User login
Preventing substance use
Substance use disorders are affecting every pediatric practice as they are major contributors to morbidity and mortality in young people. With the ongoing risks of binge drinking, the current epidemic of opioid addiction and overdose deaths in the United States, and the shifting legal status and public perception of the risk of marijuana, how to deal with substance use disorders seems to be the focus of public conversation these days. , such as parent education and early recognition in pediatric practice.
Substance abuse risk
We cannot yet predict who can safely “experiment” with substances or who will develop dependency. However, there is information that we can use to identify those at greater risk. Youth who have a first-degree relative with a substance use disorder are at greater risk for developing such a disorder themselves, and this is especially so if there is a family history of alcoholism. Youth who suffer from a psychiatric illness, particularly from anxiety and mood disorders, have a special vulnerability to abusing substances, particularly when their underlying illness is untreated or incompletely treated. Youth with ADHD are at substantially elevated risk of developing substance use disorders, although there is a complex relationship between these two problems. The evidence currently suggests that for youth who began effective treatment prior to puberty, there is no elevation in risk, but for those who did not, there is a substantially elevated risk of substance use disorders. Finally, there has been research that indicates that children with a combination of sensation-seeking, high impulsivity, anxiety-sensitivity, and hopelessness are at the highest risk for substance use disorders.2
Prevention efforts you can make: To your patients
The first step in your prevention efforts is an open conversation about drugs and alcohol. Ask your middle schoolers about whether they have tried alcohol or any drugs. Have their friends? What are kids saying about alcohol? About marijuana? Vaping? Are there other substances that kids are talking about or trying? Be genuinely curious, warm, and nonjudgmental. Find out what they think the risks of these substances may be. If appropriate, offer them some education about known risks of substances to the developing brain, to school or athletic performance, and so on. You can teach them about other trusted resources, such as the National Institute on Drug Abuse (NIDA), which has a resource specifically for teens (teens.drugabuse.gov).
For your high school students and those heading off to college, provide a safe place to talk about what they have tried and whether they (or you) have any worries about substance use. You have a unique combination of clinical authority and expertise in them as individuals, and can help them meaningfully plan how to handle their choices. You might talk about the specific risks of binge drinking, from sexual assault to alcohol poisoning and permanent cognitive effects on their developing brains. They also can benefit from hearing about the actual risks of frequent marijuana use, including impaired cognitive performance (and permanent IQ decline), and ongoing risks to their still-developing brains. Don’t be surprised if your older adolescent patients want to educate you about risks. Be curious and humble, and don’t be afraid to go together to a third party for information. You should encourage their efforts to think critically, and be empathic to their dilemma as they try to balance risks against their drive to have new experiences, to be independent, and to be strongly connected to their peers.
Adolescents should hear about your concern about their specific risks with drugs and alcohol, such as a history of traumatic brain injury (concussion), a family history of drug or alcohol dependence, or their own diagnosis of anxiety, depression, or ADHD. You might point out that because they have not tried any drugs or alcohol in high school, they may be prone to having too much to drink when they first try it. Or you might observe that because they have an anxiety disorder, they are vulnerable to becoming dependent on alcohol. Hearing about their specific level of risk equips them to make wiser choices in the context of their growing autonomy.
Prevention efforts you can make: To the parents
Your other prevention strategies should include parents. Studies have shown that when parents have clear rules and expectations about drug and alcohol use, and are consistent about enforcing consequences in their home, their children are significantly less likely than their peers to have experimented with drugs or alcohol by their senior year in high school. Parents of children headed to middle school should hear about this fact, alongside accurate information about the risks associated with alcohol and specific drugs for the developing brain.
Finally, parents need to hear that they can be effective disciplinarians, while also making clear to their children that safety comes first, and that their rules should have clear exceptions for safety. If the parents have a rule against any use of alcohol or drugs, there should be an exception if their child is out and feels unsafe. If they are drunk, or their driver has been drinking, they can call for a ride and will not be in (much) trouble. Rules don’t have to be draconian to be effective; they should always support honesty and safety first. This is a lot of territory to cover, and you do not have to be the only resource for parents. Reliable online resources, such as NIDA’s and SAMHSA’s websites, are full of useful information, and others, such as teen-safe.org, have detailed resources for parents in particular.
References
1. Hum Genet. 2012 Jun;131(6):779-89.
2. Alcohol Clin Exp Res. 2013 Jan;37(Suppl 1):E281-90.
Dr. Swick is an attending psychiatrist in the division of child psychiatry at Massachusetts General Hospital, Boston, and director of the Parenting at a Challenging Time (PACT) Program at the Vernon Cancer Center at Newton Wellesley Hospital, also in Boston. Dr. Jellinek is professor emeritus of psychiatry and pediatrics, Harvard Medical School, Boston.
Substance use disorders are affecting every pediatric practice as they are major contributors to morbidity and mortality in young people. With the ongoing risks of binge drinking, the current epidemic of opioid addiction and overdose deaths in the United States, and the shifting legal status and public perception of the risk of marijuana, how to deal with substance use disorders seems to be the focus of public conversation these days. , such as parent education and early recognition in pediatric practice.
Substance abuse risk
We cannot yet predict who can safely “experiment” with substances or who will develop dependency. However, there is information that we can use to identify those at greater risk. Youth who have a first-degree relative with a substance use disorder are at greater risk for developing such a disorder themselves, and this is especially so if there is a family history of alcoholism. Youth who suffer from a psychiatric illness, particularly from anxiety and mood disorders, have a special vulnerability to abusing substances, particularly when their underlying illness is untreated or incompletely treated. Youth with ADHD are at substantially elevated risk of developing substance use disorders, although there is a complex relationship between these two problems. The evidence currently suggests that for youth who began effective treatment prior to puberty, there is no elevation in risk, but for those who did not, there is a substantially elevated risk of substance use disorders. Finally, there has been research that indicates that children with a combination of sensation-seeking, high impulsivity, anxiety-sensitivity, and hopelessness are at the highest risk for substance use disorders.2
Prevention efforts you can make: To your patients
The first step in your prevention efforts is an open conversation about drugs and alcohol. Ask your middle schoolers about whether they have tried alcohol or any drugs. Have their friends? What are kids saying about alcohol? About marijuana? Vaping? Are there other substances that kids are talking about or trying? Be genuinely curious, warm, and nonjudgmental. Find out what they think the risks of these substances may be. If appropriate, offer them some education about known risks of substances to the developing brain, to school or athletic performance, and so on. You can teach them about other trusted resources, such as the National Institute on Drug Abuse (NIDA), which has a resource specifically for teens (teens.drugabuse.gov).
For your high school students and those heading off to college, provide a safe place to talk about what they have tried and whether they (or you) have any worries about substance use. You have a unique combination of clinical authority and expertise in them as individuals, and can help them meaningfully plan how to handle their choices. You might talk about the specific risks of binge drinking, from sexual assault to alcohol poisoning and permanent cognitive effects on their developing brains. They also can benefit from hearing about the actual risks of frequent marijuana use, including impaired cognitive performance (and permanent IQ decline), and ongoing risks to their still-developing brains. Don’t be surprised if your older adolescent patients want to educate you about risks. Be curious and humble, and don’t be afraid to go together to a third party for information. You should encourage their efforts to think critically, and be empathic to their dilemma as they try to balance risks against their drive to have new experiences, to be independent, and to be strongly connected to their peers.
Adolescents should hear about your concern about their specific risks with drugs and alcohol, such as a history of traumatic brain injury (concussion), a family history of drug or alcohol dependence, or their own diagnosis of anxiety, depression, or ADHD. You might point out that because they have not tried any drugs or alcohol in high school, they may be prone to having too much to drink when they first try it. Or you might observe that because they have an anxiety disorder, they are vulnerable to becoming dependent on alcohol. Hearing about their specific level of risk equips them to make wiser choices in the context of their growing autonomy.
Prevention efforts you can make: To the parents
Your other prevention strategies should include parents. Studies have shown that when parents have clear rules and expectations about drug and alcohol use, and are consistent about enforcing consequences in their home, their children are significantly less likely than their peers to have experimented with drugs or alcohol by their senior year in high school. Parents of children headed to middle school should hear about this fact, alongside accurate information about the risks associated with alcohol and specific drugs for the developing brain.
Finally, parents need to hear that they can be effective disciplinarians, while also making clear to their children that safety comes first, and that their rules should have clear exceptions for safety. If the parents have a rule against any use of alcohol or drugs, there should be an exception if their child is out and feels unsafe. If they are drunk, or their driver has been drinking, they can call for a ride and will not be in (much) trouble. Rules don’t have to be draconian to be effective; they should always support honesty and safety first. This is a lot of territory to cover, and you do not have to be the only resource for parents. Reliable online resources, such as NIDA’s and SAMHSA’s websites, are full of useful information, and others, such as teen-safe.org, have detailed resources for parents in particular.
References
1. Hum Genet. 2012 Jun;131(6):779-89.
2. Alcohol Clin Exp Res. 2013 Jan;37(Suppl 1):E281-90.
Dr. Swick is an attending psychiatrist in the division of child psychiatry at Massachusetts General Hospital, Boston, and director of the Parenting at a Challenging Time (PACT) Program at the Vernon Cancer Center at Newton Wellesley Hospital, also in Boston. Dr. Jellinek is professor emeritus of psychiatry and pediatrics, Harvard Medical School, Boston.
Substance use disorders are affecting every pediatric practice as they are major contributors to morbidity and mortality in young people. With the ongoing risks of binge drinking, the current epidemic of opioid addiction and overdose deaths in the United States, and the shifting legal status and public perception of the risk of marijuana, how to deal with substance use disorders seems to be the focus of public conversation these days. , such as parent education and early recognition in pediatric practice.
Substance abuse risk
We cannot yet predict who can safely “experiment” with substances or who will develop dependency. However, there is information that we can use to identify those at greater risk. Youth who have a first-degree relative with a substance use disorder are at greater risk for developing such a disorder themselves, and this is especially so if there is a family history of alcoholism. Youth who suffer from a psychiatric illness, particularly from anxiety and mood disorders, have a special vulnerability to abusing substances, particularly when their underlying illness is untreated or incompletely treated. Youth with ADHD are at substantially elevated risk of developing substance use disorders, although there is a complex relationship between these two problems. The evidence currently suggests that for youth who began effective treatment prior to puberty, there is no elevation in risk, but for those who did not, there is a substantially elevated risk of substance use disorders. Finally, there has been research that indicates that children with a combination of sensation-seeking, high impulsivity, anxiety-sensitivity, and hopelessness are at the highest risk for substance use disorders.2
Prevention efforts you can make: To your patients
The first step in your prevention efforts is an open conversation about drugs and alcohol. Ask your middle schoolers about whether they have tried alcohol or any drugs. Have their friends? What are kids saying about alcohol? About marijuana? Vaping? Are there other substances that kids are talking about or trying? Be genuinely curious, warm, and nonjudgmental. Find out what they think the risks of these substances may be. If appropriate, offer them some education about known risks of substances to the developing brain, to school or athletic performance, and so on. You can teach them about other trusted resources, such as the National Institute on Drug Abuse (NIDA), which has a resource specifically for teens (teens.drugabuse.gov).
For your high school students and those heading off to college, provide a safe place to talk about what they have tried and whether they (or you) have any worries about substance use. You have a unique combination of clinical authority and expertise in them as individuals, and can help them meaningfully plan how to handle their choices. You might talk about the specific risks of binge drinking, from sexual assault to alcohol poisoning and permanent cognitive effects on their developing brains. They also can benefit from hearing about the actual risks of frequent marijuana use, including impaired cognitive performance (and permanent IQ decline), and ongoing risks to their still-developing brains. Don’t be surprised if your older adolescent patients want to educate you about risks. Be curious and humble, and don’t be afraid to go together to a third party for information. You should encourage their efforts to think critically, and be empathic to their dilemma as they try to balance risks against their drive to have new experiences, to be independent, and to be strongly connected to their peers.
Adolescents should hear about your concern about their specific risks with drugs and alcohol, such as a history of traumatic brain injury (concussion), a family history of drug or alcohol dependence, or their own diagnosis of anxiety, depression, or ADHD. You might point out that because they have not tried any drugs or alcohol in high school, they may be prone to having too much to drink when they first try it. Or you might observe that because they have an anxiety disorder, they are vulnerable to becoming dependent on alcohol. Hearing about their specific level of risk equips them to make wiser choices in the context of their growing autonomy.
Prevention efforts you can make: To the parents
Your other prevention strategies should include parents. Studies have shown that when parents have clear rules and expectations about drug and alcohol use, and are consistent about enforcing consequences in their home, their children are significantly less likely than their peers to have experimented with drugs or alcohol by their senior year in high school. Parents of children headed to middle school should hear about this fact, alongside accurate information about the risks associated with alcohol and specific drugs for the developing brain.
Finally, parents need to hear that they can be effective disciplinarians, while also making clear to their children that safety comes first, and that their rules should have clear exceptions for safety. If the parents have a rule against any use of alcohol or drugs, there should be an exception if their child is out and feels unsafe. If they are drunk, or their driver has been drinking, they can call for a ride and will not be in (much) trouble. Rules don’t have to be draconian to be effective; they should always support honesty and safety first. This is a lot of territory to cover, and you do not have to be the only resource for parents. Reliable online resources, such as NIDA’s and SAMHSA’s websites, are full of useful information, and others, such as teen-safe.org, have detailed resources for parents in particular.
References
1. Hum Genet. 2012 Jun;131(6):779-89.
2. Alcohol Clin Exp Res. 2013 Jan;37(Suppl 1):E281-90.
Dr. Swick is an attending psychiatrist in the division of child psychiatry at Massachusetts General Hospital, Boston, and director of the Parenting at a Challenging Time (PACT) Program at the Vernon Cancer Center at Newton Wellesley Hospital, also in Boston. Dr. Jellinek is professor emeritus of psychiatry and pediatrics, Harvard Medical School, Boston.
More to psychiatry than just neuroscience; The impact of childhood trauma
More to psychiatry than just neuroscience
In his editorial “Advancing clinical neuroscience literacy among psychiatric practitioners” (From the Editor,
I find that many of my patients look for more or different drugs to fix their dysfunctional patterns in life—many of which stem from their dysfunctional and traumatic childhoods. Thus, it is more than just drugs and neurochemical pathways, more than just the “dysregulated neural circuitry,” that we need to focus on in our psychiatric practice.
I finished my psychiatric residency in 1972, before we knew much about neuroscience. Since then, we have learned so much about neuroscience and the specific neuroscience mechanisms involved in the brain and mind. Those advances have done much to aid our core understanding of psychiatric disorders. However, let us not forget that there is more to the mind than just neurochemistry, and more to our practice of psychiatry than just neuroscience.
Leonard Korn, MD
Psychiatrist
Portsmouth Regional Hospital
Portsmouth, New Hampshire
Dr. Nasrallah responds
It is now widely accepted in our field that all psychological phenomena and all human behaviors are associated with neurobiological components. All life events, especially traumatic experiences, are transduced into structural and chemical changes, often within minutes. The formation of dendritic spines to encode the memory of one’s experiences throughout waking hours is well established in neuroscience, and hundreds of studies have been published about this.
Psychotherapy is a neurobiological intervention that induces neuroplasticity and leads to structural brain repair, because talking, listening, triggering memories, inducing insight, and “connecting the dots” in one’s behavior are all biological events.1,2 There is no such thing as a purely psychological process independent of the brain. The mind is the product of ongoing complex, intricate activity of brain neurocircuits whose neurobiological activity is translated into thoughts, emotions, impulses, and behaviors. The mind is perpetually tethered to its neurological roots.
Thus, reductionism actually describes a scientific fact and is not a term with pejorative connotations used to shut down scientific discourse about the biological basis of human behavior. By advancing their clinical neuroscience literacy, psychiatric practitioners will understand that they deal with a specific brain pathology in every patient that they treat and that the medications and psychotherapeutic interventions they employ are synergistic biological treatments.3
Henry A. Nasrallah, MD
Professor and Chair
Department of Psychiatry and Behavioral Neuroscience
Saint Louis University School of Medicine
St. Louis, Missouri
References
1. Nasrallah HA. Repositioning psychotherapy as a neurobiological intervention. Current Psychiatry. 2013;12(12):18-19.
2. Nasrallah HA. Out-of-the-box questions about psychotherapy. Current Psychiatry. 2010;9(10):13-14.
3. Nasrallah HA. Medications with psychotherapy: a synergy to heal the brain. C urrent Psychiatry. 2006;5(10):11-12.
The impact of childhood trauma
I enjoyed Dr. Nasrallah’s article “Beyond DSM-5: Clinical and biologic features shared by major psychiatric syndromes” (From the Editor, Current Psychiatry. October 2017, p. 4,6-7), but there was only 1 mention of childhood trauma, which shares features with most of the commonalities he described, such as inflammation, smaller brain volumes, gene and environment interaction, shortened telomeres, and elevated cortisol levels. The Adverse Childhood Experiences Study1 taught us about the impact of childhood trauma on the entire organism. We need to focus on that commonality.
Susan Jones, MD
Child and Adolescent Psychiatrist
Virginia Treatment Center for Children
Assistant Professor
Virginia Commonwealth University
School of Medicine
Richmond, Virginia
Reference
1. Felitti VJ, Anda RF, Nordenberg D, et al. Relationship of childhood abuse and household dysfunction to many of the leading causes of death in adults. The Adverse Childhood Experiences (ACE) Study. Am J Prev Med. 1998;14(4):245-258
Dr. Nasrallah responds
It is worth pointing out that childhood trauma predominantly leads to psychotic and mood disorders in adulthood, and the criteria I mentioned would then hold true.
More to psychiatry than just neuroscience
In his editorial “Advancing clinical neuroscience literacy among psychiatric practitioners” (From the Editor,
I find that many of my patients look for more or different drugs to fix their dysfunctional patterns in life—many of which stem from their dysfunctional and traumatic childhoods. Thus, it is more than just drugs and neurochemical pathways, more than just the “dysregulated neural circuitry,” that we need to focus on in our psychiatric practice.
I finished my psychiatric residency in 1972, before we knew much about neuroscience. Since then, we have learned so much about neuroscience and the specific neuroscience mechanisms involved in the brain and mind. Those advances have done much to aid our core understanding of psychiatric disorders. However, let us not forget that there is more to the mind than just neurochemistry, and more to our practice of psychiatry than just neuroscience.
Leonard Korn, MD
Psychiatrist
Portsmouth Regional Hospital
Portsmouth, New Hampshire
Dr. Nasrallah responds
It is now widely accepted in our field that all psychological phenomena and all human behaviors are associated with neurobiological components. All life events, especially traumatic experiences, are transduced into structural and chemical changes, often within minutes. The formation of dendritic spines to encode the memory of one’s experiences throughout waking hours is well established in neuroscience, and hundreds of studies have been published about this.
Psychotherapy is a neurobiological intervention that induces neuroplasticity and leads to structural brain repair, because talking, listening, triggering memories, inducing insight, and “connecting the dots” in one’s behavior are all biological events.1,2 There is no such thing as a purely psychological process independent of the brain. The mind is the product of ongoing complex, intricate activity of brain neurocircuits whose neurobiological activity is translated into thoughts, emotions, impulses, and behaviors. The mind is perpetually tethered to its neurological roots.
Thus, reductionism actually describes a scientific fact and is not a term with pejorative connotations used to shut down scientific discourse about the biological basis of human behavior. By advancing their clinical neuroscience literacy, psychiatric practitioners will understand that they deal with a specific brain pathology in every patient that they treat and that the medications and psychotherapeutic interventions they employ are synergistic biological treatments.3
Henry A. Nasrallah, MD
Professor and Chair
Department of Psychiatry and Behavioral Neuroscience
Saint Louis University School of Medicine
St. Louis, Missouri
References
1. Nasrallah HA. Repositioning psychotherapy as a neurobiological intervention. Current Psychiatry. 2013;12(12):18-19.
2. Nasrallah HA. Out-of-the-box questions about psychotherapy. Current Psychiatry. 2010;9(10):13-14.
3. Nasrallah HA. Medications with psychotherapy: a synergy to heal the brain. C urrent Psychiatry. 2006;5(10):11-12.
The impact of childhood trauma
I enjoyed Dr. Nasrallah’s article “Beyond DSM-5: Clinical and biologic features shared by major psychiatric syndromes” (From the Editor, Current Psychiatry. October 2017, p. 4,6-7), but there was only 1 mention of childhood trauma, which shares features with most of the commonalities he described, such as inflammation, smaller brain volumes, gene and environment interaction, shortened telomeres, and elevated cortisol levels. The Adverse Childhood Experiences Study1 taught us about the impact of childhood trauma on the entire organism. We need to focus on that commonality.
Susan Jones, MD
Child and Adolescent Psychiatrist
Virginia Treatment Center for Children
Assistant Professor
Virginia Commonwealth University
School of Medicine
Richmond, Virginia
Reference
1. Felitti VJ, Anda RF, Nordenberg D, et al. Relationship of childhood abuse and household dysfunction to many of the leading causes of death in adults. The Adverse Childhood Experiences (ACE) Study. Am J Prev Med. 1998;14(4):245-258
Dr. Nasrallah responds
It is worth pointing out that childhood trauma predominantly leads to psychotic and mood disorders in adulthood, and the criteria I mentioned would then hold true.
More to psychiatry than just neuroscience
In his editorial “Advancing clinical neuroscience literacy among psychiatric practitioners” (From the Editor,
I find that many of my patients look for more or different drugs to fix their dysfunctional patterns in life—many of which stem from their dysfunctional and traumatic childhoods. Thus, it is more than just drugs and neurochemical pathways, more than just the “dysregulated neural circuitry,” that we need to focus on in our psychiatric practice.
I finished my psychiatric residency in 1972, before we knew much about neuroscience. Since then, we have learned so much about neuroscience and the specific neuroscience mechanisms involved in the brain and mind. Those advances have done much to aid our core understanding of psychiatric disorders. However, let us not forget that there is more to the mind than just neurochemistry, and more to our practice of psychiatry than just neuroscience.
Leonard Korn, MD
Psychiatrist
Portsmouth Regional Hospital
Portsmouth, New Hampshire
Dr. Nasrallah responds
It is now widely accepted in our field that all psychological phenomena and all human behaviors are associated with neurobiological components. All life events, especially traumatic experiences, are transduced into structural and chemical changes, often within minutes. The formation of dendritic spines to encode the memory of one’s experiences throughout waking hours is well established in neuroscience, and hundreds of studies have been published about this.
Psychotherapy is a neurobiological intervention that induces neuroplasticity and leads to structural brain repair, because talking, listening, triggering memories, inducing insight, and “connecting the dots” in one’s behavior are all biological events.1,2 There is no such thing as a purely psychological process independent of the brain. The mind is the product of ongoing complex, intricate activity of brain neurocircuits whose neurobiological activity is translated into thoughts, emotions, impulses, and behaviors. The mind is perpetually tethered to its neurological roots.
Thus, reductionism actually describes a scientific fact and is not a term with pejorative connotations used to shut down scientific discourse about the biological basis of human behavior. By advancing their clinical neuroscience literacy, psychiatric practitioners will understand that they deal with a specific brain pathology in every patient that they treat and that the medications and psychotherapeutic interventions they employ are synergistic biological treatments.3
Henry A. Nasrallah, MD
Professor and Chair
Department of Psychiatry and Behavioral Neuroscience
Saint Louis University School of Medicine
St. Louis, Missouri
References
1. Nasrallah HA. Repositioning psychotherapy as a neurobiological intervention. Current Psychiatry. 2013;12(12):18-19.
2. Nasrallah HA. Out-of-the-box questions about psychotherapy. Current Psychiatry. 2010;9(10):13-14.
3. Nasrallah HA. Medications with psychotherapy: a synergy to heal the brain. C urrent Psychiatry. 2006;5(10):11-12.
The impact of childhood trauma
I enjoyed Dr. Nasrallah’s article “Beyond DSM-5: Clinical and biologic features shared by major psychiatric syndromes” (From the Editor, Current Psychiatry. October 2017, p. 4,6-7), but there was only 1 mention of childhood trauma, which shares features with most of the commonalities he described, such as inflammation, smaller brain volumes, gene and environment interaction, shortened telomeres, and elevated cortisol levels. The Adverse Childhood Experiences Study1 taught us about the impact of childhood trauma on the entire organism. We need to focus on that commonality.
Susan Jones, MD
Child and Adolescent Psychiatrist
Virginia Treatment Center for Children
Assistant Professor
Virginia Commonwealth University
School of Medicine
Richmond, Virginia
Reference
1. Felitti VJ, Anda RF, Nordenberg D, et al. Relationship of childhood abuse and household dysfunction to many of the leading causes of death in adults. The Adverse Childhood Experiences (ACE) Study. Am J Prev Med. 1998;14(4):245-258
Dr. Nasrallah responds
It is worth pointing out that childhood trauma predominantly leads to psychotic and mood disorders in adulthood, and the criteria I mentioned would then hold true.
Physician wellness needs attention at personal, institutional, and cultural levels
Do you know we have record rates of physician burnout, dissatisfaction, and suicide? Ongoing shortages in primary care, without improvement in sight? Physicians exiting medicine earlier than in the past?
What about burnout? Do you know it affects patients as well as their doctors? Affects physicians’ families and friends? Increases mistakes and malpractice risk? Affects patient adherence and outcomes? Is costly to the entire system?
How do we start to fix this? : personal wellness, organizational wellness, and wellness within the culture of medicine.
The high level of physician burnout indicates that addressing wellness at the personal level is not enough. It speaks to a systemic rather than individual etiology. Organizations have begun to recognize it is in their best interest to keep their physicians happy. Losing even one physician to burnout is expensive. In addition, burned out physicians are liabilities. Mistakes increase. Productivity decreases. Patient satisfaction decreases. Ripple effects touch other members of the team, which leads to further burnout. If for no other reason, physician wellness at the organizational level matters because it affects the bottom line.
Wellness within the culture of medicine is the third level of our framework. Western medicine has its own set of customs, traditions, and values that are learned early in the course of medical training. The value of sound scientific methods, the importance placed on logic and reason, and the significance of professional integrity are examples. Hard work, sacrifice, and commitment also are included. Unhealthy values include harsh judgment, shame, a sense of superiority, and perfection.
When examining physician wellness at the cultural level, we also must address discrimination within medicine. Overt racism, misogyny, ageism, and discrimination based upon sexual orientation are everyday occurrences and affect everyone within the culture of medicine. It’s difficult to experience wellness at the same time as discrimination.
At every level, physician wellness depends upon continuous, usually low-tech activities and habits based upon individual and shared values. Identifying and shaping these shared values is not going to happen on its own. We all have an obligation to speak and act up. We need improved physician health. Our families, our communities, patients, and even the institution of medicine deserves better.
Dr. Stepien practices pediatrics in Juneau, Alaska. She is on the Pediatric News editorial advisory board. Email her at [email protected]
Do you know we have record rates of physician burnout, dissatisfaction, and suicide? Ongoing shortages in primary care, without improvement in sight? Physicians exiting medicine earlier than in the past?
What about burnout? Do you know it affects patients as well as their doctors? Affects physicians’ families and friends? Increases mistakes and malpractice risk? Affects patient adherence and outcomes? Is costly to the entire system?
How do we start to fix this? : personal wellness, organizational wellness, and wellness within the culture of medicine.
The high level of physician burnout indicates that addressing wellness at the personal level is not enough. It speaks to a systemic rather than individual etiology. Organizations have begun to recognize it is in their best interest to keep their physicians happy. Losing even one physician to burnout is expensive. In addition, burned out physicians are liabilities. Mistakes increase. Productivity decreases. Patient satisfaction decreases. Ripple effects touch other members of the team, which leads to further burnout. If for no other reason, physician wellness at the organizational level matters because it affects the bottom line.
Wellness within the culture of medicine is the third level of our framework. Western medicine has its own set of customs, traditions, and values that are learned early in the course of medical training. The value of sound scientific methods, the importance placed on logic and reason, and the significance of professional integrity are examples. Hard work, sacrifice, and commitment also are included. Unhealthy values include harsh judgment, shame, a sense of superiority, and perfection.
When examining physician wellness at the cultural level, we also must address discrimination within medicine. Overt racism, misogyny, ageism, and discrimination based upon sexual orientation are everyday occurrences and affect everyone within the culture of medicine. It’s difficult to experience wellness at the same time as discrimination.
At every level, physician wellness depends upon continuous, usually low-tech activities and habits based upon individual and shared values. Identifying and shaping these shared values is not going to happen on its own. We all have an obligation to speak and act up. We need improved physician health. Our families, our communities, patients, and even the institution of medicine deserves better.
Dr. Stepien practices pediatrics in Juneau, Alaska. She is on the Pediatric News editorial advisory board. Email her at [email protected]
Do you know we have record rates of physician burnout, dissatisfaction, and suicide? Ongoing shortages in primary care, without improvement in sight? Physicians exiting medicine earlier than in the past?
What about burnout? Do you know it affects patients as well as their doctors? Affects physicians’ families and friends? Increases mistakes and malpractice risk? Affects patient adherence and outcomes? Is costly to the entire system?
How do we start to fix this? : personal wellness, organizational wellness, and wellness within the culture of medicine.
The high level of physician burnout indicates that addressing wellness at the personal level is not enough. It speaks to a systemic rather than individual etiology. Organizations have begun to recognize it is in their best interest to keep their physicians happy. Losing even one physician to burnout is expensive. In addition, burned out physicians are liabilities. Mistakes increase. Productivity decreases. Patient satisfaction decreases. Ripple effects touch other members of the team, which leads to further burnout. If for no other reason, physician wellness at the organizational level matters because it affects the bottom line.
Wellness within the culture of medicine is the third level of our framework. Western medicine has its own set of customs, traditions, and values that are learned early in the course of medical training. The value of sound scientific methods, the importance placed on logic and reason, and the significance of professional integrity are examples. Hard work, sacrifice, and commitment also are included. Unhealthy values include harsh judgment, shame, a sense of superiority, and perfection.
When examining physician wellness at the cultural level, we also must address discrimination within medicine. Overt racism, misogyny, ageism, and discrimination based upon sexual orientation are everyday occurrences and affect everyone within the culture of medicine. It’s difficult to experience wellness at the same time as discrimination.
At every level, physician wellness depends upon continuous, usually low-tech activities and habits based upon individual and shared values. Identifying and shaping these shared values is not going to happen on its own. We all have an obligation to speak and act up. We need improved physician health. Our families, our communities, patients, and even the institution of medicine deserves better.
Dr. Stepien practices pediatrics in Juneau, Alaska. She is on the Pediatric News editorial advisory board. Email her at [email protected]
Postpartum depression: Moving toward improved screening with a new app
Over the last several years, there’s been increasing interest and ultimately a growing number of mandates across dozens of states to screen women for postpartum depression (PPD). As PPD is the most common, and often devastating, complication in modern obstetrics, screening for it is a movement that I fully support.
What’s been challenging is how to roll out screening in a widespread fashion using a standardized tool that is both easy to use and to score, and that has only a modest number of false positives (i.e., it has good specificity).
The first version of the MGHPDS app combines the Edinburgh Postpartum Depression Scale (EPDS) – the most commonly used screen for PPD – with screening tools that measure sleep disturbance, anxiety, and stress. And while the Edinburgh scale has been an enormous contribution to psychiatry, its implementation in obstetric settings and community settings using pen and pencil has been a challenge at times given the inclusion of some questions that are “reverse scored”; other problems when the EPDS has been scaled for use in large settings include rates of false positives as high as 25%.
Our app, which gives users an opportunity to let us review their scores after giving informed consent, ultimately will lead to the development of a shortened set of questions that zero in on the symptoms most commonly associated with PPD. That information will derive from a validation study looking at how well the questions on the MGHPDS correlate with major depression; we hope to launch version 2.0 in mid-2018. The second version of the app is likely to include some items from the Edinburgh scale and also selected symptoms of anxiety, sleep problems, and perceived stress. Thus, the goal of the second version will be realized: a more specific scale with targeted symptoms that correlate with the clinical diagnosis of depression.
Automatic scoring of the questionnaires leads to an app-generated result across a spectrum from “no evidence of depressive symptoms,” to a message noting concern and instructing the user to seek medical attention. There are also links to educational resources about PPD within the app.
The task of referring women with PPD for treatment and then getting them well is a huge undertaking, and one where we currently are falling short. I have been heartened across the last decade to see the focus land on the issue of PPD screening, but failing to couple screening with evidence-based treatment is an incomplete victory. So with the next version of the app, we want to include treatment tools and a way to track women over time, looking at whether they were treated and if they got well.
We want clinicians to be aware of our app and to share it with their patients. But even more importantly, we want to reach out directly to women because they will lead the way on this effort.
The stakes for unrecognized and untreated PPD are simply too great for women, children, and their families.
Dr. Cohen is the director of the Ammon-Pinizzotto Center for Women’s Mental Health at Massachusetts General Hospital in Boston, which provides information resources and conducts clinical care and research in reproductive mental health. He has been a consultant to manufacturers of psychiatric medications.
Over the last several years, there’s been increasing interest and ultimately a growing number of mandates across dozens of states to screen women for postpartum depression (PPD). As PPD is the most common, and often devastating, complication in modern obstetrics, screening for it is a movement that I fully support.
What’s been challenging is how to roll out screening in a widespread fashion using a standardized tool that is both easy to use and to score, and that has only a modest number of false positives (i.e., it has good specificity).
The first version of the MGHPDS app combines the Edinburgh Postpartum Depression Scale (EPDS) – the most commonly used screen for PPD – with screening tools that measure sleep disturbance, anxiety, and stress. And while the Edinburgh scale has been an enormous contribution to psychiatry, its implementation in obstetric settings and community settings using pen and pencil has been a challenge at times given the inclusion of some questions that are “reverse scored”; other problems when the EPDS has been scaled for use in large settings include rates of false positives as high as 25%.
Our app, which gives users an opportunity to let us review their scores after giving informed consent, ultimately will lead to the development of a shortened set of questions that zero in on the symptoms most commonly associated with PPD. That information will derive from a validation study looking at how well the questions on the MGHPDS correlate with major depression; we hope to launch version 2.0 in mid-2018. The second version of the app is likely to include some items from the Edinburgh scale and also selected symptoms of anxiety, sleep problems, and perceived stress. Thus, the goal of the second version will be realized: a more specific scale with targeted symptoms that correlate with the clinical diagnosis of depression.
Automatic scoring of the questionnaires leads to an app-generated result across a spectrum from “no evidence of depressive symptoms,” to a message noting concern and instructing the user to seek medical attention. There are also links to educational resources about PPD within the app.
The task of referring women with PPD for treatment and then getting them well is a huge undertaking, and one where we currently are falling short. I have been heartened across the last decade to see the focus land on the issue of PPD screening, but failing to couple screening with evidence-based treatment is an incomplete victory. So with the next version of the app, we want to include treatment tools and a way to track women over time, looking at whether they were treated and if they got well.
We want clinicians to be aware of our app and to share it with their patients. But even more importantly, we want to reach out directly to women because they will lead the way on this effort.
The stakes for unrecognized and untreated PPD are simply too great for women, children, and their families.
Dr. Cohen is the director of the Ammon-Pinizzotto Center for Women’s Mental Health at Massachusetts General Hospital in Boston, which provides information resources and conducts clinical care and research in reproductive mental health. He has been a consultant to manufacturers of psychiatric medications.
Over the last several years, there’s been increasing interest and ultimately a growing number of mandates across dozens of states to screen women for postpartum depression (PPD). As PPD is the most common, and often devastating, complication in modern obstetrics, screening for it is a movement that I fully support.
What’s been challenging is how to roll out screening in a widespread fashion using a standardized tool that is both easy to use and to score, and that has only a modest number of false positives (i.e., it has good specificity).
The first version of the MGHPDS app combines the Edinburgh Postpartum Depression Scale (EPDS) – the most commonly used screen for PPD – with screening tools that measure sleep disturbance, anxiety, and stress. And while the Edinburgh scale has been an enormous contribution to psychiatry, its implementation in obstetric settings and community settings using pen and pencil has been a challenge at times given the inclusion of some questions that are “reverse scored”; other problems when the EPDS has been scaled for use in large settings include rates of false positives as high as 25%.
Our app, which gives users an opportunity to let us review their scores after giving informed consent, ultimately will lead to the development of a shortened set of questions that zero in on the symptoms most commonly associated with PPD. That information will derive from a validation study looking at how well the questions on the MGHPDS correlate with major depression; we hope to launch version 2.0 in mid-2018. The second version of the app is likely to include some items from the Edinburgh scale and also selected symptoms of anxiety, sleep problems, and perceived stress. Thus, the goal of the second version will be realized: a more specific scale with targeted symptoms that correlate with the clinical diagnosis of depression.
Automatic scoring of the questionnaires leads to an app-generated result across a spectrum from “no evidence of depressive symptoms,” to a message noting concern and instructing the user to seek medical attention. There are also links to educational resources about PPD within the app.
The task of referring women with PPD for treatment and then getting them well is a huge undertaking, and one where we currently are falling short. I have been heartened across the last decade to see the focus land on the issue of PPD screening, but failing to couple screening with evidence-based treatment is an incomplete victory. So with the next version of the app, we want to include treatment tools and a way to track women over time, looking at whether they were treated and if they got well.
We want clinicians to be aware of our app and to share it with their patients. But even more importantly, we want to reach out directly to women because they will lead the way on this effort.
The stakes for unrecognized and untreated PPD are simply too great for women, children, and their families.
Dr. Cohen is the director of the Ammon-Pinizzotto Center for Women’s Mental Health at Massachusetts General Hospital in Boston, which provides information resources and conducts clinical care and research in reproductive mental health. He has been a consultant to manufacturers of psychiatric medications.
Integrating behavioral health and primary care
This is the fourth in a series of articles from the National Center for Excellence in Primary Care Research (NCEPCR) in the Agency for Healthcare Research and Quality (AHRQ). This series introduces sets of tools and resources designed to help your practice.
Many patients with anxiety, depression, behavioral problems, substance abuse, and other mental and behavioral health conditions turn to their primary care providers as their first, and often only, source of mental health care. Unfortunately, this care may not be as effective as patients and primary care personnel would hope or expect it to be. Problems exist with missed or inaccurate diagnoses, referrals and coordination of care, and other failures in detection and treatment (NIMH Integrated Care Web site, accessed Oct. 1, 2017).
Through the Academy’s web portal interested clinicians, health care administrators, quality improvement specialists, and others can access a wide range of resources related to behavioral health integration. A hallmark of the site is the Integration Playbook, developed as a guide to integrating behavioral health in primary care and other ambulatory care settings. The Playbook assists the growing number of primary care practices and health systems that are beginning to design and implement integrated behavioral health services. The Playbook’s implementation framework is designed to be meaningful at any level of integration development.
One challenge in implementing primary care and behavioral health integration is connecting the community engaged in integrated health care. Often behavioral health and primary care providers operate within the same building or organization but are not be aware of each other’s presence. One goal of the Academy is to unite these disparate efforts and direct providers towards one another in an attempt to facilitate collaboration. In the same vein, the Academy aims to offer resources to patients and the community on integration, including the identification of integrated practices they can access.
In addition, in order to measure quality of care in this new approach to health care delivery, the Academy created the Atlas of Integrated Behavioral Health Care Quality Measures. Intended for practices and teams that wish to understand whether they are providing high-quality integrated behavioral health care or are preparing to implement integrated care, the Atlas aims to support the field of integrated behavioral health care measurement by 1) presenting a framework for understanding measurement of integrated care; 2) providing a list of existing measures relevant to integrated behavioral health care; and 3) organizing the measures by the framework and by user goals to facilitate selection of measures.
Links from the NCEPCR site:
Tools and Resources for Research, Quality Improvement, and Practice
https://www.ahrq.gov/ncepcr/research-qi-practice/practice-transformation-qi.html
Academy Web Portal: https://www.integrationacademy.ahrq.gov
The Integration Playbook: https://integrationacademy.ahrq.gov/playbook/about-playbook
Lexicon: https://integrationacademy.ahrq.gov/lexicon
Atlas of Integrated Behavioral Health Care Quality Measures: https://integrationacademy.ahrq.gov/resources/ibhc-measures-atlas
These and other tools can be found at the NCEPCR Web site: https://www.ahrq.gov/ncepcr.
Dr. Genevro is a health scientist at AHRQ. Dr. Ganiats is director, National Center for Excellence in Primary Care Research, AHRQ.
This is the fourth in a series of articles from the National Center for Excellence in Primary Care Research (NCEPCR) in the Agency for Healthcare Research and Quality (AHRQ). This series introduces sets of tools and resources designed to help your practice.
Many patients with anxiety, depression, behavioral problems, substance abuse, and other mental and behavioral health conditions turn to their primary care providers as their first, and often only, source of mental health care. Unfortunately, this care may not be as effective as patients and primary care personnel would hope or expect it to be. Problems exist with missed or inaccurate diagnoses, referrals and coordination of care, and other failures in detection and treatment (NIMH Integrated Care Web site, accessed Oct. 1, 2017).
Through the Academy’s web portal interested clinicians, health care administrators, quality improvement specialists, and others can access a wide range of resources related to behavioral health integration. A hallmark of the site is the Integration Playbook, developed as a guide to integrating behavioral health in primary care and other ambulatory care settings. The Playbook assists the growing number of primary care practices and health systems that are beginning to design and implement integrated behavioral health services. The Playbook’s implementation framework is designed to be meaningful at any level of integration development.
One challenge in implementing primary care and behavioral health integration is connecting the community engaged in integrated health care. Often behavioral health and primary care providers operate within the same building or organization but are not be aware of each other’s presence. One goal of the Academy is to unite these disparate efforts and direct providers towards one another in an attempt to facilitate collaboration. In the same vein, the Academy aims to offer resources to patients and the community on integration, including the identification of integrated practices they can access.
In addition, in order to measure quality of care in this new approach to health care delivery, the Academy created the Atlas of Integrated Behavioral Health Care Quality Measures. Intended for practices and teams that wish to understand whether they are providing high-quality integrated behavioral health care or are preparing to implement integrated care, the Atlas aims to support the field of integrated behavioral health care measurement by 1) presenting a framework for understanding measurement of integrated care; 2) providing a list of existing measures relevant to integrated behavioral health care; and 3) organizing the measures by the framework and by user goals to facilitate selection of measures.
Links from the NCEPCR site:
Tools and Resources for Research, Quality Improvement, and Practice
https://www.ahrq.gov/ncepcr/research-qi-practice/practice-transformation-qi.html
Academy Web Portal: https://www.integrationacademy.ahrq.gov
The Integration Playbook: https://integrationacademy.ahrq.gov/playbook/about-playbook
Lexicon: https://integrationacademy.ahrq.gov/lexicon
Atlas of Integrated Behavioral Health Care Quality Measures: https://integrationacademy.ahrq.gov/resources/ibhc-measures-atlas
These and other tools can be found at the NCEPCR Web site: https://www.ahrq.gov/ncepcr.
Dr. Genevro is a health scientist at AHRQ. Dr. Ganiats is director, National Center for Excellence in Primary Care Research, AHRQ.
This is the fourth in a series of articles from the National Center for Excellence in Primary Care Research (NCEPCR) in the Agency for Healthcare Research and Quality (AHRQ). This series introduces sets of tools and resources designed to help your practice.
Many patients with anxiety, depression, behavioral problems, substance abuse, and other mental and behavioral health conditions turn to their primary care providers as their first, and often only, source of mental health care. Unfortunately, this care may not be as effective as patients and primary care personnel would hope or expect it to be. Problems exist with missed or inaccurate diagnoses, referrals and coordination of care, and other failures in detection and treatment (NIMH Integrated Care Web site, accessed Oct. 1, 2017).
Through the Academy’s web portal interested clinicians, health care administrators, quality improvement specialists, and others can access a wide range of resources related to behavioral health integration. A hallmark of the site is the Integration Playbook, developed as a guide to integrating behavioral health in primary care and other ambulatory care settings. The Playbook assists the growing number of primary care practices and health systems that are beginning to design and implement integrated behavioral health services. The Playbook’s implementation framework is designed to be meaningful at any level of integration development.
One challenge in implementing primary care and behavioral health integration is connecting the community engaged in integrated health care. Often behavioral health and primary care providers operate within the same building or organization but are not be aware of each other’s presence. One goal of the Academy is to unite these disparate efforts and direct providers towards one another in an attempt to facilitate collaboration. In the same vein, the Academy aims to offer resources to patients and the community on integration, including the identification of integrated practices they can access.
In addition, in order to measure quality of care in this new approach to health care delivery, the Academy created the Atlas of Integrated Behavioral Health Care Quality Measures. Intended for practices and teams that wish to understand whether they are providing high-quality integrated behavioral health care or are preparing to implement integrated care, the Atlas aims to support the field of integrated behavioral health care measurement by 1) presenting a framework for understanding measurement of integrated care; 2) providing a list of existing measures relevant to integrated behavioral health care; and 3) organizing the measures by the framework and by user goals to facilitate selection of measures.
Links from the NCEPCR site:
Tools and Resources for Research, Quality Improvement, and Practice
https://www.ahrq.gov/ncepcr/research-qi-practice/practice-transformation-qi.html
Academy Web Portal: https://www.integrationacademy.ahrq.gov
The Integration Playbook: https://integrationacademy.ahrq.gov/playbook/about-playbook
Lexicon: https://integrationacademy.ahrq.gov/lexicon
Atlas of Integrated Behavioral Health Care Quality Measures: https://integrationacademy.ahrq.gov/resources/ibhc-measures-atlas
These and other tools can be found at the NCEPCR Web site: https://www.ahrq.gov/ncepcr.
Dr. Genevro is a health scientist at AHRQ. Dr. Ganiats is director, National Center for Excellence in Primary Care Research, AHRQ.
ADHD and the role of wellness
ADHD is a very common disorder with several medication treatment options. There also are wellness and parenting strategies that can address aspects of the challenges of ADHD that are not perfectly covered by medication, such as excess symptoms, times of day that are not covered, or oppositional behavior that often develops secondarily.
Case summary
James is a 6-year-old boy who has been an active, high-energy child since preschool. He has had difficulty with wiggling around in kindergarten and preschool, talking excessively, and being unable to follow directions and pay attention. He is impulsive, disruptive, and frequently doesn’t listen to what his parents tell him to do. Parents and teachers rank him in the clinical range for hyperactivity, impulsivity, and attention problems on standardized rating scales.
Discussion
When we first discuss a new diagnosis with a family, we have the opportunity to shape the family’s expectations about that diagnosis and how it should be addressed. When I discuss ADHD with a new family, I want them to understand the symptoms of inattention, hyperactivity, and impulsiveness, and that these symptoms are not the child’s fault, but rather related to the way his brain is connected. At the same time, I also emphasize that these connections are not entirely fixed, that they mature over time, and that they are affected by experiences in life. In particular, I stress that positive experiences and wellness activities can influence the brain in a positive way. While, of course, I discuss the range of medications that can address these issues, I also deal with wellness in the treatment plan.
Exercise
Studies in humans and animals have provided background evidence that exercise increases the release of neurotransmitters such as dopamine and norepinephrine that are important in the pathophysiology of ADHD. Cerillo-Urbina et al. did a meta-analysis in 2015 of randomized controlled trials and found medium to large effect sizes for a variety of physical activity programs with respect to attention, hyperactivity, and impulsivity, although the study quality was generally low.1 Clearly we need additional more rigorous studies, but given the positive direction of outcomes, the lack of side effects, and the many other positive effects of exercise, it does not seem too soon to add exercise as a prescription for our patients with ADHD. I review this evidence with families, ask them about physical activity they like, and ask if they are willing to work toward an hour of exercise a day.
Sleep
Many children with ADHD have problems with sleep even before they start on stimulant medications, which can further affect sleep. Addressing sleep early on can improve ADHD symptoms, as well as help parents change or avoid patterns like having children fall asleep to the sound of a television. Brief sleep hygiene and cognitive-behavioral therapy interventions over three visits were demonstrated in a randomized controlled trial by Hisock et al. to improve ADHD symptoms and behavioral function.2 These psychosocial interventions clearly are the first line in addressing sleep problems in ADHD, and can benefit even sleep problems connected to medication.
Parent training
Treatment plan
1. Have the child exercise 1 hour every day. Have fun!
2. Establish a nightly bedtime routine, with a bath at 7:30 p.m., brushing of teeth, a story, and lights out at 8 with no TV in the room.
3. Check out the CHADD website for Parent to Parent.
4. Start a trial of stimulant medication.
5. Return in 2 weeks to monitor these interventions, adjust goals, and adjust medications.
When to refer
Many parents will be able to put such a plan in motion with your support and that of other parents. If they are struggling, therapists, psychologists, and psychiatrists trained in motivational and behavioral methods can provide more individualized parent training. Also consider whether the parents themselves may have ADHD and could use referral and treatment.
Dr. Hall is assistant professor of psychiatry and pediatrics at the University of Vermont, Burlington. She said she had no relevant financial disclosures.
References
1. Child Care Health Dev. 2015 Nov;41(6):779-88.
2. BMJ. 2015. doi: 10.1136/bmj.h68.
ADHD is a very common disorder with several medication treatment options. There also are wellness and parenting strategies that can address aspects of the challenges of ADHD that are not perfectly covered by medication, such as excess symptoms, times of day that are not covered, or oppositional behavior that often develops secondarily.
Case summary
James is a 6-year-old boy who has been an active, high-energy child since preschool. He has had difficulty with wiggling around in kindergarten and preschool, talking excessively, and being unable to follow directions and pay attention. He is impulsive, disruptive, and frequently doesn’t listen to what his parents tell him to do. Parents and teachers rank him in the clinical range for hyperactivity, impulsivity, and attention problems on standardized rating scales.
Discussion
When we first discuss a new diagnosis with a family, we have the opportunity to shape the family’s expectations about that diagnosis and how it should be addressed. When I discuss ADHD with a new family, I want them to understand the symptoms of inattention, hyperactivity, and impulsiveness, and that these symptoms are not the child’s fault, but rather related to the way his brain is connected. At the same time, I also emphasize that these connections are not entirely fixed, that they mature over time, and that they are affected by experiences in life. In particular, I stress that positive experiences and wellness activities can influence the brain in a positive way. While, of course, I discuss the range of medications that can address these issues, I also deal with wellness in the treatment plan.
Exercise
Studies in humans and animals have provided background evidence that exercise increases the release of neurotransmitters such as dopamine and norepinephrine that are important in the pathophysiology of ADHD. Cerillo-Urbina et al. did a meta-analysis in 2015 of randomized controlled trials and found medium to large effect sizes for a variety of physical activity programs with respect to attention, hyperactivity, and impulsivity, although the study quality was generally low.1 Clearly we need additional more rigorous studies, but given the positive direction of outcomes, the lack of side effects, and the many other positive effects of exercise, it does not seem too soon to add exercise as a prescription for our patients with ADHD. I review this evidence with families, ask them about physical activity they like, and ask if they are willing to work toward an hour of exercise a day.
Sleep
Many children with ADHD have problems with sleep even before they start on stimulant medications, which can further affect sleep. Addressing sleep early on can improve ADHD symptoms, as well as help parents change or avoid patterns like having children fall asleep to the sound of a television. Brief sleep hygiene and cognitive-behavioral therapy interventions over three visits were demonstrated in a randomized controlled trial by Hisock et al. to improve ADHD symptoms and behavioral function.2 These psychosocial interventions clearly are the first line in addressing sleep problems in ADHD, and can benefit even sleep problems connected to medication.
Parent training
Treatment plan
1. Have the child exercise 1 hour every day. Have fun!
2. Establish a nightly bedtime routine, with a bath at 7:30 p.m., brushing of teeth, a story, and lights out at 8 with no TV in the room.
3. Check out the CHADD website for Parent to Parent.
4. Start a trial of stimulant medication.
5. Return in 2 weeks to monitor these interventions, adjust goals, and adjust medications.
When to refer
Many parents will be able to put such a plan in motion with your support and that of other parents. If they are struggling, therapists, psychologists, and psychiatrists trained in motivational and behavioral methods can provide more individualized parent training. Also consider whether the parents themselves may have ADHD and could use referral and treatment.
Dr. Hall is assistant professor of psychiatry and pediatrics at the University of Vermont, Burlington. She said she had no relevant financial disclosures.
References
1. Child Care Health Dev. 2015 Nov;41(6):779-88.
2. BMJ. 2015. doi: 10.1136/bmj.h68.
ADHD is a very common disorder with several medication treatment options. There also are wellness and parenting strategies that can address aspects of the challenges of ADHD that are not perfectly covered by medication, such as excess symptoms, times of day that are not covered, or oppositional behavior that often develops secondarily.
Case summary
James is a 6-year-old boy who has been an active, high-energy child since preschool. He has had difficulty with wiggling around in kindergarten and preschool, talking excessively, and being unable to follow directions and pay attention. He is impulsive, disruptive, and frequently doesn’t listen to what his parents tell him to do. Parents and teachers rank him in the clinical range for hyperactivity, impulsivity, and attention problems on standardized rating scales.
Discussion
When we first discuss a new diagnosis with a family, we have the opportunity to shape the family’s expectations about that diagnosis and how it should be addressed. When I discuss ADHD with a new family, I want them to understand the symptoms of inattention, hyperactivity, and impulsiveness, and that these symptoms are not the child’s fault, but rather related to the way his brain is connected. At the same time, I also emphasize that these connections are not entirely fixed, that they mature over time, and that they are affected by experiences in life. In particular, I stress that positive experiences and wellness activities can influence the brain in a positive way. While, of course, I discuss the range of medications that can address these issues, I also deal with wellness in the treatment plan.
Exercise
Studies in humans and animals have provided background evidence that exercise increases the release of neurotransmitters such as dopamine and norepinephrine that are important in the pathophysiology of ADHD. Cerillo-Urbina et al. did a meta-analysis in 2015 of randomized controlled trials and found medium to large effect sizes for a variety of physical activity programs with respect to attention, hyperactivity, and impulsivity, although the study quality was generally low.1 Clearly we need additional more rigorous studies, but given the positive direction of outcomes, the lack of side effects, and the many other positive effects of exercise, it does not seem too soon to add exercise as a prescription for our patients with ADHD. I review this evidence with families, ask them about physical activity they like, and ask if they are willing to work toward an hour of exercise a day.
Sleep
Many children with ADHD have problems with sleep even before they start on stimulant medications, which can further affect sleep. Addressing sleep early on can improve ADHD symptoms, as well as help parents change or avoid patterns like having children fall asleep to the sound of a television. Brief sleep hygiene and cognitive-behavioral therapy interventions over three visits were demonstrated in a randomized controlled trial by Hisock et al. to improve ADHD symptoms and behavioral function.2 These psychosocial interventions clearly are the first line in addressing sleep problems in ADHD, and can benefit even sleep problems connected to medication.
Parent training
Treatment plan
1. Have the child exercise 1 hour every day. Have fun!
2. Establish a nightly bedtime routine, with a bath at 7:30 p.m., brushing of teeth, a story, and lights out at 8 with no TV in the room.
3. Check out the CHADD website for Parent to Parent.
4. Start a trial of stimulant medication.
5. Return in 2 weeks to monitor these interventions, adjust goals, and adjust medications.
When to refer
Many parents will be able to put such a plan in motion with your support and that of other parents. If they are struggling, therapists, psychologists, and psychiatrists trained in motivational and behavioral methods can provide more individualized parent training. Also consider whether the parents themselves may have ADHD and could use referral and treatment.
Dr. Hall is assistant professor of psychiatry and pediatrics at the University of Vermont, Burlington. She said she had no relevant financial disclosures.
References
1. Child Care Health Dev. 2015 Nov;41(6):779-88.
2. BMJ. 2015. doi: 10.1136/bmj.h68.
Ending hazing as a rite of manhood on college campuses
Is hazing a necessary rite of passage in Greek life, or a terrible tradition that needs to end once and for all?
There can be no justification for hazing, especially after the recent tragic deaths of fraternity pledges at Florida State University, Texas State University, and Louisiana State University. The horror of hazing has been brought home by the refiling of charges against several Penn State fraternity members in the torturous death last February of Timothy Piazza, which was recorded on videotape. In response to recent deaths and injuries, some colleges have suspended Greek life activities on campus. Unfortunately, hazing deaths are not new to college campuses but have a been a problem for several years, with 40 deaths in the last decade. The majority of these deaths involved the forced consumption of large amounts of alcohol, but some have involved beatings and other forms of abuse.
What exactly is hazing? According to the organization StopHazing (stophazing.org), it is “any activity expected of someone joining or participating in a group that humiliates, degrades, abuses, or endangers them regardless of a person’s willingness to participate.” Activities may involve alcohol consumption, humiliation, sleep deprivation, physical abuse, and sexual abuse. Hazing is not just a problem of fraternities; half of college students joining clubs, teams, and other organizations experience hazing. In fact, half of young adults have been hazed by the time they graduate from high school.
Given its inherent dangers, we have to wonder, why does hazing continue? The National Public Radio show 1A offered one answer to this troubling question on its Nov. 15 show, “How to Stop Hazing.” Two panel members, a filmmaker and a professor, discussed their own hazing experiences in college fraternities that included being forced to drink too much alcohol, eating noxious products, and being subjected to violence. One of the panel members talked about hazing other people. Both men admitted that the hazing process made them feel closer to their fraternity brothers: They formed lifelong bonds and also became stronger in facing adversity. In many ways, hazing was a masculine rite of passage. Neither panel member condoned the behaviors they were subjected to or participated in, and in fact suggested that college men should find new ways to bond and have a sense of belonging.
Even though the panelists were not promoting hazing, I was struck by their almost fond recollection of these experiences. I, in contrast, have no fond memory of an incident that I would consider medical hazing. During my internship when working on an internal medicine unit, I was ordered back to work after 2 days at home with the flu, although I was still febrile and coughing up a storm. That week, I was punished with an extra night of on-call duty. This incident did not leave me embracing the camaraderie and hardiness of my medical colleagues. It left me more determined than ever to treat peers and trainees with care and compassion, and never to abuse my power.
In our own practices as psychiatrists, we can play a role in helping our young adult male patients avoid hazing experiences, which have the potential to lead to depression, anxiety, posttraumatic stress disorder, and suicidal behaviors. We can work with our male patients to develop a sense of belonging and an understanding of who they are as men, without putting their lives or others’ lives at risk. In my work as a college counseling center psychiatrist for over 2 decades, I have often addressed the issues of masculinity, friendship, and peer pressure with my male patients. For those of you who work with young adult men, particularly in the college population, here are some tips:
1. Talk with your male patients about healthy versus harmful relationships. No relationship should involve the intentional infliction of physical or emotional pain. Men will acknowledge that a man hitting a girlfriend is abusive. They need to understand that male fraternity brothers hitting each other or forcing someone to drink a large volume of alcohol is equally abusive. Encourage your patients to know their limits and set boundaries if they are asked to do something dangerous to themselves or others.
2. Role play with your patients how to say no to their peers. I did that with a patient who was drinking too much in general with his fraternity brothers. He was afraid they would reject him if he drank less. He was pleasantly surprised when they did not pressure him to drink more, but instead encouraged him to do what is healthy for him.
3. Encourage your patients to have strong social connections on campus. Well-run fraternities can provide these friendship without inflicting pain. Intramural sports, singing groups, bands, and volunteer organizations all provide great ways to connect and also have a sense of accomplishment. Social connections improve grades, physical health, and emotional health.
4. Encourage your male patients to accept who they are, without embracing one stereotype of what it means to be a man. Social media often promotes unattainable physical images, and some male patients will take supplements or even steroids to build up muscle mass. Promote a healthy lifestyle without extremes in exercise and diet. Explore with your patient what it means to be a man in the 21st century, at a time when typical gender roles are being challenged.
5. Listen for cues about your patients’ relationship with their fathers, which have a large impact on how they view masculinity. Many of the male patients I see discuss how they are trying to be more in touch with and expressive about their feelings, after watching their fathers hold in their emotions or use alcohol to numb emotional pain. Some patients have been able to model and encourage a greater openness with their fathers, while others have been met with silence. As a patient is creating his own life story, his father’s history is always in the background.
Should all fraternities be shut down to end the hazing problem? I don’t believe this is the answer. Each campus has a different fraternity culture, and fraternities on many campuses can be a positive force. I have heard young men describe how fraternities encouraged them academically, discouraged excessive drinking, and promoted ethical behavior. But given that abuses have been prevalent on certain campuses, it is incumbent upon universities to enforce safe behaviors. Fraternity brothers who hurt others should be prosecuted, not protected.
The hazing on campuses needs to stop, and we as psychiatrists should talk about this important issue with our patients and sometimes their parents. We can educate our patients about this insidious form of physical and emotional abuse; we can encourage them not to be bystanders when this happens; and we can promote a culture of respect on our campuses.
Hazing is not just a campus but a national cultural problem, as we are finding from the avalanche of news reports about sexual harassment and assault in the political and entertainment worlds. Victims are exposed to abuses and then deterred from reporting them as a condition of staying in and advancing in the professions they love. Hazing is an abuse of power that we as psychiatrists must continue to fight. We should teach our young adult men the mantra that is now being used by some fraternities, “Real men don’t haze.”
Dr. Morris is an associate professor of psychiatry and associate program director for student health psychiatry at the University of Florida, Gainesville. She is the author of The Campus Cure: A Parent’s Guide to Mental Health and Wellness for College Students, which will be published by Rowman & Littlefield of Lanham, Md., in January 2018.
Is hazing a necessary rite of passage in Greek life, or a terrible tradition that needs to end once and for all?
There can be no justification for hazing, especially after the recent tragic deaths of fraternity pledges at Florida State University, Texas State University, and Louisiana State University. The horror of hazing has been brought home by the refiling of charges against several Penn State fraternity members in the torturous death last February of Timothy Piazza, which was recorded on videotape. In response to recent deaths and injuries, some colleges have suspended Greek life activities on campus. Unfortunately, hazing deaths are not new to college campuses but have a been a problem for several years, with 40 deaths in the last decade. The majority of these deaths involved the forced consumption of large amounts of alcohol, but some have involved beatings and other forms of abuse.
What exactly is hazing? According to the organization StopHazing (stophazing.org), it is “any activity expected of someone joining or participating in a group that humiliates, degrades, abuses, or endangers them regardless of a person’s willingness to participate.” Activities may involve alcohol consumption, humiliation, sleep deprivation, physical abuse, and sexual abuse. Hazing is not just a problem of fraternities; half of college students joining clubs, teams, and other organizations experience hazing. In fact, half of young adults have been hazed by the time they graduate from high school.
Given its inherent dangers, we have to wonder, why does hazing continue? The National Public Radio show 1A offered one answer to this troubling question on its Nov. 15 show, “How to Stop Hazing.” Two panel members, a filmmaker and a professor, discussed their own hazing experiences in college fraternities that included being forced to drink too much alcohol, eating noxious products, and being subjected to violence. One of the panel members talked about hazing other people. Both men admitted that the hazing process made them feel closer to their fraternity brothers: They formed lifelong bonds and also became stronger in facing adversity. In many ways, hazing was a masculine rite of passage. Neither panel member condoned the behaviors they were subjected to or participated in, and in fact suggested that college men should find new ways to bond and have a sense of belonging.
Even though the panelists were not promoting hazing, I was struck by their almost fond recollection of these experiences. I, in contrast, have no fond memory of an incident that I would consider medical hazing. During my internship when working on an internal medicine unit, I was ordered back to work after 2 days at home with the flu, although I was still febrile and coughing up a storm. That week, I was punished with an extra night of on-call duty. This incident did not leave me embracing the camaraderie and hardiness of my medical colleagues. It left me more determined than ever to treat peers and trainees with care and compassion, and never to abuse my power.
In our own practices as psychiatrists, we can play a role in helping our young adult male patients avoid hazing experiences, which have the potential to lead to depression, anxiety, posttraumatic stress disorder, and suicidal behaviors. We can work with our male patients to develop a sense of belonging and an understanding of who they are as men, without putting their lives or others’ lives at risk. In my work as a college counseling center psychiatrist for over 2 decades, I have often addressed the issues of masculinity, friendship, and peer pressure with my male patients. For those of you who work with young adult men, particularly in the college population, here are some tips:
1. Talk with your male patients about healthy versus harmful relationships. No relationship should involve the intentional infliction of physical or emotional pain. Men will acknowledge that a man hitting a girlfriend is abusive. They need to understand that male fraternity brothers hitting each other or forcing someone to drink a large volume of alcohol is equally abusive. Encourage your patients to know their limits and set boundaries if they are asked to do something dangerous to themselves or others.
2. Role play with your patients how to say no to their peers. I did that with a patient who was drinking too much in general with his fraternity brothers. He was afraid they would reject him if he drank less. He was pleasantly surprised when they did not pressure him to drink more, but instead encouraged him to do what is healthy for him.
3. Encourage your patients to have strong social connections on campus. Well-run fraternities can provide these friendship without inflicting pain. Intramural sports, singing groups, bands, and volunteer organizations all provide great ways to connect and also have a sense of accomplishment. Social connections improve grades, physical health, and emotional health.
4. Encourage your male patients to accept who they are, without embracing one stereotype of what it means to be a man. Social media often promotes unattainable physical images, and some male patients will take supplements or even steroids to build up muscle mass. Promote a healthy lifestyle without extremes in exercise and diet. Explore with your patient what it means to be a man in the 21st century, at a time when typical gender roles are being challenged.
5. Listen for cues about your patients’ relationship with their fathers, which have a large impact on how they view masculinity. Many of the male patients I see discuss how they are trying to be more in touch with and expressive about their feelings, after watching their fathers hold in their emotions or use alcohol to numb emotional pain. Some patients have been able to model and encourage a greater openness with their fathers, while others have been met with silence. As a patient is creating his own life story, his father’s history is always in the background.
Should all fraternities be shut down to end the hazing problem? I don’t believe this is the answer. Each campus has a different fraternity culture, and fraternities on many campuses can be a positive force. I have heard young men describe how fraternities encouraged them academically, discouraged excessive drinking, and promoted ethical behavior. But given that abuses have been prevalent on certain campuses, it is incumbent upon universities to enforce safe behaviors. Fraternity brothers who hurt others should be prosecuted, not protected.
The hazing on campuses needs to stop, and we as psychiatrists should talk about this important issue with our patients and sometimes their parents. We can educate our patients about this insidious form of physical and emotional abuse; we can encourage them not to be bystanders when this happens; and we can promote a culture of respect on our campuses.
Hazing is not just a campus but a national cultural problem, as we are finding from the avalanche of news reports about sexual harassment and assault in the political and entertainment worlds. Victims are exposed to abuses and then deterred from reporting them as a condition of staying in and advancing in the professions they love. Hazing is an abuse of power that we as psychiatrists must continue to fight. We should teach our young adult men the mantra that is now being used by some fraternities, “Real men don’t haze.”
Dr. Morris is an associate professor of psychiatry and associate program director for student health psychiatry at the University of Florida, Gainesville. She is the author of The Campus Cure: A Parent’s Guide to Mental Health and Wellness for College Students, which will be published by Rowman & Littlefield of Lanham, Md., in January 2018.
Is hazing a necessary rite of passage in Greek life, or a terrible tradition that needs to end once and for all?
There can be no justification for hazing, especially after the recent tragic deaths of fraternity pledges at Florida State University, Texas State University, and Louisiana State University. The horror of hazing has been brought home by the refiling of charges against several Penn State fraternity members in the torturous death last February of Timothy Piazza, which was recorded on videotape. In response to recent deaths and injuries, some colleges have suspended Greek life activities on campus. Unfortunately, hazing deaths are not new to college campuses but have a been a problem for several years, with 40 deaths in the last decade. The majority of these deaths involved the forced consumption of large amounts of alcohol, but some have involved beatings and other forms of abuse.
What exactly is hazing? According to the organization StopHazing (stophazing.org), it is “any activity expected of someone joining or participating in a group that humiliates, degrades, abuses, or endangers them regardless of a person’s willingness to participate.” Activities may involve alcohol consumption, humiliation, sleep deprivation, physical abuse, and sexual abuse. Hazing is not just a problem of fraternities; half of college students joining clubs, teams, and other organizations experience hazing. In fact, half of young adults have been hazed by the time they graduate from high school.
Given its inherent dangers, we have to wonder, why does hazing continue? The National Public Radio show 1A offered one answer to this troubling question on its Nov. 15 show, “How to Stop Hazing.” Two panel members, a filmmaker and a professor, discussed their own hazing experiences in college fraternities that included being forced to drink too much alcohol, eating noxious products, and being subjected to violence. One of the panel members talked about hazing other people. Both men admitted that the hazing process made them feel closer to their fraternity brothers: They formed lifelong bonds and also became stronger in facing adversity. In many ways, hazing was a masculine rite of passage. Neither panel member condoned the behaviors they were subjected to or participated in, and in fact suggested that college men should find new ways to bond and have a sense of belonging.
Even though the panelists were not promoting hazing, I was struck by their almost fond recollection of these experiences. I, in contrast, have no fond memory of an incident that I would consider medical hazing. During my internship when working on an internal medicine unit, I was ordered back to work after 2 days at home with the flu, although I was still febrile and coughing up a storm. That week, I was punished with an extra night of on-call duty. This incident did not leave me embracing the camaraderie and hardiness of my medical colleagues. It left me more determined than ever to treat peers and trainees with care and compassion, and never to abuse my power.
In our own practices as psychiatrists, we can play a role in helping our young adult male patients avoid hazing experiences, which have the potential to lead to depression, anxiety, posttraumatic stress disorder, and suicidal behaviors. We can work with our male patients to develop a sense of belonging and an understanding of who they are as men, without putting their lives or others’ lives at risk. In my work as a college counseling center psychiatrist for over 2 decades, I have often addressed the issues of masculinity, friendship, and peer pressure with my male patients. For those of you who work with young adult men, particularly in the college population, here are some tips:
1. Talk with your male patients about healthy versus harmful relationships. No relationship should involve the intentional infliction of physical or emotional pain. Men will acknowledge that a man hitting a girlfriend is abusive. They need to understand that male fraternity brothers hitting each other or forcing someone to drink a large volume of alcohol is equally abusive. Encourage your patients to know their limits and set boundaries if they are asked to do something dangerous to themselves or others.
2. Role play with your patients how to say no to their peers. I did that with a patient who was drinking too much in general with his fraternity brothers. He was afraid they would reject him if he drank less. He was pleasantly surprised when they did not pressure him to drink more, but instead encouraged him to do what is healthy for him.
3. Encourage your patients to have strong social connections on campus. Well-run fraternities can provide these friendship without inflicting pain. Intramural sports, singing groups, bands, and volunteer organizations all provide great ways to connect and also have a sense of accomplishment. Social connections improve grades, physical health, and emotional health.
4. Encourage your male patients to accept who they are, without embracing one stereotype of what it means to be a man. Social media often promotes unattainable physical images, and some male patients will take supplements or even steroids to build up muscle mass. Promote a healthy lifestyle without extremes in exercise and diet. Explore with your patient what it means to be a man in the 21st century, at a time when typical gender roles are being challenged.
5. Listen for cues about your patients’ relationship with their fathers, which have a large impact on how they view masculinity. Many of the male patients I see discuss how they are trying to be more in touch with and expressive about their feelings, after watching their fathers hold in their emotions or use alcohol to numb emotional pain. Some patients have been able to model and encourage a greater openness with their fathers, while others have been met with silence. As a patient is creating his own life story, his father’s history is always in the background.
Should all fraternities be shut down to end the hazing problem? I don’t believe this is the answer. Each campus has a different fraternity culture, and fraternities on many campuses can be a positive force. I have heard young men describe how fraternities encouraged them academically, discouraged excessive drinking, and promoted ethical behavior. But given that abuses have been prevalent on certain campuses, it is incumbent upon universities to enforce safe behaviors. Fraternity brothers who hurt others should be prosecuted, not protected.
The hazing on campuses needs to stop, and we as psychiatrists should talk about this important issue with our patients and sometimes their parents. We can educate our patients about this insidious form of physical and emotional abuse; we can encourage them not to be bystanders when this happens; and we can promote a culture of respect on our campuses.
Hazing is not just a campus but a national cultural problem, as we are finding from the avalanche of news reports about sexual harassment and assault in the political and entertainment worlds. Victims are exposed to abuses and then deterred from reporting them as a condition of staying in and advancing in the professions they love. Hazing is an abuse of power that we as psychiatrists must continue to fight. We should teach our young adult men the mantra that is now being used by some fraternities, “Real men don’t haze.”
Dr. Morris is an associate professor of psychiatry and associate program director for student health psychiatry at the University of Florida, Gainesville. She is the author of The Campus Cure: A Parent’s Guide to Mental Health and Wellness for College Students, which will be published by Rowman & Littlefield of Lanham, Md., in January 2018.
A program to increase flu vaccine compliance
. It won’t hurt your bottom line either and actually will help it. A flu shot program potentially can be run by a licensed practical nurse, registered nurse, physician’s assistant, or pediatric nurse practitioner, depending on your state’s law regarding vaccine administration by other than a physician, thus freeing up the physician to see well-child and sick-call patients.
It’s easy to set up a flu shot program and run it. Start preparing in June, preceding the upcoming flu season. Designate several Saturdays and or Sundays in September, October, November, December, and January as flu shot Saturdays and/or Sundays. And if Columbus day falls on a weekday, consider adding Columbus Day to your program dates as the kids often are off from school that day (check the local school calendar).
Next, prepare a postcard to be mailed to all patients on the lists your EMR produced for you. Keep the postcard simple. Announce the program, and state the dates the flu shot program is running. Ask parents to call to make an appointment for a flu vaccine only by appointment “with the program.” In addition to mailing a postcard, announce the flu shot program by sending out automated telephone calls and emails to all three lists the EMR has produced for you. The postcard mailing is your first contact, essentially announcing the program with dates and times. An automated phone call may be used to announce a specific date for which you are “now booking.” A good option when using automated phone calls is to allow the caller to press “zero” to be connected to the office to schedule a “flu shot only” appointment! Finally, emails announcing the dates of the program simply will reinforce information about the program.
Mr. Berman has been providing practice management services to physicians and other medical providers since 1983. He is the CEO of a pediatrics practice with locations in Staten Island and Brooklyn, N.Y. He holds a faculty appointment at State University of New York, Brooklyn, as a lecturer for the department of family medicine’s residency training program. He has no disclosures to report. Email him at [email protected].
. It won’t hurt your bottom line either and actually will help it. A flu shot program potentially can be run by a licensed practical nurse, registered nurse, physician’s assistant, or pediatric nurse practitioner, depending on your state’s law regarding vaccine administration by other than a physician, thus freeing up the physician to see well-child and sick-call patients.
It’s easy to set up a flu shot program and run it. Start preparing in June, preceding the upcoming flu season. Designate several Saturdays and or Sundays in September, October, November, December, and January as flu shot Saturdays and/or Sundays. And if Columbus day falls on a weekday, consider adding Columbus Day to your program dates as the kids often are off from school that day (check the local school calendar).
Next, prepare a postcard to be mailed to all patients on the lists your EMR produced for you. Keep the postcard simple. Announce the program, and state the dates the flu shot program is running. Ask parents to call to make an appointment for a flu vaccine only by appointment “with the program.” In addition to mailing a postcard, announce the flu shot program by sending out automated telephone calls and emails to all three lists the EMR has produced for you. The postcard mailing is your first contact, essentially announcing the program with dates and times. An automated phone call may be used to announce a specific date for which you are “now booking.” A good option when using automated phone calls is to allow the caller to press “zero” to be connected to the office to schedule a “flu shot only” appointment! Finally, emails announcing the dates of the program simply will reinforce information about the program.
Mr. Berman has been providing practice management services to physicians and other medical providers since 1983. He is the CEO of a pediatrics practice with locations in Staten Island and Brooklyn, N.Y. He holds a faculty appointment at State University of New York, Brooklyn, as a lecturer for the department of family medicine’s residency training program. He has no disclosures to report. Email him at [email protected].
. It won’t hurt your bottom line either and actually will help it. A flu shot program potentially can be run by a licensed practical nurse, registered nurse, physician’s assistant, or pediatric nurse practitioner, depending on your state’s law regarding vaccine administration by other than a physician, thus freeing up the physician to see well-child and sick-call patients.
It’s easy to set up a flu shot program and run it. Start preparing in June, preceding the upcoming flu season. Designate several Saturdays and or Sundays in September, October, November, December, and January as flu shot Saturdays and/or Sundays. And if Columbus day falls on a weekday, consider adding Columbus Day to your program dates as the kids often are off from school that day (check the local school calendar).
Next, prepare a postcard to be mailed to all patients on the lists your EMR produced for you. Keep the postcard simple. Announce the program, and state the dates the flu shot program is running. Ask parents to call to make an appointment for a flu vaccine only by appointment “with the program.” In addition to mailing a postcard, announce the flu shot program by sending out automated telephone calls and emails to all three lists the EMR has produced for you. The postcard mailing is your first contact, essentially announcing the program with dates and times. An automated phone call may be used to announce a specific date for which you are “now booking.” A good option when using automated phone calls is to allow the caller to press “zero” to be connected to the office to schedule a “flu shot only” appointment! Finally, emails announcing the dates of the program simply will reinforce information about the program.
Mr. Berman has been providing practice management services to physicians and other medical providers since 1983. He is the CEO of a pediatrics practice with locations in Staten Island and Brooklyn, N.Y. He holds a faculty appointment at State University of New York, Brooklyn, as a lecturer for the department of family medicine’s residency training program. He has no disclosures to report. Email him at [email protected].
Systems biology – A primer
Systems biology is relatively new. It is an interdisciplinary field that focuses on complex interactions within biological systems using a holistic approach in the pursuit of scientific discovery.
The systems biology approach seeks to integrate biological knowledge to understand how cells and molecules interact with one another. A key component is computational and mathematical modeling. The ever-increasing amount of biological data, and the judgment that this data cannot be understood by simply drawing lines between interacting cells and molecules, explains the demand for a systematic approach.
Prominent examples for biological systems are the immune system and the nervous system, which already have the word ”system” included. Although the idea of system-level understanding is not new, the growing interest in applying the systems approach has been driven by breakthrough advances in molecular biology and bioinformatics.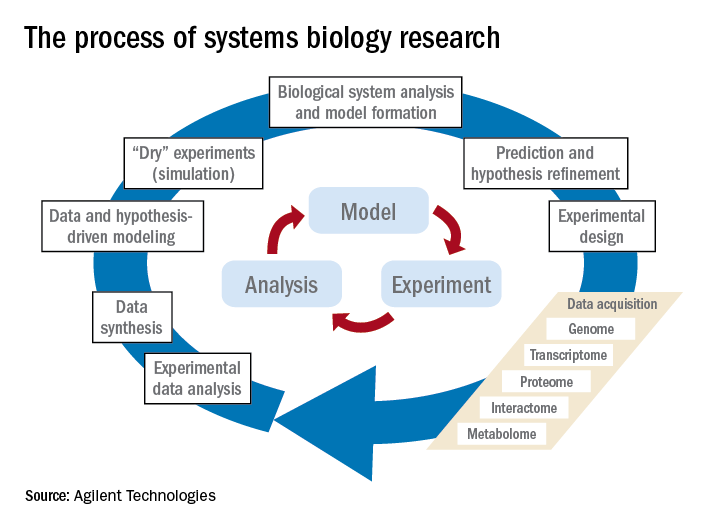
Over the past 10 years, our group has identified highly significant differences in immune functioning between the 10% of children who frequently develop acute otitis media (i.e., those who are “otitis prone”) and the children who develop AOM infrequently (60% of children) or not at all (30% of children). We also have identified a cohort of about 10% of children who fail to respond to infant vaccinations (low vaccine responders), compared with children who respond with protective immunity and establishment of immune memory. The differences in children who are prone to AOM vs. those who are not and in low vaccine responders vs. normal vaccine responders include differences in cytokine molecules in blood (providing biosignatures), reduced antibodies, immune memory, and aberrant intercellular signaling networks after otopathogen exposure (AOM prone vs. non–AOM prone) and routine pediatric vaccination (low vs. normal vaccine responders).
Dr. Pichichero, a specialist in pediatric infectious diseases, is director of the Research Institute at Rochester (N.Y.) General Hospital. He is also a pediatrician at Legacy Pediatrics in Rochester. He has no relevant financial disclosures. Email him at [email protected].
Systems biology is relatively new. It is an interdisciplinary field that focuses on complex interactions within biological systems using a holistic approach in the pursuit of scientific discovery.
The systems biology approach seeks to integrate biological knowledge to understand how cells and molecules interact with one another. A key component is computational and mathematical modeling. The ever-increasing amount of biological data, and the judgment that this data cannot be understood by simply drawing lines between interacting cells and molecules, explains the demand for a systematic approach.
Prominent examples for biological systems are the immune system and the nervous system, which already have the word ”system” included. Although the idea of system-level understanding is not new, the growing interest in applying the systems approach has been driven by breakthrough advances in molecular biology and bioinformatics.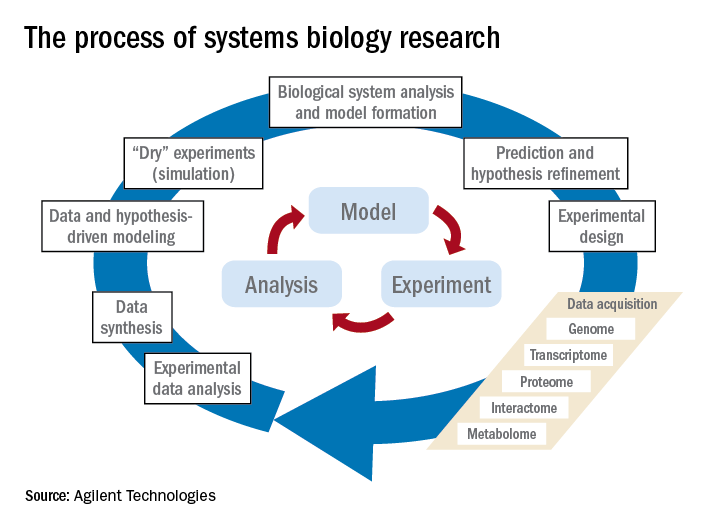
Over the past 10 years, our group has identified highly significant differences in immune functioning between the 10% of children who frequently develop acute otitis media (i.e., those who are “otitis prone”) and the children who develop AOM infrequently (60% of children) or not at all (30% of children). We also have identified a cohort of about 10% of children who fail to respond to infant vaccinations (low vaccine responders), compared with children who respond with protective immunity and establishment of immune memory. The differences in children who are prone to AOM vs. those who are not and in low vaccine responders vs. normal vaccine responders include differences in cytokine molecules in blood (providing biosignatures), reduced antibodies, immune memory, and aberrant intercellular signaling networks after otopathogen exposure (AOM prone vs. non–AOM prone) and routine pediatric vaccination (low vs. normal vaccine responders).
Dr. Pichichero, a specialist in pediatric infectious diseases, is director of the Research Institute at Rochester (N.Y.) General Hospital. He is also a pediatrician at Legacy Pediatrics in Rochester. He has no relevant financial disclosures. Email him at [email protected].
Systems biology is relatively new. It is an interdisciplinary field that focuses on complex interactions within biological systems using a holistic approach in the pursuit of scientific discovery.
The systems biology approach seeks to integrate biological knowledge to understand how cells and molecules interact with one another. A key component is computational and mathematical modeling. The ever-increasing amount of biological data, and the judgment that this data cannot be understood by simply drawing lines between interacting cells and molecules, explains the demand for a systematic approach.
Prominent examples for biological systems are the immune system and the nervous system, which already have the word ”system” included. Although the idea of system-level understanding is not new, the growing interest in applying the systems approach has been driven by breakthrough advances in molecular biology and bioinformatics.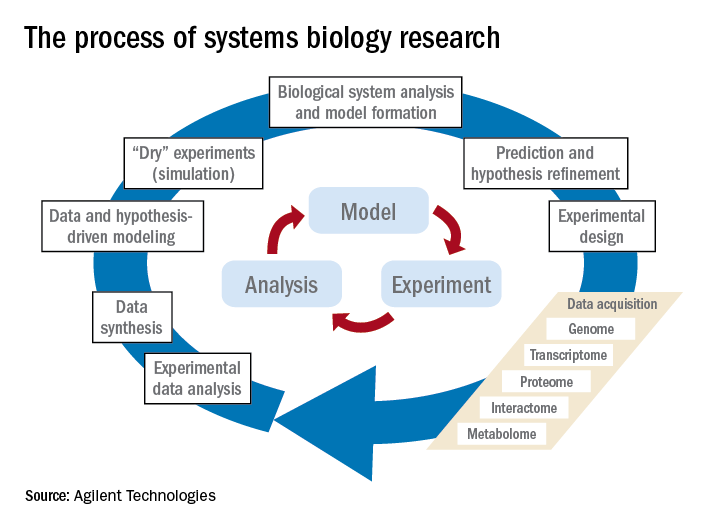
Over the past 10 years, our group has identified highly significant differences in immune functioning between the 10% of children who frequently develop acute otitis media (i.e., those who are “otitis prone”) and the children who develop AOM infrequently (60% of children) or not at all (30% of children). We also have identified a cohort of about 10% of children who fail to respond to infant vaccinations (low vaccine responders), compared with children who respond with protective immunity and establishment of immune memory. The differences in children who are prone to AOM vs. those who are not and in low vaccine responders vs. normal vaccine responders include differences in cytokine molecules in blood (providing biosignatures), reduced antibodies, immune memory, and aberrant intercellular signaling networks after otopathogen exposure (AOM prone vs. non–AOM prone) and routine pediatric vaccination (low vs. normal vaccine responders).
Dr. Pichichero, a specialist in pediatric infectious diseases, is director of the Research Institute at Rochester (N.Y.) General Hospital. He is also a pediatrician at Legacy Pediatrics in Rochester. He has no relevant financial disclosures. Email him at [email protected].
Health care panhandlers: A symptom of our system’s baked-in pressures?
A few nights a week after work I have to stop by the store for this or that.
In the last 1-2 months there’s always been a couple at the parking lot exit, both in wheelchairs, with a big sign asking for money to help one of them beat cancer. They even have the amount listed.
But, by the same token, they could be quite legitimate. The American health care system is full of cracks that seriously ill people can slip through. One recent survey found that about 30% of Americans had trouble paying their medical bills.
It’s easy to look at people like this and think, “I’ll never let that happen to me.” We assume they must be smokers, or irresponsible spenders, or some other reason that makes us feel we won’t stumble into the same pitfalls. That’s reassuring, and sometimes true, but not always. And probably more often than we want to realize.
The world is full of people and families devastated by bad luck. Through no fault of their own, they develop a terrible medical condition or suffer grievous injuries, and suddenly, decent, hard-working, previously healthy people are facing foreclosure and financial ruin. It could, quite literally, be any of us.
Case in point: My family has good insurance and has averaged $10,000 in out-of-pocket medical expenses per year for the last several years. That’s for routine stuff: meeting deductibles, copays on medications, tests, and doctor visits, a few ER trips, etc. The only real “surprise” in there was when my wife broke her leg and needed surgery.
If the panhandlers really did have legitimate medical issues, I might be willing to help out. I give to charity. My grandmother and parents stressed that value to me, and I try to teach it to my kids. But, sadly, we live in a world full of con artists who try to make money by taking advantage of caring peoples’ feelings. Look at all the scams that immediately cropped up following the recent hurricane and wildfire disasters. Without knowing the truth, I’d rather give to an organization like the Salvation Army or Red Cross, hoping they have more experience than I do in sorting out who’s really in need.
As a doctor, I also try to justify it by thinking about how much care I do for “free.” This includes uninsured hospital patients we all see on call, knowing we’ll end up writing their bill off as a loss, and bounced checks for copays and deductible portions that we know we’ll never see.
But, no matter how I try to rationalize it, it still bothers me when I see them sitting there as I leave the store. I don’t know if they’re legitimate. But if they are, they aren’t alone, and there’s something seriously wrong with our health care system.
[polldaddy:9876776]
Dr. Block has a solo neurology practice in Scottsdale, Ariz.
A few nights a week after work I have to stop by the store for this or that.
In the last 1-2 months there’s always been a couple at the parking lot exit, both in wheelchairs, with a big sign asking for money to help one of them beat cancer. They even have the amount listed.
But, by the same token, they could be quite legitimate. The American health care system is full of cracks that seriously ill people can slip through. One recent survey found that about 30% of Americans had trouble paying their medical bills.
It’s easy to look at people like this and think, “I’ll never let that happen to me.” We assume they must be smokers, or irresponsible spenders, or some other reason that makes us feel we won’t stumble into the same pitfalls. That’s reassuring, and sometimes true, but not always. And probably more often than we want to realize.
The world is full of people and families devastated by bad luck. Through no fault of their own, they develop a terrible medical condition or suffer grievous injuries, and suddenly, decent, hard-working, previously healthy people are facing foreclosure and financial ruin. It could, quite literally, be any of us.
Case in point: My family has good insurance and has averaged $10,000 in out-of-pocket medical expenses per year for the last several years. That’s for routine stuff: meeting deductibles, copays on medications, tests, and doctor visits, a few ER trips, etc. The only real “surprise” in there was when my wife broke her leg and needed surgery.
If the panhandlers really did have legitimate medical issues, I might be willing to help out. I give to charity. My grandmother and parents stressed that value to me, and I try to teach it to my kids. But, sadly, we live in a world full of con artists who try to make money by taking advantage of caring peoples’ feelings. Look at all the scams that immediately cropped up following the recent hurricane and wildfire disasters. Without knowing the truth, I’d rather give to an organization like the Salvation Army or Red Cross, hoping they have more experience than I do in sorting out who’s really in need.
As a doctor, I also try to justify it by thinking about how much care I do for “free.” This includes uninsured hospital patients we all see on call, knowing we’ll end up writing their bill off as a loss, and bounced checks for copays and deductible portions that we know we’ll never see.
But, no matter how I try to rationalize it, it still bothers me when I see them sitting there as I leave the store. I don’t know if they’re legitimate. But if they are, they aren’t alone, and there’s something seriously wrong with our health care system.
[polldaddy:9876776]
Dr. Block has a solo neurology practice in Scottsdale, Ariz.
A few nights a week after work I have to stop by the store for this or that.
In the last 1-2 months there’s always been a couple at the parking lot exit, both in wheelchairs, with a big sign asking for money to help one of them beat cancer. They even have the amount listed.
But, by the same token, they could be quite legitimate. The American health care system is full of cracks that seriously ill people can slip through. One recent survey found that about 30% of Americans had trouble paying their medical bills.
It’s easy to look at people like this and think, “I’ll never let that happen to me.” We assume they must be smokers, or irresponsible spenders, or some other reason that makes us feel we won’t stumble into the same pitfalls. That’s reassuring, and sometimes true, but not always. And probably more often than we want to realize.
The world is full of people and families devastated by bad luck. Through no fault of their own, they develop a terrible medical condition or suffer grievous injuries, and suddenly, decent, hard-working, previously healthy people are facing foreclosure and financial ruin. It could, quite literally, be any of us.
Case in point: My family has good insurance and has averaged $10,000 in out-of-pocket medical expenses per year for the last several years. That’s for routine stuff: meeting deductibles, copays on medications, tests, and doctor visits, a few ER trips, etc. The only real “surprise” in there was when my wife broke her leg and needed surgery.
If the panhandlers really did have legitimate medical issues, I might be willing to help out. I give to charity. My grandmother and parents stressed that value to me, and I try to teach it to my kids. But, sadly, we live in a world full of con artists who try to make money by taking advantage of caring peoples’ feelings. Look at all the scams that immediately cropped up following the recent hurricane and wildfire disasters. Without knowing the truth, I’d rather give to an organization like the Salvation Army or Red Cross, hoping they have more experience than I do in sorting out who’s really in need.
As a doctor, I also try to justify it by thinking about how much care I do for “free.” This includes uninsured hospital patients we all see on call, knowing we’ll end up writing their bill off as a loss, and bounced checks for copays and deductible portions that we know we’ll never see.
But, no matter how I try to rationalize it, it still bothers me when I see them sitting there as I leave the store. I don’t know if they’re legitimate. But if they are, they aren’t alone, and there’s something seriously wrong with our health care system.
[polldaddy:9876776]
Dr. Block has a solo neurology practice in Scottsdale, Ariz.
























