User login
Try to Remember …
How often do you misplace your keys or forget why you walked into a room? When I was younger, I dismissed things such as losing my train of thought (my nephew calls that a brain fart), a neglected errand (probably not important enough), or getting lost trying to go somewhere (never was good at directions anyway).
Know that I was never a “list maker.” I gave that up—because I often could not remember where I’d put it. Usually, once I wrote something down, I would eventually (in the same day) recall whatever was on it, so I wouldn’t fret about where I left that list.
Names? I could always tell you where we met, what you were wearing, and where you were sitting. But your name? Forget about it. (Those who have met me know the truth in that statement!)
During particularly stressful or busy times, if I found myself a bit more “absentminded” than usual, I would joke, “Of all the things I’ve lost, I miss my mind the most.”
Now I wonder: Just how serious are those instances of memory lapse? Yes, occasional memory lapses are part of normal aging. Just like our joints, our brains are not as young as they used to be. Even a 90-year-old with a healthy brain has experienced a loss of 10% brain cell volume.1 And let’s be honest, in celebrating major accomplishments (or failures), some of us have killed a few additional brain cells along the way (wink, wink).
We know that as we age, just as our stride has slowed, so too has the sharpness of our recall dulled. However, at what point are those misfires of our brain no longer a minor nuisance?
Data from the Administration on Aging document that in 2013, an estimated 44.7 million US residents were 65 or older.2 An estimated 5 million of them had Alzheimer disease. That translates to one in nine people—scary! This number, researchers predict, will increase to 13.8 million by 2050.3
Moreover, these statistics become more startling as we recognize that the cost of providing long-term and hospice care to people with Alzheimer disease (and other forms of dementia) is estimated to increase from $203 billion in 2013 to $1.2 trillion in 2050 (in 2013 dollars).4 Therefore, it is imperative for us, both as individuals and as health care professionals, to know the warning signs of dementia and be attentive to even seemingly subtle changes in behavior.
Early recognition that these changes are more than minor lapses in memory is important. Delays in diagnosis can result in a reduction of access to available treatments and resources. Yet, at what point do we start to consider those minor instances of forgetfulness not as normal but as indications of developing cognitive problems? My colleagues in gerontology tell us it is when those changes negatively affect activities of daily living and ability to function.
Continue for the difference between my lifelong “geographic handicap” and a form of dementia >>
What is the difference between my lifelong “geographic handicap” and a form of dementia? Would I (or any of my family or friends) recognize it? The diagnosis of dementia is not based on a sole symptom; rather, it requires the existence of at least two types of impairment that are significant and interfere with daily life.
Thankfully, I have adjusted to being “temporarily misplaced” (I don’t call it lost) and smiling at you whilst I try to remember your name. It may seem I jest or am insensitive to a grave health issue—but I am very serious about our need to pay attention to ourselves, to those we care for, and to those we care about (including neighbors). I now live in an area where a “silver alert” (missing elder) is an almost daily occurrence.
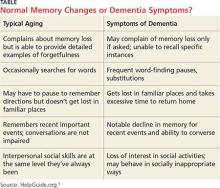
The table provides a comparison of normal-aging memory changes versus dementia symptoms; this is a tool we can use in practice and provide to our patients and their families.5 However, when changes in memory become so pervasive and severe that they are disrupting work, hobbies, social activities, and family relationships, we must recognize that they are the warning signs of Alzheimer disease.6 After reading multiple reports and guides, and witnessing the disease progression in neighbors, I share the three most significant hallmarks of the disease: impaired judgment, difficulty in recalling new information, and unusual behavior.7
It is important to remember—and to communicate to our patients—that memory loss itself does not meet the criteria for dementia. While some may be quick to fear that diagnosis, other factors that can contribute to cognitive problems are stress, depression, vitamin deficiency, thyroid disease, and even dehydration. All of these can be managed, with a resultant reversal of symptoms of memory loss.8 As always, a good health history, review of symptoms, and physical examination will guide us to an accurate diagnosis and plan of care.
There are multiple resources available for patients and families who receive a diagnosis of dementia or Alzheimer disease. Fear of the diagnosis need not blind us to the early warning signs. As NPs and PAs, despite our busy schedules, we must stop and listen to both the patient and the family, and ask the difficult questions about judgment and behavior in our aging patients.
REFERENCES
1. Doty L. Caregiving topics: early signs of dementia. http://alzonline.phhp.ufl.edu/en/reading/EarlySignsFeb08.pdf. Accessed December 11, 2015.
2. CDC. Older persons’ health. www.cdc.gov/nchs/fastats/older-american-health.htm. Accessed December 11, 2015.
3. Hebert LE, Weuve J, Scherr PA, Evans DL. Alzheimer disease in the United States (2010–2050) estimated using the 2010 census. Neurology. 2013;80:1778-1783.
4. Alzheimer’s Association. 2013 Alzheimer’s disease facts and figures. Alzheimers Dement. 2013;9(2):20-245.
5. Wayne M, White M, Smith M. Understanding dementia. www.helpguide.org/articles/alzheimers-dementia/understanding-dementia.htm. Accessed December 11, 2015.
6. Smith M, Robinson L, Segal R. Age-related memory loss. www.helpguide.org/articles/memory/age-related-memory-loss.htm. Accessed December 11, 2015.
7. A guide to coping with Alzheimer’s disease: a Harvard Medical School Special Health Report. www.health.harvard.edu/special-health-reports/a-guide-to-coping-with-alzheimers-disease. Accessed December 11, 2015.
8. HelpGuide.org. What’s causing your memory loss? www.helpguide.org/harvard/whats-causing-your-memory-loss.htm. Accessed December 11, 2015.
How often do you misplace your keys or forget why you walked into a room? When I was younger, I dismissed things such as losing my train of thought (my nephew calls that a brain fart), a neglected errand (probably not important enough), or getting lost trying to go somewhere (never was good at directions anyway).
Know that I was never a “list maker.” I gave that up—because I often could not remember where I’d put it. Usually, once I wrote something down, I would eventually (in the same day) recall whatever was on it, so I wouldn’t fret about where I left that list.
Names? I could always tell you where we met, what you were wearing, and where you were sitting. But your name? Forget about it. (Those who have met me know the truth in that statement!)
During particularly stressful or busy times, if I found myself a bit more “absentminded” than usual, I would joke, “Of all the things I’ve lost, I miss my mind the most.”
Now I wonder: Just how serious are those instances of memory lapse? Yes, occasional memory lapses are part of normal aging. Just like our joints, our brains are not as young as they used to be. Even a 90-year-old with a healthy brain has experienced a loss of 10% brain cell volume.1 And let’s be honest, in celebrating major accomplishments (or failures), some of us have killed a few additional brain cells along the way (wink, wink).
We know that as we age, just as our stride has slowed, so too has the sharpness of our recall dulled. However, at what point are those misfires of our brain no longer a minor nuisance?
Data from the Administration on Aging document that in 2013, an estimated 44.7 million US residents were 65 or older.2 An estimated 5 million of them had Alzheimer disease. That translates to one in nine people—scary! This number, researchers predict, will increase to 13.8 million by 2050.3
Moreover, these statistics become more startling as we recognize that the cost of providing long-term and hospice care to people with Alzheimer disease (and other forms of dementia) is estimated to increase from $203 billion in 2013 to $1.2 trillion in 2050 (in 2013 dollars).4 Therefore, it is imperative for us, both as individuals and as health care professionals, to know the warning signs of dementia and be attentive to even seemingly subtle changes in behavior.
Early recognition that these changes are more than minor lapses in memory is important. Delays in diagnosis can result in a reduction of access to available treatments and resources. Yet, at what point do we start to consider those minor instances of forgetfulness not as normal but as indications of developing cognitive problems? My colleagues in gerontology tell us it is when those changes negatively affect activities of daily living and ability to function.
Continue for the difference between my lifelong “geographic handicap” and a form of dementia >>
What is the difference between my lifelong “geographic handicap” and a form of dementia? Would I (or any of my family or friends) recognize it? The diagnosis of dementia is not based on a sole symptom; rather, it requires the existence of at least two types of impairment that are significant and interfere with daily life.
Thankfully, I have adjusted to being “temporarily misplaced” (I don’t call it lost) and smiling at you whilst I try to remember your name. It may seem I jest or am insensitive to a grave health issue—but I am very serious about our need to pay attention to ourselves, to those we care for, and to those we care about (including neighbors). I now live in an area where a “silver alert” (missing elder) is an almost daily occurrence.
The table provides a comparison of normal-aging memory changes versus dementia symptoms; this is a tool we can use in practice and provide to our patients and their families.5 However, when changes in memory become so pervasive and severe that they are disrupting work, hobbies, social activities, and family relationships, we must recognize that they are the warning signs of Alzheimer disease.6 After reading multiple reports and guides, and witnessing the disease progression in neighbors, I share the three most significant hallmarks of the disease: impaired judgment, difficulty in recalling new information, and unusual behavior.7
It is important to remember—and to communicate to our patients—that memory loss itself does not meet the criteria for dementia. While some may be quick to fear that diagnosis, other factors that can contribute to cognitive problems are stress, depression, vitamin deficiency, thyroid disease, and even dehydration. All of these can be managed, with a resultant reversal of symptoms of memory loss.8 As always, a good health history, review of symptoms, and physical examination will guide us to an accurate diagnosis and plan of care.
There are multiple resources available for patients and families who receive a diagnosis of dementia or Alzheimer disease. Fear of the diagnosis need not blind us to the early warning signs. As NPs and PAs, despite our busy schedules, we must stop and listen to both the patient and the family, and ask the difficult questions about judgment and behavior in our aging patients.
REFERENCES
1. Doty L. Caregiving topics: early signs of dementia. http://alzonline.phhp.ufl.edu/en/reading/EarlySignsFeb08.pdf. Accessed December 11, 2015.
2. CDC. Older persons’ health. www.cdc.gov/nchs/fastats/older-american-health.htm. Accessed December 11, 2015.
3. Hebert LE, Weuve J, Scherr PA, Evans DL. Alzheimer disease in the United States (2010–2050) estimated using the 2010 census. Neurology. 2013;80:1778-1783.
4. Alzheimer’s Association. 2013 Alzheimer’s disease facts and figures. Alzheimers Dement. 2013;9(2):20-245.
5. Wayne M, White M, Smith M. Understanding dementia. www.helpguide.org/articles/alzheimers-dementia/understanding-dementia.htm. Accessed December 11, 2015.
6. Smith M, Robinson L, Segal R. Age-related memory loss. www.helpguide.org/articles/memory/age-related-memory-loss.htm. Accessed December 11, 2015.
7. A guide to coping with Alzheimer’s disease: a Harvard Medical School Special Health Report. www.health.harvard.edu/special-health-reports/a-guide-to-coping-with-alzheimers-disease. Accessed December 11, 2015.
8. HelpGuide.org. What’s causing your memory loss? www.helpguide.org/harvard/whats-causing-your-memory-loss.htm. Accessed December 11, 2015.
How often do you misplace your keys or forget why you walked into a room? When I was younger, I dismissed things such as losing my train of thought (my nephew calls that a brain fart), a neglected errand (probably not important enough), or getting lost trying to go somewhere (never was good at directions anyway).
Know that I was never a “list maker.” I gave that up—because I often could not remember where I’d put it. Usually, once I wrote something down, I would eventually (in the same day) recall whatever was on it, so I wouldn’t fret about where I left that list.
Names? I could always tell you where we met, what you were wearing, and where you were sitting. But your name? Forget about it. (Those who have met me know the truth in that statement!)
During particularly stressful or busy times, if I found myself a bit more “absentminded” than usual, I would joke, “Of all the things I’ve lost, I miss my mind the most.”
Now I wonder: Just how serious are those instances of memory lapse? Yes, occasional memory lapses are part of normal aging. Just like our joints, our brains are not as young as they used to be. Even a 90-year-old with a healthy brain has experienced a loss of 10% brain cell volume.1 And let’s be honest, in celebrating major accomplishments (or failures), some of us have killed a few additional brain cells along the way (wink, wink).
We know that as we age, just as our stride has slowed, so too has the sharpness of our recall dulled. However, at what point are those misfires of our brain no longer a minor nuisance?
Data from the Administration on Aging document that in 2013, an estimated 44.7 million US residents were 65 or older.2 An estimated 5 million of them had Alzheimer disease. That translates to one in nine people—scary! This number, researchers predict, will increase to 13.8 million by 2050.3
Moreover, these statistics become more startling as we recognize that the cost of providing long-term and hospice care to people with Alzheimer disease (and other forms of dementia) is estimated to increase from $203 billion in 2013 to $1.2 trillion in 2050 (in 2013 dollars).4 Therefore, it is imperative for us, both as individuals and as health care professionals, to know the warning signs of dementia and be attentive to even seemingly subtle changes in behavior.
Early recognition that these changes are more than minor lapses in memory is important. Delays in diagnosis can result in a reduction of access to available treatments and resources. Yet, at what point do we start to consider those minor instances of forgetfulness not as normal but as indications of developing cognitive problems? My colleagues in gerontology tell us it is when those changes negatively affect activities of daily living and ability to function.
Continue for the difference between my lifelong “geographic handicap” and a form of dementia >>
What is the difference between my lifelong “geographic handicap” and a form of dementia? Would I (or any of my family or friends) recognize it? The diagnosis of dementia is not based on a sole symptom; rather, it requires the existence of at least two types of impairment that are significant and interfere with daily life.
Thankfully, I have adjusted to being “temporarily misplaced” (I don’t call it lost) and smiling at you whilst I try to remember your name. It may seem I jest or am insensitive to a grave health issue—but I am very serious about our need to pay attention to ourselves, to those we care for, and to those we care about (including neighbors). I now live in an area where a “silver alert” (missing elder) is an almost daily occurrence.
The table provides a comparison of normal-aging memory changes versus dementia symptoms; this is a tool we can use in practice and provide to our patients and their families.5 However, when changes in memory become so pervasive and severe that they are disrupting work, hobbies, social activities, and family relationships, we must recognize that they are the warning signs of Alzheimer disease.6 After reading multiple reports and guides, and witnessing the disease progression in neighbors, I share the three most significant hallmarks of the disease: impaired judgment, difficulty in recalling new information, and unusual behavior.7
It is important to remember—and to communicate to our patients—that memory loss itself does not meet the criteria for dementia. While some may be quick to fear that diagnosis, other factors that can contribute to cognitive problems are stress, depression, vitamin deficiency, thyroid disease, and even dehydration. All of these can be managed, with a resultant reversal of symptoms of memory loss.8 As always, a good health history, review of symptoms, and physical examination will guide us to an accurate diagnosis and plan of care.
There are multiple resources available for patients and families who receive a diagnosis of dementia or Alzheimer disease. Fear of the diagnosis need not blind us to the early warning signs. As NPs and PAs, despite our busy schedules, we must stop and listen to both the patient and the family, and ask the difficult questions about judgment and behavior in our aging patients.
REFERENCES
1. Doty L. Caregiving topics: early signs of dementia. http://alzonline.phhp.ufl.edu/en/reading/EarlySignsFeb08.pdf. Accessed December 11, 2015.
2. CDC. Older persons’ health. www.cdc.gov/nchs/fastats/older-american-health.htm. Accessed December 11, 2015.
3. Hebert LE, Weuve J, Scherr PA, Evans DL. Alzheimer disease in the United States (2010–2050) estimated using the 2010 census. Neurology. 2013;80:1778-1783.
4. Alzheimer’s Association. 2013 Alzheimer’s disease facts and figures. Alzheimers Dement. 2013;9(2):20-245.
5. Wayne M, White M, Smith M. Understanding dementia. www.helpguide.org/articles/alzheimers-dementia/understanding-dementia.htm. Accessed December 11, 2015.
6. Smith M, Robinson L, Segal R. Age-related memory loss. www.helpguide.org/articles/memory/age-related-memory-loss.htm. Accessed December 11, 2015.
7. A guide to coping with Alzheimer’s disease: a Harvard Medical School Special Health Report. www.health.harvard.edu/special-health-reports/a-guide-to-coping-with-alzheimers-disease. Accessed December 11, 2015.
8. HelpGuide.org. What’s causing your memory loss? www.helpguide.org/harvard/whats-causing-your-memory-loss.htm. Accessed December 11, 2015.
Chutzpah
Chutzpah is a Yiddish word that entered American English, joining bagel and nosh. The usual translations of chutzpah – “nerve” or “effrontery” – are correct enough, but leave out the zest implied by chutzpah’s classic case: a man who kills his parents and throws himself on the mercy of the court because he is an orphan.
We all meet patients with chutzpah, which can be amusing, impressive – even breathtaking.
Take for instance the woman who paged me one evening last month. “I visit your nurse for cosmetic stuff,” she said when I called her back. “Your prices for laser hair removal were high, though, so I went to a spa where I could use a Groupon.”
How nice, I thought.
“Anyhow,” she continued, “I went for a treatment at the spa today, and now I have little red bumps all over my thighs. I thought it might be a reaction, and since you are my dermatologist I called to ask what to do.”
Good to be needed.
Then the next week I got another call, this time from a man I hadn’t seen in a long time. “I really like you as a dermatologist,” he began.
“Thank you,” I murmured.
“I saw this spot on my leg that worried me,” he said. “I was going to show it to you, but your office is in an old building, and old buildings don’t agree with me.”
As I scratched my head, he went on. “So I went to another dermatologist who works in a newer building. He did a biopsy and told me I have skin cancer. He said I should have surgery to take it off. I consider you my dermatologist, though, so I called to ask whether you think surgery is a good idea.”
I said I thought it was. I did not add that he should look for an old surgeon in a new building.
These patients are fresh in my mind, but it doesn’t take much effort to come up with others.
“Mr. Skillman wants a refill on his steroid cream,” says my secretary.
“Sure,” I tell her. “E-scribe it over.”
“No,” she says. “He wants a hard copy mailed to him.”
“Does he have one of those mail order pharmacies that requires a written script?”
“No.”
“But it’s so much simpler to call it in or do it by computer. Why does he have to have a hard copy?”
“I don’t know. But he insists on having one.”
I could go on and on. So could you, I’m sure.
When confronted with chutzpah, you have two options: challenge the person showing it and refuse to go along with his demands, or just sigh, comply, and move on. In general, I go with option #2.
First of all, anyone pushy enough to act this way will not react well to being pushed back. (“What’s your problem? Are you too busy to write a prescription? Too stingy to mail it?”)
Second, and perhaps more to the point, many people who display chutzpah don’t know that’s what they are doing. The woman who went for laser at the Groupon spa really has no idea I’d think it odd for her to call me about a complication instead of the spa personnel who lasered her legs. On some level, she figures that they probably don’t know (look how cheap they are), and thinks I should be flattered to be asked. After all, I’m her dermatologist.
Some people with chutzpah are aggressive and difficult and don’t care if they’re being offensive. A lot more are just clueless. The fellow who bores the daylights out of everyone at dinner parties with long, pointless stories doesn’t know he’s being tedious. He just doesn’t pick up social cues.
Most patients, like most people, are polite and deferential. The rest, though, are more memorable.
My building is indeed old. One hundred years ago it was the swankiest apartment house around. Every flat had rooms for a butler, a maid, and a chauffeur for their Packard motorcar. Then the builder went belly-up during the Depression, and the new owner converted it to medical offices. Downward mobility works for me.
Faced with chutzpah, I shrug, smile, and get on with it. Enough people can still tolerate old buildings, and old dermatologists.
Dr. Rockoff practices dermatology in Brookline, Mass., and is a longtime contributor to Dermatology News. He serves on the clinical faculty at Tufts University, Boston, and has taught senior medical students and other trainees for 30 years. Write to him at [email protected].
Chutzpah is a Yiddish word that entered American English, joining bagel and nosh. The usual translations of chutzpah – “nerve” or “effrontery” – are correct enough, but leave out the zest implied by chutzpah’s classic case: a man who kills his parents and throws himself on the mercy of the court because he is an orphan.
We all meet patients with chutzpah, which can be amusing, impressive – even breathtaking.
Take for instance the woman who paged me one evening last month. “I visit your nurse for cosmetic stuff,” she said when I called her back. “Your prices for laser hair removal were high, though, so I went to a spa where I could use a Groupon.”
How nice, I thought.
“Anyhow,” she continued, “I went for a treatment at the spa today, and now I have little red bumps all over my thighs. I thought it might be a reaction, and since you are my dermatologist I called to ask what to do.”
Good to be needed.
Then the next week I got another call, this time from a man I hadn’t seen in a long time. “I really like you as a dermatologist,” he began.
“Thank you,” I murmured.
“I saw this spot on my leg that worried me,” he said. “I was going to show it to you, but your office is in an old building, and old buildings don’t agree with me.”
As I scratched my head, he went on. “So I went to another dermatologist who works in a newer building. He did a biopsy and told me I have skin cancer. He said I should have surgery to take it off. I consider you my dermatologist, though, so I called to ask whether you think surgery is a good idea.”
I said I thought it was. I did not add that he should look for an old surgeon in a new building.
These patients are fresh in my mind, but it doesn’t take much effort to come up with others.
“Mr. Skillman wants a refill on his steroid cream,” says my secretary.
“Sure,” I tell her. “E-scribe it over.”
“No,” she says. “He wants a hard copy mailed to him.”
“Does he have one of those mail order pharmacies that requires a written script?”
“No.”
“But it’s so much simpler to call it in or do it by computer. Why does he have to have a hard copy?”
“I don’t know. But he insists on having one.”
I could go on and on. So could you, I’m sure.
When confronted with chutzpah, you have two options: challenge the person showing it and refuse to go along with his demands, or just sigh, comply, and move on. In general, I go with option #2.
First of all, anyone pushy enough to act this way will not react well to being pushed back. (“What’s your problem? Are you too busy to write a prescription? Too stingy to mail it?”)
Second, and perhaps more to the point, many people who display chutzpah don’t know that’s what they are doing. The woman who went for laser at the Groupon spa really has no idea I’d think it odd for her to call me about a complication instead of the spa personnel who lasered her legs. On some level, she figures that they probably don’t know (look how cheap they are), and thinks I should be flattered to be asked. After all, I’m her dermatologist.
Some people with chutzpah are aggressive and difficult and don’t care if they’re being offensive. A lot more are just clueless. The fellow who bores the daylights out of everyone at dinner parties with long, pointless stories doesn’t know he’s being tedious. He just doesn’t pick up social cues.
Most patients, like most people, are polite and deferential. The rest, though, are more memorable.
My building is indeed old. One hundred years ago it was the swankiest apartment house around. Every flat had rooms for a butler, a maid, and a chauffeur for their Packard motorcar. Then the builder went belly-up during the Depression, and the new owner converted it to medical offices. Downward mobility works for me.
Faced with chutzpah, I shrug, smile, and get on with it. Enough people can still tolerate old buildings, and old dermatologists.
Dr. Rockoff practices dermatology in Brookline, Mass., and is a longtime contributor to Dermatology News. He serves on the clinical faculty at Tufts University, Boston, and has taught senior medical students and other trainees for 30 years. Write to him at [email protected].
Chutzpah is a Yiddish word that entered American English, joining bagel and nosh. The usual translations of chutzpah – “nerve” or “effrontery” – are correct enough, but leave out the zest implied by chutzpah’s classic case: a man who kills his parents and throws himself on the mercy of the court because he is an orphan.
We all meet patients with chutzpah, which can be amusing, impressive – even breathtaking.
Take for instance the woman who paged me one evening last month. “I visit your nurse for cosmetic stuff,” she said when I called her back. “Your prices for laser hair removal were high, though, so I went to a spa where I could use a Groupon.”
How nice, I thought.
“Anyhow,” she continued, “I went for a treatment at the spa today, and now I have little red bumps all over my thighs. I thought it might be a reaction, and since you are my dermatologist I called to ask what to do.”
Good to be needed.
Then the next week I got another call, this time from a man I hadn’t seen in a long time. “I really like you as a dermatologist,” he began.
“Thank you,” I murmured.
“I saw this spot on my leg that worried me,” he said. “I was going to show it to you, but your office is in an old building, and old buildings don’t agree with me.”
As I scratched my head, he went on. “So I went to another dermatologist who works in a newer building. He did a biopsy and told me I have skin cancer. He said I should have surgery to take it off. I consider you my dermatologist, though, so I called to ask whether you think surgery is a good idea.”
I said I thought it was. I did not add that he should look for an old surgeon in a new building.
These patients are fresh in my mind, but it doesn’t take much effort to come up with others.
“Mr. Skillman wants a refill on his steroid cream,” says my secretary.
“Sure,” I tell her. “E-scribe it over.”
“No,” she says. “He wants a hard copy mailed to him.”
“Does he have one of those mail order pharmacies that requires a written script?”
“No.”
“But it’s so much simpler to call it in or do it by computer. Why does he have to have a hard copy?”
“I don’t know. But he insists on having one.”
I could go on and on. So could you, I’m sure.
When confronted with chutzpah, you have two options: challenge the person showing it and refuse to go along with his demands, or just sigh, comply, and move on. In general, I go with option #2.
First of all, anyone pushy enough to act this way will not react well to being pushed back. (“What’s your problem? Are you too busy to write a prescription? Too stingy to mail it?”)
Second, and perhaps more to the point, many people who display chutzpah don’t know that’s what they are doing. The woman who went for laser at the Groupon spa really has no idea I’d think it odd for her to call me about a complication instead of the spa personnel who lasered her legs. On some level, she figures that they probably don’t know (look how cheap they are), and thinks I should be flattered to be asked. After all, I’m her dermatologist.
Some people with chutzpah are aggressive and difficult and don’t care if they’re being offensive. A lot more are just clueless. The fellow who bores the daylights out of everyone at dinner parties with long, pointless stories doesn’t know he’s being tedious. He just doesn’t pick up social cues.
Most patients, like most people, are polite and deferential. The rest, though, are more memorable.
My building is indeed old. One hundred years ago it was the swankiest apartment house around. Every flat had rooms for a butler, a maid, and a chauffeur for their Packard motorcar. Then the builder went belly-up during the Depression, and the new owner converted it to medical offices. Downward mobility works for me.
Faced with chutzpah, I shrug, smile, and get on with it. Enough people can still tolerate old buildings, and old dermatologists.
Dr. Rockoff practices dermatology in Brookline, Mass., and is a longtime contributor to Dermatology News. He serves on the clinical faculty at Tufts University, Boston, and has taught senior medical students and other trainees for 30 years. Write to him at [email protected].
Self-directed learning
Never before in history has medicine progressed as quickly as it does today. The half-life of knowledge and practices is shortening, and the ocean of literature continues to amass every day. In this context, it is simply not possible for training programs to teach in didactics everything residents must know to become competent, much less excellent, doctors. Self-directed learning has become a critical part of residents’ education.
How can we make self-directed learning a more successful process? Attending physicians are likely to answer with the old saying, ‘You can lead a horse to water, but you can’t make it drink!’ While this saying points to the fact that self-directed learning requires a thirsty horse, it takes for granted the role of the guide in showing where water is plentiful. We argue that residents’ self-directed learning can be made more successful by recognizing the role of attendings in this process.
In an era of infinite resources, the limiting factor to learning has become time. The more we learn, the more humbled we are by the vastness of what we don’t know. Self-directed learners must be smart in deciding what should be learned. Herein lies the value of attendings, who, whether we are aware or not, shape our learning simply by virtue of their example. We would do well to pay closer attention to them. No textbook can replace their vast experience, which allows them to hone in on relevant details, to quickly develop comprehensive differentials, or revise plans.
But this learning cannot be based on simply observing and blindly emulating our teachers. We refer to Dr. Bloom’s taxonomy for levels of cognitive learning, in saying that these steps will only get us to the most basic levels of learning, which is “knowing” a disease to the extent that we can apply that knowledge in patient care. These can be acquired without significant mental effort; just by listening to morning reports, reading quick tidbits in between taking care of patients, etc. The goal, however, should be utilizing this basic knowledge as a foundation to develop higher levels of learning, namely Analysis, Synthesis, and Evaluation.
An example for analysis would be quickly going over each of the differentials in a disease and learning what distinguishes them. Synthesis is integrating different ideas and creating a customized plan for the particular patient that is found in no book. Lastly, evaluation is the level of cognition needed to be able to appraise and critique the large volume of opinion that we come across, establish our own opinion, and be able to defend it.
Here again our attendings are valuable resources who can guide us in reaching each of these levels. We must be willing to challenge ourselves by challenging our attendings when things do not make sense. It means always questioning why your attending physician made one medical decision versus another. It means also to challenge what we think we know, in order to discover what we don’t know. … Returning to the old adage, perhaps the key to self-directed learning is for the horse to learn his masters’ ways to the well, so he may adapt to an ever-changing environment.
Dr. Hung and Dr. Ramakrishna are pediatric residents at the Metrohealth Medical Center in Cleveland, Ohio. Email them at [email protected].
Never before in history has medicine progressed as quickly as it does today. The half-life of knowledge and practices is shortening, and the ocean of literature continues to amass every day. In this context, it is simply not possible for training programs to teach in didactics everything residents must know to become competent, much less excellent, doctors. Self-directed learning has become a critical part of residents’ education.
How can we make self-directed learning a more successful process? Attending physicians are likely to answer with the old saying, ‘You can lead a horse to water, but you can’t make it drink!’ While this saying points to the fact that self-directed learning requires a thirsty horse, it takes for granted the role of the guide in showing where water is plentiful. We argue that residents’ self-directed learning can be made more successful by recognizing the role of attendings in this process.
In an era of infinite resources, the limiting factor to learning has become time. The more we learn, the more humbled we are by the vastness of what we don’t know. Self-directed learners must be smart in deciding what should be learned. Herein lies the value of attendings, who, whether we are aware or not, shape our learning simply by virtue of their example. We would do well to pay closer attention to them. No textbook can replace their vast experience, which allows them to hone in on relevant details, to quickly develop comprehensive differentials, or revise plans.
But this learning cannot be based on simply observing and blindly emulating our teachers. We refer to Dr. Bloom’s taxonomy for levels of cognitive learning, in saying that these steps will only get us to the most basic levels of learning, which is “knowing” a disease to the extent that we can apply that knowledge in patient care. These can be acquired without significant mental effort; just by listening to morning reports, reading quick tidbits in between taking care of patients, etc. The goal, however, should be utilizing this basic knowledge as a foundation to develop higher levels of learning, namely Analysis, Synthesis, and Evaluation.
An example for analysis would be quickly going over each of the differentials in a disease and learning what distinguishes them. Synthesis is integrating different ideas and creating a customized plan for the particular patient that is found in no book. Lastly, evaluation is the level of cognition needed to be able to appraise and critique the large volume of opinion that we come across, establish our own opinion, and be able to defend it.
Here again our attendings are valuable resources who can guide us in reaching each of these levels. We must be willing to challenge ourselves by challenging our attendings when things do not make sense. It means always questioning why your attending physician made one medical decision versus another. It means also to challenge what we think we know, in order to discover what we don’t know. … Returning to the old adage, perhaps the key to self-directed learning is for the horse to learn his masters’ ways to the well, so he may adapt to an ever-changing environment.
Dr. Hung and Dr. Ramakrishna are pediatric residents at the Metrohealth Medical Center in Cleveland, Ohio. Email them at [email protected].
Never before in history has medicine progressed as quickly as it does today. The half-life of knowledge and practices is shortening, and the ocean of literature continues to amass every day. In this context, it is simply not possible for training programs to teach in didactics everything residents must know to become competent, much less excellent, doctors. Self-directed learning has become a critical part of residents’ education.
How can we make self-directed learning a more successful process? Attending physicians are likely to answer with the old saying, ‘You can lead a horse to water, but you can’t make it drink!’ While this saying points to the fact that self-directed learning requires a thirsty horse, it takes for granted the role of the guide in showing where water is plentiful. We argue that residents’ self-directed learning can be made more successful by recognizing the role of attendings in this process.
In an era of infinite resources, the limiting factor to learning has become time. The more we learn, the more humbled we are by the vastness of what we don’t know. Self-directed learners must be smart in deciding what should be learned. Herein lies the value of attendings, who, whether we are aware or not, shape our learning simply by virtue of their example. We would do well to pay closer attention to them. No textbook can replace their vast experience, which allows them to hone in on relevant details, to quickly develop comprehensive differentials, or revise plans.
But this learning cannot be based on simply observing and blindly emulating our teachers. We refer to Dr. Bloom’s taxonomy for levels of cognitive learning, in saying that these steps will only get us to the most basic levels of learning, which is “knowing” a disease to the extent that we can apply that knowledge in patient care. These can be acquired without significant mental effort; just by listening to morning reports, reading quick tidbits in between taking care of patients, etc. The goal, however, should be utilizing this basic knowledge as a foundation to develop higher levels of learning, namely Analysis, Synthesis, and Evaluation.
An example for analysis would be quickly going over each of the differentials in a disease and learning what distinguishes them. Synthesis is integrating different ideas and creating a customized plan for the particular patient that is found in no book. Lastly, evaluation is the level of cognition needed to be able to appraise and critique the large volume of opinion that we come across, establish our own opinion, and be able to defend it.
Here again our attendings are valuable resources who can guide us in reaching each of these levels. We must be willing to challenge ourselves by challenging our attendings when things do not make sense. It means always questioning why your attending physician made one medical decision versus another. It means also to challenge what we think we know, in order to discover what we don’t know. … Returning to the old adage, perhaps the key to self-directed learning is for the horse to learn his masters’ ways to the well, so he may adapt to an ever-changing environment.
Dr. Hung and Dr. Ramakrishna are pediatric residents at the Metrohealth Medical Center in Cleveland, Ohio. Email them at [email protected].
Guidance for parents of LGBT youth
Two years ago, a mother of one of my patients asked me for advice. She knew that her daughter identified as lesbian, and she was fully supportive. One day, her daughter wanted to go to a sleepover at a female friend’s house. Her first reaction was to say yes, but then she had second thoughts: If her daughter were straight, and this friend were male, she would not allow her to go because of the potential for sexual activity. When she told her daughter she could not attend the sleepover, her daughter accused her of not letting her go because of her sexual orientation. And now, the dilemma: In her effort to be fair and consistent with her values, the mother is being accused of discrimination. What should she do?
Parents play an irreplaceable role in the life of any teen, especially in the lives of teens that identify as lesbian, gay, bisexual, or transgender (LGBT). But many LGBT youth face serious challenges with their parents. They face the potential of parental rejection of their sexual or gender identity. At the very worst, teens may face homelessness if they come out to homophobic parents.1 Youth whose parents are accepting, nevertheless, are less likely to have mental health problems or engage in substance use.2
As a clinical provider for children and adolescents, caregivers will ask you for advice on how to address parenting challenges. Because LGBT youth are at risk for many adverse health outcomes, and parental support is paramount in preventing them, this is an opportunity for you to help this vulnerable population.
If parents ask you how to be supportive of their LGBT children, here are some recommendations, which are based on an intervention by colleagues at the University of Utah:3
1. Let their affection show. Receiving news that a child is LGBT can be emotionally intense for parents.4 Because of this emotional intensity, parents may react negatively and neglect to show their love for their child, which is what the child is seeking. Parents showing affection is the first step in supporting their LGBT child. Remind parents to tell their child that they love them no matter what.
2. Avoid rejecting behaviors. This is sometimes hard, because some forms of rejection can be quite subtle. Avoid saying anything that may indicate a negative view of LGBT people, even if it is not intended. For example, saying that something is “gay” may seem innocent enough, but it sends the message that being gay is something to be ashamed of.
3. Express their pain away from their child. Evidence shows that minimizing a child’s exposure to parental conflict and stress is associated with better coping with these devastating events.5 Parents should avoid telling their children that news of their sexual orientation or gender identity upsets them, as this is another form of rejecting behavior.
4. Do good before they feel good. Previous studies suggest that changes in behavior can occur even though a person may feel otherwise.6 Negative feelings about a child’s sexual orientation or gender identity can last months or years.7 It’s okay to have these feelings, but showing support such as telling their child how they still love them can ultimately lead to acceptance.
Although it is important for parents to accept their child, it is only half the battle. If you remember Baumrind’s theory on parenting, there are two sides of parenting. The first side involves parents showing their affection, love, and support for their children, which I described earlier. The other side involves managing a child’s behaviors, whether parents create an environment that makes it difficult to engage in behaviors they disapprove of or teach their children how to make the right decision.8 Many LGBT youth engage in risky behaviors because it’s a way of coping in a homophobic environment. The parents’ job is to teach their children healthier coping strategies.
Research on this aspect of parenting in LGBT youth is still at its infancy, and some of it is not reassuring. One important behavior, parental monitoring, which is “a set of correlated parenting behaviors involving attention to and tracking of the child’s whereabouts, activities, and adaptations,”9 can prevent conduct disorders, substance use, and mental health problems in the typical teenager.10 Unfortunately, we don’t find the same results for sexual minorities. One study suggests that parental monitoring may not prevent high-risk sexual behavior for young gay males, even if the parent is aware of the young man’s sexual orientation.11
This doesn’t mean that parental monitoring isn’t helpful. This just means that parenting LGBT youth is different than parenting heterosexual youth. It’s not enough for parents to just accept their child’s sexual orientation. They also must help them make the right decisions taking into consideration the effect of stigma and discrimination on sexual minorities. There are a couple of things you can suggest to your parents to help them raise their LGBT children:
1. Be proactive. Join organizations that support parents of LGBT youth such as Parents, Families, and Friends of Lesbians and Gays (PFLAG). Also, parents must be aware of their children’s behavior. If they are acting depressed, seek help. Having depression or anxiety increases the chances of engaging in risky behaviors, so the earlier parents address this, the better.
2. Make their child know what their views are on high risk-behaviors, such as substance use or having unprotected sex. They need to communicate their expectations clearly. If parents believe that drinking alcohol before the legal age is wrong, they should clearly let their children know that.
3. Make it easier for their child to tell parents what’s going on in their lives. Parents have to gain their children’s trust, be accessible (don’t answer texts while talking to them!), and be an active listener. LGBT youth may not ask parents for advice because they feel that because their parents are straight or cisgender, their life experiences do not apply. Being a member of an organization like PLFAG can be helpful, because parents can ask other parents who have experience raising LGBT youth for advice that works.
4. If parents’ children do something wrong, they should talk to them about how their actions were risky. Children will listen to parents if they view their parenting as legitimate and fair, which can only happen if there is a strong parent-child relationship. Being supportive of a child’s sexual orientation or gender identity is key here. And for the next time, it’s always good to role-play a scenario (for example, what to do if someone tries to make them drink at a party).
Parents of LGBT youth face many challenges. You can help these parents by encouraging them to accept and support their child’s sexual orientation or gender identity and provide parenting strategies relevant for LGBT youth. Most important of all, encourage them to seek support through organizations like PFLAG. With this support, parents can encourage healthy development in LGBT youth.
Resources for parents of LGBT youth
• The Centers for Disease Control and Prevention (CDC) has information on the health of LGBT Youth and advice on parental monitoring in general.
• The Family Acceptance Project is a project researching ways to improve parent-child relationships in LGBT Youth.
• PFLAG is an organization that provides support for families of LGBT youth.
• Lead with Love is a film about how various types of families react to their children coming out to them.
References
1. J Sex Res. 2004 Nov;41(4):329-42.
2. Aust N Z J Psychiatry. 2010 Sep;44(9):774-83.
3. Huebner D. “Leading with Love: Interventions to Support Families of Lesbian, Gay, and Bisexual Adolescents,” The Register Report, Vol. 39. National Register of Health Service Psychologists, Spring 2013.
4. J GLBT Fam Stud. 2014 Jan;10(1-2):36-57.
5. Prof Psychol Res Pr. 2008 Apr;39(2):113-21.
6. “Behaviorism: Classic Studies” (Casper, Wyo: Endeavor Books/Mountain States Litho, 2009).
7. Journal of LGBT Issues in Counseling. 2008;2(2):126-58.
8. Genet Psychol Monogr. 1967;75(1):43-88.
9. Clin Child Fam Psychol Rev. 1998 Mar;1(1):61-75.
10. “Parental Monitoring of Adolescents: Current Perspectives for Researchers and Practitioners” (New York: Columbia University Press, 2010).
11. AIDS Behav. 2014 Aug;18(8):1604-14.
Dr. Montano is an adolescent medicine fellow at Children’s Hospital of Pittsburgh of UPMC and a postdoctoral fellow in the department of pediatrics at the University of Pittsburgh. Email him at [email protected].
Two years ago, a mother of one of my patients asked me for advice. She knew that her daughter identified as lesbian, and she was fully supportive. One day, her daughter wanted to go to a sleepover at a female friend’s house. Her first reaction was to say yes, but then she had second thoughts: If her daughter were straight, and this friend were male, she would not allow her to go because of the potential for sexual activity. When she told her daughter she could not attend the sleepover, her daughter accused her of not letting her go because of her sexual orientation. And now, the dilemma: In her effort to be fair and consistent with her values, the mother is being accused of discrimination. What should she do?
Parents play an irreplaceable role in the life of any teen, especially in the lives of teens that identify as lesbian, gay, bisexual, or transgender (LGBT). But many LGBT youth face serious challenges with their parents. They face the potential of parental rejection of their sexual or gender identity. At the very worst, teens may face homelessness if they come out to homophobic parents.1 Youth whose parents are accepting, nevertheless, are less likely to have mental health problems or engage in substance use.2
As a clinical provider for children and adolescents, caregivers will ask you for advice on how to address parenting challenges. Because LGBT youth are at risk for many adverse health outcomes, and parental support is paramount in preventing them, this is an opportunity for you to help this vulnerable population.
If parents ask you how to be supportive of their LGBT children, here are some recommendations, which are based on an intervention by colleagues at the University of Utah:3
1. Let their affection show. Receiving news that a child is LGBT can be emotionally intense for parents.4 Because of this emotional intensity, parents may react negatively and neglect to show their love for their child, which is what the child is seeking. Parents showing affection is the first step in supporting their LGBT child. Remind parents to tell their child that they love them no matter what.
2. Avoid rejecting behaviors. This is sometimes hard, because some forms of rejection can be quite subtle. Avoid saying anything that may indicate a negative view of LGBT people, even if it is not intended. For example, saying that something is “gay” may seem innocent enough, but it sends the message that being gay is something to be ashamed of.
3. Express their pain away from their child. Evidence shows that minimizing a child’s exposure to parental conflict and stress is associated with better coping with these devastating events.5 Parents should avoid telling their children that news of their sexual orientation or gender identity upsets them, as this is another form of rejecting behavior.
4. Do good before they feel good. Previous studies suggest that changes in behavior can occur even though a person may feel otherwise.6 Negative feelings about a child’s sexual orientation or gender identity can last months or years.7 It’s okay to have these feelings, but showing support such as telling their child how they still love them can ultimately lead to acceptance.
Although it is important for parents to accept their child, it is only half the battle. If you remember Baumrind’s theory on parenting, there are two sides of parenting. The first side involves parents showing their affection, love, and support for their children, which I described earlier. The other side involves managing a child’s behaviors, whether parents create an environment that makes it difficult to engage in behaviors they disapprove of or teach their children how to make the right decision.8 Many LGBT youth engage in risky behaviors because it’s a way of coping in a homophobic environment. The parents’ job is to teach their children healthier coping strategies.
Research on this aspect of parenting in LGBT youth is still at its infancy, and some of it is not reassuring. One important behavior, parental monitoring, which is “a set of correlated parenting behaviors involving attention to and tracking of the child’s whereabouts, activities, and adaptations,”9 can prevent conduct disorders, substance use, and mental health problems in the typical teenager.10 Unfortunately, we don’t find the same results for sexual minorities. One study suggests that parental monitoring may not prevent high-risk sexual behavior for young gay males, even if the parent is aware of the young man’s sexual orientation.11
This doesn’t mean that parental monitoring isn’t helpful. This just means that parenting LGBT youth is different than parenting heterosexual youth. It’s not enough for parents to just accept their child’s sexual orientation. They also must help them make the right decisions taking into consideration the effect of stigma and discrimination on sexual minorities. There are a couple of things you can suggest to your parents to help them raise their LGBT children:
1. Be proactive. Join organizations that support parents of LGBT youth such as Parents, Families, and Friends of Lesbians and Gays (PFLAG). Also, parents must be aware of their children’s behavior. If they are acting depressed, seek help. Having depression or anxiety increases the chances of engaging in risky behaviors, so the earlier parents address this, the better.
2. Make their child know what their views are on high risk-behaviors, such as substance use or having unprotected sex. They need to communicate their expectations clearly. If parents believe that drinking alcohol before the legal age is wrong, they should clearly let their children know that.
3. Make it easier for their child to tell parents what’s going on in their lives. Parents have to gain their children’s trust, be accessible (don’t answer texts while talking to them!), and be an active listener. LGBT youth may not ask parents for advice because they feel that because their parents are straight or cisgender, their life experiences do not apply. Being a member of an organization like PLFAG can be helpful, because parents can ask other parents who have experience raising LGBT youth for advice that works.
4. If parents’ children do something wrong, they should talk to them about how their actions were risky. Children will listen to parents if they view their parenting as legitimate and fair, which can only happen if there is a strong parent-child relationship. Being supportive of a child’s sexual orientation or gender identity is key here. And for the next time, it’s always good to role-play a scenario (for example, what to do if someone tries to make them drink at a party).
Parents of LGBT youth face many challenges. You can help these parents by encouraging them to accept and support their child’s sexual orientation or gender identity and provide parenting strategies relevant for LGBT youth. Most important of all, encourage them to seek support through organizations like PFLAG. With this support, parents can encourage healthy development in LGBT youth.
Resources for parents of LGBT youth
• The Centers for Disease Control and Prevention (CDC) has information on the health of LGBT Youth and advice on parental monitoring in general.
• The Family Acceptance Project is a project researching ways to improve parent-child relationships in LGBT Youth.
• PFLAG is an organization that provides support for families of LGBT youth.
• Lead with Love is a film about how various types of families react to their children coming out to them.
References
1. J Sex Res. 2004 Nov;41(4):329-42.
2. Aust N Z J Psychiatry. 2010 Sep;44(9):774-83.
3. Huebner D. “Leading with Love: Interventions to Support Families of Lesbian, Gay, and Bisexual Adolescents,” The Register Report, Vol. 39. National Register of Health Service Psychologists, Spring 2013.
4. J GLBT Fam Stud. 2014 Jan;10(1-2):36-57.
5. Prof Psychol Res Pr. 2008 Apr;39(2):113-21.
6. “Behaviorism: Classic Studies” (Casper, Wyo: Endeavor Books/Mountain States Litho, 2009).
7. Journal of LGBT Issues in Counseling. 2008;2(2):126-58.
8. Genet Psychol Monogr. 1967;75(1):43-88.
9. Clin Child Fam Psychol Rev. 1998 Mar;1(1):61-75.
10. “Parental Monitoring of Adolescents: Current Perspectives for Researchers and Practitioners” (New York: Columbia University Press, 2010).
11. AIDS Behav. 2014 Aug;18(8):1604-14.
Dr. Montano is an adolescent medicine fellow at Children’s Hospital of Pittsburgh of UPMC and a postdoctoral fellow in the department of pediatrics at the University of Pittsburgh. Email him at [email protected].
Two years ago, a mother of one of my patients asked me for advice. She knew that her daughter identified as lesbian, and she was fully supportive. One day, her daughter wanted to go to a sleepover at a female friend’s house. Her first reaction was to say yes, but then she had second thoughts: If her daughter were straight, and this friend were male, she would not allow her to go because of the potential for sexual activity. When she told her daughter she could not attend the sleepover, her daughter accused her of not letting her go because of her sexual orientation. And now, the dilemma: In her effort to be fair and consistent with her values, the mother is being accused of discrimination. What should she do?
Parents play an irreplaceable role in the life of any teen, especially in the lives of teens that identify as lesbian, gay, bisexual, or transgender (LGBT). But many LGBT youth face serious challenges with their parents. They face the potential of parental rejection of their sexual or gender identity. At the very worst, teens may face homelessness if they come out to homophobic parents.1 Youth whose parents are accepting, nevertheless, are less likely to have mental health problems or engage in substance use.2
As a clinical provider for children and adolescents, caregivers will ask you for advice on how to address parenting challenges. Because LGBT youth are at risk for many adverse health outcomes, and parental support is paramount in preventing them, this is an opportunity for you to help this vulnerable population.
If parents ask you how to be supportive of their LGBT children, here are some recommendations, which are based on an intervention by colleagues at the University of Utah:3
1. Let their affection show. Receiving news that a child is LGBT can be emotionally intense for parents.4 Because of this emotional intensity, parents may react negatively and neglect to show their love for their child, which is what the child is seeking. Parents showing affection is the first step in supporting their LGBT child. Remind parents to tell their child that they love them no matter what.
2. Avoid rejecting behaviors. This is sometimes hard, because some forms of rejection can be quite subtle. Avoid saying anything that may indicate a negative view of LGBT people, even if it is not intended. For example, saying that something is “gay” may seem innocent enough, but it sends the message that being gay is something to be ashamed of.
3. Express their pain away from their child. Evidence shows that minimizing a child’s exposure to parental conflict and stress is associated with better coping with these devastating events.5 Parents should avoid telling their children that news of their sexual orientation or gender identity upsets them, as this is another form of rejecting behavior.
4. Do good before they feel good. Previous studies suggest that changes in behavior can occur even though a person may feel otherwise.6 Negative feelings about a child’s sexual orientation or gender identity can last months or years.7 It’s okay to have these feelings, but showing support such as telling their child how they still love them can ultimately lead to acceptance.
Although it is important for parents to accept their child, it is only half the battle. If you remember Baumrind’s theory on parenting, there are two sides of parenting. The first side involves parents showing their affection, love, and support for their children, which I described earlier. The other side involves managing a child’s behaviors, whether parents create an environment that makes it difficult to engage in behaviors they disapprove of or teach their children how to make the right decision.8 Many LGBT youth engage in risky behaviors because it’s a way of coping in a homophobic environment. The parents’ job is to teach their children healthier coping strategies.
Research on this aspect of parenting in LGBT youth is still at its infancy, and some of it is not reassuring. One important behavior, parental monitoring, which is “a set of correlated parenting behaviors involving attention to and tracking of the child’s whereabouts, activities, and adaptations,”9 can prevent conduct disorders, substance use, and mental health problems in the typical teenager.10 Unfortunately, we don’t find the same results for sexual minorities. One study suggests that parental monitoring may not prevent high-risk sexual behavior for young gay males, even if the parent is aware of the young man’s sexual orientation.11
This doesn’t mean that parental monitoring isn’t helpful. This just means that parenting LGBT youth is different than parenting heterosexual youth. It’s not enough for parents to just accept their child’s sexual orientation. They also must help them make the right decisions taking into consideration the effect of stigma and discrimination on sexual minorities. There are a couple of things you can suggest to your parents to help them raise their LGBT children:
1. Be proactive. Join organizations that support parents of LGBT youth such as Parents, Families, and Friends of Lesbians and Gays (PFLAG). Also, parents must be aware of their children’s behavior. If they are acting depressed, seek help. Having depression or anxiety increases the chances of engaging in risky behaviors, so the earlier parents address this, the better.
2. Make their child know what their views are on high risk-behaviors, such as substance use or having unprotected sex. They need to communicate their expectations clearly. If parents believe that drinking alcohol before the legal age is wrong, they should clearly let their children know that.
3. Make it easier for their child to tell parents what’s going on in their lives. Parents have to gain their children’s trust, be accessible (don’t answer texts while talking to them!), and be an active listener. LGBT youth may not ask parents for advice because they feel that because their parents are straight or cisgender, their life experiences do not apply. Being a member of an organization like PLFAG can be helpful, because parents can ask other parents who have experience raising LGBT youth for advice that works.
4. If parents’ children do something wrong, they should talk to them about how their actions were risky. Children will listen to parents if they view their parenting as legitimate and fair, which can only happen if there is a strong parent-child relationship. Being supportive of a child’s sexual orientation or gender identity is key here. And for the next time, it’s always good to role-play a scenario (for example, what to do if someone tries to make them drink at a party).
Parents of LGBT youth face many challenges. You can help these parents by encouraging them to accept and support their child’s sexual orientation or gender identity and provide parenting strategies relevant for LGBT youth. Most important of all, encourage them to seek support through organizations like PFLAG. With this support, parents can encourage healthy development in LGBT youth.
Resources for parents of LGBT youth
• The Centers for Disease Control and Prevention (CDC) has information on the health of LGBT Youth and advice on parental monitoring in general.
• The Family Acceptance Project is a project researching ways to improve parent-child relationships in LGBT Youth.
• PFLAG is an organization that provides support for families of LGBT youth.
• Lead with Love is a film about how various types of families react to their children coming out to them.
References
1. J Sex Res. 2004 Nov;41(4):329-42.
2. Aust N Z J Psychiatry. 2010 Sep;44(9):774-83.
3. Huebner D. “Leading with Love: Interventions to Support Families of Lesbian, Gay, and Bisexual Adolescents,” The Register Report, Vol. 39. National Register of Health Service Psychologists, Spring 2013.
4. J GLBT Fam Stud. 2014 Jan;10(1-2):36-57.
5. Prof Psychol Res Pr. 2008 Apr;39(2):113-21.
6. “Behaviorism: Classic Studies” (Casper, Wyo: Endeavor Books/Mountain States Litho, 2009).
7. Journal of LGBT Issues in Counseling. 2008;2(2):126-58.
8. Genet Psychol Monogr. 1967;75(1):43-88.
9. Clin Child Fam Psychol Rev. 1998 Mar;1(1):61-75.
10. “Parental Monitoring of Adolescents: Current Perspectives for Researchers and Practitioners” (New York: Columbia University Press, 2010).
11. AIDS Behav. 2014 Aug;18(8):1604-14.
Dr. Montano is an adolescent medicine fellow at Children’s Hospital of Pittsburgh of UPMC and a postdoctoral fellow in the department of pediatrics at the University of Pittsburgh. Email him at [email protected].
The HPV vaccine
As physicians, we play a unique role in medicine. Drawing on research data, we provide a gateway of information to patients and families. Governing agencies use that data to make recommendations so that we can promote treatment with confidence. But we also have a responsibility if there is an ill outcome, so being well versed on vaccines and treatments is imperative.
Since the human papillomavirus (HPV) vaccines (Gardasil, Cervarix) were approved for the prevention of HPV, there has been controversy. Despite the ongoing reports of the vaccine’s success in lowering cervical cancer rates, many parents still feel that it puts their children at risk.
A 2012 study – a systematic review of parents’ knowledge of HPV – showed a decline from 2001 to 2011, with a rise in parents’ safety concerns, and fewer parents opting to have their children vaccinated (Obstet Gynecol Int. 2012. doi: 10.1155/2012/921236).
Several studies have shown the overwhelming decline in cervical cancer that is directly related to the implementation of the HPV vaccines. But there has been growing concern, as postural orthostatic hypotension (POTS), complex regional pain syndrome (CRPS), and sudden death have been cited as side effects of theses vaccines. POTS and CRPS have been in the headlines recently, since a report came out linking the vaccine to these syndromes. Although a review by the European Medicines Agency found that the evidence does not support the notion of the HPV vaccine causing POTS or CRPS, many groups still promote a ban of the vaccine.
In 2013, Japan withdrew its recommendation for administration of the HPV vaccine after reports that many girls had been seriously harmed by it, and now calls for follow-up for patients who believe they are having side effects. Researchers argue that the basis for this action is poorly founded, and that many young women are being deprived of a vaccine that would be protective. But just as many say that more investigation needs to be done before the recommendation can be reinstated, given the number of reports about women being seriously injured from the vaccine. The Japan Society of Obstetrics and Gynecology is pleading with the Japanese Health Ministry to commence recommending the HPV cancer-preventing vaccineonce again.
An Internet search of this topic shows there are several articles questioning the safety of the vaccine, and throughout the world, concerns are forcing more research to be done to ensure its safety. Although the research overwhelmingly shows that the risk-to-benefit ratio is in favor of the HPV vaccine, several sites are reporting injury.
In a study of 997,585 girls aged 10-17 years in Denmark and Sweden, among whom 296,826 received a total of 696,420 quadrivalent HPV vaccine doses, 1,043 (less than 1%) were found to have adverse reactions, compared with 11,944 (2%) of unvaccinated girls (BMJ 2013;347:f5906). Although some relationship between HPV vaccine and autoimmune disorders such as Behçet’s syndrome, Raynaud’s disease, and type 1 diabetes was apparent, no consistent evidence for a causal association was found.
“Analysis of data reported to the Vaccine Adverse Event Reporting System revealed disproportionate reporting of venous thromboembolism,” noted Dr. Lisen Arnheim-Dahlström of the Karolinska Institutet, Stockholm, lead author of the BMJ study, and associates. “A study by the Vaccine Safety Datalink, which involved eight outcomes, identified a nonsignificantly increased relative risk (1.98) of venous thromboembolism; medical record review could confirm five of the eight cases identified from databases using international classification of diseases codes, and all five had known risk factors for venous thromboembolism. In our analysis, based on 21 vaccine exposed cases, there was no significant association with venous thromboembolism within 90 days after exposure to [quadrivalent] HPV vaccine.”
These rising concerns are resulting in more parents declining the HPV vaccine, and more questions for the primary care physician to answer. Not only are parents alarmed, but so are the physicians who make the recommendations. Being aware of the most current research and reports for and against the vaccine’s use, and being able to discuss with the family the validity of this information, will help to dispel much of the anxiety.
Dr. Pearce is a pediatrician in Frankfort, Ill. To contact her, send email to [email protected].
As physicians, we play a unique role in medicine. Drawing on research data, we provide a gateway of information to patients and families. Governing agencies use that data to make recommendations so that we can promote treatment with confidence. But we also have a responsibility if there is an ill outcome, so being well versed on vaccines and treatments is imperative.
Since the human papillomavirus (HPV) vaccines (Gardasil, Cervarix) were approved for the prevention of HPV, there has been controversy. Despite the ongoing reports of the vaccine’s success in lowering cervical cancer rates, many parents still feel that it puts their children at risk.
A 2012 study – a systematic review of parents’ knowledge of HPV – showed a decline from 2001 to 2011, with a rise in parents’ safety concerns, and fewer parents opting to have their children vaccinated (Obstet Gynecol Int. 2012. doi: 10.1155/2012/921236).
Several studies have shown the overwhelming decline in cervical cancer that is directly related to the implementation of the HPV vaccines. But there has been growing concern, as postural orthostatic hypotension (POTS), complex regional pain syndrome (CRPS), and sudden death have been cited as side effects of theses vaccines. POTS and CRPS have been in the headlines recently, since a report came out linking the vaccine to these syndromes. Although a review by the European Medicines Agency found that the evidence does not support the notion of the HPV vaccine causing POTS or CRPS, many groups still promote a ban of the vaccine.
In 2013, Japan withdrew its recommendation for administration of the HPV vaccine after reports that many girls had been seriously harmed by it, and now calls for follow-up for patients who believe they are having side effects. Researchers argue that the basis for this action is poorly founded, and that many young women are being deprived of a vaccine that would be protective. But just as many say that more investigation needs to be done before the recommendation can be reinstated, given the number of reports about women being seriously injured from the vaccine. The Japan Society of Obstetrics and Gynecology is pleading with the Japanese Health Ministry to commence recommending the HPV cancer-preventing vaccineonce again.
An Internet search of this topic shows there are several articles questioning the safety of the vaccine, and throughout the world, concerns are forcing more research to be done to ensure its safety. Although the research overwhelmingly shows that the risk-to-benefit ratio is in favor of the HPV vaccine, several sites are reporting injury.
In a study of 997,585 girls aged 10-17 years in Denmark and Sweden, among whom 296,826 received a total of 696,420 quadrivalent HPV vaccine doses, 1,043 (less than 1%) were found to have adverse reactions, compared with 11,944 (2%) of unvaccinated girls (BMJ 2013;347:f5906). Although some relationship between HPV vaccine and autoimmune disorders such as Behçet’s syndrome, Raynaud’s disease, and type 1 diabetes was apparent, no consistent evidence for a causal association was found.
“Analysis of data reported to the Vaccine Adverse Event Reporting System revealed disproportionate reporting of venous thromboembolism,” noted Dr. Lisen Arnheim-Dahlström of the Karolinska Institutet, Stockholm, lead author of the BMJ study, and associates. “A study by the Vaccine Safety Datalink, which involved eight outcomes, identified a nonsignificantly increased relative risk (1.98) of venous thromboembolism; medical record review could confirm five of the eight cases identified from databases using international classification of diseases codes, and all five had known risk factors for venous thromboembolism. In our analysis, based on 21 vaccine exposed cases, there was no significant association with venous thromboembolism within 90 days after exposure to [quadrivalent] HPV vaccine.”
These rising concerns are resulting in more parents declining the HPV vaccine, and more questions for the primary care physician to answer. Not only are parents alarmed, but so are the physicians who make the recommendations. Being aware of the most current research and reports for and against the vaccine’s use, and being able to discuss with the family the validity of this information, will help to dispel much of the anxiety.
Dr. Pearce is a pediatrician in Frankfort, Ill. To contact her, send email to [email protected].
As physicians, we play a unique role in medicine. Drawing on research data, we provide a gateway of information to patients and families. Governing agencies use that data to make recommendations so that we can promote treatment with confidence. But we also have a responsibility if there is an ill outcome, so being well versed on vaccines and treatments is imperative.
Since the human papillomavirus (HPV) vaccines (Gardasil, Cervarix) were approved for the prevention of HPV, there has been controversy. Despite the ongoing reports of the vaccine’s success in lowering cervical cancer rates, many parents still feel that it puts their children at risk.
A 2012 study – a systematic review of parents’ knowledge of HPV – showed a decline from 2001 to 2011, with a rise in parents’ safety concerns, and fewer parents opting to have their children vaccinated (Obstet Gynecol Int. 2012. doi: 10.1155/2012/921236).
Several studies have shown the overwhelming decline in cervical cancer that is directly related to the implementation of the HPV vaccines. But there has been growing concern, as postural orthostatic hypotension (POTS), complex regional pain syndrome (CRPS), and sudden death have been cited as side effects of theses vaccines. POTS and CRPS have been in the headlines recently, since a report came out linking the vaccine to these syndromes. Although a review by the European Medicines Agency found that the evidence does not support the notion of the HPV vaccine causing POTS or CRPS, many groups still promote a ban of the vaccine.
In 2013, Japan withdrew its recommendation for administration of the HPV vaccine after reports that many girls had been seriously harmed by it, and now calls for follow-up for patients who believe they are having side effects. Researchers argue that the basis for this action is poorly founded, and that many young women are being deprived of a vaccine that would be protective. But just as many say that more investigation needs to be done before the recommendation can be reinstated, given the number of reports about women being seriously injured from the vaccine. The Japan Society of Obstetrics and Gynecology is pleading with the Japanese Health Ministry to commence recommending the HPV cancer-preventing vaccineonce again.
An Internet search of this topic shows there are several articles questioning the safety of the vaccine, and throughout the world, concerns are forcing more research to be done to ensure its safety. Although the research overwhelmingly shows that the risk-to-benefit ratio is in favor of the HPV vaccine, several sites are reporting injury.
In a study of 997,585 girls aged 10-17 years in Denmark and Sweden, among whom 296,826 received a total of 696,420 quadrivalent HPV vaccine doses, 1,043 (less than 1%) were found to have adverse reactions, compared with 11,944 (2%) of unvaccinated girls (BMJ 2013;347:f5906). Although some relationship between HPV vaccine and autoimmune disorders such as Behçet’s syndrome, Raynaud’s disease, and type 1 diabetes was apparent, no consistent evidence for a causal association was found.
“Analysis of data reported to the Vaccine Adverse Event Reporting System revealed disproportionate reporting of venous thromboembolism,” noted Dr. Lisen Arnheim-Dahlström of the Karolinska Institutet, Stockholm, lead author of the BMJ study, and associates. “A study by the Vaccine Safety Datalink, which involved eight outcomes, identified a nonsignificantly increased relative risk (1.98) of venous thromboembolism; medical record review could confirm five of the eight cases identified from databases using international classification of diseases codes, and all five had known risk factors for venous thromboembolism. In our analysis, based on 21 vaccine exposed cases, there was no significant association with venous thromboembolism within 90 days after exposure to [quadrivalent] HPV vaccine.”
These rising concerns are resulting in more parents declining the HPV vaccine, and more questions for the primary care physician to answer. Not only are parents alarmed, but so are the physicians who make the recommendations. Being aware of the most current research and reports for and against the vaccine’s use, and being able to discuss with the family the validity of this information, will help to dispel much of the anxiety.
Dr. Pearce is a pediatrician in Frankfort, Ill. To contact her, send email to [email protected].
Reader discussions regarding trends in minimally invasive hysterectomy
AN OPEN LETTER TO THE FDA ON MORCELLATION FOR PRESUMED UTERINE FIBROIDS
On December 8, 2015, 46 minimally invasive surgeons, gynecologic oncologists, and other experts spoke out in unison when they sent an open letter to the US Food and Drug Administration (FDA). They called into question the FDA’s estimate of the likelihood of occult leiomyosarcoma (LMS) and recommended continued use of power morcellation in appropriate cases.
An excerpt from this letter is published here. To read the letter in its entirety and the names of the signees, click here.
Letter excerpt:
If abdominal hysterectomy is recommended to women with fibroids, will women be better off?
By focusing exclusively on the risk of LMS, the FDA failed to take into account other risks associated with surgery. Laparoscopic surgery uses small incisions, is performed as an outpatient procedure (or overnight stay), has a faster recovery (2 weeks vs 4–6 weeks for open surgery), and is associated with lower mortality and fewer complications. These benefits of minimally invasive surgery are now well established in gynecologic and general surgery.
Using published best-evidence data, a recent decision analysis1 showed that, comparing 100,000 women undergoing laparoscopic hysterectomy with 100,000 undergoing open hysterectomy, the group undergoing laparoscopic surgery would experience 20 fewer perioperative deaths, 150 fewer pulmonary or venous embolus, and 4,800 fewer wound infections. Importantly, women having open surgery would have 8,000 fewer quality-of-life years.
A recently published study2 found that, in the 8 months following the FDA safety communication, utilization of laparoscopic hysterectomies decreased by 4.1% (P = .005), and abdominal and vaginal hysterectomies increased by 1.7% (P = .112) and 2.4% (P = .012), respectively. Major surgical complications (not including blood transfusions) increased from 2.2% to 2.8% (P = .015), and the rate of hospital readmission within 30 days also increased from 3.4% to 4.2% (P = .025). These observations merit consideration as women weigh the pros and cons of minimally invasive surgery with morcellation versus open surgery.
Clinical recommendations
Recent attention to surgical options for women with uterine leiomyomas and the risk of an occult LMS are positive developments in that the gynecologic community is reexamining relevant issues. We respectfully suggest that the following clinical recommendations be considered:
- The risk of LMS is higher in older postmenopausal women; greater caution should be exercised prior to recommending morcellation procedures for these women.
- Preoperative consideration of LMS is important. Women aged 35 years and older with irregular uterine bleeding and presumed fibroids should have an endometrial biopsy, which occasionally may detect LMS prior to surgery. Women should have normal results of cervical cancer screening.
- Ultrasound or MRI findings of a large irregular vascular mass, often with irregular anechoic (cystic) areas reflecting necrosis, may cause suspicion of LMS.
- Women wishing minimally invasive procedures with morcellation, including scalpel morcellation via the vagina or mini-laparotomy, or power morcellation using laparoscopic guidance, should understand the potential risk of decreased survival should LMS be present. Open procedures should be offered to all women who are considering minimally invasive procedures for “fibroids.”
- Following morcellation, careful inspection for tissue fragments should be undertaken and copious irrigation of the pelvic and abdominal cavities should be performed to minimize the risk of retained
tissue. - Further investigations of a means to identify LMS preoperatively should be supported. Likewise, investigation into the biology of LMS should be funded to better understand the propensity of tissue fragments or cells to implant and grow. With that knowledge, minimally invasive procedures could be avoided for women with LMS and women choosing minimally invasive surgery could be reassured that they do not have LMS.
Respecting women who suffer from LMS, we conclude that the FDA directive was based on a misleading analysis. Consequently, more accurate estimates regarding the prevalence of LMS among women having surgery for fibroids should be issued. Women have a right to self determination. Modification of the FDA’s current restrictive guidance regarding power morcellation would empower each woman to consider the pertinent issues and have the freedom to undertake shared decision making with her surgeon in order to select the procedure that is most appropriate for her.
References
1. Siedhoff MT, Wheeler SB, Rutstein SE, et al. Laparoscopic hysterectomy with morcellation vs abdominal hysterectomy for presumed fibroid tumors in premenopausal women: a decision analysis. Am J Obstet Gynecol. 2015;212(5):591.e1–e8.
2. Harris JA, Swenson CW, Uppal S, et al. Practice patterns and postoperative complications before and after Food and Drug Administration Safety Communication on power morcellation [published online ahead of print August 24, 2015]. Am J Obstet Gynecol. doi:10.1016/j.ajog.2015.08.047.
Choose the best approach for the patient
I cannot decrease the number of abdominal hysterectomies I perform—all of them are indicated.
Richard Hatch, MD
Augusta, Georgia
Supracervical hysterectomy: simplest is best
Supracervical hysterectomy (SCH) via a Pfannenstiel incision in women with a body mass index less than 25 kg/m2 is a great procedure for uterine pathology. SCH addresses only the uterine pathology and preserves the cervix, is a sterile procedure, requires no ancillary equipment, should take less than 30 minutes, preserves the full length of the vagina, requires only an overnight hospitalization, and has a short learning curve.
Removal of the cervix in any hysterectomy is the procedure that results in bladder and ureter injury and infection from contamination. Patients should be driving and back to nonphysical jobs in less than 1 week. As medical care becomes a truly transparent market-based business, patients will opt for SCH over higher priced alternatives. Sometimes the simplest procedures are still the best.
Joe Walsh, MD
Philadelphia, Pennsylvania
Continue to teach abdominal hysterectomy
No one can disagree with the statistics of shorter recovery and less morbidity for laparoscopic and vaginal procedures. In fact, what separates a gynecologist from other surgeons is the ability to operate in and through the vagina. There is still a place for abdominal hysterectomy for benign disease in modern gynecology.
Most programs produce good laparoscopic surgeons but ill prepared abdominal and vaginal surgeons. No gynecologist should be operating in the pelvis unless he or she is comfortable going into the retroperitoneal space if necessary. Many of the total laparoscopic hysterectomies that are performed could be done vaginally without abdominal incisions.
Now we have a generation of gynecologic surgeons who believe a robotic hysterectomy (at great extra expense) offers the patient an advantage, despite longer anesthesia and procedure times. We know morbidity has a direct correlation to operating and anesthesia time. Although I am impressed with what the next generation can do through a laparoscope, I would hate to let them continue without the experience or the ability to do an open abdominal procedure.
Allan N. Boruszak, MD
Washington, North Carolina
Dr. Barbieri’s response
I appreciate the perspectives of Drs. Hatch, Walsh, and Boruszak on the important issue of improving hysterectomy outcomes. Dr. Hatch raises the important point that gynecologists routinely select the best surgical approach for the unique needs of their patients. Based on a given gynecologist’s panel of patients and their unique medical issues, it may be difficult to change the distribution of surgical approaches to hysterectomy. Dr. Walsh advocates for a “minimally invasive” abdominal SCH, which is a valid approach to improving the outcomes of the abdominal approach. Dr. Boruszak rightly highlights the importance of teaching gynecologists to access the retroperitoneum, paravesical, and pararectal spaces in order to improve patient outcomes.
“VAGINAL HYSTERECTOMY WITH BASIC INSTRUMENTATION”
BARBARA S. LEVY, MD (OCTOBER, 2015)
Appreciates the instrument review
Dr. Levy’s article on vaginal hysterectomy using basic instruments is really wonderful. The segment on uterine reduction strategies will be especially useful. I appreciate her preference to use the Ligasure vessel-sealing device over suturing pedicles. Before we take steps to debulk the uterus, it is always essential, and better, to ligate uterine vessels, as this minimizes blood loss and makes the surgical field clearer.
R. Sasirekha
Puducherry, India
Skill should be rewarded
When I trained, vaginal hysterectomy was reserved for prolapse. After joining the Army, my eyes were opened by physicians who could morcellate a 16-week uterus or perform a 20-minute vaginal hysterectomy on a nulliparous woman for sterilization (which, of course, is controversial).
Once in private practice, incorporating these new skills into my own techniques was challenging and rewarding. Imagine my disappointment when I found out that reimbursement was a disincentive. It is easy to be altruistic, but one has to consider the incentives, too. Skill should be rewarded.
Mark B. Vizer, MD
Lansdale, Pennsylvania
A long-time proponent of vaginal hysterectomy
I appreciate the articles by Drs. Levy and Gebhart on vaginal surgical techniques. I have long been a proponent of vaginal hysterectomy as the preferred route for removal of the uterus (and tubes and ovaries, if indicated). I do most of my hysterectomies vaginally, with salpingectomies and oophorectomies if indicated. As an older surgeon, I now refer patients with uteri larger than 16 weeks, endometriosis, or suspected cancer.
Doug Tolley, MD
Yuba City, California
Share your thoughts! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
AN OPEN LETTER TO THE FDA ON MORCELLATION FOR PRESUMED UTERINE FIBROIDS
On December 8, 2015, 46 minimally invasive surgeons, gynecologic oncologists, and other experts spoke out in unison when they sent an open letter to the US Food and Drug Administration (FDA). They called into question the FDA’s estimate of the likelihood of occult leiomyosarcoma (LMS) and recommended continued use of power morcellation in appropriate cases.
An excerpt from this letter is published here. To read the letter in its entirety and the names of the signees, click here.
Letter excerpt:
If abdominal hysterectomy is recommended to women with fibroids, will women be better off?
By focusing exclusively on the risk of LMS, the FDA failed to take into account other risks associated with surgery. Laparoscopic surgery uses small incisions, is performed as an outpatient procedure (or overnight stay), has a faster recovery (2 weeks vs 4–6 weeks for open surgery), and is associated with lower mortality and fewer complications. These benefits of minimally invasive surgery are now well established in gynecologic and general surgery.
Using published best-evidence data, a recent decision analysis1 showed that, comparing 100,000 women undergoing laparoscopic hysterectomy with 100,000 undergoing open hysterectomy, the group undergoing laparoscopic surgery would experience 20 fewer perioperative deaths, 150 fewer pulmonary or venous embolus, and 4,800 fewer wound infections. Importantly, women having open surgery would have 8,000 fewer quality-of-life years.
A recently published study2 found that, in the 8 months following the FDA safety communication, utilization of laparoscopic hysterectomies decreased by 4.1% (P = .005), and abdominal and vaginal hysterectomies increased by 1.7% (P = .112) and 2.4% (P = .012), respectively. Major surgical complications (not including blood transfusions) increased from 2.2% to 2.8% (P = .015), and the rate of hospital readmission within 30 days also increased from 3.4% to 4.2% (P = .025). These observations merit consideration as women weigh the pros and cons of minimally invasive surgery with morcellation versus open surgery.
Clinical recommendations
Recent attention to surgical options for women with uterine leiomyomas and the risk of an occult LMS are positive developments in that the gynecologic community is reexamining relevant issues. We respectfully suggest that the following clinical recommendations be considered:
- The risk of LMS is higher in older postmenopausal women; greater caution should be exercised prior to recommending morcellation procedures for these women.
- Preoperative consideration of LMS is important. Women aged 35 years and older with irregular uterine bleeding and presumed fibroids should have an endometrial biopsy, which occasionally may detect LMS prior to surgery. Women should have normal results of cervical cancer screening.
- Ultrasound or MRI findings of a large irregular vascular mass, often with irregular anechoic (cystic) areas reflecting necrosis, may cause suspicion of LMS.
- Women wishing minimally invasive procedures with morcellation, including scalpel morcellation via the vagina or mini-laparotomy, or power morcellation using laparoscopic guidance, should understand the potential risk of decreased survival should LMS be present. Open procedures should be offered to all women who are considering minimally invasive procedures for “fibroids.”
- Following morcellation, careful inspection for tissue fragments should be undertaken and copious irrigation of the pelvic and abdominal cavities should be performed to minimize the risk of retained
tissue. - Further investigations of a means to identify LMS preoperatively should be supported. Likewise, investigation into the biology of LMS should be funded to better understand the propensity of tissue fragments or cells to implant and grow. With that knowledge, minimally invasive procedures could be avoided for women with LMS and women choosing minimally invasive surgery could be reassured that they do not have LMS.
Respecting women who suffer from LMS, we conclude that the FDA directive was based on a misleading analysis. Consequently, more accurate estimates regarding the prevalence of LMS among women having surgery for fibroids should be issued. Women have a right to self determination. Modification of the FDA’s current restrictive guidance regarding power morcellation would empower each woman to consider the pertinent issues and have the freedom to undertake shared decision making with her surgeon in order to select the procedure that is most appropriate for her.
References
1. Siedhoff MT, Wheeler SB, Rutstein SE, et al. Laparoscopic hysterectomy with morcellation vs abdominal hysterectomy for presumed fibroid tumors in premenopausal women: a decision analysis. Am J Obstet Gynecol. 2015;212(5):591.e1–e8.
2. Harris JA, Swenson CW, Uppal S, et al. Practice patterns and postoperative complications before and after Food and Drug Administration Safety Communication on power morcellation [published online ahead of print August 24, 2015]. Am J Obstet Gynecol. doi:10.1016/j.ajog.2015.08.047.
Choose the best approach for the patient
I cannot decrease the number of abdominal hysterectomies I perform—all of them are indicated.
Richard Hatch, MD
Augusta, Georgia
Supracervical hysterectomy: simplest is best
Supracervical hysterectomy (SCH) via a Pfannenstiel incision in women with a body mass index less than 25 kg/m2 is a great procedure for uterine pathology. SCH addresses only the uterine pathology and preserves the cervix, is a sterile procedure, requires no ancillary equipment, should take less than 30 minutes, preserves the full length of the vagina, requires only an overnight hospitalization, and has a short learning curve.
Removal of the cervix in any hysterectomy is the procedure that results in bladder and ureter injury and infection from contamination. Patients should be driving and back to nonphysical jobs in less than 1 week. As medical care becomes a truly transparent market-based business, patients will opt for SCH over higher priced alternatives. Sometimes the simplest procedures are still the best.
Joe Walsh, MD
Philadelphia, Pennsylvania
Continue to teach abdominal hysterectomy
No one can disagree with the statistics of shorter recovery and less morbidity for laparoscopic and vaginal procedures. In fact, what separates a gynecologist from other surgeons is the ability to operate in and through the vagina. There is still a place for abdominal hysterectomy for benign disease in modern gynecology.
Most programs produce good laparoscopic surgeons but ill prepared abdominal and vaginal surgeons. No gynecologist should be operating in the pelvis unless he or she is comfortable going into the retroperitoneal space if necessary. Many of the total laparoscopic hysterectomies that are performed could be done vaginally without abdominal incisions.
Now we have a generation of gynecologic surgeons who believe a robotic hysterectomy (at great extra expense) offers the patient an advantage, despite longer anesthesia and procedure times. We know morbidity has a direct correlation to operating and anesthesia time. Although I am impressed with what the next generation can do through a laparoscope, I would hate to let them continue without the experience or the ability to do an open abdominal procedure.
Allan N. Boruszak, MD
Washington, North Carolina
Dr. Barbieri’s response
I appreciate the perspectives of Drs. Hatch, Walsh, and Boruszak on the important issue of improving hysterectomy outcomes. Dr. Hatch raises the important point that gynecologists routinely select the best surgical approach for the unique needs of their patients. Based on a given gynecologist’s panel of patients and their unique medical issues, it may be difficult to change the distribution of surgical approaches to hysterectomy. Dr. Walsh advocates for a “minimally invasive” abdominal SCH, which is a valid approach to improving the outcomes of the abdominal approach. Dr. Boruszak rightly highlights the importance of teaching gynecologists to access the retroperitoneum, paravesical, and pararectal spaces in order to improve patient outcomes.
“VAGINAL HYSTERECTOMY WITH BASIC INSTRUMENTATION”
BARBARA S. LEVY, MD (OCTOBER, 2015)
Appreciates the instrument review
Dr. Levy’s article on vaginal hysterectomy using basic instruments is really wonderful. The segment on uterine reduction strategies will be especially useful. I appreciate her preference to use the Ligasure vessel-sealing device over suturing pedicles. Before we take steps to debulk the uterus, it is always essential, and better, to ligate uterine vessels, as this minimizes blood loss and makes the surgical field clearer.
R. Sasirekha
Puducherry, India
Skill should be rewarded
When I trained, vaginal hysterectomy was reserved for prolapse. After joining the Army, my eyes were opened by physicians who could morcellate a 16-week uterus or perform a 20-minute vaginal hysterectomy on a nulliparous woman for sterilization (which, of course, is controversial).
Once in private practice, incorporating these new skills into my own techniques was challenging and rewarding. Imagine my disappointment when I found out that reimbursement was a disincentive. It is easy to be altruistic, but one has to consider the incentives, too. Skill should be rewarded.
Mark B. Vizer, MD
Lansdale, Pennsylvania
A long-time proponent of vaginal hysterectomy
I appreciate the articles by Drs. Levy and Gebhart on vaginal surgical techniques. I have long been a proponent of vaginal hysterectomy as the preferred route for removal of the uterus (and tubes and ovaries, if indicated). I do most of my hysterectomies vaginally, with salpingectomies and oophorectomies if indicated. As an older surgeon, I now refer patients with uteri larger than 16 weeks, endometriosis, or suspected cancer.
Doug Tolley, MD
Yuba City, California
Share your thoughts! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
AN OPEN LETTER TO THE FDA ON MORCELLATION FOR PRESUMED UTERINE FIBROIDS
On December 8, 2015, 46 minimally invasive surgeons, gynecologic oncologists, and other experts spoke out in unison when they sent an open letter to the US Food and Drug Administration (FDA). They called into question the FDA’s estimate of the likelihood of occult leiomyosarcoma (LMS) and recommended continued use of power morcellation in appropriate cases.
An excerpt from this letter is published here. To read the letter in its entirety and the names of the signees, click here.
Letter excerpt:
If abdominal hysterectomy is recommended to women with fibroids, will women be better off?
By focusing exclusively on the risk of LMS, the FDA failed to take into account other risks associated with surgery. Laparoscopic surgery uses small incisions, is performed as an outpatient procedure (or overnight stay), has a faster recovery (2 weeks vs 4–6 weeks for open surgery), and is associated with lower mortality and fewer complications. These benefits of minimally invasive surgery are now well established in gynecologic and general surgery.
Using published best-evidence data, a recent decision analysis1 showed that, comparing 100,000 women undergoing laparoscopic hysterectomy with 100,000 undergoing open hysterectomy, the group undergoing laparoscopic surgery would experience 20 fewer perioperative deaths, 150 fewer pulmonary or venous embolus, and 4,800 fewer wound infections. Importantly, women having open surgery would have 8,000 fewer quality-of-life years.
A recently published study2 found that, in the 8 months following the FDA safety communication, utilization of laparoscopic hysterectomies decreased by 4.1% (P = .005), and abdominal and vaginal hysterectomies increased by 1.7% (P = .112) and 2.4% (P = .012), respectively. Major surgical complications (not including blood transfusions) increased from 2.2% to 2.8% (P = .015), and the rate of hospital readmission within 30 days also increased from 3.4% to 4.2% (P = .025). These observations merit consideration as women weigh the pros and cons of minimally invasive surgery with morcellation versus open surgery.
Clinical recommendations
Recent attention to surgical options for women with uterine leiomyomas and the risk of an occult LMS are positive developments in that the gynecologic community is reexamining relevant issues. We respectfully suggest that the following clinical recommendations be considered:
- The risk of LMS is higher in older postmenopausal women; greater caution should be exercised prior to recommending morcellation procedures for these women.
- Preoperative consideration of LMS is important. Women aged 35 years and older with irregular uterine bleeding and presumed fibroids should have an endometrial biopsy, which occasionally may detect LMS prior to surgery. Women should have normal results of cervical cancer screening.
- Ultrasound or MRI findings of a large irregular vascular mass, often with irregular anechoic (cystic) areas reflecting necrosis, may cause suspicion of LMS.
- Women wishing minimally invasive procedures with morcellation, including scalpel morcellation via the vagina or mini-laparotomy, or power morcellation using laparoscopic guidance, should understand the potential risk of decreased survival should LMS be present. Open procedures should be offered to all women who are considering minimally invasive procedures for “fibroids.”
- Following morcellation, careful inspection for tissue fragments should be undertaken and copious irrigation of the pelvic and abdominal cavities should be performed to minimize the risk of retained
tissue. - Further investigations of a means to identify LMS preoperatively should be supported. Likewise, investigation into the biology of LMS should be funded to better understand the propensity of tissue fragments or cells to implant and grow. With that knowledge, minimally invasive procedures could be avoided for women with LMS and women choosing minimally invasive surgery could be reassured that they do not have LMS.
Respecting women who suffer from LMS, we conclude that the FDA directive was based on a misleading analysis. Consequently, more accurate estimates regarding the prevalence of LMS among women having surgery for fibroids should be issued. Women have a right to self determination. Modification of the FDA’s current restrictive guidance regarding power morcellation would empower each woman to consider the pertinent issues and have the freedom to undertake shared decision making with her surgeon in order to select the procedure that is most appropriate for her.
References
1. Siedhoff MT, Wheeler SB, Rutstein SE, et al. Laparoscopic hysterectomy with morcellation vs abdominal hysterectomy for presumed fibroid tumors in premenopausal women: a decision analysis. Am J Obstet Gynecol. 2015;212(5):591.e1–e8.
2. Harris JA, Swenson CW, Uppal S, et al. Practice patterns and postoperative complications before and after Food and Drug Administration Safety Communication on power morcellation [published online ahead of print August 24, 2015]. Am J Obstet Gynecol. doi:10.1016/j.ajog.2015.08.047.
Choose the best approach for the patient
I cannot decrease the number of abdominal hysterectomies I perform—all of them are indicated.
Richard Hatch, MD
Augusta, Georgia
Supracervical hysterectomy: simplest is best
Supracervical hysterectomy (SCH) via a Pfannenstiel incision in women with a body mass index less than 25 kg/m2 is a great procedure for uterine pathology. SCH addresses only the uterine pathology and preserves the cervix, is a sterile procedure, requires no ancillary equipment, should take less than 30 minutes, preserves the full length of the vagina, requires only an overnight hospitalization, and has a short learning curve.
Removal of the cervix in any hysterectomy is the procedure that results in bladder and ureter injury and infection from contamination. Patients should be driving and back to nonphysical jobs in less than 1 week. As medical care becomes a truly transparent market-based business, patients will opt for SCH over higher priced alternatives. Sometimes the simplest procedures are still the best.
Joe Walsh, MD
Philadelphia, Pennsylvania
Continue to teach abdominal hysterectomy
No one can disagree with the statistics of shorter recovery and less morbidity for laparoscopic and vaginal procedures. In fact, what separates a gynecologist from other surgeons is the ability to operate in and through the vagina. There is still a place for abdominal hysterectomy for benign disease in modern gynecology.
Most programs produce good laparoscopic surgeons but ill prepared abdominal and vaginal surgeons. No gynecologist should be operating in the pelvis unless he or she is comfortable going into the retroperitoneal space if necessary. Many of the total laparoscopic hysterectomies that are performed could be done vaginally without abdominal incisions.
Now we have a generation of gynecologic surgeons who believe a robotic hysterectomy (at great extra expense) offers the patient an advantage, despite longer anesthesia and procedure times. We know morbidity has a direct correlation to operating and anesthesia time. Although I am impressed with what the next generation can do through a laparoscope, I would hate to let them continue without the experience or the ability to do an open abdominal procedure.
Allan N. Boruszak, MD
Washington, North Carolina
Dr. Barbieri’s response
I appreciate the perspectives of Drs. Hatch, Walsh, and Boruszak on the important issue of improving hysterectomy outcomes. Dr. Hatch raises the important point that gynecologists routinely select the best surgical approach for the unique needs of their patients. Based on a given gynecologist’s panel of patients and their unique medical issues, it may be difficult to change the distribution of surgical approaches to hysterectomy. Dr. Walsh advocates for a “minimally invasive” abdominal SCH, which is a valid approach to improving the outcomes of the abdominal approach. Dr. Boruszak rightly highlights the importance of teaching gynecologists to access the retroperitoneum, paravesical, and pararectal spaces in order to improve patient outcomes.
“VAGINAL HYSTERECTOMY WITH BASIC INSTRUMENTATION”
BARBARA S. LEVY, MD (OCTOBER, 2015)
Appreciates the instrument review
Dr. Levy’s article on vaginal hysterectomy using basic instruments is really wonderful. The segment on uterine reduction strategies will be especially useful. I appreciate her preference to use the Ligasure vessel-sealing device over suturing pedicles. Before we take steps to debulk the uterus, it is always essential, and better, to ligate uterine vessels, as this minimizes blood loss and makes the surgical field clearer.
R. Sasirekha
Puducherry, India
Skill should be rewarded
When I trained, vaginal hysterectomy was reserved for prolapse. After joining the Army, my eyes were opened by physicians who could morcellate a 16-week uterus or perform a 20-minute vaginal hysterectomy on a nulliparous woman for sterilization (which, of course, is controversial).
Once in private practice, incorporating these new skills into my own techniques was challenging and rewarding. Imagine my disappointment when I found out that reimbursement was a disincentive. It is easy to be altruistic, but one has to consider the incentives, too. Skill should be rewarded.
Mark B. Vizer, MD
Lansdale, Pennsylvania
A long-time proponent of vaginal hysterectomy
I appreciate the articles by Drs. Levy and Gebhart on vaginal surgical techniques. I have long been a proponent of vaginal hysterectomy as the preferred route for removal of the uterus (and tubes and ovaries, if indicated). I do most of my hysterectomies vaginally, with salpingectomies and oophorectomies if indicated. As an older surgeon, I now refer patients with uteri larger than 16 weeks, endometriosis, or suspected cancer.
Doug Tolley, MD
Yuba City, California
Share your thoughts! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
READ THESE LETTERS:
An open letter to the FDA on morcellation for presumed uterine fibroids
Choose the best approach for the patient
Continue to teach abdominal hysterectomy
Appreciates the instrument review
Skill should be rewarded
A long-time proponent of hysterectomy
Stewardship at 3 a.m.
The 3-month-old infant presents to the emergency department with a fever of 101° F. The emergency physician decides the infant looks ill enough to warrant some investigation. A urinalysis indicates a urinary tract infection. I am consulted to complete the admission to the hospital. The question arises, “Is a lumbar puncture indicated to rule out meningitis?”
I’ve been down this pathway many times. For years I have relied on a meta-analysis which corrected the bias of an old article from 1972.1 Multiple studies in the 2000-2010 time frame have shown that the risk of concurrent meningitis in a young infant with a UTI is vanishingly small. It is much less than 2%, with many studies finding 0%. So on a typical day, my answer is no tap if there is no clinical suggestion of meningitis.
Hospital medicine has recently focused on reducing overdiagnosis and overtreatment. When you only occasionally admit patients to the hospital, untoward events appear random and uncommon. When you work there day in and day out, you appreciate that all medical interventions have risks and costs.
A recent editorial raised the question of stewardship in medicine.2 It asked why physicians would choose a very expensive drug when there is little evidence of its superiority over a much cheaper predecessor. Physicians, whose actions influence a $3 trillion industry, have not embraced stewardship as a major component of their professional responsibilities. The physician does have a fiduciary duty toward the patient. The physician recommends the best care possible to achieve the patient’s goals of care. Dentistry is distinctly different in this regard. Dentists often have several ways of repairing decayed teeth. Various types of fillings are available. Gold fillings are more expensive. Newer implants are several times more expensive than crowns. Dentists routinely adjust their treatment plan based on what the patient can afford.
While most other industries have market competition and profitability as incentives to avoid extravagance, U.S. health care seems unbridled by fiscal responsibility. The news that a small pharmaceutical company had raised the price of an old generic antibiotic by 5000%3 exposed the irrationality and capriciousness4 of the pricing of medications in the United States. Many politicians decried the behavior but to little effect. Most consumer products, especially computers, become more powerful and cheaper with each decade. Health care does not follow this pattern
There are many factors that influence physician behavior. Concerns about malpractice may bias physicians toward expensive overtreatment. Modern medical research is usually published expounding on the benefits of a new technology over a previous therapy without any acknowledgment that the newer and more expensive treatment may have a downside. This biases people to use the latest and greatest treatment even though it may have only demonstrated noninferiority in its trials.
I try to use evidence-based medicine when it is available. In the clinical case described earlier, I indicate to the emergency doctor that unless there is a clinical impression of coexisting meningitis, the lumbar puncture is not indicated. I cite the meta-analysis as I have many times before. But this night is different. I am simultaneously admitting a teenager whose gastrostomy tube had become dislodged and couldn’t be replaced. This neurologically devastated child had had meningitis as an infant. He is a stark reminder of the consequences of a missed diagnosis.
The parents of that child have provided him wonderful care. His skin is in excellent condition. His moderate contractures are testimony to dedicated stretching regimens at home. It is evident that the parents love the child as he is. But I am sure they would give anything to have avoided this scenario and to reverse the consequences of that meningitis. And so, the best evidence we have, that the risk of meningitis in an infant is low, is not as reassuring to me on this night. At 3 a.m., the juxtaposition of the two patients is unsettling. Is the risk low enough? Would that new test5, serum procalcitonin, help me to make a better decision? How certain must I be that an intervention is unnecessary?
Health care policy, economics, and practice guidelines can be debated with detached objectivity around a conference table in the middle of the day. The trepidation in an emergency room at 3 a.m. is different. This is my patient. I am his doctor. That is the heart of medical ethics.
Dr. Powell is a pediatric hospitalist and clinical ethics consultant living in St. Louis. Dr. Powell said he had no relevant financial disclosures or conflicts of interest. E-mail him at [email protected].
References
1. “How common is co-existing meningitis in infants with urinary tract infection?” on Bestbets.org.
2. “Why do doctors choose a $2,000 cure when a $50 one is just as good?” by Andrew Lam, Washington Post, Dec. 10, 2015.
3. “Drug Goes From $13.50 a Tablet to $750, Overnight” by Andrew Pollack, New York Times, Sept. 20, 2015.
4. “How an $84,000 drug got its price: ‘Let’s hold our position … whatever the headlines’ ” by Carolyn Y. Johnson and Brady Dennis, Washington Post, Dec. 1, 2015.
5. JAMA Pediatr. Published online, 2015 Nov 23. doi:10.1001/jamapediatrics.2015.3267.
The 3-month-old infant presents to the emergency department with a fever of 101° F. The emergency physician decides the infant looks ill enough to warrant some investigation. A urinalysis indicates a urinary tract infection. I am consulted to complete the admission to the hospital. The question arises, “Is a lumbar puncture indicated to rule out meningitis?”
I’ve been down this pathway many times. For years I have relied on a meta-analysis which corrected the bias of an old article from 1972.1 Multiple studies in the 2000-2010 time frame have shown that the risk of concurrent meningitis in a young infant with a UTI is vanishingly small. It is much less than 2%, with many studies finding 0%. So on a typical day, my answer is no tap if there is no clinical suggestion of meningitis.
Hospital medicine has recently focused on reducing overdiagnosis and overtreatment. When you only occasionally admit patients to the hospital, untoward events appear random and uncommon. When you work there day in and day out, you appreciate that all medical interventions have risks and costs.
A recent editorial raised the question of stewardship in medicine.2 It asked why physicians would choose a very expensive drug when there is little evidence of its superiority over a much cheaper predecessor. Physicians, whose actions influence a $3 trillion industry, have not embraced stewardship as a major component of their professional responsibilities. The physician does have a fiduciary duty toward the patient. The physician recommends the best care possible to achieve the patient’s goals of care. Dentistry is distinctly different in this regard. Dentists often have several ways of repairing decayed teeth. Various types of fillings are available. Gold fillings are more expensive. Newer implants are several times more expensive than crowns. Dentists routinely adjust their treatment plan based on what the patient can afford.
While most other industries have market competition and profitability as incentives to avoid extravagance, U.S. health care seems unbridled by fiscal responsibility. The news that a small pharmaceutical company had raised the price of an old generic antibiotic by 5000%3 exposed the irrationality and capriciousness4 of the pricing of medications in the United States. Many politicians decried the behavior but to little effect. Most consumer products, especially computers, become more powerful and cheaper with each decade. Health care does not follow this pattern
There are many factors that influence physician behavior. Concerns about malpractice may bias physicians toward expensive overtreatment. Modern medical research is usually published expounding on the benefits of a new technology over a previous therapy without any acknowledgment that the newer and more expensive treatment may have a downside. This biases people to use the latest and greatest treatment even though it may have only demonstrated noninferiority in its trials.
I try to use evidence-based medicine when it is available. In the clinical case described earlier, I indicate to the emergency doctor that unless there is a clinical impression of coexisting meningitis, the lumbar puncture is not indicated. I cite the meta-analysis as I have many times before. But this night is different. I am simultaneously admitting a teenager whose gastrostomy tube had become dislodged and couldn’t be replaced. This neurologically devastated child had had meningitis as an infant. He is a stark reminder of the consequences of a missed diagnosis.
The parents of that child have provided him wonderful care. His skin is in excellent condition. His moderate contractures are testimony to dedicated stretching regimens at home. It is evident that the parents love the child as he is. But I am sure they would give anything to have avoided this scenario and to reverse the consequences of that meningitis. And so, the best evidence we have, that the risk of meningitis in an infant is low, is not as reassuring to me on this night. At 3 a.m., the juxtaposition of the two patients is unsettling. Is the risk low enough? Would that new test5, serum procalcitonin, help me to make a better decision? How certain must I be that an intervention is unnecessary?
Health care policy, economics, and practice guidelines can be debated with detached objectivity around a conference table in the middle of the day. The trepidation in an emergency room at 3 a.m. is different. This is my patient. I am his doctor. That is the heart of medical ethics.
Dr. Powell is a pediatric hospitalist and clinical ethics consultant living in St. Louis. Dr. Powell said he had no relevant financial disclosures or conflicts of interest. E-mail him at [email protected].
References
1. “How common is co-existing meningitis in infants with urinary tract infection?” on Bestbets.org.
2. “Why do doctors choose a $2,000 cure when a $50 one is just as good?” by Andrew Lam, Washington Post, Dec. 10, 2015.
3. “Drug Goes From $13.50 a Tablet to $750, Overnight” by Andrew Pollack, New York Times, Sept. 20, 2015.
4. “How an $84,000 drug got its price: ‘Let’s hold our position … whatever the headlines’ ” by Carolyn Y. Johnson and Brady Dennis, Washington Post, Dec. 1, 2015.
5. JAMA Pediatr. Published online, 2015 Nov 23. doi:10.1001/jamapediatrics.2015.3267.
The 3-month-old infant presents to the emergency department with a fever of 101° F. The emergency physician decides the infant looks ill enough to warrant some investigation. A urinalysis indicates a urinary tract infection. I am consulted to complete the admission to the hospital. The question arises, “Is a lumbar puncture indicated to rule out meningitis?”
I’ve been down this pathway many times. For years I have relied on a meta-analysis which corrected the bias of an old article from 1972.1 Multiple studies in the 2000-2010 time frame have shown that the risk of concurrent meningitis in a young infant with a UTI is vanishingly small. It is much less than 2%, with many studies finding 0%. So on a typical day, my answer is no tap if there is no clinical suggestion of meningitis.
Hospital medicine has recently focused on reducing overdiagnosis and overtreatment. When you only occasionally admit patients to the hospital, untoward events appear random and uncommon. When you work there day in and day out, you appreciate that all medical interventions have risks and costs.
A recent editorial raised the question of stewardship in medicine.2 It asked why physicians would choose a very expensive drug when there is little evidence of its superiority over a much cheaper predecessor. Physicians, whose actions influence a $3 trillion industry, have not embraced stewardship as a major component of their professional responsibilities. The physician does have a fiduciary duty toward the patient. The physician recommends the best care possible to achieve the patient’s goals of care. Dentistry is distinctly different in this regard. Dentists often have several ways of repairing decayed teeth. Various types of fillings are available. Gold fillings are more expensive. Newer implants are several times more expensive than crowns. Dentists routinely adjust their treatment plan based on what the patient can afford.
While most other industries have market competition and profitability as incentives to avoid extravagance, U.S. health care seems unbridled by fiscal responsibility. The news that a small pharmaceutical company had raised the price of an old generic antibiotic by 5000%3 exposed the irrationality and capriciousness4 of the pricing of medications in the United States. Many politicians decried the behavior but to little effect. Most consumer products, especially computers, become more powerful and cheaper with each decade. Health care does not follow this pattern
There are many factors that influence physician behavior. Concerns about malpractice may bias physicians toward expensive overtreatment. Modern medical research is usually published expounding on the benefits of a new technology over a previous therapy without any acknowledgment that the newer and more expensive treatment may have a downside. This biases people to use the latest and greatest treatment even though it may have only demonstrated noninferiority in its trials.
I try to use evidence-based medicine when it is available. In the clinical case described earlier, I indicate to the emergency doctor that unless there is a clinical impression of coexisting meningitis, the lumbar puncture is not indicated. I cite the meta-analysis as I have many times before. But this night is different. I am simultaneously admitting a teenager whose gastrostomy tube had become dislodged and couldn’t be replaced. This neurologically devastated child had had meningitis as an infant. He is a stark reminder of the consequences of a missed diagnosis.
The parents of that child have provided him wonderful care. His skin is in excellent condition. His moderate contractures are testimony to dedicated stretching regimens at home. It is evident that the parents love the child as he is. But I am sure they would give anything to have avoided this scenario and to reverse the consequences of that meningitis. And so, the best evidence we have, that the risk of meningitis in an infant is low, is not as reassuring to me on this night. At 3 a.m., the juxtaposition of the two patients is unsettling. Is the risk low enough? Would that new test5, serum procalcitonin, help me to make a better decision? How certain must I be that an intervention is unnecessary?
Health care policy, economics, and practice guidelines can be debated with detached objectivity around a conference table in the middle of the day. The trepidation in an emergency room at 3 a.m. is different. This is my patient. I am his doctor. That is the heart of medical ethics.
Dr. Powell is a pediatric hospitalist and clinical ethics consultant living in St. Louis. Dr. Powell said he had no relevant financial disclosures or conflicts of interest. E-mail him at [email protected].
References
1. “How common is co-existing meningitis in infants with urinary tract infection?” on Bestbets.org.
2. “Why do doctors choose a $2,000 cure when a $50 one is just as good?” by Andrew Lam, Washington Post, Dec. 10, 2015.
3. “Drug Goes From $13.50 a Tablet to $750, Overnight” by Andrew Pollack, New York Times, Sept. 20, 2015.
4. “How an $84,000 drug got its price: ‘Let’s hold our position … whatever the headlines’ ” by Carolyn Y. Johnson and Brady Dennis, Washington Post, Dec. 1, 2015.
5. JAMA Pediatr. Published online, 2015 Nov 23. doi:10.1001/jamapediatrics.2015.3267.
Debunking marijuana myths for teens
The annual checkup has long provided an opportunity for early adolescents to learn about the risks of alcohol and drug use from a trusted source who may be less biased than parents, teachers, or police. Parents also turn to their child’s pediatrician for guidance on how to broach this important topic with their children, or they may come with concerns about their children’s use of drugs or alcohol.
Marijuana has become an increasingly complex topic, as its legal status has rapidly changed: It’s legal to purchase marijuana in four states (Alaska, Colorado, Oregon, and Washington, as well as the District of Columbia); it is decriminalized in 20 states and the District of Columbia for certain marijuana possession offenses; and it is legal to use medical marijuana in 23 states. As its legal status changes, attitudes about its use also have shifted, and its availability, form, and potency all have changed dramatically in just the past decade. Further, we ourselves may have mixed feelings about marijuana use based on our own experience as adolescents and sampling bias. We may have seen its low-level use and minimal effects in young or mature adults, or we may have seen substantial use of marijuana have a major deleterious impact on a friend or become a gateway drug for addiction to dangerous substances.
Before addressing marijuana use with adolescent patients and dealing with their potential skepticism concerning any harm, it is worth spending a little time looking in the mirror to consider your perspective on marijuana use and your response to disbelief.
According to the National Institute on Drug Abuse’s Monitoring the Future (MTF) survey, almost 12% of 8th graders, 27% of 10th graders, and 35% of 12th graders in the United States reported having used marijuana in the past year. Among the 12th graders in that 2014 survey, almost 20% were current users of marijuana and 6% were daily users. Many surveys, including the MTF, have demonstrated that attitudes of teenagers have shifted about marijuana’s dangerousness, with a steep and steady decline in the number of teenagers believing that regular marijuana use poses a risk to their health and well-being. In 2014, less than 40% of 12th graders in the MTF survey agreed that regular use of marijuana would pose a risk to their well-being, compared with a peak of almost 80% of 12th graders in the early 1990’s.
Pediatricians have an opportunity to change their patient’s thinking about marijuana. At the checkup when you routinely ask about alcohol and drug use, ask about marijuana use in particular. You might start by asking if they have heard their friends talking about marijuana? What have they heard? Are other kids using it? Have they ever seen anyone use it? Have their friends invited them to try? You should find out if they think it is safe or dangerous, and how it compares with cigarettes, alcohol, and other drugs on this score. Then you may be able to debunk some myths you hear from them.
Myth No. 1: Marijuana is medicine
Although 23 states allow the legal sale of marijuana for “medicinal purposes,” it is important to note that there are currently no Food and Drug Administration–approved indications for medical marijuana. There is modest evidence that the active compounds in marijuana (delta-9-tetra-hydrocannabinol [THC] and other cannabinoids) can be effective in the management of the muscle spasticity associated with multiple sclerosis, the treatment of nausea associated with chemotherapy, and increasing the appetite of patients with wasting due to AIDS, and there are FDA-approved synthetic cannabinoids that can be prescribed for these symptoms. It is also important to note that there is no evidence that THC or other cannabinoids are useful in the treatment of mood or anxiety symptoms, even though these are often used as reasons for seeking medicinal marijuana. Indeed, marijuana may cause or worsen several psychiatric problems.
Myth No. 2: Marijuana is safe
Although there is consensus that moderate marijuana use in adulthood poses only limited health risks (including the known risks of smoking), there is robust evidence that marijuana use during youth (through the early 20s) causes several serious and permanent effects on the developing brain. One 2012 study showed that for youth who are dependent on marijuana before they are 18 years, there is an 8-point drop in IQ in adulthood (Proc Natl Acad Sci USA. 2012 Oct 2;109[40]:E2657-64). This IQ drop persists even if they quit smoking, and does not occur for those who first become dependent on marijuana in adulthood. A 2015 study demonstrated that even for adolescents who are light smokers (one to two times weekly) with no evidence of marijuana dependence, there are significant abnormalities in the size and shape of their amygdala and nucleus accumbens, with associated changes in their motivation, decision making, attention, functional memory, and processing of emotions(J Neurosci. 2014 Apr 16;34[16]:5529-38). These abnormalities increase with increased frequency of use, and are not seen in those who begin smoking in adulthood (mid-20s and later).
Beyond these findings of cognitive deficits, evidence is growing that adolescent marijuana use is associated with several psychiatric illnesses, including depression and anxiety. There is especially strong evidence for a causal link between marijuana use and psychotic illnesses in (genetically) vulnerable young people. Any marijuana user can experience a brief psychotic reaction if the amount ingested or smoked is great enough, but for those young people who carry a specific variant of the gene for catechol-o-methyltransferase (COMT, an enzyme that degrades neurotransmitters), smoking marijuana in adolescence nearly triples their risk of developing schizophrenia in adulthood. For youth with a variant of the AKT gene (another enzyme affecting dopamine signaling in the brain), daily use of marijuana raises their risk of developing schizophrenia sevenfold. Clearly, marijuana can be the critical environmental trigger for schizophrenia in genetically vulnerable youth. Until we have a comprehensive knowledge of the relevant genes, and routinely check every patient’s complete genetic profile, it is reasonable to assume that any young person using marijuana is significantly increasing the risk of developing schizophrenia, a chronic and disabling condition.
Myth No. 3: Marijuana has no effect on driving
Marijuana intoxication significantly affects motor coordination, reaction time, and judgment, and multiple studies have demonstrated a direct relationship between blood THC concentration and impaired driving ability. A recent meta-analysis demonstrated that the risk of being in a car accident doubled after marijuana use (Drug Alcohol Depend. 2004 Feb 7;73[2]:109-19). These studies usually involved adults, and it is reasonable to assume that the risks may be more pronounced in adolescents, particularly ones who are new to driving or have other problems that could affect their attention or reaction time (such as attention-deficit/hyperactivity disorder). Beyond letting patients know about the increased risks of accidents, it may be worth reminding them that driving while intoxicated – even with legal use marijuana – is a criminal offense.
Myth No. 4: Marijuana has no effect on schoolwork
Aside from the risks of causing long-term cognitive changes and psychiatric problems that can affect school performance, the direct effects of marijuana intoxication can linger and affect school performance well after its use. The “high” from marijuana typically lasts from 1 to 3 hours, but the drug’s effects on higher-level cognitive processes (mediated by the neocortex and hippocampus) can last for days. So a teenager who smokes on Saturday night may have lingering impairment of motivation, the ability to shift attention, the ability to learn complex tasks, and working memory. These are all critical cognitive abilities for learning, and can make studying on Sunday and performing well on a test on Monday much more difficult.
Myth No. 5: Marijuana is not addictive
Marijuana is addictive, with studies suggesting that nearly 9% of marijuana users will become addicted. Again, the risks are far greater for young people. Among people who begin using marijuana during adolescence, the rate of addiction climbs to 17%, and can be as high as 50% in daily users. Remember that addiction describes a pattern of continued use despite that use causing significant legal, social, or school and work problems. Users also may develop physical dependence, with a withdrawal syndrome that includes irritability, restlessness, insomnia, and appetite changes; these can last as long as 2 weeks.
Currently available forms of marijuana are much more potent than those that were studied and used in prior decades. On average, the potency of smoked marijuana has tripled, and there are concentrates (in oil form, for example) and hybrids with much higher potency still. More potent marijuana increases the high from even a small dose, and increases the likelihood of addiction and of other immediate and lingering complications of its use. So, parents who think they know what marijuana does to adolescents based on their own youthful experiences are significantly underestimating the risks.
When asking your patients explicitly about marijuana use, be curious and nonjudgmental, but also be frank and forthright about what is known about the risks associated with its use. Although the current legal and political changes around marijuana use may have given them the impression that marijuana use is safe, you want them to have the facts they need to make informed decisions. Even if you only discuss one of these myths with your patients, you will have equipped them with powerful information that they may use and share with their friends.
Dr. Swick is an attending psychiatrist in the division of child psychiatry at Massachusetts General Hospital, Boston, and director of the Parenting at a Challenging Time (PACT) Program at the Vernon Cancer Center at Newton (Mass.) Wellesley Hospital. Dr. Jellinek is professor of psychiatry and of pediatrics at Harvard Medical School, Boston. Email them at [email protected].
The annual checkup has long provided an opportunity for early adolescents to learn about the risks of alcohol and drug use from a trusted source who may be less biased than parents, teachers, or police. Parents also turn to their child’s pediatrician for guidance on how to broach this important topic with their children, or they may come with concerns about their children’s use of drugs or alcohol.
Marijuana has become an increasingly complex topic, as its legal status has rapidly changed: It’s legal to purchase marijuana in four states (Alaska, Colorado, Oregon, and Washington, as well as the District of Columbia); it is decriminalized in 20 states and the District of Columbia for certain marijuana possession offenses; and it is legal to use medical marijuana in 23 states. As its legal status changes, attitudes about its use also have shifted, and its availability, form, and potency all have changed dramatically in just the past decade. Further, we ourselves may have mixed feelings about marijuana use based on our own experience as adolescents and sampling bias. We may have seen its low-level use and minimal effects in young or mature adults, or we may have seen substantial use of marijuana have a major deleterious impact on a friend or become a gateway drug for addiction to dangerous substances.
Before addressing marijuana use with adolescent patients and dealing with their potential skepticism concerning any harm, it is worth spending a little time looking in the mirror to consider your perspective on marijuana use and your response to disbelief.
According to the National Institute on Drug Abuse’s Monitoring the Future (MTF) survey, almost 12% of 8th graders, 27% of 10th graders, and 35% of 12th graders in the United States reported having used marijuana in the past year. Among the 12th graders in that 2014 survey, almost 20% were current users of marijuana and 6% were daily users. Many surveys, including the MTF, have demonstrated that attitudes of teenagers have shifted about marijuana’s dangerousness, with a steep and steady decline in the number of teenagers believing that regular marijuana use poses a risk to their health and well-being. In 2014, less than 40% of 12th graders in the MTF survey agreed that regular use of marijuana would pose a risk to their well-being, compared with a peak of almost 80% of 12th graders in the early 1990’s.
Pediatricians have an opportunity to change their patient’s thinking about marijuana. At the checkup when you routinely ask about alcohol and drug use, ask about marijuana use in particular. You might start by asking if they have heard their friends talking about marijuana? What have they heard? Are other kids using it? Have they ever seen anyone use it? Have their friends invited them to try? You should find out if they think it is safe or dangerous, and how it compares with cigarettes, alcohol, and other drugs on this score. Then you may be able to debunk some myths you hear from them.
Myth No. 1: Marijuana is medicine
Although 23 states allow the legal sale of marijuana for “medicinal purposes,” it is important to note that there are currently no Food and Drug Administration–approved indications for medical marijuana. There is modest evidence that the active compounds in marijuana (delta-9-tetra-hydrocannabinol [THC] and other cannabinoids) can be effective in the management of the muscle spasticity associated with multiple sclerosis, the treatment of nausea associated with chemotherapy, and increasing the appetite of patients with wasting due to AIDS, and there are FDA-approved synthetic cannabinoids that can be prescribed for these symptoms. It is also important to note that there is no evidence that THC or other cannabinoids are useful in the treatment of mood or anxiety symptoms, even though these are often used as reasons for seeking medicinal marijuana. Indeed, marijuana may cause or worsen several psychiatric problems.
Myth No. 2: Marijuana is safe
Although there is consensus that moderate marijuana use in adulthood poses only limited health risks (including the known risks of smoking), there is robust evidence that marijuana use during youth (through the early 20s) causes several serious and permanent effects on the developing brain. One 2012 study showed that for youth who are dependent on marijuana before they are 18 years, there is an 8-point drop in IQ in adulthood (Proc Natl Acad Sci USA. 2012 Oct 2;109[40]:E2657-64). This IQ drop persists even if they quit smoking, and does not occur for those who first become dependent on marijuana in adulthood. A 2015 study demonstrated that even for adolescents who are light smokers (one to two times weekly) with no evidence of marijuana dependence, there are significant abnormalities in the size and shape of their amygdala and nucleus accumbens, with associated changes in their motivation, decision making, attention, functional memory, and processing of emotions(J Neurosci. 2014 Apr 16;34[16]:5529-38). These abnormalities increase with increased frequency of use, and are not seen in those who begin smoking in adulthood (mid-20s and later).
Beyond these findings of cognitive deficits, evidence is growing that adolescent marijuana use is associated with several psychiatric illnesses, including depression and anxiety. There is especially strong evidence for a causal link between marijuana use and psychotic illnesses in (genetically) vulnerable young people. Any marijuana user can experience a brief psychotic reaction if the amount ingested or smoked is great enough, but for those young people who carry a specific variant of the gene for catechol-o-methyltransferase (COMT, an enzyme that degrades neurotransmitters), smoking marijuana in adolescence nearly triples their risk of developing schizophrenia in adulthood. For youth with a variant of the AKT gene (another enzyme affecting dopamine signaling in the brain), daily use of marijuana raises their risk of developing schizophrenia sevenfold. Clearly, marijuana can be the critical environmental trigger for schizophrenia in genetically vulnerable youth. Until we have a comprehensive knowledge of the relevant genes, and routinely check every patient’s complete genetic profile, it is reasonable to assume that any young person using marijuana is significantly increasing the risk of developing schizophrenia, a chronic and disabling condition.
Myth No. 3: Marijuana has no effect on driving
Marijuana intoxication significantly affects motor coordination, reaction time, and judgment, and multiple studies have demonstrated a direct relationship between blood THC concentration and impaired driving ability. A recent meta-analysis demonstrated that the risk of being in a car accident doubled after marijuana use (Drug Alcohol Depend. 2004 Feb 7;73[2]:109-19). These studies usually involved adults, and it is reasonable to assume that the risks may be more pronounced in adolescents, particularly ones who are new to driving or have other problems that could affect their attention or reaction time (such as attention-deficit/hyperactivity disorder). Beyond letting patients know about the increased risks of accidents, it may be worth reminding them that driving while intoxicated – even with legal use marijuana – is a criminal offense.
Myth No. 4: Marijuana has no effect on schoolwork
Aside from the risks of causing long-term cognitive changes and psychiatric problems that can affect school performance, the direct effects of marijuana intoxication can linger and affect school performance well after its use. The “high” from marijuana typically lasts from 1 to 3 hours, but the drug’s effects on higher-level cognitive processes (mediated by the neocortex and hippocampus) can last for days. So a teenager who smokes on Saturday night may have lingering impairment of motivation, the ability to shift attention, the ability to learn complex tasks, and working memory. These are all critical cognitive abilities for learning, and can make studying on Sunday and performing well on a test on Monday much more difficult.
Myth No. 5: Marijuana is not addictive
Marijuana is addictive, with studies suggesting that nearly 9% of marijuana users will become addicted. Again, the risks are far greater for young people. Among people who begin using marijuana during adolescence, the rate of addiction climbs to 17%, and can be as high as 50% in daily users. Remember that addiction describes a pattern of continued use despite that use causing significant legal, social, or school and work problems. Users also may develop physical dependence, with a withdrawal syndrome that includes irritability, restlessness, insomnia, and appetite changes; these can last as long as 2 weeks.
Currently available forms of marijuana are much more potent than those that were studied and used in prior decades. On average, the potency of smoked marijuana has tripled, and there are concentrates (in oil form, for example) and hybrids with much higher potency still. More potent marijuana increases the high from even a small dose, and increases the likelihood of addiction and of other immediate and lingering complications of its use. So, parents who think they know what marijuana does to adolescents based on their own youthful experiences are significantly underestimating the risks.
When asking your patients explicitly about marijuana use, be curious and nonjudgmental, but also be frank and forthright about what is known about the risks associated with its use. Although the current legal and political changes around marijuana use may have given them the impression that marijuana use is safe, you want them to have the facts they need to make informed decisions. Even if you only discuss one of these myths with your patients, you will have equipped them with powerful information that they may use and share with their friends.
Dr. Swick is an attending psychiatrist in the division of child psychiatry at Massachusetts General Hospital, Boston, and director of the Parenting at a Challenging Time (PACT) Program at the Vernon Cancer Center at Newton (Mass.) Wellesley Hospital. Dr. Jellinek is professor of psychiatry and of pediatrics at Harvard Medical School, Boston. Email them at [email protected].
The annual checkup has long provided an opportunity for early adolescents to learn about the risks of alcohol and drug use from a trusted source who may be less biased than parents, teachers, or police. Parents also turn to their child’s pediatrician for guidance on how to broach this important topic with their children, or they may come with concerns about their children’s use of drugs or alcohol.
Marijuana has become an increasingly complex topic, as its legal status has rapidly changed: It’s legal to purchase marijuana in four states (Alaska, Colorado, Oregon, and Washington, as well as the District of Columbia); it is decriminalized in 20 states and the District of Columbia for certain marijuana possession offenses; and it is legal to use medical marijuana in 23 states. As its legal status changes, attitudes about its use also have shifted, and its availability, form, and potency all have changed dramatically in just the past decade. Further, we ourselves may have mixed feelings about marijuana use based on our own experience as adolescents and sampling bias. We may have seen its low-level use and minimal effects in young or mature adults, or we may have seen substantial use of marijuana have a major deleterious impact on a friend or become a gateway drug for addiction to dangerous substances.
Before addressing marijuana use with adolescent patients and dealing with their potential skepticism concerning any harm, it is worth spending a little time looking in the mirror to consider your perspective on marijuana use and your response to disbelief.
According to the National Institute on Drug Abuse’s Monitoring the Future (MTF) survey, almost 12% of 8th graders, 27% of 10th graders, and 35% of 12th graders in the United States reported having used marijuana in the past year. Among the 12th graders in that 2014 survey, almost 20% were current users of marijuana and 6% were daily users. Many surveys, including the MTF, have demonstrated that attitudes of teenagers have shifted about marijuana’s dangerousness, with a steep and steady decline in the number of teenagers believing that regular marijuana use poses a risk to their health and well-being. In 2014, less than 40% of 12th graders in the MTF survey agreed that regular use of marijuana would pose a risk to their well-being, compared with a peak of almost 80% of 12th graders in the early 1990’s.
Pediatricians have an opportunity to change their patient’s thinking about marijuana. At the checkup when you routinely ask about alcohol and drug use, ask about marijuana use in particular. You might start by asking if they have heard their friends talking about marijuana? What have they heard? Are other kids using it? Have they ever seen anyone use it? Have their friends invited them to try? You should find out if they think it is safe or dangerous, and how it compares with cigarettes, alcohol, and other drugs on this score. Then you may be able to debunk some myths you hear from them.
Myth No. 1: Marijuana is medicine
Although 23 states allow the legal sale of marijuana for “medicinal purposes,” it is important to note that there are currently no Food and Drug Administration–approved indications for medical marijuana. There is modest evidence that the active compounds in marijuana (delta-9-tetra-hydrocannabinol [THC] and other cannabinoids) can be effective in the management of the muscle spasticity associated with multiple sclerosis, the treatment of nausea associated with chemotherapy, and increasing the appetite of patients with wasting due to AIDS, and there are FDA-approved synthetic cannabinoids that can be prescribed for these symptoms. It is also important to note that there is no evidence that THC or other cannabinoids are useful in the treatment of mood or anxiety symptoms, even though these are often used as reasons for seeking medicinal marijuana. Indeed, marijuana may cause or worsen several psychiatric problems.
Myth No. 2: Marijuana is safe
Although there is consensus that moderate marijuana use in adulthood poses only limited health risks (including the known risks of smoking), there is robust evidence that marijuana use during youth (through the early 20s) causes several serious and permanent effects on the developing brain. One 2012 study showed that for youth who are dependent on marijuana before they are 18 years, there is an 8-point drop in IQ in adulthood (Proc Natl Acad Sci USA. 2012 Oct 2;109[40]:E2657-64). This IQ drop persists even if they quit smoking, and does not occur for those who first become dependent on marijuana in adulthood. A 2015 study demonstrated that even for adolescents who are light smokers (one to two times weekly) with no evidence of marijuana dependence, there are significant abnormalities in the size and shape of their amygdala and nucleus accumbens, with associated changes in their motivation, decision making, attention, functional memory, and processing of emotions(J Neurosci. 2014 Apr 16;34[16]:5529-38). These abnormalities increase with increased frequency of use, and are not seen in those who begin smoking in adulthood (mid-20s and later).
Beyond these findings of cognitive deficits, evidence is growing that adolescent marijuana use is associated with several psychiatric illnesses, including depression and anxiety. There is especially strong evidence for a causal link between marijuana use and psychotic illnesses in (genetically) vulnerable young people. Any marijuana user can experience a brief psychotic reaction if the amount ingested or smoked is great enough, but for those young people who carry a specific variant of the gene for catechol-o-methyltransferase (COMT, an enzyme that degrades neurotransmitters), smoking marijuana in adolescence nearly triples their risk of developing schizophrenia in adulthood. For youth with a variant of the AKT gene (another enzyme affecting dopamine signaling in the brain), daily use of marijuana raises their risk of developing schizophrenia sevenfold. Clearly, marijuana can be the critical environmental trigger for schizophrenia in genetically vulnerable youth. Until we have a comprehensive knowledge of the relevant genes, and routinely check every patient’s complete genetic profile, it is reasonable to assume that any young person using marijuana is significantly increasing the risk of developing schizophrenia, a chronic and disabling condition.
Myth No. 3: Marijuana has no effect on driving
Marijuana intoxication significantly affects motor coordination, reaction time, and judgment, and multiple studies have demonstrated a direct relationship between blood THC concentration and impaired driving ability. A recent meta-analysis demonstrated that the risk of being in a car accident doubled after marijuana use (Drug Alcohol Depend. 2004 Feb 7;73[2]:109-19). These studies usually involved adults, and it is reasonable to assume that the risks may be more pronounced in adolescents, particularly ones who are new to driving or have other problems that could affect their attention or reaction time (such as attention-deficit/hyperactivity disorder). Beyond letting patients know about the increased risks of accidents, it may be worth reminding them that driving while intoxicated – even with legal use marijuana – is a criminal offense.
Myth No. 4: Marijuana has no effect on schoolwork
Aside from the risks of causing long-term cognitive changes and psychiatric problems that can affect school performance, the direct effects of marijuana intoxication can linger and affect school performance well after its use. The “high” from marijuana typically lasts from 1 to 3 hours, but the drug’s effects on higher-level cognitive processes (mediated by the neocortex and hippocampus) can last for days. So a teenager who smokes on Saturday night may have lingering impairment of motivation, the ability to shift attention, the ability to learn complex tasks, and working memory. These are all critical cognitive abilities for learning, and can make studying on Sunday and performing well on a test on Monday much more difficult.
Myth No. 5: Marijuana is not addictive
Marijuana is addictive, with studies suggesting that nearly 9% of marijuana users will become addicted. Again, the risks are far greater for young people. Among people who begin using marijuana during adolescence, the rate of addiction climbs to 17%, and can be as high as 50% in daily users. Remember that addiction describes a pattern of continued use despite that use causing significant legal, social, or school and work problems. Users also may develop physical dependence, with a withdrawal syndrome that includes irritability, restlessness, insomnia, and appetite changes; these can last as long as 2 weeks.
Currently available forms of marijuana are much more potent than those that were studied and used in prior decades. On average, the potency of smoked marijuana has tripled, and there are concentrates (in oil form, for example) and hybrids with much higher potency still. More potent marijuana increases the high from even a small dose, and increases the likelihood of addiction and of other immediate and lingering complications of its use. So, parents who think they know what marijuana does to adolescents based on their own youthful experiences are significantly underestimating the risks.
When asking your patients explicitly about marijuana use, be curious and nonjudgmental, but also be frank and forthright about what is known about the risks associated with its use. Although the current legal and political changes around marijuana use may have given them the impression that marijuana use is safe, you want them to have the facts they need to make informed decisions. Even if you only discuss one of these myths with your patients, you will have equipped them with powerful information that they may use and share with their friends.
Dr. Swick is an attending psychiatrist in the division of child psychiatry at Massachusetts General Hospital, Boston, and director of the Parenting at a Challenging Time (PACT) Program at the Vernon Cancer Center at Newton (Mass.) Wellesley Hospital. Dr. Jellinek is professor of psychiatry and of pediatrics at Harvard Medical School, Boston. Email them at [email protected].
Poor sportsmanship
I try to avoid revisiting a subject I have pontificated on in the recent past, but when I encounter a situation in which scientists are behaving unscientifically it is hard to remain silent. In 2002, a Pittsburgh neuropathologist named Bennet Omalu performed an autopsy on Mike Webster, a former National Football League (NFL) lineman who had died in his 50s. Webster had been exhibiting bizarre behaviors and was developing dementia. What Dr. Omalu found in Webster’s brain was a collection of changes that have become known as chronic traumatic encephalopathy (CTE).
In the decade following the publication of Dr. Omalu’s findings in the journal Neurosurgery in 2005, there has been some unsavory back and forths between the NFL’s Mild Traumatic Brain Injury Committee and Dr. Omalu that I learned about in the Wall Street Journal (“The Doctor the NFL Tried to Silence,” by Jeanne Marie Laskas, Nov 24, 2015). The doctor’s side of the story has been published in a book, “Concussion” (New York: Penguin Random House, 2015). “Concussion,” the movie based on the book, was slated for release in December.
The tangle of he said – our experts don’t agree has involved the University of Michigan and Boston University, and the smell of conflict of interest hangs over the NFL’s choice of experts and its decisions to publish or not publish the results of various studies. It now appears that Dr. Omalu’s discovery was the tip of an iceberg of undetermined size. As happens far too often, assumptions and attributions have been made in haste based on scanty evidence from small studies that have surely failed to control for all of the possible contributors.
Considering the results of the autopsies on a few NFL players, it is probably reasonable to suspect that there is something in the culture surrounding professional football that makes some of the players vulnerable to central nervous system damage. And blows to the head are likely to be one of those factors. However, leaping to the conclusion that parents shouldn’t allow their young children to play football is another story. But that is just what Dr. Omalu has done in an op-ed piece that has appeared in the New York Times (“Don’t Let Kids Play Football,” Dec 7, 2015).
Relying heavily on the analogy with cumulative effects of cigarette smoking, Dr. Omalu continues to fan the flame that he ignited with his initial autopsy finding. The timing of the piece is interesting in light of the movie’s release date of Dec. 25. While his discovery of CTE in a professional player is important, Dr. Omalu’s case for prohibiting children from playing football is rife with half-truths and unwarranted conclusions.
For example, he states that in his 30 years as a neuropathologist he has yet to see a “neuron that naturally creates a new neuron to regenerate itself.” True, but he fails to report that there is new evidence that the long-held dictum that neurons can’t heal themselves may be wrong.
Dr. Omalu observes that “if a child who plays football is subjected to advanced radiological and neurocognitive studies during the season and several months after there can be evidence of brain damage at the cellular level even if there were no documented concussions or reported symptoms.” It took some time, but I eventually found the study to which I assume he is referring, by Dr. Christopher T. Whitlow of Wake Forest University, Winston-Salem, N.C., presented at the Radiological Society of North America meeting in December of 2014. Its lead author is careful to state that conclusions should not be drawn from this small preliminary study and observes, “it is unclear whether or not these effects will be associated with any long-term consequences.” However, Dr. Omalu asserts that “If that child continues to play over many seasons, these cellular injuries accumulate to cause irreversible brain damage.” He states this as fact without any supporting evidence.
Fortunately, the American Academy of Pediatrics has presented a more balanced perspective on allowing children to participate in football in light of what we are learning about the health of professional players (“Tackling in Youth Football” [Pediatrics. 2015;136(5)e1419-31]). Dr. William P. Meehan III and Dr. Gregory L. Landry, speaking for the Council on Sports Medicine and Fitness, point out that serious head and neck injury in young football players is very unlikely, and that by teaching proper tackling technique, these injuries can be further decreased.
The real solution to the problem that Dr. Omalu first brought to light in 2002 lies with zero tolerance for the practice of tackling headfirst at all levels of football. Although the NFL has made some feeble attempts to discipline its teams, there is still more that should be done. Every professional and college football game is being video recorded, often from multiple angles. Retrospective analysis of these images should be used to discipline players whose injury-threatening tactics have not been detected by the officials during the game. Multiple game suspensions meted out promptly, and without possibility of appeal, would go a long way to return football to being the safer sport it was when leather helmets discouraged players from using their heads as lethal weapons.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine, for nearly 40 years. He has authored several books on behavioral pediatrics including “How to Say No to Your Toddler.”
I try to avoid revisiting a subject I have pontificated on in the recent past, but when I encounter a situation in which scientists are behaving unscientifically it is hard to remain silent. In 2002, a Pittsburgh neuropathologist named Bennet Omalu performed an autopsy on Mike Webster, a former National Football League (NFL) lineman who had died in his 50s. Webster had been exhibiting bizarre behaviors and was developing dementia. What Dr. Omalu found in Webster’s brain was a collection of changes that have become known as chronic traumatic encephalopathy (CTE).
In the decade following the publication of Dr. Omalu’s findings in the journal Neurosurgery in 2005, there has been some unsavory back and forths between the NFL’s Mild Traumatic Brain Injury Committee and Dr. Omalu that I learned about in the Wall Street Journal (“The Doctor the NFL Tried to Silence,” by Jeanne Marie Laskas, Nov 24, 2015). The doctor’s side of the story has been published in a book, “Concussion” (New York: Penguin Random House, 2015). “Concussion,” the movie based on the book, was slated for release in December.
The tangle of he said – our experts don’t agree has involved the University of Michigan and Boston University, and the smell of conflict of interest hangs over the NFL’s choice of experts and its decisions to publish or not publish the results of various studies. It now appears that Dr. Omalu’s discovery was the tip of an iceberg of undetermined size. As happens far too often, assumptions and attributions have been made in haste based on scanty evidence from small studies that have surely failed to control for all of the possible contributors.
Considering the results of the autopsies on a few NFL players, it is probably reasonable to suspect that there is something in the culture surrounding professional football that makes some of the players vulnerable to central nervous system damage. And blows to the head are likely to be one of those factors. However, leaping to the conclusion that parents shouldn’t allow their young children to play football is another story. But that is just what Dr. Omalu has done in an op-ed piece that has appeared in the New York Times (“Don’t Let Kids Play Football,” Dec 7, 2015).
Relying heavily on the analogy with cumulative effects of cigarette smoking, Dr. Omalu continues to fan the flame that he ignited with his initial autopsy finding. The timing of the piece is interesting in light of the movie’s release date of Dec. 25. While his discovery of CTE in a professional player is important, Dr. Omalu’s case for prohibiting children from playing football is rife with half-truths and unwarranted conclusions.
For example, he states that in his 30 years as a neuropathologist he has yet to see a “neuron that naturally creates a new neuron to regenerate itself.” True, but he fails to report that there is new evidence that the long-held dictum that neurons can’t heal themselves may be wrong.
Dr. Omalu observes that “if a child who plays football is subjected to advanced radiological and neurocognitive studies during the season and several months after there can be evidence of brain damage at the cellular level even if there were no documented concussions or reported symptoms.” It took some time, but I eventually found the study to which I assume he is referring, by Dr. Christopher T. Whitlow of Wake Forest University, Winston-Salem, N.C., presented at the Radiological Society of North America meeting in December of 2014. Its lead author is careful to state that conclusions should not be drawn from this small preliminary study and observes, “it is unclear whether or not these effects will be associated with any long-term consequences.” However, Dr. Omalu asserts that “If that child continues to play over many seasons, these cellular injuries accumulate to cause irreversible brain damage.” He states this as fact without any supporting evidence.
Fortunately, the American Academy of Pediatrics has presented a more balanced perspective on allowing children to participate in football in light of what we are learning about the health of professional players (“Tackling in Youth Football” [Pediatrics. 2015;136(5)e1419-31]). Dr. William P. Meehan III and Dr. Gregory L. Landry, speaking for the Council on Sports Medicine and Fitness, point out that serious head and neck injury in young football players is very unlikely, and that by teaching proper tackling technique, these injuries can be further decreased.
The real solution to the problem that Dr. Omalu first brought to light in 2002 lies with zero tolerance for the practice of tackling headfirst at all levels of football. Although the NFL has made some feeble attempts to discipline its teams, there is still more that should be done. Every professional and college football game is being video recorded, often from multiple angles. Retrospective analysis of these images should be used to discipline players whose injury-threatening tactics have not been detected by the officials during the game. Multiple game suspensions meted out promptly, and without possibility of appeal, would go a long way to return football to being the safer sport it was when leather helmets discouraged players from using their heads as lethal weapons.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine, for nearly 40 years. He has authored several books on behavioral pediatrics including “How to Say No to Your Toddler.”
I try to avoid revisiting a subject I have pontificated on in the recent past, but when I encounter a situation in which scientists are behaving unscientifically it is hard to remain silent. In 2002, a Pittsburgh neuropathologist named Bennet Omalu performed an autopsy on Mike Webster, a former National Football League (NFL) lineman who had died in his 50s. Webster had been exhibiting bizarre behaviors and was developing dementia. What Dr. Omalu found in Webster’s brain was a collection of changes that have become known as chronic traumatic encephalopathy (CTE).
In the decade following the publication of Dr. Omalu’s findings in the journal Neurosurgery in 2005, there has been some unsavory back and forths between the NFL’s Mild Traumatic Brain Injury Committee and Dr. Omalu that I learned about in the Wall Street Journal (“The Doctor the NFL Tried to Silence,” by Jeanne Marie Laskas, Nov 24, 2015). The doctor’s side of the story has been published in a book, “Concussion” (New York: Penguin Random House, 2015). “Concussion,” the movie based on the book, was slated for release in December.
The tangle of he said – our experts don’t agree has involved the University of Michigan and Boston University, and the smell of conflict of interest hangs over the NFL’s choice of experts and its decisions to publish or not publish the results of various studies. It now appears that Dr. Omalu’s discovery was the tip of an iceberg of undetermined size. As happens far too often, assumptions and attributions have been made in haste based on scanty evidence from small studies that have surely failed to control for all of the possible contributors.
Considering the results of the autopsies on a few NFL players, it is probably reasonable to suspect that there is something in the culture surrounding professional football that makes some of the players vulnerable to central nervous system damage. And blows to the head are likely to be one of those factors. However, leaping to the conclusion that parents shouldn’t allow their young children to play football is another story. But that is just what Dr. Omalu has done in an op-ed piece that has appeared in the New York Times (“Don’t Let Kids Play Football,” Dec 7, 2015).
Relying heavily on the analogy with cumulative effects of cigarette smoking, Dr. Omalu continues to fan the flame that he ignited with his initial autopsy finding. The timing of the piece is interesting in light of the movie’s release date of Dec. 25. While his discovery of CTE in a professional player is important, Dr. Omalu’s case for prohibiting children from playing football is rife with half-truths and unwarranted conclusions.
For example, he states that in his 30 years as a neuropathologist he has yet to see a “neuron that naturally creates a new neuron to regenerate itself.” True, but he fails to report that there is new evidence that the long-held dictum that neurons can’t heal themselves may be wrong.
Dr. Omalu observes that “if a child who plays football is subjected to advanced radiological and neurocognitive studies during the season and several months after there can be evidence of brain damage at the cellular level even if there were no documented concussions or reported symptoms.” It took some time, but I eventually found the study to which I assume he is referring, by Dr. Christopher T. Whitlow of Wake Forest University, Winston-Salem, N.C., presented at the Radiological Society of North America meeting in December of 2014. Its lead author is careful to state that conclusions should not be drawn from this small preliminary study and observes, “it is unclear whether or not these effects will be associated with any long-term consequences.” However, Dr. Omalu asserts that “If that child continues to play over many seasons, these cellular injuries accumulate to cause irreversible brain damage.” He states this as fact without any supporting evidence.
Fortunately, the American Academy of Pediatrics has presented a more balanced perspective on allowing children to participate in football in light of what we are learning about the health of professional players (“Tackling in Youth Football” [Pediatrics. 2015;136(5)e1419-31]). Dr. William P. Meehan III and Dr. Gregory L. Landry, speaking for the Council on Sports Medicine and Fitness, point out that serious head and neck injury in young football players is very unlikely, and that by teaching proper tackling technique, these injuries can be further decreased.
The real solution to the problem that Dr. Omalu first brought to light in 2002 lies with zero tolerance for the practice of tackling headfirst at all levels of football. Although the NFL has made some feeble attempts to discipline its teams, there is still more that should be done. Every professional and college football game is being video recorded, often from multiple angles. Retrospective analysis of these images should be used to discipline players whose injury-threatening tactics have not been detected by the officials during the game. Multiple game suspensions meted out promptly, and without possibility of appeal, would go a long way to return football to being the safer sport it was when leather helmets discouraged players from using their heads as lethal weapons.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine, for nearly 40 years. He has authored several books on behavioral pediatrics including “How to Say No to Your Toddler.”
Using an Incident Command System Model for Initial Response to an Administrative Crisis at the Phoenix VA Health Care System
On April 9, 2014, allegations were made relating to delays experienced by patients accessing care at the Phoenix VA Health Care System (PVAHCS). After an in-depth investigation, multiple administrative problems were discovered related to scheduling processes at PVAHCS as well as many other VA facilities across the country. In Phoenix, there were 1,400 patients on the official electronic waiting list (EWL) in addition to 1,700 patients who had requested care but were not on any official waiting list.1
The following is a description of the use of an Incident Command System (ICS) model to provide care for these veterans in the face of an existing lack of capacity to do so. This is written from the perspective of frontline physicians representing hospital medicine, the emergency department, and primary care. The authors’ views do not necessarily reflect the official position of the VA or PVAHCS.
Under direction of the President, the VA crafted the official response to meet the needs of veterans awaiting care. The program, called the Accelerating Care Initiative (ACI), was launched on May 21, 2014. With the cooperation of the White House, the VA brought to bear substantial resources to enable PVAHCS to accomplish the task with an “all-hands-on-deck” approach. These resources included the Disaster Emergency Medical Personnel System (DEMPS), Traveling Nurse Corps (TNC), and the VA Locum Tenens program.
This situation was unprecedented, and an administrative framework was needed to organize and manage the extra personnel and resources involved in the response. The decision was made to use the ICS to achieve this aim. Most people involved in health care administration have been exposed to ICS concepts but are not accustomed to approaching an administrative problem the way emergency managers would respond to a natural disaster, such as a flood or hurricane.
According to the Federal Emergency Management Agency, ICS is “a standardized on-scene emergency management construct.”2 Incident Command System combines resources and people under a common organizational structure, using a common terminology to facilitate cooperation between any and all entities that may be involved in an incident. It is a modular concept and designed to be adaptable and scalable from isolated local events, such as a traffic accident, to regional catastrophes such as a category 5 hurricane. Incident Command System was developed in the 1970s, but it has become the standard approach for government agencies, law enforcement, first responders, and the military.
The PVAHCS adopted an ICS framework, and the chief of staff (COS) took on the incident commander role full time. The deputy assumed all other COS duties related to hospital operations. Phoenix VA Health Care System used the VA national call center to rapidly contact patients awaiting care and established the other standard ICS branches with Operations, Planning, Logistics, and Finance/Administration with appropriate task forces underneath each department. Within Operations, PVAHCS established task forces for the primary care, medical specialty care, surgical specialty care, and mental health departments.
Efficient command, control, and communication was facilitated by having twice-daily huddles with key staff members for 20 to 30 minutes to share updates and refine operational goals. This worked well and provided the situational awareness for our incident commander to rapidly channel situation reports (SITREPS) to the VA Secretary’s office in Washington without drawing focus away from creating solutions. As a midsize facility that lacks certain specialized medical and surgical services, PVAHCS already had an established system for referring veterans for these services. This enabled PVAHCS to use these channels to provide medical and surgical specialty care where demand exceeded capacity to schedule within a reasonable time frame.
Federal law, at the time, severely limited the ability of PVAHCS to outsource primary care in this fashion, which required finding new ways to create additional capacity. This was a major operational challenge due to very limited physical space as well as an insufficient number of primary care and administrative support staff. The PVAHCS made the equivalent of 5 new primary care teams operational with rotating volunteers from other VAs and our preexisting DEMPS, Locum Tenens, and TNC programs.
Medical subspecialty clinics within the primary care area were promptly moved to create space for the new primary care teams. To create this additional space, PVAHCS postponed a planned expansion of a community living center in the main hospital building complex. While PVAHCS was standing up the ICS, VA facilities from other regions loaned 3 mobile medical units. These vehicles included fully capable examination tables and telehealth capability and were used for intake appointments, new unassigned patients, and as administrative space.
In August 2014, the Veterans Choice Act (VCA) allowed veterans to access care from non-VA providers. Eligibility was based on the distance a veteran lived from a VA facility or the inability to be seen within a specified time period. The VCA provided PVACHS with an additional tool to meet veterans’ care needs as it increased the hiring of permanent staff. After about 3 months, PVAHCS succeeded in contacting > 6,000 veterans and providing > 3,200 veterans with appointments at the either PVAHCS or local civilian partners. Despite the initial successes, the preliminary gains in patient access at PVAHCS will not be sustainable, and wait times will not decrease substantially without increased permanent staff and further improvements in both the facility and its processes. Although these improvements are a priority, progress has been slow.
Efforts are underway to enhance operational integration between providers, nursing, and administrative support personnel. Congress has renewed its support of a larger and more functional health care center along with the addition of 2 more clinics within the metro Phoenix area. The PVAHCS has since stood down the ICS and ACI operations and transferred these operations to a newly created Patient Flow Committee. This group is chaired by the COS and meets monthly to supervise process improvement teams using lean modalities to address issues creating excessive waits or delays in patient care throughout the facility.
This access to care crisis was exacerbated by intense media and political attention. Further disarray resulted from the abrupt loss of several senior executives at PVAHCS—all the way up to former VA Secretary Eric K. Shinseki. Use of the ICS was highly effective in providing the necessary organizational structure for key staff to focus on solving the immediate problems locally while managing external resources that were in constant flux. The authors strongly recommend consideration of the ICS as a management framework to tackle similar problems.
Author disclosures
The authors report no actual or potential conflicts of interest with regard to this article.
Disclaimer
The opinions expressed herein are those of the authors and do not necessarily reflect those of Federal Practitioner, Frontline Medical Communications Inc., the U.S. Government, or any of its agencies.
1. VA Office of Inspector General. Veterans Health Administration Interim Report: Review of Patient Wait Times, Scheduling Practices, and Alleged Patient Deaths at the Phoenix Health Care System. U.S. Department of Veterans Affairs Website. http://www.va.gov/oig/pubs/VAOIG-14-02603-178.pdf. Published May 28, 2014. Accessed November 16, 2015.
2. U.S. Department of Homeland Security, Federal Emergency Management Agency. Developing and Maintaining Emergency Operations Plans. Comprehensive Preparedness Guide 101, Version 2.0. Federal Emergency Management Agency Website. http://www.fema.gov/media-library-data/20130726-1828-25045-0014/cpg_101_comprehensive_preparedness_guide_developing_and_maintaining_emergency_operations_plans_2010.pdf. Published November 2010. Accessed November 16, 2015.
On April 9, 2014, allegations were made relating to delays experienced by patients accessing care at the Phoenix VA Health Care System (PVAHCS). After an in-depth investigation, multiple administrative problems were discovered related to scheduling processes at PVAHCS as well as many other VA facilities across the country. In Phoenix, there were 1,400 patients on the official electronic waiting list (EWL) in addition to 1,700 patients who had requested care but were not on any official waiting list.1
The following is a description of the use of an Incident Command System (ICS) model to provide care for these veterans in the face of an existing lack of capacity to do so. This is written from the perspective of frontline physicians representing hospital medicine, the emergency department, and primary care. The authors’ views do not necessarily reflect the official position of the VA or PVAHCS.
Under direction of the President, the VA crafted the official response to meet the needs of veterans awaiting care. The program, called the Accelerating Care Initiative (ACI), was launched on May 21, 2014. With the cooperation of the White House, the VA brought to bear substantial resources to enable PVAHCS to accomplish the task with an “all-hands-on-deck” approach. These resources included the Disaster Emergency Medical Personnel System (DEMPS), Traveling Nurse Corps (TNC), and the VA Locum Tenens program.
This situation was unprecedented, and an administrative framework was needed to organize and manage the extra personnel and resources involved in the response. The decision was made to use the ICS to achieve this aim. Most people involved in health care administration have been exposed to ICS concepts but are not accustomed to approaching an administrative problem the way emergency managers would respond to a natural disaster, such as a flood or hurricane.
According to the Federal Emergency Management Agency, ICS is “a standardized on-scene emergency management construct.”2 Incident Command System combines resources and people under a common organizational structure, using a common terminology to facilitate cooperation between any and all entities that may be involved in an incident. It is a modular concept and designed to be adaptable and scalable from isolated local events, such as a traffic accident, to regional catastrophes such as a category 5 hurricane. Incident Command System was developed in the 1970s, but it has become the standard approach for government agencies, law enforcement, first responders, and the military.
The PVAHCS adopted an ICS framework, and the chief of staff (COS) took on the incident commander role full time. The deputy assumed all other COS duties related to hospital operations. Phoenix VA Health Care System used the VA national call center to rapidly contact patients awaiting care and established the other standard ICS branches with Operations, Planning, Logistics, and Finance/Administration with appropriate task forces underneath each department. Within Operations, PVAHCS established task forces for the primary care, medical specialty care, surgical specialty care, and mental health departments.
Efficient command, control, and communication was facilitated by having twice-daily huddles with key staff members for 20 to 30 minutes to share updates and refine operational goals. This worked well and provided the situational awareness for our incident commander to rapidly channel situation reports (SITREPS) to the VA Secretary’s office in Washington without drawing focus away from creating solutions. As a midsize facility that lacks certain specialized medical and surgical services, PVAHCS already had an established system for referring veterans for these services. This enabled PVAHCS to use these channels to provide medical and surgical specialty care where demand exceeded capacity to schedule within a reasonable time frame.
Federal law, at the time, severely limited the ability of PVAHCS to outsource primary care in this fashion, which required finding new ways to create additional capacity. This was a major operational challenge due to very limited physical space as well as an insufficient number of primary care and administrative support staff. The PVAHCS made the equivalent of 5 new primary care teams operational with rotating volunteers from other VAs and our preexisting DEMPS, Locum Tenens, and TNC programs.
Medical subspecialty clinics within the primary care area were promptly moved to create space for the new primary care teams. To create this additional space, PVAHCS postponed a planned expansion of a community living center in the main hospital building complex. While PVAHCS was standing up the ICS, VA facilities from other regions loaned 3 mobile medical units. These vehicles included fully capable examination tables and telehealth capability and were used for intake appointments, new unassigned patients, and as administrative space.
In August 2014, the Veterans Choice Act (VCA) allowed veterans to access care from non-VA providers. Eligibility was based on the distance a veteran lived from a VA facility or the inability to be seen within a specified time period. The VCA provided PVACHS with an additional tool to meet veterans’ care needs as it increased the hiring of permanent staff. After about 3 months, PVAHCS succeeded in contacting > 6,000 veterans and providing > 3,200 veterans with appointments at the either PVAHCS or local civilian partners. Despite the initial successes, the preliminary gains in patient access at PVAHCS will not be sustainable, and wait times will not decrease substantially without increased permanent staff and further improvements in both the facility and its processes. Although these improvements are a priority, progress has been slow.
Efforts are underway to enhance operational integration between providers, nursing, and administrative support personnel. Congress has renewed its support of a larger and more functional health care center along with the addition of 2 more clinics within the metro Phoenix area. The PVAHCS has since stood down the ICS and ACI operations and transferred these operations to a newly created Patient Flow Committee. This group is chaired by the COS and meets monthly to supervise process improvement teams using lean modalities to address issues creating excessive waits or delays in patient care throughout the facility.
This access to care crisis was exacerbated by intense media and political attention. Further disarray resulted from the abrupt loss of several senior executives at PVAHCS—all the way up to former VA Secretary Eric K. Shinseki. Use of the ICS was highly effective in providing the necessary organizational structure for key staff to focus on solving the immediate problems locally while managing external resources that were in constant flux. The authors strongly recommend consideration of the ICS as a management framework to tackle similar problems.
Author disclosures
The authors report no actual or potential conflicts of interest with regard to this article.
Disclaimer
The opinions expressed herein are those of the authors and do not necessarily reflect those of Federal Practitioner, Frontline Medical Communications Inc., the U.S. Government, or any of its agencies.
On April 9, 2014, allegations were made relating to delays experienced by patients accessing care at the Phoenix VA Health Care System (PVAHCS). After an in-depth investigation, multiple administrative problems were discovered related to scheduling processes at PVAHCS as well as many other VA facilities across the country. In Phoenix, there were 1,400 patients on the official electronic waiting list (EWL) in addition to 1,700 patients who had requested care but were not on any official waiting list.1
The following is a description of the use of an Incident Command System (ICS) model to provide care for these veterans in the face of an existing lack of capacity to do so. This is written from the perspective of frontline physicians representing hospital medicine, the emergency department, and primary care. The authors’ views do not necessarily reflect the official position of the VA or PVAHCS.
Under direction of the President, the VA crafted the official response to meet the needs of veterans awaiting care. The program, called the Accelerating Care Initiative (ACI), was launched on May 21, 2014. With the cooperation of the White House, the VA brought to bear substantial resources to enable PVAHCS to accomplish the task with an “all-hands-on-deck” approach. These resources included the Disaster Emergency Medical Personnel System (DEMPS), Traveling Nurse Corps (TNC), and the VA Locum Tenens program.
This situation was unprecedented, and an administrative framework was needed to organize and manage the extra personnel and resources involved in the response. The decision was made to use the ICS to achieve this aim. Most people involved in health care administration have been exposed to ICS concepts but are not accustomed to approaching an administrative problem the way emergency managers would respond to a natural disaster, such as a flood or hurricane.
According to the Federal Emergency Management Agency, ICS is “a standardized on-scene emergency management construct.”2 Incident Command System combines resources and people under a common organizational structure, using a common terminology to facilitate cooperation between any and all entities that may be involved in an incident. It is a modular concept and designed to be adaptable and scalable from isolated local events, such as a traffic accident, to regional catastrophes such as a category 5 hurricane. Incident Command System was developed in the 1970s, but it has become the standard approach for government agencies, law enforcement, first responders, and the military.
The PVAHCS adopted an ICS framework, and the chief of staff (COS) took on the incident commander role full time. The deputy assumed all other COS duties related to hospital operations. Phoenix VA Health Care System used the VA national call center to rapidly contact patients awaiting care and established the other standard ICS branches with Operations, Planning, Logistics, and Finance/Administration with appropriate task forces underneath each department. Within Operations, PVAHCS established task forces for the primary care, medical specialty care, surgical specialty care, and mental health departments.
Efficient command, control, and communication was facilitated by having twice-daily huddles with key staff members for 20 to 30 minutes to share updates and refine operational goals. This worked well and provided the situational awareness for our incident commander to rapidly channel situation reports (SITREPS) to the VA Secretary’s office in Washington without drawing focus away from creating solutions. As a midsize facility that lacks certain specialized medical and surgical services, PVAHCS already had an established system for referring veterans for these services. This enabled PVAHCS to use these channels to provide medical and surgical specialty care where demand exceeded capacity to schedule within a reasonable time frame.
Federal law, at the time, severely limited the ability of PVAHCS to outsource primary care in this fashion, which required finding new ways to create additional capacity. This was a major operational challenge due to very limited physical space as well as an insufficient number of primary care and administrative support staff. The PVAHCS made the equivalent of 5 new primary care teams operational with rotating volunteers from other VAs and our preexisting DEMPS, Locum Tenens, and TNC programs.
Medical subspecialty clinics within the primary care area were promptly moved to create space for the new primary care teams. To create this additional space, PVAHCS postponed a planned expansion of a community living center in the main hospital building complex. While PVAHCS was standing up the ICS, VA facilities from other regions loaned 3 mobile medical units. These vehicles included fully capable examination tables and telehealth capability and were used for intake appointments, new unassigned patients, and as administrative space.
In August 2014, the Veterans Choice Act (VCA) allowed veterans to access care from non-VA providers. Eligibility was based on the distance a veteran lived from a VA facility or the inability to be seen within a specified time period. The VCA provided PVACHS with an additional tool to meet veterans’ care needs as it increased the hiring of permanent staff. After about 3 months, PVAHCS succeeded in contacting > 6,000 veterans and providing > 3,200 veterans with appointments at the either PVAHCS or local civilian partners. Despite the initial successes, the preliminary gains in patient access at PVAHCS will not be sustainable, and wait times will not decrease substantially without increased permanent staff and further improvements in both the facility and its processes. Although these improvements are a priority, progress has been slow.
Efforts are underway to enhance operational integration between providers, nursing, and administrative support personnel. Congress has renewed its support of a larger and more functional health care center along with the addition of 2 more clinics within the metro Phoenix area. The PVAHCS has since stood down the ICS and ACI operations and transferred these operations to a newly created Patient Flow Committee. This group is chaired by the COS and meets monthly to supervise process improvement teams using lean modalities to address issues creating excessive waits or delays in patient care throughout the facility.
This access to care crisis was exacerbated by intense media and political attention. Further disarray resulted from the abrupt loss of several senior executives at PVAHCS—all the way up to former VA Secretary Eric K. Shinseki. Use of the ICS was highly effective in providing the necessary organizational structure for key staff to focus on solving the immediate problems locally while managing external resources that were in constant flux. The authors strongly recommend consideration of the ICS as a management framework to tackle similar problems.
Author disclosures
The authors report no actual or potential conflicts of interest with regard to this article.
Disclaimer
The opinions expressed herein are those of the authors and do not necessarily reflect those of Federal Practitioner, Frontline Medical Communications Inc., the U.S. Government, or any of its agencies.
1. VA Office of Inspector General. Veterans Health Administration Interim Report: Review of Patient Wait Times, Scheduling Practices, and Alleged Patient Deaths at the Phoenix Health Care System. U.S. Department of Veterans Affairs Website. http://www.va.gov/oig/pubs/VAOIG-14-02603-178.pdf. Published May 28, 2014. Accessed November 16, 2015.
2. U.S. Department of Homeland Security, Federal Emergency Management Agency. Developing and Maintaining Emergency Operations Plans. Comprehensive Preparedness Guide 101, Version 2.0. Federal Emergency Management Agency Website. http://www.fema.gov/media-library-data/20130726-1828-25045-0014/cpg_101_comprehensive_preparedness_guide_developing_and_maintaining_emergency_operations_plans_2010.pdf. Published November 2010. Accessed November 16, 2015.
1. VA Office of Inspector General. Veterans Health Administration Interim Report: Review of Patient Wait Times, Scheduling Practices, and Alleged Patient Deaths at the Phoenix Health Care System. U.S. Department of Veterans Affairs Website. http://www.va.gov/oig/pubs/VAOIG-14-02603-178.pdf. Published May 28, 2014. Accessed November 16, 2015.
2. U.S. Department of Homeland Security, Federal Emergency Management Agency. Developing and Maintaining Emergency Operations Plans. Comprehensive Preparedness Guide 101, Version 2.0. Federal Emergency Management Agency Website. http://www.fema.gov/media-library-data/20130726-1828-25045-0014/cpg_101_comprehensive_preparedness_guide_developing_and_maintaining_emergency_operations_plans_2010.pdf. Published November 2010. Accessed November 16, 2015.