User login
Domo Arigato, Mr. Roboto
A few months ago, I purchased an Amazon Echo system. The device is built on Amazon’s cloud-based voice service, Alexa, which can hear, understand, and respond to any question or command. The speaker is always listening and is activated when the user (eg, me!) says the name Alexa. For instance, I can say “Alexa, what is the weather today?” and it will provide the forecast. In fact, each morning I request my daily news briefing, and Alexa quickly tunes to NPR Radio. By linking to my Google calendar, it also tells me my agenda for the day. It researches and provides information that might otherwise take me a while to locate.
Now, I confess: I’ve had to train myself to refer to Alexa as “it” instead of “her.” Human beings have a rich history of wanting to “humanize” computers, as the science fiction film genre can attest. Go back nearly 50 years to Colossus: The Forbin Project (1970) and you have a story of two super-computers—one built by the United States, the other by Russia—that join forces and take over the world, making humans their slaves. The award-winning Bicentennial Man (1999) follows the life and times of Andrew, an NDR-114 robot originally purchased as a household appliance to perform menial tasks; when it begins to experience emotions and creative thought, the owners discover Andrew is no ordinary robot. And who can forget Hal, the computer in 2001: A Space Odyssey (1968) that takes over a space mission until a clever astronaut manages to disengage it (I almost said him), or Data, a very likable android in the successful franchise Star Trek: The Next Generation.
Let’s face it: We are both obsessed with, and leery of, new technology—particularly artificial intelligence (AI). Some detractors have denounced Alexa’s capabilities as “just a glorified smartphone.” Others have expressed grave concerns about the security of personal information and conversations, as Big Brother may be listening. (In that case, it’s not the machines that are evil; it’s those who use them!)
But—cue a John Williams score—what if we harnessed the power of AI for good and not evil? I’ll be serious now: At the recent Leadership in Healthcare Summer Institute (which I was honored to teach at), a group of doctoral students gave a presentation on the potential of AI in the identification and care of anxiety and depression. They identified a need—every 16.2 minutes, a person dies by suicide in the US—and proposed a solution. Because access to care may be limited (by provider shortages, remote locations, etc), the students suggested a hybrid AI/telehealth platform that offers 24/7 support and provider access to individuals with anxiety and depression, via a secure mobile app.1 It got me thinking: Could this technology be a positive intervention in health care?
Actually, it’s already happening. Mayo Clinic researchers have used AI to identify the genomic information of brain tumors without biopsy. At Stanford University, researchers are training an AI neural network to recognize skin cancer lesions with the accuracy of an expert dermatologist. The same deep-learning technology is being used in the field of pathology for the detection of liver lesions.2
Now, I’m sure some of you are questioning whether a machine can really match or replace a human when it comes to assessing a patient’s condition. There were many who resisted the idea of telehealth when that was the latest, greatest thing, because providers cannot do a full assessment with the required diagnostic testing and imaging from a distance. Some feel that telehealth should be reserved for situations in which, say, a remote provider is reviewing and reporting on test results, or a patient just needs to follow up with his/her provider for a minor issue.
Mental health, however, entails less “laying on of hands” and may be a good candidate for AI-based interventions—at least for follow-up and support services. (I am certainly not discounting the value of real human interaction in any sphere of health care.) We know patients benefit from early mental health intervention programs, but we also know those benefits may not be sustained over time and distance. Logistical issues that any of us may face—time, transportation, availability—are often exacerbated for those with impaired functioning due to a mental illness. If a patient with major depression cannot bring himself to get out of bed to make a cup of coffee, how is he going to travel across town (changing buses two or three times) to keep an appointment with his health care provider?
Here’s where AI might make a difference: What if there were a patient-focused e-platform that could provide cost-effective and accessible services across the continuum of care? Current Internet-based interventions rely on human mediators to deliver therapeutic content, which is then refined into a model that can interpret and respond to critical user data—resulting in tailored online therapy. But if we could integrate the user experience with sophisticated and cutting-edge AI technology, we could deliver content more effectively to redefine these interventions and improve outcomes.
A paper recently featured in Frontiers in Psychology discussed the value of doing just that. D’Alfonso and colleagues reported on an Internet-based social therapy web application that uses a series of interactive modules to help users navigate situations and develop psychosocial skills. In its current form—within a research setting—the system is utilized by small groups of users, making human-supported engagement via moderators possible. But D’Alfonso and colleagues note that the incorporation of automated suggestions within the modules would allow the technology to be rolled out to a larger audience and ensure that “interaction” is available whenever a user needs it—not just when a human moderator is “on the clock.”3
Another article, in the International Journal of Swarm Intelligence and Evolutionary Computation (2016), discussed the development of socially intelligent robotic systems, not unlike Alexa, to address social connectedness. The author proposes an autonomous assistive system (AAS) as a low-cost, standalone interventional device to reduce social isolation. This could easily be deployed in homes for the elderly or even at remote sites. The AAS has been programmed to detect isolation in patients based on data regarding skeletal movements, facial expressions, and speech patterns. In the not-so-distant future, this high-density data will be sent over the cloud to allow clinicians to monitor in real-time and intervene remotely, as appropriate (eg, by initiating a home visit).4
Of course, in any form, implementation of AI will not be simple—there are real costs to be considered, and we still have to contend with the fears that all those sci-fi films have instilled. A recent global study revealed significant concerns that would certainly apply to the health care arena. When asked which of the following participants most feared about the use of AI,
- 33% of respondents chose “It will never know me/my preferences as well as a human being”
- 24% chose “The rise of the robot and enslavement of humanity”
- 5% feared “Robots uncovering my deepest secrets.”5
Despite all this, however, respondents also expressed optimism in the power and potential of AI: Nearly 70% said they are in support of further use of AI if it helps make their lives easier.4 Wouldn’t life be easier if AI could be used to significantly reduce errors, increase access to care, and bring a fresh viewpoint to the issue of patient education?
What do you think? Would you trust a robot to be your coworker, identifying tumors and conducting mental health screenings? Is it possible to convince patients to accept help via an impersonal medium (and risk exposure of their personal health information)? Share your fears, support, or concerns about AI with me at [email protected].
1. Halabi AH. How will artificial intelligence change healthcare? June 8, 2017. www.quora.com/How-will-AI-change-healthcare. Accessed July 12, 2017.
2. Hepburn D, Francis D, Hoosier M, et al. smaRT MD2: a patient-focused e-platform for use across the continuum of care for anxiety and depression. A June 2017 presentation to Leadership in Healthcare, Summer Institute, Nova Southeastern University, Tampa, FL.
3. D’Alfonso S, Santesteban-Echarri O, Rice S, et al. Artificial intelligence-assisted online social therapy for youth mental health. Front Psychol. 2017;8(796):1-13.
4. Gulrez T, Neftimeziani S, Mc evoy P, Hodgson A. Loneliness kills: can autonomous systems and robotics assist in providing solutions? Int J Swarm Intel Evol Comput. 2016;5:1.
5. Pegasystems. What consumers really think about AI: a global study. www.pega.com/AI. Accessed July 7, 2017.
A few months ago, I purchased an Amazon Echo system. The device is built on Amazon’s cloud-based voice service, Alexa, which can hear, understand, and respond to any question or command. The speaker is always listening and is activated when the user (eg, me!) says the name Alexa. For instance, I can say “Alexa, what is the weather today?” and it will provide the forecast. In fact, each morning I request my daily news briefing, and Alexa quickly tunes to NPR Radio. By linking to my Google calendar, it also tells me my agenda for the day. It researches and provides information that might otherwise take me a while to locate.
Now, I confess: I’ve had to train myself to refer to Alexa as “it” instead of “her.” Human beings have a rich history of wanting to “humanize” computers, as the science fiction film genre can attest. Go back nearly 50 years to Colossus: The Forbin Project (1970) and you have a story of two super-computers—one built by the United States, the other by Russia—that join forces and take over the world, making humans their slaves. The award-winning Bicentennial Man (1999) follows the life and times of Andrew, an NDR-114 robot originally purchased as a household appliance to perform menial tasks; when it begins to experience emotions and creative thought, the owners discover Andrew is no ordinary robot. And who can forget Hal, the computer in 2001: A Space Odyssey (1968) that takes over a space mission until a clever astronaut manages to disengage it (I almost said him), or Data, a very likable android in the successful franchise Star Trek: The Next Generation.
Let’s face it: We are both obsessed with, and leery of, new technology—particularly artificial intelligence (AI). Some detractors have denounced Alexa’s capabilities as “just a glorified smartphone.” Others have expressed grave concerns about the security of personal information and conversations, as Big Brother may be listening. (In that case, it’s not the machines that are evil; it’s those who use them!)
But—cue a John Williams score—what if we harnessed the power of AI for good and not evil? I’ll be serious now: At the recent Leadership in Healthcare Summer Institute (which I was honored to teach at), a group of doctoral students gave a presentation on the potential of AI in the identification and care of anxiety and depression. They identified a need—every 16.2 minutes, a person dies by suicide in the US—and proposed a solution. Because access to care may be limited (by provider shortages, remote locations, etc), the students suggested a hybrid AI/telehealth platform that offers 24/7 support and provider access to individuals with anxiety and depression, via a secure mobile app.1 It got me thinking: Could this technology be a positive intervention in health care?
Actually, it’s already happening. Mayo Clinic researchers have used AI to identify the genomic information of brain tumors without biopsy. At Stanford University, researchers are training an AI neural network to recognize skin cancer lesions with the accuracy of an expert dermatologist. The same deep-learning technology is being used in the field of pathology for the detection of liver lesions.2
Now, I’m sure some of you are questioning whether a machine can really match or replace a human when it comes to assessing a patient’s condition. There were many who resisted the idea of telehealth when that was the latest, greatest thing, because providers cannot do a full assessment with the required diagnostic testing and imaging from a distance. Some feel that telehealth should be reserved for situations in which, say, a remote provider is reviewing and reporting on test results, or a patient just needs to follow up with his/her provider for a minor issue.
Mental health, however, entails less “laying on of hands” and may be a good candidate for AI-based interventions—at least for follow-up and support services. (I am certainly not discounting the value of real human interaction in any sphere of health care.) We know patients benefit from early mental health intervention programs, but we also know those benefits may not be sustained over time and distance. Logistical issues that any of us may face—time, transportation, availability—are often exacerbated for those with impaired functioning due to a mental illness. If a patient with major depression cannot bring himself to get out of bed to make a cup of coffee, how is he going to travel across town (changing buses two or three times) to keep an appointment with his health care provider?
Here’s where AI might make a difference: What if there were a patient-focused e-platform that could provide cost-effective and accessible services across the continuum of care? Current Internet-based interventions rely on human mediators to deliver therapeutic content, which is then refined into a model that can interpret and respond to critical user data—resulting in tailored online therapy. But if we could integrate the user experience with sophisticated and cutting-edge AI technology, we could deliver content more effectively to redefine these interventions and improve outcomes.
A paper recently featured in Frontiers in Psychology discussed the value of doing just that. D’Alfonso and colleagues reported on an Internet-based social therapy web application that uses a series of interactive modules to help users navigate situations and develop psychosocial skills. In its current form—within a research setting—the system is utilized by small groups of users, making human-supported engagement via moderators possible. But D’Alfonso and colleagues note that the incorporation of automated suggestions within the modules would allow the technology to be rolled out to a larger audience and ensure that “interaction” is available whenever a user needs it—not just when a human moderator is “on the clock.”3
Another article, in the International Journal of Swarm Intelligence and Evolutionary Computation (2016), discussed the development of socially intelligent robotic systems, not unlike Alexa, to address social connectedness. The author proposes an autonomous assistive system (AAS) as a low-cost, standalone interventional device to reduce social isolation. This could easily be deployed in homes for the elderly or even at remote sites. The AAS has been programmed to detect isolation in patients based on data regarding skeletal movements, facial expressions, and speech patterns. In the not-so-distant future, this high-density data will be sent over the cloud to allow clinicians to monitor in real-time and intervene remotely, as appropriate (eg, by initiating a home visit).4
Of course, in any form, implementation of AI will not be simple—there are real costs to be considered, and we still have to contend with the fears that all those sci-fi films have instilled. A recent global study revealed significant concerns that would certainly apply to the health care arena. When asked which of the following participants most feared about the use of AI,
- 33% of respondents chose “It will never know me/my preferences as well as a human being”
- 24% chose “The rise of the robot and enslavement of humanity”
- 5% feared “Robots uncovering my deepest secrets.”5
Despite all this, however, respondents also expressed optimism in the power and potential of AI: Nearly 70% said they are in support of further use of AI if it helps make their lives easier.4 Wouldn’t life be easier if AI could be used to significantly reduce errors, increase access to care, and bring a fresh viewpoint to the issue of patient education?
What do you think? Would you trust a robot to be your coworker, identifying tumors and conducting mental health screenings? Is it possible to convince patients to accept help via an impersonal medium (and risk exposure of their personal health information)? Share your fears, support, or concerns about AI with me at [email protected].
A few months ago, I purchased an Amazon Echo system. The device is built on Amazon’s cloud-based voice service, Alexa, which can hear, understand, and respond to any question or command. The speaker is always listening and is activated when the user (eg, me!) says the name Alexa. For instance, I can say “Alexa, what is the weather today?” and it will provide the forecast. In fact, each morning I request my daily news briefing, and Alexa quickly tunes to NPR Radio. By linking to my Google calendar, it also tells me my agenda for the day. It researches and provides information that might otherwise take me a while to locate.
Now, I confess: I’ve had to train myself to refer to Alexa as “it” instead of “her.” Human beings have a rich history of wanting to “humanize” computers, as the science fiction film genre can attest. Go back nearly 50 years to Colossus: The Forbin Project (1970) and you have a story of two super-computers—one built by the United States, the other by Russia—that join forces and take over the world, making humans their slaves. The award-winning Bicentennial Man (1999) follows the life and times of Andrew, an NDR-114 robot originally purchased as a household appliance to perform menial tasks; when it begins to experience emotions and creative thought, the owners discover Andrew is no ordinary robot. And who can forget Hal, the computer in 2001: A Space Odyssey (1968) that takes over a space mission until a clever astronaut manages to disengage it (I almost said him), or Data, a very likable android in the successful franchise Star Trek: The Next Generation.
Let’s face it: We are both obsessed with, and leery of, new technology—particularly artificial intelligence (AI). Some detractors have denounced Alexa’s capabilities as “just a glorified smartphone.” Others have expressed grave concerns about the security of personal information and conversations, as Big Brother may be listening. (In that case, it’s not the machines that are evil; it’s those who use them!)
But—cue a John Williams score—what if we harnessed the power of AI for good and not evil? I’ll be serious now: At the recent Leadership in Healthcare Summer Institute (which I was honored to teach at), a group of doctoral students gave a presentation on the potential of AI in the identification and care of anxiety and depression. They identified a need—every 16.2 minutes, a person dies by suicide in the US—and proposed a solution. Because access to care may be limited (by provider shortages, remote locations, etc), the students suggested a hybrid AI/telehealth platform that offers 24/7 support and provider access to individuals with anxiety and depression, via a secure mobile app.1 It got me thinking: Could this technology be a positive intervention in health care?
Actually, it’s already happening. Mayo Clinic researchers have used AI to identify the genomic information of brain tumors without biopsy. At Stanford University, researchers are training an AI neural network to recognize skin cancer lesions with the accuracy of an expert dermatologist. The same deep-learning technology is being used in the field of pathology for the detection of liver lesions.2
Now, I’m sure some of you are questioning whether a machine can really match or replace a human when it comes to assessing a patient’s condition. There were many who resisted the idea of telehealth when that was the latest, greatest thing, because providers cannot do a full assessment with the required diagnostic testing and imaging from a distance. Some feel that telehealth should be reserved for situations in which, say, a remote provider is reviewing and reporting on test results, or a patient just needs to follow up with his/her provider for a minor issue.
Mental health, however, entails less “laying on of hands” and may be a good candidate for AI-based interventions—at least for follow-up and support services. (I am certainly not discounting the value of real human interaction in any sphere of health care.) We know patients benefit from early mental health intervention programs, but we also know those benefits may not be sustained over time and distance. Logistical issues that any of us may face—time, transportation, availability—are often exacerbated for those with impaired functioning due to a mental illness. If a patient with major depression cannot bring himself to get out of bed to make a cup of coffee, how is he going to travel across town (changing buses two or three times) to keep an appointment with his health care provider?
Here’s where AI might make a difference: What if there were a patient-focused e-platform that could provide cost-effective and accessible services across the continuum of care? Current Internet-based interventions rely on human mediators to deliver therapeutic content, which is then refined into a model that can interpret and respond to critical user data—resulting in tailored online therapy. But if we could integrate the user experience with sophisticated and cutting-edge AI technology, we could deliver content more effectively to redefine these interventions and improve outcomes.
A paper recently featured in Frontiers in Psychology discussed the value of doing just that. D’Alfonso and colleagues reported on an Internet-based social therapy web application that uses a series of interactive modules to help users navigate situations and develop psychosocial skills. In its current form—within a research setting—the system is utilized by small groups of users, making human-supported engagement via moderators possible. But D’Alfonso and colleagues note that the incorporation of automated suggestions within the modules would allow the technology to be rolled out to a larger audience and ensure that “interaction” is available whenever a user needs it—not just when a human moderator is “on the clock.”3
Another article, in the International Journal of Swarm Intelligence and Evolutionary Computation (2016), discussed the development of socially intelligent robotic systems, not unlike Alexa, to address social connectedness. The author proposes an autonomous assistive system (AAS) as a low-cost, standalone interventional device to reduce social isolation. This could easily be deployed in homes for the elderly or even at remote sites. The AAS has been programmed to detect isolation in patients based on data regarding skeletal movements, facial expressions, and speech patterns. In the not-so-distant future, this high-density data will be sent over the cloud to allow clinicians to monitor in real-time and intervene remotely, as appropriate (eg, by initiating a home visit).4
Of course, in any form, implementation of AI will not be simple—there are real costs to be considered, and we still have to contend with the fears that all those sci-fi films have instilled. A recent global study revealed significant concerns that would certainly apply to the health care arena. When asked which of the following participants most feared about the use of AI,
- 33% of respondents chose “It will never know me/my preferences as well as a human being”
- 24% chose “The rise of the robot and enslavement of humanity”
- 5% feared “Robots uncovering my deepest secrets.”5
Despite all this, however, respondents also expressed optimism in the power and potential of AI: Nearly 70% said they are in support of further use of AI if it helps make their lives easier.4 Wouldn’t life be easier if AI could be used to significantly reduce errors, increase access to care, and bring a fresh viewpoint to the issue of patient education?
What do you think? Would you trust a robot to be your coworker, identifying tumors and conducting mental health screenings? Is it possible to convince patients to accept help via an impersonal medium (and risk exposure of their personal health information)? Share your fears, support, or concerns about AI with me at [email protected].
1. Halabi AH. How will artificial intelligence change healthcare? June 8, 2017. www.quora.com/How-will-AI-change-healthcare. Accessed July 12, 2017.
2. Hepburn D, Francis D, Hoosier M, et al. smaRT MD2: a patient-focused e-platform for use across the continuum of care for anxiety and depression. A June 2017 presentation to Leadership in Healthcare, Summer Institute, Nova Southeastern University, Tampa, FL.
3. D’Alfonso S, Santesteban-Echarri O, Rice S, et al. Artificial intelligence-assisted online social therapy for youth mental health. Front Psychol. 2017;8(796):1-13.
4. Gulrez T, Neftimeziani S, Mc evoy P, Hodgson A. Loneliness kills: can autonomous systems and robotics assist in providing solutions? Int J Swarm Intel Evol Comput. 2016;5:1.
5. Pegasystems. What consumers really think about AI: a global study. www.pega.com/AI. Accessed July 7, 2017.
1. Halabi AH. How will artificial intelligence change healthcare? June 8, 2017. www.quora.com/How-will-AI-change-healthcare. Accessed July 12, 2017.
2. Hepburn D, Francis D, Hoosier M, et al. smaRT MD2: a patient-focused e-platform for use across the continuum of care for anxiety and depression. A June 2017 presentation to Leadership in Healthcare, Summer Institute, Nova Southeastern University, Tampa, FL.
3. D’Alfonso S, Santesteban-Echarri O, Rice S, et al. Artificial intelligence-assisted online social therapy for youth mental health. Front Psychol. 2017;8(796):1-13.
4. Gulrez T, Neftimeziani S, Mc evoy P, Hodgson A. Loneliness kills: can autonomous systems and robotics assist in providing solutions? Int J Swarm Intel Evol Comput. 2016;5:1.
5. Pegasystems. What consumers really think about AI: a global study. www.pega.com/AI. Accessed July 7, 2017.
Adalimumab for Hidradenitis Suppurativa
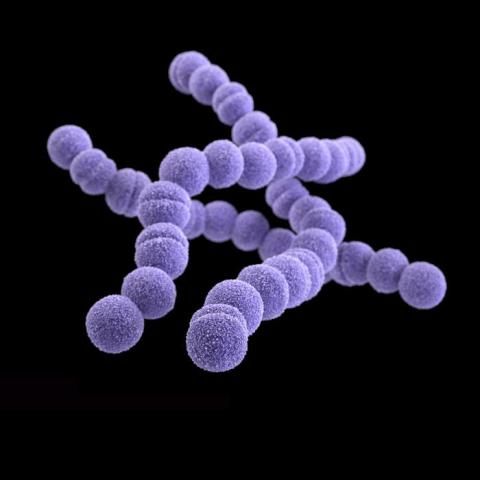
We applaud Kimball et al1 on their report that adalimumab demonstrated clinical improvement in patients with hidradenitis suppurativa (HS) versus placebo in 2 phase 3 trials. Hidradenitis suppurativa is a chronic relapsing condition with painful subcutaneous abscesses, malodorous drainage, sinus tract formation, and scarring that typically occurs in the axillae and anogenital region. It impairs the quality of life for these patients, as evidenced by higher Dermatology Life Quality Index scores compared to psoriasis, pimples, hand rash, atopic eczema, or control.2
The exact pathogenesis of HS is unknown but likely involves a complex interaction of genetic, hormonal, immunologic, and environmental factors.3 The levels of inflammatory cytokines are elevated in HS lesions, specifically IL-1β, tumor necrosis factor α, IL-10, and CXCL9, as well as monokines from IFN-γ, IL-11, and IL-17A. Additionally, the dermis of affected regions contains IL-12– and IL-23–containing macrophages along with IL-17–producing T cells.3 These findings reveal many potential therapeutic targets for the treatment of HS.
PIONEER I and PIONEER II are similarly designed 36-week phase 3 trials of 633 patients with HS who were unresponsive to oral antibiotic treatment.1 By week 12, a significantly greater proportion of patients receiving adalimumab demonstrated clinical improvement (≥50% reduction in total abscess and nodule count) compared to placebo in both trials (PIONEER I: 41.8% vs 26.0%, P=.003; PIONEER II: 58.9% vs 27.6%, P<.001). Secondary end points (inflammatory-nodule count, pain score, and disease severity) were only achieved in PIONEER II. The difference in clinical improvement between the trials is likely due to higher baseline disease severity in the HS patients in PIONEER I versus PIONEER II. No new safety risks were reported and were in accordance with prior adalimumab trials for other diseases. Notably, 10 paradoxical psoriasislike eruptions were reported.
Adalimumab is the first and only US Food and Drug Administration–approved therapy for HS. Further understanding of the pathogenesis of HS may result in additional biologic treatments for HS. We encourage the manufacturers of other biologic therapies, such as infliximab,4 ustekinumab,5 anakinra,6 secukinumab, ixekizumab, and brodalumab, to consider conducting further clinical trials in HS to enhance the therapeutic options available for this debilitating disease.
- Kimball AB, Okun MM, Williams DA, et al. Two Phase 3 trials of adalimumab for hidradenitis suppurativa. N Engl J Med. 2016;375:422-434.
- Vinding GR, Knudsen KM, Ellervik C, et al. Self-reported skin morbidities and health-related quality of life: a population-based nested case-control study. Dermatology. 2014;228:261-268.
- Deckers IE, van der Zee HH, Prens EP. Epidemiology of hidradenitis suppurativa: prevalence, pathogenesis, and factors associated with the development of HS. Curr Dermatol Rep. 2014;3:54-60.
- Ingram JR, Woo PN, Chua SL, et al. Interventions for hidradenitis suppurativa: a Cochrane systematic review incorporating GRADE assessment of evidence quality. Br J Dermatol. 2016;174:970-978.
- Blok JL, Li K, Brodmerkel C, et al. Ustekinumab in hidradenitis suppurativa: clinical results and a search for potential biomarkers in serum. Br J Dermatol. 2016;174:839-846.
- Tzanetakou V, Kanni T, Giatrakou S, et al. Safety and efficacy of anakinra in severe hidradenitis suppurativa: a randomized clinical trial. JAMA Dermatol. 2016;152:52-59.
We applaud Kimball et al1 on their report that adalimumab demonstrated clinical improvement in patients with hidradenitis suppurativa (HS) versus placebo in 2 phase 3 trials. Hidradenitis suppurativa is a chronic relapsing condition with painful subcutaneous abscesses, malodorous drainage, sinus tract formation, and scarring that typically occurs in the axillae and anogenital region. It impairs the quality of life for these patients, as evidenced by higher Dermatology Life Quality Index scores compared to psoriasis, pimples, hand rash, atopic eczema, or control.2
The exact pathogenesis of HS is unknown but likely involves a complex interaction of genetic, hormonal, immunologic, and environmental factors.3 The levels of inflammatory cytokines are elevated in HS lesions, specifically IL-1β, tumor necrosis factor α, IL-10, and CXCL9, as well as monokines from IFN-γ, IL-11, and IL-17A. Additionally, the dermis of affected regions contains IL-12– and IL-23–containing macrophages along with IL-17–producing T cells.3 These findings reveal many potential therapeutic targets for the treatment of HS.
PIONEER I and PIONEER II are similarly designed 36-week phase 3 trials of 633 patients with HS who were unresponsive to oral antibiotic treatment.1 By week 12, a significantly greater proportion of patients receiving adalimumab demonstrated clinical improvement (≥50% reduction in total abscess and nodule count) compared to placebo in both trials (PIONEER I: 41.8% vs 26.0%, P=.003; PIONEER II: 58.9% vs 27.6%, P<.001). Secondary end points (inflammatory-nodule count, pain score, and disease severity) were only achieved in PIONEER II. The difference in clinical improvement between the trials is likely due to higher baseline disease severity in the HS patients in PIONEER I versus PIONEER II. No new safety risks were reported and were in accordance with prior adalimumab trials for other diseases. Notably, 10 paradoxical psoriasislike eruptions were reported.
Adalimumab is the first and only US Food and Drug Administration–approved therapy for HS. Further understanding of the pathogenesis of HS may result in additional biologic treatments for HS. We encourage the manufacturers of other biologic therapies, such as infliximab,4 ustekinumab,5 anakinra,6 secukinumab, ixekizumab, and brodalumab, to consider conducting further clinical trials in HS to enhance the therapeutic options available for this debilitating disease.
We applaud Kimball et al1 on their report that adalimumab demonstrated clinical improvement in patients with hidradenitis suppurativa (HS) versus placebo in 2 phase 3 trials. Hidradenitis suppurativa is a chronic relapsing condition with painful subcutaneous abscesses, malodorous drainage, sinus tract formation, and scarring that typically occurs in the axillae and anogenital region. It impairs the quality of life for these patients, as evidenced by higher Dermatology Life Quality Index scores compared to psoriasis, pimples, hand rash, atopic eczema, or control.2
The exact pathogenesis of HS is unknown but likely involves a complex interaction of genetic, hormonal, immunologic, and environmental factors.3 The levels of inflammatory cytokines are elevated in HS lesions, specifically IL-1β, tumor necrosis factor α, IL-10, and CXCL9, as well as monokines from IFN-γ, IL-11, and IL-17A. Additionally, the dermis of affected regions contains IL-12– and IL-23–containing macrophages along with IL-17–producing T cells.3 These findings reveal many potential therapeutic targets for the treatment of HS.
PIONEER I and PIONEER II are similarly designed 36-week phase 3 trials of 633 patients with HS who were unresponsive to oral antibiotic treatment.1 By week 12, a significantly greater proportion of patients receiving adalimumab demonstrated clinical improvement (≥50% reduction in total abscess and nodule count) compared to placebo in both trials (PIONEER I: 41.8% vs 26.0%, P=.003; PIONEER II: 58.9% vs 27.6%, P<.001). Secondary end points (inflammatory-nodule count, pain score, and disease severity) were only achieved in PIONEER II. The difference in clinical improvement between the trials is likely due to higher baseline disease severity in the HS patients in PIONEER I versus PIONEER II. No new safety risks were reported and were in accordance with prior adalimumab trials for other diseases. Notably, 10 paradoxical psoriasislike eruptions were reported.
Adalimumab is the first and only US Food and Drug Administration–approved therapy for HS. Further understanding of the pathogenesis of HS may result in additional biologic treatments for HS. We encourage the manufacturers of other biologic therapies, such as infliximab,4 ustekinumab,5 anakinra,6 secukinumab, ixekizumab, and brodalumab, to consider conducting further clinical trials in HS to enhance the therapeutic options available for this debilitating disease.
- Kimball AB, Okun MM, Williams DA, et al. Two Phase 3 trials of adalimumab for hidradenitis suppurativa. N Engl J Med. 2016;375:422-434.
- Vinding GR, Knudsen KM, Ellervik C, et al. Self-reported skin morbidities and health-related quality of life: a population-based nested case-control study. Dermatology. 2014;228:261-268.
- Deckers IE, van der Zee HH, Prens EP. Epidemiology of hidradenitis suppurativa: prevalence, pathogenesis, and factors associated with the development of HS. Curr Dermatol Rep. 2014;3:54-60.
- Ingram JR, Woo PN, Chua SL, et al. Interventions for hidradenitis suppurativa: a Cochrane systematic review incorporating GRADE assessment of evidence quality. Br J Dermatol. 2016;174:970-978.
- Blok JL, Li K, Brodmerkel C, et al. Ustekinumab in hidradenitis suppurativa: clinical results and a search for potential biomarkers in serum. Br J Dermatol. 2016;174:839-846.
- Tzanetakou V, Kanni T, Giatrakou S, et al. Safety and efficacy of anakinra in severe hidradenitis suppurativa: a randomized clinical trial. JAMA Dermatol. 2016;152:52-59.
- Kimball AB, Okun MM, Williams DA, et al. Two Phase 3 trials of adalimumab for hidradenitis suppurativa. N Engl J Med. 2016;375:422-434.
- Vinding GR, Knudsen KM, Ellervik C, et al. Self-reported skin morbidities and health-related quality of life: a population-based nested case-control study. Dermatology. 2014;228:261-268.
- Deckers IE, van der Zee HH, Prens EP. Epidemiology of hidradenitis suppurativa: prevalence, pathogenesis, and factors associated with the development of HS. Curr Dermatol Rep. 2014;3:54-60.
- Ingram JR, Woo PN, Chua SL, et al. Interventions for hidradenitis suppurativa: a Cochrane systematic review incorporating GRADE assessment of evidence quality. Br J Dermatol. 2016;174:970-978.
- Blok JL, Li K, Brodmerkel C, et al. Ustekinumab in hidradenitis suppurativa: clinical results and a search for potential biomarkers in serum. Br J Dermatol. 2016;174:839-846.
- Tzanetakou V, Kanni T, Giatrakou S, et al. Safety and efficacy of anakinra in severe hidradenitis suppurativa: a randomized clinical trial. JAMA Dermatol. 2016;152:52-59.
Recent Controversies in Pediatric Dermatology: The Usage of General Anesthesia in Young Children
Clinicians who have attempted to perform an in-office procedure on infants or young children will recognize the difficulties that arise from the developmental inability to cooperate with procedures.1 Potential problems mentioned in the literature include but are not limited to anxiety, which is identified in all age groups of patients undergoing dermatologic procedures2; limitation of pain control3; and poor outcomes due to movement by the patient.1 In one author’s experience (N.B.S.), anxious and scared children can potentially cause injury to themselves, parents/guardians, and health care professionals by flailing and kicking; children are flexible and can wriggle out of even fine grips, and some children, especially toddlers, can be strong.
The usage of topical anesthetics can only give superficial anesthesia. They can ostensibly reduce pain and are useful for anesthesia of curettage, but their use is limited in infants and young children by the minimal amount of drug that is safe for application, as risks of absorption include methemoglobinemia and seizure
General anesthesia seems to be the best alternative due to associated amnesia of the events occurring including pain; immobilization and ability to produce more accurate biopsy sampling; better immobilization leading to superior cosmetic results; and reduced risk to patients, parents/guardians, and health care professionals from a flailing child. In the field of pediatric dermatology, general anesthesia often is used for excision of larger lesions and cosmetic repairs. Operating room privileges are not always easy to obtain, but many pediatric dermatologists take advantage of outpatient surgical centers associated with their medical center. A retrospective review of 226 children receiving 681 procedures at a single institution documented low rates of complications.1
If it was that easy, most children would be anesthetized with general anesthesia. However, there are risks associated with general anesthesia. Parents/guardians often will do what they can to avoid risk and may therefore refuse general anesthesia, but it is not completely avoidable in complicated skin disease. Despite the risks, the benefit is present in a major anomaly correction such as a cleft palate in a 6-month-old but may not be there for the treatment of a wart. When procedures are nonessential or may be conducted without anesthesia, avoidance of general anesthesia is reasonable and a combination of topical and local infiltrative anesthesia can help. In the American Academy of Dermatology guidelines on in-office anesthesia, Kouba et al5 states: “Topical agents are recommended as a first-line method of anesthesia for the repair of dermal lacerations in children and for other minor dermatologic procedures, including curettage. For skin biopsy, excision, or other cases where topical agents alone are insufficient, adjunctive use of topical anesthesia to lessen the discomfort of infiltrative anesthetic should be considered.”
A new controversy recently has emerged concerning the potential risks of anesthesia on neurocognitive development in infants and young children. These concerns regardingthe labeling changes of anesthetic and sedation drugs by the US Food and Drug Administration (FDA) in December 2016 specifically focused on these risks in children younger than 3 years with prolonged (>3 hours) and repeated exposures; however, this kind of exposure is unlikely with standard pediatric dermatologic procedures.6-9
There is compelling evidence from animal studies that exposure to all anesthetic agents in clinical use induces neurotoxicity and long-term adverse neurobehavioral deficits; however, whether these findings are applicable in human infants is unknown.6-9 Most of the studies in humans showing adverse outcomes have been retrospective observational studies subject to multiple sources of bias. Two recent large clinical studies—the GAS (General Anaesthesia compared to Spinal anaesthesia) trial10 and the PANDA (Pediatric Anesthesia and Neurodevelopment Assessment) study11—have shown no evidence of abnormal neurocognitive effects with a single brief exposure before 3 years of age (PANDA) or during infancy (GAS) in otherwise-healthy children.10,11
It is important to note that the FDA labeling change warning specifically stated that “[c]onsistent with animal studies, recent human data suggest that a single, relatively short exposure to general anesthetic and sedation drugs in infants or toddlers is unlikely to have negative effects on behavior or learning.” Moreover, the FDA emphasized that “Surgeries or procedures in children younger than 3 years should not be delayed or avoided when medically necessary.”12 Taking these points into consideration, we should offer our patients in-office care when possible and postpone elective procedures when advisable but proceed when necessary for our patients’ physical and emotional health.
- Juern AM, Cassidy LD, Lyon VB. More evidence confirming the safety of general anesthesia in pediatric dermatologic surgery. Pediatr Dermatol. 2010;27:355-360.
- Gerwels JW, Bezzant JL, Le Maire L, et al. Oral transmucosal fentanyl citrate premedication in patients undergoing outpatient dermatologic procedures. J Dermatol Surg Oncol. 1994;20:823-826.
- D’Acunto C, Raone B, Neri I, et al. Outpatient pediatric dermatologic surgery: experience in 296 patients. Pediatr Dermatol. 2015;32:424-426.
- Gunter JB. Benefit and risks of local anesthetics in infants and children. Paediatr Drugs. 2002;4:649-672.
- Kouba DJ, LoPiccolo MC, Alam M, et al. Guidelines for the use of local anesthesia in office-based dermatologic surgery [published online March 4, 2016]. J Am Acad Dermatol. 2016;74:1201-1219.
- Jevtovic-Todorovic V, Hartman RE, Izumi Y, et al. Early exposure to common anesthetic agents causes widespread neurodegeneration in the developing rat brain and persistent learning deficits. J Neurosci. 2003;23:876-882.
- Brambrink AM, Evers AS, Avidan MS, et al. Isoflurane-induced neuroapoptosis in the neonatal rhesus macaque brain. Anesthesiology. 2010;112:834-841.
- Raper J, Alvarado MC, Murphy KL, et al. Multiple anesthetic exposure in infant monkeys alters emotional reactivity to an acute stressor. Anesthesiology. 2015;123:1084-1092.
- Davidson AJ. Anesthesia and neurotoxicity to the developing brain: the clinical relevance. Paediatric Anaesthesia. 2011;21:716-721.
- Davidson AJ, Disma N, de Graaff JC, et al; GAS consortium. Neurodevelopmental outcome at 2 years of age after general anaesthesia and awake-regional anaesthesia in infancy (GAS): an international multicentre, randomised controlled trial. Lancet. 2016;387:239-250.
- Sun LS, Li G, Miller TL, et al. Association between a single general anesthesia exposure before age 36 months and neurocognitive outcomes in later childhood. JAMA. 2016;315:2312-2320.
- General anesthetic and sedation drugs: drug safety communication—new warnings for young children and pregnant women. US Food and Drug Administration website. https://www.fda.gov/safety/medwatch/safetyinformation/safetyalertsforhumanmedicalproducts/ucm533195.htm. Published December 14, 2016. Accessed July 25, 2017.
Clinicians who have attempted to perform an in-office procedure on infants or young children will recognize the difficulties that arise from the developmental inability to cooperate with procedures.1 Potential problems mentioned in the literature include but are not limited to anxiety, which is identified in all age groups of patients undergoing dermatologic procedures2; limitation of pain control3; and poor outcomes due to movement by the patient.1 In one author’s experience (N.B.S.), anxious and scared children can potentially cause injury to themselves, parents/guardians, and health care professionals by flailing and kicking; children are flexible and can wriggle out of even fine grips, and some children, especially toddlers, can be strong.
The usage of topical anesthetics can only give superficial anesthesia. They can ostensibly reduce pain and are useful for anesthesia of curettage, but their use is limited in infants and young children by the minimal amount of drug that is safe for application, as risks of absorption include methemoglobinemia and seizure
General anesthesia seems to be the best alternative due to associated amnesia of the events occurring including pain; immobilization and ability to produce more accurate biopsy sampling; better immobilization leading to superior cosmetic results; and reduced risk to patients, parents/guardians, and health care professionals from a flailing child. In the field of pediatric dermatology, general anesthesia often is used for excision of larger lesions and cosmetic repairs. Operating room privileges are not always easy to obtain, but many pediatric dermatologists take advantage of outpatient surgical centers associated with their medical center. A retrospective review of 226 children receiving 681 procedures at a single institution documented low rates of complications.1
If it was that easy, most children would be anesthetized with general anesthesia. However, there are risks associated with general anesthesia. Parents/guardians often will do what they can to avoid risk and may therefore refuse general anesthesia, but it is not completely avoidable in complicated skin disease. Despite the risks, the benefit is present in a major anomaly correction such as a cleft palate in a 6-month-old but may not be there for the treatment of a wart. When procedures are nonessential or may be conducted without anesthesia, avoidance of general anesthesia is reasonable and a combination of topical and local infiltrative anesthesia can help. In the American Academy of Dermatology guidelines on in-office anesthesia, Kouba et al5 states: “Topical agents are recommended as a first-line method of anesthesia for the repair of dermal lacerations in children and for other minor dermatologic procedures, including curettage. For skin biopsy, excision, or other cases where topical agents alone are insufficient, adjunctive use of topical anesthesia to lessen the discomfort of infiltrative anesthetic should be considered.”
A new controversy recently has emerged concerning the potential risks of anesthesia on neurocognitive development in infants and young children. These concerns regardingthe labeling changes of anesthetic and sedation drugs by the US Food and Drug Administration (FDA) in December 2016 specifically focused on these risks in children younger than 3 years with prolonged (>3 hours) and repeated exposures; however, this kind of exposure is unlikely with standard pediatric dermatologic procedures.6-9
There is compelling evidence from animal studies that exposure to all anesthetic agents in clinical use induces neurotoxicity and long-term adverse neurobehavioral deficits; however, whether these findings are applicable in human infants is unknown.6-9 Most of the studies in humans showing adverse outcomes have been retrospective observational studies subject to multiple sources of bias. Two recent large clinical studies—the GAS (General Anaesthesia compared to Spinal anaesthesia) trial10 and the PANDA (Pediatric Anesthesia and Neurodevelopment Assessment) study11—have shown no evidence of abnormal neurocognitive effects with a single brief exposure before 3 years of age (PANDA) or during infancy (GAS) in otherwise-healthy children.10,11
It is important to note that the FDA labeling change warning specifically stated that “[c]onsistent with animal studies, recent human data suggest that a single, relatively short exposure to general anesthetic and sedation drugs in infants or toddlers is unlikely to have negative effects on behavior or learning.” Moreover, the FDA emphasized that “Surgeries or procedures in children younger than 3 years should not be delayed or avoided when medically necessary.”12 Taking these points into consideration, we should offer our patients in-office care when possible and postpone elective procedures when advisable but proceed when necessary for our patients’ physical and emotional health.
Clinicians who have attempted to perform an in-office procedure on infants or young children will recognize the difficulties that arise from the developmental inability to cooperate with procedures.1 Potential problems mentioned in the literature include but are not limited to anxiety, which is identified in all age groups of patients undergoing dermatologic procedures2; limitation of pain control3; and poor outcomes due to movement by the patient.1 In one author’s experience (N.B.S.), anxious and scared children can potentially cause injury to themselves, parents/guardians, and health care professionals by flailing and kicking; children are flexible and can wriggle out of even fine grips, and some children, especially toddlers, can be strong.
The usage of topical anesthetics can only give superficial anesthesia. They can ostensibly reduce pain and are useful for anesthesia of curettage, but their use is limited in infants and young children by the minimal amount of drug that is safe for application, as risks of absorption include methemoglobinemia and seizure
General anesthesia seems to be the best alternative due to associated amnesia of the events occurring including pain; immobilization and ability to produce more accurate biopsy sampling; better immobilization leading to superior cosmetic results; and reduced risk to patients, parents/guardians, and health care professionals from a flailing child. In the field of pediatric dermatology, general anesthesia often is used for excision of larger lesions and cosmetic repairs. Operating room privileges are not always easy to obtain, but many pediatric dermatologists take advantage of outpatient surgical centers associated with their medical center. A retrospective review of 226 children receiving 681 procedures at a single institution documented low rates of complications.1
If it was that easy, most children would be anesthetized with general anesthesia. However, there are risks associated with general anesthesia. Parents/guardians often will do what they can to avoid risk and may therefore refuse general anesthesia, but it is not completely avoidable in complicated skin disease. Despite the risks, the benefit is present in a major anomaly correction such as a cleft palate in a 6-month-old but may not be there for the treatment of a wart. When procedures are nonessential or may be conducted without anesthesia, avoidance of general anesthesia is reasonable and a combination of topical and local infiltrative anesthesia can help. In the American Academy of Dermatology guidelines on in-office anesthesia, Kouba et al5 states: “Topical agents are recommended as a first-line method of anesthesia for the repair of dermal lacerations in children and for other minor dermatologic procedures, including curettage. For skin biopsy, excision, or other cases where topical agents alone are insufficient, adjunctive use of topical anesthesia to lessen the discomfort of infiltrative anesthetic should be considered.”
A new controversy recently has emerged concerning the potential risks of anesthesia on neurocognitive development in infants and young children. These concerns regardingthe labeling changes of anesthetic and sedation drugs by the US Food and Drug Administration (FDA) in December 2016 specifically focused on these risks in children younger than 3 years with prolonged (>3 hours) and repeated exposures; however, this kind of exposure is unlikely with standard pediatric dermatologic procedures.6-9
There is compelling evidence from animal studies that exposure to all anesthetic agents in clinical use induces neurotoxicity and long-term adverse neurobehavioral deficits; however, whether these findings are applicable in human infants is unknown.6-9 Most of the studies in humans showing adverse outcomes have been retrospective observational studies subject to multiple sources of bias. Two recent large clinical studies—the GAS (General Anaesthesia compared to Spinal anaesthesia) trial10 and the PANDA (Pediatric Anesthesia and Neurodevelopment Assessment) study11—have shown no evidence of abnormal neurocognitive effects with a single brief exposure before 3 years of age (PANDA) or during infancy (GAS) in otherwise-healthy children.10,11
It is important to note that the FDA labeling change warning specifically stated that “[c]onsistent with animal studies, recent human data suggest that a single, relatively short exposure to general anesthetic and sedation drugs in infants or toddlers is unlikely to have negative effects on behavior or learning.” Moreover, the FDA emphasized that “Surgeries or procedures in children younger than 3 years should not be delayed or avoided when medically necessary.”12 Taking these points into consideration, we should offer our patients in-office care when possible and postpone elective procedures when advisable but proceed when necessary for our patients’ physical and emotional health.
- Juern AM, Cassidy LD, Lyon VB. More evidence confirming the safety of general anesthesia in pediatric dermatologic surgery. Pediatr Dermatol. 2010;27:355-360.
- Gerwels JW, Bezzant JL, Le Maire L, et al. Oral transmucosal fentanyl citrate premedication in patients undergoing outpatient dermatologic procedures. J Dermatol Surg Oncol. 1994;20:823-826.
- D’Acunto C, Raone B, Neri I, et al. Outpatient pediatric dermatologic surgery: experience in 296 patients. Pediatr Dermatol. 2015;32:424-426.
- Gunter JB. Benefit and risks of local anesthetics in infants and children. Paediatr Drugs. 2002;4:649-672.
- Kouba DJ, LoPiccolo MC, Alam M, et al. Guidelines for the use of local anesthesia in office-based dermatologic surgery [published online March 4, 2016]. J Am Acad Dermatol. 2016;74:1201-1219.
- Jevtovic-Todorovic V, Hartman RE, Izumi Y, et al. Early exposure to common anesthetic agents causes widespread neurodegeneration in the developing rat brain and persistent learning deficits. J Neurosci. 2003;23:876-882.
- Brambrink AM, Evers AS, Avidan MS, et al. Isoflurane-induced neuroapoptosis in the neonatal rhesus macaque brain. Anesthesiology. 2010;112:834-841.
- Raper J, Alvarado MC, Murphy KL, et al. Multiple anesthetic exposure in infant monkeys alters emotional reactivity to an acute stressor. Anesthesiology. 2015;123:1084-1092.
- Davidson AJ. Anesthesia and neurotoxicity to the developing brain: the clinical relevance. Paediatric Anaesthesia. 2011;21:716-721.
- Davidson AJ, Disma N, de Graaff JC, et al; GAS consortium. Neurodevelopmental outcome at 2 years of age after general anaesthesia and awake-regional anaesthesia in infancy (GAS): an international multicentre, randomised controlled trial. Lancet. 2016;387:239-250.
- Sun LS, Li G, Miller TL, et al. Association between a single general anesthesia exposure before age 36 months and neurocognitive outcomes in later childhood. JAMA. 2016;315:2312-2320.
- General anesthetic and sedation drugs: drug safety communication—new warnings for young children and pregnant women. US Food and Drug Administration website. https://www.fda.gov/safety/medwatch/safetyinformation/safetyalertsforhumanmedicalproducts/ucm533195.htm. Published December 14, 2016. Accessed July 25, 2017.
- Juern AM, Cassidy LD, Lyon VB. More evidence confirming the safety of general anesthesia in pediatric dermatologic surgery. Pediatr Dermatol. 2010;27:355-360.
- Gerwels JW, Bezzant JL, Le Maire L, et al. Oral transmucosal fentanyl citrate premedication in patients undergoing outpatient dermatologic procedures. J Dermatol Surg Oncol. 1994;20:823-826.
- D’Acunto C, Raone B, Neri I, et al. Outpatient pediatric dermatologic surgery: experience in 296 patients. Pediatr Dermatol. 2015;32:424-426.
- Gunter JB. Benefit and risks of local anesthetics in infants and children. Paediatr Drugs. 2002;4:649-672.
- Kouba DJ, LoPiccolo MC, Alam M, et al. Guidelines for the use of local anesthesia in office-based dermatologic surgery [published online March 4, 2016]. J Am Acad Dermatol. 2016;74:1201-1219.
- Jevtovic-Todorovic V, Hartman RE, Izumi Y, et al. Early exposure to common anesthetic agents causes widespread neurodegeneration in the developing rat brain and persistent learning deficits. J Neurosci. 2003;23:876-882.
- Brambrink AM, Evers AS, Avidan MS, et al. Isoflurane-induced neuroapoptosis in the neonatal rhesus macaque brain. Anesthesiology. 2010;112:834-841.
- Raper J, Alvarado MC, Murphy KL, et al. Multiple anesthetic exposure in infant monkeys alters emotional reactivity to an acute stressor. Anesthesiology. 2015;123:1084-1092.
- Davidson AJ. Anesthesia and neurotoxicity to the developing brain: the clinical relevance. Paediatric Anaesthesia. 2011;21:716-721.
- Davidson AJ, Disma N, de Graaff JC, et al; GAS consortium. Neurodevelopmental outcome at 2 years of age after general anaesthesia and awake-regional anaesthesia in infancy (GAS): an international multicentre, randomised controlled trial. Lancet. 2016;387:239-250.
- Sun LS, Li G, Miller TL, et al. Association between a single general anesthesia exposure before age 36 months and neurocognitive outcomes in later childhood. JAMA. 2016;315:2312-2320.
- General anesthetic and sedation drugs: drug safety communication—new warnings for young children and pregnant women. US Food and Drug Administration website. https://www.fda.gov/safety/medwatch/safetyinformation/safetyalertsforhumanmedicalproducts/ucm533195.htm. Published December 14, 2016. Accessed July 25, 2017.
Military Brats: Members of a Lost Tribe
Some of you who are reading this column likely are military brats from one branch or another. Many of us felt the call to give back by either joining the military, PHS, or working in organizations like the VA, treating former service members. That certainly was a huge motivation for me to become a VA physician. I always felt more welcomed, even felt at home, at the VA or at a military hospital than I did at any civilian health care facility. And many of my colleagues feel the same way. Other brats have never interacted much with the military except for their being raised by family members in the armed forces; yet this designation is still a part of their identity,
The percentage of adults > 50 years old who have an immediate family member who served in the military is 77%; the percentage of those aged 30 to 49 years is 57%; and aged < 30 years, only 33%.1 Almost 5% of adult Americans are military brats. This demographic trend brings with it an increasing chance that current and former service members may feel socially isolated and that many health care professionals will struggle to relate to, and appreciate, their unique cultural background.
Authors always should acknowledge any material conflict of interest, and as a double Army brat, I am far from objective on this subject. I was born and raised on an army base. My father was a career military physician, and my mother, albeit briefly, was an army nurse. Some of my earliest memories are of being with my father and driving around Fort Sam Houston when everyone and everything stopped upon hearing the sound of a bugle (at the time, it was still a real bugle). My father and I would get out of the car. He would salute, and I would stand as still as a small active child can while we turned toward the flag being lowered over the base.
In reading about army brats, this memory seems to be a common one. Many individuals have commented on how this repeated experience from their youth instilled in them a sense of respect for our flag and country and an appreciation of order and discipline that stayed with them long after they became adults.
Obviously, while those of us claiming this identity use it positively as a phrase of winsome nostalgia and civic pride, in everyday language a brat is a pejorative reference. The online magazine Military Brat Life, defines the term as “someone, who, as a child, grows up in a family where one or more parents are ‘career’ military, and where the children move from base to base, experiencing life in several different places and possibly different countries.”2 The phrase denotes an individual whose parents at some point served full-time in the military, no duration is specified or whether the parents had to be active duty, reserve or National Guard members. The prefix for the label comes from the military branch in which the parents primarily served, though like hyphenated names some younger generations will introduce themselves as a Navy-Air Force brat. Other sites suggest that it doesn’t refer to a spoiled child at all but actually is yet another of the acronyms that proliferate in military environments. Although after I read these possible theories, many seemed retrospective attempts to jettison the negative connotations.
I learned that like others sharing similar formative experiences, military brats are considered a subculture or a third culture, in some of the literature. There is a dearth of scholarly data about the phenomenology and social psychology of adults who spent some of their formative years under the auspices of military culture. As in any foray into cultural competence, avoiding stereotypes is crucial. However, research has shown that the experience of growing up in the military is one that bestows resilience and risk.3 It is also an important piece of a patient’s narrative that health care professionals in and out of the federal system should consider to provide patient-centered care.
A childhood in a military environment is often romanticized as shaping an adult who is worldly, cosmopolitan, resilient, and tolerant. Although these are adaptive traits that children of military personnel develop, there also is a far darker side emerging in the research.4 We are all too aware of the epidemic of suicide, opioid use, and posttraumatic stress disorder that has developed in the wake of our country’s latest and lasting conflicts. The reverberations of these mental health problems are felt by the children who lived through them or who lost loved ones to war or suicide. The DoD has begun recognizing this collateral damage and is developing innovative programs to help children and adolescents.
We need to do more though, not just in this arena when the wounds occur, but also later when those wounded come to nurse practitioners and psychologists, social workers, and physicians. Our growing number of community partners through Choice and other programs also need to be aware of the potential mental health impacts of being a military brat or family member.
In the introduction to one of the best books written on the subject, Military Brats: Legacies of Childhood Inside the Fortress, author Pat Conroy wrote, “I thought I was singular in all this, one of a kind.... I discovered that I speak in the multitongued, deep-throated voice of my tribe. It’s a language I was not even aware I spoke... a secret family I did not know I had.... Military brats, my lost tribe, spent their entire youth in service to this country, and no one even knew we were there.”5
1. Pew Research Center. The military-civilian gap: fewer family connections. http://www.pewsocialtrends.org/2011/11/23/the-military-civilian-gap-fewer-family-connections. Published November 23, 2011. Accessed July 12, 2017.
2. Baker V. What is a military brat? http://militarybratlife.com/what-is-a-military-brat. Published January 22, 2015. Accessed July 13, 2017.
3. Park N. Military children and families: strengths and challenges in war and peace. Am Psychol. 2011;66(1):65-72.
4. McGuire AC, Kanesarajah J, Runge CE, Ireland R, Waller M, Dobson AJ. Effect of multiple deployments on military families: a cross-sectional study of health and well-being of partners and children. Mill Med. 2016;181(4):319-327.
5. Wertsch ME. Military Brats: Legacies of Childhood Inside the Fortress. St. Louis, MO: Brightwell Publishing; 2011.
Some of you who are reading this column likely are military brats from one branch or another. Many of us felt the call to give back by either joining the military, PHS, or working in organizations like the VA, treating former service members. That certainly was a huge motivation for me to become a VA physician. I always felt more welcomed, even felt at home, at the VA or at a military hospital than I did at any civilian health care facility. And many of my colleagues feel the same way. Other brats have never interacted much with the military except for their being raised by family members in the armed forces; yet this designation is still a part of their identity,
The percentage of adults > 50 years old who have an immediate family member who served in the military is 77%; the percentage of those aged 30 to 49 years is 57%; and aged < 30 years, only 33%.1 Almost 5% of adult Americans are military brats. This demographic trend brings with it an increasing chance that current and former service members may feel socially isolated and that many health care professionals will struggle to relate to, and appreciate, their unique cultural background.
Authors always should acknowledge any material conflict of interest, and as a double Army brat, I am far from objective on this subject. I was born and raised on an army base. My father was a career military physician, and my mother, albeit briefly, was an army nurse. Some of my earliest memories are of being with my father and driving around Fort Sam Houston when everyone and everything stopped upon hearing the sound of a bugle (at the time, it was still a real bugle). My father and I would get out of the car. He would salute, and I would stand as still as a small active child can while we turned toward the flag being lowered over the base.
In reading about army brats, this memory seems to be a common one. Many individuals have commented on how this repeated experience from their youth instilled in them a sense of respect for our flag and country and an appreciation of order and discipline that stayed with them long after they became adults.
Obviously, while those of us claiming this identity use it positively as a phrase of winsome nostalgia and civic pride, in everyday language a brat is a pejorative reference. The online magazine Military Brat Life, defines the term as “someone, who, as a child, grows up in a family where one or more parents are ‘career’ military, and where the children move from base to base, experiencing life in several different places and possibly different countries.”2 The phrase denotes an individual whose parents at some point served full-time in the military, no duration is specified or whether the parents had to be active duty, reserve or National Guard members. The prefix for the label comes from the military branch in which the parents primarily served, though like hyphenated names some younger generations will introduce themselves as a Navy-Air Force brat. Other sites suggest that it doesn’t refer to a spoiled child at all but actually is yet another of the acronyms that proliferate in military environments. Although after I read these possible theories, many seemed retrospective attempts to jettison the negative connotations.
I learned that like others sharing similar formative experiences, military brats are considered a subculture or a third culture, in some of the literature. There is a dearth of scholarly data about the phenomenology and social psychology of adults who spent some of their formative years under the auspices of military culture. As in any foray into cultural competence, avoiding stereotypes is crucial. However, research has shown that the experience of growing up in the military is one that bestows resilience and risk.3 It is also an important piece of a patient’s narrative that health care professionals in and out of the federal system should consider to provide patient-centered care.
A childhood in a military environment is often romanticized as shaping an adult who is worldly, cosmopolitan, resilient, and tolerant. Although these are adaptive traits that children of military personnel develop, there also is a far darker side emerging in the research.4 We are all too aware of the epidemic of suicide, opioid use, and posttraumatic stress disorder that has developed in the wake of our country’s latest and lasting conflicts. The reverberations of these mental health problems are felt by the children who lived through them or who lost loved ones to war or suicide. The DoD has begun recognizing this collateral damage and is developing innovative programs to help children and adolescents.
We need to do more though, not just in this arena when the wounds occur, but also later when those wounded come to nurse practitioners and psychologists, social workers, and physicians. Our growing number of community partners through Choice and other programs also need to be aware of the potential mental health impacts of being a military brat or family member.
In the introduction to one of the best books written on the subject, Military Brats: Legacies of Childhood Inside the Fortress, author Pat Conroy wrote, “I thought I was singular in all this, one of a kind.... I discovered that I speak in the multitongued, deep-throated voice of my tribe. It’s a language I was not even aware I spoke... a secret family I did not know I had.... Military brats, my lost tribe, spent their entire youth in service to this country, and no one even knew we were there.”5
Some of you who are reading this column likely are military brats from one branch or another. Many of us felt the call to give back by either joining the military, PHS, or working in organizations like the VA, treating former service members. That certainly was a huge motivation for me to become a VA physician. I always felt more welcomed, even felt at home, at the VA or at a military hospital than I did at any civilian health care facility. And many of my colleagues feel the same way. Other brats have never interacted much with the military except for their being raised by family members in the armed forces; yet this designation is still a part of their identity,
The percentage of adults > 50 years old who have an immediate family member who served in the military is 77%; the percentage of those aged 30 to 49 years is 57%; and aged < 30 years, only 33%.1 Almost 5% of adult Americans are military brats. This demographic trend brings with it an increasing chance that current and former service members may feel socially isolated and that many health care professionals will struggle to relate to, and appreciate, their unique cultural background.
Authors always should acknowledge any material conflict of interest, and as a double Army brat, I am far from objective on this subject. I was born and raised on an army base. My father was a career military physician, and my mother, albeit briefly, was an army nurse. Some of my earliest memories are of being with my father and driving around Fort Sam Houston when everyone and everything stopped upon hearing the sound of a bugle (at the time, it was still a real bugle). My father and I would get out of the car. He would salute, and I would stand as still as a small active child can while we turned toward the flag being lowered over the base.
In reading about army brats, this memory seems to be a common one. Many individuals have commented on how this repeated experience from their youth instilled in them a sense of respect for our flag and country and an appreciation of order and discipline that stayed with them long after they became adults.
Obviously, while those of us claiming this identity use it positively as a phrase of winsome nostalgia and civic pride, in everyday language a brat is a pejorative reference. The online magazine Military Brat Life, defines the term as “someone, who, as a child, grows up in a family where one or more parents are ‘career’ military, and where the children move from base to base, experiencing life in several different places and possibly different countries.”2 The phrase denotes an individual whose parents at some point served full-time in the military, no duration is specified or whether the parents had to be active duty, reserve or National Guard members. The prefix for the label comes from the military branch in which the parents primarily served, though like hyphenated names some younger generations will introduce themselves as a Navy-Air Force brat. Other sites suggest that it doesn’t refer to a spoiled child at all but actually is yet another of the acronyms that proliferate in military environments. Although after I read these possible theories, many seemed retrospective attempts to jettison the negative connotations.
I learned that like others sharing similar formative experiences, military brats are considered a subculture or a third culture, in some of the literature. There is a dearth of scholarly data about the phenomenology and social psychology of adults who spent some of their formative years under the auspices of military culture. As in any foray into cultural competence, avoiding stereotypes is crucial. However, research has shown that the experience of growing up in the military is one that bestows resilience and risk.3 It is also an important piece of a patient’s narrative that health care professionals in and out of the federal system should consider to provide patient-centered care.
A childhood in a military environment is often romanticized as shaping an adult who is worldly, cosmopolitan, resilient, and tolerant. Although these are adaptive traits that children of military personnel develop, there also is a far darker side emerging in the research.4 We are all too aware of the epidemic of suicide, opioid use, and posttraumatic stress disorder that has developed in the wake of our country’s latest and lasting conflicts. The reverberations of these mental health problems are felt by the children who lived through them or who lost loved ones to war or suicide. The DoD has begun recognizing this collateral damage and is developing innovative programs to help children and adolescents.
We need to do more though, not just in this arena when the wounds occur, but also later when those wounded come to nurse practitioners and psychologists, social workers, and physicians. Our growing number of community partners through Choice and other programs also need to be aware of the potential mental health impacts of being a military brat or family member.
In the introduction to one of the best books written on the subject, Military Brats: Legacies of Childhood Inside the Fortress, author Pat Conroy wrote, “I thought I was singular in all this, one of a kind.... I discovered that I speak in the multitongued, deep-throated voice of my tribe. It’s a language I was not even aware I spoke... a secret family I did not know I had.... Military brats, my lost tribe, spent their entire youth in service to this country, and no one even knew we were there.”5
1. Pew Research Center. The military-civilian gap: fewer family connections. http://www.pewsocialtrends.org/2011/11/23/the-military-civilian-gap-fewer-family-connections. Published November 23, 2011. Accessed July 12, 2017.
2. Baker V. What is a military brat? http://militarybratlife.com/what-is-a-military-brat. Published January 22, 2015. Accessed July 13, 2017.
3. Park N. Military children and families: strengths and challenges in war and peace. Am Psychol. 2011;66(1):65-72.
4. McGuire AC, Kanesarajah J, Runge CE, Ireland R, Waller M, Dobson AJ. Effect of multiple deployments on military families: a cross-sectional study of health and well-being of partners and children. Mill Med. 2016;181(4):319-327.
5. Wertsch ME. Military Brats: Legacies of Childhood Inside the Fortress. St. Louis, MO: Brightwell Publishing; 2011.
1. Pew Research Center. The military-civilian gap: fewer family connections. http://www.pewsocialtrends.org/2011/11/23/the-military-civilian-gap-fewer-family-connections. Published November 23, 2011. Accessed July 12, 2017.
2. Baker V. What is a military brat? http://militarybratlife.com/what-is-a-military-brat. Published January 22, 2015. Accessed July 13, 2017.
3. Park N. Military children and families: strengths and challenges in war and peace. Am Psychol. 2011;66(1):65-72.
4. McGuire AC, Kanesarajah J, Runge CE, Ireland R, Waller M, Dobson AJ. Effect of multiple deployments on military families: a cross-sectional study of health and well-being of partners and children. Mill Med. 2016;181(4):319-327.
5. Wertsch ME. Military Brats: Legacies of Childhood Inside the Fortress. St. Louis, MO: Brightwell Publishing; 2011.
Getting it right at the end of life
Although the concept of the living will was first proposed in 1969
In contrast, an informal search of PubMed reveals that at least 38 articles on advance directives and end-of-life care have been published during the first 7 months of 2017. And a feature article in this month’s issue of JFP makes one more. Why is there such strong interest now in an issue that seldom arose when I began practice in 1978?
More complex, less personalized medicine. As medical care has become more sophisticated, there is a great deal more we can do to keep people alive as they approach the end of life, and a great many more decisions to be made.
Additionally, people are much less likely today to be cared for in their dying days by a family physician who knows them, their wishes, and their family well. In my early years in small-town practice, I was present when my patients were dying, and I usually knew their family members. Family meetings were easy to arrange, and we quickly came to a consensus about what to do and what not to do. If I was not available, one of my practice partners was. We cared for our patients in the office, nursing home, and hospital. Now, most dying hospitalized patients are cared for by hospitalists who may be meeting the patient for the first time.
Getting more people to participate. Consequently, it is important to understand patients’ wishes for end-of-life care and to document those wishes in writing, using things like a POLST (Physician Orders for Life-Sustaining Treatment) form. Although randomized trials support the value of advance care planning, especially in primary care settings,3,4 two-thirds of Americans have not completed an advance directive.5 Rolnick suggests we “delegalize” the process to remove barriers and make it easier for people to execute such documents and integrate them into health care systems.6
Make it part of your office routine. A 70-year-old patient of mine with advanced COPD arrived at his office visit last month with advance directive and POLST forms in hand. We had an excellent, frank conversation, spiced with humor that he supplied, about his wishes for end-of-life care. Just like so many other tasks that we must squeeze into our busy schedules, this is one that we should hard-wire into our office systems and routines.
1. Kutner L. Due process of euthanasia: the living will, a proposal. Indiana Law J. 1969;44:539-554.
2. Schneiderman LJ, Arras JD. Counseling patients to counsel physicians on future care in the event of patient incompetence. Ann Intern Med. 1985;102:693-698.
3. Weathers E, O’Caoimh R, Cornally N, et al. Advance care planning: a systematic review of randomised controlled trials conducted with older adults. Maturitas. 2016;91:101-109.
4. Tierney WM, Dexter PR, Gramelspacher GP, et al. The effect of discussions about advance directives on patients’ satisfaction with primary care. J Gen Intern Med. 2001;16:32-40.
5. Yadav KN, Gabler NB, Cooney E, et al. Approximately one in three US adults completes any type of advance directive for end-of-life care. Health Aff (Millwood). 2017;36:1244-1251.
6. Rolnick JA, Asch DA, Halpern SD. Delegalizing advance directives—facilitating advance care planning. N Engl J Med. 2017;376:2105-2107.
Although the concept of the living will was first proposed in 1969
In contrast, an informal search of PubMed reveals that at least 38 articles on advance directives and end-of-life care have been published during the first 7 months of 2017. And a feature article in this month’s issue of JFP makes one more. Why is there such strong interest now in an issue that seldom arose when I began practice in 1978?
More complex, less personalized medicine. As medical care has become more sophisticated, there is a great deal more we can do to keep people alive as they approach the end of life, and a great many more decisions to be made.
Additionally, people are much less likely today to be cared for in their dying days by a family physician who knows them, their wishes, and their family well. In my early years in small-town practice, I was present when my patients were dying, and I usually knew their family members. Family meetings were easy to arrange, and we quickly came to a consensus about what to do and what not to do. If I was not available, one of my practice partners was. We cared for our patients in the office, nursing home, and hospital. Now, most dying hospitalized patients are cared for by hospitalists who may be meeting the patient for the first time.
Getting more people to participate. Consequently, it is important to understand patients’ wishes for end-of-life care and to document those wishes in writing, using things like a POLST (Physician Orders for Life-Sustaining Treatment) form. Although randomized trials support the value of advance care planning, especially in primary care settings,3,4 two-thirds of Americans have not completed an advance directive.5 Rolnick suggests we “delegalize” the process to remove barriers and make it easier for people to execute such documents and integrate them into health care systems.6
Make it part of your office routine. A 70-year-old patient of mine with advanced COPD arrived at his office visit last month with advance directive and POLST forms in hand. We had an excellent, frank conversation, spiced with humor that he supplied, about his wishes for end-of-life care. Just like so many other tasks that we must squeeze into our busy schedules, this is one that we should hard-wire into our office systems and routines.
Although the concept of the living will was first proposed in 1969
In contrast, an informal search of PubMed reveals that at least 38 articles on advance directives and end-of-life care have been published during the first 7 months of 2017. And a feature article in this month’s issue of JFP makes one more. Why is there such strong interest now in an issue that seldom arose when I began practice in 1978?
More complex, less personalized medicine. As medical care has become more sophisticated, there is a great deal more we can do to keep people alive as they approach the end of life, and a great many more decisions to be made.
Additionally, people are much less likely today to be cared for in their dying days by a family physician who knows them, their wishes, and their family well. In my early years in small-town practice, I was present when my patients were dying, and I usually knew their family members. Family meetings were easy to arrange, and we quickly came to a consensus about what to do and what not to do. If I was not available, one of my practice partners was. We cared for our patients in the office, nursing home, and hospital. Now, most dying hospitalized patients are cared for by hospitalists who may be meeting the patient for the first time.
Getting more people to participate. Consequently, it is important to understand patients’ wishes for end-of-life care and to document those wishes in writing, using things like a POLST (Physician Orders for Life-Sustaining Treatment) form. Although randomized trials support the value of advance care planning, especially in primary care settings,3,4 two-thirds of Americans have not completed an advance directive.5 Rolnick suggests we “delegalize” the process to remove barriers and make it easier for people to execute such documents and integrate them into health care systems.6
Make it part of your office routine. A 70-year-old patient of mine with advanced COPD arrived at his office visit last month with advance directive and POLST forms in hand. We had an excellent, frank conversation, spiced with humor that he supplied, about his wishes for end-of-life care. Just like so many other tasks that we must squeeze into our busy schedules, this is one that we should hard-wire into our office systems and routines.
1. Kutner L. Due process of euthanasia: the living will, a proposal. Indiana Law J. 1969;44:539-554.
2. Schneiderman LJ, Arras JD. Counseling patients to counsel physicians on future care in the event of patient incompetence. Ann Intern Med. 1985;102:693-698.
3. Weathers E, O’Caoimh R, Cornally N, et al. Advance care planning: a systematic review of randomised controlled trials conducted with older adults. Maturitas. 2016;91:101-109.
4. Tierney WM, Dexter PR, Gramelspacher GP, et al. The effect of discussions about advance directives on patients’ satisfaction with primary care. J Gen Intern Med. 2001;16:32-40.
5. Yadav KN, Gabler NB, Cooney E, et al. Approximately one in three US adults completes any type of advance directive for end-of-life care. Health Aff (Millwood). 2017;36:1244-1251.
6. Rolnick JA, Asch DA, Halpern SD. Delegalizing advance directives—facilitating advance care planning. N Engl J Med. 2017;376:2105-2107.
1. Kutner L. Due process of euthanasia: the living will, a proposal. Indiana Law J. 1969;44:539-554.
2. Schneiderman LJ, Arras JD. Counseling patients to counsel physicians on future care in the event of patient incompetence. Ann Intern Med. 1985;102:693-698.
3. Weathers E, O’Caoimh R, Cornally N, et al. Advance care planning: a systematic review of randomised controlled trials conducted with older adults. Maturitas. 2016;91:101-109.
4. Tierney WM, Dexter PR, Gramelspacher GP, et al. The effect of discussions about advance directives on patients’ satisfaction with primary care. J Gen Intern Med. 2001;16:32-40.
5. Yadav KN, Gabler NB, Cooney E, et al. Approximately one in three US adults completes any type of advance directive for end-of-life care. Health Aff (Millwood). 2017;36:1244-1251.
6. Rolnick JA, Asch DA, Halpern SD. Delegalizing advance directives—facilitating advance care planning. N Engl J Med. 2017;376:2105-2107.
Skin care Q and A for your staff
in helping us be more efficient with our time. I asked my staff to put together a list of the most common patient skin care questions. This column can be used as a guide for your staff when answering questions about skin care.
Q: Should my sunscreen be applied first or last?
A: The best way to remember is that medications should be applied closest to the skin and sunscreen should be applied closest to the sun. I recommend that morning skin care be applied in the following order:
Step 1. Facial cleanser
Step 2. Eye products (protect the delicate eye area from the medication)
Step 3. Treatment product (medications, or the most important active ingredients)
Step 4. Moisturizer (if needed)
Step 5. Sunscreen
Q: When can I restart my normal skin care regimen after receiving dermal fillers?
A: The morning after receiving dermal fillers, you can resume your normal facial skin care regimen.
Q: How do I treat my skin after receiving cosmetic injections such as Botox?
A: After you are injected with dermal fillers, keep the Arnica gel, Arnica pads, or post procedure product on your face until bedtime. Prior to bed, wash your face with a gentle cleanser and lukewarm water. Do not use any scrubs, facial brushes, or hydroxy acids. Apply a soothing gel or soothing moisturizer. Do not use hot water on the face for 48 hours. Avoid hot showers, saunas, facial steaming, facial massage, and exercise for 48 hours. If you must exercise, try to keep the face cool with an ice filled bottle of water. Heat makes you more likely to bruise.
Q: Will retinol make my skin sun sensitive?
A: Retinol breaks down upon sun exposure so it should only be used at night. It is a myth that retinol makes your skin sun sensitive. Retinol is a form of vitamin A that helps protect your skin from sun damage by reducing levels of an enzyme called collagenase that is produced after sun exposure. For this and other reasons, retinol can help protect your skin from sun damage. However, if your skin gets irritated from the retinol and you go into the sun, you can develop postinflammatory hyperpigmentation – or dark patches on the skin. It is a good idea to always wear sunscreen in the morning every day whether you are using retinol or not.
Q: What do I do to treat the dark circles under my eyes?
A: Dark circles can be caused by sluggish blood flow around the eyes leading to deposition of a pigment found in blood called hemosiderin. Dark circles around the eyes also can be caused by an increased amount of the pigment melanin that occurs from sun exposure, heat, estrogen, and stress. Treatments include lifestyle habits that increase blood circulation, such as smoking cessation and exercise. Supplements such as horse chestnut may help improve circulation. Ingredients such as the tyrosinase inhibitors ascorbic acid, kojic acid, arbutin, and hydroquinone will help decrease melanin production, and may improve dark circles caused by increased melanin. Wearing a daily sunscreen around the eyes is a very important part of improving the appearance of dark circles under the eyes.
Q: Do I need an eye cream?
A: Most people need an eye product whether it is a serum, gel, or cream. Eye treatment products are usually one of the first skin care products that male patients purchase. The most common indications for eye treatment products are dark circles under the eyes, puffy eyes, dryness, fine lines, or redness. Each one of these indications requires very different ingredients; therefore, most people need more than one eye product depending on what eye issues they are experiencing. Eye treatment products can protect the delicate eye area from medications such as tretinoin that gets on the pillowcase and is transferred to the eye area at night. Eye products that have humectants, such as heparan sulfate or hyaluronic acid, should be used to treat fines lines and dryness, but these may make eyes puffy. For those with dry and puffy eyes, a second eye product with vasoconstrictive ingredients should be used in the daytime while the hydrating one is used at night. Antiaging eye products with retinol and hydroxy acids may irritate sensitive skin types so they can be paired with a soothing eye product. Consider using different eye products for the morning and evening depending on what eye issues need to be treated.
Q: Will moisturizer make my acne worse?
A: Noncomedogenic moisturizers can help improve acne and speed recovery. Using the proper cleanser and moisturizer will make acne medications more tolerable. Many patients cannot tolerate their acne medications every day. The bacteria that cause acne reproduce every 12 hours. For this reason, acne medications must be used consistently twice a day. Using the proper cleanser and moisturizer makes this possible in most patients. Avoid moisturizers with coconut oil, isopropyl myristate, and other ingredients known to cause acne.
Q: Why does my face get so red after washing it?
A: Rosacea-prone skin types get red from the friction of washing the face – even if just using water. If this occurs, use skin care products with anti-inflammatory ingredients such as argan oil, green tea, fever few, chamomile, caffeine, resveratrol, and niacinamide to sooth the skin. These can be paired with prescription rosacea medications such as Rhofade (oxymetazoline hydrochloride) to reduce facial redness. People with rosacea-prone skin types should avoid facial brushes, scrubs, and vigorous exfoliation.
Q: Why is my melasma not getting better on skin lighteners?
Educating our staff on the basics of skin care can make our office much more efficient. If you liked the format of this column or have questions that you hear often from patients, please email me at [email protected].
Dr. Baumann is a private practice dermatologist, researcher, author and entrepreneur who practices in Miami. She founded the Cosmetic Dermatology Center at the University of Miami in 1997. Dr. Baumann wrote two textbooks: “Cosmetic Dermatology: Principles and Practice” (New York: McGraw-Hill, 2002), and “Cosmeceuticals and Cosmetic Ingredients,” (New York: McGraw-Hill, 2014), and a New York Times Best Sellers book for consumers, “The Skin Type Solution” (New York: Bantam Dell, 2006). Dr. Baumann has received funding for advisory boards and/or clinical research trials from Allergan, Evolus, Galderma, Aclaris, and Revance. She is the founder and CEO of Skin Type Solutions Franchise Systems LLC.
in helping us be more efficient with our time. I asked my staff to put together a list of the most common patient skin care questions. This column can be used as a guide for your staff when answering questions about skin care.
Q: Should my sunscreen be applied first or last?
A: The best way to remember is that medications should be applied closest to the skin and sunscreen should be applied closest to the sun. I recommend that morning skin care be applied in the following order:
Step 1. Facial cleanser
Step 2. Eye products (protect the delicate eye area from the medication)
Step 3. Treatment product (medications, or the most important active ingredients)
Step 4. Moisturizer (if needed)
Step 5. Sunscreen
Q: When can I restart my normal skin care regimen after receiving dermal fillers?
A: The morning after receiving dermal fillers, you can resume your normal facial skin care regimen.
Q: How do I treat my skin after receiving cosmetic injections such as Botox?
A: After you are injected with dermal fillers, keep the Arnica gel, Arnica pads, or post procedure product on your face until bedtime. Prior to bed, wash your face with a gentle cleanser and lukewarm water. Do not use any scrubs, facial brushes, or hydroxy acids. Apply a soothing gel or soothing moisturizer. Do not use hot water on the face for 48 hours. Avoid hot showers, saunas, facial steaming, facial massage, and exercise for 48 hours. If you must exercise, try to keep the face cool with an ice filled bottle of water. Heat makes you more likely to bruise.
Q: Will retinol make my skin sun sensitive?
A: Retinol breaks down upon sun exposure so it should only be used at night. It is a myth that retinol makes your skin sun sensitive. Retinol is a form of vitamin A that helps protect your skin from sun damage by reducing levels of an enzyme called collagenase that is produced after sun exposure. For this and other reasons, retinol can help protect your skin from sun damage. However, if your skin gets irritated from the retinol and you go into the sun, you can develop postinflammatory hyperpigmentation – or dark patches on the skin. It is a good idea to always wear sunscreen in the morning every day whether you are using retinol or not.
Q: What do I do to treat the dark circles under my eyes?
A: Dark circles can be caused by sluggish blood flow around the eyes leading to deposition of a pigment found in blood called hemosiderin. Dark circles around the eyes also can be caused by an increased amount of the pigment melanin that occurs from sun exposure, heat, estrogen, and stress. Treatments include lifestyle habits that increase blood circulation, such as smoking cessation and exercise. Supplements such as horse chestnut may help improve circulation. Ingredients such as the tyrosinase inhibitors ascorbic acid, kojic acid, arbutin, and hydroquinone will help decrease melanin production, and may improve dark circles caused by increased melanin. Wearing a daily sunscreen around the eyes is a very important part of improving the appearance of dark circles under the eyes.
Q: Do I need an eye cream?
A: Most people need an eye product whether it is a serum, gel, or cream. Eye treatment products are usually one of the first skin care products that male patients purchase. The most common indications for eye treatment products are dark circles under the eyes, puffy eyes, dryness, fine lines, or redness. Each one of these indications requires very different ingredients; therefore, most people need more than one eye product depending on what eye issues they are experiencing. Eye treatment products can protect the delicate eye area from medications such as tretinoin that gets on the pillowcase and is transferred to the eye area at night. Eye products that have humectants, such as heparan sulfate or hyaluronic acid, should be used to treat fines lines and dryness, but these may make eyes puffy. For those with dry and puffy eyes, a second eye product with vasoconstrictive ingredients should be used in the daytime while the hydrating one is used at night. Antiaging eye products with retinol and hydroxy acids may irritate sensitive skin types so they can be paired with a soothing eye product. Consider using different eye products for the morning and evening depending on what eye issues need to be treated.
Q: Will moisturizer make my acne worse?
A: Noncomedogenic moisturizers can help improve acne and speed recovery. Using the proper cleanser and moisturizer will make acne medications more tolerable. Many patients cannot tolerate their acne medications every day. The bacteria that cause acne reproduce every 12 hours. For this reason, acne medications must be used consistently twice a day. Using the proper cleanser and moisturizer makes this possible in most patients. Avoid moisturizers with coconut oil, isopropyl myristate, and other ingredients known to cause acne.
Q: Why does my face get so red after washing it?
A: Rosacea-prone skin types get red from the friction of washing the face – even if just using water. If this occurs, use skin care products with anti-inflammatory ingredients such as argan oil, green tea, fever few, chamomile, caffeine, resveratrol, and niacinamide to sooth the skin. These can be paired with prescription rosacea medications such as Rhofade (oxymetazoline hydrochloride) to reduce facial redness. People with rosacea-prone skin types should avoid facial brushes, scrubs, and vigorous exfoliation.
Q: Why is my melasma not getting better on skin lighteners?
Educating our staff on the basics of skin care can make our office much more efficient. If you liked the format of this column or have questions that you hear often from patients, please email me at [email protected].
Dr. Baumann is a private practice dermatologist, researcher, author and entrepreneur who practices in Miami. She founded the Cosmetic Dermatology Center at the University of Miami in 1997. Dr. Baumann wrote two textbooks: “Cosmetic Dermatology: Principles and Practice” (New York: McGraw-Hill, 2002), and “Cosmeceuticals and Cosmetic Ingredients,” (New York: McGraw-Hill, 2014), and a New York Times Best Sellers book for consumers, “The Skin Type Solution” (New York: Bantam Dell, 2006). Dr. Baumann has received funding for advisory boards and/or clinical research trials from Allergan, Evolus, Galderma, Aclaris, and Revance. She is the founder and CEO of Skin Type Solutions Franchise Systems LLC.
in helping us be more efficient with our time. I asked my staff to put together a list of the most common patient skin care questions. This column can be used as a guide for your staff when answering questions about skin care.
Q: Should my sunscreen be applied first or last?
A: The best way to remember is that medications should be applied closest to the skin and sunscreen should be applied closest to the sun. I recommend that morning skin care be applied in the following order:
Step 1. Facial cleanser
Step 2. Eye products (protect the delicate eye area from the medication)
Step 3. Treatment product (medications, or the most important active ingredients)
Step 4. Moisturizer (if needed)
Step 5. Sunscreen
Q: When can I restart my normal skin care regimen after receiving dermal fillers?
A: The morning after receiving dermal fillers, you can resume your normal facial skin care regimen.
Q: How do I treat my skin after receiving cosmetic injections such as Botox?
A: After you are injected with dermal fillers, keep the Arnica gel, Arnica pads, or post procedure product on your face until bedtime. Prior to bed, wash your face with a gentle cleanser and lukewarm water. Do not use any scrubs, facial brushes, or hydroxy acids. Apply a soothing gel or soothing moisturizer. Do not use hot water on the face for 48 hours. Avoid hot showers, saunas, facial steaming, facial massage, and exercise for 48 hours. If you must exercise, try to keep the face cool with an ice filled bottle of water. Heat makes you more likely to bruise.
Q: Will retinol make my skin sun sensitive?
A: Retinol breaks down upon sun exposure so it should only be used at night. It is a myth that retinol makes your skin sun sensitive. Retinol is a form of vitamin A that helps protect your skin from sun damage by reducing levels of an enzyme called collagenase that is produced after sun exposure. For this and other reasons, retinol can help protect your skin from sun damage. However, if your skin gets irritated from the retinol and you go into the sun, you can develop postinflammatory hyperpigmentation – or dark patches on the skin. It is a good idea to always wear sunscreen in the morning every day whether you are using retinol or not.
Q: What do I do to treat the dark circles under my eyes?
A: Dark circles can be caused by sluggish blood flow around the eyes leading to deposition of a pigment found in blood called hemosiderin. Dark circles around the eyes also can be caused by an increased amount of the pigment melanin that occurs from sun exposure, heat, estrogen, and stress. Treatments include lifestyle habits that increase blood circulation, such as smoking cessation and exercise. Supplements such as horse chestnut may help improve circulation. Ingredients such as the tyrosinase inhibitors ascorbic acid, kojic acid, arbutin, and hydroquinone will help decrease melanin production, and may improve dark circles caused by increased melanin. Wearing a daily sunscreen around the eyes is a very important part of improving the appearance of dark circles under the eyes.
Q: Do I need an eye cream?
A: Most people need an eye product whether it is a serum, gel, or cream. Eye treatment products are usually one of the first skin care products that male patients purchase. The most common indications for eye treatment products are dark circles under the eyes, puffy eyes, dryness, fine lines, or redness. Each one of these indications requires very different ingredients; therefore, most people need more than one eye product depending on what eye issues they are experiencing. Eye treatment products can protect the delicate eye area from medications such as tretinoin that gets on the pillowcase and is transferred to the eye area at night. Eye products that have humectants, such as heparan sulfate or hyaluronic acid, should be used to treat fines lines and dryness, but these may make eyes puffy. For those with dry and puffy eyes, a second eye product with vasoconstrictive ingredients should be used in the daytime while the hydrating one is used at night. Antiaging eye products with retinol and hydroxy acids may irritate sensitive skin types so they can be paired with a soothing eye product. Consider using different eye products for the morning and evening depending on what eye issues need to be treated.
Q: Will moisturizer make my acne worse?
A: Noncomedogenic moisturizers can help improve acne and speed recovery. Using the proper cleanser and moisturizer will make acne medications more tolerable. Many patients cannot tolerate their acne medications every day. The bacteria that cause acne reproduce every 12 hours. For this reason, acne medications must be used consistently twice a day. Using the proper cleanser and moisturizer makes this possible in most patients. Avoid moisturizers with coconut oil, isopropyl myristate, and other ingredients known to cause acne.
Q: Why does my face get so red after washing it?
A: Rosacea-prone skin types get red from the friction of washing the face – even if just using water. If this occurs, use skin care products with anti-inflammatory ingredients such as argan oil, green tea, fever few, chamomile, caffeine, resveratrol, and niacinamide to sooth the skin. These can be paired with prescription rosacea medications such as Rhofade (oxymetazoline hydrochloride) to reduce facial redness. People with rosacea-prone skin types should avoid facial brushes, scrubs, and vigorous exfoliation.
Q: Why is my melasma not getting better on skin lighteners?
Educating our staff on the basics of skin care can make our office much more efficient. If you liked the format of this column or have questions that you hear often from patients, please email me at [email protected].
Dr. Baumann is a private practice dermatologist, researcher, author and entrepreneur who practices in Miami. She founded the Cosmetic Dermatology Center at the University of Miami in 1997. Dr. Baumann wrote two textbooks: “Cosmetic Dermatology: Principles and Practice” (New York: McGraw-Hill, 2002), and “Cosmeceuticals and Cosmetic Ingredients,” (New York: McGraw-Hill, 2014), and a New York Times Best Sellers book for consumers, “The Skin Type Solution” (New York: Bantam Dell, 2006). Dr. Baumann has received funding for advisory boards and/or clinical research trials from Allergan, Evolus, Galderma, Aclaris, and Revance. She is the founder and CEO of Skin Type Solutions Franchise Systems LLC.
The team and I
As a physician or a patient, you probably have noticed that the quality of health care is better when there is a continuous relationship between the physician and the patient. Discontinuity can make doctor-patient communication less fluid, but familiarity can breed comfort and confidence. Patients often complain when they see a different physician at every visit. And physicians know they are less efficient when they are seeing a patient they have never seen before.
They discovered that less continuity was associated with more ambulatory sick visits and more ambulatory sensitive hospitalizations, particularly for children with chronic conditions. Interestingly, they could find no association between continuity measured at well visits and patients’ health outcomes.
With only a gut level and personal relationship with the subject, I wondered how the researchers measured something as nebulous as continuity. It turns out there are several ways to measure continuity, of which the investigators focused on two. The Usual Provider of Care is calculated by dividing the number of visits with the most common provider by the total number of primary care visits. The Bice and Boxerman Continuity of Care Index is more difficult to calculate because, rather than using a single provider, it lumps a small core of providers together (such as a team) as the most the common provider.
As a curmudgeonly, old school, egotistical kind of guy, I was surprised and disappointed to learn from this paper’s references of another study that found, in at least one scenario, the individual-based (Usual Provider of Care) and team-based (Bice and Boxerman Continuity of Care Index) methods of defining continuity yielded comparable results (Med Care. 2016 May;54[5]:e30-4). I always have assumed that, regardless of how well it had been crafted, that I could provide better continuity than a team of providers.
I know what you are thinking: This guy hasn’t bought into the maxim that “There is no I in team.” No, no, I do believe in it, but in the context of continuity of care, it seemed to me that sometimes the more links there are in the chain, the more chances there are for miscommunication. And we all know that primary care is 90% communication.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine, for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.” Email him at [email protected].
As a physician or a patient, you probably have noticed that the quality of health care is better when there is a continuous relationship between the physician and the patient. Discontinuity can make doctor-patient communication less fluid, but familiarity can breed comfort and confidence. Patients often complain when they see a different physician at every visit. And physicians know they are less efficient when they are seeing a patient they have never seen before.
They discovered that less continuity was associated with more ambulatory sick visits and more ambulatory sensitive hospitalizations, particularly for children with chronic conditions. Interestingly, they could find no association between continuity measured at well visits and patients’ health outcomes.
With only a gut level and personal relationship with the subject, I wondered how the researchers measured something as nebulous as continuity. It turns out there are several ways to measure continuity, of which the investigators focused on two. The Usual Provider of Care is calculated by dividing the number of visits with the most common provider by the total number of primary care visits. The Bice and Boxerman Continuity of Care Index is more difficult to calculate because, rather than using a single provider, it lumps a small core of providers together (such as a team) as the most the common provider.
As a curmudgeonly, old school, egotistical kind of guy, I was surprised and disappointed to learn from this paper’s references of another study that found, in at least one scenario, the individual-based (Usual Provider of Care) and team-based (Bice and Boxerman Continuity of Care Index) methods of defining continuity yielded comparable results (Med Care. 2016 May;54[5]:e30-4). I always have assumed that, regardless of how well it had been crafted, that I could provide better continuity than a team of providers.
I know what you are thinking: This guy hasn’t bought into the maxim that “There is no I in team.” No, no, I do believe in it, but in the context of continuity of care, it seemed to me that sometimes the more links there are in the chain, the more chances there are for miscommunication. And we all know that primary care is 90% communication.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine, for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.” Email him at [email protected].
As a physician or a patient, you probably have noticed that the quality of health care is better when there is a continuous relationship between the physician and the patient. Discontinuity can make doctor-patient communication less fluid, but familiarity can breed comfort and confidence. Patients often complain when they see a different physician at every visit. And physicians know they are less efficient when they are seeing a patient they have never seen before.
They discovered that less continuity was associated with more ambulatory sick visits and more ambulatory sensitive hospitalizations, particularly for children with chronic conditions. Interestingly, they could find no association between continuity measured at well visits and patients’ health outcomes.
With only a gut level and personal relationship with the subject, I wondered how the researchers measured something as nebulous as continuity. It turns out there are several ways to measure continuity, of which the investigators focused on two. The Usual Provider of Care is calculated by dividing the number of visits with the most common provider by the total number of primary care visits. The Bice and Boxerman Continuity of Care Index is more difficult to calculate because, rather than using a single provider, it lumps a small core of providers together (such as a team) as the most the common provider.
As a curmudgeonly, old school, egotistical kind of guy, I was surprised and disappointed to learn from this paper’s references of another study that found, in at least one scenario, the individual-based (Usual Provider of Care) and team-based (Bice and Boxerman Continuity of Care Index) methods of defining continuity yielded comparable results (Med Care. 2016 May;54[5]:e30-4). I always have assumed that, regardless of how well it had been crafted, that I could provide better continuity than a team of providers.
I know what you are thinking: This guy hasn’t bought into the maxim that “There is no I in team.” No, no, I do believe in it, but in the context of continuity of care, it seemed to me that sometimes the more links there are in the chain, the more chances there are for miscommunication. And we all know that primary care is 90% communication.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine, for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.” Email him at [email protected].
Successful teams
As physicians, we know, and have been taught, that success comes from being smart and answering questions correctly. By doing so, we excelled in school, scored high on standardized tests, and confidently raised our hands in class. As a result, we were chosen for plum assignments like class officer, yearbook editor, and team captain. Success bred success and we were initiated into honor societies, accepted into prestigious internships, and allowed to work on important research projects.
These achievements guaranteed further success in medical school where the tradition of competition continued as we positioned for the attention of those who would someday write our letters of recommendation. This model of individual success served us very well until we joined a hematology group to begin our practice.
When we join a group of physicians, we join a team. The team might organize around diagnoses, laboratories, or geographic location, but it is a team nonetheless. The team, of course, includes more than just physicians. As a team member, we are expected to fulfill a role that advances the mission of the team and the larger organization. That mission may include some combination of academic, educational, and clinical productivity.
As physicians trained to compete with other individuals, teamwork does not come naturally. We might think that so long as the team consists of more and mor
As Margaret Heffernan brilliantly points out in “Margaret Heffernan: Why it’s time to forget the pecking order at work,” a TED talk video posted on YouTube, teams consisting of those skilled in interpersonal relationships are much more effective, efficient, and productive than are teams consisting of those skilled in problem-solving with superior IQs. The teams that function most successfully are those that create a culture of trust and helpfulness no matter the individual talents of those on the team.
As a department chair, I try to see past the thickness of the CV to ensure that I see into the person’s ability to relate with other people. If the CV is thick and the emotional intelligence high, then that is the person I want on my team, but I would rather have the latter than the former, and so would teammates and patients.
Research has shown repeatedly that no individuals can hope to achieve on their own what a good, functional team can achieve as a group. Yet, the academic hierarchy rewards individuals, not teams. Hopefully, the rewarded individual will recognize the support and effort of the team, but that is not always the case and not always done adequately.
How can academic departments develop social capital in their teams and reward them, in addition to individuals, for their successes? Social capital grows when the relationships between people become stronger. Those bonds develop though informal interaction outside the work environment. The more the team knows each other, the more they trust each other, the more they are willing to help each other, and the more they are likely to be civil to one another. Teams of friends are much more likely to solve problems quickly for less cost than teams of strangers.
Reward and recognition for a team is not as easy as it sounds. Everyone wants individual recognition for their work, not just as an integral member of a team. The world loves All-Stars and MVPs as much as they love their teams. We do not need to change the way we reward individuals, but we do need to also include teams for reward and recognition. How can a leader determine which teams are most deserving of the highest reward? Many institutions measure employee engagement through surveys. High-functioning teams are likely to be highly engaged and high scores on surveys should be recognized and rewarded. Teams with low employee turnover help reduce training costs and should be appreciated.
Successful implementation of continuous improvement projects are an often overlooked opportunity for an expression of gratitude. I am sure there are other ways to acknowledge a team’s efforts and I hope readers will write to us with their ideas for all to share. Perhaps by doing so, we can accelerate the cultural transformation of academic medicine from one of personal achievement to one of team success.
Dr. Kalaycio is editor in chief of Hematology News. He chairs the department of hematologic oncology and blood disorders at Cleveland Clinic Taussig Cancer Institute. Contact him at [email protected].
As physicians, we know, and have been taught, that success comes from being smart and answering questions correctly. By doing so, we excelled in school, scored high on standardized tests, and confidently raised our hands in class. As a result, we were chosen for plum assignments like class officer, yearbook editor, and team captain. Success bred success and we were initiated into honor societies, accepted into prestigious internships, and allowed to work on important research projects.
These achievements guaranteed further success in medical school where the tradition of competition continued as we positioned for the attention of those who would someday write our letters of recommendation. This model of individual success served us very well until we joined a hematology group to begin our practice.
When we join a group of physicians, we join a team. The team might organize around diagnoses, laboratories, or geographic location, but it is a team nonetheless. The team, of course, includes more than just physicians. As a team member, we are expected to fulfill a role that advances the mission of the team and the larger organization. That mission may include some combination of academic, educational, and clinical productivity.
As physicians trained to compete with other individuals, teamwork does not come naturally. We might think that so long as the team consists of more and mor
As Margaret Heffernan brilliantly points out in “Margaret Heffernan: Why it’s time to forget the pecking order at work,” a TED talk video posted on YouTube, teams consisting of those skilled in interpersonal relationships are much more effective, efficient, and productive than are teams consisting of those skilled in problem-solving with superior IQs. The teams that function most successfully are those that create a culture of trust and helpfulness no matter the individual talents of those on the team.
As a department chair, I try to see past the thickness of the CV to ensure that I see into the person’s ability to relate with other people. If the CV is thick and the emotional intelligence high, then that is the person I want on my team, but I would rather have the latter than the former, and so would teammates and patients.
Research has shown repeatedly that no individuals can hope to achieve on their own what a good, functional team can achieve as a group. Yet, the academic hierarchy rewards individuals, not teams. Hopefully, the rewarded individual will recognize the support and effort of the team, but that is not always the case and not always done adequately.
How can academic departments develop social capital in their teams and reward them, in addition to individuals, for their successes? Social capital grows when the relationships between people become stronger. Those bonds develop though informal interaction outside the work environment. The more the team knows each other, the more they trust each other, the more they are willing to help each other, and the more they are likely to be civil to one another. Teams of friends are much more likely to solve problems quickly for less cost than teams of strangers.
Reward and recognition for a team is not as easy as it sounds. Everyone wants individual recognition for their work, not just as an integral member of a team. The world loves All-Stars and MVPs as much as they love their teams. We do not need to change the way we reward individuals, but we do need to also include teams for reward and recognition. How can a leader determine which teams are most deserving of the highest reward? Many institutions measure employee engagement through surveys. High-functioning teams are likely to be highly engaged and high scores on surveys should be recognized and rewarded. Teams with low employee turnover help reduce training costs and should be appreciated.
Successful implementation of continuous improvement projects are an often overlooked opportunity for an expression of gratitude. I am sure there are other ways to acknowledge a team’s efforts and I hope readers will write to us with their ideas for all to share. Perhaps by doing so, we can accelerate the cultural transformation of academic medicine from one of personal achievement to one of team success.
Dr. Kalaycio is editor in chief of Hematology News. He chairs the department of hematologic oncology and blood disorders at Cleveland Clinic Taussig Cancer Institute. Contact him at [email protected].
As physicians, we know, and have been taught, that success comes from being smart and answering questions correctly. By doing so, we excelled in school, scored high on standardized tests, and confidently raised our hands in class. As a result, we were chosen for plum assignments like class officer, yearbook editor, and team captain. Success bred success and we were initiated into honor societies, accepted into prestigious internships, and allowed to work on important research projects.
These achievements guaranteed further success in medical school where the tradition of competition continued as we positioned for the attention of those who would someday write our letters of recommendation. This model of individual success served us very well until we joined a hematology group to begin our practice.
When we join a group of physicians, we join a team. The team might organize around diagnoses, laboratories, or geographic location, but it is a team nonetheless. The team, of course, includes more than just physicians. As a team member, we are expected to fulfill a role that advances the mission of the team and the larger organization. That mission may include some combination of academic, educational, and clinical productivity.
As physicians trained to compete with other individuals, teamwork does not come naturally. We might think that so long as the team consists of more and mor
As Margaret Heffernan brilliantly points out in “Margaret Heffernan: Why it’s time to forget the pecking order at work,” a TED talk video posted on YouTube, teams consisting of those skilled in interpersonal relationships are much more effective, efficient, and productive than are teams consisting of those skilled in problem-solving with superior IQs. The teams that function most successfully are those that create a culture of trust and helpfulness no matter the individual talents of those on the team.
As a department chair, I try to see past the thickness of the CV to ensure that I see into the person’s ability to relate with other people. If the CV is thick and the emotional intelligence high, then that is the person I want on my team, but I would rather have the latter than the former, and so would teammates and patients.
Research has shown repeatedly that no individuals can hope to achieve on their own what a good, functional team can achieve as a group. Yet, the academic hierarchy rewards individuals, not teams. Hopefully, the rewarded individual will recognize the support and effort of the team, but that is not always the case and not always done adequately.
How can academic departments develop social capital in their teams and reward them, in addition to individuals, for their successes? Social capital grows when the relationships between people become stronger. Those bonds develop though informal interaction outside the work environment. The more the team knows each other, the more they trust each other, the more they are willing to help each other, and the more they are likely to be civil to one another. Teams of friends are much more likely to solve problems quickly for less cost than teams of strangers.
Reward and recognition for a team is not as easy as it sounds. Everyone wants individual recognition for their work, not just as an integral member of a team. The world loves All-Stars and MVPs as much as they love their teams. We do not need to change the way we reward individuals, but we do need to also include teams for reward and recognition. How can a leader determine which teams are most deserving of the highest reward? Many institutions measure employee engagement through surveys. High-functioning teams are likely to be highly engaged and high scores on surveys should be recognized and rewarded. Teams with low employee turnover help reduce training costs and should be appreciated.
Successful implementation of continuous improvement projects are an often overlooked opportunity for an expression of gratitude. I am sure there are other ways to acknowledge a team’s efforts and I hope readers will write to us with their ideas for all to share. Perhaps by doing so, we can accelerate the cultural transformation of academic medicine from one of personal achievement to one of team success.
Dr. Kalaycio is editor in chief of Hematology News. He chairs the department of hematologic oncology and blood disorders at Cleveland Clinic Taussig Cancer Institute. Contact him at [email protected].
PANS and PANDAS – A step forward?
In the Journal of Child and Adolescent Psychopharmacology’s July 2017 issue, a group of respected individuals representing diverse expertise published “guidelines” to support clinical management of pediatric acute-onset neuropsychiatric syndrome (PANS) and its subclass PANDAS (those associated with streptococcal infection). PANS represents an enigmatic clinical syndrome that includes abrupt onset of obsessive-compulsive disorder (OCD) or eating restriction in combination with anxiety, attention deficit, hyperkinesia, emotional lability, irritability, aggressive or oppositional behavior, or academic decline. Neurologic findings also may be present; these are most often motor or vocal tics, but choreiform movements of the finger (repetitive motions that are rapid, jerky, and involuntary), deteriorating penmanship, sleep disruptions, or urinary frequency also may be present. The clinical course most often is relapsing and remitting with overall improvement over months or years.
(J Child Adolesc Psychopharmacol. 2017 Apr 7. doi: 10.1089/cap.2016.0151).
Specific recommendations include:
1. Searching for a coexisting infectious etiology with history, exam, and appropriate laboratory testing (including ASO and ADB antibodies), and, when present, treating accordingly. Even in the absence of definitive evidence of GAS infection, they recommend an initial course of antimicrobial therapy such as that given to patients with rheumatic fever.
2. For children with PANDAS (PANS with either culture or serologic evidence of GAS), consider instituting long-term streptococcal prophylaxis. The data on its value is mixed; however, most studies find more than 40% (and as many as 75%) of exacerbations are associated with GAS, and at least one study reports a reduction in neuropsychiatric exacerbations in children on penicillin or azithromycin prophylaxis for a 1-year period. Such decisions should be individualized: In children with strong evidence of exacerbations linked to GAS, there was thought to be greater likelihood of benefit, while, in those with no evidence for prior GAS infection, the potential for benefit was thought to be insufficient to justify prophylaxis. Furthermore, the optimal duration of prophylaxis is unknown. The guidelines recommend up to 2 years, but individualization is appropriate since severe cases may warrant prolonged prophylaxis.
3. In children who present with PANDAS and a positive throat culture for GAS, follow-up should be the same as that given for rheumatic fever, with reculture at 2-7 days and retreatment if there is persistence of GAS.
4. Vigilance for GAS infection in family members is appropriate, including obtaining throat cultures from persons with pharyngitis and treating them promptly when results are positive.
5. When GAS infection is not identified, the clinician should search for alternative infectious agents, such as Mycoplasma pneumoniae (using polymerase chain reaction on throat or nasopharyngeal swab), influenza virus, or alternative infections such as sinusitis, and treat accordingly.
6. Children with PANS and PANDAS should be immunized according to Advisory Committee of Immunization Practices recommendations, which includes annual influenza immunization. The committee reported that symptom flares after immunization were uncommon, brief, and manageable with NSAIDs.
7. The committee suggested that optimization of serum vitamin D levels among children with PANS and PANDAS could be of benefit, despite limited evidence. The committee members recommended treating children with PANS/PANDAS with vitamin D3 as needed to maintain serum 25-hydroxy vitamin D levels above 30 ng/mL. No benefit for adenotonsillectomy was identified. The committee recommended that tonsillectomy and/or adenoidectomy should limited to those with traditional indications (sleep apnea, failure to thrive, and abnormally large tonsils, etc.). The committee also found no evidence to suggest that probiotics modulate this condition.
These guidelines come with an important caveat. They represent a practical clinical approach for the management of infection in the context of PANS or PANDAS and rely heavily on the clinical experience of the members of the PANS/PANDAS Consortium. They provide criteria for the retrospective diagnosis of GAS infection and recommend treatment of GAS in all patients with newly diagnosed PANS. The suggested guidelines are supported by limited data and recognize that further prospective study of the mechanistic link between infection and PANS, clarification of the risk factors for development of PANS, and definitive study of the risks and benefits of antimicrobial prophylaxis are needed.
The consortium also has published two accompanying guidelines that address psychiatric (J Child Adolesc Psychopharmacol. 2017. doi: 10.1089/cap.2016.0145) and immunomodulatory management (J Child Adolesc Psychopharmacol. 2017. doi: 10.1089/cap.2016.0148) in the same issue of the Journal of Child and Adolescent Psychopharmacology.
Proposed criteria for documenting GAS infection in PANS pediatric patients
- A rise in serial antibody level, regardless of rapid test or culture result. This definition does not require clinical pharyngitis.
- Acute pharyngitis with a positive GAS throat culture, with or without a rising antibody level.
- Pharyngitis with characteristic palatal petechiae.
- Pharyngitis with a characteristic scarlatiniform rash.
- Pharyngitis without a throat swab or serology, but intimate (usually household) exposure to a proven GAS case.
- Asymptomatic pharyngeal colonization documented after an intimate exposure.
- Asymptomatic pharyngeal colonization after a negative throat swab documented within the prior 3-4 months.
- Single ASO or ADB antibody level within 6 months after the initial onset of neuropsychiatric symptoms may be accepted as positive if it is more than 95th percentile, using the laboratory’s normal standard for children of comparable age, or provisionally ASO greater than or equal to 1:480 or ADB greater than or equal to 1:1280.
- Both ASO and ADB are elevated at more than 80% percentile for age in the same serum sample within 6 months after the initial onset of neuropsychiatric symptoms.
- Culture-documented streptococcal dermatitis.
Source: J Child Adolesc Psychopharmacol. 2017. doi: 10.1089/cap.2016.0151.
Dr. Pelton is chief of pediatric infectious disease and coordinator of the maternal-child HIV program at Boston Medical Center. Dr. Pelton said he had no relevant financial disclosures. Email him at [email protected].
In the Journal of Child and Adolescent Psychopharmacology’s July 2017 issue, a group of respected individuals representing diverse expertise published “guidelines” to support clinical management of pediatric acute-onset neuropsychiatric syndrome (PANS) and its subclass PANDAS (those associated with streptococcal infection). PANS represents an enigmatic clinical syndrome that includes abrupt onset of obsessive-compulsive disorder (OCD) or eating restriction in combination with anxiety, attention deficit, hyperkinesia, emotional lability, irritability, aggressive or oppositional behavior, or academic decline. Neurologic findings also may be present; these are most often motor or vocal tics, but choreiform movements of the finger (repetitive motions that are rapid, jerky, and involuntary), deteriorating penmanship, sleep disruptions, or urinary frequency also may be present. The clinical course most often is relapsing and remitting with overall improvement over months or years.
(J Child Adolesc Psychopharmacol. 2017 Apr 7. doi: 10.1089/cap.2016.0151).
Specific recommendations include:
1. Searching for a coexisting infectious etiology with history, exam, and appropriate laboratory testing (including ASO and ADB antibodies), and, when present, treating accordingly. Even in the absence of definitive evidence of GAS infection, they recommend an initial course of antimicrobial therapy such as that given to patients with rheumatic fever.
2. For children with PANDAS (PANS with either culture or serologic evidence of GAS), consider instituting long-term streptococcal prophylaxis. The data on its value is mixed; however, most studies find more than 40% (and as many as 75%) of exacerbations are associated with GAS, and at least one study reports a reduction in neuropsychiatric exacerbations in children on penicillin or azithromycin prophylaxis for a 1-year period. Such decisions should be individualized: In children with strong evidence of exacerbations linked to GAS, there was thought to be greater likelihood of benefit, while, in those with no evidence for prior GAS infection, the potential for benefit was thought to be insufficient to justify prophylaxis. Furthermore, the optimal duration of prophylaxis is unknown. The guidelines recommend up to 2 years, but individualization is appropriate since severe cases may warrant prolonged prophylaxis.
3. In children who present with PANDAS and a positive throat culture for GAS, follow-up should be the same as that given for rheumatic fever, with reculture at 2-7 days and retreatment if there is persistence of GAS.
4. Vigilance for GAS infection in family members is appropriate, including obtaining throat cultures from persons with pharyngitis and treating them promptly when results are positive.
5. When GAS infection is not identified, the clinician should search for alternative infectious agents, such as Mycoplasma pneumoniae (using polymerase chain reaction on throat or nasopharyngeal swab), influenza virus, or alternative infections such as sinusitis, and treat accordingly.
6. Children with PANS and PANDAS should be immunized according to Advisory Committee of Immunization Practices recommendations, which includes annual influenza immunization. The committee reported that symptom flares after immunization were uncommon, brief, and manageable with NSAIDs.
7. The committee suggested that optimization of serum vitamin D levels among children with PANS and PANDAS could be of benefit, despite limited evidence. The committee members recommended treating children with PANS/PANDAS with vitamin D3 as needed to maintain serum 25-hydroxy vitamin D levels above 30 ng/mL. No benefit for adenotonsillectomy was identified. The committee recommended that tonsillectomy and/or adenoidectomy should limited to those with traditional indications (sleep apnea, failure to thrive, and abnormally large tonsils, etc.). The committee also found no evidence to suggest that probiotics modulate this condition.
These guidelines come with an important caveat. They represent a practical clinical approach for the management of infection in the context of PANS or PANDAS and rely heavily on the clinical experience of the members of the PANS/PANDAS Consortium. They provide criteria for the retrospective diagnosis of GAS infection and recommend treatment of GAS in all patients with newly diagnosed PANS. The suggested guidelines are supported by limited data and recognize that further prospective study of the mechanistic link between infection and PANS, clarification of the risk factors for development of PANS, and definitive study of the risks and benefits of antimicrobial prophylaxis are needed.
The consortium also has published two accompanying guidelines that address psychiatric (J Child Adolesc Psychopharmacol. 2017. doi: 10.1089/cap.2016.0145) and immunomodulatory management (J Child Adolesc Psychopharmacol. 2017. doi: 10.1089/cap.2016.0148) in the same issue of the Journal of Child and Adolescent Psychopharmacology.
Proposed criteria for documenting GAS infection in PANS pediatric patients
- A rise in serial antibody level, regardless of rapid test or culture result. This definition does not require clinical pharyngitis.
- Acute pharyngitis with a positive GAS throat culture, with or without a rising antibody level.
- Pharyngitis with characteristic palatal petechiae.
- Pharyngitis with a characteristic scarlatiniform rash.
- Pharyngitis without a throat swab or serology, but intimate (usually household) exposure to a proven GAS case.
- Asymptomatic pharyngeal colonization documented after an intimate exposure.
- Asymptomatic pharyngeal colonization after a negative throat swab documented within the prior 3-4 months.
- Single ASO or ADB antibody level within 6 months after the initial onset of neuropsychiatric symptoms may be accepted as positive if it is more than 95th percentile, using the laboratory’s normal standard for children of comparable age, or provisionally ASO greater than or equal to 1:480 or ADB greater than or equal to 1:1280.
- Both ASO and ADB are elevated at more than 80% percentile for age in the same serum sample within 6 months after the initial onset of neuropsychiatric symptoms.
- Culture-documented streptococcal dermatitis.
Source: J Child Adolesc Psychopharmacol. 2017. doi: 10.1089/cap.2016.0151.
Dr. Pelton is chief of pediatric infectious disease and coordinator of the maternal-child HIV program at Boston Medical Center. Dr. Pelton said he had no relevant financial disclosures. Email him at [email protected].
In the Journal of Child and Adolescent Psychopharmacology’s July 2017 issue, a group of respected individuals representing diverse expertise published “guidelines” to support clinical management of pediatric acute-onset neuropsychiatric syndrome (PANS) and its subclass PANDAS (those associated with streptococcal infection). PANS represents an enigmatic clinical syndrome that includes abrupt onset of obsessive-compulsive disorder (OCD) or eating restriction in combination with anxiety, attention deficit, hyperkinesia, emotional lability, irritability, aggressive or oppositional behavior, or academic decline. Neurologic findings also may be present; these are most often motor or vocal tics, but choreiform movements of the finger (repetitive motions that are rapid, jerky, and involuntary), deteriorating penmanship, sleep disruptions, or urinary frequency also may be present. The clinical course most often is relapsing and remitting with overall improvement over months or years.
(J Child Adolesc Psychopharmacol. 2017 Apr 7. doi: 10.1089/cap.2016.0151).
Specific recommendations include:
1. Searching for a coexisting infectious etiology with history, exam, and appropriate laboratory testing (including ASO and ADB antibodies), and, when present, treating accordingly. Even in the absence of definitive evidence of GAS infection, they recommend an initial course of antimicrobial therapy such as that given to patients with rheumatic fever.
2. For children with PANDAS (PANS with either culture or serologic evidence of GAS), consider instituting long-term streptococcal prophylaxis. The data on its value is mixed; however, most studies find more than 40% (and as many as 75%) of exacerbations are associated with GAS, and at least one study reports a reduction in neuropsychiatric exacerbations in children on penicillin or azithromycin prophylaxis for a 1-year period. Such decisions should be individualized: In children with strong evidence of exacerbations linked to GAS, there was thought to be greater likelihood of benefit, while, in those with no evidence for prior GAS infection, the potential for benefit was thought to be insufficient to justify prophylaxis. Furthermore, the optimal duration of prophylaxis is unknown. The guidelines recommend up to 2 years, but individualization is appropriate since severe cases may warrant prolonged prophylaxis.
3. In children who present with PANDAS and a positive throat culture for GAS, follow-up should be the same as that given for rheumatic fever, with reculture at 2-7 days and retreatment if there is persistence of GAS.
4. Vigilance for GAS infection in family members is appropriate, including obtaining throat cultures from persons with pharyngitis and treating them promptly when results are positive.
5. When GAS infection is not identified, the clinician should search for alternative infectious agents, such as Mycoplasma pneumoniae (using polymerase chain reaction on throat or nasopharyngeal swab), influenza virus, or alternative infections such as sinusitis, and treat accordingly.
6. Children with PANS and PANDAS should be immunized according to Advisory Committee of Immunization Practices recommendations, which includes annual influenza immunization. The committee reported that symptom flares after immunization were uncommon, brief, and manageable with NSAIDs.
7. The committee suggested that optimization of serum vitamin D levels among children with PANS and PANDAS could be of benefit, despite limited evidence. The committee members recommended treating children with PANS/PANDAS with vitamin D3 as needed to maintain serum 25-hydroxy vitamin D levels above 30 ng/mL. No benefit for adenotonsillectomy was identified. The committee recommended that tonsillectomy and/or adenoidectomy should limited to those with traditional indications (sleep apnea, failure to thrive, and abnormally large tonsils, etc.). The committee also found no evidence to suggest that probiotics modulate this condition.
These guidelines come with an important caveat. They represent a practical clinical approach for the management of infection in the context of PANS or PANDAS and rely heavily on the clinical experience of the members of the PANS/PANDAS Consortium. They provide criteria for the retrospective diagnosis of GAS infection and recommend treatment of GAS in all patients with newly diagnosed PANS. The suggested guidelines are supported by limited data and recognize that further prospective study of the mechanistic link between infection and PANS, clarification of the risk factors for development of PANS, and definitive study of the risks and benefits of antimicrobial prophylaxis are needed.
The consortium also has published two accompanying guidelines that address psychiatric (J Child Adolesc Psychopharmacol. 2017. doi: 10.1089/cap.2016.0145) and immunomodulatory management (J Child Adolesc Psychopharmacol. 2017. doi: 10.1089/cap.2016.0148) in the same issue of the Journal of Child and Adolescent Psychopharmacology.
Proposed criteria for documenting GAS infection in PANS pediatric patients
- A rise in serial antibody level, regardless of rapid test or culture result. This definition does not require clinical pharyngitis.
- Acute pharyngitis with a positive GAS throat culture, with or without a rising antibody level.
- Pharyngitis with characteristic palatal petechiae.
- Pharyngitis with a characteristic scarlatiniform rash.
- Pharyngitis without a throat swab or serology, but intimate (usually household) exposure to a proven GAS case.
- Asymptomatic pharyngeal colonization documented after an intimate exposure.
- Asymptomatic pharyngeal colonization after a negative throat swab documented within the prior 3-4 months.
- Single ASO or ADB antibody level within 6 months after the initial onset of neuropsychiatric symptoms may be accepted as positive if it is more than 95th percentile, using the laboratory’s normal standard for children of comparable age, or provisionally ASO greater than or equal to 1:480 or ADB greater than or equal to 1:1280.
- Both ASO and ADB are elevated at more than 80% percentile for age in the same serum sample within 6 months after the initial onset of neuropsychiatric symptoms.
- Culture-documented streptococcal dermatitis.
Source: J Child Adolesc Psychopharmacol. 2017. doi: 10.1089/cap.2016.0151.
Dr. Pelton is chief of pediatric infectious disease and coordinator of the maternal-child HIV program at Boston Medical Center. Dr. Pelton said he had no relevant financial disclosures. Email him at [email protected].