User login
Rethinking the Rebels
Each month I set out on an expedition to find a topic for this column. I came across a new book Rebel Health by Susannah Fox that I thought might be a good one. It’s both a treatise on the shortcomings of healthcare and a Baedeker for patients on how to find their way to being better served. Her argument is that many patients’ needs are unmet and their conditions are often invisible to us in mainstream healthcare. We fail to find solutions to help them. Patients would benefit from more open access to their records and more resources to take control of their own health, she argues. A few chapters in, I thought, “Oh, here we go, another diatribe on doctors and how we care most about how to keep patients in their rightful, subordinate place.” The “Rebel” title is provocative and implies patients need to overthrow the status quo. Well, I am part of the establishment. I stopped reading. This book doesn’t apply to me, I thought.
After all, I’m a healthcare progressive, right? My notes and results have been open for years. I encourage shared decision-making and try to empower patients as much as treat them. The idea that I or my colleagues are unwilling to do whatever is necessary to meet our patients’ needs was maddening. We dedicate our lives to it. My young daughter often greets me in the morning by asking if I’ll be working tonight. Most nights, I am — answering patient messages, collaborating with colleagues to help patients, keeping up with medical knowledge. I was angry at what felt like unjust criticism, especially that we’d neglect patients because their problems are not obvious or worse, there is not enough money to be made helping them. Harrumph.
That’s when I realized the best thing for me was to read the entire book and digest the arguments. I pride myself on being well-read, but I fall into a common trap: the podcasts I listen to, news I consume, and books I read mostly affirm my beliefs. It is a healthy choice to seek dispositive data and contrasting stories rather than always feeding our personal opinions.
Rebel Health was not written by Robespierre. It was penned by a thoughtful, articulate patient advocate with over 20 years experience. She has far more bona fides than I could achieve in two lifetimes. In the book, she reminds us that She describes four patient archetypes: seekers, networkers, solvers, and champions, and offers a four-quadrant model to visualize how some patients are unhelped by our current healthcare system. She advocates for frictionless, open access to health data and tries to inspire patients to connect, innovate, and create to fill the voids that exist in healthcare. We have come a long way from the immured system of a decade ago; much of that is the result of patient advocates. But healthcare is still too costly, too fragmented and too many patients unhelped. “Community is a superpower,” she writes. I agree, we should assemble all the heroes in the universe for this challenge.
Fox also tells stories of patients who solved diagnostic dilemmas through their own research and advocacy. I thought of my own contrasting experiences of patients whose DIY care was based on misinformation and how their false confidence led to poorer outcomes for them. I want to share with her readers how physicians feel hurt when patients question our competence or place the opinion of an adversarial Redditor over ours. Physicians are sometimes wrong and often in doubt. Most of us care deeply about our patients regardless of how visible their diagnosis or how easy they are to appease.
We don’t have time to engage back-and-forth on an insignificantly abnormal test they find in their open chart or why B12 and hormone testing would not be helpful for their disease. It’s also not the patients’ fault. Having unfettered access to their data might add work, but it also adds value. They are trying to learn and be active in their care. Physicians are frustrated mostly because we don’t have time to meet these unmet needs. Everyone is trying their best and we all want the same thing: patients to be satisfied and well.
As for learning the skill of being open-minded, an excellent reference is Adam Grant’s Think Again. It’s inspiring and instructive of how we can all be more open, including how to have productive arguments rather than fruitless fights. We live in divisive times. Perhaps if we all put in effort to be open-minded, push down righteous indignation, and advance more honest humility we’d all be a bit better off.
Patients are the primary audience for the Rebel Health book. Yet, as we care about them and we all want to make healthcare better, it is worth reading in its entirety. I told my daughter I don’t have to work tonight because I’ve written my article this month. When she’s a little older, I’ll tell her all about it. To be successful, she’ll have to be as open-minded as she is smart. She can learn both.
I have no conflict of interest in the book.
Dr. Benabio is director of Healthcare Transformation and chief of dermatology at Kaiser Permanente San Diego. The opinions expressed in this column are his own and do not represent those of Kaiser Permanente. Dr. Benabio is @Dermdoc on Twitter. Write to him at [email protected].
Each month I set out on an expedition to find a topic for this column. I came across a new book Rebel Health by Susannah Fox that I thought might be a good one. It’s both a treatise on the shortcomings of healthcare and a Baedeker for patients on how to find their way to being better served. Her argument is that many patients’ needs are unmet and their conditions are often invisible to us in mainstream healthcare. We fail to find solutions to help them. Patients would benefit from more open access to their records and more resources to take control of their own health, she argues. A few chapters in, I thought, “Oh, here we go, another diatribe on doctors and how we care most about how to keep patients in their rightful, subordinate place.” The “Rebel” title is provocative and implies patients need to overthrow the status quo. Well, I am part of the establishment. I stopped reading. This book doesn’t apply to me, I thought.
After all, I’m a healthcare progressive, right? My notes and results have been open for years. I encourage shared decision-making and try to empower patients as much as treat them. The idea that I or my colleagues are unwilling to do whatever is necessary to meet our patients’ needs was maddening. We dedicate our lives to it. My young daughter often greets me in the morning by asking if I’ll be working tonight. Most nights, I am — answering patient messages, collaborating with colleagues to help patients, keeping up with medical knowledge. I was angry at what felt like unjust criticism, especially that we’d neglect patients because their problems are not obvious or worse, there is not enough money to be made helping them. Harrumph.
That’s when I realized the best thing for me was to read the entire book and digest the arguments. I pride myself on being well-read, but I fall into a common trap: the podcasts I listen to, news I consume, and books I read mostly affirm my beliefs. It is a healthy choice to seek dispositive data and contrasting stories rather than always feeding our personal opinions.
Rebel Health was not written by Robespierre. It was penned by a thoughtful, articulate patient advocate with over 20 years experience. She has far more bona fides than I could achieve in two lifetimes. In the book, she reminds us that She describes four patient archetypes: seekers, networkers, solvers, and champions, and offers a four-quadrant model to visualize how some patients are unhelped by our current healthcare system. She advocates for frictionless, open access to health data and tries to inspire patients to connect, innovate, and create to fill the voids that exist in healthcare. We have come a long way from the immured system of a decade ago; much of that is the result of patient advocates. But healthcare is still too costly, too fragmented and too many patients unhelped. “Community is a superpower,” she writes. I agree, we should assemble all the heroes in the universe for this challenge.
Fox also tells stories of patients who solved diagnostic dilemmas through their own research and advocacy. I thought of my own contrasting experiences of patients whose DIY care was based on misinformation and how their false confidence led to poorer outcomes for them. I want to share with her readers how physicians feel hurt when patients question our competence or place the opinion of an adversarial Redditor over ours. Physicians are sometimes wrong and often in doubt. Most of us care deeply about our patients regardless of how visible their diagnosis or how easy they are to appease.
We don’t have time to engage back-and-forth on an insignificantly abnormal test they find in their open chart or why B12 and hormone testing would not be helpful for their disease. It’s also not the patients’ fault. Having unfettered access to their data might add work, but it also adds value. They are trying to learn and be active in their care. Physicians are frustrated mostly because we don’t have time to meet these unmet needs. Everyone is trying their best and we all want the same thing: patients to be satisfied and well.
As for learning the skill of being open-minded, an excellent reference is Adam Grant’s Think Again. It’s inspiring and instructive of how we can all be more open, including how to have productive arguments rather than fruitless fights. We live in divisive times. Perhaps if we all put in effort to be open-minded, push down righteous indignation, and advance more honest humility we’d all be a bit better off.
Patients are the primary audience for the Rebel Health book. Yet, as we care about them and we all want to make healthcare better, it is worth reading in its entirety. I told my daughter I don’t have to work tonight because I’ve written my article this month. When she’s a little older, I’ll tell her all about it. To be successful, she’ll have to be as open-minded as she is smart. She can learn both.
I have no conflict of interest in the book.
Dr. Benabio is director of Healthcare Transformation and chief of dermatology at Kaiser Permanente San Diego. The opinions expressed in this column are his own and do not represent those of Kaiser Permanente. Dr. Benabio is @Dermdoc on Twitter. Write to him at [email protected].
Each month I set out on an expedition to find a topic for this column. I came across a new book Rebel Health by Susannah Fox that I thought might be a good one. It’s both a treatise on the shortcomings of healthcare and a Baedeker for patients on how to find their way to being better served. Her argument is that many patients’ needs are unmet and their conditions are often invisible to us in mainstream healthcare. We fail to find solutions to help them. Patients would benefit from more open access to their records and more resources to take control of their own health, she argues. A few chapters in, I thought, “Oh, here we go, another diatribe on doctors and how we care most about how to keep patients in their rightful, subordinate place.” The “Rebel” title is provocative and implies patients need to overthrow the status quo. Well, I am part of the establishment. I stopped reading. This book doesn’t apply to me, I thought.
After all, I’m a healthcare progressive, right? My notes and results have been open for years. I encourage shared decision-making and try to empower patients as much as treat them. The idea that I or my colleagues are unwilling to do whatever is necessary to meet our patients’ needs was maddening. We dedicate our lives to it. My young daughter often greets me in the morning by asking if I’ll be working tonight. Most nights, I am — answering patient messages, collaborating with colleagues to help patients, keeping up with medical knowledge. I was angry at what felt like unjust criticism, especially that we’d neglect patients because their problems are not obvious or worse, there is not enough money to be made helping them. Harrumph.
That’s when I realized the best thing for me was to read the entire book and digest the arguments. I pride myself on being well-read, but I fall into a common trap: the podcasts I listen to, news I consume, and books I read mostly affirm my beliefs. It is a healthy choice to seek dispositive data and contrasting stories rather than always feeding our personal opinions.
Rebel Health was not written by Robespierre. It was penned by a thoughtful, articulate patient advocate with over 20 years experience. She has far more bona fides than I could achieve in two lifetimes. In the book, she reminds us that She describes four patient archetypes: seekers, networkers, solvers, and champions, and offers a four-quadrant model to visualize how some patients are unhelped by our current healthcare system. She advocates for frictionless, open access to health data and tries to inspire patients to connect, innovate, and create to fill the voids that exist in healthcare. We have come a long way from the immured system of a decade ago; much of that is the result of patient advocates. But healthcare is still too costly, too fragmented and too many patients unhelped. “Community is a superpower,” she writes. I agree, we should assemble all the heroes in the universe for this challenge.
Fox also tells stories of patients who solved diagnostic dilemmas through their own research and advocacy. I thought of my own contrasting experiences of patients whose DIY care was based on misinformation and how their false confidence led to poorer outcomes for them. I want to share with her readers how physicians feel hurt when patients question our competence or place the opinion of an adversarial Redditor over ours. Physicians are sometimes wrong and often in doubt. Most of us care deeply about our patients regardless of how visible their diagnosis or how easy they are to appease.
We don’t have time to engage back-and-forth on an insignificantly abnormal test they find in their open chart or why B12 and hormone testing would not be helpful for their disease. It’s also not the patients’ fault. Having unfettered access to their data might add work, but it also adds value. They are trying to learn and be active in their care. Physicians are frustrated mostly because we don’t have time to meet these unmet needs. Everyone is trying their best and we all want the same thing: patients to be satisfied and well.
As for learning the skill of being open-minded, an excellent reference is Adam Grant’s Think Again. It’s inspiring and instructive of how we can all be more open, including how to have productive arguments rather than fruitless fights. We live in divisive times. Perhaps if we all put in effort to be open-minded, push down righteous indignation, and advance more honest humility we’d all be a bit better off.
Patients are the primary audience for the Rebel Health book. Yet, as we care about them and we all want to make healthcare better, it is worth reading in its entirety. I told my daughter I don’t have to work tonight because I’ve written my article this month. When she’s a little older, I’ll tell her all about it. To be successful, she’ll have to be as open-minded as she is smart. She can learn both.
I have no conflict of interest in the book.
Dr. Benabio is director of Healthcare Transformation and chief of dermatology at Kaiser Permanente San Diego. The opinions expressed in this column are his own and do not represent those of Kaiser Permanente. Dr. Benabio is @Dermdoc on Twitter. Write to him at [email protected].
Access to Perinatal Mental Healthcare: What Exactly Are The Obstacles?
The first of May is marked as the World Maternal Mental Health Day, a time for patient groups, medical societies, clinicians, and other colleagues who care for women to highlight maternal mental health and to advocate for increased awareness, enhanced access to care, decrease in stigma, and development of the most effective treatments.
In this spirit, and within the context of greater mental health awareness, I wanted to highlight the ironic dichotomy we see in reproductive psychiatry today. Namely, although we have many useful treatments available in the field to treat maternal psychiatric illness, there are barriers to accessing mental healthcare that prevent women from receiving treatment and getting well.
Thinking back on the last few years from the other side of the pandemic, when COVID concerns turned the experience of motherhood on its side in so many ways, we can only acknowledge that it is an important time in the field of reproductive psychiatry. We have seen not only the development of new pharmacologic (neurosteroids) and nonpharmacologic therapies (transcranial magnetic stimulation, cognitive-behaviorial therapy for perinatal depression), but also the focus on new digital apps for perinatal depression that may be scalable and that may help bridge the voids in access to effective treatment from the most rural to the most urban settings.
In a previous column, I wrote about the potential difficulties of identifying at-risk women with postpartum psychiatric illness, particularly within the context of disparate data collection methods and management of data. Hospital systems that favor paper screening methods rather than digital platforms pose special problems. I also noted an even larger concern: namely, once screened, it can be very challenging to engage women with postpartum depression in treatment, and women may ultimately not navigate to care for a variety of reasons. These components are but one part of the so-called “perinatal treatment cascade.” When we look at access to care, patients would ideally move from depression screening as an example and, following endorsement of significant symptoms, would receive a referral, which would result in the patient being seen, followed up, and getting well. But that is not what is happening.
A recent preliminary study published as a short communication in the Archives of Women’s Mental Health highlighted this issue. The authors used the Edinburgh Postnatal Depression Scale (EPDS) to follow symptoms of depression in 145 pregnant women in ob.gyn. services, and found that there were low levels of adherence to psychiatric screenings and referrals in the perinatal period. Another study published in the Journal of Clinical Psychiatry found 30.8% of women with postpartum depression were identified clinically, 15.8% received treatment, and 3.2% achieved remission. That is the gulf, in 2024, that we have not managed to bridge.
The findings show the difficulty women experience accessing perinatal mental health resources. While we’ve known for a long time that the “perinatal treatment cascade” is real, what we don’t understand are the variables in the mix, particularly for patients in marginalized groups. We also do not know where women fall off the curve with regard to accessing care. In my mind, if we’re going to make a difference, we need to know the answer to that question.
Part of the issue is that the research into understanding why women fall off the curve is incomplete. You cannot simply hand a sheet to a woman with an EPDS score of 12 who’s depressed and has a newborn and expect her to navigate to care. What we should really be doing is investing in care navigation for women.
The situation is analogous to diagnosing and treating cardiac abnormalities in a catheterization laboratory. If a patient has a blocked coronary artery and needs a stent, then they need to go to the cath lab. We haven’t yet figured out the process in reproductive psychiatry to optimize the likelihood that patients will be screened and then referred to receive the best available treatment.
Some of our ob.gyn. colleagues have been working to improve access to perinatal mental health services, such as offering on-site services, and offering training and services to patients and providers on screening, assessment, and treatment. At the Center for Women’s Mental Health, we are conducting the Screening and Treatment Enhancement for Postpartum Depression study, which is a universal screening and referral program for women at our center. While some progress is being made, there are still far too many women who are falling through the cracks and not receiving the care they need.
It is both ironic and sad that the growing number of available treatments in reproductive psychiatry are scalable, yet we haven’t figured out how to facilitate access to care. While we should be excited about new treatments, we also need to take the time to understand what the barriers are for at-risk women accessing mental healthcare in the postpartum period.
Dr. Cohen is the director of the Ammon-Pinizzotto Center for Women’s Mental Health at Massachusetts General Hospital in Boston, which provides information resources and conducts clinical care and research in reproductive mental health. He has been a consultant to manufacturers of psychiatric medications. STEPS for PPD is funded by the Marriott Foundation. Full disclosure information for Dr. Cohen is available at womensmentalhealth.org. Email Dr. Cohen at [email protected].
The first of May is marked as the World Maternal Mental Health Day, a time for patient groups, medical societies, clinicians, and other colleagues who care for women to highlight maternal mental health and to advocate for increased awareness, enhanced access to care, decrease in stigma, and development of the most effective treatments.
In this spirit, and within the context of greater mental health awareness, I wanted to highlight the ironic dichotomy we see in reproductive psychiatry today. Namely, although we have many useful treatments available in the field to treat maternal psychiatric illness, there are barriers to accessing mental healthcare that prevent women from receiving treatment and getting well.
Thinking back on the last few years from the other side of the pandemic, when COVID concerns turned the experience of motherhood on its side in so many ways, we can only acknowledge that it is an important time in the field of reproductive psychiatry. We have seen not only the development of new pharmacologic (neurosteroids) and nonpharmacologic therapies (transcranial magnetic stimulation, cognitive-behaviorial therapy for perinatal depression), but also the focus on new digital apps for perinatal depression that may be scalable and that may help bridge the voids in access to effective treatment from the most rural to the most urban settings.
In a previous column, I wrote about the potential difficulties of identifying at-risk women with postpartum psychiatric illness, particularly within the context of disparate data collection methods and management of data. Hospital systems that favor paper screening methods rather than digital platforms pose special problems. I also noted an even larger concern: namely, once screened, it can be very challenging to engage women with postpartum depression in treatment, and women may ultimately not navigate to care for a variety of reasons. These components are but one part of the so-called “perinatal treatment cascade.” When we look at access to care, patients would ideally move from depression screening as an example and, following endorsement of significant symptoms, would receive a referral, which would result in the patient being seen, followed up, and getting well. But that is not what is happening.
A recent preliminary study published as a short communication in the Archives of Women’s Mental Health highlighted this issue. The authors used the Edinburgh Postnatal Depression Scale (EPDS) to follow symptoms of depression in 145 pregnant women in ob.gyn. services, and found that there were low levels of adherence to psychiatric screenings and referrals in the perinatal period. Another study published in the Journal of Clinical Psychiatry found 30.8% of women with postpartum depression were identified clinically, 15.8% received treatment, and 3.2% achieved remission. That is the gulf, in 2024, that we have not managed to bridge.
The findings show the difficulty women experience accessing perinatal mental health resources. While we’ve known for a long time that the “perinatal treatment cascade” is real, what we don’t understand are the variables in the mix, particularly for patients in marginalized groups. We also do not know where women fall off the curve with regard to accessing care. In my mind, if we’re going to make a difference, we need to know the answer to that question.
Part of the issue is that the research into understanding why women fall off the curve is incomplete. You cannot simply hand a sheet to a woman with an EPDS score of 12 who’s depressed and has a newborn and expect her to navigate to care. What we should really be doing is investing in care navigation for women.
The situation is analogous to diagnosing and treating cardiac abnormalities in a catheterization laboratory. If a patient has a blocked coronary artery and needs a stent, then they need to go to the cath lab. We haven’t yet figured out the process in reproductive psychiatry to optimize the likelihood that patients will be screened and then referred to receive the best available treatment.
Some of our ob.gyn. colleagues have been working to improve access to perinatal mental health services, such as offering on-site services, and offering training and services to patients and providers on screening, assessment, and treatment. At the Center for Women’s Mental Health, we are conducting the Screening and Treatment Enhancement for Postpartum Depression study, which is a universal screening and referral program for women at our center. While some progress is being made, there are still far too many women who are falling through the cracks and not receiving the care they need.
It is both ironic and sad that the growing number of available treatments in reproductive psychiatry are scalable, yet we haven’t figured out how to facilitate access to care. While we should be excited about new treatments, we also need to take the time to understand what the barriers are for at-risk women accessing mental healthcare in the postpartum period.
Dr. Cohen is the director of the Ammon-Pinizzotto Center for Women’s Mental Health at Massachusetts General Hospital in Boston, which provides information resources and conducts clinical care and research in reproductive mental health. He has been a consultant to manufacturers of psychiatric medications. STEPS for PPD is funded by the Marriott Foundation. Full disclosure information for Dr. Cohen is available at womensmentalhealth.org. Email Dr. Cohen at [email protected].
The first of May is marked as the World Maternal Mental Health Day, a time for patient groups, medical societies, clinicians, and other colleagues who care for women to highlight maternal mental health and to advocate for increased awareness, enhanced access to care, decrease in stigma, and development of the most effective treatments.
In this spirit, and within the context of greater mental health awareness, I wanted to highlight the ironic dichotomy we see in reproductive psychiatry today. Namely, although we have many useful treatments available in the field to treat maternal psychiatric illness, there are barriers to accessing mental healthcare that prevent women from receiving treatment and getting well.
Thinking back on the last few years from the other side of the pandemic, when COVID concerns turned the experience of motherhood on its side in so many ways, we can only acknowledge that it is an important time in the field of reproductive psychiatry. We have seen not only the development of new pharmacologic (neurosteroids) and nonpharmacologic therapies (transcranial magnetic stimulation, cognitive-behaviorial therapy for perinatal depression), but also the focus on new digital apps for perinatal depression that may be scalable and that may help bridge the voids in access to effective treatment from the most rural to the most urban settings.
In a previous column, I wrote about the potential difficulties of identifying at-risk women with postpartum psychiatric illness, particularly within the context of disparate data collection methods and management of data. Hospital systems that favor paper screening methods rather than digital platforms pose special problems. I also noted an even larger concern: namely, once screened, it can be very challenging to engage women with postpartum depression in treatment, and women may ultimately not navigate to care for a variety of reasons. These components are but one part of the so-called “perinatal treatment cascade.” When we look at access to care, patients would ideally move from depression screening as an example and, following endorsement of significant symptoms, would receive a referral, which would result in the patient being seen, followed up, and getting well. But that is not what is happening.
A recent preliminary study published as a short communication in the Archives of Women’s Mental Health highlighted this issue. The authors used the Edinburgh Postnatal Depression Scale (EPDS) to follow symptoms of depression in 145 pregnant women in ob.gyn. services, and found that there were low levels of adherence to psychiatric screenings and referrals in the perinatal period. Another study published in the Journal of Clinical Psychiatry found 30.8% of women with postpartum depression were identified clinically, 15.8% received treatment, and 3.2% achieved remission. That is the gulf, in 2024, that we have not managed to bridge.
The findings show the difficulty women experience accessing perinatal mental health resources. While we’ve known for a long time that the “perinatal treatment cascade” is real, what we don’t understand are the variables in the mix, particularly for patients in marginalized groups. We also do not know where women fall off the curve with regard to accessing care. In my mind, if we’re going to make a difference, we need to know the answer to that question.
Part of the issue is that the research into understanding why women fall off the curve is incomplete. You cannot simply hand a sheet to a woman with an EPDS score of 12 who’s depressed and has a newborn and expect her to navigate to care. What we should really be doing is investing in care navigation for women.
The situation is analogous to diagnosing and treating cardiac abnormalities in a catheterization laboratory. If a patient has a blocked coronary artery and needs a stent, then they need to go to the cath lab. We haven’t yet figured out the process in reproductive psychiatry to optimize the likelihood that patients will be screened and then referred to receive the best available treatment.
Some of our ob.gyn. colleagues have been working to improve access to perinatal mental health services, such as offering on-site services, and offering training and services to patients and providers on screening, assessment, and treatment. At the Center for Women’s Mental Health, we are conducting the Screening and Treatment Enhancement for Postpartum Depression study, which is a universal screening and referral program for women at our center. While some progress is being made, there are still far too many women who are falling through the cracks and not receiving the care they need.
It is both ironic and sad that the growing number of available treatments in reproductive psychiatry are scalable, yet we haven’t figured out how to facilitate access to care. While we should be excited about new treatments, we also need to take the time to understand what the barriers are for at-risk women accessing mental healthcare in the postpartum period.
Dr. Cohen is the director of the Ammon-Pinizzotto Center for Women’s Mental Health at Massachusetts General Hospital in Boston, which provides information resources and conducts clinical care and research in reproductive mental health. He has been a consultant to manufacturers of psychiatric medications. STEPS for PPD is funded by the Marriott Foundation. Full disclosure information for Dr. Cohen is available at womensmentalhealth.org. Email Dr. Cohen at [email protected].
Will the Federal Non-Compete Ban Take Effect?
(with very limited exceptions). The final rule will not go into effect until 120 days after its publication in the Federal Register, which took place on May 7, and numerous legal challenges appear to be on the horizon.
The principal components of the rule are as follows:
- After the effective date, most non-compete agreements (which prevent departing employees from signing with a new employer for a defined period within a specific geographic area) are banned nationwide.
- The rule exempts certain “senior executives,” ie individuals who earn more than $151,164 annually and serve in policy-making positions.
- There is another major exception for non-competes connected with a sale of a business.
- While not explicitly stated, the rule arguably exempts non-profits, tax-exempt hospitals, and other tax-exempt entities.
- Employers must provide verbal and written notice to employees regarding existing agreements, which would be voided under the rule.
The final rule is the latest skirmish in an ongoing, years-long debate. Twelve states have already put non-compete bans in place, according to a recent paper, and they may serve as a harbinger of things to come should the federal ban go into effect. Each state rule varies in its specifics as states respond to local market conditions. While some states ban all non-compete agreements outright, others limit them based on variables, such as income and employment circumstances. Of course, should the federal ban take effect, it will supersede whatever rules the individual states have in place.
In drafting the rule, the FTC reasoned that non-compete clauses constitute restraint of trade, and eliminating them could potentially increase worker earnings as well as lower health care costs by billions of dollars. In its statements on the proposed ban, the FTC claimed that it could lower health spending across the board by almost $150 billion per year and return $300 million to workers each year in earnings. The agency cited a large body of research that non-competes make it harder for workers to move between jobs and can raise prices for goods and services, while suppressing wages for workers and inhibiting the creation of new businesses.
Most physicians affected by non-compete agreements heavily favor the new rule, because it would give them more control over their careers and expand their practice and income opportunities. It would allow them to get a new job with a competing organization, bucking a long-standing trend that hospitals and health care systems have heavily relied on to keep staff in place.
The rule would, however, keep in place “non-solicitation” rules that many health care organizations have put in place. That means that if a physician leaves an employer, he or she cannot reach out to former patients and colleagues to bring them along or invite them to join him or her at the new employment venue.
Within that clause, however, the FTC has specified that if such non-solicitation agreement has the “equivalent effect” of a non-compete, the agency would deem it such. That means, even if that rule stands, it could be contested and may be interpreted as violating the non-compete provision. So, there is value in reading all the fine print should the rule move forward.
Physicians in independent practices who employ physician assistants and nurse practitioners have expressed concerns that their expensively trained employees might be tempted to accept a nearby, higher-paying position. The “non-solicitation” clause would theoretically prevent them from taking patients and co-workers with them — unless it were successfully contested. Many questions remain.
Further complicating the non-compete ban issue is how it might impact nonprofit institutions. Most hospitals structured as nonprofits would theoretically be exempt from the rule, although it is not specifically stated in the rule itself, because the FTC Act gives the Commission jurisdiction over for-profit companies only. This would obviously create an unfair advantage for nonprofits, who could continue writing non-compete clauses with impunity.
All of these questions may be moot, of course, because a number of powerful entities with deep pockets have lined up in opposition to the rule. Some of them have even questioned the FTC’s authority to pass the rule at all, on the grounds that Section 5 of the FTC Act does not give it the authority to police labor markets. A lawsuit has already been filed by the US Chamber of Commerce. Other large groups in opposition are the American Medical Group Association, the American Hospital Association, and numerous large hospital and healthcare networks.
Only time will tell whether this issue will be regulated on a national level or remain the purview of each individual state.
Dr. Eastern practices dermatology and dermatologic surgery in Belleville, N.J. He is the author of numerous articles and textbook chapters, and is a longtime monthly columnist for Dermatology News. Write to him at [email protected].
(with very limited exceptions). The final rule will not go into effect until 120 days after its publication in the Federal Register, which took place on May 7, and numerous legal challenges appear to be on the horizon.
The principal components of the rule are as follows:
- After the effective date, most non-compete agreements (which prevent departing employees from signing with a new employer for a defined period within a specific geographic area) are banned nationwide.
- The rule exempts certain “senior executives,” ie individuals who earn more than $151,164 annually and serve in policy-making positions.
- There is another major exception for non-competes connected with a sale of a business.
- While not explicitly stated, the rule arguably exempts non-profits, tax-exempt hospitals, and other tax-exempt entities.
- Employers must provide verbal and written notice to employees regarding existing agreements, which would be voided under the rule.
The final rule is the latest skirmish in an ongoing, years-long debate. Twelve states have already put non-compete bans in place, according to a recent paper, and they may serve as a harbinger of things to come should the federal ban go into effect. Each state rule varies in its specifics as states respond to local market conditions. While some states ban all non-compete agreements outright, others limit them based on variables, such as income and employment circumstances. Of course, should the federal ban take effect, it will supersede whatever rules the individual states have in place.
In drafting the rule, the FTC reasoned that non-compete clauses constitute restraint of trade, and eliminating them could potentially increase worker earnings as well as lower health care costs by billions of dollars. In its statements on the proposed ban, the FTC claimed that it could lower health spending across the board by almost $150 billion per year and return $300 million to workers each year in earnings. The agency cited a large body of research that non-competes make it harder for workers to move between jobs and can raise prices for goods and services, while suppressing wages for workers and inhibiting the creation of new businesses.
Most physicians affected by non-compete agreements heavily favor the new rule, because it would give them more control over their careers and expand their practice and income opportunities. It would allow them to get a new job with a competing organization, bucking a long-standing trend that hospitals and health care systems have heavily relied on to keep staff in place.
The rule would, however, keep in place “non-solicitation” rules that many health care organizations have put in place. That means that if a physician leaves an employer, he or she cannot reach out to former patients and colleagues to bring them along or invite them to join him or her at the new employment venue.
Within that clause, however, the FTC has specified that if such non-solicitation agreement has the “equivalent effect” of a non-compete, the agency would deem it such. That means, even if that rule stands, it could be contested and may be interpreted as violating the non-compete provision. So, there is value in reading all the fine print should the rule move forward.
Physicians in independent practices who employ physician assistants and nurse practitioners have expressed concerns that their expensively trained employees might be tempted to accept a nearby, higher-paying position. The “non-solicitation” clause would theoretically prevent them from taking patients and co-workers with them — unless it were successfully contested. Many questions remain.
Further complicating the non-compete ban issue is how it might impact nonprofit institutions. Most hospitals structured as nonprofits would theoretically be exempt from the rule, although it is not specifically stated in the rule itself, because the FTC Act gives the Commission jurisdiction over for-profit companies only. This would obviously create an unfair advantage for nonprofits, who could continue writing non-compete clauses with impunity.
All of these questions may be moot, of course, because a number of powerful entities with deep pockets have lined up in opposition to the rule. Some of them have even questioned the FTC’s authority to pass the rule at all, on the grounds that Section 5 of the FTC Act does not give it the authority to police labor markets. A lawsuit has already been filed by the US Chamber of Commerce. Other large groups in opposition are the American Medical Group Association, the American Hospital Association, and numerous large hospital and healthcare networks.
Only time will tell whether this issue will be regulated on a national level or remain the purview of each individual state.
Dr. Eastern practices dermatology and dermatologic surgery in Belleville, N.J. He is the author of numerous articles and textbook chapters, and is a longtime monthly columnist for Dermatology News. Write to him at [email protected].
(with very limited exceptions). The final rule will not go into effect until 120 days after its publication in the Federal Register, which took place on May 7, and numerous legal challenges appear to be on the horizon.
The principal components of the rule are as follows:
- After the effective date, most non-compete agreements (which prevent departing employees from signing with a new employer for a defined period within a specific geographic area) are banned nationwide.
- The rule exempts certain “senior executives,” ie individuals who earn more than $151,164 annually and serve in policy-making positions.
- There is another major exception for non-competes connected with a sale of a business.
- While not explicitly stated, the rule arguably exempts non-profits, tax-exempt hospitals, and other tax-exempt entities.
- Employers must provide verbal and written notice to employees regarding existing agreements, which would be voided under the rule.
The final rule is the latest skirmish in an ongoing, years-long debate. Twelve states have already put non-compete bans in place, according to a recent paper, and they may serve as a harbinger of things to come should the federal ban go into effect. Each state rule varies in its specifics as states respond to local market conditions. While some states ban all non-compete agreements outright, others limit them based on variables, such as income and employment circumstances. Of course, should the federal ban take effect, it will supersede whatever rules the individual states have in place.
In drafting the rule, the FTC reasoned that non-compete clauses constitute restraint of trade, and eliminating them could potentially increase worker earnings as well as lower health care costs by billions of dollars. In its statements on the proposed ban, the FTC claimed that it could lower health spending across the board by almost $150 billion per year and return $300 million to workers each year in earnings. The agency cited a large body of research that non-competes make it harder for workers to move between jobs and can raise prices for goods and services, while suppressing wages for workers and inhibiting the creation of new businesses.
Most physicians affected by non-compete agreements heavily favor the new rule, because it would give them more control over their careers and expand their practice and income opportunities. It would allow them to get a new job with a competing organization, bucking a long-standing trend that hospitals and health care systems have heavily relied on to keep staff in place.
The rule would, however, keep in place “non-solicitation” rules that many health care organizations have put in place. That means that if a physician leaves an employer, he or she cannot reach out to former patients and colleagues to bring them along or invite them to join him or her at the new employment venue.
Within that clause, however, the FTC has specified that if such non-solicitation agreement has the “equivalent effect” of a non-compete, the agency would deem it such. That means, even if that rule stands, it could be contested and may be interpreted as violating the non-compete provision. So, there is value in reading all the fine print should the rule move forward.
Physicians in independent practices who employ physician assistants and nurse practitioners have expressed concerns that their expensively trained employees might be tempted to accept a nearby, higher-paying position. The “non-solicitation” clause would theoretically prevent them from taking patients and co-workers with them — unless it were successfully contested. Many questions remain.
Further complicating the non-compete ban issue is how it might impact nonprofit institutions. Most hospitals structured as nonprofits would theoretically be exempt from the rule, although it is not specifically stated in the rule itself, because the FTC Act gives the Commission jurisdiction over for-profit companies only. This would obviously create an unfair advantage for nonprofits, who could continue writing non-compete clauses with impunity.
All of these questions may be moot, of course, because a number of powerful entities with deep pockets have lined up in opposition to the rule. Some of them have even questioned the FTC’s authority to pass the rule at all, on the grounds that Section 5 of the FTC Act does not give it the authority to police labor markets. A lawsuit has already been filed by the US Chamber of Commerce. Other large groups in opposition are the American Medical Group Association, the American Hospital Association, and numerous large hospital and healthcare networks.
Only time will tell whether this issue will be regulated on a national level or remain the purview of each individual state.
Dr. Eastern practices dermatology and dermatologic surgery in Belleville, N.J. He is the author of numerous articles and textbook chapters, and is a longtime monthly columnist for Dermatology News. Write to him at [email protected].
Fluoride, Water, and Kids’ Brains: It’s Complicated
This transcript has been edited for clarity.
I recently looked back at my folder full of these medical study commentaries, this weekly video series we call Impact Factor, and realized that I’ve been doing this for a long time. More than 400 articles, believe it or not.
I’ve learned a lot in that time — about medicine, of course — but also about how people react to certain topics. If you’ve been with me this whole time, or even for just a chunk of it, you’ll know that I tend to take a measured approach to most topics. No one study is ever truly definitive, after all. But regardless of how even-keeled I may be, there are some topics that I just know in advance are going to be a bit divisive: studies about gun control; studies about vitamin D; and, of course, studies about fluoride.
Shall We Shake This Hornet’s Nest?
The fluoridation of the US water system began in 1945 with the goal of reducing cavities in the population. The CDC named water fluoridation one of the 10 great public health achievements of the 20th century, along with such inarguable achievements as the recognition of tobacco as a health hazard.
But fluoridation has never been without its detractors. One problem is that the spectrum of beliefs about the potential harm of fluoridation is huge. On one end, you have science-based concerns such as the recognition that excessive fluoride intake can cause fluorosis and stain tooth enamel. I’ll note that the EPA regulates fluoride levels — there is a fair amount of naturally occurring fluoride in water tables around the world — to prevent this. And, of course, on the other end of the spectrum, you have beliefs that are essentially conspiracy theories: “They” add fluoride to the water supply to control us.
The challenge for me is that when one “side” of a scientific debate includes the crazy theories, it can be hard to discuss that whole spectrum, since there are those who will see evidence of any adverse fluoride effect as confirmation that the conspiracy theory is true.
I can’t help this. So I’ll just say this up front: I am about to tell you about a study that shows some potential risk from fluoride exposure. I will tell you up front that there are some significant caveats to the study that call the results into question. And I will tell you up front that no one is controlling your mind, or my mind, with fluoride; they do it with social media.
Let’s Dive Into These Shark-Infested, Fluoridated Waters
We’re talking about the study, “Maternal Urinary Fluoride and Child Neurobehavior at Age 36 Months,” which appears in JAMA Network Open.
It’s a study of 229 mother-child pairs from the Los Angeles area. The moms had their urinary fluoride level measured once before 30 weeks of gestation. A neurobehavioral battery called the Preschool Child Behavior Checklist was administered to the children at age 36 months.
The main thing you’ll hear about this study — in headlines, Facebook posts, and manifestos locked in drawers somewhere — is the primary result: A 0.68-mg/L increase in urinary fluoride in the mothers, about 25 percentile points, was associated with a doubling of the risk for neurobehavioral problems in their kids when they were 3 years old.
Yikes.
But this is not a randomized trial. Researchers didn’t randomly assign some women to have high fluoride intake and some women to have low fluoride intake. They knew that other factors that might lead to neurobehavioral problems could also lead to higher fluoride intake. They represent these factors in what’s known as a directed acyclic graph, as seen here, and account for them statistically using a regression equation.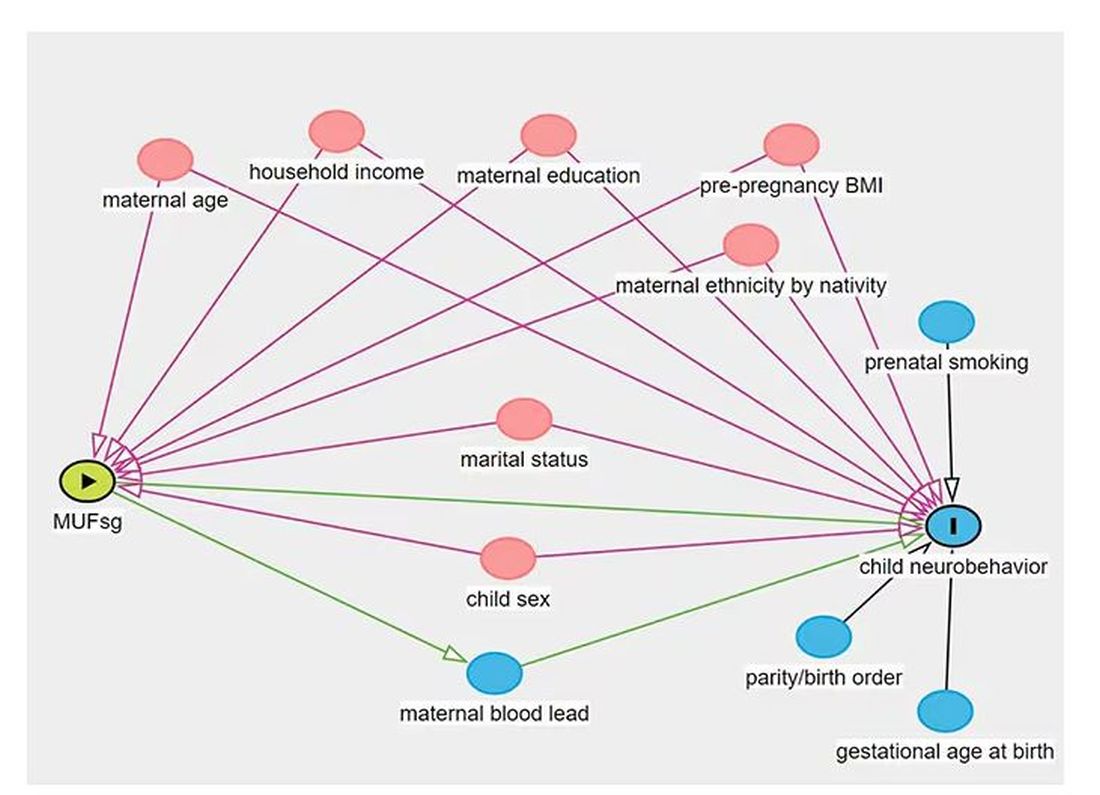
Not represented here are neighborhood characteristics. Los Angeles does not have uniformly fluoridated water, and neurobehavioral problems in kids are strongly linked to stressors in their environments. Fluoride level could be an innocent bystander.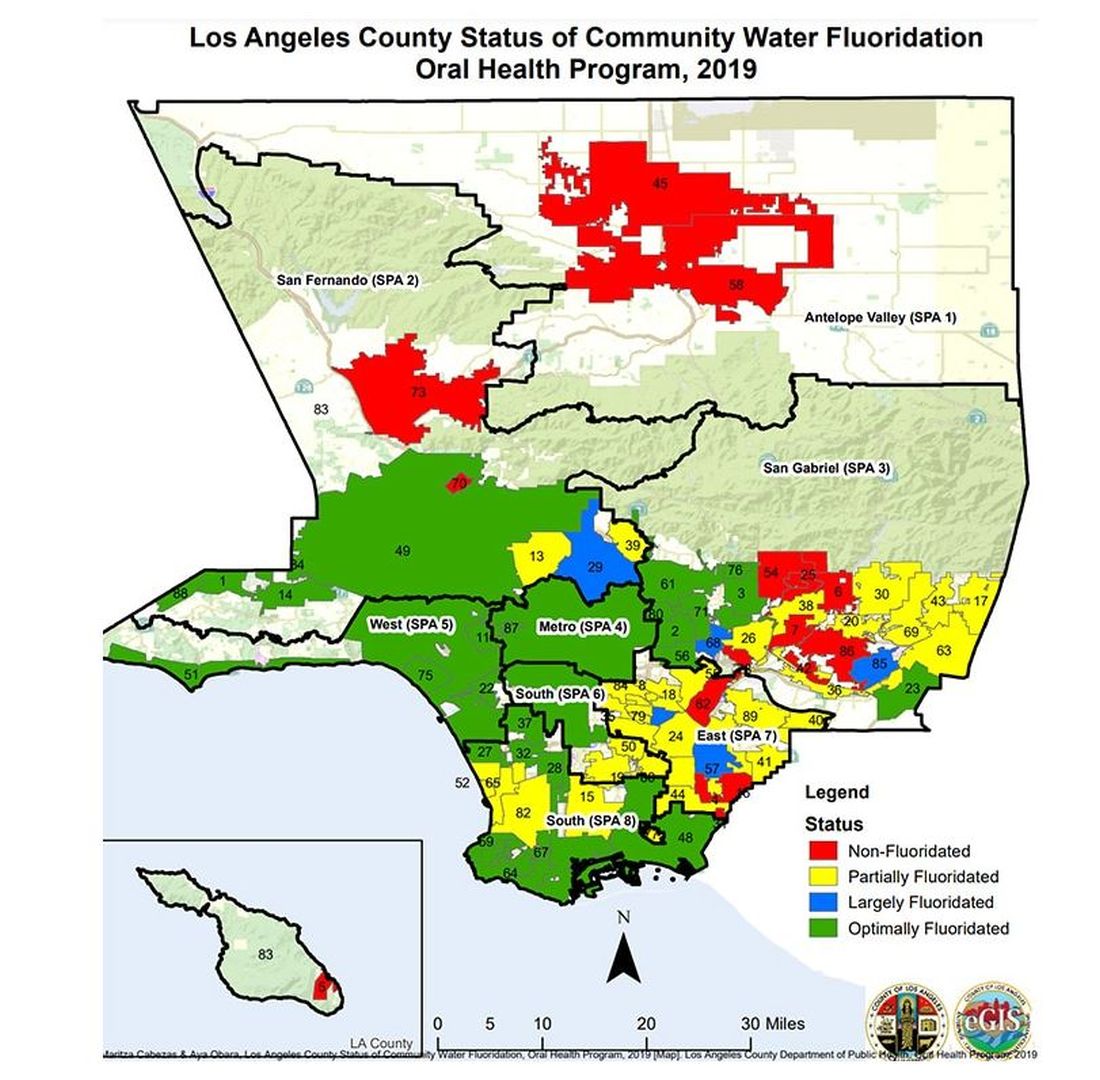
I’m really just describing the classic issue of correlation versus causation here, the bane of all observational research and — let’s be honest — a bit of a crutch that allows us to disregard the results of studies we don’t like, provided the study wasn’t a randomized trial.
But I have a deeper issue with this study than the old “failure to adjust for relevant confounders” thing, as important as that is.
The exposure of interest in this study is maternal urinary fluoride, as measured in a spot sample. It’s not often that I get to go deep on nephrology in this space, but let’s think about that for a second. Let’s assume for a moment that fluoride is toxic to the developing fetal brain, the main concern raised by the results of the study. How would that work? Presumably, mom would be ingesting fluoride from various sources (like the water supply), and that fluoride would get into her blood, and from her blood across the placenta to the baby’s blood, and into the baby’s brain.
Is Urinary Fluoride a Good Measure of Blood Fluoride?
It’s not great. Empirically, we have data that tell us that levels of urine fluoride are not all that similar to levels of serum fluoride. In 2014, a study investigated the correlation between urine and serum fluoride in a cohort of 60 schoolchildren and found a correlation coefficient of around 0.5.
Why isn’t urine fluoride a great proxy for serum fluoride? The most obvious reason is the urine concentration. Human urine concentration can range from about 50 mmol to 1200 mmol (a 24-fold difference) depending on hydration status. Over the course of 24 hours, for example, the amount of fluoride you put out in your urine may be fairly stable in relation to intake, but for a spot urine sample it would be wildly variable. The authors know this, of course, and so they divide the measured urine fluoride by the specific gravity of the urine to give a sort of “dilution adjusted” value. That’s what is actually used in this study. But specific gravity is, itself, an imperfect measure of how dilute the urine is.
This is something that comes up a lot in urinary biomarker research and it’s not that hard to get around. The best thing would be to just measure blood levels of fluoride. The second best option is 24-hour fluoride excretion. After that, the next best thing would be to adjust the spot concentration by other markers of urinary dilution — creatinine or osmolality — as sensitivity analyses. Any of these approaches would lend credence to the results of the study.
Urinary fluoride excretion is pH dependent. The more acidic the urine, the less fluoride is excreted. Many things — including, importantly, diet — affect urine pH. And it is not a stretch to think that diet may also affect the developing fetus. Neither urine pH nor dietary habits were accounted for in this study.
So, here we are. We have an observational study suggesting a harm that may be associated with fluoride. There may be a causal link here, in which case we need further studies to weigh the harm against the more well-established public health benefit. Or, this is all correlation — an illusion created by the limitations of observational data, and the unique challenges of estimating intake from a single urine sample. In other words, this study has something for everyone, fluoride boosters and skeptics alike. Let the arguments begin. But, if possible, leave me out of it.
Dr. Wilson is associate professor of medicine and public health and director of the Clinical and Translational Research Accelerator at Yale University, New Haven, Conn. He has disclosed no relevant financial relationships.
A version of this article appeared on Medscape.com.
This transcript has been edited for clarity.
I recently looked back at my folder full of these medical study commentaries, this weekly video series we call Impact Factor, and realized that I’ve been doing this for a long time. More than 400 articles, believe it or not.
I’ve learned a lot in that time — about medicine, of course — but also about how people react to certain topics. If you’ve been with me this whole time, or even for just a chunk of it, you’ll know that I tend to take a measured approach to most topics. No one study is ever truly definitive, after all. But regardless of how even-keeled I may be, there are some topics that I just know in advance are going to be a bit divisive: studies about gun control; studies about vitamin D; and, of course, studies about fluoride.
Shall We Shake This Hornet’s Nest?
The fluoridation of the US water system began in 1945 with the goal of reducing cavities in the population. The CDC named water fluoridation one of the 10 great public health achievements of the 20th century, along with such inarguable achievements as the recognition of tobacco as a health hazard.
But fluoridation has never been without its detractors. One problem is that the spectrum of beliefs about the potential harm of fluoridation is huge. On one end, you have science-based concerns such as the recognition that excessive fluoride intake can cause fluorosis and stain tooth enamel. I’ll note that the EPA regulates fluoride levels — there is a fair amount of naturally occurring fluoride in water tables around the world — to prevent this. And, of course, on the other end of the spectrum, you have beliefs that are essentially conspiracy theories: “They” add fluoride to the water supply to control us.
The challenge for me is that when one “side” of a scientific debate includes the crazy theories, it can be hard to discuss that whole spectrum, since there are those who will see evidence of any adverse fluoride effect as confirmation that the conspiracy theory is true.
I can’t help this. So I’ll just say this up front: I am about to tell you about a study that shows some potential risk from fluoride exposure. I will tell you up front that there are some significant caveats to the study that call the results into question. And I will tell you up front that no one is controlling your mind, or my mind, with fluoride; they do it with social media.
Let’s Dive Into These Shark-Infested, Fluoridated Waters
We’re talking about the study, “Maternal Urinary Fluoride and Child Neurobehavior at Age 36 Months,” which appears in JAMA Network Open.
It’s a study of 229 mother-child pairs from the Los Angeles area. The moms had their urinary fluoride level measured once before 30 weeks of gestation. A neurobehavioral battery called the Preschool Child Behavior Checklist was administered to the children at age 36 months.
The main thing you’ll hear about this study — in headlines, Facebook posts, and manifestos locked in drawers somewhere — is the primary result: A 0.68-mg/L increase in urinary fluoride in the mothers, about 25 percentile points, was associated with a doubling of the risk for neurobehavioral problems in their kids when they were 3 years old.
Yikes.
But this is not a randomized trial. Researchers didn’t randomly assign some women to have high fluoride intake and some women to have low fluoride intake. They knew that other factors that might lead to neurobehavioral problems could also lead to higher fluoride intake. They represent these factors in what’s known as a directed acyclic graph, as seen here, and account for them statistically using a regression equation.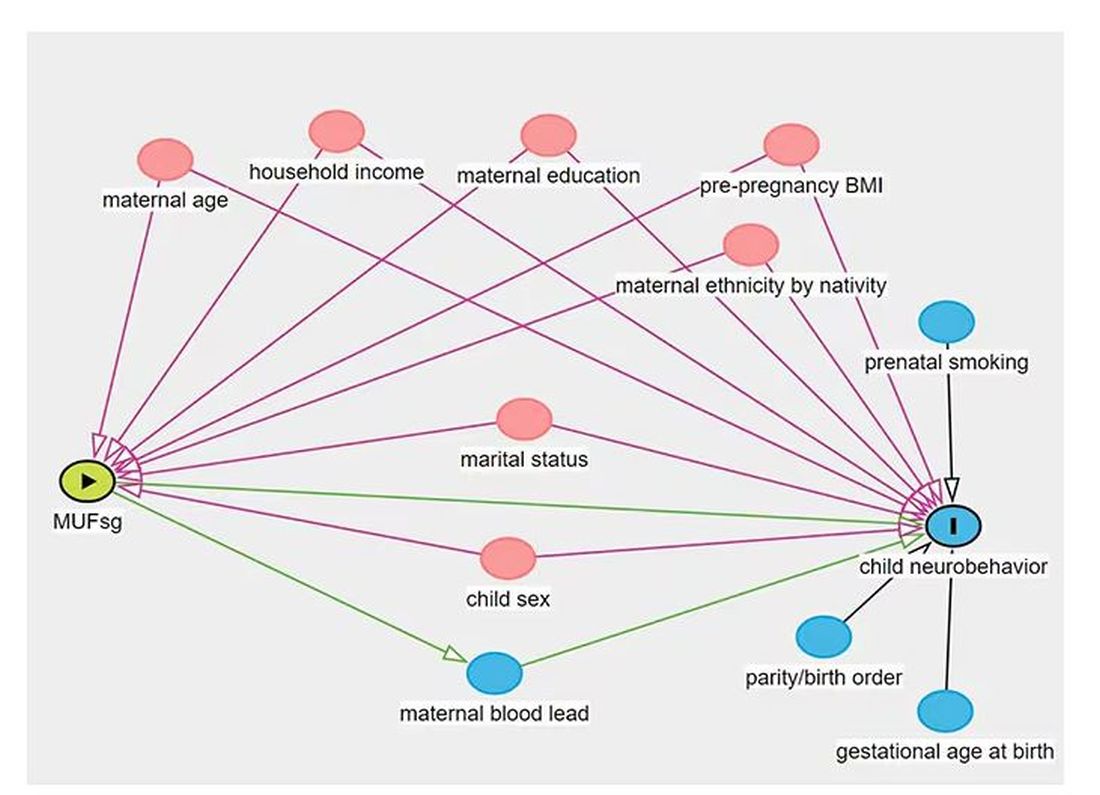
Not represented here are neighborhood characteristics. Los Angeles does not have uniformly fluoridated water, and neurobehavioral problems in kids are strongly linked to stressors in their environments. Fluoride level could be an innocent bystander.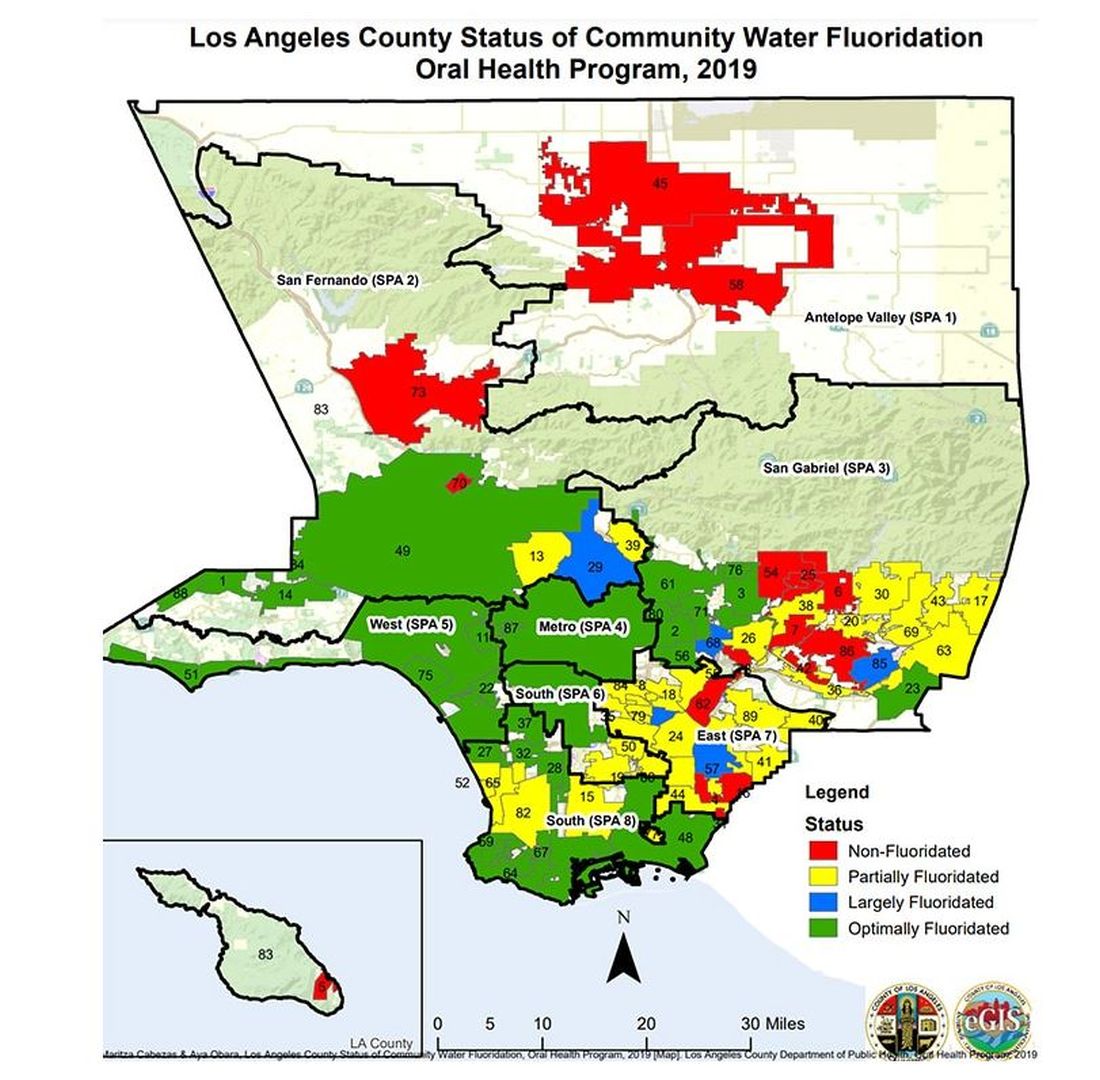
I’m really just describing the classic issue of correlation versus causation here, the bane of all observational research and — let’s be honest — a bit of a crutch that allows us to disregard the results of studies we don’t like, provided the study wasn’t a randomized trial.
But I have a deeper issue with this study than the old “failure to adjust for relevant confounders” thing, as important as that is.
The exposure of interest in this study is maternal urinary fluoride, as measured in a spot sample. It’s not often that I get to go deep on nephrology in this space, but let’s think about that for a second. Let’s assume for a moment that fluoride is toxic to the developing fetal brain, the main concern raised by the results of the study. How would that work? Presumably, mom would be ingesting fluoride from various sources (like the water supply), and that fluoride would get into her blood, and from her blood across the placenta to the baby’s blood, and into the baby’s brain.
Is Urinary Fluoride a Good Measure of Blood Fluoride?
It’s not great. Empirically, we have data that tell us that levels of urine fluoride are not all that similar to levels of serum fluoride. In 2014, a study investigated the correlation between urine and serum fluoride in a cohort of 60 schoolchildren and found a correlation coefficient of around 0.5.
Why isn’t urine fluoride a great proxy for serum fluoride? The most obvious reason is the urine concentration. Human urine concentration can range from about 50 mmol to 1200 mmol (a 24-fold difference) depending on hydration status. Over the course of 24 hours, for example, the amount of fluoride you put out in your urine may be fairly stable in relation to intake, but for a spot urine sample it would be wildly variable. The authors know this, of course, and so they divide the measured urine fluoride by the specific gravity of the urine to give a sort of “dilution adjusted” value. That’s what is actually used in this study. But specific gravity is, itself, an imperfect measure of how dilute the urine is.
This is something that comes up a lot in urinary biomarker research and it’s not that hard to get around. The best thing would be to just measure blood levels of fluoride. The second best option is 24-hour fluoride excretion. After that, the next best thing would be to adjust the spot concentration by other markers of urinary dilution — creatinine or osmolality — as sensitivity analyses. Any of these approaches would lend credence to the results of the study.
Urinary fluoride excretion is pH dependent. The more acidic the urine, the less fluoride is excreted. Many things — including, importantly, diet — affect urine pH. And it is not a stretch to think that diet may also affect the developing fetus. Neither urine pH nor dietary habits were accounted for in this study.
So, here we are. We have an observational study suggesting a harm that may be associated with fluoride. There may be a causal link here, in which case we need further studies to weigh the harm against the more well-established public health benefit. Or, this is all correlation — an illusion created by the limitations of observational data, and the unique challenges of estimating intake from a single urine sample. In other words, this study has something for everyone, fluoride boosters and skeptics alike. Let the arguments begin. But, if possible, leave me out of it.
Dr. Wilson is associate professor of medicine and public health and director of the Clinical and Translational Research Accelerator at Yale University, New Haven, Conn. He has disclosed no relevant financial relationships.
A version of this article appeared on Medscape.com.
This transcript has been edited for clarity.
I recently looked back at my folder full of these medical study commentaries, this weekly video series we call Impact Factor, and realized that I’ve been doing this for a long time. More than 400 articles, believe it or not.
I’ve learned a lot in that time — about medicine, of course — but also about how people react to certain topics. If you’ve been with me this whole time, or even for just a chunk of it, you’ll know that I tend to take a measured approach to most topics. No one study is ever truly definitive, after all. But regardless of how even-keeled I may be, there are some topics that I just know in advance are going to be a bit divisive: studies about gun control; studies about vitamin D; and, of course, studies about fluoride.
Shall We Shake This Hornet’s Nest?
The fluoridation of the US water system began in 1945 with the goal of reducing cavities in the population. The CDC named water fluoridation one of the 10 great public health achievements of the 20th century, along with such inarguable achievements as the recognition of tobacco as a health hazard.
But fluoridation has never been without its detractors. One problem is that the spectrum of beliefs about the potential harm of fluoridation is huge. On one end, you have science-based concerns such as the recognition that excessive fluoride intake can cause fluorosis and stain tooth enamel. I’ll note that the EPA regulates fluoride levels — there is a fair amount of naturally occurring fluoride in water tables around the world — to prevent this. And, of course, on the other end of the spectrum, you have beliefs that are essentially conspiracy theories: “They” add fluoride to the water supply to control us.
The challenge for me is that when one “side” of a scientific debate includes the crazy theories, it can be hard to discuss that whole spectrum, since there are those who will see evidence of any adverse fluoride effect as confirmation that the conspiracy theory is true.
I can’t help this. So I’ll just say this up front: I am about to tell you about a study that shows some potential risk from fluoride exposure. I will tell you up front that there are some significant caveats to the study that call the results into question. And I will tell you up front that no one is controlling your mind, or my mind, with fluoride; they do it with social media.
Let’s Dive Into These Shark-Infested, Fluoridated Waters
We’re talking about the study, “Maternal Urinary Fluoride and Child Neurobehavior at Age 36 Months,” which appears in JAMA Network Open.
It’s a study of 229 mother-child pairs from the Los Angeles area. The moms had their urinary fluoride level measured once before 30 weeks of gestation. A neurobehavioral battery called the Preschool Child Behavior Checklist was administered to the children at age 36 months.
The main thing you’ll hear about this study — in headlines, Facebook posts, and manifestos locked in drawers somewhere — is the primary result: A 0.68-mg/L increase in urinary fluoride in the mothers, about 25 percentile points, was associated with a doubling of the risk for neurobehavioral problems in their kids when they were 3 years old.
Yikes.
But this is not a randomized trial. Researchers didn’t randomly assign some women to have high fluoride intake and some women to have low fluoride intake. They knew that other factors that might lead to neurobehavioral problems could also lead to higher fluoride intake. They represent these factors in what’s known as a directed acyclic graph, as seen here, and account for them statistically using a regression equation.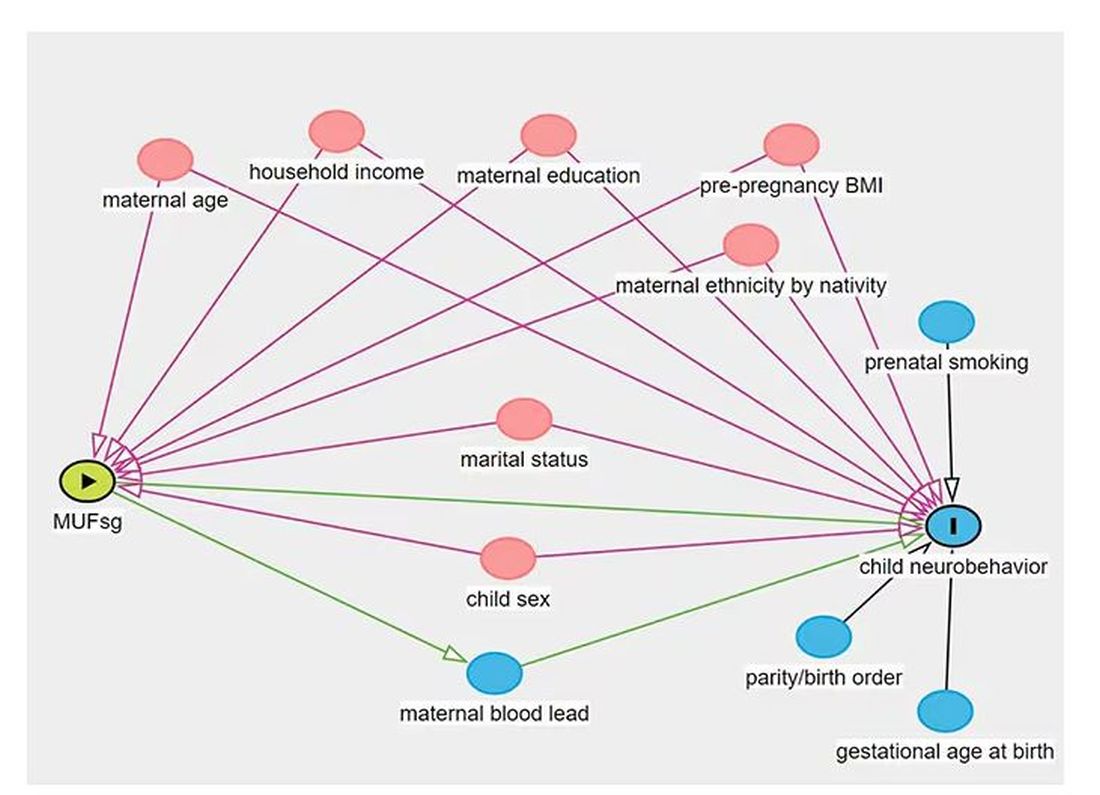
Not represented here are neighborhood characteristics. Los Angeles does not have uniformly fluoridated water, and neurobehavioral problems in kids are strongly linked to stressors in their environments. Fluoride level could be an innocent bystander.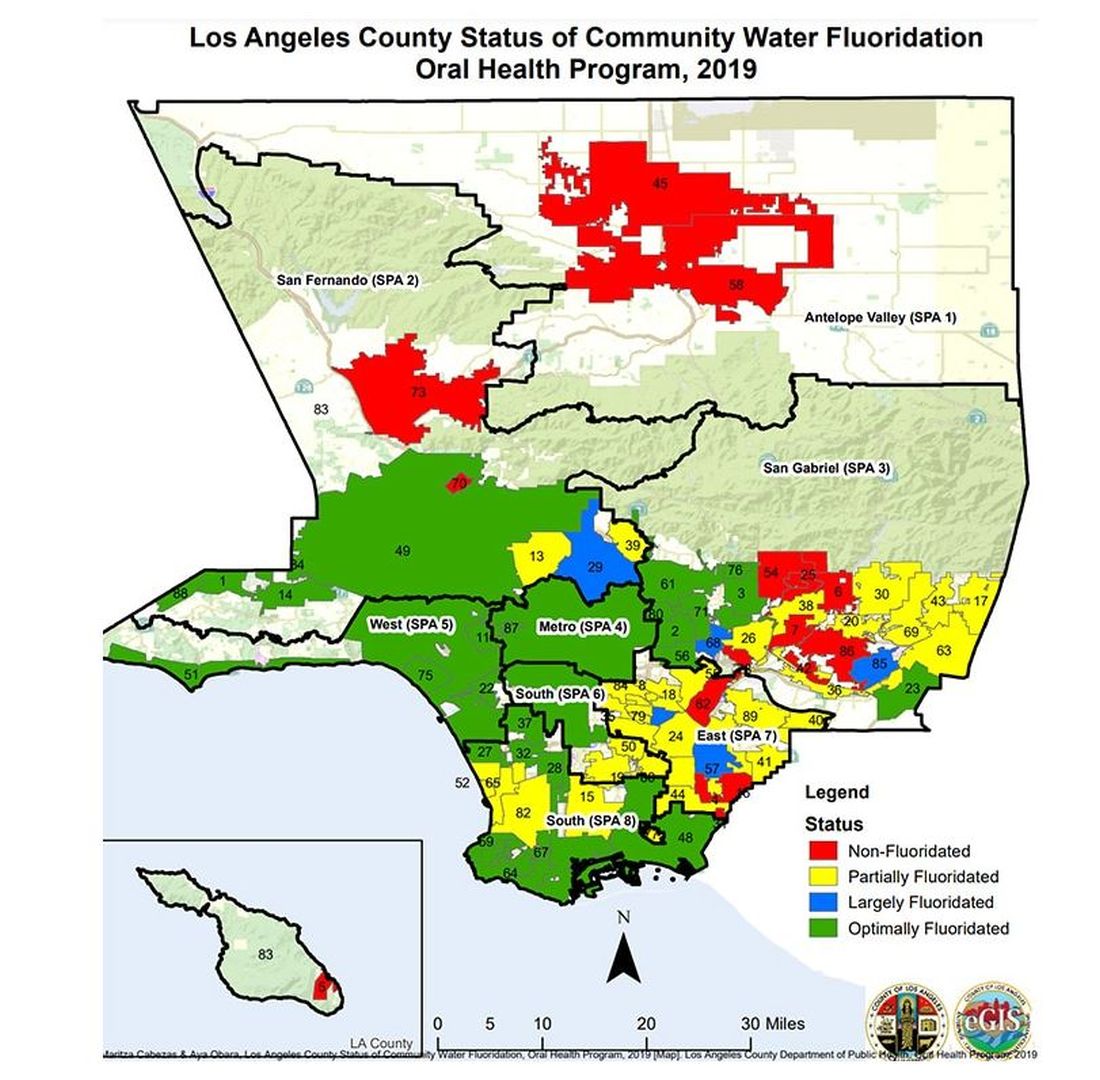
I’m really just describing the classic issue of correlation versus causation here, the bane of all observational research and — let’s be honest — a bit of a crutch that allows us to disregard the results of studies we don’t like, provided the study wasn’t a randomized trial.
But I have a deeper issue with this study than the old “failure to adjust for relevant confounders” thing, as important as that is.
The exposure of interest in this study is maternal urinary fluoride, as measured in a spot sample. It’s not often that I get to go deep on nephrology in this space, but let’s think about that for a second. Let’s assume for a moment that fluoride is toxic to the developing fetal brain, the main concern raised by the results of the study. How would that work? Presumably, mom would be ingesting fluoride from various sources (like the water supply), and that fluoride would get into her blood, and from her blood across the placenta to the baby’s blood, and into the baby’s brain.
Is Urinary Fluoride a Good Measure of Blood Fluoride?
It’s not great. Empirically, we have data that tell us that levels of urine fluoride are not all that similar to levels of serum fluoride. In 2014, a study investigated the correlation between urine and serum fluoride in a cohort of 60 schoolchildren and found a correlation coefficient of around 0.5.
Why isn’t urine fluoride a great proxy for serum fluoride? The most obvious reason is the urine concentration. Human urine concentration can range from about 50 mmol to 1200 mmol (a 24-fold difference) depending on hydration status. Over the course of 24 hours, for example, the amount of fluoride you put out in your urine may be fairly stable in relation to intake, but for a spot urine sample it would be wildly variable. The authors know this, of course, and so they divide the measured urine fluoride by the specific gravity of the urine to give a sort of “dilution adjusted” value. That’s what is actually used in this study. But specific gravity is, itself, an imperfect measure of how dilute the urine is.
This is something that comes up a lot in urinary biomarker research and it’s not that hard to get around. The best thing would be to just measure blood levels of fluoride. The second best option is 24-hour fluoride excretion. After that, the next best thing would be to adjust the spot concentration by other markers of urinary dilution — creatinine or osmolality — as sensitivity analyses. Any of these approaches would lend credence to the results of the study.
Urinary fluoride excretion is pH dependent. The more acidic the urine, the less fluoride is excreted. Many things — including, importantly, diet — affect urine pH. And it is not a stretch to think that diet may also affect the developing fetus. Neither urine pH nor dietary habits were accounted for in this study.
So, here we are. We have an observational study suggesting a harm that may be associated with fluoride. There may be a causal link here, in which case we need further studies to weigh the harm against the more well-established public health benefit. Or, this is all correlation — an illusion created by the limitations of observational data, and the unique challenges of estimating intake from a single urine sample. In other words, this study has something for everyone, fluoride boosters and skeptics alike. Let the arguments begin. But, if possible, leave me out of it.
Dr. Wilson is associate professor of medicine and public health and director of the Clinical and Translational Research Accelerator at Yale University, New Haven, Conn. He has disclosed no relevant financial relationships.
A version of this article appeared on Medscape.com.
Don’t Miss the Dx: A 24-Year-Old Man With Sudden-Onset Hematuria, Proteinuria, Edema, and Hypertension
Presentation
A 24-year-old man with no significant past medical history presents to urgent care with a 1-week history of sudden-onset dark urine, leg swelling, and unusually high blood pressure readings, with recent values around 160/100 mm Hg. Physical examination reveals pitting edema up to the mid-shins and mild periorbital edema, with an elevated blood pressure of 158/98 mm Hg. Past medical history was significant for frequent upper respiratory tract infections over the past year. Laboratory findings include hematuria, proteinuria, and a raised serum creatinine level at 1.8 mg/dL, indicating a reduced estimated glomerular filtration rate (eGFR) of 45 mL/min/1.73 m2. Other tests such as a complete blood count and comprehensive metabolic panel (except for creatinine and albumin) are within normal limits. Given these findings, the patient is referred to nephrology for further evaluation to determine the underlying cause of his renal symptoms.
Differential Diagnosis
A glomerular disease can be assumed to be present if the patient manifests glomerular hematuria, glomerular proteinuria, or both, such as in this patient.
Glomerulonephritis occurs due to inflammation in the glomeruli, which leads to blood in urine, variable degrees of protein in urine (sometimes in the nephrotic range), and white blood cells in urine without any urinary tract infection. Patients may also experience hypertension and kidney function impairment. Diagnoses to consider include:
- Postinfectious glomerulonephritis
- Crescentic glomerulonephritis
- Diffuse proliferative glomerulonephritis
- Glomerulonephritis associated with nonstreptococcal infection
- Membranoproliferative glomerulonephritis
- Membranous glomerulonephritis
- Poststreptococcal glomerulonephritis
- Rapidly Progressive glomerulonephritis
All patients presenting with proteinuria and hematuria should undergo a thorough evaluation for glomerular disease, which generally involves laboratory testing and, in most patients, a kidney biopsy to obtain a definitive diagnosis.
Diagnosis
This patient underwent a renal biopsy, which showed C3-dominant deposition by immunofluorescence; electron microscopy (EM) showed discontinuous, ill-defined intramembranous deposits; and mass spectrometry showed terminal complement components in C3 deposits. The patient was diagnosed with C3 glomerulonephritis (C3G).
The diagnosis of C3G is established by kidney biopsy demonstrating the characteristic findings on immunofluorescence microscopy or EM in a patient with suspected glomerulonephritis. In patients with biopsy-confirmed C3G, additional testing should be performed to help identify the underlying etiology of the glomerulopathy to help determine therapy.
For all patients diagnosed with C3G, especially those who are older than 50 years, it is important to rule out monoclonal gammopathy which can be done through various tests such as serum protein electrophoresis and immunofixation, serum free light chains, and urine protein electrophoresis and immunofixation. The presence of a paraprotein, including a monoclonal light chain, can activate the alternative complement cascade and may be responsible for the condition.
Expert opinion recommends a comprehensive complement evaluation for all C3 glomerulopathy patients, including overall complement activity assessment, serum levels measurement of complement proteins and their split products, and autoantibodies screening.
Complement evaluation may include:
- Serum C3 and C4
- Soluble C5b-9 (soluble membrane attack complex)
- Serum factor H
- Serum factor B, factor I, and membrane cofactor protein (MCP; CD46)
All patients with C3G should also undergo screening for autoantibodies:
- C3 nephritic factor (C3NeF)
- C5 nephritic factor (C5NeF)
- C4 nephritic factor (C4NeF)
- Other autoantibodies against factor H, factor B, and/or C3b
It is recommended that genetic testing be considered for patients with C3 glomerulopathy to screen for complement genes including C3, CFB, CFH, CFHR5, and CFI and copy number variations and rearrangements of the CFH-CFHR gene cluster. The value of genetic testing in the clinical setting is still being defined; however, it has been observed that patients with mutations in complement genes generally respond less favorably to mycophenolate mofetil (MMF) compared with those who are positive for nephritic factors.
Management
The patient was managed with an angiotensin-converting enzyme (ACE) inhibitor to treat proteinuria and hypertension and MMF for immunosuppression. Enrollment in a clinical trial of an investigational complement inhibitor was discussed with the patient.
Currently, there are no therapeutic agents specifically designed to target the underlying complement dysregulation that occurs in individuals with C3G, and an optimal treatment for C3 glomerulopathy has not been established.
Various nonspecific therapies have been used to treat C3G, including plasmapheresis, steroids, rituximab, cyclophosphamide, and MMF and have shown positive results. For patients with C3G who have a known genetic variant (eg, CFH mutation) or who have acute kidney injury, plasmapheresis and plasma exchange may be helpful. Using these agents judiciously and in conjunction with optimal blood pressure control is important for maximum benefit in treating C3G. When someone with end-stage renal disease (ESRD) caused by C3G chooses to have a kidney transplant, it is important to know that C3G is likely to return in almost all cases and is the leading cause of transplant failure in 50%-90% of recipients.
Prognosis
The prognosis of C3G varies and is affected by various clinical and histological factors. While some patients may have consistently low levels of protein in their urine and maintain stable kidney function over time, others may experience severe nephrotic syndrome or rapidly progressive glomerulonephritis, which often leads to a poor prognosis.
Progression to ESRD is a major complication of C3G, with approximately 70% of affected children and 30%-50% of adults reaching this stage. In addition, disease recurrence is common after kidney transplantation, with about 50% of patients experiencing allograft loss within 10 years. Predictive factors for disease progression, although not robustly established, include initial eGFR at diagnosis, percentage of tubular atrophy, and extent of interstitial fibrosis in the cortical area as observed on kidney biopsies.
Clinical Takeaways
For patients exhibiting symptoms like proteinuria and hematuria indicative of glomerulonephritis, a comprehensive evaluation including laboratory tests and a kidney biopsy is essential to confirm a C3G diagnosis through characteristic findings on immunofluorescence microscopy or electron microscopy.
Additional tests to rule out associated conditions like monoclonal gammopathy and comprehensive complement evaluation are also recommended to understand the underlying etiology and guide therapy.
Though there are no treatments specifically targeting the underlying complement dysregulation unique to C3G, nonspecific therapies like ACE inhibitors, immunosuppressants (eg, MMF), and plasmapheresis are commonly used.
Some anticomplement therapies are available or under investigation, which might offer more targeted intervention options.
The prognosis for patients with C3G can vary widely and factors such as initial eGFR, the extent of tubular atrophy, and interstitial fibrosis are important predictors of disease progression.
Dr. Alper is an associate professor, Nephrology, Tulane University School of Medicine, New Orleans, Louisiana. He has disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Presentation
A 24-year-old man with no significant past medical history presents to urgent care with a 1-week history of sudden-onset dark urine, leg swelling, and unusually high blood pressure readings, with recent values around 160/100 mm Hg. Physical examination reveals pitting edema up to the mid-shins and mild periorbital edema, with an elevated blood pressure of 158/98 mm Hg. Past medical history was significant for frequent upper respiratory tract infections over the past year. Laboratory findings include hematuria, proteinuria, and a raised serum creatinine level at 1.8 mg/dL, indicating a reduced estimated glomerular filtration rate (eGFR) of 45 mL/min/1.73 m2. Other tests such as a complete blood count and comprehensive metabolic panel (except for creatinine and albumin) are within normal limits. Given these findings, the patient is referred to nephrology for further evaluation to determine the underlying cause of his renal symptoms.
Differential Diagnosis
A glomerular disease can be assumed to be present if the patient manifests glomerular hematuria, glomerular proteinuria, or both, such as in this patient.
Glomerulonephritis occurs due to inflammation in the glomeruli, which leads to blood in urine, variable degrees of protein in urine (sometimes in the nephrotic range), and white blood cells in urine without any urinary tract infection. Patients may also experience hypertension and kidney function impairment. Diagnoses to consider include:
- Postinfectious glomerulonephritis
- Crescentic glomerulonephritis
- Diffuse proliferative glomerulonephritis
- Glomerulonephritis associated with nonstreptococcal infection
- Membranoproliferative glomerulonephritis
- Membranous glomerulonephritis
- Poststreptococcal glomerulonephritis
- Rapidly Progressive glomerulonephritis
All patients presenting with proteinuria and hematuria should undergo a thorough evaluation for glomerular disease, which generally involves laboratory testing and, in most patients, a kidney biopsy to obtain a definitive diagnosis.
Diagnosis
This patient underwent a renal biopsy, which showed C3-dominant deposition by immunofluorescence; electron microscopy (EM) showed discontinuous, ill-defined intramembranous deposits; and mass spectrometry showed terminal complement components in C3 deposits. The patient was diagnosed with C3 glomerulonephritis (C3G).
The diagnosis of C3G is established by kidney biopsy demonstrating the characteristic findings on immunofluorescence microscopy or EM in a patient with suspected glomerulonephritis. In patients with biopsy-confirmed C3G, additional testing should be performed to help identify the underlying etiology of the glomerulopathy to help determine therapy.
For all patients diagnosed with C3G, especially those who are older than 50 years, it is important to rule out monoclonal gammopathy which can be done through various tests such as serum protein electrophoresis and immunofixation, serum free light chains, and urine protein electrophoresis and immunofixation. The presence of a paraprotein, including a monoclonal light chain, can activate the alternative complement cascade and may be responsible for the condition.
Expert opinion recommends a comprehensive complement evaluation for all C3 glomerulopathy patients, including overall complement activity assessment, serum levels measurement of complement proteins and their split products, and autoantibodies screening.
Complement evaluation may include:
- Serum C3 and C4
- Soluble C5b-9 (soluble membrane attack complex)
- Serum factor H
- Serum factor B, factor I, and membrane cofactor protein (MCP; CD46)
All patients with C3G should also undergo screening for autoantibodies:
- C3 nephritic factor (C3NeF)
- C5 nephritic factor (C5NeF)
- C4 nephritic factor (C4NeF)
- Other autoantibodies against factor H, factor B, and/or C3b
It is recommended that genetic testing be considered for patients with C3 glomerulopathy to screen for complement genes including C3, CFB, CFH, CFHR5, and CFI and copy number variations and rearrangements of the CFH-CFHR gene cluster. The value of genetic testing in the clinical setting is still being defined; however, it has been observed that patients with mutations in complement genes generally respond less favorably to mycophenolate mofetil (MMF) compared with those who are positive for nephritic factors.
Management
The patient was managed with an angiotensin-converting enzyme (ACE) inhibitor to treat proteinuria and hypertension and MMF for immunosuppression. Enrollment in a clinical trial of an investigational complement inhibitor was discussed with the patient.
Currently, there are no therapeutic agents specifically designed to target the underlying complement dysregulation that occurs in individuals with C3G, and an optimal treatment for C3 glomerulopathy has not been established.
Various nonspecific therapies have been used to treat C3G, including plasmapheresis, steroids, rituximab, cyclophosphamide, and MMF and have shown positive results. For patients with C3G who have a known genetic variant (eg, CFH mutation) or who have acute kidney injury, plasmapheresis and plasma exchange may be helpful. Using these agents judiciously and in conjunction with optimal blood pressure control is important for maximum benefit in treating C3G. When someone with end-stage renal disease (ESRD) caused by C3G chooses to have a kidney transplant, it is important to know that C3G is likely to return in almost all cases and is the leading cause of transplant failure in 50%-90% of recipients.
Prognosis
The prognosis of C3G varies and is affected by various clinical and histological factors. While some patients may have consistently low levels of protein in their urine and maintain stable kidney function over time, others may experience severe nephrotic syndrome or rapidly progressive glomerulonephritis, which often leads to a poor prognosis.
Progression to ESRD is a major complication of C3G, with approximately 70% of affected children and 30%-50% of adults reaching this stage. In addition, disease recurrence is common after kidney transplantation, with about 50% of patients experiencing allograft loss within 10 years. Predictive factors for disease progression, although not robustly established, include initial eGFR at diagnosis, percentage of tubular atrophy, and extent of interstitial fibrosis in the cortical area as observed on kidney biopsies.
Clinical Takeaways
For patients exhibiting symptoms like proteinuria and hematuria indicative of glomerulonephritis, a comprehensive evaluation including laboratory tests and a kidney biopsy is essential to confirm a C3G diagnosis through characteristic findings on immunofluorescence microscopy or electron microscopy.
Additional tests to rule out associated conditions like monoclonal gammopathy and comprehensive complement evaluation are also recommended to understand the underlying etiology and guide therapy.
Though there are no treatments specifically targeting the underlying complement dysregulation unique to C3G, nonspecific therapies like ACE inhibitors, immunosuppressants (eg, MMF), and plasmapheresis are commonly used.
Some anticomplement therapies are available or under investigation, which might offer more targeted intervention options.
The prognosis for patients with C3G can vary widely and factors such as initial eGFR, the extent of tubular atrophy, and interstitial fibrosis are important predictors of disease progression.
Dr. Alper is an associate professor, Nephrology, Tulane University School of Medicine, New Orleans, Louisiana. He has disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Presentation
A 24-year-old man with no significant past medical history presents to urgent care with a 1-week history of sudden-onset dark urine, leg swelling, and unusually high blood pressure readings, with recent values around 160/100 mm Hg. Physical examination reveals pitting edema up to the mid-shins and mild periorbital edema, with an elevated blood pressure of 158/98 mm Hg. Past medical history was significant for frequent upper respiratory tract infections over the past year. Laboratory findings include hematuria, proteinuria, and a raised serum creatinine level at 1.8 mg/dL, indicating a reduced estimated glomerular filtration rate (eGFR) of 45 mL/min/1.73 m2. Other tests such as a complete blood count and comprehensive metabolic panel (except for creatinine and albumin) are within normal limits. Given these findings, the patient is referred to nephrology for further evaluation to determine the underlying cause of his renal symptoms.
Differential Diagnosis
A glomerular disease can be assumed to be present if the patient manifests glomerular hematuria, glomerular proteinuria, or both, such as in this patient.
Glomerulonephritis occurs due to inflammation in the glomeruli, which leads to blood in urine, variable degrees of protein in urine (sometimes in the nephrotic range), and white blood cells in urine without any urinary tract infection. Patients may also experience hypertension and kidney function impairment. Diagnoses to consider include:
- Postinfectious glomerulonephritis
- Crescentic glomerulonephritis
- Diffuse proliferative glomerulonephritis
- Glomerulonephritis associated with nonstreptococcal infection
- Membranoproliferative glomerulonephritis
- Membranous glomerulonephritis
- Poststreptococcal glomerulonephritis
- Rapidly Progressive glomerulonephritis
All patients presenting with proteinuria and hematuria should undergo a thorough evaluation for glomerular disease, which generally involves laboratory testing and, in most patients, a kidney biopsy to obtain a definitive diagnosis.
Diagnosis
This patient underwent a renal biopsy, which showed C3-dominant deposition by immunofluorescence; electron microscopy (EM) showed discontinuous, ill-defined intramembranous deposits; and mass spectrometry showed terminal complement components in C3 deposits. The patient was diagnosed with C3 glomerulonephritis (C3G).
The diagnosis of C3G is established by kidney biopsy demonstrating the characteristic findings on immunofluorescence microscopy or EM in a patient with suspected glomerulonephritis. In patients with biopsy-confirmed C3G, additional testing should be performed to help identify the underlying etiology of the glomerulopathy to help determine therapy.
For all patients diagnosed with C3G, especially those who are older than 50 years, it is important to rule out monoclonal gammopathy which can be done through various tests such as serum protein electrophoresis and immunofixation, serum free light chains, and urine protein electrophoresis and immunofixation. The presence of a paraprotein, including a monoclonal light chain, can activate the alternative complement cascade and may be responsible for the condition.
Expert opinion recommends a comprehensive complement evaluation for all C3 glomerulopathy patients, including overall complement activity assessment, serum levels measurement of complement proteins and their split products, and autoantibodies screening.
Complement evaluation may include:
- Serum C3 and C4
- Soluble C5b-9 (soluble membrane attack complex)
- Serum factor H
- Serum factor B, factor I, and membrane cofactor protein (MCP; CD46)
All patients with C3G should also undergo screening for autoantibodies:
- C3 nephritic factor (C3NeF)
- C5 nephritic factor (C5NeF)
- C4 nephritic factor (C4NeF)
- Other autoantibodies against factor H, factor B, and/or C3b
It is recommended that genetic testing be considered for patients with C3 glomerulopathy to screen for complement genes including C3, CFB, CFH, CFHR5, and CFI and copy number variations and rearrangements of the CFH-CFHR gene cluster. The value of genetic testing in the clinical setting is still being defined; however, it has been observed that patients with mutations in complement genes generally respond less favorably to mycophenolate mofetil (MMF) compared with those who are positive for nephritic factors.
Management
The patient was managed with an angiotensin-converting enzyme (ACE) inhibitor to treat proteinuria and hypertension and MMF for immunosuppression. Enrollment in a clinical trial of an investigational complement inhibitor was discussed with the patient.
Currently, there are no therapeutic agents specifically designed to target the underlying complement dysregulation that occurs in individuals with C3G, and an optimal treatment for C3 glomerulopathy has not been established.
Various nonspecific therapies have been used to treat C3G, including plasmapheresis, steroids, rituximab, cyclophosphamide, and MMF and have shown positive results. For patients with C3G who have a known genetic variant (eg, CFH mutation) or who have acute kidney injury, plasmapheresis and plasma exchange may be helpful. Using these agents judiciously and in conjunction with optimal blood pressure control is important for maximum benefit in treating C3G. When someone with end-stage renal disease (ESRD) caused by C3G chooses to have a kidney transplant, it is important to know that C3G is likely to return in almost all cases and is the leading cause of transplant failure in 50%-90% of recipients.
Prognosis
The prognosis of C3G varies and is affected by various clinical and histological factors. While some patients may have consistently low levels of protein in their urine and maintain stable kidney function over time, others may experience severe nephrotic syndrome or rapidly progressive glomerulonephritis, which often leads to a poor prognosis.
Progression to ESRD is a major complication of C3G, with approximately 70% of affected children and 30%-50% of adults reaching this stage. In addition, disease recurrence is common after kidney transplantation, with about 50% of patients experiencing allograft loss within 10 years. Predictive factors for disease progression, although not robustly established, include initial eGFR at diagnosis, percentage of tubular atrophy, and extent of interstitial fibrosis in the cortical area as observed on kidney biopsies.
Clinical Takeaways
For patients exhibiting symptoms like proteinuria and hematuria indicative of glomerulonephritis, a comprehensive evaluation including laboratory tests and a kidney biopsy is essential to confirm a C3G diagnosis through characteristic findings on immunofluorescence microscopy or electron microscopy.
Additional tests to rule out associated conditions like monoclonal gammopathy and comprehensive complement evaluation are also recommended to understand the underlying etiology and guide therapy.
Though there are no treatments specifically targeting the underlying complement dysregulation unique to C3G, nonspecific therapies like ACE inhibitors, immunosuppressants (eg, MMF), and plasmapheresis are commonly used.
Some anticomplement therapies are available or under investigation, which might offer more targeted intervention options.
The prognosis for patients with C3G can vary widely and factors such as initial eGFR, the extent of tubular atrophy, and interstitial fibrosis are important predictors of disease progression.
Dr. Alper is an associate professor, Nephrology, Tulane University School of Medicine, New Orleans, Louisiana. He has disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
An 8-year-old girl presented with papules on her bilateral eyelid margins
, with an equal distribution across genders and ethnicities.1 It is caused by mutations in the ECM1 gene2 on chromosome 1q21. This leads to the abnormal deposition of hyaline material in various tissues across different organ systems, with the classic manifestations known as the “string of pearls” sign and a hoarse cry or voice.
The rarity of lipoid proteinosis often leads to challenges in diagnosis. Particularly when deviating from the common association with consanguinity, the potential for de novo mutations or a broader genetic variability in disease expression is highlighted. Our patient presents with symptoms that are pathognomonic to LP with moniliform blepharosis and hoarseness of the voice, in addition to scarring of the extremities.
Other common clinical manifestations in patients with LP include cobblestoning of the mucosa; hyperkeratosis of the elbows, knees, and hands; and calcification of the amygdala with neuroimaging.3
Genetic testing that identifies a loss-of-function mutation in ECM1 offers diagnostic confirmation. Patients often need multidisciplinary care involving dermatology; ear, nose, throat; neurology; and genetics. Treatment of LP is mostly symptomatic with unsatisfactory resolution of cutaneous changes, with retinoids such as acitretin used as the first-line option and surgery as a consideration for laryngeal hyaline deposits.2 Although LP can affect different organ systems, patients tend to have a normal lifespan.
LP is a rare disorder that dermatologists often learn about during textbook sessions or didactics in residency but do not see in practice for decades, or if ever. This case highlights the need to review the classic presentations of rare conditions.
This case and the photos were submitted by Ms. Chang, BS, Western University of Health Sciences, College of Osteopathic Medicine, Pomona, California; Dr. Connie Chang, Verdugo Dermatology, Glendale, California; and Dr. Yuchieh Kathryn Chang, MD Anderson Cancer Center, Houston, Texas. The column was edited by Donna Bilu Martin, MD.
Dr. Bilu Martin is a board-certified dermatologist in private practice at Premier Dermatology, MD, in Aventura, Florida. More diagnostic cases are available at mdedge.com/dermatology. To submit a case for possible publication, send an email to [email protected].
References
1. Mcgrath JA. Handb Clin Neurol. 2015:132:317-22. doi: 10.1016/B978-0-444-62702-5.00023-8.
2. Hamada Tet al. Hum Mol Genet. 2002 Apr 1;11(7):833-40. doi: 10.1093/hmg/11.7.833.
3. Frenkel B et al. Clin Oral Investig. 2017 Sep;21(7):2245-51 doi: 10.1007/s00784-016-2017-7.
, with an equal distribution across genders and ethnicities.1 It is caused by mutations in the ECM1 gene2 on chromosome 1q21. This leads to the abnormal deposition of hyaline material in various tissues across different organ systems, with the classic manifestations known as the “string of pearls” sign and a hoarse cry or voice.
The rarity of lipoid proteinosis often leads to challenges in diagnosis. Particularly when deviating from the common association with consanguinity, the potential for de novo mutations or a broader genetic variability in disease expression is highlighted. Our patient presents with symptoms that are pathognomonic to LP with moniliform blepharosis and hoarseness of the voice, in addition to scarring of the extremities.
Other common clinical manifestations in patients with LP include cobblestoning of the mucosa; hyperkeratosis of the elbows, knees, and hands; and calcification of the amygdala with neuroimaging.3
Genetic testing that identifies a loss-of-function mutation in ECM1 offers diagnostic confirmation. Patients often need multidisciplinary care involving dermatology; ear, nose, throat; neurology; and genetics. Treatment of LP is mostly symptomatic with unsatisfactory resolution of cutaneous changes, with retinoids such as acitretin used as the first-line option and surgery as a consideration for laryngeal hyaline deposits.2 Although LP can affect different organ systems, patients tend to have a normal lifespan.
LP is a rare disorder that dermatologists often learn about during textbook sessions or didactics in residency but do not see in practice for decades, or if ever. This case highlights the need to review the classic presentations of rare conditions.
This case and the photos were submitted by Ms. Chang, BS, Western University of Health Sciences, College of Osteopathic Medicine, Pomona, California; Dr. Connie Chang, Verdugo Dermatology, Glendale, California; and Dr. Yuchieh Kathryn Chang, MD Anderson Cancer Center, Houston, Texas. The column was edited by Donna Bilu Martin, MD.
Dr. Bilu Martin is a board-certified dermatologist in private practice at Premier Dermatology, MD, in Aventura, Florida. More diagnostic cases are available at mdedge.com/dermatology. To submit a case for possible publication, send an email to [email protected].
References
1. Mcgrath JA. Handb Clin Neurol. 2015:132:317-22. doi: 10.1016/B978-0-444-62702-5.00023-8.
2. Hamada Tet al. Hum Mol Genet. 2002 Apr 1;11(7):833-40. doi: 10.1093/hmg/11.7.833.
3. Frenkel B et al. Clin Oral Investig. 2017 Sep;21(7):2245-51 doi: 10.1007/s00784-016-2017-7.
, with an equal distribution across genders and ethnicities.1 It is caused by mutations in the ECM1 gene2 on chromosome 1q21. This leads to the abnormal deposition of hyaline material in various tissues across different organ systems, with the classic manifestations known as the “string of pearls” sign and a hoarse cry or voice.
The rarity of lipoid proteinosis often leads to challenges in diagnosis. Particularly when deviating from the common association with consanguinity, the potential for de novo mutations or a broader genetic variability in disease expression is highlighted. Our patient presents with symptoms that are pathognomonic to LP with moniliform blepharosis and hoarseness of the voice, in addition to scarring of the extremities.
Other common clinical manifestations in patients with LP include cobblestoning of the mucosa; hyperkeratosis of the elbows, knees, and hands; and calcification of the amygdala with neuroimaging.3
Genetic testing that identifies a loss-of-function mutation in ECM1 offers diagnostic confirmation. Patients often need multidisciplinary care involving dermatology; ear, nose, throat; neurology; and genetics. Treatment of LP is mostly symptomatic with unsatisfactory resolution of cutaneous changes, with retinoids such as acitretin used as the first-line option and surgery as a consideration for laryngeal hyaline deposits.2 Although LP can affect different organ systems, patients tend to have a normal lifespan.
LP is a rare disorder that dermatologists often learn about during textbook sessions or didactics in residency but do not see in practice for decades, or if ever. This case highlights the need to review the classic presentations of rare conditions.
This case and the photos were submitted by Ms. Chang, BS, Western University of Health Sciences, College of Osteopathic Medicine, Pomona, California; Dr. Connie Chang, Verdugo Dermatology, Glendale, California; and Dr. Yuchieh Kathryn Chang, MD Anderson Cancer Center, Houston, Texas. The column was edited by Donna Bilu Martin, MD.
Dr. Bilu Martin is a board-certified dermatologist in private practice at Premier Dermatology, MD, in Aventura, Florida. More diagnostic cases are available at mdedge.com/dermatology. To submit a case for possible publication, send an email to [email protected].
References
1. Mcgrath JA. Handb Clin Neurol. 2015:132:317-22. doi: 10.1016/B978-0-444-62702-5.00023-8.
2. Hamada Tet al. Hum Mol Genet. 2002 Apr 1;11(7):833-40. doi: 10.1093/hmg/11.7.833.
3. Frenkel B et al. Clin Oral Investig. 2017 Sep;21(7):2245-51 doi: 10.1007/s00784-016-2017-7.
Guidance for Practicing Primary Care: Updated Clinical Guidelines Regarding Dry Eye Syndrome
On February 11, 2024, the American Academy of Ophthalmology (AAO) issued new guidelines regarding dry eye syndrome or keratoconjunctivitis sicca. According to the National Eye Institute, dry eye affects approximately 16 million Americans. Dry eye is a multifactorial disease with causes including excessive screen time and refractive surgery. While it may seem that dry eye is a nuisance disease, it can actually damage the cornea if not treated appropriately.
The guidelines state that dry eye can affect the quality of life as well as the outcomes of ocular surgeries such as cataract surgery. It is imperative that we discuss this potential complication before our patients undergo these procedures. As primary care physicians, we have seen that patients may not be well educated on their health conditions by other doctors. We may not be the one performing the surgery but it is likely the patient will seek our advice if any complication arises.
The guidelines say that clinical examination is the gold standard for diagnosing this disease. We need to be proficient at doing eye exams and refer to a specialist when appropriate. The treatment can likely be undertaken in the primary care office unless there are other symptoms such as loss of visual acuity. The guidelines suggest several diagnostic tests, such as the Schirmer test and tear osmolarity test, which may be outside the scope of the primary care setting. Often, clinical history will guide the diagnosis.
Treatments include several Food and Drug Administration–approved eye drops. We need to know what they are and when to prescribe them. We know they will not cure the disease but can keep it under control and improve the patient’s quality of life.
Dry eye may seem a trivial complaint in the sea of diseases we treat on a daily basis. However, it is not trivial to the patient. It can affect their vision and make their life miserable. We need to pay attention when our patients bring this to our attention. We are not just making them comfortable but protecting their corneas. This can be done in conjunction with routine ophthalmologic visits.
According to the authors of these guidelines, approximately 10% of patients with significantly dry eyes and mouth will have Sj
These guidelines also suggest a classification for dry eye including mild, moderate, and severe. Since the treatment varies depending on classification, we need to learn this classification system. They also stress follow-up visits. It is not enough just to diagnose the disease and start treatment, we need to see the patients back for follow-up.
Currently, most people work and play on electronic devices. Dry eye syndrome can make this more difficult and vice versa. While it is typically not a vision-threatening disease, it can be a life-altering one. Ocular symptoms are something we see frequently in our practices, from allergic conjunctivitis to glaucoma. Often, the patient starts seeking help in our office.
Yes, our patients may have more life-threatening diseases. Our job is not just to save lives but to help our patients live healthy lives. If their lives are being affected by any disease, we must step in and do something. Dry eye is not just an inconvenience but something that causes great suffering. Eventually we may end up referring the patient to the ophthalmologist, but if we can do something to ease their discomfort while they are waiting, we would be changing their lives. We must educate ourselves on this disease and appropriate treatments to be prescribed depending on the classification of disease.
Dr. Girgis practices family medicine in South River, N.J., and is a clinical assistant professor of family medicine at Robert Wood Johnson Medical School, New Brunswick, NJ. She has no conflicts of interest.
On February 11, 2024, the American Academy of Ophthalmology (AAO) issued new guidelines regarding dry eye syndrome or keratoconjunctivitis sicca. According to the National Eye Institute, dry eye affects approximately 16 million Americans. Dry eye is a multifactorial disease with causes including excessive screen time and refractive surgery. While it may seem that dry eye is a nuisance disease, it can actually damage the cornea if not treated appropriately.
The guidelines state that dry eye can affect the quality of life as well as the outcomes of ocular surgeries such as cataract surgery. It is imperative that we discuss this potential complication before our patients undergo these procedures. As primary care physicians, we have seen that patients may not be well educated on their health conditions by other doctors. We may not be the one performing the surgery but it is likely the patient will seek our advice if any complication arises.
The guidelines say that clinical examination is the gold standard for diagnosing this disease. We need to be proficient at doing eye exams and refer to a specialist when appropriate. The treatment can likely be undertaken in the primary care office unless there are other symptoms such as loss of visual acuity. The guidelines suggest several diagnostic tests, such as the Schirmer test and tear osmolarity test, which may be outside the scope of the primary care setting. Often, clinical history will guide the diagnosis.
Treatments include several Food and Drug Administration–approved eye drops. We need to know what they are and when to prescribe them. We know they will not cure the disease but can keep it under control and improve the patient’s quality of life.
Dry eye may seem a trivial complaint in the sea of diseases we treat on a daily basis. However, it is not trivial to the patient. It can affect their vision and make their life miserable. We need to pay attention when our patients bring this to our attention. We are not just making them comfortable but protecting their corneas. This can be done in conjunction with routine ophthalmologic visits.
According to the authors of these guidelines, approximately 10% of patients with significantly dry eyes and mouth will have Sj
These guidelines also suggest a classification for dry eye including mild, moderate, and severe. Since the treatment varies depending on classification, we need to learn this classification system. They also stress follow-up visits. It is not enough just to diagnose the disease and start treatment, we need to see the patients back for follow-up.
Currently, most people work and play on electronic devices. Dry eye syndrome can make this more difficult and vice versa. While it is typically not a vision-threatening disease, it can be a life-altering one. Ocular symptoms are something we see frequently in our practices, from allergic conjunctivitis to glaucoma. Often, the patient starts seeking help in our office.
Yes, our patients may have more life-threatening diseases. Our job is not just to save lives but to help our patients live healthy lives. If their lives are being affected by any disease, we must step in and do something. Dry eye is not just an inconvenience but something that causes great suffering. Eventually we may end up referring the patient to the ophthalmologist, but if we can do something to ease their discomfort while they are waiting, we would be changing their lives. We must educate ourselves on this disease and appropriate treatments to be prescribed depending on the classification of disease.
Dr. Girgis practices family medicine in South River, N.J., and is a clinical assistant professor of family medicine at Robert Wood Johnson Medical School, New Brunswick, NJ. She has no conflicts of interest.
On February 11, 2024, the American Academy of Ophthalmology (AAO) issued new guidelines regarding dry eye syndrome or keratoconjunctivitis sicca. According to the National Eye Institute, dry eye affects approximately 16 million Americans. Dry eye is a multifactorial disease with causes including excessive screen time and refractive surgery. While it may seem that dry eye is a nuisance disease, it can actually damage the cornea if not treated appropriately.
The guidelines state that dry eye can affect the quality of life as well as the outcomes of ocular surgeries such as cataract surgery. It is imperative that we discuss this potential complication before our patients undergo these procedures. As primary care physicians, we have seen that patients may not be well educated on their health conditions by other doctors. We may not be the one performing the surgery but it is likely the patient will seek our advice if any complication arises.
The guidelines say that clinical examination is the gold standard for diagnosing this disease. We need to be proficient at doing eye exams and refer to a specialist when appropriate. The treatment can likely be undertaken in the primary care office unless there are other symptoms such as loss of visual acuity. The guidelines suggest several diagnostic tests, such as the Schirmer test and tear osmolarity test, which may be outside the scope of the primary care setting. Often, clinical history will guide the diagnosis.
Treatments include several Food and Drug Administration–approved eye drops. We need to know what they are and when to prescribe them. We know they will not cure the disease but can keep it under control and improve the patient’s quality of life.
Dry eye may seem a trivial complaint in the sea of diseases we treat on a daily basis. However, it is not trivial to the patient. It can affect their vision and make their life miserable. We need to pay attention when our patients bring this to our attention. We are not just making them comfortable but protecting their corneas. This can be done in conjunction with routine ophthalmologic visits.
According to the authors of these guidelines, approximately 10% of patients with significantly dry eyes and mouth will have Sj
These guidelines also suggest a classification for dry eye including mild, moderate, and severe. Since the treatment varies depending on classification, we need to learn this classification system. They also stress follow-up visits. It is not enough just to diagnose the disease and start treatment, we need to see the patients back for follow-up.
Currently, most people work and play on electronic devices. Dry eye syndrome can make this more difficult and vice versa. While it is typically not a vision-threatening disease, it can be a life-altering one. Ocular symptoms are something we see frequently in our practices, from allergic conjunctivitis to glaucoma. Often, the patient starts seeking help in our office.
Yes, our patients may have more life-threatening diseases. Our job is not just to save lives but to help our patients live healthy lives. If their lives are being affected by any disease, we must step in and do something. Dry eye is not just an inconvenience but something that causes great suffering. Eventually we may end up referring the patient to the ophthalmologist, but if we can do something to ease their discomfort while they are waiting, we would be changing their lives. We must educate ourselves on this disease and appropriate treatments to be prescribed depending on the classification of disease.
Dr. Girgis practices family medicine in South River, N.J., and is a clinical assistant professor of family medicine at Robert Wood Johnson Medical School, New Brunswick, NJ. She has no conflicts of interest.
Macadamia and Sapucaia Extracts and the Skin
Macadamia (Macadamia tetraphylla) is endemic to Australia and is now commercially cultivated worldwide.1 It is closely related genetically to the other macadamia plants, including the other main one, M. integrifolia, cultivated for macadamia nuts. Known in Brazil as sapucaia or castanha-de-sapucaia, Lecythis pisonis (also referred to as “cream nut” or “monkey pot”) is a large, deciduous tropical tree and member of the Brazil nut family, Lecythidaceae.2 Various parts of both of these plants have been associated with medicinal properties, including the potential for dermatologic activity. Notably, the leaves of L. pisonis have been used in traditional medicine to treat pruritus.2 .
Macadamia
Extraction to Harness Antioxidant Activity
In 2015, Dailey and Vuong developed an aqueous extraction process to recover the phenolic content and antioxidant functionality from the skin waste of M. tetraphylla using response surface methodology. As an environmentally suitable solvent that is also cheap and safe, water was chosen to maximize the extraction scenario. They identified the proper conditions (90° C, a time of 20 min, and a sample-to-solvent ratio of 5 g/100 mL) to obtain sufficient phenolic compounds, proanthocyanidins, and flavonoids to render robust antioxidant function.1
Early in 2023, Somwongin et al. investigated various green extraction methods for viability in harnessing the cosmetic/cosmeceutical ingredients of M. integrifolia pericarps. Extracts were assessed for total phenolic content as well as antioxidant and anti–skin aging functions. They found that among the green extraction methods (ultrasound, micellar, microwave, and pulsed electric field extraction with water used as a clean solvent), the ultrasound-assisted extraction method netted the greatest yield and total phenolic content. It was also associated with the most robust antioxidant and anti–skin aging activities. Indeed, the researchers reported that its antioxidant activities were comparable to ascorbic acid and Trolox and its anti–skin aging potency on a par with epigallocatechin-3-gallate and oleanolic acid. The ultrasound-assisted extract was also deemed safe as it did not provoke irritation. The authors concluded that this environmentally suitable extraction method for M. integrifolia is appropriate for obtaining effective macadamia extracts for use in cosmetics and cosmeceuticals.3
Anti-Aging Activity
In 2017, Addy et al. set out to characterize skin surface lipid composition and differences in an age- and sex-controlled population as a foundation for developing a botanically derived skin surface lipid mimetic agent. They noted that fatty acids, triglycerides, cholesterol, steryl esters, wax esters, and squalene are the main constituents of skin surface lipids. The investigators obtained skin surface lipid samples from the foreheads of 59 healthy 22-year-old women, analyzed them, and used the raw components of M. integrifolia, Simmondsia chinensis, and Olea europaea to engineer a mimetic product. They reported that the esterification reactions of jojoba, macadamia, and tall oils, combined with squalene derived from O. europaea, yielded an appropriate skin surface lipid mimetic, which, when applied to delipidized skin, assisted in recovering barrier function, enhancing skin hydration, and improving elasticity as well as firmness in aged skin. The researchers concluded that this skin surface lipid mimetic could serve as an effective supplement to human skin surface lipids in aged skin and for conditions in which the stratum corneum is impaired.4
Two years later, Hanum et al. compared the effects of macadamia nut oil nanocream and conventional cream for treating cutaneous aging over a 4-week period. The macadamia nut oil nanocream, which contained macadamia nut oil 10%, tween 80, propylene glycol, cetyl alcohol, methylparaben, propylparaben, and distilled water, was compared with the conventional cream based on effects on moisture, evenness, pore size, melanin, and wrinkling. The macadamia nut oil was found to yield superior anti-aging activity along each parameter as compared with the conventional cream. The researchers concluded that the macadamia nut oil in nanocream can be an effective formulation for providing benefits in addressing cutaneous aging.5
Macadamia nut oil has also been used in an anti-aging emulsion that was evaluated in a small study with 11 volunteers in 2008. Akhtar et al. prepared multiple emulsions of vitamin C and wheat protein using macadamia oil for its abundant supply of palmitoleic acid. Over 4 weeks, the emulsion was found to increase skin moisture without affecting other skin parameters, such as elasticity, erythema, melanin, pH, or sebum levels.6
Sapucaia (L. pisonis), an ornamental tree that is used for timber, produces edible, nutritious nuts that are rich in tocopherols, polyphenols, and fatty acids.7,8 In 2018, Demoliner et al. identified and characterized the phenolic substances present in sapucaia nut extract and its shell. Antioxidant activity conferred by the extract was attributed to the copious supply of catechin, epicatechin, and myricetin, as well as ellagic and ferulic acids, among the 14 phenolic constituents. The shell included 22 phenolic substances along with a significant level of condensed tannins and marked antioxidant function. The authors correlated the substantial activity imparted by the shell with its higher phenolic content, and suggested this robust source of natural antioxidants could be well suited to use in cosmetic products.9
Antifungal Activity
In 2015, Vieira et al. characterized 12 fractions enriched in peptides derived from L. pisonis seeds to determine inhibitory activity against Candida albicans. The fraction that exerted the strongest activity at 10 μg/mL, suppressing C. albicans growth by 38.5% and inducing a 69.3% loss of viability, was identified as similar to plant defensins and thus dubbed “L. pisonis defensin 1 (Lp-Def1).” The investigators concluded that Lp-Def1 acts on C. albicans by slightly elevating the induction of reactive oxygen species and causing a significant reduction in mitochondrial activity. They suggested that their findings support the use of plant defensins, particularly Lp-Def1, in the formulation of antifungal products, especially to address C. albicans.10
Pruritus
In 2012, Silva et al. studied the antipruritic impact of L. pisonis leaf extracts in mice and rats. Pretreatment with the various fractions of L. pisonis as well as constituent mixed triterpenes (ursolic and oleanolic acids) significantly blocked scratching behavior provoked by compound 48/80. The degranulation of rat peritoneal mast cells caused by compound 48/80 was also substantially decreased from pretreatment with the ethanol extract of L. pisonis, ether-L. pisonis fraction, and mixed triterpenes. The L. pisonis ether fraction suppressed edema induced by carrageenan administration and the ethanol extract displayed no toxicity up to an oral dose of 2g/kg. The investigators concluded that their results strongly support the antipruritic effects of L. pisonis leaves as well as the traditional use of the plant to treat pruritus.2
Stability for Cosmetic Creams
In 2020, Rampazzo et al. assessed the stability and cytotoxicity of a cosmetic cream containing sapucaia nut oil. All three tested concentrations (1%, 5%, and 10%) of the cream were found to be stable, with an effective preservative system, and deemed safe for use on human skin. To maintain a pH appropriate for a body cream, the formulation requires a stabilizing agent. The cream with 5% nut oil was identified as the most stable and satisfying for use on the skin.7
More recently, Hertel Pereira et al. investigated the benefits of using L. pisonis pericarp extract, known to exhibit abundant antioxidants, in an all-natural skin cream. They found that formulation instability increased proportionally with the concentration of the extract, but the use of the outer pericarp of L. pisonis was well suited for the cream formulation, with physical-chemical and organoleptic qualities unchanged after the stability test.11
Conclusion
The available literature on the medical applications of macadamia and sapucaia plants is sparse. Some recent findings are promising regarding possible uses in skin health. However, much more research is necessary before considering macadamia and sapucaia as viable sources of botanical agents capable of delivering significant cutaneous benefits.
Dr. Baumann is a private practice dermatologist, researcher, author, and entrepreneur in Miami. She founded the division of cosmetic dermatology at the University of Miami in 1997. The third edition of her bestselling textbook, “Cosmetic Dermatology,” was published in 2022. Dr. Baumann has received funding for advisory boards and/or clinical research trials from Allergan, Galderma, Johnson & Johnson, and Burt’s Bees. She is the CEO of Skin Type Solutions Inc., an SaaS company used to generate skin care routines in office and as an e-commerce solution. Write to her at [email protected].
References
1. Dailey A and Vuong QV. Antioxidants (Basel). 2015 Nov 12;4(4):699-718.
2. Silva LL et al. J Ethnopharmacol. 2012 Jan 6;139(1):90-97.
3. Somwongin S et al. Ultrason Sonochem. 2023 Jan;92:106266.
4. Addy J et al. J Cosmet Sci. 2017 Jan/Feb;68(1):59-67.
5. Hanum TI et al. Open Access Maced J Med Sci. 2019 Nov 14;7(22):3917-3920.
6. Akhtar N and Yazan Y. Pak J Pharm Sci. 2008 Jan;21(1):45-50.
7. Rampazzo APS et al. J Cosmet Sci. 2020 Sep/Oct;71(5):239-250.
8. Rosa TLM et al. Food Res Int. 2020 Nov;137:109383.
9. Demoliner F et al. Food Res Int. 2018 Oct;112:434-442.
10. Vieira ME et al. Acta Biochim Biophys Sin (Shanghai). 2015 Sep;47(9):716-729.
11. Hertel Pereira AC et al. J Cosmet Sci. 2021 Mar-Apr;72(2):155-162.
Macadamia (Macadamia tetraphylla) is endemic to Australia and is now commercially cultivated worldwide.1 It is closely related genetically to the other macadamia plants, including the other main one, M. integrifolia, cultivated for macadamia nuts. Known in Brazil as sapucaia or castanha-de-sapucaia, Lecythis pisonis (also referred to as “cream nut” or “monkey pot”) is a large, deciduous tropical tree and member of the Brazil nut family, Lecythidaceae.2 Various parts of both of these plants have been associated with medicinal properties, including the potential for dermatologic activity. Notably, the leaves of L. pisonis have been used in traditional medicine to treat pruritus.2 .
Macadamia
Extraction to Harness Antioxidant Activity
In 2015, Dailey and Vuong developed an aqueous extraction process to recover the phenolic content and antioxidant functionality from the skin waste of M. tetraphylla using response surface methodology. As an environmentally suitable solvent that is also cheap and safe, water was chosen to maximize the extraction scenario. They identified the proper conditions (90° C, a time of 20 min, and a sample-to-solvent ratio of 5 g/100 mL) to obtain sufficient phenolic compounds, proanthocyanidins, and flavonoids to render robust antioxidant function.1
Early in 2023, Somwongin et al. investigated various green extraction methods for viability in harnessing the cosmetic/cosmeceutical ingredients of M. integrifolia pericarps. Extracts were assessed for total phenolic content as well as antioxidant and anti–skin aging functions. They found that among the green extraction methods (ultrasound, micellar, microwave, and pulsed electric field extraction with water used as a clean solvent), the ultrasound-assisted extraction method netted the greatest yield and total phenolic content. It was also associated with the most robust antioxidant and anti–skin aging activities. Indeed, the researchers reported that its antioxidant activities were comparable to ascorbic acid and Trolox and its anti–skin aging potency on a par with epigallocatechin-3-gallate and oleanolic acid. The ultrasound-assisted extract was also deemed safe as it did not provoke irritation. The authors concluded that this environmentally suitable extraction method for M. integrifolia is appropriate for obtaining effective macadamia extracts for use in cosmetics and cosmeceuticals.3
Anti-Aging Activity
In 2017, Addy et al. set out to characterize skin surface lipid composition and differences in an age- and sex-controlled population as a foundation for developing a botanically derived skin surface lipid mimetic agent. They noted that fatty acids, triglycerides, cholesterol, steryl esters, wax esters, and squalene are the main constituents of skin surface lipids. The investigators obtained skin surface lipid samples from the foreheads of 59 healthy 22-year-old women, analyzed them, and used the raw components of M. integrifolia, Simmondsia chinensis, and Olea europaea to engineer a mimetic product. They reported that the esterification reactions of jojoba, macadamia, and tall oils, combined with squalene derived from O. europaea, yielded an appropriate skin surface lipid mimetic, which, when applied to delipidized skin, assisted in recovering barrier function, enhancing skin hydration, and improving elasticity as well as firmness in aged skin. The researchers concluded that this skin surface lipid mimetic could serve as an effective supplement to human skin surface lipids in aged skin and for conditions in which the stratum corneum is impaired.4
Two years later, Hanum et al. compared the effects of macadamia nut oil nanocream and conventional cream for treating cutaneous aging over a 4-week period. The macadamia nut oil nanocream, which contained macadamia nut oil 10%, tween 80, propylene glycol, cetyl alcohol, methylparaben, propylparaben, and distilled water, was compared with the conventional cream based on effects on moisture, evenness, pore size, melanin, and wrinkling. The macadamia nut oil was found to yield superior anti-aging activity along each parameter as compared with the conventional cream. The researchers concluded that the macadamia nut oil in nanocream can be an effective formulation for providing benefits in addressing cutaneous aging.5
Macadamia nut oil has also been used in an anti-aging emulsion that was evaluated in a small study with 11 volunteers in 2008. Akhtar et al. prepared multiple emulsions of vitamin C and wheat protein using macadamia oil for its abundant supply of palmitoleic acid. Over 4 weeks, the emulsion was found to increase skin moisture without affecting other skin parameters, such as elasticity, erythema, melanin, pH, or sebum levels.6
Sapucaia (L. pisonis), an ornamental tree that is used for timber, produces edible, nutritious nuts that are rich in tocopherols, polyphenols, and fatty acids.7,8 In 2018, Demoliner et al. identified and characterized the phenolic substances present in sapucaia nut extract and its shell. Antioxidant activity conferred by the extract was attributed to the copious supply of catechin, epicatechin, and myricetin, as well as ellagic and ferulic acids, among the 14 phenolic constituents. The shell included 22 phenolic substances along with a significant level of condensed tannins and marked antioxidant function. The authors correlated the substantial activity imparted by the shell with its higher phenolic content, and suggested this robust source of natural antioxidants could be well suited to use in cosmetic products.9
Antifungal Activity
In 2015, Vieira et al. characterized 12 fractions enriched in peptides derived from L. pisonis seeds to determine inhibitory activity against Candida albicans. The fraction that exerted the strongest activity at 10 μg/mL, suppressing C. albicans growth by 38.5% and inducing a 69.3% loss of viability, was identified as similar to plant defensins and thus dubbed “L. pisonis defensin 1 (Lp-Def1).” The investigators concluded that Lp-Def1 acts on C. albicans by slightly elevating the induction of reactive oxygen species and causing a significant reduction in mitochondrial activity. They suggested that their findings support the use of plant defensins, particularly Lp-Def1, in the formulation of antifungal products, especially to address C. albicans.10
Pruritus
In 2012, Silva et al. studied the antipruritic impact of L. pisonis leaf extracts in mice and rats. Pretreatment with the various fractions of L. pisonis as well as constituent mixed triterpenes (ursolic and oleanolic acids) significantly blocked scratching behavior provoked by compound 48/80. The degranulation of rat peritoneal mast cells caused by compound 48/80 was also substantially decreased from pretreatment with the ethanol extract of L. pisonis, ether-L. pisonis fraction, and mixed triterpenes. The L. pisonis ether fraction suppressed edema induced by carrageenan administration and the ethanol extract displayed no toxicity up to an oral dose of 2g/kg. The investigators concluded that their results strongly support the antipruritic effects of L. pisonis leaves as well as the traditional use of the plant to treat pruritus.2
Stability for Cosmetic Creams
In 2020, Rampazzo et al. assessed the stability and cytotoxicity of a cosmetic cream containing sapucaia nut oil. All three tested concentrations (1%, 5%, and 10%) of the cream were found to be stable, with an effective preservative system, and deemed safe for use on human skin. To maintain a pH appropriate for a body cream, the formulation requires a stabilizing agent. The cream with 5% nut oil was identified as the most stable and satisfying for use on the skin.7
More recently, Hertel Pereira et al. investigated the benefits of using L. pisonis pericarp extract, known to exhibit abundant antioxidants, in an all-natural skin cream. They found that formulation instability increased proportionally with the concentration of the extract, but the use of the outer pericarp of L. pisonis was well suited for the cream formulation, with physical-chemical and organoleptic qualities unchanged after the stability test.11
Conclusion
The available literature on the medical applications of macadamia and sapucaia plants is sparse. Some recent findings are promising regarding possible uses in skin health. However, much more research is necessary before considering macadamia and sapucaia as viable sources of botanical agents capable of delivering significant cutaneous benefits.
Dr. Baumann is a private practice dermatologist, researcher, author, and entrepreneur in Miami. She founded the division of cosmetic dermatology at the University of Miami in 1997. The third edition of her bestselling textbook, “Cosmetic Dermatology,” was published in 2022. Dr. Baumann has received funding for advisory boards and/or clinical research trials from Allergan, Galderma, Johnson & Johnson, and Burt’s Bees. She is the CEO of Skin Type Solutions Inc., an SaaS company used to generate skin care routines in office and as an e-commerce solution. Write to her at [email protected].
References
1. Dailey A and Vuong QV. Antioxidants (Basel). 2015 Nov 12;4(4):699-718.
2. Silva LL et al. J Ethnopharmacol. 2012 Jan 6;139(1):90-97.
3. Somwongin S et al. Ultrason Sonochem. 2023 Jan;92:106266.
4. Addy J et al. J Cosmet Sci. 2017 Jan/Feb;68(1):59-67.
5. Hanum TI et al. Open Access Maced J Med Sci. 2019 Nov 14;7(22):3917-3920.
6. Akhtar N and Yazan Y. Pak J Pharm Sci. 2008 Jan;21(1):45-50.
7. Rampazzo APS et al. J Cosmet Sci. 2020 Sep/Oct;71(5):239-250.
8. Rosa TLM et al. Food Res Int. 2020 Nov;137:109383.
9. Demoliner F et al. Food Res Int. 2018 Oct;112:434-442.
10. Vieira ME et al. Acta Biochim Biophys Sin (Shanghai). 2015 Sep;47(9):716-729.
11. Hertel Pereira AC et al. J Cosmet Sci. 2021 Mar-Apr;72(2):155-162.
Macadamia (Macadamia tetraphylla) is endemic to Australia and is now commercially cultivated worldwide.1 It is closely related genetically to the other macadamia plants, including the other main one, M. integrifolia, cultivated for macadamia nuts. Known in Brazil as sapucaia or castanha-de-sapucaia, Lecythis pisonis (also referred to as “cream nut” or “monkey pot”) is a large, deciduous tropical tree and member of the Brazil nut family, Lecythidaceae.2 Various parts of both of these plants have been associated with medicinal properties, including the potential for dermatologic activity. Notably, the leaves of L. pisonis have been used in traditional medicine to treat pruritus.2 .
Macadamia
Extraction to Harness Antioxidant Activity
In 2015, Dailey and Vuong developed an aqueous extraction process to recover the phenolic content and antioxidant functionality from the skin waste of M. tetraphylla using response surface methodology. As an environmentally suitable solvent that is also cheap and safe, water was chosen to maximize the extraction scenario. They identified the proper conditions (90° C, a time of 20 min, and a sample-to-solvent ratio of 5 g/100 mL) to obtain sufficient phenolic compounds, proanthocyanidins, and flavonoids to render robust antioxidant function.1
Early in 2023, Somwongin et al. investigated various green extraction methods for viability in harnessing the cosmetic/cosmeceutical ingredients of M. integrifolia pericarps. Extracts were assessed for total phenolic content as well as antioxidant and anti–skin aging functions. They found that among the green extraction methods (ultrasound, micellar, microwave, and pulsed electric field extraction with water used as a clean solvent), the ultrasound-assisted extraction method netted the greatest yield and total phenolic content. It was also associated with the most robust antioxidant and anti–skin aging activities. Indeed, the researchers reported that its antioxidant activities were comparable to ascorbic acid and Trolox and its anti–skin aging potency on a par with epigallocatechin-3-gallate and oleanolic acid. The ultrasound-assisted extract was also deemed safe as it did not provoke irritation. The authors concluded that this environmentally suitable extraction method for M. integrifolia is appropriate for obtaining effective macadamia extracts for use in cosmetics and cosmeceuticals.3
Anti-Aging Activity
In 2017, Addy et al. set out to characterize skin surface lipid composition and differences in an age- and sex-controlled population as a foundation for developing a botanically derived skin surface lipid mimetic agent. They noted that fatty acids, triglycerides, cholesterol, steryl esters, wax esters, and squalene are the main constituents of skin surface lipids. The investigators obtained skin surface lipid samples from the foreheads of 59 healthy 22-year-old women, analyzed them, and used the raw components of M. integrifolia, Simmondsia chinensis, and Olea europaea to engineer a mimetic product. They reported that the esterification reactions of jojoba, macadamia, and tall oils, combined with squalene derived from O. europaea, yielded an appropriate skin surface lipid mimetic, which, when applied to delipidized skin, assisted in recovering barrier function, enhancing skin hydration, and improving elasticity as well as firmness in aged skin. The researchers concluded that this skin surface lipid mimetic could serve as an effective supplement to human skin surface lipids in aged skin and for conditions in which the stratum corneum is impaired.4
Two years later, Hanum et al. compared the effects of macadamia nut oil nanocream and conventional cream for treating cutaneous aging over a 4-week period. The macadamia nut oil nanocream, which contained macadamia nut oil 10%, tween 80, propylene glycol, cetyl alcohol, methylparaben, propylparaben, and distilled water, was compared with the conventional cream based on effects on moisture, evenness, pore size, melanin, and wrinkling. The macadamia nut oil was found to yield superior anti-aging activity along each parameter as compared with the conventional cream. The researchers concluded that the macadamia nut oil in nanocream can be an effective formulation for providing benefits in addressing cutaneous aging.5
Macadamia nut oil has also been used in an anti-aging emulsion that was evaluated in a small study with 11 volunteers in 2008. Akhtar et al. prepared multiple emulsions of vitamin C and wheat protein using macadamia oil for its abundant supply of palmitoleic acid. Over 4 weeks, the emulsion was found to increase skin moisture without affecting other skin parameters, such as elasticity, erythema, melanin, pH, or sebum levels.6
Sapucaia (L. pisonis), an ornamental tree that is used for timber, produces edible, nutritious nuts that are rich in tocopherols, polyphenols, and fatty acids.7,8 In 2018, Demoliner et al. identified and characterized the phenolic substances present in sapucaia nut extract and its shell. Antioxidant activity conferred by the extract was attributed to the copious supply of catechin, epicatechin, and myricetin, as well as ellagic and ferulic acids, among the 14 phenolic constituents. The shell included 22 phenolic substances along with a significant level of condensed tannins and marked antioxidant function. The authors correlated the substantial activity imparted by the shell with its higher phenolic content, and suggested this robust source of natural antioxidants could be well suited to use in cosmetic products.9
Antifungal Activity
In 2015, Vieira et al. characterized 12 fractions enriched in peptides derived from L. pisonis seeds to determine inhibitory activity against Candida albicans. The fraction that exerted the strongest activity at 10 μg/mL, suppressing C. albicans growth by 38.5% and inducing a 69.3% loss of viability, was identified as similar to plant defensins and thus dubbed “L. pisonis defensin 1 (Lp-Def1).” The investigators concluded that Lp-Def1 acts on C. albicans by slightly elevating the induction of reactive oxygen species and causing a significant reduction in mitochondrial activity. They suggested that their findings support the use of plant defensins, particularly Lp-Def1, in the formulation of antifungal products, especially to address C. albicans.10
Pruritus
In 2012, Silva et al. studied the antipruritic impact of L. pisonis leaf extracts in mice and rats. Pretreatment with the various fractions of L. pisonis as well as constituent mixed triterpenes (ursolic and oleanolic acids) significantly blocked scratching behavior provoked by compound 48/80. The degranulation of rat peritoneal mast cells caused by compound 48/80 was also substantially decreased from pretreatment with the ethanol extract of L. pisonis, ether-L. pisonis fraction, and mixed triterpenes. The L. pisonis ether fraction suppressed edema induced by carrageenan administration and the ethanol extract displayed no toxicity up to an oral dose of 2g/kg. The investigators concluded that their results strongly support the antipruritic effects of L. pisonis leaves as well as the traditional use of the plant to treat pruritus.2
Stability for Cosmetic Creams
In 2020, Rampazzo et al. assessed the stability and cytotoxicity of a cosmetic cream containing sapucaia nut oil. All three tested concentrations (1%, 5%, and 10%) of the cream were found to be stable, with an effective preservative system, and deemed safe for use on human skin. To maintain a pH appropriate for a body cream, the formulation requires a stabilizing agent. The cream with 5% nut oil was identified as the most stable and satisfying for use on the skin.7
More recently, Hertel Pereira et al. investigated the benefits of using L. pisonis pericarp extract, known to exhibit abundant antioxidants, in an all-natural skin cream. They found that formulation instability increased proportionally with the concentration of the extract, but the use of the outer pericarp of L. pisonis was well suited for the cream formulation, with physical-chemical and organoleptic qualities unchanged after the stability test.11
Conclusion
The available literature on the medical applications of macadamia and sapucaia plants is sparse. Some recent findings are promising regarding possible uses in skin health. However, much more research is necessary before considering macadamia and sapucaia as viable sources of botanical agents capable of delivering significant cutaneous benefits.
Dr. Baumann is a private practice dermatologist, researcher, author, and entrepreneur in Miami. She founded the division of cosmetic dermatology at the University of Miami in 1997. The third edition of her bestselling textbook, “Cosmetic Dermatology,” was published in 2022. Dr. Baumann has received funding for advisory boards and/or clinical research trials from Allergan, Galderma, Johnson & Johnson, and Burt’s Bees. She is the CEO of Skin Type Solutions Inc., an SaaS company used to generate skin care routines in office and as an e-commerce solution. Write to her at [email protected].
References
1. Dailey A and Vuong QV. Antioxidants (Basel). 2015 Nov 12;4(4):699-718.
2. Silva LL et al. J Ethnopharmacol. 2012 Jan 6;139(1):90-97.
3. Somwongin S et al. Ultrason Sonochem. 2023 Jan;92:106266.
4. Addy J et al. J Cosmet Sci. 2017 Jan/Feb;68(1):59-67.
5. Hanum TI et al. Open Access Maced J Med Sci. 2019 Nov 14;7(22):3917-3920.
6. Akhtar N and Yazan Y. Pak J Pharm Sci. 2008 Jan;21(1):45-50.
7. Rampazzo APS et al. J Cosmet Sci. 2020 Sep/Oct;71(5):239-250.
8. Rosa TLM et al. Food Res Int. 2020 Nov;137:109383.
9. Demoliner F et al. Food Res Int. 2018 Oct;112:434-442.
10. Vieira ME et al. Acta Biochim Biophys Sin (Shanghai). 2015 Sep;47(9):716-729.
11. Hertel Pereira AC et al. J Cosmet Sci. 2021 Mar-Apr;72(2):155-162.
Alcohol to Blame: Weight Regain After Bariatric Surgery
A 50-year-old woman with a history of class 3 obesity, gastroesophageal reflux disease, prediabetes, metabolic dysfunction–associated steatotic liver disease, asthma, and depression returns to our weight management clinic with weight regain 4 years after Roux-en-Y gastric bypass.
Her initial body weight was 389 lb (176.8 kg; body mass index [BMI], 65), and her nadir weight after surgery was 183 lb (83.2 kg; BMI, 30.5), representing a total weight loss of 53%. During the initial 2 years after surgery, she experienced multiple life stressors and was treated with venlafaxine for mild depression. She regained 25 lb (11.4 kg). Over the next 2 years, she gained another 20 lb (9.1 kg), for a total of 45 lb (20.5 kg) above nadir.
The patient reported increased nighttime consumption of alcohol including vodka, wine, and beer of over 20 drinks per week for the past 2 years. Her laboratory profile showed an elevated fasting glucose level (106 mg/dL, formerly 98 mg/dL), an elevated gamma-glutamyl transferase (GGT) level, and iron deficiency anemia. She admitted to regularly missing doses of postbariatric vitamins and minerals.
Ask Patients About Alcohol Use
It’s important to ask patients with significant weight regain after metabolic and bariatric surgery (MBS) about alcohol intake, because patients who have MBS are at an increased risk of developing alcohol use disorder (AUD).
The American Society for Metabolic and Bariatric Surgery recommends screening for alcohol intake both before and after MBS. Underreporting of alcohol consumption is common, but an elevated GGT level or elevated liver enzyme levels can indicate alcohol use. Depression and anxiety exacerbated by life stressors often accompany excessive alcohol intake.
Some antiobesity medications that regulate appetite may also help limit excessive alcohol intake. Naltrexone is used both for the treatment of AUD and for weight management, often in combination with bupropion). In a patient with weight regain and AUD, naltrexone alone would be a reasonable treatment option, although weight loss would probably be modest. The addition of bupropion to naltrexone would probably produce more weight loss; average total body weight loss with bupropion-naltrexone in clinical trials was about 6%. One cautionary note on bupropion: A patient’s seizure history should be elicited, because people with AUD are at increased risk for seizures in the withdrawal stage and bupropion can make those seizures more likely.
Glucagon-like peptide 1 (GLP-1) receptor agonists (eg, liraglutide and semaglutide) and dual GLP-1/GIP (glucose-dependent insulinotropic polypeptide receptor agonists) (eg, tirzepatide) are second-generation antiobesity medications that produce more weight loss than first-generation agents such as bupropion/naltrexone. Of note, prior bariatric surgery was an exclusion criterion in the clinical trials assessing the efficacy of these agents for weight loss. The use of GLP-1 receptor agonists after MBS in people with inadequate weight loss or weight regain has been an area of active research. The BARI-OPTIMISE randomized clinical trial published in 2023 assessed the safety and efficacy of liraglutide 3.0 mg daily in patients with inadequate weight loss after MBS. The mean body weight reduction was 8.82% in the liraglutide group vs 0.54% in the placebo group.
There is also emerging interest in the potential of GLP-1 receptor agonists in AUD. These medications act on the central nervous system to influence reward pathways. In rodents, studies have shown that GLP-1 receptor agonist administration reduces alcohol intake, although most studies have focused on short-term effects.
A series of experiments assessed the effects of semaglutide on alcohol intake in rodents. The authors found that semaglutide lowered the alcohol-induced release of dopamine and enhanced dopamine metabolism within the nucleus accumbens.
Evidence in humans is still limited, with only one published randomized controlled trial to date. In the 26-week study, weekly exenatide was not superior to placebo in reducing the number of heavy drinking days in patients with AUD who also received cognitive-behavioral therapy. An exploratory analysis in a subgroup of patients with obesity and AUD showed that exenatide reduced alcohol consumption. Of note, exenatide is rarely used in clinical practice because it does not produce substantial weight loss.
Liraglutide was chosen for this patient because of the established efficacy for this agent in patients with a history of MBS. In addition, patients often anecdotally report reduced desire for alcohol while taking a GLP-1 receptor agonist. Although GLP-1 receptor agonists have been shown to reduce alcohol intake in animal studies, their efficacy and safety in humans with AUD are not yet well established.
Back to Our Patient:
Given the patient’s weight regain, an upper gastrointestinal series was performed to rule out gastro-gastric fistula or other anatomic abnormalities. After fistula was ruled out, she was prescribed liraglutide for weight management, which was titrated from 0.6 mg/d to 3 mg/d per the prescribing guidelines.
With the use of liraglutide over the next year, the patient maintained a stable weight of 200 lb (90.9 kg) and noted that along with reduced appetite, her cravings for alcohol had diminished and she no longer felt the urge to drink alcohol at night. Her fasting glucose and GGT levels normalized. She began to see a nutritionist regularly and was planning to rejoin a bariatric support group.
Dr. Schmitz is an instructor in the Department of Medicine, Division of Endocrinology, Diabetes, and Metabolism, Weill Cornell Medicine, New York. She has disclosed no relevant financial relationships. Dr. Kashyap is a assistant chief of clinical affairs, Division of Endocrinology, Diabetes and Metabolism, Weill Cornell New York Presbyterian, New York. She disclosed ties to GI Dynamics.
A version of this article appeared on Medscape.com.
A 50-year-old woman with a history of class 3 obesity, gastroesophageal reflux disease, prediabetes, metabolic dysfunction–associated steatotic liver disease, asthma, and depression returns to our weight management clinic with weight regain 4 years after Roux-en-Y gastric bypass.
Her initial body weight was 389 lb (176.8 kg; body mass index [BMI], 65), and her nadir weight after surgery was 183 lb (83.2 kg; BMI, 30.5), representing a total weight loss of 53%. During the initial 2 years after surgery, she experienced multiple life stressors and was treated with venlafaxine for mild depression. She regained 25 lb (11.4 kg). Over the next 2 years, she gained another 20 lb (9.1 kg), for a total of 45 lb (20.5 kg) above nadir.
The patient reported increased nighttime consumption of alcohol including vodka, wine, and beer of over 20 drinks per week for the past 2 years. Her laboratory profile showed an elevated fasting glucose level (106 mg/dL, formerly 98 mg/dL), an elevated gamma-glutamyl transferase (GGT) level, and iron deficiency anemia. She admitted to regularly missing doses of postbariatric vitamins and minerals.
Ask Patients About Alcohol Use
It’s important to ask patients with significant weight regain after metabolic and bariatric surgery (MBS) about alcohol intake, because patients who have MBS are at an increased risk of developing alcohol use disorder (AUD).
The American Society for Metabolic and Bariatric Surgery recommends screening for alcohol intake both before and after MBS. Underreporting of alcohol consumption is common, but an elevated GGT level or elevated liver enzyme levels can indicate alcohol use. Depression and anxiety exacerbated by life stressors often accompany excessive alcohol intake.
Some antiobesity medications that regulate appetite may also help limit excessive alcohol intake. Naltrexone is used both for the treatment of AUD and for weight management, often in combination with bupropion). In a patient with weight regain and AUD, naltrexone alone would be a reasonable treatment option, although weight loss would probably be modest. The addition of bupropion to naltrexone would probably produce more weight loss; average total body weight loss with bupropion-naltrexone in clinical trials was about 6%. One cautionary note on bupropion: A patient’s seizure history should be elicited, because people with AUD are at increased risk for seizures in the withdrawal stage and bupropion can make those seizures more likely.
Glucagon-like peptide 1 (GLP-1) receptor agonists (eg, liraglutide and semaglutide) and dual GLP-1/GIP (glucose-dependent insulinotropic polypeptide receptor agonists) (eg, tirzepatide) are second-generation antiobesity medications that produce more weight loss than first-generation agents such as bupropion/naltrexone. Of note, prior bariatric surgery was an exclusion criterion in the clinical trials assessing the efficacy of these agents for weight loss. The use of GLP-1 receptor agonists after MBS in people with inadequate weight loss or weight regain has been an area of active research. The BARI-OPTIMISE randomized clinical trial published in 2023 assessed the safety and efficacy of liraglutide 3.0 mg daily in patients with inadequate weight loss after MBS. The mean body weight reduction was 8.82% in the liraglutide group vs 0.54% in the placebo group.
There is also emerging interest in the potential of GLP-1 receptor agonists in AUD. These medications act on the central nervous system to influence reward pathways. In rodents, studies have shown that GLP-1 receptor agonist administration reduces alcohol intake, although most studies have focused on short-term effects.
A series of experiments assessed the effects of semaglutide on alcohol intake in rodents. The authors found that semaglutide lowered the alcohol-induced release of dopamine and enhanced dopamine metabolism within the nucleus accumbens.
Evidence in humans is still limited, with only one published randomized controlled trial to date. In the 26-week study, weekly exenatide was not superior to placebo in reducing the number of heavy drinking days in patients with AUD who also received cognitive-behavioral therapy. An exploratory analysis in a subgroup of patients with obesity and AUD showed that exenatide reduced alcohol consumption. Of note, exenatide is rarely used in clinical practice because it does not produce substantial weight loss.
Liraglutide was chosen for this patient because of the established efficacy for this agent in patients with a history of MBS. In addition, patients often anecdotally report reduced desire for alcohol while taking a GLP-1 receptor agonist. Although GLP-1 receptor agonists have been shown to reduce alcohol intake in animal studies, their efficacy and safety in humans with AUD are not yet well established.
Back to Our Patient:
Given the patient’s weight regain, an upper gastrointestinal series was performed to rule out gastro-gastric fistula or other anatomic abnormalities. After fistula was ruled out, she was prescribed liraglutide for weight management, which was titrated from 0.6 mg/d to 3 mg/d per the prescribing guidelines.
With the use of liraglutide over the next year, the patient maintained a stable weight of 200 lb (90.9 kg) and noted that along with reduced appetite, her cravings for alcohol had diminished and she no longer felt the urge to drink alcohol at night. Her fasting glucose and GGT levels normalized. She began to see a nutritionist regularly and was planning to rejoin a bariatric support group.
Dr. Schmitz is an instructor in the Department of Medicine, Division of Endocrinology, Diabetes, and Metabolism, Weill Cornell Medicine, New York. She has disclosed no relevant financial relationships. Dr. Kashyap is a assistant chief of clinical affairs, Division of Endocrinology, Diabetes and Metabolism, Weill Cornell New York Presbyterian, New York. She disclosed ties to GI Dynamics.
A version of this article appeared on Medscape.com.
A 50-year-old woman with a history of class 3 obesity, gastroesophageal reflux disease, prediabetes, metabolic dysfunction–associated steatotic liver disease, asthma, and depression returns to our weight management clinic with weight regain 4 years after Roux-en-Y gastric bypass.
Her initial body weight was 389 lb (176.8 kg; body mass index [BMI], 65), and her nadir weight after surgery was 183 lb (83.2 kg; BMI, 30.5), representing a total weight loss of 53%. During the initial 2 years after surgery, she experienced multiple life stressors and was treated with venlafaxine for mild depression. She regained 25 lb (11.4 kg). Over the next 2 years, she gained another 20 lb (9.1 kg), for a total of 45 lb (20.5 kg) above nadir.
The patient reported increased nighttime consumption of alcohol including vodka, wine, and beer of over 20 drinks per week for the past 2 years. Her laboratory profile showed an elevated fasting glucose level (106 mg/dL, formerly 98 mg/dL), an elevated gamma-glutamyl transferase (GGT) level, and iron deficiency anemia. She admitted to regularly missing doses of postbariatric vitamins and minerals.
Ask Patients About Alcohol Use
It’s important to ask patients with significant weight regain after metabolic and bariatric surgery (MBS) about alcohol intake, because patients who have MBS are at an increased risk of developing alcohol use disorder (AUD).
The American Society for Metabolic and Bariatric Surgery recommends screening for alcohol intake both before and after MBS. Underreporting of alcohol consumption is common, but an elevated GGT level or elevated liver enzyme levels can indicate alcohol use. Depression and anxiety exacerbated by life stressors often accompany excessive alcohol intake.
Some antiobesity medications that regulate appetite may also help limit excessive alcohol intake. Naltrexone is used both for the treatment of AUD and for weight management, often in combination with bupropion). In a patient with weight regain and AUD, naltrexone alone would be a reasonable treatment option, although weight loss would probably be modest. The addition of bupropion to naltrexone would probably produce more weight loss; average total body weight loss with bupropion-naltrexone in clinical trials was about 6%. One cautionary note on bupropion: A patient’s seizure history should be elicited, because people with AUD are at increased risk for seizures in the withdrawal stage and bupropion can make those seizures more likely.
Glucagon-like peptide 1 (GLP-1) receptor agonists (eg, liraglutide and semaglutide) and dual GLP-1/GIP (glucose-dependent insulinotropic polypeptide receptor agonists) (eg, tirzepatide) are second-generation antiobesity medications that produce more weight loss than first-generation agents such as bupropion/naltrexone. Of note, prior bariatric surgery was an exclusion criterion in the clinical trials assessing the efficacy of these agents for weight loss. The use of GLP-1 receptor agonists after MBS in people with inadequate weight loss or weight regain has been an area of active research. The BARI-OPTIMISE randomized clinical trial published in 2023 assessed the safety and efficacy of liraglutide 3.0 mg daily in patients with inadequate weight loss after MBS. The mean body weight reduction was 8.82% in the liraglutide group vs 0.54% in the placebo group.
There is also emerging interest in the potential of GLP-1 receptor agonists in AUD. These medications act on the central nervous system to influence reward pathways. In rodents, studies have shown that GLP-1 receptor agonist administration reduces alcohol intake, although most studies have focused on short-term effects.
A series of experiments assessed the effects of semaglutide on alcohol intake in rodents. The authors found that semaglutide lowered the alcohol-induced release of dopamine and enhanced dopamine metabolism within the nucleus accumbens.
Evidence in humans is still limited, with only one published randomized controlled trial to date. In the 26-week study, weekly exenatide was not superior to placebo in reducing the number of heavy drinking days in patients with AUD who also received cognitive-behavioral therapy. An exploratory analysis in a subgroup of patients with obesity and AUD showed that exenatide reduced alcohol consumption. Of note, exenatide is rarely used in clinical practice because it does not produce substantial weight loss.
Liraglutide was chosen for this patient because of the established efficacy for this agent in patients with a history of MBS. In addition, patients often anecdotally report reduced desire for alcohol while taking a GLP-1 receptor agonist. Although GLP-1 receptor agonists have been shown to reduce alcohol intake in animal studies, their efficacy and safety in humans with AUD are not yet well established.
Back to Our Patient:
Given the patient’s weight regain, an upper gastrointestinal series was performed to rule out gastro-gastric fistula or other anatomic abnormalities. After fistula was ruled out, she was prescribed liraglutide for weight management, which was titrated from 0.6 mg/d to 3 mg/d per the prescribing guidelines.
With the use of liraglutide over the next year, the patient maintained a stable weight of 200 lb (90.9 kg) and noted that along with reduced appetite, her cravings for alcohol had diminished and she no longer felt the urge to drink alcohol at night. Her fasting glucose and GGT levels normalized. She began to see a nutritionist regularly and was planning to rejoin a bariatric support group.
Dr. Schmitz is an instructor in the Department of Medicine, Division of Endocrinology, Diabetes, and Metabolism, Weill Cornell Medicine, New York. She has disclosed no relevant financial relationships. Dr. Kashyap is a assistant chief of clinical affairs, Division of Endocrinology, Diabetes and Metabolism, Weill Cornell New York Presbyterian, New York. She disclosed ties to GI Dynamics.
A version of this article appeared on Medscape.com.
Specialists Are ‘Underwater’ With Some Insurance-Preferred Biosimilars
Editor’s note: This article is adapted from an explanatory statement that Dr. Feldman wrote for the Coalition of State Rheumatology Organizations (CSRO).
According to the Guinness Book of World records, the longest time someone has held their breath underwater voluntarily is 24 minutes and 37.36 seconds. While certainly an amazing feat, UnitedHealthcare, many of the Blues, and other national “payers” are expecting rheumatologists and other specialists to live “underwater” in order to take care of their patients. In other words, these insurance companies are mandating that specialists use certain provider-administered biosimilars whose acquisition cost is higher than what the insurance company is willing to reimburse them. Essentially, the insurance companies expect the rheumatologists to pay them to take care of their patients. Because of the substantial and destabilizing financial losses incurred, many practices and free-standing infusion centers have been forced to cease offering these biosimilars. Most rheumatologists will provide patients with appropriate alternatives when available and permitted by the insurer; otherwise, they must refer patients to hospital-based infusion centers. That results in delayed care and increased costs for patients and the system, because hospital-based infusion typically costs more than twice what office-based infusion costs.
Quantifying the Problem
To help quantify the magnitude of this issue, the Coalition of State Rheumatology Organizations (CSRO) recently conducted a survey of its membership. A shocking 97% of respondents reported that their practice had been affected by reimbursement rates for some biosimilars being lower than acquisition costs, with 91% of respondents stating that this issue is more pronounced for certain biosimilars than others. Across the board, respondents most frequently identified Inflectra (infliximab-dyyb) and Avsola (infliximab-axxq) as being especially affected: Over 88% and over 85% of respondents identified these two products, respectively, as being underwater. These results support the ongoing anecdotal reports CSRO continues to receive from rheumatology practices.
However, the survey results indicated that this issue is by no means confined to those two biosimilars. Truxima (rituximab-abbs) — a biosimilar for Rituxan — was frequently mentioned as well. Notably, respondents almost uniformly identified biosimilars in the infliximab and rituximab families, which illustrates that this issue is no longer confined to one or two early-to-market biosimilars but has almost become a hallmark of this particular biosimilars market. Remarkably, one respondent commented that the brand products are now cheaper to acquire than the biosimilars. Furthermore, the survey included respondents from across the country, indicating that this issue is not confined to a particular region.
How Did This Happen?
Biosimilars held promise for increasing availability and decreasing biologic costs for patients but, thus far, no patients have seen their cost go down. It appears that the only biosimilars that have made it to “preferred” status on the formulary are the ones that have made more money for the middlemen in the drug supply chain, particularly those that construct formularies. Now, we have provider-administered biosimilars whose acquisition cost exceeds the reimbursement for these drugs. This disparity was ultimately created by biosimilar manufacturers “over-rebating” their drugs to health insurance companies to gain “fail-first” status on the formulary.
For example, the manufacturer of Inflectra offered substantial rebates to health insurers for preferred formulary placement. These rebates are factored into the sales price of the medication, which then results in a rapidly declining average sales price (ASP) for the biosimilar. Unfortunately, the acquisition cost for the drug does not experience commensurate reductions, resulting in physicians being reimbursed far less for the drug than it costs to acquire. The financial losses for physicians put them underwater as a result of the acquisition costs for the preferred drugs far surpassing the reimbursement from the health insurance company that constructed the formulary.
While various factors affect ASPs and acquisition costs, this particular consequence of formulary placement based on price concessions is a major driver of the underwater situation in which physicians have found themselves with many biosimilars. Not only does that lead to a lower uptake of biosimilars, but it also results in patients being referred to the hospital outpatient infusion sites to receive this care, as freestanding infusion centers cannot treat these patients either. Hospitals incur higher costs because of facility fees and elevated rates, and this makes private rheumatology in-office infusion centers a much lower-cost option. Similarly, home infusion services, while convenient, are marginally more expensive than private practices and, in cases of biologic infusions, it is important to note that physicians’ offices have a greater safety profile than home infusion of biologics. The overall result of these “fail-first underwater drugs” is delayed and more costly care for the patient and the “system,” particularly self-insured employers.
What Is Being Done to Correct This?
Since ASPs are updated quarterly, it is possible that acquisition costs and reimbursements might stabilize over time, making the drugs affordable again to practices. However, that does not appear to be happening in the near future, so that possibility does not offer immediate relief to struggling practices. It doesn’t promise a favorable outlook for future biosimilar entries of provider-administered medications if formularies continue to prefer the highest-rebated medication.
This dynamic between ASP and acquisition cost does not happen on the pharmacy side because the price concessions on specific drug rebates and fees are proprietary. There appears to be no equivalent to a publicly known ASP on the pharmacy side, which has led to myriad pricing definitions and manipulation on the pharmacy benefit side of medications. In any event, the savings from rebates and other manufacturer price concessions on pharmacy drugs do not influence ASPs of medical benefit drugs.
The Inflation Reduction Act provided a temporary increase in the add-on payment for biosimilars from ASP+6% to ASP+8%, but as long as the biosimilar’s ASP is lower than the reference brand’s ASP, that temporary increase does not appear to make up for the large differential between ASP and acquisition cost. It should be noted that any federal attempt to artificially lower the ASP of a provider-administered drug without a pathway assuring that the acquisition cost for the provider is less than the reimbursement is going to result in loss of access for patients to those medications and/or higher hospital site of care costs.
A Few Partial Fixes, But Most Complaints Go Ignored
Considering the higher costs of hospital-based infusion, insurers should be motivated to keep patients within private practices. Perhaps through insurers’ recognition of that fact, some practices have successfully negotiated exceptions for specific patients by discussing this situation with insurers. From the feedback that CSRO has received from rheumatology practices, it appears that most insurers have been ignoring the complaints from physicians. The few who have responded have resulted in only partial fixes, with some of the biosimilars still left underwater.
Ultimate Solution?
This issue is a direct result of the “rebate game,” whereby price concessions from drug manufacturers drive formulary placement. For provider-administered medications, this results in an artificially lowered ASP, not as a consequence of free-market incentives that benefit the patient, but as a result of misaligned incentives created by Safe Harbor–protected “kickbacks,” distorting the free market and paradoxically reducing access to these medications, delaying care, and increasing prices for patients and the healthcare system.
While federal and state governments are not likely to address this particular situation in the biosimilars market, CSRO is highlighting this issue as a prime example of why the current formulary construction system urgently requires federal reform. At this time, the biosimilars most affected are Inflectra and Avsola, but if nothing changes, more and more biosimilars will fall victim to the short-sighted pricing strategy of aggressive rebating to gain formulary position, with physician purchasers and patients left to navigate the aftermath. The existing system, which necessitates drug companies purchasing formulary access from pharmacy benefit managers, has led to delayed and even denied patient access to certain provider-administered drugs. Moreover, it now appears to be hindering the adoption of biosimilars.
To address this, a multifaceted approach is required. It not only involves reevaluating the rebate system and its impact on formulary construction and ASP, but also ensuring that acquisition costs for providers are aligned with reimbursement rates. Insurers must recognize the economic and clinical value of maintaining infusions within private practices and immediately update their policies to ensure that physician in-office infusion is financially feasible for these “fail-first” biosimilars.
Ultimately, the goal should be to create a sustainable model that promotes the use of affordable biosimilars, enhances patient access to affordable care, and supports the financial viability of medical practices. Concerted efforts to reform the current formulary construction system are required to achieve a healthcare environment that is both cost effective and patient centric.
Dr. Feldman is a rheumatologist in private practice with The Rheumatology Group in New Orleans. She is the CSRO’s vice president of advocacy and government affairs and its immediate past president, as well as past chair of the Alliance for Safe Biologic Medicines and a past member of the American College of Rheumatology insurance subcommittee. You can reach her at [email protected].
Editor’s note: This article is adapted from an explanatory statement that Dr. Feldman wrote for the Coalition of State Rheumatology Organizations (CSRO).
According to the Guinness Book of World records, the longest time someone has held their breath underwater voluntarily is 24 minutes and 37.36 seconds. While certainly an amazing feat, UnitedHealthcare, many of the Blues, and other national “payers” are expecting rheumatologists and other specialists to live “underwater” in order to take care of their patients. In other words, these insurance companies are mandating that specialists use certain provider-administered biosimilars whose acquisition cost is higher than what the insurance company is willing to reimburse them. Essentially, the insurance companies expect the rheumatologists to pay them to take care of their patients. Because of the substantial and destabilizing financial losses incurred, many practices and free-standing infusion centers have been forced to cease offering these biosimilars. Most rheumatologists will provide patients with appropriate alternatives when available and permitted by the insurer; otherwise, they must refer patients to hospital-based infusion centers. That results in delayed care and increased costs for patients and the system, because hospital-based infusion typically costs more than twice what office-based infusion costs.
Quantifying the Problem
To help quantify the magnitude of this issue, the Coalition of State Rheumatology Organizations (CSRO) recently conducted a survey of its membership. A shocking 97% of respondents reported that their practice had been affected by reimbursement rates for some biosimilars being lower than acquisition costs, with 91% of respondents stating that this issue is more pronounced for certain biosimilars than others. Across the board, respondents most frequently identified Inflectra (infliximab-dyyb) and Avsola (infliximab-axxq) as being especially affected: Over 88% and over 85% of respondents identified these two products, respectively, as being underwater. These results support the ongoing anecdotal reports CSRO continues to receive from rheumatology practices.
However, the survey results indicated that this issue is by no means confined to those two biosimilars. Truxima (rituximab-abbs) — a biosimilar for Rituxan — was frequently mentioned as well. Notably, respondents almost uniformly identified biosimilars in the infliximab and rituximab families, which illustrates that this issue is no longer confined to one or two early-to-market biosimilars but has almost become a hallmark of this particular biosimilars market. Remarkably, one respondent commented that the brand products are now cheaper to acquire than the biosimilars. Furthermore, the survey included respondents from across the country, indicating that this issue is not confined to a particular region.
How Did This Happen?
Biosimilars held promise for increasing availability and decreasing biologic costs for patients but, thus far, no patients have seen their cost go down. It appears that the only biosimilars that have made it to “preferred” status on the formulary are the ones that have made more money for the middlemen in the drug supply chain, particularly those that construct formularies. Now, we have provider-administered biosimilars whose acquisition cost exceeds the reimbursement for these drugs. This disparity was ultimately created by biosimilar manufacturers “over-rebating” their drugs to health insurance companies to gain “fail-first” status on the formulary.
For example, the manufacturer of Inflectra offered substantial rebates to health insurers for preferred formulary placement. These rebates are factored into the sales price of the medication, which then results in a rapidly declining average sales price (ASP) for the biosimilar. Unfortunately, the acquisition cost for the drug does not experience commensurate reductions, resulting in physicians being reimbursed far less for the drug than it costs to acquire. The financial losses for physicians put them underwater as a result of the acquisition costs for the preferred drugs far surpassing the reimbursement from the health insurance company that constructed the formulary.
While various factors affect ASPs and acquisition costs, this particular consequence of formulary placement based on price concessions is a major driver of the underwater situation in which physicians have found themselves with many biosimilars. Not only does that lead to a lower uptake of biosimilars, but it also results in patients being referred to the hospital outpatient infusion sites to receive this care, as freestanding infusion centers cannot treat these patients either. Hospitals incur higher costs because of facility fees and elevated rates, and this makes private rheumatology in-office infusion centers a much lower-cost option. Similarly, home infusion services, while convenient, are marginally more expensive than private practices and, in cases of biologic infusions, it is important to note that physicians’ offices have a greater safety profile than home infusion of biologics. The overall result of these “fail-first underwater drugs” is delayed and more costly care for the patient and the “system,” particularly self-insured employers.
What Is Being Done to Correct This?
Since ASPs are updated quarterly, it is possible that acquisition costs and reimbursements might stabilize over time, making the drugs affordable again to practices. However, that does not appear to be happening in the near future, so that possibility does not offer immediate relief to struggling practices. It doesn’t promise a favorable outlook for future biosimilar entries of provider-administered medications if formularies continue to prefer the highest-rebated medication.
This dynamic between ASP and acquisition cost does not happen on the pharmacy side because the price concessions on specific drug rebates and fees are proprietary. There appears to be no equivalent to a publicly known ASP on the pharmacy side, which has led to myriad pricing definitions and manipulation on the pharmacy benefit side of medications. In any event, the savings from rebates and other manufacturer price concessions on pharmacy drugs do not influence ASPs of medical benefit drugs.
The Inflation Reduction Act provided a temporary increase in the add-on payment for biosimilars from ASP+6% to ASP+8%, but as long as the biosimilar’s ASP is lower than the reference brand’s ASP, that temporary increase does not appear to make up for the large differential between ASP and acquisition cost. It should be noted that any federal attempt to artificially lower the ASP of a provider-administered drug without a pathway assuring that the acquisition cost for the provider is less than the reimbursement is going to result in loss of access for patients to those medications and/or higher hospital site of care costs.
A Few Partial Fixes, But Most Complaints Go Ignored
Considering the higher costs of hospital-based infusion, insurers should be motivated to keep patients within private practices. Perhaps through insurers’ recognition of that fact, some practices have successfully negotiated exceptions for specific patients by discussing this situation with insurers. From the feedback that CSRO has received from rheumatology practices, it appears that most insurers have been ignoring the complaints from physicians. The few who have responded have resulted in only partial fixes, with some of the biosimilars still left underwater.
Ultimate Solution?
This issue is a direct result of the “rebate game,” whereby price concessions from drug manufacturers drive formulary placement. For provider-administered medications, this results in an artificially lowered ASP, not as a consequence of free-market incentives that benefit the patient, but as a result of misaligned incentives created by Safe Harbor–protected “kickbacks,” distorting the free market and paradoxically reducing access to these medications, delaying care, and increasing prices for patients and the healthcare system.
While federal and state governments are not likely to address this particular situation in the biosimilars market, CSRO is highlighting this issue as a prime example of why the current formulary construction system urgently requires federal reform. At this time, the biosimilars most affected are Inflectra and Avsola, but if nothing changes, more and more biosimilars will fall victim to the short-sighted pricing strategy of aggressive rebating to gain formulary position, with physician purchasers and patients left to navigate the aftermath. The existing system, which necessitates drug companies purchasing formulary access from pharmacy benefit managers, has led to delayed and even denied patient access to certain provider-administered drugs. Moreover, it now appears to be hindering the adoption of biosimilars.
To address this, a multifaceted approach is required. It not only involves reevaluating the rebate system and its impact on formulary construction and ASP, but also ensuring that acquisition costs for providers are aligned with reimbursement rates. Insurers must recognize the economic and clinical value of maintaining infusions within private practices and immediately update their policies to ensure that physician in-office infusion is financially feasible for these “fail-first” biosimilars.
Ultimately, the goal should be to create a sustainable model that promotes the use of affordable biosimilars, enhances patient access to affordable care, and supports the financial viability of medical practices. Concerted efforts to reform the current formulary construction system are required to achieve a healthcare environment that is both cost effective and patient centric.
Dr. Feldman is a rheumatologist in private practice with The Rheumatology Group in New Orleans. She is the CSRO’s vice president of advocacy and government affairs and its immediate past president, as well as past chair of the Alliance for Safe Biologic Medicines and a past member of the American College of Rheumatology insurance subcommittee. You can reach her at [email protected].
Editor’s note: This article is adapted from an explanatory statement that Dr. Feldman wrote for the Coalition of State Rheumatology Organizations (CSRO).
According to the Guinness Book of World records, the longest time someone has held their breath underwater voluntarily is 24 minutes and 37.36 seconds. While certainly an amazing feat, UnitedHealthcare, many of the Blues, and other national “payers” are expecting rheumatologists and other specialists to live “underwater” in order to take care of their patients. In other words, these insurance companies are mandating that specialists use certain provider-administered biosimilars whose acquisition cost is higher than what the insurance company is willing to reimburse them. Essentially, the insurance companies expect the rheumatologists to pay them to take care of their patients. Because of the substantial and destabilizing financial losses incurred, many practices and free-standing infusion centers have been forced to cease offering these biosimilars. Most rheumatologists will provide patients with appropriate alternatives when available and permitted by the insurer; otherwise, they must refer patients to hospital-based infusion centers. That results in delayed care and increased costs for patients and the system, because hospital-based infusion typically costs more than twice what office-based infusion costs.
Quantifying the Problem
To help quantify the magnitude of this issue, the Coalition of State Rheumatology Organizations (CSRO) recently conducted a survey of its membership. A shocking 97% of respondents reported that their practice had been affected by reimbursement rates for some biosimilars being lower than acquisition costs, with 91% of respondents stating that this issue is more pronounced for certain biosimilars than others. Across the board, respondents most frequently identified Inflectra (infliximab-dyyb) and Avsola (infliximab-axxq) as being especially affected: Over 88% and over 85% of respondents identified these two products, respectively, as being underwater. These results support the ongoing anecdotal reports CSRO continues to receive from rheumatology practices.
However, the survey results indicated that this issue is by no means confined to those two biosimilars. Truxima (rituximab-abbs) — a biosimilar for Rituxan — was frequently mentioned as well. Notably, respondents almost uniformly identified biosimilars in the infliximab and rituximab families, which illustrates that this issue is no longer confined to one or two early-to-market biosimilars but has almost become a hallmark of this particular biosimilars market. Remarkably, one respondent commented that the brand products are now cheaper to acquire than the biosimilars. Furthermore, the survey included respondents from across the country, indicating that this issue is not confined to a particular region.
How Did This Happen?
Biosimilars held promise for increasing availability and decreasing biologic costs for patients but, thus far, no patients have seen their cost go down. It appears that the only biosimilars that have made it to “preferred” status on the formulary are the ones that have made more money for the middlemen in the drug supply chain, particularly those that construct formularies. Now, we have provider-administered biosimilars whose acquisition cost exceeds the reimbursement for these drugs. This disparity was ultimately created by biosimilar manufacturers “over-rebating” their drugs to health insurance companies to gain “fail-first” status on the formulary.
For example, the manufacturer of Inflectra offered substantial rebates to health insurers for preferred formulary placement. These rebates are factored into the sales price of the medication, which then results in a rapidly declining average sales price (ASP) for the biosimilar. Unfortunately, the acquisition cost for the drug does not experience commensurate reductions, resulting in physicians being reimbursed far less for the drug than it costs to acquire. The financial losses for physicians put them underwater as a result of the acquisition costs for the preferred drugs far surpassing the reimbursement from the health insurance company that constructed the formulary.
While various factors affect ASPs and acquisition costs, this particular consequence of formulary placement based on price concessions is a major driver of the underwater situation in which physicians have found themselves with many biosimilars. Not only does that lead to a lower uptake of biosimilars, but it also results in patients being referred to the hospital outpatient infusion sites to receive this care, as freestanding infusion centers cannot treat these patients either. Hospitals incur higher costs because of facility fees and elevated rates, and this makes private rheumatology in-office infusion centers a much lower-cost option. Similarly, home infusion services, while convenient, are marginally more expensive than private practices and, in cases of biologic infusions, it is important to note that physicians’ offices have a greater safety profile than home infusion of biologics. The overall result of these “fail-first underwater drugs” is delayed and more costly care for the patient and the “system,” particularly self-insured employers.
What Is Being Done to Correct This?
Since ASPs are updated quarterly, it is possible that acquisition costs and reimbursements might stabilize over time, making the drugs affordable again to practices. However, that does not appear to be happening in the near future, so that possibility does not offer immediate relief to struggling practices. It doesn’t promise a favorable outlook for future biosimilar entries of provider-administered medications if formularies continue to prefer the highest-rebated medication.
This dynamic between ASP and acquisition cost does not happen on the pharmacy side because the price concessions on specific drug rebates and fees are proprietary. There appears to be no equivalent to a publicly known ASP on the pharmacy side, which has led to myriad pricing definitions and manipulation on the pharmacy benefit side of medications. In any event, the savings from rebates and other manufacturer price concessions on pharmacy drugs do not influence ASPs of medical benefit drugs.
The Inflation Reduction Act provided a temporary increase in the add-on payment for biosimilars from ASP+6% to ASP+8%, but as long as the biosimilar’s ASP is lower than the reference brand’s ASP, that temporary increase does not appear to make up for the large differential between ASP and acquisition cost. It should be noted that any federal attempt to artificially lower the ASP of a provider-administered drug without a pathway assuring that the acquisition cost for the provider is less than the reimbursement is going to result in loss of access for patients to those medications and/or higher hospital site of care costs.
A Few Partial Fixes, But Most Complaints Go Ignored
Considering the higher costs of hospital-based infusion, insurers should be motivated to keep patients within private practices. Perhaps through insurers’ recognition of that fact, some practices have successfully negotiated exceptions for specific patients by discussing this situation with insurers. From the feedback that CSRO has received from rheumatology practices, it appears that most insurers have been ignoring the complaints from physicians. The few who have responded have resulted in only partial fixes, with some of the biosimilars still left underwater.
Ultimate Solution?
This issue is a direct result of the “rebate game,” whereby price concessions from drug manufacturers drive formulary placement. For provider-administered medications, this results in an artificially lowered ASP, not as a consequence of free-market incentives that benefit the patient, but as a result of misaligned incentives created by Safe Harbor–protected “kickbacks,” distorting the free market and paradoxically reducing access to these medications, delaying care, and increasing prices for patients and the healthcare system.
While federal and state governments are not likely to address this particular situation in the biosimilars market, CSRO is highlighting this issue as a prime example of why the current formulary construction system urgently requires federal reform. At this time, the biosimilars most affected are Inflectra and Avsola, but if nothing changes, more and more biosimilars will fall victim to the short-sighted pricing strategy of aggressive rebating to gain formulary position, with physician purchasers and patients left to navigate the aftermath. The existing system, which necessitates drug companies purchasing formulary access from pharmacy benefit managers, has led to delayed and even denied patient access to certain provider-administered drugs. Moreover, it now appears to be hindering the adoption of biosimilars.
To address this, a multifaceted approach is required. It not only involves reevaluating the rebate system and its impact on formulary construction and ASP, but also ensuring that acquisition costs for providers are aligned with reimbursement rates. Insurers must recognize the economic and clinical value of maintaining infusions within private practices and immediately update their policies to ensure that physician in-office infusion is financially feasible for these “fail-first” biosimilars.
Ultimately, the goal should be to create a sustainable model that promotes the use of affordable biosimilars, enhances patient access to affordable care, and supports the financial viability of medical practices. Concerted efforts to reform the current formulary construction system are required to achieve a healthcare environment that is both cost effective and patient centric.
Dr. Feldman is a rheumatologist in private practice with The Rheumatology Group in New Orleans. She is the CSRO’s vice president of advocacy and government affairs and its immediate past president, as well as past chair of the Alliance for Safe Biologic Medicines and a past member of the American College of Rheumatology insurance subcommittee. You can reach her at [email protected].













