User login
CPAP Oversells and Underperforms
Continuous positive airway pressure (CPAP) is first-line therapy for sleep-related breathing disorders (SRBDs). Obstructive sleep apnea (OSA) is the major player in the SRBDs space, with a prevalence approaching 100% in adult men using current diagnostic criteria. Patients with OSA and comorbid cardiovascular disease (CVD) are diagnosed with OSA syndrome, and CPAP is prescribed. Primary care physicians and cardiologists are quick to refer patients with CVD to sleep docs to see whether CPAP can improve CVD-related outcomes.
What the Studies Show
There’s a problem though. Let’s do a quick review. In 2005, the CANPAP study found CPAP didn’t improve a composite CVD outcome that included mortality. A post hoc analysis found that it actually increased mortality if central apneas weren’t eliminated. The post hoc analysis also found benefit when central apneas were eliminated, but for all-comers, CPAP didn’t improve outcomes. Strike one.
Enter adaptive servo-ventilation (ASV). If CANPAP showed that success depended on eliminating central apneas, why not use ASV for all patients with CVD and central apneas or Cheyne-Stokes respirations? ASV eliminates central apneas and Cheyne-Stokes. Well, that didn’t work either. The randomized, controlled SERVE-HF trial, published in 2015, showed that ASV increases all-cause and CVD-specific mortality. Oops. That’s two trials showing that CPAP and ASV can increase mortality in patients with heart failure. Strike two.
Alright. But that’s heart failure. What about hypertension or coronary artery disease (CAD)? Shouldn’t such patients be treated with CPAP to reduce CVD risk? After all, there’s all those surrogate outcomes data for CPAP — it improves vascular tone and lowers catecholamines and all that stuff. Doesn’t it lower blood pressure too? Surely CPAP benefits patients with CVD who don’t have heart failure, right?
Not really. The RICCADSA study, published in 2016, found that CPAP didn’t reduce a composite of CVD outcomes in patients with newly revascularized CAD. The SAVE trial published the same year had a similar design with similar results. CPAP did not improve CVD-related outcomes. Most recently, the ISAACC study was negative. That’s three negative randomized controlled trials in less than 5 years showing CPAP doesn’t affect CVD-related outcomes in high-risk populations with known disease. Strike three?
CPAP provides no benefit for CVD and possible harm when treating heart failure. Surely CPAP is useful for patients with hypertension. Let’s see. The American Academy of Sleep Medicine (AASM) conducted meta-analyses for the guideline it produced recommending CPAP for patients with comorbid hypertension. They note that 24-hour blood pressure measurements are best correlated with outcomes. CPAP did lead to significant 24-hour blood pressure reduction, but guess how large it was? For systolic blood pressure, it was 1.5 mm Hg; for diastolic pressure, it was 1.6 mm Hg. That’s it.
How did the AASM summarize and interpret the above data in their 2019 guidelines for prescribing CPAP? Although covered in their detailed review, both heart failure and CVD are left out of their primary recommendations . They do provide a conditional recommendation for prescribing CPAP to patients with comorbid hypertension that states, “The majority of well-informed patients would choose the intervention over no treatment.” Really? If you were told that CPAP provides less reduction in blood pressure than dietary changes and/or medications, would you choose to wear it or take a pill once a day? Remember, you have to take the pill anyway to get your blood pressure to target unless your pressure is only 1.5-1.6 mm Hg above normal. Where does one find patients who are anxious to wear a mask to bed for minimal benefit and a 20% copay? I’ve yet to meet one.
As always, the pressure pushers are undeterred by inconvenient evidence. A secondary analysis of adherent patients in RICCADSA resorts to the “bait and switch” that’s propped up CPAP enthusiasts for decades: Compare adherent patients versus those who are not (or those who refuse treatment) to prove benefit. The flaws to this approach are obvious. First, performing a post hoc analysis that reintroduces all of the confounding that plagues existing CPAP data negates the benefits of randomization, fancy statistics notwithstanding. Second, it belies the reality that in well-controlled, well-conducted randomized trials where patients get far more support than those in the community (and sometimes are preselected for adherence), a majority simply won’t use CPAP . Excluding the nonadherent or comparing them with the adherent is the epitome of selection bias.
The editorial accompanying the ISAACC study is a tour de force in CPAP apologies. The apnea-hypopnea index (AHI) isn’t the right metric — this one’s invoked often. Never mind that the very premise that OSA causes CVD is from observational data based on the AHI. If you abandon the AHI, don’t you lose your justification for prospective trials targeting CVD with CPAP?
Even better, in an argument fit for a Twitter ban, the author suggests that patients in ISAACC, SAVE, and RICCADSA couldn’t benefit because they already have CVD. The very concept, refuted by decades of secondary prevention research in cardiology, implies that CPAP should be used for primary prevention. Only a sleep researcher could spin a negative study into an expansion of CPAP indications. Others in the AASM have made similar proposals.
Final Thoughts
The sleep field lacks unblinded realists capable of choosing wisely. A little therapeutic underconfidence is warranted. Diseases and therapies will always have champions. Prudence and restraint? Not so much. The AASM could summarize the CPAP literature in a single recommendation: “If your patient is sleepy, CPAP might help them feel better if their disease is moderate or severe.” All other indications are soft.
A version of this article first appeared on Medscape.com.
Aaron B. Holley, MD, is a professor of medicine at Uniformed Services University in Bethesda, Maryland, and a pulmonary/sleep and critical care medicine physician at MedStar Washington Hospital Center in Washington, DC. He covers a wide range of topics in pulmonary, critical care, and sleep medicine .
Continuous positive airway pressure (CPAP) is first-line therapy for sleep-related breathing disorders (SRBDs). Obstructive sleep apnea (OSA) is the major player in the SRBDs space, with a prevalence approaching 100% in adult men using current diagnostic criteria. Patients with OSA and comorbid cardiovascular disease (CVD) are diagnosed with OSA syndrome, and CPAP is prescribed. Primary care physicians and cardiologists are quick to refer patients with CVD to sleep docs to see whether CPAP can improve CVD-related outcomes.
What the Studies Show
There’s a problem though. Let’s do a quick review. In 2005, the CANPAP study found CPAP didn’t improve a composite CVD outcome that included mortality. A post hoc analysis found that it actually increased mortality if central apneas weren’t eliminated. The post hoc analysis also found benefit when central apneas were eliminated, but for all-comers, CPAP didn’t improve outcomes. Strike one.
Enter adaptive servo-ventilation (ASV). If CANPAP showed that success depended on eliminating central apneas, why not use ASV for all patients with CVD and central apneas or Cheyne-Stokes respirations? ASV eliminates central apneas and Cheyne-Stokes. Well, that didn’t work either. The randomized, controlled SERVE-HF trial, published in 2015, showed that ASV increases all-cause and CVD-specific mortality. Oops. That’s two trials showing that CPAP and ASV can increase mortality in patients with heart failure. Strike two.
Alright. But that’s heart failure. What about hypertension or coronary artery disease (CAD)? Shouldn’t such patients be treated with CPAP to reduce CVD risk? After all, there’s all those surrogate outcomes data for CPAP — it improves vascular tone and lowers catecholamines and all that stuff. Doesn’t it lower blood pressure too? Surely CPAP benefits patients with CVD who don’t have heart failure, right?
Not really. The RICCADSA study, published in 2016, found that CPAP didn’t reduce a composite of CVD outcomes in patients with newly revascularized CAD. The SAVE trial published the same year had a similar design with similar results. CPAP did not improve CVD-related outcomes. Most recently, the ISAACC study was negative. That’s three negative randomized controlled trials in less than 5 years showing CPAP doesn’t affect CVD-related outcomes in high-risk populations with known disease. Strike three?
CPAP provides no benefit for CVD and possible harm when treating heart failure. Surely CPAP is useful for patients with hypertension. Let’s see. The American Academy of Sleep Medicine (AASM) conducted meta-analyses for the guideline it produced recommending CPAP for patients with comorbid hypertension. They note that 24-hour blood pressure measurements are best correlated with outcomes. CPAP did lead to significant 24-hour blood pressure reduction, but guess how large it was? For systolic blood pressure, it was 1.5 mm Hg; for diastolic pressure, it was 1.6 mm Hg. That’s it.
How did the AASM summarize and interpret the above data in their 2019 guidelines for prescribing CPAP? Although covered in their detailed review, both heart failure and CVD are left out of their primary recommendations . They do provide a conditional recommendation for prescribing CPAP to patients with comorbid hypertension that states, “The majority of well-informed patients would choose the intervention over no treatment.” Really? If you were told that CPAP provides less reduction in blood pressure than dietary changes and/or medications, would you choose to wear it or take a pill once a day? Remember, you have to take the pill anyway to get your blood pressure to target unless your pressure is only 1.5-1.6 mm Hg above normal. Where does one find patients who are anxious to wear a mask to bed for minimal benefit and a 20% copay? I’ve yet to meet one.
As always, the pressure pushers are undeterred by inconvenient evidence. A secondary analysis of adherent patients in RICCADSA resorts to the “bait and switch” that’s propped up CPAP enthusiasts for decades: Compare adherent patients versus those who are not (or those who refuse treatment) to prove benefit. The flaws to this approach are obvious. First, performing a post hoc analysis that reintroduces all of the confounding that plagues existing CPAP data negates the benefits of randomization, fancy statistics notwithstanding. Second, it belies the reality that in well-controlled, well-conducted randomized trials where patients get far more support than those in the community (and sometimes are preselected for adherence), a majority simply won’t use CPAP . Excluding the nonadherent or comparing them with the adherent is the epitome of selection bias.
The editorial accompanying the ISAACC study is a tour de force in CPAP apologies. The apnea-hypopnea index (AHI) isn’t the right metric — this one’s invoked often. Never mind that the very premise that OSA causes CVD is from observational data based on the AHI. If you abandon the AHI, don’t you lose your justification for prospective trials targeting CVD with CPAP?
Even better, in an argument fit for a Twitter ban, the author suggests that patients in ISAACC, SAVE, and RICCADSA couldn’t benefit because they already have CVD. The very concept, refuted by decades of secondary prevention research in cardiology, implies that CPAP should be used for primary prevention. Only a sleep researcher could spin a negative study into an expansion of CPAP indications. Others in the AASM have made similar proposals.
Final Thoughts
The sleep field lacks unblinded realists capable of choosing wisely. A little therapeutic underconfidence is warranted. Diseases and therapies will always have champions. Prudence and restraint? Not so much. The AASM could summarize the CPAP literature in a single recommendation: “If your patient is sleepy, CPAP might help them feel better if their disease is moderate or severe.” All other indications are soft.
A version of this article first appeared on Medscape.com.
Aaron B. Holley, MD, is a professor of medicine at Uniformed Services University in Bethesda, Maryland, and a pulmonary/sleep and critical care medicine physician at MedStar Washington Hospital Center in Washington, DC. He covers a wide range of topics in pulmonary, critical care, and sleep medicine .
Continuous positive airway pressure (CPAP) is first-line therapy for sleep-related breathing disorders (SRBDs). Obstructive sleep apnea (OSA) is the major player in the SRBDs space, with a prevalence approaching 100% in adult men using current diagnostic criteria. Patients with OSA and comorbid cardiovascular disease (CVD) are diagnosed with OSA syndrome, and CPAP is prescribed. Primary care physicians and cardiologists are quick to refer patients with CVD to sleep docs to see whether CPAP can improve CVD-related outcomes.
What the Studies Show
There’s a problem though. Let’s do a quick review. In 2005, the CANPAP study found CPAP didn’t improve a composite CVD outcome that included mortality. A post hoc analysis found that it actually increased mortality if central apneas weren’t eliminated. The post hoc analysis also found benefit when central apneas were eliminated, but for all-comers, CPAP didn’t improve outcomes. Strike one.
Enter adaptive servo-ventilation (ASV). If CANPAP showed that success depended on eliminating central apneas, why not use ASV for all patients with CVD and central apneas or Cheyne-Stokes respirations? ASV eliminates central apneas and Cheyne-Stokes. Well, that didn’t work either. The randomized, controlled SERVE-HF trial, published in 2015, showed that ASV increases all-cause and CVD-specific mortality. Oops. That’s two trials showing that CPAP and ASV can increase mortality in patients with heart failure. Strike two.
Alright. But that’s heart failure. What about hypertension or coronary artery disease (CAD)? Shouldn’t such patients be treated with CPAP to reduce CVD risk? After all, there’s all those surrogate outcomes data for CPAP — it improves vascular tone and lowers catecholamines and all that stuff. Doesn’t it lower blood pressure too? Surely CPAP benefits patients with CVD who don’t have heart failure, right?
Not really. The RICCADSA study, published in 2016, found that CPAP didn’t reduce a composite of CVD outcomes in patients with newly revascularized CAD. The SAVE trial published the same year had a similar design with similar results. CPAP did not improve CVD-related outcomes. Most recently, the ISAACC study was negative. That’s three negative randomized controlled trials in less than 5 years showing CPAP doesn’t affect CVD-related outcomes in high-risk populations with known disease. Strike three?
CPAP provides no benefit for CVD and possible harm when treating heart failure. Surely CPAP is useful for patients with hypertension. Let’s see. The American Academy of Sleep Medicine (AASM) conducted meta-analyses for the guideline it produced recommending CPAP for patients with comorbid hypertension. They note that 24-hour blood pressure measurements are best correlated with outcomes. CPAP did lead to significant 24-hour blood pressure reduction, but guess how large it was? For systolic blood pressure, it was 1.5 mm Hg; for diastolic pressure, it was 1.6 mm Hg. That’s it.
How did the AASM summarize and interpret the above data in their 2019 guidelines for prescribing CPAP? Although covered in their detailed review, both heart failure and CVD are left out of their primary recommendations . They do provide a conditional recommendation for prescribing CPAP to patients with comorbid hypertension that states, “The majority of well-informed patients would choose the intervention over no treatment.” Really? If you were told that CPAP provides less reduction in blood pressure than dietary changes and/or medications, would you choose to wear it or take a pill once a day? Remember, you have to take the pill anyway to get your blood pressure to target unless your pressure is only 1.5-1.6 mm Hg above normal. Where does one find patients who are anxious to wear a mask to bed for minimal benefit and a 20% copay? I’ve yet to meet one.
As always, the pressure pushers are undeterred by inconvenient evidence. A secondary analysis of adherent patients in RICCADSA resorts to the “bait and switch” that’s propped up CPAP enthusiasts for decades: Compare adherent patients versus those who are not (or those who refuse treatment) to prove benefit. The flaws to this approach are obvious. First, performing a post hoc analysis that reintroduces all of the confounding that plagues existing CPAP data negates the benefits of randomization, fancy statistics notwithstanding. Second, it belies the reality that in well-controlled, well-conducted randomized trials where patients get far more support than those in the community (and sometimes are preselected for adherence), a majority simply won’t use CPAP . Excluding the nonadherent or comparing them with the adherent is the epitome of selection bias.
The editorial accompanying the ISAACC study is a tour de force in CPAP apologies. The apnea-hypopnea index (AHI) isn’t the right metric — this one’s invoked often. Never mind that the very premise that OSA causes CVD is from observational data based on the AHI. If you abandon the AHI, don’t you lose your justification for prospective trials targeting CVD with CPAP?
Even better, in an argument fit for a Twitter ban, the author suggests that patients in ISAACC, SAVE, and RICCADSA couldn’t benefit because they already have CVD. The very concept, refuted by decades of secondary prevention research in cardiology, implies that CPAP should be used for primary prevention. Only a sleep researcher could spin a negative study into an expansion of CPAP indications. Others in the AASM have made similar proposals.
Final Thoughts
The sleep field lacks unblinded realists capable of choosing wisely. A little therapeutic underconfidence is warranted. Diseases and therapies will always have champions. Prudence and restraint? Not so much. The AASM could summarize the CPAP literature in a single recommendation: “If your patient is sleepy, CPAP might help them feel better if their disease is moderate or severe.” All other indications are soft.
A version of this article first appeared on Medscape.com.
Aaron B. Holley, MD, is a professor of medicine at Uniformed Services University in Bethesda, Maryland, and a pulmonary/sleep and critical care medicine physician at MedStar Washington Hospital Center in Washington, DC. He covers a wide range of topics in pulmonary, critical care, and sleep medicine .
Too Little and Too Late with Obesity Prevention
As we begin to find our way in the new world of obesity management, questions continue to surface more quickly than answers. This isn’t surprising, as we are being asked to view obesity as a disease when for decades the general consensus has been that overweight people are simply will power deficient.
Are the new drugs as effective as we are told by the patients and physicians who have had some experience using and prescribing them? Will they continue to be effective in the very long run? Will their safety record hold up over time? And for those of us in pediatrics, what will be their role for children? As a group we tend to be cautious about drugs that haven’t been thoroughly tested in children. How many years will it take before we feel comfortable with obesity drugs? And, of course, we should be asking ourselves the same questions about bariatric surgery.
Fortunately, while the media spotlight has been focused on the treatment arm of our obesity strategy, there are still some folks looking at what has been up to now the discouraging prospects for prevention. The U.S. Preventive Services Task Force (USPSTF) has recently released a draft of its recommendations that includes evidence supporting the effectiveness of “intensive behavioral interventions” (defined as a minimum of 26 hours of counseling). In reviewing data from nearly 60 randomized controlled trials, which included more than 10,000 children, the task force found that It should be noted that the USPSTF gave the intervention package only a B grade, which means that the agency found evidence of high certainty of a moderate benefit over an unspecified time period. Certainly, not a ringing endorsement.
While I think we must applaud the diligent efforts of the task force and its commitment to prevention, I fear that the strategy is too little too late. That being said, I am willing to accept the idea that targeting age 6 for intensive counseling may qualify for the better-late-than-never category. The task force acknowledges that procuring the resources given our already understaffed mental health clinics is going to be difficult and expensive. I would add that it will be so costly in time and money as to be unrealistic.
Based on my observations of thousands of children, the scaffolding of habits, diet, and preference for inactivity that underly obesity has already been laid by age 6. Are we prepared to shoulder our already overburdened school systems in an attempt to reconfigure this foundation of an obesogenic lifestyle? An effort on this scale after children have been sent off to first grade is doomed to failure.
A recent review of data reported by the CDC and reviewed in the journal Pediatrics reveals that about 2% of children receiving federal assistance from the WIC program are severely obese. It is probably safe to say that these preschoolers represent just the tip of a very concerning iceberg.
By waiting until age 6, we would increase the risk of further stigmatizing the obese child. What will he tell his peers when he is taken out of school or misses a playdate because he has to meet with his “obesity counselor”?
If we are going to take obesity prevention seriously and spend time and money in counseling, doesn’t it make more sense to invest this effort on the parents and the home situation when the child is still under their influence? We must be prepared to unwrap and employ an “intensive behavioral package” the first time we see evidence that the child’s growth chart is heading in an unhealthy direction.
This won’t always be easy. I can recall seeing a 4-year-old whose weight had risen dramatically from her previous curve in the year since her 3-year checkup. The answer became obvious when I discovered that her grandmother, for whom baking was a passion, had taken over as her daycare provider. Arriving at a solution that kept the family on speaking terms took some tact, but it was one of my rare successes in obesity prevention. And, it worked because of early intervention.
Thank you USPSTF, but 6 years is too late.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine, for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.” Other than a Littman stethoscope he accepted as a first-year medical student in 1966, Dr. Wilkoff reports having nothing to disclose. Email him at [email protected].
As we begin to find our way in the new world of obesity management, questions continue to surface more quickly than answers. This isn’t surprising, as we are being asked to view obesity as a disease when for decades the general consensus has been that overweight people are simply will power deficient.
Are the new drugs as effective as we are told by the patients and physicians who have had some experience using and prescribing them? Will they continue to be effective in the very long run? Will their safety record hold up over time? And for those of us in pediatrics, what will be their role for children? As a group we tend to be cautious about drugs that haven’t been thoroughly tested in children. How many years will it take before we feel comfortable with obesity drugs? And, of course, we should be asking ourselves the same questions about bariatric surgery.
Fortunately, while the media spotlight has been focused on the treatment arm of our obesity strategy, there are still some folks looking at what has been up to now the discouraging prospects for prevention. The U.S. Preventive Services Task Force (USPSTF) has recently released a draft of its recommendations that includes evidence supporting the effectiveness of “intensive behavioral interventions” (defined as a minimum of 26 hours of counseling). In reviewing data from nearly 60 randomized controlled trials, which included more than 10,000 children, the task force found that It should be noted that the USPSTF gave the intervention package only a B grade, which means that the agency found evidence of high certainty of a moderate benefit over an unspecified time period. Certainly, not a ringing endorsement.
While I think we must applaud the diligent efforts of the task force and its commitment to prevention, I fear that the strategy is too little too late. That being said, I am willing to accept the idea that targeting age 6 for intensive counseling may qualify for the better-late-than-never category. The task force acknowledges that procuring the resources given our already understaffed mental health clinics is going to be difficult and expensive. I would add that it will be so costly in time and money as to be unrealistic.
Based on my observations of thousands of children, the scaffolding of habits, diet, and preference for inactivity that underly obesity has already been laid by age 6. Are we prepared to shoulder our already overburdened school systems in an attempt to reconfigure this foundation of an obesogenic lifestyle? An effort on this scale after children have been sent off to first grade is doomed to failure.
A recent review of data reported by the CDC and reviewed in the journal Pediatrics reveals that about 2% of children receiving federal assistance from the WIC program are severely obese. It is probably safe to say that these preschoolers represent just the tip of a very concerning iceberg.
By waiting until age 6, we would increase the risk of further stigmatizing the obese child. What will he tell his peers when he is taken out of school or misses a playdate because he has to meet with his “obesity counselor”?
If we are going to take obesity prevention seriously and spend time and money in counseling, doesn’t it make more sense to invest this effort on the parents and the home situation when the child is still under their influence? We must be prepared to unwrap and employ an “intensive behavioral package” the first time we see evidence that the child’s growth chart is heading in an unhealthy direction.
This won’t always be easy. I can recall seeing a 4-year-old whose weight had risen dramatically from her previous curve in the year since her 3-year checkup. The answer became obvious when I discovered that her grandmother, for whom baking was a passion, had taken over as her daycare provider. Arriving at a solution that kept the family on speaking terms took some tact, but it was one of my rare successes in obesity prevention. And, it worked because of early intervention.
Thank you USPSTF, but 6 years is too late.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine, for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.” Other than a Littman stethoscope he accepted as a first-year medical student in 1966, Dr. Wilkoff reports having nothing to disclose. Email him at [email protected].
As we begin to find our way in the new world of obesity management, questions continue to surface more quickly than answers. This isn’t surprising, as we are being asked to view obesity as a disease when for decades the general consensus has been that overweight people are simply will power deficient.
Are the new drugs as effective as we are told by the patients and physicians who have had some experience using and prescribing them? Will they continue to be effective in the very long run? Will their safety record hold up over time? And for those of us in pediatrics, what will be their role for children? As a group we tend to be cautious about drugs that haven’t been thoroughly tested in children. How many years will it take before we feel comfortable with obesity drugs? And, of course, we should be asking ourselves the same questions about bariatric surgery.
Fortunately, while the media spotlight has been focused on the treatment arm of our obesity strategy, there are still some folks looking at what has been up to now the discouraging prospects for prevention. The U.S. Preventive Services Task Force (USPSTF) has recently released a draft of its recommendations that includes evidence supporting the effectiveness of “intensive behavioral interventions” (defined as a minimum of 26 hours of counseling). In reviewing data from nearly 60 randomized controlled trials, which included more than 10,000 children, the task force found that It should be noted that the USPSTF gave the intervention package only a B grade, which means that the agency found evidence of high certainty of a moderate benefit over an unspecified time period. Certainly, not a ringing endorsement.
While I think we must applaud the diligent efforts of the task force and its commitment to prevention, I fear that the strategy is too little too late. That being said, I am willing to accept the idea that targeting age 6 for intensive counseling may qualify for the better-late-than-never category. The task force acknowledges that procuring the resources given our already understaffed mental health clinics is going to be difficult and expensive. I would add that it will be so costly in time and money as to be unrealistic.
Based on my observations of thousands of children, the scaffolding of habits, diet, and preference for inactivity that underly obesity has already been laid by age 6. Are we prepared to shoulder our already overburdened school systems in an attempt to reconfigure this foundation of an obesogenic lifestyle? An effort on this scale after children have been sent off to first grade is doomed to failure.
A recent review of data reported by the CDC and reviewed in the journal Pediatrics reveals that about 2% of children receiving federal assistance from the WIC program are severely obese. It is probably safe to say that these preschoolers represent just the tip of a very concerning iceberg.
By waiting until age 6, we would increase the risk of further stigmatizing the obese child. What will he tell his peers when he is taken out of school or misses a playdate because he has to meet with his “obesity counselor”?
If we are going to take obesity prevention seriously and spend time and money in counseling, doesn’t it make more sense to invest this effort on the parents and the home situation when the child is still under their influence? We must be prepared to unwrap and employ an “intensive behavioral package” the first time we see evidence that the child’s growth chart is heading in an unhealthy direction.
This won’t always be easy. I can recall seeing a 4-year-old whose weight had risen dramatically from her previous curve in the year since her 3-year checkup. The answer became obvious when I discovered that her grandmother, for whom baking was a passion, had taken over as her daycare provider. Arriving at a solution that kept the family on speaking terms took some tact, but it was one of my rare successes in obesity prevention. And, it worked because of early intervention.
Thank you USPSTF, but 6 years is too late.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine, for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.” Other than a Littman stethoscope he accepted as a first-year medical student in 1966, Dr. Wilkoff reports having nothing to disclose. Email him at [email protected].
DEI and C
You’re familiar with DIY and DUI, but what associations do the initials DEI trigger in your thought processor? Your college is probably influenced by it. So is your medical school, as are many of the businesses whose advertisements bombard you on television and the internet. Your professional association is definitely involved with it.
In the words of one newspaper columnist, DEI is an “ideological framework” whose most recognizable buzz words are “diversity,” “equity,” and “inclusion.” In the case of the American Academy of Pediatrics (AAP), DEI has taken the form of a hiring philosophy that accepts and respects its responsibility to create a workplace “where each person can fully contribute to the shared mission without discrimination or intimidation and each person is respected, supported, and provided the equal opportunity, regardless of race, ethnicity, ancestry, national origin, religion, gender, marital status, sexual orientation, gender identity, or expression age, veteran status, immigration status, or disability.”.
As an organization representing its members, the AAP has issued a statement: “Celebrating the diversity of children and families and promoting nurturing, inclusive environments means actively opposing intolerance, bigotry, bias and discrimination” Further, ”. Included in its recommendations to fulfill this commitment are efforts to diversify the pediatric workforce and eliminate race-based medicine.
For the AAP, its commitment to diversity, equity, and inclusion seems to be a good fit. The first line of its mission statement — “to attain optimal physical, mental, and social health and well-being for all infants, children, adolescents and young adults” — is well focused and one that its members can agree upon. However, we are beginning to see and hear that on some college and university campuses DEI has worn out its welcome.
In academia, the decision to include a broad mix of students and faculty with diverse backgrounds and at the same time provide opportunities equitably has hit some serious bumps in the road. It’s unclear how much the chaos in the Middle East is to blame, However, for several years there have been unfortunate campus incidents when the invitation of controversial guest speakers has laid bare the widely different interpretations of exactly what “free speech” means.
From its hazy inception, DEI has been missing one key ingredient — commonality. If we are going to actively seek to include individuals from a variety of backgrounds, encourage them to celebrate their diversity, and offer them equitable opportunities, then at the same time we must make it clear that our overriding goal is to seek and encourage the civil discussion of what we all have in common. Neglecting this additional step of promoting commonality is a grave mistake.
One mustn’t be surprised that a group of individuals from diverse backgrounds will have differing opinions. Finding common ground will predictably be a challenge, but it can be done. It requires compromise and a commitment to civil discussion. Regrettably, DEI as a framework places so much emphasis on the individual and diversity that the critical concept of commonality has been lost. Ironically, true inclusion and equity can’t occur without a reverence for commonality.
The AAP has done a good job of folding DEI into fulfilling the first sentence of its mission statement. However, it must not lose sight of the critical ingredient of commonality as it seeks to “support the professional needs of its members” (the second sentence of its mission). Despite a general agreement on the goal of providing care for all children, there are differences of opinion among its members when it comes to some of the details. The confusing topic of gender-affirmative care comes to mind. I am confident that as a group of thoughtful professionals, even in the face of wide differences, we can see the way to civil and productive discussions in the search for commonality.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine, for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.” Other than a Littman stethoscope he accepted as a first-year medical student in 1966, Dr. Wilkoff reports having nothing to disclose. Email him at [email protected].
You’re familiar with DIY and DUI, but what associations do the initials DEI trigger in your thought processor? Your college is probably influenced by it. So is your medical school, as are many of the businesses whose advertisements bombard you on television and the internet. Your professional association is definitely involved with it.
In the words of one newspaper columnist, DEI is an “ideological framework” whose most recognizable buzz words are “diversity,” “equity,” and “inclusion.” In the case of the American Academy of Pediatrics (AAP), DEI has taken the form of a hiring philosophy that accepts and respects its responsibility to create a workplace “where each person can fully contribute to the shared mission without discrimination or intimidation and each person is respected, supported, and provided the equal opportunity, regardless of race, ethnicity, ancestry, national origin, religion, gender, marital status, sexual orientation, gender identity, or expression age, veteran status, immigration status, or disability.”.
As an organization representing its members, the AAP has issued a statement: “Celebrating the diversity of children and families and promoting nurturing, inclusive environments means actively opposing intolerance, bigotry, bias and discrimination” Further, ”. Included in its recommendations to fulfill this commitment are efforts to diversify the pediatric workforce and eliminate race-based medicine.
For the AAP, its commitment to diversity, equity, and inclusion seems to be a good fit. The first line of its mission statement — “to attain optimal physical, mental, and social health and well-being for all infants, children, adolescents and young adults” — is well focused and one that its members can agree upon. However, we are beginning to see and hear that on some college and university campuses DEI has worn out its welcome.
In academia, the decision to include a broad mix of students and faculty with diverse backgrounds and at the same time provide opportunities equitably has hit some serious bumps in the road. It’s unclear how much the chaos in the Middle East is to blame, However, for several years there have been unfortunate campus incidents when the invitation of controversial guest speakers has laid bare the widely different interpretations of exactly what “free speech” means.
From its hazy inception, DEI has been missing one key ingredient — commonality. If we are going to actively seek to include individuals from a variety of backgrounds, encourage them to celebrate their diversity, and offer them equitable opportunities, then at the same time we must make it clear that our overriding goal is to seek and encourage the civil discussion of what we all have in common. Neglecting this additional step of promoting commonality is a grave mistake.
One mustn’t be surprised that a group of individuals from diverse backgrounds will have differing opinions. Finding common ground will predictably be a challenge, but it can be done. It requires compromise and a commitment to civil discussion. Regrettably, DEI as a framework places so much emphasis on the individual and diversity that the critical concept of commonality has been lost. Ironically, true inclusion and equity can’t occur without a reverence for commonality.
The AAP has done a good job of folding DEI into fulfilling the first sentence of its mission statement. However, it must not lose sight of the critical ingredient of commonality as it seeks to “support the professional needs of its members” (the second sentence of its mission). Despite a general agreement on the goal of providing care for all children, there are differences of opinion among its members when it comes to some of the details. The confusing topic of gender-affirmative care comes to mind. I am confident that as a group of thoughtful professionals, even in the face of wide differences, we can see the way to civil and productive discussions in the search for commonality.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine, for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.” Other than a Littman stethoscope he accepted as a first-year medical student in 1966, Dr. Wilkoff reports having nothing to disclose. Email him at [email protected].
You’re familiar with DIY and DUI, but what associations do the initials DEI trigger in your thought processor? Your college is probably influenced by it. So is your medical school, as are many of the businesses whose advertisements bombard you on television and the internet. Your professional association is definitely involved with it.
In the words of one newspaper columnist, DEI is an “ideological framework” whose most recognizable buzz words are “diversity,” “equity,” and “inclusion.” In the case of the American Academy of Pediatrics (AAP), DEI has taken the form of a hiring philosophy that accepts and respects its responsibility to create a workplace “where each person can fully contribute to the shared mission without discrimination or intimidation and each person is respected, supported, and provided the equal opportunity, regardless of race, ethnicity, ancestry, national origin, religion, gender, marital status, sexual orientation, gender identity, or expression age, veteran status, immigration status, or disability.”.
As an organization representing its members, the AAP has issued a statement: “Celebrating the diversity of children and families and promoting nurturing, inclusive environments means actively opposing intolerance, bigotry, bias and discrimination” Further, ”. Included in its recommendations to fulfill this commitment are efforts to diversify the pediatric workforce and eliminate race-based medicine.
For the AAP, its commitment to diversity, equity, and inclusion seems to be a good fit. The first line of its mission statement — “to attain optimal physical, mental, and social health and well-being for all infants, children, adolescents and young adults” — is well focused and one that its members can agree upon. However, we are beginning to see and hear that on some college and university campuses DEI has worn out its welcome.
In academia, the decision to include a broad mix of students and faculty with diverse backgrounds and at the same time provide opportunities equitably has hit some serious bumps in the road. It’s unclear how much the chaos in the Middle East is to blame, However, for several years there have been unfortunate campus incidents when the invitation of controversial guest speakers has laid bare the widely different interpretations of exactly what “free speech” means.
From its hazy inception, DEI has been missing one key ingredient — commonality. If we are going to actively seek to include individuals from a variety of backgrounds, encourage them to celebrate their diversity, and offer them equitable opportunities, then at the same time we must make it clear that our overriding goal is to seek and encourage the civil discussion of what we all have in common. Neglecting this additional step of promoting commonality is a grave mistake.
One mustn’t be surprised that a group of individuals from diverse backgrounds will have differing opinions. Finding common ground will predictably be a challenge, but it can be done. It requires compromise and a commitment to civil discussion. Regrettably, DEI as a framework places so much emphasis on the individual and diversity that the critical concept of commonality has been lost. Ironically, true inclusion and equity can’t occur without a reverence for commonality.
The AAP has done a good job of folding DEI into fulfilling the first sentence of its mission statement. However, it must not lose sight of the critical ingredient of commonality as it seeks to “support the professional needs of its members” (the second sentence of its mission). Despite a general agreement on the goal of providing care for all children, there are differences of opinion among its members when it comes to some of the details. The confusing topic of gender-affirmative care comes to mind. I am confident that as a group of thoughtful professionals, even in the face of wide differences, we can see the way to civil and productive discussions in the search for commonality.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine, for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.” Other than a Littman stethoscope he accepted as a first-year medical student in 1966, Dr. Wilkoff reports having nothing to disclose. Email him at [email protected].
MediFinders Keepers ... Unfortunately
In the last 3 months I’ve had an odd uptick in calls for foot-drop. Some of them said they’d seen other neurologists and were hoping I could help them, others that they wanted to see a specialist in foot-drop. Most called in, a few even showed up at the office wanting to be seen that day.
Now, I have nothing against seeing patients with foot-drop. It’s a relatively common issue in my field. But I’ve never claimed to be a “specialist” in foot-drop. I don’t even do my own EMG/NCVs anymore, except for the occasional carpal tunnel syndrome case.
So where were all these people coming from?
All of them had previously seen good neurologists, had the correct work-up, diagnoses, and treatment, but just hadn’t had the outcome they wanted. Now they were showing up at my little office, telling my staff that I was their last hope.
All of them had the common thread that they weren’t sent by my regular referral base. Instead, they found me on “the Internet.” Of course, none remembered where. This isn’t easy, as there are hundreds of physician listing and review sites out there. But, because of the number of calls, and the abuse that my staff and I were getting when people found out I wasn’t some magical foot-drop guru, I decided to try to find out.
After a few days of searching in my spare time, I finally had it. A site called MediFind lists me as being “advanced” in treating foot-drop, to the extent that it’s at the top of my “Areas of Expertise.” The site also says I handle “Autosomal Dominant Partial Epilepsy with Auditory Features” (no, I don’t. Try the epilepsy centers in town), “Familial Neurocardiogenic Syncope” (no), and narcolepsy (definitely not, try a sleep specialist).
I have no affiliation with MediFind. In fact, I’d never heard of them until I began tracking down this issue. How they came to have such incorrect information about me I don’t know, perhaps pulled from insurance billing data, or patient reviews, or a Magic 8 Ball.
But the foot-drop issue had, oddly, become a problem. My staff was having to tell people who called in with it that I wanted to see their previous neurology records so I didn’t waste their time. People being told I wasn’t some Ivory Tower foot-dropologist often became abusive and nasty, something I won’t tolerate (5 years ago this was rarely a problem, now it’s frighteningly common). People who made it as far as seeing me (a few when this began) were livid when I looked through their records and said I had nothing to offer that their previous neurologist(s) hadn’t done. I was accused of false advertising, misrepresenting myself, etc, even though I had nothing to do with why MediFind put that up.
So I wrote to MediFind, using the email info on their page. I told them I didn’t specialize in foot-drop, and didn’t even handle several of the other conditions on their page. I asked them to take those things out, or (preferably) simply delete my listing from their site.
I got an automated reply thanking me for writing to them and saying their team would look into it. That was almost a month ago. I haven’t heard back, and the listing is, as of this writing, still up.
The computer algorithms that create such listings have no interest in correcting their errors, and so the frustration for these patients, my staff, and myself, is going to continue for a while. It’s a waste of time for them and us.
And, as this point, I doubt there’s much I can do about it.
Dr. Block has a solo neurology practice in Scottsdale, Ariz.
In the last 3 months I’ve had an odd uptick in calls for foot-drop. Some of them said they’d seen other neurologists and were hoping I could help them, others that they wanted to see a specialist in foot-drop. Most called in, a few even showed up at the office wanting to be seen that day.
Now, I have nothing against seeing patients with foot-drop. It’s a relatively common issue in my field. But I’ve never claimed to be a “specialist” in foot-drop. I don’t even do my own EMG/NCVs anymore, except for the occasional carpal tunnel syndrome case.
So where were all these people coming from?
All of them had previously seen good neurologists, had the correct work-up, diagnoses, and treatment, but just hadn’t had the outcome they wanted. Now they were showing up at my little office, telling my staff that I was their last hope.
All of them had the common thread that they weren’t sent by my regular referral base. Instead, they found me on “the Internet.” Of course, none remembered where. This isn’t easy, as there are hundreds of physician listing and review sites out there. But, because of the number of calls, and the abuse that my staff and I were getting when people found out I wasn’t some magical foot-drop guru, I decided to try to find out.
After a few days of searching in my spare time, I finally had it. A site called MediFind lists me as being “advanced” in treating foot-drop, to the extent that it’s at the top of my “Areas of Expertise.” The site also says I handle “Autosomal Dominant Partial Epilepsy with Auditory Features” (no, I don’t. Try the epilepsy centers in town), “Familial Neurocardiogenic Syncope” (no), and narcolepsy (definitely not, try a sleep specialist).
I have no affiliation with MediFind. In fact, I’d never heard of them until I began tracking down this issue. How they came to have such incorrect information about me I don’t know, perhaps pulled from insurance billing data, or patient reviews, or a Magic 8 Ball.
But the foot-drop issue had, oddly, become a problem. My staff was having to tell people who called in with it that I wanted to see their previous neurology records so I didn’t waste their time. People being told I wasn’t some Ivory Tower foot-dropologist often became abusive and nasty, something I won’t tolerate (5 years ago this was rarely a problem, now it’s frighteningly common). People who made it as far as seeing me (a few when this began) were livid when I looked through their records and said I had nothing to offer that their previous neurologist(s) hadn’t done. I was accused of false advertising, misrepresenting myself, etc, even though I had nothing to do with why MediFind put that up.
So I wrote to MediFind, using the email info on their page. I told them I didn’t specialize in foot-drop, and didn’t even handle several of the other conditions on their page. I asked them to take those things out, or (preferably) simply delete my listing from their site.
I got an automated reply thanking me for writing to them and saying their team would look into it. That was almost a month ago. I haven’t heard back, and the listing is, as of this writing, still up.
The computer algorithms that create such listings have no interest in correcting their errors, and so the frustration for these patients, my staff, and myself, is going to continue for a while. It’s a waste of time for them and us.
And, as this point, I doubt there’s much I can do about it.
Dr. Block has a solo neurology practice in Scottsdale, Ariz.
In the last 3 months I’ve had an odd uptick in calls for foot-drop. Some of them said they’d seen other neurologists and were hoping I could help them, others that they wanted to see a specialist in foot-drop. Most called in, a few even showed up at the office wanting to be seen that day.
Now, I have nothing against seeing patients with foot-drop. It’s a relatively common issue in my field. But I’ve never claimed to be a “specialist” in foot-drop. I don’t even do my own EMG/NCVs anymore, except for the occasional carpal tunnel syndrome case.
So where were all these people coming from?
All of them had previously seen good neurologists, had the correct work-up, diagnoses, and treatment, but just hadn’t had the outcome they wanted. Now they were showing up at my little office, telling my staff that I was their last hope.
All of them had the common thread that they weren’t sent by my regular referral base. Instead, they found me on “the Internet.” Of course, none remembered where. This isn’t easy, as there are hundreds of physician listing and review sites out there. But, because of the number of calls, and the abuse that my staff and I were getting when people found out I wasn’t some magical foot-drop guru, I decided to try to find out.
After a few days of searching in my spare time, I finally had it. A site called MediFind lists me as being “advanced” in treating foot-drop, to the extent that it’s at the top of my “Areas of Expertise.” The site also says I handle “Autosomal Dominant Partial Epilepsy with Auditory Features” (no, I don’t. Try the epilepsy centers in town), “Familial Neurocardiogenic Syncope” (no), and narcolepsy (definitely not, try a sleep specialist).
I have no affiliation with MediFind. In fact, I’d never heard of them until I began tracking down this issue. How they came to have such incorrect information about me I don’t know, perhaps pulled from insurance billing data, or patient reviews, or a Magic 8 Ball.
But the foot-drop issue had, oddly, become a problem. My staff was having to tell people who called in with it that I wanted to see their previous neurology records so I didn’t waste their time. People being told I wasn’t some Ivory Tower foot-dropologist often became abusive and nasty, something I won’t tolerate (5 years ago this was rarely a problem, now it’s frighteningly common). People who made it as far as seeing me (a few when this began) were livid when I looked through their records and said I had nothing to offer that their previous neurologist(s) hadn’t done. I was accused of false advertising, misrepresenting myself, etc, even though I had nothing to do with why MediFind put that up.
So I wrote to MediFind, using the email info on their page. I told them I didn’t specialize in foot-drop, and didn’t even handle several of the other conditions on their page. I asked them to take those things out, or (preferably) simply delete my listing from their site.
I got an automated reply thanking me for writing to them and saying their team would look into it. That was almost a month ago. I haven’t heard back, and the listing is, as of this writing, still up.
The computer algorithms that create such listings have no interest in correcting their errors, and so the frustration for these patients, my staff, and myself, is going to continue for a while. It’s a waste of time for them and us.
And, as this point, I doubt there’s much I can do about it.
Dr. Block has a solo neurology practice in Scottsdale, Ariz.
Deciphering the usefulness of probiotics
The idea of the use of probiotics has a history going back more than a century when Russian scientist, Elie Metchnikoff, theorized that lactic acid bacteria may offer health benefits as well as promote longevity. In the early 1900s, intestinal disorders were frequently treated with nonpathogenic bacteria to replace gut microbes.
Today, the market is flooded with products from foods to prescription medications containing probiotics that extol their health benefits. It has been estimated that the global market for probiotics is more than $32 billion dollars annually and is expected to increase 8% per year.
As family doctors, patients come to us with many questions about the use of probiotics. Look online or on store shelves — there are so many types, doses, and brands of probiotics it is hard to decipher which are worth using. We older doctors never received much education about them.
Earlier this year, the World Gastroenterology Organization (WGO) developed recommendations around the use of probiotics and defined them as “live microbes that have been shown in controlled human studies to impart a health benefit.” Their recommendation is to use the strains that have been shown to be beneficial for the condition they claim to help and have been shown to do so in controlled studies. The dosage advised should be that shown to be useful in studies.
While this is an easy statement to make, it is much less so in clinical practice. The guidelines do a good job breaking down the conditions they help and the strains that have shown to be beneficial for specific conditions.
There have been claims that probiotics have been shown to be beneficial in colorectal cancer. While there have been some studies to show that they can improve markers associated with colorectal cancer, there are no data that probiotics actually do much in terms of prevention. Eating a healthy diet is more helpful here.
One area where probiotics have been shown to be beneficial is in the prevention of antibiotic-associated diarrhea. This makes sense since we know that antibiotics can kill the “good bacteria” lining the gut wall and probiotics work to replace them. Other conditions where these agents have been shown to be beneficial include radiation-induced diarrhea, acute diarrhea, irritable bowel syndrome, and colic in breast-fed infants.
The guideline contains good evidence of where and which types of probiotics are useful and it is good to look at the charts in the paper to see the specific strains recommended. It also contains an extensive reference section, and as primary care physicians, it is imperative that we educate ourselves on these agents.
While probiotics are typically sold as supplements, we should not dismiss them summarily. It is easy to do that when supplemental products are marketed and sold unethically with no clinical evidence of benefit. We need to remember that just because something is a supplement doesn’t necessarily mean that it was not studied.
Family physicians need to be able to educate their patients and answer their questions. When we don’t have the answers, we need to find them. Any time our patient doesn’t get good information from us, they will probably go to the Internet and get bad advice from someone else.
There is much ongoing research about the gut microbiome and the bacteria that can be found in the gut. Researchers are looking into the “gut-brain” axis but there is not much good evidence of this link yet. There is no evidence that probiotics can cure Alzheimer’s disease or Parkinsonism. The future may reveal different stories, but for now, we need to follow the evidence we have available.
There are many outlandish claims about what the gut microbiome is responsible for and can do for health. It is easy to have a knee-jerk reaction when anyone brings it up in conversation. We need to arm ourselves with the evidence. We are stewards of the health and safety of our patients.
Dr. Girgis practices family medicine in South River, N.J., and is a clinical assistant professor of family medicine at Robert Wood Johnson Medical School, New Brunswick, N.J. She was paid by Pfizer as a consultant on Paxlovid and is the editor in chief of Physician’s Weekly.
The idea of the use of probiotics has a history going back more than a century when Russian scientist, Elie Metchnikoff, theorized that lactic acid bacteria may offer health benefits as well as promote longevity. In the early 1900s, intestinal disorders were frequently treated with nonpathogenic bacteria to replace gut microbes.
Today, the market is flooded with products from foods to prescription medications containing probiotics that extol their health benefits. It has been estimated that the global market for probiotics is more than $32 billion dollars annually and is expected to increase 8% per year.
As family doctors, patients come to us with many questions about the use of probiotics. Look online or on store shelves — there are so many types, doses, and brands of probiotics it is hard to decipher which are worth using. We older doctors never received much education about them.
Earlier this year, the World Gastroenterology Organization (WGO) developed recommendations around the use of probiotics and defined them as “live microbes that have been shown in controlled human studies to impart a health benefit.” Their recommendation is to use the strains that have been shown to be beneficial for the condition they claim to help and have been shown to do so in controlled studies. The dosage advised should be that shown to be useful in studies.
While this is an easy statement to make, it is much less so in clinical practice. The guidelines do a good job breaking down the conditions they help and the strains that have shown to be beneficial for specific conditions.
There have been claims that probiotics have been shown to be beneficial in colorectal cancer. While there have been some studies to show that they can improve markers associated with colorectal cancer, there are no data that probiotics actually do much in terms of prevention. Eating a healthy diet is more helpful here.
One area where probiotics have been shown to be beneficial is in the prevention of antibiotic-associated diarrhea. This makes sense since we know that antibiotics can kill the “good bacteria” lining the gut wall and probiotics work to replace them. Other conditions where these agents have been shown to be beneficial include radiation-induced diarrhea, acute diarrhea, irritable bowel syndrome, and colic in breast-fed infants.
The guideline contains good evidence of where and which types of probiotics are useful and it is good to look at the charts in the paper to see the specific strains recommended. It also contains an extensive reference section, and as primary care physicians, it is imperative that we educate ourselves on these agents.
While probiotics are typically sold as supplements, we should not dismiss them summarily. It is easy to do that when supplemental products are marketed and sold unethically with no clinical evidence of benefit. We need to remember that just because something is a supplement doesn’t necessarily mean that it was not studied.
Family physicians need to be able to educate their patients and answer their questions. When we don’t have the answers, we need to find them. Any time our patient doesn’t get good information from us, they will probably go to the Internet and get bad advice from someone else.
There is much ongoing research about the gut microbiome and the bacteria that can be found in the gut. Researchers are looking into the “gut-brain” axis but there is not much good evidence of this link yet. There is no evidence that probiotics can cure Alzheimer’s disease or Parkinsonism. The future may reveal different stories, but for now, we need to follow the evidence we have available.
There are many outlandish claims about what the gut microbiome is responsible for and can do for health. It is easy to have a knee-jerk reaction when anyone brings it up in conversation. We need to arm ourselves with the evidence. We are stewards of the health and safety of our patients.
Dr. Girgis practices family medicine in South River, N.J., and is a clinical assistant professor of family medicine at Robert Wood Johnson Medical School, New Brunswick, N.J. She was paid by Pfizer as a consultant on Paxlovid and is the editor in chief of Physician’s Weekly.
The idea of the use of probiotics has a history going back more than a century when Russian scientist, Elie Metchnikoff, theorized that lactic acid bacteria may offer health benefits as well as promote longevity. In the early 1900s, intestinal disorders were frequently treated with nonpathogenic bacteria to replace gut microbes.
Today, the market is flooded with products from foods to prescription medications containing probiotics that extol their health benefits. It has been estimated that the global market for probiotics is more than $32 billion dollars annually and is expected to increase 8% per year.
As family doctors, patients come to us with many questions about the use of probiotics. Look online or on store shelves — there are so many types, doses, and brands of probiotics it is hard to decipher which are worth using. We older doctors never received much education about them.
Earlier this year, the World Gastroenterology Organization (WGO) developed recommendations around the use of probiotics and defined them as “live microbes that have been shown in controlled human studies to impart a health benefit.” Their recommendation is to use the strains that have been shown to be beneficial for the condition they claim to help and have been shown to do so in controlled studies. The dosage advised should be that shown to be useful in studies.
While this is an easy statement to make, it is much less so in clinical practice. The guidelines do a good job breaking down the conditions they help and the strains that have shown to be beneficial for specific conditions.
There have been claims that probiotics have been shown to be beneficial in colorectal cancer. While there have been some studies to show that they can improve markers associated with colorectal cancer, there are no data that probiotics actually do much in terms of prevention. Eating a healthy diet is more helpful here.
One area where probiotics have been shown to be beneficial is in the prevention of antibiotic-associated diarrhea. This makes sense since we know that antibiotics can kill the “good bacteria” lining the gut wall and probiotics work to replace them. Other conditions where these agents have been shown to be beneficial include radiation-induced diarrhea, acute diarrhea, irritable bowel syndrome, and colic in breast-fed infants.
The guideline contains good evidence of where and which types of probiotics are useful and it is good to look at the charts in the paper to see the specific strains recommended. It also contains an extensive reference section, and as primary care physicians, it is imperative that we educate ourselves on these agents.
While probiotics are typically sold as supplements, we should not dismiss them summarily. It is easy to do that when supplemental products are marketed and sold unethically with no clinical evidence of benefit. We need to remember that just because something is a supplement doesn’t necessarily mean that it was not studied.
Family physicians need to be able to educate their patients and answer their questions. When we don’t have the answers, we need to find them. Any time our patient doesn’t get good information from us, they will probably go to the Internet and get bad advice from someone else.
There is much ongoing research about the gut microbiome and the bacteria that can be found in the gut. Researchers are looking into the “gut-brain” axis but there is not much good evidence of this link yet. There is no evidence that probiotics can cure Alzheimer’s disease or Parkinsonism. The future may reveal different stories, but for now, we need to follow the evidence we have available.
There are many outlandish claims about what the gut microbiome is responsible for and can do for health. It is easy to have a knee-jerk reaction when anyone brings it up in conversation. We need to arm ourselves with the evidence. We are stewards of the health and safety of our patients.
Dr. Girgis practices family medicine in South River, N.J., and is a clinical assistant professor of family medicine at Robert Wood Johnson Medical School, New Brunswick, N.J. She was paid by Pfizer as a consultant on Paxlovid and is the editor in chief of Physician’s Weekly.
Sometimes well-intended mental health treatment hurts
We love psychiatry. We love the idea that someone can come to receive care from a physician to alleviate psychological suffering.
Some people experience such severe anguish that they are unable to relate to others. Some are so despondent that they are unable to make decisions. Some are so distressed that their thoughts become inconsistent with reality. We want all those people, and many more, to have access to effective psychiatric care. However, there are reasonable expectations that one should be able to have that a treatment will help, and that appropriate informed consent is given.
One recent article reminded us of this in a particularly poignant way.
The study in question is a recent publication looking at the universal use of psychotherapy for teenagers.1 At face value, we would have certainly considered this to be a benevolent and well-meaning intervention. Anyone who has been a teenager or has talked to one, is aware of the emotional instability punctuated by episodes of intense anxiety or irritability. It is age appropriate for a teenager to question and explore their identity. Teenagers are notoriously impulsive with a deep desire for validating interpersonal relationships. One could continue to list the symptoms of borderline personality disorder (BPD) and find a lot of similarity with the condition of transitioning from a child to an adult.
It is thus common sense to consider applying the most established therapy for BPD, dialectical behavioral therapy (DBT), to teenagers. The basics of DBT would seem to be helpful to anyone but appear particularly appropriate to this population. Mindfulness, the practice of paying attention to your present experience, allows one to realize that they are trapped in past or hypothetical future moments. Emotional regulation provides the tools that offer a frame for our feelings and involves recognizing feelings and understanding what they mean. Interpersonal work allows one to recognize and adapt to the feelings of others, while learning how to have a healthy voice with others. Distress tolerance is the exercise of learning to experience and contain our feelings.
The study looked at about 1,000 young adolescents, around 13 years old across high schools in Sydney, Australia: 598 adolescents were allocated to the intervention, and 566 to the control. The intervention consisted of eight weekly sessions of DBT lasting about 50 minutes. The results were “contrary to predictions.” Participants who received DBT “reported significantly increased total difficulties,” and “significant increases in depression and anxiety.” The effects were worse in males yet significant in both genders. The study concludes with “a reminder that present enthusiasm for universal dissemination of short-term DBT-based group skills training within schools, specifically in early adolescence, is ahead of the research evidence.”
We can’t help but wonder why the outcomes of the study were this way; here are some ideas:
• Society has natural ways of developing interpersonal skills, emotional regulation, and the ability to appreciate the present. Interpersonal skills are consistently fostered and tested in schools. Navigating high school parties, the process of organizing them, and getting invited to them requires significant social dexterity. Rejection from romantic interest, alienation from peers, rewards for accomplishment, and acceptance by other peers are some of the daily emotional obstacles that teenagers face. Being constantly taught by older individuals and scolded by parents is its own course in mindfulness. Those are few of the many natural processes of interpersonal growth that formalized therapy may impede.
• The universal discussion of psychological terms and psychiatric symptoms may not only destigmatize mental illness, but also normalize and possibly even promote it. While punishing or stigmatizing a child for having mental illness is obviously unacceptable and cruel, we do wonder if the compulsory psychotherapy may provide negative effects. Psychotherapies, especially manualized ones, were developed to alleviate mental suffering. It seems possible that this format normalizes pathology.
In 1961, Erving Goffman described the concept of sane people appearing insane in an asylum as “mortification.” In 2023, we have much improved, but have we done something to internalize patterns of suffering and alienation rather than dispel them? They are given forms that explain what the feeling of depression is when they may have never considered it. They are given tools to handle distress, when distress may not be present.
• Many human beings live on a fairly tight rope of suppression and the less adaptive repression. Suppression is the defense mechanism by which individuals make an effort to put distressing thoughts out of conscious awareness. After a difficult breakup a teenager may ask some friends to go out and watch a movie, making efforts to put negative feelings out of conscious awareness until there is an opportunity to cope adaptively with those stressors.
Repression is the defense mechanism by which individuals make an effort to prevent distressing thoughts from entering conscious awareness in the first place. After a difficult breakup a teenager acts like nothing happened. While not particularly adaptive, many people live with significant repression and without particular anguish. It is possible that uncovering all of those repressed and suppressed feelings through the exploratory work of therapy may destabilize individuals from their tight rope.
• A less problematic explanation could also be what was previously referred to as therapeutic regression. In psychoanalytic theory, patients are generally thought to have a compromise formation, a psychological strategy used to reconcile conflicting drives. The compromise formation is the way a patient balances their desires against moral expectations and the realities of the external world. In therapy, that compromise formation can be challenged, leading to therapeutic regression.
By uncovering and confronting deeply rooted feelings, a patient may find that their symptoms temporarily intensify. This may not be a problem, but a necessary step to growth in some patients. It is possible that a program longer than 8 weeks would have overcome a temporary worsening in outcome measures.
While it’s easy to highlight the darker moments in psychiatric history, psychiatry has grown into a field which offers well-accepted and uncontroversially promoted forms of treatment. This is evolution, exemplified by the mere consideration of the universal use of psychotherapy for teenagers. But this raises important questions about the potential unintended consequences of normalizing and formalizing therapy. It prompted us to reflect on whether psychiatric treatment is always the best solution and if it might, at times, impede natural processes of growth and coping.
In this context, the study on universal DBT-based group skills training for teenagers challenged our assumptions. The unexpected outcomes suggest that societal and educational systems may naturally foster many of the skills that formalized therapy seeks to provide, and may do so with greater efficacy than that which prescriptive psychiatric treatments have to offer. Moreover, the universal discussion of psychiatric symptoms may not only destigmatize mental illness but also normalize it, potentially leading to unnecessary pathology.
Finally, the study prompted us to consider the fine balance that people find themselves in, questioning whether we should be so certain that our interventions can always provide a better outcome than an individual’s current coping mechanisms. These findings serve as a valuable reminder that our enthusiasm for widespread psychiatric interventions should be tempered by rigorous research and a nuanced understanding of human psychology and development.
This study could be an example of the grandiose stance psychiatry has at times taken of late, suggesting the field has an intervention for all that ails you and can serve as a corrective to society’s maladaptive deviations. Rising rates of mental illness in the community are not interpreted as a failing of the field of psychiatry, but as evidence that we need more psychiatrists. Acts of gun violence, ever increasing rates suicides, and even political disagreements are met with the idea that if only we had more mental health capacity, this could be avoided.
Dr. Badre is a clinical and forensic psychiatrist in San Diego. He holds teaching positions at the University of California, San Diego, and the University of San Diego. He teaches medical education, psychopharmacology, ethics in psychiatry, and correctional care. Dr. Badre can be reached at his website, BadreMD.com. He has no conflicts of interest. Dr. ZoBell is a fourth-year senior resident at UCSD Psychiatry Residency Program. She is currently serving as the program’s Chief Resident at the VA San Diego on the inpatient psychiatric unit. Dr. ZoBell is interested in outpatient and emergency psychiatry as well as psychotherapy. Dr. Lehman is a professor of psychiatry at the University of California, San Diego. He is codirector of all acute and intensive psychiatric treatment at the Veterans Affairs Medical Center in San Diego, where he practices clinical psychiatry. He has no conflicts of interest.
Reference
1. Harvey, LJ, et al. Investigating the efficacy of a Dialectical behaviour therapy-based universal intervention on adolescent social and emotional well-being outcomes. Behav Res Ther. 2023 Oct. doi: 10.1016/j.brat.2023.104408.
We love psychiatry. We love the idea that someone can come to receive care from a physician to alleviate psychological suffering.
Some people experience such severe anguish that they are unable to relate to others. Some are so despondent that they are unable to make decisions. Some are so distressed that their thoughts become inconsistent with reality. We want all those people, and many more, to have access to effective psychiatric care. However, there are reasonable expectations that one should be able to have that a treatment will help, and that appropriate informed consent is given.
One recent article reminded us of this in a particularly poignant way.
The study in question is a recent publication looking at the universal use of psychotherapy for teenagers.1 At face value, we would have certainly considered this to be a benevolent and well-meaning intervention. Anyone who has been a teenager or has talked to one, is aware of the emotional instability punctuated by episodes of intense anxiety or irritability. It is age appropriate for a teenager to question and explore their identity. Teenagers are notoriously impulsive with a deep desire for validating interpersonal relationships. One could continue to list the symptoms of borderline personality disorder (BPD) and find a lot of similarity with the condition of transitioning from a child to an adult.
It is thus common sense to consider applying the most established therapy for BPD, dialectical behavioral therapy (DBT), to teenagers. The basics of DBT would seem to be helpful to anyone but appear particularly appropriate to this population. Mindfulness, the practice of paying attention to your present experience, allows one to realize that they are trapped in past or hypothetical future moments. Emotional regulation provides the tools that offer a frame for our feelings and involves recognizing feelings and understanding what they mean. Interpersonal work allows one to recognize and adapt to the feelings of others, while learning how to have a healthy voice with others. Distress tolerance is the exercise of learning to experience and contain our feelings.
The study looked at about 1,000 young adolescents, around 13 years old across high schools in Sydney, Australia: 598 adolescents were allocated to the intervention, and 566 to the control. The intervention consisted of eight weekly sessions of DBT lasting about 50 minutes. The results were “contrary to predictions.” Participants who received DBT “reported significantly increased total difficulties,” and “significant increases in depression and anxiety.” The effects were worse in males yet significant in both genders. The study concludes with “a reminder that present enthusiasm for universal dissemination of short-term DBT-based group skills training within schools, specifically in early adolescence, is ahead of the research evidence.”
We can’t help but wonder why the outcomes of the study were this way; here are some ideas:
• Society has natural ways of developing interpersonal skills, emotional regulation, and the ability to appreciate the present. Interpersonal skills are consistently fostered and tested in schools. Navigating high school parties, the process of organizing them, and getting invited to them requires significant social dexterity. Rejection from romantic interest, alienation from peers, rewards for accomplishment, and acceptance by other peers are some of the daily emotional obstacles that teenagers face. Being constantly taught by older individuals and scolded by parents is its own course in mindfulness. Those are few of the many natural processes of interpersonal growth that formalized therapy may impede.
• The universal discussion of psychological terms and psychiatric symptoms may not only destigmatize mental illness, but also normalize and possibly even promote it. While punishing or stigmatizing a child for having mental illness is obviously unacceptable and cruel, we do wonder if the compulsory psychotherapy may provide negative effects. Psychotherapies, especially manualized ones, were developed to alleviate mental suffering. It seems possible that this format normalizes pathology.
In 1961, Erving Goffman described the concept of sane people appearing insane in an asylum as “mortification.” In 2023, we have much improved, but have we done something to internalize patterns of suffering and alienation rather than dispel them? They are given forms that explain what the feeling of depression is when they may have never considered it. They are given tools to handle distress, when distress may not be present.
• Many human beings live on a fairly tight rope of suppression and the less adaptive repression. Suppression is the defense mechanism by which individuals make an effort to put distressing thoughts out of conscious awareness. After a difficult breakup a teenager may ask some friends to go out and watch a movie, making efforts to put negative feelings out of conscious awareness until there is an opportunity to cope adaptively with those stressors.
Repression is the defense mechanism by which individuals make an effort to prevent distressing thoughts from entering conscious awareness in the first place. After a difficult breakup a teenager acts like nothing happened. While not particularly adaptive, many people live with significant repression and without particular anguish. It is possible that uncovering all of those repressed and suppressed feelings through the exploratory work of therapy may destabilize individuals from their tight rope.
• A less problematic explanation could also be what was previously referred to as therapeutic regression. In psychoanalytic theory, patients are generally thought to have a compromise formation, a psychological strategy used to reconcile conflicting drives. The compromise formation is the way a patient balances their desires against moral expectations and the realities of the external world. In therapy, that compromise formation can be challenged, leading to therapeutic regression.
By uncovering and confronting deeply rooted feelings, a patient may find that their symptoms temporarily intensify. This may not be a problem, but a necessary step to growth in some patients. It is possible that a program longer than 8 weeks would have overcome a temporary worsening in outcome measures.
While it’s easy to highlight the darker moments in psychiatric history, psychiatry has grown into a field which offers well-accepted and uncontroversially promoted forms of treatment. This is evolution, exemplified by the mere consideration of the universal use of psychotherapy for teenagers. But this raises important questions about the potential unintended consequences of normalizing and formalizing therapy. It prompted us to reflect on whether psychiatric treatment is always the best solution and if it might, at times, impede natural processes of growth and coping.
In this context, the study on universal DBT-based group skills training for teenagers challenged our assumptions. The unexpected outcomes suggest that societal and educational systems may naturally foster many of the skills that formalized therapy seeks to provide, and may do so with greater efficacy than that which prescriptive psychiatric treatments have to offer. Moreover, the universal discussion of psychiatric symptoms may not only destigmatize mental illness but also normalize it, potentially leading to unnecessary pathology.
Finally, the study prompted us to consider the fine balance that people find themselves in, questioning whether we should be so certain that our interventions can always provide a better outcome than an individual’s current coping mechanisms. These findings serve as a valuable reminder that our enthusiasm for widespread psychiatric interventions should be tempered by rigorous research and a nuanced understanding of human psychology and development.
This study could be an example of the grandiose stance psychiatry has at times taken of late, suggesting the field has an intervention for all that ails you and can serve as a corrective to society’s maladaptive deviations. Rising rates of mental illness in the community are not interpreted as a failing of the field of psychiatry, but as evidence that we need more psychiatrists. Acts of gun violence, ever increasing rates suicides, and even political disagreements are met with the idea that if only we had more mental health capacity, this could be avoided.
Dr. Badre is a clinical and forensic psychiatrist in San Diego. He holds teaching positions at the University of California, San Diego, and the University of San Diego. He teaches medical education, psychopharmacology, ethics in psychiatry, and correctional care. Dr. Badre can be reached at his website, BadreMD.com. He has no conflicts of interest. Dr. ZoBell is a fourth-year senior resident at UCSD Psychiatry Residency Program. She is currently serving as the program’s Chief Resident at the VA San Diego on the inpatient psychiatric unit. Dr. ZoBell is interested in outpatient and emergency psychiatry as well as psychotherapy. Dr. Lehman is a professor of psychiatry at the University of California, San Diego. He is codirector of all acute and intensive psychiatric treatment at the Veterans Affairs Medical Center in San Diego, where he practices clinical psychiatry. He has no conflicts of interest.
Reference
1. Harvey, LJ, et al. Investigating the efficacy of a Dialectical behaviour therapy-based universal intervention on adolescent social and emotional well-being outcomes. Behav Res Ther. 2023 Oct. doi: 10.1016/j.brat.2023.104408.
We love psychiatry. We love the idea that someone can come to receive care from a physician to alleviate psychological suffering.
Some people experience such severe anguish that they are unable to relate to others. Some are so despondent that they are unable to make decisions. Some are so distressed that their thoughts become inconsistent with reality. We want all those people, and many more, to have access to effective psychiatric care. However, there are reasonable expectations that one should be able to have that a treatment will help, and that appropriate informed consent is given.
One recent article reminded us of this in a particularly poignant way.
The study in question is a recent publication looking at the universal use of psychotherapy for teenagers.1 At face value, we would have certainly considered this to be a benevolent and well-meaning intervention. Anyone who has been a teenager or has talked to one, is aware of the emotional instability punctuated by episodes of intense anxiety or irritability. It is age appropriate for a teenager to question and explore their identity. Teenagers are notoriously impulsive with a deep desire for validating interpersonal relationships. One could continue to list the symptoms of borderline personality disorder (BPD) and find a lot of similarity with the condition of transitioning from a child to an adult.
It is thus common sense to consider applying the most established therapy for BPD, dialectical behavioral therapy (DBT), to teenagers. The basics of DBT would seem to be helpful to anyone but appear particularly appropriate to this population. Mindfulness, the practice of paying attention to your present experience, allows one to realize that they are trapped in past or hypothetical future moments. Emotional regulation provides the tools that offer a frame for our feelings and involves recognizing feelings and understanding what they mean. Interpersonal work allows one to recognize and adapt to the feelings of others, while learning how to have a healthy voice with others. Distress tolerance is the exercise of learning to experience and contain our feelings.
The study looked at about 1,000 young adolescents, around 13 years old across high schools in Sydney, Australia: 598 adolescents were allocated to the intervention, and 566 to the control. The intervention consisted of eight weekly sessions of DBT lasting about 50 minutes. The results were “contrary to predictions.” Participants who received DBT “reported significantly increased total difficulties,” and “significant increases in depression and anxiety.” The effects were worse in males yet significant in both genders. The study concludes with “a reminder that present enthusiasm for universal dissemination of short-term DBT-based group skills training within schools, specifically in early adolescence, is ahead of the research evidence.”
We can’t help but wonder why the outcomes of the study were this way; here are some ideas:
• Society has natural ways of developing interpersonal skills, emotional regulation, and the ability to appreciate the present. Interpersonal skills are consistently fostered and tested in schools. Navigating high school parties, the process of organizing them, and getting invited to them requires significant social dexterity. Rejection from romantic interest, alienation from peers, rewards for accomplishment, and acceptance by other peers are some of the daily emotional obstacles that teenagers face. Being constantly taught by older individuals and scolded by parents is its own course in mindfulness. Those are few of the many natural processes of interpersonal growth that formalized therapy may impede.
• The universal discussion of psychological terms and psychiatric symptoms may not only destigmatize mental illness, but also normalize and possibly even promote it. While punishing or stigmatizing a child for having mental illness is obviously unacceptable and cruel, we do wonder if the compulsory psychotherapy may provide negative effects. Psychotherapies, especially manualized ones, were developed to alleviate mental suffering. It seems possible that this format normalizes pathology.
In 1961, Erving Goffman described the concept of sane people appearing insane in an asylum as “mortification.” In 2023, we have much improved, but have we done something to internalize patterns of suffering and alienation rather than dispel them? They are given forms that explain what the feeling of depression is when they may have never considered it. They are given tools to handle distress, when distress may not be present.
• Many human beings live on a fairly tight rope of suppression and the less adaptive repression. Suppression is the defense mechanism by which individuals make an effort to put distressing thoughts out of conscious awareness. After a difficult breakup a teenager may ask some friends to go out and watch a movie, making efforts to put negative feelings out of conscious awareness until there is an opportunity to cope adaptively with those stressors.
Repression is the defense mechanism by which individuals make an effort to prevent distressing thoughts from entering conscious awareness in the first place. After a difficult breakup a teenager acts like nothing happened. While not particularly adaptive, many people live with significant repression and without particular anguish. It is possible that uncovering all of those repressed and suppressed feelings through the exploratory work of therapy may destabilize individuals from their tight rope.
• A less problematic explanation could also be what was previously referred to as therapeutic regression. In psychoanalytic theory, patients are generally thought to have a compromise formation, a psychological strategy used to reconcile conflicting drives. The compromise formation is the way a patient balances their desires against moral expectations and the realities of the external world. In therapy, that compromise formation can be challenged, leading to therapeutic regression.
By uncovering and confronting deeply rooted feelings, a patient may find that their symptoms temporarily intensify. This may not be a problem, but a necessary step to growth in some patients. It is possible that a program longer than 8 weeks would have overcome a temporary worsening in outcome measures.
While it’s easy to highlight the darker moments in psychiatric history, psychiatry has grown into a field which offers well-accepted and uncontroversially promoted forms of treatment. This is evolution, exemplified by the mere consideration of the universal use of psychotherapy for teenagers. But this raises important questions about the potential unintended consequences of normalizing and formalizing therapy. It prompted us to reflect on whether psychiatric treatment is always the best solution and if it might, at times, impede natural processes of growth and coping.
In this context, the study on universal DBT-based group skills training for teenagers challenged our assumptions. The unexpected outcomes suggest that societal and educational systems may naturally foster many of the skills that formalized therapy seeks to provide, and may do so with greater efficacy than that which prescriptive psychiatric treatments have to offer. Moreover, the universal discussion of psychiatric symptoms may not only destigmatize mental illness but also normalize it, potentially leading to unnecessary pathology.
Finally, the study prompted us to consider the fine balance that people find themselves in, questioning whether we should be so certain that our interventions can always provide a better outcome than an individual’s current coping mechanisms. These findings serve as a valuable reminder that our enthusiasm for widespread psychiatric interventions should be tempered by rigorous research and a nuanced understanding of human psychology and development.
This study could be an example of the grandiose stance psychiatry has at times taken of late, suggesting the field has an intervention for all that ails you and can serve as a corrective to society’s maladaptive deviations. Rising rates of mental illness in the community are not interpreted as a failing of the field of psychiatry, but as evidence that we need more psychiatrists. Acts of gun violence, ever increasing rates suicides, and even political disagreements are met with the idea that if only we had more mental health capacity, this could be avoided.
Dr. Badre is a clinical and forensic psychiatrist in San Diego. He holds teaching positions at the University of California, San Diego, and the University of San Diego. He teaches medical education, psychopharmacology, ethics in psychiatry, and correctional care. Dr. Badre can be reached at his website, BadreMD.com. He has no conflicts of interest. Dr. ZoBell is a fourth-year senior resident at UCSD Psychiatry Residency Program. She is currently serving as the program’s Chief Resident at the VA San Diego on the inpatient psychiatric unit. Dr. ZoBell is interested in outpatient and emergency psychiatry as well as psychotherapy. Dr. Lehman is a professor of psychiatry at the University of California, San Diego. He is codirector of all acute and intensive psychiatric treatment at the Veterans Affairs Medical Center in San Diego, where he practices clinical psychiatry. He has no conflicts of interest.
Reference
1. Harvey, LJ, et al. Investigating the efficacy of a Dialectical behaviour therapy-based universal intervention on adolescent social and emotional well-being outcomes. Behav Res Ther. 2023 Oct. doi: 10.1016/j.brat.2023.104408.
Erectile Dysfunction Rx: Give It a Shot
This transcript has been edited for clarity.
I’m Dr Rachel Rubin. I am a urologist with fellowship training in sexual medicine. Today I’m going to explain why I may recommend that your patients put a needle directly into their penises for help with erectile dysfunction (ED).
I know that sounds crazy, but in a recent video when I talked about erection hardness, I acknowledged that it may not be easy to talk with patients about their penises, but it’s important.
ED can be a marker for cardiovascular disease, with 50% of our 50-year-old patients having ED. As physicians, we must do a better job of talking to our patients about ED and letting them know that it’s a marker for overall health.
How do we treat ED? Primary care doctors can do a great deal for patients with ED, and there are other things that urologists can do when you run out of options in your own toolbox.
What’s important for a healthy erection? You need three things: healthy muscle, healthy nerves, and healthy arteries. If anything goes wrong with muscles, nerves, or arteries, this is what leads to ED. Think through the algorithm of your patient’s medical history: Do they have diabetes, which can affect their nerves? Do they have high blood pressure, which can affect their arteries? Do they have problems with testosterone, which can affect the smooth muscles of the penis? Understanding your patient’s history can be really helpful when you figure out what is the best treatment strategy for your patient.
For the penis to work, those smooth muscles have to relax; therefore, your brain has to be relaxed, along with your pelvic floor muscles. The smooth muscle of the penis has to be relaxed so it can fill with blood, increase in girth and size, and hold that erection in place.
To treat ED, we have a biopsychosocial toolbox. Biology refers to the muscles, arteries, and nerves. The psychosocial component is stress: If your brain is stressed, you have a lot of adrenaline around that can tighten those smooth muscles and cause you to lose an erection.
So, what are these treatments? I’ll start with lifestyle. A healthy heart means a healthy penis, so, all of the things you already recommend for lifestyle changes can really help with ED. Sleep is important. Does your patient need a sleep study? Do they have sleep apnea? Are they exercising? Recent data show that exercise may be just as effective, if not more effective, than Viagra. How about a good diet? The Mediterranean diet seems to be the most helpful. So, encourage your patients to make dietary, exercise, sleep, and other lifestyle changes if they want to improve erectile function.
What about sex education? Most physicians didn’t get great education about sex in medical school, but it’s very important to our patients who likewise have had inadequate sex education. Ask questions, talk to them, explain what is normal.
I can’t stress enough how important mental health is to a great sex life. Everyone would benefit from sex therapy and becoming better at sex. We need to get better at communicating and educating patients and their partners to maximize their quality of life. If you need to refer to a specialist, we recommend going to psychologytoday.com or aasect.org to find a local sex therapist. Call them and use them in your referral networks.
In the “bio” component of the biopsychosocial approach, we can do a lot to treat ED with medications and hormones. Testosterone has been shown to help with low libido and erectile function. Checking the patient’s testosterone level can be very helpful. Pills — we are familiar with Viagra, Cialis, Levitra, and Stendra. The oral PDE-5 inhibitors have been around since the late 1990s and they work quite well for many people with ED. Viagra and Cialis are generic now and patients can get them fairly inexpensively with discount coupons from GoodRx or Cost Plus Drugs. They may not even have to worry about insurance coverage.
Pills relax the smooth muscle of the penis so that it fills with blood and becomes erect, but they don’t work for everybody. If pills stop working, we often talk about synergistic treatments — combining pills and devices. Devices for ED should be discussed more often, and clinicians should consider prescribing them. We commonly discuss eyeglasses and wheelchairs, but we don’t talk about the sexual health devices that could help patients have more success and fun in the bedroom.
What are the various types of devices for ED? One common device is a vacuum pump, which can be very effective. This is how they work: The penis is lubricated and placed into the pump. A button on the pump creates suction that brings blood into the penis. The patient then applies a constriction band around the base of the penis to hold that erection in place.
“Sex tech” has really expanded to help patients with ED with devices that vibrate and hold the erection in place. Vibrating devices allow for a better orgasm. We even have devices that monitor erectile fitness (like a Fitbit for the penis), gathering data to help patients understand the firmness of their erections.
Devices are helpful adjuncts, but they don’t always do enough to achieve an erect penis that’s hard enough for penetration. In those cases, we can recommend injections that increase smooth muscle relaxation of the penis. I know it sounds crazy. If the muscles, arteries, and nerves of the penis aren’t functioning well, additional smooth muscle relaxation can be achieved by injecting alprostadil (prostaglandin E1) directly into the penis. It’s a tiny needle. It doesn’t hurt. These injections can be quite helpful for our patients, and we often recommend them.
But what happens when your patient doesn’t even respond to injections or any of the synergistic treatments? They’ve tried everything. Urologists may suggest a surgical option, the penile implant. Penile implants contain a pump inside the scrotum that fills with fluid, allowing a rigid erection. Penile implants are wonderful for patients who can no longer get erections. Talking to a urologist about the pros and the cons and the risks and benefits of surgically placed implants is very important.
Finally, ED is a marker for cardiovascular disease. These patients may need a cardiology workup. They need to improve their general health. We have to ask our patients about their goals and what they care about, and find a toolbox that makes sense for each patient and couple to maximize their sexual health and quality of life. Don’t give up. If you have questions, let us know.
Rachel S. Rubin, MD, is Assistant Clinical Professor, Department of Urology, Georgetown University, Washington, DC; Private practice, Rachel Rubin MD PLLC, North Bethesda, Maryland. She disclosed ties with Sprout, Maternal Medical, Absorption Pharmaceuticals, GSK, and Endo.
A version of this article appeared on Medscape.com.
This transcript has been edited for clarity.
I’m Dr Rachel Rubin. I am a urologist with fellowship training in sexual medicine. Today I’m going to explain why I may recommend that your patients put a needle directly into their penises for help with erectile dysfunction (ED).
I know that sounds crazy, but in a recent video when I talked about erection hardness, I acknowledged that it may not be easy to talk with patients about their penises, but it’s important.
ED can be a marker for cardiovascular disease, with 50% of our 50-year-old patients having ED. As physicians, we must do a better job of talking to our patients about ED and letting them know that it’s a marker for overall health.
How do we treat ED? Primary care doctors can do a great deal for patients with ED, and there are other things that urologists can do when you run out of options in your own toolbox.
What’s important for a healthy erection? You need three things: healthy muscle, healthy nerves, and healthy arteries. If anything goes wrong with muscles, nerves, or arteries, this is what leads to ED. Think through the algorithm of your patient’s medical history: Do they have diabetes, which can affect their nerves? Do they have high blood pressure, which can affect their arteries? Do they have problems with testosterone, which can affect the smooth muscles of the penis? Understanding your patient’s history can be really helpful when you figure out what is the best treatment strategy for your patient.
For the penis to work, those smooth muscles have to relax; therefore, your brain has to be relaxed, along with your pelvic floor muscles. The smooth muscle of the penis has to be relaxed so it can fill with blood, increase in girth and size, and hold that erection in place.
To treat ED, we have a biopsychosocial toolbox. Biology refers to the muscles, arteries, and nerves. The psychosocial component is stress: If your brain is stressed, you have a lot of adrenaline around that can tighten those smooth muscles and cause you to lose an erection.
So, what are these treatments? I’ll start with lifestyle. A healthy heart means a healthy penis, so, all of the things you already recommend for lifestyle changes can really help with ED. Sleep is important. Does your patient need a sleep study? Do they have sleep apnea? Are they exercising? Recent data show that exercise may be just as effective, if not more effective, than Viagra. How about a good diet? The Mediterranean diet seems to be the most helpful. So, encourage your patients to make dietary, exercise, sleep, and other lifestyle changes if they want to improve erectile function.
What about sex education? Most physicians didn’t get great education about sex in medical school, but it’s very important to our patients who likewise have had inadequate sex education. Ask questions, talk to them, explain what is normal.
I can’t stress enough how important mental health is to a great sex life. Everyone would benefit from sex therapy and becoming better at sex. We need to get better at communicating and educating patients and their partners to maximize their quality of life. If you need to refer to a specialist, we recommend going to psychologytoday.com or aasect.org to find a local sex therapist. Call them and use them in your referral networks.
In the “bio” component of the biopsychosocial approach, we can do a lot to treat ED with medications and hormones. Testosterone has been shown to help with low libido and erectile function. Checking the patient’s testosterone level can be very helpful. Pills — we are familiar with Viagra, Cialis, Levitra, and Stendra. The oral PDE-5 inhibitors have been around since the late 1990s and they work quite well for many people with ED. Viagra and Cialis are generic now and patients can get them fairly inexpensively with discount coupons from GoodRx or Cost Plus Drugs. They may not even have to worry about insurance coverage.
Pills relax the smooth muscle of the penis so that it fills with blood and becomes erect, but they don’t work for everybody. If pills stop working, we often talk about synergistic treatments — combining pills and devices. Devices for ED should be discussed more often, and clinicians should consider prescribing them. We commonly discuss eyeglasses and wheelchairs, but we don’t talk about the sexual health devices that could help patients have more success and fun in the bedroom.
What are the various types of devices for ED? One common device is a vacuum pump, which can be very effective. This is how they work: The penis is lubricated and placed into the pump. A button on the pump creates suction that brings blood into the penis. The patient then applies a constriction band around the base of the penis to hold that erection in place.
“Sex tech” has really expanded to help patients with ED with devices that vibrate and hold the erection in place. Vibrating devices allow for a better orgasm. We even have devices that monitor erectile fitness (like a Fitbit for the penis), gathering data to help patients understand the firmness of their erections.
Devices are helpful adjuncts, but they don’t always do enough to achieve an erect penis that’s hard enough for penetration. In those cases, we can recommend injections that increase smooth muscle relaxation of the penis. I know it sounds crazy. If the muscles, arteries, and nerves of the penis aren’t functioning well, additional smooth muscle relaxation can be achieved by injecting alprostadil (prostaglandin E1) directly into the penis. It’s a tiny needle. It doesn’t hurt. These injections can be quite helpful for our patients, and we often recommend them.
But what happens when your patient doesn’t even respond to injections or any of the synergistic treatments? They’ve tried everything. Urologists may suggest a surgical option, the penile implant. Penile implants contain a pump inside the scrotum that fills with fluid, allowing a rigid erection. Penile implants are wonderful for patients who can no longer get erections. Talking to a urologist about the pros and the cons and the risks and benefits of surgically placed implants is very important.
Finally, ED is a marker for cardiovascular disease. These patients may need a cardiology workup. They need to improve their general health. We have to ask our patients about their goals and what they care about, and find a toolbox that makes sense for each patient and couple to maximize their sexual health and quality of life. Don’t give up. If you have questions, let us know.
Rachel S. Rubin, MD, is Assistant Clinical Professor, Department of Urology, Georgetown University, Washington, DC; Private practice, Rachel Rubin MD PLLC, North Bethesda, Maryland. She disclosed ties with Sprout, Maternal Medical, Absorption Pharmaceuticals, GSK, and Endo.
A version of this article appeared on Medscape.com.
This transcript has been edited for clarity.
I’m Dr Rachel Rubin. I am a urologist with fellowship training in sexual medicine. Today I’m going to explain why I may recommend that your patients put a needle directly into their penises for help with erectile dysfunction (ED).
I know that sounds crazy, but in a recent video when I talked about erection hardness, I acknowledged that it may not be easy to talk with patients about their penises, but it’s important.
ED can be a marker for cardiovascular disease, with 50% of our 50-year-old patients having ED. As physicians, we must do a better job of talking to our patients about ED and letting them know that it’s a marker for overall health.
How do we treat ED? Primary care doctors can do a great deal for patients with ED, and there are other things that urologists can do when you run out of options in your own toolbox.
What’s important for a healthy erection? You need three things: healthy muscle, healthy nerves, and healthy arteries. If anything goes wrong with muscles, nerves, or arteries, this is what leads to ED. Think through the algorithm of your patient’s medical history: Do they have diabetes, which can affect their nerves? Do they have high blood pressure, which can affect their arteries? Do they have problems with testosterone, which can affect the smooth muscles of the penis? Understanding your patient’s history can be really helpful when you figure out what is the best treatment strategy for your patient.
For the penis to work, those smooth muscles have to relax; therefore, your brain has to be relaxed, along with your pelvic floor muscles. The smooth muscle of the penis has to be relaxed so it can fill with blood, increase in girth and size, and hold that erection in place.
To treat ED, we have a biopsychosocial toolbox. Biology refers to the muscles, arteries, and nerves. The psychosocial component is stress: If your brain is stressed, you have a lot of adrenaline around that can tighten those smooth muscles and cause you to lose an erection.
So, what are these treatments? I’ll start with lifestyle. A healthy heart means a healthy penis, so, all of the things you already recommend for lifestyle changes can really help with ED. Sleep is important. Does your patient need a sleep study? Do they have sleep apnea? Are they exercising? Recent data show that exercise may be just as effective, if not more effective, than Viagra. How about a good diet? The Mediterranean diet seems to be the most helpful. So, encourage your patients to make dietary, exercise, sleep, and other lifestyle changes if they want to improve erectile function.
What about sex education? Most physicians didn’t get great education about sex in medical school, but it’s very important to our patients who likewise have had inadequate sex education. Ask questions, talk to them, explain what is normal.
I can’t stress enough how important mental health is to a great sex life. Everyone would benefit from sex therapy and becoming better at sex. We need to get better at communicating and educating patients and their partners to maximize their quality of life. If you need to refer to a specialist, we recommend going to psychologytoday.com or aasect.org to find a local sex therapist. Call them and use them in your referral networks.
In the “bio” component of the biopsychosocial approach, we can do a lot to treat ED with medications and hormones. Testosterone has been shown to help with low libido and erectile function. Checking the patient’s testosterone level can be very helpful. Pills — we are familiar with Viagra, Cialis, Levitra, and Stendra. The oral PDE-5 inhibitors have been around since the late 1990s and they work quite well for many people with ED. Viagra and Cialis are generic now and patients can get them fairly inexpensively with discount coupons from GoodRx or Cost Plus Drugs. They may not even have to worry about insurance coverage.
Pills relax the smooth muscle of the penis so that it fills with blood and becomes erect, but they don’t work for everybody. If pills stop working, we often talk about synergistic treatments — combining pills and devices. Devices for ED should be discussed more often, and clinicians should consider prescribing them. We commonly discuss eyeglasses and wheelchairs, but we don’t talk about the sexual health devices that could help patients have more success and fun in the bedroom.
What are the various types of devices for ED? One common device is a vacuum pump, which can be very effective. This is how they work: The penis is lubricated and placed into the pump. A button on the pump creates suction that brings blood into the penis. The patient then applies a constriction band around the base of the penis to hold that erection in place.
“Sex tech” has really expanded to help patients with ED with devices that vibrate and hold the erection in place. Vibrating devices allow for a better orgasm. We even have devices that monitor erectile fitness (like a Fitbit for the penis), gathering data to help patients understand the firmness of their erections.
Devices are helpful adjuncts, but they don’t always do enough to achieve an erect penis that’s hard enough for penetration. In those cases, we can recommend injections that increase smooth muscle relaxation of the penis. I know it sounds crazy. If the muscles, arteries, and nerves of the penis aren’t functioning well, additional smooth muscle relaxation can be achieved by injecting alprostadil (prostaglandin E1) directly into the penis. It’s a tiny needle. It doesn’t hurt. These injections can be quite helpful for our patients, and we often recommend them.
But what happens when your patient doesn’t even respond to injections or any of the synergistic treatments? They’ve tried everything. Urologists may suggest a surgical option, the penile implant. Penile implants contain a pump inside the scrotum that fills with fluid, allowing a rigid erection. Penile implants are wonderful for patients who can no longer get erections. Talking to a urologist about the pros and the cons and the risks and benefits of surgically placed implants is very important.
Finally, ED is a marker for cardiovascular disease. These patients may need a cardiology workup. They need to improve their general health. We have to ask our patients about their goals and what they care about, and find a toolbox that makes sense for each patient and couple to maximize their sexual health and quality of life. Don’t give up. If you have questions, let us know.
Rachel S. Rubin, MD, is Assistant Clinical Professor, Department of Urology, Georgetown University, Washington, DC; Private practice, Rachel Rubin MD PLLC, North Bethesda, Maryland. She disclosed ties with Sprout, Maternal Medical, Absorption Pharmaceuticals, GSK, and Endo.
A version of this article appeared on Medscape.com.
Supercharge your medical practice with ChatGPT: Here’s why you should upgrade
Artificial intelligence (AI) has already demonstrated its potential in various areas of healthcare, from early disease detection and drug discovery to genomics and personalized care. OpenAI’s ChatGPT, a large language model, is one AI tool that has been transforming practices across the globe, including mine.
Let me walk you through it.
ChatGPT is essentially an AI-fueled assistant, capable of interpreting and generating human-like text in response to user inputs. Imagine a well-informed and competent trainee working with you, ready to tackle tasks from handling patient inquiries to summarizing intricate medical literature.
Currently, ChatGPT works on the “freemium” pricing model; there is a free version built upon GPT-3.5 as well as a subscription “ChatGPT Plus” version based on GPT-4 which offers additional features such as the use of third-party plug-ins.
Now, you may ask, “Isn’t the free version enough?” The free version is indeed impressive, but upgrading to the paid version for $20 per month unlocks the full potential of this tool, particularly if we add plug-ins.
Here are some of the best ways to incorporate ChatGPT Plus into your practice.
Time saver and efficiency multiplier. The paid version of ChatGPT is an extraordinary time-saving tool. It can help you sort through vast amounts of medical literature in a fraction of the time it would normally take. Imagine having to sift through hundreds of articles to find the latest research relevant to a patient’s case. With the paid version of ChatGPT, you can simply ask it to provide summaries of the most recent and relevant studies, all in seconds.
Did you forget about that PowerPoint you need to make but know the potential papers you would use? No problem. ChatGPT can create slides in a few minutes. It becomes your on-demand research assistant.
Of course, you need to provide the source you find most relevant to you. Using plug-ins such as ScholarAI and Link Reader are great.
Improved patient communication. Explaining complex medical terminology and procedures to patients can sometimes be a challenge. ChatGPT can generate simplified and personalized explanations for your patients, fostering their understanding and involvement in their care process.
Epic is currently collaborating with Nuance Communications, Microsoft’s speech recognition subsidiary, to use generative AI tools for medical note-taking in the electronic health record. However, you do not need to wait for it; it just takes a prompt in ChatGPT and then copying/pasting the results into the chart.
Smoother administrative management. The premium version of ChatGPT can automate administrative tasks such as creating letters of medical necessity, clearance to other physicians for services, or even communications to staff on specific topics. This frees you to focus more on your core work: providing patient care.
Precision medicine aid. ChatGPT can be a powerful ally in the field of precision medicine. Its capabilities for analyzing large datasets and unearthing valuable insights can help deliver more personalized and potentially effective treatment plans. For example, one can prompt ChatGPT to query the reported frequency of certain genomic variants and their implications; with the upgraded version and plug-ins, the results will have fewer hallucinations — inaccurate results — and key data references.
Unlimited accessibility. Uninterrupted access is a compelling reason to upgrade. While the free version may have usage limitations, the premium version provides unrestricted, round-the-clock access. Be it a late-night research quest or an early-morning patient query, your AI assistant will always be available.
Strengthened privacy and security. The premium version of ChatGPT includes heightened privacy and security measures. Just make sure to follow HIPAA and not include identifiers when making queries.
Embracing AI tools like ChatGPT in your practice can help you stay at the cutting edge of medical care, saving you time, enhancing patient communication, and supporting you in providing personalized care.
While the free version can serve as a good starting point (there are apps for both iOS and Android), upgrading to the paid version opens up a world of possibilities that can truly supercharge your practice.
I would love to hear your comments on this column or on future topics. Contact me at [email protected].
Arturo Loaiza-Bonilla, MD, MSEd, is the cofounder and chief medical officer at Massive Bio, a company connecting patients to clinical trials using artificial intelligence. His research and professional interests focus on precision medicine, clinical trial design, digital health, entrepreneurship, and patient advocacy. Dr. Loaiza-Bonilla is Assistant Professor of Medicine, Drexel University School of Medicine, Philadelphia, Pennsylvania, and serves as medical director of oncology research at Capital Health in New Jersey, where he maintains a connection to patient care by attending to patients 2 days a week. He has financial relationships with Verify, PSI CRO, Bayer, AstraZeneca, Cardinal Health, BrightInsight, The Lynx Group, Fresenius, Pfizer, Ipsen, Guardant, Amgen, Eisai, Natera, Merck, and Bristol Myers Squibb.
A version of this article appeared on Medscape.com.
Artificial intelligence (AI) has already demonstrated its potential in various areas of healthcare, from early disease detection and drug discovery to genomics and personalized care. OpenAI’s ChatGPT, a large language model, is one AI tool that has been transforming practices across the globe, including mine.
Let me walk you through it.
ChatGPT is essentially an AI-fueled assistant, capable of interpreting and generating human-like text in response to user inputs. Imagine a well-informed and competent trainee working with you, ready to tackle tasks from handling patient inquiries to summarizing intricate medical literature.
Currently, ChatGPT works on the “freemium” pricing model; there is a free version built upon GPT-3.5 as well as a subscription “ChatGPT Plus” version based on GPT-4 which offers additional features such as the use of third-party plug-ins.
Now, you may ask, “Isn’t the free version enough?” The free version is indeed impressive, but upgrading to the paid version for $20 per month unlocks the full potential of this tool, particularly if we add plug-ins.
Here are some of the best ways to incorporate ChatGPT Plus into your practice.
Time saver and efficiency multiplier. The paid version of ChatGPT is an extraordinary time-saving tool. It can help you sort through vast amounts of medical literature in a fraction of the time it would normally take. Imagine having to sift through hundreds of articles to find the latest research relevant to a patient’s case. With the paid version of ChatGPT, you can simply ask it to provide summaries of the most recent and relevant studies, all in seconds.
Did you forget about that PowerPoint you need to make but know the potential papers you would use? No problem. ChatGPT can create slides in a few minutes. It becomes your on-demand research assistant.
Of course, you need to provide the source you find most relevant to you. Using plug-ins such as ScholarAI and Link Reader are great.
Improved patient communication. Explaining complex medical terminology and procedures to patients can sometimes be a challenge. ChatGPT can generate simplified and personalized explanations for your patients, fostering their understanding and involvement in their care process.
Epic is currently collaborating with Nuance Communications, Microsoft’s speech recognition subsidiary, to use generative AI tools for medical note-taking in the electronic health record. However, you do not need to wait for it; it just takes a prompt in ChatGPT and then copying/pasting the results into the chart.
Smoother administrative management. The premium version of ChatGPT can automate administrative tasks such as creating letters of medical necessity, clearance to other physicians for services, or even communications to staff on specific topics. This frees you to focus more on your core work: providing patient care.
Precision medicine aid. ChatGPT can be a powerful ally in the field of precision medicine. Its capabilities for analyzing large datasets and unearthing valuable insights can help deliver more personalized and potentially effective treatment plans. For example, one can prompt ChatGPT to query the reported frequency of certain genomic variants and their implications; with the upgraded version and plug-ins, the results will have fewer hallucinations — inaccurate results — and key data references.
Unlimited accessibility. Uninterrupted access is a compelling reason to upgrade. While the free version may have usage limitations, the premium version provides unrestricted, round-the-clock access. Be it a late-night research quest or an early-morning patient query, your AI assistant will always be available.
Strengthened privacy and security. The premium version of ChatGPT includes heightened privacy and security measures. Just make sure to follow HIPAA and not include identifiers when making queries.
Embracing AI tools like ChatGPT in your practice can help you stay at the cutting edge of medical care, saving you time, enhancing patient communication, and supporting you in providing personalized care.
While the free version can serve as a good starting point (there are apps for both iOS and Android), upgrading to the paid version opens up a world of possibilities that can truly supercharge your practice.
I would love to hear your comments on this column or on future topics. Contact me at [email protected].
Arturo Loaiza-Bonilla, MD, MSEd, is the cofounder and chief medical officer at Massive Bio, a company connecting patients to clinical trials using artificial intelligence. His research and professional interests focus on precision medicine, clinical trial design, digital health, entrepreneurship, and patient advocacy. Dr. Loaiza-Bonilla is Assistant Professor of Medicine, Drexel University School of Medicine, Philadelphia, Pennsylvania, and serves as medical director of oncology research at Capital Health in New Jersey, where he maintains a connection to patient care by attending to patients 2 days a week. He has financial relationships with Verify, PSI CRO, Bayer, AstraZeneca, Cardinal Health, BrightInsight, The Lynx Group, Fresenius, Pfizer, Ipsen, Guardant, Amgen, Eisai, Natera, Merck, and Bristol Myers Squibb.
A version of this article appeared on Medscape.com.
Artificial intelligence (AI) has already demonstrated its potential in various areas of healthcare, from early disease detection and drug discovery to genomics and personalized care. OpenAI’s ChatGPT, a large language model, is one AI tool that has been transforming practices across the globe, including mine.
Let me walk you through it.
ChatGPT is essentially an AI-fueled assistant, capable of interpreting and generating human-like text in response to user inputs. Imagine a well-informed and competent trainee working with you, ready to tackle tasks from handling patient inquiries to summarizing intricate medical literature.
Currently, ChatGPT works on the “freemium” pricing model; there is a free version built upon GPT-3.5 as well as a subscription “ChatGPT Plus” version based on GPT-4 which offers additional features such as the use of third-party plug-ins.
Now, you may ask, “Isn’t the free version enough?” The free version is indeed impressive, but upgrading to the paid version for $20 per month unlocks the full potential of this tool, particularly if we add plug-ins.
Here are some of the best ways to incorporate ChatGPT Plus into your practice.
Time saver and efficiency multiplier. The paid version of ChatGPT is an extraordinary time-saving tool. It can help you sort through vast amounts of medical literature in a fraction of the time it would normally take. Imagine having to sift through hundreds of articles to find the latest research relevant to a patient’s case. With the paid version of ChatGPT, you can simply ask it to provide summaries of the most recent and relevant studies, all in seconds.
Did you forget about that PowerPoint you need to make but know the potential papers you would use? No problem. ChatGPT can create slides in a few minutes. It becomes your on-demand research assistant.
Of course, you need to provide the source you find most relevant to you. Using plug-ins such as ScholarAI and Link Reader are great.
Improved patient communication. Explaining complex medical terminology and procedures to patients can sometimes be a challenge. ChatGPT can generate simplified and personalized explanations for your patients, fostering their understanding and involvement in their care process.
Epic is currently collaborating with Nuance Communications, Microsoft’s speech recognition subsidiary, to use generative AI tools for medical note-taking in the electronic health record. However, you do not need to wait for it; it just takes a prompt in ChatGPT and then copying/pasting the results into the chart.
Smoother administrative management. The premium version of ChatGPT can automate administrative tasks such as creating letters of medical necessity, clearance to other physicians for services, or even communications to staff on specific topics. This frees you to focus more on your core work: providing patient care.
Precision medicine aid. ChatGPT can be a powerful ally in the field of precision medicine. Its capabilities for analyzing large datasets and unearthing valuable insights can help deliver more personalized and potentially effective treatment plans. For example, one can prompt ChatGPT to query the reported frequency of certain genomic variants and their implications; with the upgraded version and plug-ins, the results will have fewer hallucinations — inaccurate results — and key data references.
Unlimited accessibility. Uninterrupted access is a compelling reason to upgrade. While the free version may have usage limitations, the premium version provides unrestricted, round-the-clock access. Be it a late-night research quest or an early-morning patient query, your AI assistant will always be available.
Strengthened privacy and security. The premium version of ChatGPT includes heightened privacy and security measures. Just make sure to follow HIPAA and not include identifiers when making queries.
Embracing AI tools like ChatGPT in your practice can help you stay at the cutting edge of medical care, saving you time, enhancing patient communication, and supporting you in providing personalized care.
While the free version can serve as a good starting point (there are apps for both iOS and Android), upgrading to the paid version opens up a world of possibilities that can truly supercharge your practice.
I would love to hear your comments on this column or on future topics. Contact me at [email protected].
Arturo Loaiza-Bonilla, MD, MSEd, is the cofounder and chief medical officer at Massive Bio, a company connecting patients to clinical trials using artificial intelligence. His research and professional interests focus on precision medicine, clinical trial design, digital health, entrepreneurship, and patient advocacy. Dr. Loaiza-Bonilla is Assistant Professor of Medicine, Drexel University School of Medicine, Philadelphia, Pennsylvania, and serves as medical director of oncology research at Capital Health in New Jersey, where he maintains a connection to patient care by attending to patients 2 days a week. He has financial relationships with Verify, PSI CRO, Bayer, AstraZeneca, Cardinal Health, BrightInsight, The Lynx Group, Fresenius, Pfizer, Ipsen, Guardant, Amgen, Eisai, Natera, Merck, and Bristol Myers Squibb.
A version of this article appeared on Medscape.com.
Toward a better framework for postmarketing reproductive safety surveillance of medications
For the last 30 years, the Center for Women’s Mental Health at Massachusetts General Hospital (MGH) has had as part of its mission, the conveying of accurate information about the reproductive safety of psychiatric medications. There has been a spectrum of medicines developed across psychiatric indications over the last several decades, and many studies over those decades have attempted to delineate the reproductive safety of these agents.
With the development of new antidepressants and second-generation antipsychotics has come an appreciation of the utility of these agents across a wide range of psychiatric disease states and psychiatric symptoms. More and more data demonstrate the efficacy of these medicines for mood and anxiety disorders; these agents are also used for a broad array of symptoms from insomnia, irritability, and symptoms of posttraumatic stress disorder (PTSD) just as examples — even absent formal approval by the US Food and Drug Administration (FDA) for these specific indications. With the growing use of medicines, including new antidepressants like selective serotonin reuptake inhibitors (SSRIs) and serotonin-norepinephrine reuptake inhibitors, and second-generation atypical antipsychotics, there has been a greater interest and appreciation of the need to provide women with the best information about reproductive safety of these medicines as well.
When I began working in reproductive psychiatry, the FDA was using the pregnancy labeling categories introduced in 1979. The categories were simple, but also oversimplified in terms of incompletely conveying information about reproductive safety. For instance, category labels of B and C under the old labeling system could be nebulous, containing sparse information (in the case of category B) or animal data and some conflicting human data (in the case of category C) that may not have translated into relevant or easily interpretable safety information for patients and clinicians.
It was on that basis the current Pregnancy and Lactation Labeling (PLLR) Final Rule was published in 2014, which was a shift from categorical labeling to more descriptive labeling, including updated actual information on the package insert about available reproductive safety data, animal data, and data on lactation.
Even following the publication of the PLLR, there has still been an acknowledgment in the field that our assessment tools for postmarketing reproductive safety surveillance are incomplete. A recent 2-day FDA workshop hosted by the Duke-Margolis Center for Health Policy on optimizing the use of postapproval pregnancy safety studies sought to discuss the many questions that still surround this issue. Based on presentations at this workshop, a framework emerged for the future of assessing the reproductive safety of medications, which included an effort to develop the most effective model using tools such as pregnancy registries and harnessing “big data,” whether through electronic health records or large administrative databases from public and private insurers. Together, these various sources of information can provide signals of potential concern, prompting the need for a more rigorous look at the reproductive safety of a medication, or provide reassurance if data fail to indicate the absence of a signal of risk.
FDA’s new commitments under the latest reauthorization of the Prescription Drug User Fee Act (PDUFA VII) include pregnancy-specific postmarketing safety requirements as well as the creation of a framework for how data from pregnancy-specific postmarketing studies can be used. The agency is also conducting demonstration projects, including one for assessing the performance of pregnancy registries for the potential to detect safety signals for medications early in pregnancy. FDA is expanding its Sentinel Initiative to help accomplish these aims, and is implementing an Active Risk Identification and Analysis (ARIA) system to conduct active safety surveillance of medications used during pregnancy.
Pregnancy registries have now been available for decades, and some have been more successful than others across different classes of medicines, with the most rigorous registries including prospective follow-up of women across pregnancies and careful documentation of malformations (at best with original source data and with a blinded dysmorphologist). Still, with all of its rigor, even the best-intentioned efforts with respect to pregnancy registries have limitations. As I mentioned in my testimony during the public comment portion of the workshop, the sheer volume of pregnancy data from administrative databases we now have access to is attractive, but the quality of these data needs to be good enough to ascertain a signal of risk if they are to be used as a basis for reproductive safety determination.
The flip side of using data from large administrative databases is using carefully collected data from pregnancy registries. With a pregnancy registry, accrual of a substantial number of participants can also take a considerable period of time, and initial risk estimates of outcomes can have typically large confidence intervals, which can make it difficult to discern whether a drug is safe for women of reproductive age.
Another key issue is a lack of participation from manufacturers with respect to commitment to collection of high-quality reproductive safety data. History has shown that many medication manufacturers, unless required to have a dedicated registry as part of a postmarketing requirement or commitment, will invest sparse resources to track data on safety of fetal drug exposure. Participation is typically voluntary and varies from company to company unless, as noted previously, there is a postmarketing requirement or commitment tied to the approval of a medication. Just as a recent concrete example, the manufacturer of a new medication recently approved by the FDA for the treatment of postpartum depression (which will include presumably sexually active women well into the first postpartum year) has no plan to support the collection of reproductive safety data on this new medication because it is not required to, based on current FDA guidelines and the absence of a postmarketing requirement to do so.
Looking ahead
While the PLLR was a huge step forward in the field from the old pregnancy category system that could misinform women contemplating pregnancy, it also sets the stage for the next iteration of a system that allows us to generate information more quickly about the reproductive safety of medications. In psychiatry, as many as 10% of women use SSRIs during pregnancy. With drugs like atypical antipsychotics being used across disease states — in schizophrenia, bipolar disorder, depression, anxiety, insomnia, and PTSD — and where new classes of medicine are becoming available, like with ketamine or steroids, we need to have a system by which we can more quickly ascertain reproductive safety information. This information informs treatment decisions during a critical life event of deciding to try to become pregnant or during an actual pregnancy.
In my mind, it is reassuring when a registry has even as few as 50-60 cases of fetal exposure without an increase in the risk for malformation, because it can mean we are not seeing a repeat of the past with medications like thalidomide and sodium valproate. However, patients and clinicians are starved for better data. Risk assessment is also different from clinician to clinician and patient to patient. We want to empower patients to make decisions that work for them based on more rapidly accumulating information and help inform their decisions.
To come out on the “other side” of the PLLR, , which can be confusing when study results frequently conflict. I believe we have an obligation today to do this better, because the areas of reproductive toxicology and pharmacovigilance are growing incredibly quickly, and clinicians and patients are seeing these volumes of data being published without the ability to integrate that information in a systematic way.
Dr. Cohen is the director of the Ammon-Pinizzotto Center for Women’s Mental Health at Massachusetts General Hospital (MGH) in Boston, which provides information resources and conducts clinical care and research in reproductive mental health. He has been a consultant to manufacturers of psychiatric medications. Full disclosure information for Dr. Cohen is available at womensmentalhealth.org. Email Dr. Cohen at [email protected].
For the last 30 years, the Center for Women’s Mental Health at Massachusetts General Hospital (MGH) has had as part of its mission, the conveying of accurate information about the reproductive safety of psychiatric medications. There has been a spectrum of medicines developed across psychiatric indications over the last several decades, and many studies over those decades have attempted to delineate the reproductive safety of these agents.
With the development of new antidepressants and second-generation antipsychotics has come an appreciation of the utility of these agents across a wide range of psychiatric disease states and psychiatric symptoms. More and more data demonstrate the efficacy of these medicines for mood and anxiety disorders; these agents are also used for a broad array of symptoms from insomnia, irritability, and symptoms of posttraumatic stress disorder (PTSD) just as examples — even absent formal approval by the US Food and Drug Administration (FDA) for these specific indications. With the growing use of medicines, including new antidepressants like selective serotonin reuptake inhibitors (SSRIs) and serotonin-norepinephrine reuptake inhibitors, and second-generation atypical antipsychotics, there has been a greater interest and appreciation of the need to provide women with the best information about reproductive safety of these medicines as well.
When I began working in reproductive psychiatry, the FDA was using the pregnancy labeling categories introduced in 1979. The categories were simple, but also oversimplified in terms of incompletely conveying information about reproductive safety. For instance, category labels of B and C under the old labeling system could be nebulous, containing sparse information (in the case of category B) or animal data and some conflicting human data (in the case of category C) that may not have translated into relevant or easily interpretable safety information for patients and clinicians.
It was on that basis the current Pregnancy and Lactation Labeling (PLLR) Final Rule was published in 2014, which was a shift from categorical labeling to more descriptive labeling, including updated actual information on the package insert about available reproductive safety data, animal data, and data on lactation.
Even following the publication of the PLLR, there has still been an acknowledgment in the field that our assessment tools for postmarketing reproductive safety surveillance are incomplete. A recent 2-day FDA workshop hosted by the Duke-Margolis Center for Health Policy on optimizing the use of postapproval pregnancy safety studies sought to discuss the many questions that still surround this issue. Based on presentations at this workshop, a framework emerged for the future of assessing the reproductive safety of medications, which included an effort to develop the most effective model using tools such as pregnancy registries and harnessing “big data,” whether through electronic health records or large administrative databases from public and private insurers. Together, these various sources of information can provide signals of potential concern, prompting the need for a more rigorous look at the reproductive safety of a medication, or provide reassurance if data fail to indicate the absence of a signal of risk.
FDA’s new commitments under the latest reauthorization of the Prescription Drug User Fee Act (PDUFA VII) include pregnancy-specific postmarketing safety requirements as well as the creation of a framework for how data from pregnancy-specific postmarketing studies can be used. The agency is also conducting demonstration projects, including one for assessing the performance of pregnancy registries for the potential to detect safety signals for medications early in pregnancy. FDA is expanding its Sentinel Initiative to help accomplish these aims, and is implementing an Active Risk Identification and Analysis (ARIA) system to conduct active safety surveillance of medications used during pregnancy.
Pregnancy registries have now been available for decades, and some have been more successful than others across different classes of medicines, with the most rigorous registries including prospective follow-up of women across pregnancies and careful documentation of malformations (at best with original source data and with a blinded dysmorphologist). Still, with all of its rigor, even the best-intentioned efforts with respect to pregnancy registries have limitations. As I mentioned in my testimony during the public comment portion of the workshop, the sheer volume of pregnancy data from administrative databases we now have access to is attractive, but the quality of these data needs to be good enough to ascertain a signal of risk if they are to be used as a basis for reproductive safety determination.
The flip side of using data from large administrative databases is using carefully collected data from pregnancy registries. With a pregnancy registry, accrual of a substantial number of participants can also take a considerable period of time, and initial risk estimates of outcomes can have typically large confidence intervals, which can make it difficult to discern whether a drug is safe for women of reproductive age.
Another key issue is a lack of participation from manufacturers with respect to commitment to collection of high-quality reproductive safety data. History has shown that many medication manufacturers, unless required to have a dedicated registry as part of a postmarketing requirement or commitment, will invest sparse resources to track data on safety of fetal drug exposure. Participation is typically voluntary and varies from company to company unless, as noted previously, there is a postmarketing requirement or commitment tied to the approval of a medication. Just as a recent concrete example, the manufacturer of a new medication recently approved by the FDA for the treatment of postpartum depression (which will include presumably sexually active women well into the first postpartum year) has no plan to support the collection of reproductive safety data on this new medication because it is not required to, based on current FDA guidelines and the absence of a postmarketing requirement to do so.
Looking ahead
While the PLLR was a huge step forward in the field from the old pregnancy category system that could misinform women contemplating pregnancy, it also sets the stage for the next iteration of a system that allows us to generate information more quickly about the reproductive safety of medications. In psychiatry, as many as 10% of women use SSRIs during pregnancy. With drugs like atypical antipsychotics being used across disease states — in schizophrenia, bipolar disorder, depression, anxiety, insomnia, and PTSD — and where new classes of medicine are becoming available, like with ketamine or steroids, we need to have a system by which we can more quickly ascertain reproductive safety information. This information informs treatment decisions during a critical life event of deciding to try to become pregnant or during an actual pregnancy.
In my mind, it is reassuring when a registry has even as few as 50-60 cases of fetal exposure without an increase in the risk for malformation, because it can mean we are not seeing a repeat of the past with medications like thalidomide and sodium valproate. However, patients and clinicians are starved for better data. Risk assessment is also different from clinician to clinician and patient to patient. We want to empower patients to make decisions that work for them based on more rapidly accumulating information and help inform their decisions.
To come out on the “other side” of the PLLR, , which can be confusing when study results frequently conflict. I believe we have an obligation today to do this better, because the areas of reproductive toxicology and pharmacovigilance are growing incredibly quickly, and clinicians and patients are seeing these volumes of data being published without the ability to integrate that information in a systematic way.
Dr. Cohen is the director of the Ammon-Pinizzotto Center for Women’s Mental Health at Massachusetts General Hospital (MGH) in Boston, which provides information resources and conducts clinical care and research in reproductive mental health. He has been a consultant to manufacturers of psychiatric medications. Full disclosure information for Dr. Cohen is available at womensmentalhealth.org. Email Dr. Cohen at [email protected].
For the last 30 years, the Center for Women’s Mental Health at Massachusetts General Hospital (MGH) has had as part of its mission, the conveying of accurate information about the reproductive safety of psychiatric medications. There has been a spectrum of medicines developed across psychiatric indications over the last several decades, and many studies over those decades have attempted to delineate the reproductive safety of these agents.
With the development of new antidepressants and second-generation antipsychotics has come an appreciation of the utility of these agents across a wide range of psychiatric disease states and psychiatric symptoms. More and more data demonstrate the efficacy of these medicines for mood and anxiety disorders; these agents are also used for a broad array of symptoms from insomnia, irritability, and symptoms of posttraumatic stress disorder (PTSD) just as examples — even absent formal approval by the US Food and Drug Administration (FDA) for these specific indications. With the growing use of medicines, including new antidepressants like selective serotonin reuptake inhibitors (SSRIs) and serotonin-norepinephrine reuptake inhibitors, and second-generation atypical antipsychotics, there has been a greater interest and appreciation of the need to provide women with the best information about reproductive safety of these medicines as well.
When I began working in reproductive psychiatry, the FDA was using the pregnancy labeling categories introduced in 1979. The categories were simple, but also oversimplified in terms of incompletely conveying information about reproductive safety. For instance, category labels of B and C under the old labeling system could be nebulous, containing sparse information (in the case of category B) or animal data and some conflicting human data (in the case of category C) that may not have translated into relevant or easily interpretable safety information for patients and clinicians.
It was on that basis the current Pregnancy and Lactation Labeling (PLLR) Final Rule was published in 2014, which was a shift from categorical labeling to more descriptive labeling, including updated actual information on the package insert about available reproductive safety data, animal data, and data on lactation.
Even following the publication of the PLLR, there has still been an acknowledgment in the field that our assessment tools for postmarketing reproductive safety surveillance are incomplete. A recent 2-day FDA workshop hosted by the Duke-Margolis Center for Health Policy on optimizing the use of postapproval pregnancy safety studies sought to discuss the many questions that still surround this issue. Based on presentations at this workshop, a framework emerged for the future of assessing the reproductive safety of medications, which included an effort to develop the most effective model using tools such as pregnancy registries and harnessing “big data,” whether through electronic health records or large administrative databases from public and private insurers. Together, these various sources of information can provide signals of potential concern, prompting the need for a more rigorous look at the reproductive safety of a medication, or provide reassurance if data fail to indicate the absence of a signal of risk.
FDA’s new commitments under the latest reauthorization of the Prescription Drug User Fee Act (PDUFA VII) include pregnancy-specific postmarketing safety requirements as well as the creation of a framework for how data from pregnancy-specific postmarketing studies can be used. The agency is also conducting demonstration projects, including one for assessing the performance of pregnancy registries for the potential to detect safety signals for medications early in pregnancy. FDA is expanding its Sentinel Initiative to help accomplish these aims, and is implementing an Active Risk Identification and Analysis (ARIA) system to conduct active safety surveillance of medications used during pregnancy.
Pregnancy registries have now been available for decades, and some have been more successful than others across different classes of medicines, with the most rigorous registries including prospective follow-up of women across pregnancies and careful documentation of malformations (at best with original source data and with a blinded dysmorphologist). Still, with all of its rigor, even the best-intentioned efforts with respect to pregnancy registries have limitations. As I mentioned in my testimony during the public comment portion of the workshop, the sheer volume of pregnancy data from administrative databases we now have access to is attractive, but the quality of these data needs to be good enough to ascertain a signal of risk if they are to be used as a basis for reproductive safety determination.
The flip side of using data from large administrative databases is using carefully collected data from pregnancy registries. With a pregnancy registry, accrual of a substantial number of participants can also take a considerable period of time, and initial risk estimates of outcomes can have typically large confidence intervals, which can make it difficult to discern whether a drug is safe for women of reproductive age.
Another key issue is a lack of participation from manufacturers with respect to commitment to collection of high-quality reproductive safety data. History has shown that many medication manufacturers, unless required to have a dedicated registry as part of a postmarketing requirement or commitment, will invest sparse resources to track data on safety of fetal drug exposure. Participation is typically voluntary and varies from company to company unless, as noted previously, there is a postmarketing requirement or commitment tied to the approval of a medication. Just as a recent concrete example, the manufacturer of a new medication recently approved by the FDA for the treatment of postpartum depression (which will include presumably sexually active women well into the first postpartum year) has no plan to support the collection of reproductive safety data on this new medication because it is not required to, based on current FDA guidelines and the absence of a postmarketing requirement to do so.
Looking ahead
While the PLLR was a huge step forward in the field from the old pregnancy category system that could misinform women contemplating pregnancy, it also sets the stage for the next iteration of a system that allows us to generate information more quickly about the reproductive safety of medications. In psychiatry, as many as 10% of women use SSRIs during pregnancy. With drugs like atypical antipsychotics being used across disease states — in schizophrenia, bipolar disorder, depression, anxiety, insomnia, and PTSD — and where new classes of medicine are becoming available, like with ketamine or steroids, we need to have a system by which we can more quickly ascertain reproductive safety information. This information informs treatment decisions during a critical life event of deciding to try to become pregnant or during an actual pregnancy.
In my mind, it is reassuring when a registry has even as few as 50-60 cases of fetal exposure without an increase in the risk for malformation, because it can mean we are not seeing a repeat of the past with medications like thalidomide and sodium valproate. However, patients and clinicians are starved for better data. Risk assessment is also different from clinician to clinician and patient to patient. We want to empower patients to make decisions that work for them based on more rapidly accumulating information and help inform their decisions.
To come out on the “other side” of the PLLR, , which can be confusing when study results frequently conflict. I believe we have an obligation today to do this better, because the areas of reproductive toxicology and pharmacovigilance are growing incredibly quickly, and clinicians and patients are seeing these volumes of data being published without the ability to integrate that information in a systematic way.
Dr. Cohen is the director of the Ammon-Pinizzotto Center for Women’s Mental Health at Massachusetts General Hospital (MGH) in Boston, which provides information resources and conducts clinical care and research in reproductive mental health. He has been a consultant to manufacturers of psychiatric medications. Full disclosure information for Dr. Cohen is available at womensmentalhealth.org. Email Dr. Cohen at [email protected].
How to prescribe Zepbound
December marks the advent of the approval of tirzepatide (Zepbound) for on-label treatment of obesity. In November 2023, the US Food and Drug Administration (FDA) approved it for the treatment of obesity in adults.
In May 2022, the FDA approved Mounjaro, which is tirzepatide, for type 2 diabetes. Since then, many physicians, including myself, have prescribed it off-label for obesity. As an endocrinologist treating both obesity and diabetes, 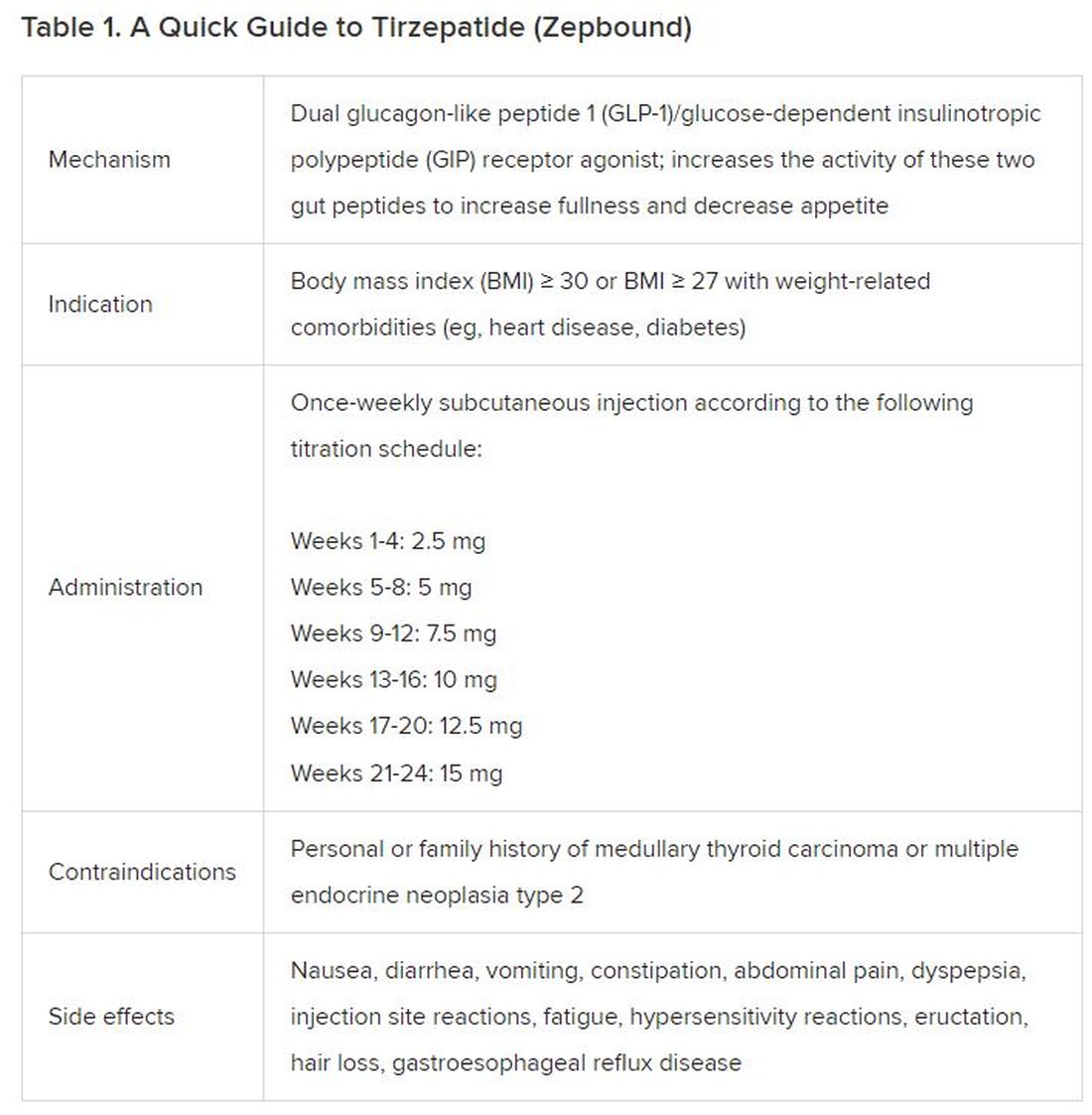
The Expertise
Because GLP-1 receptor agonists have been around since 2005, we’ve had over a decade of clinical experience with these medications. Table 2 provides more nuanced information on tirzepatide (as Zepbound, for obesity) based on our experiences with dulaglutide, liraglutide, semaglutide, and tirzepatide (as Mounjaro).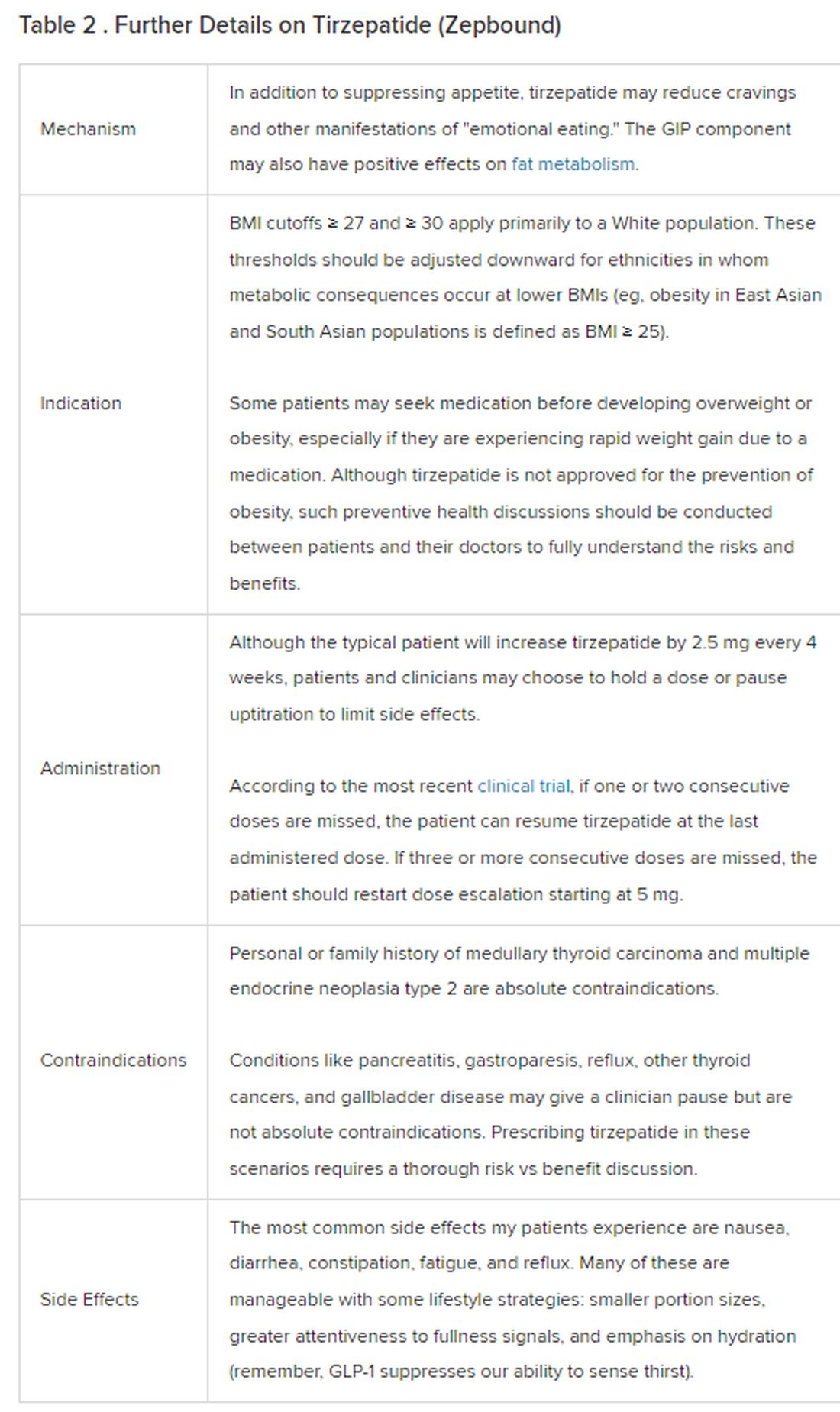
The Reality
In today’s increasingly complex healthcare system, the reality of providing high-quality obesity care is challenging. When discussing tirzepatide with patients, I use a 4 Cs schematic — comorbidities, cautions, costs, choices — to cover the most frequently asked questions.
Comorbidities
In trials, tirzepatide reduced A1c by about 2%. In one diabetes trial, tirzepatide reduced liver fat content significantly more than the comparator (insulin), and trials of tirzepatide in nonalcoholic steatohepatitis are ongoing. A prespecified meta-analysis of tirzepatide and cardiovascular disease estimated a 20% reduction in the risk for cardiovascular death, myocardial infarction, stroke, and hospitalized unstable angina. Tirzepatide as well as other GLP-1 agonists may be beneficial in alcohol use disorder. Prescribing tirzepatide to patients who have or are at risk of developing such comorbidities is an ideal way to target multiple metabolic diseases with one agent.
Cautions
The first principle of medicine is “do no harm.” Tirzepatide may be a poor option for individuals with a history of pancreatitis, gastroparesis, or severe gastroesophageal reflux disease. Because tirzepatide may interfere with the efficacy of estrogen-containing contraceptives during its uptitration phase, women should speak with their doctors about appropriate birth control options (eg, progestin-only, barrier methods). In clinical trials of tirzepatide, male participants were also advised to use reliable contraception. If patients are family-planning, tirzepatide should be discontinued 2 months (for women) and 4 months (for men) before conception, because its effects on fertility or pregnancy are currently unknown.
Costs
At a retail price of $1279 per month, Zepbound is only slightly more affordable than its main competitor, Wegovy (semaglutide 2.4 mg). Complex pharmacy negotiations may reduce this cost, but even with rebates, coupons, and commercial insurance, these costs still place tirzepatide out of reach for many patients. For patients who cannot access tirzepatide, clinicians should discuss more cost-feasible, evidence-based alternatives: for example, phentermine, phentermine-topiramate, naltrexone-bupropion, metformin, bupropion, or topiramate.
Choices
Patient preference drives much of today’s clinical decision-making. Some patients may be switching from semaglutide to tirzepatide, whether by choice or on the basis of physician recommendation. Although no head-to-head obesity trial exists, data from SURPASS-2 and SUSTAIN-FORTE can inform therapeutic equivalence:
- Semaglutide 1.0 mg to tirzepatide 2.5 mg will be a step-down; 5 mg will be a step-up
- Semaglutide 2.0 or 2.4 mg to tirzepatide 5 mg is probably equivalent
The decision to switch therapeutics may depend on weight loss goals, side effect tolerability, or insurance coverage. As with all medications, the use of tirzepatide should progress with shared decision-making, thorough discussions of risks vs benefits, and individualized regimens tailored to each patient’s needs.
The newly approved Zepbound is a valuable addition to our toolbox of obesity treatments. Patients and providers alike are excited for its potential as a highly effective antiobesity medication that can cause a degree of weight loss necessary to reverse comorbidities. The medical management of obesity with agents like tirzepatide holds great promise in addressing today’s obesity epidemic.
Dr. Tchang is Assistant Professor, Clinical Medicine, Division of Endocrinology, Diabetes, and Metabolism, Weill Cornell Medicine; Physician, Department of Medicine, Iris Cantor Women’s Health Center, Comprehensive Weight Control Center, New York, NY. She disclosed ties to Gelesis and Novo Nordisk.
A version of this article appeared on Medscape.com.
December marks the advent of the approval of tirzepatide (Zepbound) for on-label treatment of obesity. In November 2023, the US Food and Drug Administration (FDA) approved it for the treatment of obesity in adults.
In May 2022, the FDA approved Mounjaro, which is tirzepatide, for type 2 diabetes. Since then, many physicians, including myself, have prescribed it off-label for obesity. As an endocrinologist treating both obesity and diabetes, 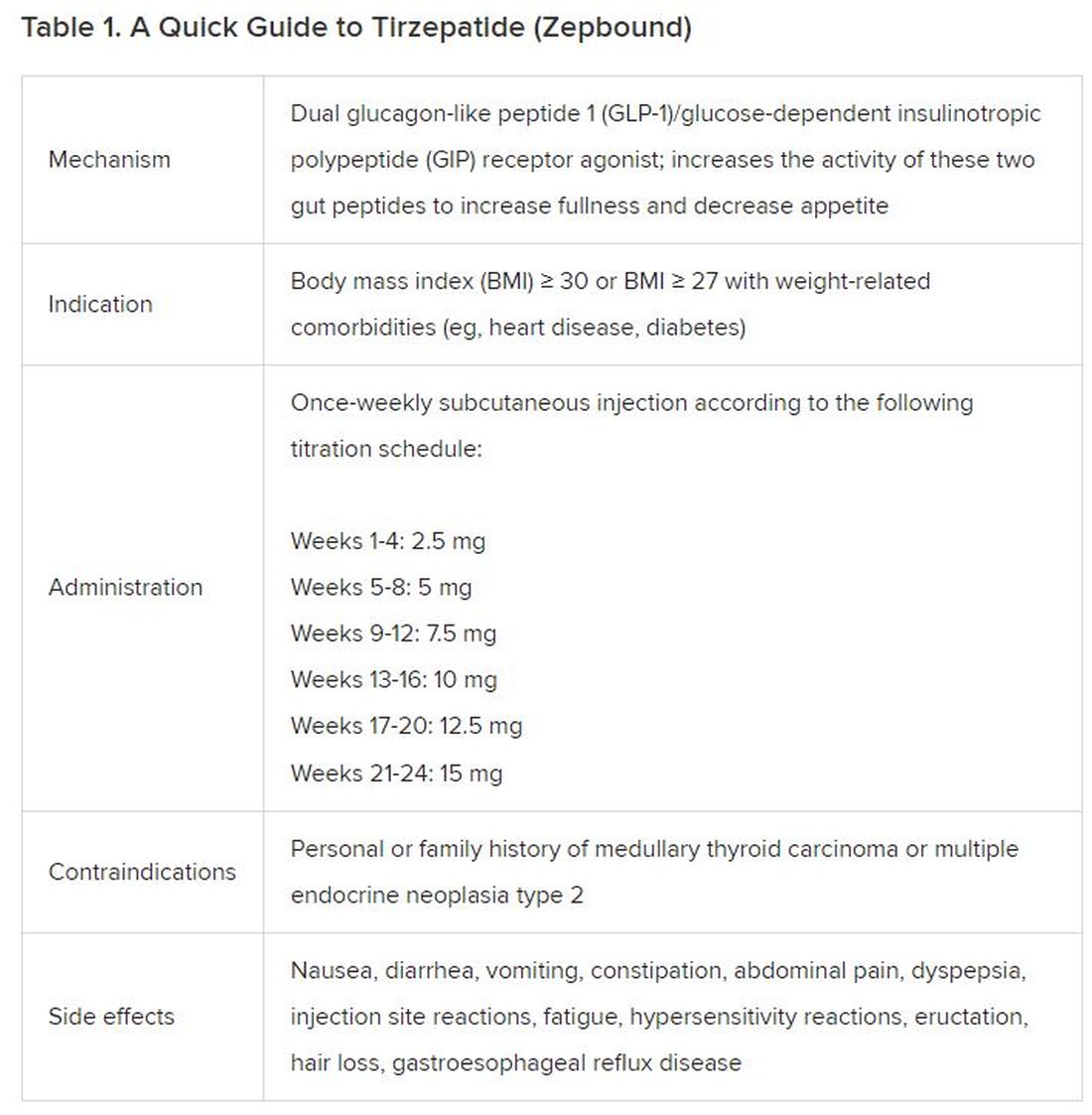
The Expertise
Because GLP-1 receptor agonists have been around since 2005, we’ve had over a decade of clinical experience with these medications. Table 2 provides more nuanced information on tirzepatide (as Zepbound, for obesity) based on our experiences with dulaglutide, liraglutide, semaglutide, and tirzepatide (as Mounjaro).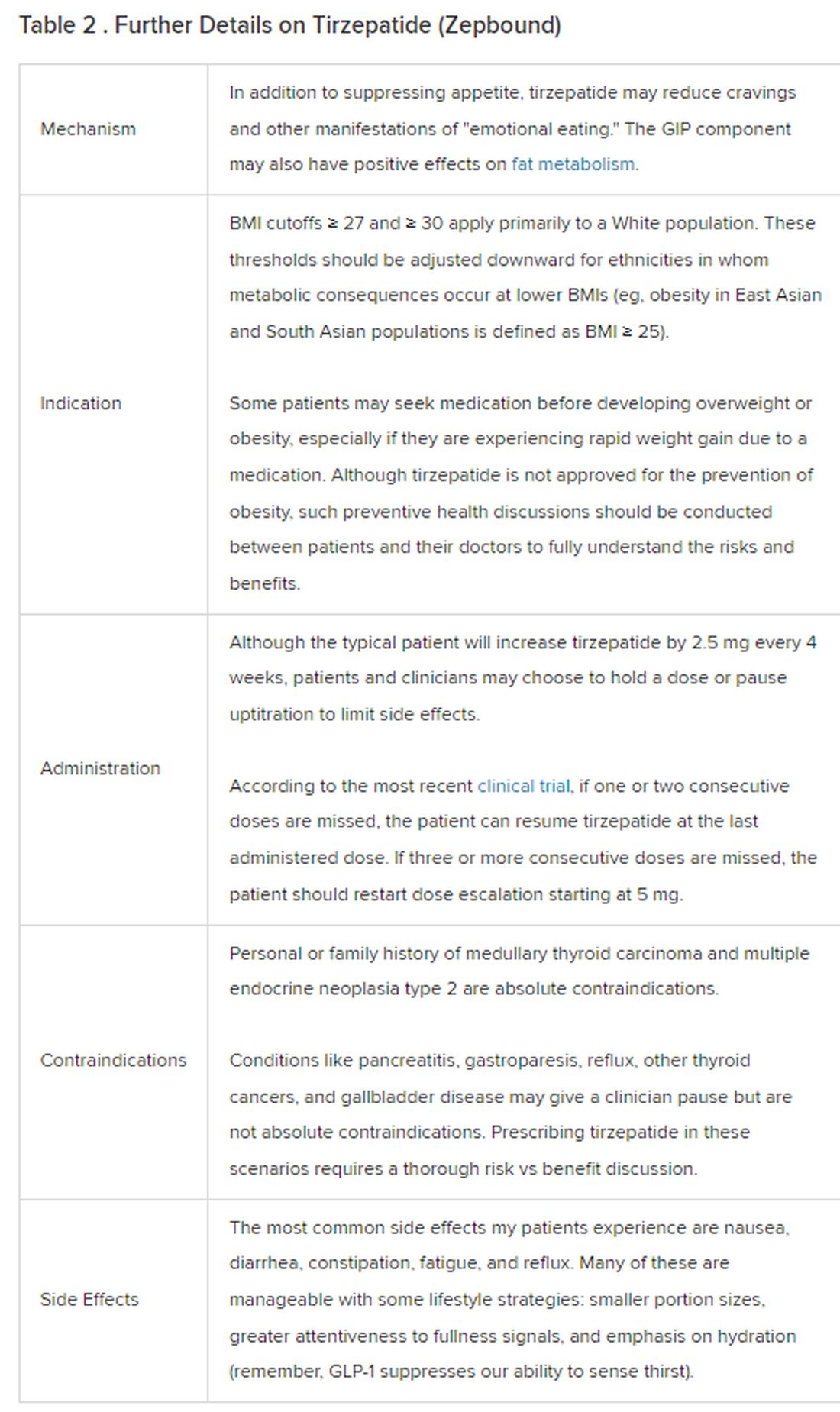
The Reality
In today’s increasingly complex healthcare system, the reality of providing high-quality obesity care is challenging. When discussing tirzepatide with patients, I use a 4 Cs schematic — comorbidities, cautions, costs, choices — to cover the most frequently asked questions.
Comorbidities
In trials, tirzepatide reduced A1c by about 2%. In one diabetes trial, tirzepatide reduced liver fat content significantly more than the comparator (insulin), and trials of tirzepatide in nonalcoholic steatohepatitis are ongoing. A prespecified meta-analysis of tirzepatide and cardiovascular disease estimated a 20% reduction in the risk for cardiovascular death, myocardial infarction, stroke, and hospitalized unstable angina. Tirzepatide as well as other GLP-1 agonists may be beneficial in alcohol use disorder. Prescribing tirzepatide to patients who have or are at risk of developing such comorbidities is an ideal way to target multiple metabolic diseases with one agent.
Cautions
The first principle of medicine is “do no harm.” Tirzepatide may be a poor option for individuals with a history of pancreatitis, gastroparesis, or severe gastroesophageal reflux disease. Because tirzepatide may interfere with the efficacy of estrogen-containing contraceptives during its uptitration phase, women should speak with their doctors about appropriate birth control options (eg, progestin-only, barrier methods). In clinical trials of tirzepatide, male participants were also advised to use reliable contraception. If patients are family-planning, tirzepatide should be discontinued 2 months (for women) and 4 months (for men) before conception, because its effects on fertility or pregnancy are currently unknown.
Costs
At a retail price of $1279 per month, Zepbound is only slightly more affordable than its main competitor, Wegovy (semaglutide 2.4 mg). Complex pharmacy negotiations may reduce this cost, but even with rebates, coupons, and commercial insurance, these costs still place tirzepatide out of reach for many patients. For patients who cannot access tirzepatide, clinicians should discuss more cost-feasible, evidence-based alternatives: for example, phentermine, phentermine-topiramate, naltrexone-bupropion, metformin, bupropion, or topiramate.
Choices
Patient preference drives much of today’s clinical decision-making. Some patients may be switching from semaglutide to tirzepatide, whether by choice or on the basis of physician recommendation. Although no head-to-head obesity trial exists, data from SURPASS-2 and SUSTAIN-FORTE can inform therapeutic equivalence:
- Semaglutide 1.0 mg to tirzepatide 2.5 mg will be a step-down; 5 mg will be a step-up
- Semaglutide 2.0 or 2.4 mg to tirzepatide 5 mg is probably equivalent
The decision to switch therapeutics may depend on weight loss goals, side effect tolerability, or insurance coverage. As with all medications, the use of tirzepatide should progress with shared decision-making, thorough discussions of risks vs benefits, and individualized regimens tailored to each patient’s needs.
The newly approved Zepbound is a valuable addition to our toolbox of obesity treatments. Patients and providers alike are excited for its potential as a highly effective antiobesity medication that can cause a degree of weight loss necessary to reverse comorbidities. The medical management of obesity with agents like tirzepatide holds great promise in addressing today’s obesity epidemic.
Dr. Tchang is Assistant Professor, Clinical Medicine, Division of Endocrinology, Diabetes, and Metabolism, Weill Cornell Medicine; Physician, Department of Medicine, Iris Cantor Women’s Health Center, Comprehensive Weight Control Center, New York, NY. She disclosed ties to Gelesis and Novo Nordisk.
A version of this article appeared on Medscape.com.
December marks the advent of the approval of tirzepatide (Zepbound) for on-label treatment of obesity. In November 2023, the US Food and Drug Administration (FDA) approved it for the treatment of obesity in adults.
In May 2022, the FDA approved Mounjaro, which is tirzepatide, for type 2 diabetes. Since then, many physicians, including myself, have prescribed it off-label for obesity. As an endocrinologist treating both obesity and diabetes, 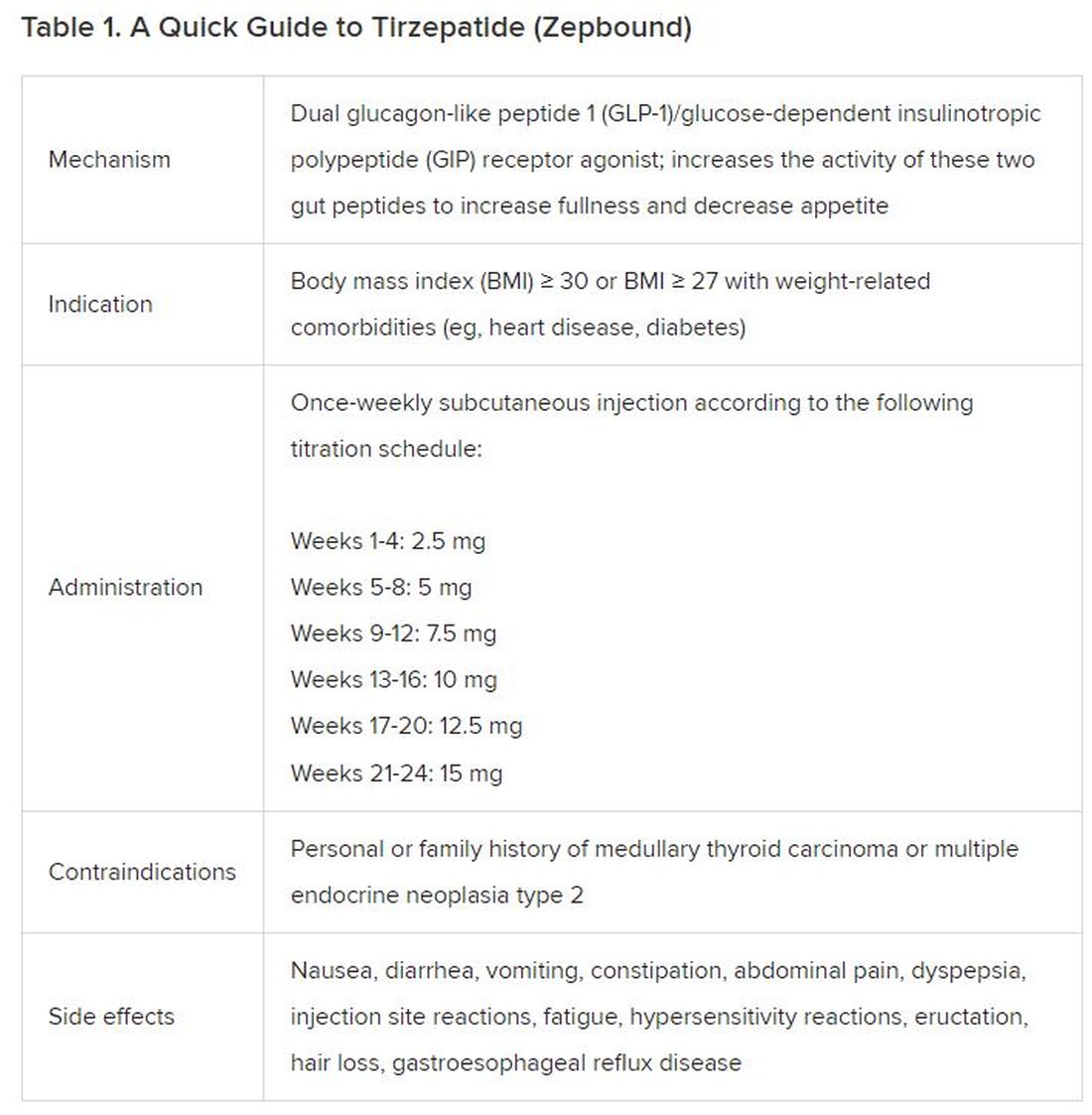
The Expertise
Because GLP-1 receptor agonists have been around since 2005, we’ve had over a decade of clinical experience with these medications. Table 2 provides more nuanced information on tirzepatide (as Zepbound, for obesity) based on our experiences with dulaglutide, liraglutide, semaglutide, and tirzepatide (as Mounjaro).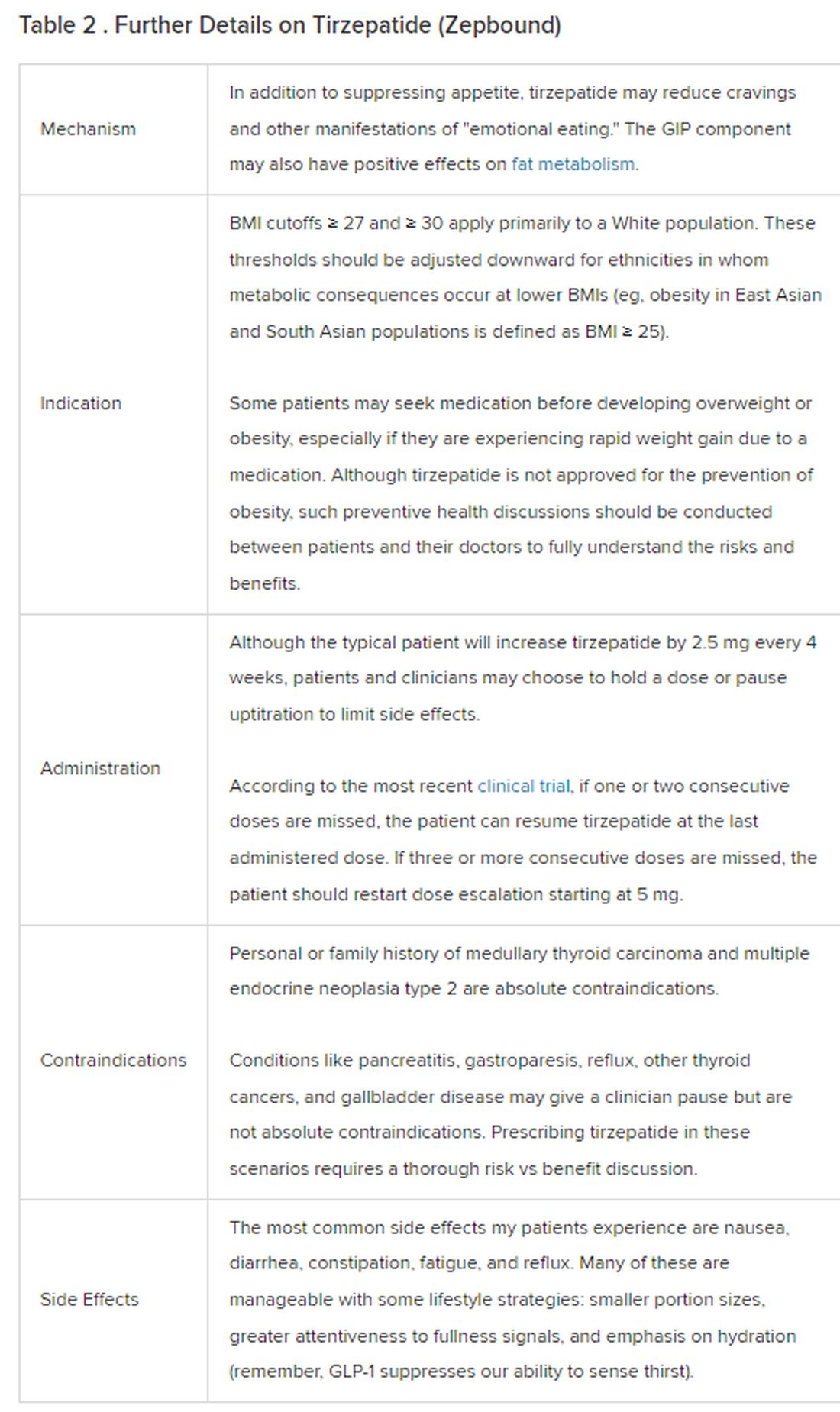
The Reality
In today’s increasingly complex healthcare system, the reality of providing high-quality obesity care is challenging. When discussing tirzepatide with patients, I use a 4 Cs schematic — comorbidities, cautions, costs, choices — to cover the most frequently asked questions.
Comorbidities
In trials, tirzepatide reduced A1c by about 2%. In one diabetes trial, tirzepatide reduced liver fat content significantly more than the comparator (insulin), and trials of tirzepatide in nonalcoholic steatohepatitis are ongoing. A prespecified meta-analysis of tirzepatide and cardiovascular disease estimated a 20% reduction in the risk for cardiovascular death, myocardial infarction, stroke, and hospitalized unstable angina. Tirzepatide as well as other GLP-1 agonists may be beneficial in alcohol use disorder. Prescribing tirzepatide to patients who have or are at risk of developing such comorbidities is an ideal way to target multiple metabolic diseases with one agent.
Cautions
The first principle of medicine is “do no harm.” Tirzepatide may be a poor option for individuals with a history of pancreatitis, gastroparesis, or severe gastroesophageal reflux disease. Because tirzepatide may interfere with the efficacy of estrogen-containing contraceptives during its uptitration phase, women should speak with their doctors about appropriate birth control options (eg, progestin-only, barrier methods). In clinical trials of tirzepatide, male participants were also advised to use reliable contraception. If patients are family-planning, tirzepatide should be discontinued 2 months (for women) and 4 months (for men) before conception, because its effects on fertility or pregnancy are currently unknown.
Costs
At a retail price of $1279 per month, Zepbound is only slightly more affordable than its main competitor, Wegovy (semaglutide 2.4 mg). Complex pharmacy negotiations may reduce this cost, but even with rebates, coupons, and commercial insurance, these costs still place tirzepatide out of reach for many patients. For patients who cannot access tirzepatide, clinicians should discuss more cost-feasible, evidence-based alternatives: for example, phentermine, phentermine-topiramate, naltrexone-bupropion, metformin, bupropion, or topiramate.
Choices
Patient preference drives much of today’s clinical decision-making. Some patients may be switching from semaglutide to tirzepatide, whether by choice or on the basis of physician recommendation. Although no head-to-head obesity trial exists, data from SURPASS-2 and SUSTAIN-FORTE can inform therapeutic equivalence:
- Semaglutide 1.0 mg to tirzepatide 2.5 mg will be a step-down; 5 mg will be a step-up
- Semaglutide 2.0 or 2.4 mg to tirzepatide 5 mg is probably equivalent
The decision to switch therapeutics may depend on weight loss goals, side effect tolerability, or insurance coverage. As with all medications, the use of tirzepatide should progress with shared decision-making, thorough discussions of risks vs benefits, and individualized regimens tailored to each patient’s needs.
The newly approved Zepbound is a valuable addition to our toolbox of obesity treatments. Patients and providers alike are excited for its potential as a highly effective antiobesity medication that can cause a degree of weight loss necessary to reverse comorbidities. The medical management of obesity with agents like tirzepatide holds great promise in addressing today’s obesity epidemic.
Dr. Tchang is Assistant Professor, Clinical Medicine, Division of Endocrinology, Diabetes, and Metabolism, Weill Cornell Medicine; Physician, Department of Medicine, Iris Cantor Women’s Health Center, Comprehensive Weight Control Center, New York, NY. She disclosed ties to Gelesis and Novo Nordisk.
A version of this article appeared on Medscape.com.











