User login
Breastfeeding and colorectal cancer
I, like every pediatrician I know, believe that breast milk is the best nutrition for human newborns. Its balance of nutritive elements and its role in preventing of a wide range of illnesses are so great that we are still learning the extent of their magnitude. It just makes sense that a mother’s milk is most well suited for her baby.
I am a bit less unambiguous about breastfeeding. By that I mean the process of providing breast milk to an infant directly from its mother’s breast. Before you yank my AAP membership card, let me make it clear that I think every woman should consider breastfeeding her infant. But we must accept that in a few situations, even with help from caring and enlightened health care providers and family members, breastfeeding doesn’t work as well as we would have hoped. Fortunately, there are alternatives.
My reservations about the process are few, and until recently I have had an unwaveringly positive attitude toward the safety of breast milk. The cause of my little bit of uncertainty arrived in a recent study by two researchers at the Dana Farber Institute in Boston, in which the A younger cohort within that larger group had a dramatic 40% increased risk of developing high-risk cancer before reaching age 55.
The population the investigators studied came from the large Nurses’ Health Study II, a well-known repository of longitudinal health data. The researchers reported that they included biometric data and a large collection of lifestyle factors including smoking, alcohol intake, and diet in their calculations. However, breastfeeding continued to register the highest association. Interestingly, the investigators found that women who were breastfed for 9 months or longer had twice the risk of colorectal cancer as those who breastfed for from 4 to 8 months.
The study population was all women and predominantly white. However, in the general population it is the non-Hispanic white population that is experiencing the greatest increase in incidence. Of course, the study could not answer whether this association with breastfeeding also existed in minority populations.
The researchers suspect that what they are seeing is a reflection of the Westernization of the American lifestyle. One of the researchers is interested in the gut biome of infants and plans to further the investigation in that direction. Could some substance from the environment be concentrating in breast milk? Or is something missing in breast milk? She points out that, while formulas are generally fortified with vitamin D, breast milk is not.
As concerning as the results of this study may sound, the authors are very careful to urge mothers to continue to breastfeed and choose it as their first choice for feeding their babies. I have been pleasantly surprised that this study has not gotten widespread media attention because bad news travels fast. I have chosen to share it with you because at some point you may begin getting questions from concerned parents.
While apparently well done, this study is just the beginning. Like any good research, it poses more questions than it answers. For us as pediatricians it means we should continue to recommend breast milk as the first food. But, we must stay alert as further research looks deeper into this association.
We should also take advantage of our special access to young parents, a demographic that less frequently sees a physician for preventive care. For whatever reason colorectal cancer is occurring at younger ages. When we have the opportunity we should be reminding 40-year-olds not to wait until age 50 to screen for colorectal cancer, particularly if they have a family history of the disease.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine, for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.” Other than a Littman stethoscope he accepted as a first-year medical student in 1966, Dr. Wilkoff reports having nothing to disclose. Email him at [email protected].
I, like every pediatrician I know, believe that breast milk is the best nutrition for human newborns. Its balance of nutritive elements and its role in preventing of a wide range of illnesses are so great that we are still learning the extent of their magnitude. It just makes sense that a mother’s milk is most well suited for her baby.
I am a bit less unambiguous about breastfeeding. By that I mean the process of providing breast milk to an infant directly from its mother’s breast. Before you yank my AAP membership card, let me make it clear that I think every woman should consider breastfeeding her infant. But we must accept that in a few situations, even with help from caring and enlightened health care providers and family members, breastfeeding doesn’t work as well as we would have hoped. Fortunately, there are alternatives.
My reservations about the process are few, and until recently I have had an unwaveringly positive attitude toward the safety of breast milk. The cause of my little bit of uncertainty arrived in a recent study by two researchers at the Dana Farber Institute in Boston, in which the A younger cohort within that larger group had a dramatic 40% increased risk of developing high-risk cancer before reaching age 55.
The population the investigators studied came from the large Nurses’ Health Study II, a well-known repository of longitudinal health data. The researchers reported that they included biometric data and a large collection of lifestyle factors including smoking, alcohol intake, and diet in their calculations. However, breastfeeding continued to register the highest association. Interestingly, the investigators found that women who were breastfed for 9 months or longer had twice the risk of colorectal cancer as those who breastfed for from 4 to 8 months.
The study population was all women and predominantly white. However, in the general population it is the non-Hispanic white population that is experiencing the greatest increase in incidence. Of course, the study could not answer whether this association with breastfeeding also existed in minority populations.
The researchers suspect that what they are seeing is a reflection of the Westernization of the American lifestyle. One of the researchers is interested in the gut biome of infants and plans to further the investigation in that direction. Could some substance from the environment be concentrating in breast milk? Or is something missing in breast milk? She points out that, while formulas are generally fortified with vitamin D, breast milk is not.
As concerning as the results of this study may sound, the authors are very careful to urge mothers to continue to breastfeed and choose it as their first choice for feeding their babies. I have been pleasantly surprised that this study has not gotten widespread media attention because bad news travels fast. I have chosen to share it with you because at some point you may begin getting questions from concerned parents.
While apparently well done, this study is just the beginning. Like any good research, it poses more questions than it answers. For us as pediatricians it means we should continue to recommend breast milk as the first food. But, we must stay alert as further research looks deeper into this association.
We should also take advantage of our special access to young parents, a demographic that less frequently sees a physician for preventive care. For whatever reason colorectal cancer is occurring at younger ages. When we have the opportunity we should be reminding 40-year-olds not to wait until age 50 to screen for colorectal cancer, particularly if they have a family history of the disease.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine, for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.” Other than a Littman stethoscope he accepted as a first-year medical student in 1966, Dr. Wilkoff reports having nothing to disclose. Email him at [email protected].
I, like every pediatrician I know, believe that breast milk is the best nutrition for human newborns. Its balance of nutritive elements and its role in preventing of a wide range of illnesses are so great that we are still learning the extent of their magnitude. It just makes sense that a mother’s milk is most well suited for her baby.
I am a bit less unambiguous about breastfeeding. By that I mean the process of providing breast milk to an infant directly from its mother’s breast. Before you yank my AAP membership card, let me make it clear that I think every woman should consider breastfeeding her infant. But we must accept that in a few situations, even with help from caring and enlightened health care providers and family members, breastfeeding doesn’t work as well as we would have hoped. Fortunately, there are alternatives.
My reservations about the process are few, and until recently I have had an unwaveringly positive attitude toward the safety of breast milk. The cause of my little bit of uncertainty arrived in a recent study by two researchers at the Dana Farber Institute in Boston, in which the A younger cohort within that larger group had a dramatic 40% increased risk of developing high-risk cancer before reaching age 55.
The population the investigators studied came from the large Nurses’ Health Study II, a well-known repository of longitudinal health data. The researchers reported that they included biometric data and a large collection of lifestyle factors including smoking, alcohol intake, and diet in their calculations. However, breastfeeding continued to register the highest association. Interestingly, the investigators found that women who were breastfed for 9 months or longer had twice the risk of colorectal cancer as those who breastfed for from 4 to 8 months.
The study population was all women and predominantly white. However, in the general population it is the non-Hispanic white population that is experiencing the greatest increase in incidence. Of course, the study could not answer whether this association with breastfeeding also existed in minority populations.
The researchers suspect that what they are seeing is a reflection of the Westernization of the American lifestyle. One of the researchers is interested in the gut biome of infants and plans to further the investigation in that direction. Could some substance from the environment be concentrating in breast milk? Or is something missing in breast milk? She points out that, while formulas are generally fortified with vitamin D, breast milk is not.
As concerning as the results of this study may sound, the authors are very careful to urge mothers to continue to breastfeed and choose it as their first choice for feeding their babies. I have been pleasantly surprised that this study has not gotten widespread media attention because bad news travels fast. I have chosen to share it with you because at some point you may begin getting questions from concerned parents.
While apparently well done, this study is just the beginning. Like any good research, it poses more questions than it answers. For us as pediatricians it means we should continue to recommend breast milk as the first food. But, we must stay alert as further research looks deeper into this association.
We should also take advantage of our special access to young parents, a demographic that less frequently sees a physician for preventive care. For whatever reason colorectal cancer is occurring at younger ages. When we have the opportunity we should be reminding 40-year-olds not to wait until age 50 to screen for colorectal cancer, particularly if they have a family history of the disease.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine, for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.” Other than a Littman stethoscope he accepted as a first-year medical student in 1966, Dr. Wilkoff reports having nothing to disclose. Email him at [email protected].
GI symptoms during menopause deserve attention
This transcript has been edited for clarity.
Welcome back to another GI Common Concerns.
Today, I want to highlight some information about menopause.
Approximately 1.5 million women in the United States per year enter into menopause. Hysterectomy is also one of the most common surgeries for women worldwide, with an estimated 20%-40% undergoing this procedure by the age of 60.
Therefore, whether it’s because of biologic onset with age or surgical induction, menopause is a very common condition, and it’s important that we understand its symptoms and the latest information around it.
Impact on GI motility
One of the clearest functional symptoms to be aware of with menopause relates to alterations in hormonal balance. This has an impact on gastrointestinal (GI) motility by increasing abdominal muscle stimulation related to different patterns of secretion and can result in a number of symptomatic changes.
One such change that can occur is food intolerance. It is believed that menopause-associated food intolerance has multiple possible causes and may be related more to alterations to the microbiome, which can be contributed to by diet, activity, sleep cycle, and other factors.
When food intolerances are triggered in the perimenopausal or menopausal patient, it may lead you to recommend the well-established FODMAP diet, which is known to reduce symptoms. But the answer for every patient is not simply placing them on a FODMAP diet and telling them they have irritable bowel syndrome.
Other approaches can be considered for addressing food intolerance in these patients. The data are quite strong that adjunctive use of a dietitian is tremendously helpful in this particular population.
When it comes to menopausal patients, however, we need to consider other changes in their activity or adverse contributors to their mental health, such as stress or anxiety. These all contribute to more of a multifactorial composite in this population, for which irritable bowel syndrome serves as a similar example.
This means that we may need to expand our horizons rather than to focus on solely on antispasmodic or diet-related interventions.
Instead, we can start to consider more of a multidimensional treatment approach consisting of education, relaxation, cognitive-behavioral therapy, and physical activity. Certainly, there are now behavioral interventions using Internet-based digital formats to increase the acceptability and sustainability among patients.
Choosing such a multidisciplinary approach can be quite helpful.
The metabolic consequences of altering hormonal balance
Recent data from a rat model study investigated the metabolic impact of changing hormonal balance.
Investigators looked at ovariectomized rats and found that there was a biologic change in the diversity of the general GI biome. There were also noteworthy associations with weight fluctuations and dramatic changes in the spatial memory and cognitive performance characteristics of these rats, which was subsequently improved by supplemental estrogen.
This indicates that we may be able to remediate these effects with the similar use of supplemental hormone replacement treatments.
Another recent study looked at nonalcoholic fatty liver disease, which is very common in the general population and has a > 20% worldwide prevalence in postmenopausal women. Albeit small in numbers, this was a very interesting study.
Investigators looked at the delivery method for menopausal hormone therapy, which was transdermal for 75 patients and oral for 293 patients. Then, they looked at ultrasound definition of nonalcoholic fatty liver disease after 1 year as the endpoint. They found an approximate 7% reduction in the patients who received the transdermal administration compared with a 4% increase in the patients who received it orally.
Again, we have to remember this is a relatively small study, but the results indicate that the route of estrogen administration may be an important consideration in nonalcoholic fatty liver disease.
Sleep disturbances: fragmentation, duration, and quality
Sleep is something that’s near and dear to my heart and is the focus of a lot of our research.
Sleep disturbances are really part and parcel of menopause and are observed with hormonal imbalances and temperature intolerances. Disturbances such as sleep fragmentation, shorter sleep duration, and poorer sleep quality have a dramatic effect not only on the biome but also on sensory thresholds.
Therefore, as we start to look at mitigating strategies here, we need to focus on sleep and ask the right questions.
In my own practice, I try not to just ask, “How did you sleep last night?” That’s because sleep can be somewhat amnestic. You may have a cognitive awakening or a noncognitive awakening but still have experienced fragmentation.
As a result, my focus is on next-day function. I ask my patients, “When you get up in the morning, are you refreshed? Do you have the ability to perform daytime activities? Do you experience early fatigue or cognitive changes that occur?”
These questions can provide good insights into the sleep efficiency of the previous night.
The effect of the microbiome on osteoporosis
One final topic I found very interesting pertains to the effects of menopause on osteoporosis.
We certainly know that postmenopausal women have a very high prevalence of osteopenia, and that osteoporosis is a progression of that, as well as that increased bone-related disease affects fractures and related morbidity and mortality.
However, there’s accumulating evidence on the osteoporotic effects of biomarker changes in menopause, which shows that the biome regulates the pathophysiologic process of at least a large degree of osteoporosis.
This starts to make sense when you look at the pro-inflammatory factors that increase with changes in biome diversity, in particular tumor necrosis factor alpha (which is something we also see in inflammatory bowel disease), interleukin-1, and increased activated osteoclasts.
Therefore, when it comes to decreasing bone loss among patients who are perimenopausal or postmenopausal, we don’t yet have a clear answer. Hormone therapy, diet, activity, vitamin D supplementation, and other things may positively change the biome. They are worthy topics for patients to bring up with their ob.gyns. or primary care doctors.
Although it may be a little bit outside the scope of gastroenterology, in my opinion there are a number of new findings relating to menopause that we as a field need to be more proactive in addressing.
Ask the right questions when these people come in to you, irrespective of why they’re there. Start to ask about the quality of their sleep. What are their other functional symptoms? What are their other potential osteoporosis-related risks?
We must do a better job about individualizing care. Rather than treating patients as disease states, we must start to do specific patient-focused care.
I hope this gives you some provocative thoughts when you have your next session with a patient in the perimenopausal or menopausal state. There are lots of things that we continue to learn.
Dr. Johnson is professor of medicine and chief of gastroenterology at Eastern Virginia Medical School in Norfolk, Va., and a past president of the American College of Gastroenterology. He serves as an adviser to ISOThrive and Johnson & Johnson.
A version of this article first appeared on Medscape.com.
This transcript has been edited for clarity.
Welcome back to another GI Common Concerns.
Today, I want to highlight some information about menopause.
Approximately 1.5 million women in the United States per year enter into menopause. Hysterectomy is also one of the most common surgeries for women worldwide, with an estimated 20%-40% undergoing this procedure by the age of 60.
Therefore, whether it’s because of biologic onset with age or surgical induction, menopause is a very common condition, and it’s important that we understand its symptoms and the latest information around it.
Impact on GI motility
One of the clearest functional symptoms to be aware of with menopause relates to alterations in hormonal balance. This has an impact on gastrointestinal (GI) motility by increasing abdominal muscle stimulation related to different patterns of secretion and can result in a number of symptomatic changes.
One such change that can occur is food intolerance. It is believed that menopause-associated food intolerance has multiple possible causes and may be related more to alterations to the microbiome, which can be contributed to by diet, activity, sleep cycle, and other factors.
When food intolerances are triggered in the perimenopausal or menopausal patient, it may lead you to recommend the well-established FODMAP diet, which is known to reduce symptoms. But the answer for every patient is not simply placing them on a FODMAP diet and telling them they have irritable bowel syndrome.
Other approaches can be considered for addressing food intolerance in these patients. The data are quite strong that adjunctive use of a dietitian is tremendously helpful in this particular population.
When it comes to menopausal patients, however, we need to consider other changes in their activity or adverse contributors to their mental health, such as stress or anxiety. These all contribute to more of a multifactorial composite in this population, for which irritable bowel syndrome serves as a similar example.
This means that we may need to expand our horizons rather than to focus on solely on antispasmodic or diet-related interventions.
Instead, we can start to consider more of a multidimensional treatment approach consisting of education, relaxation, cognitive-behavioral therapy, and physical activity. Certainly, there are now behavioral interventions using Internet-based digital formats to increase the acceptability and sustainability among patients.
Choosing such a multidisciplinary approach can be quite helpful.
The metabolic consequences of altering hormonal balance
Recent data from a rat model study investigated the metabolic impact of changing hormonal balance.
Investigators looked at ovariectomized rats and found that there was a biologic change in the diversity of the general GI biome. There were also noteworthy associations with weight fluctuations and dramatic changes in the spatial memory and cognitive performance characteristics of these rats, which was subsequently improved by supplemental estrogen.
This indicates that we may be able to remediate these effects with the similar use of supplemental hormone replacement treatments.
Another recent study looked at nonalcoholic fatty liver disease, which is very common in the general population and has a > 20% worldwide prevalence in postmenopausal women. Albeit small in numbers, this was a very interesting study.
Investigators looked at the delivery method for menopausal hormone therapy, which was transdermal for 75 patients and oral for 293 patients. Then, they looked at ultrasound definition of nonalcoholic fatty liver disease after 1 year as the endpoint. They found an approximate 7% reduction in the patients who received the transdermal administration compared with a 4% increase in the patients who received it orally.
Again, we have to remember this is a relatively small study, but the results indicate that the route of estrogen administration may be an important consideration in nonalcoholic fatty liver disease.
Sleep disturbances: fragmentation, duration, and quality
Sleep is something that’s near and dear to my heart and is the focus of a lot of our research.
Sleep disturbances are really part and parcel of menopause and are observed with hormonal imbalances and temperature intolerances. Disturbances such as sleep fragmentation, shorter sleep duration, and poorer sleep quality have a dramatic effect not only on the biome but also on sensory thresholds.
Therefore, as we start to look at mitigating strategies here, we need to focus on sleep and ask the right questions.
In my own practice, I try not to just ask, “How did you sleep last night?” That’s because sleep can be somewhat amnestic. You may have a cognitive awakening or a noncognitive awakening but still have experienced fragmentation.
As a result, my focus is on next-day function. I ask my patients, “When you get up in the morning, are you refreshed? Do you have the ability to perform daytime activities? Do you experience early fatigue or cognitive changes that occur?”
These questions can provide good insights into the sleep efficiency of the previous night.
The effect of the microbiome on osteoporosis
One final topic I found very interesting pertains to the effects of menopause on osteoporosis.
We certainly know that postmenopausal women have a very high prevalence of osteopenia, and that osteoporosis is a progression of that, as well as that increased bone-related disease affects fractures and related morbidity and mortality.
However, there’s accumulating evidence on the osteoporotic effects of biomarker changes in menopause, which shows that the biome regulates the pathophysiologic process of at least a large degree of osteoporosis.
This starts to make sense when you look at the pro-inflammatory factors that increase with changes in biome diversity, in particular tumor necrosis factor alpha (which is something we also see in inflammatory bowel disease), interleukin-1, and increased activated osteoclasts.
Therefore, when it comes to decreasing bone loss among patients who are perimenopausal or postmenopausal, we don’t yet have a clear answer. Hormone therapy, diet, activity, vitamin D supplementation, and other things may positively change the biome. They are worthy topics for patients to bring up with their ob.gyns. or primary care doctors.
Although it may be a little bit outside the scope of gastroenterology, in my opinion there are a number of new findings relating to menopause that we as a field need to be more proactive in addressing.
Ask the right questions when these people come in to you, irrespective of why they’re there. Start to ask about the quality of their sleep. What are their other functional symptoms? What are their other potential osteoporosis-related risks?
We must do a better job about individualizing care. Rather than treating patients as disease states, we must start to do specific patient-focused care.
I hope this gives you some provocative thoughts when you have your next session with a patient in the perimenopausal or menopausal state. There are lots of things that we continue to learn.
Dr. Johnson is professor of medicine and chief of gastroenterology at Eastern Virginia Medical School in Norfolk, Va., and a past president of the American College of Gastroenterology. He serves as an adviser to ISOThrive and Johnson & Johnson.
A version of this article first appeared on Medscape.com.
This transcript has been edited for clarity.
Welcome back to another GI Common Concerns.
Today, I want to highlight some information about menopause.
Approximately 1.5 million women in the United States per year enter into menopause. Hysterectomy is also one of the most common surgeries for women worldwide, with an estimated 20%-40% undergoing this procedure by the age of 60.
Therefore, whether it’s because of biologic onset with age or surgical induction, menopause is a very common condition, and it’s important that we understand its symptoms and the latest information around it.
Impact on GI motility
One of the clearest functional symptoms to be aware of with menopause relates to alterations in hormonal balance. This has an impact on gastrointestinal (GI) motility by increasing abdominal muscle stimulation related to different patterns of secretion and can result in a number of symptomatic changes.
One such change that can occur is food intolerance. It is believed that menopause-associated food intolerance has multiple possible causes and may be related more to alterations to the microbiome, which can be contributed to by diet, activity, sleep cycle, and other factors.
When food intolerances are triggered in the perimenopausal or menopausal patient, it may lead you to recommend the well-established FODMAP diet, which is known to reduce symptoms. But the answer for every patient is not simply placing them on a FODMAP diet and telling them they have irritable bowel syndrome.
Other approaches can be considered for addressing food intolerance in these patients. The data are quite strong that adjunctive use of a dietitian is tremendously helpful in this particular population.
When it comes to menopausal patients, however, we need to consider other changes in their activity or adverse contributors to their mental health, such as stress or anxiety. These all contribute to more of a multifactorial composite in this population, for which irritable bowel syndrome serves as a similar example.
This means that we may need to expand our horizons rather than to focus on solely on antispasmodic or diet-related interventions.
Instead, we can start to consider more of a multidimensional treatment approach consisting of education, relaxation, cognitive-behavioral therapy, and physical activity. Certainly, there are now behavioral interventions using Internet-based digital formats to increase the acceptability and sustainability among patients.
Choosing such a multidisciplinary approach can be quite helpful.
The metabolic consequences of altering hormonal balance
Recent data from a rat model study investigated the metabolic impact of changing hormonal balance.
Investigators looked at ovariectomized rats and found that there was a biologic change in the diversity of the general GI biome. There were also noteworthy associations with weight fluctuations and dramatic changes in the spatial memory and cognitive performance characteristics of these rats, which was subsequently improved by supplemental estrogen.
This indicates that we may be able to remediate these effects with the similar use of supplemental hormone replacement treatments.
Another recent study looked at nonalcoholic fatty liver disease, which is very common in the general population and has a > 20% worldwide prevalence in postmenopausal women. Albeit small in numbers, this was a very interesting study.
Investigators looked at the delivery method for menopausal hormone therapy, which was transdermal for 75 patients and oral for 293 patients. Then, they looked at ultrasound definition of nonalcoholic fatty liver disease after 1 year as the endpoint. They found an approximate 7% reduction in the patients who received the transdermal administration compared with a 4% increase in the patients who received it orally.
Again, we have to remember this is a relatively small study, but the results indicate that the route of estrogen administration may be an important consideration in nonalcoholic fatty liver disease.
Sleep disturbances: fragmentation, duration, and quality
Sleep is something that’s near and dear to my heart and is the focus of a lot of our research.
Sleep disturbances are really part and parcel of menopause and are observed with hormonal imbalances and temperature intolerances. Disturbances such as sleep fragmentation, shorter sleep duration, and poorer sleep quality have a dramatic effect not only on the biome but also on sensory thresholds.
Therefore, as we start to look at mitigating strategies here, we need to focus on sleep and ask the right questions.
In my own practice, I try not to just ask, “How did you sleep last night?” That’s because sleep can be somewhat amnestic. You may have a cognitive awakening or a noncognitive awakening but still have experienced fragmentation.
As a result, my focus is on next-day function. I ask my patients, “When you get up in the morning, are you refreshed? Do you have the ability to perform daytime activities? Do you experience early fatigue or cognitive changes that occur?”
These questions can provide good insights into the sleep efficiency of the previous night.
The effect of the microbiome on osteoporosis
One final topic I found very interesting pertains to the effects of menopause on osteoporosis.
We certainly know that postmenopausal women have a very high prevalence of osteopenia, and that osteoporosis is a progression of that, as well as that increased bone-related disease affects fractures and related morbidity and mortality.
However, there’s accumulating evidence on the osteoporotic effects of biomarker changes in menopause, which shows that the biome regulates the pathophysiologic process of at least a large degree of osteoporosis.
This starts to make sense when you look at the pro-inflammatory factors that increase with changes in biome diversity, in particular tumor necrosis factor alpha (which is something we also see in inflammatory bowel disease), interleukin-1, and increased activated osteoclasts.
Therefore, when it comes to decreasing bone loss among patients who are perimenopausal or postmenopausal, we don’t yet have a clear answer. Hormone therapy, diet, activity, vitamin D supplementation, and other things may positively change the biome. They are worthy topics for patients to bring up with their ob.gyns. or primary care doctors.
Although it may be a little bit outside the scope of gastroenterology, in my opinion there are a number of new findings relating to menopause that we as a field need to be more proactive in addressing.
Ask the right questions when these people come in to you, irrespective of why they’re there. Start to ask about the quality of their sleep. What are their other functional symptoms? What are their other potential osteoporosis-related risks?
We must do a better job about individualizing care. Rather than treating patients as disease states, we must start to do specific patient-focused care.
I hope this gives you some provocative thoughts when you have your next session with a patient in the perimenopausal or menopausal state. There are lots of things that we continue to learn.
Dr. Johnson is professor of medicine and chief of gastroenterology at Eastern Virginia Medical School in Norfolk, Va., and a past president of the American College of Gastroenterology. He serves as an adviser to ISOThrive and Johnson & Johnson.
A version of this article first appeared on Medscape.com.
Foreword: VA Research and COVID-19
Sylvester Norman, a 67-year-old Coast Guard veteran and retired day-care worker from Nashville, Tennessee, volunteered to participate in the US Department of Veterans Affairs (VA) Million Veteran Program (MVP). He and all 4 of his brothers had experienced kidney illness. During the pandemic, Adriana Hung, MD, MPH, an MVP researcher and associate professor of nephrology at Vanderbilt University, noticed that a disproportionate number of Black patients hospitalized with COVID-19 were dying of acute kidney failure. Dr. Hung used data from Norman and other Black veterans provided through the MVP to identify genetic variations in the APOL1 gene linked to kidney disease found in 1 of every 8 people of African descent. Her research proved that a COVID-19 viral infection can trigger these genes and drive a patient’s kidneys to go into failure. Thanks to her research and volunteers like Norman, a new drug targeting APOL1 may soon receive approval from the US Food and Drug Administration (FDA).
This is only one example of the life-saving work conducted by the Veterans Health Administration (VHA) during the pandemic. On January 21, 2020, 1 day after the first confirmed COVID-19 case in the US, the VHA quickly activated its Emergency Management Coordination Cell (EMCC) under a unified command structure with round-the-clock operations to track the evolving risk and plan a response to this once-in-a-century pandemic. A few months later, and before the US declared COVID-19 a pandemic, the VHA research program sprang into action, preparing its community of investigators to address the emerging needs and challenges of the COVID-19 public health crisis. Three years later, although the federal COVID-19 public emergency is declared over, the VHA remains diligent in observing trends and conducting necessary research on the disease as case numbers rise and fall across time.
This special issue of Federal Practitioner showcases the many ways that the VHA successfully leveraged and rapidly mobilized its research enterprise capabilities as part of the national response to COVID-19 and continues to work in this area. As the virus rapidly spread across the country, the VHA research program, overseen by the Office of Research and Development (ORD) and in partnership with other VHA offices, demonstrated the strength and agility that come from being part of a nationwide integrated health care system.
Historically, the VHA has been one of the nation’s leaders in translating medical breakthroughs to the treatment and care of veterans and the nation. Today, the VHA ensures that veterans have increased access to innovative health care solutions by promoting new medical research initiatives, training health care professionals, and developing community partnerships.
As this special issue of Federal Practitioner demonstrates, the VHA’s extraordinary research response to the COVID-19 pandemic was shaped by its ongoing transformation to a full-scale research enterprise; diversity of partnerships with academia, other federal agencies, and industry; extensive infrastructure for funding and quickly ramping up multisite clinical trials; and longstanding partnership with veterans, who volunteer to serve their country twice—first in uniform, and later by volunteering to participate in VA research.
By leveraging these and other assets, VHA investigators have conducted > 900 COVID-19 research projects across 83 VA medical centers, with nearly 3000 VA-affiliated papers published by mid-2023. We have also become a leader in long COVID, generating notable findings using our electronic health record data and filling in the picture with studies that include interviews with thousands of patients, examinations of blood markers, and exploration of the role of genetics. Along the way, the VA collaborated with federal partners, such as the US Department of Defense, by funding a longitudinal research cohort in which 2800 veterans are enrolled. Through this joint effort, researchers will learn more about the natural history and outcomes among veterans affected by COVID-19. This work continues as part of the VA commitment to the health and care of these veterans and nation as a whole.
Additionally, by partnering with veterans, the VA established a research volunteer registry. More than 58,000 veterans volunteered to be contacted to participate in studies if they were eligible. This effort was critical to the VA’s ability to contribute to the vaccine and other therapeutic trials that were seeking approval from the FDA for broader public use. This volunteerism by these veterans showed the nation that the VA is a valuable partner in times of need.
The VA research program remains tightly focused on understanding the long-term impacts of COVID-19. At the same time, the VA is committed to using lessons learned during the crisis in addressing high priorities in veterans’ health care. Among those priorities is fulfilling our mission under the Sergeant First Class Heath Robinson Honoring Our Promise to Address Comprehensive Toxics (PACT) Act of 2022 to improve care for veterans with military environmental exposures. Over the next few years, VA researchers will analyze health care and epidemiologic data to improve the identification and treatment of medical conditions potentially associated with toxic exposures. This work will include analyses of health trends of post-9/11 veterans, cancer rates among veterans, toxic exposure and mental health outcomes, and the health effects of jet fuels.
Our research program also will support the VA priority of hiring faster and more competitively. With many of the 3700 VA-funded principal investigators also serving as faculty at top universities, VA research programs position us to recruit the best and brightest professionals on the cutting edge of health care. These efforts work hand in hand with the clinical training the VA provides to 113,000 health professions trainees, creating a pipeline of clinicians and physician-researchers for the future. Further, these partnerships strengthen the VA’s ability to expand access by connecting veterans to the best, immediate care.
Finally, VA research will continue to be critical to our top clinical priority of preventing veteran suicide. This area of VA research covers a wide and critically important set of topics, such as the use of predictive modeling to determine veterans most at risk as well as studies on substance use disorders and suicidal ideation, among others.
The impressive collection of articles in this special issue provides a snapshot of the large-scale, all-hands approach the VHA adopted during the COVID-19 public health crisis. I am extremely proud of the work you are about to read.
Sylvester Norman, a 67-year-old Coast Guard veteran and retired day-care worker from Nashville, Tennessee, volunteered to participate in the US Department of Veterans Affairs (VA) Million Veteran Program (MVP). He and all 4 of his brothers had experienced kidney illness. During the pandemic, Adriana Hung, MD, MPH, an MVP researcher and associate professor of nephrology at Vanderbilt University, noticed that a disproportionate number of Black patients hospitalized with COVID-19 were dying of acute kidney failure. Dr. Hung used data from Norman and other Black veterans provided through the MVP to identify genetic variations in the APOL1 gene linked to kidney disease found in 1 of every 8 people of African descent. Her research proved that a COVID-19 viral infection can trigger these genes and drive a patient’s kidneys to go into failure. Thanks to her research and volunteers like Norman, a new drug targeting APOL1 may soon receive approval from the US Food and Drug Administration (FDA).
This is only one example of the life-saving work conducted by the Veterans Health Administration (VHA) during the pandemic. On January 21, 2020, 1 day after the first confirmed COVID-19 case in the US, the VHA quickly activated its Emergency Management Coordination Cell (EMCC) under a unified command structure with round-the-clock operations to track the evolving risk and plan a response to this once-in-a-century pandemic. A few months later, and before the US declared COVID-19 a pandemic, the VHA research program sprang into action, preparing its community of investigators to address the emerging needs and challenges of the COVID-19 public health crisis. Three years later, although the federal COVID-19 public emergency is declared over, the VHA remains diligent in observing trends and conducting necessary research on the disease as case numbers rise and fall across time.
This special issue of Federal Practitioner showcases the many ways that the VHA successfully leveraged and rapidly mobilized its research enterprise capabilities as part of the national response to COVID-19 and continues to work in this area. As the virus rapidly spread across the country, the VHA research program, overseen by the Office of Research and Development (ORD) and in partnership with other VHA offices, demonstrated the strength and agility that come from being part of a nationwide integrated health care system.
Historically, the VHA has been one of the nation’s leaders in translating medical breakthroughs to the treatment and care of veterans and the nation. Today, the VHA ensures that veterans have increased access to innovative health care solutions by promoting new medical research initiatives, training health care professionals, and developing community partnerships.
As this special issue of Federal Practitioner demonstrates, the VHA’s extraordinary research response to the COVID-19 pandemic was shaped by its ongoing transformation to a full-scale research enterprise; diversity of partnerships with academia, other federal agencies, and industry; extensive infrastructure for funding and quickly ramping up multisite clinical trials; and longstanding partnership with veterans, who volunteer to serve their country twice—first in uniform, and later by volunteering to participate in VA research.
By leveraging these and other assets, VHA investigators have conducted > 900 COVID-19 research projects across 83 VA medical centers, with nearly 3000 VA-affiliated papers published by mid-2023. We have also become a leader in long COVID, generating notable findings using our electronic health record data and filling in the picture with studies that include interviews with thousands of patients, examinations of blood markers, and exploration of the role of genetics. Along the way, the VA collaborated with federal partners, such as the US Department of Defense, by funding a longitudinal research cohort in which 2800 veterans are enrolled. Through this joint effort, researchers will learn more about the natural history and outcomes among veterans affected by COVID-19. This work continues as part of the VA commitment to the health and care of these veterans and nation as a whole.
Additionally, by partnering with veterans, the VA established a research volunteer registry. More than 58,000 veterans volunteered to be contacted to participate in studies if they were eligible. This effort was critical to the VA’s ability to contribute to the vaccine and other therapeutic trials that were seeking approval from the FDA for broader public use. This volunteerism by these veterans showed the nation that the VA is a valuable partner in times of need.
The VA research program remains tightly focused on understanding the long-term impacts of COVID-19. At the same time, the VA is committed to using lessons learned during the crisis in addressing high priorities in veterans’ health care. Among those priorities is fulfilling our mission under the Sergeant First Class Heath Robinson Honoring Our Promise to Address Comprehensive Toxics (PACT) Act of 2022 to improve care for veterans with military environmental exposures. Over the next few years, VA researchers will analyze health care and epidemiologic data to improve the identification and treatment of medical conditions potentially associated with toxic exposures. This work will include analyses of health trends of post-9/11 veterans, cancer rates among veterans, toxic exposure and mental health outcomes, and the health effects of jet fuels.
Our research program also will support the VA priority of hiring faster and more competitively. With many of the 3700 VA-funded principal investigators also serving as faculty at top universities, VA research programs position us to recruit the best and brightest professionals on the cutting edge of health care. These efforts work hand in hand with the clinical training the VA provides to 113,000 health professions trainees, creating a pipeline of clinicians and physician-researchers for the future. Further, these partnerships strengthen the VA’s ability to expand access by connecting veterans to the best, immediate care.
Finally, VA research will continue to be critical to our top clinical priority of preventing veteran suicide. This area of VA research covers a wide and critically important set of topics, such as the use of predictive modeling to determine veterans most at risk as well as studies on substance use disorders and suicidal ideation, among others.
The impressive collection of articles in this special issue provides a snapshot of the large-scale, all-hands approach the VHA adopted during the COVID-19 public health crisis. I am extremely proud of the work you are about to read.
Sylvester Norman, a 67-year-old Coast Guard veteran and retired day-care worker from Nashville, Tennessee, volunteered to participate in the US Department of Veterans Affairs (VA) Million Veteran Program (MVP). He and all 4 of his brothers had experienced kidney illness. During the pandemic, Adriana Hung, MD, MPH, an MVP researcher and associate professor of nephrology at Vanderbilt University, noticed that a disproportionate number of Black patients hospitalized with COVID-19 were dying of acute kidney failure. Dr. Hung used data from Norman and other Black veterans provided through the MVP to identify genetic variations in the APOL1 gene linked to kidney disease found in 1 of every 8 people of African descent. Her research proved that a COVID-19 viral infection can trigger these genes and drive a patient’s kidneys to go into failure. Thanks to her research and volunteers like Norman, a new drug targeting APOL1 may soon receive approval from the US Food and Drug Administration (FDA).
This is only one example of the life-saving work conducted by the Veterans Health Administration (VHA) during the pandemic. On January 21, 2020, 1 day after the first confirmed COVID-19 case in the US, the VHA quickly activated its Emergency Management Coordination Cell (EMCC) under a unified command structure with round-the-clock operations to track the evolving risk and plan a response to this once-in-a-century pandemic. A few months later, and before the US declared COVID-19 a pandemic, the VHA research program sprang into action, preparing its community of investigators to address the emerging needs and challenges of the COVID-19 public health crisis. Three years later, although the federal COVID-19 public emergency is declared over, the VHA remains diligent in observing trends and conducting necessary research on the disease as case numbers rise and fall across time.
This special issue of Federal Practitioner showcases the many ways that the VHA successfully leveraged and rapidly mobilized its research enterprise capabilities as part of the national response to COVID-19 and continues to work in this area. As the virus rapidly spread across the country, the VHA research program, overseen by the Office of Research and Development (ORD) and in partnership with other VHA offices, demonstrated the strength and agility that come from being part of a nationwide integrated health care system.
Historically, the VHA has been one of the nation’s leaders in translating medical breakthroughs to the treatment and care of veterans and the nation. Today, the VHA ensures that veterans have increased access to innovative health care solutions by promoting new medical research initiatives, training health care professionals, and developing community partnerships.
As this special issue of Federal Practitioner demonstrates, the VHA’s extraordinary research response to the COVID-19 pandemic was shaped by its ongoing transformation to a full-scale research enterprise; diversity of partnerships with academia, other federal agencies, and industry; extensive infrastructure for funding and quickly ramping up multisite clinical trials; and longstanding partnership with veterans, who volunteer to serve their country twice—first in uniform, and later by volunteering to participate in VA research.
By leveraging these and other assets, VHA investigators have conducted > 900 COVID-19 research projects across 83 VA medical centers, with nearly 3000 VA-affiliated papers published by mid-2023. We have also become a leader in long COVID, generating notable findings using our electronic health record data and filling in the picture with studies that include interviews with thousands of patients, examinations of blood markers, and exploration of the role of genetics. Along the way, the VA collaborated with federal partners, such as the US Department of Defense, by funding a longitudinal research cohort in which 2800 veterans are enrolled. Through this joint effort, researchers will learn more about the natural history and outcomes among veterans affected by COVID-19. This work continues as part of the VA commitment to the health and care of these veterans and nation as a whole.
Additionally, by partnering with veterans, the VA established a research volunteer registry. More than 58,000 veterans volunteered to be contacted to participate in studies if they were eligible. This effort was critical to the VA’s ability to contribute to the vaccine and other therapeutic trials that were seeking approval from the FDA for broader public use. This volunteerism by these veterans showed the nation that the VA is a valuable partner in times of need.
The VA research program remains tightly focused on understanding the long-term impacts of COVID-19. At the same time, the VA is committed to using lessons learned during the crisis in addressing high priorities in veterans’ health care. Among those priorities is fulfilling our mission under the Sergeant First Class Heath Robinson Honoring Our Promise to Address Comprehensive Toxics (PACT) Act of 2022 to improve care for veterans with military environmental exposures. Over the next few years, VA researchers will analyze health care and epidemiologic data to improve the identification and treatment of medical conditions potentially associated with toxic exposures. This work will include analyses of health trends of post-9/11 veterans, cancer rates among veterans, toxic exposure and mental health outcomes, and the health effects of jet fuels.
Our research program also will support the VA priority of hiring faster and more competitively. With many of the 3700 VA-funded principal investigators also serving as faculty at top universities, VA research programs position us to recruit the best and brightest professionals on the cutting edge of health care. These efforts work hand in hand with the clinical training the VA provides to 113,000 health professions trainees, creating a pipeline of clinicians and physician-researchers for the future. Further, these partnerships strengthen the VA’s ability to expand access by connecting veterans to the best, immediate care.
Finally, VA research will continue to be critical to our top clinical priority of preventing veteran suicide. This area of VA research covers a wide and critically important set of topics, such as the use of predictive modeling to determine veterans most at risk as well as studies on substance use disorders and suicidal ideation, among others.
The impressive collection of articles in this special issue provides a snapshot of the large-scale, all-hands approach the VHA adopted during the COVID-19 public health crisis. I am extremely proud of the work you are about to read.
Right under our noses
Until a couple of weeks ago I considered myself a COVID virgin. I had navigated a full 36 months without a positive test, despite cohabiting with my wife in a 2,500-square-foot house during her bout with the SARS-CoV-2 virus last year. I have been reasonably careful, a situational mask wearer, and good about avoiding poorly ventilated crowded spaces. Of course I was fully vaccinated but was waiting until we had gotten closer to a December trip before getting the newest booster.
I had always been quietly smug about my good luck. And, I was pretty sure that luck had been the major contributor to my run of good health. Nonetheless, in my private moments I often wondered if I somehow had inherited or acquired an unusual defense against the virus that had been getting the best of my peers. One rather far-fetched explanation that kept popping out of my subconscious involved my profuse and persistent runny nose.
Like a fair number in my demographic, I have what I have self-diagnosed as vasomotor rhinitis. In the cooler months and particularly when I am active outdoors, my nose runs like a faucet. I half-jokingly told my wife after a particularly drippy bike ride on a frigid November afternoon that even the most robust virus couldn’t possibly have survived the swim upstream against torrent of mucus splashing onto the handlebars of my bike.
A recent study published in the journal Cell suggests that my off-the-wall explanation for my COVID resistance wasn’t quite so hair-brained. The investigators haven’t found that septuagenarian adults with high-volume runny noses are drowning the SARS-Co- 2 virus before it can do any damage. However, the researchers did discover that, This first line of defense seems to be more effective than in adults, where the virus can more easily slip through into the bloodstream, sometimes with a dramatic release of circulating cytokines, which occasionally create problems of their own. Children also release cytokines, but this is predominantly in their nose, where it appears to be less damaging. Interestingly, in children this initial response persists for around 300 days while in adults the immune response experiences a much more rapid decline. I guess this means we have to chalk one more up for snotty nose kids.
However, the results of this study also suggest that we should be giving more attention to the development of nasal vaccines. I recall that nearly 3 years ago, at the beginning of the pandemic, scientists using a ferret model had developed an effective nasal vaccine. I’m not sure why this faded out of the picture, but it feels like it’s time to turn the spotlight on this line of research again.
I suspect that in addition to being more effective, a nasal vaccine may gain more support among the antivaxxer population, many of whom I suspect are really needle phobics hiding behind a smoke screen of anti-science double talk.
At any rate, I will continue to search for articles that support my contention that my high-flow rhinorrhea is protecting me. I have always been told that a cold nose was the sign of a healthy dog. I’m just trying to prove that the same is true for us old guys with clear runny noses.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine, for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.” Other than a Littman stethoscope he accepted as a first-year medical student in 1966, Dr. Wilkoff reports having nothing to disclose. Email him at [email protected].
Until a couple of weeks ago I considered myself a COVID virgin. I had navigated a full 36 months without a positive test, despite cohabiting with my wife in a 2,500-square-foot house during her bout with the SARS-CoV-2 virus last year. I have been reasonably careful, a situational mask wearer, and good about avoiding poorly ventilated crowded spaces. Of course I was fully vaccinated but was waiting until we had gotten closer to a December trip before getting the newest booster.
I had always been quietly smug about my good luck. And, I was pretty sure that luck had been the major contributor to my run of good health. Nonetheless, in my private moments I often wondered if I somehow had inherited or acquired an unusual defense against the virus that had been getting the best of my peers. One rather far-fetched explanation that kept popping out of my subconscious involved my profuse and persistent runny nose.
Like a fair number in my demographic, I have what I have self-diagnosed as vasomotor rhinitis. In the cooler months and particularly when I am active outdoors, my nose runs like a faucet. I half-jokingly told my wife after a particularly drippy bike ride on a frigid November afternoon that even the most robust virus couldn’t possibly have survived the swim upstream against torrent of mucus splashing onto the handlebars of my bike.
A recent study published in the journal Cell suggests that my off-the-wall explanation for my COVID resistance wasn’t quite so hair-brained. The investigators haven’t found that septuagenarian adults with high-volume runny noses are drowning the SARS-Co- 2 virus before it can do any damage. However, the researchers did discover that, This first line of defense seems to be more effective than in adults, where the virus can more easily slip through into the bloodstream, sometimes with a dramatic release of circulating cytokines, which occasionally create problems of their own. Children also release cytokines, but this is predominantly in their nose, where it appears to be less damaging. Interestingly, in children this initial response persists for around 300 days while in adults the immune response experiences a much more rapid decline. I guess this means we have to chalk one more up for snotty nose kids.
However, the results of this study also suggest that we should be giving more attention to the development of nasal vaccines. I recall that nearly 3 years ago, at the beginning of the pandemic, scientists using a ferret model had developed an effective nasal vaccine. I’m not sure why this faded out of the picture, but it feels like it’s time to turn the spotlight on this line of research again.
I suspect that in addition to being more effective, a nasal vaccine may gain more support among the antivaxxer population, many of whom I suspect are really needle phobics hiding behind a smoke screen of anti-science double talk.
At any rate, I will continue to search for articles that support my contention that my high-flow rhinorrhea is protecting me. I have always been told that a cold nose was the sign of a healthy dog. I’m just trying to prove that the same is true for us old guys with clear runny noses.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine, for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.” Other than a Littman stethoscope he accepted as a first-year medical student in 1966, Dr. Wilkoff reports having nothing to disclose. Email him at [email protected].
Until a couple of weeks ago I considered myself a COVID virgin. I had navigated a full 36 months without a positive test, despite cohabiting with my wife in a 2,500-square-foot house during her bout with the SARS-CoV-2 virus last year. I have been reasonably careful, a situational mask wearer, and good about avoiding poorly ventilated crowded spaces. Of course I was fully vaccinated but was waiting until we had gotten closer to a December trip before getting the newest booster.
I had always been quietly smug about my good luck. And, I was pretty sure that luck had been the major contributor to my run of good health. Nonetheless, in my private moments I often wondered if I somehow had inherited or acquired an unusual defense against the virus that had been getting the best of my peers. One rather far-fetched explanation that kept popping out of my subconscious involved my profuse and persistent runny nose.
Like a fair number in my demographic, I have what I have self-diagnosed as vasomotor rhinitis. In the cooler months and particularly when I am active outdoors, my nose runs like a faucet. I half-jokingly told my wife after a particularly drippy bike ride on a frigid November afternoon that even the most robust virus couldn’t possibly have survived the swim upstream against torrent of mucus splashing onto the handlebars of my bike.
A recent study published in the journal Cell suggests that my off-the-wall explanation for my COVID resistance wasn’t quite so hair-brained. The investigators haven’t found that septuagenarian adults with high-volume runny noses are drowning the SARS-Co- 2 virus before it can do any damage. However, the researchers did discover that, This first line of defense seems to be more effective than in adults, where the virus can more easily slip through into the bloodstream, sometimes with a dramatic release of circulating cytokines, which occasionally create problems of their own. Children also release cytokines, but this is predominantly in their nose, where it appears to be less damaging. Interestingly, in children this initial response persists for around 300 days while in adults the immune response experiences a much more rapid decline. I guess this means we have to chalk one more up for snotty nose kids.
However, the results of this study also suggest that we should be giving more attention to the development of nasal vaccines. I recall that nearly 3 years ago, at the beginning of the pandemic, scientists using a ferret model had developed an effective nasal vaccine. I’m not sure why this faded out of the picture, but it feels like it’s time to turn the spotlight on this line of research again.
I suspect that in addition to being more effective, a nasal vaccine may gain more support among the antivaxxer population, many of whom I suspect are really needle phobics hiding behind a smoke screen of anti-science double talk.
At any rate, I will continue to search for articles that support my contention that my high-flow rhinorrhea is protecting me. I have always been told that a cold nose was the sign of a healthy dog. I’m just trying to prove that the same is true for us old guys with clear runny noses.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine, for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.” Other than a Littman stethoscope he accepted as a first-year medical student in 1966, Dr. Wilkoff reports having nothing to disclose. Email him at [email protected].
Heart rate variability: Are we ignoring a harbinger of health?
A very long time ago, when I ran clinical labs, one of the most ordered tests was the “sed rate” (aka ESR, the erythrocyte sedimentation rate). Easy, quick, and low cost, with high sensitivity but very low specificity. If the sed rate was normal, the patient probably did not have an infectious or inflammatory disease. If it was elevated, they probably did, but no telling what. Later, the C-reactive protein (CRP) test came into common use. Same general inferences: If the CRP was low, the patient was unlikely to have an inflammatory process; if high, they were sick, but we didn’t know what with.
Could the heart rate variability (HRV) score come to be thought of similarly? Much as the sed rate and CRP are sensitivity indicators of infectious or inflammatory diseases, might the HRV score be a sensitivity indicator for nervous system (central and autonomic) and cardiovascular (especially heart rhythm) malfunctions?
A substantial and relatively old body of heart rhythm literature ties HRV alterations to posttraumatic stress disorder, physician occupational stress, sleep disorders, depression, autonomic nervous system derangements, various cardiac arrhythmias, fatigue, overexertion, medications, and age itself.
More than 100 million Americans are now believed to use smartwatches or personal fitness monitors. Some 30%-40% of these devices measure HRV. So what? Credible research about this huge mass of accumulating data from “wearables” is lacking.
What is HRV?
HRV is the variation in time between each heartbeat, in milliseconds. HRV is influenced by the autonomic nervous system, perhaps reflecting sympathetic-parasympathetic balance. Some devices measure HRV 24/7. My Fitbit Inspire 2 reports only nighttime measures during 3 hours of sustained sleep. Most trackers report averages; some calculate the root mean squares; others calculate standard deviations. All fitness trackers warn not to use the data for medical purposes.
Normal values (reference ranges) for HRV begin at an average of 100 msec in the first decade of life and decline by approximately 10 msec per decade lived. At age 30-40, the average is 70 msec; age 60-70, it’s 40 msec; and at age 90-100, it’s 10 msec.
As a long-time lab guy, I used to teach proper use of lab tests. Fitness trackers are “lab tests” of a sort. We taught never to do a lab test unless you know what you are going to do with the result, no matter what it is. We also taught “never do anything just because you can.” Curiosity, we know, is a frequent driver of lab test ordering.
That underlying philosophy gives me a hard time when it comes to wearables. I have been enamored of watching my step count, active zone minutes, resting heart rate, active heart rate, various sleep scores, and breathing rate (and, of course, a manually entered early morning daily body weight) for several years. I even check my “readiness score” (a calculation using resting heart rate, recent sleep, recent active zone minutes, and perhaps HRV) each morning and adjust my behaviors accordingly.
Why monitor HRV?
But what should we do with HRV scores? Ignore them? Try to understand them, perhaps as a screening tool? Or monitor HRV for consistency or change? “Monitoring” is a proper and common use of lab tests.
Some say we should improve the HRV score by managing stress, getting regular exercise, eating a healthy diet, getting enough sleep, and not smoking or consuming excess alcohol. Duh! I do all of that anyway.
The claims that HRV is a “simple but powerful tool that can be used to track overall health and well-being” might turn out to be true. Proper study and sharing of data will enable that determination.
To advance understanding, I offer an n-of-1, a real-world personal anecdote about HRV.
I did not request the HRV function on my Fitbit Inspire 2. It simply appeared, and I ignored it for some time.
A year or two ago, I started noticing my HRV score every morning. Initially, I did not like to see my “low” score, until I learned that the reference range was dramatically affected by age and I was in my late 80s at the time. The vast majority of my HRV readings were in the range of 17 msec to 27 msec.
Last week, I was administered the new Moderna COVID-19 Spikevax vaccine and the old folks’ influenza vaccine simultaneously. In my case, side effects from each vaccine have been modest in the past, but I never previously had both administered at the same time. My immune response was, shall we say, robust. Chills, muscle aches, headache, fatigue, deltoid swelling, fitful sleep, and increased resting heart rate.
My nightly average HRV had been running between 17 msec and 35 msec for many months. WHOA! After the shots, my overnight HRV score plummeted from 24 msec to 10 msec, my lowest ever. Instant worry. The next day, it rebounded to 28 msec, and it has been in the high teens or low 20s since then.
Off to PubMed. A recent study of HRV on the second and 10th days after administering the Pfizer mRNA vaccine to 75 healthy volunteers found that the HRV on day 2 was dramatically lower than prevaccination levels and by day 10, it had returned to prevaccination levels. Some comfort there.
Another review article has reported a rapid fall and rapid rebound of HRV after COVID-19 vaccination. A 2010 report demonstrated a significant but not dramatic short-term lowering of HRV after influenza A vaccination and correlated it with CRP changes.
Some believe that the decline in HRV after vaccination reflects an increased immune response and sympathetic nervous activity.
I don’t plan to receive my flu and COVID vaccines on the same day again.
So, I went back to review what happened to my HRV when I had COVID in 2023. My HRV was 14 msec and 12 msec on the first 2 days of symptoms, and then returned to the 20 msec range.
I received the RSV vaccine this year without adverse effects, and my HRV scores were 29 msec, 33 msec, and 32 msec on the first 3 days after vaccination. Finally, after receiving a pneumococcal vaccine in 2023, I had no adverse effects, and my HRV scores on the 5 days after vaccination were indeterminate: 19 msec, 14 msec, 18 msec, 13 msec, and 17 msec.
Of course, correlation is not causation. Cause and effect remain undetermined. But I find these observations interesting for a potentially useful screening test.
George D. Lundberg, MD, is the Editor in Chief of Cancer Commons.
A version of this article first appeared on Medscape.com.
A very long time ago, when I ran clinical labs, one of the most ordered tests was the “sed rate” (aka ESR, the erythrocyte sedimentation rate). Easy, quick, and low cost, with high sensitivity but very low specificity. If the sed rate was normal, the patient probably did not have an infectious or inflammatory disease. If it was elevated, they probably did, but no telling what. Later, the C-reactive protein (CRP) test came into common use. Same general inferences: If the CRP was low, the patient was unlikely to have an inflammatory process; if high, they were sick, but we didn’t know what with.
Could the heart rate variability (HRV) score come to be thought of similarly? Much as the sed rate and CRP are sensitivity indicators of infectious or inflammatory diseases, might the HRV score be a sensitivity indicator for nervous system (central and autonomic) and cardiovascular (especially heart rhythm) malfunctions?
A substantial and relatively old body of heart rhythm literature ties HRV alterations to posttraumatic stress disorder, physician occupational stress, sleep disorders, depression, autonomic nervous system derangements, various cardiac arrhythmias, fatigue, overexertion, medications, and age itself.
More than 100 million Americans are now believed to use smartwatches or personal fitness monitors. Some 30%-40% of these devices measure HRV. So what? Credible research about this huge mass of accumulating data from “wearables” is lacking.
What is HRV?
HRV is the variation in time between each heartbeat, in milliseconds. HRV is influenced by the autonomic nervous system, perhaps reflecting sympathetic-parasympathetic balance. Some devices measure HRV 24/7. My Fitbit Inspire 2 reports only nighttime measures during 3 hours of sustained sleep. Most trackers report averages; some calculate the root mean squares; others calculate standard deviations. All fitness trackers warn not to use the data for medical purposes.
Normal values (reference ranges) for HRV begin at an average of 100 msec in the first decade of life and decline by approximately 10 msec per decade lived. At age 30-40, the average is 70 msec; age 60-70, it’s 40 msec; and at age 90-100, it’s 10 msec.
As a long-time lab guy, I used to teach proper use of lab tests. Fitness trackers are “lab tests” of a sort. We taught never to do a lab test unless you know what you are going to do with the result, no matter what it is. We also taught “never do anything just because you can.” Curiosity, we know, is a frequent driver of lab test ordering.
That underlying philosophy gives me a hard time when it comes to wearables. I have been enamored of watching my step count, active zone minutes, resting heart rate, active heart rate, various sleep scores, and breathing rate (and, of course, a manually entered early morning daily body weight) for several years. I even check my “readiness score” (a calculation using resting heart rate, recent sleep, recent active zone minutes, and perhaps HRV) each morning and adjust my behaviors accordingly.
Why monitor HRV?
But what should we do with HRV scores? Ignore them? Try to understand them, perhaps as a screening tool? Or monitor HRV for consistency or change? “Monitoring” is a proper and common use of lab tests.
Some say we should improve the HRV score by managing stress, getting regular exercise, eating a healthy diet, getting enough sleep, and not smoking or consuming excess alcohol. Duh! I do all of that anyway.
The claims that HRV is a “simple but powerful tool that can be used to track overall health and well-being” might turn out to be true. Proper study and sharing of data will enable that determination.
To advance understanding, I offer an n-of-1, a real-world personal anecdote about HRV.
I did not request the HRV function on my Fitbit Inspire 2. It simply appeared, and I ignored it for some time.
A year or two ago, I started noticing my HRV score every morning. Initially, I did not like to see my “low” score, until I learned that the reference range was dramatically affected by age and I was in my late 80s at the time. The vast majority of my HRV readings were in the range of 17 msec to 27 msec.
Last week, I was administered the new Moderna COVID-19 Spikevax vaccine and the old folks’ influenza vaccine simultaneously. In my case, side effects from each vaccine have been modest in the past, but I never previously had both administered at the same time. My immune response was, shall we say, robust. Chills, muscle aches, headache, fatigue, deltoid swelling, fitful sleep, and increased resting heart rate.
My nightly average HRV had been running between 17 msec and 35 msec for many months. WHOA! After the shots, my overnight HRV score plummeted from 24 msec to 10 msec, my lowest ever. Instant worry. The next day, it rebounded to 28 msec, and it has been in the high teens or low 20s since then.
Off to PubMed. A recent study of HRV on the second and 10th days after administering the Pfizer mRNA vaccine to 75 healthy volunteers found that the HRV on day 2 was dramatically lower than prevaccination levels and by day 10, it had returned to prevaccination levels. Some comfort there.
Another review article has reported a rapid fall and rapid rebound of HRV after COVID-19 vaccination. A 2010 report demonstrated a significant but not dramatic short-term lowering of HRV after influenza A vaccination and correlated it with CRP changes.
Some believe that the decline in HRV after vaccination reflects an increased immune response and sympathetic nervous activity.
I don’t plan to receive my flu and COVID vaccines on the same day again.
So, I went back to review what happened to my HRV when I had COVID in 2023. My HRV was 14 msec and 12 msec on the first 2 days of symptoms, and then returned to the 20 msec range.
I received the RSV vaccine this year without adverse effects, and my HRV scores were 29 msec, 33 msec, and 32 msec on the first 3 days after vaccination. Finally, after receiving a pneumococcal vaccine in 2023, I had no adverse effects, and my HRV scores on the 5 days after vaccination were indeterminate: 19 msec, 14 msec, 18 msec, 13 msec, and 17 msec.
Of course, correlation is not causation. Cause and effect remain undetermined. But I find these observations interesting for a potentially useful screening test.
George D. Lundberg, MD, is the Editor in Chief of Cancer Commons.
A version of this article first appeared on Medscape.com.
A very long time ago, when I ran clinical labs, one of the most ordered tests was the “sed rate” (aka ESR, the erythrocyte sedimentation rate). Easy, quick, and low cost, with high sensitivity but very low specificity. If the sed rate was normal, the patient probably did not have an infectious or inflammatory disease. If it was elevated, they probably did, but no telling what. Later, the C-reactive protein (CRP) test came into common use. Same general inferences: If the CRP was low, the patient was unlikely to have an inflammatory process; if high, they were sick, but we didn’t know what with.
Could the heart rate variability (HRV) score come to be thought of similarly? Much as the sed rate and CRP are sensitivity indicators of infectious or inflammatory diseases, might the HRV score be a sensitivity indicator for nervous system (central and autonomic) and cardiovascular (especially heart rhythm) malfunctions?
A substantial and relatively old body of heart rhythm literature ties HRV alterations to posttraumatic stress disorder, physician occupational stress, sleep disorders, depression, autonomic nervous system derangements, various cardiac arrhythmias, fatigue, overexertion, medications, and age itself.
More than 100 million Americans are now believed to use smartwatches or personal fitness monitors. Some 30%-40% of these devices measure HRV. So what? Credible research about this huge mass of accumulating data from “wearables” is lacking.
What is HRV?
HRV is the variation in time between each heartbeat, in milliseconds. HRV is influenced by the autonomic nervous system, perhaps reflecting sympathetic-parasympathetic balance. Some devices measure HRV 24/7. My Fitbit Inspire 2 reports only nighttime measures during 3 hours of sustained sleep. Most trackers report averages; some calculate the root mean squares; others calculate standard deviations. All fitness trackers warn not to use the data for medical purposes.
Normal values (reference ranges) for HRV begin at an average of 100 msec in the first decade of life and decline by approximately 10 msec per decade lived. At age 30-40, the average is 70 msec; age 60-70, it’s 40 msec; and at age 90-100, it’s 10 msec.
As a long-time lab guy, I used to teach proper use of lab tests. Fitness trackers are “lab tests” of a sort. We taught never to do a lab test unless you know what you are going to do with the result, no matter what it is. We also taught “never do anything just because you can.” Curiosity, we know, is a frequent driver of lab test ordering.
That underlying philosophy gives me a hard time when it comes to wearables. I have been enamored of watching my step count, active zone minutes, resting heart rate, active heart rate, various sleep scores, and breathing rate (and, of course, a manually entered early morning daily body weight) for several years. I even check my “readiness score” (a calculation using resting heart rate, recent sleep, recent active zone minutes, and perhaps HRV) each morning and adjust my behaviors accordingly.
Why monitor HRV?
But what should we do with HRV scores? Ignore them? Try to understand them, perhaps as a screening tool? Or monitor HRV for consistency or change? “Monitoring” is a proper and common use of lab tests.
Some say we should improve the HRV score by managing stress, getting regular exercise, eating a healthy diet, getting enough sleep, and not smoking or consuming excess alcohol. Duh! I do all of that anyway.
The claims that HRV is a “simple but powerful tool that can be used to track overall health and well-being” might turn out to be true. Proper study and sharing of data will enable that determination.
To advance understanding, I offer an n-of-1, a real-world personal anecdote about HRV.
I did not request the HRV function on my Fitbit Inspire 2. It simply appeared, and I ignored it for some time.
A year or two ago, I started noticing my HRV score every morning. Initially, I did not like to see my “low” score, until I learned that the reference range was dramatically affected by age and I was in my late 80s at the time. The vast majority of my HRV readings were in the range of 17 msec to 27 msec.
Last week, I was administered the new Moderna COVID-19 Spikevax vaccine and the old folks’ influenza vaccine simultaneously. In my case, side effects from each vaccine have been modest in the past, but I never previously had both administered at the same time. My immune response was, shall we say, robust. Chills, muscle aches, headache, fatigue, deltoid swelling, fitful sleep, and increased resting heart rate.
My nightly average HRV had been running between 17 msec and 35 msec for many months. WHOA! After the shots, my overnight HRV score plummeted from 24 msec to 10 msec, my lowest ever. Instant worry. The next day, it rebounded to 28 msec, and it has been in the high teens or low 20s since then.
Off to PubMed. A recent study of HRV on the second and 10th days after administering the Pfizer mRNA vaccine to 75 healthy volunteers found that the HRV on day 2 was dramatically lower than prevaccination levels and by day 10, it had returned to prevaccination levels. Some comfort there.
Another review article has reported a rapid fall and rapid rebound of HRV after COVID-19 vaccination. A 2010 report demonstrated a significant but not dramatic short-term lowering of HRV after influenza A vaccination and correlated it with CRP changes.
Some believe that the decline in HRV after vaccination reflects an increased immune response and sympathetic nervous activity.
I don’t plan to receive my flu and COVID vaccines on the same day again.
So, I went back to review what happened to my HRV when I had COVID in 2023. My HRV was 14 msec and 12 msec on the first 2 days of symptoms, and then returned to the 20 msec range.
I received the RSV vaccine this year without adverse effects, and my HRV scores were 29 msec, 33 msec, and 32 msec on the first 3 days after vaccination. Finally, after receiving a pneumococcal vaccine in 2023, I had no adverse effects, and my HRV scores on the 5 days after vaccination were indeterminate: 19 msec, 14 msec, 18 msec, 13 msec, and 17 msec.
Of course, correlation is not causation. Cause and effect remain undetermined. But I find these observations interesting for a potentially useful screening test.
George D. Lundberg, MD, is the Editor in Chief of Cancer Commons.
A version of this article first appeared on Medscape.com.
Q&A: Cancer screening in older patients – who to screen and when to stop
More than 1 in 10 Americans over age 60 years will be diagnosed with cancer, according to the National Cancer Institute, making screening for the disease in older patients imperative. Much of the burden of cancer screening falls on primary care physicians. This news organization spoke recently with William L. Dahut, MD, chief scientific officer of the American Cancer Society, about the particular challenges of screening in older patients.
Question: How much does cancer screening change with age? What are the considerations for clinicians – what risks and comorbidities are important to consider in older populations?
Answer: We at the American Cancer Society are giving a lot of thought to how to help primary care practices keep up with screening, particularly with respect to guidelines, but also best practices where judgment is required, such as cancer screening in their older patients.
We’ve had a lot of conversations recently about cancer risk in the young, largely because data show rates are going up for colorectal and breast cancer in this population. But it’s not one size fits all. Screening for young women who have a BRCA gene, if they have dense breasts, or if they have a strong family history of breast cancer should be different from those who are at average risk of the disease.
But statistically, there are about 15 per 100,000 breast cancer diagnoses in women under the age of 40 while over the age of 65 it’s 443 per 100,000. So, the risk significantly increases with age but we should not have an arbitrary cut-off. The life expectancy of a woman at age 75 is about 13.5 years. If you’re over the age of 70 or 75, then it’s going to be comorbidities that you look at, as well as individual patient decisions. Patients may say, “I don’t want to ever go through a mammogram again, because I don’t want to have a biopsy again, and I’m not going to get treated.” Or they may say, “My mom died of metastatic breast cancer when she was 82 and I want to know.”
Q: How should primary care physicians interpret conflicting guidance from the major medical groups? For example, the American College of Gastroenterology and your own organization recommend colorectal cancer screening start at age 45 now. But the American College of Physicians recently came out and said 50. What is a well-meaning primary care physician supposed to do?
A: We make more of guideline differences than we should. Sometimes guideline differences aren’t a reflection of different judgments, but rather what data were available when the most recent update took place. For colorectal cancer screening, the ACS dropped the age to begin screening to 45 in 2018 based on a very careful consideration of disease burden data and within several years most other guideline developers reached the same conclusion.
However, I think it’s good for family practice and internal medicine doctors to know that significant GI symptoms in a young patient could be colorectal cancer. It’s not as if nobody sees a 34-year-old or 27-year-old with colorectal cancer. They should be aware that if something goes away in a day or two, that’s fine, but persistent GI symptoms need a cancer workup – colonoscopy or referral to a gastroenterologist. So that’s why I think age 45 is the time when folks should begin screening.
Q: What are the medical-legal issues for a physician who is trying to follow guideline-based care when there are different guidelines?
A: Any physician can say, “We follow the guidelines of this particular organization.” I don’t think anyone can say that an organization’s guidelines are malpractice. For individual physicians, following a set of office-based guidelines will hopefully keep them out of legal difficulty.
Q: What are the risks of overscreening, especially in breast cancer where false positives may result in invasive testing?
A: What people think of as overscreening takes a number of different forms. What one guideline would imply is overscreening is recommended screening by another guideline. I think we would all agree that in an average-risk population, beginning screening before it is recommended would be overscreening, and continuing screening when a patient has life-limiting comorbidities would constitute overscreening. Screening too frequently can constitute overscreening.
For example, many women report that their doctors still are advising a baseline mammogram at age 35. Most guideline-developing organizations would regard this as overscreening in an average-risk population.
I think we are also getting better, certainly in prostate cancer, about knowing who needs to be treated and not treated. There are a lot of cancers that would have been treated 20-30 years ago but now are being safely followed with PSA and MRI. We may be able to get to that point with breast cancer over time, too.
Q: Are you saying that there may be breast cancers for which active surveillance is appropriate? Is that already the case?
A: We’re not there yet. I think some of the DCIS breast cancers are part of the discussion on whether hormonal treatment or surgeries are done. I think people do have those discussions in the context of morbidity and life expectancy. Over time, we’re likely to have more cancers for which we won’t need surgical treatments.
Q: Why did the American Cancer Society change the upper limit for lung cancer screening from 75 to 80 years of age?
A: For an individual older than 65, screening will now continue until the patient is 80, assuming the patient is in good health. According to the previous guideline, if a patient was 65 and more than 15 years beyond smoking cessation, then screening would end. This is exactly the time when we see lung cancers increase in the population and so a curable lung cancer would not previously have been detected by a screening CT scan. *
Q: What role do the multicancer blood and DNA tests play in screening now?
A: As you know, the Exact Sciences Cologuard test is already included in major guidelines for colorectal cancer screening and covered by insurance. Our philosophy on multicancer early detection tests is that we’re supportive of Medicare reimbursement when two things occur: 1. When we know there’s clinical benefit, and 2. When the test has been approved by the FDA.
The multicancer early detection tests in development and undergoing prospective research would not now replace screening for the cancers with established screening programs, but if they are shown to have clinical utility for the cancers in their panel, we would be able to reduce deaths from cancers that mostly are diagnosed at late stages and have poor prognoses.
There’s going to be a need for expertise in primary care practices to help interpret the tests. These are new questions, which are well beyond what even the typical oncologist is trained in, much less primary care physicians. We and other organizations are working on providing those answers.
Q: While we’re on the subject of the future, how do you envision AI helping or hindering cancer screening specifically in primary care?
A: I think AI is going to help things for a couple of reasons. The ability of AI is to get through data quickly and get you information that’s personalized and useful. If AI tools could let a patient know their individual risk of a cancer in the near and long term, that would help the primary care doctor screen in an individualized way. I think AI is going to be able to improve both diagnostic radiology and pathology, and could make a very big difference in settings outside of large cancer centers that operate at high volume every day. The data look very promising for AI to contribute to risk estimation by operating like a second reader in imaging and pathology.
Q: Anything else you’d like to say on this subject that clinicians should know?
A: The questions about whether or not patients should be screened is being pushed on family practice doctors and internists and these questions require a relationship with the patient. A hard stopping point at age 70 when lots of people will live 20 years or more doesn’t make sense.
There’s very little data from randomized clinical trials of screening people over the age of 70. We know that cancer risk does obviously increase with age, particularly prostate and breast cancer. And these are the cancers that are going to be the most common in your practices. If someone has a known mutation, I think you’re going to look differently at screening them. And first-degree family members, particularly for the more aggressive cancers, should be considered for screening.
My philosophy on cancer screening in the elderly is that I think the guidelines are guidelines. If patients have very limited life expectancy, then they shouldn’t be screened. There are calculators that estimate life expectancy in the context of current age and current health status, and these can be useful for decision making and counseling. Patients never think their life expectancy is shorter than 10 years. If their life expectancy is longer than 10 years, then I think, all things being equal, they should continue screening, but the question of ongoing screening needs to be periodically revisited.
*This story was updated on Nov. 1, 2023.
More than 1 in 10 Americans over age 60 years will be diagnosed with cancer, according to the National Cancer Institute, making screening for the disease in older patients imperative. Much of the burden of cancer screening falls on primary care physicians. This news organization spoke recently with William L. Dahut, MD, chief scientific officer of the American Cancer Society, about the particular challenges of screening in older patients.
Question: How much does cancer screening change with age? What are the considerations for clinicians – what risks and comorbidities are important to consider in older populations?
Answer: We at the American Cancer Society are giving a lot of thought to how to help primary care practices keep up with screening, particularly with respect to guidelines, but also best practices where judgment is required, such as cancer screening in their older patients.
We’ve had a lot of conversations recently about cancer risk in the young, largely because data show rates are going up for colorectal and breast cancer in this population. But it’s not one size fits all. Screening for young women who have a BRCA gene, if they have dense breasts, or if they have a strong family history of breast cancer should be different from those who are at average risk of the disease.
But statistically, there are about 15 per 100,000 breast cancer diagnoses in women under the age of 40 while over the age of 65 it’s 443 per 100,000. So, the risk significantly increases with age but we should not have an arbitrary cut-off. The life expectancy of a woman at age 75 is about 13.5 years. If you’re over the age of 70 or 75, then it’s going to be comorbidities that you look at, as well as individual patient decisions. Patients may say, “I don’t want to ever go through a mammogram again, because I don’t want to have a biopsy again, and I’m not going to get treated.” Or they may say, “My mom died of metastatic breast cancer when she was 82 and I want to know.”
Q: How should primary care physicians interpret conflicting guidance from the major medical groups? For example, the American College of Gastroenterology and your own organization recommend colorectal cancer screening start at age 45 now. But the American College of Physicians recently came out and said 50. What is a well-meaning primary care physician supposed to do?
A: We make more of guideline differences than we should. Sometimes guideline differences aren’t a reflection of different judgments, but rather what data were available when the most recent update took place. For colorectal cancer screening, the ACS dropped the age to begin screening to 45 in 2018 based on a very careful consideration of disease burden data and within several years most other guideline developers reached the same conclusion.
However, I think it’s good for family practice and internal medicine doctors to know that significant GI symptoms in a young patient could be colorectal cancer. It’s not as if nobody sees a 34-year-old or 27-year-old with colorectal cancer. They should be aware that if something goes away in a day or two, that’s fine, but persistent GI symptoms need a cancer workup – colonoscopy or referral to a gastroenterologist. So that’s why I think age 45 is the time when folks should begin screening.
Q: What are the medical-legal issues for a physician who is trying to follow guideline-based care when there are different guidelines?
A: Any physician can say, “We follow the guidelines of this particular organization.” I don’t think anyone can say that an organization’s guidelines are malpractice. For individual physicians, following a set of office-based guidelines will hopefully keep them out of legal difficulty.
Q: What are the risks of overscreening, especially in breast cancer where false positives may result in invasive testing?
A: What people think of as overscreening takes a number of different forms. What one guideline would imply is overscreening is recommended screening by another guideline. I think we would all agree that in an average-risk population, beginning screening before it is recommended would be overscreening, and continuing screening when a patient has life-limiting comorbidities would constitute overscreening. Screening too frequently can constitute overscreening.
For example, many women report that their doctors still are advising a baseline mammogram at age 35. Most guideline-developing organizations would regard this as overscreening in an average-risk population.
I think we are also getting better, certainly in prostate cancer, about knowing who needs to be treated and not treated. There are a lot of cancers that would have been treated 20-30 years ago but now are being safely followed with PSA and MRI. We may be able to get to that point with breast cancer over time, too.
Q: Are you saying that there may be breast cancers for which active surveillance is appropriate? Is that already the case?
A: We’re not there yet. I think some of the DCIS breast cancers are part of the discussion on whether hormonal treatment or surgeries are done. I think people do have those discussions in the context of morbidity and life expectancy. Over time, we’re likely to have more cancers for which we won’t need surgical treatments.
Q: Why did the American Cancer Society change the upper limit for lung cancer screening from 75 to 80 years of age?
A: For an individual older than 65, screening will now continue until the patient is 80, assuming the patient is in good health. According to the previous guideline, if a patient was 65 and more than 15 years beyond smoking cessation, then screening would end. This is exactly the time when we see lung cancers increase in the population and so a curable lung cancer would not previously have been detected by a screening CT scan. *
Q: What role do the multicancer blood and DNA tests play in screening now?
A: As you know, the Exact Sciences Cologuard test is already included in major guidelines for colorectal cancer screening and covered by insurance. Our philosophy on multicancer early detection tests is that we’re supportive of Medicare reimbursement when two things occur: 1. When we know there’s clinical benefit, and 2. When the test has been approved by the FDA.
The multicancer early detection tests in development and undergoing prospective research would not now replace screening for the cancers with established screening programs, but if they are shown to have clinical utility for the cancers in their panel, we would be able to reduce deaths from cancers that mostly are diagnosed at late stages and have poor prognoses.
There’s going to be a need for expertise in primary care practices to help interpret the tests. These are new questions, which are well beyond what even the typical oncologist is trained in, much less primary care physicians. We and other organizations are working on providing those answers.
Q: While we’re on the subject of the future, how do you envision AI helping or hindering cancer screening specifically in primary care?
A: I think AI is going to help things for a couple of reasons. The ability of AI is to get through data quickly and get you information that’s personalized and useful. If AI tools could let a patient know their individual risk of a cancer in the near and long term, that would help the primary care doctor screen in an individualized way. I think AI is going to be able to improve both diagnostic radiology and pathology, and could make a very big difference in settings outside of large cancer centers that operate at high volume every day. The data look very promising for AI to contribute to risk estimation by operating like a second reader in imaging and pathology.
Q: Anything else you’d like to say on this subject that clinicians should know?
A: The questions about whether or not patients should be screened is being pushed on family practice doctors and internists and these questions require a relationship with the patient. A hard stopping point at age 70 when lots of people will live 20 years or more doesn’t make sense.
There’s very little data from randomized clinical trials of screening people over the age of 70. We know that cancer risk does obviously increase with age, particularly prostate and breast cancer. And these are the cancers that are going to be the most common in your practices. If someone has a known mutation, I think you’re going to look differently at screening them. And first-degree family members, particularly for the more aggressive cancers, should be considered for screening.
My philosophy on cancer screening in the elderly is that I think the guidelines are guidelines. If patients have very limited life expectancy, then they shouldn’t be screened. There are calculators that estimate life expectancy in the context of current age and current health status, and these can be useful for decision making and counseling. Patients never think their life expectancy is shorter than 10 years. If their life expectancy is longer than 10 years, then I think, all things being equal, they should continue screening, but the question of ongoing screening needs to be periodically revisited.
*This story was updated on Nov. 1, 2023.
More than 1 in 10 Americans over age 60 years will be diagnosed with cancer, according to the National Cancer Institute, making screening for the disease in older patients imperative. Much of the burden of cancer screening falls on primary care physicians. This news organization spoke recently with William L. Dahut, MD, chief scientific officer of the American Cancer Society, about the particular challenges of screening in older patients.
Question: How much does cancer screening change with age? What are the considerations for clinicians – what risks and comorbidities are important to consider in older populations?
Answer: We at the American Cancer Society are giving a lot of thought to how to help primary care practices keep up with screening, particularly with respect to guidelines, but also best practices where judgment is required, such as cancer screening in their older patients.
We’ve had a lot of conversations recently about cancer risk in the young, largely because data show rates are going up for colorectal and breast cancer in this population. But it’s not one size fits all. Screening for young women who have a BRCA gene, if they have dense breasts, or if they have a strong family history of breast cancer should be different from those who are at average risk of the disease.
But statistically, there are about 15 per 100,000 breast cancer diagnoses in women under the age of 40 while over the age of 65 it’s 443 per 100,000. So, the risk significantly increases with age but we should not have an arbitrary cut-off. The life expectancy of a woman at age 75 is about 13.5 years. If you’re over the age of 70 or 75, then it’s going to be comorbidities that you look at, as well as individual patient decisions. Patients may say, “I don’t want to ever go through a mammogram again, because I don’t want to have a biopsy again, and I’m not going to get treated.” Or they may say, “My mom died of metastatic breast cancer when she was 82 and I want to know.”
Q: How should primary care physicians interpret conflicting guidance from the major medical groups? For example, the American College of Gastroenterology and your own organization recommend colorectal cancer screening start at age 45 now. But the American College of Physicians recently came out and said 50. What is a well-meaning primary care physician supposed to do?
A: We make more of guideline differences than we should. Sometimes guideline differences aren’t a reflection of different judgments, but rather what data were available when the most recent update took place. For colorectal cancer screening, the ACS dropped the age to begin screening to 45 in 2018 based on a very careful consideration of disease burden data and within several years most other guideline developers reached the same conclusion.
However, I think it’s good for family practice and internal medicine doctors to know that significant GI symptoms in a young patient could be colorectal cancer. It’s not as if nobody sees a 34-year-old or 27-year-old with colorectal cancer. They should be aware that if something goes away in a day or two, that’s fine, but persistent GI symptoms need a cancer workup – colonoscopy or referral to a gastroenterologist. So that’s why I think age 45 is the time when folks should begin screening.
Q: What are the medical-legal issues for a physician who is trying to follow guideline-based care when there are different guidelines?
A: Any physician can say, “We follow the guidelines of this particular organization.” I don’t think anyone can say that an organization’s guidelines are malpractice. For individual physicians, following a set of office-based guidelines will hopefully keep them out of legal difficulty.
Q: What are the risks of overscreening, especially in breast cancer where false positives may result in invasive testing?
A: What people think of as overscreening takes a number of different forms. What one guideline would imply is overscreening is recommended screening by another guideline. I think we would all agree that in an average-risk population, beginning screening before it is recommended would be overscreening, and continuing screening when a patient has life-limiting comorbidities would constitute overscreening. Screening too frequently can constitute overscreening.
For example, many women report that their doctors still are advising a baseline mammogram at age 35. Most guideline-developing organizations would regard this as overscreening in an average-risk population.
I think we are also getting better, certainly in prostate cancer, about knowing who needs to be treated and not treated. There are a lot of cancers that would have been treated 20-30 years ago but now are being safely followed with PSA and MRI. We may be able to get to that point with breast cancer over time, too.
Q: Are you saying that there may be breast cancers for which active surveillance is appropriate? Is that already the case?
A: We’re not there yet. I think some of the DCIS breast cancers are part of the discussion on whether hormonal treatment or surgeries are done. I think people do have those discussions in the context of morbidity and life expectancy. Over time, we’re likely to have more cancers for which we won’t need surgical treatments.
Q: Why did the American Cancer Society change the upper limit for lung cancer screening from 75 to 80 years of age?
A: For an individual older than 65, screening will now continue until the patient is 80, assuming the patient is in good health. According to the previous guideline, if a patient was 65 and more than 15 years beyond smoking cessation, then screening would end. This is exactly the time when we see lung cancers increase in the population and so a curable lung cancer would not previously have been detected by a screening CT scan. *
Q: What role do the multicancer blood and DNA tests play in screening now?
A: As you know, the Exact Sciences Cologuard test is already included in major guidelines for colorectal cancer screening and covered by insurance. Our philosophy on multicancer early detection tests is that we’re supportive of Medicare reimbursement when two things occur: 1. When we know there’s clinical benefit, and 2. When the test has been approved by the FDA.
The multicancer early detection tests in development and undergoing prospective research would not now replace screening for the cancers with established screening programs, but if they are shown to have clinical utility for the cancers in their panel, we would be able to reduce deaths from cancers that mostly are diagnosed at late stages and have poor prognoses.
There’s going to be a need for expertise in primary care practices to help interpret the tests. These are new questions, which are well beyond what even the typical oncologist is trained in, much less primary care physicians. We and other organizations are working on providing those answers.
Q: While we’re on the subject of the future, how do you envision AI helping or hindering cancer screening specifically in primary care?
A: I think AI is going to help things for a couple of reasons. The ability of AI is to get through data quickly and get you information that’s personalized and useful. If AI tools could let a patient know their individual risk of a cancer in the near and long term, that would help the primary care doctor screen in an individualized way. I think AI is going to be able to improve both diagnostic radiology and pathology, and could make a very big difference in settings outside of large cancer centers that operate at high volume every day. The data look very promising for AI to contribute to risk estimation by operating like a second reader in imaging and pathology.
Q: Anything else you’d like to say on this subject that clinicians should know?
A: The questions about whether or not patients should be screened is being pushed on family practice doctors and internists and these questions require a relationship with the patient. A hard stopping point at age 70 when lots of people will live 20 years or more doesn’t make sense.
There’s very little data from randomized clinical trials of screening people over the age of 70. We know that cancer risk does obviously increase with age, particularly prostate and breast cancer. And these are the cancers that are going to be the most common in your practices. If someone has a known mutation, I think you’re going to look differently at screening them. And first-degree family members, particularly for the more aggressive cancers, should be considered for screening.
My philosophy on cancer screening in the elderly is that I think the guidelines are guidelines. If patients have very limited life expectancy, then they shouldn’t be screened. There are calculators that estimate life expectancy in the context of current age and current health status, and these can be useful for decision making and counseling. Patients never think their life expectancy is shorter than 10 years. If their life expectancy is longer than 10 years, then I think, all things being equal, they should continue screening, but the question of ongoing screening needs to be periodically revisited.
*This story was updated on Nov. 1, 2023.
My pet peeves about the current state of primary care
For this month’s column, I wanted to share some frustrations I have had about the current state of primary care. We all find those things that are going on in medicine that seem crazy and we just have to find a way to adapt to them. It is good to be able to share some of these thoughts with a community as distinguished as you readers. I know some of these are issues that you all struggle with and I wanted to give a voice to them. I wish I had answers to fix them.
Faxes from insurance companies
I find faxes from insurance companies immensely annoying. First, it takes time to go through lots of unwanted faxes but these faxes are extremely inaccurate. Today I received a fax telling me I might want to consider starting a statin in my 64-year-old HIV patient who has hypertension. He has been on a statin for 10 years.
Another fax warned me to not combine ACE inhibitors and angiotensin II receptor blockers (ARBs) in a patient who was switched from an ACE inhibitor in July to an ARB because of a cough. The fax that was sent to me has a documented end date for the ACE inhibitor before the start date of the ARB.
We only have so much time in the day and piles of faxes are not helpful.
Speaking of faxes: Why do physical therapy offices and nursing homes fax the same form every day? Physicians do not always work in clinic every single day and it increases the workload and burden when you have to sort through three copies of the same fax. I once worked in a world where these would be sent by mail, and mailed back a week later, which seemed to work just fine.
Misinformation
Our patients have many sources of health information. Much of the information they get comes from family, friends, social media posts, and Internet sites. The accuracy of the information is often questionable, and in some cases, they are victims of intentional misinformation.
It is frustrating and time consuming to counter the bogus, unsubstantiated information patients receive. It is especially difficult when patients have done their own research on proven therapies (such as statins) and do not want to use them because of the many websites they have looked at that make unscientific claims about the dangers of the proposed therapy. I share evidence-based websites with my patients for their research; my favorite is medlineplus.gov.
Access crisis
The availability of specialty care is extremely limited now. In my health care system, there is up to a 6-month wait for appointments in neurology, cardiology, and endocrinology. This puts the burden on the primary care professional to manage the patient’s health, even when the patient really needs specialty care. It also increases the calls we receive to interpret the echocardiograms, MRIs, or lab tests ordered by specialists who do not share the interpretation of the results with their patients.
What can be done to improve this situation? Automatic consults in the hospital should be limited. Every patient who has a transient ischemic attack with a negative workup does not need neurology follow-up. The same goes for patients who have chest pain but a negative cardiac workup in the hospital – they do not need follow-up by a cardiologist, nor do those who have stable, well-managed coronary disease. We have to find a way to keep our specialists seeing the patients whom they can help the most and available for consultation in a timely fashion.
Please share your pet peeves with me. I will try to give them voice in the future. Hang in there, you are the glue that keeps this flawed system together.
Dr. Paauw is professor of medicine in the division of general internal medicine at the University of Washington, Seattle, and he serves as third-year medical student clerkship director at the University of Washington. Contact Dr. Paauw at [email protected].
For this month’s column, I wanted to share some frustrations I have had about the current state of primary care. We all find those things that are going on in medicine that seem crazy and we just have to find a way to adapt to them. It is good to be able to share some of these thoughts with a community as distinguished as you readers. I know some of these are issues that you all struggle with and I wanted to give a voice to them. I wish I had answers to fix them.
Faxes from insurance companies
I find faxes from insurance companies immensely annoying. First, it takes time to go through lots of unwanted faxes but these faxes are extremely inaccurate. Today I received a fax telling me I might want to consider starting a statin in my 64-year-old HIV patient who has hypertension. He has been on a statin for 10 years.
Another fax warned me to not combine ACE inhibitors and angiotensin II receptor blockers (ARBs) in a patient who was switched from an ACE inhibitor in July to an ARB because of a cough. The fax that was sent to me has a documented end date for the ACE inhibitor before the start date of the ARB.
We only have so much time in the day and piles of faxes are not helpful.
Speaking of faxes: Why do physical therapy offices and nursing homes fax the same form every day? Physicians do not always work in clinic every single day and it increases the workload and burden when you have to sort through three copies of the same fax. I once worked in a world where these would be sent by mail, and mailed back a week later, which seemed to work just fine.
Misinformation
Our patients have many sources of health information. Much of the information they get comes from family, friends, social media posts, and Internet sites. The accuracy of the information is often questionable, and in some cases, they are victims of intentional misinformation.
It is frustrating and time consuming to counter the bogus, unsubstantiated information patients receive. It is especially difficult when patients have done their own research on proven therapies (such as statins) and do not want to use them because of the many websites they have looked at that make unscientific claims about the dangers of the proposed therapy. I share evidence-based websites with my patients for their research; my favorite is medlineplus.gov.
Access crisis
The availability of specialty care is extremely limited now. In my health care system, there is up to a 6-month wait for appointments in neurology, cardiology, and endocrinology. This puts the burden on the primary care professional to manage the patient’s health, even when the patient really needs specialty care. It also increases the calls we receive to interpret the echocardiograms, MRIs, or lab tests ordered by specialists who do not share the interpretation of the results with their patients.
What can be done to improve this situation? Automatic consults in the hospital should be limited. Every patient who has a transient ischemic attack with a negative workup does not need neurology follow-up. The same goes for patients who have chest pain but a negative cardiac workup in the hospital – they do not need follow-up by a cardiologist, nor do those who have stable, well-managed coronary disease. We have to find a way to keep our specialists seeing the patients whom they can help the most and available for consultation in a timely fashion.
Please share your pet peeves with me. I will try to give them voice in the future. Hang in there, you are the glue that keeps this flawed system together.
Dr. Paauw is professor of medicine in the division of general internal medicine at the University of Washington, Seattle, and he serves as third-year medical student clerkship director at the University of Washington. Contact Dr. Paauw at [email protected].
For this month’s column, I wanted to share some frustrations I have had about the current state of primary care. We all find those things that are going on in medicine that seem crazy and we just have to find a way to adapt to them. It is good to be able to share some of these thoughts with a community as distinguished as you readers. I know some of these are issues that you all struggle with and I wanted to give a voice to them. I wish I had answers to fix them.
Faxes from insurance companies
I find faxes from insurance companies immensely annoying. First, it takes time to go through lots of unwanted faxes but these faxes are extremely inaccurate. Today I received a fax telling me I might want to consider starting a statin in my 64-year-old HIV patient who has hypertension. He has been on a statin for 10 years.
Another fax warned me to not combine ACE inhibitors and angiotensin II receptor blockers (ARBs) in a patient who was switched from an ACE inhibitor in July to an ARB because of a cough. The fax that was sent to me has a documented end date for the ACE inhibitor before the start date of the ARB.
We only have so much time in the day and piles of faxes are not helpful.
Speaking of faxes: Why do physical therapy offices and nursing homes fax the same form every day? Physicians do not always work in clinic every single day and it increases the workload and burden when you have to sort through three copies of the same fax. I once worked in a world where these would be sent by mail, and mailed back a week later, which seemed to work just fine.
Misinformation
Our patients have many sources of health information. Much of the information they get comes from family, friends, social media posts, and Internet sites. The accuracy of the information is often questionable, and in some cases, they are victims of intentional misinformation.
It is frustrating and time consuming to counter the bogus, unsubstantiated information patients receive. It is especially difficult when patients have done their own research on proven therapies (such as statins) and do not want to use them because of the many websites they have looked at that make unscientific claims about the dangers of the proposed therapy. I share evidence-based websites with my patients for their research; my favorite is medlineplus.gov.
Access crisis
The availability of specialty care is extremely limited now. In my health care system, there is up to a 6-month wait for appointments in neurology, cardiology, and endocrinology. This puts the burden on the primary care professional to manage the patient’s health, even when the patient really needs specialty care. It also increases the calls we receive to interpret the echocardiograms, MRIs, or lab tests ordered by specialists who do not share the interpretation of the results with their patients.
What can be done to improve this situation? Automatic consults in the hospital should be limited. Every patient who has a transient ischemic attack with a negative workup does not need neurology follow-up. The same goes for patients who have chest pain but a negative cardiac workup in the hospital – they do not need follow-up by a cardiologist, nor do those who have stable, well-managed coronary disease. We have to find a way to keep our specialists seeing the patients whom they can help the most and available for consultation in a timely fashion.
Please share your pet peeves with me. I will try to give them voice in the future. Hang in there, you are the glue that keeps this flawed system together.
Dr. Paauw is professor of medicine in the division of general internal medicine at the University of Washington, Seattle, and he serves as third-year medical student clerkship director at the University of Washington. Contact Dr. Paauw at [email protected].
A focus on women with diabetes and their offspring
In 2021, diabetes and related complications was the 8th leading cause of death in the United States.1 As of 2022, more than 11% of the U.S. population had diabetes and 38% of the adult U.S. population had prediabetes.2 Diabetes is the most expensive chronic condition in the United States, where $1 of every $4 in health care costs is spent on care.3
Where this is most concerning is diabetes in pregnancy. While childbirth rates in the United States have decreased since the 2007 high of 4.32 million births4 to 3.66 million in 2021,5 the incidence of diabetes in pregnancy – both pregestational and gestational – has increased. The rate of pregestational diabetes in 2021 was 10.9 per 1,000 births, a 27% increase from 2016 (8.6 per 1,000).6 The percentage of those giving birth who also were diagnosed with gestational diabetes mellitus (GDM) was 8.3% in 2021, up from 6.0% in 2016.7
Adverse outcomes for an infant born to a mother with diabetes include a higher risk of obesity and diabetes as adults, potentially leading to a forward-feeding cycle.
We and our colleagues established the Diabetes in Pregnancy Study Group of North America in 1997 because we had witnessed too frequently the devastating diabetes-induced pregnancy complications in our patients. The mission we set forth was to provide a forum for dialogue among maternal-fetal medicine subspecialists. The three main goals we set forth to support this mission were to provide a catalyst for research, contribute to the creation and refinement of medical policies, and influence professional practices in diabetes in pregnancy.8
In the last quarter century, DPSG-NA, through its annual and biennial meetings, has brought together several hundred practitioners that include physicians, nurses, statisticians, researchers, nutritionists, and allied health professionals, among others. As a group, it has improved the detection and management of diabetes in pregnant women and their offspring through knowledge sharing and influencing policies on GDM screening, diagnosis, management, and treatment. Our members have shown that preconceptional counseling for women with diabetes can significantly reduce congenital malformation and perinatal mortality compared with those women with pregestational diabetes who receive no counseling.9,10
We have addressed a wide variety of topics including the paucity of data in determining the timing of delivery for women with diabetes and the Institute of Medicine/National Academy of Medicine recommendations of gestational weight gain and risks of not adhering to them. We have learned about new scientific discoveries that reveal underlying mechanisms to diabetes-related birth defects and potential therapeutic targets; and we have discussed the health literacy requirements, ethics, and opportunities for lifestyle intervention.11-16
But we need to do more.
Two risk factors are at play: Women continue to choose to have babies at later ages and their pregnancies continue to be complicated by the rising incidence of obesity (see Figure 1 and Figure 2). 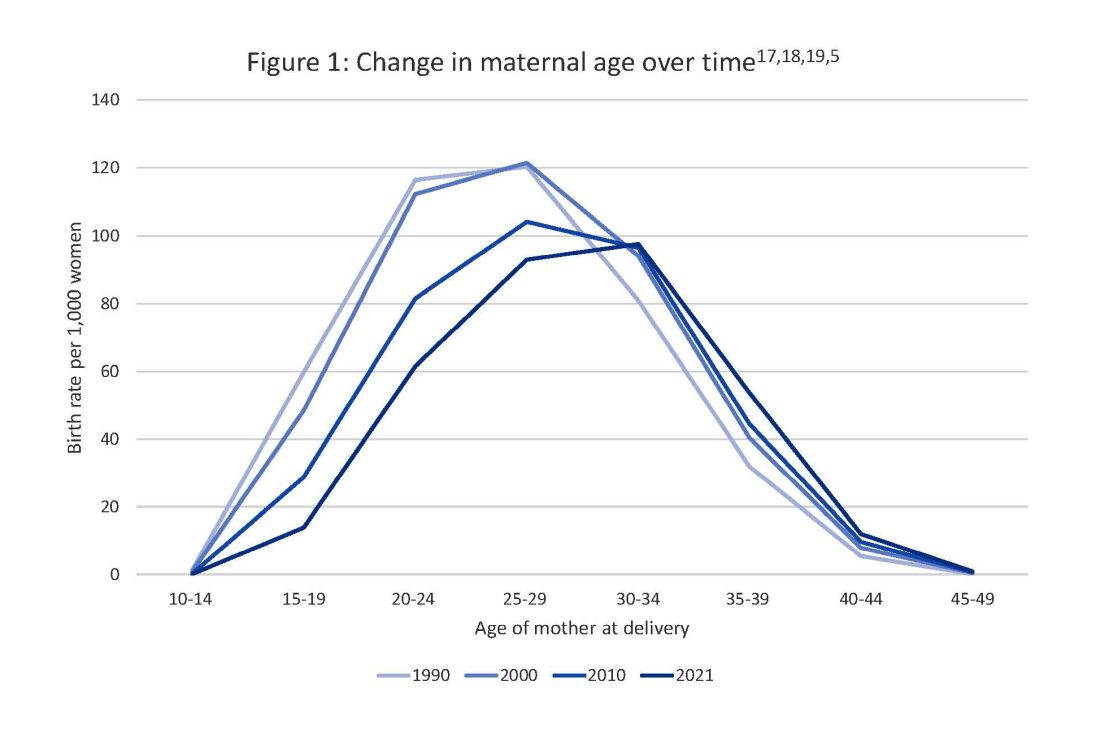
The global obesity epidemic has become a significant concern for all aspects of health and particularly for diabetes in pregnancy. 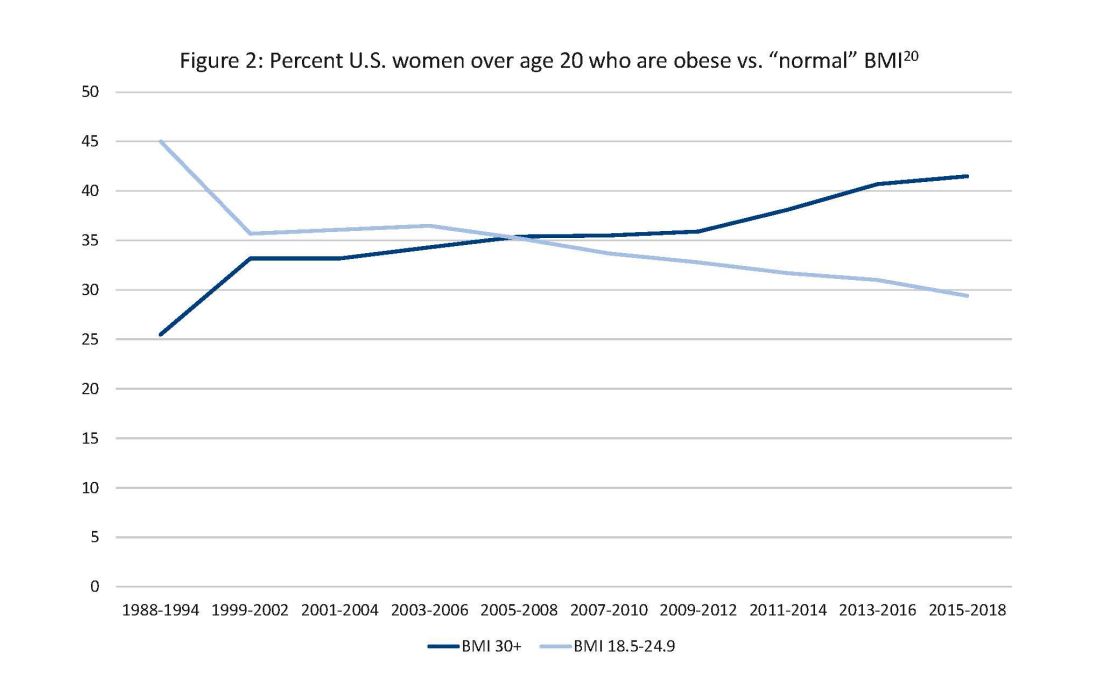
In 1990, 24.9% of women in the United States were obese; in 2010, 35.8%; and now more than 41%. Some experts project that by 2030 more than 80% of women in the United States will be overweight or obese.21
If we are to stop this cycle of diabetes begets more diabetes, now more than ever we need to come together and accelerate the research and education around the diabetes in pregnancy. Join us at this year’s DPSG-NA meeting Oct. 26-28 to take part in the knowledge sharing, discussions, and planning. More information can be found online at https://events.dpsg-na.com/home.
Dr. Miodovnik is adjunct professor of obstetrics, gynecology, and reproductive sciences at University of Maryland School of Medicine. Dr. Reece is professor of obstetrics, gynecology, and reproductive sciences and senior scientist at the Center for Birth Defects Research at University of Maryland School of Medicine.
References
1. Xu J et al. Mortality in the United States, 2021. NCHS Data Brief. 2022 Dec;(456):1-8. PMID: 36598387.
2. Centers for Disease Control and Prevention, diabetes data and statistics.
3. American Diabetes Association. The Cost of Diabetes.
4. Martin JA et al. Births: Final data for 2007. Natl Vital Stat Rep. 2010 Aug 9;58(24):1-85. PMID: 21254725.
5. Osterman MJK et al. Births: Final data for 2021. Natl Vital Stat Rep. 2023 Jan;72(1):1-53. PMID: 36723449.
6. Gregory ECW and Ely DM. Trends and characteristics in prepregnancy diabetes: United States, 2016-2021. Natl Vital Stat Rep. 2023 May;72(6):1-13. PMID: 37256333.
7. QuickStats: Percentage of mothers with gestational diabetes, by maternal age – National Vital Statistics System, United States, 2016 and 2021. MMWR Morb Mortal Wkly Rep. 2023 Jan 6;72(1):16. doi: 10.15585/mmwr.mm7201a4.
8. Langer O et al. The Diabetes in Pregnancy Study Group of North America – Introduction and summary statement. Prenat Neonat Med. 1998;3(6):514-6.
9. Willhoite MB et al. The impact of preconception counseling on pregnancy outcomes. The experience of the Maine Diabetes in Pregnancy Program. Diabetes Care. 1993 Feb;16(2):450-5. doi: 10.2337/diacare.16.2.450.
10. McElvy SS et al. A focused preconceptional and early pregnancy program in women with type 1 diabetes reduces perinatal mortality and malformation rates to general population levels. J Matern Fetal Med. 2000 Jan-Feb;9(1):14-20. doi: 10.1002/(SICI)1520-6661(200001/02)9:1<14::AID-MFM5>3.0.CO;2-K.
11. Rosen JA et al. The history and contributions of the Diabetes in Pregnancy Study Group of North America (1997-2015). Am J Perinatol. 2016 Nov;33(13):1223-6. doi: 10.1055/s-0036-1585082.
12. Driggers RW and Baschat A. The 12th meeting of the Diabetes in Pregnancy Study Group of North America (DPSG-NA): Introduction and overview. J Matern Fetal Neonatal Med. 2012 Jan;25(1):3-4. doi: 10.3109/14767058.2012.626917.
13. Langer O et al. The proceedings of the Diabetes in Pregnancy Study Group of North America 2009 conference. J Matern Fetal Neonatal Med. 2010 Mar;23(3):196-8. doi: 10.3109/14767050903550634.
14. Reece EA et al. A consensus report of the Diabetes in Pregnancy Study Group of North America Conference, Little Rock, Ark., May 2002. J Matern Fetal Neonatal Med. 2002 Dec;12(6):362-4. doi: 10.1080/jmf.12.6.362.364.
15. Reece EA and Maulik D. A consensus conference of the Diabetes in Pregnancy Study Group of North America. J Matern Fetal Neonatal Med. 2002 Dec;12(6):361. doi: 10.1080/jmf.12.6.361.361.
16. Gabbe SG. Summation of the second meeting of the Diabetes in Pregnancy Study Group of North America (DPSG-NA). J Matern Fetal Med. 2000 Jan-Feb;9(1):3-9.
17. Vital Statistics of the United States 1990: Volume I – Natality.
18. Martin JA et al. Births: final data for 2000. Natl Vital Stat Rep. 2002 Feb 12;50(5):1-101. PMID: 11876093.
19. Martin JA et al. Births: final data for 2010. Natl Vital Stat Rep. 2012 Aug 28;61(1):1-72. PMID: 24974589.
20. CDC Website. Normal weight, overweight, and obesity among adults aged 20 and over, by selected characteristics: United States.
21. Wang Y et al. Has the prevalence of overweight, obesity, and central obesity levelled off in the United States? Trends, patterns, disparities, and future projections for the obesity epidemic. Int J Epidemiol. 2020 Jun 1;49(3):810-23. doi: 10.1093/ije/dyz273.
In 2021, diabetes and related complications was the 8th leading cause of death in the United States.1 As of 2022, more than 11% of the U.S. population had diabetes and 38% of the adult U.S. population had prediabetes.2 Diabetes is the most expensive chronic condition in the United States, where $1 of every $4 in health care costs is spent on care.3
Where this is most concerning is diabetes in pregnancy. While childbirth rates in the United States have decreased since the 2007 high of 4.32 million births4 to 3.66 million in 2021,5 the incidence of diabetes in pregnancy – both pregestational and gestational – has increased. The rate of pregestational diabetes in 2021 was 10.9 per 1,000 births, a 27% increase from 2016 (8.6 per 1,000).6 The percentage of those giving birth who also were diagnosed with gestational diabetes mellitus (GDM) was 8.3% in 2021, up from 6.0% in 2016.7
Adverse outcomes for an infant born to a mother with diabetes include a higher risk of obesity and diabetes as adults, potentially leading to a forward-feeding cycle.
We and our colleagues established the Diabetes in Pregnancy Study Group of North America in 1997 because we had witnessed too frequently the devastating diabetes-induced pregnancy complications in our patients. The mission we set forth was to provide a forum for dialogue among maternal-fetal medicine subspecialists. The three main goals we set forth to support this mission were to provide a catalyst for research, contribute to the creation and refinement of medical policies, and influence professional practices in diabetes in pregnancy.8
In the last quarter century, DPSG-NA, through its annual and biennial meetings, has brought together several hundred practitioners that include physicians, nurses, statisticians, researchers, nutritionists, and allied health professionals, among others. As a group, it has improved the detection and management of diabetes in pregnant women and their offspring through knowledge sharing and influencing policies on GDM screening, diagnosis, management, and treatment. Our members have shown that preconceptional counseling for women with diabetes can significantly reduce congenital malformation and perinatal mortality compared with those women with pregestational diabetes who receive no counseling.9,10
We have addressed a wide variety of topics including the paucity of data in determining the timing of delivery for women with diabetes and the Institute of Medicine/National Academy of Medicine recommendations of gestational weight gain and risks of not adhering to them. We have learned about new scientific discoveries that reveal underlying mechanisms to diabetes-related birth defects and potential therapeutic targets; and we have discussed the health literacy requirements, ethics, and opportunities for lifestyle intervention.11-16
But we need to do more.
Two risk factors are at play: Women continue to choose to have babies at later ages and their pregnancies continue to be complicated by the rising incidence of obesity (see Figure 1 and Figure 2). 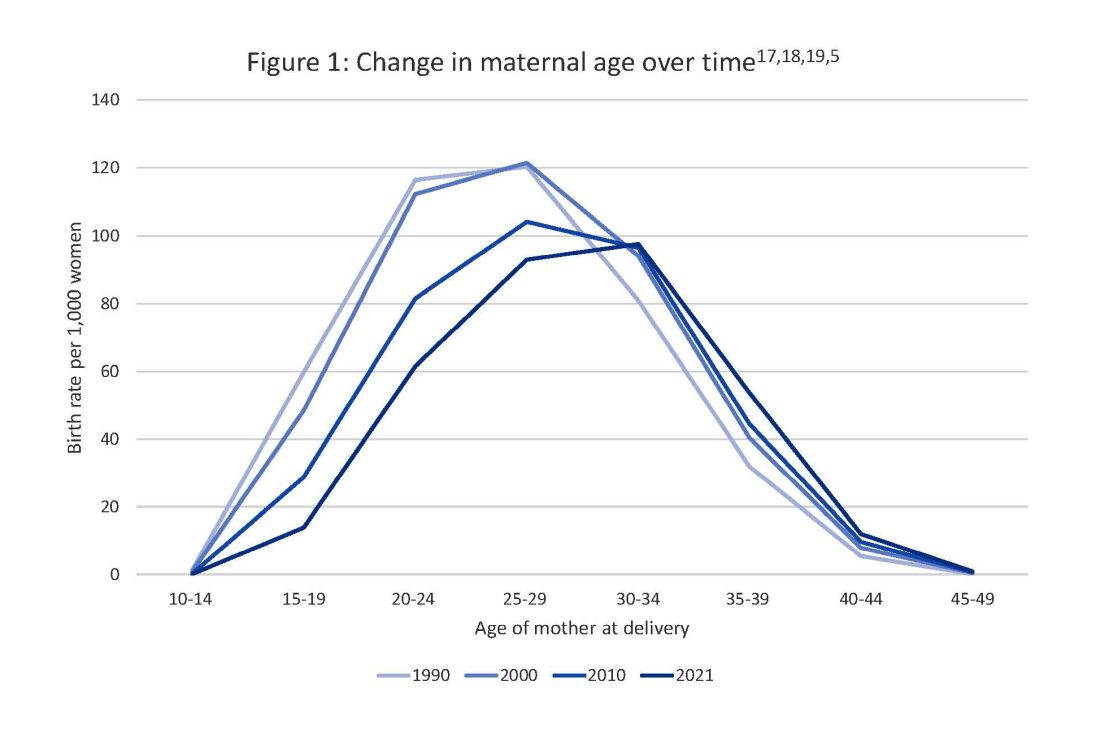
The global obesity epidemic has become a significant concern for all aspects of health and particularly for diabetes in pregnancy. 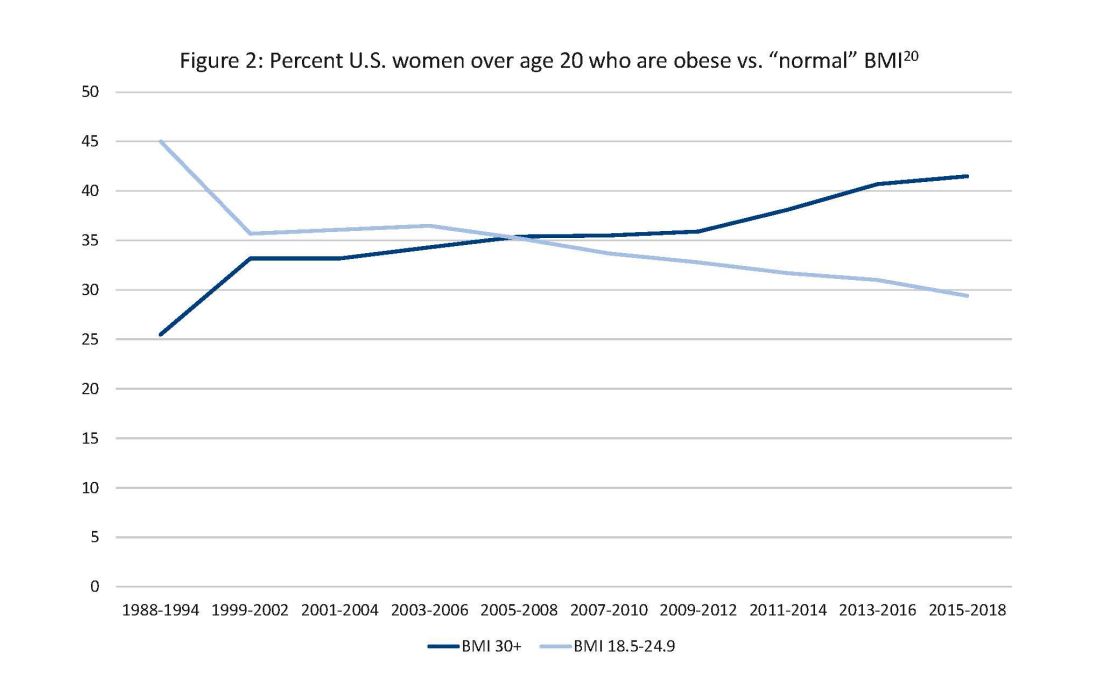
In 1990, 24.9% of women in the United States were obese; in 2010, 35.8%; and now more than 41%. Some experts project that by 2030 more than 80% of women in the United States will be overweight or obese.21
If we are to stop this cycle of diabetes begets more diabetes, now more than ever we need to come together and accelerate the research and education around the diabetes in pregnancy. Join us at this year’s DPSG-NA meeting Oct. 26-28 to take part in the knowledge sharing, discussions, and planning. More information can be found online at https://events.dpsg-na.com/home.
Dr. Miodovnik is adjunct professor of obstetrics, gynecology, and reproductive sciences at University of Maryland School of Medicine. Dr. Reece is professor of obstetrics, gynecology, and reproductive sciences and senior scientist at the Center for Birth Defects Research at University of Maryland School of Medicine.
References
1. Xu J et al. Mortality in the United States, 2021. NCHS Data Brief. 2022 Dec;(456):1-8. PMID: 36598387.
2. Centers for Disease Control and Prevention, diabetes data and statistics.
3. American Diabetes Association. The Cost of Diabetes.
4. Martin JA et al. Births: Final data for 2007. Natl Vital Stat Rep. 2010 Aug 9;58(24):1-85. PMID: 21254725.
5. Osterman MJK et al. Births: Final data for 2021. Natl Vital Stat Rep. 2023 Jan;72(1):1-53. PMID: 36723449.
6. Gregory ECW and Ely DM. Trends and characteristics in prepregnancy diabetes: United States, 2016-2021. Natl Vital Stat Rep. 2023 May;72(6):1-13. PMID: 37256333.
7. QuickStats: Percentage of mothers with gestational diabetes, by maternal age – National Vital Statistics System, United States, 2016 and 2021. MMWR Morb Mortal Wkly Rep. 2023 Jan 6;72(1):16. doi: 10.15585/mmwr.mm7201a4.
8. Langer O et al. The Diabetes in Pregnancy Study Group of North America – Introduction and summary statement. Prenat Neonat Med. 1998;3(6):514-6.
9. Willhoite MB et al. The impact of preconception counseling on pregnancy outcomes. The experience of the Maine Diabetes in Pregnancy Program. Diabetes Care. 1993 Feb;16(2):450-5. doi: 10.2337/diacare.16.2.450.
10. McElvy SS et al. A focused preconceptional and early pregnancy program in women with type 1 diabetes reduces perinatal mortality and malformation rates to general population levels. J Matern Fetal Med. 2000 Jan-Feb;9(1):14-20. doi: 10.1002/(SICI)1520-6661(200001/02)9:1<14::AID-MFM5>3.0.CO;2-K.
11. Rosen JA et al. The history and contributions of the Diabetes in Pregnancy Study Group of North America (1997-2015). Am J Perinatol. 2016 Nov;33(13):1223-6. doi: 10.1055/s-0036-1585082.
12. Driggers RW and Baschat A. The 12th meeting of the Diabetes in Pregnancy Study Group of North America (DPSG-NA): Introduction and overview. J Matern Fetal Neonatal Med. 2012 Jan;25(1):3-4. doi: 10.3109/14767058.2012.626917.
13. Langer O et al. The proceedings of the Diabetes in Pregnancy Study Group of North America 2009 conference. J Matern Fetal Neonatal Med. 2010 Mar;23(3):196-8. doi: 10.3109/14767050903550634.
14. Reece EA et al. A consensus report of the Diabetes in Pregnancy Study Group of North America Conference, Little Rock, Ark., May 2002. J Matern Fetal Neonatal Med. 2002 Dec;12(6):362-4. doi: 10.1080/jmf.12.6.362.364.
15. Reece EA and Maulik D. A consensus conference of the Diabetes in Pregnancy Study Group of North America. J Matern Fetal Neonatal Med. 2002 Dec;12(6):361. doi: 10.1080/jmf.12.6.361.361.
16. Gabbe SG. Summation of the second meeting of the Diabetes in Pregnancy Study Group of North America (DPSG-NA). J Matern Fetal Med. 2000 Jan-Feb;9(1):3-9.
17. Vital Statistics of the United States 1990: Volume I – Natality.
18. Martin JA et al. Births: final data for 2000. Natl Vital Stat Rep. 2002 Feb 12;50(5):1-101. PMID: 11876093.
19. Martin JA et al. Births: final data for 2010. Natl Vital Stat Rep. 2012 Aug 28;61(1):1-72. PMID: 24974589.
20. CDC Website. Normal weight, overweight, and obesity among adults aged 20 and over, by selected characteristics: United States.
21. Wang Y et al. Has the prevalence of overweight, obesity, and central obesity levelled off in the United States? Trends, patterns, disparities, and future projections for the obesity epidemic. Int J Epidemiol. 2020 Jun 1;49(3):810-23. doi: 10.1093/ije/dyz273.
In 2021, diabetes and related complications was the 8th leading cause of death in the United States.1 As of 2022, more than 11% of the U.S. population had diabetes and 38% of the adult U.S. population had prediabetes.2 Diabetes is the most expensive chronic condition in the United States, where $1 of every $4 in health care costs is spent on care.3
Where this is most concerning is diabetes in pregnancy. While childbirth rates in the United States have decreased since the 2007 high of 4.32 million births4 to 3.66 million in 2021,5 the incidence of diabetes in pregnancy – both pregestational and gestational – has increased. The rate of pregestational diabetes in 2021 was 10.9 per 1,000 births, a 27% increase from 2016 (8.6 per 1,000).6 The percentage of those giving birth who also were diagnosed with gestational diabetes mellitus (GDM) was 8.3% in 2021, up from 6.0% in 2016.7
Adverse outcomes for an infant born to a mother with diabetes include a higher risk of obesity and diabetes as adults, potentially leading to a forward-feeding cycle.
We and our colleagues established the Diabetes in Pregnancy Study Group of North America in 1997 because we had witnessed too frequently the devastating diabetes-induced pregnancy complications in our patients. The mission we set forth was to provide a forum for dialogue among maternal-fetal medicine subspecialists. The three main goals we set forth to support this mission were to provide a catalyst for research, contribute to the creation and refinement of medical policies, and influence professional practices in diabetes in pregnancy.8
In the last quarter century, DPSG-NA, through its annual and biennial meetings, has brought together several hundred practitioners that include physicians, nurses, statisticians, researchers, nutritionists, and allied health professionals, among others. As a group, it has improved the detection and management of diabetes in pregnant women and their offspring through knowledge sharing and influencing policies on GDM screening, diagnosis, management, and treatment. Our members have shown that preconceptional counseling for women with diabetes can significantly reduce congenital malformation and perinatal mortality compared with those women with pregestational diabetes who receive no counseling.9,10
We have addressed a wide variety of topics including the paucity of data in determining the timing of delivery for women with diabetes and the Institute of Medicine/National Academy of Medicine recommendations of gestational weight gain and risks of not adhering to them. We have learned about new scientific discoveries that reveal underlying mechanisms to diabetes-related birth defects and potential therapeutic targets; and we have discussed the health literacy requirements, ethics, and opportunities for lifestyle intervention.11-16
But we need to do more.
Two risk factors are at play: Women continue to choose to have babies at later ages and their pregnancies continue to be complicated by the rising incidence of obesity (see Figure 1 and Figure 2). 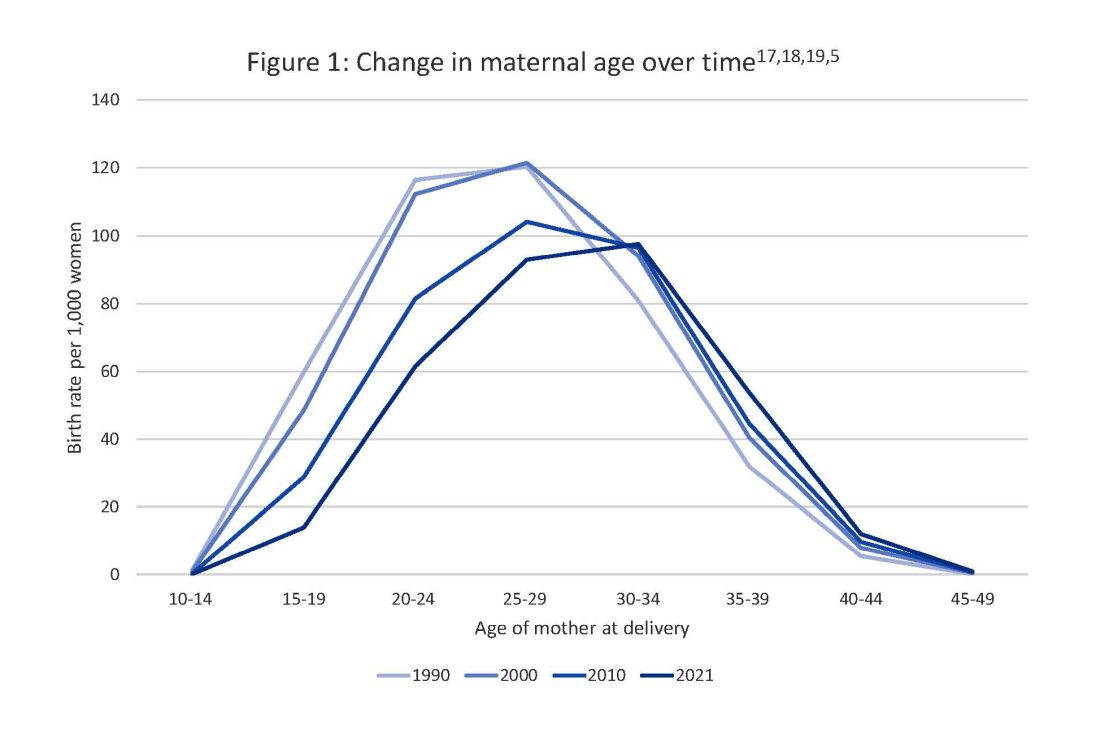
The global obesity epidemic has become a significant concern for all aspects of health and particularly for diabetes in pregnancy. 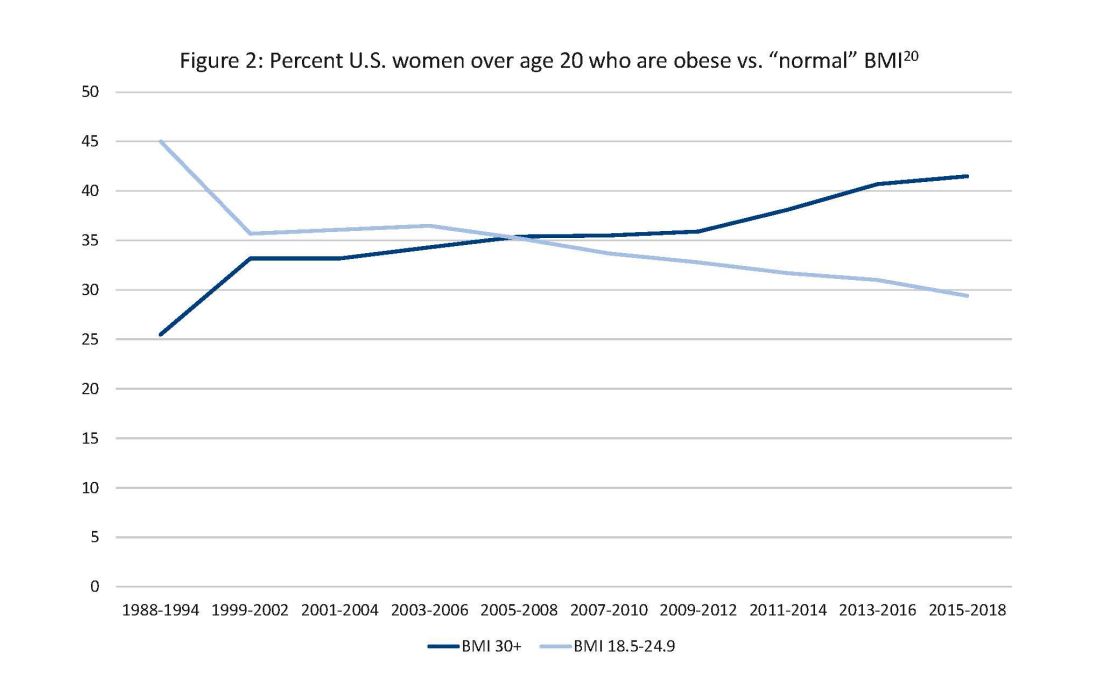
In 1990, 24.9% of women in the United States were obese; in 2010, 35.8%; and now more than 41%. Some experts project that by 2030 more than 80% of women in the United States will be overweight or obese.21
If we are to stop this cycle of diabetes begets more diabetes, now more than ever we need to come together and accelerate the research and education around the diabetes in pregnancy. Join us at this year’s DPSG-NA meeting Oct. 26-28 to take part in the knowledge sharing, discussions, and planning. More information can be found online at https://events.dpsg-na.com/home.
Dr. Miodovnik is adjunct professor of obstetrics, gynecology, and reproductive sciences at University of Maryland School of Medicine. Dr. Reece is professor of obstetrics, gynecology, and reproductive sciences and senior scientist at the Center for Birth Defects Research at University of Maryland School of Medicine.
References
1. Xu J et al. Mortality in the United States, 2021. NCHS Data Brief. 2022 Dec;(456):1-8. PMID: 36598387.
2. Centers for Disease Control and Prevention, diabetes data and statistics.
3. American Diabetes Association. The Cost of Diabetes.
4. Martin JA et al. Births: Final data for 2007. Natl Vital Stat Rep. 2010 Aug 9;58(24):1-85. PMID: 21254725.
5. Osterman MJK et al. Births: Final data for 2021. Natl Vital Stat Rep. 2023 Jan;72(1):1-53. PMID: 36723449.
6. Gregory ECW and Ely DM. Trends and characteristics in prepregnancy diabetes: United States, 2016-2021. Natl Vital Stat Rep. 2023 May;72(6):1-13. PMID: 37256333.
7. QuickStats: Percentage of mothers with gestational diabetes, by maternal age – National Vital Statistics System, United States, 2016 and 2021. MMWR Morb Mortal Wkly Rep. 2023 Jan 6;72(1):16. doi: 10.15585/mmwr.mm7201a4.
8. Langer O et al. The Diabetes in Pregnancy Study Group of North America – Introduction and summary statement. Prenat Neonat Med. 1998;3(6):514-6.
9. Willhoite MB et al. The impact of preconception counseling on pregnancy outcomes. The experience of the Maine Diabetes in Pregnancy Program. Diabetes Care. 1993 Feb;16(2):450-5. doi: 10.2337/diacare.16.2.450.
10. McElvy SS et al. A focused preconceptional and early pregnancy program in women with type 1 diabetes reduces perinatal mortality and malformation rates to general population levels. J Matern Fetal Med. 2000 Jan-Feb;9(1):14-20. doi: 10.1002/(SICI)1520-6661(200001/02)9:1<14::AID-MFM5>3.0.CO;2-K.
11. Rosen JA et al. The history and contributions of the Diabetes in Pregnancy Study Group of North America (1997-2015). Am J Perinatol. 2016 Nov;33(13):1223-6. doi: 10.1055/s-0036-1585082.
12. Driggers RW and Baschat A. The 12th meeting of the Diabetes in Pregnancy Study Group of North America (DPSG-NA): Introduction and overview. J Matern Fetal Neonatal Med. 2012 Jan;25(1):3-4. doi: 10.3109/14767058.2012.626917.
13. Langer O et al. The proceedings of the Diabetes in Pregnancy Study Group of North America 2009 conference. J Matern Fetal Neonatal Med. 2010 Mar;23(3):196-8. doi: 10.3109/14767050903550634.
14. Reece EA et al. A consensus report of the Diabetes in Pregnancy Study Group of North America Conference, Little Rock, Ark., May 2002. J Matern Fetal Neonatal Med. 2002 Dec;12(6):362-4. doi: 10.1080/jmf.12.6.362.364.
15. Reece EA and Maulik D. A consensus conference of the Diabetes in Pregnancy Study Group of North America. J Matern Fetal Neonatal Med. 2002 Dec;12(6):361. doi: 10.1080/jmf.12.6.361.361.
16. Gabbe SG. Summation of the second meeting of the Diabetes in Pregnancy Study Group of North America (DPSG-NA). J Matern Fetal Med. 2000 Jan-Feb;9(1):3-9.
17. Vital Statistics of the United States 1990: Volume I – Natality.
18. Martin JA et al. Births: final data for 2000. Natl Vital Stat Rep. 2002 Feb 12;50(5):1-101. PMID: 11876093.
19. Martin JA et al. Births: final data for 2010. Natl Vital Stat Rep. 2012 Aug 28;61(1):1-72. PMID: 24974589.
20. CDC Website. Normal weight, overweight, and obesity among adults aged 20 and over, by selected characteristics: United States.
21. Wang Y et al. Has the prevalence of overweight, obesity, and central obesity levelled off in the United States? Trends, patterns, disparities, and future projections for the obesity epidemic. Int J Epidemiol. 2020 Jun 1;49(3):810-23. doi: 10.1093/ije/dyz273.
Neoadjuvant advantages: Treating locally advanced lung cancer
Many of you saw the press release from Merck announcing that their randomized trial comparing chemo with chemo plus pembrolizumab in the neoadjuvant setting led to improved event-free survival and also improved pathologic complete response rate.
This comes in addition to the data from the AstraZeneca trial with durvalumab saying they’ve already achieved their endpoint of higher pathologic complete response rate vs. chemotherapy alone and also the data with nivolumab from Bristol-Myers Squibb saying that nivolumab plus chemotherapy leads to a better event-free survival and a better pathologic complete response rate. That information has led to Food and Drug Administration approval for their regimen.
We’re running the table with these very positive data, and I think it’s just a sign that the approach is safe and effective.
A huge question has come up. I just came from a meeting of lung cancer experts asking what to do if you have a patient with a small tumor, for example, a 3-cm tumor. Do you recommend immediate surgery followed by adjuvant therapy, chemotherapy, and then a checkpoint inhibitor if appropriate? Or do you proceed with neoadjuvant therapy if appropriate? The truth is that it’s a very difficult decision.
We have overwhelming data that the neoadjuvant approach works for that patient. Please remember that this is a clinically staged patient. This is not the patient after their surgery, where I think we have a very clear path. We have adjuvant data and adjuvant trials for those patients.
For the patient who’s in your office with a small tumor or a small tumor and only hilar lymphadenopathy, the decision there isn’t data driven, but rather it is experience driven. The data that are out there right now suggest that neoadjuvant therapy is a better way to go. Why is that?
Well, I think that the first reason is that it is probably a better regimen. I think many of you saw the recent clinical trial by Patel and colleagues in the New England Journal of Medicine with melanoma. It was an interesting trial. They gave a checkpoint inhibitor for 18 doses after surgery for melanoma versus three doses of checkpoint inhibitor, surgery, and then 15 doses of the checkpoint inhibitor.
It was 18 doses versus 18 doses, with the only difference being the three doses before surgery. Lo and behold, the three doses before surgery led to a better event-free survival.
There are preclinical data in lung cancer demonstrating that the same thing is true. Tina Cascone published on that years ago. We could talk about why, but it appears that neoadjuvant is just better.
There are other advantages to it as well. I think a big one is that all the information shows that it’s better tolerated, so you’re more likely to give all the drug. You can see if the drug isn’t working, and you can stop the drug. Also, if the drug is causing a side effect, you can see whether it’s working or not and use that decision to stop. It’s different than when you’re giving a drug in the adjuvant setting where you don’t really know whether it is working or not.
I think that it’s time to change some of our standards. When patients appear with lung cancers other than tiny ones that might be detected through screening, you need to convene your multidisciplinary group. You need to weigh the pros and cons I think that it’s time to change some of our standards. When patients appear with lung cancers other than tiny ones that might be detected through screening, you need to convene your multidisciplinary group coming in. It’s already an FDA-approved regimen with nivolumab and chemotherapy, and I think we’re moving to making that our standard of care now.
The way to handle it today, though, is to convene your multidisciplinary panel about every patient other than those with the tiniest of lung cancers and put your heads together to see what the best treatment is for that patient.
Dr. Kris is professor of medicine, Weill Cornell Medicine, and the William and Joy Ruane Chair in Thoracic Oncology, Memorial Sloan Kettering Cancer Center, both in New York. He disclosed ties with Ariad Pharmaceuticals, AstraZeneca, Pfizer, PUMA, and Roche/Genentech.
A version of this article appeared on Medscape.com.
Many of you saw the press release from Merck announcing that their randomized trial comparing chemo with chemo plus pembrolizumab in the neoadjuvant setting led to improved event-free survival and also improved pathologic complete response rate.
This comes in addition to the data from the AstraZeneca trial with durvalumab saying they’ve already achieved their endpoint of higher pathologic complete response rate vs. chemotherapy alone and also the data with nivolumab from Bristol-Myers Squibb saying that nivolumab plus chemotherapy leads to a better event-free survival and a better pathologic complete response rate. That information has led to Food and Drug Administration approval for their regimen.
We’re running the table with these very positive data, and I think it’s just a sign that the approach is safe and effective.
A huge question has come up. I just came from a meeting of lung cancer experts asking what to do if you have a patient with a small tumor, for example, a 3-cm tumor. Do you recommend immediate surgery followed by adjuvant therapy, chemotherapy, and then a checkpoint inhibitor if appropriate? Or do you proceed with neoadjuvant therapy if appropriate? The truth is that it’s a very difficult decision.
We have overwhelming data that the neoadjuvant approach works for that patient. Please remember that this is a clinically staged patient. This is not the patient after their surgery, where I think we have a very clear path. We have adjuvant data and adjuvant trials for those patients.
For the patient who’s in your office with a small tumor or a small tumor and only hilar lymphadenopathy, the decision there isn’t data driven, but rather it is experience driven. The data that are out there right now suggest that neoadjuvant therapy is a better way to go. Why is that?
Well, I think that the first reason is that it is probably a better regimen. I think many of you saw the recent clinical trial by Patel and colleagues in the New England Journal of Medicine with melanoma. It was an interesting trial. They gave a checkpoint inhibitor for 18 doses after surgery for melanoma versus three doses of checkpoint inhibitor, surgery, and then 15 doses of the checkpoint inhibitor.
It was 18 doses versus 18 doses, with the only difference being the three doses before surgery. Lo and behold, the three doses before surgery led to a better event-free survival.
There are preclinical data in lung cancer demonstrating that the same thing is true. Tina Cascone published on that years ago. We could talk about why, but it appears that neoadjuvant is just better.
There are other advantages to it as well. I think a big one is that all the information shows that it’s better tolerated, so you’re more likely to give all the drug. You can see if the drug isn’t working, and you can stop the drug. Also, if the drug is causing a side effect, you can see whether it’s working or not and use that decision to stop. It’s different than when you’re giving a drug in the adjuvant setting where you don’t really know whether it is working or not.
I think that it’s time to change some of our standards. When patients appear with lung cancers other than tiny ones that might be detected through screening, you need to convene your multidisciplinary group. You need to weigh the pros and cons I think that it’s time to change some of our standards. When patients appear with lung cancers other than tiny ones that might be detected through screening, you need to convene your multidisciplinary group coming in. It’s already an FDA-approved regimen with nivolumab and chemotherapy, and I think we’re moving to making that our standard of care now.
The way to handle it today, though, is to convene your multidisciplinary panel about every patient other than those with the tiniest of lung cancers and put your heads together to see what the best treatment is for that patient.
Dr. Kris is professor of medicine, Weill Cornell Medicine, and the William and Joy Ruane Chair in Thoracic Oncology, Memorial Sloan Kettering Cancer Center, both in New York. He disclosed ties with Ariad Pharmaceuticals, AstraZeneca, Pfizer, PUMA, and Roche/Genentech.
A version of this article appeared on Medscape.com.
Many of you saw the press release from Merck announcing that their randomized trial comparing chemo with chemo plus pembrolizumab in the neoadjuvant setting led to improved event-free survival and also improved pathologic complete response rate.
This comes in addition to the data from the AstraZeneca trial with durvalumab saying they’ve already achieved their endpoint of higher pathologic complete response rate vs. chemotherapy alone and also the data with nivolumab from Bristol-Myers Squibb saying that nivolumab plus chemotherapy leads to a better event-free survival and a better pathologic complete response rate. That information has led to Food and Drug Administration approval for their regimen.
We’re running the table with these very positive data, and I think it’s just a sign that the approach is safe and effective.
A huge question has come up. I just came from a meeting of lung cancer experts asking what to do if you have a patient with a small tumor, for example, a 3-cm tumor. Do you recommend immediate surgery followed by adjuvant therapy, chemotherapy, and then a checkpoint inhibitor if appropriate? Or do you proceed with neoadjuvant therapy if appropriate? The truth is that it’s a very difficult decision.
We have overwhelming data that the neoadjuvant approach works for that patient. Please remember that this is a clinically staged patient. This is not the patient after their surgery, where I think we have a very clear path. We have adjuvant data and adjuvant trials for those patients.
For the patient who’s in your office with a small tumor or a small tumor and only hilar lymphadenopathy, the decision there isn’t data driven, but rather it is experience driven. The data that are out there right now suggest that neoadjuvant therapy is a better way to go. Why is that?
Well, I think that the first reason is that it is probably a better regimen. I think many of you saw the recent clinical trial by Patel and colleagues in the New England Journal of Medicine with melanoma. It was an interesting trial. They gave a checkpoint inhibitor for 18 doses after surgery for melanoma versus three doses of checkpoint inhibitor, surgery, and then 15 doses of the checkpoint inhibitor.
It was 18 doses versus 18 doses, with the only difference being the three doses before surgery. Lo and behold, the three doses before surgery led to a better event-free survival.
There are preclinical data in lung cancer demonstrating that the same thing is true. Tina Cascone published on that years ago. We could talk about why, but it appears that neoadjuvant is just better.
There are other advantages to it as well. I think a big one is that all the information shows that it’s better tolerated, so you’re more likely to give all the drug. You can see if the drug isn’t working, and you can stop the drug. Also, if the drug is causing a side effect, you can see whether it’s working or not and use that decision to stop. It’s different than when you’re giving a drug in the adjuvant setting where you don’t really know whether it is working or not.
I think that it’s time to change some of our standards. When patients appear with lung cancers other than tiny ones that might be detected through screening, you need to convene your multidisciplinary group. You need to weigh the pros and cons I think that it’s time to change some of our standards. When patients appear with lung cancers other than tiny ones that might be detected through screening, you need to convene your multidisciplinary group coming in. It’s already an FDA-approved regimen with nivolumab and chemotherapy, and I think we’re moving to making that our standard of care now.
The way to handle it today, though, is to convene your multidisciplinary panel about every patient other than those with the tiniest of lung cancers and put your heads together to see what the best treatment is for that patient.
Dr. Kris is professor of medicine, Weill Cornell Medicine, and the William and Joy Ruane Chair in Thoracic Oncology, Memorial Sloan Kettering Cancer Center, both in New York. He disclosed ties with Ariad Pharmaceuticals, AstraZeneca, Pfizer, PUMA, and Roche/Genentech.
A version of this article appeared on Medscape.com.
Suits or joggers? A doctor’s dress code
Look at this guy – NFL Chargers jersey and shorts with a RVCA hat on backward. And next to him, a woman wearing her spin-class-Lulu gear. There’s also a guy sporting a 2016 San Diego Rock ‘n Roll Marathon Tee. And that young woman is actually wearing slippers. A visitor from the 1950s would be thunderstruck to see such casual wear on people waiting to board a plane. Photos from that era show men buttoned up in white shirt and tie and women wearing Chanel with hats and white gloves. This dramatic transformation from formal to unfussy wear cuts through all social situations, including in my office. As a new doc out of residency, I used to wear a tie and shoes that could hold a shine. Now I wear jogger scrubs and sneakers. Rather than be offended by the lack of formality though, patients seem to appreciate it. Should they?
At first glance this seems to be a modern phenomenon. The reasons for casual wear today are manifold: about one-third of people work from home, Millennials are taking over with their TikTok values and general irreverence, COVID made us all fat and lazy. Heck, even the U.S. Senate briefly abolished the requirement to wear suits on the Senate floor. But getting dressed up was never to signal that you are elite or superior to others. It’s the opposite. To get dressed is a signal that you are serving others, a tradition that is as old as society.
Think of Downton Abbey as an example. The servants were always required to be smartly dressed when working, whereas members of the family could be dressed up or not. It’s clear who is serving whom. This tradition lives today in the hospitality industry. When you mosey into the lobby of a luxury hotel in your Rainbow sandals you can expect everyone who greets you will be in finery, signaling that they put in effort to serve you. You’ll find the same for all staff at the Mayo Clinic in Rochester, Minn., which is no coincidence.
Suits used to be standard in medicine. In the 19th century, physicians wore formal black-tie when seeing patients. Unlike hospitality however, we had good reason to eschew the tradition: germs. Once we figured out that our pus-stained ties and jackets were doing harm, we switched to wearing sanitized uniforms. Casual wear for doctors isn’t a modern phenomenon after all, then. For proof, compare Thomas Eakins painting “The Gross Clinic” (1875) with his later “The Agnew Clinic” (1889). In the former, Dr. Gross is portrayed in formal black wear, bloody hand and all. In the latter, Dr. Agnew is wearing white FIGS (or the 1890’s equivalent anyway). Similarly, nurses uniforms traditionally resembled kitchen servants, with criss-cross aprons and floor length skirts. It wasn’t until the 1980’s that nurses stopped wearing dresses and white caps.
In the operating theater it’s obviously critical that we wear sanitized scrubs to mitigate the risk of infection. Originally white to signal cleanliness, scrubs were changed to blue-green because surgeons were blinded by the lights bouncing off the uniforms. (Green is also opposite red on the color wheel, supposedly enhancing the ability to distinguish shades of red).
But Over time we’ve lost significant autonomy in our practice and lost a little respect from our patients. Payers tell us what to do. Patients question our expertise. Choosing what we wear is one of the few bits of medicine we still have agency. Pewter or pink, joggers or cargo pants, we get to choose.
The last time I flew British Airways everyone was in lounge wear, except the flight crew, of course. They were all smartly dressed. Recently British Airways rolled out updated, slightly more relaxed dress codes. Very modern, but I wonder if in a way we’re not all just a bit worse off.
Dr. Benabio is director of Healthcare Transformation and chief of dermatology at Kaiser Permanente San Diego. The opinions expressed in this column are his own and do not represent those of Kaiser Permanente. Dr. Benabio is @Dermdoc on Twitter. Write to him at [email protected]
Look at this guy – NFL Chargers jersey and shorts with a RVCA hat on backward. And next to him, a woman wearing her spin-class-Lulu gear. There’s also a guy sporting a 2016 San Diego Rock ‘n Roll Marathon Tee. And that young woman is actually wearing slippers. A visitor from the 1950s would be thunderstruck to see such casual wear on people waiting to board a plane. Photos from that era show men buttoned up in white shirt and tie and women wearing Chanel with hats and white gloves. This dramatic transformation from formal to unfussy wear cuts through all social situations, including in my office. As a new doc out of residency, I used to wear a tie and shoes that could hold a shine. Now I wear jogger scrubs and sneakers. Rather than be offended by the lack of formality though, patients seem to appreciate it. Should they?
At first glance this seems to be a modern phenomenon. The reasons for casual wear today are manifold: about one-third of people work from home, Millennials are taking over with their TikTok values and general irreverence, COVID made us all fat and lazy. Heck, even the U.S. Senate briefly abolished the requirement to wear suits on the Senate floor. But getting dressed up was never to signal that you are elite or superior to others. It’s the opposite. To get dressed is a signal that you are serving others, a tradition that is as old as society.
Think of Downton Abbey as an example. The servants were always required to be smartly dressed when working, whereas members of the family could be dressed up or not. It’s clear who is serving whom. This tradition lives today in the hospitality industry. When you mosey into the lobby of a luxury hotel in your Rainbow sandals you can expect everyone who greets you will be in finery, signaling that they put in effort to serve you. You’ll find the same for all staff at the Mayo Clinic in Rochester, Minn., which is no coincidence.
Suits used to be standard in medicine. In the 19th century, physicians wore formal black-tie when seeing patients. Unlike hospitality however, we had good reason to eschew the tradition: germs. Once we figured out that our pus-stained ties and jackets were doing harm, we switched to wearing sanitized uniforms. Casual wear for doctors isn’t a modern phenomenon after all, then. For proof, compare Thomas Eakins painting “The Gross Clinic” (1875) with his later “The Agnew Clinic” (1889). In the former, Dr. Gross is portrayed in formal black wear, bloody hand and all. In the latter, Dr. Agnew is wearing white FIGS (or the 1890’s equivalent anyway). Similarly, nurses uniforms traditionally resembled kitchen servants, with criss-cross aprons and floor length skirts. It wasn’t until the 1980’s that nurses stopped wearing dresses and white caps.
In the operating theater it’s obviously critical that we wear sanitized scrubs to mitigate the risk of infection. Originally white to signal cleanliness, scrubs were changed to blue-green because surgeons were blinded by the lights bouncing off the uniforms. (Green is also opposite red on the color wheel, supposedly enhancing the ability to distinguish shades of red).
But Over time we’ve lost significant autonomy in our practice and lost a little respect from our patients. Payers tell us what to do. Patients question our expertise. Choosing what we wear is one of the few bits of medicine we still have agency. Pewter or pink, joggers or cargo pants, we get to choose.
The last time I flew British Airways everyone was in lounge wear, except the flight crew, of course. They were all smartly dressed. Recently British Airways rolled out updated, slightly more relaxed dress codes. Very modern, but I wonder if in a way we’re not all just a bit worse off.
Dr. Benabio is director of Healthcare Transformation and chief of dermatology at Kaiser Permanente San Diego. The opinions expressed in this column are his own and do not represent those of Kaiser Permanente. Dr. Benabio is @Dermdoc on Twitter. Write to him at [email protected]
Look at this guy – NFL Chargers jersey and shorts with a RVCA hat on backward. And next to him, a woman wearing her spin-class-Lulu gear. There’s also a guy sporting a 2016 San Diego Rock ‘n Roll Marathon Tee. And that young woman is actually wearing slippers. A visitor from the 1950s would be thunderstruck to see such casual wear on people waiting to board a plane. Photos from that era show men buttoned up in white shirt and tie and women wearing Chanel with hats and white gloves. This dramatic transformation from formal to unfussy wear cuts through all social situations, including in my office. As a new doc out of residency, I used to wear a tie and shoes that could hold a shine. Now I wear jogger scrubs and sneakers. Rather than be offended by the lack of formality though, patients seem to appreciate it. Should they?
At first glance this seems to be a modern phenomenon. The reasons for casual wear today are manifold: about one-third of people work from home, Millennials are taking over with their TikTok values and general irreverence, COVID made us all fat and lazy. Heck, even the U.S. Senate briefly abolished the requirement to wear suits on the Senate floor. But getting dressed up was never to signal that you are elite or superior to others. It’s the opposite. To get dressed is a signal that you are serving others, a tradition that is as old as society.
Think of Downton Abbey as an example. The servants were always required to be smartly dressed when working, whereas members of the family could be dressed up or not. It’s clear who is serving whom. This tradition lives today in the hospitality industry. When you mosey into the lobby of a luxury hotel in your Rainbow sandals you can expect everyone who greets you will be in finery, signaling that they put in effort to serve you. You’ll find the same for all staff at the Mayo Clinic in Rochester, Minn., which is no coincidence.
Suits used to be standard in medicine. In the 19th century, physicians wore formal black-tie when seeing patients. Unlike hospitality however, we had good reason to eschew the tradition: germs. Once we figured out that our pus-stained ties and jackets were doing harm, we switched to wearing sanitized uniforms. Casual wear for doctors isn’t a modern phenomenon after all, then. For proof, compare Thomas Eakins painting “The Gross Clinic” (1875) with his later “The Agnew Clinic” (1889). In the former, Dr. Gross is portrayed in formal black wear, bloody hand and all. In the latter, Dr. Agnew is wearing white FIGS (or the 1890’s equivalent anyway). Similarly, nurses uniforms traditionally resembled kitchen servants, with criss-cross aprons and floor length skirts. It wasn’t until the 1980’s that nurses stopped wearing dresses and white caps.
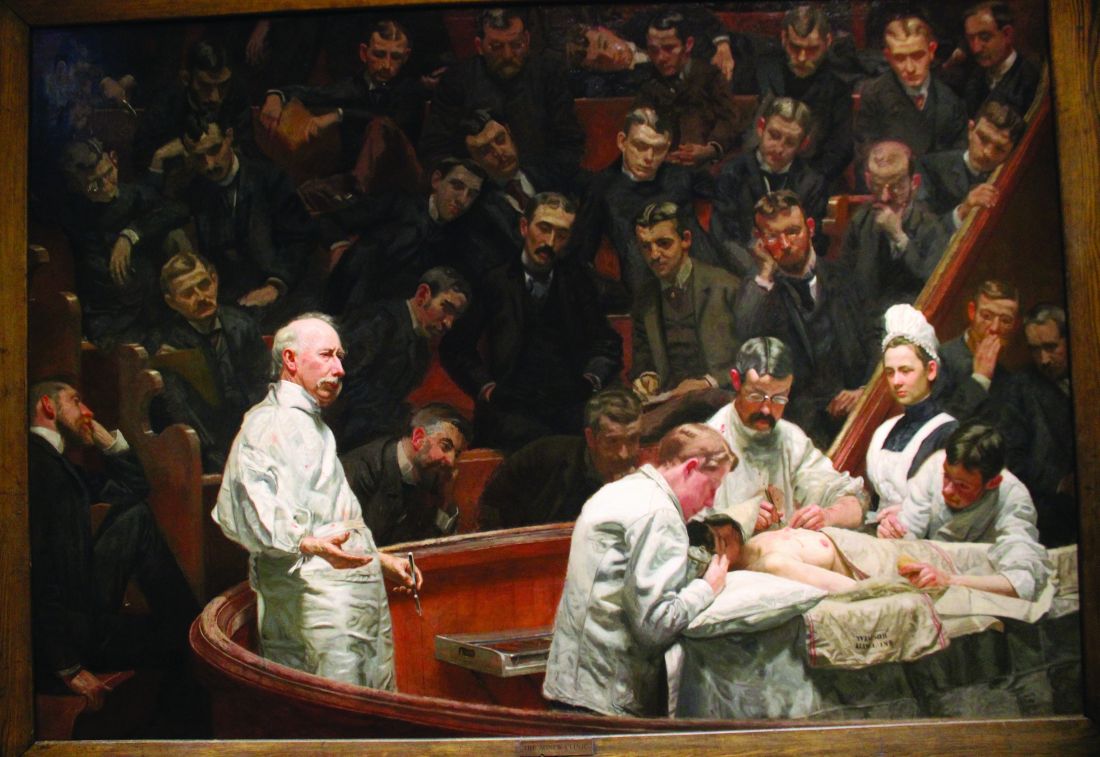
In the operating theater it’s obviously critical that we wear sanitized scrubs to mitigate the risk of infection. Originally white to signal cleanliness, scrubs were changed to blue-green because surgeons were blinded by the lights bouncing off the uniforms. (Green is also opposite red on the color wheel, supposedly enhancing the ability to distinguish shades of red).
But Over time we’ve lost significant autonomy in our practice and lost a little respect from our patients. Payers tell us what to do. Patients question our expertise. Choosing what we wear is one of the few bits of medicine we still have agency. Pewter or pink, joggers or cargo pants, we get to choose.
The last time I flew British Airways everyone was in lounge wear, except the flight crew, of course. They were all smartly dressed. Recently British Airways rolled out updated, slightly more relaxed dress codes. Very modern, but I wonder if in a way we’re not all just a bit worse off.
Dr. Benabio is director of Healthcare Transformation and chief of dermatology at Kaiser Permanente San Diego. The opinions expressed in this column are his own and do not represent those of Kaiser Permanente. Dr. Benabio is @Dermdoc on Twitter. Write to him at [email protected]







