User login
A closing column
As the year comes to an end, I have decided – after 9 years of writing for Pediatric News – to bring my column to a close. It has been a great joy to be a part of the pediatric community in this way, and I have been grateful for those of you who approach me at meetings, saying, “Hey, I recognize you – I really like your column!” or tell me you appreciated a particular topic or piece of advice.
As I reflected on the columns I have written, I realized there were two themes that repeatedly emerged as most meaningful to me. While these thoughts are nothing new, I thought they would be a fitting way to sum up my writings over the years.
First, and most important, is that patients and families are the best partners we have in the care we give. When we take the time to listen to them, involve them in decision making and think past what we see on the surface, kids are healthier. This is just as true for preventative “well-baby” care as it is for acute and specialty care. Understanding a family’s priorities, values, and the context in which they live is just as important as our medical knowledge and skills when taking care of patients. Pediatricians are expert at bringing all of these things together, grounded in the best and most up-to-date evidence available, and in doing so elevate the care of children.
Which leads me to the second theme – pediatricians are a strong and important voice for children, and it is important for us to learn to lead. Through our work, we have a window into the lives of children, both when they are healthy and when they are sick. That is a great privilege but also a great responsibility. We see the things that work well in our systems and the things that do not. We see the amazing things children are capable of, but also troubling and pervasive inequities in care, access, and education. We see children who aren’t having their basic needs met – things like food, shelter, and a safe place to play. We see how these inequities impact health and wellness – both now and as children grow into adults. These observations, and the things we learn by caring for children and families day in and day out, can be translated into action. For each of us that will mean something different, but it is imperative that we develop our talents as advocates and leaders so that we can catalyze change. Our best hope for making things better is if we each do our part to create solutions. And when that happens, children – a lot of children – are healthier.
Since I began my first column 9 years ago, a lot has changed for me, and I suspect for many of you. When I first began writing, my now tall, confident tween (who already wears the same shoe size as me!) was barely walking. Thank you to all who have listened and encouraged me along the way – it has been a fun journey, and I’ve appreciated your time.
Dr. Beers is assistant professor of pediatrics at Children’s National Medical Center and the George Washington University Medical Center, both in Washington. She is chair of the American Academy of Pediatrics Committee on Residency Scholarships and immediate past president of the District of Columbia chapter of the American Academy of Pediatrics.
As the year comes to an end, I have decided – after 9 years of writing for Pediatric News – to bring my column to a close. It has been a great joy to be a part of the pediatric community in this way, and I have been grateful for those of you who approach me at meetings, saying, “Hey, I recognize you – I really like your column!” or tell me you appreciated a particular topic or piece of advice.
As I reflected on the columns I have written, I realized there were two themes that repeatedly emerged as most meaningful to me. While these thoughts are nothing new, I thought they would be a fitting way to sum up my writings over the years.
First, and most important, is that patients and families are the best partners we have in the care we give. When we take the time to listen to them, involve them in decision making and think past what we see on the surface, kids are healthier. This is just as true for preventative “well-baby” care as it is for acute and specialty care. Understanding a family’s priorities, values, and the context in which they live is just as important as our medical knowledge and skills when taking care of patients. Pediatricians are expert at bringing all of these things together, grounded in the best and most up-to-date evidence available, and in doing so elevate the care of children.
Which leads me to the second theme – pediatricians are a strong and important voice for children, and it is important for us to learn to lead. Through our work, we have a window into the lives of children, both when they are healthy and when they are sick. That is a great privilege but also a great responsibility. We see the things that work well in our systems and the things that do not. We see the amazing things children are capable of, but also troubling and pervasive inequities in care, access, and education. We see children who aren’t having their basic needs met – things like food, shelter, and a safe place to play. We see how these inequities impact health and wellness – both now and as children grow into adults. These observations, and the things we learn by caring for children and families day in and day out, can be translated into action. For each of us that will mean something different, but it is imperative that we develop our talents as advocates and leaders so that we can catalyze change. Our best hope for making things better is if we each do our part to create solutions. And when that happens, children – a lot of children – are healthier.
Since I began my first column 9 years ago, a lot has changed for me, and I suspect for many of you. When I first began writing, my now tall, confident tween (who already wears the same shoe size as me!) was barely walking. Thank you to all who have listened and encouraged me along the way – it has been a fun journey, and I’ve appreciated your time.
Dr. Beers is assistant professor of pediatrics at Children’s National Medical Center and the George Washington University Medical Center, both in Washington. She is chair of the American Academy of Pediatrics Committee on Residency Scholarships and immediate past president of the District of Columbia chapter of the American Academy of Pediatrics.
As the year comes to an end, I have decided – after 9 years of writing for Pediatric News – to bring my column to a close. It has been a great joy to be a part of the pediatric community in this way, and I have been grateful for those of you who approach me at meetings, saying, “Hey, I recognize you – I really like your column!” or tell me you appreciated a particular topic or piece of advice.
As I reflected on the columns I have written, I realized there were two themes that repeatedly emerged as most meaningful to me. While these thoughts are nothing new, I thought they would be a fitting way to sum up my writings over the years.
First, and most important, is that patients and families are the best partners we have in the care we give. When we take the time to listen to them, involve them in decision making and think past what we see on the surface, kids are healthier. This is just as true for preventative “well-baby” care as it is for acute and specialty care. Understanding a family’s priorities, values, and the context in which they live is just as important as our medical knowledge and skills when taking care of patients. Pediatricians are expert at bringing all of these things together, grounded in the best and most up-to-date evidence available, and in doing so elevate the care of children.
Which leads me to the second theme – pediatricians are a strong and important voice for children, and it is important for us to learn to lead. Through our work, we have a window into the lives of children, both when they are healthy and when they are sick. That is a great privilege but also a great responsibility. We see the things that work well in our systems and the things that do not. We see the amazing things children are capable of, but also troubling and pervasive inequities in care, access, and education. We see children who aren’t having their basic needs met – things like food, shelter, and a safe place to play. We see how these inequities impact health and wellness – both now and as children grow into adults. These observations, and the things we learn by caring for children and families day in and day out, can be translated into action. For each of us that will mean something different, but it is imperative that we develop our talents as advocates and leaders so that we can catalyze change. Our best hope for making things better is if we each do our part to create solutions. And when that happens, children – a lot of children – are healthier.
Since I began my first column 9 years ago, a lot has changed for me, and I suspect for many of you. When I first began writing, my now tall, confident tween (who already wears the same shoe size as me!) was barely walking. Thank you to all who have listened and encouraged me along the way – it has been a fun journey, and I’ve appreciated your time.
Dr. Beers is assistant professor of pediatrics at Children’s National Medical Center and the George Washington University Medical Center, both in Washington. She is chair of the American Academy of Pediatrics Committee on Residency Scholarships and immediate past president of the District of Columbia chapter of the American Academy of Pediatrics.
The Optum termination thunderbolt
One afternoon, after seeing your last patient, you’re doing the old-school thing, with your feet up, opening and reading your paper mail after a hard day’s work at the dermatology ranch. You see an odd form letter – a green sticker on the outside, certified mail – stating that you have been terminated from a Medicare advantage plan, no reason given.
At first, you don’t care so much. After all, this plan pays you only 95% of Medicare. Then you think about it and realize that this plan represents 50% of all Medicare beneficiaries in your area. You start to freak out, and you immediately go to the American Academy of Dermatology website where you read Rob Portman’s article about how to fight a termination notice and respond expeditiously.
Later that night, your spouse asks why you were singled out. “Are you a bad doctor? What did you do wrong? Can the kids still go to college?
The answer, most often, is that you did nothing wrong. You’ve just been caught up in the insurer’s network management software, Optum 360.
Optum 360 is a large health care information and management subsidiary of UnitedHealthcare. It was created as a joint venture by the Optum insight (health technology) unit of UnitedHealthcare, and Dignity Health (claims processing), forming Optum 360.
Optum claims that its software measures the efficiency of providers, saving insurers money and improving the quality of care – the Valhalla of health care managers everywhere. Unfortunately, Optum doesn’t deliver this vision of heaven on earth, at least not for dermatology.
Optum 360does little more than aggregate and average the costs of individual providers with no recognition of severity of disease or case mix. The physician with the most reimbursement during an episode of care for a given ICD-9 code (now for a group of ICD-10 codes) gets credited with all the expenses under that code. For example, you do two stages of Mohs surgery on a big basal cell on the nose that you send to plastics for repair. If the reimbursement for the Mohs surgery exceeds the plastics reimbursement, the Optum software designates you as the responsible provider. The cost of the plastics repair accrues to you; the hospital OR facility charges accrue to you (facilities are not considered a provider); and the anesthesiologist charges are credited to you. In addition, the superficial basal cell carcinoma on the patient’s back, treated a week later by the referring doctor, is also attributed to you as part of the original episode of care. There are no quality parameters and no subspecialty recognition.
If your patient load regularly includes patients who have Mohs surgery, the dermatologist down the street who does Mohs only once a week looks much better to Optum than you do. The referral-only medical dermatologist in town, who treats very sick patients and routinely prescribes biologics, and (heaven forbid) intravenous immunoglobulin, is similarly tagged for termination from the insurer’s network.
So it looks as though dermatologists who handle the toughest patients lose out. But who really loses the most? The sickest patients! The dermatologist can always fill the schedule with patients with other insurance coverage and reduce the backlog or, if worse comes to worse, he can take the Canadian cure and go on vacation. The sickest patients, however, get eliminated from the system when their doctors get eliminated by UnitedHealthcare’s software. Then patients often cannot find another doctor because most insurer’s physician rosters are 70% inaccurate (JAMA Dermatol. 2014 Dec;150[12]:1290-7).
In some circumstances, the sickest patients have reported either being unable to find other dermatologists willing to provide the special service they need or having to wait up to 6 months for an open appointment. These patients then try to drop back into fee-for-service Medicare, only to find they cannot afford the gap insurance, which costs five times as much. Why? Because those patients now have a preexisting condition. Yes, preexisting conditions still apply in the world of gap insurance.
This is obviously not optimal nor even acceptable. To quote Michael Keaton from the 1982 movie “Night Shift”: “Is this a great country or what?” The answer is a resounding “yes” for medical insurance companies who are booking record profits, but “no” for the sickest patients.
Dr. Coldiron is a past president of the American Academy of Dermatology. He is currently in private practice, but maintains a clinical assistant professorship at the University of Cincinnati. He cares for patients, teaches medical students and residents, and has several active clinical research projects. Dr. Coldiron is the author of more than 80 scientific letters, papers, and several book chapters, and he speaks frequently on a variety of topics. Reach him at [email protected].
One afternoon, after seeing your last patient, you’re doing the old-school thing, with your feet up, opening and reading your paper mail after a hard day’s work at the dermatology ranch. You see an odd form letter – a green sticker on the outside, certified mail – stating that you have been terminated from a Medicare advantage plan, no reason given.
At first, you don’t care so much. After all, this plan pays you only 95% of Medicare. Then you think about it and realize that this plan represents 50% of all Medicare beneficiaries in your area. You start to freak out, and you immediately go to the American Academy of Dermatology website where you read Rob Portman’s article about how to fight a termination notice and respond expeditiously.
Later that night, your spouse asks why you were singled out. “Are you a bad doctor? What did you do wrong? Can the kids still go to college?
The answer, most often, is that you did nothing wrong. You’ve just been caught up in the insurer’s network management software, Optum 360.
Optum 360 is a large health care information and management subsidiary of UnitedHealthcare. It was created as a joint venture by the Optum insight (health technology) unit of UnitedHealthcare, and Dignity Health (claims processing), forming Optum 360.
Optum claims that its software measures the efficiency of providers, saving insurers money and improving the quality of care – the Valhalla of health care managers everywhere. Unfortunately, Optum doesn’t deliver this vision of heaven on earth, at least not for dermatology.
Optum 360does little more than aggregate and average the costs of individual providers with no recognition of severity of disease or case mix. The physician with the most reimbursement during an episode of care for a given ICD-9 code (now for a group of ICD-10 codes) gets credited with all the expenses under that code. For example, you do two stages of Mohs surgery on a big basal cell on the nose that you send to plastics for repair. If the reimbursement for the Mohs surgery exceeds the plastics reimbursement, the Optum software designates you as the responsible provider. The cost of the plastics repair accrues to you; the hospital OR facility charges accrue to you (facilities are not considered a provider); and the anesthesiologist charges are credited to you. In addition, the superficial basal cell carcinoma on the patient’s back, treated a week later by the referring doctor, is also attributed to you as part of the original episode of care. There are no quality parameters and no subspecialty recognition.
If your patient load regularly includes patients who have Mohs surgery, the dermatologist down the street who does Mohs only once a week looks much better to Optum than you do. The referral-only medical dermatologist in town, who treats very sick patients and routinely prescribes biologics, and (heaven forbid) intravenous immunoglobulin, is similarly tagged for termination from the insurer’s network.
So it looks as though dermatologists who handle the toughest patients lose out. But who really loses the most? The sickest patients! The dermatologist can always fill the schedule with patients with other insurance coverage and reduce the backlog or, if worse comes to worse, he can take the Canadian cure and go on vacation. The sickest patients, however, get eliminated from the system when their doctors get eliminated by UnitedHealthcare’s software. Then patients often cannot find another doctor because most insurer’s physician rosters are 70% inaccurate (JAMA Dermatol. 2014 Dec;150[12]:1290-7).
In some circumstances, the sickest patients have reported either being unable to find other dermatologists willing to provide the special service they need or having to wait up to 6 months for an open appointment. These patients then try to drop back into fee-for-service Medicare, only to find they cannot afford the gap insurance, which costs five times as much. Why? Because those patients now have a preexisting condition. Yes, preexisting conditions still apply in the world of gap insurance.
This is obviously not optimal nor even acceptable. To quote Michael Keaton from the 1982 movie “Night Shift”: “Is this a great country or what?” The answer is a resounding “yes” for medical insurance companies who are booking record profits, but “no” for the sickest patients.
Dr. Coldiron is a past president of the American Academy of Dermatology. He is currently in private practice, but maintains a clinical assistant professorship at the University of Cincinnati. He cares for patients, teaches medical students and residents, and has several active clinical research projects. Dr. Coldiron is the author of more than 80 scientific letters, papers, and several book chapters, and he speaks frequently on a variety of topics. Reach him at [email protected].
One afternoon, after seeing your last patient, you’re doing the old-school thing, with your feet up, opening and reading your paper mail after a hard day’s work at the dermatology ranch. You see an odd form letter – a green sticker on the outside, certified mail – stating that you have been terminated from a Medicare advantage plan, no reason given.
At first, you don’t care so much. After all, this plan pays you only 95% of Medicare. Then you think about it and realize that this plan represents 50% of all Medicare beneficiaries in your area. You start to freak out, and you immediately go to the American Academy of Dermatology website where you read Rob Portman’s article about how to fight a termination notice and respond expeditiously.
Later that night, your spouse asks why you were singled out. “Are you a bad doctor? What did you do wrong? Can the kids still go to college?
The answer, most often, is that you did nothing wrong. You’ve just been caught up in the insurer’s network management software, Optum 360.
Optum 360 is a large health care information and management subsidiary of UnitedHealthcare. It was created as a joint venture by the Optum insight (health technology) unit of UnitedHealthcare, and Dignity Health (claims processing), forming Optum 360.
Optum claims that its software measures the efficiency of providers, saving insurers money and improving the quality of care – the Valhalla of health care managers everywhere. Unfortunately, Optum doesn’t deliver this vision of heaven on earth, at least not for dermatology.
Optum 360does little more than aggregate and average the costs of individual providers with no recognition of severity of disease or case mix. The physician with the most reimbursement during an episode of care for a given ICD-9 code (now for a group of ICD-10 codes) gets credited with all the expenses under that code. For example, you do two stages of Mohs surgery on a big basal cell on the nose that you send to plastics for repair. If the reimbursement for the Mohs surgery exceeds the plastics reimbursement, the Optum software designates you as the responsible provider. The cost of the plastics repair accrues to you; the hospital OR facility charges accrue to you (facilities are not considered a provider); and the anesthesiologist charges are credited to you. In addition, the superficial basal cell carcinoma on the patient’s back, treated a week later by the referring doctor, is also attributed to you as part of the original episode of care. There are no quality parameters and no subspecialty recognition.
If your patient load regularly includes patients who have Mohs surgery, the dermatologist down the street who does Mohs only once a week looks much better to Optum than you do. The referral-only medical dermatologist in town, who treats very sick patients and routinely prescribes biologics, and (heaven forbid) intravenous immunoglobulin, is similarly tagged for termination from the insurer’s network.
So it looks as though dermatologists who handle the toughest patients lose out. But who really loses the most? The sickest patients! The dermatologist can always fill the schedule with patients with other insurance coverage and reduce the backlog or, if worse comes to worse, he can take the Canadian cure and go on vacation. The sickest patients, however, get eliminated from the system when their doctors get eliminated by UnitedHealthcare’s software. Then patients often cannot find another doctor because most insurer’s physician rosters are 70% inaccurate (JAMA Dermatol. 2014 Dec;150[12]:1290-7).
In some circumstances, the sickest patients have reported either being unable to find other dermatologists willing to provide the special service they need or having to wait up to 6 months for an open appointment. These patients then try to drop back into fee-for-service Medicare, only to find they cannot afford the gap insurance, which costs five times as much. Why? Because those patients now have a preexisting condition. Yes, preexisting conditions still apply in the world of gap insurance.
This is obviously not optimal nor even acceptable. To quote Michael Keaton from the 1982 movie “Night Shift”: “Is this a great country or what?” The answer is a resounding “yes” for medical insurance companies who are booking record profits, but “no” for the sickest patients.
Dr. Coldiron is a past president of the American Academy of Dermatology. He is currently in private practice, but maintains a clinical assistant professorship at the University of Cincinnati. He cares for patients, teaches medical students and residents, and has several active clinical research projects. Dr. Coldiron is the author of more than 80 scientific letters, papers, and several book chapters, and he speaks frequently on a variety of topics. Reach him at [email protected].
Career Development: A Focused Plan or Serendipity?
Fifth grade is a wonderful school year and fifth graders are interesting, enthusiastic, and busy people, but conflicts can arise amidst their many activities. We discovered that our fifth grader could not finish his homework, play on 3 sports teams, take bass lessons (and practice), join the city chorus, play outside with his friends, walk his dog, spend quality time with his parents, and do his chores—much less eat and sleep. Choices needed to be made. Unfortunately, in our community dropping out of the premier soccer club probably limits future possibilities in the sport; nevertheless, it would entail 6 to 8 hours of game and practice time per week (plus travel), as well as multiple 3-day tournaments. Therefore our son dropped soccer, as we decided the best strategy for our fifth grader to develop and mature was to do his personal best at his schoolwork while also exploring a greater variety of less intensive extracurricular experiences.
Most dermatologists appropriately adopt a different strategy during medical school and dermatology training. An intensive, single-minded focus gets us through hours in the anatomy laboratory, the first difficult clinical rotations, sleepless nights, grand rounds quizzing, and board examinations. Completion of our training does not, however, signal that development and maturation are complete; rather, we must then choose among a new set of options, such as the basic questions of whether to practice in an academic setting or group or solo practice and whether to emphasize a subspecialty. These choices involve some mutually exclusive options and exist in a milieu of adult (ie, nonacademic) dilemmas concerning family life, community and spiritual life, avocations, exercise regimens, housing and material goods, and other routine aspects of life. The professional options that are available may be limited by the lack of community opportunities, geographic need, or job availability in a preferred location or institution.
So how do dermatologists manage to start their careers, then develop and maintain them? A best practice is to be both introspective as well as aware of our external environments. Good questions to ask ourselves periodically (having different answers at different stages is highly recommended!) include: What are my core values and what do I want to accomplish? Pay attention to your gut. When do you lose track of time and what makes you want to scream in frustration? Regularly take an inventory of your strengths and find opportunities to acquire the competencies that can take you to the next level. What skill do I need to finesse and how do I finesse it? Do an external scan and understand limiting factors such as geographic saturation in your desired practice type or the lack of appropriate collaborators in your preferred area of interest. Search out people who are doing what you’d like to do and then identify their paths and what you can use from their experiences to help with your career development.
Once you have identified a few professional goals to pursue, utilize all the resources you can find. You might find helpful seminars at an academic institution or at conferences. Do you want to become the regional expert in sarcoidosis? Check out what has been written and find other experts in the subject and where they are speaking. Many organizations have practice management or leadership development courses and seminars. There also are books for everything—those that I have found most useful include Douglas Stone’s Difficult Conversations: How to Discuss What Matters Most1 and William L. Fisher and Roger Ury’s classic, Getting to Yes: Negotiating Agreement Without Giving In.2 Have to give a talk? There is a PowerPoint 2016 for Dummies.3 The same series also includes a book on the Microsoft® Excel spreadsheet. Also check out my all-time favorite—Brian Tracy’s Eat That Frog! 21 Ways to Stop Procrastinating and Get More Done in Less Time.4
It is important to experiment with different professional experiences and have an open mind when a new activity presents itself. Look for opportunities for new side ventures or interesting projects that will not take up much time so you can continue to do your best at your daily work. When I was a senior resident, a dermatologist from Maine asked me if I would help him find a dermatologist who would work regularly at a rural clinic in the northern part of the state. My answer was, why not me? For 8 years I worked in that clinic once to twice per month, seeing as many patients as I could for 8 to 12 hours a day on Friday, Saturday, and Sunday, and then returning to Boston, Massachusetts, for my normal work week. I even took my 2 youngest children (who were born during that time) with me and found a family there who took excellent care of them while I worked. It ended up being one of the most important experiences, both intellectually and emotionally, of my professional career. I learned how to diagnose difficult and complex dermatology problems by myself in an environment with few resources (the closest dermatologist was 150 miles away), how to use primary care providers to manage patients remotely, how to set up a clinic and manage staff (I hired other part-time staff to help me), and how to lead an effort that I felt passionate about. I sometimes even took on residents, which helped me finesse my teaching and supervision style.
Unlike the achievement of becoming a board-certified dermatologist, a dermatology career does not develop in a straight line, and rarely at a steady pace. It seems to me that a shift from a single-minded focus during residency to the fifth-grade strategy of doing our personal best at the main tasks of everyday work as well as participating in a variety of other experiences successfully develops a career that encompasses excellence, enthusiasm, and the fulfillment of personal needs along with those of our practice or institution. When we do our personal best on the day-to-day matters, people will be beating down the doors to offer other valuable experiences. To paraphrase an old truism, if you want something done well, find a busy person who does other things well. Some of the experiences presented to us may question our basic assumptions and redirect our careers; others will fizzle out, but not before they garner self-confidence or even indirectly lead to something more substantial in our careers. Sometimes all that an experience teaches us is that we do not want to continue down that path.
Career development is a dynamic process. Strive for excellence in everything that you do, keep your eyes open for broadening experiences, and maintain your fifth-grade enthusiasm! I am not sure what I will be doing in 5 years, but I hope it will be fresh, varied, and exciting. Do dermatology careers develop through a focused plan or serendipity? At my mature age, with a well-developed career, my answer is mostly serendipity.
1. Stone D, Patton B, Heen S. Difficult Conversations: How to Discuss What Matters Most. New York, NY: Penguin Books; 2010.
2. Fisher R, Ury W, Patton B. Getting to Yes: Negotiating Agreement Without Giving In. New York, NY: Penguin Books; 2011.
3. Lowe D. PowerPoint 2016 for Dummies. Hoboken, NJ: John Wiley & Sons; 2015.
4. Tracy B. Eat That Frog! 21 Ways to Stop Procrastinating and Get More Done in Less Time. 2nd ed. San Francisco, CA: Berrett-Koehler Publishers; 2007.
Fifth grade is a wonderful school year and fifth graders are interesting, enthusiastic, and busy people, but conflicts can arise amidst their many activities. We discovered that our fifth grader could not finish his homework, play on 3 sports teams, take bass lessons (and practice), join the city chorus, play outside with his friends, walk his dog, spend quality time with his parents, and do his chores—much less eat and sleep. Choices needed to be made. Unfortunately, in our community dropping out of the premier soccer club probably limits future possibilities in the sport; nevertheless, it would entail 6 to 8 hours of game and practice time per week (plus travel), as well as multiple 3-day tournaments. Therefore our son dropped soccer, as we decided the best strategy for our fifth grader to develop and mature was to do his personal best at his schoolwork while also exploring a greater variety of less intensive extracurricular experiences.
Most dermatologists appropriately adopt a different strategy during medical school and dermatology training. An intensive, single-minded focus gets us through hours in the anatomy laboratory, the first difficult clinical rotations, sleepless nights, grand rounds quizzing, and board examinations. Completion of our training does not, however, signal that development and maturation are complete; rather, we must then choose among a new set of options, such as the basic questions of whether to practice in an academic setting or group or solo practice and whether to emphasize a subspecialty. These choices involve some mutually exclusive options and exist in a milieu of adult (ie, nonacademic) dilemmas concerning family life, community and spiritual life, avocations, exercise regimens, housing and material goods, and other routine aspects of life. The professional options that are available may be limited by the lack of community opportunities, geographic need, or job availability in a preferred location or institution.
So how do dermatologists manage to start their careers, then develop and maintain them? A best practice is to be both introspective as well as aware of our external environments. Good questions to ask ourselves periodically (having different answers at different stages is highly recommended!) include: What are my core values and what do I want to accomplish? Pay attention to your gut. When do you lose track of time and what makes you want to scream in frustration? Regularly take an inventory of your strengths and find opportunities to acquire the competencies that can take you to the next level. What skill do I need to finesse and how do I finesse it? Do an external scan and understand limiting factors such as geographic saturation in your desired practice type or the lack of appropriate collaborators in your preferred area of interest. Search out people who are doing what you’d like to do and then identify their paths and what you can use from their experiences to help with your career development.
Once you have identified a few professional goals to pursue, utilize all the resources you can find. You might find helpful seminars at an academic institution or at conferences. Do you want to become the regional expert in sarcoidosis? Check out what has been written and find other experts in the subject and where they are speaking. Many organizations have practice management or leadership development courses and seminars. There also are books for everything—those that I have found most useful include Douglas Stone’s Difficult Conversations: How to Discuss What Matters Most1 and William L. Fisher and Roger Ury’s classic, Getting to Yes: Negotiating Agreement Without Giving In.2 Have to give a talk? There is a PowerPoint 2016 for Dummies.3 The same series also includes a book on the Microsoft® Excel spreadsheet. Also check out my all-time favorite—Brian Tracy’s Eat That Frog! 21 Ways to Stop Procrastinating and Get More Done in Less Time.4
It is important to experiment with different professional experiences and have an open mind when a new activity presents itself. Look for opportunities for new side ventures or interesting projects that will not take up much time so you can continue to do your best at your daily work. When I was a senior resident, a dermatologist from Maine asked me if I would help him find a dermatologist who would work regularly at a rural clinic in the northern part of the state. My answer was, why not me? For 8 years I worked in that clinic once to twice per month, seeing as many patients as I could for 8 to 12 hours a day on Friday, Saturday, and Sunday, and then returning to Boston, Massachusetts, for my normal work week. I even took my 2 youngest children (who were born during that time) with me and found a family there who took excellent care of them while I worked. It ended up being one of the most important experiences, both intellectually and emotionally, of my professional career. I learned how to diagnose difficult and complex dermatology problems by myself in an environment with few resources (the closest dermatologist was 150 miles away), how to use primary care providers to manage patients remotely, how to set up a clinic and manage staff (I hired other part-time staff to help me), and how to lead an effort that I felt passionate about. I sometimes even took on residents, which helped me finesse my teaching and supervision style.
Unlike the achievement of becoming a board-certified dermatologist, a dermatology career does not develop in a straight line, and rarely at a steady pace. It seems to me that a shift from a single-minded focus during residency to the fifth-grade strategy of doing our personal best at the main tasks of everyday work as well as participating in a variety of other experiences successfully develops a career that encompasses excellence, enthusiasm, and the fulfillment of personal needs along with those of our practice or institution. When we do our personal best on the day-to-day matters, people will be beating down the doors to offer other valuable experiences. To paraphrase an old truism, if you want something done well, find a busy person who does other things well. Some of the experiences presented to us may question our basic assumptions and redirect our careers; others will fizzle out, but not before they garner self-confidence or even indirectly lead to something more substantial in our careers. Sometimes all that an experience teaches us is that we do not want to continue down that path.
Career development is a dynamic process. Strive for excellence in everything that you do, keep your eyes open for broadening experiences, and maintain your fifth-grade enthusiasm! I am not sure what I will be doing in 5 years, but I hope it will be fresh, varied, and exciting. Do dermatology careers develop through a focused plan or serendipity? At my mature age, with a well-developed career, my answer is mostly serendipity.
Fifth grade is a wonderful school year and fifth graders are interesting, enthusiastic, and busy people, but conflicts can arise amidst their many activities. We discovered that our fifth grader could not finish his homework, play on 3 sports teams, take bass lessons (and practice), join the city chorus, play outside with his friends, walk his dog, spend quality time with his parents, and do his chores—much less eat and sleep. Choices needed to be made. Unfortunately, in our community dropping out of the premier soccer club probably limits future possibilities in the sport; nevertheless, it would entail 6 to 8 hours of game and practice time per week (plus travel), as well as multiple 3-day tournaments. Therefore our son dropped soccer, as we decided the best strategy for our fifth grader to develop and mature was to do his personal best at his schoolwork while also exploring a greater variety of less intensive extracurricular experiences.
Most dermatologists appropriately adopt a different strategy during medical school and dermatology training. An intensive, single-minded focus gets us through hours in the anatomy laboratory, the first difficult clinical rotations, sleepless nights, grand rounds quizzing, and board examinations. Completion of our training does not, however, signal that development and maturation are complete; rather, we must then choose among a new set of options, such as the basic questions of whether to practice in an academic setting or group or solo practice and whether to emphasize a subspecialty. These choices involve some mutually exclusive options and exist in a milieu of adult (ie, nonacademic) dilemmas concerning family life, community and spiritual life, avocations, exercise regimens, housing and material goods, and other routine aspects of life. The professional options that are available may be limited by the lack of community opportunities, geographic need, or job availability in a preferred location or institution.
So how do dermatologists manage to start their careers, then develop and maintain them? A best practice is to be both introspective as well as aware of our external environments. Good questions to ask ourselves periodically (having different answers at different stages is highly recommended!) include: What are my core values and what do I want to accomplish? Pay attention to your gut. When do you lose track of time and what makes you want to scream in frustration? Regularly take an inventory of your strengths and find opportunities to acquire the competencies that can take you to the next level. What skill do I need to finesse and how do I finesse it? Do an external scan and understand limiting factors such as geographic saturation in your desired practice type or the lack of appropriate collaborators in your preferred area of interest. Search out people who are doing what you’d like to do and then identify their paths and what you can use from their experiences to help with your career development.
Once you have identified a few professional goals to pursue, utilize all the resources you can find. You might find helpful seminars at an academic institution or at conferences. Do you want to become the regional expert in sarcoidosis? Check out what has been written and find other experts in the subject and where they are speaking. Many organizations have practice management or leadership development courses and seminars. There also are books for everything—those that I have found most useful include Douglas Stone’s Difficult Conversations: How to Discuss What Matters Most1 and William L. Fisher and Roger Ury’s classic, Getting to Yes: Negotiating Agreement Without Giving In.2 Have to give a talk? There is a PowerPoint 2016 for Dummies.3 The same series also includes a book on the Microsoft® Excel spreadsheet. Also check out my all-time favorite—Brian Tracy’s Eat That Frog! 21 Ways to Stop Procrastinating and Get More Done in Less Time.4
It is important to experiment with different professional experiences and have an open mind when a new activity presents itself. Look for opportunities for new side ventures or interesting projects that will not take up much time so you can continue to do your best at your daily work. When I was a senior resident, a dermatologist from Maine asked me if I would help him find a dermatologist who would work regularly at a rural clinic in the northern part of the state. My answer was, why not me? For 8 years I worked in that clinic once to twice per month, seeing as many patients as I could for 8 to 12 hours a day on Friday, Saturday, and Sunday, and then returning to Boston, Massachusetts, for my normal work week. I even took my 2 youngest children (who were born during that time) with me and found a family there who took excellent care of them while I worked. It ended up being one of the most important experiences, both intellectually and emotionally, of my professional career. I learned how to diagnose difficult and complex dermatology problems by myself in an environment with few resources (the closest dermatologist was 150 miles away), how to use primary care providers to manage patients remotely, how to set up a clinic and manage staff (I hired other part-time staff to help me), and how to lead an effort that I felt passionate about. I sometimes even took on residents, which helped me finesse my teaching and supervision style.
Unlike the achievement of becoming a board-certified dermatologist, a dermatology career does not develop in a straight line, and rarely at a steady pace. It seems to me that a shift from a single-minded focus during residency to the fifth-grade strategy of doing our personal best at the main tasks of everyday work as well as participating in a variety of other experiences successfully develops a career that encompasses excellence, enthusiasm, and the fulfillment of personal needs along with those of our practice or institution. When we do our personal best on the day-to-day matters, people will be beating down the doors to offer other valuable experiences. To paraphrase an old truism, if you want something done well, find a busy person who does other things well. Some of the experiences presented to us may question our basic assumptions and redirect our careers; others will fizzle out, but not before they garner self-confidence or even indirectly lead to something more substantial in our careers. Sometimes all that an experience teaches us is that we do not want to continue down that path.
Career development is a dynamic process. Strive for excellence in everything that you do, keep your eyes open for broadening experiences, and maintain your fifth-grade enthusiasm! I am not sure what I will be doing in 5 years, but I hope it will be fresh, varied, and exciting. Do dermatology careers develop through a focused plan or serendipity? At my mature age, with a well-developed career, my answer is mostly serendipity.
1. Stone D, Patton B, Heen S. Difficult Conversations: How to Discuss What Matters Most. New York, NY: Penguin Books; 2010.
2. Fisher R, Ury W, Patton B. Getting to Yes: Negotiating Agreement Without Giving In. New York, NY: Penguin Books; 2011.
3. Lowe D. PowerPoint 2016 for Dummies. Hoboken, NJ: John Wiley & Sons; 2015.
4. Tracy B. Eat That Frog! 21 Ways to Stop Procrastinating and Get More Done in Less Time. 2nd ed. San Francisco, CA: Berrett-Koehler Publishers; 2007.
1. Stone D, Patton B, Heen S. Difficult Conversations: How to Discuss What Matters Most. New York, NY: Penguin Books; 2010.
2. Fisher R, Ury W, Patton B. Getting to Yes: Negotiating Agreement Without Giving In. New York, NY: Penguin Books; 2011.
3. Lowe D. PowerPoint 2016 for Dummies. Hoboken, NJ: John Wiley & Sons; 2015.
4. Tracy B. Eat That Frog! 21 Ways to Stop Procrastinating and Get More Done in Less Time. 2nd ed. San Francisco, CA: Berrett-Koehler Publishers; 2007.
Judicious antibiotic use key in ambulatory settings
I was recently asked to evaluate a young child with a urinary tract infection caused by an extended spectrum beta-lactamase (ESBL)–producing Escherichia coli.
I’d just broken the bad news to the mother: There was no oral medication available to treat the baby, so she’d have to stay in the hospital for a full intravenous course.
“Has your child been treated with antibiotics recently?” I asked the mother, wondering how the baby had come to have such a resistant infection.
“She had a couple days of runny nose and a low-grade fever a couple of weeks ago,” she told me. “Her doctor treated her for a sinus infection.”
In 2011, doctors in outpatient settings across the United States wrote 262.5 million prescriptions for antibiotics – 73.7 million for children – and according to the Centers for Disease Control and Prevention, about 50% of these were completely unnecessary because they were prescribed for viral respiratory tract infections (Clin Infect Dis. 2015 May 1;60[9]:1308-16).
Prescribing practices varied by region, with the highest rates in the South. Don’t think I’m judging. I live in Kentucky, the state with the highest rate of antibiotic prescribing at 1,281 prescriptions per 1,000 persons. Is it any wonder that we’re seeing kids with very resistant infections?
The CDC estimates that at least two million people in the United States are infected annually with antibiotic-resistant bacteria and at least 23,000 of them die as a result of these infections. It is estimated that prevention strategies that include better antibiotic prescribing could prevent as many as 619,000 infections and 37,000 deaths over 5 years. Fortunately, my little patient recovered fully, but it has made me think about antimicrobial stewardship, especially its role in the outpatient setting.
According the American Academy of Pediatrics, the goal of antimicrobial stewardship is “to optimize antimicrobial use, with the aim of decreasing inappropriate use that leads to unwarranted toxicity and to selection and spread of resistant organisms.”
Antimicrobial stewardship programs (ASPs) are increasingly common in inpatient settings and have been shown to reduce antibiotic use. These programs can take many forms. The hospital where I work relies primarily on clinical guidelines emphasizing appropriate empiric therapy for a variety of common conditions. Other hospitals employ prospective audit and feedback, as well as a restricted formulary. Medicare and Medicaid Conditions of Participation will soon require hospitals that receive funds from the Centers for Medicare and Medicaid Services have an ASP.
Comparatively little has been published about ASPs in the outpatient setting. The American Academy of Pediatrics suggests that effective strategies include patient education, provider education, provider audit and feedback, and clinical decision support. We have at least some data that these work, at least in a research setting.
From 2000 to 2003, a controlled, cluster-randomized trial in 16 Massachusetts communities demonstrated that a 3-year, multifaceted, community-level intervention was “modestly successful” in reducing antibiotic use (Pediatrics. 2008 Jan;121[1]:e15-23). As a part of this intervention, parents received education via direct mail and in primary care settings, pharmacies, and child care centers while physicians received small-group education, frequent updates and educational materials, and prescribing feedback. Antibiotic prescribing was measured via health insurance claims data from all children who were 6 years of age or younger and resided in study communities, and were insured by one of four participating health plans. Coincident with the intervention, there was 4.2% decrease in antibiotic prescribing among children aged 24 to <48 months and a 6.7% decrease among those aged 48-72 months. The effect was greatest among Medicaid-insured children.
More recently, 18 primary care practices in Pennsylvania and New Jersey were randomized to an intervention that consisted of a 1-hour, on-site education session followed by 1 year of personalized, quarterly audit and feedback of prescribing for bacterial and viral acute respiratory tract infections (ARTIs), or usual practice (JAMA. 2013 Jun 12;309[22]:2345-52). The prescribing practices of 162 clinicians were included in the analysis.
Broad spectrum–antibiotic prescribing decreased in intervention practices, compared with controls (26.8% to 14.3% among intervention practices vs. 28.4% to 22.6% in controls), as did “off-guideline” prescribing for pneumonia and acute sinusitis. Antibiotic prescribing for viral infections was relatively low at baseline and did not change. The authors concluded that “extending antimicrobial stewardship to the ambulatory setting, where such programs have generally not been implemented, may have important health benefits.” Unfortunately, the positive effect in these practices was not sustained after the audit and feedback stopped (JAMA. 2014 Dec 17;312[23]:2569-70).
Not all antimicrobial stewardship interventions need to be time- and resource-intensive. Investigators in California found that providers who publicly pledged to reducing inappropriate antibiotic use for ARTIs by signing and posting a commitment letter in exam rooms actually prescribed fewer inappropriate antibiotic courses for their adult patients (JAMA Intern Med. 2014 Mar;174[3]:425-31).
“When you have a cough, sore throat, or other illness, your doctor will help you select the best possible treatments. If an antibiotic would do more harm than good, your doctor will explain this to you, and may offer other treatments that are better for you,” the letter read in part. There was a 19.7 absolute percentage reduction in inappropriate antibiotic prescribing for ARTIs among clinicians randomized to the commitment letter invention relative to controls.
Can antimicrobial strategies work in the “real” world, in a busy pediatrician’s office? According to Dr. Patricia Purcell, a physician with East Louisville Pediatrics in Louisville, Ky., the answer is “yes.”
“We actually start with education in the newborn period,” Dr. Purcell said. “We let parents know that we are not going to call in antibiotics over the phone, and we’re not going to prescribe them for an upper respiratory tract infection.”
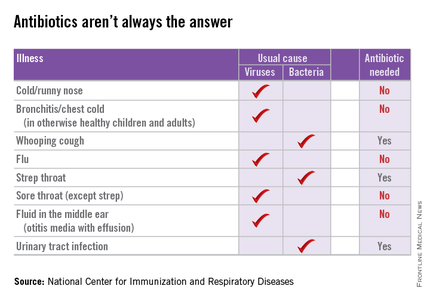
Dr. Purcell and her partners have committed to following evidence-based guidelines for antibiotic practices, such as the AAP’s guidelines for otitis media and sinusitis. She also noted that at least one major insurance company is starting to provide the group feedback about their antibiotic-prescribing practices. “They want to make sure we are not prescribing antibiotics for viruses,” she said.
Still, the message that antibiotics are not always the answer can be a bitter pill for some parents to swallow. A pediatrician friend in Alabama notes: “I have these conversations every day, and a lot of parents are mad at me for not prescribing antibiotics for their child’s ‘terrible cold.’” Another friend notes that watchful waiting can be a burden for parents who have high copays or difficulties with transportation.
Still, many parents would welcome a frank discussion about the risks and benefits of antibiotics. After I shared some of the CDC information for parents with a nursing colleague, she told me that her daughter recently had a febrile illness and was diagnosed with otitis media. “I don’t like giving my kids meds they don’t need,” she told me. “However, if the doc says they need antibiotics and they prescribe them, I give them. I never say, ‘Do we really need antibiotics for that?’”
Now she is rethinking that approach. “Was 10 days of amoxicillin necessary for a ‘red’ eardrum?! I’m just a mom. ... I don’t know the answer to that! Was her ear red because she had been crying or because of her fever? Did she get ‘treatment’ she did not need? Did the doctor give me antibiotics without education because she assumed that is why I brought her in?”
This year’s “Get Smart About Antibiotics Week” was Nov. 16-22. This annual 1-week observance is intended to raise awareness of the threat of antibiotic resistance and the importance of appropriate prescribing and use. Kudos if you celebrated this in your office. If you missed it, it’s not too late to check out some of the activities suggested by the CDC, and try one or two in your own practice. Email me with your ideas about stewardship in the outpatient setting, and I’ll try to feature at least some of them in a future column.
Dr. Bryant is a pediatrician specializing in infectious diseases at the University of Louisville (Ky.) and Kosair Children’s Hospital, also in Louisville. Dr. Bryant disclosed that she has been an investigator for clinical trials funded by Pfizer for the past 2 years. Email her at [email protected].
I was recently asked to evaluate a young child with a urinary tract infection caused by an extended spectrum beta-lactamase (ESBL)–producing Escherichia coli.
I’d just broken the bad news to the mother: There was no oral medication available to treat the baby, so she’d have to stay in the hospital for a full intravenous course.
“Has your child been treated with antibiotics recently?” I asked the mother, wondering how the baby had come to have such a resistant infection.
“She had a couple days of runny nose and a low-grade fever a couple of weeks ago,” she told me. “Her doctor treated her for a sinus infection.”
In 2011, doctors in outpatient settings across the United States wrote 262.5 million prescriptions for antibiotics – 73.7 million for children – and according to the Centers for Disease Control and Prevention, about 50% of these were completely unnecessary because they were prescribed for viral respiratory tract infections (Clin Infect Dis. 2015 May 1;60[9]:1308-16).
Prescribing practices varied by region, with the highest rates in the South. Don’t think I’m judging. I live in Kentucky, the state with the highest rate of antibiotic prescribing at 1,281 prescriptions per 1,000 persons. Is it any wonder that we’re seeing kids with very resistant infections?
The CDC estimates that at least two million people in the United States are infected annually with antibiotic-resistant bacteria and at least 23,000 of them die as a result of these infections. It is estimated that prevention strategies that include better antibiotic prescribing could prevent as many as 619,000 infections and 37,000 deaths over 5 years. Fortunately, my little patient recovered fully, but it has made me think about antimicrobial stewardship, especially its role in the outpatient setting.
According the American Academy of Pediatrics, the goal of antimicrobial stewardship is “to optimize antimicrobial use, with the aim of decreasing inappropriate use that leads to unwarranted toxicity and to selection and spread of resistant organisms.”
Antimicrobial stewardship programs (ASPs) are increasingly common in inpatient settings and have been shown to reduce antibiotic use. These programs can take many forms. The hospital where I work relies primarily on clinical guidelines emphasizing appropriate empiric therapy for a variety of common conditions. Other hospitals employ prospective audit and feedback, as well as a restricted formulary. Medicare and Medicaid Conditions of Participation will soon require hospitals that receive funds from the Centers for Medicare and Medicaid Services have an ASP.
Comparatively little has been published about ASPs in the outpatient setting. The American Academy of Pediatrics suggests that effective strategies include patient education, provider education, provider audit and feedback, and clinical decision support. We have at least some data that these work, at least in a research setting.
From 2000 to 2003, a controlled, cluster-randomized trial in 16 Massachusetts communities demonstrated that a 3-year, multifaceted, community-level intervention was “modestly successful” in reducing antibiotic use (Pediatrics. 2008 Jan;121[1]:e15-23). As a part of this intervention, parents received education via direct mail and in primary care settings, pharmacies, and child care centers while physicians received small-group education, frequent updates and educational materials, and prescribing feedback. Antibiotic prescribing was measured via health insurance claims data from all children who were 6 years of age or younger and resided in study communities, and were insured by one of four participating health plans. Coincident with the intervention, there was 4.2% decrease in antibiotic prescribing among children aged 24 to <48 months and a 6.7% decrease among those aged 48-72 months. The effect was greatest among Medicaid-insured children.
More recently, 18 primary care practices in Pennsylvania and New Jersey were randomized to an intervention that consisted of a 1-hour, on-site education session followed by 1 year of personalized, quarterly audit and feedback of prescribing for bacterial and viral acute respiratory tract infections (ARTIs), or usual practice (JAMA. 2013 Jun 12;309[22]:2345-52). The prescribing practices of 162 clinicians were included in the analysis.
Broad spectrum–antibiotic prescribing decreased in intervention practices, compared with controls (26.8% to 14.3% among intervention practices vs. 28.4% to 22.6% in controls), as did “off-guideline” prescribing for pneumonia and acute sinusitis. Antibiotic prescribing for viral infections was relatively low at baseline and did not change. The authors concluded that “extending antimicrobial stewardship to the ambulatory setting, where such programs have generally not been implemented, may have important health benefits.” Unfortunately, the positive effect in these practices was not sustained after the audit and feedback stopped (JAMA. 2014 Dec 17;312[23]:2569-70).
Not all antimicrobial stewardship interventions need to be time- and resource-intensive. Investigators in California found that providers who publicly pledged to reducing inappropriate antibiotic use for ARTIs by signing and posting a commitment letter in exam rooms actually prescribed fewer inappropriate antibiotic courses for their adult patients (JAMA Intern Med. 2014 Mar;174[3]:425-31).
“When you have a cough, sore throat, or other illness, your doctor will help you select the best possible treatments. If an antibiotic would do more harm than good, your doctor will explain this to you, and may offer other treatments that are better for you,” the letter read in part. There was a 19.7 absolute percentage reduction in inappropriate antibiotic prescribing for ARTIs among clinicians randomized to the commitment letter invention relative to controls.
Can antimicrobial strategies work in the “real” world, in a busy pediatrician’s office? According to Dr. Patricia Purcell, a physician with East Louisville Pediatrics in Louisville, Ky., the answer is “yes.”
“We actually start with education in the newborn period,” Dr. Purcell said. “We let parents know that we are not going to call in antibiotics over the phone, and we’re not going to prescribe them for an upper respiratory tract infection.”
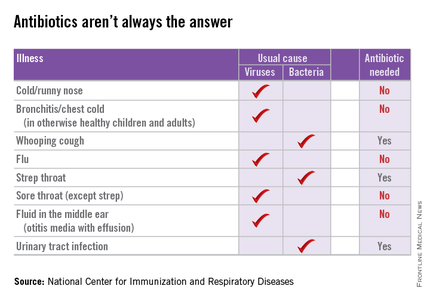
Dr. Purcell and her partners have committed to following evidence-based guidelines for antibiotic practices, such as the AAP’s guidelines for otitis media and sinusitis. She also noted that at least one major insurance company is starting to provide the group feedback about their antibiotic-prescribing practices. “They want to make sure we are not prescribing antibiotics for viruses,” she said.
Still, the message that antibiotics are not always the answer can be a bitter pill for some parents to swallow. A pediatrician friend in Alabama notes: “I have these conversations every day, and a lot of parents are mad at me for not prescribing antibiotics for their child’s ‘terrible cold.’” Another friend notes that watchful waiting can be a burden for parents who have high copays or difficulties with transportation.
Still, many parents would welcome a frank discussion about the risks and benefits of antibiotics. After I shared some of the CDC information for parents with a nursing colleague, she told me that her daughter recently had a febrile illness and was diagnosed with otitis media. “I don’t like giving my kids meds they don’t need,” she told me. “However, if the doc says they need antibiotics and they prescribe them, I give them. I never say, ‘Do we really need antibiotics for that?’”
Now she is rethinking that approach. “Was 10 days of amoxicillin necessary for a ‘red’ eardrum?! I’m just a mom. ... I don’t know the answer to that! Was her ear red because she had been crying or because of her fever? Did she get ‘treatment’ she did not need? Did the doctor give me antibiotics without education because she assumed that is why I brought her in?”
This year’s “Get Smart About Antibiotics Week” was Nov. 16-22. This annual 1-week observance is intended to raise awareness of the threat of antibiotic resistance and the importance of appropriate prescribing and use. Kudos if you celebrated this in your office. If you missed it, it’s not too late to check out some of the activities suggested by the CDC, and try one or two in your own practice. Email me with your ideas about stewardship in the outpatient setting, and I’ll try to feature at least some of them in a future column.
Dr. Bryant is a pediatrician specializing in infectious diseases at the University of Louisville (Ky.) and Kosair Children’s Hospital, also in Louisville. Dr. Bryant disclosed that she has been an investigator for clinical trials funded by Pfizer for the past 2 years. Email her at [email protected].
I was recently asked to evaluate a young child with a urinary tract infection caused by an extended spectrum beta-lactamase (ESBL)–producing Escherichia coli.
I’d just broken the bad news to the mother: There was no oral medication available to treat the baby, so she’d have to stay in the hospital for a full intravenous course.
“Has your child been treated with antibiotics recently?” I asked the mother, wondering how the baby had come to have such a resistant infection.
“She had a couple days of runny nose and a low-grade fever a couple of weeks ago,” she told me. “Her doctor treated her for a sinus infection.”
In 2011, doctors in outpatient settings across the United States wrote 262.5 million prescriptions for antibiotics – 73.7 million for children – and according to the Centers for Disease Control and Prevention, about 50% of these were completely unnecessary because they were prescribed for viral respiratory tract infections (Clin Infect Dis. 2015 May 1;60[9]:1308-16).
Prescribing practices varied by region, with the highest rates in the South. Don’t think I’m judging. I live in Kentucky, the state with the highest rate of antibiotic prescribing at 1,281 prescriptions per 1,000 persons. Is it any wonder that we’re seeing kids with very resistant infections?
The CDC estimates that at least two million people in the United States are infected annually with antibiotic-resistant bacteria and at least 23,000 of them die as a result of these infections. It is estimated that prevention strategies that include better antibiotic prescribing could prevent as many as 619,000 infections and 37,000 deaths over 5 years. Fortunately, my little patient recovered fully, but it has made me think about antimicrobial stewardship, especially its role in the outpatient setting.
According the American Academy of Pediatrics, the goal of antimicrobial stewardship is “to optimize antimicrobial use, with the aim of decreasing inappropriate use that leads to unwarranted toxicity and to selection and spread of resistant organisms.”
Antimicrobial stewardship programs (ASPs) are increasingly common in inpatient settings and have been shown to reduce antibiotic use. These programs can take many forms. The hospital where I work relies primarily on clinical guidelines emphasizing appropriate empiric therapy for a variety of common conditions. Other hospitals employ prospective audit and feedback, as well as a restricted formulary. Medicare and Medicaid Conditions of Participation will soon require hospitals that receive funds from the Centers for Medicare and Medicaid Services have an ASP.
Comparatively little has been published about ASPs in the outpatient setting. The American Academy of Pediatrics suggests that effective strategies include patient education, provider education, provider audit and feedback, and clinical decision support. We have at least some data that these work, at least in a research setting.
From 2000 to 2003, a controlled, cluster-randomized trial in 16 Massachusetts communities demonstrated that a 3-year, multifaceted, community-level intervention was “modestly successful” in reducing antibiotic use (Pediatrics. 2008 Jan;121[1]:e15-23). As a part of this intervention, parents received education via direct mail and in primary care settings, pharmacies, and child care centers while physicians received small-group education, frequent updates and educational materials, and prescribing feedback. Antibiotic prescribing was measured via health insurance claims data from all children who were 6 years of age or younger and resided in study communities, and were insured by one of four participating health plans. Coincident with the intervention, there was 4.2% decrease in antibiotic prescribing among children aged 24 to <48 months and a 6.7% decrease among those aged 48-72 months. The effect was greatest among Medicaid-insured children.
More recently, 18 primary care practices in Pennsylvania and New Jersey were randomized to an intervention that consisted of a 1-hour, on-site education session followed by 1 year of personalized, quarterly audit and feedback of prescribing for bacterial and viral acute respiratory tract infections (ARTIs), or usual practice (JAMA. 2013 Jun 12;309[22]:2345-52). The prescribing practices of 162 clinicians were included in the analysis.
Broad spectrum–antibiotic prescribing decreased in intervention practices, compared with controls (26.8% to 14.3% among intervention practices vs. 28.4% to 22.6% in controls), as did “off-guideline” prescribing for pneumonia and acute sinusitis. Antibiotic prescribing for viral infections was relatively low at baseline and did not change. The authors concluded that “extending antimicrobial stewardship to the ambulatory setting, where such programs have generally not been implemented, may have important health benefits.” Unfortunately, the positive effect in these practices was not sustained after the audit and feedback stopped (JAMA. 2014 Dec 17;312[23]:2569-70).
Not all antimicrobial stewardship interventions need to be time- and resource-intensive. Investigators in California found that providers who publicly pledged to reducing inappropriate antibiotic use for ARTIs by signing and posting a commitment letter in exam rooms actually prescribed fewer inappropriate antibiotic courses for their adult patients (JAMA Intern Med. 2014 Mar;174[3]:425-31).
“When you have a cough, sore throat, or other illness, your doctor will help you select the best possible treatments. If an antibiotic would do more harm than good, your doctor will explain this to you, and may offer other treatments that are better for you,” the letter read in part. There was a 19.7 absolute percentage reduction in inappropriate antibiotic prescribing for ARTIs among clinicians randomized to the commitment letter invention relative to controls.
Can antimicrobial strategies work in the “real” world, in a busy pediatrician’s office? According to Dr. Patricia Purcell, a physician with East Louisville Pediatrics in Louisville, Ky., the answer is “yes.”
“We actually start with education in the newborn period,” Dr. Purcell said. “We let parents know that we are not going to call in antibiotics over the phone, and we’re not going to prescribe them for an upper respiratory tract infection.”
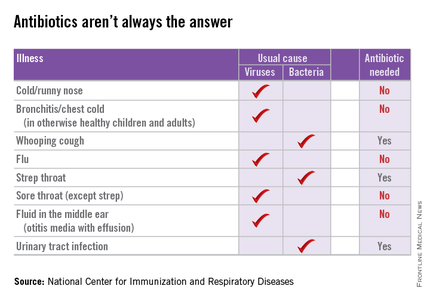
Dr. Purcell and her partners have committed to following evidence-based guidelines for antibiotic practices, such as the AAP’s guidelines for otitis media and sinusitis. She also noted that at least one major insurance company is starting to provide the group feedback about their antibiotic-prescribing practices. “They want to make sure we are not prescribing antibiotics for viruses,” she said.
Still, the message that antibiotics are not always the answer can be a bitter pill for some parents to swallow. A pediatrician friend in Alabama notes: “I have these conversations every day, and a lot of parents are mad at me for not prescribing antibiotics for their child’s ‘terrible cold.’” Another friend notes that watchful waiting can be a burden for parents who have high copays or difficulties with transportation.
Still, many parents would welcome a frank discussion about the risks and benefits of antibiotics. After I shared some of the CDC information for parents with a nursing colleague, she told me that her daughter recently had a febrile illness and was diagnosed with otitis media. “I don’t like giving my kids meds they don’t need,” she told me. “However, if the doc says they need antibiotics and they prescribe them, I give them. I never say, ‘Do we really need antibiotics for that?’”
Now she is rethinking that approach. “Was 10 days of amoxicillin necessary for a ‘red’ eardrum?! I’m just a mom. ... I don’t know the answer to that! Was her ear red because she had been crying or because of her fever? Did she get ‘treatment’ she did not need? Did the doctor give me antibiotics without education because she assumed that is why I brought her in?”
This year’s “Get Smart About Antibiotics Week” was Nov. 16-22. This annual 1-week observance is intended to raise awareness of the threat of antibiotic resistance and the importance of appropriate prescribing and use. Kudos if you celebrated this in your office. If you missed it, it’s not too late to check out some of the activities suggested by the CDC, and try one or two in your own practice. Email me with your ideas about stewardship in the outpatient setting, and I’ll try to feature at least some of them in a future column.
Dr. Bryant is a pediatrician specializing in infectious diseases at the University of Louisville (Ky.) and Kosair Children’s Hospital, also in Louisville. Dr. Bryant disclosed that she has been an investigator for clinical trials funded by Pfizer for the past 2 years. Email her at [email protected].
Assessment of High Staphylococcus aureus MIC and Poor Patient Outcomes
Staphylococcus aureus (S aureus) is a common cause of infection within the hospital and in the community.1 Treatment is based on the organism’s susceptibility to methicillin and is referred to as either MRSA (methicillin-resistant S aureus) or MSSA (methicillin-susceptible S aureus). As antibiotic resistance has evolved, patients with S aureus (especially MRSA) infections have become more difficult to treat. Susceptibility testing guides treatment of these infections and determines the minimum inhibitory concentration (MIC) for each antibiotic. A MIC is the minimum concentration of an antibiotic that will inhibit the visible growth of the organism after incubation.
Related: Experts Debate Infection Control Merits of ‘Bare Beneath the Elbows’
Vancomycin has remained the mainstay for treatment of patients with MRSA infections. An increasing number of infections with high documented MICs to vancomycin are raising concern that resistance may be developing. Clinical controversy exists within the infectious disease community as to whether vancomycin is less effective against S aureus infections with a vancomycin MIC of ≥ 2 µg/mL, contributing to poor patient outcomes.2
The Clinical and Laboratory Standards Institute (CLSI) lowered the breakpoint for vancomycin in 2006 from > 4 µg/mL to > 2 µg/mL.3 Breakpoints delineate MIC values that are considered susceptible, nonsusceptible, or resistant to an antibiotic. The CLSI breakpoint change points to an increase in vancomycin resistance and supports the need for further discussion and insight.
A 2012 meta-analysis was conducted to determine whether an association exists between S aureus infections with vancomycin MIC values ≥ 2 µg/mL and the effectiveness of the therapy.2 Twenty-two studies were included with a primary outcome of 30-day mortality. A review of MRSA data revealed a statistically significant association between high vancomycin MICs (≥ 1.5 µg/mL) and increased mortality (P < .01), regardless of the source of infection. When limiting the data to Etest (bioMérieux, Marcy L’Etoile, France) MIC testing for MRSA bloodstream infections (BSIs), a vancomycin MIC ≥ 1.5 µg/mL was not associated with increased mortality (P = .08). Comparing data for MIC ≥ 2 µg/mL and ≤ 1.5 µg/mL, found that MICs ≥ 2 µg/mL were associated with increased mortality (P < .01). Analysis of the 11 studies that included data on treatment failure concluded that S aureus infections with a vancomycin MIC ≥ 1.5 µg/mL were associated with an increased risk of treatment failure in both MSSA and MRSA infections (P < .01) and that treatment failure was more likely in MRSA BSIs than in non-BSIs (P < .01).Evidence to support a possible correlation between high S aureus vancomycin MICs and poor patient outcomes came from a 2013 meta-analysis.3 The specific aim of this study was to examine the correlations between vancomycin MIC, patient mortality, and treatment failure. A MIC ≥ 1.5 µg/mL and ≥ 1.0 µg/mL were used to classify MICs as high when determined by Etest and broth microdilution (BMD), respectively. Analysis revealed an association between high vancomycin MICs and increased risk of treatment failure (relative risk [RR] 1.40, 95% confidence interval [CI] 1.15-1.71) and overall mortality (RR 1.42, 95% CI 1.08-1.87). Similarly, a sensitivity analysis on S aureus BSIs with high vancomycin MICs revealed an increased risk of mortality (RR 1.46, 95% CI 1.06-2.01) and treatment failure (RR 1.37, 95% CI 1.09-1.73).
Related: The Importance of an Antimicrobial Stewardship Program
The most recent meta-analysis (published in 2014) included patients with S aureus bacteremia and evaluated the association of high S aureus vancomycin MIC with an increased risk of mortality.4 A high MIC was defined as ≥ 1.5 µg/mL by Etest and ≥ 2.0 µg/mL by BMD. The analysis of 38 studies found a nonstatistically significant difference in mortality risk (P = .43). Further analysis was performed to determine whether the vancomycin MIC cutoff plays a role in increased mortality. No statistically significant difference in mortality was found when using a vancomycin MIC ≥ 1.5 µg/mL, ≥ 2.0 µg/mL, ≥ 4.0 µg/mL, or ≥ 8.0 µg/mL. The authors argued that their differing conclusions from other meta-analyses may be due to the inclusion of only bacteremias rather than all infection types, and although there was not a statistically significant difference, increased risk of mortality could not be excluded.
Related: Results Mixed in Hospital Efforts to Tackle Antimicrobial Resistance
Although conclusions of published meta-analyses differ, the results highlight the necessity of using clinical judgment in treating patients with S aureus infections with high MIC values and to consider the primary source and severity of infection. A confounding factor to direct comparison of the literature is the variations based on the method of MIC determination and testing (Etest vs BMD).
Additionally, all 3 studies addressed the importance of considering clinical patient factors that may lead to poorer prognosis as well as the difficultly in achieving necessary vancomycin levels with limited toxicity. The risk of increased mortality in patients with high vancomycin MICs cannot be ruled out at this time. Therefore, additional patient factors as well as the potential toxicities that may result from vancomycin therapy should be considered when using vancomycin in treating patients with S aureus infections.
Additional Note
An earlier version of this article appeared in the Pharmacy Related Newsletter: The Capsule, of the William S. Middleton Memorial Veterans Hospital.
Author disclosures
The authors report no actual or potential conflicts of interest with regard to this article.
Disclaimer
The opinions expressed herein are those of the authors and do not necessarily reflect those of Federal Practitioner, Frontline Medical Communications Inc., the U.S. Government, or any of its agencies. This article may discuss unlabeled or investigational use of certain drugs. Please review complete prescribing information for specific drugs or drug combinations—including indications, contraindications, warnings, and adverse effects—before administering pharmacologic therapy to patients.
1. Martin JH, Norris R, Barras M, et al. Therapeutic monitoring of vancomycin in adult patients: a consensus review of the American Society of Health-System Pharmacists, the Infectious Diseases Society of America, and the Society of Infectious Diseases Pharmacists. Clin Biochem Rev. 2010;31(1):21-24.
2. van Hal SJ, Lodise TP, Paterson DL. The clinical significance of vancomycin minimum inhibitory concentration in Staphylococcus aureus infections: a systematic review and meta-analysis. Clin Infect Dis. 2012;54(6):755-771.
3. Jacob JT, DiazGranados CA. High vancomycin minimum inhibitory concentration and clinical outcomes in adults with methicillin-resistant Staphylococcus aureus infections: a meta-analysis. Int J Infect Dis. 2013;17(2):e93-e100.
4. Kalil AC, Van Schooneveld TC, Fey PD, Rupp ME. Association between vancomycin minimum inhibitory concentration and mortality among patients with Staphylococcus aureus bloodstream infections: a systematic review and meta-analysis. JAMA. 2014;312(15):1552-1564.
Staphylococcus aureus (S aureus) is a common cause of infection within the hospital and in the community.1 Treatment is based on the organism’s susceptibility to methicillin and is referred to as either MRSA (methicillin-resistant S aureus) or MSSA (methicillin-susceptible S aureus). As antibiotic resistance has evolved, patients with S aureus (especially MRSA) infections have become more difficult to treat. Susceptibility testing guides treatment of these infections and determines the minimum inhibitory concentration (MIC) for each antibiotic. A MIC is the minimum concentration of an antibiotic that will inhibit the visible growth of the organism after incubation.
Related: Experts Debate Infection Control Merits of ‘Bare Beneath the Elbows’
Vancomycin has remained the mainstay for treatment of patients with MRSA infections. An increasing number of infections with high documented MICs to vancomycin are raising concern that resistance may be developing. Clinical controversy exists within the infectious disease community as to whether vancomycin is less effective against S aureus infections with a vancomycin MIC of ≥ 2 µg/mL, contributing to poor patient outcomes.2
The Clinical and Laboratory Standards Institute (CLSI) lowered the breakpoint for vancomycin in 2006 from > 4 µg/mL to > 2 µg/mL.3 Breakpoints delineate MIC values that are considered susceptible, nonsusceptible, or resistant to an antibiotic. The CLSI breakpoint change points to an increase in vancomycin resistance and supports the need for further discussion and insight.
A 2012 meta-analysis was conducted to determine whether an association exists between S aureus infections with vancomycin MIC values ≥ 2 µg/mL and the effectiveness of the therapy.2 Twenty-two studies were included with a primary outcome of 30-day mortality. A review of MRSA data revealed a statistically significant association between high vancomycin MICs (≥ 1.5 µg/mL) and increased mortality (P < .01), regardless of the source of infection. When limiting the data to Etest (bioMérieux, Marcy L’Etoile, France) MIC testing for MRSA bloodstream infections (BSIs), a vancomycin MIC ≥ 1.5 µg/mL was not associated with increased mortality (P = .08). Comparing data for MIC ≥ 2 µg/mL and ≤ 1.5 µg/mL, found that MICs ≥ 2 µg/mL were associated with increased mortality (P < .01). Analysis of the 11 studies that included data on treatment failure concluded that S aureus infections with a vancomycin MIC ≥ 1.5 µg/mL were associated with an increased risk of treatment failure in both MSSA and MRSA infections (P < .01) and that treatment failure was more likely in MRSA BSIs than in non-BSIs (P < .01).Evidence to support a possible correlation between high S aureus vancomycin MICs and poor patient outcomes came from a 2013 meta-analysis.3 The specific aim of this study was to examine the correlations between vancomycin MIC, patient mortality, and treatment failure. A MIC ≥ 1.5 µg/mL and ≥ 1.0 µg/mL were used to classify MICs as high when determined by Etest and broth microdilution (BMD), respectively. Analysis revealed an association between high vancomycin MICs and increased risk of treatment failure (relative risk [RR] 1.40, 95% confidence interval [CI] 1.15-1.71) and overall mortality (RR 1.42, 95% CI 1.08-1.87). Similarly, a sensitivity analysis on S aureus BSIs with high vancomycin MICs revealed an increased risk of mortality (RR 1.46, 95% CI 1.06-2.01) and treatment failure (RR 1.37, 95% CI 1.09-1.73).
Related: The Importance of an Antimicrobial Stewardship Program
The most recent meta-analysis (published in 2014) included patients with S aureus bacteremia and evaluated the association of high S aureus vancomycin MIC with an increased risk of mortality.4 A high MIC was defined as ≥ 1.5 µg/mL by Etest and ≥ 2.0 µg/mL by BMD. The analysis of 38 studies found a nonstatistically significant difference in mortality risk (P = .43). Further analysis was performed to determine whether the vancomycin MIC cutoff plays a role in increased mortality. No statistically significant difference in mortality was found when using a vancomycin MIC ≥ 1.5 µg/mL, ≥ 2.0 µg/mL, ≥ 4.0 µg/mL, or ≥ 8.0 µg/mL. The authors argued that their differing conclusions from other meta-analyses may be due to the inclusion of only bacteremias rather than all infection types, and although there was not a statistically significant difference, increased risk of mortality could not be excluded.
Related: Results Mixed in Hospital Efforts to Tackle Antimicrobial Resistance
Although conclusions of published meta-analyses differ, the results highlight the necessity of using clinical judgment in treating patients with S aureus infections with high MIC values and to consider the primary source and severity of infection. A confounding factor to direct comparison of the literature is the variations based on the method of MIC determination and testing (Etest vs BMD).
Additionally, all 3 studies addressed the importance of considering clinical patient factors that may lead to poorer prognosis as well as the difficultly in achieving necessary vancomycin levels with limited toxicity. The risk of increased mortality in patients with high vancomycin MICs cannot be ruled out at this time. Therefore, additional patient factors as well as the potential toxicities that may result from vancomycin therapy should be considered when using vancomycin in treating patients with S aureus infections.
Additional Note
An earlier version of this article appeared in the Pharmacy Related Newsletter: The Capsule, of the William S. Middleton Memorial Veterans Hospital.
Author disclosures
The authors report no actual or potential conflicts of interest with regard to this article.
Disclaimer
The opinions expressed herein are those of the authors and do not necessarily reflect those of Federal Practitioner, Frontline Medical Communications Inc., the U.S. Government, or any of its agencies. This article may discuss unlabeled or investigational use of certain drugs. Please review complete prescribing information for specific drugs or drug combinations—including indications, contraindications, warnings, and adverse effects—before administering pharmacologic therapy to patients.
Staphylococcus aureus (S aureus) is a common cause of infection within the hospital and in the community.1 Treatment is based on the organism’s susceptibility to methicillin and is referred to as either MRSA (methicillin-resistant S aureus) or MSSA (methicillin-susceptible S aureus). As antibiotic resistance has evolved, patients with S aureus (especially MRSA) infections have become more difficult to treat. Susceptibility testing guides treatment of these infections and determines the minimum inhibitory concentration (MIC) for each antibiotic. A MIC is the minimum concentration of an antibiotic that will inhibit the visible growth of the organism after incubation.
Related: Experts Debate Infection Control Merits of ‘Bare Beneath the Elbows’
Vancomycin has remained the mainstay for treatment of patients with MRSA infections. An increasing number of infections with high documented MICs to vancomycin are raising concern that resistance may be developing. Clinical controversy exists within the infectious disease community as to whether vancomycin is less effective against S aureus infections with a vancomycin MIC of ≥ 2 µg/mL, contributing to poor patient outcomes.2
The Clinical and Laboratory Standards Institute (CLSI) lowered the breakpoint for vancomycin in 2006 from > 4 µg/mL to > 2 µg/mL.3 Breakpoints delineate MIC values that are considered susceptible, nonsusceptible, or resistant to an antibiotic. The CLSI breakpoint change points to an increase in vancomycin resistance and supports the need for further discussion and insight.
A 2012 meta-analysis was conducted to determine whether an association exists between S aureus infections with vancomycin MIC values ≥ 2 µg/mL and the effectiveness of the therapy.2 Twenty-two studies were included with a primary outcome of 30-day mortality. A review of MRSA data revealed a statistically significant association between high vancomycin MICs (≥ 1.5 µg/mL) and increased mortality (P < .01), regardless of the source of infection. When limiting the data to Etest (bioMérieux, Marcy L’Etoile, France) MIC testing for MRSA bloodstream infections (BSIs), a vancomycin MIC ≥ 1.5 µg/mL was not associated with increased mortality (P = .08). Comparing data for MIC ≥ 2 µg/mL and ≤ 1.5 µg/mL, found that MICs ≥ 2 µg/mL were associated with increased mortality (P < .01). Analysis of the 11 studies that included data on treatment failure concluded that S aureus infections with a vancomycin MIC ≥ 1.5 µg/mL were associated with an increased risk of treatment failure in both MSSA and MRSA infections (P < .01) and that treatment failure was more likely in MRSA BSIs than in non-BSIs (P < .01).Evidence to support a possible correlation between high S aureus vancomycin MICs and poor patient outcomes came from a 2013 meta-analysis.3 The specific aim of this study was to examine the correlations between vancomycin MIC, patient mortality, and treatment failure. A MIC ≥ 1.5 µg/mL and ≥ 1.0 µg/mL were used to classify MICs as high when determined by Etest and broth microdilution (BMD), respectively. Analysis revealed an association between high vancomycin MICs and increased risk of treatment failure (relative risk [RR] 1.40, 95% confidence interval [CI] 1.15-1.71) and overall mortality (RR 1.42, 95% CI 1.08-1.87). Similarly, a sensitivity analysis on S aureus BSIs with high vancomycin MICs revealed an increased risk of mortality (RR 1.46, 95% CI 1.06-2.01) and treatment failure (RR 1.37, 95% CI 1.09-1.73).
Related: The Importance of an Antimicrobial Stewardship Program
The most recent meta-analysis (published in 2014) included patients with S aureus bacteremia and evaluated the association of high S aureus vancomycin MIC with an increased risk of mortality.4 A high MIC was defined as ≥ 1.5 µg/mL by Etest and ≥ 2.0 µg/mL by BMD. The analysis of 38 studies found a nonstatistically significant difference in mortality risk (P = .43). Further analysis was performed to determine whether the vancomycin MIC cutoff plays a role in increased mortality. No statistically significant difference in mortality was found when using a vancomycin MIC ≥ 1.5 µg/mL, ≥ 2.0 µg/mL, ≥ 4.0 µg/mL, or ≥ 8.0 µg/mL. The authors argued that their differing conclusions from other meta-analyses may be due to the inclusion of only bacteremias rather than all infection types, and although there was not a statistically significant difference, increased risk of mortality could not be excluded.
Related: Results Mixed in Hospital Efforts to Tackle Antimicrobial Resistance
Although conclusions of published meta-analyses differ, the results highlight the necessity of using clinical judgment in treating patients with S aureus infections with high MIC values and to consider the primary source and severity of infection. A confounding factor to direct comparison of the literature is the variations based on the method of MIC determination and testing (Etest vs BMD).
Additionally, all 3 studies addressed the importance of considering clinical patient factors that may lead to poorer prognosis as well as the difficultly in achieving necessary vancomycin levels with limited toxicity. The risk of increased mortality in patients with high vancomycin MICs cannot be ruled out at this time. Therefore, additional patient factors as well as the potential toxicities that may result from vancomycin therapy should be considered when using vancomycin in treating patients with S aureus infections.
Additional Note
An earlier version of this article appeared in the Pharmacy Related Newsletter: The Capsule, of the William S. Middleton Memorial Veterans Hospital.
Author disclosures
The authors report no actual or potential conflicts of interest with regard to this article.
Disclaimer
The opinions expressed herein are those of the authors and do not necessarily reflect those of Federal Practitioner, Frontline Medical Communications Inc., the U.S. Government, or any of its agencies. This article may discuss unlabeled or investigational use of certain drugs. Please review complete prescribing information for specific drugs or drug combinations—including indications, contraindications, warnings, and adverse effects—before administering pharmacologic therapy to patients.
1. Martin JH, Norris R, Barras M, et al. Therapeutic monitoring of vancomycin in adult patients: a consensus review of the American Society of Health-System Pharmacists, the Infectious Diseases Society of America, and the Society of Infectious Diseases Pharmacists. Clin Biochem Rev. 2010;31(1):21-24.
2. van Hal SJ, Lodise TP, Paterson DL. The clinical significance of vancomycin minimum inhibitory concentration in Staphylococcus aureus infections: a systematic review and meta-analysis. Clin Infect Dis. 2012;54(6):755-771.
3. Jacob JT, DiazGranados CA. High vancomycin minimum inhibitory concentration and clinical outcomes in adults with methicillin-resistant Staphylococcus aureus infections: a meta-analysis. Int J Infect Dis. 2013;17(2):e93-e100.
4. Kalil AC, Van Schooneveld TC, Fey PD, Rupp ME. Association between vancomycin minimum inhibitory concentration and mortality among patients with Staphylococcus aureus bloodstream infections: a systematic review and meta-analysis. JAMA. 2014;312(15):1552-1564.
1. Martin JH, Norris R, Barras M, et al. Therapeutic monitoring of vancomycin in adult patients: a consensus review of the American Society of Health-System Pharmacists, the Infectious Diseases Society of America, and the Society of Infectious Diseases Pharmacists. Clin Biochem Rev. 2010;31(1):21-24.
2. van Hal SJ, Lodise TP, Paterson DL. The clinical significance of vancomycin minimum inhibitory concentration in Staphylococcus aureus infections: a systematic review and meta-analysis. Clin Infect Dis. 2012;54(6):755-771.
3. Jacob JT, DiazGranados CA. High vancomycin minimum inhibitory concentration and clinical outcomes in adults with methicillin-resistant Staphylococcus aureus infections: a meta-analysis. Int J Infect Dis. 2013;17(2):e93-e100.
4. Kalil AC, Van Schooneveld TC, Fey PD, Rupp ME. Association between vancomycin minimum inhibitory concentration and mortality among patients with Staphylococcus aureus bloodstream infections: a systematic review and meta-analysis. JAMA. 2014;312(15):1552-1564.
Assessing longer-term effects of SSRI exposure in pregnancy
Over the last 2 decades, the medical community has accumulated more information regarding fetal exposure to selective serotonin reuptake inhibitors than almost any medicine that women take during pregnancy.
Data on the risks for major congenital malformations and even specific malformations, such as cardiac defects, are so vast that they can be confusing for clinicians and researchers alike to digest. Yet the consensus among experts in reproductive safety is that the risk of teratogenesis following fetal exposure to SSRIs is small in terms of absolute risks (N Engl J Med. 2007;356:2732-3.).
But women and their partners are worried about more than the risk of malformations. They also are concerned about how fetal exposure to SSRIs will impact long-term neurobehavioral sequelae. It turns out that is a much more challenging question, and the data available to inform our answers still are relatively sparse.
Research gaps
There have been several reports in the literature that suggest there are modest effects on motor function in children whose mothers used SSRIs during pregnancy, but these reports have not been particularly systematic and have excluded some relevant variables, such as the presence or absence of a psychiatric disorder during pregnancy.
In what is considered a seminal examination of this topic performed more than a decade ago, Dr. Irena Nulman and her colleagues at the Motherisk program in Toronto demonstrated the importance of accounting for postpartum maternal depression and mood. Among a group of children exposed to fluoxetine (Prozac) or tricyclic antidepressants throughout pregnancy, there were no differences in IQ or language development, compared with unexposed children between 15 and 71 months of age. However, children with lower cognitive and language achievement were more likely to have mothers with higher ratings of postpartum mood disturbance (Am J Psychiatry. 2002 Nov;159[11]:1889-95.).
The charge to the field is to tackle this next clinical research frontier: the longer-term effects of fetal exposure to antidepressants and maternal psychiatric illness. Only by factoring in both of these important variables will we be able to get a true model of risk for this very critical issue of longer-term behavioral function.
Recently, researchers attempted to look at this question using data from the Norwegian Mother and Child Cohort study, a large population-based, prospective pregnancy cohort study. Children were assessed at age 3 years and motor development was assessed by maternal reports of fine and gross motor development using items from the Ages and Stages Questionnaire (ASQ). Maternal ASQ scores were compared with data from another Norwegian study in which clinicians assessed motor development using the gross and fine motor Mullen Scales of Early Learning (MSEL).
The strength of the study is that it included a very large number of children – more than 50,000 – although it is noteworthy that only a small percentage of women actually used SSRIs during pregnancy. A total of 381 women reported the use of SSRIs during pregnancy, with about half of the women reporting prolonged use (defined as exposure at two points of observation in the study).
The findings are noteworthy. The study showed that children with prolonged SSRI exposure were more likely to exhibit delays in fine motor development, compared with children with no fetal exposure to SSRIs (odds ratio, 1.42; 95% confidence interval, 1.07-1.87). The association persisted even after adjusting for symptoms of anxiety and depression before and during pregnancy. The severity of maternal depression provided only a partial explanation for the association, and depression after pregnancy appeared to have no impact on the estimated effect of SSRIs during pregnancy (BJOG. 2015 Sep 15. doi: 10.1111/1471-0528.13582).
Personal medicine
So how does the clinician translate these findings into practice? While the study indicates that prolonged prenatal exposure to SSRIs was associated with delayed motor development at age 3 years, the association was very weak, and only a few children had clinically significant impairment in motor development. The finding should be reassuring to many women who are faced with this decision.
The researchers should be commended for trying to at least begin to tackle this critical frontier with respect to the risk-benefit decision in using these medicines during pregnancy. The problem is that in the absence of robust data quantifying the exposure to maternal psychiatric illness, the quality of the data still is somewhat limited.
So far the data indicate that there is not a major signal for neurobehavioral dysregulation associated with fetal exposure to SSRIs. That being said, to adequately answer the question for the field it will be important to conduct a single, prospective study where we can accurately quantify exposure to medicine and exposure to maternal psychiatric illness during pregnancy. That type of study will allow us to assess the relative exposures and come up with a much more refined risk estimate. We also will be able to fold in a critical piece – the role of genomics.
Genomics will play a significant role in determining risk because vulnerability to potential disruption in central nervous system development may be a factor in determining the development of the brain in utero. We know, for example, that prenatal stress affects neuromodulation in the brain, and that vulnerability to disruption will be variable from patient to patient. Prospective studies where we not only quantify what medicines women are taking and the severity of psychiatric illness, but also vulnerability to central nervous system disruption, if any, at the level of the genome will be a critical missing piece for future investigators.
Even similar exposure to medicine and psychiatric disorders may have variable effects on the developing brain. If we can identify that variability at the level of the genome, then we will be able to create a refined model of risk that will dictate personalized medicine with respect to reproductive psychopharmacology.
Dr. Cohen is the director of the Center for Women’s Mental Health at Massachusetts General Hospital in Boston, which provides information resources and conducts clinical care and research in reproductive mental health. He has been a consultant to manufacturers of psychiatric medications. To comment, email him at [email protected].
Over the last 2 decades, the medical community has accumulated more information regarding fetal exposure to selective serotonin reuptake inhibitors than almost any medicine that women take during pregnancy.
Data on the risks for major congenital malformations and even specific malformations, such as cardiac defects, are so vast that they can be confusing for clinicians and researchers alike to digest. Yet the consensus among experts in reproductive safety is that the risk of teratogenesis following fetal exposure to SSRIs is small in terms of absolute risks (N Engl J Med. 2007;356:2732-3.).
But women and their partners are worried about more than the risk of malformations. They also are concerned about how fetal exposure to SSRIs will impact long-term neurobehavioral sequelae. It turns out that is a much more challenging question, and the data available to inform our answers still are relatively sparse.
Research gaps
There have been several reports in the literature that suggest there are modest effects on motor function in children whose mothers used SSRIs during pregnancy, but these reports have not been particularly systematic and have excluded some relevant variables, such as the presence or absence of a psychiatric disorder during pregnancy.
In what is considered a seminal examination of this topic performed more than a decade ago, Dr. Irena Nulman and her colleagues at the Motherisk program in Toronto demonstrated the importance of accounting for postpartum maternal depression and mood. Among a group of children exposed to fluoxetine (Prozac) or tricyclic antidepressants throughout pregnancy, there were no differences in IQ or language development, compared with unexposed children between 15 and 71 months of age. However, children with lower cognitive and language achievement were more likely to have mothers with higher ratings of postpartum mood disturbance (Am J Psychiatry. 2002 Nov;159[11]:1889-95.).
The charge to the field is to tackle this next clinical research frontier: the longer-term effects of fetal exposure to antidepressants and maternal psychiatric illness. Only by factoring in both of these important variables will we be able to get a true model of risk for this very critical issue of longer-term behavioral function.
Recently, researchers attempted to look at this question using data from the Norwegian Mother and Child Cohort study, a large population-based, prospective pregnancy cohort study. Children were assessed at age 3 years and motor development was assessed by maternal reports of fine and gross motor development using items from the Ages and Stages Questionnaire (ASQ). Maternal ASQ scores were compared with data from another Norwegian study in which clinicians assessed motor development using the gross and fine motor Mullen Scales of Early Learning (MSEL).
The strength of the study is that it included a very large number of children – more than 50,000 – although it is noteworthy that only a small percentage of women actually used SSRIs during pregnancy. A total of 381 women reported the use of SSRIs during pregnancy, with about half of the women reporting prolonged use (defined as exposure at two points of observation in the study).
The findings are noteworthy. The study showed that children with prolonged SSRI exposure were more likely to exhibit delays in fine motor development, compared with children with no fetal exposure to SSRIs (odds ratio, 1.42; 95% confidence interval, 1.07-1.87). The association persisted even after adjusting for symptoms of anxiety and depression before and during pregnancy. The severity of maternal depression provided only a partial explanation for the association, and depression after pregnancy appeared to have no impact on the estimated effect of SSRIs during pregnancy (BJOG. 2015 Sep 15. doi: 10.1111/1471-0528.13582).
Personal medicine
So how does the clinician translate these findings into practice? While the study indicates that prolonged prenatal exposure to SSRIs was associated with delayed motor development at age 3 years, the association was very weak, and only a few children had clinically significant impairment in motor development. The finding should be reassuring to many women who are faced with this decision.
The researchers should be commended for trying to at least begin to tackle this critical frontier with respect to the risk-benefit decision in using these medicines during pregnancy. The problem is that in the absence of robust data quantifying the exposure to maternal psychiatric illness, the quality of the data still is somewhat limited.
So far the data indicate that there is not a major signal for neurobehavioral dysregulation associated with fetal exposure to SSRIs. That being said, to adequately answer the question for the field it will be important to conduct a single, prospective study where we can accurately quantify exposure to medicine and exposure to maternal psychiatric illness during pregnancy. That type of study will allow us to assess the relative exposures and come up with a much more refined risk estimate. We also will be able to fold in a critical piece – the role of genomics.
Genomics will play a significant role in determining risk because vulnerability to potential disruption in central nervous system development may be a factor in determining the development of the brain in utero. We know, for example, that prenatal stress affects neuromodulation in the brain, and that vulnerability to disruption will be variable from patient to patient. Prospective studies where we not only quantify what medicines women are taking and the severity of psychiatric illness, but also vulnerability to central nervous system disruption, if any, at the level of the genome will be a critical missing piece for future investigators.
Even similar exposure to medicine and psychiatric disorders may have variable effects on the developing brain. If we can identify that variability at the level of the genome, then we will be able to create a refined model of risk that will dictate personalized medicine with respect to reproductive psychopharmacology.
Dr. Cohen is the director of the Center for Women’s Mental Health at Massachusetts General Hospital in Boston, which provides information resources and conducts clinical care and research in reproductive mental health. He has been a consultant to manufacturers of psychiatric medications. To comment, email him at [email protected].
Over the last 2 decades, the medical community has accumulated more information regarding fetal exposure to selective serotonin reuptake inhibitors than almost any medicine that women take during pregnancy.
Data on the risks for major congenital malformations and even specific malformations, such as cardiac defects, are so vast that they can be confusing for clinicians and researchers alike to digest. Yet the consensus among experts in reproductive safety is that the risk of teratogenesis following fetal exposure to SSRIs is small in terms of absolute risks (N Engl J Med. 2007;356:2732-3.).
But women and their partners are worried about more than the risk of malformations. They also are concerned about how fetal exposure to SSRIs will impact long-term neurobehavioral sequelae. It turns out that is a much more challenging question, and the data available to inform our answers still are relatively sparse.
Research gaps
There have been several reports in the literature that suggest there are modest effects on motor function in children whose mothers used SSRIs during pregnancy, but these reports have not been particularly systematic and have excluded some relevant variables, such as the presence or absence of a psychiatric disorder during pregnancy.
In what is considered a seminal examination of this topic performed more than a decade ago, Dr. Irena Nulman and her colleagues at the Motherisk program in Toronto demonstrated the importance of accounting for postpartum maternal depression and mood. Among a group of children exposed to fluoxetine (Prozac) or tricyclic antidepressants throughout pregnancy, there were no differences in IQ or language development, compared with unexposed children between 15 and 71 months of age. However, children with lower cognitive and language achievement were more likely to have mothers with higher ratings of postpartum mood disturbance (Am J Psychiatry. 2002 Nov;159[11]:1889-95.).
The charge to the field is to tackle this next clinical research frontier: the longer-term effects of fetal exposure to antidepressants and maternal psychiatric illness. Only by factoring in both of these important variables will we be able to get a true model of risk for this very critical issue of longer-term behavioral function.
Recently, researchers attempted to look at this question using data from the Norwegian Mother and Child Cohort study, a large population-based, prospective pregnancy cohort study. Children were assessed at age 3 years and motor development was assessed by maternal reports of fine and gross motor development using items from the Ages and Stages Questionnaire (ASQ). Maternal ASQ scores were compared with data from another Norwegian study in which clinicians assessed motor development using the gross and fine motor Mullen Scales of Early Learning (MSEL).
The strength of the study is that it included a very large number of children – more than 50,000 – although it is noteworthy that only a small percentage of women actually used SSRIs during pregnancy. A total of 381 women reported the use of SSRIs during pregnancy, with about half of the women reporting prolonged use (defined as exposure at two points of observation in the study).
The findings are noteworthy. The study showed that children with prolonged SSRI exposure were more likely to exhibit delays in fine motor development, compared with children with no fetal exposure to SSRIs (odds ratio, 1.42; 95% confidence interval, 1.07-1.87). The association persisted even after adjusting for symptoms of anxiety and depression before and during pregnancy. The severity of maternal depression provided only a partial explanation for the association, and depression after pregnancy appeared to have no impact on the estimated effect of SSRIs during pregnancy (BJOG. 2015 Sep 15. doi: 10.1111/1471-0528.13582).
Personal medicine
So how does the clinician translate these findings into practice? While the study indicates that prolonged prenatal exposure to SSRIs was associated with delayed motor development at age 3 years, the association was very weak, and only a few children had clinically significant impairment in motor development. The finding should be reassuring to many women who are faced with this decision.
The researchers should be commended for trying to at least begin to tackle this critical frontier with respect to the risk-benefit decision in using these medicines during pregnancy. The problem is that in the absence of robust data quantifying the exposure to maternal psychiatric illness, the quality of the data still is somewhat limited.
So far the data indicate that there is not a major signal for neurobehavioral dysregulation associated with fetal exposure to SSRIs. That being said, to adequately answer the question for the field it will be important to conduct a single, prospective study where we can accurately quantify exposure to medicine and exposure to maternal psychiatric illness during pregnancy. That type of study will allow us to assess the relative exposures and come up with a much more refined risk estimate. We also will be able to fold in a critical piece – the role of genomics.
Genomics will play a significant role in determining risk because vulnerability to potential disruption in central nervous system development may be a factor in determining the development of the brain in utero. We know, for example, that prenatal stress affects neuromodulation in the brain, and that vulnerability to disruption will be variable from patient to patient. Prospective studies where we not only quantify what medicines women are taking and the severity of psychiatric illness, but also vulnerability to central nervous system disruption, if any, at the level of the genome will be a critical missing piece for future investigators.
Even similar exposure to medicine and psychiatric disorders may have variable effects on the developing brain. If we can identify that variability at the level of the genome, then we will be able to create a refined model of risk that will dictate personalized medicine with respect to reproductive psychopharmacology.
Dr. Cohen is the director of the Center for Women’s Mental Health at Massachusetts General Hospital in Boston, which provides information resources and conducts clinical care and research in reproductive mental health. He has been a consultant to manufacturers of psychiatric medications. To comment, email him at [email protected].
Brothers and sisters, unite!
In this month’s Vascular Specialist, there are two letters to the editor that seem to imply a division in the SVS membership. The letters indirectly suggest that the SVS comprises two camps, on the one hand, academics, and on the other, community-based physicians. Further, although the majority of the membership comprises primarily of nonacademic surgeons, the leadership is, and will remain, predominantly composed of University-employed physicians. Implicit also is that there may not be a common agenda.
However, many questions come to mind: Are we truly a house divided? If so, how did this come about? Do community and academic surgeons indeed have different concerns that split us into camps? If so, how can we come together because the aphorism “United we stand, divided we fall” will have critical implications for the future of our specialty.
Dennis Gable writes that “the SVS is often (and historically) thought of as a society reserved for academic surgeons” because it is regarded solely as a vehicle to arrange a national academic meeting (the VAM). However, he counters that incorrect assessment by describing many fundamentally important roles that the SVS plays in the daily lives of practicing vascular surgeons. He encourages members to go online (at www.vascularweb.org) and see for themselves all that the SVS is doing for vascular surgery, vascular surgeons and their patients. The Society’s strong advocacy efforts on reimbursement issues, for example, have prevented millions of dollars in payment cuts, something hugely important to members in community practice.
However, many older surgeons will recall a period when only a select few could join the Society for Vascular Surgery as it was then constituted. Entry was reserved for nationally recognized researchers or those with an extensive list of publications. At that time, it was even difficult to become a member of the International Society for Cardiovascular Surgery. Community surgeons who had limited or few current publications were almost totally excluded. That was the impetus for community surgeons to form the Society for Clinical Vascular Surgery. However, some years back the SVS expanded beyond just the meeting and sought to be inclusive rather than restrictive. Membership is now virtually guaranteed to all board-certified vascular surgeons in good standing. Even members of allied health groups such as nurse practitioners and physician assistants are encouraged to become affiliate members. The SVS inspires female and minority medical students to become vascular surgeons and future members.
Further, 7 years ago, current President Bruce Perler, then chair of the Clinical Practice Council, initiated the Community Practice Advisory Committee in an effort to address the concerns of community members. I had the privilege of being its first chairperson. The current chairperson of that committee, Richard Lynn, now serves on the Board of the Society. Additionally, the SVS has made a concerted effort to add community surgeons to all of its committees.
Even the annual meeting has increasingly added multiple sessions addressing topics of interest to community surgeons. As attendance at these session proves, academic and employed physicians have found them to be equally informative. This is the result of the changing economic and health care environment that has blurred the lines between academic and nonacademic practices. Is there, then, any real division that separates the university surgeon from his or her community counterpart? Personally I believe there is none. If there is, it is simply a historical memory that has failed to disappear when confronted with the reality of the present.
However, Carlo Dall’Olmo and Dennis Gable, community surgeons who have been very active in SVS leadership positions (Carlo as Chair of the PAC and Dennis as Membership Chair), both recognize the absence of community surgeons on the SVS Executive Committee. Does this imply a conspiracy? Of course not! Rather, it is a result of the many factors briefly outlined in their letters. I have had the benefit of discussions with both men, as well as current and past SVS Presidents, so perhaps I can paraphrase their thoughts on this issue.
Carlo suggests that it is a result of a governance structure that rewards leadership positions based not only on service to the Society but also on academic achievements. He, as well as many others, suggests that our leaders should be elected, based not only on their publications and research, but also they must have proven dedication to the Society as well as providing a manifesto or platform explaining their goals for its future. Indeed, most if not all current and past executive members have been some of the most prolific researchers and have also effectively served on multiple committees over many years. If not for their hard work (unpaid and purely voluntary), our Society would never be in the viable situation it is now. We certainly owe a great deal of gratitude to the many academics who have so effectively stewarded our organization.
Some also have questioned whether busy community practice surgeons will be equally able to comply with the time-consuming demands of the Executive Committee. The presidency is almost a full-time position, yet it remains unpaid. Accordingly, a private-practice surgeon will need the backing of his or her partners or sufficient finances to counter the loss of income. Academic surgeons also have busy lives running departments, lecturing students, and operating on the most-challenging cases. Surely then, if candidates have proven themselves through years of conscientious labor on SVS committees, the manner of their employment or source of income should not influence their electability.
Dennis also explains that many private practice surgeons have a laissez-faire attitude leaving the multitude of committee appointments to these dedicated academic surgeons. On the contrary, I have spoken with numerous community surgeons who claim to have volunteered for committee or leadership positions and have not yet been appointed. Perhaps it is a self-fulfilling situation. The composition of the SVS Nominating Committee, which proposes the slate for SVS officers, originally comprised the immediate past, current, and future presidents. The composition was changed several years ago and now includes the two immediate past presidents, a representative from the affiliated vascular societies, a representative from the SVS Councils, and recently, an at-large member elected by the SVS membership. The objective was to encourage participation from someone, possibly a community practice surgeon, who had the support of the general membership.
However, it is problematic for community surgeons to gain sufficient exposure or national recognition to be elected unless they publish and lecture prolifically. Since the nominating committee has always consisted of academic surgeons, it could be argued that they would necessarily favor academics. On the other hand, such favoritism may be based simply on the fact that they are more familiar with one another. It is conceivable that as more community surgeons prove their organizational skills by serving on various committees, some will become well known and electable. As yet, the current pool of eligible community surgeons is small, whereas there are many academic surgeons clearly deserving of appointment.
Interestingly, there are now academic members of the current Executive Committee who were formerly in private practice or are currently in situations that can be regarded as both academic and community based. This suggests that the lines between academic and community practice have blurred sufficiently enough that we should no longer consider ourselves as belonging to different camps. Also, for the last 3 years, I have been a guest at the SVS Board of Directors meetings, where I have witnessed intense deliberation on multiple issues of equal concern to both academic and private surgeons. In fact, some current leaders are so certain that we are all the same that they question whether the addition of community surgeons will add new insights that might modify the daily function and future agenda of the SVS.
Consistent with the necessity for full disclosure, I am a community-practice surgeon, although I was in full-time academics for the first 6 years of my practice and now hold a position as a clinical professor at Florida State University Medical School in Tallahassee. With this background, I suggest that negating the value of community input is an incorrect concept. Private practice has many challenges, which include diverse issues such as maintaining IT departments, staffing, electronic medical records, Stark issues, malpractice insurance requirements, PQRS requirements, contract issues, partnership contracts, and competition with other specialists and hospital groups. Even current training paradigms are affecting private practitioners. Accordingly, it is imperative that their concerns are heard at the highest level. Perhaps, too, having community-practice representation on the Executive would be seen as a positive impetus to encourage more unaffiliated community doctors to join the Society.In September, Pope Francis visited America. During his speech to the United Nations, he made the following statement: “The contemporary world, with its open wounds which affect so many of our brothers and sisters, commands that we confront every form of polarization which would divide it into these two camps.”
Vascular surgeons and the Society for Vascular Surgery would do well to heed his words.
Dr. Samson is a clinical professor of surgery (vascular) at Florida State University Medical School, is president of Mote Vascular Foundation, and an attending vascular surgeon, Sarasota (Fla.) Vascular Specialists. Dr. Samson also considers himself a member of his proposed American College of Vascular Surgery.
In this month’s Vascular Specialist, there are two letters to the editor that seem to imply a division in the SVS membership. The letters indirectly suggest that the SVS comprises two camps, on the one hand, academics, and on the other, community-based physicians. Further, although the majority of the membership comprises primarily of nonacademic surgeons, the leadership is, and will remain, predominantly composed of University-employed physicians. Implicit also is that there may not be a common agenda.
However, many questions come to mind: Are we truly a house divided? If so, how did this come about? Do community and academic surgeons indeed have different concerns that split us into camps? If so, how can we come together because the aphorism “United we stand, divided we fall” will have critical implications for the future of our specialty.
Dennis Gable writes that “the SVS is often (and historically) thought of as a society reserved for academic surgeons” because it is regarded solely as a vehicle to arrange a national academic meeting (the VAM). However, he counters that incorrect assessment by describing many fundamentally important roles that the SVS plays in the daily lives of practicing vascular surgeons. He encourages members to go online (at www.vascularweb.org) and see for themselves all that the SVS is doing for vascular surgery, vascular surgeons and their patients. The Society’s strong advocacy efforts on reimbursement issues, for example, have prevented millions of dollars in payment cuts, something hugely important to members in community practice.
However, many older surgeons will recall a period when only a select few could join the Society for Vascular Surgery as it was then constituted. Entry was reserved for nationally recognized researchers or those with an extensive list of publications. At that time, it was even difficult to become a member of the International Society for Cardiovascular Surgery. Community surgeons who had limited or few current publications were almost totally excluded. That was the impetus for community surgeons to form the Society for Clinical Vascular Surgery. However, some years back the SVS expanded beyond just the meeting and sought to be inclusive rather than restrictive. Membership is now virtually guaranteed to all board-certified vascular surgeons in good standing. Even members of allied health groups such as nurse practitioners and physician assistants are encouraged to become affiliate members. The SVS inspires female and minority medical students to become vascular surgeons and future members.
Further, 7 years ago, current President Bruce Perler, then chair of the Clinical Practice Council, initiated the Community Practice Advisory Committee in an effort to address the concerns of community members. I had the privilege of being its first chairperson. The current chairperson of that committee, Richard Lynn, now serves on the Board of the Society. Additionally, the SVS has made a concerted effort to add community surgeons to all of its committees.
Even the annual meeting has increasingly added multiple sessions addressing topics of interest to community surgeons. As attendance at these session proves, academic and employed physicians have found them to be equally informative. This is the result of the changing economic and health care environment that has blurred the lines between academic and nonacademic practices. Is there, then, any real division that separates the university surgeon from his or her community counterpart? Personally I believe there is none. If there is, it is simply a historical memory that has failed to disappear when confronted with the reality of the present.
However, Carlo Dall’Olmo and Dennis Gable, community surgeons who have been very active in SVS leadership positions (Carlo as Chair of the PAC and Dennis as Membership Chair), both recognize the absence of community surgeons on the SVS Executive Committee. Does this imply a conspiracy? Of course not! Rather, it is a result of the many factors briefly outlined in their letters. I have had the benefit of discussions with both men, as well as current and past SVS Presidents, so perhaps I can paraphrase their thoughts on this issue.
Carlo suggests that it is a result of a governance structure that rewards leadership positions based not only on service to the Society but also on academic achievements. He, as well as many others, suggests that our leaders should be elected, based not only on their publications and research, but also they must have proven dedication to the Society as well as providing a manifesto or platform explaining their goals for its future. Indeed, most if not all current and past executive members have been some of the most prolific researchers and have also effectively served on multiple committees over many years. If not for their hard work (unpaid and purely voluntary), our Society would never be in the viable situation it is now. We certainly owe a great deal of gratitude to the many academics who have so effectively stewarded our organization.
Some also have questioned whether busy community practice surgeons will be equally able to comply with the time-consuming demands of the Executive Committee. The presidency is almost a full-time position, yet it remains unpaid. Accordingly, a private-practice surgeon will need the backing of his or her partners or sufficient finances to counter the loss of income. Academic surgeons also have busy lives running departments, lecturing students, and operating on the most-challenging cases. Surely then, if candidates have proven themselves through years of conscientious labor on SVS committees, the manner of their employment or source of income should not influence their electability.
Dennis also explains that many private practice surgeons have a laissez-faire attitude leaving the multitude of committee appointments to these dedicated academic surgeons. On the contrary, I have spoken with numerous community surgeons who claim to have volunteered for committee or leadership positions and have not yet been appointed. Perhaps it is a self-fulfilling situation. The composition of the SVS Nominating Committee, which proposes the slate for SVS officers, originally comprised the immediate past, current, and future presidents. The composition was changed several years ago and now includes the two immediate past presidents, a representative from the affiliated vascular societies, a representative from the SVS Councils, and recently, an at-large member elected by the SVS membership. The objective was to encourage participation from someone, possibly a community practice surgeon, who had the support of the general membership.
However, it is problematic for community surgeons to gain sufficient exposure or national recognition to be elected unless they publish and lecture prolifically. Since the nominating committee has always consisted of academic surgeons, it could be argued that they would necessarily favor academics. On the other hand, such favoritism may be based simply on the fact that they are more familiar with one another. It is conceivable that as more community surgeons prove their organizational skills by serving on various committees, some will become well known and electable. As yet, the current pool of eligible community surgeons is small, whereas there are many academic surgeons clearly deserving of appointment.
Interestingly, there are now academic members of the current Executive Committee who were formerly in private practice or are currently in situations that can be regarded as both academic and community based. This suggests that the lines between academic and community practice have blurred sufficiently enough that we should no longer consider ourselves as belonging to different camps. Also, for the last 3 years, I have been a guest at the SVS Board of Directors meetings, where I have witnessed intense deliberation on multiple issues of equal concern to both academic and private surgeons. In fact, some current leaders are so certain that we are all the same that they question whether the addition of community surgeons will add new insights that might modify the daily function and future agenda of the SVS.
Consistent with the necessity for full disclosure, I am a community-practice surgeon, although I was in full-time academics for the first 6 years of my practice and now hold a position as a clinical professor at Florida State University Medical School in Tallahassee. With this background, I suggest that negating the value of community input is an incorrect concept. Private practice has many challenges, which include diverse issues such as maintaining IT departments, staffing, electronic medical records, Stark issues, malpractice insurance requirements, PQRS requirements, contract issues, partnership contracts, and competition with other specialists and hospital groups. Even current training paradigms are affecting private practitioners. Accordingly, it is imperative that their concerns are heard at the highest level. Perhaps, too, having community-practice representation on the Executive would be seen as a positive impetus to encourage more unaffiliated community doctors to join the Society.In September, Pope Francis visited America. During his speech to the United Nations, he made the following statement: “The contemporary world, with its open wounds which affect so many of our brothers and sisters, commands that we confront every form of polarization which would divide it into these two camps.”
Vascular surgeons and the Society for Vascular Surgery would do well to heed his words.
Dr. Samson is a clinical professor of surgery (vascular) at Florida State University Medical School, is president of Mote Vascular Foundation, and an attending vascular surgeon, Sarasota (Fla.) Vascular Specialists. Dr. Samson also considers himself a member of his proposed American College of Vascular Surgery.
In this month’s Vascular Specialist, there are two letters to the editor that seem to imply a division in the SVS membership. The letters indirectly suggest that the SVS comprises two camps, on the one hand, academics, and on the other, community-based physicians. Further, although the majority of the membership comprises primarily of nonacademic surgeons, the leadership is, and will remain, predominantly composed of University-employed physicians. Implicit also is that there may not be a common agenda.
However, many questions come to mind: Are we truly a house divided? If so, how did this come about? Do community and academic surgeons indeed have different concerns that split us into camps? If so, how can we come together because the aphorism “United we stand, divided we fall” will have critical implications for the future of our specialty.
Dennis Gable writes that “the SVS is often (and historically) thought of as a society reserved for academic surgeons” because it is regarded solely as a vehicle to arrange a national academic meeting (the VAM). However, he counters that incorrect assessment by describing many fundamentally important roles that the SVS plays in the daily lives of practicing vascular surgeons. He encourages members to go online (at www.vascularweb.org) and see for themselves all that the SVS is doing for vascular surgery, vascular surgeons and their patients. The Society’s strong advocacy efforts on reimbursement issues, for example, have prevented millions of dollars in payment cuts, something hugely important to members in community practice.
However, many older surgeons will recall a period when only a select few could join the Society for Vascular Surgery as it was then constituted. Entry was reserved for nationally recognized researchers or those with an extensive list of publications. At that time, it was even difficult to become a member of the International Society for Cardiovascular Surgery. Community surgeons who had limited or few current publications were almost totally excluded. That was the impetus for community surgeons to form the Society for Clinical Vascular Surgery. However, some years back the SVS expanded beyond just the meeting and sought to be inclusive rather than restrictive. Membership is now virtually guaranteed to all board-certified vascular surgeons in good standing. Even members of allied health groups such as nurse practitioners and physician assistants are encouraged to become affiliate members. The SVS inspires female and minority medical students to become vascular surgeons and future members.
Further, 7 years ago, current President Bruce Perler, then chair of the Clinical Practice Council, initiated the Community Practice Advisory Committee in an effort to address the concerns of community members. I had the privilege of being its first chairperson. The current chairperson of that committee, Richard Lynn, now serves on the Board of the Society. Additionally, the SVS has made a concerted effort to add community surgeons to all of its committees.
Even the annual meeting has increasingly added multiple sessions addressing topics of interest to community surgeons. As attendance at these session proves, academic and employed physicians have found them to be equally informative. This is the result of the changing economic and health care environment that has blurred the lines between academic and nonacademic practices. Is there, then, any real division that separates the university surgeon from his or her community counterpart? Personally I believe there is none. If there is, it is simply a historical memory that has failed to disappear when confronted with the reality of the present.
However, Carlo Dall’Olmo and Dennis Gable, community surgeons who have been very active in SVS leadership positions (Carlo as Chair of the PAC and Dennis as Membership Chair), both recognize the absence of community surgeons on the SVS Executive Committee. Does this imply a conspiracy? Of course not! Rather, it is a result of the many factors briefly outlined in their letters. I have had the benefit of discussions with both men, as well as current and past SVS Presidents, so perhaps I can paraphrase their thoughts on this issue.
Carlo suggests that it is a result of a governance structure that rewards leadership positions based not only on service to the Society but also on academic achievements. He, as well as many others, suggests that our leaders should be elected, based not only on their publications and research, but also they must have proven dedication to the Society as well as providing a manifesto or platform explaining their goals for its future. Indeed, most if not all current and past executive members have been some of the most prolific researchers and have also effectively served on multiple committees over many years. If not for their hard work (unpaid and purely voluntary), our Society would never be in the viable situation it is now. We certainly owe a great deal of gratitude to the many academics who have so effectively stewarded our organization.
Some also have questioned whether busy community practice surgeons will be equally able to comply with the time-consuming demands of the Executive Committee. The presidency is almost a full-time position, yet it remains unpaid. Accordingly, a private-practice surgeon will need the backing of his or her partners or sufficient finances to counter the loss of income. Academic surgeons also have busy lives running departments, lecturing students, and operating on the most-challenging cases. Surely then, if candidates have proven themselves through years of conscientious labor on SVS committees, the manner of their employment or source of income should not influence their electability.
Dennis also explains that many private practice surgeons have a laissez-faire attitude leaving the multitude of committee appointments to these dedicated academic surgeons. On the contrary, I have spoken with numerous community surgeons who claim to have volunteered for committee or leadership positions and have not yet been appointed. Perhaps it is a self-fulfilling situation. The composition of the SVS Nominating Committee, which proposes the slate for SVS officers, originally comprised the immediate past, current, and future presidents. The composition was changed several years ago and now includes the two immediate past presidents, a representative from the affiliated vascular societies, a representative from the SVS Councils, and recently, an at-large member elected by the SVS membership. The objective was to encourage participation from someone, possibly a community practice surgeon, who had the support of the general membership.
However, it is problematic for community surgeons to gain sufficient exposure or national recognition to be elected unless they publish and lecture prolifically. Since the nominating committee has always consisted of academic surgeons, it could be argued that they would necessarily favor academics. On the other hand, such favoritism may be based simply on the fact that they are more familiar with one another. It is conceivable that as more community surgeons prove their organizational skills by serving on various committees, some will become well known and electable. As yet, the current pool of eligible community surgeons is small, whereas there are many academic surgeons clearly deserving of appointment.
Interestingly, there are now academic members of the current Executive Committee who were formerly in private practice or are currently in situations that can be regarded as both academic and community based. This suggests that the lines between academic and community practice have blurred sufficiently enough that we should no longer consider ourselves as belonging to different camps. Also, for the last 3 years, I have been a guest at the SVS Board of Directors meetings, where I have witnessed intense deliberation on multiple issues of equal concern to both academic and private surgeons. In fact, some current leaders are so certain that we are all the same that they question whether the addition of community surgeons will add new insights that might modify the daily function and future agenda of the SVS.
Consistent with the necessity for full disclosure, I am a community-practice surgeon, although I was in full-time academics for the first 6 years of my practice and now hold a position as a clinical professor at Florida State University Medical School in Tallahassee. With this background, I suggest that negating the value of community input is an incorrect concept. Private practice has many challenges, which include diverse issues such as maintaining IT departments, staffing, electronic medical records, Stark issues, malpractice insurance requirements, PQRS requirements, contract issues, partnership contracts, and competition with other specialists and hospital groups. Even current training paradigms are affecting private practitioners. Accordingly, it is imperative that their concerns are heard at the highest level. Perhaps, too, having community-practice representation on the Executive would be seen as a positive impetus to encourage more unaffiliated community doctors to join the Society.In September, Pope Francis visited America. During his speech to the United Nations, he made the following statement: “The contemporary world, with its open wounds which affect so many of our brothers and sisters, commands that we confront every form of polarization which would divide it into these two camps.”
Vascular surgeons and the Society for Vascular Surgery would do well to heed his words.
Dr. Samson is a clinical professor of surgery (vascular) at Florida State University Medical School, is president of Mote Vascular Foundation, and an attending vascular surgeon, Sarasota (Fla.) Vascular Specialists. Dr. Samson also considers himself a member of his proposed American College of Vascular Surgery.
Aunt Tillie and electronic health records
I’m lost, but I’m making record time.
– A pilot, somewhere over the Pacific Ocean
The other day I was reading the printout of an electronic medical record of a patient transferred to our practice. The record reminded me a lot of my Aunt Tillie. Aunt Tillie was the aunt whom everyone would avoid at family gatherings when I was young because the minute she started talking you could be sure of two things: first, that it would be a long time till she stopped talking, and second, that most of what she had to say simply was not relevant to what anyone was interested in hearing. She was interested in what she was interested in and seemed to care little about the needs of anyone else in the room.
The patient in question was 32 years old and had gone to an emergency room for headache and chest pain. Headache and chest pain can be challenging problems, but there are still certain things in both the history and on physical exam that are relevant and informative. It was hard to find those things in this medical record. After a relatively short history of present illness (HPI) that said my patient had presented with 1 day of headache and chest pain. The HPI on this record took up less than three lines. The assessment scales went on for over two pages. When we see records like this, driven by a system that desires to document every question or scale that every possible insurer might be looking for on every possible patient, we fear that common sense has died.
Among the extraneous information in the EHR was a Morse Fall Scale score. The Morse scale and point system were carefully laid out with the actions to be taken at various levels of risk, from bed in the lowest position to when to use skid-proof slipper socks. Then the Braden Scale for Predicting Pressure Sore Risk was recorded, followed by the Domestic Violence Score, complete with indication of whether the patient was under immediate threat and whether police, social services, and mental health professionals were notified. There also was a pain assessment that was filled out with an area indicating that the patient and her family were instructed to tell someone if her level of pain changed. Seriously. The pain assessment scale was located right after the suicide risk assessment and the depression scale, presumably because if the depression assessment occurred any later in the visit the patient might have scored higher out of desperation.
The death of common sense is neither pretty nor fast. As we fill out scales that answer neither evidence-based preventive health interventions nor meet the current needs of the patient, we have become concerned that we, as physicians, have chosen a path that seems to be the clearest – including all possible questions on all possible patients – but is actually fraught with peril.
We have become so concerned about not missing any potential source of reimbursement and protecting ourselves from any source of liability that our visits take longer and our focus has become distracted from the real problems that patients bring to us. By so doing we end up not accomplishing our goal of maximizing reimbursement because we move slower through our visits, filling out information that is not meaningful to either patient or physician. We also do not protect ourselves from liability when we are distracted by the need to fill out irrelevant information and are subsequently left with less time to get through the important parts of our visit, leaving us to take a less detailed history than we might otherwise have performed.
In 1995, Phillip K. Howard wrote a book about the legal system, The Death of Common Sense (Random House). In it, he argues that the desire to have clear rules that allow uniformity in the operation of law has resulted in a system that is inefficient and “precludes the exercise of judgment.” Mr. Howard argues that, no matter how detailed, laws cannot anticipate all of society’s needs. He goes on to state that “law can’t think, and so law must be entrusted to humans and they must take responsibility for their interpretation of it.”
We find a similar case to what Mr. Howard described to be occurring in medicine today. Patients present as individuals, with complex problems that require well-trained clinicians who can prioritize among the many concerns and determine which algorithms of diagnosis and treatment are appropriate to a given visit on a given day. When each visit follows a rote format, no visit follows the format that best serves the patient.
The argument that each visit is unique is not an argument for chaos in the organization of our visits and record – the visits need to be organized and recorded in a standard fashion. It is, rather, recognition that patients typically present with atypical symptoms and that all patients and visits are different from one another. To provide excellent medical care requires that well-trained clinicians make choices about what should be addressed at any given visit and that our charts and electronic record systems must be driven by patient needs and outcomes, not checkboxes derived from potential needs that are divorced from common sense for the visit at hand.
As we reflect further on this issue, we have come to the conclusion that the difference between our EHR systems and Aunt Tillie is that, when Thanksgiving came, we could avoid Aunt Tillie.
Dr. Notte is a family physician and clinical informaticist for Abington (Pa.) Memorial Hospital. He is a partner in EHR Practice Consultants, a firm that aids physicians in adopting electronic health records. Dr. Skolnik is associate director of the family medicine residency program at Abington Memorial Hospital and professor of family and community medicine at Temple University in Philadelphia.
I’m lost, but I’m making record time.
– A pilot, somewhere over the Pacific Ocean
The other day I was reading the printout of an electronic medical record of a patient transferred to our practice. The record reminded me a lot of my Aunt Tillie. Aunt Tillie was the aunt whom everyone would avoid at family gatherings when I was young because the minute she started talking you could be sure of two things: first, that it would be a long time till she stopped talking, and second, that most of what she had to say simply was not relevant to what anyone was interested in hearing. She was interested in what she was interested in and seemed to care little about the needs of anyone else in the room.
The patient in question was 32 years old and had gone to an emergency room for headache and chest pain. Headache and chest pain can be challenging problems, but there are still certain things in both the history and on physical exam that are relevant and informative. It was hard to find those things in this medical record. After a relatively short history of present illness (HPI) that said my patient had presented with 1 day of headache and chest pain. The HPI on this record took up less than three lines. The assessment scales went on for over two pages. When we see records like this, driven by a system that desires to document every question or scale that every possible insurer might be looking for on every possible patient, we fear that common sense has died.
Among the extraneous information in the EHR was a Morse Fall Scale score. The Morse scale and point system were carefully laid out with the actions to be taken at various levels of risk, from bed in the lowest position to when to use skid-proof slipper socks. Then the Braden Scale for Predicting Pressure Sore Risk was recorded, followed by the Domestic Violence Score, complete with indication of whether the patient was under immediate threat and whether police, social services, and mental health professionals were notified. There also was a pain assessment that was filled out with an area indicating that the patient and her family were instructed to tell someone if her level of pain changed. Seriously. The pain assessment scale was located right after the suicide risk assessment and the depression scale, presumably because if the depression assessment occurred any later in the visit the patient might have scored higher out of desperation.
The death of common sense is neither pretty nor fast. As we fill out scales that answer neither evidence-based preventive health interventions nor meet the current needs of the patient, we have become concerned that we, as physicians, have chosen a path that seems to be the clearest – including all possible questions on all possible patients – but is actually fraught with peril.
We have become so concerned about not missing any potential source of reimbursement and protecting ourselves from any source of liability that our visits take longer and our focus has become distracted from the real problems that patients bring to us. By so doing we end up not accomplishing our goal of maximizing reimbursement because we move slower through our visits, filling out information that is not meaningful to either patient or physician. We also do not protect ourselves from liability when we are distracted by the need to fill out irrelevant information and are subsequently left with less time to get through the important parts of our visit, leaving us to take a less detailed history than we might otherwise have performed.
In 1995, Phillip K. Howard wrote a book about the legal system, The Death of Common Sense (Random House). In it, he argues that the desire to have clear rules that allow uniformity in the operation of law has resulted in a system that is inefficient and “precludes the exercise of judgment.” Mr. Howard argues that, no matter how detailed, laws cannot anticipate all of society’s needs. He goes on to state that “law can’t think, and so law must be entrusted to humans and they must take responsibility for their interpretation of it.”
We find a similar case to what Mr. Howard described to be occurring in medicine today. Patients present as individuals, with complex problems that require well-trained clinicians who can prioritize among the many concerns and determine which algorithms of diagnosis and treatment are appropriate to a given visit on a given day. When each visit follows a rote format, no visit follows the format that best serves the patient.
The argument that each visit is unique is not an argument for chaos in the organization of our visits and record – the visits need to be organized and recorded in a standard fashion. It is, rather, recognition that patients typically present with atypical symptoms and that all patients and visits are different from one another. To provide excellent medical care requires that well-trained clinicians make choices about what should be addressed at any given visit and that our charts and electronic record systems must be driven by patient needs and outcomes, not checkboxes derived from potential needs that are divorced from common sense for the visit at hand.
As we reflect further on this issue, we have come to the conclusion that the difference between our EHR systems and Aunt Tillie is that, when Thanksgiving came, we could avoid Aunt Tillie.
Dr. Notte is a family physician and clinical informaticist for Abington (Pa.) Memorial Hospital. He is a partner in EHR Practice Consultants, a firm that aids physicians in adopting electronic health records. Dr. Skolnik is associate director of the family medicine residency program at Abington Memorial Hospital and professor of family and community medicine at Temple University in Philadelphia.
I’m lost, but I’m making record time.
– A pilot, somewhere over the Pacific Ocean
The other day I was reading the printout of an electronic medical record of a patient transferred to our practice. The record reminded me a lot of my Aunt Tillie. Aunt Tillie was the aunt whom everyone would avoid at family gatherings when I was young because the minute she started talking you could be sure of two things: first, that it would be a long time till she stopped talking, and second, that most of what she had to say simply was not relevant to what anyone was interested in hearing. She was interested in what she was interested in and seemed to care little about the needs of anyone else in the room.
The patient in question was 32 years old and had gone to an emergency room for headache and chest pain. Headache and chest pain can be challenging problems, but there are still certain things in both the history and on physical exam that are relevant and informative. It was hard to find those things in this medical record. After a relatively short history of present illness (HPI) that said my patient had presented with 1 day of headache and chest pain. The HPI on this record took up less than three lines. The assessment scales went on for over two pages. When we see records like this, driven by a system that desires to document every question or scale that every possible insurer might be looking for on every possible patient, we fear that common sense has died.
Among the extraneous information in the EHR was a Morse Fall Scale score. The Morse scale and point system were carefully laid out with the actions to be taken at various levels of risk, from bed in the lowest position to when to use skid-proof slipper socks. Then the Braden Scale for Predicting Pressure Sore Risk was recorded, followed by the Domestic Violence Score, complete with indication of whether the patient was under immediate threat and whether police, social services, and mental health professionals were notified. There also was a pain assessment that was filled out with an area indicating that the patient and her family were instructed to tell someone if her level of pain changed. Seriously. The pain assessment scale was located right after the suicide risk assessment and the depression scale, presumably because if the depression assessment occurred any later in the visit the patient might have scored higher out of desperation.
The death of common sense is neither pretty nor fast. As we fill out scales that answer neither evidence-based preventive health interventions nor meet the current needs of the patient, we have become concerned that we, as physicians, have chosen a path that seems to be the clearest – including all possible questions on all possible patients – but is actually fraught with peril.
We have become so concerned about not missing any potential source of reimbursement and protecting ourselves from any source of liability that our visits take longer and our focus has become distracted from the real problems that patients bring to us. By so doing we end up not accomplishing our goal of maximizing reimbursement because we move slower through our visits, filling out information that is not meaningful to either patient or physician. We also do not protect ourselves from liability when we are distracted by the need to fill out irrelevant information and are subsequently left with less time to get through the important parts of our visit, leaving us to take a less detailed history than we might otherwise have performed.
In 1995, Phillip K. Howard wrote a book about the legal system, The Death of Common Sense (Random House). In it, he argues that the desire to have clear rules that allow uniformity in the operation of law has resulted in a system that is inefficient and “precludes the exercise of judgment.” Mr. Howard argues that, no matter how detailed, laws cannot anticipate all of society’s needs. He goes on to state that “law can’t think, and so law must be entrusted to humans and they must take responsibility for their interpretation of it.”
We find a similar case to what Mr. Howard described to be occurring in medicine today. Patients present as individuals, with complex problems that require well-trained clinicians who can prioritize among the many concerns and determine which algorithms of diagnosis and treatment are appropriate to a given visit on a given day. When each visit follows a rote format, no visit follows the format that best serves the patient.
The argument that each visit is unique is not an argument for chaos in the organization of our visits and record – the visits need to be organized and recorded in a standard fashion. It is, rather, recognition that patients typically present with atypical symptoms and that all patients and visits are different from one another. To provide excellent medical care requires that well-trained clinicians make choices about what should be addressed at any given visit and that our charts and electronic record systems must be driven by patient needs and outcomes, not checkboxes derived from potential needs that are divorced from common sense for the visit at hand.
As we reflect further on this issue, we have come to the conclusion that the difference between our EHR systems and Aunt Tillie is that, when Thanksgiving came, we could avoid Aunt Tillie.
Dr. Notte is a family physician and clinical informaticist for Abington (Pa.) Memorial Hospital. He is a partner in EHR Practice Consultants, a firm that aids physicians in adopting electronic health records. Dr. Skolnik is associate director of the family medicine residency program at Abington Memorial Hospital and professor of family and community medicine at Temple University in Philadelphia.
Drinking while pregnant: Not worth the risk
Recent findings by the American Academy of Pediatrics (AAP) regarding alcohol consumption during pregnancy are quite clear: Don’t drink at all while pregnant. This warning from the AAP is consistent with advice from the American College of Obstetricians and Gynecologists (ACOG) and the Centers for Disease Control and Prevention: No safe level of alcohol consumption during pregnancy has been identified, and no period during pregnancy appears to be safe for alcohol consumption.
In fact, ACOG has recommended screening for alcohol use early in pregnancy since 1977. However, the CDC reports that 1 in 10 pregnant women aged 18-44 years has consumed alcohol in the past 30 days. Some recent studies claim that a small number of drinks during pregnancy could be safe, and I’ve even seen some reports of ob.gyns. allowing alcohol use during pregnancy.
With such disparities between recommendations and patient behavior, the role of the obstetrician is more crucial than ever. Education, prevention, and intervention are essential to good health for mother and baby.
It has long been recognized that heavy drinking during pregnancy is associated with Fetal Alcohol Syndrome, but there are more subtle effects that fall under the umbrella of Fetal Alcohol Spectrum Disorders. These effects may include physical, mental, behavioral, and learning disabilities with lifelong implications and may not be detected until a child starts school.
Screening for alcohol use is of the utmost importance. Three simple steps have been proven effective in identifying women who drink at risky levels and engage them in changing behavior to reduce their risk for an alcohol-exposed pregnancy. These steps include asking about alcohol use, providing brief motivation-enhancing interventions, and follow-up for women who engage in risky drinking. See ACOG’s Fetal Alcohol Syndrome Prevention Tool Kit for more detail.
It is worth noting that a positive screen does not always mean a woman needs to be referred to treatment. Brief intervention by an ob.gyn. is effective and has been shown to reduce risky behavior by 70%. Randomized studies reported significant reductions in alcohol use and improved newborn outcomes after intervention.
Prenatal exposure to alcohol is one of the leading preventable causes of birth defects. With so many risk factors out of a mother’s control during pregnancy, why risk it?
Dr. Conry is assistant physician in chief at the Permanente Medical Group in Roseville, Calif., and associate clinical professor of ob.gyn. at the University of California, Davis. She has been a practicing ob.gyn. with the Permanente Medical Group for more than 20 years. She is a past president of the American College of Obstetricians and Gynecologists.
Recent findings by the American Academy of Pediatrics (AAP) regarding alcohol consumption during pregnancy are quite clear: Don’t drink at all while pregnant. This warning from the AAP is consistent with advice from the American College of Obstetricians and Gynecologists (ACOG) and the Centers for Disease Control and Prevention: No safe level of alcohol consumption during pregnancy has been identified, and no period during pregnancy appears to be safe for alcohol consumption.
In fact, ACOG has recommended screening for alcohol use early in pregnancy since 1977. However, the CDC reports that 1 in 10 pregnant women aged 18-44 years has consumed alcohol in the past 30 days. Some recent studies claim that a small number of drinks during pregnancy could be safe, and I’ve even seen some reports of ob.gyns. allowing alcohol use during pregnancy.
With such disparities between recommendations and patient behavior, the role of the obstetrician is more crucial than ever. Education, prevention, and intervention are essential to good health for mother and baby.
It has long been recognized that heavy drinking during pregnancy is associated with Fetal Alcohol Syndrome, but there are more subtle effects that fall under the umbrella of Fetal Alcohol Spectrum Disorders. These effects may include physical, mental, behavioral, and learning disabilities with lifelong implications and may not be detected until a child starts school.
Screening for alcohol use is of the utmost importance. Three simple steps have been proven effective in identifying women who drink at risky levels and engage them in changing behavior to reduce their risk for an alcohol-exposed pregnancy. These steps include asking about alcohol use, providing brief motivation-enhancing interventions, and follow-up for women who engage in risky drinking. See ACOG’s Fetal Alcohol Syndrome Prevention Tool Kit for more detail.
It is worth noting that a positive screen does not always mean a woman needs to be referred to treatment. Brief intervention by an ob.gyn. is effective and has been shown to reduce risky behavior by 70%. Randomized studies reported significant reductions in alcohol use and improved newborn outcomes after intervention.
Prenatal exposure to alcohol is one of the leading preventable causes of birth defects. With so many risk factors out of a mother’s control during pregnancy, why risk it?
Dr. Conry is assistant physician in chief at the Permanente Medical Group in Roseville, Calif., and associate clinical professor of ob.gyn. at the University of California, Davis. She has been a practicing ob.gyn. with the Permanente Medical Group for more than 20 years. She is a past president of the American College of Obstetricians and Gynecologists.
Recent findings by the American Academy of Pediatrics (AAP) regarding alcohol consumption during pregnancy are quite clear: Don’t drink at all while pregnant. This warning from the AAP is consistent with advice from the American College of Obstetricians and Gynecologists (ACOG) and the Centers for Disease Control and Prevention: No safe level of alcohol consumption during pregnancy has been identified, and no period during pregnancy appears to be safe for alcohol consumption.
In fact, ACOG has recommended screening for alcohol use early in pregnancy since 1977. However, the CDC reports that 1 in 10 pregnant women aged 18-44 years has consumed alcohol in the past 30 days. Some recent studies claim that a small number of drinks during pregnancy could be safe, and I’ve even seen some reports of ob.gyns. allowing alcohol use during pregnancy.
With such disparities between recommendations and patient behavior, the role of the obstetrician is more crucial than ever. Education, prevention, and intervention are essential to good health for mother and baby.
It has long been recognized that heavy drinking during pregnancy is associated with Fetal Alcohol Syndrome, but there are more subtle effects that fall under the umbrella of Fetal Alcohol Spectrum Disorders. These effects may include physical, mental, behavioral, and learning disabilities with lifelong implications and may not be detected until a child starts school.
Screening for alcohol use is of the utmost importance. Three simple steps have been proven effective in identifying women who drink at risky levels and engage them in changing behavior to reduce their risk for an alcohol-exposed pregnancy. These steps include asking about alcohol use, providing brief motivation-enhancing interventions, and follow-up for women who engage in risky drinking. See ACOG’s Fetal Alcohol Syndrome Prevention Tool Kit for more detail.
It is worth noting that a positive screen does not always mean a woman needs to be referred to treatment. Brief intervention by an ob.gyn. is effective and has been shown to reduce risky behavior by 70%. Randomized studies reported significant reductions in alcohol use and improved newborn outcomes after intervention.
Prenatal exposure to alcohol is one of the leading preventable causes of birth defects. With so many risk factors out of a mother’s control during pregnancy, why risk it?
Dr. Conry is assistant physician in chief at the Permanente Medical Group in Roseville, Calif., and associate clinical professor of ob.gyn. at the University of California, Davis. She has been a practicing ob.gyn. with the Permanente Medical Group for more than 20 years. She is a past president of the American College of Obstetricians and Gynecologists.
Providing ambivalent medical advice
When did some doctors become so wishy-washy?
A large part of what we do is guide people through an often-confusing maze of test results and treatment options. I respect patients’ right to make their own decisions, but it came as a surprise to me to find that some doctors are turning such things over to the patients. After all, doctors are the ones who went through over a decade of training to understand the risks, benefits, and goals of each step for them. Granted, I live in Arizona, where you don’t need a doctor’s order to have labs done. You can research whatever you want on Google, decide what work-up you need, and go get whatever labs you want done.
But back to my original point. Recently, one of my patients was admitted to the hospital, then followed up with me in the office. I looked through his test results and told him what I felt the next step should be, ordered a few things, and wrote an instruction sheet to start daily aspirin. I commented that it surprised me the last hadn’t been done as an inpatient.
His answer? “They said I could if I wanted to, but didn’t make a clear suggestion.” I figured this was a simple miscommunication, so I pulled up the hospital chart on my computer. There I found a note from the attending that said, “The patient was told he may or may not want to take a daily aspirin, and that doing so might or might not be to his benefit.” What on Earth?
I understand there are no guarantees in this job. There’s no crystal ball to know for sure that what we’re doing is right. Any drug can cause serious and unexpected complications. We take calculated risks and hope we come out ahead. But to phrase it like this? Where the patient isn’t given the guidance we’re supposed to provide? What’s the point of even being a doctor?
Since then, I’ve noticed similar phrasing in other charts: “We discussed doing a brain MRI, and she’ll let me know what she decides” and “I told her that starting Lamictal may or may not prevent seizures, and to consider it as something she should or shouldn’t do.”
I’m sure some of it is part of the hurried flight-of-ideas dictations we all do when we’re busy at the hospital. There’s also a component of legalese to make sure that we documented discussing risks with the patient.
But I still don’t get the ambivalence. In similar situations, I provide guidance and advice and tell people what I think they should do. I’m not going to force anyone to do anything they don’t want to. If they disagree, I note it and make whatever suggestions I think will help. In the end, it’s their decision. I get that.
When I take my car to get fixed, I don’t want the mechanic to tell me what may or may not need to be repaired, and I hope patients see me the same way.
Dr. Block has a solo neurology practice in Scottsdale, Ariz.
When did some doctors become so wishy-washy?
A large part of what we do is guide people through an often-confusing maze of test results and treatment options. I respect patients’ right to make their own decisions, but it came as a surprise to me to find that some doctors are turning such things over to the patients. After all, doctors are the ones who went through over a decade of training to understand the risks, benefits, and goals of each step for them. Granted, I live in Arizona, where you don’t need a doctor’s order to have labs done. You can research whatever you want on Google, decide what work-up you need, and go get whatever labs you want done.
But back to my original point. Recently, one of my patients was admitted to the hospital, then followed up with me in the office. I looked through his test results and told him what I felt the next step should be, ordered a few things, and wrote an instruction sheet to start daily aspirin. I commented that it surprised me the last hadn’t been done as an inpatient.
His answer? “They said I could if I wanted to, but didn’t make a clear suggestion.” I figured this was a simple miscommunication, so I pulled up the hospital chart on my computer. There I found a note from the attending that said, “The patient was told he may or may not want to take a daily aspirin, and that doing so might or might not be to his benefit.” What on Earth?
I understand there are no guarantees in this job. There’s no crystal ball to know for sure that what we’re doing is right. Any drug can cause serious and unexpected complications. We take calculated risks and hope we come out ahead. But to phrase it like this? Where the patient isn’t given the guidance we’re supposed to provide? What’s the point of even being a doctor?
Since then, I’ve noticed similar phrasing in other charts: “We discussed doing a brain MRI, and she’ll let me know what she decides” and “I told her that starting Lamictal may or may not prevent seizures, and to consider it as something she should or shouldn’t do.”
I’m sure some of it is part of the hurried flight-of-ideas dictations we all do when we’re busy at the hospital. There’s also a component of legalese to make sure that we documented discussing risks with the patient.
But I still don’t get the ambivalence. In similar situations, I provide guidance and advice and tell people what I think they should do. I’m not going to force anyone to do anything they don’t want to. If they disagree, I note it and make whatever suggestions I think will help. In the end, it’s their decision. I get that.
When I take my car to get fixed, I don’t want the mechanic to tell me what may or may not need to be repaired, and I hope patients see me the same way.
Dr. Block has a solo neurology practice in Scottsdale, Ariz.
When did some doctors become so wishy-washy?
A large part of what we do is guide people through an often-confusing maze of test results and treatment options. I respect patients’ right to make their own decisions, but it came as a surprise to me to find that some doctors are turning such things over to the patients. After all, doctors are the ones who went through over a decade of training to understand the risks, benefits, and goals of each step for them. Granted, I live in Arizona, where you don’t need a doctor’s order to have labs done. You can research whatever you want on Google, decide what work-up you need, and go get whatever labs you want done.
But back to my original point. Recently, one of my patients was admitted to the hospital, then followed up with me in the office. I looked through his test results and told him what I felt the next step should be, ordered a few things, and wrote an instruction sheet to start daily aspirin. I commented that it surprised me the last hadn’t been done as an inpatient.
His answer? “They said I could if I wanted to, but didn’t make a clear suggestion.” I figured this was a simple miscommunication, so I pulled up the hospital chart on my computer. There I found a note from the attending that said, “The patient was told he may or may not want to take a daily aspirin, and that doing so might or might not be to his benefit.” What on Earth?
I understand there are no guarantees in this job. There’s no crystal ball to know for sure that what we’re doing is right. Any drug can cause serious and unexpected complications. We take calculated risks and hope we come out ahead. But to phrase it like this? Where the patient isn’t given the guidance we’re supposed to provide? What’s the point of even being a doctor?
Since then, I’ve noticed similar phrasing in other charts: “We discussed doing a brain MRI, and she’ll let me know what she decides” and “I told her that starting Lamictal may or may not prevent seizures, and to consider it as something she should or shouldn’t do.”
I’m sure some of it is part of the hurried flight-of-ideas dictations we all do when we’re busy at the hospital. There’s also a component of legalese to make sure that we documented discussing risks with the patient.
But I still don’t get the ambivalence. In similar situations, I provide guidance and advice and tell people what I think they should do. I’m not going to force anyone to do anything they don’t want to. If they disagree, I note it and make whatever suggestions I think will help. In the end, it’s their decision. I get that.
When I take my car to get fixed, I don’t want the mechanic to tell me what may or may not need to be repaired, and I hope patients see me the same way.
Dr. Block has a solo neurology practice in Scottsdale, Ariz.














