User login
Insulin pumps: Great devices, but you still have to press the button
In this issue of the Journal, Millstein et al provide an elegant, practical, and up-to-date review of insulin pump therapy (also known as continuous subcutaneous insulin infusion), emphasizing its benefits and comparing it with multiple daily insulin injections.1
NOT FOR EVERYONE
While insulin pumps make the lives of many patients much easier, we should be careful when generalizing their indications. These devices have been with us for 4 decades, during which they have progressively been made more precise and more intelligent—and smaller. The technology may be attractive to some patients but undesirable to others (Table 1).
Many healthcare providers are unfamiliar with pump technology, and some are intimidated by it because it involves a dynamic device-user interface that is more complex than that of other concealed programmed devices such as pacemakers. Inadequate glycemic management is complex and may result from factors such as fear of hypoglycemia, difficulty with insulin dose adjustment, and poor math skills.2
Unfortunately, some patients are given a pump without proper screening and education, and they tend to call the pump manufacturer’s help line or their provider often for help with technical problems. Selecting the right patient for this technology is more important than the converse.
Indications for an insulin pump vary by country. In some countries, a pump is started as soon as type 1 diabetes is diagnosed. In the United States, the indications are very rigorous and restrictive, especially for patients with type 2 diabetes, in whom a lack of endogenous insulin production must first be proved.
There is no question that a pump should be offered to every patient with type 1 diabetes who demonstrates good motivation to improve his or her glucose control, but only after a rigorous education program. This option is too costly to be tried just to see if the patient likes it.
ADVERSE EVENTS WITH INSULIN PUMPS: MORE DATA NEEDED
A worrisome aspect of continuous subcutaneous insulin infusion at a population level is a lack of information on the root causes of adverse events (diabetic ketoacidosis or severe hypoglycemia) in patients who use it. These events may be serious and sometimes even fatal.
Outside of a controlled environment, it is difficult to ascertain whether an adverse event represents device error or user error, since pumps contain different components (electronic, mechanical, and pharmacologic) that interface with the human user.3 How adverse events are tracked or categorized is unclear, and given the risks associated with this technology, better postmarketing evaluation is needed. Furthermore, we do not know if the precision of insulin delivery decreases over the life of a pump.
While most pump manufacturers have good customer service and make every effort to provide the patient with a replacement pump in case of failure, we do not know if anyone maintains a database of such failures or adverse events, and if those failures can be analyzed to improve safety.3
INTERFACES ARE NOT STANDARD
When one buys a new car, little time is needed to learn how to operate it because most cars use the same basic features.
The situation is different with insulin pumps. To compete with each other, pump manufacturers create different looks, different insulin delivery methods, and different ways of administering a bolus. Switching from one pump to another is difficult without detailed education on the “bells and whistles” of the new pump.
Most patients use just a few features of the pump. They look at it as more of a convenience. They sometimes forget they are wearing it, and even forget to take a bolus before a meal.
PATIENT SATISFACTION DEPENDS ON THE PATIENT
For years, we thought insulin pumps were better at improving hypoglycemia awareness. But in a prospective study, multiple daily injections with frequent self-monitoring of blood glucose provided identical outcomes without worsening hemoglobin A1c compared with continuous infusion with real-time continuous glucose monitoring, although satisfaction with treatment was better in the latter group.4
Patients’ satisfaction with continuous subcutaneous insulin infusion depends on their baseline hemoglobin A1c level. Patients with relatively low hemoglobin A1c tend to take an active approach to self-care, describe the pump as a tool for meeting glycemic goals, and say the pump makes them feel more normal. Patients with high hemoglobin A1c tend to have a more passive approach to their self-care and have more negative experiences with the pump. Women are more concerned than men with the effect of the pump on body image and social acceptance.5
DOLLARS AND CENTS
According to 2012 estimates, 29 million Americans had diabetes mellitus, of whom 1.25 million had type 1. The direct medical costs of diabetes are estimated at $176 billion, of which 12% covers overall pharmacy costs.6 About 31% of adults with diabetes use insulin.7
For a device that costs $6,000, has a life span of only 4 years, and requires supplies that cost $300 per month, rigorous interpretation of superiority data would be needed to confirm that this technology would have a positive impact on public health if every insulin-using patient with diabetes were to say yes to it. It is true that switching from multiple daily injections to a pump leads to a significant reduction in insulin expenditures in patients with type 2 diabetes, according to a retrospective analysis of claims data.8
However, not all studies comparing pumps and multiple daily injections in type 2 diabetes have shown an advantage of one over the other in terms of a reduction in fasting glucose, hemoglobin A1c, or incidence of hypoglycemia.9 A meta-analysis10 found that the two therapies had similar effects on glycemic control and hypoglycemia. Continuous infusion had a more favorable effect in adults with type 1 diabetes.10
Neither continuous infusion nor multiple daily injections can mimic physiologic endogenous insulin secretion. Endogenous insulin is secreted into the portal system, and its main site of action is the liver. As a result, there is more hepatic glucose uptake and thus a lower peripheral plasma insulin concentration with endogenous secretion than with systemic administration. Endogenous insulin secretion also suppresses hepatic glucose production and reduces the risk of hypoglycemia.11
PROGRESS, BUT NOT PERFECTION
Diabetes mellitus constitutes a big burden on patients and on society. The discovery of insulin was a giant leap forward; the insulin pump was another great advance. We are getting closer to an integrated bionic pancreas. We are far from achieving a perfect system, but we are much better off than we were 50 or 80 years ago. And although insulin pump technology is sophisticated and precise, it still interfaces with a human user, and the human user still must press its buttons.
- Millstein R, Mora Becerra N, Shubrook JH. Insulin pumps: beyond basal-bolus. Cleve Clin J Med 2015; 82:835–842.
- Cavan DA, Ziegler R, Cranston I, et al. Automated bolus advisor control and usability study (ABACUS): does use of an insulin bolus advisor improve glycaemic control in patients failing multiple daily insulin injection (MDI) therapy? [NCT01460446]. BMC Fam Pract 2012; 13:102.
- Heinemann L, Fleming GA, Petrie JR, Holl RW, Bergenstal RM, Peters AL. Insulin pump risks and benefits: a clinical appraisal of pump safety standards, adverse event reporting, and research needs: a joint statement of the European Association for the Study of Diabetes and the American Diabetes Association Diabetes Technology Working Group. Diabetes Care 2015; 38:716–722.
- Little SA, Leelarathna L, Walkinshaw E, et al. Recovery of hypoglycemia awareness in long-standing type 1 diabetes: a multicenter 2 × 2 factorial randomized controlled trial comparing insulin pump with multiple daily injections and continuous with conventional glucose self-monitoring (HypoCOMPaSS). Diabetes Care 2014; 37:2114–2122.
- Ritholz MD, Smaldone A, Lee J, Castillo A, Wolpert H, Weinger K. Perceptions of psychosocial factors and the insulin pump. Diabetes Care 2007; 30:549–554.
- American Diabetes Association. Statistics about diabetes. Overall numbers, diabetes and prediabetes. www.diabetes.org/diabetes-basics/statistics/. Accessed November 4, 2015.
- Centers for Disease Control and Prevention (CDC). Age-adjusted percentage of adults with diabetes using diabetes medication, by type of medication, United States, 1997–2011. www.cdc.gov/diabetes/statistics/meduse/fig2.htm. Accessed November 4, 2015.
- David G, Gill M, Gunnarsson C, Shafiroff J, Edelman S. Switching from multiple daily injections to CSII pump therapy: insulin expenditures in type 2 diabetes. Am J Manag Care; 20:e490–e497.
- Gao GQ, Heng XY, Wang YL, et al. Comparison of continuous subcutaneous insulin infusion and insulin glargine-based multiple daily insulin aspart injections with preferential adjustment of basal insulin in patients with type 2 diabetes. Exp Ther Med 2014; 8:1191–1196.
- Yeh HC, Brown TT, Maruthur N, et al. Comparative effectiveness and safety of methods of insulin delivery and glucose monitoring for diabetes mellitus: a systematic review and meta-analysis. Ann Intern Med 2012; 157:336–347.
- Logtenberg SJ, van Ballegooie E, Israêl-Bultman H, van Linde A, Bilo HJ. Glycaemic control, health status and treatment satisfaction with continuous intraperitoneal insulin infusion. Neth J Med 2007; 65:65–70.
In this issue of the Journal, Millstein et al provide an elegant, practical, and up-to-date review of insulin pump therapy (also known as continuous subcutaneous insulin infusion), emphasizing its benefits and comparing it with multiple daily insulin injections.1
NOT FOR EVERYONE
While insulin pumps make the lives of many patients much easier, we should be careful when generalizing their indications. These devices have been with us for 4 decades, during which they have progressively been made more precise and more intelligent—and smaller. The technology may be attractive to some patients but undesirable to others (Table 1).
Many healthcare providers are unfamiliar with pump technology, and some are intimidated by it because it involves a dynamic device-user interface that is more complex than that of other concealed programmed devices such as pacemakers. Inadequate glycemic management is complex and may result from factors such as fear of hypoglycemia, difficulty with insulin dose adjustment, and poor math skills.2
Unfortunately, some patients are given a pump without proper screening and education, and they tend to call the pump manufacturer’s help line or their provider often for help with technical problems. Selecting the right patient for this technology is more important than the converse.
Indications for an insulin pump vary by country. In some countries, a pump is started as soon as type 1 diabetes is diagnosed. In the United States, the indications are very rigorous and restrictive, especially for patients with type 2 diabetes, in whom a lack of endogenous insulin production must first be proved.
There is no question that a pump should be offered to every patient with type 1 diabetes who demonstrates good motivation to improve his or her glucose control, but only after a rigorous education program. This option is too costly to be tried just to see if the patient likes it.
ADVERSE EVENTS WITH INSULIN PUMPS: MORE DATA NEEDED
A worrisome aspect of continuous subcutaneous insulin infusion at a population level is a lack of information on the root causes of adverse events (diabetic ketoacidosis or severe hypoglycemia) in patients who use it. These events may be serious and sometimes even fatal.
Outside of a controlled environment, it is difficult to ascertain whether an adverse event represents device error or user error, since pumps contain different components (electronic, mechanical, and pharmacologic) that interface with the human user.3 How adverse events are tracked or categorized is unclear, and given the risks associated with this technology, better postmarketing evaluation is needed. Furthermore, we do not know if the precision of insulin delivery decreases over the life of a pump.
While most pump manufacturers have good customer service and make every effort to provide the patient with a replacement pump in case of failure, we do not know if anyone maintains a database of such failures or adverse events, and if those failures can be analyzed to improve safety.3
INTERFACES ARE NOT STANDARD
When one buys a new car, little time is needed to learn how to operate it because most cars use the same basic features.
The situation is different with insulin pumps. To compete with each other, pump manufacturers create different looks, different insulin delivery methods, and different ways of administering a bolus. Switching from one pump to another is difficult without detailed education on the “bells and whistles” of the new pump.
Most patients use just a few features of the pump. They look at it as more of a convenience. They sometimes forget they are wearing it, and even forget to take a bolus before a meal.
PATIENT SATISFACTION DEPENDS ON THE PATIENT
For years, we thought insulin pumps were better at improving hypoglycemia awareness. But in a prospective study, multiple daily injections with frequent self-monitoring of blood glucose provided identical outcomes without worsening hemoglobin A1c compared with continuous infusion with real-time continuous glucose monitoring, although satisfaction with treatment was better in the latter group.4
Patients’ satisfaction with continuous subcutaneous insulin infusion depends on their baseline hemoglobin A1c level. Patients with relatively low hemoglobin A1c tend to take an active approach to self-care, describe the pump as a tool for meeting glycemic goals, and say the pump makes them feel more normal. Patients with high hemoglobin A1c tend to have a more passive approach to their self-care and have more negative experiences with the pump. Women are more concerned than men with the effect of the pump on body image and social acceptance.5
DOLLARS AND CENTS
According to 2012 estimates, 29 million Americans had diabetes mellitus, of whom 1.25 million had type 1. The direct medical costs of diabetes are estimated at $176 billion, of which 12% covers overall pharmacy costs.6 About 31% of adults with diabetes use insulin.7
For a device that costs $6,000, has a life span of only 4 years, and requires supplies that cost $300 per month, rigorous interpretation of superiority data would be needed to confirm that this technology would have a positive impact on public health if every insulin-using patient with diabetes were to say yes to it. It is true that switching from multiple daily injections to a pump leads to a significant reduction in insulin expenditures in patients with type 2 diabetes, according to a retrospective analysis of claims data.8
However, not all studies comparing pumps and multiple daily injections in type 2 diabetes have shown an advantage of one over the other in terms of a reduction in fasting glucose, hemoglobin A1c, or incidence of hypoglycemia.9 A meta-analysis10 found that the two therapies had similar effects on glycemic control and hypoglycemia. Continuous infusion had a more favorable effect in adults with type 1 diabetes.10
Neither continuous infusion nor multiple daily injections can mimic physiologic endogenous insulin secretion. Endogenous insulin is secreted into the portal system, and its main site of action is the liver. As a result, there is more hepatic glucose uptake and thus a lower peripheral plasma insulin concentration with endogenous secretion than with systemic administration. Endogenous insulin secretion also suppresses hepatic glucose production and reduces the risk of hypoglycemia.11
PROGRESS, BUT NOT PERFECTION
Diabetes mellitus constitutes a big burden on patients and on society. The discovery of insulin was a giant leap forward; the insulin pump was another great advance. We are getting closer to an integrated bionic pancreas. We are far from achieving a perfect system, but we are much better off than we were 50 or 80 years ago. And although insulin pump technology is sophisticated and precise, it still interfaces with a human user, and the human user still must press its buttons.
In this issue of the Journal, Millstein et al provide an elegant, practical, and up-to-date review of insulin pump therapy (also known as continuous subcutaneous insulin infusion), emphasizing its benefits and comparing it with multiple daily insulin injections.1
NOT FOR EVERYONE
While insulin pumps make the lives of many patients much easier, we should be careful when generalizing their indications. These devices have been with us for 4 decades, during which they have progressively been made more precise and more intelligent—and smaller. The technology may be attractive to some patients but undesirable to others (Table 1).
Many healthcare providers are unfamiliar with pump technology, and some are intimidated by it because it involves a dynamic device-user interface that is more complex than that of other concealed programmed devices such as pacemakers. Inadequate glycemic management is complex and may result from factors such as fear of hypoglycemia, difficulty with insulin dose adjustment, and poor math skills.2
Unfortunately, some patients are given a pump without proper screening and education, and they tend to call the pump manufacturer’s help line or their provider often for help with technical problems. Selecting the right patient for this technology is more important than the converse.
Indications for an insulin pump vary by country. In some countries, a pump is started as soon as type 1 diabetes is diagnosed. In the United States, the indications are very rigorous and restrictive, especially for patients with type 2 diabetes, in whom a lack of endogenous insulin production must first be proved.
There is no question that a pump should be offered to every patient with type 1 diabetes who demonstrates good motivation to improve his or her glucose control, but only after a rigorous education program. This option is too costly to be tried just to see if the patient likes it.
ADVERSE EVENTS WITH INSULIN PUMPS: MORE DATA NEEDED
A worrisome aspect of continuous subcutaneous insulin infusion at a population level is a lack of information on the root causes of adverse events (diabetic ketoacidosis or severe hypoglycemia) in patients who use it. These events may be serious and sometimes even fatal.
Outside of a controlled environment, it is difficult to ascertain whether an adverse event represents device error or user error, since pumps contain different components (electronic, mechanical, and pharmacologic) that interface with the human user.3 How adverse events are tracked or categorized is unclear, and given the risks associated with this technology, better postmarketing evaluation is needed. Furthermore, we do not know if the precision of insulin delivery decreases over the life of a pump.
While most pump manufacturers have good customer service and make every effort to provide the patient with a replacement pump in case of failure, we do not know if anyone maintains a database of such failures or adverse events, and if those failures can be analyzed to improve safety.3
INTERFACES ARE NOT STANDARD
When one buys a new car, little time is needed to learn how to operate it because most cars use the same basic features.
The situation is different with insulin pumps. To compete with each other, pump manufacturers create different looks, different insulin delivery methods, and different ways of administering a bolus. Switching from one pump to another is difficult without detailed education on the “bells and whistles” of the new pump.
Most patients use just a few features of the pump. They look at it as more of a convenience. They sometimes forget they are wearing it, and even forget to take a bolus before a meal.
PATIENT SATISFACTION DEPENDS ON THE PATIENT
For years, we thought insulin pumps were better at improving hypoglycemia awareness. But in a prospective study, multiple daily injections with frequent self-monitoring of blood glucose provided identical outcomes without worsening hemoglobin A1c compared with continuous infusion with real-time continuous glucose monitoring, although satisfaction with treatment was better in the latter group.4
Patients’ satisfaction with continuous subcutaneous insulin infusion depends on their baseline hemoglobin A1c level. Patients with relatively low hemoglobin A1c tend to take an active approach to self-care, describe the pump as a tool for meeting glycemic goals, and say the pump makes them feel more normal. Patients with high hemoglobin A1c tend to have a more passive approach to their self-care and have more negative experiences with the pump. Women are more concerned than men with the effect of the pump on body image and social acceptance.5
DOLLARS AND CENTS
According to 2012 estimates, 29 million Americans had diabetes mellitus, of whom 1.25 million had type 1. The direct medical costs of diabetes are estimated at $176 billion, of which 12% covers overall pharmacy costs.6 About 31% of adults with diabetes use insulin.7
For a device that costs $6,000, has a life span of only 4 years, and requires supplies that cost $300 per month, rigorous interpretation of superiority data would be needed to confirm that this technology would have a positive impact on public health if every insulin-using patient with diabetes were to say yes to it. It is true that switching from multiple daily injections to a pump leads to a significant reduction in insulin expenditures in patients with type 2 diabetes, according to a retrospective analysis of claims data.8
However, not all studies comparing pumps and multiple daily injections in type 2 diabetes have shown an advantage of one over the other in terms of a reduction in fasting glucose, hemoglobin A1c, or incidence of hypoglycemia.9 A meta-analysis10 found that the two therapies had similar effects on glycemic control and hypoglycemia. Continuous infusion had a more favorable effect in adults with type 1 diabetes.10
Neither continuous infusion nor multiple daily injections can mimic physiologic endogenous insulin secretion. Endogenous insulin is secreted into the portal system, and its main site of action is the liver. As a result, there is more hepatic glucose uptake and thus a lower peripheral plasma insulin concentration with endogenous secretion than with systemic administration. Endogenous insulin secretion also suppresses hepatic glucose production and reduces the risk of hypoglycemia.11
PROGRESS, BUT NOT PERFECTION
Diabetes mellitus constitutes a big burden on patients and on society. The discovery of insulin was a giant leap forward; the insulin pump was another great advance. We are getting closer to an integrated bionic pancreas. We are far from achieving a perfect system, but we are much better off than we were 50 or 80 years ago. And although insulin pump technology is sophisticated and precise, it still interfaces with a human user, and the human user still must press its buttons.
- Millstein R, Mora Becerra N, Shubrook JH. Insulin pumps: beyond basal-bolus. Cleve Clin J Med 2015; 82:835–842.
- Cavan DA, Ziegler R, Cranston I, et al. Automated bolus advisor control and usability study (ABACUS): does use of an insulin bolus advisor improve glycaemic control in patients failing multiple daily insulin injection (MDI) therapy? [NCT01460446]. BMC Fam Pract 2012; 13:102.
- Heinemann L, Fleming GA, Petrie JR, Holl RW, Bergenstal RM, Peters AL. Insulin pump risks and benefits: a clinical appraisal of pump safety standards, adverse event reporting, and research needs: a joint statement of the European Association for the Study of Diabetes and the American Diabetes Association Diabetes Technology Working Group. Diabetes Care 2015; 38:716–722.
- Little SA, Leelarathna L, Walkinshaw E, et al. Recovery of hypoglycemia awareness in long-standing type 1 diabetes: a multicenter 2 × 2 factorial randomized controlled trial comparing insulin pump with multiple daily injections and continuous with conventional glucose self-monitoring (HypoCOMPaSS). Diabetes Care 2014; 37:2114–2122.
- Ritholz MD, Smaldone A, Lee J, Castillo A, Wolpert H, Weinger K. Perceptions of psychosocial factors and the insulin pump. Diabetes Care 2007; 30:549–554.
- American Diabetes Association. Statistics about diabetes. Overall numbers, diabetes and prediabetes. www.diabetes.org/diabetes-basics/statistics/. Accessed November 4, 2015.
- Centers for Disease Control and Prevention (CDC). Age-adjusted percentage of adults with diabetes using diabetes medication, by type of medication, United States, 1997–2011. www.cdc.gov/diabetes/statistics/meduse/fig2.htm. Accessed November 4, 2015.
- David G, Gill M, Gunnarsson C, Shafiroff J, Edelman S. Switching from multiple daily injections to CSII pump therapy: insulin expenditures in type 2 diabetes. Am J Manag Care; 20:e490–e497.
- Gao GQ, Heng XY, Wang YL, et al. Comparison of continuous subcutaneous insulin infusion and insulin glargine-based multiple daily insulin aspart injections with preferential adjustment of basal insulin in patients with type 2 diabetes. Exp Ther Med 2014; 8:1191–1196.
- Yeh HC, Brown TT, Maruthur N, et al. Comparative effectiveness and safety of methods of insulin delivery and glucose monitoring for diabetes mellitus: a systematic review and meta-analysis. Ann Intern Med 2012; 157:336–347.
- Logtenberg SJ, van Ballegooie E, Israêl-Bultman H, van Linde A, Bilo HJ. Glycaemic control, health status and treatment satisfaction with continuous intraperitoneal insulin infusion. Neth J Med 2007; 65:65–70.
- Millstein R, Mora Becerra N, Shubrook JH. Insulin pumps: beyond basal-bolus. Cleve Clin J Med 2015; 82:835–842.
- Cavan DA, Ziegler R, Cranston I, et al. Automated bolus advisor control and usability study (ABACUS): does use of an insulin bolus advisor improve glycaemic control in patients failing multiple daily insulin injection (MDI) therapy? [NCT01460446]. BMC Fam Pract 2012; 13:102.
- Heinemann L, Fleming GA, Petrie JR, Holl RW, Bergenstal RM, Peters AL. Insulin pump risks and benefits: a clinical appraisal of pump safety standards, adverse event reporting, and research needs: a joint statement of the European Association for the Study of Diabetes and the American Diabetes Association Diabetes Technology Working Group. Diabetes Care 2015; 38:716–722.
- Little SA, Leelarathna L, Walkinshaw E, et al. Recovery of hypoglycemia awareness in long-standing type 1 diabetes: a multicenter 2 × 2 factorial randomized controlled trial comparing insulin pump with multiple daily injections and continuous with conventional glucose self-monitoring (HypoCOMPaSS). Diabetes Care 2014; 37:2114–2122.
- Ritholz MD, Smaldone A, Lee J, Castillo A, Wolpert H, Weinger K. Perceptions of psychosocial factors and the insulin pump. Diabetes Care 2007; 30:549–554.
- American Diabetes Association. Statistics about diabetes. Overall numbers, diabetes and prediabetes. www.diabetes.org/diabetes-basics/statistics/. Accessed November 4, 2015.
- Centers for Disease Control and Prevention (CDC). Age-adjusted percentage of adults with diabetes using diabetes medication, by type of medication, United States, 1997–2011. www.cdc.gov/diabetes/statistics/meduse/fig2.htm. Accessed November 4, 2015.
- David G, Gill M, Gunnarsson C, Shafiroff J, Edelman S. Switching from multiple daily injections to CSII pump therapy: insulin expenditures in type 2 diabetes. Am J Manag Care; 20:e490–e497.
- Gao GQ, Heng XY, Wang YL, et al. Comparison of continuous subcutaneous insulin infusion and insulin glargine-based multiple daily insulin aspart injections with preferential adjustment of basal insulin in patients with type 2 diabetes. Exp Ther Med 2014; 8:1191–1196.
- Yeh HC, Brown TT, Maruthur N, et al. Comparative effectiveness and safety of methods of insulin delivery and glucose monitoring for diabetes mellitus: a systematic review and meta-analysis. Ann Intern Med 2012; 157:336–347.
- Logtenberg SJ, van Ballegooie E, Israêl-Bultman H, van Linde A, Bilo HJ. Glycaemic control, health status and treatment satisfaction with continuous intraperitoneal insulin infusion. Neth J Med 2007; 65:65–70.
Breast milk: Good? Better? Best?
When you finish reading this column … on second thought, stop now and read the Oct. 17, 2015, opinion piece titled “Overselling Breast-Feeding.” You will discover a well-researched and thoughtfully crafted article by Courtney Jung, a political science professor at the University of Toronto, in which she dares to carefully dissect one of our most revered sacred cows. The result is a convincing argument for rethinking how we present and promote breastfeeding. I won’t attempt to reconstruct her rationale. You can read it for yourself. But, I suspect that if you spend any part of your day trying to help new parents navigate the choppy waters of those first 6 months, you will find what she has to say strikes more than a few familiar chords.
Like most of you, what I learned about breastfeeding came as on the job training. Marilyn and I started our family while I was still in medical school, giving me the advantage of having watched the process bump along twice before I found myself on the frontline of private practice. I had been taught in school about all the advantages breast milk, but it didn’t take long in the real world to discover that breastfeeding could have a dark side.
I had to become a chameleon. I needed to be strong advocate for the advantages of breast milk and support new mothers as they tried to match the American Academy of Pediatrics’ guidelines. However, there were situations in which despite everyone’s best efforts, the handwriting on the wall said, “This isn’t working.” Then it was time to change my colors and convincingly convey the new truth that even a baby that isn’t breastfed is going to be fine. That a woman who doesn’t breastfeed can and will be a mother every bit as good as one who doesn’t breastfed her baby for 6 months or a year.
The tension between the party line and reality became so great that in frustration I decided to write my third book about breastfeeding. The result was “The Maternity Leave Breastfeeding Plan” (New York: Simon and Schuster, 2002). The watered-down title was chosen by the publisher. The subtitle, “How to Enjoy Nursing for 3 Months and Go Back to Work Guilt-Free,” was a better reflection of my message that there can be some serious challenges to breastfeeding and not to worry if it doesn’t work. Surprisingly, it found itself on a La Leche League list of recommended books – that is until someone in the organization actually read it.
Although I had always harbored doubts that many of the studies purporting to show the advantages of breastfeeding were poorly controlled, in 2002, I couldn’t find any data to support my concerns. But over the last decade those studies have begun to emerge and Professor Jung has found them and included them in her new book, “Lactivism: How Feminists and Fundamentalists, Hippies and Yuppies, and Physicians and Politicians Made Breastfeeding Big Business and Bad Policy” (New York: Basic Books, 2015).
It will be interesting to see how her observations play to the wider audience it deserves. The discussions may be lively and heated, and public opinion may shift a bit. But what won’t change is that those of us who deal with mothers and babies in a very personal way will still have to struggle with promoting a good product that isn’t always easy to obtain.
Breast milk is good … but it isn’t always better or best.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine, for nearly 40 years. He has authored several books on behavioral pediatrics including “How to Say No to Your Toddler.”
When you finish reading this column … on second thought, stop now and read the Oct. 17, 2015, opinion piece titled “Overselling Breast-Feeding.” You will discover a well-researched and thoughtfully crafted article by Courtney Jung, a political science professor at the University of Toronto, in which she dares to carefully dissect one of our most revered sacred cows. The result is a convincing argument for rethinking how we present and promote breastfeeding. I won’t attempt to reconstruct her rationale. You can read it for yourself. But, I suspect that if you spend any part of your day trying to help new parents navigate the choppy waters of those first 6 months, you will find what she has to say strikes more than a few familiar chords.
Like most of you, what I learned about breastfeeding came as on the job training. Marilyn and I started our family while I was still in medical school, giving me the advantage of having watched the process bump along twice before I found myself on the frontline of private practice. I had been taught in school about all the advantages breast milk, but it didn’t take long in the real world to discover that breastfeeding could have a dark side.
I had to become a chameleon. I needed to be strong advocate for the advantages of breast milk and support new mothers as they tried to match the American Academy of Pediatrics’ guidelines. However, there were situations in which despite everyone’s best efforts, the handwriting on the wall said, “This isn’t working.” Then it was time to change my colors and convincingly convey the new truth that even a baby that isn’t breastfed is going to be fine. That a woman who doesn’t breastfeed can and will be a mother every bit as good as one who doesn’t breastfed her baby for 6 months or a year.
The tension between the party line and reality became so great that in frustration I decided to write my third book about breastfeeding. The result was “The Maternity Leave Breastfeeding Plan” (New York: Simon and Schuster, 2002). The watered-down title was chosen by the publisher. The subtitle, “How to Enjoy Nursing for 3 Months and Go Back to Work Guilt-Free,” was a better reflection of my message that there can be some serious challenges to breastfeeding and not to worry if it doesn’t work. Surprisingly, it found itself on a La Leche League list of recommended books – that is until someone in the organization actually read it.
Although I had always harbored doubts that many of the studies purporting to show the advantages of breastfeeding were poorly controlled, in 2002, I couldn’t find any data to support my concerns. But over the last decade those studies have begun to emerge and Professor Jung has found them and included them in her new book, “Lactivism: How Feminists and Fundamentalists, Hippies and Yuppies, and Physicians and Politicians Made Breastfeeding Big Business and Bad Policy” (New York: Basic Books, 2015).
It will be interesting to see how her observations play to the wider audience it deserves. The discussions may be lively and heated, and public opinion may shift a bit. But what won’t change is that those of us who deal with mothers and babies in a very personal way will still have to struggle with promoting a good product that isn’t always easy to obtain.
Breast milk is good … but it isn’t always better or best.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine, for nearly 40 years. He has authored several books on behavioral pediatrics including “How to Say No to Your Toddler.”
When you finish reading this column … on second thought, stop now and read the Oct. 17, 2015, opinion piece titled “Overselling Breast-Feeding.” You will discover a well-researched and thoughtfully crafted article by Courtney Jung, a political science professor at the University of Toronto, in which she dares to carefully dissect one of our most revered sacred cows. The result is a convincing argument for rethinking how we present and promote breastfeeding. I won’t attempt to reconstruct her rationale. You can read it for yourself. But, I suspect that if you spend any part of your day trying to help new parents navigate the choppy waters of those first 6 months, you will find what she has to say strikes more than a few familiar chords.
Like most of you, what I learned about breastfeeding came as on the job training. Marilyn and I started our family while I was still in medical school, giving me the advantage of having watched the process bump along twice before I found myself on the frontline of private practice. I had been taught in school about all the advantages breast milk, but it didn’t take long in the real world to discover that breastfeeding could have a dark side.
I had to become a chameleon. I needed to be strong advocate for the advantages of breast milk and support new mothers as they tried to match the American Academy of Pediatrics’ guidelines. However, there were situations in which despite everyone’s best efforts, the handwriting on the wall said, “This isn’t working.” Then it was time to change my colors and convincingly convey the new truth that even a baby that isn’t breastfed is going to be fine. That a woman who doesn’t breastfeed can and will be a mother every bit as good as one who doesn’t breastfed her baby for 6 months or a year.
The tension between the party line and reality became so great that in frustration I decided to write my third book about breastfeeding. The result was “The Maternity Leave Breastfeeding Plan” (New York: Simon and Schuster, 2002). The watered-down title was chosen by the publisher. The subtitle, “How to Enjoy Nursing for 3 Months and Go Back to Work Guilt-Free,” was a better reflection of my message that there can be some serious challenges to breastfeeding and not to worry if it doesn’t work. Surprisingly, it found itself on a La Leche League list of recommended books – that is until someone in the organization actually read it.
Although I had always harbored doubts that many of the studies purporting to show the advantages of breastfeeding were poorly controlled, in 2002, I couldn’t find any data to support my concerns. But over the last decade those studies have begun to emerge and Professor Jung has found them and included them in her new book, “Lactivism: How Feminists and Fundamentalists, Hippies and Yuppies, and Physicians and Politicians Made Breastfeeding Big Business and Bad Policy” (New York: Basic Books, 2015).
It will be interesting to see how her observations play to the wider audience it deserves. The discussions may be lively and heated, and public opinion may shift a bit. But what won’t change is that those of us who deal with mothers and babies in a very personal way will still have to struggle with promoting a good product that isn’t always easy to obtain.
Breast milk is good … but it isn’t always better or best.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine, for nearly 40 years. He has authored several books on behavioral pediatrics including “How to Say No to Your Toddler.”
Let’s roll!
Imagine yourself in a small community hospital standing at the bedside of a tiny preemie waiting for the neonatal transport team to return your call for help.
With one eye shifting between the clock and the oximeter, you have the other one looking out the window hoping that the predicted snow and freezing rain will hold out for another hour. You have done everything you can do, but clearly it’s not going to be enough to rescue this little person who had the misfortune of exiting the birth canal several months too early.
You have been able to insert an umbilical vein catheter and miraculously have threaded an endotracheal tube into a trachea that looked no bigger than a piece of spaghetti, or maybe you have failed and the nurses are taking turns bagging. The transport team returns your call for help and with apologies reports that they are tied up with a similar scenario further south; they predict that it may be an hour and a half before they will be able to get back to their hospital, which is a half hour down the road from you.
They suggest some things that you have already done. Should you wait for more skilled hands and their equipment or transport the patient yourself and get on the road before it becomes a skating rink? There is an antique transport isolette gathering dust in the storage room down the hall, and the local fire department ambulance crew with whom you are on a first-name basis is always ready to help. Is it time to gather the troops and tell them, “Let’s roll!” ?
If you have ever lived through a similar scenario, you may find a recent study interesting (Ann Intern Med. 2015;163[9]:681-90). What these investigators found was that for adults who had suffered major trauma, stroke, respiratory failure, and acute myocardial infarction, those who were transported by crews with basic life support (BLS) skills had significantly better long-term survival and neurologic outcomes than did those victims transported by crews with advanced life support (ALS) skills.
In the flurry of comments that circulated following the release of the study were a few questions about the methodology, but most commentators were searching for an explanation. Was critical time lost by the ALS crews doing stuff when the better course of action would have been to get the ambulance rolling to the hospital and more definitive care? Does the temptation to do things because you can do them sometimes cloud the decision-making process?
Although I have lived the scenario I described, it is less likely to happen now. Backup teams from other institutions may be activated. The teams are so well equipped and trained that the gaps between their capabilities and the neonatal intensive care unit have narrowed, but there is no question that they remain and are significant.
The other thing that hasn’t changed is the weather here in Maine. While we have beautiful summers that prompt us to put “Vacationland” on our license plates, our winters are a challenge. In addition to the patient’s condition and the availability of resources, the decision of whether to invest time in stabilization or get moving toward the referral center also must include the risk to the patient and staff who will be traveling on weather-threatened roads.
On the other hand, we can’t ignore the elephant that occasionally finds its way into the room when decisions are made about how thoroughly a critically ill patient is stabilized and how speedily he is transferred. And, that ponderous pachyderm is the hot potato factor and sometimes answers to its acronym, NIMBY (“not in my back yard”). You know as well as I do that despite the Emergency Medical Treatment and Active Labor Act (EMTALA) regulations, there are cases when a patient is hustled out the door without being appropriately stabilized primarily to avoid having that patient die in the referring hospital. We must continue to ask ourselves if we have done everything that we can do to stabilize the patient before we say, “Let’s roll!”
William G. Wilkoff, M.D., practiced primary care pediatrics in Brunswick, Maine, for nearly 40 years. He has authored several books on behavioral pediatrics including “How to Say No to Your Toddler.”
Imagine yourself in a small community hospital standing at the bedside of a tiny preemie waiting for the neonatal transport team to return your call for help.
With one eye shifting between the clock and the oximeter, you have the other one looking out the window hoping that the predicted snow and freezing rain will hold out for another hour. You have done everything you can do, but clearly it’s not going to be enough to rescue this little person who had the misfortune of exiting the birth canal several months too early.
You have been able to insert an umbilical vein catheter and miraculously have threaded an endotracheal tube into a trachea that looked no bigger than a piece of spaghetti, or maybe you have failed and the nurses are taking turns bagging. The transport team returns your call for help and with apologies reports that they are tied up with a similar scenario further south; they predict that it may be an hour and a half before they will be able to get back to their hospital, which is a half hour down the road from you.
They suggest some things that you have already done. Should you wait for more skilled hands and their equipment or transport the patient yourself and get on the road before it becomes a skating rink? There is an antique transport isolette gathering dust in the storage room down the hall, and the local fire department ambulance crew with whom you are on a first-name basis is always ready to help. Is it time to gather the troops and tell them, “Let’s roll!” ?
If you have ever lived through a similar scenario, you may find a recent study interesting (Ann Intern Med. 2015;163[9]:681-90). What these investigators found was that for adults who had suffered major trauma, stroke, respiratory failure, and acute myocardial infarction, those who were transported by crews with basic life support (BLS) skills had significantly better long-term survival and neurologic outcomes than did those victims transported by crews with advanced life support (ALS) skills.
In the flurry of comments that circulated following the release of the study were a few questions about the methodology, but most commentators were searching for an explanation. Was critical time lost by the ALS crews doing stuff when the better course of action would have been to get the ambulance rolling to the hospital and more definitive care? Does the temptation to do things because you can do them sometimes cloud the decision-making process?
Although I have lived the scenario I described, it is less likely to happen now. Backup teams from other institutions may be activated. The teams are so well equipped and trained that the gaps between their capabilities and the neonatal intensive care unit have narrowed, but there is no question that they remain and are significant.
The other thing that hasn’t changed is the weather here in Maine. While we have beautiful summers that prompt us to put “Vacationland” on our license plates, our winters are a challenge. In addition to the patient’s condition and the availability of resources, the decision of whether to invest time in stabilization or get moving toward the referral center also must include the risk to the patient and staff who will be traveling on weather-threatened roads.
On the other hand, we can’t ignore the elephant that occasionally finds its way into the room when decisions are made about how thoroughly a critically ill patient is stabilized and how speedily he is transferred. And, that ponderous pachyderm is the hot potato factor and sometimes answers to its acronym, NIMBY (“not in my back yard”). You know as well as I do that despite the Emergency Medical Treatment and Active Labor Act (EMTALA) regulations, there are cases when a patient is hustled out the door without being appropriately stabilized primarily to avoid having that patient die in the referring hospital. We must continue to ask ourselves if we have done everything that we can do to stabilize the patient before we say, “Let’s roll!”
William G. Wilkoff, M.D., practiced primary care pediatrics in Brunswick, Maine, for nearly 40 years. He has authored several books on behavioral pediatrics including “How to Say No to Your Toddler.”
Imagine yourself in a small community hospital standing at the bedside of a tiny preemie waiting for the neonatal transport team to return your call for help.
With one eye shifting between the clock and the oximeter, you have the other one looking out the window hoping that the predicted snow and freezing rain will hold out for another hour. You have done everything you can do, but clearly it’s not going to be enough to rescue this little person who had the misfortune of exiting the birth canal several months too early.
You have been able to insert an umbilical vein catheter and miraculously have threaded an endotracheal tube into a trachea that looked no bigger than a piece of spaghetti, or maybe you have failed and the nurses are taking turns bagging. The transport team returns your call for help and with apologies reports that they are tied up with a similar scenario further south; they predict that it may be an hour and a half before they will be able to get back to their hospital, which is a half hour down the road from you.
They suggest some things that you have already done. Should you wait for more skilled hands and their equipment or transport the patient yourself and get on the road before it becomes a skating rink? There is an antique transport isolette gathering dust in the storage room down the hall, and the local fire department ambulance crew with whom you are on a first-name basis is always ready to help. Is it time to gather the troops and tell them, “Let’s roll!” ?
If you have ever lived through a similar scenario, you may find a recent study interesting (Ann Intern Med. 2015;163[9]:681-90). What these investigators found was that for adults who had suffered major trauma, stroke, respiratory failure, and acute myocardial infarction, those who were transported by crews with basic life support (BLS) skills had significantly better long-term survival and neurologic outcomes than did those victims transported by crews with advanced life support (ALS) skills.
In the flurry of comments that circulated following the release of the study were a few questions about the methodology, but most commentators were searching for an explanation. Was critical time lost by the ALS crews doing stuff when the better course of action would have been to get the ambulance rolling to the hospital and more definitive care? Does the temptation to do things because you can do them sometimes cloud the decision-making process?
Although I have lived the scenario I described, it is less likely to happen now. Backup teams from other institutions may be activated. The teams are so well equipped and trained that the gaps between their capabilities and the neonatal intensive care unit have narrowed, but there is no question that they remain and are significant.
The other thing that hasn’t changed is the weather here in Maine. While we have beautiful summers that prompt us to put “Vacationland” on our license plates, our winters are a challenge. In addition to the patient’s condition and the availability of resources, the decision of whether to invest time in stabilization or get moving toward the referral center also must include the risk to the patient and staff who will be traveling on weather-threatened roads.
On the other hand, we can’t ignore the elephant that occasionally finds its way into the room when decisions are made about how thoroughly a critically ill patient is stabilized and how speedily he is transferred. And, that ponderous pachyderm is the hot potato factor and sometimes answers to its acronym, NIMBY (“not in my back yard”). You know as well as I do that despite the Emergency Medical Treatment and Active Labor Act (EMTALA) regulations, there are cases when a patient is hustled out the door without being appropriately stabilized primarily to avoid having that patient die in the referring hospital. We must continue to ask ourselves if we have done everything that we can do to stabilize the patient before we say, “Let’s roll!”
William G. Wilkoff, M.D., practiced primary care pediatrics in Brunswick, Maine, for nearly 40 years. He has authored several books on behavioral pediatrics including “How to Say No to Your Toddler.”
Rising death rates of white midlife Americans
Princeton University Professor of Economics and Public Affairs Anne Case, Ph.D., and 2015 Nobel Prize winner in economics Angus Deaton, Ph.D., recently made headlines with an article in the Proceedings of the National Academy of Sciences that showed a remarkable anomaly in global death rates.
The steady decline in death rates seen across the world for age-specific cohorts held true in the United States with one exception: White men and women aged 45-54 years and only in the period of 1999 to 2013. The rising death rates in this cohort were concentrated most intensely among those with less than a high school education and among men. This finding was not seen in cohorts from other countries or in this age group in the United States before 1999.
Many explanations have been given for this focused finding, from income inequality to the stubbornly slow recovery from the recent economic recession. But none of these speculations explains why the upturn in death rates was not seen among Hispanics or blacks in this age cohort – or why it was not seen in the decade before 2000.
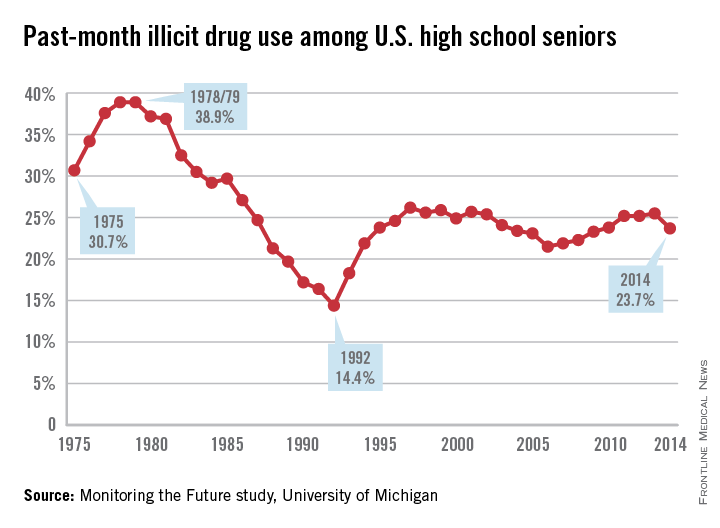
Several clues provide insight. The first is that the increase in deaths was mostly the result of rising rates of drug overdose, suicide, and chronic liver disease, including cirrhosis of the liver. In 1978, the peak of the modern drug epidemic, this cohort was aged 10-24 years. This sharp drug abuse epidemic was distinctly American and more prevalent among white males than among white females or other males. The annual Monitoring the Future study, funded by the National Institute on Drug Abuse and conducted by the University of Michigan, Ann Arbor, has chronicled the patterns of substance use for American 12th graders from 1975 to the present. It provides a snapshot of the patterns of adolescent drug use in this cohort. During the peak of the national drug epidemic, this cohort was at the most vulnerable age for starting drug use.
The second clue to this puzzle is that in recent decades, there has been a breakdown in the health and social capital of whites having lower educations, as author and political scientist author Charles Murray, Ph.D., recounted in a recent book (“Coming Apart: The State of White America, 1960-2010,” [New York: Crown Forum, 2012]). This might have resulted in an increased vulnerability in midlife within this cohort to adverse health effects and in less resiliency in mitigating those effects.
A third relevant clue is that the adverse health effects of adolescent drug use are not limited to adolescence. Substance use disorders most commonly begin in the teenage years (Nature. 2015 Jun;[522]:S46-7). Early drug use is a predictor of lifelong serious co-occurring health problems, including addiction to alcohol and other drugs.
Thus, in addition to the explanations already put forth in response to the Case-Deaton findings, an additional factor has significance. The leading edge of the Baby Boom generation not only sparked the modern drug abuse epidemic in their teen years but also carries with it a substantially heightened lifelong health risk for overdose death, suicide, and chronic liver disease.
This finding is significant not only for the health of this aging cohort but also for young people today. The delayed consequences of adolescent drug and alcohol use provide another good reason to refocus public health efforts to encourage youth to grow up without using alcohol, tobacco, marijuana, and other drugs.
Dr. DuPont is president of the Institute for Behavior and Health, Rockville, Md., and was the first director of the National Institute on Drug Abuse (1973-1978).
Princeton University Professor of Economics and Public Affairs Anne Case, Ph.D., and 2015 Nobel Prize winner in economics Angus Deaton, Ph.D., recently made headlines with an article in the Proceedings of the National Academy of Sciences that showed a remarkable anomaly in global death rates.
The steady decline in death rates seen across the world for age-specific cohorts held true in the United States with one exception: White men and women aged 45-54 years and only in the period of 1999 to 2013. The rising death rates in this cohort were concentrated most intensely among those with less than a high school education and among men. This finding was not seen in cohorts from other countries or in this age group in the United States before 1999.
Many explanations have been given for this focused finding, from income inequality to the stubbornly slow recovery from the recent economic recession. But none of these speculations explains why the upturn in death rates was not seen among Hispanics or blacks in this age cohort – or why it was not seen in the decade before 2000.
Several clues provide insight. The first is that the increase in deaths was mostly the result of rising rates of drug overdose, suicide, and chronic liver disease, including cirrhosis of the liver. In 1978, the peak of the modern drug epidemic, this cohort was aged 10-24 years. This sharp drug abuse epidemic was distinctly American and more prevalent among white males than among white females or other males. The annual Monitoring the Future study, funded by the National Institute on Drug Abuse and conducted by the University of Michigan, Ann Arbor, has chronicled the patterns of substance use for American 12th graders from 1975 to the present. It provides a snapshot of the patterns of adolescent drug use in this cohort. During the peak of the national drug epidemic, this cohort was at the most vulnerable age for starting drug use.
The second clue to this puzzle is that in recent decades, there has been a breakdown in the health and social capital of whites having lower educations, as author and political scientist author Charles Murray, Ph.D., recounted in a recent book (“Coming Apart: The State of White America, 1960-2010,” [New York: Crown Forum, 2012]). This might have resulted in an increased vulnerability in midlife within this cohort to adverse health effects and in less resiliency in mitigating those effects.
A third relevant clue is that the adverse health effects of adolescent drug use are not limited to adolescence. Substance use disorders most commonly begin in the teenage years (Nature. 2015 Jun;[522]:S46-7). Early drug use is a predictor of lifelong serious co-occurring health problems, including addiction to alcohol and other drugs.
Thus, in addition to the explanations already put forth in response to the Case-Deaton findings, an additional factor has significance. The leading edge of the Baby Boom generation not only sparked the modern drug abuse epidemic in their teen years but also carries with it a substantially heightened lifelong health risk for overdose death, suicide, and chronic liver disease.
This finding is significant not only for the health of this aging cohort but also for young people today. The delayed consequences of adolescent drug and alcohol use provide another good reason to refocus public health efforts to encourage youth to grow up without using alcohol, tobacco, marijuana, and other drugs.
Dr. DuPont is president of the Institute for Behavior and Health, Rockville, Md., and was the first director of the National Institute on Drug Abuse (1973-1978).
Princeton University Professor of Economics and Public Affairs Anne Case, Ph.D., and 2015 Nobel Prize winner in economics Angus Deaton, Ph.D., recently made headlines with an article in the Proceedings of the National Academy of Sciences that showed a remarkable anomaly in global death rates.
The steady decline in death rates seen across the world for age-specific cohorts held true in the United States with one exception: White men and women aged 45-54 years and only in the period of 1999 to 2013. The rising death rates in this cohort were concentrated most intensely among those with less than a high school education and among men. This finding was not seen in cohorts from other countries or in this age group in the United States before 1999.
Many explanations have been given for this focused finding, from income inequality to the stubbornly slow recovery from the recent economic recession. But none of these speculations explains why the upturn in death rates was not seen among Hispanics or blacks in this age cohort – or why it was not seen in the decade before 2000.
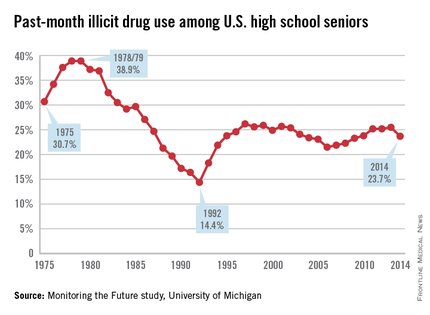
Several clues provide insight. The first is that the increase in deaths was mostly the result of rising rates of drug overdose, suicide, and chronic liver disease, including cirrhosis of the liver. In 1978, the peak of the modern drug epidemic, this cohort was aged 10-24 years. This sharp drug abuse epidemic was distinctly American and more prevalent among white males than among white females or other males. The annual Monitoring the Future study, funded by the National Institute on Drug Abuse and conducted by the University of Michigan, Ann Arbor, has chronicled the patterns of substance use for American 12th graders from 1975 to the present. It provides a snapshot of the patterns of adolescent drug use in this cohort. During the peak of the national drug epidemic, this cohort was at the most vulnerable age for starting drug use.
The second clue to this puzzle is that in recent decades, there has been a breakdown in the health and social capital of whites having lower educations, as author and political scientist author Charles Murray, Ph.D., recounted in a recent book (“Coming Apart: The State of White America, 1960-2010,” [New York: Crown Forum, 2012]). This might have resulted in an increased vulnerability in midlife within this cohort to adverse health effects and in less resiliency in mitigating those effects.
A third relevant clue is that the adverse health effects of adolescent drug use are not limited to adolescence. Substance use disorders most commonly begin in the teenage years (Nature. 2015 Jun;[522]:S46-7). Early drug use is a predictor of lifelong serious co-occurring health problems, including addiction to alcohol and other drugs.
Thus, in addition to the explanations already put forth in response to the Case-Deaton findings, an additional factor has significance. The leading edge of the Baby Boom generation not only sparked the modern drug abuse epidemic in their teen years but also carries with it a substantially heightened lifelong health risk for overdose death, suicide, and chronic liver disease.
This finding is significant not only for the health of this aging cohort but also for young people today. The delayed consequences of adolescent drug and alcohol use provide another good reason to refocus public health efforts to encourage youth to grow up without using alcohol, tobacco, marijuana, and other drugs.
Dr. DuPont is president of the Institute for Behavior and Health, Rockville, Md., and was the first director of the National Institute on Drug Abuse (1973-1978).
Defying Gravity
Last week, I fell in the driveway. I was taking the trash to the curb when I tripped and fell into the large blue recycling bin. Although it was 6 AM, I jumped up and looked around, horrified that someone may have seen my episode of gracelessness. I did bump my head and spent the rest of the day feeling stupid while rubbing the sore spot.
This incident, though more ego-bruising than anything, really conveyed to me the concerns of falling—not only for the elderly, but for all of us. So, not to be confused with the signature song from the musical Wicked sung by Elphaba (the Wicked Witch of the West) who has a desire to live without limits, my editorial this month discusses sobering limits in our everyday lives. And it does implicate gravity!
According to the National Council on Aging, about 1 in 3 adults ages 65 and older fall each year.1 Unintentional falls are the leading cause of nonfatal and fatal injuries (eg, hip fractures, head trauma) for older adults and result in about 57 fall-related deaths per 100,000 people per year.1,2 In 2013, more than 25,000 elderly individuals in the United States died from unintentional fall injuries.3
Who falls? Who doesn’t? But data indicate that among community-dwelling individuals older than 65, women fall more frequently than their male counterparts.4 But while injury and mortality rates rise dramatically for both sexes, regardless of race, after age 85, men in this age-group are more likely to die from a fall than are women.5
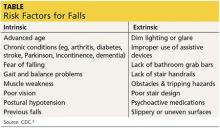
There are many risk factors that contribute to falling (see the table6), with gait and balance problems reported as the most significant contributor to falls among older adults.7 In addition, researchers report an increase in diseases linked to falls: diabetes, heart disease, stroke, arthritis, and Parkinson disease. In many cases, the medication used to treat the disease increases the risk for falling.8 It behooves every clinician to assess for and address any modifiable risk factors at each patient visit; one valuable resource is the CDC’s Compendium of Effective Fall Interventions: What Works for Community-Dwelling Older Adults.9
The issue of falling must be addressed on a larger scale, though. In response to the sobering statistics about falls, retirement communities, assisted living facilities, and nursing homes are trying to balance safety with their residents’ desire to live as they choose. They are hiring architects, interior designers, and engineers to find better ways to create safe living spaces, including installing floor lighting (similar to that on airplanes) that automatically illuminates a pathway to the bathroom when a resident gets out of bed.10
Continue for fall prevention in the community >>
But what about fall prevention in the community? A cost-benefit analysis revealed that community-based fall interventions are feasible and effective and provide a positive return on investment—no small consideration, given our current circumstances: Every 13 seconds, an older adult is treated in the emergency department for a fall, and every 29 minutes, an older adult dies from a fall-related injury.4,5 These estimates will likely rise as the population ages. The financial repercussions of falls and resultant morbidity and mortality may exceed $59 billion by 2020, according to the National Council on Aging.1 However, a 2013 report to Congress by the Centers for Medicare & Medicaid Services indicated that older adults’ participation in a falls prevention program has resulted in reduced health care costs.11
Over the decades, many different approaches have been used to enhance older adults’ participation in such programs. I am proud to report that my university is among the many organizations to address this issue. A.T. Still University of Health Sciences (ATSU) was recently awarded a $95,000 grant by the Baptist Hospitals and Health Systems (BHHS) to support the university’s Fall Prevention Outreach program—the largest university-based fall-prevention initiative in the country.12
Since the program began in 2008, more than 2,000 Arizonans have completed the eight-week curriculum, which gives older adults the tools they need to prevent falls and manage the often-paralyzing fear of falling that comes with growing older. Since injuries sustained from falls are the leading cause of accidental injury deaths in Arizonans ages 65 and older, according to the state’s Department of Health Services, this program gives us an opportunity to have a direct impact on our community.
ATSU uses A Matter of Balance, a nationally recognized fall-prevention curriculum developed by Boston University.13 After receiving special training, teams of ATSU physician assistant, physical therapy, occupational therapy, athletic training, and audiology students offer the curriculum, at no cost, to older citizens at 41 community sites in the Greater Phoenix area. Collaborations with partners ranging from local municipalities to assisted-living communities make the program possible.
Part of the BHHS grant funded the certification of 15 master trainers who teach the two-day A Matter of Balance curriculum to the ATSU students and the community volunteers who will, in turn, lead the sessions. The grant also funded the expansion of the program to an additional 24 sites, for a total of 65.12
For those who wish to identify appropriate evidence-based fall prevention programs in their community, the CDC developed a new guide, Preventing Falls: A Guide to Implementing Effective Community-Based Fall Prevention Programs.14 This “how-to” outlines how community-based organizations initiate and maintain effective programs. It focuses on implementation of fall prevention programs and offers strategies on program planning, development, implementation, and evaluation. This resource provides a solid starting point for those seeking to address this increasingly prevalent issue.
How do you investigate the risk for falls with your patients? I would be interested in hearing from you what resources are available in your community. You can contact me at [email protected].
REFERENCES
1. Cameron K, Schneider E, Childress D, Gilchrist C. (2015). National Council on Aging Falls Free® National Action Plan (2015). www.ncoa.org/FallsFreeNAP. Accessed November 5, 2015.
2. CDC. Important Facts about Falls. www.cdc.gov/homeandrecreationalsafety/falls/adultfalls.html. Accessed November 5, 2015.
3. CDC National Center for Injury Prevention and Control. Injury Prevention & Control: Data & Statistics (WISQARSTM). www.cdc.gov/injury/wisqars/. Accessed August 15, 2013.
4. Carande-Kulis I, Stevens JA, Florence CS, et al. Special Report from the CDC: a cost-benefit analysis of three older adult fall prevention interventions. J Safety Res. 2015;52:65-70.
5. CDC. WISQARS leading causes of nonfatal injury reports: 2006. Accessed November 13, 2006.
6. CDC. Risk factors for falls. http://www.cdc.gov/steadi/pdf/risk_factors_for_falls-a.pdf. Accessed November 4, 2015.
7. Hausdorff JM, Rios DA, Edelberg HK. Gait variability and fall risk in community-living older adults: a 1-year prospective study. Arch Phys Med Rehabil. 2001;82(8):1050-1056.
8. Ambrose AF, Paul G, Hausdorff JM. Risk factors for falls among older adults: a review of the literature. Maturitas. 2013;75(1):51-61.
9. CDC. Compendium of Effective Fall Interventions: What Works for Community-Dwelling Older Adults. 3rd ed. www.cdc.gov/homeandrecreationalsafety/Falls/compendium.html. Accessed November 4, 2015.
10. Hafner K. Bracing for the falls of an aging nation. New York Times. November 2, 2014. www.nytimes.com/interactive/2014/11/03/health/bracing-for-the-falls-of-an-aging-nation.html?emc=edit_na_20141102&_r=0. Accessed November 4, 2015.
11. Houry D. The White House Conference on Aging and keeping older adults STEADI and free from falls. www.whitehouseconferenceonaging.gov/blog/post/the-white-house-conference-on-aging-and-keeping-older-adults-steadi-and-free-from-falls1.aspx. Accessed November 4, 2015.
12. Scott K. ATSU receives $95,000 grant to expand Fall Prevention Outreach program [news release]. October 1, 2015. http://news.atsu.edu/index.php/archives/category/arizona-campus. Accessed November 4, 2015.
13. MaineHealth Partnership for Healthy Aging. A Matter of Balance: Managing Concerns About Falls. www.mainehealth.org/AMatterofBalanceFrequentlyAskedQuestions#mob. Accessed November 4, 2015.
14. CDC. Preventing Falls: A Guide to Implementing Effective Community-Based Fall Prevention Programs. www.cdc.gov/HomeandRecreationalSafetyFalls/community_preventfalls.html. Accessed November 4, 2015.
Last week, I fell in the driveway. I was taking the trash to the curb when I tripped and fell into the large blue recycling bin. Although it was 6 AM, I jumped up and looked around, horrified that someone may have seen my episode of gracelessness. I did bump my head and spent the rest of the day feeling stupid while rubbing the sore spot.
This incident, though more ego-bruising than anything, really conveyed to me the concerns of falling—not only for the elderly, but for all of us. So, not to be confused with the signature song from the musical Wicked sung by Elphaba (the Wicked Witch of the West) who has a desire to live without limits, my editorial this month discusses sobering limits in our everyday lives. And it does implicate gravity!
According to the National Council on Aging, about 1 in 3 adults ages 65 and older fall each year.1 Unintentional falls are the leading cause of nonfatal and fatal injuries (eg, hip fractures, head trauma) for older adults and result in about 57 fall-related deaths per 100,000 people per year.1,2 In 2013, more than 25,000 elderly individuals in the United States died from unintentional fall injuries.3
Who falls? Who doesn’t? But data indicate that among community-dwelling individuals older than 65, women fall more frequently than their male counterparts.4 But while injury and mortality rates rise dramatically for both sexes, regardless of race, after age 85, men in this age-group are more likely to die from a fall than are women.5
There are many risk factors that contribute to falling (see the table6), with gait and balance problems reported as the most significant contributor to falls among older adults.7 In addition, researchers report an increase in diseases linked to falls: diabetes, heart disease, stroke, arthritis, and Parkinson disease. In many cases, the medication used to treat the disease increases the risk for falling.8 It behooves every clinician to assess for and address any modifiable risk factors at each patient visit; one valuable resource is the CDC’s Compendium of Effective Fall Interventions: What Works for Community-Dwelling Older Adults.9
The issue of falling must be addressed on a larger scale, though. In response to the sobering statistics about falls, retirement communities, assisted living facilities, and nursing homes are trying to balance safety with their residents’ desire to live as they choose. They are hiring architects, interior designers, and engineers to find better ways to create safe living spaces, including installing floor lighting (similar to that on airplanes) that automatically illuminates a pathway to the bathroom when a resident gets out of bed.10
Continue for fall prevention in the community >>
But what about fall prevention in the community? A cost-benefit analysis revealed that community-based fall interventions are feasible and effective and provide a positive return on investment—no small consideration, given our current circumstances: Every 13 seconds, an older adult is treated in the emergency department for a fall, and every 29 minutes, an older adult dies from a fall-related injury.4,5 These estimates will likely rise as the population ages. The financial repercussions of falls and resultant morbidity and mortality may exceed $59 billion by 2020, according to the National Council on Aging.1 However, a 2013 report to Congress by the Centers for Medicare & Medicaid Services indicated that older adults’ participation in a falls prevention program has resulted in reduced health care costs.11
Over the decades, many different approaches have been used to enhance older adults’ participation in such programs. I am proud to report that my university is among the many organizations to address this issue. A.T. Still University of Health Sciences (ATSU) was recently awarded a $95,000 grant by the Baptist Hospitals and Health Systems (BHHS) to support the university’s Fall Prevention Outreach program—the largest university-based fall-prevention initiative in the country.12
Since the program began in 2008, more than 2,000 Arizonans have completed the eight-week curriculum, which gives older adults the tools they need to prevent falls and manage the often-paralyzing fear of falling that comes with growing older. Since injuries sustained from falls are the leading cause of accidental injury deaths in Arizonans ages 65 and older, according to the state’s Department of Health Services, this program gives us an opportunity to have a direct impact on our community.
ATSU uses A Matter of Balance, a nationally recognized fall-prevention curriculum developed by Boston University.13 After receiving special training, teams of ATSU physician assistant, physical therapy, occupational therapy, athletic training, and audiology students offer the curriculum, at no cost, to older citizens at 41 community sites in the Greater Phoenix area. Collaborations with partners ranging from local municipalities to assisted-living communities make the program possible.
Part of the BHHS grant funded the certification of 15 master trainers who teach the two-day A Matter of Balance curriculum to the ATSU students and the community volunteers who will, in turn, lead the sessions. The grant also funded the expansion of the program to an additional 24 sites, for a total of 65.12
For those who wish to identify appropriate evidence-based fall prevention programs in their community, the CDC developed a new guide, Preventing Falls: A Guide to Implementing Effective Community-Based Fall Prevention Programs.14 This “how-to” outlines how community-based organizations initiate and maintain effective programs. It focuses on implementation of fall prevention programs and offers strategies on program planning, development, implementation, and evaluation. This resource provides a solid starting point for those seeking to address this increasingly prevalent issue.
How do you investigate the risk for falls with your patients? I would be interested in hearing from you what resources are available in your community. You can contact me at [email protected].
REFERENCES
1. Cameron K, Schneider E, Childress D, Gilchrist C. (2015). National Council on Aging Falls Free® National Action Plan (2015). www.ncoa.org/FallsFreeNAP. Accessed November 5, 2015.
2. CDC. Important Facts about Falls. www.cdc.gov/homeandrecreationalsafety/falls/adultfalls.html. Accessed November 5, 2015.
3. CDC National Center for Injury Prevention and Control. Injury Prevention & Control: Data & Statistics (WISQARSTM). www.cdc.gov/injury/wisqars/. Accessed August 15, 2013.
4. Carande-Kulis I, Stevens JA, Florence CS, et al. Special Report from the CDC: a cost-benefit analysis of three older adult fall prevention interventions. J Safety Res. 2015;52:65-70.
5. CDC. WISQARS leading causes of nonfatal injury reports: 2006. Accessed November 13, 2006.
6. CDC. Risk factors for falls. http://www.cdc.gov/steadi/pdf/risk_factors_for_falls-a.pdf. Accessed November 4, 2015.
7. Hausdorff JM, Rios DA, Edelberg HK. Gait variability and fall risk in community-living older adults: a 1-year prospective study. Arch Phys Med Rehabil. 2001;82(8):1050-1056.
8. Ambrose AF, Paul G, Hausdorff JM. Risk factors for falls among older adults: a review of the literature. Maturitas. 2013;75(1):51-61.
9. CDC. Compendium of Effective Fall Interventions: What Works for Community-Dwelling Older Adults. 3rd ed. www.cdc.gov/homeandrecreationalsafety/Falls/compendium.html. Accessed November 4, 2015.
10. Hafner K. Bracing for the falls of an aging nation. New York Times. November 2, 2014. www.nytimes.com/interactive/2014/11/03/health/bracing-for-the-falls-of-an-aging-nation.html?emc=edit_na_20141102&_r=0. Accessed November 4, 2015.
11. Houry D. The White House Conference on Aging and keeping older adults STEADI and free from falls. www.whitehouseconferenceonaging.gov/blog/post/the-white-house-conference-on-aging-and-keeping-older-adults-steadi-and-free-from-falls1.aspx. Accessed November 4, 2015.
12. Scott K. ATSU receives $95,000 grant to expand Fall Prevention Outreach program [news release]. October 1, 2015. http://news.atsu.edu/index.php/archives/category/arizona-campus. Accessed November 4, 2015.
13. MaineHealth Partnership for Healthy Aging. A Matter of Balance: Managing Concerns About Falls. www.mainehealth.org/AMatterofBalanceFrequentlyAskedQuestions#mob. Accessed November 4, 2015.
14. CDC. Preventing Falls: A Guide to Implementing Effective Community-Based Fall Prevention Programs. www.cdc.gov/HomeandRecreationalSafetyFalls/community_preventfalls.html. Accessed November 4, 2015.
Last week, I fell in the driveway. I was taking the trash to the curb when I tripped and fell into the large blue recycling bin. Although it was 6 AM, I jumped up and looked around, horrified that someone may have seen my episode of gracelessness. I did bump my head and spent the rest of the day feeling stupid while rubbing the sore spot.
This incident, though more ego-bruising than anything, really conveyed to me the concerns of falling—not only for the elderly, but for all of us. So, not to be confused with the signature song from the musical Wicked sung by Elphaba (the Wicked Witch of the West) who has a desire to live without limits, my editorial this month discusses sobering limits in our everyday lives. And it does implicate gravity!
According to the National Council on Aging, about 1 in 3 adults ages 65 and older fall each year.1 Unintentional falls are the leading cause of nonfatal and fatal injuries (eg, hip fractures, head trauma) for older adults and result in about 57 fall-related deaths per 100,000 people per year.1,2 In 2013, more than 25,000 elderly individuals in the United States died from unintentional fall injuries.3
Who falls? Who doesn’t? But data indicate that among community-dwelling individuals older than 65, women fall more frequently than their male counterparts.4 But while injury and mortality rates rise dramatically for both sexes, regardless of race, after age 85, men in this age-group are more likely to die from a fall than are women.5
There are many risk factors that contribute to falling (see the table6), with gait and balance problems reported as the most significant contributor to falls among older adults.7 In addition, researchers report an increase in diseases linked to falls: diabetes, heart disease, stroke, arthritis, and Parkinson disease. In many cases, the medication used to treat the disease increases the risk for falling.8 It behooves every clinician to assess for and address any modifiable risk factors at each patient visit; one valuable resource is the CDC’s Compendium of Effective Fall Interventions: What Works for Community-Dwelling Older Adults.9
The issue of falling must be addressed on a larger scale, though. In response to the sobering statistics about falls, retirement communities, assisted living facilities, and nursing homes are trying to balance safety with their residents’ desire to live as they choose. They are hiring architects, interior designers, and engineers to find better ways to create safe living spaces, including installing floor lighting (similar to that on airplanes) that automatically illuminates a pathway to the bathroom when a resident gets out of bed.10
Continue for fall prevention in the community >>
But what about fall prevention in the community? A cost-benefit analysis revealed that community-based fall interventions are feasible and effective and provide a positive return on investment—no small consideration, given our current circumstances: Every 13 seconds, an older adult is treated in the emergency department for a fall, and every 29 minutes, an older adult dies from a fall-related injury.4,5 These estimates will likely rise as the population ages. The financial repercussions of falls and resultant morbidity and mortality may exceed $59 billion by 2020, according to the National Council on Aging.1 However, a 2013 report to Congress by the Centers for Medicare & Medicaid Services indicated that older adults’ participation in a falls prevention program has resulted in reduced health care costs.11
Over the decades, many different approaches have been used to enhance older adults’ participation in such programs. I am proud to report that my university is among the many organizations to address this issue. A.T. Still University of Health Sciences (ATSU) was recently awarded a $95,000 grant by the Baptist Hospitals and Health Systems (BHHS) to support the university’s Fall Prevention Outreach program—the largest university-based fall-prevention initiative in the country.12
Since the program began in 2008, more than 2,000 Arizonans have completed the eight-week curriculum, which gives older adults the tools they need to prevent falls and manage the often-paralyzing fear of falling that comes with growing older. Since injuries sustained from falls are the leading cause of accidental injury deaths in Arizonans ages 65 and older, according to the state’s Department of Health Services, this program gives us an opportunity to have a direct impact on our community.
ATSU uses A Matter of Balance, a nationally recognized fall-prevention curriculum developed by Boston University.13 After receiving special training, teams of ATSU physician assistant, physical therapy, occupational therapy, athletic training, and audiology students offer the curriculum, at no cost, to older citizens at 41 community sites in the Greater Phoenix area. Collaborations with partners ranging from local municipalities to assisted-living communities make the program possible.
Part of the BHHS grant funded the certification of 15 master trainers who teach the two-day A Matter of Balance curriculum to the ATSU students and the community volunteers who will, in turn, lead the sessions. The grant also funded the expansion of the program to an additional 24 sites, for a total of 65.12
For those who wish to identify appropriate evidence-based fall prevention programs in their community, the CDC developed a new guide, Preventing Falls: A Guide to Implementing Effective Community-Based Fall Prevention Programs.14 This “how-to” outlines how community-based organizations initiate and maintain effective programs. It focuses on implementation of fall prevention programs and offers strategies on program planning, development, implementation, and evaluation. This resource provides a solid starting point for those seeking to address this increasingly prevalent issue.
How do you investigate the risk for falls with your patients? I would be interested in hearing from you what resources are available in your community. You can contact me at [email protected].
REFERENCES
1. Cameron K, Schneider E, Childress D, Gilchrist C. (2015). National Council on Aging Falls Free® National Action Plan (2015). www.ncoa.org/FallsFreeNAP. Accessed November 5, 2015.
2. CDC. Important Facts about Falls. www.cdc.gov/homeandrecreationalsafety/falls/adultfalls.html. Accessed November 5, 2015.
3. CDC National Center for Injury Prevention and Control. Injury Prevention & Control: Data & Statistics (WISQARSTM). www.cdc.gov/injury/wisqars/. Accessed August 15, 2013.
4. Carande-Kulis I, Stevens JA, Florence CS, et al. Special Report from the CDC: a cost-benefit analysis of three older adult fall prevention interventions. J Safety Res. 2015;52:65-70.
5. CDC. WISQARS leading causes of nonfatal injury reports: 2006. Accessed November 13, 2006.
6. CDC. Risk factors for falls. http://www.cdc.gov/steadi/pdf/risk_factors_for_falls-a.pdf. Accessed November 4, 2015.
7. Hausdorff JM, Rios DA, Edelberg HK. Gait variability and fall risk in community-living older adults: a 1-year prospective study. Arch Phys Med Rehabil. 2001;82(8):1050-1056.
8. Ambrose AF, Paul G, Hausdorff JM. Risk factors for falls among older adults: a review of the literature. Maturitas. 2013;75(1):51-61.
9. CDC. Compendium of Effective Fall Interventions: What Works for Community-Dwelling Older Adults. 3rd ed. www.cdc.gov/homeandrecreationalsafety/Falls/compendium.html. Accessed November 4, 2015.
10. Hafner K. Bracing for the falls of an aging nation. New York Times. November 2, 2014. www.nytimes.com/interactive/2014/11/03/health/bracing-for-the-falls-of-an-aging-nation.html?emc=edit_na_20141102&_r=0. Accessed November 4, 2015.
11. Houry D. The White House Conference on Aging and keeping older adults STEADI and free from falls. www.whitehouseconferenceonaging.gov/blog/post/the-white-house-conference-on-aging-and-keeping-older-adults-steadi-and-free-from-falls1.aspx. Accessed November 4, 2015.
12. Scott K. ATSU receives $95,000 grant to expand Fall Prevention Outreach program [news release]. October 1, 2015. http://news.atsu.edu/index.php/archives/category/arizona-campus. Accessed November 4, 2015.
13. MaineHealth Partnership for Healthy Aging. A Matter of Balance: Managing Concerns About Falls. www.mainehealth.org/AMatterofBalanceFrequentlyAskedQuestions#mob. Accessed November 4, 2015.
14. CDC. Preventing Falls: A Guide to Implementing Effective Community-Based Fall Prevention Programs. www.cdc.gov/HomeandRecreationalSafetyFalls/community_preventfalls.html. Accessed November 4, 2015.
30 Years of psychiatry, with no fundamental progress
It is helpful, when evaluating any scientific proposal, to first examine underlying assumptions. In the editorial outlining 10 foundations of advanced care for psychiatrists (Do you practice sophisticated psychiatry? 10 Proposed foundations of care, Current Psychiatry, From the Editor, August 2015, p. 12-13), there are a number of assumptions that warrant discussion. I want to discuss just one of those assumptions: that psychiatric practice is better now than it was 30 years ago.
I argue that psychiatric care in America, as a whole, is much worse now than when I finished training in 1990, primarily because of changes in healthcare reimbursement. When I was in training, it was common for patients to stay in the hospital for a month or longer. One reason for the longer stays was because it takes weeks for anti depressants and antipsychotics to reveal their effectiveness. If, after 10 days, no improvement was seen, there was time to change medications.
With a hospital stay now averaging less than a week, today’s inpatient psychiatrists must rely on faith that the first treatment will work; the patient must hope that he (she) does not fall through the cracks after discharge; and the outpatient psychiatrist, short on time and psychotherapeutic training, might feel more like an assembly line worker than a professional.
Longer stays also meant more intense and extended periods of psychotherapy and psychosocial support than is possible now. It was common, when I was in training, for the biological camp to dismiss the benefits of psychotherapy therapy. After several decades of research, that position is no longer tenable—yet hospital stays remain impractically short.
If all of the medications developed since 1990 disappeared, I believe I could be as effective a psychiatrist as I am today. The simple, sad fact is that there have been no major psychopharmacotherapeutic advances in the past 30 years. Yes, there have been changes in side-effect profiles and improvements around the edges, so to speak, but no fundamental changes in effectiveness since the introduction of clozapine.
What about advances in treating negative symptoms of schizophrenia, you ask? I have not been impressed.
The worst change in psychiatric practice in the last 30 years, and the one that threatens to undermine our profession the most, is relinquishing psychotherapy as a major component of our practice. I do not mean cognitive-behavioral therapy (CBT), although that paint-by-the-numbers set of tools is better than nothing. I mean psychoanalytic psychotherapy, because it is the only comprehensive developmental theory of the mind and its pathology. There is no CBT of development, for example.
To practice and research most effectively, we need good theories of both mind and brain. For all our advances, we are no closer to explaining the mind through a brain-based theory than when Sigmund Freud tried with his Project for a Scientific Psychology.
Ours is, by far, the hardest, most intellectually challenging medical profession. We must be masters of neuroscience to bring forth a future when something such as a Project for a Scientific Psychology will be possible; we must do the best by our patients with available somatic treatments; but we also must be masters at understanding human emotional development and the intricacies of relationships and how these influence the function and epigenetics of our brains. We must reinforce our understanding of the mind through doing psychotherapy with a significant fraction of our patients to further that understanding and its associated skills—or we risk becoming assembly line psychiatrists.
Over the past 25 years of practice, I have learned that the 2 most important tools we have are time and our evolutionarily determined empathic capacity to enter another human’s subjective world. The first session should not be about ordering medical tests and gathering family history; it should be about establishing a relationship. It is on the strength of that relationship that the success of understanding and treatment, whether somatic or psychological, rests.
Thirty years ago, we had all the time we needed. That was, in some ways, a Golden Age of psychiatry. Imagine if we could bring together the greater availability of time of that era with the increasing biological and psychoanalytic understanding of the present. Then, we might have a new Golden Age. For that to happen, we must fight to change the reimbursement system. The quickest way—maybe the only way—to do that is to stop accepting reimbursement from healthcare insurance companies.
Jule P. Miller III, MD
Private Practice
Biloxi, Mississippi
Dr. Nasrallah responds
Dr. Miller is correct: Insurance has defiled psychiatric care, both inpatient and outpatient, including minimizing hospital days of care and reducing psychiatric visits to med-checks with no time to provide even rudimentary psychotherapy—psychodynamic or otherwise. I believe that the optimal medical model of psychiatric care must incorporate empathic capacity, which establishes the indispensable therapeutic alliance with each patient we see.
Dr. Miller is harsh on the lack of psychiatric advances since completing training 25 years ago. I have been in academia throughout those years and I am thrilled by how much neuroscience we have discovered that is directly related to disorders of affect, thought, cognition, and behavior. The challenge continues to be in translating those discoveries into practical therapeutic interventions, which proves the point that psychiatry is the most challenging medical specialty, consistent with the brain (and its mind) being, by far, the most complex organ.
We cannot abdicate insurance reimbursement except for our well-to-do patients. Patients with severe and disabling mental disorders, who need our services the most, cannot afford to pay for care, and depend on Medicare and Medicaid, whose modest reimbursement would impoverish non-salaried psychiatrists. Because of the severe shortage of psychiatrists, who are the only specialists who can competently manage neurobiological disorders such as schizophrenia, bipolar disorder, and severe depression, I believe we should deploy our resources for those vulnerable patients and leave the worried well and walking wounded to other mental health professionals.
Henry A. Nasrallah, MD
Professor and Chairman
Department of Psychiatry
Saint Louis University School of Medicine
St. Louis, Missouri
It is helpful, when evaluating any scientific proposal, to first examine underlying assumptions. In the editorial outlining 10 foundations of advanced care for psychiatrists (Do you practice sophisticated psychiatry? 10 Proposed foundations of care, Current Psychiatry, From the Editor, August 2015, p. 12-13), there are a number of assumptions that warrant discussion. I want to discuss just one of those assumptions: that psychiatric practice is better now than it was 30 years ago.
I argue that psychiatric care in America, as a whole, is much worse now than when I finished training in 1990, primarily because of changes in healthcare reimbursement. When I was in training, it was common for patients to stay in the hospital for a month or longer. One reason for the longer stays was because it takes weeks for anti depressants and antipsychotics to reveal their effectiveness. If, after 10 days, no improvement was seen, there was time to change medications.
With a hospital stay now averaging less than a week, today’s inpatient psychiatrists must rely on faith that the first treatment will work; the patient must hope that he (she) does not fall through the cracks after discharge; and the outpatient psychiatrist, short on time and psychotherapeutic training, might feel more like an assembly line worker than a professional.
Longer stays also meant more intense and extended periods of psychotherapy and psychosocial support than is possible now. It was common, when I was in training, for the biological camp to dismiss the benefits of psychotherapy therapy. After several decades of research, that position is no longer tenable—yet hospital stays remain impractically short.
If all of the medications developed since 1990 disappeared, I believe I could be as effective a psychiatrist as I am today. The simple, sad fact is that there have been no major psychopharmacotherapeutic advances in the past 30 years. Yes, there have been changes in side-effect profiles and improvements around the edges, so to speak, but no fundamental changes in effectiveness since the introduction of clozapine.
What about advances in treating negative symptoms of schizophrenia, you ask? I have not been impressed.
The worst change in psychiatric practice in the last 30 years, and the one that threatens to undermine our profession the most, is relinquishing psychotherapy as a major component of our practice. I do not mean cognitive-behavioral therapy (CBT), although that paint-by-the-numbers set of tools is better than nothing. I mean psychoanalytic psychotherapy, because it is the only comprehensive developmental theory of the mind and its pathology. There is no CBT of development, for example.
To practice and research most effectively, we need good theories of both mind and brain. For all our advances, we are no closer to explaining the mind through a brain-based theory than when Sigmund Freud tried with his Project for a Scientific Psychology.
Ours is, by far, the hardest, most intellectually challenging medical profession. We must be masters of neuroscience to bring forth a future when something such as a Project for a Scientific Psychology will be possible; we must do the best by our patients with available somatic treatments; but we also must be masters at understanding human emotional development and the intricacies of relationships and how these influence the function and epigenetics of our brains. We must reinforce our understanding of the mind through doing psychotherapy with a significant fraction of our patients to further that understanding and its associated skills—or we risk becoming assembly line psychiatrists.
Over the past 25 years of practice, I have learned that the 2 most important tools we have are time and our evolutionarily determined empathic capacity to enter another human’s subjective world. The first session should not be about ordering medical tests and gathering family history; it should be about establishing a relationship. It is on the strength of that relationship that the success of understanding and treatment, whether somatic or psychological, rests.
Thirty years ago, we had all the time we needed. That was, in some ways, a Golden Age of psychiatry. Imagine if we could bring together the greater availability of time of that era with the increasing biological and psychoanalytic understanding of the present. Then, we might have a new Golden Age. For that to happen, we must fight to change the reimbursement system. The quickest way—maybe the only way—to do that is to stop accepting reimbursement from healthcare insurance companies.
Jule P. Miller III, MD
Private Practice
Biloxi, Mississippi
Dr. Nasrallah responds
Dr. Miller is correct: Insurance has defiled psychiatric care, both inpatient and outpatient, including minimizing hospital days of care and reducing psychiatric visits to med-checks with no time to provide even rudimentary psychotherapy—psychodynamic or otherwise. I believe that the optimal medical model of psychiatric care must incorporate empathic capacity, which establishes the indispensable therapeutic alliance with each patient we see.
Dr. Miller is harsh on the lack of psychiatric advances since completing training 25 years ago. I have been in academia throughout those years and I am thrilled by how much neuroscience we have discovered that is directly related to disorders of affect, thought, cognition, and behavior. The challenge continues to be in translating those discoveries into practical therapeutic interventions, which proves the point that psychiatry is the most challenging medical specialty, consistent with the brain (and its mind) being, by far, the most complex organ.
We cannot abdicate insurance reimbursement except for our well-to-do patients. Patients with severe and disabling mental disorders, who need our services the most, cannot afford to pay for care, and depend on Medicare and Medicaid, whose modest reimbursement would impoverish non-salaried psychiatrists. Because of the severe shortage of psychiatrists, who are the only specialists who can competently manage neurobiological disorders such as schizophrenia, bipolar disorder, and severe depression, I believe we should deploy our resources for those vulnerable patients and leave the worried well and walking wounded to other mental health professionals.
Henry A. Nasrallah, MD
Professor and Chairman
Department of Psychiatry
Saint Louis University School of Medicine
St. Louis, Missouri
It is helpful, when evaluating any scientific proposal, to first examine underlying assumptions. In the editorial outlining 10 foundations of advanced care for psychiatrists (Do you practice sophisticated psychiatry? 10 Proposed foundations of care, Current Psychiatry, From the Editor, August 2015, p. 12-13), there are a number of assumptions that warrant discussion. I want to discuss just one of those assumptions: that psychiatric practice is better now than it was 30 years ago.
I argue that psychiatric care in America, as a whole, is much worse now than when I finished training in 1990, primarily because of changes in healthcare reimbursement. When I was in training, it was common for patients to stay in the hospital for a month or longer. One reason for the longer stays was because it takes weeks for anti depressants and antipsychotics to reveal their effectiveness. If, after 10 days, no improvement was seen, there was time to change medications.
With a hospital stay now averaging less than a week, today’s inpatient psychiatrists must rely on faith that the first treatment will work; the patient must hope that he (she) does not fall through the cracks after discharge; and the outpatient psychiatrist, short on time and psychotherapeutic training, might feel more like an assembly line worker than a professional.
Longer stays also meant more intense and extended periods of psychotherapy and psychosocial support than is possible now. It was common, when I was in training, for the biological camp to dismiss the benefits of psychotherapy therapy. After several decades of research, that position is no longer tenable—yet hospital stays remain impractically short.
If all of the medications developed since 1990 disappeared, I believe I could be as effective a psychiatrist as I am today. The simple, sad fact is that there have been no major psychopharmacotherapeutic advances in the past 30 years. Yes, there have been changes in side-effect profiles and improvements around the edges, so to speak, but no fundamental changes in effectiveness since the introduction of clozapine.
What about advances in treating negative symptoms of schizophrenia, you ask? I have not been impressed.
The worst change in psychiatric practice in the last 30 years, and the one that threatens to undermine our profession the most, is relinquishing psychotherapy as a major component of our practice. I do not mean cognitive-behavioral therapy (CBT), although that paint-by-the-numbers set of tools is better than nothing. I mean psychoanalytic psychotherapy, because it is the only comprehensive developmental theory of the mind and its pathology. There is no CBT of development, for example.
To practice and research most effectively, we need good theories of both mind and brain. For all our advances, we are no closer to explaining the mind through a brain-based theory than when Sigmund Freud tried with his Project for a Scientific Psychology.
Ours is, by far, the hardest, most intellectually challenging medical profession. We must be masters of neuroscience to bring forth a future when something such as a Project for a Scientific Psychology will be possible; we must do the best by our patients with available somatic treatments; but we also must be masters at understanding human emotional development and the intricacies of relationships and how these influence the function and epigenetics of our brains. We must reinforce our understanding of the mind through doing psychotherapy with a significant fraction of our patients to further that understanding and its associated skills—or we risk becoming assembly line psychiatrists.
Over the past 25 years of practice, I have learned that the 2 most important tools we have are time and our evolutionarily determined empathic capacity to enter another human’s subjective world. The first session should not be about ordering medical tests and gathering family history; it should be about establishing a relationship. It is on the strength of that relationship that the success of understanding and treatment, whether somatic or psychological, rests.
Thirty years ago, we had all the time we needed. That was, in some ways, a Golden Age of psychiatry. Imagine if we could bring together the greater availability of time of that era with the increasing biological and psychoanalytic understanding of the present. Then, we might have a new Golden Age. For that to happen, we must fight to change the reimbursement system. The quickest way—maybe the only way—to do that is to stop accepting reimbursement from healthcare insurance companies.
Jule P. Miller III, MD
Private Practice
Biloxi, Mississippi
Dr. Nasrallah responds
Dr. Miller is correct: Insurance has defiled psychiatric care, both inpatient and outpatient, including minimizing hospital days of care and reducing psychiatric visits to med-checks with no time to provide even rudimentary psychotherapy—psychodynamic or otherwise. I believe that the optimal medical model of psychiatric care must incorporate empathic capacity, which establishes the indispensable therapeutic alliance with each patient we see.
Dr. Miller is harsh on the lack of psychiatric advances since completing training 25 years ago. I have been in academia throughout those years and I am thrilled by how much neuroscience we have discovered that is directly related to disorders of affect, thought, cognition, and behavior. The challenge continues to be in translating those discoveries into practical therapeutic interventions, which proves the point that psychiatry is the most challenging medical specialty, consistent with the brain (and its mind) being, by far, the most complex organ.
We cannot abdicate insurance reimbursement except for our well-to-do patients. Patients with severe and disabling mental disorders, who need our services the most, cannot afford to pay for care, and depend on Medicare and Medicaid, whose modest reimbursement would impoverish non-salaried psychiatrists. Because of the severe shortage of psychiatrists, who are the only specialists who can competently manage neurobiological disorders such as schizophrenia, bipolar disorder, and severe depression, I believe we should deploy our resources for those vulnerable patients and leave the worried well and walking wounded to other mental health professionals.
Henry A. Nasrallah, MD
Professor and Chairman
Department of Psychiatry
Saint Louis University School of Medicine
St. Louis, Missouri
Design thinking
Design thinking isn’t only for products such as the Apple watch. It is a methodology used to improve customer experiences not only with products but also with services. Much in the same way that the SOAP note shaped our thinking about diagnosis and treatment, design thinking provides a scaffold to help us better understand the needs and wants of customers, or in our case, patients.
Design thinking uses specific tools and methodologies to understand experiences from others’ perspectives. From its roots in Silicon Valley, design thinking has grown steadily in its influence. Its first high priests were people such as Steve Jobs and David Kelly, who famously designed the computer mouse. The principles learned or applied to increasingly complicated products and services led to the growth of an entire industry in Palo Alto, Calif., with companies such as IDEO and gurus such as IDEO CEO and President Tim Brown of Stanford (Calif.) University has an entire graduate school program on design thinking called d.school while Coursera offers online courses on design thinking.
The principles are simple: The better you understand your customers and their needs, the better you can design your services. There are many toolkits that are available for you to try for free. Empathy Mapping is an easy one you could apply to your practice to enhance your patients’ experience.
The idea behind this technique is to immerse yourself in your patient’s world. Pick a time when your practice is closed. Then take a journey through your office as if you were a patient. It’s important that you keep the experience as close to reality as possible. Start before you even arrive at your office. What is the experience like driving to your office? Do patients have to fight traffic to get to you? Is parking easy to find? How far must they walk from their car to get to your office? What is your check-in process like? Are patients greeted by name? Are they first handed paperwork to complete? Or are they introduced and warmly welcomed to your practice first?
What’s the experience like in the waiting room? Take note of not only what your patients see but also what they hear, smell, touch, and say. What experience does your furniture give patients? What type of magazines are available to them? Do you have Wi-Fi? Is there a television? If so, is it showing simply an advertisement, or is it something that your patients would connect with? Is there music playing?
Using the same process, continue your journey through an entire patient visit. Make note of what the experience is like walking back to your exam rooms. What do your patients see and smell while sitting in an exam room waiting for you? Does it smell of isopropyl alcohol? Is it cold or hot? What’s it like to sit in your room wearing nothing but a patient gown? Are there instruments such as cryo guns that could be intimidating to patients? All of these factors can be modified and thus “designed” to optimize the experience for your patients. Continue this journey including a physical exam and discussion with the doctor and other providers and assistants.
This is a great exercise not only for you but more importantly for your staff. Ask your staff to take notes as they walk through the same empathy mapping journey. It will give them an entirely new and valuable perspective on what it’s like to be a patient in your office. Once you’ve completed your empathy mapping, sit with your team and brainstorm about opportunities to improve the experience for your patients. Ask yourselves what things surprised you. What things do you feel could have the largest impact on your patients’ experience in your office? In what ways can you modify the spaces in your office to optimize your patients’ experience?
Having done this exercise in my own clinic, I found it highly impactful. It gave me a deeper understanding of and appreciation for my patients and caused me to make several minor but important changes in my exam room and to my and my staff’s interactions with patients. I hope you have a similarly informative experience.
If you’re interested in learning more about design thinking, then check out the following books and articles:
• “Change by Design: How Design Thinking Transforms Organization and Inspires Innovation,” by Tim Brown (New York: Harper Business, 2009).
• “The Art of Innovation,” by Tom Kelley (New York: A Currency Book, Doubleday, Random House, 2001).
• Design Thinking Comes of Age, by Jon Kolko (Harv Bus Rev. Sep 2015;pp 66-71).
Dr. Benabio is a partner physician in the department of dermatology of the Southern California Permanente Group in San Diego, and a volunteer clinical assistant professor at the University of California, San Diego. Dr. Benabio is @dermdoc on Twitter.
Design thinking isn’t only for products such as the Apple watch. It is a methodology used to improve customer experiences not only with products but also with services. Much in the same way that the SOAP note shaped our thinking about diagnosis and treatment, design thinking provides a scaffold to help us better understand the needs and wants of customers, or in our case, patients.
Design thinking uses specific tools and methodologies to understand experiences from others’ perspectives. From its roots in Silicon Valley, design thinking has grown steadily in its influence. Its first high priests were people such as Steve Jobs and David Kelly, who famously designed the computer mouse. The principles learned or applied to increasingly complicated products and services led to the growth of an entire industry in Palo Alto, Calif., with companies such as IDEO and gurus such as IDEO CEO and President Tim Brown of Stanford (Calif.) University has an entire graduate school program on design thinking called d.school while Coursera offers online courses on design thinking.
The principles are simple: The better you understand your customers and their needs, the better you can design your services. There are many toolkits that are available for you to try for free. Empathy Mapping is an easy one you could apply to your practice to enhance your patients’ experience.
The idea behind this technique is to immerse yourself in your patient’s world. Pick a time when your practice is closed. Then take a journey through your office as if you were a patient. It’s important that you keep the experience as close to reality as possible. Start before you even arrive at your office. What is the experience like driving to your office? Do patients have to fight traffic to get to you? Is parking easy to find? How far must they walk from their car to get to your office? What is your check-in process like? Are patients greeted by name? Are they first handed paperwork to complete? Or are they introduced and warmly welcomed to your practice first?
What’s the experience like in the waiting room? Take note of not only what your patients see but also what they hear, smell, touch, and say. What experience does your furniture give patients? What type of magazines are available to them? Do you have Wi-Fi? Is there a television? If so, is it showing simply an advertisement, or is it something that your patients would connect with? Is there music playing?
Using the same process, continue your journey through an entire patient visit. Make note of what the experience is like walking back to your exam rooms. What do your patients see and smell while sitting in an exam room waiting for you? Does it smell of isopropyl alcohol? Is it cold or hot? What’s it like to sit in your room wearing nothing but a patient gown? Are there instruments such as cryo guns that could be intimidating to patients? All of these factors can be modified and thus “designed” to optimize the experience for your patients. Continue this journey including a physical exam and discussion with the doctor and other providers and assistants.
This is a great exercise not only for you but more importantly for your staff. Ask your staff to take notes as they walk through the same empathy mapping journey. It will give them an entirely new and valuable perspective on what it’s like to be a patient in your office. Once you’ve completed your empathy mapping, sit with your team and brainstorm about opportunities to improve the experience for your patients. Ask yourselves what things surprised you. What things do you feel could have the largest impact on your patients’ experience in your office? In what ways can you modify the spaces in your office to optimize your patients’ experience?
Having done this exercise in my own clinic, I found it highly impactful. It gave me a deeper understanding of and appreciation for my patients and caused me to make several minor but important changes in my exam room and to my and my staff’s interactions with patients. I hope you have a similarly informative experience.
If you’re interested in learning more about design thinking, then check out the following books and articles:
• “Change by Design: How Design Thinking Transforms Organization and Inspires Innovation,” by Tim Brown (New York: Harper Business, 2009).
• “The Art of Innovation,” by Tom Kelley (New York: A Currency Book, Doubleday, Random House, 2001).
• Design Thinking Comes of Age, by Jon Kolko (Harv Bus Rev. Sep 2015;pp 66-71).
Dr. Benabio is a partner physician in the department of dermatology of the Southern California Permanente Group in San Diego, and a volunteer clinical assistant professor at the University of California, San Diego. Dr. Benabio is @dermdoc on Twitter.
Design thinking isn’t only for products such as the Apple watch. It is a methodology used to improve customer experiences not only with products but also with services. Much in the same way that the SOAP note shaped our thinking about diagnosis and treatment, design thinking provides a scaffold to help us better understand the needs and wants of customers, or in our case, patients.
Design thinking uses specific tools and methodologies to understand experiences from others’ perspectives. From its roots in Silicon Valley, design thinking has grown steadily in its influence. Its first high priests were people such as Steve Jobs and David Kelly, who famously designed the computer mouse. The principles learned or applied to increasingly complicated products and services led to the growth of an entire industry in Palo Alto, Calif., with companies such as IDEO and gurus such as IDEO CEO and President Tim Brown of Stanford (Calif.) University has an entire graduate school program on design thinking called d.school while Coursera offers online courses on design thinking.
The principles are simple: The better you understand your customers and their needs, the better you can design your services. There are many toolkits that are available for you to try for free. Empathy Mapping is an easy one you could apply to your practice to enhance your patients’ experience.
The idea behind this technique is to immerse yourself in your patient’s world. Pick a time when your practice is closed. Then take a journey through your office as if you were a patient. It’s important that you keep the experience as close to reality as possible. Start before you even arrive at your office. What is the experience like driving to your office? Do patients have to fight traffic to get to you? Is parking easy to find? How far must they walk from their car to get to your office? What is your check-in process like? Are patients greeted by name? Are they first handed paperwork to complete? Or are they introduced and warmly welcomed to your practice first?
What’s the experience like in the waiting room? Take note of not only what your patients see but also what they hear, smell, touch, and say. What experience does your furniture give patients? What type of magazines are available to them? Do you have Wi-Fi? Is there a television? If so, is it showing simply an advertisement, or is it something that your patients would connect with? Is there music playing?
Using the same process, continue your journey through an entire patient visit. Make note of what the experience is like walking back to your exam rooms. What do your patients see and smell while sitting in an exam room waiting for you? Does it smell of isopropyl alcohol? Is it cold or hot? What’s it like to sit in your room wearing nothing but a patient gown? Are there instruments such as cryo guns that could be intimidating to patients? All of these factors can be modified and thus “designed” to optimize the experience for your patients. Continue this journey including a physical exam and discussion with the doctor and other providers and assistants.
This is a great exercise not only for you but more importantly for your staff. Ask your staff to take notes as they walk through the same empathy mapping journey. It will give them an entirely new and valuable perspective on what it’s like to be a patient in your office. Once you’ve completed your empathy mapping, sit with your team and brainstorm about opportunities to improve the experience for your patients. Ask yourselves what things surprised you. What things do you feel could have the largest impact on your patients’ experience in your office? In what ways can you modify the spaces in your office to optimize your patients’ experience?
Having done this exercise in my own clinic, I found it highly impactful. It gave me a deeper understanding of and appreciation for my patients and caused me to make several minor but important changes in my exam room and to my and my staff’s interactions with patients. I hope you have a similarly informative experience.
If you’re interested in learning more about design thinking, then check out the following books and articles:
• “Change by Design: How Design Thinking Transforms Organization and Inspires Innovation,” by Tim Brown (New York: Harper Business, 2009).
• “The Art of Innovation,” by Tom Kelley (New York: A Currency Book, Doubleday, Random House, 2001).
• Design Thinking Comes of Age, by Jon Kolko (Harv Bus Rev. Sep 2015;pp 66-71).
Dr. Benabio is a partner physician in the department of dermatology of the Southern California Permanente Group in San Diego, and a volunteer clinical assistant professor at the University of California, San Diego. Dr. Benabio is @dermdoc on Twitter.
Myth of the Month: Does Colace work?
Myth: Docusate is a stool softener and helps with constipation.
A 60-year-old man is injured in a fall and breaks four ribs. He is in severe pain and is prescribed oxycodone and naproxen for pain. What treatment would you prescribe to help decrease problems with constipation?
A. Docusate.
B. Docusate and polyethylene glycol.
C. Psyllium.
D. Polyethylene glycol.
Constipation is extremely common, occurring in up to 20%-25% of the elderly population and 90% of patients treated with opioids. The formal definition of constipation is fewer than three bowel movements per week. Patients are concerned with other symptoms as well, including hard stool consistency and the feeling of incomplete evacuation.
An extremely commonly prescribed medication for patients with symptoms of constipation/hard stool passage is docusate (Colace). This medication is often a part of bowel programs for institutionalized/hospitalized patients, as well as being frequently prescribed when patients are treated with opiates.
Does it work?
Docusate is frequently prescribed as a “stool softener,” but does it increase water content in stool? In a randomized, controlled trial of docusate vs. psyllium, 170 adult patients with chronic constipation received either 5.1 g twice a day of psyllium or 100 mg twice a day of docusate (Aliment Pharmacol Ther. 1998 May;12[5]:491-7).
Psyllium was superior in its effect on stool frequency, stool water content, total stool output, and the combination of several objective measures of constipation. Compared with baseline, psyllium increased stool water content by 2.33%, vs .01% for docusate (P =. 007), and stool weight was increased in the group treated with psyllium, compared with docusate-treated patients (359.9 g/week vs. 271.9 g/week, respectively; P = .005). Docusate does not appear to have any effect on stool water content or amount of stool.
In a study of constipation treatment in patients receiving opioids, Dr. Yoko Tarumi and her colleagues studied 74 patients admitted to hospice units (J Pain Symptom Manage. 2013 Jan;45[1]:2-13). A total of 74 patients were randomized to receive docusate 100 mg twice a day plus senna, or placebo plus senna. Once the study was started, inclusion criteria were broadened to include hospice patients with nonmalignant disease and patients who were not on opioids.
Almost all patients in the study did receive opioids (94% of the docusate patients and 100% of placebo-treated patients). There were no significant between the groups in stool volume, frequency, consistency, or in perceived completeness of evacuation.
In a randomized, controlled study of elderly patients on a medicine ward, 34 patients were randomized to docusate or control (no laxatives)(J Chronic Dis. 1976 Jan;29[1]:59-63). There was no difference in frequency or quality of stools between groups.
A systematic review of the usefulness of docusate in chronically ill patients concluded that the widespread use of docusate for the treatment of constipation in palliative-care patients is based on inadequate experimental evidence (J Pain Symptom Manage. 2000 Feb;19[2]:130-6).
The Canadian Agency for Drugs and Technologies in Health concluded “the available evidence suggests that docusate is no more effective than placebo in the prevention or management of constipation” (Dioctyl sulfosuccinate or docusate [calcium or sodium] for the prevention or management of constipation: a review of the clinical effectiveness. Canadian Agency for Drugs and Technologies in Health; 2014 Jun 26).
Dr. Davendra Ramkumar and his colleagues published a systematic review of drug trials for the treatment of constipation in 2005 (Am J Gastroenterol. 2005 Apr;100[4]:936-71). Only polyethylene glycol and tegaserod received grade A evidence for published trials. Psyllium and lactulose received grade B evidence. Docusate received a level 3, grade C for evidence (poor quality evidence, poor evidence to support a recommendation for or against the use of the modality).
I have been surprised at how docusate has been the most commonly prescribed laxative agent. Polyethylene glycol or psyllium are better evidence-based options. Docusate is often prescribed as a stool softener, and it has even less evidence that it softens stool than its poor evidence as a laxative.
Acknowledgments
My thanks to the late Dr. David Saunders for teaching me 30 years ago that docusate was not a helpful option for the management of constipation, and to Sarah Steinkruger for doing much of the research that was used in this column.
Dr. Paauw is professor of medicine in the division of general internal medicine at the University of Washington, Seattle, and he serves as third-year medical student clerkship director at the University of Washington. Contact Dr. Paauw at [email protected].
Myth: Docusate is a stool softener and helps with constipation.
A 60-year-old man is injured in a fall and breaks four ribs. He is in severe pain and is prescribed oxycodone and naproxen for pain. What treatment would you prescribe to help decrease problems with constipation?
A. Docusate.
B. Docusate and polyethylene glycol.
C. Psyllium.
D. Polyethylene glycol.
Constipation is extremely common, occurring in up to 20%-25% of the elderly population and 90% of patients treated with opioids. The formal definition of constipation is fewer than three bowel movements per week. Patients are concerned with other symptoms as well, including hard stool consistency and the feeling of incomplete evacuation.
An extremely commonly prescribed medication for patients with symptoms of constipation/hard stool passage is docusate (Colace). This medication is often a part of bowel programs for institutionalized/hospitalized patients, as well as being frequently prescribed when patients are treated with opiates.
Does it work?
Docusate is frequently prescribed as a “stool softener,” but does it increase water content in stool? In a randomized, controlled trial of docusate vs. psyllium, 170 adult patients with chronic constipation received either 5.1 g twice a day of psyllium or 100 mg twice a day of docusate (Aliment Pharmacol Ther. 1998 May;12[5]:491-7).
Psyllium was superior in its effect on stool frequency, stool water content, total stool output, and the combination of several objective measures of constipation. Compared with baseline, psyllium increased stool water content by 2.33%, vs .01% for docusate (P =. 007), and stool weight was increased in the group treated with psyllium, compared with docusate-treated patients (359.9 g/week vs. 271.9 g/week, respectively; P = .005). Docusate does not appear to have any effect on stool water content or amount of stool.
In a study of constipation treatment in patients receiving opioids, Dr. Yoko Tarumi and her colleagues studied 74 patients admitted to hospice units (J Pain Symptom Manage. 2013 Jan;45[1]:2-13). A total of 74 patients were randomized to receive docusate 100 mg twice a day plus senna, or placebo plus senna. Once the study was started, inclusion criteria were broadened to include hospice patients with nonmalignant disease and patients who were not on opioids.
Almost all patients in the study did receive opioids (94% of the docusate patients and 100% of placebo-treated patients). There were no significant between the groups in stool volume, frequency, consistency, or in perceived completeness of evacuation.
In a randomized, controlled study of elderly patients on a medicine ward, 34 patients were randomized to docusate or control (no laxatives)(J Chronic Dis. 1976 Jan;29[1]:59-63). There was no difference in frequency or quality of stools between groups.
A systematic review of the usefulness of docusate in chronically ill patients concluded that the widespread use of docusate for the treatment of constipation in palliative-care patients is based on inadequate experimental evidence (J Pain Symptom Manage. 2000 Feb;19[2]:130-6).
The Canadian Agency for Drugs and Technologies in Health concluded “the available evidence suggests that docusate is no more effective than placebo in the prevention or management of constipation” (Dioctyl sulfosuccinate or docusate [calcium or sodium] for the prevention or management of constipation: a review of the clinical effectiveness. Canadian Agency for Drugs and Technologies in Health; 2014 Jun 26).
Dr. Davendra Ramkumar and his colleagues published a systematic review of drug trials for the treatment of constipation in 2005 (Am J Gastroenterol. 2005 Apr;100[4]:936-71). Only polyethylene glycol and tegaserod received grade A evidence for published trials. Psyllium and lactulose received grade B evidence. Docusate received a level 3, grade C for evidence (poor quality evidence, poor evidence to support a recommendation for or against the use of the modality).
I have been surprised at how docusate has been the most commonly prescribed laxative agent. Polyethylene glycol or psyllium are better evidence-based options. Docusate is often prescribed as a stool softener, and it has even less evidence that it softens stool than its poor evidence as a laxative.
Acknowledgments
My thanks to the late Dr. David Saunders for teaching me 30 years ago that docusate was not a helpful option for the management of constipation, and to Sarah Steinkruger for doing much of the research that was used in this column.
Dr. Paauw is professor of medicine in the division of general internal medicine at the University of Washington, Seattle, and he serves as third-year medical student clerkship director at the University of Washington. Contact Dr. Paauw at [email protected].
Myth: Docusate is a stool softener and helps with constipation.
A 60-year-old man is injured in a fall and breaks four ribs. He is in severe pain and is prescribed oxycodone and naproxen for pain. What treatment would you prescribe to help decrease problems with constipation?
A. Docusate.
B. Docusate and polyethylene glycol.
C. Psyllium.
D. Polyethylene glycol.
Constipation is extremely common, occurring in up to 20%-25% of the elderly population and 90% of patients treated with opioids. The formal definition of constipation is fewer than three bowel movements per week. Patients are concerned with other symptoms as well, including hard stool consistency and the feeling of incomplete evacuation.
An extremely commonly prescribed medication for patients with symptoms of constipation/hard stool passage is docusate (Colace). This medication is often a part of bowel programs for institutionalized/hospitalized patients, as well as being frequently prescribed when patients are treated with opiates.
Does it work?
Docusate is frequently prescribed as a “stool softener,” but does it increase water content in stool? In a randomized, controlled trial of docusate vs. psyllium, 170 adult patients with chronic constipation received either 5.1 g twice a day of psyllium or 100 mg twice a day of docusate (Aliment Pharmacol Ther. 1998 May;12[5]:491-7).
Psyllium was superior in its effect on stool frequency, stool water content, total stool output, and the combination of several objective measures of constipation. Compared with baseline, psyllium increased stool water content by 2.33%, vs .01% for docusate (P =. 007), and stool weight was increased in the group treated with psyllium, compared with docusate-treated patients (359.9 g/week vs. 271.9 g/week, respectively; P = .005). Docusate does not appear to have any effect on stool water content or amount of stool.
In a study of constipation treatment in patients receiving opioids, Dr. Yoko Tarumi and her colleagues studied 74 patients admitted to hospice units (J Pain Symptom Manage. 2013 Jan;45[1]:2-13). A total of 74 patients were randomized to receive docusate 100 mg twice a day plus senna, or placebo plus senna. Once the study was started, inclusion criteria were broadened to include hospice patients with nonmalignant disease and patients who were not on opioids.
Almost all patients in the study did receive opioids (94% of the docusate patients and 100% of placebo-treated patients). There were no significant between the groups in stool volume, frequency, consistency, or in perceived completeness of evacuation.
In a randomized, controlled study of elderly patients on a medicine ward, 34 patients were randomized to docusate or control (no laxatives)(J Chronic Dis. 1976 Jan;29[1]:59-63). There was no difference in frequency or quality of stools between groups.
A systematic review of the usefulness of docusate in chronically ill patients concluded that the widespread use of docusate for the treatment of constipation in palliative-care patients is based on inadequate experimental evidence (J Pain Symptom Manage. 2000 Feb;19[2]:130-6).
The Canadian Agency for Drugs and Technologies in Health concluded “the available evidence suggests that docusate is no more effective than placebo in the prevention or management of constipation” (Dioctyl sulfosuccinate or docusate [calcium or sodium] for the prevention or management of constipation: a review of the clinical effectiveness. Canadian Agency for Drugs and Technologies in Health; 2014 Jun 26).
Dr. Davendra Ramkumar and his colleagues published a systematic review of drug trials for the treatment of constipation in 2005 (Am J Gastroenterol. 2005 Apr;100[4]:936-71). Only polyethylene glycol and tegaserod received grade A evidence for published trials. Psyllium and lactulose received grade B evidence. Docusate received a level 3, grade C for evidence (poor quality evidence, poor evidence to support a recommendation for or against the use of the modality).
I have been surprised at how docusate has been the most commonly prescribed laxative agent. Polyethylene glycol or psyllium are better evidence-based options. Docusate is often prescribed as a stool softener, and it has even less evidence that it softens stool than its poor evidence as a laxative.
Acknowledgments
My thanks to the late Dr. David Saunders for teaching me 30 years ago that docusate was not a helpful option for the management of constipation, and to Sarah Steinkruger for doing much of the research that was used in this column.
Dr. Paauw is professor of medicine in the division of general internal medicine at the University of Washington, Seattle, and he serves as third-year medical student clerkship director at the University of Washington. Contact Dr. Paauw at [email protected].
Law & Medicine: To whom do doctors owe a duty?
Question: A doctor may owe a duty of care in the setting of:
A. A cyber relationship.
B. A special relationship.
C. Both A and B.
D. Neither A nor B.
Answer: C. Ascertaining whether a defendant owes a duty to a claimant is the first inquiry in the tort of negligence. To say there is no duty owed is to deny liability altogether, however obvious the breach or horrendous the foreseeable injuries.
Thus, duty is used as a filter mechanism to reduce frivolous suits or otherwise control the tide of litigation, to prevent “liability in an indeterminate amount for an indeterminate time to an indeterminate class.”
Duty in the context of medical negligence is not usually in dispute, as it is plainly owed by a doctor to his or her patient. It arises out of the doctor-patient relationship. Whether a relationship has been formed in the first place is a threshold inquiry. Where a doctor accepts a patient who is seeking his or her services, the relationship is readily evident. Duty is also established when the doctor begins the evaluation process in a typical encounter.
However, a phone inquiry by a potential patient, without more, may be insufficient to create this relationship, although this may depend on the nature of the phone conversation and the doctor’s response.
Likewise, a “curbside” consultation sought by a colleague does not normally translate into a duty for the doctor offering the opinion. Presumably casual advice given freely and understood as such at social gatherings does not add up to a doctor-patient relationship, and courts will look to reasonableness as the touchstone in deciding whether such a relationship was ever formed.
Still, there are some medical situations where a legitimate question of duty can be raised. With the growth of electronic medical records and communication, medical encounters in cyberspace will emerge as an increasing source of litigation.
Internet liability can be far reaching. In addition to risks governing negligence, informed consent, and privacy/confidentiality, there are additional issues of product liability, cross-border jurisdictional conflicts, and others.
The threshold question when assessing cyberspace liability arising, for example, from the use of doctor-operated medical websites concerns duty, because its existence or denial will determine whether the case can go forward in the first place. Although not the typical office or hospital patient, a plaintiff may argue successfully that a doctor-patient relationship had nonetheless been formed in cyberspace.
It is possible that such a relationship will be found in some circumstances, relevant factors being knowledge of names of subscribers, frequency of interactions, specificity of queries, and so on. In particular, a subscription fee is likely to be construed as evidence of soliciting and accepting a more committed interaction, so it places the operator of the website at greater legal risk. A specific disclaimer is a standard precaution but may not be enough to definitively protect against a lawsuit.
Courts have ruled in favor of plaintiffs despite the absence of face-to-face interaction with a physician. In one case, a doctor speaking to a patient from the emergency department was deemed to have formed a doctor-patient relationship (O’Neill v. Montefiore Hospital, 11 A.D.2d 132 (N.Y.A.D. 1 Dept. 1960). In another, an on-call neurologist’s telephone advice to the treating doctor likewise raised the issue of legal duty (Lection v. Dyll, 65 S.W.3d 696 (Tex. App. Dallas 2001).
The state of Hawaii now permits telehealth services to be reimbursable, notwithstanding the absence of face-to-face contact (HI Rev Stat § 431:10A-116.3[a]). With this law, an online encounter will likely translate into a professional relationship – with corresponding legal duty of due care.
In the case of a Good Samaritan physician – i.e., one who offers gratuitous aid to a stranger in need of medical assistance – courts are unlikely to find a professional relationship, because there is no common law duty to help a stranger.
However, once treatment has begun, there is a duty not to make matters worse. So, all 50 states have enacted Good Samaritan statutes, which protect against liability arising out of negligent rescue. Note that statutory protection is generally excluded for Good Samaritan acts performed within a hospital setting, under the theory that doctors have an ongoing relationship with the hospital and are already obligated to provide emergency care within its walls.
Another category of legal duty concerns nonpatient third parties. The complaint may relate to a failure to warn family members of a patient’s contagious disease, or the transmissible condition may have been missed and an innocent third party was injured as a result.
Another situation where duty to a third party might arise is the learning of a credible threat of harm directed at a named individual. This is famously known as the Tarasoff doctrine, after a California case in which the court imposed a duty on a college psychologist to directly warn an intended victim of harm by his patient – even though that meant breaching confidentiality of a professional relationship, and the victim was a nonpatient third party (Tarasoff v. Regents of University of California, 551 P.2d 334 [Cal. 1976]).
A doctor may also incur liability for automobile injuries sustained by one other than his or her own patient. In a Hawaii case, a car suddenly veered across five lanes of traffic, striking an 11-year-old bystander. The driver alleged that the prescription medication prazosin caused him to lose control of the car.
In ruling that the health care provider was liable to the injured bystander, the Hawaii Supreme Court held that physicians have a duty to warn their patients of potential adverse medication effects, and this responsibility should extend to third parties (McKenzie v. Hawaii Permanente Medical Group, 47 P.3d 1209 [Haw. 2002]).
A foreseeable and unreasonable risk of harm is an important factor, but not the only decisive factor, in construing the existence of a legal duty. Under some circumstances, the term “special relationship” has been employed based on a consideration of “existing social values, customs, and considerations of policy.”
In a Massachusetts case, a family practitioner had failed to warn his patient of the risk of diabetic drugs when operating a vehicle. Just 45 minutes after the patient’s discharge from the hospital, he developed hypoglycemia, losing consciousness and injuring a motorcyclist who then sued the doctor. The court used the “special relationship” rationale in ruling that the doctor owed a duty to the motorcyclist (Arsenault v. McConarty, 21 Mass. L. Rptr. 500 [2006]).
Dr. Tan is emeritus professor of medicine and former adjunct professor of law at the University of Hawaii, and currently directs the St. Francis International Center for Healthcare Ethics in Honolulu. This article is meant to be educational and does not constitute medical, ethical, or legal advice. Some of the articles in this series are adapted from the author’s 2006 book, “Medical Malpractice: Understanding the Law, Managing the Risk,” and his 2012 Halsbury treatise, “Medical Negligence and Professional Misconduct.” For additional information, readers may contact the author at [email protected].
Question: A doctor may owe a duty of care in the setting of:
A. A cyber relationship.
B. A special relationship.
C. Both A and B.
D. Neither A nor B.
Answer: C. Ascertaining whether a defendant owes a duty to a claimant is the first inquiry in the tort of negligence. To say there is no duty owed is to deny liability altogether, however obvious the breach or horrendous the foreseeable injuries.
Thus, duty is used as a filter mechanism to reduce frivolous suits or otherwise control the tide of litigation, to prevent “liability in an indeterminate amount for an indeterminate time to an indeterminate class.”
Duty in the context of medical negligence is not usually in dispute, as it is plainly owed by a doctor to his or her patient. It arises out of the doctor-patient relationship. Whether a relationship has been formed in the first place is a threshold inquiry. Where a doctor accepts a patient who is seeking his or her services, the relationship is readily evident. Duty is also established when the doctor begins the evaluation process in a typical encounter.
However, a phone inquiry by a potential patient, without more, may be insufficient to create this relationship, although this may depend on the nature of the phone conversation and the doctor’s response.
Likewise, a “curbside” consultation sought by a colleague does not normally translate into a duty for the doctor offering the opinion. Presumably casual advice given freely and understood as such at social gatherings does not add up to a doctor-patient relationship, and courts will look to reasonableness as the touchstone in deciding whether such a relationship was ever formed.
Still, there are some medical situations where a legitimate question of duty can be raised. With the growth of electronic medical records and communication, medical encounters in cyberspace will emerge as an increasing source of litigation.
Internet liability can be far reaching. In addition to risks governing negligence, informed consent, and privacy/confidentiality, there are additional issues of product liability, cross-border jurisdictional conflicts, and others.
The threshold question when assessing cyberspace liability arising, for example, from the use of doctor-operated medical websites concerns duty, because its existence or denial will determine whether the case can go forward in the first place. Although not the typical office or hospital patient, a plaintiff may argue successfully that a doctor-patient relationship had nonetheless been formed in cyberspace.
It is possible that such a relationship will be found in some circumstances, relevant factors being knowledge of names of subscribers, frequency of interactions, specificity of queries, and so on. In particular, a subscription fee is likely to be construed as evidence of soliciting and accepting a more committed interaction, so it places the operator of the website at greater legal risk. A specific disclaimer is a standard precaution but may not be enough to definitively protect against a lawsuit.
Courts have ruled in favor of plaintiffs despite the absence of face-to-face interaction with a physician. In one case, a doctor speaking to a patient from the emergency department was deemed to have formed a doctor-patient relationship (O’Neill v. Montefiore Hospital, 11 A.D.2d 132 (N.Y.A.D. 1 Dept. 1960). In another, an on-call neurologist’s telephone advice to the treating doctor likewise raised the issue of legal duty (Lection v. Dyll, 65 S.W.3d 696 (Tex. App. Dallas 2001).
The state of Hawaii now permits telehealth services to be reimbursable, notwithstanding the absence of face-to-face contact (HI Rev Stat § 431:10A-116.3[a]). With this law, an online encounter will likely translate into a professional relationship – with corresponding legal duty of due care.
In the case of a Good Samaritan physician – i.e., one who offers gratuitous aid to a stranger in need of medical assistance – courts are unlikely to find a professional relationship, because there is no common law duty to help a stranger.
However, once treatment has begun, there is a duty not to make matters worse. So, all 50 states have enacted Good Samaritan statutes, which protect against liability arising out of negligent rescue. Note that statutory protection is generally excluded for Good Samaritan acts performed within a hospital setting, under the theory that doctors have an ongoing relationship with the hospital and are already obligated to provide emergency care within its walls.
Another category of legal duty concerns nonpatient third parties. The complaint may relate to a failure to warn family members of a patient’s contagious disease, or the transmissible condition may have been missed and an innocent third party was injured as a result.
Another situation where duty to a third party might arise is the learning of a credible threat of harm directed at a named individual. This is famously known as the Tarasoff doctrine, after a California case in which the court imposed a duty on a college psychologist to directly warn an intended victim of harm by his patient – even though that meant breaching confidentiality of a professional relationship, and the victim was a nonpatient third party (Tarasoff v. Regents of University of California, 551 P.2d 334 [Cal. 1976]).
A doctor may also incur liability for automobile injuries sustained by one other than his or her own patient. In a Hawaii case, a car suddenly veered across five lanes of traffic, striking an 11-year-old bystander. The driver alleged that the prescription medication prazosin caused him to lose control of the car.
In ruling that the health care provider was liable to the injured bystander, the Hawaii Supreme Court held that physicians have a duty to warn their patients of potential adverse medication effects, and this responsibility should extend to third parties (McKenzie v. Hawaii Permanente Medical Group, 47 P.3d 1209 [Haw. 2002]).
A foreseeable and unreasonable risk of harm is an important factor, but not the only decisive factor, in construing the existence of a legal duty. Under some circumstances, the term “special relationship” has been employed based on a consideration of “existing social values, customs, and considerations of policy.”
In a Massachusetts case, a family practitioner had failed to warn his patient of the risk of diabetic drugs when operating a vehicle. Just 45 minutes after the patient’s discharge from the hospital, he developed hypoglycemia, losing consciousness and injuring a motorcyclist who then sued the doctor. The court used the “special relationship” rationale in ruling that the doctor owed a duty to the motorcyclist (Arsenault v. McConarty, 21 Mass. L. Rptr. 500 [2006]).
Dr. Tan is emeritus professor of medicine and former adjunct professor of law at the University of Hawaii, and currently directs the St. Francis International Center for Healthcare Ethics in Honolulu. This article is meant to be educational and does not constitute medical, ethical, or legal advice. Some of the articles in this series are adapted from the author’s 2006 book, “Medical Malpractice: Understanding the Law, Managing the Risk,” and his 2012 Halsbury treatise, “Medical Negligence and Professional Misconduct.” For additional information, readers may contact the author at [email protected].
Question: A doctor may owe a duty of care in the setting of:
A. A cyber relationship.
B. A special relationship.
C. Both A and B.
D. Neither A nor B.
Answer: C. Ascertaining whether a defendant owes a duty to a claimant is the first inquiry in the tort of negligence. To say there is no duty owed is to deny liability altogether, however obvious the breach or horrendous the foreseeable injuries.
Thus, duty is used as a filter mechanism to reduce frivolous suits or otherwise control the tide of litigation, to prevent “liability in an indeterminate amount for an indeterminate time to an indeterminate class.”
Duty in the context of medical negligence is not usually in dispute, as it is plainly owed by a doctor to his or her patient. It arises out of the doctor-patient relationship. Whether a relationship has been formed in the first place is a threshold inquiry. Where a doctor accepts a patient who is seeking his or her services, the relationship is readily evident. Duty is also established when the doctor begins the evaluation process in a typical encounter.
However, a phone inquiry by a potential patient, without more, may be insufficient to create this relationship, although this may depend on the nature of the phone conversation and the doctor’s response.
Likewise, a “curbside” consultation sought by a colleague does not normally translate into a duty for the doctor offering the opinion. Presumably casual advice given freely and understood as such at social gatherings does not add up to a doctor-patient relationship, and courts will look to reasonableness as the touchstone in deciding whether such a relationship was ever formed.
Still, there are some medical situations where a legitimate question of duty can be raised. With the growth of electronic medical records and communication, medical encounters in cyberspace will emerge as an increasing source of litigation.
Internet liability can be far reaching. In addition to risks governing negligence, informed consent, and privacy/confidentiality, there are additional issues of product liability, cross-border jurisdictional conflicts, and others.
The threshold question when assessing cyberspace liability arising, for example, from the use of doctor-operated medical websites concerns duty, because its existence or denial will determine whether the case can go forward in the first place. Although not the typical office or hospital patient, a plaintiff may argue successfully that a doctor-patient relationship had nonetheless been formed in cyberspace.
It is possible that such a relationship will be found in some circumstances, relevant factors being knowledge of names of subscribers, frequency of interactions, specificity of queries, and so on. In particular, a subscription fee is likely to be construed as evidence of soliciting and accepting a more committed interaction, so it places the operator of the website at greater legal risk. A specific disclaimer is a standard precaution but may not be enough to definitively protect against a lawsuit.
Courts have ruled in favor of plaintiffs despite the absence of face-to-face interaction with a physician. In one case, a doctor speaking to a patient from the emergency department was deemed to have formed a doctor-patient relationship (O’Neill v. Montefiore Hospital, 11 A.D.2d 132 (N.Y.A.D. 1 Dept. 1960). In another, an on-call neurologist’s telephone advice to the treating doctor likewise raised the issue of legal duty (Lection v. Dyll, 65 S.W.3d 696 (Tex. App. Dallas 2001).
The state of Hawaii now permits telehealth services to be reimbursable, notwithstanding the absence of face-to-face contact (HI Rev Stat § 431:10A-116.3[a]). With this law, an online encounter will likely translate into a professional relationship – with corresponding legal duty of due care.
In the case of a Good Samaritan physician – i.e., one who offers gratuitous aid to a stranger in need of medical assistance – courts are unlikely to find a professional relationship, because there is no common law duty to help a stranger.
However, once treatment has begun, there is a duty not to make matters worse. So, all 50 states have enacted Good Samaritan statutes, which protect against liability arising out of negligent rescue. Note that statutory protection is generally excluded for Good Samaritan acts performed within a hospital setting, under the theory that doctors have an ongoing relationship with the hospital and are already obligated to provide emergency care within its walls.
Another category of legal duty concerns nonpatient third parties. The complaint may relate to a failure to warn family members of a patient’s contagious disease, or the transmissible condition may have been missed and an innocent third party was injured as a result.
Another situation where duty to a third party might arise is the learning of a credible threat of harm directed at a named individual. This is famously known as the Tarasoff doctrine, after a California case in which the court imposed a duty on a college psychologist to directly warn an intended victim of harm by his patient – even though that meant breaching confidentiality of a professional relationship, and the victim was a nonpatient third party (Tarasoff v. Regents of University of California, 551 P.2d 334 [Cal. 1976]).
A doctor may also incur liability for automobile injuries sustained by one other than his or her own patient. In a Hawaii case, a car suddenly veered across five lanes of traffic, striking an 11-year-old bystander. The driver alleged that the prescription medication prazosin caused him to lose control of the car.
In ruling that the health care provider was liable to the injured bystander, the Hawaii Supreme Court held that physicians have a duty to warn their patients of potential adverse medication effects, and this responsibility should extend to third parties (McKenzie v. Hawaii Permanente Medical Group, 47 P.3d 1209 [Haw. 2002]).
A foreseeable and unreasonable risk of harm is an important factor, but not the only decisive factor, in construing the existence of a legal duty. Under some circumstances, the term “special relationship” has been employed based on a consideration of “existing social values, customs, and considerations of policy.”
In a Massachusetts case, a family practitioner had failed to warn his patient of the risk of diabetic drugs when operating a vehicle. Just 45 minutes after the patient’s discharge from the hospital, he developed hypoglycemia, losing consciousness and injuring a motorcyclist who then sued the doctor. The court used the “special relationship” rationale in ruling that the doctor owed a duty to the motorcyclist (Arsenault v. McConarty, 21 Mass. L. Rptr. 500 [2006]).
Dr. Tan is emeritus professor of medicine and former adjunct professor of law at the University of Hawaii, and currently directs the St. Francis International Center for Healthcare Ethics in Honolulu. This article is meant to be educational and does not constitute medical, ethical, or legal advice. Some of the articles in this series are adapted from the author’s 2006 book, “Medical Malpractice: Understanding the Law, Managing the Risk,” and his 2012 Halsbury treatise, “Medical Negligence and Professional Misconduct.” For additional information, readers may contact the author at [email protected].
A good night’s sleep with placebo
Is it just me? I don’t think that I have visited with a single patient this week who’s not struggling with sleep. Our heavily caffeinated, media-obsessed, melatonin-killing, computer-screen-staring, tragic work-life imbalances explain away a lot of it. Knowing that, though, patients in front of me seek immediate relief.
A prescription takes substantially less effort than does training patients on sleep hygiene or sleep restriction. The problem with “z” drugs is, of course, that tolerance can develop within 4 weeks with daily use. These drugs have been associated with mood and cognitive changes and increased mortality. Many of my patients cannot use them sparingly, because relief of insomnia is something of which they cannot get enough. Then we are either back to square one or playing the dose-escalation game.
I have always wondered how much of this is the “placebo effect” and how we could use this to our clinical advantage. This is certainly what I hear from my cynical colleagues when I recommend melatonin – which, by the way, I personally believe is an extremely effective and underutilized intervention. We should remind ourselves to be cognizant of the “if I can’t prescribe it, it can’t work that well” mentality.
Alexander Winkler and Winfried Rief of the University of Marburg, Germany, conducted a brilliant systematic review examining the effect of placebo conditions in randomized trials including polysomnography addressing primary insomnia (Sleep. 2015 Jun 1;38[6]:925-31).
The investigators identified 32 studies with almost 4,000 patients in 82 treatment conditions: The studies were published between 1992 and 2012. Of those 82 treatment conditions, 17 included hypnotic drugs.
Results suggest that 64% of drug response to medications for primary insomnia is achieved in the placebo group.
So what does this mean clinically? I think the first thing it means is that we should consider (re)launching frank discourse about the ethics surrounding the use of placebo in clinical medicine. Are we all too horrified to think that patients may get better despite us rather than because of us to dig too deeply here?
The second thing it means is that patients should be instructed to use the medications only when needed. If a minority of the drug effect for insomnia is from the drug itself, we should minimize the buildup of tolerance by using it sparingly. Studies that have alternated a hypnotic with a placebo show that this works just as well as using a hypnotic every night.
Patients should be encouraged to alternate therapy, such as trying melatonin first and resorting to a “z” drug only if sleep remains elusive. Alternating drug therapy may also enhance the efficacy of the medication.
Always try to combine pharmacotherapy with good sleep hygiene to maximize benefits.
Dr. Ebbert is professor of medicine, a general internist at the Mayo Clinic in Rochester, Minn., and a diplomate of the American Board of Addiction Medicine. The opinions expressed are those of the author and do not necessarily represent the views and opinions of the Mayo Clinic. The opinions expressed in this article should not be used to diagnose or treat any medical condition nor should they be used as a substitute for medical advice from a qualified, board-certified practicing clinician. Dr. Ebbert has no relevant financial disclosures about this article. Follow him on Twitter @jonebbert.
Is it just me? I don’t think that I have visited with a single patient this week who’s not struggling with sleep. Our heavily caffeinated, media-obsessed, melatonin-killing, computer-screen-staring, tragic work-life imbalances explain away a lot of it. Knowing that, though, patients in front of me seek immediate relief.
A prescription takes substantially less effort than does training patients on sleep hygiene or sleep restriction. The problem with “z” drugs is, of course, that tolerance can develop within 4 weeks with daily use. These drugs have been associated with mood and cognitive changes and increased mortality. Many of my patients cannot use them sparingly, because relief of insomnia is something of which they cannot get enough. Then we are either back to square one or playing the dose-escalation game.
I have always wondered how much of this is the “placebo effect” and how we could use this to our clinical advantage. This is certainly what I hear from my cynical colleagues when I recommend melatonin – which, by the way, I personally believe is an extremely effective and underutilized intervention. We should remind ourselves to be cognizant of the “if I can’t prescribe it, it can’t work that well” mentality.
Alexander Winkler and Winfried Rief of the University of Marburg, Germany, conducted a brilliant systematic review examining the effect of placebo conditions in randomized trials including polysomnography addressing primary insomnia (Sleep. 2015 Jun 1;38[6]:925-31).
The investigators identified 32 studies with almost 4,000 patients in 82 treatment conditions: The studies were published between 1992 and 2012. Of those 82 treatment conditions, 17 included hypnotic drugs.
Results suggest that 64% of drug response to medications for primary insomnia is achieved in the placebo group.
So what does this mean clinically? I think the first thing it means is that we should consider (re)launching frank discourse about the ethics surrounding the use of placebo in clinical medicine. Are we all too horrified to think that patients may get better despite us rather than because of us to dig too deeply here?
The second thing it means is that patients should be instructed to use the medications only when needed. If a minority of the drug effect for insomnia is from the drug itself, we should minimize the buildup of tolerance by using it sparingly. Studies that have alternated a hypnotic with a placebo show that this works just as well as using a hypnotic every night.
Patients should be encouraged to alternate therapy, such as trying melatonin first and resorting to a “z” drug only if sleep remains elusive. Alternating drug therapy may also enhance the efficacy of the medication.
Always try to combine pharmacotherapy with good sleep hygiene to maximize benefits.
Dr. Ebbert is professor of medicine, a general internist at the Mayo Clinic in Rochester, Minn., and a diplomate of the American Board of Addiction Medicine. The opinions expressed are those of the author and do not necessarily represent the views and opinions of the Mayo Clinic. The opinions expressed in this article should not be used to diagnose or treat any medical condition nor should they be used as a substitute for medical advice from a qualified, board-certified practicing clinician. Dr. Ebbert has no relevant financial disclosures about this article. Follow him on Twitter @jonebbert.
Is it just me? I don’t think that I have visited with a single patient this week who’s not struggling with sleep. Our heavily caffeinated, media-obsessed, melatonin-killing, computer-screen-staring, tragic work-life imbalances explain away a lot of it. Knowing that, though, patients in front of me seek immediate relief.
A prescription takes substantially less effort than does training patients on sleep hygiene or sleep restriction. The problem with “z” drugs is, of course, that tolerance can develop within 4 weeks with daily use. These drugs have been associated with mood and cognitive changes and increased mortality. Many of my patients cannot use them sparingly, because relief of insomnia is something of which they cannot get enough. Then we are either back to square one or playing the dose-escalation game.
I have always wondered how much of this is the “placebo effect” and how we could use this to our clinical advantage. This is certainly what I hear from my cynical colleagues when I recommend melatonin – which, by the way, I personally believe is an extremely effective and underutilized intervention. We should remind ourselves to be cognizant of the “if I can’t prescribe it, it can’t work that well” mentality.
Alexander Winkler and Winfried Rief of the University of Marburg, Germany, conducted a brilliant systematic review examining the effect of placebo conditions in randomized trials including polysomnography addressing primary insomnia (Sleep. 2015 Jun 1;38[6]:925-31).
The investigators identified 32 studies with almost 4,000 patients in 82 treatment conditions: The studies were published between 1992 and 2012. Of those 82 treatment conditions, 17 included hypnotic drugs.
Results suggest that 64% of drug response to medications for primary insomnia is achieved in the placebo group.
So what does this mean clinically? I think the first thing it means is that we should consider (re)launching frank discourse about the ethics surrounding the use of placebo in clinical medicine. Are we all too horrified to think that patients may get better despite us rather than because of us to dig too deeply here?
The second thing it means is that patients should be instructed to use the medications only when needed. If a minority of the drug effect for insomnia is from the drug itself, we should minimize the buildup of tolerance by using it sparingly. Studies that have alternated a hypnotic with a placebo show that this works just as well as using a hypnotic every night.
Patients should be encouraged to alternate therapy, such as trying melatonin first and resorting to a “z” drug only if sleep remains elusive. Alternating drug therapy may also enhance the efficacy of the medication.
Always try to combine pharmacotherapy with good sleep hygiene to maximize benefits.
Dr. Ebbert is professor of medicine, a general internist at the Mayo Clinic in Rochester, Minn., and a diplomate of the American Board of Addiction Medicine. The opinions expressed are those of the author and do not necessarily represent the views and opinions of the Mayo Clinic. The opinions expressed in this article should not be used to diagnose or treat any medical condition nor should they be used as a substitute for medical advice from a qualified, board-certified practicing clinician. Dr. Ebbert has no relevant financial disclosures about this article. Follow him on Twitter @jonebbert.