User login
How a medical recoding may limit cancer patients’ options for breast reconstruction
On June 1, the Centers for Medicare & Medicaid Services plans to reexamine how doctors are paid for a type of breast reconstruction known as DIEP flap, in which skin, fat, and blood vessels are harvested from a woman’s abdomen to create a new breast.
The procedure offers potential advantages over implants and operations that take muscle from the abdomen. But it’s also more expensive. If patients go outside an insurance network for the operation, it can cost more than $50,000. And, if insurers pay significantly less for the surgery as a result of the government’s decision, some in-network surgeons would stop offering it, a plastic surgeons group has argued.
The DIEP flap controversy, spotlighted by CBS News in January, illustrates arcane and indirect ways the federal government can influence which medical options are available – even to people with private insurance. Often, the answers come down to billing codes – which identify specific medical services on forms doctors submit for reimbursement – and the competing pleas of groups whose interests are riding on them.
Medical coding is the backbone for “how business gets done in medicine,” said Karen Joynt Maddox, MD, MPH, a physician at Washington University in St. Louis who researches health economics and policy.
CMS, the agency overseeing Medicare and Medicaid, maintains a list of codes representing thousands of medical services and products. It regularly evaluates whether to add codes or revise or remove existing ones. In 2022, it decided to eliminate a code that has enabled doctors to collect much more money for DIEP flap operations than for simpler types of breast reconstruction.
In 2006, CMS established an “S” code – S2068 – for what was then a relatively new procedure: breast reconstructions with deep inferior epigastric perforator flap (DIEP flap). S codes temporarily fill gaps in a parallel system of billing codes known as CPT codes, which are maintained by the American Medical Association.
Codes don’t dictate the amounts private insurers pay for medical services; those reimbursements are generally worked out between insurance companies and medical providers. However, using the narrowly targeted S code, doctors and hospitals have been able to distinguish DIEP flap surgeries, which require complex microsurgical skills, from other forms of breast reconstruction that take less time to perform and generally yield lower insurance reimbursements.
CMS announced in 2022 that it planned to eliminate the S code at the end of 2024 – a move some doctors say would slash the amount surgeons are paid. (To be precise, CMS announced it would eliminate a series of three S codes for similar procedures, but some of the more outspoken critics have focused on one of them, S2068.) The agency’s decision is already changing the landscape of reconstructive surgery and creating anxiety for breast cancer patients.
Kate Getz, a single mother in Morton, Ill., learned she had cancer in January at age 30. As she grappled with her diagnosis, it was overwhelming to think about what her body would look like over the long term. She pictured herself getting married one day and wondered “how on earth I would be able to wear a wedding dress with only having one breast left,” she said.
She thought a DIEP flap was her best option and worried about having to undergo repeated surgeries if she got implants instead. Implants generally need to be replaced every 10 years or so. But after she spent more than a month trying to get answers about how her DIEP flap surgery would be covered, Ms. Getz’s insurer, Cigna, informed her it would use a lower-paying CPT code to reimburse her physician, Ms. Getz said. As far as she could see, that would have made it impossible for Ms. Getz to obtain the surgery.
Paying out of pocket was “not even an option.”
“I’m a single mom. We get by, right? But I’m not, not wealthy by any means,” she said.
Cost is not necessarily the only hurdle patients seeking DIEP flaps must overcome. Citing the complexity of the procedure, Ms. Getz said, a local plastic surgeon told her it would be difficult for him to perform. She ended up traveling from Illinois to Texas for the surgery.
The government’s plan to eliminate the three S codes was driven by the Blue Cross Blue Shield Association, a major lobbying organization for health insurance companies. In 2021, the group asked CMS to discontinue the codes, arguing that they were no longer needed because the AMA had updated a CPT code to explicitly include DIEP flap surgery and the related operations, according to a CMS document.
For years, the AMA advised doctors that the CPT code was appropriate for DIEP flap procedures. But after the government’s decision, at least two major insurance companies told doctors they would no longer reimburse them under the higher-paying codes, prompting a backlash.
Physicians and advocacy groups for breast cancer patients, such as the nonprofit organization Susan G. Komen, have argued that many plastic surgeons would stop providing DIEP flap procedures for women with private insurance because they wouldn’t get paid enough.
Lawmakers from both parties have asked the agency to keep the S code, including Rep. Debbie Wasserman Schultz (D-Fla.) and Sen. Amy Klobuchar (D-Minn.), who have had breast cancer, and Sen. Marsha Blackburn (R-Tenn.).
CMS at its June 1 meeting will consider whether to keep the three S codes or delay their expiration.
In a May 30 statement, Blue Cross Blue Shield Association spokesperson Kelly Parsons reiterated the organization’s view that “there is no longer a need to keep the S codes.”
In a profit-driven health care system, there’s a tug of war over reimbursements between providers and insurance companies, often at the expense of patients, said Dr. Joynt Maddox.
“We’re in this sort of constant battle” between hospital chains and insurance companies “about who’s going to wield more power at the bargaining table,” Dr. Joynt Maddox said. “And the clinical piece of that often gets lost, because it’s not often the clinical benefit and the clinical priority and the patient centeredness that’s at the middle of these conversations.”
Elisabeth Potter, MD, a plastic surgeon who specializes in DIEP flap surgeries, decided to perform Ms. Getz’s surgery at whatever price Cigna would pay.
According to Fair Health, a nonprofit that provides information on health care costs, in Austin, Tex. – where Dr. Potter is based – an insurer might pay an in-network doctor $9,323 for the surgery when it’s billed using the CPT code and $18,037 under the S code. Those amounts are not averages; rather, Fair Health estimated that 80% of payment rates are lower than or equal to those amounts.
Dr. Potter said her Cigna reimbursement “is significantly lower.”
Weeks before her May surgery, Ms. Getz received big news – Cigna had reversed itself and would cover her surgery under the S code. It “felt like a real victory,” she said.
But she still fears for other patients.
“I’m still asking these companies to do right by women,” Ms. Getz said. “I’m still asking them to provide the procedures we need to reimburse them at rates where women have access to them regardless of their wealth.”
In a statement, Cigna spokesperson Justine Sessions said the insurer remains “committed to ensuring that our customers have affordable coverage and access to the full range of breast reconstruction procedures and to quality surgeons who perform these complex surgeries.”
Medical costs that health insurers cover generally are passed along to consumers in the form of premiums, deductibles, and other out-of-pocket expenses.
For any type of breast reconstruction, there are benefits, risks, and trade-offs. A 2018 paper published in JAMA Surgery found that women who underwent DIEP flap surgery had higher odds of developing “reoperative complications” within 2 years than those who received artificial implants. However, DIEP flaps had lower odds of infection than implants.
Implants carry risks of additional surgery, pain, rupture, and even an uncommon type of immune system cancer.
Other flap procedures that take muscle from the abdomen can leave women with weakened abdominal walls and increase their risk of developing a hernia.
Academic research shows that insurance reimbursement affects which women can access DIEP flap breast reconstruction, creating a two-tiered system for private health insurance versus government programs like Medicare and Medicaid. Private insurance generally pays physicians more than government coverage, and Medicare doesn’t use S codes.
Lynn Damitz, a physician and board vice president of health policy and advocacy for the American Society of Plastic Surgeons, said the group supports continuing the S code temporarily or indefinitely. If reimbursements drop, some doctors won’t perform DIEP flaps anymore.
A study published in February found that, of patients who used their own tissue for breast reconstruction, privately insured patients were more likely than publicly insured patients to receive DIEP flap reconstruction.
To Dr. Potter, that shows what will happen if private insurance payments plummet. “If you’re a Medicare provider and you’re not paid to do DIEP flaps, you never tell a patient that it’s an option. You won’t perform it,” Dr. Potter said. “If you take private insurance and all of a sudden your reimbursement rate is cut from $15,000 down to $3,500, you’re not going to do that surgery. And I’m not saying that that’s the right thing to do, but that’s what happens.”
KHN (Kaiser Health News) is a national newsroom that produces in-depth journalism about health issues. Together with Policy Analysis and Polling, KHN is one of the three major operating programs at KFF (Kaiser Family Foundation). KFF is an endowed nonprofit organization providing information on health issues to the nation.
On June 1, the Centers for Medicare & Medicaid Services plans to reexamine how doctors are paid for a type of breast reconstruction known as DIEP flap, in which skin, fat, and blood vessels are harvested from a woman’s abdomen to create a new breast.
The procedure offers potential advantages over implants and operations that take muscle from the abdomen. But it’s also more expensive. If patients go outside an insurance network for the operation, it can cost more than $50,000. And, if insurers pay significantly less for the surgery as a result of the government’s decision, some in-network surgeons would stop offering it, a plastic surgeons group has argued.
The DIEP flap controversy, spotlighted by CBS News in January, illustrates arcane and indirect ways the federal government can influence which medical options are available – even to people with private insurance. Often, the answers come down to billing codes – which identify specific medical services on forms doctors submit for reimbursement – and the competing pleas of groups whose interests are riding on them.
Medical coding is the backbone for “how business gets done in medicine,” said Karen Joynt Maddox, MD, MPH, a physician at Washington University in St. Louis who researches health economics and policy.
CMS, the agency overseeing Medicare and Medicaid, maintains a list of codes representing thousands of medical services and products. It regularly evaluates whether to add codes or revise or remove existing ones. In 2022, it decided to eliminate a code that has enabled doctors to collect much more money for DIEP flap operations than for simpler types of breast reconstruction.
In 2006, CMS established an “S” code – S2068 – for what was then a relatively new procedure: breast reconstructions with deep inferior epigastric perforator flap (DIEP flap). S codes temporarily fill gaps in a parallel system of billing codes known as CPT codes, which are maintained by the American Medical Association.
Codes don’t dictate the amounts private insurers pay for medical services; those reimbursements are generally worked out between insurance companies and medical providers. However, using the narrowly targeted S code, doctors and hospitals have been able to distinguish DIEP flap surgeries, which require complex microsurgical skills, from other forms of breast reconstruction that take less time to perform and generally yield lower insurance reimbursements.
CMS announced in 2022 that it planned to eliminate the S code at the end of 2024 – a move some doctors say would slash the amount surgeons are paid. (To be precise, CMS announced it would eliminate a series of three S codes for similar procedures, but some of the more outspoken critics have focused on one of them, S2068.) The agency’s decision is already changing the landscape of reconstructive surgery and creating anxiety for breast cancer patients.
Kate Getz, a single mother in Morton, Ill., learned she had cancer in January at age 30. As she grappled with her diagnosis, it was overwhelming to think about what her body would look like over the long term. She pictured herself getting married one day and wondered “how on earth I would be able to wear a wedding dress with only having one breast left,” she said.
She thought a DIEP flap was her best option and worried about having to undergo repeated surgeries if she got implants instead. Implants generally need to be replaced every 10 years or so. But after she spent more than a month trying to get answers about how her DIEP flap surgery would be covered, Ms. Getz’s insurer, Cigna, informed her it would use a lower-paying CPT code to reimburse her physician, Ms. Getz said. As far as she could see, that would have made it impossible for Ms. Getz to obtain the surgery.
Paying out of pocket was “not even an option.”
“I’m a single mom. We get by, right? But I’m not, not wealthy by any means,” she said.
Cost is not necessarily the only hurdle patients seeking DIEP flaps must overcome. Citing the complexity of the procedure, Ms. Getz said, a local plastic surgeon told her it would be difficult for him to perform. She ended up traveling from Illinois to Texas for the surgery.
The government’s plan to eliminate the three S codes was driven by the Blue Cross Blue Shield Association, a major lobbying organization for health insurance companies. In 2021, the group asked CMS to discontinue the codes, arguing that they were no longer needed because the AMA had updated a CPT code to explicitly include DIEP flap surgery and the related operations, according to a CMS document.
For years, the AMA advised doctors that the CPT code was appropriate for DIEP flap procedures. But after the government’s decision, at least two major insurance companies told doctors they would no longer reimburse them under the higher-paying codes, prompting a backlash.
Physicians and advocacy groups for breast cancer patients, such as the nonprofit organization Susan G. Komen, have argued that many plastic surgeons would stop providing DIEP flap procedures for women with private insurance because they wouldn’t get paid enough.
Lawmakers from both parties have asked the agency to keep the S code, including Rep. Debbie Wasserman Schultz (D-Fla.) and Sen. Amy Klobuchar (D-Minn.), who have had breast cancer, and Sen. Marsha Blackburn (R-Tenn.).
CMS at its June 1 meeting will consider whether to keep the three S codes or delay their expiration.
In a May 30 statement, Blue Cross Blue Shield Association spokesperson Kelly Parsons reiterated the organization’s view that “there is no longer a need to keep the S codes.”
In a profit-driven health care system, there’s a tug of war over reimbursements between providers and insurance companies, often at the expense of patients, said Dr. Joynt Maddox.
“We’re in this sort of constant battle” between hospital chains and insurance companies “about who’s going to wield more power at the bargaining table,” Dr. Joynt Maddox said. “And the clinical piece of that often gets lost, because it’s not often the clinical benefit and the clinical priority and the patient centeredness that’s at the middle of these conversations.”
Elisabeth Potter, MD, a plastic surgeon who specializes in DIEP flap surgeries, decided to perform Ms. Getz’s surgery at whatever price Cigna would pay.
According to Fair Health, a nonprofit that provides information on health care costs, in Austin, Tex. – where Dr. Potter is based – an insurer might pay an in-network doctor $9,323 for the surgery when it’s billed using the CPT code and $18,037 under the S code. Those amounts are not averages; rather, Fair Health estimated that 80% of payment rates are lower than or equal to those amounts.
Dr. Potter said her Cigna reimbursement “is significantly lower.”
Weeks before her May surgery, Ms. Getz received big news – Cigna had reversed itself and would cover her surgery under the S code. It “felt like a real victory,” she said.
But she still fears for other patients.
“I’m still asking these companies to do right by women,” Ms. Getz said. “I’m still asking them to provide the procedures we need to reimburse them at rates where women have access to them regardless of their wealth.”
In a statement, Cigna spokesperson Justine Sessions said the insurer remains “committed to ensuring that our customers have affordable coverage and access to the full range of breast reconstruction procedures and to quality surgeons who perform these complex surgeries.”
Medical costs that health insurers cover generally are passed along to consumers in the form of premiums, deductibles, and other out-of-pocket expenses.
For any type of breast reconstruction, there are benefits, risks, and trade-offs. A 2018 paper published in JAMA Surgery found that women who underwent DIEP flap surgery had higher odds of developing “reoperative complications” within 2 years than those who received artificial implants. However, DIEP flaps had lower odds of infection than implants.
Implants carry risks of additional surgery, pain, rupture, and even an uncommon type of immune system cancer.
Other flap procedures that take muscle from the abdomen can leave women with weakened abdominal walls and increase their risk of developing a hernia.
Academic research shows that insurance reimbursement affects which women can access DIEP flap breast reconstruction, creating a two-tiered system for private health insurance versus government programs like Medicare and Medicaid. Private insurance generally pays physicians more than government coverage, and Medicare doesn’t use S codes.
Lynn Damitz, a physician and board vice president of health policy and advocacy for the American Society of Plastic Surgeons, said the group supports continuing the S code temporarily or indefinitely. If reimbursements drop, some doctors won’t perform DIEP flaps anymore.
A study published in February found that, of patients who used their own tissue for breast reconstruction, privately insured patients were more likely than publicly insured patients to receive DIEP flap reconstruction.
To Dr. Potter, that shows what will happen if private insurance payments plummet. “If you’re a Medicare provider and you’re not paid to do DIEP flaps, you never tell a patient that it’s an option. You won’t perform it,” Dr. Potter said. “If you take private insurance and all of a sudden your reimbursement rate is cut from $15,000 down to $3,500, you’re not going to do that surgery. And I’m not saying that that’s the right thing to do, but that’s what happens.”
KHN (Kaiser Health News) is a national newsroom that produces in-depth journalism about health issues. Together with Policy Analysis and Polling, KHN is one of the three major operating programs at KFF (Kaiser Family Foundation). KFF is an endowed nonprofit organization providing information on health issues to the nation.
On June 1, the Centers for Medicare & Medicaid Services plans to reexamine how doctors are paid for a type of breast reconstruction known as DIEP flap, in which skin, fat, and blood vessels are harvested from a woman’s abdomen to create a new breast.
The procedure offers potential advantages over implants and operations that take muscle from the abdomen. But it’s also more expensive. If patients go outside an insurance network for the operation, it can cost more than $50,000. And, if insurers pay significantly less for the surgery as a result of the government’s decision, some in-network surgeons would stop offering it, a plastic surgeons group has argued.
The DIEP flap controversy, spotlighted by CBS News in January, illustrates arcane and indirect ways the federal government can influence which medical options are available – even to people with private insurance. Often, the answers come down to billing codes – which identify specific medical services on forms doctors submit for reimbursement – and the competing pleas of groups whose interests are riding on them.
Medical coding is the backbone for “how business gets done in medicine,” said Karen Joynt Maddox, MD, MPH, a physician at Washington University in St. Louis who researches health economics and policy.
CMS, the agency overseeing Medicare and Medicaid, maintains a list of codes representing thousands of medical services and products. It regularly evaluates whether to add codes or revise or remove existing ones. In 2022, it decided to eliminate a code that has enabled doctors to collect much more money for DIEP flap operations than for simpler types of breast reconstruction.
In 2006, CMS established an “S” code – S2068 – for what was then a relatively new procedure: breast reconstructions with deep inferior epigastric perforator flap (DIEP flap). S codes temporarily fill gaps in a parallel system of billing codes known as CPT codes, which are maintained by the American Medical Association.
Codes don’t dictate the amounts private insurers pay for medical services; those reimbursements are generally worked out between insurance companies and medical providers. However, using the narrowly targeted S code, doctors and hospitals have been able to distinguish DIEP flap surgeries, which require complex microsurgical skills, from other forms of breast reconstruction that take less time to perform and generally yield lower insurance reimbursements.
CMS announced in 2022 that it planned to eliminate the S code at the end of 2024 – a move some doctors say would slash the amount surgeons are paid. (To be precise, CMS announced it would eliminate a series of three S codes for similar procedures, but some of the more outspoken critics have focused on one of them, S2068.) The agency’s decision is already changing the landscape of reconstructive surgery and creating anxiety for breast cancer patients.
Kate Getz, a single mother in Morton, Ill., learned she had cancer in January at age 30. As she grappled with her diagnosis, it was overwhelming to think about what her body would look like over the long term. She pictured herself getting married one day and wondered “how on earth I would be able to wear a wedding dress with only having one breast left,” she said.
She thought a DIEP flap was her best option and worried about having to undergo repeated surgeries if she got implants instead. Implants generally need to be replaced every 10 years or so. But after she spent more than a month trying to get answers about how her DIEP flap surgery would be covered, Ms. Getz’s insurer, Cigna, informed her it would use a lower-paying CPT code to reimburse her physician, Ms. Getz said. As far as she could see, that would have made it impossible for Ms. Getz to obtain the surgery.
Paying out of pocket was “not even an option.”
“I’m a single mom. We get by, right? But I’m not, not wealthy by any means,” she said.
Cost is not necessarily the only hurdle patients seeking DIEP flaps must overcome. Citing the complexity of the procedure, Ms. Getz said, a local plastic surgeon told her it would be difficult for him to perform. She ended up traveling from Illinois to Texas for the surgery.
The government’s plan to eliminate the three S codes was driven by the Blue Cross Blue Shield Association, a major lobbying organization for health insurance companies. In 2021, the group asked CMS to discontinue the codes, arguing that they were no longer needed because the AMA had updated a CPT code to explicitly include DIEP flap surgery and the related operations, according to a CMS document.
For years, the AMA advised doctors that the CPT code was appropriate for DIEP flap procedures. But after the government’s decision, at least two major insurance companies told doctors they would no longer reimburse them under the higher-paying codes, prompting a backlash.
Physicians and advocacy groups for breast cancer patients, such as the nonprofit organization Susan G. Komen, have argued that many plastic surgeons would stop providing DIEP flap procedures for women with private insurance because they wouldn’t get paid enough.
Lawmakers from both parties have asked the agency to keep the S code, including Rep. Debbie Wasserman Schultz (D-Fla.) and Sen. Amy Klobuchar (D-Minn.), who have had breast cancer, and Sen. Marsha Blackburn (R-Tenn.).
CMS at its June 1 meeting will consider whether to keep the three S codes or delay their expiration.
In a May 30 statement, Blue Cross Blue Shield Association spokesperson Kelly Parsons reiterated the organization’s view that “there is no longer a need to keep the S codes.”
In a profit-driven health care system, there’s a tug of war over reimbursements between providers and insurance companies, often at the expense of patients, said Dr. Joynt Maddox.
“We’re in this sort of constant battle” between hospital chains and insurance companies “about who’s going to wield more power at the bargaining table,” Dr. Joynt Maddox said. “And the clinical piece of that often gets lost, because it’s not often the clinical benefit and the clinical priority and the patient centeredness that’s at the middle of these conversations.”
Elisabeth Potter, MD, a plastic surgeon who specializes in DIEP flap surgeries, decided to perform Ms. Getz’s surgery at whatever price Cigna would pay.
According to Fair Health, a nonprofit that provides information on health care costs, in Austin, Tex. – where Dr. Potter is based – an insurer might pay an in-network doctor $9,323 for the surgery when it’s billed using the CPT code and $18,037 under the S code. Those amounts are not averages; rather, Fair Health estimated that 80% of payment rates are lower than or equal to those amounts.
Dr. Potter said her Cigna reimbursement “is significantly lower.”
Weeks before her May surgery, Ms. Getz received big news – Cigna had reversed itself and would cover her surgery under the S code. It “felt like a real victory,” she said.
But she still fears for other patients.
“I’m still asking these companies to do right by women,” Ms. Getz said. “I’m still asking them to provide the procedures we need to reimburse them at rates where women have access to them regardless of their wealth.”
In a statement, Cigna spokesperson Justine Sessions said the insurer remains “committed to ensuring that our customers have affordable coverage and access to the full range of breast reconstruction procedures and to quality surgeons who perform these complex surgeries.”
Medical costs that health insurers cover generally are passed along to consumers in the form of premiums, deductibles, and other out-of-pocket expenses.
For any type of breast reconstruction, there are benefits, risks, and trade-offs. A 2018 paper published in JAMA Surgery found that women who underwent DIEP flap surgery had higher odds of developing “reoperative complications” within 2 years than those who received artificial implants. However, DIEP flaps had lower odds of infection than implants.
Implants carry risks of additional surgery, pain, rupture, and even an uncommon type of immune system cancer.
Other flap procedures that take muscle from the abdomen can leave women with weakened abdominal walls and increase their risk of developing a hernia.
Academic research shows that insurance reimbursement affects which women can access DIEP flap breast reconstruction, creating a two-tiered system for private health insurance versus government programs like Medicare and Medicaid. Private insurance generally pays physicians more than government coverage, and Medicare doesn’t use S codes.
Lynn Damitz, a physician and board vice president of health policy and advocacy for the American Society of Plastic Surgeons, said the group supports continuing the S code temporarily or indefinitely. If reimbursements drop, some doctors won’t perform DIEP flaps anymore.
A study published in February found that, of patients who used their own tissue for breast reconstruction, privately insured patients were more likely than publicly insured patients to receive DIEP flap reconstruction.
To Dr. Potter, that shows what will happen if private insurance payments plummet. “If you’re a Medicare provider and you’re not paid to do DIEP flaps, you never tell a patient that it’s an option. You won’t perform it,” Dr. Potter said. “If you take private insurance and all of a sudden your reimbursement rate is cut from $15,000 down to $3,500, you’re not going to do that surgery. And I’m not saying that that’s the right thing to do, but that’s what happens.”
KHN (Kaiser Health News) is a national newsroom that produces in-depth journalism about health issues. Together with Policy Analysis and Polling, KHN is one of the three major operating programs at KFF (Kaiser Family Foundation). KFF is an endowed nonprofit organization providing information on health issues to the nation.
Ancient plague, cyclical pandemics … history lesson?
Even the plague wanted to visit Stonehenge
We’re about to blow your mind: The history you learned in school was often inaccurate. Shocking, we know, so we’ll give you a minute to process this incredible news.
Better? Good. Now, let’s look back at high school European history. The Black Death, specifically. The common narrative is that the Mongols, while besieging a Crimean city belonging to the Genoese, catapulted dead bodies infected with some mystery disease that turned out to be the plague. The Genoese then brought the plague back to Italy, and from there, we all know the rest of the story.
The Black Death was certainly extremely important to the development of modern Europe as we know it, but the history books gloss over the much longer history of the plague. Yersinia pestis did not suddenly appear unbidden in a Mongol war camp in 1347. The Black Death wasn’t even the first horrific, continent-wide pandemic caused by the plague; the Plague of Justinian 800 years earlier crippled the Byzantine Empire during an expansionist phase and killed anywhere between 15 million and 100 million.
Today, though, LOTME looks even deeper into history, nearly beyond even history itself, back into the depths of early Bronze Age northern Europe. Specifically, to two ancient burial sites in England, where researchers have identified three 4,000-year-old cases of Y. pestis, the first recorded incidence of the disease in Britain.
Two of the individuals, identified through analysis of dental pulp, were young children buried at a mass grave in Somerset, while the third, a middle-aged woman, was found in a ring cairn in Cumbria. These sites are hundreds of miles apart, yet carbon dating suggests all three people lived and died at roughly the same time. The strain found is very similar to other samples of plague found across central and western Europe starting around 3,000 BCE, suggesting a single, easily spread disease affecting a large area in a relatively small period of time. In other words, a pandemic. Even in these ancient times, the world was connected. Not even the island of Britain could escape.
Beyond that though, the research helps confirm the cyclical nature of the plague; over time, it loses its effectiveness and goes into hiding, only to mutate and come roaring back. This is a story with absolutely no relevance at all to the modern world. Nope, no plagues or pandemics going around right now, no viruses fading into the background in any way. What a ridiculous inference to make.
Uncovering the invisible with artificial intelligence
This week in “What Else Can AI Do?” new research shows that a computer program can reveal brain injury that couldn’t be seen before with typical MRI.
The hot new AI, birthed by researchers at New York University, could potentially be a game changer by linking repeated head impacts with tiny, structural changes in the brains of athletes who have not been diagnosed with a concussion. By using machine learning to train the AI, the researchers were, for the first time, able to distinguish the brain of athletes who played contact sports (football, soccer, lacrosse) from those participating in noncontact sports such as baseball, basketball, and cross-country.
How did they do it? The investigators “designed statistical techniques that gave their computer program the ability to ‘learn’ how to predict exposure to repeated head impacts using mathematical models,” they explained in a written statement. Adding in data from the MRI scans of 81 male athletes with no known concussion diagnosis and the ability to identify unusual brain features between athletes with and without head trauma allowed the AI to predict results with accuracy even Miss Cleo would envy.
“This method may provide an important diagnostic tool not only for concussion, but also for detecting the damage that stems from subtler and more frequent head impacts,” said lead author Junbo Chen, an engineering doctoral candidate at NYU. That could make this new AI a valuable asset to science and medicine.
There are many things the human brain can do that AI can’t, and delegation could be one of them. Examining the data that represent the human brain in minute detail? Maybe we leave that to the machine.
Talk about your field promotions
If you’re a surgeon doing an amputation, the list of possible assistants pretty much starts and ends in only one place: Not the closest available janitor.
That may seem like an oddly obvious thing for us to say, but there’s at least one former Mainz (Germany) University Hospital physician who really needed to get this bit of advice before he attempted an unassisted toe amputation back in October of 2020. Yes, that does seem like kind of a long time ago for us to be reporting it now, but the details of the incident only just came to light a few days ago, thanks to German public broadcaster SWR.
Since it was just a toe, the surgeon thought he could perform the operation without any help. The toe, unfortunately, had other plans. The partially anesthetized patient got restless in the operating room, but with no actual trained nurse in the vicinity, the surgeon asked the closest available person – that would be the janitor – to lend a hand.
The surgical manager heard about these goings-on and got to the operating room too late to stop the procedure but soon enough to see the cleaning staffer “at the operating table with a bloody suction cup and a bloody compress in their hands,” SWR recently reported.
The incident was reported to the hospital’s medical director and the surgeon was fired, but since the patient experienced no complications not much fuss was made about it at the time.
Well, guess what? It’s toe-tally our job to make a fuss about these kinds of things. Or could it be that our job, much like the surgeon’s employment and the patient’s digit, is here toe-day and gone toe-morrow?
Even the plague wanted to visit Stonehenge
We’re about to blow your mind: The history you learned in school was often inaccurate. Shocking, we know, so we’ll give you a minute to process this incredible news.
Better? Good. Now, let’s look back at high school European history. The Black Death, specifically. The common narrative is that the Mongols, while besieging a Crimean city belonging to the Genoese, catapulted dead bodies infected with some mystery disease that turned out to be the plague. The Genoese then brought the plague back to Italy, and from there, we all know the rest of the story.
The Black Death was certainly extremely important to the development of modern Europe as we know it, but the history books gloss over the much longer history of the plague. Yersinia pestis did not suddenly appear unbidden in a Mongol war camp in 1347. The Black Death wasn’t even the first horrific, continent-wide pandemic caused by the plague; the Plague of Justinian 800 years earlier crippled the Byzantine Empire during an expansionist phase and killed anywhere between 15 million and 100 million.
Today, though, LOTME looks even deeper into history, nearly beyond even history itself, back into the depths of early Bronze Age northern Europe. Specifically, to two ancient burial sites in England, where researchers have identified three 4,000-year-old cases of Y. pestis, the first recorded incidence of the disease in Britain.
Two of the individuals, identified through analysis of dental pulp, were young children buried at a mass grave in Somerset, while the third, a middle-aged woman, was found in a ring cairn in Cumbria. These sites are hundreds of miles apart, yet carbon dating suggests all three people lived and died at roughly the same time. The strain found is very similar to other samples of plague found across central and western Europe starting around 3,000 BCE, suggesting a single, easily spread disease affecting a large area in a relatively small period of time. In other words, a pandemic. Even in these ancient times, the world was connected. Not even the island of Britain could escape.
Beyond that though, the research helps confirm the cyclical nature of the plague; over time, it loses its effectiveness and goes into hiding, only to mutate and come roaring back. This is a story with absolutely no relevance at all to the modern world. Nope, no plagues or pandemics going around right now, no viruses fading into the background in any way. What a ridiculous inference to make.
Uncovering the invisible with artificial intelligence
This week in “What Else Can AI Do?” new research shows that a computer program can reveal brain injury that couldn’t be seen before with typical MRI.
The hot new AI, birthed by researchers at New York University, could potentially be a game changer by linking repeated head impacts with tiny, structural changes in the brains of athletes who have not been diagnosed with a concussion. By using machine learning to train the AI, the researchers were, for the first time, able to distinguish the brain of athletes who played contact sports (football, soccer, lacrosse) from those participating in noncontact sports such as baseball, basketball, and cross-country.
How did they do it? The investigators “designed statistical techniques that gave their computer program the ability to ‘learn’ how to predict exposure to repeated head impacts using mathematical models,” they explained in a written statement. Adding in data from the MRI scans of 81 male athletes with no known concussion diagnosis and the ability to identify unusual brain features between athletes with and without head trauma allowed the AI to predict results with accuracy even Miss Cleo would envy.
“This method may provide an important diagnostic tool not only for concussion, but also for detecting the damage that stems from subtler and more frequent head impacts,” said lead author Junbo Chen, an engineering doctoral candidate at NYU. That could make this new AI a valuable asset to science and medicine.
There are many things the human brain can do that AI can’t, and delegation could be one of them. Examining the data that represent the human brain in minute detail? Maybe we leave that to the machine.
Talk about your field promotions
If you’re a surgeon doing an amputation, the list of possible assistants pretty much starts and ends in only one place: Not the closest available janitor.
That may seem like an oddly obvious thing for us to say, but there’s at least one former Mainz (Germany) University Hospital physician who really needed to get this bit of advice before he attempted an unassisted toe amputation back in October of 2020. Yes, that does seem like kind of a long time ago for us to be reporting it now, but the details of the incident only just came to light a few days ago, thanks to German public broadcaster SWR.
Since it was just a toe, the surgeon thought he could perform the operation without any help. The toe, unfortunately, had other plans. The partially anesthetized patient got restless in the operating room, but with no actual trained nurse in the vicinity, the surgeon asked the closest available person – that would be the janitor – to lend a hand.
The surgical manager heard about these goings-on and got to the operating room too late to stop the procedure but soon enough to see the cleaning staffer “at the operating table with a bloody suction cup and a bloody compress in their hands,” SWR recently reported.
The incident was reported to the hospital’s medical director and the surgeon was fired, but since the patient experienced no complications not much fuss was made about it at the time.
Well, guess what? It’s toe-tally our job to make a fuss about these kinds of things. Or could it be that our job, much like the surgeon’s employment and the patient’s digit, is here toe-day and gone toe-morrow?
Even the plague wanted to visit Stonehenge
We’re about to blow your mind: The history you learned in school was often inaccurate. Shocking, we know, so we’ll give you a minute to process this incredible news.
Better? Good. Now, let’s look back at high school European history. The Black Death, specifically. The common narrative is that the Mongols, while besieging a Crimean city belonging to the Genoese, catapulted dead bodies infected with some mystery disease that turned out to be the plague. The Genoese then brought the plague back to Italy, and from there, we all know the rest of the story.
The Black Death was certainly extremely important to the development of modern Europe as we know it, but the history books gloss over the much longer history of the plague. Yersinia pestis did not suddenly appear unbidden in a Mongol war camp in 1347. The Black Death wasn’t even the first horrific, continent-wide pandemic caused by the plague; the Plague of Justinian 800 years earlier crippled the Byzantine Empire during an expansionist phase and killed anywhere between 15 million and 100 million.
Today, though, LOTME looks even deeper into history, nearly beyond even history itself, back into the depths of early Bronze Age northern Europe. Specifically, to two ancient burial sites in England, where researchers have identified three 4,000-year-old cases of Y. pestis, the first recorded incidence of the disease in Britain.
Two of the individuals, identified through analysis of dental pulp, were young children buried at a mass grave in Somerset, while the third, a middle-aged woman, was found in a ring cairn in Cumbria. These sites are hundreds of miles apart, yet carbon dating suggests all three people lived and died at roughly the same time. The strain found is very similar to other samples of plague found across central and western Europe starting around 3,000 BCE, suggesting a single, easily spread disease affecting a large area in a relatively small period of time. In other words, a pandemic. Even in these ancient times, the world was connected. Not even the island of Britain could escape.
Beyond that though, the research helps confirm the cyclical nature of the plague; over time, it loses its effectiveness and goes into hiding, only to mutate and come roaring back. This is a story with absolutely no relevance at all to the modern world. Nope, no plagues or pandemics going around right now, no viruses fading into the background in any way. What a ridiculous inference to make.
Uncovering the invisible with artificial intelligence
This week in “What Else Can AI Do?” new research shows that a computer program can reveal brain injury that couldn’t be seen before with typical MRI.
The hot new AI, birthed by researchers at New York University, could potentially be a game changer by linking repeated head impacts with tiny, structural changes in the brains of athletes who have not been diagnosed with a concussion. By using machine learning to train the AI, the researchers were, for the first time, able to distinguish the brain of athletes who played contact sports (football, soccer, lacrosse) from those participating in noncontact sports such as baseball, basketball, and cross-country.
How did they do it? The investigators “designed statistical techniques that gave their computer program the ability to ‘learn’ how to predict exposure to repeated head impacts using mathematical models,” they explained in a written statement. Adding in data from the MRI scans of 81 male athletes with no known concussion diagnosis and the ability to identify unusual brain features between athletes with and without head trauma allowed the AI to predict results with accuracy even Miss Cleo would envy.
“This method may provide an important diagnostic tool not only for concussion, but also for detecting the damage that stems from subtler and more frequent head impacts,” said lead author Junbo Chen, an engineering doctoral candidate at NYU. That could make this new AI a valuable asset to science and medicine.
There are many things the human brain can do that AI can’t, and delegation could be one of them. Examining the data that represent the human brain in minute detail? Maybe we leave that to the machine.
Talk about your field promotions
If you’re a surgeon doing an amputation, the list of possible assistants pretty much starts and ends in only one place: Not the closest available janitor.
That may seem like an oddly obvious thing for us to say, but there’s at least one former Mainz (Germany) University Hospital physician who really needed to get this bit of advice before he attempted an unassisted toe amputation back in October of 2020. Yes, that does seem like kind of a long time ago for us to be reporting it now, but the details of the incident only just came to light a few days ago, thanks to German public broadcaster SWR.
Since it was just a toe, the surgeon thought he could perform the operation without any help. The toe, unfortunately, had other plans. The partially anesthetized patient got restless in the operating room, but with no actual trained nurse in the vicinity, the surgeon asked the closest available person – that would be the janitor – to lend a hand.
The surgical manager heard about these goings-on and got to the operating room too late to stop the procedure but soon enough to see the cleaning staffer “at the operating table with a bloody suction cup and a bloody compress in their hands,” SWR recently reported.
The incident was reported to the hospital’s medical director and the surgeon was fired, but since the patient experienced no complications not much fuss was made about it at the time.
Well, guess what? It’s toe-tally our job to make a fuss about these kinds of things. Or could it be that our job, much like the surgeon’s employment and the patient’s digit, is here toe-day and gone toe-morrow?
Survey: Family medicine earnings steady despite overall growth for physicians
according to the results of the Medscape Family Physician Compensation Report 2023.
Average compensation for the specialty, which has risen by 31% since 2015, was stagnant in 2022, showing no growth from the previous year. COVID, at least, had less of an effect on earnings, as 48% of family physicians cited pandemic-related income losses, compared with 64% in 2021, according to those who responded to Medscape’s annual survey, which was conducted from Oct. 2, 2022, to Jan. 17, 2023.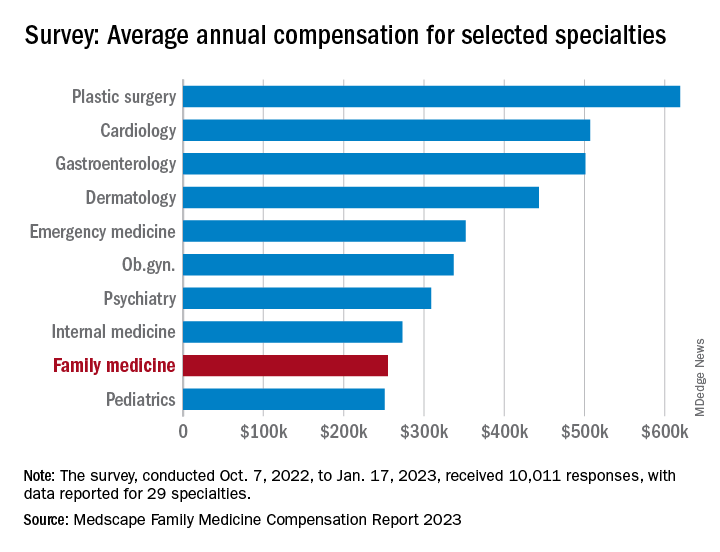
Comments from those respondents covered several areas that were already concerning physicians before the pandemic. One wrote that “decreasing Medicare reimbursement and poor payor mix destroy our income,” and another said that “patients have become rude and come with poor information from social media.” One respondent described the situation this way: “Overwhelming burnout. I had to reduce my hours to keep myself from quitting medicine completely.”
Overall physician compensation in 2022 was up by about 4% from 2021. For the 12% of the 10,011 respondents who practice family medicine, the average held at $255,000, where it had been the year before. Among the other primary care specialists, internists’ earnings were up by almost 4% and pediatricians did almost as well with a 3% increase, while ob.gyns. joined family physicians in the no-growth club, the Medscape results show.
For all physicians, average compensation in 2022 was $352,000, an increase of almost 18% since 2018. “Supply and demand is the biggest driver,” Mike Belkin, JD, of physician recruitment firm Merritt Hawkins, said in an interview. “Organizations understand it’s not getting any easier to get good candidates, and so for the most part, physicians are getting good offers.”
The lack of increase in FPs earnings among internists also included a decline of note: The disparity between mens’ and womens’ compensation dropped from 26% in 2021 to 23% in 2022. The 2022 disparity was only 16% for internists, however, even though family medicine has a considerably larger share of women (49% vs. 40%) among those surveyed, Medscape said.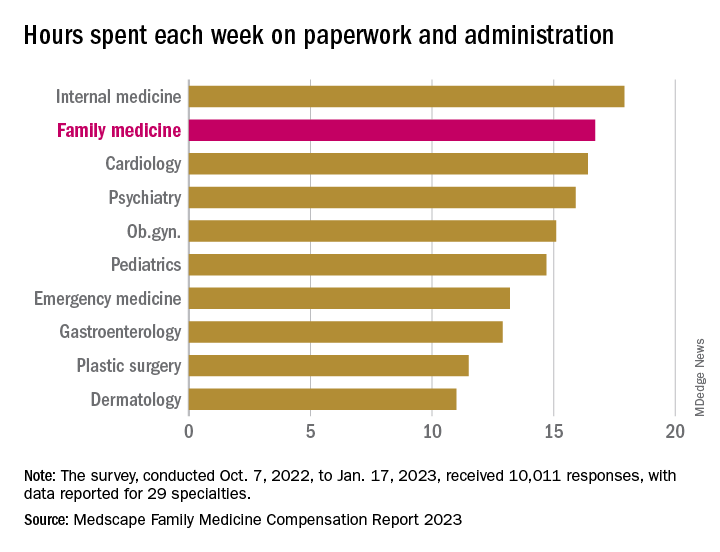
Satisfaction with their compensation, on the other hand, was higher among the family physicians (50%), compared with internists (43%). In 2022, 55% of family physicians said that they had been fairly paid.
In 2022, FP respondents reported spending an average of 16.7 hours (up from 15.6 hours in 2021) each week on paperwork and administration, just below the survey leaders, physical medicine and rehabilitation (18.5 hours) and nephrology (18.1 hours) but well above anesthesiology, lowest of the 29 specialties at 9.0 hours, and the 2022 average of 15.5 hours for all physicians, Medscape said.
When asked if they would choose medicine again, 72% of family physician respondents and 73% of all physicians said yes, with emergency medicine (65%) and dermatology (86%) representing the two extremes. A question about specialty choice showed that 66% of FPs would choose it again, putting them 28th of the 29 included specialties in their eagerness to follow the same path, above only the internists (61%), Medscape reported.
Commenters among the survey respondents were not identified by specialty, but dissatisfaction on many fronts was a definite theme:
- “Our costs go up, and our reimbursement does not.”
- “Our practice was acquired by venture capital firms; they slashed costs.”
- “My productivity bonus should have come to $45,000. Instead I was paid only $15,000. Yet cardiologists and administrators who were working from home part of the year received their full bonus.”
- “I will no longer practice cookbook mediocrity.”
according to the results of the Medscape Family Physician Compensation Report 2023.
Average compensation for the specialty, which has risen by 31% since 2015, was stagnant in 2022, showing no growth from the previous year. COVID, at least, had less of an effect on earnings, as 48% of family physicians cited pandemic-related income losses, compared with 64% in 2021, according to those who responded to Medscape’s annual survey, which was conducted from Oct. 2, 2022, to Jan. 17, 2023.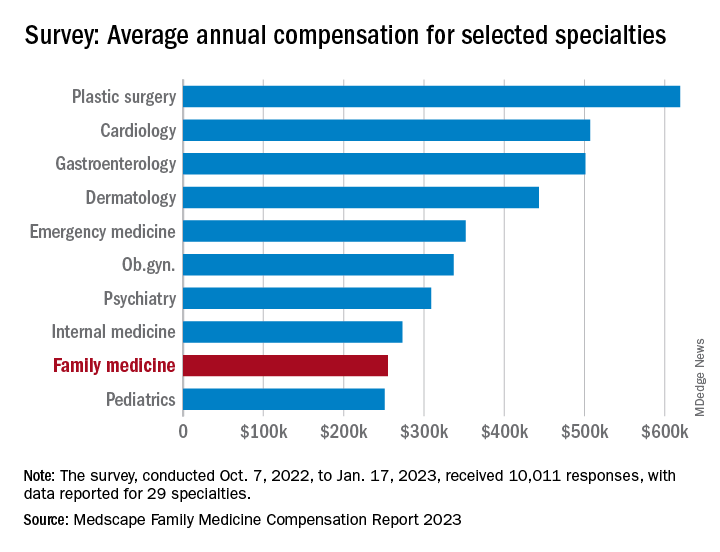
Comments from those respondents covered several areas that were already concerning physicians before the pandemic. One wrote that “decreasing Medicare reimbursement and poor payor mix destroy our income,” and another said that “patients have become rude and come with poor information from social media.” One respondent described the situation this way: “Overwhelming burnout. I had to reduce my hours to keep myself from quitting medicine completely.”
Overall physician compensation in 2022 was up by about 4% from 2021. For the 12% of the 10,011 respondents who practice family medicine, the average held at $255,000, where it had been the year before. Among the other primary care specialists, internists’ earnings were up by almost 4% and pediatricians did almost as well with a 3% increase, while ob.gyns. joined family physicians in the no-growth club, the Medscape results show.
For all physicians, average compensation in 2022 was $352,000, an increase of almost 18% since 2018. “Supply and demand is the biggest driver,” Mike Belkin, JD, of physician recruitment firm Merritt Hawkins, said in an interview. “Organizations understand it’s not getting any easier to get good candidates, and so for the most part, physicians are getting good offers.”
The lack of increase in FPs earnings among internists also included a decline of note: The disparity between mens’ and womens’ compensation dropped from 26% in 2021 to 23% in 2022. The 2022 disparity was only 16% for internists, however, even though family medicine has a considerably larger share of women (49% vs. 40%) among those surveyed, Medscape said.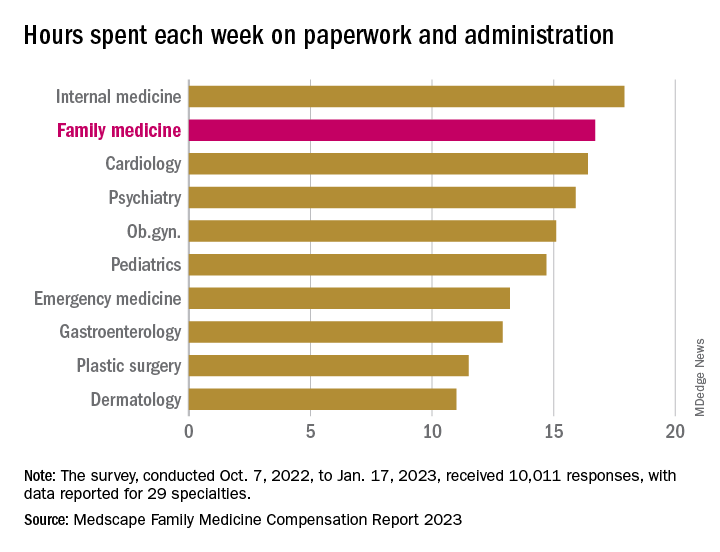
Satisfaction with their compensation, on the other hand, was higher among the family physicians (50%), compared with internists (43%). In 2022, 55% of family physicians said that they had been fairly paid.
In 2022, FP respondents reported spending an average of 16.7 hours (up from 15.6 hours in 2021) each week on paperwork and administration, just below the survey leaders, physical medicine and rehabilitation (18.5 hours) and nephrology (18.1 hours) but well above anesthesiology, lowest of the 29 specialties at 9.0 hours, and the 2022 average of 15.5 hours for all physicians, Medscape said.
When asked if they would choose medicine again, 72% of family physician respondents and 73% of all physicians said yes, with emergency medicine (65%) and dermatology (86%) representing the two extremes. A question about specialty choice showed that 66% of FPs would choose it again, putting them 28th of the 29 included specialties in their eagerness to follow the same path, above only the internists (61%), Medscape reported.
Commenters among the survey respondents were not identified by specialty, but dissatisfaction on many fronts was a definite theme:
- “Our costs go up, and our reimbursement does not.”
- “Our practice was acquired by venture capital firms; they slashed costs.”
- “My productivity bonus should have come to $45,000. Instead I was paid only $15,000. Yet cardiologists and administrators who were working from home part of the year received their full bonus.”
- “I will no longer practice cookbook mediocrity.”
according to the results of the Medscape Family Physician Compensation Report 2023.
Average compensation for the specialty, which has risen by 31% since 2015, was stagnant in 2022, showing no growth from the previous year. COVID, at least, had less of an effect on earnings, as 48% of family physicians cited pandemic-related income losses, compared with 64% in 2021, according to those who responded to Medscape’s annual survey, which was conducted from Oct. 2, 2022, to Jan. 17, 2023.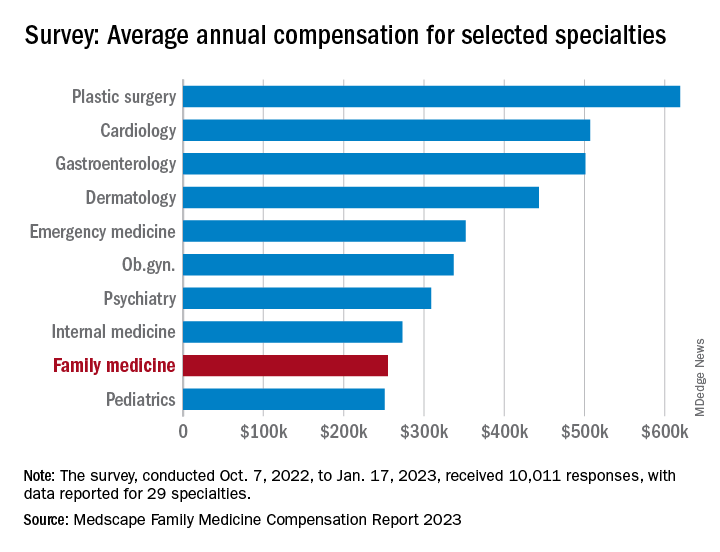
Comments from those respondents covered several areas that were already concerning physicians before the pandemic. One wrote that “decreasing Medicare reimbursement and poor payor mix destroy our income,” and another said that “patients have become rude and come with poor information from social media.” One respondent described the situation this way: “Overwhelming burnout. I had to reduce my hours to keep myself from quitting medicine completely.”
Overall physician compensation in 2022 was up by about 4% from 2021. For the 12% of the 10,011 respondents who practice family medicine, the average held at $255,000, where it had been the year before. Among the other primary care specialists, internists’ earnings were up by almost 4% and pediatricians did almost as well with a 3% increase, while ob.gyns. joined family physicians in the no-growth club, the Medscape results show.
For all physicians, average compensation in 2022 was $352,000, an increase of almost 18% since 2018. “Supply and demand is the biggest driver,” Mike Belkin, JD, of physician recruitment firm Merritt Hawkins, said in an interview. “Organizations understand it’s not getting any easier to get good candidates, and so for the most part, physicians are getting good offers.”
The lack of increase in FPs earnings among internists also included a decline of note: The disparity between mens’ and womens’ compensation dropped from 26% in 2021 to 23% in 2022. The 2022 disparity was only 16% for internists, however, even though family medicine has a considerably larger share of women (49% vs. 40%) among those surveyed, Medscape said.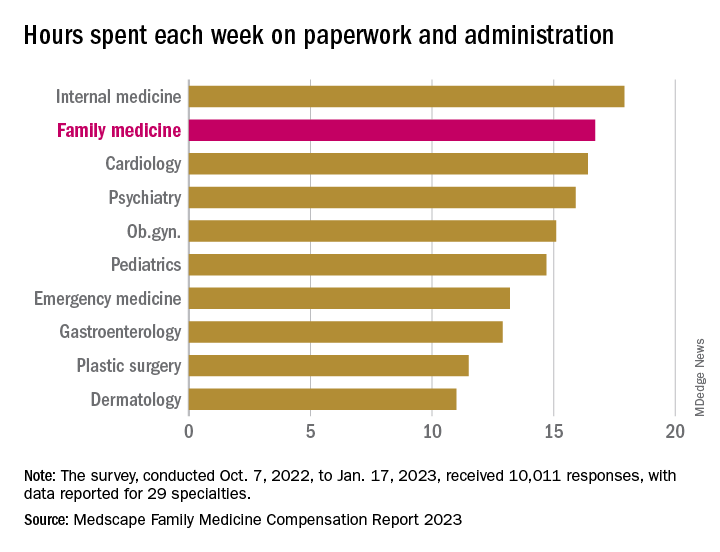
Satisfaction with their compensation, on the other hand, was higher among the family physicians (50%), compared with internists (43%). In 2022, 55% of family physicians said that they had been fairly paid.
In 2022, FP respondents reported spending an average of 16.7 hours (up from 15.6 hours in 2021) each week on paperwork and administration, just below the survey leaders, physical medicine and rehabilitation (18.5 hours) and nephrology (18.1 hours) but well above anesthesiology, lowest of the 29 specialties at 9.0 hours, and the 2022 average of 15.5 hours for all physicians, Medscape said.
When asked if they would choose medicine again, 72% of family physician respondents and 73% of all physicians said yes, with emergency medicine (65%) and dermatology (86%) representing the two extremes. A question about specialty choice showed that 66% of FPs would choose it again, putting them 28th of the 29 included specialties in their eagerness to follow the same path, above only the internists (61%), Medscape reported.
Commenters among the survey respondents were not identified by specialty, but dissatisfaction on many fronts was a definite theme:
- “Our costs go up, and our reimbursement does not.”
- “Our practice was acquired by venture capital firms; they slashed costs.”
- “My productivity bonus should have come to $45,000. Instead I was paid only $15,000. Yet cardiologists and administrators who were working from home part of the year received their full bonus.”
- “I will no longer practice cookbook mediocrity.”
Blood cancer patient takes on bias and ‘gaslighting’
Diagnosed with Hodgkin lymphoma in 2021, Ms. Ngon underwent port surgery to allow chemotherapy to be administered. Her right arm lost circulation and went numb, so she sought guidance from her blood cancer specialist. He dismissed her worries, saying that her tumors were pinching a nerve. She’d get better, he predicted, after more chemo.

“I knew in my body that something was wrong,” Ms. Ngon recalled. When the oncologist continued to downplay her concerns, she and a fellow communications specialist sat down together in the hospital lobby to draft an email to her physician. “We were trying to articulate the urgency in an email that expresses that I’m not being dramatic. We had to do it in a way that didn’t insult his intelligence: ‘Respectfully, you’re the doctor, but I know something is wrong.’ ”
In essence, Ms. Ngon was trying to be diplomatic and not trigger her oncologist’s defenses, while still convincing him to take action. Her approach to getting her doctor’s attention worked. He referred Ms. Ngon to a radiologist, who discovered that she had blood clots in her arm. Ms. Ngon then landed in the ICU for a week, as clinicians tried to break up the clots.
“I was the perfect person for this to happen to, because of my job and education. But it makes me sad because I understand I was in a fortunate position, with a background in communication. Most people don’t have that,” Ms. Ngon said.
This and other negative experiences during her medical saga inspired Ms. Ngon to partner with the Lymphoma Research Foundation in order to spread the word about unique challenges facing patients like her: people of color.
Ms. Ngon, who is Black, said her goal as a patient advocate is to “empower communities of color to speak up for themselves and hold oncologists responsible for listening and understanding differences across cultures.” And she wants to take a stand against the “gaslighting” of patients.
African Americans with hematologic disease like Ms. Ngon face a higher risk of poor outcomes than Whites, even as they are less likely than Whites to develop certain blood cancers. The reasons for this disparity aren’t clear, but researchers suspect they’re related to factors such as poverty, lack of insurance, genetics, and limited access to high-quality care.
Some researchers have blamed another factor: racism. A 2022 study sought to explain why Black and Hispanic patients with acute myeloid leukemia in urban areas have higher mortality rates than Whites, “despite more favorable genetics and younger age” (hazard ratio, 1.59, 95% confidence interval, 1.15-2.22 and HR, 1.25; 95% CI, 0.88-1.79). The study authors determined that “structural racism” – which they measured by examining segregation and “disadvantage” in neighborhoods where patients lived – accounted for nearly all of the disparities.
Ms. Ngon said her experiences and her awareness about poorer outcomes in medicine for African Americans – such as higher death rates for Black women during pregnancy – affect how she interacts with clinicians. “I automatically assume a barrier between me and my doctors, and it’s their responsibility to dismantle it.”
Making an connection with a physician can make a huge difference, she said. “I walked into my primary care doctor’s office and saw that she was a Latino woman. My guard went down, and I could feel her care for me as a human being. Whether that was because she was also a woman of color or not, I don’t know. But I did feel more cared for.”
However, Ms. Ngon could not find a Black oncologist to care for her in New York City, and that’s no surprise.
Ethnic and gender diversity remains an immense challenge in the hematology/oncology field. According to the American Society of Clinical Oncology, only about a third of oncologists are women, and the percentages identifying themselves as Black/African American and Hispanic are just 2.3% and 5.8%, respectively.
These numbers don’t seem likely to budge much any time soon. An analysis of medical students in U.S. oncology training programs from 2015-2020 found that just 3.8% identified themselves as Black/African American and 5.1% as Hispanic/Latino versus 52.15% as White and 31% as Asian/Pacific Islander/Native Hawaiian.
Ms. Ngon encountered challenges on other fronts during her cancer care. When she needed a wig during chemotherapy, a list of insurer-approved shops didn’t include any that catered to African Americans. Essentially, she said, she was being told that she couldn’t “purchase a wig from a place that makes you feel comfortable and from a woman who understand your needs as a Black woman. It needs to be from these specific shops that really don’t cater to my community.”
She also found it difficult to find fellow patients who shared her unique challenges. “I remember when I was diagnosed, I was looking through the support groups on Facebook, trying to find someone Black to ask about whether braiding my hair might stop it from falling out.”
Now, Ms. Ngon is in remission. And she’s happy with her oncologist, who’s White. “He listened to me, and he promised me that I would have the most boring recovery process ever, after everything I’d experienced. That explains a lot of why I felt so comfortable with him.”
She hopes to use her partnership with the Lymphoma Research Foundation to be a resource for people of color and alert them to the support that’s available for them. “I would love to let them know how to advocate for themselves as patients, how to trust their bodies, how to push back if they feel like they’re not getting the care that they deserve.”
Ms. Ngon would also like to see more support for medical students of color. “I hope to exist in a world one day where it wouldn’t be so hard to find an oncologist who looks like me in a city as large as this one,” she said.
As for oncologists, she urged them to “go the extra mile and really, really listen to what patients are saying. It’s easier said than done because there are natural biases in this world, and it’s hard to overcome those obstacles. But to not be heard and have to push every time. It was just exhausting to do that on top of trying to beat cancer.”
Diagnosed with Hodgkin lymphoma in 2021, Ms. Ngon underwent port surgery to allow chemotherapy to be administered. Her right arm lost circulation and went numb, so she sought guidance from her blood cancer specialist. He dismissed her worries, saying that her tumors were pinching a nerve. She’d get better, he predicted, after more chemo.

“I knew in my body that something was wrong,” Ms. Ngon recalled. When the oncologist continued to downplay her concerns, she and a fellow communications specialist sat down together in the hospital lobby to draft an email to her physician. “We were trying to articulate the urgency in an email that expresses that I’m not being dramatic. We had to do it in a way that didn’t insult his intelligence: ‘Respectfully, you’re the doctor, but I know something is wrong.’ ”
In essence, Ms. Ngon was trying to be diplomatic and not trigger her oncologist’s defenses, while still convincing him to take action. Her approach to getting her doctor’s attention worked. He referred Ms. Ngon to a radiologist, who discovered that she had blood clots in her arm. Ms. Ngon then landed in the ICU for a week, as clinicians tried to break up the clots.
“I was the perfect person for this to happen to, because of my job and education. But it makes me sad because I understand I was in a fortunate position, with a background in communication. Most people don’t have that,” Ms. Ngon said.
This and other negative experiences during her medical saga inspired Ms. Ngon to partner with the Lymphoma Research Foundation in order to spread the word about unique challenges facing patients like her: people of color.
Ms. Ngon, who is Black, said her goal as a patient advocate is to “empower communities of color to speak up for themselves and hold oncologists responsible for listening and understanding differences across cultures.” And she wants to take a stand against the “gaslighting” of patients.
African Americans with hematologic disease like Ms. Ngon face a higher risk of poor outcomes than Whites, even as they are less likely than Whites to develop certain blood cancers. The reasons for this disparity aren’t clear, but researchers suspect they’re related to factors such as poverty, lack of insurance, genetics, and limited access to high-quality care.
Some researchers have blamed another factor: racism. A 2022 study sought to explain why Black and Hispanic patients with acute myeloid leukemia in urban areas have higher mortality rates than Whites, “despite more favorable genetics and younger age” (hazard ratio, 1.59, 95% confidence interval, 1.15-2.22 and HR, 1.25; 95% CI, 0.88-1.79). The study authors determined that “structural racism” – which they measured by examining segregation and “disadvantage” in neighborhoods where patients lived – accounted for nearly all of the disparities.
Ms. Ngon said her experiences and her awareness about poorer outcomes in medicine for African Americans – such as higher death rates for Black women during pregnancy – affect how she interacts with clinicians. “I automatically assume a barrier between me and my doctors, and it’s their responsibility to dismantle it.”
Making an connection with a physician can make a huge difference, she said. “I walked into my primary care doctor’s office and saw that she was a Latino woman. My guard went down, and I could feel her care for me as a human being. Whether that was because she was also a woman of color or not, I don’t know. But I did feel more cared for.”
However, Ms. Ngon could not find a Black oncologist to care for her in New York City, and that’s no surprise.
Ethnic and gender diversity remains an immense challenge in the hematology/oncology field. According to the American Society of Clinical Oncology, only about a third of oncologists are women, and the percentages identifying themselves as Black/African American and Hispanic are just 2.3% and 5.8%, respectively.
These numbers don’t seem likely to budge much any time soon. An analysis of medical students in U.S. oncology training programs from 2015-2020 found that just 3.8% identified themselves as Black/African American and 5.1% as Hispanic/Latino versus 52.15% as White and 31% as Asian/Pacific Islander/Native Hawaiian.
Ms. Ngon encountered challenges on other fronts during her cancer care. When she needed a wig during chemotherapy, a list of insurer-approved shops didn’t include any that catered to African Americans. Essentially, she said, she was being told that she couldn’t “purchase a wig from a place that makes you feel comfortable and from a woman who understand your needs as a Black woman. It needs to be from these specific shops that really don’t cater to my community.”
She also found it difficult to find fellow patients who shared her unique challenges. “I remember when I was diagnosed, I was looking through the support groups on Facebook, trying to find someone Black to ask about whether braiding my hair might stop it from falling out.”
Now, Ms. Ngon is in remission. And she’s happy with her oncologist, who’s White. “He listened to me, and he promised me that I would have the most boring recovery process ever, after everything I’d experienced. That explains a lot of why I felt so comfortable with him.”
She hopes to use her partnership with the Lymphoma Research Foundation to be a resource for people of color and alert them to the support that’s available for them. “I would love to let them know how to advocate for themselves as patients, how to trust their bodies, how to push back if they feel like they’re not getting the care that they deserve.”
Ms. Ngon would also like to see more support for medical students of color. “I hope to exist in a world one day where it wouldn’t be so hard to find an oncologist who looks like me in a city as large as this one,” she said.
As for oncologists, she urged them to “go the extra mile and really, really listen to what patients are saying. It’s easier said than done because there are natural biases in this world, and it’s hard to overcome those obstacles. But to not be heard and have to push every time. It was just exhausting to do that on top of trying to beat cancer.”
Diagnosed with Hodgkin lymphoma in 2021, Ms. Ngon underwent port surgery to allow chemotherapy to be administered. Her right arm lost circulation and went numb, so she sought guidance from her blood cancer specialist. He dismissed her worries, saying that her tumors were pinching a nerve. She’d get better, he predicted, after more chemo.

“I knew in my body that something was wrong,” Ms. Ngon recalled. When the oncologist continued to downplay her concerns, she and a fellow communications specialist sat down together in the hospital lobby to draft an email to her physician. “We were trying to articulate the urgency in an email that expresses that I’m not being dramatic. We had to do it in a way that didn’t insult his intelligence: ‘Respectfully, you’re the doctor, but I know something is wrong.’ ”
In essence, Ms. Ngon was trying to be diplomatic and not trigger her oncologist’s defenses, while still convincing him to take action. Her approach to getting her doctor’s attention worked. He referred Ms. Ngon to a radiologist, who discovered that she had blood clots in her arm. Ms. Ngon then landed in the ICU for a week, as clinicians tried to break up the clots.
“I was the perfect person for this to happen to, because of my job and education. But it makes me sad because I understand I was in a fortunate position, with a background in communication. Most people don’t have that,” Ms. Ngon said.
This and other negative experiences during her medical saga inspired Ms. Ngon to partner with the Lymphoma Research Foundation in order to spread the word about unique challenges facing patients like her: people of color.
Ms. Ngon, who is Black, said her goal as a patient advocate is to “empower communities of color to speak up for themselves and hold oncologists responsible for listening and understanding differences across cultures.” And she wants to take a stand against the “gaslighting” of patients.
African Americans with hematologic disease like Ms. Ngon face a higher risk of poor outcomes than Whites, even as they are less likely than Whites to develop certain blood cancers. The reasons for this disparity aren’t clear, but researchers suspect they’re related to factors such as poverty, lack of insurance, genetics, and limited access to high-quality care.
Some researchers have blamed another factor: racism. A 2022 study sought to explain why Black and Hispanic patients with acute myeloid leukemia in urban areas have higher mortality rates than Whites, “despite more favorable genetics and younger age” (hazard ratio, 1.59, 95% confidence interval, 1.15-2.22 and HR, 1.25; 95% CI, 0.88-1.79). The study authors determined that “structural racism” – which they measured by examining segregation and “disadvantage” in neighborhoods where patients lived – accounted for nearly all of the disparities.
Ms. Ngon said her experiences and her awareness about poorer outcomes in medicine for African Americans – such as higher death rates for Black women during pregnancy – affect how she interacts with clinicians. “I automatically assume a barrier between me and my doctors, and it’s their responsibility to dismantle it.”
Making an connection with a physician can make a huge difference, she said. “I walked into my primary care doctor’s office and saw that she was a Latino woman. My guard went down, and I could feel her care for me as a human being. Whether that was because she was also a woman of color or not, I don’t know. But I did feel more cared for.”
However, Ms. Ngon could not find a Black oncologist to care for her in New York City, and that’s no surprise.
Ethnic and gender diversity remains an immense challenge in the hematology/oncology field. According to the American Society of Clinical Oncology, only about a third of oncologists are women, and the percentages identifying themselves as Black/African American and Hispanic are just 2.3% and 5.8%, respectively.
These numbers don’t seem likely to budge much any time soon. An analysis of medical students in U.S. oncology training programs from 2015-2020 found that just 3.8% identified themselves as Black/African American and 5.1% as Hispanic/Latino versus 52.15% as White and 31% as Asian/Pacific Islander/Native Hawaiian.
Ms. Ngon encountered challenges on other fronts during her cancer care. When she needed a wig during chemotherapy, a list of insurer-approved shops didn’t include any that catered to African Americans. Essentially, she said, she was being told that she couldn’t “purchase a wig from a place that makes you feel comfortable and from a woman who understand your needs as a Black woman. It needs to be from these specific shops that really don’t cater to my community.”
She also found it difficult to find fellow patients who shared her unique challenges. “I remember when I was diagnosed, I was looking through the support groups on Facebook, trying to find someone Black to ask about whether braiding my hair might stop it from falling out.”
Now, Ms. Ngon is in remission. And she’s happy with her oncologist, who’s White. “He listened to me, and he promised me that I would have the most boring recovery process ever, after everything I’d experienced. That explains a lot of why I felt so comfortable with him.”
She hopes to use her partnership with the Lymphoma Research Foundation to be a resource for people of color and alert them to the support that’s available for them. “I would love to let them know how to advocate for themselves as patients, how to trust their bodies, how to push back if they feel like they’re not getting the care that they deserve.”
Ms. Ngon would also like to see more support for medical students of color. “I hope to exist in a world one day where it wouldn’t be so hard to find an oncologist who looks like me in a city as large as this one,” she said.
As for oncologists, she urged them to “go the extra mile and really, really listen to what patients are saying. It’s easier said than done because there are natural biases in this world, and it’s hard to overcome those obstacles. But to not be heard and have to push every time. It was just exhausting to do that on top of trying to beat cancer.”
Exercise and empathy can help back pain patients in primary care
Treatment of chronic back pain remains a challenge for primary care physicians, and a new Cochrane Review confirms previous studies suggesting that analgesics and antidepressants fall short in terms of relief.
Data from another Cochrane Review support the value of exercise for chronic low back pain, although it is often underused, and the Food and Drug Administration’s recent approval of a spinal cord stimulation device for chronic back pain opens the door for another alternative.
Regardless of treatment type, however, patients report that empathy and clear communication from their doctors go a long way in their satisfaction with pain management, according to another recent study.
Exercise helps when patients adhere
The objective of the Cochrane Review on “Exercise therapy for chronic low back pain” was to determine whether exercise improves pain and functioning for people with chronic low back pain, compared with no treatment, usual care, or other common treatments, corresponding author Jill Hayden, PhD, of Dalhousie University, Halifax, N.S., said in an interview.
When back pain is chronic, it is expensive in terms of health care costs and lost work hours, said Dr. Hayden. “Exercise is promoted in many guidelines and is often recommended for, and used by, people with chronic low back pain.” However, “systematic reviews have found only small treatment effects, with considerable variation across individual trials.”
The 2021 review is one of the largest in the Cochrane Library, and included 249 trials and 24,486 study participants. However, Dr. Hayden said she had been disappointed by the methodological limitations of many of the trials. “The field is saturated with small exercise trials, many of which suffer from poor planning, conduct, and reporting due to limited resources.”
In the current review, “we found that exercise is likely to be effective for chronic low back pain. Overall, 3 months after the start of treatment, people receiving exercise treatment rated their pain an average of 15 points better on a scale of 0-100, and functional limitations were 7 points better, compared to people who had no treatment or usual care,” said Dr. Hayden.
Barriers to the use of exercise to treat pain may include fear of movement on the part of patients, she noted.
“Although our related network meta-analysis found some differences between specific types of exercise, we found all exercise types are more effective than minimal treatment,” she said. “People with chronic low back pain should be encouraged to do exercises that they enjoy and will do consistently to promote adherence.”
Limitations of medications
Both the safety and effectiveness of analgesics and antidepressants for pain in general and back pain in particular have come under scrutiny in recent research. A study published online in the British Medical Journal of patients with acute low back pain found that, although some medications were associated with large reductions in pain intensity, compared with placebo, the quality of the studies was “low or very low confidence,” according to a Medscape report on the findings.
This conclusion was supported in a large-scale analysis of the safety and effectiveness of antidepressants in chronic pain conditions, including back pain.
A new Cochrane Review led by a team of researchers in the United Kingdom found inadequate evidence to support the effectiveness of most antidepressants used for chronic pain, including amitriptyline, fluoxetine, citalopram, paroxetine, sertraline, and duloxetine.
“While chronic pain remains one of the top causes of daily disability worldwide, clinicians’ choices at offering interventions are getting fewer, especially if they tend toward a medical model and want a pharmacological solution,” corresponding author Tamar Pincus, PhD, of the University of Southampton (England), said in an interview. “We now know that opioids harm patients, and the evidence for common analgesics such as paracetamol and ibuprofen, for some conditions such as back pain, suggest they are not effective and might cause harm. This leaves clinicians with few options, and the most common prescription, supported by guidelines, is antidepressants.”
The study found moderate evidence that duloxetine can reduce pain in the short term and improve physical activity and some evidence that milnacipran might also be effective, Dr. Pincus said. “For all other antidepressants, including the commonly prescribed amitriptyline, the evidence was poor. Of importance, the average length of trials was 10 weeks, so long-term effects for all antidepressants remain unknown, and side effects and adverse events were reported poorly, so we also don’t know if any antidepressants are harmful.”
The takeaway message for the management of back pain in particular? “If a clinician and a patient decide together that it would be a good idea to try an antidepressant to reduce pain, they should consider starting with duloxetine, the drug with supporting evidence,” she said.
Physician attitude matters
Antidepressants may not have much impact on chronic pain, but a physician’s empathy and support do, according to data from a registry study of more than 1,300 individuals.
Despite efforts and guidelines from multiple medical organizations to promote optimal pain management, “much remains unknown regarding how the patient-physician interaction affects the process of delivering medical care for chronic low back pain and, ultimately, patient satisfaction,” John C. Licciardone, DO, of the University of North Texas Health Science Center, Fort Worth, and colleagues wrote in Annals of Family Medicine.
Previous studies have examined the relationship between clinical outcomes and patient satisfaction, but data on patient satisfaction with medical care for chronic low back pain specifically are limited, they said.
The researchers reviewed data from a national pain registry of adults aged 21-79 years that included self-reported measures of physician communication and empathy, prescribing data for opioids, and outcomes data for pain intensity, physical function, and health-related quality of life.
In a multivariate analysis, physician empathy and physician communication showed the strongest associations with patient satisfaction (P < .001).
The researchers found a negligible correlation between opioid prescription and perceived physician empathy and communication, “although current physician prescribing of opioids was also associated with patient satisfaction,” they wrote.
“Our findings pertaining to physician empathy are intriguing because they do not necessarily involve a therapeutic alliance with the patient based on collaborative communication or the expectation of a therapeutic effect via pharmacotherapy,” the researchers wrote .
The findings were limited by several factors including the cross-sectional design that prevented conclusions about cause and effect, the researchers noted. “It is possible that prior improvements in pain intensity, physical function, or [health-related quality of life] might have prompted participants to report more favorable ratings for physician empathy, physician communication, or patient satisfaction at registry enrollment.” However, the study supports the view that patients with low back pain in particular value physicians who validate their concerns and symptoms, and who make an effort to communicate treatment plans clearly.
Back pain patients continue to challenge primary care
“Back pain is a major issue in U.S. health care, in part because too many people have tough physical jobs or longstanding injuries that become chronic,” William Golden, MD, professor of medicine and public health at the University of Arkansas for Medical Sciences, Little Rock, said in an interview.
“There are no magic bullets for a lot of back pain patients, so empathy and support are key drivers,” he noted. “Helping patients maximize functionality as opposed to seeking mythical cures is the stronger line of visit discussions, but that takes a bit of time and skill in interviewing.
“It is fairly well established that duloxetine is useful in pain management, especially when present with mood disorders, either primary or secondary to the back-related disability,” said Dr. Golden. “Greater dissemination of its utility is probably useful, as is the side effect profile of the drug as well,” given the “nasty discontinuation syndrome when the treatment is reduced or stopped.”
Looking ahead, “more research is needed about microsurgery, namely for whom and for what anatomic presentations,” said Dr. Golden. Other topics for further research include a better understanding about medical marijuana and pain management and its interactions and side effects with other opioids and muscle relaxants. “Polypharmacy is still an issue in this class of patient,” and many of these patients are frustrated and angry “so the psychosocial skills of the PCP can be greatly tested as well,” he said.
Empathy promotes patient adherence to treatment
The new opioid prescription guidelines have increased interest among clinicians in how to improve patient satisfaction with the care for back pain provided, Noel Deep, MD, said in an interview. “These studies address this concern and bring forth an important aspect of the physician-patient relationship, namely the human touch and empathy.”
“I have been a strong proponent of the trust and relationship between a physician and patient; displaying empathy and increased and transparent communication between the physician and the patient has always resulted in better relationships and better outcomes for patients, especially those dealing with chronic health concerns,” said Dr. Deep, who is a general internist in a multispecialty group practice with Aspirus Antigo (Wisc.) Clinic and the chief medical officer and a staff physician at Aspirus Langlade Hospital, also in Antigo.
Potential barriers to effective pain management include beliefs and attitudes on the part of patients, Dr. Deep noted. “Physicians lacking adequate time to communicate effectively with the patient and describe nonopioid and nonsurgical interventions would be another potential barrier.” Other issues include the time and effort, as well as cost, associated with interventions such as physical therapy and other nondrug and nonsurgical interventions. Issues with family and social support and health literacy are also potential barriers to pain management.
Clinical takeaways
Low back pain is one of the most common reasons for a visit in primary care and can be “chronic and debilitating,” Grace Lin, MD, an internal medicine physician and primary care provider at the University of California, San Francisco, said in an interview.
“One issue with the Cochrane Review on exercise is that the studies on exercise were heterogeneous, so it’s difficult to know whether there is a particular kind of exercise that would be most effective and should be recommended to patients,” she said.
Furthermore, she said, “there is a physical therapist shortage in the U.S. I practice in a major city with a large health care system, and it can still take months to get an appointment with a physical therapist.” Also, insurance coverage may limit which therapists a patient can see and how many visits they can have.
“On the clinician side, I think physicians need to be better informed about the evidence base for back pain treatment, namely that exercise is effective and that, long term, analgesics are not,” Dr. Lin said. “This might decrease overprescription of ineffective analgesics and encourage more education about and referrals to physical therapy.”
“Physicians should continue to educate patients that physical therapy is the first-line treatment for back pain and that pain medications are secondary,” she said. “I think that analgesics can be effective for the short term to get people to a point where they feel well enough to do physical therapy. Duloxetine also appears to be moderately effective for chronic low back pain, in part because it may also help address coexisting depression and anxiety,” but these options should be reserved for adjuncts to physical therapy for back pain.
The findings from the study on empathy and communication suggest that the main challenges to these behaviors are systemic, said Dr. Lin.
“Our health care system is not conducive to treating chronic back pain,” she said. Primary care visits that last for 15 or 20 minutes are not long enough to diagnose and counsel patients on such a complex problem as chronic low back pain. Since back pain is usually not the only issue the primary care physician is dealing with during that visit, this can lead to patients feeling like their doctor isn’t listening to them and doesn’t care about their pain.
“We need to better understand the mechanisms by which people develop chronic, debilitating back pain,” Dr. Lin said. “I think if we understood this better, more effective and targeted treatments, both pharmacological and nonpharmacological, could be developed.”
The Annals of Family Medicine study received no outside funding, and the researchers had no financial conflicts to disclose. The Cochrane Reviews was supported by the National Institute for Health and Care Research’s Health Technology Assessment program, and the authors had no financial conflicts to disclose. Dr. Golden and Dr. Deep had no financial conflicts to disclose and serve on the editorial advisory board of Internal Medicine News. Dr. Lin disclosed receiving research funding from the Institute for Clinical and Economic Review and the National Institutes of Health.
Treatment of chronic back pain remains a challenge for primary care physicians, and a new Cochrane Review confirms previous studies suggesting that analgesics and antidepressants fall short in terms of relief.
Data from another Cochrane Review support the value of exercise for chronic low back pain, although it is often underused, and the Food and Drug Administration’s recent approval of a spinal cord stimulation device for chronic back pain opens the door for another alternative.
Regardless of treatment type, however, patients report that empathy and clear communication from their doctors go a long way in their satisfaction with pain management, according to another recent study.
Exercise helps when patients adhere
The objective of the Cochrane Review on “Exercise therapy for chronic low back pain” was to determine whether exercise improves pain and functioning for people with chronic low back pain, compared with no treatment, usual care, or other common treatments, corresponding author Jill Hayden, PhD, of Dalhousie University, Halifax, N.S., said in an interview.
When back pain is chronic, it is expensive in terms of health care costs and lost work hours, said Dr. Hayden. “Exercise is promoted in many guidelines and is often recommended for, and used by, people with chronic low back pain.” However, “systematic reviews have found only small treatment effects, with considerable variation across individual trials.”
The 2021 review is one of the largest in the Cochrane Library, and included 249 trials and 24,486 study participants. However, Dr. Hayden said she had been disappointed by the methodological limitations of many of the trials. “The field is saturated with small exercise trials, many of which suffer from poor planning, conduct, and reporting due to limited resources.”
In the current review, “we found that exercise is likely to be effective for chronic low back pain. Overall, 3 months after the start of treatment, people receiving exercise treatment rated their pain an average of 15 points better on a scale of 0-100, and functional limitations were 7 points better, compared to people who had no treatment or usual care,” said Dr. Hayden.
Barriers to the use of exercise to treat pain may include fear of movement on the part of patients, she noted.
“Although our related network meta-analysis found some differences between specific types of exercise, we found all exercise types are more effective than minimal treatment,” she said. “People with chronic low back pain should be encouraged to do exercises that they enjoy and will do consistently to promote adherence.”
Limitations of medications
Both the safety and effectiveness of analgesics and antidepressants for pain in general and back pain in particular have come under scrutiny in recent research. A study published online in the British Medical Journal of patients with acute low back pain found that, although some medications were associated with large reductions in pain intensity, compared with placebo, the quality of the studies was “low or very low confidence,” according to a Medscape report on the findings.
This conclusion was supported in a large-scale analysis of the safety and effectiveness of antidepressants in chronic pain conditions, including back pain.
A new Cochrane Review led by a team of researchers in the United Kingdom found inadequate evidence to support the effectiveness of most antidepressants used for chronic pain, including amitriptyline, fluoxetine, citalopram, paroxetine, sertraline, and duloxetine.
“While chronic pain remains one of the top causes of daily disability worldwide, clinicians’ choices at offering interventions are getting fewer, especially if they tend toward a medical model and want a pharmacological solution,” corresponding author Tamar Pincus, PhD, of the University of Southampton (England), said in an interview. “We now know that opioids harm patients, and the evidence for common analgesics such as paracetamol and ibuprofen, for some conditions such as back pain, suggest they are not effective and might cause harm. This leaves clinicians with few options, and the most common prescription, supported by guidelines, is antidepressants.”
The study found moderate evidence that duloxetine can reduce pain in the short term and improve physical activity and some evidence that milnacipran might also be effective, Dr. Pincus said. “For all other antidepressants, including the commonly prescribed amitriptyline, the evidence was poor. Of importance, the average length of trials was 10 weeks, so long-term effects for all antidepressants remain unknown, and side effects and adverse events were reported poorly, so we also don’t know if any antidepressants are harmful.”
The takeaway message for the management of back pain in particular? “If a clinician and a patient decide together that it would be a good idea to try an antidepressant to reduce pain, they should consider starting with duloxetine, the drug with supporting evidence,” she said.
Physician attitude matters
Antidepressants may not have much impact on chronic pain, but a physician’s empathy and support do, according to data from a registry study of more than 1,300 individuals.
Despite efforts and guidelines from multiple medical organizations to promote optimal pain management, “much remains unknown regarding how the patient-physician interaction affects the process of delivering medical care for chronic low back pain and, ultimately, patient satisfaction,” John C. Licciardone, DO, of the University of North Texas Health Science Center, Fort Worth, and colleagues wrote in Annals of Family Medicine.
Previous studies have examined the relationship between clinical outcomes and patient satisfaction, but data on patient satisfaction with medical care for chronic low back pain specifically are limited, they said.
The researchers reviewed data from a national pain registry of adults aged 21-79 years that included self-reported measures of physician communication and empathy, prescribing data for opioids, and outcomes data for pain intensity, physical function, and health-related quality of life.
In a multivariate analysis, physician empathy and physician communication showed the strongest associations with patient satisfaction (P < .001).
The researchers found a negligible correlation between opioid prescription and perceived physician empathy and communication, “although current physician prescribing of opioids was also associated with patient satisfaction,” they wrote.
“Our findings pertaining to physician empathy are intriguing because they do not necessarily involve a therapeutic alliance with the patient based on collaborative communication or the expectation of a therapeutic effect via pharmacotherapy,” the researchers wrote .
The findings were limited by several factors including the cross-sectional design that prevented conclusions about cause and effect, the researchers noted. “It is possible that prior improvements in pain intensity, physical function, or [health-related quality of life] might have prompted participants to report more favorable ratings for physician empathy, physician communication, or patient satisfaction at registry enrollment.” However, the study supports the view that patients with low back pain in particular value physicians who validate their concerns and symptoms, and who make an effort to communicate treatment plans clearly.
Back pain patients continue to challenge primary care
“Back pain is a major issue in U.S. health care, in part because too many people have tough physical jobs or longstanding injuries that become chronic,” William Golden, MD, professor of medicine and public health at the University of Arkansas for Medical Sciences, Little Rock, said in an interview.
“There are no magic bullets for a lot of back pain patients, so empathy and support are key drivers,” he noted. “Helping patients maximize functionality as opposed to seeking mythical cures is the stronger line of visit discussions, but that takes a bit of time and skill in interviewing.
“It is fairly well established that duloxetine is useful in pain management, especially when present with mood disorders, either primary or secondary to the back-related disability,” said Dr. Golden. “Greater dissemination of its utility is probably useful, as is the side effect profile of the drug as well,” given the “nasty discontinuation syndrome when the treatment is reduced or stopped.”
Looking ahead, “more research is needed about microsurgery, namely for whom and for what anatomic presentations,” said Dr. Golden. Other topics for further research include a better understanding about medical marijuana and pain management and its interactions and side effects with other opioids and muscle relaxants. “Polypharmacy is still an issue in this class of patient,” and many of these patients are frustrated and angry “so the psychosocial skills of the PCP can be greatly tested as well,” he said.
Empathy promotes patient adherence to treatment
The new opioid prescription guidelines have increased interest among clinicians in how to improve patient satisfaction with the care for back pain provided, Noel Deep, MD, said in an interview. “These studies address this concern and bring forth an important aspect of the physician-patient relationship, namely the human touch and empathy.”
“I have been a strong proponent of the trust and relationship between a physician and patient; displaying empathy and increased and transparent communication between the physician and the patient has always resulted in better relationships and better outcomes for patients, especially those dealing with chronic health concerns,” said Dr. Deep, who is a general internist in a multispecialty group practice with Aspirus Antigo (Wisc.) Clinic and the chief medical officer and a staff physician at Aspirus Langlade Hospital, also in Antigo.
Potential barriers to effective pain management include beliefs and attitudes on the part of patients, Dr. Deep noted. “Physicians lacking adequate time to communicate effectively with the patient and describe nonopioid and nonsurgical interventions would be another potential barrier.” Other issues include the time and effort, as well as cost, associated with interventions such as physical therapy and other nondrug and nonsurgical interventions. Issues with family and social support and health literacy are also potential barriers to pain management.
Clinical takeaways
Low back pain is one of the most common reasons for a visit in primary care and can be “chronic and debilitating,” Grace Lin, MD, an internal medicine physician and primary care provider at the University of California, San Francisco, said in an interview.
“One issue with the Cochrane Review on exercise is that the studies on exercise were heterogeneous, so it’s difficult to know whether there is a particular kind of exercise that would be most effective and should be recommended to patients,” she said.
Furthermore, she said, “there is a physical therapist shortage in the U.S. I practice in a major city with a large health care system, and it can still take months to get an appointment with a physical therapist.” Also, insurance coverage may limit which therapists a patient can see and how many visits they can have.
“On the clinician side, I think physicians need to be better informed about the evidence base for back pain treatment, namely that exercise is effective and that, long term, analgesics are not,” Dr. Lin said. “This might decrease overprescription of ineffective analgesics and encourage more education about and referrals to physical therapy.”
“Physicians should continue to educate patients that physical therapy is the first-line treatment for back pain and that pain medications are secondary,” she said. “I think that analgesics can be effective for the short term to get people to a point where they feel well enough to do physical therapy. Duloxetine also appears to be moderately effective for chronic low back pain, in part because it may also help address coexisting depression and anxiety,” but these options should be reserved for adjuncts to physical therapy for back pain.
The findings from the study on empathy and communication suggest that the main challenges to these behaviors are systemic, said Dr. Lin.
“Our health care system is not conducive to treating chronic back pain,” she said. Primary care visits that last for 15 or 20 minutes are not long enough to diagnose and counsel patients on such a complex problem as chronic low back pain. Since back pain is usually not the only issue the primary care physician is dealing with during that visit, this can lead to patients feeling like their doctor isn’t listening to them and doesn’t care about their pain.
“We need to better understand the mechanisms by which people develop chronic, debilitating back pain,” Dr. Lin said. “I think if we understood this better, more effective and targeted treatments, both pharmacological and nonpharmacological, could be developed.”
The Annals of Family Medicine study received no outside funding, and the researchers had no financial conflicts to disclose. The Cochrane Reviews was supported by the National Institute for Health and Care Research’s Health Technology Assessment program, and the authors had no financial conflicts to disclose. Dr. Golden and Dr. Deep had no financial conflicts to disclose and serve on the editorial advisory board of Internal Medicine News. Dr. Lin disclosed receiving research funding from the Institute for Clinical and Economic Review and the National Institutes of Health.
Treatment of chronic back pain remains a challenge for primary care physicians, and a new Cochrane Review confirms previous studies suggesting that analgesics and antidepressants fall short in terms of relief.
Data from another Cochrane Review support the value of exercise for chronic low back pain, although it is often underused, and the Food and Drug Administration’s recent approval of a spinal cord stimulation device for chronic back pain opens the door for another alternative.
Regardless of treatment type, however, patients report that empathy and clear communication from their doctors go a long way in their satisfaction with pain management, according to another recent study.
Exercise helps when patients adhere
The objective of the Cochrane Review on “Exercise therapy for chronic low back pain” was to determine whether exercise improves pain and functioning for people with chronic low back pain, compared with no treatment, usual care, or other common treatments, corresponding author Jill Hayden, PhD, of Dalhousie University, Halifax, N.S., said in an interview.
When back pain is chronic, it is expensive in terms of health care costs and lost work hours, said Dr. Hayden. “Exercise is promoted in many guidelines and is often recommended for, and used by, people with chronic low back pain.” However, “systematic reviews have found only small treatment effects, with considerable variation across individual trials.”
The 2021 review is one of the largest in the Cochrane Library, and included 249 trials and 24,486 study participants. However, Dr. Hayden said she had been disappointed by the methodological limitations of many of the trials. “The field is saturated with small exercise trials, many of which suffer from poor planning, conduct, and reporting due to limited resources.”
In the current review, “we found that exercise is likely to be effective for chronic low back pain. Overall, 3 months after the start of treatment, people receiving exercise treatment rated their pain an average of 15 points better on a scale of 0-100, and functional limitations were 7 points better, compared to people who had no treatment or usual care,” said Dr. Hayden.
Barriers to the use of exercise to treat pain may include fear of movement on the part of patients, she noted.
“Although our related network meta-analysis found some differences between specific types of exercise, we found all exercise types are more effective than minimal treatment,” she said. “People with chronic low back pain should be encouraged to do exercises that they enjoy and will do consistently to promote adherence.”
Limitations of medications
Both the safety and effectiveness of analgesics and antidepressants for pain in general and back pain in particular have come under scrutiny in recent research. A study published online in the British Medical Journal of patients with acute low back pain found that, although some medications were associated with large reductions in pain intensity, compared with placebo, the quality of the studies was “low or very low confidence,” according to a Medscape report on the findings.
This conclusion was supported in a large-scale analysis of the safety and effectiveness of antidepressants in chronic pain conditions, including back pain.
A new Cochrane Review led by a team of researchers in the United Kingdom found inadequate evidence to support the effectiveness of most antidepressants used for chronic pain, including amitriptyline, fluoxetine, citalopram, paroxetine, sertraline, and duloxetine.
“While chronic pain remains one of the top causes of daily disability worldwide, clinicians’ choices at offering interventions are getting fewer, especially if they tend toward a medical model and want a pharmacological solution,” corresponding author Tamar Pincus, PhD, of the University of Southampton (England), said in an interview. “We now know that opioids harm patients, and the evidence for common analgesics such as paracetamol and ibuprofen, for some conditions such as back pain, suggest they are not effective and might cause harm. This leaves clinicians with few options, and the most common prescription, supported by guidelines, is antidepressants.”
The study found moderate evidence that duloxetine can reduce pain in the short term and improve physical activity and some evidence that milnacipran might also be effective, Dr. Pincus said. “For all other antidepressants, including the commonly prescribed amitriptyline, the evidence was poor. Of importance, the average length of trials was 10 weeks, so long-term effects for all antidepressants remain unknown, and side effects and adverse events were reported poorly, so we also don’t know if any antidepressants are harmful.”
The takeaway message for the management of back pain in particular? “If a clinician and a patient decide together that it would be a good idea to try an antidepressant to reduce pain, they should consider starting with duloxetine, the drug with supporting evidence,” she said.
Physician attitude matters
Antidepressants may not have much impact on chronic pain, but a physician’s empathy and support do, according to data from a registry study of more than 1,300 individuals.
Despite efforts and guidelines from multiple medical organizations to promote optimal pain management, “much remains unknown regarding how the patient-physician interaction affects the process of delivering medical care for chronic low back pain and, ultimately, patient satisfaction,” John C. Licciardone, DO, of the University of North Texas Health Science Center, Fort Worth, and colleagues wrote in Annals of Family Medicine.
Previous studies have examined the relationship between clinical outcomes and patient satisfaction, but data on patient satisfaction with medical care for chronic low back pain specifically are limited, they said.
The researchers reviewed data from a national pain registry of adults aged 21-79 years that included self-reported measures of physician communication and empathy, prescribing data for opioids, and outcomes data for pain intensity, physical function, and health-related quality of life.
In a multivariate analysis, physician empathy and physician communication showed the strongest associations with patient satisfaction (P < .001).
The researchers found a negligible correlation between opioid prescription and perceived physician empathy and communication, “although current physician prescribing of opioids was also associated with patient satisfaction,” they wrote.
“Our findings pertaining to physician empathy are intriguing because they do not necessarily involve a therapeutic alliance with the patient based on collaborative communication or the expectation of a therapeutic effect via pharmacotherapy,” the researchers wrote .
The findings were limited by several factors including the cross-sectional design that prevented conclusions about cause and effect, the researchers noted. “It is possible that prior improvements in pain intensity, physical function, or [health-related quality of life] might have prompted participants to report more favorable ratings for physician empathy, physician communication, or patient satisfaction at registry enrollment.” However, the study supports the view that patients with low back pain in particular value physicians who validate their concerns and symptoms, and who make an effort to communicate treatment plans clearly.
Back pain patients continue to challenge primary care
“Back pain is a major issue in U.S. health care, in part because too many people have tough physical jobs or longstanding injuries that become chronic,” William Golden, MD, professor of medicine and public health at the University of Arkansas for Medical Sciences, Little Rock, said in an interview.
“There are no magic bullets for a lot of back pain patients, so empathy and support are key drivers,” he noted. “Helping patients maximize functionality as opposed to seeking mythical cures is the stronger line of visit discussions, but that takes a bit of time and skill in interviewing.
“It is fairly well established that duloxetine is useful in pain management, especially when present with mood disorders, either primary or secondary to the back-related disability,” said Dr. Golden. “Greater dissemination of its utility is probably useful, as is the side effect profile of the drug as well,” given the “nasty discontinuation syndrome when the treatment is reduced or stopped.”
Looking ahead, “more research is needed about microsurgery, namely for whom and for what anatomic presentations,” said Dr. Golden. Other topics for further research include a better understanding about medical marijuana and pain management and its interactions and side effects with other opioids and muscle relaxants. “Polypharmacy is still an issue in this class of patient,” and many of these patients are frustrated and angry “so the psychosocial skills of the PCP can be greatly tested as well,” he said.
Empathy promotes patient adherence to treatment
The new opioid prescription guidelines have increased interest among clinicians in how to improve patient satisfaction with the care for back pain provided, Noel Deep, MD, said in an interview. “These studies address this concern and bring forth an important aspect of the physician-patient relationship, namely the human touch and empathy.”
“I have been a strong proponent of the trust and relationship between a physician and patient; displaying empathy and increased and transparent communication between the physician and the patient has always resulted in better relationships and better outcomes for patients, especially those dealing with chronic health concerns,” said Dr. Deep, who is a general internist in a multispecialty group practice with Aspirus Antigo (Wisc.) Clinic and the chief medical officer and a staff physician at Aspirus Langlade Hospital, also in Antigo.
Potential barriers to effective pain management include beliefs and attitudes on the part of patients, Dr. Deep noted. “Physicians lacking adequate time to communicate effectively with the patient and describe nonopioid and nonsurgical interventions would be another potential barrier.” Other issues include the time and effort, as well as cost, associated with interventions such as physical therapy and other nondrug and nonsurgical interventions. Issues with family and social support and health literacy are also potential barriers to pain management.
Clinical takeaways
Low back pain is one of the most common reasons for a visit in primary care and can be “chronic and debilitating,” Grace Lin, MD, an internal medicine physician and primary care provider at the University of California, San Francisco, said in an interview.
“One issue with the Cochrane Review on exercise is that the studies on exercise were heterogeneous, so it’s difficult to know whether there is a particular kind of exercise that would be most effective and should be recommended to patients,” she said.
Furthermore, she said, “there is a physical therapist shortage in the U.S. I practice in a major city with a large health care system, and it can still take months to get an appointment with a physical therapist.” Also, insurance coverage may limit which therapists a patient can see and how many visits they can have.
“On the clinician side, I think physicians need to be better informed about the evidence base for back pain treatment, namely that exercise is effective and that, long term, analgesics are not,” Dr. Lin said. “This might decrease overprescription of ineffective analgesics and encourage more education about and referrals to physical therapy.”
“Physicians should continue to educate patients that physical therapy is the first-line treatment for back pain and that pain medications are secondary,” she said. “I think that analgesics can be effective for the short term to get people to a point where they feel well enough to do physical therapy. Duloxetine also appears to be moderately effective for chronic low back pain, in part because it may also help address coexisting depression and anxiety,” but these options should be reserved for adjuncts to physical therapy for back pain.
The findings from the study on empathy and communication suggest that the main challenges to these behaviors are systemic, said Dr. Lin.
“Our health care system is not conducive to treating chronic back pain,” she said. Primary care visits that last for 15 or 20 minutes are not long enough to diagnose and counsel patients on such a complex problem as chronic low back pain. Since back pain is usually not the only issue the primary care physician is dealing with during that visit, this can lead to patients feeling like their doctor isn’t listening to them and doesn’t care about their pain.
“We need to better understand the mechanisms by which people develop chronic, debilitating back pain,” Dr. Lin said. “I think if we understood this better, more effective and targeted treatments, both pharmacological and nonpharmacological, could be developed.”
The Annals of Family Medicine study received no outside funding, and the researchers had no financial conflicts to disclose. The Cochrane Reviews was supported by the National Institute for Health and Care Research’s Health Technology Assessment program, and the authors had no financial conflicts to disclose. Dr. Golden and Dr. Deep had no financial conflicts to disclose and serve on the editorial advisory board of Internal Medicine News. Dr. Lin disclosed receiving research funding from the Institute for Clinical and Economic Review and the National Institutes of Health.
Internists in 2022: Increased earnings can’t stop rising dissatisfaction
Internists experienced many of the usual ups and downs regarding nonclinical matters in 2022: Compensation was up, but satisfaction with compensation was down; the percentage of internists who would choose another specialty was up and time spent on paperwork and administration was down only slightly.
A year that began with the COVID-19 Omicron surge ended with many of the same old issues regaining the attention of physicians, according to those who responded to Medscape’s annual compensation survey, which was conducted from Oct. 2, 2022, to Jan. 17, 2023.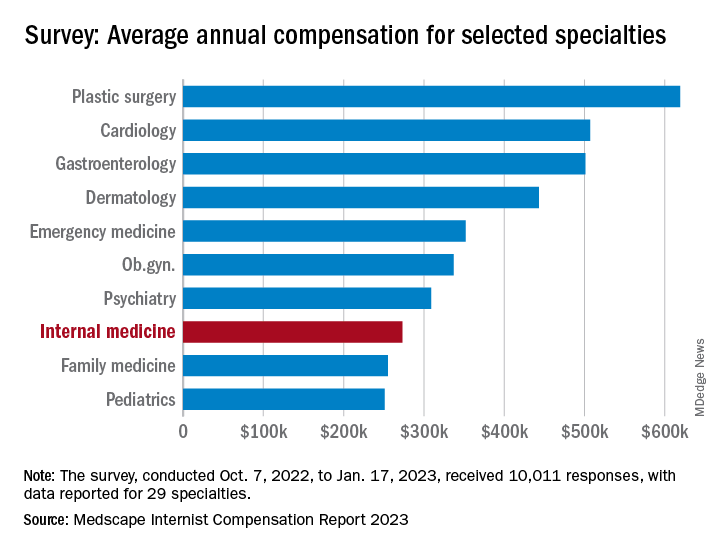
“Decreasing Medicare reimbursement and poor payor mix destroy our income,” one physician wrote, and another said that “patients have become rude and come with poor information from social media.” One respondent described the situation this way: “Overwhelming burnout. I had to reduce my hours to keep myself from quitting medicine completely.”
For internists at least, some of the survey results were positive. For the 13% of the 10,011 respondents who practice internal medicine, average compensation went from $264,000 in 2021 to $273,000 in 2022, an increase of almost 4% that matched the average for all physicians. Among the other primary care specialists, pediatricians did almost as well with a 3% increase, but ob.gyns. and family physicians only managed to keep their 2022 earnings at 2021 levels.
Overall physician compensation for 2022 was $352,000, an increase of almost 18% since 2018. “Supply and demand is the biggest driver,” Mike Belkin, JD, of physician recruitment firm Merritt Hawkins, said in an interview. “Organizations understand it’s not getting any easier to get good candidates, and so for the most part, physicians are getting good offers.”
The latest increase in earnings among internists also included a decline: The disparity between mens’ and womens’ compensation dropped from 24% in 2021 to 16% in 2022. The gap was slightly larger for all physicians in 2022, with men earning about 19% more than women, and larger again among specialists at 27%, but both of those figures are lower than in recent years, Medscape said.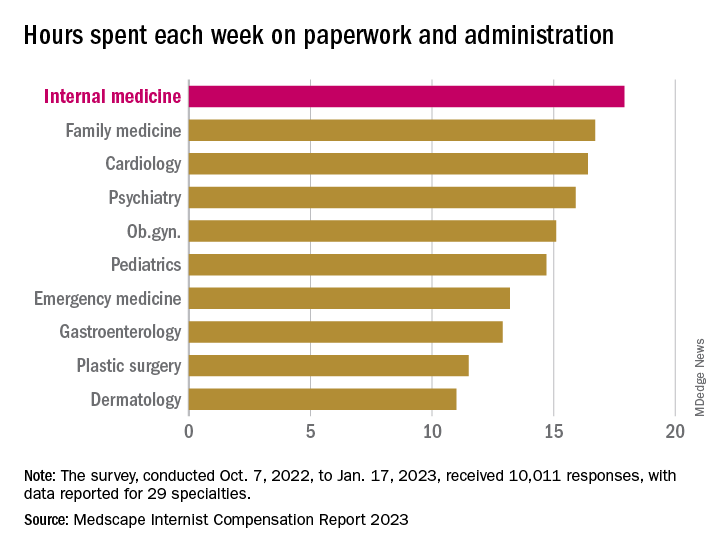
Satisfaction with their compensation, however, was not high for internists: Only 43% feel that they are fairly paid, coming in above only ophthalmology (42%) and infectious diseases (35%) and well below psychiatry (68%) at the top of the list, the Medscape data show. In the 2022 report, 49% of internists said that they had been fairly paid.
In another source of potential dissatisfaction, internist respondents reported spending an average of 17.9 hours each week on paperwork and administration, just below the survey leaders, physical medicine and rehabilitation (18.5 hours) and nephrology (18.1 hours) and well above anesthesiology, which was the lowest of the 29 specialties at 9.0 hours, and the 2022 average of 15.5 hours for all physicians, Medscape said. A small bright spot comes in the form of a decline from the internists’ time of 18.7 hours per week in 2021.
When asked if they would choose medicine again, 72% of internist respondents and 73% of all physicians said yes, with emergency medicine (65%) and dermatology (86%) representing the two extremes. A question about specialty choice showed internists to be the least likely of the 29 included specialties to follow the same path, with 61% (down from 63% in 2022) approving their initial selection, versus 97% for plastic surgeons, Medscape reported.
Commenters among the survey respondents were not identified by specialty, but dissatisfaction on many fronts was a definite theme:
- “Our costs go up, and our reimbursement does not.”
- “Our practice was acquired by venture capital firms; they slashed costs.”
- “My productivity bonus should have come to $45,000. Instead I was paid only $15,000. Yet cardiologists and administrators who were working from home part of the year received their full bonus.”
- “I will no longer practice cookbook mediocrity.”
Internists experienced many of the usual ups and downs regarding nonclinical matters in 2022: Compensation was up, but satisfaction with compensation was down; the percentage of internists who would choose another specialty was up and time spent on paperwork and administration was down only slightly.
A year that began with the COVID-19 Omicron surge ended with many of the same old issues regaining the attention of physicians, according to those who responded to Medscape’s annual compensation survey, which was conducted from Oct. 2, 2022, to Jan. 17, 2023.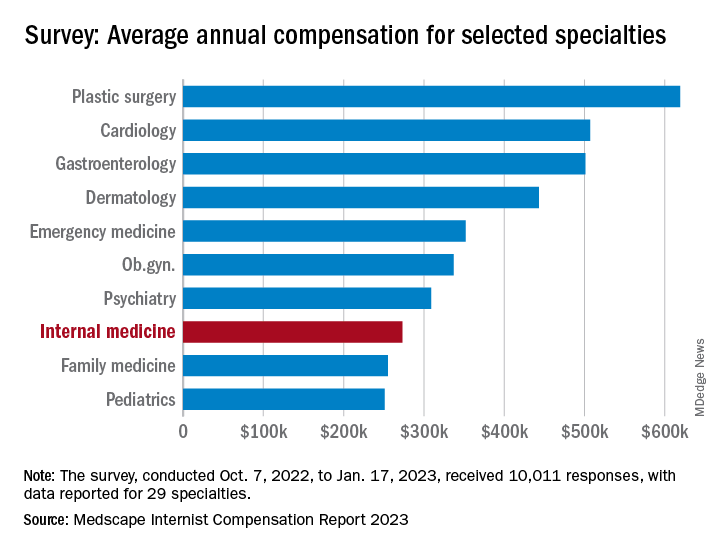
“Decreasing Medicare reimbursement and poor payor mix destroy our income,” one physician wrote, and another said that “patients have become rude and come with poor information from social media.” One respondent described the situation this way: “Overwhelming burnout. I had to reduce my hours to keep myself from quitting medicine completely.”
For internists at least, some of the survey results were positive. For the 13% of the 10,011 respondents who practice internal medicine, average compensation went from $264,000 in 2021 to $273,000 in 2022, an increase of almost 4% that matched the average for all physicians. Among the other primary care specialists, pediatricians did almost as well with a 3% increase, but ob.gyns. and family physicians only managed to keep their 2022 earnings at 2021 levels.
Overall physician compensation for 2022 was $352,000, an increase of almost 18% since 2018. “Supply and demand is the biggest driver,” Mike Belkin, JD, of physician recruitment firm Merritt Hawkins, said in an interview. “Organizations understand it’s not getting any easier to get good candidates, and so for the most part, physicians are getting good offers.”
The latest increase in earnings among internists also included a decline: The disparity between mens’ and womens’ compensation dropped from 24% in 2021 to 16% in 2022. The gap was slightly larger for all physicians in 2022, with men earning about 19% more than women, and larger again among specialists at 27%, but both of those figures are lower than in recent years, Medscape said.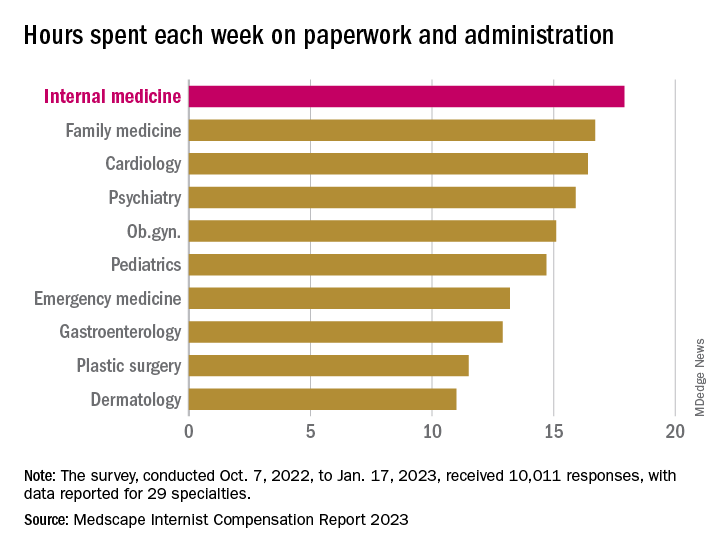
Satisfaction with their compensation, however, was not high for internists: Only 43% feel that they are fairly paid, coming in above only ophthalmology (42%) and infectious diseases (35%) and well below psychiatry (68%) at the top of the list, the Medscape data show. In the 2022 report, 49% of internists said that they had been fairly paid.
In another source of potential dissatisfaction, internist respondents reported spending an average of 17.9 hours each week on paperwork and administration, just below the survey leaders, physical medicine and rehabilitation (18.5 hours) and nephrology (18.1 hours) and well above anesthesiology, which was the lowest of the 29 specialties at 9.0 hours, and the 2022 average of 15.5 hours for all physicians, Medscape said. A small bright spot comes in the form of a decline from the internists’ time of 18.7 hours per week in 2021.
When asked if they would choose medicine again, 72% of internist respondents and 73% of all physicians said yes, with emergency medicine (65%) and dermatology (86%) representing the two extremes. A question about specialty choice showed internists to be the least likely of the 29 included specialties to follow the same path, with 61% (down from 63% in 2022) approving their initial selection, versus 97% for plastic surgeons, Medscape reported.
Commenters among the survey respondents were not identified by specialty, but dissatisfaction on many fronts was a definite theme:
- “Our costs go up, and our reimbursement does not.”
- “Our practice was acquired by venture capital firms; they slashed costs.”
- “My productivity bonus should have come to $45,000. Instead I was paid only $15,000. Yet cardiologists and administrators who were working from home part of the year received their full bonus.”
- “I will no longer practice cookbook mediocrity.”
Internists experienced many of the usual ups and downs regarding nonclinical matters in 2022: Compensation was up, but satisfaction with compensation was down; the percentage of internists who would choose another specialty was up and time spent on paperwork and administration was down only slightly.
A year that began with the COVID-19 Omicron surge ended with many of the same old issues regaining the attention of physicians, according to those who responded to Medscape’s annual compensation survey, which was conducted from Oct. 2, 2022, to Jan. 17, 2023.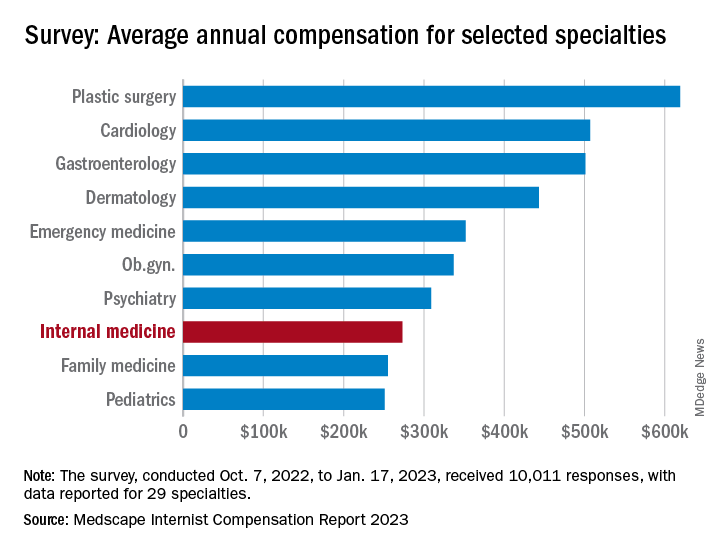
“Decreasing Medicare reimbursement and poor payor mix destroy our income,” one physician wrote, and another said that “patients have become rude and come with poor information from social media.” One respondent described the situation this way: “Overwhelming burnout. I had to reduce my hours to keep myself from quitting medicine completely.”
For internists at least, some of the survey results were positive. For the 13% of the 10,011 respondents who practice internal medicine, average compensation went from $264,000 in 2021 to $273,000 in 2022, an increase of almost 4% that matched the average for all physicians. Among the other primary care specialists, pediatricians did almost as well with a 3% increase, but ob.gyns. and family physicians only managed to keep their 2022 earnings at 2021 levels.
Overall physician compensation for 2022 was $352,000, an increase of almost 18% since 2018. “Supply and demand is the biggest driver,” Mike Belkin, JD, of physician recruitment firm Merritt Hawkins, said in an interview. “Organizations understand it’s not getting any easier to get good candidates, and so for the most part, physicians are getting good offers.”
The latest increase in earnings among internists also included a decline: The disparity between mens’ and womens’ compensation dropped from 24% in 2021 to 16% in 2022. The gap was slightly larger for all physicians in 2022, with men earning about 19% more than women, and larger again among specialists at 27%, but both of those figures are lower than in recent years, Medscape said.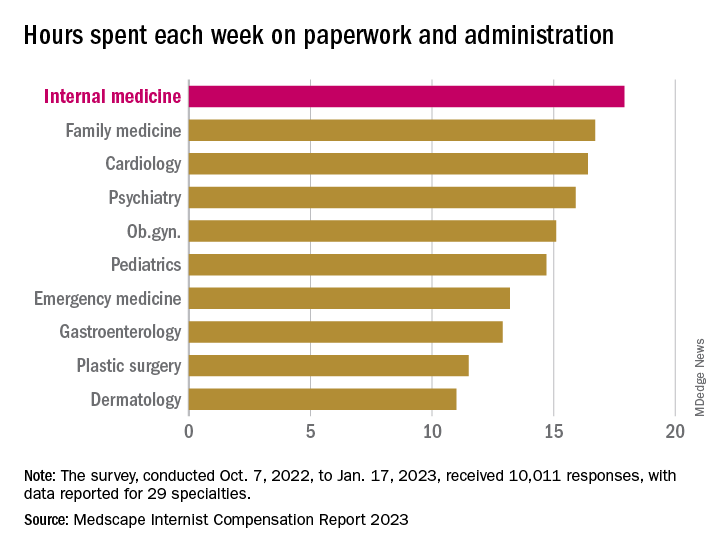
Satisfaction with their compensation, however, was not high for internists: Only 43% feel that they are fairly paid, coming in above only ophthalmology (42%) and infectious diseases (35%) and well below psychiatry (68%) at the top of the list, the Medscape data show. In the 2022 report, 49% of internists said that they had been fairly paid.
In another source of potential dissatisfaction, internist respondents reported spending an average of 17.9 hours each week on paperwork and administration, just below the survey leaders, physical medicine and rehabilitation (18.5 hours) and nephrology (18.1 hours) and well above anesthesiology, which was the lowest of the 29 specialties at 9.0 hours, and the 2022 average of 15.5 hours for all physicians, Medscape said. A small bright spot comes in the form of a decline from the internists’ time of 18.7 hours per week in 2021.
When asked if they would choose medicine again, 72% of internist respondents and 73% of all physicians said yes, with emergency medicine (65%) and dermatology (86%) representing the two extremes. A question about specialty choice showed internists to be the least likely of the 29 included specialties to follow the same path, with 61% (down from 63% in 2022) approving their initial selection, versus 97% for plastic surgeons, Medscape reported.
Commenters among the survey respondents were not identified by specialty, but dissatisfaction on many fronts was a definite theme:
- “Our costs go up, and our reimbursement does not.”
- “Our practice was acquired by venture capital firms; they slashed costs.”
- “My productivity bonus should have come to $45,000. Instead I was paid only $15,000. Yet cardiologists and administrators who were working from home part of the year received their full bonus.”
- “I will no longer practice cookbook mediocrity.”
States move to curb insurers’ prior authorization requirements as federal reforms lag
Amid growing criticism of health insurers’ onerous prior authorization practices, lawmakers in 30 states have introduced bills this year that aim to rein in insurer gatekeeping and improve patient care.
“This is something that goes on in every doctor’s office every day; the frustrations, the delays, and the use of office staff time are just unbelievable,” said Steven Orland, MD, a board-certified urologist and president of the Medical Society of New Jersey.
The bills, which cover private health plans and insurers that states regulate, may provide some relief for physicians as federal efforts to streamline prior authorization for some Medicare patients have lagged.
Last year, Congress failed to pass the Improving Seniors’ Timely Access to Care Act of 2021, despite 326 co-sponsors. The bill would have compelled insurers covering Medicare Advantage enrollees to speed up prior authorizations, make the process more transparent, and remove obstacles such as requiring fax machine submissions.
Last month, however, the Centers for Medicare & Medicaid Services issued a final rule that will improve some aspects of prior authorizations in Medicare Advantage insurance plans and ensure that enrollees have the same access to necessary care as traditional Medicare enrollees.
The insurance industry has long defended prior authorization requirements and opposed legislation that would limit them.
America’s Health Insurance Plans (AHIP) and the Blue Cross Blue Shield Association said in a 2019 letter to a congressional committee when the federal legislation was first introduced, “Prior authorizations enforce best practices and guidelines for care management and help physicians identify and avoid care techniques that would harm patient outcomes, such as designating prescriptions that could feed into an opioid addiction.” AHIP didn’t respond to repeated requests for comment.
But some major insurers now appear willing to compromise and voluntarily reduce the volume of prior authorizations they require. Days before the federal final rule was released, three major insurers – United HealthCare, Cigna, and Aetna CVS Health – announced they plan to drop some prior authorization requirements and automate processes.
United HealthCare said it will eliminate almost 20% of its prior authorizations for some nonurgent surgeries and procedures starting this summer. It also will create a national Gold Card program in 2024 for physicians who meet its eligibility requirements, which would eliminate prior authorization requirements for most procedures. Both initiatives will apply to commercial, Medicare Advantage, and Medicaid businesses, said the insurer in a statement.
However, United HealthCare also announced that in June it will start requiring prior authorization for diagnostic (not screening) gastrointestinal endoscopies for its nearly 27 million privately insured patients, citing data it says shows potentially harmful overuse of scopes. Physician groups have publicly criticized the move, saying it could delay lifesaving treatment, and have asked the insurer to reconsider.
Cigna and Aetna also have moved to pare back prior authorization processes. Scott Josephs, national medical officer for Cigna, told Healthcare Dive that Cigna has removed prior authorization reviews from nearly 500 services since 2020.
An Aetna spokesperson told Healthcare Dive that the CVS-owned payer has implemented a gold card program and rolled back prior authorization requirements on cataract surgeries, video EEGs, and home infusion for some drugs, according to Healthcare Dive.
Cigna has faced increased scrutiny from some state regulators since a ProPublica/The Capitol Forum article revealed in March that its doctors were denying claims without opening patients’ files, contrary to what insurance laws and regulations require in many states.
Over a period of 2 months last year, Cigna doctors denied over 300,000 requests for payments using this method, spending an average of 1.2 seconds on each case, the investigation found. In a written response, Cigna said the reporting by ProPublica and The Capitol Forum was “biased and incomplete.”
States aim to reduce prior authorization volume
The American Medical Association said it has been tracking nearly 90 prior authorization reform bills in 30 states. More than a dozen bills are still being considered in this legislative session, including in Arkansas, California, New Jersey, North Carolina, Maryland, and Washington, D.C.
“The groundswell of activity in the states reflects how big a problem this is,” said an AMA legislative expert. “The issue used to be ‘how can we automate and streamline processes’; now the issue is focused on reducing the volume of prior authorizations and the harm that can cause patients.”
The state bills use different strategies to reduce excessive prior authorization requirements. Maryland’s proposed bill, for example, would require just one prior authorization to stay on a prescription drug, if the insurer has previously approved the drug and the patient continues to successfully be treated by the drug.
Washington, D.C. and New Jersey have introduced comprehensive reform bills that include a “grace period” of 60 days, to ensure continuity of care when a patient switches health plans. They also would eliminate repeat authorizations for chronic and long-term conditions, set explicit timelines for insurers to respond to prior authorization requests and appeals, and require that practicing physicians review denials that are appealed.
Many state bills also would require insurers to be more transparent by posting information on their websites about which services and drugs require prior authorization and what their approval rates are for them, said AMA’s legislative expert.
“There’s a black hole of information that insurers have access to. We would really like to know how many prior authorization requests are denied, the time it takes to deny them, and the reasons for denial,” said Josh Bengal, JD, the director of government relations for the Medical Society of New Jersey.
The legislation in New Jersey and other states faces stiff opposition from the insurance lobby, especially state associations of health plans affiliated with AHIP. The California Association of Health Plans, for example, opposes a “gold card” bill (SB 598), introduced in February, that would allow a select group of high-performing doctors to skip prior authorizations for 1 year.
The CAHP states, “Californians deserve safe, high quality, high-value health care. Yet SB 598 will derail the progress we have made in our health care system by lowering the value and safety that Californians should expect from their health care providers,” according to a fact sheet.
The fact-sheet defines “low-value care” as medical services for which there is little to no benefit and poses potential physical or financial harm to patients, such as unnecessary CT scans or MRIs for uncomplicated conditions.
California is one of about a dozen states that have introduced gold card legislation this year. If enacted, they would join five states with gold card laws: West Virginia, Texas, Vermont, Michigan, and Louisiana.
How do gold cards work?
Physicians who achieve a high approval rate of prior authorizations from insurers for 1 year are eligible to be exempted from obtaining prior authorizations the following year.
The approval rate is at least 90% for a certain number of eligible health services, but the number of prior authorizations required to qualify can range from 5 to 30, depending on the state law.
Gold card legislation typically also gives the treating physician the right to have an appeal of a prior authorization denial by a physician peer of the same or similar specialty.
California’s bill would also apply to all covered health services, which is broader than what United HealthCare has proposed for its gold card exemption. The bill would also require a plan or insurer to annually monitor rates of prior authorization approval, modification, appeal, and denial, and to discontinue services, items, and supplies that are approved 95% of the time.
“These are important reforms that will help ensure that patients can receive the care they need, when they need it,” said CMA president Donaldo Hernandez, MD.
However, it’s not clear how many physicians will meet “gold card” status based on Texas’ recent experience with its own “gold card” law.
The Texas Department of Insurance estimated that only 3.3% of licensed physicians in the state have met “gold card” status since the bill became law in 2021, said Zeke Silva, MD, an interventional radiologist who serves on the Council of Legislation for the Texas Medical Association.
He noted that the legislation has had a limited effect for several reasons. Commercial health plans only make up only about 20% of all health plans in Texas. Also, the final regulations didn’t go into effect until last May and physicians are evaluated by health plans for “gold card” status every 6 months, said Dr. Silva.
In addition, physicians must have at least five prior authorizations approved for the same health service, which the law left up to the health plans to define, said Dr. Silva.
Now, the Texas Medical Association is lobbying for legislative improvements. “We want to reduce the number of eligible services that health plans require for prior authorizations and have more oversight of prior authorization denials by the Texas Department of Insurance and the Texas Medical Board,” said Dr. Silva.
He’s optimistic that if the bill becomes law, the number of physicians eligible for gold cards may increase.
Meanwhile, the AMA’s legislative expert, who declined to be identified because of organization policy, acknowledged the possibility that some prior authorization bills will die in state legislatures this year.
“We remain hopeful, but it’s an uphill battle. The state medical associations face a lot of opposition from health plans who don’t want to see these reforms become law.”
A version of this article originally appeared on Medscape.com.
Amid growing criticism of health insurers’ onerous prior authorization practices, lawmakers in 30 states have introduced bills this year that aim to rein in insurer gatekeeping and improve patient care.
“This is something that goes on in every doctor’s office every day; the frustrations, the delays, and the use of office staff time are just unbelievable,” said Steven Orland, MD, a board-certified urologist and president of the Medical Society of New Jersey.
The bills, which cover private health plans and insurers that states regulate, may provide some relief for physicians as federal efforts to streamline prior authorization for some Medicare patients have lagged.
Last year, Congress failed to pass the Improving Seniors’ Timely Access to Care Act of 2021, despite 326 co-sponsors. The bill would have compelled insurers covering Medicare Advantage enrollees to speed up prior authorizations, make the process more transparent, and remove obstacles such as requiring fax machine submissions.
Last month, however, the Centers for Medicare & Medicaid Services issued a final rule that will improve some aspects of prior authorizations in Medicare Advantage insurance plans and ensure that enrollees have the same access to necessary care as traditional Medicare enrollees.
The insurance industry has long defended prior authorization requirements and opposed legislation that would limit them.
America’s Health Insurance Plans (AHIP) and the Blue Cross Blue Shield Association said in a 2019 letter to a congressional committee when the federal legislation was first introduced, “Prior authorizations enforce best practices and guidelines for care management and help physicians identify and avoid care techniques that would harm patient outcomes, such as designating prescriptions that could feed into an opioid addiction.” AHIP didn’t respond to repeated requests for comment.
But some major insurers now appear willing to compromise and voluntarily reduce the volume of prior authorizations they require. Days before the federal final rule was released, three major insurers – United HealthCare, Cigna, and Aetna CVS Health – announced they plan to drop some prior authorization requirements and automate processes.
United HealthCare said it will eliminate almost 20% of its prior authorizations for some nonurgent surgeries and procedures starting this summer. It also will create a national Gold Card program in 2024 for physicians who meet its eligibility requirements, which would eliminate prior authorization requirements for most procedures. Both initiatives will apply to commercial, Medicare Advantage, and Medicaid businesses, said the insurer in a statement.
However, United HealthCare also announced that in June it will start requiring prior authorization for diagnostic (not screening) gastrointestinal endoscopies for its nearly 27 million privately insured patients, citing data it says shows potentially harmful overuse of scopes. Physician groups have publicly criticized the move, saying it could delay lifesaving treatment, and have asked the insurer to reconsider.
Cigna and Aetna also have moved to pare back prior authorization processes. Scott Josephs, national medical officer for Cigna, told Healthcare Dive that Cigna has removed prior authorization reviews from nearly 500 services since 2020.
An Aetna spokesperson told Healthcare Dive that the CVS-owned payer has implemented a gold card program and rolled back prior authorization requirements on cataract surgeries, video EEGs, and home infusion for some drugs, according to Healthcare Dive.
Cigna has faced increased scrutiny from some state regulators since a ProPublica/The Capitol Forum article revealed in March that its doctors were denying claims without opening patients’ files, contrary to what insurance laws and regulations require in many states.
Over a period of 2 months last year, Cigna doctors denied over 300,000 requests for payments using this method, spending an average of 1.2 seconds on each case, the investigation found. In a written response, Cigna said the reporting by ProPublica and The Capitol Forum was “biased and incomplete.”
States aim to reduce prior authorization volume
The American Medical Association said it has been tracking nearly 90 prior authorization reform bills in 30 states. More than a dozen bills are still being considered in this legislative session, including in Arkansas, California, New Jersey, North Carolina, Maryland, and Washington, D.C.
“The groundswell of activity in the states reflects how big a problem this is,” said an AMA legislative expert. “The issue used to be ‘how can we automate and streamline processes’; now the issue is focused on reducing the volume of prior authorizations and the harm that can cause patients.”
The state bills use different strategies to reduce excessive prior authorization requirements. Maryland’s proposed bill, for example, would require just one prior authorization to stay on a prescription drug, if the insurer has previously approved the drug and the patient continues to successfully be treated by the drug.
Washington, D.C. and New Jersey have introduced comprehensive reform bills that include a “grace period” of 60 days, to ensure continuity of care when a patient switches health plans. They also would eliminate repeat authorizations for chronic and long-term conditions, set explicit timelines for insurers to respond to prior authorization requests and appeals, and require that practicing physicians review denials that are appealed.
Many state bills also would require insurers to be more transparent by posting information on their websites about which services and drugs require prior authorization and what their approval rates are for them, said AMA’s legislative expert.
“There’s a black hole of information that insurers have access to. We would really like to know how many prior authorization requests are denied, the time it takes to deny them, and the reasons for denial,” said Josh Bengal, JD, the director of government relations for the Medical Society of New Jersey.
The legislation in New Jersey and other states faces stiff opposition from the insurance lobby, especially state associations of health plans affiliated with AHIP. The California Association of Health Plans, for example, opposes a “gold card” bill (SB 598), introduced in February, that would allow a select group of high-performing doctors to skip prior authorizations for 1 year.
The CAHP states, “Californians deserve safe, high quality, high-value health care. Yet SB 598 will derail the progress we have made in our health care system by lowering the value and safety that Californians should expect from their health care providers,” according to a fact sheet.
The fact-sheet defines “low-value care” as medical services for which there is little to no benefit and poses potential physical or financial harm to patients, such as unnecessary CT scans or MRIs for uncomplicated conditions.
California is one of about a dozen states that have introduced gold card legislation this year. If enacted, they would join five states with gold card laws: West Virginia, Texas, Vermont, Michigan, and Louisiana.
How do gold cards work?
Physicians who achieve a high approval rate of prior authorizations from insurers for 1 year are eligible to be exempted from obtaining prior authorizations the following year.
The approval rate is at least 90% for a certain number of eligible health services, but the number of prior authorizations required to qualify can range from 5 to 30, depending on the state law.
Gold card legislation typically also gives the treating physician the right to have an appeal of a prior authorization denial by a physician peer of the same or similar specialty.
California’s bill would also apply to all covered health services, which is broader than what United HealthCare has proposed for its gold card exemption. The bill would also require a plan or insurer to annually monitor rates of prior authorization approval, modification, appeal, and denial, and to discontinue services, items, and supplies that are approved 95% of the time.
“These are important reforms that will help ensure that patients can receive the care they need, when they need it,” said CMA president Donaldo Hernandez, MD.
However, it’s not clear how many physicians will meet “gold card” status based on Texas’ recent experience with its own “gold card” law.
The Texas Department of Insurance estimated that only 3.3% of licensed physicians in the state have met “gold card” status since the bill became law in 2021, said Zeke Silva, MD, an interventional radiologist who serves on the Council of Legislation for the Texas Medical Association.
He noted that the legislation has had a limited effect for several reasons. Commercial health plans only make up only about 20% of all health plans in Texas. Also, the final regulations didn’t go into effect until last May and physicians are evaluated by health plans for “gold card” status every 6 months, said Dr. Silva.
In addition, physicians must have at least five prior authorizations approved for the same health service, which the law left up to the health plans to define, said Dr. Silva.
Now, the Texas Medical Association is lobbying for legislative improvements. “We want to reduce the number of eligible services that health plans require for prior authorizations and have more oversight of prior authorization denials by the Texas Department of Insurance and the Texas Medical Board,” said Dr. Silva.
He’s optimistic that if the bill becomes law, the number of physicians eligible for gold cards may increase.
Meanwhile, the AMA’s legislative expert, who declined to be identified because of organization policy, acknowledged the possibility that some prior authorization bills will die in state legislatures this year.
“We remain hopeful, but it’s an uphill battle. The state medical associations face a lot of opposition from health plans who don’t want to see these reforms become law.”
A version of this article originally appeared on Medscape.com.
Amid growing criticism of health insurers’ onerous prior authorization practices, lawmakers in 30 states have introduced bills this year that aim to rein in insurer gatekeeping and improve patient care.
“This is something that goes on in every doctor’s office every day; the frustrations, the delays, and the use of office staff time are just unbelievable,” said Steven Orland, MD, a board-certified urologist and president of the Medical Society of New Jersey.
The bills, which cover private health plans and insurers that states regulate, may provide some relief for physicians as federal efforts to streamline prior authorization for some Medicare patients have lagged.
Last year, Congress failed to pass the Improving Seniors’ Timely Access to Care Act of 2021, despite 326 co-sponsors. The bill would have compelled insurers covering Medicare Advantage enrollees to speed up prior authorizations, make the process more transparent, and remove obstacles such as requiring fax machine submissions.
Last month, however, the Centers for Medicare & Medicaid Services issued a final rule that will improve some aspects of prior authorizations in Medicare Advantage insurance plans and ensure that enrollees have the same access to necessary care as traditional Medicare enrollees.
The insurance industry has long defended prior authorization requirements and opposed legislation that would limit them.
America’s Health Insurance Plans (AHIP) and the Blue Cross Blue Shield Association said in a 2019 letter to a congressional committee when the federal legislation was first introduced, “Prior authorizations enforce best practices and guidelines for care management and help physicians identify and avoid care techniques that would harm patient outcomes, such as designating prescriptions that could feed into an opioid addiction.” AHIP didn’t respond to repeated requests for comment.
But some major insurers now appear willing to compromise and voluntarily reduce the volume of prior authorizations they require. Days before the federal final rule was released, three major insurers – United HealthCare, Cigna, and Aetna CVS Health – announced they plan to drop some prior authorization requirements and automate processes.
United HealthCare said it will eliminate almost 20% of its prior authorizations for some nonurgent surgeries and procedures starting this summer. It also will create a national Gold Card program in 2024 for physicians who meet its eligibility requirements, which would eliminate prior authorization requirements for most procedures. Both initiatives will apply to commercial, Medicare Advantage, and Medicaid businesses, said the insurer in a statement.
However, United HealthCare also announced that in June it will start requiring prior authorization for diagnostic (not screening) gastrointestinal endoscopies for its nearly 27 million privately insured patients, citing data it says shows potentially harmful overuse of scopes. Physician groups have publicly criticized the move, saying it could delay lifesaving treatment, and have asked the insurer to reconsider.
Cigna and Aetna also have moved to pare back prior authorization processes. Scott Josephs, national medical officer for Cigna, told Healthcare Dive that Cigna has removed prior authorization reviews from nearly 500 services since 2020.
An Aetna spokesperson told Healthcare Dive that the CVS-owned payer has implemented a gold card program and rolled back prior authorization requirements on cataract surgeries, video EEGs, and home infusion for some drugs, according to Healthcare Dive.
Cigna has faced increased scrutiny from some state regulators since a ProPublica/The Capitol Forum article revealed in March that its doctors were denying claims without opening patients’ files, contrary to what insurance laws and regulations require in many states.
Over a period of 2 months last year, Cigna doctors denied over 300,000 requests for payments using this method, spending an average of 1.2 seconds on each case, the investigation found. In a written response, Cigna said the reporting by ProPublica and The Capitol Forum was “biased and incomplete.”
States aim to reduce prior authorization volume
The American Medical Association said it has been tracking nearly 90 prior authorization reform bills in 30 states. More than a dozen bills are still being considered in this legislative session, including in Arkansas, California, New Jersey, North Carolina, Maryland, and Washington, D.C.
“The groundswell of activity in the states reflects how big a problem this is,” said an AMA legislative expert. “The issue used to be ‘how can we automate and streamline processes’; now the issue is focused on reducing the volume of prior authorizations and the harm that can cause patients.”
The state bills use different strategies to reduce excessive prior authorization requirements. Maryland’s proposed bill, for example, would require just one prior authorization to stay on a prescription drug, if the insurer has previously approved the drug and the patient continues to successfully be treated by the drug.
Washington, D.C. and New Jersey have introduced comprehensive reform bills that include a “grace period” of 60 days, to ensure continuity of care when a patient switches health plans. They also would eliminate repeat authorizations for chronic and long-term conditions, set explicit timelines for insurers to respond to prior authorization requests and appeals, and require that practicing physicians review denials that are appealed.
Many state bills also would require insurers to be more transparent by posting information on their websites about which services and drugs require prior authorization and what their approval rates are for them, said AMA’s legislative expert.
“There’s a black hole of information that insurers have access to. We would really like to know how many prior authorization requests are denied, the time it takes to deny them, and the reasons for denial,” said Josh Bengal, JD, the director of government relations for the Medical Society of New Jersey.
The legislation in New Jersey and other states faces stiff opposition from the insurance lobby, especially state associations of health plans affiliated with AHIP. The California Association of Health Plans, for example, opposes a “gold card” bill (SB 598), introduced in February, that would allow a select group of high-performing doctors to skip prior authorizations for 1 year.
The CAHP states, “Californians deserve safe, high quality, high-value health care. Yet SB 598 will derail the progress we have made in our health care system by lowering the value and safety that Californians should expect from their health care providers,” according to a fact sheet.
The fact-sheet defines “low-value care” as medical services for which there is little to no benefit and poses potential physical or financial harm to patients, such as unnecessary CT scans or MRIs for uncomplicated conditions.
California is one of about a dozen states that have introduced gold card legislation this year. If enacted, they would join five states with gold card laws: West Virginia, Texas, Vermont, Michigan, and Louisiana.
How do gold cards work?
Physicians who achieve a high approval rate of prior authorizations from insurers for 1 year are eligible to be exempted from obtaining prior authorizations the following year.
The approval rate is at least 90% for a certain number of eligible health services, but the number of prior authorizations required to qualify can range from 5 to 30, depending on the state law.
Gold card legislation typically also gives the treating physician the right to have an appeal of a prior authorization denial by a physician peer of the same or similar specialty.
California’s bill would also apply to all covered health services, which is broader than what United HealthCare has proposed for its gold card exemption. The bill would also require a plan or insurer to annually monitor rates of prior authorization approval, modification, appeal, and denial, and to discontinue services, items, and supplies that are approved 95% of the time.
“These are important reforms that will help ensure that patients can receive the care they need, when they need it,” said CMA president Donaldo Hernandez, MD.
However, it’s not clear how many physicians will meet “gold card” status based on Texas’ recent experience with its own “gold card” law.
The Texas Department of Insurance estimated that only 3.3% of licensed physicians in the state have met “gold card” status since the bill became law in 2021, said Zeke Silva, MD, an interventional radiologist who serves on the Council of Legislation for the Texas Medical Association.
He noted that the legislation has had a limited effect for several reasons. Commercial health plans only make up only about 20% of all health plans in Texas. Also, the final regulations didn’t go into effect until last May and physicians are evaluated by health plans for “gold card” status every 6 months, said Dr. Silva.
In addition, physicians must have at least five prior authorizations approved for the same health service, which the law left up to the health plans to define, said Dr. Silva.
Now, the Texas Medical Association is lobbying for legislative improvements. “We want to reduce the number of eligible services that health plans require for prior authorizations and have more oversight of prior authorization denials by the Texas Department of Insurance and the Texas Medical Board,” said Dr. Silva.
He’s optimistic that if the bill becomes law, the number of physicians eligible for gold cards may increase.
Meanwhile, the AMA’s legislative expert, who declined to be identified because of organization policy, acknowledged the possibility that some prior authorization bills will die in state legislatures this year.
“We remain hopeful, but it’s an uphill battle. The state medical associations face a lot of opposition from health plans who don’t want to see these reforms become law.”
A version of this article originally appeared on Medscape.com.
The weird world of hydrogels: How they’ll change health care
Imagine a day when a simple injection prompts a broken bone to heal. When tiny, ingestible devices linger in the body, unnoticed, tracking our health or delivering life-saving medications. When brain and heart implants mesh with flesh so seamlessly that the body thinks they’ve been there all along.
These are the dreams of materials scientists who have toiled for decades to mimic the complex architecture of the human body in hopes of replacing broken parts or treating disease.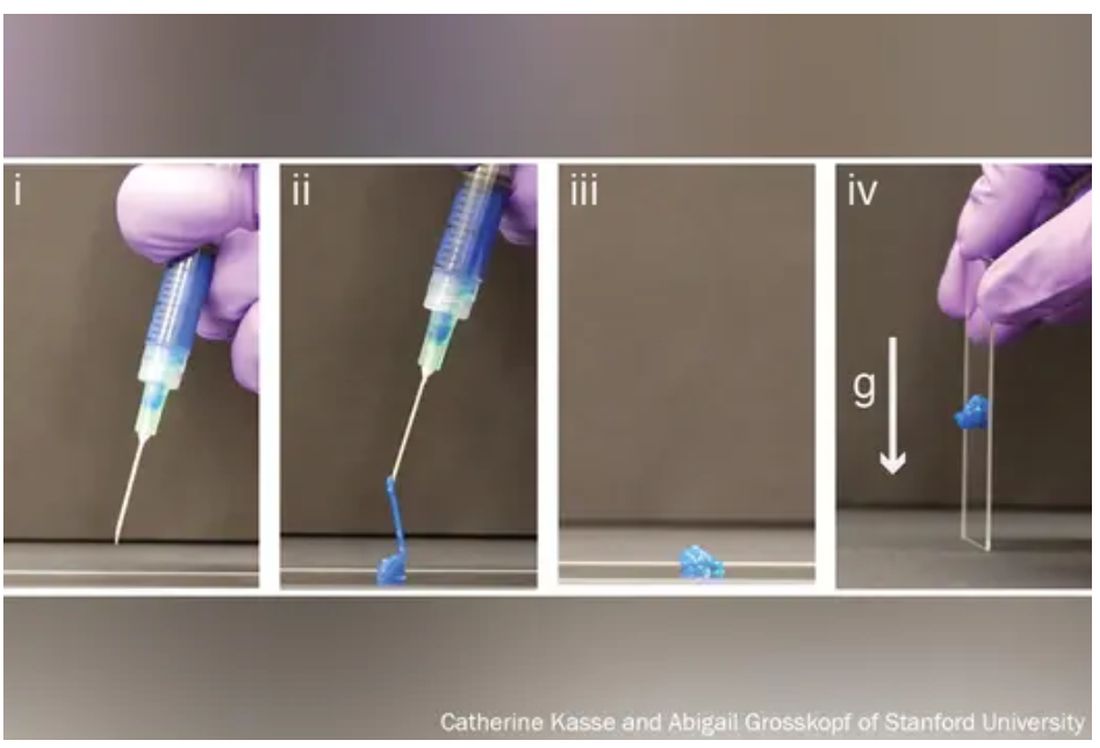
The problem, say bioengineers, is that most replacement and corrective parts – from prosthetics to pacemakers – are made of hard, dry, lifeless materials, like metal or plastic, while biological tissue is soft, wet, and living.
The body knows the difference and tends to reject imitations.
Enter hydrogels, three-dimensional networks of molecules swollen with – by definition – water.
First described in 1960 by creators of soft contact lenses, these weird, shape-shifting substances are able to morph from liquid to solid to a squishy in-between. (Early, simple uses include hair gel or Jell-O.). Slow to gain attention, growing to just 1,000 studies published by 1982, they’ve become the subject of intense study recently, with 100,000 papers published by 2020, and 3,800 already this year alone.
As chemists, biologists, and engineers begin to work more with one another and with medical doctors,
“We are, essentially, hydrogels,” said Benjamin Wiley, PhD, a chemistry professor at Duke University in Durham, N.C. “As people develop new hydrogels that more closely match the tissues in our body, we’ll be able to treat a whole host of ailments we couldn’t treat before.”
From contact lenses to brain implants
Put simply, a hydrogel is like a mesh bag of water.
The mesh is made of polymers, or spaghetti-like strands of molecules, stitched together in a repeating pattern and swollen with H2O, much like the way 3D matrixes in our body surround, support, and give structure to our cells and tissues.
“Imagine a soccer net, with all of these long fibers woven together to create the net,” said Eric Appel, PhD, associate professor of materials science and engineering at Stanford (Calif.) University.
While the broader category of “gels” could be filled with anything, including chemical solvents, water is the key ingredient that sets hydrogels apart, making them ideal for, as some scientists put it, “merging humans and machines.”
Human bones are about 25% water, while muscles hover around 70% and the brain is 85%. The precious liquid plays a host of critical roles, from shuttling nutrients in and waste out to helping cells talk to each other.
Lab-made hydrogels can be loaded with cargo (like a ball in the net), including cells or drugs that help mimic some of those functions.
Hydrogels are soft and pliable like flesh. So, if used in implants, they may be less likely to damage surrounding tissue.
“Think about a metal spoon in your bowl of pudding. As you’re shaking the bowl, the spoon doesn’t stay in place, and you get scarring around the spoon,” said Christina Tringides, PhD, a materials scientist who studies neural engineering. That, she says, is exactly what happens to brain implants when patients breathe or move. “It’s a mechanical mismatch. But with hydrogels, you could get perfect mechanical matching.”
Hydrogels also tend to be nontoxic, so the immune system may be less likely to attack them as foreign bodies.
All this has made hydrogels the new darling of the bioengineering world.
“There has been an absolute explosion of interest in these materials,” Dr. Appel said.
Smarter drug delivery and ingestible electronics
Early versions of hydrogels were thick and gooey, making it hard to get them inside the body.
“Think of a block of Jell-O. You couldn’t inject something like that,” Dr. Appel said.
But Dr. Appel, whose lab develops new drug delivery systems, has been tinkering with gel formulas for years in hopes that these high-tech globs could someday ferry timed-release drugs to just the right spot in the body.
His new hydrogels start as fully formed gels (which help preserve the drug contents) inside a syringe. But once the plunger is pushed, they magically shape-shift to a liquid thin enough to flow easily through a standard needle. Upon exit, they immediately reform into gels, protecting the inherent cargo from degrading.
This could be a game changer at a time when many cutting-edge drugs – think Humira for arthritis or Ozempic for type 2 diabetes – are made of quickly degrading proteins too large and complex to simply jam into a pill. Instead, they must be injected, often frequently.
“Because the gel takes months to dissolve, it slowly delivers the drug over time,” Dr. Appel said. “You could conceivably go from a shot once a week to once every 4 months.”
Such slow-release hydrogels could make vaccines last longer, in turn teaching the body to better resist emerging virus variants, and deliver tumor-busting therapies more precisely, said Dr. Appel, who has formed a startup and hopes to fast-track the first hydrogel drug delivery system to clinical trials within a few years.
Meanwhile, another team at the Massachusetts Institute of Technology has taken a different approach, developing a standard-sized ingestible hydrogel pill that swells up like a puffer fish in the stomach, lasting a month and slowly releasing drugs all the while. To remove the pill, a patient simply drinks a salt-based solution that shrivels the ping-pong ball–sized device so it can be passed out of the body.
In a paper in Nature Communications, the scientists showed the puffer fish pill could also be loaded with tiny cameras or monitors to track conditions like ulcers or cancer.
“The dream is to have a Jell-O-like smart pill that, once swallowed, stays in the stomach and monitors the patient’s health,” said Xuanhe Zhao, PhD, a researcher on the project and associate professor of mechanical engineering at MIT.
Building joints and regrowing bones
Since the 1970s, researchers have mulled using hydrogels to replace human cartilage, a remarkably strong and flexible tissue made of about 90% water but able to withstand the weight of a car on an area about the size of a coin.
Until recently, those efforts have largely failed. Meaning when knee cartilage wears down, things like cartilage transplants, drilling holes to stimulate new growth, or total joint replacements – all of which require lengthy rehab – are the only options.
But that may be about to change.
Dr. Wiley and his colleagues at Duke recently reported that they’d developed the first gel-based cartilage substitute even stronger and more durable than the real thing.
By attaching their hydrogel to a titanium backing to help stick it in place, they hope to repair damaged cartilage “much like a dentist fills a cavity” long before surgery is necessary.
They too have partnered with industry to bring their hydrogel to market – starting with knees.
“Ultimately, the goal is to do any joint – hips, ankles, fingers, and toes,” Dr. Wiley said.
At the University of Toronto, chemist Karina Carneiro, PhD, and dentist Christopher McCulloch, DDS, are also thinking big.
In a recent paper in Proceedings of the National Academy of Sciences, they describe a hydrogel, designed by Dr. Carneiro and made of DNA, that can be injected, migrate to a defect in bone – an irreparable break, hole from surgery, or jawbone withered by age – and fill in the gap like putty. But not only does it patch the hole, it prompts the bone to regenerate.
In rats with holes in their skulls due to surgery, they found that the treatment did not work as well as the existing gold standard for repairing holes in bone – grafting bone from elsewhere in the body. But it did work.
“These are very early days for DNA hydrogels,” cautioned Dr. McCulloch, a study coauthor and professor in the Faculty of Dentistry, noting that it will likely be a decade or more before such technology could be available to patients. “But there is the potential that DNA hydrogel could someday grow bone without having to have highly invasive surgical procedures. That’s a significant advancement.”
A sci-fi future
Perhaps the wildest, and weirdest, potential applications of hydrogels come in the realm of human-machine interaction.
Numerous companies are already dabbling in neural prosthetic or brain computer interfaces that might someday, for instance, let someone who is paralyzed and can’t speak write on a laptop using their thoughts.
The spoon-in-the-Jell-O problem has been a major stumbling block.
But Dr. Tringides, who recently earned her PhD in biophysics from Harvard, is working on it.
She and her team have developed a seaweed-based hydrogel loaded with tiny flecks of nanomaterials that can not only meld nicely into squishy brain tissue but also conduct electricity.
Within a decade, she says, this could replace the clunky platinum metal discs used for electrocorticography – recording electrical activity in the brain to identify where seizures start or doing precise brain surgery.
In 30 to 50 years? Let your imagination run wild.
“I’m a skeptic. I like to take research step by step,” she said. “But things are definitely progressing in an interesting direction.”
A version of this article first appeared on WebMD.com.
Imagine a day when a simple injection prompts a broken bone to heal. When tiny, ingestible devices linger in the body, unnoticed, tracking our health or delivering life-saving medications. When brain and heart implants mesh with flesh so seamlessly that the body thinks they’ve been there all along.
These are the dreams of materials scientists who have toiled for decades to mimic the complex architecture of the human body in hopes of replacing broken parts or treating disease.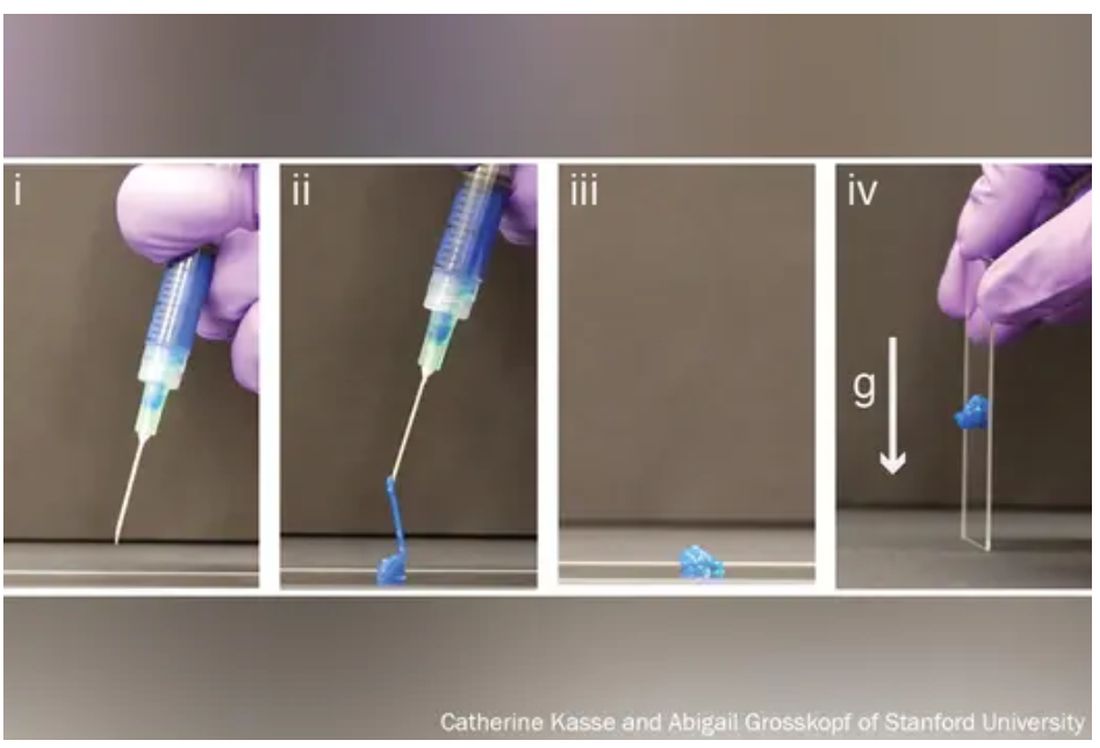
The problem, say bioengineers, is that most replacement and corrective parts – from prosthetics to pacemakers – are made of hard, dry, lifeless materials, like metal or plastic, while biological tissue is soft, wet, and living.
The body knows the difference and tends to reject imitations.
Enter hydrogels, three-dimensional networks of molecules swollen with – by definition – water.
First described in 1960 by creators of soft contact lenses, these weird, shape-shifting substances are able to morph from liquid to solid to a squishy in-between. (Early, simple uses include hair gel or Jell-O.). Slow to gain attention, growing to just 1,000 studies published by 1982, they’ve become the subject of intense study recently, with 100,000 papers published by 2020, and 3,800 already this year alone.
As chemists, biologists, and engineers begin to work more with one another and with medical doctors,
“We are, essentially, hydrogels,” said Benjamin Wiley, PhD, a chemistry professor at Duke University in Durham, N.C. “As people develop new hydrogels that more closely match the tissues in our body, we’ll be able to treat a whole host of ailments we couldn’t treat before.”
From contact lenses to brain implants
Put simply, a hydrogel is like a mesh bag of water.
The mesh is made of polymers, or spaghetti-like strands of molecules, stitched together in a repeating pattern and swollen with H2O, much like the way 3D matrixes in our body surround, support, and give structure to our cells and tissues.
“Imagine a soccer net, with all of these long fibers woven together to create the net,” said Eric Appel, PhD, associate professor of materials science and engineering at Stanford (Calif.) University.
While the broader category of “gels” could be filled with anything, including chemical solvents, water is the key ingredient that sets hydrogels apart, making them ideal for, as some scientists put it, “merging humans and machines.”
Human bones are about 25% water, while muscles hover around 70% and the brain is 85%. The precious liquid plays a host of critical roles, from shuttling nutrients in and waste out to helping cells talk to each other.
Lab-made hydrogels can be loaded with cargo (like a ball in the net), including cells or drugs that help mimic some of those functions.
Hydrogels are soft and pliable like flesh. So, if used in implants, they may be less likely to damage surrounding tissue.
“Think about a metal spoon in your bowl of pudding. As you’re shaking the bowl, the spoon doesn’t stay in place, and you get scarring around the spoon,” said Christina Tringides, PhD, a materials scientist who studies neural engineering. That, she says, is exactly what happens to brain implants when patients breathe or move. “It’s a mechanical mismatch. But with hydrogels, you could get perfect mechanical matching.”
Hydrogels also tend to be nontoxic, so the immune system may be less likely to attack them as foreign bodies.
All this has made hydrogels the new darling of the bioengineering world.
“There has been an absolute explosion of interest in these materials,” Dr. Appel said.
Smarter drug delivery and ingestible electronics
Early versions of hydrogels were thick and gooey, making it hard to get them inside the body.
“Think of a block of Jell-O. You couldn’t inject something like that,” Dr. Appel said.
But Dr. Appel, whose lab develops new drug delivery systems, has been tinkering with gel formulas for years in hopes that these high-tech globs could someday ferry timed-release drugs to just the right spot in the body.
His new hydrogels start as fully formed gels (which help preserve the drug contents) inside a syringe. But once the plunger is pushed, they magically shape-shift to a liquid thin enough to flow easily through a standard needle. Upon exit, they immediately reform into gels, protecting the inherent cargo from degrading.
This could be a game changer at a time when many cutting-edge drugs – think Humira for arthritis or Ozempic for type 2 diabetes – are made of quickly degrading proteins too large and complex to simply jam into a pill. Instead, they must be injected, often frequently.
“Because the gel takes months to dissolve, it slowly delivers the drug over time,” Dr. Appel said. “You could conceivably go from a shot once a week to once every 4 months.”
Such slow-release hydrogels could make vaccines last longer, in turn teaching the body to better resist emerging virus variants, and deliver tumor-busting therapies more precisely, said Dr. Appel, who has formed a startup and hopes to fast-track the first hydrogel drug delivery system to clinical trials within a few years.
Meanwhile, another team at the Massachusetts Institute of Technology has taken a different approach, developing a standard-sized ingestible hydrogel pill that swells up like a puffer fish in the stomach, lasting a month and slowly releasing drugs all the while. To remove the pill, a patient simply drinks a salt-based solution that shrivels the ping-pong ball–sized device so it can be passed out of the body.
In a paper in Nature Communications, the scientists showed the puffer fish pill could also be loaded with tiny cameras or monitors to track conditions like ulcers or cancer.
“The dream is to have a Jell-O-like smart pill that, once swallowed, stays in the stomach and monitors the patient’s health,” said Xuanhe Zhao, PhD, a researcher on the project and associate professor of mechanical engineering at MIT.
Building joints and regrowing bones
Since the 1970s, researchers have mulled using hydrogels to replace human cartilage, a remarkably strong and flexible tissue made of about 90% water but able to withstand the weight of a car on an area about the size of a coin.
Until recently, those efforts have largely failed. Meaning when knee cartilage wears down, things like cartilage transplants, drilling holes to stimulate new growth, or total joint replacements – all of which require lengthy rehab – are the only options.
But that may be about to change.
Dr. Wiley and his colleagues at Duke recently reported that they’d developed the first gel-based cartilage substitute even stronger and more durable than the real thing.
By attaching their hydrogel to a titanium backing to help stick it in place, they hope to repair damaged cartilage “much like a dentist fills a cavity” long before surgery is necessary.
They too have partnered with industry to bring their hydrogel to market – starting with knees.
“Ultimately, the goal is to do any joint – hips, ankles, fingers, and toes,” Dr. Wiley said.
At the University of Toronto, chemist Karina Carneiro, PhD, and dentist Christopher McCulloch, DDS, are also thinking big.
In a recent paper in Proceedings of the National Academy of Sciences, they describe a hydrogel, designed by Dr. Carneiro and made of DNA, that can be injected, migrate to a defect in bone – an irreparable break, hole from surgery, or jawbone withered by age – and fill in the gap like putty. But not only does it patch the hole, it prompts the bone to regenerate.
In rats with holes in their skulls due to surgery, they found that the treatment did not work as well as the existing gold standard for repairing holes in bone – grafting bone from elsewhere in the body. But it did work.
“These are very early days for DNA hydrogels,” cautioned Dr. McCulloch, a study coauthor and professor in the Faculty of Dentistry, noting that it will likely be a decade or more before such technology could be available to patients. “But there is the potential that DNA hydrogel could someday grow bone without having to have highly invasive surgical procedures. That’s a significant advancement.”
A sci-fi future
Perhaps the wildest, and weirdest, potential applications of hydrogels come in the realm of human-machine interaction.
Numerous companies are already dabbling in neural prosthetic or brain computer interfaces that might someday, for instance, let someone who is paralyzed and can’t speak write on a laptop using their thoughts.
The spoon-in-the-Jell-O problem has been a major stumbling block.
But Dr. Tringides, who recently earned her PhD in biophysics from Harvard, is working on it.
She and her team have developed a seaweed-based hydrogel loaded with tiny flecks of nanomaterials that can not only meld nicely into squishy brain tissue but also conduct electricity.
Within a decade, she says, this could replace the clunky platinum metal discs used for electrocorticography – recording electrical activity in the brain to identify where seizures start or doing precise brain surgery.
In 30 to 50 years? Let your imagination run wild.
“I’m a skeptic. I like to take research step by step,” she said. “But things are definitely progressing in an interesting direction.”
A version of this article first appeared on WebMD.com.
Imagine a day when a simple injection prompts a broken bone to heal. When tiny, ingestible devices linger in the body, unnoticed, tracking our health or delivering life-saving medications. When brain and heart implants mesh with flesh so seamlessly that the body thinks they’ve been there all along.
These are the dreams of materials scientists who have toiled for decades to mimic the complex architecture of the human body in hopes of replacing broken parts or treating disease.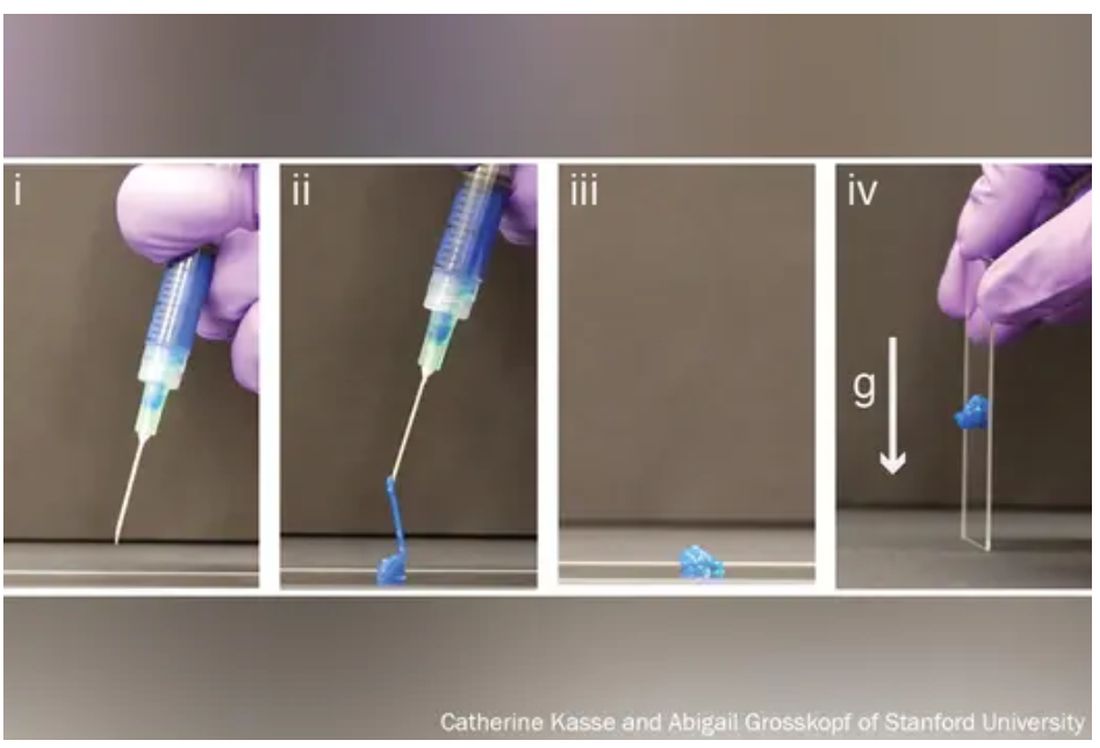
The problem, say bioengineers, is that most replacement and corrective parts – from prosthetics to pacemakers – are made of hard, dry, lifeless materials, like metal or plastic, while biological tissue is soft, wet, and living.
The body knows the difference and tends to reject imitations.
Enter hydrogels, three-dimensional networks of molecules swollen with – by definition – water.
First described in 1960 by creators of soft contact lenses, these weird, shape-shifting substances are able to morph from liquid to solid to a squishy in-between. (Early, simple uses include hair gel or Jell-O.). Slow to gain attention, growing to just 1,000 studies published by 1982, they’ve become the subject of intense study recently, with 100,000 papers published by 2020, and 3,800 already this year alone.
As chemists, biologists, and engineers begin to work more with one another and with medical doctors,
“We are, essentially, hydrogels,” said Benjamin Wiley, PhD, a chemistry professor at Duke University in Durham, N.C. “As people develop new hydrogels that more closely match the tissues in our body, we’ll be able to treat a whole host of ailments we couldn’t treat before.”
From contact lenses to brain implants
Put simply, a hydrogel is like a mesh bag of water.
The mesh is made of polymers, or spaghetti-like strands of molecules, stitched together in a repeating pattern and swollen with H2O, much like the way 3D matrixes in our body surround, support, and give structure to our cells and tissues.
“Imagine a soccer net, with all of these long fibers woven together to create the net,” said Eric Appel, PhD, associate professor of materials science and engineering at Stanford (Calif.) University.
While the broader category of “gels” could be filled with anything, including chemical solvents, water is the key ingredient that sets hydrogels apart, making them ideal for, as some scientists put it, “merging humans and machines.”
Human bones are about 25% water, while muscles hover around 70% and the brain is 85%. The precious liquid plays a host of critical roles, from shuttling nutrients in and waste out to helping cells talk to each other.
Lab-made hydrogels can be loaded with cargo (like a ball in the net), including cells or drugs that help mimic some of those functions.
Hydrogels are soft and pliable like flesh. So, if used in implants, they may be less likely to damage surrounding tissue.
“Think about a metal spoon in your bowl of pudding. As you’re shaking the bowl, the spoon doesn’t stay in place, and you get scarring around the spoon,” said Christina Tringides, PhD, a materials scientist who studies neural engineering. That, she says, is exactly what happens to brain implants when patients breathe or move. “It’s a mechanical mismatch. But with hydrogels, you could get perfect mechanical matching.”
Hydrogels also tend to be nontoxic, so the immune system may be less likely to attack them as foreign bodies.
All this has made hydrogels the new darling of the bioengineering world.
“There has been an absolute explosion of interest in these materials,” Dr. Appel said.
Smarter drug delivery and ingestible electronics
Early versions of hydrogels were thick and gooey, making it hard to get them inside the body.
“Think of a block of Jell-O. You couldn’t inject something like that,” Dr. Appel said.
But Dr. Appel, whose lab develops new drug delivery systems, has been tinkering with gel formulas for years in hopes that these high-tech globs could someday ferry timed-release drugs to just the right spot in the body.
His new hydrogels start as fully formed gels (which help preserve the drug contents) inside a syringe. But once the plunger is pushed, they magically shape-shift to a liquid thin enough to flow easily through a standard needle. Upon exit, they immediately reform into gels, protecting the inherent cargo from degrading.
This could be a game changer at a time when many cutting-edge drugs – think Humira for arthritis or Ozempic for type 2 diabetes – are made of quickly degrading proteins too large and complex to simply jam into a pill. Instead, they must be injected, often frequently.
“Because the gel takes months to dissolve, it slowly delivers the drug over time,” Dr. Appel said. “You could conceivably go from a shot once a week to once every 4 months.”
Such slow-release hydrogels could make vaccines last longer, in turn teaching the body to better resist emerging virus variants, and deliver tumor-busting therapies more precisely, said Dr. Appel, who has formed a startup and hopes to fast-track the first hydrogel drug delivery system to clinical trials within a few years.
Meanwhile, another team at the Massachusetts Institute of Technology has taken a different approach, developing a standard-sized ingestible hydrogel pill that swells up like a puffer fish in the stomach, lasting a month and slowly releasing drugs all the while. To remove the pill, a patient simply drinks a salt-based solution that shrivels the ping-pong ball–sized device so it can be passed out of the body.
In a paper in Nature Communications, the scientists showed the puffer fish pill could also be loaded with tiny cameras or monitors to track conditions like ulcers or cancer.
“The dream is to have a Jell-O-like smart pill that, once swallowed, stays in the stomach and monitors the patient’s health,” said Xuanhe Zhao, PhD, a researcher on the project and associate professor of mechanical engineering at MIT.
Building joints and regrowing bones
Since the 1970s, researchers have mulled using hydrogels to replace human cartilage, a remarkably strong and flexible tissue made of about 90% water but able to withstand the weight of a car on an area about the size of a coin.
Until recently, those efforts have largely failed. Meaning when knee cartilage wears down, things like cartilage transplants, drilling holes to stimulate new growth, or total joint replacements – all of which require lengthy rehab – are the only options.
But that may be about to change.
Dr. Wiley and his colleagues at Duke recently reported that they’d developed the first gel-based cartilage substitute even stronger and more durable than the real thing.
By attaching their hydrogel to a titanium backing to help stick it in place, they hope to repair damaged cartilage “much like a dentist fills a cavity” long before surgery is necessary.
They too have partnered with industry to bring their hydrogel to market – starting with knees.
“Ultimately, the goal is to do any joint – hips, ankles, fingers, and toes,” Dr. Wiley said.
At the University of Toronto, chemist Karina Carneiro, PhD, and dentist Christopher McCulloch, DDS, are also thinking big.
In a recent paper in Proceedings of the National Academy of Sciences, they describe a hydrogel, designed by Dr. Carneiro and made of DNA, that can be injected, migrate to a defect in bone – an irreparable break, hole from surgery, or jawbone withered by age – and fill in the gap like putty. But not only does it patch the hole, it prompts the bone to regenerate.
In rats with holes in their skulls due to surgery, they found that the treatment did not work as well as the existing gold standard for repairing holes in bone – grafting bone from elsewhere in the body. But it did work.
“These are very early days for DNA hydrogels,” cautioned Dr. McCulloch, a study coauthor and professor in the Faculty of Dentistry, noting that it will likely be a decade or more before such technology could be available to patients. “But there is the potential that DNA hydrogel could someday grow bone without having to have highly invasive surgical procedures. That’s a significant advancement.”
A sci-fi future
Perhaps the wildest, and weirdest, potential applications of hydrogels come in the realm of human-machine interaction.
Numerous companies are already dabbling in neural prosthetic or brain computer interfaces that might someday, for instance, let someone who is paralyzed and can’t speak write on a laptop using their thoughts.
The spoon-in-the-Jell-O problem has been a major stumbling block.
But Dr. Tringides, who recently earned her PhD in biophysics from Harvard, is working on it.
She and her team have developed a seaweed-based hydrogel loaded with tiny flecks of nanomaterials that can not only meld nicely into squishy brain tissue but also conduct electricity.
Within a decade, she says, this could replace the clunky platinum metal discs used for electrocorticography – recording electrical activity in the brain to identify where seizures start or doing precise brain surgery.
In 30 to 50 years? Let your imagination run wild.
“I’m a skeptic. I like to take research step by step,” she said. “But things are definitely progressing in an interesting direction.”
A version of this article first appeared on WebMD.com.
People still want their medical intelligence in human form
Doctors or AI? Lukewarm vote of confidence goes to …
Well, we’ve got some good news for the physicians out there, and we’ve got some bad news. Which do you want first? Okay, we’re mostly hearing good news, so here goes: Most people would choose a human doctor over artificial intelligence for the diagnosis and treatment of their medical conditions.
And the bad news? In the survey we’re talking about, “most” was 53%, so not exactly a huge victory for the carbon-based life forms. Yup, about 47% of the 2,472 respondents said they would prefer an AI-based clinic over a human specialist, and that number went up if individuals were told that their primary care physicians were on board with AI, “or otherwise nudged to consider AI as good,” the research team said in a written statement released by the University of Arizona, Tucson.
They went on to add that “this signaled the significance of the human physician in guiding a patient’s decision.” So patients will still need their doctors in the future to … um … this is a bit awkward … tell them how good the AI is?
And yes, we know that ChatGPT is already doing the same thing to journalists, but could it write a medical-humor column? Not a chance. Probably can’t even tell a joke.
How do ghosts get rid of wrinkles? Boo-tox. There, let’s see ChatGPT do that.
Explaining the joke makes it funnier, right?
Here at LOTME headquarters, we live by one simple rule, passed down directly from the Buddha himself: “Never let a good presurgical assessment of refractory epilepsy go to waste. Also, don’t believe everything you read on the Internet.”
This human-created joke has been brought to you by the leading theory of humor, which states that comedy stems from our brain reacting to an incongruous part of reality in a positive way. These positive emotions light up our neurons in a specific fashion, and boom, comedy is achieved.
Previous studies into the science of comedy have typically used functional MRI to analyze the brain while it was gripped in the throes of a comedic reaction. Unfortunately, fMRI cannot detect the entirety of the electromagnetic spectrum generated by the brain during these moments, so observing scientists have been, quite literally, missing out on some of the joke. And that’s where a new study from France comes in.
In the study, the researchers showed a group of patients with epilepsy who were hooked up to deep brain electrodes and a high-tech neuroimaging machine – part of the aforementioned presurgical assessment – a 3-minute excerpt from a Charlie Chaplin movie and analyzed their brain activity. Why Charlie Chaplin? Simple. Slapstick is perhaps the most accessible form of comedy across cultures. We can all appreciate a man getting hit in the head with a coconut. The world’s oldest bar joke or whatever this is? Not so much.
During the funniest scenes, all study participants showed increased high-frequency gamma waves (indicating high cognitive engagement) and a decrease in low-frequency waves (indicating reduced inattention and introspection). During unfunny scenes, such as transition moments, the opposite occurred. Importantly, this inverse relationship occurred in the temporal lobe but not in other regions, supporting previous research that indicated humor was mainly processed in the temporal lobe.
The investigators suggested future research should focus on longer videos with more complex forms of comedy, such as jokes, irony, sarcasm, or reference humor. So, uh, a guy getting hit in the head with two coconuts? That’s high-brow stuff right there.
Hot take: Humans aren’t that special
We humans have always prided ourselves on being different from “the animals” in an exceptional way. News flash! We aren’t. We may be the apex predator, but new research shows that humans, as part of the animal kingdom, just aren’t special.
Not special? How can they say that? Are gorillas doing open-heart surgery? Do wolverines tell jokes? At a more basic level, though, the way we operate as mammals in societies is not unique or even new. Elephants are known to mourn their deceased and to have funeral-like practices, ants invented agriculture, and we’re certainly not the only species that has figured out how to use tools.
This new research just demonstrates another way we aren’t exceptional, and that’s in our mating practices and outcomes.
“Humans appear to resemble mammals that live in monogamous partnerships and to some extent, those classified as cooperative breeders, where breeding individuals have to rely on the help of others to raise their offspring,” Monique Borgerhoff Mulder, PhD, professor emerita of anthropology at the University of California, Davis, said in a written statement.
The research team, which consisted of over 100 investigators, looked at 90 human populations based on data from over 80,000 people globally and compared the human data with 49 different nonhuman mammal species. In polygynous societies in which men take several wives, they found, women have more access to resources like food, shelter, and parenting help. Monogamy, on the other hand, “can drive significant inequalities among women,” Dr. Borgerhoff Mulder said, by promoting large differences in the number of children couples produce.
Human day-to-day behavior and child-rearing habits – one parent taking a daughter to ballet class and fixing dinner so the other parent can get to exercise class before picking up the son from soccer practice – may have us thinking that we are part of an evolved society, but really we are not much different than other mammals that hunt, forage for food, and rear and teach their children, the researchers suggested.
So, yes, humans can travel to the moon, create a vaccine for smallpox, and hit other humans with coconuts, but when it comes to simply having offspring or raising them, we’re not all that special. Get over it.
Doctors or AI? Lukewarm vote of confidence goes to …
Well, we’ve got some good news for the physicians out there, and we’ve got some bad news. Which do you want first? Okay, we’re mostly hearing good news, so here goes: Most people would choose a human doctor over artificial intelligence for the diagnosis and treatment of their medical conditions.
And the bad news? In the survey we’re talking about, “most” was 53%, so not exactly a huge victory for the carbon-based life forms. Yup, about 47% of the 2,472 respondents said they would prefer an AI-based clinic over a human specialist, and that number went up if individuals were told that their primary care physicians were on board with AI, “or otherwise nudged to consider AI as good,” the research team said in a written statement released by the University of Arizona, Tucson.
They went on to add that “this signaled the significance of the human physician in guiding a patient’s decision.” So patients will still need their doctors in the future to … um … this is a bit awkward … tell them how good the AI is?
And yes, we know that ChatGPT is already doing the same thing to journalists, but could it write a medical-humor column? Not a chance. Probably can’t even tell a joke.
How do ghosts get rid of wrinkles? Boo-tox. There, let’s see ChatGPT do that.
Explaining the joke makes it funnier, right?
Here at LOTME headquarters, we live by one simple rule, passed down directly from the Buddha himself: “Never let a good presurgical assessment of refractory epilepsy go to waste. Also, don’t believe everything you read on the Internet.”
This human-created joke has been brought to you by the leading theory of humor, which states that comedy stems from our brain reacting to an incongruous part of reality in a positive way. These positive emotions light up our neurons in a specific fashion, and boom, comedy is achieved.
Previous studies into the science of comedy have typically used functional MRI to analyze the brain while it was gripped in the throes of a comedic reaction. Unfortunately, fMRI cannot detect the entirety of the electromagnetic spectrum generated by the brain during these moments, so observing scientists have been, quite literally, missing out on some of the joke. And that’s where a new study from France comes in.
In the study, the researchers showed a group of patients with epilepsy who were hooked up to deep brain electrodes and a high-tech neuroimaging machine – part of the aforementioned presurgical assessment – a 3-minute excerpt from a Charlie Chaplin movie and analyzed their brain activity. Why Charlie Chaplin? Simple. Slapstick is perhaps the most accessible form of comedy across cultures. We can all appreciate a man getting hit in the head with a coconut. The world’s oldest bar joke or whatever this is? Not so much.
During the funniest scenes, all study participants showed increased high-frequency gamma waves (indicating high cognitive engagement) and a decrease in low-frequency waves (indicating reduced inattention and introspection). During unfunny scenes, such as transition moments, the opposite occurred. Importantly, this inverse relationship occurred in the temporal lobe but not in other regions, supporting previous research that indicated humor was mainly processed in the temporal lobe.
The investigators suggested future research should focus on longer videos with more complex forms of comedy, such as jokes, irony, sarcasm, or reference humor. So, uh, a guy getting hit in the head with two coconuts? That’s high-brow stuff right there.
Hot take: Humans aren’t that special
We humans have always prided ourselves on being different from “the animals” in an exceptional way. News flash! We aren’t. We may be the apex predator, but new research shows that humans, as part of the animal kingdom, just aren’t special.
Not special? How can they say that? Are gorillas doing open-heart surgery? Do wolverines tell jokes? At a more basic level, though, the way we operate as mammals in societies is not unique or even new. Elephants are known to mourn their deceased and to have funeral-like practices, ants invented agriculture, and we’re certainly not the only species that has figured out how to use tools.
This new research just demonstrates another way we aren’t exceptional, and that’s in our mating practices and outcomes.
“Humans appear to resemble mammals that live in monogamous partnerships and to some extent, those classified as cooperative breeders, where breeding individuals have to rely on the help of others to raise their offspring,” Monique Borgerhoff Mulder, PhD, professor emerita of anthropology at the University of California, Davis, said in a written statement.
The research team, which consisted of over 100 investigators, looked at 90 human populations based on data from over 80,000 people globally and compared the human data with 49 different nonhuman mammal species. In polygynous societies in which men take several wives, they found, women have more access to resources like food, shelter, and parenting help. Monogamy, on the other hand, “can drive significant inequalities among women,” Dr. Borgerhoff Mulder said, by promoting large differences in the number of children couples produce.
Human day-to-day behavior and child-rearing habits – one parent taking a daughter to ballet class and fixing dinner so the other parent can get to exercise class before picking up the son from soccer practice – may have us thinking that we are part of an evolved society, but really we are not much different than other mammals that hunt, forage for food, and rear and teach their children, the researchers suggested.
So, yes, humans can travel to the moon, create a vaccine for smallpox, and hit other humans with coconuts, but when it comes to simply having offspring or raising them, we’re not all that special. Get over it.
Doctors or AI? Lukewarm vote of confidence goes to …
Well, we’ve got some good news for the physicians out there, and we’ve got some bad news. Which do you want first? Okay, we’re mostly hearing good news, so here goes: Most people would choose a human doctor over artificial intelligence for the diagnosis and treatment of their medical conditions.
And the bad news? In the survey we’re talking about, “most” was 53%, so not exactly a huge victory for the carbon-based life forms. Yup, about 47% of the 2,472 respondents said they would prefer an AI-based clinic over a human specialist, and that number went up if individuals were told that their primary care physicians were on board with AI, “or otherwise nudged to consider AI as good,” the research team said in a written statement released by the University of Arizona, Tucson.
They went on to add that “this signaled the significance of the human physician in guiding a patient’s decision.” So patients will still need their doctors in the future to … um … this is a bit awkward … tell them how good the AI is?
And yes, we know that ChatGPT is already doing the same thing to journalists, but could it write a medical-humor column? Not a chance. Probably can’t even tell a joke.
How do ghosts get rid of wrinkles? Boo-tox. There, let’s see ChatGPT do that.
Explaining the joke makes it funnier, right?
Here at LOTME headquarters, we live by one simple rule, passed down directly from the Buddha himself: “Never let a good presurgical assessment of refractory epilepsy go to waste. Also, don’t believe everything you read on the Internet.”
This human-created joke has been brought to you by the leading theory of humor, which states that comedy stems from our brain reacting to an incongruous part of reality in a positive way. These positive emotions light up our neurons in a specific fashion, and boom, comedy is achieved.
Previous studies into the science of comedy have typically used functional MRI to analyze the brain while it was gripped in the throes of a comedic reaction. Unfortunately, fMRI cannot detect the entirety of the electromagnetic spectrum generated by the brain during these moments, so observing scientists have been, quite literally, missing out on some of the joke. And that’s where a new study from France comes in.
In the study, the researchers showed a group of patients with epilepsy who were hooked up to deep brain electrodes and a high-tech neuroimaging machine – part of the aforementioned presurgical assessment – a 3-minute excerpt from a Charlie Chaplin movie and analyzed their brain activity. Why Charlie Chaplin? Simple. Slapstick is perhaps the most accessible form of comedy across cultures. We can all appreciate a man getting hit in the head with a coconut. The world’s oldest bar joke or whatever this is? Not so much.
During the funniest scenes, all study participants showed increased high-frequency gamma waves (indicating high cognitive engagement) and a decrease in low-frequency waves (indicating reduced inattention and introspection). During unfunny scenes, such as transition moments, the opposite occurred. Importantly, this inverse relationship occurred in the temporal lobe but not in other regions, supporting previous research that indicated humor was mainly processed in the temporal lobe.
The investigators suggested future research should focus on longer videos with more complex forms of comedy, such as jokes, irony, sarcasm, or reference humor. So, uh, a guy getting hit in the head with two coconuts? That’s high-brow stuff right there.
Hot take: Humans aren’t that special
We humans have always prided ourselves on being different from “the animals” in an exceptional way. News flash! We aren’t. We may be the apex predator, but new research shows that humans, as part of the animal kingdom, just aren’t special.
Not special? How can they say that? Are gorillas doing open-heart surgery? Do wolverines tell jokes? At a more basic level, though, the way we operate as mammals in societies is not unique or even new. Elephants are known to mourn their deceased and to have funeral-like practices, ants invented agriculture, and we’re certainly not the only species that has figured out how to use tools.
This new research just demonstrates another way we aren’t exceptional, and that’s in our mating practices and outcomes.
“Humans appear to resemble mammals that live in monogamous partnerships and to some extent, those classified as cooperative breeders, where breeding individuals have to rely on the help of others to raise their offspring,” Monique Borgerhoff Mulder, PhD, professor emerita of anthropology at the University of California, Davis, said in a written statement.
The research team, which consisted of over 100 investigators, looked at 90 human populations based on data from over 80,000 people globally and compared the human data with 49 different nonhuman mammal species. In polygynous societies in which men take several wives, they found, women have more access to resources like food, shelter, and parenting help. Monogamy, on the other hand, “can drive significant inequalities among women,” Dr. Borgerhoff Mulder said, by promoting large differences in the number of children couples produce.
Human day-to-day behavior and child-rearing habits – one parent taking a daughter to ballet class and fixing dinner so the other parent can get to exercise class before picking up the son from soccer practice – may have us thinking that we are part of an evolved society, but really we are not much different than other mammals that hunt, forage for food, and rear and teach their children, the researchers suggested.
So, yes, humans can travel to the moon, create a vaccine for smallpox, and hit other humans with coconuts, but when it comes to simply having offspring or raising them, we’re not all that special. Get over it.
COVID emergency over, but hundreds are still dying weekly
Traci Sikes’s older sister Debbie had survived several health setbacks in life – a heart attack, a cancer diagnosis, and a couple of botched surgeries for a bad back. But by early 2023, the 68-year-old from Brownwood, Tex., was in remission from lymphoma, feeling stronger, and celebrating a birthday for one of her 11 beloved grandchildren.
Then Debbie caught COVID-19. Less than 2 months later, in March, she died of severe lung damage caused by the coronavirus.
Traci was able to make the trip from her home in Washington state to Texas to be with Debbie before she died. She was grateful that she arrived while her sister was still lucid and to hear her sister’s last word – “love” – spoken to one of her grandchildren before she took her final breath.
“My sister was wonderful,” Sikes said. “And she shouldn’t be gone.”
Just 6 months after President Joe Biden declared last fall that “the pandemic is over,” Just as both the World Health Organization and U.S. government recently ended the 3-year-old coronavirus public health emergency, COVID is still killing more than 100 people every day in the U.S., according to the CDC, and amid widespread efforts to move on and drop protective measures, the country’s most vulnerable people are still at significant risk.
The prevailing attitude that we need to learn to live with the current level of risk feels like a “slap in the face,” for COVID grievers who have already paid the price,” said Sabila Khan, who cofounded a Facebook group for COVID loss support, which now has more than 14,000 members.
It also minimizes the continuing loss of life and that so many people are still dying traumatic and unnecessary deaths, she said.
“It feels like it’s been brushed aside,” she said. “Like, ‘It’s business as usual. It’s over. Take off your mask.’ My family and I are still masked, and we’re probably the only ones masked in any given room.”
The abandoning of protective measures also fails to recognize the ongoing and catastrophic risks of long COVID and the experiences of an estimated 26 million people in the U.S. living with long COVID.
“It’s been drummed into us that death is the only serious outcome [of the virus] and we still haven’t made enough space for the idea that long COVID is a very serious outcome,” said David Putrino, PhD, director of rehabilitation innovation for the Mount Sinai Health System in New York, who has helped care for thousands of patients with long COVID.
Historic drop in life expectancy
More than 1.1 million Americans have died from COVID over the past 3 years, and experts say the official numbers are likely underestimated because of errors in death certificate reporting. Although deaths have waned from earlier in the pandemic, the disease has become the fourth leading cause of death in the United States after heart disease, cancer, and “unintentional injury” such as drug overdoses.
What makes these deaths all the more tragic is that COVID is a preventable disease, said Carla Sevin, MD, a critical care doctor and director of the Pulmonary Patient Care Center at Vanderbilt University Medical Center in Nashville, Tenn. Masking, available vaccines, and social distancing have all been shown to significantly lower the risk of spreading and catching the virus. New drugs have also made it possible for infected people to survive COVID.
“It’s possible to not spread COVID,” she said. “It’s possible to protect yourself against COVID. It’s possible to treat COVID. And we’re doing all of those things imperfectly.”
By the end of 2021, Americans overall were dying 3 years sooner, on average, than they were before the pandemic, with life expectancy dropping from 79 years to 76 years, the largest decline in a century.
Globally, the COVID death toll is nearing 7 million. Across all ages, on average, each person who died passed away 10 years younger than they otherwise would have. That’s tens of millions of years wiped away.
As U.S. surgeon and health researcher Atul Gawande, MD, put it in a New York Times essay about the pandemic response: “Human development has been pushed into reverse.”
What is an acceptable threshold of death?
In the United States, more than 80% of deaths from the disease have been in people age 65 and older. Underlying medical conditions and disabilities also raise the risk of severe illness and dying from COVID.
The virus is also disproportionately killing Black, Hispanic, and Indigenous people and those with less access to health care. Racialized groups are dying from COVID at younger ages. COVID advocates and Americans who’ve lost loved ones to the disease say our willingness to accept these facts and the current mortality rate amounts to health-based discrimination.
“Would politicians be approaching this differently had it mostly affected rich white people?” Ms. Khan said.
Ms. Khan’s dad, Shafqat, was an advocate and community organizer for Pakistani immigrants. After contracting COVID, he was rushed to a hospital near his daughter’s Jersey City, N.J., home from a rehab facility where he was being treated for an aggressive form of Parkinson’s disease. For the 8 days her father was in the hospital, she and other family members couldn’t visit him, and he wasn’t even well enough to talk on the phone. He died from COVID in April 2020.
“My father was an extraordinary person who did so much good and he died alone, terrified in a hospital,” she said. “I can’t even wrap my head around that and how he deserved more. No one deserves that.”
At Vanderbilt University Medical Center, where she works as a critical care doctor, COVID deaths are now different from those in the early days of the pandemic, Dr. Sevin said. Most patients now in the intensive care unit are older and immunocompromised – and they tend to blend in more with others in the intensive care unit. That makes the impact of COVID even more hidden and easily ignored.
“It’s easy not to value somebody who’s an invisible number you don’t know,” she said. “You don’t see them writing their will and talking to their best friend. You don’t see the tears rolling down their face because they know what’s going to happen to them and they’re going to asphyxiate to death.”
One COVID patient who died recently in Dr. Sevin’s ICU ward was an older woman who had no living relatives. “She was very, very lonely, and we would always stand outside the door on rounds, and she would motion for us to come in, but we had to then all gown up,” Dr. Sevin said. “It just breaks your heart that people are still having to go through it.”
Dr. Sevin finds it frustrating that so many of the measures that public health officials fought so hard for over the last 3 years – including masking guidelines, government-funded vaccine clinics, and access to potentially life-saving antiviral medications – are now going away because of the lifting of the pandemic emergency declaration.
What makes matters worse, she said, is that public consciousness about taking precautions to protect others is starting to disappear in favor of an “all or nothing attitude” about the continued risks.
“Like either I’m going to stay home and be a hermit, or I’m going to just throw caution to the wind and go to bars and let people yell in my face,” she said. “We learned some hard lessons, and I wish we could hold onto those.”
Americans like Traci Sikes who’ve lost loved ones and health care workers on the front lines say it is particularly frustrating that so many people are framing the current response to the risks of COVID as “personal choice” over responsibility to others, as well as a sense of fatalism and lack of urgent care.
“Why does nobody seem to be angry about this?” Ms. Sikes said. “People talk about COVID like it’s just another thing to die from. But my sister didn’t have to die from it at all.”
A version of this article first appeared on WebMD.com.
Traci Sikes’s older sister Debbie had survived several health setbacks in life – a heart attack, a cancer diagnosis, and a couple of botched surgeries for a bad back. But by early 2023, the 68-year-old from Brownwood, Tex., was in remission from lymphoma, feeling stronger, and celebrating a birthday for one of her 11 beloved grandchildren.
Then Debbie caught COVID-19. Less than 2 months later, in March, she died of severe lung damage caused by the coronavirus.
Traci was able to make the trip from her home in Washington state to Texas to be with Debbie before she died. She was grateful that she arrived while her sister was still lucid and to hear her sister’s last word – “love” – spoken to one of her grandchildren before she took her final breath.
“My sister was wonderful,” Sikes said. “And she shouldn’t be gone.”
Just 6 months after President Joe Biden declared last fall that “the pandemic is over,” Just as both the World Health Organization and U.S. government recently ended the 3-year-old coronavirus public health emergency, COVID is still killing more than 100 people every day in the U.S., according to the CDC, and amid widespread efforts to move on and drop protective measures, the country’s most vulnerable people are still at significant risk.
The prevailing attitude that we need to learn to live with the current level of risk feels like a “slap in the face,” for COVID grievers who have already paid the price,” said Sabila Khan, who cofounded a Facebook group for COVID loss support, which now has more than 14,000 members.
It also minimizes the continuing loss of life and that so many people are still dying traumatic and unnecessary deaths, she said.
“It feels like it’s been brushed aside,” she said. “Like, ‘It’s business as usual. It’s over. Take off your mask.’ My family and I are still masked, and we’re probably the only ones masked in any given room.”
The abandoning of protective measures also fails to recognize the ongoing and catastrophic risks of long COVID and the experiences of an estimated 26 million people in the U.S. living with long COVID.
“It’s been drummed into us that death is the only serious outcome [of the virus] and we still haven’t made enough space for the idea that long COVID is a very serious outcome,” said David Putrino, PhD, director of rehabilitation innovation for the Mount Sinai Health System in New York, who has helped care for thousands of patients with long COVID.
Historic drop in life expectancy
More than 1.1 million Americans have died from COVID over the past 3 years, and experts say the official numbers are likely underestimated because of errors in death certificate reporting. Although deaths have waned from earlier in the pandemic, the disease has become the fourth leading cause of death in the United States after heart disease, cancer, and “unintentional injury” such as drug overdoses.
What makes these deaths all the more tragic is that COVID is a preventable disease, said Carla Sevin, MD, a critical care doctor and director of the Pulmonary Patient Care Center at Vanderbilt University Medical Center in Nashville, Tenn. Masking, available vaccines, and social distancing have all been shown to significantly lower the risk of spreading and catching the virus. New drugs have also made it possible for infected people to survive COVID.
“It’s possible to not spread COVID,” she said. “It’s possible to protect yourself against COVID. It’s possible to treat COVID. And we’re doing all of those things imperfectly.”
By the end of 2021, Americans overall were dying 3 years sooner, on average, than they were before the pandemic, with life expectancy dropping from 79 years to 76 years, the largest decline in a century.
Globally, the COVID death toll is nearing 7 million. Across all ages, on average, each person who died passed away 10 years younger than they otherwise would have. That’s tens of millions of years wiped away.
As U.S. surgeon and health researcher Atul Gawande, MD, put it in a New York Times essay about the pandemic response: “Human development has been pushed into reverse.”
What is an acceptable threshold of death?
In the United States, more than 80% of deaths from the disease have been in people age 65 and older. Underlying medical conditions and disabilities also raise the risk of severe illness and dying from COVID.
The virus is also disproportionately killing Black, Hispanic, and Indigenous people and those with less access to health care. Racialized groups are dying from COVID at younger ages. COVID advocates and Americans who’ve lost loved ones to the disease say our willingness to accept these facts and the current mortality rate amounts to health-based discrimination.
“Would politicians be approaching this differently had it mostly affected rich white people?” Ms. Khan said.
Ms. Khan’s dad, Shafqat, was an advocate and community organizer for Pakistani immigrants. After contracting COVID, he was rushed to a hospital near his daughter’s Jersey City, N.J., home from a rehab facility where he was being treated for an aggressive form of Parkinson’s disease. For the 8 days her father was in the hospital, she and other family members couldn’t visit him, and he wasn’t even well enough to talk on the phone. He died from COVID in April 2020.
“My father was an extraordinary person who did so much good and he died alone, terrified in a hospital,” she said. “I can’t even wrap my head around that and how he deserved more. No one deserves that.”
At Vanderbilt University Medical Center, where she works as a critical care doctor, COVID deaths are now different from those in the early days of the pandemic, Dr. Sevin said. Most patients now in the intensive care unit are older and immunocompromised – and they tend to blend in more with others in the intensive care unit. That makes the impact of COVID even more hidden and easily ignored.
“It’s easy not to value somebody who’s an invisible number you don’t know,” she said. “You don’t see them writing their will and talking to their best friend. You don’t see the tears rolling down their face because they know what’s going to happen to them and they’re going to asphyxiate to death.”
One COVID patient who died recently in Dr. Sevin’s ICU ward was an older woman who had no living relatives. “She was very, very lonely, and we would always stand outside the door on rounds, and she would motion for us to come in, but we had to then all gown up,” Dr. Sevin said. “It just breaks your heart that people are still having to go through it.”
Dr. Sevin finds it frustrating that so many of the measures that public health officials fought so hard for over the last 3 years – including masking guidelines, government-funded vaccine clinics, and access to potentially life-saving antiviral medications – are now going away because of the lifting of the pandemic emergency declaration.
What makes matters worse, she said, is that public consciousness about taking precautions to protect others is starting to disappear in favor of an “all or nothing attitude” about the continued risks.
“Like either I’m going to stay home and be a hermit, or I’m going to just throw caution to the wind and go to bars and let people yell in my face,” she said. “We learned some hard lessons, and I wish we could hold onto those.”
Americans like Traci Sikes who’ve lost loved ones and health care workers on the front lines say it is particularly frustrating that so many people are framing the current response to the risks of COVID as “personal choice” over responsibility to others, as well as a sense of fatalism and lack of urgent care.
“Why does nobody seem to be angry about this?” Ms. Sikes said. “People talk about COVID like it’s just another thing to die from. But my sister didn’t have to die from it at all.”
A version of this article first appeared on WebMD.com.
Traci Sikes’s older sister Debbie had survived several health setbacks in life – a heart attack, a cancer diagnosis, and a couple of botched surgeries for a bad back. But by early 2023, the 68-year-old from Brownwood, Tex., was in remission from lymphoma, feeling stronger, and celebrating a birthday for one of her 11 beloved grandchildren.
Then Debbie caught COVID-19. Less than 2 months later, in March, she died of severe lung damage caused by the coronavirus.
Traci was able to make the trip from her home in Washington state to Texas to be with Debbie before she died. She was grateful that she arrived while her sister was still lucid and to hear her sister’s last word – “love” – spoken to one of her grandchildren before she took her final breath.
“My sister was wonderful,” Sikes said. “And she shouldn’t be gone.”
Just 6 months after President Joe Biden declared last fall that “the pandemic is over,” Just as both the World Health Organization and U.S. government recently ended the 3-year-old coronavirus public health emergency, COVID is still killing more than 100 people every day in the U.S., according to the CDC, and amid widespread efforts to move on and drop protective measures, the country’s most vulnerable people are still at significant risk.
The prevailing attitude that we need to learn to live with the current level of risk feels like a “slap in the face,” for COVID grievers who have already paid the price,” said Sabila Khan, who cofounded a Facebook group for COVID loss support, which now has more than 14,000 members.
It also minimizes the continuing loss of life and that so many people are still dying traumatic and unnecessary deaths, she said.
“It feels like it’s been brushed aside,” she said. “Like, ‘It’s business as usual. It’s over. Take off your mask.’ My family and I are still masked, and we’re probably the only ones masked in any given room.”
The abandoning of protective measures also fails to recognize the ongoing and catastrophic risks of long COVID and the experiences of an estimated 26 million people in the U.S. living with long COVID.
“It’s been drummed into us that death is the only serious outcome [of the virus] and we still haven’t made enough space for the idea that long COVID is a very serious outcome,” said David Putrino, PhD, director of rehabilitation innovation for the Mount Sinai Health System in New York, who has helped care for thousands of patients with long COVID.
Historic drop in life expectancy
More than 1.1 million Americans have died from COVID over the past 3 years, and experts say the official numbers are likely underestimated because of errors in death certificate reporting. Although deaths have waned from earlier in the pandemic, the disease has become the fourth leading cause of death in the United States after heart disease, cancer, and “unintentional injury” such as drug overdoses.
What makes these deaths all the more tragic is that COVID is a preventable disease, said Carla Sevin, MD, a critical care doctor and director of the Pulmonary Patient Care Center at Vanderbilt University Medical Center in Nashville, Tenn. Masking, available vaccines, and social distancing have all been shown to significantly lower the risk of spreading and catching the virus. New drugs have also made it possible for infected people to survive COVID.
“It’s possible to not spread COVID,” she said. “It’s possible to protect yourself against COVID. It’s possible to treat COVID. And we’re doing all of those things imperfectly.”
By the end of 2021, Americans overall were dying 3 years sooner, on average, than they were before the pandemic, with life expectancy dropping from 79 years to 76 years, the largest decline in a century.
Globally, the COVID death toll is nearing 7 million. Across all ages, on average, each person who died passed away 10 years younger than they otherwise would have. That’s tens of millions of years wiped away.
As U.S. surgeon and health researcher Atul Gawande, MD, put it in a New York Times essay about the pandemic response: “Human development has been pushed into reverse.”
What is an acceptable threshold of death?
In the United States, more than 80% of deaths from the disease have been in people age 65 and older. Underlying medical conditions and disabilities also raise the risk of severe illness and dying from COVID.
The virus is also disproportionately killing Black, Hispanic, and Indigenous people and those with less access to health care. Racialized groups are dying from COVID at younger ages. COVID advocates and Americans who’ve lost loved ones to the disease say our willingness to accept these facts and the current mortality rate amounts to health-based discrimination.
“Would politicians be approaching this differently had it mostly affected rich white people?” Ms. Khan said.
Ms. Khan’s dad, Shafqat, was an advocate and community organizer for Pakistani immigrants. After contracting COVID, he was rushed to a hospital near his daughter’s Jersey City, N.J., home from a rehab facility where he was being treated for an aggressive form of Parkinson’s disease. For the 8 days her father was in the hospital, she and other family members couldn’t visit him, and he wasn’t even well enough to talk on the phone. He died from COVID in April 2020.
“My father was an extraordinary person who did so much good and he died alone, terrified in a hospital,” she said. “I can’t even wrap my head around that and how he deserved more. No one deserves that.”
At Vanderbilt University Medical Center, where she works as a critical care doctor, COVID deaths are now different from those in the early days of the pandemic, Dr. Sevin said. Most patients now in the intensive care unit are older and immunocompromised – and they tend to blend in more with others in the intensive care unit. That makes the impact of COVID even more hidden and easily ignored.
“It’s easy not to value somebody who’s an invisible number you don’t know,” she said. “You don’t see them writing their will and talking to their best friend. You don’t see the tears rolling down their face because they know what’s going to happen to them and they’re going to asphyxiate to death.”
One COVID patient who died recently in Dr. Sevin’s ICU ward was an older woman who had no living relatives. “She was very, very lonely, and we would always stand outside the door on rounds, and she would motion for us to come in, but we had to then all gown up,” Dr. Sevin said. “It just breaks your heart that people are still having to go through it.”
Dr. Sevin finds it frustrating that so many of the measures that public health officials fought so hard for over the last 3 years – including masking guidelines, government-funded vaccine clinics, and access to potentially life-saving antiviral medications – are now going away because of the lifting of the pandemic emergency declaration.
What makes matters worse, she said, is that public consciousness about taking precautions to protect others is starting to disappear in favor of an “all or nothing attitude” about the continued risks.
“Like either I’m going to stay home and be a hermit, or I’m going to just throw caution to the wind and go to bars and let people yell in my face,” she said. “We learned some hard lessons, and I wish we could hold onto those.”
Americans like Traci Sikes who’ve lost loved ones and health care workers on the front lines say it is particularly frustrating that so many people are framing the current response to the risks of COVID as “personal choice” over responsibility to others, as well as a sense of fatalism and lack of urgent care.
“Why does nobody seem to be angry about this?” Ms. Sikes said. “People talk about COVID like it’s just another thing to die from. But my sister didn’t have to die from it at all.”
A version of this article first appeared on WebMD.com.








