User login
Dr. Carl Bell always asked the hard questions
Carl C. Bell, MD, started his career by asking the hard questions that no one dared to ask. His curiosity, courage, and compassion for all communities would lead him to impact the world in ways that few psychiatrists could ever imagine.
His accomplishments were many and far-reaching, dating back over 4 decades of service and research. He was a prolific author and researcher, having written more than 400 books, chapters, and articles. His research covered a lot of ground, but four critical areas of focus were childhood trauma, violence prevention, criminal justice reform, and most recently, fetal alcohol spectrum disorders.
The word “visionary” is frequently overused. But when we apply it to Dr. Carl Bell, the word does not do him justice. If you take a closer look at all four of those areas, you can see a common thread: What are the elements of a society that can tear communities apart?
When I look at Dr. Bell’s research, I see a man with a dedicated vision to addressing each of those elements in systematic way, and a determination to bring the results of that research into his Southside Chicago community in numerous ways, including by serving as president and CEO of the Community Mental Health Council, and as director of the Institute for Juvenile Research at the University of Illinois at Chicago.
Dr. Bell was a leader for his patients as well as for black psychiatrists. He was a founding member of Black Psychiatrists of America and served as a mentor in some way to the vast majority of black psychiatrists currently practicing in the country. As a black male psychiatrist, I saw Dr. Bell as a source of inspiration in my career and the standard by which I measured myself. I’m not talking about awards or accomplishments, as Dr. Bell has countless accolades, including most recently, being presented this year with the American Psychiatric Association’s Adolph Meyer Award for Lifetime Achievement in Psychiatric Research and the National Medical Association’s Scroll of Merit. I am referring to Dr. Bell’s willingness to walk away from something he thought was wrong.
For every accolade he won or prestigious committee he served on, I would wager that he declined or stepped way from just as many. Dr. Bell’s character and vision for psychiatry in general, and the mental health of African American communities specifically, would not allow him to pay lip service to agendas that were self-serving, and did not push the field and communities forward.
During his service as an editorial advisory board member for Clinical Psychiatry News, Dr. Bell could always be relied upon to offer an insightful perspective to any discussion, ranging from violence prevention to the social determinants of health and their role in fetal alcohol spectrum disorders.
What I will remember most about Dr. Bell is his strong character. My guess is that he was never shy about stating the truth to a patient or a president of the United States. He possessed the intellect to back up any of his views while also having the humility of a dedicated community psychiatrist who worked for no other reason than to serve his patients.
When I first met Dr. Bell, he was giving a grand rounds at the George Washington University department of psychiatry. He was wearing a hat during the lecture and a belt with the Superman logo. I thought to myself, “Whoa, this is a different type of guy,” then I sat and listened to the talk, and was utterly astounded by his intellect, humor, honesty, and passion for his patients. I had never heard a psychiatrist speak with a combination of such command and approachability, and again, I thought to myself, “Whoa, this is a different type of guy.”
Little did I know that Dr. Bell and I would end up serving together on the editorial board of CPN. I loved seeing Dr. Bell, and catching up and gleaning from his wisdom. I was very humbled by how generous Dr. Bell was with his time and the extent to which he would make himself available as a mentor. During a CPN board meeting, we were trying to come up with a mantra that would capture the mission of the new MDedge Psychiatry website. Dr. Bell (in a hat, of course) let everyone else talk, and then, in a calm voice, said: “We ask the hard questions.” As editor in chief of MDedge Psychiatry, I knew this had to be the mantra. It was aspirational, gave us an identity, and held our feet to the fire – to always ask hard questions in the service of patients and readers. I looked forward to discussing the evolution of the site, seeing him at meetings and conferences, brainstorming the implications of new advances in the field, and simply walking down the street and laughing.
Those events will never occur again, because Carl left us on Thursday, Aug 1. Carl has left us with a legacy of work that we are still coming to appreciate. He left us with a mandate to pursue the truth and make an impact in our communities. He taught black psychiatrists what it meant to stand up unapologetically for your community and society. As I reflect on the scope of his life, I have one last hard question for Carl: “Why did you have to leave us so soon?”
Dr. Norris is assistant professor of psychiatry and behavioral sciences at George Washington University, Washington. He also serves as assistant dean of student affairs at the university, and medical director of psychiatric and behavioral sciences at GWU Hospital. Dr. Norris also is host of the MDedge Psychcast.
Carl C. Bell, MD, started his career by asking the hard questions that no one dared to ask. His curiosity, courage, and compassion for all communities would lead him to impact the world in ways that few psychiatrists could ever imagine.
His accomplishments were many and far-reaching, dating back over 4 decades of service and research. He was a prolific author and researcher, having written more than 400 books, chapters, and articles. His research covered a lot of ground, but four critical areas of focus were childhood trauma, violence prevention, criminal justice reform, and most recently, fetal alcohol spectrum disorders.
The word “visionary” is frequently overused. But when we apply it to Dr. Carl Bell, the word does not do him justice. If you take a closer look at all four of those areas, you can see a common thread: What are the elements of a society that can tear communities apart?
When I look at Dr. Bell’s research, I see a man with a dedicated vision to addressing each of those elements in systematic way, and a determination to bring the results of that research into his Southside Chicago community in numerous ways, including by serving as president and CEO of the Community Mental Health Council, and as director of the Institute for Juvenile Research at the University of Illinois at Chicago.
Dr. Bell was a leader for his patients as well as for black psychiatrists. He was a founding member of Black Psychiatrists of America and served as a mentor in some way to the vast majority of black psychiatrists currently practicing in the country. As a black male psychiatrist, I saw Dr. Bell as a source of inspiration in my career and the standard by which I measured myself. I’m not talking about awards or accomplishments, as Dr. Bell has countless accolades, including most recently, being presented this year with the American Psychiatric Association’s Adolph Meyer Award for Lifetime Achievement in Psychiatric Research and the National Medical Association’s Scroll of Merit. I am referring to Dr. Bell’s willingness to walk away from something he thought was wrong.
For every accolade he won or prestigious committee he served on, I would wager that he declined or stepped way from just as many. Dr. Bell’s character and vision for psychiatry in general, and the mental health of African American communities specifically, would not allow him to pay lip service to agendas that were self-serving, and did not push the field and communities forward.
During his service as an editorial advisory board member for Clinical Psychiatry News, Dr. Bell could always be relied upon to offer an insightful perspective to any discussion, ranging from violence prevention to the social determinants of health and their role in fetal alcohol spectrum disorders.
What I will remember most about Dr. Bell is his strong character. My guess is that he was never shy about stating the truth to a patient or a president of the United States. He possessed the intellect to back up any of his views while also having the humility of a dedicated community psychiatrist who worked for no other reason than to serve his patients.
When I first met Dr. Bell, he was giving a grand rounds at the George Washington University department of psychiatry. He was wearing a hat during the lecture and a belt with the Superman logo. I thought to myself, “Whoa, this is a different type of guy,” then I sat and listened to the talk, and was utterly astounded by his intellect, humor, honesty, and passion for his patients. I had never heard a psychiatrist speak with a combination of such command and approachability, and again, I thought to myself, “Whoa, this is a different type of guy.”
Little did I know that Dr. Bell and I would end up serving together on the editorial board of CPN. I loved seeing Dr. Bell, and catching up and gleaning from his wisdom. I was very humbled by how generous Dr. Bell was with his time and the extent to which he would make himself available as a mentor. During a CPN board meeting, we were trying to come up with a mantra that would capture the mission of the new MDedge Psychiatry website. Dr. Bell (in a hat, of course) let everyone else talk, and then, in a calm voice, said: “We ask the hard questions.” As editor in chief of MDedge Psychiatry, I knew this had to be the mantra. It was aspirational, gave us an identity, and held our feet to the fire – to always ask hard questions in the service of patients and readers. I looked forward to discussing the evolution of the site, seeing him at meetings and conferences, brainstorming the implications of new advances in the field, and simply walking down the street and laughing.
Those events will never occur again, because Carl left us on Thursday, Aug 1. Carl has left us with a legacy of work that we are still coming to appreciate. He left us with a mandate to pursue the truth and make an impact in our communities. He taught black psychiatrists what it meant to stand up unapologetically for your community and society. As I reflect on the scope of his life, I have one last hard question for Carl: “Why did you have to leave us so soon?”
Dr. Norris is assistant professor of psychiatry and behavioral sciences at George Washington University, Washington. He also serves as assistant dean of student affairs at the university, and medical director of psychiatric and behavioral sciences at GWU Hospital. Dr. Norris also is host of the MDedge Psychcast.
Carl C. Bell, MD, started his career by asking the hard questions that no one dared to ask. His curiosity, courage, and compassion for all communities would lead him to impact the world in ways that few psychiatrists could ever imagine.
His accomplishments were many and far-reaching, dating back over 4 decades of service and research. He was a prolific author and researcher, having written more than 400 books, chapters, and articles. His research covered a lot of ground, but four critical areas of focus were childhood trauma, violence prevention, criminal justice reform, and most recently, fetal alcohol spectrum disorders.
The word “visionary” is frequently overused. But when we apply it to Dr. Carl Bell, the word does not do him justice. If you take a closer look at all four of those areas, you can see a common thread: What are the elements of a society that can tear communities apart?
When I look at Dr. Bell’s research, I see a man with a dedicated vision to addressing each of those elements in systematic way, and a determination to bring the results of that research into his Southside Chicago community in numerous ways, including by serving as president and CEO of the Community Mental Health Council, and as director of the Institute for Juvenile Research at the University of Illinois at Chicago.
Dr. Bell was a leader for his patients as well as for black psychiatrists. He was a founding member of Black Psychiatrists of America and served as a mentor in some way to the vast majority of black psychiatrists currently practicing in the country. As a black male psychiatrist, I saw Dr. Bell as a source of inspiration in my career and the standard by which I measured myself. I’m not talking about awards or accomplishments, as Dr. Bell has countless accolades, including most recently, being presented this year with the American Psychiatric Association’s Adolph Meyer Award for Lifetime Achievement in Psychiatric Research and the National Medical Association’s Scroll of Merit. I am referring to Dr. Bell’s willingness to walk away from something he thought was wrong.
For every accolade he won or prestigious committee he served on, I would wager that he declined or stepped way from just as many. Dr. Bell’s character and vision for psychiatry in general, and the mental health of African American communities specifically, would not allow him to pay lip service to agendas that were self-serving, and did not push the field and communities forward.
During his service as an editorial advisory board member for Clinical Psychiatry News, Dr. Bell could always be relied upon to offer an insightful perspective to any discussion, ranging from violence prevention to the social determinants of health and their role in fetal alcohol spectrum disorders.
What I will remember most about Dr. Bell is his strong character. My guess is that he was never shy about stating the truth to a patient or a president of the United States. He possessed the intellect to back up any of his views while also having the humility of a dedicated community psychiatrist who worked for no other reason than to serve his patients.
When I first met Dr. Bell, he was giving a grand rounds at the George Washington University department of psychiatry. He was wearing a hat during the lecture and a belt with the Superman logo. I thought to myself, “Whoa, this is a different type of guy,” then I sat and listened to the talk, and was utterly astounded by his intellect, humor, honesty, and passion for his patients. I had never heard a psychiatrist speak with a combination of such command and approachability, and again, I thought to myself, “Whoa, this is a different type of guy.”
Little did I know that Dr. Bell and I would end up serving together on the editorial board of CPN. I loved seeing Dr. Bell, and catching up and gleaning from his wisdom. I was very humbled by how generous Dr. Bell was with his time and the extent to which he would make himself available as a mentor. During a CPN board meeting, we were trying to come up with a mantra that would capture the mission of the new MDedge Psychiatry website. Dr. Bell (in a hat, of course) let everyone else talk, and then, in a calm voice, said: “We ask the hard questions.” As editor in chief of MDedge Psychiatry, I knew this had to be the mantra. It was aspirational, gave us an identity, and held our feet to the fire – to always ask hard questions in the service of patients and readers. I looked forward to discussing the evolution of the site, seeing him at meetings and conferences, brainstorming the implications of new advances in the field, and simply walking down the street and laughing.
Those events will never occur again, because Carl left us on Thursday, Aug 1. Carl has left us with a legacy of work that we are still coming to appreciate. He left us with a mandate to pursue the truth and make an impact in our communities. He taught black psychiatrists what it meant to stand up unapologetically for your community and society. As I reflect on the scope of his life, I have one last hard question for Carl: “Why did you have to leave us so soon?”
Dr. Norris is assistant professor of psychiatry and behavioral sciences at George Washington University, Washington. He also serves as assistant dean of student affairs at the university, and medical director of psychiatric and behavioral sciences at GWU Hospital. Dr. Norris also is host of the MDedge Psychcast.
In memory of Dr. Carl Compton Bell
It was a simple message in the body of an email: “A strong voice in and for psychiatry is now silent.”
That is how I shared the news of the passing of Carl Compton Bell, MD, with the leadership of the American Psychiatric Association and what I think Carl would have approved be shared. Although he was a member of APA, he was never interested in the trappings of leadership there or any other organizations of which he was a longtime member, really. He preferred to “do the work” and was known to not suffer fools who were in it to promote themselves. He was always ready, willing, and able to offer guidance or assistance in your work and never failed to have an opinion on what else you needed to do. Some of my favorite memories of Carl are the talks he initiated at the drop of a hat where he “dropped some knowledge” about what he was doing or what you should be doing.
Upon hearing of his death, I described him to someone as fearless, unapologetic, smart, and ready to advocate for black people at the drop of one of the many hats he wore over the years. In fact, his decades of wardrobes is one the other things many of us will remember – the CMHC baseball cap with the “Stop Black on Black” crime T-shirt, the Obama cap paired with an assortment of message T-shirts (depending on what issue he was focused on at the time), and, most recently, the longer hair sticking out from under the wide brim leather cowboy hat with the highway patrol polarized sunglasses.
And whether it was the Surgeon General or an audience at the Carter Center, the message was consistent and powerful. An international researcher, clinician, teacher, and author of more than 500 books, chapters, and articles, he spent most of his career directly addressing issues of violence and HIV prevention, misdiagnosis of psychiatric disorders in African Americans, and the psychological effects on children exposed to violence.
Honoring the legacy of Carl Bell is about more than how we can all follow in his footsteps and more about being like him – unapologetically fearless and focused on improving the health, mental health, and overall well-being of black people. He was very clear that his talents, his skills, his focus – whether it was clinical care, training, or research – would be on black people, and he was often amused at the response, mostly from white people, when he stated clearly that this was his focus. He was often challenged by them, and his response as I frequently heard him say was: “I care about black people; I want to help black people.” I think he basically felt that, if it was good for black people, it would also benefit everyone else.
So, there’s a lesson for us as we heap on the well-deserved accolades on him and his life’s work, and reminisce about our personal encounters and experiences with him over the decades. As we reflect on what he meant to each of us as a friend, a colleague, and a history maker, I think the lesson is that if Carl were here today, he’d say: “OK, that’s all good, thank you for the nice words but what are you doing for black people today? What are you doing to improve their health and life condition today?” I think if we really want to honor his legacy and continue his work, we must be as fearless and focused as he was as we follow his lead and carry on with the work that promotes mental health in the black community. And when we are challenged for wanting to do this work, we must be just as unapologetic and thoughtful as he was, even channeling our own “Carl Bell” moment if needed. As a lifelong martial arts practitioner, I will end with this: “The bamboo which bends in the wind is stronger than the mighty oak which breaks in a storm.” Carl was the bamboo, and he’s with the Ancestors now, encouraging us to do the work and bend not break. Rest, my brother; job well done!
Dr. Stewart is immediate past president of the American Psychiatric Association.
It was a simple message in the body of an email: “A strong voice in and for psychiatry is now silent.”
That is how I shared the news of the passing of Carl Compton Bell, MD, with the leadership of the American Psychiatric Association and what I think Carl would have approved be shared. Although he was a member of APA, he was never interested in the trappings of leadership there or any other organizations of which he was a longtime member, really. He preferred to “do the work” and was known to not suffer fools who were in it to promote themselves. He was always ready, willing, and able to offer guidance or assistance in your work and never failed to have an opinion on what else you needed to do. Some of my favorite memories of Carl are the talks he initiated at the drop of a hat where he “dropped some knowledge” about what he was doing or what you should be doing.
Upon hearing of his death, I described him to someone as fearless, unapologetic, smart, and ready to advocate for black people at the drop of one of the many hats he wore over the years. In fact, his decades of wardrobes is one the other things many of us will remember – the CMHC baseball cap with the “Stop Black on Black” crime T-shirt, the Obama cap paired with an assortment of message T-shirts (depending on what issue he was focused on at the time), and, most recently, the longer hair sticking out from under the wide brim leather cowboy hat with the highway patrol polarized sunglasses.
And whether it was the Surgeon General or an audience at the Carter Center, the message was consistent and powerful. An international researcher, clinician, teacher, and author of more than 500 books, chapters, and articles, he spent most of his career directly addressing issues of violence and HIV prevention, misdiagnosis of psychiatric disorders in African Americans, and the psychological effects on children exposed to violence.
Honoring the legacy of Carl Bell is about more than how we can all follow in his footsteps and more about being like him – unapologetically fearless and focused on improving the health, mental health, and overall well-being of black people. He was very clear that his talents, his skills, his focus – whether it was clinical care, training, or research – would be on black people, and he was often amused at the response, mostly from white people, when he stated clearly that this was his focus. He was often challenged by them, and his response as I frequently heard him say was: “I care about black people; I want to help black people.” I think he basically felt that, if it was good for black people, it would also benefit everyone else.
So, there’s a lesson for us as we heap on the well-deserved accolades on him and his life’s work, and reminisce about our personal encounters and experiences with him over the decades. As we reflect on what he meant to each of us as a friend, a colleague, and a history maker, I think the lesson is that if Carl were here today, he’d say: “OK, that’s all good, thank you for the nice words but what are you doing for black people today? What are you doing to improve their health and life condition today?” I think if we really want to honor his legacy and continue his work, we must be as fearless and focused as he was as we follow his lead and carry on with the work that promotes mental health in the black community. And when we are challenged for wanting to do this work, we must be just as unapologetic and thoughtful as he was, even channeling our own “Carl Bell” moment if needed. As a lifelong martial arts practitioner, I will end with this: “The bamboo which bends in the wind is stronger than the mighty oak which breaks in a storm.” Carl was the bamboo, and he’s with the Ancestors now, encouraging us to do the work and bend not break. Rest, my brother; job well done!
Dr. Stewart is immediate past president of the American Psychiatric Association.
It was a simple message in the body of an email: “A strong voice in and for psychiatry is now silent.”
That is how I shared the news of the passing of Carl Compton Bell, MD, with the leadership of the American Psychiatric Association and what I think Carl would have approved be shared. Although he was a member of APA, he was never interested in the trappings of leadership there or any other organizations of which he was a longtime member, really. He preferred to “do the work” and was known to not suffer fools who were in it to promote themselves. He was always ready, willing, and able to offer guidance or assistance in your work and never failed to have an opinion on what else you needed to do. Some of my favorite memories of Carl are the talks he initiated at the drop of a hat where he “dropped some knowledge” about what he was doing or what you should be doing.
Upon hearing of his death, I described him to someone as fearless, unapologetic, smart, and ready to advocate for black people at the drop of one of the many hats he wore over the years. In fact, his decades of wardrobes is one the other things many of us will remember – the CMHC baseball cap with the “Stop Black on Black” crime T-shirt, the Obama cap paired with an assortment of message T-shirts (depending on what issue he was focused on at the time), and, most recently, the longer hair sticking out from under the wide brim leather cowboy hat with the highway patrol polarized sunglasses.
And whether it was the Surgeon General or an audience at the Carter Center, the message was consistent and powerful. An international researcher, clinician, teacher, and author of more than 500 books, chapters, and articles, he spent most of his career directly addressing issues of violence and HIV prevention, misdiagnosis of psychiatric disorders in African Americans, and the psychological effects on children exposed to violence.
Honoring the legacy of Carl Bell is about more than how we can all follow in his footsteps and more about being like him – unapologetically fearless and focused on improving the health, mental health, and overall well-being of black people. He was very clear that his talents, his skills, his focus – whether it was clinical care, training, or research – would be on black people, and he was often amused at the response, mostly from white people, when he stated clearly that this was his focus. He was often challenged by them, and his response as I frequently heard him say was: “I care about black people; I want to help black people.” I think he basically felt that, if it was good for black people, it would also benefit everyone else.
So, there’s a lesson for us as we heap on the well-deserved accolades on him and his life’s work, and reminisce about our personal encounters and experiences with him over the decades. As we reflect on what he meant to each of us as a friend, a colleague, and a history maker, I think the lesson is that if Carl were here today, he’d say: “OK, that’s all good, thank you for the nice words but what are you doing for black people today? What are you doing to improve their health and life condition today?” I think if we really want to honor his legacy and continue his work, we must be as fearless and focused as he was as we follow his lead and carry on with the work that promotes mental health in the black community. And when we are challenged for wanting to do this work, we must be just as unapologetic and thoughtful as he was, even channeling our own “Carl Bell” moment if needed. As a lifelong martial arts practitioner, I will end with this: “The bamboo which bends in the wind is stronger than the mighty oak which breaks in a storm.” Carl was the bamboo, and he’s with the Ancestors now, encouraging us to do the work and bend not break. Rest, my brother; job well done!
Dr. Stewart is immediate past president of the American Psychiatric Association.
Why do so many women aged 65 years and older die of cervical cancer?
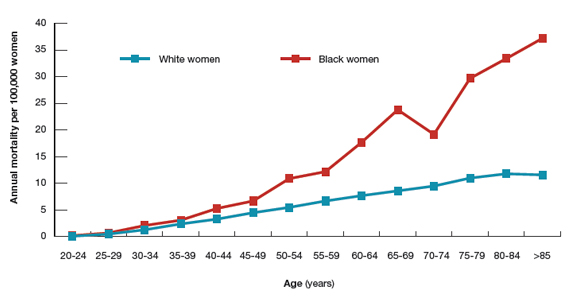
Surprisingly, the cervical cancer death rate is greater among women aged >65 years than among younger women1,2 (FIGURE). Paradoxically, most of our screening programs focus on women <65 years of age. A nationwide study from Denmark estimated that the cervical cancer death rate per 100,000 women at ages 40 to 44 and 65 to 69 was 3.8 and 9.0, respectively.1 In other words, the cervical cancer death rate at age 65 to 69 years was 2.36 times higher than at age 40 to 44 years.1
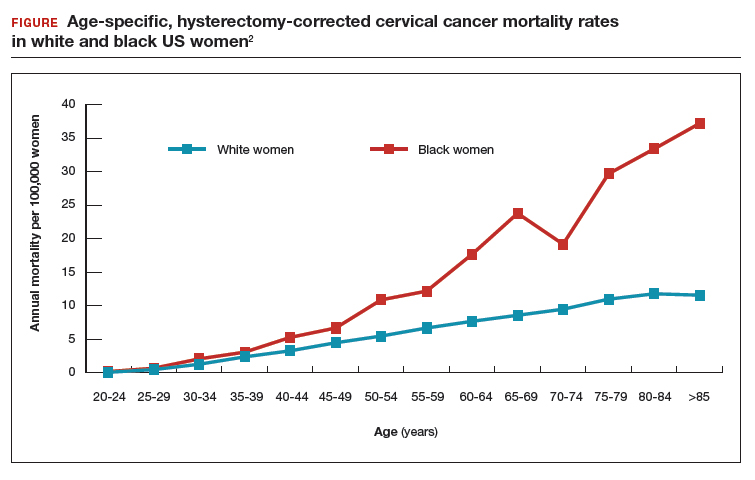
A study from the United States estimated that the cervical cancer death rate per 100,000 white women at ages 40 to 44 and 65 to 69 was 3.3 and 8.6, respectively,2 very similar to the findings from Denmark. The same US study estimated that the cervical cancer death rate per 100,000 black women at ages 40 to 44 and 65 to 69 was 5.3 and 23.8, highlighting the fact that, in the United States, cervical cancer disease burden is disproportionately greater among black than among white women.2 In addition, the cervical cancer death rate among black women at age 65 to 69 was 4.49 times higher than at age 40 to 44 years.2
Given the high death rate from cervical cancer in women >65 years of age, it is paradoxical that most professional society guidelines recommend discontinuing cervical cancer screening at 65 years of age, if previous cervical cancer screening is normal.3,4 Is the problem due to an inability to implement the current guidelines? Or is the problem that the guidelines are not optimally designed to reduce cervical cancer risk in women >65 years of age?
The American College of Obstetricians and Gynecologists (ACOG) and the US Preventive Services Task Force (USPSTF) recommend against cervical cancer screening in women >65 years of age who have had adequate prior screening and are not otherwise at high risk for cervical cancer. However, ACOG and the USPSTF caution that there are many groups of women that may benefit from continued screening after 65 years of age, including women with HIV infection, a compromised immune system, or previous high-grade precancerous lesion or cervicalcancer; women with limited access to care; women from racial/ethnic minority groups; and migrant women.4 Many clinicians remember the guidance, “discontinue cervical cancer screening at 65 years” but do not recall all the clinical factors that might warrant continued screening past age 65. Of special concern is that black,2 Hispanic,5 and migrant women6 are at much higher risk for invasive cervical cancer than white or US-born women.
The optimal implementation of the ACOG and USPSTF guidelines are undermined by a fractured health care system, where key pieces of information may be unavailable to the clinician tasked with making a decision about discontinuing cervical cancer screening. Imagine the case in which a 65-year-old woman pre‑sents to her primary care physician for cervical cancer screening. The clinician performs a cervical cytology test and obtains a report of “no intraepithelial lesion or malignancy.” The clinician then recommends that the patient discontinue cervical cancer screening. Unbeknownst to the clinician, the patient had a positive HPV 16/18/45 test within the past 10 years in another health system. In this case, it would be inappropriate to terminate the patient from cervical cancer screening.
Continue to: Testing for hrHPV is superior to cervical cytology in women >65 years...
Testing for hrHPV is superior to cervical cytology in women >65 years
In Sweden, about 30% of cervical cancer cases occur in women aged >60 years.7 To assess the prevalence of oncogenic high-risk HPV (hrHPV), women at ages 60, 65, 70, and 75 years were invited to send sequential self-collected vaginal samples for nucleic acid testing for hrHPV. The prevalence of hrHPV was found to be 4.4%. Women with a second positive, self-collected, hrHPV test were invited for colposcopy, cervical biopsy, and cytology testing. Among the women with two positive hrHPV tests, cervical biopsy revealed 7 cases of cervical intraepithelial neoplasia grade 2 (CIN2), 6 cases of CIN1, and 4 biopsies without CIN. In these women 94% of the cervical cytology samples returned, “no intraepithelial lesion or malignancy” and 6% revealed atypical squamous cells of undetermined significance. This study suggests that, in women aged >65 years, cervical cytology may have a high rate of false-negative results, possibly due to epithelial atrophy. An evolving clinical pearl is that, when using the current cervical cancer screening guidelines, the final screen for cervical cancer must include a nucleic acid test for hrHPV.
In women 65 to 90 years, the prevalence of hrHPV is approximately 5%
In a study of 40,382 women aged 14 to 95 years, the prevalence of hrHPV was 46% in 20- to 23-year-old women and 5.7% in women older than 65 years of age.8 In a study of more than 108,000 women aged 69 to >89 years the prevalence of hrHPV was 4.3%, and similar prevalence rates were seen across all ages from 69 to >89 years.9 The carcinogenic role of persistent hrHPV infection in women >65 years is an important area for future research.
Latent HPV virus infection
Following a primary varicella-zoster infection (chickenpox), the virus may remain in a latent state in sensory ganglia, reactivating later in life to cause shingles. Thirty percent of people who have a primary chickenpox infection eventually will develop a case of shingles. Immunocompromised populations are at an increased risk of developing shingles because of reduced T-cell mediated immunity.
A recent hypothesis is that in immunocompromised and older women, latent HPV can reactivate and cause clinically significant infection.10 Following renal transplantation investigators have reported a significant increase in the prevalence of genital HPV, without a change in sexual behavior.11 In cervical tissue from women with no evidence of active HPV infection, highly sensitive PCR-based assays detected HPV16 virus in a latent state in some women, possibly due to disruption of the viral E2 gene.12 If latent HPV infection is a valid biological concept, it suggests that there is no “safe age” at which to discontinue screening for HPV infection because the virus cannot be detected in screening samples while it is latent.
Options for cervical cancer screening in women >65 years
Three options might reduce the morbidity and mortality associated with cervical cancer in women >65 years.
Option 1: Double-down on trying to effectively implement current guidelines. The high rate of cervical cancer mortality in women >65 years of age indicates that the current guidelines, as implemented in real clinical practice, are not working. A problem with the current screening guidelines is that clinicians are expected to be capable of finding all relevant cervical cancer test results and properly interpreting the results. Clinicians are over-taxed and fallible, and the current approach is not likely to be successful unless additional information technology solutions are implemented.
Continue to: Health systems could use information...
Health systems could use information technology to mitigate these problems. For example, health systems could deploy software to assemble every cervical screening result on each woman and pre‑sent those results to clinicians in a single integrated view in the electronic record. Additionally, once all lifetime screening results are consolidated in one view, artificial intelligence systems could be used to analyze the totality of results and identify women who would benefit by continued screening past age 65 and women who could safely discontinue screening.
Option 2: Adopt the Australian approach to cervical cancer screening. The current Australian approach to cervical cancer screening is built on 3 pillars: 1) school-based vaccination of all children against hrHPV, 2) screening all women from 25 to 74 years of age every 5 years using nucleic acid testing for hrHPV, and 3) providing a system for the testing of samples self-collected by women who are reluctant to visit a clinician for screening.13 Australia has one of the lowest cervical cancer death rates in the world.
Option 3: Continue screening most women past age 65. Women >65 years of age are known to be infected with hrHPV genotypes. hrHPV infection causes cervical cancer. Cervical cancer causes many deaths in women aged >65 years. There is no strong rationale for ignoring these three facts. hrHPV screening every 5 years as long as the woman is healthy and has a reasonable life expectancy is an option that could be evaluated in randomized studies.
Given the high rate of cervical cancer death in women >65 years of age, I plan to be very cautious about discontinuing cervical cancer screening until I can personally ensure that my patient has no evidence of hrHPV infection.
In 2008, Harald zur Hausen, MD, received the Nobel Prize in Physiology or Medicine for discovering that human papilloma virus (HPV) caused cervical cancer. In a recent study, 74% of cervical cancers were associated with HPV 16 or 18 infections. A total of 89% of the cancers were associated with one of the high-risk HPV genotypes, including HPV 16/18/31/33/45/52/58.1
Recently, HPV has been shown to be a major cause of oropharyngeal cancer. The Centers for Disease Control and Prevention calculated that in CY2015 in the United States there were 18,917 cases of HPV-associated oropharyngeal squamous cell cancer and 11,788 cases of cervical cancer.2 Most cases of HPV-associated oropharyngeal cancer occur in men, and HPV vaccination of boys may help to prevent this cancer type. Oncogenic HPV produce two proteins (E6 and E7) that promote viral replication and squamous cell growth by inhibiting the function of p53 and retinoblastoma protein. The immortalized HeLa cell line, derived from Ms. Henrietta Lack's cervical cancer, contains integrated HPV18 nucleic acid sequences.3,4
The discovery that HPV causes cancer catalyzed the development of nucleic acid tests to identify high-risk oncogenic HPV and vaccines against high-risk oncogenic HPV genotypes that prevent cervical cancer. From a public health perspective, it is more effective to vaccinate the population against oncogenic HPV genotypes than to screen and treat cancer. In the United States, vaccination rates range from a high of 92% (District of Columbia) and 89% (Rhode Island) to a low of 47% (Wyoming) and 50% (Kentucky and Mississippi).5 To reduce HPV-associated cancer mortality, the gap in vaccination compliance must be closed.
References
- Kjaer SK, Munk C, Junge J, et al. Carcinogenic HPV prevalence and age-specific type distribution in 40,382 women with normal cervical cytology, ACSUC/LSIL, HSIL, or cervical cancer: what is the potential for prevention? Cancer Causes Control. 2014;25:179-189.
- Van Dyne EA, Henley SJ, Saraiya M, et al. Trends in human papillomavirus-associated cancers - United States, 1999-2015. MMWR Morb Mortal Wkly Rep. 2018;67:918-924.
- Rosl F, Westphal EM, zur Hausen H. Chromatin structure and transcriptional regulation of human papillomavirus type 18 DNA in HeLa cells. Mol Carcinog. 1989;2:72-80.
- Adey A, Burton JN, Kitzman, et al. The haplotype-resolved genome and epigenome of the aneuploid HeLa cancer cell line. Nature. 2013;500:207-211.
- Walker TY, Elam-Evans LD, Singleton JA, et al. National, regional, state, and selected local area vaccination coverage among adolescents aged 13-17 years - United States, 2016. MMWR Morb Mortal Wkly Rep. 2017;66:874-882.
- Hammer A, Kahlert J, Gravitt PE, et al. Hysterectomy-corrected cervical cancer mortality rates in Denmark during 2002-2015: a registry-based cohort study. Acta Obstet Gynecol Scand. 2019;98:1063-1069.
- Beavis AL, Gravitt PE, Rositch AF. Hysterectomy-corrected cervical cancer mortality rates reveal a larger racial disparity in the United States. Cancer. 2017;123:1044-1050.
- American College of Obstetricians and Gynecologists Committee on Practice Bulletins--Gynecology. Practice Bulletin No. 168: cervical cancer screening and prevention. Obstet Gynecol. 2016;128:e111-30.
- Curry SJ, Krist AH, Owens DK, et al; US Preventive Services Task Force. Screening for cervical cancer: US Preventive Services Task Force recommendation statement. JAMA. 2018;320:674-686.
- Stang A, Hawk H, Knowlton R, et al. Hysterectomy-corrected incidence rates of cervical and uterine cancers in Massachusetts, 1995-2010. Ann Epidemiol. 2014;24:849-854.
- Hallowell BD, Endeshaw M, McKenna MT, et al. Cervical cancer death rates among U.S.- and foreign-born women: U.S., 2005-2014. Am J Prev Med. 2019;56:869-874.
- Lindström AK, Hermansson RS, Gustavsson I, et al. Cervical dysplasia in elderly women performing repeated self-sampling for HPV testing. PLoS One. 2018;13:e0207714.
- Kjaer SK, Munk C, Junge J, et al. Carcinogenic HPV prevalence and age-specific type distribution in 40,382 women with normal cervical cytology, ACSUC/LSIL, HSIL, or cervical cancer: what is the potential for prevention? Cancer Causes Control. 2014;25:179-189.
- Andersen B, Christensen BS, Christensen J, et al. HPV-prevalence in elderly women in Denmark. Gynecol Oncol. 2019;154:118-123.
- Gravitt PE, Winer RL. Natural history of HPV infection across the lifespan: role of viral latency. Viruses. 2017;9:E267.
- Hinten F, Hilbrands LB, Meeuwis KAP, et al. Reactivation of latent HPV infections after renal transplantation. Am J Transplant. 2017;17:1563-1573.
- Leonard SM, Pereira M, Roberts S, et al. Evidence of disrupted high-risk human papillomavirus DNA in morphologically normal cervices of older women. Sci Rep. 2016;6:20847.
- Cervical cancer screening. Cancer Council website. https://www.cancer.org.au/about-cancer/early-detection/screening-programs/cervical-cancer-screening.html. Updated March 15, 2019. Accessed July 23, 2019.
Surprisingly, the cervical cancer death rate is greater among women aged >65 years than among younger women1,2 (FIGURE). Paradoxically, most of our screening programs focus on women <65 years of age. A nationwide study from Denmark estimated that the cervical cancer death rate per 100,000 women at ages 40 to 44 and 65 to 69 was 3.8 and 9.0, respectively.1 In other words, the cervical cancer death rate at age 65 to 69 years was 2.36 times higher than at age 40 to 44 years.1
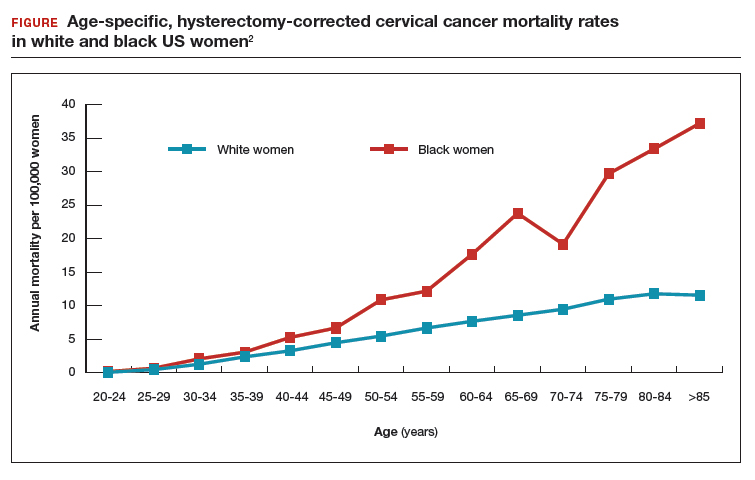
A study from the United States estimated that the cervical cancer death rate per 100,000 white women at ages 40 to 44 and 65 to 69 was 3.3 and 8.6, respectively,2 very similar to the findings from Denmark. The same US study estimated that the cervical cancer death rate per 100,000 black women at ages 40 to 44 and 65 to 69 was 5.3 and 23.8, highlighting the fact that, in the United States, cervical cancer disease burden is disproportionately greater among black than among white women.2 In addition, the cervical cancer death rate among black women at age 65 to 69 was 4.49 times higher than at age 40 to 44 years.2
Given the high death rate from cervical cancer in women >65 years of age, it is paradoxical that most professional society guidelines recommend discontinuing cervical cancer screening at 65 years of age, if previous cervical cancer screening is normal.3,4 Is the problem due to an inability to implement the current guidelines? Or is the problem that the guidelines are not optimally designed to reduce cervical cancer risk in women >65 years of age?
The American College of Obstetricians and Gynecologists (ACOG) and the US Preventive Services Task Force (USPSTF) recommend against cervical cancer screening in women >65 years of age who have had adequate prior screening and are not otherwise at high risk for cervical cancer. However, ACOG and the USPSTF caution that there are many groups of women that may benefit from continued screening after 65 years of age, including women with HIV infection, a compromised immune system, or previous high-grade precancerous lesion or cervicalcancer; women with limited access to care; women from racial/ethnic minority groups; and migrant women.4 Many clinicians remember the guidance, “discontinue cervical cancer screening at 65 years” but do not recall all the clinical factors that might warrant continued screening past age 65. Of special concern is that black,2 Hispanic,5 and migrant women6 are at much higher risk for invasive cervical cancer than white or US-born women.
The optimal implementation of the ACOG and USPSTF guidelines are undermined by a fractured health care system, where key pieces of information may be unavailable to the clinician tasked with making a decision about discontinuing cervical cancer screening. Imagine the case in which a 65-year-old woman pre‑sents to her primary care physician for cervical cancer screening. The clinician performs a cervical cytology test and obtains a report of “no intraepithelial lesion or malignancy.” The clinician then recommends that the patient discontinue cervical cancer screening. Unbeknownst to the clinician, the patient had a positive HPV 16/18/45 test within the past 10 years in another health system. In this case, it would be inappropriate to terminate the patient from cervical cancer screening.
Continue to: Testing for hrHPV is superior to cervical cytology in women >65 years...
Testing for hrHPV is superior to cervical cytology in women >65 years
In Sweden, about 30% of cervical cancer cases occur in women aged >60 years.7 To assess the prevalence of oncogenic high-risk HPV (hrHPV), women at ages 60, 65, 70, and 75 years were invited to send sequential self-collected vaginal samples for nucleic acid testing for hrHPV. The prevalence of hrHPV was found to be 4.4%. Women with a second positive, self-collected, hrHPV test were invited for colposcopy, cervical biopsy, and cytology testing. Among the women with two positive hrHPV tests, cervical biopsy revealed 7 cases of cervical intraepithelial neoplasia grade 2 (CIN2), 6 cases of CIN1, and 4 biopsies without CIN. In these women 94% of the cervical cytology samples returned, “no intraepithelial lesion or malignancy” and 6% revealed atypical squamous cells of undetermined significance. This study suggests that, in women aged >65 years, cervical cytology may have a high rate of false-negative results, possibly due to epithelial atrophy. An evolving clinical pearl is that, when using the current cervical cancer screening guidelines, the final screen for cervical cancer must include a nucleic acid test for hrHPV.
In women 65 to 90 years, the prevalence of hrHPV is approximately 5%
In a study of 40,382 women aged 14 to 95 years, the prevalence of hrHPV was 46% in 20- to 23-year-old women and 5.7% in women older than 65 years of age.8 In a study of more than 108,000 women aged 69 to >89 years the prevalence of hrHPV was 4.3%, and similar prevalence rates were seen across all ages from 69 to >89 years.9 The carcinogenic role of persistent hrHPV infection in women >65 years is an important area for future research.
Latent HPV virus infection
Following a primary varicella-zoster infection (chickenpox), the virus may remain in a latent state in sensory ganglia, reactivating later in life to cause shingles. Thirty percent of people who have a primary chickenpox infection eventually will develop a case of shingles. Immunocompromised populations are at an increased risk of developing shingles because of reduced T-cell mediated immunity.
A recent hypothesis is that in immunocompromised and older women, latent HPV can reactivate and cause clinically significant infection.10 Following renal transplantation investigators have reported a significant increase in the prevalence of genital HPV, without a change in sexual behavior.11 In cervical tissue from women with no evidence of active HPV infection, highly sensitive PCR-based assays detected HPV16 virus in a latent state in some women, possibly due to disruption of the viral E2 gene.12 If latent HPV infection is a valid biological concept, it suggests that there is no “safe age” at which to discontinue screening for HPV infection because the virus cannot be detected in screening samples while it is latent.
Options for cervical cancer screening in women >65 years
Three options might reduce the morbidity and mortality associated with cervical cancer in women >65 years.
Option 1: Double-down on trying to effectively implement current guidelines. The high rate of cervical cancer mortality in women >65 years of age indicates that the current guidelines, as implemented in real clinical practice, are not working. A problem with the current screening guidelines is that clinicians are expected to be capable of finding all relevant cervical cancer test results and properly interpreting the results. Clinicians are over-taxed and fallible, and the current approach is not likely to be successful unless additional information technology solutions are implemented.
Continue to: Health systems could use information...
Health systems could use information technology to mitigate these problems. For example, health systems could deploy software to assemble every cervical screening result on each woman and pre‑sent those results to clinicians in a single integrated view in the electronic record. Additionally, once all lifetime screening results are consolidated in one view, artificial intelligence systems could be used to analyze the totality of results and identify women who would benefit by continued screening past age 65 and women who could safely discontinue screening.
Option 2: Adopt the Australian approach to cervical cancer screening. The current Australian approach to cervical cancer screening is built on 3 pillars: 1) school-based vaccination of all children against hrHPV, 2) screening all women from 25 to 74 years of age every 5 years using nucleic acid testing for hrHPV, and 3) providing a system for the testing of samples self-collected by women who are reluctant to visit a clinician for screening.13 Australia has one of the lowest cervical cancer death rates in the world.
Option 3: Continue screening most women past age 65. Women >65 years of age are known to be infected with hrHPV genotypes. hrHPV infection causes cervical cancer. Cervical cancer causes many deaths in women aged >65 years. There is no strong rationale for ignoring these three facts. hrHPV screening every 5 years as long as the woman is healthy and has a reasonable life expectancy is an option that could be evaluated in randomized studies.
Given the high rate of cervical cancer death in women >65 years of age, I plan to be very cautious about discontinuing cervical cancer screening until I can personally ensure that my patient has no evidence of hrHPV infection.
In 2008, Harald zur Hausen, MD, received the Nobel Prize in Physiology or Medicine for discovering that human papilloma virus (HPV) caused cervical cancer. In a recent study, 74% of cervical cancers were associated with HPV 16 or 18 infections. A total of 89% of the cancers were associated with one of the high-risk HPV genotypes, including HPV 16/18/31/33/45/52/58.1
Recently, HPV has been shown to be a major cause of oropharyngeal cancer. The Centers for Disease Control and Prevention calculated that in CY2015 in the United States there were 18,917 cases of HPV-associated oropharyngeal squamous cell cancer and 11,788 cases of cervical cancer.2 Most cases of HPV-associated oropharyngeal cancer occur in men, and HPV vaccination of boys may help to prevent this cancer type. Oncogenic HPV produce two proteins (E6 and E7) that promote viral replication and squamous cell growth by inhibiting the function of p53 and retinoblastoma protein. The immortalized HeLa cell line, derived from Ms. Henrietta Lack's cervical cancer, contains integrated HPV18 nucleic acid sequences.3,4
The discovery that HPV causes cancer catalyzed the development of nucleic acid tests to identify high-risk oncogenic HPV and vaccines against high-risk oncogenic HPV genotypes that prevent cervical cancer. From a public health perspective, it is more effective to vaccinate the population against oncogenic HPV genotypes than to screen and treat cancer. In the United States, vaccination rates range from a high of 92% (District of Columbia) and 89% (Rhode Island) to a low of 47% (Wyoming) and 50% (Kentucky and Mississippi).5 To reduce HPV-associated cancer mortality, the gap in vaccination compliance must be closed.
References
- Kjaer SK, Munk C, Junge J, et al. Carcinogenic HPV prevalence and age-specific type distribution in 40,382 women with normal cervical cytology, ACSUC/LSIL, HSIL, or cervical cancer: what is the potential for prevention? Cancer Causes Control. 2014;25:179-189.
- Van Dyne EA, Henley SJ, Saraiya M, et al. Trends in human papillomavirus-associated cancers - United States, 1999-2015. MMWR Morb Mortal Wkly Rep. 2018;67:918-924.
- Rosl F, Westphal EM, zur Hausen H. Chromatin structure and transcriptional regulation of human papillomavirus type 18 DNA in HeLa cells. Mol Carcinog. 1989;2:72-80.
- Adey A, Burton JN, Kitzman, et al. The haplotype-resolved genome and epigenome of the aneuploid HeLa cancer cell line. Nature. 2013;500:207-211.
- Walker TY, Elam-Evans LD, Singleton JA, et al. National, regional, state, and selected local area vaccination coverage among adolescents aged 13-17 years - United States, 2016. MMWR Morb Mortal Wkly Rep. 2017;66:874-882.
Surprisingly, the cervical cancer death rate is greater among women aged >65 years than among younger women1,2 (FIGURE). Paradoxically, most of our screening programs focus on women <65 years of age. A nationwide study from Denmark estimated that the cervical cancer death rate per 100,000 women at ages 40 to 44 and 65 to 69 was 3.8 and 9.0, respectively.1 In other words, the cervical cancer death rate at age 65 to 69 years was 2.36 times higher than at age 40 to 44 years.1
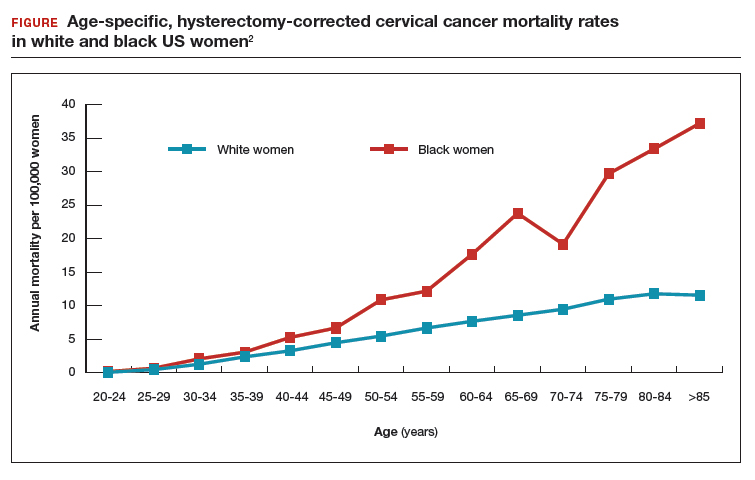
A study from the United States estimated that the cervical cancer death rate per 100,000 white women at ages 40 to 44 and 65 to 69 was 3.3 and 8.6, respectively,2 very similar to the findings from Denmark. The same US study estimated that the cervical cancer death rate per 100,000 black women at ages 40 to 44 and 65 to 69 was 5.3 and 23.8, highlighting the fact that, in the United States, cervical cancer disease burden is disproportionately greater among black than among white women.2 In addition, the cervical cancer death rate among black women at age 65 to 69 was 4.49 times higher than at age 40 to 44 years.2
Given the high death rate from cervical cancer in women >65 years of age, it is paradoxical that most professional society guidelines recommend discontinuing cervical cancer screening at 65 years of age, if previous cervical cancer screening is normal.3,4 Is the problem due to an inability to implement the current guidelines? Or is the problem that the guidelines are not optimally designed to reduce cervical cancer risk in women >65 years of age?
The American College of Obstetricians and Gynecologists (ACOG) and the US Preventive Services Task Force (USPSTF) recommend against cervical cancer screening in women >65 years of age who have had adequate prior screening and are not otherwise at high risk for cervical cancer. However, ACOG and the USPSTF caution that there are many groups of women that may benefit from continued screening after 65 years of age, including women with HIV infection, a compromised immune system, or previous high-grade precancerous lesion or cervicalcancer; women with limited access to care; women from racial/ethnic minority groups; and migrant women.4 Many clinicians remember the guidance, “discontinue cervical cancer screening at 65 years” but do not recall all the clinical factors that might warrant continued screening past age 65. Of special concern is that black,2 Hispanic,5 and migrant women6 are at much higher risk for invasive cervical cancer than white or US-born women.
The optimal implementation of the ACOG and USPSTF guidelines are undermined by a fractured health care system, where key pieces of information may be unavailable to the clinician tasked with making a decision about discontinuing cervical cancer screening. Imagine the case in which a 65-year-old woman pre‑sents to her primary care physician for cervical cancer screening. The clinician performs a cervical cytology test and obtains a report of “no intraepithelial lesion or malignancy.” The clinician then recommends that the patient discontinue cervical cancer screening. Unbeknownst to the clinician, the patient had a positive HPV 16/18/45 test within the past 10 years in another health system. In this case, it would be inappropriate to terminate the patient from cervical cancer screening.
Continue to: Testing for hrHPV is superior to cervical cytology in women >65 years...
Testing for hrHPV is superior to cervical cytology in women >65 years
In Sweden, about 30% of cervical cancer cases occur in women aged >60 years.7 To assess the prevalence of oncogenic high-risk HPV (hrHPV), women at ages 60, 65, 70, and 75 years were invited to send sequential self-collected vaginal samples for nucleic acid testing for hrHPV. The prevalence of hrHPV was found to be 4.4%. Women with a second positive, self-collected, hrHPV test were invited for colposcopy, cervical biopsy, and cytology testing. Among the women with two positive hrHPV tests, cervical biopsy revealed 7 cases of cervical intraepithelial neoplasia grade 2 (CIN2), 6 cases of CIN1, and 4 biopsies without CIN. In these women 94% of the cervical cytology samples returned, “no intraepithelial lesion or malignancy” and 6% revealed atypical squamous cells of undetermined significance. This study suggests that, in women aged >65 years, cervical cytology may have a high rate of false-negative results, possibly due to epithelial atrophy. An evolving clinical pearl is that, when using the current cervical cancer screening guidelines, the final screen for cervical cancer must include a nucleic acid test for hrHPV.
In women 65 to 90 years, the prevalence of hrHPV is approximately 5%
In a study of 40,382 women aged 14 to 95 years, the prevalence of hrHPV was 46% in 20- to 23-year-old women and 5.7% in women older than 65 years of age.8 In a study of more than 108,000 women aged 69 to >89 years the prevalence of hrHPV was 4.3%, and similar prevalence rates were seen across all ages from 69 to >89 years.9 The carcinogenic role of persistent hrHPV infection in women >65 years is an important area for future research.
Latent HPV virus infection
Following a primary varicella-zoster infection (chickenpox), the virus may remain in a latent state in sensory ganglia, reactivating later in life to cause shingles. Thirty percent of people who have a primary chickenpox infection eventually will develop a case of shingles. Immunocompromised populations are at an increased risk of developing shingles because of reduced T-cell mediated immunity.
A recent hypothesis is that in immunocompromised and older women, latent HPV can reactivate and cause clinically significant infection.10 Following renal transplantation investigators have reported a significant increase in the prevalence of genital HPV, without a change in sexual behavior.11 In cervical tissue from women with no evidence of active HPV infection, highly sensitive PCR-based assays detected HPV16 virus in a latent state in some women, possibly due to disruption of the viral E2 gene.12 If latent HPV infection is a valid biological concept, it suggests that there is no “safe age” at which to discontinue screening for HPV infection because the virus cannot be detected in screening samples while it is latent.
Options for cervical cancer screening in women >65 years
Three options might reduce the morbidity and mortality associated with cervical cancer in women >65 years.
Option 1: Double-down on trying to effectively implement current guidelines. The high rate of cervical cancer mortality in women >65 years of age indicates that the current guidelines, as implemented in real clinical practice, are not working. A problem with the current screening guidelines is that clinicians are expected to be capable of finding all relevant cervical cancer test results and properly interpreting the results. Clinicians are over-taxed and fallible, and the current approach is not likely to be successful unless additional information technology solutions are implemented.
Continue to: Health systems could use information...
Health systems could use information technology to mitigate these problems. For example, health systems could deploy software to assemble every cervical screening result on each woman and pre‑sent those results to clinicians in a single integrated view in the electronic record. Additionally, once all lifetime screening results are consolidated in one view, artificial intelligence systems could be used to analyze the totality of results and identify women who would benefit by continued screening past age 65 and women who could safely discontinue screening.
Option 2: Adopt the Australian approach to cervical cancer screening. The current Australian approach to cervical cancer screening is built on 3 pillars: 1) school-based vaccination of all children against hrHPV, 2) screening all women from 25 to 74 years of age every 5 years using nucleic acid testing for hrHPV, and 3) providing a system for the testing of samples self-collected by women who are reluctant to visit a clinician for screening.13 Australia has one of the lowest cervical cancer death rates in the world.
Option 3: Continue screening most women past age 65. Women >65 years of age are known to be infected with hrHPV genotypes. hrHPV infection causes cervical cancer. Cervical cancer causes many deaths in women aged >65 years. There is no strong rationale for ignoring these three facts. hrHPV screening every 5 years as long as the woman is healthy and has a reasonable life expectancy is an option that could be evaluated in randomized studies.
Given the high rate of cervical cancer death in women >65 years of age, I plan to be very cautious about discontinuing cervical cancer screening until I can personally ensure that my patient has no evidence of hrHPV infection.
In 2008, Harald zur Hausen, MD, received the Nobel Prize in Physiology or Medicine for discovering that human papilloma virus (HPV) caused cervical cancer. In a recent study, 74% of cervical cancers were associated with HPV 16 or 18 infections. A total of 89% of the cancers were associated with one of the high-risk HPV genotypes, including HPV 16/18/31/33/45/52/58.1
Recently, HPV has been shown to be a major cause of oropharyngeal cancer. The Centers for Disease Control and Prevention calculated that in CY2015 in the United States there were 18,917 cases of HPV-associated oropharyngeal squamous cell cancer and 11,788 cases of cervical cancer.2 Most cases of HPV-associated oropharyngeal cancer occur in men, and HPV vaccination of boys may help to prevent this cancer type. Oncogenic HPV produce two proteins (E6 and E7) that promote viral replication and squamous cell growth by inhibiting the function of p53 and retinoblastoma protein. The immortalized HeLa cell line, derived from Ms. Henrietta Lack's cervical cancer, contains integrated HPV18 nucleic acid sequences.3,4
The discovery that HPV causes cancer catalyzed the development of nucleic acid tests to identify high-risk oncogenic HPV and vaccines against high-risk oncogenic HPV genotypes that prevent cervical cancer. From a public health perspective, it is more effective to vaccinate the population against oncogenic HPV genotypes than to screen and treat cancer. In the United States, vaccination rates range from a high of 92% (District of Columbia) and 89% (Rhode Island) to a low of 47% (Wyoming) and 50% (Kentucky and Mississippi).5 To reduce HPV-associated cancer mortality, the gap in vaccination compliance must be closed.
References
- Kjaer SK, Munk C, Junge J, et al. Carcinogenic HPV prevalence and age-specific type distribution in 40,382 women with normal cervical cytology, ACSUC/LSIL, HSIL, or cervical cancer: what is the potential for prevention? Cancer Causes Control. 2014;25:179-189.
- Van Dyne EA, Henley SJ, Saraiya M, et al. Trends in human papillomavirus-associated cancers - United States, 1999-2015. MMWR Morb Mortal Wkly Rep. 2018;67:918-924.
- Rosl F, Westphal EM, zur Hausen H. Chromatin structure and transcriptional regulation of human papillomavirus type 18 DNA in HeLa cells. Mol Carcinog. 1989;2:72-80.
- Adey A, Burton JN, Kitzman, et al. The haplotype-resolved genome and epigenome of the aneuploid HeLa cancer cell line. Nature. 2013;500:207-211.
- Walker TY, Elam-Evans LD, Singleton JA, et al. National, regional, state, and selected local area vaccination coverage among adolescents aged 13-17 years - United States, 2016. MMWR Morb Mortal Wkly Rep. 2017;66:874-882.
- Hammer A, Kahlert J, Gravitt PE, et al. Hysterectomy-corrected cervical cancer mortality rates in Denmark during 2002-2015: a registry-based cohort study. Acta Obstet Gynecol Scand. 2019;98:1063-1069.
- Beavis AL, Gravitt PE, Rositch AF. Hysterectomy-corrected cervical cancer mortality rates reveal a larger racial disparity in the United States. Cancer. 2017;123:1044-1050.
- American College of Obstetricians and Gynecologists Committee on Practice Bulletins--Gynecology. Practice Bulletin No. 168: cervical cancer screening and prevention. Obstet Gynecol. 2016;128:e111-30.
- Curry SJ, Krist AH, Owens DK, et al; US Preventive Services Task Force. Screening for cervical cancer: US Preventive Services Task Force recommendation statement. JAMA. 2018;320:674-686.
- Stang A, Hawk H, Knowlton R, et al. Hysterectomy-corrected incidence rates of cervical and uterine cancers in Massachusetts, 1995-2010. Ann Epidemiol. 2014;24:849-854.
- Hallowell BD, Endeshaw M, McKenna MT, et al. Cervical cancer death rates among U.S.- and foreign-born women: U.S., 2005-2014. Am J Prev Med. 2019;56:869-874.
- Lindström AK, Hermansson RS, Gustavsson I, et al. Cervical dysplasia in elderly women performing repeated self-sampling for HPV testing. PLoS One. 2018;13:e0207714.
- Kjaer SK, Munk C, Junge J, et al. Carcinogenic HPV prevalence and age-specific type distribution in 40,382 women with normal cervical cytology, ACSUC/LSIL, HSIL, or cervical cancer: what is the potential for prevention? Cancer Causes Control. 2014;25:179-189.
- Andersen B, Christensen BS, Christensen J, et al. HPV-prevalence in elderly women in Denmark. Gynecol Oncol. 2019;154:118-123.
- Gravitt PE, Winer RL. Natural history of HPV infection across the lifespan: role of viral latency. Viruses. 2017;9:E267.
- Hinten F, Hilbrands LB, Meeuwis KAP, et al. Reactivation of latent HPV infections after renal transplantation. Am J Transplant. 2017;17:1563-1573.
- Leonard SM, Pereira M, Roberts S, et al. Evidence of disrupted high-risk human papillomavirus DNA in morphologically normal cervices of older women. Sci Rep. 2016;6:20847.
- Cervical cancer screening. Cancer Council website. https://www.cancer.org.au/about-cancer/early-detection/screening-programs/cervical-cancer-screening.html. Updated March 15, 2019. Accessed July 23, 2019.
- Hammer A, Kahlert J, Gravitt PE, et al. Hysterectomy-corrected cervical cancer mortality rates in Denmark during 2002-2015: a registry-based cohort study. Acta Obstet Gynecol Scand. 2019;98:1063-1069.
- Beavis AL, Gravitt PE, Rositch AF. Hysterectomy-corrected cervical cancer mortality rates reveal a larger racial disparity in the United States. Cancer. 2017;123:1044-1050.
- American College of Obstetricians and Gynecologists Committee on Practice Bulletins--Gynecology. Practice Bulletin No. 168: cervical cancer screening and prevention. Obstet Gynecol. 2016;128:e111-30.
- Curry SJ, Krist AH, Owens DK, et al; US Preventive Services Task Force. Screening for cervical cancer: US Preventive Services Task Force recommendation statement. JAMA. 2018;320:674-686.
- Stang A, Hawk H, Knowlton R, et al. Hysterectomy-corrected incidence rates of cervical and uterine cancers in Massachusetts, 1995-2010. Ann Epidemiol. 2014;24:849-854.
- Hallowell BD, Endeshaw M, McKenna MT, et al. Cervical cancer death rates among U.S.- and foreign-born women: U.S., 2005-2014. Am J Prev Med. 2019;56:869-874.
- Lindström AK, Hermansson RS, Gustavsson I, et al. Cervical dysplasia in elderly women performing repeated self-sampling for HPV testing. PLoS One. 2018;13:e0207714.
- Kjaer SK, Munk C, Junge J, et al. Carcinogenic HPV prevalence and age-specific type distribution in 40,382 women with normal cervical cytology, ACSUC/LSIL, HSIL, or cervical cancer: what is the potential for prevention? Cancer Causes Control. 2014;25:179-189.
- Andersen B, Christensen BS, Christensen J, et al. HPV-prevalence in elderly women in Denmark. Gynecol Oncol. 2019;154:118-123.
- Gravitt PE, Winer RL. Natural history of HPV infection across the lifespan: role of viral latency. Viruses. 2017;9:E267.
- Hinten F, Hilbrands LB, Meeuwis KAP, et al. Reactivation of latent HPV infections after renal transplantation. Am J Transplant. 2017;17:1563-1573.
- Leonard SM, Pereira M, Roberts S, et al. Evidence of disrupted high-risk human papillomavirus DNA in morphologically normal cervices of older women. Sci Rep. 2016;6:20847.
- Cervical cancer screening. Cancer Council website. https://www.cancer.org.au/about-cancer/early-detection/screening-programs/cervical-cancer-screening.html. Updated March 15, 2019. Accessed July 23, 2019.
Technology, counseling, and CBT apps for primary care
There is probably no area where human contact is more important than in the area of counseling and psychotherapy. Or so most of us have thought. It turns out that, even in behavioral medicine, technology has made fantastic inroads in helping patients achieve real improvement in troublesome behavioral symptoms. We will not go over that evidence in this column, other than to say that the evidence is there, but rather we will review some of the best apps that those of us in primary care can utilize in the care of our patients. It is our opinion that these apps are best used in conjunction with our care to supplement the counseling we are giving our patients in the office. Many of the apps listed may be used for both anxiety and depression, as well as in areas related to problem solving, self-esteem, anger management, creating lifestyle changes, and coping with uncertainty.
MoodKit
MoodKit is a CBT app with four main tools: a collection of activities focused on coping self-efficacy (a person’s belief in success in specific situations) that includes individual productivity, social relationships, physical activity, and healthy habits; a thought checker; mood tracker; and journal. MoodKit is accessed in an unstructured way and can be used as an unguided self-help app. It is useful in patient interactions to access interventions in areas such as social engagement and options for choosing a healthy lifestyle. It is available in Apple’s App Store, and it costs $4.99.
Moodnotes
Based on CBT and positive psychology, Moodnotes assists in recognizing and learning about “traps” in thinking, as well as emphasizing healthier thinking habits. Traps in thinking include “catastrophic thinking” where patients with depression may think that a small error or behavioral indiscretion may lead to a consequence that far exceeds what is likely, or “mind-reading” where a person assumes that others are critical of them without actually having evidence that this is the case. Moodnotes tracks mood over a period of time while identifying factors that influence it. It is helpful in between visits to aid clinicians in gaining perspective on mood patterns. It is available in the App Store; it costs $4.99.
MoodMission
This app recommends strategies based in CBT after input of low moods or feelings of anxiety. MoodMission provides five “missions” to engage in that promote confidence in handling stressors and promotes coping self-efficacy. The app learns what style works best and tailors techniques according to when a patient uses it most frequently. Rewards in the app are used to promote motivation and to increase pleasure and self-confidence. It is useful for patients who could use a lift in mood or decrease in symptoms of anxiety and depression. It available in the App Store and Google Play, and it’s free.
What’s Up
In line with its development based on principles from CBT and Acceptance and Commitment Therapy (ACT), What’s Up identifies common negative thinking patterns and methods to overcome them with useful metaphors, a catastrophe scale, grounding techniques, and breathing exercises. What’s Up syncs data across multiple devices and uses a unique passcode to protect this information. One of the abilities that separates it from other apps is that it can become active in forums where people discuss similar feelings and strategies that have been useful for them. It is available in the App Store and Google Play, and it’s free.
Moodpath
Moodpath uses daily screenings to create better understanding of thoughts, feelings, and emotions. If needed, it provides a discussion guide to talking with a medical professional based on answers to its daily screenings. Included in the app are over 150 psychological exercises and videos to promote and strengthen overall mental health. It is useful in introducing how to discuss mental health with a professional. It is available in the App Store and Google Play free of cost.
MindShift CBT
Designed to assist youth and young adults in coping with anxiety, MindShift constructs an individualized toolbox to help individuals deal with test anxiety, perfectionism, social anxiety, worry, panic, and conflict. The app includes directions on how to construct “belief experiments” to test common beliefs that fuel anxiety, guided relaxation, as well as tools and tips to help set and accomplish goals. It is useful in helping teens and young adults learn about helpful and unhelpful anxiety, as well as to overcome fears by gradually facing them in manageable steps. It is available in the App Store and Google Play for free.
CBT-i Coach
CBT-i Coach, based on principles of cognitive behavioral therapy for insomnia (CBT-i), is a structured program to learn about sleep, develop positive sleep routines, and improve sleep environment. The CBT methods used attempt to change behaviors, which in turn provides confidence that patients will sleep better on a regular basis. It useful as a first-line intervention in treating symptoms of insomnia. It is available in the App Store and Google Play for no cost.
Getselfhelp.co.uk
This website provides free self-help and therapy resources grounded in methods that teach the change agents in CBT that can influence negative and destructive thought patterns. Negative thought patterns include thinking in terms of all or nothing: “Nothing ever works out for me,” fortune telling: “I shouldn’t even try,” and overgeneralization: “This didn’t work so this will not either.” Getselfhelp.co.uk provides handouts on a wide array of symptoms related to anxiety, depression, low self-esteem, panic attacks, social disorder, and more. The solution section of the website supplies interventions that can be printed and saved for future use. It is helpful for clinicians and patients in identifying an area of need and creating an action plan. It is also useful for clinicians to have as an augmented supplement for counseling and is free of cost.
The bottom line
When used correctly the resources that we have reviewed can essentially be deployed in a manner similar to how we use finger-stick blood sugar monitoring in the treatment of diabetes. Each of these technologies works best when combined with clinician input and periodic review. When used to supplement clinician counseling, the apps may help sustain motivation and provide insights and exercises that improve patient engagement and supplement the effect of counseling and/or medications that are prescribed in the office.
Dr. Skolnik is professor of family and community medicine at Jefferson Medical College, Philadelphia, and an associate director of the family medicine residency program at Abington (Pa.) Jefferson Health. Aaron Sutton is a behavioral health consultant and faculty member in the family medicine residency program at Abington Jefferson Health.
There is probably no area where human contact is more important than in the area of counseling and psychotherapy. Or so most of us have thought. It turns out that, even in behavioral medicine, technology has made fantastic inroads in helping patients achieve real improvement in troublesome behavioral symptoms. We will not go over that evidence in this column, other than to say that the evidence is there, but rather we will review some of the best apps that those of us in primary care can utilize in the care of our patients. It is our opinion that these apps are best used in conjunction with our care to supplement the counseling we are giving our patients in the office. Many of the apps listed may be used for both anxiety and depression, as well as in areas related to problem solving, self-esteem, anger management, creating lifestyle changes, and coping with uncertainty.
MoodKit
MoodKit is a CBT app with four main tools: a collection of activities focused on coping self-efficacy (a person’s belief in success in specific situations) that includes individual productivity, social relationships, physical activity, and healthy habits; a thought checker; mood tracker; and journal. MoodKit is accessed in an unstructured way and can be used as an unguided self-help app. It is useful in patient interactions to access interventions in areas such as social engagement and options for choosing a healthy lifestyle. It is available in Apple’s App Store, and it costs $4.99.
Moodnotes
Based on CBT and positive psychology, Moodnotes assists in recognizing and learning about “traps” in thinking, as well as emphasizing healthier thinking habits. Traps in thinking include “catastrophic thinking” where patients with depression may think that a small error or behavioral indiscretion may lead to a consequence that far exceeds what is likely, or “mind-reading” where a person assumes that others are critical of them without actually having evidence that this is the case. Moodnotes tracks mood over a period of time while identifying factors that influence it. It is helpful in between visits to aid clinicians in gaining perspective on mood patterns. It is available in the App Store; it costs $4.99.
MoodMission
This app recommends strategies based in CBT after input of low moods or feelings of anxiety. MoodMission provides five “missions” to engage in that promote confidence in handling stressors and promotes coping self-efficacy. The app learns what style works best and tailors techniques according to when a patient uses it most frequently. Rewards in the app are used to promote motivation and to increase pleasure and self-confidence. It is useful for patients who could use a lift in mood or decrease in symptoms of anxiety and depression. It available in the App Store and Google Play, and it’s free.
What’s Up
In line with its development based on principles from CBT and Acceptance and Commitment Therapy (ACT), What’s Up identifies common negative thinking patterns and methods to overcome them with useful metaphors, a catastrophe scale, grounding techniques, and breathing exercises. What’s Up syncs data across multiple devices and uses a unique passcode to protect this information. One of the abilities that separates it from other apps is that it can become active in forums where people discuss similar feelings and strategies that have been useful for them. It is available in the App Store and Google Play, and it’s free.
Moodpath
Moodpath uses daily screenings to create better understanding of thoughts, feelings, and emotions. If needed, it provides a discussion guide to talking with a medical professional based on answers to its daily screenings. Included in the app are over 150 psychological exercises and videos to promote and strengthen overall mental health. It is useful in introducing how to discuss mental health with a professional. It is available in the App Store and Google Play free of cost.
MindShift CBT
Designed to assist youth and young adults in coping with anxiety, MindShift constructs an individualized toolbox to help individuals deal with test anxiety, perfectionism, social anxiety, worry, panic, and conflict. The app includes directions on how to construct “belief experiments” to test common beliefs that fuel anxiety, guided relaxation, as well as tools and tips to help set and accomplish goals. It is useful in helping teens and young adults learn about helpful and unhelpful anxiety, as well as to overcome fears by gradually facing them in manageable steps. It is available in the App Store and Google Play for free.
CBT-i Coach
CBT-i Coach, based on principles of cognitive behavioral therapy for insomnia (CBT-i), is a structured program to learn about sleep, develop positive sleep routines, and improve sleep environment. The CBT methods used attempt to change behaviors, which in turn provides confidence that patients will sleep better on a regular basis. It useful as a first-line intervention in treating symptoms of insomnia. It is available in the App Store and Google Play for no cost.
Getselfhelp.co.uk
This website provides free self-help and therapy resources grounded in methods that teach the change agents in CBT that can influence negative and destructive thought patterns. Negative thought patterns include thinking in terms of all or nothing: “Nothing ever works out for me,” fortune telling: “I shouldn’t even try,” and overgeneralization: “This didn’t work so this will not either.” Getselfhelp.co.uk provides handouts on a wide array of symptoms related to anxiety, depression, low self-esteem, panic attacks, social disorder, and more. The solution section of the website supplies interventions that can be printed and saved for future use. It is helpful for clinicians and patients in identifying an area of need and creating an action plan. It is also useful for clinicians to have as an augmented supplement for counseling and is free of cost.
The bottom line
When used correctly the resources that we have reviewed can essentially be deployed in a manner similar to how we use finger-stick blood sugar monitoring in the treatment of diabetes. Each of these technologies works best when combined with clinician input and periodic review. When used to supplement clinician counseling, the apps may help sustain motivation and provide insights and exercises that improve patient engagement and supplement the effect of counseling and/or medications that are prescribed in the office.
Dr. Skolnik is professor of family and community medicine at Jefferson Medical College, Philadelphia, and an associate director of the family medicine residency program at Abington (Pa.) Jefferson Health. Aaron Sutton is a behavioral health consultant and faculty member in the family medicine residency program at Abington Jefferson Health.
There is probably no area where human contact is more important than in the area of counseling and psychotherapy. Or so most of us have thought. It turns out that, even in behavioral medicine, technology has made fantastic inroads in helping patients achieve real improvement in troublesome behavioral symptoms. We will not go over that evidence in this column, other than to say that the evidence is there, but rather we will review some of the best apps that those of us in primary care can utilize in the care of our patients. It is our opinion that these apps are best used in conjunction with our care to supplement the counseling we are giving our patients in the office. Many of the apps listed may be used for both anxiety and depression, as well as in areas related to problem solving, self-esteem, anger management, creating lifestyle changes, and coping with uncertainty.
MoodKit
MoodKit is a CBT app with four main tools: a collection of activities focused on coping self-efficacy (a person’s belief in success in specific situations) that includes individual productivity, social relationships, physical activity, and healthy habits; a thought checker; mood tracker; and journal. MoodKit is accessed in an unstructured way and can be used as an unguided self-help app. It is useful in patient interactions to access interventions in areas such as social engagement and options for choosing a healthy lifestyle. It is available in Apple’s App Store, and it costs $4.99.
Moodnotes
Based on CBT and positive psychology, Moodnotes assists in recognizing and learning about “traps” in thinking, as well as emphasizing healthier thinking habits. Traps in thinking include “catastrophic thinking” where patients with depression may think that a small error or behavioral indiscretion may lead to a consequence that far exceeds what is likely, or “mind-reading” where a person assumes that others are critical of them without actually having evidence that this is the case. Moodnotes tracks mood over a period of time while identifying factors that influence it. It is helpful in between visits to aid clinicians in gaining perspective on mood patterns. It is available in the App Store; it costs $4.99.
MoodMission
This app recommends strategies based in CBT after input of low moods or feelings of anxiety. MoodMission provides five “missions” to engage in that promote confidence in handling stressors and promotes coping self-efficacy. The app learns what style works best and tailors techniques according to when a patient uses it most frequently. Rewards in the app are used to promote motivation and to increase pleasure and self-confidence. It is useful for patients who could use a lift in mood or decrease in symptoms of anxiety and depression. It available in the App Store and Google Play, and it’s free.
What’s Up
In line with its development based on principles from CBT and Acceptance and Commitment Therapy (ACT), What’s Up identifies common negative thinking patterns and methods to overcome them with useful metaphors, a catastrophe scale, grounding techniques, and breathing exercises. What’s Up syncs data across multiple devices and uses a unique passcode to protect this information. One of the abilities that separates it from other apps is that it can become active in forums where people discuss similar feelings and strategies that have been useful for them. It is available in the App Store and Google Play, and it’s free.
Moodpath
Moodpath uses daily screenings to create better understanding of thoughts, feelings, and emotions. If needed, it provides a discussion guide to talking with a medical professional based on answers to its daily screenings. Included in the app are over 150 psychological exercises and videos to promote and strengthen overall mental health. It is useful in introducing how to discuss mental health with a professional. It is available in the App Store and Google Play free of cost.
MindShift CBT
Designed to assist youth and young adults in coping with anxiety, MindShift constructs an individualized toolbox to help individuals deal with test anxiety, perfectionism, social anxiety, worry, panic, and conflict. The app includes directions on how to construct “belief experiments” to test common beliefs that fuel anxiety, guided relaxation, as well as tools and tips to help set and accomplish goals. It is useful in helping teens and young adults learn about helpful and unhelpful anxiety, as well as to overcome fears by gradually facing them in manageable steps. It is available in the App Store and Google Play for free.
CBT-i Coach
CBT-i Coach, based on principles of cognitive behavioral therapy for insomnia (CBT-i), is a structured program to learn about sleep, develop positive sleep routines, and improve sleep environment. The CBT methods used attempt to change behaviors, which in turn provides confidence that patients will sleep better on a regular basis. It useful as a first-line intervention in treating symptoms of insomnia. It is available in the App Store and Google Play for no cost.
Getselfhelp.co.uk
This website provides free self-help and therapy resources grounded in methods that teach the change agents in CBT that can influence negative and destructive thought patterns. Negative thought patterns include thinking in terms of all or nothing: “Nothing ever works out for me,” fortune telling: “I shouldn’t even try,” and overgeneralization: “This didn’t work so this will not either.” Getselfhelp.co.uk provides handouts on a wide array of symptoms related to anxiety, depression, low self-esteem, panic attacks, social disorder, and more. The solution section of the website supplies interventions that can be printed and saved for future use. It is helpful for clinicians and patients in identifying an area of need and creating an action plan. It is also useful for clinicians to have as an augmented supplement for counseling and is free of cost.
The bottom line
When used correctly the resources that we have reviewed can essentially be deployed in a manner similar to how we use finger-stick blood sugar monitoring in the treatment of diabetes. Each of these technologies works best when combined with clinician input and periodic review. When used to supplement clinician counseling, the apps may help sustain motivation and provide insights and exercises that improve patient engagement and supplement the effect of counseling and/or medications that are prescribed in the office.
Dr. Skolnik is professor of family and community medicine at Jefferson Medical College, Philadelphia, and an associate director of the family medicine residency program at Abington (Pa.) Jefferson Health. Aaron Sutton is a behavioral health consultant and faculty member in the family medicine residency program at Abington Jefferson Health.
Primary care: Practice meets technology
Technology has infiltrated all parts of our everyday lives, including healthcare. Patients can make and cancel appointments, send e-mails directly to their physician, and request prescription refills—all through electronic portals. Physicians and healthcare providers must adjust to these changes in care-delivery models. Primary care providers must also adapt as younger generations seek access for their health needs outside of the doctor’s office.
And so it is with everyday life. Online banking and bill-paying is common. Groceries can be bought online and delivered within an hour. Connecting with family or friends around the world can be done with the touch of a button. In the United States, 90% of adults own a cell phone; many do not have a land line. More than 65% of adult Americans under age 75 own a smart phone, and 50% of the public owns a tablet computer.1
DRIVERS OF CHANGE: THE MILLENNIALS
The development and use of new technology is driven by the coming of age of the youngest adult population, ie, “Generation Y” or millennials, ie, persons born between 1981 and 1996.2 They now account for 28% of the US adult population, surpassing the baby boomers (born 1946 to 1964) by 8 million.3
Millennials have grown up with the World Wide Web at their fingertips. They are accustomed to an environment full of choices and unlimited, instantly available information.4
Millennials are cost-conscious shoppers who desire convenience and quick access. As patients, they often forgo traditional doctor’s office visits, turning instead to the Internet for quick answers to their questions in blogs and websites.5 A Kaiser Family Foundation survey in 2018 indicated that only a quarter of millennials see a primary care physician for healthcare needs.6
The shortage of primary care physicians
There are several reasons for this. Primary care physicians are in short supply, more Americans have insurance after the passage of the Affordable Care Act, and more physicians are working part-time or retiring earlier than in previous generations. There will be a continued shortfall of 15,000 to 49,000 full-time-equivalent primary care physicians by 2030.7 A survey of 15 large metropolitan markets found that the average wait time for a primary care new patient appointment increased to 24.1 days—a 30% increase from 2014. In some cities, the wait time can be 3 to 4 months.8
Older patients of the baby-boomer generation tend to discuss medical issues with their primary care physician, often relying on their feedback to improve their health lifestyle choices.9 Baby boomers who are Medicare subscribers tend to see their regular doctor at least once or twice a year10; trust is built with this continuity in care.
The rise of pharmacy clinics
But the shortage of primary care physicians and the desire of younger patients for immediate access to care have fueled the growth of new options for access, such as retail clinics in large pharmacies. These clinics are mostly found in the South and Midwest and are staffed by nurse practitioners,11 and 90% of their billing falls under 10 common diagnoses, including urinary tract and upper respiratory infections. More than 40% of patients seeking care at retail pharmacy clinics are 18 to 44 years of age, and less than 25% of this group have a primary care provider.11 These clinics have shorter wait times and limited out-of-pocket costs, and they are more convenient. In a study of adults visiting these clinics for vaccination, 30% did so during evening, weekend, and holiday hours, when traditional doctors’ offices are closed.12
Telemedicine’s foothold
Telemedicine has also taken a foothold in healthcare. Initially used for episodic illnesses, there is now growing acceptance of telemedicine for management of chronic physical and mental health problems. Accessibility to a doctor via a mobile device while at home has proven to be helpful to young, elderly, and minority patients living in rural areas,13 although reimbursement and legal issues continue to constrain its growth.14 Telemedicine is predicted to grow by nearly 15% from now to 2025, especially in North America and Europe, where technology has kept pace and government initiatives are encouraging its advancement.15
The American College of Physicians has published recommendations on how best to use telemedicine, especially when there is already an established patient-physician relationship. Telemedicine can bridge the divide for those who lack access to care because of geographic constraints or who cannot afford a regular doctor’s office appointment.16 It can also allow healthcare “extenders” like social workers, nutritionists, pharmacists, and nurses to work collaboratively with the primary care physician to improve patient education and outcomes.17
Wearable devices
The wearable device market continues to expand, in large part due to the increased availability and utilization of mobile technology. These gadgets can record steps, sleep, and heart rate. Consumer fitness trackers can give patients insight into their activity levels and encourage them to modify their behavior, ie, get up and move around more.17 The Deloitte Center for Health Solutions survey in 2018 showed that 62% of millennials use consumer fitness trackers to help meet their wellness goals, compared with 16% of seniors and 25% of baby boomers.18 There are few studies showing that these devices improve overall health promotion or decrease healthcare costs,17,19 but research is ongoing.
And the “generation gap” in technology’s uptake is slowly closing: 81% of American adults own a smartphone, and the rate in people over age 50 increased from 53% in 2015 to 67% in 2018.20 By comparison, 92% of millennials own a smartphone.1
Smartphone apps
A 2015 survey of more than 1,600 US adults found that 58% had downloaded an application to their smartphone to track their health needs, with 41% using more than 5 health-related apps; the most commonly downloaded apps tracked physical activity, food intake, exercise programs or weight loss progress.21
Users of mobile health apps are generally younger and more highly educated than nonusers.22 However, baby boomers are willing to try mobile health apps if the apps are intuitive, accessible, and effective; this is important, especially since this group accounts for more than 20% of US healthcare expenditures.23 Engaging and empowering baby boomers to use this technology may allow them to remain independent, live healthier, and avoid unnecessary office visits, thus decreasing strain on the limited healthcare workforce.23
ADAPTING TO THE GENERATIONAL SHIFT
Physicians and physician educators should be aware of this generational shift. Millennial-aged doctors will continue to embrace technology to achieve their work-life balance in order to avoid burnout and maintain robust primary care practices whether in the office or outside of it.
Medical school curricula
Medical schools need to adjust their curricula to prepare the next generation of physicians to engage with these new healthcare delivery models and technology. Practicing telemedicine, assessing mobile app safety and utility, and effectively integrating data from patient-specific devices represent a new skill set that is considerably different from the typical face-to-face encounters learners experience today.
Recognizing this, more than 50% of medical schools have added telemedicine and digital health to the curriculum,24 with suggestions to include telemedicine-related content in the Accreditation Council for Graduate Medical Education core competencies.25
Improving the electronic medical record
Maximizing the efficiency of electronic medical records will also be important because physicians currently spend more than 50% of their workday on documentation and administrative tasks; for every 1 hour of patient contact, physicians spend 2 hours in front of the electronic medical record.26 End-users (doctors, nurses, pharmacists, scribes) should interact or engage with developers of electronic medical record systems to promote platforms that enhance workflow, increase connectivity to mobile apps, foster team collaboration, and provide consistency in patient safety and privacy.27
Early and continuous education on use of the electronic medical record should be routine, as proficiency improves work-life balance, physician job satisfaction, and patient care by reducing after-hours note completion and in-box tasks leading to burnout.28
Technology-enabled primary care
Technology-enabled healthcare is here to stay and will continue to evolve, incorporating telehealth, smartphones, mobile apps, in-home and wearable devices, and online video communication.17 Clinicians will need to be adept at working with these technologies to advance quality care in population health. It will require clinician training and professional development, advances in technology, and revised reimbursement policies.17 But despite the increased use of mobile apps, there remain concerns about the possible dangers associated with their use, including breaches in confidentiality, conflicts of interest, and lack of professional medical involvement and evidence in their design.29
THE IMPORTANCE OF BEING SAVVY
There is a growing need for primary care providers to be technologically savvy and readily accessible via e-mail, healthcare portals, or in the office to keep up with the generational shifts and expectations occurring in this decade. Healthcare systems should have the right infrastructure in place, including efficient Web platforms to support telemedicine or to synchronize digital tracking devices, as well as a trained workforce to understand and implement these revolutionary changes into everyday practice. Educators will need to provide training in these changing platforms to medical students and residents. Primary care will evolve to redefine its role within the context of these emerging technologies17 and to adjust to these market demands in order to stay relevant.
- Jiang J. Millennials stand out for their technology use, but older generations also embrace digital life. Pew Research Center. www.pewresearch.org/fact-tank/2018/05/02/millennials-stand-out-for-their-technology-use-but-older-generations-also-embrace-digital-life. Accessed April 2, 2019.
- Dimock, M. Defining generations: Where Millennials end and post-Millennials begin. Pew Research Center. www.pewresearch.org/fact-tank/2019/01/17/where-millennials-end-and-generation-z-begins. Accessed April 2, 2019.
- The Generation Gap in American Politics. Pew Research Center. www.people-press.org/2018/03/01/the-generation-gap-in-american-politics. Accessed April 2, 2019.
- Hopkins L, Hampton BS, Abbott, JF, et al. To the point: medical education, technology and the millennial learner. Am J Obstet Gynecol 2018; 218(2):188–192. doi:10.1016/j.ajog.2017.06.001
- DuPuis R. Courting the impatient patient: providers must embrace millennial’s health care expectations. Central Penn Business Journal. www.cpbj.com/courting-the-impatient-patient-providers-must-embrace-millennials-health-care-expectations. Accessed April 2, 2019.
- Boodman SG. Spurred by convenience, Millennials often spurn the “family doctor” model. Kaiser Health News. khn.org/news/spurred-by-convenience-millennials-often-spurn-the-family-doctor-model. Accessed April 2, 2019.
- Association of American Medical Colleges. 2018 update: the complexities of physician supply and demand: projections from 2016 to 2030. aamc-black.global.ssl.fastly.net/production/media/filer_public/31/13/3113ee5c-a038-4c16-89af-294a69826650/2019_update_-_the_complexities_of_physician_supply_and_demand_-_projections_from_2017-2032.pdf. Accessed April 2, 2019.
- Merritt Hawkins. 2017 Survey of physician appointment wait times and Medicare and Medicaid acceptance rates. www.merritthawkins.com/uploadedFiles/MerrittHawkins/Content/Pdf/mha2017waittimesurveyPDF.pdf. Accessed April 2, 2019.
- SSRN. Employee Benefit Research Institute. Consumer engagement in health care among Millennials, Baby Boomers, and Generation X: findings from the 2017 Consumer Engagement in Health Care Survey. papers.ssrn.com/sol3/papers.cfm?abstract_id=3160059. Accessed April 2, 2019.
- Centers for Disease Control and Prevention (CDC). Summary health statistics: national health interview survey, 2016, Table A–18c. ftp.cdc.gov/pub/Health_Statistics/NCHS/NHIS/SHS/2016_SHS_Table_A-18.pdf. Accessed April 2, 2019.
- Rand Corporation. The evolving role of retail clinics. www.rand.org/content/dam/rand/pubs/research_briefs/RB9400/RB9491-2/RAND_RB9491-2.pdf. Accessed April 2, 2019.
- Goad JA, Taitel MS, Fensterheim LE, Cannon, AE. Vaccinations administered during off-clinic hours at a national community pharmacy: implications for increasing patient access and convenience. Ann Fam Med 2013; 11(5):429–436. doi:10.1370/afm.1542
- Hansen MR, Okuda DT. Multiple sclerosis in the contemporary age: understanding the Millennial patient with multiple sclerosis to create next-generation care, Neurol Clin 2018; 36(1):219–230. doi:10.1016/j.ncl.2017.08.012
- Dorsey ER, Topol EJ. State of telehealth. N Engl J Med 2016; 375(2):154–161. doi:10.1056/NEJMra1601705
- Landi, H. Report: telehealth market estimated to reach $19.5B by 2025. Healthcare Informatics. www.healthcare-informatics.com/news-item/telemedicine/report-telehealth-market-estimated-reach-195b-2025. Accessed April 2, 2019.
- Daniel H, Sulmasy LS; Health and Public Policy Committee of the American College of Physicians. Policy recommendations to guide the use of telemedicine in primary care settings: an American College of Physicians position paper. Ann Intern Med 2015; 163(10):787–789. doi:10.7326/M15-0498
- Young HM, Nesbitt TS. Increasing the capacity of primary care through enabling technology. J Gen Intern Med 2017; 32(4):398–403. doi:10.1007/s11606-016-3952-3
- Abrams K, Korba C. Consumers are on board with virtual health options. Deloitte Insights, www2.deloitte.com/insights/us/en/industry/health-care/virtual-health-care-consumer-experience-survey.html. Accessed April 2, 2019.
- Coughlin SS, Stewart J. Use of consumer wearable devices to promote physical activity: a review of health intervention studies. J Environ Health Sci 2016; 2(6). doi:10.15436/2378-6841.16.1123
- Taylor K, Silver L. Smartphone ownership is growing rapidly around the world but not always equally. Pew Research Center. www.pewglobal.org/2019/02/05/smartphone-ownership-is-growing-rapidly-around-the-world-but-not-always-equally. Accessed April 2, 2019.
- Krebs P, Duncan DT. Health app use among us mobile phone owners: a national survey. JMIR Mhealth Uhealth 2015; 3(4):e101. doi:10.2196/mhealth.4924
- Carroll JK, Moorhead A, Bond R, LeBlanc WG, Petrella RJ, Fiscella K. Who uses mobile health apps and does use matter? A secondary data analytics approach. J Med Internet Res 2017; 19(4):e125. doi:10.2196/jmir.5604
- Kruse CS, Mileski M, Moreno J. Mobile health solutions for the aging population: a systematic narrative analysis. J Telemed Telecare 2017; 23(4):439–451. doi:10.1177/1357633X16649790
- Warshaw R. From bedside to webside: future doctors learn to practice remotely. AAMC News. news.aamc.org/medical-education/article/future-doctors-learn-practice-remotely. Accessed April 2, 2019.
- DeJong C, Lucey CR, Dudley RA. Incorporating a new technology while doing no harm, virtually. JAMA 2015; 314(22):2351–2352. doi:10.1001/jama.2015.13572
- Sinsky C, Colligan L, Li L, Prgomet M, Reynolds S, et al. Allocation of physician time in ambulatory practice: a time and motion study in 4 specialties. Ann Intern Med 2016; 165(11):753–760. doi:10.7326/M16-0961
- Kim MS. Improving electronic health records training through usability evaluation in primary care. J Health and Med Informat 2013; 4(5) e110. doi:10.4172/2157-7420.1000e110
- Robertson SL, Robinson MD, Reid A. Electronic health record effects on work-life balance and burnout within the i3 population collaborative. J Grad Med Educ 2017; 9(4):479–484. doi:10.4300/JGME-D-16-00123.1
- Buijink AW, Visser BJ, Marshall L. Medical apps for smartphones: lack of evidence undermines quality and safety. Evid Based Med 2013; 18(3):90–92. doi:10.1136/eb-2012-100885
Technology has infiltrated all parts of our everyday lives, including healthcare. Patients can make and cancel appointments, send e-mails directly to their physician, and request prescription refills—all through electronic portals. Physicians and healthcare providers must adjust to these changes in care-delivery models. Primary care providers must also adapt as younger generations seek access for their health needs outside of the doctor’s office.
And so it is with everyday life. Online banking and bill-paying is common. Groceries can be bought online and delivered within an hour. Connecting with family or friends around the world can be done with the touch of a button. In the United States, 90% of adults own a cell phone; many do not have a land line. More than 65% of adult Americans under age 75 own a smart phone, and 50% of the public owns a tablet computer.1
DRIVERS OF CHANGE: THE MILLENNIALS
The development and use of new technology is driven by the coming of age of the youngest adult population, ie, “Generation Y” or millennials, ie, persons born between 1981 and 1996.2 They now account for 28% of the US adult population, surpassing the baby boomers (born 1946 to 1964) by 8 million.3
Millennials have grown up with the World Wide Web at their fingertips. They are accustomed to an environment full of choices and unlimited, instantly available information.4
Millennials are cost-conscious shoppers who desire convenience and quick access. As patients, they often forgo traditional doctor’s office visits, turning instead to the Internet for quick answers to their questions in blogs and websites.5 A Kaiser Family Foundation survey in 2018 indicated that only a quarter of millennials see a primary care physician for healthcare needs.6
The shortage of primary care physicians
There are several reasons for this. Primary care physicians are in short supply, more Americans have insurance after the passage of the Affordable Care Act, and more physicians are working part-time or retiring earlier than in previous generations. There will be a continued shortfall of 15,000 to 49,000 full-time-equivalent primary care physicians by 2030.7 A survey of 15 large metropolitan markets found that the average wait time for a primary care new patient appointment increased to 24.1 days—a 30% increase from 2014. In some cities, the wait time can be 3 to 4 months.8
Older patients of the baby-boomer generation tend to discuss medical issues with their primary care physician, often relying on their feedback to improve their health lifestyle choices.9 Baby boomers who are Medicare subscribers tend to see their regular doctor at least once or twice a year10; trust is built with this continuity in care.
The rise of pharmacy clinics
But the shortage of primary care physicians and the desire of younger patients for immediate access to care have fueled the growth of new options for access, such as retail clinics in large pharmacies. These clinics are mostly found in the South and Midwest and are staffed by nurse practitioners,11 and 90% of their billing falls under 10 common diagnoses, including urinary tract and upper respiratory infections. More than 40% of patients seeking care at retail pharmacy clinics are 18 to 44 years of age, and less than 25% of this group have a primary care provider.11 These clinics have shorter wait times and limited out-of-pocket costs, and they are more convenient. In a study of adults visiting these clinics for vaccination, 30% did so during evening, weekend, and holiday hours, when traditional doctors’ offices are closed.12
Telemedicine’s foothold
Telemedicine has also taken a foothold in healthcare. Initially used for episodic illnesses, there is now growing acceptance of telemedicine for management of chronic physical and mental health problems. Accessibility to a doctor via a mobile device while at home has proven to be helpful to young, elderly, and minority patients living in rural areas,13 although reimbursement and legal issues continue to constrain its growth.14 Telemedicine is predicted to grow by nearly 15% from now to 2025, especially in North America and Europe, where technology has kept pace and government initiatives are encouraging its advancement.15
The American College of Physicians has published recommendations on how best to use telemedicine, especially when there is already an established patient-physician relationship. Telemedicine can bridge the divide for those who lack access to care because of geographic constraints or who cannot afford a regular doctor’s office appointment.16 It can also allow healthcare “extenders” like social workers, nutritionists, pharmacists, and nurses to work collaboratively with the primary care physician to improve patient education and outcomes.17
Wearable devices
The wearable device market continues to expand, in large part due to the increased availability and utilization of mobile technology. These gadgets can record steps, sleep, and heart rate. Consumer fitness trackers can give patients insight into their activity levels and encourage them to modify their behavior, ie, get up and move around more.17 The Deloitte Center for Health Solutions survey in 2018 showed that 62% of millennials use consumer fitness trackers to help meet their wellness goals, compared with 16% of seniors and 25% of baby boomers.18 There are few studies showing that these devices improve overall health promotion or decrease healthcare costs,17,19 but research is ongoing.
And the “generation gap” in technology’s uptake is slowly closing: 81% of American adults own a smartphone, and the rate in people over age 50 increased from 53% in 2015 to 67% in 2018.20 By comparison, 92% of millennials own a smartphone.1
Smartphone apps
A 2015 survey of more than 1,600 US adults found that 58% had downloaded an application to their smartphone to track their health needs, with 41% using more than 5 health-related apps; the most commonly downloaded apps tracked physical activity, food intake, exercise programs or weight loss progress.21
Users of mobile health apps are generally younger and more highly educated than nonusers.22 However, baby boomers are willing to try mobile health apps if the apps are intuitive, accessible, and effective; this is important, especially since this group accounts for more than 20% of US healthcare expenditures.23 Engaging and empowering baby boomers to use this technology may allow them to remain independent, live healthier, and avoid unnecessary office visits, thus decreasing strain on the limited healthcare workforce.23
ADAPTING TO THE GENERATIONAL SHIFT
Physicians and physician educators should be aware of this generational shift. Millennial-aged doctors will continue to embrace technology to achieve their work-life balance in order to avoid burnout and maintain robust primary care practices whether in the office or outside of it.
Medical school curricula
Medical schools need to adjust their curricula to prepare the next generation of physicians to engage with these new healthcare delivery models and technology. Practicing telemedicine, assessing mobile app safety and utility, and effectively integrating data from patient-specific devices represent a new skill set that is considerably different from the typical face-to-face encounters learners experience today.
Recognizing this, more than 50% of medical schools have added telemedicine and digital health to the curriculum,24 with suggestions to include telemedicine-related content in the Accreditation Council for Graduate Medical Education core competencies.25
Improving the electronic medical record
Maximizing the efficiency of electronic medical records will also be important because physicians currently spend more than 50% of their workday on documentation and administrative tasks; for every 1 hour of patient contact, physicians spend 2 hours in front of the electronic medical record.26 End-users (doctors, nurses, pharmacists, scribes) should interact or engage with developers of electronic medical record systems to promote platforms that enhance workflow, increase connectivity to mobile apps, foster team collaboration, and provide consistency in patient safety and privacy.27
Early and continuous education on use of the electronic medical record should be routine, as proficiency improves work-life balance, physician job satisfaction, and patient care by reducing after-hours note completion and in-box tasks leading to burnout.28
Technology-enabled primary care
Technology-enabled healthcare is here to stay and will continue to evolve, incorporating telehealth, smartphones, mobile apps, in-home and wearable devices, and online video communication.17 Clinicians will need to be adept at working with these technologies to advance quality care in population health. It will require clinician training and professional development, advances in technology, and revised reimbursement policies.17 But despite the increased use of mobile apps, there remain concerns about the possible dangers associated with their use, including breaches in confidentiality, conflicts of interest, and lack of professional medical involvement and evidence in their design.29
THE IMPORTANCE OF BEING SAVVY
There is a growing need for primary care providers to be technologically savvy and readily accessible via e-mail, healthcare portals, or in the office to keep up with the generational shifts and expectations occurring in this decade. Healthcare systems should have the right infrastructure in place, including efficient Web platforms to support telemedicine or to synchronize digital tracking devices, as well as a trained workforce to understand and implement these revolutionary changes into everyday practice. Educators will need to provide training in these changing platforms to medical students and residents. Primary care will evolve to redefine its role within the context of these emerging technologies17 and to adjust to these market demands in order to stay relevant.
Technology has infiltrated all parts of our everyday lives, including healthcare. Patients can make and cancel appointments, send e-mails directly to their physician, and request prescription refills—all through electronic portals. Physicians and healthcare providers must adjust to these changes in care-delivery models. Primary care providers must also adapt as younger generations seek access for their health needs outside of the doctor’s office.
And so it is with everyday life. Online banking and bill-paying is common. Groceries can be bought online and delivered within an hour. Connecting with family or friends around the world can be done with the touch of a button. In the United States, 90% of adults own a cell phone; many do not have a land line. More than 65% of adult Americans under age 75 own a smart phone, and 50% of the public owns a tablet computer.1
DRIVERS OF CHANGE: THE MILLENNIALS
The development and use of new technology is driven by the coming of age of the youngest adult population, ie, “Generation Y” or millennials, ie, persons born between 1981 and 1996.2 They now account for 28% of the US adult population, surpassing the baby boomers (born 1946 to 1964) by 8 million.3
Millennials have grown up with the World Wide Web at their fingertips. They are accustomed to an environment full of choices and unlimited, instantly available information.4
Millennials are cost-conscious shoppers who desire convenience and quick access. As patients, they often forgo traditional doctor’s office visits, turning instead to the Internet for quick answers to their questions in blogs and websites.5 A Kaiser Family Foundation survey in 2018 indicated that only a quarter of millennials see a primary care physician for healthcare needs.6
The shortage of primary care physicians
There are several reasons for this. Primary care physicians are in short supply, more Americans have insurance after the passage of the Affordable Care Act, and more physicians are working part-time or retiring earlier than in previous generations. There will be a continued shortfall of 15,000 to 49,000 full-time-equivalent primary care physicians by 2030.7 A survey of 15 large metropolitan markets found that the average wait time for a primary care new patient appointment increased to 24.1 days—a 30% increase from 2014. In some cities, the wait time can be 3 to 4 months.8
Older patients of the baby-boomer generation tend to discuss medical issues with their primary care physician, often relying on their feedback to improve their health lifestyle choices.9 Baby boomers who are Medicare subscribers tend to see their regular doctor at least once or twice a year10; trust is built with this continuity in care.
The rise of pharmacy clinics
But the shortage of primary care physicians and the desire of younger patients for immediate access to care have fueled the growth of new options for access, such as retail clinics in large pharmacies. These clinics are mostly found in the South and Midwest and are staffed by nurse practitioners,11 and 90% of their billing falls under 10 common diagnoses, including urinary tract and upper respiratory infections. More than 40% of patients seeking care at retail pharmacy clinics are 18 to 44 years of age, and less than 25% of this group have a primary care provider.11 These clinics have shorter wait times and limited out-of-pocket costs, and they are more convenient. In a study of adults visiting these clinics for vaccination, 30% did so during evening, weekend, and holiday hours, when traditional doctors’ offices are closed.12
Telemedicine’s foothold
Telemedicine has also taken a foothold in healthcare. Initially used for episodic illnesses, there is now growing acceptance of telemedicine for management of chronic physical and mental health problems. Accessibility to a doctor via a mobile device while at home has proven to be helpful to young, elderly, and minority patients living in rural areas,13 although reimbursement and legal issues continue to constrain its growth.14 Telemedicine is predicted to grow by nearly 15% from now to 2025, especially in North America and Europe, where technology has kept pace and government initiatives are encouraging its advancement.15
The American College of Physicians has published recommendations on how best to use telemedicine, especially when there is already an established patient-physician relationship. Telemedicine can bridge the divide for those who lack access to care because of geographic constraints or who cannot afford a regular doctor’s office appointment.16 It can also allow healthcare “extenders” like social workers, nutritionists, pharmacists, and nurses to work collaboratively with the primary care physician to improve patient education and outcomes.17
Wearable devices
The wearable device market continues to expand, in large part due to the increased availability and utilization of mobile technology. These gadgets can record steps, sleep, and heart rate. Consumer fitness trackers can give patients insight into their activity levels and encourage them to modify their behavior, ie, get up and move around more.17 The Deloitte Center for Health Solutions survey in 2018 showed that 62% of millennials use consumer fitness trackers to help meet their wellness goals, compared with 16% of seniors and 25% of baby boomers.18 There are few studies showing that these devices improve overall health promotion or decrease healthcare costs,17,19 but research is ongoing.
And the “generation gap” in technology’s uptake is slowly closing: 81% of American adults own a smartphone, and the rate in people over age 50 increased from 53% in 2015 to 67% in 2018.20 By comparison, 92% of millennials own a smartphone.1
Smartphone apps
A 2015 survey of more than 1,600 US adults found that 58% had downloaded an application to their smartphone to track their health needs, with 41% using more than 5 health-related apps; the most commonly downloaded apps tracked physical activity, food intake, exercise programs or weight loss progress.21
Users of mobile health apps are generally younger and more highly educated than nonusers.22 However, baby boomers are willing to try mobile health apps if the apps are intuitive, accessible, and effective; this is important, especially since this group accounts for more than 20% of US healthcare expenditures.23 Engaging and empowering baby boomers to use this technology may allow them to remain independent, live healthier, and avoid unnecessary office visits, thus decreasing strain on the limited healthcare workforce.23
ADAPTING TO THE GENERATIONAL SHIFT
Physicians and physician educators should be aware of this generational shift. Millennial-aged doctors will continue to embrace technology to achieve their work-life balance in order to avoid burnout and maintain robust primary care practices whether in the office or outside of it.
Medical school curricula
Medical schools need to adjust their curricula to prepare the next generation of physicians to engage with these new healthcare delivery models and technology. Practicing telemedicine, assessing mobile app safety and utility, and effectively integrating data from patient-specific devices represent a new skill set that is considerably different from the typical face-to-face encounters learners experience today.
Recognizing this, more than 50% of medical schools have added telemedicine and digital health to the curriculum,24 with suggestions to include telemedicine-related content in the Accreditation Council for Graduate Medical Education core competencies.25
Improving the electronic medical record
Maximizing the efficiency of electronic medical records will also be important because physicians currently spend more than 50% of their workday on documentation and administrative tasks; for every 1 hour of patient contact, physicians spend 2 hours in front of the electronic medical record.26 End-users (doctors, nurses, pharmacists, scribes) should interact or engage with developers of electronic medical record systems to promote platforms that enhance workflow, increase connectivity to mobile apps, foster team collaboration, and provide consistency in patient safety and privacy.27
Early and continuous education on use of the electronic medical record should be routine, as proficiency improves work-life balance, physician job satisfaction, and patient care by reducing after-hours note completion and in-box tasks leading to burnout.28
Technology-enabled primary care
Technology-enabled healthcare is here to stay and will continue to evolve, incorporating telehealth, smartphones, mobile apps, in-home and wearable devices, and online video communication.17 Clinicians will need to be adept at working with these technologies to advance quality care in population health. It will require clinician training and professional development, advances in technology, and revised reimbursement policies.17 But despite the increased use of mobile apps, there remain concerns about the possible dangers associated with their use, including breaches in confidentiality, conflicts of interest, and lack of professional medical involvement and evidence in their design.29
THE IMPORTANCE OF BEING SAVVY
There is a growing need for primary care providers to be technologically savvy and readily accessible via e-mail, healthcare portals, or in the office to keep up with the generational shifts and expectations occurring in this decade. Healthcare systems should have the right infrastructure in place, including efficient Web platforms to support telemedicine or to synchronize digital tracking devices, as well as a trained workforce to understand and implement these revolutionary changes into everyday practice. Educators will need to provide training in these changing platforms to medical students and residents. Primary care will evolve to redefine its role within the context of these emerging technologies17 and to adjust to these market demands in order to stay relevant.
- Jiang J. Millennials stand out for their technology use, but older generations also embrace digital life. Pew Research Center. www.pewresearch.org/fact-tank/2018/05/02/millennials-stand-out-for-their-technology-use-but-older-generations-also-embrace-digital-life. Accessed April 2, 2019.
- Dimock, M. Defining generations: Where Millennials end and post-Millennials begin. Pew Research Center. www.pewresearch.org/fact-tank/2019/01/17/where-millennials-end-and-generation-z-begins. Accessed April 2, 2019.
- The Generation Gap in American Politics. Pew Research Center. www.people-press.org/2018/03/01/the-generation-gap-in-american-politics. Accessed April 2, 2019.
- Hopkins L, Hampton BS, Abbott, JF, et al. To the point: medical education, technology and the millennial learner. Am J Obstet Gynecol 2018; 218(2):188–192. doi:10.1016/j.ajog.2017.06.001
- DuPuis R. Courting the impatient patient: providers must embrace millennial’s health care expectations. Central Penn Business Journal. www.cpbj.com/courting-the-impatient-patient-providers-must-embrace-millennials-health-care-expectations. Accessed April 2, 2019.
- Boodman SG. Spurred by convenience, Millennials often spurn the “family doctor” model. Kaiser Health News. khn.org/news/spurred-by-convenience-millennials-often-spurn-the-family-doctor-model. Accessed April 2, 2019.
- Association of American Medical Colleges. 2018 update: the complexities of physician supply and demand: projections from 2016 to 2030. aamc-black.global.ssl.fastly.net/production/media/filer_public/31/13/3113ee5c-a038-4c16-89af-294a69826650/2019_update_-_the_complexities_of_physician_supply_and_demand_-_projections_from_2017-2032.pdf. Accessed April 2, 2019.
- Merritt Hawkins. 2017 Survey of physician appointment wait times and Medicare and Medicaid acceptance rates. www.merritthawkins.com/uploadedFiles/MerrittHawkins/Content/Pdf/mha2017waittimesurveyPDF.pdf. Accessed April 2, 2019.
- SSRN. Employee Benefit Research Institute. Consumer engagement in health care among Millennials, Baby Boomers, and Generation X: findings from the 2017 Consumer Engagement in Health Care Survey. papers.ssrn.com/sol3/papers.cfm?abstract_id=3160059. Accessed April 2, 2019.
- Centers for Disease Control and Prevention (CDC). Summary health statistics: national health interview survey, 2016, Table A–18c. ftp.cdc.gov/pub/Health_Statistics/NCHS/NHIS/SHS/2016_SHS_Table_A-18.pdf. Accessed April 2, 2019.
- Rand Corporation. The evolving role of retail clinics. www.rand.org/content/dam/rand/pubs/research_briefs/RB9400/RB9491-2/RAND_RB9491-2.pdf. Accessed April 2, 2019.
- Goad JA, Taitel MS, Fensterheim LE, Cannon, AE. Vaccinations administered during off-clinic hours at a national community pharmacy: implications for increasing patient access and convenience. Ann Fam Med 2013; 11(5):429–436. doi:10.1370/afm.1542
- Hansen MR, Okuda DT. Multiple sclerosis in the contemporary age: understanding the Millennial patient with multiple sclerosis to create next-generation care, Neurol Clin 2018; 36(1):219–230. doi:10.1016/j.ncl.2017.08.012
- Dorsey ER, Topol EJ. State of telehealth. N Engl J Med 2016; 375(2):154–161. doi:10.1056/NEJMra1601705
- Landi, H. Report: telehealth market estimated to reach $19.5B by 2025. Healthcare Informatics. www.healthcare-informatics.com/news-item/telemedicine/report-telehealth-market-estimated-reach-195b-2025. Accessed April 2, 2019.
- Daniel H, Sulmasy LS; Health and Public Policy Committee of the American College of Physicians. Policy recommendations to guide the use of telemedicine in primary care settings: an American College of Physicians position paper. Ann Intern Med 2015; 163(10):787–789. doi:10.7326/M15-0498
- Young HM, Nesbitt TS. Increasing the capacity of primary care through enabling technology. J Gen Intern Med 2017; 32(4):398–403. doi:10.1007/s11606-016-3952-3
- Abrams K, Korba C. Consumers are on board with virtual health options. Deloitte Insights, www2.deloitte.com/insights/us/en/industry/health-care/virtual-health-care-consumer-experience-survey.html. Accessed April 2, 2019.
- Coughlin SS, Stewart J. Use of consumer wearable devices to promote physical activity: a review of health intervention studies. J Environ Health Sci 2016; 2(6). doi:10.15436/2378-6841.16.1123
- Taylor K, Silver L. Smartphone ownership is growing rapidly around the world but not always equally. Pew Research Center. www.pewglobal.org/2019/02/05/smartphone-ownership-is-growing-rapidly-around-the-world-but-not-always-equally. Accessed April 2, 2019.
- Krebs P, Duncan DT. Health app use among us mobile phone owners: a national survey. JMIR Mhealth Uhealth 2015; 3(4):e101. doi:10.2196/mhealth.4924
- Carroll JK, Moorhead A, Bond R, LeBlanc WG, Petrella RJ, Fiscella K. Who uses mobile health apps and does use matter? A secondary data analytics approach. J Med Internet Res 2017; 19(4):e125. doi:10.2196/jmir.5604
- Kruse CS, Mileski M, Moreno J. Mobile health solutions for the aging population: a systematic narrative analysis. J Telemed Telecare 2017; 23(4):439–451. doi:10.1177/1357633X16649790
- Warshaw R. From bedside to webside: future doctors learn to practice remotely. AAMC News. news.aamc.org/medical-education/article/future-doctors-learn-practice-remotely. Accessed April 2, 2019.
- DeJong C, Lucey CR, Dudley RA. Incorporating a new technology while doing no harm, virtually. JAMA 2015; 314(22):2351–2352. doi:10.1001/jama.2015.13572
- Sinsky C, Colligan L, Li L, Prgomet M, Reynolds S, et al. Allocation of physician time in ambulatory practice: a time and motion study in 4 specialties. Ann Intern Med 2016; 165(11):753–760. doi:10.7326/M16-0961
- Kim MS. Improving electronic health records training through usability evaluation in primary care. J Health and Med Informat 2013; 4(5) e110. doi:10.4172/2157-7420.1000e110
- Robertson SL, Robinson MD, Reid A. Electronic health record effects on work-life balance and burnout within the i3 population collaborative. J Grad Med Educ 2017; 9(4):479–484. doi:10.4300/JGME-D-16-00123.1
- Buijink AW, Visser BJ, Marshall L. Medical apps for smartphones: lack of evidence undermines quality and safety. Evid Based Med 2013; 18(3):90–92. doi:10.1136/eb-2012-100885
- Jiang J. Millennials stand out for their technology use, but older generations also embrace digital life. Pew Research Center. www.pewresearch.org/fact-tank/2018/05/02/millennials-stand-out-for-their-technology-use-but-older-generations-also-embrace-digital-life. Accessed April 2, 2019.
- Dimock, M. Defining generations: Where Millennials end and post-Millennials begin. Pew Research Center. www.pewresearch.org/fact-tank/2019/01/17/where-millennials-end-and-generation-z-begins. Accessed April 2, 2019.
- The Generation Gap in American Politics. Pew Research Center. www.people-press.org/2018/03/01/the-generation-gap-in-american-politics. Accessed April 2, 2019.
- Hopkins L, Hampton BS, Abbott, JF, et al. To the point: medical education, technology and the millennial learner. Am J Obstet Gynecol 2018; 218(2):188–192. doi:10.1016/j.ajog.2017.06.001
- DuPuis R. Courting the impatient patient: providers must embrace millennial’s health care expectations. Central Penn Business Journal. www.cpbj.com/courting-the-impatient-patient-providers-must-embrace-millennials-health-care-expectations. Accessed April 2, 2019.
- Boodman SG. Spurred by convenience, Millennials often spurn the “family doctor” model. Kaiser Health News. khn.org/news/spurred-by-convenience-millennials-often-spurn-the-family-doctor-model. Accessed April 2, 2019.
- Association of American Medical Colleges. 2018 update: the complexities of physician supply and demand: projections from 2016 to 2030. aamc-black.global.ssl.fastly.net/production/media/filer_public/31/13/3113ee5c-a038-4c16-89af-294a69826650/2019_update_-_the_complexities_of_physician_supply_and_demand_-_projections_from_2017-2032.pdf. Accessed April 2, 2019.
- Merritt Hawkins. 2017 Survey of physician appointment wait times and Medicare and Medicaid acceptance rates. www.merritthawkins.com/uploadedFiles/MerrittHawkins/Content/Pdf/mha2017waittimesurveyPDF.pdf. Accessed April 2, 2019.
- SSRN. Employee Benefit Research Institute. Consumer engagement in health care among Millennials, Baby Boomers, and Generation X: findings from the 2017 Consumer Engagement in Health Care Survey. papers.ssrn.com/sol3/papers.cfm?abstract_id=3160059. Accessed April 2, 2019.
- Centers for Disease Control and Prevention (CDC). Summary health statistics: national health interview survey, 2016, Table A–18c. ftp.cdc.gov/pub/Health_Statistics/NCHS/NHIS/SHS/2016_SHS_Table_A-18.pdf. Accessed April 2, 2019.
- Rand Corporation. The evolving role of retail clinics. www.rand.org/content/dam/rand/pubs/research_briefs/RB9400/RB9491-2/RAND_RB9491-2.pdf. Accessed April 2, 2019.
- Goad JA, Taitel MS, Fensterheim LE, Cannon, AE. Vaccinations administered during off-clinic hours at a national community pharmacy: implications for increasing patient access and convenience. Ann Fam Med 2013; 11(5):429–436. doi:10.1370/afm.1542
- Hansen MR, Okuda DT. Multiple sclerosis in the contemporary age: understanding the Millennial patient with multiple sclerosis to create next-generation care, Neurol Clin 2018; 36(1):219–230. doi:10.1016/j.ncl.2017.08.012
- Dorsey ER, Topol EJ. State of telehealth. N Engl J Med 2016; 375(2):154–161. doi:10.1056/NEJMra1601705
- Landi, H. Report: telehealth market estimated to reach $19.5B by 2025. Healthcare Informatics. www.healthcare-informatics.com/news-item/telemedicine/report-telehealth-market-estimated-reach-195b-2025. Accessed April 2, 2019.
- Daniel H, Sulmasy LS; Health and Public Policy Committee of the American College of Physicians. Policy recommendations to guide the use of telemedicine in primary care settings: an American College of Physicians position paper. Ann Intern Med 2015; 163(10):787–789. doi:10.7326/M15-0498
- Young HM, Nesbitt TS. Increasing the capacity of primary care through enabling technology. J Gen Intern Med 2017; 32(4):398–403. doi:10.1007/s11606-016-3952-3
- Abrams K, Korba C. Consumers are on board with virtual health options. Deloitte Insights, www2.deloitte.com/insights/us/en/industry/health-care/virtual-health-care-consumer-experience-survey.html. Accessed April 2, 2019.
- Coughlin SS, Stewart J. Use of consumer wearable devices to promote physical activity: a review of health intervention studies. J Environ Health Sci 2016; 2(6). doi:10.15436/2378-6841.16.1123
- Taylor K, Silver L. Smartphone ownership is growing rapidly around the world but not always equally. Pew Research Center. www.pewglobal.org/2019/02/05/smartphone-ownership-is-growing-rapidly-around-the-world-but-not-always-equally. Accessed April 2, 2019.
- Krebs P, Duncan DT. Health app use among us mobile phone owners: a national survey. JMIR Mhealth Uhealth 2015; 3(4):e101. doi:10.2196/mhealth.4924
- Carroll JK, Moorhead A, Bond R, LeBlanc WG, Petrella RJ, Fiscella K. Who uses mobile health apps and does use matter? A secondary data analytics approach. J Med Internet Res 2017; 19(4):e125. doi:10.2196/jmir.5604
- Kruse CS, Mileski M, Moreno J. Mobile health solutions for the aging population: a systematic narrative analysis. J Telemed Telecare 2017; 23(4):439–451. doi:10.1177/1357633X16649790
- Warshaw R. From bedside to webside: future doctors learn to practice remotely. AAMC News. news.aamc.org/medical-education/article/future-doctors-learn-practice-remotely. Accessed April 2, 2019.
- DeJong C, Lucey CR, Dudley RA. Incorporating a new technology while doing no harm, virtually. JAMA 2015; 314(22):2351–2352. doi:10.1001/jama.2015.13572
- Sinsky C, Colligan L, Li L, Prgomet M, Reynolds S, et al. Allocation of physician time in ambulatory practice: a time and motion study in 4 specialties. Ann Intern Med 2016; 165(11):753–760. doi:10.7326/M16-0961
- Kim MS. Improving electronic health records training through usability evaluation in primary care. J Health and Med Informat 2013; 4(5) e110. doi:10.4172/2157-7420.1000e110
- Robertson SL, Robinson MD, Reid A. Electronic health record effects on work-life balance and burnout within the i3 population collaborative. J Grad Med Educ 2017; 9(4):479–484. doi:10.4300/JGME-D-16-00123.1
- Buijink AW, Visser BJ, Marshall L. Medical apps for smartphones: lack of evidence undermines quality and safety. Evid Based Med 2013; 18(3):90–92. doi:10.1136/eb-2012-100885
Beyond ‘selfies’: An epidemic of acquired narcissism
Narcissism has an evil reputation. But is it justified? A modicum of narcissism is actually healthy. It can bolster self-confidence, assertiveness, and success in business and in the sociobiology of mating. Perhaps that’s why narcissism as a trait has a survival value from an evolutionary perspective.
Taking an excessive number of “selfies” with a smartphone is probably the most common and relatively benign form of mild narcissism (and not in DSM-5, yet). Narcissistic personality disorder (NPD), with a prevalence of 1%, is on the extreme end of the narcissism continuum. It has become tainted with such an intensely negative halo that it has become a despised trait, an insult, and even a vile epithet, like a 4-letter word. But as psychiatrists and other mental health professionals, we clinically relate to patients with NPD as being afflicted with a serious neuropsychiatric disorder, not as despicable individuals. Many people outside the mental health profession abhor persons with NPD because of their gargantuan hubris, insufferable selfishness, self-aggrandizement, emotional abuse of others, and irremediable vanity. Narcissistic personality disorder deprives its sufferers of the prosocial capacity for empathy, which leads them to belittle others or treat competent individuals with disdain, never as equals. They also seem to be incapable of experiencing shame as they inflate their self-importance and megalomania at the expense of those they degrade. They cannot tolerate any success by others because it threatens to overshadow their own exaggerated achievements. They can be mercilessly harsh towards their underlings. They are incapable of fostering warm, long-term loving relationships, where bidirectional respect is essential. Their lives often are replete with brief, broken-up relationships because they emotionally, physically, or sexually abuse their intimate partners.
Primary NPD has been shown in twin studies to be highly genetic, and more strongly heritable than 17 other personality dimensions.1 It is also resistant to any effective psychotherapeutic, pharmacologic, or somatic treatments. This is particularly relevant given the proclivity of individuals with NPD to experience a crushing disappointment, commonly known as “narcissistic injury,” following a real or imagined failure. This could lead to a painful depression or an outburst of “narcissistic rage” directed at anyone perceived as undermining them, and may even lead to violent behavior.2
Apart from heritable narcissism, there is also another form of narcissism that can develop in some individuals following life events. That hazardous condition, known as “acquired narcissism,” is most often associated with achieving the coveted status of an exalted celebrity. At risk for this acquired personality affliction are famous actors, singers, movie directors, TV anchors, or politicians (although some politicians are natural-born narcissists, driven to seek the powers of public office), and less frequently physicians (perhaps because the practice of medicine is not done in front of spectators) or scientists (because research, no matter how momentous, rarely procures the glamour or public adulation of the entertainment industry). The ardent fans of those “celebs” shower them with such intense attention and adulation that it malignantly transforms previously “normal” individuals into narcissists who start believing they are indeed “very special” and superior to the rest of us mortals (especially as their earning power balloons into the millions after growing up with humble social or economic roots).
Social media has become a catalyst for acquired narcissism, with millions of followers on Twitter, Facebook, or YouTube. Cable TV also caters to politicians, some of whom morph into narcissists, intoxicated with their newfound eminence and stature among their partisan followers, and become genuinely convinced that they have supreme power or influence over the masses. They get carried away with their own exaggerated self-importance as oracles of the “truth,” regardless of how extreme their views may be. Celebrity, politics, social media, and cable TV have converged into a combustible mix, a crucible for acquired narcissism.
An interesting feature of acquired narcissism is “collective narcissism,” in which celebrities coalesce to consolidate their imagined superhuman attributes that go beyond the technical skills of their professions such as acting, singing, sports, or politics. Thus, entertainers or star athletes believe they can enunciate radical statements about contemporary social, political, or environmental issues (at both ends of the debate) as though their artistic success renders them wise arbiters of the truth. What complicates matters is their delirious fans, who revere and mimic whatever their idols say (and their fashion or their tattoos), which further intensifies the grandiosity and megalomania of acquired narcissism. Celebrity triggers mindless idolatry, fueling the narcissism of individuals who are blessed (or cursed?) with runaway personal success. Neuroscientists should conduct research into how the brain is neurobiologically altered by fame, but there are many more urgent questions that demand their attention. It would be important to know if it is reversible or enduring, even as fame inevitably dims.
Continue to: The pursuit of wealth and fame...
The pursuit of wealth and fame is widely prevalent and can be healthy if it is not all-consuming. But if achieved beyond the aspirer’s wildest dreams, he/she may reach an inflection point conducive to a pathologic degree of acquired narcissism. That’s what the French refer to as “les risques du métier” (ie, occupational hazard). I recall reading about celebrities who became enraged when a policeman “dared” to stop their car for some driving violation, confronting the officer with “Do you know who I am?” That question may be a clinical biomarker of acquired narcissism.
Interestingly, several years ago, when the American Psychiatry Association last revised the DSM—sometimes referred to as the “bible” of psychiatric nosology—it came close to dropping NPD from its listed disorders, but then reverted and kept it as one of the 275 diagnostic categories included in DSM-5.3 Had the NPD diagnosis been discarded, one wonders if the mythical god of narcissism would have suffered a transcendental “narcissistic injury”…
1. Livesley WJ, Jang KL, Jackson DN, et al. Genetic and environmental contributions to dimensions of personality disorder. Am J Psychiatry. 1993;150(12):1826-1831
2. Malmquist CP. Homicide: a psychiatric perspective. Washington, DC: American Psychiatric Publishing, Inc.; 2006:181-182.
3. Diagnostic and statistical manual of mental disorders, 5th ed. Washington, DC: American Psychiatric Association; 2013.
Narcissism has an evil reputation. But is it justified? A modicum of narcissism is actually healthy. It can bolster self-confidence, assertiveness, and success in business and in the sociobiology of mating. Perhaps that’s why narcissism as a trait has a survival value from an evolutionary perspective.
Taking an excessive number of “selfies” with a smartphone is probably the most common and relatively benign form of mild narcissism (and not in DSM-5, yet). Narcissistic personality disorder (NPD), with a prevalence of 1%, is on the extreme end of the narcissism continuum. It has become tainted with such an intensely negative halo that it has become a despised trait, an insult, and even a vile epithet, like a 4-letter word. But as psychiatrists and other mental health professionals, we clinically relate to patients with NPD as being afflicted with a serious neuropsychiatric disorder, not as despicable individuals. Many people outside the mental health profession abhor persons with NPD because of their gargantuan hubris, insufferable selfishness, self-aggrandizement, emotional abuse of others, and irremediable vanity. Narcissistic personality disorder deprives its sufferers of the prosocial capacity for empathy, which leads them to belittle others or treat competent individuals with disdain, never as equals. They also seem to be incapable of experiencing shame as they inflate their self-importance and megalomania at the expense of those they degrade. They cannot tolerate any success by others because it threatens to overshadow their own exaggerated achievements. They can be mercilessly harsh towards their underlings. They are incapable of fostering warm, long-term loving relationships, where bidirectional respect is essential. Their lives often are replete with brief, broken-up relationships because they emotionally, physically, or sexually abuse their intimate partners.
Primary NPD has been shown in twin studies to be highly genetic, and more strongly heritable than 17 other personality dimensions.1 It is also resistant to any effective psychotherapeutic, pharmacologic, or somatic treatments. This is particularly relevant given the proclivity of individuals with NPD to experience a crushing disappointment, commonly known as “narcissistic injury,” following a real or imagined failure. This could lead to a painful depression or an outburst of “narcissistic rage” directed at anyone perceived as undermining them, and may even lead to violent behavior.2
Apart from heritable narcissism, there is also another form of narcissism that can develop in some individuals following life events. That hazardous condition, known as “acquired narcissism,” is most often associated with achieving the coveted status of an exalted celebrity. At risk for this acquired personality affliction are famous actors, singers, movie directors, TV anchors, or politicians (although some politicians are natural-born narcissists, driven to seek the powers of public office), and less frequently physicians (perhaps because the practice of medicine is not done in front of spectators) or scientists (because research, no matter how momentous, rarely procures the glamour or public adulation of the entertainment industry). The ardent fans of those “celebs” shower them with such intense attention and adulation that it malignantly transforms previously “normal” individuals into narcissists who start believing they are indeed “very special” and superior to the rest of us mortals (especially as their earning power balloons into the millions after growing up with humble social or economic roots).
Social media has become a catalyst for acquired narcissism, with millions of followers on Twitter, Facebook, or YouTube. Cable TV also caters to politicians, some of whom morph into narcissists, intoxicated with their newfound eminence and stature among their partisan followers, and become genuinely convinced that they have supreme power or influence over the masses. They get carried away with their own exaggerated self-importance as oracles of the “truth,” regardless of how extreme their views may be. Celebrity, politics, social media, and cable TV have converged into a combustible mix, a crucible for acquired narcissism.
An interesting feature of acquired narcissism is “collective narcissism,” in which celebrities coalesce to consolidate their imagined superhuman attributes that go beyond the technical skills of their professions such as acting, singing, sports, or politics. Thus, entertainers or star athletes believe they can enunciate radical statements about contemporary social, political, or environmental issues (at both ends of the debate) as though their artistic success renders them wise arbiters of the truth. What complicates matters is their delirious fans, who revere and mimic whatever their idols say (and their fashion or their tattoos), which further intensifies the grandiosity and megalomania of acquired narcissism. Celebrity triggers mindless idolatry, fueling the narcissism of individuals who are blessed (or cursed?) with runaway personal success. Neuroscientists should conduct research into how the brain is neurobiologically altered by fame, but there are many more urgent questions that demand their attention. It would be important to know if it is reversible or enduring, even as fame inevitably dims.
Continue to: The pursuit of wealth and fame...
The pursuit of wealth and fame is widely prevalent and can be healthy if it is not all-consuming. But if achieved beyond the aspirer’s wildest dreams, he/she may reach an inflection point conducive to a pathologic degree of acquired narcissism. That’s what the French refer to as “les risques du métier” (ie, occupational hazard). I recall reading about celebrities who became enraged when a policeman “dared” to stop their car for some driving violation, confronting the officer with “Do you know who I am?” That question may be a clinical biomarker of acquired narcissism.
Interestingly, several years ago, when the American Psychiatry Association last revised the DSM—sometimes referred to as the “bible” of psychiatric nosology—it came close to dropping NPD from its listed disorders, but then reverted and kept it as one of the 275 diagnostic categories included in DSM-5.3 Had the NPD diagnosis been discarded, one wonders if the mythical god of narcissism would have suffered a transcendental “narcissistic injury”…
Narcissism has an evil reputation. But is it justified? A modicum of narcissism is actually healthy. It can bolster self-confidence, assertiveness, and success in business and in the sociobiology of mating. Perhaps that’s why narcissism as a trait has a survival value from an evolutionary perspective.
Taking an excessive number of “selfies” with a smartphone is probably the most common and relatively benign form of mild narcissism (and not in DSM-5, yet). Narcissistic personality disorder (NPD), with a prevalence of 1%, is on the extreme end of the narcissism continuum. It has become tainted with such an intensely negative halo that it has become a despised trait, an insult, and even a vile epithet, like a 4-letter word. But as psychiatrists and other mental health professionals, we clinically relate to patients with NPD as being afflicted with a serious neuropsychiatric disorder, not as despicable individuals. Many people outside the mental health profession abhor persons with NPD because of their gargantuan hubris, insufferable selfishness, self-aggrandizement, emotional abuse of others, and irremediable vanity. Narcissistic personality disorder deprives its sufferers of the prosocial capacity for empathy, which leads them to belittle others or treat competent individuals with disdain, never as equals. They also seem to be incapable of experiencing shame as they inflate their self-importance and megalomania at the expense of those they degrade. They cannot tolerate any success by others because it threatens to overshadow their own exaggerated achievements. They can be mercilessly harsh towards their underlings. They are incapable of fostering warm, long-term loving relationships, where bidirectional respect is essential. Their lives often are replete with brief, broken-up relationships because they emotionally, physically, or sexually abuse their intimate partners.
Primary NPD has been shown in twin studies to be highly genetic, and more strongly heritable than 17 other personality dimensions.1 It is also resistant to any effective psychotherapeutic, pharmacologic, or somatic treatments. This is particularly relevant given the proclivity of individuals with NPD to experience a crushing disappointment, commonly known as “narcissistic injury,” following a real or imagined failure. This could lead to a painful depression or an outburst of “narcissistic rage” directed at anyone perceived as undermining them, and may even lead to violent behavior.2
Apart from heritable narcissism, there is also another form of narcissism that can develop in some individuals following life events. That hazardous condition, known as “acquired narcissism,” is most often associated with achieving the coveted status of an exalted celebrity. At risk for this acquired personality affliction are famous actors, singers, movie directors, TV anchors, or politicians (although some politicians are natural-born narcissists, driven to seek the powers of public office), and less frequently physicians (perhaps because the practice of medicine is not done in front of spectators) or scientists (because research, no matter how momentous, rarely procures the glamour or public adulation of the entertainment industry). The ardent fans of those “celebs” shower them with such intense attention and adulation that it malignantly transforms previously “normal” individuals into narcissists who start believing they are indeed “very special” and superior to the rest of us mortals (especially as their earning power balloons into the millions after growing up with humble social or economic roots).
Social media has become a catalyst for acquired narcissism, with millions of followers on Twitter, Facebook, or YouTube. Cable TV also caters to politicians, some of whom morph into narcissists, intoxicated with their newfound eminence and stature among their partisan followers, and become genuinely convinced that they have supreme power or influence over the masses. They get carried away with their own exaggerated self-importance as oracles of the “truth,” regardless of how extreme their views may be. Celebrity, politics, social media, and cable TV have converged into a combustible mix, a crucible for acquired narcissism.
An interesting feature of acquired narcissism is “collective narcissism,” in which celebrities coalesce to consolidate their imagined superhuman attributes that go beyond the technical skills of their professions such as acting, singing, sports, or politics. Thus, entertainers or star athletes believe they can enunciate radical statements about contemporary social, political, or environmental issues (at both ends of the debate) as though their artistic success renders them wise arbiters of the truth. What complicates matters is their delirious fans, who revere and mimic whatever their idols say (and their fashion or their tattoos), which further intensifies the grandiosity and megalomania of acquired narcissism. Celebrity triggers mindless idolatry, fueling the narcissism of individuals who are blessed (or cursed?) with runaway personal success. Neuroscientists should conduct research into how the brain is neurobiologically altered by fame, but there are many more urgent questions that demand their attention. It would be important to know if it is reversible or enduring, even as fame inevitably dims.
Continue to: The pursuit of wealth and fame...
The pursuit of wealth and fame is widely prevalent and can be healthy if it is not all-consuming. But if achieved beyond the aspirer’s wildest dreams, he/she may reach an inflection point conducive to a pathologic degree of acquired narcissism. That’s what the French refer to as “les risques du métier” (ie, occupational hazard). I recall reading about celebrities who became enraged when a policeman “dared” to stop their car for some driving violation, confronting the officer with “Do you know who I am?” That question may be a clinical biomarker of acquired narcissism.
Interestingly, several years ago, when the American Psychiatry Association last revised the DSM—sometimes referred to as the “bible” of psychiatric nosology—it came close to dropping NPD from its listed disorders, but then reverted and kept it as one of the 275 diagnostic categories included in DSM-5.3 Had the NPD diagnosis been discarded, one wonders if the mythical god of narcissism would have suffered a transcendental “narcissistic injury”…
1. Livesley WJ, Jang KL, Jackson DN, et al. Genetic and environmental contributions to dimensions of personality disorder. Am J Psychiatry. 1993;150(12):1826-1831
2. Malmquist CP. Homicide: a psychiatric perspective. Washington, DC: American Psychiatric Publishing, Inc.; 2006:181-182.
3. Diagnostic and statistical manual of mental disorders, 5th ed. Washington, DC: American Psychiatric Association; 2013.
1. Livesley WJ, Jang KL, Jackson DN, et al. Genetic and environmental contributions to dimensions of personality disorder. Am J Psychiatry. 1993;150(12):1826-1831
2. Malmquist CP. Homicide: a psychiatric perspective. Washington, DC: American Psychiatric Publishing, Inc.; 2006:181-182.
3. Diagnostic and statistical manual of mental disorders, 5th ed. Washington, DC: American Psychiatric Association; 2013.
Backlash against using rating scales
I strongly disagree with the editorial by Ahmed A. Aboraya, MD, DrPH, and Henry A. Nasrallah, MD, (“It’s time to implement measurement-based care in psychiatric practice,” From the Editor,
We do not have much more to lose before it’s a checklist, vital signs, and a script. I now refer to our profession as “McMedicine.” If you don’t have what is on the menu, you cannot get served. Diseases are rarely treated, symptoms are treated. This is not the profession of medicine. We are not fixing much; we are mostly providing consumers for pharmaceutical companies.
Few psychiatric disorders have been subjected to more measurement than depression. Quite a while ago, someone tried to compare depression scales. They correlated scale scores with the results of evaluations by board-certified psychiatrists. The best scale was a single question: “Are you depressed?” This had been included as a control. Can you do better?
Furthermore, the “paper and numbers” people can’t wait to get an “objective” wrench to tighten the screws and apply the principles of the industrial revolution to squeeze more money out of the system. They will find some way to turn patients into standardized products.
John L. Schenkel, MD
Retired psychiatrist
Peru, NY
With the use of an electronic medical record, what should be a simple 1-page note is transformed into a 5-page note of details. Doctors no longer attend to their patients but rather to their computers. Has this raised consciousness—the most important metric, according to Dr. David Hawkins? I doubt it.
In the words of my great professor, Dr. James Gustafson, I will continue to start my interview with what concerns the patient. Most of the time, they implicitly know.
Our focus should instead be on bringing down the cost of health care. This is what angers our patients most, and yet we do not make it a priority.
Psychiatrist
Glenbeigh Hospital
Rock Creek, Ohio
Signature Health
Ashtabula, Ohio
Behavioral Wellness Group
Mentor, Ohio
Continue to: The authors respond
The authors respond
We appreciate Drs. Schenkel’s and Primc’s comments on our editorial regarding measurement-based care (MBC). However, MBC will not increase the workload of psychiatrists; rather, it will streamline the evaluation of patients and measure the severity of their symptoms or adverse effects as well as the degree of their improvement. The proper use of scales with the appropriate patient populations may actually help clinicians to reduce the extensive amount of details that go into medical records.
The following quote, an excerpt from another article we wrote on MBC,1 speaks to Dr. Primc’s concerns:
“…measures in psychiatry could be considered the equivalent of a thermometer and a stethoscope to a physician.
Ahmed A. Aboraya, MD, DrPH
Assistant Professor
Department of Behavioral Medicine and Psychiatry
Chief of Psychiatry
Sharpe Hospital West Virginia University
Weston, West Virginia
Henry A. Nasrallah, MD
Professor of Psychiatry, Neurology, and Neuroscience
Medical Director: Neuropsychiatry
Director, Schizophrenia and Neuropsychiatry Programs
University of Cincinnati College of Medicine
Cincinnati, Ohio
Professor Emeritus, Saint Louis University
St. Louis, Missouri
Reference
1. Aboraya A, Nasrallah HA, Elswick DE, et al. Measurement-based care in psychiatry-past, present, and future. Innov Clin Neurosci. 2018;15(11-12):13-26.
I strongly disagree with the editorial by Ahmed A. Aboraya, MD, DrPH, and Henry A. Nasrallah, MD, (“It’s time to implement measurement-based care in psychiatric practice,” From the Editor,
We do not have much more to lose before it’s a checklist, vital signs, and a script. I now refer to our profession as “McMedicine.” If you don’t have what is on the menu, you cannot get served. Diseases are rarely treated, symptoms are treated. This is not the profession of medicine. We are not fixing much; we are mostly providing consumers for pharmaceutical companies.
Few psychiatric disorders have been subjected to more measurement than depression. Quite a while ago, someone tried to compare depression scales. They correlated scale scores with the results of evaluations by board-certified psychiatrists. The best scale was a single question: “Are you depressed?” This had been included as a control. Can you do better?
Furthermore, the “paper and numbers” people can’t wait to get an “objective” wrench to tighten the screws and apply the principles of the industrial revolution to squeeze more money out of the system. They will find some way to turn patients into standardized products.
John L. Schenkel, MD
Retired psychiatrist
Peru, NY
With the use of an electronic medical record, what should be a simple 1-page note is transformed into a 5-page note of details. Doctors no longer attend to their patients but rather to their computers. Has this raised consciousness—the most important metric, according to Dr. David Hawkins? I doubt it.
In the words of my great professor, Dr. James Gustafson, I will continue to start my interview with what concerns the patient. Most of the time, they implicitly know.
Our focus should instead be on bringing down the cost of health care. This is what angers our patients most, and yet we do not make it a priority.
Psychiatrist
Glenbeigh Hospital
Rock Creek, Ohio
Signature Health
Ashtabula, Ohio
Behavioral Wellness Group
Mentor, Ohio
Continue to: The authors respond
The authors respond
We appreciate Drs. Schenkel’s and Primc’s comments on our editorial regarding measurement-based care (MBC). However, MBC will not increase the workload of psychiatrists; rather, it will streamline the evaluation of patients and measure the severity of their symptoms or adverse effects as well as the degree of their improvement. The proper use of scales with the appropriate patient populations may actually help clinicians to reduce the extensive amount of details that go into medical records.
The following quote, an excerpt from another article we wrote on MBC,1 speaks to Dr. Primc’s concerns:
“…measures in psychiatry could be considered the equivalent of a thermometer and a stethoscope to a physician.
Ahmed A. Aboraya, MD, DrPH
Assistant Professor
Department of Behavioral Medicine and Psychiatry
Chief of Psychiatry
Sharpe Hospital West Virginia University
Weston, West Virginia
Henry A. Nasrallah, MD
Professor of Psychiatry, Neurology, and Neuroscience
Medical Director: Neuropsychiatry
Director, Schizophrenia and Neuropsychiatry Programs
University of Cincinnati College of Medicine
Cincinnati, Ohio
Professor Emeritus, Saint Louis University
St. Louis, Missouri
Reference
1. Aboraya A, Nasrallah HA, Elswick DE, et al. Measurement-based care in psychiatry-past, present, and future. Innov Clin Neurosci. 2018;15(11-12):13-26.
I strongly disagree with the editorial by Ahmed A. Aboraya, MD, DrPH, and Henry A. Nasrallah, MD, (“It’s time to implement measurement-based care in psychiatric practice,” From the Editor,
We do not have much more to lose before it’s a checklist, vital signs, and a script. I now refer to our profession as “McMedicine.” If you don’t have what is on the menu, you cannot get served. Diseases are rarely treated, symptoms are treated. This is not the profession of medicine. We are not fixing much; we are mostly providing consumers for pharmaceutical companies.
Few psychiatric disorders have been subjected to more measurement than depression. Quite a while ago, someone tried to compare depression scales. They correlated scale scores with the results of evaluations by board-certified psychiatrists. The best scale was a single question: “Are you depressed?” This had been included as a control. Can you do better?
Furthermore, the “paper and numbers” people can’t wait to get an “objective” wrench to tighten the screws and apply the principles of the industrial revolution to squeeze more money out of the system. They will find some way to turn patients into standardized products.
John L. Schenkel, MD
Retired psychiatrist
Peru, NY
With the use of an electronic medical record, what should be a simple 1-page note is transformed into a 5-page note of details. Doctors no longer attend to their patients but rather to their computers. Has this raised consciousness—the most important metric, according to Dr. David Hawkins? I doubt it.
In the words of my great professor, Dr. James Gustafson, I will continue to start my interview with what concerns the patient. Most of the time, they implicitly know.
Our focus should instead be on bringing down the cost of health care. This is what angers our patients most, and yet we do not make it a priority.
Psychiatrist
Glenbeigh Hospital
Rock Creek, Ohio
Signature Health
Ashtabula, Ohio
Behavioral Wellness Group
Mentor, Ohio
Continue to: The authors respond
The authors respond
We appreciate Drs. Schenkel’s and Primc’s comments on our editorial regarding measurement-based care (MBC). However, MBC will not increase the workload of psychiatrists; rather, it will streamline the evaluation of patients and measure the severity of their symptoms or adverse effects as well as the degree of their improvement. The proper use of scales with the appropriate patient populations may actually help clinicians to reduce the extensive amount of details that go into medical records.
The following quote, an excerpt from another article we wrote on MBC,1 speaks to Dr. Primc’s concerns:
“…measures in psychiatry could be considered the equivalent of a thermometer and a stethoscope to a physician.
Ahmed A. Aboraya, MD, DrPH
Assistant Professor
Department of Behavioral Medicine and Psychiatry
Chief of Psychiatry
Sharpe Hospital West Virginia University
Weston, West Virginia
Henry A. Nasrallah, MD
Professor of Psychiatry, Neurology, and Neuroscience
Medical Director: Neuropsychiatry
Director, Schizophrenia and Neuropsychiatry Programs
University of Cincinnati College of Medicine
Cincinnati, Ohio
Professor Emeritus, Saint Louis University
St. Louis, Missouri
Reference
1. Aboraya A, Nasrallah HA, Elswick DE, et al. Measurement-based care in psychiatry-past, present, and future. Innov Clin Neurosci. 2018;15(11-12):13-26.
We owe a lot to scientists like Henry Lynch
It is with great sadness that we note the passing (June 2, 2019; age 91) of Dr. Henry Lynch. Dr. Lynch almost singlehandedly brought attention to the genetic syndrome that bears his name. In 1913 Aldred Warthin (pathology chair at the University of Michigan) first described family “G”, the family of his seamstress who had told him that her family all dies of cancer. She herself succumbed to endometrial cancer. A plaque commemorating Dr. Warthin hangs down the hallway from my office at Michigan. His report fell into obscurity until the 1960s when Dr. Lynch arranged a reunion of family G in Ann Arbor, leading to a detailed update of the family in 1971. He recognized the autosomal dominance of the pedigree pattern.
In 1973, C. Richard Boland, MD, AGAF (past AGA President), wrote a medical school thesis entitled “A Familial Cancer Syndrome” and subsequently published two papers in which he first used the term “Lynch syndrome (I and II). Dr. Boland (whose family also carried a Lynch syndrome variant) spent his career adding to our molecular and clinical knowledge about nonpolyposis colon cancer syndromes. In the 1990s Vogelstein and others first described the molecular pathways that lead to colon cancer – and the rest is history.
I was a young faculty gastroenterologist at the Minneapolis VA Medical Center when one day my phone rang; it was Henry Lynch. He wanted to alert me that one of his patients was coming to me for surveillance colonoscopy. He explained the importance of what I was to do and how I should follow this man. I was overwhelmed by his attention to his patient (one of thousands) and his kindness to me. I had the privilege of traveling with him as visiting professors on a trip to South America. He was one of the kindest, most intelligent, and gracious persons I had ever met. I never forgot that experience.
We owe a lot to scientists, clinicians, and thought leaders like Henry Lynch who provide us the scientific basis of the care we give our patients.
John I. Allen, MD, MBA, AGAF
Editor in Chief
It is with great sadness that we note the passing (June 2, 2019; age 91) of Dr. Henry Lynch. Dr. Lynch almost singlehandedly brought attention to the genetic syndrome that bears his name. In 1913 Aldred Warthin (pathology chair at the University of Michigan) first described family “G”, the family of his seamstress who had told him that her family all dies of cancer. She herself succumbed to endometrial cancer. A plaque commemorating Dr. Warthin hangs down the hallway from my office at Michigan. His report fell into obscurity until the 1960s when Dr. Lynch arranged a reunion of family G in Ann Arbor, leading to a detailed update of the family in 1971. He recognized the autosomal dominance of the pedigree pattern.
In 1973, C. Richard Boland, MD, AGAF (past AGA President), wrote a medical school thesis entitled “A Familial Cancer Syndrome” and subsequently published two papers in which he first used the term “Lynch syndrome (I and II). Dr. Boland (whose family also carried a Lynch syndrome variant) spent his career adding to our molecular and clinical knowledge about nonpolyposis colon cancer syndromes. In the 1990s Vogelstein and others first described the molecular pathways that lead to colon cancer – and the rest is history.
I was a young faculty gastroenterologist at the Minneapolis VA Medical Center when one day my phone rang; it was Henry Lynch. He wanted to alert me that one of his patients was coming to me for surveillance colonoscopy. He explained the importance of what I was to do and how I should follow this man. I was overwhelmed by his attention to his patient (one of thousands) and his kindness to me. I had the privilege of traveling with him as visiting professors on a trip to South America. He was one of the kindest, most intelligent, and gracious persons I had ever met. I never forgot that experience.
We owe a lot to scientists, clinicians, and thought leaders like Henry Lynch who provide us the scientific basis of the care we give our patients.
John I. Allen, MD, MBA, AGAF
Editor in Chief
It is with great sadness that we note the passing (June 2, 2019; age 91) of Dr. Henry Lynch. Dr. Lynch almost singlehandedly brought attention to the genetic syndrome that bears his name. In 1913 Aldred Warthin (pathology chair at the University of Michigan) first described family “G”, the family of his seamstress who had told him that her family all dies of cancer. She herself succumbed to endometrial cancer. A plaque commemorating Dr. Warthin hangs down the hallway from my office at Michigan. His report fell into obscurity until the 1960s when Dr. Lynch arranged a reunion of family G in Ann Arbor, leading to a detailed update of the family in 1971. He recognized the autosomal dominance of the pedigree pattern.
In 1973, C. Richard Boland, MD, AGAF (past AGA President), wrote a medical school thesis entitled “A Familial Cancer Syndrome” and subsequently published two papers in which he first used the term “Lynch syndrome (I and II). Dr. Boland (whose family also carried a Lynch syndrome variant) spent his career adding to our molecular and clinical knowledge about nonpolyposis colon cancer syndromes. In the 1990s Vogelstein and others first described the molecular pathways that lead to colon cancer – and the rest is history.
I was a young faculty gastroenterologist at the Minneapolis VA Medical Center when one day my phone rang; it was Henry Lynch. He wanted to alert me that one of his patients was coming to me for surveillance colonoscopy. He explained the importance of what I was to do and how I should follow this man. I was overwhelmed by his attention to his patient (one of thousands) and his kindness to me. I had the privilege of traveling with him as visiting professors on a trip to South America. He was one of the kindest, most intelligent, and gracious persons I had ever met. I never forgot that experience.
We owe a lot to scientists, clinicians, and thought leaders like Henry Lynch who provide us the scientific basis of the care we give our patients.
John I. Allen, MD, MBA, AGAF
Editor in Chief
A solution for reducing referrals (and malpractice suits)
I agree with Dr. Hickner’s editorial “To refer—or not?” (J Fam Pract. 2019;68:8) that family physicians could manage about 30% of the patients they refer to specialists. Still, it’s worth noting that many referrals are motivated by the threat of unmerited malpractice suits. Until the medical liability system becomes less adversarial and unmerited suits are eliminated, all primary care doctors—not just family physicians—will continue to send patients to specialists—even when these physicians are themselves capable of treating such patients.
What might help mitigate malpractice suits? There could be benefit from oversight of health courts, which would be presided over by judges with special training in medical malpractice. Being nonadversarial, health courts would cut down on legal wrangling, settle suits, and get awards to patients quicker. They would also cut down on attorney and court fees, which account for almost half of the total amount spent on litigation. These courts wouldn’t completely eliminate unnecessary referrals to specialists, but they could help make a difference.
Edward Volpintesta, MD
Bethel, Conn
I agree with Dr. Hickner’s editorial “To refer—or not?” (J Fam Pract. 2019;68:8) that family physicians could manage about 30% of the patients they refer to specialists. Still, it’s worth noting that many referrals are motivated by the threat of unmerited malpractice suits. Until the medical liability system becomes less adversarial and unmerited suits are eliminated, all primary care doctors—not just family physicians—will continue to send patients to specialists—even when these physicians are themselves capable of treating such patients.
What might help mitigate malpractice suits? There could be benefit from oversight of health courts, which would be presided over by judges with special training in medical malpractice. Being nonadversarial, health courts would cut down on legal wrangling, settle suits, and get awards to patients quicker. They would also cut down on attorney and court fees, which account for almost half of the total amount spent on litigation. These courts wouldn’t completely eliminate unnecessary referrals to specialists, but they could help make a difference.
Edward Volpintesta, MD
Bethel, Conn
I agree with Dr. Hickner’s editorial “To refer—or not?” (J Fam Pract. 2019;68:8) that family physicians could manage about 30% of the patients they refer to specialists. Still, it’s worth noting that many referrals are motivated by the threat of unmerited malpractice suits. Until the medical liability system becomes less adversarial and unmerited suits are eliminated, all primary care doctors—not just family physicians—will continue to send patients to specialists—even when these physicians are themselves capable of treating such patients.
What might help mitigate malpractice suits? There could be benefit from oversight of health courts, which would be presided over by judges with special training in medical malpractice. Being nonadversarial, health courts would cut down on legal wrangling, settle suits, and get awards to patients quicker. They would also cut down on attorney and court fees, which account for almost half of the total amount spent on litigation. These courts wouldn’t completely eliminate unnecessary referrals to specialists, but they could help make a difference.
Edward Volpintesta, MD
Bethel, Conn