User login
Too little time and too many worries for social media
I’m not on Facebook, either professionally or personally.
My office doesn’t have a Twitter account.
In fact, my only nod to social media at all is a rarely updated LinkedIn page, which is really just a public CV.
Why, in this age of connectedness, do I hide from these things? One reason is time. There isn’t much of it in the course of a day. Between my practice (patients, dictations, forms, returning calls, reviewing tests, rinse, wash, repeat), my family (wife, kids, dogs, house), and all the other things that make up a day (driving, finances, bathing, sleep), I don’t have much extra time. I really have no desire to see what others had for breakfast, look at pictures of a distant cousin’s kids, or have an online political argument with in-laws.
Another reason is privacy. Most patients are good people, but there are scary ones, too. I don’t want them knowing my kids’ names, or what school they go to, or seeing their pictures. In this age trying to have a degree of personal privacy is hard enough. I don’t want to make it any easier for someone looking to cause trouble.
I have nothing against my patients. I like the majority of them. But I don’t want to be online friends with them, either. Practicing objective medicine requires a degree of emotional distance, and I don’t want to do anything to shorten that. Social media connections with someone may also clue you into their personal and political beliefs, and, as I’ve said before, I think knowing those about patients (and them knowing mine) can only make the relationship difficult.
And the last is from a medical-legal view. The definition of what constitutes medical advice seems to be quite vague, and I worry anything I innocuously post or tweet could be taken to mean that I had an established treating medical relationship with someone or that my malpractice carrier could raise my rates by saying I was doing online medicine.
There’s also the simple fact that anything can be interpreted in any way. I worry that something I might put up could be used against me in court. Let’s say a patient dies while I’m on vacation, and the family decides to sue. Pictures of me relaxing with my kids on the trip could be used to make me look like an uncaring, callous doctor, even if I had no idea what was going on back home.
I’ll keep my somewhat under-the-radar personal existence as it is. Others may feel I’m missing out on the wonders of the social age, but I’m happy with keeping my home life just that – at home.
Dr. Block has a solo neurology practice in Scottsdale, Ariz.
I’m not on Facebook, either professionally or personally.
My office doesn’t have a Twitter account.
In fact, my only nod to social media at all is a rarely updated LinkedIn page, which is really just a public CV.
Why, in this age of connectedness, do I hide from these things? One reason is time. There isn’t much of it in the course of a day. Between my practice (patients, dictations, forms, returning calls, reviewing tests, rinse, wash, repeat), my family (wife, kids, dogs, house), and all the other things that make up a day (driving, finances, bathing, sleep), I don’t have much extra time. I really have no desire to see what others had for breakfast, look at pictures of a distant cousin’s kids, or have an online political argument with in-laws.
Another reason is privacy. Most patients are good people, but there are scary ones, too. I don’t want them knowing my kids’ names, or what school they go to, or seeing their pictures. In this age trying to have a degree of personal privacy is hard enough. I don’t want to make it any easier for someone looking to cause trouble.
I have nothing against my patients. I like the majority of them. But I don’t want to be online friends with them, either. Practicing objective medicine requires a degree of emotional distance, and I don’t want to do anything to shorten that. Social media connections with someone may also clue you into their personal and political beliefs, and, as I’ve said before, I think knowing those about patients (and them knowing mine) can only make the relationship difficult.
And the last is from a medical-legal view. The definition of what constitutes medical advice seems to be quite vague, and I worry anything I innocuously post or tweet could be taken to mean that I had an established treating medical relationship with someone or that my malpractice carrier could raise my rates by saying I was doing online medicine.
There’s also the simple fact that anything can be interpreted in any way. I worry that something I might put up could be used against me in court. Let’s say a patient dies while I’m on vacation, and the family decides to sue. Pictures of me relaxing with my kids on the trip could be used to make me look like an uncaring, callous doctor, even if I had no idea what was going on back home.
I’ll keep my somewhat under-the-radar personal existence as it is. Others may feel I’m missing out on the wonders of the social age, but I’m happy with keeping my home life just that – at home.
Dr. Block has a solo neurology practice in Scottsdale, Ariz.
I’m not on Facebook, either professionally or personally.
My office doesn’t have a Twitter account.
In fact, my only nod to social media at all is a rarely updated LinkedIn page, which is really just a public CV.
Why, in this age of connectedness, do I hide from these things? One reason is time. There isn’t much of it in the course of a day. Between my practice (patients, dictations, forms, returning calls, reviewing tests, rinse, wash, repeat), my family (wife, kids, dogs, house), and all the other things that make up a day (driving, finances, bathing, sleep), I don’t have much extra time. I really have no desire to see what others had for breakfast, look at pictures of a distant cousin’s kids, or have an online political argument with in-laws.
Another reason is privacy. Most patients are good people, but there are scary ones, too. I don’t want them knowing my kids’ names, or what school they go to, or seeing their pictures. In this age trying to have a degree of personal privacy is hard enough. I don’t want to make it any easier for someone looking to cause trouble.
I have nothing against my patients. I like the majority of them. But I don’t want to be online friends with them, either. Practicing objective medicine requires a degree of emotional distance, and I don’t want to do anything to shorten that. Social media connections with someone may also clue you into their personal and political beliefs, and, as I’ve said before, I think knowing those about patients (and them knowing mine) can only make the relationship difficult.
And the last is from a medical-legal view. The definition of what constitutes medical advice seems to be quite vague, and I worry anything I innocuously post or tweet could be taken to mean that I had an established treating medical relationship with someone or that my malpractice carrier could raise my rates by saying I was doing online medicine.
There’s also the simple fact that anything can be interpreted in any way. I worry that something I might put up could be used against me in court. Let’s say a patient dies while I’m on vacation, and the family decides to sue. Pictures of me relaxing with my kids on the trip could be used to make me look like an uncaring, callous doctor, even if I had no idea what was going on back home.
I’ll keep my somewhat under-the-radar personal existence as it is. Others may feel I’m missing out on the wonders of the social age, but I’m happy with keeping my home life just that – at home.
Dr. Block has a solo neurology practice in Scottsdale, Ariz.
It's All About the Spit!
Remember eighth grade, when you were taught the correlation between pH and saliva? You learned that testing saliva provides information on whether the mouth is an acidic, basic, or neutral environment. But did you ever suspect then that saliva would become a formidable instrument for medical diagnosis, health, and research?
It’s true, friends and colleagues: Spit is the latest, greatest trend in health care! This important physiologic fluid, which contains a highly complex assortment of substances, is rapidly gaining notice as a diagnostic tool. Don’t believe it? Read on!
The oral cavity, according to Dr. Jack Dillenberg, the inaugural dean of the Arizona School of Dentistry and Oral Health (ASDOH), “is the gateway and window into health in our body. The signs of nutritional deficiencies, general infections, and systemic diseases that affect the entire body may first become apparent in the oral cavity via lesions or other oral problems. Saliva plays a significant role in maintaining oral health and has a strong correlation to tooth decay.”1
Yes, we’ve known for a while that an adequate amount of saliva serves as a pH buffer; when plaque pH drops below 5.5, dental caries can occur. But according to researchers at The Johns Hopkins University’s Center for Interdisciplinary Salivary Bioscience Research (yes, a research center dedicated to spit!), saliva holds a wealth of data that is easily collected and economically analyzed and may be a key to many mysteries of human biology and genetics, as well as a helpful tool to combat disease. “There’s lots of potential in exploring what’s in saliva,” according to Dr. Doug Granger, the center’s director and a psychoneuroendocrinologist (what a mouthful—pun intended!) at Arizona State University.2
Saliva in the mouth forms a thin film that protects against dental caries, erosion, attrition, abrasion, periodontal diseases, candidiasis, and abrasive mucosal lesions. Studies suggest saliva may be useful in detecting heart disease, acid reflux, and diabetes; it is already being used for rapid HIV testing.3-5 Researchers have also reported encouraging results in the use of saliva for the diagnosis of autoimmune disorders, breast cancer, oral cancers, gum disease, and cardiovascular, endocrine, and infectious diseases.6,7
Is saliva screening the new "blood test"?
So is saliva screening the new “blood test”? Blood testing, performed as an aid to diagnosis, has its drawbacks: Samples are often uncomfortable to obtain, a lab visit may be necessary, and processing takes time. Finding a reasonable alternative would be beneficial, but there are several steps to such a process.
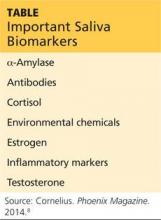
The capacity to monitor health status, disease onset and progression, and treatment outcomes through noninvasive means is a goal in health care promotion and delivery. For this to occur, three things must happen: first, specific biomarkers associated with a health or disease state must be established; second, a noninvasive manner to detect and monitor those biomarkers must be developed; and third, a mechanism to differentiate between the results is needed. Dr. Granger’s team has been studying the possibilities for several years now. Some of the key biomarkers measurable via saliva are listed in the Table below.8
Meanwhile, Dr. Tony Hashemian and colleagues at the ASDOH have developed a diagnostic tool based on pH. The purpose of their pH of Oral Health (pH2OH) initiative is to deliver new technology for pH saliva testing.9 This innovation uses a mobile phone application to capture time-sensitive data and to communicate with a server (in compliance with HIPAA regulations, of course).
Next page: Saliva-testing examination tool >>
A saliva-testing examination tool is used by the dental team to educate patients, inform preventive treatment planning, and assist with proper selection of dental materials to initiate changes in the patient’s oral hygiene. Dental teams measure saliva pH with test strips—the litmus paper we used even as kids in school. It is simply a strip of colored paper that, when soaked in sample saliva, turns a different color depending on the pH level. The color scale ranges from red (indicating a strong acidic state [pH < 3]) to dark blue or purple (indicating a strong alkaline state [pH > 11]).
The free iPhone or Android app developed by Dr. Hashemian’s team is designed to capture the pH value for a patient. The app can manually set the value, or you can take a picture of a test strip and auto-calculate the pH using color-coding analysis. Once set, the app will allow you to save the data and track improvements to oral pH over time.9
With improvements in immunology, microbiology, and biochemistry, salivary testing—in both research and clinical settings—may prove to be an applied and reliable means of recognizing oral signs of systemic illness and exposure to risk factors.10 Salivary diagnostics will be the next great breakthrough in improving the general health of the public. Stay tuned.
What are your thoughts about how “spit” could be applied clinically? Contact me at [email protected].
REFERENCES
1. Personal communication. February 17, 2015.
2. Walker AK. Researchers eye saliva for patient testing. Baltimore Sun. May 23, 2012.
3. Devi TJ. Saliva: a potential diagnostic tool. J Dental Med Sci. 2014;13(2):52-57.
4. Giannobile WV, Beikler T, Kinney JS, et al. Saliva as a diagnostic tool for periodontal disease: current state and future directions. Periodontol 2000. 2009;50:52-64.
5. Gopinath VK, Arzreanne AR. Saliva as a diagnostic tool for assessment of dental caries. Arch Orofacial Sci. 2006;1:57-59.
6. Streckfus CF, Bigler LR. Salivary glands and saliva: saliva as a diagnostic fluid. Oral Dis. 2002;8:69-76.
7. Lee JM, Garon E, Wong DR. Salivary diagnostics. Orthod Cranioffac Res. 2009;12:206211.
8. Cornelius K. Spit, polished. Phoenix Magazine. November 2014; 38.
9. AT Still University, Arizona School of Dentistry and Oral Health. pH2OH. www.ph2oh.com/apps/. Accessed March 21, 2015.
10. Lawrence HP. Salivary markers of systemic disease: noninvasive diagnosis of disease and monitoring of general health. J Can Dent Assoc. 2002;68(3):170-174.
Remember eighth grade, when you were taught the correlation between pH and saliva? You learned that testing saliva provides information on whether the mouth is an acidic, basic, or neutral environment. But did you ever suspect then that saliva would become a formidable instrument for medical diagnosis, health, and research?
It’s true, friends and colleagues: Spit is the latest, greatest trend in health care! This important physiologic fluid, which contains a highly complex assortment of substances, is rapidly gaining notice as a diagnostic tool. Don’t believe it? Read on!
The oral cavity, according to Dr. Jack Dillenberg, the inaugural dean of the Arizona School of Dentistry and Oral Health (ASDOH), “is the gateway and window into health in our body. The signs of nutritional deficiencies, general infections, and systemic diseases that affect the entire body may first become apparent in the oral cavity via lesions or other oral problems. Saliva plays a significant role in maintaining oral health and has a strong correlation to tooth decay.”1
Yes, we’ve known for a while that an adequate amount of saliva serves as a pH buffer; when plaque pH drops below 5.5, dental caries can occur. But according to researchers at The Johns Hopkins University’s Center for Interdisciplinary Salivary Bioscience Research (yes, a research center dedicated to spit!), saliva holds a wealth of data that is easily collected and economically analyzed and may be a key to many mysteries of human biology and genetics, as well as a helpful tool to combat disease. “There’s lots of potential in exploring what’s in saliva,” according to Dr. Doug Granger, the center’s director and a psychoneuroendocrinologist (what a mouthful—pun intended!) at Arizona State University.2
Saliva in the mouth forms a thin film that protects against dental caries, erosion, attrition, abrasion, periodontal diseases, candidiasis, and abrasive mucosal lesions. Studies suggest saliva may be useful in detecting heart disease, acid reflux, and diabetes; it is already being used for rapid HIV testing.3-5 Researchers have also reported encouraging results in the use of saliva for the diagnosis of autoimmune disorders, breast cancer, oral cancers, gum disease, and cardiovascular, endocrine, and infectious diseases.6,7
Is saliva screening the new "blood test"?
So is saliva screening the new “blood test”? Blood testing, performed as an aid to diagnosis, has its drawbacks: Samples are often uncomfortable to obtain, a lab visit may be necessary, and processing takes time. Finding a reasonable alternative would be beneficial, but there are several steps to such a process.
The capacity to monitor health status, disease onset and progression, and treatment outcomes through noninvasive means is a goal in health care promotion and delivery. For this to occur, three things must happen: first, specific biomarkers associated with a health or disease state must be established; second, a noninvasive manner to detect and monitor those biomarkers must be developed; and third, a mechanism to differentiate between the results is needed. Dr. Granger’s team has been studying the possibilities for several years now. Some of the key biomarkers measurable via saliva are listed in the Table below.8
Meanwhile, Dr. Tony Hashemian and colleagues at the ASDOH have developed a diagnostic tool based on pH. The purpose of their pH of Oral Health (pH2OH) initiative is to deliver new technology for pH saliva testing.9 This innovation uses a mobile phone application to capture time-sensitive data and to communicate with a server (in compliance with HIPAA regulations, of course).
Next page: Saliva-testing examination tool >>
A saliva-testing examination tool is used by the dental team to educate patients, inform preventive treatment planning, and assist with proper selection of dental materials to initiate changes in the patient’s oral hygiene. Dental teams measure saliva pH with test strips—the litmus paper we used even as kids in school. It is simply a strip of colored paper that, when soaked in sample saliva, turns a different color depending on the pH level. The color scale ranges from red (indicating a strong acidic state [pH < 3]) to dark blue or purple (indicating a strong alkaline state [pH > 11]).
The free iPhone or Android app developed by Dr. Hashemian’s team is designed to capture the pH value for a patient. The app can manually set the value, or you can take a picture of a test strip and auto-calculate the pH using color-coding analysis. Once set, the app will allow you to save the data and track improvements to oral pH over time.9
With improvements in immunology, microbiology, and biochemistry, salivary testing—in both research and clinical settings—may prove to be an applied and reliable means of recognizing oral signs of systemic illness and exposure to risk factors.10 Salivary diagnostics will be the next great breakthrough in improving the general health of the public. Stay tuned.
What are your thoughts about how “spit” could be applied clinically? Contact me at [email protected].
REFERENCES
1. Personal communication. February 17, 2015.
2. Walker AK. Researchers eye saliva for patient testing. Baltimore Sun. May 23, 2012.
3. Devi TJ. Saliva: a potential diagnostic tool. J Dental Med Sci. 2014;13(2):52-57.
4. Giannobile WV, Beikler T, Kinney JS, et al. Saliva as a diagnostic tool for periodontal disease: current state and future directions. Periodontol 2000. 2009;50:52-64.
5. Gopinath VK, Arzreanne AR. Saliva as a diagnostic tool for assessment of dental caries. Arch Orofacial Sci. 2006;1:57-59.
6. Streckfus CF, Bigler LR. Salivary glands and saliva: saliva as a diagnostic fluid. Oral Dis. 2002;8:69-76.
7. Lee JM, Garon E, Wong DR. Salivary diagnostics. Orthod Cranioffac Res. 2009;12:206211.
8. Cornelius K. Spit, polished. Phoenix Magazine. November 2014; 38.
9. AT Still University, Arizona School of Dentistry and Oral Health. pH2OH. www.ph2oh.com/apps/. Accessed March 21, 2015.
10. Lawrence HP. Salivary markers of systemic disease: noninvasive diagnosis of disease and monitoring of general health. J Can Dent Assoc. 2002;68(3):170-174.
Remember eighth grade, when you were taught the correlation between pH and saliva? You learned that testing saliva provides information on whether the mouth is an acidic, basic, or neutral environment. But did you ever suspect then that saliva would become a formidable instrument for medical diagnosis, health, and research?
It’s true, friends and colleagues: Spit is the latest, greatest trend in health care! This important physiologic fluid, which contains a highly complex assortment of substances, is rapidly gaining notice as a diagnostic tool. Don’t believe it? Read on!
The oral cavity, according to Dr. Jack Dillenberg, the inaugural dean of the Arizona School of Dentistry and Oral Health (ASDOH), “is the gateway and window into health in our body. The signs of nutritional deficiencies, general infections, and systemic diseases that affect the entire body may first become apparent in the oral cavity via lesions or other oral problems. Saliva plays a significant role in maintaining oral health and has a strong correlation to tooth decay.”1
Yes, we’ve known for a while that an adequate amount of saliva serves as a pH buffer; when plaque pH drops below 5.5, dental caries can occur. But according to researchers at The Johns Hopkins University’s Center for Interdisciplinary Salivary Bioscience Research (yes, a research center dedicated to spit!), saliva holds a wealth of data that is easily collected and economically analyzed and may be a key to many mysteries of human biology and genetics, as well as a helpful tool to combat disease. “There’s lots of potential in exploring what’s in saliva,” according to Dr. Doug Granger, the center’s director and a psychoneuroendocrinologist (what a mouthful—pun intended!) at Arizona State University.2
Saliva in the mouth forms a thin film that protects against dental caries, erosion, attrition, abrasion, periodontal diseases, candidiasis, and abrasive mucosal lesions. Studies suggest saliva may be useful in detecting heart disease, acid reflux, and diabetes; it is already being used for rapid HIV testing.3-5 Researchers have also reported encouraging results in the use of saliva for the diagnosis of autoimmune disorders, breast cancer, oral cancers, gum disease, and cardiovascular, endocrine, and infectious diseases.6,7
Is saliva screening the new "blood test"?
So is saliva screening the new “blood test”? Blood testing, performed as an aid to diagnosis, has its drawbacks: Samples are often uncomfortable to obtain, a lab visit may be necessary, and processing takes time. Finding a reasonable alternative would be beneficial, but there are several steps to such a process.
The capacity to monitor health status, disease onset and progression, and treatment outcomes through noninvasive means is a goal in health care promotion and delivery. For this to occur, three things must happen: first, specific biomarkers associated with a health or disease state must be established; second, a noninvasive manner to detect and monitor those biomarkers must be developed; and third, a mechanism to differentiate between the results is needed. Dr. Granger’s team has been studying the possibilities for several years now. Some of the key biomarkers measurable via saliva are listed in the Table below.8
Meanwhile, Dr. Tony Hashemian and colleagues at the ASDOH have developed a diagnostic tool based on pH. The purpose of their pH of Oral Health (pH2OH) initiative is to deliver new technology for pH saliva testing.9 This innovation uses a mobile phone application to capture time-sensitive data and to communicate with a server (in compliance with HIPAA regulations, of course).
Next page: Saliva-testing examination tool >>
A saliva-testing examination tool is used by the dental team to educate patients, inform preventive treatment planning, and assist with proper selection of dental materials to initiate changes in the patient’s oral hygiene. Dental teams measure saliva pH with test strips—the litmus paper we used even as kids in school. It is simply a strip of colored paper that, when soaked in sample saliva, turns a different color depending on the pH level. The color scale ranges from red (indicating a strong acidic state [pH < 3]) to dark blue or purple (indicating a strong alkaline state [pH > 11]).
The free iPhone or Android app developed by Dr. Hashemian’s team is designed to capture the pH value for a patient. The app can manually set the value, or you can take a picture of a test strip and auto-calculate the pH using color-coding analysis. Once set, the app will allow you to save the data and track improvements to oral pH over time.9
With improvements in immunology, microbiology, and biochemistry, salivary testing—in both research and clinical settings—may prove to be an applied and reliable means of recognizing oral signs of systemic illness and exposure to risk factors.10 Salivary diagnostics will be the next great breakthrough in improving the general health of the public. Stay tuned.
What are your thoughts about how “spit” could be applied clinically? Contact me at [email protected].
REFERENCES
1. Personal communication. February 17, 2015.
2. Walker AK. Researchers eye saliva for patient testing. Baltimore Sun. May 23, 2012.
3. Devi TJ. Saliva: a potential diagnostic tool. J Dental Med Sci. 2014;13(2):52-57.
4. Giannobile WV, Beikler T, Kinney JS, et al. Saliva as a diagnostic tool for periodontal disease: current state and future directions. Periodontol 2000. 2009;50:52-64.
5. Gopinath VK, Arzreanne AR. Saliva as a diagnostic tool for assessment of dental caries. Arch Orofacial Sci. 2006;1:57-59.
6. Streckfus CF, Bigler LR. Salivary glands and saliva: saliva as a diagnostic fluid. Oral Dis. 2002;8:69-76.
7. Lee JM, Garon E, Wong DR. Salivary diagnostics. Orthod Cranioffac Res. 2009;12:206211.
8. Cornelius K. Spit, polished. Phoenix Magazine. November 2014; 38.
9. AT Still University, Arizona School of Dentistry and Oral Health. pH2OH. www.ph2oh.com/apps/. Accessed March 21, 2015.
10. Lawrence HP. Salivary markers of systemic disease: noninvasive diagnosis of disease and monitoring of general health. J Can Dent Assoc. 2002;68(3):170-174.
Poison plants
After a long, cold, snowy winter, I actually cheered at the first site of a purple crocus emerging from my front yard. Spring brings with it warmer weather, outdoor sports, blooming flowers, and trees full of leaves. Unfortunately, it also brings some less-desirable plants with it as well, such as poison ivy, poison oak, and poison sumac. As your patients happily emerge from their houses to play outside, some will inevitably end up in your offices itching and uncomfortable from contact dermatitis. As many as 50% of people who come in contact with these plants will have a reaction.
As with most illnesses, prevention is the best cure. Once a child (or adult, for that matter) has been exposed to poison ivy, oak, or sumac, from the genus Toxicodendron, the best you can do is try and relieve symptoms until the dermatitis resolves on its own.
The first step in prevention is recognition. The old adage, “Leaves of three, let them be” – describing three leaflets, often with small black dots, arising from a reddish stem – is generally accurate; however, there are some exceptions to this rule depending on the type of plant (particularly poison sumac) and geographic location. If you aren’t already aware of the species in your area, it is worth spending a few minutes researching what types of plants are common locally (www.cdc.gov/niosh/topics/plants).
Avoiding all contact with these plants is best; long pants, shirt sleeves, and gloves help avoid exposure, but this is often not practical for a child playing outside, and urushiol (the allergenic substance on the surface of these plants) adheres to clothes, and pets, and other things. … If known or potential exposure has happened, it is best to wash all areas of your skin as soon as possible, particularly focusing on hands and under your fingernails. There are a variety of products such as Tecnu, Zanfel, and Goop Hand Cleaner, which are effective at preventing reactions after exposure has occurred (and, in the case of Zanfel, can also relieve symptoms if a reaction occurs); however, these products can be pricey and not always on hand when you need them. Topical dish washing soap has been found in one study to be an effective alternative (Dial Ultra Dish washing Soap [no longer available] was the product used, but any surfactant-based dish washing detergent is likely effective).*
However, speaking from experience, even the best efforts to avoid or minimize exposure are not always successful. Symptoms usually occur within the first 4 days of exposure, with lesions cropping up at different times depending on the location and type of skin and intensity of exposure to urushiol. Lesions are typically very itchy and can be plaques, papules, vesicles, or bullae. It is commonly believed that the lesions can be “spread” through contact with the fluid inside these vesicles or other parts of the lesions; however, this is not in fact true. This misperception likely stems from the fact, as noted, that the lesions do appear at different times after exposure to the plant, which can make it seem as if they are spreading from one site to another. Reactions can peak anywhere from 1 day to 2 weeks after exposure and can last for several weeks. Again, speaking from experience, this is a long time to be itchy and uncomfortable, especially for young children, so management of symptoms is very important.
There are many strategies and commercial products that can help reduce itching and irritation. First, it is important to keep the skin clean and not to cause breaks in the skin through itching, hard as that may be, in order to avoid bacterial superinfection. Gentle interventions such as oatmeal baths or cool wet compresses may be helpful; swimming may also provide relief. Topical medications can play a role – topical corticosteroids, particularly higher dose, can be helpful in relief of symptoms. Calamine lotion, products containing menthol, and topical astringents are other effective options. Oral antihistamines are not terribly effective, as the itching is not caused by histamine, however, the sedating effects can help patients get some rest at night. For severe cases, oral corticosteroids are sometimes used, but care must be taken to give a long enough course to avoid rebound. And, perhaps most importantly, provide reassurance that this will get better eventually! As with most things in pediatrics, preventative measures and supportive care are key to making sure your patients enjoy their spring and summer without too much discomfort!
Dr. Beers is an assistant professor of pediatrics at Children’s National Medical Center and the George Washington University Medical Center, Washington. She is chair of the American Academy of Pediatrics Committee on Residency Scholarships and immediate past president of the District of Columbia chapter of the American Academy of Pediatrics. E-mail Dr. Beers at [email protected].
* This story was updated 3/26/2015.
After a long, cold, snowy winter, I actually cheered at the first site of a purple crocus emerging from my front yard. Spring brings with it warmer weather, outdoor sports, blooming flowers, and trees full of leaves. Unfortunately, it also brings some less-desirable plants with it as well, such as poison ivy, poison oak, and poison sumac. As your patients happily emerge from their houses to play outside, some will inevitably end up in your offices itching and uncomfortable from contact dermatitis. As many as 50% of people who come in contact with these plants will have a reaction.
As with most illnesses, prevention is the best cure. Once a child (or adult, for that matter) has been exposed to poison ivy, oak, or sumac, from the genus Toxicodendron, the best you can do is try and relieve symptoms until the dermatitis resolves on its own.
The first step in prevention is recognition. The old adage, “Leaves of three, let them be” – describing three leaflets, often with small black dots, arising from a reddish stem – is generally accurate; however, there are some exceptions to this rule depending on the type of plant (particularly poison sumac) and geographic location. If you aren’t already aware of the species in your area, it is worth spending a few minutes researching what types of plants are common locally (www.cdc.gov/niosh/topics/plants).
Avoiding all contact with these plants is best; long pants, shirt sleeves, and gloves help avoid exposure, but this is often not practical for a child playing outside, and urushiol (the allergenic substance on the surface of these plants) adheres to clothes, and pets, and other things. … If known or potential exposure has happened, it is best to wash all areas of your skin as soon as possible, particularly focusing on hands and under your fingernails. There are a variety of products such as Tecnu, Zanfel, and Goop Hand Cleaner, which are effective at preventing reactions after exposure has occurred (and, in the case of Zanfel, can also relieve symptoms if a reaction occurs); however, these products can be pricey and not always on hand when you need them. Topical dish washing soap has been found in one study to be an effective alternative (Dial Ultra Dish washing Soap [no longer available] was the product used, but any surfactant-based dish washing detergent is likely effective).*
However, speaking from experience, even the best efforts to avoid or minimize exposure are not always successful. Symptoms usually occur within the first 4 days of exposure, with lesions cropping up at different times depending on the location and type of skin and intensity of exposure to urushiol. Lesions are typically very itchy and can be plaques, papules, vesicles, or bullae. It is commonly believed that the lesions can be “spread” through contact with the fluid inside these vesicles or other parts of the lesions; however, this is not in fact true. This misperception likely stems from the fact, as noted, that the lesions do appear at different times after exposure to the plant, which can make it seem as if they are spreading from one site to another. Reactions can peak anywhere from 1 day to 2 weeks after exposure and can last for several weeks. Again, speaking from experience, this is a long time to be itchy and uncomfortable, especially for young children, so management of symptoms is very important.
There are many strategies and commercial products that can help reduce itching and irritation. First, it is important to keep the skin clean and not to cause breaks in the skin through itching, hard as that may be, in order to avoid bacterial superinfection. Gentle interventions such as oatmeal baths or cool wet compresses may be helpful; swimming may also provide relief. Topical medications can play a role – topical corticosteroids, particularly higher dose, can be helpful in relief of symptoms. Calamine lotion, products containing menthol, and topical astringents are other effective options. Oral antihistamines are not terribly effective, as the itching is not caused by histamine, however, the sedating effects can help patients get some rest at night. For severe cases, oral corticosteroids are sometimes used, but care must be taken to give a long enough course to avoid rebound. And, perhaps most importantly, provide reassurance that this will get better eventually! As with most things in pediatrics, preventative measures and supportive care are key to making sure your patients enjoy their spring and summer without too much discomfort!
Dr. Beers is an assistant professor of pediatrics at Children’s National Medical Center and the George Washington University Medical Center, Washington. She is chair of the American Academy of Pediatrics Committee on Residency Scholarships and immediate past president of the District of Columbia chapter of the American Academy of Pediatrics. E-mail Dr. Beers at [email protected].
* This story was updated 3/26/2015.
After a long, cold, snowy winter, I actually cheered at the first site of a purple crocus emerging from my front yard. Spring brings with it warmer weather, outdoor sports, blooming flowers, and trees full of leaves. Unfortunately, it also brings some less-desirable plants with it as well, such as poison ivy, poison oak, and poison sumac. As your patients happily emerge from their houses to play outside, some will inevitably end up in your offices itching and uncomfortable from contact dermatitis. As many as 50% of people who come in contact with these plants will have a reaction.
As with most illnesses, prevention is the best cure. Once a child (or adult, for that matter) has been exposed to poison ivy, oak, or sumac, from the genus Toxicodendron, the best you can do is try and relieve symptoms until the dermatitis resolves on its own.
The first step in prevention is recognition. The old adage, “Leaves of three, let them be” – describing three leaflets, often with small black dots, arising from a reddish stem – is generally accurate; however, there are some exceptions to this rule depending on the type of plant (particularly poison sumac) and geographic location. If you aren’t already aware of the species in your area, it is worth spending a few minutes researching what types of plants are common locally (www.cdc.gov/niosh/topics/plants).
Avoiding all contact with these plants is best; long pants, shirt sleeves, and gloves help avoid exposure, but this is often not practical for a child playing outside, and urushiol (the allergenic substance on the surface of these plants) adheres to clothes, and pets, and other things. … If known or potential exposure has happened, it is best to wash all areas of your skin as soon as possible, particularly focusing on hands and under your fingernails. There are a variety of products such as Tecnu, Zanfel, and Goop Hand Cleaner, which are effective at preventing reactions after exposure has occurred (and, in the case of Zanfel, can also relieve symptoms if a reaction occurs); however, these products can be pricey and not always on hand when you need them. Topical dish washing soap has been found in one study to be an effective alternative (Dial Ultra Dish washing Soap [no longer available] was the product used, but any surfactant-based dish washing detergent is likely effective).*
However, speaking from experience, even the best efforts to avoid or minimize exposure are not always successful. Symptoms usually occur within the first 4 days of exposure, with lesions cropping up at different times depending on the location and type of skin and intensity of exposure to urushiol. Lesions are typically very itchy and can be plaques, papules, vesicles, or bullae. It is commonly believed that the lesions can be “spread” through contact with the fluid inside these vesicles or other parts of the lesions; however, this is not in fact true. This misperception likely stems from the fact, as noted, that the lesions do appear at different times after exposure to the plant, which can make it seem as if they are spreading from one site to another. Reactions can peak anywhere from 1 day to 2 weeks after exposure and can last for several weeks. Again, speaking from experience, this is a long time to be itchy and uncomfortable, especially for young children, so management of symptoms is very important.
There are many strategies and commercial products that can help reduce itching and irritation. First, it is important to keep the skin clean and not to cause breaks in the skin through itching, hard as that may be, in order to avoid bacterial superinfection. Gentle interventions such as oatmeal baths or cool wet compresses may be helpful; swimming may also provide relief. Topical medications can play a role – topical corticosteroids, particularly higher dose, can be helpful in relief of symptoms. Calamine lotion, products containing menthol, and topical astringents are other effective options. Oral antihistamines are not terribly effective, as the itching is not caused by histamine, however, the sedating effects can help patients get some rest at night. For severe cases, oral corticosteroids are sometimes used, but care must be taken to give a long enough course to avoid rebound. And, perhaps most importantly, provide reassurance that this will get better eventually! As with most things in pediatrics, preventative measures and supportive care are key to making sure your patients enjoy their spring and summer without too much discomfort!
Dr. Beers is an assistant professor of pediatrics at Children’s National Medical Center and the George Washington University Medical Center, Washington. She is chair of the American Academy of Pediatrics Committee on Residency Scholarships and immediate past president of the District of Columbia chapter of the American Academy of Pediatrics. E-mail Dr. Beers at [email protected].
* This story was updated 3/26/2015.
How I responded to a nonvaccinating parent
Practicing pediatrics in California, where the measles outbreak occurred at Disneyland in December, has been an interesting experience. Suddenly, families are calling in a panic, wondering if their kids have had the vaccine, if they need the second one, if they should go to Disneyland with their infant or at all. This also seemed to me the perfect opportunity to again broach the benefit of vaccines with one of the few nonvaccinating families in my practice.
“So, has this measles outbreak made you reconsider vaccinating the kids with the MMR vaccine?” I asked my patient’s mother. “Actually, it has reinforced my beliefs,” she replied. “How is that?” I questioned. “Well, the more I read the Vaccine Adverse Event Reporting System (VAERS) reports, the more I realize that more people actually have died from the MMR vaccine than from measles in the past 10 years.” Having not reviewed the VAERS reports myself, I could not really argue intelligently, so I replied, “I’m not aware of that being true, and I will have to review the information and get back to you.”
The following is my response to her.
Dear nonvaccinating parent,
I wanted to follow up our discussion about immunizations from your visit last week. As a physician, my first duty to my patients is to first, do no harm. When you expressed your concerns regarding the VAERS data and said how more deaths were occurring from immunizations than from the measles virus itself, I felt a need to further investigate.
I reviewed the information, specifically deaths reported that were associated with the MMR vaccine on the Centers for Disease Control and Prevention VAERS website (wonder.cdc.gov/vaers.html). As you are aware, this site has been open since June of 1990 and everyone, health providers as well as parents, can report an adverse event following any vaccine at any point in time. The report yielded 65 events with regards to death and MMR vaccine over the past 25 years. Of the 65 reports, 4 of them were repeat reports of the same person, 18 had other causes that could explain death aside from the vaccine, such as leukemia diagnosed the same day, and some were associated with the vaccine, but no direct cause.
The death rate from measles has declined in recent years. According to the CDC web site, prior to the vaccine being available in 1963, in the United States alone, there were 500 deaths per year and some 4,000 cases of encephalitis. In the year 2000, the United States eliminated measles from the country (no cases in over 12 months). The last documented death from measles in the United States was in 2005, according to the CDC. This is in large part due to our vaccination rates. Worldwide, according to the World Health Organization web site, there were still 145,700 deaths in 2013.
It is interesting to me how two people can look at the same data and come to such different conclusions. You see the deaths reported on VAERS as so many deaths caused by the vaccine, and I see how many lives have been saved by vaccinating. According to the CDC data, about 85% of children are being immunized. We can extrapolate that at least 85 million children have been vaccinated in the past 25 years, and only 65 deaths have been reported to VAERS. So the death rate from measles is 1/500 and the death rate from vaccines is 1/1,000,000.
You also must keep in mind that as more and more people choose not to vaccinate, the benefit of the herd immunity your children are experiencing right now will be lost and the rate of deaths will climb again.
Sincerely,
Nazzi Mojibi, M.D.
Dr. Mojibi practices pediatrics in Fresno, Calif. She said that she had no relevant financial disclosures. E-mail her at [email protected].
Practicing pediatrics in California, where the measles outbreak occurred at Disneyland in December, has been an interesting experience. Suddenly, families are calling in a panic, wondering if their kids have had the vaccine, if they need the second one, if they should go to Disneyland with their infant or at all. This also seemed to me the perfect opportunity to again broach the benefit of vaccines with one of the few nonvaccinating families in my practice.
“So, has this measles outbreak made you reconsider vaccinating the kids with the MMR vaccine?” I asked my patient’s mother. “Actually, it has reinforced my beliefs,” she replied. “How is that?” I questioned. “Well, the more I read the Vaccine Adverse Event Reporting System (VAERS) reports, the more I realize that more people actually have died from the MMR vaccine than from measles in the past 10 years.” Having not reviewed the VAERS reports myself, I could not really argue intelligently, so I replied, “I’m not aware of that being true, and I will have to review the information and get back to you.”
The following is my response to her.
Dear nonvaccinating parent,
I wanted to follow up our discussion about immunizations from your visit last week. As a physician, my first duty to my patients is to first, do no harm. When you expressed your concerns regarding the VAERS data and said how more deaths were occurring from immunizations than from the measles virus itself, I felt a need to further investigate.
I reviewed the information, specifically deaths reported that were associated with the MMR vaccine on the Centers for Disease Control and Prevention VAERS website (wonder.cdc.gov/vaers.html). As you are aware, this site has been open since June of 1990 and everyone, health providers as well as parents, can report an adverse event following any vaccine at any point in time. The report yielded 65 events with regards to death and MMR vaccine over the past 25 years. Of the 65 reports, 4 of them were repeat reports of the same person, 18 had other causes that could explain death aside from the vaccine, such as leukemia diagnosed the same day, and some were associated with the vaccine, but no direct cause.
The death rate from measles has declined in recent years. According to the CDC web site, prior to the vaccine being available in 1963, in the United States alone, there were 500 deaths per year and some 4,000 cases of encephalitis. In the year 2000, the United States eliminated measles from the country (no cases in over 12 months). The last documented death from measles in the United States was in 2005, according to the CDC. This is in large part due to our vaccination rates. Worldwide, according to the World Health Organization web site, there were still 145,700 deaths in 2013.
It is interesting to me how two people can look at the same data and come to such different conclusions. You see the deaths reported on VAERS as so many deaths caused by the vaccine, and I see how many lives have been saved by vaccinating. According to the CDC data, about 85% of children are being immunized. We can extrapolate that at least 85 million children have been vaccinated in the past 25 years, and only 65 deaths have been reported to VAERS. So the death rate from measles is 1/500 and the death rate from vaccines is 1/1,000,000.
You also must keep in mind that as more and more people choose not to vaccinate, the benefit of the herd immunity your children are experiencing right now will be lost and the rate of deaths will climb again.
Sincerely,
Nazzi Mojibi, M.D.
Dr. Mojibi practices pediatrics in Fresno, Calif. She said that she had no relevant financial disclosures. E-mail her at [email protected].
Practicing pediatrics in California, where the measles outbreak occurred at Disneyland in December, has been an interesting experience. Suddenly, families are calling in a panic, wondering if their kids have had the vaccine, if they need the second one, if they should go to Disneyland with their infant or at all. This also seemed to me the perfect opportunity to again broach the benefit of vaccines with one of the few nonvaccinating families in my practice.
“So, has this measles outbreak made you reconsider vaccinating the kids with the MMR vaccine?” I asked my patient’s mother. “Actually, it has reinforced my beliefs,” she replied. “How is that?” I questioned. “Well, the more I read the Vaccine Adverse Event Reporting System (VAERS) reports, the more I realize that more people actually have died from the MMR vaccine than from measles in the past 10 years.” Having not reviewed the VAERS reports myself, I could not really argue intelligently, so I replied, “I’m not aware of that being true, and I will have to review the information and get back to you.”
The following is my response to her.
Dear nonvaccinating parent,
I wanted to follow up our discussion about immunizations from your visit last week. As a physician, my first duty to my patients is to first, do no harm. When you expressed your concerns regarding the VAERS data and said how more deaths were occurring from immunizations than from the measles virus itself, I felt a need to further investigate.
I reviewed the information, specifically deaths reported that were associated with the MMR vaccine on the Centers for Disease Control and Prevention VAERS website (wonder.cdc.gov/vaers.html). As you are aware, this site has been open since June of 1990 and everyone, health providers as well as parents, can report an adverse event following any vaccine at any point in time. The report yielded 65 events with regards to death and MMR vaccine over the past 25 years. Of the 65 reports, 4 of them were repeat reports of the same person, 18 had other causes that could explain death aside from the vaccine, such as leukemia diagnosed the same day, and some were associated with the vaccine, but no direct cause.
The death rate from measles has declined in recent years. According to the CDC web site, prior to the vaccine being available in 1963, in the United States alone, there were 500 deaths per year and some 4,000 cases of encephalitis. In the year 2000, the United States eliminated measles from the country (no cases in over 12 months). The last documented death from measles in the United States was in 2005, according to the CDC. This is in large part due to our vaccination rates. Worldwide, according to the World Health Organization web site, there were still 145,700 deaths in 2013.
It is interesting to me how two people can look at the same data and come to such different conclusions. You see the deaths reported on VAERS as so many deaths caused by the vaccine, and I see how many lives have been saved by vaccinating. According to the CDC data, about 85% of children are being immunized. We can extrapolate that at least 85 million children have been vaccinated in the past 25 years, and only 65 deaths have been reported to VAERS. So the death rate from measles is 1/500 and the death rate from vaccines is 1/1,000,000.
You also must keep in mind that as more and more people choose not to vaccinate, the benefit of the herd immunity your children are experiencing right now will be lost and the rate of deaths will climb again.
Sincerely,
Nazzi Mojibi, M.D.
Dr. Mojibi practices pediatrics in Fresno, Calif. She said that she had no relevant financial disclosures. E-mail her at [email protected].
Dos and don’ts for handling common sling complications
Large-scale randomized trials have not only documented the efficacy of minimally invasive midurethral slings for stress urinary continence, they have also provided more adequate data on the incidence of complications. In practice, meanwhile, we are seeing more complications as the number of midurethral sling placements increases.
Often times, complications can be significantly more impactful than the original urinary incontinence. It is important to take the complications of sling placement seriously. Let patients know that their symptoms matter, and that there are ways to manage complications.
With more long-term data and experience, we have learned more about what to do, and what not to do, to prevent, diagnose, and manage the complications associated with midurethral slings. Here is my approach to the complications most commonly encountered, including bladder perforation, voiding dysfunction, erosion, pain, and recurrent stress urinary incontinence.
I will not address vascular injury in this article, but certainly, this is a surgical emergency that needs to be handled as such. As described in the February 2015 edition of Master Class on midurethral sling technique, accurate visualization toward the ipsilateral shoulder during needle passage is an essential part of preventing vascular injuries during retropubic sling placement.
Bladder perforation
Bladder perforation has consistently been shown to be significantly more common with retropubic slings than with transobturator slings. Reported incidence has ranged from 0.8% to 34% for tension-free vaginal tape (TVT) procedures, with the higher rates seen mainly in teaching institutions. Most commonly, the reported incidence is less than 10%.
Bladder perforation has no effect on the efficacy of the treatment, and no apparent long-term consequences, as long as the injury is identified. Especially with a retropubic sling, cystoscopy should be performed after both needles are placed but prior to advancing the needles all the way through the retropubic space. Simply withdrawing a needle will cause little bladder injury while retracting deployed mesh is significantly more consequential.
I recommend filling the bladder to approximately 300 cc, or to the point where you can see evidence of full distension such as flattened urethral orifices. This confirms that the bladder is under enough distension to preclude any mucosal wrinkles or folds that can hide a trocar injury.
The first step upon recognition of a perforation is to stay calm. In the vast majority of cases, simply withdrawing the needle, replacing it, and verifying correct replacement will prevent any long-term consequences. On the other hand, you must be fully alert to the possibility that the needle wandered away from the pubic bone, and consequently may have entered a space such as the peritoneum. Suspicion for visceral injury should be increased.
Resist the temptation to replace the needle more laterally. This course correction is often an unhelpful instinct, because a more lateral replacement will not move the needle farther from the bladder; it will instead bring it closer to the iliac vessels. Vascular injuries resulting from the surgeon’s attempts at needle replacement are unfortunate, as a minor complication becomes a major one. The key is to be as distal as possible – as close to the pubic bone as possible – and not to replace the needles more laterally.
Postoperative drainage for 1-2 days may be considered, but there is nothing in the literature to require this, and many surgeons do not employ any sort of extra catheterization after surgery where perforation has been observed.
Voiding dysfunction
Some degree of voiding dysfunction is not uncommon in the short term, but when a patient is still unable to void normally or completely after several days, an evaluation is warranted. As with bladder perforation, reported incidence of voiding dysfunction has varied widely, from 2% to 45% with the newer midurethral slings. Generally, the need for surgical revision is about 2%.
There are two reasons for urinary retention: Insufficient contraction force in the bladder or too much resistance. If retention persists beyond a week – in the 7-10 day postop time period – I assess whether the problem is resulting from too much obstruction from the sling, some form of hypotonic bladder, other surgery performed in conjunction with sling placement, medications, or something else.
Difficulty in passing a small urethra catheter in the office may indicate excessive obstruction, for instance, and there may be indications on vaginal examination or through cystoscopy that the sling is too tight. A midurethral “speed bump,” or elevation at the midpoint, with either catheterization or the scope is consistent with over-correction.
Do not dilate or pull down on the sling with any kind of urethra dilator. The sling is more robust than the urethral mucosa, and we now appreciate that this practice is associated with urethral erosion.
If the problem is deemed to be excessive obstruction or over-resistance, and it is fewer than 10 days postop, the patient may be offered a minor revision; the original incision is reopened, the sling material is identified, and the sling arms (lateral to the urethra) are grasped with clamps. Gentle downward traction can loosen the sling.
The sling should be grasped laterally and not at the midpoint; some sling materials will stretch and fracture where the force is applied. A little bit of gentle downward traction (3-5 mm) will often give you the needed amount of space for relieving some of the obstruction.
Beyond 10 days postop, tissue in-growth makes such a sling adjustment difficult, if not impossible. At this point, I recommend transecting the entire sling in the midline.There is differing opinion about whether a portion of the mesh should be resected; I believe that such a resection is usually unnecessary, and that a simple midline release procedure is the best approach.
A study we performed more than a decade ago on surgical release of TVT showed that persistent post-TVT voiding dysfunction can be successfully managed with a simple midline release. Of 1,175 women who underwent TVT placement for stress urinary incontinence and/or intrinsic sphincter deficiency, 23 (1.9%) had persistent voiding dysfunction. All cases of impaired emptying were completely resolved with a release of the tape, and the majority remained cured in terms of their continence or went from “cured” to “improved” over baseline. Three patients (13%) had recurrence of stress incontinence (Obstet. Gynecol. 2002;100:898-902).
We used to wait longer before revising the sling out of fear of losing the entire benefit of the sling. As it turns out, a simple midline release (leaving most, if not all, of the mesh in place) is usually just enough to treat the new complaint while still providing enough lateral support so that the patient retains most or all of the continence achieved with the sling.
Complaints of de novo urge incontinence, or overactive bladder, should be taken seriously. Urge incontinence has even more significant associations with depression and poor quality of life than stress incontinence. In the absence of retention, usual first-line therapies for overactive bladder can be employed, including anticholinergic medications, behavioral therapies, and physical therapy. Failing these interventions, my assessment for this complaint will be similar to that for retention; I’ll look for evidence of too much resistance, such as difficulty in passing a catheter, a “speed bump” cystoscopically, or an elevated pDet on pressure-flow studies, for instance.
If any of these are present, I usually offer sling release first. If, on the other hand, there is no evidence of over resistance in a patient who has de novo urge incontinence or overactive bladder and is refractory to conservative measures, a trial of sacral neuromodulation or botox injections is considered the next step.
Erosion
Erosion remains a difficult complication to understand. Long-term follow-up data show that it occurs after 3%-4% of sling placements, rather than 1% as originally believed. Data are inconsistent, but there probably is a slightly higher incidence of vaginal erosion with a transobturator sling, given more contact between the sling and the anterior vaginal wall.
There are hints in the literature that erosion may be related to technique – perhaps to the depth of dissection during surgery – but this is difficult to quantify. Moreover, many of the reported cases of erosion occur several years, or longer, after surgery. It is hard to blame surgical technique for such delayed erosion.
As we’ve seen with previous generations of mesh, there does not appear to be any window of time after which erosion is no longer a risk. We need to recognize that there is a medium- and long-term risk of erosion and appreciate its presenting symptoms: Recurrent urinary tract infection, pain with voiding, urgency, urinary incontinence, and microscopic hematuria of new onset.
Prevention may well entail preoperative estrogenization. The science looking at the effect of estrogen on sling placement is becoming more robust. While there are uncertainties, I believe that studies likely will show that topical estrogen in the preoperative and perioperative phases plays an important role in preventing erosion from occurring. Personally, I am using it much more than I was 10 years ago.
I like the convenience of the Vagifem tablet (Novo Nordisk Inc., Plainsboro, N.J.), and am reassured by data on systemic absorption with the 10-mcg dose, but any vaginal cream or compounded suppository can be used. I usually advise 4-6 weeks of preoperative preparation, with nightly use for 2 weeks followed by 2-3 nights per week thereafter. Smoking is also a likely risk factor. Data are not entirely consistent, but I believe we should provide counseling and encourage smoking cessation before the implant of mesh.
Management is dependent on when the erosion occurs or is recognized. When erosion occurs within 6 weeks post operatively, primary repair is an option. When erosion is detected after the 6-week window and is causing symptoms, a conservative trim of bristles poking through the vaginal mucosa is worth a try. I do not advise more than one such conservative trim, however, as repeated attempts and series of small resections can make the sling exceedingly difficult to remove if more complete resection is ultimately needed. After one unsuccessful trim, I usually remove the whole sling belly, or most of the vaginal part of the sling.
For slings made of type 1 macroporous mesh, resection of the retropubic or transobturator portions of the mesh usually is not required. In the more rare situation where those pelvic areas of the mesh are associated with pain, I favor a laparoscopic approach to the retropubic space to facilitate minimally invasive removal.
Postop pain, sling failure
Groin pain, or thigh pain, sometimes occurs after placement of a transobturator sling. As I discussed in the previous Master Class on midurethral sling technique, I have seen a significant decrease in groin pain in my patients – without any reduction in benefit – with the use of a shorter transobturator sling that does not leave mesh in the adductor compartment of the thigh and groin.
For persistent groin pain, I favor the use of trigger point injection. Sometimes one injection will impact the inflammatory cycle such that the patient derives long-term benefit. At other times, the trigger point injection will serve as a diagnostic; if pain returns after a period of benefit, I am inclined to resect that part of the mesh.
Pain inside the pelvis, especially on the pelvic sidewall (obturator or puborectalis complex) usually is related to mechanical tension. In my experience, this type of discomfort is slightly more likely to occur with the transobturator slings, which penetrate through the muscular pelvic sidewall and lead to more fibrosis and scar tissue formation.
In most cases of pain and discomfort, attempting to reproduce the patient’s symptoms by putting tension on particular parts of the sling during the office exam helps guide management. If I find that palpating or putting the sling on tension recreates her complaints, and conservative injections have provided temporary or inadequate relief, I usually advocate resecting the vaginal portion of the mesh to relieve that tension.
In cases of recurrent stress urinary incontinence (when the sling has failed), a TVT or repeat TVT is often warranted. The TVT sling has been demonstrated to work after nearly every other previous kind of anti-incontinence procedure, even after a previous retropubic sling. There is little data on mesh removal in such cases. I believe that unless a previously placed but failed sling is causing symptoms, there is no need to resect it. Mesh removal is significantly more traumatic than mesh placement, and in most cases it is not necessary.
Dr. Rardin reported that he has no relevant financial disclosures.
Large-scale randomized trials have not only documented the efficacy of minimally invasive midurethral slings for stress urinary continence, they have also provided more adequate data on the incidence of complications. In practice, meanwhile, we are seeing more complications as the number of midurethral sling placements increases.
Often times, complications can be significantly more impactful than the original urinary incontinence. It is important to take the complications of sling placement seriously. Let patients know that their symptoms matter, and that there are ways to manage complications.
With more long-term data and experience, we have learned more about what to do, and what not to do, to prevent, diagnose, and manage the complications associated with midurethral slings. Here is my approach to the complications most commonly encountered, including bladder perforation, voiding dysfunction, erosion, pain, and recurrent stress urinary incontinence.
I will not address vascular injury in this article, but certainly, this is a surgical emergency that needs to be handled as such. As described in the February 2015 edition of Master Class on midurethral sling technique, accurate visualization toward the ipsilateral shoulder during needle passage is an essential part of preventing vascular injuries during retropubic sling placement.
Bladder perforation
Bladder perforation has consistently been shown to be significantly more common with retropubic slings than with transobturator slings. Reported incidence has ranged from 0.8% to 34% for tension-free vaginal tape (TVT) procedures, with the higher rates seen mainly in teaching institutions. Most commonly, the reported incidence is less than 10%.
Bladder perforation has no effect on the efficacy of the treatment, and no apparent long-term consequences, as long as the injury is identified. Especially with a retropubic sling, cystoscopy should be performed after both needles are placed but prior to advancing the needles all the way through the retropubic space. Simply withdrawing a needle will cause little bladder injury while retracting deployed mesh is significantly more consequential.
I recommend filling the bladder to approximately 300 cc, or to the point where you can see evidence of full distension such as flattened urethral orifices. This confirms that the bladder is under enough distension to preclude any mucosal wrinkles or folds that can hide a trocar injury.
The first step upon recognition of a perforation is to stay calm. In the vast majority of cases, simply withdrawing the needle, replacing it, and verifying correct replacement will prevent any long-term consequences. On the other hand, you must be fully alert to the possibility that the needle wandered away from the pubic bone, and consequently may have entered a space such as the peritoneum. Suspicion for visceral injury should be increased.
Resist the temptation to replace the needle more laterally. This course correction is often an unhelpful instinct, because a more lateral replacement will not move the needle farther from the bladder; it will instead bring it closer to the iliac vessels. Vascular injuries resulting from the surgeon’s attempts at needle replacement are unfortunate, as a minor complication becomes a major one. The key is to be as distal as possible – as close to the pubic bone as possible – and not to replace the needles more laterally.
Postoperative drainage for 1-2 days may be considered, but there is nothing in the literature to require this, and many surgeons do not employ any sort of extra catheterization after surgery where perforation has been observed.
Voiding dysfunction
Some degree of voiding dysfunction is not uncommon in the short term, but when a patient is still unable to void normally or completely after several days, an evaluation is warranted. As with bladder perforation, reported incidence of voiding dysfunction has varied widely, from 2% to 45% with the newer midurethral slings. Generally, the need for surgical revision is about 2%.
There are two reasons for urinary retention: Insufficient contraction force in the bladder or too much resistance. If retention persists beyond a week – in the 7-10 day postop time period – I assess whether the problem is resulting from too much obstruction from the sling, some form of hypotonic bladder, other surgery performed in conjunction with sling placement, medications, or something else.
Difficulty in passing a small urethra catheter in the office may indicate excessive obstruction, for instance, and there may be indications on vaginal examination or through cystoscopy that the sling is too tight. A midurethral “speed bump,” or elevation at the midpoint, with either catheterization or the scope is consistent with over-correction.
Do not dilate or pull down on the sling with any kind of urethra dilator. The sling is more robust than the urethral mucosa, and we now appreciate that this practice is associated with urethral erosion.
If the problem is deemed to be excessive obstruction or over-resistance, and it is fewer than 10 days postop, the patient may be offered a minor revision; the original incision is reopened, the sling material is identified, and the sling arms (lateral to the urethra) are grasped with clamps. Gentle downward traction can loosen the sling.
The sling should be grasped laterally and not at the midpoint; some sling materials will stretch and fracture where the force is applied. A little bit of gentle downward traction (3-5 mm) will often give you the needed amount of space for relieving some of the obstruction.
Beyond 10 days postop, tissue in-growth makes such a sling adjustment difficult, if not impossible. At this point, I recommend transecting the entire sling in the midline.There is differing opinion about whether a portion of the mesh should be resected; I believe that such a resection is usually unnecessary, and that a simple midline release procedure is the best approach.
A study we performed more than a decade ago on surgical release of TVT showed that persistent post-TVT voiding dysfunction can be successfully managed with a simple midline release. Of 1,175 women who underwent TVT placement for stress urinary incontinence and/or intrinsic sphincter deficiency, 23 (1.9%) had persistent voiding dysfunction. All cases of impaired emptying were completely resolved with a release of the tape, and the majority remained cured in terms of their continence or went from “cured” to “improved” over baseline. Three patients (13%) had recurrence of stress incontinence (Obstet. Gynecol. 2002;100:898-902).
We used to wait longer before revising the sling out of fear of losing the entire benefit of the sling. As it turns out, a simple midline release (leaving most, if not all, of the mesh in place) is usually just enough to treat the new complaint while still providing enough lateral support so that the patient retains most or all of the continence achieved with the sling.
Complaints of de novo urge incontinence, or overactive bladder, should be taken seriously. Urge incontinence has even more significant associations with depression and poor quality of life than stress incontinence. In the absence of retention, usual first-line therapies for overactive bladder can be employed, including anticholinergic medications, behavioral therapies, and physical therapy. Failing these interventions, my assessment for this complaint will be similar to that for retention; I’ll look for evidence of too much resistance, such as difficulty in passing a catheter, a “speed bump” cystoscopically, or an elevated pDet on pressure-flow studies, for instance.
If any of these are present, I usually offer sling release first. If, on the other hand, there is no evidence of over resistance in a patient who has de novo urge incontinence or overactive bladder and is refractory to conservative measures, a trial of sacral neuromodulation or botox injections is considered the next step.
Erosion
Erosion remains a difficult complication to understand. Long-term follow-up data show that it occurs after 3%-4% of sling placements, rather than 1% as originally believed. Data are inconsistent, but there probably is a slightly higher incidence of vaginal erosion with a transobturator sling, given more contact between the sling and the anterior vaginal wall.
There are hints in the literature that erosion may be related to technique – perhaps to the depth of dissection during surgery – but this is difficult to quantify. Moreover, many of the reported cases of erosion occur several years, or longer, after surgery. It is hard to blame surgical technique for such delayed erosion.
As we’ve seen with previous generations of mesh, there does not appear to be any window of time after which erosion is no longer a risk. We need to recognize that there is a medium- and long-term risk of erosion and appreciate its presenting symptoms: Recurrent urinary tract infection, pain with voiding, urgency, urinary incontinence, and microscopic hematuria of new onset.
Prevention may well entail preoperative estrogenization. The science looking at the effect of estrogen on sling placement is becoming more robust. While there are uncertainties, I believe that studies likely will show that topical estrogen in the preoperative and perioperative phases plays an important role in preventing erosion from occurring. Personally, I am using it much more than I was 10 years ago.
I like the convenience of the Vagifem tablet (Novo Nordisk Inc., Plainsboro, N.J.), and am reassured by data on systemic absorption with the 10-mcg dose, but any vaginal cream or compounded suppository can be used. I usually advise 4-6 weeks of preoperative preparation, with nightly use for 2 weeks followed by 2-3 nights per week thereafter. Smoking is also a likely risk factor. Data are not entirely consistent, but I believe we should provide counseling and encourage smoking cessation before the implant of mesh.
Management is dependent on when the erosion occurs or is recognized. When erosion occurs within 6 weeks post operatively, primary repair is an option. When erosion is detected after the 6-week window and is causing symptoms, a conservative trim of bristles poking through the vaginal mucosa is worth a try. I do not advise more than one such conservative trim, however, as repeated attempts and series of small resections can make the sling exceedingly difficult to remove if more complete resection is ultimately needed. After one unsuccessful trim, I usually remove the whole sling belly, or most of the vaginal part of the sling.
For slings made of type 1 macroporous mesh, resection of the retropubic or transobturator portions of the mesh usually is not required. In the more rare situation where those pelvic areas of the mesh are associated with pain, I favor a laparoscopic approach to the retropubic space to facilitate minimally invasive removal.
Postop pain, sling failure
Groin pain, or thigh pain, sometimes occurs after placement of a transobturator sling. As I discussed in the previous Master Class on midurethral sling technique, I have seen a significant decrease in groin pain in my patients – without any reduction in benefit – with the use of a shorter transobturator sling that does not leave mesh in the adductor compartment of the thigh and groin.
For persistent groin pain, I favor the use of trigger point injection. Sometimes one injection will impact the inflammatory cycle such that the patient derives long-term benefit. At other times, the trigger point injection will serve as a diagnostic; if pain returns after a period of benefit, I am inclined to resect that part of the mesh.
Pain inside the pelvis, especially on the pelvic sidewall (obturator or puborectalis complex) usually is related to mechanical tension. In my experience, this type of discomfort is slightly more likely to occur with the transobturator slings, which penetrate through the muscular pelvic sidewall and lead to more fibrosis and scar tissue formation.
In most cases of pain and discomfort, attempting to reproduce the patient’s symptoms by putting tension on particular parts of the sling during the office exam helps guide management. If I find that palpating or putting the sling on tension recreates her complaints, and conservative injections have provided temporary or inadequate relief, I usually advocate resecting the vaginal portion of the mesh to relieve that tension.
In cases of recurrent stress urinary incontinence (when the sling has failed), a TVT or repeat TVT is often warranted. The TVT sling has been demonstrated to work after nearly every other previous kind of anti-incontinence procedure, even after a previous retropubic sling. There is little data on mesh removal in such cases. I believe that unless a previously placed but failed sling is causing symptoms, there is no need to resect it. Mesh removal is significantly more traumatic than mesh placement, and in most cases it is not necessary.
Dr. Rardin reported that he has no relevant financial disclosures.
Large-scale randomized trials have not only documented the efficacy of minimally invasive midurethral slings for stress urinary continence, they have also provided more adequate data on the incidence of complications. In practice, meanwhile, we are seeing more complications as the number of midurethral sling placements increases.
Often times, complications can be significantly more impactful than the original urinary incontinence. It is important to take the complications of sling placement seriously. Let patients know that their symptoms matter, and that there are ways to manage complications.
With more long-term data and experience, we have learned more about what to do, and what not to do, to prevent, diagnose, and manage the complications associated with midurethral slings. Here is my approach to the complications most commonly encountered, including bladder perforation, voiding dysfunction, erosion, pain, and recurrent stress urinary incontinence.
I will not address vascular injury in this article, but certainly, this is a surgical emergency that needs to be handled as such. As described in the February 2015 edition of Master Class on midurethral sling technique, accurate visualization toward the ipsilateral shoulder during needle passage is an essential part of preventing vascular injuries during retropubic sling placement.
Bladder perforation
Bladder perforation has consistently been shown to be significantly more common with retropubic slings than with transobturator slings. Reported incidence has ranged from 0.8% to 34% for tension-free vaginal tape (TVT) procedures, with the higher rates seen mainly in teaching institutions. Most commonly, the reported incidence is less than 10%.
Bladder perforation has no effect on the efficacy of the treatment, and no apparent long-term consequences, as long as the injury is identified. Especially with a retropubic sling, cystoscopy should be performed after both needles are placed but prior to advancing the needles all the way through the retropubic space. Simply withdrawing a needle will cause little bladder injury while retracting deployed mesh is significantly more consequential.
I recommend filling the bladder to approximately 300 cc, or to the point where you can see evidence of full distension such as flattened urethral orifices. This confirms that the bladder is under enough distension to preclude any mucosal wrinkles or folds that can hide a trocar injury.
The first step upon recognition of a perforation is to stay calm. In the vast majority of cases, simply withdrawing the needle, replacing it, and verifying correct replacement will prevent any long-term consequences. On the other hand, you must be fully alert to the possibility that the needle wandered away from the pubic bone, and consequently may have entered a space such as the peritoneum. Suspicion for visceral injury should be increased.
Resist the temptation to replace the needle more laterally. This course correction is often an unhelpful instinct, because a more lateral replacement will not move the needle farther from the bladder; it will instead bring it closer to the iliac vessels. Vascular injuries resulting from the surgeon’s attempts at needle replacement are unfortunate, as a minor complication becomes a major one. The key is to be as distal as possible – as close to the pubic bone as possible – and not to replace the needles more laterally.
Postoperative drainage for 1-2 days may be considered, but there is nothing in the literature to require this, and many surgeons do not employ any sort of extra catheterization after surgery where perforation has been observed.
Voiding dysfunction
Some degree of voiding dysfunction is not uncommon in the short term, but when a patient is still unable to void normally or completely after several days, an evaluation is warranted. As with bladder perforation, reported incidence of voiding dysfunction has varied widely, from 2% to 45% with the newer midurethral slings. Generally, the need for surgical revision is about 2%.
There are two reasons for urinary retention: Insufficient contraction force in the bladder or too much resistance. If retention persists beyond a week – in the 7-10 day postop time period – I assess whether the problem is resulting from too much obstruction from the sling, some form of hypotonic bladder, other surgery performed in conjunction with sling placement, medications, or something else.
Difficulty in passing a small urethra catheter in the office may indicate excessive obstruction, for instance, and there may be indications on vaginal examination or through cystoscopy that the sling is too tight. A midurethral “speed bump,” or elevation at the midpoint, with either catheterization or the scope is consistent with over-correction.
Do not dilate or pull down on the sling with any kind of urethra dilator. The sling is more robust than the urethral mucosa, and we now appreciate that this practice is associated with urethral erosion.
If the problem is deemed to be excessive obstruction or over-resistance, and it is fewer than 10 days postop, the patient may be offered a minor revision; the original incision is reopened, the sling material is identified, and the sling arms (lateral to the urethra) are grasped with clamps. Gentle downward traction can loosen the sling.
The sling should be grasped laterally and not at the midpoint; some sling materials will stretch and fracture where the force is applied. A little bit of gentle downward traction (3-5 mm) will often give you the needed amount of space for relieving some of the obstruction.
Beyond 10 days postop, tissue in-growth makes such a sling adjustment difficult, if not impossible. At this point, I recommend transecting the entire sling in the midline.There is differing opinion about whether a portion of the mesh should be resected; I believe that such a resection is usually unnecessary, and that a simple midline release procedure is the best approach.
A study we performed more than a decade ago on surgical release of TVT showed that persistent post-TVT voiding dysfunction can be successfully managed with a simple midline release. Of 1,175 women who underwent TVT placement for stress urinary incontinence and/or intrinsic sphincter deficiency, 23 (1.9%) had persistent voiding dysfunction. All cases of impaired emptying were completely resolved with a release of the tape, and the majority remained cured in terms of their continence or went from “cured” to “improved” over baseline. Three patients (13%) had recurrence of stress incontinence (Obstet. Gynecol. 2002;100:898-902).
We used to wait longer before revising the sling out of fear of losing the entire benefit of the sling. As it turns out, a simple midline release (leaving most, if not all, of the mesh in place) is usually just enough to treat the new complaint while still providing enough lateral support so that the patient retains most or all of the continence achieved with the sling.
Complaints of de novo urge incontinence, or overactive bladder, should be taken seriously. Urge incontinence has even more significant associations with depression and poor quality of life than stress incontinence. In the absence of retention, usual first-line therapies for overactive bladder can be employed, including anticholinergic medications, behavioral therapies, and physical therapy. Failing these interventions, my assessment for this complaint will be similar to that for retention; I’ll look for evidence of too much resistance, such as difficulty in passing a catheter, a “speed bump” cystoscopically, or an elevated pDet on pressure-flow studies, for instance.
If any of these are present, I usually offer sling release first. If, on the other hand, there is no evidence of over resistance in a patient who has de novo urge incontinence or overactive bladder and is refractory to conservative measures, a trial of sacral neuromodulation or botox injections is considered the next step.
Erosion
Erosion remains a difficult complication to understand. Long-term follow-up data show that it occurs after 3%-4% of sling placements, rather than 1% as originally believed. Data are inconsistent, but there probably is a slightly higher incidence of vaginal erosion with a transobturator sling, given more contact between the sling and the anterior vaginal wall.
There are hints in the literature that erosion may be related to technique – perhaps to the depth of dissection during surgery – but this is difficult to quantify. Moreover, many of the reported cases of erosion occur several years, or longer, after surgery. It is hard to blame surgical technique for such delayed erosion.
As we’ve seen with previous generations of mesh, there does not appear to be any window of time after which erosion is no longer a risk. We need to recognize that there is a medium- and long-term risk of erosion and appreciate its presenting symptoms: Recurrent urinary tract infection, pain with voiding, urgency, urinary incontinence, and microscopic hematuria of new onset.
Prevention may well entail preoperative estrogenization. The science looking at the effect of estrogen on sling placement is becoming more robust. While there are uncertainties, I believe that studies likely will show that topical estrogen in the preoperative and perioperative phases plays an important role in preventing erosion from occurring. Personally, I am using it much more than I was 10 years ago.
I like the convenience of the Vagifem tablet (Novo Nordisk Inc., Plainsboro, N.J.), and am reassured by data on systemic absorption with the 10-mcg dose, but any vaginal cream or compounded suppository can be used. I usually advise 4-6 weeks of preoperative preparation, with nightly use for 2 weeks followed by 2-3 nights per week thereafter. Smoking is also a likely risk factor. Data are not entirely consistent, but I believe we should provide counseling and encourage smoking cessation before the implant of mesh.
Management is dependent on when the erosion occurs or is recognized. When erosion occurs within 6 weeks post operatively, primary repair is an option. When erosion is detected after the 6-week window and is causing symptoms, a conservative trim of bristles poking through the vaginal mucosa is worth a try. I do not advise more than one such conservative trim, however, as repeated attempts and series of small resections can make the sling exceedingly difficult to remove if more complete resection is ultimately needed. After one unsuccessful trim, I usually remove the whole sling belly, or most of the vaginal part of the sling.
For slings made of type 1 macroporous mesh, resection of the retropubic or transobturator portions of the mesh usually is not required. In the more rare situation where those pelvic areas of the mesh are associated with pain, I favor a laparoscopic approach to the retropubic space to facilitate minimally invasive removal.
Postop pain, sling failure
Groin pain, or thigh pain, sometimes occurs after placement of a transobturator sling. As I discussed in the previous Master Class on midurethral sling technique, I have seen a significant decrease in groin pain in my patients – without any reduction in benefit – with the use of a shorter transobturator sling that does not leave mesh in the adductor compartment of the thigh and groin.
For persistent groin pain, I favor the use of trigger point injection. Sometimes one injection will impact the inflammatory cycle such that the patient derives long-term benefit. At other times, the trigger point injection will serve as a diagnostic; if pain returns after a period of benefit, I am inclined to resect that part of the mesh.
Pain inside the pelvis, especially on the pelvic sidewall (obturator or puborectalis complex) usually is related to mechanical tension. In my experience, this type of discomfort is slightly more likely to occur with the transobturator slings, which penetrate through the muscular pelvic sidewall and lead to more fibrosis and scar tissue formation.
In most cases of pain and discomfort, attempting to reproduce the patient’s symptoms by putting tension on particular parts of the sling during the office exam helps guide management. If I find that palpating or putting the sling on tension recreates her complaints, and conservative injections have provided temporary or inadequate relief, I usually advocate resecting the vaginal portion of the mesh to relieve that tension.
In cases of recurrent stress urinary incontinence (when the sling has failed), a TVT or repeat TVT is often warranted. The TVT sling has been demonstrated to work after nearly every other previous kind of anti-incontinence procedure, even after a previous retropubic sling. There is little data on mesh removal in such cases. I believe that unless a previously placed but failed sling is causing symptoms, there is no need to resect it. Mesh removal is significantly more traumatic than mesh placement, and in most cases it is not necessary.
Dr. Rardin reported that he has no relevant financial disclosures.
Tackling midurethral sling complications
Over the past 2 decades, midurethral slings, both via a retropubic and a transobturator approach have become the first-line therapy for the surgical correction of female stress urinary incontinence. Not only are cure rates excellent for both techniques, but the incidence of complications are low.
Intraoperatively, major concerns include vascular lesions, nerve injuries, and injuries to the bowel. More minor concerns are related to the bladder.
Perioperative complications include retropubic hematoma, blood loss, urinary tract infection, and spondylitis. Postoperative risks include transient versus permanent urinary retention, vaginal versus urethral erosion, de novo urgency, bladder erosion, and urethral obstruction.
In this edition of Master Class in gynecologic surgery, I am pleased to solicit the help of Dr. Charles Rardin, who will make recommendations regarding the management of some of the most common complications related to midurethral sling procedures.
Dr. Rardin is the director of the Robotic Surgery Program at Women & Infants Hospital of Rhode Island, in Providence; a surgeon in Women & Infants’ division of urogynecology and Reconstructive Pelvic Surgery; and is the director of the hospital’s fellowship urogynecology and reconstructive pelvic surgery.
Dr. Miller is clinical associate professor at the University of Illinois at Chicago, immediate past president of the International Society for Gynecologic Endoscopy (ISGE), and a past president of the AAGL. He is a reproductive endocrinologist and minimally invasive gynecologic surgeon in private practice in Naperville, Ill., and Schaumburg, Ill.; the director of minimally invasive gynecologic surgery and the director of the AAGL/SRS fellowship in minimally invasive gynecologic surgery at Advocate Lutheran General Hospital, Park Ridge, Ill.; and the medical editor of this column, Master Class. Dr. Miller is a consultant and on the speaker’s bureau for Ethicon.
Over the past 2 decades, midurethral slings, both via a retropubic and a transobturator approach have become the first-line therapy for the surgical correction of female stress urinary incontinence. Not only are cure rates excellent for both techniques, but the incidence of complications are low.
Intraoperatively, major concerns include vascular lesions, nerve injuries, and injuries to the bowel. More minor concerns are related to the bladder.
Perioperative complications include retropubic hematoma, blood loss, urinary tract infection, and spondylitis. Postoperative risks include transient versus permanent urinary retention, vaginal versus urethral erosion, de novo urgency, bladder erosion, and urethral obstruction.
In this edition of Master Class in gynecologic surgery, I am pleased to solicit the help of Dr. Charles Rardin, who will make recommendations regarding the management of some of the most common complications related to midurethral sling procedures.
Dr. Rardin is the director of the Robotic Surgery Program at Women & Infants Hospital of Rhode Island, in Providence; a surgeon in Women & Infants’ division of urogynecology and Reconstructive Pelvic Surgery; and is the director of the hospital’s fellowship urogynecology and reconstructive pelvic surgery.
Dr. Miller is clinical associate professor at the University of Illinois at Chicago, immediate past president of the International Society for Gynecologic Endoscopy (ISGE), and a past president of the AAGL. He is a reproductive endocrinologist and minimally invasive gynecologic surgeon in private practice in Naperville, Ill., and Schaumburg, Ill.; the director of minimally invasive gynecologic surgery and the director of the AAGL/SRS fellowship in minimally invasive gynecologic surgery at Advocate Lutheran General Hospital, Park Ridge, Ill.; and the medical editor of this column, Master Class. Dr. Miller is a consultant and on the speaker’s bureau for Ethicon.
Over the past 2 decades, midurethral slings, both via a retropubic and a transobturator approach have become the first-line therapy for the surgical correction of female stress urinary incontinence. Not only are cure rates excellent for both techniques, but the incidence of complications are low.
Intraoperatively, major concerns include vascular lesions, nerve injuries, and injuries to the bowel. More minor concerns are related to the bladder.
Perioperative complications include retropubic hematoma, blood loss, urinary tract infection, and spondylitis. Postoperative risks include transient versus permanent urinary retention, vaginal versus urethral erosion, de novo urgency, bladder erosion, and urethral obstruction.
In this edition of Master Class in gynecologic surgery, I am pleased to solicit the help of Dr. Charles Rardin, who will make recommendations regarding the management of some of the most common complications related to midurethral sling procedures.
Dr. Rardin is the director of the Robotic Surgery Program at Women & Infants Hospital of Rhode Island, in Providence; a surgeon in Women & Infants’ division of urogynecology and Reconstructive Pelvic Surgery; and is the director of the hospital’s fellowship urogynecology and reconstructive pelvic surgery.
Dr. Miller is clinical associate professor at the University of Illinois at Chicago, immediate past president of the International Society for Gynecologic Endoscopy (ISGE), and a past president of the AAGL. He is a reproductive endocrinologist and minimally invasive gynecologic surgeon in private practice in Naperville, Ill., and Schaumburg, Ill.; the director of minimally invasive gynecologic surgery and the director of the AAGL/SRS fellowship in minimally invasive gynecologic surgery at Advocate Lutheran General Hospital, Park Ridge, Ill.; and the medical editor of this column, Master Class. Dr. Miller is a consultant and on the speaker’s bureau for Ethicon.
The Value of National and Hospital Registries
Following Dr. Sarmiento’s commentary, “Orthopedic Registries: Second Thoughts,” we agree that it is important and appropriate to question the value of any new additions to the orthopedic field, and registries are no exception. We thank Dr. Sarmiento for his comments on the viability of registries and the need for continued critical evaluation. Before joint registries, however, we had to rely on small-cohort analyses to assess outcomes and complications. Now, national and hospital registries, specifically joint registries, may be an invaluable source of information for orthopedic surgeons, patients, health care administrators, regulators, and implant suppliers.1,2
Contrary to Dr. Sarmiento’s belief that registry data results are likely to have been reported in the literature, it is difficult to refute the value of recent years’ registry data in helping surgeons shape their practice. For example, according to Lewallen and Etkin,3 the National Joint Registry of England and Wales information has provided orthopedic surgeons with crucial findings regarding the outcomes of metal-on-metal hip arthroplasties. Using the England and Wales registry data from more than 400,000 primary total hip arthroplasties, Smith and colleagues4 noted that metal-on-metal stemmed articulations led to poor implant survival, particularly in young women with large-diameter heads, and indicated these articulations should not be used. Australian registry data on metal-on-metal devices and reports of failure rates up to 11%5 led one manufacturer to recall its implants.6 In addition, the Norwegian Arthroplasty Register evaluated survival rates and reasons for revision for 7 types of cemented primary total knee arthroplasty (TKA) between 1994 and 2009.7 Data on more than 17,000 primary TKAs allowed Plate and colleagues8 to confidently determine that aseptic loosening was related to certain TKA designs. Using registry information, they identified patients at risk for dislocation in total hip arthroplasty and concluded that large-diameter femoral head articulations could reduce dislocation rates.
Obtaining such large cohorts of patients in individual studies is not only difficult but highly unlikely. Unlike registry data, these studies are often impractical in evaluating factors of low incidence, such as revision rates, as it is often difficult to find significant differences in small populations.9 Furthermore, these controlled trials homogenize patients—using exclusion and inclusion criteria to eliminate potential confounders—and thus poorly represent the heterogeneity of a typical hospital’s patient population.10 Although the literature may indeed have alluded to such complications, only a database as extensive as a registry can allow us to fully comprehend the outcomes of particular implants and devices.
Dr. Sarmiento points to the AO Swiss Fracture Registry as being of little benefit and raises the concern that the American Joint Replacement Registry (AJRR) may follow with the same results. However, realizing a registry’s benefits may take time and the gradual accumulation of data. Supporting this, Hübschle and colleagues11 recently used AO Swiss Fracture Registry data to validate use of balloon kyphoplasty for vertebral compression fractures and concluded that the technique is safe and effective in reducing pain—thus possibly providing the federal office with the evidence needed for reimbursement for this intervention. Therefore, this registry is now providing useful information.
We can never truly know the veracity of participating surgeons, but it is naïve to assume that this issue arises only vis-à-vis registries. If we were to debate the ethical and professional standards of colleagues in our field, such questions could extend to all studies performed, even peer-reviewed studies. Therefore, we do not think this is reason to exclude the patient data and outcomes found in registries. We must emphasize that ultimately registry data are often most useful in highlighting trends and determining triggers for further study rather than in arriving at conclusions.1 In particular, registry data may be used in cohort studies that evaluate the risk factors for and incidence of certain outcomes. Focused higher-level interventional studies can then follow the trends observed.1 However, registry data are also valuable on their own, when higher-level, randomized controlled trials may be impractical or unethical.12
Dr. Sarmiento refers to corrupt relationships between companies and orthopedists as “representing a widespread loss of professionalism in our ranks.” Despite a US Justice Department investigation into these relationships, only a few doctors were found to have had inappropriate relationships.13 In addition, the investigation and prosecution of companies led to an agreement requiring federal monitoring and new corporate compliance procedures, which should ensure stricter adherence to regulations.14 We do not believe this should undermine the value of registries and the work that has been contributed by thousands of surgeons hoping to improve the field of orthopedics. In addition, concerns about the influence of well-known individuals may be better directed at individual institution–based research, particularly as these specific authors also often have conflicts of interest that may skew the presentation of results. The strength of registry data is in providing collective data and large samples from a multitude of surgeons rather than from just high-volume surgeons, and therefore registry data provide a better overall picture of patients and their procedures.15 Furthermore, trends observed in national registries in countries such as New Zealand16 may aid in effectively reducing the revision rate, possibly up to 10%.17 If a US national joint registry is marginally as effective, then we may see considerable savings for our health care services.17,18
We wholeheartedly agree that a yearly review of registries may be constructive. Dr. Sarmiento suggests an annual publication summarizing peer-reviewed articles and the opportunity for orthopedists to decide for themselves what treatments to choose based on reports from independent investigators. Although this sounds feasible, it would be difficult to decide which articles should be selected as pertinent for this type of publication. Any selection would be biased, and not all studies with high-level evidence are necessarily important or relevant. Therefore, selecting what is most appropriate to cite is not without its difficulties. We appreciate that there are problems in standardizing data reporting among registries. However, to improve interregistry collaboration, the US Food and Drug Administration is sponsoring the International Consortium of Orthopaedic Registries (ICOR) to facilitate data presentation.19 ICOR aims to increase cooperation, standardize analyses, and improve reporting, which will only strengthen the data available to us. Such efforts will ultimately enhance coordination and international collaboration among registries.15 In addition, incorporating patient-reported outcomes into our national registry will aid in quantifying arthroplasty outcomes from the patient’s perspective and will continue to improve total joint arthroplasties.20
Overall, this debate is useful and highly relevant in highlighting potential issues with registries. Although registries are not without their flaws, like all aspects of orthopedics they are ever evolving, and they must be continually modified and improved. However, disregard for the potential value of AJRR, which has benefits for orthopedists and patients alike, is premature. Once again, we thank Dr. Sarmiento for starting this discussion, which will allow us to continue to evaluate and improve our registries.
1. Konan S, Haddad FS. Joint registries: a Ptolemaic model of data interpretation? Bone Joint J Br. 2013;95(12):1585-1586.
2. Banerjee S, Cafri G, Isaacs AJ, et al. A distributed health data network analysis of survival outcomes: the International Consortium of Orthopaedic Registries perspective. J Bone Joint Surg Am. 2014;96(suppl 1):7-11.
3. Lewallen DG, Etkin CD. The need for a national total joint registry. Orthop Nurs. 2013;32(1):4-5.
4. Smith AJ, Dieppe P, Vernon K, Porter M, Blom AW; National Joint Registry of England and Wales. Failure rates of stemmed metal-on-metal hip replacements: analysis of data from the National Joint Registry of England and Wales. Lancet. 2012;379(9822):1199-1204.
5. de Steiger RN, Hang JR, Miller LN, Graves SE, Davidson DC. Five-year results of the ASR XL Acetabular System and the ASR Hip Resurfacing System: an analysis from the Australian Orthopaedic Association National Joint Replacement Registry. J Bone Joint Surg Am. 2011;93(24):2287-2293.
6. Hug KT, Watters TS, Vail TP, Bolognesi MP. The withdrawn ASR™ THA and hip resurfacing systems: how have our patients fared over 1 to 6 years? Clin Orthop. 2013;471(2):430-438.
7. Gøthesen O, Espehaug B, Havelin L, et al. Survival rates and causes of revision in cemented primary total knee replacement: a report from the Norwegian Arthroplasty Register 1994–2009. Bone Joint J Br. 2013;95(5):636-642.
8. Plate JF, Seyler TM, Stroh DA, Issa K, Akbar M, Mont MA. Risk of dislocation using large- vs. small-diameter femoral heads in total hip arthroplasty. BMC Res Notes. 2012;5:553.
9. Daruwalla ZJ, Wong KL, Pillay KR, Leong KM, Murphy DP. Does ageing Singapore need an electronic database of hip fracture patients? The value and role of a national joint registry and an electronic database of intertrochanteric and femoral neck fractures. Singapore Med J. 2014;55(5):287-288.
10. Rasmussen JV, Olsen BS, Fevang BT, et al. A review of national shoulder and elbow joint replacement registries. J Shoulder Elbow Surg. 2012;21(10):1328-1335.
11. Hübschle L, Borgström F, Olafsson G, et al. Real-life results of balloon kyphoplasty for vertebral compression fractures from the SWISSspine registry. Spine J. 2014;14(9):2063-2077.
12. Ahn H, Court-Brown CM, McQueen MM, Schemitsch EH. The use of hospital registries in orthopaedic surgery. J Bone Joint Surg Am. 2009;91(suppl 3):68-72.
13. Youngstrom N. Swept up in major medical device case, physician pays $650,000 to settle kickback charges. AIS Health Business Daily. May 3, 2010.
14. Five companies in hip and knee replacement industry avoid prosecution by agreeing to compliance rules and monitoring [press release]. US Department of Justice website. http://www.justice.gov/usao/nj/Press/files/pdffiles/Older/hips0927.rel.pdf. Published September 27, 2007. Accessed February 19, 2015.
15. Namba RS, Inacio MC, Paxton EW, Robertsson O, Graves SE. The role of registry data in the evaluation of mobile-bearing total knee arthroplasty. J Bone Joint Surg Am. 2011;93(suppl 3):48-50.
16. Insull PJ, Cobbett H, Frampton CM, Munro JT. The use of a lipped acetabular liner decreases the rate of revision for instability after total hip replacement: a study using data from the New Zealand Joint Registry. Bone Joint J Br. 2014;96(7):884-888.
17. Rankin EA. AJRR: becoming a national US joint registry. Orthopedics. 2013;36(3):175-176.
18. American Joint Replacement Registry website. https://teamwork.aaos.org/ajrr/SitePages/About%20Us.aspx. Accessed February 19, 2015.
19. International Consortium of Orthopaedic Registries website. http://www.icor-initiative.org. Accessed February 19, 2015.
20. Franklin PD, Harrold L, Ayers DC. Incorporating patient-reported outcomes in total joint arthroplasty registries: challenges and opportunities. Clin Orthop. 2013;471(11):3482-3488.
Following Dr. Sarmiento’s commentary, “Orthopedic Registries: Second Thoughts,” we agree that it is important and appropriate to question the value of any new additions to the orthopedic field, and registries are no exception. We thank Dr. Sarmiento for his comments on the viability of registries and the need for continued critical evaluation. Before joint registries, however, we had to rely on small-cohort analyses to assess outcomes and complications. Now, national and hospital registries, specifically joint registries, may be an invaluable source of information for orthopedic surgeons, patients, health care administrators, regulators, and implant suppliers.1,2
Contrary to Dr. Sarmiento’s belief that registry data results are likely to have been reported in the literature, it is difficult to refute the value of recent years’ registry data in helping surgeons shape their practice. For example, according to Lewallen and Etkin,3 the National Joint Registry of England and Wales information has provided orthopedic surgeons with crucial findings regarding the outcomes of metal-on-metal hip arthroplasties. Using the England and Wales registry data from more than 400,000 primary total hip arthroplasties, Smith and colleagues4 noted that metal-on-metal stemmed articulations led to poor implant survival, particularly in young women with large-diameter heads, and indicated these articulations should not be used. Australian registry data on metal-on-metal devices and reports of failure rates up to 11%5 led one manufacturer to recall its implants.6 In addition, the Norwegian Arthroplasty Register evaluated survival rates and reasons for revision for 7 types of cemented primary total knee arthroplasty (TKA) between 1994 and 2009.7 Data on more than 17,000 primary TKAs allowed Plate and colleagues8 to confidently determine that aseptic loosening was related to certain TKA designs. Using registry information, they identified patients at risk for dislocation in total hip arthroplasty and concluded that large-diameter femoral head articulations could reduce dislocation rates.
Obtaining such large cohorts of patients in individual studies is not only difficult but highly unlikely. Unlike registry data, these studies are often impractical in evaluating factors of low incidence, such as revision rates, as it is often difficult to find significant differences in small populations.9 Furthermore, these controlled trials homogenize patients—using exclusion and inclusion criteria to eliminate potential confounders—and thus poorly represent the heterogeneity of a typical hospital’s patient population.10 Although the literature may indeed have alluded to such complications, only a database as extensive as a registry can allow us to fully comprehend the outcomes of particular implants and devices.
Dr. Sarmiento points to the AO Swiss Fracture Registry as being of little benefit and raises the concern that the American Joint Replacement Registry (AJRR) may follow with the same results. However, realizing a registry’s benefits may take time and the gradual accumulation of data. Supporting this, Hübschle and colleagues11 recently used AO Swiss Fracture Registry data to validate use of balloon kyphoplasty for vertebral compression fractures and concluded that the technique is safe and effective in reducing pain—thus possibly providing the federal office with the evidence needed for reimbursement for this intervention. Therefore, this registry is now providing useful information.
We can never truly know the veracity of participating surgeons, but it is naïve to assume that this issue arises only vis-à-vis registries. If we were to debate the ethical and professional standards of colleagues in our field, such questions could extend to all studies performed, even peer-reviewed studies. Therefore, we do not think this is reason to exclude the patient data and outcomes found in registries. We must emphasize that ultimately registry data are often most useful in highlighting trends and determining triggers for further study rather than in arriving at conclusions.1 In particular, registry data may be used in cohort studies that evaluate the risk factors for and incidence of certain outcomes. Focused higher-level interventional studies can then follow the trends observed.1 However, registry data are also valuable on their own, when higher-level, randomized controlled trials may be impractical or unethical.12
Dr. Sarmiento refers to corrupt relationships between companies and orthopedists as “representing a widespread loss of professionalism in our ranks.” Despite a US Justice Department investigation into these relationships, only a few doctors were found to have had inappropriate relationships.13 In addition, the investigation and prosecution of companies led to an agreement requiring federal monitoring and new corporate compliance procedures, which should ensure stricter adherence to regulations.14 We do not believe this should undermine the value of registries and the work that has been contributed by thousands of surgeons hoping to improve the field of orthopedics. In addition, concerns about the influence of well-known individuals may be better directed at individual institution–based research, particularly as these specific authors also often have conflicts of interest that may skew the presentation of results. The strength of registry data is in providing collective data and large samples from a multitude of surgeons rather than from just high-volume surgeons, and therefore registry data provide a better overall picture of patients and their procedures.15 Furthermore, trends observed in national registries in countries such as New Zealand16 may aid in effectively reducing the revision rate, possibly up to 10%.17 If a US national joint registry is marginally as effective, then we may see considerable savings for our health care services.17,18
We wholeheartedly agree that a yearly review of registries may be constructive. Dr. Sarmiento suggests an annual publication summarizing peer-reviewed articles and the opportunity for orthopedists to decide for themselves what treatments to choose based on reports from independent investigators. Although this sounds feasible, it would be difficult to decide which articles should be selected as pertinent for this type of publication. Any selection would be biased, and not all studies with high-level evidence are necessarily important or relevant. Therefore, selecting what is most appropriate to cite is not without its difficulties. We appreciate that there are problems in standardizing data reporting among registries. However, to improve interregistry collaboration, the US Food and Drug Administration is sponsoring the International Consortium of Orthopaedic Registries (ICOR) to facilitate data presentation.19 ICOR aims to increase cooperation, standardize analyses, and improve reporting, which will only strengthen the data available to us. Such efforts will ultimately enhance coordination and international collaboration among registries.15 In addition, incorporating patient-reported outcomes into our national registry will aid in quantifying arthroplasty outcomes from the patient’s perspective and will continue to improve total joint arthroplasties.20
Overall, this debate is useful and highly relevant in highlighting potential issues with registries. Although registries are not without their flaws, like all aspects of orthopedics they are ever evolving, and they must be continually modified and improved. However, disregard for the potential value of AJRR, which has benefits for orthopedists and patients alike, is premature. Once again, we thank Dr. Sarmiento for starting this discussion, which will allow us to continue to evaluate and improve our registries.
Following Dr. Sarmiento’s commentary, “Orthopedic Registries: Second Thoughts,” we agree that it is important and appropriate to question the value of any new additions to the orthopedic field, and registries are no exception. We thank Dr. Sarmiento for his comments on the viability of registries and the need for continued critical evaluation. Before joint registries, however, we had to rely on small-cohort analyses to assess outcomes and complications. Now, national and hospital registries, specifically joint registries, may be an invaluable source of information for orthopedic surgeons, patients, health care administrators, regulators, and implant suppliers.1,2
Contrary to Dr. Sarmiento’s belief that registry data results are likely to have been reported in the literature, it is difficult to refute the value of recent years’ registry data in helping surgeons shape their practice. For example, according to Lewallen and Etkin,3 the National Joint Registry of England and Wales information has provided orthopedic surgeons with crucial findings regarding the outcomes of metal-on-metal hip arthroplasties. Using the England and Wales registry data from more than 400,000 primary total hip arthroplasties, Smith and colleagues4 noted that metal-on-metal stemmed articulations led to poor implant survival, particularly in young women with large-diameter heads, and indicated these articulations should not be used. Australian registry data on metal-on-metal devices and reports of failure rates up to 11%5 led one manufacturer to recall its implants.6 In addition, the Norwegian Arthroplasty Register evaluated survival rates and reasons for revision for 7 types of cemented primary total knee arthroplasty (TKA) between 1994 and 2009.7 Data on more than 17,000 primary TKAs allowed Plate and colleagues8 to confidently determine that aseptic loosening was related to certain TKA designs. Using registry information, they identified patients at risk for dislocation in total hip arthroplasty and concluded that large-diameter femoral head articulations could reduce dislocation rates.
Obtaining such large cohorts of patients in individual studies is not only difficult but highly unlikely. Unlike registry data, these studies are often impractical in evaluating factors of low incidence, such as revision rates, as it is often difficult to find significant differences in small populations.9 Furthermore, these controlled trials homogenize patients—using exclusion and inclusion criteria to eliminate potential confounders—and thus poorly represent the heterogeneity of a typical hospital’s patient population.10 Although the literature may indeed have alluded to such complications, only a database as extensive as a registry can allow us to fully comprehend the outcomes of particular implants and devices.
Dr. Sarmiento points to the AO Swiss Fracture Registry as being of little benefit and raises the concern that the American Joint Replacement Registry (AJRR) may follow with the same results. However, realizing a registry’s benefits may take time and the gradual accumulation of data. Supporting this, Hübschle and colleagues11 recently used AO Swiss Fracture Registry data to validate use of balloon kyphoplasty for vertebral compression fractures and concluded that the technique is safe and effective in reducing pain—thus possibly providing the federal office with the evidence needed for reimbursement for this intervention. Therefore, this registry is now providing useful information.
We can never truly know the veracity of participating surgeons, but it is naïve to assume that this issue arises only vis-à-vis registries. If we were to debate the ethical and professional standards of colleagues in our field, such questions could extend to all studies performed, even peer-reviewed studies. Therefore, we do not think this is reason to exclude the patient data and outcomes found in registries. We must emphasize that ultimately registry data are often most useful in highlighting trends and determining triggers for further study rather than in arriving at conclusions.1 In particular, registry data may be used in cohort studies that evaluate the risk factors for and incidence of certain outcomes. Focused higher-level interventional studies can then follow the trends observed.1 However, registry data are also valuable on their own, when higher-level, randomized controlled trials may be impractical or unethical.12
Dr. Sarmiento refers to corrupt relationships between companies and orthopedists as “representing a widespread loss of professionalism in our ranks.” Despite a US Justice Department investigation into these relationships, only a few doctors were found to have had inappropriate relationships.13 In addition, the investigation and prosecution of companies led to an agreement requiring federal monitoring and new corporate compliance procedures, which should ensure stricter adherence to regulations.14 We do not believe this should undermine the value of registries and the work that has been contributed by thousands of surgeons hoping to improve the field of orthopedics. In addition, concerns about the influence of well-known individuals may be better directed at individual institution–based research, particularly as these specific authors also often have conflicts of interest that may skew the presentation of results. The strength of registry data is in providing collective data and large samples from a multitude of surgeons rather than from just high-volume surgeons, and therefore registry data provide a better overall picture of patients and their procedures.15 Furthermore, trends observed in national registries in countries such as New Zealand16 may aid in effectively reducing the revision rate, possibly up to 10%.17 If a US national joint registry is marginally as effective, then we may see considerable savings for our health care services.17,18
We wholeheartedly agree that a yearly review of registries may be constructive. Dr. Sarmiento suggests an annual publication summarizing peer-reviewed articles and the opportunity for orthopedists to decide for themselves what treatments to choose based on reports from independent investigators. Although this sounds feasible, it would be difficult to decide which articles should be selected as pertinent for this type of publication. Any selection would be biased, and not all studies with high-level evidence are necessarily important or relevant. Therefore, selecting what is most appropriate to cite is not without its difficulties. We appreciate that there are problems in standardizing data reporting among registries. However, to improve interregistry collaboration, the US Food and Drug Administration is sponsoring the International Consortium of Orthopaedic Registries (ICOR) to facilitate data presentation.19 ICOR aims to increase cooperation, standardize analyses, and improve reporting, which will only strengthen the data available to us. Such efforts will ultimately enhance coordination and international collaboration among registries.15 In addition, incorporating patient-reported outcomes into our national registry will aid in quantifying arthroplasty outcomes from the patient’s perspective and will continue to improve total joint arthroplasties.20
Overall, this debate is useful and highly relevant in highlighting potential issues with registries. Although registries are not without their flaws, like all aspects of orthopedics they are ever evolving, and they must be continually modified and improved. However, disregard for the potential value of AJRR, which has benefits for orthopedists and patients alike, is premature. Once again, we thank Dr. Sarmiento for starting this discussion, which will allow us to continue to evaluate and improve our registries.
1. Konan S, Haddad FS. Joint registries: a Ptolemaic model of data interpretation? Bone Joint J Br. 2013;95(12):1585-1586.
2. Banerjee S, Cafri G, Isaacs AJ, et al. A distributed health data network analysis of survival outcomes: the International Consortium of Orthopaedic Registries perspective. J Bone Joint Surg Am. 2014;96(suppl 1):7-11.
3. Lewallen DG, Etkin CD. The need for a national total joint registry. Orthop Nurs. 2013;32(1):4-5.
4. Smith AJ, Dieppe P, Vernon K, Porter M, Blom AW; National Joint Registry of England and Wales. Failure rates of stemmed metal-on-metal hip replacements: analysis of data from the National Joint Registry of England and Wales. Lancet. 2012;379(9822):1199-1204.
5. de Steiger RN, Hang JR, Miller LN, Graves SE, Davidson DC. Five-year results of the ASR XL Acetabular System and the ASR Hip Resurfacing System: an analysis from the Australian Orthopaedic Association National Joint Replacement Registry. J Bone Joint Surg Am. 2011;93(24):2287-2293.
6. Hug KT, Watters TS, Vail TP, Bolognesi MP. The withdrawn ASR™ THA and hip resurfacing systems: how have our patients fared over 1 to 6 years? Clin Orthop. 2013;471(2):430-438.
7. Gøthesen O, Espehaug B, Havelin L, et al. Survival rates and causes of revision in cemented primary total knee replacement: a report from the Norwegian Arthroplasty Register 1994–2009. Bone Joint J Br. 2013;95(5):636-642.
8. Plate JF, Seyler TM, Stroh DA, Issa K, Akbar M, Mont MA. Risk of dislocation using large- vs. small-diameter femoral heads in total hip arthroplasty. BMC Res Notes. 2012;5:553.
9. Daruwalla ZJ, Wong KL, Pillay KR, Leong KM, Murphy DP. Does ageing Singapore need an electronic database of hip fracture patients? The value and role of a national joint registry and an electronic database of intertrochanteric and femoral neck fractures. Singapore Med J. 2014;55(5):287-288.
10. Rasmussen JV, Olsen BS, Fevang BT, et al. A review of national shoulder and elbow joint replacement registries. J Shoulder Elbow Surg. 2012;21(10):1328-1335.
11. Hübschle L, Borgström F, Olafsson G, et al. Real-life results of balloon kyphoplasty for vertebral compression fractures from the SWISSspine registry. Spine J. 2014;14(9):2063-2077.
12. Ahn H, Court-Brown CM, McQueen MM, Schemitsch EH. The use of hospital registries in orthopaedic surgery. J Bone Joint Surg Am. 2009;91(suppl 3):68-72.
13. Youngstrom N. Swept up in major medical device case, physician pays $650,000 to settle kickback charges. AIS Health Business Daily. May 3, 2010.
14. Five companies in hip and knee replacement industry avoid prosecution by agreeing to compliance rules and monitoring [press release]. US Department of Justice website. http://www.justice.gov/usao/nj/Press/files/pdffiles/Older/hips0927.rel.pdf. Published September 27, 2007. Accessed February 19, 2015.
15. Namba RS, Inacio MC, Paxton EW, Robertsson O, Graves SE. The role of registry data in the evaluation of mobile-bearing total knee arthroplasty. J Bone Joint Surg Am. 2011;93(suppl 3):48-50.
16. Insull PJ, Cobbett H, Frampton CM, Munro JT. The use of a lipped acetabular liner decreases the rate of revision for instability after total hip replacement: a study using data from the New Zealand Joint Registry. Bone Joint J Br. 2014;96(7):884-888.
17. Rankin EA. AJRR: becoming a national US joint registry. Orthopedics. 2013;36(3):175-176.
18. American Joint Replacement Registry website. https://teamwork.aaos.org/ajrr/SitePages/About%20Us.aspx. Accessed February 19, 2015.
19. International Consortium of Orthopaedic Registries website. http://www.icor-initiative.org. Accessed February 19, 2015.
20. Franklin PD, Harrold L, Ayers DC. Incorporating patient-reported outcomes in total joint arthroplasty registries: challenges and opportunities. Clin Orthop. 2013;471(11):3482-3488.
1. Konan S, Haddad FS. Joint registries: a Ptolemaic model of data interpretation? Bone Joint J Br. 2013;95(12):1585-1586.
2. Banerjee S, Cafri G, Isaacs AJ, et al. A distributed health data network analysis of survival outcomes: the International Consortium of Orthopaedic Registries perspective. J Bone Joint Surg Am. 2014;96(suppl 1):7-11.
3. Lewallen DG, Etkin CD. The need for a national total joint registry. Orthop Nurs. 2013;32(1):4-5.
4. Smith AJ, Dieppe P, Vernon K, Porter M, Blom AW; National Joint Registry of England and Wales. Failure rates of stemmed metal-on-metal hip replacements: analysis of data from the National Joint Registry of England and Wales. Lancet. 2012;379(9822):1199-1204.
5. de Steiger RN, Hang JR, Miller LN, Graves SE, Davidson DC. Five-year results of the ASR XL Acetabular System and the ASR Hip Resurfacing System: an analysis from the Australian Orthopaedic Association National Joint Replacement Registry. J Bone Joint Surg Am. 2011;93(24):2287-2293.
6. Hug KT, Watters TS, Vail TP, Bolognesi MP. The withdrawn ASR™ THA and hip resurfacing systems: how have our patients fared over 1 to 6 years? Clin Orthop. 2013;471(2):430-438.
7. Gøthesen O, Espehaug B, Havelin L, et al. Survival rates and causes of revision in cemented primary total knee replacement: a report from the Norwegian Arthroplasty Register 1994–2009. Bone Joint J Br. 2013;95(5):636-642.
8. Plate JF, Seyler TM, Stroh DA, Issa K, Akbar M, Mont MA. Risk of dislocation using large- vs. small-diameter femoral heads in total hip arthroplasty. BMC Res Notes. 2012;5:553.
9. Daruwalla ZJ, Wong KL, Pillay KR, Leong KM, Murphy DP. Does ageing Singapore need an electronic database of hip fracture patients? The value and role of a national joint registry and an electronic database of intertrochanteric and femoral neck fractures. Singapore Med J. 2014;55(5):287-288.
10. Rasmussen JV, Olsen BS, Fevang BT, et al. A review of national shoulder and elbow joint replacement registries. J Shoulder Elbow Surg. 2012;21(10):1328-1335.
11. Hübschle L, Borgström F, Olafsson G, et al. Real-life results of balloon kyphoplasty for vertebral compression fractures from the SWISSspine registry. Spine J. 2014;14(9):2063-2077.
12. Ahn H, Court-Brown CM, McQueen MM, Schemitsch EH. The use of hospital registries in orthopaedic surgery. J Bone Joint Surg Am. 2009;91(suppl 3):68-72.
13. Youngstrom N. Swept up in major medical device case, physician pays $650,000 to settle kickback charges. AIS Health Business Daily. May 3, 2010.
14. Five companies in hip and knee replacement industry avoid prosecution by agreeing to compliance rules and monitoring [press release]. US Department of Justice website. http://www.justice.gov/usao/nj/Press/files/pdffiles/Older/hips0927.rel.pdf. Published September 27, 2007. Accessed February 19, 2015.
15. Namba RS, Inacio MC, Paxton EW, Robertsson O, Graves SE. The role of registry data in the evaluation of mobile-bearing total knee arthroplasty. J Bone Joint Surg Am. 2011;93(suppl 3):48-50.
16. Insull PJ, Cobbett H, Frampton CM, Munro JT. The use of a lipped acetabular liner decreases the rate of revision for instability after total hip replacement: a study using data from the New Zealand Joint Registry. Bone Joint J Br. 2014;96(7):884-888.
17. Rankin EA. AJRR: becoming a national US joint registry. Orthopedics. 2013;36(3):175-176.
18. American Joint Replacement Registry website. https://teamwork.aaos.org/ajrr/SitePages/About%20Us.aspx. Accessed February 19, 2015.
19. International Consortium of Orthopaedic Registries website. http://www.icor-initiative.org. Accessed February 19, 2015.
20. Franklin PD, Harrold L, Ayers DC. Incorporating patient-reported outcomes in total joint arthroplasty registries: challenges and opportunities. Clin Orthop. 2013;471(11):3482-3488.
Orthopedic Registries: Second Thoughts
Many assume that the American Joint Replacement Registry (AJRR) is moving forward as originally planned. No one has reported any obstacles that may cast doubt on its continued progress.
Despite the enthusiasm for AJRR, we must be realistic and admit that the project may not in the final analysis bring about its anticipated results. Therefore, periodic sober assessments of its course should be carried out, as they might result in identifying possible flaws and strengths. It is imperative to continue to express doubts regarding the true long-term value of this registry.
Much of the original support for an ongoing registry came from the example provided by the Swedish national registry. The Scandinavian registry had been said to dramatically reduce the number of complications and halve the revision rate for total hip arthroplasties. We need to question the claim that this reduction was solely the result of information produced by the registry. It is hard to believe that the literature had failed to report on those complications long before the registry publicized its findings.
As we take a fresh look at AJRR, it is perhaps wise to keep in mind the history of the AO Swiss Fracture Registry, founded by Maurice Müller and heavily subsidized by industry. Apparently, after gathering millions of pieces of information, primarily about equipment used for fracture fixation, the Swiss registry has failed to produce the greater benefits it had expected. Given the similarities between the Swiss Fracture Registry and AJRR, it is logical to assume that the latter may suffer the same fate.
I base my concerns on factors that, carefully analyzed, might be important in determining the future of AJRR. One major consideration is the difficulty in guaranteeing the veracity of data submitted—a factor shared by all registries.1 To assume that all participating surgeons adhere to high ethical and professional standards is naïve. Some surgeons who stand to make large profits from their ownership of implants or equipment are submitting false and erroneous information. Other unscrupulous orthopedists are receiving large kickbacks for helping the industry market its implants. These people will be tempted to embellish and falsify information about successes and failures and submit it to the registry.1-3
Militating against the “guaranteed success” of AJRR is this tainted relationship between the implant manufacturing industry and some members of the orthopedics community. A 2002–2006 investigation by the US Justice Department found egregious unethical transgressions and corrupt relationships between 5 companies and hundreds of orthopedists—representing a widespread loss of professionalism in our ranks.4 More recently, the Centers for Medicare & Medicaid Services5 disclosed that, in the last 5 months of 2013, $3.5 billion were paid by medical device companies to doctors and leading hospitals. As stated in a newspaper article, “‘Open Payments does not identify which financial relationships … could cause conflicts of interest,’ said Shantanu Agrawal, the agency official overseeing the project. ‘It simply makes the data available to the public.’”6 Further, “an initial Associated Press analysis found that orthopedists, cardiologists and adult medicine specialists were among the likeliest to receive payments from drug and device companies. Most of the contributions came in the form of cash payments, followed by in-kind gifts and services, and stock options.”6
This official government revelation is disturbing. Although the number of people who are deliberately committing clear infractions may be small, some of these people are likely well-known, and their influence should not be underestimated, particularly with regard to AJRR publications. Some in the orthopedic community do not question the accuracy of these publications but accept their conclusions as fact, and such may be the case with orthopedic guidelines.7
Given these concerns and the facts of the situation, can AJRR solve real problems that traditional systems have so far failed to solve? We have enough journals and scientific meetings informing us of the failures and successes of implants. I suspect it is wrong to believe that the AJRR data on 1 million patients’ arthroplasties are necessarily superior to the data from a 20,000-patient registry. Such an erroneous conclusion ignores the fact that, with clinical issues such as the one currently being addressed by AJRR, having a larger registry and more patients does not necessarily imply more meaningful information. In addition, follow-ups longer than those used with traditional methods are not possible—death will continue to intervene. No matter how many patients are included in the system, the maximum follow-up will forever remain the same.
Financing of AJRR is expensive, time-consuming, and likely to be terminated if clear evidence of the true value of the registry is not provided within the next few years. In light of such an outcome, we should replace the current system with a more effective mechanism. For example, we could produce an annual publication that summarizes the peer-reviewed articles published on joint replacement, with an emphasis on controversial topics. Orthopedic fellows, rather than readily accepting AJRR findings and recommendations, will instead be able to decide for themselves what treatment to use for each particular patient and situation, based on information provided by a number of independent investigators.
Meaningful progress in managing clinical conditions, such as the ones we are discussing, is achieved not by expanding the size of a registry but by being committed as individuals to making improvements. A cursory glance at the history of hip arthroplasty easily proves the point. Registries, guidelines, and other popular systems sometimes inadvertently create an environment that inhibits independent thinking. When powerful nonmedical economic and political bodies become involved in medical issues in order to ensure their continued profit, our autonomy is lost or compromised in major ways. Such scenarios must be avoided as forcefully as possible.8
Questioning the future of AJRR does not derive from rigid thinking or from a lack of awareness or understanding of the registry’s nature, procedures, benefits, goals, or highly altruistic and noble origins. However, pointing out a lack of evidence of success is not a crime. It is incumbent on us to look at this area and others with open minds while recognizing that honest and sincere scrutiny often helps make a better future a reality. The United States is working to achieve major goals for health care—access for all, lower costs, and fewer abuses of the system. Our involvement is a mandate to be followed enthusiastically.
1. Carr AJ. Which research is to be believed? The ethics of industrial funding of orthopaedic research. J Bone Joint Surg Br. 2005;87(11):1452-1453.
2. Callahan D. False Hopes: Overcoming the Obstacles to a Sustainable, Affordable Medicine. New Brunswick, NJ: Rutgers University Press; 1999.
3. Relman AS. A Second Opinion: Rescuing America’s Healthcare: A Plan for Universal Coverage Serving Patients Over Profit. New York: Public Affairs; 2007.
4. Five companies in hip and knee replacement industry avoid prosecution by agreeing to compliance rules and monitoring [press release]. US Department of Justice website. http://www.justice.gov/usao/nj/Press/files/pdffiles/Older/hips0927.rel.pdf. Published September 27, 2007. Accessed February 19, 2015.
5. CMS makes first wave of drug & device company payments to teaching hospitals and physicians public [press release]. Centers for Medicare & Medicaid Services website. http://www.cms.gov/Newsroom/MediaReleaseDatabase/Press-releases/2014-Press-releases-items/2014-09-30.html. Published September 30, 2014. Accessed February 19, 2015.
6. Alonso-Zaldivar R, Gillum J. Drug, device firms paid $3.5B to care providers. The Big Story. Associated Press website. http://bigstory.ap.org/article/c80ae51828a0497e87beda7f9ff60ac8/govt-reveal-drug-company-payments-doctors. Published September 30, 2014. Accessed February 19, 2015.
7. Sarmiento A. Thoughts on orthopedic guidelines. Am J Orthop. 2010;39(8):373-374.
8. Sarmiento A. Infringing on freedom of speech. J Bone Joint Surg Am. 2011;93(2):222.
Many assume that the American Joint Replacement Registry (AJRR) is moving forward as originally planned. No one has reported any obstacles that may cast doubt on its continued progress.
Despite the enthusiasm for AJRR, we must be realistic and admit that the project may not in the final analysis bring about its anticipated results. Therefore, periodic sober assessments of its course should be carried out, as they might result in identifying possible flaws and strengths. It is imperative to continue to express doubts regarding the true long-term value of this registry.
Much of the original support for an ongoing registry came from the example provided by the Swedish national registry. The Scandinavian registry had been said to dramatically reduce the number of complications and halve the revision rate for total hip arthroplasties. We need to question the claim that this reduction was solely the result of information produced by the registry. It is hard to believe that the literature had failed to report on those complications long before the registry publicized its findings.
As we take a fresh look at AJRR, it is perhaps wise to keep in mind the history of the AO Swiss Fracture Registry, founded by Maurice Müller and heavily subsidized by industry. Apparently, after gathering millions of pieces of information, primarily about equipment used for fracture fixation, the Swiss registry has failed to produce the greater benefits it had expected. Given the similarities between the Swiss Fracture Registry and AJRR, it is logical to assume that the latter may suffer the same fate.
I base my concerns on factors that, carefully analyzed, might be important in determining the future of AJRR. One major consideration is the difficulty in guaranteeing the veracity of data submitted—a factor shared by all registries.1 To assume that all participating surgeons adhere to high ethical and professional standards is naïve. Some surgeons who stand to make large profits from their ownership of implants or equipment are submitting false and erroneous information. Other unscrupulous orthopedists are receiving large kickbacks for helping the industry market its implants. These people will be tempted to embellish and falsify information about successes and failures and submit it to the registry.1-3
Militating against the “guaranteed success” of AJRR is this tainted relationship between the implant manufacturing industry and some members of the orthopedics community. A 2002–2006 investigation by the US Justice Department found egregious unethical transgressions and corrupt relationships between 5 companies and hundreds of orthopedists—representing a widespread loss of professionalism in our ranks.4 More recently, the Centers for Medicare & Medicaid Services5 disclosed that, in the last 5 months of 2013, $3.5 billion were paid by medical device companies to doctors and leading hospitals. As stated in a newspaper article, “‘Open Payments does not identify which financial relationships … could cause conflicts of interest,’ said Shantanu Agrawal, the agency official overseeing the project. ‘It simply makes the data available to the public.’”6 Further, “an initial Associated Press analysis found that orthopedists, cardiologists and adult medicine specialists were among the likeliest to receive payments from drug and device companies. Most of the contributions came in the form of cash payments, followed by in-kind gifts and services, and stock options.”6
This official government revelation is disturbing. Although the number of people who are deliberately committing clear infractions may be small, some of these people are likely well-known, and their influence should not be underestimated, particularly with regard to AJRR publications. Some in the orthopedic community do not question the accuracy of these publications but accept their conclusions as fact, and such may be the case with orthopedic guidelines.7
Given these concerns and the facts of the situation, can AJRR solve real problems that traditional systems have so far failed to solve? We have enough journals and scientific meetings informing us of the failures and successes of implants. I suspect it is wrong to believe that the AJRR data on 1 million patients’ arthroplasties are necessarily superior to the data from a 20,000-patient registry. Such an erroneous conclusion ignores the fact that, with clinical issues such as the one currently being addressed by AJRR, having a larger registry and more patients does not necessarily imply more meaningful information. In addition, follow-ups longer than those used with traditional methods are not possible—death will continue to intervene. No matter how many patients are included in the system, the maximum follow-up will forever remain the same.
Financing of AJRR is expensive, time-consuming, and likely to be terminated if clear evidence of the true value of the registry is not provided within the next few years. In light of such an outcome, we should replace the current system with a more effective mechanism. For example, we could produce an annual publication that summarizes the peer-reviewed articles published on joint replacement, with an emphasis on controversial topics. Orthopedic fellows, rather than readily accepting AJRR findings and recommendations, will instead be able to decide for themselves what treatment to use for each particular patient and situation, based on information provided by a number of independent investigators.
Meaningful progress in managing clinical conditions, such as the ones we are discussing, is achieved not by expanding the size of a registry but by being committed as individuals to making improvements. A cursory glance at the history of hip arthroplasty easily proves the point. Registries, guidelines, and other popular systems sometimes inadvertently create an environment that inhibits independent thinking. When powerful nonmedical economic and political bodies become involved in medical issues in order to ensure their continued profit, our autonomy is lost or compromised in major ways. Such scenarios must be avoided as forcefully as possible.8
Questioning the future of AJRR does not derive from rigid thinking or from a lack of awareness or understanding of the registry’s nature, procedures, benefits, goals, or highly altruistic and noble origins. However, pointing out a lack of evidence of success is not a crime. It is incumbent on us to look at this area and others with open minds while recognizing that honest and sincere scrutiny often helps make a better future a reality. The United States is working to achieve major goals for health care—access for all, lower costs, and fewer abuses of the system. Our involvement is a mandate to be followed enthusiastically.
Many assume that the American Joint Replacement Registry (AJRR) is moving forward as originally planned. No one has reported any obstacles that may cast doubt on its continued progress.
Despite the enthusiasm for AJRR, we must be realistic and admit that the project may not in the final analysis bring about its anticipated results. Therefore, periodic sober assessments of its course should be carried out, as they might result in identifying possible flaws and strengths. It is imperative to continue to express doubts regarding the true long-term value of this registry.
Much of the original support for an ongoing registry came from the example provided by the Swedish national registry. The Scandinavian registry had been said to dramatically reduce the number of complications and halve the revision rate for total hip arthroplasties. We need to question the claim that this reduction was solely the result of information produced by the registry. It is hard to believe that the literature had failed to report on those complications long before the registry publicized its findings.
As we take a fresh look at AJRR, it is perhaps wise to keep in mind the history of the AO Swiss Fracture Registry, founded by Maurice Müller and heavily subsidized by industry. Apparently, after gathering millions of pieces of information, primarily about equipment used for fracture fixation, the Swiss registry has failed to produce the greater benefits it had expected. Given the similarities between the Swiss Fracture Registry and AJRR, it is logical to assume that the latter may suffer the same fate.
I base my concerns on factors that, carefully analyzed, might be important in determining the future of AJRR. One major consideration is the difficulty in guaranteeing the veracity of data submitted—a factor shared by all registries.1 To assume that all participating surgeons adhere to high ethical and professional standards is naïve. Some surgeons who stand to make large profits from their ownership of implants or equipment are submitting false and erroneous information. Other unscrupulous orthopedists are receiving large kickbacks for helping the industry market its implants. These people will be tempted to embellish and falsify information about successes and failures and submit it to the registry.1-3
Militating against the “guaranteed success” of AJRR is this tainted relationship between the implant manufacturing industry and some members of the orthopedics community. A 2002–2006 investigation by the US Justice Department found egregious unethical transgressions and corrupt relationships between 5 companies and hundreds of orthopedists—representing a widespread loss of professionalism in our ranks.4 More recently, the Centers for Medicare & Medicaid Services5 disclosed that, in the last 5 months of 2013, $3.5 billion were paid by medical device companies to doctors and leading hospitals. As stated in a newspaper article, “‘Open Payments does not identify which financial relationships … could cause conflicts of interest,’ said Shantanu Agrawal, the agency official overseeing the project. ‘It simply makes the data available to the public.’”6 Further, “an initial Associated Press analysis found that orthopedists, cardiologists and adult medicine specialists were among the likeliest to receive payments from drug and device companies. Most of the contributions came in the form of cash payments, followed by in-kind gifts and services, and stock options.”6
This official government revelation is disturbing. Although the number of people who are deliberately committing clear infractions may be small, some of these people are likely well-known, and their influence should not be underestimated, particularly with regard to AJRR publications. Some in the orthopedic community do not question the accuracy of these publications but accept their conclusions as fact, and such may be the case with orthopedic guidelines.7
Given these concerns and the facts of the situation, can AJRR solve real problems that traditional systems have so far failed to solve? We have enough journals and scientific meetings informing us of the failures and successes of implants. I suspect it is wrong to believe that the AJRR data on 1 million patients’ arthroplasties are necessarily superior to the data from a 20,000-patient registry. Such an erroneous conclusion ignores the fact that, with clinical issues such as the one currently being addressed by AJRR, having a larger registry and more patients does not necessarily imply more meaningful information. In addition, follow-ups longer than those used with traditional methods are not possible—death will continue to intervene. No matter how many patients are included in the system, the maximum follow-up will forever remain the same.
Financing of AJRR is expensive, time-consuming, and likely to be terminated if clear evidence of the true value of the registry is not provided within the next few years. In light of such an outcome, we should replace the current system with a more effective mechanism. For example, we could produce an annual publication that summarizes the peer-reviewed articles published on joint replacement, with an emphasis on controversial topics. Orthopedic fellows, rather than readily accepting AJRR findings and recommendations, will instead be able to decide for themselves what treatment to use for each particular patient and situation, based on information provided by a number of independent investigators.
Meaningful progress in managing clinical conditions, such as the ones we are discussing, is achieved not by expanding the size of a registry but by being committed as individuals to making improvements. A cursory glance at the history of hip arthroplasty easily proves the point. Registries, guidelines, and other popular systems sometimes inadvertently create an environment that inhibits independent thinking. When powerful nonmedical economic and political bodies become involved in medical issues in order to ensure their continued profit, our autonomy is lost or compromised in major ways. Such scenarios must be avoided as forcefully as possible.8
Questioning the future of AJRR does not derive from rigid thinking or from a lack of awareness or understanding of the registry’s nature, procedures, benefits, goals, or highly altruistic and noble origins. However, pointing out a lack of evidence of success is not a crime. It is incumbent on us to look at this area and others with open minds while recognizing that honest and sincere scrutiny often helps make a better future a reality. The United States is working to achieve major goals for health care—access for all, lower costs, and fewer abuses of the system. Our involvement is a mandate to be followed enthusiastically.
1. Carr AJ. Which research is to be believed? The ethics of industrial funding of orthopaedic research. J Bone Joint Surg Br. 2005;87(11):1452-1453.
2. Callahan D. False Hopes: Overcoming the Obstacles to a Sustainable, Affordable Medicine. New Brunswick, NJ: Rutgers University Press; 1999.
3. Relman AS. A Second Opinion: Rescuing America’s Healthcare: A Plan for Universal Coverage Serving Patients Over Profit. New York: Public Affairs; 2007.
4. Five companies in hip and knee replacement industry avoid prosecution by agreeing to compliance rules and monitoring [press release]. US Department of Justice website. http://www.justice.gov/usao/nj/Press/files/pdffiles/Older/hips0927.rel.pdf. Published September 27, 2007. Accessed February 19, 2015.
5. CMS makes first wave of drug & device company payments to teaching hospitals and physicians public [press release]. Centers for Medicare & Medicaid Services website. http://www.cms.gov/Newsroom/MediaReleaseDatabase/Press-releases/2014-Press-releases-items/2014-09-30.html. Published September 30, 2014. Accessed February 19, 2015.
6. Alonso-Zaldivar R, Gillum J. Drug, device firms paid $3.5B to care providers. The Big Story. Associated Press website. http://bigstory.ap.org/article/c80ae51828a0497e87beda7f9ff60ac8/govt-reveal-drug-company-payments-doctors. Published September 30, 2014. Accessed February 19, 2015.
7. Sarmiento A. Thoughts on orthopedic guidelines. Am J Orthop. 2010;39(8):373-374.
8. Sarmiento A. Infringing on freedom of speech. J Bone Joint Surg Am. 2011;93(2):222.
1. Carr AJ. Which research is to be believed? The ethics of industrial funding of orthopaedic research. J Bone Joint Surg Br. 2005;87(11):1452-1453.
2. Callahan D. False Hopes: Overcoming the Obstacles to a Sustainable, Affordable Medicine. New Brunswick, NJ: Rutgers University Press; 1999.
3. Relman AS. A Second Opinion: Rescuing America’s Healthcare: A Plan for Universal Coverage Serving Patients Over Profit. New York: Public Affairs; 2007.
4. Five companies in hip and knee replacement industry avoid prosecution by agreeing to compliance rules and monitoring [press release]. US Department of Justice website. http://www.justice.gov/usao/nj/Press/files/pdffiles/Older/hips0927.rel.pdf. Published September 27, 2007. Accessed February 19, 2015.
5. CMS makes first wave of drug & device company payments to teaching hospitals and physicians public [press release]. Centers for Medicare & Medicaid Services website. http://www.cms.gov/Newsroom/MediaReleaseDatabase/Press-releases/2014-Press-releases-items/2014-09-30.html. Published September 30, 2014. Accessed February 19, 2015.
6. Alonso-Zaldivar R, Gillum J. Drug, device firms paid $3.5B to care providers. The Big Story. Associated Press website. http://bigstory.ap.org/article/c80ae51828a0497e87beda7f9ff60ac8/govt-reveal-drug-company-payments-doctors. Published September 30, 2014. Accessed February 19, 2015.
7. Sarmiento A. Thoughts on orthopedic guidelines. Am J Orthop. 2010;39(8):373-374.
8. Sarmiento A. Infringing on freedom of speech. J Bone Joint Surg Am. 2011;93(2):222.
We Can Do Better for Our Veterans’ Health Care
The mission statement of the US Department of Veterans Affairs (VA) reiterates Abraham Lincoln’s promise, “to care for him who shall have borne the battle, and for his widow, and his orphan,” by serving the men and women who are American veterans.1 Robert A. McDonald is the current Secretary of Veterans Affairs. He was recently appointed after the scheduling scandal at the VA. He was the previous Chairman and Chief Executive Officer of Procter & Gamble and is a graduate of West Point. Mr. McDonald has recently been criticized for some public misstatements after only being on the job for a few months.2,3 His staff includes a wide variety of numerous secretaries, deputies, councils, and assistant associates. The budget for 2016 that was recently submitted was $169 billion.4 The scandalous scheduling fiasco in the entire VA system blatantly shows the neglect of our servicemen and servicewomen and is a permanent blemish on a government-run system. Despite claims of numerous firings, only 8 people have been dismissed out of an employee pool of over 300,000.3
I have been a volunteer physician for just under 40 years at the VA Hospital in La Jolla, California, which is also an associated teaching hospital for the University of California, San Diego. Many of my reflections are from personal experience. I am also a veteran. I have a deep affection for our veterans and their families, and write this column in the hope of some possible change in their care. The physicians and health care providers in this system are dedicated and professional individuals caught up in a tangled bureaucratic web that, in most cases, handcuffs the delivery of the health care that our veterans deserve.
When one goes to the VA website, it appears that there are a myriad of services available, but, as with all government agencies, more time is spent in the creation of the website and structure of the agency than is spent in servicing the patient. Picture trying to get your health care through the local Department of Motor Vehicles office. The VA system is a huge bureaucratic overregulated agency currently out of control and lacking efficiency. From the clinic to the operating room, the process is frustrating to all involved. There are clinics staffed with medical doctors, nurse practitioners, physician assistants, medical students, residents, and fellows. Generally, they can only process 10 to 12 patients per half-day clinic because of the endless paperwork and regulatory requirements.
The operating rooms have been a formidable frustration to the surgeon. It is routine for a 7:30 am case to start at 9 am and then be followed by a 2½-hour turnover time until the second case could be scheduled. Cases cannot be scheduled that could potentially start after 3 pm. Most data would probably suggest that the operating room efficiency in terms of numbers of cases is approximately 50% to 60% of what can be done in the private environment. Staffing for all facets of the hospital operation is about double what is necessary in the outside world. Physicians must take tests on a very frequent basis on subjects that are totally unrelated to health care. Examinations on American history, electrical safety, and sexual harassment in the workplace are commonplace topics. These tests must be taken and passed in order to maintain one’s privileges at the hospital.
Is there an answer to this government-run system? Perhaps. Here is a potential solution. Over a 5-year period, divest all VA facilities, sell or rent them, and sell or rent the land. Use the proceeds, in combination with the normal budget for the VA, to create a private health care system. Veterans and their families would then receive a veteran-based private policy that would have no deductibles or copays and would allow them to seek medical care from any provider. For more complex situations such as quadriplegia, posttraumatic stress disorder (PTSD), or complex amputations, private entities would bid on a local basis, assuming they pass a strict credentialing process. These private entities would be required to pay strict attention to protocol, deliver prompt service, and produce outcomes that are acceptable in the medical workplace. The newly created system would be run by a private board composed of retired military, business executives, and entrepreneurs with no political affiliations. The trust fund would not be susceptible to any other allocation other than the medical care of veterans.
I have seen far too many spouses and families of deployed servicemen and servicewomen whose care has been neglected while their spouses are serving in a foreign land. There are far too many homeless veterans that are in need of psychiatric care and suffering from PTSD. It is estimated that 11% of the current homeless population are veterans.5 Their housing needs have been completely neglected. These are not acceptable statistics. The government now provides some burial services and headstones for our deceased veterans instead of delivering the health care for them and their families while they are still alive.
1. Mission, vision, core values & goals. US Department of Veterans Affairs website. http://www.va.gov/about_va/mission.asp. Updated April 1, 2014. Accessed March 6, 2015.
2. VA Secretary apologizes for “misspeaking” about Special Forces service. Fox News Insider website. http://insider.foxnews.com/2015/02/24/va-secretary-robert-mcdonald-apologizes-misspeaking-about-special-forces-service. Published February 24, 2015. Accessed March 6, 2015.
3. Lee MYH. No, the VA has not fired 60 people for manipulating wait-time data. Washington Post website. http://www.washingtonpost.com/blogs/fact-checker/wp/2015/02/18/no-the-va-has-not-fired-60-people-for-manipulating-wait-time-data. Published February 18, 2015. Accessed March 6, 2015.
4. Annual budget submission. US Department of Veterans Affairs website. http://www.va.gov/budget/products.asp. Updated February 3, 2015. Accessed March 6, 2015.
5. Henry M, Cortes A, Shivji A, Buck K; US Department of Housing and Urban Development, Office of Community Planning and Development. The 2014 Annual Homeless Assessment Report (AHAR) to Congress, October 2014: Part 1, Point-in-Time Estimates of Homelessness. HUD Exchange website. https://www.hudexchange.info/resources/documents/2014-AHAR-Part1.pdf. Published December 2014. Accessed March 6, 2015.
The mission statement of the US Department of Veterans Affairs (VA) reiterates Abraham Lincoln’s promise, “to care for him who shall have borne the battle, and for his widow, and his orphan,” by serving the men and women who are American veterans.1 Robert A. McDonald is the current Secretary of Veterans Affairs. He was recently appointed after the scheduling scandal at the VA. He was the previous Chairman and Chief Executive Officer of Procter & Gamble and is a graduate of West Point. Mr. McDonald has recently been criticized for some public misstatements after only being on the job for a few months.2,3 His staff includes a wide variety of numerous secretaries, deputies, councils, and assistant associates. The budget for 2016 that was recently submitted was $169 billion.4 The scandalous scheduling fiasco in the entire VA system blatantly shows the neglect of our servicemen and servicewomen and is a permanent blemish on a government-run system. Despite claims of numerous firings, only 8 people have been dismissed out of an employee pool of over 300,000.3
I have been a volunteer physician for just under 40 years at the VA Hospital in La Jolla, California, which is also an associated teaching hospital for the University of California, San Diego. Many of my reflections are from personal experience. I am also a veteran. I have a deep affection for our veterans and their families, and write this column in the hope of some possible change in their care. The physicians and health care providers in this system are dedicated and professional individuals caught up in a tangled bureaucratic web that, in most cases, handcuffs the delivery of the health care that our veterans deserve.
When one goes to the VA website, it appears that there are a myriad of services available, but, as with all government agencies, more time is spent in the creation of the website and structure of the agency than is spent in servicing the patient. Picture trying to get your health care through the local Department of Motor Vehicles office. The VA system is a huge bureaucratic overregulated agency currently out of control and lacking efficiency. From the clinic to the operating room, the process is frustrating to all involved. There are clinics staffed with medical doctors, nurse practitioners, physician assistants, medical students, residents, and fellows. Generally, they can only process 10 to 12 patients per half-day clinic because of the endless paperwork and regulatory requirements.
The operating rooms have been a formidable frustration to the surgeon. It is routine for a 7:30 am case to start at 9 am and then be followed by a 2½-hour turnover time until the second case could be scheduled. Cases cannot be scheduled that could potentially start after 3 pm. Most data would probably suggest that the operating room efficiency in terms of numbers of cases is approximately 50% to 60% of what can be done in the private environment. Staffing for all facets of the hospital operation is about double what is necessary in the outside world. Physicians must take tests on a very frequent basis on subjects that are totally unrelated to health care. Examinations on American history, electrical safety, and sexual harassment in the workplace are commonplace topics. These tests must be taken and passed in order to maintain one’s privileges at the hospital.
Is there an answer to this government-run system? Perhaps. Here is a potential solution. Over a 5-year period, divest all VA facilities, sell or rent them, and sell or rent the land. Use the proceeds, in combination with the normal budget for the VA, to create a private health care system. Veterans and their families would then receive a veteran-based private policy that would have no deductibles or copays and would allow them to seek medical care from any provider. For more complex situations such as quadriplegia, posttraumatic stress disorder (PTSD), or complex amputations, private entities would bid on a local basis, assuming they pass a strict credentialing process. These private entities would be required to pay strict attention to protocol, deliver prompt service, and produce outcomes that are acceptable in the medical workplace. The newly created system would be run by a private board composed of retired military, business executives, and entrepreneurs with no political affiliations. The trust fund would not be susceptible to any other allocation other than the medical care of veterans.
I have seen far too many spouses and families of deployed servicemen and servicewomen whose care has been neglected while their spouses are serving in a foreign land. There are far too many homeless veterans that are in need of psychiatric care and suffering from PTSD. It is estimated that 11% of the current homeless population are veterans.5 Their housing needs have been completely neglected. These are not acceptable statistics. The government now provides some burial services and headstones for our deceased veterans instead of delivering the health care for them and their families while they are still alive.
The mission statement of the US Department of Veterans Affairs (VA) reiterates Abraham Lincoln’s promise, “to care for him who shall have borne the battle, and for his widow, and his orphan,” by serving the men and women who are American veterans.1 Robert A. McDonald is the current Secretary of Veterans Affairs. He was recently appointed after the scheduling scandal at the VA. He was the previous Chairman and Chief Executive Officer of Procter & Gamble and is a graduate of West Point. Mr. McDonald has recently been criticized for some public misstatements after only being on the job for a few months.2,3 His staff includes a wide variety of numerous secretaries, deputies, councils, and assistant associates. The budget for 2016 that was recently submitted was $169 billion.4 The scandalous scheduling fiasco in the entire VA system blatantly shows the neglect of our servicemen and servicewomen and is a permanent blemish on a government-run system. Despite claims of numerous firings, only 8 people have been dismissed out of an employee pool of over 300,000.3
I have been a volunteer physician for just under 40 years at the VA Hospital in La Jolla, California, which is also an associated teaching hospital for the University of California, San Diego. Many of my reflections are from personal experience. I am also a veteran. I have a deep affection for our veterans and their families, and write this column in the hope of some possible change in their care. The physicians and health care providers in this system are dedicated and professional individuals caught up in a tangled bureaucratic web that, in most cases, handcuffs the delivery of the health care that our veterans deserve.
When one goes to the VA website, it appears that there are a myriad of services available, but, as with all government agencies, more time is spent in the creation of the website and structure of the agency than is spent in servicing the patient. Picture trying to get your health care through the local Department of Motor Vehicles office. The VA system is a huge bureaucratic overregulated agency currently out of control and lacking efficiency. From the clinic to the operating room, the process is frustrating to all involved. There are clinics staffed with medical doctors, nurse practitioners, physician assistants, medical students, residents, and fellows. Generally, they can only process 10 to 12 patients per half-day clinic because of the endless paperwork and regulatory requirements.
The operating rooms have been a formidable frustration to the surgeon. It is routine for a 7:30 am case to start at 9 am and then be followed by a 2½-hour turnover time until the second case could be scheduled. Cases cannot be scheduled that could potentially start after 3 pm. Most data would probably suggest that the operating room efficiency in terms of numbers of cases is approximately 50% to 60% of what can be done in the private environment. Staffing for all facets of the hospital operation is about double what is necessary in the outside world. Physicians must take tests on a very frequent basis on subjects that are totally unrelated to health care. Examinations on American history, electrical safety, and sexual harassment in the workplace are commonplace topics. These tests must be taken and passed in order to maintain one’s privileges at the hospital.
Is there an answer to this government-run system? Perhaps. Here is a potential solution. Over a 5-year period, divest all VA facilities, sell or rent them, and sell or rent the land. Use the proceeds, in combination with the normal budget for the VA, to create a private health care system. Veterans and their families would then receive a veteran-based private policy that would have no deductibles or copays and would allow them to seek medical care from any provider. For more complex situations such as quadriplegia, posttraumatic stress disorder (PTSD), or complex amputations, private entities would bid on a local basis, assuming they pass a strict credentialing process. These private entities would be required to pay strict attention to protocol, deliver prompt service, and produce outcomes that are acceptable in the medical workplace. The newly created system would be run by a private board composed of retired military, business executives, and entrepreneurs with no political affiliations. The trust fund would not be susceptible to any other allocation other than the medical care of veterans.
I have seen far too many spouses and families of deployed servicemen and servicewomen whose care has been neglected while their spouses are serving in a foreign land. There are far too many homeless veterans that are in need of psychiatric care and suffering from PTSD. It is estimated that 11% of the current homeless population are veterans.5 Their housing needs have been completely neglected. These are not acceptable statistics. The government now provides some burial services and headstones for our deceased veterans instead of delivering the health care for them and their families while they are still alive.
1. Mission, vision, core values & goals. US Department of Veterans Affairs website. http://www.va.gov/about_va/mission.asp. Updated April 1, 2014. Accessed March 6, 2015.
2. VA Secretary apologizes for “misspeaking” about Special Forces service. Fox News Insider website. http://insider.foxnews.com/2015/02/24/va-secretary-robert-mcdonald-apologizes-misspeaking-about-special-forces-service. Published February 24, 2015. Accessed March 6, 2015.
3. Lee MYH. No, the VA has not fired 60 people for manipulating wait-time data. Washington Post website. http://www.washingtonpost.com/blogs/fact-checker/wp/2015/02/18/no-the-va-has-not-fired-60-people-for-manipulating-wait-time-data. Published February 18, 2015. Accessed March 6, 2015.
4. Annual budget submission. US Department of Veterans Affairs website. http://www.va.gov/budget/products.asp. Updated February 3, 2015. Accessed March 6, 2015.
5. Henry M, Cortes A, Shivji A, Buck K; US Department of Housing and Urban Development, Office of Community Planning and Development. The 2014 Annual Homeless Assessment Report (AHAR) to Congress, October 2014: Part 1, Point-in-Time Estimates of Homelessness. HUD Exchange website. https://www.hudexchange.info/resources/documents/2014-AHAR-Part1.pdf. Published December 2014. Accessed March 6, 2015.
1. Mission, vision, core values & goals. US Department of Veterans Affairs website. http://www.va.gov/about_va/mission.asp. Updated April 1, 2014. Accessed March 6, 2015.
2. VA Secretary apologizes for “misspeaking” about Special Forces service. Fox News Insider website. http://insider.foxnews.com/2015/02/24/va-secretary-robert-mcdonald-apologizes-misspeaking-about-special-forces-service. Published February 24, 2015. Accessed March 6, 2015.
3. Lee MYH. No, the VA has not fired 60 people for manipulating wait-time data. Washington Post website. http://www.washingtonpost.com/blogs/fact-checker/wp/2015/02/18/no-the-va-has-not-fired-60-people-for-manipulating-wait-time-data. Published February 18, 2015. Accessed March 6, 2015.
4. Annual budget submission. US Department of Veterans Affairs website. http://www.va.gov/budget/products.asp. Updated February 3, 2015. Accessed March 6, 2015.
5. Henry M, Cortes A, Shivji A, Buck K; US Department of Housing and Urban Development, Office of Community Planning and Development. The 2014 Annual Homeless Assessment Report (AHAR) to Congress, October 2014: Part 1, Point-in-Time Estimates of Homelessness. HUD Exchange website. https://www.hudexchange.info/resources/documents/2014-AHAR-Part1.pdf. Published December 2014. Accessed March 6, 2015.
From the editors
Editor’s Note: The associate editors of Vascular Specialist were asked to provide their perspectives on the stenting controversy. Here is a selection.
Dr. Frank J. Veith: The recent lead article in the New York Times on excessive implantation of lower extremity stents highlights one key point. Vascular surgeons and all vascular specialists who treat lower extremity occlusive disease should always clearly inform patients with intermittent claudication that one acceptable treatment option is medical and lipid-lowering therapy without any invasive treatment of their arterial blockage. They should be informed that the condition almost never leads to limb loss and that invasive treatment can safely be delayed until such progression occurs.
Given such honest reassurance and the option to choose their treatment, most patients with claudication will choose a conservative rather than an invasive approach, and unnecessary stent/angioplasty and other lower extremity interventional procedures, as described in the Times article, will be minimized.
Dr. John F. Eidt: The truth is we all bear responsibility. The treatment of lower extremity peripheral artery disease (PAD) has largely defied prior efforts to define appropriate care. Even the SVS document recommending risk factor modification in the initial management of intermittent claudication leaves substantial room for individualized judgment.
The appropriateness of intervention is largely in the eye of the beholder. “Lifestyle-limiting” claudication can be invoked as justification for intervention in virtually anyone. But I do believe that vascular surgeons are more wary of the adverse consequences of vascular intervention for one important reason – we do amputations. We are unique among vascular specialists in that we deal with the tragedies of unwarranted vascular procedures. For vascular surgeons, failure of intervention means more than binary restenosis or increased target lesion revascularization. Performing an amputation after failed intervention in a claudicant leaves an indelible mark on each of us and may underlie our inherently conservative approach to PAD. But we need to be fearless in speaking the truth and serving as advocates for exemplary patient care. Continuing a relationship with a source of carotid and aortic referrals while turning a blind eye to meddlesome lower extremity intervention sends the wrong message. Our silence constitutes tacit approval. Too frequently I hear a patient say “my cardiologist says there is nothing else he can do, go see a vascular surgeon.” Despite years of branding efforts by the SVS, surveys of primary care providers and the public alike confirm that many remain uncertain of our skills. We need to do a better job of spreading the word that vascular surgeons are “leaders in the minimally invasive treatment of PAD.” Not the last resort.
Dr. Frank Pomposelli: I could not agree more with Dr. Eidt. It’s easy to indict the outpatient labs for obvious reasons but I personally agree that the root of the problem lies in the overly aggressive posture being taken toward treatment of claudication.
It just so happens that outpatient labs are filled with claudicants since they are most likely to have the least complex disease – match made in heaven or hell, depending on your perspective.
One cardiologist quoted in the N.Y. Times piece said patients with claudication have been “grossly under treated” – a convenient posture to take when billing Medicare $4.5 million a year. The other cardiologist who was the focus of the investigation called the charges “baseless and fiction” and stated his center had the lowest rate of amputation in the country.
It gets back to Dr. Eidt’s point how it’s easy for the nonsurgeon to dismiss amputation as an occasional unfortunate byproduct of a busy practice when you never have had to tell a patient they need one and suffer with them through the emotional and physical trauma that always follows. I was taught like many of you, I suspect, that any amputation after treatment for claudication should be considered not only an unacceptable complication but also a failure of the trust the patient placed in me. My mentor was a militant nihilist when it came to surgery for claudication but that concept is always in my mind whenever I treat a patient and has always tempered my decision making.
I like to think our recently published practice guidelines will help but am skeptical that it will make a positive impact where it is most needed; on those who are primarily driven by financial gain. I’d also point out that Dr. Darren B. Schneider was quoted as a member of the Society for Vascular Medicine. I guess we need to work harder on our branding.
Dr. Mark Morasch: Remember, all politics are local, and any meaningful change needs to come from the grass roots.
Experts can write guidelines, specialty societies can make statements, and newspapers can print articles but the most influential transaction occurs in the exam room when we are face to face with our patients.
Remember, even though we are a small group, we can have great influence when we always, always, always do what we know is right.
Dr. Alan M. Dietzek: Dear Patient, Let me introduce myself. I am a Board-Certified Vascular Surgeon. My specialty is unique in that I am well versed and formally trained in both the medical and surgical management of peripheral vascular disease. No other specialist can make this claim.
Most often, vascular problems can be managed conservatively with a combination of risk factor and lifestyle modification, and occasionally prescription medications, all of which I can outline and or prescribe for you. When necessary, however, I am prepared to treat your vascular problem with either a minimally invasive procedure or open surgery depending on which treatment will provide you with the best outcomes. Again, only a vascular surgeon is capable of offering you these treatment options. I am dedicated to your well-being. I am a Board-Certified Vascular Surgeon
Dr. Murray L. Shames: The recent New York Times article, “Medicare payments surge for stents to unblock blood vessels in limbs,” brings up a critical issue in how we train our residents to think and practice in the future.
Our current generation of residents is faced with a tremendous financial burden of medical school debt, and they are being offered highly competitive salaries after graduation.
The motivation to join groups with outpatient vascular centers is certainly attractive: Why not have autonomy from the hospital, control your work environment, and increase efficiency. As educators we must continue to use clinical evidence and societal guidelines (J. Vasc. Surg. 2015:1-40) to guide our clinical practice.
As vascular surgeons we have been trained to manage asymptomatic PAD and intermittent claudication nonoperatively due to it’s relatively benign natural history; endovascular interventions have dramatically increased the treatment of claudication, even in our own hands. We must continue to teach our residents restraint and to consider the impact of the interventions we perform. That way we can maintain our status as the leaders in vascular disease management and not just “interventionalists” that treat lesions.
Dr. Joann Lohr: The presence of a stenotic lesion does not mandate treatment either with a stent or surgical intervention but needs critical assessment of the impact on the patient’s quality of life. Risk factor modification needs to be undertaken before any intervention and will improve outcomes and durability of repairs. The only outcome that matters is the patient’s.
“How does treatment of this lesion change my lifestyle?” is a question that needs to be answered for each patient. Treating physicians need to establish long-term relationships.
Never be afraid to tell patients a procedure is not the first line of treatment. Thoughtful application of new technology is needed in all areas of medicine. Just because we can, should we? Appropriate individualized treatment plans and goals need to be established for each patient we treat.
Dr. Larry Kraiss: Vascular surgeons provide the full spectrum of care for PAD from medical management through intervention to the unfortunate situations when amputation is necessary.
The more sobering of these experiences have imbued most of us with a healthy respect for how an intervention can go wrong. If you haven’t had to explain to a patient or family why an amputation is necessary, you probably don’t have the same concern.
Thus, many of us have a very conservative approach to PAD intervention; primum non nocere is the governing principle. This principle is supposed to guide the actions of all physicians but I can’t help but wonder if something happened to primum non nocere on the way to the outpatient endovascular center.
When physicians become financial stakeholders in these enterprises, a pernicious incentive is introduced that is almost impossible to exclude from daily clinical decision making. Hospital-based physicians are also subject to temptation to perform unnecessary yet lucrative procedures but at least these are being done more in the open.
I suspect that the development of these centers has allowed much activity to occur that would rightly be condemned under the scrutiny of one’s hospital peers.
Dr. Laura Drudi: It really comes down to adequately informing the patient. I always find it astounding how many patients I encounter asking me in a timid tone, “What exactly did I have done on my leg?” I question what patients actually understand and retain after being overwhelmed by the informed consent we have prior to an intervention.
I see first hand the catastrophic failures of intervening on severe claudication leading to limb loss and worsening of quality of life. It’s disheartening to see adverse outcomes following vascular interventions either by vascular surgeons or other interventionalists, but I believe that if you are performing an intervention you should have the expertise and technical skills to deal with the complications.
The best interventionalists know when not to intervene and that should be the mantra we live by. We should be advocates for our patients at a local institutional level as well as a public level. I believe that following the New York Times article the public will be more aware of the potential for inappropriate or unnecessary interventions, many of which are being performed by specialists other than vascular surgeons.
The Society and individual vascular surgeons should capitalize on this opportunity to educate patients as to the benefits of consulting with a vascular surgeon before undertaking any endovascular procedure.
Dr. Elliot L. Chaikof: Both government and private payers have a vested interest in ensuring that patients receive the highest quality care, while reducing the unsustainable rate of increase in health care costs. In Massachusetts and elsewhere in the United States, this has led to the introduction of new risk contracting models that features a global payment with incentives linked to efficiency and quality.
At our institution, approximately 60% of patients are now in such risk contracts. Primary care physicians are most directly incentivized and, along with government and private payors, are highly motivated to ensure that our population of patients receives the right care, at the right time, from the right physician. The U.S. health care system continues to be in a state of flux with substantial regional variations in the delivery of care and how that care is financed.
Despite these challenges, the Society for Vascular Surgery can best serve our patients through advocacy and education, including promoting the need for full transparency of costs to our patients and their physicians. This would be most effective in active partnership with primary care providers, along with regional and national payors.
Dr. Erica L. Mitchell: The line separating a business from a profession is not entirely clear when professionals engage in business practices that serve to benefit the individual financially.
One crucial difference distinguishing the profession of medicine from other professions is that physicians have a fiduciary duty toward those whom they serve. This means that we have a legal duty to provide services to our patients that place the patient’s interest above our own financial interest.
This article highlights how legal and ethical issues arise if health care professionals forgo their fiduciary duties for personal gain. Unethical physicians should be held accountable for unethical practices.
Dr. Larry Scher: The recent article by Julie Creswell and Reed Abelson in the Jan. 29, 2015, New York Times highlights a recent problem in the care of patients with peripheral vascular disease. Vascular surgeons have been treating peripheral arterial disease for over 50 years and have generally adopted a conservative approach toward patients with claudication, emphasizing risk factor modification and exercise.
This is based on an understanding that the disease is benign, rarely progressive, and only occasionally disabling to the point that intervention is indicated for symptom relief.
With new minimally invasive techniques available and specialists other than vascular surgeons performing peripheral catheter based procedures we seem to have forgotten all that vascular surgeons have learned over the past 5 decades.
Most patients with claudication do not benefit from and may be harmed by interventions when long-term rather than short-term outcomes are analyzed. Although practitioners such as those identified in this article may believe they are pioneers in the treatment of peripheral arterial disease and specifically claudication, I would consider them cowboys who have forgotten the lessons of the past.
Editor’s Note: The associate editors of Vascular Specialist were asked to provide their perspectives on the stenting controversy. Here is a selection.
Dr. Frank J. Veith: The recent lead article in the New York Times on excessive implantation of lower extremity stents highlights one key point. Vascular surgeons and all vascular specialists who treat lower extremity occlusive disease should always clearly inform patients with intermittent claudication that one acceptable treatment option is medical and lipid-lowering therapy without any invasive treatment of their arterial blockage. They should be informed that the condition almost never leads to limb loss and that invasive treatment can safely be delayed until such progression occurs.
Given such honest reassurance and the option to choose their treatment, most patients with claudication will choose a conservative rather than an invasive approach, and unnecessary stent/angioplasty and other lower extremity interventional procedures, as described in the Times article, will be minimized.
Dr. John F. Eidt: The truth is we all bear responsibility. The treatment of lower extremity peripheral artery disease (PAD) has largely defied prior efforts to define appropriate care. Even the SVS document recommending risk factor modification in the initial management of intermittent claudication leaves substantial room for individualized judgment.
The appropriateness of intervention is largely in the eye of the beholder. “Lifestyle-limiting” claudication can be invoked as justification for intervention in virtually anyone. But I do believe that vascular surgeons are more wary of the adverse consequences of vascular intervention for one important reason – we do amputations. We are unique among vascular specialists in that we deal with the tragedies of unwarranted vascular procedures. For vascular surgeons, failure of intervention means more than binary restenosis or increased target lesion revascularization. Performing an amputation after failed intervention in a claudicant leaves an indelible mark on each of us and may underlie our inherently conservative approach to PAD. But we need to be fearless in speaking the truth and serving as advocates for exemplary patient care. Continuing a relationship with a source of carotid and aortic referrals while turning a blind eye to meddlesome lower extremity intervention sends the wrong message. Our silence constitutes tacit approval. Too frequently I hear a patient say “my cardiologist says there is nothing else he can do, go see a vascular surgeon.” Despite years of branding efforts by the SVS, surveys of primary care providers and the public alike confirm that many remain uncertain of our skills. We need to do a better job of spreading the word that vascular surgeons are “leaders in the minimally invasive treatment of PAD.” Not the last resort.
Dr. Frank Pomposelli: I could not agree more with Dr. Eidt. It’s easy to indict the outpatient labs for obvious reasons but I personally agree that the root of the problem lies in the overly aggressive posture being taken toward treatment of claudication.
It just so happens that outpatient labs are filled with claudicants since they are most likely to have the least complex disease – match made in heaven or hell, depending on your perspective.
One cardiologist quoted in the N.Y. Times piece said patients with claudication have been “grossly under treated” – a convenient posture to take when billing Medicare $4.5 million a year. The other cardiologist who was the focus of the investigation called the charges “baseless and fiction” and stated his center had the lowest rate of amputation in the country.
It gets back to Dr. Eidt’s point how it’s easy for the nonsurgeon to dismiss amputation as an occasional unfortunate byproduct of a busy practice when you never have had to tell a patient they need one and suffer with them through the emotional and physical trauma that always follows. I was taught like many of you, I suspect, that any amputation after treatment for claudication should be considered not only an unacceptable complication but also a failure of the trust the patient placed in me. My mentor was a militant nihilist when it came to surgery for claudication but that concept is always in my mind whenever I treat a patient and has always tempered my decision making.
I like to think our recently published practice guidelines will help but am skeptical that it will make a positive impact where it is most needed; on those who are primarily driven by financial gain. I’d also point out that Dr. Darren B. Schneider was quoted as a member of the Society for Vascular Medicine. I guess we need to work harder on our branding.
Dr. Mark Morasch: Remember, all politics are local, and any meaningful change needs to come from the grass roots.
Experts can write guidelines, specialty societies can make statements, and newspapers can print articles but the most influential transaction occurs in the exam room when we are face to face with our patients.
Remember, even though we are a small group, we can have great influence when we always, always, always do what we know is right.
Dr. Alan M. Dietzek: Dear Patient, Let me introduce myself. I am a Board-Certified Vascular Surgeon. My specialty is unique in that I am well versed and formally trained in both the medical and surgical management of peripheral vascular disease. No other specialist can make this claim.
Most often, vascular problems can be managed conservatively with a combination of risk factor and lifestyle modification, and occasionally prescription medications, all of which I can outline and or prescribe for you. When necessary, however, I am prepared to treat your vascular problem with either a minimally invasive procedure or open surgery depending on which treatment will provide you with the best outcomes. Again, only a vascular surgeon is capable of offering you these treatment options. I am dedicated to your well-being. I am a Board-Certified Vascular Surgeon
Dr. Murray L. Shames: The recent New York Times article, “Medicare payments surge for stents to unblock blood vessels in limbs,” brings up a critical issue in how we train our residents to think and practice in the future.
Our current generation of residents is faced with a tremendous financial burden of medical school debt, and they are being offered highly competitive salaries after graduation.
The motivation to join groups with outpatient vascular centers is certainly attractive: Why not have autonomy from the hospital, control your work environment, and increase efficiency. As educators we must continue to use clinical evidence and societal guidelines (J. Vasc. Surg. 2015:1-40) to guide our clinical practice.
As vascular surgeons we have been trained to manage asymptomatic PAD and intermittent claudication nonoperatively due to it’s relatively benign natural history; endovascular interventions have dramatically increased the treatment of claudication, even in our own hands. We must continue to teach our residents restraint and to consider the impact of the interventions we perform. That way we can maintain our status as the leaders in vascular disease management and not just “interventionalists” that treat lesions.
Dr. Joann Lohr: The presence of a stenotic lesion does not mandate treatment either with a stent or surgical intervention but needs critical assessment of the impact on the patient’s quality of life. Risk factor modification needs to be undertaken before any intervention and will improve outcomes and durability of repairs. The only outcome that matters is the patient’s.
“How does treatment of this lesion change my lifestyle?” is a question that needs to be answered for each patient. Treating physicians need to establish long-term relationships.
Never be afraid to tell patients a procedure is not the first line of treatment. Thoughtful application of new technology is needed in all areas of medicine. Just because we can, should we? Appropriate individualized treatment plans and goals need to be established for each patient we treat.
Dr. Larry Kraiss: Vascular surgeons provide the full spectrum of care for PAD from medical management through intervention to the unfortunate situations when amputation is necessary.
The more sobering of these experiences have imbued most of us with a healthy respect for how an intervention can go wrong. If you haven’t had to explain to a patient or family why an amputation is necessary, you probably don’t have the same concern.
Thus, many of us have a very conservative approach to PAD intervention; primum non nocere is the governing principle. This principle is supposed to guide the actions of all physicians but I can’t help but wonder if something happened to primum non nocere on the way to the outpatient endovascular center.
When physicians become financial stakeholders in these enterprises, a pernicious incentive is introduced that is almost impossible to exclude from daily clinical decision making. Hospital-based physicians are also subject to temptation to perform unnecessary yet lucrative procedures but at least these are being done more in the open.
I suspect that the development of these centers has allowed much activity to occur that would rightly be condemned under the scrutiny of one’s hospital peers.
Dr. Laura Drudi: It really comes down to adequately informing the patient. I always find it astounding how many patients I encounter asking me in a timid tone, “What exactly did I have done on my leg?” I question what patients actually understand and retain after being overwhelmed by the informed consent we have prior to an intervention.
I see first hand the catastrophic failures of intervening on severe claudication leading to limb loss and worsening of quality of life. It’s disheartening to see adverse outcomes following vascular interventions either by vascular surgeons or other interventionalists, but I believe that if you are performing an intervention you should have the expertise and technical skills to deal with the complications.
The best interventionalists know when not to intervene and that should be the mantra we live by. We should be advocates for our patients at a local institutional level as well as a public level. I believe that following the New York Times article the public will be more aware of the potential for inappropriate or unnecessary interventions, many of which are being performed by specialists other than vascular surgeons.
The Society and individual vascular surgeons should capitalize on this opportunity to educate patients as to the benefits of consulting with a vascular surgeon before undertaking any endovascular procedure.
Dr. Elliot L. Chaikof: Both government and private payers have a vested interest in ensuring that patients receive the highest quality care, while reducing the unsustainable rate of increase in health care costs. In Massachusetts and elsewhere in the United States, this has led to the introduction of new risk contracting models that features a global payment with incentives linked to efficiency and quality.
At our institution, approximately 60% of patients are now in such risk contracts. Primary care physicians are most directly incentivized and, along with government and private payors, are highly motivated to ensure that our population of patients receives the right care, at the right time, from the right physician. The U.S. health care system continues to be in a state of flux with substantial regional variations in the delivery of care and how that care is financed.
Despite these challenges, the Society for Vascular Surgery can best serve our patients through advocacy and education, including promoting the need for full transparency of costs to our patients and their physicians. This would be most effective in active partnership with primary care providers, along with regional and national payors.
Dr. Erica L. Mitchell: The line separating a business from a profession is not entirely clear when professionals engage in business practices that serve to benefit the individual financially.
One crucial difference distinguishing the profession of medicine from other professions is that physicians have a fiduciary duty toward those whom they serve. This means that we have a legal duty to provide services to our patients that place the patient’s interest above our own financial interest.
This article highlights how legal and ethical issues arise if health care professionals forgo their fiduciary duties for personal gain. Unethical physicians should be held accountable for unethical practices.
Dr. Larry Scher: The recent article by Julie Creswell and Reed Abelson in the Jan. 29, 2015, New York Times highlights a recent problem in the care of patients with peripheral vascular disease. Vascular surgeons have been treating peripheral arterial disease for over 50 years and have generally adopted a conservative approach toward patients with claudication, emphasizing risk factor modification and exercise.
This is based on an understanding that the disease is benign, rarely progressive, and only occasionally disabling to the point that intervention is indicated for symptom relief.
With new minimally invasive techniques available and specialists other than vascular surgeons performing peripheral catheter based procedures we seem to have forgotten all that vascular surgeons have learned over the past 5 decades.
Most patients with claudication do not benefit from and may be harmed by interventions when long-term rather than short-term outcomes are analyzed. Although practitioners such as those identified in this article may believe they are pioneers in the treatment of peripheral arterial disease and specifically claudication, I would consider them cowboys who have forgotten the lessons of the past.
Editor’s Note: The associate editors of Vascular Specialist were asked to provide their perspectives on the stenting controversy. Here is a selection.
Dr. Frank J. Veith: The recent lead article in the New York Times on excessive implantation of lower extremity stents highlights one key point. Vascular surgeons and all vascular specialists who treat lower extremity occlusive disease should always clearly inform patients with intermittent claudication that one acceptable treatment option is medical and lipid-lowering therapy without any invasive treatment of their arterial blockage. They should be informed that the condition almost never leads to limb loss and that invasive treatment can safely be delayed until such progression occurs.
Given such honest reassurance and the option to choose their treatment, most patients with claudication will choose a conservative rather than an invasive approach, and unnecessary stent/angioplasty and other lower extremity interventional procedures, as described in the Times article, will be minimized.
Dr. John F. Eidt: The truth is we all bear responsibility. The treatment of lower extremity peripheral artery disease (PAD) has largely defied prior efforts to define appropriate care. Even the SVS document recommending risk factor modification in the initial management of intermittent claudication leaves substantial room for individualized judgment.
The appropriateness of intervention is largely in the eye of the beholder. “Lifestyle-limiting” claudication can be invoked as justification for intervention in virtually anyone. But I do believe that vascular surgeons are more wary of the adverse consequences of vascular intervention for one important reason – we do amputations. We are unique among vascular specialists in that we deal with the tragedies of unwarranted vascular procedures. For vascular surgeons, failure of intervention means more than binary restenosis or increased target lesion revascularization. Performing an amputation after failed intervention in a claudicant leaves an indelible mark on each of us and may underlie our inherently conservative approach to PAD. But we need to be fearless in speaking the truth and serving as advocates for exemplary patient care. Continuing a relationship with a source of carotid and aortic referrals while turning a blind eye to meddlesome lower extremity intervention sends the wrong message. Our silence constitutes tacit approval. Too frequently I hear a patient say “my cardiologist says there is nothing else he can do, go see a vascular surgeon.” Despite years of branding efforts by the SVS, surveys of primary care providers and the public alike confirm that many remain uncertain of our skills. We need to do a better job of spreading the word that vascular surgeons are “leaders in the minimally invasive treatment of PAD.” Not the last resort.
Dr. Frank Pomposelli: I could not agree more with Dr. Eidt. It’s easy to indict the outpatient labs for obvious reasons but I personally agree that the root of the problem lies in the overly aggressive posture being taken toward treatment of claudication.
It just so happens that outpatient labs are filled with claudicants since they are most likely to have the least complex disease – match made in heaven or hell, depending on your perspective.
One cardiologist quoted in the N.Y. Times piece said patients with claudication have been “grossly under treated” – a convenient posture to take when billing Medicare $4.5 million a year. The other cardiologist who was the focus of the investigation called the charges “baseless and fiction” and stated his center had the lowest rate of amputation in the country.
It gets back to Dr. Eidt’s point how it’s easy for the nonsurgeon to dismiss amputation as an occasional unfortunate byproduct of a busy practice when you never have had to tell a patient they need one and suffer with them through the emotional and physical trauma that always follows. I was taught like many of you, I suspect, that any amputation after treatment for claudication should be considered not only an unacceptable complication but also a failure of the trust the patient placed in me. My mentor was a militant nihilist when it came to surgery for claudication but that concept is always in my mind whenever I treat a patient and has always tempered my decision making.
I like to think our recently published practice guidelines will help but am skeptical that it will make a positive impact where it is most needed; on those who are primarily driven by financial gain. I’d also point out that Dr. Darren B. Schneider was quoted as a member of the Society for Vascular Medicine. I guess we need to work harder on our branding.
Dr. Mark Morasch: Remember, all politics are local, and any meaningful change needs to come from the grass roots.
Experts can write guidelines, specialty societies can make statements, and newspapers can print articles but the most influential transaction occurs in the exam room when we are face to face with our patients.
Remember, even though we are a small group, we can have great influence when we always, always, always do what we know is right.
Dr. Alan M. Dietzek: Dear Patient, Let me introduce myself. I am a Board-Certified Vascular Surgeon. My specialty is unique in that I am well versed and formally trained in both the medical and surgical management of peripheral vascular disease. No other specialist can make this claim.
Most often, vascular problems can be managed conservatively with a combination of risk factor and lifestyle modification, and occasionally prescription medications, all of which I can outline and or prescribe for you. When necessary, however, I am prepared to treat your vascular problem with either a minimally invasive procedure or open surgery depending on which treatment will provide you with the best outcomes. Again, only a vascular surgeon is capable of offering you these treatment options. I am dedicated to your well-being. I am a Board-Certified Vascular Surgeon
Dr. Murray L. Shames: The recent New York Times article, “Medicare payments surge for stents to unblock blood vessels in limbs,” brings up a critical issue in how we train our residents to think and practice in the future.
Our current generation of residents is faced with a tremendous financial burden of medical school debt, and they are being offered highly competitive salaries after graduation.
The motivation to join groups with outpatient vascular centers is certainly attractive: Why not have autonomy from the hospital, control your work environment, and increase efficiency. As educators we must continue to use clinical evidence and societal guidelines (J. Vasc. Surg. 2015:1-40) to guide our clinical practice.
As vascular surgeons we have been trained to manage asymptomatic PAD and intermittent claudication nonoperatively due to it’s relatively benign natural history; endovascular interventions have dramatically increased the treatment of claudication, even in our own hands. We must continue to teach our residents restraint and to consider the impact of the interventions we perform. That way we can maintain our status as the leaders in vascular disease management and not just “interventionalists” that treat lesions.
Dr. Joann Lohr: The presence of a stenotic lesion does not mandate treatment either with a stent or surgical intervention but needs critical assessment of the impact on the patient’s quality of life. Risk factor modification needs to be undertaken before any intervention and will improve outcomes and durability of repairs. The only outcome that matters is the patient’s.
“How does treatment of this lesion change my lifestyle?” is a question that needs to be answered for each patient. Treating physicians need to establish long-term relationships.
Never be afraid to tell patients a procedure is not the first line of treatment. Thoughtful application of new technology is needed in all areas of medicine. Just because we can, should we? Appropriate individualized treatment plans and goals need to be established for each patient we treat.
Dr. Larry Kraiss: Vascular surgeons provide the full spectrum of care for PAD from medical management through intervention to the unfortunate situations when amputation is necessary.
The more sobering of these experiences have imbued most of us with a healthy respect for how an intervention can go wrong. If you haven’t had to explain to a patient or family why an amputation is necessary, you probably don’t have the same concern.
Thus, many of us have a very conservative approach to PAD intervention; primum non nocere is the governing principle. This principle is supposed to guide the actions of all physicians but I can’t help but wonder if something happened to primum non nocere on the way to the outpatient endovascular center.
When physicians become financial stakeholders in these enterprises, a pernicious incentive is introduced that is almost impossible to exclude from daily clinical decision making. Hospital-based physicians are also subject to temptation to perform unnecessary yet lucrative procedures but at least these are being done more in the open.
I suspect that the development of these centers has allowed much activity to occur that would rightly be condemned under the scrutiny of one’s hospital peers.
Dr. Laura Drudi: It really comes down to adequately informing the patient. I always find it astounding how many patients I encounter asking me in a timid tone, “What exactly did I have done on my leg?” I question what patients actually understand and retain after being overwhelmed by the informed consent we have prior to an intervention.
I see first hand the catastrophic failures of intervening on severe claudication leading to limb loss and worsening of quality of life. It’s disheartening to see adverse outcomes following vascular interventions either by vascular surgeons or other interventionalists, but I believe that if you are performing an intervention you should have the expertise and technical skills to deal with the complications.
The best interventionalists know when not to intervene and that should be the mantra we live by. We should be advocates for our patients at a local institutional level as well as a public level. I believe that following the New York Times article the public will be more aware of the potential for inappropriate or unnecessary interventions, many of which are being performed by specialists other than vascular surgeons.
The Society and individual vascular surgeons should capitalize on this opportunity to educate patients as to the benefits of consulting with a vascular surgeon before undertaking any endovascular procedure.
Dr. Elliot L. Chaikof: Both government and private payers have a vested interest in ensuring that patients receive the highest quality care, while reducing the unsustainable rate of increase in health care costs. In Massachusetts and elsewhere in the United States, this has led to the introduction of new risk contracting models that features a global payment with incentives linked to efficiency and quality.
At our institution, approximately 60% of patients are now in such risk contracts. Primary care physicians are most directly incentivized and, along with government and private payors, are highly motivated to ensure that our population of patients receives the right care, at the right time, from the right physician. The U.S. health care system continues to be in a state of flux with substantial regional variations in the delivery of care and how that care is financed.
Despite these challenges, the Society for Vascular Surgery can best serve our patients through advocacy and education, including promoting the need for full transparency of costs to our patients and their physicians. This would be most effective in active partnership with primary care providers, along with regional and national payors.
Dr. Erica L. Mitchell: The line separating a business from a profession is not entirely clear when professionals engage in business practices that serve to benefit the individual financially.
One crucial difference distinguishing the profession of medicine from other professions is that physicians have a fiduciary duty toward those whom they serve. This means that we have a legal duty to provide services to our patients that place the patient’s interest above our own financial interest.
This article highlights how legal and ethical issues arise if health care professionals forgo their fiduciary duties for personal gain. Unethical physicians should be held accountable for unethical practices.
Dr. Larry Scher: The recent article by Julie Creswell and Reed Abelson in the Jan. 29, 2015, New York Times highlights a recent problem in the care of patients with peripheral vascular disease. Vascular surgeons have been treating peripheral arterial disease for over 50 years and have generally adopted a conservative approach toward patients with claudication, emphasizing risk factor modification and exercise.
This is based on an understanding that the disease is benign, rarely progressive, and only occasionally disabling to the point that intervention is indicated for symptom relief.
With new minimally invasive techniques available and specialists other than vascular surgeons performing peripheral catheter based procedures we seem to have forgotten all that vascular surgeons have learned over the past 5 decades.
Most patients with claudication do not benefit from and may be harmed by interventions when long-term rather than short-term outcomes are analyzed. Although practitioners such as those identified in this article may believe they are pioneers in the treatment of peripheral arterial disease and specifically claudication, I would consider them cowboys who have forgotten the lessons of the past.