User login
Examine the patient, not just the evidence
Dr. Hickner’s editorial “Let’s talk about the evidence” (J Fam Pract. 2015;64:337) struck a chord with me. I am very supportive of evidence-based medicine (EBM), but am often dismayed by the lack of humility expressed by EBM leaders, including the US Preventive Services Task Force. We have so little evidence about much of what we do in family medicine, and most evidence comes from studies that are narrow by nature (reductionist research).
For example, doing a physical exam is part of “laying on of hands” that is part of the art of medicine. Abraham Verghese, MD, MACP, has written and spoken about the importance of examining the patient and not just depending on data.1 Yet elements of the physical exam, such as the pelvic exam example Dr. Hickner mentioned in his editorial, do not stand up well in EBM due to a lack of diagnostic accuracy. I’ll ask this: Who has studied the harm that may be caused by not examining our patients?
My physical exam “ritual” takes less than 10 minutes, and the value in the relationship I have with patients is more than a diagnostic exercise. Increasingly, I see patients become annoyed and critical of physicians who do not examine them.
Joseph E. Scherger, MD, MPH
Rancho Mirage, Calif
1. TED Talks. Abraham Verghese: A Doctor’s Touch. TED Web site. Available at: http://www.ted.com/talks/abraham_verghese_a_doctor_s_touch. Accessed July 20, 2015.
Author’s response:
Dr. Scherger makes an excellent point about the importance of physical touch for the doctor-patient relationship. The question is: What touching is appropriate? In my own experience, I have noticed that most—but not all—of the women I see are quite relieved that they don’t need yearly pelvic exams, and women I see for pap smears do not seem put off if I do not do a bimanual exam. The data are actually quite strong that routine pelvic exams in asymptomatic women lead to more harm than good. They uncover way too many false positives and almost no true positive findings, leading to unnecessary testing and treatment.1,2
John Hickner, MD, MSc
Chicago, Ill
Dr. Hickner is the editor-in-chief of The Journal of Family Practice
1. Ebell MH, Culp M, Lastinger K, et al. A systematic review of the bimanual examination as a test for ovarian cancer. Am J Prev Med. 2015;48:350–356.
2. Well-woman visit. Committee Opinion No. 534. American College of Obstetricians and Gynecologists. Obstet Gynecol. 2012;120:421-424.
Dr. Hickner’s editorial “Let’s talk about the evidence” (J Fam Pract. 2015;64:337) struck a chord with me. I am very supportive of evidence-based medicine (EBM), but am often dismayed by the lack of humility expressed by EBM leaders, including the US Preventive Services Task Force. We have so little evidence about much of what we do in family medicine, and most evidence comes from studies that are narrow by nature (reductionist research).
For example, doing a physical exam is part of “laying on of hands” that is part of the art of medicine. Abraham Verghese, MD, MACP, has written and spoken about the importance of examining the patient and not just depending on data.1 Yet elements of the physical exam, such as the pelvic exam example Dr. Hickner mentioned in his editorial, do not stand up well in EBM due to a lack of diagnostic accuracy. I’ll ask this: Who has studied the harm that may be caused by not examining our patients?
My physical exam “ritual” takes less than 10 minutes, and the value in the relationship I have with patients is more than a diagnostic exercise. Increasingly, I see patients become annoyed and critical of physicians who do not examine them.
Joseph E. Scherger, MD, MPH
Rancho Mirage, Calif
1. TED Talks. Abraham Verghese: A Doctor’s Touch. TED Web site. Available at: http://www.ted.com/talks/abraham_verghese_a_doctor_s_touch. Accessed July 20, 2015.
Author’s response:
Dr. Scherger makes an excellent point about the importance of physical touch for the doctor-patient relationship. The question is: What touching is appropriate? In my own experience, I have noticed that most—but not all—of the women I see are quite relieved that they don’t need yearly pelvic exams, and women I see for pap smears do not seem put off if I do not do a bimanual exam. The data are actually quite strong that routine pelvic exams in asymptomatic women lead to more harm than good. They uncover way too many false positives and almost no true positive findings, leading to unnecessary testing and treatment.1,2
John Hickner, MD, MSc
Chicago, Ill
Dr. Hickner is the editor-in-chief of The Journal of Family Practice
1. Ebell MH, Culp M, Lastinger K, et al. A systematic review of the bimanual examination as a test for ovarian cancer. Am J Prev Med. 2015;48:350–356.
2. Well-woman visit. Committee Opinion No. 534. American College of Obstetricians and Gynecologists. Obstet Gynecol. 2012;120:421-424.
Dr. Hickner’s editorial “Let’s talk about the evidence” (J Fam Pract. 2015;64:337) struck a chord with me. I am very supportive of evidence-based medicine (EBM), but am often dismayed by the lack of humility expressed by EBM leaders, including the US Preventive Services Task Force. We have so little evidence about much of what we do in family medicine, and most evidence comes from studies that are narrow by nature (reductionist research).
For example, doing a physical exam is part of “laying on of hands” that is part of the art of medicine. Abraham Verghese, MD, MACP, has written and spoken about the importance of examining the patient and not just depending on data.1 Yet elements of the physical exam, such as the pelvic exam example Dr. Hickner mentioned in his editorial, do not stand up well in EBM due to a lack of diagnostic accuracy. I’ll ask this: Who has studied the harm that may be caused by not examining our patients?
My physical exam “ritual” takes less than 10 minutes, and the value in the relationship I have with patients is more than a diagnostic exercise. Increasingly, I see patients become annoyed and critical of physicians who do not examine them.
Joseph E. Scherger, MD, MPH
Rancho Mirage, Calif
1. TED Talks. Abraham Verghese: A Doctor’s Touch. TED Web site. Available at: http://www.ted.com/talks/abraham_verghese_a_doctor_s_touch. Accessed July 20, 2015.
Author’s response:
Dr. Scherger makes an excellent point about the importance of physical touch for the doctor-patient relationship. The question is: What touching is appropriate? In my own experience, I have noticed that most—but not all—of the women I see are quite relieved that they don’t need yearly pelvic exams, and women I see for pap smears do not seem put off if I do not do a bimanual exam. The data are actually quite strong that routine pelvic exams in asymptomatic women lead to more harm than good. They uncover way too many false positives and almost no true positive findings, leading to unnecessary testing and treatment.1,2
John Hickner, MD, MSc
Chicago, Ill
Dr. Hickner is the editor-in-chief of The Journal of Family Practice
1. Ebell MH, Culp M, Lastinger K, et al. A systematic review of the bimanual examination as a test for ovarian cancer. Am J Prev Med. 2015;48:350–356.
2. Well-woman visit. Committee Opinion No. 534. American College of Obstetricians and Gynecologists. Obstet Gynecol. 2012;120:421-424.
Failure to reproduce
In my struggle to keep abreast of all things pediatric, I sample a variety of sources.
Of course each month I scan almost all of the abstracts in the journal Pediatrics. But to get a sense of what the nonmedical community is reading, I begin each morning with a cruise through the electronic versions of the New York Times and the Portland (Maine) Press Herald.
By lunch time I usually have hopscotched my way through the Wall Street Journal. And during our evening adult beverage quiet time, I amuse myself with our local daily. If a news story includes a link to an original article, I usually bore down deep enough to at least read the abstract. Keep in mind that this whole process of keeping current takes little more than a half an hour, 45 minutes tops.
It seems that psychology-related topics dominate the science and medicine stories that I encounter. This shouldn’t surprise you because most of us want to know more about why humans behave the way we do. We also wonder if animal behavior may provide some clues.
It may be because I was trained by careful and skeptical “hard” scientists that I have always read psychosocial and behavioral studies with several grains of salt. Despite my skepticism, I am not beneath embracing the odd study that seems to support one of my biases. The studies that don’t sync with my world view I quickly cast on the rubbish heap because the “sample group was too small,” or the “variables were not adequately controlled for,” or simply because I thought the study was poorly done.
It turns out that my skepticism has not only been well founded, but should have been broader in scope. In a recent study published in the journal Science, three young psychologists undertook a heroic and courageous effort to reproduce 100 studies from three leading psychology journals (Science 2015 Aug 28. doi:10.1126/science.aac4716). Chosen from a larger group, these studies were thought to reflect the core knowledge from which psychologists develop their understanding of such basics as learning, memory, and relationships.
The investigators found that in more than half the studies, they were unable to reproduce the results reported in the original studies despite the fact that in many cases, they were assisted by the original investigators in their attempts to replicate the conditions of the initial studies.
The authors quickly assert that their findings do not suggest that the original investigators were attempting to deceive. Nor does the failure to reproduce results necessarily mean that other future studies might confirm the original findings. Their primary point is that evaluating reproducibility is difficult.
However, this new study is troubling for two reasons. First, it casts even more doubt on the decision to expand the MCAT (Medical College Admission Test) by adding several hours of questions based on psychosocial topics in hopes of creating physicians who are more in tune with the emotional needs and social challenges of their future patients. If the results of more than half of the studies that might be considered the underpinnings of modern psychology can’t be reproduced, are we just asking aspiring medical students to learn a larger collection of half truths? And thus have medical students spend less time learning basic science and developing better critical thinking skills? There are better ways to sort for more empathetic and sensitive physicians than by building an unevenly weighted exam.
Second, although this study highlights the core of what makes science such a powerful and effective tool for discovering the truth, the anti-science folks will point to it as just another example of how we shouldn’t trust anything science tells us.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine, for nearly 40 years. He has authored several books on behavioral pediatrics, including “Coping with a Picky Eater.” Email him at [email protected].
In my struggle to keep abreast of all things pediatric, I sample a variety of sources.
Of course each month I scan almost all of the abstracts in the journal Pediatrics. But to get a sense of what the nonmedical community is reading, I begin each morning with a cruise through the electronic versions of the New York Times and the Portland (Maine) Press Herald.
By lunch time I usually have hopscotched my way through the Wall Street Journal. And during our evening adult beverage quiet time, I amuse myself with our local daily. If a news story includes a link to an original article, I usually bore down deep enough to at least read the abstract. Keep in mind that this whole process of keeping current takes little more than a half an hour, 45 minutes tops.
It seems that psychology-related topics dominate the science and medicine stories that I encounter. This shouldn’t surprise you because most of us want to know more about why humans behave the way we do. We also wonder if animal behavior may provide some clues.
It may be because I was trained by careful and skeptical “hard” scientists that I have always read psychosocial and behavioral studies with several grains of salt. Despite my skepticism, I am not beneath embracing the odd study that seems to support one of my biases. The studies that don’t sync with my world view I quickly cast on the rubbish heap because the “sample group was too small,” or the “variables were not adequately controlled for,” or simply because I thought the study was poorly done.
It turns out that my skepticism has not only been well founded, but should have been broader in scope. In a recent study published in the journal Science, three young psychologists undertook a heroic and courageous effort to reproduce 100 studies from three leading psychology journals (Science 2015 Aug 28. doi:10.1126/science.aac4716). Chosen from a larger group, these studies were thought to reflect the core knowledge from which psychologists develop their understanding of such basics as learning, memory, and relationships.
The investigators found that in more than half the studies, they were unable to reproduce the results reported in the original studies despite the fact that in many cases, they were assisted by the original investigators in their attempts to replicate the conditions of the initial studies.
The authors quickly assert that their findings do not suggest that the original investigators were attempting to deceive. Nor does the failure to reproduce results necessarily mean that other future studies might confirm the original findings. Their primary point is that evaluating reproducibility is difficult.
However, this new study is troubling for two reasons. First, it casts even more doubt on the decision to expand the MCAT (Medical College Admission Test) by adding several hours of questions based on psychosocial topics in hopes of creating physicians who are more in tune with the emotional needs and social challenges of their future patients. If the results of more than half of the studies that might be considered the underpinnings of modern psychology can’t be reproduced, are we just asking aspiring medical students to learn a larger collection of half truths? And thus have medical students spend less time learning basic science and developing better critical thinking skills? There are better ways to sort for more empathetic and sensitive physicians than by building an unevenly weighted exam.
Second, although this study highlights the core of what makes science such a powerful and effective tool for discovering the truth, the anti-science folks will point to it as just another example of how we shouldn’t trust anything science tells us.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine, for nearly 40 years. He has authored several books on behavioral pediatrics, including “Coping with a Picky Eater.” Email him at [email protected].
In my struggle to keep abreast of all things pediatric, I sample a variety of sources.
Of course each month I scan almost all of the abstracts in the journal Pediatrics. But to get a sense of what the nonmedical community is reading, I begin each morning with a cruise through the electronic versions of the New York Times and the Portland (Maine) Press Herald.
By lunch time I usually have hopscotched my way through the Wall Street Journal. And during our evening adult beverage quiet time, I amuse myself with our local daily. If a news story includes a link to an original article, I usually bore down deep enough to at least read the abstract. Keep in mind that this whole process of keeping current takes little more than a half an hour, 45 minutes tops.
It seems that psychology-related topics dominate the science and medicine stories that I encounter. This shouldn’t surprise you because most of us want to know more about why humans behave the way we do. We also wonder if animal behavior may provide some clues.
It may be because I was trained by careful and skeptical “hard” scientists that I have always read psychosocial and behavioral studies with several grains of salt. Despite my skepticism, I am not beneath embracing the odd study that seems to support one of my biases. The studies that don’t sync with my world view I quickly cast on the rubbish heap because the “sample group was too small,” or the “variables were not adequately controlled for,” or simply because I thought the study was poorly done.
It turns out that my skepticism has not only been well founded, but should have been broader in scope. In a recent study published in the journal Science, three young psychologists undertook a heroic and courageous effort to reproduce 100 studies from three leading psychology journals (Science 2015 Aug 28. doi:10.1126/science.aac4716). Chosen from a larger group, these studies were thought to reflect the core knowledge from which psychologists develop their understanding of such basics as learning, memory, and relationships.
The investigators found that in more than half the studies, they were unable to reproduce the results reported in the original studies despite the fact that in many cases, they were assisted by the original investigators in their attempts to replicate the conditions of the initial studies.
The authors quickly assert that their findings do not suggest that the original investigators were attempting to deceive. Nor does the failure to reproduce results necessarily mean that other future studies might confirm the original findings. Their primary point is that evaluating reproducibility is difficult.
However, this new study is troubling for two reasons. First, it casts even more doubt on the decision to expand the MCAT (Medical College Admission Test) by adding several hours of questions based on psychosocial topics in hopes of creating physicians who are more in tune with the emotional needs and social challenges of their future patients. If the results of more than half of the studies that might be considered the underpinnings of modern psychology can’t be reproduced, are we just asking aspiring medical students to learn a larger collection of half truths? And thus have medical students spend less time learning basic science and developing better critical thinking skills? There are better ways to sort for more empathetic and sensitive physicians than by building an unevenly weighted exam.
Second, although this study highlights the core of what makes science such a powerful and effective tool for discovering the truth, the anti-science folks will point to it as just another example of how we shouldn’t trust anything science tells us.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine, for nearly 40 years. He has authored several books on behavioral pediatrics, including “Coping with a Picky Eater.” Email him at [email protected].
Med students: Look up from your EMRs
“I have acute appendicitis,” I told my wife. “I need to go to the radiologist.”
A computed tomography (CT) scan of my abdomen confirmed my suspicion. After learning that I also had leukocytosis, we headed to the emergency department. The ED doctor was pleasantly surprised that someone had come to his facility completely evaluated. All he had to do was call the surgeon. But first he introduced me to a 4th-year medical student who was participating in a surgical rotation.
Prioritizing the EMR over the patient
The student wheeled his large computer to the side of my gurney and began to question me about my abdominal pain. Within 5 minutes, this unsupervised student had somehow acquired all the information he needed for my admission. He thanked me for my time and told me that he would see me in the operating room.
Unfortunately for him, I was not about to let him leave my cubicle without a redirect. I told him I have type 1 diabetes and several comorbidities. I wear an insulin pump and continuous glucose sensor that alerts me to impending hypoglycemia. I take 11 medications to successfully manage my metabolic disorders.
The student wheeled his machine back to the side of my gurney.
With his eyes fixed squarely on his computer and his finger on a mouse, he asked me to list all of my medications. He had never heard of a rapid-acting insulin analogue, nor was he familiar with my GLP-1 receptor agonist or SGLT2 inhibitor. And the pump and sensor? There were no check boxes for these devices in his electronic medical record (EMR).
He—like several of the doctors I met during my subsequent stay—suggested that I remove the pump and meter so that they could manage my diabetes.
Still in considerable pain, I suggested to the student and anyone else who would listen that my pump and sensor were off limits. As long as I was conscious, I would self-manage my diabetes.
I also told him that his history and physical exam were deficient. Although he did listen to my bowel sounds (or lack thereof) through a blanket and hospital gown, he overlooked examining my heart, lungs, eyes, mouth, and feet.
“You failed to ask me about my medical history or my diabetes," I said. The student searched his EMR for the appropriate questions to ask, but to no avail. Stunned, he appeared to be at a loss of words. I suggested that he ask about the type of diabetes I had, the duration of the disease, how well my glucose levels were controlled, my most recent HbA1c, and if I had developed any long-term microvascular or macrovascular complications. He politely thanked me, moved the mouse around on his computer stand, and began to wheel his computer away.
“Wait!” I thought. “Don’t you think you should examine my eyes, mouth, and feet?” I reminded myself that this student hadn’t evaluated me for peritoneal signs. So why should I insist that he look at non-critical parts of my body?
My physical pain was increasing and I was becoming increasingly distressed. The student was more interested in inputting data into the EMR than learning about acute abdomens and type 1 diabetes.
Postop: From bad to worse
My postoperative course was dreadful. I nearly died from complications that included acute renal failure, dehydration, hypokalemia, and a postoperative ileus that persisted for 8 days. My blood glucose levels, however, were perfect. Still, the Attendings and the students blamed my complications on diabetes.
“Yeah, I see this all the time,” said the hospitalist who was caring for me. “Diabetes causes gastroparesis. What we should do is have you take off that pump and sensor device. We’ll have the pharmacist help you manage your diabetes.” The hospitalist who suggested this course of action was immediately relieved of his duties by my wife as I drifted in and out of consciousness in the intensive care unit (ICU).
Despite the state of my health, I began to provide professional guidance for my own care. I demanded that the nurse give me a 250 cc rider of normal saline and increase my IV flow rate from 50 cc to 150 cc. The nasogastric tube was removed and I began using IV erythromycin, which increases gastric motility. I received oral and IV potassium.
While in the ICU, I was questioned by physicians and medical students, but never examined. I am convinced that had I not been an experienced family physician, I would have suffered a fatal postoperative event. The medical students assigned to my care would not have known that I died, unless they received a notification via Twitter.
Providing care in a digital age
My experience as a patient was in stark contrast to the way I practice medicine.
I use an EMR only to e-prescribe, and have chosen not to participate in submitting meaningful use data to the government. Rather than spending 2 hours a day making eye contact with an EMR, I prefer to use that time to listen to my patients’ concerns about their health. I know how to conduct a review of systems and I touch my patients at each visit. I look at their feet, skin, and eyes, listen to their heart and lungs, and palpate their abdomen. I perform a rectal exam on every patient who presents with abdominal pain.
I have learned to communicate my suspicions and thoughts (both positive and negative) to all of my patients. I take notes on scratch paper, not on a computer, just as my grandfather and father used to do when they were practicing medicine. I only order tests to confirm a suspected diagnosis, not as a primary means of evaluating patients.
Could my hospital experience lead to change?
Upon my discharge from the hospital, I reached out to the director of clinical studies at the local medical school and explained the deficiencies I’d encountered. I explained that the 4th-year medical students were ill-equipped to perform an adequate history or physical exam. They lacked knowledge of basic pharmacology. And they failed to appropriately follow a patient during the perioperative period.
The director appreciated my concern and provided me with the details of a corrective action plan that she had been working on.
“We need to implement our patient simulation computer program designed to teach our students how to appropriately interact with their distressed patients,” she said.
Really?
I suggested that the medical students needed to unplug their smartphones, computers, and iPads. Let them spend a day or 2 with one of us “old-time docs” who still work with our hands—hands that are skilled at evaluating patients, rather than texting and data entry. We’ll show these students how to become caring, intelligent, and dedicated clinicians.
“I have acute appendicitis,” I told my wife. “I need to go to the radiologist.”
A computed tomography (CT) scan of my abdomen confirmed my suspicion. After learning that I also had leukocytosis, we headed to the emergency department. The ED doctor was pleasantly surprised that someone had come to his facility completely evaluated. All he had to do was call the surgeon. But first he introduced me to a 4th-year medical student who was participating in a surgical rotation.
Prioritizing the EMR over the patient
The student wheeled his large computer to the side of my gurney and began to question me about my abdominal pain. Within 5 minutes, this unsupervised student had somehow acquired all the information he needed for my admission. He thanked me for my time and told me that he would see me in the operating room.
Unfortunately for him, I was not about to let him leave my cubicle without a redirect. I told him I have type 1 diabetes and several comorbidities. I wear an insulin pump and continuous glucose sensor that alerts me to impending hypoglycemia. I take 11 medications to successfully manage my metabolic disorders.
The student wheeled his machine back to the side of my gurney.
With his eyes fixed squarely on his computer and his finger on a mouse, he asked me to list all of my medications. He had never heard of a rapid-acting insulin analogue, nor was he familiar with my GLP-1 receptor agonist or SGLT2 inhibitor. And the pump and sensor? There were no check boxes for these devices in his electronic medical record (EMR).
He—like several of the doctors I met during my subsequent stay—suggested that I remove the pump and meter so that they could manage my diabetes.
Still in considerable pain, I suggested to the student and anyone else who would listen that my pump and sensor were off limits. As long as I was conscious, I would self-manage my diabetes.
I also told him that his history and physical exam were deficient. Although he did listen to my bowel sounds (or lack thereof) through a blanket and hospital gown, he overlooked examining my heart, lungs, eyes, mouth, and feet.
“You failed to ask me about my medical history or my diabetes," I said. The student searched his EMR for the appropriate questions to ask, but to no avail. Stunned, he appeared to be at a loss of words. I suggested that he ask about the type of diabetes I had, the duration of the disease, how well my glucose levels were controlled, my most recent HbA1c, and if I had developed any long-term microvascular or macrovascular complications. He politely thanked me, moved the mouse around on his computer stand, and began to wheel his computer away.
“Wait!” I thought. “Don’t you think you should examine my eyes, mouth, and feet?” I reminded myself that this student hadn’t evaluated me for peritoneal signs. So why should I insist that he look at non-critical parts of my body?
My physical pain was increasing and I was becoming increasingly distressed. The student was more interested in inputting data into the EMR than learning about acute abdomens and type 1 diabetes.
Postop: From bad to worse
My postoperative course was dreadful. I nearly died from complications that included acute renal failure, dehydration, hypokalemia, and a postoperative ileus that persisted for 8 days. My blood glucose levels, however, were perfect. Still, the Attendings and the students blamed my complications on diabetes.
“Yeah, I see this all the time,” said the hospitalist who was caring for me. “Diabetes causes gastroparesis. What we should do is have you take off that pump and sensor device. We’ll have the pharmacist help you manage your diabetes.” The hospitalist who suggested this course of action was immediately relieved of his duties by my wife as I drifted in and out of consciousness in the intensive care unit (ICU).
Despite the state of my health, I began to provide professional guidance for my own care. I demanded that the nurse give me a 250 cc rider of normal saline and increase my IV flow rate from 50 cc to 150 cc. The nasogastric tube was removed and I began using IV erythromycin, which increases gastric motility. I received oral and IV potassium.
While in the ICU, I was questioned by physicians and medical students, but never examined. I am convinced that had I not been an experienced family physician, I would have suffered a fatal postoperative event. The medical students assigned to my care would not have known that I died, unless they received a notification via Twitter.
Providing care in a digital age
My experience as a patient was in stark contrast to the way I practice medicine.
I use an EMR only to e-prescribe, and have chosen not to participate in submitting meaningful use data to the government. Rather than spending 2 hours a day making eye contact with an EMR, I prefer to use that time to listen to my patients’ concerns about their health. I know how to conduct a review of systems and I touch my patients at each visit. I look at their feet, skin, and eyes, listen to their heart and lungs, and palpate their abdomen. I perform a rectal exam on every patient who presents with abdominal pain.
I have learned to communicate my suspicions and thoughts (both positive and negative) to all of my patients. I take notes on scratch paper, not on a computer, just as my grandfather and father used to do when they were practicing medicine. I only order tests to confirm a suspected diagnosis, not as a primary means of evaluating patients.
Could my hospital experience lead to change?
Upon my discharge from the hospital, I reached out to the director of clinical studies at the local medical school and explained the deficiencies I’d encountered. I explained that the 4th-year medical students were ill-equipped to perform an adequate history or physical exam. They lacked knowledge of basic pharmacology. And they failed to appropriately follow a patient during the perioperative period.
The director appreciated my concern and provided me with the details of a corrective action plan that she had been working on.
“We need to implement our patient simulation computer program designed to teach our students how to appropriately interact with their distressed patients,” she said.
Really?
I suggested that the medical students needed to unplug their smartphones, computers, and iPads. Let them spend a day or 2 with one of us “old-time docs” who still work with our hands—hands that are skilled at evaluating patients, rather than texting and data entry. We’ll show these students how to become caring, intelligent, and dedicated clinicians.
“I have acute appendicitis,” I told my wife. “I need to go to the radiologist.”
A computed tomography (CT) scan of my abdomen confirmed my suspicion. After learning that I also had leukocytosis, we headed to the emergency department. The ED doctor was pleasantly surprised that someone had come to his facility completely evaluated. All he had to do was call the surgeon. But first he introduced me to a 4th-year medical student who was participating in a surgical rotation.
Prioritizing the EMR over the patient
The student wheeled his large computer to the side of my gurney and began to question me about my abdominal pain. Within 5 minutes, this unsupervised student had somehow acquired all the information he needed for my admission. He thanked me for my time and told me that he would see me in the operating room.
Unfortunately for him, I was not about to let him leave my cubicle without a redirect. I told him I have type 1 diabetes and several comorbidities. I wear an insulin pump and continuous glucose sensor that alerts me to impending hypoglycemia. I take 11 medications to successfully manage my metabolic disorders.
The student wheeled his machine back to the side of my gurney.
With his eyes fixed squarely on his computer and his finger on a mouse, he asked me to list all of my medications. He had never heard of a rapid-acting insulin analogue, nor was he familiar with my GLP-1 receptor agonist or SGLT2 inhibitor. And the pump and sensor? There were no check boxes for these devices in his electronic medical record (EMR).
He—like several of the doctors I met during my subsequent stay—suggested that I remove the pump and meter so that they could manage my diabetes.
Still in considerable pain, I suggested to the student and anyone else who would listen that my pump and sensor were off limits. As long as I was conscious, I would self-manage my diabetes.
I also told him that his history and physical exam were deficient. Although he did listen to my bowel sounds (or lack thereof) through a blanket and hospital gown, he overlooked examining my heart, lungs, eyes, mouth, and feet.
“You failed to ask me about my medical history or my diabetes," I said. The student searched his EMR for the appropriate questions to ask, but to no avail. Stunned, he appeared to be at a loss of words. I suggested that he ask about the type of diabetes I had, the duration of the disease, how well my glucose levels were controlled, my most recent HbA1c, and if I had developed any long-term microvascular or macrovascular complications. He politely thanked me, moved the mouse around on his computer stand, and began to wheel his computer away.
“Wait!” I thought. “Don’t you think you should examine my eyes, mouth, and feet?” I reminded myself that this student hadn’t evaluated me for peritoneal signs. So why should I insist that he look at non-critical parts of my body?
My physical pain was increasing and I was becoming increasingly distressed. The student was more interested in inputting data into the EMR than learning about acute abdomens and type 1 diabetes.
Postop: From bad to worse
My postoperative course was dreadful. I nearly died from complications that included acute renal failure, dehydration, hypokalemia, and a postoperative ileus that persisted for 8 days. My blood glucose levels, however, were perfect. Still, the Attendings and the students blamed my complications on diabetes.
“Yeah, I see this all the time,” said the hospitalist who was caring for me. “Diabetes causes gastroparesis. What we should do is have you take off that pump and sensor device. We’ll have the pharmacist help you manage your diabetes.” The hospitalist who suggested this course of action was immediately relieved of his duties by my wife as I drifted in and out of consciousness in the intensive care unit (ICU).
Despite the state of my health, I began to provide professional guidance for my own care. I demanded that the nurse give me a 250 cc rider of normal saline and increase my IV flow rate from 50 cc to 150 cc. The nasogastric tube was removed and I began using IV erythromycin, which increases gastric motility. I received oral and IV potassium.
While in the ICU, I was questioned by physicians and medical students, but never examined. I am convinced that had I not been an experienced family physician, I would have suffered a fatal postoperative event. The medical students assigned to my care would not have known that I died, unless they received a notification via Twitter.
Providing care in a digital age
My experience as a patient was in stark contrast to the way I practice medicine.
I use an EMR only to e-prescribe, and have chosen not to participate in submitting meaningful use data to the government. Rather than spending 2 hours a day making eye contact with an EMR, I prefer to use that time to listen to my patients’ concerns about their health. I know how to conduct a review of systems and I touch my patients at each visit. I look at their feet, skin, and eyes, listen to their heart and lungs, and palpate their abdomen. I perform a rectal exam on every patient who presents with abdominal pain.
I have learned to communicate my suspicions and thoughts (both positive and negative) to all of my patients. I take notes on scratch paper, not on a computer, just as my grandfather and father used to do when they were practicing medicine. I only order tests to confirm a suspected diagnosis, not as a primary means of evaluating patients.
Could my hospital experience lead to change?
Upon my discharge from the hospital, I reached out to the director of clinical studies at the local medical school and explained the deficiencies I’d encountered. I explained that the 4th-year medical students were ill-equipped to perform an adequate history or physical exam. They lacked knowledge of basic pharmacology. And they failed to appropriately follow a patient during the perioperative period.
The director appreciated my concern and provided me with the details of a corrective action plan that she had been working on.
“We need to implement our patient simulation computer program designed to teach our students how to appropriately interact with their distressed patients,” she said.
Really?
I suggested that the medical students needed to unplug their smartphones, computers, and iPads. Let them spend a day or 2 with one of us “old-time docs” who still work with our hands—hands that are skilled at evaluating patients, rather than texting and data entry. We’ll show these students how to become caring, intelligent, and dedicated clinicians.
High dose folic acid promising in preventing cardiac malformations
When most physicians and patients hear about folic acid, they automatically think about its role in preventing spina bifida and other neural tube defects. But there are now more than 20 years of data that point toward a larger role for folic acid in preventing common, and in some cases devastating, congenital heart defects.
The various published studies leave little doubt that folic acid can significantly reduce the risk for many common cardiac malformations, but other questions remain. For instance, what is the minimum dose for protection? And should health authorities around the world consider recommending a much higher dose of folic acid for short-term use in pregnant women and those trying to conceive?
Early research on cardiac malformations
One of the early studies showing the promise of folic acid beyond neural tube defects was published in 1996. The randomized, double-blind controlled trial in Hungary compared the effect of periconceptional multivitamin supplements containing 0.8 mg of folic acid versus trace element supplements on neural tube defects and other congenital abnormalities. The multivitamin supplement group had a significant reduction in urinary tract abnormalities, and in the rate of sporadic cardiovascular malformations, specifically ventricular septal defects (Am J Med Genet. 1996 Mar 15;62 [2]:179-83.).
In 2004, the same researchers confirmed their results using a controlled, cohort trial that matched pregnant women from regional antenatal care clinics who did not take vitamin supplements to pregnant women who did take supplements containing 0.8 mg folic acid. The results were similar. From a total of 3,056 offspring evaluated, 31 congenital cardiovascular malformations occurred in the group with folic acid supplementation, compared with 50 in the group without, for a 40% lower risk overall, although the main impact was seen among ventricular septal defects (Birth Defects Res A Clin Mol Teratol. 2004 Nov;70[11]:853-61.).
Our own group examined the evidence in a meta-analysis published in 2006 and found significant support for an expanded role for folic acid (J Obstet Gynaecol Can. 2006 Aug;28[8]:680-9.).
The major issue with the available studies is the lack of highest-quality evidence. While some of the studies were randomized trials, you can no longer conduct a true randomized design and withhold folic acid from women; it’s simply not ethical knowing what we know about the preventive benefits of folic acid for neural tube defects. But the literature – which includes quality cohort and case-controlled studies – is convincing.
High dose best?
While some studies have shown a protective effect of folic acid in congenital heart defects at low levels, such as the 0.8 mg used in the early Hungarian studies, other studies indicate that more is better.
A review of 13 studies published in the Lancet shows that for every 0.1 mg/day increase in folic acid intake in women aged 20-35 years, there is a corresponding 0.94 ng/mL increase in serum folate concentrations and that translates into reduced risk of defects, at least in terms of neural tube defects (Lancet. 2001 Dec 15;358[9298]:2069-73.).
Most recently, some of the same researchers that published the early reports out of Hungary on protection against congenital heart defects showed evidence that a variety of congenital heart defects could be reduced with folic acid supplementation of between 3 mg and 6 mg daily (Eur J Obstet Gynecol Reprod Biol. 2015 Jul 9;193:34-9.).
The study evaluated 3,567 infants with various congenital heart defects and 5,395 matched controls. The researchers excluded women taking multivitamins that contained folic acid and stratified the women taking folic acid alone into three subgroups: those who took folic acid anytime during pregnancy, those who took it during the “critical period” for development of malformations based on medical records and self-reported information, and those who took it during the “critical period” based on medical records alone.
During the study period, there was only one type of folic acid tablet available in Hungary – a 3-mg tablet. On average, the daily dose was 5.6 mg.
Most women began folic acid supplementation around 6-11 weeks’ gestation, coinciding with their first prenatal visit. There was a significant drop in the prevalence of cases with ventricular septal defect (odds ratio, 0.57), tetralogy of Fallot (OR, 0.53), d-transposition of great arteries (OR, 0.47), and atrial septal defect secundum (OR, 0.63) when pregnant women took high doses of folic acid during the critical period for congenital heart defect development.
Overall, the researchers concluded that about 40% of severe congenital heart defects could be prevented using high doses of folic acid during the critical period.
This is a significant reduction for a common and serious problem among pregnant women. While it’s true that there are more surgical solutions available today, cardiac malformations are still a major source of morbidity and mortality among children, and it can be the motivation for parents to terminate a pregnancy in cases where there are serious, complicated malformations.
Prevention is always the best option and this research suggests, once again, that folic acid may offer even more benefits.
The study also shows that there was no clear difference in reduction of congenital heart defects based on either a 3-mg or 6-mg dose, except with atrial septal defect secundum. In that case, the 3-mg dose reduced risk by only 10%, compared with more than 40% at 6 mg. But the researchers were quick to point out that more research is needed to look at the dose-response relationship.
The 5.6-mg average daily dose is significant because it is far above the 0.4-mg level recommended by the Centers for Disease Control and Prevention and the level frequently prescribed for pregnant women – 0.8 mg to 1 mg.
We know that some women may benefit from more folic acid, such as women who have previously given birth to a child with neural tube defects. But there are more subgroups that could benefit from higher doses of folic acid, including women taking antifolate medications such as antiepileptic drugs, methotrexate, and sulfonamides. Women who don’t consume enough vegetables and don’t take a multivitamin could benefit from high doses, as well would obese women, smokers, and women with diabetes.
For years the concern has been that folic acid at higher levels could increase the risk for certain cancers, but the evidence there is uncertain. Additionally, that risk would be triggered only after years of exposure, while the benefits of high-dose folic acid could be achieved in a matter of months. I don’t think the evidence of harm is convincing enough to stop us from considering that high-dose folic acid could be used in the general population.
One of the encouraging aspects of using folic acid to prevent congenital heart defects is that the critical window for influencing malformations is larger than with neural tube defects. While folic acid must be given in the first 28 days of pregnancy to have a benefit, the window of opportunity is 1-2 months longer for cardiac malformations.
The bottom line is that high-dose folic acid to prevent congenital heart defects is a target ripe for further research. While randomized controlled trials aren’t possible, there are plenty of high-quality studies that could be conducted to provide clinicians with the information they need to prevent these devastating malformations.
Dr. Koren is professor of pharmacology and pharmacy at the University of Toronto. He is the founding director of the Motherisk Program. He received grant support to conduct studies on folic acid from Duchesnay. He has been a consultant to several companies that produce vitamins in the context of pregnancy, including Bayer. Email him at [email protected].
When most physicians and patients hear about folic acid, they automatically think about its role in preventing spina bifida and other neural tube defects. But there are now more than 20 years of data that point toward a larger role for folic acid in preventing common, and in some cases devastating, congenital heart defects.
The various published studies leave little doubt that folic acid can significantly reduce the risk for many common cardiac malformations, but other questions remain. For instance, what is the minimum dose for protection? And should health authorities around the world consider recommending a much higher dose of folic acid for short-term use in pregnant women and those trying to conceive?
Early research on cardiac malformations
One of the early studies showing the promise of folic acid beyond neural tube defects was published in 1996. The randomized, double-blind controlled trial in Hungary compared the effect of periconceptional multivitamin supplements containing 0.8 mg of folic acid versus trace element supplements on neural tube defects and other congenital abnormalities. The multivitamin supplement group had a significant reduction in urinary tract abnormalities, and in the rate of sporadic cardiovascular malformations, specifically ventricular septal defects (Am J Med Genet. 1996 Mar 15;62 [2]:179-83.).
In 2004, the same researchers confirmed their results using a controlled, cohort trial that matched pregnant women from regional antenatal care clinics who did not take vitamin supplements to pregnant women who did take supplements containing 0.8 mg folic acid. The results were similar. From a total of 3,056 offspring evaluated, 31 congenital cardiovascular malformations occurred in the group with folic acid supplementation, compared with 50 in the group without, for a 40% lower risk overall, although the main impact was seen among ventricular septal defects (Birth Defects Res A Clin Mol Teratol. 2004 Nov;70[11]:853-61.).
Our own group examined the evidence in a meta-analysis published in 2006 and found significant support for an expanded role for folic acid (J Obstet Gynaecol Can. 2006 Aug;28[8]:680-9.).
The major issue with the available studies is the lack of highest-quality evidence. While some of the studies were randomized trials, you can no longer conduct a true randomized design and withhold folic acid from women; it’s simply not ethical knowing what we know about the preventive benefits of folic acid for neural tube defects. But the literature – which includes quality cohort and case-controlled studies – is convincing.
High dose best?
While some studies have shown a protective effect of folic acid in congenital heart defects at low levels, such as the 0.8 mg used in the early Hungarian studies, other studies indicate that more is better.
A review of 13 studies published in the Lancet shows that for every 0.1 mg/day increase in folic acid intake in women aged 20-35 years, there is a corresponding 0.94 ng/mL increase in serum folate concentrations and that translates into reduced risk of defects, at least in terms of neural tube defects (Lancet. 2001 Dec 15;358[9298]:2069-73.).
Most recently, some of the same researchers that published the early reports out of Hungary on protection against congenital heart defects showed evidence that a variety of congenital heart defects could be reduced with folic acid supplementation of between 3 mg and 6 mg daily (Eur J Obstet Gynecol Reprod Biol. 2015 Jul 9;193:34-9.).
The study evaluated 3,567 infants with various congenital heart defects and 5,395 matched controls. The researchers excluded women taking multivitamins that contained folic acid and stratified the women taking folic acid alone into three subgroups: those who took folic acid anytime during pregnancy, those who took it during the “critical period” for development of malformations based on medical records and self-reported information, and those who took it during the “critical period” based on medical records alone.
During the study period, there was only one type of folic acid tablet available in Hungary – a 3-mg tablet. On average, the daily dose was 5.6 mg.
Most women began folic acid supplementation around 6-11 weeks’ gestation, coinciding with their first prenatal visit. There was a significant drop in the prevalence of cases with ventricular septal defect (odds ratio, 0.57), tetralogy of Fallot (OR, 0.53), d-transposition of great arteries (OR, 0.47), and atrial septal defect secundum (OR, 0.63) when pregnant women took high doses of folic acid during the critical period for congenital heart defect development.
Overall, the researchers concluded that about 40% of severe congenital heart defects could be prevented using high doses of folic acid during the critical period.
This is a significant reduction for a common and serious problem among pregnant women. While it’s true that there are more surgical solutions available today, cardiac malformations are still a major source of morbidity and mortality among children, and it can be the motivation for parents to terminate a pregnancy in cases where there are serious, complicated malformations.
Prevention is always the best option and this research suggests, once again, that folic acid may offer even more benefits.
The study also shows that there was no clear difference in reduction of congenital heart defects based on either a 3-mg or 6-mg dose, except with atrial septal defect secundum. In that case, the 3-mg dose reduced risk by only 10%, compared with more than 40% at 6 mg. But the researchers were quick to point out that more research is needed to look at the dose-response relationship.
The 5.6-mg average daily dose is significant because it is far above the 0.4-mg level recommended by the Centers for Disease Control and Prevention and the level frequently prescribed for pregnant women – 0.8 mg to 1 mg.
We know that some women may benefit from more folic acid, such as women who have previously given birth to a child with neural tube defects. But there are more subgroups that could benefit from higher doses of folic acid, including women taking antifolate medications such as antiepileptic drugs, methotrexate, and sulfonamides. Women who don’t consume enough vegetables and don’t take a multivitamin could benefit from high doses, as well would obese women, smokers, and women with diabetes.
For years the concern has been that folic acid at higher levels could increase the risk for certain cancers, but the evidence there is uncertain. Additionally, that risk would be triggered only after years of exposure, while the benefits of high-dose folic acid could be achieved in a matter of months. I don’t think the evidence of harm is convincing enough to stop us from considering that high-dose folic acid could be used in the general population.
One of the encouraging aspects of using folic acid to prevent congenital heart defects is that the critical window for influencing malformations is larger than with neural tube defects. While folic acid must be given in the first 28 days of pregnancy to have a benefit, the window of opportunity is 1-2 months longer for cardiac malformations.
The bottom line is that high-dose folic acid to prevent congenital heart defects is a target ripe for further research. While randomized controlled trials aren’t possible, there are plenty of high-quality studies that could be conducted to provide clinicians with the information they need to prevent these devastating malformations.
Dr. Koren is professor of pharmacology and pharmacy at the University of Toronto. He is the founding director of the Motherisk Program. He received grant support to conduct studies on folic acid from Duchesnay. He has been a consultant to several companies that produce vitamins in the context of pregnancy, including Bayer. Email him at [email protected].
When most physicians and patients hear about folic acid, they automatically think about its role in preventing spina bifida and other neural tube defects. But there are now more than 20 years of data that point toward a larger role for folic acid in preventing common, and in some cases devastating, congenital heart defects.
The various published studies leave little doubt that folic acid can significantly reduce the risk for many common cardiac malformations, but other questions remain. For instance, what is the minimum dose for protection? And should health authorities around the world consider recommending a much higher dose of folic acid for short-term use in pregnant women and those trying to conceive?
Early research on cardiac malformations
One of the early studies showing the promise of folic acid beyond neural tube defects was published in 1996. The randomized, double-blind controlled trial in Hungary compared the effect of periconceptional multivitamin supplements containing 0.8 mg of folic acid versus trace element supplements on neural tube defects and other congenital abnormalities. The multivitamin supplement group had a significant reduction in urinary tract abnormalities, and in the rate of sporadic cardiovascular malformations, specifically ventricular septal defects (Am J Med Genet. 1996 Mar 15;62 [2]:179-83.).
In 2004, the same researchers confirmed their results using a controlled, cohort trial that matched pregnant women from regional antenatal care clinics who did not take vitamin supplements to pregnant women who did take supplements containing 0.8 mg folic acid. The results were similar. From a total of 3,056 offspring evaluated, 31 congenital cardiovascular malformations occurred in the group with folic acid supplementation, compared with 50 in the group without, for a 40% lower risk overall, although the main impact was seen among ventricular septal defects (Birth Defects Res A Clin Mol Teratol. 2004 Nov;70[11]:853-61.).
Our own group examined the evidence in a meta-analysis published in 2006 and found significant support for an expanded role for folic acid (J Obstet Gynaecol Can. 2006 Aug;28[8]:680-9.).
The major issue with the available studies is the lack of highest-quality evidence. While some of the studies were randomized trials, you can no longer conduct a true randomized design and withhold folic acid from women; it’s simply not ethical knowing what we know about the preventive benefits of folic acid for neural tube defects. But the literature – which includes quality cohort and case-controlled studies – is convincing.
High dose best?
While some studies have shown a protective effect of folic acid in congenital heart defects at low levels, such as the 0.8 mg used in the early Hungarian studies, other studies indicate that more is better.
A review of 13 studies published in the Lancet shows that for every 0.1 mg/day increase in folic acid intake in women aged 20-35 years, there is a corresponding 0.94 ng/mL increase in serum folate concentrations and that translates into reduced risk of defects, at least in terms of neural tube defects (Lancet. 2001 Dec 15;358[9298]:2069-73.).
Most recently, some of the same researchers that published the early reports out of Hungary on protection against congenital heart defects showed evidence that a variety of congenital heart defects could be reduced with folic acid supplementation of between 3 mg and 6 mg daily (Eur J Obstet Gynecol Reprod Biol. 2015 Jul 9;193:34-9.).
The study evaluated 3,567 infants with various congenital heart defects and 5,395 matched controls. The researchers excluded women taking multivitamins that contained folic acid and stratified the women taking folic acid alone into three subgroups: those who took folic acid anytime during pregnancy, those who took it during the “critical period” for development of malformations based on medical records and self-reported information, and those who took it during the “critical period” based on medical records alone.
During the study period, there was only one type of folic acid tablet available in Hungary – a 3-mg tablet. On average, the daily dose was 5.6 mg.
Most women began folic acid supplementation around 6-11 weeks’ gestation, coinciding with their first prenatal visit. There was a significant drop in the prevalence of cases with ventricular septal defect (odds ratio, 0.57), tetralogy of Fallot (OR, 0.53), d-transposition of great arteries (OR, 0.47), and atrial septal defect secundum (OR, 0.63) when pregnant women took high doses of folic acid during the critical period for congenital heart defect development.
Overall, the researchers concluded that about 40% of severe congenital heart defects could be prevented using high doses of folic acid during the critical period.
This is a significant reduction for a common and serious problem among pregnant women. While it’s true that there are more surgical solutions available today, cardiac malformations are still a major source of morbidity and mortality among children, and it can be the motivation for parents to terminate a pregnancy in cases where there are serious, complicated malformations.
Prevention is always the best option and this research suggests, once again, that folic acid may offer even more benefits.
The study also shows that there was no clear difference in reduction of congenital heart defects based on either a 3-mg or 6-mg dose, except with atrial septal defect secundum. In that case, the 3-mg dose reduced risk by only 10%, compared with more than 40% at 6 mg. But the researchers were quick to point out that more research is needed to look at the dose-response relationship.
The 5.6-mg average daily dose is significant because it is far above the 0.4-mg level recommended by the Centers for Disease Control and Prevention and the level frequently prescribed for pregnant women – 0.8 mg to 1 mg.
We know that some women may benefit from more folic acid, such as women who have previously given birth to a child with neural tube defects. But there are more subgroups that could benefit from higher doses of folic acid, including women taking antifolate medications such as antiepileptic drugs, methotrexate, and sulfonamides. Women who don’t consume enough vegetables and don’t take a multivitamin could benefit from high doses, as well would obese women, smokers, and women with diabetes.
For years the concern has been that folic acid at higher levels could increase the risk for certain cancers, but the evidence there is uncertain. Additionally, that risk would be triggered only after years of exposure, while the benefits of high-dose folic acid could be achieved in a matter of months. I don’t think the evidence of harm is convincing enough to stop us from considering that high-dose folic acid could be used in the general population.
One of the encouraging aspects of using folic acid to prevent congenital heart defects is that the critical window for influencing malformations is larger than with neural tube defects. While folic acid must be given in the first 28 days of pregnancy to have a benefit, the window of opportunity is 1-2 months longer for cardiac malformations.
The bottom line is that high-dose folic acid to prevent congenital heart defects is a target ripe for further research. While randomized controlled trials aren’t possible, there are plenty of high-quality studies that could be conducted to provide clinicians with the information they need to prevent these devastating malformations.
Dr. Koren is professor of pharmacology and pharmacy at the University of Toronto. He is the founding director of the Motherisk Program. He received grant support to conduct studies on folic acid from Duchesnay. He has been a consultant to several companies that produce vitamins in the context of pregnancy, including Bayer. Email him at [email protected].
Liar, liar ...
Okay, I admit that from time to time I have embellished the anecdotes that I include in these letters. Sometimes, I feel I need to make sure that you are paying attention. But this time, I am relating this story in its true, unvarnished state.
Two mature women with whom I am acquainted (No, one was not my wife!) had just finished their habitual Saturday morning walk through a wooded upper middle class neighborhood here in town. It was nine o’clock in the morning and the sun was shining. Suddenly, a mangy-looking fox trotted out of the woods and down the road toward them. Aware that from time to time local raccoons, skunks, and foxes have tested positive for rabies, these women began to run and flagged down the first car they saw, and without a word hopped in the back seat.
The surprised occupants of the vehicle were two mature men. You might call them strangers, but here in Maine, we don’t have any strangers. We have tourists. If a fellow Mainer doesn’t know you, he probably knows two people with whom you are acquainted.
As the women began to breathlessly explain their actions, one of the women felt a searing pain in her right thigh and assumed she had torn a muscle as she sprinted away from the fox. Within a few hundred yards, the car began to fill with smoke. Believing that the vehicle was on fire, all four occupants tumbled out into the street like four carnival clowns.
It quickly became clear that the cause of the smoke and the searing pain was that the woman’s pants were on fire. Throwing all caution and modesty to the wind, she quickly shed her pants in the middle of the road and in full view of these men, with whom it turns out she does share several acquaintances.
The source of the fire was the woman’s cell phone. The resulting injury was a palm-size, painful, deep, second-degree burn of her anterior thigh. In a quick Internet search, you will discover several very similar stories – minus the fox and the strangers. Some of the victims were children.
It turns out some cell phones have a tendency to spontaneously explode and/or catch fire. There seems to be no common factor in the events, although some of the ultrathin and flexible cell phones may be more prone to conflagration. However, the victim in our scenario has a storied past with cell phones. She has dropped them in the toilet at least once (history is a little unclear here on the exact number). On another occasion, she placed one in the sink of a public restroom, we can assume to prevent a second or third toilet submersion. As she approached the sink to retrieve it, the clever water-saving faucet – sensing her presence – turned itself on. But in the fox and fire incident, she denies any previous submersions or unusual events with this particular phone. A lawyer is now involved.
So while you and I as pediatricians may be concerned about the relationship between cell phones and health of our patients primarily because cell phones can be a dangerous distraction for young drivers, cyclists, and pedestrians, I share this anecdote to make you aware of another of their health hazards. You also may want to reconsider where you carry your cell phone.
I am not worried myself. I have a little flip phone for which I pay $100 for 500 minutes of usage a year, way more than I need or use. It couldn’t be considered a smartphone as its only noteworthy skill is taking pictures of the inside of my pants pocket. I suspect that its battery must be so small and impotent that even if it decides to self-immolate, I doubt I will notice. However, I do worry about scraggly-looking foxes meandering through my neighborhood.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine, for nearly 40 years. He has authored several books on behavioral pediatrics, including “Coping with a Picky Eater.” Email him at [email protected].
Okay, I admit that from time to time I have embellished the anecdotes that I include in these letters. Sometimes, I feel I need to make sure that you are paying attention. But this time, I am relating this story in its true, unvarnished state.
Two mature women with whom I am acquainted (No, one was not my wife!) had just finished their habitual Saturday morning walk through a wooded upper middle class neighborhood here in town. It was nine o’clock in the morning and the sun was shining. Suddenly, a mangy-looking fox trotted out of the woods and down the road toward them. Aware that from time to time local raccoons, skunks, and foxes have tested positive for rabies, these women began to run and flagged down the first car they saw, and without a word hopped in the back seat.
The surprised occupants of the vehicle were two mature men. You might call them strangers, but here in Maine, we don’t have any strangers. We have tourists. If a fellow Mainer doesn’t know you, he probably knows two people with whom you are acquainted.
As the women began to breathlessly explain their actions, one of the women felt a searing pain in her right thigh and assumed she had torn a muscle as she sprinted away from the fox. Within a few hundred yards, the car began to fill with smoke. Believing that the vehicle was on fire, all four occupants tumbled out into the street like four carnival clowns.
It quickly became clear that the cause of the smoke and the searing pain was that the woman’s pants were on fire. Throwing all caution and modesty to the wind, she quickly shed her pants in the middle of the road and in full view of these men, with whom it turns out she does share several acquaintances.
The source of the fire was the woman’s cell phone. The resulting injury was a palm-size, painful, deep, second-degree burn of her anterior thigh. In a quick Internet search, you will discover several very similar stories – minus the fox and the strangers. Some of the victims were children.
It turns out some cell phones have a tendency to spontaneously explode and/or catch fire. There seems to be no common factor in the events, although some of the ultrathin and flexible cell phones may be more prone to conflagration. However, the victim in our scenario has a storied past with cell phones. She has dropped them in the toilet at least once (history is a little unclear here on the exact number). On another occasion, she placed one in the sink of a public restroom, we can assume to prevent a second or third toilet submersion. As she approached the sink to retrieve it, the clever water-saving faucet – sensing her presence – turned itself on. But in the fox and fire incident, she denies any previous submersions or unusual events with this particular phone. A lawyer is now involved.
So while you and I as pediatricians may be concerned about the relationship between cell phones and health of our patients primarily because cell phones can be a dangerous distraction for young drivers, cyclists, and pedestrians, I share this anecdote to make you aware of another of their health hazards. You also may want to reconsider where you carry your cell phone.
I am not worried myself. I have a little flip phone for which I pay $100 for 500 minutes of usage a year, way more than I need or use. It couldn’t be considered a smartphone as its only noteworthy skill is taking pictures of the inside of my pants pocket. I suspect that its battery must be so small and impotent that even if it decides to self-immolate, I doubt I will notice. However, I do worry about scraggly-looking foxes meandering through my neighborhood.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine, for nearly 40 years. He has authored several books on behavioral pediatrics, including “Coping with a Picky Eater.” Email him at [email protected].
Okay, I admit that from time to time I have embellished the anecdotes that I include in these letters. Sometimes, I feel I need to make sure that you are paying attention. But this time, I am relating this story in its true, unvarnished state.
Two mature women with whom I am acquainted (No, one was not my wife!) had just finished their habitual Saturday morning walk through a wooded upper middle class neighborhood here in town. It was nine o’clock in the morning and the sun was shining. Suddenly, a mangy-looking fox trotted out of the woods and down the road toward them. Aware that from time to time local raccoons, skunks, and foxes have tested positive for rabies, these women began to run and flagged down the first car they saw, and without a word hopped in the back seat.
The surprised occupants of the vehicle were two mature men. You might call them strangers, but here in Maine, we don’t have any strangers. We have tourists. If a fellow Mainer doesn’t know you, he probably knows two people with whom you are acquainted.
As the women began to breathlessly explain their actions, one of the women felt a searing pain in her right thigh and assumed she had torn a muscle as she sprinted away from the fox. Within a few hundred yards, the car began to fill with smoke. Believing that the vehicle was on fire, all four occupants tumbled out into the street like four carnival clowns.
It quickly became clear that the cause of the smoke and the searing pain was that the woman’s pants were on fire. Throwing all caution and modesty to the wind, she quickly shed her pants in the middle of the road and in full view of these men, with whom it turns out she does share several acquaintances.
The source of the fire was the woman’s cell phone. The resulting injury was a palm-size, painful, deep, second-degree burn of her anterior thigh. In a quick Internet search, you will discover several very similar stories – minus the fox and the strangers. Some of the victims were children.
It turns out some cell phones have a tendency to spontaneously explode and/or catch fire. There seems to be no common factor in the events, although some of the ultrathin and flexible cell phones may be more prone to conflagration. However, the victim in our scenario has a storied past with cell phones. She has dropped them in the toilet at least once (history is a little unclear here on the exact number). On another occasion, she placed one in the sink of a public restroom, we can assume to prevent a second or third toilet submersion. As she approached the sink to retrieve it, the clever water-saving faucet – sensing her presence – turned itself on. But in the fox and fire incident, she denies any previous submersions or unusual events with this particular phone. A lawyer is now involved.
So while you and I as pediatricians may be concerned about the relationship between cell phones and health of our patients primarily because cell phones can be a dangerous distraction for young drivers, cyclists, and pedestrians, I share this anecdote to make you aware of another of their health hazards. You also may want to reconsider where you carry your cell phone.
I am not worried myself. I have a little flip phone for which I pay $100 for 500 minutes of usage a year, way more than I need or use. It couldn’t be considered a smartphone as its only noteworthy skill is taking pictures of the inside of my pants pocket. I suspect that its battery must be so small and impotent that even if it decides to self-immolate, I doubt I will notice. However, I do worry about scraggly-looking foxes meandering through my neighborhood.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine, for nearly 40 years. He has authored several books on behavioral pediatrics, including “Coping with a Picky Eater.” Email him at [email protected].
Sharing the Journey of a Transgender Patient
Joe was referred to me by a colleague in a women’s care clinic who knew of my interest in transgender health. He greeted me with, “I heard you’re interested in transgender care—I can be your guinea pig!”
Joe told me about his long-held desire to transition from being a woman to a man and asked me to be his partner in this journey. His honesty and openness about striving for an authentic life was the beginning of my own story about how a special patient can broaden understanding and change the way you practice.
Several years ago at the American Association of Nurse Practitioners National Conference, an NP from Connecticut spoke about her extensive experience with transgender patients. Her presentation was an excellent summary of the basics of gender identity and health implications. This topic seemed important to learn about, an area in which I could make a difference in my practice. Since becoming a nurse, I have felt drawn to helping the most vulnerable populations, and transgender persons experience marginalization in our society.
I never thought I could become an expert, but the speaker said that didn’t matter. She noted that her transgender patients usually teach her more than she teaches them. What is important is including transgender care in your primary care knowledge base,1 since it has been recommended that primary care providers, at the frontlines in patient-centered care, coordinate and partner with transgender patients.2
I was so fortunate to meet Joe. He was open to answering my questions about his interest in a female-to-male (FTM) transition and what the process would entail. Despite my eagerness to help, I was admittedly nervous about portraying myself as a professional, knowing that my experience with transgender issues was limited. I didn’t want to say the wrong thing or use the wrong pronoun. What I discovered is that it’s OK to feel like a novice. It just takes practice to get the wording right, but your patients will appreciate your efforts.
Joe proved to be an excellent guide on this journey; at our first visit, he offered me resources, including information about an upcoming local transgender conference, evidence-based materials, and supportive readings. As I reviewed the literature to educate myself, I discovered that despite a paucity of research, there is a growing understanding of transgender issues and an increasing body of evidence to study.
One of the keys for many people, but especially for transgender persons, is psychological support. Often, transgender people have had a tough road, struggling with gender identity, isolation from friends and family, rejection issues, discrimination, and violence. Depression and suicide are all too common in this patient population.
The Endocrine Society’s Clinical Practice Guidelines recommend that patients secure a good working relationship with a mental health provider for their journey before moving forward with hormonal treatments and surgical interventions.3 Mental health professionals can also help families of transgender persons work through difficult psychosocial issues.
Joe was already regularly meeting with a psychologist and had an excellent support network in place. He was ready for the next step, and I was onboard to help him take it. I did some research to identify professionals in my community who were accepting transgender patients, as well as community resources available for this population. In speaking with colleagues, I was able to find a local endocrinologist who would prescribe hormones, a gynecologist who was comfortable with FTM transition, and a local plastic surgeon who was experienced with FTM chest reconstruction.
During my search for appropriate referrals, I would simply call the office and leave my name and a general question about whether the practice provided transgender care. If I received a “yes” response, I would then follow up with more personal contact with the provider. I did encounter some providers who were not comfortable providing transgender health care. I don’t know if this was an individual or organizational decision, or if it reflected personal beliefs or a lack of experience—but it has affected my further referrals to those offices.
I facilitated referrals for Joe to the endocrinologist, gynecologist, and plastic surgeon. He confirmed after the visits that these providers were professional, prepared, and welcoming, so they could be referral sources for other transgender persons in the future. And for those who might not be as far along their journey as Joe was when we met, several psychiatric NP colleagues directed me to a group of qualified and experienced counselors and therapists with expertise in gender-identity issues. I also discovered that the local university has a great support group for transgender people, as well as their friends and families. With these resources, I am equipped to help my transgender patients navigate their transitions.
As Joe’s primary care provider, though, my role is about more than just providing appropriate referrals. Some of the most important conversations we had addressed the implications of his transition for future preventive health screenings. These include breast exams, which are recommended after an FTM chest reconstruction, and pelvic exams, which are recommended if the uterus and cervix remain in place.4 The World Professional Association for Transgender Health has established standards of care that are helpful for providers and patients navigating this journey.5
Together, Joe and I developed a plan of care for the transition, with Joe making informed decisions. For example, we agreed that endocrinology would initiate hormone therapy, but I would manage it after a certain point.
The support and care that I can provide to my transgender patients is obvious. But what working with them does for me is equally invaluable. On any given day in the clinic, I can feel a little deflated and think, “Did I really help anyone today?” My experiences with transgender patients are refreshing, because I know they appreciate my support whether I am an expert or not; it is truly a gift to work with them. The experience has taught me that I can put new information I learn into practice, that I am an expert in preventive care and complex case coordination, and that I can be a competent and caring part of a health care team for transgender persons.
A transition is a process—a different journey for each individual. It is also a journey for each health care provider. Other health care professionals, like myself, can educate themselves about transgender issues and even become champions for this population in their communities. I hope to assist my colleagues in becoming more educated about transgender issues in the future. Please consider sharing your thoughts with me by writing to [email protected].
REFERENCES
1. Alegria CA. Transgender identity and health care: implications for psychological and physical evaluation. J Am Acad Nurse Pract. 2011;23(4):175-182.
2. Deutsch MB, Feldman JL. Updated recommendations from the World Professional Association for Transgender Health standards of care. Am Fam Phys. 2013;87(2):89-93.
3. Hembree WC, Cohen-Kettenis P, Delemarre-van de Waal HA, et al. Endocrine treatment of transsexual persons: an Endocrine Society clinical practice guideline. J Clin Endocrinol Metab. 2009;94(9):3132-3154.
4. University of California, San Francisco Center of Excellence for Transgender Health. Primary care protocol for transgender patient care (2011). http://transhealth.ucsf.edu/protocols. Accessed August 24, 2015.
5. World Professional Association for Transgender Health. Standards of care for the health of transsexual, transgender, and gender nonconforming people (7th version; 2015). www.wpath.org/site_page.cfm?pk_association_webpage_menu=1351. Accessed August 24, 2015.
Joe was referred to me by a colleague in a women’s care clinic who knew of my interest in transgender health. He greeted me with, “I heard you’re interested in transgender care—I can be your guinea pig!”
Joe told me about his long-held desire to transition from being a woman to a man and asked me to be his partner in this journey. His honesty and openness about striving for an authentic life was the beginning of my own story about how a special patient can broaden understanding and change the way you practice.
Several years ago at the American Association of Nurse Practitioners National Conference, an NP from Connecticut spoke about her extensive experience with transgender patients. Her presentation was an excellent summary of the basics of gender identity and health implications. This topic seemed important to learn about, an area in which I could make a difference in my practice. Since becoming a nurse, I have felt drawn to helping the most vulnerable populations, and transgender persons experience marginalization in our society.
I never thought I could become an expert, but the speaker said that didn’t matter. She noted that her transgender patients usually teach her more than she teaches them. What is important is including transgender care in your primary care knowledge base,1 since it has been recommended that primary care providers, at the frontlines in patient-centered care, coordinate and partner with transgender patients.2
I was so fortunate to meet Joe. He was open to answering my questions about his interest in a female-to-male (FTM) transition and what the process would entail. Despite my eagerness to help, I was admittedly nervous about portraying myself as a professional, knowing that my experience with transgender issues was limited. I didn’t want to say the wrong thing or use the wrong pronoun. What I discovered is that it’s OK to feel like a novice. It just takes practice to get the wording right, but your patients will appreciate your efforts.
Joe proved to be an excellent guide on this journey; at our first visit, he offered me resources, including information about an upcoming local transgender conference, evidence-based materials, and supportive readings. As I reviewed the literature to educate myself, I discovered that despite a paucity of research, there is a growing understanding of transgender issues and an increasing body of evidence to study.
One of the keys for many people, but especially for transgender persons, is psychological support. Often, transgender people have had a tough road, struggling with gender identity, isolation from friends and family, rejection issues, discrimination, and violence. Depression and suicide are all too common in this patient population.
The Endocrine Society’s Clinical Practice Guidelines recommend that patients secure a good working relationship with a mental health provider for their journey before moving forward with hormonal treatments and surgical interventions.3 Mental health professionals can also help families of transgender persons work through difficult psychosocial issues.
Joe was already regularly meeting with a psychologist and had an excellent support network in place. He was ready for the next step, and I was onboard to help him take it. I did some research to identify professionals in my community who were accepting transgender patients, as well as community resources available for this population. In speaking with colleagues, I was able to find a local endocrinologist who would prescribe hormones, a gynecologist who was comfortable with FTM transition, and a local plastic surgeon who was experienced with FTM chest reconstruction.
During my search for appropriate referrals, I would simply call the office and leave my name and a general question about whether the practice provided transgender care. If I received a “yes” response, I would then follow up with more personal contact with the provider. I did encounter some providers who were not comfortable providing transgender health care. I don’t know if this was an individual or organizational decision, or if it reflected personal beliefs or a lack of experience—but it has affected my further referrals to those offices.
I facilitated referrals for Joe to the endocrinologist, gynecologist, and plastic surgeon. He confirmed after the visits that these providers were professional, prepared, and welcoming, so they could be referral sources for other transgender persons in the future. And for those who might not be as far along their journey as Joe was when we met, several psychiatric NP colleagues directed me to a group of qualified and experienced counselors and therapists with expertise in gender-identity issues. I also discovered that the local university has a great support group for transgender people, as well as their friends and families. With these resources, I am equipped to help my transgender patients navigate their transitions.
As Joe’s primary care provider, though, my role is about more than just providing appropriate referrals. Some of the most important conversations we had addressed the implications of his transition for future preventive health screenings. These include breast exams, which are recommended after an FTM chest reconstruction, and pelvic exams, which are recommended if the uterus and cervix remain in place.4 The World Professional Association for Transgender Health has established standards of care that are helpful for providers and patients navigating this journey.5
Together, Joe and I developed a plan of care for the transition, with Joe making informed decisions. For example, we agreed that endocrinology would initiate hormone therapy, but I would manage it after a certain point.
The support and care that I can provide to my transgender patients is obvious. But what working with them does for me is equally invaluable. On any given day in the clinic, I can feel a little deflated and think, “Did I really help anyone today?” My experiences with transgender patients are refreshing, because I know they appreciate my support whether I am an expert or not; it is truly a gift to work with them. The experience has taught me that I can put new information I learn into practice, that I am an expert in preventive care and complex case coordination, and that I can be a competent and caring part of a health care team for transgender persons.
A transition is a process—a different journey for each individual. It is also a journey for each health care provider. Other health care professionals, like myself, can educate themselves about transgender issues and even become champions for this population in their communities. I hope to assist my colleagues in becoming more educated about transgender issues in the future. Please consider sharing your thoughts with me by writing to [email protected].
REFERENCES
1. Alegria CA. Transgender identity and health care: implications for psychological and physical evaluation. J Am Acad Nurse Pract. 2011;23(4):175-182.
2. Deutsch MB, Feldman JL. Updated recommendations from the World Professional Association for Transgender Health standards of care. Am Fam Phys. 2013;87(2):89-93.
3. Hembree WC, Cohen-Kettenis P, Delemarre-van de Waal HA, et al. Endocrine treatment of transsexual persons: an Endocrine Society clinical practice guideline. J Clin Endocrinol Metab. 2009;94(9):3132-3154.
4. University of California, San Francisco Center of Excellence for Transgender Health. Primary care protocol for transgender patient care (2011). http://transhealth.ucsf.edu/protocols. Accessed August 24, 2015.
5. World Professional Association for Transgender Health. Standards of care for the health of transsexual, transgender, and gender nonconforming people (7th version; 2015). www.wpath.org/site_page.cfm?pk_association_webpage_menu=1351. Accessed August 24, 2015.
Joe was referred to me by a colleague in a women’s care clinic who knew of my interest in transgender health. He greeted me with, “I heard you’re interested in transgender care—I can be your guinea pig!”
Joe told me about his long-held desire to transition from being a woman to a man and asked me to be his partner in this journey. His honesty and openness about striving for an authentic life was the beginning of my own story about how a special patient can broaden understanding and change the way you practice.
Several years ago at the American Association of Nurse Practitioners National Conference, an NP from Connecticut spoke about her extensive experience with transgender patients. Her presentation was an excellent summary of the basics of gender identity and health implications. This topic seemed important to learn about, an area in which I could make a difference in my practice. Since becoming a nurse, I have felt drawn to helping the most vulnerable populations, and transgender persons experience marginalization in our society.
I never thought I could become an expert, but the speaker said that didn’t matter. She noted that her transgender patients usually teach her more than she teaches them. What is important is including transgender care in your primary care knowledge base,1 since it has been recommended that primary care providers, at the frontlines in patient-centered care, coordinate and partner with transgender patients.2
I was so fortunate to meet Joe. He was open to answering my questions about his interest in a female-to-male (FTM) transition and what the process would entail. Despite my eagerness to help, I was admittedly nervous about portraying myself as a professional, knowing that my experience with transgender issues was limited. I didn’t want to say the wrong thing or use the wrong pronoun. What I discovered is that it’s OK to feel like a novice. It just takes practice to get the wording right, but your patients will appreciate your efforts.
Joe proved to be an excellent guide on this journey; at our first visit, he offered me resources, including information about an upcoming local transgender conference, evidence-based materials, and supportive readings. As I reviewed the literature to educate myself, I discovered that despite a paucity of research, there is a growing understanding of transgender issues and an increasing body of evidence to study.
One of the keys for many people, but especially for transgender persons, is psychological support. Often, transgender people have had a tough road, struggling with gender identity, isolation from friends and family, rejection issues, discrimination, and violence. Depression and suicide are all too common in this patient population.
The Endocrine Society’s Clinical Practice Guidelines recommend that patients secure a good working relationship with a mental health provider for their journey before moving forward with hormonal treatments and surgical interventions.3 Mental health professionals can also help families of transgender persons work through difficult psychosocial issues.
Joe was already regularly meeting with a psychologist and had an excellent support network in place. He was ready for the next step, and I was onboard to help him take it. I did some research to identify professionals in my community who were accepting transgender patients, as well as community resources available for this population. In speaking with colleagues, I was able to find a local endocrinologist who would prescribe hormones, a gynecologist who was comfortable with FTM transition, and a local plastic surgeon who was experienced with FTM chest reconstruction.
During my search for appropriate referrals, I would simply call the office and leave my name and a general question about whether the practice provided transgender care. If I received a “yes” response, I would then follow up with more personal contact with the provider. I did encounter some providers who were not comfortable providing transgender health care. I don’t know if this was an individual or organizational decision, or if it reflected personal beliefs or a lack of experience—but it has affected my further referrals to those offices.
I facilitated referrals for Joe to the endocrinologist, gynecologist, and plastic surgeon. He confirmed after the visits that these providers were professional, prepared, and welcoming, so they could be referral sources for other transgender persons in the future. And for those who might not be as far along their journey as Joe was when we met, several psychiatric NP colleagues directed me to a group of qualified and experienced counselors and therapists with expertise in gender-identity issues. I also discovered that the local university has a great support group for transgender people, as well as their friends and families. With these resources, I am equipped to help my transgender patients navigate their transitions.
As Joe’s primary care provider, though, my role is about more than just providing appropriate referrals. Some of the most important conversations we had addressed the implications of his transition for future preventive health screenings. These include breast exams, which are recommended after an FTM chest reconstruction, and pelvic exams, which are recommended if the uterus and cervix remain in place.4 The World Professional Association for Transgender Health has established standards of care that are helpful for providers and patients navigating this journey.5
Together, Joe and I developed a plan of care for the transition, with Joe making informed decisions. For example, we agreed that endocrinology would initiate hormone therapy, but I would manage it after a certain point.
The support and care that I can provide to my transgender patients is obvious. But what working with them does for me is equally invaluable. On any given day in the clinic, I can feel a little deflated and think, “Did I really help anyone today?” My experiences with transgender patients are refreshing, because I know they appreciate my support whether I am an expert or not; it is truly a gift to work with them. The experience has taught me that I can put new information I learn into practice, that I am an expert in preventive care and complex case coordination, and that I can be a competent and caring part of a health care team for transgender persons.
A transition is a process—a different journey for each individual. It is also a journey for each health care provider. Other health care professionals, like myself, can educate themselves about transgender issues and even become champions for this population in their communities. I hope to assist my colleagues in becoming more educated about transgender issues in the future. Please consider sharing your thoughts with me by writing to [email protected].
REFERENCES
1. Alegria CA. Transgender identity and health care: implications for psychological and physical evaluation. J Am Acad Nurse Pract. 2011;23(4):175-182.
2. Deutsch MB, Feldman JL. Updated recommendations from the World Professional Association for Transgender Health standards of care. Am Fam Phys. 2013;87(2):89-93.
3. Hembree WC, Cohen-Kettenis P, Delemarre-van de Waal HA, et al. Endocrine treatment of transsexual persons: an Endocrine Society clinical practice guideline. J Clin Endocrinol Metab. 2009;94(9):3132-3154.
4. University of California, San Francisco Center of Excellence for Transgender Health. Primary care protocol for transgender patient care (2011). http://transhealth.ucsf.edu/protocols. Accessed August 24, 2015.
5. World Professional Association for Transgender Health. Standards of care for the health of transsexual, transgender, and gender nonconforming people (7th version; 2015). www.wpath.org/site_page.cfm?pk_association_webpage_menu=1351. Accessed August 24, 2015.
Protecting pregnant women, infants from infections
Infectious disease morbidity and mortality continue to disproportionately impact pregnant women and young infants.
In California, the incidence of pertussis approximates 100 cases per 100,000 in infants less than 5 months of age; a rate threefold greater than any other age group. Seven of nine (77%) deaths in 2013/2014 occurred in infants less than 3 months of age (California Department of Public Health Pertussis Report, Aug. 3, 2015).
Influenza severity and mortality is increased in pregnant women, and there is a greater risk of fetal morbidity and wastage. In the 2009 H1N1 pandemic, there was a 20% case fatality rate in women sick enough to be admitted to the ICU. The incidence of low birth weight also was increased among pregnant women delivering while hospitalized for influenza-related illness. These examples highlight the burden of vaccine-preventable disease in two vulnerable populations, pregnant women and infants too young to be protected by vaccines mandated by the U.S.immunization program.
The American College of Obstetricians and Gynecologists, the American Academy of Pediatrics, the Centers for Disease Control and Prevention, and many other national and state organizations endorse immunization of pregnant women to improve women’s and infants’ outcomes. Recent studies demonstrate that infants born to women vaccinated with influenza are 45%-48% less likely to be hospitalized for culture-proven influenza.
Benowitz et al. reported a 91.5% effectiveness for maternal influenza vaccination for prevention of hospitalization of infants caused by influenza in the first 6 months of life. The presumed mechanisms of protection are both the transplacental transfer of protective antibody as well as indirect protection from disease prevention in the mother (Clin Infect Dis. 2010 Dec 15;51(12):1355-61). The recommendation is that inactivated influenza vaccine can be given at any time during pregnancy; however, live attenuated influenza vaccine (LAIV; FluMist) is contraindicated, as are all live-virus vaccines. In contrast, Tdap is recommended for use either during pregnancy or post partum.
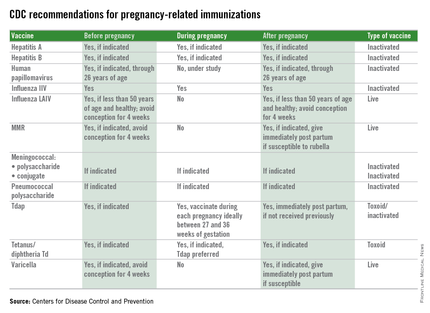
However, Healy et al. (Pediatr Infect Dis J. 2015;34(1):22-60) failed to demonstrate a benefit to postpartum immunization and cocooning for reducing pertussis illness in infants 6 months of age or younger. The likely explanation for this failure is revealed in a recent study in infant baboons where immunization with Tdap failed to decrease colonization or transmission of Bordetella pertussis, compared with natural disease or whole-cell pertussis. Thus, even though protective against disease, Tdap failure to prevent transmission within the community still occurs. The current Advisory Committee on Immunization Practices recommendation, immunization between 27 and 36 weeks, is designed to ensure high antibody concentrations in both mother and newborn at the time of birth and bridge the time period until infant immunization can elicit protective antibody.
The benefits achieved with maternal immunization must be weighed against potential for adverse events. There is no evidence of risk to either mother or infant from inactivated vaccines administered during pregnancy. Still, the recommendations for influenza and Tdap vaccine incorporate the high likelihood of exposure, the risk of morbidity or mortality from the infectious agent, and the likelihood of harm. During the H1N1 epidemic, a cohort study by Chambers et al. of H1N1 vaccine in exposed and unexposed pregnant women concluded that there was no increase in risk for major congenital defects, spontaneous abortion, or small for gestational age (Vaccine. 2013 Oct 17;31(44):5026-32). There was a signal for increase in prematurity, but the difference between H1N1-vaccinated and unvaccinated pregnancies was 3 days. In addition, a review of 11 studies, including one of 10,428 pregnant women, concluded there were no harmful maternal or fetal effects.
Additionally, no adverse risks have been identified in women who were inadvertently vaccinated during pregnancy with live-attenuated rubella, influenza, and yellow fever vaccines. Tetanus vaccination has been administered safely to several millions of pregnant women without documented serious adverse outcomes. Ongoing postmarketing surveillance continues as an important tool for identification of potential adverse effects.
One potential limitation is the blunting of infant immune responses to vaccination due to high serum antibody concentrations at the time of primary immunizations. Some studies have found lower antibody concentrations prior to booster vaccinations at 1 year of age. However, as morbidity and mortality is greater in the first months of life for many infectious diseases, this may be an acceptable trade off if high morbidity and mortality can be reduced in the first months of life.
Immunization during pregnancy represents only one aspect of prevention of vaccine preventable diseases. Preconception, prenatal, and postpartum visits with health care professionals represents an opportune time to discuss the benefits of immunization and their contribution to a healthy pregnancy outcome. Inactivated vaccines are safe for administration during pregnancy, live virus vaccines, despite being attenuated, are a theoretical risk if spread to the fetus occurs and therefore are contraindicated and should be administered during preconception counseling if indicated. The table below outlines vaccines that can be administered before, during, and after pregnancy.
Although once considered potentially contraindicated in pregnant women, evidence now supports specific vaccines as both safe for a pregnant woman and her fetus and effective for preventing serious disease in both. Universal immunization with influenza vaccine and Tdap, as recommended by multiple national professional medical organizations, will improve the outcome of pregnancy by prevention of morbidity and mortality from common community pathogens.
Dr. Pelton is chief of pediatric infectious disease and coordinator of the maternal-child HIV program at Boston Medical Center. E-mail him at [email protected].
Infectious disease morbidity and mortality continue to disproportionately impact pregnant women and young infants.
In California, the incidence of pertussis approximates 100 cases per 100,000 in infants less than 5 months of age; a rate threefold greater than any other age group. Seven of nine (77%) deaths in 2013/2014 occurred in infants less than 3 months of age (California Department of Public Health Pertussis Report, Aug. 3, 2015).
Influenza severity and mortality is increased in pregnant women, and there is a greater risk of fetal morbidity and wastage. In the 2009 H1N1 pandemic, there was a 20% case fatality rate in women sick enough to be admitted to the ICU. The incidence of low birth weight also was increased among pregnant women delivering while hospitalized for influenza-related illness. These examples highlight the burden of vaccine-preventable disease in two vulnerable populations, pregnant women and infants too young to be protected by vaccines mandated by the U.S.immunization program.
The American College of Obstetricians and Gynecologists, the American Academy of Pediatrics, the Centers for Disease Control and Prevention, and many other national and state organizations endorse immunization of pregnant women to improve women’s and infants’ outcomes. Recent studies demonstrate that infants born to women vaccinated with influenza are 45%-48% less likely to be hospitalized for culture-proven influenza.
Benowitz et al. reported a 91.5% effectiveness for maternal influenza vaccination for prevention of hospitalization of infants caused by influenza in the first 6 months of life. The presumed mechanisms of protection are both the transplacental transfer of protective antibody as well as indirect protection from disease prevention in the mother (Clin Infect Dis. 2010 Dec 15;51(12):1355-61). The recommendation is that inactivated influenza vaccine can be given at any time during pregnancy; however, live attenuated influenza vaccine (LAIV; FluMist) is contraindicated, as are all live-virus vaccines. In contrast, Tdap is recommended for use either during pregnancy or post partum.
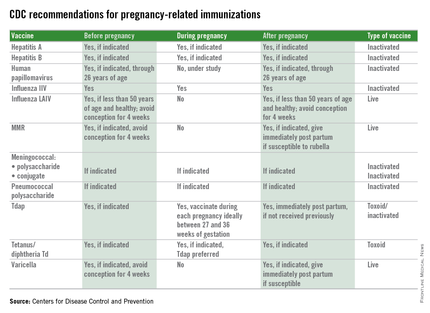
However, Healy et al. (Pediatr Infect Dis J. 2015;34(1):22-60) failed to demonstrate a benefit to postpartum immunization and cocooning for reducing pertussis illness in infants 6 months of age or younger. The likely explanation for this failure is revealed in a recent study in infant baboons where immunization with Tdap failed to decrease colonization or transmission of Bordetella pertussis, compared with natural disease or whole-cell pertussis. Thus, even though protective against disease, Tdap failure to prevent transmission within the community still occurs. The current Advisory Committee on Immunization Practices recommendation, immunization between 27 and 36 weeks, is designed to ensure high antibody concentrations in both mother and newborn at the time of birth and bridge the time period until infant immunization can elicit protective antibody.
The benefits achieved with maternal immunization must be weighed against potential for adverse events. There is no evidence of risk to either mother or infant from inactivated vaccines administered during pregnancy. Still, the recommendations for influenza and Tdap vaccine incorporate the high likelihood of exposure, the risk of morbidity or mortality from the infectious agent, and the likelihood of harm. During the H1N1 epidemic, a cohort study by Chambers et al. of H1N1 vaccine in exposed and unexposed pregnant women concluded that there was no increase in risk for major congenital defects, spontaneous abortion, or small for gestational age (Vaccine. 2013 Oct 17;31(44):5026-32). There was a signal for increase in prematurity, but the difference between H1N1-vaccinated and unvaccinated pregnancies was 3 days. In addition, a review of 11 studies, including one of 10,428 pregnant women, concluded there were no harmful maternal or fetal effects.
Additionally, no adverse risks have been identified in women who were inadvertently vaccinated during pregnancy with live-attenuated rubella, influenza, and yellow fever vaccines. Tetanus vaccination has been administered safely to several millions of pregnant women without documented serious adverse outcomes. Ongoing postmarketing surveillance continues as an important tool for identification of potential adverse effects.
One potential limitation is the blunting of infant immune responses to vaccination due to high serum antibody concentrations at the time of primary immunizations. Some studies have found lower antibody concentrations prior to booster vaccinations at 1 year of age. However, as morbidity and mortality is greater in the first months of life for many infectious diseases, this may be an acceptable trade off if high morbidity and mortality can be reduced in the first months of life.
Immunization during pregnancy represents only one aspect of prevention of vaccine preventable diseases. Preconception, prenatal, and postpartum visits with health care professionals represents an opportune time to discuss the benefits of immunization and their contribution to a healthy pregnancy outcome. Inactivated vaccines are safe for administration during pregnancy, live virus vaccines, despite being attenuated, are a theoretical risk if spread to the fetus occurs and therefore are contraindicated and should be administered during preconception counseling if indicated. The table below outlines vaccines that can be administered before, during, and after pregnancy.
Although once considered potentially contraindicated in pregnant women, evidence now supports specific vaccines as both safe for a pregnant woman and her fetus and effective for preventing serious disease in both. Universal immunization with influenza vaccine and Tdap, as recommended by multiple national professional medical organizations, will improve the outcome of pregnancy by prevention of morbidity and mortality from common community pathogens.
Dr. Pelton is chief of pediatric infectious disease and coordinator of the maternal-child HIV program at Boston Medical Center. E-mail him at [email protected].
Infectious disease morbidity and mortality continue to disproportionately impact pregnant women and young infants.
In California, the incidence of pertussis approximates 100 cases per 100,000 in infants less than 5 months of age; a rate threefold greater than any other age group. Seven of nine (77%) deaths in 2013/2014 occurred in infants less than 3 months of age (California Department of Public Health Pertussis Report, Aug. 3, 2015).
Influenza severity and mortality is increased in pregnant women, and there is a greater risk of fetal morbidity and wastage. In the 2009 H1N1 pandemic, there was a 20% case fatality rate in women sick enough to be admitted to the ICU. The incidence of low birth weight also was increased among pregnant women delivering while hospitalized for influenza-related illness. These examples highlight the burden of vaccine-preventable disease in two vulnerable populations, pregnant women and infants too young to be protected by vaccines mandated by the U.S.immunization program.
The American College of Obstetricians and Gynecologists, the American Academy of Pediatrics, the Centers for Disease Control and Prevention, and many other national and state organizations endorse immunization of pregnant women to improve women’s and infants’ outcomes. Recent studies demonstrate that infants born to women vaccinated with influenza are 45%-48% less likely to be hospitalized for culture-proven influenza.
Benowitz et al. reported a 91.5% effectiveness for maternal influenza vaccination for prevention of hospitalization of infants caused by influenza in the first 6 months of life. The presumed mechanisms of protection are both the transplacental transfer of protective antibody as well as indirect protection from disease prevention in the mother (Clin Infect Dis. 2010 Dec 15;51(12):1355-61). The recommendation is that inactivated influenza vaccine can be given at any time during pregnancy; however, live attenuated influenza vaccine (LAIV; FluMist) is contraindicated, as are all live-virus vaccines. In contrast, Tdap is recommended for use either during pregnancy or post partum.
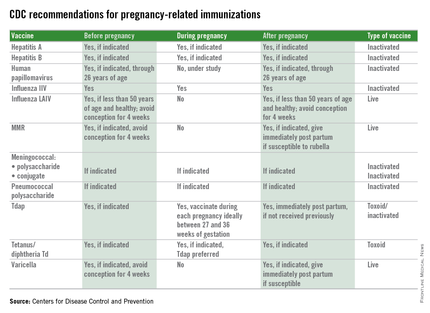
However, Healy et al. (Pediatr Infect Dis J. 2015;34(1):22-60) failed to demonstrate a benefit to postpartum immunization and cocooning for reducing pertussis illness in infants 6 months of age or younger. The likely explanation for this failure is revealed in a recent study in infant baboons where immunization with Tdap failed to decrease colonization or transmission of Bordetella pertussis, compared with natural disease or whole-cell pertussis. Thus, even though protective against disease, Tdap failure to prevent transmission within the community still occurs. The current Advisory Committee on Immunization Practices recommendation, immunization between 27 and 36 weeks, is designed to ensure high antibody concentrations in both mother and newborn at the time of birth and bridge the time period until infant immunization can elicit protective antibody.
The benefits achieved with maternal immunization must be weighed against potential for adverse events. There is no evidence of risk to either mother or infant from inactivated vaccines administered during pregnancy. Still, the recommendations for influenza and Tdap vaccine incorporate the high likelihood of exposure, the risk of morbidity or mortality from the infectious agent, and the likelihood of harm. During the H1N1 epidemic, a cohort study by Chambers et al. of H1N1 vaccine in exposed and unexposed pregnant women concluded that there was no increase in risk for major congenital defects, spontaneous abortion, or small for gestational age (Vaccine. 2013 Oct 17;31(44):5026-32). There was a signal for increase in prematurity, but the difference between H1N1-vaccinated and unvaccinated pregnancies was 3 days. In addition, a review of 11 studies, including one of 10,428 pregnant women, concluded there were no harmful maternal or fetal effects.
Additionally, no adverse risks have been identified in women who were inadvertently vaccinated during pregnancy with live-attenuated rubella, influenza, and yellow fever vaccines. Tetanus vaccination has been administered safely to several millions of pregnant women without documented serious adverse outcomes. Ongoing postmarketing surveillance continues as an important tool for identification of potential adverse effects.
One potential limitation is the blunting of infant immune responses to vaccination due to high serum antibody concentrations at the time of primary immunizations. Some studies have found lower antibody concentrations prior to booster vaccinations at 1 year of age. However, as morbidity and mortality is greater in the first months of life for many infectious diseases, this may be an acceptable trade off if high morbidity and mortality can be reduced in the first months of life.
Immunization during pregnancy represents only one aspect of prevention of vaccine preventable diseases. Preconception, prenatal, and postpartum visits with health care professionals represents an opportune time to discuss the benefits of immunization and their contribution to a healthy pregnancy outcome. Inactivated vaccines are safe for administration during pregnancy, live virus vaccines, despite being attenuated, are a theoretical risk if spread to the fetus occurs and therefore are contraindicated and should be administered during preconception counseling if indicated. The table below outlines vaccines that can be administered before, during, and after pregnancy.
Although once considered potentially contraindicated in pregnant women, evidence now supports specific vaccines as both safe for a pregnant woman and her fetus and effective for preventing serious disease in both. Universal immunization with influenza vaccine and Tdap, as recommended by multiple national professional medical organizations, will improve the outcome of pregnancy by prevention of morbidity and mortality from common community pathogens.
Dr. Pelton is chief of pediatric infectious disease and coordinator of the maternal-child HIV program at Boston Medical Center. E-mail him at [email protected].
Unsung Heroes: ED Social Workers
When we think of essential nonphysician ED staff and the roles they play in the successful management of our patients, we tend to think of nurses, nurse practitioners, physician assistants, technicians, pharmacists, patient representatives, and even transporters, housekeepers, and clerks. But we typically overlook the ED social worker, without whose efforts the modern ED would come to a grinding halt. In the early years after emergency medicine (EM) became a specialty, few, if any, EDs were staffed around the clock by social workers. This was true even in the county and municipal acute care hospitals now referred to as “safety net” hospitals.
In those days, the role of the ED social worker frequently centered around contacting the appropriate agencies for cases of child abuse and sexual assault and arranging transportation or shelter for patients who were to be discharged from the ED.
But just as the roles of EM and EDs have evolved and expanded enormously in recent decades, so too has the role of and need for ED social workers. The presence of a skilled ED social worker will almost always make it possible to safely discharge several patients a day to their homes—with arrangements made for the services and medical equipment needed—instead of admitting them to inpatient beds. Such needed services include physical and occupational therapists, visiting nurses for wound care, medication management, blood work, intravenous infusions, and meal preparation and delivery (“Meals on Wheels,” etc). Durable medical equipment needs include bedside commodes, rails, grab bars, and hospital beds. Even preventive medicine is now initiated by the ED social worker, who arranges for age-appropriate home-safety assessments and equipment installations for the increasing number of elderly who have “aged in place” in the same dwelling over many years.
As the percentage of ED patients over the age of 65—currently 18%—continues to rise during the next 40 to 50 years, the need for skilled ED social workers is increasing exponentially. There is frequently a need to temporarily relocate older discharged ED patients with families or friends when they are alone, for assessing whether a spouse or family member is capable of caring for a discharged patient at home, and even for arranging care of a pet for patients who live alone and require admission. Another way of looking at the current situation is that EDs now serve two clients—our patients and the hospital and healthcare system. Many patients who were formerly admitted to hospitals are now expected to be sent home from the ED to avoid diminishing hospital reimbursement for short-stay “observation services,” or denials. At the same time, the complex range and degree of health insurance coverage that patients have, and the scarce availability of appropriate, timely physician follow-up, are beyond the ability of an EP to deal with while continuing to care for other patients.
As the number of ED patients eligible for Medicare and Medicaid continues to rise, and the benefits are linked to changing requirements for length and type of care (“two-midnight rule” and observation services, for example), the 24/7 ED social worker has become a truly essential member of the ED staff—and now is the time to start ramping up the coverage.
Acknowledgments
We wish to thank NewYork Presbyterian/Weill Cornell Medical Center ED Social Workers, George Haskell, LMSW, and Laura Kramer, LMSW, for providing details regarding the home services and equipment they arrange for patients discharged from our ED.
When we think of essential nonphysician ED staff and the roles they play in the successful management of our patients, we tend to think of nurses, nurse practitioners, physician assistants, technicians, pharmacists, patient representatives, and even transporters, housekeepers, and clerks. But we typically overlook the ED social worker, without whose efforts the modern ED would come to a grinding halt. In the early years after emergency medicine (EM) became a specialty, few, if any, EDs were staffed around the clock by social workers. This was true even in the county and municipal acute care hospitals now referred to as “safety net” hospitals.
In those days, the role of the ED social worker frequently centered around contacting the appropriate agencies for cases of child abuse and sexual assault and arranging transportation or shelter for patients who were to be discharged from the ED.
But just as the roles of EM and EDs have evolved and expanded enormously in recent decades, so too has the role of and need for ED social workers. The presence of a skilled ED social worker will almost always make it possible to safely discharge several patients a day to their homes—with arrangements made for the services and medical equipment needed—instead of admitting them to inpatient beds. Such needed services include physical and occupational therapists, visiting nurses for wound care, medication management, blood work, intravenous infusions, and meal preparation and delivery (“Meals on Wheels,” etc). Durable medical equipment needs include bedside commodes, rails, grab bars, and hospital beds. Even preventive medicine is now initiated by the ED social worker, who arranges for age-appropriate home-safety assessments and equipment installations for the increasing number of elderly who have “aged in place” in the same dwelling over many years.
As the percentage of ED patients over the age of 65—currently 18%—continues to rise during the next 40 to 50 years, the need for skilled ED social workers is increasing exponentially. There is frequently a need to temporarily relocate older discharged ED patients with families or friends when they are alone, for assessing whether a spouse or family member is capable of caring for a discharged patient at home, and even for arranging care of a pet for patients who live alone and require admission. Another way of looking at the current situation is that EDs now serve two clients—our patients and the hospital and healthcare system. Many patients who were formerly admitted to hospitals are now expected to be sent home from the ED to avoid diminishing hospital reimbursement for short-stay “observation services,” or denials. At the same time, the complex range and degree of health insurance coverage that patients have, and the scarce availability of appropriate, timely physician follow-up, are beyond the ability of an EP to deal with while continuing to care for other patients.
As the number of ED patients eligible for Medicare and Medicaid continues to rise, and the benefits are linked to changing requirements for length and type of care (“two-midnight rule” and observation services, for example), the 24/7 ED social worker has become a truly essential member of the ED staff—and now is the time to start ramping up the coverage.
Acknowledgments
We wish to thank NewYork Presbyterian/Weill Cornell Medical Center ED Social Workers, George Haskell, LMSW, and Laura Kramer, LMSW, for providing details regarding the home services and equipment they arrange for patients discharged from our ED.
When we think of essential nonphysician ED staff and the roles they play in the successful management of our patients, we tend to think of nurses, nurse practitioners, physician assistants, technicians, pharmacists, patient representatives, and even transporters, housekeepers, and clerks. But we typically overlook the ED social worker, without whose efforts the modern ED would come to a grinding halt. In the early years after emergency medicine (EM) became a specialty, few, if any, EDs were staffed around the clock by social workers. This was true even in the county and municipal acute care hospitals now referred to as “safety net” hospitals.
In those days, the role of the ED social worker frequently centered around contacting the appropriate agencies for cases of child abuse and sexual assault and arranging transportation or shelter for patients who were to be discharged from the ED.
But just as the roles of EM and EDs have evolved and expanded enormously in recent decades, so too has the role of and need for ED social workers. The presence of a skilled ED social worker will almost always make it possible to safely discharge several patients a day to their homes—with arrangements made for the services and medical equipment needed—instead of admitting them to inpatient beds. Such needed services include physical and occupational therapists, visiting nurses for wound care, medication management, blood work, intravenous infusions, and meal preparation and delivery (“Meals on Wheels,” etc). Durable medical equipment needs include bedside commodes, rails, grab bars, and hospital beds. Even preventive medicine is now initiated by the ED social worker, who arranges for age-appropriate home-safety assessments and equipment installations for the increasing number of elderly who have “aged in place” in the same dwelling over many years.
As the percentage of ED patients over the age of 65—currently 18%—continues to rise during the next 40 to 50 years, the need for skilled ED social workers is increasing exponentially. There is frequently a need to temporarily relocate older discharged ED patients with families or friends when they are alone, for assessing whether a spouse or family member is capable of caring for a discharged patient at home, and even for arranging care of a pet for patients who live alone and require admission. Another way of looking at the current situation is that EDs now serve two clients—our patients and the hospital and healthcare system. Many patients who were formerly admitted to hospitals are now expected to be sent home from the ED to avoid diminishing hospital reimbursement for short-stay “observation services,” or denials. At the same time, the complex range and degree of health insurance coverage that patients have, and the scarce availability of appropriate, timely physician follow-up, are beyond the ability of an EP to deal with while continuing to care for other patients.
As the number of ED patients eligible for Medicare and Medicaid continues to rise, and the benefits are linked to changing requirements for length and type of care (“two-midnight rule” and observation services, for example), the 24/7 ED social worker has become a truly essential member of the ED staff—and now is the time to start ramping up the coverage.
Acknowledgments
We wish to thank NewYork Presbyterian/Weill Cornell Medical Center ED Social Workers, George Haskell, LMSW, and Laura Kramer, LMSW, for providing details regarding the home services and equipment they arrange for patients discharged from our ED.
“Present”: Ebola’s Impact on PAs in Liberia
In November 2012 and January 2014, I traveled to Liberia to conduct a needs assessment of the health care system there on behalf of a company that was interested in supporting efforts to rebuild the country’s infrastructure. I discovered that the physician assistant profession has been in existence in Liberia since 1965—the same year that it started in the United States.
During my time in Liberia, I became close friends with Jerry Kollie, PA, President of the Liberia National Physician Assistants Association (LINPAA). I recently interviewed him to learn more about his organization and the PA profession in Liberia, where they have spent almost a year and a half dealing with the worst Ebola virus outbreak in history.
Editor’s note: The following excerpt focuses on the Ebola outbreak. Please visit our website (http://bit.ly/1NgHX2Q) to learn more about the PA profession in Liberia.
John Oliphant: What impact has the Ebola epidemic had on PAs’ clinical practice in Liberia?
Jerry Kollie: The Ebola epidemic has had a serious impact on us in many ways. It created fear among many PAs about continued clinical practice. Some of our students have lost interest in the profession for fear of contracting the virus and dying after graduation.
Workforce is also an issue. Training has been delayed, which means there are fewer PAs available in the various health facilities providing services to people. Many PAs died and others were ill with Ebola, which increased the workload in our health facilities.
The outbreak also created fear among patients; many of them stopped going to health facilities for care. As a result, PAs would go to work and not see any patients.
JO: Do you know how many PAs in Liberia lost their lives due to Ebola? And how many contracted the virus but survived?
JK: A total of 26 PAs were affected by Ebola virus disease. Many contracted the virus at their workplaces and were taken to various Ebola Treatment Units (ETUs), where some died while others survived. Of the total number, 14 died (see box on page 42 for a list of their names), nine survived, and three were quarantined but did not contract the virus. Those three PAs spent 21 days in quarantine after unknowingly attending to patients who were later confirmed to have Ebola. As God would have it, they all went through the quarantine without experiencing or developing signs or symptoms.
JO: What has been your greatest leadership challenge as the President of LINPAA during the Ebola epidemic?
JK: My greatest challenge was the stress of responding to the demands of PAs who were in the various ETUs seeking medical care; responding to the numerous calls from family members, relatives, and friends wanting me to advocate for their well-being; creating awareness and informing other PAs of the status of their colleagues; and also informing the world at large of the situation we were in. I had many sleepless days and nights, with most of those happening in the months of August, September, and October 2014, when I could not sleep at my own house. I just kept moving from one ETU, radio station, or office to another, advocating and soliciting assistance for the well-being of the health care providers—especially for PAs.
Continue for the aftermath >>
AFTERMATH
On May 9, 2015, the World Health Organization declared Liberia free of Ebola after 42 consecutive days without a new case. That changed on June 29, when Liberia experienced its first new case of Ebola virus since March 20.
In the neighboring countries of Guinea and Sierra Leone, Ebola cases are still regularly occurring (although fewer than at the peak of the outbreak).
As of August 19, 2015, 880 health care workers have become infected with the Ebola virus in Liberia, Guinea, and Sierra Leone; 512 have reportedly died. In Liberia alone, 192 health care worker deaths have been attributed to Ebola.1
REFERENCES
1. World Health Organization. Ebola Situation Report, 19 August, 2015. http://apps.who.int/ebola/current-situation/ebola-situation-report-19-august-2015. Accessed August 24, 2015.
In November 2012 and January 2014, I traveled to Liberia to conduct a needs assessment of the health care system there on behalf of a company that was interested in supporting efforts to rebuild the country’s infrastructure. I discovered that the physician assistant profession has been in existence in Liberia since 1965—the same year that it started in the United States.
During my time in Liberia, I became close friends with Jerry Kollie, PA, President of the Liberia National Physician Assistants Association (LINPAA). I recently interviewed him to learn more about his organization and the PA profession in Liberia, where they have spent almost a year and a half dealing with the worst Ebola virus outbreak in history.
Editor’s note: The following excerpt focuses on the Ebola outbreak. Please visit our website (http://bit.ly/1NgHX2Q) to learn more about the PA profession in Liberia.
John Oliphant: What impact has the Ebola epidemic had on PAs’ clinical practice in Liberia?
Jerry Kollie: The Ebola epidemic has had a serious impact on us in many ways. It created fear among many PAs about continued clinical practice. Some of our students have lost interest in the profession for fear of contracting the virus and dying after graduation.
Workforce is also an issue. Training has been delayed, which means there are fewer PAs available in the various health facilities providing services to people. Many PAs died and others were ill with Ebola, which increased the workload in our health facilities.
The outbreak also created fear among patients; many of them stopped going to health facilities for care. As a result, PAs would go to work and not see any patients.
JO: Do you know how many PAs in Liberia lost their lives due to Ebola? And how many contracted the virus but survived?
JK: A total of 26 PAs were affected by Ebola virus disease. Many contracted the virus at their workplaces and were taken to various Ebola Treatment Units (ETUs), where some died while others survived. Of the total number, 14 died (see box on page 42 for a list of their names), nine survived, and three were quarantined but did not contract the virus. Those three PAs spent 21 days in quarantine after unknowingly attending to patients who were later confirmed to have Ebola. As God would have it, they all went through the quarantine without experiencing or developing signs or symptoms.
JO: What has been your greatest leadership challenge as the President of LINPAA during the Ebola epidemic?
JK: My greatest challenge was the stress of responding to the demands of PAs who were in the various ETUs seeking medical care; responding to the numerous calls from family members, relatives, and friends wanting me to advocate for their well-being; creating awareness and informing other PAs of the status of their colleagues; and also informing the world at large of the situation we were in. I had many sleepless days and nights, with most of those happening in the months of August, September, and October 2014, when I could not sleep at my own house. I just kept moving from one ETU, radio station, or office to another, advocating and soliciting assistance for the well-being of the health care providers—especially for PAs.
Continue for the aftermath >>
AFTERMATH
On May 9, 2015, the World Health Organization declared Liberia free of Ebola after 42 consecutive days without a new case. That changed on June 29, when Liberia experienced its first new case of Ebola virus since March 20.
In the neighboring countries of Guinea and Sierra Leone, Ebola cases are still regularly occurring (although fewer than at the peak of the outbreak).
As of August 19, 2015, 880 health care workers have become infected with the Ebola virus in Liberia, Guinea, and Sierra Leone; 512 have reportedly died. In Liberia alone, 192 health care worker deaths have been attributed to Ebola.1
REFERENCES
1. World Health Organization. Ebola Situation Report, 19 August, 2015. http://apps.who.int/ebola/current-situation/ebola-situation-report-19-august-2015. Accessed August 24, 2015.
In November 2012 and January 2014, I traveled to Liberia to conduct a needs assessment of the health care system there on behalf of a company that was interested in supporting efforts to rebuild the country’s infrastructure. I discovered that the physician assistant profession has been in existence in Liberia since 1965—the same year that it started in the United States.
During my time in Liberia, I became close friends with Jerry Kollie, PA, President of the Liberia National Physician Assistants Association (LINPAA). I recently interviewed him to learn more about his organization and the PA profession in Liberia, where they have spent almost a year and a half dealing with the worst Ebola virus outbreak in history.
Editor’s note: The following excerpt focuses on the Ebola outbreak. Please visit our website (http://bit.ly/1NgHX2Q) to learn more about the PA profession in Liberia.
John Oliphant: What impact has the Ebola epidemic had on PAs’ clinical practice in Liberia?
Jerry Kollie: The Ebola epidemic has had a serious impact on us in many ways. It created fear among many PAs about continued clinical practice. Some of our students have lost interest in the profession for fear of contracting the virus and dying after graduation.
Workforce is also an issue. Training has been delayed, which means there are fewer PAs available in the various health facilities providing services to people. Many PAs died and others were ill with Ebola, which increased the workload in our health facilities.
The outbreak also created fear among patients; many of them stopped going to health facilities for care. As a result, PAs would go to work and not see any patients.
JO: Do you know how many PAs in Liberia lost their lives due to Ebola? And how many contracted the virus but survived?
JK: A total of 26 PAs were affected by Ebola virus disease. Many contracted the virus at their workplaces and were taken to various Ebola Treatment Units (ETUs), where some died while others survived. Of the total number, 14 died (see box on page 42 for a list of their names), nine survived, and three were quarantined but did not contract the virus. Those three PAs spent 21 days in quarantine after unknowingly attending to patients who were later confirmed to have Ebola. As God would have it, they all went through the quarantine without experiencing or developing signs or symptoms.
JO: What has been your greatest leadership challenge as the President of LINPAA during the Ebola epidemic?
JK: My greatest challenge was the stress of responding to the demands of PAs who were in the various ETUs seeking medical care; responding to the numerous calls from family members, relatives, and friends wanting me to advocate for their well-being; creating awareness and informing other PAs of the status of their colleagues; and also informing the world at large of the situation we were in. I had many sleepless days and nights, with most of those happening in the months of August, September, and October 2014, when I could not sleep at my own house. I just kept moving from one ETU, radio station, or office to another, advocating and soliciting assistance for the well-being of the health care providers—especially for PAs.
Continue for the aftermath >>
AFTERMATH
On May 9, 2015, the World Health Organization declared Liberia free of Ebola after 42 consecutive days without a new case. That changed on June 29, when Liberia experienced its first new case of Ebola virus since March 20.
In the neighboring countries of Guinea and Sierra Leone, Ebola cases are still regularly occurring (although fewer than at the peak of the outbreak).
As of August 19, 2015, 880 health care workers have become infected with the Ebola virus in Liberia, Guinea, and Sierra Leone; 512 have reportedly died. In Liberia alone, 192 health care worker deaths have been attributed to Ebola.1
REFERENCES
1. World Health Organization. Ebola Situation Report, 19 August, 2015. http://apps.who.int/ebola/current-situation/ebola-situation-report-19-august-2015. Accessed August 24, 2015.
Cases of liver failure linked to “fat-burning” supplement
In late 2013, there were 45 cases of acute liver failure (ALF) in Hawaii, and 29 of those people reported taking OxyELITE Pro (an herbal dietary supplement marketed for weight reduction and “fat-burning”) 60 days before illness onset. Of 8 initial cases, 2 patients needed urgent liver transplants, one died, and 5 eventually recovered.1 The manufacturer of OxyELITE Pro voluntarily recalled the product after receiving a warning letter from the US Food and Drug Administration (FDA).
One way to prevent situations like this from occurring might be to ban the sale of weight loss or sports enhancement supplements unless they are rigorously tested and approved by the FDA. Voluntary reporting to the FDA is time-consuming and it takes time for the FDA to follow up on these reports.
As primary care physicians, we need to consistently ask patients about their use of supplements, educate them about the potential dangers, and identify those who are experiencing adverse reactions. While we can’t put a stop to the harm that some herbal dietary supplements might inflict on a public eager to embrace quick fixes for weight loss and improved strength, we can be the best first responders.
Linda L. Wong, MD
Honolulu, Hawaii
Reference
1. Centers for Disease Control and Prevention (CDC). Notes from the field: acute hepatitis and liver failure following the use of a dietary supplement intended for weight loss or muscle building—May-October 2013. MMWR Morb Mortal Wkly Rep. 2013;62:817-819.
In late 2013, there were 45 cases of acute liver failure (ALF) in Hawaii, and 29 of those people reported taking OxyELITE Pro (an herbal dietary supplement marketed for weight reduction and “fat-burning”) 60 days before illness onset. Of 8 initial cases, 2 patients needed urgent liver transplants, one died, and 5 eventually recovered.1 The manufacturer of OxyELITE Pro voluntarily recalled the product after receiving a warning letter from the US Food and Drug Administration (FDA).
One way to prevent situations like this from occurring might be to ban the sale of weight loss or sports enhancement supplements unless they are rigorously tested and approved by the FDA. Voluntary reporting to the FDA is time-consuming and it takes time for the FDA to follow up on these reports.
As primary care physicians, we need to consistently ask patients about their use of supplements, educate them about the potential dangers, and identify those who are experiencing adverse reactions. While we can’t put a stop to the harm that some herbal dietary supplements might inflict on a public eager to embrace quick fixes for weight loss and improved strength, we can be the best first responders.
Linda L. Wong, MD
Honolulu, Hawaii
In late 2013, there were 45 cases of acute liver failure (ALF) in Hawaii, and 29 of those people reported taking OxyELITE Pro (an herbal dietary supplement marketed for weight reduction and “fat-burning”) 60 days before illness onset. Of 8 initial cases, 2 patients needed urgent liver transplants, one died, and 5 eventually recovered.1 The manufacturer of OxyELITE Pro voluntarily recalled the product after receiving a warning letter from the US Food and Drug Administration (FDA).
One way to prevent situations like this from occurring might be to ban the sale of weight loss or sports enhancement supplements unless they are rigorously tested and approved by the FDA. Voluntary reporting to the FDA is time-consuming and it takes time for the FDA to follow up on these reports.
As primary care physicians, we need to consistently ask patients about their use of supplements, educate them about the potential dangers, and identify those who are experiencing adverse reactions. While we can’t put a stop to the harm that some herbal dietary supplements might inflict on a public eager to embrace quick fixes for weight loss and improved strength, we can be the best first responders.
Linda L. Wong, MD
Honolulu, Hawaii
Reference
1. Centers for Disease Control and Prevention (CDC). Notes from the field: acute hepatitis and liver failure following the use of a dietary supplement intended for weight loss or muscle building—May-October 2013. MMWR Morb Mortal Wkly Rep. 2013;62:817-819.
Reference
1. Centers for Disease Control and Prevention (CDC). Notes from the field: acute hepatitis and liver failure following the use of a dietary supplement intended for weight loss or muscle building—May-October 2013. MMWR Morb Mortal Wkly Rep. 2013;62:817-819.