User login
How to Navigate Challenging Patient Encounters in Dermatology Residency
Dermatologists in training are exposed to many different clinical scenarios—from the quick 15-minute encounter to diagnose a case of atopic dermatitis to hours of digging through a medical record to identify a culprit medication in a hospitalized patient with a life-threatening cutaneous drug reaction. Amidst the day-to-day clinical work that we do, there inevitably are interactions we have with patients that are less than ideal. These challenging encounters—whether they be subtle microaggressions that unfortunately enter the workplace or blatant quarrels between providers and patients that leave both parties dissatisfied—are notable contributors to physician stress levels and can lead to burnout.1,2 However, there are positive lessons to be learned from these challenging patient encounters if we manage to withstand them. When we start to understand the factors contributing to difficult clinical encounters, we can begin to develop and apply effective communication tools to productively navigate these experiences.
Defining the Difficult Patient
In 2017, the Global Burden of Disease study revealed that skin disease is the fourth leading cause of nonfatal disease burden worldwide.3 Based on this statistic, it is easy to see how some patients may experience frustration associated with their condition and subsequently displace their discontent on the physician. In one study, nearly 1 of every 6 (16.7%) outpatient encounters was considered difficult by physicians.4 Family medicine physicians defined the difficult patient as one who is violent, demanding, aggressive, and rude.5 Others in primary care specialties have considered difficult patients to have characteristics that include mental health problems, more than 5 somatic symptoms, and abrasive personalities.4,6
Situational and Physician-Centered Factors in Difficult Patient Encounters
In our medical system, the narrative often is focused on the patient, for better or worse—the patient was difficult, thereby making the encounter difficult. However, it is important to remember that difficult encounters can be attributed to several different factors, including those related to the physician, the clinical situation, or both. For example, dermatology residents juggle their clinical duties; academic work including studying, teaching, and/or research; and systemic and personal pressures at all times, whether they are cognizant of it or not. For better or worse, by virtue of being human, residents bring these factors with them to each clinical encounter. The delicate balance of these components can have a considerable impact on our delivery of good health care. This is particularly relevant in dermatology, where residents are subject to limited time during visits, work culture among clinic staff that is out of our control, and prominent complex social issues (for those of us practicing in medically underserved areas). Poor communication skills, underlying bias toward specific health conditions, limited knowledge as a trainee, and our own personal stressors also may play large roles in perceiving a clinical encounter as difficult during dermatology residency.7
Strategies to Mitigate Difficult Encounters
As a resident, if you make a statement that sparks a negative response from the patient, acknowledge their negative emotion, try to offer help, or rephrase the original statement to quickly dispel the tension. Validating a patient’s emotions and helping them embrace uncertainty can go a long way in the therapeutic relationship, especially in dermatology where so many of our diseases are chronic and without a definite cure.8 Additionally, it is important to apply strategies to redirect and de-escalate the situation during emotionally charged conversations, such as active listening, validating and empathizing with emotions, exploring alternative solutions, and providing closure to the conversation. Consensus recommendations for managing challenging encounters established by the American Academy of Family Physicians in 2013 include setting boundaries or modifying schedules, as needed, to handle difficult encounters; employing empathetic listening skills and a nonjudgmental attitude to facilitate trust and adherence to treatment; and assessing for underlying psychological illnesses with referral for appropriate diagnosis and treatment. Finally, the CALMER method—catalyst for change, alter thoughts to change feelings, listen and then make a diagnosis, make an agreement, education and follow-up, reach out and discuss feelings—is another approach that may be useful.7 In dermatology, this approach may not only dissipate unwanted tension but also make progress toward a therapeutic relationship. We cannot control the patient’s behavior in a visit, but we need to keep in mind that we are in control of our own reactions to said behavior.9 After first acknowledging this, we can then guide patients to take steps toward overcoming the issue. Within the time restrictions of a dermatology clinic visit, residents may use this approach to quickly feel more in control of a distressing situation and remain calm to better care for the patient.
Final Thoughts
Difficult patient encounters are impossible to avoid in any field of medicine, and dermatology is no exception. It will only benefit residents to recognize the multiple factors impacting a challenging encounter now and learn or enhance conflict resolution and communication skills to navigate these dissatisfying and uncomfortable situations, as they are inevitable in our careers.
- Bodner S. Stress management in the difficult patient encounter. Dent Clin North Am. 2008;52:579-603, ix-xx. doi:10.1016/j.cden.2008.02.012
- West CP, Dyrbye LN, Shanafelt TD. Physician burnout: contributors, consequences and solutions. J Intern Med. 2018;283:516-529. doi:10.1111/joim.12752
- Seth D, Cheldize K, Brown D, et al. Global burden of skin disease: inequities and innovations. Curr Dermatol Rep. 2017;6:204-210. doi:10.1007/s13671-017-0192-7
- An PGRabatin JSManwell LB, et al. Burden of difficult encounters in primary care: data from the minimizing error, maximizing outcomes study. Arch Intern Med. 2009;169:410-414. doi:10.1001/archinternmed.2008.549
- Steinmetz D, Tabenkin H. The ‘difficult patient’ as perceived by family physicians. Fam Pract. 2001;18:495-500. doi:10.1093/fampra/18.5.495
- Breuner CC, Moreno MA. Approaches to the difficult patient/parent encounter. Pediatrics. 2011;127:163-169. doi:10.1542/peds.2010-0072
- Cannarella Lorenzetti R, Jacques CH, Donovan C, et al. Managing difficult encounters: understanding physician, patient, and situational factors. Am Fam Physician. 2013;87:419-425.
- Bailey J, Martin SA, Bangs A. Managing difficult patient encounters. Am Fam Physician. 2023;108:494-500.
- Pomm HA, Shahady E, Pomm RM. The CALMER approach: teaching learners six steps to serenity when dealing with difficult patients. Fam Med. 2004;36:467-469.
Dermatologists in training are exposed to many different clinical scenarios—from the quick 15-minute encounter to diagnose a case of atopic dermatitis to hours of digging through a medical record to identify a culprit medication in a hospitalized patient with a life-threatening cutaneous drug reaction. Amidst the day-to-day clinical work that we do, there inevitably are interactions we have with patients that are less than ideal. These challenging encounters—whether they be subtle microaggressions that unfortunately enter the workplace or blatant quarrels between providers and patients that leave both parties dissatisfied—are notable contributors to physician stress levels and can lead to burnout.1,2 However, there are positive lessons to be learned from these challenging patient encounters if we manage to withstand them. When we start to understand the factors contributing to difficult clinical encounters, we can begin to develop and apply effective communication tools to productively navigate these experiences.
Defining the Difficult Patient
In 2017, the Global Burden of Disease study revealed that skin disease is the fourth leading cause of nonfatal disease burden worldwide.3 Based on this statistic, it is easy to see how some patients may experience frustration associated with their condition and subsequently displace their discontent on the physician. In one study, nearly 1 of every 6 (16.7%) outpatient encounters was considered difficult by physicians.4 Family medicine physicians defined the difficult patient as one who is violent, demanding, aggressive, and rude.5 Others in primary care specialties have considered difficult patients to have characteristics that include mental health problems, more than 5 somatic symptoms, and abrasive personalities.4,6
Situational and Physician-Centered Factors in Difficult Patient Encounters
In our medical system, the narrative often is focused on the patient, for better or worse—the patient was difficult, thereby making the encounter difficult. However, it is important to remember that difficult encounters can be attributed to several different factors, including those related to the physician, the clinical situation, or both. For example, dermatology residents juggle their clinical duties; academic work including studying, teaching, and/or research; and systemic and personal pressures at all times, whether they are cognizant of it or not. For better or worse, by virtue of being human, residents bring these factors with them to each clinical encounter. The delicate balance of these components can have a considerable impact on our delivery of good health care. This is particularly relevant in dermatology, where residents are subject to limited time during visits, work culture among clinic staff that is out of our control, and prominent complex social issues (for those of us practicing in medically underserved areas). Poor communication skills, underlying bias toward specific health conditions, limited knowledge as a trainee, and our own personal stressors also may play large roles in perceiving a clinical encounter as difficult during dermatology residency.7
Strategies to Mitigate Difficult Encounters
As a resident, if you make a statement that sparks a negative response from the patient, acknowledge their negative emotion, try to offer help, or rephrase the original statement to quickly dispel the tension. Validating a patient’s emotions and helping them embrace uncertainty can go a long way in the therapeutic relationship, especially in dermatology where so many of our diseases are chronic and without a definite cure.8 Additionally, it is important to apply strategies to redirect and de-escalate the situation during emotionally charged conversations, such as active listening, validating and empathizing with emotions, exploring alternative solutions, and providing closure to the conversation. Consensus recommendations for managing challenging encounters established by the American Academy of Family Physicians in 2013 include setting boundaries or modifying schedules, as needed, to handle difficult encounters; employing empathetic listening skills and a nonjudgmental attitude to facilitate trust and adherence to treatment; and assessing for underlying psychological illnesses with referral for appropriate diagnosis and treatment. Finally, the CALMER method—catalyst for change, alter thoughts to change feelings, listen and then make a diagnosis, make an agreement, education and follow-up, reach out and discuss feelings—is another approach that may be useful.7 In dermatology, this approach may not only dissipate unwanted tension but also make progress toward a therapeutic relationship. We cannot control the patient’s behavior in a visit, but we need to keep in mind that we are in control of our own reactions to said behavior.9 After first acknowledging this, we can then guide patients to take steps toward overcoming the issue. Within the time restrictions of a dermatology clinic visit, residents may use this approach to quickly feel more in control of a distressing situation and remain calm to better care for the patient.
Final Thoughts
Difficult patient encounters are impossible to avoid in any field of medicine, and dermatology is no exception. It will only benefit residents to recognize the multiple factors impacting a challenging encounter now and learn or enhance conflict resolution and communication skills to navigate these dissatisfying and uncomfortable situations, as they are inevitable in our careers.
Dermatologists in training are exposed to many different clinical scenarios—from the quick 15-minute encounter to diagnose a case of atopic dermatitis to hours of digging through a medical record to identify a culprit medication in a hospitalized patient with a life-threatening cutaneous drug reaction. Amidst the day-to-day clinical work that we do, there inevitably are interactions we have with patients that are less than ideal. These challenging encounters—whether they be subtle microaggressions that unfortunately enter the workplace or blatant quarrels between providers and patients that leave both parties dissatisfied—are notable contributors to physician stress levels and can lead to burnout.1,2 However, there are positive lessons to be learned from these challenging patient encounters if we manage to withstand them. When we start to understand the factors contributing to difficult clinical encounters, we can begin to develop and apply effective communication tools to productively navigate these experiences.
Defining the Difficult Patient
In 2017, the Global Burden of Disease study revealed that skin disease is the fourth leading cause of nonfatal disease burden worldwide.3 Based on this statistic, it is easy to see how some patients may experience frustration associated with their condition and subsequently displace their discontent on the physician. In one study, nearly 1 of every 6 (16.7%) outpatient encounters was considered difficult by physicians.4 Family medicine physicians defined the difficult patient as one who is violent, demanding, aggressive, and rude.5 Others in primary care specialties have considered difficult patients to have characteristics that include mental health problems, more than 5 somatic symptoms, and abrasive personalities.4,6
Situational and Physician-Centered Factors in Difficult Patient Encounters
In our medical system, the narrative often is focused on the patient, for better or worse—the patient was difficult, thereby making the encounter difficult. However, it is important to remember that difficult encounters can be attributed to several different factors, including those related to the physician, the clinical situation, or both. For example, dermatology residents juggle their clinical duties; academic work including studying, teaching, and/or research; and systemic and personal pressures at all times, whether they are cognizant of it or not. For better or worse, by virtue of being human, residents bring these factors with them to each clinical encounter. The delicate balance of these components can have a considerable impact on our delivery of good health care. This is particularly relevant in dermatology, where residents are subject to limited time during visits, work culture among clinic staff that is out of our control, and prominent complex social issues (for those of us practicing in medically underserved areas). Poor communication skills, underlying bias toward specific health conditions, limited knowledge as a trainee, and our own personal stressors also may play large roles in perceiving a clinical encounter as difficult during dermatology residency.7
Strategies to Mitigate Difficult Encounters
As a resident, if you make a statement that sparks a negative response from the patient, acknowledge their negative emotion, try to offer help, or rephrase the original statement to quickly dispel the tension. Validating a patient’s emotions and helping them embrace uncertainty can go a long way in the therapeutic relationship, especially in dermatology where so many of our diseases are chronic and without a definite cure.8 Additionally, it is important to apply strategies to redirect and de-escalate the situation during emotionally charged conversations, such as active listening, validating and empathizing with emotions, exploring alternative solutions, and providing closure to the conversation. Consensus recommendations for managing challenging encounters established by the American Academy of Family Physicians in 2013 include setting boundaries or modifying schedules, as needed, to handle difficult encounters; employing empathetic listening skills and a nonjudgmental attitude to facilitate trust and adherence to treatment; and assessing for underlying psychological illnesses with referral for appropriate diagnosis and treatment. Finally, the CALMER method—catalyst for change, alter thoughts to change feelings, listen and then make a diagnosis, make an agreement, education and follow-up, reach out and discuss feelings—is another approach that may be useful.7 In dermatology, this approach may not only dissipate unwanted tension but also make progress toward a therapeutic relationship. We cannot control the patient’s behavior in a visit, but we need to keep in mind that we are in control of our own reactions to said behavior.9 After first acknowledging this, we can then guide patients to take steps toward overcoming the issue. Within the time restrictions of a dermatology clinic visit, residents may use this approach to quickly feel more in control of a distressing situation and remain calm to better care for the patient.
Final Thoughts
Difficult patient encounters are impossible to avoid in any field of medicine, and dermatology is no exception. It will only benefit residents to recognize the multiple factors impacting a challenging encounter now and learn or enhance conflict resolution and communication skills to navigate these dissatisfying and uncomfortable situations, as they are inevitable in our careers.
- Bodner S. Stress management in the difficult patient encounter. Dent Clin North Am. 2008;52:579-603, ix-xx. doi:10.1016/j.cden.2008.02.012
- West CP, Dyrbye LN, Shanafelt TD. Physician burnout: contributors, consequences and solutions. J Intern Med. 2018;283:516-529. doi:10.1111/joim.12752
- Seth D, Cheldize K, Brown D, et al. Global burden of skin disease: inequities and innovations. Curr Dermatol Rep. 2017;6:204-210. doi:10.1007/s13671-017-0192-7
- An PGRabatin JSManwell LB, et al. Burden of difficult encounters in primary care: data from the minimizing error, maximizing outcomes study. Arch Intern Med. 2009;169:410-414. doi:10.1001/archinternmed.2008.549
- Steinmetz D, Tabenkin H. The ‘difficult patient’ as perceived by family physicians. Fam Pract. 2001;18:495-500. doi:10.1093/fampra/18.5.495
- Breuner CC, Moreno MA. Approaches to the difficult patient/parent encounter. Pediatrics. 2011;127:163-169. doi:10.1542/peds.2010-0072
- Cannarella Lorenzetti R, Jacques CH, Donovan C, et al. Managing difficult encounters: understanding physician, patient, and situational factors. Am Fam Physician. 2013;87:419-425.
- Bailey J, Martin SA, Bangs A. Managing difficult patient encounters. Am Fam Physician. 2023;108:494-500.
- Pomm HA, Shahady E, Pomm RM. The CALMER approach: teaching learners six steps to serenity when dealing with difficult patients. Fam Med. 2004;36:467-469.
- Bodner S. Stress management in the difficult patient encounter. Dent Clin North Am. 2008;52:579-603, ix-xx. doi:10.1016/j.cden.2008.02.012
- West CP, Dyrbye LN, Shanafelt TD. Physician burnout: contributors, consequences and solutions. J Intern Med. 2018;283:516-529. doi:10.1111/joim.12752
- Seth D, Cheldize K, Brown D, et al. Global burden of skin disease: inequities and innovations. Curr Dermatol Rep. 2017;6:204-210. doi:10.1007/s13671-017-0192-7
- An PGRabatin JSManwell LB, et al. Burden of difficult encounters in primary care: data from the minimizing error, maximizing outcomes study. Arch Intern Med. 2009;169:410-414. doi:10.1001/archinternmed.2008.549
- Steinmetz D, Tabenkin H. The ‘difficult patient’ as perceived by family physicians. Fam Pract. 2001;18:495-500. doi:10.1093/fampra/18.5.495
- Breuner CC, Moreno MA. Approaches to the difficult patient/parent encounter. Pediatrics. 2011;127:163-169. doi:10.1542/peds.2010-0072
- Cannarella Lorenzetti R, Jacques CH, Donovan C, et al. Managing difficult encounters: understanding physician, patient, and situational factors. Am Fam Physician. 2013;87:419-425.
- Bailey J, Martin SA, Bangs A. Managing difficult patient encounters. Am Fam Physician. 2023;108:494-500.
- Pomm HA, Shahady E, Pomm RM. The CALMER approach: teaching learners six steps to serenity when dealing with difficult patients. Fam Med. 2004;36:467-469.
RESIDENT PEARLS
- Challenging patient encounters are inevitable in our work as dermatology residents. Both physician- and patient-related factors can contribute.
- Setting boundaries, active listening, and addressing emotions during and after the visit can help to mitigate challenging encounters.
Navigating Hair Loss in Medical School: Experiences of 2 Young Black Women
As medical students, we often assume we are exempt from the diagnoses we learn about. During the first 2 years of medical school, we learn about alopecia as a condition that may be associated with stress, hormonal imbalances, nutrient deficiencies, and aging. However, our curricula do not explore the subtypes, psychosocial impact, or even the overwhelming number of Black women who are disproportionately affected by alopecia. For Black women, hair is a colossal part of their cultural identity, learning from a young age how to nurture and style natural coils. It becomes devastating when women begin to lose them.
The diagnosis of alopecia subtypes in Black women has been explored in the literature; however, understanding the unique experiences of young Black women is an important part of patient care, as alopecia often is destructive to the patient’s self-image. Therefore, it is important to shed light on these experiences so others feel empowered and supported in their journeys. Herein, we share the experiences of 2 authors (J.D. and C.A.V.O.)—both young Black women—who navigated unexpected hair loss in medical school.
Jewell’s Story
During my first year of medical school, I noticed my hair was shedding more than usual, and my ponytail was not as thick as it once was. I also had an area in my crown that was abnormally thin. My parents suggested that it was a consequence of stress, but I knew something was not right. With only 1 Black dermatologist within 2 hours of Nashville, Tennessee, I remember worrying about seeing a dermatologist who did not understand Black hair. I still scheduled an appointment, but I remember debating if I should straighten my hair or wear my naturally curly Afro. The first dermatologist I saw diagnosed me with seborrheic dermatitis—without even examining my scalp. She told me that I had a “full head of hair” and that I had nothing to worry about. I was unconvinced. Weeks later, I met with another dermatologist who took the time to listen to my concerns. After a scalp biopsy and laboratory work, she diagnosed me with telogen effluvium and androgenetic alopecia. Months later, I had the opportunity to visit the Black dermatologist, and she diagnosed me with central centrifugal cicatricial alopecia. I am grateful for the earlier dermatologists I saw, but I finally feel at ease with my diagnosis and treatment plan after being seen by the latter.
Chidubem’s Story
From a young age, I was conditioned to think my hair was thick, unmanageable, and a nuisance. I grew accustomed to people yanking on my hair, and my gentle whispers of “this hurts” and “the braid is too tight” being ignored. That continued into adulthood. While studying for the US Medical Licensing Examination, I noticed a burning sensation on my scalp. I decided to ignore it. However, as the days progressed, the slight burning sensation turned into intense burning and itching. I still ignored it. Not only did I lack the funds for a dermatology appointment, but my licensing examination was approaching, and it was more important than anything related to my hair. After the examination, I eventually made an appointment with my primary care physician, who attributed my symptoms to the stressors of medical school. “I think you are having migraines,” she told me. So, I continued to ignore my symptoms. A year passed, and a hair braider pointed out that I had 2 well-defined bald patches on my scalp. I remember feeling angry and confused as to how I missed those findings. I could no longer ignore it—it bothered me less when no one else knew about it. I quickly made a dermatology appointment. Although I opted out of a biopsy, we decided to treat my hair loss empirically, and I have experienced drastic improvement.
Final Thoughts
We are 2 Black women living more than 500 miles away from each other at different medical institutions, yet we share the same experience, which many other women unfortunately face alone. It is not uncommon for us to feel unheard, dismissed, or misdiagnosed. We write this for the Black woman sorting through the feelings of confusion and shock as she traces the hairless spot on her scalp. We write this for the medical student ignoring their symptoms until after their examination. We even write this for any nondermatologists uncomfortable with diagnosing and treating textured hair. To improve patient satisfaction and overall health outcomes, physicians must approach patients with both knowledge and cultural competency. Most importantly, dermatologists (and other physicians) should be appropriately trained in not only the structural differences of textured hair but also the unique practices and beliefs among Black women in relation to their hair.
Acknowledgments—Jewell Dinkins is the inaugural recipient of the Janssen–Skin of Color Research Fellowship at Howard University (Washington, DC), and Chidubem A.V. Okeke is the inaugural recipient of the Women’s Dermatologic Society–La Roche-Posay dermatology fellowship at Howard University.
As medical students, we often assume we are exempt from the diagnoses we learn about. During the first 2 years of medical school, we learn about alopecia as a condition that may be associated with stress, hormonal imbalances, nutrient deficiencies, and aging. However, our curricula do not explore the subtypes, psychosocial impact, or even the overwhelming number of Black women who are disproportionately affected by alopecia. For Black women, hair is a colossal part of their cultural identity, learning from a young age how to nurture and style natural coils. It becomes devastating when women begin to lose them.
The diagnosis of alopecia subtypes in Black women has been explored in the literature; however, understanding the unique experiences of young Black women is an important part of patient care, as alopecia often is destructive to the patient’s self-image. Therefore, it is important to shed light on these experiences so others feel empowered and supported in their journeys. Herein, we share the experiences of 2 authors (J.D. and C.A.V.O.)—both young Black women—who navigated unexpected hair loss in medical school.
Jewell’s Story
During my first year of medical school, I noticed my hair was shedding more than usual, and my ponytail was not as thick as it once was. I also had an area in my crown that was abnormally thin. My parents suggested that it was a consequence of stress, but I knew something was not right. With only 1 Black dermatologist within 2 hours of Nashville, Tennessee, I remember worrying about seeing a dermatologist who did not understand Black hair. I still scheduled an appointment, but I remember debating if I should straighten my hair or wear my naturally curly Afro. The first dermatologist I saw diagnosed me with seborrheic dermatitis—without even examining my scalp. She told me that I had a “full head of hair” and that I had nothing to worry about. I was unconvinced. Weeks later, I met with another dermatologist who took the time to listen to my concerns. After a scalp biopsy and laboratory work, she diagnosed me with telogen effluvium and androgenetic alopecia. Months later, I had the opportunity to visit the Black dermatologist, and she diagnosed me with central centrifugal cicatricial alopecia. I am grateful for the earlier dermatologists I saw, but I finally feel at ease with my diagnosis and treatment plan after being seen by the latter.
Chidubem’s Story
From a young age, I was conditioned to think my hair was thick, unmanageable, and a nuisance. I grew accustomed to people yanking on my hair, and my gentle whispers of “this hurts” and “the braid is too tight” being ignored. That continued into adulthood. While studying for the US Medical Licensing Examination, I noticed a burning sensation on my scalp. I decided to ignore it. However, as the days progressed, the slight burning sensation turned into intense burning and itching. I still ignored it. Not only did I lack the funds for a dermatology appointment, but my licensing examination was approaching, and it was more important than anything related to my hair. After the examination, I eventually made an appointment with my primary care physician, who attributed my symptoms to the stressors of medical school. “I think you are having migraines,” she told me. So, I continued to ignore my symptoms. A year passed, and a hair braider pointed out that I had 2 well-defined bald patches on my scalp. I remember feeling angry and confused as to how I missed those findings. I could no longer ignore it—it bothered me less when no one else knew about it. I quickly made a dermatology appointment. Although I opted out of a biopsy, we decided to treat my hair loss empirically, and I have experienced drastic improvement.
Final Thoughts
We are 2 Black women living more than 500 miles away from each other at different medical institutions, yet we share the same experience, which many other women unfortunately face alone. It is not uncommon for us to feel unheard, dismissed, or misdiagnosed. We write this for the Black woman sorting through the feelings of confusion and shock as she traces the hairless spot on her scalp. We write this for the medical student ignoring their symptoms until after their examination. We even write this for any nondermatologists uncomfortable with diagnosing and treating textured hair. To improve patient satisfaction and overall health outcomes, physicians must approach patients with both knowledge and cultural competency. Most importantly, dermatologists (and other physicians) should be appropriately trained in not only the structural differences of textured hair but also the unique practices and beliefs among Black women in relation to their hair.
Acknowledgments—Jewell Dinkins is the inaugural recipient of the Janssen–Skin of Color Research Fellowship at Howard University (Washington, DC), and Chidubem A.V. Okeke is the inaugural recipient of the Women’s Dermatologic Society–La Roche-Posay dermatology fellowship at Howard University.
As medical students, we often assume we are exempt from the diagnoses we learn about. During the first 2 years of medical school, we learn about alopecia as a condition that may be associated with stress, hormonal imbalances, nutrient deficiencies, and aging. However, our curricula do not explore the subtypes, psychosocial impact, or even the overwhelming number of Black women who are disproportionately affected by alopecia. For Black women, hair is a colossal part of their cultural identity, learning from a young age how to nurture and style natural coils. It becomes devastating when women begin to lose them.
The diagnosis of alopecia subtypes in Black women has been explored in the literature; however, understanding the unique experiences of young Black women is an important part of patient care, as alopecia often is destructive to the patient’s self-image. Therefore, it is important to shed light on these experiences so others feel empowered and supported in their journeys. Herein, we share the experiences of 2 authors (J.D. and C.A.V.O.)—both young Black women—who navigated unexpected hair loss in medical school.
Jewell’s Story
During my first year of medical school, I noticed my hair was shedding more than usual, and my ponytail was not as thick as it once was. I also had an area in my crown that was abnormally thin. My parents suggested that it was a consequence of stress, but I knew something was not right. With only 1 Black dermatologist within 2 hours of Nashville, Tennessee, I remember worrying about seeing a dermatologist who did not understand Black hair. I still scheduled an appointment, but I remember debating if I should straighten my hair or wear my naturally curly Afro. The first dermatologist I saw diagnosed me with seborrheic dermatitis—without even examining my scalp. She told me that I had a “full head of hair” and that I had nothing to worry about. I was unconvinced. Weeks later, I met with another dermatologist who took the time to listen to my concerns. After a scalp biopsy and laboratory work, she diagnosed me with telogen effluvium and androgenetic alopecia. Months later, I had the opportunity to visit the Black dermatologist, and she diagnosed me with central centrifugal cicatricial alopecia. I am grateful for the earlier dermatologists I saw, but I finally feel at ease with my diagnosis and treatment plan after being seen by the latter.
Chidubem’s Story
From a young age, I was conditioned to think my hair was thick, unmanageable, and a nuisance. I grew accustomed to people yanking on my hair, and my gentle whispers of “this hurts” and “the braid is too tight” being ignored. That continued into adulthood. While studying for the US Medical Licensing Examination, I noticed a burning sensation on my scalp. I decided to ignore it. However, as the days progressed, the slight burning sensation turned into intense burning and itching. I still ignored it. Not only did I lack the funds for a dermatology appointment, but my licensing examination was approaching, and it was more important than anything related to my hair. After the examination, I eventually made an appointment with my primary care physician, who attributed my symptoms to the stressors of medical school. “I think you are having migraines,” she told me. So, I continued to ignore my symptoms. A year passed, and a hair braider pointed out that I had 2 well-defined bald patches on my scalp. I remember feeling angry and confused as to how I missed those findings. I could no longer ignore it—it bothered me less when no one else knew about it. I quickly made a dermatology appointment. Although I opted out of a biopsy, we decided to treat my hair loss empirically, and I have experienced drastic improvement.
Final Thoughts
We are 2 Black women living more than 500 miles away from each other at different medical institutions, yet we share the same experience, which many other women unfortunately face alone. It is not uncommon for us to feel unheard, dismissed, or misdiagnosed. We write this for the Black woman sorting through the feelings of confusion and shock as she traces the hairless spot on her scalp. We write this for the medical student ignoring their symptoms until after their examination. We even write this for any nondermatologists uncomfortable with diagnosing and treating textured hair. To improve patient satisfaction and overall health outcomes, physicians must approach patients with both knowledge and cultural competency. Most importantly, dermatologists (and other physicians) should be appropriately trained in not only the structural differences of textured hair but also the unique practices and beliefs among Black women in relation to their hair.
Acknowledgments—Jewell Dinkins is the inaugural recipient of the Janssen–Skin of Color Research Fellowship at Howard University (Washington, DC), and Chidubem A.V. Okeke is the inaugural recipient of the Women’s Dermatologic Society–La Roche-Posay dermatology fellowship at Howard University.
Practice Points
- Hair loss is a common dermatologic concern among Black women and can represent a diagnostic challenge to dermatologists who may not be familiar with textured hair.
- Dermatologists should practice cultural sensitivity and provide relevant recommendations to Black patients dealing with hair loss.
Novel Solutions Needed to Attract Residents to Pediatric Rheumatology
Pediatric rheumatologists are calling a “Code (p)RED” — a pediatric rheumatology educational deficit.
There are too few pediatric rheumatologists to meet patient demand in the United States, and projections suggest that gap will continue to widen. Disappointing match trends also reflect issues with recruitment: Since 2019, only 50%-75% of pediatric rheumatology fellowship positions have been filled each year. For 2024, the subspecialty filled 32 of 52 positions.
Lack of exposure during medical school and residency, financial concerns, and a lengthy, research-focused fellowship are seen as major contributors to the workforce shortage, and novel solutions are needed to close the gap, experts argued in a recent presentation at the annual meeting of the American College of Rheumatology.
“It’s so important now to get ahead of this because what I’m afraid of is in 10-20 years, we’re not going to have a field,” Colleen Correll, MD, MPH, an associate professor in the division of pediatric rheumatology at the University of Minnesota Medical School in Minneapolis, told this news organization.
Growing Demand, Falling Supply
Because the subspecialty was officially recognized by the American Board of Pediatrics in 1991, “it’s always been a small group of providers,” Dr. Correll said. “It’s honestly always been a recognized issue in our field.”
But a 2022 report by the ACR on the pediatric workforce has brought more attention to the issue. Dr. Correll led the study and is the chair of ACR›s Pediatric Rheumatology Committee. According to the report, an estimated 287 pediatric rheumatologists were working as full-time clinicians in 2015, while the estimated demand was 382 providers. By 2030, this projected supply of pediatric rheumatologists fell to 261, while demand rose to 461 full-time providers.
The distribution of pediatric rheumatologists is also an issue. It’s generally thought that there should be at least one pediatric rheumatologist per 100,000 children, Dr. Correll explained. According to ACR estimates, the northeast region had approximately 0.83 pediatric rheumatologists per 100,000 in 2015, while the south central and southwest regions had 0.17 and 0.20 providers per 100,000 children, respectively. Projected estimates for 2030 dipped to 0.04 or lower for the south central, southwest, and southeast regions.
A separate study from the American Board of Pediatrics, also led by Dr. Correll, that is still under review offered more optimistic projections, suggesting that there would be a 75% increase in pediatric rheumatologists from 0.27 per 100,000 children in 2020 to 0.47 per 100,000 children in 2040.
“This does look better than the ACR study, though 0.47 is still a really small number and an inadequate number to treat our children in need,” she said during her presentation at the annual meeting of the American College of Rheumatology.
Lack of Exposure During Medical Education
Few medical schools have pediatric rheumatology built into their curriculum, whether that is a whole course or a single lecture, said Jay Mehta, MD, who directs the pediatric rheumatology fellowship at the Children’s Hospital of Philadelphia. Dr. Mehta, for example, did not know that pediatric rheumatology was a field before entering residency, he said. But residencies can also lack exposure: An estimated one third of residencies do not have a single pediatric rheumatologist on staff, he said.
“Those are places where people aren’t necessarily getting exposure to pediatric rheumatology,” he told this news organization, “and we know that if you’re not exposed to a field, it’s very, very unlikely that you will go into that field.”
The ACR’s Pediatric Rheumatology Residency Program is one way that the organization is working to address this issue. The program sends pediatric residents with an interest in rheumatology to the ACR annual meeting. The Rheumatology Research Foundation also runs a visiting professorship program, where a pediatric rheumatologist conducts a rheumatology education forum at an institution with no pediatric rheumatology program.
“I’ve done it a couple of times,” Dr. Mehta said during his presentation at the annual meeting. “It’s one of the most rewarding things I’ve done.”
Financial Concerns
Additionally, although pediatric rheumatology requires more training, these subspecialists will likely make less than their general pediatric colleagues over their career. According to one study in Pediatrics, a pediatric resident pursuing rheumatology is projected to make $1.2 million dollars less over the course of their career compared with someone who started their career in general pediatrics immediately after residency. (Negative financial returns were also found for all pediatric subspecialities except for cardiology, critical care, and neonatology.)
This lower earning potential is likely a deterrent, especially for those with educational debt. In one analysis published in October, medical students with at least $200,000 in education debt were 43% more likely to go into higher-paying pediatric subspecialities than those with no debt. Nearly three out of four medical graduates have education debt, according to the American Association of Medical Colleges, with a median debt of $200,000.
While the Pediatric Specialty Loan Repayment Program was specifically designed to aid pediatric subspecialists with their educational debt, qualifying for the program is difficult for pediatric rheumatologists, explained Kristen N. Hayward, MD, of Seattle Children’s in Washington. The program provides up to $100,000 in loan forgiveness in exchange for 3 years of practicing in an underserved area; however, the program stipulates that providers must provide full-time (40 hours per week) clinical care. At academic institutions, where most pediatric rheumatologists practice, there is usually a research component to their position, and even if a provider works the equivalent of 40 hours per week in a clinic in addition to their research, they don’t qualify for the program, Dr. Hayward said.
“It’s very difficult to find someone who’s actually only doing clinical work,” she said.
The ACR has worked to combat some of these economic constraints by demonstrating the direct and downstream value of rheumatologic care, Dr. Hayward said. In a recent white paper, it was estimated that including office visits, consultations, lab testing, and radiology services, one full-time equivalent rheumatologist generates $3.5 million in revenue every year and saves health systems more than $2700 per patient per year.
In addition to placing greater value on rheumatologic care, the healthcare system also needs to recognize the current nonbillable hours that pediatric rheumatologists spend taking care of patients, Dr. Hayward noted.
Especially with electronic medical records (EMRs) and online communication with patients, “there is increasingly a lot of patient care that happens outside of clinic and that takes a lot of time,” Dr. Hayward said. For example, she spends between 1 and 2 hours every day in the EMR refilling medications and responding to patient concerns, and “that all is done in my spare time,” she said. “That’s not billed to the patient in anyway.”
Length of Fellowship
The pediatric rheumatology fellowship is a 3-year program — like other pediatric subspecialities — with a research requirement. By comparison, adult rheumatology fellowships are 2 years, and fellows can pursue additional research training if they have a strong interest.
“It sounds like just 1 more year, but I think it’s coming at a really pivotal point in people’s lives, and that 1 year can make a huge difference,” Dr. Hayward explained.
The 2 years of research might also be a deterrent for individuals who know they are only interested in clinical work, she added. About half of pediatric subspecialists only pursue clinical work after graduation, according to a recent report by the National Academies of Sciences, Engineering, and Medicine (NASEM) focused on the future pediatric physician workforce.
Additionally, only 17% of pediatric rheumatologists spend more than half of their time in research, said Fred Rivara, MD, MPH, chair of the NASEM report, in a statement included in Dr. Hayward’s ACR presentation. The report, which recommended strategies to bolster the pediatric workforce, argued that the American Board of Pediatrics should develop alternative training pathways, including 2-year, clinically heavy fellowships.
The ACR workforce team is also exploring alternative training models like competency-based education, Dr. Hayward said. The Education in Pediatrics Across the Continuum project is already using this approach from medical school to pediatric residency. While this type of outcome-based program has not been tried at the fellowship level, «this has been done, it could be done, and I think we could learn from our colleagues about how they have done this successfully,» she noted.
Ultimately, Dr. Hayward emphasized that there needs to be a “sea change” to close the workforce gap — with multiple interventions addressing these individual challenges.
“Unless we all pitch in and find one way that we can all move this issue forward, we are going to be drowning in a sea of Epic inbox messages,” she said, “and never get to see the patients we want to see.”
Dr. Hayward previously owned stock/stock options for AbbVie/Abbott, Cigna/Express Scripts, Merck, and Teva and has received an educational grant from Pfizer. Dr. Correll and Dr. Mehta had no relevant disclosures.
A version of this article appeared on Medscape.com.
Pediatric rheumatologists are calling a “Code (p)RED” — a pediatric rheumatology educational deficit.
There are too few pediatric rheumatologists to meet patient demand in the United States, and projections suggest that gap will continue to widen. Disappointing match trends also reflect issues with recruitment: Since 2019, only 50%-75% of pediatric rheumatology fellowship positions have been filled each year. For 2024, the subspecialty filled 32 of 52 positions.
Lack of exposure during medical school and residency, financial concerns, and a lengthy, research-focused fellowship are seen as major contributors to the workforce shortage, and novel solutions are needed to close the gap, experts argued in a recent presentation at the annual meeting of the American College of Rheumatology.
“It’s so important now to get ahead of this because what I’m afraid of is in 10-20 years, we’re not going to have a field,” Colleen Correll, MD, MPH, an associate professor in the division of pediatric rheumatology at the University of Minnesota Medical School in Minneapolis, told this news organization.
Growing Demand, Falling Supply
Because the subspecialty was officially recognized by the American Board of Pediatrics in 1991, “it’s always been a small group of providers,” Dr. Correll said. “It’s honestly always been a recognized issue in our field.”
But a 2022 report by the ACR on the pediatric workforce has brought more attention to the issue. Dr. Correll led the study and is the chair of ACR›s Pediatric Rheumatology Committee. According to the report, an estimated 287 pediatric rheumatologists were working as full-time clinicians in 2015, while the estimated demand was 382 providers. By 2030, this projected supply of pediatric rheumatologists fell to 261, while demand rose to 461 full-time providers.
The distribution of pediatric rheumatologists is also an issue. It’s generally thought that there should be at least one pediatric rheumatologist per 100,000 children, Dr. Correll explained. According to ACR estimates, the northeast region had approximately 0.83 pediatric rheumatologists per 100,000 in 2015, while the south central and southwest regions had 0.17 and 0.20 providers per 100,000 children, respectively. Projected estimates for 2030 dipped to 0.04 or lower for the south central, southwest, and southeast regions.
A separate study from the American Board of Pediatrics, also led by Dr. Correll, that is still under review offered more optimistic projections, suggesting that there would be a 75% increase in pediatric rheumatologists from 0.27 per 100,000 children in 2020 to 0.47 per 100,000 children in 2040.
“This does look better than the ACR study, though 0.47 is still a really small number and an inadequate number to treat our children in need,” she said during her presentation at the annual meeting of the American College of Rheumatology.
Lack of Exposure During Medical Education
Few medical schools have pediatric rheumatology built into their curriculum, whether that is a whole course or a single lecture, said Jay Mehta, MD, who directs the pediatric rheumatology fellowship at the Children’s Hospital of Philadelphia. Dr. Mehta, for example, did not know that pediatric rheumatology was a field before entering residency, he said. But residencies can also lack exposure: An estimated one third of residencies do not have a single pediatric rheumatologist on staff, he said.
“Those are places where people aren’t necessarily getting exposure to pediatric rheumatology,” he told this news organization, “and we know that if you’re not exposed to a field, it’s very, very unlikely that you will go into that field.”
The ACR’s Pediatric Rheumatology Residency Program is one way that the organization is working to address this issue. The program sends pediatric residents with an interest in rheumatology to the ACR annual meeting. The Rheumatology Research Foundation also runs a visiting professorship program, where a pediatric rheumatologist conducts a rheumatology education forum at an institution with no pediatric rheumatology program.
“I’ve done it a couple of times,” Dr. Mehta said during his presentation at the annual meeting. “It’s one of the most rewarding things I’ve done.”
Financial Concerns
Additionally, although pediatric rheumatology requires more training, these subspecialists will likely make less than their general pediatric colleagues over their career. According to one study in Pediatrics, a pediatric resident pursuing rheumatology is projected to make $1.2 million dollars less over the course of their career compared with someone who started their career in general pediatrics immediately after residency. (Negative financial returns were also found for all pediatric subspecialities except for cardiology, critical care, and neonatology.)
This lower earning potential is likely a deterrent, especially for those with educational debt. In one analysis published in October, medical students with at least $200,000 in education debt were 43% more likely to go into higher-paying pediatric subspecialities than those with no debt. Nearly three out of four medical graduates have education debt, according to the American Association of Medical Colleges, with a median debt of $200,000.
While the Pediatric Specialty Loan Repayment Program was specifically designed to aid pediatric subspecialists with their educational debt, qualifying for the program is difficult for pediatric rheumatologists, explained Kristen N. Hayward, MD, of Seattle Children’s in Washington. The program provides up to $100,000 in loan forgiveness in exchange for 3 years of practicing in an underserved area; however, the program stipulates that providers must provide full-time (40 hours per week) clinical care. At academic institutions, where most pediatric rheumatologists practice, there is usually a research component to their position, and even if a provider works the equivalent of 40 hours per week in a clinic in addition to their research, they don’t qualify for the program, Dr. Hayward said.
“It’s very difficult to find someone who’s actually only doing clinical work,” she said.
The ACR has worked to combat some of these economic constraints by demonstrating the direct and downstream value of rheumatologic care, Dr. Hayward said. In a recent white paper, it was estimated that including office visits, consultations, lab testing, and radiology services, one full-time equivalent rheumatologist generates $3.5 million in revenue every year and saves health systems more than $2700 per patient per year.
In addition to placing greater value on rheumatologic care, the healthcare system also needs to recognize the current nonbillable hours that pediatric rheumatologists spend taking care of patients, Dr. Hayward noted.
Especially with electronic medical records (EMRs) and online communication with patients, “there is increasingly a lot of patient care that happens outside of clinic and that takes a lot of time,” Dr. Hayward said. For example, she spends between 1 and 2 hours every day in the EMR refilling medications and responding to patient concerns, and “that all is done in my spare time,” she said. “That’s not billed to the patient in anyway.”
Length of Fellowship
The pediatric rheumatology fellowship is a 3-year program — like other pediatric subspecialities — with a research requirement. By comparison, adult rheumatology fellowships are 2 years, and fellows can pursue additional research training if they have a strong interest.
“It sounds like just 1 more year, but I think it’s coming at a really pivotal point in people’s lives, and that 1 year can make a huge difference,” Dr. Hayward explained.
The 2 years of research might also be a deterrent for individuals who know they are only interested in clinical work, she added. About half of pediatric subspecialists only pursue clinical work after graduation, according to a recent report by the National Academies of Sciences, Engineering, and Medicine (NASEM) focused on the future pediatric physician workforce.
Additionally, only 17% of pediatric rheumatologists spend more than half of their time in research, said Fred Rivara, MD, MPH, chair of the NASEM report, in a statement included in Dr. Hayward’s ACR presentation. The report, which recommended strategies to bolster the pediatric workforce, argued that the American Board of Pediatrics should develop alternative training pathways, including 2-year, clinically heavy fellowships.
The ACR workforce team is also exploring alternative training models like competency-based education, Dr. Hayward said. The Education in Pediatrics Across the Continuum project is already using this approach from medical school to pediatric residency. While this type of outcome-based program has not been tried at the fellowship level, «this has been done, it could be done, and I think we could learn from our colleagues about how they have done this successfully,» she noted.
Ultimately, Dr. Hayward emphasized that there needs to be a “sea change” to close the workforce gap — with multiple interventions addressing these individual challenges.
“Unless we all pitch in and find one way that we can all move this issue forward, we are going to be drowning in a sea of Epic inbox messages,” she said, “and never get to see the patients we want to see.”
Dr. Hayward previously owned stock/stock options for AbbVie/Abbott, Cigna/Express Scripts, Merck, and Teva and has received an educational grant from Pfizer. Dr. Correll and Dr. Mehta had no relevant disclosures.
A version of this article appeared on Medscape.com.
Pediatric rheumatologists are calling a “Code (p)RED” — a pediatric rheumatology educational deficit.
There are too few pediatric rheumatologists to meet patient demand in the United States, and projections suggest that gap will continue to widen. Disappointing match trends also reflect issues with recruitment: Since 2019, only 50%-75% of pediatric rheumatology fellowship positions have been filled each year. For 2024, the subspecialty filled 32 of 52 positions.
Lack of exposure during medical school and residency, financial concerns, and a lengthy, research-focused fellowship are seen as major contributors to the workforce shortage, and novel solutions are needed to close the gap, experts argued in a recent presentation at the annual meeting of the American College of Rheumatology.
“It’s so important now to get ahead of this because what I’m afraid of is in 10-20 years, we’re not going to have a field,” Colleen Correll, MD, MPH, an associate professor in the division of pediatric rheumatology at the University of Minnesota Medical School in Minneapolis, told this news organization.
Growing Demand, Falling Supply
Because the subspecialty was officially recognized by the American Board of Pediatrics in 1991, “it’s always been a small group of providers,” Dr. Correll said. “It’s honestly always been a recognized issue in our field.”
But a 2022 report by the ACR on the pediatric workforce has brought more attention to the issue. Dr. Correll led the study and is the chair of ACR›s Pediatric Rheumatology Committee. According to the report, an estimated 287 pediatric rheumatologists were working as full-time clinicians in 2015, while the estimated demand was 382 providers. By 2030, this projected supply of pediatric rheumatologists fell to 261, while demand rose to 461 full-time providers.
The distribution of pediatric rheumatologists is also an issue. It’s generally thought that there should be at least one pediatric rheumatologist per 100,000 children, Dr. Correll explained. According to ACR estimates, the northeast region had approximately 0.83 pediatric rheumatologists per 100,000 in 2015, while the south central and southwest regions had 0.17 and 0.20 providers per 100,000 children, respectively. Projected estimates for 2030 dipped to 0.04 or lower for the south central, southwest, and southeast regions.
A separate study from the American Board of Pediatrics, also led by Dr. Correll, that is still under review offered more optimistic projections, suggesting that there would be a 75% increase in pediatric rheumatologists from 0.27 per 100,000 children in 2020 to 0.47 per 100,000 children in 2040.
“This does look better than the ACR study, though 0.47 is still a really small number and an inadequate number to treat our children in need,” she said during her presentation at the annual meeting of the American College of Rheumatology.
Lack of Exposure During Medical Education
Few medical schools have pediatric rheumatology built into their curriculum, whether that is a whole course or a single lecture, said Jay Mehta, MD, who directs the pediatric rheumatology fellowship at the Children’s Hospital of Philadelphia. Dr. Mehta, for example, did not know that pediatric rheumatology was a field before entering residency, he said. But residencies can also lack exposure: An estimated one third of residencies do not have a single pediatric rheumatologist on staff, he said.
“Those are places where people aren’t necessarily getting exposure to pediatric rheumatology,” he told this news organization, “and we know that if you’re not exposed to a field, it’s very, very unlikely that you will go into that field.”
The ACR’s Pediatric Rheumatology Residency Program is one way that the organization is working to address this issue. The program sends pediatric residents with an interest in rheumatology to the ACR annual meeting. The Rheumatology Research Foundation also runs a visiting professorship program, where a pediatric rheumatologist conducts a rheumatology education forum at an institution with no pediatric rheumatology program.
“I’ve done it a couple of times,” Dr. Mehta said during his presentation at the annual meeting. “It’s one of the most rewarding things I’ve done.”
Financial Concerns
Additionally, although pediatric rheumatology requires more training, these subspecialists will likely make less than their general pediatric colleagues over their career. According to one study in Pediatrics, a pediatric resident pursuing rheumatology is projected to make $1.2 million dollars less over the course of their career compared with someone who started their career in general pediatrics immediately after residency. (Negative financial returns were also found for all pediatric subspecialities except for cardiology, critical care, and neonatology.)
This lower earning potential is likely a deterrent, especially for those with educational debt. In one analysis published in October, medical students with at least $200,000 in education debt were 43% more likely to go into higher-paying pediatric subspecialities than those with no debt. Nearly three out of four medical graduates have education debt, according to the American Association of Medical Colleges, with a median debt of $200,000.
While the Pediatric Specialty Loan Repayment Program was specifically designed to aid pediatric subspecialists with their educational debt, qualifying for the program is difficult for pediatric rheumatologists, explained Kristen N. Hayward, MD, of Seattle Children’s in Washington. The program provides up to $100,000 in loan forgiveness in exchange for 3 years of practicing in an underserved area; however, the program stipulates that providers must provide full-time (40 hours per week) clinical care. At academic institutions, where most pediatric rheumatologists practice, there is usually a research component to their position, and even if a provider works the equivalent of 40 hours per week in a clinic in addition to their research, they don’t qualify for the program, Dr. Hayward said.
“It’s very difficult to find someone who’s actually only doing clinical work,” she said.
The ACR has worked to combat some of these economic constraints by demonstrating the direct and downstream value of rheumatologic care, Dr. Hayward said. In a recent white paper, it was estimated that including office visits, consultations, lab testing, and radiology services, one full-time equivalent rheumatologist generates $3.5 million in revenue every year and saves health systems more than $2700 per patient per year.
In addition to placing greater value on rheumatologic care, the healthcare system also needs to recognize the current nonbillable hours that pediatric rheumatologists spend taking care of patients, Dr. Hayward noted.
Especially with electronic medical records (EMRs) and online communication with patients, “there is increasingly a lot of patient care that happens outside of clinic and that takes a lot of time,” Dr. Hayward said. For example, she spends between 1 and 2 hours every day in the EMR refilling medications and responding to patient concerns, and “that all is done in my spare time,” she said. “That’s not billed to the patient in anyway.”
Length of Fellowship
The pediatric rheumatology fellowship is a 3-year program — like other pediatric subspecialities — with a research requirement. By comparison, adult rheumatology fellowships are 2 years, and fellows can pursue additional research training if they have a strong interest.
“It sounds like just 1 more year, but I think it’s coming at a really pivotal point in people’s lives, and that 1 year can make a huge difference,” Dr. Hayward explained.
The 2 years of research might also be a deterrent for individuals who know they are only interested in clinical work, she added. About half of pediatric subspecialists only pursue clinical work after graduation, according to a recent report by the National Academies of Sciences, Engineering, and Medicine (NASEM) focused on the future pediatric physician workforce.
Additionally, only 17% of pediatric rheumatologists spend more than half of their time in research, said Fred Rivara, MD, MPH, chair of the NASEM report, in a statement included in Dr. Hayward’s ACR presentation. The report, which recommended strategies to bolster the pediatric workforce, argued that the American Board of Pediatrics should develop alternative training pathways, including 2-year, clinically heavy fellowships.
The ACR workforce team is also exploring alternative training models like competency-based education, Dr. Hayward said. The Education in Pediatrics Across the Continuum project is already using this approach from medical school to pediatric residency. While this type of outcome-based program has not been tried at the fellowship level, «this has been done, it could be done, and I think we could learn from our colleagues about how they have done this successfully,» she noted.
Ultimately, Dr. Hayward emphasized that there needs to be a “sea change” to close the workforce gap — with multiple interventions addressing these individual challenges.
“Unless we all pitch in and find one way that we can all move this issue forward, we are going to be drowning in a sea of Epic inbox messages,” she said, “and never get to see the patients we want to see.”
Dr. Hayward previously owned stock/stock options for AbbVie/Abbott, Cigna/Express Scripts, Merck, and Teva and has received an educational grant from Pfizer. Dr. Correll and Dr. Mehta had no relevant disclosures.
A version of this article appeared on Medscape.com.
FROM ACR 2023
Fellowships in Complex Medical Dermatology
Complex medical dermatology has become an emerging field in dermatology. Although a rather protean and broad term, complex medical dermatology encompasses patients with autoimmune conditions, bullous disease, connective tissue disease, vasculitis, severe dermatoses requiring immunomodulation, and inpatient consultations. Importantly, dermatology inpatient consultations aid in lowering health care costs due to accurate diagnoses, correct treatment, and decreased hospital stays.1 A fellowship is not required for holding an inpatient role in the hospital system as a dermatologist but can be beneficial. There are combined internal medicine–dermatology programs available for medical students applying to dermatology residency, but a complex medical dermatology fellowship is an option after residency for those who are interested. I believe that a focused complex medical dermatology fellowship differs from the training offered in combined internal medicine–dermatology residency. My fellow colleagues in combined internal medicine–dermatology programs are exposed to systemic manifestations of cutaneous disease and are experts in the interplay between the skin and other organ systems. However, the focus of their programs is with the intention of becoming double boarded in internal medicine and dermatology with comprehensive exposure to both fields. In my fellowship, I am able to tailor my schedule to focus on any dermatologic disease such as connective tissue disease, pruritus, graft vs host disease, and Merkel cell carcinoma. I ultimately can determine a niche in dermatology and hone my skills for a year under supervision.
Available Fellowships
Fellowship Locations—Importantly, the complex medical dermatology fellowship is not accredited by the Accreditation Council for Graduate Medical Education, which can make it difficult to identify and apply to programs. The complex medical dermatology fellowship is different than a rheumatology-dermatology fellowship, cutaneous oncology fellowship, pediatric dermatology fellowship, or other subspecialty fellowships such as those in itch or autoimmune blistering diseases. The fellowship often encompasses gaining clinical expertise in many of these conditions. I performed a thorough search online and spoke with complex medical dermatologists to compile a list of programs that offer a complex medical dermatology fellowship: Brigham and Women’s Hospital (Boston, Massachusetts); University of California San Francisco (San Francisco, California); University of Pennsylvania (Philadelphia, Pennsylvania); Cleveland Clinic (Cleveland, Ohio); and New York University (New York, New York)(Table). Only 1 spot is offered at each of these programs.
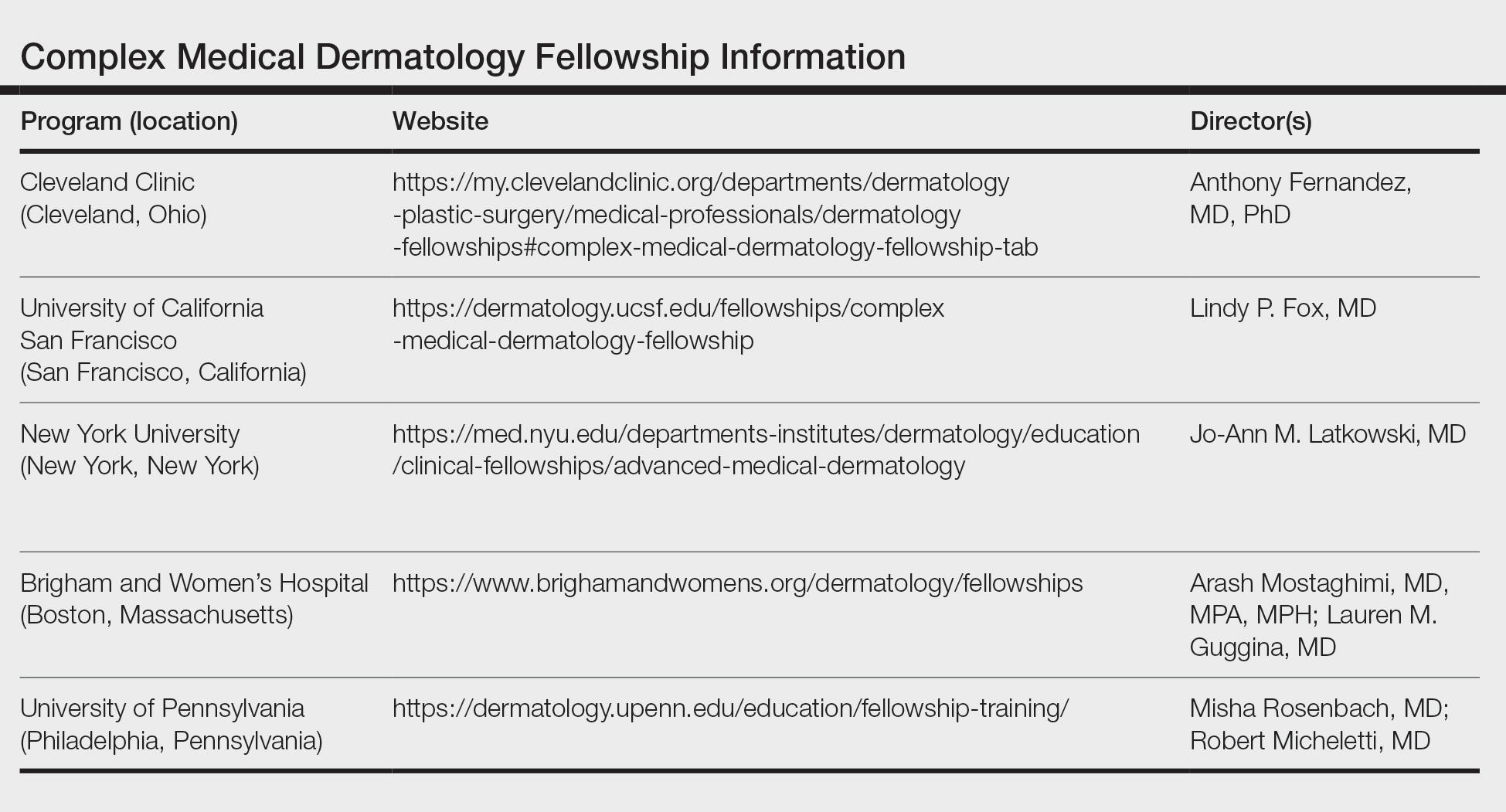
Reason to Pursue the Fellowship—There are many reasons to pursue a fellowship in complex medical dermatology such as a desire to enhance exposure to the field, to practice in an academic center and develop a niche within dermatology, to practice dermatology in an inpatient setting, to improve delivery of health care to medically challenging populations in a community setting, and to become an expert on cutaneous manifestations of internal and systemic disease.
Application—There is no standardized application or deadline for this fellowship; however, there is a concerted attempt from some of the programs to offer interviews and decisions at a similar time. Deadlines and contact information are listed on the program websites, along with more details (Table).
Recommendations—I would recommend reaching out at the beginning of postgraduate year (PGY) 4 to these programs and voicing your interest in the fellowship. It is possible to set up an away rotation at some of the programs, and if your program offers elective time, pursuing an away rotation during PGY-3 or early in PGY-4 can prove to be advantageous. Furthermore, during my application cycle I toured the University of California San Francisco, University of Pennsylvania, and Brigham and Women’s Hospital to gain further insight into each program.
Brigham and Women’s Complex Medical Dermatology Fellowship
I am currently the complex medical dermatology fellow at Brigham and Women’s Hospital, and it has been an outstanding experience thus far. The program offers numerous subspecialty clinics focusing solely on cutaneous-oncodermatology, psoriasis, rheumatology-dermatology, skin of color, mole mapping backed by artificial intelligence, cosmetics, high-risk skin cancer, neutrophilic dermatoses, patch testing, phototherapy, psychodermatology, and transplant dermatology. In addition to a wide variety of subspecialty clinics, fellows have the opportunity to participate in inpatient dermatology rounds and act as a junior attending. I appreciate the flexibility of this program combined with the ability to work alongside worldwide experts. There are numerous teaching opportunities, and all of the faculty are amiable and intelligent and emphasize wellness, education, and autonomy. Overall, my experience and decision to pursue a complex medical dermatology fellowship has been extremely rewarding and invaluable. I am gaining additional skills to aid medically challenging patients while pursuing my true passion in dermatology.
1. Sahni DR. Inpatient dermatology consultation services in hospital institutions. Cutis. 2023;111:E11-E12. doi:10.12788/cutis.0776.
Complex medical dermatology has become an emerging field in dermatology. Although a rather protean and broad term, complex medical dermatology encompasses patients with autoimmune conditions, bullous disease, connective tissue disease, vasculitis, severe dermatoses requiring immunomodulation, and inpatient consultations. Importantly, dermatology inpatient consultations aid in lowering health care costs due to accurate diagnoses, correct treatment, and decreased hospital stays.1 A fellowship is not required for holding an inpatient role in the hospital system as a dermatologist but can be beneficial. There are combined internal medicine–dermatology programs available for medical students applying to dermatology residency, but a complex medical dermatology fellowship is an option after residency for those who are interested. I believe that a focused complex medical dermatology fellowship differs from the training offered in combined internal medicine–dermatology residency. My fellow colleagues in combined internal medicine–dermatology programs are exposed to systemic manifestations of cutaneous disease and are experts in the interplay between the skin and other organ systems. However, the focus of their programs is with the intention of becoming double boarded in internal medicine and dermatology with comprehensive exposure to both fields. In my fellowship, I am able to tailor my schedule to focus on any dermatologic disease such as connective tissue disease, pruritus, graft vs host disease, and Merkel cell carcinoma. I ultimately can determine a niche in dermatology and hone my skills for a year under supervision.
Available Fellowships
Fellowship Locations—Importantly, the complex medical dermatology fellowship is not accredited by the Accreditation Council for Graduate Medical Education, which can make it difficult to identify and apply to programs. The complex medical dermatology fellowship is different than a rheumatology-dermatology fellowship, cutaneous oncology fellowship, pediatric dermatology fellowship, or other subspecialty fellowships such as those in itch or autoimmune blistering diseases. The fellowship often encompasses gaining clinical expertise in many of these conditions. I performed a thorough search online and spoke with complex medical dermatologists to compile a list of programs that offer a complex medical dermatology fellowship: Brigham and Women’s Hospital (Boston, Massachusetts); University of California San Francisco (San Francisco, California); University of Pennsylvania (Philadelphia, Pennsylvania); Cleveland Clinic (Cleveland, Ohio); and New York University (New York, New York)(Table). Only 1 spot is offered at each of these programs.
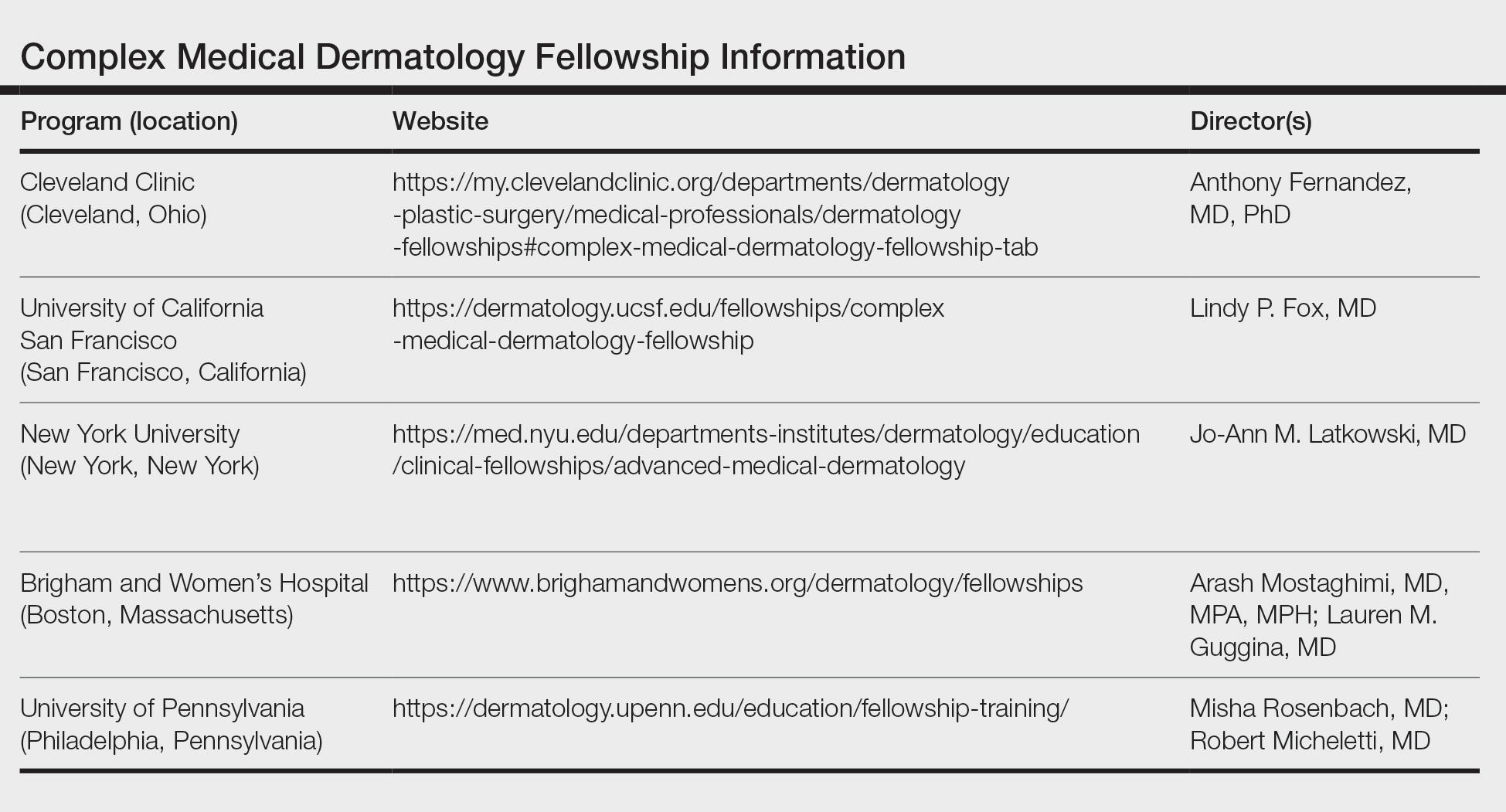
Reason to Pursue the Fellowship—There are many reasons to pursue a fellowship in complex medical dermatology such as a desire to enhance exposure to the field, to practice in an academic center and develop a niche within dermatology, to practice dermatology in an inpatient setting, to improve delivery of health care to medically challenging populations in a community setting, and to become an expert on cutaneous manifestations of internal and systemic disease.
Application—There is no standardized application or deadline for this fellowship; however, there is a concerted attempt from some of the programs to offer interviews and decisions at a similar time. Deadlines and contact information are listed on the program websites, along with more details (Table).
Recommendations—I would recommend reaching out at the beginning of postgraduate year (PGY) 4 to these programs and voicing your interest in the fellowship. It is possible to set up an away rotation at some of the programs, and if your program offers elective time, pursuing an away rotation during PGY-3 or early in PGY-4 can prove to be advantageous. Furthermore, during my application cycle I toured the University of California San Francisco, University of Pennsylvania, and Brigham and Women’s Hospital to gain further insight into each program.
Brigham and Women’s Complex Medical Dermatology Fellowship
I am currently the complex medical dermatology fellow at Brigham and Women’s Hospital, and it has been an outstanding experience thus far. The program offers numerous subspecialty clinics focusing solely on cutaneous-oncodermatology, psoriasis, rheumatology-dermatology, skin of color, mole mapping backed by artificial intelligence, cosmetics, high-risk skin cancer, neutrophilic dermatoses, patch testing, phototherapy, psychodermatology, and transplant dermatology. In addition to a wide variety of subspecialty clinics, fellows have the opportunity to participate in inpatient dermatology rounds and act as a junior attending. I appreciate the flexibility of this program combined with the ability to work alongside worldwide experts. There are numerous teaching opportunities, and all of the faculty are amiable and intelligent and emphasize wellness, education, and autonomy. Overall, my experience and decision to pursue a complex medical dermatology fellowship has been extremely rewarding and invaluable. I am gaining additional skills to aid medically challenging patients while pursuing my true passion in dermatology.
Complex medical dermatology has become an emerging field in dermatology. Although a rather protean and broad term, complex medical dermatology encompasses patients with autoimmune conditions, bullous disease, connective tissue disease, vasculitis, severe dermatoses requiring immunomodulation, and inpatient consultations. Importantly, dermatology inpatient consultations aid in lowering health care costs due to accurate diagnoses, correct treatment, and decreased hospital stays.1 A fellowship is not required for holding an inpatient role in the hospital system as a dermatologist but can be beneficial. There are combined internal medicine–dermatology programs available for medical students applying to dermatology residency, but a complex medical dermatology fellowship is an option after residency for those who are interested. I believe that a focused complex medical dermatology fellowship differs from the training offered in combined internal medicine–dermatology residency. My fellow colleagues in combined internal medicine–dermatology programs are exposed to systemic manifestations of cutaneous disease and are experts in the interplay between the skin and other organ systems. However, the focus of their programs is with the intention of becoming double boarded in internal medicine and dermatology with comprehensive exposure to both fields. In my fellowship, I am able to tailor my schedule to focus on any dermatologic disease such as connective tissue disease, pruritus, graft vs host disease, and Merkel cell carcinoma. I ultimately can determine a niche in dermatology and hone my skills for a year under supervision.
Available Fellowships
Fellowship Locations—Importantly, the complex medical dermatology fellowship is not accredited by the Accreditation Council for Graduate Medical Education, which can make it difficult to identify and apply to programs. The complex medical dermatology fellowship is different than a rheumatology-dermatology fellowship, cutaneous oncology fellowship, pediatric dermatology fellowship, or other subspecialty fellowships such as those in itch or autoimmune blistering diseases. The fellowship often encompasses gaining clinical expertise in many of these conditions. I performed a thorough search online and spoke with complex medical dermatologists to compile a list of programs that offer a complex medical dermatology fellowship: Brigham and Women’s Hospital (Boston, Massachusetts); University of California San Francisco (San Francisco, California); University of Pennsylvania (Philadelphia, Pennsylvania); Cleveland Clinic (Cleveland, Ohio); and New York University (New York, New York)(Table). Only 1 spot is offered at each of these programs.
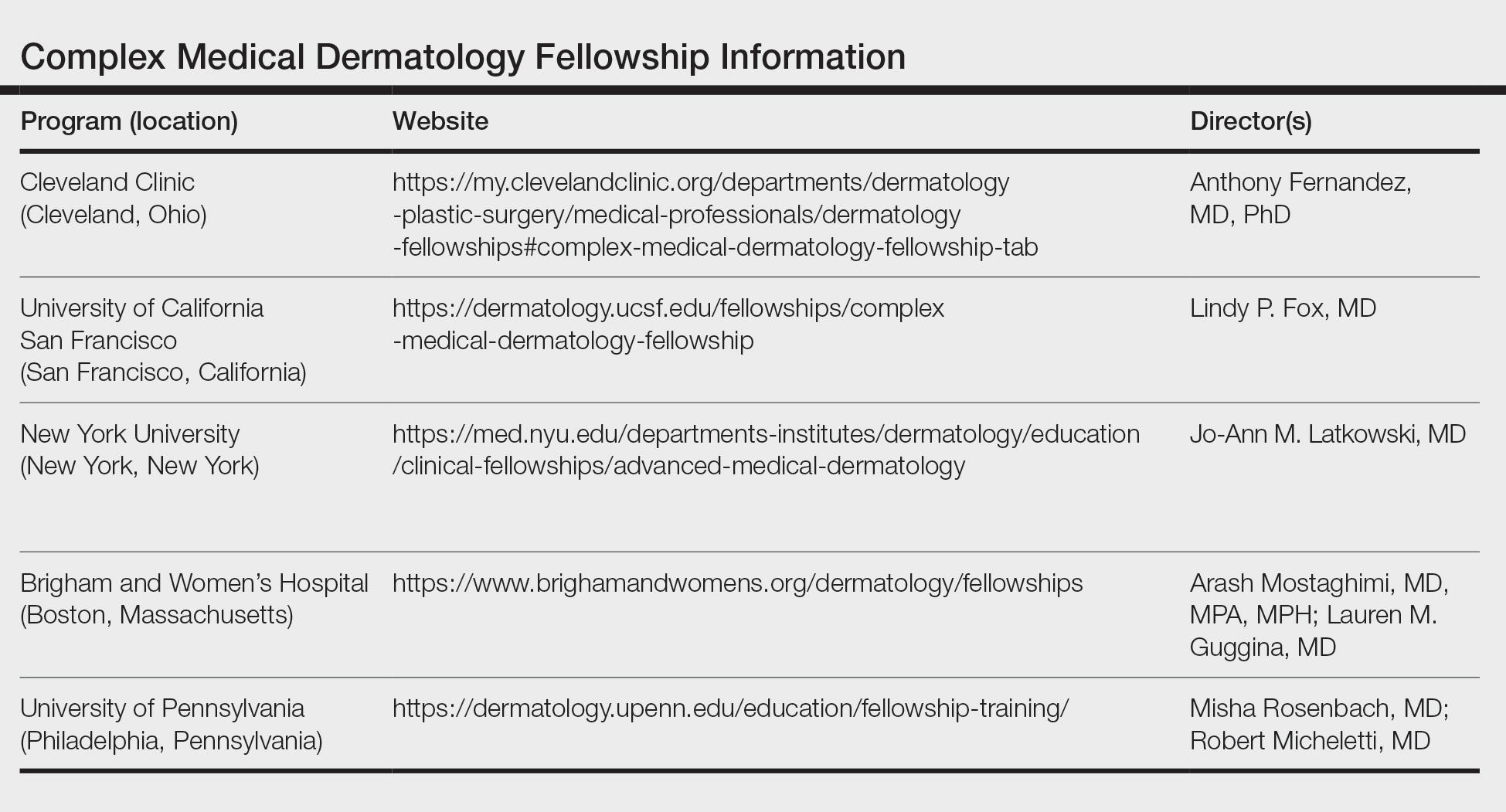
Reason to Pursue the Fellowship—There are many reasons to pursue a fellowship in complex medical dermatology such as a desire to enhance exposure to the field, to practice in an academic center and develop a niche within dermatology, to practice dermatology in an inpatient setting, to improve delivery of health care to medically challenging populations in a community setting, and to become an expert on cutaneous manifestations of internal and systemic disease.
Application—There is no standardized application or deadline for this fellowship; however, there is a concerted attempt from some of the programs to offer interviews and decisions at a similar time. Deadlines and contact information are listed on the program websites, along with more details (Table).
Recommendations—I would recommend reaching out at the beginning of postgraduate year (PGY) 4 to these programs and voicing your interest in the fellowship. It is possible to set up an away rotation at some of the programs, and if your program offers elective time, pursuing an away rotation during PGY-3 or early in PGY-4 can prove to be advantageous. Furthermore, during my application cycle I toured the University of California San Francisco, University of Pennsylvania, and Brigham and Women’s Hospital to gain further insight into each program.
Brigham and Women’s Complex Medical Dermatology Fellowship
I am currently the complex medical dermatology fellow at Brigham and Women’s Hospital, and it has been an outstanding experience thus far. The program offers numerous subspecialty clinics focusing solely on cutaneous-oncodermatology, psoriasis, rheumatology-dermatology, skin of color, mole mapping backed by artificial intelligence, cosmetics, high-risk skin cancer, neutrophilic dermatoses, patch testing, phototherapy, psychodermatology, and transplant dermatology. In addition to a wide variety of subspecialty clinics, fellows have the opportunity to participate in inpatient dermatology rounds and act as a junior attending. I appreciate the flexibility of this program combined with the ability to work alongside worldwide experts. There are numerous teaching opportunities, and all of the faculty are amiable and intelligent and emphasize wellness, education, and autonomy. Overall, my experience and decision to pursue a complex medical dermatology fellowship has been extremely rewarding and invaluable. I am gaining additional skills to aid medically challenging patients while pursuing my true passion in dermatology.
1. Sahni DR. Inpatient dermatology consultation services in hospital institutions. Cutis. 2023;111:E11-E12. doi:10.12788/cutis.0776.
1. Sahni DR. Inpatient dermatology consultation services in hospital institutions. Cutis. 2023;111:E11-E12. doi:10.12788/cutis.0776.
RESIDENT PEARL
- Complex medical dermatology is a rewarding and fascinating subspecialty of dermatology, and additional training can be accomplished through a fellowship at a variety of prestigious institutions.
Brick and mortar: Changes in the therapeutic relationship in a postvirtual world
My colleagues and I entered the realm of outpatient psychiatry during residency at a logistically and dynamically interesting time. At the beginning of our third year in training (July 2022), almost all of the outpatients we were treating were still being seen virtually. For much of the year, they remained that way. However, with the reinstatement of the Ryan Haight Act in May 2023, I began to meet patients in person for the first time—the same patients whom I had known only virtually for the first 10 months of our therapeutic relationship. I observed vast changes in the dynamic of the room; many of these patients opened up more in their first in-person session than they had all year over Zoom.
Once in-person sessions resumed, patients who during virtual visits had assured me for almost a year that their home situation was optimized had a plethora of new things to share about their seemingly straightforward living situations. Relationships that appeared stable had more layers to reveal once the half of the relationship I was treating was now comfortably seated within the walls of my office. Problems that had previously seemed biologically based suddenly had complex sociocultural elements that were divulged for the first time. Some patients felt freer to be unrestricted in their affect, in contrast to the logistical (and metaphorical) buttoned-up virtual environment. Emotions ranged from cathartic (“It’s so great to see you in person!”) to bemused (“You’re taller/shorter, older/younger than I thought!”). The screen was gone, and the tangibility of it all breathed a different air into the room.
Virtual vs in-person: Crabs on a beach
The virtual treatment space could be envisioned as crabs in shells scattered on a beach, in which 2 crabs situated in their own shells, not necessarily adjacent to each other, could communicate. This certainly had benefits, such as the convenience of not having to move to another shell, as well as the brief but telling opportunity to gaze into their home shell environment. However, sometimes there would be disadvantages, such as interference with the connection due to static in the sand; at other times, there was the potential for other crabs to overhear and inadvertently learn of each other’s presence, thus affecting the openness of the communication. In this analogy, perhaps the equivalent of an in-person meeting would be 1 crab meandering over and the 2 crabs cohabiting a conch for the first time—it’s spacious (enough), all-enveloping, and within the harkened privacy of a shared sacred space.
A unique training experience
My co-residents and I are uniquely positioned to observe this novel phenomenon due to the timing of having entered our outpatient psychiatry training during the COVID-19 pandemic. Previous generations of residents—as well as practicing psychiatrists who had initially met their patients in person and were forced to switch to virtual sessions during the pandemic—had certain perspectives and challenges of their own, but they had a known dynamic of in-person interactions at baseline. Accordingly, residents who practiced peak- and mid-pandemic and graduated without being required to treat patients face-to-face (the classes of 2022 and 2023) might have spent entire therapeutic relationships having never met their patients in person. My class (2024) was situated in this time- and situation-bound frame in which we started virtually, and by requirements of the law, later met our patients in person. Being not only an observer but an active participant in a treatment dyad within the context of this phenomenon taught me astutely about transference, countertransference, and the holding environment. Training in psychodynamic psychotherapy has taught me about the act of listening deeply and qualities of therapeutic communication. Having the opportunity to enact these principles in such a dichotomy of treatment settings has been invaluable in my education, in getting to know different facets of my patients, and in understanding the nuances of the human experience.
My colleagues and I entered the realm of outpatient psychiatry during residency at a logistically and dynamically interesting time. At the beginning of our third year in training (July 2022), almost all of the outpatients we were treating were still being seen virtually. For much of the year, they remained that way. However, with the reinstatement of the Ryan Haight Act in May 2023, I began to meet patients in person for the first time—the same patients whom I had known only virtually for the first 10 months of our therapeutic relationship. I observed vast changes in the dynamic of the room; many of these patients opened up more in their first in-person session than they had all year over Zoom.
Once in-person sessions resumed, patients who during virtual visits had assured me for almost a year that their home situation was optimized had a plethora of new things to share about their seemingly straightforward living situations. Relationships that appeared stable had more layers to reveal once the half of the relationship I was treating was now comfortably seated within the walls of my office. Problems that had previously seemed biologically based suddenly had complex sociocultural elements that were divulged for the first time. Some patients felt freer to be unrestricted in their affect, in contrast to the logistical (and metaphorical) buttoned-up virtual environment. Emotions ranged from cathartic (“It’s so great to see you in person!”) to bemused (“You’re taller/shorter, older/younger than I thought!”). The screen was gone, and the tangibility of it all breathed a different air into the room.
Virtual vs in-person: Crabs on a beach
The virtual treatment space could be envisioned as crabs in shells scattered on a beach, in which 2 crabs situated in their own shells, not necessarily adjacent to each other, could communicate. This certainly had benefits, such as the convenience of not having to move to another shell, as well as the brief but telling opportunity to gaze into their home shell environment. However, sometimes there would be disadvantages, such as interference with the connection due to static in the sand; at other times, there was the potential for other crabs to overhear and inadvertently learn of each other’s presence, thus affecting the openness of the communication. In this analogy, perhaps the equivalent of an in-person meeting would be 1 crab meandering over and the 2 crabs cohabiting a conch for the first time—it’s spacious (enough), all-enveloping, and within the harkened privacy of a shared sacred space.
A unique training experience
My co-residents and I are uniquely positioned to observe this novel phenomenon due to the timing of having entered our outpatient psychiatry training during the COVID-19 pandemic. Previous generations of residents—as well as practicing psychiatrists who had initially met their patients in person and were forced to switch to virtual sessions during the pandemic—had certain perspectives and challenges of their own, but they had a known dynamic of in-person interactions at baseline. Accordingly, residents who practiced peak- and mid-pandemic and graduated without being required to treat patients face-to-face (the classes of 2022 and 2023) might have spent entire therapeutic relationships having never met their patients in person. My class (2024) was situated in this time- and situation-bound frame in which we started virtually, and by requirements of the law, later met our patients in person. Being not only an observer but an active participant in a treatment dyad within the context of this phenomenon taught me astutely about transference, countertransference, and the holding environment. Training in psychodynamic psychotherapy has taught me about the act of listening deeply and qualities of therapeutic communication. Having the opportunity to enact these principles in such a dichotomy of treatment settings has been invaluable in my education, in getting to know different facets of my patients, and in understanding the nuances of the human experience.
My colleagues and I entered the realm of outpatient psychiatry during residency at a logistically and dynamically interesting time. At the beginning of our third year in training (July 2022), almost all of the outpatients we were treating were still being seen virtually. For much of the year, they remained that way. However, with the reinstatement of the Ryan Haight Act in May 2023, I began to meet patients in person for the first time—the same patients whom I had known only virtually for the first 10 months of our therapeutic relationship. I observed vast changes in the dynamic of the room; many of these patients opened up more in their first in-person session than they had all year over Zoom.
Once in-person sessions resumed, patients who during virtual visits had assured me for almost a year that their home situation was optimized had a plethora of new things to share about their seemingly straightforward living situations. Relationships that appeared stable had more layers to reveal once the half of the relationship I was treating was now comfortably seated within the walls of my office. Problems that had previously seemed biologically based suddenly had complex sociocultural elements that were divulged for the first time. Some patients felt freer to be unrestricted in their affect, in contrast to the logistical (and metaphorical) buttoned-up virtual environment. Emotions ranged from cathartic (“It’s so great to see you in person!”) to bemused (“You’re taller/shorter, older/younger than I thought!”). The screen was gone, and the tangibility of it all breathed a different air into the room.
Virtual vs in-person: Crabs on a beach
The virtual treatment space could be envisioned as crabs in shells scattered on a beach, in which 2 crabs situated in their own shells, not necessarily adjacent to each other, could communicate. This certainly had benefits, such as the convenience of not having to move to another shell, as well as the brief but telling opportunity to gaze into their home shell environment. However, sometimes there would be disadvantages, such as interference with the connection due to static in the sand; at other times, there was the potential for other crabs to overhear and inadvertently learn of each other’s presence, thus affecting the openness of the communication. In this analogy, perhaps the equivalent of an in-person meeting would be 1 crab meandering over and the 2 crabs cohabiting a conch for the first time—it’s spacious (enough), all-enveloping, and within the harkened privacy of a shared sacred space.
A unique training experience
My co-residents and I are uniquely positioned to observe this novel phenomenon due to the timing of having entered our outpatient psychiatry training during the COVID-19 pandemic. Previous generations of residents—as well as practicing psychiatrists who had initially met their patients in person and were forced to switch to virtual sessions during the pandemic—had certain perspectives and challenges of their own, but they had a known dynamic of in-person interactions at baseline. Accordingly, residents who practiced peak- and mid-pandemic and graduated without being required to treat patients face-to-face (the classes of 2022 and 2023) might have spent entire therapeutic relationships having never met their patients in person. My class (2024) was situated in this time- and situation-bound frame in which we started virtually, and by requirements of the law, later met our patients in person. Being not only an observer but an active participant in a treatment dyad within the context of this phenomenon taught me astutely about transference, countertransference, and the holding environment. Training in psychodynamic psychotherapy has taught me about the act of listening deeply and qualities of therapeutic communication. Having the opportunity to enact these principles in such a dichotomy of treatment settings has been invaluable in my education, in getting to know different facets of my patients, and in understanding the nuances of the human experience.
A new doctor in a COVID mask
As a 2020 graduate, my medical school experience was largely untouched by the coronavirus. However, when I transitioned to residency, the world was 4 months into the COVID-19 pandemic, and I was required to wear an N95 mask. Just as I started calling myself Dr. Petteruti, I stopped seeing my patients’ entire face, and they stopped seeing mine. In this article, I share my reflections on wearing a mask during residency.
Even after 3 years of daily practice, I have found that wearing a mask brings an acute awareness of my face. As a community physician, the spheres of personal and public life intersect as I treat patients. Learning to navigate this is an important and shared experience across many community-based residency programs. However, during the first few years of residency, I have been able to shop at a local grocery store or eat at a nearby restaurant without any concerns of being recognized by a patient. Until recently, my patients had never seen my face. That has now changed.
For a new intern, a mask can be a savior. It can hide most of what is on your face from your patient. It is remarkable how the brain fills in the gaps of the visage and, by extension, aspects of the person. Many times, I was thankful to have my morning yawn or facial expression covered during provoking conversations with patients. Furthermore, masks gave me an opportunity to examine my own reactions, emotions, affect, and countertransference of each interaction on my own time.
The mask mandate also protected some features that illustrated my youth. For the patient, a mask can add a dry, clinical distance to the physician, often emitting a professional interpretation to the encounter. For the physician, the mask serves as a concrete barrier to the otherwise effortless acts of observation. Early in my career, I had to set reminders to have patients who were taking antipsychotic medications remove their masks to assess for tardive dyskinesia. Sometimes this surprised the patient, who was hesitant to expose themselves physically and psychologically. Alternatively, mask wearing has proved to be an additional data point on some patients, such as those with disorganized behavior. If the mask is located on the patient’s head, chin, or eyes, or is otherwise inappropriately placed, this provides the clinician with supplemental information.
After spending most of my third year of residency in an outpatient office diligently learning how to build a sturdy therapeutic patient alliance, the mask mandate was lifted. Patients’ transference began to change right before my newly bared face. People often relate age to wisdom and experience, so my lack of age—and thus, possible perceived lack of knowledge—became glaringly apparent. During our initial encounters without masks, patients I had known for most of the year began discussing their symptoms and treatments with more hesitancy. My established patients suddenly had a noticeable change in the intensity of their eye contact. Some even asked if I had cut my hair or what had changed about my appearance since our previous visit. This change in affect and behavior offers a unique experience for the resident; renovating the patient-doctor relationship based on the physician’s appearance.
As psychiatrists, we would generally assume mask wearing has an undesirable effect on the therapeutic alliance and increases skewed inferences in our evaluations. This held true for my experience in residency. In psychotherapy, we work to help patients remove their own metaphorical “masks” of defense and security in self-exploration. However, as young physicians, rather than creating barriers between us and our patients, the mask mandate seemed to have created a sense of credibility in our practice and trustworthiness in our decisions.
Some questions remain. As clinicians, what are we missing when we can only see our patient’s eyes and forehead? How will the COVID-19 pandemic affect my training and career as a psychiatrist? These may remain unanswered for my generation of trainees for some time, as society will look back and contemplate this period for decades. Though we entered our career in uncertain times, with an increased risk of morbidity and death and high demand for proper personal protective equipment, we were and still are thankful for our masks and for the limited infection exposure afforded by the nature of our specialty.
As a 2020 graduate, my medical school experience was largely untouched by the coronavirus. However, when I transitioned to residency, the world was 4 months into the COVID-19 pandemic, and I was required to wear an N95 mask. Just as I started calling myself Dr. Petteruti, I stopped seeing my patients’ entire face, and they stopped seeing mine. In this article, I share my reflections on wearing a mask during residency.
Even after 3 years of daily practice, I have found that wearing a mask brings an acute awareness of my face. As a community physician, the spheres of personal and public life intersect as I treat patients. Learning to navigate this is an important and shared experience across many community-based residency programs. However, during the first few years of residency, I have been able to shop at a local grocery store or eat at a nearby restaurant without any concerns of being recognized by a patient. Until recently, my patients had never seen my face. That has now changed.
For a new intern, a mask can be a savior. It can hide most of what is on your face from your patient. It is remarkable how the brain fills in the gaps of the visage and, by extension, aspects of the person. Many times, I was thankful to have my morning yawn or facial expression covered during provoking conversations with patients. Furthermore, masks gave me an opportunity to examine my own reactions, emotions, affect, and countertransference of each interaction on my own time.
The mask mandate also protected some features that illustrated my youth. For the patient, a mask can add a dry, clinical distance to the physician, often emitting a professional interpretation to the encounter. For the physician, the mask serves as a concrete barrier to the otherwise effortless acts of observation. Early in my career, I had to set reminders to have patients who were taking antipsychotic medications remove their masks to assess for tardive dyskinesia. Sometimes this surprised the patient, who was hesitant to expose themselves physically and psychologically. Alternatively, mask wearing has proved to be an additional data point on some patients, such as those with disorganized behavior. If the mask is located on the patient’s head, chin, or eyes, or is otherwise inappropriately placed, this provides the clinician with supplemental information.
After spending most of my third year of residency in an outpatient office diligently learning how to build a sturdy therapeutic patient alliance, the mask mandate was lifted. Patients’ transference began to change right before my newly bared face. People often relate age to wisdom and experience, so my lack of age—and thus, possible perceived lack of knowledge—became glaringly apparent. During our initial encounters without masks, patients I had known for most of the year began discussing their symptoms and treatments with more hesitancy. My established patients suddenly had a noticeable change in the intensity of their eye contact. Some even asked if I had cut my hair or what had changed about my appearance since our previous visit. This change in affect and behavior offers a unique experience for the resident; renovating the patient-doctor relationship based on the physician’s appearance.
As psychiatrists, we would generally assume mask wearing has an undesirable effect on the therapeutic alliance and increases skewed inferences in our evaluations. This held true for my experience in residency. In psychotherapy, we work to help patients remove their own metaphorical “masks” of defense and security in self-exploration. However, as young physicians, rather than creating barriers between us and our patients, the mask mandate seemed to have created a sense of credibility in our practice and trustworthiness in our decisions.
Some questions remain. As clinicians, what are we missing when we can only see our patient’s eyes and forehead? How will the COVID-19 pandemic affect my training and career as a psychiatrist? These may remain unanswered for my generation of trainees for some time, as society will look back and contemplate this period for decades. Though we entered our career in uncertain times, with an increased risk of morbidity and death and high demand for proper personal protective equipment, we were and still are thankful for our masks and for the limited infection exposure afforded by the nature of our specialty.
As a 2020 graduate, my medical school experience was largely untouched by the coronavirus. However, when I transitioned to residency, the world was 4 months into the COVID-19 pandemic, and I was required to wear an N95 mask. Just as I started calling myself Dr. Petteruti, I stopped seeing my patients’ entire face, and they stopped seeing mine. In this article, I share my reflections on wearing a mask during residency.
Even after 3 years of daily practice, I have found that wearing a mask brings an acute awareness of my face. As a community physician, the spheres of personal and public life intersect as I treat patients. Learning to navigate this is an important and shared experience across many community-based residency programs. However, during the first few years of residency, I have been able to shop at a local grocery store or eat at a nearby restaurant without any concerns of being recognized by a patient. Until recently, my patients had never seen my face. That has now changed.
For a new intern, a mask can be a savior. It can hide most of what is on your face from your patient. It is remarkable how the brain fills in the gaps of the visage and, by extension, aspects of the person. Many times, I was thankful to have my morning yawn or facial expression covered during provoking conversations with patients. Furthermore, masks gave me an opportunity to examine my own reactions, emotions, affect, and countertransference of each interaction on my own time.
The mask mandate also protected some features that illustrated my youth. For the patient, a mask can add a dry, clinical distance to the physician, often emitting a professional interpretation to the encounter. For the physician, the mask serves as a concrete barrier to the otherwise effortless acts of observation. Early in my career, I had to set reminders to have patients who were taking antipsychotic medications remove their masks to assess for tardive dyskinesia. Sometimes this surprised the patient, who was hesitant to expose themselves physically and psychologically. Alternatively, mask wearing has proved to be an additional data point on some patients, such as those with disorganized behavior. If the mask is located on the patient’s head, chin, or eyes, or is otherwise inappropriately placed, this provides the clinician with supplemental information.
After spending most of my third year of residency in an outpatient office diligently learning how to build a sturdy therapeutic patient alliance, the mask mandate was lifted. Patients’ transference began to change right before my newly bared face. People often relate age to wisdom and experience, so my lack of age—and thus, possible perceived lack of knowledge—became glaringly apparent. During our initial encounters without masks, patients I had known for most of the year began discussing their symptoms and treatments with more hesitancy. My established patients suddenly had a noticeable change in the intensity of their eye contact. Some even asked if I had cut my hair or what had changed about my appearance since our previous visit. This change in affect and behavior offers a unique experience for the resident; renovating the patient-doctor relationship based on the physician’s appearance.
As psychiatrists, we would generally assume mask wearing has an undesirable effect on the therapeutic alliance and increases skewed inferences in our evaluations. This held true for my experience in residency. In psychotherapy, we work to help patients remove their own metaphorical “masks” of defense and security in self-exploration. However, as young physicians, rather than creating barriers between us and our patients, the mask mandate seemed to have created a sense of credibility in our practice and trustworthiness in our decisions.
Some questions remain. As clinicians, what are we missing when we can only see our patient’s eyes and forehead? How will the COVID-19 pandemic affect my training and career as a psychiatrist? These may remain unanswered for my generation of trainees for some time, as society will look back and contemplate this period for decades. Though we entered our career in uncertain times, with an increased risk of morbidity and death and high demand for proper personal protective equipment, we were and still are thankful for our masks and for the limited infection exposure afforded by the nature of our specialty.
Rheumatology Match Day results for 2024 follow trends of past years
While adult rheumatology programs continue to have high match rates, pediatric rheumatology programs remain less popular.
The National Residency Matching Program (NRMP) reported on Nov. 29 that rheumatology filled 124 of 127 programs (97.6%), with 273 (98.9%) of 276 positions filled. Comparatively, pediatric rheumatology filled 21 out of 38 programs (55%) and 32 (61.5%) of 52 positions.
This year, the number of programs and positions across all specialties rose by 3%, whereas the number of applications only rose by 0.4% (35 additional applicants).
“The growth of fellowship programs and positions in the Match reflect training opportunities and the future workforce trends of medical subspecialties,” said NRMP President Donna Lamb, DHSc, MBA, BSN, in a statement. “While the increase in applicant numbers did not keep pace with the increase in positions this year, the Match rate for applicants remains strong at 82%.”
In adult rheumatology, matched applicants included 117 MD graduates, 86 foreign applicants, 38 DO graduates, and 32 U.S. citizen international medical graduates. A total of 348 applicants preferred the specialty, and 78% matched to rheumatology, whereas 2% matched to a different specialty. Another 70 applicants (20%) did not match to any program.
In pediatric rheumatology, matched applicants included 23 MD graduates, 6 DO graduates, and 3 foreign applicants. All applicants who preferred pediatric rheumatology matched to a program.
Adult rheumatology was one of several specialties that filled over 95% of positions. The other specialties that matched at that rate were allergy and immunology, cardiovascular disease, clinical cardiac electrophysiology, critical care medicine, gastroenterology, hematology and oncology, and pulmonary/critical care. Interventional Pulmonology and Oncology was the only specialty to achieve a 100% fill rate.
A version of this article first appeared on Medscape.com.
While adult rheumatology programs continue to have high match rates, pediatric rheumatology programs remain less popular.
The National Residency Matching Program (NRMP) reported on Nov. 29 that rheumatology filled 124 of 127 programs (97.6%), with 273 (98.9%) of 276 positions filled. Comparatively, pediatric rheumatology filled 21 out of 38 programs (55%) and 32 (61.5%) of 52 positions.
This year, the number of programs and positions across all specialties rose by 3%, whereas the number of applications only rose by 0.4% (35 additional applicants).
“The growth of fellowship programs and positions in the Match reflect training opportunities and the future workforce trends of medical subspecialties,” said NRMP President Donna Lamb, DHSc, MBA, BSN, in a statement. “While the increase in applicant numbers did not keep pace with the increase in positions this year, the Match rate for applicants remains strong at 82%.”
In adult rheumatology, matched applicants included 117 MD graduates, 86 foreign applicants, 38 DO graduates, and 32 U.S. citizen international medical graduates. A total of 348 applicants preferred the specialty, and 78% matched to rheumatology, whereas 2% matched to a different specialty. Another 70 applicants (20%) did not match to any program.
In pediatric rheumatology, matched applicants included 23 MD graduates, 6 DO graduates, and 3 foreign applicants. All applicants who preferred pediatric rheumatology matched to a program.
Adult rheumatology was one of several specialties that filled over 95% of positions. The other specialties that matched at that rate were allergy and immunology, cardiovascular disease, clinical cardiac electrophysiology, critical care medicine, gastroenterology, hematology and oncology, and pulmonary/critical care. Interventional Pulmonology and Oncology was the only specialty to achieve a 100% fill rate.
A version of this article first appeared on Medscape.com.
While adult rheumatology programs continue to have high match rates, pediatric rheumatology programs remain less popular.
The National Residency Matching Program (NRMP) reported on Nov. 29 that rheumatology filled 124 of 127 programs (97.6%), with 273 (98.9%) of 276 positions filled. Comparatively, pediatric rheumatology filled 21 out of 38 programs (55%) and 32 (61.5%) of 52 positions.
This year, the number of programs and positions across all specialties rose by 3%, whereas the number of applications only rose by 0.4% (35 additional applicants).
“The growth of fellowship programs and positions in the Match reflect training opportunities and the future workforce trends of medical subspecialties,” said NRMP President Donna Lamb, DHSc, MBA, BSN, in a statement. “While the increase in applicant numbers did not keep pace with the increase in positions this year, the Match rate for applicants remains strong at 82%.”
In adult rheumatology, matched applicants included 117 MD graduates, 86 foreign applicants, 38 DO graduates, and 32 U.S. citizen international medical graduates. A total of 348 applicants preferred the specialty, and 78% matched to rheumatology, whereas 2% matched to a different specialty. Another 70 applicants (20%) did not match to any program.
In pediatric rheumatology, matched applicants included 23 MD graduates, 6 DO graduates, and 3 foreign applicants. All applicants who preferred pediatric rheumatology matched to a program.
Adult rheumatology was one of several specialties that filled over 95% of positions. The other specialties that matched at that rate were allergy and immunology, cardiovascular disease, clinical cardiac electrophysiology, critical care medicine, gastroenterology, hematology and oncology, and pulmonary/critical care. Interventional Pulmonology and Oncology was the only specialty to achieve a 100% fill rate.
A version of this article first appeared on Medscape.com.
Supervising residents in an outpatient setting: 6 tips for success
The Accreditation Council for Graduate Medical Education (ACGME) requires supervision of residents “provides safe and effective care to patients; ensures each resident’s development of the skills, knowledge, and attitudes required to enter the unsupervised practice of medicine; and establishes a foundation for continued professional growth.”1 Beyond delineating supervision types (direct, indirect, or oversight), best practices for outpatient supervision are lacking, which perhaps contributes to challenges and discrepancies in experiences involving both trainees and supervisors.2 In this article, I provide 6 practical recommendations for supervisors to address and overcome these challenges.
1. Don’t skip orientation
Resist the pressure to jump directly into clinical care. Devote the first supervision session to learner orientation about expectations (eg, documentation and between-visit patient outreach), logistics (eg, electronic health record or absences), clinic workflow and processes (eg, no-shows or referrals), and team members. Provide this verbally and in writing; the former fosters additional discussion and prompts questions, while the latter serves as a useful reference.
2. Plan for the end at the beginning
Plan ahead for end-of-rotation issues (eg, transfers of care or clinician sign-out), particularly because handoffs are known patient safety risks.3 Provide a written sign-out template or example, set a deadline for the first draft, and ensure known verbal sign-out occurs to both you and any trainees coming into the rotation.
3. Facilitate self-identification of strengths, weaknesses, and goals
Individual learning plans (ILPs) are a fundamental component of adult learning theory, allowing for self-directed learning and ongoing assessment by trainee and supervisor. Complete the ILP together at the beginning of the rotation and regularly devote time to revisit and revise it. This process ensures targeted feedback, which will reduce the stress and potential surprises often associated with end-of-rotation evaluations.
4. Consider the homework you assign
Be intentional about assigned readings. Consider their frequency and length, highlight where you want learners to focus, provide self-reflection questions/prompts, and take time to discuss during supervision. If you use a structured curriculum, maintain flexibility so your trainees’ interests, topics arising in real-time clinical care, and relevant in-press articles can be included.
5. Use direct observation
Whenever possible, directly observe clinical care, particularly a patient’s intake. To reduce trainee (and patient) anxiety and preserve independence, state, “I’m the attending physician supervising Dr. (NAME), who will be your doctor. We provide feedback to trainees right up to graduation so I’m here to observe and will be quiet in the background.” While direct observation is associated with early learners and inpatient settings, it is also preferred by senior outpatient psychiatry residents4 and associated with positive educational and patient outcomes.5
6. Offer supplemental experiences
If feasible, offer additional interdisciplinary supervision (eg, social workers, psychologists, or peer support), scholarly opportunities (eg, case report collaboration or clinic talk), psychotherapy cases, or meeting with patients on your caseload (eg, patients with a rare diagnosis or unique presentation). These align with ACGME’s broad supervision requirements and offer much-appreciated individualized learning tailored to the trainee.
1. Accreditation Council for Graduate Medical Education. Common Program Requirements (Residency). Updated July 1, 2022. Accessed September 6, 2023. https://www.acgme.org/globalassets/pfassets/programrequirements/cprresidency_2022v3.pdf
2. Newman M, Ravindranath D, Figueroa S, et al. Perceptions of supervision in an outpatient psychiatry clinic. Acad Psychiatry. 2016;40(1):153-156. doi:10.1007/s40596-014-0191-y
3. The Joint Commission. Inadequate hand-off communication. Sentinel Event Alert. Issue 58. September 12, 2017. Accessed September 11, 2023. https://www.jointcommission.org/-/media/tjc/documents/resources/patient-safety-topics/sentinel-event/sea_58_hand_off_comms_9_6_17_final_(1).pdf
4. Tan LL, Kam CJW. How psychiatry residents perceive clinical teaching effectiveness with or without direct supervision. The Asia-Pacific Scholar. 2020;5(2):14-21.
5. Galanter CA, Nikolov R, Green N, et al. Direct supervision in outpatient psychiatric graduate medical education. Acad Psychiatry. 2016;40(1):157-163. doi:10.1007/s40596-014-0247-z
The Accreditation Council for Graduate Medical Education (ACGME) requires supervision of residents “provides safe and effective care to patients; ensures each resident’s development of the skills, knowledge, and attitudes required to enter the unsupervised practice of medicine; and establishes a foundation for continued professional growth.”1 Beyond delineating supervision types (direct, indirect, or oversight), best practices for outpatient supervision are lacking, which perhaps contributes to challenges and discrepancies in experiences involving both trainees and supervisors.2 In this article, I provide 6 practical recommendations for supervisors to address and overcome these challenges.
1. Don’t skip orientation
Resist the pressure to jump directly into clinical care. Devote the first supervision session to learner orientation about expectations (eg, documentation and between-visit patient outreach), logistics (eg, electronic health record or absences), clinic workflow and processes (eg, no-shows or referrals), and team members. Provide this verbally and in writing; the former fosters additional discussion and prompts questions, while the latter serves as a useful reference.
2. Plan for the end at the beginning
Plan ahead for end-of-rotation issues (eg, transfers of care or clinician sign-out), particularly because handoffs are known patient safety risks.3 Provide a written sign-out template or example, set a deadline for the first draft, and ensure known verbal sign-out occurs to both you and any trainees coming into the rotation.
3. Facilitate self-identification of strengths, weaknesses, and goals
Individual learning plans (ILPs) are a fundamental component of adult learning theory, allowing for self-directed learning and ongoing assessment by trainee and supervisor. Complete the ILP together at the beginning of the rotation and regularly devote time to revisit and revise it. This process ensures targeted feedback, which will reduce the stress and potential surprises often associated with end-of-rotation evaluations.
4. Consider the homework you assign
Be intentional about assigned readings. Consider their frequency and length, highlight where you want learners to focus, provide self-reflection questions/prompts, and take time to discuss during supervision. If you use a structured curriculum, maintain flexibility so your trainees’ interests, topics arising in real-time clinical care, and relevant in-press articles can be included.
5. Use direct observation
Whenever possible, directly observe clinical care, particularly a patient’s intake. To reduce trainee (and patient) anxiety and preserve independence, state, “I’m the attending physician supervising Dr. (NAME), who will be your doctor. We provide feedback to trainees right up to graduation so I’m here to observe and will be quiet in the background.” While direct observation is associated with early learners and inpatient settings, it is also preferred by senior outpatient psychiatry residents4 and associated with positive educational and patient outcomes.5
6. Offer supplemental experiences
If feasible, offer additional interdisciplinary supervision (eg, social workers, psychologists, or peer support), scholarly opportunities (eg, case report collaboration or clinic talk), psychotherapy cases, or meeting with patients on your caseload (eg, patients with a rare diagnosis or unique presentation). These align with ACGME’s broad supervision requirements and offer much-appreciated individualized learning tailored to the trainee.
The Accreditation Council for Graduate Medical Education (ACGME) requires supervision of residents “provides safe and effective care to patients; ensures each resident’s development of the skills, knowledge, and attitudes required to enter the unsupervised practice of medicine; and establishes a foundation for continued professional growth.”1 Beyond delineating supervision types (direct, indirect, or oversight), best practices for outpatient supervision are lacking, which perhaps contributes to challenges and discrepancies in experiences involving both trainees and supervisors.2 In this article, I provide 6 practical recommendations for supervisors to address and overcome these challenges.
1. Don’t skip orientation
Resist the pressure to jump directly into clinical care. Devote the first supervision session to learner orientation about expectations (eg, documentation and between-visit patient outreach), logistics (eg, electronic health record or absences), clinic workflow and processes (eg, no-shows or referrals), and team members. Provide this verbally and in writing; the former fosters additional discussion and prompts questions, while the latter serves as a useful reference.
2. Plan for the end at the beginning
Plan ahead for end-of-rotation issues (eg, transfers of care or clinician sign-out), particularly because handoffs are known patient safety risks.3 Provide a written sign-out template or example, set a deadline for the first draft, and ensure known verbal sign-out occurs to both you and any trainees coming into the rotation.
3. Facilitate self-identification of strengths, weaknesses, and goals
Individual learning plans (ILPs) are a fundamental component of adult learning theory, allowing for self-directed learning and ongoing assessment by trainee and supervisor. Complete the ILP together at the beginning of the rotation and regularly devote time to revisit and revise it. This process ensures targeted feedback, which will reduce the stress and potential surprises often associated with end-of-rotation evaluations.
4. Consider the homework you assign
Be intentional about assigned readings. Consider their frequency and length, highlight where you want learners to focus, provide self-reflection questions/prompts, and take time to discuss during supervision. If you use a structured curriculum, maintain flexibility so your trainees’ interests, topics arising in real-time clinical care, and relevant in-press articles can be included.
5. Use direct observation
Whenever possible, directly observe clinical care, particularly a patient’s intake. To reduce trainee (and patient) anxiety and preserve independence, state, “I’m the attending physician supervising Dr. (NAME), who will be your doctor. We provide feedback to trainees right up to graduation so I’m here to observe and will be quiet in the background.” While direct observation is associated with early learners and inpatient settings, it is also preferred by senior outpatient psychiatry residents4 and associated with positive educational and patient outcomes.5
6. Offer supplemental experiences
If feasible, offer additional interdisciplinary supervision (eg, social workers, psychologists, or peer support), scholarly opportunities (eg, case report collaboration or clinic talk), psychotherapy cases, or meeting with patients on your caseload (eg, patients with a rare diagnosis or unique presentation). These align with ACGME’s broad supervision requirements and offer much-appreciated individualized learning tailored to the trainee.
1. Accreditation Council for Graduate Medical Education. Common Program Requirements (Residency). Updated July 1, 2022. Accessed September 6, 2023. https://www.acgme.org/globalassets/pfassets/programrequirements/cprresidency_2022v3.pdf
2. Newman M, Ravindranath D, Figueroa S, et al. Perceptions of supervision in an outpatient psychiatry clinic. Acad Psychiatry. 2016;40(1):153-156. doi:10.1007/s40596-014-0191-y
3. The Joint Commission. Inadequate hand-off communication. Sentinel Event Alert. Issue 58. September 12, 2017. Accessed September 11, 2023. https://www.jointcommission.org/-/media/tjc/documents/resources/patient-safety-topics/sentinel-event/sea_58_hand_off_comms_9_6_17_final_(1).pdf
4. Tan LL, Kam CJW. How psychiatry residents perceive clinical teaching effectiveness with or without direct supervision. The Asia-Pacific Scholar. 2020;5(2):14-21.
5. Galanter CA, Nikolov R, Green N, et al. Direct supervision in outpatient psychiatric graduate medical education. Acad Psychiatry. 2016;40(1):157-163. doi:10.1007/s40596-014-0247-z
1. Accreditation Council for Graduate Medical Education. Common Program Requirements (Residency). Updated July 1, 2022. Accessed September 6, 2023. https://www.acgme.org/globalassets/pfassets/programrequirements/cprresidency_2022v3.pdf
2. Newman M, Ravindranath D, Figueroa S, et al. Perceptions of supervision in an outpatient psychiatry clinic. Acad Psychiatry. 2016;40(1):153-156. doi:10.1007/s40596-014-0191-y
3. The Joint Commission. Inadequate hand-off communication. Sentinel Event Alert. Issue 58. September 12, 2017. Accessed September 11, 2023. https://www.jointcommission.org/-/media/tjc/documents/resources/patient-safety-topics/sentinel-event/sea_58_hand_off_comms_9_6_17_final_(1).pdf
4. Tan LL, Kam CJW. How psychiatry residents perceive clinical teaching effectiveness with or without direct supervision. The Asia-Pacific Scholar. 2020;5(2):14-21.
5. Galanter CA, Nikolov R, Green N, et al. Direct supervision in outpatient psychiatric graduate medical education. Acad Psychiatry. 2016;40(1):157-163. doi:10.1007/s40596-014-0247-z
Analysis of Internal Dermatology Matches Following the COVID-19 Pandemic
Dermatology residencies continue to be among the most competitive, with only 66% of seniors in US medical schools (MD programs) successfully matching to a dermatology residency in 2023, according to the National Resident Matching Program. In 2023, there were 141 dermatology residency programs accepting applications, with a total of 499 positions offered. Of 578 medical school senior applicants, 384 of those applicants successfully matched. In contrast, of the 79 senior applicants from osteopathic medical schools, only 34 successfully matched, according to the National Resident Matching Program. A higher number of students match to either their home institution or an institution at which they completed an away (external) rotation, likely because faculty members are more comfortable matching future residents with whom they have worked because of greater familiarity with these applicants, and because applicants are more comfortable with programs familiar to them.1
Prior to the COVID-19 pandemic, the Association of Professors of Dermatology published an official statement discouraging programs from offering in-person external electives to applicants in the 2020-2021 cycle. As the pandemic progressed, this evolved: for the 2021-2022 cycle, applicants were encouraged to complete only 1 away rotation, and for the 2022-2023 cycle, applicants were encouraged to complete up to 3 away rotations.2 This most recent recommendation reflects applicant experience before the pandemic, with some students having a personal connection to up to 4 programs, including their home and away programs.
A cross-sectional study published in early 2023 analyzed internal matches prior to and until the second year of the pandemic. The prepandemic rate of internal matches—applicants who matched at their home programs—was 26.7%. This rate increased to 40.3% in the 2020-2021 cycle and was 33.5% in the 2021-2022 cycle.2,3 The increase in internal matches is likely multifactorial, including the emergence of virtual interviews, the addition of program and geographic signals, and the regulation of away rotations. Notably, the rate of internal matches inversely correlates with the number of external programs to which students have connections.
We conducted a cross-sectional study to analyze the rates of internal and regional dermatology matches in the post–COVID-19 pandemic era (2022-2023) vs prepandemic and pandemic rates.
Methods
Data were obtained from publicly available online match lists from 65 US medical schools that detailed programs where dermatology applicants matched. The data reflected the postpandemic residency application cycle (2022-2023). These data were then compared to previous match rates for the prepandemic (2020-2021) and pandemic (2021-2022) application cycles. Medical schools without corresponding dermatology residency programs were excluded from the study. Regions were determined using the Association of American Medical Colleges Residency Explorer tool. The Northeast region included schools from Vermont; Pennsylvania; New Hampshire; New Jersey; Rhode Island; Maryland; Massachusetts; New York; Connecticut; and Washington, DC. The Southern region included schools from Florida, Georgia, Kentucky, Louisiana, Arkansas, North Carolina, Alabama, South Carolina, Mississippi, Tennessee, Texas, Oklahoma, and Virginia. The Western region included schools from Oregon, New Mexico, Utah, Colorado, Arizona, Washington, and California. The Central region included schools from Illinois, Indiana, Michigan, Ohio, Wisconsin, Iowa, Kansas, Minnesota, Missouri, and Nebraska. The data collected included the number of applicants who matched into dermatology, the number of applicants who matched at their home institutions, and the regions in which applicants matched. Rates of matching were calculated as percentages, and Pearson χ2 tests were used to compare internal and regional match rates between different time periods.
Results
Results for the 2022-2023 residency cycle are summarized in the Table. Of 210 matches, 80 (38.10%) of the applicants matched at their home institution. In prepandemic cycles, 26.7% of applicants matched at their home institutions, which increased to 38.1% after the pandemic (P=.028). During the pandemic, 40.3% of applicants matched at their home institutions (P=.827).2 One hundred forty-nine of 210 (70.95%) applicants matched in the same region as their home institutions. The Western region had the highest rate of both internal matches (47.06%) and same-region matches (76.47%). However, the Central and Northeast regions were a close second (43.55% for home matches and 75.81% for same-region matches) and third (42.31% for home matches and 75.00% for same-region matches) for both rates, respectively. The Southern region had the lowest rates overall, with 29.11% for home matches and 63.29% for same-region matches.
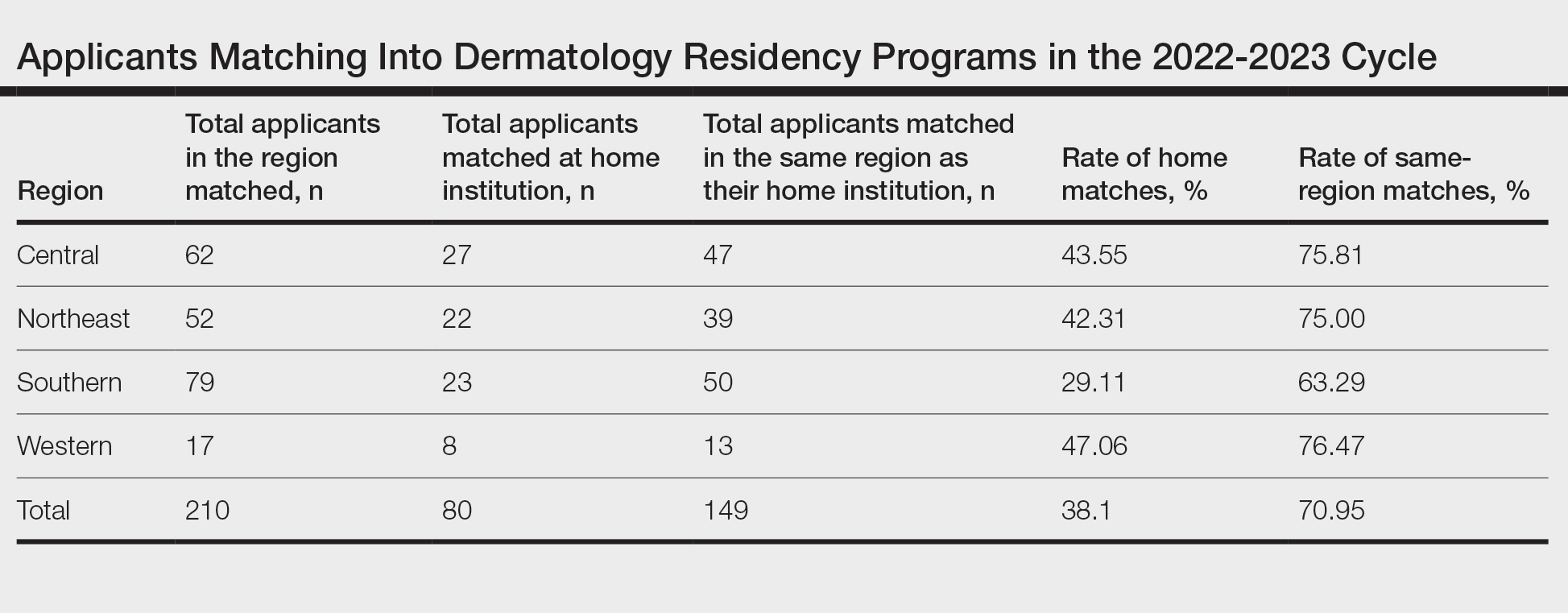
Comment
The changes to the match process resulting from the COVID-19 pandemic have had a profound impact on match outcomes since 2020. During the first year of the pandemic, internal matches increased to 40%; during the second year, the rate decreased to 33%.2 The difference between the current postpandemic internal match rate of 38.1% and the prepandemic internal match rate of 26.7% was statistically significant (P=.028). Conversely, the difference between the postpandemic internal match rate and the pandemic internal match rate was not significant (P=.827). These findings suggest that that pandemic trends have continued despite the return to multiple away rotations for students, perhaps suggesting that virtual interviews, which have been maintained at most programs despite the end of the pandemic, may be the driving force behind the increased home match rate. During the second year of the pandemic, there were greater odds (odds ratio, 2.3) of a dermatology program matching at least 1 internal applicant vs the years prior to 2020.4
The prepandemic regional match rate was 61.6% and increased to 67.5% during the pandemic.3 Following the pandemic, 70.95% of applicants matched in the same region as their home program. A study completed in 2022 using the Texas Seeking Transparency in Application to Residency database found that there was no difference in the percentage of applicants who had a geographic connection to their program when comparing the 2021 cycle to 2018-2020 cycles.5 Frequently, applicants prefer to stay within their regions due to social factors. Although applicants can again travel for external rotations, the regional match rate has stayed relatively constant before and after the pandemic, though it has trended upward throughout the latest application cycles.
During the 2022-2023 cycle, applicants were able to send preference signals to 3 programs. A survey reflecting the 2021-2022 cycle showed that 21.1% of applicants who sent a preference signal to a program were interviewed by that program, whereas only 3.7% of applicants who did not send a preference signal were interviewed. Furthermore, 19% of matched applicants sent a preference signal to the program at which they ultimately matched.6 Survey respondents included 40 accredited dermatology residency programs who reported an average of 506 applications per program. Preference signals were developed to allow applicants to connect with programs at which they were not able to rotate. It is unclear how preference signals are affecting internal or regional match rates, but similar to virtual interviewing, they may be contributing to the higher rates of internal matching.
This study is limited in the number of programs with match data publicly available for analysis. Additionally, there were no official data on how many students match at programs at which they completed external rotations. Furthermore, these data do not include reapplicants or osteopathic applicants who match within their regions. Importantly, all US medical schools were not represented in these data. Many programs, specifically in the Western region, did not have publicly available match lists. Self-reported match lists were not included in this study to avoid discrepancies. Regional rates reported here may not be representative of actual regional rates, as there were more applicants and internal matches in each region than were included in this study.
Conclusion
Although applicants were able to participate in external rotations as of the last 2 application cycles, there was still an increase in the rate of internal dermatology matches during the 2022-2023 cycle. This trend suggests an underlying disadvantage in matching for students without a home program. For the 2023-2024 cycle, applicants are recommended to complete up to 2 external rotations and may consider up to 3 if they do not have a home program. This recommended limitation in external rotations aims to allow students without a home program to develop connections with more programs.
- Luu Y, Gao W, Han J, et al. Personal connections and preference signaling: a cross-sectional analysis of the dermatology residency match during COVID-19. J Am Acad Dermatol. 2023;88:1381-1383. doi:10.1016/j.jaad.2023.01.032
- Dowdle TS, Ryan MP, Tarbox MB, et al. An analysis of internal and regional dermatology matches during the second year of the COVID-19 pandemic: a cross-sectional study. J Am Acad Dermatol. 2023;88:207-209. doi:10.1016/j.jaad.2022.04.036
- Dowdle TS, Ryan MP, Wagner RF. Internal and geographic dermatology match trends in the age of COVID-19. J Am Acad Dermatol. 2021;85:1364-1366. doi:10.1016/j.jaad.2021.08.004
- Abdelwahab R, Antezana LA, Xie KZ, et al. Cross-sectional study of dermatology residency home match incidence during the COVID-19 pandemic. J Am Acad Dermatol. 2022;87:886-888. doi:10.1016/j.jaad.2021.12.004
- Williams GE, Zimmerman JM, Wiggins CJ, et al. The indelible marks on dermatology: impacts of COVID-19 on dermatology residency Match using the Texas STAR database. Clin Dermatol. 2023;41:215-218. doi:10.1016/j.clindermatol.2022.12.001
- Dirr MA, Brownstone N, Zakria D, et al. Dermatology match preference signaling tokens: impact and implications. Dermatol Surg. 2022;48:1367-1368. doi:10.1097/DSS.0000000000003645
Dermatology residencies continue to be among the most competitive, with only 66% of seniors in US medical schools (MD programs) successfully matching to a dermatology residency in 2023, according to the National Resident Matching Program. In 2023, there were 141 dermatology residency programs accepting applications, with a total of 499 positions offered. Of 578 medical school senior applicants, 384 of those applicants successfully matched. In contrast, of the 79 senior applicants from osteopathic medical schools, only 34 successfully matched, according to the National Resident Matching Program. A higher number of students match to either their home institution or an institution at which they completed an away (external) rotation, likely because faculty members are more comfortable matching future residents with whom they have worked because of greater familiarity with these applicants, and because applicants are more comfortable with programs familiar to them.1
Prior to the COVID-19 pandemic, the Association of Professors of Dermatology published an official statement discouraging programs from offering in-person external electives to applicants in the 2020-2021 cycle. As the pandemic progressed, this evolved: for the 2021-2022 cycle, applicants were encouraged to complete only 1 away rotation, and for the 2022-2023 cycle, applicants were encouraged to complete up to 3 away rotations.2 This most recent recommendation reflects applicant experience before the pandemic, with some students having a personal connection to up to 4 programs, including their home and away programs.
A cross-sectional study published in early 2023 analyzed internal matches prior to and until the second year of the pandemic. The prepandemic rate of internal matches—applicants who matched at their home programs—was 26.7%. This rate increased to 40.3% in the 2020-2021 cycle and was 33.5% in the 2021-2022 cycle.2,3 The increase in internal matches is likely multifactorial, including the emergence of virtual interviews, the addition of program and geographic signals, and the regulation of away rotations. Notably, the rate of internal matches inversely correlates with the number of external programs to which students have connections.
We conducted a cross-sectional study to analyze the rates of internal and regional dermatology matches in the post–COVID-19 pandemic era (2022-2023) vs prepandemic and pandemic rates.
Methods
Data were obtained from publicly available online match lists from 65 US medical schools that detailed programs where dermatology applicants matched. The data reflected the postpandemic residency application cycle (2022-2023). These data were then compared to previous match rates for the prepandemic (2020-2021) and pandemic (2021-2022) application cycles. Medical schools without corresponding dermatology residency programs were excluded from the study. Regions were determined using the Association of American Medical Colleges Residency Explorer tool. The Northeast region included schools from Vermont; Pennsylvania; New Hampshire; New Jersey; Rhode Island; Maryland; Massachusetts; New York; Connecticut; and Washington, DC. The Southern region included schools from Florida, Georgia, Kentucky, Louisiana, Arkansas, North Carolina, Alabama, South Carolina, Mississippi, Tennessee, Texas, Oklahoma, and Virginia. The Western region included schools from Oregon, New Mexico, Utah, Colorado, Arizona, Washington, and California. The Central region included schools from Illinois, Indiana, Michigan, Ohio, Wisconsin, Iowa, Kansas, Minnesota, Missouri, and Nebraska. The data collected included the number of applicants who matched into dermatology, the number of applicants who matched at their home institutions, and the regions in which applicants matched. Rates of matching were calculated as percentages, and Pearson χ2 tests were used to compare internal and regional match rates between different time periods.
Results
Results for the 2022-2023 residency cycle are summarized in the Table. Of 210 matches, 80 (38.10%) of the applicants matched at their home institution. In prepandemic cycles, 26.7% of applicants matched at their home institutions, which increased to 38.1% after the pandemic (P=.028). During the pandemic, 40.3% of applicants matched at their home institutions (P=.827).2 One hundred forty-nine of 210 (70.95%) applicants matched in the same region as their home institutions. The Western region had the highest rate of both internal matches (47.06%) and same-region matches (76.47%). However, the Central and Northeast regions were a close second (43.55% for home matches and 75.81% for same-region matches) and third (42.31% for home matches and 75.00% for same-region matches) for both rates, respectively. The Southern region had the lowest rates overall, with 29.11% for home matches and 63.29% for same-region matches.
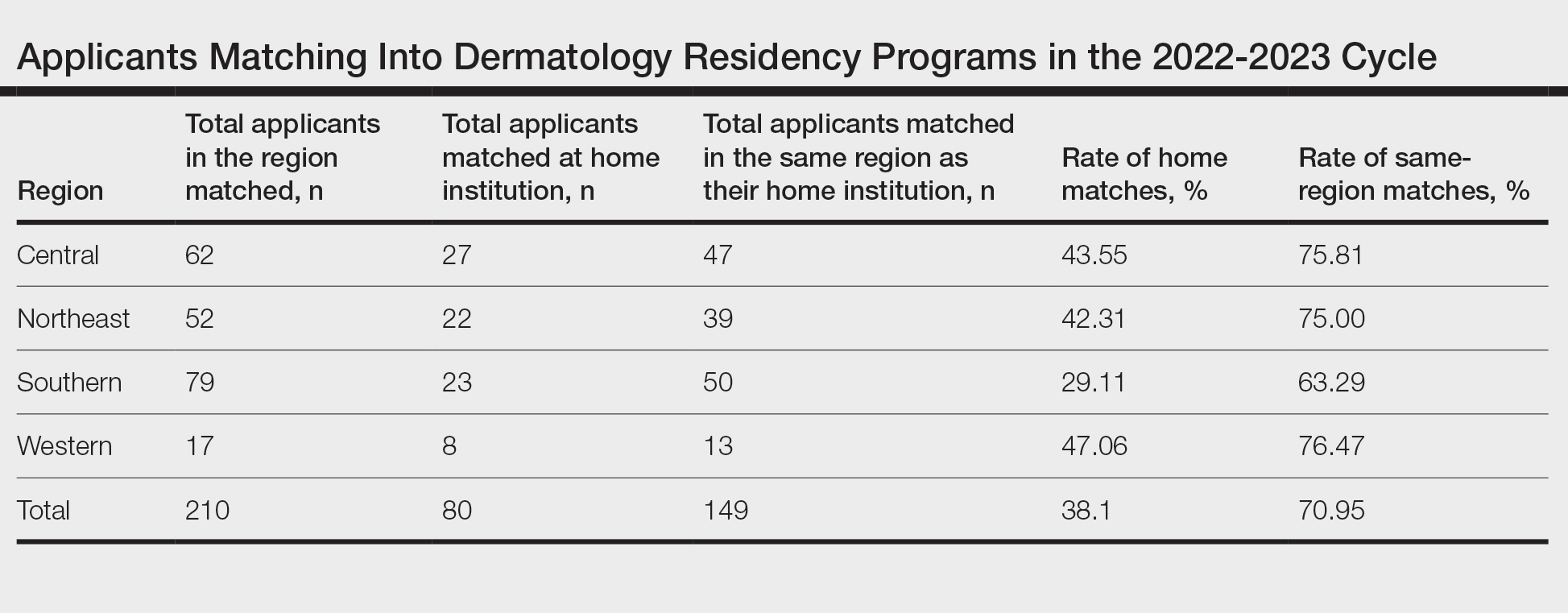
Comment
The changes to the match process resulting from the COVID-19 pandemic have had a profound impact on match outcomes since 2020. During the first year of the pandemic, internal matches increased to 40%; during the second year, the rate decreased to 33%.2 The difference between the current postpandemic internal match rate of 38.1% and the prepandemic internal match rate of 26.7% was statistically significant (P=.028). Conversely, the difference between the postpandemic internal match rate and the pandemic internal match rate was not significant (P=.827). These findings suggest that that pandemic trends have continued despite the return to multiple away rotations for students, perhaps suggesting that virtual interviews, which have been maintained at most programs despite the end of the pandemic, may be the driving force behind the increased home match rate. During the second year of the pandemic, there were greater odds (odds ratio, 2.3) of a dermatology program matching at least 1 internal applicant vs the years prior to 2020.4
The prepandemic regional match rate was 61.6% and increased to 67.5% during the pandemic.3 Following the pandemic, 70.95% of applicants matched in the same region as their home program. A study completed in 2022 using the Texas Seeking Transparency in Application to Residency database found that there was no difference in the percentage of applicants who had a geographic connection to their program when comparing the 2021 cycle to 2018-2020 cycles.5 Frequently, applicants prefer to stay within their regions due to social factors. Although applicants can again travel for external rotations, the regional match rate has stayed relatively constant before and after the pandemic, though it has trended upward throughout the latest application cycles.
During the 2022-2023 cycle, applicants were able to send preference signals to 3 programs. A survey reflecting the 2021-2022 cycle showed that 21.1% of applicants who sent a preference signal to a program were interviewed by that program, whereas only 3.7% of applicants who did not send a preference signal were interviewed. Furthermore, 19% of matched applicants sent a preference signal to the program at which they ultimately matched.6 Survey respondents included 40 accredited dermatology residency programs who reported an average of 506 applications per program. Preference signals were developed to allow applicants to connect with programs at which they were not able to rotate. It is unclear how preference signals are affecting internal or regional match rates, but similar to virtual interviewing, they may be contributing to the higher rates of internal matching.
This study is limited in the number of programs with match data publicly available for analysis. Additionally, there were no official data on how many students match at programs at which they completed external rotations. Furthermore, these data do not include reapplicants or osteopathic applicants who match within their regions. Importantly, all US medical schools were not represented in these data. Many programs, specifically in the Western region, did not have publicly available match lists. Self-reported match lists were not included in this study to avoid discrepancies. Regional rates reported here may not be representative of actual regional rates, as there were more applicants and internal matches in each region than were included in this study.
Conclusion
Although applicants were able to participate in external rotations as of the last 2 application cycles, there was still an increase in the rate of internal dermatology matches during the 2022-2023 cycle. This trend suggests an underlying disadvantage in matching for students without a home program. For the 2023-2024 cycle, applicants are recommended to complete up to 2 external rotations and may consider up to 3 if they do not have a home program. This recommended limitation in external rotations aims to allow students without a home program to develop connections with more programs.
Dermatology residencies continue to be among the most competitive, with only 66% of seniors in US medical schools (MD programs) successfully matching to a dermatology residency in 2023, according to the National Resident Matching Program. In 2023, there were 141 dermatology residency programs accepting applications, with a total of 499 positions offered. Of 578 medical school senior applicants, 384 of those applicants successfully matched. In contrast, of the 79 senior applicants from osteopathic medical schools, only 34 successfully matched, according to the National Resident Matching Program. A higher number of students match to either their home institution or an institution at which they completed an away (external) rotation, likely because faculty members are more comfortable matching future residents with whom they have worked because of greater familiarity with these applicants, and because applicants are more comfortable with programs familiar to them.1
Prior to the COVID-19 pandemic, the Association of Professors of Dermatology published an official statement discouraging programs from offering in-person external electives to applicants in the 2020-2021 cycle. As the pandemic progressed, this evolved: for the 2021-2022 cycle, applicants were encouraged to complete only 1 away rotation, and for the 2022-2023 cycle, applicants were encouraged to complete up to 3 away rotations.2 This most recent recommendation reflects applicant experience before the pandemic, with some students having a personal connection to up to 4 programs, including their home and away programs.
A cross-sectional study published in early 2023 analyzed internal matches prior to and until the second year of the pandemic. The prepandemic rate of internal matches—applicants who matched at their home programs—was 26.7%. This rate increased to 40.3% in the 2020-2021 cycle and was 33.5% in the 2021-2022 cycle.2,3 The increase in internal matches is likely multifactorial, including the emergence of virtual interviews, the addition of program and geographic signals, and the regulation of away rotations. Notably, the rate of internal matches inversely correlates with the number of external programs to which students have connections.
We conducted a cross-sectional study to analyze the rates of internal and regional dermatology matches in the post–COVID-19 pandemic era (2022-2023) vs prepandemic and pandemic rates.
Methods
Data were obtained from publicly available online match lists from 65 US medical schools that detailed programs where dermatology applicants matched. The data reflected the postpandemic residency application cycle (2022-2023). These data were then compared to previous match rates for the prepandemic (2020-2021) and pandemic (2021-2022) application cycles. Medical schools without corresponding dermatology residency programs were excluded from the study. Regions were determined using the Association of American Medical Colleges Residency Explorer tool. The Northeast region included schools from Vermont; Pennsylvania; New Hampshire; New Jersey; Rhode Island; Maryland; Massachusetts; New York; Connecticut; and Washington, DC. The Southern region included schools from Florida, Georgia, Kentucky, Louisiana, Arkansas, North Carolina, Alabama, South Carolina, Mississippi, Tennessee, Texas, Oklahoma, and Virginia. The Western region included schools from Oregon, New Mexico, Utah, Colorado, Arizona, Washington, and California. The Central region included schools from Illinois, Indiana, Michigan, Ohio, Wisconsin, Iowa, Kansas, Minnesota, Missouri, and Nebraska. The data collected included the number of applicants who matched into dermatology, the number of applicants who matched at their home institutions, and the regions in which applicants matched. Rates of matching were calculated as percentages, and Pearson χ2 tests were used to compare internal and regional match rates between different time periods.
Results
Results for the 2022-2023 residency cycle are summarized in the Table. Of 210 matches, 80 (38.10%) of the applicants matched at their home institution. In prepandemic cycles, 26.7% of applicants matched at their home institutions, which increased to 38.1% after the pandemic (P=.028). During the pandemic, 40.3% of applicants matched at their home institutions (P=.827).2 One hundred forty-nine of 210 (70.95%) applicants matched in the same region as their home institutions. The Western region had the highest rate of both internal matches (47.06%) and same-region matches (76.47%). However, the Central and Northeast regions were a close second (43.55% for home matches and 75.81% for same-region matches) and third (42.31% for home matches and 75.00% for same-region matches) for both rates, respectively. The Southern region had the lowest rates overall, with 29.11% for home matches and 63.29% for same-region matches.
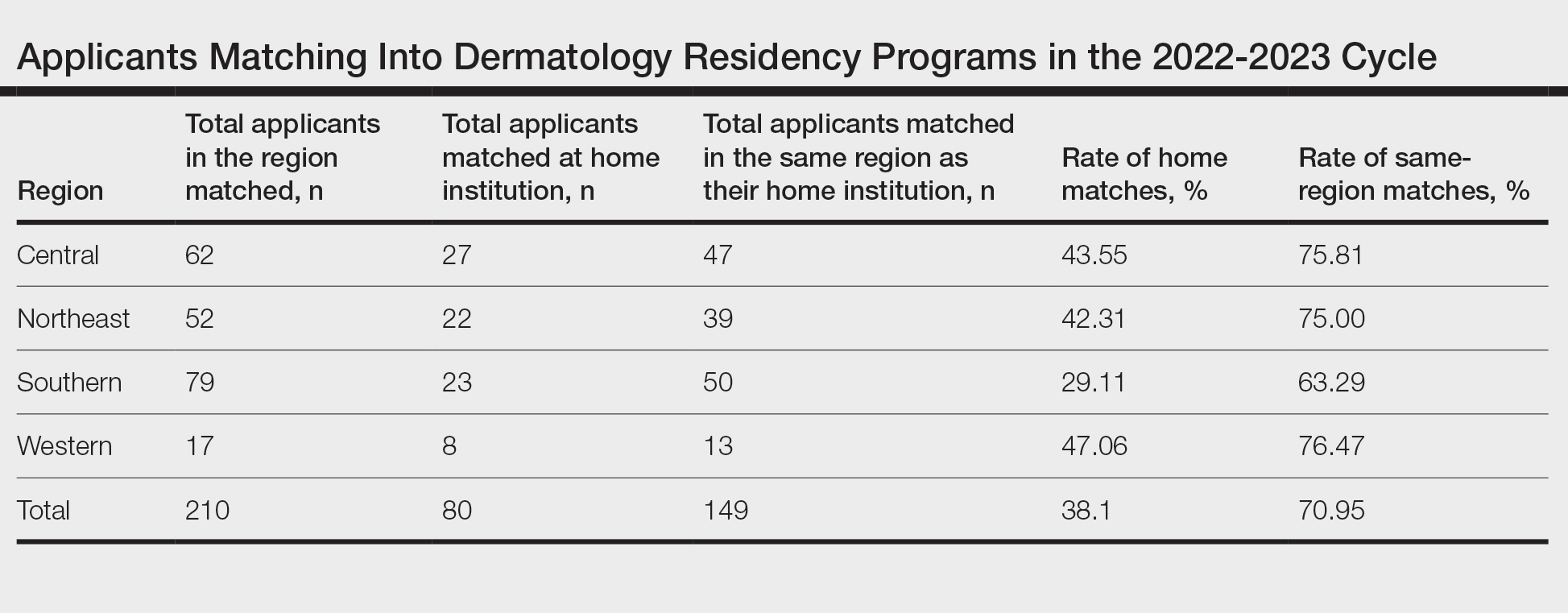
Comment
The changes to the match process resulting from the COVID-19 pandemic have had a profound impact on match outcomes since 2020. During the first year of the pandemic, internal matches increased to 40%; during the second year, the rate decreased to 33%.2 The difference between the current postpandemic internal match rate of 38.1% and the prepandemic internal match rate of 26.7% was statistically significant (P=.028). Conversely, the difference between the postpandemic internal match rate and the pandemic internal match rate was not significant (P=.827). These findings suggest that that pandemic trends have continued despite the return to multiple away rotations for students, perhaps suggesting that virtual interviews, which have been maintained at most programs despite the end of the pandemic, may be the driving force behind the increased home match rate. During the second year of the pandemic, there were greater odds (odds ratio, 2.3) of a dermatology program matching at least 1 internal applicant vs the years prior to 2020.4
The prepandemic regional match rate was 61.6% and increased to 67.5% during the pandemic.3 Following the pandemic, 70.95% of applicants matched in the same region as their home program. A study completed in 2022 using the Texas Seeking Transparency in Application to Residency database found that there was no difference in the percentage of applicants who had a geographic connection to their program when comparing the 2021 cycle to 2018-2020 cycles.5 Frequently, applicants prefer to stay within their regions due to social factors. Although applicants can again travel for external rotations, the regional match rate has stayed relatively constant before and after the pandemic, though it has trended upward throughout the latest application cycles.
During the 2022-2023 cycle, applicants were able to send preference signals to 3 programs. A survey reflecting the 2021-2022 cycle showed that 21.1% of applicants who sent a preference signal to a program were interviewed by that program, whereas only 3.7% of applicants who did not send a preference signal were interviewed. Furthermore, 19% of matched applicants sent a preference signal to the program at which they ultimately matched.6 Survey respondents included 40 accredited dermatology residency programs who reported an average of 506 applications per program. Preference signals were developed to allow applicants to connect with programs at which they were not able to rotate. It is unclear how preference signals are affecting internal or regional match rates, but similar to virtual interviewing, they may be contributing to the higher rates of internal matching.
This study is limited in the number of programs with match data publicly available for analysis. Additionally, there were no official data on how many students match at programs at which they completed external rotations. Furthermore, these data do not include reapplicants or osteopathic applicants who match within their regions. Importantly, all US medical schools were not represented in these data. Many programs, specifically in the Western region, did not have publicly available match lists. Self-reported match lists were not included in this study to avoid discrepancies. Regional rates reported here may not be representative of actual regional rates, as there were more applicants and internal matches in each region than were included in this study.
Conclusion
Although applicants were able to participate in external rotations as of the last 2 application cycles, there was still an increase in the rate of internal dermatology matches during the 2022-2023 cycle. This trend suggests an underlying disadvantage in matching for students without a home program. For the 2023-2024 cycle, applicants are recommended to complete up to 2 external rotations and may consider up to 3 if they do not have a home program. This recommended limitation in external rotations aims to allow students without a home program to develop connections with more programs.
- Luu Y, Gao W, Han J, et al. Personal connections and preference signaling: a cross-sectional analysis of the dermatology residency match during COVID-19. J Am Acad Dermatol. 2023;88:1381-1383. doi:10.1016/j.jaad.2023.01.032
- Dowdle TS, Ryan MP, Tarbox MB, et al. An analysis of internal and regional dermatology matches during the second year of the COVID-19 pandemic: a cross-sectional study. J Am Acad Dermatol. 2023;88:207-209. doi:10.1016/j.jaad.2022.04.036
- Dowdle TS, Ryan MP, Wagner RF. Internal and geographic dermatology match trends in the age of COVID-19. J Am Acad Dermatol. 2021;85:1364-1366. doi:10.1016/j.jaad.2021.08.004
- Abdelwahab R, Antezana LA, Xie KZ, et al. Cross-sectional study of dermatology residency home match incidence during the COVID-19 pandemic. J Am Acad Dermatol. 2022;87:886-888. doi:10.1016/j.jaad.2021.12.004
- Williams GE, Zimmerman JM, Wiggins CJ, et al. The indelible marks on dermatology: impacts of COVID-19 on dermatology residency Match using the Texas STAR database. Clin Dermatol. 2023;41:215-218. doi:10.1016/j.clindermatol.2022.12.001
- Dirr MA, Brownstone N, Zakria D, et al. Dermatology match preference signaling tokens: impact and implications. Dermatol Surg. 2022;48:1367-1368. doi:10.1097/DSS.0000000000003645
- Luu Y, Gao W, Han J, et al. Personal connections and preference signaling: a cross-sectional analysis of the dermatology residency match during COVID-19. J Am Acad Dermatol. 2023;88:1381-1383. doi:10.1016/j.jaad.2023.01.032
- Dowdle TS, Ryan MP, Tarbox MB, et al. An analysis of internal and regional dermatology matches during the second year of the COVID-19 pandemic: a cross-sectional study. J Am Acad Dermatol. 2023;88:207-209. doi:10.1016/j.jaad.2022.04.036
- Dowdle TS, Ryan MP, Wagner RF. Internal and geographic dermatology match trends in the age of COVID-19. J Am Acad Dermatol. 2021;85:1364-1366. doi:10.1016/j.jaad.2021.08.004
- Abdelwahab R, Antezana LA, Xie KZ, et al. Cross-sectional study of dermatology residency home match incidence during the COVID-19 pandemic. J Am Acad Dermatol. 2022;87:886-888. doi:10.1016/j.jaad.2021.12.004
- Williams GE, Zimmerman JM, Wiggins CJ, et al. The indelible marks on dermatology: impacts of COVID-19 on dermatology residency Match using the Texas STAR database. Clin Dermatol. 2023;41:215-218. doi:10.1016/j.clindermatol.2022.12.001
- Dirr MA, Brownstone N, Zakria D, et al. Dermatology match preference signaling tokens: impact and implications. Dermatol Surg. 2022;48:1367-1368. doi:10.1097/DSS.0000000000003645
PRACTICE POINTS
- Following the COVID-19 pandemic, affiliation with a home program is even more impactful in successful application to dermatology residency. Applicants from institutions without dermatology programs should consider completing additional externships.
- The high rate of applicants matching to the same regions as their home programs is due to several factors. Applicants may have a larger social support system near their home institution. Additionally, programs are more comfortable matching applicants within their own regions.
Video-Based Coaching for Dermatology Resident Surgical Education
To the Editor:
Video-based coaching (VBC) involves a surgeon recording a surgery and then reviewing the video with a surgical coach; it is a form of education that is gaining popularity among surgical specialties.1 Video-based education is underutilized in dermatology residency training.2 We conducted a pilot study at our dermatology residency program to evaluate the efficacy and feasibility of VBC.
The University of Texas at Austin Dell Medical School institutional review board approved this study. All 4 first-year dermatology residents were recruited to participate in this study. Participants filled out a prestudy survey assessing their surgical experience, confidence in performing surgery, and attitudes on VBC. Participants used a head-mounted point-of-view camera to record themselves performing a wide local excision on the trunk or extremities of a live human patient. Participants then reviewed the recording on their own and scored themselves using the Objective Structured Assessment of Technical Skills (OSATS) scoring table (scored from 1 to 5, with 5 being the highest possible score for each element), which is a validated tool for assessing surgical skills (eTable 1).3 Given that there were no assistants participating in the surgery, this element of the OSATS scoring table was excluded, making a maximum possible score of 30 and a minimum possible score of 6. After scoring themselves, participants then had a 1-on-1 coaching session with a fellowship-trained dermatologic surgeon (M.F. or T.H.) via online teleconferencing.
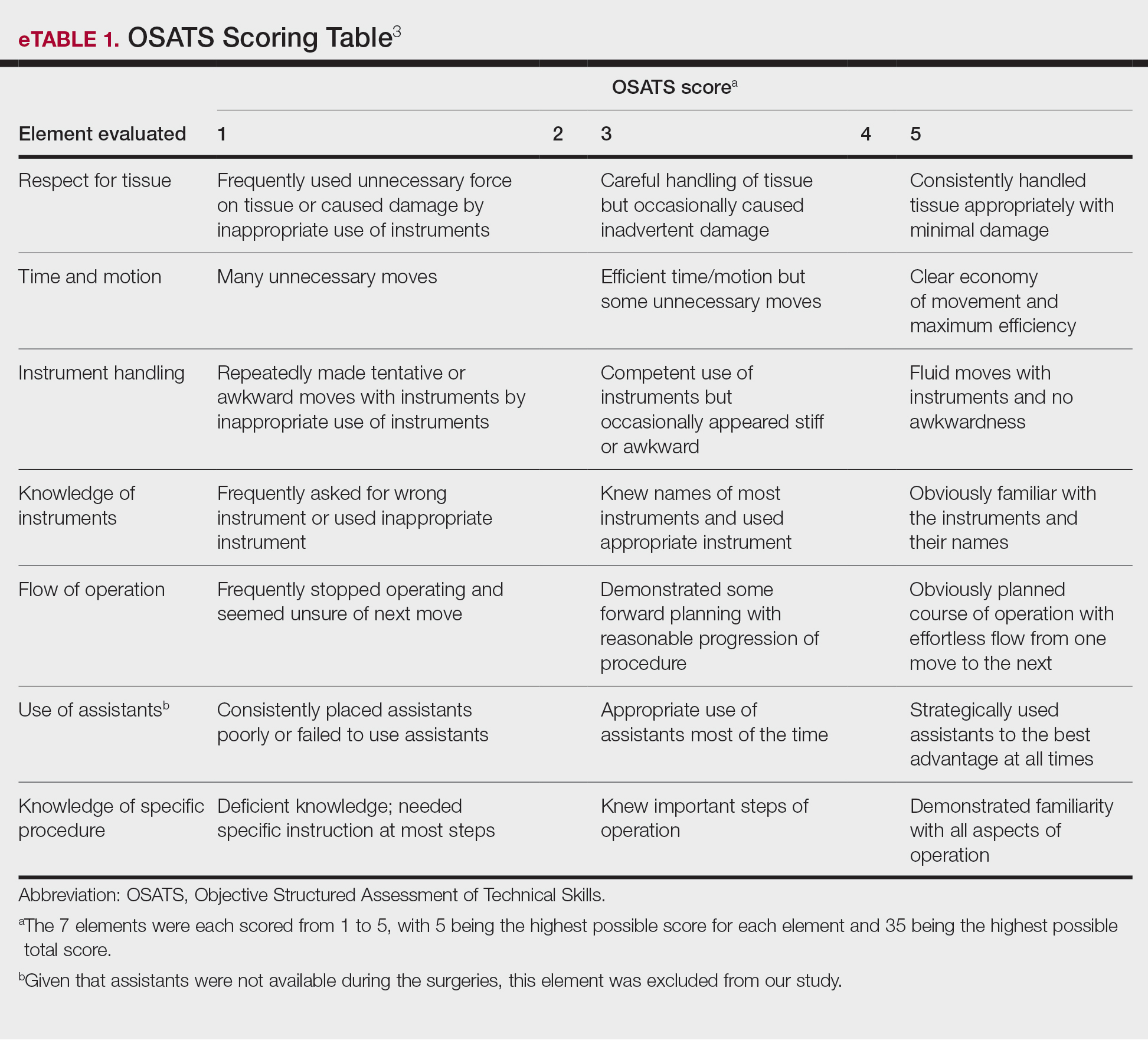
During the coaching session, participants and coaches reviewed the video. The surgical coaches also scored the residents using the OSATS, then residents and coaches discussed how the resident could improve using the OSATS scores as a guide. The residents then completed a poststudy survey assessing their surgical experience, confidence in performing surgery, and attitudes on VBC. Descriptive statistics were reported.
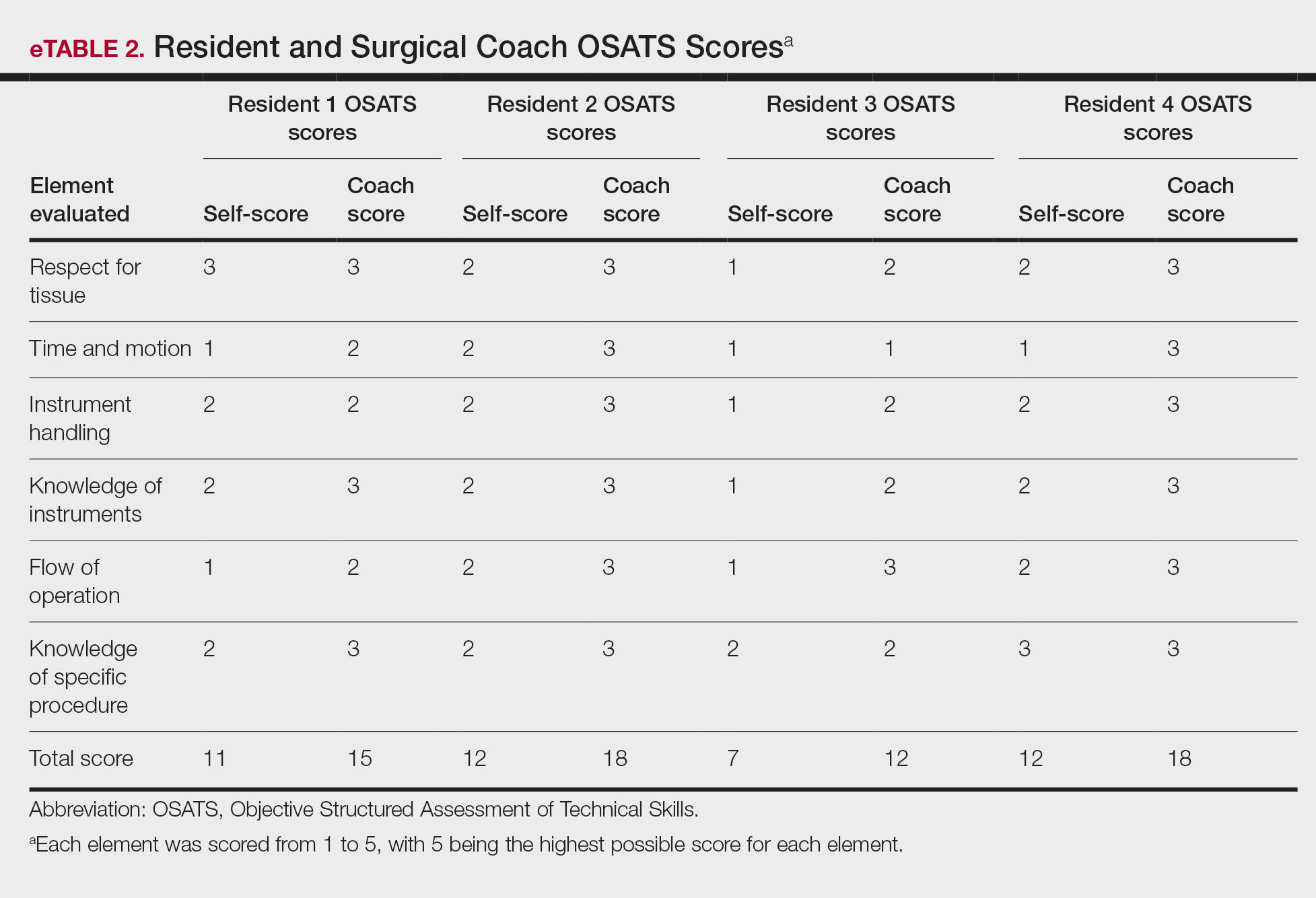
On average, residents spent 31.3 minutes reviewing their own surgeries and scoring themselves. The average time for a coaching session, which included time spent scoring, was 13.8 minutes. Residents scored themselves lower than the surgical coaches did by an average of 5.25 points (eTable 2). Residents gave themselves an average total score of 10.5, while their respective surgical coaches gave the residents an average score of 15.75. There was a trend of residents with greater surgical experience having higher OSATS scores (Figure). After the coaching session, 3 of 4 residents reported that they felt more confident in their surgical skills. All residents felt more confident in assessing their surgical skills and felt that VBC was an effective teaching measure. All residents agreed that VBC should be continued as part of their residency training.
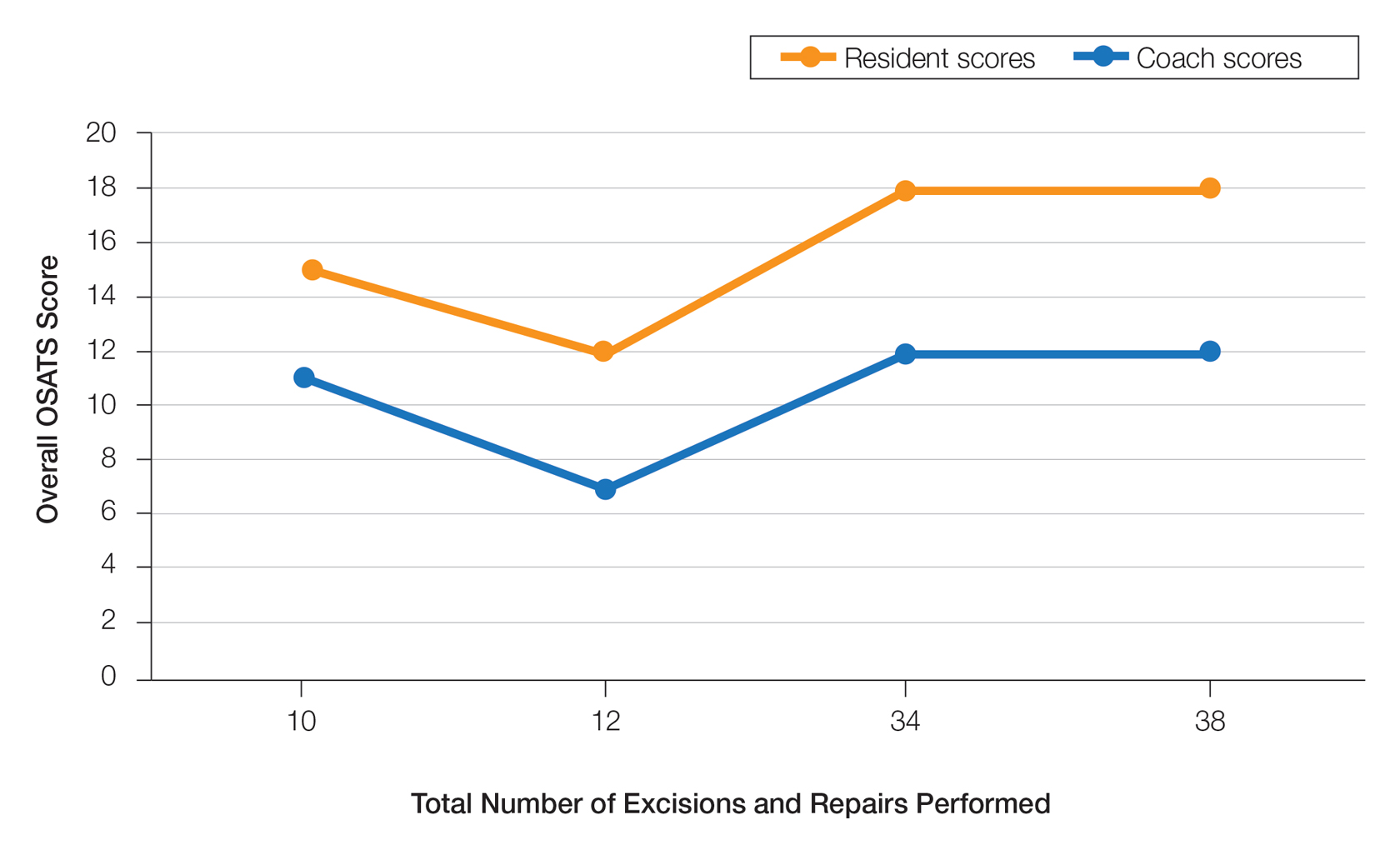
Video-based coaching has the potential to provide several benefits for dermatology trainees. Because receiving feedback intraoperatively often can be distracting and incomplete, video review can instead allow the surgeon to focus on performing the surgery and then later focus on learning while reviewing the video.1,4 Feedback also can be more comprehensive and delivered without concern for time constraints or disturbing clinic flow as well as without the additional concern of the patient overhearing comments and feedback.3 Although independent video review in the absence of coaching can lead to improvement in surgical skills, the addition of VBC provides even greater potential educational benefit.4 During the COVID-19 pandemic, VBC allowed coaches to provide feedback without additional exposures. We utilized dermatologic surgery faculty as coaches, but this format of training also would apply to general dermatology faculty.
Another goal of VBC is to enhance a trainee’s ability to perform self-directed learning, which requires accurate self-assessment.4 Accurately assessing one’s own strengths empowers a trainee to act with appropriate confidence, while understanding one’s own weaknesses allows a trainee to effectively balance confidence and caution in daily practice.5 Interestingly, in our study all residents scored themselves lower than surgical coaches, but with 1 coaching session, the residents subsequently reported greater surgical confidence.
Time constraints can be a potential barrier to surgical coaching.4 Our study demonstrates that VBC requires minimal time investment. Increasing the speed of video playback allowed for efficient evaluation of resident surgeries without compromising the coach’s ability to provide comprehensive feedback. Our feedback sessions were performed virtually, which allowed for ease of scheduling between trainees and coaches.
Our pilot study demonstrated that VBC is relatively easy to implement in a dermatology residency training setting, leveraging relatively low-cost technologies and allowing for a means of learning that residents felt was effective. Video-based coaching requires minimal time investment from both trainees and coaches and has the potential to enhance surgical confidence. Our current study is limited by its small sample size. Future studies should include follow-up recordings and assess the efficacy of VBC in enhancing surgical skills.
- Greenberg CC, Dombrowski J, Dimick JB. Video-based surgical coaching: an emerging approach to performance improvement. JAMA Surg. 2016;151:282-283.
- Dai J, Bordeaux JS, Miller CJ, et al. Assessing surgical training and deliberate practice methods in dermatology residency: a survey of dermatology program directors. Dermatol Surg. 2016;42:977-984.
- Chitgopeker P, Sidey K, Aronson A, et al. Surgical skills video-based assessment tool for dermatology residents: a prospective pilot study. J Am Acad Dermatol. 2020;83:614-616.
- Bull NB, Silverman CD, Bonrath EM. Targeted surgical coaching can improve operative self-assessment ability: a single-blinded nonrandomized trial. Surgery. 2020;167:308-313.
- Eva KW, Regehr G. Self-assessment in the health professions: a reformulation and research agenda. Acad Med. 2005;80(10 suppl):S46-S54.
To the Editor:
Video-based coaching (VBC) involves a surgeon recording a surgery and then reviewing the video with a surgical coach; it is a form of education that is gaining popularity among surgical specialties.1 Video-based education is underutilized in dermatology residency training.2 We conducted a pilot study at our dermatology residency program to evaluate the efficacy and feasibility of VBC.
The University of Texas at Austin Dell Medical School institutional review board approved this study. All 4 first-year dermatology residents were recruited to participate in this study. Participants filled out a prestudy survey assessing their surgical experience, confidence in performing surgery, and attitudes on VBC. Participants used a head-mounted point-of-view camera to record themselves performing a wide local excision on the trunk or extremities of a live human patient. Participants then reviewed the recording on their own and scored themselves using the Objective Structured Assessment of Technical Skills (OSATS) scoring table (scored from 1 to 5, with 5 being the highest possible score for each element), which is a validated tool for assessing surgical skills (eTable 1).3 Given that there were no assistants participating in the surgery, this element of the OSATS scoring table was excluded, making a maximum possible score of 30 and a minimum possible score of 6. After scoring themselves, participants then had a 1-on-1 coaching session with a fellowship-trained dermatologic surgeon (M.F. or T.H.) via online teleconferencing.
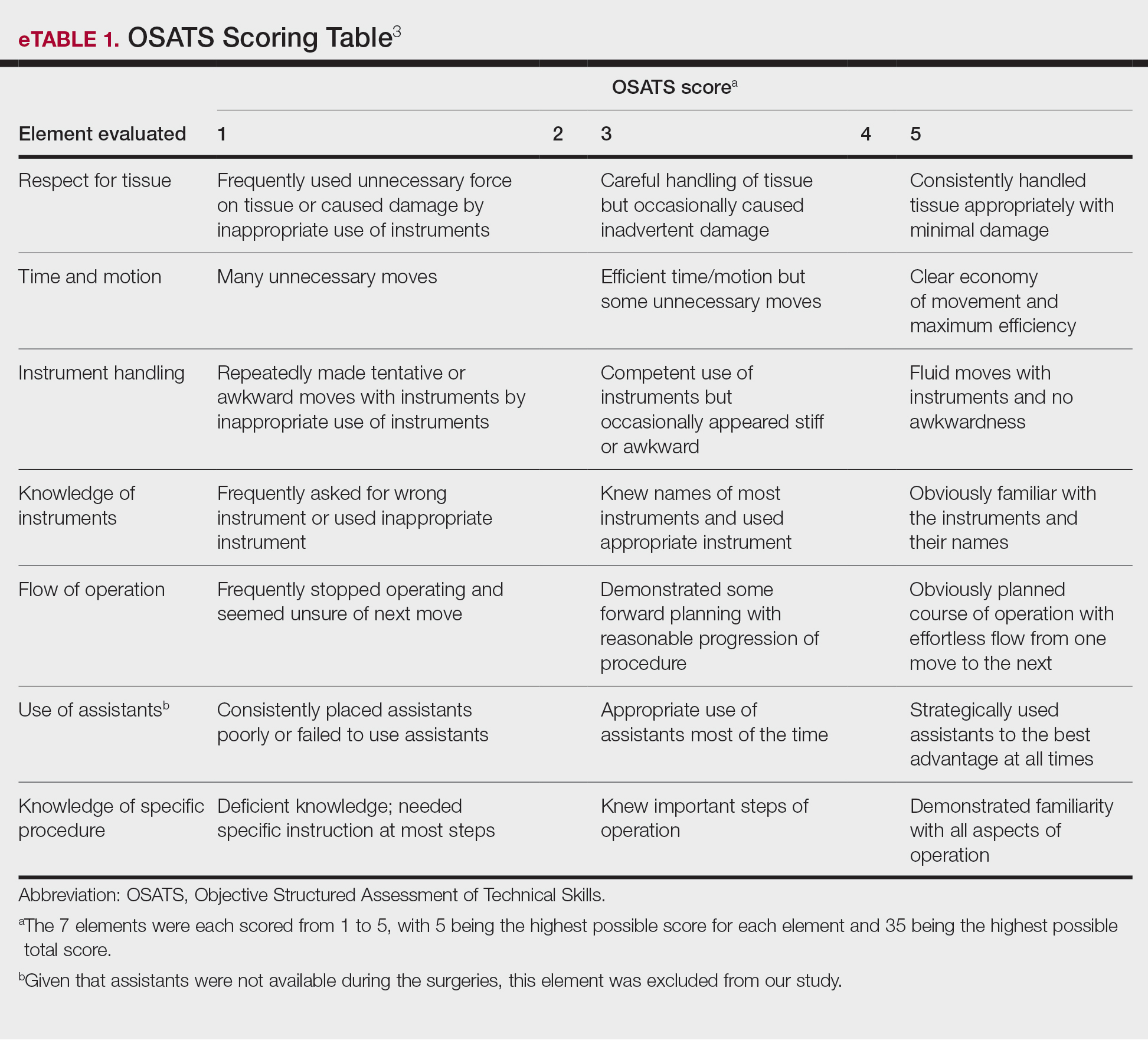
During the coaching session, participants and coaches reviewed the video. The surgical coaches also scored the residents using the OSATS, then residents and coaches discussed how the resident could improve using the OSATS scores as a guide. The residents then completed a poststudy survey assessing their surgical experience, confidence in performing surgery, and attitudes on VBC. Descriptive statistics were reported.
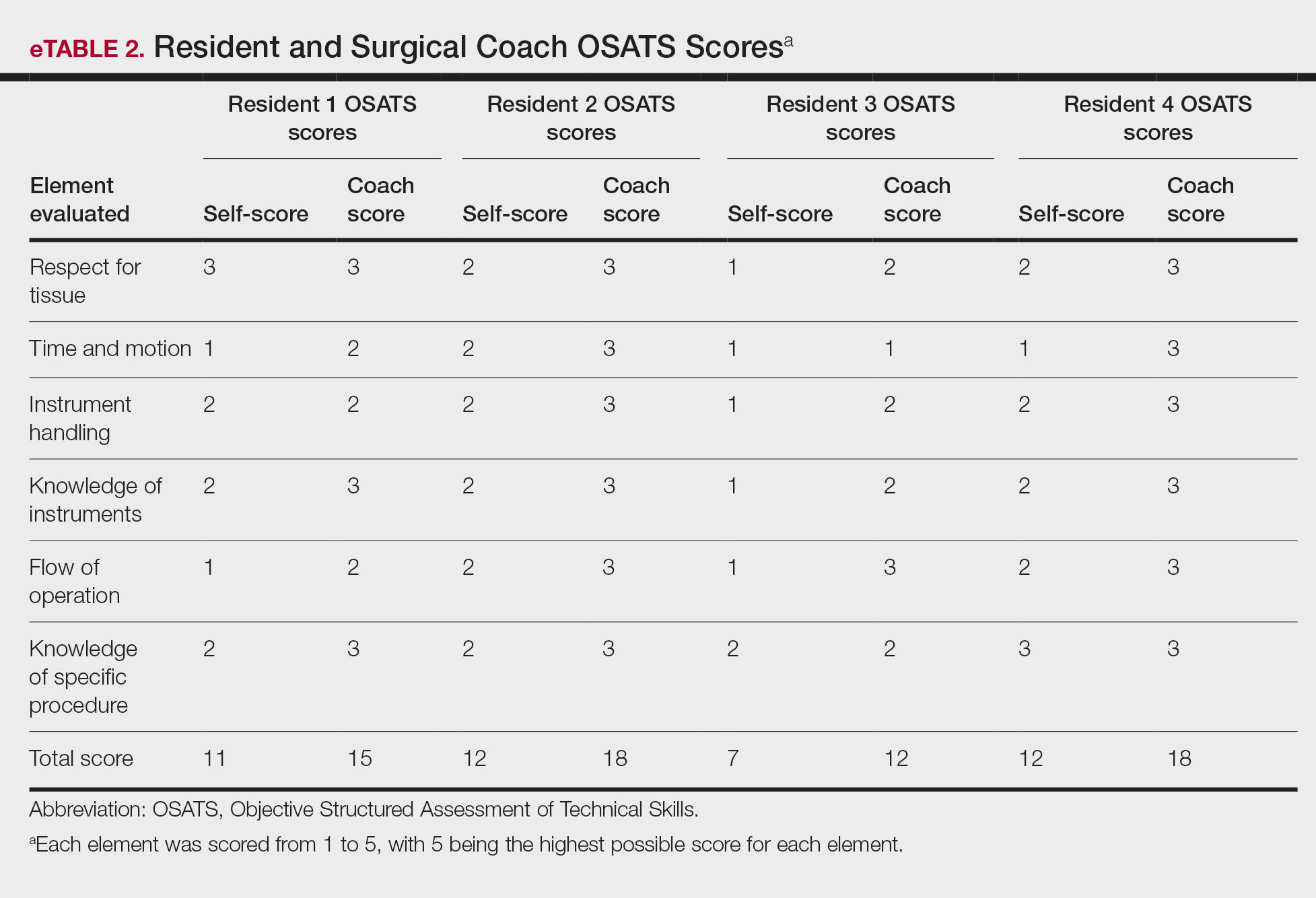
On average, residents spent 31.3 minutes reviewing their own surgeries and scoring themselves. The average time for a coaching session, which included time spent scoring, was 13.8 minutes. Residents scored themselves lower than the surgical coaches did by an average of 5.25 points (eTable 2). Residents gave themselves an average total score of 10.5, while their respective surgical coaches gave the residents an average score of 15.75. There was a trend of residents with greater surgical experience having higher OSATS scores (Figure). After the coaching session, 3 of 4 residents reported that they felt more confident in their surgical skills. All residents felt more confident in assessing their surgical skills and felt that VBC was an effective teaching measure. All residents agreed that VBC should be continued as part of their residency training.
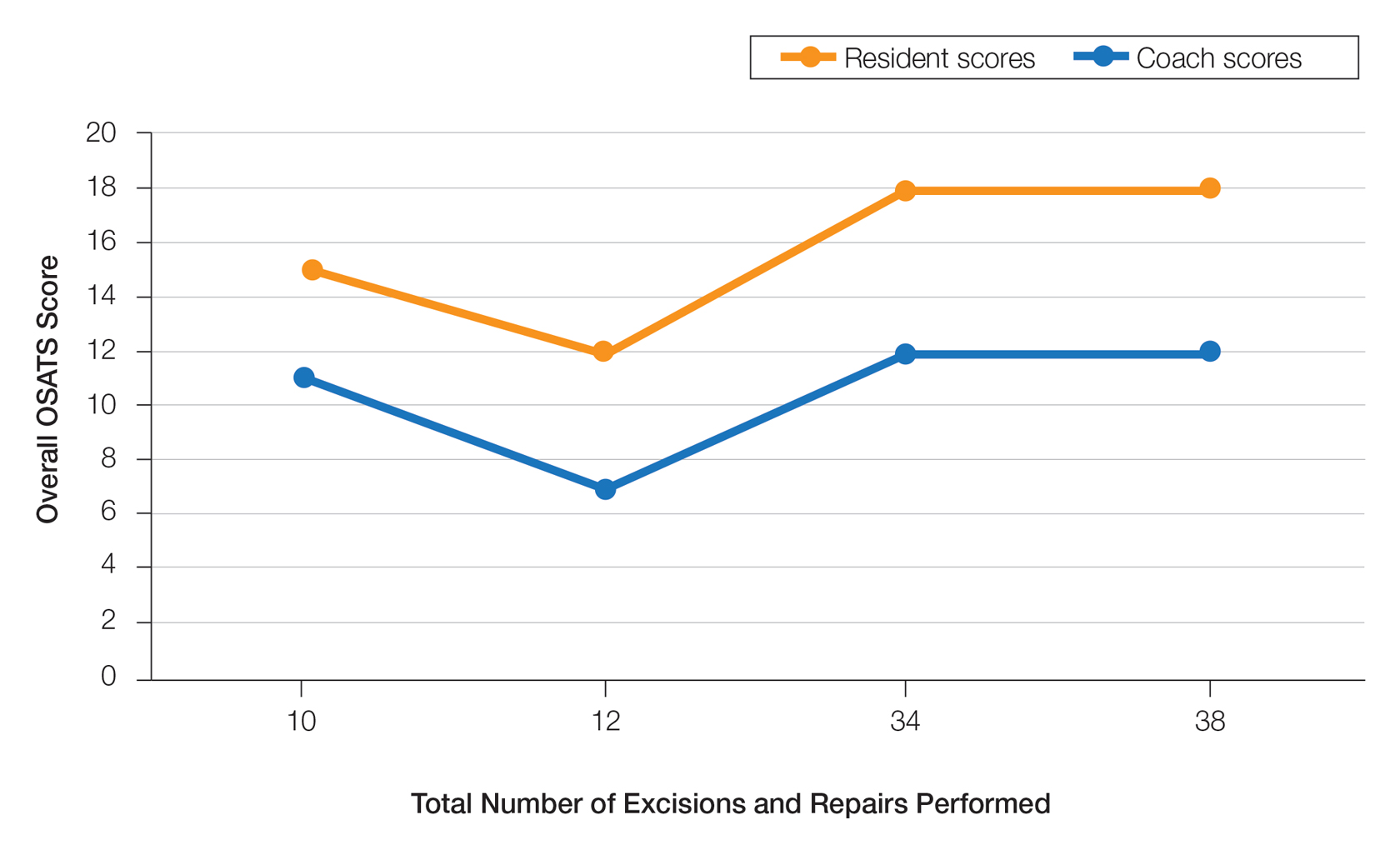
Video-based coaching has the potential to provide several benefits for dermatology trainees. Because receiving feedback intraoperatively often can be distracting and incomplete, video review can instead allow the surgeon to focus on performing the surgery and then later focus on learning while reviewing the video.1,4 Feedback also can be more comprehensive and delivered without concern for time constraints or disturbing clinic flow as well as without the additional concern of the patient overhearing comments and feedback.3 Although independent video review in the absence of coaching can lead to improvement in surgical skills, the addition of VBC provides even greater potential educational benefit.4 During the COVID-19 pandemic, VBC allowed coaches to provide feedback without additional exposures. We utilized dermatologic surgery faculty as coaches, but this format of training also would apply to general dermatology faculty.
Another goal of VBC is to enhance a trainee’s ability to perform self-directed learning, which requires accurate self-assessment.4 Accurately assessing one’s own strengths empowers a trainee to act with appropriate confidence, while understanding one’s own weaknesses allows a trainee to effectively balance confidence and caution in daily practice.5 Interestingly, in our study all residents scored themselves lower than surgical coaches, but with 1 coaching session, the residents subsequently reported greater surgical confidence.
Time constraints can be a potential barrier to surgical coaching.4 Our study demonstrates that VBC requires minimal time investment. Increasing the speed of video playback allowed for efficient evaluation of resident surgeries without compromising the coach’s ability to provide comprehensive feedback. Our feedback sessions were performed virtually, which allowed for ease of scheduling between trainees and coaches.
Our pilot study demonstrated that VBC is relatively easy to implement in a dermatology residency training setting, leveraging relatively low-cost technologies and allowing for a means of learning that residents felt was effective. Video-based coaching requires minimal time investment from both trainees and coaches and has the potential to enhance surgical confidence. Our current study is limited by its small sample size. Future studies should include follow-up recordings and assess the efficacy of VBC in enhancing surgical skills.
To the Editor:
Video-based coaching (VBC) involves a surgeon recording a surgery and then reviewing the video with a surgical coach; it is a form of education that is gaining popularity among surgical specialties.1 Video-based education is underutilized in dermatology residency training.2 We conducted a pilot study at our dermatology residency program to evaluate the efficacy and feasibility of VBC.
The University of Texas at Austin Dell Medical School institutional review board approved this study. All 4 first-year dermatology residents were recruited to participate in this study. Participants filled out a prestudy survey assessing their surgical experience, confidence in performing surgery, and attitudes on VBC. Participants used a head-mounted point-of-view camera to record themselves performing a wide local excision on the trunk or extremities of a live human patient. Participants then reviewed the recording on their own and scored themselves using the Objective Structured Assessment of Technical Skills (OSATS) scoring table (scored from 1 to 5, with 5 being the highest possible score for each element), which is a validated tool for assessing surgical skills (eTable 1).3 Given that there were no assistants participating in the surgery, this element of the OSATS scoring table was excluded, making a maximum possible score of 30 and a minimum possible score of 6. After scoring themselves, participants then had a 1-on-1 coaching session with a fellowship-trained dermatologic surgeon (M.F. or T.H.) via online teleconferencing.
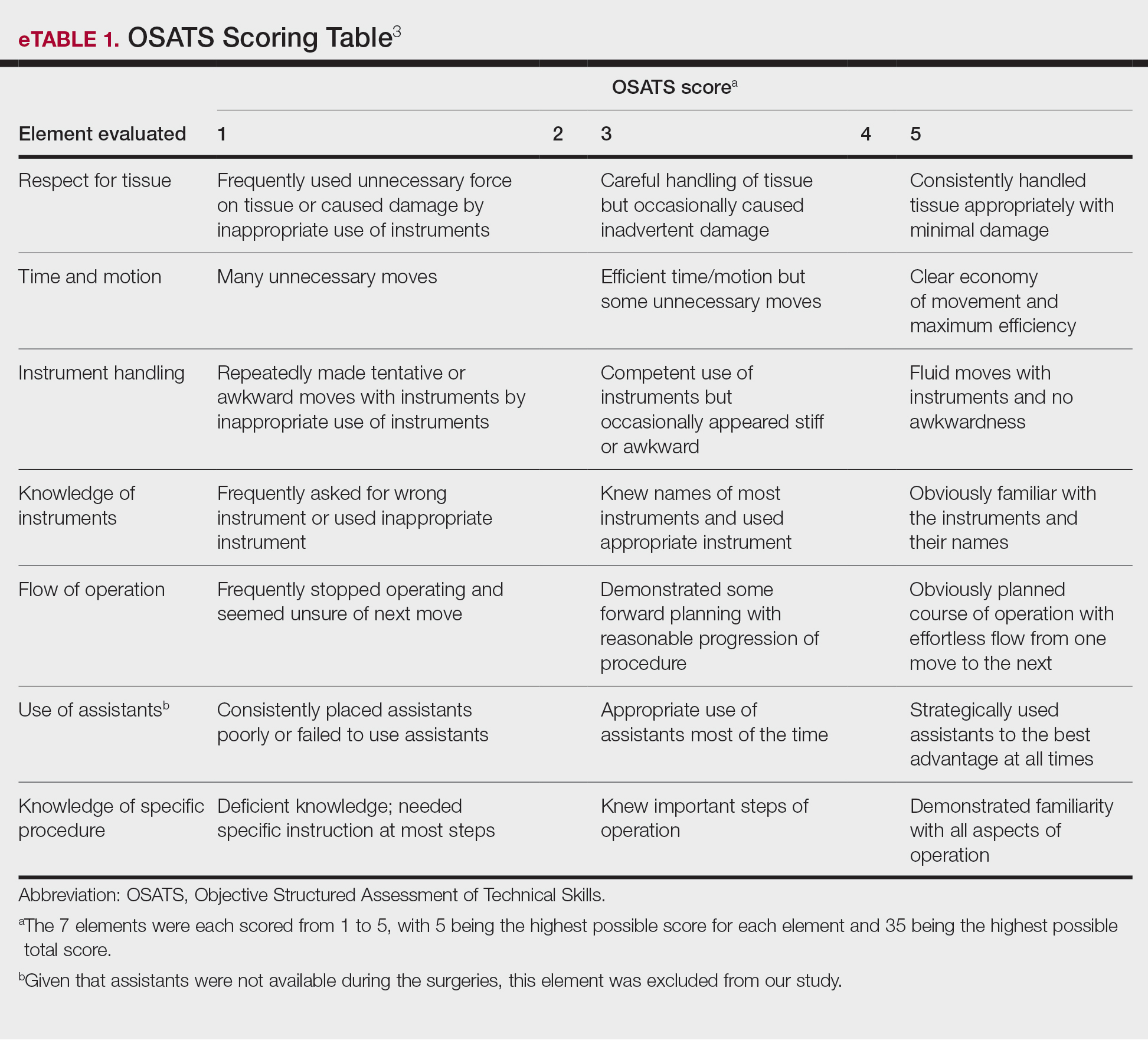
During the coaching session, participants and coaches reviewed the video. The surgical coaches also scored the residents using the OSATS, then residents and coaches discussed how the resident could improve using the OSATS scores as a guide. The residents then completed a poststudy survey assessing their surgical experience, confidence in performing surgery, and attitudes on VBC. Descriptive statistics were reported.
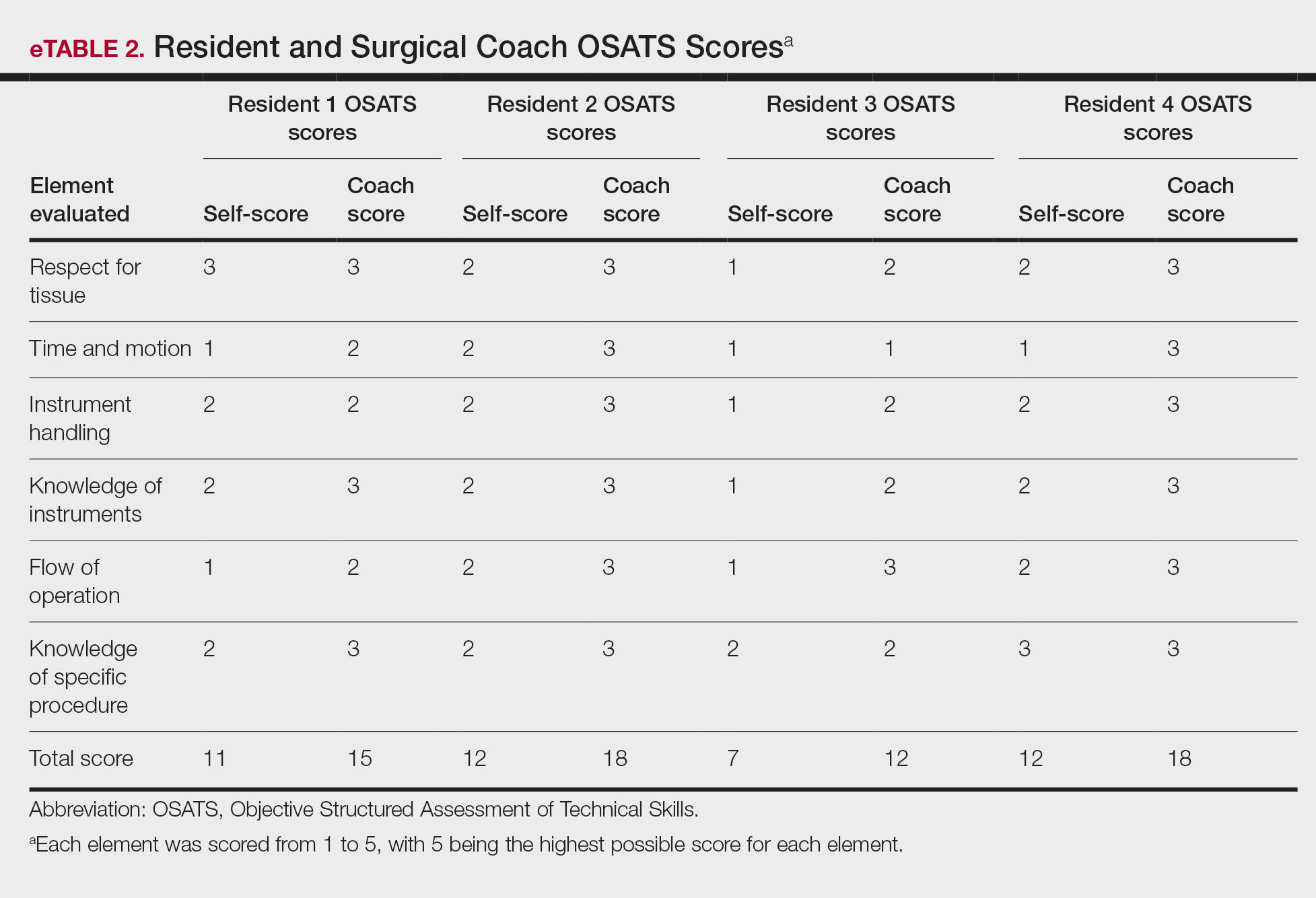
On average, residents spent 31.3 minutes reviewing their own surgeries and scoring themselves. The average time for a coaching session, which included time spent scoring, was 13.8 minutes. Residents scored themselves lower than the surgical coaches did by an average of 5.25 points (eTable 2). Residents gave themselves an average total score of 10.5, while their respective surgical coaches gave the residents an average score of 15.75. There was a trend of residents with greater surgical experience having higher OSATS scores (Figure). After the coaching session, 3 of 4 residents reported that they felt more confident in their surgical skills. All residents felt more confident in assessing their surgical skills and felt that VBC was an effective teaching measure. All residents agreed that VBC should be continued as part of their residency training.
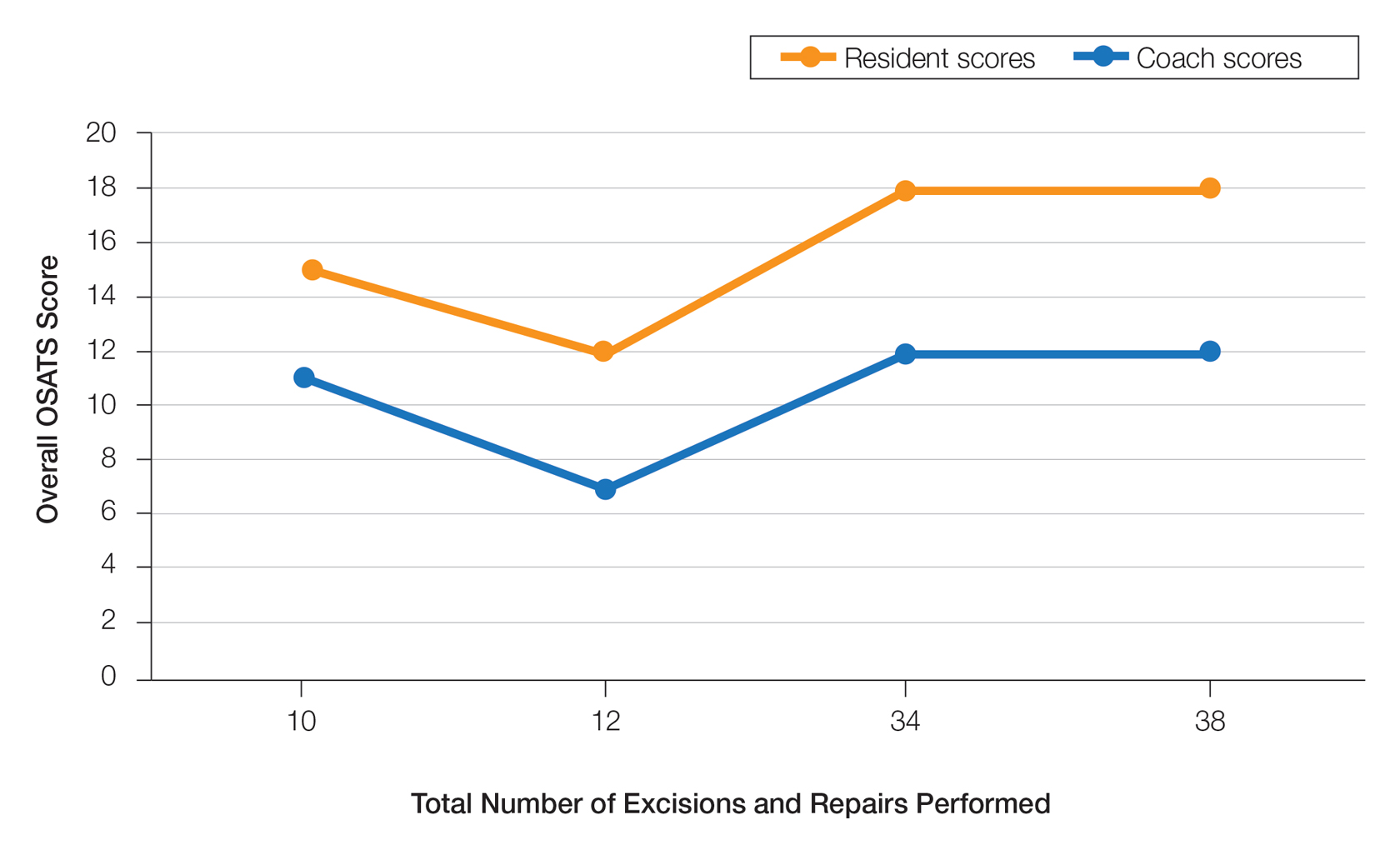
Video-based coaching has the potential to provide several benefits for dermatology trainees. Because receiving feedback intraoperatively often can be distracting and incomplete, video review can instead allow the surgeon to focus on performing the surgery and then later focus on learning while reviewing the video.1,4 Feedback also can be more comprehensive and delivered without concern for time constraints or disturbing clinic flow as well as without the additional concern of the patient overhearing comments and feedback.3 Although independent video review in the absence of coaching can lead to improvement in surgical skills, the addition of VBC provides even greater potential educational benefit.4 During the COVID-19 pandemic, VBC allowed coaches to provide feedback without additional exposures. We utilized dermatologic surgery faculty as coaches, but this format of training also would apply to general dermatology faculty.
Another goal of VBC is to enhance a trainee’s ability to perform self-directed learning, which requires accurate self-assessment.4 Accurately assessing one’s own strengths empowers a trainee to act with appropriate confidence, while understanding one’s own weaknesses allows a trainee to effectively balance confidence and caution in daily practice.5 Interestingly, in our study all residents scored themselves lower than surgical coaches, but with 1 coaching session, the residents subsequently reported greater surgical confidence.
Time constraints can be a potential barrier to surgical coaching.4 Our study demonstrates that VBC requires minimal time investment. Increasing the speed of video playback allowed for efficient evaluation of resident surgeries without compromising the coach’s ability to provide comprehensive feedback. Our feedback sessions were performed virtually, which allowed for ease of scheduling between trainees and coaches.
Our pilot study demonstrated that VBC is relatively easy to implement in a dermatology residency training setting, leveraging relatively low-cost technologies and allowing for a means of learning that residents felt was effective. Video-based coaching requires minimal time investment from both trainees and coaches and has the potential to enhance surgical confidence. Our current study is limited by its small sample size. Future studies should include follow-up recordings and assess the efficacy of VBC in enhancing surgical skills.
- Greenberg CC, Dombrowski J, Dimick JB. Video-based surgical coaching: an emerging approach to performance improvement. JAMA Surg. 2016;151:282-283.
- Dai J, Bordeaux JS, Miller CJ, et al. Assessing surgical training and deliberate practice methods in dermatology residency: a survey of dermatology program directors. Dermatol Surg. 2016;42:977-984.
- Chitgopeker P, Sidey K, Aronson A, et al. Surgical skills video-based assessment tool for dermatology residents: a prospective pilot study. J Am Acad Dermatol. 2020;83:614-616.
- Bull NB, Silverman CD, Bonrath EM. Targeted surgical coaching can improve operative self-assessment ability: a single-blinded nonrandomized trial. Surgery. 2020;167:308-313.
- Eva KW, Regehr G. Self-assessment in the health professions: a reformulation and research agenda. Acad Med. 2005;80(10 suppl):S46-S54.
- Greenberg CC, Dombrowski J, Dimick JB. Video-based surgical coaching: an emerging approach to performance improvement. JAMA Surg. 2016;151:282-283.
- Dai J, Bordeaux JS, Miller CJ, et al. Assessing surgical training and deliberate practice methods in dermatology residency: a survey of dermatology program directors. Dermatol Surg. 2016;42:977-984.
- Chitgopeker P, Sidey K, Aronson A, et al. Surgical skills video-based assessment tool for dermatology residents: a prospective pilot study. J Am Acad Dermatol. 2020;83:614-616.
- Bull NB, Silverman CD, Bonrath EM. Targeted surgical coaching can improve operative self-assessment ability: a single-blinded nonrandomized trial. Surgery. 2020;167:308-313.
- Eva KW, Regehr G. Self-assessment in the health professions: a reformulation and research agenda. Acad Med. 2005;80(10 suppl):S46-S54.
PRACTICE POINTS
- Video-based coaching (VBC) for surgical procedures is an up-and-coming form of medical education that allows a “coach” to provide thoughtful and in-depth feedback while reviewing a recording with the surgeon in a private setting. This format has potential utility in teaching dermatology resident surgeons being coached by a dermatology faculty member.
- We performed a pilot study demonstrating that VBC can be performed easily with a minimal time investment for both the surgeon and the coach. Dermatology residents not only felt that VBC was an effective teaching method but also should become a formal part of their education.







