User login
High-Value, Cost-Conscious Evaluation for PCOS: Which Tests Should Be Routinely Ordered in Acne Patients?
The adult female patient presenting with severe acne vulgaris may raise special diagnostic concerns, including consideration of an underlying hormonal disorder. Polycystic ovary syndrome (PCOS) is the most common endocrine disorder in women of reproductive age with an estimated prevalence as high as 12%.1 Many women with undiagnosed PCOS may be referred to dermatologists for evaluation of its cutaneous manifestations of hyperandrogenism including acne, hirsutism, and androgenic alopecia.2 Given the prevalence of PCOS and its long-term health implications, dermatologists can play an important role in the initial evaluation of these patients. Acne and androgenic alopecia, however, are quite common, and in the absence of red flags such as menstrual irregularities, virilization, visual field deficits, or signs of Cushing syndrome,3 clinicians must decide when to pursue limited versus comprehensive evaluation.
Despite being common in patients with PCOS, a recent study suggests that acne is an unreliable marker of biochemical hyperandrogenism, and specific features of acne (ie, lesion counts, lesional types, distribution) cannot reliably discriminate women who meet PCOS diagnostic criteria from those who do not.4 Similarly, the study found that androgenic alopecia was not associated with biochemical hyperandrogenism and was no more common in women with PCOS than women of similar age in a high-risk population. Unlike acne and androgenic alopecia, however, the study identified hirsutism, especially truncal hirsutism, as a reliable indicator of hyperandrogenemia and PCOS. Hirsutism also is associated with metabolic sequelae of PCOS. These findings suggest that hirsutism, but not acne or androgenic alopecia, in a female of reproductive age warrants a workup for PCOS.4 This report is consistent with a recommendation from the Androgen Excess and Polycystic Ovary Syndrome Society (AE-PCOS) to pursue a diagnostic evaluation in any woman presenting with hirsutism.5 Acanthosis nigricans also was found to be a reliable indicator of hyperandrogenemia, PCOS, and associated metabolic derangement. Thus, although recent evidence indicates that acne as an isolated cutaneous finding does not warrant further diagnostic evaluation, acne in the setting of hirsutism, acanthosis nigricans, menstrual irregularities, or additional specific signs of endocrine dysregulation should prompt focused workup.4
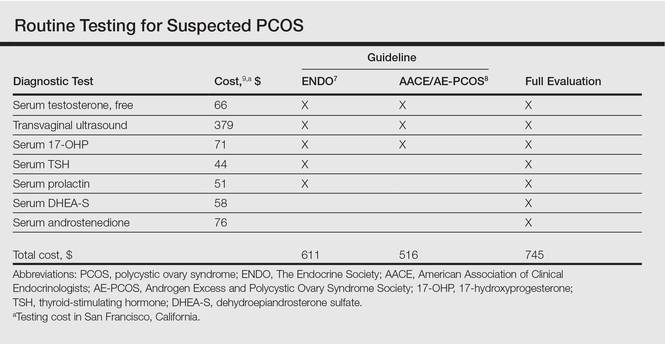
Multiple clinical practice guidelines for the evaluation of hirsutism and PCOS based on literature review and expert opinion have been proposed5-8; however, these guidelines vary in recommendations for routine diagnostic steps to exclude mimickers of PCOS such as prolactinoma/pituitary adenoma and congenital adrenal hyperplasia (CAH)(Table). In 2009, an AE-PCOS task force suggested that routine testing of thyroid function and serum prolactin in the absence of additional clinical signs may not be necessary based on the low prevalence of thyroid disorders and hyperprolactinemia in patients presenting with hyperandrogenism.6 In 2013, the Endocrine Society’s (ENDO) clinical guideline, however, recommended routine measurement of serum thyroid-stimulating hormone (TSH) to exclude thyroid disease and serum prolactin to exclude hyperprolactinemia in all women before making a diagnosis of PCOS.7 In 2015, the AE-PCOS collaborated with the American Association of Clinical Endocrinologists (AACE) and American College of Endocrinology to publish an updated guideline for best practices, which was consistent with the prior AE-PCOS recommendation in 2009 for routine screening including to test 17-hydroxyprogesterone to exclude nonclassical CAH.8
Importantly, these recommendations for routine testing for mimickers of PCOS are based on the rare prevalence of these etiologies in multiple studies of women presenting for hyperandrogenism. One study included 873 women presenting to an academic reproductive endocrine clinic for evaluation of symptoms potentially related to androgen excess. In addition to cutaneous manifestations of hirsutism, acne, and alopecia, the study also included women presenting with oligomenorrhea/amenorrhea, ovulatory dysfunction, and even virilization.10 A second study included 950 women presenting to academic endocrine departments with hirsutism, acne, or androgenic alopecia.11 Both studies defined hirsutism as having a modified Ferriman-Gallwey score of 6 or greater. Both studies also only measured serum prolactin or TSH when clinically indicated (ie, patients with ovulatory dysfunction).10,11
The diagnostic yield of tests for mimickers of PCOS was exceedingly low in both studies. For example, of the patients evaluated, only 0.4% to 0.7% had thyroid dysfunction, 0% to 0.3% had hyperprolactinemia, 0.2% had androgen-secreting neoplasms, 2.1% to 4.3% had nonclassical CAH, 0.7% had CAH, and 3.8% had HAIR-AN (hyperandrogenism, insulin resistance, and acanthosis nigricans) syndrome.10,11 Because patients in both studies were only tested for hyperprolactinemia and thyroid dysfunction when clinically indicated, it is probable that routine screening without clinical indication would result in even lower yields.
Given the increasing importance of high-value, cost-conscious care,12 clinicians must consider the costs associated with testing in the face of low pretest probability. Although some studies have examined the cost-effectiveness of fertility treatments in PCOS,13,14 no studies have examined the cost-effectiveness of diagnostic strategies for PCOS. Cost-effectiveness studies are emerging to provide important guidance on high-value, cost-conscious diagnostic evaluation and monitoring15 and are much needed in dermatology.16,17
In the case of PCOS, the costs of some diagnostic tests are relatively low. For example, based on estimates from Healthcare Bluebook,9 serum TSH and prolactin tests in San Francisco, California, are $44 and $51, respectively. However, the cumulative costs for even the most stringent routine workup for PCOS recommended in the AACE/AE-PCOS guideline consisting of a free testosterone measurement, 17-hydroxyprogesterone, and transvaginal ultrasound would still cost a total of $516. Additional TSH and prolactin tests recommended by ENDO would increase the cost of PCOS testing by approximately 18%. Routine testing for additional serum androgens—dehydroepiandrosterone sulfate (DHEA-S) and androstenedione—would further increase this amount by an additional $134 to a total cost of $745. The ENDO guideline only recommends DHEA-S testing to assist in the diagnosis of an androgen-secreting tumor when signs of virilization are present, while the AACE/AE-PCOS guideline discourages routine testing for DHEA-S and androstenedione based on the low frequency of cases in which these androgens are elevated in isolation.7,8
Although the selection of tests influences total cost, the setting of tests (ie, hospitals, physician offices, independent test settings) also can contribute to wide variations in cost. For example, Healthcare Bluebook’s estimates for transvaginal ultrasound in Chicago, Illinois, range from $236 to more than $740.9 When the separate physician visit fees are included, the total cost of a routine diagnostic evaluation of a patient with acne or hirsutism concerning for PCOS is not trivial.
Large national clinical registries and formal cost-effectiveness analyses are necessary to shed light on this issue, but it is clear that clinicians should rely on their clinical judgment when ordering laboratory tests in the evaluation for PCOS given the apparent low yield of routine screening for PCOS mimickers in the absence of clinical indications. For example, a TSH would not be warranted in a patient without evidence of thyroid dysfunction (ie, weight gain, fatigue, constipation, menstrual irregularities). Similarly, clinicians should routinely consider the principle of high-value care: whether the results of a test will change management of the patient. For example, a woman with amenorrhea and severe acne who already meets diagnostic criteria for PCOS would benefit from a combined oral contraceptive for both acne and endometrial protection. An ovarian ultrasound may not be needed to confirm the diagnosis unless there is suspicion for an ovarian condition other than PCOS causing the symptoms.
Finally, clinicians should discuss testing options and involve patients in decisions around testing. Although PCOS treatments generally target individual symptoms rather than the syndrome as a whole, confirmation of a PCOS diagnosis importantly informs women of their risk for cardiovascular and metabolic disease. The ENDO recommends screening for impaired glucose tolerance, type 2 diabetes mellitus, obesity, family history of early cardiovascular disease, tobacco use, hypertension, dyslipidemia, and obstructive sleep apnea in all women with PCOS, including nonobese patients.7 Ongoing efforts to gain and understand evidence to support high-value, cost-conscious care should be prioritized and kept in balance with shared decision-making in individual patients suspected of having PCOS.
- March WA, Moore VM, Willson KJ, et al. The prevalence of polycystic ovary syndrome in a community sample assessed under contrasting diagnostic criteria. Hum Reprod. 2010;25:544-551.
- Sivayoganathan D, Maruthini D, Glanville JM, et al. Full investigation of patients with polycystic ovary syndrome (PCOS) presenting to four different clinical specialties reveals significant differences and undiagnosed morbidity. Hum Fertil. 2011;14:261-265.
- Schmidt TH, Shinkai K. Evidence-based approach to cutaneous hyperandrogenism in women. J Am Acad Dermatol. 2015;73:672-690.
- Schmidt TH, Khanijow K, Cedars MI, et al. Cutaneous findings and systemic associations in women with polycystic ovary syndrome. JAMA Dermatol. 2015;152:391-398.
- Escobar-Morreale HF, Carmina E, Dewailly D, et al. Epidemiology, diagnosis and management of hirsutism: a consensus statement by the Androgen Excess and Polycystic Ovary Syndrome Society. Hum Reprod Update. 2012;18:146-170.
- Azziz R, Carmina E, Dewailly D, et al. The Androgen Excess and PCOS Society criteria for the polycystic ovary syndrome: the complete task force report. Fertil Steril. 2009;91:456-488.
- Legro RS, Arslanian SA, Ehermann DA, et al. Diagnosis and treatment of polycystic ovary syndrome: an Endocrine Society clinical practice guideline [published online October 22, 2013]. J Clin Endocrinol Metab. 2013;98:4565-4592.
- Goodman NF, Cobin RH, Futterweit W, et al. American Association of Clinical Endocrinologists, American College of Endocrinology, and Androgen Excess and PCOS Society disease state clinical review: guide to the best practices in the evaluation and treatment of polycystic ovary syndrome—part 1. Endocr Pract. 2015;21:1291-1300.
- Healthcare Bluebook. https://healthcarebluebook.com. Accessed June 13, 2016.
- Azziz R, Sanchez LA, Knochenhauer ES, et al. Androgen excess in women: experience with over 1000 consecutive patients. J Clin Endocrinol Metab. 2004;89:453-462.
- Carmina E, Rosato F, Jannì A, et al. Relative prevalence of different androgen excess disorders in 950 women referred because of clinical hyperandrogenism [published online November 1, 2005]. J Clin Endocrinol Metab. 2006;91:2-6.
- Owens DK, Qaseem A, Chou R, et al. High-value, cost-conscious health care: concepts for clinicians to evaluate the benefits, harms, and costs of medical interventions. Ann Intern Med. 2011;154:174-180.
- Nahuis MJ, Oude Lohuis E, Kose N, et al. Long-term follow-up of laparoscopic electrocautery of the ovaries versus ovulation induction with recombinant FSH in clomiphene citrate-resistant women with polycystic ovary syndrome: an economic evaluation. Hum Reprod Oxf Engl. 2012;27:3577-3582.
- Moolenaar LM, Nahuis MJ, Hompes PG, et al. Cost-effectiveness of treatment strategies in women with PCOS who do not conceive after six cycles of clomiphene citrate. Reprod Biomed Online. 2014;28:606-613.
- Chogle A, Saps M. Yield and cost of performing screening tests for constipation in children. Can J Gastroenterol. 2013;27:E35-E38.
- Lee YH, Scharnitz TP, Muscat J, et al. Laboratory monitoring during isotretinoin therapy for acne: a systematic review and meta-analysis. JAMA Dermatol. 2016;152:35-44.
- Shinkai K, McMichael A, Linos E. Isotretinoin laboratory test monitoring—a call to decrease testing in an era of high-value, cost-conscious care. JAMA Dermatol. 2016;152:17-19.
The adult female patient presenting with severe acne vulgaris may raise special diagnostic concerns, including consideration of an underlying hormonal disorder. Polycystic ovary syndrome (PCOS) is the most common endocrine disorder in women of reproductive age with an estimated prevalence as high as 12%.1 Many women with undiagnosed PCOS may be referred to dermatologists for evaluation of its cutaneous manifestations of hyperandrogenism including acne, hirsutism, and androgenic alopecia.2 Given the prevalence of PCOS and its long-term health implications, dermatologists can play an important role in the initial evaluation of these patients. Acne and androgenic alopecia, however, are quite common, and in the absence of red flags such as menstrual irregularities, virilization, visual field deficits, or signs of Cushing syndrome,3 clinicians must decide when to pursue limited versus comprehensive evaluation.
Despite being common in patients with PCOS, a recent study suggests that acne is an unreliable marker of biochemical hyperandrogenism, and specific features of acne (ie, lesion counts, lesional types, distribution) cannot reliably discriminate women who meet PCOS diagnostic criteria from those who do not.4 Similarly, the study found that androgenic alopecia was not associated with biochemical hyperandrogenism and was no more common in women with PCOS than women of similar age in a high-risk population. Unlike acne and androgenic alopecia, however, the study identified hirsutism, especially truncal hirsutism, as a reliable indicator of hyperandrogenemia and PCOS. Hirsutism also is associated with metabolic sequelae of PCOS. These findings suggest that hirsutism, but not acne or androgenic alopecia, in a female of reproductive age warrants a workup for PCOS.4 This report is consistent with a recommendation from the Androgen Excess and Polycystic Ovary Syndrome Society (AE-PCOS) to pursue a diagnostic evaluation in any woman presenting with hirsutism.5 Acanthosis nigricans also was found to be a reliable indicator of hyperandrogenemia, PCOS, and associated metabolic derangement. Thus, although recent evidence indicates that acne as an isolated cutaneous finding does not warrant further diagnostic evaluation, acne in the setting of hirsutism, acanthosis nigricans, menstrual irregularities, or additional specific signs of endocrine dysregulation should prompt focused workup.4
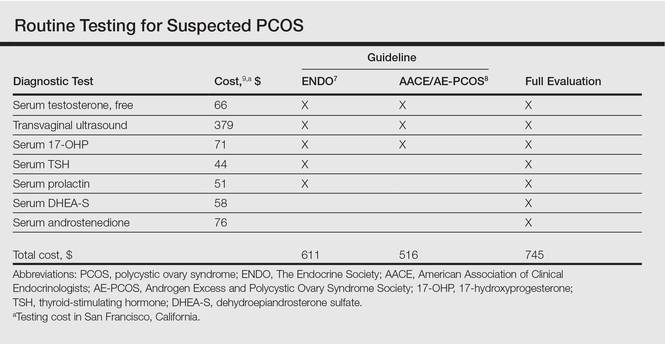
Multiple clinical practice guidelines for the evaluation of hirsutism and PCOS based on literature review and expert opinion have been proposed5-8; however, these guidelines vary in recommendations for routine diagnostic steps to exclude mimickers of PCOS such as prolactinoma/pituitary adenoma and congenital adrenal hyperplasia (CAH)(Table). In 2009, an AE-PCOS task force suggested that routine testing of thyroid function and serum prolactin in the absence of additional clinical signs may not be necessary based on the low prevalence of thyroid disorders and hyperprolactinemia in patients presenting with hyperandrogenism.6 In 2013, the Endocrine Society’s (ENDO) clinical guideline, however, recommended routine measurement of serum thyroid-stimulating hormone (TSH) to exclude thyroid disease and serum prolactin to exclude hyperprolactinemia in all women before making a diagnosis of PCOS.7 In 2015, the AE-PCOS collaborated with the American Association of Clinical Endocrinologists (AACE) and American College of Endocrinology to publish an updated guideline for best practices, which was consistent with the prior AE-PCOS recommendation in 2009 for routine screening including to test 17-hydroxyprogesterone to exclude nonclassical CAH.8
Importantly, these recommendations for routine testing for mimickers of PCOS are based on the rare prevalence of these etiologies in multiple studies of women presenting for hyperandrogenism. One study included 873 women presenting to an academic reproductive endocrine clinic for evaluation of symptoms potentially related to androgen excess. In addition to cutaneous manifestations of hirsutism, acne, and alopecia, the study also included women presenting with oligomenorrhea/amenorrhea, ovulatory dysfunction, and even virilization.10 A second study included 950 women presenting to academic endocrine departments with hirsutism, acne, or androgenic alopecia.11 Both studies defined hirsutism as having a modified Ferriman-Gallwey score of 6 or greater. Both studies also only measured serum prolactin or TSH when clinically indicated (ie, patients with ovulatory dysfunction).10,11
The diagnostic yield of tests for mimickers of PCOS was exceedingly low in both studies. For example, of the patients evaluated, only 0.4% to 0.7% had thyroid dysfunction, 0% to 0.3% had hyperprolactinemia, 0.2% had androgen-secreting neoplasms, 2.1% to 4.3% had nonclassical CAH, 0.7% had CAH, and 3.8% had HAIR-AN (hyperandrogenism, insulin resistance, and acanthosis nigricans) syndrome.10,11 Because patients in both studies were only tested for hyperprolactinemia and thyroid dysfunction when clinically indicated, it is probable that routine screening without clinical indication would result in even lower yields.
Given the increasing importance of high-value, cost-conscious care,12 clinicians must consider the costs associated with testing in the face of low pretest probability. Although some studies have examined the cost-effectiveness of fertility treatments in PCOS,13,14 no studies have examined the cost-effectiveness of diagnostic strategies for PCOS. Cost-effectiveness studies are emerging to provide important guidance on high-value, cost-conscious diagnostic evaluation and monitoring15 and are much needed in dermatology.16,17
In the case of PCOS, the costs of some diagnostic tests are relatively low. For example, based on estimates from Healthcare Bluebook,9 serum TSH and prolactin tests in San Francisco, California, are $44 and $51, respectively. However, the cumulative costs for even the most stringent routine workup for PCOS recommended in the AACE/AE-PCOS guideline consisting of a free testosterone measurement, 17-hydroxyprogesterone, and transvaginal ultrasound would still cost a total of $516. Additional TSH and prolactin tests recommended by ENDO would increase the cost of PCOS testing by approximately 18%. Routine testing for additional serum androgens—dehydroepiandrosterone sulfate (DHEA-S) and androstenedione—would further increase this amount by an additional $134 to a total cost of $745. The ENDO guideline only recommends DHEA-S testing to assist in the diagnosis of an androgen-secreting tumor when signs of virilization are present, while the AACE/AE-PCOS guideline discourages routine testing for DHEA-S and androstenedione based on the low frequency of cases in which these androgens are elevated in isolation.7,8
Although the selection of tests influences total cost, the setting of tests (ie, hospitals, physician offices, independent test settings) also can contribute to wide variations in cost. For example, Healthcare Bluebook’s estimates for transvaginal ultrasound in Chicago, Illinois, range from $236 to more than $740.9 When the separate physician visit fees are included, the total cost of a routine diagnostic evaluation of a patient with acne or hirsutism concerning for PCOS is not trivial.
Large national clinical registries and formal cost-effectiveness analyses are necessary to shed light on this issue, but it is clear that clinicians should rely on their clinical judgment when ordering laboratory tests in the evaluation for PCOS given the apparent low yield of routine screening for PCOS mimickers in the absence of clinical indications. For example, a TSH would not be warranted in a patient without evidence of thyroid dysfunction (ie, weight gain, fatigue, constipation, menstrual irregularities). Similarly, clinicians should routinely consider the principle of high-value care: whether the results of a test will change management of the patient. For example, a woman with amenorrhea and severe acne who already meets diagnostic criteria for PCOS would benefit from a combined oral contraceptive for both acne and endometrial protection. An ovarian ultrasound may not be needed to confirm the diagnosis unless there is suspicion for an ovarian condition other than PCOS causing the symptoms.
Finally, clinicians should discuss testing options and involve patients in decisions around testing. Although PCOS treatments generally target individual symptoms rather than the syndrome as a whole, confirmation of a PCOS diagnosis importantly informs women of their risk for cardiovascular and metabolic disease. The ENDO recommends screening for impaired glucose tolerance, type 2 diabetes mellitus, obesity, family history of early cardiovascular disease, tobacco use, hypertension, dyslipidemia, and obstructive sleep apnea in all women with PCOS, including nonobese patients.7 Ongoing efforts to gain and understand evidence to support high-value, cost-conscious care should be prioritized and kept in balance with shared decision-making in individual patients suspected of having PCOS.
The adult female patient presenting with severe acne vulgaris may raise special diagnostic concerns, including consideration of an underlying hormonal disorder. Polycystic ovary syndrome (PCOS) is the most common endocrine disorder in women of reproductive age with an estimated prevalence as high as 12%.1 Many women with undiagnosed PCOS may be referred to dermatologists for evaluation of its cutaneous manifestations of hyperandrogenism including acne, hirsutism, and androgenic alopecia.2 Given the prevalence of PCOS and its long-term health implications, dermatologists can play an important role in the initial evaluation of these patients. Acne and androgenic alopecia, however, are quite common, and in the absence of red flags such as menstrual irregularities, virilization, visual field deficits, or signs of Cushing syndrome,3 clinicians must decide when to pursue limited versus comprehensive evaluation.
Despite being common in patients with PCOS, a recent study suggests that acne is an unreliable marker of biochemical hyperandrogenism, and specific features of acne (ie, lesion counts, lesional types, distribution) cannot reliably discriminate women who meet PCOS diagnostic criteria from those who do not.4 Similarly, the study found that androgenic alopecia was not associated with biochemical hyperandrogenism and was no more common in women with PCOS than women of similar age in a high-risk population. Unlike acne and androgenic alopecia, however, the study identified hirsutism, especially truncal hirsutism, as a reliable indicator of hyperandrogenemia and PCOS. Hirsutism also is associated with metabolic sequelae of PCOS. These findings suggest that hirsutism, but not acne or androgenic alopecia, in a female of reproductive age warrants a workup for PCOS.4 This report is consistent with a recommendation from the Androgen Excess and Polycystic Ovary Syndrome Society (AE-PCOS) to pursue a diagnostic evaluation in any woman presenting with hirsutism.5 Acanthosis nigricans also was found to be a reliable indicator of hyperandrogenemia, PCOS, and associated metabolic derangement. Thus, although recent evidence indicates that acne as an isolated cutaneous finding does not warrant further diagnostic evaluation, acne in the setting of hirsutism, acanthosis nigricans, menstrual irregularities, or additional specific signs of endocrine dysregulation should prompt focused workup.4
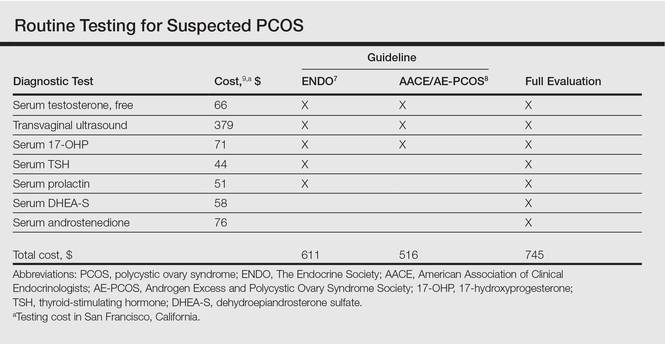
Multiple clinical practice guidelines for the evaluation of hirsutism and PCOS based on literature review and expert opinion have been proposed5-8; however, these guidelines vary in recommendations for routine diagnostic steps to exclude mimickers of PCOS such as prolactinoma/pituitary adenoma and congenital adrenal hyperplasia (CAH)(Table). In 2009, an AE-PCOS task force suggested that routine testing of thyroid function and serum prolactin in the absence of additional clinical signs may not be necessary based on the low prevalence of thyroid disorders and hyperprolactinemia in patients presenting with hyperandrogenism.6 In 2013, the Endocrine Society’s (ENDO) clinical guideline, however, recommended routine measurement of serum thyroid-stimulating hormone (TSH) to exclude thyroid disease and serum prolactin to exclude hyperprolactinemia in all women before making a diagnosis of PCOS.7 In 2015, the AE-PCOS collaborated with the American Association of Clinical Endocrinologists (AACE) and American College of Endocrinology to publish an updated guideline for best practices, which was consistent with the prior AE-PCOS recommendation in 2009 for routine screening including to test 17-hydroxyprogesterone to exclude nonclassical CAH.8
Importantly, these recommendations for routine testing for mimickers of PCOS are based on the rare prevalence of these etiologies in multiple studies of women presenting for hyperandrogenism. One study included 873 women presenting to an academic reproductive endocrine clinic for evaluation of symptoms potentially related to androgen excess. In addition to cutaneous manifestations of hirsutism, acne, and alopecia, the study also included women presenting with oligomenorrhea/amenorrhea, ovulatory dysfunction, and even virilization.10 A second study included 950 women presenting to academic endocrine departments with hirsutism, acne, or androgenic alopecia.11 Both studies defined hirsutism as having a modified Ferriman-Gallwey score of 6 or greater. Both studies also only measured serum prolactin or TSH when clinically indicated (ie, patients with ovulatory dysfunction).10,11
The diagnostic yield of tests for mimickers of PCOS was exceedingly low in both studies. For example, of the patients evaluated, only 0.4% to 0.7% had thyroid dysfunction, 0% to 0.3% had hyperprolactinemia, 0.2% had androgen-secreting neoplasms, 2.1% to 4.3% had nonclassical CAH, 0.7% had CAH, and 3.8% had HAIR-AN (hyperandrogenism, insulin resistance, and acanthosis nigricans) syndrome.10,11 Because patients in both studies were only tested for hyperprolactinemia and thyroid dysfunction when clinically indicated, it is probable that routine screening without clinical indication would result in even lower yields.
Given the increasing importance of high-value, cost-conscious care,12 clinicians must consider the costs associated with testing in the face of low pretest probability. Although some studies have examined the cost-effectiveness of fertility treatments in PCOS,13,14 no studies have examined the cost-effectiveness of diagnostic strategies for PCOS. Cost-effectiveness studies are emerging to provide important guidance on high-value, cost-conscious diagnostic evaluation and monitoring15 and are much needed in dermatology.16,17
In the case of PCOS, the costs of some diagnostic tests are relatively low. For example, based on estimates from Healthcare Bluebook,9 serum TSH and prolactin tests in San Francisco, California, are $44 and $51, respectively. However, the cumulative costs for even the most stringent routine workup for PCOS recommended in the AACE/AE-PCOS guideline consisting of a free testosterone measurement, 17-hydroxyprogesterone, and transvaginal ultrasound would still cost a total of $516. Additional TSH and prolactin tests recommended by ENDO would increase the cost of PCOS testing by approximately 18%. Routine testing for additional serum androgens—dehydroepiandrosterone sulfate (DHEA-S) and androstenedione—would further increase this amount by an additional $134 to a total cost of $745. The ENDO guideline only recommends DHEA-S testing to assist in the diagnosis of an androgen-secreting tumor when signs of virilization are present, while the AACE/AE-PCOS guideline discourages routine testing for DHEA-S and androstenedione based on the low frequency of cases in which these androgens are elevated in isolation.7,8
Although the selection of tests influences total cost, the setting of tests (ie, hospitals, physician offices, independent test settings) also can contribute to wide variations in cost. For example, Healthcare Bluebook’s estimates for transvaginal ultrasound in Chicago, Illinois, range from $236 to more than $740.9 When the separate physician visit fees are included, the total cost of a routine diagnostic evaluation of a patient with acne or hirsutism concerning for PCOS is not trivial.
Large national clinical registries and formal cost-effectiveness analyses are necessary to shed light on this issue, but it is clear that clinicians should rely on their clinical judgment when ordering laboratory tests in the evaluation for PCOS given the apparent low yield of routine screening for PCOS mimickers in the absence of clinical indications. For example, a TSH would not be warranted in a patient without evidence of thyroid dysfunction (ie, weight gain, fatigue, constipation, menstrual irregularities). Similarly, clinicians should routinely consider the principle of high-value care: whether the results of a test will change management of the patient. For example, a woman with amenorrhea and severe acne who already meets diagnostic criteria for PCOS would benefit from a combined oral contraceptive for both acne and endometrial protection. An ovarian ultrasound may not be needed to confirm the diagnosis unless there is suspicion for an ovarian condition other than PCOS causing the symptoms.
Finally, clinicians should discuss testing options and involve patients in decisions around testing. Although PCOS treatments generally target individual symptoms rather than the syndrome as a whole, confirmation of a PCOS diagnosis importantly informs women of their risk for cardiovascular and metabolic disease. The ENDO recommends screening for impaired glucose tolerance, type 2 diabetes mellitus, obesity, family history of early cardiovascular disease, tobacco use, hypertension, dyslipidemia, and obstructive sleep apnea in all women with PCOS, including nonobese patients.7 Ongoing efforts to gain and understand evidence to support high-value, cost-conscious care should be prioritized and kept in balance with shared decision-making in individual patients suspected of having PCOS.
- March WA, Moore VM, Willson KJ, et al. The prevalence of polycystic ovary syndrome in a community sample assessed under contrasting diagnostic criteria. Hum Reprod. 2010;25:544-551.
- Sivayoganathan D, Maruthini D, Glanville JM, et al. Full investigation of patients with polycystic ovary syndrome (PCOS) presenting to four different clinical specialties reveals significant differences and undiagnosed morbidity. Hum Fertil. 2011;14:261-265.
- Schmidt TH, Shinkai K. Evidence-based approach to cutaneous hyperandrogenism in women. J Am Acad Dermatol. 2015;73:672-690.
- Schmidt TH, Khanijow K, Cedars MI, et al. Cutaneous findings and systemic associations in women with polycystic ovary syndrome. JAMA Dermatol. 2015;152:391-398.
- Escobar-Morreale HF, Carmina E, Dewailly D, et al. Epidemiology, diagnosis and management of hirsutism: a consensus statement by the Androgen Excess and Polycystic Ovary Syndrome Society. Hum Reprod Update. 2012;18:146-170.
- Azziz R, Carmina E, Dewailly D, et al. The Androgen Excess and PCOS Society criteria for the polycystic ovary syndrome: the complete task force report. Fertil Steril. 2009;91:456-488.
- Legro RS, Arslanian SA, Ehermann DA, et al. Diagnosis and treatment of polycystic ovary syndrome: an Endocrine Society clinical practice guideline [published online October 22, 2013]. J Clin Endocrinol Metab. 2013;98:4565-4592.
- Goodman NF, Cobin RH, Futterweit W, et al. American Association of Clinical Endocrinologists, American College of Endocrinology, and Androgen Excess and PCOS Society disease state clinical review: guide to the best practices in the evaluation and treatment of polycystic ovary syndrome—part 1. Endocr Pract. 2015;21:1291-1300.
- Healthcare Bluebook. https://healthcarebluebook.com. Accessed June 13, 2016.
- Azziz R, Sanchez LA, Knochenhauer ES, et al. Androgen excess in women: experience with over 1000 consecutive patients. J Clin Endocrinol Metab. 2004;89:453-462.
- Carmina E, Rosato F, Jannì A, et al. Relative prevalence of different androgen excess disorders in 950 women referred because of clinical hyperandrogenism [published online November 1, 2005]. J Clin Endocrinol Metab. 2006;91:2-6.
- Owens DK, Qaseem A, Chou R, et al. High-value, cost-conscious health care: concepts for clinicians to evaluate the benefits, harms, and costs of medical interventions. Ann Intern Med. 2011;154:174-180.
- Nahuis MJ, Oude Lohuis E, Kose N, et al. Long-term follow-up of laparoscopic electrocautery of the ovaries versus ovulation induction with recombinant FSH in clomiphene citrate-resistant women with polycystic ovary syndrome: an economic evaluation. Hum Reprod Oxf Engl. 2012;27:3577-3582.
- Moolenaar LM, Nahuis MJ, Hompes PG, et al. Cost-effectiveness of treatment strategies in women with PCOS who do not conceive after six cycles of clomiphene citrate. Reprod Biomed Online. 2014;28:606-613.
- Chogle A, Saps M. Yield and cost of performing screening tests for constipation in children. Can J Gastroenterol. 2013;27:E35-E38.
- Lee YH, Scharnitz TP, Muscat J, et al. Laboratory monitoring during isotretinoin therapy for acne: a systematic review and meta-analysis. JAMA Dermatol. 2016;152:35-44.
- Shinkai K, McMichael A, Linos E. Isotretinoin laboratory test monitoring—a call to decrease testing in an era of high-value, cost-conscious care. JAMA Dermatol. 2016;152:17-19.
- March WA, Moore VM, Willson KJ, et al. The prevalence of polycystic ovary syndrome in a community sample assessed under contrasting diagnostic criteria. Hum Reprod. 2010;25:544-551.
- Sivayoganathan D, Maruthini D, Glanville JM, et al. Full investigation of patients with polycystic ovary syndrome (PCOS) presenting to four different clinical specialties reveals significant differences and undiagnosed morbidity. Hum Fertil. 2011;14:261-265.
- Schmidt TH, Shinkai K. Evidence-based approach to cutaneous hyperandrogenism in women. J Am Acad Dermatol. 2015;73:672-690.
- Schmidt TH, Khanijow K, Cedars MI, et al. Cutaneous findings and systemic associations in women with polycystic ovary syndrome. JAMA Dermatol. 2015;152:391-398.
- Escobar-Morreale HF, Carmina E, Dewailly D, et al. Epidemiology, diagnosis and management of hirsutism: a consensus statement by the Androgen Excess and Polycystic Ovary Syndrome Society. Hum Reprod Update. 2012;18:146-170.
- Azziz R, Carmina E, Dewailly D, et al. The Androgen Excess and PCOS Society criteria for the polycystic ovary syndrome: the complete task force report. Fertil Steril. 2009;91:456-488.
- Legro RS, Arslanian SA, Ehermann DA, et al. Diagnosis and treatment of polycystic ovary syndrome: an Endocrine Society clinical practice guideline [published online October 22, 2013]. J Clin Endocrinol Metab. 2013;98:4565-4592.
- Goodman NF, Cobin RH, Futterweit W, et al. American Association of Clinical Endocrinologists, American College of Endocrinology, and Androgen Excess and PCOS Society disease state clinical review: guide to the best practices in the evaluation and treatment of polycystic ovary syndrome—part 1. Endocr Pract. 2015;21:1291-1300.
- Healthcare Bluebook. https://healthcarebluebook.com. Accessed June 13, 2016.
- Azziz R, Sanchez LA, Knochenhauer ES, et al. Androgen excess in women: experience with over 1000 consecutive patients. J Clin Endocrinol Metab. 2004;89:453-462.
- Carmina E, Rosato F, Jannì A, et al. Relative prevalence of different androgen excess disorders in 950 women referred because of clinical hyperandrogenism [published online November 1, 2005]. J Clin Endocrinol Metab. 2006;91:2-6.
- Owens DK, Qaseem A, Chou R, et al. High-value, cost-conscious health care: concepts for clinicians to evaluate the benefits, harms, and costs of medical interventions. Ann Intern Med. 2011;154:174-180.
- Nahuis MJ, Oude Lohuis E, Kose N, et al. Long-term follow-up of laparoscopic electrocautery of the ovaries versus ovulation induction with recombinant FSH in clomiphene citrate-resistant women with polycystic ovary syndrome: an economic evaluation. Hum Reprod Oxf Engl. 2012;27:3577-3582.
- Moolenaar LM, Nahuis MJ, Hompes PG, et al. Cost-effectiveness of treatment strategies in women with PCOS who do not conceive after six cycles of clomiphene citrate. Reprod Biomed Online. 2014;28:606-613.
- Chogle A, Saps M. Yield and cost of performing screening tests for constipation in children. Can J Gastroenterol. 2013;27:E35-E38.
- Lee YH, Scharnitz TP, Muscat J, et al. Laboratory monitoring during isotretinoin therapy for acne: a systematic review and meta-analysis. JAMA Dermatol. 2016;152:35-44.
- Shinkai K, McMichael A, Linos E. Isotretinoin laboratory test monitoring—a call to decrease testing in an era of high-value, cost-conscious care. JAMA Dermatol. 2016;152:17-19.
The hospitalist perspective on opioid prescribing
In the United States, we are currently experiencing an opioid epidemic. The rate of opioid-related overdose deaths has reached an all-time high. Hospitalists manage a large number of patients admitted to hospitals in the U.S., and pain is a frequent symptom among these patients.
My colleagues and I wanted to explore hospitalists’ attitudes, beliefs, and practices associated with opioid prescribing during hospitalization and at discharge. In this way, we can begin a conversation about how opioids have impacted the physician’s day to day clinical practice.
For our study, published in the Journal of Hospital Medicine (doi: 10.1002/jhm.2602), we recruited and interviewed 25 hospitalists working in a variety of hospital settings, including two university hospitals, a safety-net hospital, a Veterans Affairs hospital, and a private hospital, located in Colorado and South Carolina. All 25 hospitalists were trained in internal medicine and the majority of them had completed residency within the past 5 to 10 years (48%).
Hospitalists perceived limited success in managing acute exacerbations of chronic pain with opioids, but felt confident in their ability to control acute pain with opioids. They recounted negative sentinel events with their patients that impacted their opioid prescribing practices. Hospitalists described prescribing opioids as a pragmatic tool to facilitate hospital discharges or prevent readmissions, which left them feeling conflicted about how this practice could impact their patients over the long term.
Hospitalists also described feeling uncomfortable treating hospitalized patients with acute exacerbations of a chronic pain condition. One physician said of his experience, “You never get an adequate level of pain control and you keep adding the doses up, and they get habituated.” Another physician described his challenge with controlling chronic pain in hospitalized patients. He said, “Of course their pain is not controlled, because their pain is never going to be less than 5 out of 10. And no opioid is going to get them there, unless they are unconscious.”
Negative sentinel events influenced how hospitalists prescribed opioids in their clinical practice. One physician reflected on an avoidable in-hospital overdose death, which left her more guarded when prescribing opioids. “I’ve had an experience where my patient overdosed,” she said. “She crushed up the oxycodone we were giving her in the hospital, shot it up in her central line, and died.”
Hospitalists described past experiences with patients who altered opioid prescriptions for personal gain. One hospitalist recounted such an experience, saying the patient had “forged my script and changed it from 18 pills to 180 pills.” The physician added, “I got a call from the DEA... I think she [the patient] is in prison now.”
These experiences inspired hospitalists to adopt strategies around opioid prescribing that would make it hard for a patient to jeopardize their DEA license. One physician said, “When I write the prescription, I put the name of the patient on the paper prescription with the patient’s sticker on top. I don’t want the patients to pull it off and sell the prescriptions. Especially when it is my license.”
Hospitalists felt institutional pressure to reduce hospital readmissions and to facilitate discharges. Uncontrolled pain often prolongs a hospital admission. Physicians viewed opioid prescriptions as a pragmatic tool to buffer against readmission or long hospital stays, in order to save health care dollars. On physician described his thoughts on opioid prescribing and efficiency: “If the patient comes back [to the hospital] and gets readmitted when they don’t have pain medicine, it’s a $3,000, 2-day stay in the hospital. When they have pain medicine, they stay out of the hospital. That is utterly pragmatic.”
While opioid prescribing at discharge may improve efficiency and reduce health care costs, one hospitalist also described his discomfort with the practice: “At times, especially when a patient lacks a diagnosis which is known to cause pain [opioid prescribing to prevent readmissions], it can feel cheap and dirty.”
Our study concluded that strategies to provide adequate pain relief to hospitalized patients, which allowed hospitalists to safely and optimally prescribe opioids while maintaining current standards of efficiency, are urgently needed.
Currently, our group is developing predictive tools to be embedded within the electronic medical record to inform physicians about their patient’s future risk for chronic opioid use or opioid use disorders. The goal is to inform physicians, to assist them in making safe, patient-centered, and informed opioid prescribing decisions.
Dr. Calcaterra practices in the Department of Hospital Medicine, Denver Health Medical Center, and is Assistant Professor of Medicine at the University of Colorado School of Medicine, Aurora. She reported having no financial disclosures.
In the United States, we are currently experiencing an opioid epidemic. The rate of opioid-related overdose deaths has reached an all-time high. Hospitalists manage a large number of patients admitted to hospitals in the U.S., and pain is a frequent symptom among these patients.
My colleagues and I wanted to explore hospitalists’ attitudes, beliefs, and practices associated with opioid prescribing during hospitalization and at discharge. In this way, we can begin a conversation about how opioids have impacted the physician’s day to day clinical practice.
For our study, published in the Journal of Hospital Medicine (doi: 10.1002/jhm.2602), we recruited and interviewed 25 hospitalists working in a variety of hospital settings, including two university hospitals, a safety-net hospital, a Veterans Affairs hospital, and a private hospital, located in Colorado and South Carolina. All 25 hospitalists were trained in internal medicine and the majority of them had completed residency within the past 5 to 10 years (48%).
Hospitalists perceived limited success in managing acute exacerbations of chronic pain with opioids, but felt confident in their ability to control acute pain with opioids. They recounted negative sentinel events with their patients that impacted their opioid prescribing practices. Hospitalists described prescribing opioids as a pragmatic tool to facilitate hospital discharges or prevent readmissions, which left them feeling conflicted about how this practice could impact their patients over the long term.
Hospitalists also described feeling uncomfortable treating hospitalized patients with acute exacerbations of a chronic pain condition. One physician said of his experience, “You never get an adequate level of pain control and you keep adding the doses up, and they get habituated.” Another physician described his challenge with controlling chronic pain in hospitalized patients. He said, “Of course their pain is not controlled, because their pain is never going to be less than 5 out of 10. And no opioid is going to get them there, unless they are unconscious.”
Negative sentinel events influenced how hospitalists prescribed opioids in their clinical practice. One physician reflected on an avoidable in-hospital overdose death, which left her more guarded when prescribing opioids. “I’ve had an experience where my patient overdosed,” she said. “She crushed up the oxycodone we were giving her in the hospital, shot it up in her central line, and died.”
Hospitalists described past experiences with patients who altered opioid prescriptions for personal gain. One hospitalist recounted such an experience, saying the patient had “forged my script and changed it from 18 pills to 180 pills.” The physician added, “I got a call from the DEA... I think she [the patient] is in prison now.”
These experiences inspired hospitalists to adopt strategies around opioid prescribing that would make it hard for a patient to jeopardize their DEA license. One physician said, “When I write the prescription, I put the name of the patient on the paper prescription with the patient’s sticker on top. I don’t want the patients to pull it off and sell the prescriptions. Especially when it is my license.”
Hospitalists felt institutional pressure to reduce hospital readmissions and to facilitate discharges. Uncontrolled pain often prolongs a hospital admission. Physicians viewed opioid prescriptions as a pragmatic tool to buffer against readmission or long hospital stays, in order to save health care dollars. On physician described his thoughts on opioid prescribing and efficiency: “If the patient comes back [to the hospital] and gets readmitted when they don’t have pain medicine, it’s a $3,000, 2-day stay in the hospital. When they have pain medicine, they stay out of the hospital. That is utterly pragmatic.”
While opioid prescribing at discharge may improve efficiency and reduce health care costs, one hospitalist also described his discomfort with the practice: “At times, especially when a patient lacks a diagnosis which is known to cause pain [opioid prescribing to prevent readmissions], it can feel cheap and dirty.”
Our study concluded that strategies to provide adequate pain relief to hospitalized patients, which allowed hospitalists to safely and optimally prescribe opioids while maintaining current standards of efficiency, are urgently needed.
Currently, our group is developing predictive tools to be embedded within the electronic medical record to inform physicians about their patient’s future risk for chronic opioid use or opioid use disorders. The goal is to inform physicians, to assist them in making safe, patient-centered, and informed opioid prescribing decisions.
Dr. Calcaterra practices in the Department of Hospital Medicine, Denver Health Medical Center, and is Assistant Professor of Medicine at the University of Colorado School of Medicine, Aurora. She reported having no financial disclosures.
In the United States, we are currently experiencing an opioid epidemic. The rate of opioid-related overdose deaths has reached an all-time high. Hospitalists manage a large number of patients admitted to hospitals in the U.S., and pain is a frequent symptom among these patients.
My colleagues and I wanted to explore hospitalists’ attitudes, beliefs, and practices associated with opioid prescribing during hospitalization and at discharge. In this way, we can begin a conversation about how opioids have impacted the physician’s day to day clinical practice.
For our study, published in the Journal of Hospital Medicine (doi: 10.1002/jhm.2602), we recruited and interviewed 25 hospitalists working in a variety of hospital settings, including two university hospitals, a safety-net hospital, a Veterans Affairs hospital, and a private hospital, located in Colorado and South Carolina. All 25 hospitalists were trained in internal medicine and the majority of them had completed residency within the past 5 to 10 years (48%).
Hospitalists perceived limited success in managing acute exacerbations of chronic pain with opioids, but felt confident in their ability to control acute pain with opioids. They recounted negative sentinel events with their patients that impacted their opioid prescribing practices. Hospitalists described prescribing opioids as a pragmatic tool to facilitate hospital discharges or prevent readmissions, which left them feeling conflicted about how this practice could impact their patients over the long term.
Hospitalists also described feeling uncomfortable treating hospitalized patients with acute exacerbations of a chronic pain condition. One physician said of his experience, “You never get an adequate level of pain control and you keep adding the doses up, and they get habituated.” Another physician described his challenge with controlling chronic pain in hospitalized patients. He said, “Of course their pain is not controlled, because their pain is never going to be less than 5 out of 10. And no opioid is going to get them there, unless they are unconscious.”
Negative sentinel events influenced how hospitalists prescribed opioids in their clinical practice. One physician reflected on an avoidable in-hospital overdose death, which left her more guarded when prescribing opioids. “I’ve had an experience where my patient overdosed,” she said. “She crushed up the oxycodone we were giving her in the hospital, shot it up in her central line, and died.”
Hospitalists described past experiences with patients who altered opioid prescriptions for personal gain. One hospitalist recounted such an experience, saying the patient had “forged my script and changed it from 18 pills to 180 pills.” The physician added, “I got a call from the DEA... I think she [the patient] is in prison now.”
These experiences inspired hospitalists to adopt strategies around opioid prescribing that would make it hard for a patient to jeopardize their DEA license. One physician said, “When I write the prescription, I put the name of the patient on the paper prescription with the patient’s sticker on top. I don’t want the patients to pull it off and sell the prescriptions. Especially when it is my license.”
Hospitalists felt institutional pressure to reduce hospital readmissions and to facilitate discharges. Uncontrolled pain often prolongs a hospital admission. Physicians viewed opioid prescriptions as a pragmatic tool to buffer against readmission or long hospital stays, in order to save health care dollars. On physician described his thoughts on opioid prescribing and efficiency: “If the patient comes back [to the hospital] and gets readmitted when they don’t have pain medicine, it’s a $3,000, 2-day stay in the hospital. When they have pain medicine, they stay out of the hospital. That is utterly pragmatic.”
While opioid prescribing at discharge may improve efficiency and reduce health care costs, one hospitalist also described his discomfort with the practice: “At times, especially when a patient lacks a diagnosis which is known to cause pain [opioid prescribing to prevent readmissions], it can feel cheap and dirty.”
Our study concluded that strategies to provide adequate pain relief to hospitalized patients, which allowed hospitalists to safely and optimally prescribe opioids while maintaining current standards of efficiency, are urgently needed.
Currently, our group is developing predictive tools to be embedded within the electronic medical record to inform physicians about their patient’s future risk for chronic opioid use or opioid use disorders. The goal is to inform physicians, to assist them in making safe, patient-centered, and informed opioid prescribing decisions.
Dr. Calcaterra practices in the Department of Hospital Medicine, Denver Health Medical Center, and is Assistant Professor of Medicine at the University of Colorado School of Medicine, Aurora. She reported having no financial disclosures.
Editorial Board Biographies
Struan H. Coleman, MD, PhD
Associate Editor for Practice Management/Economics
Dr. Coleman is a board-certified orthopedic surgeon specializing in hip preservation and sports medicine at the Hospital for Special Surgery in New York and the Vincera Institute in Philadelphia, and currently is the Head Team Physician for the New York Mets. He earned a medical degree from Columbia College of Physicians and Surgeons and holds a D.Phil in Microbiology from Oxford University in England. He completed his residency in Orthopedic Surgery and a fellowship in Sports Medicine at the Hospital for Special Surgery. Dr. Coleman focuses on the treatment of sports-related injuries of the hip, knee, and shoulder with a particular interest in hip arthroscopy and hip preservation. He has published multiple articles and book chapters, and holds numerous patents for technologies that are utilized by sports medicine physicians and surgeons.
Jack Farr II, MD
Associate Editor for Patellofemoral
Dr. Farr is a board-certified orthopedic surgeon and has a subspecialty practice in knee and cartilage restoration. He is affiliated with the OrthoIndy Hospital and Community Hospital South. He is also the Vice President of the Patellofemoral Foundation, is on the board for the International Cartilage Repair Society, holds a board position with the Cartilage Research Foundation, and holds a voluntary clinical full professorship in Orthopedic Surgery at the Indiana University Medical Center. Dr. Farr earned his medical degree from Indiana University, and completed his Orthopedic Surgery residency at Indiana University Medical Center. He was a design surgeon for a meniscal allograft transplant system and 2 knee patellofemoral osteotomy systems. He is also a member of the American Academy of Orthopaedic Surgeons (AAOS), the Arthroscopy Association of North America (AANA), and the European Society of Sports Traumatology, Knee Surgery and Arthroscopy (ESSKA).
Kenneth Montgomery, MD
Associate Editor for Professional Sports
Dr. Montgomery is an orthopedic surgeon who is fellowship-trained in sports medicine and hand and upper extremity surgery. He is currently practicing at Tri-County Orthopedics and Sports Medicine in Morristown, New Jersey. He is also the Head Team Physician and Medical Director for the New York Jets. He served as a team orthopedist with the New York Islanders from 1997-2009, and was formerly the section chief of Sports Medicine at ProHEALTH Care Associates in Lake Success, New York. Dr. Montgomery completed his residency in Orthopedic Surgery at the Hospital for Special Surgery, and completed a Sports Medicine fellowship at Lenox Hill Hospital. He also completed a Hand and Upper Extremity fellowship at Harvard. He is one of the founders for OrthoNations, a nonprofit organization that helps educate orthopedic surgeons in developing countries. He is also one of the founding surgeons for Cayenne Medical, a medical device company specializing in sports medicine implants.
Struan H. Coleman, MD, PhD
Associate Editor for Practice Management/Economics
Dr. Coleman is a board-certified orthopedic surgeon specializing in hip preservation and sports medicine at the Hospital for Special Surgery in New York and the Vincera Institute in Philadelphia, and currently is the Head Team Physician for the New York Mets. He earned a medical degree from Columbia College of Physicians and Surgeons and holds a D.Phil in Microbiology from Oxford University in England. He completed his residency in Orthopedic Surgery and a fellowship in Sports Medicine at the Hospital for Special Surgery. Dr. Coleman focuses on the treatment of sports-related injuries of the hip, knee, and shoulder with a particular interest in hip arthroscopy and hip preservation. He has published multiple articles and book chapters, and holds numerous patents for technologies that are utilized by sports medicine physicians and surgeons.
Jack Farr II, MD
Associate Editor for Patellofemoral
Dr. Farr is a board-certified orthopedic surgeon and has a subspecialty practice in knee and cartilage restoration. He is affiliated with the OrthoIndy Hospital and Community Hospital South. He is also the Vice President of the Patellofemoral Foundation, is on the board for the International Cartilage Repair Society, holds a board position with the Cartilage Research Foundation, and holds a voluntary clinical full professorship in Orthopedic Surgery at the Indiana University Medical Center. Dr. Farr earned his medical degree from Indiana University, and completed his Orthopedic Surgery residency at Indiana University Medical Center. He was a design surgeon for a meniscal allograft transplant system and 2 knee patellofemoral osteotomy systems. He is also a member of the American Academy of Orthopaedic Surgeons (AAOS), the Arthroscopy Association of North America (AANA), and the European Society of Sports Traumatology, Knee Surgery and Arthroscopy (ESSKA).
Kenneth Montgomery, MD
Associate Editor for Professional Sports
Dr. Montgomery is an orthopedic surgeon who is fellowship-trained in sports medicine and hand and upper extremity surgery. He is currently practicing at Tri-County Orthopedics and Sports Medicine in Morristown, New Jersey. He is also the Head Team Physician and Medical Director for the New York Jets. He served as a team orthopedist with the New York Islanders from 1997-2009, and was formerly the section chief of Sports Medicine at ProHEALTH Care Associates in Lake Success, New York. Dr. Montgomery completed his residency in Orthopedic Surgery at the Hospital for Special Surgery, and completed a Sports Medicine fellowship at Lenox Hill Hospital. He also completed a Hand and Upper Extremity fellowship at Harvard. He is one of the founders for OrthoNations, a nonprofit organization that helps educate orthopedic surgeons in developing countries. He is also one of the founding surgeons for Cayenne Medical, a medical device company specializing in sports medicine implants.
Struan H. Coleman, MD, PhD
Associate Editor for Practice Management/Economics
Dr. Coleman is a board-certified orthopedic surgeon specializing in hip preservation and sports medicine at the Hospital for Special Surgery in New York and the Vincera Institute in Philadelphia, and currently is the Head Team Physician for the New York Mets. He earned a medical degree from Columbia College of Physicians and Surgeons and holds a D.Phil in Microbiology from Oxford University in England. He completed his residency in Orthopedic Surgery and a fellowship in Sports Medicine at the Hospital for Special Surgery. Dr. Coleman focuses on the treatment of sports-related injuries of the hip, knee, and shoulder with a particular interest in hip arthroscopy and hip preservation. He has published multiple articles and book chapters, and holds numerous patents for technologies that are utilized by sports medicine physicians and surgeons.
Jack Farr II, MD
Associate Editor for Patellofemoral
Dr. Farr is a board-certified orthopedic surgeon and has a subspecialty practice in knee and cartilage restoration. He is affiliated with the OrthoIndy Hospital and Community Hospital South. He is also the Vice President of the Patellofemoral Foundation, is on the board for the International Cartilage Repair Society, holds a board position with the Cartilage Research Foundation, and holds a voluntary clinical full professorship in Orthopedic Surgery at the Indiana University Medical Center. Dr. Farr earned his medical degree from Indiana University, and completed his Orthopedic Surgery residency at Indiana University Medical Center. He was a design surgeon for a meniscal allograft transplant system and 2 knee patellofemoral osteotomy systems. He is also a member of the American Academy of Orthopaedic Surgeons (AAOS), the Arthroscopy Association of North America (AANA), and the European Society of Sports Traumatology, Knee Surgery and Arthroscopy (ESSKA).
Kenneth Montgomery, MD
Associate Editor for Professional Sports
Dr. Montgomery is an orthopedic surgeon who is fellowship-trained in sports medicine and hand and upper extremity surgery. He is currently practicing at Tri-County Orthopedics and Sports Medicine in Morristown, New Jersey. He is also the Head Team Physician and Medical Director for the New York Jets. He served as a team orthopedist with the New York Islanders from 1997-2009, and was formerly the section chief of Sports Medicine at ProHEALTH Care Associates in Lake Success, New York. Dr. Montgomery completed his residency in Orthopedic Surgery at the Hospital for Special Surgery, and completed a Sports Medicine fellowship at Lenox Hill Hospital. He also completed a Hand and Upper Extremity fellowship at Harvard. He is one of the founders for OrthoNations, a nonprofit organization that helps educate orthopedic surgeons in developing countries. He is also one of the founding surgeons for Cayenne Medical, a medical device company specializing in sports medicine implants.
Clinical Guidelines: Update in acne treatment
Acne affects 85% of teenagers but can frequently persist into adulthood. It causes significant physical and psychological effects for patients including facial scarring, depression, and decreased self-esteem. The initial approach to acne is determined according to presenting severity, emphasizing topical treatment for milder disease and the addition of oral therapy as disease becomes more severe.
Treatment of mild acne can begin with either benzoyl peroxide (BP) or a topical retinoid (TR). Another option for slightly more severe acne is to start with the initially suggested treatment for moderately severe acne, which is topical combination therapy with BP plus a topical antibiotic; TR plus BP; or TR plus BP in combination with a topical antibiotic. Combination therapy can be given either with separate application of the different medicines or by using fixed combination products that include the separate components in one formulation.
BP is an antibacterial agent, with mild comedolytic properties, and it often is added to topical antibiotic therapy to increase effectiveness and reduce the development of resistance. BP is available in strengths from 2.5% to 10% and in a variety of formulations, which can be used as leave-on or wash-off agents. Common side effects include dose dependent skin irritation and bleaching of fabric.
Topical antibiotics, including clindamycin and erythromycin, work through both their antimicrobial and anti-inflammatory affects. Monotherapy with topical antibiotics is no longer recommended; instead they should be used in combination with BP to prevent bacterial resistance. The preferred topical antibiotic is clindamycin 1% solution or gel. Clindamycin is available in a combination with BP, which may enhance compliance with the treatment regimen.
Topical retinoids are vitamin A derivatives that are the core of treatment. They are effective for all forms of acne and should always be used in the treatment of comedonal acne. There are currently three active agents available: tretinoin (0.025%-0.1% in cream, gel, or microsphere gel vehicles), adapalene (0.1% and 0.3% cream or 0.1% lotion), and tazarotene (0.05% and 0.1% cream, gel, or foam). Combination products are available containing clindamycin and BP. The main side effects of retinoids include dryness, peeling, erythema, and skin irritation. Reducing the frequency of application or potency used may be helpful for limiting these side effects. Topical retinoids increase the risk of photosensitivity, so patients should be counseled on daily sunscreen use, and their use is contraindicated in pregnancy.
Dapsone is an alternative topical treatment for mild acne. Topical dapsone is primarily effective in reducing inflammatory lesions, and seems to be more beneficial for female patients. Dapsone can be combined with topical retinoids if comedonal lesions are present.
Moderate acne can be treated with either topical combination therapy as described above, or systemic antibiotics plus a TR and BP, with or without the addition of a topical antibiotic as well. Female patients may also consider combined oral contraceptives or spironolactone for the treatment of moderate acne.
Systemic antibiotics have been used in the treatment of acne vulgaris for many years, and they are indicated for use in moderate to severe acne. They should always be used in combination with topical therapies, specifically a retinoid or BP. Generally, systemic antibiotics should be used for the shortest possible duration, often 3 months, to prevent the development of bacterial resistance. Tetracyclines and macrolides have the strongest evidence for efficacy. Doxycycline and minocycline are considered equally effective and are the preferred first-line oral antibiotics. Azithromycin has been studied in a variety of pulse dose regimens, and is a good alternative for patients who are not candidates for tetracyclines.
Combined oral contraceptive pills (COCs) are another option for the treatment of acne in female patients. COCs improve acne through their antiandrogenic effects. Spironolactone also has antiandrogen properties, and while it is not FDA approved for the treatment of acne, the AAD guidelines support selective use in women. Spironolactone has been studied at doses from 50 to 200 mg daily and has shown clinically significant improvement in acne. Side effects include diuresis, menstrual irregularities, breast tenderness, and rare hyperkalemia.
Severe acne is treated with an oral antibiotic plus topical combination therapy, or oral isotretinoin, with the addition where appropriate of COCs or oral spironolactone.
Oral isotretinoin, an isomer of retinoic acid, is approved by the FDA for the treatment of severe recalcitrant acne. It causes decreased sebum production, acne lesions, and scarring. It can also be considered in the treatment of moderate acne that is resistant to other treatments, relapses quickly, or produces significant scarring or psychosocial distress. Serum cholesterol, triglycerides, and transaminases can rise during treatment, and should be monitored. Because of the risk of teratogenic effects, the FDA has mandated that all patients receiving isotretinoin must participate in the iPLEDGE risk management program, which requires abstinence or two forms of birth control. While isotretinoin requires monitoring and carries the possibility of significant side effects, it is an effective treatment option for patients with severe recalcitrant acne.
The bottom line
Acne is commonly treated by primary care physicians. A clear approach of graded treatment based on severity of disease yields improvement in outcomes. Mild acne should be treated with benzoyl peroxide, retinoids or a combinations of topical treatments. Systemic antibiotics should be combined with topical therapies for moderate to severe acne. Female patients may also consider using combined oral contraceptives and spironolactone. Oral isotretinoin is an effective option for severe acne, but requires close monitoring.
References
Guidelines of care for the management of acne vulgaris (J Am Acad Dermatol. 2016;74[5]:945-73.e33. doi: 10.1016/j.jaad.2015.12.037. Epub 2016 Feb 17).
Dr. Skolnik is associate director of the family medicine residency program at Abington (Pa.) Memorial Hospital. Dr. Marriott is an attending family physician at Capital Health Primary Care in Hamilton, N.J.
Acne affects 85% of teenagers but can frequently persist into adulthood. It causes significant physical and psychological effects for patients including facial scarring, depression, and decreased self-esteem. The initial approach to acne is determined according to presenting severity, emphasizing topical treatment for milder disease and the addition of oral therapy as disease becomes more severe.
Treatment of mild acne can begin with either benzoyl peroxide (BP) or a topical retinoid (TR). Another option for slightly more severe acne is to start with the initially suggested treatment for moderately severe acne, which is topical combination therapy with BP plus a topical antibiotic; TR plus BP; or TR plus BP in combination with a topical antibiotic. Combination therapy can be given either with separate application of the different medicines or by using fixed combination products that include the separate components in one formulation.
BP is an antibacterial agent, with mild comedolytic properties, and it often is added to topical antibiotic therapy to increase effectiveness and reduce the development of resistance. BP is available in strengths from 2.5% to 10% and in a variety of formulations, which can be used as leave-on or wash-off agents. Common side effects include dose dependent skin irritation and bleaching of fabric.
Topical antibiotics, including clindamycin and erythromycin, work through both their antimicrobial and anti-inflammatory affects. Monotherapy with topical antibiotics is no longer recommended; instead they should be used in combination with BP to prevent bacterial resistance. The preferred topical antibiotic is clindamycin 1% solution or gel. Clindamycin is available in a combination with BP, which may enhance compliance with the treatment regimen.
Topical retinoids are vitamin A derivatives that are the core of treatment. They are effective for all forms of acne and should always be used in the treatment of comedonal acne. There are currently three active agents available: tretinoin (0.025%-0.1% in cream, gel, or microsphere gel vehicles), adapalene (0.1% and 0.3% cream or 0.1% lotion), and tazarotene (0.05% and 0.1% cream, gel, or foam). Combination products are available containing clindamycin and BP. The main side effects of retinoids include dryness, peeling, erythema, and skin irritation. Reducing the frequency of application or potency used may be helpful for limiting these side effects. Topical retinoids increase the risk of photosensitivity, so patients should be counseled on daily sunscreen use, and their use is contraindicated in pregnancy.
Dapsone is an alternative topical treatment for mild acne. Topical dapsone is primarily effective in reducing inflammatory lesions, and seems to be more beneficial for female patients. Dapsone can be combined with topical retinoids if comedonal lesions are present.
Moderate acne can be treated with either topical combination therapy as described above, or systemic antibiotics plus a TR and BP, with or without the addition of a topical antibiotic as well. Female patients may also consider combined oral contraceptives or spironolactone for the treatment of moderate acne.
Systemic antibiotics have been used in the treatment of acne vulgaris for many years, and they are indicated for use in moderate to severe acne. They should always be used in combination with topical therapies, specifically a retinoid or BP. Generally, systemic antibiotics should be used for the shortest possible duration, often 3 months, to prevent the development of bacterial resistance. Tetracyclines and macrolides have the strongest evidence for efficacy. Doxycycline and minocycline are considered equally effective and are the preferred first-line oral antibiotics. Azithromycin has been studied in a variety of pulse dose regimens, and is a good alternative for patients who are not candidates for tetracyclines.
Combined oral contraceptive pills (COCs) are another option for the treatment of acne in female patients. COCs improve acne through their antiandrogenic effects. Spironolactone also has antiandrogen properties, and while it is not FDA approved for the treatment of acne, the AAD guidelines support selective use in women. Spironolactone has been studied at doses from 50 to 200 mg daily and has shown clinically significant improvement in acne. Side effects include diuresis, menstrual irregularities, breast tenderness, and rare hyperkalemia.
Severe acne is treated with an oral antibiotic plus topical combination therapy, or oral isotretinoin, with the addition where appropriate of COCs or oral spironolactone.
Oral isotretinoin, an isomer of retinoic acid, is approved by the FDA for the treatment of severe recalcitrant acne. It causes decreased sebum production, acne lesions, and scarring. It can also be considered in the treatment of moderate acne that is resistant to other treatments, relapses quickly, or produces significant scarring or psychosocial distress. Serum cholesterol, triglycerides, and transaminases can rise during treatment, and should be monitored. Because of the risk of teratogenic effects, the FDA has mandated that all patients receiving isotretinoin must participate in the iPLEDGE risk management program, which requires abstinence or two forms of birth control. While isotretinoin requires monitoring and carries the possibility of significant side effects, it is an effective treatment option for patients with severe recalcitrant acne.
The bottom line
Acne is commonly treated by primary care physicians. A clear approach of graded treatment based on severity of disease yields improvement in outcomes. Mild acne should be treated with benzoyl peroxide, retinoids or a combinations of topical treatments. Systemic antibiotics should be combined with topical therapies for moderate to severe acne. Female patients may also consider using combined oral contraceptives and spironolactone. Oral isotretinoin is an effective option for severe acne, but requires close monitoring.
References
Guidelines of care for the management of acne vulgaris (J Am Acad Dermatol. 2016;74[5]:945-73.e33. doi: 10.1016/j.jaad.2015.12.037. Epub 2016 Feb 17).
Dr. Skolnik is associate director of the family medicine residency program at Abington (Pa.) Memorial Hospital. Dr. Marriott is an attending family physician at Capital Health Primary Care in Hamilton, N.J.
Acne affects 85% of teenagers but can frequently persist into adulthood. It causes significant physical and psychological effects for patients including facial scarring, depression, and decreased self-esteem. The initial approach to acne is determined according to presenting severity, emphasizing topical treatment for milder disease and the addition of oral therapy as disease becomes more severe.
Treatment of mild acne can begin with either benzoyl peroxide (BP) or a topical retinoid (TR). Another option for slightly more severe acne is to start with the initially suggested treatment for moderately severe acne, which is topical combination therapy with BP plus a topical antibiotic; TR plus BP; or TR plus BP in combination with a topical antibiotic. Combination therapy can be given either with separate application of the different medicines or by using fixed combination products that include the separate components in one formulation.
BP is an antibacterial agent, with mild comedolytic properties, and it often is added to topical antibiotic therapy to increase effectiveness and reduce the development of resistance. BP is available in strengths from 2.5% to 10% and in a variety of formulations, which can be used as leave-on or wash-off agents. Common side effects include dose dependent skin irritation and bleaching of fabric.
Topical antibiotics, including clindamycin and erythromycin, work through both their antimicrobial and anti-inflammatory affects. Monotherapy with topical antibiotics is no longer recommended; instead they should be used in combination with BP to prevent bacterial resistance. The preferred topical antibiotic is clindamycin 1% solution or gel. Clindamycin is available in a combination with BP, which may enhance compliance with the treatment regimen.
Topical retinoids are vitamin A derivatives that are the core of treatment. They are effective for all forms of acne and should always be used in the treatment of comedonal acne. There are currently three active agents available: tretinoin (0.025%-0.1% in cream, gel, or microsphere gel vehicles), adapalene (0.1% and 0.3% cream or 0.1% lotion), and tazarotene (0.05% and 0.1% cream, gel, or foam). Combination products are available containing clindamycin and BP. The main side effects of retinoids include dryness, peeling, erythema, and skin irritation. Reducing the frequency of application or potency used may be helpful for limiting these side effects. Topical retinoids increase the risk of photosensitivity, so patients should be counseled on daily sunscreen use, and their use is contraindicated in pregnancy.
Dapsone is an alternative topical treatment for mild acne. Topical dapsone is primarily effective in reducing inflammatory lesions, and seems to be more beneficial for female patients. Dapsone can be combined with topical retinoids if comedonal lesions are present.
Moderate acne can be treated with either topical combination therapy as described above, or systemic antibiotics plus a TR and BP, with or without the addition of a topical antibiotic as well. Female patients may also consider combined oral contraceptives or spironolactone for the treatment of moderate acne.
Systemic antibiotics have been used in the treatment of acne vulgaris for many years, and they are indicated for use in moderate to severe acne. They should always be used in combination with topical therapies, specifically a retinoid or BP. Generally, systemic antibiotics should be used for the shortest possible duration, often 3 months, to prevent the development of bacterial resistance. Tetracyclines and macrolides have the strongest evidence for efficacy. Doxycycline and minocycline are considered equally effective and are the preferred first-line oral antibiotics. Azithromycin has been studied in a variety of pulse dose regimens, and is a good alternative for patients who are not candidates for tetracyclines.
Combined oral contraceptive pills (COCs) are another option for the treatment of acne in female patients. COCs improve acne through their antiandrogenic effects. Spironolactone also has antiandrogen properties, and while it is not FDA approved for the treatment of acne, the AAD guidelines support selective use in women. Spironolactone has been studied at doses from 50 to 200 mg daily and has shown clinically significant improvement in acne. Side effects include diuresis, menstrual irregularities, breast tenderness, and rare hyperkalemia.
Severe acne is treated with an oral antibiotic plus topical combination therapy, or oral isotretinoin, with the addition where appropriate of COCs or oral spironolactone.
Oral isotretinoin, an isomer of retinoic acid, is approved by the FDA for the treatment of severe recalcitrant acne. It causes decreased sebum production, acne lesions, and scarring. It can also be considered in the treatment of moderate acne that is resistant to other treatments, relapses quickly, or produces significant scarring or psychosocial distress. Serum cholesterol, triglycerides, and transaminases can rise during treatment, and should be monitored. Because of the risk of teratogenic effects, the FDA has mandated that all patients receiving isotretinoin must participate in the iPLEDGE risk management program, which requires abstinence or two forms of birth control. While isotretinoin requires monitoring and carries the possibility of significant side effects, it is an effective treatment option for patients with severe recalcitrant acne.
The bottom line
Acne is commonly treated by primary care physicians. A clear approach of graded treatment based on severity of disease yields improvement in outcomes. Mild acne should be treated with benzoyl peroxide, retinoids or a combinations of topical treatments. Systemic antibiotics should be combined with topical therapies for moderate to severe acne. Female patients may also consider using combined oral contraceptives and spironolactone. Oral isotretinoin is an effective option for severe acne, but requires close monitoring.
References
Guidelines of care for the management of acne vulgaris (J Am Acad Dermatol. 2016;74[5]:945-73.e33. doi: 10.1016/j.jaad.2015.12.037. Epub 2016 Feb 17).
Dr. Skolnik is associate director of the family medicine residency program at Abington (Pa.) Memorial Hospital. Dr. Marriott is an attending family physician at Capital Health Primary Care in Hamilton, N.J.
Clinical Guidelines: Update in acne treatment
Acne affects 85% of teenagers but can frequently persist into adulthood. It causes significant physical and psychological effects for patients including facial scarring, depression, and decreased self-esteem. The initial approach to acne is determined according to presenting severity, emphasizing topical treatment for milder disease and the addition of oral therapy as disease becomes more severe.
Treatment of mild acne can begin with either benzoyl peroxide (BP) or a topical retinoid (TR). Another option for slightly more severe acne is to start with the initially suggested treatment for moderately severe acne, which is topical combination therapy with BP plus a topical antibiotic; TR plus BP; or TR plus BP in combination with a topical antibiotic. Combination therapy can be given either with separate application of the different medicines or by using fixed combination products that include the separate components in one formulation.
BP is an antibacterial agent, with mild comedolytic properties, and it often is added to topical antibiotic therapy to increase effectiveness and reduce the development of resistance. BP is available in strengths from 2.5% to 10% and in a variety of formulations, which can be used as leave-on or wash-off agents. Common side effects include dose dependent skin irritation and bleaching of fabric.
Topical antibiotics, including clindamycin and erythromycin, work through both their antimicrobial and anti-inflammatory affects. Monotherapy with topical antibiotics is no longer recommended; instead they should be used in combination with BP to prevent bacterial resistance. The preferred topical antibiotic is clindamycin 1% solution or gel. Clindamycin is available in a combination with BP, which may enhance compliance with the treatment regimen.
Topical retinoids are vitamin A derivatives that are the core of treatment. They are effective for all forms of acne and should always be used in the treatment of comedonal acne. There are currently three active agents available: tretinoin (0.025%-0.1% in cream, gel, or microsphere gel vehicles), adapalene (0.1% and 0.3% cream or 0.1% lotion), and tazarotene (0.05% and 0.1% cream, gel, or foam). Combination products are available containing clindamycin and BP. The main side effects of retinoids include dryness, peeling, erythema, and skin irritation. Reducing the frequency of application or potency used may be helpful for limiting these side effects. Topical retinoids increase the risk of photosensitivity, so patients should be counseled on daily sunscreen use, and their use is contraindicated in pregnancy.
Dapsone is an alternative topical treatment for mild acne. Topical dapsone is primarily effective in reducing inflammatory lesions, and seems to be more beneficial for female patients. Dapsone can be combined with topical retinoids if comedonal lesions are present.
Moderate acne can be treated with either topical combination therapy as described above, or systemic antibiotics plus a TR and BP, with or without the addition of a topical antibiotic as well. Female patients may also consider combined oral contraceptives or spironolactone for the treatment of moderate acne.
Systemic antibiotics have been used in the treatment of acne vulgaris for many years, and they are indicated for use in moderate to severe acne. They should always be used in combination with topical therapies, specifically a retinoid or BP. Generally, systemic antibiotics should be used for the shortest possible duration, often 3 months, to prevent the development of bacterial resistance. Tetracyclines and macrolides have the strongest evidence for efficacy. Doxycycline and minocycline are considered equally effective and are the preferred first-line oral antibiotics. Azithromycin has been studied in a variety of pulse dose regimens, and is a good alternative for patients who are not candidates for tetracyclines.
Combined oral contraceptive pills (COCs) are another option for the treatment of acne in female patients. COCs improve acne through their antiandrogenic effects. Spironolactone also has antiandrogen properties, and while it is not FDA approved for the treatment of acne, the AAD guidelines support selective use in women. Spironolactone has been studied at doses from 50 to 200 mg daily and has shown clinically significant improvement in acne. Side effects include diuresis, menstrual irregularities, breast tenderness, and rare hyperkalemia.
Severe acne is treated with an oral antibiotic plus topical combination therapy, or oral isotretinoin, with the addition where appropriate of COCs or oral spironolactone.
Oral isotretinoin, an isomer of retinoic acid, is approved by the FDA for the treatment of severe recalcitrant acne. It causes decreased sebum production, acne lesions, and scarring. It can also be considered in the treatment of moderate acne that is resistant to other treatments, relapses quickly, or produces significant scarring or psychosocial distress. Serum cholesterol, triglycerides, and transaminases can rise during treatment, and should be monitored. Because of the risk of teratogenic effects, the FDA has mandated that all patients receiving isotretinoin must participate in the iPLEDGE risk management program, which requires abstinence or two forms of birth control. While isotretinoin requires monitoring and carries the possibility of significant side effects, it is an effective treatment option for patients with severe recalcitrant acne.
The bottom line
Acne is commonly treated by primary care physicians. A clear approach of graded treatment based on severity of disease yields improvement in outcomes. Mild acne should be treated with benzoyl peroxide, retinoids or a combinations of topical treatments. Systemic antibiotics should be combined with topical therapies for moderate to severe acne. Female patients may also consider using combined oral contraceptives and spironolactone. Oral isotretinoin is an effective option for severe acne, but requires close monitoring.
References
Guidelines of care for the management of acne vulgaris (J Am Acad Dermatol. 2016;74[5]:945-73.e33. doi: 10.1016/j.jaad.2015.12.037. Epub 2016 Feb 17).
Dr. Skolnik is associate director of the family medicine residency program at Abington (Pa.) Memorial Hospital. Dr. Marriott is an attending family physician at Capital Health Primary Care in Hamilton, N.J.
Acne affects 85% of teenagers but can frequently persist into adulthood. It causes significant physical and psychological effects for patients including facial scarring, depression, and decreased self-esteem. The initial approach to acne is determined according to presenting severity, emphasizing topical treatment for milder disease and the addition of oral therapy as disease becomes more severe.
Treatment of mild acne can begin with either benzoyl peroxide (BP) or a topical retinoid (TR). Another option for slightly more severe acne is to start with the initially suggested treatment for moderately severe acne, which is topical combination therapy with BP plus a topical antibiotic; TR plus BP; or TR plus BP in combination with a topical antibiotic. Combination therapy can be given either with separate application of the different medicines or by using fixed combination products that include the separate components in one formulation.
BP is an antibacterial agent, with mild comedolytic properties, and it often is added to topical antibiotic therapy to increase effectiveness and reduce the development of resistance. BP is available in strengths from 2.5% to 10% and in a variety of formulations, which can be used as leave-on or wash-off agents. Common side effects include dose dependent skin irritation and bleaching of fabric.
Topical antibiotics, including clindamycin and erythromycin, work through both their antimicrobial and anti-inflammatory affects. Monotherapy with topical antibiotics is no longer recommended; instead they should be used in combination with BP to prevent bacterial resistance. The preferred topical antibiotic is clindamycin 1% solution or gel. Clindamycin is available in a combination with BP, which may enhance compliance with the treatment regimen.
Topical retinoids are vitamin A derivatives that are the core of treatment. They are effective for all forms of acne and should always be used in the treatment of comedonal acne. There are currently three active agents available: tretinoin (0.025%-0.1% in cream, gel, or microsphere gel vehicles), adapalene (0.1% and 0.3% cream or 0.1% lotion), and tazarotene (0.05% and 0.1% cream, gel, or foam). Combination products are available containing clindamycin and BP. The main side effects of retinoids include dryness, peeling, erythema, and skin irritation. Reducing the frequency of application or potency used may be helpful for limiting these side effects. Topical retinoids increase the risk of photosensitivity, so patients should be counseled on daily sunscreen use, and their use is contraindicated in pregnancy.
Dapsone is an alternative topical treatment for mild acne. Topical dapsone is primarily effective in reducing inflammatory lesions, and seems to be more beneficial for female patients. Dapsone can be combined with topical retinoids if comedonal lesions are present.
Moderate acne can be treated with either topical combination therapy as described above, or systemic antibiotics plus a TR and BP, with or without the addition of a topical antibiotic as well. Female patients may also consider combined oral contraceptives or spironolactone for the treatment of moderate acne.
Systemic antibiotics have been used in the treatment of acne vulgaris for many years, and they are indicated for use in moderate to severe acne. They should always be used in combination with topical therapies, specifically a retinoid or BP. Generally, systemic antibiotics should be used for the shortest possible duration, often 3 months, to prevent the development of bacterial resistance. Tetracyclines and macrolides have the strongest evidence for efficacy. Doxycycline and minocycline are considered equally effective and are the preferred first-line oral antibiotics. Azithromycin has been studied in a variety of pulse dose regimens, and is a good alternative for patients who are not candidates for tetracyclines.
Combined oral contraceptive pills (COCs) are another option for the treatment of acne in female patients. COCs improve acne through their antiandrogenic effects. Spironolactone also has antiandrogen properties, and while it is not FDA approved for the treatment of acne, the AAD guidelines support selective use in women. Spironolactone has been studied at doses from 50 to 200 mg daily and has shown clinically significant improvement in acne. Side effects include diuresis, menstrual irregularities, breast tenderness, and rare hyperkalemia.
Severe acne is treated with an oral antibiotic plus topical combination therapy, or oral isotretinoin, with the addition where appropriate of COCs or oral spironolactone.
Oral isotretinoin, an isomer of retinoic acid, is approved by the FDA for the treatment of severe recalcitrant acne. It causes decreased sebum production, acne lesions, and scarring. It can also be considered in the treatment of moderate acne that is resistant to other treatments, relapses quickly, or produces significant scarring or psychosocial distress. Serum cholesterol, triglycerides, and transaminases can rise during treatment, and should be monitored. Because of the risk of teratogenic effects, the FDA has mandated that all patients receiving isotretinoin must participate in the iPLEDGE risk management program, which requires abstinence or two forms of birth control. While isotretinoin requires monitoring and carries the possibility of significant side effects, it is an effective treatment option for patients with severe recalcitrant acne.
The bottom line
Acne is commonly treated by primary care physicians. A clear approach of graded treatment based on severity of disease yields improvement in outcomes. Mild acne should be treated with benzoyl peroxide, retinoids or a combinations of topical treatments. Systemic antibiotics should be combined with topical therapies for moderate to severe acne. Female patients may also consider using combined oral contraceptives and spironolactone. Oral isotretinoin is an effective option for severe acne, but requires close monitoring.
References
Guidelines of care for the management of acne vulgaris (J Am Acad Dermatol. 2016;74[5]:945-73.e33. doi: 10.1016/j.jaad.2015.12.037. Epub 2016 Feb 17).
Dr. Skolnik is associate director of the family medicine residency program at Abington (Pa.) Memorial Hospital. Dr. Marriott is an attending family physician at Capital Health Primary Care in Hamilton, N.J.
Acne affects 85% of teenagers but can frequently persist into adulthood. It causes significant physical and psychological effects for patients including facial scarring, depression, and decreased self-esteem. The initial approach to acne is determined according to presenting severity, emphasizing topical treatment for milder disease and the addition of oral therapy as disease becomes more severe.
Treatment of mild acne can begin with either benzoyl peroxide (BP) or a topical retinoid (TR). Another option for slightly more severe acne is to start with the initially suggested treatment for moderately severe acne, which is topical combination therapy with BP plus a topical antibiotic; TR plus BP; or TR plus BP in combination with a topical antibiotic. Combination therapy can be given either with separate application of the different medicines or by using fixed combination products that include the separate components in one formulation.
BP is an antibacterial agent, with mild comedolytic properties, and it often is added to topical antibiotic therapy to increase effectiveness and reduce the development of resistance. BP is available in strengths from 2.5% to 10% and in a variety of formulations, which can be used as leave-on or wash-off agents. Common side effects include dose dependent skin irritation and bleaching of fabric.
Topical antibiotics, including clindamycin and erythromycin, work through both their antimicrobial and anti-inflammatory affects. Monotherapy with topical antibiotics is no longer recommended; instead they should be used in combination with BP to prevent bacterial resistance. The preferred topical antibiotic is clindamycin 1% solution or gel. Clindamycin is available in a combination with BP, which may enhance compliance with the treatment regimen.
Topical retinoids are vitamin A derivatives that are the core of treatment. They are effective for all forms of acne and should always be used in the treatment of comedonal acne. There are currently three active agents available: tretinoin (0.025%-0.1% in cream, gel, or microsphere gel vehicles), adapalene (0.1% and 0.3% cream or 0.1% lotion), and tazarotene (0.05% and 0.1% cream, gel, or foam). Combination products are available containing clindamycin and BP. The main side effects of retinoids include dryness, peeling, erythema, and skin irritation. Reducing the frequency of application or potency used may be helpful for limiting these side effects. Topical retinoids increase the risk of photosensitivity, so patients should be counseled on daily sunscreen use, and their use is contraindicated in pregnancy.
Dapsone is an alternative topical treatment for mild acne. Topical dapsone is primarily effective in reducing inflammatory lesions, and seems to be more beneficial for female patients. Dapsone can be combined with topical retinoids if comedonal lesions are present.
Moderate acne can be treated with either topical combination therapy as described above, or systemic antibiotics plus a TR and BP, with or without the addition of a topical antibiotic as well. Female patients may also consider combined oral contraceptives or spironolactone for the treatment of moderate acne.
Systemic antibiotics have been used in the treatment of acne vulgaris for many years, and they are indicated for use in moderate to severe acne. They should always be used in combination with topical therapies, specifically a retinoid or BP. Generally, systemic antibiotics should be used for the shortest possible duration, often 3 months, to prevent the development of bacterial resistance. Tetracyclines and macrolides have the strongest evidence for efficacy. Doxycycline and minocycline are considered equally effective and are the preferred first-line oral antibiotics. Azithromycin has been studied in a variety of pulse dose regimens, and is a good alternative for patients who are not candidates for tetracyclines.
Combined oral contraceptive pills (COCs) are another option for the treatment of acne in female patients. COCs improve acne through their antiandrogenic effects. Spironolactone also has antiandrogen properties, and while it is not FDA approved for the treatment of acne, the AAD guidelines support selective use in women. Spironolactone has been studied at doses from 50 to 200 mg daily and has shown clinically significant improvement in acne. Side effects include diuresis, menstrual irregularities, breast tenderness, and rare hyperkalemia.
Severe acne is treated with an oral antibiotic plus topical combination therapy, or oral isotretinoin, with the addition where appropriate of COCs or oral spironolactone.
Oral isotretinoin, an isomer of retinoic acid, is approved by the FDA for the treatment of severe recalcitrant acne. It causes decreased sebum production, acne lesions, and scarring. It can also be considered in the treatment of moderate acne that is resistant to other treatments, relapses quickly, or produces significant scarring or psychosocial distress. Serum cholesterol, triglycerides, and transaminases can rise during treatment, and should be monitored. Because of the risk of teratogenic effects, the FDA has mandated that all patients receiving isotretinoin must participate in the iPLEDGE risk management program, which requires abstinence or two forms of birth control. While isotretinoin requires monitoring and carries the possibility of significant side effects, it is an effective treatment option for patients with severe recalcitrant acne.
The bottom line
Acne is commonly treated by primary care physicians. A clear approach of graded treatment based on severity of disease yields improvement in outcomes. Mild acne should be treated with benzoyl peroxide, retinoids or a combinations of topical treatments. Systemic antibiotics should be combined with topical therapies for moderate to severe acne. Female patients may also consider using combined oral contraceptives and spironolactone. Oral isotretinoin is an effective option for severe acne, but requires close monitoring.
References
Guidelines of care for the management of acne vulgaris (J Am Acad Dermatol. 2016;74[5]:945-73.e33. doi: 10.1016/j.jaad.2015.12.037. Epub 2016 Feb 17).
Dr. Skolnik is associate director of the family medicine residency program at Abington (Pa.) Memorial Hospital. Dr. Marriott is an attending family physician at Capital Health Primary Care in Hamilton, N.J.
Scopolamine-induced mania: ‘Theoretically possible, but statistically improbable'
Dr. Emjay Tan’s case study of a 36-year-old man who became “Manic after taking a vacation” (Cases That Test Your Skills, Current Psychiatry. April 2016, p. 45-50) is off the mark by attributing the manic episode to scopolamine—theoretically possible, but statistically improbable.
Dr. Tan may be unaware of a more frequent event: vacation hypomania. About one-third of my bipolar disorder patients had their first manic episode while on an overseas vacation or upon their return. It isn’t the fun, excitement, or novelty of a vacation that triggers the episode, but sleep deprivation, which is part and parcel of such events, particularly when they involve a holiday in a substantially different time zone.
Few people get to sleep more than a few hours the night before departing on a vacation; there’s so much to do: packing, getting to the airport hours before the flight, etc. Not many people sleep soundly on the plane, and many experience the effects of jet lag both during the first few days of vacation and when the vacationer returns home. Many vacations come with substantial and protracted sleep deprivation, and sleep deprivation is an excellent way to trigger a hypomanic episode. I suspect that is why Dr. Tan’s patient, who did not have a history of psychiatric symptoms, but who might have been genetically predisposed, became manifestly symptomatic shortly following his return from an overseas holiday.
Of course, it isn’t just first episodes of hypomania that are triggered by sleep deprivation in patients with undiagnosed bipolar disorder; the event is common in the lives of people who already receive treatment. Accordingly, my patients know that I might increase their lithium dosage for at least a few days to give them added protection as they head overseas, coupled with advice to do their best to get proper sleep.
Despite such prophylaxis, many of my bipolar disorder patients have taken a long flight overseas and, then, after half a day in the air, continued “flying.” To the best of my knowledge, none ever took scopolamine.
Martin Blinder, MD
Past Assistant Clinical Professor of Psychiatry
University of California, San Francisco
Past Adjunct Professor of Law
University of California
Hastings College of Law
San Francisco, California
Dr. Emjay Tan’s case study of a 36-year-old man who became “Manic after taking a vacation” (Cases That Test Your Skills, Current Psychiatry. April 2016, p. 45-50) is off the mark by attributing the manic episode to scopolamine—theoretically possible, but statistically improbable.
Dr. Tan may be unaware of a more frequent event: vacation hypomania. About one-third of my bipolar disorder patients had their first manic episode while on an overseas vacation or upon their return. It isn’t the fun, excitement, or novelty of a vacation that triggers the episode, but sleep deprivation, which is part and parcel of such events, particularly when they involve a holiday in a substantially different time zone.
Few people get to sleep more than a few hours the night before departing on a vacation; there’s so much to do: packing, getting to the airport hours before the flight, etc. Not many people sleep soundly on the plane, and many experience the effects of jet lag both during the first few days of vacation and when the vacationer returns home. Many vacations come with substantial and protracted sleep deprivation, and sleep deprivation is an excellent way to trigger a hypomanic episode. I suspect that is why Dr. Tan’s patient, who did not have a history of psychiatric symptoms, but who might have been genetically predisposed, became manifestly symptomatic shortly following his return from an overseas holiday.
Of course, it isn’t just first episodes of hypomania that are triggered by sleep deprivation in patients with undiagnosed bipolar disorder; the event is common in the lives of people who already receive treatment. Accordingly, my patients know that I might increase their lithium dosage for at least a few days to give them added protection as they head overseas, coupled with advice to do their best to get proper sleep.
Despite such prophylaxis, many of my bipolar disorder patients have taken a long flight overseas and, then, after half a day in the air, continued “flying.” To the best of my knowledge, none ever took scopolamine.
Martin Blinder, MD
Past Assistant Clinical Professor of Psychiatry
University of California, San Francisco
Past Adjunct Professor of Law
University of California
Hastings College of Law
San Francisco, California
Dr. Emjay Tan’s case study of a 36-year-old man who became “Manic after taking a vacation” (Cases That Test Your Skills, Current Psychiatry. April 2016, p. 45-50) is off the mark by attributing the manic episode to scopolamine—theoretically possible, but statistically improbable.
Dr. Tan may be unaware of a more frequent event: vacation hypomania. About one-third of my bipolar disorder patients had their first manic episode while on an overseas vacation or upon their return. It isn’t the fun, excitement, or novelty of a vacation that triggers the episode, but sleep deprivation, which is part and parcel of such events, particularly when they involve a holiday in a substantially different time zone.
Few people get to sleep more than a few hours the night before departing on a vacation; there’s so much to do: packing, getting to the airport hours before the flight, etc. Not many people sleep soundly on the plane, and many experience the effects of jet lag both during the first few days of vacation and when the vacationer returns home. Many vacations come with substantial and protracted sleep deprivation, and sleep deprivation is an excellent way to trigger a hypomanic episode. I suspect that is why Dr. Tan’s patient, who did not have a history of psychiatric symptoms, but who might have been genetically predisposed, became manifestly symptomatic shortly following his return from an overseas holiday.
Of course, it isn’t just first episodes of hypomania that are triggered by sleep deprivation in patients with undiagnosed bipolar disorder; the event is common in the lives of people who already receive treatment. Accordingly, my patients know that I might increase their lithium dosage for at least a few days to give them added protection as they head overseas, coupled with advice to do their best to get proper sleep.
Despite such prophylaxis, many of my bipolar disorder patients have taken a long flight overseas and, then, after half a day in the air, continued “flying.” To the best of my knowledge, none ever took scopolamine.
Martin Blinder, MD
Past Assistant Clinical Professor of Psychiatry
University of California, San Francisco
Past Adjunct Professor of Law
University of California
Hastings College of Law
San Francisco, California
“I Want What Kobe Had”: A Comprehensive Guide to Giving Your Patients the Biologic Solutions They Crave
The sun has finally set on Kobe Bryant’s magnificent career. After all the tributes and tearful goodbyes, he has finally played his last game and become a part of basketball history. Ever since his field trip to Germany for interleukin-1 receptor antagonist protein (IRAP) treatments to his knee, and his subsequent return to high-level play, I’ve been under siege in the office by patients who “want what Kobe had.” I’ve had to explain, time and time again, that IRAP treatment is not available in the United States and that platelet-rich plasma (PRP) is the closest alternative treatment, convince them that PRP may be even better, and then let them know that it’s considered experimental and not covered by insurance.
In the last issue, we discussed the future of orthopedics, which in my opinion will rely heavily on the biologic therapies now considered experimental. In this issue, we will look into our crystal balls and imagine what that future might look like. To do so, we should first consider what we hope to accomplish through the incorporation of biologic therapies.
The regeneration of articular cartilage, acceleration of fracture and tissue healing, and faster incorporation of tendon grafts to bone have long been considered the Holy Grail of Orthopedics. In his best seller, The Da Vinci Code, Dan Brown makes a compelling argument that the Holy Grail, the chalice thought to have held the blood of Christ, was in fact a mistranslated reference to his living descendants. Whenever I have a visitor or student in the operating room, I focus the scope on the synovial capillaries so they can see the individual red blood cells passing single-file through the vessels on their way to supply cells with the nutrients they need.
Perhaps, like in The Da Vinci Code, the solution to our greatest biologic challenges lies in the blood, already there, just waiting to be unlocked.
PRP has been utilized for everything from tendinopathy to arthropathy, with varied results in the literature. The lack of standardization of PRP preparations, which vary in inclusion of white cells and absolute platelet count, confounds these results even further. In this issue, we review its use in sports medicine and knee arthritis, taking a closer look at partial ulnar collateral ligament tears in baseball players.
In “Tips of the Trade,” we present a technique for “superior capsular reconstruction” that provides a novel solution for patients with pseudoparalysis from massive rotator cuff tears with little other options beside reverse total shoulder arthroplasty.
The one absolute statement I can make regarding biologics is that we currently have more questions than answers, and every hypothesis we prove simply begets more questions. More randomized controlled studies are needed in virtually every aspect of biologics, and we should all consider taking part. While the solutions our patients crave may not arrive during our careers, or even our lifetimes, the groundwork we do now will set the stage for future generations to enjoy biologically enhanced outcomes.
The sun has finally set on Kobe Bryant’s magnificent career. After all the tributes and tearful goodbyes, he has finally played his last game and become a part of basketball history. Ever since his field trip to Germany for interleukin-1 receptor antagonist protein (IRAP) treatments to his knee, and his subsequent return to high-level play, I’ve been under siege in the office by patients who “want what Kobe had.” I’ve had to explain, time and time again, that IRAP treatment is not available in the United States and that platelet-rich plasma (PRP) is the closest alternative treatment, convince them that PRP may be even better, and then let them know that it’s considered experimental and not covered by insurance.
In the last issue, we discussed the future of orthopedics, which in my opinion will rely heavily on the biologic therapies now considered experimental. In this issue, we will look into our crystal balls and imagine what that future might look like. To do so, we should first consider what we hope to accomplish through the incorporation of biologic therapies.
The regeneration of articular cartilage, acceleration of fracture and tissue healing, and faster incorporation of tendon grafts to bone have long been considered the Holy Grail of Orthopedics. In his best seller, The Da Vinci Code, Dan Brown makes a compelling argument that the Holy Grail, the chalice thought to have held the blood of Christ, was in fact a mistranslated reference to his living descendants. Whenever I have a visitor or student in the operating room, I focus the scope on the synovial capillaries so they can see the individual red blood cells passing single-file through the vessels on their way to supply cells with the nutrients they need.
Perhaps, like in The Da Vinci Code, the solution to our greatest biologic challenges lies in the blood, already there, just waiting to be unlocked.
PRP has been utilized for everything from tendinopathy to arthropathy, with varied results in the literature. The lack of standardization of PRP preparations, which vary in inclusion of white cells and absolute platelet count, confounds these results even further. In this issue, we review its use in sports medicine and knee arthritis, taking a closer look at partial ulnar collateral ligament tears in baseball players.
In “Tips of the Trade,” we present a technique for “superior capsular reconstruction” that provides a novel solution for patients with pseudoparalysis from massive rotator cuff tears with little other options beside reverse total shoulder arthroplasty.
The one absolute statement I can make regarding biologics is that we currently have more questions than answers, and every hypothesis we prove simply begets more questions. More randomized controlled studies are needed in virtually every aspect of biologics, and we should all consider taking part. While the solutions our patients crave may not arrive during our careers, or even our lifetimes, the groundwork we do now will set the stage for future generations to enjoy biologically enhanced outcomes.
The sun has finally set on Kobe Bryant’s magnificent career. After all the tributes and tearful goodbyes, he has finally played his last game and become a part of basketball history. Ever since his field trip to Germany for interleukin-1 receptor antagonist protein (IRAP) treatments to his knee, and his subsequent return to high-level play, I’ve been under siege in the office by patients who “want what Kobe had.” I’ve had to explain, time and time again, that IRAP treatment is not available in the United States and that platelet-rich plasma (PRP) is the closest alternative treatment, convince them that PRP may be even better, and then let them know that it’s considered experimental and not covered by insurance.
In the last issue, we discussed the future of orthopedics, which in my opinion will rely heavily on the biologic therapies now considered experimental. In this issue, we will look into our crystal balls and imagine what that future might look like. To do so, we should first consider what we hope to accomplish through the incorporation of biologic therapies.
The regeneration of articular cartilage, acceleration of fracture and tissue healing, and faster incorporation of tendon grafts to bone have long been considered the Holy Grail of Orthopedics. In his best seller, The Da Vinci Code, Dan Brown makes a compelling argument that the Holy Grail, the chalice thought to have held the blood of Christ, was in fact a mistranslated reference to his living descendants. Whenever I have a visitor or student in the operating room, I focus the scope on the synovial capillaries so they can see the individual red blood cells passing single-file through the vessels on their way to supply cells with the nutrients they need.
Perhaps, like in The Da Vinci Code, the solution to our greatest biologic challenges lies in the blood, already there, just waiting to be unlocked.
PRP has been utilized for everything from tendinopathy to arthropathy, with varied results in the literature. The lack of standardization of PRP preparations, which vary in inclusion of white cells and absolute platelet count, confounds these results even further. In this issue, we review its use in sports medicine and knee arthritis, taking a closer look at partial ulnar collateral ligament tears in baseball players.
In “Tips of the Trade,” we present a technique for “superior capsular reconstruction” that provides a novel solution for patients with pseudoparalysis from massive rotator cuff tears with little other options beside reverse total shoulder arthroplasty.
The one absolute statement I can make regarding biologics is that we currently have more questions than answers, and every hypothesis we prove simply begets more questions. More randomized controlled studies are needed in virtually every aspect of biologics, and we should all consider taking part. While the solutions our patients crave may not arrive during our careers, or even our lifetimes, the groundwork we do now will set the stage for future generations to enjoy biologically enhanced outcomes.
Why be a vascular surgeon?
This edition of Vascular Specialist is being published early to coincide with the VAM. Since medical students will be attending the meeting I thought this would be a good opportunity to describe an often overlooked reason why, after all my years in practice, I still enjoy being a vascular surgeon. By doing so I hope to encourage these young people to consider a career in vascular surgery.
Some vascular surgeons, with the same goal, have volunteered to mentor these students at the VAM. I suspect most mentors would extoll vascular surgery as unique amongst surgical specialties. They will describe the variety of complex operations as well as advanced endovascular procedures that we perform. Proudly, some mentors will mention that other practitioners turn to us for help when they encounter uncontrollable hemorrhage. They will emphasize that we are the one specialty that covers the gamut of vascular interventions from open surgery and endovascular procedures to medical management. Perhaps some mentors will incorporate my mantra that vascular surgeons “Operate, Dilate, and Medicate.”
However, I suggest that the most satisfying aspect of our profession is not the procedures that we perform but rather the interaction we have with our patients. After all, most of us entered the medical profession to take care of patients, and vascular patients are very special indeed. However, sometimes we established vascular surgeons become too enthralled by technical advances to remember the more humanistic reasons for our being. Also, changes in medical practice and reimbursement have resulted in many being so overworked that we do not have time to enjoy relationships with our patients. Perhaps those who are so burdened should take heed from the stories mentors will relate to inspire these students.
Based on my personal experience I suspect the mentors will say something along the following lines: “Vascular conditions are chronic and are wont to afflict more than one part of the body. Accordingly, we are required to follow most patients for their whole lives (or ours!). Not only do we treat these patients but we also become intimately involved with their families, often treating them as well. Often our ‘treatment’ will not be procedural but rather will involve emotional support of these relatives as they deal with their recuperating or debilitated spouse, sibling, or parent. Those of us who have been in practice for many years will fondly recall patients who have become an integral part of our lives. The patient who undergoes a vascular procedure will return every 6 or 12 months to have their bypass checked or their other carotid assessed.
“We follow asymptomatic small abdominal aneurysms and claudicants. A venous ulcer often recurs and a dialysis patient may require a new intervention. Some patients come to the office so they can be made more secure that their condition has not deteriorated, and the lonely just because we are the only human they interact with on a regular basis. They bring with them their varied life stories and these vignettes become a part of our own fiction. Perhaps we will share with them our own life story. Contrast that to the general surgeon who repairs a hernia and after a few post op visits may never see the patient again.
“Vascular patients may be very young or more commonly very old and come from all walks of life. So the vascular surgeon will learn to calm the crying infant. She will provide careful optimism to allay the fears of a mother who brings in her daughter scarred by a cavernous hemangioma. He or she will reassure the young girl, mortified by embarrassing spider veins, that she will be able to wear a dress to her high school prom. Together with the obstetrician, the vascular surgeon will guide a pregnant woman with a DVT through her entire pregnancy assuring her that both she and her baby will be safe.”
The mentor will re-count how special it was to get a hug from an old lady who he operated on 25 years previously when he was a young surgeon. Or the gratification one gets when a father, after a successful limb revascularization, shows a video of himself walking down the aisle at his daughter’s wedding. Perhaps the mentor will confide her sense of dismay every time a young dialysis patient is admitted for revision of a fistula and the joy she feels when told that her patient has finally received a viable transplant. Year after year the vascular surgeon will follow a patient with early onset, widespread vascular disease whose parents died young from the ravages of familial hyperlipidemia.
He will provide encouragement to help the patient stop smoking and commiserate when a sibling dies from a heart attack. The mentor might relate how she felt when she saved the leg of a soldier injured by a land mine or how she was amazed by the 80-year-old ballroom dancer who danced a few weeks after a below knee amputation.
Mentors will also describe getting to know a patient’s daily routine so they can informatively advise a patient whether it is worth having a procedure to improve quality of life. Or the thrill we get when that patient thanks us for relieving the claudication that prevented gainful employment. We are relieved when a longstanding patient wakes up neurologically intact from an endarterectomy.
However, we are filled with remorse when we inform a family that they have lost their loved one who died from a ruptured aneurysm. Of course, our failures may be devastating but they reinforce our humility when we acknowledge that we have been defeated by a disease that resisted our every effort.
The mentor may also share that “Every Xmas you will collect cards thanking you for saving a life or, out of the blue, receive a carton of fruit from the orchard of a farmer who finally was able to walk amongst her crop. You will pass tissues to the sobbing husband whose wife always accompanied him to his yearly physical, but who recently passed from incurable cancer. You will listen to stories from veterans of past wars. You will see pictures of patients’ children and you will remark how they have grown through the years. A patient will make you look admiringly at their latest puppy or prize-winning pig. You will be given stock advice by a millionaire and you will pay for a taxi for the indigent to get home from your office. You may keep patients waiting while you hear intriguing gossip or wonder just how you can stop the little old lady rambling on about lost loves. You will be charmed by the 98-year-old who makes sure that she has her hair and makeup done prior to coming to see you, and how her face lights up when you pronounce her more beautiful than ever.
“Dear student, the technical aspects of vascular surgery are indeed demanding and exciting. We are invigorated by the knowledge that our expertise saved a life or limb, prevented a stroke or provided the nephrotic with a working fistula. Even the more simple cosmetic procedures give us pleasure. If you still need inspiration to embark on a vascular surgical career I encourage you to read the Presidential address Dr. Bruce J. Brener gave to the Society for Clinical Vascular Surgery in March 1996. His eloquent portrayal of the vascular surgical experience is unmatched (Amer J Surg, 1996; 172:97-9). However, it is our daily and often lifelong interaction with our wonderful patients that so intimately reinforces our humanity and makes this profession so uniquely satisfying.”
This edition of Vascular Specialist is being published early to coincide with the VAM. Since medical students will be attending the meeting I thought this would be a good opportunity to describe an often overlooked reason why, after all my years in practice, I still enjoy being a vascular surgeon. By doing so I hope to encourage these young people to consider a career in vascular surgery.
Some vascular surgeons, with the same goal, have volunteered to mentor these students at the VAM. I suspect most mentors would extoll vascular surgery as unique amongst surgical specialties. They will describe the variety of complex operations as well as advanced endovascular procedures that we perform. Proudly, some mentors will mention that other practitioners turn to us for help when they encounter uncontrollable hemorrhage. They will emphasize that we are the one specialty that covers the gamut of vascular interventions from open surgery and endovascular procedures to medical management. Perhaps some mentors will incorporate my mantra that vascular surgeons “Operate, Dilate, and Medicate.”
However, I suggest that the most satisfying aspect of our profession is not the procedures that we perform but rather the interaction we have with our patients. After all, most of us entered the medical profession to take care of patients, and vascular patients are very special indeed. However, sometimes we established vascular surgeons become too enthralled by technical advances to remember the more humanistic reasons for our being. Also, changes in medical practice and reimbursement have resulted in many being so overworked that we do not have time to enjoy relationships with our patients. Perhaps those who are so burdened should take heed from the stories mentors will relate to inspire these students.
Based on my personal experience I suspect the mentors will say something along the following lines: “Vascular conditions are chronic and are wont to afflict more than one part of the body. Accordingly, we are required to follow most patients for their whole lives (or ours!). Not only do we treat these patients but we also become intimately involved with their families, often treating them as well. Often our ‘treatment’ will not be procedural but rather will involve emotional support of these relatives as they deal with their recuperating or debilitated spouse, sibling, or parent. Those of us who have been in practice for many years will fondly recall patients who have become an integral part of our lives. The patient who undergoes a vascular procedure will return every 6 or 12 months to have their bypass checked or their other carotid assessed.
“We follow asymptomatic small abdominal aneurysms and claudicants. A venous ulcer often recurs and a dialysis patient may require a new intervention. Some patients come to the office so they can be made more secure that their condition has not deteriorated, and the lonely just because we are the only human they interact with on a regular basis. They bring with them their varied life stories and these vignettes become a part of our own fiction. Perhaps we will share with them our own life story. Contrast that to the general surgeon who repairs a hernia and after a few post op visits may never see the patient again.
“Vascular patients may be very young or more commonly very old and come from all walks of life. So the vascular surgeon will learn to calm the crying infant. She will provide careful optimism to allay the fears of a mother who brings in her daughter scarred by a cavernous hemangioma. He or she will reassure the young girl, mortified by embarrassing spider veins, that she will be able to wear a dress to her high school prom. Together with the obstetrician, the vascular surgeon will guide a pregnant woman with a DVT through her entire pregnancy assuring her that both she and her baby will be safe.”
The mentor will re-count how special it was to get a hug from an old lady who he operated on 25 years previously when he was a young surgeon. Or the gratification one gets when a father, after a successful limb revascularization, shows a video of himself walking down the aisle at his daughter’s wedding. Perhaps the mentor will confide her sense of dismay every time a young dialysis patient is admitted for revision of a fistula and the joy she feels when told that her patient has finally received a viable transplant. Year after year the vascular surgeon will follow a patient with early onset, widespread vascular disease whose parents died young from the ravages of familial hyperlipidemia.
He will provide encouragement to help the patient stop smoking and commiserate when a sibling dies from a heart attack. The mentor might relate how she felt when she saved the leg of a soldier injured by a land mine or how she was amazed by the 80-year-old ballroom dancer who danced a few weeks after a below knee amputation.
Mentors will also describe getting to know a patient’s daily routine so they can informatively advise a patient whether it is worth having a procedure to improve quality of life. Or the thrill we get when that patient thanks us for relieving the claudication that prevented gainful employment. We are relieved when a longstanding patient wakes up neurologically intact from an endarterectomy.
However, we are filled with remorse when we inform a family that they have lost their loved one who died from a ruptured aneurysm. Of course, our failures may be devastating but they reinforce our humility when we acknowledge that we have been defeated by a disease that resisted our every effort.
The mentor may also share that “Every Xmas you will collect cards thanking you for saving a life or, out of the blue, receive a carton of fruit from the orchard of a farmer who finally was able to walk amongst her crop. You will pass tissues to the sobbing husband whose wife always accompanied him to his yearly physical, but who recently passed from incurable cancer. You will listen to stories from veterans of past wars. You will see pictures of patients’ children and you will remark how they have grown through the years. A patient will make you look admiringly at their latest puppy or prize-winning pig. You will be given stock advice by a millionaire and you will pay for a taxi for the indigent to get home from your office. You may keep patients waiting while you hear intriguing gossip or wonder just how you can stop the little old lady rambling on about lost loves. You will be charmed by the 98-year-old who makes sure that she has her hair and makeup done prior to coming to see you, and how her face lights up when you pronounce her more beautiful than ever.
“Dear student, the technical aspects of vascular surgery are indeed demanding and exciting. We are invigorated by the knowledge that our expertise saved a life or limb, prevented a stroke or provided the nephrotic with a working fistula. Even the more simple cosmetic procedures give us pleasure. If you still need inspiration to embark on a vascular surgical career I encourage you to read the Presidential address Dr. Bruce J. Brener gave to the Society for Clinical Vascular Surgery in March 1996. His eloquent portrayal of the vascular surgical experience is unmatched (Amer J Surg, 1996; 172:97-9). However, it is our daily and often lifelong interaction with our wonderful patients that so intimately reinforces our humanity and makes this profession so uniquely satisfying.”
This edition of Vascular Specialist is being published early to coincide with the VAM. Since medical students will be attending the meeting I thought this would be a good opportunity to describe an often overlooked reason why, after all my years in practice, I still enjoy being a vascular surgeon. By doing so I hope to encourage these young people to consider a career in vascular surgery.
Some vascular surgeons, with the same goal, have volunteered to mentor these students at the VAM. I suspect most mentors would extoll vascular surgery as unique amongst surgical specialties. They will describe the variety of complex operations as well as advanced endovascular procedures that we perform. Proudly, some mentors will mention that other practitioners turn to us for help when they encounter uncontrollable hemorrhage. They will emphasize that we are the one specialty that covers the gamut of vascular interventions from open surgery and endovascular procedures to medical management. Perhaps some mentors will incorporate my mantra that vascular surgeons “Operate, Dilate, and Medicate.”
However, I suggest that the most satisfying aspect of our profession is not the procedures that we perform but rather the interaction we have with our patients. After all, most of us entered the medical profession to take care of patients, and vascular patients are very special indeed. However, sometimes we established vascular surgeons become too enthralled by technical advances to remember the more humanistic reasons for our being. Also, changes in medical practice and reimbursement have resulted in many being so overworked that we do not have time to enjoy relationships with our patients. Perhaps those who are so burdened should take heed from the stories mentors will relate to inspire these students.
Based on my personal experience I suspect the mentors will say something along the following lines: “Vascular conditions are chronic and are wont to afflict more than one part of the body. Accordingly, we are required to follow most patients for their whole lives (or ours!). Not only do we treat these patients but we also become intimately involved with their families, often treating them as well. Often our ‘treatment’ will not be procedural but rather will involve emotional support of these relatives as they deal with their recuperating or debilitated spouse, sibling, or parent. Those of us who have been in practice for many years will fondly recall patients who have become an integral part of our lives. The patient who undergoes a vascular procedure will return every 6 or 12 months to have their bypass checked or their other carotid assessed.
“We follow asymptomatic small abdominal aneurysms and claudicants. A venous ulcer often recurs and a dialysis patient may require a new intervention. Some patients come to the office so they can be made more secure that their condition has not deteriorated, and the lonely just because we are the only human they interact with on a regular basis. They bring with them their varied life stories and these vignettes become a part of our own fiction. Perhaps we will share with them our own life story. Contrast that to the general surgeon who repairs a hernia and after a few post op visits may never see the patient again.
“Vascular patients may be very young or more commonly very old and come from all walks of life. So the vascular surgeon will learn to calm the crying infant. She will provide careful optimism to allay the fears of a mother who brings in her daughter scarred by a cavernous hemangioma. He or she will reassure the young girl, mortified by embarrassing spider veins, that she will be able to wear a dress to her high school prom. Together with the obstetrician, the vascular surgeon will guide a pregnant woman with a DVT through her entire pregnancy assuring her that both she and her baby will be safe.”
The mentor will re-count how special it was to get a hug from an old lady who he operated on 25 years previously when he was a young surgeon. Or the gratification one gets when a father, after a successful limb revascularization, shows a video of himself walking down the aisle at his daughter’s wedding. Perhaps the mentor will confide her sense of dismay every time a young dialysis patient is admitted for revision of a fistula and the joy she feels when told that her patient has finally received a viable transplant. Year after year the vascular surgeon will follow a patient with early onset, widespread vascular disease whose parents died young from the ravages of familial hyperlipidemia.
He will provide encouragement to help the patient stop smoking and commiserate when a sibling dies from a heart attack. The mentor might relate how she felt when she saved the leg of a soldier injured by a land mine or how she was amazed by the 80-year-old ballroom dancer who danced a few weeks after a below knee amputation.
Mentors will also describe getting to know a patient’s daily routine so they can informatively advise a patient whether it is worth having a procedure to improve quality of life. Or the thrill we get when that patient thanks us for relieving the claudication that prevented gainful employment. We are relieved when a longstanding patient wakes up neurologically intact from an endarterectomy.
However, we are filled with remorse when we inform a family that they have lost their loved one who died from a ruptured aneurysm. Of course, our failures may be devastating but they reinforce our humility when we acknowledge that we have been defeated by a disease that resisted our every effort.
The mentor may also share that “Every Xmas you will collect cards thanking you for saving a life or, out of the blue, receive a carton of fruit from the orchard of a farmer who finally was able to walk amongst her crop. You will pass tissues to the sobbing husband whose wife always accompanied him to his yearly physical, but who recently passed from incurable cancer. You will listen to stories from veterans of past wars. You will see pictures of patients’ children and you will remark how they have grown through the years. A patient will make you look admiringly at their latest puppy or prize-winning pig. You will be given stock advice by a millionaire and you will pay for a taxi for the indigent to get home from your office. You may keep patients waiting while you hear intriguing gossip or wonder just how you can stop the little old lady rambling on about lost loves. You will be charmed by the 98-year-old who makes sure that she has her hair and makeup done prior to coming to see you, and how her face lights up when you pronounce her more beautiful than ever.
“Dear student, the technical aspects of vascular surgery are indeed demanding and exciting. We are invigorated by the knowledge that our expertise saved a life or limb, prevented a stroke or provided the nephrotic with a working fistula. Even the more simple cosmetic procedures give us pleasure. If you still need inspiration to embark on a vascular surgical career I encourage you to read the Presidential address Dr. Bruce J. Brener gave to the Society for Clinical Vascular Surgery in March 1996. His eloquent portrayal of the vascular surgical experience is unmatched (Amer J Surg, 1996; 172:97-9). However, it is our daily and often lifelong interaction with our wonderful patients that so intimately reinforces our humanity and makes this profession so uniquely satisfying.”
The ACA: Here Are (Mostly) Reasons Why Not
Politics and Points to Ponder
Your commentary on the ACA “six years later” provides an insightful historical perspective, discussion of the current political dilemma, and overview of this, as you put it, “step in the right direction.” I hope all NPs and PAs will consider their political agendas in terms of the rights of our citizenry, along with their rights to practice: the right to health care, to choose health care providers, to change their social determinants of health, and to the preservation, promotion, prevention, and protection of their family’s and community’s health, as well as their own. All in the national and public interest!
Loretta C. Ford, EdD, PNP, FAAN, FAANP
Wildwood, FL
Continue for Doc, Cure My Boredom >>
Doc, Cure My Boredom
I am a seasoned, dedicated, and (according to my colleagues and patients) terrific clinician. I have been practicing as an APRN since the mid-80s. I cut my teeth in primary care and geriatrics for more than 10 years, then spent the next 14 in cardiology. With the enactment of the ACA and the shifted focus on primary care, I returned to primary care practice in 2012.
After three years back in primary care in rural Vermont, where I had my own panel of patients, I finally had enough. I was recruited by our local VA to develop a heart failure program; I have been with them since the beginning of this year. (What a godsend! I love my job again.)
The problems in health care, especially primary care, were more than I could sustain. My younger, less experienced colleagues were dropping like flies. I agree the ACA is a first step. But in our rural state, it resulted in many people with health care coverage (a very good thing) but the majority on Medicaid (not a good thing). At the risk of sounding unsympathetic, the problems lie with the government’s control of this enterprise. These patients deserve health care, but they don’t deserve an open checkbook. With our help (I can assure you, in Vermont, there are tremendous resources to help the poor), patients need to take some responsibility for their health.
Despite biweekly office visits, case managers, home care, and social work involvement, patients get bored and decide to visit the emergency department (ED) for minor issues. Medicaid pays for it, no questions asked. One patient, for example, came to my office in the morning, where I did tests and outlined a plan of care. She went home and one hour later presented to the ED for the same (nonacute) issue, because she didn’t want to wait for the plan to work. Unhappy with that visit, she presented to our local tertiary medical center later that day. Since that hospital doesn’t access our records, this patient underwent yet a third evaluation (including x-rays) on the same day, with the exact same plan of care outlined. Medicaid paid for every single thing—my tax dollars at work.
This isn’t an anomaly. Every day, I had endless encounters with this “open checkbook” approach and patients’ need for immediate gratification (despite being educated on their health problem, its expected duration, and a clear plan of care). Our culture has become centered on immediate gratification, and there is a lack of personal responsibility for one’s health. Patients—all of us—need to take responsibility for our health.
With so many people on state-sponsored plans as a result of the ACA, patients have no “skin in the game,” so to speak. They are poor, and I sympathize with that. Yet, unless they are made aware of the cost of these “boredom ED visits” and expensive tests, etc, this behavior will only continue to bankrupt the system.
Unfettered health care expenditures are not only unsustainable, they are also beyond aggravating for my many patients who pay exorbitant amounts of money on high-deductible plans. Those are the people I worry about most. They are being priced out of their health care!
So yes, the ACA is a first step—but not a good one. It simply didn’t go far enough, and it has led to burnout and chaos in the frontlines, increasing costs, and a boon to the insurance companies.
Until we eliminate private insurance companies from the equation, put every citizen on a level playing field, and expect a collaborative approach with our patients (as well as ownership of their health), it will only get worse.
Peg Sullivan, MSN, APRN
Windsor, VT
Continue for Good Concept, Poor Execution >>
Good Concept, Poor Execution
I feel you are looking at the issue incorrectly; the failure of the ACA is due not to the opponents but to the proponents. Passed by a one-party vote, it has been opposed by an ever-increasing majority since its inception in 2009. Its passage can only be defended by those who benefitted monetarily (such as the administrators of AARP, insurance companies, and politicians from districts with large entitlement constituents.)
You direct your defense from a conceptual bias—that 60% of Americans polled would like to see some form of legislated health care. They do not want this particular piece of legislation, which was written by insurance companies and validated by this administration.
Why do you think it’s opposed by so many? “Unconstitutional overreach” to some, but the argument that 30 million people were without insurance was fiction. Many were covered by their spouse yet counted as uninsured, some were not citizens, some were between jobs and employer health insurance, and all had access to the ED.
Rethink your premise for this article. You defend a worthy concept, but a bad law.
Gerard Fischer, PA-C
Naples, FL
Continue for Rural Health Care: Dearly Departed >>
Rural Health Care: Dearly Departed
I’d like to get you up to date on the rural health care crisis that the ACA has directly caused, as you make no mention of this tragic disaster in your editorial. My wife and I are an MD/PA team and have been the only medical providers in our town since 2003. More than 90% of our patient base was federally designated poor folks, but the ACA forced us to close our doors in August 2014.
The National Rural Health Association has been tracking rural hospital closures, but no one is tracking the hundreds of clinics like mine that closed as a direct result of the ACA. I know of seven practices within a 30-mile radius that have closed. One of our hospitals, with a payroll of $11.3 million, recently closed. All of these clinicians will now be on unemployment, further increasing our deficit.
In our community, 11,000 people now must drive long distances or use the ED for health care. People who do not live rurally do not understand the situation—and many don’t care, as the focus is on urban and city medicine. Early in my career, I worked with the National Health Service Corps to pay off student loans; our entire county in Minnesota had a population of only 10,000—a thousand people less than the northern California town my clinic was in. But we had a full hospital and clinic (albeit with little in the way of funds to support them).
The President could have assembled a Healthcare Advisory Taskforce of city, urban, and rural CEOs, docs, advanced practice providers, etc, to evaluate how the ACA would impact each sector. Instead, we now have a rural health care crisis as a result of “health care reform.”
Don Sakal, MMSc, PA-C
Magalia, CA
Politics and Points to Ponder
Your commentary on the ACA “six years later” provides an insightful historical perspective, discussion of the current political dilemma, and overview of this, as you put it, “step in the right direction.” I hope all NPs and PAs will consider their political agendas in terms of the rights of our citizenry, along with their rights to practice: the right to health care, to choose health care providers, to change their social determinants of health, and to the preservation, promotion, prevention, and protection of their family’s and community’s health, as well as their own. All in the national and public interest!
Loretta C. Ford, EdD, PNP, FAAN, FAANP
Wildwood, FL
Continue for Doc, Cure My Boredom >>
Doc, Cure My Boredom
I am a seasoned, dedicated, and (according to my colleagues and patients) terrific clinician. I have been practicing as an APRN since the mid-80s. I cut my teeth in primary care and geriatrics for more than 10 years, then spent the next 14 in cardiology. With the enactment of the ACA and the shifted focus on primary care, I returned to primary care practice in 2012.
After three years back in primary care in rural Vermont, where I had my own panel of patients, I finally had enough. I was recruited by our local VA to develop a heart failure program; I have been with them since the beginning of this year. (What a godsend! I love my job again.)
The problems in health care, especially primary care, were more than I could sustain. My younger, less experienced colleagues were dropping like flies. I agree the ACA is a first step. But in our rural state, it resulted in many people with health care coverage (a very good thing) but the majority on Medicaid (not a good thing). At the risk of sounding unsympathetic, the problems lie with the government’s control of this enterprise. These patients deserve health care, but they don’t deserve an open checkbook. With our help (I can assure you, in Vermont, there are tremendous resources to help the poor), patients need to take some responsibility for their health.
Despite biweekly office visits, case managers, home care, and social work involvement, patients get bored and decide to visit the emergency department (ED) for minor issues. Medicaid pays for it, no questions asked. One patient, for example, came to my office in the morning, where I did tests and outlined a plan of care. She went home and one hour later presented to the ED for the same (nonacute) issue, because she didn’t want to wait for the plan to work. Unhappy with that visit, she presented to our local tertiary medical center later that day. Since that hospital doesn’t access our records, this patient underwent yet a third evaluation (including x-rays) on the same day, with the exact same plan of care outlined. Medicaid paid for every single thing—my tax dollars at work.
This isn’t an anomaly. Every day, I had endless encounters with this “open checkbook” approach and patients’ need for immediate gratification (despite being educated on their health problem, its expected duration, and a clear plan of care). Our culture has become centered on immediate gratification, and there is a lack of personal responsibility for one’s health. Patients—all of us—need to take responsibility for our health.
With so many people on state-sponsored plans as a result of the ACA, patients have no “skin in the game,” so to speak. They are poor, and I sympathize with that. Yet, unless they are made aware of the cost of these “boredom ED visits” and expensive tests, etc, this behavior will only continue to bankrupt the system.
Unfettered health care expenditures are not only unsustainable, they are also beyond aggravating for my many patients who pay exorbitant amounts of money on high-deductible plans. Those are the people I worry about most. They are being priced out of their health care!
So yes, the ACA is a first step—but not a good one. It simply didn’t go far enough, and it has led to burnout and chaos in the frontlines, increasing costs, and a boon to the insurance companies.
Until we eliminate private insurance companies from the equation, put every citizen on a level playing field, and expect a collaborative approach with our patients (as well as ownership of their health), it will only get worse.
Peg Sullivan, MSN, APRN
Windsor, VT
Continue for Good Concept, Poor Execution >>
Good Concept, Poor Execution
I feel you are looking at the issue incorrectly; the failure of the ACA is due not to the opponents but to the proponents. Passed by a one-party vote, it has been opposed by an ever-increasing majority since its inception in 2009. Its passage can only be defended by those who benefitted monetarily (such as the administrators of AARP, insurance companies, and politicians from districts with large entitlement constituents.)
You direct your defense from a conceptual bias—that 60% of Americans polled would like to see some form of legislated health care. They do not want this particular piece of legislation, which was written by insurance companies and validated by this administration.
Why do you think it’s opposed by so many? “Unconstitutional overreach” to some, but the argument that 30 million people were without insurance was fiction. Many were covered by their spouse yet counted as uninsured, some were not citizens, some were between jobs and employer health insurance, and all had access to the ED.
Rethink your premise for this article. You defend a worthy concept, but a bad law.
Gerard Fischer, PA-C
Naples, FL
Continue for Rural Health Care: Dearly Departed >>
Rural Health Care: Dearly Departed
I’d like to get you up to date on the rural health care crisis that the ACA has directly caused, as you make no mention of this tragic disaster in your editorial. My wife and I are an MD/PA team and have been the only medical providers in our town since 2003. More than 90% of our patient base was federally designated poor folks, but the ACA forced us to close our doors in August 2014.
The National Rural Health Association has been tracking rural hospital closures, but no one is tracking the hundreds of clinics like mine that closed as a direct result of the ACA. I know of seven practices within a 30-mile radius that have closed. One of our hospitals, with a payroll of $11.3 million, recently closed. All of these clinicians will now be on unemployment, further increasing our deficit.
In our community, 11,000 people now must drive long distances or use the ED for health care. People who do not live rurally do not understand the situation—and many don’t care, as the focus is on urban and city medicine. Early in my career, I worked with the National Health Service Corps to pay off student loans; our entire county in Minnesota had a population of only 10,000—a thousand people less than the northern California town my clinic was in. But we had a full hospital and clinic (albeit with little in the way of funds to support them).
The President could have assembled a Healthcare Advisory Taskforce of city, urban, and rural CEOs, docs, advanced practice providers, etc, to evaluate how the ACA would impact each sector. Instead, we now have a rural health care crisis as a result of “health care reform.”
Don Sakal, MMSc, PA-C
Magalia, CA
Politics and Points to Ponder
Your commentary on the ACA “six years later” provides an insightful historical perspective, discussion of the current political dilemma, and overview of this, as you put it, “step in the right direction.” I hope all NPs and PAs will consider their political agendas in terms of the rights of our citizenry, along with their rights to practice: the right to health care, to choose health care providers, to change their social determinants of health, and to the preservation, promotion, prevention, and protection of their family’s and community’s health, as well as their own. All in the national and public interest!
Loretta C. Ford, EdD, PNP, FAAN, FAANP
Wildwood, FL
Continue for Doc, Cure My Boredom >>
Doc, Cure My Boredom
I am a seasoned, dedicated, and (according to my colleagues and patients) terrific clinician. I have been practicing as an APRN since the mid-80s. I cut my teeth in primary care and geriatrics for more than 10 years, then spent the next 14 in cardiology. With the enactment of the ACA and the shifted focus on primary care, I returned to primary care practice in 2012.
After three years back in primary care in rural Vermont, where I had my own panel of patients, I finally had enough. I was recruited by our local VA to develop a heart failure program; I have been with them since the beginning of this year. (What a godsend! I love my job again.)
The problems in health care, especially primary care, were more than I could sustain. My younger, less experienced colleagues were dropping like flies. I agree the ACA is a first step. But in our rural state, it resulted in many people with health care coverage (a very good thing) but the majority on Medicaid (not a good thing). At the risk of sounding unsympathetic, the problems lie with the government’s control of this enterprise. These patients deserve health care, but they don’t deserve an open checkbook. With our help (I can assure you, in Vermont, there are tremendous resources to help the poor), patients need to take some responsibility for their health.
Despite biweekly office visits, case managers, home care, and social work involvement, patients get bored and decide to visit the emergency department (ED) for minor issues. Medicaid pays for it, no questions asked. One patient, for example, came to my office in the morning, where I did tests and outlined a plan of care. She went home and one hour later presented to the ED for the same (nonacute) issue, because she didn’t want to wait for the plan to work. Unhappy with that visit, she presented to our local tertiary medical center later that day. Since that hospital doesn’t access our records, this patient underwent yet a third evaluation (including x-rays) on the same day, with the exact same plan of care outlined. Medicaid paid for every single thing—my tax dollars at work.
This isn’t an anomaly. Every day, I had endless encounters with this “open checkbook” approach and patients’ need for immediate gratification (despite being educated on their health problem, its expected duration, and a clear plan of care). Our culture has become centered on immediate gratification, and there is a lack of personal responsibility for one’s health. Patients—all of us—need to take responsibility for our health.
With so many people on state-sponsored plans as a result of the ACA, patients have no “skin in the game,” so to speak. They are poor, and I sympathize with that. Yet, unless they are made aware of the cost of these “boredom ED visits” and expensive tests, etc, this behavior will only continue to bankrupt the system.
Unfettered health care expenditures are not only unsustainable, they are also beyond aggravating for my many patients who pay exorbitant amounts of money on high-deductible plans. Those are the people I worry about most. They are being priced out of their health care!
So yes, the ACA is a first step—but not a good one. It simply didn’t go far enough, and it has led to burnout and chaos in the frontlines, increasing costs, and a boon to the insurance companies.
Until we eliminate private insurance companies from the equation, put every citizen on a level playing field, and expect a collaborative approach with our patients (as well as ownership of their health), it will only get worse.
Peg Sullivan, MSN, APRN
Windsor, VT
Continue for Good Concept, Poor Execution >>
Good Concept, Poor Execution
I feel you are looking at the issue incorrectly; the failure of the ACA is due not to the opponents but to the proponents. Passed by a one-party vote, it has been opposed by an ever-increasing majority since its inception in 2009. Its passage can only be defended by those who benefitted monetarily (such as the administrators of AARP, insurance companies, and politicians from districts with large entitlement constituents.)
You direct your defense from a conceptual bias—that 60% of Americans polled would like to see some form of legislated health care. They do not want this particular piece of legislation, which was written by insurance companies and validated by this administration.
Why do you think it’s opposed by so many? “Unconstitutional overreach” to some, but the argument that 30 million people were without insurance was fiction. Many were covered by their spouse yet counted as uninsured, some were not citizens, some were between jobs and employer health insurance, and all had access to the ED.
Rethink your premise for this article. You defend a worthy concept, but a bad law.
Gerard Fischer, PA-C
Naples, FL
Continue for Rural Health Care: Dearly Departed >>
Rural Health Care: Dearly Departed
I’d like to get you up to date on the rural health care crisis that the ACA has directly caused, as you make no mention of this tragic disaster in your editorial. My wife and I are an MD/PA team and have been the only medical providers in our town since 2003. More than 90% of our patient base was federally designated poor folks, but the ACA forced us to close our doors in August 2014.
The National Rural Health Association has been tracking rural hospital closures, but no one is tracking the hundreds of clinics like mine that closed as a direct result of the ACA. I know of seven practices within a 30-mile radius that have closed. One of our hospitals, with a payroll of $11.3 million, recently closed. All of these clinicians will now be on unemployment, further increasing our deficit.
In our community, 11,000 people now must drive long distances or use the ED for health care. People who do not live rurally do not understand the situation—and many don’t care, as the focus is on urban and city medicine. Early in my career, I worked with the National Health Service Corps to pay off student loans; our entire county in Minnesota had a population of only 10,000—a thousand people less than the northern California town my clinic was in. But we had a full hospital and clinic (albeit with little in the way of funds to support them).
The President could have assembled a Healthcare Advisory Taskforce of city, urban, and rural CEOs, docs, advanced practice providers, etc, to evaluate how the ACA would impact each sector. Instead, we now have a rural health care crisis as a result of “health care reform.”
Don Sakal, MMSc, PA-C
Magalia, CA
Precepting: Holding Students and Programs Accountable
Randy Danielsen’s editorial on the topic of precepting (April 2016) elicited a flurry of responses from our NP readers.1 The influx of feedback prompted me as an educator, an NP, and a former preceptor to wonder: Why the paucity of preceptors? Are there too many programs and too many students? And are we dropping the ball when it comes to engendering professional responsibility as a “social contract”?1
Let me start with a query: Are we requiring students to uphold their social contracts? That is, are they engaged in professional networking to enrich their own clinical experiences? Are they responsible for establishing relationships with providers in their communities in preparation for clinical rotations? Aren’t these all components of their social contracts as students?
In my PNP program, we found our own preceptors (there were no clinical coordinators “back in the day”). As a component of that, we often had to educate our preceptors on the role of the NP. Thankfully, the pediatric community was aware of the NP; in the Boston area, at least, many settings already had NPs (and PAs) as providers. Still, when I reflect back, the experience of finding a preceptor augmented my professional education. It also instilled in me responsibility for my own professional development.
When it was my turn, I agreed to precept as my contribution to the profession. However, my first foray into precepting was not a pleasant one. As some of our email authors attested to experiencing, my student was completely unprepared for her clinical rotation. I found myself teaching basic assessment skills (to a student in her final semester!), which takes considerable time in the office setting. Subsequently, I required students to have at least three years of RN experience and demonstrate a full H&P prior to acceptance. This proviso raised some eyebrows among my colleagues, but as I saw it, my role as a preceptor was to help students to improve their skills—not teach them the basics. The result: a happy preceptor and long-standing relationships with the precepted students.
Even so, like many of the clinicians who responded to Dr. Danielsen’s editorial, I must admit I eventually stopped precepting. My decision was based on several factors, but the primary reason was that the students and faculty recruiting me were somewhat cavalier in their responsibility for preparedness to practice.
Among the readers who shared their precepting experiences, many cited inexperience in the RN role as a significant issue, as well as the rapidity with which students progress through their NP programs. Some commented that there is too much material to understand and process and not enough time to master the skills. These observations lead me back to the idea of “too many programs and students.” I know I risk offending my colleagues in academia with that statement. But I also know, from conversations with colleagues and the volume of emails we received on this topic, that many preceptors are frustrated by some students’ lack of responsibility, motivation, and preparation for their clinical rotations.
Some chalk up this shortcoming to being “millennials.” Others suggest that online programs do not hold students accountable for the “real world” demands of the job. On the latter point, I would submit that the “brick and mortar” programs have similar issues with students. And while both of these points have some validity, I think the problem is more complicated.
We face a perfect storm in NP education: The demand for NPs has increased as a result of the implementation of the ACA. In response to this demand, the number of NP programs has grown, and so has the need for NP preceptors. Yet, at this critical time, the number of preceptors is dwindling (in volume, yes, but also in willingness).
To resolve this conundrum, we must take a closer look at ways we can reverse the declining interest in preceptorship. Increasing the number of available preceptors requires overcoming perceived barriers. One of these, as noted by Barker and Pittman, is the detrimental effect precepting has on productivity.2 To illustrate this, they presented findings from a study of community physicians that documented an increase in the time taken to see patients and a decrease in the number of patients seen when the physician was precepting students.3 Additional time and reduced productivity are not tolerated in today’s work environment, and patients, who increasingly see themselves as health care consumers (who can take their “business” elsewhere), don’t appreciate waiting to see their health care provider when they have an appointment.
In their research, Logan, Kovacs, and Barry also found that productivity expectations (or should I say, the expectation of reduced productivity) impeded willingness to precept.4 They identified lack of time in the workday as a major barrier. This point is difficult to counter, I admit. But they also presented two other deterrents that, conversely, I view as potential opportunities for increasing the number of willing preceptors:
Lack of training for preceptors. Preceptors must learn how to fulfill this role on their own, without any training or support. This is a significant problem, not only for nascent preceptors but also for seasoned ones, who often precept students from different programs with a variety of requirements and expectations (and paperwork!). In an editorial, a new preceptor expressed concern about her ability to “get it right” and give her student what was needed to accomplish the goals for the rotation.5 Training and supportive testimonies are essential for successful precepting. A simple approach would be for program faculty to “mentor” new preceptors: Spend time orienting them to the expectations of the program and explaining how to evaluate students. Be proactive—establish weekly conference calls and share both strategies for successful precepting relationships and the “pitfalls to avoid.”
Student preparation. The other problem discussed by Logan, Kovacs, and Barry—and attested to by many of our readers—was the skill level and readiness of students on the first day of their clinical experience. While this responsibility lies with the student (rightfully so), I believe awareness of this problem, and understanding of how it affects practitioners’ willingness to precept, offers an opportunity for our education programs. Students may not know what they don’t know, or some may be too timid to speak up if they feel unprepared to step into a clinical arena (not to confuse that unease with “first-day jitters”). It is incumbent on the program faculty to ensure their students—who are representatives of that program and the faculty—are ready for clinical rotations. What do they need to do? Conduct an assessment of skills and readiness, which would assist all parties—the student, the preceptor, and the faculty—in gauging the progress of skill improvement and student competency and capability as a provider. It is also imperative that any remediation be provided by the program (prior to the student’s entrance into the clinical setting) and not the preceptor.
The bottom line is that precepting is a partnership between the skilled practitioner, the NP faculty, and the focused student.2 The responsibility for a mutually enjoyable and rewarding experience lies with all parties involved. As seasoned NPs, we must be active participants in preparing the next generation of our colleagues. That is our professional responsibility—our fulfillment of the “social contract.” We owe it to them, we owe it to our patients, and we owe it to ourselves—because someday, down the road, these clinicians will be taking care of us!
When a topic merits two editorials, there is clearly much to discuss. What steps do you suggest we undertake to mitigate this conundrum? Share your ideas by writing to me at [email protected].
References
1. Danielsen RD. The death of altruism, or, can I get a preceptor please? Clin Rev. 2016;26(4):10,13-14.
2. Barker ER, Pittman O. Becoming a super preceptor: a practical guide to preceptorship in today’s clinical climate. J Am Acad Nurse Pract. 2010;22(3):144-149.
3. Levy BT, Gjerde CL, Albrecht LA. The effects of precepting on and the support desired by community-based preceptors in Iowa. Acad Med. 1997;72(5):382-384.
4. Logan BL, Kovacs KA, Barry TL. Precepting nurse practitioner students: one medical center’s efforts to improve the precepting process. J Am Assoc Nurse Pract. 2015;27(12):676-682.
5. Aktan NM. Clinical preceptoring: what’s in it for me? J Nurse Pract. 2010;6(2):159-160.
Randy Danielsen’s editorial on the topic of precepting (April 2016) elicited a flurry of responses from our NP readers.1 The influx of feedback prompted me as an educator, an NP, and a former preceptor to wonder: Why the paucity of preceptors? Are there too many programs and too many students? And are we dropping the ball when it comes to engendering professional responsibility as a “social contract”?1
Let me start with a query: Are we requiring students to uphold their social contracts? That is, are they engaged in professional networking to enrich their own clinical experiences? Are they responsible for establishing relationships with providers in their communities in preparation for clinical rotations? Aren’t these all components of their social contracts as students?
In my PNP program, we found our own preceptors (there were no clinical coordinators “back in the day”). As a component of that, we often had to educate our preceptors on the role of the NP. Thankfully, the pediatric community was aware of the NP; in the Boston area, at least, many settings already had NPs (and PAs) as providers. Still, when I reflect back, the experience of finding a preceptor augmented my professional education. It also instilled in me responsibility for my own professional development.
When it was my turn, I agreed to precept as my contribution to the profession. However, my first foray into precepting was not a pleasant one. As some of our email authors attested to experiencing, my student was completely unprepared for her clinical rotation. I found myself teaching basic assessment skills (to a student in her final semester!), which takes considerable time in the office setting. Subsequently, I required students to have at least three years of RN experience and demonstrate a full H&P prior to acceptance. This proviso raised some eyebrows among my colleagues, but as I saw it, my role as a preceptor was to help students to improve their skills—not teach them the basics. The result: a happy preceptor and long-standing relationships with the precepted students.
Even so, like many of the clinicians who responded to Dr. Danielsen’s editorial, I must admit I eventually stopped precepting. My decision was based on several factors, but the primary reason was that the students and faculty recruiting me were somewhat cavalier in their responsibility for preparedness to practice.
Among the readers who shared their precepting experiences, many cited inexperience in the RN role as a significant issue, as well as the rapidity with which students progress through their NP programs. Some commented that there is too much material to understand and process and not enough time to master the skills. These observations lead me back to the idea of “too many programs and students.” I know I risk offending my colleagues in academia with that statement. But I also know, from conversations with colleagues and the volume of emails we received on this topic, that many preceptors are frustrated by some students’ lack of responsibility, motivation, and preparation for their clinical rotations.
Some chalk up this shortcoming to being “millennials.” Others suggest that online programs do not hold students accountable for the “real world” demands of the job. On the latter point, I would submit that the “brick and mortar” programs have similar issues with students. And while both of these points have some validity, I think the problem is more complicated.
We face a perfect storm in NP education: The demand for NPs has increased as a result of the implementation of the ACA. In response to this demand, the number of NP programs has grown, and so has the need for NP preceptors. Yet, at this critical time, the number of preceptors is dwindling (in volume, yes, but also in willingness).
To resolve this conundrum, we must take a closer look at ways we can reverse the declining interest in preceptorship. Increasing the number of available preceptors requires overcoming perceived barriers. One of these, as noted by Barker and Pittman, is the detrimental effect precepting has on productivity.2 To illustrate this, they presented findings from a study of community physicians that documented an increase in the time taken to see patients and a decrease in the number of patients seen when the physician was precepting students.3 Additional time and reduced productivity are not tolerated in today’s work environment, and patients, who increasingly see themselves as health care consumers (who can take their “business” elsewhere), don’t appreciate waiting to see their health care provider when they have an appointment.
In their research, Logan, Kovacs, and Barry also found that productivity expectations (or should I say, the expectation of reduced productivity) impeded willingness to precept.4 They identified lack of time in the workday as a major barrier. This point is difficult to counter, I admit. But they also presented two other deterrents that, conversely, I view as potential opportunities for increasing the number of willing preceptors:
Lack of training for preceptors. Preceptors must learn how to fulfill this role on their own, without any training or support. This is a significant problem, not only for nascent preceptors but also for seasoned ones, who often precept students from different programs with a variety of requirements and expectations (and paperwork!). In an editorial, a new preceptor expressed concern about her ability to “get it right” and give her student what was needed to accomplish the goals for the rotation.5 Training and supportive testimonies are essential for successful precepting. A simple approach would be for program faculty to “mentor” new preceptors: Spend time orienting them to the expectations of the program and explaining how to evaluate students. Be proactive—establish weekly conference calls and share both strategies for successful precepting relationships and the “pitfalls to avoid.”
Student preparation. The other problem discussed by Logan, Kovacs, and Barry—and attested to by many of our readers—was the skill level and readiness of students on the first day of their clinical experience. While this responsibility lies with the student (rightfully so), I believe awareness of this problem, and understanding of how it affects practitioners’ willingness to precept, offers an opportunity for our education programs. Students may not know what they don’t know, or some may be too timid to speak up if they feel unprepared to step into a clinical arena (not to confuse that unease with “first-day jitters”). It is incumbent on the program faculty to ensure their students—who are representatives of that program and the faculty—are ready for clinical rotations. What do they need to do? Conduct an assessment of skills and readiness, which would assist all parties—the student, the preceptor, and the faculty—in gauging the progress of skill improvement and student competency and capability as a provider. It is also imperative that any remediation be provided by the program (prior to the student’s entrance into the clinical setting) and not the preceptor.
The bottom line is that precepting is a partnership between the skilled practitioner, the NP faculty, and the focused student.2 The responsibility for a mutually enjoyable and rewarding experience lies with all parties involved. As seasoned NPs, we must be active participants in preparing the next generation of our colleagues. That is our professional responsibility—our fulfillment of the “social contract.” We owe it to them, we owe it to our patients, and we owe it to ourselves—because someday, down the road, these clinicians will be taking care of us!
When a topic merits two editorials, there is clearly much to discuss. What steps do you suggest we undertake to mitigate this conundrum? Share your ideas by writing to me at [email protected].
References
1. Danielsen RD. The death of altruism, or, can I get a preceptor please? Clin Rev. 2016;26(4):10,13-14.
2. Barker ER, Pittman O. Becoming a super preceptor: a practical guide to preceptorship in today’s clinical climate. J Am Acad Nurse Pract. 2010;22(3):144-149.
3. Levy BT, Gjerde CL, Albrecht LA. The effects of precepting on and the support desired by community-based preceptors in Iowa. Acad Med. 1997;72(5):382-384.
4. Logan BL, Kovacs KA, Barry TL. Precepting nurse practitioner students: one medical center’s efforts to improve the precepting process. J Am Assoc Nurse Pract. 2015;27(12):676-682.
5. Aktan NM. Clinical preceptoring: what’s in it for me? J Nurse Pract. 2010;6(2):159-160.
Randy Danielsen’s editorial on the topic of precepting (April 2016) elicited a flurry of responses from our NP readers.1 The influx of feedback prompted me as an educator, an NP, and a former preceptor to wonder: Why the paucity of preceptors? Are there too many programs and too many students? And are we dropping the ball when it comes to engendering professional responsibility as a “social contract”?1
Let me start with a query: Are we requiring students to uphold their social contracts? That is, are they engaged in professional networking to enrich their own clinical experiences? Are they responsible for establishing relationships with providers in their communities in preparation for clinical rotations? Aren’t these all components of their social contracts as students?
In my PNP program, we found our own preceptors (there were no clinical coordinators “back in the day”). As a component of that, we often had to educate our preceptors on the role of the NP. Thankfully, the pediatric community was aware of the NP; in the Boston area, at least, many settings already had NPs (and PAs) as providers. Still, when I reflect back, the experience of finding a preceptor augmented my professional education. It also instilled in me responsibility for my own professional development.
When it was my turn, I agreed to precept as my contribution to the profession. However, my first foray into precepting was not a pleasant one. As some of our email authors attested to experiencing, my student was completely unprepared for her clinical rotation. I found myself teaching basic assessment skills (to a student in her final semester!), which takes considerable time in the office setting. Subsequently, I required students to have at least three years of RN experience and demonstrate a full H&P prior to acceptance. This proviso raised some eyebrows among my colleagues, but as I saw it, my role as a preceptor was to help students to improve their skills—not teach them the basics. The result: a happy preceptor and long-standing relationships with the precepted students.
Even so, like many of the clinicians who responded to Dr. Danielsen’s editorial, I must admit I eventually stopped precepting. My decision was based on several factors, but the primary reason was that the students and faculty recruiting me were somewhat cavalier in their responsibility for preparedness to practice.
Among the readers who shared their precepting experiences, many cited inexperience in the RN role as a significant issue, as well as the rapidity with which students progress through their NP programs. Some commented that there is too much material to understand and process and not enough time to master the skills. These observations lead me back to the idea of “too many programs and students.” I know I risk offending my colleagues in academia with that statement. But I also know, from conversations with colleagues and the volume of emails we received on this topic, that many preceptors are frustrated by some students’ lack of responsibility, motivation, and preparation for their clinical rotations.
Some chalk up this shortcoming to being “millennials.” Others suggest that online programs do not hold students accountable for the “real world” demands of the job. On the latter point, I would submit that the “brick and mortar” programs have similar issues with students. And while both of these points have some validity, I think the problem is more complicated.
We face a perfect storm in NP education: The demand for NPs has increased as a result of the implementation of the ACA. In response to this demand, the number of NP programs has grown, and so has the need for NP preceptors. Yet, at this critical time, the number of preceptors is dwindling (in volume, yes, but also in willingness).
To resolve this conundrum, we must take a closer look at ways we can reverse the declining interest in preceptorship. Increasing the number of available preceptors requires overcoming perceived barriers. One of these, as noted by Barker and Pittman, is the detrimental effect precepting has on productivity.2 To illustrate this, they presented findings from a study of community physicians that documented an increase in the time taken to see patients and a decrease in the number of patients seen when the physician was precepting students.3 Additional time and reduced productivity are not tolerated in today’s work environment, and patients, who increasingly see themselves as health care consumers (who can take their “business” elsewhere), don’t appreciate waiting to see their health care provider when they have an appointment.
In their research, Logan, Kovacs, and Barry also found that productivity expectations (or should I say, the expectation of reduced productivity) impeded willingness to precept.4 They identified lack of time in the workday as a major barrier. This point is difficult to counter, I admit. But they also presented two other deterrents that, conversely, I view as potential opportunities for increasing the number of willing preceptors:
Lack of training for preceptors. Preceptors must learn how to fulfill this role on their own, without any training or support. This is a significant problem, not only for nascent preceptors but also for seasoned ones, who often precept students from different programs with a variety of requirements and expectations (and paperwork!). In an editorial, a new preceptor expressed concern about her ability to “get it right” and give her student what was needed to accomplish the goals for the rotation.5 Training and supportive testimonies are essential for successful precepting. A simple approach would be for program faculty to “mentor” new preceptors: Spend time orienting them to the expectations of the program and explaining how to evaluate students. Be proactive—establish weekly conference calls and share both strategies for successful precepting relationships and the “pitfalls to avoid.”
Student preparation. The other problem discussed by Logan, Kovacs, and Barry—and attested to by many of our readers—was the skill level and readiness of students on the first day of their clinical experience. While this responsibility lies with the student (rightfully so), I believe awareness of this problem, and understanding of how it affects practitioners’ willingness to precept, offers an opportunity for our education programs. Students may not know what they don’t know, or some may be too timid to speak up if they feel unprepared to step into a clinical arena (not to confuse that unease with “first-day jitters”). It is incumbent on the program faculty to ensure their students—who are representatives of that program and the faculty—are ready for clinical rotations. What do they need to do? Conduct an assessment of skills and readiness, which would assist all parties—the student, the preceptor, and the faculty—in gauging the progress of skill improvement and student competency and capability as a provider. It is also imperative that any remediation be provided by the program (prior to the student’s entrance into the clinical setting) and not the preceptor.
The bottom line is that precepting is a partnership between the skilled practitioner, the NP faculty, and the focused student.2 The responsibility for a mutually enjoyable and rewarding experience lies with all parties involved. As seasoned NPs, we must be active participants in preparing the next generation of our colleagues. That is our professional responsibility—our fulfillment of the “social contract.” We owe it to them, we owe it to our patients, and we owe it to ourselves—because someday, down the road, these clinicians will be taking care of us!
When a topic merits two editorials, there is clearly much to discuss. What steps do you suggest we undertake to mitigate this conundrum? Share your ideas by writing to me at [email protected].
References
1. Danielsen RD. The death of altruism, or, can I get a preceptor please? Clin Rev. 2016;26(4):10,13-14.
2. Barker ER, Pittman O. Becoming a super preceptor: a practical guide to preceptorship in today’s clinical climate. J Am Acad Nurse Pract. 2010;22(3):144-149.
3. Levy BT, Gjerde CL, Albrecht LA. The effects of precepting on and the support desired by community-based preceptors in Iowa. Acad Med. 1997;72(5):382-384.
4. Logan BL, Kovacs KA, Barry TL. Precepting nurse practitioner students: one medical center’s efforts to improve the precepting process. J Am Assoc Nurse Pract. 2015;27(12):676-682.
5. Aktan NM. Clinical preceptoring: what’s in it for me? J Nurse Pract. 2010;6(2):159-160.