User login
An unexplained exacerbation of depression, anxiety, and panic
CASE Depression, anxiety, and panic attacks
At the urging of his parents Mr. P, age 33, presents to the partial hospitalization program (PHP) for worsening depression and anxiety, daily panic attacks with accompanying diaphoresis and headache, and the possibility that he may have taken an overdose of zolpidem. Mr. P denies taking an intentional overdose of zolpidem, claiming instead that he was having a sleep-walking episode and did not realize how many pills he took.
In addition to daily panic attacks, Mr. P reports having trouble falling asleep, overwhelming sadness, and daily passive suicidal ideation without a plan or active intent.
Mr. P cannot identify a specific trigger to this most recent exacerbation of depressed/anxious mood, but instead describes it as slowly building over the past 6 to 8 months. Mr. P says the panic attacks occur without warning and states, “I feel like my heart is going to jump out of my chest; I get a terrible headache, and I sweat like crazy. Sometimes I just feel like I’m about to pass out or die.” Although these episodes had been present for approximately 2 years, they now occur almost daily.
HISTORY Inconsistent adherence
For the last year, Mr. P had been taking alprazolam, 0.5 mg twice daily, and paroxetine, 20 mg/d, and these medications provided moderate relief of his depressive/anxious symptoms. However, he stopped taking both medications approximately 3 or 4 weeks ago when he ran out. He also takes propranolol, 20 mg/d, sporadically, for hypertension. In the past, he had been prescribed carvedilol, clonidine, and lisinopril—all with varying degrees of relief of his hypertension. He denies a family history of hypertension or any other chronic or acute health problems. He reports that he has been sober from alcohol for 19 months but smokes 1 to 2 marijuana cigarettes a day.
EVALUATION Elevated blood pressure and pulse
Mr. P’s physical examination and medical review of systems are unremarkable, except for an elevated blood pressure (190/110 mm Hg) and pulse (92 beats per minute); he also has a headache. A repeat blood pressure test later in the day is 172/94 mm Hg, with a pulse of 100 beats per minute. His urine drug screen is positive only for delta-9-tetrahydrocannabinol (THC).
[polldaddy:10558304]
The author’s observations
A CBC with differential is helpful for ruling out infection and anemia as causes of anxiety and depression.1 In Mr. P’s case, there were no concerning symptoms that pointed to anemia or infection as likely causes of his anxiety, depression, or panic attacks. A TSH level also would be reasonable, because hyperthyroidism can present as anxiety, while hyperthyroidism or hypothyroidism each can present as depression.1 However, both Mr. P’s medical history and physical examination were not concerning for thyroid disease, making it unlikely that he had either of those conditions. A review of Mr. P’s medical records indicated that within the past 6 months, his primary care physician (PCP) had ordered a CBC and TSH test; the results of both were within normal limits.
Serum porphyrin tests can exclude porphyria as a contributor to Mr. P’s anxiety and depression. Porphyrias are a group of 8 inherited disorders that involve accumulation of heme precursors (porphyrins) in the CNS and subcutaneous tissue.2 Collectively, porphyrias affect approximately 1 in 200,000 people.2 Anxiety and depression are strongly associated with porphyria, but do not occur secondary to the illness; depression and anxiety appear to be intrinsic personality features in people with porphyria.3 Skin lesions and abdominal pain are the most common symptoms,3 and there is a higher incidence of hypertension in people with porphyria than in the general population.4 Mr. P does not report any heritable disorders, nor does he appear to have any CNS disturbance or unusual cutaneous lesions, which makes it unlikely that this disorder is related to his psychiatric symptoms.
Continue to: A serum metanephrines test measures...
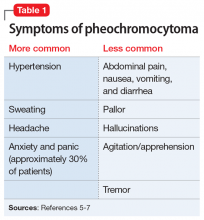
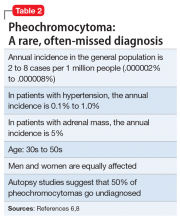
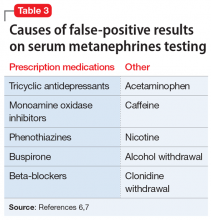
A serum metanephrines test measures the metabolites of epinephrine and norepinephrine. These catecholamines are produced in excess by an adrenal or extra-adrenal tumor seen in pheochromocytoma. The classic triad of symptoms of pheochromocytoma are hypertension, sweating, and headache; approximately 30% of patients report significant anxiety and panic (Table 15-7). This type of tumor is rare, with an annual incidence of only 2 to 8 cases per 1 million individuals. Among people with hypertension, the annual incidence is 0.1% to 1.0%, and for those with an adrenal mass, the annual incidence is 5% (Table 26,8). Autopsy studies suggest that up to 50% of pheochromocytomas are undiagnosed.8 Left untreated, pheochromocytoma can result in hypertensive crisis, arrhythmia, myocardial infarction, multisystem organ failure, and premature death.7 Table 36,7 highlights some causes of false-positive serum on metanephrines testing.
EVALUATION Metanephrines testing
Mr. P has what appears to be treatment-resistant hypertension, accompanied by the classic symptoms observed in most patients with pheochromocytoma. Because Mr. P is participating in the PHP 6 days per week for 6 hours each day, visiting his PCP would be inconvenient, so the treatment team orders the serum metanephrines test. If a positive result is found, Mr. P will be referred to his PCP for further assessment and follow-up care with endocrinology.
TREATMENT Pharmacotherapy to target anxiety and panic
Next, the treatment team establishes a safety plan for Mr. P, and restarts paroxetine, 20 mg/d, to target his depressed and anxious mood. Alprazolam, 0.5 mg twice daily, is started to target anxious mood and panic symptoms, and to allow time for the anxiolytic properties of the paroxetine to become fully effective. The alprazolam will be tapered and stopped after 2 weeks. Mr. P is started on hydroxyzine, 1 to 2 25-mg tablets 2 to 3 times daily as needed for anxious mood and panic symptoms.
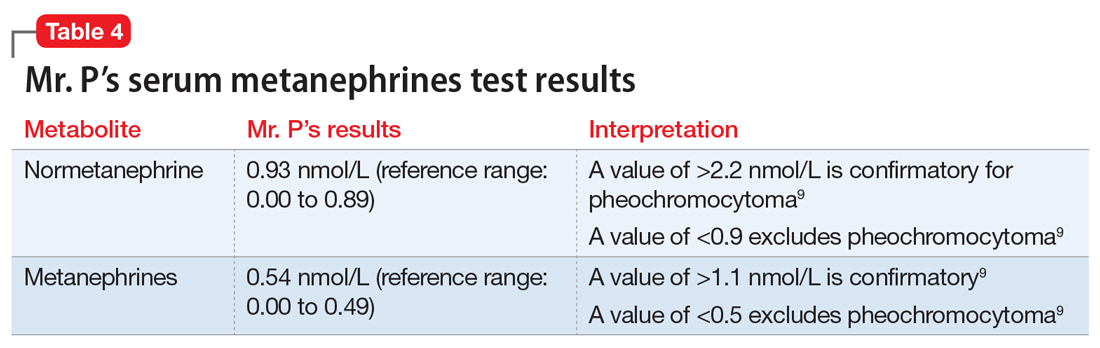
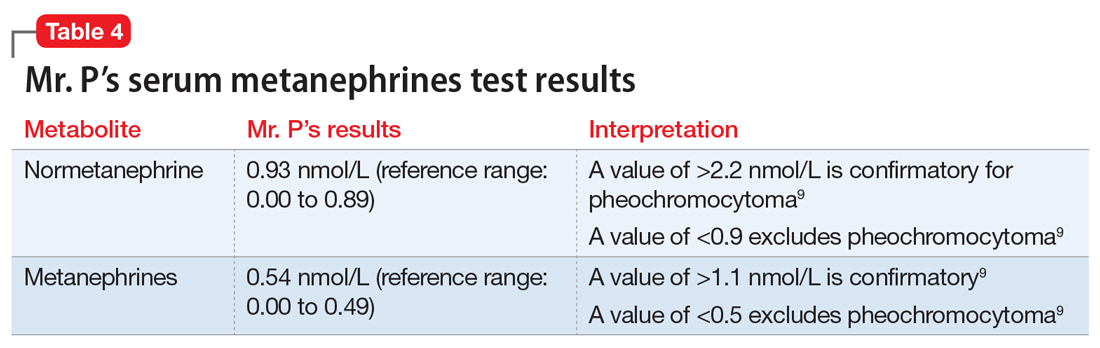
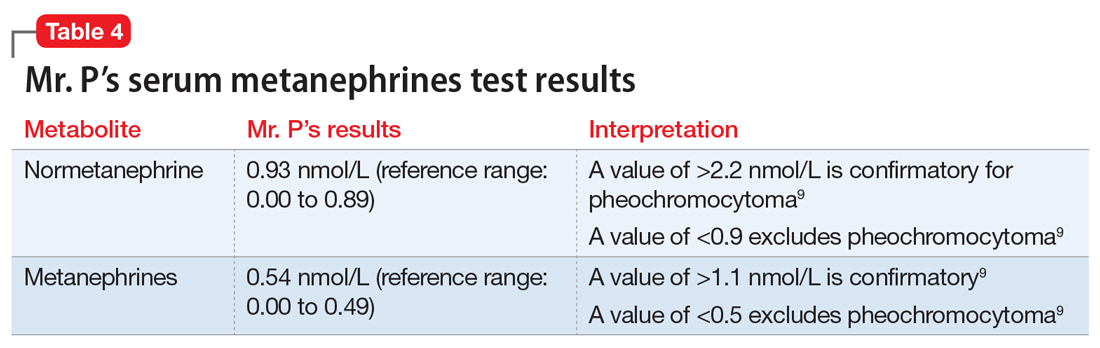
The serum metanephrines test results are equivocal, with a slight elevation of both epinephrine and norepinephrine that is too low to confirm a diagnosis of pheochromocytoma but too elevated to exclude it (Table 49). With Mr. P’s consent, the treatment team contacts his PCP and convey the results of this test. Mr. P schedules an appointment with his PCP for the following week for further assessment and confirmatory pheochromocytoma testing.
After 1 week, Mr. P remains anxious, with a slight reduction in panic attacks from multiple attacks each day to 3 or 4 attacks per week. The team considers adding an additional anxiolytic agent.
[polldaddy:10558305]
Continue to: The author's observations
The author’s observations
The triad of symptoms in pheochromocytoma results directly from the intermittent release of catecholamines into systemic circulation. Surges of epinephrine and norepinephrine lead to headaches, palpitations, diaphoresis, and (less commonly) gastrointestinal symptoms such as nausea, vomiting, and constipation. Persistent or episodic hypertension may be present, with 13% of patients maintaining a normal blood pressure.5-7 Patients with pheochromocytoma-related anxiety typically have substantial or complete resolution of anxiety and panic attacks after tumor resection.6,8,10
Because of their ability to raise catecholamine levels, several medications, including some psychotropics, can lead to false-positive results on serum and urine metanephrines testing. Tricyclic antidepressants and beta-blockers can cause false-positive results on plasma assays, while buspirone can cause false-positives on urinalysis assays.5 Trazodone, on the other hand, exhibits no catecholaminergic activity and its alpha-1 adrenergic antagonism may actually have some benefit in pheochromocytoma.11 Alpha-1 adrenergic antagonism with doxazosin, prazosin, or terazosin is the first-line of treatment in reducing pheochromocytoma-related hypertension.7 Treatment with a beta-blocker is safe only after alpha-adrenergic blockade occurs. While beta-blockers are useful for reducing the palpitations and anxiety observed in patients with pheochromocytoma, they must not be used alone due to the risk of hypertensive crisis resulting from unopposed alpha-adrenergic agonist activated vasoconstriction.5,7
TREATMENT CBT provides benefit
Mr. P decides against receiving an additional agent for anxiety and instead decides to wait for the outcome of the confirmatory pheochromocytoma testing. He continues to take alprazolam, and both his depressed mood and anxiety improve. His panic attacks continue to lessen, and he appears to benefit from cognitive-behavioral therapy provided during group therapy. Mr. P is advised by his PCP to taper and stop the alprazolam 3 to 5 days before his 24-hour urine metanephrines test because benzodiazepines can lead to false-positive results on a urinalysis assay.7
OUTCOME Remission of anxiety and depression
Mr. P has a repeat serum metanephrines test and a 24-hour urinalysis assay. Both are negative for pheochromocytoma. His PCP refers him to cardiology for management of treatment-resistant hypertension. He is discharged from the PHP and continues psychotherapy for depression and anxiety in an intensive outpatient program (IOP). Throughout his PHP and IOP treatments, he continues to take paroxetine and hydroxyzine. He achieves a successful remission of his anxiety and depression, with partial but significant remission of his panic attacks.
The author’s observations
Although Mr. P did not have pheochromocytoma, it is important to rule out this rare condition in patients who present with treatment-resistant hypertension and/or treatment-resistant anxiety.
Continue to: Bottom Line
Bottom Line
Pheochromocytoma is a tumor of the adrenal gland. The classic triad of symptoms of this rare condition is hypertension, sweating, and headache; approximately 30% of patients report significant anxiety and panic. Several medications, including tricyclic antidepressants, beta-blockers, and buspirone, can lead to false-positive results on the serum and urine metanephrines testing used to diagnose pheochromocytoma.
Related Resources
- National Organization for Rare Disorders. Rare Disease Database: pheochromocytoma. www.rarediseases.org/rare-diseases/pheochromocytoma/.
- Young WF Jr. Clinical presentation and diagnosis of pheochromocytoma. UpToDate. www.uptodate.com/contents/clinical-presentation-and-diagnosis-of-pheochromocytoma. Published January 2020.
Drug Brand Names
Alprazolam • Xanax
Amitriptyline • Elavil
Buspirone • Buspar
Carvedilol • Coreg
Clonidine • Catapres
Doxazosin • Cardura
Hydroxyzine • Vistaril
Lisinopril • Prinivil, Zestril
Paroxetine • Paxil
Prazosin • Minipress
Propranolol • Inderal
Terazosin • Hytrin
Trazodone • Desyrel
Zolpidem • Ambien
1. Morrison J. When psychological problems mask medical disorders: a guide for psychotherapists. 2nd ed. New York, NY: The Guilford Press; 2015.
2. American Porphyria Foundation. About porphyria. https://porphyriafoundation.org/patients/about-porphyria. Accessed May 13, 2020.
3. Millward L, Kelly P, King A, et al. Anxiety and depression in the acute porphyrias. J Inherit Metab Dis. 2005;28(6):1099-1107.
4. Bonkovsky H, Maddukuri VC, Yazici C, et al. Acute porphyrias in the USA: features of 108 subjects from porphyria consortium. Am J Med. 2014;127(12):1233-1241.
5. Tsirlin A, Oo Y, Sharma R, et al. Pheochromocytoma: a review. Maturitas. 2014;77(3):229-238.
6. Leung A, Zun L, Nordstrom K, et al. Psychiatric emergencies for physicians: clinical management and approach to distinguishing pheochromocytoma from psychiatric and thyrotoxic diseases in the emergency room. J Emerg Med. 2017;53(5):712-716.
7. Garg M, Kharb S, Brar KS, et al. Medical management of pheochromocytoma: role of the endocrinologist. Indian J Endocrinol and Metab. 2011;15(suppl 4):S329-S336. doi: 10.4103/2230-8210.86976.
8. Zardawi I. Phaeochromocytoma masquerading as anxiety and depression. Am J Case Rep. 2013;14:161-163.
9. ARUP Laboratories. Test directory. https://www.aruplab.com. Accessed February 11, 2020.
10. Sriram P, Raghavan V. Pheochromocytoma presenting as anxiety disorder: a case report. Asian J Psychiatr. 2017;29:83-84.
11. Stahl SM. Stahl’s essential psychopharmacology: neuroscientific basis and practical applications. Cambridge, UK: Cambridge University Press; 2013.
CASE Depression, anxiety, and panic attacks
At the urging of his parents Mr. P, age 33, presents to the partial hospitalization program (PHP) for worsening depression and anxiety, daily panic attacks with accompanying diaphoresis and headache, and the possibility that he may have taken an overdose of zolpidem. Mr. P denies taking an intentional overdose of zolpidem, claiming instead that he was having a sleep-walking episode and did not realize how many pills he took.
In addition to daily panic attacks, Mr. P reports having trouble falling asleep, overwhelming sadness, and daily passive suicidal ideation without a plan or active intent.
Mr. P cannot identify a specific trigger to this most recent exacerbation of depressed/anxious mood, but instead describes it as slowly building over the past 6 to 8 months. Mr. P says the panic attacks occur without warning and states, “I feel like my heart is going to jump out of my chest; I get a terrible headache, and I sweat like crazy. Sometimes I just feel like I’m about to pass out or die.” Although these episodes had been present for approximately 2 years, they now occur almost daily.
HISTORY Inconsistent adherence
For the last year, Mr. P had been taking alprazolam, 0.5 mg twice daily, and paroxetine, 20 mg/d, and these medications provided moderate relief of his depressive/anxious symptoms. However, he stopped taking both medications approximately 3 or 4 weeks ago when he ran out. He also takes propranolol, 20 mg/d, sporadically, for hypertension. In the past, he had been prescribed carvedilol, clonidine, and lisinopril—all with varying degrees of relief of his hypertension. He denies a family history of hypertension or any other chronic or acute health problems. He reports that he has been sober from alcohol for 19 months but smokes 1 to 2 marijuana cigarettes a day.
EVALUATION Elevated blood pressure and pulse
Mr. P’s physical examination and medical review of systems are unremarkable, except for an elevated blood pressure (190/110 mm Hg) and pulse (92 beats per minute); he also has a headache. A repeat blood pressure test later in the day is 172/94 mm Hg, with a pulse of 100 beats per minute. His urine drug screen is positive only for delta-9-tetrahydrocannabinol (THC).
[polldaddy:10558304]
The author’s observations
A CBC with differential is helpful for ruling out infection and anemia as causes of anxiety and depression.1 In Mr. P’s case, there were no concerning symptoms that pointed to anemia or infection as likely causes of his anxiety, depression, or panic attacks. A TSH level also would be reasonable, because hyperthyroidism can present as anxiety, while hyperthyroidism or hypothyroidism each can present as depression.1 However, both Mr. P’s medical history and physical examination were not concerning for thyroid disease, making it unlikely that he had either of those conditions. A review of Mr. P’s medical records indicated that within the past 6 months, his primary care physician (PCP) had ordered a CBC and TSH test; the results of both were within normal limits.
Serum porphyrin tests can exclude porphyria as a contributor to Mr. P’s anxiety and depression. Porphyrias are a group of 8 inherited disorders that involve accumulation of heme precursors (porphyrins) in the CNS and subcutaneous tissue.2 Collectively, porphyrias affect approximately 1 in 200,000 people.2 Anxiety and depression are strongly associated with porphyria, but do not occur secondary to the illness; depression and anxiety appear to be intrinsic personality features in people with porphyria.3 Skin lesions and abdominal pain are the most common symptoms,3 and there is a higher incidence of hypertension in people with porphyria than in the general population.4 Mr. P does not report any heritable disorders, nor does he appear to have any CNS disturbance or unusual cutaneous lesions, which makes it unlikely that this disorder is related to his psychiatric symptoms.
Continue to: A serum metanephrines test measures...
A serum metanephrines test measures the metabolites of epinephrine and norepinephrine. These catecholamines are produced in excess by an adrenal or extra-adrenal tumor seen in pheochromocytoma. The classic triad of symptoms of pheochromocytoma are hypertension, sweating, and headache; approximately 30% of patients report significant anxiety and panic (Table 15-7). This type of tumor is rare, with an annual incidence of only 2 to 8 cases per 1 million individuals. Among people with hypertension, the annual incidence is 0.1% to 1.0%, and for those with an adrenal mass, the annual incidence is 5% (Table 26,8). Autopsy studies suggest that up to 50% of pheochromocytomas are undiagnosed.8 Left untreated, pheochromocytoma can result in hypertensive crisis, arrhythmia, myocardial infarction, multisystem organ failure, and premature death.7 Table 36,7 highlights some causes of false-positive serum on metanephrines testing.
EVALUATION Metanephrines testing
Mr. P has what appears to be treatment-resistant hypertension, accompanied by the classic symptoms observed in most patients with pheochromocytoma. Because Mr. P is participating in the PHP 6 days per week for 6 hours each day, visiting his PCP would be inconvenient, so the treatment team orders the serum metanephrines test. If a positive result is found, Mr. P will be referred to his PCP for further assessment and follow-up care with endocrinology.
TREATMENT Pharmacotherapy to target anxiety and panic
Next, the treatment team establishes a safety plan for Mr. P, and restarts paroxetine, 20 mg/d, to target his depressed and anxious mood. Alprazolam, 0.5 mg twice daily, is started to target anxious mood and panic symptoms, and to allow time for the anxiolytic properties of the paroxetine to become fully effective. The alprazolam will be tapered and stopped after 2 weeks. Mr. P is started on hydroxyzine, 1 to 2 25-mg tablets 2 to 3 times daily as needed for anxious mood and panic symptoms.
The serum metanephrines test results are equivocal, with a slight elevation of both epinephrine and norepinephrine that is too low to confirm a diagnosis of pheochromocytoma but too elevated to exclude it (Table 49). With Mr. P’s consent, the treatment team contacts his PCP and convey the results of this test. Mr. P schedules an appointment with his PCP for the following week for further assessment and confirmatory pheochromocytoma testing.
After 1 week, Mr. P remains anxious, with a slight reduction in panic attacks from multiple attacks each day to 3 or 4 attacks per week. The team considers adding an additional anxiolytic agent.
[polldaddy:10558305]
Continue to: The author's observations
The author’s observations
The triad of symptoms in pheochromocytoma results directly from the intermittent release of catecholamines into systemic circulation. Surges of epinephrine and norepinephrine lead to headaches, palpitations, diaphoresis, and (less commonly) gastrointestinal symptoms such as nausea, vomiting, and constipation. Persistent or episodic hypertension may be present, with 13% of patients maintaining a normal blood pressure.5-7 Patients with pheochromocytoma-related anxiety typically have substantial or complete resolution of anxiety and panic attacks after tumor resection.6,8,10
Because of their ability to raise catecholamine levels, several medications, including some psychotropics, can lead to false-positive results on serum and urine metanephrines testing. Tricyclic antidepressants and beta-blockers can cause false-positive results on plasma assays, while buspirone can cause false-positives on urinalysis assays.5 Trazodone, on the other hand, exhibits no catecholaminergic activity and its alpha-1 adrenergic antagonism may actually have some benefit in pheochromocytoma.11 Alpha-1 adrenergic antagonism with doxazosin, prazosin, or terazosin is the first-line of treatment in reducing pheochromocytoma-related hypertension.7 Treatment with a beta-blocker is safe only after alpha-adrenergic blockade occurs. While beta-blockers are useful for reducing the palpitations and anxiety observed in patients with pheochromocytoma, they must not be used alone due to the risk of hypertensive crisis resulting from unopposed alpha-adrenergic agonist activated vasoconstriction.5,7
TREATMENT CBT provides benefit
Mr. P decides against receiving an additional agent for anxiety and instead decides to wait for the outcome of the confirmatory pheochromocytoma testing. He continues to take alprazolam, and both his depressed mood and anxiety improve. His panic attacks continue to lessen, and he appears to benefit from cognitive-behavioral therapy provided during group therapy. Mr. P is advised by his PCP to taper and stop the alprazolam 3 to 5 days before his 24-hour urine metanephrines test because benzodiazepines can lead to false-positive results on a urinalysis assay.7
OUTCOME Remission of anxiety and depression
Mr. P has a repeat serum metanephrines test and a 24-hour urinalysis assay. Both are negative for pheochromocytoma. His PCP refers him to cardiology for management of treatment-resistant hypertension. He is discharged from the PHP and continues psychotherapy for depression and anxiety in an intensive outpatient program (IOP). Throughout his PHP and IOP treatments, he continues to take paroxetine and hydroxyzine. He achieves a successful remission of his anxiety and depression, with partial but significant remission of his panic attacks.
The author’s observations
Although Mr. P did not have pheochromocytoma, it is important to rule out this rare condition in patients who present with treatment-resistant hypertension and/or treatment-resistant anxiety.
Continue to: Bottom Line
Bottom Line
Pheochromocytoma is a tumor of the adrenal gland. The classic triad of symptoms of this rare condition is hypertension, sweating, and headache; approximately 30% of patients report significant anxiety and panic. Several medications, including tricyclic antidepressants, beta-blockers, and buspirone, can lead to false-positive results on the serum and urine metanephrines testing used to diagnose pheochromocytoma.
Related Resources
- National Organization for Rare Disorders. Rare Disease Database: pheochromocytoma. www.rarediseases.org/rare-diseases/pheochromocytoma/.
- Young WF Jr. Clinical presentation and diagnosis of pheochromocytoma. UpToDate. www.uptodate.com/contents/clinical-presentation-and-diagnosis-of-pheochromocytoma. Published January 2020.
Drug Brand Names
Alprazolam • Xanax
Amitriptyline • Elavil
Buspirone • Buspar
Carvedilol • Coreg
Clonidine • Catapres
Doxazosin • Cardura
Hydroxyzine • Vistaril
Lisinopril • Prinivil, Zestril
Paroxetine • Paxil
Prazosin • Minipress
Propranolol • Inderal
Terazosin • Hytrin
Trazodone • Desyrel
Zolpidem • Ambien
CASE Depression, anxiety, and panic attacks
At the urging of his parents Mr. P, age 33, presents to the partial hospitalization program (PHP) for worsening depression and anxiety, daily panic attacks with accompanying diaphoresis and headache, and the possibility that he may have taken an overdose of zolpidem. Mr. P denies taking an intentional overdose of zolpidem, claiming instead that he was having a sleep-walking episode and did not realize how many pills he took.
In addition to daily panic attacks, Mr. P reports having trouble falling asleep, overwhelming sadness, and daily passive suicidal ideation without a plan or active intent.
Mr. P cannot identify a specific trigger to this most recent exacerbation of depressed/anxious mood, but instead describes it as slowly building over the past 6 to 8 months. Mr. P says the panic attacks occur without warning and states, “I feel like my heart is going to jump out of my chest; I get a terrible headache, and I sweat like crazy. Sometimes I just feel like I’m about to pass out or die.” Although these episodes had been present for approximately 2 years, they now occur almost daily.
HISTORY Inconsistent adherence
For the last year, Mr. P had been taking alprazolam, 0.5 mg twice daily, and paroxetine, 20 mg/d, and these medications provided moderate relief of his depressive/anxious symptoms. However, he stopped taking both medications approximately 3 or 4 weeks ago when he ran out. He also takes propranolol, 20 mg/d, sporadically, for hypertension. In the past, he had been prescribed carvedilol, clonidine, and lisinopril—all with varying degrees of relief of his hypertension. He denies a family history of hypertension or any other chronic or acute health problems. He reports that he has been sober from alcohol for 19 months but smokes 1 to 2 marijuana cigarettes a day.
EVALUATION Elevated blood pressure and pulse
Mr. P’s physical examination and medical review of systems are unremarkable, except for an elevated blood pressure (190/110 mm Hg) and pulse (92 beats per minute); he also has a headache. A repeat blood pressure test later in the day is 172/94 mm Hg, with a pulse of 100 beats per minute. His urine drug screen is positive only for delta-9-tetrahydrocannabinol (THC).
[polldaddy:10558304]
The author’s observations
A CBC with differential is helpful for ruling out infection and anemia as causes of anxiety and depression.1 In Mr. P’s case, there were no concerning symptoms that pointed to anemia or infection as likely causes of his anxiety, depression, or panic attacks. A TSH level also would be reasonable, because hyperthyroidism can present as anxiety, while hyperthyroidism or hypothyroidism each can present as depression.1 However, both Mr. P’s medical history and physical examination were not concerning for thyroid disease, making it unlikely that he had either of those conditions. A review of Mr. P’s medical records indicated that within the past 6 months, his primary care physician (PCP) had ordered a CBC and TSH test; the results of both were within normal limits.
Serum porphyrin tests can exclude porphyria as a contributor to Mr. P’s anxiety and depression. Porphyrias are a group of 8 inherited disorders that involve accumulation of heme precursors (porphyrins) in the CNS and subcutaneous tissue.2 Collectively, porphyrias affect approximately 1 in 200,000 people.2 Anxiety and depression are strongly associated with porphyria, but do not occur secondary to the illness; depression and anxiety appear to be intrinsic personality features in people with porphyria.3 Skin lesions and abdominal pain are the most common symptoms,3 and there is a higher incidence of hypertension in people with porphyria than in the general population.4 Mr. P does not report any heritable disorders, nor does he appear to have any CNS disturbance or unusual cutaneous lesions, which makes it unlikely that this disorder is related to his psychiatric symptoms.
Continue to: A serum metanephrines test measures...
A serum metanephrines test measures the metabolites of epinephrine and norepinephrine. These catecholamines are produced in excess by an adrenal or extra-adrenal tumor seen in pheochromocytoma. The classic triad of symptoms of pheochromocytoma are hypertension, sweating, and headache; approximately 30% of patients report significant anxiety and panic (Table 15-7). This type of tumor is rare, with an annual incidence of only 2 to 8 cases per 1 million individuals. Among people with hypertension, the annual incidence is 0.1% to 1.0%, and for those with an adrenal mass, the annual incidence is 5% (Table 26,8). Autopsy studies suggest that up to 50% of pheochromocytomas are undiagnosed.8 Left untreated, pheochromocytoma can result in hypertensive crisis, arrhythmia, myocardial infarction, multisystem organ failure, and premature death.7 Table 36,7 highlights some causes of false-positive serum on metanephrines testing.
EVALUATION Metanephrines testing
Mr. P has what appears to be treatment-resistant hypertension, accompanied by the classic symptoms observed in most patients with pheochromocytoma. Because Mr. P is participating in the PHP 6 days per week for 6 hours each day, visiting his PCP would be inconvenient, so the treatment team orders the serum metanephrines test. If a positive result is found, Mr. P will be referred to his PCP for further assessment and follow-up care with endocrinology.
TREATMENT Pharmacotherapy to target anxiety and panic
Next, the treatment team establishes a safety plan for Mr. P, and restarts paroxetine, 20 mg/d, to target his depressed and anxious mood. Alprazolam, 0.5 mg twice daily, is started to target anxious mood and panic symptoms, and to allow time for the anxiolytic properties of the paroxetine to become fully effective. The alprazolam will be tapered and stopped after 2 weeks. Mr. P is started on hydroxyzine, 1 to 2 25-mg tablets 2 to 3 times daily as needed for anxious mood and panic symptoms.
The serum metanephrines test results are equivocal, with a slight elevation of both epinephrine and norepinephrine that is too low to confirm a diagnosis of pheochromocytoma but too elevated to exclude it (Table 49). With Mr. P’s consent, the treatment team contacts his PCP and convey the results of this test. Mr. P schedules an appointment with his PCP for the following week for further assessment and confirmatory pheochromocytoma testing.
After 1 week, Mr. P remains anxious, with a slight reduction in panic attacks from multiple attacks each day to 3 or 4 attacks per week. The team considers adding an additional anxiolytic agent.
[polldaddy:10558305]
Continue to: The author's observations
The author’s observations
The triad of symptoms in pheochromocytoma results directly from the intermittent release of catecholamines into systemic circulation. Surges of epinephrine and norepinephrine lead to headaches, palpitations, diaphoresis, and (less commonly) gastrointestinal symptoms such as nausea, vomiting, and constipation. Persistent or episodic hypertension may be present, with 13% of patients maintaining a normal blood pressure.5-7 Patients with pheochromocytoma-related anxiety typically have substantial or complete resolution of anxiety and panic attacks after tumor resection.6,8,10
Because of their ability to raise catecholamine levels, several medications, including some psychotropics, can lead to false-positive results on serum and urine metanephrines testing. Tricyclic antidepressants and beta-blockers can cause false-positive results on plasma assays, while buspirone can cause false-positives on urinalysis assays.5 Trazodone, on the other hand, exhibits no catecholaminergic activity and its alpha-1 adrenergic antagonism may actually have some benefit in pheochromocytoma.11 Alpha-1 adrenergic antagonism with doxazosin, prazosin, or terazosin is the first-line of treatment in reducing pheochromocytoma-related hypertension.7 Treatment with a beta-blocker is safe only after alpha-adrenergic blockade occurs. While beta-blockers are useful for reducing the palpitations and anxiety observed in patients with pheochromocytoma, they must not be used alone due to the risk of hypertensive crisis resulting from unopposed alpha-adrenergic agonist activated vasoconstriction.5,7
TREATMENT CBT provides benefit
Mr. P decides against receiving an additional agent for anxiety and instead decides to wait for the outcome of the confirmatory pheochromocytoma testing. He continues to take alprazolam, and both his depressed mood and anxiety improve. His panic attacks continue to lessen, and he appears to benefit from cognitive-behavioral therapy provided during group therapy. Mr. P is advised by his PCP to taper and stop the alprazolam 3 to 5 days before his 24-hour urine metanephrines test because benzodiazepines can lead to false-positive results on a urinalysis assay.7
OUTCOME Remission of anxiety and depression
Mr. P has a repeat serum metanephrines test and a 24-hour urinalysis assay. Both are negative for pheochromocytoma. His PCP refers him to cardiology for management of treatment-resistant hypertension. He is discharged from the PHP and continues psychotherapy for depression and anxiety in an intensive outpatient program (IOP). Throughout his PHP and IOP treatments, he continues to take paroxetine and hydroxyzine. He achieves a successful remission of his anxiety and depression, with partial but significant remission of his panic attacks.
The author’s observations
Although Mr. P did not have pheochromocytoma, it is important to rule out this rare condition in patients who present with treatment-resistant hypertension and/or treatment-resistant anxiety.
Continue to: Bottom Line
Bottom Line
Pheochromocytoma is a tumor of the adrenal gland. The classic triad of symptoms of this rare condition is hypertension, sweating, and headache; approximately 30% of patients report significant anxiety and panic. Several medications, including tricyclic antidepressants, beta-blockers, and buspirone, can lead to false-positive results on the serum and urine metanephrines testing used to diagnose pheochromocytoma.
Related Resources
- National Organization for Rare Disorders. Rare Disease Database: pheochromocytoma. www.rarediseases.org/rare-diseases/pheochromocytoma/.
- Young WF Jr. Clinical presentation and diagnosis of pheochromocytoma. UpToDate. www.uptodate.com/contents/clinical-presentation-and-diagnosis-of-pheochromocytoma. Published January 2020.
Drug Brand Names
Alprazolam • Xanax
Amitriptyline • Elavil
Buspirone • Buspar
Carvedilol • Coreg
Clonidine • Catapres
Doxazosin • Cardura
Hydroxyzine • Vistaril
Lisinopril • Prinivil, Zestril
Paroxetine • Paxil
Prazosin • Minipress
Propranolol • Inderal
Terazosin • Hytrin
Trazodone • Desyrel
Zolpidem • Ambien
1. Morrison J. When psychological problems mask medical disorders: a guide for psychotherapists. 2nd ed. New York, NY: The Guilford Press; 2015.
2. American Porphyria Foundation. About porphyria. https://porphyriafoundation.org/patients/about-porphyria. Accessed May 13, 2020.
3. Millward L, Kelly P, King A, et al. Anxiety and depression in the acute porphyrias. J Inherit Metab Dis. 2005;28(6):1099-1107.
4. Bonkovsky H, Maddukuri VC, Yazici C, et al. Acute porphyrias in the USA: features of 108 subjects from porphyria consortium. Am J Med. 2014;127(12):1233-1241.
5. Tsirlin A, Oo Y, Sharma R, et al. Pheochromocytoma: a review. Maturitas. 2014;77(3):229-238.
6. Leung A, Zun L, Nordstrom K, et al. Psychiatric emergencies for physicians: clinical management and approach to distinguishing pheochromocytoma from psychiatric and thyrotoxic diseases in the emergency room. J Emerg Med. 2017;53(5):712-716.
7. Garg M, Kharb S, Brar KS, et al. Medical management of pheochromocytoma: role of the endocrinologist. Indian J Endocrinol and Metab. 2011;15(suppl 4):S329-S336. doi: 10.4103/2230-8210.86976.
8. Zardawi I. Phaeochromocytoma masquerading as anxiety and depression. Am J Case Rep. 2013;14:161-163.
9. ARUP Laboratories. Test directory. https://www.aruplab.com. Accessed February 11, 2020.
10. Sriram P, Raghavan V. Pheochromocytoma presenting as anxiety disorder: a case report. Asian J Psychiatr. 2017;29:83-84.
11. Stahl SM. Stahl’s essential psychopharmacology: neuroscientific basis and practical applications. Cambridge, UK: Cambridge University Press; 2013.
1. Morrison J. When psychological problems mask medical disorders: a guide for psychotherapists. 2nd ed. New York, NY: The Guilford Press; 2015.
2. American Porphyria Foundation. About porphyria. https://porphyriafoundation.org/patients/about-porphyria. Accessed May 13, 2020.
3. Millward L, Kelly P, King A, et al. Anxiety and depression in the acute porphyrias. J Inherit Metab Dis. 2005;28(6):1099-1107.
4. Bonkovsky H, Maddukuri VC, Yazici C, et al. Acute porphyrias in the USA: features of 108 subjects from porphyria consortium. Am J Med. 2014;127(12):1233-1241.
5. Tsirlin A, Oo Y, Sharma R, et al. Pheochromocytoma: a review. Maturitas. 2014;77(3):229-238.
6. Leung A, Zun L, Nordstrom K, et al. Psychiatric emergencies for physicians: clinical management and approach to distinguishing pheochromocytoma from psychiatric and thyrotoxic diseases in the emergency room. J Emerg Med. 2017;53(5):712-716.
7. Garg M, Kharb S, Brar KS, et al. Medical management of pheochromocytoma: role of the endocrinologist. Indian J Endocrinol and Metab. 2011;15(suppl 4):S329-S336. doi: 10.4103/2230-8210.86976.
8. Zardawi I. Phaeochromocytoma masquerading as anxiety and depression. Am J Case Rep. 2013;14:161-163.
9. ARUP Laboratories. Test directory. https://www.aruplab.com. Accessed February 11, 2020.
10. Sriram P, Raghavan V. Pheochromocytoma presenting as anxiety disorder: a case report. Asian J Psychiatr. 2017;29:83-84.
11. Stahl SM. Stahl’s essential psychopharmacology: neuroscientific basis and practical applications. Cambridge, UK: Cambridge University Press; 2013.
COVID-19 and Mental Health Awareness Month
#howareyoureally challenge seeks to increase access to care
We are months into the COVID-19 crisis, and mental health issues are proving to be rampant. In every crisis, there is opportunity, and this one is no different. The opportunity is clear. For Mental Health Awareness Month and beyond, we must convey a powerful message that mental health is key to our well-being and must be actively addressed. Because almost everyone has felt excess anxiety these last months, we have a unique chance to engage a wider audience.
To address the urgent need, the Mental Health Coalition was formed with the understanding that the mental health crisis is fueled by a pervasive and devastating stigma, preventing millions of individuals from being able to seek the critical treatment they need. Spearheaded by social activist and fashion designer, Kenneth Cole, it is a coalition of leading mental health organizations, brands, celebrities, and advocates who have joined forces to end the stigma surrounding mental health and to change the way people talk about, and care for, mental illness. The group’s mission listed on its website states: “We must increase the conversation around mental health. We must act to end silence, reduce stigma, and engage our community to inspire hope at this essential moment.”
As most of the United States has been under stay-at-home orders, our traditional relationships have been radically disrupted. New types of relationships are forming as we are relying even more on technology to connect us. Social media seems to be on the only “social” we can now safely engage in.
The coalition’s campaign, “#howareyoureally?” is harnessing the power of social media and creating a storytelling platform to allow users to more genuinely share their feelings in these unprecedented times. Celebrities include Whoopi Goldberg, Kendall Jenner, Chris Cuomo, Deepak Chopra, Kesha, and many more have already shared their stories.
“How Are You, Really?” challenges people to answer this question using social media in an open and honest fashion while still providing hope.
The second component of the initiative is to increase access to care, and they have a long list of collaborators, including leading mental health organizations such as the American Foundation for Suicide Prevention, Anxiety and Depression Association of America, Child Mind Institute, Depression and Bipolar Support Alliance, Didi Hirsch Mental Health Services, National Alliance on Mental Illness, and many more.
We have a unique opportunity this Mental Health Awareness Month, and As a community, we must be prepared to meet the escalating needs of our population.
Dr. Ritvo, a psychiatrist with more than 25 years’ experience, practices in Miami Beach, Fla. She is the author of “Bekindr – The Transformative Power of Kindness” (Hellertown, Pa.: Momosa Publishing, 2018) and is the founder of the Bekindr Global Initiative, a movement aimed at cultivating kindness in the world. Dr. Ritvo also is the cofounder of the Bold Beauty Project, a nonprofit group that pairs women with disabilities with photographers who create art exhibitions to raise awareness.
#howareyoureally challenge seeks to increase access to care
#howareyoureally challenge seeks to increase access to care
We are months into the COVID-19 crisis, and mental health issues are proving to be rampant. In every crisis, there is opportunity, and this one is no different. The opportunity is clear. For Mental Health Awareness Month and beyond, we must convey a powerful message that mental health is key to our well-being and must be actively addressed. Because almost everyone has felt excess anxiety these last months, we have a unique chance to engage a wider audience.
To address the urgent need, the Mental Health Coalition was formed with the understanding that the mental health crisis is fueled by a pervasive and devastating stigma, preventing millions of individuals from being able to seek the critical treatment they need. Spearheaded by social activist and fashion designer, Kenneth Cole, it is a coalition of leading mental health organizations, brands, celebrities, and advocates who have joined forces to end the stigma surrounding mental health and to change the way people talk about, and care for, mental illness. The group’s mission listed on its website states: “We must increase the conversation around mental health. We must act to end silence, reduce stigma, and engage our community to inspire hope at this essential moment.”
As most of the United States has been under stay-at-home orders, our traditional relationships have been radically disrupted. New types of relationships are forming as we are relying even more on technology to connect us. Social media seems to be on the only “social” we can now safely engage in.
The coalition’s campaign, “#howareyoureally?” is harnessing the power of social media and creating a storytelling platform to allow users to more genuinely share their feelings in these unprecedented times. Celebrities include Whoopi Goldberg, Kendall Jenner, Chris Cuomo, Deepak Chopra, Kesha, and many more have already shared their stories.
“How Are You, Really?” challenges people to answer this question using social media in an open and honest fashion while still providing hope.
The second component of the initiative is to increase access to care, and they have a long list of collaborators, including leading mental health organizations such as the American Foundation for Suicide Prevention, Anxiety and Depression Association of America, Child Mind Institute, Depression and Bipolar Support Alliance, Didi Hirsch Mental Health Services, National Alliance on Mental Illness, and many more.
We have a unique opportunity this Mental Health Awareness Month, and As a community, we must be prepared to meet the escalating needs of our population.
Dr. Ritvo, a psychiatrist with more than 25 years’ experience, practices in Miami Beach, Fla. She is the author of “Bekindr – The Transformative Power of Kindness” (Hellertown, Pa.: Momosa Publishing, 2018) and is the founder of the Bekindr Global Initiative, a movement aimed at cultivating kindness in the world. Dr. Ritvo also is the cofounder of the Bold Beauty Project, a nonprofit group that pairs women with disabilities with photographers who create art exhibitions to raise awareness.
We are months into the COVID-19 crisis, and mental health issues are proving to be rampant. In every crisis, there is opportunity, and this one is no different. The opportunity is clear. For Mental Health Awareness Month and beyond, we must convey a powerful message that mental health is key to our well-being and must be actively addressed. Because almost everyone has felt excess anxiety these last months, we have a unique chance to engage a wider audience.
To address the urgent need, the Mental Health Coalition was formed with the understanding that the mental health crisis is fueled by a pervasive and devastating stigma, preventing millions of individuals from being able to seek the critical treatment they need. Spearheaded by social activist and fashion designer, Kenneth Cole, it is a coalition of leading mental health organizations, brands, celebrities, and advocates who have joined forces to end the stigma surrounding mental health and to change the way people talk about, and care for, mental illness. The group’s mission listed on its website states: “We must increase the conversation around mental health. We must act to end silence, reduce stigma, and engage our community to inspire hope at this essential moment.”
As most of the United States has been under stay-at-home orders, our traditional relationships have been radically disrupted. New types of relationships are forming as we are relying even more on technology to connect us. Social media seems to be on the only “social” we can now safely engage in.
The coalition’s campaign, “#howareyoureally?” is harnessing the power of social media and creating a storytelling platform to allow users to more genuinely share their feelings in these unprecedented times. Celebrities include Whoopi Goldberg, Kendall Jenner, Chris Cuomo, Deepak Chopra, Kesha, and many more have already shared their stories.
“How Are You, Really?” challenges people to answer this question using social media in an open and honest fashion while still providing hope.
The second component of the initiative is to increase access to care, and they have a long list of collaborators, including leading mental health organizations such as the American Foundation for Suicide Prevention, Anxiety and Depression Association of America, Child Mind Institute, Depression and Bipolar Support Alliance, Didi Hirsch Mental Health Services, National Alliance on Mental Illness, and many more.
We have a unique opportunity this Mental Health Awareness Month, and As a community, we must be prepared to meet the escalating needs of our population.
Dr. Ritvo, a psychiatrist with more than 25 years’ experience, practices in Miami Beach, Fla. She is the author of “Bekindr – The Transformative Power of Kindness” (Hellertown, Pa.: Momosa Publishing, 2018) and is the founder of the Bekindr Global Initiative, a movement aimed at cultivating kindness in the world. Dr. Ritvo also is the cofounder of the Bold Beauty Project, a nonprofit group that pairs women with disabilities with photographers who create art exhibitions to raise awareness.
COVID-19: Delirium first, depression, anxiety, insomnia later?
Severe COVID-19 may cause delirium in the acute stage of illness, followed by the possibility of depression, anxiety, fatigue, insomnia, and posttraumatic stress disorder (PTSD) over the longer term, new research suggests.
Results from “the first systematic review and meta-analysis of the psychiatric consequences of coronavirus infection” showed that previous coronavirus epidemics were associated with a significant psychiatric burden in both the acute and post-illness stages.
“Most people with COVID-19 will not develop any mental health problems, even among those with severe cases requiring hospitalization, but given the huge numbers of people getting sick, the global impact on mental health could be considerable,” co–lead investigator Jonathan Rogers, MRCPsych, Department of Psychiatry, University College London, United Kingdom, said in a news release.
The study was published online May 18 in Lancet Psychiatry.
Need for Monitoring, Support
The researchers analyzed 65 peer-reviewed studies and seven preprint articles with data on acute and post-illness psychiatric and neuropsychiatric features of patients who had been hospitalized with COVID-19, as well as two other diseases caused by coronaviruses – severe acute respiratory syndrome (SARS), in 2002–2004, and Middle East respiratory syndrome (MERS), in 2012.
“Our main findings are that signs suggestive of delirium are common in the acute stage of SARS, MERS, and COVID-19; there is evidence of depression, anxiety, fatigue, and post-traumatic stress disorder in the post-illness stage of previous coronavirus epidemics, but there are few data yet on COVID-19,” the investigators write.
The data show that among patients acutely ill with SARS and MERS, 28% experienced confusion, 33% had depressed mood, 36% had anxiety, 34% suffered from impaired memory, and 42% had insomnia.
After recovery from SARS and MERS, sleep disorder, frequent recall of traumatic memories, emotional lability, impaired concentration, fatigue, and impaired memory were reported in more than 15% of patients during a follow-up period that ranged from 6 weeks to 39 months.
In a meta-analysis, the point prevalence in the post-illness stage was 32% for PTSD and about 15% for depression and anxiety.
In patients acutely ill with severe COVID-19, available data suggest that 65% experience delirium, 69% have agitation after withdrawal of sedation, and 21% have altered consciousness.
In one study, 33% of patients had a dysexecutive syndrome at discharge, characterized by symptoms such as inattention, disorientation, or poorly organized movements in response to command. Currently, data are very limited regarding patients who have recovered from COVID-19, the investigators caution.
“, and monitored after they recover to ensure they do not develop mental illnesses, and are able to access treatment if needed,” senior author Anthony David, FMedSci, from UCL Institute of Mental Health, said in a news release.
“While most people with COVID-19 will recover without experiencing mental illness, we need to research which factors may contribute to enduring mental health problems, and develop interventions to prevent and treat them,” he added.
Be Prepared
The coauthors of a linked commentary say it makes sense, from a biological perspective, to merge data on these three coronavirus diseases, given the degree to which they resemble each other.
They caution, however, that treatment of COVID-19 seems to be different from treatment of SARS and MERS. In addition, the social and economic situation of COVID-19 survivors’ return is completely different from that of SARS and MERS survivors.
Findings from previous coronavirus outbreaks are “useful, but might not be exact predictors of prevalences of psychiatric complications for patients with COVID-19,” write Iris Sommer, MD, PhD, from University Medical Center Groningen, the Netherlands, and P. Roberto Bakker, MD, PhD, from Maastricht University Medical Center, the Netherlands.
“The warning from [this study] that we should prepare to treat large numbers of patients with COVID-19 who go on to develop delirium, post-traumatic stress disorder, anxiety, and depression is an important message for the psychiatric community,” they add.
Sommer and Bakker also say the reported estimates of prevalence in this study should be interpreted with caution, “as true numbers of both acute and long-term psychiatric disorders for patients with COVID-19 might be considerably higher.”
Funding for the study was provided by the Wellcome Trust, the UK National Institute for Health Research (NIHR), the UK Medical Research Council, the NIHR Biomedical Research Center at the University College London Hospitals NHS Foundation Trust, and the University College London. The authors of the study and the commentary have disclosed no relevant financial relationships.
This article first appeared on Medscape.com.
Severe COVID-19 may cause delirium in the acute stage of illness, followed by the possibility of depression, anxiety, fatigue, insomnia, and posttraumatic stress disorder (PTSD) over the longer term, new research suggests.
Results from “the first systematic review and meta-analysis of the psychiatric consequences of coronavirus infection” showed that previous coronavirus epidemics were associated with a significant psychiatric burden in both the acute and post-illness stages.
“Most people with COVID-19 will not develop any mental health problems, even among those with severe cases requiring hospitalization, but given the huge numbers of people getting sick, the global impact on mental health could be considerable,” co–lead investigator Jonathan Rogers, MRCPsych, Department of Psychiatry, University College London, United Kingdom, said in a news release.
The study was published online May 18 in Lancet Psychiatry.
Need for Monitoring, Support
The researchers analyzed 65 peer-reviewed studies and seven preprint articles with data on acute and post-illness psychiatric and neuropsychiatric features of patients who had been hospitalized with COVID-19, as well as two other diseases caused by coronaviruses – severe acute respiratory syndrome (SARS), in 2002–2004, and Middle East respiratory syndrome (MERS), in 2012.
“Our main findings are that signs suggestive of delirium are common in the acute stage of SARS, MERS, and COVID-19; there is evidence of depression, anxiety, fatigue, and post-traumatic stress disorder in the post-illness stage of previous coronavirus epidemics, but there are few data yet on COVID-19,” the investigators write.
The data show that among patients acutely ill with SARS and MERS, 28% experienced confusion, 33% had depressed mood, 36% had anxiety, 34% suffered from impaired memory, and 42% had insomnia.
After recovery from SARS and MERS, sleep disorder, frequent recall of traumatic memories, emotional lability, impaired concentration, fatigue, and impaired memory were reported in more than 15% of patients during a follow-up period that ranged from 6 weeks to 39 months.
In a meta-analysis, the point prevalence in the post-illness stage was 32% for PTSD and about 15% for depression and anxiety.
In patients acutely ill with severe COVID-19, available data suggest that 65% experience delirium, 69% have agitation after withdrawal of sedation, and 21% have altered consciousness.
In one study, 33% of patients had a dysexecutive syndrome at discharge, characterized by symptoms such as inattention, disorientation, or poorly organized movements in response to command. Currently, data are very limited regarding patients who have recovered from COVID-19, the investigators caution.
“, and monitored after they recover to ensure they do not develop mental illnesses, and are able to access treatment if needed,” senior author Anthony David, FMedSci, from UCL Institute of Mental Health, said in a news release.
“While most people with COVID-19 will recover without experiencing mental illness, we need to research which factors may contribute to enduring mental health problems, and develop interventions to prevent and treat them,” he added.
Be Prepared
The coauthors of a linked commentary say it makes sense, from a biological perspective, to merge data on these three coronavirus diseases, given the degree to which they resemble each other.
They caution, however, that treatment of COVID-19 seems to be different from treatment of SARS and MERS. In addition, the social and economic situation of COVID-19 survivors’ return is completely different from that of SARS and MERS survivors.
Findings from previous coronavirus outbreaks are “useful, but might not be exact predictors of prevalences of psychiatric complications for patients with COVID-19,” write Iris Sommer, MD, PhD, from University Medical Center Groningen, the Netherlands, and P. Roberto Bakker, MD, PhD, from Maastricht University Medical Center, the Netherlands.
“The warning from [this study] that we should prepare to treat large numbers of patients with COVID-19 who go on to develop delirium, post-traumatic stress disorder, anxiety, and depression is an important message for the psychiatric community,” they add.
Sommer and Bakker also say the reported estimates of prevalence in this study should be interpreted with caution, “as true numbers of both acute and long-term psychiatric disorders for patients with COVID-19 might be considerably higher.”
Funding for the study was provided by the Wellcome Trust, the UK National Institute for Health Research (NIHR), the UK Medical Research Council, the NIHR Biomedical Research Center at the University College London Hospitals NHS Foundation Trust, and the University College London. The authors of the study and the commentary have disclosed no relevant financial relationships.
This article first appeared on Medscape.com.
Severe COVID-19 may cause delirium in the acute stage of illness, followed by the possibility of depression, anxiety, fatigue, insomnia, and posttraumatic stress disorder (PTSD) over the longer term, new research suggests.
Results from “the first systematic review and meta-analysis of the psychiatric consequences of coronavirus infection” showed that previous coronavirus epidemics were associated with a significant psychiatric burden in both the acute and post-illness stages.
“Most people with COVID-19 will not develop any mental health problems, even among those with severe cases requiring hospitalization, but given the huge numbers of people getting sick, the global impact on mental health could be considerable,” co–lead investigator Jonathan Rogers, MRCPsych, Department of Psychiatry, University College London, United Kingdom, said in a news release.
The study was published online May 18 in Lancet Psychiatry.
Need for Monitoring, Support
The researchers analyzed 65 peer-reviewed studies and seven preprint articles with data on acute and post-illness psychiatric and neuropsychiatric features of patients who had been hospitalized with COVID-19, as well as two other diseases caused by coronaviruses – severe acute respiratory syndrome (SARS), in 2002–2004, and Middle East respiratory syndrome (MERS), in 2012.
“Our main findings are that signs suggestive of delirium are common in the acute stage of SARS, MERS, and COVID-19; there is evidence of depression, anxiety, fatigue, and post-traumatic stress disorder in the post-illness stage of previous coronavirus epidemics, but there are few data yet on COVID-19,” the investigators write.
The data show that among patients acutely ill with SARS and MERS, 28% experienced confusion, 33% had depressed mood, 36% had anxiety, 34% suffered from impaired memory, and 42% had insomnia.
After recovery from SARS and MERS, sleep disorder, frequent recall of traumatic memories, emotional lability, impaired concentration, fatigue, and impaired memory were reported in more than 15% of patients during a follow-up period that ranged from 6 weeks to 39 months.
In a meta-analysis, the point prevalence in the post-illness stage was 32% for PTSD and about 15% for depression and anxiety.
In patients acutely ill with severe COVID-19, available data suggest that 65% experience delirium, 69% have agitation after withdrawal of sedation, and 21% have altered consciousness.
In one study, 33% of patients had a dysexecutive syndrome at discharge, characterized by symptoms such as inattention, disorientation, or poorly organized movements in response to command. Currently, data are very limited regarding patients who have recovered from COVID-19, the investigators caution.
“, and monitored after they recover to ensure they do not develop mental illnesses, and are able to access treatment if needed,” senior author Anthony David, FMedSci, from UCL Institute of Mental Health, said in a news release.
“While most people with COVID-19 will recover without experiencing mental illness, we need to research which factors may contribute to enduring mental health problems, and develop interventions to prevent and treat them,” he added.
Be Prepared
The coauthors of a linked commentary say it makes sense, from a biological perspective, to merge data on these three coronavirus diseases, given the degree to which they resemble each other.
They caution, however, that treatment of COVID-19 seems to be different from treatment of SARS and MERS. In addition, the social and economic situation of COVID-19 survivors’ return is completely different from that of SARS and MERS survivors.
Findings from previous coronavirus outbreaks are “useful, but might not be exact predictors of prevalences of psychiatric complications for patients with COVID-19,” write Iris Sommer, MD, PhD, from University Medical Center Groningen, the Netherlands, and P. Roberto Bakker, MD, PhD, from Maastricht University Medical Center, the Netherlands.
“The warning from [this study] that we should prepare to treat large numbers of patients with COVID-19 who go on to develop delirium, post-traumatic stress disorder, anxiety, and depression is an important message for the psychiatric community,” they add.
Sommer and Bakker also say the reported estimates of prevalence in this study should be interpreted with caution, “as true numbers of both acute and long-term psychiatric disorders for patients with COVID-19 might be considerably higher.”
Funding for the study was provided by the Wellcome Trust, the UK National Institute for Health Research (NIHR), the UK Medical Research Council, the NIHR Biomedical Research Center at the University College London Hospitals NHS Foundation Trust, and the University College London. The authors of the study and the commentary have disclosed no relevant financial relationships.
This article first appeared on Medscape.com.
COVID-19 exacerbating challenges for Latino patients
Disproportionate burden of pandemic complicates mental health care
Pamela Montano, MD, recalls the recent case of a patient with bipolar II disorder who was improving after treatment with medication and therapy when her life was upended by the COVID-19 pandemic.
The patient, who is Puerto Rican, lost two cousins to the virus, two of her brothers fell ill, and her sister became sick with coronavirus, said Dr. Montano, director of the Latino Bicultural Clinic at Gouverneur Health in New York. The patient was then left to care for her sister’s toddlers along with the patient’s own children, one of whom has special needs.
“After this happened, it increased her anxiety,” Dr. Montano said in an interview. “She’s not sleeping, and she started having panic attacks. My main concern was how to help her cope.”
Across the country, clinicians who treat mental illness and behavioral disorders in Latino patients are facing similar experiences and challenges associated with COVID-19 and the ensuing pandemic response. Current data suggest a disproportionate burden of illness and death from the novel coronavirus among racial and ethnic groups, particularly black and Hispanic patients. The disparities are likely attributable to economic and social conditions more common among such populations, compared with non-Hispanic whites, in addition to isolation from resources, according to the Centers for Disease Control and Prevention.
A recent New York City Department of Health study based on data that were available in late April found that deaths from COVID-19 were substantially higher for black and Hispanic/Latino patients than for white and Asian patients. The death rate per 100,000 population was 209.4 for blacks, 195.3 for Hispanics/Latinos, 107.7 for whites, and 90.8 for Asians.
“The COVID pandemic has highlighted the structural inequities that affect the Latino population [both] immigrant and nonimmigrant,” said Dr. Montano, a board member of the American Society of Hispanic Psychiatry and the officer of infrastructure and advocacy for the Hispanic Caucus of the American Psychiatric Association. “This includes income inequality, poor nutrition, history of trauma and discrimination, employment issues, quality education, access to technology, and overall access to appropriate cultural linguistic health care.”
Navigating challenges
For mental health professionals treating Latino patients, COVID-19 and the pandemic response have generated a range of treatment obstacles.
The transition to telehealth for example, has not been easy for some patients, said Jacqueline Posada, MD, consultation-liaison psychiatry fellow at the Inova Fairfax Hospital–George Washington University program in Falls Church, Va., and an APA Substance Abuse and Mental Health Services Administration minority fellow. Some patients lack Internet services, others forget virtual visits, and some do not have working phones, she said.
“I’ve had to be very flexible,” she said in an interview. “Ideally, I’d love to see everybody via video chat, but a lot of people either don’t have a stable Internet connection or Internet, so I meet the patient where they are. Whatever they have available, that’s what I’m going to use. If they don’t answer on the first call, I will call again at least three to five times in the first 15 minutes to make sure I’m giving them an opportunity to pick up the phone.”
In addition, Dr. Posada has encountered disconnected phones when calling patients for appointments. In such cases, Dr. Posada contacts the patient’s primary care physician to relay medication recommendations in case the patient resurfaces at the clinic.
In other instances, patients are not familiar with video technology, or they must travel to a friend or neighbor’s house to access the technology, said Hector Colón-Rivera, MD, an addiction psychiatrist and medical director of the Asociación Puertorriqueños en Marcha Behavioral Health Program, a nonprofit organization based in the Philadelphia area. Telehealth visits frequently include appearances by children, family members, barking dogs, and other distractions, said Dr. Colón-Rivera, president of the APA Hispanic Caucus.
“We’re seeing things that we didn’t used to see when they came to our office – for good or for bad,” said Dr. Colón-Rivera, an attending telemedicine physician at the University of Pittsburgh Medical Center. “It could be a good chance to meet our patient in a different way. Of course, it creates different stressors. If you have five kids on top of you and you’re the only one at home, it’s hard to do therapy.”
Psychiatrists are also seeing prior health conditions in patients exacerbated by COVID-19 fears and new health problems arising from the current pandemic environment. Dr. Posada recalls a patient whom she successfully treated for premenstrual dysphoric disorder who recently descended into severe clinical depression. The patient, from Colombia, was attending school in the United States on a student visa and supporting herself through child care jobs.
“So much of her depression was based on her social circumstance,” Dr. Posada said. “She had lost her job, her sister had lost her job so they were scraping by on her sister’s husband’s income, and the thing that brought her joy, which was going to school and studying so she could make a different life for herself than what her parents had in Colombia, also seemed like it was out of reach.”
Dr. Colón-Rivera recently received a call from a hospital where one of his patients was admitted after becoming delusional and psychotic. The patient was correctly taking medication prescribed by Dr. Colón-Rivera, but her diabetes had become uncontrolled because she was unable to reach her primary care doctor and couldn’t access the pharmacy. Her blood sugar level became elevated, leading to the delusions.
“A patient that was perfectly stable now is unstable,” he said. “Her diet has not been good enough through the pandemic, exacerbating her diabetes. She was admitted to the hospital for delirium.
Compounding of traumas
For many Latino patients, the adverse impacts of the pandemic comes on top of multiple prior traumas, such as violence exposures, discrimination, and economic issues, said Lisa Fortuna, MD, MPH, MDiv, chief of psychiatry and vice chair at Zuckerberg San Francisco General Hospital. A 2017 analysis found that nearly four in five Latino youth face at least one traumatic childhood experience, like poverty or abuse, and that about 29% of Latino youth experience four or more of these traumas.
Immigrants in particular, may have faced trauma in their home country and/or immigration trauma, Dr. Fortuna added. A 2013 study on immigrant Latino adolescents for example, found that 29% of foreign-born adolescents and 34% of foreign-born parents experienced trauma during the migration process (Int Migr Rev. 2013 Dec;47(4):10).
“All of these things are cumulative,” Dr. Fortuna said. “Then when you’re hit with a pandemic, all of the disparities that you already have and all the stress that you already have are compounded. This is for the kids, too, who have been exposed to a lot of stressors and now maybe have family members that have been ill or have died. All of these things definitely put people at risk for increased depression [and] the worsening of any preexisting posttraumatic stress disorder. We’ve seen this in previous disasters, and I expect that’s what we’re going to see more of with the COVID-19 pandemic.”
At the same time, a central cultural value of many Latinos is family unity, Dr. Montano said, a foundation that is now being strained by social distancing and severed connections.
“This has separated many families,” she said. “There has been a lot of loneliness and grief.”
Mistrust and fear toward the government, public agencies, and even the health system itself act as further hurdles for some Latinos in the face of COVID-19. In areas with large immigrant populations such as San Francisco, Dr. Fortuna noted, it’s not uncommon for undocumented patients to avoid accessing medical care and social services, or visiting emergency departments for needed care for fear of drawing attention to themselves or possible detainment.
“The fact that so many people showed up at our hospital so ill and ended up in the ICU – that could be a combination of factors. Because the population has high rates of diabetes and hypertension, that might have put people at increased risk for severe illness,” she said. “But some people may have been holding out for care because they wanted to avoid being in places out of fear of immigration scrutiny.”
Overcoming language barriers
Compounding the challenging pandemic landscape for Latino patients is the fact that many state resources about COVID-19 have not been translated to Spanish, Dr. Colón-Rivera said. He was troubled recently when he went to several state websites and found limited to no information in Spanish about the coronavirus. Some data about COVID-19 from the federal government were not translated to Spanish until officials received pushback, he added. Even now, press releases and other information disseminated by the federal government about the virus appear to be translated by an automated service – and lack sense and context.
The state agencies in Pennsylvania have been alerted to the absence of Spanish information, but change has been slow, he noted.
“In Philadelphia, 23% speaks a language other than English,” he said. “So we missed a lot of critical information that could have helped to avoid spreading the illness and access support.”
Dr. Fortuna said that California has done better with providing COVID-19–related information in Spanish, compared with some other states, but misinformation about the virus and lingering myths have still been a problem among the Latino community. The University of California, San Francisco, recently launched a Latino Task Force resource website for the Latino community that includes information in English, Spanish, and Yucatec Maya about COVID-19, health and wellness tips, and resources for various assistance needs.
The concerning lack of COVID-19 information translated to Spanish led Dr. Montano to start a Facebook page in Spanish about mental health tips and guidance for managing COVID-19–related issues. She and her team of clinicians share information, videos, relaxation exercises, and community resources on the page, among other posts. “There is also general info and recommendations about COVID-19 that I think can be useful for the community,” she said. “The idea is that patients, the general community, and providers can have share information, hope messages, and ask questions in Spanish.”
Feeling ‘helpless’
A central part of caring for Latino patients during the COVID-19 crisis has been referring them to outside agencies and social services, psychiatrists say. But finding the right resources amid a pandemic and ensuring that patients connect with the correct aid has been an uphill battle.
“We sometimes feel like our hands are tied,” Dr. Colón-Rivera said. “Sometimes, we need to call a place to bring food. Some of the state agencies and nonprofits don’t have delivery systems, so the patient has to go pick up for food or medication. Some of our patients don’t want to go outside. Some do not have cars.”
As a clinician, it can be easy to feel helpless when trying to navigate new challenges posed by the pandemic in addition to other longstanding barriers, Dr. Posada said.
“Already, mental health disorders are so influenced by social situations like poverty, job insecurity, or family issues, and now it just seems those obstacles are even more insurmountable,” she said. “At the end of the day, I can feel like: ‘Did I make a difference?’ That’s a big struggle.”
Dr. Montano’s team, which includes psychiatrists, psychologists, and social workers, have come to rely on virtual debriefings to vent, express frustrations, and support one another, she said. She also recently joined a virtual mind-body skills group as a participant.
“I recognize the importance of getting additional support and ways to alleviate burnout,” she said. “We need to take care of ourselves or we won’t be able to help others.”
Focusing on resilience during the current crisis can be beneficial for both patients and providers in coping and drawing strength, Dr. Posada said.
“When it comes to fostering resilience during times of hardship, I think it’s most helpful to reflect on what skills or attributes have helped during past crises and apply those now – whether it’s turning to comfort from close relationships, looking to religion and spirituality, practicing self-care like rest or exercise, or really tapping into one’s purpose and reason for practicing psychiatry and being a physician,” she said. “The same advice goes for clinicians: We’ve all been through hard times in the past, it’s part of the human condition and we’ve also witnessed a lot of suffering in our patients, so now is the time to practice those skills that have gotten us through hard times in the past.”
Learning lessons from COVID-19
Despite the challenges with moving to telehealth, Dr. Fortuna said the tool has proved beneficial overall for mental health care. For Dr. Fortuna’s team for example, telehealth by phone has decreased the no-show rate, compared with clinic visits, and improved care access.
“We need to figure out how to maintain that,” she said. “If we can build ways for equity and access to Internet, especially equipment, I think that’s going to help.”
In addition, more data are needed about the ways in which COVID-19 is affecting Latino patients, Dr. Colón-Rivera said. Mortality statistics have been published, but information is needed about the rates of infection and manifestation of illness.
Most importantly, the COVID-19 crisis has emphasized the critical need to address and improve the underlying inequity issues among Latino patients, psychiatrists say.
“We really need to think about how there can be partnerships, in terms of community-based Latino business and leaders, multisector resources, trying to think about how we can improve conditions both work and safety for Latinos,” Dr. Fortuna said. “How can schools get support in integrating mental health and support for families, especially now after COVID-19? And really looking at some of these underlying inequities that are the underpinnings of why people were at risk for the disproportionate effects of the COVID-19 pandemic.”
Disproportionate burden of pandemic complicates mental health care
Disproportionate burden of pandemic complicates mental health care
Pamela Montano, MD, recalls the recent case of a patient with bipolar II disorder who was improving after treatment with medication and therapy when her life was upended by the COVID-19 pandemic.
The patient, who is Puerto Rican, lost two cousins to the virus, two of her brothers fell ill, and her sister became sick with coronavirus, said Dr. Montano, director of the Latino Bicultural Clinic at Gouverneur Health in New York. The patient was then left to care for her sister’s toddlers along with the patient’s own children, one of whom has special needs.
“After this happened, it increased her anxiety,” Dr. Montano said in an interview. “She’s not sleeping, and she started having panic attacks. My main concern was how to help her cope.”
Across the country, clinicians who treat mental illness and behavioral disorders in Latino patients are facing similar experiences and challenges associated with COVID-19 and the ensuing pandemic response. Current data suggest a disproportionate burden of illness and death from the novel coronavirus among racial and ethnic groups, particularly black and Hispanic patients. The disparities are likely attributable to economic and social conditions more common among such populations, compared with non-Hispanic whites, in addition to isolation from resources, according to the Centers for Disease Control and Prevention.
A recent New York City Department of Health study based on data that were available in late April found that deaths from COVID-19 were substantially higher for black and Hispanic/Latino patients than for white and Asian patients. The death rate per 100,000 population was 209.4 for blacks, 195.3 for Hispanics/Latinos, 107.7 for whites, and 90.8 for Asians.
“The COVID pandemic has highlighted the structural inequities that affect the Latino population [both] immigrant and nonimmigrant,” said Dr. Montano, a board member of the American Society of Hispanic Psychiatry and the officer of infrastructure and advocacy for the Hispanic Caucus of the American Psychiatric Association. “This includes income inequality, poor nutrition, history of trauma and discrimination, employment issues, quality education, access to technology, and overall access to appropriate cultural linguistic health care.”
Navigating challenges
For mental health professionals treating Latino patients, COVID-19 and the pandemic response have generated a range of treatment obstacles.
The transition to telehealth for example, has not been easy for some patients, said Jacqueline Posada, MD, consultation-liaison psychiatry fellow at the Inova Fairfax Hospital–George Washington University program in Falls Church, Va., and an APA Substance Abuse and Mental Health Services Administration minority fellow. Some patients lack Internet services, others forget virtual visits, and some do not have working phones, she said.
“I’ve had to be very flexible,” she said in an interview. “Ideally, I’d love to see everybody via video chat, but a lot of people either don’t have a stable Internet connection or Internet, so I meet the patient where they are. Whatever they have available, that’s what I’m going to use. If they don’t answer on the first call, I will call again at least three to five times in the first 15 minutes to make sure I’m giving them an opportunity to pick up the phone.”
In addition, Dr. Posada has encountered disconnected phones when calling patients for appointments. In such cases, Dr. Posada contacts the patient’s primary care physician to relay medication recommendations in case the patient resurfaces at the clinic.
In other instances, patients are not familiar with video technology, or they must travel to a friend or neighbor’s house to access the technology, said Hector Colón-Rivera, MD, an addiction psychiatrist and medical director of the Asociación Puertorriqueños en Marcha Behavioral Health Program, a nonprofit organization based in the Philadelphia area. Telehealth visits frequently include appearances by children, family members, barking dogs, and other distractions, said Dr. Colón-Rivera, president of the APA Hispanic Caucus.
“We’re seeing things that we didn’t used to see when they came to our office – for good or for bad,” said Dr. Colón-Rivera, an attending telemedicine physician at the University of Pittsburgh Medical Center. “It could be a good chance to meet our patient in a different way. Of course, it creates different stressors. If you have five kids on top of you and you’re the only one at home, it’s hard to do therapy.”
Psychiatrists are also seeing prior health conditions in patients exacerbated by COVID-19 fears and new health problems arising from the current pandemic environment. Dr. Posada recalls a patient whom she successfully treated for premenstrual dysphoric disorder who recently descended into severe clinical depression. The patient, from Colombia, was attending school in the United States on a student visa and supporting herself through child care jobs.
“So much of her depression was based on her social circumstance,” Dr. Posada said. “She had lost her job, her sister had lost her job so they were scraping by on her sister’s husband’s income, and the thing that brought her joy, which was going to school and studying so she could make a different life for herself than what her parents had in Colombia, also seemed like it was out of reach.”
Dr. Colón-Rivera recently received a call from a hospital where one of his patients was admitted after becoming delusional and psychotic. The patient was correctly taking medication prescribed by Dr. Colón-Rivera, but her diabetes had become uncontrolled because she was unable to reach her primary care doctor and couldn’t access the pharmacy. Her blood sugar level became elevated, leading to the delusions.
“A patient that was perfectly stable now is unstable,” he said. “Her diet has not been good enough through the pandemic, exacerbating her diabetes. She was admitted to the hospital for delirium.
Compounding of traumas
For many Latino patients, the adverse impacts of the pandemic comes on top of multiple prior traumas, such as violence exposures, discrimination, and economic issues, said Lisa Fortuna, MD, MPH, MDiv, chief of psychiatry and vice chair at Zuckerberg San Francisco General Hospital. A 2017 analysis found that nearly four in five Latino youth face at least one traumatic childhood experience, like poverty or abuse, and that about 29% of Latino youth experience four or more of these traumas.
Immigrants in particular, may have faced trauma in their home country and/or immigration trauma, Dr. Fortuna added. A 2013 study on immigrant Latino adolescents for example, found that 29% of foreign-born adolescents and 34% of foreign-born parents experienced trauma during the migration process (Int Migr Rev. 2013 Dec;47(4):10).
“All of these things are cumulative,” Dr. Fortuna said. “Then when you’re hit with a pandemic, all of the disparities that you already have and all the stress that you already have are compounded. This is for the kids, too, who have been exposed to a lot of stressors and now maybe have family members that have been ill or have died. All of these things definitely put people at risk for increased depression [and] the worsening of any preexisting posttraumatic stress disorder. We’ve seen this in previous disasters, and I expect that’s what we’re going to see more of with the COVID-19 pandemic.”
At the same time, a central cultural value of many Latinos is family unity, Dr. Montano said, a foundation that is now being strained by social distancing and severed connections.
“This has separated many families,” she said. “There has been a lot of loneliness and grief.”
Mistrust and fear toward the government, public agencies, and even the health system itself act as further hurdles for some Latinos in the face of COVID-19. In areas with large immigrant populations such as San Francisco, Dr. Fortuna noted, it’s not uncommon for undocumented patients to avoid accessing medical care and social services, or visiting emergency departments for needed care for fear of drawing attention to themselves or possible detainment.
“The fact that so many people showed up at our hospital so ill and ended up in the ICU – that could be a combination of factors. Because the population has high rates of diabetes and hypertension, that might have put people at increased risk for severe illness,” she said. “But some people may have been holding out for care because they wanted to avoid being in places out of fear of immigration scrutiny.”
Overcoming language barriers
Compounding the challenging pandemic landscape for Latino patients is the fact that many state resources about COVID-19 have not been translated to Spanish, Dr. Colón-Rivera said. He was troubled recently when he went to several state websites and found limited to no information in Spanish about the coronavirus. Some data about COVID-19 from the federal government were not translated to Spanish until officials received pushback, he added. Even now, press releases and other information disseminated by the federal government about the virus appear to be translated by an automated service – and lack sense and context.
The state agencies in Pennsylvania have been alerted to the absence of Spanish information, but change has been slow, he noted.
“In Philadelphia, 23% speaks a language other than English,” he said. “So we missed a lot of critical information that could have helped to avoid spreading the illness and access support.”
Dr. Fortuna said that California has done better with providing COVID-19–related information in Spanish, compared with some other states, but misinformation about the virus and lingering myths have still been a problem among the Latino community. The University of California, San Francisco, recently launched a Latino Task Force resource website for the Latino community that includes information in English, Spanish, and Yucatec Maya about COVID-19, health and wellness tips, and resources for various assistance needs.
The concerning lack of COVID-19 information translated to Spanish led Dr. Montano to start a Facebook page in Spanish about mental health tips and guidance for managing COVID-19–related issues. She and her team of clinicians share information, videos, relaxation exercises, and community resources on the page, among other posts. “There is also general info and recommendations about COVID-19 that I think can be useful for the community,” she said. “The idea is that patients, the general community, and providers can have share information, hope messages, and ask questions in Spanish.”
Feeling ‘helpless’
A central part of caring for Latino patients during the COVID-19 crisis has been referring them to outside agencies and social services, psychiatrists say. But finding the right resources amid a pandemic and ensuring that patients connect with the correct aid has been an uphill battle.
“We sometimes feel like our hands are tied,” Dr. Colón-Rivera said. “Sometimes, we need to call a place to bring food. Some of the state agencies and nonprofits don’t have delivery systems, so the patient has to go pick up for food or medication. Some of our patients don’t want to go outside. Some do not have cars.”
As a clinician, it can be easy to feel helpless when trying to navigate new challenges posed by the pandemic in addition to other longstanding barriers, Dr. Posada said.
“Already, mental health disorders are so influenced by social situations like poverty, job insecurity, or family issues, and now it just seems those obstacles are even more insurmountable,” she said. “At the end of the day, I can feel like: ‘Did I make a difference?’ That’s a big struggle.”
Dr. Montano’s team, which includes psychiatrists, psychologists, and social workers, have come to rely on virtual debriefings to vent, express frustrations, and support one another, she said. She also recently joined a virtual mind-body skills group as a participant.
“I recognize the importance of getting additional support and ways to alleviate burnout,” she said. “We need to take care of ourselves or we won’t be able to help others.”
Focusing on resilience during the current crisis can be beneficial for both patients and providers in coping and drawing strength, Dr. Posada said.
“When it comes to fostering resilience during times of hardship, I think it’s most helpful to reflect on what skills or attributes have helped during past crises and apply those now – whether it’s turning to comfort from close relationships, looking to religion and spirituality, practicing self-care like rest or exercise, or really tapping into one’s purpose and reason for practicing psychiatry and being a physician,” she said. “The same advice goes for clinicians: We’ve all been through hard times in the past, it’s part of the human condition and we’ve also witnessed a lot of suffering in our patients, so now is the time to practice those skills that have gotten us through hard times in the past.”
Learning lessons from COVID-19
Despite the challenges with moving to telehealth, Dr. Fortuna said the tool has proved beneficial overall for mental health care. For Dr. Fortuna’s team for example, telehealth by phone has decreased the no-show rate, compared with clinic visits, and improved care access.
“We need to figure out how to maintain that,” she said. “If we can build ways for equity and access to Internet, especially equipment, I think that’s going to help.”
In addition, more data are needed about the ways in which COVID-19 is affecting Latino patients, Dr. Colón-Rivera said. Mortality statistics have been published, but information is needed about the rates of infection and manifestation of illness.
Most importantly, the COVID-19 crisis has emphasized the critical need to address and improve the underlying inequity issues among Latino patients, psychiatrists say.
“We really need to think about how there can be partnerships, in terms of community-based Latino business and leaders, multisector resources, trying to think about how we can improve conditions both work and safety for Latinos,” Dr. Fortuna said. “How can schools get support in integrating mental health and support for families, especially now after COVID-19? And really looking at some of these underlying inequities that are the underpinnings of why people were at risk for the disproportionate effects of the COVID-19 pandemic.”
Pamela Montano, MD, recalls the recent case of a patient with bipolar II disorder who was improving after treatment with medication and therapy when her life was upended by the COVID-19 pandemic.
The patient, who is Puerto Rican, lost two cousins to the virus, two of her brothers fell ill, and her sister became sick with coronavirus, said Dr. Montano, director of the Latino Bicultural Clinic at Gouverneur Health in New York. The patient was then left to care for her sister’s toddlers along with the patient’s own children, one of whom has special needs.
“After this happened, it increased her anxiety,” Dr. Montano said in an interview. “She’s not sleeping, and she started having panic attacks. My main concern was how to help her cope.”
Across the country, clinicians who treat mental illness and behavioral disorders in Latino patients are facing similar experiences and challenges associated with COVID-19 and the ensuing pandemic response. Current data suggest a disproportionate burden of illness and death from the novel coronavirus among racial and ethnic groups, particularly black and Hispanic patients. The disparities are likely attributable to economic and social conditions more common among such populations, compared with non-Hispanic whites, in addition to isolation from resources, according to the Centers for Disease Control and Prevention.
A recent New York City Department of Health study based on data that were available in late April found that deaths from COVID-19 were substantially higher for black and Hispanic/Latino patients than for white and Asian patients. The death rate per 100,000 population was 209.4 for blacks, 195.3 for Hispanics/Latinos, 107.7 for whites, and 90.8 for Asians.
“The COVID pandemic has highlighted the structural inequities that affect the Latino population [both] immigrant and nonimmigrant,” said Dr. Montano, a board member of the American Society of Hispanic Psychiatry and the officer of infrastructure and advocacy for the Hispanic Caucus of the American Psychiatric Association. “This includes income inequality, poor nutrition, history of trauma and discrimination, employment issues, quality education, access to technology, and overall access to appropriate cultural linguistic health care.”
Navigating challenges
For mental health professionals treating Latino patients, COVID-19 and the pandemic response have generated a range of treatment obstacles.
The transition to telehealth for example, has not been easy for some patients, said Jacqueline Posada, MD, consultation-liaison psychiatry fellow at the Inova Fairfax Hospital–George Washington University program in Falls Church, Va., and an APA Substance Abuse and Mental Health Services Administration minority fellow. Some patients lack Internet services, others forget virtual visits, and some do not have working phones, she said.
“I’ve had to be very flexible,” she said in an interview. “Ideally, I’d love to see everybody via video chat, but a lot of people either don’t have a stable Internet connection or Internet, so I meet the patient where they are. Whatever they have available, that’s what I’m going to use. If they don’t answer on the first call, I will call again at least three to five times in the first 15 minutes to make sure I’m giving them an opportunity to pick up the phone.”
In addition, Dr. Posada has encountered disconnected phones when calling patients for appointments. In such cases, Dr. Posada contacts the patient’s primary care physician to relay medication recommendations in case the patient resurfaces at the clinic.
In other instances, patients are not familiar with video technology, or they must travel to a friend or neighbor’s house to access the technology, said Hector Colón-Rivera, MD, an addiction psychiatrist and medical director of the Asociación Puertorriqueños en Marcha Behavioral Health Program, a nonprofit organization based in the Philadelphia area. Telehealth visits frequently include appearances by children, family members, barking dogs, and other distractions, said Dr. Colón-Rivera, president of the APA Hispanic Caucus.
“We’re seeing things that we didn’t used to see when they came to our office – for good or for bad,” said Dr. Colón-Rivera, an attending telemedicine physician at the University of Pittsburgh Medical Center. “It could be a good chance to meet our patient in a different way. Of course, it creates different stressors. If you have five kids on top of you and you’re the only one at home, it’s hard to do therapy.”
Psychiatrists are also seeing prior health conditions in patients exacerbated by COVID-19 fears and new health problems arising from the current pandemic environment. Dr. Posada recalls a patient whom she successfully treated for premenstrual dysphoric disorder who recently descended into severe clinical depression. The patient, from Colombia, was attending school in the United States on a student visa and supporting herself through child care jobs.
“So much of her depression was based on her social circumstance,” Dr. Posada said. “She had lost her job, her sister had lost her job so they were scraping by on her sister’s husband’s income, and the thing that brought her joy, which was going to school and studying so she could make a different life for herself than what her parents had in Colombia, also seemed like it was out of reach.”
Dr. Colón-Rivera recently received a call from a hospital where one of his patients was admitted after becoming delusional and psychotic. The patient was correctly taking medication prescribed by Dr. Colón-Rivera, but her diabetes had become uncontrolled because she was unable to reach her primary care doctor and couldn’t access the pharmacy. Her blood sugar level became elevated, leading to the delusions.
“A patient that was perfectly stable now is unstable,” he said. “Her diet has not been good enough through the pandemic, exacerbating her diabetes. She was admitted to the hospital for delirium.
Compounding of traumas
For many Latino patients, the adverse impacts of the pandemic comes on top of multiple prior traumas, such as violence exposures, discrimination, and economic issues, said Lisa Fortuna, MD, MPH, MDiv, chief of psychiatry and vice chair at Zuckerberg San Francisco General Hospital. A 2017 analysis found that nearly four in five Latino youth face at least one traumatic childhood experience, like poverty or abuse, and that about 29% of Latino youth experience four or more of these traumas.
Immigrants in particular, may have faced trauma in their home country and/or immigration trauma, Dr. Fortuna added. A 2013 study on immigrant Latino adolescents for example, found that 29% of foreign-born adolescents and 34% of foreign-born parents experienced trauma during the migration process (Int Migr Rev. 2013 Dec;47(4):10).
“All of these things are cumulative,” Dr. Fortuna said. “Then when you’re hit with a pandemic, all of the disparities that you already have and all the stress that you already have are compounded. This is for the kids, too, who have been exposed to a lot of stressors and now maybe have family members that have been ill or have died. All of these things definitely put people at risk for increased depression [and] the worsening of any preexisting posttraumatic stress disorder. We’ve seen this in previous disasters, and I expect that’s what we’re going to see more of with the COVID-19 pandemic.”
At the same time, a central cultural value of many Latinos is family unity, Dr. Montano said, a foundation that is now being strained by social distancing and severed connections.
“This has separated many families,” she said. “There has been a lot of loneliness and grief.”
Mistrust and fear toward the government, public agencies, and even the health system itself act as further hurdles for some Latinos in the face of COVID-19. In areas with large immigrant populations such as San Francisco, Dr. Fortuna noted, it’s not uncommon for undocumented patients to avoid accessing medical care and social services, or visiting emergency departments for needed care for fear of drawing attention to themselves or possible detainment.
“The fact that so many people showed up at our hospital so ill and ended up in the ICU – that could be a combination of factors. Because the population has high rates of diabetes and hypertension, that might have put people at increased risk for severe illness,” she said. “But some people may have been holding out for care because they wanted to avoid being in places out of fear of immigration scrutiny.”
Overcoming language barriers
Compounding the challenging pandemic landscape for Latino patients is the fact that many state resources about COVID-19 have not been translated to Spanish, Dr. Colón-Rivera said. He was troubled recently when he went to several state websites and found limited to no information in Spanish about the coronavirus. Some data about COVID-19 from the federal government were not translated to Spanish until officials received pushback, he added. Even now, press releases and other information disseminated by the federal government about the virus appear to be translated by an automated service – and lack sense and context.
The state agencies in Pennsylvania have been alerted to the absence of Spanish information, but change has been slow, he noted.
“In Philadelphia, 23% speaks a language other than English,” he said. “So we missed a lot of critical information that could have helped to avoid spreading the illness and access support.”
Dr. Fortuna said that California has done better with providing COVID-19–related information in Spanish, compared with some other states, but misinformation about the virus and lingering myths have still been a problem among the Latino community. The University of California, San Francisco, recently launched a Latino Task Force resource website for the Latino community that includes information in English, Spanish, and Yucatec Maya about COVID-19, health and wellness tips, and resources for various assistance needs.
The concerning lack of COVID-19 information translated to Spanish led Dr. Montano to start a Facebook page in Spanish about mental health tips and guidance for managing COVID-19–related issues. She and her team of clinicians share information, videos, relaxation exercises, and community resources on the page, among other posts. “There is also general info and recommendations about COVID-19 that I think can be useful for the community,” she said. “The idea is that patients, the general community, and providers can have share information, hope messages, and ask questions in Spanish.”
Feeling ‘helpless’
A central part of caring for Latino patients during the COVID-19 crisis has been referring them to outside agencies and social services, psychiatrists say. But finding the right resources amid a pandemic and ensuring that patients connect with the correct aid has been an uphill battle.
“We sometimes feel like our hands are tied,” Dr. Colón-Rivera said. “Sometimes, we need to call a place to bring food. Some of the state agencies and nonprofits don’t have delivery systems, so the patient has to go pick up for food or medication. Some of our patients don’t want to go outside. Some do not have cars.”
As a clinician, it can be easy to feel helpless when trying to navigate new challenges posed by the pandemic in addition to other longstanding barriers, Dr. Posada said.
“Already, mental health disorders are so influenced by social situations like poverty, job insecurity, or family issues, and now it just seems those obstacles are even more insurmountable,” she said. “At the end of the day, I can feel like: ‘Did I make a difference?’ That’s a big struggle.”
Dr. Montano’s team, which includes psychiatrists, psychologists, and social workers, have come to rely on virtual debriefings to vent, express frustrations, and support one another, she said. She also recently joined a virtual mind-body skills group as a participant.
“I recognize the importance of getting additional support and ways to alleviate burnout,” she said. “We need to take care of ourselves or we won’t be able to help others.”
Focusing on resilience during the current crisis can be beneficial for both patients and providers in coping and drawing strength, Dr. Posada said.
“When it comes to fostering resilience during times of hardship, I think it’s most helpful to reflect on what skills or attributes have helped during past crises and apply those now – whether it’s turning to comfort from close relationships, looking to religion and spirituality, practicing self-care like rest or exercise, or really tapping into one’s purpose and reason for practicing psychiatry and being a physician,” she said. “The same advice goes for clinicians: We’ve all been through hard times in the past, it’s part of the human condition and we’ve also witnessed a lot of suffering in our patients, so now is the time to practice those skills that have gotten us through hard times in the past.”
Learning lessons from COVID-19
Despite the challenges with moving to telehealth, Dr. Fortuna said the tool has proved beneficial overall for mental health care. For Dr. Fortuna’s team for example, telehealth by phone has decreased the no-show rate, compared with clinic visits, and improved care access.
“We need to figure out how to maintain that,” she said. “If we can build ways for equity and access to Internet, especially equipment, I think that’s going to help.”
In addition, more data are needed about the ways in which COVID-19 is affecting Latino patients, Dr. Colón-Rivera said. Mortality statistics have been published, but information is needed about the rates of infection and manifestation of illness.
Most importantly, the COVID-19 crisis has emphasized the critical need to address and improve the underlying inequity issues among Latino patients, psychiatrists say.
“We really need to think about how there can be partnerships, in terms of community-based Latino business and leaders, multisector resources, trying to think about how we can improve conditions both work and safety for Latinos,” Dr. Fortuna said. “How can schools get support in integrating mental health and support for families, especially now after COVID-19? And really looking at some of these underlying inequities that are the underpinnings of why people were at risk for the disproportionate effects of the COVID-19 pandemic.”
New ‘atlas’ maps links between mental disorders, physical illnesses
Mental illnesses are associated with a significantly increased risk of subsequent physical diseases, new research shows.
An international team of researchers has created an “atlas” that maps the relationship between specific mental disorders and the risk of subsequent physical illnesses.
The researchers found that, following the diagnosis of a mental disorder, psychiatric patients are significantly more likely than the general population to develop potentially life-threatening conditions, including heart disease and stroke.
These findings, the investigators noted, highlight the need for better medical care in this vulnerable population. They have created a website with detailed information about the risks of specific physical ailments and the link to particular mental disorders.
“We found that women with anxiety disorders have a 50% increased risk of developing a heart condition or stroke – over 15 years, one in three women with anxiety disorders will develop these medical disorders,” lead investigator John McGrath, MD, PhD, University of Queensland’s Brain Institute, Brisbane, Australia, and Aarhus (Denmark) University, said in a statement.
“We also looked at men with substance use disorders such as alcohol-related disorders and found they have a 400% increased risk of gut or liver disorders, while over 15 years, one in five of them will develop gut or liver conditions,” he added.
The study was published in the New England Journal of Medicine.
New ‘atlas’
It’s well known that patients with mental disorders have decreased quality of life, increased health care utilization, and a shorter life expectancy than individuals in the general population – about 10 years for men and 7 years for women.
However, the investigators noted, previous research examining the relationship between mental disorders and medical conditions only focused on “particular pairs or a small set of mental disorders and medical conditions.”
“We needed a comprehensive study to map the links between different types of mental disorders versus different types of general medical conditions. Our study has provided this atlas,” Dr. McGrath said in an interview.
The clinical utility of such a map could provide comprehensive data on relative and absolute risks of various medical conditions after a diagnosis of a mental disorder. This information, the researchers noted, would “help clinicians and health care planners identify the primary prevention needs of their patients.”
The study included 5.9 million people born in Denmark between 1900 and 2015 and followed them from 2000 to 2016, a total of 83.9 million person-years. The researchers followed patients for up to 17 years (2000-2016) for medical diagnoses and up to 48 years (1969-2016) for diagnoses of mental disorders.
The study’s large sample size allowed investigators to assess 10 broad types of mental disorders and 9 broad categories of medical conditions that encompassed 31 specific conditions.
Categories of medical conditions included circulatory, endocrine, pulmonary, gastrointestinal, urogenital, musculoskeletal, hematologic, neurologic, and cancer. Mental disorder categories included organic disorders such as Alzheimer’s, substance abuse disorders, schizophrenia, mood disorders, neurotic disorders, eating disorders, personality disorders, developmental disorders, behavioral/emotional disorders, and intellectual disabilities.
The researchers estimated associations between 90 pairs of mental disorders and broad-category medical conditions, as well as 310 pairs of mental disorders and specific medical conditions.
‘Curious’ finding
Individuals with mental disorders showed a higher risk of medical conditions in 76 out of 90 specific mental disorder–medical condition pairs.
After adjusting for sex, age, calendar time, and previous coexisting mental disorders, the median hazard ratio for a subsequent medical condition was 1.37 in patients with a mental disorder.
The lowest HR was 0.82 for organic mental disorders and the broad category of cancer (95% confidence interval, 0.80-0.84), and the highest was 3.62 for eating disorders and urogenital conditions (95% CI, 3.11-4.22). On the other hand, schizophrenia was associated with a reduced risk of developing musculoskeletal conditions (HR, 0.87; 95% CI, 0.84-0.91).
Dr. McGrath described this finding as “curious” and speculated it “may be related to underlying genetic risk factors.”
compared with the matched reference group without a mood disorder (40.9% vs. 32.6%, respectively).
The risk of developing subsequent medical conditions after a mental disorder diagnosis did not remain steady over time. For instance, although mood disorders were associated with an increased risk of developing circulatory problems (HR, 1.32; 95% CI, 1.31-1.34), the highest risk occurred during the first 6 months following diagnosis and gradually decreased over the next 15 years (HR, 2.39; 95% CI, 2.29-2.48 and HR, 1.18; 95% CI, 1.17-1.20, respectively).
“Many people with mental disorders have unhealthy lifestyle, including low exercise, poor diet, smoking, and alcohol, which may account for the increased risk of physical illness, and also they may not seek and/or may not get quick treatment for their health conditions,” said Dr. McGrath.
Additionally, “perhaps some genetic and early life exposures, such as trauma, may increase the risk of both medical conditions and mental disorders,” he added. “We need better treatments for mental disorders, so that they do not slip into unemployment or poverty.”
A strong case
In a comment, Roger McIntyre, MD, professor of psychiatry and pharmacology at the University of Toronto and head of the mood disorders psychopharmacology unit, University Health Network, said that the research “really makes a strong case for the fact that persons who have mental disorders are at higher risk of chronic diseases, and it’s the chronic diseases that decrease their lifespan.”
Dr. McIntyre, who is also director of the Depression and Bipolar Support Alliance, said that the “takeaway message is that mental disorders are not just brain disorders but are multisystem disorders.”
For this reason, “the most appropriate way to provide care would be to provide a holistic approach to treat and prevent the chronic diseases that lead to increase in mortality,” recommended Dr. McIntyre, who was not involved with the current study.
The study was supported by grants from the Danish National Research Foundation, the National Health and Medical Research Council, the Novo Nordisk Foundation , the European Union’s Horizon 2020 Research and Innovation Program, the Aarhus University Research Foundation, the Lundbeck Foundation, the National Institutes of Health, the European Commission, Helsefonden, the Danish Council for Independent Research, the Independent Research Fund Denmark, the National Health and Medical Research Council of Australia, and the National Institute on Drug Abuse.
Dr. McGrath has disclosed no relevant financial relationships. The other authors’ disclosures are listed on the original paper. Dr. McIntyre reports receiving grants from Stanley Medical Research Institute; the Canadian Institutes of Health Research/Global Alliance for Chronic Diseases/Chinese National Natural Research Foundation; and receiving speaking/consultation fees from Lundbeck, Janssen, Shire, Purdue, Pfizer, Otsuka, Allergan, Takeda, Neurocrine, Sunovion, and Minerva.
A version of this article originally appeared on Medscape.com.
Mental illnesses are associated with a significantly increased risk of subsequent physical diseases, new research shows.
An international team of researchers has created an “atlas” that maps the relationship between specific mental disorders and the risk of subsequent physical illnesses.
The researchers found that, following the diagnosis of a mental disorder, psychiatric patients are significantly more likely than the general population to develop potentially life-threatening conditions, including heart disease and stroke.
These findings, the investigators noted, highlight the need for better medical care in this vulnerable population. They have created a website with detailed information about the risks of specific physical ailments and the link to particular mental disorders.
“We found that women with anxiety disorders have a 50% increased risk of developing a heart condition or stroke – over 15 years, one in three women with anxiety disorders will develop these medical disorders,” lead investigator John McGrath, MD, PhD, University of Queensland’s Brain Institute, Brisbane, Australia, and Aarhus (Denmark) University, said in a statement.
“We also looked at men with substance use disorders such as alcohol-related disorders and found they have a 400% increased risk of gut or liver disorders, while over 15 years, one in five of them will develop gut or liver conditions,” he added.
The study was published in the New England Journal of Medicine.
New ‘atlas’
It’s well known that patients with mental disorders have decreased quality of life, increased health care utilization, and a shorter life expectancy than individuals in the general population – about 10 years for men and 7 years for women.
However, the investigators noted, previous research examining the relationship between mental disorders and medical conditions only focused on “particular pairs or a small set of mental disorders and medical conditions.”
“We needed a comprehensive study to map the links between different types of mental disorders versus different types of general medical conditions. Our study has provided this atlas,” Dr. McGrath said in an interview.
The clinical utility of such a map could provide comprehensive data on relative and absolute risks of various medical conditions after a diagnosis of a mental disorder. This information, the researchers noted, would “help clinicians and health care planners identify the primary prevention needs of their patients.”
The study included 5.9 million people born in Denmark between 1900 and 2015 and followed them from 2000 to 2016, a total of 83.9 million person-years. The researchers followed patients for up to 17 years (2000-2016) for medical diagnoses and up to 48 years (1969-2016) for diagnoses of mental disorders.
The study’s large sample size allowed investigators to assess 10 broad types of mental disorders and 9 broad categories of medical conditions that encompassed 31 specific conditions.
Categories of medical conditions included circulatory, endocrine, pulmonary, gastrointestinal, urogenital, musculoskeletal, hematologic, neurologic, and cancer. Mental disorder categories included organic disorders such as Alzheimer’s, substance abuse disorders, schizophrenia, mood disorders, neurotic disorders, eating disorders, personality disorders, developmental disorders, behavioral/emotional disorders, and intellectual disabilities.
The researchers estimated associations between 90 pairs of mental disorders and broad-category medical conditions, as well as 310 pairs of mental disorders and specific medical conditions.
‘Curious’ finding
Individuals with mental disorders showed a higher risk of medical conditions in 76 out of 90 specific mental disorder–medical condition pairs.
After adjusting for sex, age, calendar time, and previous coexisting mental disorders, the median hazard ratio for a subsequent medical condition was 1.37 in patients with a mental disorder.
The lowest HR was 0.82 for organic mental disorders and the broad category of cancer (95% confidence interval, 0.80-0.84), and the highest was 3.62 for eating disorders and urogenital conditions (95% CI, 3.11-4.22). On the other hand, schizophrenia was associated with a reduced risk of developing musculoskeletal conditions (HR, 0.87; 95% CI, 0.84-0.91).
Dr. McGrath described this finding as “curious” and speculated it “may be related to underlying genetic risk factors.”
compared with the matched reference group without a mood disorder (40.9% vs. 32.6%, respectively).
The risk of developing subsequent medical conditions after a mental disorder diagnosis did not remain steady over time. For instance, although mood disorders were associated with an increased risk of developing circulatory problems (HR, 1.32; 95% CI, 1.31-1.34), the highest risk occurred during the first 6 months following diagnosis and gradually decreased over the next 15 years (HR, 2.39; 95% CI, 2.29-2.48 and HR, 1.18; 95% CI, 1.17-1.20, respectively).
“Many people with mental disorders have unhealthy lifestyle, including low exercise, poor diet, smoking, and alcohol, which may account for the increased risk of physical illness, and also they may not seek and/or may not get quick treatment for their health conditions,” said Dr. McGrath.
Additionally, “perhaps some genetic and early life exposures, such as trauma, may increase the risk of both medical conditions and mental disorders,” he added. “We need better treatments for mental disorders, so that they do not slip into unemployment or poverty.”
A strong case
In a comment, Roger McIntyre, MD, professor of psychiatry and pharmacology at the University of Toronto and head of the mood disorders psychopharmacology unit, University Health Network, said that the research “really makes a strong case for the fact that persons who have mental disorders are at higher risk of chronic diseases, and it’s the chronic diseases that decrease their lifespan.”
Dr. McIntyre, who is also director of the Depression and Bipolar Support Alliance, said that the “takeaway message is that mental disorders are not just brain disorders but are multisystem disorders.”
For this reason, “the most appropriate way to provide care would be to provide a holistic approach to treat and prevent the chronic diseases that lead to increase in mortality,” recommended Dr. McIntyre, who was not involved with the current study.
The study was supported by grants from the Danish National Research Foundation, the National Health and Medical Research Council, the Novo Nordisk Foundation , the European Union’s Horizon 2020 Research and Innovation Program, the Aarhus University Research Foundation, the Lundbeck Foundation, the National Institutes of Health, the European Commission, Helsefonden, the Danish Council for Independent Research, the Independent Research Fund Denmark, the National Health and Medical Research Council of Australia, and the National Institute on Drug Abuse.
Dr. McGrath has disclosed no relevant financial relationships. The other authors’ disclosures are listed on the original paper. Dr. McIntyre reports receiving grants from Stanley Medical Research Institute; the Canadian Institutes of Health Research/Global Alliance for Chronic Diseases/Chinese National Natural Research Foundation; and receiving speaking/consultation fees from Lundbeck, Janssen, Shire, Purdue, Pfizer, Otsuka, Allergan, Takeda, Neurocrine, Sunovion, and Minerva.
A version of this article originally appeared on Medscape.com.
Mental illnesses are associated with a significantly increased risk of subsequent physical diseases, new research shows.
An international team of researchers has created an “atlas” that maps the relationship between specific mental disorders and the risk of subsequent physical illnesses.
The researchers found that, following the diagnosis of a mental disorder, psychiatric patients are significantly more likely than the general population to develop potentially life-threatening conditions, including heart disease and stroke.
These findings, the investigators noted, highlight the need for better medical care in this vulnerable population. They have created a website with detailed information about the risks of specific physical ailments and the link to particular mental disorders.
“We found that women with anxiety disorders have a 50% increased risk of developing a heart condition or stroke – over 15 years, one in three women with anxiety disorders will develop these medical disorders,” lead investigator John McGrath, MD, PhD, University of Queensland’s Brain Institute, Brisbane, Australia, and Aarhus (Denmark) University, said in a statement.
“We also looked at men with substance use disorders such as alcohol-related disorders and found they have a 400% increased risk of gut or liver disorders, while over 15 years, one in five of them will develop gut or liver conditions,” he added.
The study was published in the New England Journal of Medicine.
New ‘atlas’
It’s well known that patients with mental disorders have decreased quality of life, increased health care utilization, and a shorter life expectancy than individuals in the general population – about 10 years for men and 7 years for women.
However, the investigators noted, previous research examining the relationship between mental disorders and medical conditions only focused on “particular pairs or a small set of mental disorders and medical conditions.”
“We needed a comprehensive study to map the links between different types of mental disorders versus different types of general medical conditions. Our study has provided this atlas,” Dr. McGrath said in an interview.
The clinical utility of such a map could provide comprehensive data on relative and absolute risks of various medical conditions after a diagnosis of a mental disorder. This information, the researchers noted, would “help clinicians and health care planners identify the primary prevention needs of their patients.”
The study included 5.9 million people born in Denmark between 1900 and 2015 and followed them from 2000 to 2016, a total of 83.9 million person-years. The researchers followed patients for up to 17 years (2000-2016) for medical diagnoses and up to 48 years (1969-2016) for diagnoses of mental disorders.
The study’s large sample size allowed investigators to assess 10 broad types of mental disorders and 9 broad categories of medical conditions that encompassed 31 specific conditions.
Categories of medical conditions included circulatory, endocrine, pulmonary, gastrointestinal, urogenital, musculoskeletal, hematologic, neurologic, and cancer. Mental disorder categories included organic disorders such as Alzheimer’s, substance abuse disorders, schizophrenia, mood disorders, neurotic disorders, eating disorders, personality disorders, developmental disorders, behavioral/emotional disorders, and intellectual disabilities.
The researchers estimated associations between 90 pairs of mental disorders and broad-category medical conditions, as well as 310 pairs of mental disorders and specific medical conditions.
‘Curious’ finding
Individuals with mental disorders showed a higher risk of medical conditions in 76 out of 90 specific mental disorder–medical condition pairs.
After adjusting for sex, age, calendar time, and previous coexisting mental disorders, the median hazard ratio for a subsequent medical condition was 1.37 in patients with a mental disorder.
The lowest HR was 0.82 for organic mental disorders and the broad category of cancer (95% confidence interval, 0.80-0.84), and the highest was 3.62 for eating disorders and urogenital conditions (95% CI, 3.11-4.22). On the other hand, schizophrenia was associated with a reduced risk of developing musculoskeletal conditions (HR, 0.87; 95% CI, 0.84-0.91).
Dr. McGrath described this finding as “curious” and speculated it “may be related to underlying genetic risk factors.”
compared with the matched reference group without a mood disorder (40.9% vs. 32.6%, respectively).
The risk of developing subsequent medical conditions after a mental disorder diagnosis did not remain steady over time. For instance, although mood disorders were associated with an increased risk of developing circulatory problems (HR, 1.32; 95% CI, 1.31-1.34), the highest risk occurred during the first 6 months following diagnosis and gradually decreased over the next 15 years (HR, 2.39; 95% CI, 2.29-2.48 and HR, 1.18; 95% CI, 1.17-1.20, respectively).
“Many people with mental disorders have unhealthy lifestyle, including low exercise, poor diet, smoking, and alcohol, which may account for the increased risk of physical illness, and also they may not seek and/or may not get quick treatment for their health conditions,” said Dr. McGrath.
Additionally, “perhaps some genetic and early life exposures, such as trauma, may increase the risk of both medical conditions and mental disorders,” he added. “We need better treatments for mental disorders, so that they do not slip into unemployment or poverty.”
A strong case
In a comment, Roger McIntyre, MD, professor of psychiatry and pharmacology at the University of Toronto and head of the mood disorders psychopharmacology unit, University Health Network, said that the research “really makes a strong case for the fact that persons who have mental disorders are at higher risk of chronic diseases, and it’s the chronic diseases that decrease their lifespan.”
Dr. McIntyre, who is also director of the Depression and Bipolar Support Alliance, said that the “takeaway message is that mental disorders are not just brain disorders but are multisystem disorders.”
For this reason, “the most appropriate way to provide care would be to provide a holistic approach to treat and prevent the chronic diseases that lead to increase in mortality,” recommended Dr. McIntyre, who was not involved with the current study.
The study was supported by grants from the Danish National Research Foundation, the National Health and Medical Research Council, the Novo Nordisk Foundation , the European Union’s Horizon 2020 Research and Innovation Program, the Aarhus University Research Foundation, the Lundbeck Foundation, the National Institutes of Health, the European Commission, Helsefonden, the Danish Council for Independent Research, the Independent Research Fund Denmark, the National Health and Medical Research Council of Australia, and the National Institute on Drug Abuse.
Dr. McGrath has disclosed no relevant financial relationships. The other authors’ disclosures are listed on the original paper. Dr. McIntyre reports receiving grants from Stanley Medical Research Institute; the Canadian Institutes of Health Research/Global Alliance for Chronic Diseases/Chinese National Natural Research Foundation; and receiving speaking/consultation fees from Lundbeck, Janssen, Shire, Purdue, Pfizer, Otsuka, Allergan, Takeda, Neurocrine, Sunovion, and Minerva.
A version of this article originally appeared on Medscape.com.
For Indigenous communities, climate crisis could prove calamitous
Drought, fires, and pandemics lead to anxiety, depression, trauma
Kind wishes and donations worldwide came to help Australian communities and wildlife affected by the extreme drought and uncontrollable bushfires. Indeed, Australians have become a warning beacon for the planet to recognize how factors associated with global warming can morph rapidly into runaway national emergencies.
Little attention, however, has addressed the extreme vulnerability of Australia’s First Nations people, the Aboriginal & Torres Strait Islander communities, to the climate crisis. U.N. reports conclude that “Indigenous people with close emotional and ancestral ties to the land are also likely to be disproportionately affected by environmental change and extreme weather events.”1
In fact, Indigenous peoples, whether living traditionally or assimilated, are among the first to be adversely affected by climate change. This is because, in part, of extreme poverty, inadequate housing, unemployment and other social determinants, transgenerational cultural losses of life and culture, dislocations, traumatic experiences of child removal, overrepresentation in the prison system, and chronic diseases already leading to dramatic disparities in life expectancy and other health outcomes.
Research confirms that rural and remote Aboriginal communities will be Australia’s first mass climate refugees. “Without action to stop climate change, people will be forced to leave their country and leave behind much of what makes them Aboriginal.”2 This is because of hotter temperatures, poorly built and unstable homes more vulnerable to heat, and longer and drier droughts. Their communities, in fire-prone townships, are running out of water. Abject poverty severely limits their options, aggravated by government inaction because of ideological climate change denialism. And now we have the overlay of COVID-19 threatening these communities.3
Human pandemics are potentially more likely to occur with climate change. Pandemics also are more apt to be associated with population growth, human settlement encroaching on forests, increasing wild animal or intermediary vector contact, and growth in global travel.
Subsequently, Spatial separation is difficult in overcrowded, multigenerational households. It is hard to keep your hands washed with soap where reliable water supply is sometimes only communal. Their health workers’ access to protective and lifesaving ICU equipment and expertise may be extremely limited or erratic.
Much of the population is classified as highly vulnerable to COVID-19 because of chronic health disorders (for example, cardiovascular, respiratory, and renal issues; diabetes, and suicidality) and preexisting much shorter life expectancies. Their health workers’ access to protective and lifesaving ICU equipment and expertise is extremely limited. There are fears that, if COVID-19 gains a foothold, they may lose a whole generation of revered elders, who often are also the last fluent tribal language speakers and carriers of life-enhancing cultural stories, traditions, and rites. More urban-living Indigenous families may yet have a rough time avoiding these ravages.
In Australia, COVID-19 has been largely held at bay so far by state and territory governments that have closed borders, restricted nonessential travel, and discouraged or excluded outsiders from visiting remote Indigenous communities wherever possible. There have been complaints that such restrictions occasionally had been applied in these communities in a heavy-handed way by police and other authorities, and may be resisted if enforced unilaterally. They will work only if applied with cultural sensitivity, full Indigenous community consultation, and collaboration. So far, COVID-19 infection rates have been kept very low, with no Indigenous deaths. In Brazil, by contrast, infections and deaths are more than double the national average, itinerant missionaries have only just been excluded from Amazonian tribal lands so far by independent judicial intervention, while loggers and miners come and go freely, as sources of contagion.4 Some Indigenous peoples in the United States have experienced among the highest COVID-19 infection and death rates in the country (for example, the Navajo Nation in New Mexico, Arizona, and Utah), amounting to catastrophic loss and grief.
"Black Lives Matter" marches protesting the filmed police killing of George Floyd in the USA have spread worldwide, in the wake of ultra-high rates of police brutality and killings with impunity of non-white individuals.
Many Australians, including considerable numbers of Indigenous people, marched here in sympathy, despite their infective risk and vulnerabilities. They were also protesting the excessive rates of Aboriginal imprisonment, deaths in custody, and police killings without consequences. Both internationally and here, there was an apparent sense of release of pent-up anger and frustrations at both these injustices and the extra susceptibility of poor and non-white people to severe illness, death and dire economic consequences because of the pandemic. It is a deceptive myth that "we are all in this together." So it is encouraging that there is also forming a widespread sense of collective purpose and determination to get governments to address these iniquities and inequities at last.*
I have worked as a community psychiatrist in Barkinje Aboriginal tribal lands of the Far West region of New South Wales (NSW) regularly for 35 years, much of this time while also leading Royal North Shore University General Hospital & Community Mental Health Services in Sydney. Barkinje translates as “River People,” but local media mainly talk about the impact of prolonged drought on farmers and ranchers, who certainly are deeply affected by it. However, the media rarely mention the calamitous impacts on Aboriginal communities. The drought effects are exacerbated by multinational corporate irrigators that divert and allegedly steal river water with tacit encouragement from ostensibly responsible government ministers. The rivers dry up into algal ponds with millions of bloated, rotting dead fish, and entire communities’ water supplies fail.
Researchers have reported on the mental health impacts of prolonged drought and diversion of river water on rural and remote indigenous communities throughout the state of NSW.5 We have heard Barkinje and neighboring Wiradjuri people say, “if the land is sick, we are sick,” and, “if the river dries up, there’s nowhere to meet.” Fishing, a popular recreational activity and source of nutrition is now denied to these communities. Unlike farmers, they receive no governmental exceptional circumstance compensation payments during droughts. Instead, they lose their farming jobs, so there is no disposable income and loss of capacity to travel to connect to their extended kinship system and cultural roots (e.g., for funerals or football matches) in other remote townships. Such droughts exacerbate wildfires, loss of fish and birdlife, some of which are sacred spiritual totems; dying of traditional “lifeblood” rivers, decimating precious ancient red-river gumtrees that line the shores; and irreversible damage to other sacred sites (e.g., melting ancient rock art).
So, loss of sustainable food sources, meaningful livelihood, and cultural and leisure pursuits could create an existential threat to Aboriginal identity. However, rural Indigenous communities also told us “whatever you do to us, we will survive and persist, as we have done in the past.”6 This is comparable with the tenacity and resilience of other ancient cultures that have suffered genocidal persecution and discrimination in the past, and have stubbornly regrown and persisted and regrown into the future.
They yearn to care for their lands, rivers, and seas of their traditions and upbringing, whether as “saltwater” coastal or “freshwater” inland peoples. They value their extended families, honor their elders and their collective wisdom, while also living in “two worlds.” They often encourage their children to get educated and pursue individualistic aspirations to help their communities by training as tradespeople and professionals who may be better trusted to look after their own. As Charles Perkins, a most celebrated Aboriginal role model for living in both worlds, famously said: “We know we can’t live in the past, but the past lives in us.”
As anxiety and depression, psychological trauma, drug and alcohol misuse, family and communal violence, ecological grief,and suicidal vulnerability are precipitated or exacerbated by the stress of extreme environmental adversity, significant investment in ameliorating these harms is essential, not just for farmers, town businesspeople and their families, but for all those affected, especially these most vulnerable members of the community.7 We must provide more essential community services controlled by Aboriginal community members themselves. We must also train and support more Aboriginal mental health workers, healers, mental health educators, peer workers and Aboriginal liaison officers, to work alongside other mental health, and health and social service professionals. Aboriginal people need stable local employment opportunities in their communities. There is a huge opportunity to synergize traditional indigenous fire management with Western techniques, creating and consolidating more valued jobs and respected land management roles for Aboriginal rangers, vital for the future of both Aboriginal and wider communities. Pilot programs are emerging.
Aboriginal communities also need a more preventive, whole-of-life approach to social determinants, lifestyle factors, trauma, and political decisions associated with compromised neurodevelopment, and increased subsequent incidence and severity of mental illnesses in their communities.7
As Alexander Solzhenitsyn observed: “On our crowded planet there are no longer any ‘internal affairs.’ ”8 Climate change is the ultimate form of globalization: What we each do about it affects all others’ lives. We can only insist that, alongside adequate resourcing of our most evidence-based methods of fire, water, and climate control, our governments consult and listen to our Indigenous elders about applying climate management methods. These have been demonstrated to be sustainable and effective, possibly over 60,000 years – which is the longest established record of continuous Indigenous culture worldwide.
References
1. Ten impacts of the Australian bushfires. U.N. Environment Programme. 2020 Jan 20.
2. Allam L, Evershed N. “Too hot for humans? First Nations people fear becoming Australia’s first climate refugees.” The Guardian. 2019 Dec 17.
3. National Indigenous Australians Agency. “Coronavirus (COVID-19).”
4. Phillips D. “Brazil: Judge bans missionaries from Indigenous reserve over COVID-19 fears.” The Guardian. 2020 Apr 17.
5. Rigby CW et al. Aust J Rural Health. 2011 Oct;19(5):249-54.
6. Cunsolo A, Ellis NR. Nature Clim Change. 2018 Apr 3;8:275-81.
7. Gynther B et al. EClinicalMedicine. 2019 Apr 26;10:68-77.
8. Solzhenitsyn A. “Warning to the West,” speech delivered 30 Jun 1975. New York: Fararr, Straux & Girous, 1976.
Dr. Rosen, an officer of the Order of Australia and a Fellow of the Royal Australian and New Zealand College of Psychiatrists, is affiliated with the Brain & Mind Centre, University of Sydney, and the Institute of Mental Health at the University of Wollongong (Australia). He also is a community psychiatrist in a remote region of New South Wales. Dr. Rosen has no conflicts of interest.
*This article was updated 6/16/2020.
Drought, fires, and pandemics lead to anxiety, depression, trauma
Drought, fires, and pandemics lead to anxiety, depression, trauma
Kind wishes and donations worldwide came to help Australian communities and wildlife affected by the extreme drought and uncontrollable bushfires. Indeed, Australians have become a warning beacon for the planet to recognize how factors associated with global warming can morph rapidly into runaway national emergencies.
Little attention, however, has addressed the extreme vulnerability of Australia’s First Nations people, the Aboriginal & Torres Strait Islander communities, to the climate crisis. U.N. reports conclude that “Indigenous people with close emotional and ancestral ties to the land are also likely to be disproportionately affected by environmental change and extreme weather events.”1
In fact, Indigenous peoples, whether living traditionally or assimilated, are among the first to be adversely affected by climate change. This is because, in part, of extreme poverty, inadequate housing, unemployment and other social determinants, transgenerational cultural losses of life and culture, dislocations, traumatic experiences of child removal, overrepresentation in the prison system, and chronic diseases already leading to dramatic disparities in life expectancy and other health outcomes.
Research confirms that rural and remote Aboriginal communities will be Australia’s first mass climate refugees. “Without action to stop climate change, people will be forced to leave their country and leave behind much of what makes them Aboriginal.”2 This is because of hotter temperatures, poorly built and unstable homes more vulnerable to heat, and longer and drier droughts. Their communities, in fire-prone townships, are running out of water. Abject poverty severely limits their options, aggravated by government inaction because of ideological climate change denialism. And now we have the overlay of COVID-19 threatening these communities.3
Human pandemics are potentially more likely to occur with climate change. Pandemics also are more apt to be associated with population growth, human settlement encroaching on forests, increasing wild animal or intermediary vector contact, and growth in global travel.
Subsequently, Spatial separation is difficult in overcrowded, multigenerational households. It is hard to keep your hands washed with soap where reliable water supply is sometimes only communal. Their health workers’ access to protective and lifesaving ICU equipment and expertise may be extremely limited or erratic.
Much of the population is classified as highly vulnerable to COVID-19 because of chronic health disorders (for example, cardiovascular, respiratory, and renal issues; diabetes, and suicidality) and preexisting much shorter life expectancies. Their health workers’ access to protective and lifesaving ICU equipment and expertise is extremely limited. There are fears that, if COVID-19 gains a foothold, they may lose a whole generation of revered elders, who often are also the last fluent tribal language speakers and carriers of life-enhancing cultural stories, traditions, and rites. More urban-living Indigenous families may yet have a rough time avoiding these ravages.
In Australia, COVID-19 has been largely held at bay so far by state and territory governments that have closed borders, restricted nonessential travel, and discouraged or excluded outsiders from visiting remote Indigenous communities wherever possible. There have been complaints that such restrictions occasionally had been applied in these communities in a heavy-handed way by police and other authorities, and may be resisted if enforced unilaterally. They will work only if applied with cultural sensitivity, full Indigenous community consultation, and collaboration. So far, COVID-19 infection rates have been kept very low, with no Indigenous deaths. In Brazil, by contrast, infections and deaths are more than double the national average, itinerant missionaries have only just been excluded from Amazonian tribal lands so far by independent judicial intervention, while loggers and miners come and go freely, as sources of contagion.4 Some Indigenous peoples in the United States have experienced among the highest COVID-19 infection and death rates in the country (for example, the Navajo Nation in New Mexico, Arizona, and Utah), amounting to catastrophic loss and grief.
"Black Lives Matter" marches protesting the filmed police killing of George Floyd in the USA have spread worldwide, in the wake of ultra-high rates of police brutality and killings with impunity of non-white individuals.
Many Australians, including considerable numbers of Indigenous people, marched here in sympathy, despite their infective risk and vulnerabilities. They were also protesting the excessive rates of Aboriginal imprisonment, deaths in custody, and police killings without consequences. Both internationally and here, there was an apparent sense of release of pent-up anger and frustrations at both these injustices and the extra susceptibility of poor and non-white people to severe illness, death and dire economic consequences because of the pandemic. It is a deceptive myth that "we are all in this together." So it is encouraging that there is also forming a widespread sense of collective purpose and determination to get governments to address these iniquities and inequities at last.*
I have worked as a community psychiatrist in Barkinje Aboriginal tribal lands of the Far West region of New South Wales (NSW) regularly for 35 years, much of this time while also leading Royal North Shore University General Hospital & Community Mental Health Services in Sydney. Barkinje translates as “River People,” but local media mainly talk about the impact of prolonged drought on farmers and ranchers, who certainly are deeply affected by it. However, the media rarely mention the calamitous impacts on Aboriginal communities. The drought effects are exacerbated by multinational corporate irrigators that divert and allegedly steal river water with tacit encouragement from ostensibly responsible government ministers. The rivers dry up into algal ponds with millions of bloated, rotting dead fish, and entire communities’ water supplies fail.
Researchers have reported on the mental health impacts of prolonged drought and diversion of river water on rural and remote indigenous communities throughout the state of NSW.5 We have heard Barkinje and neighboring Wiradjuri people say, “if the land is sick, we are sick,” and, “if the river dries up, there’s nowhere to meet.” Fishing, a popular recreational activity and source of nutrition is now denied to these communities. Unlike farmers, they receive no governmental exceptional circumstance compensation payments during droughts. Instead, they lose their farming jobs, so there is no disposable income and loss of capacity to travel to connect to their extended kinship system and cultural roots (e.g., for funerals or football matches) in other remote townships. Such droughts exacerbate wildfires, loss of fish and birdlife, some of which are sacred spiritual totems; dying of traditional “lifeblood” rivers, decimating precious ancient red-river gumtrees that line the shores; and irreversible damage to other sacred sites (e.g., melting ancient rock art).
So, loss of sustainable food sources, meaningful livelihood, and cultural and leisure pursuits could create an existential threat to Aboriginal identity. However, rural Indigenous communities also told us “whatever you do to us, we will survive and persist, as we have done in the past.”6 This is comparable with the tenacity and resilience of other ancient cultures that have suffered genocidal persecution and discrimination in the past, and have stubbornly regrown and persisted and regrown into the future.
They yearn to care for their lands, rivers, and seas of their traditions and upbringing, whether as “saltwater” coastal or “freshwater” inland peoples. They value their extended families, honor their elders and their collective wisdom, while also living in “two worlds.” They often encourage their children to get educated and pursue individualistic aspirations to help their communities by training as tradespeople and professionals who may be better trusted to look after their own. As Charles Perkins, a most celebrated Aboriginal role model for living in both worlds, famously said: “We know we can’t live in the past, but the past lives in us.”
As anxiety and depression, psychological trauma, drug and alcohol misuse, family and communal violence, ecological grief,and suicidal vulnerability are precipitated or exacerbated by the stress of extreme environmental adversity, significant investment in ameliorating these harms is essential, not just for farmers, town businesspeople and their families, but for all those affected, especially these most vulnerable members of the community.7 We must provide more essential community services controlled by Aboriginal community members themselves. We must also train and support more Aboriginal mental health workers, healers, mental health educators, peer workers and Aboriginal liaison officers, to work alongside other mental health, and health and social service professionals. Aboriginal people need stable local employment opportunities in their communities. There is a huge opportunity to synergize traditional indigenous fire management with Western techniques, creating and consolidating more valued jobs and respected land management roles for Aboriginal rangers, vital for the future of both Aboriginal and wider communities. Pilot programs are emerging.
Aboriginal communities also need a more preventive, whole-of-life approach to social determinants, lifestyle factors, trauma, and political decisions associated with compromised neurodevelopment, and increased subsequent incidence and severity of mental illnesses in their communities.7
As Alexander Solzhenitsyn observed: “On our crowded planet there are no longer any ‘internal affairs.’ ”8 Climate change is the ultimate form of globalization: What we each do about it affects all others’ lives. We can only insist that, alongside adequate resourcing of our most evidence-based methods of fire, water, and climate control, our governments consult and listen to our Indigenous elders about applying climate management methods. These have been demonstrated to be sustainable and effective, possibly over 60,000 years – which is the longest established record of continuous Indigenous culture worldwide.
References
1. Ten impacts of the Australian bushfires. U.N. Environment Programme. 2020 Jan 20.
2. Allam L, Evershed N. “Too hot for humans? First Nations people fear becoming Australia’s first climate refugees.” The Guardian. 2019 Dec 17.
3. National Indigenous Australians Agency. “Coronavirus (COVID-19).”
4. Phillips D. “Brazil: Judge bans missionaries from Indigenous reserve over COVID-19 fears.” The Guardian. 2020 Apr 17.
5. Rigby CW et al. Aust J Rural Health. 2011 Oct;19(5):249-54.
6. Cunsolo A, Ellis NR. Nature Clim Change. 2018 Apr 3;8:275-81.
7. Gynther B et al. EClinicalMedicine. 2019 Apr 26;10:68-77.
8. Solzhenitsyn A. “Warning to the West,” speech delivered 30 Jun 1975. New York: Fararr, Straux & Girous, 1976.
Dr. Rosen, an officer of the Order of Australia and a Fellow of the Royal Australian and New Zealand College of Psychiatrists, is affiliated with the Brain & Mind Centre, University of Sydney, and the Institute of Mental Health at the University of Wollongong (Australia). He also is a community psychiatrist in a remote region of New South Wales. Dr. Rosen has no conflicts of interest.
*This article was updated 6/16/2020.
Kind wishes and donations worldwide came to help Australian communities and wildlife affected by the extreme drought and uncontrollable bushfires. Indeed, Australians have become a warning beacon for the planet to recognize how factors associated with global warming can morph rapidly into runaway national emergencies.
Little attention, however, has addressed the extreme vulnerability of Australia’s First Nations people, the Aboriginal & Torres Strait Islander communities, to the climate crisis. U.N. reports conclude that “Indigenous people with close emotional and ancestral ties to the land are also likely to be disproportionately affected by environmental change and extreme weather events.”1
In fact, Indigenous peoples, whether living traditionally or assimilated, are among the first to be adversely affected by climate change. This is because, in part, of extreme poverty, inadequate housing, unemployment and other social determinants, transgenerational cultural losses of life and culture, dislocations, traumatic experiences of child removal, overrepresentation in the prison system, and chronic diseases already leading to dramatic disparities in life expectancy and other health outcomes.
Research confirms that rural and remote Aboriginal communities will be Australia’s first mass climate refugees. “Without action to stop climate change, people will be forced to leave their country and leave behind much of what makes them Aboriginal.”2 This is because of hotter temperatures, poorly built and unstable homes more vulnerable to heat, and longer and drier droughts. Their communities, in fire-prone townships, are running out of water. Abject poverty severely limits their options, aggravated by government inaction because of ideological climate change denialism. And now we have the overlay of COVID-19 threatening these communities.3
Human pandemics are potentially more likely to occur with climate change. Pandemics also are more apt to be associated with population growth, human settlement encroaching on forests, increasing wild animal or intermediary vector contact, and growth in global travel.
Subsequently, Spatial separation is difficult in overcrowded, multigenerational households. It is hard to keep your hands washed with soap where reliable water supply is sometimes only communal. Their health workers’ access to protective and lifesaving ICU equipment and expertise may be extremely limited or erratic.
Much of the population is classified as highly vulnerable to COVID-19 because of chronic health disorders (for example, cardiovascular, respiratory, and renal issues; diabetes, and suicidality) and preexisting much shorter life expectancies. Their health workers’ access to protective and lifesaving ICU equipment and expertise is extremely limited. There are fears that, if COVID-19 gains a foothold, they may lose a whole generation of revered elders, who often are also the last fluent tribal language speakers and carriers of life-enhancing cultural stories, traditions, and rites. More urban-living Indigenous families may yet have a rough time avoiding these ravages.
In Australia, COVID-19 has been largely held at bay so far by state and territory governments that have closed borders, restricted nonessential travel, and discouraged or excluded outsiders from visiting remote Indigenous communities wherever possible. There have been complaints that such restrictions occasionally had been applied in these communities in a heavy-handed way by police and other authorities, and may be resisted if enforced unilaterally. They will work only if applied with cultural sensitivity, full Indigenous community consultation, and collaboration. So far, COVID-19 infection rates have been kept very low, with no Indigenous deaths. In Brazil, by contrast, infections and deaths are more than double the national average, itinerant missionaries have only just been excluded from Amazonian tribal lands so far by independent judicial intervention, while loggers and miners come and go freely, as sources of contagion.4 Some Indigenous peoples in the United States have experienced among the highest COVID-19 infection and death rates in the country (for example, the Navajo Nation in New Mexico, Arizona, and Utah), amounting to catastrophic loss and grief.
"Black Lives Matter" marches protesting the filmed police killing of George Floyd in the USA have spread worldwide, in the wake of ultra-high rates of police brutality and killings with impunity of non-white individuals.
Many Australians, including considerable numbers of Indigenous people, marched here in sympathy, despite their infective risk and vulnerabilities. They were also protesting the excessive rates of Aboriginal imprisonment, deaths in custody, and police killings without consequences. Both internationally and here, there was an apparent sense of release of pent-up anger and frustrations at both these injustices and the extra susceptibility of poor and non-white people to severe illness, death and dire economic consequences because of the pandemic. It is a deceptive myth that "we are all in this together." So it is encouraging that there is also forming a widespread sense of collective purpose and determination to get governments to address these iniquities and inequities at last.*
I have worked as a community psychiatrist in Barkinje Aboriginal tribal lands of the Far West region of New South Wales (NSW) regularly for 35 years, much of this time while also leading Royal North Shore University General Hospital & Community Mental Health Services in Sydney. Barkinje translates as “River People,” but local media mainly talk about the impact of prolonged drought on farmers and ranchers, who certainly are deeply affected by it. However, the media rarely mention the calamitous impacts on Aboriginal communities. The drought effects are exacerbated by multinational corporate irrigators that divert and allegedly steal river water with tacit encouragement from ostensibly responsible government ministers. The rivers dry up into algal ponds with millions of bloated, rotting dead fish, and entire communities’ water supplies fail.
Researchers have reported on the mental health impacts of prolonged drought and diversion of river water on rural and remote indigenous communities throughout the state of NSW.5 We have heard Barkinje and neighboring Wiradjuri people say, “if the land is sick, we are sick,” and, “if the river dries up, there’s nowhere to meet.” Fishing, a popular recreational activity and source of nutrition is now denied to these communities. Unlike farmers, they receive no governmental exceptional circumstance compensation payments during droughts. Instead, they lose their farming jobs, so there is no disposable income and loss of capacity to travel to connect to their extended kinship system and cultural roots (e.g., for funerals or football matches) in other remote townships. Such droughts exacerbate wildfires, loss of fish and birdlife, some of which are sacred spiritual totems; dying of traditional “lifeblood” rivers, decimating precious ancient red-river gumtrees that line the shores; and irreversible damage to other sacred sites (e.g., melting ancient rock art).
So, loss of sustainable food sources, meaningful livelihood, and cultural and leisure pursuits could create an existential threat to Aboriginal identity. However, rural Indigenous communities also told us “whatever you do to us, we will survive and persist, as we have done in the past.”6 This is comparable with the tenacity and resilience of other ancient cultures that have suffered genocidal persecution and discrimination in the past, and have stubbornly regrown and persisted and regrown into the future.
They yearn to care for their lands, rivers, and seas of their traditions and upbringing, whether as “saltwater” coastal or “freshwater” inland peoples. They value their extended families, honor their elders and their collective wisdom, while also living in “two worlds.” They often encourage their children to get educated and pursue individualistic aspirations to help their communities by training as tradespeople and professionals who may be better trusted to look after their own. As Charles Perkins, a most celebrated Aboriginal role model for living in both worlds, famously said: “We know we can’t live in the past, but the past lives in us.”
As anxiety and depression, psychological trauma, drug and alcohol misuse, family and communal violence, ecological grief,and suicidal vulnerability are precipitated or exacerbated by the stress of extreme environmental adversity, significant investment in ameliorating these harms is essential, not just for farmers, town businesspeople and their families, but for all those affected, especially these most vulnerable members of the community.7 We must provide more essential community services controlled by Aboriginal community members themselves. We must also train and support more Aboriginal mental health workers, healers, mental health educators, peer workers and Aboriginal liaison officers, to work alongside other mental health, and health and social service professionals. Aboriginal people need stable local employment opportunities in their communities. There is a huge opportunity to synergize traditional indigenous fire management with Western techniques, creating and consolidating more valued jobs and respected land management roles for Aboriginal rangers, vital for the future of both Aboriginal and wider communities. Pilot programs are emerging.
Aboriginal communities also need a more preventive, whole-of-life approach to social determinants, lifestyle factors, trauma, and political decisions associated with compromised neurodevelopment, and increased subsequent incidence and severity of mental illnesses in their communities.7
As Alexander Solzhenitsyn observed: “On our crowded planet there are no longer any ‘internal affairs.’ ”8 Climate change is the ultimate form of globalization: What we each do about it affects all others’ lives. We can only insist that, alongside adequate resourcing of our most evidence-based methods of fire, water, and climate control, our governments consult and listen to our Indigenous elders about applying climate management methods. These have been demonstrated to be sustainable and effective, possibly over 60,000 years – which is the longest established record of continuous Indigenous culture worldwide.
References
1. Ten impacts of the Australian bushfires. U.N. Environment Programme. 2020 Jan 20.
2. Allam L, Evershed N. “Too hot for humans? First Nations people fear becoming Australia’s first climate refugees.” The Guardian. 2019 Dec 17.
3. National Indigenous Australians Agency. “Coronavirus (COVID-19).”
4. Phillips D. “Brazil: Judge bans missionaries from Indigenous reserve over COVID-19 fears.” The Guardian. 2020 Apr 17.
5. Rigby CW et al. Aust J Rural Health. 2011 Oct;19(5):249-54.
6. Cunsolo A, Ellis NR. Nature Clim Change. 2018 Apr 3;8:275-81.
7. Gynther B et al. EClinicalMedicine. 2019 Apr 26;10:68-77.
8. Solzhenitsyn A. “Warning to the West,” speech delivered 30 Jun 1975. New York: Fararr, Straux & Girous, 1976.
Dr. Rosen, an officer of the Order of Australia and a Fellow of the Royal Australian and New Zealand College of Psychiatrists, is affiliated with the Brain & Mind Centre, University of Sydney, and the Institute of Mental Health at the University of Wollongong (Australia). He also is a community psychiatrist in a remote region of New South Wales. Dr. Rosen has no conflicts of interest.
*This article was updated 6/16/2020.
Plan now to address the COVID-19 mental health fallout
COVID-19 affects the physical, psychological, and social health of people around the world. In the United States, newly reported cases are rising at alarming rates.
As of early May, more than 1.3 million people were confirmed to be COVID-19 infected in the United States and more than 4 million cases were reported globally.1
According to new internal projections from the Centers for Disease Control and Prevention, by June 1, the number of daily deaths could reach about 3,000. By the end of June, a draft CDC report projects that the United States will see 200,000 new cases each day.2
COVID-19 undeniably harms mental health. It gravely instills uncertainty and anxiety, sometimes compounded by the grief of losing loved ones and not being able to mourn those losses in traditional ways. The pandemic also has led to occupational and/or financial losses. Physical distancing and shelter-in-place practices make it even harder to cope with those stresses, although those practices mitigate the dangers. The fears tied to those practices are thought to be keeping some patients with health problems from seeking needed care from hospital EDs.3 In light of the mental health crisis emerging because of the profound impact of this pandemic on all aspects of life, clinicians should start working with public health and political leaders to develop plans to address these issues now.
Known impact of previous outbreaks
Previous disease outbreaks evidence a similar pattern of heightened anxiety as the patterns seen with COVID-19. For example, during the 2009 swine flu outbreak, 36 surveys of more than 3,000 participants in the United Kingdom found that 9.6%-32.9% of the participants were “very” or “fairly” worried about the possibility of contracting swine flu.4 The 1995 Ebola outbreak in the Democratic Republic of the Congo produced stigmatization tied to the illness. That outbreak provided many lessons for physicians.5
The metaphors ascribed to different diseases affect communities’ responses to it. The SARS virus has been particularly insidious and has been thought of as a “plague.”6 Epidemics of all kinds cause fears, not only of contracting the disease and dying, but also of social exclusion.7 The emotional responses to COVID-19 can precipitate anxiety, depression, insomnia, and somatic symptoms.
Repeated exposure to news media about the disease adds to theses stresss.10 Constant news consumption can result in panicky hoarding of resources, such as masks; gloves; first-aid kits; alcohol hand rubs; and daily necessities such as food, water, and toilet paper.
Who is most affected by outbreaks?
Those most affected after a disease outbreak are patients, their families, and medical personnel. In one study, researchers who conducted an online survey of 1,210 respondents in 194 cities in China during the early phase of the outbreak found that the psychological effects were worst among women, students, and vulnerable populations.11
Meanwhile, a 2003 cross-sectional survey of 1,115 ethnic Chinese adults in Hong Kong who responded to the SARS outbreak found that the respondents most likely to heed precautionary measures against the infection were “older, female, more educated people as well as those with a positive contact history and SARS-like symptoms.”12
Negative mental health consequences of a disease outbreak might persist long after the infection has dissipated. An increased association has been found between people with mental illness and posttraumatic stress following many disasters.13,14,15
Political and health care leaders should develop plans aimed at helping people copewith pandemics.16 Such strategies should include prioritizing treatment of the physical and mental health needs of patients infected with COVID-19 and of the general population. Screening for anxiety, depression, and suicidal thoughts ought to be implemented, and specialized psychiatric care teams should be assigned.17 We know that psychiatrists and other physicians turned to telemedicine to provide support, psychotherapy, and medical attention to patients soon after physical distancing measures were put into place. Those kinds of quick responses are important for our patients.
Fear of contagious diseases often creates social divisions. Governments should offer accurate information to reduce the detrimental effect of rumors and false propaganda.18 “Social distancing” is a misleading term; these practices should be referred to as “physical distancing.” We should encourage patients to maintain interpersonal contacts – albeit at a distance – to reach out to those in need, and to support one another during these troubled times.19
References
1. World Health Organization. Situation Report–107. 2020 May 6.
2. Centers for Disease Control and Prevention. Situation Update. 2020 Apr 30.
3. O’Brien M. “Are Americans in medical crisis avoiding the ER due to coronavirus?” PBS Newshour. 2020 May 6.
4. Rubin G et al. Health Technol Assess. 2010 Jul;14(340):183-266.
5. Hall R et al. Gen Hosp Psychiatry. 2008 Sep-Oct;30(5):466-52.
6. Verghese A. Clin Infect Dis. 2004;38:932-3.
7. Interagency Standing Committee. Briefing note on addressing health and psychosocial aspects of COVID-19 Outbreak – Version 11. 2020 Feb.
8. Sim K et al. J Psychosom Res. 2010;68:195-202.
9. Shigemura J et al. Psychiatry Clin Neurosci. 2020;74:281-2.
10. Garfin DR et al. Health Psychol. 2020 May;39(5):355-7.
11. Wang C et al. Int J Environ Res Public Health. 2020 Mar 6. doi: 10.3390/ijerph1751729.
12. Leung GM et al. J Epidemiol Community Health. 2003 Nov;57(1):857-63.
13. Xiang Y et al. Int J Biol Sci. 2020;16:1741-4.
14. Alvarez J, Hunt M. J Trauma Stress. 2005 Oct 18(5);18:497-505.
15. Cukor J et al. Depress Anxiety. 2011 Mar;28(3):210-7.
16. Horton R. Lancet. 2020 Feb;395(10222):400.
17. Xiang Y-T et al. Lancet Psychiatry. 2020 Feb 4;7:228-9.
18. World Health Organization. “Rational use of personal protective equipment (PPE) for coronavirus (COVID-19).” Interim Guidance. 2020 Mar.
19. Brooks S et al. Lancet 2020 Mar 14;395:912-20.
Dr. Doppalapudi is affiliated with Griffin Memorial Hospital in Norman, Okla. Dr. Lippmann is emeritus professor of psychiatry and also in family medicine at the University of Louisville (Ky.) Dr. Doppalapudi and Dr. Lippmann disclosed no conflicts of interest.
COVID-19 affects the physical, psychological, and social health of people around the world. In the United States, newly reported cases are rising at alarming rates.
As of early May, more than 1.3 million people were confirmed to be COVID-19 infected in the United States and more than 4 million cases were reported globally.1
According to new internal projections from the Centers for Disease Control and Prevention, by June 1, the number of daily deaths could reach about 3,000. By the end of June, a draft CDC report projects that the United States will see 200,000 new cases each day.2
COVID-19 undeniably harms mental health. It gravely instills uncertainty and anxiety, sometimes compounded by the grief of losing loved ones and not being able to mourn those losses in traditional ways. The pandemic also has led to occupational and/or financial losses. Physical distancing and shelter-in-place practices make it even harder to cope with those stresses, although those practices mitigate the dangers. The fears tied to those practices are thought to be keeping some patients with health problems from seeking needed care from hospital EDs.3 In light of the mental health crisis emerging because of the profound impact of this pandemic on all aspects of life, clinicians should start working with public health and political leaders to develop plans to address these issues now.
Known impact of previous outbreaks
Previous disease outbreaks evidence a similar pattern of heightened anxiety as the patterns seen with COVID-19. For example, during the 2009 swine flu outbreak, 36 surveys of more than 3,000 participants in the United Kingdom found that 9.6%-32.9% of the participants were “very” or “fairly” worried about the possibility of contracting swine flu.4 The 1995 Ebola outbreak in the Democratic Republic of the Congo produced stigmatization tied to the illness. That outbreak provided many lessons for physicians.5
The metaphors ascribed to different diseases affect communities’ responses to it. The SARS virus has been particularly insidious and has been thought of as a “plague.”6 Epidemics of all kinds cause fears, not only of contracting the disease and dying, but also of social exclusion.7 The emotional responses to COVID-19 can precipitate anxiety, depression, insomnia, and somatic symptoms.
Repeated exposure to news media about the disease adds to theses stresss.10 Constant news consumption can result in panicky hoarding of resources, such as masks; gloves; first-aid kits; alcohol hand rubs; and daily necessities such as food, water, and toilet paper.
Who is most affected by outbreaks?
Those most affected after a disease outbreak are patients, their families, and medical personnel. In one study, researchers who conducted an online survey of 1,210 respondents in 194 cities in China during the early phase of the outbreak found that the psychological effects were worst among women, students, and vulnerable populations.11
Meanwhile, a 2003 cross-sectional survey of 1,115 ethnic Chinese adults in Hong Kong who responded to the SARS outbreak found that the respondents most likely to heed precautionary measures against the infection were “older, female, more educated people as well as those with a positive contact history and SARS-like symptoms.”12
Negative mental health consequences of a disease outbreak might persist long after the infection has dissipated. An increased association has been found between people with mental illness and posttraumatic stress following many disasters.13,14,15
Political and health care leaders should develop plans aimed at helping people copewith pandemics.16 Such strategies should include prioritizing treatment of the physical and mental health needs of patients infected with COVID-19 and of the general population. Screening for anxiety, depression, and suicidal thoughts ought to be implemented, and specialized psychiatric care teams should be assigned.17 We know that psychiatrists and other physicians turned to telemedicine to provide support, psychotherapy, and medical attention to patients soon after physical distancing measures were put into place. Those kinds of quick responses are important for our patients.
Fear of contagious diseases often creates social divisions. Governments should offer accurate information to reduce the detrimental effect of rumors and false propaganda.18 “Social distancing” is a misleading term; these practices should be referred to as “physical distancing.” We should encourage patients to maintain interpersonal contacts – albeit at a distance – to reach out to those in need, and to support one another during these troubled times.19
References
1. World Health Organization. Situation Report–107. 2020 May 6.
2. Centers for Disease Control and Prevention. Situation Update. 2020 Apr 30.
3. O’Brien M. “Are Americans in medical crisis avoiding the ER due to coronavirus?” PBS Newshour. 2020 May 6.
4. Rubin G et al. Health Technol Assess. 2010 Jul;14(340):183-266.
5. Hall R et al. Gen Hosp Psychiatry. 2008 Sep-Oct;30(5):466-52.
6. Verghese A. Clin Infect Dis. 2004;38:932-3.
7. Interagency Standing Committee. Briefing note on addressing health and psychosocial aspects of COVID-19 Outbreak – Version 11. 2020 Feb.
8. Sim K et al. J Psychosom Res. 2010;68:195-202.
9. Shigemura J et al. Psychiatry Clin Neurosci. 2020;74:281-2.
10. Garfin DR et al. Health Psychol. 2020 May;39(5):355-7.
11. Wang C et al. Int J Environ Res Public Health. 2020 Mar 6. doi: 10.3390/ijerph1751729.
12. Leung GM et al. J Epidemiol Community Health. 2003 Nov;57(1):857-63.
13. Xiang Y et al. Int J Biol Sci. 2020;16:1741-4.
14. Alvarez J, Hunt M. J Trauma Stress. 2005 Oct 18(5);18:497-505.
15. Cukor J et al. Depress Anxiety. 2011 Mar;28(3):210-7.
16. Horton R. Lancet. 2020 Feb;395(10222):400.
17. Xiang Y-T et al. Lancet Psychiatry. 2020 Feb 4;7:228-9.
18. World Health Organization. “Rational use of personal protective equipment (PPE) for coronavirus (COVID-19).” Interim Guidance. 2020 Mar.
19. Brooks S et al. Lancet 2020 Mar 14;395:912-20.
Dr. Doppalapudi is affiliated with Griffin Memorial Hospital in Norman, Okla. Dr. Lippmann is emeritus professor of psychiatry and also in family medicine at the University of Louisville (Ky.) Dr. Doppalapudi and Dr. Lippmann disclosed no conflicts of interest.
COVID-19 affects the physical, psychological, and social health of people around the world. In the United States, newly reported cases are rising at alarming rates.
As of early May, more than 1.3 million people were confirmed to be COVID-19 infected in the United States and more than 4 million cases were reported globally.1
According to new internal projections from the Centers for Disease Control and Prevention, by June 1, the number of daily deaths could reach about 3,000. By the end of June, a draft CDC report projects that the United States will see 200,000 new cases each day.2
COVID-19 undeniably harms mental health. It gravely instills uncertainty and anxiety, sometimes compounded by the grief of losing loved ones and not being able to mourn those losses in traditional ways. The pandemic also has led to occupational and/or financial losses. Physical distancing and shelter-in-place practices make it even harder to cope with those stresses, although those practices mitigate the dangers. The fears tied to those practices are thought to be keeping some patients with health problems from seeking needed care from hospital EDs.3 In light of the mental health crisis emerging because of the profound impact of this pandemic on all aspects of life, clinicians should start working with public health and political leaders to develop plans to address these issues now.
Known impact of previous outbreaks
Previous disease outbreaks evidence a similar pattern of heightened anxiety as the patterns seen with COVID-19. For example, during the 2009 swine flu outbreak, 36 surveys of more than 3,000 participants in the United Kingdom found that 9.6%-32.9% of the participants were “very” or “fairly” worried about the possibility of contracting swine flu.4 The 1995 Ebola outbreak in the Democratic Republic of the Congo produced stigmatization tied to the illness. That outbreak provided many lessons for physicians.5
The metaphors ascribed to different diseases affect communities’ responses to it. The SARS virus has been particularly insidious and has been thought of as a “plague.”6 Epidemics of all kinds cause fears, not only of contracting the disease and dying, but also of social exclusion.7 The emotional responses to COVID-19 can precipitate anxiety, depression, insomnia, and somatic symptoms.
Repeated exposure to news media about the disease adds to theses stresss.10 Constant news consumption can result in panicky hoarding of resources, such as masks; gloves; first-aid kits; alcohol hand rubs; and daily necessities such as food, water, and toilet paper.
Who is most affected by outbreaks?
Those most affected after a disease outbreak are patients, their families, and medical personnel. In one study, researchers who conducted an online survey of 1,210 respondents in 194 cities in China during the early phase of the outbreak found that the psychological effects were worst among women, students, and vulnerable populations.11
Meanwhile, a 2003 cross-sectional survey of 1,115 ethnic Chinese adults in Hong Kong who responded to the SARS outbreak found that the respondents most likely to heed precautionary measures against the infection were “older, female, more educated people as well as those with a positive contact history and SARS-like symptoms.”12
Negative mental health consequences of a disease outbreak might persist long after the infection has dissipated. An increased association has been found between people with mental illness and posttraumatic stress following many disasters.13,14,15
Political and health care leaders should develop plans aimed at helping people copewith pandemics.16 Such strategies should include prioritizing treatment of the physical and mental health needs of patients infected with COVID-19 and of the general population. Screening for anxiety, depression, and suicidal thoughts ought to be implemented, and specialized psychiatric care teams should be assigned.17 We know that psychiatrists and other physicians turned to telemedicine to provide support, psychotherapy, and medical attention to patients soon after physical distancing measures were put into place. Those kinds of quick responses are important for our patients.
Fear of contagious diseases often creates social divisions. Governments should offer accurate information to reduce the detrimental effect of rumors and false propaganda.18 “Social distancing” is a misleading term; these practices should be referred to as “physical distancing.” We should encourage patients to maintain interpersonal contacts – albeit at a distance – to reach out to those in need, and to support one another during these troubled times.19
References
1. World Health Organization. Situation Report–107. 2020 May 6.
2. Centers for Disease Control and Prevention. Situation Update. 2020 Apr 30.
3. O’Brien M. “Are Americans in medical crisis avoiding the ER due to coronavirus?” PBS Newshour. 2020 May 6.
4. Rubin G et al. Health Technol Assess. 2010 Jul;14(340):183-266.
5. Hall R et al. Gen Hosp Psychiatry. 2008 Sep-Oct;30(5):466-52.
6. Verghese A. Clin Infect Dis. 2004;38:932-3.
7. Interagency Standing Committee. Briefing note on addressing health and psychosocial aspects of COVID-19 Outbreak – Version 11. 2020 Feb.
8. Sim K et al. J Psychosom Res. 2010;68:195-202.
9. Shigemura J et al. Psychiatry Clin Neurosci. 2020;74:281-2.
10. Garfin DR et al. Health Psychol. 2020 May;39(5):355-7.
11. Wang C et al. Int J Environ Res Public Health. 2020 Mar 6. doi: 10.3390/ijerph1751729.
12. Leung GM et al. J Epidemiol Community Health. 2003 Nov;57(1):857-63.
13. Xiang Y et al. Int J Biol Sci. 2020;16:1741-4.
14. Alvarez J, Hunt M. J Trauma Stress. 2005 Oct 18(5);18:497-505.
15. Cukor J et al. Depress Anxiety. 2011 Mar;28(3):210-7.
16. Horton R. Lancet. 2020 Feb;395(10222):400.
17. Xiang Y-T et al. Lancet Psychiatry. 2020 Feb 4;7:228-9.
18. World Health Organization. “Rational use of personal protective equipment (PPE) for coronavirus (COVID-19).” Interim Guidance. 2020 Mar.
19. Brooks S et al. Lancet 2020 Mar 14;395:912-20.
Dr. Doppalapudi is affiliated with Griffin Memorial Hospital in Norman, Okla. Dr. Lippmann is emeritus professor of psychiatry and also in family medicine at the University of Louisville (Ky.) Dr. Doppalapudi and Dr. Lippmann disclosed no conflicts of interest.
‘Milestone’ study shows promise for pedophilic disorder
Testosterone-suppressing treatment with the gonadotropin-releasing hormone (GnRH) antagonist degarelix may reduce dynamic risk factors for sexual offense in men with pedophilic disorder, new research suggests.
In a first-of-its-kind randomized, controlled trial of 52 help-seeking men with the disorder, degarelix versus placebo significantly dampened two critical risk factors for committing abuse: high sexual desire and sexual attraction to children. In addition, effects were noticeable within 2 weeks.
“The medicine is quick-acting, not only on biological systems but also on thoughts and behavior,” coinvestigator and corresponding author Christoffer Rahm, MD, of the Centre for Psychiatry Research at Karolinska Institutet, Stockholm, said in an interview.
“The effect lasts and increases after 10 weeks, and especially so in the small group of high-risk individuals,” Dr. Rahm added.
The study findings were published in JAMA Psychiatry.
Opportunity for prevention
Although all men with pedophilic disorder do not commit a sexual offense, those who do generally report struggling with their sexual urges for 10 years before committing a sexual crime, the investigators noted.
This presents an opportunity for prevention by treating high-risk individuals without prior convictions. Effective treatment could prevent child sexual abuse and reduce psychosocial stress for the individual with pedophilic disorder, the researchers wrote.
GnRH antagonists are considered effective in reducing paraphilic symptoms, but their use has been limited to correctional settings. – and not just convicted men from prison and the probation system.
“It means the conclusions from the study are applicable to the patients you meet on sexual medicine and general psychiatry clinics too,” Dr. Rahm said.
The study included 52 men with a pedophilic disorder diagnosis and no contraindications to the intervention. All had contacted PrevenTell, the Swedish national telephone helpline for unwanted sexuality.
Half of the participants were randomly assigned to receive two subcutaneous 120-mg injections of degarelix acetate, while the other half received an equal volume of placebo.
The primary endpoint was efficacy at 2 weeks after injection in reducing a composite risk score of five domains for committing child sexual abuse; this risk score ranged from 0 to 15 points (each domain could be rated 0-3). Secondary endpoints included efficacy at 2 and 10 weeks in the composite score, each risk domain, quality of life, self-reported effects, and adverse events.
‘Positive effects’
At 2 weeks, the composite risk score decreased from 7.4 to 4.4 in the degarelix group and from 7.8 to 6.6 in the placebo group, which was a mean between-group difference of –1.8 (95% confidence interval, –3.2 to –0.5; P = .01).
Compared with placebo, the degarelix group also showed a decrease in the composite score at 10 weeks (−2.2; 95% CI, −3.6 to −0.7), in the domains of pedophilic disorder at 2 weeks (−0.7; 95% CI, −1.4 to 0.0) and 10 weeks (−1.1; 95% CI, −1.8 to −0.4), and in sexual preoccupation at 2 weeks (−0.7; 95% CI, −1.2 to −0.3) and 10 weeks (−0.8; 95% CI, −1.3 to −0.3).
There were no between-group differences in the other domains of self-rated risk, low empathy, and impaired self-regulation at 2 or 10 weeks, or in quality of life.
Injection-site reactions were more common with degarelix than placebo (88% vs. 4%, respectively), as were elevations in hepatobiliary enzyme levels (44% vs. 8%). Two patients in the degarelix group were hospitalized as a result of increased suicidal ideation, suggesting “vigilance for the risk of exacerbating suicidality in predisposed individuals is warranted,” the researchers wrote.
“Most patients tolerated it well, many experienced what they thought were positive effects on sexuality, and a majority wanted to continue with the medicine after the study was over and have another injection,” Dr. Rahm said.
Sexual science milestone
In an accompanying editorial, Peer Briken, MD, of the Institute for Sex Research, Sexual Medicine, and Forensic Psychiatry at University Medical Centre, Hamburg, Germany, wrote that the innovative potential of this study should “not be underestimated.”
It has previously been thought that randomized, controlled trials were not possible because it might be unethical to withhold therapy from high-risk participants and thus risk sexual assaults on children in a control group, Dr. Briken noted.
With the current study, “the situation has changed, which marks a milestone in clinical sexual science and the field of forensic psychiatry,” he wrote.
However, the “great benefit” of the study, which is the proof of feasibility of a randomized, controlled trial in this special group of patients and use of a new drug, comes with some “important limitations,” he added.
Only three participants in each treatment group were in the high-risk subgroup. In addition, the most important long-term outcome criterion – reduction in recidivism in high-risk individuals – could not be investigated, he said.
Dr. Briken agreed with the investigators that risk of suicidal tendencies during rapid testosterone withdrawal requires attention.
Despite its limitations, this study is “certainly the most important contribution to the field of pharmacotherapy of pedophilic disorders since Rösler and Witztum’s study on GnRH agonists in 1998. Also, a relevant number of the study participants (58%) were in favor of further application,” he concluded.
The study was funded by the Swedish Society of Medicine, the Söderström-Königska Foundation, the Fredrik and Ingrid Thuring Foundation, the Centre for Psychiatric Research at Karolinska Institutet, the Gothenburg Society of Medicine, Skaraborg Hospital research unit, Region Stockholm, and the Swedish Society for Medical Research. Dr. Rahm and Dr. Briken have disclosed no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
Testosterone-suppressing treatment with the gonadotropin-releasing hormone (GnRH) antagonist degarelix may reduce dynamic risk factors for sexual offense in men with pedophilic disorder, new research suggests.
In a first-of-its-kind randomized, controlled trial of 52 help-seeking men with the disorder, degarelix versus placebo significantly dampened two critical risk factors for committing abuse: high sexual desire and sexual attraction to children. In addition, effects were noticeable within 2 weeks.
“The medicine is quick-acting, not only on biological systems but also on thoughts and behavior,” coinvestigator and corresponding author Christoffer Rahm, MD, of the Centre for Psychiatry Research at Karolinska Institutet, Stockholm, said in an interview.
“The effect lasts and increases after 10 weeks, and especially so in the small group of high-risk individuals,” Dr. Rahm added.
The study findings were published in JAMA Psychiatry.
Opportunity for prevention
Although all men with pedophilic disorder do not commit a sexual offense, those who do generally report struggling with their sexual urges for 10 years before committing a sexual crime, the investigators noted.
This presents an opportunity for prevention by treating high-risk individuals without prior convictions. Effective treatment could prevent child sexual abuse and reduce psychosocial stress for the individual with pedophilic disorder, the researchers wrote.
GnRH antagonists are considered effective in reducing paraphilic symptoms, but their use has been limited to correctional settings. – and not just convicted men from prison and the probation system.
“It means the conclusions from the study are applicable to the patients you meet on sexual medicine and general psychiatry clinics too,” Dr. Rahm said.
The study included 52 men with a pedophilic disorder diagnosis and no contraindications to the intervention. All had contacted PrevenTell, the Swedish national telephone helpline for unwanted sexuality.
Half of the participants were randomly assigned to receive two subcutaneous 120-mg injections of degarelix acetate, while the other half received an equal volume of placebo.
The primary endpoint was efficacy at 2 weeks after injection in reducing a composite risk score of five domains for committing child sexual abuse; this risk score ranged from 0 to 15 points (each domain could be rated 0-3). Secondary endpoints included efficacy at 2 and 10 weeks in the composite score, each risk domain, quality of life, self-reported effects, and adverse events.
‘Positive effects’
At 2 weeks, the composite risk score decreased from 7.4 to 4.4 in the degarelix group and from 7.8 to 6.6 in the placebo group, which was a mean between-group difference of –1.8 (95% confidence interval, –3.2 to –0.5; P = .01).
Compared with placebo, the degarelix group also showed a decrease in the composite score at 10 weeks (−2.2; 95% CI, −3.6 to −0.7), in the domains of pedophilic disorder at 2 weeks (−0.7; 95% CI, −1.4 to 0.0) and 10 weeks (−1.1; 95% CI, −1.8 to −0.4), and in sexual preoccupation at 2 weeks (−0.7; 95% CI, −1.2 to −0.3) and 10 weeks (−0.8; 95% CI, −1.3 to −0.3).
There were no between-group differences in the other domains of self-rated risk, low empathy, and impaired self-regulation at 2 or 10 weeks, or in quality of life.
Injection-site reactions were more common with degarelix than placebo (88% vs. 4%, respectively), as were elevations in hepatobiliary enzyme levels (44% vs. 8%). Two patients in the degarelix group were hospitalized as a result of increased suicidal ideation, suggesting “vigilance for the risk of exacerbating suicidality in predisposed individuals is warranted,” the researchers wrote.
“Most patients tolerated it well, many experienced what they thought were positive effects on sexuality, and a majority wanted to continue with the medicine after the study was over and have another injection,” Dr. Rahm said.
Sexual science milestone
In an accompanying editorial, Peer Briken, MD, of the Institute for Sex Research, Sexual Medicine, and Forensic Psychiatry at University Medical Centre, Hamburg, Germany, wrote that the innovative potential of this study should “not be underestimated.”
It has previously been thought that randomized, controlled trials were not possible because it might be unethical to withhold therapy from high-risk participants and thus risk sexual assaults on children in a control group, Dr. Briken noted.
With the current study, “the situation has changed, which marks a milestone in clinical sexual science and the field of forensic psychiatry,” he wrote.
However, the “great benefit” of the study, which is the proof of feasibility of a randomized, controlled trial in this special group of patients and use of a new drug, comes with some “important limitations,” he added.
Only three participants in each treatment group were in the high-risk subgroup. In addition, the most important long-term outcome criterion – reduction in recidivism in high-risk individuals – could not be investigated, he said.
Dr. Briken agreed with the investigators that risk of suicidal tendencies during rapid testosterone withdrawal requires attention.
Despite its limitations, this study is “certainly the most important contribution to the field of pharmacotherapy of pedophilic disorders since Rösler and Witztum’s study on GnRH agonists in 1998. Also, a relevant number of the study participants (58%) were in favor of further application,” he concluded.
The study was funded by the Swedish Society of Medicine, the Söderström-Königska Foundation, the Fredrik and Ingrid Thuring Foundation, the Centre for Psychiatric Research at Karolinska Institutet, the Gothenburg Society of Medicine, Skaraborg Hospital research unit, Region Stockholm, and the Swedish Society for Medical Research. Dr. Rahm and Dr. Briken have disclosed no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
Testosterone-suppressing treatment with the gonadotropin-releasing hormone (GnRH) antagonist degarelix may reduce dynamic risk factors for sexual offense in men with pedophilic disorder, new research suggests.
In a first-of-its-kind randomized, controlled trial of 52 help-seeking men with the disorder, degarelix versus placebo significantly dampened two critical risk factors for committing abuse: high sexual desire and sexual attraction to children. In addition, effects were noticeable within 2 weeks.
“The medicine is quick-acting, not only on biological systems but also on thoughts and behavior,” coinvestigator and corresponding author Christoffer Rahm, MD, of the Centre for Psychiatry Research at Karolinska Institutet, Stockholm, said in an interview.
“The effect lasts and increases after 10 weeks, and especially so in the small group of high-risk individuals,” Dr. Rahm added.
The study findings were published in JAMA Psychiatry.
Opportunity for prevention
Although all men with pedophilic disorder do not commit a sexual offense, those who do generally report struggling with their sexual urges for 10 years before committing a sexual crime, the investigators noted.
This presents an opportunity for prevention by treating high-risk individuals without prior convictions. Effective treatment could prevent child sexual abuse and reduce psychosocial stress for the individual with pedophilic disorder, the researchers wrote.
GnRH antagonists are considered effective in reducing paraphilic symptoms, but their use has been limited to correctional settings. – and not just convicted men from prison and the probation system.
“It means the conclusions from the study are applicable to the patients you meet on sexual medicine and general psychiatry clinics too,” Dr. Rahm said.
The study included 52 men with a pedophilic disorder diagnosis and no contraindications to the intervention. All had contacted PrevenTell, the Swedish national telephone helpline for unwanted sexuality.
Half of the participants were randomly assigned to receive two subcutaneous 120-mg injections of degarelix acetate, while the other half received an equal volume of placebo.
The primary endpoint was efficacy at 2 weeks after injection in reducing a composite risk score of five domains for committing child sexual abuse; this risk score ranged from 0 to 15 points (each domain could be rated 0-3). Secondary endpoints included efficacy at 2 and 10 weeks in the composite score, each risk domain, quality of life, self-reported effects, and adverse events.
‘Positive effects’
At 2 weeks, the composite risk score decreased from 7.4 to 4.4 in the degarelix group and from 7.8 to 6.6 in the placebo group, which was a mean between-group difference of –1.8 (95% confidence interval, –3.2 to –0.5; P = .01).
Compared with placebo, the degarelix group also showed a decrease in the composite score at 10 weeks (−2.2; 95% CI, −3.6 to −0.7), in the domains of pedophilic disorder at 2 weeks (−0.7; 95% CI, −1.4 to 0.0) and 10 weeks (−1.1; 95% CI, −1.8 to −0.4), and in sexual preoccupation at 2 weeks (−0.7; 95% CI, −1.2 to −0.3) and 10 weeks (−0.8; 95% CI, −1.3 to −0.3).
There were no between-group differences in the other domains of self-rated risk, low empathy, and impaired self-regulation at 2 or 10 weeks, or in quality of life.
Injection-site reactions were more common with degarelix than placebo (88% vs. 4%, respectively), as were elevations in hepatobiliary enzyme levels (44% vs. 8%). Two patients in the degarelix group were hospitalized as a result of increased suicidal ideation, suggesting “vigilance for the risk of exacerbating suicidality in predisposed individuals is warranted,” the researchers wrote.
“Most patients tolerated it well, many experienced what they thought were positive effects on sexuality, and a majority wanted to continue with the medicine after the study was over and have another injection,” Dr. Rahm said.
Sexual science milestone
In an accompanying editorial, Peer Briken, MD, of the Institute for Sex Research, Sexual Medicine, and Forensic Psychiatry at University Medical Centre, Hamburg, Germany, wrote that the innovative potential of this study should “not be underestimated.”
It has previously been thought that randomized, controlled trials were not possible because it might be unethical to withhold therapy from high-risk participants and thus risk sexual assaults on children in a control group, Dr. Briken noted.
With the current study, “the situation has changed, which marks a milestone in clinical sexual science and the field of forensic psychiatry,” he wrote.
However, the “great benefit” of the study, which is the proof of feasibility of a randomized, controlled trial in this special group of patients and use of a new drug, comes with some “important limitations,” he added.
Only three participants in each treatment group were in the high-risk subgroup. In addition, the most important long-term outcome criterion – reduction in recidivism in high-risk individuals – could not be investigated, he said.
Dr. Briken agreed with the investigators that risk of suicidal tendencies during rapid testosterone withdrawal requires attention.
Despite its limitations, this study is “certainly the most important contribution to the field of pharmacotherapy of pedophilic disorders since Rösler and Witztum’s study on GnRH agonists in 1998. Also, a relevant number of the study participants (58%) were in favor of further application,” he concluded.
The study was funded by the Swedish Society of Medicine, the Söderström-Königska Foundation, the Fredrik and Ingrid Thuring Foundation, the Centre for Psychiatric Research at Karolinska Institutet, the Gothenburg Society of Medicine, Skaraborg Hospital research unit, Region Stockholm, and the Swedish Society for Medical Research. Dr. Rahm and Dr. Briken have disclosed no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
COVID-19: Social distancing with young children
Emma just celebrated her second birthday, and she has been working on the usual things that children start to master at this age: potty training, making friends, exerting her will through both actions and words, and generally enjoying life as the center of attention for both her parents and grandparents. Like everyone else in Maryland, Emma’s life changed suddenly with the coronavirus stay-at-home order that was issued on March 30. There is no more day care and her parents work from home while caring for her. Her grandparents visit, but only outside and only from a distance – there are no more hugs and there is no more sitting in her grandfather’s lap while he reads stories.
One afternoon a few weeks ago, Emma was looking out the window when she saw her friend, Max, walk by with his parents. Before her parents could stop her, Emma bolted out the door, and she and little Max wrapped each other in a tight embrace. Their parents snapped a photo of the smiling toddlers hugging before they separated the children. The photo is adorable, but as all struggle with social distancing, the poignance of two innocent toddlers in a forbidden embrace is a bit heartbreaking.
Everyone who has ever observed children knows that social distancing is not in their nature. Children play, they hug, they wrestle and tackle and poke, and sometimes even bite. And every student of social psychology has been taught about Harry Harlow’s experiments with rhesus macaques who were separated from their mothers and given access to an inanimate object to serve as a surrogate mother. The Harlow studies, while controversial, were revolutionary in demonstrating that early interactions with both a mother and with playmates were essential in the development of normal social relationships.
Regine Galanti, PhD, is a clinical psychologist at Long Island Behavioral Psychology, Cedarhurst, N.Y., who specializes in the treatment of anxiety and behavior problems. With young children she uses parent-child interaction therapy (PCIT) to help build relationships and discipline. Dr. Galanti said: “I don’t think we’re well prepared as a field to answer questions about the long-term effects of social distancing. If you need young children to socially distance, the responsibility has to fall on the adults. It’s important to explain to children what’s going on and to be honest in a developmentally appropriate way.”
Dr. Galanti has noticed that the issues that people had before COVID-19 are exacerbated by the stress of the current situation. What we do know is that young children thrive on structure.”
Tovah P. Klein, PhD, is the author of “How Toddlers Thrive” (Touchstone, 2015) and is the director of the Barnard College Center for Toddler Development in Manhattan. “When this started, we thought we would be closed for a few weeks,” Dr. Klein said. “We wanted to maintain a connection to the children, so we made videos for the parents to show to the kids, just to say ‘We’re still here.’ But as time went on and we realized it was going to be a while, we felt it was important to provide connection, so we launched a virtual program.”
Dr. Klein said that the teachers meet with their classes of 13 2-year-olds over Zoom, and when they first started, she asked the teachers to try to meet for 10 minutes. They are now meeting for 40 minutes twice a week. The children like seeing their teachers in their homes and they like seeing each other. In addition, the teachers make videos to send home and they are currently working on one to demystify masks. “We’re working on normalizing masks and showing children that when you put the mask on, you’re still there underneath.”
The center has existed for 48 years. There have been struggles for some of the children who attend; some of the parents have been hospitalized with the virus, and some work on the front line and so parents may be living away from a child.
“We’ve seen more challenging behaviors during this time, more tantrums, toileting issues, night awakenings, and more fragility. But as the new normal takes hold, things are settling in. Parents have been good about getting new routines and it helps if parents can handle their own stress,” Dr. Klein said. She also pointed out that for parents working at home while caring for their children, this can be particularly difficult on a young child. “The child knows the parent is home, but isn’t spending time with him, and he sees it as a rejection.”
Margaret Adams, MD, is a child psychiatrist in Maryland who works with very young children and their parents. She says that some of the children are thriving with the extra attention from their parents. “I often have seen difficulties with readjustment to the routine of separations to day care after a family vacation of a week, or sometimes even a weekend, even for those young ones who seem to love the social aspects of day care. I think it is likely a big impact will come upon return, depending on the developmental stage of the child,” Dr. Adams noted.
Despite the hardships of the moment, all three experts expressed hopefulness about the future for these children.
“Young children are super-resilient and that’s the blessing of this,” Dr. Galanti said. “I think they will be okay.”
Emma is home for now with her parents, who are expecting another child soon. Her mother notes: “The days are long and balancing work is an impossible challenge, but being with Emma has been a total blessing, and when would I ever have this much time to spend with my kid? She’s at such a fun age – so curious and adventurous – it’s amazing to watch her language and skills progress. I wish we weren’t in the midst of a pandemic, but Emma is definitely the bright spot.”
Dr. Miller is coauthor with Annette Hanson, MD, of “Committed: The Battle Over Involuntary Psychiatric Care” (Baltimore: Johns Hopkins University Press, 2016). She has a private practice and is assistant professor of psychiatry and behavioral sciences at Johns Hopkins, both in Baltimore. Dr. Miller has no disclosures.
Emma just celebrated her second birthday, and she has been working on the usual things that children start to master at this age: potty training, making friends, exerting her will through both actions and words, and generally enjoying life as the center of attention for both her parents and grandparents. Like everyone else in Maryland, Emma’s life changed suddenly with the coronavirus stay-at-home order that was issued on March 30. There is no more day care and her parents work from home while caring for her. Her grandparents visit, but only outside and only from a distance – there are no more hugs and there is no more sitting in her grandfather’s lap while he reads stories.
One afternoon a few weeks ago, Emma was looking out the window when she saw her friend, Max, walk by with his parents. Before her parents could stop her, Emma bolted out the door, and she and little Max wrapped each other in a tight embrace. Their parents snapped a photo of the smiling toddlers hugging before they separated the children. The photo is adorable, but as all struggle with social distancing, the poignance of two innocent toddlers in a forbidden embrace is a bit heartbreaking.
Everyone who has ever observed children knows that social distancing is not in their nature. Children play, they hug, they wrestle and tackle and poke, and sometimes even bite. And every student of social psychology has been taught about Harry Harlow’s experiments with rhesus macaques who were separated from their mothers and given access to an inanimate object to serve as a surrogate mother. The Harlow studies, while controversial, were revolutionary in demonstrating that early interactions with both a mother and with playmates were essential in the development of normal social relationships.
Regine Galanti, PhD, is a clinical psychologist at Long Island Behavioral Psychology, Cedarhurst, N.Y., who specializes in the treatment of anxiety and behavior problems. With young children she uses parent-child interaction therapy (PCIT) to help build relationships and discipline. Dr. Galanti said: “I don’t think we’re well prepared as a field to answer questions about the long-term effects of social distancing. If you need young children to socially distance, the responsibility has to fall on the adults. It’s important to explain to children what’s going on and to be honest in a developmentally appropriate way.”
Dr. Galanti has noticed that the issues that people had before COVID-19 are exacerbated by the stress of the current situation. What we do know is that young children thrive on structure.”
Tovah P. Klein, PhD, is the author of “How Toddlers Thrive” (Touchstone, 2015) and is the director of the Barnard College Center for Toddler Development in Manhattan. “When this started, we thought we would be closed for a few weeks,” Dr. Klein said. “We wanted to maintain a connection to the children, so we made videos for the parents to show to the kids, just to say ‘We’re still here.’ But as time went on and we realized it was going to be a while, we felt it was important to provide connection, so we launched a virtual program.”
Dr. Klein said that the teachers meet with their classes of 13 2-year-olds over Zoom, and when they first started, she asked the teachers to try to meet for 10 minutes. They are now meeting for 40 minutes twice a week. The children like seeing their teachers in their homes and they like seeing each other. In addition, the teachers make videos to send home and they are currently working on one to demystify masks. “We’re working on normalizing masks and showing children that when you put the mask on, you’re still there underneath.”
The center has existed for 48 years. There have been struggles for some of the children who attend; some of the parents have been hospitalized with the virus, and some work on the front line and so parents may be living away from a child.
“We’ve seen more challenging behaviors during this time, more tantrums, toileting issues, night awakenings, and more fragility. But as the new normal takes hold, things are settling in. Parents have been good about getting new routines and it helps if parents can handle their own stress,” Dr. Klein said. She also pointed out that for parents working at home while caring for their children, this can be particularly difficult on a young child. “The child knows the parent is home, but isn’t spending time with him, and he sees it as a rejection.”
Margaret Adams, MD, is a child psychiatrist in Maryland who works with very young children and their parents. She says that some of the children are thriving with the extra attention from their parents. “I often have seen difficulties with readjustment to the routine of separations to day care after a family vacation of a week, or sometimes even a weekend, even for those young ones who seem to love the social aspects of day care. I think it is likely a big impact will come upon return, depending on the developmental stage of the child,” Dr. Adams noted.
Despite the hardships of the moment, all three experts expressed hopefulness about the future for these children.
“Young children are super-resilient and that’s the blessing of this,” Dr. Galanti said. “I think they will be okay.”
Emma is home for now with her parents, who are expecting another child soon. Her mother notes: “The days are long and balancing work is an impossible challenge, but being with Emma has been a total blessing, and when would I ever have this much time to spend with my kid? She’s at such a fun age – so curious and adventurous – it’s amazing to watch her language and skills progress. I wish we weren’t in the midst of a pandemic, but Emma is definitely the bright spot.”
Dr. Miller is coauthor with Annette Hanson, MD, of “Committed: The Battle Over Involuntary Psychiatric Care” (Baltimore: Johns Hopkins University Press, 2016). She has a private practice and is assistant professor of psychiatry and behavioral sciences at Johns Hopkins, both in Baltimore. Dr. Miller has no disclosures.
Emma just celebrated her second birthday, and she has been working on the usual things that children start to master at this age: potty training, making friends, exerting her will through both actions and words, and generally enjoying life as the center of attention for both her parents and grandparents. Like everyone else in Maryland, Emma’s life changed suddenly with the coronavirus stay-at-home order that was issued on March 30. There is no more day care and her parents work from home while caring for her. Her grandparents visit, but only outside and only from a distance – there are no more hugs and there is no more sitting in her grandfather’s lap while he reads stories.
One afternoon a few weeks ago, Emma was looking out the window when she saw her friend, Max, walk by with his parents. Before her parents could stop her, Emma bolted out the door, and she and little Max wrapped each other in a tight embrace. Their parents snapped a photo of the smiling toddlers hugging before they separated the children. The photo is adorable, but as all struggle with social distancing, the poignance of two innocent toddlers in a forbidden embrace is a bit heartbreaking.
Everyone who has ever observed children knows that social distancing is not in their nature. Children play, they hug, they wrestle and tackle and poke, and sometimes even bite. And every student of social psychology has been taught about Harry Harlow’s experiments with rhesus macaques who were separated from their mothers and given access to an inanimate object to serve as a surrogate mother. The Harlow studies, while controversial, were revolutionary in demonstrating that early interactions with both a mother and with playmates were essential in the development of normal social relationships.
Regine Galanti, PhD, is a clinical psychologist at Long Island Behavioral Psychology, Cedarhurst, N.Y., who specializes in the treatment of anxiety and behavior problems. With young children she uses parent-child interaction therapy (PCIT) to help build relationships and discipline. Dr. Galanti said: “I don’t think we’re well prepared as a field to answer questions about the long-term effects of social distancing. If you need young children to socially distance, the responsibility has to fall on the adults. It’s important to explain to children what’s going on and to be honest in a developmentally appropriate way.”
Dr. Galanti has noticed that the issues that people had before COVID-19 are exacerbated by the stress of the current situation. What we do know is that young children thrive on structure.”
Tovah P. Klein, PhD, is the author of “How Toddlers Thrive” (Touchstone, 2015) and is the director of the Barnard College Center for Toddler Development in Manhattan. “When this started, we thought we would be closed for a few weeks,” Dr. Klein said. “We wanted to maintain a connection to the children, so we made videos for the parents to show to the kids, just to say ‘We’re still here.’ But as time went on and we realized it was going to be a while, we felt it was important to provide connection, so we launched a virtual program.”
Dr. Klein said that the teachers meet with their classes of 13 2-year-olds over Zoom, and when they first started, she asked the teachers to try to meet for 10 minutes. They are now meeting for 40 minutes twice a week. The children like seeing their teachers in their homes and they like seeing each other. In addition, the teachers make videos to send home and they are currently working on one to demystify masks. “We’re working on normalizing masks and showing children that when you put the mask on, you’re still there underneath.”
The center has existed for 48 years. There have been struggles for some of the children who attend; some of the parents have been hospitalized with the virus, and some work on the front line and so parents may be living away from a child.
“We’ve seen more challenging behaviors during this time, more tantrums, toileting issues, night awakenings, and more fragility. But as the new normal takes hold, things are settling in. Parents have been good about getting new routines and it helps if parents can handle their own stress,” Dr. Klein said. She also pointed out that for parents working at home while caring for their children, this can be particularly difficult on a young child. “The child knows the parent is home, but isn’t spending time with him, and he sees it as a rejection.”
Margaret Adams, MD, is a child psychiatrist in Maryland who works with very young children and their parents. She says that some of the children are thriving with the extra attention from their parents. “I often have seen difficulties with readjustment to the routine of separations to day care after a family vacation of a week, or sometimes even a weekend, even for those young ones who seem to love the social aspects of day care. I think it is likely a big impact will come upon return, depending on the developmental stage of the child,” Dr. Adams noted.
Despite the hardships of the moment, all three experts expressed hopefulness about the future for these children.
“Young children are super-resilient and that’s the blessing of this,” Dr. Galanti said. “I think they will be okay.”
Emma is home for now with her parents, who are expecting another child soon. Her mother notes: “The days are long and balancing work is an impossible challenge, but being with Emma has been a total blessing, and when would I ever have this much time to spend with my kid? She’s at such a fun age – so curious and adventurous – it’s amazing to watch her language and skills progress. I wish we weren’t in the midst of a pandemic, but Emma is definitely the bright spot.”
Dr. Miller is coauthor with Annette Hanson, MD, of “Committed: The Battle Over Involuntary Psychiatric Care” (Baltimore: Johns Hopkins University Press, 2016). She has a private practice and is assistant professor of psychiatry and behavioral sciences at Johns Hopkins, both in Baltimore. Dr. Miller has no disclosures.
COVID-19: To have and to hold ... in quarantine
Tips for marriage survival during a pandemic
Most married couples vowed to stay with their partners during sickness and health, but none of us vowed to remain trapped with our loved ones behind the same four walls, all day, every day, for an unknown period of time. We didn’t sign up for this! Some romantics may be titillated by the prospect, while more independent partners may panic at the mere thought of spending all day and night with their loved ones.
Because of the swift implementation of the lifestyle-altering restrictions, couples did not have ample time to mentally and physically prepare. A lack of preparation and loss of control heightens our emotions. It can make couples more susceptible to engage in unhealthy styles of communication and destructive behaviors that are harmful to their relationships.
There are psychological reasons that “absence makes the heart grow fonder.” Distance from your partner is not just a clever way to make your partner appreciate and desire you more. It is human nature to habituate to what is part of your daily life. For instance, when your partner is away from you while on a work trip, you may find the first night or two alone relaxing; but by day 3, you begin to miss your partner’s hugs and kisses, smell, and touch. And after many days apart, you may even miss the incessant nagging that secretly motivates you. Physical distance from our partners essentially gives us the ability to long for and appreciate each other. Our brains are wired to pay more attention to things that are novel and exciting and less interested in what is in our everyday lives.
Separation gives us the ability to miss our partners, while quarantine does the complete opposite.
To avoid contemplating how to murder one’s spouse before quarantine ends, partners can strengthen their relationships by using the strategies I’ve outlined below, which are loosely based on dialectical behavior therapy (DBT). These strategies can be useful for anyone – providers and patients alike – going through these struggles.
Dialectical behavior therapy was developed by psychologist Marsha Linehan PhD, to help regulate emotions for people diagnosed with borderline personality disorder. These skills help to identify thoughts and feelings, to accept one’s inner emotional world and outward behaviors. The idea is that, once you can recognize and accept, then change is possible. The “dialectic” in dialectical behavior therapy implies that one is attempting to find a balance between acceptance and change. All of us can benefit from these skills, especially emotionally volatile couples who are trapped together in quarantine.
Radically accept what is uncertain in your lives
Radical acceptance is a practice used in DBT in situations that are out of our control, such as the COVID-19 pandemic. Radically accept that you and your partner are trapped in quarantine without attempting to place blame on our government, your spouse, your boss, and even yourself. Radical acceptance is exactly what the name implies. Accept your current situation for what it is and not what you hoped it to be.
Accept the unknown and unanswered questions such as when will this quarantine end? Will there be a summer camp? Will I get back to my office this summer? Will my children even return to school in the fall? The acceptance of what is out of your control will ultimately decrease your mental time spent worrying and obsessing about the uncertainties of your post-quarantine life and instead provide you more time to be present with your spouse.
Remain mindful during all communication with your spouse. To stay in the moment, you need to be aware of your bodily reactions to distress and notice when your heart rate increases, breathing becomes more shallow, stomach muscles tighten, and when your thoughts become more negative. Mindfulness skills enable us to use physiological changes in our body to become aware of our emotions. You can use your partner’s nonverbal body language and tone of voice to gauge that person’s emotional reactivity.
The practice of mindfulness leads to an increased emotional intelligence. The goal is to have enough self-awareness and emotional understanding of your partner and enough empathy to know when a conversation is becoming too emotionally charged and to let it go and back off. Mindfulness is not nagging your partner to remember to change the heating unit filters with a reminder of what happened years ago when this wasn’t done promptly – without first checking in to make sure your partner is emotionally ready for this type of conversation.
When we have strong emotions, we are using the more primitive parts of our brain that induce a fight or flight reaction. These emotional reactions overshadow the more advanced prefrontal region of our brain that stores our rational thoughts and reasoning skills, a concept identified by psychologist Daniel Goleman as “emotional hijacking.”
Use distress tolerance skills to deal with negative emotions
Distress tolerance is an individual’s ability to manage feelings in response to stress. Distress tolerance skills are aimed at helping one manage intense emotions without worsening a situation by engaging in behaviors that are destructive and may exacerbate the problem. The goal is to tolerate the stress while with your partner and not respond negatively or in a way that is harmful to the integrity of your relationship.
To prioritize your relationship, this may mean that you choose not to react negatively when your partner makes a passive-aggressive comment on how you spent your day during quarantine since you still have a pile of laundry on your bedroom floor and overflowing dishes in the kitchen sink. A high level of distress tolerance will enable you to not overreact or withdraw from your spouse when flooded with emotions of anger or sadness.
Distraction techniques are a type of distress tolerance skill. You can engage in activities that keep you distracted and require your full attention. When things get heated between you and your spouse during quarantine, try to obtain some distance from each other to cool down and engage in an activity that involves your full concentration.
Many of us have been surprised by our hidden talents that were discovered during the quarantine. Use the time away from your partner to distract yourself with your new passion for writing, baking, organizing, and even your newfound love of balloon artistry. Do an activity that engages your mind and provides you the necessary physical and mental time away from your partner to deescalate. You can always revisit the initial cause of the conflict when both you and your partner are not emotionally charged. You can also distract yourself with self-soothing tactics such as taking a warm bath or a reading good book. Perhaps distract yourself by giving back to others and spending time planning a drive-by surprise party for your sister’s birthday next month. It can be helpful to distract yourself by comparing yourself to others less fortunate than you or a time in your life when you and your partner were struggling much worse than now, to provide perspective. The goal is not to add to your distress but instead, provide yourself a sense of perspective.
Use interpersonal effectiveness skills to establish a healthy relationship
Be gentle in all your communications with your partner, think about your spouse’s perspective, show empathy and interest in what your partner has to say by your verbal communication or body language, such as maintaining eye contact, and offer recognitional cues, such as “uh-huh” and “oh, really.” Avoid communication that is at all invalidating. Never start a sentence with “YOU” while having heated conversations with your spouse; instead, use “I feel” statements. This type of communication avoids the blame game that gets many couples into trouble.
Instead, communicate how you feel while not necessarily blaming your spouse but rather expressing your emotions. This will ultimately lead to less defensive communication from your partner. Remember that not all communication is for the sole purpose of communicating. Much of the time, communication is used as an attempt for one partner to connect with the other partner. Couples may say that they have difficulty with communication when it is not the communication that is the issue but instead the underlying disconnect of the couple.
This disconnect usually manifests while couples are communicating, and therefore, can be misconstrued as solely a communication issue by the couple. When your partner asks you to stop staring at your phone during dinner, it is not necessarily that your spouse is attempting to control you or wants to engage in some deep conversation, but more likely a bid to try to connect with you. Your partner is attempting to tell you that he or she feels disconnected, misses you, and wants to reconnect.
Provide validation and acceptance to your partner
Focus on your partner’s strengths and accept the weaknesses. Accept that your partner is scattered, disorganized, and takes at least 20 minutes to find the phone and keys every morning. Remember that during your courtship days, you found your partner’s flighty attributes to be endearing. Do the same for your strengths and weaknesses.
Accept that the pandemic is unpredictable and that you may need to strengthen your ability to be flexible and more adaptable. This will ultimately lead to feeling less disappointment by your partner and more accepting of shortcomings. Acceptance of your imperfections will improve your sense of worth and confidence and lessen negative emotions, such as guilt, regret, and shame.
Accept the fact that, as similar as we all are, we use different methods to recharge ourselves. In contrast, your spouse needs alone time without distractions to reboot mentally and prepare for the following day. In the pre-pandemic world, if there were a mismatch in what a couple needed to feel rejuvenated, they could independently compensate and search for fulfillment outside of the home. Before stay-at-home orders were rolled out throughout the country, spouses had ample opportunities to spend time away from their partners at work, dinner with friends, or while squeezing in a 7 p.m. yoga sculpt class – barely getting home in time to kiss our children goodnight – with a few minutes to spare to engage in mundane conversation with our partners before our nighttime routine of TV commenced. Unfortunately, COVID-19 has made it very hard for couples to carve out that time for compensatory activities outside of the home.
Remember that you are a team
Remind yourself of the reason why you initially fell in love with your partner. Teammates do not keep score or compete with one another. They support each other when one player is not feeling well, and they make sacrifices for the betterment of the team.
Your marriage vows included “through sickness and health” and now should include “through quarantine.”
Dr. Abraham is a psychiatrist in private practice in Philadelphia. She has no disclosures.
Tips for marriage survival during a pandemic
Tips for marriage survival during a pandemic
Most married couples vowed to stay with their partners during sickness and health, but none of us vowed to remain trapped with our loved ones behind the same four walls, all day, every day, for an unknown period of time. We didn’t sign up for this! Some romantics may be titillated by the prospect, while more independent partners may panic at the mere thought of spending all day and night with their loved ones.
Because of the swift implementation of the lifestyle-altering restrictions, couples did not have ample time to mentally and physically prepare. A lack of preparation and loss of control heightens our emotions. It can make couples more susceptible to engage in unhealthy styles of communication and destructive behaviors that are harmful to their relationships.
There are psychological reasons that “absence makes the heart grow fonder.” Distance from your partner is not just a clever way to make your partner appreciate and desire you more. It is human nature to habituate to what is part of your daily life. For instance, when your partner is away from you while on a work trip, you may find the first night or two alone relaxing; but by day 3, you begin to miss your partner’s hugs and kisses, smell, and touch. And after many days apart, you may even miss the incessant nagging that secretly motivates you. Physical distance from our partners essentially gives us the ability to long for and appreciate each other. Our brains are wired to pay more attention to things that are novel and exciting and less interested in what is in our everyday lives.
Separation gives us the ability to miss our partners, while quarantine does the complete opposite.
To avoid contemplating how to murder one’s spouse before quarantine ends, partners can strengthen their relationships by using the strategies I’ve outlined below, which are loosely based on dialectical behavior therapy (DBT). These strategies can be useful for anyone – providers and patients alike – going through these struggles.
Dialectical behavior therapy was developed by psychologist Marsha Linehan PhD, to help regulate emotions for people diagnosed with borderline personality disorder. These skills help to identify thoughts and feelings, to accept one’s inner emotional world and outward behaviors. The idea is that, once you can recognize and accept, then change is possible. The “dialectic” in dialectical behavior therapy implies that one is attempting to find a balance between acceptance and change. All of us can benefit from these skills, especially emotionally volatile couples who are trapped together in quarantine.
Radically accept what is uncertain in your lives
Radical acceptance is a practice used in DBT in situations that are out of our control, such as the COVID-19 pandemic. Radically accept that you and your partner are trapped in quarantine without attempting to place blame on our government, your spouse, your boss, and even yourself. Radical acceptance is exactly what the name implies. Accept your current situation for what it is and not what you hoped it to be.
Accept the unknown and unanswered questions such as when will this quarantine end? Will there be a summer camp? Will I get back to my office this summer? Will my children even return to school in the fall? The acceptance of what is out of your control will ultimately decrease your mental time spent worrying and obsessing about the uncertainties of your post-quarantine life and instead provide you more time to be present with your spouse.
Remain mindful during all communication with your spouse. To stay in the moment, you need to be aware of your bodily reactions to distress and notice when your heart rate increases, breathing becomes more shallow, stomach muscles tighten, and when your thoughts become more negative. Mindfulness skills enable us to use physiological changes in our body to become aware of our emotions. You can use your partner’s nonverbal body language and tone of voice to gauge that person’s emotional reactivity.
The practice of mindfulness leads to an increased emotional intelligence. The goal is to have enough self-awareness and emotional understanding of your partner and enough empathy to know when a conversation is becoming too emotionally charged and to let it go and back off. Mindfulness is not nagging your partner to remember to change the heating unit filters with a reminder of what happened years ago when this wasn’t done promptly – without first checking in to make sure your partner is emotionally ready for this type of conversation.
When we have strong emotions, we are using the more primitive parts of our brain that induce a fight or flight reaction. These emotional reactions overshadow the more advanced prefrontal region of our brain that stores our rational thoughts and reasoning skills, a concept identified by psychologist Daniel Goleman as “emotional hijacking.”
Use distress tolerance skills to deal with negative emotions
Distress tolerance is an individual’s ability to manage feelings in response to stress. Distress tolerance skills are aimed at helping one manage intense emotions without worsening a situation by engaging in behaviors that are destructive and may exacerbate the problem. The goal is to tolerate the stress while with your partner and not respond negatively or in a way that is harmful to the integrity of your relationship.
To prioritize your relationship, this may mean that you choose not to react negatively when your partner makes a passive-aggressive comment on how you spent your day during quarantine since you still have a pile of laundry on your bedroom floor and overflowing dishes in the kitchen sink. A high level of distress tolerance will enable you to not overreact or withdraw from your spouse when flooded with emotions of anger or sadness.
Distraction techniques are a type of distress tolerance skill. You can engage in activities that keep you distracted and require your full attention. When things get heated between you and your spouse during quarantine, try to obtain some distance from each other to cool down and engage in an activity that involves your full concentration.
Many of us have been surprised by our hidden talents that were discovered during the quarantine. Use the time away from your partner to distract yourself with your new passion for writing, baking, organizing, and even your newfound love of balloon artistry. Do an activity that engages your mind and provides you the necessary physical and mental time away from your partner to deescalate. You can always revisit the initial cause of the conflict when both you and your partner are not emotionally charged. You can also distract yourself with self-soothing tactics such as taking a warm bath or a reading good book. Perhaps distract yourself by giving back to others and spending time planning a drive-by surprise party for your sister’s birthday next month. It can be helpful to distract yourself by comparing yourself to others less fortunate than you or a time in your life when you and your partner were struggling much worse than now, to provide perspective. The goal is not to add to your distress but instead, provide yourself a sense of perspective.
Use interpersonal effectiveness skills to establish a healthy relationship
Be gentle in all your communications with your partner, think about your spouse’s perspective, show empathy and interest in what your partner has to say by your verbal communication or body language, such as maintaining eye contact, and offer recognitional cues, such as “uh-huh” and “oh, really.” Avoid communication that is at all invalidating. Never start a sentence with “YOU” while having heated conversations with your spouse; instead, use “I feel” statements. This type of communication avoids the blame game that gets many couples into trouble.
Instead, communicate how you feel while not necessarily blaming your spouse but rather expressing your emotions. This will ultimately lead to less defensive communication from your partner. Remember that not all communication is for the sole purpose of communicating. Much of the time, communication is used as an attempt for one partner to connect with the other partner. Couples may say that they have difficulty with communication when it is not the communication that is the issue but instead the underlying disconnect of the couple.
This disconnect usually manifests while couples are communicating, and therefore, can be misconstrued as solely a communication issue by the couple. When your partner asks you to stop staring at your phone during dinner, it is not necessarily that your spouse is attempting to control you or wants to engage in some deep conversation, but more likely a bid to try to connect with you. Your partner is attempting to tell you that he or she feels disconnected, misses you, and wants to reconnect.
Provide validation and acceptance to your partner
Focus on your partner’s strengths and accept the weaknesses. Accept that your partner is scattered, disorganized, and takes at least 20 minutes to find the phone and keys every morning. Remember that during your courtship days, you found your partner’s flighty attributes to be endearing. Do the same for your strengths and weaknesses.
Accept that the pandemic is unpredictable and that you may need to strengthen your ability to be flexible and more adaptable. This will ultimately lead to feeling less disappointment by your partner and more accepting of shortcomings. Acceptance of your imperfections will improve your sense of worth and confidence and lessen negative emotions, such as guilt, regret, and shame.
Accept the fact that, as similar as we all are, we use different methods to recharge ourselves. In contrast, your spouse needs alone time without distractions to reboot mentally and prepare for the following day. In the pre-pandemic world, if there were a mismatch in what a couple needed to feel rejuvenated, they could independently compensate and search for fulfillment outside of the home. Before stay-at-home orders were rolled out throughout the country, spouses had ample opportunities to spend time away from their partners at work, dinner with friends, or while squeezing in a 7 p.m. yoga sculpt class – barely getting home in time to kiss our children goodnight – with a few minutes to spare to engage in mundane conversation with our partners before our nighttime routine of TV commenced. Unfortunately, COVID-19 has made it very hard for couples to carve out that time for compensatory activities outside of the home.
Remember that you are a team
Remind yourself of the reason why you initially fell in love with your partner. Teammates do not keep score or compete with one another. They support each other when one player is not feeling well, and they make sacrifices for the betterment of the team.
Your marriage vows included “through sickness and health” and now should include “through quarantine.”
Dr. Abraham is a psychiatrist in private practice in Philadelphia. She has no disclosures.
Most married couples vowed to stay with their partners during sickness and health, but none of us vowed to remain trapped with our loved ones behind the same four walls, all day, every day, for an unknown period of time. We didn’t sign up for this! Some romantics may be titillated by the prospect, while more independent partners may panic at the mere thought of spending all day and night with their loved ones.
Because of the swift implementation of the lifestyle-altering restrictions, couples did not have ample time to mentally and physically prepare. A lack of preparation and loss of control heightens our emotions. It can make couples more susceptible to engage in unhealthy styles of communication and destructive behaviors that are harmful to their relationships.
There are psychological reasons that “absence makes the heart grow fonder.” Distance from your partner is not just a clever way to make your partner appreciate and desire you more. It is human nature to habituate to what is part of your daily life. For instance, when your partner is away from you while on a work trip, you may find the first night or two alone relaxing; but by day 3, you begin to miss your partner’s hugs and kisses, smell, and touch. And after many days apart, you may even miss the incessant nagging that secretly motivates you. Physical distance from our partners essentially gives us the ability to long for and appreciate each other. Our brains are wired to pay more attention to things that are novel and exciting and less interested in what is in our everyday lives.
Separation gives us the ability to miss our partners, while quarantine does the complete opposite.
To avoid contemplating how to murder one’s spouse before quarantine ends, partners can strengthen their relationships by using the strategies I’ve outlined below, which are loosely based on dialectical behavior therapy (DBT). These strategies can be useful for anyone – providers and patients alike – going through these struggles.
Dialectical behavior therapy was developed by psychologist Marsha Linehan PhD, to help regulate emotions for people diagnosed with borderline personality disorder. These skills help to identify thoughts and feelings, to accept one’s inner emotional world and outward behaviors. The idea is that, once you can recognize and accept, then change is possible. The “dialectic” in dialectical behavior therapy implies that one is attempting to find a balance between acceptance and change. All of us can benefit from these skills, especially emotionally volatile couples who are trapped together in quarantine.
Radically accept what is uncertain in your lives
Radical acceptance is a practice used in DBT in situations that are out of our control, such as the COVID-19 pandemic. Radically accept that you and your partner are trapped in quarantine without attempting to place blame on our government, your spouse, your boss, and even yourself. Radical acceptance is exactly what the name implies. Accept your current situation for what it is and not what you hoped it to be.
Accept the unknown and unanswered questions such as when will this quarantine end? Will there be a summer camp? Will I get back to my office this summer? Will my children even return to school in the fall? The acceptance of what is out of your control will ultimately decrease your mental time spent worrying and obsessing about the uncertainties of your post-quarantine life and instead provide you more time to be present with your spouse.
Remain mindful during all communication with your spouse. To stay in the moment, you need to be aware of your bodily reactions to distress and notice when your heart rate increases, breathing becomes more shallow, stomach muscles tighten, and when your thoughts become more negative. Mindfulness skills enable us to use physiological changes in our body to become aware of our emotions. You can use your partner’s nonverbal body language and tone of voice to gauge that person’s emotional reactivity.
The practice of mindfulness leads to an increased emotional intelligence. The goal is to have enough self-awareness and emotional understanding of your partner and enough empathy to know when a conversation is becoming too emotionally charged and to let it go and back off. Mindfulness is not nagging your partner to remember to change the heating unit filters with a reminder of what happened years ago when this wasn’t done promptly – without first checking in to make sure your partner is emotionally ready for this type of conversation.
When we have strong emotions, we are using the more primitive parts of our brain that induce a fight or flight reaction. These emotional reactions overshadow the more advanced prefrontal region of our brain that stores our rational thoughts and reasoning skills, a concept identified by psychologist Daniel Goleman as “emotional hijacking.”
Use distress tolerance skills to deal with negative emotions
Distress tolerance is an individual’s ability to manage feelings in response to stress. Distress tolerance skills are aimed at helping one manage intense emotions without worsening a situation by engaging in behaviors that are destructive and may exacerbate the problem. The goal is to tolerate the stress while with your partner and not respond negatively or in a way that is harmful to the integrity of your relationship.
To prioritize your relationship, this may mean that you choose not to react negatively when your partner makes a passive-aggressive comment on how you spent your day during quarantine since you still have a pile of laundry on your bedroom floor and overflowing dishes in the kitchen sink. A high level of distress tolerance will enable you to not overreact or withdraw from your spouse when flooded with emotions of anger or sadness.
Distraction techniques are a type of distress tolerance skill. You can engage in activities that keep you distracted and require your full attention. When things get heated between you and your spouse during quarantine, try to obtain some distance from each other to cool down and engage in an activity that involves your full concentration.
Many of us have been surprised by our hidden talents that were discovered during the quarantine. Use the time away from your partner to distract yourself with your new passion for writing, baking, organizing, and even your newfound love of balloon artistry. Do an activity that engages your mind and provides you the necessary physical and mental time away from your partner to deescalate. You can always revisit the initial cause of the conflict when both you and your partner are not emotionally charged. You can also distract yourself with self-soothing tactics such as taking a warm bath or a reading good book. Perhaps distract yourself by giving back to others and spending time planning a drive-by surprise party for your sister’s birthday next month. It can be helpful to distract yourself by comparing yourself to others less fortunate than you or a time in your life when you and your partner were struggling much worse than now, to provide perspective. The goal is not to add to your distress but instead, provide yourself a sense of perspective.
Use interpersonal effectiveness skills to establish a healthy relationship
Be gentle in all your communications with your partner, think about your spouse’s perspective, show empathy and interest in what your partner has to say by your verbal communication or body language, such as maintaining eye contact, and offer recognitional cues, such as “uh-huh” and “oh, really.” Avoid communication that is at all invalidating. Never start a sentence with “YOU” while having heated conversations with your spouse; instead, use “I feel” statements. This type of communication avoids the blame game that gets many couples into trouble.
Instead, communicate how you feel while not necessarily blaming your spouse but rather expressing your emotions. This will ultimately lead to less defensive communication from your partner. Remember that not all communication is for the sole purpose of communicating. Much of the time, communication is used as an attempt for one partner to connect with the other partner. Couples may say that they have difficulty with communication when it is not the communication that is the issue but instead the underlying disconnect of the couple.
This disconnect usually manifests while couples are communicating, and therefore, can be misconstrued as solely a communication issue by the couple. When your partner asks you to stop staring at your phone during dinner, it is not necessarily that your spouse is attempting to control you or wants to engage in some deep conversation, but more likely a bid to try to connect with you. Your partner is attempting to tell you that he or she feels disconnected, misses you, and wants to reconnect.
Provide validation and acceptance to your partner
Focus on your partner’s strengths and accept the weaknesses. Accept that your partner is scattered, disorganized, and takes at least 20 minutes to find the phone and keys every morning. Remember that during your courtship days, you found your partner’s flighty attributes to be endearing. Do the same for your strengths and weaknesses.
Accept that the pandemic is unpredictable and that you may need to strengthen your ability to be flexible and more adaptable. This will ultimately lead to feeling less disappointment by your partner and more accepting of shortcomings. Acceptance of your imperfections will improve your sense of worth and confidence and lessen negative emotions, such as guilt, regret, and shame.
Accept the fact that, as similar as we all are, we use different methods to recharge ourselves. In contrast, your spouse needs alone time without distractions to reboot mentally and prepare for the following day. In the pre-pandemic world, if there were a mismatch in what a couple needed to feel rejuvenated, they could independently compensate and search for fulfillment outside of the home. Before stay-at-home orders were rolled out throughout the country, spouses had ample opportunities to spend time away from their partners at work, dinner with friends, or while squeezing in a 7 p.m. yoga sculpt class – barely getting home in time to kiss our children goodnight – with a few minutes to spare to engage in mundane conversation with our partners before our nighttime routine of TV commenced. Unfortunately, COVID-19 has made it very hard for couples to carve out that time for compensatory activities outside of the home.
Remember that you are a team
Remind yourself of the reason why you initially fell in love with your partner. Teammates do not keep score or compete with one another. They support each other when one player is not feeling well, and they make sacrifices for the betterment of the team.
Your marriage vows included “through sickness and health” and now should include “through quarantine.”
Dr. Abraham is a psychiatrist in private practice in Philadelphia. She has no disclosures.