:181-189.
A note of thanks
I am a 74-year-old ObGyn who finished training at the University of North Carolina in 1979. Currently, I am working at a rural health group 2 days a week as a source of in-house gyn referral for 17 primary care physicians and mid-level providers. Our patients are almost all underserved and self-pay. The bulk of my work is related to evaluating abnormal uterine bleeding and abnormal Pap tests. Your publication of OBG Management serves now as one of my main sources of information. I just wanted to thank you and let you know that the publication is important. Keep up the good work and best wishes.
Julian Brantley, MD
Rocky Mountain, North Carolina
Dr. Barbieri responds
I thank Dr. Brantley for taking time from a busy practice to write about how OBG Management provides practical information relevant to practice. Each issue of OBG Management is built on a foundation of insights from expert clinicians, which is crafted into a finished product by a superb editorial team. Our goal is to enhance the quality of women’s health care and the professional development of obstetrician-gynecologists and all women’s health care clinicians. ●
CAN WE RETURN TO THE ABCS OF CRAFTING A MEDICAL RECORD NOTE?
ROBERT L. BARBIERI, MD (OCTOBER 2021)
Physicians can help provide EMR fixes
I appreciate Dr. Barbieri’s editorials and insight on many issues facing our profession. I would like to offer my comments on a recent article.
If you want your brakes fixed, don’t go to a shoe maker. Physicians seem to have lost our sense of who is most competent in determining the best way to practice and communicate medical care. Somehow we have turned this over to the bureaucrats, who seem to find ways to complicate the lives of both providers and patients. Maybe we are too busy caring for patients and trying to find ways to alleviate the burden placed on our time by the electronic medical record (EMR) system, which was touted as an improvement in medical care and increasing provider efficiency. Most of the time I hear my colleagues describing ways to “work around” an EMR system that has immense deficiencies in providing accurate information in a way that is easily digested by whomever is viewing the record. The universal ability to transfer information is simply not true. One colleague had the same office version of Cerner as was used in the hospital setting but was unable to send information back and forth due to the danger of the potential to corrupt the system.
Dr. Barbieri mentioned his work around to make the record easier for the patient to read. I ask, what about the coding descriptions, which most systems are now requiring physicians to put in at the time of the encounter? In the past this was done by certified coders, who undergo a 1- to 2-year training program, and is now being performed by physicians who have minimal to no training in coding. (And who, by the way, can be fined for both under- and over coding.) The example Dr. Barbieri put forth for obesity comes to mind and is part of the medical record in all cases. The terminology used by ICD10 is not so kind and requires some imagination when trying to find the right code for many diagnoses.
When will we stop allowing others, who know little about medicine and caring for patients, to tell us how to provide the care that we have trained for 7-12 years on how best to deliver?
William Sutton, MD
Muncie, Indiana
Dr. Barbieri responds
I thank Dr. Sutton for providing his experience with the electronic medical record. I agree with him that bureaucrats often create health care rules that do more to hinder than help patients. With regard to coding and billing, I use ICD-10 codes and usually bill based on time, which includes both face-to-face time with the patient and time spent reviewing the patient’s medical records. Now that federal regulations require medical notes to be shared with patients, I craft my history, assessment, and plan with language that is easy for a patient to accept and understand, avoiding medical terms that patients might misinterpret.
Should microscopy be replaced?
I agree with many points Dr. Barbieri made in his editorial. However, I do not agree that the microscopic examination of the vaginal discharge should be replaced. NAAT offers some advantages, but it does not offer a complete assessment of the vaginal ecosystem and microbiome. I believe that NAAT should be used in conjunction with the pelvic examination and microscopic examination of the vaginal discharge.
Microscopic examination of the vaginal discharge can reveal:
- whether or not the squamous epithelial cells are estrogenized. The absence of estrogen will, along with physical findings, indicate the possibility that the patient is experiencing atrophic vaginitis.
- the presence of estrogenized squamous epithelial cells. Plus, a finding of erythema of the vaginal epithelium indicates that the patient has an inflammatory condition and vaginitis, suggesting a possible infection in addition to vaginitis.
- the presence of white blood cells >5/40X magnification, which indicates the possible presence of infection in addition to vaginitis (eg, BV).
I agree that NAAT can confirm an initial diagnosis or refute it. In the latter case, the physician can change treatment accordingly. In the absence or in conjunction with the presence of a sexually transmitted infection, the composition of the vaginal microbiome is significant (ie, determining if vaginal dysbiosis is present). Performing a comprehensive evaluation, determining if the most common pathogens are present in aerobic vaginitis and/or BV, plus completing a Lactobacillus panel can be expensive. If insurance companies do not pay for such testing, patients will be reluctant to pay out of pocket for these tests.
My final comment addresses the administration of NAAT for aerobic vaginitis, and for BV, it is probably an ineffective treatment. Vaginal dysbiosis is based on whether the appropriate species of Lactobacillus is present, and the concentration. Treatment most likely will be based on replenishing or restoring the appropriate species of Lactobacillus to dominance.
Sebastian Faro, MD, PhD
Houston, Texas
Dr. Barbieri responds
I agree with Dr. Faro; when used by highly trained clinicians, microscopy is an excellent tool for evaluating vaginal specimens. Expert clinicians, such as Dr. Faro, with a focus on infectious diseases do not need to rely on NAAT testing except for identifying cases of T vaginalis infection. However, in standard clinical practice, microscopy performs poorly, resulting in misdiagnosis.1 In the average clinical practice, NAAT testing may help improve patient outcomes.
1. Gaydos CA, Beqaj S, Schwebke JR, et al. Clinical validation of a test for the diagnosis of vaginitis. Obstet Gynecol. 2017;130:181-189.
A note of thanks
I am a 74-year-old ObGyn who finished training at the University of North Carolina in 1979. Currently, I am working at a rural health group 2 days a week as a source of in-house gyn referral for 17 primary care physicians and mid-level providers. Our patients are almost all underserved and self-pay. The bulk of my work is related to evaluating abnormal uterine bleeding and abnormal Pap tests. Your publication of OBG Management serves now as one of my main sources of information. I just wanted to thank you and let you know that the publication is important. Keep up the good work and best wishes.
Julian Brantley, MD
Rocky Mountain, North Carolina
Dr. Barbieri responds
I thank Dr. Brantley for taking time from a busy practice to write about how OBG Management provides practical information relevant to practice. Each issue of OBG Management is built on a foundation of insights from expert clinicians, which is crafted into a finished product by a superb editorial team. Our goal is to enhance the quality of women’s health care and the professional development of obstetrician-gynecologists and all women’s health care clinicians. ●
CAN WE RETURN TO THE ABCS OF CRAFTING A MEDICAL RECORD NOTE?
ROBERT L. BARBIERI, MD (OCTOBER 2021)
Physicians can help provide EMR fixes
I appreciate Dr. Barbieri’s editorials and insight on many issues facing our profession. I would like to offer my comments on a recent article.
If you want your brakes fixed, don’t go to a shoe maker. Physicians seem to have lost our sense of who is most competent in determining the best way to practice and communicate medical care. Somehow we have turned this over to the bureaucrats, who seem to find ways to complicate the lives of both providers and patients. Maybe we are too busy caring for patients and trying to find ways to alleviate the burden placed on our time by the electronic medical record (EMR) system, which was touted as an improvement in medical care and increasing provider efficiency. Most of the time I hear my colleagues describing ways to “work around” an EMR system that has immense deficiencies in providing accurate information in a way that is easily digested by whomever is viewing the record. The universal ability to transfer information is simply not true. One colleague had the same office version of Cerner as was used in the hospital setting but was unable to send information back and forth due to the danger of the potential to corrupt the system.
Dr. Barbieri mentioned his work around to make the record easier for the patient to read. I ask, what about the coding descriptions, which most systems are now requiring physicians to put in at the time of the encounter? In the past this was done by certified coders, who undergo a 1- to 2-year training program, and is now being performed by physicians who have minimal to no training in coding. (And who, by the way, can be fined for both under- and over coding.) The example Dr. Barbieri put forth for obesity comes to mind and is part of the medical record in all cases. The terminology used by ICD10 is not so kind and requires some imagination when trying to find the right code for many diagnoses.
When will we stop allowing others, who know little about medicine and caring for patients, to tell us how to provide the care that we have trained for 7-12 years on how best to deliver?
William Sutton, MD
Muncie, Indiana
Dr. Barbieri responds
I thank Dr. Sutton for providing his experience with the electronic medical record. I agree with him that bureaucrats often create health care rules that do more to hinder than help patients. With regard to coding and billing, I use ICD-10 codes and usually bill based on time, which includes both face-to-face time with the patient and time spent reviewing the patient’s medical records. Now that federal regulations require medical notes to be shared with patients, I craft my history, assessment, and plan with language that is easy for a patient to accept and understand, avoiding medical terms that patients might misinterpret.
Should microscopy be replaced?
I agree with many points Dr. Barbieri made in his editorial. However, I do not agree that the microscopic examination of the vaginal discharge should be replaced. NAAT offers some advantages, but it does not offer a complete assessment of the vaginal ecosystem and microbiome. I believe that NAAT should be used in conjunction with the pelvic examination and microscopic examination of the vaginal discharge.
Microscopic examination of the vaginal discharge can reveal:
- whether or not the squamous epithelial cells are estrogenized. The absence of estrogen will, along with physical findings, indicate the possibility that the patient is experiencing atrophic vaginitis.
- the presence of estrogenized squamous epithelial cells. Plus, a finding of erythema of the vaginal epithelium indicates that the patient has an inflammatory condition and vaginitis, suggesting a possible infection in addition to vaginitis.
- the presence of white blood cells >5/40X magnification, which indicates the possible presence of infection in addition to vaginitis (eg, BV).
I agree that NAAT can confirm an initial diagnosis or refute it. In the latter case, the physician can change treatment accordingly. In the absence or in conjunction with the presence of a sexually transmitted infection, the composition of the vaginal microbiome is significant (ie, determining if vaginal dysbiosis is present). Performing a comprehensive evaluation, determining if the most common pathogens are present in aerobic vaginitis and/or BV, plus completing a Lactobacillus panel can be expensive. If insurance companies do not pay for such testing, patients will be reluctant to pay out of pocket for these tests.
My final comment addresses the administration of NAAT for aerobic vaginitis, and for BV, it is probably an ineffective treatment. Vaginal dysbiosis is based on whether the appropriate species of Lactobacillus is present, and the concentration. Treatment most likely will be based on replenishing or restoring the appropriate species of Lactobacillus to dominance.
Sebastian Faro, MD, PhD
Houston, Texas
Dr. Barbieri responds
I agree with Dr. Faro; when used by highly trained clinicians, microscopy is an excellent tool for evaluating vaginal specimens. Expert clinicians, such as Dr. Faro, with a focus on infectious diseases do not need to rely on NAAT testing except for identifying cases of T vaginalis infection. However, in standard clinical practice, microscopy performs poorly, resulting in misdiagnosis.1 In the average clinical practice, NAAT testing may help improve patient outcomes.
1. Gaydos CA, Beqaj S, Schwebke JR, et al. Clinical validation of a test for the diagnosis of vaginitis. Obstet Gynecol. 2017;130:181-189.
A note of thanks
I am a 74-year-old ObGyn who finished training at the University of North Carolina in 1979. Currently, I am working at a rural health group 2 days a week as a source of in-house gyn referral for 17 primary care physicians and mid-level providers. Our patients are almost all underserved and self-pay. The bulk of my work is related to evaluating abnormal uterine bleeding and abnormal Pap tests. Your publication of OBG Management serves now as one of my main sources of information. I just wanted to thank you and let you know that the publication is important. Keep up the good work and best wishes.
Julian Brantley, MD
Rocky Mountain, North Carolina
Dr. Barbieri responds
I thank Dr. Brantley for taking time from a busy practice to write about how OBG Management provides practical information relevant to practice. Each issue of OBG Management is built on a foundation of insights from expert clinicians, which is crafted into a finished product by a superb editorial team. Our goal is to enhance the quality of women’s health care and the professional development of obstetrician-gynecologists and all women’s health care clinicians. ●
How to make the best of your worst reviews
I have a love-hate relationship with patient reviews and satisfaction scores. I love good reviews and hate bad ones. Actually, I skim good reviews and then dwell for days on the negative ones, trying to rack my brain as to what I did wrong. Like everyone else, I have off days when I’m tired or distracted or just overwhelmed. Though I try to bring my A game to every patient visit, realistically, I know that I don’t always achieve this. But, for me, the difference in my best visits and good-enough visits is the difference between a 4-star and 5-star review. What’s up with those 1-star reviews?
Many, many years ago, when patient satisfaction scores were in their infancy, our clinic rewarded any physician who got a 100% satisfaction score. On the surface that makes perfect sense – of course, our patients should be satisfied 100% of the time, right? When I asked one of the winners of this competition how he did it (I never scored 100%), he told me, “I just do whatever the patient wants me to do.” Yikes, I thought at the time. That may be the recipe for an A+ for patient satisfaction but not for quality or outcomes.
Sometimes, I know that they are going to be unhappy, such as when I decline to refill their drug of abuse. Other times, I have to exercise my best medical judgment and hope that my explanation does not alienate the patient. After all, when I say “no” to a patient request, it is with their overall health and well-being in mind. But I would be lying if I said that I have matured to the point that I’m not bothered by a negative review or a patient choosing to take their care elsewhere.
Most of us seek and welcome feedback. Over time, I’ve learned to do this during the visit by asking “Am I giving you too much information?” or “What do you think of the plan?” or “What’s most important to you?” There are times when I conclude the visit and know that the patient is not satisfied but remain unable to ferret out where I let them down – even, on occasion, when I ask them directly. Ideally, any feedback we get from our patients, positive or negative, would be specific and actionable. It rarely is.
There is no doubt we have entered the era of consumer medicine. Everything from the physical appearance of our clinics to the response time to electronic messages is fair game in how patients judge us. As we all know, patients assume competence – they are not usually impressed by your training or quality outcomes because they already believe you are clinically competent (or arguably they’d never set foot in your office). Instead of judging us how we often judge ourselves, patients form opinions about us by how we enter the room, whether we sit or stand, how long they wait in the exam room before we come in, or whether they like the nurse with whom we work. So many subtle things – many of which are outside of our control.
I often struggle with staying on time. When I am invariably walking into the room late, I make a point of thanking patients for their patience. When I’m very late, I offer a more detailed, HIPAA-compliant explanation. What I wish my patients saw was that I am often accommodating a patient who arrives late for their appointment or who wants me to address every concern they’ve had for the past 5 years. While I aspire to not allow the patient’s perception of the visit to unduly influence how I handle the visit, it inevitably does. I do want to have patients who are happy with their experience.
One of my friends is enviously pragmatic in her view on patient experience. “I’m not their friend and they don’t have to like me.” She emphasizes the clinical care she is providing and does not allow patients who are upset with some aspect of the care to weigh heavy on her. It may be that specialists are more likely to enjoy the luxury of putting aside how patients feel about them personally. In primary care, the patient-physician relationship is so central to what we do that ignoring your “likability” has the potential to threaten your professional viability.
I conclude this blog much like I started it. My desire is to allow the negative reviews, particularly if they have nothing actionable in them, to roll off my back and to keep my focus on the clinical care that I am providing. In actuality, I care deeply about how my patients experience their visit with me and will likely continue to take my reviews to heart.
Dr. Frank is a family physician in Neenah, Wisc. She disclosed no relevant conflicts of interest.
A version of this article first appeared on Medscape.com.
I have a love-hate relationship with patient reviews and satisfaction scores. I love good reviews and hate bad ones. Actually, I skim good reviews and then dwell for days on the negative ones, trying to rack my brain as to what I did wrong. Like everyone else, I have off days when I’m tired or distracted or just overwhelmed. Though I try to bring my A game to every patient visit, realistically, I know that I don’t always achieve this. But, for me, the difference in my best visits and good-enough visits is the difference between a 4-star and 5-star review. What’s up with those 1-star reviews?
Many, many years ago, when patient satisfaction scores were in their infancy, our clinic rewarded any physician who got a 100% satisfaction score. On the surface that makes perfect sense – of course, our patients should be satisfied 100% of the time, right? When I asked one of the winners of this competition how he did it (I never scored 100%), he told me, “I just do whatever the patient wants me to do.” Yikes, I thought at the time. That may be the recipe for an A+ for patient satisfaction but not for quality or outcomes.
Sometimes, I know that they are going to be unhappy, such as when I decline to refill their drug of abuse. Other times, I have to exercise my best medical judgment and hope that my explanation does not alienate the patient. After all, when I say “no” to a patient request, it is with their overall health and well-being in mind. But I would be lying if I said that I have matured to the point that I’m not bothered by a negative review or a patient choosing to take their care elsewhere.
Most of us seek and welcome feedback. Over time, I’ve learned to do this during the visit by asking “Am I giving you too much information?” or “What do you think of the plan?” or “What’s most important to you?” There are times when I conclude the visit and know that the patient is not satisfied but remain unable to ferret out where I let them down – even, on occasion, when I ask them directly. Ideally, any feedback we get from our patients, positive or negative, would be specific and actionable. It rarely is.
There is no doubt we have entered the era of consumer medicine. Everything from the physical appearance of our clinics to the response time to electronic messages is fair game in how patients judge us. As we all know, patients assume competence – they are not usually impressed by your training or quality outcomes because they already believe you are clinically competent (or arguably they’d never set foot in your office). Instead of judging us how we often judge ourselves, patients form opinions about us by how we enter the room, whether we sit or stand, how long they wait in the exam room before we come in, or whether they like the nurse with whom we work. So many subtle things – many of which are outside of our control.
I often struggle with staying on time. When I am invariably walking into the room late, I make a point of thanking patients for their patience. When I’m very late, I offer a more detailed, HIPAA-compliant explanation. What I wish my patients saw was that I am often accommodating a patient who arrives late for their appointment or who wants me to address every concern they’ve had for the past 5 years. While I aspire to not allow the patient’s perception of the visit to unduly influence how I handle the visit, it inevitably does. I do want to have patients who are happy with their experience.
One of my friends is enviously pragmatic in her view on patient experience. “I’m not their friend and they don’t have to like me.” She emphasizes the clinical care she is providing and does not allow patients who are upset with some aspect of the care to weigh heavy on her. It may be that specialists are more likely to enjoy the luxury of putting aside how patients feel about them personally. In primary care, the patient-physician relationship is so central to what we do that ignoring your “likability” has the potential to threaten your professional viability.
I conclude this blog much like I started it. My desire is to allow the negative reviews, particularly if they have nothing actionable in them, to roll off my back and to keep my focus on the clinical care that I am providing. In actuality, I care deeply about how my patients experience their visit with me and will likely continue to take my reviews to heart.
Dr. Frank is a family physician in Neenah, Wisc. She disclosed no relevant conflicts of interest.
A version of this article first appeared on Medscape.com.
I have a love-hate relationship with patient reviews and satisfaction scores. I love good reviews and hate bad ones. Actually, I skim good reviews and then dwell for days on the negative ones, trying to rack my brain as to what I did wrong. Like everyone else, I have off days when I’m tired or distracted or just overwhelmed. Though I try to bring my A game to every patient visit, realistically, I know that I don’t always achieve this. But, for me, the difference in my best visits and good-enough visits is the difference between a 4-star and 5-star review. What’s up with those 1-star reviews?
Many, many years ago, when patient satisfaction scores were in their infancy, our clinic rewarded any physician who got a 100% satisfaction score. On the surface that makes perfect sense – of course, our patients should be satisfied 100% of the time, right? When I asked one of the winners of this competition how he did it (I never scored 100%), he told me, “I just do whatever the patient wants me to do.” Yikes, I thought at the time. That may be the recipe for an A+ for patient satisfaction but not for quality or outcomes.
Sometimes, I know that they are going to be unhappy, such as when I decline to refill their drug of abuse. Other times, I have to exercise my best medical judgment and hope that my explanation does not alienate the patient. After all, when I say “no” to a patient request, it is with their overall health and well-being in mind. But I would be lying if I said that I have matured to the point that I’m not bothered by a negative review or a patient choosing to take their care elsewhere.
Most of us seek and welcome feedback. Over time, I’ve learned to do this during the visit by asking “Am I giving you too much information?” or “What do you think of the plan?” or “What’s most important to you?” There are times when I conclude the visit and know that the patient is not satisfied but remain unable to ferret out where I let them down – even, on occasion, when I ask them directly. Ideally, any feedback we get from our patients, positive or negative, would be specific and actionable. It rarely is.
There is no doubt we have entered the era of consumer medicine. Everything from the physical appearance of our clinics to the response time to electronic messages is fair game in how patients judge us. As we all know, patients assume competence – they are not usually impressed by your training or quality outcomes because they already believe you are clinically competent (or arguably they’d never set foot in your office). Instead of judging us how we often judge ourselves, patients form opinions about us by how we enter the room, whether we sit or stand, how long they wait in the exam room before we come in, or whether they like the nurse with whom we work. So many subtle things – many of which are outside of our control.
I often struggle with staying on time. When I am invariably walking into the room late, I make a point of thanking patients for their patience. When I’m very late, I offer a more detailed, HIPAA-compliant explanation. What I wish my patients saw was that I am often accommodating a patient who arrives late for their appointment or who wants me to address every concern they’ve had for the past 5 years. While I aspire to not allow the patient’s perception of the visit to unduly influence how I handle the visit, it inevitably does. I do want to have patients who are happy with their experience.
One of my friends is enviously pragmatic in her view on patient experience. “I’m not their friend and they don’t have to like me.” She emphasizes the clinical care she is providing and does not allow patients who are upset with some aspect of the care to weigh heavy on her. It may be that specialists are more likely to enjoy the luxury of putting aside how patients feel about them personally. In primary care, the patient-physician relationship is so central to what we do that ignoring your “likability” has the potential to threaten your professional viability.
I conclude this blog much like I started it. My desire is to allow the negative reviews, particularly if they have nothing actionable in them, to roll off my back and to keep my focus on the clinical care that I am providing. In actuality, I care deeply about how my patients experience their visit with me and will likely continue to take my reviews to heart.
Dr. Frank is a family physician in Neenah, Wisc. She disclosed no relevant conflicts of interest.
A version of this article first appeared on Medscape.com.
Is corporate telepsychiatry the solution to access to care problems?
When Sue W’s mother died in 2018, she struggled terribly. She was already seeing a psychotherapist and was taking duloxetine, prescribed by her primary care physician. But her grief was profound, and her depression became paralyzing. She needed to see a psychiatrist, and there were many available in or near her hometown, a Connecticut suburb of New York City, but neither Sue, her therapist, nor her primary care doctor could find a psychiatrist who participated with her insurance. Finally, she was given the name of a psychiatrist in Manhattan who practiced online, and she made an appointment on the Skypiatrist (a telepsychiatry group founded in 2016) website.
“I hesitated about it at first,” Sue said. “The doctor was nice, and I liked the convenience. Appointments were 15 minutes long, although the first session was longer. He focused on the medications, which was okay because I already have a therapist. And it was really easy. I made appointments on their website and I saw the doctor through the same site, and I really liked that I could send him messages.” The psychiatrist was responsive when Sue had trouble coming off duloxetine, and he gave her instructions for a slower taper. The treatment was affordable and accessible, and she got better.
When you also consider that many private-practice psychiatrists do not participate with insurance panels, online companies that do accept insurance may add value, convenience, and access.
Cerebral, the largest online psychiatric service in the country, began seeing patients in January 2020, offering medications and psychotherapy. They participate with a number of commercial insurers, and this varies by state, but not with Medicaid or Medicare. Patients pay a monthly fee, and an initial 30-minute medication evaluation session is conducted, often with a nurse practitioner. They advertise wait times of less than 7 days.
Another company, Done, offers treatment specifically for ADHD. They don’t accept insurance for appointments; patients must submit their own claims for reimbursement. Their pricing structure involves a fee of $199 for the first month, then $79 a month thereafter, which does not include medications. Hims – another online company – targets men with a variety of health issues, including mental health problems.
Some of these internet companies have been in the news recently for concerns related to quality of care and prescribing practices. A The Wall Street Journal article of March 26, 2022, quoted clinicians who had previously worked for Cerebral and Done who left because they felt pressured to see patients quickly and to prescribe stimulants. Not all of the prescribers were unhappy, however. Yina Cruz-Harris, a nurse practitioner at Done who has a doctorate in nursing practice, said that she manages 2,300 patients with ADHD for Done. Virtually all are on stimulants. She renews each patient’s monthly prescription from her New Jersey home, based mostly on online forms filled out by the patients. She’s fast, doing two renewals per minute, and Done pays her almost $10 per patient, working out to around $20,000 in monthly earnings.
In May, the Department of Justice began looking into Cerebral’s practices around controlled substances and more recently, Cerebral has been in the news for complaints from patients that they have been unable to reach their prescribers when problems arise. Some pharmacy chains have refused to fill prescriptions for controlled medications from online telehealth providers, and some online providers, including Cerebral, are no longer prescribing controlled substances. A front-page The Wall Street Journal article on Aug. 19, 2022, told the story of a man with a history of addiction who was prescribed stimulants after a brief appointment with a prescriber at Done. Family and friends in his sober house believe that the stimulants triggered a relapse, and he died of an opioid overdose.
During the early days of the pandemic, nonemergency psychiatric care was shut down and we all became virtual psychiatrists. Many of us saw new patients and prescribed controlled medications to people we had never met in real life.
“John Brown,” MD, PhD, spoke with me on the condition that I don’t use his real name or the name of the practice he left. He was hired by a traditional group practice with a multidisciplinary staff and several offices in his state. Most of the clinicians worked part time and were contractual employees, and Dr. Brown was hired to develop a specialty service. He soon learned that the practice – which participates with a number of insurance plans – was not financially stable, and it was acquired by an investment firm with no medical experience.
“They wanted everyone to work 40-hour weeks and see 14 patients a day, including 3-4 new patients, and suddenly everyone was overextended and exhausted. Overnight, most of the therapists left, and they hired nurse practitioners to replace many of the psychiatrists. People weren’t getting good care.” While this was not a telepsychiatry startup, it was a corporate takeover of a traditional practice that was unable to remain financially solvent while participating with insurance panels.
Like Sue W, Elizabeth K struggled to get treatment for ADHD even before the pandemic.
“I work multiple part-time jobs, don’t own a car, and don’t have insurance. Before telehealth became available, it was difficult and discouraging for me to maintain consistent treatment. It took me months to get initial appointments with a doctor and I live in one of the largest cities in the country.” She was pleased with the care she received by Done.
“I was pleasantly surprised by the authenticity and thoroughness of my first telehealth provider,” Elizabeth noted. “She remembered and considered more about me, my medical history, and details of my personal life than nearly every psychiatric doctor I’ve ever seen. They informed me of the long-term effects of medications and the importance of routine cardiovascular check-ups. Also, they wouldn’t prescribe more than 5 mg of Adderall (even though I had been prescribed 30-90 mg a day for most of my life) until I completed a medical check-up with blood pressure and blood test results.”
Corporate telepsychiatry may fill an important void and provide care to many people who have been unable to access traditional treatment. Something, however, has to account for the fact that care is more affordable through startups than through traditional psychiatric practices. Startups have expensive technological and infrastructure costs and added layers of administration. This translates to either higher volumes with shorter appointments, less compensation for prescribers, or both. How this will affect the future of psychiatric care remains to be seen.
Dr. Miller, is a coauthor of “Committed: The Battle Over Involuntary Psychiatric Care” (Johns Hopkins University Press, 2016). She has a private practice and is assistant professor of psychiatry and behavioral sciences at Johns Hopkins University, Baltimore. She has disclosed no relevant financial relationships. A version of this article first appeared on Medscape.com.
When Sue W’s mother died in 2018, she struggled terribly. She was already seeing a psychotherapist and was taking duloxetine, prescribed by her primary care physician. But her grief was profound, and her depression became paralyzing. She needed to see a psychiatrist, and there were many available in or near her hometown, a Connecticut suburb of New York City, but neither Sue, her therapist, nor her primary care doctor could find a psychiatrist who participated with her insurance. Finally, she was given the name of a psychiatrist in Manhattan who practiced online, and she made an appointment on the Skypiatrist (a telepsychiatry group founded in 2016) website.
“I hesitated about it at first,” Sue said. “The doctor was nice, and I liked the convenience. Appointments were 15 minutes long, although the first session was longer. He focused on the medications, which was okay because I already have a therapist. And it was really easy. I made appointments on their website and I saw the doctor through the same site, and I really liked that I could send him messages.” The psychiatrist was responsive when Sue had trouble coming off duloxetine, and he gave her instructions for a slower taper. The treatment was affordable and accessible, and she got better.
When you also consider that many private-practice psychiatrists do not participate with insurance panels, online companies that do accept insurance may add value, convenience, and access.
Cerebral, the largest online psychiatric service in the country, began seeing patients in January 2020, offering medications and psychotherapy. They participate with a number of commercial insurers, and this varies by state, but not with Medicaid or Medicare. Patients pay a monthly fee, and an initial 30-minute medication evaluation session is conducted, often with a nurse practitioner. They advertise wait times of less than 7 days.
Another company, Done, offers treatment specifically for ADHD. They don’t accept insurance for appointments; patients must submit their own claims for reimbursement. Their pricing structure involves a fee of $199 for the first month, then $79 a month thereafter, which does not include medications. Hims – another online company – targets men with a variety of health issues, including mental health problems.
Some of these internet companies have been in the news recently for concerns related to quality of care and prescribing practices. A The Wall Street Journal article of March 26, 2022, quoted clinicians who had previously worked for Cerebral and Done who left because they felt pressured to see patients quickly and to prescribe stimulants. Not all of the prescribers were unhappy, however. Yina Cruz-Harris, a nurse practitioner at Done who has a doctorate in nursing practice, said that she manages 2,300 patients with ADHD for Done. Virtually all are on stimulants. She renews each patient’s monthly prescription from her New Jersey home, based mostly on online forms filled out by the patients. She’s fast, doing two renewals per minute, and Done pays her almost $10 per patient, working out to around $20,000 in monthly earnings.
In May, the Department of Justice began looking into Cerebral’s practices around controlled substances and more recently, Cerebral has been in the news for complaints from patients that they have been unable to reach their prescribers when problems arise. Some pharmacy chains have refused to fill prescriptions for controlled medications from online telehealth providers, and some online providers, including Cerebral, are no longer prescribing controlled substances. A front-page The Wall Street Journal article on Aug. 19, 2022, told the story of a man with a history of addiction who was prescribed stimulants after a brief appointment with a prescriber at Done. Family and friends in his sober house believe that the stimulants triggered a relapse, and he died of an opioid overdose.
During the early days of the pandemic, nonemergency psychiatric care was shut down and we all became virtual psychiatrists. Many of us saw new patients and prescribed controlled medications to people we had never met in real life.
“John Brown,” MD, PhD, spoke with me on the condition that I don’t use his real name or the name of the practice he left. He was hired by a traditional group practice with a multidisciplinary staff and several offices in his state. Most of the clinicians worked part time and were contractual employees, and Dr. Brown was hired to develop a specialty service. He soon learned that the practice – which participates with a number of insurance plans – was not financially stable, and it was acquired by an investment firm with no medical experience.
“They wanted everyone to work 40-hour weeks and see 14 patients a day, including 3-4 new patients, and suddenly everyone was overextended and exhausted. Overnight, most of the therapists left, and they hired nurse practitioners to replace many of the psychiatrists. People weren’t getting good care.” While this was not a telepsychiatry startup, it was a corporate takeover of a traditional practice that was unable to remain financially solvent while participating with insurance panels.
Like Sue W, Elizabeth K struggled to get treatment for ADHD even before the pandemic.
“I work multiple part-time jobs, don’t own a car, and don’t have insurance. Before telehealth became available, it was difficult and discouraging for me to maintain consistent treatment. It took me months to get initial appointments with a doctor and I live in one of the largest cities in the country.” She was pleased with the care she received by Done.
“I was pleasantly surprised by the authenticity and thoroughness of my first telehealth provider,” Elizabeth noted. “She remembered and considered more about me, my medical history, and details of my personal life than nearly every psychiatric doctor I’ve ever seen. They informed me of the long-term effects of medications and the importance of routine cardiovascular check-ups. Also, they wouldn’t prescribe more than 5 mg of Adderall (even though I had been prescribed 30-90 mg a day for most of my life) until I completed a medical check-up with blood pressure and blood test results.”
Corporate telepsychiatry may fill an important void and provide care to many people who have been unable to access traditional treatment. Something, however, has to account for the fact that care is more affordable through startups than through traditional psychiatric practices. Startups have expensive technological and infrastructure costs and added layers of administration. This translates to either higher volumes with shorter appointments, less compensation for prescribers, or both. How this will affect the future of psychiatric care remains to be seen.
Dr. Miller, is a coauthor of “Committed: The Battle Over Involuntary Psychiatric Care” (Johns Hopkins University Press, 2016). She has a private practice and is assistant professor of psychiatry and behavioral sciences at Johns Hopkins University, Baltimore. She has disclosed no relevant financial relationships. A version of this article first appeared on Medscape.com.
When Sue W’s mother died in 2018, she struggled terribly. She was already seeing a psychotherapist and was taking duloxetine, prescribed by her primary care physician. But her grief was profound, and her depression became paralyzing. She needed to see a psychiatrist, and there were many available in or near her hometown, a Connecticut suburb of New York City, but neither Sue, her therapist, nor her primary care doctor could find a psychiatrist who participated with her insurance. Finally, she was given the name of a psychiatrist in Manhattan who practiced online, and she made an appointment on the Skypiatrist (a telepsychiatry group founded in 2016) website.
“I hesitated about it at first,” Sue said. “The doctor was nice, and I liked the convenience. Appointments were 15 minutes long, although the first session was longer. He focused on the medications, which was okay because I already have a therapist. And it was really easy. I made appointments on their website and I saw the doctor through the same site, and I really liked that I could send him messages.” The psychiatrist was responsive when Sue had trouble coming off duloxetine, and he gave her instructions for a slower taper. The treatment was affordable and accessible, and she got better.
When you also consider that many private-practice psychiatrists do not participate with insurance panels, online companies that do accept insurance may add value, convenience, and access.
Cerebral, the largest online psychiatric service in the country, began seeing patients in January 2020, offering medications and psychotherapy. They participate with a number of commercial insurers, and this varies by state, but not with Medicaid or Medicare. Patients pay a monthly fee, and an initial 30-minute medication evaluation session is conducted, often with a nurse practitioner. They advertise wait times of less than 7 days.
Another company, Done, offers treatment specifically for ADHD. They don’t accept insurance for appointments; patients must submit their own claims for reimbursement. Their pricing structure involves a fee of $199 for the first month, then $79 a month thereafter, which does not include medications. Hims – another online company – targets men with a variety of health issues, including mental health problems.
Some of these internet companies have been in the news recently for concerns related to quality of care and prescribing practices. A The Wall Street Journal article of March 26, 2022, quoted clinicians who had previously worked for Cerebral and Done who left because they felt pressured to see patients quickly and to prescribe stimulants. Not all of the prescribers were unhappy, however. Yina Cruz-Harris, a nurse practitioner at Done who has a doctorate in nursing practice, said that she manages 2,300 patients with ADHD for Done. Virtually all are on stimulants. She renews each patient’s monthly prescription from her New Jersey home, based mostly on online forms filled out by the patients. She’s fast, doing two renewals per minute, and Done pays her almost $10 per patient, working out to around $20,000 in monthly earnings.
In May, the Department of Justice began looking into Cerebral’s practices around controlled substances and more recently, Cerebral has been in the news for complaints from patients that they have been unable to reach their prescribers when problems arise. Some pharmacy chains have refused to fill prescriptions for controlled medications from online telehealth providers, and some online providers, including Cerebral, are no longer prescribing controlled substances. A front-page The Wall Street Journal article on Aug. 19, 2022, told the story of a man with a history of addiction who was prescribed stimulants after a brief appointment with a prescriber at Done. Family and friends in his sober house believe that the stimulants triggered a relapse, and he died of an opioid overdose.
During the early days of the pandemic, nonemergency psychiatric care was shut down and we all became virtual psychiatrists. Many of us saw new patients and prescribed controlled medications to people we had never met in real life.
“John Brown,” MD, PhD, spoke with me on the condition that I don’t use his real name or the name of the practice he left. He was hired by a traditional group practice with a multidisciplinary staff and several offices in his state. Most of the clinicians worked part time and were contractual employees, and Dr. Brown was hired to develop a specialty service. He soon learned that the practice – which participates with a number of insurance plans – was not financially stable, and it was acquired by an investment firm with no medical experience.
“They wanted everyone to work 40-hour weeks and see 14 patients a day, including 3-4 new patients, and suddenly everyone was overextended and exhausted. Overnight, most of the therapists left, and they hired nurse practitioners to replace many of the psychiatrists. People weren’t getting good care.” While this was not a telepsychiatry startup, it was a corporate takeover of a traditional practice that was unable to remain financially solvent while participating with insurance panels.
Like Sue W, Elizabeth K struggled to get treatment for ADHD even before the pandemic.
“I work multiple part-time jobs, don’t own a car, and don’t have insurance. Before telehealth became available, it was difficult and discouraging for me to maintain consistent treatment. It took me months to get initial appointments with a doctor and I live in one of the largest cities in the country.” She was pleased with the care she received by Done.
“I was pleasantly surprised by the authenticity and thoroughness of my first telehealth provider,” Elizabeth noted. “She remembered and considered more about me, my medical history, and details of my personal life than nearly every psychiatric doctor I’ve ever seen. They informed me of the long-term effects of medications and the importance of routine cardiovascular check-ups. Also, they wouldn’t prescribe more than 5 mg of Adderall (even though I had been prescribed 30-90 mg a day for most of my life) until I completed a medical check-up with blood pressure and blood test results.”
Corporate telepsychiatry may fill an important void and provide care to many people who have been unable to access traditional treatment. Something, however, has to account for the fact that care is more affordable through startups than through traditional psychiatric practices. Startups have expensive technological and infrastructure costs and added layers of administration. This translates to either higher volumes with shorter appointments, less compensation for prescribers, or both. How this will affect the future of psychiatric care remains to be seen.
Dr. Miller, is a coauthor of “Committed: The Battle Over Involuntary Psychiatric Care” (Johns Hopkins University Press, 2016). She has a private practice and is assistant professor of psychiatry and behavioral sciences at Johns Hopkins University, Baltimore. She has disclosed no relevant financial relationships. A version of this article first appeared on Medscape.com.
Do lipid labs need to be fasting?
When I worked as a scribe prior to starting medical school, it was commonplace for patients to have fasting labs. I always felt terrible for the patients we saw late in the afternoon that had somehow fasted all day. For many other patients, there was the challenge of finding a time when they could return to have fasting labs drawn.
However, I have still observed instances when patients need to have fasting labs. We can look at an example case to better understand when and why patients do and do not need to fast prior to having their lipids checked.
Case
A 57-year-old woman presents for an annual wellness visit. She has been healthy this past year with no new concerns. Her blood pressure has been well controlled, and she continues on a statin for hyperlipidemia. She is due for annual labs. She ate breakfast this morning. Which of the following do you recommend?
A. Obtain lipids with her other blood work now.
B. Have her return tomorrow to obtain fasting labs.
In this situation, A is the correct answer. The patient is due for routine screening labs and there are no current indications that fasting labs are necessary.
Studies of fasting vs. nonfasting lipids
Sidhu and Naugler performed a cross-sectional analysis comparing lipid values at fasting intervals of 1 hour to 16 hours.1 They found the mean total cholesterol and HDL cholesterol values differed by greater than 2%. For LDL cholesterol, the values differed by less than 10% and triglycerides values differed by less than 20%. With this information, the researchers concluded fasting for routine lipids is generally unnecessary.
Mora and colleagues performed a post hoc prospective follow-up of a randomized control
trial to assess if nonfasting lipid measurements could cause misclassification of cardiovascular risk assessment.2 Based on 8,270 participants, coronary events associated with fasting vs. nonfasting lipid values were similar when adjusted hazard ratios were compared. They also found an agreement of 94.8% when classifying participants into ASCVD risk categories for fasting and nonfasting lipid values. These outcomes led them to support the use of nonfasting lipid labs for routine cardiovascular risk assessment.
Rahman and colleagues performed a systematic review and found the use of nonfasting lipid values can reliably determine statin management in most situations.3 Circumstances where fasting labs should be used are if patients have a genetic dyslipidemia, if patients have severe hypertriglyceridemia (greater than 500 mg/dL), and if patients have pancreatitis. Triglyceride values fluctuate the most between the fasting and nonfasting state as seen above from Sidhu and Naugler. This could impact triglyceride disorder management and the accuracy of LDL cholesterol estimation (calculated by the Friedewald equation: LDL cholesterol = total cholesterol – HDL cholesterol – triglycerides/5 in mg/dL).3
Benefits of nonfasting lipid labs
There are many benefits of nonfasting labs. For the patients, they do not have to come to their appointments hungry, we can reduce the risk of hypoglycemia for those with diabetes, and they do not have to come back at a later date if they ate something earlier in the day.
For the lab, we can improve efficiency and decrease early morning congestion when patients typically come in for fasting labs.
Lastly, for the provider, nonfasting labs can improve workflow and help decrease the number of patients lost to follow-up who were unable to complete fasting labs the same day as their appointment.
Summary
Patients do not need to fast prior to having lipid levels drawn for routine screening. Fasting labs should be considered for patients who have a genetic dyslipidemia or if there is concern for hypertriglyceridemia.
Per the ACC/AHA guidelines, nonfasting lipids can be used to assess ASCVD risk and to establish a baseline LDL cholesterol in adults 20 years and older. If a patient has nonfasting triglycerides greater than 400 mg/dL, repeat fasting lipids should be drawn to assess fasting triglycerides and to establish a baseline LDL cholesterol.4
Ms. Ervin is a fourth-year medical student at the University of Washington, Seattle. She has no conflicts to disclose. Dr. Paauw is professor of medicine in the division of general internal medicine at the University of Washington, and he serves as third-year medical student clerkship director at the university. He is a member of the editorial advisory board of Internal Medicine News. Dr. Paauw has no conflicts to disclose. Contact him at [email protected].
References
1. Rahman F et al. Curr Atheroscler Rep. 2018;20(3):14. Published 2018 Feb 17.
2. Mora S et al. JAMA Intern Med. 2019;179(7):898-905.
3. Sidhu D and Naugler C. Arch Intern Med. 2012;172(22):1707-10.
4. Hoover LE. Am Fam Physician. 2019 May 1;99(9):589-91.
When I worked as a scribe prior to starting medical school, it was commonplace for patients to have fasting labs. I always felt terrible for the patients we saw late in the afternoon that had somehow fasted all day. For many other patients, there was the challenge of finding a time when they could return to have fasting labs drawn.
However, I have still observed instances when patients need to have fasting labs. We can look at an example case to better understand when and why patients do and do not need to fast prior to having their lipids checked.
Case
A 57-year-old woman presents for an annual wellness visit. She has been healthy this past year with no new concerns. Her blood pressure has been well controlled, and she continues on a statin for hyperlipidemia. She is due for annual labs. She ate breakfast this morning. Which of the following do you recommend?
A. Obtain lipids with her other blood work now.
B. Have her return tomorrow to obtain fasting labs.
In this situation, A is the correct answer. The patient is due for routine screening labs and there are no current indications that fasting labs are necessary.
Studies of fasting vs. nonfasting lipids
Sidhu and Naugler performed a cross-sectional analysis comparing lipid values at fasting intervals of 1 hour to 16 hours.1 They found the mean total cholesterol and HDL cholesterol values differed by greater than 2%. For LDL cholesterol, the values differed by less than 10% and triglycerides values differed by less than 20%. With this information, the researchers concluded fasting for routine lipids is generally unnecessary.
Mora and colleagues performed a post hoc prospective follow-up of a randomized control
trial to assess if nonfasting lipid measurements could cause misclassification of cardiovascular risk assessment.2 Based on 8,270 participants, coronary events associated with fasting vs. nonfasting lipid values were similar when adjusted hazard ratios were compared. They also found an agreement of 94.8% when classifying participants into ASCVD risk categories for fasting and nonfasting lipid values. These outcomes led them to support the use of nonfasting lipid labs for routine cardiovascular risk assessment.
Rahman and colleagues performed a systematic review and found the use of nonfasting lipid values can reliably determine statin management in most situations.3 Circumstances where fasting labs should be used are if patients have a genetic dyslipidemia, if patients have severe hypertriglyceridemia (greater than 500 mg/dL), and if patients have pancreatitis. Triglyceride values fluctuate the most between the fasting and nonfasting state as seen above from Sidhu and Naugler. This could impact triglyceride disorder management and the accuracy of LDL cholesterol estimation (calculated by the Friedewald equation: LDL cholesterol = total cholesterol – HDL cholesterol – triglycerides/5 in mg/dL).3
Benefits of nonfasting lipid labs
There are many benefits of nonfasting labs. For the patients, they do not have to come to their appointments hungry, we can reduce the risk of hypoglycemia for those with diabetes, and they do not have to come back at a later date if they ate something earlier in the day.
For the lab, we can improve efficiency and decrease early morning congestion when patients typically come in for fasting labs.
Lastly, for the provider, nonfasting labs can improve workflow and help decrease the number of patients lost to follow-up who were unable to complete fasting labs the same day as their appointment.
Summary
Patients do not need to fast prior to having lipid levels drawn for routine screening. Fasting labs should be considered for patients who have a genetic dyslipidemia or if there is concern for hypertriglyceridemia.
Per the ACC/AHA guidelines, nonfasting lipids can be used to assess ASCVD risk and to establish a baseline LDL cholesterol in adults 20 years and older. If a patient has nonfasting triglycerides greater than 400 mg/dL, repeat fasting lipids should be drawn to assess fasting triglycerides and to establish a baseline LDL cholesterol.4
Ms. Ervin is a fourth-year medical student at the University of Washington, Seattle. She has no conflicts to disclose. Dr. Paauw is professor of medicine in the division of general internal medicine at the University of Washington, and he serves as third-year medical student clerkship director at the university. He is a member of the editorial advisory board of Internal Medicine News. Dr. Paauw has no conflicts to disclose. Contact him at [email protected].
References
1. Rahman F et al. Curr Atheroscler Rep. 2018;20(3):14. Published 2018 Feb 17.
2. Mora S et al. JAMA Intern Med. 2019;179(7):898-905.
3. Sidhu D and Naugler C. Arch Intern Med. 2012;172(22):1707-10.
4. Hoover LE. Am Fam Physician. 2019 May 1;99(9):589-91.
When I worked as a scribe prior to starting medical school, it was commonplace for patients to have fasting labs. I always felt terrible for the patients we saw late in the afternoon that had somehow fasted all day. For many other patients, there was the challenge of finding a time when they could return to have fasting labs drawn.
However, I have still observed instances when patients need to have fasting labs. We can look at an example case to better understand when and why patients do and do not need to fast prior to having their lipids checked.
Case
A 57-year-old woman presents for an annual wellness visit. She has been healthy this past year with no new concerns. Her blood pressure has been well controlled, and she continues on a statin for hyperlipidemia. She is due for annual labs. She ate breakfast this morning. Which of the following do you recommend?
A. Obtain lipids with her other blood work now.
B. Have her return tomorrow to obtain fasting labs.
In this situation, A is the correct answer. The patient is due for routine screening labs and there are no current indications that fasting labs are necessary.
Studies of fasting vs. nonfasting lipids
Sidhu and Naugler performed a cross-sectional analysis comparing lipid values at fasting intervals of 1 hour to 16 hours.1 They found the mean total cholesterol and HDL cholesterol values differed by greater than 2%. For LDL cholesterol, the values differed by less than 10% and triglycerides values differed by less than 20%. With this information, the researchers concluded fasting for routine lipids is generally unnecessary.
Mora and colleagues performed a post hoc prospective follow-up of a randomized control
trial to assess if nonfasting lipid measurements could cause misclassification of cardiovascular risk assessment.2 Based on 8,270 participants, coronary events associated with fasting vs. nonfasting lipid values were similar when adjusted hazard ratios were compared. They also found an agreement of 94.8% when classifying participants into ASCVD risk categories for fasting and nonfasting lipid values. These outcomes led them to support the use of nonfasting lipid labs for routine cardiovascular risk assessment.
Rahman and colleagues performed a systematic review and found the use of nonfasting lipid values can reliably determine statin management in most situations.3 Circumstances where fasting labs should be used are if patients have a genetic dyslipidemia, if patients have severe hypertriglyceridemia (greater than 500 mg/dL), and if patients have pancreatitis. Triglyceride values fluctuate the most between the fasting and nonfasting state as seen above from Sidhu and Naugler. This could impact triglyceride disorder management and the accuracy of LDL cholesterol estimation (calculated by the Friedewald equation: LDL cholesterol = total cholesterol – HDL cholesterol – triglycerides/5 in mg/dL).3
Benefits of nonfasting lipid labs
There are many benefits of nonfasting labs. For the patients, they do not have to come to their appointments hungry, we can reduce the risk of hypoglycemia for those with diabetes, and they do not have to come back at a later date if they ate something earlier in the day.
For the lab, we can improve efficiency and decrease early morning congestion when patients typically come in for fasting labs.
Lastly, for the provider, nonfasting labs can improve workflow and help decrease the number of patients lost to follow-up who were unable to complete fasting labs the same day as their appointment.
Summary
Patients do not need to fast prior to having lipid levels drawn for routine screening. Fasting labs should be considered for patients who have a genetic dyslipidemia or if there is concern for hypertriglyceridemia.
Per the ACC/AHA guidelines, nonfasting lipids can be used to assess ASCVD risk and to establish a baseline LDL cholesterol in adults 20 years and older. If a patient has nonfasting triglycerides greater than 400 mg/dL, repeat fasting lipids should be drawn to assess fasting triglycerides and to establish a baseline LDL cholesterol.4
Ms. Ervin is a fourth-year medical student at the University of Washington, Seattle. She has no conflicts to disclose. Dr. Paauw is professor of medicine in the division of general internal medicine at the University of Washington, and he serves as third-year medical student clerkship director at the university. He is a member of the editorial advisory board of Internal Medicine News. Dr. Paauw has no conflicts to disclose. Contact him at [email protected].
References
1. Rahman F et al. Curr Atheroscler Rep. 2018;20(3):14. Published 2018 Feb 17.
2. Mora S et al. JAMA Intern Med. 2019;179(7):898-905.
3. Sidhu D and Naugler C. Arch Intern Med. 2012;172(22):1707-10.
4. Hoover LE. Am Fam Physician. 2019 May 1;99(9):589-91.
Dignity
Queen Elizabeth is everywhere. She was even on the last slide of a presentation on COVID, monkeypox, and influenza vaccines given by our physician in charge of quality. This was odd. The presenter wasn’t English. The Queen had nothing to do with vaccines. Nor apparently would she have said even if she did have an opinion about them. But there we were, an audience of physicians and staff pausing for a moment of remembrance of her.
I’m not a Monarchist – except perhaps for the Kennedys. I grew up in New England. I don’t have an opinion on whether or not the British Crown should endure. But I do marvel at the astounding effect Queen Elizabeth’s passing had on so many around the world. Her personal qualities, particularly her steadiness and humane sympathy, might explain why so many are sad hearing the news. But also I think there was something in her role that we all wished for: Not the owning of palaces and sceptres, but rather, the respect that was given to her.
She was a stateswoman of “unmatched dignity,” the White House wrote. That was true, but it seems being the Queen might have been the last job on earth where such dignity is still possible. Certainly in politics, education, and even health care, there doesn’t seem to be much left lately.
The same day of that presentation I walked into the room of a patient 22 minutes late, she held her arm forth tapping her watch to indicate the time and my tardiness. Unnecessary, if not impertinent. Covering for one of my female physician colleagues, I read an email from a patient which began, “Dear Julie, With all due respect …” Another patient submitted a photo for us to review that was clearly taken from her car while waiting at a stop light. Hardly the consideration a clinical encounter should be given.
Much has been lost for patients. too. There are patients trying to make appointments lately who are told: “There are none. Call back later.” . There is no dignified way to remove exam paper stuck to your backside before introducing yourself to the doctor. Maybe that last slide of Her Majesty was in fact for us to have a moment of silence for what we’ve all lost.
Walter Bagehot (pronounce it “Baj-et” if you tell this story to your Harlan wine friends) was a political writer and editor of The Economist in the 1860s. He famously said that the secret to the English government was having two kinds of institutions, the dignified and the efficient. The efficient, Parliament, was responsible for all the work. The dignified, the Crown, gives significance and holds everyone’s respect. If medicine ever once was both dignified and efficient, we aren’t lately. We push to reduce backlogs, offer same-time virtual care, work to reduce costs. We’ve driven medicine to the efficient and left little of the dignity it seems.
The Queen will be remembered for her lifelong dedication to the laborious service of others. Even though each of us in medicine pledges the same, we also mourn this week the loss of dignity that once came with it.
Dr. Benabio is director of Healthcare Transformation and chief of dermatology at Kaiser Permanente San Diego. The opinions expressed in this column are his own and do not represent those of Kaiser Permanente. Dr. Benabio is @Dermdoc on Twitter. Write to him at [email protected].
Queen Elizabeth is everywhere. She was even on the last slide of a presentation on COVID, monkeypox, and influenza vaccines given by our physician in charge of quality. This was odd. The presenter wasn’t English. The Queen had nothing to do with vaccines. Nor apparently would she have said even if she did have an opinion about them. But there we were, an audience of physicians and staff pausing for a moment of remembrance of her.
I’m not a Monarchist – except perhaps for the Kennedys. I grew up in New England. I don’t have an opinion on whether or not the British Crown should endure. But I do marvel at the astounding effect Queen Elizabeth’s passing had on so many around the world. Her personal qualities, particularly her steadiness and humane sympathy, might explain why so many are sad hearing the news. But also I think there was something in her role that we all wished for: Not the owning of palaces and sceptres, but rather, the respect that was given to her.
She was a stateswoman of “unmatched dignity,” the White House wrote. That was true, but it seems being the Queen might have been the last job on earth where such dignity is still possible. Certainly in politics, education, and even health care, there doesn’t seem to be much left lately.
The same day of that presentation I walked into the room of a patient 22 minutes late, she held her arm forth tapping her watch to indicate the time and my tardiness. Unnecessary, if not impertinent. Covering for one of my female physician colleagues, I read an email from a patient which began, “Dear Julie, With all due respect …” Another patient submitted a photo for us to review that was clearly taken from her car while waiting at a stop light. Hardly the consideration a clinical encounter should be given.
Much has been lost for patients. too. There are patients trying to make appointments lately who are told: “There are none. Call back later.” . There is no dignified way to remove exam paper stuck to your backside before introducing yourself to the doctor. Maybe that last slide of Her Majesty was in fact for us to have a moment of silence for what we’ve all lost.
Walter Bagehot (pronounce it “Baj-et” if you tell this story to your Harlan wine friends) was a political writer and editor of The Economist in the 1860s. He famously said that the secret to the English government was having two kinds of institutions, the dignified and the efficient. The efficient, Parliament, was responsible for all the work. The dignified, the Crown, gives significance and holds everyone’s respect. If medicine ever once was both dignified and efficient, we aren’t lately. We push to reduce backlogs, offer same-time virtual care, work to reduce costs. We’ve driven medicine to the efficient and left little of the dignity it seems.
The Queen will be remembered for her lifelong dedication to the laborious service of others. Even though each of us in medicine pledges the same, we also mourn this week the loss of dignity that once came with it.
Dr. Benabio is director of Healthcare Transformation and chief of dermatology at Kaiser Permanente San Diego. The opinions expressed in this column are his own and do not represent those of Kaiser Permanente. Dr. Benabio is @Dermdoc on Twitter. Write to him at [email protected].
Queen Elizabeth is everywhere. She was even on the last slide of a presentation on COVID, monkeypox, and influenza vaccines given by our physician in charge of quality. This was odd. The presenter wasn’t English. The Queen had nothing to do with vaccines. Nor apparently would she have said even if she did have an opinion about them. But there we were, an audience of physicians and staff pausing for a moment of remembrance of her.
I’m not a Monarchist – except perhaps for the Kennedys. I grew up in New England. I don’t have an opinion on whether or not the British Crown should endure. But I do marvel at the astounding effect Queen Elizabeth’s passing had on so many around the world. Her personal qualities, particularly her steadiness and humane sympathy, might explain why so many are sad hearing the news. But also I think there was something in her role that we all wished for: Not the owning of palaces and sceptres, but rather, the respect that was given to her.
She was a stateswoman of “unmatched dignity,” the White House wrote. That was true, but it seems being the Queen might have been the last job on earth where such dignity is still possible. Certainly in politics, education, and even health care, there doesn’t seem to be much left lately.
The same day of that presentation I walked into the room of a patient 22 minutes late, she held her arm forth tapping her watch to indicate the time and my tardiness. Unnecessary, if not impertinent. Covering for one of my female physician colleagues, I read an email from a patient which began, “Dear Julie, With all due respect …” Another patient submitted a photo for us to review that was clearly taken from her car while waiting at a stop light. Hardly the consideration a clinical encounter should be given.
Much has been lost for patients. too. There are patients trying to make appointments lately who are told: “There are none. Call back later.” . There is no dignified way to remove exam paper stuck to your backside before introducing yourself to the doctor. Maybe that last slide of Her Majesty was in fact for us to have a moment of silence for what we’ve all lost.
Walter Bagehot (pronounce it “Baj-et” if you tell this story to your Harlan wine friends) was a political writer and editor of The Economist in the 1860s. He famously said that the secret to the English government was having two kinds of institutions, the dignified and the efficient. The efficient, Parliament, was responsible for all the work. The dignified, the Crown, gives significance and holds everyone’s respect. If medicine ever once was both dignified and efficient, we aren’t lately. We push to reduce backlogs, offer same-time virtual care, work to reduce costs. We’ve driven medicine to the efficient and left little of the dignity it seems.
The Queen will be remembered for her lifelong dedication to the laborious service of others. Even though each of us in medicine pledges the same, we also mourn this week the loss of dignity that once came with it.
Dr. Benabio is director of Healthcare Transformation and chief of dermatology at Kaiser Permanente San Diego. The opinions expressed in this column are his own and do not represent those of Kaiser Permanente. Dr. Benabio is @Dermdoc on Twitter. Write to him at [email protected].
Me, my spouse, and COVID
Managing family conflict and cohesion
I watched you in the garage, with your wipes and your mask, your gloves and bottles of sprays and potions. I admired your fealty to CNN’s Dr. Sanjay Gupta as he demonstrated the proper technique for disinfecting groceries. I watched sterile protocol being broken and quietly closed the garage door.
I listened to your descriptions of the agility of the virus with each exhalation of breath, and how far the virus could travel with a tailwind and in cold dry air. I listen as closely and with the same intention as I listen to my yoga teacher’s explication of the benefits of attention to the breath.
Relatives and friends came prepared to be entertained outdoors. Even masked, you eschewed the world. Your version of science clashes with my laissez-faire attitude. We blow up as a couple. Then we settle down and learn how to cope with the stress, as a team, together.
The COVID factor
In the first few months of any stressor, family and couple functioning must reorganize to manage well.
During lockdown, social scientists accessed an eager public ready to participate in their studies. With nowhere to go, many people, especially women, completed online COVID surveys. Community-based tools such as the Centers for Disease Control and Prevention’s Social Vulnerability Index identified populations of high social vulnerability (as caused by external stresses on human health, such as unemployment, overcrowding, presence of an individual with caregiving needs, and low educational attainment). It is assumed that such populations will experience more stress and have more difficulty coping and adjusting.
In a study by a team at the University of Miami, social vulnerability was associated with more disrupted family functioning, except when households with children (n = 2,666) were compared to households without children (n = 1,456).1 What allowed these families with children to enjoy better functioning?
Looking more closely at the Miami study, what can we find? It is a large survey study (n = 4,122), disseminated through professional networks and social media via purchased Facebook and Instagram ads. Data were logged in REDCap, and participants had the option of taking the survey in English or Spanish. Most participants were female (93.5%), 55.7% responded in English, and 44.3% in Spanish. There were few differences between the women who had and did not have children, in terms of their age, employment status, and education level. The number of children in the household did not affect the results.
This study used a new tool called the COVID-19 Household Environment Scale. This tool has 25 items measuring individual and household characteristics, and associated COVID-19 stressors. This tool also includes two family functioning measures: conflict and cohesion, asking the respondent to reflect on the change in “conflict” or “togetherness,” as it relates to household experiences and activities, compared with the period before social distancing.
The surprising finding was that even though households with children reported more conflict than before the start of the pandemic, they also reported more cohesion. This syncs with my experience. My niece and nephew found that having their teenage children at home brought them closer as a family, cut down on some of the extracurricular activities they did not support, and generally “slowed the world down.”
However, in a study in Germany, survey respondents (n = 1,042) noted that having children up to 17 years old was associated with decreases in satisfaction with family life, although this was not related to changes in family demands. The study assessed changes over 6 months and underscores the fact that perceptions of family demands and family well-being are independent of each other.2
These findings also resonate with prior research that measured burden and reward in couples. High burden is not associated with low reward; these two constructs are independent of each other.3
What about couples?
It is no surprise that poor relationships begat poor coping. In an online Belgian survey of 1,491 cohabiting couples during the shutdown, both men and women felt significantly more stress than before, because they felt restricted in their relationship.4
However, only women reported significantly more stress during the lockdown than before, because of relationship conflicts, such as feeling neglected by their partner. These feelings had predated lockdown.
In another lockdown online survey of 782 U.S. adults (89.8% White, 84.5% female), cohabitating intimate partners reported that there were higher thoughts of separation if the participants were younger, or if there was higher verbal aggression, higher relationship invalidation, and lower relationship satisfaction. Higher relationship satisfaction was reported when there was lower money stress, higher sexual fulfillment, lower relationship invalidation, and higher perceived fairness of relationship power. High relationship satisfaction was also reported where there were no children in the home.5
It should be noted that none of these relationship variables was measured in the Miami study discussed above, and this study did not measure perceived conflict or perceived cohesion, so we know less about these aspects of the family unit.
What about teens?
The COVID-19 lockdown had a positive effect on the dynamics in some families, according to a naturalistic study of adolescents (n = 155) who completed surveys at two time periods (initial and 8 weeks).6
These adolescents reported a reduction in perceived psychological control by their mothers, and no change in autonomy support. The changes did not vary according to gender or the mother’s employment situation. The decrease in psychological control was greater with higher initial levels of satisfaction with the mother, and lower levels of the teens disobeying their parents.
What about hospital settings?
The worst of the COVID experience was in the hospital. The pain was displayed on the faces of the staff as they labored to figure out how to care for the dying patients who had no contact with their families. Hospitals, out of fear of contamination and viral dissemination, excluded visitors. In those early days of uncertainty, the stress among staff, patients, and family members was high.
In response to family members feeling disconnected from the health care team and the psychological and moral distress of the staff, Nadine J. Kaslow and colleagues revised policies and procedures at Emory University, Atlanta, facilities to reprioritize patient- and family-centered care.7
The guiding principles focus on providing safe yet compassionate and ethical care, balancing community health and the mitigation of viral transmission, while appreciating family members as essential partners in care; fostering communication between patients and their families; and promoting interactions and decision-making among health care providers, patients, and families.
COVID continues to intrude in many of our lives. Many people are mourning family members and friends who died after contracting the disease. Many people choose to ignore their risk and live their lives as before. Many people, like my spouse and me, continue to debate the merits of venturing into public spaces. Personally, COVID has given me time to read many more books than I could ever have imagined and allowed my spouse to explore the delicate nuances of cooking.
Dr. Heru is professor of psychiatry at the University of Colorado at Denver, Aurora. She is editor of “Working With Families in Medical Settings: A Multidisciplinary Guide for Psychiatrists and Other Health Professionals” (New York: Routledge, 2013). She has no conflicts of interest to disclose. Contact Dr. Heru at [email protected].
References
1. Chavez JV et al. Assessing the impact of COVID-19 social distancing and social vulnerability on family functioning in an international sample of households with and without children. Couple Fam Psychol: Res Pract. 2021 Dec;10(4): 233-48. doi: 10.1037/cfp0000166.
2. Rudolph CW, Zacher H. Family demands and satisfaction with family life during the COVID-19 pandemic. Couple Fam Psychol: Res Pract. 2021 Dec;10(4): 249-59. doi: 10.1037/cfp0000170.
3. Heru AM et al. Family functioning in the caregivers of patients with dementia. Int J Geriatr Psychiatry. 2004 Jun;19(6):533-7. doi: 10.1002/gps.1119.
4. Schokkenbroek JM et al. Partners in lockdown: Relationship stress in men and women during the COVID-19 pandemic. Couple Fam Psychol: Res Pract. 2021 Sept;10(3): 149-57. doi: 10.1037/cfp0000172.
5. Eubanks Fleming CJ, Franzese AT. Should I stay or should I go? Evaluating intimate relationship outcomes during the 2020 pandemic shutdown. Couple Fam Psychol: Res Pract. 2021 Sept;10(3): 158-67. doi: 10.1037/cfp0000169.
6. Bacikova-Sleskova M,et al. Did perceived parenting in adolescence change as a result of the COVID-19 lockdown? A natural experiment. Couple Fam Psychol: Res Pract. 2021 Dec;10(4): 271-80. doi: 10.1037/cfp0000167.
7. Kaslow NJ et al. A roadmap for patient- and family-centered care during the pandemic. Couple Fam Psychol: Res Pract. 2021 Sept;10(3): 223-32. doi: 10.1037/cfp0000176.
Managing family conflict and cohesion
Managing family conflict and cohesion
I watched you in the garage, with your wipes and your mask, your gloves and bottles of sprays and potions. I admired your fealty to CNN’s Dr. Sanjay Gupta as he demonstrated the proper technique for disinfecting groceries. I watched sterile protocol being broken and quietly closed the garage door.
I listened to your descriptions of the agility of the virus with each exhalation of breath, and how far the virus could travel with a tailwind and in cold dry air. I listen as closely and with the same intention as I listen to my yoga teacher’s explication of the benefits of attention to the breath.
Relatives and friends came prepared to be entertained outdoors. Even masked, you eschewed the world. Your version of science clashes with my laissez-faire attitude. We blow up as a couple. Then we settle down and learn how to cope with the stress, as a team, together.
The COVID factor
In the first few months of any stressor, family and couple functioning must reorganize to manage well.
During lockdown, social scientists accessed an eager public ready to participate in their studies. With nowhere to go, many people, especially women, completed online COVID surveys. Community-based tools such as the Centers for Disease Control and Prevention’s Social Vulnerability Index identified populations of high social vulnerability (as caused by external stresses on human health, such as unemployment, overcrowding, presence of an individual with caregiving needs, and low educational attainment). It is assumed that such populations will experience more stress and have more difficulty coping and adjusting.
In a study by a team at the University of Miami, social vulnerability was associated with more disrupted family functioning, except when households with children (n = 2,666) were compared to households without children (n = 1,456).1 What allowed these families with children to enjoy better functioning?
Looking more closely at the Miami study, what can we find? It is a large survey study (n = 4,122), disseminated through professional networks and social media via purchased Facebook and Instagram ads. Data were logged in REDCap, and participants had the option of taking the survey in English or Spanish. Most participants were female (93.5%), 55.7% responded in English, and 44.3% in Spanish. There were few differences between the women who had and did not have children, in terms of their age, employment status, and education level. The number of children in the household did not affect the results.
This study used a new tool called the COVID-19 Household Environment Scale. This tool has 25 items measuring individual and household characteristics, and associated COVID-19 stressors. This tool also includes two family functioning measures: conflict and cohesion, asking the respondent to reflect on the change in “conflict” or “togetherness,” as it relates to household experiences and activities, compared with the period before social distancing.
The surprising finding was that even though households with children reported more conflict than before the start of the pandemic, they also reported more cohesion. This syncs with my experience. My niece and nephew found that having their teenage children at home brought them closer as a family, cut down on some of the extracurricular activities they did not support, and generally “slowed the world down.”
However, in a study in Germany, survey respondents (n = 1,042) noted that having children up to 17 years old was associated with decreases in satisfaction with family life, although this was not related to changes in family demands. The study assessed changes over 6 months and underscores the fact that perceptions of family demands and family well-being are independent of each other.2
These findings also resonate with prior research that measured burden and reward in couples. High burden is not associated with low reward; these two constructs are independent of each other.3
What about couples?
It is no surprise that poor relationships begat poor coping. In an online Belgian survey of 1,491 cohabiting couples during the shutdown, both men and women felt significantly more stress than before, because they felt restricted in their relationship.4
However, only women reported significantly more stress during the lockdown than before, because of relationship conflicts, such as feeling neglected by their partner. These feelings had predated lockdown.
In another lockdown online survey of 782 U.S. adults (89.8% White, 84.5% female), cohabitating intimate partners reported that there were higher thoughts of separation if the participants were younger, or if there was higher verbal aggression, higher relationship invalidation, and lower relationship satisfaction. Higher relationship satisfaction was reported when there was lower money stress, higher sexual fulfillment, lower relationship invalidation, and higher perceived fairness of relationship power. High relationship satisfaction was also reported where there were no children in the home.5
It should be noted that none of these relationship variables was measured in the Miami study discussed above, and this study did not measure perceived conflict or perceived cohesion, so we know less about these aspects of the family unit.
What about teens?
The COVID-19 lockdown had a positive effect on the dynamics in some families, according to a naturalistic study of adolescents (n = 155) who completed surveys at two time periods (initial and 8 weeks).6
These adolescents reported a reduction in perceived psychological control by their mothers, and no change in autonomy support. The changes did not vary according to gender or the mother’s employment situation. The decrease in psychological control was greater with higher initial levels of satisfaction with the mother, and lower levels of the teens disobeying their parents.
What about hospital settings?
The worst of the COVID experience was in the hospital. The pain was displayed on the faces of the staff as they labored to figure out how to care for the dying patients who had no contact with their families. Hospitals, out of fear of contamination and viral dissemination, excluded visitors. In those early days of uncertainty, the stress among staff, patients, and family members was high.
In response to family members feeling disconnected from the health care team and the psychological and moral distress of the staff, Nadine J. Kaslow and colleagues revised policies and procedures at Emory University, Atlanta, facilities to reprioritize patient- and family-centered care.7
The guiding principles focus on providing safe yet compassionate and ethical care, balancing community health and the mitigation of viral transmission, while appreciating family members as essential partners in care; fostering communication between patients and their families; and promoting interactions and decision-making among health care providers, patients, and families.
COVID continues to intrude in many of our lives. Many people are mourning family members and friends who died after contracting the disease. Many people choose to ignore their risk and live their lives as before. Many people, like my spouse and me, continue to debate the merits of venturing into public spaces. Personally, COVID has given me time to read many more books than I could ever have imagined and allowed my spouse to explore the delicate nuances of cooking.
Dr. Heru is professor of psychiatry at the University of Colorado at Denver, Aurora. She is editor of “Working With Families in Medical Settings: A Multidisciplinary Guide for Psychiatrists and Other Health Professionals” (New York: Routledge, 2013). She has no conflicts of interest to disclose. Contact Dr. Heru at [email protected].
References
1. Chavez JV et al. Assessing the impact of COVID-19 social distancing and social vulnerability on family functioning in an international sample of households with and without children. Couple Fam Psychol: Res Pract. 2021 Dec;10(4): 233-48. doi: 10.1037/cfp0000166.
2. Rudolph CW, Zacher H. Family demands and satisfaction with family life during the COVID-19 pandemic. Couple Fam Psychol: Res Pract. 2021 Dec;10(4): 249-59. doi: 10.1037/cfp0000170.
3. Heru AM et al. Family functioning in the caregivers of patients with dementia. Int J Geriatr Psychiatry. 2004 Jun;19(6):533-7. doi: 10.1002/gps.1119.
4. Schokkenbroek JM et al. Partners in lockdown: Relationship stress in men and women during the COVID-19 pandemic. Couple Fam Psychol: Res Pract. 2021 Sept;10(3): 149-57. doi: 10.1037/cfp0000172.
5. Eubanks Fleming CJ, Franzese AT. Should I stay or should I go? Evaluating intimate relationship outcomes during the 2020 pandemic shutdown. Couple Fam Psychol: Res Pract. 2021 Sept;10(3): 158-67. doi: 10.1037/cfp0000169.
6. Bacikova-Sleskova M,et al. Did perceived parenting in adolescence change as a result of the COVID-19 lockdown? A natural experiment. Couple Fam Psychol: Res Pract. 2021 Dec;10(4): 271-80. doi: 10.1037/cfp0000167.
7. Kaslow NJ et al. A roadmap for patient- and family-centered care during the pandemic. Couple Fam Psychol: Res Pract. 2021 Sept;10(3): 223-32. doi: 10.1037/cfp0000176.
I watched you in the garage, with your wipes and your mask, your gloves and bottles of sprays and potions. I admired your fealty to CNN’s Dr. Sanjay Gupta as he demonstrated the proper technique for disinfecting groceries. I watched sterile protocol being broken and quietly closed the garage door.
I listened to your descriptions of the agility of the virus with each exhalation of breath, and how far the virus could travel with a tailwind and in cold dry air. I listen as closely and with the same intention as I listen to my yoga teacher’s explication of the benefits of attention to the breath.
Relatives and friends came prepared to be entertained outdoors. Even masked, you eschewed the world. Your version of science clashes with my laissez-faire attitude. We blow up as a couple. Then we settle down and learn how to cope with the stress, as a team, together.
The COVID factor
In the first few months of any stressor, family and couple functioning must reorganize to manage well.
During lockdown, social scientists accessed an eager public ready to participate in their studies. With nowhere to go, many people, especially women, completed online COVID surveys. Community-based tools such as the Centers for Disease Control and Prevention’s Social Vulnerability Index identified populations of high social vulnerability (as caused by external stresses on human health, such as unemployment, overcrowding, presence of an individual with caregiving needs, and low educational attainment). It is assumed that such populations will experience more stress and have more difficulty coping and adjusting.
In a study by a team at the University of Miami, social vulnerability was associated with more disrupted family functioning, except when households with children (n = 2,666) were compared to households without children (n = 1,456).1 What allowed these families with children to enjoy better functioning?
Looking more closely at the Miami study, what can we find? It is a large survey study (n = 4,122), disseminated through professional networks and social media via purchased Facebook and Instagram ads. Data were logged in REDCap, and participants had the option of taking the survey in English or Spanish. Most participants were female (93.5%), 55.7% responded in English, and 44.3% in Spanish. There were few differences between the women who had and did not have children, in terms of their age, employment status, and education level. The number of children in the household did not affect the results.
This study used a new tool called the COVID-19 Household Environment Scale. This tool has 25 items measuring individual and household characteristics, and associated COVID-19 stressors. This tool also includes two family functioning measures: conflict and cohesion, asking the respondent to reflect on the change in “conflict” or “togetherness,” as it relates to household experiences and activities, compared with the period before social distancing.
The surprising finding was that even though households with children reported more conflict than before the start of the pandemic, they also reported more cohesion. This syncs with my experience. My niece and nephew found that having their teenage children at home brought them closer as a family, cut down on some of the extracurricular activities they did not support, and generally “slowed the world down.”
However, in a study in Germany, survey respondents (n = 1,042) noted that having children up to 17 years old was associated with decreases in satisfaction with family life, although this was not related to changes in family demands. The study assessed changes over 6 months and underscores the fact that perceptions of family demands and family well-being are independent of each other.2
These findings also resonate with prior research that measured burden and reward in couples. High burden is not associated with low reward; these two constructs are independent of each other.3
What about couples?
It is no surprise that poor relationships begat poor coping. In an online Belgian survey of 1,491 cohabiting couples during the shutdown, both men and women felt significantly more stress than before, because they felt restricted in their relationship.4
However, only women reported significantly more stress during the lockdown than before, because of relationship conflicts, such as feeling neglected by their partner. These feelings had predated lockdown.
In another lockdown online survey of 782 U.S. adults (89.8% White, 84.5% female), cohabitating intimate partners reported that there were higher thoughts of separation if the participants were younger, or if there was higher verbal aggression, higher relationship invalidation, and lower relationship satisfaction. Higher relationship satisfaction was reported when there was lower money stress, higher sexual fulfillment, lower relationship invalidation, and higher perceived fairness of relationship power. High relationship satisfaction was also reported where there were no children in the home.5
It should be noted that none of these relationship variables was measured in the Miami study discussed above, and this study did not measure perceived conflict or perceived cohesion, so we know less about these aspects of the family unit.
What about teens?
The COVID-19 lockdown had a positive effect on the dynamics in some families, according to a naturalistic study of adolescents (n = 155) who completed surveys at two time periods (initial and 8 weeks).6
These adolescents reported a reduction in perceived psychological control by their mothers, and no change in autonomy support. The changes did not vary according to gender or the mother’s employment situation. The decrease in psychological control was greater with higher initial levels of satisfaction with the mother, and lower levels of the teens disobeying their parents.
What about hospital settings?
The worst of the COVID experience was in the hospital. The pain was displayed on the faces of the staff as they labored to figure out how to care for the dying patients who had no contact with their families. Hospitals, out of fear of contamination and viral dissemination, excluded visitors. In those early days of uncertainty, the stress among staff, patients, and family members was high.
In response to family members feeling disconnected from the health care team and the psychological and moral distress of the staff, Nadine J. Kaslow and colleagues revised policies and procedures at Emory University, Atlanta, facilities to reprioritize patient- and family-centered care.7
The guiding principles focus on providing safe yet compassionate and ethical care, balancing community health and the mitigation of viral transmission, while appreciating family members as essential partners in care; fostering communication between patients and their families; and promoting interactions and decision-making among health care providers, patients, and families.
COVID continues to intrude in many of our lives. Many people are mourning family members and friends who died after contracting the disease. Many people choose to ignore their risk and live their lives as before. Many people, like my spouse and me, continue to debate the merits of venturing into public spaces. Personally, COVID has given me time to read many more books than I could ever have imagined and allowed my spouse to explore the delicate nuances of cooking.
Dr. Heru is professor of psychiatry at the University of Colorado at Denver, Aurora. She is editor of “Working With Families in Medical Settings: A Multidisciplinary Guide for Psychiatrists and Other Health Professionals” (New York: Routledge, 2013). She has no conflicts of interest to disclose. Contact Dr. Heru at [email protected].
References
1. Chavez JV et al. Assessing the impact of COVID-19 social distancing and social vulnerability on family functioning in an international sample of households with and without children. Couple Fam Psychol: Res Pract. 2021 Dec;10(4): 233-48. doi: 10.1037/cfp0000166.
2. Rudolph CW, Zacher H. Family demands and satisfaction with family life during the COVID-19 pandemic. Couple Fam Psychol: Res Pract. 2021 Dec;10(4): 249-59. doi: 10.1037/cfp0000170.
3. Heru AM et al. Family functioning in the caregivers of patients with dementia. Int J Geriatr Psychiatry. 2004 Jun;19(6):533-7. doi: 10.1002/gps.1119.
4. Schokkenbroek JM et al. Partners in lockdown: Relationship stress in men and women during the COVID-19 pandemic. Couple Fam Psychol: Res Pract. 2021 Sept;10(3): 149-57. doi: 10.1037/cfp0000172.
5. Eubanks Fleming CJ, Franzese AT. Should I stay or should I go? Evaluating intimate relationship outcomes during the 2020 pandemic shutdown. Couple Fam Psychol: Res Pract. 2021 Sept;10(3): 158-67. doi: 10.1037/cfp0000169.
6. Bacikova-Sleskova M,et al. Did perceived parenting in adolescence change as a result of the COVID-19 lockdown? A natural experiment. Couple Fam Psychol: Res Pract. 2021 Dec;10(4): 271-80. doi: 10.1037/cfp0000167.
7. Kaslow NJ et al. A roadmap for patient- and family-centered care during the pandemic. Couple Fam Psychol: Res Pract. 2021 Sept;10(3): 223-32. doi: 10.1037/cfp0000176.









