User login
The Best of DDW 2022: Feel the history
“The Best of DDW” elicits in the minds of most readers a compilation of the most important clinical and scientific content presented at DDW.
But I am not referring to that.
The “Best of DDW 2022” was the American Gastroenterological Association Presidential Plenary Session thanks to the humanity and vision of outgoing AGA President John Inadomi, MD.1 I sat in the audience, misty eyed, as each presenter addressed issues that strike deep into our humanity – the social determinants of health that have festered for far too long, leading to intolerable differences in health outcomes based on accidents of birth, and amplified by racism.
As the table on stage slowly filled in, an amazing picture took shape. A majority of the speakers were Black gastroenterologists and hepatologists, and among them many were young women. As I watched the video of a group of young Black gastroenterologists and hepatologists reaching out to the community, I asked myself “Has anything like this ever happened at a major national medical association meeting in the United States? Ever?” And then it occurred to me: “And just imagine, this exactly 2 days before the 2-year anniversary of the death of George Floyd.”
The plenary session happened on May 23, and I was conscious about the dates because I will never forget that George Floyd was killed on May 25, 2020 – my 55th birthday. The juxtaposition of his death and my birthday 2 years ago shook me profoundly, prompting me to write down my reflections and my hope that, in the national reactions that followed, we were seeing the beginning of true change.2 Two years later, despite our national divisions and serious challenges, I have reasons for hope.
On May 24, I ran into a colleague who was a Black woman. I have stopped being afraid to bring up previously untouchable subjects. I asked her what she thought about the remarkable AGA Plenary. She said she was glad that she is here to see it – that her parents never got the chance.
I admitted to her that I often ask myself what more I could and should be doing. I’m trying to do what I can in recruitment, education, in my personal life. What more? She said that one thing we really need is for people who look like me to amplify the message.
So here it is: Readers, listen to the plenary talks if you were not there. At minimum, behold the following line-up of speakers and topics. Feel the history.
This was the Best of DDW 2022:
- Julius Friedenwald Recognition of Timothy Wang. – John Inadomi.
- Presidential Address: Don’t Talk: Act. The relevance of DEI to gastroenterologists and hepatologists and the imperative for action. – John Inadomi.
- AGA Equity Project: Accomplishments and what lies ahead. – Byron L. Cryer, Sandra M. Quezada.
- The genesis and goals of the Association of Black Gastroenterologists and Hepatologists. – Sophie M. Balzora.
- Increasing racial and ethnic diversity in clinical trials: What we need to do. – Monica Webb Hooper.
- Reducing disparities in colorectal cancer. – Rachel Blankson Issaka.
- Reducing disparities in liver disease. – Lauren Nephew.
- Reducing disparities in IBD. – Fernando Velayos.
Uri Ladabaum, MD, MS, is with the division of gastroenterology and hepatology in the department of medicine at Stanford (Calif.) University. He reports serving on the advisory board for UniversalDx and Lean Medical and as a consultant for Medtronic, Clinical Genomics, Guardant Health, and Freenome. Dr. Ladabaum made these comments during the AGA Institute Presidential Plenary at the annual Digestive Disease Week®.
References
1. Inadomi JM. Gastroenterology. 2022 Jun;162(7):1855-7.
2. Ladabaum U. Ann Intern Med. 2020 Dec 1;173(11):938-9.
“The Best of DDW” elicits in the minds of most readers a compilation of the most important clinical and scientific content presented at DDW.
But I am not referring to that.
The “Best of DDW 2022” was the American Gastroenterological Association Presidential Plenary Session thanks to the humanity and vision of outgoing AGA President John Inadomi, MD.1 I sat in the audience, misty eyed, as each presenter addressed issues that strike deep into our humanity – the social determinants of health that have festered for far too long, leading to intolerable differences in health outcomes based on accidents of birth, and amplified by racism.
As the table on stage slowly filled in, an amazing picture took shape. A majority of the speakers were Black gastroenterologists and hepatologists, and among them many were young women. As I watched the video of a group of young Black gastroenterologists and hepatologists reaching out to the community, I asked myself “Has anything like this ever happened at a major national medical association meeting in the United States? Ever?” And then it occurred to me: “And just imagine, this exactly 2 days before the 2-year anniversary of the death of George Floyd.”
The plenary session happened on May 23, and I was conscious about the dates because I will never forget that George Floyd was killed on May 25, 2020 – my 55th birthday. The juxtaposition of his death and my birthday 2 years ago shook me profoundly, prompting me to write down my reflections and my hope that, in the national reactions that followed, we were seeing the beginning of true change.2 Two years later, despite our national divisions and serious challenges, I have reasons for hope.
On May 24, I ran into a colleague who was a Black woman. I have stopped being afraid to bring up previously untouchable subjects. I asked her what she thought about the remarkable AGA Plenary. She said she was glad that she is here to see it – that her parents never got the chance.
I admitted to her that I often ask myself what more I could and should be doing. I’m trying to do what I can in recruitment, education, in my personal life. What more? She said that one thing we really need is for people who look like me to amplify the message.
So here it is: Readers, listen to the plenary talks if you were not there. At minimum, behold the following line-up of speakers and topics. Feel the history.
This was the Best of DDW 2022:
- Julius Friedenwald Recognition of Timothy Wang. – John Inadomi.
- Presidential Address: Don’t Talk: Act. The relevance of DEI to gastroenterologists and hepatologists and the imperative for action. – John Inadomi.
- AGA Equity Project: Accomplishments and what lies ahead. – Byron L. Cryer, Sandra M. Quezada.
- The genesis and goals of the Association of Black Gastroenterologists and Hepatologists. – Sophie M. Balzora.
- Increasing racial and ethnic diversity in clinical trials: What we need to do. – Monica Webb Hooper.
- Reducing disparities in colorectal cancer. – Rachel Blankson Issaka.
- Reducing disparities in liver disease. – Lauren Nephew.
- Reducing disparities in IBD. – Fernando Velayos.
Uri Ladabaum, MD, MS, is with the division of gastroenterology and hepatology in the department of medicine at Stanford (Calif.) University. He reports serving on the advisory board for UniversalDx and Lean Medical and as a consultant for Medtronic, Clinical Genomics, Guardant Health, and Freenome. Dr. Ladabaum made these comments during the AGA Institute Presidential Plenary at the annual Digestive Disease Week®.
References
1. Inadomi JM. Gastroenterology. 2022 Jun;162(7):1855-7.
2. Ladabaum U. Ann Intern Med. 2020 Dec 1;173(11):938-9.
“The Best of DDW” elicits in the minds of most readers a compilation of the most important clinical and scientific content presented at DDW.
But I am not referring to that.
The “Best of DDW 2022” was the American Gastroenterological Association Presidential Plenary Session thanks to the humanity and vision of outgoing AGA President John Inadomi, MD.1 I sat in the audience, misty eyed, as each presenter addressed issues that strike deep into our humanity – the social determinants of health that have festered for far too long, leading to intolerable differences in health outcomes based on accidents of birth, and amplified by racism.
As the table on stage slowly filled in, an amazing picture took shape. A majority of the speakers were Black gastroenterologists and hepatologists, and among them many were young women. As I watched the video of a group of young Black gastroenterologists and hepatologists reaching out to the community, I asked myself “Has anything like this ever happened at a major national medical association meeting in the United States? Ever?” And then it occurred to me: “And just imagine, this exactly 2 days before the 2-year anniversary of the death of George Floyd.”
The plenary session happened on May 23, and I was conscious about the dates because I will never forget that George Floyd was killed on May 25, 2020 – my 55th birthday. The juxtaposition of his death and my birthday 2 years ago shook me profoundly, prompting me to write down my reflections and my hope that, in the national reactions that followed, we were seeing the beginning of true change.2 Two years later, despite our national divisions and serious challenges, I have reasons for hope.
On May 24, I ran into a colleague who was a Black woman. I have stopped being afraid to bring up previously untouchable subjects. I asked her what she thought about the remarkable AGA Plenary. She said she was glad that she is here to see it – that her parents never got the chance.
I admitted to her that I often ask myself what more I could and should be doing. I’m trying to do what I can in recruitment, education, in my personal life. What more? She said that one thing we really need is for people who look like me to amplify the message.
So here it is: Readers, listen to the plenary talks if you were not there. At minimum, behold the following line-up of speakers and topics. Feel the history.
This was the Best of DDW 2022:
- Julius Friedenwald Recognition of Timothy Wang. – John Inadomi.
- Presidential Address: Don’t Talk: Act. The relevance of DEI to gastroenterologists and hepatologists and the imperative for action. – John Inadomi.
- AGA Equity Project: Accomplishments and what lies ahead. – Byron L. Cryer, Sandra M. Quezada.
- The genesis and goals of the Association of Black Gastroenterologists and Hepatologists. – Sophie M. Balzora.
- Increasing racial and ethnic diversity in clinical trials: What we need to do. – Monica Webb Hooper.
- Reducing disparities in colorectal cancer. – Rachel Blankson Issaka.
- Reducing disparities in liver disease. – Lauren Nephew.
- Reducing disparities in IBD. – Fernando Velayos.
Uri Ladabaum, MD, MS, is with the division of gastroenterology and hepatology in the department of medicine at Stanford (Calif.) University. He reports serving on the advisory board for UniversalDx and Lean Medical and as a consultant for Medtronic, Clinical Genomics, Guardant Health, and Freenome. Dr. Ladabaum made these comments during the AGA Institute Presidential Plenary at the annual Digestive Disease Week®.
References
1. Inadomi JM. Gastroenterology. 2022 Jun;162(7):1855-7.
2. Ladabaum U. Ann Intern Med. 2020 Dec 1;173(11):938-9.
Reversing depression: A plethora of therapeutic strategies and mechanisms
Despite much progress, major depressive disorder (MDD) continues to be a challenging and life-threatening neuropsychiatric disorder. It is highly prevalent and afflicts tens of millions of Americans.
It is also ranked as the No. 1 disabling medical (not just psychiatric) condition by the World Health Organization.1 A significant proportion of patients with MDD do not respond adequately to several rounds of antidepressant medications,2 and many are labeled as having “treatment-resistant depression” (TRD).
In a previous article, I provocatively proposed that TRD is a myth.3 What I meant is that in a heterogeneous syndrome such as depression, failure to respond to 1, 2, or even 3 antidepressants should not imply TRD, because there is a “right treatment” that has not yet been identified for a given depressed patient. Most of those labeled as TRD have simply not yet received the pharmacotherapy or somatic therapy with the requisite mechanism of action for their variant of depression within a heterogeneous syndrome. IV ketamine, which, astonishingly, often reverses severe TRD of chronic duration within a few hours, is a prime example of why the term TRD is often used prematurely. Ketamine’s mechanism of action (immediate neuroplasticity via glutamate N-methyl-
Some clinicians may not be aware of the abundance of mechanisms of action currently available for the treatment of MDD as well as bipolar depression. Many practitioners, in both psychiatry and primary care, usually start the treatment of depression with a selective serotonin reuptake inhibitor, and if that does not produce a response or remission, they might switch to a serotonin-norepinephrine reuptake inhibitor. If that does not control the patient’s depressive symptoms, they start entertaining the notion that the patient may have TRD, not realizing that they have barely scratched the surface of the many therapeutic options and mechanisms of action, one of which could be the “best match” for a given patient.4
There will come a day when “precision psychiatry” finally arrives, and specific biomarkers will be developed to identify the “right” treatment for each patient within the heterogenous syndrome of depression.5 Until that day arrives, the treatment of depression will continue to be a process of trial and error, and hit or miss. But research will eventually discover genetic, neurochemical, neurophysiological, neuroimaging, or neuroimmune biomarkers that will rapidly guide clinicians to the correct treatment. This is critical to avoid inordinate delays in achieving remission and avert the ever-present risk of suicidal behavior.
The Table6 provides an overview of the numerous treatments currently available to manage depression. All increase brain-derived neurotrophic factor and restore healthy neuroplasticity and neurogenesis, which are impaired in MDD and currently believed to be a final common pathway for all depression treatments.7
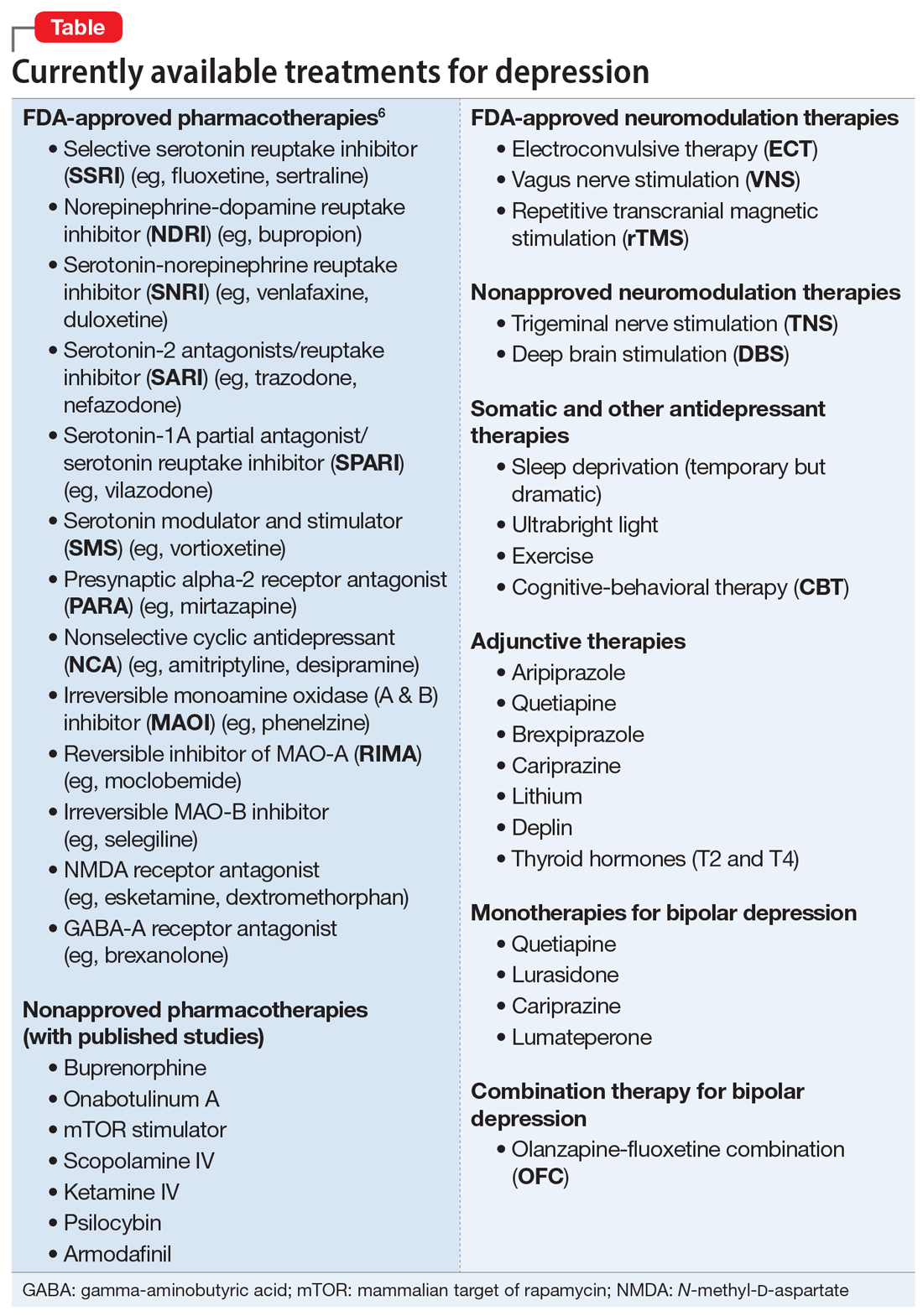
These 41 therapeutic approaches to treating MDD or bipolar depression reflect the heterogeneity of mechanisms of action to address an equally heterogeneous syndrome. This implies that clinicians have a wide array of on-label options to manage patients with depression, aiming for remission, not just a good response, which typically is defined as a ≥50% reduction in total score on one of the validated rating scales used to quantify depression severity, such as the Montgomery-Åsberg Depression Rating Scale, Hamilton Depression Rating Scale, or Calgary Depression Scale for Schizophrenia.
Continue to: When several FDA-approved pharmacotherapies...
When several FDA-approved pharmacotherapies fall short and produce a suboptimal response, clinicians can resort to other treatment options known to have a higher efficacy than oral antidepressants. These include electroconvulsive therapy, repetitive transcranial magnetic stimulation, and vagus nerve stimulation. Other on-label options include adjunctive therapy with one of the approved second-generation antipsychotic agents or with adjunctive esketamine.
But if the patient still does not improve, one of many emerging off-label treatment options may work. One of the exciting new discoveries is the hallucinogen psilocybin, whose mechanism of action is truly unique. Unlike standard antidepressant medications, which modulate neurotransmitters, psilocybin increases the brain’s network flexibility, decreases the modularity of several key brain networks (especially the default-brain network, or DMN), and alters the dark and distorted mental perspective of depression to a much healthier and optimistic outlook about the self and the world.8 Such novel breakthroughs in the treatment of severe depression will shed some unprecedented insights into the core neurobiology of depression, and may lead to early intervention and prevention.
As the saying goes, all roads lead to Rome. Psychiatric clinicians should rejoice that there are abundant approaches and therapeutic mechanisms to relieve their severely melancholic (and often suicidal) patients from the grips of this disabling and life-altering brain syndrome.
1. World Health Organization. Depression: let’s talk says WHO, as depression tops list of causes of ill health. March 30, 2017. Accessed July 5, 2022. www.who.int/news/item/30-03-2017--depression-let-s-talk-says-who-as-depression-tops-list-of-causes-of-ill-health
2. Trivedi MH, Fava M, Wisniewski SR, et al. Medication augmentation after the failure of SSRIs for depression. N Eng J Med. 2006;354(12)1243-1252.
3. Nasrallah HA. Treatment resistance is a myth! Current Psychiatry. 2021;20(3):14-16,28.
4. Nasrallah HA. 10 Recent paradigm shifts in the neurobiology and treatment of depression. Current Psychiatry. 2015;14(2):10-13.
5. Nasrallah HA. Biomarkers in neuropsychiatric disorders: translating research to clinical applications. Biomarkers in Neuropsychiatry. 2019;1:100001. doi:10.1016/j.bionps.2019.100001
6. Procyshyn RM, Bezchlibnyk-Butler KZ, Jeffries JJ. Clinical Handbook of Psychotropic Drugs. 23rd ed. Hogrefe; 2019.
7. Tartt AN, Mariani, MB, Hen R, et al. Dysregulation of adult hippocampal neuroplasticity in major depression: pathogenesis and therapeutic implications. Mol Psychiatry. 2022;27(6):2689-2699.
8. Lowe H, Toyang N, Steele B, et al. The therapeutic potential of psilocybin. Molecules. 2021;26(10):2948. doi: 10.3390/molecules26102948
Despite much progress, major depressive disorder (MDD) continues to be a challenging and life-threatening neuropsychiatric disorder. It is highly prevalent and afflicts tens of millions of Americans.
It is also ranked as the No. 1 disabling medical (not just psychiatric) condition by the World Health Organization.1 A significant proportion of patients with MDD do not respond adequately to several rounds of antidepressant medications,2 and many are labeled as having “treatment-resistant depression” (TRD).
In a previous article, I provocatively proposed that TRD is a myth.3 What I meant is that in a heterogeneous syndrome such as depression, failure to respond to 1, 2, or even 3 antidepressants should not imply TRD, because there is a “right treatment” that has not yet been identified for a given depressed patient. Most of those labeled as TRD have simply not yet received the pharmacotherapy or somatic therapy with the requisite mechanism of action for their variant of depression within a heterogeneous syndrome. IV ketamine, which, astonishingly, often reverses severe TRD of chronic duration within a few hours, is a prime example of why the term TRD is often used prematurely. Ketamine’s mechanism of action (immediate neuroplasticity via glutamate N-methyl-
Some clinicians may not be aware of the abundance of mechanisms of action currently available for the treatment of MDD as well as bipolar depression. Many practitioners, in both psychiatry and primary care, usually start the treatment of depression with a selective serotonin reuptake inhibitor, and if that does not produce a response or remission, they might switch to a serotonin-norepinephrine reuptake inhibitor. If that does not control the patient’s depressive symptoms, they start entertaining the notion that the patient may have TRD, not realizing that they have barely scratched the surface of the many therapeutic options and mechanisms of action, one of which could be the “best match” for a given patient.4
There will come a day when “precision psychiatry” finally arrives, and specific biomarkers will be developed to identify the “right” treatment for each patient within the heterogenous syndrome of depression.5 Until that day arrives, the treatment of depression will continue to be a process of trial and error, and hit or miss. But research will eventually discover genetic, neurochemical, neurophysiological, neuroimaging, or neuroimmune biomarkers that will rapidly guide clinicians to the correct treatment. This is critical to avoid inordinate delays in achieving remission and avert the ever-present risk of suicidal behavior.
The Table6 provides an overview of the numerous treatments currently available to manage depression. All increase brain-derived neurotrophic factor and restore healthy neuroplasticity and neurogenesis, which are impaired in MDD and currently believed to be a final common pathway for all depression treatments.7
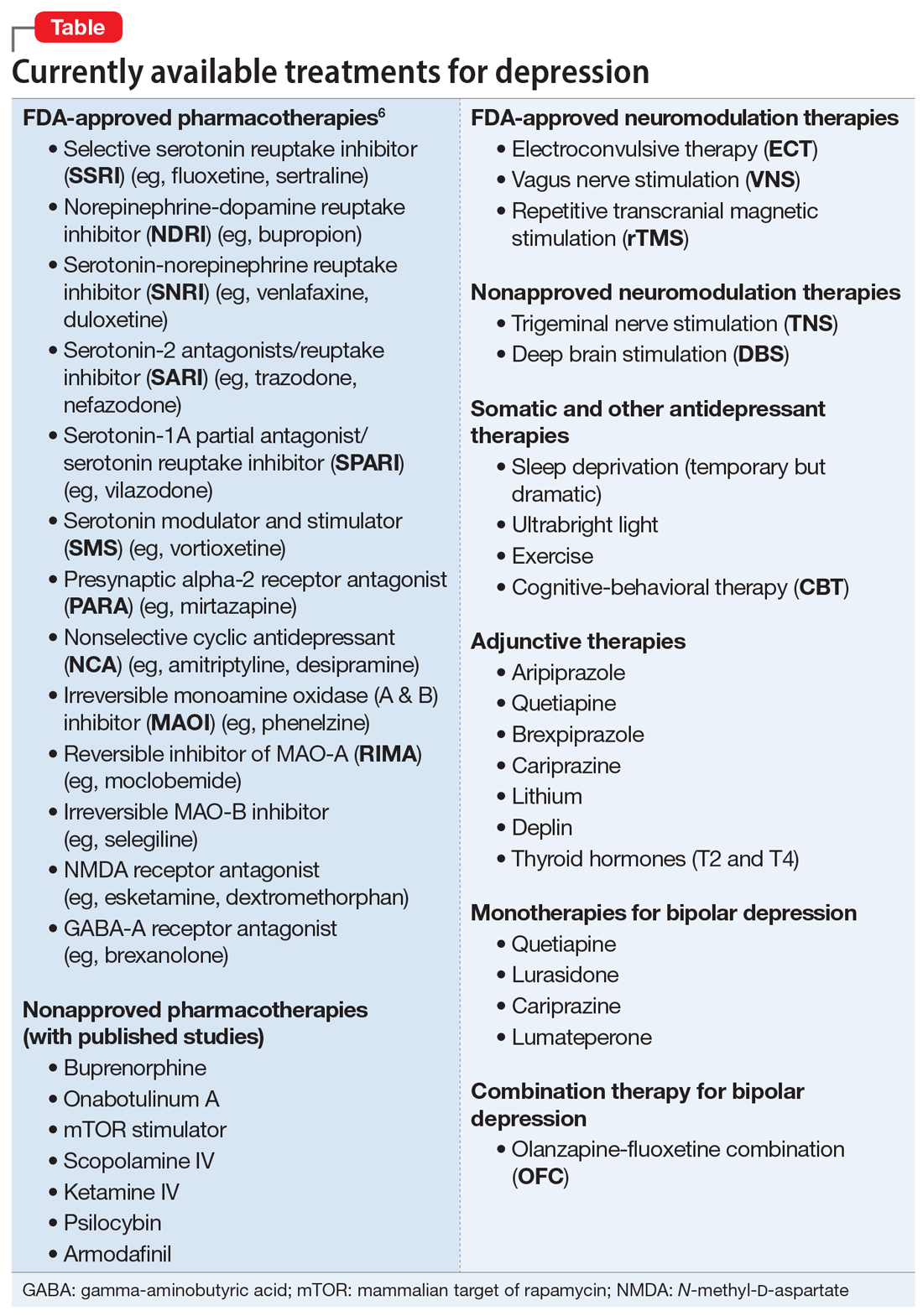
These 41 therapeutic approaches to treating MDD or bipolar depression reflect the heterogeneity of mechanisms of action to address an equally heterogeneous syndrome. This implies that clinicians have a wide array of on-label options to manage patients with depression, aiming for remission, not just a good response, which typically is defined as a ≥50% reduction in total score on one of the validated rating scales used to quantify depression severity, such as the Montgomery-Åsberg Depression Rating Scale, Hamilton Depression Rating Scale, or Calgary Depression Scale for Schizophrenia.
Continue to: When several FDA-approved pharmacotherapies...
When several FDA-approved pharmacotherapies fall short and produce a suboptimal response, clinicians can resort to other treatment options known to have a higher efficacy than oral antidepressants. These include electroconvulsive therapy, repetitive transcranial magnetic stimulation, and vagus nerve stimulation. Other on-label options include adjunctive therapy with one of the approved second-generation antipsychotic agents or with adjunctive esketamine.
But if the patient still does not improve, one of many emerging off-label treatment options may work. One of the exciting new discoveries is the hallucinogen psilocybin, whose mechanism of action is truly unique. Unlike standard antidepressant medications, which modulate neurotransmitters, psilocybin increases the brain’s network flexibility, decreases the modularity of several key brain networks (especially the default-brain network, or DMN), and alters the dark and distorted mental perspective of depression to a much healthier and optimistic outlook about the self and the world.8 Such novel breakthroughs in the treatment of severe depression will shed some unprecedented insights into the core neurobiology of depression, and may lead to early intervention and prevention.
As the saying goes, all roads lead to Rome. Psychiatric clinicians should rejoice that there are abundant approaches and therapeutic mechanisms to relieve their severely melancholic (and often suicidal) patients from the grips of this disabling and life-altering brain syndrome.
Despite much progress, major depressive disorder (MDD) continues to be a challenging and life-threatening neuropsychiatric disorder. It is highly prevalent and afflicts tens of millions of Americans.
It is also ranked as the No. 1 disabling medical (not just psychiatric) condition by the World Health Organization.1 A significant proportion of patients with MDD do not respond adequately to several rounds of antidepressant medications,2 and many are labeled as having “treatment-resistant depression” (TRD).
In a previous article, I provocatively proposed that TRD is a myth.3 What I meant is that in a heterogeneous syndrome such as depression, failure to respond to 1, 2, or even 3 antidepressants should not imply TRD, because there is a “right treatment” that has not yet been identified for a given depressed patient. Most of those labeled as TRD have simply not yet received the pharmacotherapy or somatic therapy with the requisite mechanism of action for their variant of depression within a heterogeneous syndrome. IV ketamine, which, astonishingly, often reverses severe TRD of chronic duration within a few hours, is a prime example of why the term TRD is often used prematurely. Ketamine’s mechanism of action (immediate neuroplasticity via glutamate N-methyl-
Some clinicians may not be aware of the abundance of mechanisms of action currently available for the treatment of MDD as well as bipolar depression. Many practitioners, in both psychiatry and primary care, usually start the treatment of depression with a selective serotonin reuptake inhibitor, and if that does not produce a response or remission, they might switch to a serotonin-norepinephrine reuptake inhibitor. If that does not control the patient’s depressive symptoms, they start entertaining the notion that the patient may have TRD, not realizing that they have barely scratched the surface of the many therapeutic options and mechanisms of action, one of which could be the “best match” for a given patient.4
There will come a day when “precision psychiatry” finally arrives, and specific biomarkers will be developed to identify the “right” treatment for each patient within the heterogenous syndrome of depression.5 Until that day arrives, the treatment of depression will continue to be a process of trial and error, and hit or miss. But research will eventually discover genetic, neurochemical, neurophysiological, neuroimaging, or neuroimmune biomarkers that will rapidly guide clinicians to the correct treatment. This is critical to avoid inordinate delays in achieving remission and avert the ever-present risk of suicidal behavior.
The Table6 provides an overview of the numerous treatments currently available to manage depression. All increase brain-derived neurotrophic factor and restore healthy neuroplasticity and neurogenesis, which are impaired in MDD and currently believed to be a final common pathway for all depression treatments.7
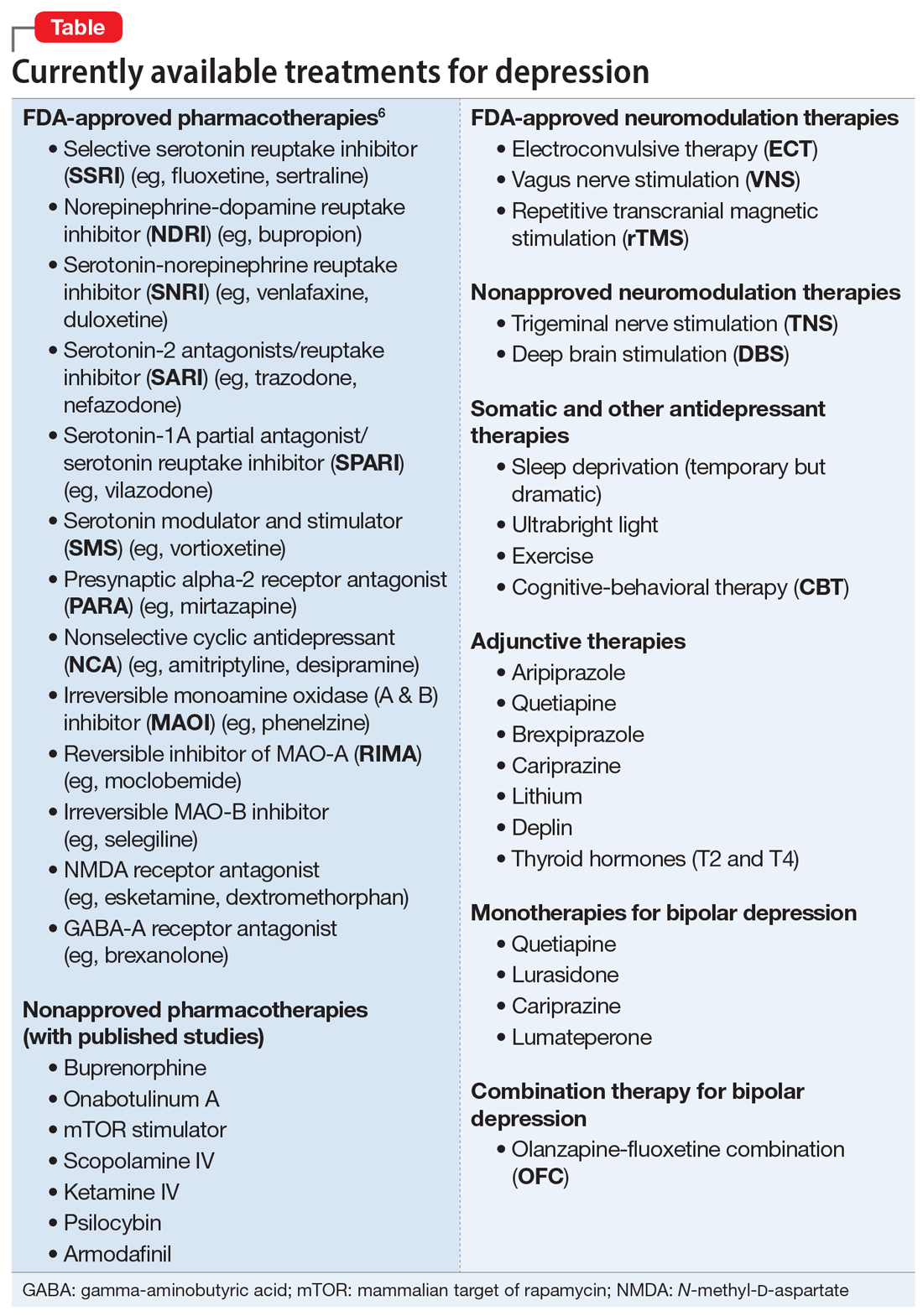
These 41 therapeutic approaches to treating MDD or bipolar depression reflect the heterogeneity of mechanisms of action to address an equally heterogeneous syndrome. This implies that clinicians have a wide array of on-label options to manage patients with depression, aiming for remission, not just a good response, which typically is defined as a ≥50% reduction in total score on one of the validated rating scales used to quantify depression severity, such as the Montgomery-Åsberg Depression Rating Scale, Hamilton Depression Rating Scale, or Calgary Depression Scale for Schizophrenia.
Continue to: When several FDA-approved pharmacotherapies...
When several FDA-approved pharmacotherapies fall short and produce a suboptimal response, clinicians can resort to other treatment options known to have a higher efficacy than oral antidepressants. These include electroconvulsive therapy, repetitive transcranial magnetic stimulation, and vagus nerve stimulation. Other on-label options include adjunctive therapy with one of the approved second-generation antipsychotic agents or with adjunctive esketamine.
But if the patient still does not improve, one of many emerging off-label treatment options may work. One of the exciting new discoveries is the hallucinogen psilocybin, whose mechanism of action is truly unique. Unlike standard antidepressant medications, which modulate neurotransmitters, psilocybin increases the brain’s network flexibility, decreases the modularity of several key brain networks (especially the default-brain network, or DMN), and alters the dark and distorted mental perspective of depression to a much healthier and optimistic outlook about the self and the world.8 Such novel breakthroughs in the treatment of severe depression will shed some unprecedented insights into the core neurobiology of depression, and may lead to early intervention and prevention.
As the saying goes, all roads lead to Rome. Psychiatric clinicians should rejoice that there are abundant approaches and therapeutic mechanisms to relieve their severely melancholic (and often suicidal) patients from the grips of this disabling and life-altering brain syndrome.
1. World Health Organization. Depression: let’s talk says WHO, as depression tops list of causes of ill health. March 30, 2017. Accessed July 5, 2022. www.who.int/news/item/30-03-2017--depression-let-s-talk-says-who-as-depression-tops-list-of-causes-of-ill-health
2. Trivedi MH, Fava M, Wisniewski SR, et al. Medication augmentation after the failure of SSRIs for depression. N Eng J Med. 2006;354(12)1243-1252.
3. Nasrallah HA. Treatment resistance is a myth! Current Psychiatry. 2021;20(3):14-16,28.
4. Nasrallah HA. 10 Recent paradigm shifts in the neurobiology and treatment of depression. Current Psychiatry. 2015;14(2):10-13.
5. Nasrallah HA. Biomarkers in neuropsychiatric disorders: translating research to clinical applications. Biomarkers in Neuropsychiatry. 2019;1:100001. doi:10.1016/j.bionps.2019.100001
6. Procyshyn RM, Bezchlibnyk-Butler KZ, Jeffries JJ. Clinical Handbook of Psychotropic Drugs. 23rd ed. Hogrefe; 2019.
7. Tartt AN, Mariani, MB, Hen R, et al. Dysregulation of adult hippocampal neuroplasticity in major depression: pathogenesis and therapeutic implications. Mol Psychiatry. 2022;27(6):2689-2699.
8. Lowe H, Toyang N, Steele B, et al. The therapeutic potential of psilocybin. Molecules. 2021;26(10):2948. doi: 10.3390/molecules26102948
1. World Health Organization. Depression: let’s talk says WHO, as depression tops list of causes of ill health. March 30, 2017. Accessed July 5, 2022. www.who.int/news/item/30-03-2017--depression-let-s-talk-says-who-as-depression-tops-list-of-causes-of-ill-health
2. Trivedi MH, Fava M, Wisniewski SR, et al. Medication augmentation after the failure of SSRIs for depression. N Eng J Med. 2006;354(12)1243-1252.
3. Nasrallah HA. Treatment resistance is a myth! Current Psychiatry. 2021;20(3):14-16,28.
4. Nasrallah HA. 10 Recent paradigm shifts in the neurobiology and treatment of depression. Current Psychiatry. 2015;14(2):10-13.
5. Nasrallah HA. Biomarkers in neuropsychiatric disorders: translating research to clinical applications. Biomarkers in Neuropsychiatry. 2019;1:100001. doi:10.1016/j.bionps.2019.100001
6. Procyshyn RM, Bezchlibnyk-Butler KZ, Jeffries JJ. Clinical Handbook of Psychotropic Drugs. 23rd ed. Hogrefe; 2019.
7. Tartt AN, Mariani, MB, Hen R, et al. Dysregulation of adult hippocampal neuroplasticity in major depression: pathogenesis and therapeutic implications. Mol Psychiatry. 2022;27(6):2689-2699.
8. Lowe H, Toyang N, Steele B, et al. The therapeutic potential of psilocybin. Molecules. 2021;26(10):2948. doi: 10.3390/molecules26102948
Hope, help, and humor when facing a life-threatening illness
Editor’s note: Readers’ Forum is a department for correspondence from readers that is not in response to articles published in
My father, Morty Sosland, MD, was a psychiatrist in a community health setting when he was diagnosed with amyotrophic lateral sclerosis (ALS; Lou Gehrig’s disease) in April 2020. He continued to work until February 2021 and credits his ongoing resilience to what he refers to as “the 3 Hs”: hope, help, and humor. Although he can no longer speak, I was able to interview him over the advanced technology that is text messaging.
Sarah: Hi, Dad.
Morty: It’s Doctor Dad to you.
Sarah: I guess we are starting with humor, then?
Humor
Research has demonstrated that humor can have serious health benefits, such as decreasing stress-making hormones and altering dopamine activity.1 For individuals facing a life-threatening illness, humor can help them gain a sense of perspective in a situation that would otherwise feel overwhelming.
Sarah: I feel like a lot of the humor you used with patients was to help them gain perspective.
Continue to: Morty
Morty: Yes. I’d have to know the client well enough, though—and timing is important. My patients would come to me with a long list of challenges they had faced in the week, and I would say, “But besides that, everything’s good?”
Sarah: And besides the ALS, everything’s good?
Morty: Exactly. I’d also use magic or math tricks to make kids like coming to therapy or to reinforce important concepts.
Sarah: How has humor helped you cope?
Morty: Thinking about things in humorous ways has always been helpful. I used to say my Olympic sport was walking to the dining room with my walker. Unfortunately, I can’t do that anymore, so now my Olympic sport is getting out of bed. It’s a team sport.
Sarah: And that’s a good segue to…
Help
Countless studies have shown the impact of social support on health. Good social support can increase resilience, protect against mental illness, and even increase life expectancy.2 Support becomes even more critical when you are physically dependent on others due to illness.
Continue to: Sarah
Sarah: Was it difficult for you to accept help at first?
Morty: I would say yes—but at the same time, I accepted it because the illness was so shocking. I learned early on this was a fight that my family would also fight alongside me.
Sarah: I remember you would quote Fred Rogers.
Morty: Actually, it was Fred Rogers’ mother. She would tell her son during hard times, “Look for the helpers. You will always find people who are helping.” Helpers can be family members, friends, doctors, and aides, as well as others who have the same illness.
Hope
In the face of all life’s challenges, hope is important, but in the face of a life-threatening illness, hope must be multifaceted.3 In addition to hope for a cure, patients may focus their hopes on deepening relationships, maintaining dignity, or living each day to its fullest.
Morty: Early on in this illness, I chose to set a positive tone when I told people. I would say I have the top doctors and there is more research now than ever. Years ago, I wrote a children’s book with the mantra, “I say I can, I make a plan, I get right to it and then I do it.”4 My plan is to be around for at least 30 more years.
Sarah: Do you think it’s possible to hold acceptance and hope at the same time?
Morty: Acceptance and hope are not easy, but possible. I get down about this illness. In my dreams, I walk and talk, and most mornings I wake up and see my wheelchair and I think this is absurd or a different choice word. But I focus on the things I still can do, and that gives me a feeling of hope. I can read the latest research, I can enjoy moments of laughter, and I can spend time with my family and close friends.
1. Yim J. Therapeutic benefits of laughter in mental health: a theoretical review. Tohoku J Exp Med. 2016;239(3):243-249. doi:10.1620/tjem.239.243
2. Ozbay F, Johnson DC, Dimoulas E, et al. Social support and resilience to stress: from neurobiology to clinical practice. Psychiatry (Edgmont). 2007;4(5):35-40.
3. Hill DL, Feudnter C. Hope in the midst of terminal illness. In: Gallagher MW, Lopez SJ, eds. The Oxford Handbook of Hope. Oxford University Press; 2018:191-206.
4. Sosland MD. The Can Do Duck: A Story About Believing in Yourself. Can Do Duck Publishing; 2019.
Editor’s note: Readers’ Forum is a department for correspondence from readers that is not in response to articles published in
My father, Morty Sosland, MD, was a psychiatrist in a community health setting when he was diagnosed with amyotrophic lateral sclerosis (ALS; Lou Gehrig’s disease) in April 2020. He continued to work until February 2021 and credits his ongoing resilience to what he refers to as “the 3 Hs”: hope, help, and humor. Although he can no longer speak, I was able to interview him over the advanced technology that is text messaging.
Sarah: Hi, Dad.
Morty: It’s Doctor Dad to you.
Sarah: I guess we are starting with humor, then?
Humor
Research has demonstrated that humor can have serious health benefits, such as decreasing stress-making hormones and altering dopamine activity.1 For individuals facing a life-threatening illness, humor can help them gain a sense of perspective in a situation that would otherwise feel overwhelming.
Sarah: I feel like a lot of the humor you used with patients was to help them gain perspective.
Continue to: Morty
Morty: Yes. I’d have to know the client well enough, though—and timing is important. My patients would come to me with a long list of challenges they had faced in the week, and I would say, “But besides that, everything’s good?”
Sarah: And besides the ALS, everything’s good?
Morty: Exactly. I’d also use magic or math tricks to make kids like coming to therapy or to reinforce important concepts.
Sarah: How has humor helped you cope?
Morty: Thinking about things in humorous ways has always been helpful. I used to say my Olympic sport was walking to the dining room with my walker. Unfortunately, I can’t do that anymore, so now my Olympic sport is getting out of bed. It’s a team sport.
Sarah: And that’s a good segue to…
Help
Countless studies have shown the impact of social support on health. Good social support can increase resilience, protect against mental illness, and even increase life expectancy.2 Support becomes even more critical when you are physically dependent on others due to illness.
Continue to: Sarah
Sarah: Was it difficult for you to accept help at first?
Morty: I would say yes—but at the same time, I accepted it because the illness was so shocking. I learned early on this was a fight that my family would also fight alongside me.
Sarah: I remember you would quote Fred Rogers.
Morty: Actually, it was Fred Rogers’ mother. She would tell her son during hard times, “Look for the helpers. You will always find people who are helping.” Helpers can be family members, friends, doctors, and aides, as well as others who have the same illness.
Hope
In the face of all life’s challenges, hope is important, but in the face of a life-threatening illness, hope must be multifaceted.3 In addition to hope for a cure, patients may focus their hopes on deepening relationships, maintaining dignity, or living each day to its fullest.
Morty: Early on in this illness, I chose to set a positive tone when I told people. I would say I have the top doctors and there is more research now than ever. Years ago, I wrote a children’s book with the mantra, “I say I can, I make a plan, I get right to it and then I do it.”4 My plan is to be around for at least 30 more years.
Sarah: Do you think it’s possible to hold acceptance and hope at the same time?
Morty: Acceptance and hope are not easy, but possible. I get down about this illness. In my dreams, I walk and talk, and most mornings I wake up and see my wheelchair and I think this is absurd or a different choice word. But I focus on the things I still can do, and that gives me a feeling of hope. I can read the latest research, I can enjoy moments of laughter, and I can spend time with my family and close friends.
Editor’s note: Readers’ Forum is a department for correspondence from readers that is not in response to articles published in
My father, Morty Sosland, MD, was a psychiatrist in a community health setting when he was diagnosed with amyotrophic lateral sclerosis (ALS; Lou Gehrig’s disease) in April 2020. He continued to work until February 2021 and credits his ongoing resilience to what he refers to as “the 3 Hs”: hope, help, and humor. Although he can no longer speak, I was able to interview him over the advanced technology that is text messaging.
Sarah: Hi, Dad.
Morty: It’s Doctor Dad to you.
Sarah: I guess we are starting with humor, then?
Humor
Research has demonstrated that humor can have serious health benefits, such as decreasing stress-making hormones and altering dopamine activity.1 For individuals facing a life-threatening illness, humor can help them gain a sense of perspective in a situation that would otherwise feel overwhelming.
Sarah: I feel like a lot of the humor you used with patients was to help them gain perspective.
Continue to: Morty
Morty: Yes. I’d have to know the client well enough, though—and timing is important. My patients would come to me with a long list of challenges they had faced in the week, and I would say, “But besides that, everything’s good?”
Sarah: And besides the ALS, everything’s good?
Morty: Exactly. I’d also use magic or math tricks to make kids like coming to therapy or to reinforce important concepts.
Sarah: How has humor helped you cope?
Morty: Thinking about things in humorous ways has always been helpful. I used to say my Olympic sport was walking to the dining room with my walker. Unfortunately, I can’t do that anymore, so now my Olympic sport is getting out of bed. It’s a team sport.
Sarah: And that’s a good segue to…
Help
Countless studies have shown the impact of social support on health. Good social support can increase resilience, protect against mental illness, and even increase life expectancy.2 Support becomes even more critical when you are physically dependent on others due to illness.
Continue to: Sarah
Sarah: Was it difficult for you to accept help at first?
Morty: I would say yes—but at the same time, I accepted it because the illness was so shocking. I learned early on this was a fight that my family would also fight alongside me.
Sarah: I remember you would quote Fred Rogers.
Morty: Actually, it was Fred Rogers’ mother. She would tell her son during hard times, “Look for the helpers. You will always find people who are helping.” Helpers can be family members, friends, doctors, and aides, as well as others who have the same illness.
Hope
In the face of all life’s challenges, hope is important, but in the face of a life-threatening illness, hope must be multifaceted.3 In addition to hope for a cure, patients may focus their hopes on deepening relationships, maintaining dignity, or living each day to its fullest.
Morty: Early on in this illness, I chose to set a positive tone when I told people. I would say I have the top doctors and there is more research now than ever. Years ago, I wrote a children’s book with the mantra, “I say I can, I make a plan, I get right to it and then I do it.”4 My plan is to be around for at least 30 more years.
Sarah: Do you think it’s possible to hold acceptance and hope at the same time?
Morty: Acceptance and hope are not easy, but possible. I get down about this illness. In my dreams, I walk and talk, and most mornings I wake up and see my wheelchair and I think this is absurd or a different choice word. But I focus on the things I still can do, and that gives me a feeling of hope. I can read the latest research, I can enjoy moments of laughter, and I can spend time with my family and close friends.
1. Yim J. Therapeutic benefits of laughter in mental health: a theoretical review. Tohoku J Exp Med. 2016;239(3):243-249. doi:10.1620/tjem.239.243
2. Ozbay F, Johnson DC, Dimoulas E, et al. Social support and resilience to stress: from neurobiology to clinical practice. Psychiatry (Edgmont). 2007;4(5):35-40.
3. Hill DL, Feudnter C. Hope in the midst of terminal illness. In: Gallagher MW, Lopez SJ, eds. The Oxford Handbook of Hope. Oxford University Press; 2018:191-206.
4. Sosland MD. The Can Do Duck: A Story About Believing in Yourself. Can Do Duck Publishing; 2019.
1. Yim J. Therapeutic benefits of laughter in mental health: a theoretical review. Tohoku J Exp Med. 2016;239(3):243-249. doi:10.1620/tjem.239.243
2. Ozbay F, Johnson DC, Dimoulas E, et al. Social support and resilience to stress: from neurobiology to clinical practice. Psychiatry (Edgmont). 2007;4(5):35-40.
3. Hill DL, Feudnter C. Hope in the midst of terminal illness. In: Gallagher MW, Lopez SJ, eds. The Oxford Handbook of Hope. Oxford University Press; 2018:191-206.
4. Sosland MD. The Can Do Duck: A Story About Believing in Yourself. Can Do Duck Publishing; 2019.
The impact of COVID-19 on adolescents’ mental health
While the COVID-19 pandemic has impacted the mental health of a wide range of individuals, its adverse effects have been particularly detrimental to adolescents. In this article, I discuss evidence that shows the effects of the pandemic on adolescent patients, potential reasons for this increased distress, and what types of coping mechanisms adolescents have used to counter these effects.
Increases in multiple measures of psychopathology
Multiple online surveys and other studies have documented the pandemic’s impact on younger individuals. In the United States, visits to emergency departments by pediatric patients increased in the months after the first lockdown period.1 Several studies found increased rates of anxiety and depression among adolescents during the COVID-19 pandemic.2,3 In an online survey of 359 children and 3,254 adolescents in China, 22% of respondents reported that they experienced depressive symptoms.3 In an online survey of 1,054 Canadian adolescents, 43% said they were “very concerned” about the pandemic.4 In an online survey of 7,353 adolescents in the United States, 37% reported suicidal ideation during the pandemic compared to 17% in 2017.5 A Chinese study found that smartphone and internet addiction was significantly associated with increased levels of depressive symptoms during the pandemic.3 In a survey in the Philippines, 16.3% of adolescents reported moderate-to-severe psychological impairment during the pandemic; the rates of COVID-19–related anxiety were higher among girls vs boys.6 Alcohol and cannabis use increased among Canadian adolescents during the pandemic, according to an online survey.7 Adolescents with anorexia nervosa reported a 70% increase in poor eating habits and more thoughts associated with eating disorders during the pandemic.8 A Danish study found that children and adolescents newly diagnosed with obsessive-compulsive disorder (OCD) or who had completed treatment exhibited worsening OCD, anxiety, and depressive symptoms during the pandemic.9 An online survey of 6,196 Chinese adolescents found that those with a higher number of pre-pandemic adverse childhood experiences, such as abuse and neglect, had elevated posttraumatic stress symptoms and anxiety during the onset of the pandemic.10
Underlying causes of pandemic-induced distress
Limited social connectedness during the pandemic is a major reason for distress among adolescents. A review of 80 studies found that social isolation and loneliness as a result of social distancing and quarantining were associated with an increased risk of depression, anxiety, suicidal ideation, and self-harm.11 Parents’ stress about the risks of COVID-19 was correlated with worsening mental health in their adolescent children.12 A Chinese study found that the amount of time students spent on smartphones and social media doubled during the pandemic.13 In an online survey of 7,890 Chinese adolescents, greater social media, internet, and smartphone use was associated with increased anxiety and depression.14 This may be in part the result of adolescents spending time reading COVID-related news.
Coping mechanisms to increase well-being
Researchers have identified several positive coping mechanisms adolescents employed during the pandemic. Although some data suggest that increased internet use raises the risk of COVID-related distress, for certain adolescents, using social media to stay connected with friends and relatives was a buffer for feelings of loneliness and might have increased mental well-being.15 Other common coping mechanisms include relying on faith, volunteering, and starting new hobbies.16 During the pandemic, there were higher rates of playing outside and increased physical activity, which correlated with positive mental health outcomes.16 An online survey of 1,040 adolescents found that those who looked to the future optimistically and confidently had a higher health-related quality of life.17
Continuing an emphasis on adolescent well-being
Although data are limited, adolescents can continue to use these coping mechanisms to maintain their well-being, even if COVID-related restrictions are lifted or reimplemented. During these difficult times, it is imperative for adolescents to get the mental health services they need, and for psychiatric clinicians to continue to find avenues to promote resilience and mental wellness among young patients.
1. Leeb RT, Bitsko RH, Radhakrishnan L, et al. Mental health–related emergency department visits among children aged <18 years during the COVID-19 pandemic—United States, January 1-October 17, 2020. MMWR Morb Mortal Wkly Rep. 2020;69(45):1675-1680. doi:10.15585/mmwr.mm6945a3
2. Oosterhoff B, Palmer CA, Wilson J, et al. Adolescents’ motivations to engage in social distancing during the COVID-19 pandemic: associations with mental and social health. J Adolesc Health. 2020;67(2):179-185. doi:10.1016/j.jadohealth.2020.05.004
3. Duan L, Shao X, Wang Y, et al. An investigation of mental health status of children and adolescents in China during the outbreak of COVID-19. J Affect Disord. 2020;275:112-118. doi:10.1016/j.jad.2020.06.029
4. Ellis WE, Dumas TM, Forbes LM. Physically isolated but socially connected: psychological adjustment and stress among adolescents during the initial COVID-19 crisis. Can J Behav Sci. 2020;52(3):177-187. doi:10.1037/cbs0000215
5. Murata S, Rezeppa T, Thoma B, et al. The psychiatric sequelae of the COVID-19 pandemic in adolescents, adults, and health care workers. Depress Anxiety. 2021;38(2):233-246. doi:10.1002/da.23120
6. Tee ML, Tee CA, Anlacan JP, et al. Psychological impact of COVID-19 pandemic in the Philippines. J Affect Disord. 2020;277:379-391. doi:10.1016/j.jad.2020.08.043
7. Dumas TM, Ellis W, Litt DM. What does adolescent substance use look like during the COVID-19 pandemic? Examining changes in frequency, social contexts, and pandemic-related predictors. J Adolesc Health. 2020;67(3):354-361. doi:10.1016/j.jadohealth.2020.06.018
8. Schlegl S, Maier J, Meule A, et al. Eating disorders in times of the COVID-19 pandemic—results from an online survey of patients with anorexia nervosa. Int J Eat Disord. 2020;53:1791-1800. doi:10.1002/eat.23374.
9. Nissen JB, Højgaard D, Thomsen PH. The immediate effect of COVID-19 pandemic on children and adolescents with obsessive compulsive disorder. BMC Psychiatry. 2020;20(1):511. doi:10.1186/s12888-020-02905-5
10. Guo J, Fu M, Liu D, et al. Is the psychological impact of exposure to COVID-19 stronger in adolescents with pre-pandemic maltreatment experiences? A survey of rural Chinese adolescents. Child Abuse Negl. 2020;110(Pt 2):104667. doi:10.1016/j.chiabu.2020.104667
11. Loades ME, Chatburn E, Higson-Sweeney N, et al. Rapid Systematic Review: The impact of social isolation and loneliness on the mental health of children and adolescents in the context of COVID-19. J Am Acad Child Adolesc Psychiatry. 2020;59(11):1218-1239.e3. doi:10.1016/j.jaac.2020.05.009
12. Spinelli M, Lionetti F, Setti A, et al. Parenting stress during the COVID-19 outbreak: socioeconomic and environmental risk factors and implications for children emotion regulation. Fam Process. 2021;60(2):639-653. doi:10.1111/famp.12601
13. Chen IH, Chen CY, Pakpour AH, et al. Internet-related behaviors and psychological distress among schoolchildren during COVID-19 school suspension. J Am Acad Child Adolesc Psychiatry. 2020;59(10):1099-1102.e1. doi:10.1016/j.jaac.2020.06.007
14. Li W, Zhang Y, Wang J, et al. Association of home quarantine and mental health among teenagers in Wuhan, China, during the COVID-19 pandemic. JAMA Pediatr. 2021;175(3):313-316. doi:10.1001/jamapediatrics.2020.5499
15. Janssen, LHC, Kullberg, MJ, Verkuil B, et al. Does the COVID-19 pandemic impact parents’ and adolescents’ well-being? An EMA-study on daily affect and parenting. PLoS One. 2020;15(10):e0240962. doi:10.1371/journal.pone.0240962
16. Banati P, Jones N, Youssef S. Intersecting vulnerabilities: the impacts of COVID-19 on the psycho-emotional lives of young people in low- and middle-income countries. Eur J Dev Res. 2020;32(5):1613-1638. doi:10.1057/s41287-020-00325-5
17. Ravens-Sieberer U, Kaman A, Otto C, et al. Mental health and quality of life in children and adolescents during the COVID-19 pandemic—results of the COPSY study. Dtsch Arztebl Int. 2020;117(48):828-829. doi:10.3238/arztebl.2020.0828
While the COVID-19 pandemic has impacted the mental health of a wide range of individuals, its adverse effects have been particularly detrimental to adolescents. In this article, I discuss evidence that shows the effects of the pandemic on adolescent patients, potential reasons for this increased distress, and what types of coping mechanisms adolescents have used to counter these effects.
Increases in multiple measures of psychopathology
Multiple online surveys and other studies have documented the pandemic’s impact on younger individuals. In the United States, visits to emergency departments by pediatric patients increased in the months after the first lockdown period.1 Several studies found increased rates of anxiety and depression among adolescents during the COVID-19 pandemic.2,3 In an online survey of 359 children and 3,254 adolescents in China, 22% of respondents reported that they experienced depressive symptoms.3 In an online survey of 1,054 Canadian adolescents, 43% said they were “very concerned” about the pandemic.4 In an online survey of 7,353 adolescents in the United States, 37% reported suicidal ideation during the pandemic compared to 17% in 2017.5 A Chinese study found that smartphone and internet addiction was significantly associated with increased levels of depressive symptoms during the pandemic.3 In a survey in the Philippines, 16.3% of adolescents reported moderate-to-severe psychological impairment during the pandemic; the rates of COVID-19–related anxiety were higher among girls vs boys.6 Alcohol and cannabis use increased among Canadian adolescents during the pandemic, according to an online survey.7 Adolescents with anorexia nervosa reported a 70% increase in poor eating habits and more thoughts associated with eating disorders during the pandemic.8 A Danish study found that children and adolescents newly diagnosed with obsessive-compulsive disorder (OCD) or who had completed treatment exhibited worsening OCD, anxiety, and depressive symptoms during the pandemic.9 An online survey of 6,196 Chinese adolescents found that those with a higher number of pre-pandemic adverse childhood experiences, such as abuse and neglect, had elevated posttraumatic stress symptoms and anxiety during the onset of the pandemic.10
Underlying causes of pandemic-induced distress
Limited social connectedness during the pandemic is a major reason for distress among adolescents. A review of 80 studies found that social isolation and loneliness as a result of social distancing and quarantining were associated with an increased risk of depression, anxiety, suicidal ideation, and self-harm.11 Parents’ stress about the risks of COVID-19 was correlated with worsening mental health in their adolescent children.12 A Chinese study found that the amount of time students spent on smartphones and social media doubled during the pandemic.13 In an online survey of 7,890 Chinese adolescents, greater social media, internet, and smartphone use was associated with increased anxiety and depression.14 This may be in part the result of adolescents spending time reading COVID-related news.
Coping mechanisms to increase well-being
Researchers have identified several positive coping mechanisms adolescents employed during the pandemic. Although some data suggest that increased internet use raises the risk of COVID-related distress, for certain adolescents, using social media to stay connected with friends and relatives was a buffer for feelings of loneliness and might have increased mental well-being.15 Other common coping mechanisms include relying on faith, volunteering, and starting new hobbies.16 During the pandemic, there were higher rates of playing outside and increased physical activity, which correlated with positive mental health outcomes.16 An online survey of 1,040 adolescents found that those who looked to the future optimistically and confidently had a higher health-related quality of life.17
Continuing an emphasis on adolescent well-being
Although data are limited, adolescents can continue to use these coping mechanisms to maintain their well-being, even if COVID-related restrictions are lifted or reimplemented. During these difficult times, it is imperative for adolescents to get the mental health services they need, and for psychiatric clinicians to continue to find avenues to promote resilience and mental wellness among young patients.
While the COVID-19 pandemic has impacted the mental health of a wide range of individuals, its adverse effects have been particularly detrimental to adolescents. In this article, I discuss evidence that shows the effects of the pandemic on adolescent patients, potential reasons for this increased distress, and what types of coping mechanisms adolescents have used to counter these effects.
Increases in multiple measures of psychopathology
Multiple online surveys and other studies have documented the pandemic’s impact on younger individuals. In the United States, visits to emergency departments by pediatric patients increased in the months after the first lockdown period.1 Several studies found increased rates of anxiety and depression among adolescents during the COVID-19 pandemic.2,3 In an online survey of 359 children and 3,254 adolescents in China, 22% of respondents reported that they experienced depressive symptoms.3 In an online survey of 1,054 Canadian adolescents, 43% said they were “very concerned” about the pandemic.4 In an online survey of 7,353 adolescents in the United States, 37% reported suicidal ideation during the pandemic compared to 17% in 2017.5 A Chinese study found that smartphone and internet addiction was significantly associated with increased levels of depressive symptoms during the pandemic.3 In a survey in the Philippines, 16.3% of adolescents reported moderate-to-severe psychological impairment during the pandemic; the rates of COVID-19–related anxiety were higher among girls vs boys.6 Alcohol and cannabis use increased among Canadian adolescents during the pandemic, according to an online survey.7 Adolescents with anorexia nervosa reported a 70% increase in poor eating habits and more thoughts associated with eating disorders during the pandemic.8 A Danish study found that children and adolescents newly diagnosed with obsessive-compulsive disorder (OCD) or who had completed treatment exhibited worsening OCD, anxiety, and depressive symptoms during the pandemic.9 An online survey of 6,196 Chinese adolescents found that those with a higher number of pre-pandemic adverse childhood experiences, such as abuse and neglect, had elevated posttraumatic stress symptoms and anxiety during the onset of the pandemic.10
Underlying causes of pandemic-induced distress
Limited social connectedness during the pandemic is a major reason for distress among adolescents. A review of 80 studies found that social isolation and loneliness as a result of social distancing and quarantining were associated with an increased risk of depression, anxiety, suicidal ideation, and self-harm.11 Parents’ stress about the risks of COVID-19 was correlated with worsening mental health in their adolescent children.12 A Chinese study found that the amount of time students spent on smartphones and social media doubled during the pandemic.13 In an online survey of 7,890 Chinese adolescents, greater social media, internet, and smartphone use was associated with increased anxiety and depression.14 This may be in part the result of adolescents spending time reading COVID-related news.
Coping mechanisms to increase well-being
Researchers have identified several positive coping mechanisms adolescents employed during the pandemic. Although some data suggest that increased internet use raises the risk of COVID-related distress, for certain adolescents, using social media to stay connected with friends and relatives was a buffer for feelings of loneliness and might have increased mental well-being.15 Other common coping mechanisms include relying on faith, volunteering, and starting new hobbies.16 During the pandemic, there were higher rates of playing outside and increased physical activity, which correlated with positive mental health outcomes.16 An online survey of 1,040 adolescents found that those who looked to the future optimistically and confidently had a higher health-related quality of life.17
Continuing an emphasis on adolescent well-being
Although data are limited, adolescents can continue to use these coping mechanisms to maintain their well-being, even if COVID-related restrictions are lifted or reimplemented. During these difficult times, it is imperative for adolescents to get the mental health services they need, and for psychiatric clinicians to continue to find avenues to promote resilience and mental wellness among young patients.
1. Leeb RT, Bitsko RH, Radhakrishnan L, et al. Mental health–related emergency department visits among children aged <18 years during the COVID-19 pandemic—United States, January 1-October 17, 2020. MMWR Morb Mortal Wkly Rep. 2020;69(45):1675-1680. doi:10.15585/mmwr.mm6945a3
2. Oosterhoff B, Palmer CA, Wilson J, et al. Adolescents’ motivations to engage in social distancing during the COVID-19 pandemic: associations with mental and social health. J Adolesc Health. 2020;67(2):179-185. doi:10.1016/j.jadohealth.2020.05.004
3. Duan L, Shao X, Wang Y, et al. An investigation of mental health status of children and adolescents in China during the outbreak of COVID-19. J Affect Disord. 2020;275:112-118. doi:10.1016/j.jad.2020.06.029
4. Ellis WE, Dumas TM, Forbes LM. Physically isolated but socially connected: psychological adjustment and stress among adolescents during the initial COVID-19 crisis. Can J Behav Sci. 2020;52(3):177-187. doi:10.1037/cbs0000215
5. Murata S, Rezeppa T, Thoma B, et al. The psychiatric sequelae of the COVID-19 pandemic in adolescents, adults, and health care workers. Depress Anxiety. 2021;38(2):233-246. doi:10.1002/da.23120
6. Tee ML, Tee CA, Anlacan JP, et al. Psychological impact of COVID-19 pandemic in the Philippines. J Affect Disord. 2020;277:379-391. doi:10.1016/j.jad.2020.08.043
7. Dumas TM, Ellis W, Litt DM. What does adolescent substance use look like during the COVID-19 pandemic? Examining changes in frequency, social contexts, and pandemic-related predictors. J Adolesc Health. 2020;67(3):354-361. doi:10.1016/j.jadohealth.2020.06.018
8. Schlegl S, Maier J, Meule A, et al. Eating disorders in times of the COVID-19 pandemic—results from an online survey of patients with anorexia nervosa. Int J Eat Disord. 2020;53:1791-1800. doi:10.1002/eat.23374.
9. Nissen JB, Højgaard D, Thomsen PH. The immediate effect of COVID-19 pandemic on children and adolescents with obsessive compulsive disorder. BMC Psychiatry. 2020;20(1):511. doi:10.1186/s12888-020-02905-5
10. Guo J, Fu M, Liu D, et al. Is the psychological impact of exposure to COVID-19 stronger in adolescents with pre-pandemic maltreatment experiences? A survey of rural Chinese adolescents. Child Abuse Negl. 2020;110(Pt 2):104667. doi:10.1016/j.chiabu.2020.104667
11. Loades ME, Chatburn E, Higson-Sweeney N, et al. Rapid Systematic Review: The impact of social isolation and loneliness on the mental health of children and adolescents in the context of COVID-19. J Am Acad Child Adolesc Psychiatry. 2020;59(11):1218-1239.e3. doi:10.1016/j.jaac.2020.05.009
12. Spinelli M, Lionetti F, Setti A, et al. Parenting stress during the COVID-19 outbreak: socioeconomic and environmental risk factors and implications for children emotion regulation. Fam Process. 2021;60(2):639-653. doi:10.1111/famp.12601
13. Chen IH, Chen CY, Pakpour AH, et al. Internet-related behaviors and psychological distress among schoolchildren during COVID-19 school suspension. J Am Acad Child Adolesc Psychiatry. 2020;59(10):1099-1102.e1. doi:10.1016/j.jaac.2020.06.007
14. Li W, Zhang Y, Wang J, et al. Association of home quarantine and mental health among teenagers in Wuhan, China, during the COVID-19 pandemic. JAMA Pediatr. 2021;175(3):313-316. doi:10.1001/jamapediatrics.2020.5499
15. Janssen, LHC, Kullberg, MJ, Verkuil B, et al. Does the COVID-19 pandemic impact parents’ and adolescents’ well-being? An EMA-study on daily affect and parenting. PLoS One. 2020;15(10):e0240962. doi:10.1371/journal.pone.0240962
16. Banati P, Jones N, Youssef S. Intersecting vulnerabilities: the impacts of COVID-19 on the psycho-emotional lives of young people in low- and middle-income countries. Eur J Dev Res. 2020;32(5):1613-1638. doi:10.1057/s41287-020-00325-5
17. Ravens-Sieberer U, Kaman A, Otto C, et al. Mental health and quality of life in children and adolescents during the COVID-19 pandemic—results of the COPSY study. Dtsch Arztebl Int. 2020;117(48):828-829. doi:10.3238/arztebl.2020.0828
1. Leeb RT, Bitsko RH, Radhakrishnan L, et al. Mental health–related emergency department visits among children aged <18 years during the COVID-19 pandemic—United States, January 1-October 17, 2020. MMWR Morb Mortal Wkly Rep. 2020;69(45):1675-1680. doi:10.15585/mmwr.mm6945a3
2. Oosterhoff B, Palmer CA, Wilson J, et al. Adolescents’ motivations to engage in social distancing during the COVID-19 pandemic: associations with mental and social health. J Adolesc Health. 2020;67(2):179-185. doi:10.1016/j.jadohealth.2020.05.004
3. Duan L, Shao X, Wang Y, et al. An investigation of mental health status of children and adolescents in China during the outbreak of COVID-19. J Affect Disord. 2020;275:112-118. doi:10.1016/j.jad.2020.06.029
4. Ellis WE, Dumas TM, Forbes LM. Physically isolated but socially connected: psychological adjustment and stress among adolescents during the initial COVID-19 crisis. Can J Behav Sci. 2020;52(3):177-187. doi:10.1037/cbs0000215
5. Murata S, Rezeppa T, Thoma B, et al. The psychiatric sequelae of the COVID-19 pandemic in adolescents, adults, and health care workers. Depress Anxiety. 2021;38(2):233-246. doi:10.1002/da.23120
6. Tee ML, Tee CA, Anlacan JP, et al. Psychological impact of COVID-19 pandemic in the Philippines. J Affect Disord. 2020;277:379-391. doi:10.1016/j.jad.2020.08.043
7. Dumas TM, Ellis W, Litt DM. What does adolescent substance use look like during the COVID-19 pandemic? Examining changes in frequency, social contexts, and pandemic-related predictors. J Adolesc Health. 2020;67(3):354-361. doi:10.1016/j.jadohealth.2020.06.018
8. Schlegl S, Maier J, Meule A, et al. Eating disorders in times of the COVID-19 pandemic—results from an online survey of patients with anorexia nervosa. Int J Eat Disord. 2020;53:1791-1800. doi:10.1002/eat.23374.
9. Nissen JB, Højgaard D, Thomsen PH. The immediate effect of COVID-19 pandemic on children and adolescents with obsessive compulsive disorder. BMC Psychiatry. 2020;20(1):511. doi:10.1186/s12888-020-02905-5
10. Guo J, Fu M, Liu D, et al. Is the psychological impact of exposure to COVID-19 stronger in adolescents with pre-pandemic maltreatment experiences? A survey of rural Chinese adolescents. Child Abuse Negl. 2020;110(Pt 2):104667. doi:10.1016/j.chiabu.2020.104667
11. Loades ME, Chatburn E, Higson-Sweeney N, et al. Rapid Systematic Review: The impact of social isolation and loneliness on the mental health of children and adolescents in the context of COVID-19. J Am Acad Child Adolesc Psychiatry. 2020;59(11):1218-1239.e3. doi:10.1016/j.jaac.2020.05.009
12. Spinelli M, Lionetti F, Setti A, et al. Parenting stress during the COVID-19 outbreak: socioeconomic and environmental risk factors and implications for children emotion regulation. Fam Process. 2021;60(2):639-653. doi:10.1111/famp.12601
13. Chen IH, Chen CY, Pakpour AH, et al. Internet-related behaviors and psychological distress among schoolchildren during COVID-19 school suspension. J Am Acad Child Adolesc Psychiatry. 2020;59(10):1099-1102.e1. doi:10.1016/j.jaac.2020.06.007
14. Li W, Zhang Y, Wang J, et al. Association of home quarantine and mental health among teenagers in Wuhan, China, during the COVID-19 pandemic. JAMA Pediatr. 2021;175(3):313-316. doi:10.1001/jamapediatrics.2020.5499
15. Janssen, LHC, Kullberg, MJ, Verkuil B, et al. Does the COVID-19 pandemic impact parents’ and adolescents’ well-being? An EMA-study on daily affect and parenting. PLoS One. 2020;15(10):e0240962. doi:10.1371/journal.pone.0240962
16. Banati P, Jones N, Youssef S. Intersecting vulnerabilities: the impacts of COVID-19 on the psycho-emotional lives of young people in low- and middle-income countries. Eur J Dev Res. 2020;32(5):1613-1638. doi:10.1057/s41287-020-00325-5
17. Ravens-Sieberer U, Kaman A, Otto C, et al. Mental health and quality of life in children and adolescents during the COVID-19 pandemic—results of the COPSY study. Dtsch Arztebl Int. 2020;117(48):828-829. doi:10.3238/arztebl.2020.0828
More on stigma
I just finished reading your editorial “A PSYCHIATRIC MANIFESTO: Stigma is hate speech and a hate crime” (
Our son went from an honor roll student before the pandemic to a child I barely recognized. Approximately 6 months into the pandemic, he was using drugs, vaping nicotine, destroying our property, and eloping at night. The journey of watching his decline and getting him help was agonizing. But the stigma around what was happening to him was an entirely separate animal.
Our society vilifies, ridicules, dismisses, and often makes fun of those with mental health issues. I experience it daily with my son and am on constant guard to shoot down any comments and to calmly teach those who say such cruel things. But the shame my son feels is the most devastating part. Although we keep reminding him that his condition is a medical condition like diabetes or heart disease, for a teenage boy, that makes no sense. He just wants to be “normal.” And living in a world that rarely represents mental illness this way, it’s almost a lost cause to get him to let go of this shame. All we can do is love him, be there for him, support him, and do what we can to educate those around us about the stigma of mental illness.
What a powerful and accurate article. Thank you for putting into words what I have been thinking and feeling, and for being as outraged as we are at how this vulnerable population is treated. My husband is a psychiatrist and we live in an affluent urban area, so we are not in the middle of nowhere with no knowledge of what is happening to our son. And despite that, we still suffer from the stigma.
Thank you, Dr. Nasrallah.
Name withheld
I need to take a moment to thank you for your editorial about stigma being hate speech and a hate crime. I really agree with you, and I think the way you formulated and articulated this message is very compelling.
I have focused on normalizing mental health differences among entrepreneurs as a destigmatization strategy (see https://www.sciencedirect.com/science/article/pii/S0883902622000027 and https://link.springer.com/article/10.1007/s11187-018-0059-8). Entrepreneurs clearly illustrate the fallacy of stigma. As a simple example, Elon Musk—the wealthiest person in the world—talks openly about being autistic, and possibly bipolar. These mental health differences help him create jobs and contribute to our shared prosperity. Nothing to be ashamed of there.
Thanks again for being such an effective advocate.
Michael A. Freeman, MD
Kentfield, California
Continue to: Thank you...
Thank you so much for your “Psychiatric Manifesto.” I will do my best to disseminate it amongst colleagues, patients, friends, family, and as many others as possible.
Daniel N. Pistone, MD
San Francisco, California
Once again, your words hit the pin on the head.
Robert W. Pollack, MD, ABPN, DLFAPA
Fort Myers, Florida
I just finished reading your editorial “A PSYCHIATRIC MANIFESTO: Stigma is hate speech and a hate crime” (
Our son went from an honor roll student before the pandemic to a child I barely recognized. Approximately 6 months into the pandemic, he was using drugs, vaping nicotine, destroying our property, and eloping at night. The journey of watching his decline and getting him help was agonizing. But the stigma around what was happening to him was an entirely separate animal.
Our society vilifies, ridicules, dismisses, and often makes fun of those with mental health issues. I experience it daily with my son and am on constant guard to shoot down any comments and to calmly teach those who say such cruel things. But the shame my son feels is the most devastating part. Although we keep reminding him that his condition is a medical condition like diabetes or heart disease, for a teenage boy, that makes no sense. He just wants to be “normal.” And living in a world that rarely represents mental illness this way, it’s almost a lost cause to get him to let go of this shame. All we can do is love him, be there for him, support him, and do what we can to educate those around us about the stigma of mental illness.
What a powerful and accurate article. Thank you for putting into words what I have been thinking and feeling, and for being as outraged as we are at how this vulnerable population is treated. My husband is a psychiatrist and we live in an affluent urban area, so we are not in the middle of nowhere with no knowledge of what is happening to our son. And despite that, we still suffer from the stigma.
Thank you, Dr. Nasrallah.
Name withheld
I need to take a moment to thank you for your editorial about stigma being hate speech and a hate crime. I really agree with you, and I think the way you formulated and articulated this message is very compelling.
I have focused on normalizing mental health differences among entrepreneurs as a destigmatization strategy (see https://www.sciencedirect.com/science/article/pii/S0883902622000027 and https://link.springer.com/article/10.1007/s11187-018-0059-8). Entrepreneurs clearly illustrate the fallacy of stigma. As a simple example, Elon Musk—the wealthiest person in the world—talks openly about being autistic, and possibly bipolar. These mental health differences help him create jobs and contribute to our shared prosperity. Nothing to be ashamed of there.
Thanks again for being such an effective advocate.
Michael A. Freeman, MD
Kentfield, California
Continue to: Thank you...
Thank you so much for your “Psychiatric Manifesto.” I will do my best to disseminate it amongst colleagues, patients, friends, family, and as many others as possible.
Daniel N. Pistone, MD
San Francisco, California
Once again, your words hit the pin on the head.
Robert W. Pollack, MD, ABPN, DLFAPA
Fort Myers, Florida
I just finished reading your editorial “A PSYCHIATRIC MANIFESTO: Stigma is hate speech and a hate crime” (
Our son went from an honor roll student before the pandemic to a child I barely recognized. Approximately 6 months into the pandemic, he was using drugs, vaping nicotine, destroying our property, and eloping at night. The journey of watching his decline and getting him help was agonizing. But the stigma around what was happening to him was an entirely separate animal.
Our society vilifies, ridicules, dismisses, and often makes fun of those with mental health issues. I experience it daily with my son and am on constant guard to shoot down any comments and to calmly teach those who say such cruel things. But the shame my son feels is the most devastating part. Although we keep reminding him that his condition is a medical condition like diabetes or heart disease, for a teenage boy, that makes no sense. He just wants to be “normal.” And living in a world that rarely represents mental illness this way, it’s almost a lost cause to get him to let go of this shame. All we can do is love him, be there for him, support him, and do what we can to educate those around us about the stigma of mental illness.
What a powerful and accurate article. Thank you for putting into words what I have been thinking and feeling, and for being as outraged as we are at how this vulnerable population is treated. My husband is a psychiatrist and we live in an affluent urban area, so we are not in the middle of nowhere with no knowledge of what is happening to our son. And despite that, we still suffer from the stigma.
Thank you, Dr. Nasrallah.
Name withheld
I need to take a moment to thank you for your editorial about stigma being hate speech and a hate crime. I really agree with you, and I think the way you formulated and articulated this message is very compelling.
I have focused on normalizing mental health differences among entrepreneurs as a destigmatization strategy (see https://www.sciencedirect.com/science/article/pii/S0883902622000027 and https://link.springer.com/article/10.1007/s11187-018-0059-8). Entrepreneurs clearly illustrate the fallacy of stigma. As a simple example, Elon Musk—the wealthiest person in the world—talks openly about being autistic, and possibly bipolar. These mental health differences help him create jobs and contribute to our shared prosperity. Nothing to be ashamed of there.
Thanks again for being such an effective advocate.
Michael A. Freeman, MD
Kentfield, California
Continue to: Thank you...
Thank you so much for your “Psychiatric Manifesto.” I will do my best to disseminate it amongst colleagues, patients, friends, family, and as many others as possible.
Daniel N. Pistone, MD
San Francisco, California
Once again, your words hit the pin on the head.
Robert W. Pollack, MD, ABPN, DLFAPA
Fort Myers, Florida
Then and now: Inflammatory bowel diseases
(IBD) creating a whole new landscape for the disease.
In 2007, IBD seemed to be primarily a disease of Caucasian and Jewish ancestry. While prevalence of IBD is still highest in the Western world, there is now increasing incidence, even accounting for detection bias, in people of all other ancestries globally. Incidence of IBD in children under the age of 18 years is also rising. Patients with IBD are living longer and, despite the notion that IBD is a disease primarily of younger adults, nearly one-third of Americans with IBD are 60 years and older.
“Adalimumab aids in Crohn’s disease” read the front page of the inaugural issue of GI & Hepatology News in January 2007. The article highlighted the GAIN study, which demonstrated that patients who lost response to infliximab responded to adalimumab, the second anti-tumor necrosis factor (TNF) agent approved for the treatment of Crohn’s disease and subsequently ulcerative colitis. Over the subsequent 15 years, the armamentarium of treatment options for Crohn’s disease and ulcerative colitis have rapidly proliferated: there are now four anti–tumor necrosis factor (TNF) agents, two anti-integrin agents, two anti-interleukin agents, two Janus kinase inhibitors and a sphingosine-1 receptor modulator approved for the treatment of IBD. Many more promising treatment options are in trials. Other mechanisms are under investigation as well, including antimicrobial therapies for ulcerative colitis and stem cell therapeutics for the treatment of refractory perianal fistulizing Crohn’s disease. Perhaps even more novel – dietary therapies are more rigorously under investigation.
“Ulcerative colitis guidelines endorse combined therapy” reads another headline from the inaugural GI & Hepatology News issue. The article discusses the European Crohn’s and Colitis Organisation’s consensus guideline that topical and systemic agents used together are superior to either used alone, referring specifically to mesalamine, both systemic and topical as well as the additional of topical corticosteroid to systemic mesalamine. Combination therapy has a completely new meaning in modern times. With the publication of the SONIC trial in 2010, combination therapy referred to an anti-TNF in combination with an immunomodulator for the ensuing decade. However, in this new era of IBD treatment, combination therapy could also mean a biologic with a small molecule or even combination biologics, for which there is an ongoing randomized controlled trial. On the topic of treatment strategies, one of the biggest shifts in the IBD treatment paradigm is the bottom-up versus top-down approach of treatment, with increasing evidence to suggest that early biologic initiation is more effective, especially in patients with Crohn’s disease. Therapeutic drug monitoring is mainstream. Treat-to-target strategies to achieve more stringent outcomes, such as biomarker, endoscopic and histologic normalization, especially in ulcerative colitis, have evolved to become the norm in 2022.
The combination of increased treatment options, decreased reliance on corticosteroids and stringent treatment strategies have resulted in improved outcomes: IBD-related hospitalizations, surgeries, and even mortality have declined since 2007. The growing recognition and focus on extra-intestinal manifestations, including fatigue, and the gut-brain axis are important steps to improving the overall quality of life of patients with IBD. Beyond treating the disease, we are now learning how to treat the patient. We will be developing personalized strategies to identify the right patient for the right treatment, including patient-level clinical and biologic markers. We need to identify those who are at risk for IBD to prevent the disease at a preclinical phase. Concomitantly, we must continue the quest to cure the disease!
Dr. Kochar is a gastroenterologist and inflammatory bowel disease specialist at Massachusetts General Hospital and a physician investigator in the clinical and translational epidemiology unit at The Mongan Institute, both in Boston. She has no relevant disclosures.
(IBD) creating a whole new landscape for the disease.
In 2007, IBD seemed to be primarily a disease of Caucasian and Jewish ancestry. While prevalence of IBD is still highest in the Western world, there is now increasing incidence, even accounting for detection bias, in people of all other ancestries globally. Incidence of IBD in children under the age of 18 years is also rising. Patients with IBD are living longer and, despite the notion that IBD is a disease primarily of younger adults, nearly one-third of Americans with IBD are 60 years and older.
“Adalimumab aids in Crohn’s disease” read the front page of the inaugural issue of GI & Hepatology News in January 2007. The article highlighted the GAIN study, which demonstrated that patients who lost response to infliximab responded to adalimumab, the second anti-tumor necrosis factor (TNF) agent approved for the treatment of Crohn’s disease and subsequently ulcerative colitis. Over the subsequent 15 years, the armamentarium of treatment options for Crohn’s disease and ulcerative colitis have rapidly proliferated: there are now four anti–tumor necrosis factor (TNF) agents, two anti-integrin agents, two anti-interleukin agents, two Janus kinase inhibitors and a sphingosine-1 receptor modulator approved for the treatment of IBD. Many more promising treatment options are in trials. Other mechanisms are under investigation as well, including antimicrobial therapies for ulcerative colitis and stem cell therapeutics for the treatment of refractory perianal fistulizing Crohn’s disease. Perhaps even more novel – dietary therapies are more rigorously under investigation.
“Ulcerative colitis guidelines endorse combined therapy” reads another headline from the inaugural GI & Hepatology News issue. The article discusses the European Crohn’s and Colitis Organisation’s consensus guideline that topical and systemic agents used together are superior to either used alone, referring specifically to mesalamine, both systemic and topical as well as the additional of topical corticosteroid to systemic mesalamine. Combination therapy has a completely new meaning in modern times. With the publication of the SONIC trial in 2010, combination therapy referred to an anti-TNF in combination with an immunomodulator for the ensuing decade. However, in this new era of IBD treatment, combination therapy could also mean a biologic with a small molecule or even combination biologics, for which there is an ongoing randomized controlled trial. On the topic of treatment strategies, one of the biggest shifts in the IBD treatment paradigm is the bottom-up versus top-down approach of treatment, with increasing evidence to suggest that early biologic initiation is more effective, especially in patients with Crohn’s disease. Therapeutic drug monitoring is mainstream. Treat-to-target strategies to achieve more stringent outcomes, such as biomarker, endoscopic and histologic normalization, especially in ulcerative colitis, have evolved to become the norm in 2022.
The combination of increased treatment options, decreased reliance on corticosteroids and stringent treatment strategies have resulted in improved outcomes: IBD-related hospitalizations, surgeries, and even mortality have declined since 2007. The growing recognition and focus on extra-intestinal manifestations, including fatigue, and the gut-brain axis are important steps to improving the overall quality of life of patients with IBD. Beyond treating the disease, we are now learning how to treat the patient. We will be developing personalized strategies to identify the right patient for the right treatment, including patient-level clinical and biologic markers. We need to identify those who are at risk for IBD to prevent the disease at a preclinical phase. Concomitantly, we must continue the quest to cure the disease!
Dr. Kochar is a gastroenterologist and inflammatory bowel disease specialist at Massachusetts General Hospital and a physician investigator in the clinical and translational epidemiology unit at The Mongan Institute, both in Boston. She has no relevant disclosures.
(IBD) creating a whole new landscape for the disease.
In 2007, IBD seemed to be primarily a disease of Caucasian and Jewish ancestry. While prevalence of IBD is still highest in the Western world, there is now increasing incidence, even accounting for detection bias, in people of all other ancestries globally. Incidence of IBD in children under the age of 18 years is also rising. Patients with IBD are living longer and, despite the notion that IBD is a disease primarily of younger adults, nearly one-third of Americans with IBD are 60 years and older.
“Adalimumab aids in Crohn’s disease” read the front page of the inaugural issue of GI & Hepatology News in January 2007. The article highlighted the GAIN study, which demonstrated that patients who lost response to infliximab responded to adalimumab, the second anti-tumor necrosis factor (TNF) agent approved for the treatment of Crohn’s disease and subsequently ulcerative colitis. Over the subsequent 15 years, the armamentarium of treatment options for Crohn’s disease and ulcerative colitis have rapidly proliferated: there are now four anti–tumor necrosis factor (TNF) agents, two anti-integrin agents, two anti-interleukin agents, two Janus kinase inhibitors and a sphingosine-1 receptor modulator approved for the treatment of IBD. Many more promising treatment options are in trials. Other mechanisms are under investigation as well, including antimicrobial therapies for ulcerative colitis and stem cell therapeutics for the treatment of refractory perianal fistulizing Crohn’s disease. Perhaps even more novel – dietary therapies are more rigorously under investigation.
“Ulcerative colitis guidelines endorse combined therapy” reads another headline from the inaugural GI & Hepatology News issue. The article discusses the European Crohn’s and Colitis Organisation’s consensus guideline that topical and systemic agents used together are superior to either used alone, referring specifically to mesalamine, both systemic and topical as well as the additional of topical corticosteroid to systemic mesalamine. Combination therapy has a completely new meaning in modern times. With the publication of the SONIC trial in 2010, combination therapy referred to an anti-TNF in combination with an immunomodulator for the ensuing decade. However, in this new era of IBD treatment, combination therapy could also mean a biologic with a small molecule or even combination biologics, for which there is an ongoing randomized controlled trial. On the topic of treatment strategies, one of the biggest shifts in the IBD treatment paradigm is the bottom-up versus top-down approach of treatment, with increasing evidence to suggest that early biologic initiation is more effective, especially in patients with Crohn’s disease. Therapeutic drug monitoring is mainstream. Treat-to-target strategies to achieve more stringent outcomes, such as biomarker, endoscopic and histologic normalization, especially in ulcerative colitis, have evolved to become the norm in 2022.
The combination of increased treatment options, decreased reliance on corticosteroids and stringent treatment strategies have resulted in improved outcomes: IBD-related hospitalizations, surgeries, and even mortality have declined since 2007. The growing recognition and focus on extra-intestinal manifestations, including fatigue, and the gut-brain axis are important steps to improving the overall quality of life of patients with IBD. Beyond treating the disease, we are now learning how to treat the patient. We will be developing personalized strategies to identify the right patient for the right treatment, including patient-level clinical and biologic markers. We need to identify those who are at risk for IBD to prevent the disease at a preclinical phase. Concomitantly, we must continue the quest to cure the disease!
Dr. Kochar is a gastroenterologist and inflammatory bowel disease specialist at Massachusetts General Hospital and a physician investigator in the clinical and translational epidemiology unit at The Mongan Institute, both in Boston. She has no relevant disclosures.
A valuable learning experience
It was a pleasure to serve as editor-in-chief (EIC) of GI & Hepatology News from 2011 to 2016. As the second EIC of the newspaper, I was preceded by Dr. Charles Lightdale – big shoes to fill! I was fortunate to attract a strong group of associate editors who covered many key areas of interest for the paper’s readership. With the enthusiastic support of American Gastroenterological Association staff members, we published once-monthly and received generally positive feedback from readers – predominantly U.S.-based AGA members.
Serving as EIC was also a learning opportunity for me. A number of potentially newsworthy items were brought to my attention – some of which I would not otherwise have seen. Although not all were of direct relevance to the readership, I believe that most of those we published were of value.
One rewarding aspect of the editorship was the opportunity to liaise with those experts from whom I solicited commentaries on some of our featured items. These busy individuals were consistently generous with their time and expertise, and I believe that their contributions added to the paper’s overall appeal.
I initiated the inclusion of two DDSEP questions per edition, and am pleased that this feature continues. One less successful venture was the attempt at a Correspondence section, which ultimately proved too cumbersome to maintain.
I congratulate the AGA on the 15th anniversary of GIHN, and I wish the current EIC, Dr. Megan Adams, and her editorial colleagues continued success in providing this benefit to AGA members.
Colin W. Howden, MD, AGAF, is professor emeritus in the division of gastroenterology, department of medicine, at the University of Tennessee, Memphis. He is a consultant for Allakos, Ironwood, Phathom, and RedHill Biopharma. He is a member of speakers’ bureaus for Alnylam, RedHill Biopharma, and Sanofi/Genzyme. He owns stock in Antibe Therapeutics.
It was a pleasure to serve as editor-in-chief (EIC) of GI & Hepatology News from 2011 to 2016. As the second EIC of the newspaper, I was preceded by Dr. Charles Lightdale – big shoes to fill! I was fortunate to attract a strong group of associate editors who covered many key areas of interest for the paper’s readership. With the enthusiastic support of American Gastroenterological Association staff members, we published once-monthly and received generally positive feedback from readers – predominantly U.S.-based AGA members.
Serving as EIC was also a learning opportunity for me. A number of potentially newsworthy items were brought to my attention – some of which I would not otherwise have seen. Although not all were of direct relevance to the readership, I believe that most of those we published were of value.
One rewarding aspect of the editorship was the opportunity to liaise with those experts from whom I solicited commentaries on some of our featured items. These busy individuals were consistently generous with their time and expertise, and I believe that their contributions added to the paper’s overall appeal.
I initiated the inclusion of two DDSEP questions per edition, and am pleased that this feature continues. One less successful venture was the attempt at a Correspondence section, which ultimately proved too cumbersome to maintain.
I congratulate the AGA on the 15th anniversary of GIHN, and I wish the current EIC, Dr. Megan Adams, and her editorial colleagues continued success in providing this benefit to AGA members.
Colin W. Howden, MD, AGAF, is professor emeritus in the division of gastroenterology, department of medicine, at the University of Tennessee, Memphis. He is a consultant for Allakos, Ironwood, Phathom, and RedHill Biopharma. He is a member of speakers’ bureaus for Alnylam, RedHill Biopharma, and Sanofi/Genzyme. He owns stock in Antibe Therapeutics.
It was a pleasure to serve as editor-in-chief (EIC) of GI & Hepatology News from 2011 to 2016. As the second EIC of the newspaper, I was preceded by Dr. Charles Lightdale – big shoes to fill! I was fortunate to attract a strong group of associate editors who covered many key areas of interest for the paper’s readership. With the enthusiastic support of American Gastroenterological Association staff members, we published once-monthly and received generally positive feedback from readers – predominantly U.S.-based AGA members.
Serving as EIC was also a learning opportunity for me. A number of potentially newsworthy items were brought to my attention – some of which I would not otherwise have seen. Although not all were of direct relevance to the readership, I believe that most of those we published were of value.
One rewarding aspect of the editorship was the opportunity to liaise with those experts from whom I solicited commentaries on some of our featured items. These busy individuals were consistently generous with their time and expertise, and I believe that their contributions added to the paper’s overall appeal.
I initiated the inclusion of two DDSEP questions per edition, and am pleased that this feature continues. One less successful venture was the attempt at a Correspondence section, which ultimately proved too cumbersome to maintain.
I congratulate the AGA on the 15th anniversary of GIHN, and I wish the current EIC, Dr. Megan Adams, and her editorial colleagues continued success in providing this benefit to AGA members.
Colin W. Howden, MD, AGAF, is professor emeritus in the division of gastroenterology, department of medicine, at the University of Tennessee, Memphis. He is a consultant for Allakos, Ironwood, Phathom, and RedHill Biopharma. He is a member of speakers’ bureaus for Alnylam, RedHill Biopharma, and Sanofi/Genzyme. He owns stock in Antibe Therapeutics.
Legal abortion is a matter of public health
On June 24, the U.S. Supreme Court overturned Roe v. Wade, a decision that was issued in 1973. From now on, each state will be able to choose the laws that it wants to put in place regarding abortion. Several states have already decided to ban abortion altogether. As a physician, but also as a woman, I am stunned to see this opposition to a right that, in my opinion, is also a matter of public health.
International data
In Belgium, voluntary termination of pregnancy (VTP) has been allowed since 1990. Except in the case of a serious medical problem, the abortion must take place before the end of the 12th week after conception. So, 14 weeks from the last menstrual period (LMP).
Beyond that time frame, a VTP can be performed only when the continuation of the pregnancy endangers the health of the woman or when it is certain that the unborn child will be affected by a condition of particular gravity and recognized as incurable at the time of diagnosis. This is referred to as termination for medical reasons (TFMR).
First observation
The annual number of VTPs did not climb following legalization. For the past 20 years in Belgium, that number has remained stable, hovering around 19,000. Abortion continues to be an action – neither trivialized nor minimized – that is difficult for any woman to take, no matter what her reason.
Second observation
Over 60% of women who had an abortion were using a form of contraception. So, while the burden of contraception still rests almost exclusively on the woman, it cannot be said that those who had a VTP did not use some method of birth control.
Even more important, legal abortions have very few complications, either physical or psychological. Studies show that pregnancy itself carries a higher risk for psychopathological manifestations than a VTP. These VTPs are safe, and women quickly recover from them. The most sensitive time seems to be the period before the abortion, and it’s at this stage that most of the psychological and psychopathological manifestations accumulate. The majority of women facing a VTP experience feelings of relief, and only a minority develop psychological problems, usually when there is already a history of mental disorder. The literature shows that the levels of anxiety and depression decrease in the month following the abortion. Being denied a VTP, on the other hand, significantly increases the woman’s risk of developing a mental disorder.
Should a VTP be denied, a woman, if she determines that she doesn’t have any other choice, may then end up turning to a back-alley abortion. The methods used for this are medieval, dangerous, and may not prove successful – things like using chemicals, piercing the amniotic sac with a needle or sharp object (the famous coat hanger), eating or drinking abortifacient herbs, taking large quantities of medication, punching the stomach, falling down stairs, and engaging in intense physical exercise.
From there, these risky methods inevitably lead to numerous complications: Incomplete abortions, infections, septicemia, breakthrough bleeding, subsequent sterility, laceration of the uterine wall, or death.
Around one-third of women who undergo risky abortions develop complications, while less than half receive care.
The World Health Organization estimates that back-alley abortions represent 49% of abortions worldwide. It puts the number of illegal abortions performed each year at 20 million.
Each year, around 60,000 women worldwide die as a result of an unsafe VTP. That’s one woman every 9 minutes. And odds are that these figures are underestimated.
Making the decision to resort to a VTP is always difficult. Ideally, you should be able to discuss it with your partner, when there is one, and with your close friends and family, to have someone go with you as support, to weigh the pros and cons, and to make a choice in line with your convictions and your conscience. But first and foremost, the law must guarantee the right to be able to ask oneself this question, because guaranteeing this right is also guaranteeing the health and safety of women, and that is why this remains a public health imperative.
A version of this article first appeared on Medscape.com. This article was translated from MediQuality.
On June 24, the U.S. Supreme Court overturned Roe v. Wade, a decision that was issued in 1973. From now on, each state will be able to choose the laws that it wants to put in place regarding abortion. Several states have already decided to ban abortion altogether. As a physician, but also as a woman, I am stunned to see this opposition to a right that, in my opinion, is also a matter of public health.
International data
In Belgium, voluntary termination of pregnancy (VTP) has been allowed since 1990. Except in the case of a serious medical problem, the abortion must take place before the end of the 12th week after conception. So, 14 weeks from the last menstrual period (LMP).
Beyond that time frame, a VTP can be performed only when the continuation of the pregnancy endangers the health of the woman or when it is certain that the unborn child will be affected by a condition of particular gravity and recognized as incurable at the time of diagnosis. This is referred to as termination for medical reasons (TFMR).
First observation
The annual number of VTPs did not climb following legalization. For the past 20 years in Belgium, that number has remained stable, hovering around 19,000. Abortion continues to be an action – neither trivialized nor minimized – that is difficult for any woman to take, no matter what her reason.
Second observation
Over 60% of women who had an abortion were using a form of contraception. So, while the burden of contraception still rests almost exclusively on the woman, it cannot be said that those who had a VTP did not use some method of birth control.
Even more important, legal abortions have very few complications, either physical or psychological. Studies show that pregnancy itself carries a higher risk for psychopathological manifestations than a VTP. These VTPs are safe, and women quickly recover from them. The most sensitive time seems to be the period before the abortion, and it’s at this stage that most of the psychological and psychopathological manifestations accumulate. The majority of women facing a VTP experience feelings of relief, and only a minority develop psychological problems, usually when there is already a history of mental disorder. The literature shows that the levels of anxiety and depression decrease in the month following the abortion. Being denied a VTP, on the other hand, significantly increases the woman’s risk of developing a mental disorder.
Should a VTP be denied, a woman, if she determines that she doesn’t have any other choice, may then end up turning to a back-alley abortion. The methods used for this are medieval, dangerous, and may not prove successful – things like using chemicals, piercing the amniotic sac with a needle or sharp object (the famous coat hanger), eating or drinking abortifacient herbs, taking large quantities of medication, punching the stomach, falling down stairs, and engaging in intense physical exercise.
From there, these risky methods inevitably lead to numerous complications: Incomplete abortions, infections, septicemia, breakthrough bleeding, subsequent sterility, laceration of the uterine wall, or death.
Around one-third of women who undergo risky abortions develop complications, while less than half receive care.
The World Health Organization estimates that back-alley abortions represent 49% of abortions worldwide. It puts the number of illegal abortions performed each year at 20 million.
Each year, around 60,000 women worldwide die as a result of an unsafe VTP. That’s one woman every 9 minutes. And odds are that these figures are underestimated.
Making the decision to resort to a VTP is always difficult. Ideally, you should be able to discuss it with your partner, when there is one, and with your close friends and family, to have someone go with you as support, to weigh the pros and cons, and to make a choice in line with your convictions and your conscience. But first and foremost, the law must guarantee the right to be able to ask oneself this question, because guaranteeing this right is also guaranteeing the health and safety of women, and that is why this remains a public health imperative.
A version of this article first appeared on Medscape.com. This article was translated from MediQuality.
On June 24, the U.S. Supreme Court overturned Roe v. Wade, a decision that was issued in 1973. From now on, each state will be able to choose the laws that it wants to put in place regarding abortion. Several states have already decided to ban abortion altogether. As a physician, but also as a woman, I am stunned to see this opposition to a right that, in my opinion, is also a matter of public health.
International data
In Belgium, voluntary termination of pregnancy (VTP) has been allowed since 1990. Except in the case of a serious medical problem, the abortion must take place before the end of the 12th week after conception. So, 14 weeks from the last menstrual period (LMP).
Beyond that time frame, a VTP can be performed only when the continuation of the pregnancy endangers the health of the woman or when it is certain that the unborn child will be affected by a condition of particular gravity and recognized as incurable at the time of diagnosis. This is referred to as termination for medical reasons (TFMR).
First observation
The annual number of VTPs did not climb following legalization. For the past 20 years in Belgium, that number has remained stable, hovering around 19,000. Abortion continues to be an action – neither trivialized nor minimized – that is difficult for any woman to take, no matter what her reason.
Second observation
Over 60% of women who had an abortion were using a form of contraception. So, while the burden of contraception still rests almost exclusively on the woman, it cannot be said that those who had a VTP did not use some method of birth control.
Even more important, legal abortions have very few complications, either physical or psychological. Studies show that pregnancy itself carries a higher risk for psychopathological manifestations than a VTP. These VTPs are safe, and women quickly recover from them. The most sensitive time seems to be the period before the abortion, and it’s at this stage that most of the psychological and psychopathological manifestations accumulate. The majority of women facing a VTP experience feelings of relief, and only a minority develop psychological problems, usually when there is already a history of mental disorder. The literature shows that the levels of anxiety and depression decrease in the month following the abortion. Being denied a VTP, on the other hand, significantly increases the woman’s risk of developing a mental disorder.
Should a VTP be denied, a woman, if she determines that she doesn’t have any other choice, may then end up turning to a back-alley abortion. The methods used for this are medieval, dangerous, and may not prove successful – things like using chemicals, piercing the amniotic sac with a needle or sharp object (the famous coat hanger), eating or drinking abortifacient herbs, taking large quantities of medication, punching the stomach, falling down stairs, and engaging in intense physical exercise.
From there, these risky methods inevitably lead to numerous complications: Incomplete abortions, infections, septicemia, breakthrough bleeding, subsequent sterility, laceration of the uterine wall, or death.
Around one-third of women who undergo risky abortions develop complications, while less than half receive care.
The World Health Organization estimates that back-alley abortions represent 49% of abortions worldwide. It puts the number of illegal abortions performed each year at 20 million.
Each year, around 60,000 women worldwide die as a result of an unsafe VTP. That’s one woman every 9 minutes. And odds are that these figures are underestimated.
Making the decision to resort to a VTP is always difficult. Ideally, you should be able to discuss it with your partner, when there is one, and with your close friends and family, to have someone go with you as support, to weigh the pros and cons, and to make a choice in line with your convictions and your conscience. But first and foremost, the law must guarantee the right to be able to ask oneself this question, because guaranteeing this right is also guaranteeing the health and safety of women, and that is why this remains a public health imperative.
A version of this article first appeared on Medscape.com. This article was translated from MediQuality.
How does radiofrequency microneedling work?
Technology in the field of aesthetic dermatology continues to advance over time. Microneedling, largely used to improve textural changes of the skin associated with photoaging and acne scarring, has evolved over time from the use of dermarollers and microneedling skin pens to energy-based devices that deliver radiofrequency (RF) energy though microneedles that are used today.
.
Unlike prior radiofrequency energy-based devices that deliver radiofrequency energy on the skin surface to allow bulk thermal energy (or heat) to stimulate collagen remodeling and tissue tightening, RF microneedling devices deliver the same RF or thermal energy via needles. RF, measured in Hertz (Hz) is part of the electromagnetic spectrum, with most devices delivering thermal energy at around 1-2 MHz, which is less than most typical RF only devices (at around 4-6 MHz), but with potentially more precise depth and delivery. For comparison, the RF of household electrical currents are around 60 Hz; traditional electrosurgical units, 50Hz -300 kHz; AM radio, 500 KHz; and microwaves, 2500 MHz.
When delivered to the skin, RF energy produces a change in the electrical charge of the skin, resulting in movement of electrons. The impedance (or resistance) of the tissue to the electron movement is what generates heat. Different factors, including tissue thickness, pressure applied to the tissue, hydration, bipolar versus monopolar delivery, and the number of needles are several factors than can affect the impedance.
Bipolar RF means that the current passes between two electrodes, whereas monopolar RF means that the electrical current is between an active treatment electrode and a passive grounding electrode (or grounding pad typically placed on the patient’s back). With bipolar RF, the current is limited to the area between the two electrodes. The depth of penetration is half of the distance between the electrodes, thus resulting in shallow (but potentially more aggressive) tissue heating. With monopolar RF, deeper tissue penetration occurs that is also often less uncomfortable to the patient.
The desired result of the energy delivery is collagen remodeling and strengthening of elastin. RF microneedling and microneedling in general may also have potential for use in enhancing topical product delivery.
Depending on the device, settings can be tailored to affect the energy delivery, including the type of needle (insulated vs. uninsulated vs. semi-insulated), Hz, number of needles, depth of needles, and time of exposure. In general, insulated needle tips provide less heat accumulation and potential injury to the skin surface, whereas uninsulated needles allow for more heat accumulation. Insulated needles, longer time of exposure, and lower energies (Hz) are safer options for darker skin types and those who hyperpigment easily.
Immediately after treatment, expected clinical endpoints can include erythema, edema, and possibly pinpoint bleeding that may last approximately several days to 2 weeks depending on the intensity of treatment. Potential side effects include infection, pigmentary alteration, folliculitis, prolonged grid marks, and scarring. Contraindications to treatment include having a pacemaker, history of keloid formation, active skin infections, prior gold threads in the treatment area, pregnancy and breastfeeding, metal implants in the treatment area, embedded electronic devices that cannot be turned off, isotretinoin use in the past 6 months, and allergy to any of the components of treatment.
Caution should be taken with tattoos in the treatment area or grounding pad (including cosmetic tattoos as tattoo ink may often contain metals that may absorb some of the heat, increasing the risk for injury or extrusion of the ink), a history of cold sores or herpes simplex virus in the treatment area (if so, a prophylactic antiviral would be indicated prior to treatment), use of topical retinoids in the past 7 days, having received neurotoxin or fillers in the prior 2 weeks, autoimmune disease, bleeding disorders, neuropathy, and history of poor healing.
Depending on the device and area being treated, most RF microneedling treatments require two to five treatments, typically 4-6 weeks apart. If improvement is seen, it may be noticeable after one to two treatments, and as with laser resurfacing, continued improvement may be noticeable over the following 6-12 months post treatment.
Dr. Wesley and Dr. Lily Talakoub are cocontributors to this column. Dr. Wesley practices dermatology in Beverly Hills, Calif. Dr. Talakoub is in private practice in McLean, Va. This month’s column is by Dr. Wesley. Write to them at [email protected]. Dr. Wesley has no relevant disclosures.
Technology in the field of aesthetic dermatology continues to advance over time. Microneedling, largely used to improve textural changes of the skin associated with photoaging and acne scarring, has evolved over time from the use of dermarollers and microneedling skin pens to energy-based devices that deliver radiofrequency (RF) energy though microneedles that are used today.
.
Unlike prior radiofrequency energy-based devices that deliver radiofrequency energy on the skin surface to allow bulk thermal energy (or heat) to stimulate collagen remodeling and tissue tightening, RF microneedling devices deliver the same RF or thermal energy via needles. RF, measured in Hertz (Hz) is part of the electromagnetic spectrum, with most devices delivering thermal energy at around 1-2 MHz, which is less than most typical RF only devices (at around 4-6 MHz), but with potentially more precise depth and delivery. For comparison, the RF of household electrical currents are around 60 Hz; traditional electrosurgical units, 50Hz -300 kHz; AM radio, 500 KHz; and microwaves, 2500 MHz.
When delivered to the skin, RF energy produces a change in the electrical charge of the skin, resulting in movement of electrons. The impedance (or resistance) of the tissue to the electron movement is what generates heat. Different factors, including tissue thickness, pressure applied to the tissue, hydration, bipolar versus monopolar delivery, and the number of needles are several factors than can affect the impedance.
Bipolar RF means that the current passes between two electrodes, whereas monopolar RF means that the electrical current is between an active treatment electrode and a passive grounding electrode (or grounding pad typically placed on the patient’s back). With bipolar RF, the current is limited to the area between the two electrodes. The depth of penetration is half of the distance between the electrodes, thus resulting in shallow (but potentially more aggressive) tissue heating. With monopolar RF, deeper tissue penetration occurs that is also often less uncomfortable to the patient.
The desired result of the energy delivery is collagen remodeling and strengthening of elastin. RF microneedling and microneedling in general may also have potential for use in enhancing topical product delivery.
Depending on the device, settings can be tailored to affect the energy delivery, including the type of needle (insulated vs. uninsulated vs. semi-insulated), Hz, number of needles, depth of needles, and time of exposure. In general, insulated needle tips provide less heat accumulation and potential injury to the skin surface, whereas uninsulated needles allow for more heat accumulation. Insulated needles, longer time of exposure, and lower energies (Hz) are safer options for darker skin types and those who hyperpigment easily.
Immediately after treatment, expected clinical endpoints can include erythema, edema, and possibly pinpoint bleeding that may last approximately several days to 2 weeks depending on the intensity of treatment. Potential side effects include infection, pigmentary alteration, folliculitis, prolonged grid marks, and scarring. Contraindications to treatment include having a pacemaker, history of keloid formation, active skin infections, prior gold threads in the treatment area, pregnancy and breastfeeding, metal implants in the treatment area, embedded electronic devices that cannot be turned off, isotretinoin use in the past 6 months, and allergy to any of the components of treatment.
Caution should be taken with tattoos in the treatment area or grounding pad (including cosmetic tattoos as tattoo ink may often contain metals that may absorb some of the heat, increasing the risk for injury or extrusion of the ink), a history of cold sores or herpes simplex virus in the treatment area (if so, a prophylactic antiviral would be indicated prior to treatment), use of topical retinoids in the past 7 days, having received neurotoxin or fillers in the prior 2 weeks, autoimmune disease, bleeding disorders, neuropathy, and history of poor healing.
Depending on the device and area being treated, most RF microneedling treatments require two to five treatments, typically 4-6 weeks apart. If improvement is seen, it may be noticeable after one to two treatments, and as with laser resurfacing, continued improvement may be noticeable over the following 6-12 months post treatment.
Dr. Wesley and Dr. Lily Talakoub are cocontributors to this column. Dr. Wesley practices dermatology in Beverly Hills, Calif. Dr. Talakoub is in private practice in McLean, Va. This month’s column is by Dr. Wesley. Write to them at [email protected]. Dr. Wesley has no relevant disclosures.
Technology in the field of aesthetic dermatology continues to advance over time. Microneedling, largely used to improve textural changes of the skin associated with photoaging and acne scarring, has evolved over time from the use of dermarollers and microneedling skin pens to energy-based devices that deliver radiofrequency (RF) energy though microneedles that are used today.
.
Unlike prior radiofrequency energy-based devices that deliver radiofrequency energy on the skin surface to allow bulk thermal energy (or heat) to stimulate collagen remodeling and tissue tightening, RF microneedling devices deliver the same RF or thermal energy via needles. RF, measured in Hertz (Hz) is part of the electromagnetic spectrum, with most devices delivering thermal energy at around 1-2 MHz, which is less than most typical RF only devices (at around 4-6 MHz), but with potentially more precise depth and delivery. For comparison, the RF of household electrical currents are around 60 Hz; traditional electrosurgical units, 50Hz -300 kHz; AM radio, 500 KHz; and microwaves, 2500 MHz.
When delivered to the skin, RF energy produces a change in the electrical charge of the skin, resulting in movement of electrons. The impedance (or resistance) of the tissue to the electron movement is what generates heat. Different factors, including tissue thickness, pressure applied to the tissue, hydration, bipolar versus monopolar delivery, and the number of needles are several factors than can affect the impedance.
Bipolar RF means that the current passes between two electrodes, whereas monopolar RF means that the electrical current is between an active treatment electrode and a passive grounding electrode (or grounding pad typically placed on the patient’s back). With bipolar RF, the current is limited to the area between the two electrodes. The depth of penetration is half of the distance between the electrodes, thus resulting in shallow (but potentially more aggressive) tissue heating. With monopolar RF, deeper tissue penetration occurs that is also often less uncomfortable to the patient.
The desired result of the energy delivery is collagen remodeling and strengthening of elastin. RF microneedling and microneedling in general may also have potential for use in enhancing topical product delivery.
Depending on the device, settings can be tailored to affect the energy delivery, including the type of needle (insulated vs. uninsulated vs. semi-insulated), Hz, number of needles, depth of needles, and time of exposure. In general, insulated needle tips provide less heat accumulation and potential injury to the skin surface, whereas uninsulated needles allow for more heat accumulation. Insulated needles, longer time of exposure, and lower energies (Hz) are safer options for darker skin types and those who hyperpigment easily.
Immediately after treatment, expected clinical endpoints can include erythema, edema, and possibly pinpoint bleeding that may last approximately several days to 2 weeks depending on the intensity of treatment. Potential side effects include infection, pigmentary alteration, folliculitis, prolonged grid marks, and scarring. Contraindications to treatment include having a pacemaker, history of keloid formation, active skin infections, prior gold threads in the treatment area, pregnancy and breastfeeding, metal implants in the treatment area, embedded electronic devices that cannot be turned off, isotretinoin use in the past 6 months, and allergy to any of the components of treatment.
Caution should be taken with tattoos in the treatment area or grounding pad (including cosmetic tattoos as tattoo ink may often contain metals that may absorb some of the heat, increasing the risk for injury or extrusion of the ink), a history of cold sores or herpes simplex virus in the treatment area (if so, a prophylactic antiviral would be indicated prior to treatment), use of topical retinoids in the past 7 days, having received neurotoxin or fillers in the prior 2 weeks, autoimmune disease, bleeding disorders, neuropathy, and history of poor healing.
Depending on the device and area being treated, most RF microneedling treatments require two to five treatments, typically 4-6 weeks apart. If improvement is seen, it may be noticeable after one to two treatments, and as with laser resurfacing, continued improvement may be noticeable over the following 6-12 months post treatment.
Dr. Wesley and Dr. Lily Talakoub are cocontributors to this column. Dr. Wesley practices dermatology in Beverly Hills, Calif. Dr. Talakoub is in private practice in McLean, Va. This month’s column is by Dr. Wesley. Write to them at [email protected]. Dr. Wesley has no relevant disclosures.









