User login
Fetal alcohol spectrum disorders and suicidality
As psychiatrists, we understand that behavior is complex and determined by multiple factors. However, despite our understanding that behavior is cultural, sociological, psychological, and biological, we often lose sight of the biological perspective because the brain is such a complex organ and because we are inundated with psychological theories of behavior. As I have said before, we cannot abdicate our role of being biologists in the reflection of mental health and wellness.
Accordingly, I feel it is my duty to bring our attention to a biologic etiology of suicidal behavior. I came across an article on the life expectancy of individuals afflicted with fetal alcohol syndrome in the Journal of Population Therapeutics and Clinical Pharmacology (2016;23[1]:e53-9). The findings were astonishing. As it turns out, the life expectancy of people with fetal alcohol syndrome is 34 years of age on average, and the leading causes of death were “external causes,” which accounted for 44% of the deaths. Suicide was responsible for 15% of those deaths, accidents for 14%, poisoning by illegal drugs or alcohol for 7%, and other external causes for another 7%, according to the article.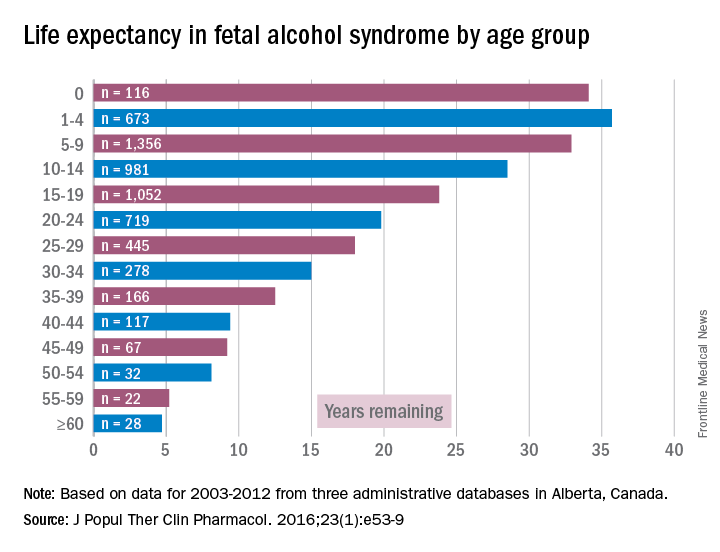
While working in a general hospital in a low-income African American environment where there are high rates of fetal alcohol exposure, I see at least 3-4 suicide attempts a week on the medical-surgical/psychiatric inpatient units where I serve. I am always looking for patients who have ND-PAE because determining such a diagnosis is critical to those patients’ medical-surgical care. For example, there was one woman with ND-PAE who had operable breast carcinoma but did not come in for a return visit until after her carcinoma had become inoperable (she forgot how important it was to get timely treatment). There was a patient who always had out-of-control diabetes because he did not know how to use his glucometer. There was a patient who was taking his antipsychotic medication during the day instead of as prescribed – at bedtime – because he could not read the instructions on his medication bottle. (I have altered several key aspects of my patients’ stories to protect their confidentiality.)
However, until I read that suicide was responsible for 15% of deaths with external causes among patients with fetal alcohol syndrome – patients whose life expectancy averages only 34 years – it did not occur to me that affect dysregulation also was likely to lead to suicide attempts among patients with ND-PAE.
When several of us who were working on the issue of suicide prevention while part of the Committee on Psychopathology & Prevention of Adolescent & Adult Suicide produced our report called “Reducing Suicide: A National Perspective” in 2002, the idea that paying attention to fetal environments and birth outcomes could inform the area of suicide prevention was an alien one. Now, it is a serious consideration because this dynamic just might explain part of the complex phenomena of some suicidal behaviors.
Dr. Bell is a staff psychiatrist at Jackson Park Hospital Family Medicine Clinic in Chicago; clinical psychiatrist emeritus in the department of psychiatry at the University of Illinois at Chicago; former president/CEO of Community Mental Health Council; and former director of the Institute for Juvenile Research (birthplace of child psychiatry), also in Chicago.
As psychiatrists, we understand that behavior is complex and determined by multiple factors. However, despite our understanding that behavior is cultural, sociological, psychological, and biological, we often lose sight of the biological perspective because the brain is such a complex organ and because we are inundated with psychological theories of behavior. As I have said before, we cannot abdicate our role of being biologists in the reflection of mental health and wellness.
Accordingly, I feel it is my duty to bring our attention to a biologic etiology of suicidal behavior. I came across an article on the life expectancy of individuals afflicted with fetal alcohol syndrome in the Journal of Population Therapeutics and Clinical Pharmacology (2016;23[1]:e53-9). The findings were astonishing. As it turns out, the life expectancy of people with fetal alcohol syndrome is 34 years of age on average, and the leading causes of death were “external causes,” which accounted for 44% of the deaths. Suicide was responsible for 15% of those deaths, accidents for 14%, poisoning by illegal drugs or alcohol for 7%, and other external causes for another 7%, according to the article.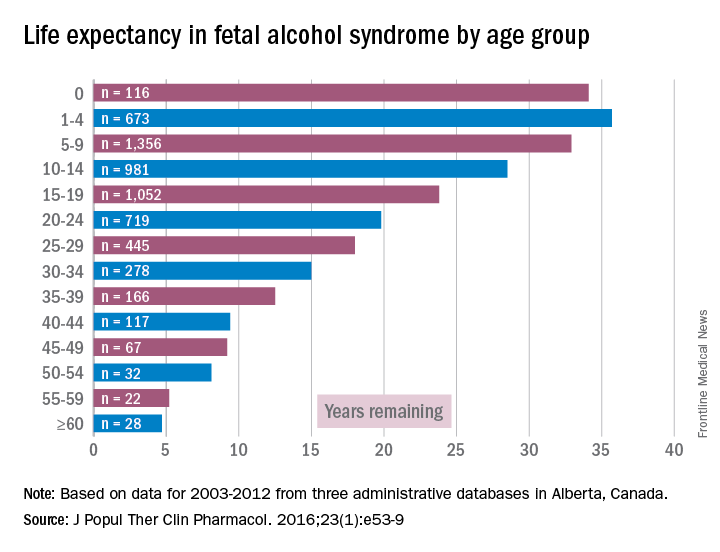
While working in a general hospital in a low-income African American environment where there are high rates of fetal alcohol exposure, I see at least 3-4 suicide attempts a week on the medical-surgical/psychiatric inpatient units where I serve. I am always looking for patients who have ND-PAE because determining such a diagnosis is critical to those patients’ medical-surgical care. For example, there was one woman with ND-PAE who had operable breast carcinoma but did not come in for a return visit until after her carcinoma had become inoperable (she forgot how important it was to get timely treatment). There was a patient who always had out-of-control diabetes because he did not know how to use his glucometer. There was a patient who was taking his antipsychotic medication during the day instead of as prescribed – at bedtime – because he could not read the instructions on his medication bottle. (I have altered several key aspects of my patients’ stories to protect their confidentiality.)
However, until I read that suicide was responsible for 15% of deaths with external causes among patients with fetal alcohol syndrome – patients whose life expectancy averages only 34 years – it did not occur to me that affect dysregulation also was likely to lead to suicide attempts among patients with ND-PAE.
When several of us who were working on the issue of suicide prevention while part of the Committee on Psychopathology & Prevention of Adolescent & Adult Suicide produced our report called “Reducing Suicide: A National Perspective” in 2002, the idea that paying attention to fetal environments and birth outcomes could inform the area of suicide prevention was an alien one. Now, it is a serious consideration because this dynamic just might explain part of the complex phenomena of some suicidal behaviors.
Dr. Bell is a staff psychiatrist at Jackson Park Hospital Family Medicine Clinic in Chicago; clinical psychiatrist emeritus in the department of psychiatry at the University of Illinois at Chicago; former president/CEO of Community Mental Health Council; and former director of the Institute for Juvenile Research (birthplace of child psychiatry), also in Chicago.
As psychiatrists, we understand that behavior is complex and determined by multiple factors. However, despite our understanding that behavior is cultural, sociological, psychological, and biological, we often lose sight of the biological perspective because the brain is such a complex organ and because we are inundated with psychological theories of behavior. As I have said before, we cannot abdicate our role of being biologists in the reflection of mental health and wellness.
Accordingly, I feel it is my duty to bring our attention to a biologic etiology of suicidal behavior. I came across an article on the life expectancy of individuals afflicted with fetal alcohol syndrome in the Journal of Population Therapeutics and Clinical Pharmacology (2016;23[1]:e53-9). The findings were astonishing. As it turns out, the life expectancy of people with fetal alcohol syndrome is 34 years of age on average, and the leading causes of death were “external causes,” which accounted for 44% of the deaths. Suicide was responsible for 15% of those deaths, accidents for 14%, poisoning by illegal drugs or alcohol for 7%, and other external causes for another 7%, according to the article.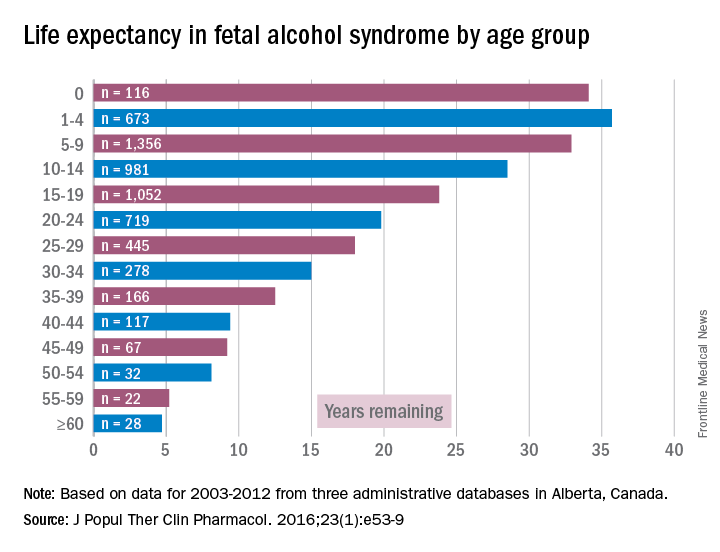
While working in a general hospital in a low-income African American environment where there are high rates of fetal alcohol exposure, I see at least 3-4 suicide attempts a week on the medical-surgical/psychiatric inpatient units where I serve. I am always looking for patients who have ND-PAE because determining such a diagnosis is critical to those patients’ medical-surgical care. For example, there was one woman with ND-PAE who had operable breast carcinoma but did not come in for a return visit until after her carcinoma had become inoperable (she forgot how important it was to get timely treatment). There was a patient who always had out-of-control diabetes because he did not know how to use his glucometer. There was a patient who was taking his antipsychotic medication during the day instead of as prescribed – at bedtime – because he could not read the instructions on his medication bottle. (I have altered several key aspects of my patients’ stories to protect their confidentiality.)
However, until I read that suicide was responsible for 15% of deaths with external causes among patients with fetal alcohol syndrome – patients whose life expectancy averages only 34 years – it did not occur to me that affect dysregulation also was likely to lead to suicide attempts among patients with ND-PAE.
When several of us who were working on the issue of suicide prevention while part of the Committee on Psychopathology & Prevention of Adolescent & Adult Suicide produced our report called “Reducing Suicide: A National Perspective” in 2002, the idea that paying attention to fetal environments and birth outcomes could inform the area of suicide prevention was an alien one. Now, it is a serious consideration because this dynamic just might explain part of the complex phenomena of some suicidal behaviors.
Dr. Bell is a staff psychiatrist at Jackson Park Hospital Family Medicine Clinic in Chicago; clinical psychiatrist emeritus in the department of psychiatry at the University of Illinois at Chicago; former president/CEO of Community Mental Health Council; and former director of the Institute for Juvenile Research (birthplace of child psychiatry), also in Chicago.
Identity crisis
The provider has received “advanced-level education in pharmacology, pathophysiology, and physical assessment, diagnosis, and management” and provides patient care in a medical home “in a holistic fashion including physical care, therapeutic treatments, education, and coordination of services.”
This quote comes from a recent story in Pediatric News about collaborative practice. Was the author offering a job description of a) a chiropractor, b) a nurse practitioner, c) a pediatric oncologist, or d) a primary care physician?
Based on my personal experience working with nurse practitioners, both in hospital and office settings, I wholeheartedly concur with Dr. Haut’s list of their qualifications and capabilities. My problem is that she doesn’t list, nor can I comfortably imagine, the additional skills that a physician should have in his or her toolbox to complete the complementary relationships in a primary care practice that Dr. Haut envisions.
From my perspective, nurse practitioners and primary care physicians share the same job description, the one I listed in the first paragraph of this column. They both provide face-to-face, usually hands-on, medical care. At that critical interface between patient and provider, how do their roles differ? What other skills does a physician need to complement those of a competent and already experienced nurse practitioner?
Does being a physician guarantee that he or she has more experience than a nurse practitioner? You know as well as I do that you finished your training pretty wet behind the ears, and the first 5 years or more of your practice career were when you really began to feel like a competent provider. If my child has an earache, I would probably be more comfortable, or at least as comfortable, with her seeing a nurse practitioner with 5 years of experience in a busy practice than a newly minted, board-eligible pediatrician.
Is the breadth of a physician’s training in medical school an asset? Does the 2-month rotation he or she did on the adult neurology service taking care of stroke victims give the physician an advantage when it comes to taking care of pediatric patients with asthma?
Actually, I can imagine a suite of skills that a physician might bring to a collaborative practice that a nurse practitioner may not have, or more likely may have chosen not to pursue. Those skills have little to do with direct patient care, but can be critical for survival in today’s medical care environment. Here I am thinking of things such as negotiating with third-party payers, and leading and/or administering the complexities of a medium-sized or larger medical group. Does having a degree from a medical school automatically mean that the graduate is a skilled leader or administrator?
I can envision that over time a physician and a nurse practitioner might create an arrangement in which one of them focuses on the patients with asthma and attention-deficit/hyperactivity disorder, and the other develops an expertise in breastfeeding management and picky eating. That kind of relationship fits my definition of complementary. However, a relationship in which the doctor is the boss and the nurse practitioner is not doesn’t feel complementary or collaborative to me.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine, for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.”
The provider has received “advanced-level education in pharmacology, pathophysiology, and physical assessment, diagnosis, and management” and provides patient care in a medical home “in a holistic fashion including physical care, therapeutic treatments, education, and coordination of services.”
This quote comes from a recent story in Pediatric News about collaborative practice. Was the author offering a job description of a) a chiropractor, b) a nurse practitioner, c) a pediatric oncologist, or d) a primary care physician?
Based on my personal experience working with nurse practitioners, both in hospital and office settings, I wholeheartedly concur with Dr. Haut’s list of their qualifications and capabilities. My problem is that she doesn’t list, nor can I comfortably imagine, the additional skills that a physician should have in his or her toolbox to complete the complementary relationships in a primary care practice that Dr. Haut envisions.
From my perspective, nurse practitioners and primary care physicians share the same job description, the one I listed in the first paragraph of this column. They both provide face-to-face, usually hands-on, medical care. At that critical interface between patient and provider, how do their roles differ? What other skills does a physician need to complement those of a competent and already experienced nurse practitioner?
Does being a physician guarantee that he or she has more experience than a nurse practitioner? You know as well as I do that you finished your training pretty wet behind the ears, and the first 5 years or more of your practice career were when you really began to feel like a competent provider. If my child has an earache, I would probably be more comfortable, or at least as comfortable, with her seeing a nurse practitioner with 5 years of experience in a busy practice than a newly minted, board-eligible pediatrician.
Is the breadth of a physician’s training in medical school an asset? Does the 2-month rotation he or she did on the adult neurology service taking care of stroke victims give the physician an advantage when it comes to taking care of pediatric patients with asthma?
Actually, I can imagine a suite of skills that a physician might bring to a collaborative practice that a nurse practitioner may not have, or more likely may have chosen not to pursue. Those skills have little to do with direct patient care, but can be critical for survival in today’s medical care environment. Here I am thinking of things such as negotiating with third-party payers, and leading and/or administering the complexities of a medium-sized or larger medical group. Does having a degree from a medical school automatically mean that the graduate is a skilled leader or administrator?
I can envision that over time a physician and a nurse practitioner might create an arrangement in which one of them focuses on the patients with asthma and attention-deficit/hyperactivity disorder, and the other develops an expertise in breastfeeding management and picky eating. That kind of relationship fits my definition of complementary. However, a relationship in which the doctor is the boss and the nurse practitioner is not doesn’t feel complementary or collaborative to me.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine, for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.”
The provider has received “advanced-level education in pharmacology, pathophysiology, and physical assessment, diagnosis, and management” and provides patient care in a medical home “in a holistic fashion including physical care, therapeutic treatments, education, and coordination of services.”
This quote comes from a recent story in Pediatric News about collaborative practice. Was the author offering a job description of a) a chiropractor, b) a nurse practitioner, c) a pediatric oncologist, or d) a primary care physician?
Based on my personal experience working with nurse practitioners, both in hospital and office settings, I wholeheartedly concur with Dr. Haut’s list of their qualifications and capabilities. My problem is that she doesn’t list, nor can I comfortably imagine, the additional skills that a physician should have in his or her toolbox to complete the complementary relationships in a primary care practice that Dr. Haut envisions.
From my perspective, nurse practitioners and primary care physicians share the same job description, the one I listed in the first paragraph of this column. They both provide face-to-face, usually hands-on, medical care. At that critical interface between patient and provider, how do their roles differ? What other skills does a physician need to complement those of a competent and already experienced nurse practitioner?
Does being a physician guarantee that he or she has more experience than a nurse practitioner? You know as well as I do that you finished your training pretty wet behind the ears, and the first 5 years or more of your practice career were when you really began to feel like a competent provider. If my child has an earache, I would probably be more comfortable, or at least as comfortable, with her seeing a nurse practitioner with 5 years of experience in a busy practice than a newly minted, board-eligible pediatrician.
Is the breadth of a physician’s training in medical school an asset? Does the 2-month rotation he or she did on the adult neurology service taking care of stroke victims give the physician an advantage when it comes to taking care of pediatric patients with asthma?
Actually, I can imagine a suite of skills that a physician might bring to a collaborative practice that a nurse practitioner may not have, or more likely may have chosen not to pursue. Those skills have little to do with direct patient care, but can be critical for survival in today’s medical care environment. Here I am thinking of things such as negotiating with third-party payers, and leading and/or administering the complexities of a medium-sized or larger medical group. Does having a degree from a medical school automatically mean that the graduate is a skilled leader or administrator?
I can envision that over time a physician and a nurse practitioner might create an arrangement in which one of them focuses on the patients with asthma and attention-deficit/hyperactivity disorder, and the other develops an expertise in breastfeeding management and picky eating. That kind of relationship fits my definition of complementary. However, a relationship in which the doctor is the boss and the nurse practitioner is not doesn’t feel complementary or collaborative to me.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine, for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.”
Typhoid isn’t covered??!!
My wife and I decided to visit Morocco, to test the maxim that my fellow columnist Joe Eastern often cites: The words you won’t say on your deathbed are, “If only I had spent more time at the office.”
Though I’m not convinced he’s right about that – he’s never even seen my office – I thought I’d give being away a try. My office manager comes from near Marrakesh. While bound for Morocco, we could check out her hometown, even if there is no obvious tax angle.
As I contemplated exotic travel, the first things that came to mind of course were what rare diseases I might catch, which vaccines could prevent them, and how to get insurance to pay for getting immunized. Alexa helped me find CDC recommendations for immunizations for travel to Morocco, which included:
• Typhoid ... contaminated food or water.
• Hepatitis A ... contaminated food or water.
• Hepatitis B ... contaminated body fluids (sex, needles, etc.).
• Cholera ... contaminated food or water.
• Rabies ... infected animals.
• Influenza ... airborne droplets.
This trip was indeed starting to sound like an awful lot of fun.
My PCP called in several of the relevant vaccines to my local pharmacy, who informed me that typhoid vaccine is not covered by my health insurance. This spurred the following (somewhat embellished) dialogue with my insurer:
“Why is typhoid not covered?”
“Contractual exclusion. We don’t cover anything starting with “typ-,” including typhoid, typhus, typical, and typographic.”
“Do you cover bubonic plague?”
“Only for high-risk travel.”
“Such as?”
“Such as if you travel to Europe during the 14th century.”
“How about Hepatitis B and rabies?”
“That would depend.”
“On what?”
“On whether you plan to have sex with rabid bats, or rabid sex with placid bats.”
“I wouldn’t say I have plans. But, you know, in the moment ...”
“Sorry, not covered.”
“How about cholera?”
“Have you ever been threatened by cholera?
“Not exactly. But I did have a cranky uncle. When he was irritated, he often said, ‘May cholera grab you!’ ”
“You’re not covered. Your uncle might be.”
“We’ve decided on a side trip to Tanzania. As long as we’re already in Africa ...”
“Do you suffer from Sleeping Sickness?”
“Only at Grand Rounds.”
“We do cover eflornithine, but there is a problem ...”
“What problem?”
“Our only eflornithine manufacturing facility is in Bangladesh, where it takes up two floors of a factory that also makes designer jeans. That factory is closed for safety and child-labor violations.”
“For how long?”
“Indefinitely”
“Then what can I do?”
“You can apply eflornithine cream for your Sleeping Sickness and hope for the best.”
“Eflornithine cream?”
“Vaniqa. It may not help your sleeping symptoms, but you’ll need fewer haircuts.”
“Oh, thanks. What about River Blindness? Do you cover ivermectin?”
“Only if the preferred formulary alternatives have been exhausted.”
“What are those?”
“Metronidazole and azelaic acid.”
“Hold on! Are you looking at the page for onchocerciasis or the one for rosacea?”
“Yes. Did Montezuma ever make it to Morocco?”
“I don’t have that information. You’ll have to ask Alexa. Anything else?”
“No, I’m all set. Just remind me what you said about bats?”
In the end a family situation came up, and we had to cancel our trip. Instead, we watched the movie “Casablanca.” That is an excellent movie, with many pungent and memorable lines. Not only that but watching it does not cause jet lag.
As for the typhoid vaccine, in the end, it was not covered by insurance. Nevertheless, I haven’t had a bit of typhoid, so the vaccine seems to be working very well.
Dr. Rockoff practices dermatology in Brookline, Mass., and is a longtime contributor to Dermatology News. He serves on the clinical faculty at Tufts University, Boston, and has taught senior medical students and other trainees for 30 years. His second book, “Act Like a Doctor, Think Like a Patient,” is available at amazon.com and barnesandnoble.com. Write to him at [email protected].
My wife and I decided to visit Morocco, to test the maxim that my fellow columnist Joe Eastern often cites: The words you won’t say on your deathbed are, “If only I had spent more time at the office.”
Though I’m not convinced he’s right about that – he’s never even seen my office – I thought I’d give being away a try. My office manager comes from near Marrakesh. While bound for Morocco, we could check out her hometown, even if there is no obvious tax angle.
As I contemplated exotic travel, the first things that came to mind of course were what rare diseases I might catch, which vaccines could prevent them, and how to get insurance to pay for getting immunized. Alexa helped me find CDC recommendations for immunizations for travel to Morocco, which included:
• Typhoid ... contaminated food or water.
• Hepatitis A ... contaminated food or water.
• Hepatitis B ... contaminated body fluids (sex, needles, etc.).
• Cholera ... contaminated food or water.
• Rabies ... infected animals.
• Influenza ... airborne droplets.
This trip was indeed starting to sound like an awful lot of fun.
My PCP called in several of the relevant vaccines to my local pharmacy, who informed me that typhoid vaccine is not covered by my health insurance. This spurred the following (somewhat embellished) dialogue with my insurer:
“Why is typhoid not covered?”
“Contractual exclusion. We don’t cover anything starting with “typ-,” including typhoid, typhus, typical, and typographic.”
“Do you cover bubonic plague?”
“Only for high-risk travel.”
“Such as?”
“Such as if you travel to Europe during the 14th century.”
“How about Hepatitis B and rabies?”
“That would depend.”
“On what?”
“On whether you plan to have sex with rabid bats, or rabid sex with placid bats.”
“I wouldn’t say I have plans. But, you know, in the moment ...”
“Sorry, not covered.”
“How about cholera?”
“Have you ever been threatened by cholera?
“Not exactly. But I did have a cranky uncle. When he was irritated, he often said, ‘May cholera grab you!’ ”
“You’re not covered. Your uncle might be.”
“We’ve decided on a side trip to Tanzania. As long as we’re already in Africa ...”
“Do you suffer from Sleeping Sickness?”
“Only at Grand Rounds.”
“We do cover eflornithine, but there is a problem ...”
“What problem?”
“Our only eflornithine manufacturing facility is in Bangladesh, where it takes up two floors of a factory that also makes designer jeans. That factory is closed for safety and child-labor violations.”
“For how long?”
“Indefinitely”
“Then what can I do?”
“You can apply eflornithine cream for your Sleeping Sickness and hope for the best.”
“Eflornithine cream?”
“Vaniqa. It may not help your sleeping symptoms, but you’ll need fewer haircuts.”
“Oh, thanks. What about River Blindness? Do you cover ivermectin?”
“Only if the preferred formulary alternatives have been exhausted.”
“What are those?”
“Metronidazole and azelaic acid.”
“Hold on! Are you looking at the page for onchocerciasis or the one for rosacea?”
“Yes. Did Montezuma ever make it to Morocco?”
“I don’t have that information. You’ll have to ask Alexa. Anything else?”
“No, I’m all set. Just remind me what you said about bats?”
In the end a family situation came up, and we had to cancel our trip. Instead, we watched the movie “Casablanca.” That is an excellent movie, with many pungent and memorable lines. Not only that but watching it does not cause jet lag.
As for the typhoid vaccine, in the end, it was not covered by insurance. Nevertheless, I haven’t had a bit of typhoid, so the vaccine seems to be working very well.
Dr. Rockoff practices dermatology in Brookline, Mass., and is a longtime contributor to Dermatology News. He serves on the clinical faculty at Tufts University, Boston, and has taught senior medical students and other trainees for 30 years. His second book, “Act Like a Doctor, Think Like a Patient,” is available at amazon.com and barnesandnoble.com. Write to him at [email protected].
My wife and I decided to visit Morocco, to test the maxim that my fellow columnist Joe Eastern often cites: The words you won’t say on your deathbed are, “If only I had spent more time at the office.”
Though I’m not convinced he’s right about that – he’s never even seen my office – I thought I’d give being away a try. My office manager comes from near Marrakesh. While bound for Morocco, we could check out her hometown, even if there is no obvious tax angle.
As I contemplated exotic travel, the first things that came to mind of course were what rare diseases I might catch, which vaccines could prevent them, and how to get insurance to pay for getting immunized. Alexa helped me find CDC recommendations for immunizations for travel to Morocco, which included:
• Typhoid ... contaminated food or water.
• Hepatitis A ... contaminated food or water.
• Hepatitis B ... contaminated body fluids (sex, needles, etc.).
• Cholera ... contaminated food or water.
• Rabies ... infected animals.
• Influenza ... airborne droplets.
This trip was indeed starting to sound like an awful lot of fun.
My PCP called in several of the relevant vaccines to my local pharmacy, who informed me that typhoid vaccine is not covered by my health insurance. This spurred the following (somewhat embellished) dialogue with my insurer:
“Why is typhoid not covered?”
“Contractual exclusion. We don’t cover anything starting with “typ-,” including typhoid, typhus, typical, and typographic.”
“Do you cover bubonic plague?”
“Only for high-risk travel.”
“Such as?”
“Such as if you travel to Europe during the 14th century.”
“How about Hepatitis B and rabies?”
“That would depend.”
“On what?”
“On whether you plan to have sex with rabid bats, or rabid sex with placid bats.”
“I wouldn’t say I have plans. But, you know, in the moment ...”
“Sorry, not covered.”
“How about cholera?”
“Have you ever been threatened by cholera?
“Not exactly. But I did have a cranky uncle. When he was irritated, he often said, ‘May cholera grab you!’ ”
“You’re not covered. Your uncle might be.”
“We’ve decided on a side trip to Tanzania. As long as we’re already in Africa ...”
“Do you suffer from Sleeping Sickness?”
“Only at Grand Rounds.”
“We do cover eflornithine, but there is a problem ...”
“What problem?”
“Our only eflornithine manufacturing facility is in Bangladesh, where it takes up two floors of a factory that also makes designer jeans. That factory is closed for safety and child-labor violations.”
“For how long?”
“Indefinitely”
“Then what can I do?”
“You can apply eflornithine cream for your Sleeping Sickness and hope for the best.”
“Eflornithine cream?”
“Vaniqa. It may not help your sleeping symptoms, but you’ll need fewer haircuts.”
“Oh, thanks. What about River Blindness? Do you cover ivermectin?”
“Only if the preferred formulary alternatives have been exhausted.”
“What are those?”
“Metronidazole and azelaic acid.”
“Hold on! Are you looking at the page for onchocerciasis or the one for rosacea?”
“Yes. Did Montezuma ever make it to Morocco?”
“I don’t have that information. You’ll have to ask Alexa. Anything else?”
“No, I’m all set. Just remind me what you said about bats?”
In the end a family situation came up, and we had to cancel our trip. Instead, we watched the movie “Casablanca.” That is an excellent movie, with many pungent and memorable lines. Not only that but watching it does not cause jet lag.
As for the typhoid vaccine, in the end, it was not covered by insurance. Nevertheless, I haven’t had a bit of typhoid, so the vaccine seems to be working very well.
Dr. Rockoff practices dermatology in Brookline, Mass., and is a longtime contributor to Dermatology News. He serves on the clinical faculty at Tufts University, Boston, and has taught senior medical students and other trainees for 30 years. His second book, “Act Like a Doctor, Think Like a Patient,” is available at amazon.com and barnesandnoble.com. Write to him at [email protected].
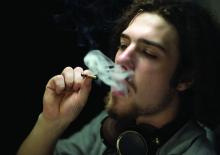
When cannabis use becomes another disorder
Despite the justified concern about rising opiate use in the United States, cannabis remains the most commonly used substance in the 12- to 17-year-old population.1 Cannabis use is widespread, particularly in states in which it has been decriminalized or legalized. While use of alcohol and nicotine has fallen among high school students from the years 2010 to 2015, marijuana use has remained relatively constant.2 In addition, the potency of cannabis with regard to tetrahydrocannabinol (THC) content has increased over the years. Despite the common belief among the public that cannabis use is benign, accumulating research is revealing a number of concerning consequences, especially in vulnerable populations and those who use cannabis regularly.
Case summary
Case discussion
Treatment for these adverse effects of cannabis is cessation of the drug. This can be accomplished through hard work with a counselor, who may recommend any of a number of treatments, including contingency management, cognitive behavioral therapy, systematic multidimensional family therapy, and motivational enhancement therapy, among others.5 While common lore is that it is impossible to stop cannabis use, the effect sizes of these treatments is in the moderate to large range. There are viable options to stop cannabis use, especially when it becomes problematic.
Dr. Althoff is associate professor of psychiatry, psychology, and pediatrics at the University of Vermont, Burlington. He is director of the division of behavioral genetics and conducts research on the development of self-regulation in children. Email him at [email protected].
References
1. “Results from the 2013 National Survey on Drug Use and Health: Summary of National Findings,” Substance Abuse and Mental Health Services Administration Center for Behavioral Health Statistics and Quality, 2013.
2. “Monitoring the Future Survey, 2015,” National Institute on Drug Abuse.
3. Pharmaceuticals (Basel). 2012 Jul;5(7):719-26.
4. Nat Rev Neurosci. 2007 Nov;8(11):885-95.
5. Dtsch Arztebl Int. 2016 Sep;113(39): 653-9.
Despite the justified concern about rising opiate use in the United States, cannabis remains the most commonly used substance in the 12- to 17-year-old population.1 Cannabis use is widespread, particularly in states in which it has been decriminalized or legalized. While use of alcohol and nicotine has fallen among high school students from the years 2010 to 2015, marijuana use has remained relatively constant.2 In addition, the potency of cannabis with regard to tetrahydrocannabinol (THC) content has increased over the years. Despite the common belief among the public that cannabis use is benign, accumulating research is revealing a number of concerning consequences, especially in vulnerable populations and those who use cannabis regularly.
Case summary
Case discussion
Treatment for these adverse effects of cannabis is cessation of the drug. This can be accomplished through hard work with a counselor, who may recommend any of a number of treatments, including contingency management, cognitive behavioral therapy, systematic multidimensional family therapy, and motivational enhancement therapy, among others.5 While common lore is that it is impossible to stop cannabis use, the effect sizes of these treatments is in the moderate to large range. There are viable options to stop cannabis use, especially when it becomes problematic.
Dr. Althoff is associate professor of psychiatry, psychology, and pediatrics at the University of Vermont, Burlington. He is director of the division of behavioral genetics and conducts research on the development of self-regulation in children. Email him at [email protected].
References
1. “Results from the 2013 National Survey on Drug Use and Health: Summary of National Findings,” Substance Abuse and Mental Health Services Administration Center for Behavioral Health Statistics and Quality, 2013.
2. “Monitoring the Future Survey, 2015,” National Institute on Drug Abuse.
3. Pharmaceuticals (Basel). 2012 Jul;5(7):719-26.
4. Nat Rev Neurosci. 2007 Nov;8(11):885-95.
5. Dtsch Arztebl Int. 2016 Sep;113(39): 653-9.
Despite the justified concern about rising opiate use in the United States, cannabis remains the most commonly used substance in the 12- to 17-year-old population.1 Cannabis use is widespread, particularly in states in which it has been decriminalized or legalized. While use of alcohol and nicotine has fallen among high school students from the years 2010 to 2015, marijuana use has remained relatively constant.2 In addition, the potency of cannabis with regard to tetrahydrocannabinol (THC) content has increased over the years. Despite the common belief among the public that cannabis use is benign, accumulating research is revealing a number of concerning consequences, especially in vulnerable populations and those who use cannabis regularly.
Case summary
Case discussion
Treatment for these adverse effects of cannabis is cessation of the drug. This can be accomplished through hard work with a counselor, who may recommend any of a number of treatments, including contingency management, cognitive behavioral therapy, systematic multidimensional family therapy, and motivational enhancement therapy, among others.5 While common lore is that it is impossible to stop cannabis use, the effect sizes of these treatments is in the moderate to large range. There are viable options to stop cannabis use, especially when it becomes problematic.
Dr. Althoff is associate professor of psychiatry, psychology, and pediatrics at the University of Vermont, Burlington. He is director of the division of behavioral genetics and conducts research on the development of self-regulation in children. Email him at [email protected].
References
1. “Results from the 2013 National Survey on Drug Use and Health: Summary of National Findings,” Substance Abuse and Mental Health Services Administration Center for Behavioral Health Statistics and Quality, 2013.
2. “Monitoring the Future Survey, 2015,” National Institute on Drug Abuse.
3. Pharmaceuticals (Basel). 2012 Jul;5(7):719-26.
4. Nat Rev Neurosci. 2007 Nov;8(11):885-95.
5. Dtsch Arztebl Int. 2016 Sep;113(39): 653-9.
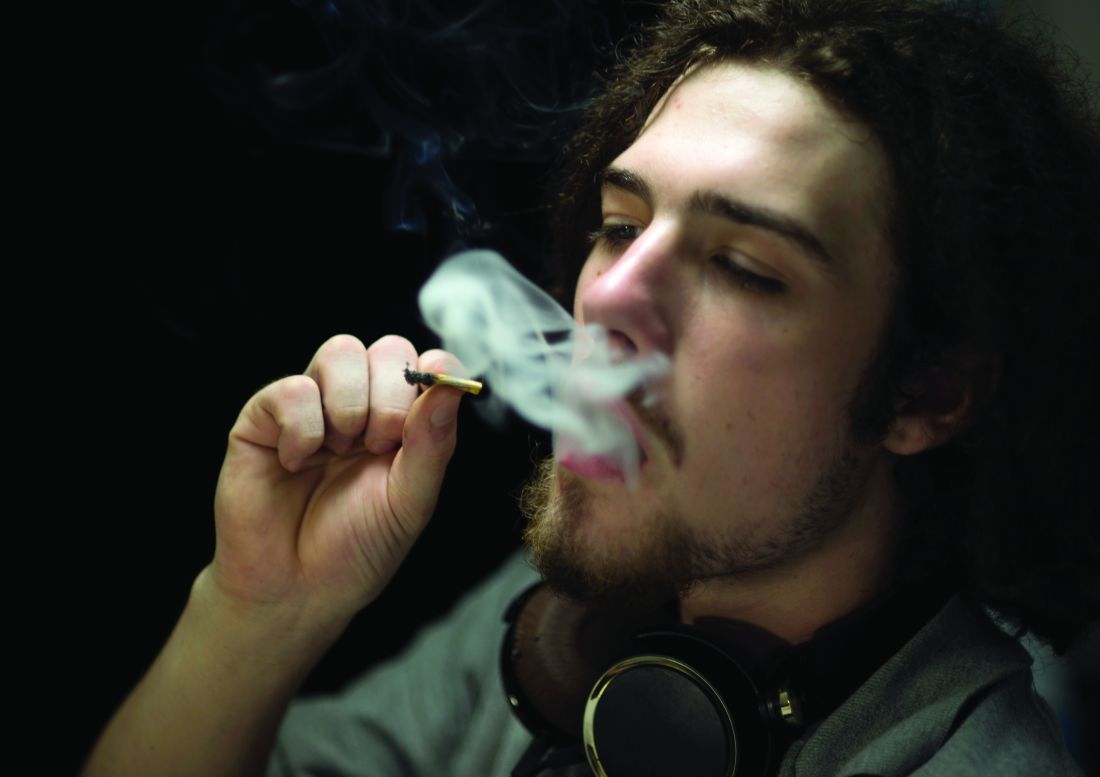
Sleepless in adolescence
One thing that constantly surprises me about adolescent sleep is that neither the teen nor the parent is as concerned about it as I am. Instead, they complain about irritability, dropping grades, anxiety, depression, obesity, oppositionality, fatigue, and even substance use – all documented effects of sleep debt.
Inadequate sleep changes the brain, resulting in thinner gray matter, less neuroplasticity, poorer higher-level cognitive abilities (attention, working memory, inhibition, judgment, decision-making), lower motivation, and poorer academic functioning. None of these are losses teens can afford!
While sleep problems are more common in those with mental health disorders, poor sleep precedes anxiety and depression more than the reverse. Sleep problems increase the risk of depression, and depression relapses. Insomnia predicts risk behaviors – drinking and driving, smoking, delinquency. Getting less than 8 hours of sleep is associated with a threefold higher risk of suicide attempts.
Despite these pervasive threats to health and development, instead of concern, I find a lot of resistance in families and teens to taking action to improve sleep.
Teens don’t believe in problems from inadequate sleep. After all, they say, their peers are “all” getting the same amount of sleep. And they are largely correct – 75% of U.S. 12th graders get less than 8 hours of sleep. But the data are clear that children aged 12-18 years need 8.25-9.25 hours of sleep.
Parents generally are not aware of how little sleep their teens are getting because they go to bed on their own. If parents do check, any teenagers worth the label can growl their way out of supervision, “promise” to shut off the lights, or feign sleep. Having the house, pantry, and electronics to themselves at night is worth the risk of a consequence, especially for those who would rather avoid interacting.
The social forces keeping teens up at night are their “life”: the hours required for homework can be the reason for inadequate sleep. In subgroups of teens, sports practices, employment, or family responsibilities may extend the day past a bedtime needed for optimal sleep.
But use of electronics – the lifeline of adolescents – is responsible for much of their sleep debt. Electronic devices both delay sleep onset and reduce sleep duration. After 9:00 p.m., 34% of children aged older than 12 years are text messaging, 44% are talking, 55% are online, and 24% are playing computer games. Use of a TV or tablet at bedtime results in reduced sleep, and increased poor quality of sleep. Three or more hours of TV result not only in difficulty falling asleep and frequent awakenings, but also sleep issues later as adults. Shooter video games result in lower sleepiness, longer sleep latency, and shorter REM sleep. Even the low level light from electronic devices alters circadian rhythm and suppresses nocturnal melatonin secretion.
Keep in mind the biological reasons teens go to bed later. One is the typical emotional hyperarousal of being a teen. But other biological forces are at work in adolescence, such as reduction in the accumulation of sleep pressure during wakefulness and delaying the melatonin release that produces sleepiness. Teens (and parents) think sleeping in on weekends takes care of inadequate weekday sleep, but this so-called “recovery sleep” tends to occur at an inappropriate time in the circadian phase and further delays melatonin production, as well as reducing sleep pressure, making it even harder to fall asleep.
In some cases, medications we prescribe – such as stimulants, theophylline, antihistamines, or anticonvulsants – are at fault for delaying or disturbing sleep. But more often it is self-administered substances that are part of the teen’s attempt to stay awake – including nicotine, alcohol, and caffeine – that produce shorter sleep duration, increased latency to sleep, more wake time during sleep, and increased daytime sleepiness; it results in a vicious cycle. Sleep disruption may explain the association of these substances with less memory consolidation, poorer academic performance, and higher rates of risk behaviors.
We adults also are a cause of teen sleep debt. We are the ones allowing the early school start times for teens, primarily to allow for after school sports programs that glorify the school and bring kudos to some at the expense of all the students. A 65-minute earlier start in 10th grade resulted in less than half of students getting 7 hours of sleep or more. The level of resulting sleepiness is equal to that of narcolepsy.
As primary care clinicians, we can and need to detect, educate about, and treat sleep debt and sleep disorders. Sleep questionnaires can help. Treatment of sleep includes coaching for: having a cool, dark room used mainly for sleep; a regular schedule 7 days per week; avoiding exercise within 2 hours of bedtime; avoiding stimulants such as caffeine, tea, nicotine, and medications at least 3 hours before bedtime; keeping to a routine with no daytime naps; and especially no media in the bedroom! For teens already not able to sleep until early morning, you can recommend that they work bedtime back or forward by 1 hour per day until hitting a time that will allow 9 hours of sleep. Alternatively, have them stay up all night to reset their biological clock. Subsequently, the sleep schedule has to stay within 1 hour for sleep and waking 7 days per week. Anxious teens, besides needing therapy, may need a soothing routine, no visible clock, and a plan to get back up for 1 hour every time it takes longer than 10 minutes to fall asleep.
If sleepy teens report adequate time in bed, then we need to understand pathologies such as obstructive sleep apnea, restless legs syndrome, menstruation-related or primary hypersomnias, and narcolepsy to diagnose and resolve the problem.
Parents may have given up protecting their teens from inadequate sleep so we as health providers need to do so.
Dr. Howard is assistant professor of pediatrics at Johns Hopkins University, Baltimore, and creator of CHADIS (www.CHADIS.com). She had no other relevant disclosures. Dr. Howard’s contribution to this publication was as a paid expert to Frontline Medical News. E-mail her at [email protected].
One thing that constantly surprises me about adolescent sleep is that neither the teen nor the parent is as concerned about it as I am. Instead, they complain about irritability, dropping grades, anxiety, depression, obesity, oppositionality, fatigue, and even substance use – all documented effects of sleep debt.
Inadequate sleep changes the brain, resulting in thinner gray matter, less neuroplasticity, poorer higher-level cognitive abilities (attention, working memory, inhibition, judgment, decision-making), lower motivation, and poorer academic functioning. None of these are losses teens can afford!
While sleep problems are more common in those with mental health disorders, poor sleep precedes anxiety and depression more than the reverse. Sleep problems increase the risk of depression, and depression relapses. Insomnia predicts risk behaviors – drinking and driving, smoking, delinquency. Getting less than 8 hours of sleep is associated with a threefold higher risk of suicide attempts.
Despite these pervasive threats to health and development, instead of concern, I find a lot of resistance in families and teens to taking action to improve sleep.
Teens don’t believe in problems from inadequate sleep. After all, they say, their peers are “all” getting the same amount of sleep. And they are largely correct – 75% of U.S. 12th graders get less than 8 hours of sleep. But the data are clear that children aged 12-18 years need 8.25-9.25 hours of sleep.
Parents generally are not aware of how little sleep their teens are getting because they go to bed on their own. If parents do check, any teenagers worth the label can growl their way out of supervision, “promise” to shut off the lights, or feign sleep. Having the house, pantry, and electronics to themselves at night is worth the risk of a consequence, especially for those who would rather avoid interacting.
The social forces keeping teens up at night are their “life”: the hours required for homework can be the reason for inadequate sleep. In subgroups of teens, sports practices, employment, or family responsibilities may extend the day past a bedtime needed for optimal sleep.
But use of electronics – the lifeline of adolescents – is responsible for much of their sleep debt. Electronic devices both delay sleep onset and reduce sleep duration. After 9:00 p.m., 34% of children aged older than 12 years are text messaging, 44% are talking, 55% are online, and 24% are playing computer games. Use of a TV or tablet at bedtime results in reduced sleep, and increased poor quality of sleep. Three or more hours of TV result not only in difficulty falling asleep and frequent awakenings, but also sleep issues later as adults. Shooter video games result in lower sleepiness, longer sleep latency, and shorter REM sleep. Even the low level light from electronic devices alters circadian rhythm and suppresses nocturnal melatonin secretion.
Keep in mind the biological reasons teens go to bed later. One is the typical emotional hyperarousal of being a teen. But other biological forces are at work in adolescence, such as reduction in the accumulation of sleep pressure during wakefulness and delaying the melatonin release that produces sleepiness. Teens (and parents) think sleeping in on weekends takes care of inadequate weekday sleep, but this so-called “recovery sleep” tends to occur at an inappropriate time in the circadian phase and further delays melatonin production, as well as reducing sleep pressure, making it even harder to fall asleep.
In some cases, medications we prescribe – such as stimulants, theophylline, antihistamines, or anticonvulsants – are at fault for delaying or disturbing sleep. But more often it is self-administered substances that are part of the teen’s attempt to stay awake – including nicotine, alcohol, and caffeine – that produce shorter sleep duration, increased latency to sleep, more wake time during sleep, and increased daytime sleepiness; it results in a vicious cycle. Sleep disruption may explain the association of these substances with less memory consolidation, poorer academic performance, and higher rates of risk behaviors.
We adults also are a cause of teen sleep debt. We are the ones allowing the early school start times for teens, primarily to allow for after school sports programs that glorify the school and bring kudos to some at the expense of all the students. A 65-minute earlier start in 10th grade resulted in less than half of students getting 7 hours of sleep or more. The level of resulting sleepiness is equal to that of narcolepsy.
As primary care clinicians, we can and need to detect, educate about, and treat sleep debt and sleep disorders. Sleep questionnaires can help. Treatment of sleep includes coaching for: having a cool, dark room used mainly for sleep; a regular schedule 7 days per week; avoiding exercise within 2 hours of bedtime; avoiding stimulants such as caffeine, tea, nicotine, and medications at least 3 hours before bedtime; keeping to a routine with no daytime naps; and especially no media in the bedroom! For teens already not able to sleep until early morning, you can recommend that they work bedtime back or forward by 1 hour per day until hitting a time that will allow 9 hours of sleep. Alternatively, have them stay up all night to reset their biological clock. Subsequently, the sleep schedule has to stay within 1 hour for sleep and waking 7 days per week. Anxious teens, besides needing therapy, may need a soothing routine, no visible clock, and a plan to get back up for 1 hour every time it takes longer than 10 minutes to fall asleep.
If sleepy teens report adequate time in bed, then we need to understand pathologies such as obstructive sleep apnea, restless legs syndrome, menstruation-related or primary hypersomnias, and narcolepsy to diagnose and resolve the problem.
Parents may have given up protecting their teens from inadequate sleep so we as health providers need to do so.
Dr. Howard is assistant professor of pediatrics at Johns Hopkins University, Baltimore, and creator of CHADIS (www.CHADIS.com). She had no other relevant disclosures. Dr. Howard’s contribution to this publication was as a paid expert to Frontline Medical News. E-mail her at [email protected].
One thing that constantly surprises me about adolescent sleep is that neither the teen nor the parent is as concerned about it as I am. Instead, they complain about irritability, dropping grades, anxiety, depression, obesity, oppositionality, fatigue, and even substance use – all documented effects of sleep debt.
Inadequate sleep changes the brain, resulting in thinner gray matter, less neuroplasticity, poorer higher-level cognitive abilities (attention, working memory, inhibition, judgment, decision-making), lower motivation, and poorer academic functioning. None of these are losses teens can afford!
While sleep problems are more common in those with mental health disorders, poor sleep precedes anxiety and depression more than the reverse. Sleep problems increase the risk of depression, and depression relapses. Insomnia predicts risk behaviors – drinking and driving, smoking, delinquency. Getting less than 8 hours of sleep is associated with a threefold higher risk of suicide attempts.
Despite these pervasive threats to health and development, instead of concern, I find a lot of resistance in families and teens to taking action to improve sleep.
Teens don’t believe in problems from inadequate sleep. After all, they say, their peers are “all” getting the same amount of sleep. And they are largely correct – 75% of U.S. 12th graders get less than 8 hours of sleep. But the data are clear that children aged 12-18 years need 8.25-9.25 hours of sleep.
Parents generally are not aware of how little sleep their teens are getting because they go to bed on their own. If parents do check, any teenagers worth the label can growl their way out of supervision, “promise” to shut off the lights, or feign sleep. Having the house, pantry, and electronics to themselves at night is worth the risk of a consequence, especially for those who would rather avoid interacting.
The social forces keeping teens up at night are their “life”: the hours required for homework can be the reason for inadequate sleep. In subgroups of teens, sports practices, employment, or family responsibilities may extend the day past a bedtime needed for optimal sleep.
But use of electronics – the lifeline of adolescents – is responsible for much of their sleep debt. Electronic devices both delay sleep onset and reduce sleep duration. After 9:00 p.m., 34% of children aged older than 12 years are text messaging, 44% are talking, 55% are online, and 24% are playing computer games. Use of a TV or tablet at bedtime results in reduced sleep, and increased poor quality of sleep. Three or more hours of TV result not only in difficulty falling asleep and frequent awakenings, but also sleep issues later as adults. Shooter video games result in lower sleepiness, longer sleep latency, and shorter REM sleep. Even the low level light from electronic devices alters circadian rhythm and suppresses nocturnal melatonin secretion.
Keep in mind the biological reasons teens go to bed later. One is the typical emotional hyperarousal of being a teen. But other biological forces are at work in adolescence, such as reduction in the accumulation of sleep pressure during wakefulness and delaying the melatonin release that produces sleepiness. Teens (and parents) think sleeping in on weekends takes care of inadequate weekday sleep, but this so-called “recovery sleep” tends to occur at an inappropriate time in the circadian phase and further delays melatonin production, as well as reducing sleep pressure, making it even harder to fall asleep.
In some cases, medications we prescribe – such as stimulants, theophylline, antihistamines, or anticonvulsants – are at fault for delaying or disturbing sleep. But more often it is self-administered substances that are part of the teen’s attempt to stay awake – including nicotine, alcohol, and caffeine – that produce shorter sleep duration, increased latency to sleep, more wake time during sleep, and increased daytime sleepiness; it results in a vicious cycle. Sleep disruption may explain the association of these substances with less memory consolidation, poorer academic performance, and higher rates of risk behaviors.
We adults also are a cause of teen sleep debt. We are the ones allowing the early school start times for teens, primarily to allow for after school sports programs that glorify the school and bring kudos to some at the expense of all the students. A 65-minute earlier start in 10th grade resulted in less than half of students getting 7 hours of sleep or more. The level of resulting sleepiness is equal to that of narcolepsy.
As primary care clinicians, we can and need to detect, educate about, and treat sleep debt and sleep disorders. Sleep questionnaires can help. Treatment of sleep includes coaching for: having a cool, dark room used mainly for sleep; a regular schedule 7 days per week; avoiding exercise within 2 hours of bedtime; avoiding stimulants such as caffeine, tea, nicotine, and medications at least 3 hours before bedtime; keeping to a routine with no daytime naps; and especially no media in the bedroom! For teens already not able to sleep until early morning, you can recommend that they work bedtime back or forward by 1 hour per day until hitting a time that will allow 9 hours of sleep. Alternatively, have them stay up all night to reset their biological clock. Subsequently, the sleep schedule has to stay within 1 hour for sleep and waking 7 days per week. Anxious teens, besides needing therapy, may need a soothing routine, no visible clock, and a plan to get back up for 1 hour every time it takes longer than 10 minutes to fall asleep.
If sleepy teens report adequate time in bed, then we need to understand pathologies such as obstructive sleep apnea, restless legs syndrome, menstruation-related or primary hypersomnias, and narcolepsy to diagnose and resolve the problem.
Parents may have given up protecting their teens from inadequate sleep so we as health providers need to do so.
Dr. Howard is assistant professor of pediatrics at Johns Hopkins University, Baltimore, and creator of CHADIS (www.CHADIS.com). She had no other relevant disclosures. Dr. Howard’s contribution to this publication was as a paid expert to Frontline Medical News. E-mail her at [email protected].
Practice changing events of 2017
Members of the Pediatric News Editorial Advisory Board share some of the events and findings of 2017 that they believe have or will have the most impact on pediatric practice.
Francis Rushton Jr., MD, practiced pediatrics in Beaufort, S.C. for 32 years, and currently is the medical director of S.C. Quality through Technology and Innovation in Pediatrics (QTIP), funded by the South Carolina Department of Health and Human Services.
Dropping the human papillomavirus (HPV) regimen to two shots from three shots, as recommended by the Centers for Disease Control and Prevention, appears to have really improved uptake of HPV immunization.
Preventive oral health in the pediatrician’s office is not really a new recommendation from 2017; we have been talking about fluoride varnish for over a decade. What is new is that we gradually are seeing fluoride varnish move into practice, up from 1,000 applications in pediatric offices in 2011 to close to 20,000 applications in South Carolina alone.
Pediatricians are being asked to screen more and more. We’re asked to do developmental screening, postpartum depression screening, autism screening, behavioral health screening, social determinants of health screening, parental concerns screening, etc. As a result, we now have multiple different screens with different schedules. The Survey of Well-Being of Young Children screening tool does it all – one screen at each preschool well visit from birth to age 5 years.
A different approach is to use CHADIS (Child Health and Development Interactive System), a for-profit venture where all the screens are loaded electronically.
Howard Smart, MD, is chairman of pediatrics at Sharp Rees-Stealy Medical Group, San Diego.
The switch to a two-dose schedule for HPV vaccination has improved both acceptance of the vaccine and the likelihood of timely completion of the HPV series.
Kelly Curran, MD, MA, is an assistant professor of pediatrics at the University of Oklahoma Health Sciences Center, Oklahoma City, practicing adolescent medicine.
The news from Australia is that the older meningitis B vaccine (MeNZB) provides some protection against Neisseria gonorrhoeae, as reported in the Lancet (2017 July 10. doi: 10.1016/S0140-6736[17]31449-6)! The newer version of the meningitis B vaccine Bexsero also contains the same outer membrane vesicle antigen. Given increasing bacterial resistance – and pan-resistant gonorrhea organisms already in some parts of the world – this is exciting news for the future!
The increased use of the reverse screening algorithm for syphilis is exciting. Although this has been “available” for several years, increasingly more physicians/laboratories are using this in practice. Our academic center – in a relatively high prevalence area for syphilis – recently switched to this screening method.
M. Susan Jay, MD, is a professor of pediatrics and section chief of adolescent medicine at the Medical College of Wisconsin and program director of adolescent health and medicine at the Children’s Hospital of Wisconsin, both in Milwaukee.
In adolescent medicine, the addition of long-acting reversible contraceptives has been wonderful as an aid to both menstrual management and contraception. Specifically, Liletta, a new IUD that is smaller in size and remains in place for 5 years as well as being considerably more cost effective, has changed care for adolescent females.
Suzanne C. Boulter, MD, is adjunct professor of pediatrics and community and family medicine at the Geisel School of Medicine at Dartmouth in Hanover, N.H.
I was very impressed with the recent American Academy of Pediatrics policy on human trafficking published in Pediatrics (2017 November. doi: 10.1542/peds.2017-3138), and think this is a new area of knowledge of which pediatricians need to be aware.
With all the news and social media about sexual misconduct by persons in power, I’m a bit concerned that there could be a fallout on pediatricians performing appropriate examinations on their patients that could be interpreted as something else.
Timothy J. Joos, MD, MPH, is a practicing clinician in combined internal medicine/pediatrics in Seattle. For the last decade, he has worked at a federally qualified community health center in Seattle serving a largely low-income and immigrant population.
With regard to practice-changing events for 2017, I don’t wish to downplay the numerous research advances over the year, but the advances cannot be made without funding, and they are not going to be practice-changing if they can’t reach the patients. We can’t ignore the uncertainty that the current political situation in 2017 has caused for our patients and their families, as well as for research and for the health care industry in general.
It is impossible to deny the important role government health care programs play in the health of our own patients and the health of the whole country. According to numbers from the Kaiser Family Foundation website, currently 38% of the estimated 74 million kids in this country are covered by Medicaid and CHIP programs. The numbers of uninsured children are at all-time lows at 5% (adults 10%). The current uncertainty of government funding is felt strongly by safety net providers such as community health centers that have traditionally seen the uninsured patients. The community health center where I work went from 35% of its patients being uninsured before the Affordable Care Act to about 15% now.
Efforts to dismantle the Affordable Care Act and reverse Medicaid expansions, as well as delays on funding to the CHIP program, have created uncertainty and anxiety across health care from the administrators and insurance companies to us – the providers – and the families we take care of. In addition, National Institutes of Health funding is threatened to be cut by 20%. 2017 will go down in history as the year of health care toxic stress (that is, unless 2018 is worse). As we celebrate the end of the year, we all deserve a Xanax and a Zantac.
Members of the Pediatric News Editorial Advisory Board share some of the events and findings of 2017 that they believe have or will have the most impact on pediatric practice.
Francis Rushton Jr., MD, practiced pediatrics in Beaufort, S.C. for 32 years, and currently is the medical director of S.C. Quality through Technology and Innovation in Pediatrics (QTIP), funded by the South Carolina Department of Health and Human Services.
Dropping the human papillomavirus (HPV) regimen to two shots from three shots, as recommended by the Centers for Disease Control and Prevention, appears to have really improved uptake of HPV immunization.
Preventive oral health in the pediatrician’s office is not really a new recommendation from 2017; we have been talking about fluoride varnish for over a decade. What is new is that we gradually are seeing fluoride varnish move into practice, up from 1,000 applications in pediatric offices in 2011 to close to 20,000 applications in South Carolina alone.
Pediatricians are being asked to screen more and more. We’re asked to do developmental screening, postpartum depression screening, autism screening, behavioral health screening, social determinants of health screening, parental concerns screening, etc. As a result, we now have multiple different screens with different schedules. The Survey of Well-Being of Young Children screening tool does it all – one screen at each preschool well visit from birth to age 5 years.
A different approach is to use CHADIS (Child Health and Development Interactive System), a for-profit venture where all the screens are loaded electronically.
Howard Smart, MD, is chairman of pediatrics at Sharp Rees-Stealy Medical Group, San Diego.
The switch to a two-dose schedule for HPV vaccination has improved both acceptance of the vaccine and the likelihood of timely completion of the HPV series.
Kelly Curran, MD, MA, is an assistant professor of pediatrics at the University of Oklahoma Health Sciences Center, Oklahoma City, practicing adolescent medicine.
The news from Australia is that the older meningitis B vaccine (MeNZB) provides some protection against Neisseria gonorrhoeae, as reported in the Lancet (2017 July 10. doi: 10.1016/S0140-6736[17]31449-6)! The newer version of the meningitis B vaccine Bexsero also contains the same outer membrane vesicle antigen. Given increasing bacterial resistance – and pan-resistant gonorrhea organisms already in some parts of the world – this is exciting news for the future!
The increased use of the reverse screening algorithm for syphilis is exciting. Although this has been “available” for several years, increasingly more physicians/laboratories are using this in practice. Our academic center – in a relatively high prevalence area for syphilis – recently switched to this screening method.
M. Susan Jay, MD, is a professor of pediatrics and section chief of adolescent medicine at the Medical College of Wisconsin and program director of adolescent health and medicine at the Children’s Hospital of Wisconsin, both in Milwaukee.
In adolescent medicine, the addition of long-acting reversible contraceptives has been wonderful as an aid to both menstrual management and contraception. Specifically, Liletta, a new IUD that is smaller in size and remains in place for 5 years as well as being considerably more cost effective, has changed care for adolescent females.
Suzanne C. Boulter, MD, is adjunct professor of pediatrics and community and family medicine at the Geisel School of Medicine at Dartmouth in Hanover, N.H.
I was very impressed with the recent American Academy of Pediatrics policy on human trafficking published in Pediatrics (2017 November. doi: 10.1542/peds.2017-3138), and think this is a new area of knowledge of which pediatricians need to be aware.
With all the news and social media about sexual misconduct by persons in power, I’m a bit concerned that there could be a fallout on pediatricians performing appropriate examinations on their patients that could be interpreted as something else.
Timothy J. Joos, MD, MPH, is a practicing clinician in combined internal medicine/pediatrics in Seattle. For the last decade, he has worked at a federally qualified community health center in Seattle serving a largely low-income and immigrant population.
With regard to practice-changing events for 2017, I don’t wish to downplay the numerous research advances over the year, but the advances cannot be made without funding, and they are not going to be practice-changing if they can’t reach the patients. We can’t ignore the uncertainty that the current political situation in 2017 has caused for our patients and their families, as well as for research and for the health care industry in general.
It is impossible to deny the important role government health care programs play in the health of our own patients and the health of the whole country. According to numbers from the Kaiser Family Foundation website, currently 38% of the estimated 74 million kids in this country are covered by Medicaid and CHIP programs. The numbers of uninsured children are at all-time lows at 5% (adults 10%). The current uncertainty of government funding is felt strongly by safety net providers such as community health centers that have traditionally seen the uninsured patients. The community health center where I work went from 35% of its patients being uninsured before the Affordable Care Act to about 15% now.
Efforts to dismantle the Affordable Care Act and reverse Medicaid expansions, as well as delays on funding to the CHIP program, have created uncertainty and anxiety across health care from the administrators and insurance companies to us – the providers – and the families we take care of. In addition, National Institutes of Health funding is threatened to be cut by 20%. 2017 will go down in history as the year of health care toxic stress (that is, unless 2018 is worse). As we celebrate the end of the year, we all deserve a Xanax and a Zantac.
Members of the Pediatric News Editorial Advisory Board share some of the events and findings of 2017 that they believe have or will have the most impact on pediatric practice.
Francis Rushton Jr., MD, practiced pediatrics in Beaufort, S.C. for 32 years, and currently is the medical director of S.C. Quality through Technology and Innovation in Pediatrics (QTIP), funded by the South Carolina Department of Health and Human Services.
Dropping the human papillomavirus (HPV) regimen to two shots from three shots, as recommended by the Centers for Disease Control and Prevention, appears to have really improved uptake of HPV immunization.
Preventive oral health in the pediatrician’s office is not really a new recommendation from 2017; we have been talking about fluoride varnish for over a decade. What is new is that we gradually are seeing fluoride varnish move into practice, up from 1,000 applications in pediatric offices in 2011 to close to 20,000 applications in South Carolina alone.
Pediatricians are being asked to screen more and more. We’re asked to do developmental screening, postpartum depression screening, autism screening, behavioral health screening, social determinants of health screening, parental concerns screening, etc. As a result, we now have multiple different screens with different schedules. The Survey of Well-Being of Young Children screening tool does it all – one screen at each preschool well visit from birth to age 5 years.
A different approach is to use CHADIS (Child Health and Development Interactive System), a for-profit venture where all the screens are loaded electronically.
Howard Smart, MD, is chairman of pediatrics at Sharp Rees-Stealy Medical Group, San Diego.
The switch to a two-dose schedule for HPV vaccination has improved both acceptance of the vaccine and the likelihood of timely completion of the HPV series.
Kelly Curran, MD, MA, is an assistant professor of pediatrics at the University of Oklahoma Health Sciences Center, Oklahoma City, practicing adolescent medicine.
The news from Australia is that the older meningitis B vaccine (MeNZB) provides some protection against Neisseria gonorrhoeae, as reported in the Lancet (2017 July 10. doi: 10.1016/S0140-6736[17]31449-6)! The newer version of the meningitis B vaccine Bexsero also contains the same outer membrane vesicle antigen. Given increasing bacterial resistance – and pan-resistant gonorrhea organisms already in some parts of the world – this is exciting news for the future!
The increased use of the reverse screening algorithm for syphilis is exciting. Although this has been “available” for several years, increasingly more physicians/laboratories are using this in practice. Our academic center – in a relatively high prevalence area for syphilis – recently switched to this screening method.
M. Susan Jay, MD, is a professor of pediatrics and section chief of adolescent medicine at the Medical College of Wisconsin and program director of adolescent health and medicine at the Children’s Hospital of Wisconsin, both in Milwaukee.
In adolescent medicine, the addition of long-acting reversible contraceptives has been wonderful as an aid to both menstrual management and contraception. Specifically, Liletta, a new IUD that is smaller in size and remains in place for 5 years as well as being considerably more cost effective, has changed care for adolescent females.
Suzanne C. Boulter, MD, is adjunct professor of pediatrics and community and family medicine at the Geisel School of Medicine at Dartmouth in Hanover, N.H.
I was very impressed with the recent American Academy of Pediatrics policy on human trafficking published in Pediatrics (2017 November. doi: 10.1542/peds.2017-3138), and think this is a new area of knowledge of which pediatricians need to be aware.
With all the news and social media about sexual misconduct by persons in power, I’m a bit concerned that there could be a fallout on pediatricians performing appropriate examinations on their patients that could be interpreted as something else.
Timothy J. Joos, MD, MPH, is a practicing clinician in combined internal medicine/pediatrics in Seattle. For the last decade, he has worked at a federally qualified community health center in Seattle serving a largely low-income and immigrant population.
With regard to practice-changing events for 2017, I don’t wish to downplay the numerous research advances over the year, but the advances cannot be made without funding, and they are not going to be practice-changing if they can’t reach the patients. We can’t ignore the uncertainty that the current political situation in 2017 has caused for our patients and their families, as well as for research and for the health care industry in general.
It is impossible to deny the important role government health care programs play in the health of our own patients and the health of the whole country. According to numbers from the Kaiser Family Foundation website, currently 38% of the estimated 74 million kids in this country are covered by Medicaid and CHIP programs. The numbers of uninsured children are at all-time lows at 5% (adults 10%). The current uncertainty of government funding is felt strongly by safety net providers such as community health centers that have traditionally seen the uninsured patients. The community health center where I work went from 35% of its patients being uninsured before the Affordable Care Act to about 15% now.
Efforts to dismantle the Affordable Care Act and reverse Medicaid expansions, as well as delays on funding to the CHIP program, have created uncertainty and anxiety across health care from the administrators and insurance companies to us – the providers – and the families we take care of. In addition, National Institutes of Health funding is threatened to be cut by 20%. 2017 will go down in history as the year of health care toxic stress (that is, unless 2018 is worse). As we celebrate the end of the year, we all deserve a Xanax and a Zantac.
Preexposure prophylaxis among LGBT youth
Every prevention effort or treatment has its own risks. Gynecologists must consider the risk for blood clots from using estrogen-containing oral contraceptives versus the risk of blood clots from pregnancy. Endocrinologists must weigh the risk of decreased bone mineral density versus premature closure of growth plates when starting pubertal blockers for children suffering from precocious puberty. Psychologists and primary care providers must consider the risk for increased suicidal thoughts while on selective serotonin reuptake inhibitors versus the risk of completed suicide if the depression remains untreated.
In the United States alone, 22% of HIV infections occur in people aged 13-24 years. Among those with HIV infection, 81% are young men who have sex with men (MSM).1 Among those new infections, young MSM of color are nearly four times as likely to have HIV, compared with white young MSM.2 Moreover, the incidence of HIV infection among transgender individuals is three times higher than the national average.3
What further hampers public health prevention efforts is the stigma and discrimination LGBT youth face in trying to prevent HIV infections: 84% of those aged 15-24 years report recognizing stigma around HIV in the United States.4 In addition, black MSM were more likely than other MSMs to report this kind of stigma.5 And it isn’t enough that LGBT youth have to face stigma and discrimination. In fact, because of it, they often face serious financial challenges. It is estimated that 50% of homeless youth identify as LGBT, and 40% of them were forced out of their homes because of their sexual orientation or gender identity.6 Also, transgender youth have difficulty finding employment because of their gender identity.7 A combination of homelessness or chronic unemployment has driven many LGBT youth to survival sex or sex for money, which puts them at higher risk for HIV infection.7,8 The risk for HIV infection is so high that we should be using all available resources, including PrEP, to address these profound health disparities.
Studies, however, are forthcoming. One study by Hosek et al. that was published in September suggested that PrEP among adolescents can be safe and well tolerated, may not increase the rate of high-risk sexual behaviors, and may not increase the risk of other STDs such as gonorrhea and chlamydia. It must be noted, however, that incidence of HIV was fairly high – the HIV seroconversion rate was 6.4 per 100 person-years. Nevertheless, researchers found the rate of HIV seroconversion was higher among those with lower levels of Truvada in their bodies, compared with the seroconversion rate in those with higher levels of the medication. This suggests that adherence is key in using PrEP to prevent HIV infection.10 Although far from definitive, this small study provides some solid evidence that PrEP is safe and effective in preventing HIV among LGBT youth. More studies that will eventually support its effectiveness and safety are on the way.11
Dr. Montano is an assistant professor of pediatrics at the University of Pittsburgh and an adolescent medicine physician at Children’s Hospital of Pittsburgh of UPMC. Email him at [email protected].
Resource
CDC website on PrEP: https://www.cdc.gov/hiv/risk/prep/index.html, with provider guidelines.
References
1. Centers for Disease Control and Prevention. HIV Among Youth fact sheet, April 2017.
2. Centers for Disease Control and Prevention. HIV Surveillance Report, 2015; vol. 27.
3. Centers for Disease Control and Prevention. HIV Among Transgender People.
4. Kaiser Family Foundation. National survey of teens and young adults on HIV/AIDS, Nov. 1, 2012. .
5. J Acquir Immune Defic Syndr. 2016;73(5):547-55.
6. Serving our youth: Findings from a national survey of services providers working with lesbian, gay, bisexual and transgender youth who are homeless or at risk of becoming homeless (The Williams Institute with True Colors and The Palette Fund, 2012).
7. Injustice at every turn: A report of the national transgender discrimination survey (National Center for Transgender Equality and National Gay and Lesbian Task Force, 2011).
8. J Acquir Immune Defic Syndr. 2010 Apr;53(5):661-4.
9. Centers for Disease Control and Prevention. Preexposure prophylaxis for the prevention of HIV infection in the United States: A clinical practice guideline, 2014.
10. JAMA Pediatr. 2017;171(11):1063-71.
11. J Int AIDS Soc. 2016;19. doi: 10.7448/IAS.19.7.21107.
Every prevention effort or treatment has its own risks. Gynecologists must consider the risk for blood clots from using estrogen-containing oral contraceptives versus the risk of blood clots from pregnancy. Endocrinologists must weigh the risk of decreased bone mineral density versus premature closure of growth plates when starting pubertal blockers for children suffering from precocious puberty. Psychologists and primary care providers must consider the risk for increased suicidal thoughts while on selective serotonin reuptake inhibitors versus the risk of completed suicide if the depression remains untreated.
In the United States alone, 22% of HIV infections occur in people aged 13-24 years. Among those with HIV infection, 81% are young men who have sex with men (MSM).1 Among those new infections, young MSM of color are nearly four times as likely to have HIV, compared with white young MSM.2 Moreover, the incidence of HIV infection among transgender individuals is three times higher than the national average.3
What further hampers public health prevention efforts is the stigma and discrimination LGBT youth face in trying to prevent HIV infections: 84% of those aged 15-24 years report recognizing stigma around HIV in the United States.4 In addition, black MSM were more likely than other MSMs to report this kind of stigma.5 And it isn’t enough that LGBT youth have to face stigma and discrimination. In fact, because of it, they often face serious financial challenges. It is estimated that 50% of homeless youth identify as LGBT, and 40% of them were forced out of their homes because of their sexual orientation or gender identity.6 Also, transgender youth have difficulty finding employment because of their gender identity.7 A combination of homelessness or chronic unemployment has driven many LGBT youth to survival sex or sex for money, which puts them at higher risk for HIV infection.7,8 The risk for HIV infection is so high that we should be using all available resources, including PrEP, to address these profound health disparities.
Studies, however, are forthcoming. One study by Hosek et al. that was published in September suggested that PrEP among adolescents can be safe and well tolerated, may not increase the rate of high-risk sexual behaviors, and may not increase the risk of other STDs such as gonorrhea and chlamydia. It must be noted, however, that incidence of HIV was fairly high – the HIV seroconversion rate was 6.4 per 100 person-years. Nevertheless, researchers found the rate of HIV seroconversion was higher among those with lower levels of Truvada in their bodies, compared with the seroconversion rate in those with higher levels of the medication. This suggests that adherence is key in using PrEP to prevent HIV infection.10 Although far from definitive, this small study provides some solid evidence that PrEP is safe and effective in preventing HIV among LGBT youth. More studies that will eventually support its effectiveness and safety are on the way.11
Dr. Montano is an assistant professor of pediatrics at the University of Pittsburgh and an adolescent medicine physician at Children’s Hospital of Pittsburgh of UPMC. Email him at [email protected].
Resource
CDC website on PrEP: https://www.cdc.gov/hiv/risk/prep/index.html, with provider guidelines.
References
1. Centers for Disease Control and Prevention. HIV Among Youth fact sheet, April 2017.
2. Centers for Disease Control and Prevention. HIV Surveillance Report, 2015; vol. 27.
3. Centers for Disease Control and Prevention. HIV Among Transgender People.
4. Kaiser Family Foundation. National survey of teens and young adults on HIV/AIDS, Nov. 1, 2012. .
5. J Acquir Immune Defic Syndr. 2016;73(5):547-55.
6. Serving our youth: Findings from a national survey of services providers working with lesbian, gay, bisexual and transgender youth who are homeless or at risk of becoming homeless (The Williams Institute with True Colors and The Palette Fund, 2012).
7. Injustice at every turn: A report of the national transgender discrimination survey (National Center for Transgender Equality and National Gay and Lesbian Task Force, 2011).
8. J Acquir Immune Defic Syndr. 2010 Apr;53(5):661-4.
9. Centers for Disease Control and Prevention. Preexposure prophylaxis for the prevention of HIV infection in the United States: A clinical practice guideline, 2014.
10. JAMA Pediatr. 2017;171(11):1063-71.
11. J Int AIDS Soc. 2016;19. doi: 10.7448/IAS.19.7.21107.
Every prevention effort or treatment has its own risks. Gynecologists must consider the risk for blood clots from using estrogen-containing oral contraceptives versus the risk of blood clots from pregnancy. Endocrinologists must weigh the risk of decreased bone mineral density versus premature closure of growth plates when starting pubertal blockers for children suffering from precocious puberty. Psychologists and primary care providers must consider the risk for increased suicidal thoughts while on selective serotonin reuptake inhibitors versus the risk of completed suicide if the depression remains untreated.
In the United States alone, 22% of HIV infections occur in people aged 13-24 years. Among those with HIV infection, 81% are young men who have sex with men (MSM).1 Among those new infections, young MSM of color are nearly four times as likely to have HIV, compared with white young MSM.2 Moreover, the incidence of HIV infection among transgender individuals is three times higher than the national average.3
What further hampers public health prevention efforts is the stigma and discrimination LGBT youth face in trying to prevent HIV infections: 84% of those aged 15-24 years report recognizing stigma around HIV in the United States.4 In addition, black MSM were more likely than other MSMs to report this kind of stigma.5 And it isn’t enough that LGBT youth have to face stigma and discrimination. In fact, because of it, they often face serious financial challenges. It is estimated that 50% of homeless youth identify as LGBT, and 40% of them were forced out of their homes because of their sexual orientation or gender identity.6 Also, transgender youth have difficulty finding employment because of their gender identity.7 A combination of homelessness or chronic unemployment has driven many LGBT youth to survival sex or sex for money, which puts them at higher risk for HIV infection.7,8 The risk for HIV infection is so high that we should be using all available resources, including PrEP, to address these profound health disparities.
Studies, however, are forthcoming. One study by Hosek et al. that was published in September suggested that PrEP among adolescents can be safe and well tolerated, may not increase the rate of high-risk sexual behaviors, and may not increase the risk of other STDs such as gonorrhea and chlamydia. It must be noted, however, that incidence of HIV was fairly high – the HIV seroconversion rate was 6.4 per 100 person-years. Nevertheless, researchers found the rate of HIV seroconversion was higher among those with lower levels of Truvada in their bodies, compared with the seroconversion rate in those with higher levels of the medication. This suggests that adherence is key in using PrEP to prevent HIV infection.10 Although far from definitive, this small study provides some solid evidence that PrEP is safe and effective in preventing HIV among LGBT youth. More studies that will eventually support its effectiveness and safety are on the way.11
Dr. Montano is an assistant professor of pediatrics at the University of Pittsburgh and an adolescent medicine physician at Children’s Hospital of Pittsburgh of UPMC. Email him at [email protected].
Resource
CDC website on PrEP: https://www.cdc.gov/hiv/risk/prep/index.html, with provider guidelines.
References
1. Centers for Disease Control and Prevention. HIV Among Youth fact sheet, April 2017.
2. Centers for Disease Control and Prevention. HIV Surveillance Report, 2015; vol. 27.
3. Centers for Disease Control and Prevention. HIV Among Transgender People.
4. Kaiser Family Foundation. National survey of teens and young adults on HIV/AIDS, Nov. 1, 2012. .
5. J Acquir Immune Defic Syndr. 2016;73(5):547-55.
6. Serving our youth: Findings from a national survey of services providers working with lesbian, gay, bisexual and transgender youth who are homeless or at risk of becoming homeless (The Williams Institute with True Colors and The Palette Fund, 2012).
7. Injustice at every turn: A report of the national transgender discrimination survey (National Center for Transgender Equality and National Gay and Lesbian Task Force, 2011).
8. J Acquir Immune Defic Syndr. 2010 Apr;53(5):661-4.
9. Centers for Disease Control and Prevention. Preexposure prophylaxis for the prevention of HIV infection in the United States: A clinical practice guideline, 2014.
10. JAMA Pediatr. 2017;171(11):1063-71.
11. J Int AIDS Soc. 2016;19. doi: 10.7448/IAS.19.7.21107.
Toy stethoscopes
Many of my articles are inspired when I observe discordant things juxtaposed. As we move deep into winter, once again I am confronted with the issue of infection control in the office and on the ward. Hospitals have gowns, gloves, masks, and toy stethoscopes. My outpatient offices rarely used more than the sink. In urgent care clinic, each evening I would swab three or four throats for strep, with one or two turning positive. I thought nothing of it, other than being glad when gagging a patient that I wear glasses. In the hospital, I must gown, glove, and mask for a patient with strep throat. The variations in practice between hospitals (I’ve been credentialed in 30) do not make me confident in the evidence base for infection control practices. I mentioned the Red Book to a second-year resident last week. He said he had seen it on a shelf but never actually used it.
In medical school, I was taught that the most important part of a stethoscope is between the ears. I believe that statement is true, but in a similar way to how I choose wines. My palate can’t tell the difference between a $15 and a $50 bottle of wine, so buying more expensive wine is a waste. However, a $3 bottle of wine is clearly inferior, if not undrinkable. There are oenophiles (one a distant cousin in Norway) who have trained their palates to tell the difference in wines, just as there are audiophiles who support the sales of $1,000 stereo speakers. Some fraction of those snobs may have justification. So, if cardiologists have strong opinions on stethoscopes, I won’t begrudge them their choice of a more expensive model. Their tastes do not mean that the average person should spend that much on wine, speakers, or stethoscopes. I will assert that there was a time when I could tell a day or two in advance that my otoscope bulb was going to burn out. The color balance was wrong. I carried a pocket otoscope for a few years when rounding in the hospital, but never found it as accurate as my original one. Every craftsman gets accustomed to their best tools.
A professional should be aware of the minimum quality of tool needed to get the job done.
Toy isolation stethoscopes ($3 each retail in bulk) add nothing to my discernment of an infant with bronchiolitis who is distressed, so I consider that equipment a waste of money and polluting to the environment. I typically use my stethoscope and foam it on leaving the room. There is evidence that either foam or alcohol pads are effective1 in killing germs, but no proof that this hygiene makes a difference clinically.2 The myriad researchers who have published about stethoscope contamination have stopped at padding their academic portfolios with something easy to publish, which basically is a high school science project using agar plates. They then make insinuations about policy, without any cost-benefit analysis. They really haven’t been bothered enough to advance the science of clinical medicine and actually measure a clinical impact of these policies. It is a corruption of science created by the publish-or-perish environment.
One survey found that 45% of physicians disinfect their stethoscope annually or less. Laundering of white coats follows a similar pattern, which is why the British National Health Service banned lab coats for physicians 10 years ago. No ties or long sleeve shirts either. I am smug knowing that my sartorial sense was ahead of my time in this regard.
The quality-improvement work of Ignaz Semmelweis should be required reading for all physicians. The control chart3 he published on puerperal fever in Vienna in the 1840s is spectacular. Infection control is important. Modern medical science cannot produce a similar control chart to justify the amount of dollars spent annually on gowns, gloves, masks, and toy stethoscopes. Sad.
Dr. Powell is a pediatric hospitalist and clinical ethics consultant living in St. Louis. Email him at [email protected].
References
1. Am J Infect Control. 2009 Apr;37(3):241-3.
2. J Hosp Infect. 2015 Sep;91(1):1-7.
3. https://en.wikipedia.org/wiki/Historical_mortality_rates_of_puerperal_fever
Many of my articles are inspired when I observe discordant things juxtaposed. As we move deep into winter, once again I am confronted with the issue of infection control in the office and on the ward. Hospitals have gowns, gloves, masks, and toy stethoscopes. My outpatient offices rarely used more than the sink. In urgent care clinic, each evening I would swab three or four throats for strep, with one or two turning positive. I thought nothing of it, other than being glad when gagging a patient that I wear glasses. In the hospital, I must gown, glove, and mask for a patient with strep throat. The variations in practice between hospitals (I’ve been credentialed in 30) do not make me confident in the evidence base for infection control practices. I mentioned the Red Book to a second-year resident last week. He said he had seen it on a shelf but never actually used it.
In medical school, I was taught that the most important part of a stethoscope is between the ears. I believe that statement is true, but in a similar way to how I choose wines. My palate can’t tell the difference between a $15 and a $50 bottle of wine, so buying more expensive wine is a waste. However, a $3 bottle of wine is clearly inferior, if not undrinkable. There are oenophiles (one a distant cousin in Norway) who have trained their palates to tell the difference in wines, just as there are audiophiles who support the sales of $1,000 stereo speakers. Some fraction of those snobs may have justification. So, if cardiologists have strong opinions on stethoscopes, I won’t begrudge them their choice of a more expensive model. Their tastes do not mean that the average person should spend that much on wine, speakers, or stethoscopes. I will assert that there was a time when I could tell a day or two in advance that my otoscope bulb was going to burn out. The color balance was wrong. I carried a pocket otoscope for a few years when rounding in the hospital, but never found it as accurate as my original one. Every craftsman gets accustomed to their best tools.
A professional should be aware of the minimum quality of tool needed to get the job done.
Toy isolation stethoscopes ($3 each retail in bulk) add nothing to my discernment of an infant with bronchiolitis who is distressed, so I consider that equipment a waste of money and polluting to the environment. I typically use my stethoscope and foam it on leaving the room. There is evidence that either foam or alcohol pads are effective1 in killing germs, but no proof that this hygiene makes a difference clinically.2 The myriad researchers who have published about stethoscope contamination have stopped at padding their academic portfolios with something easy to publish, which basically is a high school science project using agar plates. They then make insinuations about policy, without any cost-benefit analysis. They really haven’t been bothered enough to advance the science of clinical medicine and actually measure a clinical impact of these policies. It is a corruption of science created by the publish-or-perish environment.
One survey found that 45% of physicians disinfect their stethoscope annually or less. Laundering of white coats follows a similar pattern, which is why the British National Health Service banned lab coats for physicians 10 years ago. No ties or long sleeve shirts either. I am smug knowing that my sartorial sense was ahead of my time in this regard.
The quality-improvement work of Ignaz Semmelweis should be required reading for all physicians. The control chart3 he published on puerperal fever in Vienna in the 1840s is spectacular. Infection control is important. Modern medical science cannot produce a similar control chart to justify the amount of dollars spent annually on gowns, gloves, masks, and toy stethoscopes. Sad.
Dr. Powell is a pediatric hospitalist and clinical ethics consultant living in St. Louis. Email him at [email protected].
References
1. Am J Infect Control. 2009 Apr;37(3):241-3.
2. J Hosp Infect. 2015 Sep;91(1):1-7.
3. https://en.wikipedia.org/wiki/Historical_mortality_rates_of_puerperal_fever
Many of my articles are inspired when I observe discordant things juxtaposed. As we move deep into winter, once again I am confronted with the issue of infection control in the office and on the ward. Hospitals have gowns, gloves, masks, and toy stethoscopes. My outpatient offices rarely used more than the sink. In urgent care clinic, each evening I would swab three or four throats for strep, with one or two turning positive. I thought nothing of it, other than being glad when gagging a patient that I wear glasses. In the hospital, I must gown, glove, and mask for a patient with strep throat. The variations in practice between hospitals (I’ve been credentialed in 30) do not make me confident in the evidence base for infection control practices. I mentioned the Red Book to a second-year resident last week. He said he had seen it on a shelf but never actually used it.
In medical school, I was taught that the most important part of a stethoscope is between the ears. I believe that statement is true, but in a similar way to how I choose wines. My palate can’t tell the difference between a $15 and a $50 bottle of wine, so buying more expensive wine is a waste. However, a $3 bottle of wine is clearly inferior, if not undrinkable. There are oenophiles (one a distant cousin in Norway) who have trained their palates to tell the difference in wines, just as there are audiophiles who support the sales of $1,000 stereo speakers. Some fraction of those snobs may have justification. So, if cardiologists have strong opinions on stethoscopes, I won’t begrudge them their choice of a more expensive model. Their tastes do not mean that the average person should spend that much on wine, speakers, or stethoscopes. I will assert that there was a time when I could tell a day or two in advance that my otoscope bulb was going to burn out. The color balance was wrong. I carried a pocket otoscope for a few years when rounding in the hospital, but never found it as accurate as my original one. Every craftsman gets accustomed to their best tools.
A professional should be aware of the minimum quality of tool needed to get the job done.
Toy isolation stethoscopes ($3 each retail in bulk) add nothing to my discernment of an infant with bronchiolitis who is distressed, so I consider that equipment a waste of money and polluting to the environment. I typically use my stethoscope and foam it on leaving the room. There is evidence that either foam or alcohol pads are effective1 in killing germs, but no proof that this hygiene makes a difference clinically.2 The myriad researchers who have published about stethoscope contamination have stopped at padding their academic portfolios with something easy to publish, which basically is a high school science project using agar plates. They then make insinuations about policy, without any cost-benefit analysis. They really haven’t been bothered enough to advance the science of clinical medicine and actually measure a clinical impact of these policies. It is a corruption of science created by the publish-or-perish environment.
One survey found that 45% of physicians disinfect their stethoscope annually or less. Laundering of white coats follows a similar pattern, which is why the British National Health Service banned lab coats for physicians 10 years ago. No ties or long sleeve shirts either. I am smug knowing that my sartorial sense was ahead of my time in this regard.
The quality-improvement work of Ignaz Semmelweis should be required reading for all physicians. The control chart3 he published on puerperal fever in Vienna in the 1840s is spectacular. Infection control is important. Modern medical science cannot produce a similar control chart to justify the amount of dollars spent annually on gowns, gloves, masks, and toy stethoscopes. Sad.
Dr. Powell is a pediatric hospitalist and clinical ethics consultant living in St. Louis. Email him at [email protected].
References
1. Am J Infect Control. 2009 Apr;37(3):241-3.
2. J Hosp Infect. 2015 Sep;91(1):1-7.
3. https://en.wikipedia.org/wiki/Historical_mortality_rates_of_puerperal_fever
The National Kidney Foundation Names Clinician Reviews® Recipient of the 2018 Nostradamus Award
Frontline Medical Communications today announced that its journal, Clinician Reviews (CR), dedicated to nurse practitioners and physician assistants, has been named recipient of the 2018 Nostradamus Award.
Annually, National Kidney Foundation’s Council of Advanced Practitioners (CAP) presents this award to an individual, group, or organization that, through forethought and vision, recognizes, supports, and promotes the contributions of Advance Practitioners in nephrology. Clinician Reviews is being recognized for its Q&A feature Renal Consult, which provides expert advice to help clinicians address the complexities of renal diseases.
“Clinician Reviews joins a list of outstanding winners, including nephrologists, a United States senator, and others who have recognized CAP’s worth and supported its advancement,” said Karen Clemments, Editorial Director of clinical publications and Editor of Clinician Reviews. She continued, “We are excited to be among an esteemed group of past recipients for our ongoing endeavors to educate advanced practitioners in support of their clinical, professional needs in preventing, diagnosing, and treating kidney diseases.”
In announcing the award, Ms. Clemments noted that Renal Consult aligns with CAP’s goal to improve patient outcomes by enhancing advanced practitioners’ knowledge base and skills that will have a direct impact on clinical practice in a variety of settings. Renal Consult appears quarterly in print and online in CR’s robust, interactive website, digital edition, and mobile app.
The National Kidney Foundation is the leading organization in the United States dedicated to the awareness, prevention, and treatment of kidney disease for hundreds of thousands of healthcare professionals, millions of patients and their families, and tens of millions of Americans at risk. Clinician Reviews will be recognized during an awards luncheon at the NKF 2018 Spring Clinical Meeting in April.
Frontline Medical Communications today announced that its journal, Clinician Reviews (CR), dedicated to nurse practitioners and physician assistants, has been named recipient of the 2018 Nostradamus Award.
Annually, National Kidney Foundation’s Council of Advanced Practitioners (CAP) presents this award to an individual, group, or organization that, through forethought and vision, recognizes, supports, and promotes the contributions of Advance Practitioners in nephrology. Clinician Reviews is being recognized for its Q&A feature Renal Consult, which provides expert advice to help clinicians address the complexities of renal diseases.
“Clinician Reviews joins a list of outstanding winners, including nephrologists, a United States senator, and others who have recognized CAP’s worth and supported its advancement,” said Karen Clemments, Editorial Director of clinical publications and Editor of Clinician Reviews. She continued, “We are excited to be among an esteemed group of past recipients for our ongoing endeavors to educate advanced practitioners in support of their clinical, professional needs in preventing, diagnosing, and treating kidney diseases.”
In announcing the award, Ms. Clemments noted that Renal Consult aligns with CAP’s goal to improve patient outcomes by enhancing advanced practitioners’ knowledge base and skills that will have a direct impact on clinical practice in a variety of settings. Renal Consult appears quarterly in print and online in CR’s robust, interactive website, digital edition, and mobile app.
The National Kidney Foundation is the leading organization in the United States dedicated to the awareness, prevention, and treatment of kidney disease for hundreds of thousands of healthcare professionals, millions of patients and their families, and tens of millions of Americans at risk. Clinician Reviews will be recognized during an awards luncheon at the NKF 2018 Spring Clinical Meeting in April.
Frontline Medical Communications today announced that its journal, Clinician Reviews (CR), dedicated to nurse practitioners and physician assistants, has been named recipient of the 2018 Nostradamus Award.
Annually, National Kidney Foundation’s Council of Advanced Practitioners (CAP) presents this award to an individual, group, or organization that, through forethought and vision, recognizes, supports, and promotes the contributions of Advance Practitioners in nephrology. Clinician Reviews is being recognized for its Q&A feature Renal Consult, which provides expert advice to help clinicians address the complexities of renal diseases.
“Clinician Reviews joins a list of outstanding winners, including nephrologists, a United States senator, and others who have recognized CAP’s worth and supported its advancement,” said Karen Clemments, Editorial Director of clinical publications and Editor of Clinician Reviews. She continued, “We are excited to be among an esteemed group of past recipients for our ongoing endeavors to educate advanced practitioners in support of their clinical, professional needs in preventing, diagnosing, and treating kidney diseases.”
In announcing the award, Ms. Clemments noted that Renal Consult aligns with CAP’s goal to improve patient outcomes by enhancing advanced practitioners’ knowledge base and skills that will have a direct impact on clinical practice in a variety of settings. Renal Consult appears quarterly in print and online in CR’s robust, interactive website, digital edition, and mobile app.
The National Kidney Foundation is the leading organization in the United States dedicated to the awareness, prevention, and treatment of kidney disease for hundreds of thousands of healthcare professionals, millions of patients and their families, and tens of millions of Americans at risk. Clinician Reviews will be recognized during an awards luncheon at the NKF 2018 Spring Clinical Meeting in April.