User login
Improving our crystal ball: prognostication in neuroscience ICUs
The most difficult decisions in neuroscience intensive care units often involve patients’ ultimate goals of care. Oftentimes, family members of a brain-injured patient with an apparently poor neurologic prognosis must weigh whether their loved one would have preferred prolongation of aggressive ICU and post-ICU care, often with little to no chance for “meaningful” recovery, or death via the institution of comfort measures only. Proper prognostication is crucial to the family when making such decisions. However, the process of formulating and talking about prognosis for our most severely affected patients is subject to physician and family biases, families’ insufficient understanding of projected outcomes, and sometimes clinical nihilism by the physicians.
The process of predicting the outcomes of patients with traumatic brain injury (TBI) serves as an example of these issues. Moderate to severe TBI continues to be a leading cause of death and disability in the United States.1 Most deaths of patients with moderate to severe TBI follow decisions by doctors and families to pursue comfort care only. However, these decisions occur at a disconcertingly highly variable rate at different trauma centers, with the variation seemingly unrelated to patients’ disease severity, age, or previously diagnosed comorbidities.2 These patients are at risk for their care being influenced by a self-fulfilling prophecy: That is, the impression of a poor prognosis communicated by clinicians to a patient’s family, whether correct or incorrect, affects the aggressiveness of the care that a patient receives and determines the patient’s outcome.3
Remedying these issues through a family or health care proxy decision support intervention (“decision aid”) that could improve and standardize the way TBI prognosis is communicated may lead to better informed decisions for these critically ill patients, with potentially less decisional regret and post-ICU stress disorders in families, and decisions more in line with the patient’s values and preferences.4 A recent Cochrane review showed that for a decision aid to be effective and integrated into routine clinical care, it must contain disease-specific data tailored to patients and their families/proxies, and be simple and time efficient for physicians to use.5 Taking these factors into account, researchers at the University of Massachusetts are developing a National Institutes of Health–funded pilot decision aid for goals-of-care decisions in critically-ill TBI patients.
While the field of TBI has tools such as the IMPACT calculator that can be used to estimate a patient’s long-term prognosis based on how patients with similar clinical characteristics in large clinical databases have done, the fundamental uncertainty of prognosis remains a difficult challenge.6 Arguably, this challenge is even more daunting when estimating prognosis for patients with severe ischemic stroke and intracerebral hemorrhage (ICH). The use of ischemic stroke outcome prediction tools is complicated, as many of them are based on population databases with wide variations in whether included patients received intravenous tissue plasminogen activator, endovascular therapy, both, or neither. Furthermore, a recent study comparing the accuracy of the ICH score for predicting 3-month outcome for ICH patients to the subjective predictions of clinicians made within 24 hours of patient admission found that the educated guesses of physicians and nurses overall seemed to correlate with actual outcomes more closely than the ICH score output.7 This finding highlights the challenge of using available outcome “calculators” for individual patients in ICUs.
Ultimately, the decisions made about the goals of care for ICU patients come down not only to what their expected outcomes are, but also whether their surrogate decision makers believe that those outcomes would be acceptable to the patient.8 Potential pitfalls abound with regard to this issue as well. Decision makers are often not made aware of the fact that many times patients with significant disability may nevertheless report a reasonable quality of life. By their very nature, conversations regarding patient prognosis inevitably focus on what future disabilities one might expect; accounting for a patient’s possible adaptation to disability is both easy to overlook and hard to accomplish even when given adequate attention.9 Improvements in the field of neuroprognostication may not only depend on the development of new shared decision making tools for physicians and families but also on increasing awareness of the limitations of prognostic scales and the cognitive biases that may exist when discussing the possibilities of future disability.
References
1. Traumatic Brain Injury Statistics [online]. Available at: http://www.cdc.gov/traumaticbraininjury/statistics.html. Accessed Nov. 1.
3. Neurocrit Care. 2013;19:347-63.
4. Col NF. Chapter 17: Shared Decision Making. In: Communicating Risks and Benefits: An Evidence-Based User’s Guide [online]. Available at http://www.fda.gov/downloads/AboutFDA/ReportsManualsForms/Reports/UCM268069.pdf.
5. Cochrane Database Syst Rev. 2011 Oct 5;(10):CD001431.
6. PLoS Med. 2008 Aug;5(8):e165; discussion e168.
8. Neurocrit Care. 2015;23:131-41.
Dr. Muehlschlegel is associate professor of neurology (neurocritical care), anesthesia/critical care, and surgery at the University of Massachusetts, Worcester. Dr. Hwang is assistant professor of neurology in the division of neurocritical care and emergency neurology at Yale University, New Haven, Conn. Dr. Muehlschlegel reported receiving a grant from the National Institutes of Health for her research in developing a pilot decision aid for goals-of-care decisions in critically-ill TBI patients. Dr. Hwang reported receiving research funding from the American Brain Foundation, the Apple Pickers Foundation, the National Institute on Aging, and the Neurocritical Care Society.
The most difficult decisions in neuroscience intensive care units often involve patients’ ultimate goals of care. Oftentimes, family members of a brain-injured patient with an apparently poor neurologic prognosis must weigh whether their loved one would have preferred prolongation of aggressive ICU and post-ICU care, often with little to no chance for “meaningful” recovery, or death via the institution of comfort measures only. Proper prognostication is crucial to the family when making such decisions. However, the process of formulating and talking about prognosis for our most severely affected patients is subject to physician and family biases, families’ insufficient understanding of projected outcomes, and sometimes clinical nihilism by the physicians.
The process of predicting the outcomes of patients with traumatic brain injury (TBI) serves as an example of these issues. Moderate to severe TBI continues to be a leading cause of death and disability in the United States.1 Most deaths of patients with moderate to severe TBI follow decisions by doctors and families to pursue comfort care only. However, these decisions occur at a disconcertingly highly variable rate at different trauma centers, with the variation seemingly unrelated to patients’ disease severity, age, or previously diagnosed comorbidities.2 These patients are at risk for their care being influenced by a self-fulfilling prophecy: That is, the impression of a poor prognosis communicated by clinicians to a patient’s family, whether correct or incorrect, affects the aggressiveness of the care that a patient receives and determines the patient’s outcome.3
Remedying these issues through a family or health care proxy decision support intervention (“decision aid”) that could improve and standardize the way TBI prognosis is communicated may lead to better informed decisions for these critically ill patients, with potentially less decisional regret and post-ICU stress disorders in families, and decisions more in line with the patient’s values and preferences.4 A recent Cochrane review showed that for a decision aid to be effective and integrated into routine clinical care, it must contain disease-specific data tailored to patients and their families/proxies, and be simple and time efficient for physicians to use.5 Taking these factors into account, researchers at the University of Massachusetts are developing a National Institutes of Health–funded pilot decision aid for goals-of-care decisions in critically-ill TBI patients.
While the field of TBI has tools such as the IMPACT calculator that can be used to estimate a patient’s long-term prognosis based on how patients with similar clinical characteristics in large clinical databases have done, the fundamental uncertainty of prognosis remains a difficult challenge.6 Arguably, this challenge is even more daunting when estimating prognosis for patients with severe ischemic stroke and intracerebral hemorrhage (ICH). The use of ischemic stroke outcome prediction tools is complicated, as many of them are based on population databases with wide variations in whether included patients received intravenous tissue plasminogen activator, endovascular therapy, both, or neither. Furthermore, a recent study comparing the accuracy of the ICH score for predicting 3-month outcome for ICH patients to the subjective predictions of clinicians made within 24 hours of patient admission found that the educated guesses of physicians and nurses overall seemed to correlate with actual outcomes more closely than the ICH score output.7 This finding highlights the challenge of using available outcome “calculators” for individual patients in ICUs.
Ultimately, the decisions made about the goals of care for ICU patients come down not only to what their expected outcomes are, but also whether their surrogate decision makers believe that those outcomes would be acceptable to the patient.8 Potential pitfalls abound with regard to this issue as well. Decision makers are often not made aware of the fact that many times patients with significant disability may nevertheless report a reasonable quality of life. By their very nature, conversations regarding patient prognosis inevitably focus on what future disabilities one might expect; accounting for a patient’s possible adaptation to disability is both easy to overlook and hard to accomplish even when given adequate attention.9 Improvements in the field of neuroprognostication may not only depend on the development of new shared decision making tools for physicians and families but also on increasing awareness of the limitations of prognostic scales and the cognitive biases that may exist when discussing the possibilities of future disability.
References
1. Traumatic Brain Injury Statistics [online]. Available at: http://www.cdc.gov/traumaticbraininjury/statistics.html. Accessed Nov. 1.
3. Neurocrit Care. 2013;19:347-63.
4. Col NF. Chapter 17: Shared Decision Making. In: Communicating Risks and Benefits: An Evidence-Based User’s Guide [online]. Available at http://www.fda.gov/downloads/AboutFDA/ReportsManualsForms/Reports/UCM268069.pdf.
5. Cochrane Database Syst Rev. 2011 Oct 5;(10):CD001431.
6. PLoS Med. 2008 Aug;5(8):e165; discussion e168.
8. Neurocrit Care. 2015;23:131-41.
Dr. Muehlschlegel is associate professor of neurology (neurocritical care), anesthesia/critical care, and surgery at the University of Massachusetts, Worcester. Dr. Hwang is assistant professor of neurology in the division of neurocritical care and emergency neurology at Yale University, New Haven, Conn. Dr. Muehlschlegel reported receiving a grant from the National Institutes of Health for her research in developing a pilot decision aid for goals-of-care decisions in critically-ill TBI patients. Dr. Hwang reported receiving research funding from the American Brain Foundation, the Apple Pickers Foundation, the National Institute on Aging, and the Neurocritical Care Society.
The most difficult decisions in neuroscience intensive care units often involve patients’ ultimate goals of care. Oftentimes, family members of a brain-injured patient with an apparently poor neurologic prognosis must weigh whether their loved one would have preferred prolongation of aggressive ICU and post-ICU care, often with little to no chance for “meaningful” recovery, or death via the institution of comfort measures only. Proper prognostication is crucial to the family when making such decisions. However, the process of formulating and talking about prognosis for our most severely affected patients is subject to physician and family biases, families’ insufficient understanding of projected outcomes, and sometimes clinical nihilism by the physicians.
The process of predicting the outcomes of patients with traumatic brain injury (TBI) serves as an example of these issues. Moderate to severe TBI continues to be a leading cause of death and disability in the United States.1 Most deaths of patients with moderate to severe TBI follow decisions by doctors and families to pursue comfort care only. However, these decisions occur at a disconcertingly highly variable rate at different trauma centers, with the variation seemingly unrelated to patients’ disease severity, age, or previously diagnosed comorbidities.2 These patients are at risk for their care being influenced by a self-fulfilling prophecy: That is, the impression of a poor prognosis communicated by clinicians to a patient’s family, whether correct or incorrect, affects the aggressiveness of the care that a patient receives and determines the patient’s outcome.3
Remedying these issues through a family or health care proxy decision support intervention (“decision aid”) that could improve and standardize the way TBI prognosis is communicated may lead to better informed decisions for these critically ill patients, with potentially less decisional regret and post-ICU stress disorders in families, and decisions more in line with the patient’s values and preferences.4 A recent Cochrane review showed that for a decision aid to be effective and integrated into routine clinical care, it must contain disease-specific data tailored to patients and their families/proxies, and be simple and time efficient for physicians to use.5 Taking these factors into account, researchers at the University of Massachusetts are developing a National Institutes of Health–funded pilot decision aid for goals-of-care decisions in critically-ill TBI patients.
While the field of TBI has tools such as the IMPACT calculator that can be used to estimate a patient’s long-term prognosis based on how patients with similar clinical characteristics in large clinical databases have done, the fundamental uncertainty of prognosis remains a difficult challenge.6 Arguably, this challenge is even more daunting when estimating prognosis for patients with severe ischemic stroke and intracerebral hemorrhage (ICH). The use of ischemic stroke outcome prediction tools is complicated, as many of them are based on population databases with wide variations in whether included patients received intravenous tissue plasminogen activator, endovascular therapy, both, or neither. Furthermore, a recent study comparing the accuracy of the ICH score for predicting 3-month outcome for ICH patients to the subjective predictions of clinicians made within 24 hours of patient admission found that the educated guesses of physicians and nurses overall seemed to correlate with actual outcomes more closely than the ICH score output.7 This finding highlights the challenge of using available outcome “calculators” for individual patients in ICUs.
Ultimately, the decisions made about the goals of care for ICU patients come down not only to what their expected outcomes are, but also whether their surrogate decision makers believe that those outcomes would be acceptable to the patient.8 Potential pitfalls abound with regard to this issue as well. Decision makers are often not made aware of the fact that many times patients with significant disability may nevertheless report a reasonable quality of life. By their very nature, conversations regarding patient prognosis inevitably focus on what future disabilities one might expect; accounting for a patient’s possible adaptation to disability is both easy to overlook and hard to accomplish even when given adequate attention.9 Improvements in the field of neuroprognostication may not only depend on the development of new shared decision making tools for physicians and families but also on increasing awareness of the limitations of prognostic scales and the cognitive biases that may exist when discussing the possibilities of future disability.
References
1. Traumatic Brain Injury Statistics [online]. Available at: http://www.cdc.gov/traumaticbraininjury/statistics.html. Accessed Nov. 1.
3. Neurocrit Care. 2013;19:347-63.
4. Col NF. Chapter 17: Shared Decision Making. In: Communicating Risks and Benefits: An Evidence-Based User’s Guide [online]. Available at http://www.fda.gov/downloads/AboutFDA/ReportsManualsForms/Reports/UCM268069.pdf.
5. Cochrane Database Syst Rev. 2011 Oct 5;(10):CD001431.
6. PLoS Med. 2008 Aug;5(8):e165; discussion e168.
8. Neurocrit Care. 2015;23:131-41.
Dr. Muehlschlegel is associate professor of neurology (neurocritical care), anesthesia/critical care, and surgery at the University of Massachusetts, Worcester. Dr. Hwang is assistant professor of neurology in the division of neurocritical care and emergency neurology at Yale University, New Haven, Conn. Dr. Muehlschlegel reported receiving a grant from the National Institutes of Health for her research in developing a pilot decision aid for goals-of-care decisions in critically-ill TBI patients. Dr. Hwang reported receiving research funding from the American Brain Foundation, the Apple Pickers Foundation, the National Institute on Aging, and the Neurocritical Care Society.
Racing against burnout
At 6 a.m., after eight admissions back to back, I feel like I can’t stay awake any longer. I desperately need a nap. I have 30 minutes before my next admission, but I know I’m not going to rest. I close my eyes, and I only see charts. I’m trying not to collapse, but I still have three more patients to admit before I go home. And I can’t rest.
I’m scared that I’ll make a mistake. While I write my history of presenting illness, I imagine the day team reading my notes and hoping they don’t notice that I was about to crash on the desk. I check my documentation multiple times to make sure I don’t miss anything, and I know that won’t relieve my anxiety. When I leave, I will still feel the failure of not being able to give my best for my patient or for my night team, because I’m too tired. I know this frustration is going to give room to the emptiness – that indifference of being so beaten up that you can’t feel anymore.
And eventually, shame comes in. I’m ashamed of how I feel, because somehow, it means I am weak. All these feelings threaten to cripple me. Then I get home and cry till I fall asleep.
Recently, I read an article about a young physician contemplating suicide in her first year of practice. She described the dread of going into work and the emptiness left at the end of the day. Halfway through my second year of residency, I could relate to those feelings. I dealt with the anxiety of wondering what type of shift I was going to walk into, and experienced the stress of not wanting to disappoint the team, my peers, the patient, or myself.
Being constantly afraid of making a mistake is tiring. Sometimes, I get the pat on the back from senior physicians, saying I will survive. But it’s not enough. I can’t blame them. It’s human nature to forget how bad it hurt and just remember being strong enough to bear it. I count the days til I have a day off or the weeks til my next vacation. I try not to complain as much because nobody wants to hear it, and nothing is going to change. I feel deeply alone, like nobody cares.
And in the end I put myself onto this path. I knew what I was getting myself into. And I get myself out of it. I hold on to the smiles my staff give me when I walk in. I experience that 10-minute interview with someone whose thought process was so disorganized, and I realize that it took some skill to connect with that patient.
I am heartened by my ability to deescalate a patient who was about to become violent because I know Spanish. I notice that I am able to work faster than I did just a year ago. So I hold on. The trick was to find what made me want to hold on and what motivates me.
I’m not going to write about socializing or finding a hobby outside of medicine. But I must acknowledge that I have a wonderful book club, supportive boyfriend, and family. I lose myself in books, TV shows, cooking. I even started reading comic books. Plenty of articles are out there about how to beat physician burnout. They all help. I tried knitting, coloring, you name it, but for me, those activities were just not enough. I had to try to find meaning behind the work I do. I had to grab all those small moments during a shift and knit them together to build a bridge to where my passion lies. Then I started by reminding myself why I wanted to practice medicine and why psychiatry.
What inspires me is learning how to decipher what hides behind a symptom – why patient A’s anxiety is different from patient B’s. I find psychodynamics fascinating, so I read. I read literature, articles, and books with subjects around my interests. So when I see a patient at 4 a.m. for 5 minutes, I can knit it together with what I read. So it has meaning. And then it’s easier to hold on. Because the 12-hour overnight shift becomes hours of learning about my passion. Because I feel a step closer. And even though last night’s shift was so hard, I’m happy to be back at work today. When I read about the psychopathology of depression and then admit five patients with suicidal ideation, it stops being the same story over and over. It turns into an exploration, and it becomes fascinating. I won’t hear the same story again. So many times, attendings told me to read, and I had to be at my breaking point to understand why it was so essential. Now I’m motivated, and I plan to keep pushing myself to the limit to find a new challenge and to surprise myself in the middle of my beat-up tiredness when I see something in my patient that so many have written about. The adrenaline rush comes on the path of becoming that psychiatrist I aim to be, not in the diploma I will get 2 years from now.
I am racing against burnout, but I’m winning. And I wanted to share my experience to remind others that we are not alone on this path, and we should not have higher suicide rates than other professional groups.
If you are a resident or more experienced physician, know that you are not alone. Many others just like you are stretching themselves thin. Follow the tips of how to beat burnout that you’ve seen around. Find what works for you and dig into yourself, into what drove you in this direction, into where your passion lies. Find the meaning behind this hard work, and connect it to the passion that motivates you. Think of what made you want to become a doctor! I’m not sure it works 100% of the time.
Ask me again in 6 months.
Dr. Serrano is a PGY2 psychiatry resident at the Einstein Medical Center in Philadelphia.
At 6 a.m., after eight admissions back to back, I feel like I can’t stay awake any longer. I desperately need a nap. I have 30 minutes before my next admission, but I know I’m not going to rest. I close my eyes, and I only see charts. I’m trying not to collapse, but I still have three more patients to admit before I go home. And I can’t rest.
I’m scared that I’ll make a mistake. While I write my history of presenting illness, I imagine the day team reading my notes and hoping they don’t notice that I was about to crash on the desk. I check my documentation multiple times to make sure I don’t miss anything, and I know that won’t relieve my anxiety. When I leave, I will still feel the failure of not being able to give my best for my patient or for my night team, because I’m too tired. I know this frustration is going to give room to the emptiness – that indifference of being so beaten up that you can’t feel anymore.
And eventually, shame comes in. I’m ashamed of how I feel, because somehow, it means I am weak. All these feelings threaten to cripple me. Then I get home and cry till I fall asleep.
Recently, I read an article about a young physician contemplating suicide in her first year of practice. She described the dread of going into work and the emptiness left at the end of the day. Halfway through my second year of residency, I could relate to those feelings. I dealt with the anxiety of wondering what type of shift I was going to walk into, and experienced the stress of not wanting to disappoint the team, my peers, the patient, or myself.
Being constantly afraid of making a mistake is tiring. Sometimes, I get the pat on the back from senior physicians, saying I will survive. But it’s not enough. I can’t blame them. It’s human nature to forget how bad it hurt and just remember being strong enough to bear it. I count the days til I have a day off or the weeks til my next vacation. I try not to complain as much because nobody wants to hear it, and nothing is going to change. I feel deeply alone, like nobody cares.
And in the end I put myself onto this path. I knew what I was getting myself into. And I get myself out of it. I hold on to the smiles my staff give me when I walk in. I experience that 10-minute interview with someone whose thought process was so disorganized, and I realize that it took some skill to connect with that patient.
I am heartened by my ability to deescalate a patient who was about to become violent because I know Spanish. I notice that I am able to work faster than I did just a year ago. So I hold on. The trick was to find what made me want to hold on and what motivates me.
I’m not going to write about socializing or finding a hobby outside of medicine. But I must acknowledge that I have a wonderful book club, supportive boyfriend, and family. I lose myself in books, TV shows, cooking. I even started reading comic books. Plenty of articles are out there about how to beat physician burnout. They all help. I tried knitting, coloring, you name it, but for me, those activities were just not enough. I had to try to find meaning behind the work I do. I had to grab all those small moments during a shift and knit them together to build a bridge to where my passion lies. Then I started by reminding myself why I wanted to practice medicine and why psychiatry.
What inspires me is learning how to decipher what hides behind a symptom – why patient A’s anxiety is different from patient B’s. I find psychodynamics fascinating, so I read. I read literature, articles, and books with subjects around my interests. So when I see a patient at 4 a.m. for 5 minutes, I can knit it together with what I read. So it has meaning. And then it’s easier to hold on. Because the 12-hour overnight shift becomes hours of learning about my passion. Because I feel a step closer. And even though last night’s shift was so hard, I’m happy to be back at work today. When I read about the psychopathology of depression and then admit five patients with suicidal ideation, it stops being the same story over and over. It turns into an exploration, and it becomes fascinating. I won’t hear the same story again. So many times, attendings told me to read, and I had to be at my breaking point to understand why it was so essential. Now I’m motivated, and I plan to keep pushing myself to the limit to find a new challenge and to surprise myself in the middle of my beat-up tiredness when I see something in my patient that so many have written about. The adrenaline rush comes on the path of becoming that psychiatrist I aim to be, not in the diploma I will get 2 years from now.
I am racing against burnout, but I’m winning. And I wanted to share my experience to remind others that we are not alone on this path, and we should not have higher suicide rates than other professional groups.
If you are a resident or more experienced physician, know that you are not alone. Many others just like you are stretching themselves thin. Follow the tips of how to beat burnout that you’ve seen around. Find what works for you and dig into yourself, into what drove you in this direction, into where your passion lies. Find the meaning behind this hard work, and connect it to the passion that motivates you. Think of what made you want to become a doctor! I’m not sure it works 100% of the time.
Ask me again in 6 months.
Dr. Serrano is a PGY2 psychiatry resident at the Einstein Medical Center in Philadelphia.
At 6 a.m., after eight admissions back to back, I feel like I can’t stay awake any longer. I desperately need a nap. I have 30 minutes before my next admission, but I know I’m not going to rest. I close my eyes, and I only see charts. I’m trying not to collapse, but I still have three more patients to admit before I go home. And I can’t rest.
I’m scared that I’ll make a mistake. While I write my history of presenting illness, I imagine the day team reading my notes and hoping they don’t notice that I was about to crash on the desk. I check my documentation multiple times to make sure I don’t miss anything, and I know that won’t relieve my anxiety. When I leave, I will still feel the failure of not being able to give my best for my patient or for my night team, because I’m too tired. I know this frustration is going to give room to the emptiness – that indifference of being so beaten up that you can’t feel anymore.
And eventually, shame comes in. I’m ashamed of how I feel, because somehow, it means I am weak. All these feelings threaten to cripple me. Then I get home and cry till I fall asleep.
Recently, I read an article about a young physician contemplating suicide in her first year of practice. She described the dread of going into work and the emptiness left at the end of the day. Halfway through my second year of residency, I could relate to those feelings. I dealt with the anxiety of wondering what type of shift I was going to walk into, and experienced the stress of not wanting to disappoint the team, my peers, the patient, or myself.
Being constantly afraid of making a mistake is tiring. Sometimes, I get the pat on the back from senior physicians, saying I will survive. But it’s not enough. I can’t blame them. It’s human nature to forget how bad it hurt and just remember being strong enough to bear it. I count the days til I have a day off or the weeks til my next vacation. I try not to complain as much because nobody wants to hear it, and nothing is going to change. I feel deeply alone, like nobody cares.
And in the end I put myself onto this path. I knew what I was getting myself into. And I get myself out of it. I hold on to the smiles my staff give me when I walk in. I experience that 10-minute interview with someone whose thought process was so disorganized, and I realize that it took some skill to connect with that patient.
I am heartened by my ability to deescalate a patient who was about to become violent because I know Spanish. I notice that I am able to work faster than I did just a year ago. So I hold on. The trick was to find what made me want to hold on and what motivates me.
I’m not going to write about socializing or finding a hobby outside of medicine. But I must acknowledge that I have a wonderful book club, supportive boyfriend, and family. I lose myself in books, TV shows, cooking. I even started reading comic books. Plenty of articles are out there about how to beat physician burnout. They all help. I tried knitting, coloring, you name it, but for me, those activities were just not enough. I had to try to find meaning behind the work I do. I had to grab all those small moments during a shift and knit them together to build a bridge to where my passion lies. Then I started by reminding myself why I wanted to practice medicine and why psychiatry.
What inspires me is learning how to decipher what hides behind a symptom – why patient A’s anxiety is different from patient B’s. I find psychodynamics fascinating, so I read. I read literature, articles, and books with subjects around my interests. So when I see a patient at 4 a.m. for 5 minutes, I can knit it together with what I read. So it has meaning. And then it’s easier to hold on. Because the 12-hour overnight shift becomes hours of learning about my passion. Because I feel a step closer. And even though last night’s shift was so hard, I’m happy to be back at work today. When I read about the psychopathology of depression and then admit five patients with suicidal ideation, it stops being the same story over and over. It turns into an exploration, and it becomes fascinating. I won’t hear the same story again. So many times, attendings told me to read, and I had to be at my breaking point to understand why it was so essential. Now I’m motivated, and I plan to keep pushing myself to the limit to find a new challenge and to surprise myself in the middle of my beat-up tiredness when I see something in my patient that so many have written about. The adrenaline rush comes on the path of becoming that psychiatrist I aim to be, not in the diploma I will get 2 years from now.
I am racing against burnout, but I’m winning. And I wanted to share my experience to remind others that we are not alone on this path, and we should not have higher suicide rates than other professional groups.
If you are a resident or more experienced physician, know that you are not alone. Many others just like you are stretching themselves thin. Follow the tips of how to beat burnout that you’ve seen around. Find what works for you and dig into yourself, into what drove you in this direction, into where your passion lies. Find the meaning behind this hard work, and connect it to the passion that motivates you. Think of what made you want to become a doctor! I’m not sure it works 100% of the time.
Ask me again in 6 months.
Dr. Serrano is a PGY2 psychiatry resident at the Einstein Medical Center in Philadelphia.
Transitions
A few years ago I accepted an offer to work in a small community hospital. It was the only medical facility in a small town and was located in a semirural area. The nearest referral center was about 75 miles away.
At that time the hospital employed a single full-time vascular surgeon who for obvious reasons was expected to provide round-the-clock coverage and who had rather limited opportunities for educational and recreational escapes. Leaving town meant transferring his patients to the “hospitalist” service for their postop care. Patients who truly needed vascular services had to be transferred to a tertiary care facility by ambulance. Alternatively, the hospital might seek locum tenens coverage if any were even available. However, the cost was substantial, and the productivity was minimal.
Up to that point I had spent most of my career in major high-volume teaching hospitals, along with a stint in solo practice running on the 24/7 never-take-a-holiday treadmill. At age 60+ I was by no means ready to hang up my scalpel, but I was more than willing to earn less money in return for less work (and less stress).
I then had the opportunity to meet this surgeon and representatives of the hospital administration. We discussed a plan to satisfy the interests of all participants. The hospital hired me as a permanent but part-time employee. For a half salary I would work 26 weeks per year, generally 2 weeks on duty at a time and 2 weeks off. As the bureaucrats would put it, I was a 0.5 FTE.
Overall, the arrangement worked pretty well. The surgeon was finally able to turn off his pager, go to meetings, and take vacations. He even enjoyed the small bonus of finally having a colleague to talk to. The hospital now had blanket coverage of the vascular service and even saw a moderate uptick in volume. The patients finally had rational continuity of care. I was able to remain fully engaged with a somewhat smaller practice. I could schedule elective case and provide long-term follow-up care relatively seamlessly despite my limited hours. And of course, I now had more free time.
I would also often engage friends and colleagues in my own cohort of aging practitioners, especially at conferences and seminars. They generally expressed considerable interest in my new practice arrangements. The reaction I received with surprising regularity was “Where do I sign up?”
Where indeed? I had apparently tapped into a reservoir of interest among fellow senior surgeons for a way to more gradually wind down their remaining years in practice. Yet few were in situations that offered or even allowed that level of flexibility. For most, the late career practice paradigm remained the all-too-familiar one of galloping along at full speed until the last suture was tied, then quitting cold turkey. Take all the skill, experience, and passion and place it all into the back of a golf cart.
The particulars of my situation would clearly not be universally applicable. However, I do believe that scaled-down practice options can and should be both productive and cost effective under a variety of circumstances. If we were to think more creatively, more careers might wind up more gracefully. In fact, I believe that kinder and gentler transitions at both ends of our careers would not only provide added satisfaction to the elders but could also expand mentoring opportunities for our colleagues just entering practice.
The current debate about the preparedness of new graduates is based upon the presumption that a specific number of years or a specific number of cases suddenly qualifies someone to function with total autonomy. This myth has never really been true and may or may not be even less so now. As it is currently fashionable to compare OR practices with aviation safety, allow me to suggest as an analogy that no one would confuse the final readiness for solo flight with the ability to captain a 747. What better way to guide the maturation of a professional than to have an experienced copilot? But that is probably a subject for another essay.
Dr. Rivers is a former associate professor of surgery at Albert Einstein College of Medicine, Bronx, New York.
A few years ago I accepted an offer to work in a small community hospital. It was the only medical facility in a small town and was located in a semirural area. The nearest referral center was about 75 miles away.
At that time the hospital employed a single full-time vascular surgeon who for obvious reasons was expected to provide round-the-clock coverage and who had rather limited opportunities for educational and recreational escapes. Leaving town meant transferring his patients to the “hospitalist” service for their postop care. Patients who truly needed vascular services had to be transferred to a tertiary care facility by ambulance. Alternatively, the hospital might seek locum tenens coverage if any were even available. However, the cost was substantial, and the productivity was minimal.
Up to that point I had spent most of my career in major high-volume teaching hospitals, along with a stint in solo practice running on the 24/7 never-take-a-holiday treadmill. At age 60+ I was by no means ready to hang up my scalpel, but I was more than willing to earn less money in return for less work (and less stress).
I then had the opportunity to meet this surgeon and representatives of the hospital administration. We discussed a plan to satisfy the interests of all participants. The hospital hired me as a permanent but part-time employee. For a half salary I would work 26 weeks per year, generally 2 weeks on duty at a time and 2 weeks off. As the bureaucrats would put it, I was a 0.5 FTE.
Overall, the arrangement worked pretty well. The surgeon was finally able to turn off his pager, go to meetings, and take vacations. He even enjoyed the small bonus of finally having a colleague to talk to. The hospital now had blanket coverage of the vascular service and even saw a moderate uptick in volume. The patients finally had rational continuity of care. I was able to remain fully engaged with a somewhat smaller practice. I could schedule elective case and provide long-term follow-up care relatively seamlessly despite my limited hours. And of course, I now had more free time.
I would also often engage friends and colleagues in my own cohort of aging practitioners, especially at conferences and seminars. They generally expressed considerable interest in my new practice arrangements. The reaction I received with surprising regularity was “Where do I sign up?”
Where indeed? I had apparently tapped into a reservoir of interest among fellow senior surgeons for a way to more gradually wind down their remaining years in practice. Yet few were in situations that offered or even allowed that level of flexibility. For most, the late career practice paradigm remained the all-too-familiar one of galloping along at full speed until the last suture was tied, then quitting cold turkey. Take all the skill, experience, and passion and place it all into the back of a golf cart.
The particulars of my situation would clearly not be universally applicable. However, I do believe that scaled-down practice options can and should be both productive and cost effective under a variety of circumstances. If we were to think more creatively, more careers might wind up more gracefully. In fact, I believe that kinder and gentler transitions at both ends of our careers would not only provide added satisfaction to the elders but could also expand mentoring opportunities for our colleagues just entering practice.
The current debate about the preparedness of new graduates is based upon the presumption that a specific number of years or a specific number of cases suddenly qualifies someone to function with total autonomy. This myth has never really been true and may or may not be even less so now. As it is currently fashionable to compare OR practices with aviation safety, allow me to suggest as an analogy that no one would confuse the final readiness for solo flight with the ability to captain a 747. What better way to guide the maturation of a professional than to have an experienced copilot? But that is probably a subject for another essay.
Dr. Rivers is a former associate professor of surgery at Albert Einstein College of Medicine, Bronx, New York.
A few years ago I accepted an offer to work in a small community hospital. It was the only medical facility in a small town and was located in a semirural area. The nearest referral center was about 75 miles away.
At that time the hospital employed a single full-time vascular surgeon who for obvious reasons was expected to provide round-the-clock coverage and who had rather limited opportunities for educational and recreational escapes. Leaving town meant transferring his patients to the “hospitalist” service for their postop care. Patients who truly needed vascular services had to be transferred to a tertiary care facility by ambulance. Alternatively, the hospital might seek locum tenens coverage if any were even available. However, the cost was substantial, and the productivity was minimal.
Up to that point I had spent most of my career in major high-volume teaching hospitals, along with a stint in solo practice running on the 24/7 never-take-a-holiday treadmill. At age 60+ I was by no means ready to hang up my scalpel, but I was more than willing to earn less money in return for less work (and less stress).
I then had the opportunity to meet this surgeon and representatives of the hospital administration. We discussed a plan to satisfy the interests of all participants. The hospital hired me as a permanent but part-time employee. For a half salary I would work 26 weeks per year, generally 2 weeks on duty at a time and 2 weeks off. As the bureaucrats would put it, I was a 0.5 FTE.
Overall, the arrangement worked pretty well. The surgeon was finally able to turn off his pager, go to meetings, and take vacations. He even enjoyed the small bonus of finally having a colleague to talk to. The hospital now had blanket coverage of the vascular service and even saw a moderate uptick in volume. The patients finally had rational continuity of care. I was able to remain fully engaged with a somewhat smaller practice. I could schedule elective case and provide long-term follow-up care relatively seamlessly despite my limited hours. And of course, I now had more free time.
I would also often engage friends and colleagues in my own cohort of aging practitioners, especially at conferences and seminars. They generally expressed considerable interest in my new practice arrangements. The reaction I received with surprising regularity was “Where do I sign up?”
Where indeed? I had apparently tapped into a reservoir of interest among fellow senior surgeons for a way to more gradually wind down their remaining years in practice. Yet few were in situations that offered or even allowed that level of flexibility. For most, the late career practice paradigm remained the all-too-familiar one of galloping along at full speed until the last suture was tied, then quitting cold turkey. Take all the skill, experience, and passion and place it all into the back of a golf cart.
The particulars of my situation would clearly not be universally applicable. However, I do believe that scaled-down practice options can and should be both productive and cost effective under a variety of circumstances. If we were to think more creatively, more careers might wind up more gracefully. In fact, I believe that kinder and gentler transitions at both ends of our careers would not only provide added satisfaction to the elders but could also expand mentoring opportunities for our colleagues just entering practice.
The current debate about the preparedness of new graduates is based upon the presumption that a specific number of years or a specific number of cases suddenly qualifies someone to function with total autonomy. This myth has never really been true and may or may not be even less so now. As it is currently fashionable to compare OR practices with aviation safety, allow me to suggest as an analogy that no one would confuse the final readiness for solo flight with the ability to captain a 747. What better way to guide the maturation of a professional than to have an experienced copilot? But that is probably a subject for another essay.
Dr. Rivers is a former associate professor of surgery at Albert Einstein College of Medicine, Bronx, New York.
How to be a better negotiator
One of the most valuable things I learned in business school was how to be a better negotiator. Negotiation skills are helpful not only for job contracts, but also for many areas of life. Negotiating with your vendors, employees, health plans, and even spouse or children can be a fruitful experience. Indeed, using good negotiation techniques with your patients can help you optimize the best care with the best service whether in person or virtually.
The three principles I want you to understand are:
1. Negotiate on interests, not positions.
2. Frame or be framed.
3. Win/Win is not only possible; it is the most likely outcome of good negotiating.
Let’s use an example to illustrate each of these: If a patient comes to you asking for Vicodin (hydrocodone and acetaminophen) because you froze actinic keratoses, your first instinct might be to think this patient is a drug seeker and that he is not going to be satisfied unless you give in to his demand. You are a conscientious doctor and never prescribe narcotics for liquid nitrogen treatments. Here, you’ve just locked into a position, and there is no opportunity for negotiation. Instead, take a different approach – consider interests, not positions.
Positions are what you’ve decided. Interests, in contrast, are the reasons why you came to that decision. Think about both your interests and your patient’s interests. The patient wants something to block pain. You want to provide appropriate, safe care. In this instance, ask him why he wants Vicodin; probe about issues that might underlie his request. Keep asking until you feel you understand his interests. This is critical to good negotiation. Then think about your interests. You don’t want your patient to be in pain, and you don’t want to feed a patient’s dependency problem or risk your license for inappropriate drug dispensing.
Second, frame the problem (as you see it) or risk being framed by your patient. Your patient might see you as uncaring and unwilling to help him. You can change this by reframing yourself as the doctor who actually does care. For example, you might say, “I’m concerned about you. Taking Vicodin for this is not normal, and this drug is notorious for leading people into drug dependency. I don’t want to expose you to that risk.” Here, you have taken control of the frame and presented yourself as concerned rather than uncaring.
Third, in almost every negotiation there is an opportunity to expand the pie. That is, each party can offer something that was not in the original discussion but would benefit both. In this instance, you might offer to give the patient samples of a topical treatment for actinic keratoses. The patient, sensing your genuine concern, might offer to bring his mother to you for skin cancer treatment as she, too, is particularly sensitive to pain.
Of course, not all negotiations end in agreement. Sometimes your best option is to reject the request. If your patient is unwilling to compromise, then your best course of action might be to not treat him at all. Before doing so, remember that you will often have a better outcome if you try to reach agreement and that using sound negotiating practice will be a significant advantage. (Please, just don’t tell my wife about this column.)
Dr. Benabio is a partner physician in the department of dermatology of the Southern California Permanente Group in San Diego and a volunteer clinical assistant professor at the University of California, San Diego. Dr. Benabio is @dermdoc on Twitter. Write to him at [email protected].
One of the most valuable things I learned in business school was how to be a better negotiator. Negotiation skills are helpful not only for job contracts, but also for many areas of life. Negotiating with your vendors, employees, health plans, and even spouse or children can be a fruitful experience. Indeed, using good negotiation techniques with your patients can help you optimize the best care with the best service whether in person or virtually.
The three principles I want you to understand are:
1. Negotiate on interests, not positions.
2. Frame or be framed.
3. Win/Win is not only possible; it is the most likely outcome of good negotiating.
Let’s use an example to illustrate each of these: If a patient comes to you asking for Vicodin (hydrocodone and acetaminophen) because you froze actinic keratoses, your first instinct might be to think this patient is a drug seeker and that he is not going to be satisfied unless you give in to his demand. You are a conscientious doctor and never prescribe narcotics for liquid nitrogen treatments. Here, you’ve just locked into a position, and there is no opportunity for negotiation. Instead, take a different approach – consider interests, not positions.
Positions are what you’ve decided. Interests, in contrast, are the reasons why you came to that decision. Think about both your interests and your patient’s interests. The patient wants something to block pain. You want to provide appropriate, safe care. In this instance, ask him why he wants Vicodin; probe about issues that might underlie his request. Keep asking until you feel you understand his interests. This is critical to good negotiation. Then think about your interests. You don’t want your patient to be in pain, and you don’t want to feed a patient’s dependency problem or risk your license for inappropriate drug dispensing.
Second, frame the problem (as you see it) or risk being framed by your patient. Your patient might see you as uncaring and unwilling to help him. You can change this by reframing yourself as the doctor who actually does care. For example, you might say, “I’m concerned about you. Taking Vicodin for this is not normal, and this drug is notorious for leading people into drug dependency. I don’t want to expose you to that risk.” Here, you have taken control of the frame and presented yourself as concerned rather than uncaring.
Third, in almost every negotiation there is an opportunity to expand the pie. That is, each party can offer something that was not in the original discussion but would benefit both. In this instance, you might offer to give the patient samples of a topical treatment for actinic keratoses. The patient, sensing your genuine concern, might offer to bring his mother to you for skin cancer treatment as she, too, is particularly sensitive to pain.
Of course, not all negotiations end in agreement. Sometimes your best option is to reject the request. If your patient is unwilling to compromise, then your best course of action might be to not treat him at all. Before doing so, remember that you will often have a better outcome if you try to reach agreement and that using sound negotiating practice will be a significant advantage. (Please, just don’t tell my wife about this column.)
Dr. Benabio is a partner physician in the department of dermatology of the Southern California Permanente Group in San Diego and a volunteer clinical assistant professor at the University of California, San Diego. Dr. Benabio is @dermdoc on Twitter. Write to him at [email protected].
One of the most valuable things I learned in business school was how to be a better negotiator. Negotiation skills are helpful not only for job contracts, but also for many areas of life. Negotiating with your vendors, employees, health plans, and even spouse or children can be a fruitful experience. Indeed, using good negotiation techniques with your patients can help you optimize the best care with the best service whether in person or virtually.
The three principles I want you to understand are:
1. Negotiate on interests, not positions.
2. Frame or be framed.
3. Win/Win is not only possible; it is the most likely outcome of good negotiating.
Let’s use an example to illustrate each of these: If a patient comes to you asking for Vicodin (hydrocodone and acetaminophen) because you froze actinic keratoses, your first instinct might be to think this patient is a drug seeker and that he is not going to be satisfied unless you give in to his demand. You are a conscientious doctor and never prescribe narcotics for liquid nitrogen treatments. Here, you’ve just locked into a position, and there is no opportunity for negotiation. Instead, take a different approach – consider interests, not positions.
Positions are what you’ve decided. Interests, in contrast, are the reasons why you came to that decision. Think about both your interests and your patient’s interests. The patient wants something to block pain. You want to provide appropriate, safe care. In this instance, ask him why he wants Vicodin; probe about issues that might underlie his request. Keep asking until you feel you understand his interests. This is critical to good negotiation. Then think about your interests. You don’t want your patient to be in pain, and you don’t want to feed a patient’s dependency problem or risk your license for inappropriate drug dispensing.
Second, frame the problem (as you see it) or risk being framed by your patient. Your patient might see you as uncaring and unwilling to help him. You can change this by reframing yourself as the doctor who actually does care. For example, you might say, “I’m concerned about you. Taking Vicodin for this is not normal, and this drug is notorious for leading people into drug dependency. I don’t want to expose you to that risk.” Here, you have taken control of the frame and presented yourself as concerned rather than uncaring.
Third, in almost every negotiation there is an opportunity to expand the pie. That is, each party can offer something that was not in the original discussion but would benefit both. In this instance, you might offer to give the patient samples of a topical treatment for actinic keratoses. The patient, sensing your genuine concern, might offer to bring his mother to you for skin cancer treatment as she, too, is particularly sensitive to pain.
Of course, not all negotiations end in agreement. Sometimes your best option is to reject the request. If your patient is unwilling to compromise, then your best course of action might be to not treat him at all. Before doing so, remember that you will often have a better outcome if you try to reach agreement and that using sound negotiating practice will be a significant advantage. (Please, just don’t tell my wife about this column.)
Dr. Benabio is a partner physician in the department of dermatology of the Southern California Permanente Group in San Diego and a volunteer clinical assistant professor at the University of California, San Diego. Dr. Benabio is @dermdoc on Twitter. Write to him at [email protected].
EHR Report: Smith vs. Smith: Errors in the era of EHRs
George Smith (DOB 2/12/51) is a 65-year-old male patient with a history of hypertension and hyperlipidemia who presents to his local emergency department complaining of worsening dyspnea. He has been suffering with a “chest cold” for the past week, and has also noticed a gradual increase in chest discomfort. The patient is unsure if this is related to exertion or due to his nonproductive cough, but describes the sensation as a “tightness that seems to be getting worse.” The emergency physician is appropriately concerned about a cardiac cause for his symptoms, but is reassured after a check of his electronic health record reveals a recent nuclear treadmill stress test showing normal myocardial perfusion and excellent exercise tolerance, with a low probability of coronary disease.
The only problem is that George Smith never had a stress test. In fact, it’s his twin brother James Smith – also with a birth date of 2/12/51 and a home in the same city – who just had the study done in preparation for surgery. The mix-up in the records began 3 weeks ago, when a tech in the cardiac testing department made an error registering James for his stress test, and now the results of his study have filed into the chart of his twin brother. Fortunately for George, the primary care physician who cares for both brothers happens to be in the emergency department seeing a different patient. He is “curbsided” by the ED doc and recognizes the identification error before the patient is to be discharged home.
This alarming situation – a fictionalized version of a story that happens regularly in hospitals all across the United States – highlights several serious problems with electronic health records. With all of their claimed advantages, EHRs have created a tremendous number of new complications. Some are obvious, such as increased documentation time, connectivity issues, hardware failures, and superfluous “overdocumentation.” But the more troubling issues with electronic records are the ones that are much subtler. Specifically, as the case above highlights, there is the tendency to “lose the forest in the trees” of the EHR, and actually make mistakes that can have devastating consequences. This month we want to cast a light on how electronic tools designed to improve quality and safety actually can compromise them, beginning with the unfortunate reality that …
Modern conveniences can make errors more convenient as well
One of the great advantages of a well-designed electronic record is the ease of locating information when you need it; by entering a few pieces of information such as a last name and date of birth, we can find the needed data in seconds. Unfortunately, this simple and elegant system has exposed a weakness in the people using it: confirmation bias – the idea that we all tend to see what we want to see. This is an adaptive behavior that we all develop to improve efficiency and successfully navigate all of the conscious and subconscious decisions we make throughout the day. Typically, confirmation bias serves to make our lives easier, but in the case above, it didn’t help Mr. Smith; on the contrary, it almost led to disastrous consequences. The error was fortunately recognized by his astute primary care physician, but this case could have ended much differently. The experience should serve as a reminder to us that …
We can easily lose the big picture
The days of hunting for missing patient charts are thankfully long gone, but there are a few critical aspects of paper records that have been lost in the translation to electronic form. One such missing piece was noted by a colleague when first transitioning to an EHR. After a day or two of struggling with the new software, he lamented “I’m missing the big picture!” He had lost the advantage of glancing at a paper chart and instantly recalling the details about his patients that he had compiled over many years of care. For many physicians like him, this may mean reviewing handwritten notes or jottings in the margin of the chart, but sometimes just the appearance of the chart itself is enough to trigger an intellectual or emotional response.
This notion simply doesn’t exist in the world of electronic “charts,” which are all uniform by design. In the quest to simplify workflow and encourage muscle memory, EHR designers have eschewed the intangible experience of holding a yellowing, dog-eared, overflowing patient folder. Instead, physicians now find themselves holding the same PC or tablet as they walk into every patient encounter, left with only a name and date of birth to distinguish one patient from the next. Even worse, the mere definition of a patient chart has moved from a physical construct to a metaphysical one. Charts can be anywhere and everywhere, and can be edited by any end user at virtually any point of care. This opens up almost limitless opportunities for error, and unfortunately …
Errors can last a lifetime
With each episode of care, the charts of the two Mr. Smiths could become more enmeshed, and the histories harder to untangle. (In this case, a passing reference to the stress test results in the ED intern’s history and physical of George Smith may perpetuate the mistake, even though the error has been caught this time.) When mistakes like this are identified, hundreds of collective staff hours can be required to unweave comingled medical records, even when they don’t result in patient harm. It is therefore critical to develop safeguards to prevent them from occurring in the first place, with efforts that include training programs, workflow process improvement, and technology enhancement.
Ultimately, it may be impossible to prevent all documentation errors. However, by focusing on the big picture and considering patient safety first, we can raise awareness of these and other critical issues and develop the tools and training necessary to make mistakes possible to avoid.
Dr. Notte is a family physician and clinical informaticist for Abington (Pa.) Memorial Hospital. He is also a partner in EHR Practice Consultants, a firm that aids physicians in adopting electronic health records. Dr. Skolnik is associate director of the family medicine residency program at Abington (Pa.) Memorial Hospital and professor of family and community medicine at Temple University, Philadelphia.
George Smith (DOB 2/12/51) is a 65-year-old male patient with a history of hypertension and hyperlipidemia who presents to his local emergency department complaining of worsening dyspnea. He has been suffering with a “chest cold” for the past week, and has also noticed a gradual increase in chest discomfort. The patient is unsure if this is related to exertion or due to his nonproductive cough, but describes the sensation as a “tightness that seems to be getting worse.” The emergency physician is appropriately concerned about a cardiac cause for his symptoms, but is reassured after a check of his electronic health record reveals a recent nuclear treadmill stress test showing normal myocardial perfusion and excellent exercise tolerance, with a low probability of coronary disease.
The only problem is that George Smith never had a stress test. In fact, it’s his twin brother James Smith – also with a birth date of 2/12/51 and a home in the same city – who just had the study done in preparation for surgery. The mix-up in the records began 3 weeks ago, when a tech in the cardiac testing department made an error registering James for his stress test, and now the results of his study have filed into the chart of his twin brother. Fortunately for George, the primary care physician who cares for both brothers happens to be in the emergency department seeing a different patient. He is “curbsided” by the ED doc and recognizes the identification error before the patient is to be discharged home.
This alarming situation – a fictionalized version of a story that happens regularly in hospitals all across the United States – highlights several serious problems with electronic health records. With all of their claimed advantages, EHRs have created a tremendous number of new complications. Some are obvious, such as increased documentation time, connectivity issues, hardware failures, and superfluous “overdocumentation.” But the more troubling issues with electronic records are the ones that are much subtler. Specifically, as the case above highlights, there is the tendency to “lose the forest in the trees” of the EHR, and actually make mistakes that can have devastating consequences. This month we want to cast a light on how electronic tools designed to improve quality and safety actually can compromise them, beginning with the unfortunate reality that …
Modern conveniences can make errors more convenient as well
One of the great advantages of a well-designed electronic record is the ease of locating information when you need it; by entering a few pieces of information such as a last name and date of birth, we can find the needed data in seconds. Unfortunately, this simple and elegant system has exposed a weakness in the people using it: confirmation bias – the idea that we all tend to see what we want to see. This is an adaptive behavior that we all develop to improve efficiency and successfully navigate all of the conscious and subconscious decisions we make throughout the day. Typically, confirmation bias serves to make our lives easier, but in the case above, it didn’t help Mr. Smith; on the contrary, it almost led to disastrous consequences. The error was fortunately recognized by his astute primary care physician, but this case could have ended much differently. The experience should serve as a reminder to us that …
We can easily lose the big picture
The days of hunting for missing patient charts are thankfully long gone, but there are a few critical aspects of paper records that have been lost in the translation to electronic form. One such missing piece was noted by a colleague when first transitioning to an EHR. After a day or two of struggling with the new software, he lamented “I’m missing the big picture!” He had lost the advantage of glancing at a paper chart and instantly recalling the details about his patients that he had compiled over many years of care. For many physicians like him, this may mean reviewing handwritten notes or jottings in the margin of the chart, but sometimes just the appearance of the chart itself is enough to trigger an intellectual or emotional response.
This notion simply doesn’t exist in the world of electronic “charts,” which are all uniform by design. In the quest to simplify workflow and encourage muscle memory, EHR designers have eschewed the intangible experience of holding a yellowing, dog-eared, overflowing patient folder. Instead, physicians now find themselves holding the same PC or tablet as they walk into every patient encounter, left with only a name and date of birth to distinguish one patient from the next. Even worse, the mere definition of a patient chart has moved from a physical construct to a metaphysical one. Charts can be anywhere and everywhere, and can be edited by any end user at virtually any point of care. This opens up almost limitless opportunities for error, and unfortunately …
Errors can last a lifetime
With each episode of care, the charts of the two Mr. Smiths could become more enmeshed, and the histories harder to untangle. (In this case, a passing reference to the stress test results in the ED intern’s history and physical of George Smith may perpetuate the mistake, even though the error has been caught this time.) When mistakes like this are identified, hundreds of collective staff hours can be required to unweave comingled medical records, even when they don’t result in patient harm. It is therefore critical to develop safeguards to prevent them from occurring in the first place, with efforts that include training programs, workflow process improvement, and technology enhancement.
Ultimately, it may be impossible to prevent all documentation errors. However, by focusing on the big picture and considering patient safety first, we can raise awareness of these and other critical issues and develop the tools and training necessary to make mistakes possible to avoid.
Dr. Notte is a family physician and clinical informaticist for Abington (Pa.) Memorial Hospital. He is also a partner in EHR Practice Consultants, a firm that aids physicians in adopting electronic health records. Dr. Skolnik is associate director of the family medicine residency program at Abington (Pa.) Memorial Hospital and professor of family and community medicine at Temple University, Philadelphia.
George Smith (DOB 2/12/51) is a 65-year-old male patient with a history of hypertension and hyperlipidemia who presents to his local emergency department complaining of worsening dyspnea. He has been suffering with a “chest cold” for the past week, and has also noticed a gradual increase in chest discomfort. The patient is unsure if this is related to exertion or due to his nonproductive cough, but describes the sensation as a “tightness that seems to be getting worse.” The emergency physician is appropriately concerned about a cardiac cause for his symptoms, but is reassured after a check of his electronic health record reveals a recent nuclear treadmill stress test showing normal myocardial perfusion and excellent exercise tolerance, with a low probability of coronary disease.
The only problem is that George Smith never had a stress test. In fact, it’s his twin brother James Smith – also with a birth date of 2/12/51 and a home in the same city – who just had the study done in preparation for surgery. The mix-up in the records began 3 weeks ago, when a tech in the cardiac testing department made an error registering James for his stress test, and now the results of his study have filed into the chart of his twin brother. Fortunately for George, the primary care physician who cares for both brothers happens to be in the emergency department seeing a different patient. He is “curbsided” by the ED doc and recognizes the identification error before the patient is to be discharged home.
This alarming situation – a fictionalized version of a story that happens regularly in hospitals all across the United States – highlights several serious problems with electronic health records. With all of their claimed advantages, EHRs have created a tremendous number of new complications. Some are obvious, such as increased documentation time, connectivity issues, hardware failures, and superfluous “overdocumentation.” But the more troubling issues with electronic records are the ones that are much subtler. Specifically, as the case above highlights, there is the tendency to “lose the forest in the trees” of the EHR, and actually make mistakes that can have devastating consequences. This month we want to cast a light on how electronic tools designed to improve quality and safety actually can compromise them, beginning with the unfortunate reality that …
Modern conveniences can make errors more convenient as well
One of the great advantages of a well-designed electronic record is the ease of locating information when you need it; by entering a few pieces of information such as a last name and date of birth, we can find the needed data in seconds. Unfortunately, this simple and elegant system has exposed a weakness in the people using it: confirmation bias – the idea that we all tend to see what we want to see. This is an adaptive behavior that we all develop to improve efficiency and successfully navigate all of the conscious and subconscious decisions we make throughout the day. Typically, confirmation bias serves to make our lives easier, but in the case above, it didn’t help Mr. Smith; on the contrary, it almost led to disastrous consequences. The error was fortunately recognized by his astute primary care physician, but this case could have ended much differently. The experience should serve as a reminder to us that …
We can easily lose the big picture
The days of hunting for missing patient charts are thankfully long gone, but there are a few critical aspects of paper records that have been lost in the translation to electronic form. One such missing piece was noted by a colleague when first transitioning to an EHR. After a day or two of struggling with the new software, he lamented “I’m missing the big picture!” He had lost the advantage of glancing at a paper chart and instantly recalling the details about his patients that he had compiled over many years of care. For many physicians like him, this may mean reviewing handwritten notes or jottings in the margin of the chart, but sometimes just the appearance of the chart itself is enough to trigger an intellectual or emotional response.
This notion simply doesn’t exist in the world of electronic “charts,” which are all uniform by design. In the quest to simplify workflow and encourage muscle memory, EHR designers have eschewed the intangible experience of holding a yellowing, dog-eared, overflowing patient folder. Instead, physicians now find themselves holding the same PC or tablet as they walk into every patient encounter, left with only a name and date of birth to distinguish one patient from the next. Even worse, the mere definition of a patient chart has moved from a physical construct to a metaphysical one. Charts can be anywhere and everywhere, and can be edited by any end user at virtually any point of care. This opens up almost limitless opportunities for error, and unfortunately …
Errors can last a lifetime
With each episode of care, the charts of the two Mr. Smiths could become more enmeshed, and the histories harder to untangle. (In this case, a passing reference to the stress test results in the ED intern’s history and physical of George Smith may perpetuate the mistake, even though the error has been caught this time.) When mistakes like this are identified, hundreds of collective staff hours can be required to unweave comingled medical records, even when they don’t result in patient harm. It is therefore critical to develop safeguards to prevent them from occurring in the first place, with efforts that include training programs, workflow process improvement, and technology enhancement.
Ultimately, it may be impossible to prevent all documentation errors. However, by focusing on the big picture and considering patient safety first, we can raise awareness of these and other critical issues and develop the tools and training necessary to make mistakes possible to avoid.
Dr. Notte is a family physician and clinical informaticist for Abington (Pa.) Memorial Hospital. He is also a partner in EHR Practice Consultants, a firm that aids physicians in adopting electronic health records. Dr. Skolnik is associate director of the family medicine residency program at Abington (Pa.) Memorial Hospital and professor of family and community medicine at Temple University, Philadelphia.
Law & Medicine: Locality rule
Question: An injured patient alleges that her eye doctor was negligent in failing to adhere to national treatment guidelines and in not using modern medical equipment. The encounter took place in a rural setting, with the nearest hospital 100 miles away.
In her malpractice lawsuit, which of the following choices is incorrect?
A. One of the doctor’s defenses may be the locality rule.
B. The plaintiff’s strongest argument is that community standards should parallel national standards for a specialist doctor such as an ophthalmologist.
C. Her expert witness must be a practicing ophthalmologist from the area.
D. The expert must be familiar with the local standards but does not have to practice there.
E. It all depends on what the state statute says, because the locality rule is not uniform settled law.
Answer: C. In traditional medical tort law, courts would rely on the standard of the particular locale where the tortious act took place, the so-called locality rule. This was based on the belief that different standards of care were applicable in different areas of the country, e.g., urban vs. rural. The rule can be traced to Small v. Howard,1 an 1880 Massachusetts opinion, which was subsequently overruled in 1968.
Factors favoring the trend away from a local standard toward a national standard include conformity in medical school and residency curricula, and prescribed board certification requirements. Internet access and telemedicine have further propagated this uniformity. Finally, two additional facets of modern medicine – continuing medical education and published clinical practice guidelines – are at odds with a rule geared toward local standards.
One argument against the locality rule is that undue reliance on an outdated mode of practice will perpetuate substandard care. In an older New York malpractice case where a newborn became blind, the pediatrician cited local custom to defend the prolonged use of oxygen to treat preterm infants, despite evidence that this practice might have serious consequences. However, the court of appeals held that the pediatrician’s superior knowledge of the increased risk of hyperoxygenation should have enabled him to use his best judgment instead of relying on the indefensible local custom.
Under a strict version of the locality rule, otherwise qualified expert witnesses may be excluded if they are not practitioners in the locale in question. Still, some courts may allow out-of-state experts to offer their opinions. This has been especially helpful to plaintiffs who are far less likely to be able to secure willing local experts, given the reluctance of many physicians to testify against a fellow doctor in their community.
Take Tennessee as an example. It once excluded the expert testimony of an orthopedic surgeon from Johnson City because the expert witness testified about the national standard and did not have actual knowledge of the standard of care in Nashville, the community where the alleged malpractice occurred.
The Tennessee Court of Appeals later ruled that expert witnesses had to have “personal” or “firsthand knowledge” of the community standard of care, and that interviewing other physicians in the area did not suffice. It subsequently clarified that an expert witness need not actually practice in the same or similar locale, and that professional contact with physicians from comparable communities, such as through referrals, would be acceptable.
Two well-known cases touching on the locality rule bear summarizing: In Swink v. Weintraub,2 Mrs. Swink bled into her pericardium during repair of a defective pacemaker electric lead. She died as a result, and her family pursued a wrongful death action, alleging negligence including delayed pericardiocentesis and surgical intervention.
The jury returned a verdict for the plaintiff, awarding damages in the amount of $1,047,732.20. On appeal, the defendants argued that North Carolina’s locality rule extended to all aspects of a negligence action, and that the trial court erred in admitting expert opinions without regard to whether those opinions reflected the “same or similar community” standard of care.
But the court of appeals disagreed, emphasizing that compliance with the “same or similar community” standard does not necessarily exonerate a defendant from an allegation of medical negligence. The court said liability can be established if the defendant did not exercise his “best judgment” in the treatment of the patient or if the defendant failed to use “reasonable care and diligence” in his efforts to render medical assistance.
In McClure v. Inova Medical Group, a Virginia jury found that a family practice resident had failed to meet the Virginia community standard of care when he did not order the prostate-specific antigen (PSA) test in a 53-year-old patient who was subsequently diagnosed with prostate cancer. The doctor had discussed the risks and benefits of PSA testing, but the patient declined taking the test. Jurors sided with the plaintiff’s argument that according to the local or statewide standard, Virginia doctors simply ordered the test as a matter of routine for men older than 50 years without necessarily discussing risks and benefits. The court awarded $1 million to the patient.3
Although the majority of jurisdictions have abandoned the locality rule, several continue to adhere to either a strict or modified version.4 Examples are Arizona, Idaho, New York, Tennessee, Virginia, and Washington. A modified rule exists in Louisiana, which holds general practitioners to a community standard and specialists to a national standard.
Finally, many authors have recommended a narrowly constructed rule based not on geographic boundaries, but on the availability of local resources. Courts would then look at the totality of circumstances, but remember that there is always the duty to refer or transfer to an available specialist/facility – and that the failure to do so may form the basis of liability.
As one physician put it: Location should not come into play with respect to the knowledge or skill of the treating physician; and even if a physician may not have the facilities to perform an emergency cesarean section, he or she should still know when it’s called for.
References
1. Small v. Howard, 128 Mass 131 (1880).
2. Swink v. Weintraub, 672 S.E.2d 53 (N.C. Court of Appeals 2009).
3. JAMA. 2004 Jan 7;291(1):15-6.
4. JAMA. 2007 Jun 20;297(23):2633-7.
Dr. Tan is professor emeritus of medicine and former adjunct professor of law at the University of Hawaii, and currently directs the St. Francis International Center for Healthcare Ethics in Honolulu. This article is meant to be educational and does not constitute medical, ethical, or legal advice. Some of the articles in this series are adapted from the author’s 2006 book, “Medical Malpractice: Understanding the Law, Managing the Risk,” and his 2012 Halsbury treatise, “Medical Negligence and Professional Misconduct.” For additional information, readers may contact the author at [email protected].
Question: An injured patient alleges that her eye doctor was negligent in failing to adhere to national treatment guidelines and in not using modern medical equipment. The encounter took place in a rural setting, with the nearest hospital 100 miles away.
In her malpractice lawsuit, which of the following choices is incorrect?
A. One of the doctor’s defenses may be the locality rule.
B. The plaintiff’s strongest argument is that community standards should parallel national standards for a specialist doctor such as an ophthalmologist.
C. Her expert witness must be a practicing ophthalmologist from the area.
D. The expert must be familiar with the local standards but does not have to practice there.
E. It all depends on what the state statute says, because the locality rule is not uniform settled law.
Answer: C. In traditional medical tort law, courts would rely on the standard of the particular locale where the tortious act took place, the so-called locality rule. This was based on the belief that different standards of care were applicable in different areas of the country, e.g., urban vs. rural. The rule can be traced to Small v. Howard,1 an 1880 Massachusetts opinion, which was subsequently overruled in 1968.
Factors favoring the trend away from a local standard toward a national standard include conformity in medical school and residency curricula, and prescribed board certification requirements. Internet access and telemedicine have further propagated this uniformity. Finally, two additional facets of modern medicine – continuing medical education and published clinical practice guidelines – are at odds with a rule geared toward local standards.
One argument against the locality rule is that undue reliance on an outdated mode of practice will perpetuate substandard care. In an older New York malpractice case where a newborn became blind, the pediatrician cited local custom to defend the prolonged use of oxygen to treat preterm infants, despite evidence that this practice might have serious consequences. However, the court of appeals held that the pediatrician’s superior knowledge of the increased risk of hyperoxygenation should have enabled him to use his best judgment instead of relying on the indefensible local custom.
Under a strict version of the locality rule, otherwise qualified expert witnesses may be excluded if they are not practitioners in the locale in question. Still, some courts may allow out-of-state experts to offer their opinions. This has been especially helpful to plaintiffs who are far less likely to be able to secure willing local experts, given the reluctance of many physicians to testify against a fellow doctor in their community.
Take Tennessee as an example. It once excluded the expert testimony of an orthopedic surgeon from Johnson City because the expert witness testified about the national standard and did not have actual knowledge of the standard of care in Nashville, the community where the alleged malpractice occurred.
The Tennessee Court of Appeals later ruled that expert witnesses had to have “personal” or “firsthand knowledge” of the community standard of care, and that interviewing other physicians in the area did not suffice. It subsequently clarified that an expert witness need not actually practice in the same or similar locale, and that professional contact with physicians from comparable communities, such as through referrals, would be acceptable.
Two well-known cases touching on the locality rule bear summarizing: In Swink v. Weintraub,2 Mrs. Swink bled into her pericardium during repair of a defective pacemaker electric lead. She died as a result, and her family pursued a wrongful death action, alleging negligence including delayed pericardiocentesis and surgical intervention.
The jury returned a verdict for the plaintiff, awarding damages in the amount of $1,047,732.20. On appeal, the defendants argued that North Carolina’s locality rule extended to all aspects of a negligence action, and that the trial court erred in admitting expert opinions without regard to whether those opinions reflected the “same or similar community” standard of care.
But the court of appeals disagreed, emphasizing that compliance with the “same or similar community” standard does not necessarily exonerate a defendant from an allegation of medical negligence. The court said liability can be established if the defendant did not exercise his “best judgment” in the treatment of the patient or if the defendant failed to use “reasonable care and diligence” in his efforts to render medical assistance.
In McClure v. Inova Medical Group, a Virginia jury found that a family practice resident had failed to meet the Virginia community standard of care when he did not order the prostate-specific antigen (PSA) test in a 53-year-old patient who was subsequently diagnosed with prostate cancer. The doctor had discussed the risks and benefits of PSA testing, but the patient declined taking the test. Jurors sided with the plaintiff’s argument that according to the local or statewide standard, Virginia doctors simply ordered the test as a matter of routine for men older than 50 years without necessarily discussing risks and benefits. The court awarded $1 million to the patient.3
Although the majority of jurisdictions have abandoned the locality rule, several continue to adhere to either a strict or modified version.4 Examples are Arizona, Idaho, New York, Tennessee, Virginia, and Washington. A modified rule exists in Louisiana, which holds general practitioners to a community standard and specialists to a national standard.
Finally, many authors have recommended a narrowly constructed rule based not on geographic boundaries, but on the availability of local resources. Courts would then look at the totality of circumstances, but remember that there is always the duty to refer or transfer to an available specialist/facility – and that the failure to do so may form the basis of liability.
As one physician put it: Location should not come into play with respect to the knowledge or skill of the treating physician; and even if a physician may not have the facilities to perform an emergency cesarean section, he or she should still know when it’s called for.
References
1. Small v. Howard, 128 Mass 131 (1880).
2. Swink v. Weintraub, 672 S.E.2d 53 (N.C. Court of Appeals 2009).
3. JAMA. 2004 Jan 7;291(1):15-6.
4. JAMA. 2007 Jun 20;297(23):2633-7.
Dr. Tan is professor emeritus of medicine and former adjunct professor of law at the University of Hawaii, and currently directs the St. Francis International Center for Healthcare Ethics in Honolulu. This article is meant to be educational and does not constitute medical, ethical, or legal advice. Some of the articles in this series are adapted from the author’s 2006 book, “Medical Malpractice: Understanding the Law, Managing the Risk,” and his 2012 Halsbury treatise, “Medical Negligence and Professional Misconduct.” For additional information, readers may contact the author at [email protected].
Question: An injured patient alleges that her eye doctor was negligent in failing to adhere to national treatment guidelines and in not using modern medical equipment. The encounter took place in a rural setting, with the nearest hospital 100 miles away.
In her malpractice lawsuit, which of the following choices is incorrect?
A. One of the doctor’s defenses may be the locality rule.
B. The plaintiff’s strongest argument is that community standards should parallel national standards for a specialist doctor such as an ophthalmologist.
C. Her expert witness must be a practicing ophthalmologist from the area.
D. The expert must be familiar with the local standards but does not have to practice there.
E. It all depends on what the state statute says, because the locality rule is not uniform settled law.
Answer: C. In traditional medical tort law, courts would rely on the standard of the particular locale where the tortious act took place, the so-called locality rule. This was based on the belief that different standards of care were applicable in different areas of the country, e.g., urban vs. rural. The rule can be traced to Small v. Howard,1 an 1880 Massachusetts opinion, which was subsequently overruled in 1968.
Factors favoring the trend away from a local standard toward a national standard include conformity in medical school and residency curricula, and prescribed board certification requirements. Internet access and telemedicine have further propagated this uniformity. Finally, two additional facets of modern medicine – continuing medical education and published clinical practice guidelines – are at odds with a rule geared toward local standards.
One argument against the locality rule is that undue reliance on an outdated mode of practice will perpetuate substandard care. In an older New York malpractice case where a newborn became blind, the pediatrician cited local custom to defend the prolonged use of oxygen to treat preterm infants, despite evidence that this practice might have serious consequences. However, the court of appeals held that the pediatrician’s superior knowledge of the increased risk of hyperoxygenation should have enabled him to use his best judgment instead of relying on the indefensible local custom.
Under a strict version of the locality rule, otherwise qualified expert witnesses may be excluded if they are not practitioners in the locale in question. Still, some courts may allow out-of-state experts to offer their opinions. This has been especially helpful to plaintiffs who are far less likely to be able to secure willing local experts, given the reluctance of many physicians to testify against a fellow doctor in their community.
Take Tennessee as an example. It once excluded the expert testimony of an orthopedic surgeon from Johnson City because the expert witness testified about the national standard and did not have actual knowledge of the standard of care in Nashville, the community where the alleged malpractice occurred.
The Tennessee Court of Appeals later ruled that expert witnesses had to have “personal” or “firsthand knowledge” of the community standard of care, and that interviewing other physicians in the area did not suffice. It subsequently clarified that an expert witness need not actually practice in the same or similar locale, and that professional contact with physicians from comparable communities, such as through referrals, would be acceptable.
Two well-known cases touching on the locality rule bear summarizing: In Swink v. Weintraub,2 Mrs. Swink bled into her pericardium during repair of a defective pacemaker electric lead. She died as a result, and her family pursued a wrongful death action, alleging negligence including delayed pericardiocentesis and surgical intervention.
The jury returned a verdict for the plaintiff, awarding damages in the amount of $1,047,732.20. On appeal, the defendants argued that North Carolina’s locality rule extended to all aspects of a negligence action, and that the trial court erred in admitting expert opinions without regard to whether those opinions reflected the “same or similar community” standard of care.
But the court of appeals disagreed, emphasizing that compliance with the “same or similar community” standard does not necessarily exonerate a defendant from an allegation of medical negligence. The court said liability can be established if the defendant did not exercise his “best judgment” in the treatment of the patient or if the defendant failed to use “reasonable care and diligence” in his efforts to render medical assistance.
In McClure v. Inova Medical Group, a Virginia jury found that a family practice resident had failed to meet the Virginia community standard of care when he did not order the prostate-specific antigen (PSA) test in a 53-year-old patient who was subsequently diagnosed with prostate cancer. The doctor had discussed the risks and benefits of PSA testing, but the patient declined taking the test. Jurors sided with the plaintiff’s argument that according to the local or statewide standard, Virginia doctors simply ordered the test as a matter of routine for men older than 50 years without necessarily discussing risks and benefits. The court awarded $1 million to the patient.3
Although the majority of jurisdictions have abandoned the locality rule, several continue to adhere to either a strict or modified version.4 Examples are Arizona, Idaho, New York, Tennessee, Virginia, and Washington. A modified rule exists in Louisiana, which holds general practitioners to a community standard and specialists to a national standard.
Finally, many authors have recommended a narrowly constructed rule based not on geographic boundaries, but on the availability of local resources. Courts would then look at the totality of circumstances, but remember that there is always the duty to refer or transfer to an available specialist/facility – and that the failure to do so may form the basis of liability.
As one physician put it: Location should not come into play with respect to the knowledge or skill of the treating physician; and even if a physician may not have the facilities to perform an emergency cesarean section, he or she should still know when it’s called for.
References
1. Small v. Howard, 128 Mass 131 (1880).
2. Swink v. Weintraub, 672 S.E.2d 53 (N.C. Court of Appeals 2009).
3. JAMA. 2004 Jan 7;291(1):15-6.
4. JAMA. 2007 Jun 20;297(23):2633-7.
Dr. Tan is professor emeritus of medicine and former adjunct professor of law at the University of Hawaii, and currently directs the St. Francis International Center for Healthcare Ethics in Honolulu. This article is meant to be educational and does not constitute medical, ethical, or legal advice. Some of the articles in this series are adapted from the author’s 2006 book, “Medical Malpractice: Understanding the Law, Managing the Risk,” and his 2012 Halsbury treatise, “Medical Negligence and Professional Misconduct.” For additional information, readers may contact the author at [email protected].
From the Washington Office: Brave new world of acronyms
Just over a year ago, Congress passed and the President signed into law the MACRA legislation, which will serve as the basis for Medicare physician payment beginning in 2019. At the recent Leadership and Advocacy Summit, it became apparent to me that a “refresher” on seven key acronyms would be useful for surgeons as they gear up to understand and effectively participate in this “brave new world” which is rapidly approaching.
Accordingly, let us start at the beginning. MACRA stands for the Medicare Access and CHIP (Children’s Health Insurance Program) Reauthorization Act of 2015. As noted above, this legislation, signed into law by President Obama on April 16, 2015, replaces the flawed sustainable growth rate formula and will be the template utilized to determine Medicare physician payment beginning in 2019. However, it is important to note that it is anticipated that the data to be utilized as the basis for payment in 2019 will likely be collected sometime in 2017.
MACRA provides modest but stable positive updates of 0.5 percent/year for the 5-year period of 2015-2019. Fellows may remember that this provision was included in the legislation as a direct result of objections made by the leadership of the ACS to the original draft legislation, which contained no provision for a positive update. In addition, MACRA provides for the elimination, after 2018, of the current-law penalties associated with the existing Medicare quality programs, including the PQRS (Physician Quality Reporting System), the VBM (Value-Based Modifier) program and the EHR-MU (Electronic Health Record–Meaningful Use) program. That said, and as outlined below, we will not be saying goodbye to these programs completely. Accordingly, surgeons need to remain, or become, familiar with those acronyms and the programs they represent.
MACRA has two payment pathways. Physicians will choose to participate in one or the other. Those choices are: 1) MIPS (Merit-based Incentive Payment System) and 2) APMs (Alternative Payment Models).
Beginning in 2019, the PQRS (Physician Quality Reporting System), the VBM (Value-Based Modifier) program and the EHR-MU (Electronic Health Record–Meaningful Use) program will be combined into MIPS (Merit-based Incentive Payment System). In this program, it is possible for all surgeons to receive an annual positive update based on their individual performance in the four categories of Quality, Resource Use, Electronic Health Record–Meaningful Use, and lastly the newly created category of Clinical Practice Improvement Activities (CPIA).
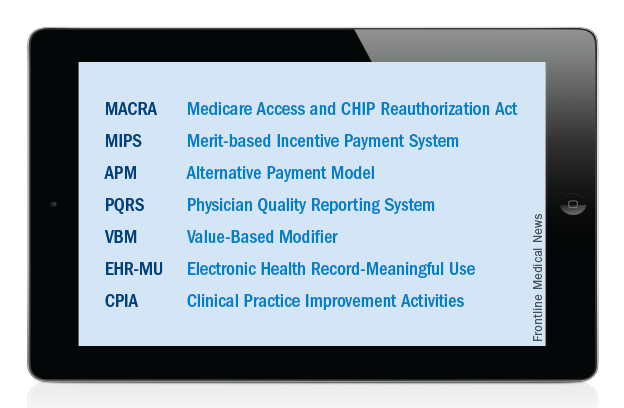
Individual surgeons’ performance in the four categories will be combined into a composite score. Each individual composite score will then be compared with a performance threshold. The threshold will be set as either the mean or median of the composite performance scores for all MIPS-eligible professionals from a prior performance period. The threshold will reset every year. Those with an individual composite performance score above the threshold will receive a positive payment adjustment while those with an individual composite performance score below the threshold will receive a negative payment adjustment.
The Quality component of the MIPS will consist of quality measures currently used in existing quality performance programs namely, the PQRS (Physician Quality Reporting System), the VBM (Value-Based Modifier program), and EHR-MU (Electronic Health Record–Meaningful Use), as well as measures developed by stakeholders to meet the needs of specialties lacking meaningful measures in the current programs. The RESOURCE USE component of MIPS will include the cost measures used in the current VBM (Value-Based Modifier) program. With regard to the Electronic Health Record–Meaningful Use (EHR-MU) component of MIPS, current EHR-MU requirements will continue to apply but are expected to be modified significantly. ACS continues to advocate for changes to the EHR-MU program to make it easier for surgeons to comply with requirements. Evidence of the effectiveness of our advocacy in this area is found in the success achieved in obtaining a blanket exception for the 2015 reporting period, Stage 2 Meaningful Use rule about which I wrote in the December 2015 and January 2016 editions of this column.
The CPIA (Clinical Practice Improvement Activities) are designed to assess surgeons’ effort toward improving their clinical practice and/or their preparation toward participating in APMs (Alternative Payment Models). The menu of specific, approved activities has yet to be firmly established. ACS provided significant input on the CPIA component of MIPS in our November 2015 response to the request for information issued by the Centers for Medicare & Medicaid Services (CMS) last fall. The MACRA legislation specifies that the CPIA be applicable to all specialties and be attainable for small practices and professionals in rural and underserved areas.
Those Fellows interested in knowing specifically the areas on which CMS requested input in the process of drafting the first proposed rule on MACRA and how ACS responded to same may find the letter sent in response to CMS at https://www.facs.org/~/media/files/advocacy/medicare/cms%20mips%20apm%20rfi%20final.ashx.
The new law takes concerted steps to incentivize and encourage providers to develop and participate in APMs (Alternative Payment Models). As with the CPIA discussed above, the details of APMs are not yet fully clear and are currently being developed. ACS is actively working on behalf of surgeons to develop APMs as part of the policy efforts of the Division of Advocacy and Health Policy. In general, these programs will require quality measures, the inclusion of elements of upside and downside financial risk for providers and use of certified electronic health record technology. For those surgeons who receive a significant share of their revenue from an APM, an annual 5% bonus will be available for each of the years 2019-2024. To qualify for that bonus, surgeons must receive 25% of their Medicare revenue from an APM in the years 2019 and 2020. That threshold requirement subsequently increases to 50% in 2021 and ultimately to 75% beginning in 2023.
As MACRA specifies that providers participate in either MIPS or APMs, surgeons who meet the aforementioned threshold of payment from a qualified APM will be exempted from many of the MIPS reporting requirements and receive the 5% bonus in lieu of the previously described MIPS payment adjustment. Those who participate in APMs but fail to meet the threshold necessary to receive the 5% bonus will receive credit for their participation in the CPIA component of their MIPS composite score but will not receive the 5% incentive.
While it is completely understandable that acronyms add to surgeons’ collective frustration, I am confident that all Fellows can, with relative ease, master the seven acronyms above and thus be well on their way to both understanding and successfully participating in the new Medicare physician payment system.
Until next month …
Dr. Patrick V. Bailey is an ACS Fellow, a pediatric surgeon, and Medical Director, Advocacy, for the Division of Advocacy and Health Policy, in the ACS offices in Washington, D.C.
Just over a year ago, Congress passed and the President signed into law the MACRA legislation, which will serve as the basis for Medicare physician payment beginning in 2019. At the recent Leadership and Advocacy Summit, it became apparent to me that a “refresher” on seven key acronyms would be useful for surgeons as they gear up to understand and effectively participate in this “brave new world” which is rapidly approaching.
Accordingly, let us start at the beginning. MACRA stands for the Medicare Access and CHIP (Children’s Health Insurance Program) Reauthorization Act of 2015. As noted above, this legislation, signed into law by President Obama on April 16, 2015, replaces the flawed sustainable growth rate formula and will be the template utilized to determine Medicare physician payment beginning in 2019. However, it is important to note that it is anticipated that the data to be utilized as the basis for payment in 2019 will likely be collected sometime in 2017.
MACRA provides modest but stable positive updates of 0.5 percent/year for the 5-year period of 2015-2019. Fellows may remember that this provision was included in the legislation as a direct result of objections made by the leadership of the ACS to the original draft legislation, which contained no provision for a positive update. In addition, MACRA provides for the elimination, after 2018, of the current-law penalties associated with the existing Medicare quality programs, including the PQRS (Physician Quality Reporting System), the VBM (Value-Based Modifier) program and the EHR-MU (Electronic Health Record–Meaningful Use) program. That said, and as outlined below, we will not be saying goodbye to these programs completely. Accordingly, surgeons need to remain, or become, familiar with those acronyms and the programs they represent.
MACRA has two payment pathways. Physicians will choose to participate in one or the other. Those choices are: 1) MIPS (Merit-based Incentive Payment System) and 2) APMs (Alternative Payment Models).
Beginning in 2019, the PQRS (Physician Quality Reporting System), the VBM (Value-Based Modifier) program and the EHR-MU (Electronic Health Record–Meaningful Use) program will be combined into MIPS (Merit-based Incentive Payment System). In this program, it is possible for all surgeons to receive an annual positive update based on their individual performance in the four categories of Quality, Resource Use, Electronic Health Record–Meaningful Use, and lastly the newly created category of Clinical Practice Improvement Activities (CPIA).
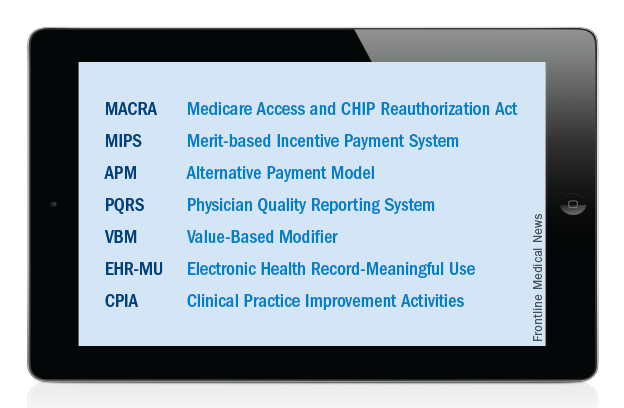
Individual surgeons’ performance in the four categories will be combined into a composite score. Each individual composite score will then be compared with a performance threshold. The threshold will be set as either the mean or median of the composite performance scores for all MIPS-eligible professionals from a prior performance period. The threshold will reset every year. Those with an individual composite performance score above the threshold will receive a positive payment adjustment while those with an individual composite performance score below the threshold will receive a negative payment adjustment.
The Quality component of the MIPS will consist of quality measures currently used in existing quality performance programs namely, the PQRS (Physician Quality Reporting System), the VBM (Value-Based Modifier program), and EHR-MU (Electronic Health Record–Meaningful Use), as well as measures developed by stakeholders to meet the needs of specialties lacking meaningful measures in the current programs. The RESOURCE USE component of MIPS will include the cost measures used in the current VBM (Value-Based Modifier) program. With regard to the Electronic Health Record–Meaningful Use (EHR-MU) component of MIPS, current EHR-MU requirements will continue to apply but are expected to be modified significantly. ACS continues to advocate for changes to the EHR-MU program to make it easier for surgeons to comply with requirements. Evidence of the effectiveness of our advocacy in this area is found in the success achieved in obtaining a blanket exception for the 2015 reporting period, Stage 2 Meaningful Use rule about which I wrote in the December 2015 and January 2016 editions of this column.
The CPIA (Clinical Practice Improvement Activities) are designed to assess surgeons’ effort toward improving their clinical practice and/or their preparation toward participating in APMs (Alternative Payment Models). The menu of specific, approved activities has yet to be firmly established. ACS provided significant input on the CPIA component of MIPS in our November 2015 response to the request for information issued by the Centers for Medicare & Medicaid Services (CMS) last fall. The MACRA legislation specifies that the CPIA be applicable to all specialties and be attainable for small practices and professionals in rural and underserved areas.
Those Fellows interested in knowing specifically the areas on which CMS requested input in the process of drafting the first proposed rule on MACRA and how ACS responded to same may find the letter sent in response to CMS at https://www.facs.org/~/media/files/advocacy/medicare/cms%20mips%20apm%20rfi%20final.ashx.
The new law takes concerted steps to incentivize and encourage providers to develop and participate in APMs (Alternative Payment Models). As with the CPIA discussed above, the details of APMs are not yet fully clear and are currently being developed. ACS is actively working on behalf of surgeons to develop APMs as part of the policy efforts of the Division of Advocacy and Health Policy. In general, these programs will require quality measures, the inclusion of elements of upside and downside financial risk for providers and use of certified electronic health record technology. For those surgeons who receive a significant share of their revenue from an APM, an annual 5% bonus will be available for each of the years 2019-2024. To qualify for that bonus, surgeons must receive 25% of their Medicare revenue from an APM in the years 2019 and 2020. That threshold requirement subsequently increases to 50% in 2021 and ultimately to 75% beginning in 2023.
As MACRA specifies that providers participate in either MIPS or APMs, surgeons who meet the aforementioned threshold of payment from a qualified APM will be exempted from many of the MIPS reporting requirements and receive the 5% bonus in lieu of the previously described MIPS payment adjustment. Those who participate in APMs but fail to meet the threshold necessary to receive the 5% bonus will receive credit for their participation in the CPIA component of their MIPS composite score but will not receive the 5% incentive.
While it is completely understandable that acronyms add to surgeons’ collective frustration, I am confident that all Fellows can, with relative ease, master the seven acronyms above and thus be well on their way to both understanding and successfully participating in the new Medicare physician payment system.
Until next month …
Dr. Patrick V. Bailey is an ACS Fellow, a pediatric surgeon, and Medical Director, Advocacy, for the Division of Advocacy and Health Policy, in the ACS offices in Washington, D.C.
Just over a year ago, Congress passed and the President signed into law the MACRA legislation, which will serve as the basis for Medicare physician payment beginning in 2019. At the recent Leadership and Advocacy Summit, it became apparent to me that a “refresher” on seven key acronyms would be useful for surgeons as they gear up to understand and effectively participate in this “brave new world” which is rapidly approaching.
Accordingly, let us start at the beginning. MACRA stands for the Medicare Access and CHIP (Children’s Health Insurance Program) Reauthorization Act of 2015. As noted above, this legislation, signed into law by President Obama on April 16, 2015, replaces the flawed sustainable growth rate formula and will be the template utilized to determine Medicare physician payment beginning in 2019. However, it is important to note that it is anticipated that the data to be utilized as the basis for payment in 2019 will likely be collected sometime in 2017.
MACRA provides modest but stable positive updates of 0.5 percent/year for the 5-year period of 2015-2019. Fellows may remember that this provision was included in the legislation as a direct result of objections made by the leadership of the ACS to the original draft legislation, which contained no provision for a positive update. In addition, MACRA provides for the elimination, after 2018, of the current-law penalties associated with the existing Medicare quality programs, including the PQRS (Physician Quality Reporting System), the VBM (Value-Based Modifier) program and the EHR-MU (Electronic Health Record–Meaningful Use) program. That said, and as outlined below, we will not be saying goodbye to these programs completely. Accordingly, surgeons need to remain, or become, familiar with those acronyms and the programs they represent.
MACRA has two payment pathways. Physicians will choose to participate in one or the other. Those choices are: 1) MIPS (Merit-based Incentive Payment System) and 2) APMs (Alternative Payment Models).
Beginning in 2019, the PQRS (Physician Quality Reporting System), the VBM (Value-Based Modifier) program and the EHR-MU (Electronic Health Record–Meaningful Use) program will be combined into MIPS (Merit-based Incentive Payment System). In this program, it is possible for all surgeons to receive an annual positive update based on their individual performance in the four categories of Quality, Resource Use, Electronic Health Record–Meaningful Use, and lastly the newly created category of Clinical Practice Improvement Activities (CPIA).
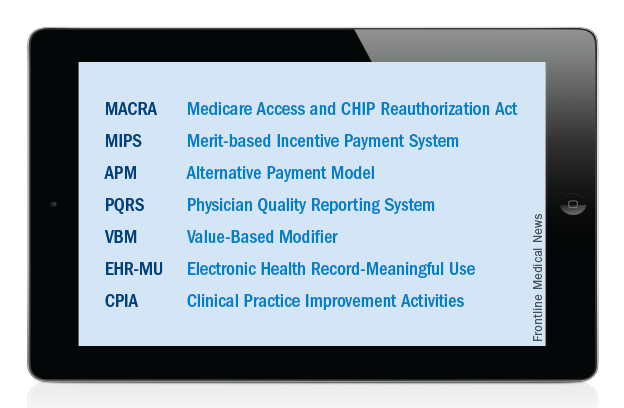
Individual surgeons’ performance in the four categories will be combined into a composite score. Each individual composite score will then be compared with a performance threshold. The threshold will be set as either the mean or median of the composite performance scores for all MIPS-eligible professionals from a prior performance period. The threshold will reset every year. Those with an individual composite performance score above the threshold will receive a positive payment adjustment while those with an individual composite performance score below the threshold will receive a negative payment adjustment.
The Quality component of the MIPS will consist of quality measures currently used in existing quality performance programs namely, the PQRS (Physician Quality Reporting System), the VBM (Value-Based Modifier program), and EHR-MU (Electronic Health Record–Meaningful Use), as well as measures developed by stakeholders to meet the needs of specialties lacking meaningful measures in the current programs. The RESOURCE USE component of MIPS will include the cost measures used in the current VBM (Value-Based Modifier) program. With regard to the Electronic Health Record–Meaningful Use (EHR-MU) component of MIPS, current EHR-MU requirements will continue to apply but are expected to be modified significantly. ACS continues to advocate for changes to the EHR-MU program to make it easier for surgeons to comply with requirements. Evidence of the effectiveness of our advocacy in this area is found in the success achieved in obtaining a blanket exception for the 2015 reporting period, Stage 2 Meaningful Use rule about which I wrote in the December 2015 and January 2016 editions of this column.
The CPIA (Clinical Practice Improvement Activities) are designed to assess surgeons’ effort toward improving their clinical practice and/or their preparation toward participating in APMs (Alternative Payment Models). The menu of specific, approved activities has yet to be firmly established. ACS provided significant input on the CPIA component of MIPS in our November 2015 response to the request for information issued by the Centers for Medicare & Medicaid Services (CMS) last fall. The MACRA legislation specifies that the CPIA be applicable to all specialties and be attainable for small practices and professionals in rural and underserved areas.
Those Fellows interested in knowing specifically the areas on which CMS requested input in the process of drafting the first proposed rule on MACRA and how ACS responded to same may find the letter sent in response to CMS at https://www.facs.org/~/media/files/advocacy/medicare/cms%20mips%20apm%20rfi%20final.ashx.
The new law takes concerted steps to incentivize and encourage providers to develop and participate in APMs (Alternative Payment Models). As with the CPIA discussed above, the details of APMs are not yet fully clear and are currently being developed. ACS is actively working on behalf of surgeons to develop APMs as part of the policy efforts of the Division of Advocacy and Health Policy. In general, these programs will require quality measures, the inclusion of elements of upside and downside financial risk for providers and use of certified electronic health record technology. For those surgeons who receive a significant share of their revenue from an APM, an annual 5% bonus will be available for each of the years 2019-2024. To qualify for that bonus, surgeons must receive 25% of their Medicare revenue from an APM in the years 2019 and 2020. That threshold requirement subsequently increases to 50% in 2021 and ultimately to 75% beginning in 2023.
As MACRA specifies that providers participate in either MIPS or APMs, surgeons who meet the aforementioned threshold of payment from a qualified APM will be exempted from many of the MIPS reporting requirements and receive the 5% bonus in lieu of the previously described MIPS payment adjustment. Those who participate in APMs but fail to meet the threshold necessary to receive the 5% bonus will receive credit for their participation in the CPIA component of their MIPS composite score but will not receive the 5% incentive.
While it is completely understandable that acronyms add to surgeons’ collective frustration, I am confident that all Fellows can, with relative ease, master the seven acronyms above and thus be well on their way to both understanding and successfully participating in the new Medicare physician payment system.
Until next month …
Dr. Patrick V. Bailey is an ACS Fellow, a pediatric surgeon, and Medical Director, Advocacy, for the Division of Advocacy and Health Policy, in the ACS offices in Washington, D.C.
Dealing with compassion fatigue
It was close to 2 decades ago, but it is still as clear as if it had been yesterday. I sat in the intensive care unit, fresh from my residency, tears streaming down my face, which was firmly nestled between my hands as I tried to hide my pain from every soul around me – doctors, nurses, patients’ family members – anyone and everyone.
I had just lost a very dear patient and emotions were running high. I only hoped no one at the nurses’ station would notice me, at least until I had a chance to regain my composure. After all, who would expect to see, or even respect, a doctor found sobbing like a child over a patient who died? Isn’t that all part of the job? Don’t we anticipate the death of some of our most critically ill patients?
Almost paralyzed with grief, I had a hard decision to make.
Option one: I could sit firmly planted in my seat and deal with my personal loss, the loss of my patient with chart number 0001 – yes, my very first patient in private practice. Over time, she and I had developed a very warm, loving relationship, almost like that of a mother and daughter as she was several decades my elder. I had a right to grieve my loss just as anyone else would grieve after losing someone they cared for, didn’t I?
Option two: I could bury my personal feelings and deal with them later in the comfort of my home, safe from the incessant pages from nurses calling about other patients’ urgent needs, hidden from accusing, sometimes condescending glances from other medical professionals who could never understand why I would react so strongly to the death of a patient – especially in a place surrounded by the watchful eyes of others who hold physicians to such a high standard.
Not so much to save face, but for the sake of other critically ill patients who needed a calm, clear-thinking physician to make prudent decisions regarding their care, I chose option two.
As hospitalists, our work is exciting and extremely rewarding, yet with all the suffering and death we see, we must be very careful to guard our hearts and minds, lest we fall into a state of perpetual inner turmoil and stress, and find ourselves seeking counseling or even prescription medication to cope. Compassion satisfaction and compassion fatigue are two ends of a spectrum that caregivers, including medical professionals, often experience. As the names suggest, the former refers to the positive feelings of helping others in need, while the latter refers to a potentially pathologic psychological adaptation to the suffering we experience.
Dr. Charles Figley, director of the Tulane Traumatology Institute in New Orleans, describes compassion fatigue as “a state experienced by those helping people or animals in distress; it is an extreme state of tension and preoccupation with the suffering of those being helped to the degree that it can create a secondary traumatic stress for the helper.”
We all have different coping mechanisms. Some hospitalists are so focused on the art of healing the sick that they have learned to dissociate themselves from the suffering of the individuals they serve, while still delivering excellent care to each and every patient. Not everyone has reached that level.
“Striking the right work-life balance helps me,” said Dr. Marianne Cunanan-Bush, medical director of the inpatient team at Baltimore Washington Medical Center in Glen Burnie, Md. “The first part of my day is spent in personal quiet time, [so] I can just relax and let my mind go free. And my family life is vital. My husband and I play tennis with our children and do other fun things as a family and that helps keep me grounded.”
Dr. Jiayan Chen, a hospitalist at Baltimore Washington Medical Center, finds it almost impossible to completely avoid compassion fatigue. “As hospitalists, I think we can only try to minimize it,” she said. “Try to be sympathetic to patient and family but remain neutral to avoid too high compassion fatigue. Talk to colleagues a couple of times a day, give yourself a few small breaks, including lunch time, drink a cup of water, anything to help break the tension of care during the day.”
Whatever your personal style or inner make-up, be true to yourself. It’s okay to be stoic and to cry sometimes, but if you need help dealing with the trauma and stress this profession sometimes brings, don’t be ashamed to seek the counsel of friends, family members, or even professionals. Two useful resources for help in dealing with, and preventing, compassion fatigue are the Compassion Fatigue Awareness Project and ProQOL.org.
Those of you with small children will appreciate this more than others: As the words of a popular song sung by little girls from coast to coast say, “Let it go, let it go. Don’t hold it back anymore!”
Dr. Hester is a hospitalist at Baltimore Washington Medical Center in Glen Burnie, Md. She is the creator of the Patient Whiz, a patient-engagement app for iOS. Reach her at [email protected].
It was close to 2 decades ago, but it is still as clear as if it had been yesterday. I sat in the intensive care unit, fresh from my residency, tears streaming down my face, which was firmly nestled between my hands as I tried to hide my pain from every soul around me – doctors, nurses, patients’ family members – anyone and everyone.
I had just lost a very dear patient and emotions were running high. I only hoped no one at the nurses’ station would notice me, at least until I had a chance to regain my composure. After all, who would expect to see, or even respect, a doctor found sobbing like a child over a patient who died? Isn’t that all part of the job? Don’t we anticipate the death of some of our most critically ill patients?
Almost paralyzed with grief, I had a hard decision to make.
Option one: I could sit firmly planted in my seat and deal with my personal loss, the loss of my patient with chart number 0001 – yes, my very first patient in private practice. Over time, she and I had developed a very warm, loving relationship, almost like that of a mother and daughter as she was several decades my elder. I had a right to grieve my loss just as anyone else would grieve after losing someone they cared for, didn’t I?
Option two: I could bury my personal feelings and deal with them later in the comfort of my home, safe from the incessant pages from nurses calling about other patients’ urgent needs, hidden from accusing, sometimes condescending glances from other medical professionals who could never understand why I would react so strongly to the death of a patient – especially in a place surrounded by the watchful eyes of others who hold physicians to such a high standard.
Not so much to save face, but for the sake of other critically ill patients who needed a calm, clear-thinking physician to make prudent decisions regarding their care, I chose option two.
As hospitalists, our work is exciting and extremely rewarding, yet with all the suffering and death we see, we must be very careful to guard our hearts and minds, lest we fall into a state of perpetual inner turmoil and stress, and find ourselves seeking counseling or even prescription medication to cope. Compassion satisfaction and compassion fatigue are two ends of a spectrum that caregivers, including medical professionals, often experience. As the names suggest, the former refers to the positive feelings of helping others in need, while the latter refers to a potentially pathologic psychological adaptation to the suffering we experience.
Dr. Charles Figley, director of the Tulane Traumatology Institute in New Orleans, describes compassion fatigue as “a state experienced by those helping people or animals in distress; it is an extreme state of tension and preoccupation with the suffering of those being helped to the degree that it can create a secondary traumatic stress for the helper.”
We all have different coping mechanisms. Some hospitalists are so focused on the art of healing the sick that they have learned to dissociate themselves from the suffering of the individuals they serve, while still delivering excellent care to each and every patient. Not everyone has reached that level.
“Striking the right work-life balance helps me,” said Dr. Marianne Cunanan-Bush, medical director of the inpatient team at Baltimore Washington Medical Center in Glen Burnie, Md. “The first part of my day is spent in personal quiet time, [so] I can just relax and let my mind go free. And my family life is vital. My husband and I play tennis with our children and do other fun things as a family and that helps keep me grounded.”
Dr. Jiayan Chen, a hospitalist at Baltimore Washington Medical Center, finds it almost impossible to completely avoid compassion fatigue. “As hospitalists, I think we can only try to minimize it,” she said. “Try to be sympathetic to patient and family but remain neutral to avoid too high compassion fatigue. Talk to colleagues a couple of times a day, give yourself a few small breaks, including lunch time, drink a cup of water, anything to help break the tension of care during the day.”
Whatever your personal style or inner make-up, be true to yourself. It’s okay to be stoic and to cry sometimes, but if you need help dealing with the trauma and stress this profession sometimes brings, don’t be ashamed to seek the counsel of friends, family members, or even professionals. Two useful resources for help in dealing with, and preventing, compassion fatigue are the Compassion Fatigue Awareness Project and ProQOL.org.
Those of you with small children will appreciate this more than others: As the words of a popular song sung by little girls from coast to coast say, “Let it go, let it go. Don’t hold it back anymore!”
Dr. Hester is a hospitalist at Baltimore Washington Medical Center in Glen Burnie, Md. She is the creator of the Patient Whiz, a patient-engagement app for iOS. Reach her at [email protected].
It was close to 2 decades ago, but it is still as clear as if it had been yesterday. I sat in the intensive care unit, fresh from my residency, tears streaming down my face, which was firmly nestled between my hands as I tried to hide my pain from every soul around me – doctors, nurses, patients’ family members – anyone and everyone.
I had just lost a very dear patient and emotions were running high. I only hoped no one at the nurses’ station would notice me, at least until I had a chance to regain my composure. After all, who would expect to see, or even respect, a doctor found sobbing like a child over a patient who died? Isn’t that all part of the job? Don’t we anticipate the death of some of our most critically ill patients?
Almost paralyzed with grief, I had a hard decision to make.
Option one: I could sit firmly planted in my seat and deal with my personal loss, the loss of my patient with chart number 0001 – yes, my very first patient in private practice. Over time, she and I had developed a very warm, loving relationship, almost like that of a mother and daughter as she was several decades my elder. I had a right to grieve my loss just as anyone else would grieve after losing someone they cared for, didn’t I?
Option two: I could bury my personal feelings and deal with them later in the comfort of my home, safe from the incessant pages from nurses calling about other patients’ urgent needs, hidden from accusing, sometimes condescending glances from other medical professionals who could never understand why I would react so strongly to the death of a patient – especially in a place surrounded by the watchful eyes of others who hold physicians to such a high standard.
Not so much to save face, but for the sake of other critically ill patients who needed a calm, clear-thinking physician to make prudent decisions regarding their care, I chose option two.
As hospitalists, our work is exciting and extremely rewarding, yet with all the suffering and death we see, we must be very careful to guard our hearts and minds, lest we fall into a state of perpetual inner turmoil and stress, and find ourselves seeking counseling or even prescription medication to cope. Compassion satisfaction and compassion fatigue are two ends of a spectrum that caregivers, including medical professionals, often experience. As the names suggest, the former refers to the positive feelings of helping others in need, while the latter refers to a potentially pathologic psychological adaptation to the suffering we experience.
Dr. Charles Figley, director of the Tulane Traumatology Institute in New Orleans, describes compassion fatigue as “a state experienced by those helping people or animals in distress; it is an extreme state of tension and preoccupation with the suffering of those being helped to the degree that it can create a secondary traumatic stress for the helper.”
We all have different coping mechanisms. Some hospitalists are so focused on the art of healing the sick that they have learned to dissociate themselves from the suffering of the individuals they serve, while still delivering excellent care to each and every patient. Not everyone has reached that level.
“Striking the right work-life balance helps me,” said Dr. Marianne Cunanan-Bush, medical director of the inpatient team at Baltimore Washington Medical Center in Glen Burnie, Md. “The first part of my day is spent in personal quiet time, [so] I can just relax and let my mind go free. And my family life is vital. My husband and I play tennis with our children and do other fun things as a family and that helps keep me grounded.”
Dr. Jiayan Chen, a hospitalist at Baltimore Washington Medical Center, finds it almost impossible to completely avoid compassion fatigue. “As hospitalists, I think we can only try to minimize it,” she said. “Try to be sympathetic to patient and family but remain neutral to avoid too high compassion fatigue. Talk to colleagues a couple of times a day, give yourself a few small breaks, including lunch time, drink a cup of water, anything to help break the tension of care during the day.”
Whatever your personal style or inner make-up, be true to yourself. It’s okay to be stoic and to cry sometimes, but if you need help dealing with the trauma and stress this profession sometimes brings, don’t be ashamed to seek the counsel of friends, family members, or even professionals. Two useful resources for help in dealing with, and preventing, compassion fatigue are the Compassion Fatigue Awareness Project and ProQOL.org.
Those of you with small children will appreciate this more than others: As the words of a popular song sung by little girls from coast to coast say, “Let it go, let it go. Don’t hold it back anymore!”
Dr. Hester is a hospitalist at Baltimore Washington Medical Center in Glen Burnie, Md. She is the creator of the Patient Whiz, a patient-engagement app for iOS. Reach her at [email protected].
What standards do insurance companies hold themselves to?
My newest iteration of a VIP, or very ill patient, is a lovely middle-aged gentleman who has been sick for a year with a multisystem disorder. It started with severely swollen hands and feet along with significant anemia and fatigue. One year, many imaging studies, a couple of biopsies, and a latent tuberculosis infection later, he is still very sick. Throughout his ordeal he has often said to me: “You are the quarterback.” I’ve taken that to heart.
I don’t know why this surprises me, but insurance companies are being increasingly difficult. They’re passing more of the cost of health care to patients, and they’re less willing to cover medications and procedures. I have patients who can’t get physical therapy because they can’t afford the $45 copay for each visit. One patient stopped her hydroxychloroquine because it went from $4/month to $90/month. A couple of patients have opted not to take risedronate because the copay per month is $200 – that’s $200 for one generic pill.
At a recent morbidity and mortality conference, the attendees, nonrheumatologists all, were incredulous that cyclophosphamide, which has been around for ages and should be generic, is not covered by Medicare. Our patient with granulomatosis with polyangiitis and alveolar hemorrhage was on the hook for several hundred dollars per month, which he couldn’t afford.
Insurers also have been giving me more pushback for medications. For example, I recently tried to start one of my patients on etanercept for rheumatoid arthritis. His insurance company wrote to say etanercept was not their “preferred” first-line biologic. I explained that their preferred anti-TNF agents all carried the potential for developing anti-drug antibodies when used without methotrexate, which was contraindicated in my patient. They were unmoved.
I had a similar experience with my VIP. He was denied tocilizumab because he had not yet tried and failed two anti-TNF agents. I appealed the decision because I thought etanercept had caused a side effect that might be a class effect. To my surprise, rather than getting an approval, I received instead a request for medical literature to support my theory. Who knew that the decision-bots were so sophisticated?
Ultimately, I got the drug approved, but of course this process was an inconvenience to me, adding unnecessarily to the work of doctoring. More importantly, it was time wasted for my patient who was suffering tremendously.
My point is this: The idea of me as quarterback is quaint. Ultimately, it is the insurance company that dictates testing, treatment, physician, and facility.
There is an expectation that physicians are perfect, and we have internalized that expectation to some degree, holding ourselves to exacting standards, guided by what’s in the patient’s best interest. I want to know what sort of standards insurance companies hold themselves to, because I think they – out of all of us involved in health care – they who have the greatest resources should be absolutely unimpeachable.
Dr. Chan practices rheumatology in Pawtucket, R.I.
My newest iteration of a VIP, or very ill patient, is a lovely middle-aged gentleman who has been sick for a year with a multisystem disorder. It started with severely swollen hands and feet along with significant anemia and fatigue. One year, many imaging studies, a couple of biopsies, and a latent tuberculosis infection later, he is still very sick. Throughout his ordeal he has often said to me: “You are the quarterback.” I’ve taken that to heart.
I don’t know why this surprises me, but insurance companies are being increasingly difficult. They’re passing more of the cost of health care to patients, and they’re less willing to cover medications and procedures. I have patients who can’t get physical therapy because they can’t afford the $45 copay for each visit. One patient stopped her hydroxychloroquine because it went from $4/month to $90/month. A couple of patients have opted not to take risedronate because the copay per month is $200 – that’s $200 for one generic pill.
At a recent morbidity and mortality conference, the attendees, nonrheumatologists all, were incredulous that cyclophosphamide, which has been around for ages and should be generic, is not covered by Medicare. Our patient with granulomatosis with polyangiitis and alveolar hemorrhage was on the hook for several hundred dollars per month, which he couldn’t afford.
Insurers also have been giving me more pushback for medications. For example, I recently tried to start one of my patients on etanercept for rheumatoid arthritis. His insurance company wrote to say etanercept was not their “preferred” first-line biologic. I explained that their preferred anti-TNF agents all carried the potential for developing anti-drug antibodies when used without methotrexate, which was contraindicated in my patient. They were unmoved.
I had a similar experience with my VIP. He was denied tocilizumab because he had not yet tried and failed two anti-TNF agents. I appealed the decision because I thought etanercept had caused a side effect that might be a class effect. To my surprise, rather than getting an approval, I received instead a request for medical literature to support my theory. Who knew that the decision-bots were so sophisticated?
Ultimately, I got the drug approved, but of course this process was an inconvenience to me, adding unnecessarily to the work of doctoring. More importantly, it was time wasted for my patient who was suffering tremendously.
My point is this: The idea of me as quarterback is quaint. Ultimately, it is the insurance company that dictates testing, treatment, physician, and facility.
There is an expectation that physicians are perfect, and we have internalized that expectation to some degree, holding ourselves to exacting standards, guided by what’s in the patient’s best interest. I want to know what sort of standards insurance companies hold themselves to, because I think they – out of all of us involved in health care – they who have the greatest resources should be absolutely unimpeachable.
Dr. Chan practices rheumatology in Pawtucket, R.I.
My newest iteration of a VIP, or very ill patient, is a lovely middle-aged gentleman who has been sick for a year with a multisystem disorder. It started with severely swollen hands and feet along with significant anemia and fatigue. One year, many imaging studies, a couple of biopsies, and a latent tuberculosis infection later, he is still very sick. Throughout his ordeal he has often said to me: “You are the quarterback.” I’ve taken that to heart.
I don’t know why this surprises me, but insurance companies are being increasingly difficult. They’re passing more of the cost of health care to patients, and they’re less willing to cover medications and procedures. I have patients who can’t get physical therapy because they can’t afford the $45 copay for each visit. One patient stopped her hydroxychloroquine because it went from $4/month to $90/month. A couple of patients have opted not to take risedronate because the copay per month is $200 – that’s $200 for one generic pill.
At a recent morbidity and mortality conference, the attendees, nonrheumatologists all, were incredulous that cyclophosphamide, which has been around for ages and should be generic, is not covered by Medicare. Our patient with granulomatosis with polyangiitis and alveolar hemorrhage was on the hook for several hundred dollars per month, which he couldn’t afford.
Insurers also have been giving me more pushback for medications. For example, I recently tried to start one of my patients on etanercept for rheumatoid arthritis. His insurance company wrote to say etanercept was not their “preferred” first-line biologic. I explained that their preferred anti-TNF agents all carried the potential for developing anti-drug antibodies when used without methotrexate, which was contraindicated in my patient. They were unmoved.
I had a similar experience with my VIP. He was denied tocilizumab because he had not yet tried and failed two anti-TNF agents. I appealed the decision because I thought etanercept had caused a side effect that might be a class effect. To my surprise, rather than getting an approval, I received instead a request for medical literature to support my theory. Who knew that the decision-bots were so sophisticated?
Ultimately, I got the drug approved, but of course this process was an inconvenience to me, adding unnecessarily to the work of doctoring. More importantly, it was time wasted for my patient who was suffering tremendously.
My point is this: The idea of me as quarterback is quaint. Ultimately, it is the insurance company that dictates testing, treatment, physician, and facility.
There is an expectation that physicians are perfect, and we have internalized that expectation to some degree, holding ourselves to exacting standards, guided by what’s in the patient’s best interest. I want to know what sort of standards insurance companies hold themselves to, because I think they – out of all of us involved in health care – they who have the greatest resources should be absolutely unimpeachable.
Dr. Chan practices rheumatology in Pawtucket, R.I.
Aesthetic Dermatology: Effects of climate change on skin
Global climate appears to be changing at an unprecedented rate. Climate change can be caused by many factors, including variations in solar radiation received by the earth, oceanic circulation, plate tectonics, as well as human-induced alterations of the natural world. Many human activities, such as the use of fossil fuel and the consequent accumulation of greenhouse gases in the atmosphere, land consumption, deforestation, industrial processes, as well as some agriculture practices, are contributing to global climate change. Many have reported on the current trend toward global warming (average surface temperature has augmented by 0.6°C over the past 100 years), decreased precipitation, atmospheric humidity changes, and the rise in global extreme climatic events. The magnitude and cause of these changes and their impact on human activity have become important matters of debate worldwide, representing climate change as one of the greatest challenges of the modern age.
Although many articles have been written based on observations and various predictive models of how climate change could affect social, economic, and health systems, only a few studies exist about the effects of this change on skin and skin disease. However, the skin is the most highly exposed organ to the environment; therefore, cutaneous conditions are inclined to respond to changes in climate.
Skin cancer
The World Health Organization predicts that the depletion of the ozone layer could lead to further increased rates of melanoma and nonmelanoma skin cancer. In humans, it has been speculated that a long-term rise of temperature by 2°C could increase the carcinogenic effectiveness of solar UV by 10%.
Strictly speaking, stratospheric ozone depletion is not part of “global climate change,” which occurs in the troposphere. There are, however, several recently described interactions between ozone depletion and greenhouse gas–induced warming. Stratospheric ozone absorbs much of the incoming solar ultraviolet radiation, especially the biologically more damaging, shorter-wavelength UVB wavelengths. We now know that various industrial halogenated chemicals such as the chlorofluorocarbons or CFCs (used in refrigeration, insulation, and spray-can propellants) and methyl bromide, while inert at ambient Earth-surface temperatures, react with ozone in the extremely cold polar stratosphere. This destruction of ozone occurs especially in late winter and early spring.
During the 1980s and 1990s at northern midlatitudes (such as Europe), the average year-round ozone concentration declined by around 4% per decade; over the southern regions of Australia, New Zealand, Argentina, and South Africa, the figure approximated 6%-7%. UV exposures at northern midlatitudes are likely to peak around 2020, with an estimated 10% increase in effective ultraviolet radiation relative to 1980s levels.
The modeling of future ozone levels and UV radiation (UVR) exposures has estimated that, in consequence, a ‘European’ population living at around 45 degrees North will experience, by 2050, an approximate 5% excess of total skin cancer incidence (assuming, conservatively, no change in age distribution). The equivalent estimation for the U.S. population is for a 10% increase in skin cancer incidence by around 2050.
In the mid-1980s, governments recognized the emerging hazard from ozone depletion. The Montreal Protocol of 1987 was adopted, and the phasing out of major ozone-destroying gases began. Some anticipate a slow but near-complete recovery of stratospheric ozone by the middle of the twenty-first century; the Environmental Protection Agency (EPA) estimates recovery by 2065 with strict adherence to protection protocols.
Increased exposure to UVR also leads to increased rates of lens opacification, cataracts, and whole-body immunosuppression. UVR-induced immunosuppression could influence patterns of infectious disease. It may also influence the occurrence and progression of various autoimmune diseases and, less certainly, vaccine efficacy.
Extreme weather events
The International Society of Dermatology Task Force on Climate Change reports that weather phenomena such as El Niño also result in changes to dermatologic conditions. The El Niño Southern Oscillation (ENSO) is a complex climate phenomenon occurring in the Pacific Ocean at intervals of 2-7 years. The term refers to fluctuations in ocean temperatures in the tropical eastern Pacific Ocean (El Niño, the warm phase of ENSO, and La Niña, the cool phase of ENSO) and in atmospheric pressure across the Pacific basin (Southern Oscillation). This weather pattern is attributed with causing climate change in certain parts of the world and is associated with disease outbreaks.
El Niño has been associated with increases in the occurrence of actinic keratosis, tinea, pityriasis versicolor, miliaria, folliculitis, rosacea, dermatitis caused by Paederus irritans and Paederus sabaeus, and certain vector-borne and waterborne diseases (such as dengue fever, leishmaniasis, Chagas disease, Barmah Forest virus, and leptospirosis), and with decreases in the occurrence of dermatitis, scabies, psoriasis, and papular urticaria. La Niña has been associated with increases in the occurrence of varicella; hand, foot, and mouth disease; and Ross River virus (in certain areas), and decreases in viral warts and leishmaniasis.
Separately, global warming is expected to affect the start, duration, and intensity of the pollen season, and secondarily the rate of asthma exacerbations due to air pollution, respiratory infections, and/or cold air inhalation, with probable increases in eczema and other atopy-related conditions as well.
Vector-borne diseases
In the past year, the largest Ebola virus outbreak in West Africa has resulted in importation of the virus to other countries and secondary local transmission. Autochthonous transmission of Chikungunya virus has occurred in nonendemic areas, including Europe, the Caribbean, and the Americas. Zika virus has re-emerged in the Pacific with local transmission from imported cases. Climate change, deforestation, and changes in precipitation have been linked to variations in the geographical distribution of vectors of some infectious diseases (leishmaniasis, Lyme disease, and now Zika virus) by changing their spread. A warm and humid environment from global warming can also encourage the colonization of the skin by bacteria and fungi.
Finally, there is a wider, ecological dimension to consider. UV radiation impairs the molecular chemistry of photosynthesis both on land (terrestrial plants) and at sea (phytoplankton). This could affect world food production, at least marginally, and thus contribute to nutritional and health problems in food-insecure populations.
Another reason of many, but from a dermatologist’s point of view, to be mindful of taking care of the planet and our environment.
References
1. World Health Organization (WHO).
2. Photochem Photobiol Sci. 2002 May;1(5):324-6.
3. G Ital Dermatol Venereol. 2013 Feb;148(1):135-46.
4. Int J Dermatol. 2012 Jun;51(6):656-61.
5. Int J Dermatol. 2015 Dec;54(12):1343-51.
6. Curr Opin Infect Dis. 2015 Apr;28(2):139-50.
Dr. Wesley and Dr. Talakoub are co-contributors to this column. Dr. Talakoub is in private practice in McLean, Va. Dr. Wesley practices dermatology in Beverly Hills, Calif. This month’s column is by Dr. Wesley. Write to them at [email protected].
Global climate appears to be changing at an unprecedented rate. Climate change can be caused by many factors, including variations in solar radiation received by the earth, oceanic circulation, plate tectonics, as well as human-induced alterations of the natural world. Many human activities, such as the use of fossil fuel and the consequent accumulation of greenhouse gases in the atmosphere, land consumption, deforestation, industrial processes, as well as some agriculture practices, are contributing to global climate change. Many have reported on the current trend toward global warming (average surface temperature has augmented by 0.6°C over the past 100 years), decreased precipitation, atmospheric humidity changes, and the rise in global extreme climatic events. The magnitude and cause of these changes and their impact on human activity have become important matters of debate worldwide, representing climate change as one of the greatest challenges of the modern age.
Although many articles have been written based on observations and various predictive models of how climate change could affect social, economic, and health systems, only a few studies exist about the effects of this change on skin and skin disease. However, the skin is the most highly exposed organ to the environment; therefore, cutaneous conditions are inclined to respond to changes in climate.
Skin cancer
The World Health Organization predicts that the depletion of the ozone layer could lead to further increased rates of melanoma and nonmelanoma skin cancer. In humans, it has been speculated that a long-term rise of temperature by 2°C could increase the carcinogenic effectiveness of solar UV by 10%.
Strictly speaking, stratospheric ozone depletion is not part of “global climate change,” which occurs in the troposphere. There are, however, several recently described interactions between ozone depletion and greenhouse gas–induced warming. Stratospheric ozone absorbs much of the incoming solar ultraviolet radiation, especially the biologically more damaging, shorter-wavelength UVB wavelengths. We now know that various industrial halogenated chemicals such as the chlorofluorocarbons or CFCs (used in refrigeration, insulation, and spray-can propellants) and methyl bromide, while inert at ambient Earth-surface temperatures, react with ozone in the extremely cold polar stratosphere. This destruction of ozone occurs especially in late winter and early spring.
During the 1980s and 1990s at northern midlatitudes (such as Europe), the average year-round ozone concentration declined by around 4% per decade; over the southern regions of Australia, New Zealand, Argentina, and South Africa, the figure approximated 6%-7%. UV exposures at northern midlatitudes are likely to peak around 2020, with an estimated 10% increase in effective ultraviolet radiation relative to 1980s levels.
The modeling of future ozone levels and UV radiation (UVR) exposures has estimated that, in consequence, a ‘European’ population living at around 45 degrees North will experience, by 2050, an approximate 5% excess of total skin cancer incidence (assuming, conservatively, no change in age distribution). The equivalent estimation for the U.S. population is for a 10% increase in skin cancer incidence by around 2050.
In the mid-1980s, governments recognized the emerging hazard from ozone depletion. The Montreal Protocol of 1987 was adopted, and the phasing out of major ozone-destroying gases began. Some anticipate a slow but near-complete recovery of stratospheric ozone by the middle of the twenty-first century; the Environmental Protection Agency (EPA) estimates recovery by 2065 with strict adherence to protection protocols.
Increased exposure to UVR also leads to increased rates of lens opacification, cataracts, and whole-body immunosuppression. UVR-induced immunosuppression could influence patterns of infectious disease. It may also influence the occurrence and progression of various autoimmune diseases and, less certainly, vaccine efficacy.
Extreme weather events
The International Society of Dermatology Task Force on Climate Change reports that weather phenomena such as El Niño also result in changes to dermatologic conditions. The El Niño Southern Oscillation (ENSO) is a complex climate phenomenon occurring in the Pacific Ocean at intervals of 2-7 years. The term refers to fluctuations in ocean temperatures in the tropical eastern Pacific Ocean (El Niño, the warm phase of ENSO, and La Niña, the cool phase of ENSO) and in atmospheric pressure across the Pacific basin (Southern Oscillation). This weather pattern is attributed with causing climate change in certain parts of the world and is associated with disease outbreaks.
El Niño has been associated with increases in the occurrence of actinic keratosis, tinea, pityriasis versicolor, miliaria, folliculitis, rosacea, dermatitis caused by Paederus irritans and Paederus sabaeus, and certain vector-borne and waterborne diseases (such as dengue fever, leishmaniasis, Chagas disease, Barmah Forest virus, and leptospirosis), and with decreases in the occurrence of dermatitis, scabies, psoriasis, and papular urticaria. La Niña has been associated with increases in the occurrence of varicella; hand, foot, and mouth disease; and Ross River virus (in certain areas), and decreases in viral warts and leishmaniasis.
Separately, global warming is expected to affect the start, duration, and intensity of the pollen season, and secondarily the rate of asthma exacerbations due to air pollution, respiratory infections, and/or cold air inhalation, with probable increases in eczema and other atopy-related conditions as well.
Vector-borne diseases
In the past year, the largest Ebola virus outbreak in West Africa has resulted in importation of the virus to other countries and secondary local transmission. Autochthonous transmission of Chikungunya virus has occurred in nonendemic areas, including Europe, the Caribbean, and the Americas. Zika virus has re-emerged in the Pacific with local transmission from imported cases. Climate change, deforestation, and changes in precipitation have been linked to variations in the geographical distribution of vectors of some infectious diseases (leishmaniasis, Lyme disease, and now Zika virus) by changing their spread. A warm and humid environment from global warming can also encourage the colonization of the skin by bacteria and fungi.
Finally, there is a wider, ecological dimension to consider. UV radiation impairs the molecular chemistry of photosynthesis both on land (terrestrial plants) and at sea (phytoplankton). This could affect world food production, at least marginally, and thus contribute to nutritional and health problems in food-insecure populations.
Another reason of many, but from a dermatologist’s point of view, to be mindful of taking care of the planet and our environment.
References
1. World Health Organization (WHO).
2. Photochem Photobiol Sci. 2002 May;1(5):324-6.
3. G Ital Dermatol Venereol. 2013 Feb;148(1):135-46.
4. Int J Dermatol. 2012 Jun;51(6):656-61.
5. Int J Dermatol. 2015 Dec;54(12):1343-51.
6. Curr Opin Infect Dis. 2015 Apr;28(2):139-50.
Dr. Wesley and Dr. Talakoub are co-contributors to this column. Dr. Talakoub is in private practice in McLean, Va. Dr. Wesley practices dermatology in Beverly Hills, Calif. This month’s column is by Dr. Wesley. Write to them at [email protected].
Global climate appears to be changing at an unprecedented rate. Climate change can be caused by many factors, including variations in solar radiation received by the earth, oceanic circulation, plate tectonics, as well as human-induced alterations of the natural world. Many human activities, such as the use of fossil fuel and the consequent accumulation of greenhouse gases in the atmosphere, land consumption, deforestation, industrial processes, as well as some agriculture practices, are contributing to global climate change. Many have reported on the current trend toward global warming (average surface temperature has augmented by 0.6°C over the past 100 years), decreased precipitation, atmospheric humidity changes, and the rise in global extreme climatic events. The magnitude and cause of these changes and their impact on human activity have become important matters of debate worldwide, representing climate change as one of the greatest challenges of the modern age.
Although many articles have been written based on observations and various predictive models of how climate change could affect social, economic, and health systems, only a few studies exist about the effects of this change on skin and skin disease. However, the skin is the most highly exposed organ to the environment; therefore, cutaneous conditions are inclined to respond to changes in climate.
Skin cancer
The World Health Organization predicts that the depletion of the ozone layer could lead to further increased rates of melanoma and nonmelanoma skin cancer. In humans, it has been speculated that a long-term rise of temperature by 2°C could increase the carcinogenic effectiveness of solar UV by 10%.
Strictly speaking, stratospheric ozone depletion is not part of “global climate change,” which occurs in the troposphere. There are, however, several recently described interactions between ozone depletion and greenhouse gas–induced warming. Stratospheric ozone absorbs much of the incoming solar ultraviolet radiation, especially the biologically more damaging, shorter-wavelength UVB wavelengths. We now know that various industrial halogenated chemicals such as the chlorofluorocarbons or CFCs (used in refrigeration, insulation, and spray-can propellants) and methyl bromide, while inert at ambient Earth-surface temperatures, react with ozone in the extremely cold polar stratosphere. This destruction of ozone occurs especially in late winter and early spring.
During the 1980s and 1990s at northern midlatitudes (such as Europe), the average year-round ozone concentration declined by around 4% per decade; over the southern regions of Australia, New Zealand, Argentina, and South Africa, the figure approximated 6%-7%. UV exposures at northern midlatitudes are likely to peak around 2020, with an estimated 10% increase in effective ultraviolet radiation relative to 1980s levels.
The modeling of future ozone levels and UV radiation (UVR) exposures has estimated that, in consequence, a ‘European’ population living at around 45 degrees North will experience, by 2050, an approximate 5% excess of total skin cancer incidence (assuming, conservatively, no change in age distribution). The equivalent estimation for the U.S. population is for a 10% increase in skin cancer incidence by around 2050.
In the mid-1980s, governments recognized the emerging hazard from ozone depletion. The Montreal Protocol of 1987 was adopted, and the phasing out of major ozone-destroying gases began. Some anticipate a slow but near-complete recovery of stratospheric ozone by the middle of the twenty-first century; the Environmental Protection Agency (EPA) estimates recovery by 2065 with strict adherence to protection protocols.
Increased exposure to UVR also leads to increased rates of lens opacification, cataracts, and whole-body immunosuppression. UVR-induced immunosuppression could influence patterns of infectious disease. It may also influence the occurrence and progression of various autoimmune diseases and, less certainly, vaccine efficacy.
Extreme weather events
The International Society of Dermatology Task Force on Climate Change reports that weather phenomena such as El Niño also result in changes to dermatologic conditions. The El Niño Southern Oscillation (ENSO) is a complex climate phenomenon occurring in the Pacific Ocean at intervals of 2-7 years. The term refers to fluctuations in ocean temperatures in the tropical eastern Pacific Ocean (El Niño, the warm phase of ENSO, and La Niña, the cool phase of ENSO) and in atmospheric pressure across the Pacific basin (Southern Oscillation). This weather pattern is attributed with causing climate change in certain parts of the world and is associated with disease outbreaks.
El Niño has been associated with increases in the occurrence of actinic keratosis, tinea, pityriasis versicolor, miliaria, folliculitis, rosacea, dermatitis caused by Paederus irritans and Paederus sabaeus, and certain vector-borne and waterborne diseases (such as dengue fever, leishmaniasis, Chagas disease, Barmah Forest virus, and leptospirosis), and with decreases in the occurrence of dermatitis, scabies, psoriasis, and papular urticaria. La Niña has been associated with increases in the occurrence of varicella; hand, foot, and mouth disease; and Ross River virus (in certain areas), and decreases in viral warts and leishmaniasis.
Separately, global warming is expected to affect the start, duration, and intensity of the pollen season, and secondarily the rate of asthma exacerbations due to air pollution, respiratory infections, and/or cold air inhalation, with probable increases in eczema and other atopy-related conditions as well.
Vector-borne diseases
In the past year, the largest Ebola virus outbreak in West Africa has resulted in importation of the virus to other countries and secondary local transmission. Autochthonous transmission of Chikungunya virus has occurred in nonendemic areas, including Europe, the Caribbean, and the Americas. Zika virus has re-emerged in the Pacific with local transmission from imported cases. Climate change, deforestation, and changes in precipitation have been linked to variations in the geographical distribution of vectors of some infectious diseases (leishmaniasis, Lyme disease, and now Zika virus) by changing their spread. A warm and humid environment from global warming can also encourage the colonization of the skin by bacteria and fungi.
Finally, there is a wider, ecological dimension to consider. UV radiation impairs the molecular chemistry of photosynthesis both on land (terrestrial plants) and at sea (phytoplankton). This could affect world food production, at least marginally, and thus contribute to nutritional and health problems in food-insecure populations.
Another reason of many, but from a dermatologist’s point of view, to be mindful of taking care of the planet and our environment.
References
1. World Health Organization (WHO).
2. Photochem Photobiol Sci. 2002 May;1(5):324-6.
3. G Ital Dermatol Venereol. 2013 Feb;148(1):135-46.
4. Int J Dermatol. 2012 Jun;51(6):656-61.
5. Int J Dermatol. 2015 Dec;54(12):1343-51.
6. Curr Opin Infect Dis. 2015 Apr;28(2):139-50.
Dr. Wesley and Dr. Talakoub are co-contributors to this column. Dr. Talakoub is in private practice in McLean, Va. Dr. Wesley practices dermatology in Beverly Hills, Calif. This month’s column is by Dr. Wesley. Write to them at [email protected].