User login
The Ethical Implications of Dermatology Residents Treating Attending Physicians
Residents are confronted daily with situations in clinic that require a foundation in medical ethics to assist in decision-making. Attending physicians require health care services and at times may seek care from resident physicians. If the attending physician has direct oversight over the resident, however, the ethics of the resident treating them need to be addressed. Although patients have autonomy to choose whoever they want as a physician, nonmaleficence dictates that the resident may forego treatment due to concerns for providing suboptimal care; however, this same attending may be treated under specific circumstances. This column explores the ethical implications of both situations.
The Ethical Dilemma of Treating an Attending
Imagine this scenario: You are in your resident general dermatology clinic seeing patients with an attending overseeing your clinical decisions following each encounter. You look on your schedule and see that the next patient is one of your pediatric dermatology attendings for a total-body skin examination (TBSE). You have never treated a physician that oversees you, and you ponder whether you should perform the examination or fetch your attending to perform the encounter alone.
This conundrum then brings other questions to mind: Would changing the reason for the appointment (ie, an acute problem vs a TBSE) alter your decision as to whether or not you would treat this attending? Would the situation be different if this was an attending in a different department?
Ethics Curriculum for Residents
Medical providers face ethical dilemmas daily, and dermatologists and dermatology residents are not excluded. Dermatoethics can provide a framework for the best approach to this hypothetical situation. To equip residents with resources on ethics and a cognitive framework to approach similar situations, the American Board of Dermatology has created an ethics curriculum for residents to learn over their 3 years of training.1
One study that analyzed the ethical themes portrayed in essays by fourth-year medical students showed that the most common themes included autonomy, social justice, nonmaleficence, beneficence, honesty, and respect.2 These themes must be considered in different permutations throughout ethical conundrums.
In the situation of an attending physician who supervises a resident in another clinic voluntarily attending the resident clinic, the physician is aware of the resident’s skills and qualifications and knows that supervision is being provided by an attending physician, which allows informed consent to be made, as a study by Unruh et al3 shows. The patient’s autonomy allows them to choose their treating provider.
However, there are several reasons why the resident may be hesitant to enter the room. One concern may be that during a TBSE the provider usually examines the patient’s genitals, rectum, and breasts.4 Because the resident knows the individual personally, the patient and/or the provider may be uncomfortable checking these areas, leaving a portion of the examination unperformed. This neglect may harm the patient (eg, a genital melanoma is missed), violating the tenant of nonmaleficence.
The effect of the medical hierarchy also should be considered. The de facto hierarchy of attendings supervising residents, interns, and medical students, with each group having some oversight over the next, can have positive effects on education and appropriate patient management but also can prove to be detrimental to the patient and provider in some circumstances. Studies have shown that residents may be less willing to disagree with their superior’s opinions for fear of negative reactions and harmful effects on their future careers.5-7 The hierarchy of medicine also can affect a resident’s moral judgement by intimidating the practitioner to perform tasks or make diagnoses they may not wish to make.5,6,8,9 For example, the resident may send a prescription for a medication that the attending requested despite no clear indication of need. This mingling of patient and supervisor roles can result in a resident treating their attending physician inconsistently with their standard of care.
Navigating the Ethics of Treating Family Members
The American Medical Association Code of Medical Ethics Opinions on Patient-Physician Relationships highlights treating family members as an important ethical topic. Although most residents and attendings are not biologically related, a familial-style relationship exists in many dermatology programs between attendings and residents due to the close-knit nature of dermatology programs. Diagnostic and treatment accuracy may be diminished by the discomfort or disbelief that a condition could affect someone the resident cares about.10
The American Medical Association also states that a physician can treat family members in an emergency situation or for short-term minor problems. If these 2 exceptions were to be extrapolated to apply to situations involving residents and attendings in addition to family, there would be situations where a dermatology resident could ethically treat their attending physician.10 If the attending physician was worried about a problem that was deemed potentially life-threatening, such as a rapidly progressive bullous eruption concerning for Stevens-Johnson syndrome following the initiation of a new medication, and they wanted an urgent evaluation and biopsy, an ethicist could argue that urgent treatment is medically indicated as deferring treatment could have negative consequences on the patient’s health. In addition, if the attending found a splinter in their finger following yardwork and needed assistance in removal, this also could be treated by their resident, as it is minimally invasive and has a finite conclusion.
Treating Nonsupervisory Attendings
In the case of performing a TBSE on an attending from another specialty, it would be acceptable and less ethically ambiguous if no close personal relationship existed between the two practitioners, as this patient would have no direct oversight over the resident physician.
Final Thoughts
Each situation that residents face may carry ethical implications with perspectives from the patient, provider, and bystanders. The above scenarios highlight specific instances that a dermatology resident may face and provide insight into how they may approach the situations. At the same time, it is important to remember that every situation is different and requires a unique approach. Fortunately,physicians—specifically dermatologists—are provided many resources to help navigate challenging scenarios.
Acknowledgments—The author thanks Jane M. Grant-Kels, MD (Farmington, Connecticut), for reviewing this paper and providing feedback to improve its content, as well as Warren R. Heymann, MD (Camden, New Jersey), for assisting in the creation of this topic and article.
- Dermatoethics. American Board of Dermatology website. Accessed August 9, 2022. https://www.abderm.org/residents-and-fellows/dermatoethics
- House JB, Theyyunni N, Barnosky AR, et al. Understanding ethical dilemmas in the emergency department: views from medical students’ essays. J Emerg Med. 2015;48:492-498.
- Unruh KP, Dhulipala SC, Holt GE. Patient understanding of the role of the orthopedic resident. J Surg Educ. 2013;70:345-349.
- Grandhi R, Grant-Kels JM. Naked and vulnerable: the ethics of chaperoning full-body skin examinations. J Am Acad Dermatol. 2017;76:1221-1223.
- Salehi PP, Jacobs D, Suhail-Sindhu T, et al. Consequences of medical hierarchy on medical students, residents, and medical education in otolaryngology. Otolaryngol Head Neck Surg. 2020;163:906-914.
- Lomis KD, Carpenter RO, Miller BM. Moral distress in the third year of medical school: a descriptive review of student case reflections. Am J Surg. 2009;197:107-112.
- Troughton R, Mariano V, Campbell A, et al. Understanding determinants of infection control practices in surgery: the role of shared ownership and team hierarchy. Antimicrob Resist Infect Control. 2019;8:116.
- Chiu PP, Hilliard RI, Azzie G, et al. Experience of moral distress among pediatric surgery trainees. J Pediatr Surg. 2008;43:986-993.
- Martinez W, Lo B. Medical students’ experiences with medical errors: an analysis of medical student essays. Med Educ. 2008;42:733-741.
- Chapter 1. opinions on patient-physician relationships. American Medical Association website. Accessed on August 9, 2022. https://www.ama-assn.org/system/files/code-of-medical-ethics-chapter-1.pdf
Residents are confronted daily with situations in clinic that require a foundation in medical ethics to assist in decision-making. Attending physicians require health care services and at times may seek care from resident physicians. If the attending physician has direct oversight over the resident, however, the ethics of the resident treating them need to be addressed. Although patients have autonomy to choose whoever they want as a physician, nonmaleficence dictates that the resident may forego treatment due to concerns for providing suboptimal care; however, this same attending may be treated under specific circumstances. This column explores the ethical implications of both situations.
The Ethical Dilemma of Treating an Attending
Imagine this scenario: You are in your resident general dermatology clinic seeing patients with an attending overseeing your clinical decisions following each encounter. You look on your schedule and see that the next patient is one of your pediatric dermatology attendings for a total-body skin examination (TBSE). You have never treated a physician that oversees you, and you ponder whether you should perform the examination or fetch your attending to perform the encounter alone.
This conundrum then brings other questions to mind: Would changing the reason for the appointment (ie, an acute problem vs a TBSE) alter your decision as to whether or not you would treat this attending? Would the situation be different if this was an attending in a different department?
Ethics Curriculum for Residents
Medical providers face ethical dilemmas daily, and dermatologists and dermatology residents are not excluded. Dermatoethics can provide a framework for the best approach to this hypothetical situation. To equip residents with resources on ethics and a cognitive framework to approach similar situations, the American Board of Dermatology has created an ethics curriculum for residents to learn over their 3 years of training.1
One study that analyzed the ethical themes portrayed in essays by fourth-year medical students showed that the most common themes included autonomy, social justice, nonmaleficence, beneficence, honesty, and respect.2 These themes must be considered in different permutations throughout ethical conundrums.
In the situation of an attending physician who supervises a resident in another clinic voluntarily attending the resident clinic, the physician is aware of the resident’s skills and qualifications and knows that supervision is being provided by an attending physician, which allows informed consent to be made, as a study by Unruh et al3 shows. The patient’s autonomy allows them to choose their treating provider.
However, there are several reasons why the resident may be hesitant to enter the room. One concern may be that during a TBSE the provider usually examines the patient’s genitals, rectum, and breasts.4 Because the resident knows the individual personally, the patient and/or the provider may be uncomfortable checking these areas, leaving a portion of the examination unperformed. This neglect may harm the patient (eg, a genital melanoma is missed), violating the tenant of nonmaleficence.
The effect of the medical hierarchy also should be considered. The de facto hierarchy of attendings supervising residents, interns, and medical students, with each group having some oversight over the next, can have positive effects on education and appropriate patient management but also can prove to be detrimental to the patient and provider in some circumstances. Studies have shown that residents may be less willing to disagree with their superior’s opinions for fear of negative reactions and harmful effects on their future careers.5-7 The hierarchy of medicine also can affect a resident’s moral judgement by intimidating the practitioner to perform tasks or make diagnoses they may not wish to make.5,6,8,9 For example, the resident may send a prescription for a medication that the attending requested despite no clear indication of need. This mingling of patient and supervisor roles can result in a resident treating their attending physician inconsistently with their standard of care.
Navigating the Ethics of Treating Family Members
The American Medical Association Code of Medical Ethics Opinions on Patient-Physician Relationships highlights treating family members as an important ethical topic. Although most residents and attendings are not biologically related, a familial-style relationship exists in many dermatology programs between attendings and residents due to the close-knit nature of dermatology programs. Diagnostic and treatment accuracy may be diminished by the discomfort or disbelief that a condition could affect someone the resident cares about.10
The American Medical Association also states that a physician can treat family members in an emergency situation or for short-term minor problems. If these 2 exceptions were to be extrapolated to apply to situations involving residents and attendings in addition to family, there would be situations where a dermatology resident could ethically treat their attending physician.10 If the attending physician was worried about a problem that was deemed potentially life-threatening, such as a rapidly progressive bullous eruption concerning for Stevens-Johnson syndrome following the initiation of a new medication, and they wanted an urgent evaluation and biopsy, an ethicist could argue that urgent treatment is medically indicated as deferring treatment could have negative consequences on the patient’s health. In addition, if the attending found a splinter in their finger following yardwork and needed assistance in removal, this also could be treated by their resident, as it is minimally invasive and has a finite conclusion.
Treating Nonsupervisory Attendings
In the case of performing a TBSE on an attending from another specialty, it would be acceptable and less ethically ambiguous if no close personal relationship existed between the two practitioners, as this patient would have no direct oversight over the resident physician.
Final Thoughts
Each situation that residents face may carry ethical implications with perspectives from the patient, provider, and bystanders. The above scenarios highlight specific instances that a dermatology resident may face and provide insight into how they may approach the situations. At the same time, it is important to remember that every situation is different and requires a unique approach. Fortunately,physicians—specifically dermatologists—are provided many resources to help navigate challenging scenarios.
Acknowledgments—The author thanks Jane M. Grant-Kels, MD (Farmington, Connecticut), for reviewing this paper and providing feedback to improve its content, as well as Warren R. Heymann, MD (Camden, New Jersey), for assisting in the creation of this topic and article.
Residents are confronted daily with situations in clinic that require a foundation in medical ethics to assist in decision-making. Attending physicians require health care services and at times may seek care from resident physicians. If the attending physician has direct oversight over the resident, however, the ethics of the resident treating them need to be addressed. Although patients have autonomy to choose whoever they want as a physician, nonmaleficence dictates that the resident may forego treatment due to concerns for providing suboptimal care; however, this same attending may be treated under specific circumstances. This column explores the ethical implications of both situations.
The Ethical Dilemma of Treating an Attending
Imagine this scenario: You are in your resident general dermatology clinic seeing patients with an attending overseeing your clinical decisions following each encounter. You look on your schedule and see that the next patient is one of your pediatric dermatology attendings for a total-body skin examination (TBSE). You have never treated a physician that oversees you, and you ponder whether you should perform the examination or fetch your attending to perform the encounter alone.
This conundrum then brings other questions to mind: Would changing the reason for the appointment (ie, an acute problem vs a TBSE) alter your decision as to whether or not you would treat this attending? Would the situation be different if this was an attending in a different department?
Ethics Curriculum for Residents
Medical providers face ethical dilemmas daily, and dermatologists and dermatology residents are not excluded. Dermatoethics can provide a framework for the best approach to this hypothetical situation. To equip residents with resources on ethics and a cognitive framework to approach similar situations, the American Board of Dermatology has created an ethics curriculum for residents to learn over their 3 years of training.1
One study that analyzed the ethical themes portrayed in essays by fourth-year medical students showed that the most common themes included autonomy, social justice, nonmaleficence, beneficence, honesty, and respect.2 These themes must be considered in different permutations throughout ethical conundrums.
In the situation of an attending physician who supervises a resident in another clinic voluntarily attending the resident clinic, the physician is aware of the resident’s skills and qualifications and knows that supervision is being provided by an attending physician, which allows informed consent to be made, as a study by Unruh et al3 shows. The patient’s autonomy allows them to choose their treating provider.
However, there are several reasons why the resident may be hesitant to enter the room. One concern may be that during a TBSE the provider usually examines the patient’s genitals, rectum, and breasts.4 Because the resident knows the individual personally, the patient and/or the provider may be uncomfortable checking these areas, leaving a portion of the examination unperformed. This neglect may harm the patient (eg, a genital melanoma is missed), violating the tenant of nonmaleficence.
The effect of the medical hierarchy also should be considered. The de facto hierarchy of attendings supervising residents, interns, and medical students, with each group having some oversight over the next, can have positive effects on education and appropriate patient management but also can prove to be detrimental to the patient and provider in some circumstances. Studies have shown that residents may be less willing to disagree with their superior’s opinions for fear of negative reactions and harmful effects on their future careers.5-7 The hierarchy of medicine also can affect a resident’s moral judgement by intimidating the practitioner to perform tasks or make diagnoses they may not wish to make.5,6,8,9 For example, the resident may send a prescription for a medication that the attending requested despite no clear indication of need. This mingling of patient and supervisor roles can result in a resident treating their attending physician inconsistently with their standard of care.
Navigating the Ethics of Treating Family Members
The American Medical Association Code of Medical Ethics Opinions on Patient-Physician Relationships highlights treating family members as an important ethical topic. Although most residents and attendings are not biologically related, a familial-style relationship exists in many dermatology programs between attendings and residents due to the close-knit nature of dermatology programs. Diagnostic and treatment accuracy may be diminished by the discomfort or disbelief that a condition could affect someone the resident cares about.10
The American Medical Association also states that a physician can treat family members in an emergency situation or for short-term minor problems. If these 2 exceptions were to be extrapolated to apply to situations involving residents and attendings in addition to family, there would be situations where a dermatology resident could ethically treat their attending physician.10 If the attending physician was worried about a problem that was deemed potentially life-threatening, such as a rapidly progressive bullous eruption concerning for Stevens-Johnson syndrome following the initiation of a new medication, and they wanted an urgent evaluation and biopsy, an ethicist could argue that urgent treatment is medically indicated as deferring treatment could have negative consequences on the patient’s health. In addition, if the attending found a splinter in their finger following yardwork and needed assistance in removal, this also could be treated by their resident, as it is minimally invasive and has a finite conclusion.
Treating Nonsupervisory Attendings
In the case of performing a TBSE on an attending from another specialty, it would be acceptable and less ethically ambiguous if no close personal relationship existed between the two practitioners, as this patient would have no direct oversight over the resident physician.
Final Thoughts
Each situation that residents face may carry ethical implications with perspectives from the patient, provider, and bystanders. The above scenarios highlight specific instances that a dermatology resident may face and provide insight into how they may approach the situations. At the same time, it is important to remember that every situation is different and requires a unique approach. Fortunately,physicians—specifically dermatologists—are provided many resources to help navigate challenging scenarios.
Acknowledgments—The author thanks Jane M. Grant-Kels, MD (Farmington, Connecticut), for reviewing this paper and providing feedback to improve its content, as well as Warren R. Heymann, MD (Camden, New Jersey), for assisting in the creation of this topic and article.
- Dermatoethics. American Board of Dermatology website. Accessed August 9, 2022. https://www.abderm.org/residents-and-fellows/dermatoethics
- House JB, Theyyunni N, Barnosky AR, et al. Understanding ethical dilemmas in the emergency department: views from medical students’ essays. J Emerg Med. 2015;48:492-498.
- Unruh KP, Dhulipala SC, Holt GE. Patient understanding of the role of the orthopedic resident. J Surg Educ. 2013;70:345-349.
- Grandhi R, Grant-Kels JM. Naked and vulnerable: the ethics of chaperoning full-body skin examinations. J Am Acad Dermatol. 2017;76:1221-1223.
- Salehi PP, Jacobs D, Suhail-Sindhu T, et al. Consequences of medical hierarchy on medical students, residents, and medical education in otolaryngology. Otolaryngol Head Neck Surg. 2020;163:906-914.
- Lomis KD, Carpenter RO, Miller BM. Moral distress in the third year of medical school: a descriptive review of student case reflections. Am J Surg. 2009;197:107-112.
- Troughton R, Mariano V, Campbell A, et al. Understanding determinants of infection control practices in surgery: the role of shared ownership and team hierarchy. Antimicrob Resist Infect Control. 2019;8:116.
- Chiu PP, Hilliard RI, Azzie G, et al. Experience of moral distress among pediatric surgery trainees. J Pediatr Surg. 2008;43:986-993.
- Martinez W, Lo B. Medical students’ experiences with medical errors: an analysis of medical student essays. Med Educ. 2008;42:733-741.
- Chapter 1. opinions on patient-physician relationships. American Medical Association website. Accessed on August 9, 2022. https://www.ama-assn.org/system/files/code-of-medical-ethics-chapter-1.pdf
- Dermatoethics. American Board of Dermatology website. Accessed August 9, 2022. https://www.abderm.org/residents-and-fellows/dermatoethics
- House JB, Theyyunni N, Barnosky AR, et al. Understanding ethical dilemmas in the emergency department: views from medical students’ essays. J Emerg Med. 2015;48:492-498.
- Unruh KP, Dhulipala SC, Holt GE. Patient understanding of the role of the orthopedic resident. J Surg Educ. 2013;70:345-349.
- Grandhi R, Grant-Kels JM. Naked and vulnerable: the ethics of chaperoning full-body skin examinations. J Am Acad Dermatol. 2017;76:1221-1223.
- Salehi PP, Jacobs D, Suhail-Sindhu T, et al. Consequences of medical hierarchy on medical students, residents, and medical education in otolaryngology. Otolaryngol Head Neck Surg. 2020;163:906-914.
- Lomis KD, Carpenter RO, Miller BM. Moral distress in the third year of medical school: a descriptive review of student case reflections. Am J Surg. 2009;197:107-112.
- Troughton R, Mariano V, Campbell A, et al. Understanding determinants of infection control practices in surgery: the role of shared ownership and team hierarchy. Antimicrob Resist Infect Control. 2019;8:116.
- Chiu PP, Hilliard RI, Azzie G, et al. Experience of moral distress among pediatric surgery trainees. J Pediatr Surg. 2008;43:986-993.
- Martinez W, Lo B. Medical students’ experiences with medical errors: an analysis of medical student essays. Med Educ. 2008;42:733-741.
- Chapter 1. opinions on patient-physician relationships. American Medical Association website. Accessed on August 9, 2022. https://www.ama-assn.org/system/files/code-of-medical-ethics-chapter-1.pdf
Resident Pearls
- Dermatology residents should not perform total-body skin examinations on or provide long-term care to attending physicians that directly oversee them.
- Residents should only provide care to their attending physicians if the attending’s life is in imminent danger from delay of treatment or if it is a self-limited, minor problem.
Applications for the CUTIS 2023 Resident Corner Column
The Cutis Editorial Board is now accepting applications for the 2023 Resident Corner column. The Editorial Board will select 2 to 3 residents to serve as the Resident Corner columnists for 1 year. Articles are posted online only at www.mdedge.com/dermatology but will be referenced in Index Medicus. All applicants must be current residents and will be in residency throughout 2023.
For consideration, send your curriculum vitae along with a brief (not to exceed 500 words) statement of why you enjoy Cutis and what you can offer your fellow residents in contributing a monthly column.
A signed letter of recommendation from the Director of the dermatology residency program also should be supplied.
All materials should be submitted via email to Melissa Sears ([email protected]) by October 28. The residents who are selected to write the column for the upcoming year will be notified by November 4.
We look forward to continuing to educate dermatology residents on topics that are most important to them!
The Cutis Editorial Board is now accepting applications for the 2023 Resident Corner column. The Editorial Board will select 2 to 3 residents to serve as the Resident Corner columnists for 1 year. Articles are posted online only at www.mdedge.com/dermatology but will be referenced in Index Medicus. All applicants must be current residents and will be in residency throughout 2023.
For consideration, send your curriculum vitae along with a brief (not to exceed 500 words) statement of why you enjoy Cutis and what you can offer your fellow residents in contributing a monthly column.
A signed letter of recommendation from the Director of the dermatology residency program also should be supplied.
All materials should be submitted via email to Melissa Sears ([email protected]) by October 28. The residents who are selected to write the column for the upcoming year will be notified by November 4.
We look forward to continuing to educate dermatology residents on topics that are most important to them!
The Cutis Editorial Board is now accepting applications for the 2023 Resident Corner column. The Editorial Board will select 2 to 3 residents to serve as the Resident Corner columnists for 1 year. Articles are posted online only at www.mdedge.com/dermatology but will be referenced in Index Medicus. All applicants must be current residents and will be in residency throughout 2023.
For consideration, send your curriculum vitae along with a brief (not to exceed 500 words) statement of why you enjoy Cutis and what you can offer your fellow residents in contributing a monthly column.
A signed letter of recommendation from the Director of the dermatology residency program also should be supplied.
All materials should be submitted via email to Melissa Sears ([email protected]) by October 28. The residents who are selected to write the column for the upcoming year will be notified by November 4.
We look forward to continuing to educate dermatology residents on topics that are most important to them!
Perceptions of Community Service in Dermatology Residency Training Programs: A Survey-Based Study of Program Directors, Residents, and Recent Dermatology Residency Graduates
Community service (CS) or service learning in dermatology (eg, free skin cancer screenings, providing care through free clinics, free teledermatology consultations) is instrumental in mitigating disparities and improving access to equitable dermatologic care. With the rate of underinsured and uninsured patients on the rise, free and federally qualified clinics frequently are the sole means by which patients access specialty care such as dermatology.1 Contributing to the economic gap in access, the geographic disparity of dermatologists in the United States continues to climb, and many marginalized communities remain without dermatologists.2 Nearly 30% of the total US population resides in geographic areas that are underserved by dermatologists, while there appears to be an oversupply of dermatologists in urban areas.3 Dermatologists practicing in rural areas make up only 10% of the dermatology workforce,4 whereas 40% of all dermatologists practice in the most densely populated US cities.5 Consequently, patients in these underserved communities face longer wait times6 and are less likely to utilize dermatology services than patients in dermatologist-dense geographic areas.7
Service opportunities have become increasingly integrated into graduate medical education.8 These service activities help bridge the health care access gap while fulfilling Accreditation Council of Graduate Medical Education (ACGME) requirements. Our study assessed the importance of CS to dermatology residency program directors (PDs), dermatology residents, and recent dermatology residency graduates. Herein, we describe the perceptions of CS within dermatology residency training among PDs and residents.
Methods
In this study, CS is defined as participation in activities to increase dermatologic access, education, and resources to underserved communities. Using the approved Association of Professors of Dermatology listserve and direct email communication, we surveyed 142 PDs of ACGME-accredited dermatology residency training programs. The deidentified respondents voluntarily completed a 17-question Qualtrics survey with a 5-point Likert scale (extremely, very, moderately, slightly, or not at all), yes/no/undecided, and qualitative responses.
We also surveyed current dermatology residents and recent graduates of ACGME-accredited dermatology residency programs via PDs nationwide. The deidentified respondents voluntarily completed a 19-question Qualtrics survey with a 5-point Likert scale (extremely, very, moderately, slightly, or not at all), yes/no/undecided, and qualitative responses.
Descriptive statistics were used for data analysis for both Qualtrics surveys. The University of Pittsburgh institutional review board deemed this study exempt.

Results
Feedback From PDs—Of the 142 PDs, we received 78 responses (54.9%). For selection of dermatology residents, CS was moderately to extremely important to 64 (82.1%) PDs, and 63 (80.8%) PDs stated CS was moderately to extremely important to their dermatology residency program at large. For dermatology residency training, 66 (84.6%) PDs believed CS is important, whereas 3 (3.8%) believed it is not important, and 9 (11.5%) remained undecided (Figure 1). Notably, 17 (21.8%) programs required CS as part of the dermatology educational curriculum, with most of these programs requiring 10 hours or less during the 3 years of residency training. Of the programs with required CS, 15 (88.2%) had dermatology-specific CS requirements, with 10 (58.8%) programs involved in CS at free and/or underserved clinics and some programs participating in other CS activities, such as advocacy, mentorship, educational outreach, or sports (Figure 2A).

Community service opportunities were offered to dermatology residents by 69 (88.5%) programs, including the 17 programs that required CS as part of the dermatology educational curriculum. Among these programs with optional CS, 43 (82.7%) PDs reported CS opportunities at free and/or underserved clinics, and 30 (57.7%) reported CS opportunities through global health initiatives (Figure 2B). Other CS opportunities offered included partnerships with community outreach organizations and mentoring underprivileged students. Patient populations that benefit from CS offered by these dermatology residency programs included 55 (79.7%) underserved, 33 (47.8%) minority, 31 (44.9%) immigrant, 14 (20.3%) pediatric, 14 (20.3%) elderly, and 10 (14.5%) rural populations (Figure 2C). At dermatology residency programs with optional CS opportunities, 22 (42.3%) PDs endorsed at least 50% of their residents participating in these activities.
Qualitative responses revealed that some PDs view CS as “a way for residents to stay connected to what drew them to medicine” and “essential to improving perceptions by physicians and patients about dermatology.” Program directors perceived lack of available time, initiative, and resources as well as minimal resident interest, malpractice coverage, and lack of educational opportunities as potential barriers to CS involvement by residents (Table). Forty-six (59.0%) PDs believed that CS should not be an ACGME requirement for dermatology training, 23 (29.5%) believed it should be required, and 9 (11.5%) were undecided.

Feedback From Residents—We received responses from 92 current dermatology residents and recent dermatology residency graduates; 86 (93.5%) respondents were trainees or recent graduates from academic dermatology residency training programs, and 6 (6.5%) were from community-based training programs. Community service was perceived to be an important part of dermatology training by 68 (73.9%) respondents, and dermatology-specific CS opportunities were available to 65 (70.7%) respondents (Figure 1). Although CS was required of only 7 (7.6%) respondents, 36 (39.1%) respondents volunteered at a free dermatology clinic during residency training. Among respondents who were not provided CS opportunities through their residency program, 23 (85.2%) stated they would have participated if given the opportunity.
Dermatology residents listed increased access to care for marginalized populations, increased sense of purpose, increased competence, and decreased burnout as perceived benefits of participation in CS. Of the dermatology residents who volunteered at a free dermatology clinic during training, 27 (75.0%) regarded the experience as a “high-yield learning opportunity.” Additionally, 29 (80.6%) residents stated their participation in a free dermatology clinic increased their awareness of health disparities and societal factors affecting dermatologic care in underserved patient populations. These respondents affirmed that their participation motivated them to become more involved in outreach targeting underserved populations throughout the duration of their careers.
Comment
The results of this nationwide survey have several important implications for dermatology residency programs, with a focus on programs in well-resourced and high socioeconomic status areas. Although most PDs believe that CS is important for dermatology resident training, few programs have CS requirements, and the majority are opposed to ACGME-mandated CS. Dermatology residents and recent graduates overwhelmingly conveyed that participation in a free dermatology clinic during residency training increased their knowledge base surrounding socioeconomic determinants of health and practicing in resource-limited settings. Furthermore, most trainees expressed that CS participation as a resident motivated them to continue to partake in CS for the underserved as an attending physician. The discordance between perceived value of CS by residents and the lack of CS requirements and opportunities by residency programs represents a realistic opportunity for residency training programs to integrate CS into the curriculum.
Residency programs that integrate service for the underserved into their program goals are 3 times more successful in graduating dermatology residents who practice in underserved communities.9 Patients in marginalized communities and those from lower socioeconomic backgrounds face many barriers to accessing dermatologic care including longer wait times and higher practice rejection rates than patients with private insurance.6 Through increased CS opportunities, dermatology residency programs can strengthen the local health care infrastructure and bridge the gap in access to dermatologic care.
By establishing a formal CS rotation in dermatology residency programs, residents will experience invaluable first-hand educational opportunities, provide comprehensive care for patients in resource-limited settings, and hopefully continue to serve in marginalized communities. Incorporating service for the underserved into the dermatology residency curriculum not only enhances the cultural competency of trainees but also mandates that skin health equity be made a priority. By exposing dermatology residents to the diverse patient populations often served by free clinics, residents will increase their knowledge of skin disease presentation in patients with darker skin tones, which has historically been deficient in medical education.10,11
The limitations of this survey study included recall bias, the response rate of PDs (54.9%), and the inability to determine response rate of residents, as we were unable to establish the total number of residents who received our survey. Based on geographic location, some dermatology residency programs may treat a high percentage of medically underserved patients, which already improves access to dermatology. For this reason, follow-up studies correlating PD and resident responses with region, program size, and university/community affiliation will increase our understanding of CS participation and perceptions.
Conclusion
Dermatology residency program participation in CS helps reduce barriers to access for patients in marginalized communities. Incorporating CS into the dermatology residency program curriculum creates a rewarding training environment that increases skin health equity, fosters an interest in health disparities, and enhances the cultural competency of its trainees.
- Buster KJ, Stevens EI, Elmets CA. Dermatologic health disparities. Dermatol Clin. 2012;30:53-59.
- Vaidya T, Zubritsky L, Alikhan A, et al. Socioeconomic and geographic barriers to dermatology care in urban and rural US populations. J Am Acad Dermatol. 2018;78:406-408.
- Suneja T, Smith ED, Chen GJ, et al. Waiting times to see a dermatologist are perceived as too long by dermatologists: implications for the dermatology workforce. Arch Dermatol. 2001;137:1303-1307.
- Resneck J, Kimball AB. The dermatology workforce shortage. J Am Acad Dermatol. 2004;50:50-54.
- Yoo JY, Rigel DS. Trends in dermatology: geographic density of US dermatologists. Arch Dermatol. 2010;146:779.
- Resneck J, Pletcher MJ, Lozano N. Medicare, Medicaid, and access to dermatologists: the effect of patient insurance on appointment access and wait times. J Am Acad Dermatol. 2004;50:85-92.
- Tripathi R, Knusel KD, Ezaldein HH, et al. Association of demographic and socioeconomic characteristics with differences in use of outpatient dermatology services in the United States. JAMA Dermatol. 2018;154:1286-1291.
- Vance MC, Kennedy KG. Developing an advocacy curriculum: lessons learned from a national survey of psychiatric residency programs. Acad Psychiatry. 2020;44:283-288.
- Blanco G, Vasquez R, Nezafati K, et al. How residency programs can foster practice for the underserved. J Am Acad Dermatol. 2012;67:158-159.
- Ebede T, Papier A. Disparities in dermatology educational resources.J Am Acad Dermatol. 2006;55:687-690.
- Nijhawan RI, Jacob SE, Woolery-Lloyd H. Skin of color education in dermatology residency programs: does residency training reflect the changing demographics of the United States? J Am Acad Dermatol. 2008;59:615-618.
Community service (CS) or service learning in dermatology (eg, free skin cancer screenings, providing care through free clinics, free teledermatology consultations) is instrumental in mitigating disparities and improving access to equitable dermatologic care. With the rate of underinsured and uninsured patients on the rise, free and federally qualified clinics frequently are the sole means by which patients access specialty care such as dermatology.1 Contributing to the economic gap in access, the geographic disparity of dermatologists in the United States continues to climb, and many marginalized communities remain without dermatologists.2 Nearly 30% of the total US population resides in geographic areas that are underserved by dermatologists, while there appears to be an oversupply of dermatologists in urban areas.3 Dermatologists practicing in rural areas make up only 10% of the dermatology workforce,4 whereas 40% of all dermatologists practice in the most densely populated US cities.5 Consequently, patients in these underserved communities face longer wait times6 and are less likely to utilize dermatology services than patients in dermatologist-dense geographic areas.7
Service opportunities have become increasingly integrated into graduate medical education.8 These service activities help bridge the health care access gap while fulfilling Accreditation Council of Graduate Medical Education (ACGME) requirements. Our study assessed the importance of CS to dermatology residency program directors (PDs), dermatology residents, and recent dermatology residency graduates. Herein, we describe the perceptions of CS within dermatology residency training among PDs and residents.
Methods
In this study, CS is defined as participation in activities to increase dermatologic access, education, and resources to underserved communities. Using the approved Association of Professors of Dermatology listserve and direct email communication, we surveyed 142 PDs of ACGME-accredited dermatology residency training programs. The deidentified respondents voluntarily completed a 17-question Qualtrics survey with a 5-point Likert scale (extremely, very, moderately, slightly, or not at all), yes/no/undecided, and qualitative responses.
We also surveyed current dermatology residents and recent graduates of ACGME-accredited dermatology residency programs via PDs nationwide. The deidentified respondents voluntarily completed a 19-question Qualtrics survey with a 5-point Likert scale (extremely, very, moderately, slightly, or not at all), yes/no/undecided, and qualitative responses.
Descriptive statistics were used for data analysis for both Qualtrics surveys. The University of Pittsburgh institutional review board deemed this study exempt.

Results
Feedback From PDs—Of the 142 PDs, we received 78 responses (54.9%). For selection of dermatology residents, CS was moderately to extremely important to 64 (82.1%) PDs, and 63 (80.8%) PDs stated CS was moderately to extremely important to their dermatology residency program at large. For dermatology residency training, 66 (84.6%) PDs believed CS is important, whereas 3 (3.8%) believed it is not important, and 9 (11.5%) remained undecided (Figure 1). Notably, 17 (21.8%) programs required CS as part of the dermatology educational curriculum, with most of these programs requiring 10 hours or less during the 3 years of residency training. Of the programs with required CS, 15 (88.2%) had dermatology-specific CS requirements, with 10 (58.8%) programs involved in CS at free and/or underserved clinics and some programs participating in other CS activities, such as advocacy, mentorship, educational outreach, or sports (Figure 2A).

Community service opportunities were offered to dermatology residents by 69 (88.5%) programs, including the 17 programs that required CS as part of the dermatology educational curriculum. Among these programs with optional CS, 43 (82.7%) PDs reported CS opportunities at free and/or underserved clinics, and 30 (57.7%) reported CS opportunities through global health initiatives (Figure 2B). Other CS opportunities offered included partnerships with community outreach organizations and mentoring underprivileged students. Patient populations that benefit from CS offered by these dermatology residency programs included 55 (79.7%) underserved, 33 (47.8%) minority, 31 (44.9%) immigrant, 14 (20.3%) pediatric, 14 (20.3%) elderly, and 10 (14.5%) rural populations (Figure 2C). At dermatology residency programs with optional CS opportunities, 22 (42.3%) PDs endorsed at least 50% of their residents participating in these activities.
Qualitative responses revealed that some PDs view CS as “a way for residents to stay connected to what drew them to medicine” and “essential to improving perceptions by physicians and patients about dermatology.” Program directors perceived lack of available time, initiative, and resources as well as minimal resident interest, malpractice coverage, and lack of educational opportunities as potential barriers to CS involvement by residents (Table). Forty-six (59.0%) PDs believed that CS should not be an ACGME requirement for dermatology training, 23 (29.5%) believed it should be required, and 9 (11.5%) were undecided.

Feedback From Residents—We received responses from 92 current dermatology residents and recent dermatology residency graduates; 86 (93.5%) respondents were trainees or recent graduates from academic dermatology residency training programs, and 6 (6.5%) were from community-based training programs. Community service was perceived to be an important part of dermatology training by 68 (73.9%) respondents, and dermatology-specific CS opportunities were available to 65 (70.7%) respondents (Figure 1). Although CS was required of only 7 (7.6%) respondents, 36 (39.1%) respondents volunteered at a free dermatology clinic during residency training. Among respondents who were not provided CS opportunities through their residency program, 23 (85.2%) stated they would have participated if given the opportunity.
Dermatology residents listed increased access to care for marginalized populations, increased sense of purpose, increased competence, and decreased burnout as perceived benefits of participation in CS. Of the dermatology residents who volunteered at a free dermatology clinic during training, 27 (75.0%) regarded the experience as a “high-yield learning opportunity.” Additionally, 29 (80.6%) residents stated their participation in a free dermatology clinic increased their awareness of health disparities and societal factors affecting dermatologic care in underserved patient populations. These respondents affirmed that their participation motivated them to become more involved in outreach targeting underserved populations throughout the duration of their careers.
Comment
The results of this nationwide survey have several important implications for dermatology residency programs, with a focus on programs in well-resourced and high socioeconomic status areas. Although most PDs believe that CS is important for dermatology resident training, few programs have CS requirements, and the majority are opposed to ACGME-mandated CS. Dermatology residents and recent graduates overwhelmingly conveyed that participation in a free dermatology clinic during residency training increased their knowledge base surrounding socioeconomic determinants of health and practicing in resource-limited settings. Furthermore, most trainees expressed that CS participation as a resident motivated them to continue to partake in CS for the underserved as an attending physician. The discordance between perceived value of CS by residents and the lack of CS requirements and opportunities by residency programs represents a realistic opportunity for residency training programs to integrate CS into the curriculum.
Residency programs that integrate service for the underserved into their program goals are 3 times more successful in graduating dermatology residents who practice in underserved communities.9 Patients in marginalized communities and those from lower socioeconomic backgrounds face many barriers to accessing dermatologic care including longer wait times and higher practice rejection rates than patients with private insurance.6 Through increased CS opportunities, dermatology residency programs can strengthen the local health care infrastructure and bridge the gap in access to dermatologic care.
By establishing a formal CS rotation in dermatology residency programs, residents will experience invaluable first-hand educational opportunities, provide comprehensive care for patients in resource-limited settings, and hopefully continue to serve in marginalized communities. Incorporating service for the underserved into the dermatology residency curriculum not only enhances the cultural competency of trainees but also mandates that skin health equity be made a priority. By exposing dermatology residents to the diverse patient populations often served by free clinics, residents will increase their knowledge of skin disease presentation in patients with darker skin tones, which has historically been deficient in medical education.10,11
The limitations of this survey study included recall bias, the response rate of PDs (54.9%), and the inability to determine response rate of residents, as we were unable to establish the total number of residents who received our survey. Based on geographic location, some dermatology residency programs may treat a high percentage of medically underserved patients, which already improves access to dermatology. For this reason, follow-up studies correlating PD and resident responses with region, program size, and university/community affiliation will increase our understanding of CS participation and perceptions.
Conclusion
Dermatology residency program participation in CS helps reduce barriers to access for patients in marginalized communities. Incorporating CS into the dermatology residency program curriculum creates a rewarding training environment that increases skin health equity, fosters an interest in health disparities, and enhances the cultural competency of its trainees.
Community service (CS) or service learning in dermatology (eg, free skin cancer screenings, providing care through free clinics, free teledermatology consultations) is instrumental in mitigating disparities and improving access to equitable dermatologic care. With the rate of underinsured and uninsured patients on the rise, free and federally qualified clinics frequently are the sole means by which patients access specialty care such as dermatology.1 Contributing to the economic gap in access, the geographic disparity of dermatologists in the United States continues to climb, and many marginalized communities remain without dermatologists.2 Nearly 30% of the total US population resides in geographic areas that are underserved by dermatologists, while there appears to be an oversupply of dermatologists in urban areas.3 Dermatologists practicing in rural areas make up only 10% of the dermatology workforce,4 whereas 40% of all dermatologists practice in the most densely populated US cities.5 Consequently, patients in these underserved communities face longer wait times6 and are less likely to utilize dermatology services than patients in dermatologist-dense geographic areas.7
Service opportunities have become increasingly integrated into graduate medical education.8 These service activities help bridge the health care access gap while fulfilling Accreditation Council of Graduate Medical Education (ACGME) requirements. Our study assessed the importance of CS to dermatology residency program directors (PDs), dermatology residents, and recent dermatology residency graduates. Herein, we describe the perceptions of CS within dermatology residency training among PDs and residents.
Methods
In this study, CS is defined as participation in activities to increase dermatologic access, education, and resources to underserved communities. Using the approved Association of Professors of Dermatology listserve and direct email communication, we surveyed 142 PDs of ACGME-accredited dermatology residency training programs. The deidentified respondents voluntarily completed a 17-question Qualtrics survey with a 5-point Likert scale (extremely, very, moderately, slightly, or not at all), yes/no/undecided, and qualitative responses.
We also surveyed current dermatology residents and recent graduates of ACGME-accredited dermatology residency programs via PDs nationwide. The deidentified respondents voluntarily completed a 19-question Qualtrics survey with a 5-point Likert scale (extremely, very, moderately, slightly, or not at all), yes/no/undecided, and qualitative responses.
Descriptive statistics were used for data analysis for both Qualtrics surveys. The University of Pittsburgh institutional review board deemed this study exempt.

Results
Feedback From PDs—Of the 142 PDs, we received 78 responses (54.9%). For selection of dermatology residents, CS was moderately to extremely important to 64 (82.1%) PDs, and 63 (80.8%) PDs stated CS was moderately to extremely important to their dermatology residency program at large. For dermatology residency training, 66 (84.6%) PDs believed CS is important, whereas 3 (3.8%) believed it is not important, and 9 (11.5%) remained undecided (Figure 1). Notably, 17 (21.8%) programs required CS as part of the dermatology educational curriculum, with most of these programs requiring 10 hours or less during the 3 years of residency training. Of the programs with required CS, 15 (88.2%) had dermatology-specific CS requirements, with 10 (58.8%) programs involved in CS at free and/or underserved clinics and some programs participating in other CS activities, such as advocacy, mentorship, educational outreach, or sports (Figure 2A).

Community service opportunities were offered to dermatology residents by 69 (88.5%) programs, including the 17 programs that required CS as part of the dermatology educational curriculum. Among these programs with optional CS, 43 (82.7%) PDs reported CS opportunities at free and/or underserved clinics, and 30 (57.7%) reported CS opportunities through global health initiatives (Figure 2B). Other CS opportunities offered included partnerships with community outreach organizations and mentoring underprivileged students. Patient populations that benefit from CS offered by these dermatology residency programs included 55 (79.7%) underserved, 33 (47.8%) minority, 31 (44.9%) immigrant, 14 (20.3%) pediatric, 14 (20.3%) elderly, and 10 (14.5%) rural populations (Figure 2C). At dermatology residency programs with optional CS opportunities, 22 (42.3%) PDs endorsed at least 50% of their residents participating in these activities.
Qualitative responses revealed that some PDs view CS as “a way for residents to stay connected to what drew them to medicine” and “essential to improving perceptions by physicians and patients about dermatology.” Program directors perceived lack of available time, initiative, and resources as well as minimal resident interest, malpractice coverage, and lack of educational opportunities as potential barriers to CS involvement by residents (Table). Forty-six (59.0%) PDs believed that CS should not be an ACGME requirement for dermatology training, 23 (29.5%) believed it should be required, and 9 (11.5%) were undecided.

Feedback From Residents—We received responses from 92 current dermatology residents and recent dermatology residency graduates; 86 (93.5%) respondents were trainees or recent graduates from academic dermatology residency training programs, and 6 (6.5%) were from community-based training programs. Community service was perceived to be an important part of dermatology training by 68 (73.9%) respondents, and dermatology-specific CS opportunities were available to 65 (70.7%) respondents (Figure 1). Although CS was required of only 7 (7.6%) respondents, 36 (39.1%) respondents volunteered at a free dermatology clinic during residency training. Among respondents who were not provided CS opportunities through their residency program, 23 (85.2%) stated they would have participated if given the opportunity.
Dermatology residents listed increased access to care for marginalized populations, increased sense of purpose, increased competence, and decreased burnout as perceived benefits of participation in CS. Of the dermatology residents who volunteered at a free dermatology clinic during training, 27 (75.0%) regarded the experience as a “high-yield learning opportunity.” Additionally, 29 (80.6%) residents stated their participation in a free dermatology clinic increased their awareness of health disparities and societal factors affecting dermatologic care in underserved patient populations. These respondents affirmed that their participation motivated them to become more involved in outreach targeting underserved populations throughout the duration of their careers.
Comment
The results of this nationwide survey have several important implications for dermatology residency programs, with a focus on programs in well-resourced and high socioeconomic status areas. Although most PDs believe that CS is important for dermatology resident training, few programs have CS requirements, and the majority are opposed to ACGME-mandated CS. Dermatology residents and recent graduates overwhelmingly conveyed that participation in a free dermatology clinic during residency training increased their knowledge base surrounding socioeconomic determinants of health and practicing in resource-limited settings. Furthermore, most trainees expressed that CS participation as a resident motivated them to continue to partake in CS for the underserved as an attending physician. The discordance between perceived value of CS by residents and the lack of CS requirements and opportunities by residency programs represents a realistic opportunity for residency training programs to integrate CS into the curriculum.
Residency programs that integrate service for the underserved into their program goals are 3 times more successful in graduating dermatology residents who practice in underserved communities.9 Patients in marginalized communities and those from lower socioeconomic backgrounds face many barriers to accessing dermatologic care including longer wait times and higher practice rejection rates than patients with private insurance.6 Through increased CS opportunities, dermatology residency programs can strengthen the local health care infrastructure and bridge the gap in access to dermatologic care.
By establishing a formal CS rotation in dermatology residency programs, residents will experience invaluable first-hand educational opportunities, provide comprehensive care for patients in resource-limited settings, and hopefully continue to serve in marginalized communities. Incorporating service for the underserved into the dermatology residency curriculum not only enhances the cultural competency of trainees but also mandates that skin health equity be made a priority. By exposing dermatology residents to the diverse patient populations often served by free clinics, residents will increase their knowledge of skin disease presentation in patients with darker skin tones, which has historically been deficient in medical education.10,11
The limitations of this survey study included recall bias, the response rate of PDs (54.9%), and the inability to determine response rate of residents, as we were unable to establish the total number of residents who received our survey. Based on geographic location, some dermatology residency programs may treat a high percentage of medically underserved patients, which already improves access to dermatology. For this reason, follow-up studies correlating PD and resident responses with region, program size, and university/community affiliation will increase our understanding of CS participation and perceptions.
Conclusion
Dermatology residency program participation in CS helps reduce barriers to access for patients in marginalized communities. Incorporating CS into the dermatology residency program curriculum creates a rewarding training environment that increases skin health equity, fosters an interest in health disparities, and enhances the cultural competency of its trainees.
- Buster KJ, Stevens EI, Elmets CA. Dermatologic health disparities. Dermatol Clin. 2012;30:53-59.
- Vaidya T, Zubritsky L, Alikhan A, et al. Socioeconomic and geographic barriers to dermatology care in urban and rural US populations. J Am Acad Dermatol. 2018;78:406-408.
- Suneja T, Smith ED, Chen GJ, et al. Waiting times to see a dermatologist are perceived as too long by dermatologists: implications for the dermatology workforce. Arch Dermatol. 2001;137:1303-1307.
- Resneck J, Kimball AB. The dermatology workforce shortage. J Am Acad Dermatol. 2004;50:50-54.
- Yoo JY, Rigel DS. Trends in dermatology: geographic density of US dermatologists. Arch Dermatol. 2010;146:779.
- Resneck J, Pletcher MJ, Lozano N. Medicare, Medicaid, and access to dermatologists: the effect of patient insurance on appointment access and wait times. J Am Acad Dermatol. 2004;50:85-92.
- Tripathi R, Knusel KD, Ezaldein HH, et al. Association of demographic and socioeconomic characteristics with differences in use of outpatient dermatology services in the United States. JAMA Dermatol. 2018;154:1286-1291.
- Vance MC, Kennedy KG. Developing an advocacy curriculum: lessons learned from a national survey of psychiatric residency programs. Acad Psychiatry. 2020;44:283-288.
- Blanco G, Vasquez R, Nezafati K, et al. How residency programs can foster practice for the underserved. J Am Acad Dermatol. 2012;67:158-159.
- Ebede T, Papier A. Disparities in dermatology educational resources.J Am Acad Dermatol. 2006;55:687-690.
- Nijhawan RI, Jacob SE, Woolery-Lloyd H. Skin of color education in dermatology residency programs: does residency training reflect the changing demographics of the United States? J Am Acad Dermatol. 2008;59:615-618.
- Buster KJ, Stevens EI, Elmets CA. Dermatologic health disparities. Dermatol Clin. 2012;30:53-59.
- Vaidya T, Zubritsky L, Alikhan A, et al. Socioeconomic and geographic barriers to dermatology care in urban and rural US populations. J Am Acad Dermatol. 2018;78:406-408.
- Suneja T, Smith ED, Chen GJ, et al. Waiting times to see a dermatologist are perceived as too long by dermatologists: implications for the dermatology workforce. Arch Dermatol. 2001;137:1303-1307.
- Resneck J, Kimball AB. The dermatology workforce shortage. J Am Acad Dermatol. 2004;50:50-54.
- Yoo JY, Rigel DS. Trends in dermatology: geographic density of US dermatologists. Arch Dermatol. 2010;146:779.
- Resneck J, Pletcher MJ, Lozano N. Medicare, Medicaid, and access to dermatologists: the effect of patient insurance on appointment access and wait times. J Am Acad Dermatol. 2004;50:85-92.
- Tripathi R, Knusel KD, Ezaldein HH, et al. Association of demographic and socioeconomic characteristics with differences in use of outpatient dermatology services in the United States. JAMA Dermatol. 2018;154:1286-1291.
- Vance MC, Kennedy KG. Developing an advocacy curriculum: lessons learned from a national survey of psychiatric residency programs. Acad Psychiatry. 2020;44:283-288.
- Blanco G, Vasquez R, Nezafati K, et al. How residency programs can foster practice for the underserved. J Am Acad Dermatol. 2012;67:158-159.
- Ebede T, Papier A. Disparities in dermatology educational resources.J Am Acad Dermatol. 2006;55:687-690.
- Nijhawan RI, Jacob SE, Woolery-Lloyd H. Skin of color education in dermatology residency programs: does residency training reflect the changing demographics of the United States? J Am Acad Dermatol. 2008;59:615-618.
Practice Points
- Participation of dermatology residents in service-learning experiences increases awareness of health disparities and social factors impacting dermatologic care and promotes a lifelong commitment to serving vulnerable populations.
- Integrating service learning into the dermatology residency program curriculum enhances trainees’ cultural sensitivity and encourages the prioritization of skin health equity.
- Service learning will help bridge the gap in access to dermatologic care for patients in medically marginalized communities.
Nail Salon Safety: From Nail Dystrophy to Acrylate Contact Allergies
As residents, it is important to understand the steps of the manicuring process and be able to inform patients on how to maintain optimal nail health while continuing to go to nail salons. Most patients are not aware of the possible allergic, traumatic, and/or infectious complications of manicuring their nails. There are practical steps that can be taken to prevent nail issues, such as avoiding cutting one’s cuticles or using allergen-free nail polishes. These simple fixes can make a big difference in long-term nail health in our patients.
Nail Polish Application Process
The nails are first soaked in a warm soapy solution to soften the nail plate and cuticles.1 Then the nail tips and plates are filed and occasionally are smoothed with a drill. The cuticles are cut with a cuticle cutter. Nail polish—base coat, color enamel, and top coat—is then applied to the nail. Acrylic or sculptured nails and gel and dip manicures are composed of chemical monomers and polymers that harden either at room temperature or through UV or light-emitting diode (LED) exposure. The chemicals in these products can damage nails and cause allergic reactions.
Contact Dermatitis
Approximately 2% of individuals have been found to have allergic or irritant contact dermatitis to nail care products. The top 5 allergens implicated in nail products are (1) 2-hydroxyethyl methacrylate, (2) methyl methacrylate, (3) ethyl acrylate, (4) ethyl-2-cyanoacrylate, and (5) tosylamide.2 Methyl methacrylate was banned in 1974 by the US Food and Drug Administration due to reports of severe contact dermatitis, paronychia, and nail dystrophy.3 Due to their potent sensitizing effects, acrylates were named the contact allergen of the year in 2012 by the American Contact Dermatitis Society.3
Acrylates are plastic products formed by polymerization of acrylic or methacrylic acid.4 Artificial sculptured nails are created by mixing powdered polymethyl methacrylate polymers and liquid ethyl or isobutyl methacrylate monomers and then applying this mixture to the nail plate.5 Gel and powder nails employ a mixture that is similar to acrylic powders, which require UV or LED radiation to polymerize and harden on the nail plate.
Tosylamide, or tosylamide formaldehyde resin, is another potent allergen that promotes adhesion of the enamel to the nail.6 It is important to note that sensitization may develop months to years after using artificial nails.
Clinical features of contact allergy secondary to nail polish can vary. Some patients experience severe periungual dermatitis. Others can present with facial or eyelid dermatitis due to exposure to airborne particles of acrylates or from contact with fingertips bearing acrylic nails.6,7 If inhaled, acrylates also can cause wheezing asthma or allergic rhinoconjunctivitis.
Common Onychodystrophies
Damage to the natural nail plate is inevitable with continued wear of sculptured nails. With 2 to 4 months of consecutive wear, the natural nails turn yellow, brittle, and weak.5 One study noted that the thickness of an individual’s left thumb nail plate thinned from 0.059 cm to 0.03 cm after a gel manicure was removed from the nail.8 Nail injuries due to manicuring include keratin granulations, onycholysis, pincer nail deformities, pseudopsoriatic nails, lamellar onychoschizia, transverse leukonychia, and ingrown nails.6 One interesting nail dystrophy reported secondary to gel manicures is pterygium inversum unguis or a ventral pterygium that causes an abnormal painful adherence of the hyponychium to the ventral surface of the nail plate. Patients prone to developing pterygium inversum unguis can experience sensitivity, pain, or burning sensations during LED or UVA light exposure.9
Infections
In addition to contact allergies and nail dystrophies, each step of the manicuring process, such as cutting cuticles, presents opportunities for infectious agents to enter the nail fold. Acute or chronic paronychia, or inflammation of the nail fold, most commonly is caused by bacterial infections with Staphylococcus aureus. Green nail syndrome caused by Pseudomonas aeruginosa also is common.1 Onychomycosis due to Trichophyton rubrum is one of the most frequent fungal infections contracted at nail salons. Mycobacteria such as Mycobacterium fortuitum also have been implicated in infections from salons, as they can be found in the jets of pedicure spas, which are not sanitized regularly.10
Final Thoughts
Nail cosmetics are an integral part of many patients’ lives. Being able to educate yourself and your patients on the hazards of nail salons can help them avoid painful infections, contact allergies, and acute to chronic nail deformities. It is important for residents to be aware of the different dermatoses that can arise in men and women who frequent nail salons as the popularity of the nail beauty industry continues to rise.
- Reinecke JK, Hinshaw MA. Nail health in women. Int J Womens Dermatol. 2020;6:73-79. doi:10.1016/j.ijwd.2020.01.006
- Warshaw EM, Voller LM, Silverberg JI, et al. Contact dermatitis associated with nail care products: retrospective analysis of North American Contact Dermatitis Group data, 2001-2016. Dermatitis. 2020;31:191-201. doi:10.1097/DER.0000000000000583
- Militello M, Hu S, Laughter M, et al. American Contact Dermatitis Society allergens of the year 2000 to 2020 [published online April 25, 2020]. Dermatol Clin. 2020;38:309-320. doi:10.1016/j.det.2020.02.011
- Kucharczyk M, Słowik-Rylska M, Cyran-Stemplewska S, et al. Acrylates as a significant cause of allergic contact dermatitis: new sources of exposure. Postepy Dermatol Alergol. 2021;38:555-560. doi:10.5114/ada.2020.95848
- Draelos ZD. Cosmetics and cosmeceuticals. In: Bolognia J, Schaffer JV, Cerroni L, eds. Dermatology. 4th ed. Elsevier; 2018:2587-2588.
- Iorizzo M, Piraccini BM, Tosti A. Nail cosmetics in nail disorders.J Cosmet Dermatol. 2007;6:53-58. doi:10.1111/j.1473-2165.2007.00290.x
- Maio P, Carvalho R, Amaro C, et al. Letter: allergic contact dermatitis from sculptured acrylic nails: special presentation with a possible airborne pattern. Dermatol Online J. 2012;18:13.
- Chen AF, Chimento SM, Hu S, et al. Nail damage from gel polish manicure. J Cosmet Dermatol. 2012;11:27-29. doi:10.1111/j.1473-2165.2011.00595.x
- Cervantes J, Sanchez M, Eber AE, et al. Pterygium inversum unguis secondary to gel polish [published online October 16, 2017]. J Eur Acad Dermatol Venereol. 2018;32:160-163. doi:10.1111/jdv.14603
- Vugia DJ, Jang Y, Zizek C, et al. Mycobacteria in nail salon whirlpool footbaths, California. Emerg Infect Dis. 2005;11:616-618. doi:10.3201/eid1104.040936
As residents, it is important to understand the steps of the manicuring process and be able to inform patients on how to maintain optimal nail health while continuing to go to nail salons. Most patients are not aware of the possible allergic, traumatic, and/or infectious complications of manicuring their nails. There are practical steps that can be taken to prevent nail issues, such as avoiding cutting one’s cuticles or using allergen-free nail polishes. These simple fixes can make a big difference in long-term nail health in our patients.
Nail Polish Application Process
The nails are first soaked in a warm soapy solution to soften the nail plate and cuticles.1 Then the nail tips and plates are filed and occasionally are smoothed with a drill. The cuticles are cut with a cuticle cutter. Nail polish—base coat, color enamel, and top coat—is then applied to the nail. Acrylic or sculptured nails and gel and dip manicures are composed of chemical monomers and polymers that harden either at room temperature or through UV or light-emitting diode (LED) exposure. The chemicals in these products can damage nails and cause allergic reactions.
Contact Dermatitis
Approximately 2% of individuals have been found to have allergic or irritant contact dermatitis to nail care products. The top 5 allergens implicated in nail products are (1) 2-hydroxyethyl methacrylate, (2) methyl methacrylate, (3) ethyl acrylate, (4) ethyl-2-cyanoacrylate, and (5) tosylamide.2 Methyl methacrylate was banned in 1974 by the US Food and Drug Administration due to reports of severe contact dermatitis, paronychia, and nail dystrophy.3 Due to their potent sensitizing effects, acrylates were named the contact allergen of the year in 2012 by the American Contact Dermatitis Society.3
Acrylates are plastic products formed by polymerization of acrylic or methacrylic acid.4 Artificial sculptured nails are created by mixing powdered polymethyl methacrylate polymers and liquid ethyl or isobutyl methacrylate monomers and then applying this mixture to the nail plate.5 Gel and powder nails employ a mixture that is similar to acrylic powders, which require UV or LED radiation to polymerize and harden on the nail plate.
Tosylamide, or tosylamide formaldehyde resin, is another potent allergen that promotes adhesion of the enamel to the nail.6 It is important to note that sensitization may develop months to years after using artificial nails.
Clinical features of contact allergy secondary to nail polish can vary. Some patients experience severe periungual dermatitis. Others can present with facial or eyelid dermatitis due to exposure to airborne particles of acrylates or from contact with fingertips bearing acrylic nails.6,7 If inhaled, acrylates also can cause wheezing asthma or allergic rhinoconjunctivitis.
Common Onychodystrophies
Damage to the natural nail plate is inevitable with continued wear of sculptured nails. With 2 to 4 months of consecutive wear, the natural nails turn yellow, brittle, and weak.5 One study noted that the thickness of an individual’s left thumb nail plate thinned from 0.059 cm to 0.03 cm after a gel manicure was removed from the nail.8 Nail injuries due to manicuring include keratin granulations, onycholysis, pincer nail deformities, pseudopsoriatic nails, lamellar onychoschizia, transverse leukonychia, and ingrown nails.6 One interesting nail dystrophy reported secondary to gel manicures is pterygium inversum unguis or a ventral pterygium that causes an abnormal painful adherence of the hyponychium to the ventral surface of the nail plate. Patients prone to developing pterygium inversum unguis can experience sensitivity, pain, or burning sensations during LED or UVA light exposure.9
Infections
In addition to contact allergies and nail dystrophies, each step of the manicuring process, such as cutting cuticles, presents opportunities for infectious agents to enter the nail fold. Acute or chronic paronychia, or inflammation of the nail fold, most commonly is caused by bacterial infections with Staphylococcus aureus. Green nail syndrome caused by Pseudomonas aeruginosa also is common.1 Onychomycosis due to Trichophyton rubrum is one of the most frequent fungal infections contracted at nail salons. Mycobacteria such as Mycobacterium fortuitum also have been implicated in infections from salons, as they can be found in the jets of pedicure spas, which are not sanitized regularly.10
Final Thoughts
Nail cosmetics are an integral part of many patients’ lives. Being able to educate yourself and your patients on the hazards of nail salons can help them avoid painful infections, contact allergies, and acute to chronic nail deformities. It is important for residents to be aware of the different dermatoses that can arise in men and women who frequent nail salons as the popularity of the nail beauty industry continues to rise.
As residents, it is important to understand the steps of the manicuring process and be able to inform patients on how to maintain optimal nail health while continuing to go to nail salons. Most patients are not aware of the possible allergic, traumatic, and/or infectious complications of manicuring their nails. There are practical steps that can be taken to prevent nail issues, such as avoiding cutting one’s cuticles or using allergen-free nail polishes. These simple fixes can make a big difference in long-term nail health in our patients.
Nail Polish Application Process
The nails are first soaked in a warm soapy solution to soften the nail plate and cuticles.1 Then the nail tips and plates are filed and occasionally are smoothed with a drill. The cuticles are cut with a cuticle cutter. Nail polish—base coat, color enamel, and top coat—is then applied to the nail. Acrylic or sculptured nails and gel and dip manicures are composed of chemical monomers and polymers that harden either at room temperature or through UV or light-emitting diode (LED) exposure. The chemicals in these products can damage nails and cause allergic reactions.
Contact Dermatitis
Approximately 2% of individuals have been found to have allergic or irritant contact dermatitis to nail care products. The top 5 allergens implicated in nail products are (1) 2-hydroxyethyl methacrylate, (2) methyl methacrylate, (3) ethyl acrylate, (4) ethyl-2-cyanoacrylate, and (5) tosylamide.2 Methyl methacrylate was banned in 1974 by the US Food and Drug Administration due to reports of severe contact dermatitis, paronychia, and nail dystrophy.3 Due to their potent sensitizing effects, acrylates were named the contact allergen of the year in 2012 by the American Contact Dermatitis Society.3
Acrylates are plastic products formed by polymerization of acrylic or methacrylic acid.4 Artificial sculptured nails are created by mixing powdered polymethyl methacrylate polymers and liquid ethyl or isobutyl methacrylate monomers and then applying this mixture to the nail plate.5 Gel and powder nails employ a mixture that is similar to acrylic powders, which require UV or LED radiation to polymerize and harden on the nail plate.
Tosylamide, or tosylamide formaldehyde resin, is another potent allergen that promotes adhesion of the enamel to the nail.6 It is important to note that sensitization may develop months to years after using artificial nails.
Clinical features of contact allergy secondary to nail polish can vary. Some patients experience severe periungual dermatitis. Others can present with facial or eyelid dermatitis due to exposure to airborne particles of acrylates or from contact with fingertips bearing acrylic nails.6,7 If inhaled, acrylates also can cause wheezing asthma or allergic rhinoconjunctivitis.
Common Onychodystrophies
Damage to the natural nail plate is inevitable with continued wear of sculptured nails. With 2 to 4 months of consecutive wear, the natural nails turn yellow, brittle, and weak.5 One study noted that the thickness of an individual’s left thumb nail plate thinned from 0.059 cm to 0.03 cm after a gel manicure was removed from the nail.8 Nail injuries due to manicuring include keratin granulations, onycholysis, pincer nail deformities, pseudopsoriatic nails, lamellar onychoschizia, transverse leukonychia, and ingrown nails.6 One interesting nail dystrophy reported secondary to gel manicures is pterygium inversum unguis or a ventral pterygium that causes an abnormal painful adherence of the hyponychium to the ventral surface of the nail plate. Patients prone to developing pterygium inversum unguis can experience sensitivity, pain, or burning sensations during LED or UVA light exposure.9
Infections
In addition to contact allergies and nail dystrophies, each step of the manicuring process, such as cutting cuticles, presents opportunities for infectious agents to enter the nail fold. Acute or chronic paronychia, or inflammation of the nail fold, most commonly is caused by bacterial infections with Staphylococcus aureus. Green nail syndrome caused by Pseudomonas aeruginosa also is common.1 Onychomycosis due to Trichophyton rubrum is one of the most frequent fungal infections contracted at nail salons. Mycobacteria such as Mycobacterium fortuitum also have been implicated in infections from salons, as they can be found in the jets of pedicure spas, which are not sanitized regularly.10
Final Thoughts
Nail cosmetics are an integral part of many patients’ lives. Being able to educate yourself and your patients on the hazards of nail salons can help them avoid painful infections, contact allergies, and acute to chronic nail deformities. It is important for residents to be aware of the different dermatoses that can arise in men and women who frequent nail salons as the popularity of the nail beauty industry continues to rise.
- Reinecke JK, Hinshaw MA. Nail health in women. Int J Womens Dermatol. 2020;6:73-79. doi:10.1016/j.ijwd.2020.01.006
- Warshaw EM, Voller LM, Silverberg JI, et al. Contact dermatitis associated with nail care products: retrospective analysis of North American Contact Dermatitis Group data, 2001-2016. Dermatitis. 2020;31:191-201. doi:10.1097/DER.0000000000000583
- Militello M, Hu S, Laughter M, et al. American Contact Dermatitis Society allergens of the year 2000 to 2020 [published online April 25, 2020]. Dermatol Clin. 2020;38:309-320. doi:10.1016/j.det.2020.02.011
- Kucharczyk M, Słowik-Rylska M, Cyran-Stemplewska S, et al. Acrylates as a significant cause of allergic contact dermatitis: new sources of exposure. Postepy Dermatol Alergol. 2021;38:555-560. doi:10.5114/ada.2020.95848
- Draelos ZD. Cosmetics and cosmeceuticals. In: Bolognia J, Schaffer JV, Cerroni L, eds. Dermatology. 4th ed. Elsevier; 2018:2587-2588.
- Iorizzo M, Piraccini BM, Tosti A. Nail cosmetics in nail disorders.J Cosmet Dermatol. 2007;6:53-58. doi:10.1111/j.1473-2165.2007.00290.x
- Maio P, Carvalho R, Amaro C, et al. Letter: allergic contact dermatitis from sculptured acrylic nails: special presentation with a possible airborne pattern. Dermatol Online J. 2012;18:13.
- Chen AF, Chimento SM, Hu S, et al. Nail damage from gel polish manicure. J Cosmet Dermatol. 2012;11:27-29. doi:10.1111/j.1473-2165.2011.00595.x
- Cervantes J, Sanchez M, Eber AE, et al. Pterygium inversum unguis secondary to gel polish [published online October 16, 2017]. J Eur Acad Dermatol Venereol. 2018;32:160-163. doi:10.1111/jdv.14603
- Vugia DJ, Jang Y, Zizek C, et al. Mycobacteria in nail salon whirlpool footbaths, California. Emerg Infect Dis. 2005;11:616-618. doi:10.3201/eid1104.040936
- Reinecke JK, Hinshaw MA. Nail health in women. Int J Womens Dermatol. 2020;6:73-79. doi:10.1016/j.ijwd.2020.01.006
- Warshaw EM, Voller LM, Silverberg JI, et al. Contact dermatitis associated with nail care products: retrospective analysis of North American Contact Dermatitis Group data, 2001-2016. Dermatitis. 2020;31:191-201. doi:10.1097/DER.0000000000000583
- Militello M, Hu S, Laughter M, et al. American Contact Dermatitis Society allergens of the year 2000 to 2020 [published online April 25, 2020]. Dermatol Clin. 2020;38:309-320. doi:10.1016/j.det.2020.02.011
- Kucharczyk M, Słowik-Rylska M, Cyran-Stemplewska S, et al. Acrylates as a significant cause of allergic contact dermatitis: new sources of exposure. Postepy Dermatol Alergol. 2021;38:555-560. doi:10.5114/ada.2020.95848
- Draelos ZD. Cosmetics and cosmeceuticals. In: Bolognia J, Schaffer JV, Cerroni L, eds. Dermatology. 4th ed. Elsevier; 2018:2587-2588.
- Iorizzo M, Piraccini BM, Tosti A. Nail cosmetics in nail disorders.J Cosmet Dermatol. 2007;6:53-58. doi:10.1111/j.1473-2165.2007.00290.x
- Maio P, Carvalho R, Amaro C, et al. Letter: allergic contact dermatitis from sculptured acrylic nails: special presentation with a possible airborne pattern. Dermatol Online J. 2012;18:13.
- Chen AF, Chimento SM, Hu S, et al. Nail damage from gel polish manicure. J Cosmet Dermatol. 2012;11:27-29. doi:10.1111/j.1473-2165.2011.00595.x
- Cervantes J, Sanchez M, Eber AE, et al. Pterygium inversum unguis secondary to gel polish [published online October 16, 2017]. J Eur Acad Dermatol Venereol. 2018;32:160-163. doi:10.1111/jdv.14603
- Vugia DJ, Jang Y, Zizek C, et al. Mycobacteria in nail salon whirlpool footbaths, California. Emerg Infect Dis. 2005;11:616-618. doi:10.3201/eid1104.040936
Resident Pearls
- Every step of the nail manicuring process presents opportunities for nail trauma, infections, and contact dermatitis.
- As residents, it is important to be aware of the hazards associated with nail salons and educate our patients accordingly.
- Nail health is essential to optimizing everyday work for our patients—whether it entails taking care of children, typing, or other hands-on activities.
The impact of COVID-19 on adolescents’ mental health
While the COVID-19 pandemic has impacted the mental health of a wide range of individuals, its adverse effects have been particularly detrimental to adolescents. In this article, I discuss evidence that shows the effects of the pandemic on adolescent patients, potential reasons for this increased distress, and what types of coping mechanisms adolescents have used to counter these effects.
Increases in multiple measures of psychopathology
Multiple online surveys and other studies have documented the pandemic’s impact on younger individuals. In the United States, visits to emergency departments by pediatric patients increased in the months after the first lockdown period.1 Several studies found increased rates of anxiety and depression among adolescents during the COVID-19 pandemic.2,3 In an online survey of 359 children and 3,254 adolescents in China, 22% of respondents reported that they experienced depressive symptoms.3 In an online survey of 1,054 Canadian adolescents, 43% said they were “very concerned” about the pandemic.4 In an online survey of 7,353 adolescents in the United States, 37% reported suicidal ideation during the pandemic compared to 17% in 2017.5 A Chinese study found that smartphone and internet addiction was significantly associated with increased levels of depressive symptoms during the pandemic.3 In a survey in the Philippines, 16.3% of adolescents reported moderate-to-severe psychological impairment during the pandemic; the rates of COVID-19–related anxiety were higher among girls vs boys.6 Alcohol and cannabis use increased among Canadian adolescents during the pandemic, according to an online survey.7 Adolescents with anorexia nervosa reported a 70% increase in poor eating habits and more thoughts associated with eating disorders during the pandemic.8 A Danish study found that children and adolescents newly diagnosed with obsessive-compulsive disorder (OCD) or who had completed treatment exhibited worsening OCD, anxiety, and depressive symptoms during the pandemic.9 An online survey of 6,196 Chinese adolescents found that those with a higher number of pre-pandemic adverse childhood experiences, such as abuse and neglect, had elevated posttraumatic stress symptoms and anxiety during the onset of the pandemic.10
Underlying causes of pandemic-induced distress
Limited social connectedness during the pandemic is a major reason for distress among adolescents. A review of 80 studies found that social isolation and loneliness as a result of social distancing and quarantining were associated with an increased risk of depression, anxiety, suicidal ideation, and self-harm.11 Parents’ stress about the risks of COVID-19 was correlated with worsening mental health in their adolescent children.12 A Chinese study found that the amount of time students spent on smartphones and social media doubled during the pandemic.13 In an online survey of 7,890 Chinese adolescents, greater social media, internet, and smartphone use was associated with increased anxiety and depression.14 This may be in part the result of adolescents spending time reading COVID-related news.
Coping mechanisms to increase well-being
Researchers have identified several positive coping mechanisms adolescents employed during the pandemic. Although some data suggest that increased internet use raises the risk of COVID-related distress, for certain adolescents, using social media to stay connected with friends and relatives was a buffer for feelings of loneliness and might have increased mental well-being.15 Other common coping mechanisms include relying on faith, volunteering, and starting new hobbies.16 During the pandemic, there were higher rates of playing outside and increased physical activity, which correlated with positive mental health outcomes.16 An online survey of 1,040 adolescents found that those who looked to the future optimistically and confidently had a higher health-related quality of life.17
Continuing an emphasis on adolescent well-being
Although data are limited, adolescents can continue to use these coping mechanisms to maintain their well-being, even if COVID-related restrictions are lifted or reimplemented. During these difficult times, it is imperative for adolescents to get the mental health services they need, and for psychiatric clinicians to continue to find avenues to promote resilience and mental wellness among young patients.
1. Leeb RT, Bitsko RH, Radhakrishnan L, et al. Mental health–related emergency department visits among children aged <18 years during the COVID-19 pandemic—United States, January 1-October 17, 2020. MMWR Morb Mortal Wkly Rep. 2020;69(45):1675-1680. doi:10.15585/mmwr.mm6945a3
2. Oosterhoff B, Palmer CA, Wilson J, et al. Adolescents’ motivations to engage in social distancing during the COVID-19 pandemic: associations with mental and social health. J Adolesc Health. 2020;67(2):179-185. doi:10.1016/j.jadohealth.2020.05.004
3. Duan L, Shao X, Wang Y, et al. An investigation of mental health status of children and adolescents in China during the outbreak of COVID-19. J Affect Disord. 2020;275:112-118. doi:10.1016/j.jad.2020.06.029
4. Ellis WE, Dumas TM, Forbes LM. Physically isolated but socially connected: psychological adjustment and stress among adolescents during the initial COVID-19 crisis. Can J Behav Sci. 2020;52(3):177-187. doi:10.1037/cbs0000215
5. Murata S, Rezeppa T, Thoma B, et al. The psychiatric sequelae of the COVID-19 pandemic in adolescents, adults, and health care workers. Depress Anxiety. 2021;38(2):233-246. doi:10.1002/da.23120
6. Tee ML, Tee CA, Anlacan JP, et al. Psychological impact of COVID-19 pandemic in the Philippines. J Affect Disord. 2020;277:379-391. doi:10.1016/j.jad.2020.08.043
7. Dumas TM, Ellis W, Litt DM. What does adolescent substance use look like during the COVID-19 pandemic? Examining changes in frequency, social contexts, and pandemic-related predictors. J Adolesc Health. 2020;67(3):354-361. doi:10.1016/j.jadohealth.2020.06.018
8. Schlegl S, Maier J, Meule A, et al. Eating disorders in times of the COVID-19 pandemic—results from an online survey of patients with anorexia nervosa. Int J Eat Disord. 2020;53:1791-1800. doi:10.1002/eat.23374.
9. Nissen JB, Højgaard D, Thomsen PH. The immediate effect of COVID-19 pandemic on children and adolescents with obsessive compulsive disorder. BMC Psychiatry. 2020;20(1):511. doi:10.1186/s12888-020-02905-5
10. Guo J, Fu M, Liu D, et al. Is the psychological impact of exposure to COVID-19 stronger in adolescents with pre-pandemic maltreatment experiences? A survey of rural Chinese adolescents. Child Abuse Negl. 2020;110(Pt 2):104667. doi:10.1016/j.chiabu.2020.104667
11. Loades ME, Chatburn E, Higson-Sweeney N, et al. Rapid Systematic Review: The impact of social isolation and loneliness on the mental health of children and adolescents in the context of COVID-19. J Am Acad Child Adolesc Psychiatry. 2020;59(11):1218-1239.e3. doi:10.1016/j.jaac.2020.05.009
12. Spinelli M, Lionetti F, Setti A, et al. Parenting stress during the COVID-19 outbreak: socioeconomic and environmental risk factors and implications for children emotion regulation. Fam Process. 2021;60(2):639-653. doi:10.1111/famp.12601
13. Chen IH, Chen CY, Pakpour AH, et al. Internet-related behaviors and psychological distress among schoolchildren during COVID-19 school suspension. J Am Acad Child Adolesc Psychiatry. 2020;59(10):1099-1102.e1. doi:10.1016/j.jaac.2020.06.007
14. Li W, Zhang Y, Wang J, et al. Association of home quarantine and mental health among teenagers in Wuhan, China, during the COVID-19 pandemic. JAMA Pediatr. 2021;175(3):313-316. doi:10.1001/jamapediatrics.2020.5499
15. Janssen, LHC, Kullberg, MJ, Verkuil B, et al. Does the COVID-19 pandemic impact parents’ and adolescents’ well-being? An EMA-study on daily affect and parenting. PLoS One. 2020;15(10):e0240962. doi:10.1371/journal.pone.0240962
16. Banati P, Jones N, Youssef S. Intersecting vulnerabilities: the impacts of COVID-19 on the psycho-emotional lives of young people in low- and middle-income countries. Eur J Dev Res. 2020;32(5):1613-1638. doi:10.1057/s41287-020-00325-5
17. Ravens-Sieberer U, Kaman A, Otto C, et al. Mental health and quality of life in children and adolescents during the COVID-19 pandemic—results of the COPSY study. Dtsch Arztebl Int. 2020;117(48):828-829. doi:10.3238/arztebl.2020.0828
While the COVID-19 pandemic has impacted the mental health of a wide range of individuals, its adverse effects have been particularly detrimental to adolescents. In this article, I discuss evidence that shows the effects of the pandemic on adolescent patients, potential reasons for this increased distress, and what types of coping mechanisms adolescents have used to counter these effects.
Increases in multiple measures of psychopathology
Multiple online surveys and other studies have documented the pandemic’s impact on younger individuals. In the United States, visits to emergency departments by pediatric patients increased in the months after the first lockdown period.1 Several studies found increased rates of anxiety and depression among adolescents during the COVID-19 pandemic.2,3 In an online survey of 359 children and 3,254 adolescents in China, 22% of respondents reported that they experienced depressive symptoms.3 In an online survey of 1,054 Canadian adolescents, 43% said they were “very concerned” about the pandemic.4 In an online survey of 7,353 adolescents in the United States, 37% reported suicidal ideation during the pandemic compared to 17% in 2017.5 A Chinese study found that smartphone and internet addiction was significantly associated with increased levels of depressive symptoms during the pandemic.3 In a survey in the Philippines, 16.3% of adolescents reported moderate-to-severe psychological impairment during the pandemic; the rates of COVID-19–related anxiety were higher among girls vs boys.6 Alcohol and cannabis use increased among Canadian adolescents during the pandemic, according to an online survey.7 Adolescents with anorexia nervosa reported a 70% increase in poor eating habits and more thoughts associated with eating disorders during the pandemic.8 A Danish study found that children and adolescents newly diagnosed with obsessive-compulsive disorder (OCD) or who had completed treatment exhibited worsening OCD, anxiety, and depressive symptoms during the pandemic.9 An online survey of 6,196 Chinese adolescents found that those with a higher number of pre-pandemic adverse childhood experiences, such as abuse and neglect, had elevated posttraumatic stress symptoms and anxiety during the onset of the pandemic.10
Underlying causes of pandemic-induced distress
Limited social connectedness during the pandemic is a major reason for distress among adolescents. A review of 80 studies found that social isolation and loneliness as a result of social distancing and quarantining were associated with an increased risk of depression, anxiety, suicidal ideation, and self-harm.11 Parents’ stress about the risks of COVID-19 was correlated with worsening mental health in their adolescent children.12 A Chinese study found that the amount of time students spent on smartphones and social media doubled during the pandemic.13 In an online survey of 7,890 Chinese adolescents, greater social media, internet, and smartphone use was associated with increased anxiety and depression.14 This may be in part the result of adolescents spending time reading COVID-related news.
Coping mechanisms to increase well-being
Researchers have identified several positive coping mechanisms adolescents employed during the pandemic. Although some data suggest that increased internet use raises the risk of COVID-related distress, for certain adolescents, using social media to stay connected with friends and relatives was a buffer for feelings of loneliness and might have increased mental well-being.15 Other common coping mechanisms include relying on faith, volunteering, and starting new hobbies.16 During the pandemic, there were higher rates of playing outside and increased physical activity, which correlated with positive mental health outcomes.16 An online survey of 1,040 adolescents found that those who looked to the future optimistically and confidently had a higher health-related quality of life.17
Continuing an emphasis on adolescent well-being
Although data are limited, adolescents can continue to use these coping mechanisms to maintain their well-being, even if COVID-related restrictions are lifted or reimplemented. During these difficult times, it is imperative for adolescents to get the mental health services they need, and for psychiatric clinicians to continue to find avenues to promote resilience and mental wellness among young patients.
While the COVID-19 pandemic has impacted the mental health of a wide range of individuals, its adverse effects have been particularly detrimental to adolescents. In this article, I discuss evidence that shows the effects of the pandemic on adolescent patients, potential reasons for this increased distress, and what types of coping mechanisms adolescents have used to counter these effects.
Increases in multiple measures of psychopathology
Multiple online surveys and other studies have documented the pandemic’s impact on younger individuals. In the United States, visits to emergency departments by pediatric patients increased in the months after the first lockdown period.1 Several studies found increased rates of anxiety and depression among adolescents during the COVID-19 pandemic.2,3 In an online survey of 359 children and 3,254 adolescents in China, 22% of respondents reported that they experienced depressive symptoms.3 In an online survey of 1,054 Canadian adolescents, 43% said they were “very concerned” about the pandemic.4 In an online survey of 7,353 adolescents in the United States, 37% reported suicidal ideation during the pandemic compared to 17% in 2017.5 A Chinese study found that smartphone and internet addiction was significantly associated with increased levels of depressive symptoms during the pandemic.3 In a survey in the Philippines, 16.3% of adolescents reported moderate-to-severe psychological impairment during the pandemic; the rates of COVID-19–related anxiety were higher among girls vs boys.6 Alcohol and cannabis use increased among Canadian adolescents during the pandemic, according to an online survey.7 Adolescents with anorexia nervosa reported a 70% increase in poor eating habits and more thoughts associated with eating disorders during the pandemic.8 A Danish study found that children and adolescents newly diagnosed with obsessive-compulsive disorder (OCD) or who had completed treatment exhibited worsening OCD, anxiety, and depressive symptoms during the pandemic.9 An online survey of 6,196 Chinese adolescents found that those with a higher number of pre-pandemic adverse childhood experiences, such as abuse and neglect, had elevated posttraumatic stress symptoms and anxiety during the onset of the pandemic.10
Underlying causes of pandemic-induced distress
Limited social connectedness during the pandemic is a major reason for distress among adolescents. A review of 80 studies found that social isolation and loneliness as a result of social distancing and quarantining were associated with an increased risk of depression, anxiety, suicidal ideation, and self-harm.11 Parents’ stress about the risks of COVID-19 was correlated with worsening mental health in their adolescent children.12 A Chinese study found that the amount of time students spent on smartphones and social media doubled during the pandemic.13 In an online survey of 7,890 Chinese adolescents, greater social media, internet, and smartphone use was associated with increased anxiety and depression.14 This may be in part the result of adolescents spending time reading COVID-related news.
Coping mechanisms to increase well-being
Researchers have identified several positive coping mechanisms adolescents employed during the pandemic. Although some data suggest that increased internet use raises the risk of COVID-related distress, for certain adolescents, using social media to stay connected with friends and relatives was a buffer for feelings of loneliness and might have increased mental well-being.15 Other common coping mechanisms include relying on faith, volunteering, and starting new hobbies.16 During the pandemic, there were higher rates of playing outside and increased physical activity, which correlated with positive mental health outcomes.16 An online survey of 1,040 adolescents found that those who looked to the future optimistically and confidently had a higher health-related quality of life.17
Continuing an emphasis on adolescent well-being
Although data are limited, adolescents can continue to use these coping mechanisms to maintain their well-being, even if COVID-related restrictions are lifted or reimplemented. During these difficult times, it is imperative for adolescents to get the mental health services they need, and for psychiatric clinicians to continue to find avenues to promote resilience and mental wellness among young patients.
1. Leeb RT, Bitsko RH, Radhakrishnan L, et al. Mental health–related emergency department visits among children aged <18 years during the COVID-19 pandemic—United States, January 1-October 17, 2020. MMWR Morb Mortal Wkly Rep. 2020;69(45):1675-1680. doi:10.15585/mmwr.mm6945a3
2. Oosterhoff B, Palmer CA, Wilson J, et al. Adolescents’ motivations to engage in social distancing during the COVID-19 pandemic: associations with mental and social health. J Adolesc Health. 2020;67(2):179-185. doi:10.1016/j.jadohealth.2020.05.004
3. Duan L, Shao X, Wang Y, et al. An investigation of mental health status of children and adolescents in China during the outbreak of COVID-19. J Affect Disord. 2020;275:112-118. doi:10.1016/j.jad.2020.06.029
4. Ellis WE, Dumas TM, Forbes LM. Physically isolated but socially connected: psychological adjustment and stress among adolescents during the initial COVID-19 crisis. Can J Behav Sci. 2020;52(3):177-187. doi:10.1037/cbs0000215
5. Murata S, Rezeppa T, Thoma B, et al. The psychiatric sequelae of the COVID-19 pandemic in adolescents, adults, and health care workers. Depress Anxiety. 2021;38(2):233-246. doi:10.1002/da.23120
6. Tee ML, Tee CA, Anlacan JP, et al. Psychological impact of COVID-19 pandemic in the Philippines. J Affect Disord. 2020;277:379-391. doi:10.1016/j.jad.2020.08.043
7. Dumas TM, Ellis W, Litt DM. What does adolescent substance use look like during the COVID-19 pandemic? Examining changes in frequency, social contexts, and pandemic-related predictors. J Adolesc Health. 2020;67(3):354-361. doi:10.1016/j.jadohealth.2020.06.018
8. Schlegl S, Maier J, Meule A, et al. Eating disorders in times of the COVID-19 pandemic—results from an online survey of patients with anorexia nervosa. Int J Eat Disord. 2020;53:1791-1800. doi:10.1002/eat.23374.
9. Nissen JB, Højgaard D, Thomsen PH. The immediate effect of COVID-19 pandemic on children and adolescents with obsessive compulsive disorder. BMC Psychiatry. 2020;20(1):511. doi:10.1186/s12888-020-02905-5
10. Guo J, Fu M, Liu D, et al. Is the psychological impact of exposure to COVID-19 stronger in adolescents with pre-pandemic maltreatment experiences? A survey of rural Chinese adolescents. Child Abuse Negl. 2020;110(Pt 2):104667. doi:10.1016/j.chiabu.2020.104667
11. Loades ME, Chatburn E, Higson-Sweeney N, et al. Rapid Systematic Review: The impact of social isolation and loneliness on the mental health of children and adolescents in the context of COVID-19. J Am Acad Child Adolesc Psychiatry. 2020;59(11):1218-1239.e3. doi:10.1016/j.jaac.2020.05.009
12. Spinelli M, Lionetti F, Setti A, et al. Parenting stress during the COVID-19 outbreak: socioeconomic and environmental risk factors and implications for children emotion regulation. Fam Process. 2021;60(2):639-653. doi:10.1111/famp.12601
13. Chen IH, Chen CY, Pakpour AH, et al. Internet-related behaviors and psychological distress among schoolchildren during COVID-19 school suspension. J Am Acad Child Adolesc Psychiatry. 2020;59(10):1099-1102.e1. doi:10.1016/j.jaac.2020.06.007
14. Li W, Zhang Y, Wang J, et al. Association of home quarantine and mental health among teenagers in Wuhan, China, during the COVID-19 pandemic. JAMA Pediatr. 2021;175(3):313-316. doi:10.1001/jamapediatrics.2020.5499
15. Janssen, LHC, Kullberg, MJ, Verkuil B, et al. Does the COVID-19 pandemic impact parents’ and adolescents’ well-being? An EMA-study on daily affect and parenting. PLoS One. 2020;15(10):e0240962. doi:10.1371/journal.pone.0240962
16. Banati P, Jones N, Youssef S. Intersecting vulnerabilities: the impacts of COVID-19 on the psycho-emotional lives of young people in low- and middle-income countries. Eur J Dev Res. 2020;32(5):1613-1638. doi:10.1057/s41287-020-00325-5
17. Ravens-Sieberer U, Kaman A, Otto C, et al. Mental health and quality of life in children and adolescents during the COVID-19 pandemic—results of the COPSY study. Dtsch Arztebl Int. 2020;117(48):828-829. doi:10.3238/arztebl.2020.0828
1. Leeb RT, Bitsko RH, Radhakrishnan L, et al. Mental health–related emergency department visits among children aged <18 years during the COVID-19 pandemic—United States, January 1-October 17, 2020. MMWR Morb Mortal Wkly Rep. 2020;69(45):1675-1680. doi:10.15585/mmwr.mm6945a3
2. Oosterhoff B, Palmer CA, Wilson J, et al. Adolescents’ motivations to engage in social distancing during the COVID-19 pandemic: associations with mental and social health. J Adolesc Health. 2020;67(2):179-185. doi:10.1016/j.jadohealth.2020.05.004
3. Duan L, Shao X, Wang Y, et al. An investigation of mental health status of children and adolescents in China during the outbreak of COVID-19. J Affect Disord. 2020;275:112-118. doi:10.1016/j.jad.2020.06.029
4. Ellis WE, Dumas TM, Forbes LM. Physically isolated but socially connected: psychological adjustment and stress among adolescents during the initial COVID-19 crisis. Can J Behav Sci. 2020;52(3):177-187. doi:10.1037/cbs0000215
5. Murata S, Rezeppa T, Thoma B, et al. The psychiatric sequelae of the COVID-19 pandemic in adolescents, adults, and health care workers. Depress Anxiety. 2021;38(2):233-246. doi:10.1002/da.23120
6. Tee ML, Tee CA, Anlacan JP, et al. Psychological impact of COVID-19 pandemic in the Philippines. J Affect Disord. 2020;277:379-391. doi:10.1016/j.jad.2020.08.043
7. Dumas TM, Ellis W, Litt DM. What does adolescent substance use look like during the COVID-19 pandemic? Examining changes in frequency, social contexts, and pandemic-related predictors. J Adolesc Health. 2020;67(3):354-361. doi:10.1016/j.jadohealth.2020.06.018
8. Schlegl S, Maier J, Meule A, et al. Eating disorders in times of the COVID-19 pandemic—results from an online survey of patients with anorexia nervosa. Int J Eat Disord. 2020;53:1791-1800. doi:10.1002/eat.23374.
9. Nissen JB, Højgaard D, Thomsen PH. The immediate effect of COVID-19 pandemic on children and adolescents with obsessive compulsive disorder. BMC Psychiatry. 2020;20(1):511. doi:10.1186/s12888-020-02905-5
10. Guo J, Fu M, Liu D, et al. Is the psychological impact of exposure to COVID-19 stronger in adolescents with pre-pandemic maltreatment experiences? A survey of rural Chinese adolescents. Child Abuse Negl. 2020;110(Pt 2):104667. doi:10.1016/j.chiabu.2020.104667
11. Loades ME, Chatburn E, Higson-Sweeney N, et al. Rapid Systematic Review: The impact of social isolation and loneliness on the mental health of children and adolescents in the context of COVID-19. J Am Acad Child Adolesc Psychiatry. 2020;59(11):1218-1239.e3. doi:10.1016/j.jaac.2020.05.009
12. Spinelli M, Lionetti F, Setti A, et al. Parenting stress during the COVID-19 outbreak: socioeconomic and environmental risk factors and implications for children emotion regulation. Fam Process. 2021;60(2):639-653. doi:10.1111/famp.12601
13. Chen IH, Chen CY, Pakpour AH, et al. Internet-related behaviors and psychological distress among schoolchildren during COVID-19 school suspension. J Am Acad Child Adolesc Psychiatry. 2020;59(10):1099-1102.e1. doi:10.1016/j.jaac.2020.06.007
14. Li W, Zhang Y, Wang J, et al. Association of home quarantine and mental health among teenagers in Wuhan, China, during the COVID-19 pandemic. JAMA Pediatr. 2021;175(3):313-316. doi:10.1001/jamapediatrics.2020.5499
15. Janssen, LHC, Kullberg, MJ, Verkuil B, et al. Does the COVID-19 pandemic impact parents’ and adolescents’ well-being? An EMA-study on daily affect and parenting. PLoS One. 2020;15(10):e0240962. doi:10.1371/journal.pone.0240962
16. Banati P, Jones N, Youssef S. Intersecting vulnerabilities: the impacts of COVID-19 on the psycho-emotional lives of young people in low- and middle-income countries. Eur J Dev Res. 2020;32(5):1613-1638. doi:10.1057/s41287-020-00325-5
17. Ravens-Sieberer U, Kaman A, Otto C, et al. Mental health and quality of life in children and adolescents during the COVID-19 pandemic—results of the COPSY study. Dtsch Arztebl Int. 2020;117(48):828-829. doi:10.3238/arztebl.2020.0828
Nonphysician Clinicians in Dermatology Residencies: Cross-sectional Survey on Residency Education
To the Editor:
There is increasing demand for medical care in the United States due to expanded health care coverage; an aging population; and advancements in diagnostics, treatment, and technology.1 It is predicted that by 2050 the number of dermatologists will be 24.4% short of the expected estimate of demand.2
Accordingly, dermatologists are increasingly practicing in team-based care delivery models that incorporate nonphysician clinicians (NPCs), including nurse practitioners and physician assistants.1 Despite recognition that NPCs are taking a larger role in medical teams, there is, to our knowledge, limited training for dermatologists and dermatologists in-training to optimize this professional alliance.
The objectives of this study included (1) determining whether residency programs adequately prepare residents to work with or supervise NPCs and (2) understanding the relationship between NPCs and dermatology residents across residency programs in the United States.
An anonymous cross-sectional, Internet-based survey designed using Google Forms survey creation and administration software was distributed to 117 dermatology residency program directors through email, with a request for further dissemination to residents through self-maintained listserves. Four email reminders about completing and disseminating the survey were sent to program directors between August and November 2020. The study was approved by the Emory University institutional review board. All respondents consented to participate in this survey prior to completing it.
The survey included questions pertaining to demographic information, residents’ experiences working with NPCs, residency program training specific to working with NPCs, and residents’ and residency program directors’ opinions on NPCs’ impact on education and patient care. Program directors were asked to respond N/A to 6 questions on the survey because data from those questions represented residents’ opinions only. Questions relating to residents’ and residency program directors’ opinions were based on a 5-point scale of impact (1=strongly impact in a negative way; 5=strongly impact in a positive way) or importance (1=not at all important; 5=extremely important). The survey was not previously validated.
Descriptive analysis and a paired t test were conducted when appropriate. Missing data were excluded.
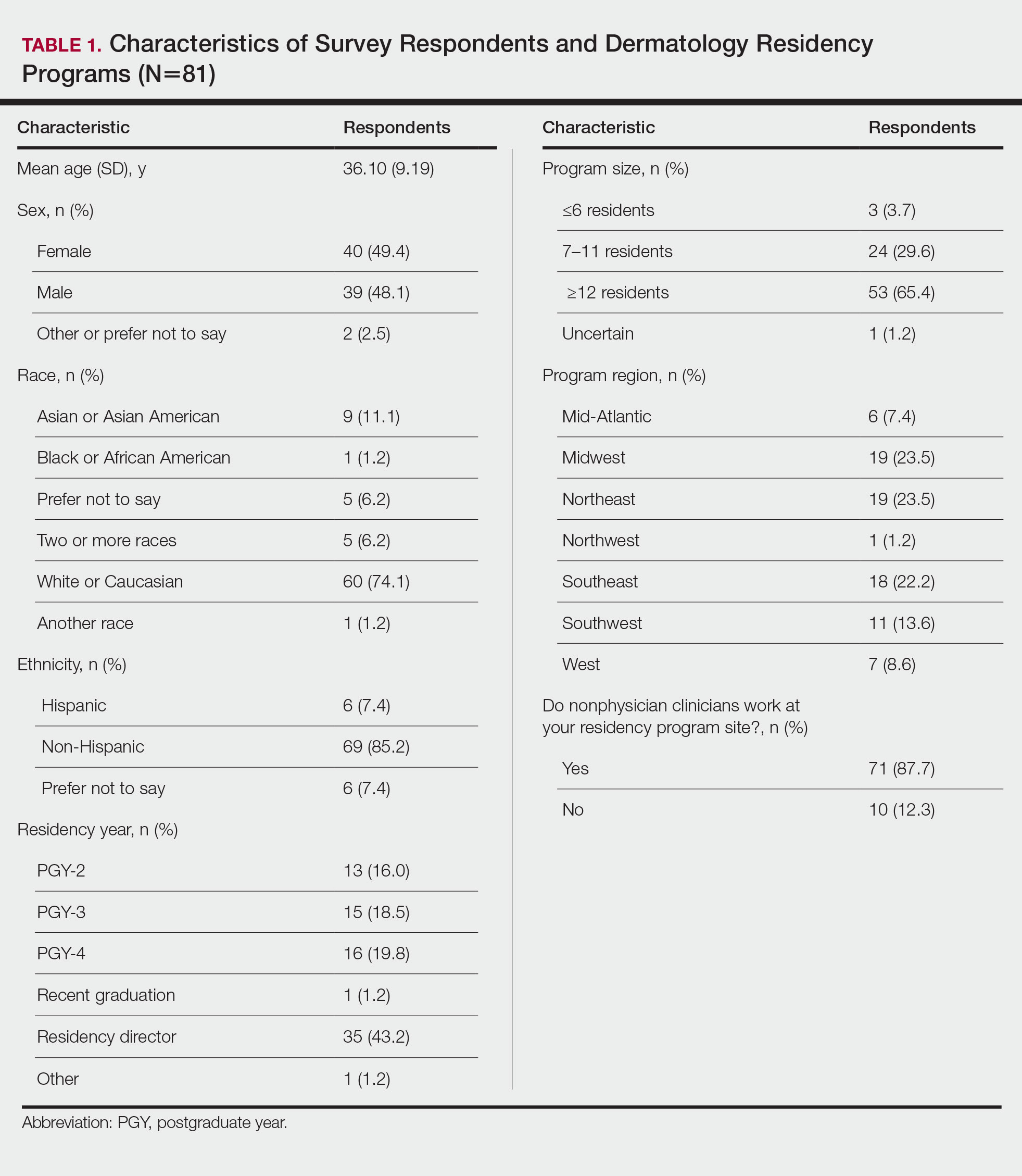
There were 81 respondents to the survey. Demographic information is shown Table 1. Thirty-five dermatology residency program directors (29.9% of 117 programs) responded. Of the 45 residents or recent graduates, 29 (64.4%) reported that they foresaw the need to work with or supervise NPCs in the future (Table 2). Currently, 29 (64.4%) residents also reported that (1) they do not feel adequately trained to provide supervision of or to work with NPCs or (2) were uncertain whether they could do so. Sixty-five (80.2%) respondents stated that there was no formalized training in their program for supervising or working with NPCs; 45 (55.6%) respondents noted that they do not think that their program provided adequate training in supervising NPCs.
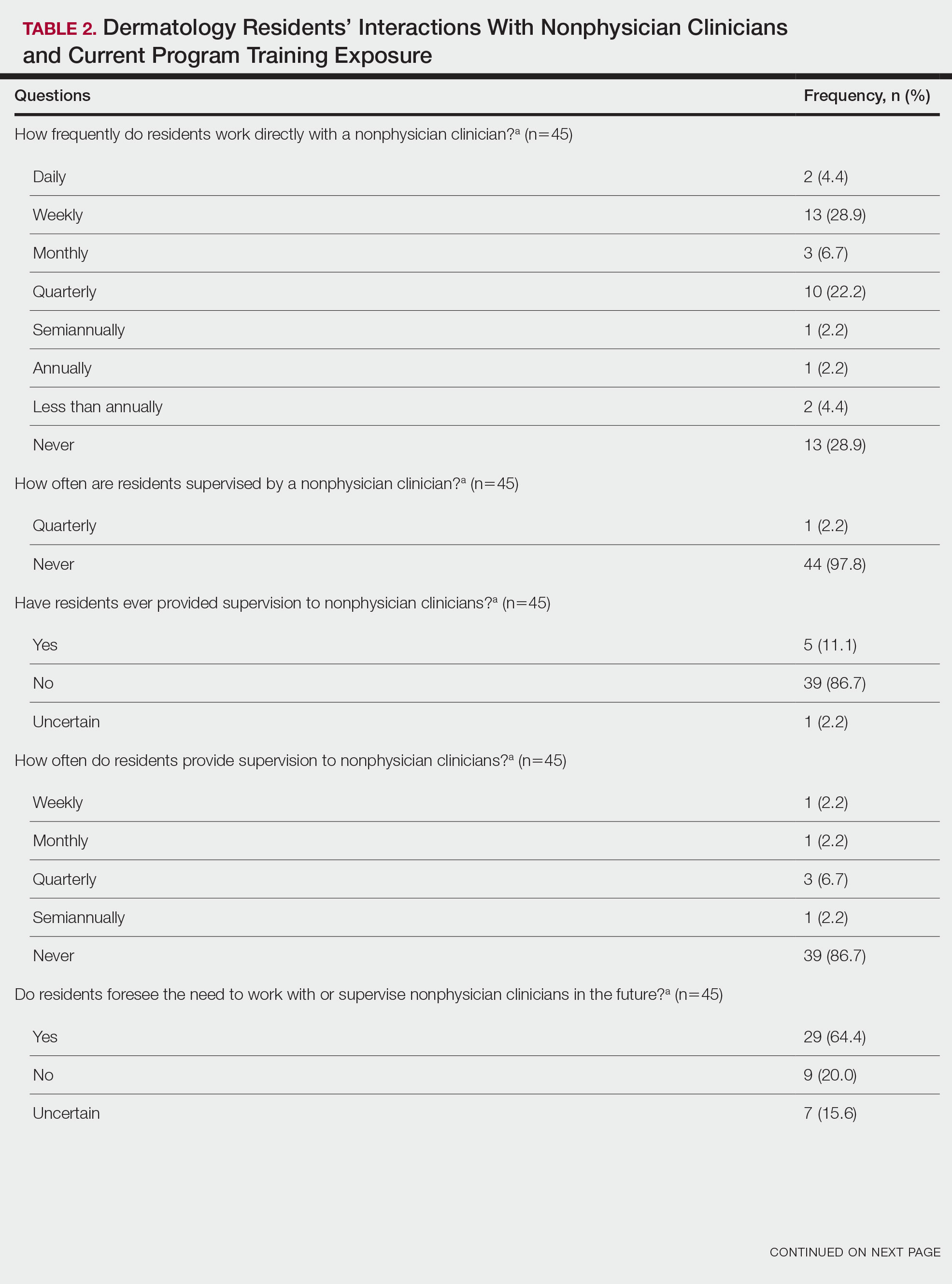
Regarding NPCs impact on care, residency program directors who completed the survey were more likely to rank NPCs as having a more significant positive impact on patient care than residents (mean score, 3.43 vs 2.78; P=.043; 95% CI, –1.28 to –0.20)(Table 3).
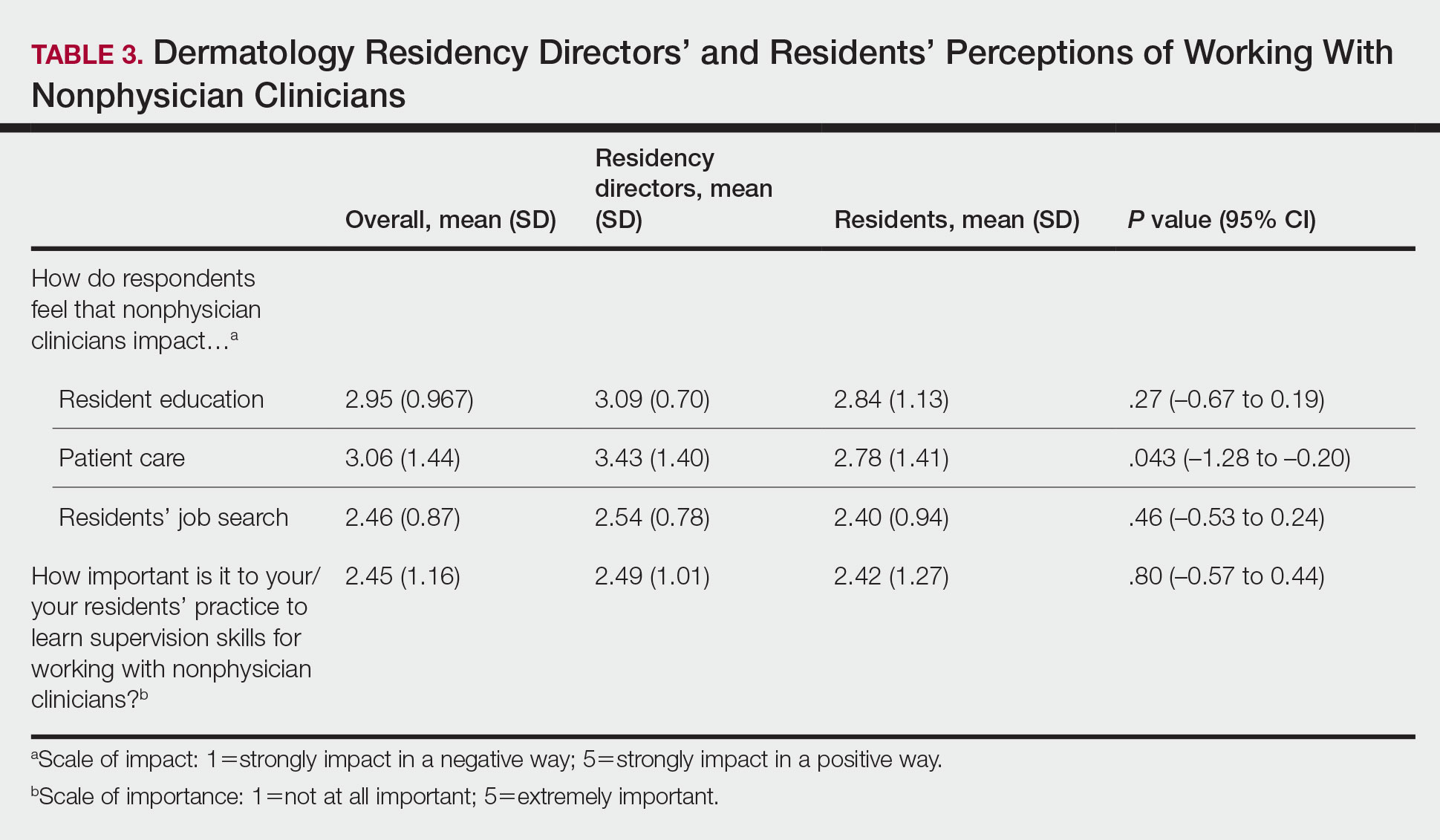
This study demonstrated a lack of dermatology training related to working with NPCs in a professional setting and highlighted residents’ perception that formal education in working with and supervising NPCs could be of benefit to their education. Furthermore, residency directors perceived NPCs as having a greater positive impact on patient care than residents did, underscoring the importance of the continued need to educate residents on working synergistically with NPCs to optimize patient care. Ultimately, these results suggest a potential area for further development of residency curricula.
There are approximately 360,000 NPCs serving as integral members of interdisciplinary medical teams across the United States.3,4 In a 2014 survey, 46% of 2001 dermatologists noted that they already employed 1 or more NPCs, a number that has increased over time and is likely to continue to do so.5 Although the number of NPCs in dermatology has increased, there remain limited formal training and certificate programs for these providers.1,6
Furthermore, the American Academy of Dermatology recommends that “[w]hen practicing in a dermatological setting, non-dermatologist physicians and non-physician clinicians . . . should be directly supervised by a board-certified dermatologist.”7 Therefore, the responsibility for a dermatology-specific education can fall on the dermatologist, necessitating adequate supervision and training of NPCs.
The findings of this study were limited by a small sample size; response bias because distribution of the survey relied on program directors disseminating the instrument to their residents, thereby limiting generalizability; and a lack of predissemination validation of the survey. Additional research in this area should focus on survey validation and distribution directly to dermatology residents, instead of relying on dermatology program directors to disseminate the survey.
- Sargen MR, Shi L, Hooker RS, et al. Future growth of physicians and non-physician providers within the U.S. Dermatology workforce. Dermatol Online J. 2017;23:13030/qt840223q6
- The current and projected dermatology workforce in the United States. J Am Acad Dermatol. 2016;74(suppl 1):AB122. doi:10.1016/j.jaad.2016.02.478
- Nurse anesthetists, nurse midwives, and nurse practitioners.Occupational Outlook Handbook. Washington, DC: US Department of Labor. Updated April 18, 2022. Accessed July 14, 2022. https://www.bls.gov/ooh/health care/nurse-anesthetists-nurse-midwives-and-nurse-practitioners.htm
- Physician assistants. Occupational Outlook Handbook. Washington, DC: US Department of Labor. Updated April 18, 2022. Accessed July 14, 2022. https://www.bls.gov/ooh/healthcare/physician-assistants.htm
- Ehrlich A, Kostecki J, Olkaba H. Trends in dermatology practices and the implications for the workforce. J Am Acad Dermatol. 2017;77:746-752. doi:10.1016/j.jaad.2017.06.030
- Anderson AM, Matsumoto M, Saul MI, et al. Accuracy of skin cancer diagnosis by physician assistants compared with dermatologists in a large health care system. JAMA Dermatol. 2018;154:569-573. doi:10.1001/jamadermatol.2018.0212s
- American Academy of Dermatology Association. Position statement on the practice of dermatology: protecting and preserving patient safety and quality care. Revised May 21, 2016. Accessed July 14, 2022. https://server.aad.org/Forms/Policies/Uploads/PS/PS-Practice of Dermatology-Protecting Preserving Patient Safety Quality Care.pdf?
To the Editor:
There is increasing demand for medical care in the United States due to expanded health care coverage; an aging population; and advancements in diagnostics, treatment, and technology.1 It is predicted that by 2050 the number of dermatologists will be 24.4% short of the expected estimate of demand.2
Accordingly, dermatologists are increasingly practicing in team-based care delivery models that incorporate nonphysician clinicians (NPCs), including nurse practitioners and physician assistants.1 Despite recognition that NPCs are taking a larger role in medical teams, there is, to our knowledge, limited training for dermatologists and dermatologists in-training to optimize this professional alliance.
The objectives of this study included (1) determining whether residency programs adequately prepare residents to work with or supervise NPCs and (2) understanding the relationship between NPCs and dermatology residents across residency programs in the United States.
An anonymous cross-sectional, Internet-based survey designed using Google Forms survey creation and administration software was distributed to 117 dermatology residency program directors through email, with a request for further dissemination to residents through self-maintained listserves. Four email reminders about completing and disseminating the survey were sent to program directors between August and November 2020. The study was approved by the Emory University institutional review board. All respondents consented to participate in this survey prior to completing it.
The survey included questions pertaining to demographic information, residents’ experiences working with NPCs, residency program training specific to working with NPCs, and residents’ and residency program directors’ opinions on NPCs’ impact on education and patient care. Program directors were asked to respond N/A to 6 questions on the survey because data from those questions represented residents’ opinions only. Questions relating to residents’ and residency program directors’ opinions were based on a 5-point scale of impact (1=strongly impact in a negative way; 5=strongly impact in a positive way) or importance (1=not at all important; 5=extremely important). The survey was not previously validated.
Descriptive analysis and a paired t test were conducted when appropriate. Missing data were excluded.
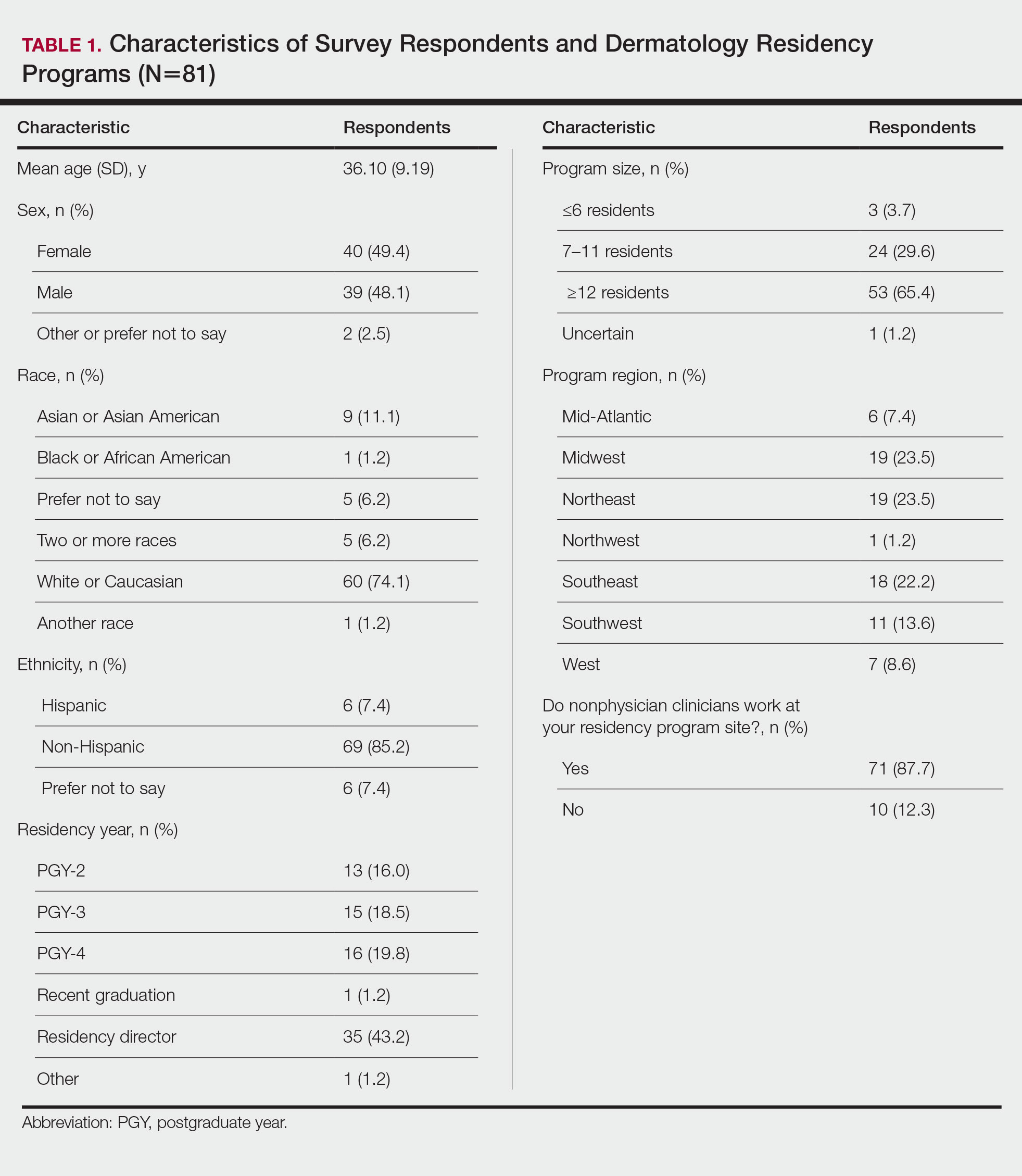
There were 81 respondents to the survey. Demographic information is shown Table 1. Thirty-five dermatology residency program directors (29.9% of 117 programs) responded. Of the 45 residents or recent graduates, 29 (64.4%) reported that they foresaw the need to work with or supervise NPCs in the future (Table 2). Currently, 29 (64.4%) residents also reported that (1) they do not feel adequately trained to provide supervision of or to work with NPCs or (2) were uncertain whether they could do so. Sixty-five (80.2%) respondents stated that there was no formalized training in their program for supervising or working with NPCs; 45 (55.6%) respondents noted that they do not think that their program provided adequate training in supervising NPCs.
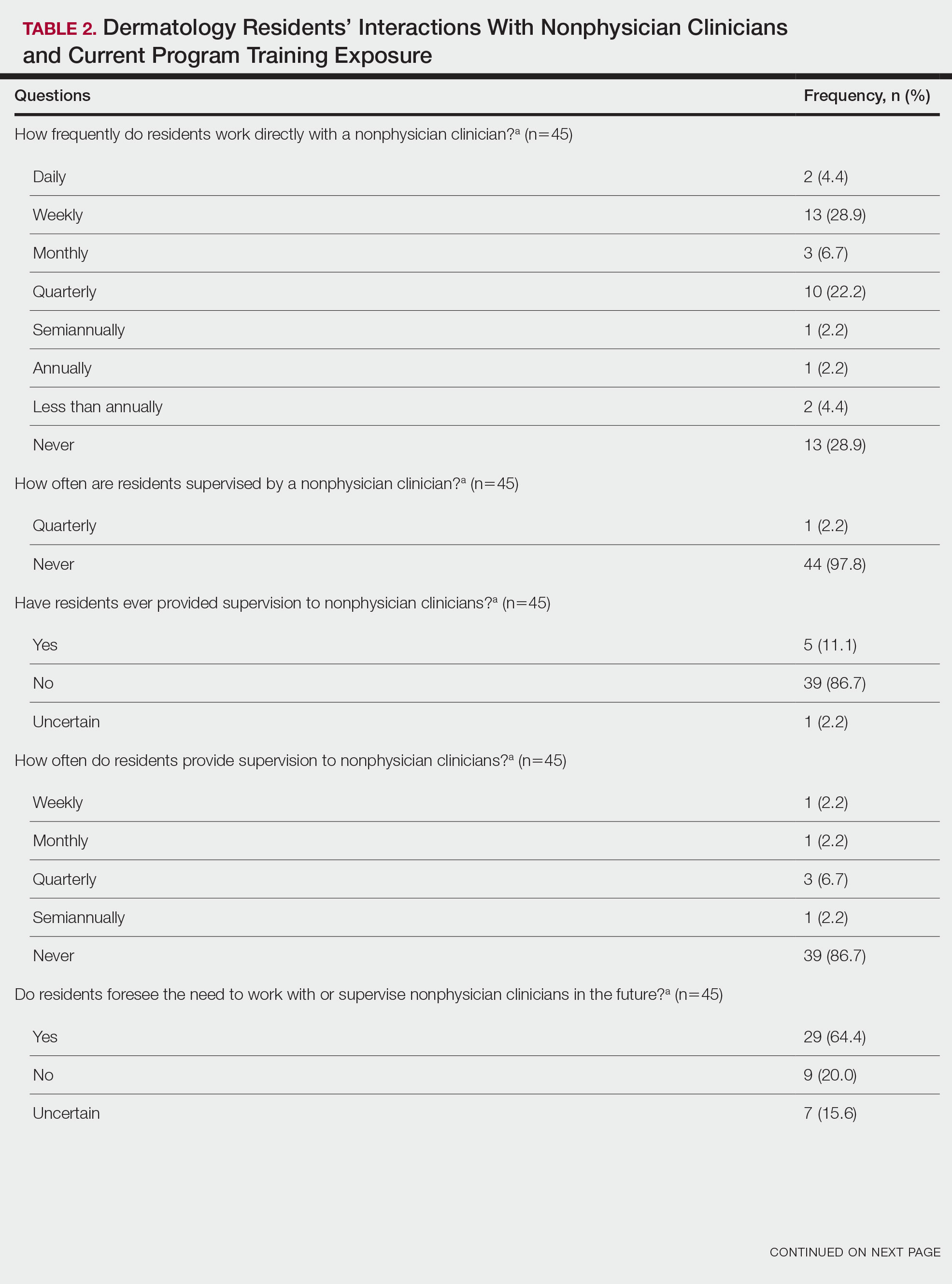
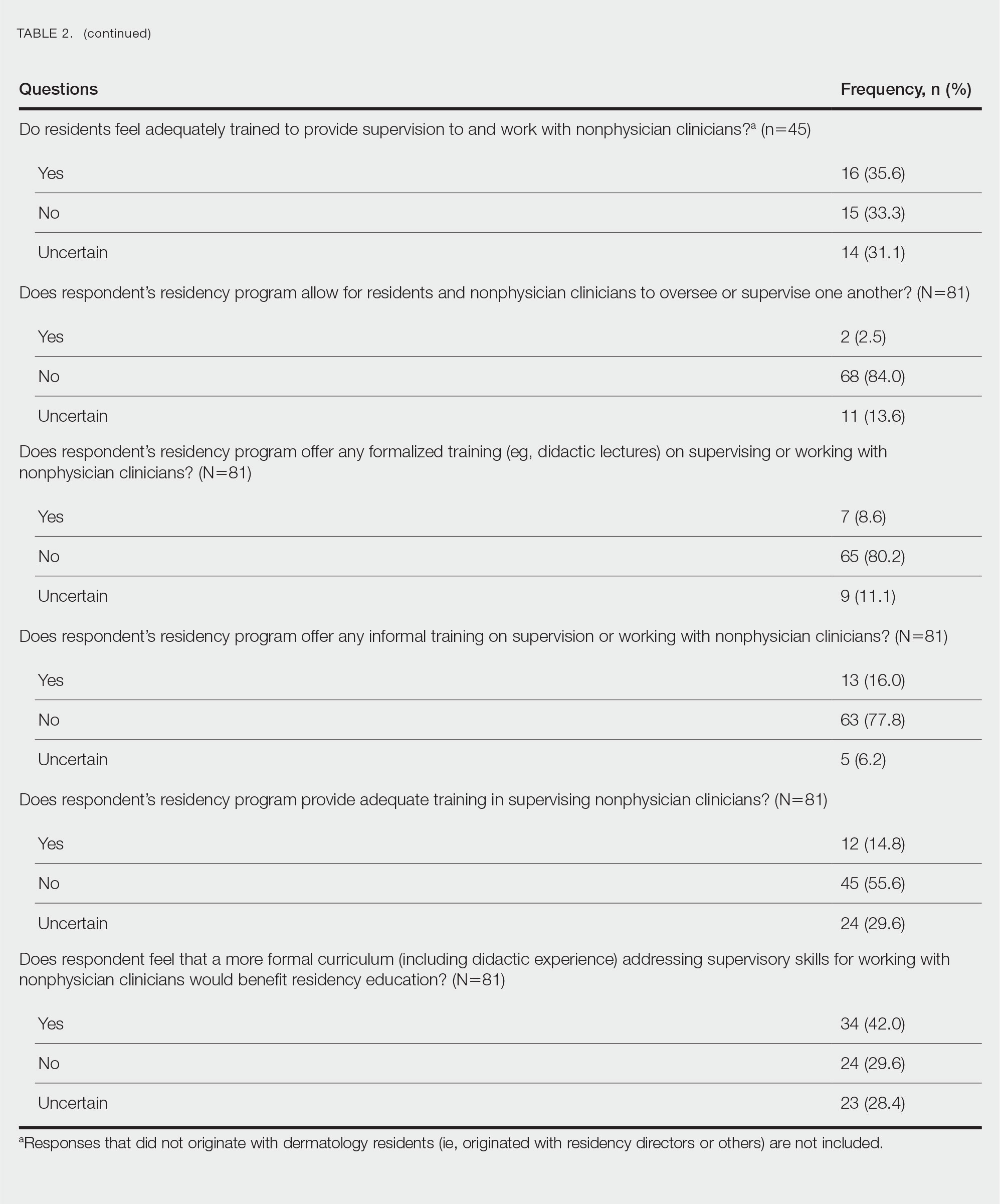
Regarding NPCs impact on care, residency program directors who completed the survey were more likely to rank NPCs as having a more significant positive impact on patient care than residents (mean score, 3.43 vs 2.78; P=.043; 95% CI, –1.28 to –0.20)(Table 3).
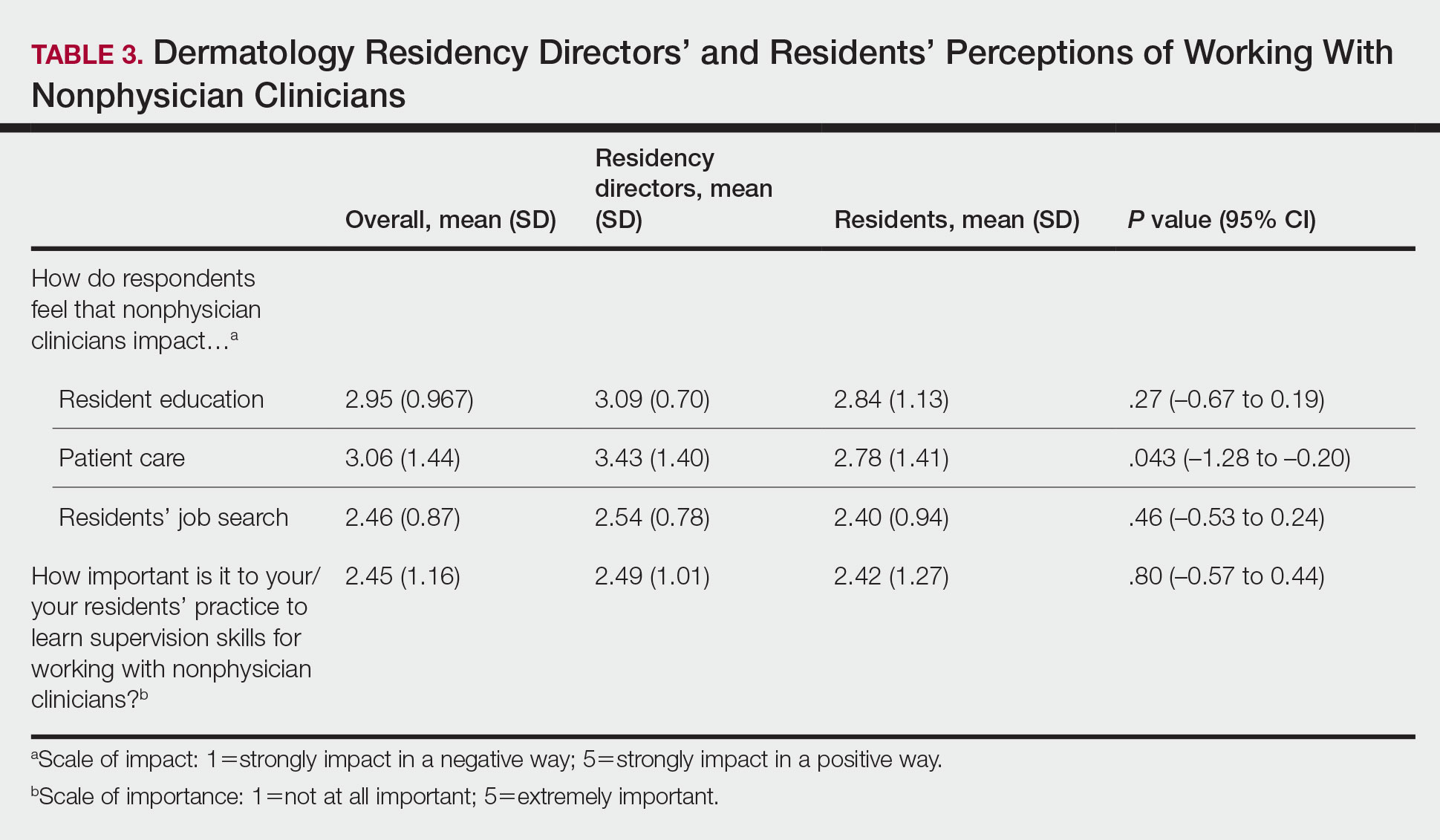
This study demonstrated a lack of dermatology training related to working with NPCs in a professional setting and highlighted residents’ perception that formal education in working with and supervising NPCs could be of benefit to their education. Furthermore, residency directors perceived NPCs as having a greater positive impact on patient care than residents did, underscoring the importance of the continued need to educate residents on working synergistically with NPCs to optimize patient care. Ultimately, these results suggest a potential area for further development of residency curricula.
There are approximately 360,000 NPCs serving as integral members of interdisciplinary medical teams across the United States.3,4 In a 2014 survey, 46% of 2001 dermatologists noted that they already employed 1 or more NPCs, a number that has increased over time and is likely to continue to do so.5 Although the number of NPCs in dermatology has increased, there remain limited formal training and certificate programs for these providers.1,6
Furthermore, the American Academy of Dermatology recommends that “[w]hen practicing in a dermatological setting, non-dermatologist physicians and non-physician clinicians . . . should be directly supervised by a board-certified dermatologist.”7 Therefore, the responsibility for a dermatology-specific education can fall on the dermatologist, necessitating adequate supervision and training of NPCs.
The findings of this study were limited by a small sample size; response bias because distribution of the survey relied on program directors disseminating the instrument to their residents, thereby limiting generalizability; and a lack of predissemination validation of the survey. Additional research in this area should focus on survey validation and distribution directly to dermatology residents, instead of relying on dermatology program directors to disseminate the survey.
To the Editor:
There is increasing demand for medical care in the United States due to expanded health care coverage; an aging population; and advancements in diagnostics, treatment, and technology.1 It is predicted that by 2050 the number of dermatologists will be 24.4% short of the expected estimate of demand.2
Accordingly, dermatologists are increasingly practicing in team-based care delivery models that incorporate nonphysician clinicians (NPCs), including nurse practitioners and physician assistants.1 Despite recognition that NPCs are taking a larger role in medical teams, there is, to our knowledge, limited training for dermatologists and dermatologists in-training to optimize this professional alliance.
The objectives of this study included (1) determining whether residency programs adequately prepare residents to work with or supervise NPCs and (2) understanding the relationship between NPCs and dermatology residents across residency programs in the United States.
An anonymous cross-sectional, Internet-based survey designed using Google Forms survey creation and administration software was distributed to 117 dermatology residency program directors through email, with a request for further dissemination to residents through self-maintained listserves. Four email reminders about completing and disseminating the survey were sent to program directors between August and November 2020. The study was approved by the Emory University institutional review board. All respondents consented to participate in this survey prior to completing it.
The survey included questions pertaining to demographic information, residents’ experiences working with NPCs, residency program training specific to working with NPCs, and residents’ and residency program directors’ opinions on NPCs’ impact on education and patient care. Program directors were asked to respond N/A to 6 questions on the survey because data from those questions represented residents’ opinions only. Questions relating to residents’ and residency program directors’ opinions were based on a 5-point scale of impact (1=strongly impact in a negative way; 5=strongly impact in a positive way) or importance (1=not at all important; 5=extremely important). The survey was not previously validated.
Descriptive analysis and a paired t test were conducted when appropriate. Missing data were excluded.
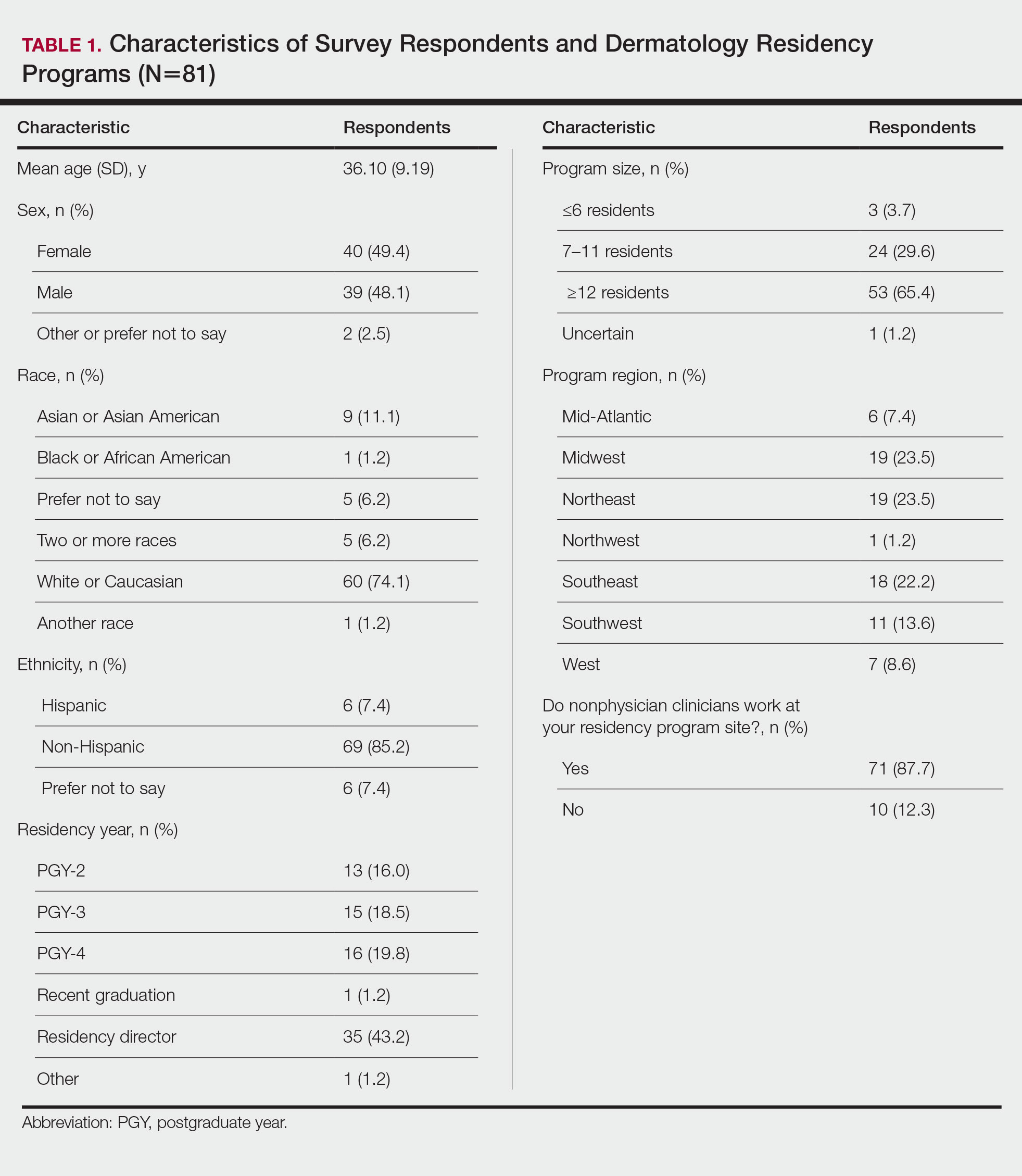
There were 81 respondents to the survey. Demographic information is shown Table 1. Thirty-five dermatology residency program directors (29.9% of 117 programs) responded. Of the 45 residents or recent graduates, 29 (64.4%) reported that they foresaw the need to work with or supervise NPCs in the future (Table 2). Currently, 29 (64.4%) residents also reported that (1) they do not feel adequately trained to provide supervision of or to work with NPCs or (2) were uncertain whether they could do so. Sixty-five (80.2%) respondents stated that there was no formalized training in their program for supervising or working with NPCs; 45 (55.6%) respondents noted that they do not think that their program provided adequate training in supervising NPCs.
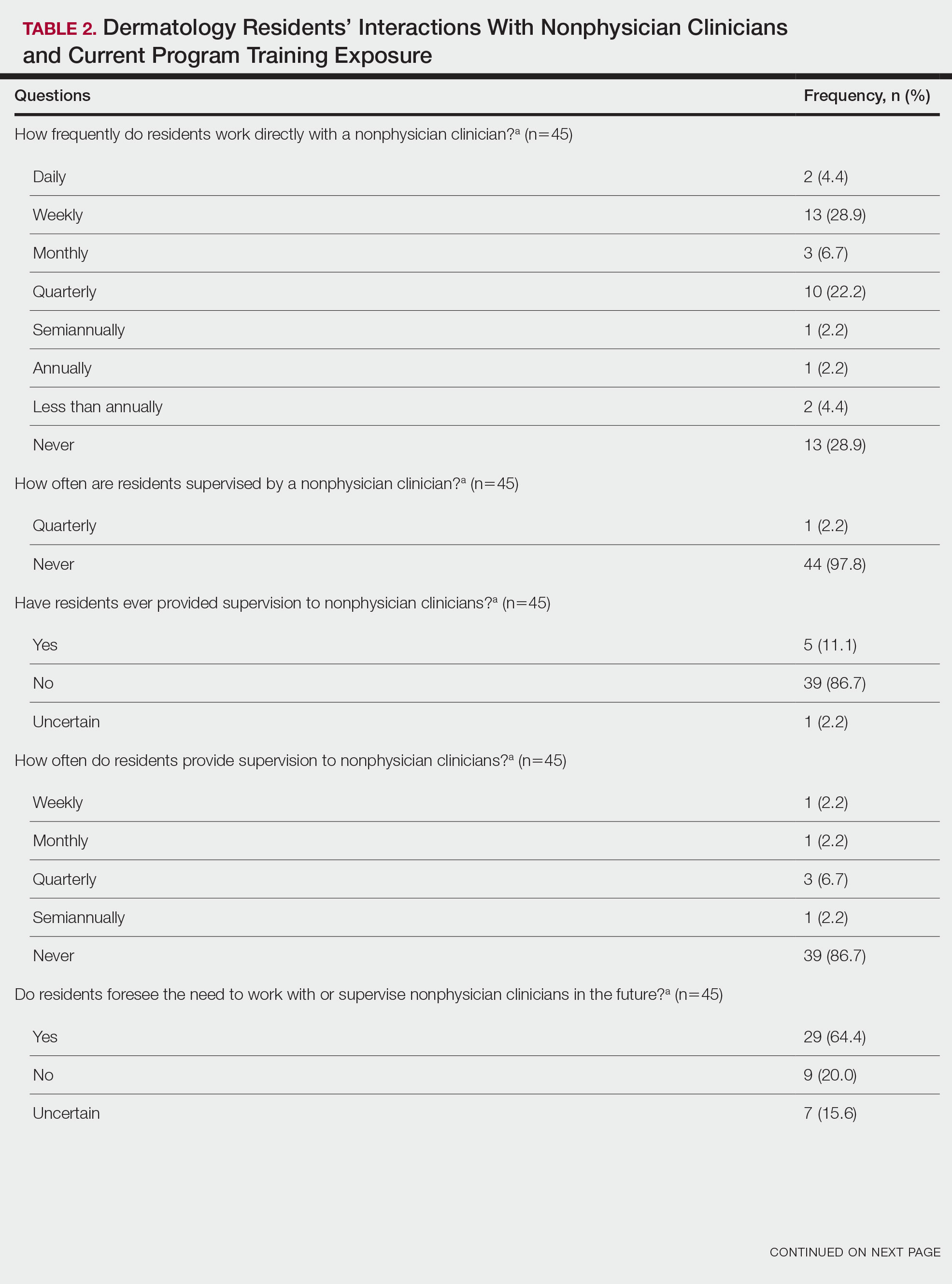
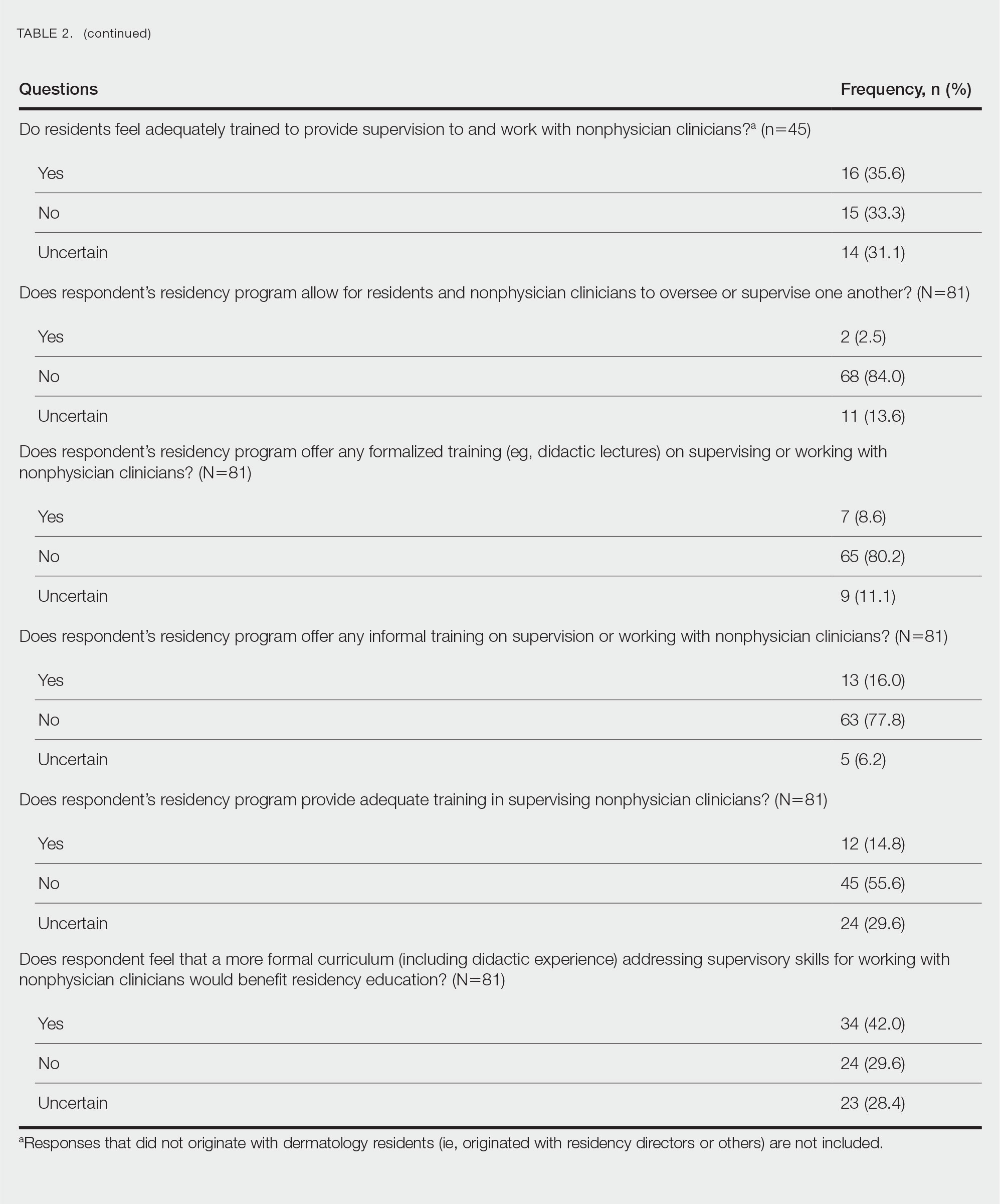
Regarding NPCs impact on care, residency program directors who completed the survey were more likely to rank NPCs as having a more significant positive impact on patient care than residents (mean score, 3.43 vs 2.78; P=.043; 95% CI, –1.28 to –0.20)(Table 3).
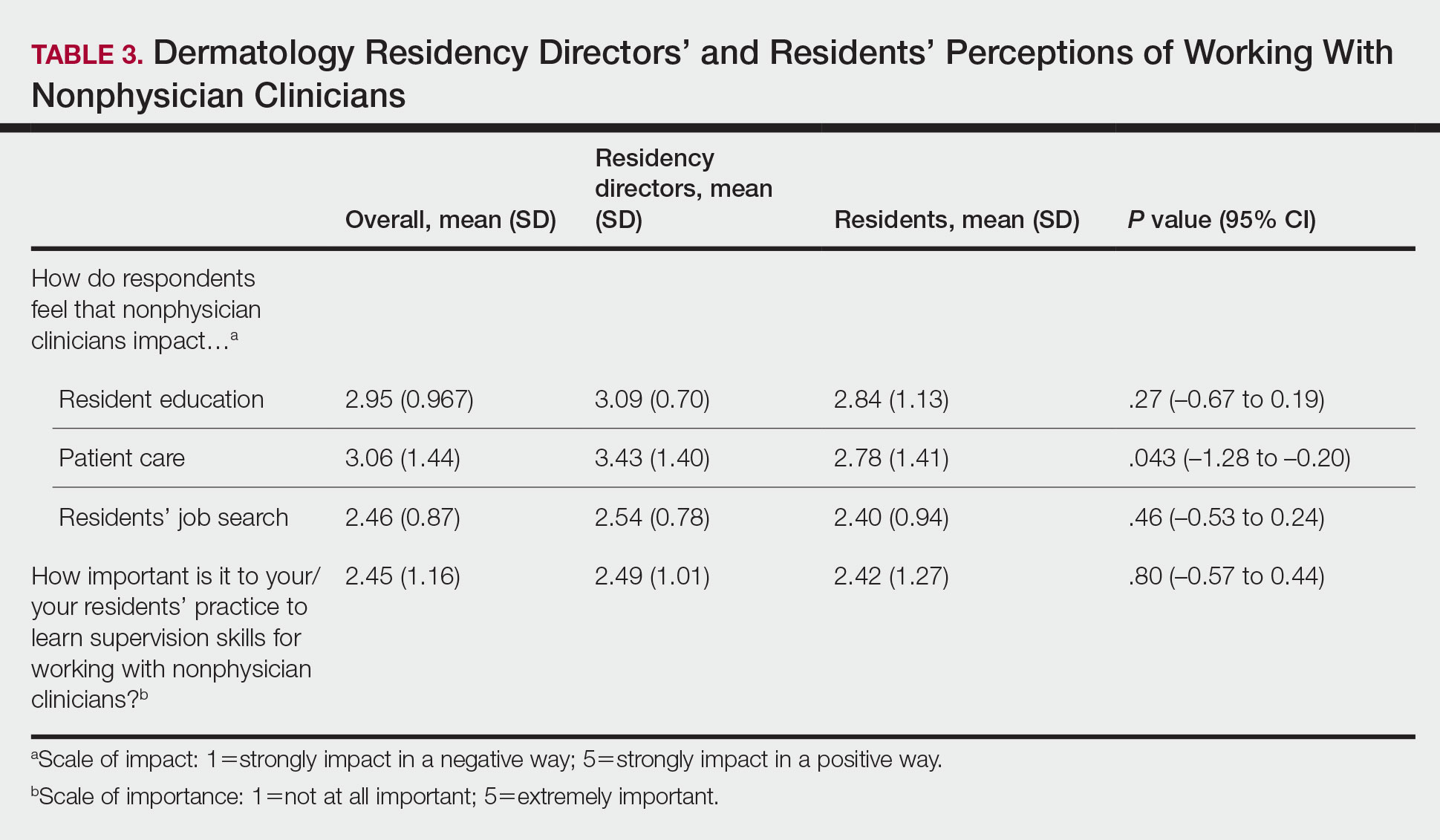
This study demonstrated a lack of dermatology training related to working with NPCs in a professional setting and highlighted residents’ perception that formal education in working with and supervising NPCs could be of benefit to their education. Furthermore, residency directors perceived NPCs as having a greater positive impact on patient care than residents did, underscoring the importance of the continued need to educate residents on working synergistically with NPCs to optimize patient care. Ultimately, these results suggest a potential area for further development of residency curricula.
There are approximately 360,000 NPCs serving as integral members of interdisciplinary medical teams across the United States.3,4 In a 2014 survey, 46% of 2001 dermatologists noted that they already employed 1 or more NPCs, a number that has increased over time and is likely to continue to do so.5 Although the number of NPCs in dermatology has increased, there remain limited formal training and certificate programs for these providers.1,6
Furthermore, the American Academy of Dermatology recommends that “[w]hen practicing in a dermatological setting, non-dermatologist physicians and non-physician clinicians . . . should be directly supervised by a board-certified dermatologist.”7 Therefore, the responsibility for a dermatology-specific education can fall on the dermatologist, necessitating adequate supervision and training of NPCs.
The findings of this study were limited by a small sample size; response bias because distribution of the survey relied on program directors disseminating the instrument to their residents, thereby limiting generalizability; and a lack of predissemination validation of the survey. Additional research in this area should focus on survey validation and distribution directly to dermatology residents, instead of relying on dermatology program directors to disseminate the survey.
- Sargen MR, Shi L, Hooker RS, et al. Future growth of physicians and non-physician providers within the U.S. Dermatology workforce. Dermatol Online J. 2017;23:13030/qt840223q6
- The current and projected dermatology workforce in the United States. J Am Acad Dermatol. 2016;74(suppl 1):AB122. doi:10.1016/j.jaad.2016.02.478
- Nurse anesthetists, nurse midwives, and nurse practitioners.Occupational Outlook Handbook. Washington, DC: US Department of Labor. Updated April 18, 2022. Accessed July 14, 2022. https://www.bls.gov/ooh/health care/nurse-anesthetists-nurse-midwives-and-nurse-practitioners.htm
- Physician assistants. Occupational Outlook Handbook. Washington, DC: US Department of Labor. Updated April 18, 2022. Accessed July 14, 2022. https://www.bls.gov/ooh/healthcare/physician-assistants.htm
- Ehrlich A, Kostecki J, Olkaba H. Trends in dermatology practices and the implications for the workforce. J Am Acad Dermatol. 2017;77:746-752. doi:10.1016/j.jaad.2017.06.030
- Anderson AM, Matsumoto M, Saul MI, et al. Accuracy of skin cancer diagnosis by physician assistants compared with dermatologists in a large health care system. JAMA Dermatol. 2018;154:569-573. doi:10.1001/jamadermatol.2018.0212s
- American Academy of Dermatology Association. Position statement on the practice of dermatology: protecting and preserving patient safety and quality care. Revised May 21, 2016. Accessed July 14, 2022. https://server.aad.org/Forms/Policies/Uploads/PS/PS-Practice of Dermatology-Protecting Preserving Patient Safety Quality Care.pdf?
- Sargen MR, Shi L, Hooker RS, et al. Future growth of physicians and non-physician providers within the U.S. Dermatology workforce. Dermatol Online J. 2017;23:13030/qt840223q6
- The current and projected dermatology workforce in the United States. J Am Acad Dermatol. 2016;74(suppl 1):AB122. doi:10.1016/j.jaad.2016.02.478
- Nurse anesthetists, nurse midwives, and nurse practitioners.Occupational Outlook Handbook. Washington, DC: US Department of Labor. Updated April 18, 2022. Accessed July 14, 2022. https://www.bls.gov/ooh/health care/nurse-anesthetists-nurse-midwives-and-nurse-practitioners.htm
- Physician assistants. Occupational Outlook Handbook. Washington, DC: US Department of Labor. Updated April 18, 2022. Accessed July 14, 2022. https://www.bls.gov/ooh/healthcare/physician-assistants.htm
- Ehrlich A, Kostecki J, Olkaba H. Trends in dermatology practices and the implications for the workforce. J Am Acad Dermatol. 2017;77:746-752. doi:10.1016/j.jaad.2017.06.030
- Anderson AM, Matsumoto M, Saul MI, et al. Accuracy of skin cancer diagnosis by physician assistants compared with dermatologists in a large health care system. JAMA Dermatol. 2018;154:569-573. doi:10.1001/jamadermatol.2018.0212s
- American Academy of Dermatology Association. Position statement on the practice of dermatology: protecting and preserving patient safety and quality care. Revised May 21, 2016. Accessed July 14, 2022. https://server.aad.org/Forms/Policies/Uploads/PS/PS-Practice of Dermatology-Protecting Preserving Patient Safety Quality Care.pdf?
Practice Points
- Most dermatology residency programs do not offer training on working with and supervising nonphysician clinicians.
- Dermatology residents think that formal training in supervising nonphysician clinicians would be a beneficial addition to the residency curriculum.
What influences a trainee’s decision to choose pediatric dermatology as a career?
INDIANAPOLIS – Three during and after fellowship.
Those are key findings from a survey of current and prior pediatric dermatology fellows, which sought to investigate what factors influence their career decisions.
According to the study’s principal investigator, Lucia Z. Diaz, MD, pediatric dermatology suffers from workforce shortages and geographic maldistribution as a subspecialty in the United States. She also noted that, from 2016 to 2021, 100% of pediatric dermatology applicants matched, yet about 15 of every 31 positions remained unfilled during each of those years. This suggests that there may be a lack of trainee mentorship secondary to a lack of available pediatric dermatologists.
“Somewhere along the way, we lose trainees to general dermatology, or they may go through a pediatric dermatology fellowship but not actually see children upon completion of their training,” Dr. Diaz, chief of pediatric dermatology at the University of Texas at Austin, said in an interview at the annual meeting of the Society for Pediatric Dermatology, where the study was presented during a poster session. “We wanted to find out factors influencing this.”
For the study, Dr. Diaz, Courtney N. Haller, MD, a first-year dermatology resident at the University of Texas at Austin, and their colleagues emailed a 37-item survey to 59 current and prior pediatric dermatology fellows who trained in the United States in the past 4 years (classes of 2019-2022). Current fellows were asked to share their future plans, and past fellows were asked to share details about their current practice situation including practice type (such as academics, private practice, and a mix of adult and pediatrics), and the researchers used descriptive statistics and chi-square analyses to evaluate qualitative data.
In all, 41 survey participants gave complete responses, and 3 gave partial responses. Of these, 8 were current fellows, 36 were past fellows, and 38 were female. The researchers found that 67% of survey respondents first became interested in pediatric dermatology in medical school, while the decision to pursue a fellowship occurred then (33%) or during their third year of dermatology residency (33%). Early exposure to pediatric dermatology, from medical school through dermatology PGY-2, was significantly associated with an early decision to pursue a pediatric dermatology career (P = .004).
In addition, respondents at institutions with two or more pediatric dermatology faculty were significantly more likely to cite home institution mentorship as an influencing factor in their career decision (P = .035).
“I thought that the interest in pediatric dermatology would peak early on during dermatology residency, but it primarily happens during medical school,” said Dr. Diaz, who is also associate director of the dermatology residency program at the medical school. “Mentorship and early exposure to pediatric dermatology during medical school are really important.”
The top three factors that discouraged respondents from pursuing a pediatric dermatology fellowship included a lack of salary benefit with additional training (83%), additional time required to complete training (73%), and geographic relocation (20%). After fellowship, 51% of respondents said they plan to or currently work in academic settings, while 88% said they plan to work full time or currently were working full time.
Interestingly, fellows with additional pediatric training such as an internship or residency were not more likely to see a greater percentage of pediatric patients in practice than those without this training (P = .14). The top 3 reasons for not seeing pediatric patients 100% of the clinical time were interest in seeing adult patients (67%), financial factors (56%), and interest in performing more procedures (56%).
In other findings, the top three factors in deciding practice location were proximity to extended family (63%), practice type (59%), and income (51%).
Adelaide A. Hebert, MD, who was asked to comment on the study, said that the lack of salary benefit from additional training is a sticking point for many fellows. “The market trends of supply and demand do not work in pediatric dermatology,” said Dr. Hebert, professor of dermatology and pediatrics, and chief of pediatric dermatology at the University of Texas, Houston. “You would think that, because there are fewer of us, we should be paid more, but it does not work that way.”
She characterized the overall study findings as “a real testament to what the challenges are” in recruiting trainees to pediatric dermatology. “The influence of mentors resonates in this assessment, but influences that are somewhat beyond our control also play a role, such as lack of salary benefit from additional training, interest in seeing adult patients, and financial factors.”
Neither the researchers nor Dr. Hebert reported having relevant financial disclosures.
INDIANAPOLIS – Three during and after fellowship.
Those are key findings from a survey of current and prior pediatric dermatology fellows, which sought to investigate what factors influence their career decisions.
According to the study’s principal investigator, Lucia Z. Diaz, MD, pediatric dermatology suffers from workforce shortages and geographic maldistribution as a subspecialty in the United States. She also noted that, from 2016 to 2021, 100% of pediatric dermatology applicants matched, yet about 15 of every 31 positions remained unfilled during each of those years. This suggests that there may be a lack of trainee mentorship secondary to a lack of available pediatric dermatologists.
“Somewhere along the way, we lose trainees to general dermatology, or they may go through a pediatric dermatology fellowship but not actually see children upon completion of their training,” Dr. Diaz, chief of pediatric dermatology at the University of Texas at Austin, said in an interview at the annual meeting of the Society for Pediatric Dermatology, where the study was presented during a poster session. “We wanted to find out factors influencing this.”
For the study, Dr. Diaz, Courtney N. Haller, MD, a first-year dermatology resident at the University of Texas at Austin, and their colleagues emailed a 37-item survey to 59 current and prior pediatric dermatology fellows who trained in the United States in the past 4 years (classes of 2019-2022). Current fellows were asked to share their future plans, and past fellows were asked to share details about their current practice situation including practice type (such as academics, private practice, and a mix of adult and pediatrics), and the researchers used descriptive statistics and chi-square analyses to evaluate qualitative data.
In all, 41 survey participants gave complete responses, and 3 gave partial responses. Of these, 8 were current fellows, 36 were past fellows, and 38 were female. The researchers found that 67% of survey respondents first became interested in pediatric dermatology in medical school, while the decision to pursue a fellowship occurred then (33%) or during their third year of dermatology residency (33%). Early exposure to pediatric dermatology, from medical school through dermatology PGY-2, was significantly associated with an early decision to pursue a pediatric dermatology career (P = .004).
In addition, respondents at institutions with two or more pediatric dermatology faculty were significantly more likely to cite home institution mentorship as an influencing factor in their career decision (P = .035).
“I thought that the interest in pediatric dermatology would peak early on during dermatology residency, but it primarily happens during medical school,” said Dr. Diaz, who is also associate director of the dermatology residency program at the medical school. “Mentorship and early exposure to pediatric dermatology during medical school are really important.”
The top three factors that discouraged respondents from pursuing a pediatric dermatology fellowship included a lack of salary benefit with additional training (83%), additional time required to complete training (73%), and geographic relocation (20%). After fellowship, 51% of respondents said they plan to or currently work in academic settings, while 88% said they plan to work full time or currently were working full time.
Interestingly, fellows with additional pediatric training such as an internship or residency were not more likely to see a greater percentage of pediatric patients in practice than those without this training (P = .14). The top 3 reasons for not seeing pediatric patients 100% of the clinical time were interest in seeing adult patients (67%), financial factors (56%), and interest in performing more procedures (56%).
In other findings, the top three factors in deciding practice location were proximity to extended family (63%), practice type (59%), and income (51%).
Adelaide A. Hebert, MD, who was asked to comment on the study, said that the lack of salary benefit from additional training is a sticking point for many fellows. “The market trends of supply and demand do not work in pediatric dermatology,” said Dr. Hebert, professor of dermatology and pediatrics, and chief of pediatric dermatology at the University of Texas, Houston. “You would think that, because there are fewer of us, we should be paid more, but it does not work that way.”
She characterized the overall study findings as “a real testament to what the challenges are” in recruiting trainees to pediatric dermatology. “The influence of mentors resonates in this assessment, but influences that are somewhat beyond our control also play a role, such as lack of salary benefit from additional training, interest in seeing adult patients, and financial factors.”
Neither the researchers nor Dr. Hebert reported having relevant financial disclosures.
INDIANAPOLIS – Three during and after fellowship.
Those are key findings from a survey of current and prior pediatric dermatology fellows, which sought to investigate what factors influence their career decisions.
According to the study’s principal investigator, Lucia Z. Diaz, MD, pediatric dermatology suffers from workforce shortages and geographic maldistribution as a subspecialty in the United States. She also noted that, from 2016 to 2021, 100% of pediatric dermatology applicants matched, yet about 15 of every 31 positions remained unfilled during each of those years. This suggests that there may be a lack of trainee mentorship secondary to a lack of available pediatric dermatologists.
“Somewhere along the way, we lose trainees to general dermatology, or they may go through a pediatric dermatology fellowship but not actually see children upon completion of their training,” Dr. Diaz, chief of pediatric dermatology at the University of Texas at Austin, said in an interview at the annual meeting of the Society for Pediatric Dermatology, where the study was presented during a poster session. “We wanted to find out factors influencing this.”
For the study, Dr. Diaz, Courtney N. Haller, MD, a first-year dermatology resident at the University of Texas at Austin, and their colleagues emailed a 37-item survey to 59 current and prior pediatric dermatology fellows who trained in the United States in the past 4 years (classes of 2019-2022). Current fellows were asked to share their future plans, and past fellows were asked to share details about their current practice situation including practice type (such as academics, private practice, and a mix of adult and pediatrics), and the researchers used descriptive statistics and chi-square analyses to evaluate qualitative data.
In all, 41 survey participants gave complete responses, and 3 gave partial responses. Of these, 8 were current fellows, 36 were past fellows, and 38 were female. The researchers found that 67% of survey respondents first became interested in pediatric dermatology in medical school, while the decision to pursue a fellowship occurred then (33%) or during their third year of dermatology residency (33%). Early exposure to pediatric dermatology, from medical school through dermatology PGY-2, was significantly associated with an early decision to pursue a pediatric dermatology career (P = .004).
In addition, respondents at institutions with two or more pediatric dermatology faculty were significantly more likely to cite home institution mentorship as an influencing factor in their career decision (P = .035).
“I thought that the interest in pediatric dermatology would peak early on during dermatology residency, but it primarily happens during medical school,” said Dr. Diaz, who is also associate director of the dermatology residency program at the medical school. “Mentorship and early exposure to pediatric dermatology during medical school are really important.”
The top three factors that discouraged respondents from pursuing a pediatric dermatology fellowship included a lack of salary benefit with additional training (83%), additional time required to complete training (73%), and geographic relocation (20%). After fellowship, 51% of respondents said they plan to or currently work in academic settings, while 88% said they plan to work full time or currently were working full time.
Interestingly, fellows with additional pediatric training such as an internship or residency were not more likely to see a greater percentage of pediatric patients in practice than those without this training (P = .14). The top 3 reasons for not seeing pediatric patients 100% of the clinical time were interest in seeing adult patients (67%), financial factors (56%), and interest in performing more procedures (56%).
In other findings, the top three factors in deciding practice location were proximity to extended family (63%), practice type (59%), and income (51%).
Adelaide A. Hebert, MD, who was asked to comment on the study, said that the lack of salary benefit from additional training is a sticking point for many fellows. “The market trends of supply and demand do not work in pediatric dermatology,” said Dr. Hebert, professor of dermatology and pediatrics, and chief of pediatric dermatology at the University of Texas, Houston. “You would think that, because there are fewer of us, we should be paid more, but it does not work that way.”
She characterized the overall study findings as “a real testament to what the challenges are” in recruiting trainees to pediatric dermatology. “The influence of mentors resonates in this assessment, but influences that are somewhat beyond our control also play a role, such as lack of salary benefit from additional training, interest in seeing adult patients, and financial factors.”
Neither the researchers nor Dr. Hebert reported having relevant financial disclosures.
AT SPD 2022
Simple Intraoperative Technique to Improve Wound Edge Approximation for Residents
Practice Gap
Dermatology residents can struggle with surgical closure early in their training years. Although experienced dermatologic surgeons may intuitively be able to align edges for maximal cosmesis, doing so can prove challenging in the context of learning basic surgical techniques for early residents.
Furthermore, local anesthesia can distort cutaneous anatomy and surgical landmarks, requiring the surgeon to reexamine their closure technique. Patients may require position changes or may make involuntary movements, both of which require dynamic thinking and planning on the part of the dermatologic surgeon to achieve optimal outcomes.
The Technique
We propose the use of sutures to intraoperatively guide placement of the dermal needle. This technique can be used for various closure types; here, we demonstrate its use in a standard elliptical excision.
To begin, a standard length to width ellipse ratio of 3:1 is drawn with appropriate margins around a neoplasm.1 After excision and appropriate undermining of the ellipse, we typically use deep sutures to close the deep space. The first pass of the needle through tissue can be performed in a place of the surgeon’s preference but typically abides by the rule of halves or the zipper method (Figure 1A). To determine optimal placement of the second needle pass through tissue, we recommend applying gentle opposing traction forces to the wound apices to approximate the linear outcome of the wound edges. The surgeon can use a skin hook to guide placement of the needle to the contralateral wound edge in an unassisted method of this technique (Figure 1B). The surgeon’s assistant also can aid in applying cutaneous traction along the length of the excision if the surgeon wishes to free their hands (Figure 1C). Because the risk of needlestick injury at this step is small, it is prudent for the surgeon to advise the assistant to avoid needlestick injury by keeping their hands away from the needle path in the surgical site.
Although traction is being applied to the wound apices, the deep suture should extend across the wound with just enough pressure to leave a serosanguineous notched mark in the contralateral tissue edge (Figure 1D). After releasing traction on the wound edges, the surgeon can effortlessly visualize the target for needle placement and make a throw through the tissue accordingly.

This process can be continued until wound closure is complete (Figure 2). Top sutures or adhesive strips can be placed afterward for completing approximation of the wound edges superficially.
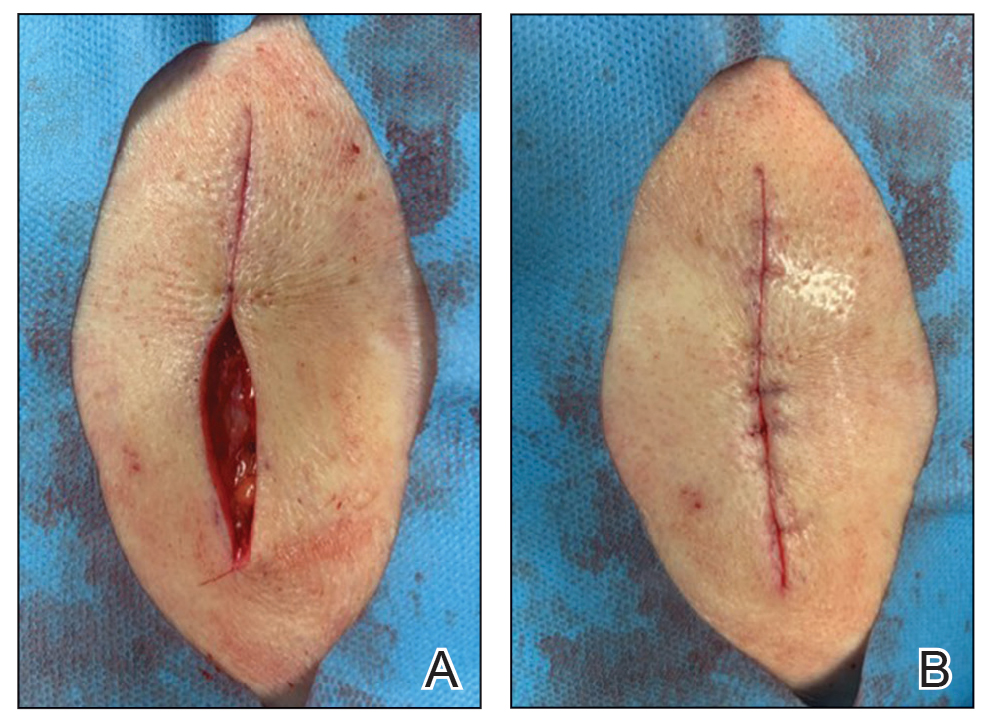
Practice Implications
By using this technique to align wound edges intraoperatively, the surgeon can have a functional guide for needle placement. The technique allows improvement of function and cosmesis of surgical wounds, while also accounting for topographical variations in the patient’s surgical site. Approximation of the wound edges is particularly important at the beginning of closure, as the wound edges align and approximate more with each subsequent stitch, with decreasing tension.2
In addition, when operating on a curvilinear or challenging topographical surface of the body, this technique can provide a clear template for guiding suture placement for approximating wound edges. Furthermore, local biodynamic anatomy might become distorted after excision of the tissue specimen due to release of centripetal tangential forces that were present in the pre-excised skin.1 Local change in biodynamic forces may be difficult to plan for preoperatively using other techniques.3
Although this technique can be utilized for all suture placements in closure, it is of greatest value when placing the first few sutures and when operating on nonplanar surfaces that might become distorted after excision. To ensure the best outcome, it is important to be certain that the area has been properly cleaned prior to surgery and a sterile technique is used.
- Paul SP. Biodynamic excisional skin tension lines for excisional surgery of the lower limb and the technique of using parallel relaxing incisions to further reduce wound tension. Plast Reconstr Surg Glob Open. 2017;5:E1614. doi:10.1097/GOX.0000000000001614
- Miller CJ, Antunes MB, Sobanko JF. Surgical technique for optimal outcomes: part II. repairing tissue: suturing. J Am Acad Dermatol. 2015;72:389-402. doi:10.1016/j.jaad.2014.08.006
- Parikh SA, Sloan B. Clinical pearl: a simple and effective technique for improving surgical closures for the early-learning resident. Cutis. 2017;100:338-339.
Practice Gap
Dermatology residents can struggle with surgical closure early in their training years. Although experienced dermatologic surgeons may intuitively be able to align edges for maximal cosmesis, doing so can prove challenging in the context of learning basic surgical techniques for early residents.
Furthermore, local anesthesia can distort cutaneous anatomy and surgical landmarks, requiring the surgeon to reexamine their closure technique. Patients may require position changes or may make involuntary movements, both of which require dynamic thinking and planning on the part of the dermatologic surgeon to achieve optimal outcomes.
The Technique
We propose the use of sutures to intraoperatively guide placement of the dermal needle. This technique can be used for various closure types; here, we demonstrate its use in a standard elliptical excision.
To begin, a standard length to width ellipse ratio of 3:1 is drawn with appropriate margins around a neoplasm.1 After excision and appropriate undermining of the ellipse, we typically use deep sutures to close the deep space. The first pass of the needle through tissue can be performed in a place of the surgeon’s preference but typically abides by the rule of halves or the zipper method (Figure 1A). To determine optimal placement of the second needle pass through tissue, we recommend applying gentle opposing traction forces to the wound apices to approximate the linear outcome of the wound edges. The surgeon can use a skin hook to guide placement of the needle to the contralateral wound edge in an unassisted method of this technique (Figure 1B). The surgeon’s assistant also can aid in applying cutaneous traction along the length of the excision if the surgeon wishes to free their hands (Figure 1C). Because the risk of needlestick injury at this step is small, it is prudent for the surgeon to advise the assistant to avoid needlestick injury by keeping their hands away from the needle path in the surgical site.
Although traction is being applied to the wound apices, the deep suture should extend across the wound with just enough pressure to leave a serosanguineous notched mark in the contralateral tissue edge (Figure 1D). After releasing traction on the wound edges, the surgeon can effortlessly visualize the target for needle placement and make a throw through the tissue accordingly.

This process can be continued until wound closure is complete (Figure 2). Top sutures or adhesive strips can be placed afterward for completing approximation of the wound edges superficially.
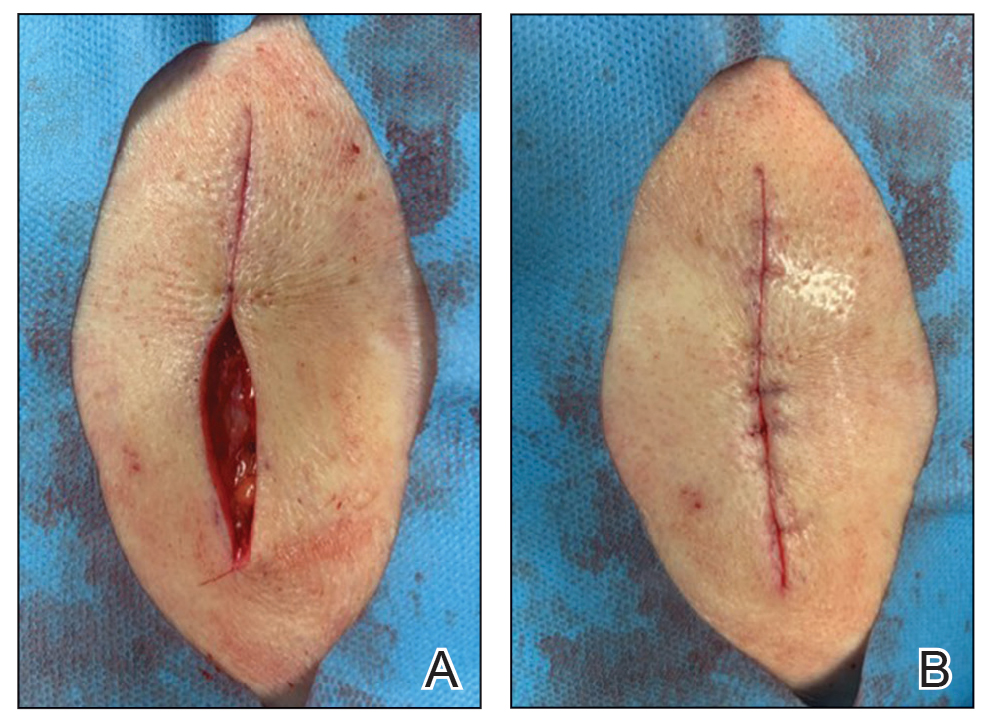
Practice Implications
By using this technique to align wound edges intraoperatively, the surgeon can have a functional guide for needle placement. The technique allows improvement of function and cosmesis of surgical wounds, while also accounting for topographical variations in the patient’s surgical site. Approximation of the wound edges is particularly important at the beginning of closure, as the wound edges align and approximate more with each subsequent stitch, with decreasing tension.2
In addition, when operating on a curvilinear or challenging topographical surface of the body, this technique can provide a clear template for guiding suture placement for approximating wound edges. Furthermore, local biodynamic anatomy might become distorted after excision of the tissue specimen due to release of centripetal tangential forces that were present in the pre-excised skin.1 Local change in biodynamic forces may be difficult to plan for preoperatively using other techniques.3
Although this technique can be utilized for all suture placements in closure, it is of greatest value when placing the first few sutures and when operating on nonplanar surfaces that might become distorted after excision. To ensure the best outcome, it is important to be certain that the area has been properly cleaned prior to surgery and a sterile technique is used.
Practice Gap
Dermatology residents can struggle with surgical closure early in their training years. Although experienced dermatologic surgeons may intuitively be able to align edges for maximal cosmesis, doing so can prove challenging in the context of learning basic surgical techniques for early residents.
Furthermore, local anesthesia can distort cutaneous anatomy and surgical landmarks, requiring the surgeon to reexamine their closure technique. Patients may require position changes or may make involuntary movements, both of which require dynamic thinking and planning on the part of the dermatologic surgeon to achieve optimal outcomes.
The Technique
We propose the use of sutures to intraoperatively guide placement of the dermal needle. This technique can be used for various closure types; here, we demonstrate its use in a standard elliptical excision.
To begin, a standard length to width ellipse ratio of 3:1 is drawn with appropriate margins around a neoplasm.1 After excision and appropriate undermining of the ellipse, we typically use deep sutures to close the deep space. The first pass of the needle through tissue can be performed in a place of the surgeon’s preference but typically abides by the rule of halves or the zipper method (Figure 1A). To determine optimal placement of the second needle pass through tissue, we recommend applying gentle opposing traction forces to the wound apices to approximate the linear outcome of the wound edges. The surgeon can use a skin hook to guide placement of the needle to the contralateral wound edge in an unassisted method of this technique (Figure 1B). The surgeon’s assistant also can aid in applying cutaneous traction along the length of the excision if the surgeon wishes to free their hands (Figure 1C). Because the risk of needlestick injury at this step is small, it is prudent for the surgeon to advise the assistant to avoid needlestick injury by keeping their hands away from the needle path in the surgical site.
Although traction is being applied to the wound apices, the deep suture should extend across the wound with just enough pressure to leave a serosanguineous notched mark in the contralateral tissue edge (Figure 1D). After releasing traction on the wound edges, the surgeon can effortlessly visualize the target for needle placement and make a throw through the tissue accordingly.

This process can be continued until wound closure is complete (Figure 2). Top sutures or adhesive strips can be placed afterward for completing approximation of the wound edges superficially.
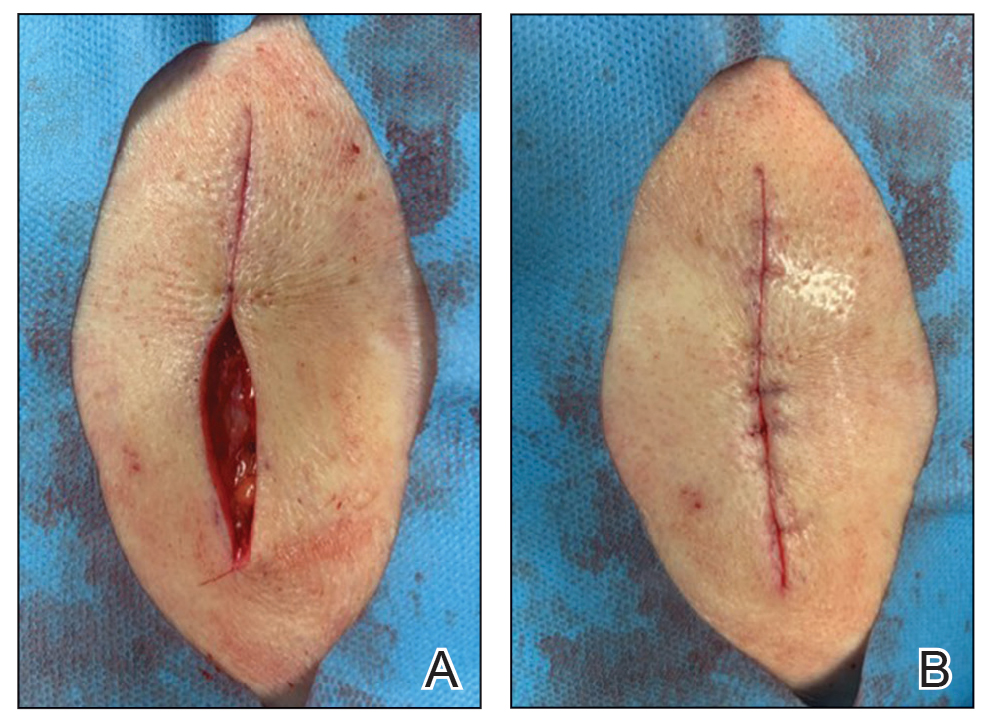
Practice Implications
By using this technique to align wound edges intraoperatively, the surgeon can have a functional guide for needle placement. The technique allows improvement of function and cosmesis of surgical wounds, while also accounting for topographical variations in the patient’s surgical site. Approximation of the wound edges is particularly important at the beginning of closure, as the wound edges align and approximate more with each subsequent stitch, with decreasing tension.2
In addition, when operating on a curvilinear or challenging topographical surface of the body, this technique can provide a clear template for guiding suture placement for approximating wound edges. Furthermore, local biodynamic anatomy might become distorted after excision of the tissue specimen due to release of centripetal tangential forces that were present in the pre-excised skin.1 Local change in biodynamic forces may be difficult to plan for preoperatively using other techniques.3
Although this technique can be utilized for all suture placements in closure, it is of greatest value when placing the first few sutures and when operating on nonplanar surfaces that might become distorted after excision. To ensure the best outcome, it is important to be certain that the area has been properly cleaned prior to surgery and a sterile technique is used.
- Paul SP. Biodynamic excisional skin tension lines for excisional surgery of the lower limb and the technique of using parallel relaxing incisions to further reduce wound tension. Plast Reconstr Surg Glob Open. 2017;5:E1614. doi:10.1097/GOX.0000000000001614
- Miller CJ, Antunes MB, Sobanko JF. Surgical technique for optimal outcomes: part II. repairing tissue: suturing. J Am Acad Dermatol. 2015;72:389-402. doi:10.1016/j.jaad.2014.08.006
- Parikh SA, Sloan B. Clinical pearl: a simple and effective technique for improving surgical closures for the early-learning resident. Cutis. 2017;100:338-339.
- Paul SP. Biodynamic excisional skin tension lines for excisional surgery of the lower limb and the technique of using parallel relaxing incisions to further reduce wound tension. Plast Reconstr Surg Glob Open. 2017;5:E1614. doi:10.1097/GOX.0000000000001614
- Miller CJ, Antunes MB, Sobanko JF. Surgical technique for optimal outcomes: part II. repairing tissue: suturing. J Am Acad Dermatol. 2015;72:389-402. doi:10.1016/j.jaad.2014.08.006
- Parikh SA, Sloan B. Clinical pearl: a simple and effective technique for improving surgical closures for the early-learning resident. Cutis. 2017;100:338-339.
Why we should be scrutinizing the rising prevalence of adult ADHD
In patients with attention-deficit/hyperactivity disorder (ADHD), stimulants reduce impulsivity and improve attention and focus. In individuals who do not have this disorder, stimulants are believed to enhance cognition, attention, and physical performance. In this article, I describe how a patient whose intermittent use of stimulants for motivation and cognitive enhancement shaped my approach to the diagnosis of ADHD.
Instant gratification and quick solutions
I asked him questions to confirm the diagnosis, but he rushed to reassure me that he had already been diagnosed with ADHD and had been doing well on dextroamphetamine and amphetamine for many years. I was inclined to question his diagnosis of ADHD after learning of his “as-needed” use of stimulants as brain enhancers. His medical record reflecting the diagnosis of ADHD dated back to when he was a first-year dental student. The diagnosis was based on the patient’s report of procrastination for as long as he could remember. It also hinged on difficulties learning a second language and math being a challenging subject for him. Despite this, he managed to do well in school and earn an undergraduate degree, well enough to later pursue dentistry at a reputable university.
I thought, “Isn’t it normal to lose motivation and have doubts when preparing for a high-stakes exam like the boards? Aren’t these negative thoughts distracting enough to render sustained focus impossible? Doesn’t everyone struggle with procrastination, especially when they need to study? If learning a new language requires devotion, consistency, and sacrifice, isn’t it inherently challenging? Doesn’t good performance in math depend on multiple factors (ie, a strong foundation, cumulative learning, frequent practice), and thus leaves many students struggling?”
This interaction and many similar ones made me scrutinize the diagnosis of ADHD in patients I encounter in clinical settings. We live in a society where instant gratification is cherished, and quick fixes are pursued with little contemplation of pitfalls. Students use stimulants to cram for exams, high-functioning professionals use them to meet deadlines, and athletes use them to enhance performance and improve reaction times. Psychiatry seems to be drawn into the demands of society and may be fueling the “quick-fix” mentality by prescribing stimulants to healthy individuals who want to improve their focus, and then diagnosing them with ADHD to align the prescription with an appropriate diagnosis. Research on the adverse effects of stimulant use in adults is not convincing nor conclusive enough to sway prescribers from denying the average adult patient a stimulant to enhance cognitive function before a high-stakes exam or a critical, career-shaping project if they present with some ADHD traits, which the patient might even hyperbolize to secure the desired prescription. All of this may contribute to the perceived rising prevalence of ADHD among adults.
As for my 30-year-old dental student, I reasoned that continuing his medication, for now, would help me establish rapport and trust. This would allow me to counsel him on the long-term adverse effects of stimulants, and develop a plan to optimize his sleep, focus, and time management skills, eventually improving his cognition and attention naturally. Unfortunately, he did not show up to future appointments after I sent him the refill.
In patients with attention-deficit/hyperactivity disorder (ADHD), stimulants reduce impulsivity and improve attention and focus. In individuals who do not have this disorder, stimulants are believed to enhance cognition, attention, and physical performance. In this article, I describe how a patient whose intermittent use of stimulants for motivation and cognitive enhancement shaped my approach to the diagnosis of ADHD.
Instant gratification and quick solutions
I asked him questions to confirm the diagnosis, but he rushed to reassure me that he had already been diagnosed with ADHD and had been doing well on dextroamphetamine and amphetamine for many years. I was inclined to question his diagnosis of ADHD after learning of his “as-needed” use of stimulants as brain enhancers. His medical record reflecting the diagnosis of ADHD dated back to when he was a first-year dental student. The diagnosis was based on the patient’s report of procrastination for as long as he could remember. It also hinged on difficulties learning a second language and math being a challenging subject for him. Despite this, he managed to do well in school and earn an undergraduate degree, well enough to later pursue dentistry at a reputable university.
I thought, “Isn’t it normal to lose motivation and have doubts when preparing for a high-stakes exam like the boards? Aren’t these negative thoughts distracting enough to render sustained focus impossible? Doesn’t everyone struggle with procrastination, especially when they need to study? If learning a new language requires devotion, consistency, and sacrifice, isn’t it inherently challenging? Doesn’t good performance in math depend on multiple factors (ie, a strong foundation, cumulative learning, frequent practice), and thus leaves many students struggling?”
This interaction and many similar ones made me scrutinize the diagnosis of ADHD in patients I encounter in clinical settings. We live in a society where instant gratification is cherished, and quick fixes are pursued with little contemplation of pitfalls. Students use stimulants to cram for exams, high-functioning professionals use them to meet deadlines, and athletes use them to enhance performance and improve reaction times. Psychiatry seems to be drawn into the demands of society and may be fueling the “quick-fix” mentality by prescribing stimulants to healthy individuals who want to improve their focus, and then diagnosing them with ADHD to align the prescription with an appropriate diagnosis. Research on the adverse effects of stimulant use in adults is not convincing nor conclusive enough to sway prescribers from denying the average adult patient a stimulant to enhance cognitive function before a high-stakes exam or a critical, career-shaping project if they present with some ADHD traits, which the patient might even hyperbolize to secure the desired prescription. All of this may contribute to the perceived rising prevalence of ADHD among adults.
As for my 30-year-old dental student, I reasoned that continuing his medication, for now, would help me establish rapport and trust. This would allow me to counsel him on the long-term adverse effects of stimulants, and develop a plan to optimize his sleep, focus, and time management skills, eventually improving his cognition and attention naturally. Unfortunately, he did not show up to future appointments after I sent him the refill.
In patients with attention-deficit/hyperactivity disorder (ADHD), stimulants reduce impulsivity and improve attention and focus. In individuals who do not have this disorder, stimulants are believed to enhance cognition, attention, and physical performance. In this article, I describe how a patient whose intermittent use of stimulants for motivation and cognitive enhancement shaped my approach to the diagnosis of ADHD.
Instant gratification and quick solutions
I asked him questions to confirm the diagnosis, but he rushed to reassure me that he had already been diagnosed with ADHD and had been doing well on dextroamphetamine and amphetamine for many years. I was inclined to question his diagnosis of ADHD after learning of his “as-needed” use of stimulants as brain enhancers. His medical record reflecting the diagnosis of ADHD dated back to when he was a first-year dental student. The diagnosis was based on the patient’s report of procrastination for as long as he could remember. It also hinged on difficulties learning a second language and math being a challenging subject for him. Despite this, he managed to do well in school and earn an undergraduate degree, well enough to later pursue dentistry at a reputable university.
I thought, “Isn’t it normal to lose motivation and have doubts when preparing for a high-stakes exam like the boards? Aren’t these negative thoughts distracting enough to render sustained focus impossible? Doesn’t everyone struggle with procrastination, especially when they need to study? If learning a new language requires devotion, consistency, and sacrifice, isn’t it inherently challenging? Doesn’t good performance in math depend on multiple factors (ie, a strong foundation, cumulative learning, frequent practice), and thus leaves many students struggling?”
This interaction and many similar ones made me scrutinize the diagnosis of ADHD in patients I encounter in clinical settings. We live in a society where instant gratification is cherished, and quick fixes are pursued with little contemplation of pitfalls. Students use stimulants to cram for exams, high-functioning professionals use them to meet deadlines, and athletes use them to enhance performance and improve reaction times. Psychiatry seems to be drawn into the demands of society and may be fueling the “quick-fix” mentality by prescribing stimulants to healthy individuals who want to improve their focus, and then diagnosing them with ADHD to align the prescription with an appropriate diagnosis. Research on the adverse effects of stimulant use in adults is not convincing nor conclusive enough to sway prescribers from denying the average adult patient a stimulant to enhance cognitive function before a high-stakes exam or a critical, career-shaping project if they present with some ADHD traits, which the patient might even hyperbolize to secure the desired prescription. All of this may contribute to the perceived rising prevalence of ADHD among adults.
As for my 30-year-old dental student, I reasoned that continuing his medication, for now, would help me establish rapport and trust. This would allow me to counsel him on the long-term adverse effects of stimulants, and develop a plan to optimize his sleep, focus, and time management skills, eventually improving his cognition and attention naturally. Unfortunately, he did not show up to future appointments after I sent him the refill.
Prioritizing Mental Health in Residency
The World Health Organization declared COVID-19 a pandemic on March 11, 2020, just 4 months before the start of a new residency cycle. Referred to as “COVID interns,” PGY-1 residents transitioning out of medical school in 2020 faced an unprecedented challenge of doctoring within a confused and ill-prepared health care system, while senior residents scrambled to adjust to their rapidly changing training programs. Each subsequent week brought more sobering news of increasing hospitalizations, intensive care unit admissions, and deaths; hospitals across the country resorted to the redeployment of residents across all specialties to buffer the growing need within their internal medicine and critical care units.1 And while the news and social media blurred into a collage of ventilator shortages, politicization of science, and “#healthcareheroes,” one study showed53.7% of medical interns (N=108) were struggling with mild to extremely severe depression, while 63.9% reported mild to severe anxiety.2
Many shortcomings of our health care system—ill preparedness, racial disparity, health illiteracy—were highlighted during the COVID-19 pandemic, and providers’ mental health was no exception.3 Classic psychosocial risk factors, such as high demands, lack of control, lack of institutional support, and absence of reward defined the workplace, leading Theorell4 to call it “a randomized trial for maximal worsening of the work environment.” Stress and burnout during residency are not novel concepts. A 2002 survey including 415 medical residency programs with a response from more than 4000 residents found depressive symptoms in 35% of respondents, paired with feelings of increased cynicism and decreased humanism despite major curricular reforms and duty hour limitations.5 Unfortunately, the statistics in the coming years hardly budged and, in the wake of the pandemic, culminated to more than 50% to 76% of physicians worldwide reporting burnout in 2020.6-8
As a COVID intern at Brigham and Women’s Hospital (Boston, Massachusetts), I also experienced the demanding workload and witnessed the struggle of my colleagues firsthand. Brigham and Women’s Hospital, similar to many of its peer institutions, implemented frequent mental health check-ins within its curriculum. Known as the Intern Humanistic Curriculum, these check-ins essentially were an echo chamber to unload the psychological burdens of our workdays, and we eagerly shared what made us angry, sad, hopeful, and hopeless. During one such session, I learned about moral injury, a term originating in the military defined as the psychological stress resulting from actions—or the lack of actions—that violates one’s moral or ethical code.9 With the onslaught of patient deaths for which most of us felt unprepared, we had all endured varying degrees of moral injury. Greenberg et al9 described 2 potential outcomes after moral injury: (1) the development of mental health disorders such as depression and posttraumatic stress disorder, or (2) posttraumatic growth, which is the bolstering of psychological resilience. Notably, the outcome is based on the way someone is supported before, during, and after the challenging incident.9
With the aim of psychological growth and developing resilience, residents should prioritize mental health throughout their training. To this end, several resources are readily available, many of which I actively use or frequently revisit, which are reviewed here.
Mindfulness Meditation App
Calm (https://www.calm.com/) is one of several popular mobile applications (apps) that delivers mindfulness mediation—the practice of attending to experiences, thoughts, and emotions without bias or judgment. With more than 100 million downloads, Calm includes meditation tutorials, breathing exercises, nature scenes and sounds, and audio programs taught by mindfulness experts for $69.99 a year or $14.99 a month. Systemic reviews have demonstrated reduced sleep disturbance, decreased ruminative thoughts and emotional reactivity, and increased awareness and acceptance in those practicing mindfulness meditation. Calm users have reported these benefits, with many able to forego the time- and cost-intensive cognitive behavioral therapy that requires highly trained therapists.10-12
Exercise to Relieve Stress
Both aerobic and anaerobic exercises are antidepressive and anxiolytic and also lower one’s overall sensitivity to stress. Whether it is governed by neurotransmitters such as the activation of the opioid systems or the release of endogenous endorphins or time spent focusing on a different task at hand, the benefits of exercise against mental stressors have been extensively studied and established.13 Consider obtaining a new gym membership at the start of residency or joining an intramural team. Both have the added benefit of expanding your social circle.
Socialize With Others
Social isolation and perceived loneliness are key stressors linked to neuroendocrine disturbances that underlie depression, anxiety, and even schizophrenia.14,15 Throughout residency there will be several social events and opportunities to gather with colleagues—inside or outside of the work environment—and residents should attend as time allows. Even virtual social interactions were found to reduce stress and help in the treatment of social anxiety disorder.14
Communicate About Stressors
Open up to your co-residents, friends, and family about any struggles that may be invisible on the outside. Even attendings can empathize with the struggles of residency, and the mentors in place are actively trained to prioritize resident wellness. If verbal communication is not your strength, try journaling. Writing helps to untangle and better define underlying stressors and is itself meditative.16,17 However, ensure that your journaling is focused on positive emotional responses and aims to determine the positive benefits within any stressful event; those solely expressing negative emotions were found to have higher levels of stress and anxiety afterward than they had before.17
Seek a Mental Health Specialist
As with all other human ailments, severe mental health disorders require specialists and proper medication. Unfortunately, substantial stigma accompanying mental health continues to permeate medicine, creating considerable barriers for residents in need of care.18 A 2016 survey of more than 2000 physicians found that those with mental illnesses did not seek treatment due to limited time, fear of being reported to a medical licensing board, concern over obtaining licensure, and shame or embarrassment at the diagnosis.19 Besides urging residents to seek care, more effort should be invested in addressing the stigma and ensuring confidentiality. In 2021, the internal medicine and medicine-pediatrics residency at the University of Colorado Anschutz Medical Campus (Aurora, Colorado) developed a confidential opt-out, rather than opt-in, mental health program, and appointments were made for all 80 interns in advance. In doing so, they found increased participation and self-reported wellness at a relatively low cost and simple implementation.20 For trainees without such access, online or mobile therapy platforms offering electronic mental health treatment or telepsychiatry also have been employed.21,22 The onus ultimately is still on the individual to seek the care they need. Although only an anecdotal piece of evidence, I have found the prevalence of physicians taking selective serotonin reuptake inhibitors such as escitalopram, sertraline, or fluoxetine to be strikingly common and quite beneficial.
Final Thoughts
Residency remains rife with financial, emotional, and physical stressors; even as the dust settles on the COVID-19 pandemic, the light shed on the importance of trainee mental health must remain illuminated. For the aforementioned resources to have an impact, residents need to be empowered to openly discuss mental health issues and to seek help if necessary. Finally, in 2018, the Journal of Graduate Medical Education published a 10-year prospective cohort study that found that emotional distress during residency persists in professional practice even 10 years after residency and is associated with future burnout.23 Trainees should consider prioritizing their mental health to not only improve their quality of life in the present but also as an investment for their future.
- Spiegelman J, Praiss A, Syeda S, et al. Preparation and redeployment of house staff during a pandemic. Semin Perinatol. 2020;44:151297.
- Debnath PR, Islam MS, Karmakar PK, et al. Mental health concerns, insomnia, and loneliness among intern doctors amidst the COVID-19 pandemic: evidence from a large tertiary care hospital in Bangladesh. Int J Ment Health Addict. 2021:1-21. doi:10.1007/s11469-021-00690-0
- O’Reilly-Shah VN, Gentry KR, Van Cleve W, et al. The COVID-19 pandemic highlights shortcomings in US health care informatics infrastructure: a call to action. Anesth Analg. 2020;131:340-344.
- Theorell T. COVID-19 and working conditions in health care. Psychother Psychosom. 2020;89:193-194.
- Collier VU, McCue JD, Markus A, et al. Stress in medical residency: status quo after a decade of reform? Ann Intern Med. 2002;136:384-390.
- AbuDujain NM, Almuhaideb QA, Alrumaihi NA, et al. The impact of the COVID-19 pandemic on medical interns’ education, training, and mental health: a cross-sectional study. Cureus. 2021;13:E19250.
- Amanullah S, Ramesh Shankar R. The impact of COVID-19 on physician burnout globally: a review. Healthcare (Basel). 2020;8:421.
- Lebares CC, Guvva EV, Ascher NL, et al. Burnout and stress among US surgery residents: psychological distress and resilience. J Am Coll Surg. 2018;226:80-90.
- Greenberg N, Docherty M, Gnanapragasam S, et al. Managing mental health challenges faced by healthcare workers during COVID-19 pandemic. BMJ. 2020;368:m1211.
- Gal E, Stefan S, Cristea IA. The efficacy of mindfulness meditation apps in enhancing users’ well-being and mental health related outcomes: a meta-analysis of randomized controlled trials. J Affect Disord. 2021;279:131-142.
- Huberty J, Green J, Glissmann C, et al. Efficacy of the mindfulness meditation mobile app “Calm” to reduce stress among college students: randomized controlled trial. JMIR Mhealth Uhealth. 2019;7:E14273.
- Huberty J, Puzia ME, Larkey L, et al. Can a meditation app help my sleep? a cross-sectional survey of Calm users. PLoS One. 2021;16:E0257518.
- Salmon P. Effects of physical exercise on anxiety, depression, and sensitivity to stress: a unifying theory. Clin Psychol Rev. 2001;21:33-61.
- Kampmann IL, Emmelkamp PM, Hartanto D, et al. Exposure to virtual social interactions in the treatment of social anxiety disorder: a randomized controlled trial. Behav Res Ther. 2016;77:147-156.
- Mumtaz F, Khan MI, Zubair M, et al. Neurobiology and consequences of social isolation stress in animal model-A comprehensive review. Biomed Pharmacother. 2018;105:1205-1222.
- Khanna P, Singh K. Stress management training and gratitude journaling in the classroom: an initial investigation in Indian context. Curr Psychol. 2021;40:5737-5748.
- Ullrich PM, Lutgendorf SK. Journaling about stressful events: effects of cognitive processing and emotional expression. Ann Behav Med. 2002;24:244-250.
- Outhoff K. Depression in doctors: a bitter pill to swallow. S Afr Fam Pract. 2019;61(suppl 1):S11-S14.
- Gold KJ, Andrew LB, Goldman EB, et al. “I would never want to have a mental health diagnosis on my record”: a survey of female physicians on mental health diagnosis, treatment, and reporting. Gen Hosp Psychiatry. 2016;43:51-57.
- Major A, Williams JG, McGuire WC, et al. Removing barriers: a confidential opt-out mental health pilot program for internal medicine interns. Acad Med. 2021;96:686-689.
- Greenhalgh T, Wherton J. Telepsychiatry: learning from the pandemic. Br J Psychiatry. 2022;220:1-5.
- Timakum T, Xie Q, Song M. Analysis of E-mental health research: mapping the relationship between information technology and mental healthcare. BMC Psychiatry. 2022;22:57.
- Raimo J, LaVine S, Spielmann K, et al. The correlation of stress in residency with future stress and burnout: a 10-year prospective cohort study. J Grad Med Educ. 2018;10:524-531.
The World Health Organization declared COVID-19 a pandemic on March 11, 2020, just 4 months before the start of a new residency cycle. Referred to as “COVID interns,” PGY-1 residents transitioning out of medical school in 2020 faced an unprecedented challenge of doctoring within a confused and ill-prepared health care system, while senior residents scrambled to adjust to their rapidly changing training programs. Each subsequent week brought more sobering news of increasing hospitalizations, intensive care unit admissions, and deaths; hospitals across the country resorted to the redeployment of residents across all specialties to buffer the growing need within their internal medicine and critical care units.1 And while the news and social media blurred into a collage of ventilator shortages, politicization of science, and “#healthcareheroes,” one study showed53.7% of medical interns (N=108) were struggling with mild to extremely severe depression, while 63.9% reported mild to severe anxiety.2
Many shortcomings of our health care system—ill preparedness, racial disparity, health illiteracy—were highlighted during the COVID-19 pandemic, and providers’ mental health was no exception.3 Classic psychosocial risk factors, such as high demands, lack of control, lack of institutional support, and absence of reward defined the workplace, leading Theorell4 to call it “a randomized trial for maximal worsening of the work environment.” Stress and burnout during residency are not novel concepts. A 2002 survey including 415 medical residency programs with a response from more than 4000 residents found depressive symptoms in 35% of respondents, paired with feelings of increased cynicism and decreased humanism despite major curricular reforms and duty hour limitations.5 Unfortunately, the statistics in the coming years hardly budged and, in the wake of the pandemic, culminated to more than 50% to 76% of physicians worldwide reporting burnout in 2020.6-8
As a COVID intern at Brigham and Women’s Hospital (Boston, Massachusetts), I also experienced the demanding workload and witnessed the struggle of my colleagues firsthand. Brigham and Women’s Hospital, similar to many of its peer institutions, implemented frequent mental health check-ins within its curriculum. Known as the Intern Humanistic Curriculum, these check-ins essentially were an echo chamber to unload the psychological burdens of our workdays, and we eagerly shared what made us angry, sad, hopeful, and hopeless. During one such session, I learned about moral injury, a term originating in the military defined as the psychological stress resulting from actions—or the lack of actions—that violates one’s moral or ethical code.9 With the onslaught of patient deaths for which most of us felt unprepared, we had all endured varying degrees of moral injury. Greenberg et al9 described 2 potential outcomes after moral injury: (1) the development of mental health disorders such as depression and posttraumatic stress disorder, or (2) posttraumatic growth, which is the bolstering of psychological resilience. Notably, the outcome is based on the way someone is supported before, during, and after the challenging incident.9
With the aim of psychological growth and developing resilience, residents should prioritize mental health throughout their training. To this end, several resources are readily available, many of which I actively use or frequently revisit, which are reviewed here.
Mindfulness Meditation App
Calm (https://www.calm.com/) is one of several popular mobile applications (apps) that delivers mindfulness mediation—the practice of attending to experiences, thoughts, and emotions without bias or judgment. With more than 100 million downloads, Calm includes meditation tutorials, breathing exercises, nature scenes and sounds, and audio programs taught by mindfulness experts for $69.99 a year or $14.99 a month. Systemic reviews have demonstrated reduced sleep disturbance, decreased ruminative thoughts and emotional reactivity, and increased awareness and acceptance in those practicing mindfulness meditation. Calm users have reported these benefits, with many able to forego the time- and cost-intensive cognitive behavioral therapy that requires highly trained therapists.10-12
Exercise to Relieve Stress
Both aerobic and anaerobic exercises are antidepressive and anxiolytic and also lower one’s overall sensitivity to stress. Whether it is governed by neurotransmitters such as the activation of the opioid systems or the release of endogenous endorphins or time spent focusing on a different task at hand, the benefits of exercise against mental stressors have been extensively studied and established.13 Consider obtaining a new gym membership at the start of residency or joining an intramural team. Both have the added benefit of expanding your social circle.
Socialize With Others
Social isolation and perceived loneliness are key stressors linked to neuroendocrine disturbances that underlie depression, anxiety, and even schizophrenia.14,15 Throughout residency there will be several social events and opportunities to gather with colleagues—inside or outside of the work environment—and residents should attend as time allows. Even virtual social interactions were found to reduce stress and help in the treatment of social anxiety disorder.14
Communicate About Stressors
Open up to your co-residents, friends, and family about any struggles that may be invisible on the outside. Even attendings can empathize with the struggles of residency, and the mentors in place are actively trained to prioritize resident wellness. If verbal communication is not your strength, try journaling. Writing helps to untangle and better define underlying stressors and is itself meditative.16,17 However, ensure that your journaling is focused on positive emotional responses and aims to determine the positive benefits within any stressful event; those solely expressing negative emotions were found to have higher levels of stress and anxiety afterward than they had before.17
Seek a Mental Health Specialist
As with all other human ailments, severe mental health disorders require specialists and proper medication. Unfortunately, substantial stigma accompanying mental health continues to permeate medicine, creating considerable barriers for residents in need of care.18 A 2016 survey of more than 2000 physicians found that those with mental illnesses did not seek treatment due to limited time, fear of being reported to a medical licensing board, concern over obtaining licensure, and shame or embarrassment at the diagnosis.19 Besides urging residents to seek care, more effort should be invested in addressing the stigma and ensuring confidentiality. In 2021, the internal medicine and medicine-pediatrics residency at the University of Colorado Anschutz Medical Campus (Aurora, Colorado) developed a confidential opt-out, rather than opt-in, mental health program, and appointments were made for all 80 interns in advance. In doing so, they found increased participation and self-reported wellness at a relatively low cost and simple implementation.20 For trainees without such access, online or mobile therapy platforms offering electronic mental health treatment or telepsychiatry also have been employed.21,22 The onus ultimately is still on the individual to seek the care they need. Although only an anecdotal piece of evidence, I have found the prevalence of physicians taking selective serotonin reuptake inhibitors such as escitalopram, sertraline, or fluoxetine to be strikingly common and quite beneficial.
Final Thoughts
Residency remains rife with financial, emotional, and physical stressors; even as the dust settles on the COVID-19 pandemic, the light shed on the importance of trainee mental health must remain illuminated. For the aforementioned resources to have an impact, residents need to be empowered to openly discuss mental health issues and to seek help if necessary. Finally, in 2018, the Journal of Graduate Medical Education published a 10-year prospective cohort study that found that emotional distress during residency persists in professional practice even 10 years after residency and is associated with future burnout.23 Trainees should consider prioritizing their mental health to not only improve their quality of life in the present but also as an investment for their future.
The World Health Organization declared COVID-19 a pandemic on March 11, 2020, just 4 months before the start of a new residency cycle. Referred to as “COVID interns,” PGY-1 residents transitioning out of medical school in 2020 faced an unprecedented challenge of doctoring within a confused and ill-prepared health care system, while senior residents scrambled to adjust to their rapidly changing training programs. Each subsequent week brought more sobering news of increasing hospitalizations, intensive care unit admissions, and deaths; hospitals across the country resorted to the redeployment of residents across all specialties to buffer the growing need within their internal medicine and critical care units.1 And while the news and social media blurred into a collage of ventilator shortages, politicization of science, and “#healthcareheroes,” one study showed53.7% of medical interns (N=108) were struggling with mild to extremely severe depression, while 63.9% reported mild to severe anxiety.2
Many shortcomings of our health care system—ill preparedness, racial disparity, health illiteracy—were highlighted during the COVID-19 pandemic, and providers’ mental health was no exception.3 Classic psychosocial risk factors, such as high demands, lack of control, lack of institutional support, and absence of reward defined the workplace, leading Theorell4 to call it “a randomized trial for maximal worsening of the work environment.” Stress and burnout during residency are not novel concepts. A 2002 survey including 415 medical residency programs with a response from more than 4000 residents found depressive symptoms in 35% of respondents, paired with feelings of increased cynicism and decreased humanism despite major curricular reforms and duty hour limitations.5 Unfortunately, the statistics in the coming years hardly budged and, in the wake of the pandemic, culminated to more than 50% to 76% of physicians worldwide reporting burnout in 2020.6-8
As a COVID intern at Brigham and Women’s Hospital (Boston, Massachusetts), I also experienced the demanding workload and witnessed the struggle of my colleagues firsthand. Brigham and Women’s Hospital, similar to many of its peer institutions, implemented frequent mental health check-ins within its curriculum. Known as the Intern Humanistic Curriculum, these check-ins essentially were an echo chamber to unload the psychological burdens of our workdays, and we eagerly shared what made us angry, sad, hopeful, and hopeless. During one such session, I learned about moral injury, a term originating in the military defined as the psychological stress resulting from actions—or the lack of actions—that violates one’s moral or ethical code.9 With the onslaught of patient deaths for which most of us felt unprepared, we had all endured varying degrees of moral injury. Greenberg et al9 described 2 potential outcomes after moral injury: (1) the development of mental health disorders such as depression and posttraumatic stress disorder, or (2) posttraumatic growth, which is the bolstering of psychological resilience. Notably, the outcome is based on the way someone is supported before, during, and after the challenging incident.9
With the aim of psychological growth and developing resilience, residents should prioritize mental health throughout their training. To this end, several resources are readily available, many of which I actively use or frequently revisit, which are reviewed here.
Mindfulness Meditation App
Calm (https://www.calm.com/) is one of several popular mobile applications (apps) that delivers mindfulness mediation—the practice of attending to experiences, thoughts, and emotions without bias or judgment. With more than 100 million downloads, Calm includes meditation tutorials, breathing exercises, nature scenes and sounds, and audio programs taught by mindfulness experts for $69.99 a year or $14.99 a month. Systemic reviews have demonstrated reduced sleep disturbance, decreased ruminative thoughts and emotional reactivity, and increased awareness and acceptance in those practicing mindfulness meditation. Calm users have reported these benefits, with many able to forego the time- and cost-intensive cognitive behavioral therapy that requires highly trained therapists.10-12
Exercise to Relieve Stress
Both aerobic and anaerobic exercises are antidepressive and anxiolytic and also lower one’s overall sensitivity to stress. Whether it is governed by neurotransmitters such as the activation of the opioid systems or the release of endogenous endorphins or time spent focusing on a different task at hand, the benefits of exercise against mental stressors have been extensively studied and established.13 Consider obtaining a new gym membership at the start of residency or joining an intramural team. Both have the added benefit of expanding your social circle.
Socialize With Others
Social isolation and perceived loneliness are key stressors linked to neuroendocrine disturbances that underlie depression, anxiety, and even schizophrenia.14,15 Throughout residency there will be several social events and opportunities to gather with colleagues—inside or outside of the work environment—and residents should attend as time allows. Even virtual social interactions were found to reduce stress and help in the treatment of social anxiety disorder.14
Communicate About Stressors
Open up to your co-residents, friends, and family about any struggles that may be invisible on the outside. Even attendings can empathize with the struggles of residency, and the mentors in place are actively trained to prioritize resident wellness. If verbal communication is not your strength, try journaling. Writing helps to untangle and better define underlying stressors and is itself meditative.16,17 However, ensure that your journaling is focused on positive emotional responses and aims to determine the positive benefits within any stressful event; those solely expressing negative emotions were found to have higher levels of stress and anxiety afterward than they had before.17
Seek a Mental Health Specialist
As with all other human ailments, severe mental health disorders require specialists and proper medication. Unfortunately, substantial stigma accompanying mental health continues to permeate medicine, creating considerable barriers for residents in need of care.18 A 2016 survey of more than 2000 physicians found that those with mental illnesses did not seek treatment due to limited time, fear of being reported to a medical licensing board, concern over obtaining licensure, and shame or embarrassment at the diagnosis.19 Besides urging residents to seek care, more effort should be invested in addressing the stigma and ensuring confidentiality. In 2021, the internal medicine and medicine-pediatrics residency at the University of Colorado Anschutz Medical Campus (Aurora, Colorado) developed a confidential opt-out, rather than opt-in, mental health program, and appointments were made for all 80 interns in advance. In doing so, they found increased participation and self-reported wellness at a relatively low cost and simple implementation.20 For trainees without such access, online or mobile therapy platforms offering electronic mental health treatment or telepsychiatry also have been employed.21,22 The onus ultimately is still on the individual to seek the care they need. Although only an anecdotal piece of evidence, I have found the prevalence of physicians taking selective serotonin reuptake inhibitors such as escitalopram, sertraline, or fluoxetine to be strikingly common and quite beneficial.
Final Thoughts
Residency remains rife with financial, emotional, and physical stressors; even as the dust settles on the COVID-19 pandemic, the light shed on the importance of trainee mental health must remain illuminated. For the aforementioned resources to have an impact, residents need to be empowered to openly discuss mental health issues and to seek help if necessary. Finally, in 2018, the Journal of Graduate Medical Education published a 10-year prospective cohort study that found that emotional distress during residency persists in professional practice even 10 years after residency and is associated with future burnout.23 Trainees should consider prioritizing their mental health to not only improve their quality of life in the present but also as an investment for their future.
- Spiegelman J, Praiss A, Syeda S, et al. Preparation and redeployment of house staff during a pandemic. Semin Perinatol. 2020;44:151297.
- Debnath PR, Islam MS, Karmakar PK, et al. Mental health concerns, insomnia, and loneliness among intern doctors amidst the COVID-19 pandemic: evidence from a large tertiary care hospital in Bangladesh. Int J Ment Health Addict. 2021:1-21. doi:10.1007/s11469-021-00690-0
- O’Reilly-Shah VN, Gentry KR, Van Cleve W, et al. The COVID-19 pandemic highlights shortcomings in US health care informatics infrastructure: a call to action. Anesth Analg. 2020;131:340-344.
- Theorell T. COVID-19 and working conditions in health care. Psychother Psychosom. 2020;89:193-194.
- Collier VU, McCue JD, Markus A, et al. Stress in medical residency: status quo after a decade of reform? Ann Intern Med. 2002;136:384-390.
- AbuDujain NM, Almuhaideb QA, Alrumaihi NA, et al. The impact of the COVID-19 pandemic on medical interns’ education, training, and mental health: a cross-sectional study. Cureus. 2021;13:E19250.
- Amanullah S, Ramesh Shankar R. The impact of COVID-19 on physician burnout globally: a review. Healthcare (Basel). 2020;8:421.
- Lebares CC, Guvva EV, Ascher NL, et al. Burnout and stress among US surgery residents: psychological distress and resilience. J Am Coll Surg. 2018;226:80-90.
- Greenberg N, Docherty M, Gnanapragasam S, et al. Managing mental health challenges faced by healthcare workers during COVID-19 pandemic. BMJ. 2020;368:m1211.
- Gal E, Stefan S, Cristea IA. The efficacy of mindfulness meditation apps in enhancing users’ well-being and mental health related outcomes: a meta-analysis of randomized controlled trials. J Affect Disord. 2021;279:131-142.
- Huberty J, Green J, Glissmann C, et al. Efficacy of the mindfulness meditation mobile app “Calm” to reduce stress among college students: randomized controlled trial. JMIR Mhealth Uhealth. 2019;7:E14273.
- Huberty J, Puzia ME, Larkey L, et al. Can a meditation app help my sleep? a cross-sectional survey of Calm users. PLoS One. 2021;16:E0257518.
- Salmon P. Effects of physical exercise on anxiety, depression, and sensitivity to stress: a unifying theory. Clin Psychol Rev. 2001;21:33-61.
- Kampmann IL, Emmelkamp PM, Hartanto D, et al. Exposure to virtual social interactions in the treatment of social anxiety disorder: a randomized controlled trial. Behav Res Ther. 2016;77:147-156.
- Mumtaz F, Khan MI, Zubair M, et al. Neurobiology and consequences of social isolation stress in animal model-A comprehensive review. Biomed Pharmacother. 2018;105:1205-1222.
- Khanna P, Singh K. Stress management training and gratitude journaling in the classroom: an initial investigation in Indian context. Curr Psychol. 2021;40:5737-5748.
- Ullrich PM, Lutgendorf SK. Journaling about stressful events: effects of cognitive processing and emotional expression. Ann Behav Med. 2002;24:244-250.
- Outhoff K. Depression in doctors: a bitter pill to swallow. S Afr Fam Pract. 2019;61(suppl 1):S11-S14.
- Gold KJ, Andrew LB, Goldman EB, et al. “I would never want to have a mental health diagnosis on my record”: a survey of female physicians on mental health diagnosis, treatment, and reporting. Gen Hosp Psychiatry. 2016;43:51-57.
- Major A, Williams JG, McGuire WC, et al. Removing barriers: a confidential opt-out mental health pilot program for internal medicine interns. Acad Med. 2021;96:686-689.
- Greenhalgh T, Wherton J. Telepsychiatry: learning from the pandemic. Br J Psychiatry. 2022;220:1-5.
- Timakum T, Xie Q, Song M. Analysis of E-mental health research: mapping the relationship between information technology and mental healthcare. BMC Psychiatry. 2022;22:57.
- Raimo J, LaVine S, Spielmann K, et al. The correlation of stress in residency with future stress and burnout: a 10-year prospective cohort study. J Grad Med Educ. 2018;10:524-531.
- Spiegelman J, Praiss A, Syeda S, et al. Preparation and redeployment of house staff during a pandemic. Semin Perinatol. 2020;44:151297.
- Debnath PR, Islam MS, Karmakar PK, et al. Mental health concerns, insomnia, and loneliness among intern doctors amidst the COVID-19 pandemic: evidence from a large tertiary care hospital in Bangladesh. Int J Ment Health Addict. 2021:1-21. doi:10.1007/s11469-021-00690-0
- O’Reilly-Shah VN, Gentry KR, Van Cleve W, et al. The COVID-19 pandemic highlights shortcomings in US health care informatics infrastructure: a call to action. Anesth Analg. 2020;131:340-344.
- Theorell T. COVID-19 and working conditions in health care. Psychother Psychosom. 2020;89:193-194.
- Collier VU, McCue JD, Markus A, et al. Stress in medical residency: status quo after a decade of reform? Ann Intern Med. 2002;136:384-390.
- AbuDujain NM, Almuhaideb QA, Alrumaihi NA, et al. The impact of the COVID-19 pandemic on medical interns’ education, training, and mental health: a cross-sectional study. Cureus. 2021;13:E19250.
- Amanullah S, Ramesh Shankar R. The impact of COVID-19 on physician burnout globally: a review. Healthcare (Basel). 2020;8:421.
- Lebares CC, Guvva EV, Ascher NL, et al. Burnout and stress among US surgery residents: psychological distress and resilience. J Am Coll Surg. 2018;226:80-90.
- Greenberg N, Docherty M, Gnanapragasam S, et al. Managing mental health challenges faced by healthcare workers during COVID-19 pandemic. BMJ. 2020;368:m1211.
- Gal E, Stefan S, Cristea IA. The efficacy of mindfulness meditation apps in enhancing users’ well-being and mental health related outcomes: a meta-analysis of randomized controlled trials. J Affect Disord. 2021;279:131-142.
- Huberty J, Green J, Glissmann C, et al. Efficacy of the mindfulness meditation mobile app “Calm” to reduce stress among college students: randomized controlled trial. JMIR Mhealth Uhealth. 2019;7:E14273.
- Huberty J, Puzia ME, Larkey L, et al. Can a meditation app help my sleep? a cross-sectional survey of Calm users. PLoS One. 2021;16:E0257518.
- Salmon P. Effects of physical exercise on anxiety, depression, and sensitivity to stress: a unifying theory. Clin Psychol Rev. 2001;21:33-61.
- Kampmann IL, Emmelkamp PM, Hartanto D, et al. Exposure to virtual social interactions in the treatment of social anxiety disorder: a randomized controlled trial. Behav Res Ther. 2016;77:147-156.
- Mumtaz F, Khan MI, Zubair M, et al. Neurobiology and consequences of social isolation stress in animal model-A comprehensive review. Biomed Pharmacother. 2018;105:1205-1222.
- Khanna P, Singh K. Stress management training and gratitude journaling in the classroom: an initial investigation in Indian context. Curr Psychol. 2021;40:5737-5748.
- Ullrich PM, Lutgendorf SK. Journaling about stressful events: effects of cognitive processing and emotional expression. Ann Behav Med. 2002;24:244-250.
- Outhoff K. Depression in doctors: a bitter pill to swallow. S Afr Fam Pract. 2019;61(suppl 1):S11-S14.
- Gold KJ, Andrew LB, Goldman EB, et al. “I would never want to have a mental health diagnosis on my record”: a survey of female physicians on mental health diagnosis, treatment, and reporting. Gen Hosp Psychiatry. 2016;43:51-57.
- Major A, Williams JG, McGuire WC, et al. Removing barriers: a confidential opt-out mental health pilot program for internal medicine interns. Acad Med. 2021;96:686-689.
- Greenhalgh T, Wherton J. Telepsychiatry: learning from the pandemic. Br J Psychiatry. 2022;220:1-5.
- Timakum T, Xie Q, Song M. Analysis of E-mental health research: mapping the relationship between information technology and mental healthcare. BMC Psychiatry. 2022;22:57.
- Raimo J, LaVine S, Spielmann K, et al. The correlation of stress in residency with future stress and burnout: a 10-year prospective cohort study. J Grad Med Educ. 2018;10:524-531.
Resident Pearl
- Although institution-sponsored wellness programs exist to promote the mental health of trainees, rates of anxiety and depression remain high among residents, which was further highlighted during the COVID-19 pandemic. Instead of passively engaging with wellness messages, residents must actively prioritize their own mental health to avoid stress and burnout.