User login
Video etiquette
FaceTime with my mother would be better described as ForeheadTime. She loves to use video for our Sunday calls, yet when she does, she always talks into her iPhone as if it’s a speakerphone. As a result, all I see is the top of her head. “Mom. Lower the phone. Mom, I can’t see you,” I must repeat weekly.
Video provides a richer experience compared with telephone. It allows for a deeper, emotional connection. That’s why moms like mine prefer it to telephone conversations. In medicine, video visits are uncommon, but that’s changing as payers are now reimbursing and patients are demanding the service. For many, they offer a far more convenient and still effective method to receive medical care. Psychiatry is an obvious example. Less obvious, but still effective examples, include endocrinology, pediatrics, primary care, surgery (post operatively), and dermatology.
Like the example with my mom, quality of the experience matters, and issues often arise not from the technology, but from the technique. Making eye contact is more difficult on video, and not looking patients in the eye can harm doctor-patient bonding. Here are a few basic tips when using video with your patients:
• Be sure the light source is in front of you. Having windows behind you often puts you in shadow.
• The best place for the camera is at the top of your screen. It’s nearly impossible to look into the camera and see the patient if the camera is next to the screen instead of above.
• Remember, to look directly at the patient, you have to look into the camera. This is tricky and easy to forget.
• Be sure your entire head and upper torso are in the frame. Talking heads can be intimidating.
• When possible, use a headset with a microphone. Headsets help both you and your patient hear better and give the patient an increased sense of privacy.
• Generally speaking, video visits take as long or longer than in-person visits. Remember to be patient as some of your patients may experience technical difficulties. Our IT colleagues have a word for it: “picnic,” which stands for “Problem In Chair Not In Computer.” You should also train your staff to aid you and the patients. For instance, if a patient is struggling with the computer, you might have your assistant help him or her while you move on to the next patient.
• Although the patient can be home, it is best for you to be in your office. It’s possible to do video consults from home, but it is more difficult because you have to ensure that both your technology and your environment are secure and private. Otherwise, you risk violating HIPAA or other compliance requirements.
• Be sure to get the appropriate consent before conducting a virtual visit. In California, it requires only verbal consent, but your state’s requirements might be different.
• As for your appearance, there’s a reason why Kennedy won the Kennedy-Nixon debates. Video does reveal details that you might not want emphasized. A two-day beard might appear hip in person but unkempt and uncaring online. Bold stripes or checks on your shirt sometimes appear distorted, so opt for solids in soft shades. Scrubs are okay, but be sure to check your neckline, particularly as you move about. Whether it’s clothing or accessories, avoid anything overly distracting.
Video visits have had a long, slow ramp-up, but they seem to be gaining momentum. You may not use them in your practice now, but it’s likely we all will someday. Soon.
Dr. Benabio is a partner physician in the department of dermatology of the Southern California Permanente Group in San Diego, and a volunteer clinical assistant professor at the University of California, San Diego. He is @dermdoc on Twitter.
FaceTime with my mother would be better described as ForeheadTime. She loves to use video for our Sunday calls, yet when she does, she always talks into her iPhone as if it’s a speakerphone. As a result, all I see is the top of her head. “Mom. Lower the phone. Mom, I can’t see you,” I must repeat weekly.
Video provides a richer experience compared with telephone. It allows for a deeper, emotional connection. That’s why moms like mine prefer it to telephone conversations. In medicine, video visits are uncommon, but that’s changing as payers are now reimbursing and patients are demanding the service. For many, they offer a far more convenient and still effective method to receive medical care. Psychiatry is an obvious example. Less obvious, but still effective examples, include endocrinology, pediatrics, primary care, surgery (post operatively), and dermatology.
Like the example with my mom, quality of the experience matters, and issues often arise not from the technology, but from the technique. Making eye contact is more difficult on video, and not looking patients in the eye can harm doctor-patient bonding. Here are a few basic tips when using video with your patients:
• Be sure the light source is in front of you. Having windows behind you often puts you in shadow.
• The best place for the camera is at the top of your screen. It’s nearly impossible to look into the camera and see the patient if the camera is next to the screen instead of above.
• Remember, to look directly at the patient, you have to look into the camera. This is tricky and easy to forget.
• Be sure your entire head and upper torso are in the frame. Talking heads can be intimidating.
• When possible, use a headset with a microphone. Headsets help both you and your patient hear better and give the patient an increased sense of privacy.
• Generally speaking, video visits take as long or longer than in-person visits. Remember to be patient as some of your patients may experience technical difficulties. Our IT colleagues have a word for it: “picnic,” which stands for “Problem In Chair Not In Computer.” You should also train your staff to aid you and the patients. For instance, if a patient is struggling with the computer, you might have your assistant help him or her while you move on to the next patient.
• Although the patient can be home, it is best for you to be in your office. It’s possible to do video consults from home, but it is more difficult because you have to ensure that both your technology and your environment are secure and private. Otherwise, you risk violating HIPAA or other compliance requirements.
• Be sure to get the appropriate consent before conducting a virtual visit. In California, it requires only verbal consent, but your state’s requirements might be different.
• As for your appearance, there’s a reason why Kennedy won the Kennedy-Nixon debates. Video does reveal details that you might not want emphasized. A two-day beard might appear hip in person but unkempt and uncaring online. Bold stripes or checks on your shirt sometimes appear distorted, so opt for solids in soft shades. Scrubs are okay, but be sure to check your neckline, particularly as you move about. Whether it’s clothing or accessories, avoid anything overly distracting.
Video visits have had a long, slow ramp-up, but they seem to be gaining momentum. You may not use them in your practice now, but it’s likely we all will someday. Soon.
Dr. Benabio is a partner physician in the department of dermatology of the Southern California Permanente Group in San Diego, and a volunteer clinical assistant professor at the University of California, San Diego. He is @dermdoc on Twitter.
FaceTime with my mother would be better described as ForeheadTime. She loves to use video for our Sunday calls, yet when she does, she always talks into her iPhone as if it’s a speakerphone. As a result, all I see is the top of her head. “Mom. Lower the phone. Mom, I can’t see you,” I must repeat weekly.
Video provides a richer experience compared with telephone. It allows for a deeper, emotional connection. That’s why moms like mine prefer it to telephone conversations. In medicine, video visits are uncommon, but that’s changing as payers are now reimbursing and patients are demanding the service. For many, they offer a far more convenient and still effective method to receive medical care. Psychiatry is an obvious example. Less obvious, but still effective examples, include endocrinology, pediatrics, primary care, surgery (post operatively), and dermatology.
Like the example with my mom, quality of the experience matters, and issues often arise not from the technology, but from the technique. Making eye contact is more difficult on video, and not looking patients in the eye can harm doctor-patient bonding. Here are a few basic tips when using video with your patients:
• Be sure the light source is in front of you. Having windows behind you often puts you in shadow.
• The best place for the camera is at the top of your screen. It’s nearly impossible to look into the camera and see the patient if the camera is next to the screen instead of above.
• Remember, to look directly at the patient, you have to look into the camera. This is tricky and easy to forget.
• Be sure your entire head and upper torso are in the frame. Talking heads can be intimidating.
• When possible, use a headset with a microphone. Headsets help both you and your patient hear better and give the patient an increased sense of privacy.
• Generally speaking, video visits take as long or longer than in-person visits. Remember to be patient as some of your patients may experience technical difficulties. Our IT colleagues have a word for it: “picnic,” which stands for “Problem In Chair Not In Computer.” You should also train your staff to aid you and the patients. For instance, if a patient is struggling with the computer, you might have your assistant help him or her while you move on to the next patient.
• Although the patient can be home, it is best for you to be in your office. It’s possible to do video consults from home, but it is more difficult because you have to ensure that both your technology and your environment are secure and private. Otherwise, you risk violating HIPAA or other compliance requirements.
• Be sure to get the appropriate consent before conducting a virtual visit. In California, it requires only verbal consent, but your state’s requirements might be different.
• As for your appearance, there’s a reason why Kennedy won the Kennedy-Nixon debates. Video does reveal details that you might not want emphasized. A two-day beard might appear hip in person but unkempt and uncaring online. Bold stripes or checks on your shirt sometimes appear distorted, so opt for solids in soft shades. Scrubs are okay, but be sure to check your neckline, particularly as you move about. Whether it’s clothing or accessories, avoid anything overly distracting.
Video visits have had a long, slow ramp-up, but they seem to be gaining momentum. You may not use them in your practice now, but it’s likely we all will someday. Soon.
Dr. Benabio is a partner physician in the department of dermatology of the Southern California Permanente Group in San Diego, and a volunteer clinical assistant professor at the University of California, San Diego. He is @dermdoc on Twitter.
Neurosurgery at the End of Life
The juxtaposition between my first 2 days of neurosurgery could not have been more profound. On my first day as a third-year medical student, the attending and chief resident let me take the lead on the first case: a straightforward brain biopsy. I got to make the incision, drill the burr hole, and perform the needle biopsy. I still remember the thrill of the technical challenge, the controlled violence of drilling into the skull, and the finesse of accessing the tumor core.
The buzz was so strong that I barely registered the diagnosis that was called back from the pathologist: glioblastoma. It was not until I saw the face of the disease the next morning that I understood the reality of a GBM diagnosis. That face belonged to a 47-year-old man who hadn’t slept all night, wide eyed with apprehension at what news I might bring. He beseeched me with questions, and though his aphasia left him stammering to get the words out, I knew exactly what he was asking: Would he live or die? It was a question I was in no position to answer. Instead, I reassured him that we were waiting on the final pathology, all the while trying to forget the fact that the frozen section suggested an aggressive subtype, surely heralding a poor prognosis.
In his poignant memoir, “Do No Harm: Stories of Life, Death and Brain Surgery” (New York: Thomas Dunne Book, 2015), Dr. Henry Marsh writes beautifully about how difficult it can be to find the balance between optimism and realism. In one memorable passage, Dr. Marsh shows a house officer a scan of a highly malignant brain tumor and asks him what he would say to the patient. The trainee reflexively hides behind jargon, skirting around what he knew to be the truth: This tumor would kill her. Marsh presses him to admit that he’s lying, before lamenting at how hard it is to improve these critical communication skills: “When I have had to break bad news I never know whether I have done it well or not. The patients aren’t going to ring me up afterward and say, ‘Mr. Marsh, I really liked the way you told me that I was going to die,’ or ‘Mr. Marsh, you were crap.’ You can only hope that you haven’t made too much of a mess of it.”
I could certainly relate to Dr. Marsh’s house officer as I walked away from my own patient. I felt almost deceitful withholding diagnostic information from him, even if I did the “right” thing. It made me wonder, why did I want to become a neurosurgeon? Surely to help people through some of the most difficult moments of their lives. But is it possible to be a source of comfort when you are required so often to be a harbinger of death? The answer depends on whether one can envision a role for the neurosurgeon beyond the mandate of “life at all costs.”
While the field has become known for its life-saving procedures, neurosurgeons are called just as often to preside over the end of their patient’s lives – work that requires just as much skill as any technical procedure. Dr. Marsh recognized the tremendous human cost of neglecting that work. For cases that appear “hopeless,” he writes, “We often end up operating because it’s easier than being honest, and it means that we can avoid a painful conversation.”
We are only beginning to understand the many issues that neurosurgical patients face at the end of life, but so far it is clear that neurosurgical trainees require substantive training in prognostication, communication, and palliation (Crit Care Med. 2015 Sep;43[9]:1964-77 1,2; J Neurooncol. 2009 Jan;91[1]:39-43). Is there room in the current training paradigm for more formal education in these domains? As we move further into the 21st century, we must embrace the need for masterful clinicians outside of the operating room if we are to ever challenge the axiom set forth by the renowned French surgeon, René Leriche, some 65 years ago: “Every surgeon carries within himself a small cemetery, where from time to time he goes to pray – a place of bitterness and regret, where he must look for an explanation for his failures.” Let us look forward to the day when this is no longer the case.
Stephen Miranda is a medical student from the University of Rochester, who is now working as a research fellow at Ariadne Labs, a joint center for health systems innovation at Brigham & Women’s Hospital and Harvard T.H. Chan School of Public Health, both in Boston.
The juxtaposition between my first 2 days of neurosurgery could not have been more profound. On my first day as a third-year medical student, the attending and chief resident let me take the lead on the first case: a straightforward brain biopsy. I got to make the incision, drill the burr hole, and perform the needle biopsy. I still remember the thrill of the technical challenge, the controlled violence of drilling into the skull, and the finesse of accessing the tumor core.
The buzz was so strong that I barely registered the diagnosis that was called back from the pathologist: glioblastoma. It was not until I saw the face of the disease the next morning that I understood the reality of a GBM diagnosis. That face belonged to a 47-year-old man who hadn’t slept all night, wide eyed with apprehension at what news I might bring. He beseeched me with questions, and though his aphasia left him stammering to get the words out, I knew exactly what he was asking: Would he live or die? It was a question I was in no position to answer. Instead, I reassured him that we were waiting on the final pathology, all the while trying to forget the fact that the frozen section suggested an aggressive subtype, surely heralding a poor prognosis.
In his poignant memoir, “Do No Harm: Stories of Life, Death and Brain Surgery” (New York: Thomas Dunne Book, 2015), Dr. Henry Marsh writes beautifully about how difficult it can be to find the balance between optimism and realism. In one memorable passage, Dr. Marsh shows a house officer a scan of a highly malignant brain tumor and asks him what he would say to the patient. The trainee reflexively hides behind jargon, skirting around what he knew to be the truth: This tumor would kill her. Marsh presses him to admit that he’s lying, before lamenting at how hard it is to improve these critical communication skills: “When I have had to break bad news I never know whether I have done it well or not. The patients aren’t going to ring me up afterward and say, ‘Mr. Marsh, I really liked the way you told me that I was going to die,’ or ‘Mr. Marsh, you were crap.’ You can only hope that you haven’t made too much of a mess of it.”
I could certainly relate to Dr. Marsh’s house officer as I walked away from my own patient. I felt almost deceitful withholding diagnostic information from him, even if I did the “right” thing. It made me wonder, why did I want to become a neurosurgeon? Surely to help people through some of the most difficult moments of their lives. But is it possible to be a source of comfort when you are required so often to be a harbinger of death? The answer depends on whether one can envision a role for the neurosurgeon beyond the mandate of “life at all costs.”
While the field has become known for its life-saving procedures, neurosurgeons are called just as often to preside over the end of their patient’s lives – work that requires just as much skill as any technical procedure. Dr. Marsh recognized the tremendous human cost of neglecting that work. For cases that appear “hopeless,” he writes, “We often end up operating because it’s easier than being honest, and it means that we can avoid a painful conversation.”
We are only beginning to understand the many issues that neurosurgical patients face at the end of life, but so far it is clear that neurosurgical trainees require substantive training in prognostication, communication, and palliation (Crit Care Med. 2015 Sep;43[9]:1964-77 1,2; J Neurooncol. 2009 Jan;91[1]:39-43). Is there room in the current training paradigm for more formal education in these domains? As we move further into the 21st century, we must embrace the need for masterful clinicians outside of the operating room if we are to ever challenge the axiom set forth by the renowned French surgeon, René Leriche, some 65 years ago: “Every surgeon carries within himself a small cemetery, where from time to time he goes to pray – a place of bitterness and regret, where he must look for an explanation for his failures.” Let us look forward to the day when this is no longer the case.
Stephen Miranda is a medical student from the University of Rochester, who is now working as a research fellow at Ariadne Labs, a joint center for health systems innovation at Brigham & Women’s Hospital and Harvard T.H. Chan School of Public Health, both in Boston.
The juxtaposition between my first 2 days of neurosurgery could not have been more profound. On my first day as a third-year medical student, the attending and chief resident let me take the lead on the first case: a straightforward brain biopsy. I got to make the incision, drill the burr hole, and perform the needle biopsy. I still remember the thrill of the technical challenge, the controlled violence of drilling into the skull, and the finesse of accessing the tumor core.
The buzz was so strong that I barely registered the diagnosis that was called back from the pathologist: glioblastoma. It was not until I saw the face of the disease the next morning that I understood the reality of a GBM diagnosis. That face belonged to a 47-year-old man who hadn’t slept all night, wide eyed with apprehension at what news I might bring. He beseeched me with questions, and though his aphasia left him stammering to get the words out, I knew exactly what he was asking: Would he live or die? It was a question I was in no position to answer. Instead, I reassured him that we were waiting on the final pathology, all the while trying to forget the fact that the frozen section suggested an aggressive subtype, surely heralding a poor prognosis.
In his poignant memoir, “Do No Harm: Stories of Life, Death and Brain Surgery” (New York: Thomas Dunne Book, 2015), Dr. Henry Marsh writes beautifully about how difficult it can be to find the balance between optimism and realism. In one memorable passage, Dr. Marsh shows a house officer a scan of a highly malignant brain tumor and asks him what he would say to the patient. The trainee reflexively hides behind jargon, skirting around what he knew to be the truth: This tumor would kill her. Marsh presses him to admit that he’s lying, before lamenting at how hard it is to improve these critical communication skills: “When I have had to break bad news I never know whether I have done it well or not. The patients aren’t going to ring me up afterward and say, ‘Mr. Marsh, I really liked the way you told me that I was going to die,’ or ‘Mr. Marsh, you were crap.’ You can only hope that you haven’t made too much of a mess of it.”
I could certainly relate to Dr. Marsh’s house officer as I walked away from my own patient. I felt almost deceitful withholding diagnostic information from him, even if I did the “right” thing. It made me wonder, why did I want to become a neurosurgeon? Surely to help people through some of the most difficult moments of their lives. But is it possible to be a source of comfort when you are required so often to be a harbinger of death? The answer depends on whether one can envision a role for the neurosurgeon beyond the mandate of “life at all costs.”
While the field has become known for its life-saving procedures, neurosurgeons are called just as often to preside over the end of their patient’s lives – work that requires just as much skill as any technical procedure. Dr. Marsh recognized the tremendous human cost of neglecting that work. For cases that appear “hopeless,” he writes, “We often end up operating because it’s easier than being honest, and it means that we can avoid a painful conversation.”
We are only beginning to understand the many issues that neurosurgical patients face at the end of life, but so far it is clear that neurosurgical trainees require substantive training in prognostication, communication, and palliation (Crit Care Med. 2015 Sep;43[9]:1964-77 1,2; J Neurooncol. 2009 Jan;91[1]:39-43). Is there room in the current training paradigm for more formal education in these domains? As we move further into the 21st century, we must embrace the need for masterful clinicians outside of the operating room if we are to ever challenge the axiom set forth by the renowned French surgeon, René Leriche, some 65 years ago: “Every surgeon carries within himself a small cemetery, where from time to time he goes to pray – a place of bitterness and regret, where he must look for an explanation for his failures.” Let us look forward to the day when this is no longer the case.
Stephen Miranda is a medical student from the University of Rochester, who is now working as a research fellow at Ariadne Labs, a joint center for health systems innovation at Brigham & Women’s Hospital and Harvard T.H. Chan School of Public Health, both in Boston.
A new year, a new wish list
It’s 2016. Where am I?
2015 was a mixed year for neurologists and doctors in general. The Sustainable Growth Rate was repealed in a rare moment of bipartisan cooperation. Whether this will stem the tide of doctors leaving Medicare remains to be seen. In my area, it seems like another internist changes to concierge practice every week.
Even with these changes, I can’t say the reimbursement rates have returned to previous levels. Neurologists, in a primarily thinking field, often take the brunt of cuts on the few procedures we have. Like other fields, we try to cram more things into limited time and hope it all somehow works out.
2016 brings an election year, and again doctors will be in the unenviable position of ping-pong balls whacked between both sides to score political points. It would be nice to have political parties willing to work out what’s best for the health of Americans as a whole rather than trying to fire up the extreme ends of the political spectrum.
2015 was the year a new International Classification of Diseases system was foisted on us for reasons I still don’t understand. With it came a whole new wave of codes and modifiers to learn. This in turn takes a lot of time, for which we aren’t paid. Time is something I, and most docs, don’t have a lot of. I’d like to focus on caring for patients, and nothing more, but the powers that be appear to have a dim view of such silliness. This brings me back to watching internists gradually shift to cash-pay models and wondering how big the demand would be for a general neurologist in that world. The only one I know who actually did it shut down in a few months.
What’s on my wish list in 2016? Obviously, the health and welfare of myself and those around me comes first. For my patients, it’s some breakthroughs for the terrible diseases we still have no real treatments for. For my practice, it’s staying strong enough to remain independent. Some better reimbursement and non–snake oil sources of revenue are always nice. I’m hoping that in 1 year I’ll be able to write something more optimistic.
Wishing you all a great 2016!
Dr. Block has a solo neurology practice in Scottsdale, Ariz.
It’s 2016. Where am I?
2015 was a mixed year for neurologists and doctors in general. The Sustainable Growth Rate was repealed in a rare moment of bipartisan cooperation. Whether this will stem the tide of doctors leaving Medicare remains to be seen. In my area, it seems like another internist changes to concierge practice every week.
Even with these changes, I can’t say the reimbursement rates have returned to previous levels. Neurologists, in a primarily thinking field, often take the brunt of cuts on the few procedures we have. Like other fields, we try to cram more things into limited time and hope it all somehow works out.
2016 brings an election year, and again doctors will be in the unenviable position of ping-pong balls whacked between both sides to score political points. It would be nice to have political parties willing to work out what’s best for the health of Americans as a whole rather than trying to fire up the extreme ends of the political spectrum.
2015 was the year a new International Classification of Diseases system was foisted on us for reasons I still don’t understand. With it came a whole new wave of codes and modifiers to learn. This in turn takes a lot of time, for which we aren’t paid. Time is something I, and most docs, don’t have a lot of. I’d like to focus on caring for patients, and nothing more, but the powers that be appear to have a dim view of such silliness. This brings me back to watching internists gradually shift to cash-pay models and wondering how big the demand would be for a general neurologist in that world. The only one I know who actually did it shut down in a few months.
What’s on my wish list in 2016? Obviously, the health and welfare of myself and those around me comes first. For my patients, it’s some breakthroughs for the terrible diseases we still have no real treatments for. For my practice, it’s staying strong enough to remain independent. Some better reimbursement and non–snake oil sources of revenue are always nice. I’m hoping that in 1 year I’ll be able to write something more optimistic.
Wishing you all a great 2016!
Dr. Block has a solo neurology practice in Scottsdale, Ariz.
It’s 2016. Where am I?
2015 was a mixed year for neurologists and doctors in general. The Sustainable Growth Rate was repealed in a rare moment of bipartisan cooperation. Whether this will stem the tide of doctors leaving Medicare remains to be seen. In my area, it seems like another internist changes to concierge practice every week.
Even with these changes, I can’t say the reimbursement rates have returned to previous levels. Neurologists, in a primarily thinking field, often take the brunt of cuts on the few procedures we have. Like other fields, we try to cram more things into limited time and hope it all somehow works out.
2016 brings an election year, and again doctors will be in the unenviable position of ping-pong balls whacked between both sides to score political points. It would be nice to have political parties willing to work out what’s best for the health of Americans as a whole rather than trying to fire up the extreme ends of the political spectrum.
2015 was the year a new International Classification of Diseases system was foisted on us for reasons I still don’t understand. With it came a whole new wave of codes and modifiers to learn. This in turn takes a lot of time, for which we aren’t paid. Time is something I, and most docs, don’t have a lot of. I’d like to focus on caring for patients, and nothing more, but the powers that be appear to have a dim view of such silliness. This brings me back to watching internists gradually shift to cash-pay models and wondering how big the demand would be for a general neurologist in that world. The only one I know who actually did it shut down in a few months.
What’s on my wish list in 2016? Obviously, the health and welfare of myself and those around me comes first. For my patients, it’s some breakthroughs for the terrible diseases we still have no real treatments for. For my practice, it’s staying strong enough to remain independent. Some better reimbursement and non–snake oil sources of revenue are always nice. I’m hoping that in 1 year I’ll be able to write something more optimistic.
Wishing you all a great 2016!
Dr. Block has a solo neurology practice in Scottsdale, Ariz.
Myth of the Month: Beta-blocker myths
A 59-year-old man is admitted to the ICU with a myocardial infarction. He is discharged after 5 days on enalapril, metoprolol, simvastatin, and aspirin. At a 3-month follow-up, he is noted to have marked anhedonia, complaints of insomnia, feelings of worthlessness, and psychomotor retardation.
What would you do?
A) Stop the enalapril.
B) Stop the metoprolol.
C) Stop the simvastatin.
D) Begin a tricyclic antidepressant.
E) Begin an SSRI.
When I was in medical school, the dogma was to never give beta-blockers to patients with systolic heart failure, because it would worsen the heart failure.1 As we all know, this dogma completely reversed, and beta-blocker therapy is a cornerstone of treatment of patients with systolic heart failure, with improvements in morbidity and mortality.2 Underutilization of beta-blockers for indicated conditions is likely due to fear of beta-blocker side effects.2
There has long been concern that beta-blockers can cause, or worsen, depression. As a result, beta-blockers are sometimes withheld from patients with a history of depression who may benefit, or beta-blockers are stopped in patients who develop depression.
Early reports of possible beta-blocker–induced depression surfaced soon after the beta-blocker propranolol became available in the 1960s. A frequently cited reference is a letter to the British Medical Journal in which H.J. Waal reported that 20 of 89 patients on propranolol volunteered or exhibited depressive symptoms.3 Almost half of those patients were diagnosed with grade I depression – symptoms of irritability, insomnia, nightmares, and fatigue. No control group of patients was evaluated to ascertain the prevalence of those symptoms in patients treated with other antihypertensives, or in nonhypertensive patients.
M. H. Pollack and colleagues reported on a series of three patients who developed symptoms of depression after starting propranolol, and the researchers concluded that depression following the administration of propranolol was a real phenomenon.4
Many subsequent studies have cast doubt on the association of beta-blockers and depression. Depression is common following myocardial infarction and in patients with coronary artery disease. Several studies have looked closely for association with beta-blocker use in this population.
Dr. Steven J. Schleifer and colleagues evaluated 190 patients who had sustained a myocardial infarction for evidence of depression. The patients were interviewed 8-10 days after the infarct and again at 3 months. No antianginal or antihypertensive medications, including beta-blockers, were associated with an increase in depression.5
Dr. Joost P. van Melle and colleagues participated in a multicenter study that looked at patients following myocardial infarction, assessing for depressive symptoms at baseline and at 3, 6, 9, and 12 months using the Beck depression inventory.6 A total of 254 patients receiving beta-blockers were matched with 127 control patients post MI not receiving beta-blockers. No significant differences were found between non–beta-blocker users and beta-blocker users on the presence of depressive symptoms.
Robert Carney, Ph.D., and colleagues evaluated 75 patients undergoing elective cardiac catheterization with psychiatric interview and psychological assessments.7 Half of the patients in the study were receiving beta-blockers. Thirty-three percent of the patients who were not receiving beta-blockers met DSM-III criteria for depression, and 21% of the beta-blocker–treated patients met criteria for depression.
Dr. Linda Battes and colleagues reported that beta-blocker use actually decreased the risk of depression in patients who had undergone a percutaneous intervention, with a risk reduction of 49% for depression in beta-blocker–treated patients.8 In a study of elderly patients, Dr. Hendrika Luijendijk and colleagues followed 5,104 elderly persons for episodes of incident depression. They found that beta-blocker use did not increase the risk of developing depression.9
Beta-blockers often have been avoided in patients with obstructive pulmonary disease – both in patients with asthma and those with COPD – because of concern for worsening obstructive pulmonary disease. There is strong evidence now that beta-blocker use is not problematic in patients with COPD.
Dr. Surya Bhatt and colleagues found that beta-blocker use decreased COPD exacerbations.10 Almost 3,500 patients were included. During a median of 2.1 years of follow-up, beta-blocker use was associated with a significantly lower rate of total exacerbations (incidence risk ratio, 0.73; 95% confidence interval, 0.60-0.90; P = .003) and severe exacerbations (IRR, 0.67, 95% CI, 0.48-0.93; P = .016).
Dr. Qingxia Du and colleagues found that beta-blocker use in patients with COPD both reduced exacerbations and reduced mortality.11 In another study, the use of beta-blockers in patients hospitalized for acute exacerbations of COPD reduced mortality.12 Most of the patients receiving beta-blockers in that study had severe cardiovascular disease.
There are far fewer data on beta-blocker use in patients with asthma. In general, beta-blockers are routinely avoided in patients with asthma. In one small study of asthmatic patients receiving propranolol, there was no effect on methacholine challenge response, histamine responsiveness, or asthma control questionnaire results.13 In a murine model of asthma, long-term administration of beta-blockers resulted in a decrease in airway hyperresponsiveness, suggesting an anti-inflammatory effect.14 This topic is an area of interest for further study in asthma control.
So much of what we thought we knew about beta-blockers has turned out to not be so. We keep our eyes open and welcome further enlightenment.
References
1. Circulation. 1983 Jun;67(6 Pt 2):I91.
2. Expert Opin Drug Saf. 2015 Dec;14(12):1855-63.
3. Br Med J. 1967 Apr 1;2(5543):50.
4. J Nerv Ment Dis. 1985 Feb;173(2):118-9.
5. Am Heart J. 1991 May;121(5):1397-402.
6. J Am Coll Cardiol. 2006 Dec 5;48(11):2209-14.
7. Am J Med. 1987 Aug;83(2):223-6.
8. J Affect Disord. 2012 Feb;136(3):751-7.
9. J Clin Psychopharmacol. 2011 Feb;31(1):45-50.
10. Thorax. 2016 Jan;71(1):8-14.
12. Thorax. 2008 Apr;63(4):301-5.
13. Am J Respir Crit Care Med. 2013 Jun 15;187(12):1308-14.
14. Int J Gen Med. 2013 Jul 8;6:549-55.
Dr. Paauw is professor of medicine in the division of general internal medicine at the University of Washington, Seattle, and he serves as third-year medical student clerkship director at the University of Washington. Contact Dr. Paauw at [email protected].
A 59-year-old man is admitted to the ICU with a myocardial infarction. He is discharged after 5 days on enalapril, metoprolol, simvastatin, and aspirin. At a 3-month follow-up, he is noted to have marked anhedonia, complaints of insomnia, feelings of worthlessness, and psychomotor retardation.
What would you do?
A) Stop the enalapril.
B) Stop the metoprolol.
C) Stop the simvastatin.
D) Begin a tricyclic antidepressant.
E) Begin an SSRI.
When I was in medical school, the dogma was to never give beta-blockers to patients with systolic heart failure, because it would worsen the heart failure.1 As we all know, this dogma completely reversed, and beta-blocker therapy is a cornerstone of treatment of patients with systolic heart failure, with improvements in morbidity and mortality.2 Underutilization of beta-blockers for indicated conditions is likely due to fear of beta-blocker side effects.2
There has long been concern that beta-blockers can cause, or worsen, depression. As a result, beta-blockers are sometimes withheld from patients with a history of depression who may benefit, or beta-blockers are stopped in patients who develop depression.
Early reports of possible beta-blocker–induced depression surfaced soon after the beta-blocker propranolol became available in the 1960s. A frequently cited reference is a letter to the British Medical Journal in which H.J. Waal reported that 20 of 89 patients on propranolol volunteered or exhibited depressive symptoms.3 Almost half of those patients were diagnosed with grade I depression – symptoms of irritability, insomnia, nightmares, and fatigue. No control group of patients was evaluated to ascertain the prevalence of those symptoms in patients treated with other antihypertensives, or in nonhypertensive patients.
M. H. Pollack and colleagues reported on a series of three patients who developed symptoms of depression after starting propranolol, and the researchers concluded that depression following the administration of propranolol was a real phenomenon.4
Many subsequent studies have cast doubt on the association of beta-blockers and depression. Depression is common following myocardial infarction and in patients with coronary artery disease. Several studies have looked closely for association with beta-blocker use in this population.
Dr. Steven J. Schleifer and colleagues evaluated 190 patients who had sustained a myocardial infarction for evidence of depression. The patients were interviewed 8-10 days after the infarct and again at 3 months. No antianginal or antihypertensive medications, including beta-blockers, were associated with an increase in depression.5
Dr. Joost P. van Melle and colleagues participated in a multicenter study that looked at patients following myocardial infarction, assessing for depressive symptoms at baseline and at 3, 6, 9, and 12 months using the Beck depression inventory.6 A total of 254 patients receiving beta-blockers were matched with 127 control patients post MI not receiving beta-blockers. No significant differences were found between non–beta-blocker users and beta-blocker users on the presence of depressive symptoms.
Robert Carney, Ph.D., and colleagues evaluated 75 patients undergoing elective cardiac catheterization with psychiatric interview and psychological assessments.7 Half of the patients in the study were receiving beta-blockers. Thirty-three percent of the patients who were not receiving beta-blockers met DSM-III criteria for depression, and 21% of the beta-blocker–treated patients met criteria for depression.
Dr. Linda Battes and colleagues reported that beta-blocker use actually decreased the risk of depression in patients who had undergone a percutaneous intervention, with a risk reduction of 49% for depression in beta-blocker–treated patients.8 In a study of elderly patients, Dr. Hendrika Luijendijk and colleagues followed 5,104 elderly persons for episodes of incident depression. They found that beta-blocker use did not increase the risk of developing depression.9
Beta-blockers often have been avoided in patients with obstructive pulmonary disease – both in patients with asthma and those with COPD – because of concern for worsening obstructive pulmonary disease. There is strong evidence now that beta-blocker use is not problematic in patients with COPD.
Dr. Surya Bhatt and colleagues found that beta-blocker use decreased COPD exacerbations.10 Almost 3,500 patients were included. During a median of 2.1 years of follow-up, beta-blocker use was associated with a significantly lower rate of total exacerbations (incidence risk ratio, 0.73; 95% confidence interval, 0.60-0.90; P = .003) and severe exacerbations (IRR, 0.67, 95% CI, 0.48-0.93; P = .016).
Dr. Qingxia Du and colleagues found that beta-blocker use in patients with COPD both reduced exacerbations and reduced mortality.11 In another study, the use of beta-blockers in patients hospitalized for acute exacerbations of COPD reduced mortality.12 Most of the patients receiving beta-blockers in that study had severe cardiovascular disease.
There are far fewer data on beta-blocker use in patients with asthma. In general, beta-blockers are routinely avoided in patients with asthma. In one small study of asthmatic patients receiving propranolol, there was no effect on methacholine challenge response, histamine responsiveness, or asthma control questionnaire results.13 In a murine model of asthma, long-term administration of beta-blockers resulted in a decrease in airway hyperresponsiveness, suggesting an anti-inflammatory effect.14 This topic is an area of interest for further study in asthma control.
So much of what we thought we knew about beta-blockers has turned out to not be so. We keep our eyes open and welcome further enlightenment.
References
1. Circulation. 1983 Jun;67(6 Pt 2):I91.
2. Expert Opin Drug Saf. 2015 Dec;14(12):1855-63.
3. Br Med J. 1967 Apr 1;2(5543):50.
4. J Nerv Ment Dis. 1985 Feb;173(2):118-9.
5. Am Heart J. 1991 May;121(5):1397-402.
6. J Am Coll Cardiol. 2006 Dec 5;48(11):2209-14.
7. Am J Med. 1987 Aug;83(2):223-6.
8. J Affect Disord. 2012 Feb;136(3):751-7.
9. J Clin Psychopharmacol. 2011 Feb;31(1):45-50.
10. Thorax. 2016 Jan;71(1):8-14.
12. Thorax. 2008 Apr;63(4):301-5.
13. Am J Respir Crit Care Med. 2013 Jun 15;187(12):1308-14.
14. Int J Gen Med. 2013 Jul 8;6:549-55.
Dr. Paauw is professor of medicine in the division of general internal medicine at the University of Washington, Seattle, and he serves as third-year medical student clerkship director at the University of Washington. Contact Dr. Paauw at [email protected].
A 59-year-old man is admitted to the ICU with a myocardial infarction. He is discharged after 5 days on enalapril, metoprolol, simvastatin, and aspirin. At a 3-month follow-up, he is noted to have marked anhedonia, complaints of insomnia, feelings of worthlessness, and psychomotor retardation.
What would you do?
A) Stop the enalapril.
B) Stop the metoprolol.
C) Stop the simvastatin.
D) Begin a tricyclic antidepressant.
E) Begin an SSRI.
When I was in medical school, the dogma was to never give beta-blockers to patients with systolic heart failure, because it would worsen the heart failure.1 As we all know, this dogma completely reversed, and beta-blocker therapy is a cornerstone of treatment of patients with systolic heart failure, with improvements in morbidity and mortality.2 Underutilization of beta-blockers for indicated conditions is likely due to fear of beta-blocker side effects.2
There has long been concern that beta-blockers can cause, or worsen, depression. As a result, beta-blockers are sometimes withheld from patients with a history of depression who may benefit, or beta-blockers are stopped in patients who develop depression.
Early reports of possible beta-blocker–induced depression surfaced soon after the beta-blocker propranolol became available in the 1960s. A frequently cited reference is a letter to the British Medical Journal in which H.J. Waal reported that 20 of 89 patients on propranolol volunteered or exhibited depressive symptoms.3 Almost half of those patients were diagnosed with grade I depression – symptoms of irritability, insomnia, nightmares, and fatigue. No control group of patients was evaluated to ascertain the prevalence of those symptoms in patients treated with other antihypertensives, or in nonhypertensive patients.
M. H. Pollack and colleagues reported on a series of three patients who developed symptoms of depression after starting propranolol, and the researchers concluded that depression following the administration of propranolol was a real phenomenon.4
Many subsequent studies have cast doubt on the association of beta-blockers and depression. Depression is common following myocardial infarction and in patients with coronary artery disease. Several studies have looked closely for association with beta-blocker use in this population.
Dr. Steven J. Schleifer and colleagues evaluated 190 patients who had sustained a myocardial infarction for evidence of depression. The patients were interviewed 8-10 days after the infarct and again at 3 months. No antianginal or antihypertensive medications, including beta-blockers, were associated with an increase in depression.5
Dr. Joost P. van Melle and colleagues participated in a multicenter study that looked at patients following myocardial infarction, assessing for depressive symptoms at baseline and at 3, 6, 9, and 12 months using the Beck depression inventory.6 A total of 254 patients receiving beta-blockers were matched with 127 control patients post MI not receiving beta-blockers. No significant differences were found between non–beta-blocker users and beta-blocker users on the presence of depressive symptoms.
Robert Carney, Ph.D., and colleagues evaluated 75 patients undergoing elective cardiac catheterization with psychiatric interview and psychological assessments.7 Half of the patients in the study were receiving beta-blockers. Thirty-three percent of the patients who were not receiving beta-blockers met DSM-III criteria for depression, and 21% of the beta-blocker–treated patients met criteria for depression.
Dr. Linda Battes and colleagues reported that beta-blocker use actually decreased the risk of depression in patients who had undergone a percutaneous intervention, with a risk reduction of 49% for depression in beta-blocker–treated patients.8 In a study of elderly patients, Dr. Hendrika Luijendijk and colleagues followed 5,104 elderly persons for episodes of incident depression. They found that beta-blocker use did not increase the risk of developing depression.9
Beta-blockers often have been avoided in patients with obstructive pulmonary disease – both in patients with asthma and those with COPD – because of concern for worsening obstructive pulmonary disease. There is strong evidence now that beta-blocker use is not problematic in patients with COPD.
Dr. Surya Bhatt and colleagues found that beta-blocker use decreased COPD exacerbations.10 Almost 3,500 patients were included. During a median of 2.1 years of follow-up, beta-blocker use was associated with a significantly lower rate of total exacerbations (incidence risk ratio, 0.73; 95% confidence interval, 0.60-0.90; P = .003) and severe exacerbations (IRR, 0.67, 95% CI, 0.48-0.93; P = .016).
Dr. Qingxia Du and colleagues found that beta-blocker use in patients with COPD both reduced exacerbations and reduced mortality.11 In another study, the use of beta-blockers in patients hospitalized for acute exacerbations of COPD reduced mortality.12 Most of the patients receiving beta-blockers in that study had severe cardiovascular disease.
There are far fewer data on beta-blocker use in patients with asthma. In general, beta-blockers are routinely avoided in patients with asthma. In one small study of asthmatic patients receiving propranolol, there was no effect on methacholine challenge response, histamine responsiveness, or asthma control questionnaire results.13 In a murine model of asthma, long-term administration of beta-blockers resulted in a decrease in airway hyperresponsiveness, suggesting an anti-inflammatory effect.14 This topic is an area of interest for further study in asthma control.
So much of what we thought we knew about beta-blockers has turned out to not be so. We keep our eyes open and welcome further enlightenment.
References
1. Circulation. 1983 Jun;67(6 Pt 2):I91.
2. Expert Opin Drug Saf. 2015 Dec;14(12):1855-63.
3. Br Med J. 1967 Apr 1;2(5543):50.
4. J Nerv Ment Dis. 1985 Feb;173(2):118-9.
5. Am Heart J. 1991 May;121(5):1397-402.
6. J Am Coll Cardiol. 2006 Dec 5;48(11):2209-14.
7. Am J Med. 1987 Aug;83(2):223-6.
8. J Affect Disord. 2012 Feb;136(3):751-7.
9. J Clin Psychopharmacol. 2011 Feb;31(1):45-50.
10. Thorax. 2016 Jan;71(1):8-14.
12. Thorax. 2008 Apr;63(4):301-5.
13. Am J Respir Crit Care Med. 2013 Jun 15;187(12):1308-14.
14. Int J Gen Med. 2013 Jul 8;6:549-55.
Dr. Paauw is professor of medicine in the division of general internal medicine at the University of Washington, Seattle, and he serves as third-year medical student clerkship director at the University of Washington. Contact Dr. Paauw at [email protected].
The scribe in the room and the scribe in the sky
A core feature of all electronic health records is the necessity of data input into discrete fields in the chart. This is most frequently accomplished by a combination of typing the information that is needed and selecting, by clicking, the discrete information that is required, such as specific diagnoses and lab and radiology studies. The need to efficiently and effectively input a large amount of information has presented perhaps the greatest challenge of going digital for many physicians, particularly those over 40 years of age who do not type very well.
A number of innovative solutions are now available to address this issue, none perfect, and all offering alternatives to traditional means of documentation. We will briefly review three of these alternative methods, along with some thoughts about the advantages and disadvantages of each method. Let us also say that a challenge for all the methods we will discuss is the cost of the methods, and an advantage that all these assistive technologies offer is the ability for physicians to save time and lessen aggravation. Proponents of all strategies that charge money to save physicians time state that the time saved is equal to revenue earned seeing more patients, which in turn more than pays for the cost of the solution.
Transcription software, the most popular of which is Dragon, has been available for quite some time. This software can accurately transcribe the physician’s dictated notes into the appropriate section of the EHR. Many of the most popular EHRs now have the ability to have speech recognition fully integrated into the workflow of documentation of the EHR. The benefit of transcription software is that the physician directly determines what is going to be documented in the chart and retains complete control of the note. The disadvantage is that the physician still takes time organizing the note and inputting data.
To address the issue of the physician’s needing to take time to input information into the EHR, some practices have begun to use medical “scribes” in the form of a person who is in the room during the visit and is trained to write a note as the doctor sees the patient. The scribe will also order labs and x-rays as requested by the physician. An advantage of the scribe is that the physician can focus on the patient and does not need to navigate the EHR or worry about inputting data at all. In addition, feedback is usually given to the scribe on an ongoing basis so the scribe learns the preferences of the physician. The disadvantage is that the scribe is in the room during the visit, which can be awkward for patients, particularly if sensitive information is being shared about psychological problems, family planning, STDs, or any of many other issues that are routinely discussed at primary care office visits.
Finally, a California company, Augmedix, is trying to blend a 20th-century concept with 21st-century technology, seeing and paying attention to patients while doing electronic documentation. We want to disclose that we have no personal or financial interests in the company. Augmedix is essentially a scribe service with a modern twist. The physician wears a small head-mounted computer that includes a microphone, camera, and transparent display. This allows visual and auditory data from the patient visit to be transmitted to a scribe (a real, live human) located remotely in one of Augmedix’s data centers. The scribe is “logged in” to a copy of the physician’s electronic record and documents the visit in the appropriate place in the chart. This occurs in real time, so when the physician is finished seeing the patient, the note is complete and ready to be signed off. The benefit here is that there is no additional person in the room during the visit, yet just as when a scribe is in the room, the physician does not have to deal with negotiating the complexities of input into the EHR. In addition, through a feature the company calls “concierge service,” Augmedix scribes have the ability to display data to the physician upon request. For example, if the provider says “show me the blood pressure from our last visit” or “bring up Mrs. Smith’s x-ray results,” the scribe can send the requested information right to the tiny display on the headset. This allows the clinician to be “untethered” from the computer.
The concept raises a number of technical and philosophical questions. Foremost among these questions is that of privacy. Pelu Tran, president, CCO, and cofounder, explained that the technology is completely secure and compliant with all privacy laws. The data feeds transmitted through the headset are encrypted and are not permanently stored on any of Augmedix’s servers. Once the documentation is complete, the information is destroyed. HIPAA laws allow for this arrangement in the same way other transcription services are allowed. One disadvantage is likely to be cost, but Mr. Tran states that internal data show that a typical primary care physician can have about one to three additional patient visits per day using this tool and that the added revenue from seeing more patients should cover the cost of the service. Another potential disadvantage is a question of whether the note will reflect the ideas of the physician versus becoming a transcript of the visit, including the important as well as extraneous information that might be difficult to wade through when looking back at a note.
As for us, we are still typing our notes into the EHR, for now. We remain intrigued by the range of approaches that are beginning to appear, offering options for solutions that improve the quality of physicians’ lives with attention to maintaining and improving the physician-patient relationship.
Dr. Notte is a family physician and clinical informaticist for Abington (Pa.) Memorial Hospital. He is a partner in EHR Practice Consultants, a firm that aids physicians in adopting electronic health records. Dr. Skolnik is associate director of the family medicine residency program at Abington Memorial Hospital and professor of family and community medicine at Temple University in Philadelphia.
A core feature of all electronic health records is the necessity of data input into discrete fields in the chart. This is most frequently accomplished by a combination of typing the information that is needed and selecting, by clicking, the discrete information that is required, such as specific diagnoses and lab and radiology studies. The need to efficiently and effectively input a large amount of information has presented perhaps the greatest challenge of going digital for many physicians, particularly those over 40 years of age who do not type very well.
A number of innovative solutions are now available to address this issue, none perfect, and all offering alternatives to traditional means of documentation. We will briefly review three of these alternative methods, along with some thoughts about the advantages and disadvantages of each method. Let us also say that a challenge for all the methods we will discuss is the cost of the methods, and an advantage that all these assistive technologies offer is the ability for physicians to save time and lessen aggravation. Proponents of all strategies that charge money to save physicians time state that the time saved is equal to revenue earned seeing more patients, which in turn more than pays for the cost of the solution.
Transcription software, the most popular of which is Dragon, has been available for quite some time. This software can accurately transcribe the physician’s dictated notes into the appropriate section of the EHR. Many of the most popular EHRs now have the ability to have speech recognition fully integrated into the workflow of documentation of the EHR. The benefit of transcription software is that the physician directly determines what is going to be documented in the chart and retains complete control of the note. The disadvantage is that the physician still takes time organizing the note and inputting data.
To address the issue of the physician’s needing to take time to input information into the EHR, some practices have begun to use medical “scribes” in the form of a person who is in the room during the visit and is trained to write a note as the doctor sees the patient. The scribe will also order labs and x-rays as requested by the physician. An advantage of the scribe is that the physician can focus on the patient and does not need to navigate the EHR or worry about inputting data at all. In addition, feedback is usually given to the scribe on an ongoing basis so the scribe learns the preferences of the physician. The disadvantage is that the scribe is in the room during the visit, which can be awkward for patients, particularly if sensitive information is being shared about psychological problems, family planning, STDs, or any of many other issues that are routinely discussed at primary care office visits.
Finally, a California company, Augmedix, is trying to blend a 20th-century concept with 21st-century technology, seeing and paying attention to patients while doing electronic documentation. We want to disclose that we have no personal or financial interests in the company. Augmedix is essentially a scribe service with a modern twist. The physician wears a small head-mounted computer that includes a microphone, camera, and transparent display. This allows visual and auditory data from the patient visit to be transmitted to a scribe (a real, live human) located remotely in one of Augmedix’s data centers. The scribe is “logged in” to a copy of the physician’s electronic record and documents the visit in the appropriate place in the chart. This occurs in real time, so when the physician is finished seeing the patient, the note is complete and ready to be signed off. The benefit here is that there is no additional person in the room during the visit, yet just as when a scribe is in the room, the physician does not have to deal with negotiating the complexities of input into the EHR. In addition, through a feature the company calls “concierge service,” Augmedix scribes have the ability to display data to the physician upon request. For example, if the provider says “show me the blood pressure from our last visit” or “bring up Mrs. Smith’s x-ray results,” the scribe can send the requested information right to the tiny display on the headset. This allows the clinician to be “untethered” from the computer.
The concept raises a number of technical and philosophical questions. Foremost among these questions is that of privacy. Pelu Tran, president, CCO, and cofounder, explained that the technology is completely secure and compliant with all privacy laws. The data feeds transmitted through the headset are encrypted and are not permanently stored on any of Augmedix’s servers. Once the documentation is complete, the information is destroyed. HIPAA laws allow for this arrangement in the same way other transcription services are allowed. One disadvantage is likely to be cost, but Mr. Tran states that internal data show that a typical primary care physician can have about one to three additional patient visits per day using this tool and that the added revenue from seeing more patients should cover the cost of the service. Another potential disadvantage is a question of whether the note will reflect the ideas of the physician versus becoming a transcript of the visit, including the important as well as extraneous information that might be difficult to wade through when looking back at a note.
As for us, we are still typing our notes into the EHR, for now. We remain intrigued by the range of approaches that are beginning to appear, offering options for solutions that improve the quality of physicians’ lives with attention to maintaining and improving the physician-patient relationship.
Dr. Notte is a family physician and clinical informaticist for Abington (Pa.) Memorial Hospital. He is a partner in EHR Practice Consultants, a firm that aids physicians in adopting electronic health records. Dr. Skolnik is associate director of the family medicine residency program at Abington Memorial Hospital and professor of family and community medicine at Temple University in Philadelphia.
A core feature of all electronic health records is the necessity of data input into discrete fields in the chart. This is most frequently accomplished by a combination of typing the information that is needed and selecting, by clicking, the discrete information that is required, such as specific diagnoses and lab and radiology studies. The need to efficiently and effectively input a large amount of information has presented perhaps the greatest challenge of going digital for many physicians, particularly those over 40 years of age who do not type very well.
A number of innovative solutions are now available to address this issue, none perfect, and all offering alternatives to traditional means of documentation. We will briefly review three of these alternative methods, along with some thoughts about the advantages and disadvantages of each method. Let us also say that a challenge for all the methods we will discuss is the cost of the methods, and an advantage that all these assistive technologies offer is the ability for physicians to save time and lessen aggravation. Proponents of all strategies that charge money to save physicians time state that the time saved is equal to revenue earned seeing more patients, which in turn more than pays for the cost of the solution.
Transcription software, the most popular of which is Dragon, has been available for quite some time. This software can accurately transcribe the physician’s dictated notes into the appropriate section of the EHR. Many of the most popular EHRs now have the ability to have speech recognition fully integrated into the workflow of documentation of the EHR. The benefit of transcription software is that the physician directly determines what is going to be documented in the chart and retains complete control of the note. The disadvantage is that the physician still takes time organizing the note and inputting data.
To address the issue of the physician’s needing to take time to input information into the EHR, some practices have begun to use medical “scribes” in the form of a person who is in the room during the visit and is trained to write a note as the doctor sees the patient. The scribe will also order labs and x-rays as requested by the physician. An advantage of the scribe is that the physician can focus on the patient and does not need to navigate the EHR or worry about inputting data at all. In addition, feedback is usually given to the scribe on an ongoing basis so the scribe learns the preferences of the physician. The disadvantage is that the scribe is in the room during the visit, which can be awkward for patients, particularly if sensitive information is being shared about psychological problems, family planning, STDs, or any of many other issues that are routinely discussed at primary care office visits.
Finally, a California company, Augmedix, is trying to blend a 20th-century concept with 21st-century technology, seeing and paying attention to patients while doing electronic documentation. We want to disclose that we have no personal or financial interests in the company. Augmedix is essentially a scribe service with a modern twist. The physician wears a small head-mounted computer that includes a microphone, camera, and transparent display. This allows visual and auditory data from the patient visit to be transmitted to a scribe (a real, live human) located remotely in one of Augmedix’s data centers. The scribe is “logged in” to a copy of the physician’s electronic record and documents the visit in the appropriate place in the chart. This occurs in real time, so when the physician is finished seeing the patient, the note is complete and ready to be signed off. The benefit here is that there is no additional person in the room during the visit, yet just as when a scribe is in the room, the physician does not have to deal with negotiating the complexities of input into the EHR. In addition, through a feature the company calls “concierge service,” Augmedix scribes have the ability to display data to the physician upon request. For example, if the provider says “show me the blood pressure from our last visit” or “bring up Mrs. Smith’s x-ray results,” the scribe can send the requested information right to the tiny display on the headset. This allows the clinician to be “untethered” from the computer.
The concept raises a number of technical and philosophical questions. Foremost among these questions is that of privacy. Pelu Tran, president, CCO, and cofounder, explained that the technology is completely secure and compliant with all privacy laws. The data feeds transmitted through the headset are encrypted and are not permanently stored on any of Augmedix’s servers. Once the documentation is complete, the information is destroyed. HIPAA laws allow for this arrangement in the same way other transcription services are allowed. One disadvantage is likely to be cost, but Mr. Tran states that internal data show that a typical primary care physician can have about one to three additional patient visits per day using this tool and that the added revenue from seeing more patients should cover the cost of the service. Another potential disadvantage is a question of whether the note will reflect the ideas of the physician versus becoming a transcript of the visit, including the important as well as extraneous information that might be difficult to wade through when looking back at a note.
As for us, we are still typing our notes into the EHR, for now. We remain intrigued by the range of approaches that are beginning to appear, offering options for solutions that improve the quality of physicians’ lives with attention to maintaining and improving the physician-patient relationship.
Dr. Notte is a family physician and clinical informaticist for Abington (Pa.) Memorial Hospital. He is a partner in EHR Practice Consultants, a firm that aids physicians in adopting electronic health records. Dr. Skolnik is associate director of the family medicine residency program at Abington Memorial Hospital and professor of family and community medicine at Temple University in Philadelphia.
Medical Roundtable: Peripheral T-Cell Lymphomas: A Practical Approach to Newly Diagnosed and Relapsed Patients
Moderator: Steven M. Horwitz, MD1
Discussants: Alison Moskowitz, MD1; Michelle Fanale, MD2; Andrei Shustov, MD3
From Memorial Sloan Kettering Cancer Center, New York, NY1; MD Anderson Cancer Center, Houston, TX2; University of Washington Medical Center, Seattle, WA3
Address for correspondence: Steven M. Horwitz, MD, Memorial Sloan Kettering Cancer Center, 1275 York Avenue, New York, NY 10065
E-mail: [email protected]
DR. HORWITZ: My name is Dr. Steven Horwitz from Memorial Sloan-Kettering Cancer Center. I’m joined today by Drs. Alison Moskowitz, Memorial Sloan-Kettering, Michelle Fanale of MD Anderson, and Andrei Shustov, University of Washington in Seattle. Thank you all for joining us for this conversation on T-cell lymphoma. My colleagues are all well known as experts in T-cell lymphomas. Those of you who treat these diseases recognize the systemic T-cell lymphomas as one of our greater challenges in hematologic malignancies in terms of the treatment options for patients and the frequent lack of definitive data to guide our decisions.
I thought what we would do today is have a very practical discussion about the way we think about these diseases, the decisions we make, and the way we make those decisions. I'll start off by asking when you get a referral of a patient with a new diagnosis of peripheral T-cell lymphoma (PTCL), what are some of the basic things that you first think about in terms of approaching a new patient?
DR. SHUSTOV: I think one of the biggest challenges in T-cell lymphomas still remains making the proper diagnosis. In general, pathologists in the United States have a pretty good idea when they see T-cell lymphomas, however, subclassification remains a challenge even for expert hematopathologists due to frequent histologic overlap between the subtypes of PTCL, and even with non-malignant autoimmune disorders. I frequently see patients who are diagnosed with or misdiagnosed with a different subtype of T-cell lymphoma. The most challenging is differentiation between angioimmunoblastic T-cell lymphoma (AITL), anaplastic large cell T-cell lymphoma (ALCL), and PTCL not otherwise specified (PTCL-NOS), especially when the latter patients have high expression of CD30 and/or bear features resembling AITL.
Sometimes they are a slam-dunk diagnosis, but frequently our hematopathologists reverse the diagnosis after doing additional studies on the biopsy material. The most recent case I've seen in my clinic for consultation was a patient with a diagnosis of extranodal NK-cell lymphoma that was reclassified as a gamma-delta T-cell lymphoma after additional work-up. I truly believe that it is advisable that majority, if not all PTCL cases are reviewed by expert hematopathology teams at academic centers that see large volumes of these cases.
I think it's very important to educate community physicians and patients about a proper PTCL diagnosis, especially now that more targeted therapies are being developed and the gene expression profiling techniques will probably lead to identification of specific pathways that are amenable to therapy with specific biologic agents.
DR. FANALE: I'd like to expand upon what Andrei just said. For me the next step after confirming the pathology diagnosis is to think about two things. To think about whether or not this patient is a patient who might be eligible for an ongoing front-line trial, typically if the patient meets eligibility criteria for one of our ongoing front-line trials I would really recommend to the patient to consider being enrolled in that trial, and I also think about whether the patient, if he or she enters into remission with front-line therapy, can be considered for a consolidative autologous stem cell transplant.
I think it's very important to educate community physicians and patients about a proper PTCL diagnosis. Right now, our ongoing front-line trial is the ECHELON-2 trial which is evaluating brentuximab vedotin (BV) plus cyclophosphamide, doxorubicin, prednisone (CHP [BV-CHP]) chemotherapy compared to standard of care cyclophosphamide, doxorubicin, vincristine, prednisone (CHOP) chemotherapy, and that trial is based on the promising data that we've seen in the initial phase I trial that combined BV plus CHP chemotherapy followed by maintenance BV which demonstrated both high and durable complete remission (CR) rates.1 BV is an antibody drug conjugate that's targeted at CD30 and carries initial US Food and Drug Administration approval for patients who have relapsed or refractory ALCL which has a 100% level of CD30 positivity and then also has a National Comprehensive Cancer Network listing for treating other types of relapsed or refractory CD30 positive PTCL as well.
Also there is another upcoming front-line trial, which is to combine pralatrexate plus CHOP. If a patient isn't eligible for a clinical trial or it's just not feasible for that patient to enroll in a clinical trial, I will then look further at what would be potentially the best standard of care option for that patient.
I'll look at the patient's age and performance status and if they are generally less than age 65 or so and if otherwise well, I'll preferentially treat that patient with CHOEP which is CHOP plus etoposide. And then, for a patient who's either older than this or has multiple other comorbidities, I would treat that patient typically with CHOP alone.
DR. HORWITZ: Thank you, we'll go further into the selection of initial therapies but first circle back, I was curious as to how often your center comes to a different diagnosis than the referring center, and are there pitfalls you see that alert you to be suspicious of diagnosis.
DR. SHUSTOV: I'd say probably 10% of cases that we see at our center will be reclassified by our hematopathologists. In most cases, they do not necessarily reverse the diagnosis, but provide further clarification. It is occurring to me that in the community, pathologists are less likely to call the subtype of T-cell lymphoma and limit the report to the general description of T-cell lymphoprolipherative disorder, or state something like “consistent with T-cell lymphoma with features of AITL, or with features of anaplastic lymphoma.” I would admit though, that sometimes it's very difficult to identify the specific subtype of PTCL even in the expert hands; but I'd say these cases would constitute no more than 5% of PTCL patients.
DR. HORWITZ: And in your experience is it mostly fine tuning a T-cell lymphoma diagnosis, or do you see totally different diagnoses?
DR. MOSKOWITZ: Usually review by expert hematopathologists simply leads to fine-tuning the T-cell lymphoma diagnosis, however, I occasionally see significant changes in diagnosis. Often, alterations or clarification of a diagnosis are made possible only after we provide the pathologist with clinical history. For example, a lymph node biopsy may be interpreted as ALCL, however the knowledge that the particular patient has a history of mycosis fungoides would lead the pathologist to consider the diagnosis of large cell transformation of mycosis fungoides rather than ALCL. In such a case, molecular studies are helpful in confirming that the lymph node findings originate from the same clone as that in the original mycosis fungoides lesions, rather than representing a second primary.
DR. FANALE: Very occasionally, I've seen patients truly “with a misdiagnosis and a complete revision of diagnosis” and, usually, those pitfalls that I've seen them occasionally have been the young patients—the young patients who generally have disease in the thorax and neck, who are treated as though they have classical Hodgkin lymphoma, who have very significant progression of disease on standard of care treatment. So it's important that not all cases that have CD30 positivity are classical Hodgkin lymphoma even if the patient is young.
DR. HORWITZ: I often think the systemic T-cell lymphomas usually behave in an aggressive fashion so when the clinical picture and the diagnosis don't really fit, I think about getting a second biopsy before we finalize the diagnosis. Of course, when people are ill with obviously progressing disease, you may need to move more quickly.
I often think the systemic T-cell lymphomas usually behave in an aggressive fashion so when the clinical picture and the diagnosis don't really fit, I think about getting a second biopsy before we finalize the diagnosis. To move on, when you first see a patient, what is the decision tree in your mind in terms of picking therapy or planning therapy, or what kind of things do you consider?
DR. MOSKOWITZ: The first thing I think about when deciding upon treatment for a patient with T-cell lymphoma is whether or not I plan to use a curative approach to therapy. As was mentioned by Michelle, this decision is partly based upon the patients’ comorbidities and age. For patients who are eligible for curative therapy, our frontline approach for the most common types of T-cell lymphoma is to use CHOP with or without etoposide followed by consideration for autologous stem cell transplant in first remission. There are certainly individuals for whom such an aggressive strategy would not be appropriate due to age or co-morbidities. In these individuals, we may consider CHOP-based therapy alone or sometimes even milder approaches aimed at disease control.
DR. HORWITZ: Andrei, are you similar in the CHOP/CHOEP paradigm? And if so, what do you think of those data? How do you decide between the two and when do you do that regimen versus something different?
DR. SHUSTOV: I think I will double or triple what Michelle and Alison just said; for me, the two most important decisions that I have to make in the first encounter with patients with newly diagnosed PTCL are: 1) whether we're going to pursue curative approach strategy; and 2) whether the patient can tolerate the intensity of treatments that would provide him/her with the best chance of cure or long term remission. Patients who are elderly and have high risk disease would be very hard to cure, especially considering that the consolidative transplant might carry high rates of morbidity or mortality; more conservative strategies might be appropriate in these cases. On the other hand, younger and more fit patients might benefit more from intensified initial regimens—ie, CHOEP—followed by high-dose therapy and either autologous or allogeneic stem cell transplant (ALLO).
I usually have a long initial discussion with patients and families during which we decide on the intent of treatment and what to expect from certain regimens in terms of toxicities. I typically choose CHOEP regimen (or infusional version, etoposide, prednisone, vincristine, cyclophosphamide, doxorubicin [EPOCH]) for younger patients based on recent German data, even though this was a retrospective study and benefit of adding etoposide only approached statistical significance for the majority of PTCL subtypes.2 In older patients, I try to avoid anthracyclines, especially in the palliative intent setting, based on the retrospective analysis by the International T-Cell Lymphoma Project, and frequently use CEOP regimen (CHOEP minus anthracycline).3 I find that the majority of older patients tolerate this treatment somewhat better than anthracycline-containing combinations like CHOP.
In the very elderly and frail patients, I try to avoid combination chemotherapy all together. It is a somewhat easier decision for patients with AITL. Some of them are more indolent than other sub-types, and I would treat such patients with immunomodulatory approach, ie with a combination of prednisone and cyclosporine; then, I would consider single agent therapy with one of the recently approved agents for relapsed and refractory PTCL. I would also double what Michelle said in regard to making the best attempt to enroll patients into open clinical trials, because the current standards are not really satisfactory for many T-cell lymphoma patients.
DR. HORWITZ: It sounds like we all approach a new patient similarly. However, several of our up front trials are randomized against CHOP as opposed to CHOEP. When you're consenting a patient to those trials, how do you explain it to a patient or how important do you think the etoposide is?
DR. SHUSTOV: I share your frustration with quite a few of the current study designs for that exact reason. Some of these are confirmatory trials after conditional approvals of the new agents and are important. However, as often happens, in the confirmatory trials, we use controls that are a default from a lot of historical data, or the “common” way that the majority of patients are being treated. It is really a challenge when you consent patients to studies where a control arm is something that you think might not be quite adequate.
Having said that, the CHOEP study that was mentioned several times is a retrospective subgroup analysis and the addition of etoposide had marginal benefit that approached significance, but certainly was not a home run. I don't think we are ready to say that etoposide provides survival advantage in T-cell lymphoma patients and dismiss clinical trials in favor of just giving a patient the CHOEP, even though CHOP is admittedly not the best comparator. I discuss this controversy with patients and tell them frankly that the data that we base addition of etoposide on are not the best evidence one may have. Then, I ask patients to decide which approach sounds more reasonable to them and they make their choice.
DR. FANALE: To expand just slightly upon what Andrei said, I do emphasize to the patient and to the referring doctors that if you look at National Comprehensive Cancer Network guidelines, CHOP, CHOEP, EPOCH, all of these are potential options. So there's really not yet one trial that would say that one is clearly superior to the other at this time. I also emphasize to the patient and to the referring clinician that the only way, let's say, the patient could get the targeted agent plus the chemotherapy and have that 50% chance of, potentially, receiving that combination is really through the randomized clinical trial.
DR. HORWITZ: That was excellent, thank you. So you have alluded to this a bit. How much does subtype specific treatment come into play?
DR. MOSKOWITZ: At this point in time, outside of a clinical trial, for PTCL-NOS, AITL, and ALCL, the front-line approach would typically be CHOEP followed by autologous stem cell transplant. As Michelle mentioned, for a patient with ALCL, I would offer enrollment on the ECHELON-2 study in which patients are randomized to CHOP or BV-CHP, in order to give patients the option of potentially receiving BV.
For AITL, we are now obtaining molecular testing for certain mutations, particularly IDH2, because we currently have a study open with an IDH2 inhibitor that specifically enrolls patients with IDH2-mutant AITL. Because the testing takes some time to get back, we typically test patients’ biopsies at the time of diagnosis, so that we know if they're eligible for future clinical trials in case their disease does not respond to upfront therapy.
There are T-cell lymphoma subtypes that we treat quite differently from the entities discussed so far. For human T-lymphotropic virus-1 associated adult T-cell lymphoma, for example, the data with CHOP are really not good and we typically used EPOCH with the aim to consolidate with an allogeneic stem cell transplant.
Likewise, for hepatosplenic T-cell lymphoma, we have not observed good responses with the CHOP-based therapy and therefore we typically use platinum-based or ifosfamide-based therapy upfront with the aim to consolidate with allogeneic stem cell transplant. Extranodal NK/T-cell lymphoma is another entity for which CHOP is typically not effective and we have adopted asparaginase-based regimens, such as dexamethasone, methotrexate, ifosfamide, L-asparaginase, etoposide (SMILE) for this disease.
DR. SHUSTOV: I completely agree with Alison; for more common nodal lymphomas it is really hard at this point to base a treatment decision on histology, at least, in the front-line setting. However, some of the rare and unique subtypes, we generally treat with a completely different approach (ie, extranodal NK-cell lymphomas, enteropathy-associated T-cell lymphomas, adult T-cell leukemia/lymphomas).
DR. HORWITZ: Excellent. I’m curious, in a patient with ALCL who refused randomization of the ECHELON-2 trial, would you give them BV-CHP off study or would you discuss that as an alternative were they not to participate in the trial?
DR. FANALE: No. I don't urge treatment that's not approved for a particular line of therapy off clinical protocol with the exception that, let's say, if a patient is not a candidate for chemotherapy in second line setting for a particular lymphoma such as Hodgkin lymphoma—then, I would reference published data like Alison's data for a second line use of BV say for classical Hodgkin lymphoma and work with the insurance company to get the drug approved for that patient population, but if a patient just doesn't want to go on trial because they don't like the 50/50 chance of receiving BV-CHP compared to CHOP and they say, “I really want the 100% chance. Why don't you just contact my insurance?” I will explain to them the rationale of why the trial is being conducted including the hope that if the endpoints are met and the regimen is approved for front-line therapy then patients in the future can get BV-CHP at any oncology clinic, but I tell them for now it is a protocol based treatment option.
DR. HORWITZ: That's a very good answer. Can we now touch on the idea of transplant vs no transplant in first remission. Always, sometimes, never; how do you all think about that?
DR. SHUSTOV: I think that the idea of consolidative transplant is very heavily debated and discussed at the majority of specialized PTCL meetings. The reason for that is controversial nature of current clinical evidence. In the absence of randomized trials it is very hard to compare prospective phase II trial data to historical controls. You can interpret this in two ways; you might say, well, these are good data, outcome numbers look better than historical controls, and all patients with PTCL should have a consolidative transplant; or you can say, well, I don't have randomized data, and only a randomized study would really tell us whether post-induction consolidative transplant improves survival.
That is why it is such a controversial subject, and we agree that the phase II perspective studies of transplantation are hampered by significant bias; patients who are able and willing to travel to academic centers, were more robust and able to tolerate high dose therapy. They also have chemosensitive disease and that puts them in a completely different category than those you see in populational or retrospective studies, or other historical control trials.
Having said that, when I talk to patients, and I think that this is where I involve patients into treatment decision very heavily, I present them with the data and say that it is not wrong to do or not do the transplant in first CR. I make patients and family a big part of the decision. When they ask me what would give the patient the best chance being in remission five years from today, my answer is transplant, however, the data are not perfect, and the curative potential of autologous transplant in PTCL is not known.
DR. FANALE: So typically here, we would refer most patients on for front-line consolidative autologous stem cell transplant, I think, some exceptions are the ones that Andrei already touched on. If we're seeing a patient who has PTCL-NOS and this patient is the very rare patient who has early stage disease, with really no significant risk factors, that patient, unless there were pathologic features that showed a higher level of aggressiveness as Alison commented on, this patient might be one where we might defer doing the consolidative stem cell transplant for particularly if the patient’s disease entered into remission very quickly, but this still is controversial.
I'm not sure how you practice within each of your centers, but another patient, or where we would potentially defer, is a patient with fairly limited nasal NK/T-cell lymphoma, a patient that we’ve treated, let's say, with the dexamethasone, etoposide, ifosfamide, carboplatin (DeVIC) chemotherapy regimen plus a concomitant high-dose radiation, we typically historically here have deferred doing consolidative stem cell transplant for that patient population.
In terms of what Andrei commented on for when we might consider an ALLO and for a frontline consolidation, here we typically would not. The exception to that rule is that I've had a couple of patients here who have PTCL with a secondary hemophagocytic lymphohistiocytosis syndrome and then, for those patients because the concern is that the autologous stem cell transplant probably wouldn't be enough and for those patients given that they have such a dismal prognosis from the secondary hemophagocytic lymphohistiocytosis, we send those patients on for an ALLO.
DR. MOSKOWITZ: To expand upon early stage extranodal NK/T-cell lymphoma, I agree with Michelle that we wouldn't use an autologous stem cell transplant in first remission. Typically, for patients with localized disease, we recommend 2 cycles of SMILE followed by involved field radiation. Our patients treated with this approach have typically done quite well without needing a transplant.
DR. HORWITZ: That was great. If there are no further comments on upfront therapy, we can move over to relapse setting. When you see a patient at relapse, what are your strategies and how do you approach that patient?
DR. MOSKOWITZ: The first question in my mind when a patient is either not responding to or relapsing following front-line therapy is: what is my ultimate goal? For a patient who is fit and refractory to CHOP or has relapsed after CHOP or autologous stem cell transplant, my ultimate goal would be to try to get them to an ALLO. My choice of treatment following front-line therapy depends upon whether or not we are aiming for an ALLO as well as whether a donor has been identified for the patient.
Usually, if a patient just relapsed following front-line therapy, we are not necessarily ready to proceed quickly to ALLO. This may be because a donor has not yet been identified or because the patients’ eligibility for an ALLO is not clear. In this situation, my choice of treatment would be something that can be continued, potentially for several months, while we get things in place for the transplant. Treatment options in this situation would include the approved single agents for T-cell lymphoma, such as romidepsin, belinostat, pralatrexate, as well as BV (which would be specific for ALCL). In addition, I would consider enrollment on a promising clinical trial. Among these options, my choice of treatment typically depends upon the side effect profile and/or schedule, which is individualized for the patient. The one caveat would be that I typically will aim to use a histone deacetylase inhibitor (HDAC) inhibitor as my first choice for a patient with AITL.
Usually, if a patient just relapsed following front-line therapy, we are not necessarily ready to proceed quickly to ALLO. This may be because a donor has not yet been identified or because the patients’ eligibility for an ALLO is not clear. If my patient has a donor available and we are ready to move quickly to transplant, I would use one of the multi-agent regimens, such as ifosfamide, carboplatin, etoposide (ICE) or cisplatin, cytosine arabinoside, dexamethasone (DHAP), with the aim to try to get them into remission and relatively quickly proceed to transplant. The problem with using one of these types of regimens for everyone in the second-line setting is that the treatment cannot be continued indefinitely due to cumulative toxicity; therefore we need to know that we are ready to proceed to transplant if we are going to use one of the more intense regimens.
DR. HORWITZ: How do the others approach relapse?
DR. FANALE: Generally, a lot of similarities with what Alison discussed. Typically, it's if we're going to be sending the patient on for consideration for ALLO, I think the favor would be to try to use a regimen that has a high CR rate knowing that there is a trend toward improved progression free survival for the patient who enters into CR when compared to those who did not. I think the only slight difference might be just the timing and the selection, so, typically, here, even if the patient doesn't actually have a definite established donor quite yet we'll typically favor a combination type of a treatment approach, so whether or not that would be a platinum-based regimen such as ICE, as Alison mentioned, or gemcitabine-based chemotherapy regimen or similar.
I would generally favor one of those options, usually, over a single-agent therapeutic approach just knowing that the CR rates, generally, with exception of BV for ALCL are, generally, ranging about the 10%–15% range. And then, of course, first priority would be if there is a clinical trial available whether that's with a doublet of targeted agents or with the targeted agent plus chemotherapy in the relapse setting, we would typically favor that approach for a patient being considered for a stem cell transplant, ALLO approach.
DR. SHUSTOV: I'll consolidate what Michelle and Alison just said. I think we're on the same page. To me, the most important decision (even more important in the relapse setting) is to figure out whether we are still going to try to cure the lymphoma or we will pursue a palliative approach for which now we have several treatment options. So again, I’d have a long discussion with the patient, whether we're going to try and cure the disease, or we will pursue a palliative approach.
If this is a curative approach strategy and we're heading toward ALLO, we would start searching for the donor immediately. The choice of salvage therapy depends on duration of first remission. Primary refractory disease patients who failed CHOP, CHOEP, or EPOCH outright or within 3 months, I typically consider using the single agent approach, because even ICE and DHAP type regimens don’t work well for these patients. I put my “money” into HDAC inhibitors or antifolates, or other targeted therapy, if this is anaplastic lymphoma.
For patients who had at least 6 months remission from the initial therapy, younger patients who are still fit, I agree, I would consider standard salvage regimens like DHAP, etoposide, methylprednisolone, high-dosecytarabine, cisplatin (ESHAP) and ICE, and then, follow this with allograft.
DR. HORWITZ: You have all talked about allografting, I have two questions. What is your best guess in terms of percentage of patients you see with relapsed T-cell lymphoma who actually undergo ALLO at some point and do you ever consider autologous transplantation in those who didn't have it as part of their initial therapy?
DR. SHUSTOV: It certainly depends on the type of the academic center that patients are referred to, and we all practice at academic institutions with very strong ALLO programs. In patients who we select for a curative approach (one half to two thirds) we will at least make the best effort to take them to allogeneic grafting. Patients might fall off this track if they don't respond to salvage therapies or develop significant treatment/disease-related complications, ie fungal infections, organ toxicities, poor performance status, etc. Overall, I'd say that we successfully take about half of the patients with relapsed PTCL that are willing to pursue curative approach to allograft.
In addition, I consider autologous stem cell transplant in relapse setting for three situations. One is relapsed ALK-positive ALCL, some patients with ALK-negative ALCL who have had long initial remission and after relapse, and achieved second remission with BV or other salvage therapy. Finally, I’d consider auto-transplant in patients with AITL who achieved second CR with salvage therapy.
DR. HORWITZ: In terms of the relapse setting—some of you talked about angioimmunoblastic and HDAC inhibitors or BV for ALCL—when you have a relapse patient with PTCL-NOS, how do you pick a second line agent if you're not going directly to transplant, and are there new drugs that you're particularly excited about?
DR. FANALE: To answer your questions in terms of how I might choose a targeted agent for a patient who has PTCL-NOS and doesn't have AITL or ALCL, if the patient isn't eligible for trial or trial isn't feasible for that patient, I'll typically look at schedule, and then I'll look at side effect profile. For instance, for comparison, there are two HDAC inhibitor drugs right now approved, romidepsin and belinostat, so I think that potentially in a private practice setting, belinostat might be one when you look at the efficacy, being generally, around equivalent on where a patient might prefer that regimen because of the fact that they come in for five days in a row and then, their treatment is done for that cycle.
At a larger referral center to which patients are often traveling back and forth, it can be quite difficult for a patient to stay in town to do five days of treatment in a row. Often, these patients will prefer the romidepsin schedule because of the fact that they're coming back in once per week for three weeks in a row per cycle. The other way that I'll look at it is side effect profile, so, let's say, pralatrexate compared to the HDAC inhibitors, I will usually favor the HDAC inhibitors because of the potential side effect of mucositis with pralatrexate, although I have been able to manage through the mucositis by giving the patients more of a cutaneous T-cell lymphoma dosing format.
There had been a high level of interest in new emerging agents such as the aurora A-kinase inhibitors, alisertib, and that trial is now complete and the data are to be presented at The American Society of Hematology’s Annual Meeting this year.4 Other new therapies that are emerging are the PI3K inhibitors such as duvelisib and others. One advantage for many of the drugs in current trials is that they are oral agents.
My interest also lies in the combination approach, such as two or three targeted agent combinations, with the goal that if you see favorable CR rates and progression-free survival rates in the relapsed setting that you can then potentially move these treatments to the front-line setting to potentially move beyond the CHOP-based platform of therapies.
DR. SHUSTOV: For patients outside anaplastic lymphoma where, obviously, most of us would likely use BV, given the response rate to this agent, the decision is really based on convenience of the schedule, toxicity profile, and—sometimes—patient’s preference. So, toxicity and quality of life become kind of more decision-driving factors than disease biology. I’d have a discussion with patients about all three drugs, how they are administered, and what toxicities can be expected. Four-hour infusion of romidepsin might not be acceptable for some patients who have to travel long distances to treatment centers. They may prefer more rapid infusion (they would favor a trial of pralatrexate; or, as Alison mentioned, patient prefers a five-day/daily versus weekly administration.
It's kind of a coin toss decision outside clinical trials. Certainly, participation in studies in relapse setting is the high priority. We are all really looking forward to developing doublet combinations of novel agents, ie studies like the one Michelle is running at MD Anderson with a combination of alisertib and romidepsin.
DR. MOSKOWITZ: I'll echo what both Andrei and Michelle said that our choice of treatment is individualized and depends upon side-effect profile and the schedule. With regard to novel agents, I am also very excited about the studies that will be opening with the PI-3 kinase inhibitor, IPI-145. There have been promising results seen with single-agent IPI-1455 and we will be opening a study evaluating it in combination with bortezomib or romidepsin.
In addition, I mentioned earlier the IDH2 inhibitor, which we're studying right now in patients with AITL that is characterized by the presence of the IDH2 mutation. It would be exciting to see if targeting a specific mutation in this disease translates into responses.
DR. HORWITZ: Great, I think that was fantastic. I would like to thank Drs. Moskowitz, Shustov, and Fanale for a very thorough impractical discussion on how they approach and manage patients with T-cell lymphoma. I’m impressed that there is significant consistency among these experts in terms of how they manage these uncommon and often challenging lymphomas in terms of upfront combination chemotherapy approaches, combination considerations for the use of transplantation, as well as their enthusiasm for and dedication to incorporating clinical trials as part of everyday management.
References
1. Fanale MA, Horwitz SM, Forero-Torres A, et al. Brentuximab vedotin in the front-line treatment of patients with CD30+ peripheral T-cell lymphomas: results of a phase I study. J Clin Oncol. 2014;32(28):3137–3143.
2. Schmitz N, Trümper L, Ziepert M, et al. Treatment and prognosis of mature T-cell and NK-cell lymphoma: an analysis of patients with T-cell lymphoma treated in studies of the German High-Grade Non-Hodgkin Lymphoma Study Group. Blood. 2010;116(18):3418–3425. doi: 10.1182/blood-2010-02-270785. Epub 2010 Jul 21.
3. Vose J, Armitage J, Weisenburger D, for the International T-Cell Lymphoma Project. J Clin Oncol. 2008;26(25):4124–4130. doi: 10.1200/JCO.2008.16.4558. Epub 2008 Jul 14.
4. O’Connor OA, Ozcan M, Jacobsen ED, et al. First multicenter, randomized phase 3 study in patients with relapsed/refractory peripheral T-cell lymphoma: alisertib versus investigator’s choice. Paper to be presented at: American Society of Hematology 57th Annual Meeting & Exposition; December 5–8, 2015; Orlando, FL.
5. Horwitz SM, Porcu P, Flinn I, et al. Duvelisib (IPI-145), a phosphoinositide-3-kinsae-γδ inhibitor, shows activity in patients with relapsed/refractory T-cell lymphoma. Paper presented at: American Society of Hematology 56th Annual Meeting & Exposition; December 6–9, 2014; San Francisco, CA.
Moderator: Steven M. Horwitz, MD1
Discussants: Alison Moskowitz, MD1; Michelle Fanale, MD2; Andrei Shustov, MD3
From Memorial Sloan Kettering Cancer Center, New York, NY1; MD Anderson Cancer Center, Houston, TX2; University of Washington Medical Center, Seattle, WA3
Address for correspondence: Steven M. Horwitz, MD, Memorial Sloan Kettering Cancer Center, 1275 York Avenue, New York, NY 10065
E-mail: [email protected]
DR. HORWITZ: My name is Dr. Steven Horwitz from Memorial Sloan-Kettering Cancer Center. I’m joined today by Drs. Alison Moskowitz, Memorial Sloan-Kettering, Michelle Fanale of MD Anderson, and Andrei Shustov, University of Washington in Seattle. Thank you all for joining us for this conversation on T-cell lymphoma. My colleagues are all well known as experts in T-cell lymphomas. Those of you who treat these diseases recognize the systemic T-cell lymphomas as one of our greater challenges in hematologic malignancies in terms of the treatment options for patients and the frequent lack of definitive data to guide our decisions.
I thought what we would do today is have a very practical discussion about the way we think about these diseases, the decisions we make, and the way we make those decisions. I'll start off by asking when you get a referral of a patient with a new diagnosis of peripheral T-cell lymphoma (PTCL), what are some of the basic things that you first think about in terms of approaching a new patient?
DR. SHUSTOV: I think one of the biggest challenges in T-cell lymphomas still remains making the proper diagnosis. In general, pathologists in the United States have a pretty good idea when they see T-cell lymphomas, however, subclassification remains a challenge even for expert hematopathologists due to frequent histologic overlap between the subtypes of PTCL, and even with non-malignant autoimmune disorders. I frequently see patients who are diagnosed with or misdiagnosed with a different subtype of T-cell lymphoma. The most challenging is differentiation between angioimmunoblastic T-cell lymphoma (AITL), anaplastic large cell T-cell lymphoma (ALCL), and PTCL not otherwise specified (PTCL-NOS), especially when the latter patients have high expression of CD30 and/or bear features resembling AITL.
Sometimes they are a slam-dunk diagnosis, but frequently our hematopathologists reverse the diagnosis after doing additional studies on the biopsy material. The most recent case I've seen in my clinic for consultation was a patient with a diagnosis of extranodal NK-cell lymphoma that was reclassified as a gamma-delta T-cell lymphoma after additional work-up. I truly believe that it is advisable that majority, if not all PTCL cases are reviewed by expert hematopathology teams at academic centers that see large volumes of these cases.
I think it's very important to educate community physicians and patients about a proper PTCL diagnosis, especially now that more targeted therapies are being developed and the gene expression profiling techniques will probably lead to identification of specific pathways that are amenable to therapy with specific biologic agents.
DR. FANALE: I'd like to expand upon what Andrei just said. For me the next step after confirming the pathology diagnosis is to think about two things. To think about whether or not this patient is a patient who might be eligible for an ongoing front-line trial, typically if the patient meets eligibility criteria for one of our ongoing front-line trials I would really recommend to the patient to consider being enrolled in that trial, and I also think about whether the patient, if he or she enters into remission with front-line therapy, can be considered for a consolidative autologous stem cell transplant.
I think it's very important to educate community physicians and patients about a proper PTCL diagnosis. Right now, our ongoing front-line trial is the ECHELON-2 trial which is evaluating brentuximab vedotin (BV) plus cyclophosphamide, doxorubicin, prednisone (CHP [BV-CHP]) chemotherapy compared to standard of care cyclophosphamide, doxorubicin, vincristine, prednisone (CHOP) chemotherapy, and that trial is based on the promising data that we've seen in the initial phase I trial that combined BV plus CHP chemotherapy followed by maintenance BV which demonstrated both high and durable complete remission (CR) rates.1 BV is an antibody drug conjugate that's targeted at CD30 and carries initial US Food and Drug Administration approval for patients who have relapsed or refractory ALCL which has a 100% level of CD30 positivity and then also has a National Comprehensive Cancer Network listing for treating other types of relapsed or refractory CD30 positive PTCL as well.
Also there is another upcoming front-line trial, which is to combine pralatrexate plus CHOP. If a patient isn't eligible for a clinical trial or it's just not feasible for that patient to enroll in a clinical trial, I will then look further at what would be potentially the best standard of care option for that patient.
I'll look at the patient's age and performance status and if they are generally less than age 65 or so and if otherwise well, I'll preferentially treat that patient with CHOEP which is CHOP plus etoposide. And then, for a patient who's either older than this or has multiple other comorbidities, I would treat that patient typically with CHOP alone.
DR. HORWITZ: Thank you, we'll go further into the selection of initial therapies but first circle back, I was curious as to how often your center comes to a different diagnosis than the referring center, and are there pitfalls you see that alert you to be suspicious of diagnosis.
DR. SHUSTOV: I'd say probably 10% of cases that we see at our center will be reclassified by our hematopathologists. In most cases, they do not necessarily reverse the diagnosis, but provide further clarification. It is occurring to me that in the community, pathologists are less likely to call the subtype of T-cell lymphoma and limit the report to the general description of T-cell lymphoprolipherative disorder, or state something like “consistent with T-cell lymphoma with features of AITL, or with features of anaplastic lymphoma.” I would admit though, that sometimes it's very difficult to identify the specific subtype of PTCL even in the expert hands; but I'd say these cases would constitute no more than 5% of PTCL patients.
DR. HORWITZ: And in your experience is it mostly fine tuning a T-cell lymphoma diagnosis, or do you see totally different diagnoses?
DR. MOSKOWITZ: Usually review by expert hematopathologists simply leads to fine-tuning the T-cell lymphoma diagnosis, however, I occasionally see significant changes in diagnosis. Often, alterations or clarification of a diagnosis are made possible only after we provide the pathologist with clinical history. For example, a lymph node biopsy may be interpreted as ALCL, however the knowledge that the particular patient has a history of mycosis fungoides would lead the pathologist to consider the diagnosis of large cell transformation of mycosis fungoides rather than ALCL. In such a case, molecular studies are helpful in confirming that the lymph node findings originate from the same clone as that in the original mycosis fungoides lesions, rather than representing a second primary.
DR. FANALE: Very occasionally, I've seen patients truly “with a misdiagnosis and a complete revision of diagnosis” and, usually, those pitfalls that I've seen them occasionally have been the young patients—the young patients who generally have disease in the thorax and neck, who are treated as though they have classical Hodgkin lymphoma, who have very significant progression of disease on standard of care treatment. So it's important that not all cases that have CD30 positivity are classical Hodgkin lymphoma even if the patient is young.
DR. HORWITZ: I often think the systemic T-cell lymphomas usually behave in an aggressive fashion so when the clinical picture and the diagnosis don't really fit, I think about getting a second biopsy before we finalize the diagnosis. Of course, when people are ill with obviously progressing disease, you may need to move more quickly.
I often think the systemic T-cell lymphomas usually behave in an aggressive fashion so when the clinical picture and the diagnosis don't really fit, I think about getting a second biopsy before we finalize the diagnosis. To move on, when you first see a patient, what is the decision tree in your mind in terms of picking therapy or planning therapy, or what kind of things do you consider?
DR. MOSKOWITZ: The first thing I think about when deciding upon treatment for a patient with T-cell lymphoma is whether or not I plan to use a curative approach to therapy. As was mentioned by Michelle, this decision is partly based upon the patients’ comorbidities and age. For patients who are eligible for curative therapy, our frontline approach for the most common types of T-cell lymphoma is to use CHOP with or without etoposide followed by consideration for autologous stem cell transplant in first remission. There are certainly individuals for whom such an aggressive strategy would not be appropriate due to age or co-morbidities. In these individuals, we may consider CHOP-based therapy alone or sometimes even milder approaches aimed at disease control.
DR. HORWITZ: Andrei, are you similar in the CHOP/CHOEP paradigm? And if so, what do you think of those data? How do you decide between the two and when do you do that regimen versus something different?
DR. SHUSTOV: I think I will double or triple what Michelle and Alison just said; for me, the two most important decisions that I have to make in the first encounter with patients with newly diagnosed PTCL are: 1) whether we're going to pursue curative approach strategy; and 2) whether the patient can tolerate the intensity of treatments that would provide him/her with the best chance of cure or long term remission. Patients who are elderly and have high risk disease would be very hard to cure, especially considering that the consolidative transplant might carry high rates of morbidity or mortality; more conservative strategies might be appropriate in these cases. On the other hand, younger and more fit patients might benefit more from intensified initial regimens—ie, CHOEP—followed by high-dose therapy and either autologous or allogeneic stem cell transplant (ALLO).
I usually have a long initial discussion with patients and families during which we decide on the intent of treatment and what to expect from certain regimens in terms of toxicities. I typically choose CHOEP regimen (or infusional version, etoposide, prednisone, vincristine, cyclophosphamide, doxorubicin [EPOCH]) for younger patients based on recent German data, even though this was a retrospective study and benefit of adding etoposide only approached statistical significance for the majority of PTCL subtypes.2 In older patients, I try to avoid anthracyclines, especially in the palliative intent setting, based on the retrospective analysis by the International T-Cell Lymphoma Project, and frequently use CEOP regimen (CHOEP minus anthracycline).3 I find that the majority of older patients tolerate this treatment somewhat better than anthracycline-containing combinations like CHOP.
In the very elderly and frail patients, I try to avoid combination chemotherapy all together. It is a somewhat easier decision for patients with AITL. Some of them are more indolent than other sub-types, and I would treat such patients with immunomodulatory approach, ie with a combination of prednisone and cyclosporine; then, I would consider single agent therapy with one of the recently approved agents for relapsed and refractory PTCL. I would also double what Michelle said in regard to making the best attempt to enroll patients into open clinical trials, because the current standards are not really satisfactory for many T-cell lymphoma patients.
DR. HORWITZ: It sounds like we all approach a new patient similarly. However, several of our up front trials are randomized against CHOP as opposed to CHOEP. When you're consenting a patient to those trials, how do you explain it to a patient or how important do you think the etoposide is?
DR. SHUSTOV: I share your frustration with quite a few of the current study designs for that exact reason. Some of these are confirmatory trials after conditional approvals of the new agents and are important. However, as often happens, in the confirmatory trials, we use controls that are a default from a lot of historical data, or the “common” way that the majority of patients are being treated. It is really a challenge when you consent patients to studies where a control arm is something that you think might not be quite adequate.
Having said that, the CHOEP study that was mentioned several times is a retrospective subgroup analysis and the addition of etoposide had marginal benefit that approached significance, but certainly was not a home run. I don't think we are ready to say that etoposide provides survival advantage in T-cell lymphoma patients and dismiss clinical trials in favor of just giving a patient the CHOEP, even though CHOP is admittedly not the best comparator. I discuss this controversy with patients and tell them frankly that the data that we base addition of etoposide on are not the best evidence one may have. Then, I ask patients to decide which approach sounds more reasonable to them and they make their choice.
DR. FANALE: To expand just slightly upon what Andrei said, I do emphasize to the patient and to the referring doctors that if you look at National Comprehensive Cancer Network guidelines, CHOP, CHOEP, EPOCH, all of these are potential options. So there's really not yet one trial that would say that one is clearly superior to the other at this time. I also emphasize to the patient and to the referring clinician that the only way, let's say, the patient could get the targeted agent plus the chemotherapy and have that 50% chance of, potentially, receiving that combination is really through the randomized clinical trial.
DR. HORWITZ: That was excellent, thank you. So you have alluded to this a bit. How much does subtype specific treatment come into play?
DR. MOSKOWITZ: At this point in time, outside of a clinical trial, for PTCL-NOS, AITL, and ALCL, the front-line approach would typically be CHOEP followed by autologous stem cell transplant. As Michelle mentioned, for a patient with ALCL, I would offer enrollment on the ECHELON-2 study in which patients are randomized to CHOP or BV-CHP, in order to give patients the option of potentially receiving BV.
For AITL, we are now obtaining molecular testing for certain mutations, particularly IDH2, because we currently have a study open with an IDH2 inhibitor that specifically enrolls patients with IDH2-mutant AITL. Because the testing takes some time to get back, we typically test patients’ biopsies at the time of diagnosis, so that we know if they're eligible for future clinical trials in case their disease does not respond to upfront therapy.
There are T-cell lymphoma subtypes that we treat quite differently from the entities discussed so far. For human T-lymphotropic virus-1 associated adult T-cell lymphoma, for example, the data with CHOP are really not good and we typically used EPOCH with the aim to consolidate with an allogeneic stem cell transplant.
Likewise, for hepatosplenic T-cell lymphoma, we have not observed good responses with the CHOP-based therapy and therefore we typically use platinum-based or ifosfamide-based therapy upfront with the aim to consolidate with allogeneic stem cell transplant. Extranodal NK/T-cell lymphoma is another entity for which CHOP is typically not effective and we have adopted asparaginase-based regimens, such as dexamethasone, methotrexate, ifosfamide, L-asparaginase, etoposide (SMILE) for this disease.
DR. SHUSTOV: I completely agree with Alison; for more common nodal lymphomas it is really hard at this point to base a treatment decision on histology, at least, in the front-line setting. However, some of the rare and unique subtypes, we generally treat with a completely different approach (ie, extranodal NK-cell lymphomas, enteropathy-associated T-cell lymphomas, adult T-cell leukemia/lymphomas).
DR. HORWITZ: Excellent. I’m curious, in a patient with ALCL who refused randomization of the ECHELON-2 trial, would you give them BV-CHP off study or would you discuss that as an alternative were they not to participate in the trial?
DR. FANALE: No. I don't urge treatment that's not approved for a particular line of therapy off clinical protocol with the exception that, let's say, if a patient is not a candidate for chemotherapy in second line setting for a particular lymphoma such as Hodgkin lymphoma—then, I would reference published data like Alison's data for a second line use of BV say for classical Hodgkin lymphoma and work with the insurance company to get the drug approved for that patient population, but if a patient just doesn't want to go on trial because they don't like the 50/50 chance of receiving BV-CHP compared to CHOP and they say, “I really want the 100% chance. Why don't you just contact my insurance?” I will explain to them the rationale of why the trial is being conducted including the hope that if the endpoints are met and the regimen is approved for front-line therapy then patients in the future can get BV-CHP at any oncology clinic, but I tell them for now it is a protocol based treatment option.
DR. HORWITZ: That's a very good answer. Can we now touch on the idea of transplant vs no transplant in first remission. Always, sometimes, never; how do you all think about that?
DR. SHUSTOV: I think that the idea of consolidative transplant is very heavily debated and discussed at the majority of specialized PTCL meetings. The reason for that is controversial nature of current clinical evidence. In the absence of randomized trials it is very hard to compare prospective phase II trial data to historical controls. You can interpret this in two ways; you might say, well, these are good data, outcome numbers look better than historical controls, and all patients with PTCL should have a consolidative transplant; or you can say, well, I don't have randomized data, and only a randomized study would really tell us whether post-induction consolidative transplant improves survival.
That is why it is such a controversial subject, and we agree that the phase II perspective studies of transplantation are hampered by significant bias; patients who are able and willing to travel to academic centers, were more robust and able to tolerate high dose therapy. They also have chemosensitive disease and that puts them in a completely different category than those you see in populational or retrospective studies, or other historical control trials.
Having said that, when I talk to patients, and I think that this is where I involve patients into treatment decision very heavily, I present them with the data and say that it is not wrong to do or not do the transplant in first CR. I make patients and family a big part of the decision. When they ask me what would give the patient the best chance being in remission five years from today, my answer is transplant, however, the data are not perfect, and the curative potential of autologous transplant in PTCL is not known.
DR. FANALE: So typically here, we would refer most patients on for front-line consolidative autologous stem cell transplant, I think, some exceptions are the ones that Andrei already touched on. If we're seeing a patient who has PTCL-NOS and this patient is the very rare patient who has early stage disease, with really no significant risk factors, that patient, unless there were pathologic features that showed a higher level of aggressiveness as Alison commented on, this patient might be one where we might defer doing the consolidative stem cell transplant for particularly if the patient’s disease entered into remission very quickly, but this still is controversial.
I'm not sure how you practice within each of your centers, but another patient, or where we would potentially defer, is a patient with fairly limited nasal NK/T-cell lymphoma, a patient that we’ve treated, let's say, with the dexamethasone, etoposide, ifosfamide, carboplatin (DeVIC) chemotherapy regimen plus a concomitant high-dose radiation, we typically historically here have deferred doing consolidative stem cell transplant for that patient population.
In terms of what Andrei commented on for when we might consider an ALLO and for a frontline consolidation, here we typically would not. The exception to that rule is that I've had a couple of patients here who have PTCL with a secondary hemophagocytic lymphohistiocytosis syndrome and then, for those patients because the concern is that the autologous stem cell transplant probably wouldn't be enough and for those patients given that they have such a dismal prognosis from the secondary hemophagocytic lymphohistiocytosis, we send those patients on for an ALLO.
DR. MOSKOWITZ: To expand upon early stage extranodal NK/T-cell lymphoma, I agree with Michelle that we wouldn't use an autologous stem cell transplant in first remission. Typically, for patients with localized disease, we recommend 2 cycles of SMILE followed by involved field radiation. Our patients treated with this approach have typically done quite well without needing a transplant.
DR. HORWITZ: That was great. If there are no further comments on upfront therapy, we can move over to relapse setting. When you see a patient at relapse, what are your strategies and how do you approach that patient?
DR. MOSKOWITZ: The first question in my mind when a patient is either not responding to or relapsing following front-line therapy is: what is my ultimate goal? For a patient who is fit and refractory to CHOP or has relapsed after CHOP or autologous stem cell transplant, my ultimate goal would be to try to get them to an ALLO. My choice of treatment following front-line therapy depends upon whether or not we are aiming for an ALLO as well as whether a donor has been identified for the patient.
Usually, if a patient just relapsed following front-line therapy, we are not necessarily ready to proceed quickly to ALLO. This may be because a donor has not yet been identified or because the patients’ eligibility for an ALLO is not clear. In this situation, my choice of treatment would be something that can be continued, potentially for several months, while we get things in place for the transplant. Treatment options in this situation would include the approved single agents for T-cell lymphoma, such as romidepsin, belinostat, pralatrexate, as well as BV (which would be specific for ALCL). In addition, I would consider enrollment on a promising clinical trial. Among these options, my choice of treatment typically depends upon the side effect profile and/or schedule, which is individualized for the patient. The one caveat would be that I typically will aim to use a histone deacetylase inhibitor (HDAC) inhibitor as my first choice for a patient with AITL.
Usually, if a patient just relapsed following front-line therapy, we are not necessarily ready to proceed quickly to ALLO. This may be because a donor has not yet been identified or because the patients’ eligibility for an ALLO is not clear. If my patient has a donor available and we are ready to move quickly to transplant, I would use one of the multi-agent regimens, such as ifosfamide, carboplatin, etoposide (ICE) or cisplatin, cytosine arabinoside, dexamethasone (DHAP), with the aim to try to get them into remission and relatively quickly proceed to transplant. The problem with using one of these types of regimens for everyone in the second-line setting is that the treatment cannot be continued indefinitely due to cumulative toxicity; therefore we need to know that we are ready to proceed to transplant if we are going to use one of the more intense regimens.
DR. HORWITZ: How do the others approach relapse?
DR. FANALE: Generally, a lot of similarities with what Alison discussed. Typically, it's if we're going to be sending the patient on for consideration for ALLO, I think the favor would be to try to use a regimen that has a high CR rate knowing that there is a trend toward improved progression free survival for the patient who enters into CR when compared to those who did not. I think the only slight difference might be just the timing and the selection, so, typically, here, even if the patient doesn't actually have a definite established donor quite yet we'll typically favor a combination type of a treatment approach, so whether or not that would be a platinum-based regimen such as ICE, as Alison mentioned, or gemcitabine-based chemotherapy regimen or similar.
I would generally favor one of those options, usually, over a single-agent therapeutic approach just knowing that the CR rates, generally, with exception of BV for ALCL are, generally, ranging about the 10%–15% range. And then, of course, first priority would be if there is a clinical trial available whether that's with a doublet of targeted agents or with the targeted agent plus chemotherapy in the relapse setting, we would typically favor that approach for a patient being considered for a stem cell transplant, ALLO approach.
DR. SHUSTOV: I'll consolidate what Michelle and Alison just said. I think we're on the same page. To me, the most important decision (even more important in the relapse setting) is to figure out whether we are still going to try to cure the lymphoma or we will pursue a palliative approach for which now we have several treatment options. So again, I’d have a long discussion with the patient, whether we're going to try and cure the disease, or we will pursue a palliative approach.
If this is a curative approach strategy and we're heading toward ALLO, we would start searching for the donor immediately. The choice of salvage therapy depends on duration of first remission. Primary refractory disease patients who failed CHOP, CHOEP, or EPOCH outright or within 3 months, I typically consider using the single agent approach, because even ICE and DHAP type regimens don’t work well for these patients. I put my “money” into HDAC inhibitors or antifolates, or other targeted therapy, if this is anaplastic lymphoma.
For patients who had at least 6 months remission from the initial therapy, younger patients who are still fit, I agree, I would consider standard salvage regimens like DHAP, etoposide, methylprednisolone, high-dosecytarabine, cisplatin (ESHAP) and ICE, and then, follow this with allograft.
DR. HORWITZ: You have all talked about allografting, I have two questions. What is your best guess in terms of percentage of patients you see with relapsed T-cell lymphoma who actually undergo ALLO at some point and do you ever consider autologous transplantation in those who didn't have it as part of their initial therapy?
DR. SHUSTOV: It certainly depends on the type of the academic center that patients are referred to, and we all practice at academic institutions with very strong ALLO programs. In patients who we select for a curative approach (one half to two thirds) we will at least make the best effort to take them to allogeneic grafting. Patients might fall off this track if they don't respond to salvage therapies or develop significant treatment/disease-related complications, ie fungal infections, organ toxicities, poor performance status, etc. Overall, I'd say that we successfully take about half of the patients with relapsed PTCL that are willing to pursue curative approach to allograft.
In addition, I consider autologous stem cell transplant in relapse setting for three situations. One is relapsed ALK-positive ALCL, some patients with ALK-negative ALCL who have had long initial remission and after relapse, and achieved second remission with BV or other salvage therapy. Finally, I’d consider auto-transplant in patients with AITL who achieved second CR with salvage therapy.
DR. HORWITZ: In terms of the relapse setting—some of you talked about angioimmunoblastic and HDAC inhibitors or BV for ALCL—when you have a relapse patient with PTCL-NOS, how do you pick a second line agent if you're not going directly to transplant, and are there new drugs that you're particularly excited about?
DR. FANALE: To answer your questions in terms of how I might choose a targeted agent for a patient who has PTCL-NOS and doesn't have AITL or ALCL, if the patient isn't eligible for trial or trial isn't feasible for that patient, I'll typically look at schedule, and then I'll look at side effect profile. For instance, for comparison, there are two HDAC inhibitor drugs right now approved, romidepsin and belinostat, so I think that potentially in a private practice setting, belinostat might be one when you look at the efficacy, being generally, around equivalent on where a patient might prefer that regimen because of the fact that they come in for five days in a row and then, their treatment is done for that cycle.
At a larger referral center to which patients are often traveling back and forth, it can be quite difficult for a patient to stay in town to do five days of treatment in a row. Often, these patients will prefer the romidepsin schedule because of the fact that they're coming back in once per week for three weeks in a row per cycle. The other way that I'll look at it is side effect profile, so, let's say, pralatrexate compared to the HDAC inhibitors, I will usually favor the HDAC inhibitors because of the potential side effect of mucositis with pralatrexate, although I have been able to manage through the mucositis by giving the patients more of a cutaneous T-cell lymphoma dosing format.
There had been a high level of interest in new emerging agents such as the aurora A-kinase inhibitors, alisertib, and that trial is now complete and the data are to be presented at The American Society of Hematology’s Annual Meeting this year.4 Other new therapies that are emerging are the PI3K inhibitors such as duvelisib and others. One advantage for many of the drugs in current trials is that they are oral agents.
My interest also lies in the combination approach, such as two or three targeted agent combinations, with the goal that if you see favorable CR rates and progression-free survival rates in the relapsed setting that you can then potentially move these treatments to the front-line setting to potentially move beyond the CHOP-based platform of therapies.
DR. SHUSTOV: For patients outside anaplastic lymphoma where, obviously, most of us would likely use BV, given the response rate to this agent, the decision is really based on convenience of the schedule, toxicity profile, and—sometimes—patient’s preference. So, toxicity and quality of life become kind of more decision-driving factors than disease biology. I’d have a discussion with patients about all three drugs, how they are administered, and what toxicities can be expected. Four-hour infusion of romidepsin might not be acceptable for some patients who have to travel long distances to treatment centers. They may prefer more rapid infusion (they would favor a trial of pralatrexate; or, as Alison mentioned, patient prefers a five-day/daily versus weekly administration.
It's kind of a coin toss decision outside clinical trials. Certainly, participation in studies in relapse setting is the high priority. We are all really looking forward to developing doublet combinations of novel agents, ie studies like the one Michelle is running at MD Anderson with a combination of alisertib and romidepsin.
DR. MOSKOWITZ: I'll echo what both Andrei and Michelle said that our choice of treatment is individualized and depends upon side-effect profile and the schedule. With regard to novel agents, I am also very excited about the studies that will be opening with the PI-3 kinase inhibitor, IPI-145. There have been promising results seen with single-agent IPI-1455 and we will be opening a study evaluating it in combination with bortezomib or romidepsin.
In addition, I mentioned earlier the IDH2 inhibitor, which we're studying right now in patients with AITL that is characterized by the presence of the IDH2 mutation. It would be exciting to see if targeting a specific mutation in this disease translates into responses.
DR. HORWITZ: Great, I think that was fantastic. I would like to thank Drs. Moskowitz, Shustov, and Fanale for a very thorough impractical discussion on how they approach and manage patients with T-cell lymphoma. I’m impressed that there is significant consistency among these experts in terms of how they manage these uncommon and often challenging lymphomas in terms of upfront combination chemotherapy approaches, combination considerations for the use of transplantation, as well as their enthusiasm for and dedication to incorporating clinical trials as part of everyday management.
References
1. Fanale MA, Horwitz SM, Forero-Torres A, et al. Brentuximab vedotin in the front-line treatment of patients with CD30+ peripheral T-cell lymphomas: results of a phase I study. J Clin Oncol. 2014;32(28):3137–3143.
2. Schmitz N, Trümper L, Ziepert M, et al. Treatment and prognosis of mature T-cell and NK-cell lymphoma: an analysis of patients with T-cell lymphoma treated in studies of the German High-Grade Non-Hodgkin Lymphoma Study Group. Blood. 2010;116(18):3418–3425. doi: 10.1182/blood-2010-02-270785. Epub 2010 Jul 21.
3. Vose J, Armitage J, Weisenburger D, for the International T-Cell Lymphoma Project. J Clin Oncol. 2008;26(25):4124–4130. doi: 10.1200/JCO.2008.16.4558. Epub 2008 Jul 14.
4. O’Connor OA, Ozcan M, Jacobsen ED, et al. First multicenter, randomized phase 3 study in patients with relapsed/refractory peripheral T-cell lymphoma: alisertib versus investigator’s choice. Paper to be presented at: American Society of Hematology 57th Annual Meeting & Exposition; December 5–8, 2015; Orlando, FL.
5. Horwitz SM, Porcu P, Flinn I, et al. Duvelisib (IPI-145), a phosphoinositide-3-kinsae-γδ inhibitor, shows activity in patients with relapsed/refractory T-cell lymphoma. Paper presented at: American Society of Hematology 56th Annual Meeting & Exposition; December 6–9, 2014; San Francisco, CA.
Moderator: Steven M. Horwitz, MD1
Discussants: Alison Moskowitz, MD1; Michelle Fanale, MD2; Andrei Shustov, MD3
From Memorial Sloan Kettering Cancer Center, New York, NY1; MD Anderson Cancer Center, Houston, TX2; University of Washington Medical Center, Seattle, WA3
Address for correspondence: Steven M. Horwitz, MD, Memorial Sloan Kettering Cancer Center, 1275 York Avenue, New York, NY 10065
E-mail: [email protected]
DR. HORWITZ: My name is Dr. Steven Horwitz from Memorial Sloan-Kettering Cancer Center. I’m joined today by Drs. Alison Moskowitz, Memorial Sloan-Kettering, Michelle Fanale of MD Anderson, and Andrei Shustov, University of Washington in Seattle. Thank you all for joining us for this conversation on T-cell lymphoma. My colleagues are all well known as experts in T-cell lymphomas. Those of you who treat these diseases recognize the systemic T-cell lymphomas as one of our greater challenges in hematologic malignancies in terms of the treatment options for patients and the frequent lack of definitive data to guide our decisions.
I thought what we would do today is have a very practical discussion about the way we think about these diseases, the decisions we make, and the way we make those decisions. I'll start off by asking when you get a referral of a patient with a new diagnosis of peripheral T-cell lymphoma (PTCL), what are some of the basic things that you first think about in terms of approaching a new patient?
DR. SHUSTOV: I think one of the biggest challenges in T-cell lymphomas still remains making the proper diagnosis. In general, pathologists in the United States have a pretty good idea when they see T-cell lymphomas, however, subclassification remains a challenge even for expert hematopathologists due to frequent histologic overlap between the subtypes of PTCL, and even with non-malignant autoimmune disorders. I frequently see patients who are diagnosed with or misdiagnosed with a different subtype of T-cell lymphoma. The most challenging is differentiation between angioimmunoblastic T-cell lymphoma (AITL), anaplastic large cell T-cell lymphoma (ALCL), and PTCL not otherwise specified (PTCL-NOS), especially when the latter patients have high expression of CD30 and/or bear features resembling AITL.
Sometimes they are a slam-dunk diagnosis, but frequently our hematopathologists reverse the diagnosis after doing additional studies on the biopsy material. The most recent case I've seen in my clinic for consultation was a patient with a diagnosis of extranodal NK-cell lymphoma that was reclassified as a gamma-delta T-cell lymphoma after additional work-up. I truly believe that it is advisable that majority, if not all PTCL cases are reviewed by expert hematopathology teams at academic centers that see large volumes of these cases.
I think it's very important to educate community physicians and patients about a proper PTCL diagnosis, especially now that more targeted therapies are being developed and the gene expression profiling techniques will probably lead to identification of specific pathways that are amenable to therapy with specific biologic agents.
DR. FANALE: I'd like to expand upon what Andrei just said. For me the next step after confirming the pathology diagnosis is to think about two things. To think about whether or not this patient is a patient who might be eligible for an ongoing front-line trial, typically if the patient meets eligibility criteria for one of our ongoing front-line trials I would really recommend to the patient to consider being enrolled in that trial, and I also think about whether the patient, if he or she enters into remission with front-line therapy, can be considered for a consolidative autologous stem cell transplant.
I think it's very important to educate community physicians and patients about a proper PTCL diagnosis. Right now, our ongoing front-line trial is the ECHELON-2 trial which is evaluating brentuximab vedotin (BV) plus cyclophosphamide, doxorubicin, prednisone (CHP [BV-CHP]) chemotherapy compared to standard of care cyclophosphamide, doxorubicin, vincristine, prednisone (CHOP) chemotherapy, and that trial is based on the promising data that we've seen in the initial phase I trial that combined BV plus CHP chemotherapy followed by maintenance BV which demonstrated both high and durable complete remission (CR) rates.1 BV is an antibody drug conjugate that's targeted at CD30 and carries initial US Food and Drug Administration approval for patients who have relapsed or refractory ALCL which has a 100% level of CD30 positivity and then also has a National Comprehensive Cancer Network listing for treating other types of relapsed or refractory CD30 positive PTCL as well.
Also there is another upcoming front-line trial, which is to combine pralatrexate plus CHOP. If a patient isn't eligible for a clinical trial or it's just not feasible for that patient to enroll in a clinical trial, I will then look further at what would be potentially the best standard of care option for that patient.
I'll look at the patient's age and performance status and if they are generally less than age 65 or so and if otherwise well, I'll preferentially treat that patient with CHOEP which is CHOP plus etoposide. And then, for a patient who's either older than this or has multiple other comorbidities, I would treat that patient typically with CHOP alone.
DR. HORWITZ: Thank you, we'll go further into the selection of initial therapies but first circle back, I was curious as to how often your center comes to a different diagnosis than the referring center, and are there pitfalls you see that alert you to be suspicious of diagnosis.
DR. SHUSTOV: I'd say probably 10% of cases that we see at our center will be reclassified by our hematopathologists. In most cases, they do not necessarily reverse the diagnosis, but provide further clarification. It is occurring to me that in the community, pathologists are less likely to call the subtype of T-cell lymphoma and limit the report to the general description of T-cell lymphoprolipherative disorder, or state something like “consistent with T-cell lymphoma with features of AITL, or with features of anaplastic lymphoma.” I would admit though, that sometimes it's very difficult to identify the specific subtype of PTCL even in the expert hands; but I'd say these cases would constitute no more than 5% of PTCL patients.
DR. HORWITZ: And in your experience is it mostly fine tuning a T-cell lymphoma diagnosis, or do you see totally different diagnoses?
DR. MOSKOWITZ: Usually review by expert hematopathologists simply leads to fine-tuning the T-cell lymphoma diagnosis, however, I occasionally see significant changes in diagnosis. Often, alterations or clarification of a diagnosis are made possible only after we provide the pathologist with clinical history. For example, a lymph node biopsy may be interpreted as ALCL, however the knowledge that the particular patient has a history of mycosis fungoides would lead the pathologist to consider the diagnosis of large cell transformation of mycosis fungoides rather than ALCL. In such a case, molecular studies are helpful in confirming that the lymph node findings originate from the same clone as that in the original mycosis fungoides lesions, rather than representing a second primary.
DR. FANALE: Very occasionally, I've seen patients truly “with a misdiagnosis and a complete revision of diagnosis” and, usually, those pitfalls that I've seen them occasionally have been the young patients—the young patients who generally have disease in the thorax and neck, who are treated as though they have classical Hodgkin lymphoma, who have very significant progression of disease on standard of care treatment. So it's important that not all cases that have CD30 positivity are classical Hodgkin lymphoma even if the patient is young.
DR. HORWITZ: I often think the systemic T-cell lymphomas usually behave in an aggressive fashion so when the clinical picture and the diagnosis don't really fit, I think about getting a second biopsy before we finalize the diagnosis. Of course, when people are ill with obviously progressing disease, you may need to move more quickly.
I often think the systemic T-cell lymphomas usually behave in an aggressive fashion so when the clinical picture and the diagnosis don't really fit, I think about getting a second biopsy before we finalize the diagnosis. To move on, when you first see a patient, what is the decision tree in your mind in terms of picking therapy or planning therapy, or what kind of things do you consider?
DR. MOSKOWITZ: The first thing I think about when deciding upon treatment for a patient with T-cell lymphoma is whether or not I plan to use a curative approach to therapy. As was mentioned by Michelle, this decision is partly based upon the patients’ comorbidities and age. For patients who are eligible for curative therapy, our frontline approach for the most common types of T-cell lymphoma is to use CHOP with or without etoposide followed by consideration for autologous stem cell transplant in first remission. There are certainly individuals for whom such an aggressive strategy would not be appropriate due to age or co-morbidities. In these individuals, we may consider CHOP-based therapy alone or sometimes even milder approaches aimed at disease control.
DR. HORWITZ: Andrei, are you similar in the CHOP/CHOEP paradigm? And if so, what do you think of those data? How do you decide between the two and when do you do that regimen versus something different?
DR. SHUSTOV: I think I will double or triple what Michelle and Alison just said; for me, the two most important decisions that I have to make in the first encounter with patients with newly diagnosed PTCL are: 1) whether we're going to pursue curative approach strategy; and 2) whether the patient can tolerate the intensity of treatments that would provide him/her with the best chance of cure or long term remission. Patients who are elderly and have high risk disease would be very hard to cure, especially considering that the consolidative transplant might carry high rates of morbidity or mortality; more conservative strategies might be appropriate in these cases. On the other hand, younger and more fit patients might benefit more from intensified initial regimens—ie, CHOEP—followed by high-dose therapy and either autologous or allogeneic stem cell transplant (ALLO).
I usually have a long initial discussion with patients and families during which we decide on the intent of treatment and what to expect from certain regimens in terms of toxicities. I typically choose CHOEP regimen (or infusional version, etoposide, prednisone, vincristine, cyclophosphamide, doxorubicin [EPOCH]) for younger patients based on recent German data, even though this was a retrospective study and benefit of adding etoposide only approached statistical significance for the majority of PTCL subtypes.2 In older patients, I try to avoid anthracyclines, especially in the palliative intent setting, based on the retrospective analysis by the International T-Cell Lymphoma Project, and frequently use CEOP regimen (CHOEP minus anthracycline).3 I find that the majority of older patients tolerate this treatment somewhat better than anthracycline-containing combinations like CHOP.
In the very elderly and frail patients, I try to avoid combination chemotherapy all together. It is a somewhat easier decision for patients with AITL. Some of them are more indolent than other sub-types, and I would treat such patients with immunomodulatory approach, ie with a combination of prednisone and cyclosporine; then, I would consider single agent therapy with one of the recently approved agents for relapsed and refractory PTCL. I would also double what Michelle said in regard to making the best attempt to enroll patients into open clinical trials, because the current standards are not really satisfactory for many T-cell lymphoma patients.
DR. HORWITZ: It sounds like we all approach a new patient similarly. However, several of our up front trials are randomized against CHOP as opposed to CHOEP. When you're consenting a patient to those trials, how do you explain it to a patient or how important do you think the etoposide is?
DR. SHUSTOV: I share your frustration with quite a few of the current study designs for that exact reason. Some of these are confirmatory trials after conditional approvals of the new agents and are important. However, as often happens, in the confirmatory trials, we use controls that are a default from a lot of historical data, or the “common” way that the majority of patients are being treated. It is really a challenge when you consent patients to studies where a control arm is something that you think might not be quite adequate.
Having said that, the CHOEP study that was mentioned several times is a retrospective subgroup analysis and the addition of etoposide had marginal benefit that approached significance, but certainly was not a home run. I don't think we are ready to say that etoposide provides survival advantage in T-cell lymphoma patients and dismiss clinical trials in favor of just giving a patient the CHOEP, even though CHOP is admittedly not the best comparator. I discuss this controversy with patients and tell them frankly that the data that we base addition of etoposide on are not the best evidence one may have. Then, I ask patients to decide which approach sounds more reasonable to them and they make their choice.
DR. FANALE: To expand just slightly upon what Andrei said, I do emphasize to the patient and to the referring doctors that if you look at National Comprehensive Cancer Network guidelines, CHOP, CHOEP, EPOCH, all of these are potential options. So there's really not yet one trial that would say that one is clearly superior to the other at this time. I also emphasize to the patient and to the referring clinician that the only way, let's say, the patient could get the targeted agent plus the chemotherapy and have that 50% chance of, potentially, receiving that combination is really through the randomized clinical trial.
DR. HORWITZ: That was excellent, thank you. So you have alluded to this a bit. How much does subtype specific treatment come into play?
DR. MOSKOWITZ: At this point in time, outside of a clinical trial, for PTCL-NOS, AITL, and ALCL, the front-line approach would typically be CHOEP followed by autologous stem cell transplant. As Michelle mentioned, for a patient with ALCL, I would offer enrollment on the ECHELON-2 study in which patients are randomized to CHOP or BV-CHP, in order to give patients the option of potentially receiving BV.
For AITL, we are now obtaining molecular testing for certain mutations, particularly IDH2, because we currently have a study open with an IDH2 inhibitor that specifically enrolls patients with IDH2-mutant AITL. Because the testing takes some time to get back, we typically test patients’ biopsies at the time of diagnosis, so that we know if they're eligible for future clinical trials in case their disease does not respond to upfront therapy.
There are T-cell lymphoma subtypes that we treat quite differently from the entities discussed so far. For human T-lymphotropic virus-1 associated adult T-cell lymphoma, for example, the data with CHOP are really not good and we typically used EPOCH with the aim to consolidate with an allogeneic stem cell transplant.
Likewise, for hepatosplenic T-cell lymphoma, we have not observed good responses with the CHOP-based therapy and therefore we typically use platinum-based or ifosfamide-based therapy upfront with the aim to consolidate with allogeneic stem cell transplant. Extranodal NK/T-cell lymphoma is another entity for which CHOP is typically not effective and we have adopted asparaginase-based regimens, such as dexamethasone, methotrexate, ifosfamide, L-asparaginase, etoposide (SMILE) for this disease.
DR. SHUSTOV: I completely agree with Alison; for more common nodal lymphomas it is really hard at this point to base a treatment decision on histology, at least, in the front-line setting. However, some of the rare and unique subtypes, we generally treat with a completely different approach (ie, extranodal NK-cell lymphomas, enteropathy-associated T-cell lymphomas, adult T-cell leukemia/lymphomas).
DR. HORWITZ: Excellent. I’m curious, in a patient with ALCL who refused randomization of the ECHELON-2 trial, would you give them BV-CHP off study or would you discuss that as an alternative were they not to participate in the trial?
DR. FANALE: No. I don't urge treatment that's not approved for a particular line of therapy off clinical protocol with the exception that, let's say, if a patient is not a candidate for chemotherapy in second line setting for a particular lymphoma such as Hodgkin lymphoma—then, I would reference published data like Alison's data for a second line use of BV say for classical Hodgkin lymphoma and work with the insurance company to get the drug approved for that patient population, but if a patient just doesn't want to go on trial because they don't like the 50/50 chance of receiving BV-CHP compared to CHOP and they say, “I really want the 100% chance. Why don't you just contact my insurance?” I will explain to them the rationale of why the trial is being conducted including the hope that if the endpoints are met and the regimen is approved for front-line therapy then patients in the future can get BV-CHP at any oncology clinic, but I tell them for now it is a protocol based treatment option.
DR. HORWITZ: That's a very good answer. Can we now touch on the idea of transplant vs no transplant in first remission. Always, sometimes, never; how do you all think about that?
DR. SHUSTOV: I think that the idea of consolidative transplant is very heavily debated and discussed at the majority of specialized PTCL meetings. The reason for that is controversial nature of current clinical evidence. In the absence of randomized trials it is very hard to compare prospective phase II trial data to historical controls. You can interpret this in two ways; you might say, well, these are good data, outcome numbers look better than historical controls, and all patients with PTCL should have a consolidative transplant; or you can say, well, I don't have randomized data, and only a randomized study would really tell us whether post-induction consolidative transplant improves survival.
That is why it is such a controversial subject, and we agree that the phase II perspective studies of transplantation are hampered by significant bias; patients who are able and willing to travel to academic centers, were more robust and able to tolerate high dose therapy. They also have chemosensitive disease and that puts them in a completely different category than those you see in populational or retrospective studies, or other historical control trials.
Having said that, when I talk to patients, and I think that this is where I involve patients into treatment decision very heavily, I present them with the data and say that it is not wrong to do or not do the transplant in first CR. I make patients and family a big part of the decision. When they ask me what would give the patient the best chance being in remission five years from today, my answer is transplant, however, the data are not perfect, and the curative potential of autologous transplant in PTCL is not known.
DR. FANALE: So typically here, we would refer most patients on for front-line consolidative autologous stem cell transplant, I think, some exceptions are the ones that Andrei already touched on. If we're seeing a patient who has PTCL-NOS and this patient is the very rare patient who has early stage disease, with really no significant risk factors, that patient, unless there were pathologic features that showed a higher level of aggressiveness as Alison commented on, this patient might be one where we might defer doing the consolidative stem cell transplant for particularly if the patient’s disease entered into remission very quickly, but this still is controversial.
I'm not sure how you practice within each of your centers, but another patient, or where we would potentially defer, is a patient with fairly limited nasal NK/T-cell lymphoma, a patient that we’ve treated, let's say, with the dexamethasone, etoposide, ifosfamide, carboplatin (DeVIC) chemotherapy regimen plus a concomitant high-dose radiation, we typically historically here have deferred doing consolidative stem cell transplant for that patient population.
In terms of what Andrei commented on for when we might consider an ALLO and for a frontline consolidation, here we typically would not. The exception to that rule is that I've had a couple of patients here who have PTCL with a secondary hemophagocytic lymphohistiocytosis syndrome and then, for those patients because the concern is that the autologous stem cell transplant probably wouldn't be enough and for those patients given that they have such a dismal prognosis from the secondary hemophagocytic lymphohistiocytosis, we send those patients on for an ALLO.
DR. MOSKOWITZ: To expand upon early stage extranodal NK/T-cell lymphoma, I agree with Michelle that we wouldn't use an autologous stem cell transplant in first remission. Typically, for patients with localized disease, we recommend 2 cycles of SMILE followed by involved field radiation. Our patients treated with this approach have typically done quite well without needing a transplant.
DR. HORWITZ: That was great. If there are no further comments on upfront therapy, we can move over to relapse setting. When you see a patient at relapse, what are your strategies and how do you approach that patient?
DR. MOSKOWITZ: The first question in my mind when a patient is either not responding to or relapsing following front-line therapy is: what is my ultimate goal? For a patient who is fit and refractory to CHOP or has relapsed after CHOP or autologous stem cell transplant, my ultimate goal would be to try to get them to an ALLO. My choice of treatment following front-line therapy depends upon whether or not we are aiming for an ALLO as well as whether a donor has been identified for the patient.
Usually, if a patient just relapsed following front-line therapy, we are not necessarily ready to proceed quickly to ALLO. This may be because a donor has not yet been identified or because the patients’ eligibility for an ALLO is not clear. In this situation, my choice of treatment would be something that can be continued, potentially for several months, while we get things in place for the transplant. Treatment options in this situation would include the approved single agents for T-cell lymphoma, such as romidepsin, belinostat, pralatrexate, as well as BV (which would be specific for ALCL). In addition, I would consider enrollment on a promising clinical trial. Among these options, my choice of treatment typically depends upon the side effect profile and/or schedule, which is individualized for the patient. The one caveat would be that I typically will aim to use a histone deacetylase inhibitor (HDAC) inhibitor as my first choice for a patient with AITL.
Usually, if a patient just relapsed following front-line therapy, we are not necessarily ready to proceed quickly to ALLO. This may be because a donor has not yet been identified or because the patients’ eligibility for an ALLO is not clear. If my patient has a donor available and we are ready to move quickly to transplant, I would use one of the multi-agent regimens, such as ifosfamide, carboplatin, etoposide (ICE) or cisplatin, cytosine arabinoside, dexamethasone (DHAP), with the aim to try to get them into remission and relatively quickly proceed to transplant. The problem with using one of these types of regimens for everyone in the second-line setting is that the treatment cannot be continued indefinitely due to cumulative toxicity; therefore we need to know that we are ready to proceed to transplant if we are going to use one of the more intense regimens.
DR. HORWITZ: How do the others approach relapse?
DR. FANALE: Generally, a lot of similarities with what Alison discussed. Typically, it's if we're going to be sending the patient on for consideration for ALLO, I think the favor would be to try to use a regimen that has a high CR rate knowing that there is a trend toward improved progression free survival for the patient who enters into CR when compared to those who did not. I think the only slight difference might be just the timing and the selection, so, typically, here, even if the patient doesn't actually have a definite established donor quite yet we'll typically favor a combination type of a treatment approach, so whether or not that would be a platinum-based regimen such as ICE, as Alison mentioned, or gemcitabine-based chemotherapy regimen or similar.
I would generally favor one of those options, usually, over a single-agent therapeutic approach just knowing that the CR rates, generally, with exception of BV for ALCL are, generally, ranging about the 10%–15% range. And then, of course, first priority would be if there is a clinical trial available whether that's with a doublet of targeted agents or with the targeted agent plus chemotherapy in the relapse setting, we would typically favor that approach for a patient being considered for a stem cell transplant, ALLO approach.
DR. SHUSTOV: I'll consolidate what Michelle and Alison just said. I think we're on the same page. To me, the most important decision (even more important in the relapse setting) is to figure out whether we are still going to try to cure the lymphoma or we will pursue a palliative approach for which now we have several treatment options. So again, I’d have a long discussion with the patient, whether we're going to try and cure the disease, or we will pursue a palliative approach.
If this is a curative approach strategy and we're heading toward ALLO, we would start searching for the donor immediately. The choice of salvage therapy depends on duration of first remission. Primary refractory disease patients who failed CHOP, CHOEP, or EPOCH outright or within 3 months, I typically consider using the single agent approach, because even ICE and DHAP type regimens don’t work well for these patients. I put my “money” into HDAC inhibitors or antifolates, or other targeted therapy, if this is anaplastic lymphoma.
For patients who had at least 6 months remission from the initial therapy, younger patients who are still fit, I agree, I would consider standard salvage regimens like DHAP, etoposide, methylprednisolone, high-dosecytarabine, cisplatin (ESHAP) and ICE, and then, follow this with allograft.
DR. HORWITZ: You have all talked about allografting, I have two questions. What is your best guess in terms of percentage of patients you see with relapsed T-cell lymphoma who actually undergo ALLO at some point and do you ever consider autologous transplantation in those who didn't have it as part of their initial therapy?
DR. SHUSTOV: It certainly depends on the type of the academic center that patients are referred to, and we all practice at academic institutions with very strong ALLO programs. In patients who we select for a curative approach (one half to two thirds) we will at least make the best effort to take them to allogeneic grafting. Patients might fall off this track if they don't respond to salvage therapies or develop significant treatment/disease-related complications, ie fungal infections, organ toxicities, poor performance status, etc. Overall, I'd say that we successfully take about half of the patients with relapsed PTCL that are willing to pursue curative approach to allograft.
In addition, I consider autologous stem cell transplant in relapse setting for three situations. One is relapsed ALK-positive ALCL, some patients with ALK-negative ALCL who have had long initial remission and after relapse, and achieved second remission with BV or other salvage therapy. Finally, I’d consider auto-transplant in patients with AITL who achieved second CR with salvage therapy.
DR. HORWITZ: In terms of the relapse setting—some of you talked about angioimmunoblastic and HDAC inhibitors or BV for ALCL—when you have a relapse patient with PTCL-NOS, how do you pick a second line agent if you're not going directly to transplant, and are there new drugs that you're particularly excited about?
DR. FANALE: To answer your questions in terms of how I might choose a targeted agent for a patient who has PTCL-NOS and doesn't have AITL or ALCL, if the patient isn't eligible for trial or trial isn't feasible for that patient, I'll typically look at schedule, and then I'll look at side effect profile. For instance, for comparison, there are two HDAC inhibitor drugs right now approved, romidepsin and belinostat, so I think that potentially in a private practice setting, belinostat might be one when you look at the efficacy, being generally, around equivalent on where a patient might prefer that regimen because of the fact that they come in for five days in a row and then, their treatment is done for that cycle.
At a larger referral center to which patients are often traveling back and forth, it can be quite difficult for a patient to stay in town to do five days of treatment in a row. Often, these patients will prefer the romidepsin schedule because of the fact that they're coming back in once per week for three weeks in a row per cycle. The other way that I'll look at it is side effect profile, so, let's say, pralatrexate compared to the HDAC inhibitors, I will usually favor the HDAC inhibitors because of the potential side effect of mucositis with pralatrexate, although I have been able to manage through the mucositis by giving the patients more of a cutaneous T-cell lymphoma dosing format.
There had been a high level of interest in new emerging agents such as the aurora A-kinase inhibitors, alisertib, and that trial is now complete and the data are to be presented at The American Society of Hematology’s Annual Meeting this year.4 Other new therapies that are emerging are the PI3K inhibitors such as duvelisib and others. One advantage for many of the drugs in current trials is that they are oral agents.
My interest also lies in the combination approach, such as two or three targeted agent combinations, with the goal that if you see favorable CR rates and progression-free survival rates in the relapsed setting that you can then potentially move these treatments to the front-line setting to potentially move beyond the CHOP-based platform of therapies.
DR. SHUSTOV: For patients outside anaplastic lymphoma where, obviously, most of us would likely use BV, given the response rate to this agent, the decision is really based on convenience of the schedule, toxicity profile, and—sometimes—patient’s preference. So, toxicity and quality of life become kind of more decision-driving factors than disease biology. I’d have a discussion with patients about all three drugs, how they are administered, and what toxicities can be expected. Four-hour infusion of romidepsin might not be acceptable for some patients who have to travel long distances to treatment centers. They may prefer more rapid infusion (they would favor a trial of pralatrexate; or, as Alison mentioned, patient prefers a five-day/daily versus weekly administration.
It's kind of a coin toss decision outside clinical trials. Certainly, participation in studies in relapse setting is the high priority. We are all really looking forward to developing doublet combinations of novel agents, ie studies like the one Michelle is running at MD Anderson with a combination of alisertib and romidepsin.
DR. MOSKOWITZ: I'll echo what both Andrei and Michelle said that our choice of treatment is individualized and depends upon side-effect profile and the schedule. With regard to novel agents, I am also very excited about the studies that will be opening with the PI-3 kinase inhibitor, IPI-145. There have been promising results seen with single-agent IPI-1455 and we will be opening a study evaluating it in combination with bortezomib or romidepsin.
In addition, I mentioned earlier the IDH2 inhibitor, which we're studying right now in patients with AITL that is characterized by the presence of the IDH2 mutation. It would be exciting to see if targeting a specific mutation in this disease translates into responses.
DR. HORWITZ: Great, I think that was fantastic. I would like to thank Drs. Moskowitz, Shustov, and Fanale for a very thorough impractical discussion on how they approach and manage patients with T-cell lymphoma. I’m impressed that there is significant consistency among these experts in terms of how they manage these uncommon and often challenging lymphomas in terms of upfront combination chemotherapy approaches, combination considerations for the use of transplantation, as well as their enthusiasm for and dedication to incorporating clinical trials as part of everyday management.
References
1. Fanale MA, Horwitz SM, Forero-Torres A, et al. Brentuximab vedotin in the front-line treatment of patients with CD30+ peripheral T-cell lymphomas: results of a phase I study. J Clin Oncol. 2014;32(28):3137–3143.
2. Schmitz N, Trümper L, Ziepert M, et al. Treatment and prognosis of mature T-cell and NK-cell lymphoma: an analysis of patients with T-cell lymphoma treated in studies of the German High-Grade Non-Hodgkin Lymphoma Study Group. Blood. 2010;116(18):3418–3425. doi: 10.1182/blood-2010-02-270785. Epub 2010 Jul 21.
3. Vose J, Armitage J, Weisenburger D, for the International T-Cell Lymphoma Project. J Clin Oncol. 2008;26(25):4124–4130. doi: 10.1200/JCO.2008.16.4558. Epub 2008 Jul 14.
4. O’Connor OA, Ozcan M, Jacobsen ED, et al. First multicenter, randomized phase 3 study in patients with relapsed/refractory peripheral T-cell lymphoma: alisertib versus investigator’s choice. Paper to be presented at: American Society of Hematology 57th Annual Meeting & Exposition; December 5–8, 2015; Orlando, FL.
5. Horwitz SM, Porcu P, Flinn I, et al. Duvelisib (IPI-145), a phosphoinositide-3-kinsae-γδ inhibitor, shows activity in patients with relapsed/refractory T-cell lymphoma. Paper presented at: American Society of Hematology 56th Annual Meeting & Exposition; December 6–9, 2014; San Francisco, CA.
The "Bottom Line" - Part II
Continuing last month’s review of quotes and analogies from past editorials illustrating key points, I found similarities between a scripted exchange from a now famous aviation emergency and a fundamental principle of emergency-medicine practice and resident education. When his aircraft suddenly lost both engines to a flock of geese upon take-off, Captain Chesley Sullenberger immediately took control from his copilot by placing his hand on the controls and announcing “my aircraft.” He then safely brought the plane down on the Hudson River 4 minutes later, saving all 155 passengers and crew on board (“My Patient” Emerg Med. 2009;41[3]:5 and Emerg Med. 2013;45[4]:1). I wrote: “…for some potentially catastrophic medical occurrences, everything depends on who is operating and who is standing a few feet away, ready to take over the controls on a moment’s notice. Emergency Medicine is one of an increasing number of specialties that have found the resources to adopt the concept of “my patient” at all hours.…”
The typical first question on ED patient satisfaction questionnaires is “apart from the wait, how would you rate your overall experience?” To me, this sounded very much like asking “apart from that Mrs Lincoln, how did you enjoy the play?” (“Patient Satisfaction,” Emerg Med. 2010;42[7]:5).
Although the Affordable Care Act of 2010 promised millions of Americans access to timely care, there were no provisions to increase the number of health care providers. As a result, ED visits continued to increase, along with the risk of compromising care due to overcrowding—even in so-called “safety-net” hospitals. “[With] the large and growing number of patients vying for space to land on the safety net, it is inevitable that some will hit the rim or miss the net entirely.”
“A National Disgrace” (Emerg Med. 2012;44[8]:2 and Emerg Med. 2015;47[7]:292), referred to continuing nationwide medication shortages, recalling “cold war images of empty shelves in Russian supermarkets which still remain vivid reminders of a failed system of government. So who would have predicted that in the 21st-century the mighty United States of America… would have hospital pharmacy shelves bereft of essential medications, including many of the sterile, injectable, crash cart meds that we rely on during resuscitations?”
“A Wintry Mix of Patients” (Emerg Med. 2013;45[3]:1 and Emerg Med. 2015;47[7]:101) considered the terrible, inexcusable plight of patients who require acute psychiatric inpatient care, waiting days or weeks in EDs for beds. It ended with “as a nation, if we cannot recognize the seriousness of this problem and if we do nothing to fix it immediately, lack of bed [capacity] is not the only lack of capacity from which we suffer.”
“Will You Still Need Me, Will You Still Feed Me…?” (Emerg Med. 2013;45[5]:1) called for age-appropriate reductions in EP night shift requirements, pointing out that “the greatest professional baseball players cannot play professionally in their 50s or 60s…”, and suggested that “staffing and running attached or satellite urgent care centers could utilize the interpersonal and clinical skills EPs have acquired over years of EM practice, while allowing their ED group to maintain financial viability…”
“We Told You So! Now What?” (Emerg Med. 2014;46[1]:5 1/14) noted that published data confirmed our prediction that the Affordable Care Act would not reduce the numbers of ED visits; and asked “…why do so many people continue to go to EDs despite the overcrowding and all of the efforts to dissuade them?” The question was answered by paraphrasing … Winston Churchill on democracy as a form of government: “for many, many people and many, many problems, EDs may be the worst form of care, except for all of the others.”
Finally, in “’Tis the Season” (Emerg Med. 2014;46[12]:5), we asked readers if they “would be able to diagnose the first case of Ebola in a febrile patient who has no travel history and presents to an ED during flu season.” Referencing some famous advice to internists who must be able to recognize rare diseases, but more frequently favor more common diagnoses, we suggested that “determining when hoofbeats are caused by a horse and when they are caused by a zebra is one of the most difficult challenges of emergency medicine.”
Before you gallop off on your own horse or zebra, we once again wish you a happy and healthy New Year.
Continuing last month’s review of quotes and analogies from past editorials illustrating key points, I found similarities between a scripted exchange from a now famous aviation emergency and a fundamental principle of emergency-medicine practice and resident education. When his aircraft suddenly lost both engines to a flock of geese upon take-off, Captain Chesley Sullenberger immediately took control from his copilot by placing his hand on the controls and announcing “my aircraft.” He then safely brought the plane down on the Hudson River 4 minutes later, saving all 155 passengers and crew on board (“My Patient” Emerg Med. 2009;41[3]:5 and Emerg Med. 2013;45[4]:1). I wrote: “…for some potentially catastrophic medical occurrences, everything depends on who is operating and who is standing a few feet away, ready to take over the controls on a moment’s notice. Emergency Medicine is one of an increasing number of specialties that have found the resources to adopt the concept of “my patient” at all hours.…”
The typical first question on ED patient satisfaction questionnaires is “apart from the wait, how would you rate your overall experience?” To me, this sounded very much like asking “apart from that Mrs Lincoln, how did you enjoy the play?” (“Patient Satisfaction,” Emerg Med. 2010;42[7]:5).
Although the Affordable Care Act of 2010 promised millions of Americans access to timely care, there were no provisions to increase the number of health care providers. As a result, ED visits continued to increase, along with the risk of compromising care due to overcrowding—even in so-called “safety-net” hospitals. “[With] the large and growing number of patients vying for space to land on the safety net, it is inevitable that some will hit the rim or miss the net entirely.”
“A National Disgrace” (Emerg Med. 2012;44[8]:2 and Emerg Med. 2015;47[7]:292), referred to continuing nationwide medication shortages, recalling “cold war images of empty shelves in Russian supermarkets which still remain vivid reminders of a failed system of government. So who would have predicted that in the 21st-century the mighty United States of America… would have hospital pharmacy shelves bereft of essential medications, including many of the sterile, injectable, crash cart meds that we rely on during resuscitations?”
“A Wintry Mix of Patients” (Emerg Med. 2013;45[3]:1 and Emerg Med. 2015;47[7]:101) considered the terrible, inexcusable plight of patients who require acute psychiatric inpatient care, waiting days or weeks in EDs for beds. It ended with “as a nation, if we cannot recognize the seriousness of this problem and if we do nothing to fix it immediately, lack of bed [capacity] is not the only lack of capacity from which we suffer.”
“Will You Still Need Me, Will You Still Feed Me…?” (Emerg Med. 2013;45[5]:1) called for age-appropriate reductions in EP night shift requirements, pointing out that “the greatest professional baseball players cannot play professionally in their 50s or 60s…”, and suggested that “staffing and running attached or satellite urgent care centers could utilize the interpersonal and clinical skills EPs have acquired over years of EM practice, while allowing their ED group to maintain financial viability…”
“We Told You So! Now What?” (Emerg Med. 2014;46[1]:5 1/14) noted that published data confirmed our prediction that the Affordable Care Act would not reduce the numbers of ED visits; and asked “…why do so many people continue to go to EDs despite the overcrowding and all of the efforts to dissuade them?” The question was answered by paraphrasing … Winston Churchill on democracy as a form of government: “for many, many people and many, many problems, EDs may be the worst form of care, except for all of the others.”
Finally, in “’Tis the Season” (Emerg Med. 2014;46[12]:5), we asked readers if they “would be able to diagnose the first case of Ebola in a febrile patient who has no travel history and presents to an ED during flu season.” Referencing some famous advice to internists who must be able to recognize rare diseases, but more frequently favor more common diagnoses, we suggested that “determining when hoofbeats are caused by a horse and when they are caused by a zebra is one of the most difficult challenges of emergency medicine.”
Before you gallop off on your own horse or zebra, we once again wish you a happy and healthy New Year.
Continuing last month’s review of quotes and analogies from past editorials illustrating key points, I found similarities between a scripted exchange from a now famous aviation emergency and a fundamental principle of emergency-medicine practice and resident education. When his aircraft suddenly lost both engines to a flock of geese upon take-off, Captain Chesley Sullenberger immediately took control from his copilot by placing his hand on the controls and announcing “my aircraft.” He then safely brought the plane down on the Hudson River 4 minutes later, saving all 155 passengers and crew on board (“My Patient” Emerg Med. 2009;41[3]:5 and Emerg Med. 2013;45[4]:1). I wrote: “…for some potentially catastrophic medical occurrences, everything depends on who is operating and who is standing a few feet away, ready to take over the controls on a moment’s notice. Emergency Medicine is one of an increasing number of specialties that have found the resources to adopt the concept of “my patient” at all hours.…”
The typical first question on ED patient satisfaction questionnaires is “apart from the wait, how would you rate your overall experience?” To me, this sounded very much like asking “apart from that Mrs Lincoln, how did you enjoy the play?” (“Patient Satisfaction,” Emerg Med. 2010;42[7]:5).
Although the Affordable Care Act of 2010 promised millions of Americans access to timely care, there were no provisions to increase the number of health care providers. As a result, ED visits continued to increase, along with the risk of compromising care due to overcrowding—even in so-called “safety-net” hospitals. “[With] the large and growing number of patients vying for space to land on the safety net, it is inevitable that some will hit the rim or miss the net entirely.”
“A National Disgrace” (Emerg Med. 2012;44[8]:2 and Emerg Med. 2015;47[7]:292), referred to continuing nationwide medication shortages, recalling “cold war images of empty shelves in Russian supermarkets which still remain vivid reminders of a failed system of government. So who would have predicted that in the 21st-century the mighty United States of America… would have hospital pharmacy shelves bereft of essential medications, including many of the sterile, injectable, crash cart meds that we rely on during resuscitations?”
“A Wintry Mix of Patients” (Emerg Med. 2013;45[3]:1 and Emerg Med. 2015;47[7]:101) considered the terrible, inexcusable plight of patients who require acute psychiatric inpatient care, waiting days or weeks in EDs for beds. It ended with “as a nation, if we cannot recognize the seriousness of this problem and if we do nothing to fix it immediately, lack of bed [capacity] is not the only lack of capacity from which we suffer.”
“Will You Still Need Me, Will You Still Feed Me…?” (Emerg Med. 2013;45[5]:1) called for age-appropriate reductions in EP night shift requirements, pointing out that “the greatest professional baseball players cannot play professionally in their 50s or 60s…”, and suggested that “staffing and running attached or satellite urgent care centers could utilize the interpersonal and clinical skills EPs have acquired over years of EM practice, while allowing their ED group to maintain financial viability…”
“We Told You So! Now What?” (Emerg Med. 2014;46[1]:5 1/14) noted that published data confirmed our prediction that the Affordable Care Act would not reduce the numbers of ED visits; and asked “…why do so many people continue to go to EDs despite the overcrowding and all of the efforts to dissuade them?” The question was answered by paraphrasing … Winston Churchill on democracy as a form of government: “for many, many people and many, many problems, EDs may be the worst form of care, except for all of the others.”
Finally, in “’Tis the Season” (Emerg Med. 2014;46[12]:5), we asked readers if they “would be able to diagnose the first case of Ebola in a febrile patient who has no travel history and presents to an ED during flu season.” Referencing some famous advice to internists who must be able to recognize rare diseases, but more frequently favor more common diagnoses, we suggested that “determining when hoofbeats are caused by a horse and when they are caused by a zebra is one of the most difficult challenges of emergency medicine.”
Before you gallop off on your own horse or zebra, we once again wish you a happy and healthy New Year.
Dispelling four myths about the FDA
Does the U.S. Food and Drug Administration control the price of drugs? Do other countries approve drugs faster than the United States? Can the FDA tell doctors how to prescribe drugs? There is a lot of misinformation about exactly what the FDA does and doesn’t do. Here are the top four FDA myths … BUSTED!
Myth 1: Patients cannot get access to drugs they need because the FDA is too slow in approving drugs.
FACT: The FDA approves drugs faster on average than all other developed nations. That is 40 days faster than Japan; 70 days faster than Canada; and 174 days faster than the European Union (EU).1
People often say that drugs are being developed and made available to patients in other countries before they are marketed here in the United States. Physicians often gripe that their patients can’t get access to medicines that are available to others overseas. These anecdotes have led to the urban legend that the FDA evaluates and approves drugs at a slower rate than foreign agencies, especially the European Medicines Agency (EMA).
In a recent report by the British-based Centre for Innovation in Regulatory Science, “over 75% of the new drugs approved by Japan, EU, Canada, Australia, Switzerland, and FDA, from 2004 to 2013, were approved first by FDA.” The FDA continues to lead among regulatory agencies in drug approvals that ensure patients get access to the lifesaving medicines they need.
The U.S. Food and Drug Administration has significantly increased the speed by which new drugs reach patients in need. Between 2006 and 2010, three out of four new drugs approved in both Europe and the U.S. were first approved by the FDA. In the specific example of cancer, the FDA also approved 32 of the 35 prospective cancer drugs between 2003-2010, whereas the EMA only approved 26. Among those cancer drugs approved, over 90% were first approved by the FDA. Just last year, almost two-thirds of the novel drugs approved by the FDA (26 of 41 or about 63%) were approved in the United States before receiving approval in any other country.2
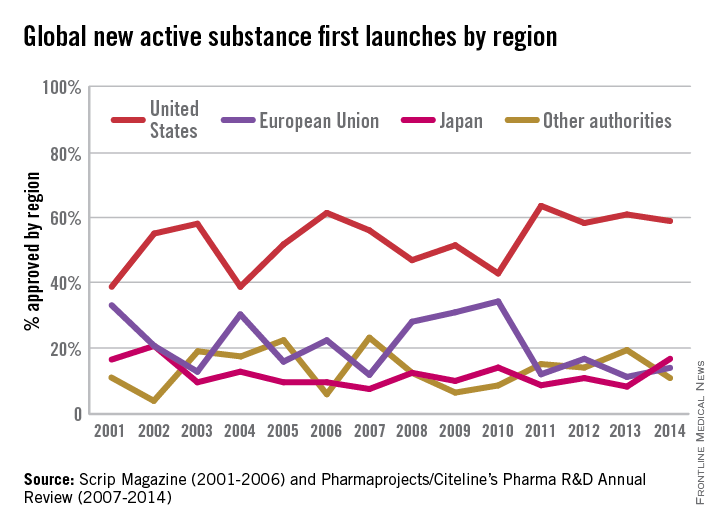
Myth 2: The FDA controls drug prices.
FACT: The FDA has no legal authority whatsoever to investigate or control the prices charged for marketed drugs. Manufacturers, distributors, and retailers establish these prices.
Drug prices do have a direct impact on the ability of people to cope with their illnesses as well as meet other expenses and the FDA recognizes that other factors beyond its purview, including insurance coverage and drug pricing, can determine patient access to drugs. However, the FDA has no legal authority whatsoever to investigate or control the prices charged for marketed drugs. Manufacturers, distributors, and retailers establish these prices.
The FDA is responsible for assuring the American public that the drugs approved today are safe and effective. In carrying out this responsibility, the FDA also works under the law to make medicines accessible to doctors and their patients through strategies such as expanding access to generic medicines, reducing the time and cost of bringing new medicines to market, as well as ensuring safe use practices and the most up-to-date information for health care professionals and patients.
Myth 3: The FDA conducts clinical trials.
FACT: The FDA does not develop, manufacture, or test drugs. The FDA does oversee the testing of new drugs to evaluate the safety and effectiveness profile in clinical trials.
Drug manufacturers submit full reports on the drug so that the FDA can evaluate their data. These studies are conducted to answer whether the drug in study works for the proposed indication. By completing a full review and analysis of the submitted data, the FDA assesses the benefit and risk of each drug to determine if the drug will be approved.
Companies must submit an investigational new drug (IND) application to the FDA before testing can begin. The IND is the means through which the sponsor obtains an exemption from the FDA to begin testing and legally transporting or distributing a drug under investigation across state lines.
The FDA’s role in the development of a new drug begins when the drug sponsor (usually the manufacturer or potential marketer) wants to test the diagnostic or therapeutic potential in humans (after having screened the new molecule for pharmacological activity and acute toxicity potential in animals). It is at this point that the molecule changes in legal status under the Federal Food, Drug, and Cosmetic Act and becomes a new drug subject to specific requirements of the drug regulatory system.3
Myth 4: The FDA regulates the practice of medicine.
FACT: The FDA regulates the approval of a drug, but not how it is prescribed. Doctors are permitted to prescribe a drug for any reason they think is medically appropriate.
The FDA creates the “drug label” in conjunction with the drug company to ensure that promotional claims are not false or misleading. The drug label of FDA-approved drugs provides information about the drug, including the approved doses and how the drug should be given to treat the medical condition for which it was approved.
However, physicians often use drugs in a way that is different from that described in the FDA-approved drug label, an “off-label” use. This can mean that the drug is:
• Used for a different disease or medical condition.
• Given in a different way (such as by a different route).
• Given in a different dose.
Off-label is also called “nonapproved” or “unapproved” use of a drug. Because drug makers have not put their drugs through the studies required by the FDA to officially approve the drug for new uses, new uses for these drugs should be taken with caution as the FDA has not reviewed the clinical evidence to support the new use. Any off-label drug usage should include a detailed conversation between physician and patient.4
Dr. John J. Whyte is the director of Professional Affairs and Stakeholder Engagement (PASE) in the FDA’s Center for Drug Evaluation and Research (CDER).
Does the U.S. Food and Drug Administration control the price of drugs? Do other countries approve drugs faster than the United States? Can the FDA tell doctors how to prescribe drugs? There is a lot of misinformation about exactly what the FDA does and doesn’t do. Here are the top four FDA myths … BUSTED!
Myth 1: Patients cannot get access to drugs they need because the FDA is too slow in approving drugs.
FACT: The FDA approves drugs faster on average than all other developed nations. That is 40 days faster than Japan; 70 days faster than Canada; and 174 days faster than the European Union (EU).1
People often say that drugs are being developed and made available to patients in other countries before they are marketed here in the United States. Physicians often gripe that their patients can’t get access to medicines that are available to others overseas. These anecdotes have led to the urban legend that the FDA evaluates and approves drugs at a slower rate than foreign agencies, especially the European Medicines Agency (EMA).
In a recent report by the British-based Centre for Innovation in Regulatory Science, “over 75% of the new drugs approved by Japan, EU, Canada, Australia, Switzerland, and FDA, from 2004 to 2013, were approved first by FDA.” The FDA continues to lead among regulatory agencies in drug approvals that ensure patients get access to the lifesaving medicines they need.
The U.S. Food and Drug Administration has significantly increased the speed by which new drugs reach patients in need. Between 2006 and 2010, three out of four new drugs approved in both Europe and the U.S. were first approved by the FDA. In the specific example of cancer, the FDA also approved 32 of the 35 prospective cancer drugs between 2003-2010, whereas the EMA only approved 26. Among those cancer drugs approved, over 90% were first approved by the FDA. Just last year, almost two-thirds of the novel drugs approved by the FDA (26 of 41 or about 63%) were approved in the United States before receiving approval in any other country.2
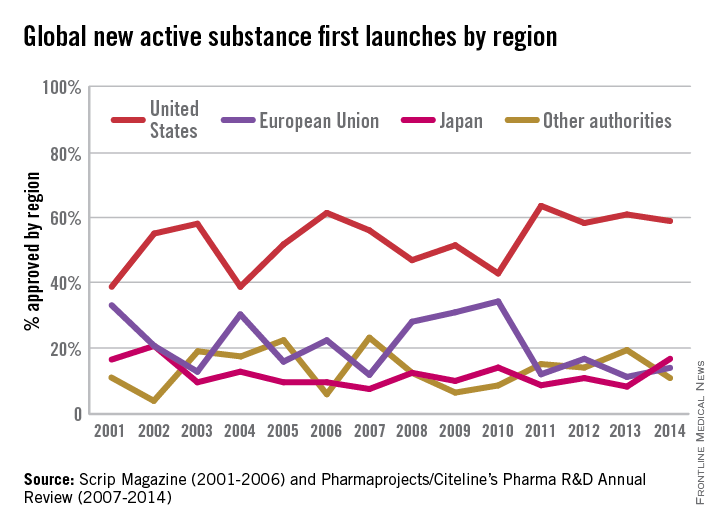
Myth 2: The FDA controls drug prices.
FACT: The FDA has no legal authority whatsoever to investigate or control the prices charged for marketed drugs. Manufacturers, distributors, and retailers establish these prices.
Drug prices do have a direct impact on the ability of people to cope with their illnesses as well as meet other expenses and the FDA recognizes that other factors beyond its purview, including insurance coverage and drug pricing, can determine patient access to drugs. However, the FDA has no legal authority whatsoever to investigate or control the prices charged for marketed drugs. Manufacturers, distributors, and retailers establish these prices.
The FDA is responsible for assuring the American public that the drugs approved today are safe and effective. In carrying out this responsibility, the FDA also works under the law to make medicines accessible to doctors and their patients through strategies such as expanding access to generic medicines, reducing the time and cost of bringing new medicines to market, as well as ensuring safe use practices and the most up-to-date information for health care professionals and patients.
Myth 3: The FDA conducts clinical trials.
FACT: The FDA does not develop, manufacture, or test drugs. The FDA does oversee the testing of new drugs to evaluate the safety and effectiveness profile in clinical trials.
Drug manufacturers submit full reports on the drug so that the FDA can evaluate their data. These studies are conducted to answer whether the drug in study works for the proposed indication. By completing a full review and analysis of the submitted data, the FDA assesses the benefit and risk of each drug to determine if the drug will be approved.
Companies must submit an investigational new drug (IND) application to the FDA before testing can begin. The IND is the means through which the sponsor obtains an exemption from the FDA to begin testing and legally transporting or distributing a drug under investigation across state lines.
The FDA’s role in the development of a new drug begins when the drug sponsor (usually the manufacturer or potential marketer) wants to test the diagnostic or therapeutic potential in humans (after having screened the new molecule for pharmacological activity and acute toxicity potential in animals). It is at this point that the molecule changes in legal status under the Federal Food, Drug, and Cosmetic Act and becomes a new drug subject to specific requirements of the drug regulatory system.3
Myth 4: The FDA regulates the practice of medicine.
FACT: The FDA regulates the approval of a drug, but not how it is prescribed. Doctors are permitted to prescribe a drug for any reason they think is medically appropriate.
The FDA creates the “drug label” in conjunction with the drug company to ensure that promotional claims are not false or misleading. The drug label of FDA-approved drugs provides information about the drug, including the approved doses and how the drug should be given to treat the medical condition for which it was approved.
However, physicians often use drugs in a way that is different from that described in the FDA-approved drug label, an “off-label” use. This can mean that the drug is:
• Used for a different disease or medical condition.
• Given in a different way (such as by a different route).
• Given in a different dose.
Off-label is also called “nonapproved” or “unapproved” use of a drug. Because drug makers have not put their drugs through the studies required by the FDA to officially approve the drug for new uses, new uses for these drugs should be taken with caution as the FDA has not reviewed the clinical evidence to support the new use. Any off-label drug usage should include a detailed conversation between physician and patient.4
Dr. John J. Whyte is the director of Professional Affairs and Stakeholder Engagement (PASE) in the FDA’s Center for Drug Evaluation and Research (CDER).
Does the U.S. Food and Drug Administration control the price of drugs? Do other countries approve drugs faster than the United States? Can the FDA tell doctors how to prescribe drugs? There is a lot of misinformation about exactly what the FDA does and doesn’t do. Here are the top four FDA myths … BUSTED!
Myth 1: Patients cannot get access to drugs they need because the FDA is too slow in approving drugs.
FACT: The FDA approves drugs faster on average than all other developed nations. That is 40 days faster than Japan; 70 days faster than Canada; and 174 days faster than the European Union (EU).1
People often say that drugs are being developed and made available to patients in other countries before they are marketed here in the United States. Physicians often gripe that their patients can’t get access to medicines that are available to others overseas. These anecdotes have led to the urban legend that the FDA evaluates and approves drugs at a slower rate than foreign agencies, especially the European Medicines Agency (EMA).
In a recent report by the British-based Centre for Innovation in Regulatory Science, “over 75% of the new drugs approved by Japan, EU, Canada, Australia, Switzerland, and FDA, from 2004 to 2013, were approved first by FDA.” The FDA continues to lead among regulatory agencies in drug approvals that ensure patients get access to the lifesaving medicines they need.
The U.S. Food and Drug Administration has significantly increased the speed by which new drugs reach patients in need. Between 2006 and 2010, three out of four new drugs approved in both Europe and the U.S. were first approved by the FDA. In the specific example of cancer, the FDA also approved 32 of the 35 prospective cancer drugs between 2003-2010, whereas the EMA only approved 26. Among those cancer drugs approved, over 90% were first approved by the FDA. Just last year, almost two-thirds of the novel drugs approved by the FDA (26 of 41 or about 63%) were approved in the United States before receiving approval in any other country.2
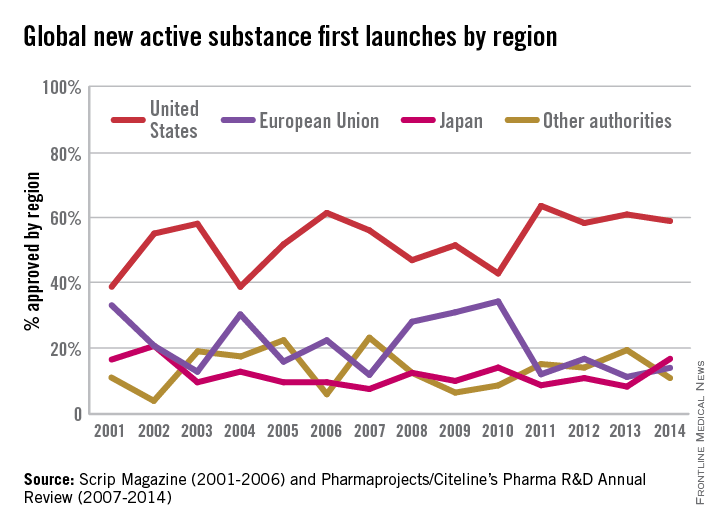
Myth 2: The FDA controls drug prices.
FACT: The FDA has no legal authority whatsoever to investigate or control the prices charged for marketed drugs. Manufacturers, distributors, and retailers establish these prices.
Drug prices do have a direct impact on the ability of people to cope with their illnesses as well as meet other expenses and the FDA recognizes that other factors beyond its purview, including insurance coverage and drug pricing, can determine patient access to drugs. However, the FDA has no legal authority whatsoever to investigate or control the prices charged for marketed drugs. Manufacturers, distributors, and retailers establish these prices.
The FDA is responsible for assuring the American public that the drugs approved today are safe and effective. In carrying out this responsibility, the FDA also works under the law to make medicines accessible to doctors and their patients through strategies such as expanding access to generic medicines, reducing the time and cost of bringing new medicines to market, as well as ensuring safe use practices and the most up-to-date information for health care professionals and patients.
Myth 3: The FDA conducts clinical trials.
FACT: The FDA does not develop, manufacture, or test drugs. The FDA does oversee the testing of new drugs to evaluate the safety and effectiveness profile in clinical trials.
Drug manufacturers submit full reports on the drug so that the FDA can evaluate their data. These studies are conducted to answer whether the drug in study works for the proposed indication. By completing a full review and analysis of the submitted data, the FDA assesses the benefit and risk of each drug to determine if the drug will be approved.
Companies must submit an investigational new drug (IND) application to the FDA before testing can begin. The IND is the means through which the sponsor obtains an exemption from the FDA to begin testing and legally transporting or distributing a drug under investigation across state lines.
The FDA’s role in the development of a new drug begins when the drug sponsor (usually the manufacturer or potential marketer) wants to test the diagnostic or therapeutic potential in humans (after having screened the new molecule for pharmacological activity and acute toxicity potential in animals). It is at this point that the molecule changes in legal status under the Federal Food, Drug, and Cosmetic Act and becomes a new drug subject to specific requirements of the drug regulatory system.3
Myth 4: The FDA regulates the practice of medicine.
FACT: The FDA regulates the approval of a drug, but not how it is prescribed. Doctors are permitted to prescribe a drug for any reason they think is medically appropriate.
The FDA creates the “drug label” in conjunction with the drug company to ensure that promotional claims are not false or misleading. The drug label of FDA-approved drugs provides information about the drug, including the approved doses and how the drug should be given to treat the medical condition for which it was approved.
However, physicians often use drugs in a way that is different from that described in the FDA-approved drug label, an “off-label” use. This can mean that the drug is:
• Used for a different disease or medical condition.
• Given in a different way (such as by a different route).
• Given in a different dose.
Off-label is also called “nonapproved” or “unapproved” use of a drug. Because drug makers have not put their drugs through the studies required by the FDA to officially approve the drug for new uses, new uses for these drugs should be taken with caution as the FDA has not reviewed the clinical evidence to support the new use. Any off-label drug usage should include a detailed conversation between physician and patient.4
Dr. John J. Whyte is the director of Professional Affairs and Stakeholder Engagement (PASE) in the FDA’s Center for Drug Evaluation and Research (CDER).
What if we are all they have?
I recently attended a CME conference at Johns Hopkins University titled “Infectious Diseases Update for Primary Care and Hospital Medicine.” As one would assume, some things were highly germane to my practice as a hospitalist, while others were, well, not relevant at all.
Don’t get me wrong, the conference was excellent and very thought provoking. It not only taught me clinically useful information, it challenged me to do more than I am used to doing for my patients; thus, I pass this challenge along to you.
One expert presented a case of an otherwise healthy patient who was found to have mildly elevated liver function tests on routine lab work done for life insurance purposes. His ALT and AST were 73 and 36, respectively, numbers that many of us would simply defer to the primary care provider to follow. But what if there is no primary care doctor? What if we are all they have?
Upon further evaluation, this patient was found to have hepatitis C. A more detailed history revealed that he had injected drugs with friends a few times over 20 years ago. The conference presenter shared statistics showing there are 2.7 million to 5 million people living with chronic HCV in America, and an estimated 45% to 60% of them are unaware of their disease – a disease that responds so well to treatment that simply screening baby boomers has the potential to prevent over 120,000 HCV-related deaths! It’s mind boggling to imagine how many people of all ages will die from this disease alone, completely oblivious to its existence.
Many people have obtained health insurance as a direct result of the Affordable Care Act, yet there are still many Americans who remain uninsured. When they are hospitalized for an acute illness, it may be the only encounter they have had with a medical professional in years. So, I ask the question again: What if we are all they have?
We can design all the elaborate hand-offs, discharge summaries, and patient instruction forms we want, but what if patients are unable to actually act on our “easy-to-understand” recommendations? Many of our patients will, out of embarrassment, nod their heads in agreement when we stress the extreme importance of following up with a primary care doctor and getting their prescriptions filled, knowing all the while that they simply don’t have the means to do so. I don’t think I will ever forget how out of touch I felt after giving a patient my spiel about taking his medication as prescribed to decrease his risk of a heart attack. He looked straight into my eyes and frankly, yet ever so respectively said, “Dr. Hester, I can either buy my medicine or I can eat.”
Sometimes it’s just that simple.
We all feel the urgency to provide high-quality care while keeping that care cost effective and time efficient, but hospitalists have a unique opportunity to not only serve our patients’ acute needs when they present via EMS to the ED, but to protect them from unforeseen catastrophes in the future. An extra (needed) test here and there, a little more time spent counseling on lifestyle changes, a few more minutes spent trying to help coordinate affordable (or free) follow-up care can all pay big dividends, and you may never have to see those patients in the hospital again. Isn’t that the goal?
Dr. Hester is a hospitalist at Baltimore-Washington Medical Center in Glen Burnie, Md. She is the creator of the Patient Whiz, a patient-engagement app for iOS. Reach her at [email protected].
I recently attended a CME conference at Johns Hopkins University titled “Infectious Diseases Update for Primary Care and Hospital Medicine.” As one would assume, some things were highly germane to my practice as a hospitalist, while others were, well, not relevant at all.
Don’t get me wrong, the conference was excellent and very thought provoking. It not only taught me clinically useful information, it challenged me to do more than I am used to doing for my patients; thus, I pass this challenge along to you.
One expert presented a case of an otherwise healthy patient who was found to have mildly elevated liver function tests on routine lab work done for life insurance purposes. His ALT and AST were 73 and 36, respectively, numbers that many of us would simply defer to the primary care provider to follow. But what if there is no primary care doctor? What if we are all they have?
Upon further evaluation, this patient was found to have hepatitis C. A more detailed history revealed that he had injected drugs with friends a few times over 20 years ago. The conference presenter shared statistics showing there are 2.7 million to 5 million people living with chronic HCV in America, and an estimated 45% to 60% of them are unaware of their disease – a disease that responds so well to treatment that simply screening baby boomers has the potential to prevent over 120,000 HCV-related deaths! It’s mind boggling to imagine how many people of all ages will die from this disease alone, completely oblivious to its existence.
Many people have obtained health insurance as a direct result of the Affordable Care Act, yet there are still many Americans who remain uninsured. When they are hospitalized for an acute illness, it may be the only encounter they have had with a medical professional in years. So, I ask the question again: What if we are all they have?
We can design all the elaborate hand-offs, discharge summaries, and patient instruction forms we want, but what if patients are unable to actually act on our “easy-to-understand” recommendations? Many of our patients will, out of embarrassment, nod their heads in agreement when we stress the extreme importance of following up with a primary care doctor and getting their prescriptions filled, knowing all the while that they simply don’t have the means to do so. I don’t think I will ever forget how out of touch I felt after giving a patient my spiel about taking his medication as prescribed to decrease his risk of a heart attack. He looked straight into my eyes and frankly, yet ever so respectively said, “Dr. Hester, I can either buy my medicine or I can eat.”
Sometimes it’s just that simple.
We all feel the urgency to provide high-quality care while keeping that care cost effective and time efficient, but hospitalists have a unique opportunity to not only serve our patients’ acute needs when they present via EMS to the ED, but to protect them from unforeseen catastrophes in the future. An extra (needed) test here and there, a little more time spent counseling on lifestyle changes, a few more minutes spent trying to help coordinate affordable (or free) follow-up care can all pay big dividends, and you may never have to see those patients in the hospital again. Isn’t that the goal?
Dr. Hester is a hospitalist at Baltimore-Washington Medical Center in Glen Burnie, Md. She is the creator of the Patient Whiz, a patient-engagement app for iOS. Reach her at [email protected].
I recently attended a CME conference at Johns Hopkins University titled “Infectious Diseases Update for Primary Care and Hospital Medicine.” As one would assume, some things were highly germane to my practice as a hospitalist, while others were, well, not relevant at all.
Don’t get me wrong, the conference was excellent and very thought provoking. It not only taught me clinically useful information, it challenged me to do more than I am used to doing for my patients; thus, I pass this challenge along to you.
One expert presented a case of an otherwise healthy patient who was found to have mildly elevated liver function tests on routine lab work done for life insurance purposes. His ALT and AST were 73 and 36, respectively, numbers that many of us would simply defer to the primary care provider to follow. But what if there is no primary care doctor? What if we are all they have?
Upon further evaluation, this patient was found to have hepatitis C. A more detailed history revealed that he had injected drugs with friends a few times over 20 years ago. The conference presenter shared statistics showing there are 2.7 million to 5 million people living with chronic HCV in America, and an estimated 45% to 60% of them are unaware of their disease – a disease that responds so well to treatment that simply screening baby boomers has the potential to prevent over 120,000 HCV-related deaths! It’s mind boggling to imagine how many people of all ages will die from this disease alone, completely oblivious to its existence.
Many people have obtained health insurance as a direct result of the Affordable Care Act, yet there are still many Americans who remain uninsured. When they are hospitalized for an acute illness, it may be the only encounter they have had with a medical professional in years. So, I ask the question again: What if we are all they have?
We can design all the elaborate hand-offs, discharge summaries, and patient instruction forms we want, but what if patients are unable to actually act on our “easy-to-understand” recommendations? Many of our patients will, out of embarrassment, nod their heads in agreement when we stress the extreme importance of following up with a primary care doctor and getting their prescriptions filled, knowing all the while that they simply don’t have the means to do so. I don’t think I will ever forget how out of touch I felt after giving a patient my spiel about taking his medication as prescribed to decrease his risk of a heart attack. He looked straight into my eyes and frankly, yet ever so respectively said, “Dr. Hester, I can either buy my medicine or I can eat.”
Sometimes it’s just that simple.
We all feel the urgency to provide high-quality care while keeping that care cost effective and time efficient, but hospitalists have a unique opportunity to not only serve our patients’ acute needs when they present via EMS to the ED, but to protect them from unforeseen catastrophes in the future. An extra (needed) test here and there, a little more time spent counseling on lifestyle changes, a few more minutes spent trying to help coordinate affordable (or free) follow-up care can all pay big dividends, and you may never have to see those patients in the hospital again. Isn’t that the goal?
Dr. Hester is a hospitalist at Baltimore-Washington Medical Center in Glen Burnie, Md. She is the creator of the Patient Whiz, a patient-engagement app for iOS. Reach her at [email protected].
Finally, an extra set of hands
In September 2015, the Centers for Medicare & Medicaid Services (CMS) launched a promising 4-year program called the "Transforming Clinical Practice Initiative" to lighten the load for family physicians.1 The central figures in this program are skilled and trained quality improvement advisors (QIA) who will work directly with physicians and their staffs to assist with the heavy lifting of practice improvement. The Oklahoma Physicians Research and Resources Network has used QIAs, which it calls practice enhancement assistants (PEAs), for more than 20 years to help Oklahoma family physicians improve various aspects of their practices, including testing processes, diabetes care, and preventive services. The PEAs have been enormously helpful.2
For this new CMS program, the feds awarded $685 million to 39 national and regional collaborative health care transformation networks and supporting organizations to develop peer-based learning networks to facilitate practice improvements.1 The program is designed to help more than 140,000 primary care physicians improve their practices by providing an extra set of skilled hands.
The American Board of Family Medicine (ABFM) and the American Academy of Family Physicians (AAFP) have teamed up to assist with this national effort. ABFM will cover the cost for the first 6000 family physicians who enroll in one of the regional Practice Transformation Networks to use their newly developed chronic disease registry called PRIME. This registry will extract clinical quality data from diverse electronic health records and report back to practices. The registry will meet the new federal quality measures reporting requirements and will also be a path for maintenance of certification.
The CMS Transforming Clinical Practice Initiative is a great opportunity to get that extra set of skilled hands you need to help meet new quality mandates and make your office more efficient and enjoyable for you, your staff, and your patients. Contact the ABFM (www.theabfm.org) to find out which organization is running the Practice Transformation Network in your area.
1. Centers for Medicare & Medicaid Services (CMS). Transforming clinical practice initiative awards. CMS Web site. Available at: https://www.cms.gov/Newsroom/MediaReleaseDatabase/Fact-sheets/2015-Fact-sheets-items/2015-09-29.html. Accessed December 15, 2015.
2. Nagykaldi Z, Mold JW, Robinson A, et al. Practice facilitators and practice-based research networks. J Am Board Fam Med. 2006;19:506-510.
In September 2015, the Centers for Medicare & Medicaid Services (CMS) launched a promising 4-year program called the "Transforming Clinical Practice Initiative" to lighten the load for family physicians.1 The central figures in this program are skilled and trained quality improvement advisors (QIA) who will work directly with physicians and their staffs to assist with the heavy lifting of practice improvement. The Oklahoma Physicians Research and Resources Network has used QIAs, which it calls practice enhancement assistants (PEAs), for more than 20 years to help Oklahoma family physicians improve various aspects of their practices, including testing processes, diabetes care, and preventive services. The PEAs have been enormously helpful.2
For this new CMS program, the feds awarded $685 million to 39 national and regional collaborative health care transformation networks and supporting organizations to develop peer-based learning networks to facilitate practice improvements.1 The program is designed to help more than 140,000 primary care physicians improve their practices by providing an extra set of skilled hands.
The American Board of Family Medicine (ABFM) and the American Academy of Family Physicians (AAFP) have teamed up to assist with this national effort. ABFM will cover the cost for the first 6000 family physicians who enroll in one of the regional Practice Transformation Networks to use their newly developed chronic disease registry called PRIME. This registry will extract clinical quality data from diverse electronic health records and report back to practices. The registry will meet the new federal quality measures reporting requirements and will also be a path for maintenance of certification.
The CMS Transforming Clinical Practice Initiative is a great opportunity to get that extra set of skilled hands you need to help meet new quality mandates and make your office more efficient and enjoyable for you, your staff, and your patients. Contact the ABFM (www.theabfm.org) to find out which organization is running the Practice Transformation Network in your area.
In September 2015, the Centers for Medicare & Medicaid Services (CMS) launched a promising 4-year program called the "Transforming Clinical Practice Initiative" to lighten the load for family physicians.1 The central figures in this program are skilled and trained quality improvement advisors (QIA) who will work directly with physicians and their staffs to assist with the heavy lifting of practice improvement. The Oklahoma Physicians Research and Resources Network has used QIAs, which it calls practice enhancement assistants (PEAs), for more than 20 years to help Oklahoma family physicians improve various aspects of their practices, including testing processes, diabetes care, and preventive services. The PEAs have been enormously helpful.2
For this new CMS program, the feds awarded $685 million to 39 national and regional collaborative health care transformation networks and supporting organizations to develop peer-based learning networks to facilitate practice improvements.1 The program is designed to help more than 140,000 primary care physicians improve their practices by providing an extra set of skilled hands.
The American Board of Family Medicine (ABFM) and the American Academy of Family Physicians (AAFP) have teamed up to assist with this national effort. ABFM will cover the cost for the first 6000 family physicians who enroll in one of the regional Practice Transformation Networks to use their newly developed chronic disease registry called PRIME. This registry will extract clinical quality data from diverse electronic health records and report back to practices. The registry will meet the new federal quality measures reporting requirements and will also be a path for maintenance of certification.
The CMS Transforming Clinical Practice Initiative is a great opportunity to get that extra set of skilled hands you need to help meet new quality mandates and make your office more efficient and enjoyable for you, your staff, and your patients. Contact the ABFM (www.theabfm.org) to find out which organization is running the Practice Transformation Network in your area.
1. Centers for Medicare & Medicaid Services (CMS). Transforming clinical practice initiative awards. CMS Web site. Available at: https://www.cms.gov/Newsroom/MediaReleaseDatabase/Fact-sheets/2015-Fact-sheets-items/2015-09-29.html. Accessed December 15, 2015.
2. Nagykaldi Z, Mold JW, Robinson A, et al. Practice facilitators and practice-based research networks. J Am Board Fam Med. 2006;19:506-510.
1. Centers for Medicare & Medicaid Services (CMS). Transforming clinical practice initiative awards. CMS Web site. Available at: https://www.cms.gov/Newsroom/MediaReleaseDatabase/Fact-sheets/2015-Fact-sheets-items/2015-09-29.html. Accessed December 15, 2015.
2. Nagykaldi Z, Mold JW, Robinson A, et al. Practice facilitators and practice-based research networks. J Am Board Fam Med. 2006;19:506-510.