User login
Cognitive-behavioral therapy a standout for better immune function
Psychosocial interventions, particularly cognitive-behavioral therapy (CBT), are associated with enhanced immune system function, new research suggests.
Results of a systematic review and meta-analysis that included 56 randomized controlled trials and more than 4,000 participants showed that over time, psychosocial interventions appeared to augment beneficial immune system function while concurrently decreasing harmful immune system function in comparison with control conditions.
“These associations were most reliable for cognitive-behavioral therapy and multiple or combined interventions and for studies that assessed proinflammatory cytokines or markers, which are key indicators of inflammation in the body,” study investigator George M. Slavich, PhD, said in an interview.
“The analysis helps address the question of which types of psychosocial interventions are most consistently associated with changes in immune system function, under what conditions, and for whom. This knowledge could, in turn, be used to inform research efforts and public policy aimed at using psychosocial interventions to improve immune-related health outcomes,” added Dr. Slavich, director of the Laboratory for Stress Assessment and Research, University of California, Los Angeles.
The study was published online June 3 in JAMA Psychiatry.
Link to serious physical, mental illnesses
There is substantial evidence that the immune system plays a role in a variety of mental and physical health problems. Such problems include anxiety disorders, depression, suicide, schizophrenia, cardiovascular disease, autoimmune disorders, and neurodegenerative diseases. It has been recently suggested that more than half of all deaths worldwide are attributable to inflammation-related conditions.
Although pharmacologic interventions can play a role in addressing inflammation, they are not without drawbacks, most notably, cost and adverse side effects.
The World Health Organization, the National Academy of Medicine, the National Institutes of Health, and other groups have emphasized the importance of addressing global disease burden through psychosocial interventions when possible.
Such recommendations are supported by scientific evidence. Previous research has shown that immune system processes are influenced by a variety of social, neurocognitive, and behavioral factors.
Given such findings, researchers have examined the effects of interventions that reduce stress or bolster psychological resources on immune system function.
However, such research has yielded conflicting findings. Some studies show that psychosocial interventions clearly enhance immunity, whereas others do not.
In addition, questions remain regarding which types of interventions reliably improve immune system function, under what conditions, and for whom.
“Research has shown that psychological factors – such as life stress, negative emotions, and social support – are associated with changes in immune system function,” Dr. Slavich noted.
“In addition, there is growing appreciation that immune system processes involved in inflammation may contribute to peoples’ risk for several major mental and physical health problems, including anxiety disorders, depression, heart disease, and autoimmune and neurodegenerative disorders.”
First study of its kind
To shed light on these potential links, the researchers conducted what they believe is the first systematic review and meta-analysis of randomized clinical trials of the effects of psychosocial interventions on immune system outcomes.
As part of the review, Dr. Slavich and colleagues estimated the associations between eight psychosocial interventions and seven markers of immune system function.
The eight psychosocial interventions were behavior therapy, cognitive therapy, CBT, CBT plus additive treatment or mode of delivery, bereavement or supportive therapy, multiple or combined interventions, other psychotherapy, and psychoeducation.
The seven immune outcomes that might be influenced by these interventions are proinflammatory cytokines and markers, anti-inflammatory cytokines, antibodies, immune cell counts, natural killer cell activity, viral load, and other immune outcomes.
The researchers also examined nine potential factors that might moderate the associations between psychosocial interventions and immune system function.
They searched a variety of databases for all relevant randomized controlled trials published through Dec. 31, 2018. Studies were eligible for inclusion if they included a psychosocial intervention and immune outcome, as well as preintervention and postintervention immunologic assessments.
The researchers identified 4,621 studies. Of these studies, 62 were eligible for inclusion; 56, which included 4,060 patients, were included in the final meta-analysis.
Results showed that psychosocial interventions were associated with enhanced immune system function (P < .001). There was relatively low heterogeneity between studies in these effect sizes, which, the investigators said, indicates that the association was relatively consistent across studies and conditions.
The meta-analysis showed that individuals who were assigned to a psychosocial intervention condition demonstrated a 14.7% improvement (95% confidence interval [CI], 5.7%–23.8%) in beneficial immune system function compared with their counterparts who were assigned to a control condition.
Similarly, participants who received psychosocial interventions demonstrated an 18.0% decrease (95% CI, 7.2%–28.8%) in harmful immune system function over time.
A standout
Regarding the effect of the type of intervention on the association, only CBT (31 studies; P < .001) and multiple or combined interventions (seven studies; P = .01) were significantly associated with changes in immune system outcomes.
The analysis also found that interventions that included a group component were more consistently associated with enhanced immune function than were those that did not include a group component. Nevertheless, this difference did not reach statistical significance (P = .06).
Contrary to the researchers’ expectations, the analysis also revealed that intervention length did not moderate the association between psychosocial interventions and immune system function (P = .93).
With respect to the type of immune marker studied, the meta-analysis found that psychosocial interventions had significantly different associations with the various immune markers studied. Of the seven immune outcomes investigated, only proinflammatory cytokine or marker levels (33 studies; P < .001) and immune cell counts (27 studies; P < .001) were significantly associated with the psychosocial interventions examined.
and were robust across age, sex, and intervention duration.
These results suggest that psychosocial interventions – particularly CBT and multiple or combined psychotherapeutic modalities – may play an important role in improving immune-related health outcomes.
Such interventions may not only be effective, they may also prove to be affordable alternatives to current therapeutic options. The mean length of a CBT intervention in the meta-analysis was 10.4 weeks, which the investigators equated with a total cost of $1,560 per patient.
“By comparison, the cost of using infliximab to reduce inflammation in persons with an autoimmune disorder is approximately $25,000 per patient per year,” they wrote.
“The results suggest the possibility that psychotherapy may be helpful for reducing inflammation and improving immune-related health in certain circumstances,” Dr. Slavich concluded. “However, the studies that we examined differed in terms of their quality, and we did not examine health outcomes in the present investigation.
“Therefore, more research needs to be done to determine how the present findings might be translated into treatment options or public policy.”
A path to better health
In an accompanying editorial, Veronika Engert, PhD, Joshua A. Grant, PhD, and Bernhard Strauss, PhD, noted that although infectious disease was once the primary cause of death in society, it has been supplanted by other complex and chronic illnesses, which often do not follow simple cause-and-effect associations.
“Rather,” they wrote, “these illnesses develop from a complex milieu of biological, psychological, and social factors that may also influence the disease progress and its prognosis. Against this backdrop, the meta-analysis by Shields and colleagues is an important confirmation of the biopsychosocial model.”
The editorialists explained that recent psychophysiological, neurobiological, and epigenetic research offers a glimpse into the relationship between psychological and social factors in pathogenesis. Nevertheless, the authors noted that a comprehensive examination of the potential effects of psychosocial interventions on immune parameters in various physical health conditions has been lacking.
“The evidence provided by Shields et al. is exactly what is needed to more fully shift treatment from an illness-centered to a patient-centered approach,” they wrote. “To that end, this meta-analysis may serve as a guide for policy makers aiming to improve immune-associated health.”
The research was supported by a Society in Science–Branco Weiss Fellowship, Brain and Behavior Research, and the National Institutes of Health. Dr. Slavich, Dr. Engert, Dr. Grant, and Dr. Strauss have disclosed no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
Psychosocial interventions, particularly cognitive-behavioral therapy (CBT), are associated with enhanced immune system function, new research suggests.
Results of a systematic review and meta-analysis that included 56 randomized controlled trials and more than 4,000 participants showed that over time, psychosocial interventions appeared to augment beneficial immune system function while concurrently decreasing harmful immune system function in comparison with control conditions.
“These associations were most reliable for cognitive-behavioral therapy and multiple or combined interventions and for studies that assessed proinflammatory cytokines or markers, which are key indicators of inflammation in the body,” study investigator George M. Slavich, PhD, said in an interview.
“The analysis helps address the question of which types of psychosocial interventions are most consistently associated with changes in immune system function, under what conditions, and for whom. This knowledge could, in turn, be used to inform research efforts and public policy aimed at using psychosocial interventions to improve immune-related health outcomes,” added Dr. Slavich, director of the Laboratory for Stress Assessment and Research, University of California, Los Angeles.
The study was published online June 3 in JAMA Psychiatry.
Link to serious physical, mental illnesses
There is substantial evidence that the immune system plays a role in a variety of mental and physical health problems. Such problems include anxiety disorders, depression, suicide, schizophrenia, cardiovascular disease, autoimmune disorders, and neurodegenerative diseases. It has been recently suggested that more than half of all deaths worldwide are attributable to inflammation-related conditions.
Although pharmacologic interventions can play a role in addressing inflammation, they are not without drawbacks, most notably, cost and adverse side effects.
The World Health Organization, the National Academy of Medicine, the National Institutes of Health, and other groups have emphasized the importance of addressing global disease burden through psychosocial interventions when possible.
Such recommendations are supported by scientific evidence. Previous research has shown that immune system processes are influenced by a variety of social, neurocognitive, and behavioral factors.
Given such findings, researchers have examined the effects of interventions that reduce stress or bolster psychological resources on immune system function.
However, such research has yielded conflicting findings. Some studies show that psychosocial interventions clearly enhance immunity, whereas others do not.
In addition, questions remain regarding which types of interventions reliably improve immune system function, under what conditions, and for whom.
“Research has shown that psychological factors – such as life stress, negative emotions, and social support – are associated with changes in immune system function,” Dr. Slavich noted.
“In addition, there is growing appreciation that immune system processes involved in inflammation may contribute to peoples’ risk for several major mental and physical health problems, including anxiety disorders, depression, heart disease, and autoimmune and neurodegenerative disorders.”
First study of its kind
To shed light on these potential links, the researchers conducted what they believe is the first systematic review and meta-analysis of randomized clinical trials of the effects of psychosocial interventions on immune system outcomes.
As part of the review, Dr. Slavich and colleagues estimated the associations between eight psychosocial interventions and seven markers of immune system function.
The eight psychosocial interventions were behavior therapy, cognitive therapy, CBT, CBT plus additive treatment or mode of delivery, bereavement or supportive therapy, multiple or combined interventions, other psychotherapy, and psychoeducation.
The seven immune outcomes that might be influenced by these interventions are proinflammatory cytokines and markers, anti-inflammatory cytokines, antibodies, immune cell counts, natural killer cell activity, viral load, and other immune outcomes.
The researchers also examined nine potential factors that might moderate the associations between psychosocial interventions and immune system function.
They searched a variety of databases for all relevant randomized controlled trials published through Dec. 31, 2018. Studies were eligible for inclusion if they included a psychosocial intervention and immune outcome, as well as preintervention and postintervention immunologic assessments.
The researchers identified 4,621 studies. Of these studies, 62 were eligible for inclusion; 56, which included 4,060 patients, were included in the final meta-analysis.
Results showed that psychosocial interventions were associated with enhanced immune system function (P < .001). There was relatively low heterogeneity between studies in these effect sizes, which, the investigators said, indicates that the association was relatively consistent across studies and conditions.
The meta-analysis showed that individuals who were assigned to a psychosocial intervention condition demonstrated a 14.7% improvement (95% confidence interval [CI], 5.7%–23.8%) in beneficial immune system function compared with their counterparts who were assigned to a control condition.
Similarly, participants who received psychosocial interventions demonstrated an 18.0% decrease (95% CI, 7.2%–28.8%) in harmful immune system function over time.
A standout
Regarding the effect of the type of intervention on the association, only CBT (31 studies; P < .001) and multiple or combined interventions (seven studies; P = .01) were significantly associated with changes in immune system outcomes.
The analysis also found that interventions that included a group component were more consistently associated with enhanced immune function than were those that did not include a group component. Nevertheless, this difference did not reach statistical significance (P = .06).
Contrary to the researchers’ expectations, the analysis also revealed that intervention length did not moderate the association between psychosocial interventions and immune system function (P = .93).
With respect to the type of immune marker studied, the meta-analysis found that psychosocial interventions had significantly different associations with the various immune markers studied. Of the seven immune outcomes investigated, only proinflammatory cytokine or marker levels (33 studies; P < .001) and immune cell counts (27 studies; P < .001) were significantly associated with the psychosocial interventions examined.
and were robust across age, sex, and intervention duration.
These results suggest that psychosocial interventions – particularly CBT and multiple or combined psychotherapeutic modalities – may play an important role in improving immune-related health outcomes.
Such interventions may not only be effective, they may also prove to be affordable alternatives to current therapeutic options. The mean length of a CBT intervention in the meta-analysis was 10.4 weeks, which the investigators equated with a total cost of $1,560 per patient.
“By comparison, the cost of using infliximab to reduce inflammation in persons with an autoimmune disorder is approximately $25,000 per patient per year,” they wrote.
“The results suggest the possibility that psychotherapy may be helpful for reducing inflammation and improving immune-related health in certain circumstances,” Dr. Slavich concluded. “However, the studies that we examined differed in terms of their quality, and we did not examine health outcomes in the present investigation.
“Therefore, more research needs to be done to determine how the present findings might be translated into treatment options or public policy.”
A path to better health
In an accompanying editorial, Veronika Engert, PhD, Joshua A. Grant, PhD, and Bernhard Strauss, PhD, noted that although infectious disease was once the primary cause of death in society, it has been supplanted by other complex and chronic illnesses, which often do not follow simple cause-and-effect associations.
“Rather,” they wrote, “these illnesses develop from a complex milieu of biological, psychological, and social factors that may also influence the disease progress and its prognosis. Against this backdrop, the meta-analysis by Shields and colleagues is an important confirmation of the biopsychosocial model.”
The editorialists explained that recent psychophysiological, neurobiological, and epigenetic research offers a glimpse into the relationship between psychological and social factors in pathogenesis. Nevertheless, the authors noted that a comprehensive examination of the potential effects of psychosocial interventions on immune parameters in various physical health conditions has been lacking.
“The evidence provided by Shields et al. is exactly what is needed to more fully shift treatment from an illness-centered to a patient-centered approach,” they wrote. “To that end, this meta-analysis may serve as a guide for policy makers aiming to improve immune-associated health.”
The research was supported by a Society in Science–Branco Weiss Fellowship, Brain and Behavior Research, and the National Institutes of Health. Dr. Slavich, Dr. Engert, Dr. Grant, and Dr. Strauss have disclosed no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
Psychosocial interventions, particularly cognitive-behavioral therapy (CBT), are associated with enhanced immune system function, new research suggests.
Results of a systematic review and meta-analysis that included 56 randomized controlled trials and more than 4,000 participants showed that over time, psychosocial interventions appeared to augment beneficial immune system function while concurrently decreasing harmful immune system function in comparison with control conditions.
“These associations were most reliable for cognitive-behavioral therapy and multiple or combined interventions and for studies that assessed proinflammatory cytokines or markers, which are key indicators of inflammation in the body,” study investigator George M. Slavich, PhD, said in an interview.
“The analysis helps address the question of which types of psychosocial interventions are most consistently associated with changes in immune system function, under what conditions, and for whom. This knowledge could, in turn, be used to inform research efforts and public policy aimed at using psychosocial interventions to improve immune-related health outcomes,” added Dr. Slavich, director of the Laboratory for Stress Assessment and Research, University of California, Los Angeles.
The study was published online June 3 in JAMA Psychiatry.
Link to serious physical, mental illnesses
There is substantial evidence that the immune system plays a role in a variety of mental and physical health problems. Such problems include anxiety disorders, depression, suicide, schizophrenia, cardiovascular disease, autoimmune disorders, and neurodegenerative diseases. It has been recently suggested that more than half of all deaths worldwide are attributable to inflammation-related conditions.
Although pharmacologic interventions can play a role in addressing inflammation, they are not without drawbacks, most notably, cost and adverse side effects.
The World Health Organization, the National Academy of Medicine, the National Institutes of Health, and other groups have emphasized the importance of addressing global disease burden through psychosocial interventions when possible.
Such recommendations are supported by scientific evidence. Previous research has shown that immune system processes are influenced by a variety of social, neurocognitive, and behavioral factors.
Given such findings, researchers have examined the effects of interventions that reduce stress or bolster psychological resources on immune system function.
However, such research has yielded conflicting findings. Some studies show that psychosocial interventions clearly enhance immunity, whereas others do not.
In addition, questions remain regarding which types of interventions reliably improve immune system function, under what conditions, and for whom.
“Research has shown that psychological factors – such as life stress, negative emotions, and social support – are associated with changes in immune system function,” Dr. Slavich noted.
“In addition, there is growing appreciation that immune system processes involved in inflammation may contribute to peoples’ risk for several major mental and physical health problems, including anxiety disorders, depression, heart disease, and autoimmune and neurodegenerative disorders.”
First study of its kind
To shed light on these potential links, the researchers conducted what they believe is the first systematic review and meta-analysis of randomized clinical trials of the effects of psychosocial interventions on immune system outcomes.
As part of the review, Dr. Slavich and colleagues estimated the associations between eight psychosocial interventions and seven markers of immune system function.
The eight psychosocial interventions were behavior therapy, cognitive therapy, CBT, CBT plus additive treatment or mode of delivery, bereavement or supportive therapy, multiple or combined interventions, other psychotherapy, and psychoeducation.
The seven immune outcomes that might be influenced by these interventions are proinflammatory cytokines and markers, anti-inflammatory cytokines, antibodies, immune cell counts, natural killer cell activity, viral load, and other immune outcomes.
The researchers also examined nine potential factors that might moderate the associations between psychosocial interventions and immune system function.
They searched a variety of databases for all relevant randomized controlled trials published through Dec. 31, 2018. Studies were eligible for inclusion if they included a psychosocial intervention and immune outcome, as well as preintervention and postintervention immunologic assessments.
The researchers identified 4,621 studies. Of these studies, 62 were eligible for inclusion; 56, which included 4,060 patients, were included in the final meta-analysis.
Results showed that psychosocial interventions were associated with enhanced immune system function (P < .001). There was relatively low heterogeneity between studies in these effect sizes, which, the investigators said, indicates that the association was relatively consistent across studies and conditions.
The meta-analysis showed that individuals who were assigned to a psychosocial intervention condition demonstrated a 14.7% improvement (95% confidence interval [CI], 5.7%–23.8%) in beneficial immune system function compared with their counterparts who were assigned to a control condition.
Similarly, participants who received psychosocial interventions demonstrated an 18.0% decrease (95% CI, 7.2%–28.8%) in harmful immune system function over time.
A standout
Regarding the effect of the type of intervention on the association, only CBT (31 studies; P < .001) and multiple or combined interventions (seven studies; P = .01) were significantly associated with changes in immune system outcomes.
The analysis also found that interventions that included a group component were more consistently associated with enhanced immune function than were those that did not include a group component. Nevertheless, this difference did not reach statistical significance (P = .06).
Contrary to the researchers’ expectations, the analysis also revealed that intervention length did not moderate the association between psychosocial interventions and immune system function (P = .93).
With respect to the type of immune marker studied, the meta-analysis found that psychosocial interventions had significantly different associations with the various immune markers studied. Of the seven immune outcomes investigated, only proinflammatory cytokine or marker levels (33 studies; P < .001) and immune cell counts (27 studies; P < .001) were significantly associated with the psychosocial interventions examined.
and were robust across age, sex, and intervention duration.
These results suggest that psychosocial interventions – particularly CBT and multiple or combined psychotherapeutic modalities – may play an important role in improving immune-related health outcomes.
Such interventions may not only be effective, they may also prove to be affordable alternatives to current therapeutic options. The mean length of a CBT intervention in the meta-analysis was 10.4 weeks, which the investigators equated with a total cost of $1,560 per patient.
“By comparison, the cost of using infliximab to reduce inflammation in persons with an autoimmune disorder is approximately $25,000 per patient per year,” they wrote.
“The results suggest the possibility that psychotherapy may be helpful for reducing inflammation and improving immune-related health in certain circumstances,” Dr. Slavich concluded. “However, the studies that we examined differed in terms of their quality, and we did not examine health outcomes in the present investigation.
“Therefore, more research needs to be done to determine how the present findings might be translated into treatment options or public policy.”
A path to better health
In an accompanying editorial, Veronika Engert, PhD, Joshua A. Grant, PhD, and Bernhard Strauss, PhD, noted that although infectious disease was once the primary cause of death in society, it has been supplanted by other complex and chronic illnesses, which often do not follow simple cause-and-effect associations.
“Rather,” they wrote, “these illnesses develop from a complex milieu of biological, psychological, and social factors that may also influence the disease progress and its prognosis. Against this backdrop, the meta-analysis by Shields and colleagues is an important confirmation of the biopsychosocial model.”
The editorialists explained that recent psychophysiological, neurobiological, and epigenetic research offers a glimpse into the relationship between psychological and social factors in pathogenesis. Nevertheless, the authors noted that a comprehensive examination of the potential effects of psychosocial interventions on immune parameters in various physical health conditions has been lacking.
“The evidence provided by Shields et al. is exactly what is needed to more fully shift treatment from an illness-centered to a patient-centered approach,” they wrote. “To that end, this meta-analysis may serve as a guide for policy makers aiming to improve immune-associated health.”
The research was supported by a Society in Science–Branco Weiss Fellowship, Brain and Behavior Research, and the National Institutes of Health. Dr. Slavich, Dr. Engert, Dr. Grant, and Dr. Strauss have disclosed no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
Addressing suicide prevention among South Asian Americans
Multifaceted strategies are needed to address unique cultural factors
On first glance, the age-adjusted rate of suicide for Asian and Pacific Islander populations living in the United States looks comparatively low.
Over the past 2 decades in the United States, for example, the overall rate increased by 35%, from, 10.5 to 14.2 per 100,000 individuals. That compares with a rate of 7.0 per 100,000 among Asian and Pacific Islander communities.1
However, because of the aggregate nature (national suicide mortality data combine people of Asian, Native Hawaiian, and other Pacific Islander descent into a single group) in which these data are reported, a significant amount of salient information on subgroups of Asian Americans is lost.2 There is a growing body of research on the mental health of Asian Americans, but the dearth of information and research on suicide in South Asians is striking.3 In fact, a review of literature finds fewer than 10 articles on the topic that have been published in peer-reviewed journals in the last decade. to provide effective, culturally sensitive care.
Diverse group
There are 3.4 million individuals of South Asian descent in the United States. Geographically, South Asians may have familial and cultural/historical roots in Bangladesh, Bhutan, India, Maldives, Nepal, and Pakistan.4 They enjoy a rich diversity in terms of cultural and religious beliefs, language, socioeconomic status, modes of acculturation, and immigration patterns. Asian Indians are the largest group of South Asians in the United States. They are highly educated, with a larger proportion of them pursuing an undergraduate and/or graduate level education than the general population. The median household income of Asian Indians is also higher than the national average.5
In general, suicide, like all mental health issues, is a stigmatized and taboo topic in the South Asian community.6 Also, South Asian Americans are hesitant to seek mental health care because of a perceived inability of Western health care professionals to understand their cultural views. Extrapolation from data on South Asians in the United Kingdom, aggregate statistics for Asian Americans and Pacific Islanders, and studies on South Asians in the United States highlight two South Asian subgroups that are particularly vulnerable to suicide. These are young adults (aged 18-24 years) and women.7
Suicide is the second-leading cause of death for young Asian American men in the United States. Rates of lifetime suicidal ideation and attempts are higher among younger Asian Americans (aged 18-24 years) than among older Asian American adults. Young Asian American adults have been found to have higher levels of suicidal ideation than their white counterparts.8,9 Acculturation or assimilating into a different culture, familial violence as a child, hopelessness or a thought pattern with a pessimistic outlook, depression, and childhood sexual abuse have all been found to be positively correlated with suicidal ideation and attempted suicide in South Asian Americans. One study that conducted0 in-group analysis on undergraduate university students of South Asian descent living in New York found higher levels of hopelessness and depression in Asian Indians relative to Bangladeshi or Pakistani Americans.10
In addition, higher levels of suicidal ideation are reported in Asian Indians relative to Bangladeshi or Pakistani Americans. These results resemble findings from similar studies in the United Kingdom. A posited reason for these findings is a difference in religious beliefs. Pakistani and Bangladeshi Americans are predominantly Muslim, have stronger moral beliefs against suicide, and consider it a sin as defined by Islamic beliefs. Asian Indians, in contrast, are majority Hindu and believe in reincarnation – a context that might make suicide seem more permissible.11
South Asian women are particularly vulnerable to domestic violence, childhood sexual abuse, intimate partner violence, and/or familial violence. Cultural gender norms, traditional norms, and patriarchal ideology in the South Asian community make quantifying the level of childhood sexual abuse and familial violence a challenge. Furthermore, culturally, South Asian women are often considered subordinate relative to men, and discussion around family violence and childhood sexual abuse is avoided. Studies from the United Kingdom find a lack of knowledge around, disclosure of, and fear of reporting childhood sexual abuse in South Asian women. A study of a sample of representative South Asian American women found that 25.2% had experienced some form of childhood sexual abuse.12
Research also suggests that South Asians in the United States have some of the highest rates of intimate partner violence. Another study in the United States found that two out of five South Asian women have experienced physical and/or sexual intimate partner violence. This is much higher than the rate found in representative general U.S. population samples.
Literature suggests that exposure to these factors increases womens’ risk for suicidal ideation and attempted suicide. In the United Kingdom, research on South Asian women (aged 18-24 years) has found rates of attempted suicide to be three times higher than those of their white counterparts. Research from the United Kingdom and the United States suggests that younger married South Asian women are exposed to emotional and/or physical abuse from their spouse or in-laws, which is often a mediating factor in their increased risk for suicide.
Attempts to address suicide in the South Asian American community have to be multifaceted. An ideal approach would consist of educating, and connecting with, the community through ethnic media and trusted community sources, such as primary care doctors, caregivers, and social workers. In line with established American Psychological Association guidelines on caring for individuals of immigrant origin, health care professionals should document the patient’s number of generations in the country, number of years in the country, language fluency, family and community support, educational level, social status changes related to immigration, intimate relationships with people of different backgrounds, and stress related to acculturation. Special attention should be paid to South Asian women. Health care professionals should screen South Asian women for past and current intimate partner violence, provide culturally appropriate intimate partner violence resources, and be prepared to refer them to legal counseling services. Also, South Asian women should be screened for a history of exposure to familial violence and childhood sexual abuse.1
To adequately serve this population, there is a need to build capacity in the provision of culturally appropriate mental health services. Access to mental health care professionals through settings such as shelters for abused women, South Asian community–based organizations, youth centers, college counseling, and senior centers would encourage individuals to seek care without the threat of being stigmatized.
References
1. Hedegaard H et al. Suicide mortality in the United States, 1999–2017. NCHS Data Brief, No. 330. 2018 Nov.
2. Ahmad-Stout DJ and Nath SR. J College Stud Psychother. 2013 Jan 10;27(1):43-61.
3. Li H and Keshavan M. Asian J Psychiatry. 2011;4(1):1.
4. Nagaraj NC et al. J Immigr Minor Health. 2019 Oct;21(5):978-1003.
5. Nagaraj NC et al. J Comm Health. 2018;43(3):543-51.
6. Cao KO. Generations. 2014;30(4):82-5.
7. Hurwitz EJ et al. J Immigr Minor Health. 2006;8(3):251-61.
8. Polanco-Roman L et al. Cultur Divers Ethnic Minor Psychol. 2019 Dec 23. doi: 10.1037/cpd0000313.
9. Erausquin JT et al. J Youth Adolesc. 2019 Sep;48(9):1796-1805.
10. Lane R et al. Asian Am J Psychol. 2016;7(2):120-8.
11. Nath SR et al. Asian Am J Psychol. 2018;9(4):334-343.
12. Robertson HA et al. J Immigr Minor Health. 2016 Jul 31;18(4):921-7.
Mr. Kaleka is a medical student in the class of 2021 at Central Michigan University (CMU) College of Medicine, Mt. Pleasant. He has no disclosures. Mr. Kaleka would like to thank his mentor, Furhut Janssen, DO, for her continued guidance and support in research on mental health in immigrant populations.
Multifaceted strategies are needed to address unique cultural factors
Multifaceted strategies are needed to address unique cultural factors
On first glance, the age-adjusted rate of suicide for Asian and Pacific Islander populations living in the United States looks comparatively low.
Over the past 2 decades in the United States, for example, the overall rate increased by 35%, from, 10.5 to 14.2 per 100,000 individuals. That compares with a rate of 7.0 per 100,000 among Asian and Pacific Islander communities.1
However, because of the aggregate nature (national suicide mortality data combine people of Asian, Native Hawaiian, and other Pacific Islander descent into a single group) in which these data are reported, a significant amount of salient information on subgroups of Asian Americans is lost.2 There is a growing body of research on the mental health of Asian Americans, but the dearth of information and research on suicide in South Asians is striking.3 In fact, a review of literature finds fewer than 10 articles on the topic that have been published in peer-reviewed journals in the last decade. to provide effective, culturally sensitive care.
Diverse group
There are 3.4 million individuals of South Asian descent in the United States. Geographically, South Asians may have familial and cultural/historical roots in Bangladesh, Bhutan, India, Maldives, Nepal, and Pakistan.4 They enjoy a rich diversity in terms of cultural and religious beliefs, language, socioeconomic status, modes of acculturation, and immigration patterns. Asian Indians are the largest group of South Asians in the United States. They are highly educated, with a larger proportion of them pursuing an undergraduate and/or graduate level education than the general population. The median household income of Asian Indians is also higher than the national average.5
In general, suicide, like all mental health issues, is a stigmatized and taboo topic in the South Asian community.6 Also, South Asian Americans are hesitant to seek mental health care because of a perceived inability of Western health care professionals to understand their cultural views. Extrapolation from data on South Asians in the United Kingdom, aggregate statistics for Asian Americans and Pacific Islanders, and studies on South Asians in the United States highlight two South Asian subgroups that are particularly vulnerable to suicide. These are young adults (aged 18-24 years) and women.7
Suicide is the second-leading cause of death for young Asian American men in the United States. Rates of lifetime suicidal ideation and attempts are higher among younger Asian Americans (aged 18-24 years) than among older Asian American adults. Young Asian American adults have been found to have higher levels of suicidal ideation than their white counterparts.8,9 Acculturation or assimilating into a different culture, familial violence as a child, hopelessness or a thought pattern with a pessimistic outlook, depression, and childhood sexual abuse have all been found to be positively correlated with suicidal ideation and attempted suicide in South Asian Americans. One study that conducted0 in-group analysis on undergraduate university students of South Asian descent living in New York found higher levels of hopelessness and depression in Asian Indians relative to Bangladeshi or Pakistani Americans.10
In addition, higher levels of suicidal ideation are reported in Asian Indians relative to Bangladeshi or Pakistani Americans. These results resemble findings from similar studies in the United Kingdom. A posited reason for these findings is a difference in religious beliefs. Pakistani and Bangladeshi Americans are predominantly Muslim, have stronger moral beliefs against suicide, and consider it a sin as defined by Islamic beliefs. Asian Indians, in contrast, are majority Hindu and believe in reincarnation – a context that might make suicide seem more permissible.11
South Asian women are particularly vulnerable to domestic violence, childhood sexual abuse, intimate partner violence, and/or familial violence. Cultural gender norms, traditional norms, and patriarchal ideology in the South Asian community make quantifying the level of childhood sexual abuse and familial violence a challenge. Furthermore, culturally, South Asian women are often considered subordinate relative to men, and discussion around family violence and childhood sexual abuse is avoided. Studies from the United Kingdom find a lack of knowledge around, disclosure of, and fear of reporting childhood sexual abuse in South Asian women. A study of a sample of representative South Asian American women found that 25.2% had experienced some form of childhood sexual abuse.12
Research also suggests that South Asians in the United States have some of the highest rates of intimate partner violence. Another study in the United States found that two out of five South Asian women have experienced physical and/or sexual intimate partner violence. This is much higher than the rate found in representative general U.S. population samples.
Literature suggests that exposure to these factors increases womens’ risk for suicidal ideation and attempted suicide. In the United Kingdom, research on South Asian women (aged 18-24 years) has found rates of attempted suicide to be three times higher than those of their white counterparts. Research from the United Kingdom and the United States suggests that younger married South Asian women are exposed to emotional and/or physical abuse from their spouse or in-laws, which is often a mediating factor in their increased risk for suicide.
Attempts to address suicide in the South Asian American community have to be multifaceted. An ideal approach would consist of educating, and connecting with, the community through ethnic media and trusted community sources, such as primary care doctors, caregivers, and social workers. In line with established American Psychological Association guidelines on caring for individuals of immigrant origin, health care professionals should document the patient’s number of generations in the country, number of years in the country, language fluency, family and community support, educational level, social status changes related to immigration, intimate relationships with people of different backgrounds, and stress related to acculturation. Special attention should be paid to South Asian women. Health care professionals should screen South Asian women for past and current intimate partner violence, provide culturally appropriate intimate partner violence resources, and be prepared to refer them to legal counseling services. Also, South Asian women should be screened for a history of exposure to familial violence and childhood sexual abuse.1
To adequately serve this population, there is a need to build capacity in the provision of culturally appropriate mental health services. Access to mental health care professionals through settings such as shelters for abused women, South Asian community–based organizations, youth centers, college counseling, and senior centers would encourage individuals to seek care without the threat of being stigmatized.
References
1. Hedegaard H et al. Suicide mortality in the United States, 1999–2017. NCHS Data Brief, No. 330. 2018 Nov.
2. Ahmad-Stout DJ and Nath SR. J College Stud Psychother. 2013 Jan 10;27(1):43-61.
3. Li H and Keshavan M. Asian J Psychiatry. 2011;4(1):1.
4. Nagaraj NC et al. J Immigr Minor Health. 2019 Oct;21(5):978-1003.
5. Nagaraj NC et al. J Comm Health. 2018;43(3):543-51.
6. Cao KO. Generations. 2014;30(4):82-5.
7. Hurwitz EJ et al. J Immigr Minor Health. 2006;8(3):251-61.
8. Polanco-Roman L et al. Cultur Divers Ethnic Minor Psychol. 2019 Dec 23. doi: 10.1037/cpd0000313.
9. Erausquin JT et al. J Youth Adolesc. 2019 Sep;48(9):1796-1805.
10. Lane R et al. Asian Am J Psychol. 2016;7(2):120-8.
11. Nath SR et al. Asian Am J Psychol. 2018;9(4):334-343.
12. Robertson HA et al. J Immigr Minor Health. 2016 Jul 31;18(4):921-7.
Mr. Kaleka is a medical student in the class of 2021 at Central Michigan University (CMU) College of Medicine, Mt. Pleasant. He has no disclosures. Mr. Kaleka would like to thank his mentor, Furhut Janssen, DO, for her continued guidance and support in research on mental health in immigrant populations.
On first glance, the age-adjusted rate of suicide for Asian and Pacific Islander populations living in the United States looks comparatively low.
Over the past 2 decades in the United States, for example, the overall rate increased by 35%, from, 10.5 to 14.2 per 100,000 individuals. That compares with a rate of 7.0 per 100,000 among Asian and Pacific Islander communities.1
However, because of the aggregate nature (national suicide mortality data combine people of Asian, Native Hawaiian, and other Pacific Islander descent into a single group) in which these data are reported, a significant amount of salient information on subgroups of Asian Americans is lost.2 There is a growing body of research on the mental health of Asian Americans, but the dearth of information and research on suicide in South Asians is striking.3 In fact, a review of literature finds fewer than 10 articles on the topic that have been published in peer-reviewed journals in the last decade. to provide effective, culturally sensitive care.
Diverse group
There are 3.4 million individuals of South Asian descent in the United States. Geographically, South Asians may have familial and cultural/historical roots in Bangladesh, Bhutan, India, Maldives, Nepal, and Pakistan.4 They enjoy a rich diversity in terms of cultural and religious beliefs, language, socioeconomic status, modes of acculturation, and immigration patterns. Asian Indians are the largest group of South Asians in the United States. They are highly educated, with a larger proportion of them pursuing an undergraduate and/or graduate level education than the general population. The median household income of Asian Indians is also higher than the national average.5
In general, suicide, like all mental health issues, is a stigmatized and taboo topic in the South Asian community.6 Also, South Asian Americans are hesitant to seek mental health care because of a perceived inability of Western health care professionals to understand their cultural views. Extrapolation from data on South Asians in the United Kingdom, aggregate statistics for Asian Americans and Pacific Islanders, and studies on South Asians in the United States highlight two South Asian subgroups that are particularly vulnerable to suicide. These are young adults (aged 18-24 years) and women.7
Suicide is the second-leading cause of death for young Asian American men in the United States. Rates of lifetime suicidal ideation and attempts are higher among younger Asian Americans (aged 18-24 years) than among older Asian American adults. Young Asian American adults have been found to have higher levels of suicidal ideation than their white counterparts.8,9 Acculturation or assimilating into a different culture, familial violence as a child, hopelessness or a thought pattern with a pessimistic outlook, depression, and childhood sexual abuse have all been found to be positively correlated with suicidal ideation and attempted suicide in South Asian Americans. One study that conducted0 in-group analysis on undergraduate university students of South Asian descent living in New York found higher levels of hopelessness and depression in Asian Indians relative to Bangladeshi or Pakistani Americans.10
In addition, higher levels of suicidal ideation are reported in Asian Indians relative to Bangladeshi or Pakistani Americans. These results resemble findings from similar studies in the United Kingdom. A posited reason for these findings is a difference in religious beliefs. Pakistani and Bangladeshi Americans are predominantly Muslim, have stronger moral beliefs against suicide, and consider it a sin as defined by Islamic beliefs. Asian Indians, in contrast, are majority Hindu and believe in reincarnation – a context that might make suicide seem more permissible.11
South Asian women are particularly vulnerable to domestic violence, childhood sexual abuse, intimate partner violence, and/or familial violence. Cultural gender norms, traditional norms, and patriarchal ideology in the South Asian community make quantifying the level of childhood sexual abuse and familial violence a challenge. Furthermore, culturally, South Asian women are often considered subordinate relative to men, and discussion around family violence and childhood sexual abuse is avoided. Studies from the United Kingdom find a lack of knowledge around, disclosure of, and fear of reporting childhood sexual abuse in South Asian women. A study of a sample of representative South Asian American women found that 25.2% had experienced some form of childhood sexual abuse.12
Research also suggests that South Asians in the United States have some of the highest rates of intimate partner violence. Another study in the United States found that two out of five South Asian women have experienced physical and/or sexual intimate partner violence. This is much higher than the rate found in representative general U.S. population samples.
Literature suggests that exposure to these factors increases womens’ risk for suicidal ideation and attempted suicide. In the United Kingdom, research on South Asian women (aged 18-24 years) has found rates of attempted suicide to be three times higher than those of their white counterparts. Research from the United Kingdom and the United States suggests that younger married South Asian women are exposed to emotional and/or physical abuse from their spouse or in-laws, which is often a mediating factor in their increased risk for suicide.
Attempts to address suicide in the South Asian American community have to be multifaceted. An ideal approach would consist of educating, and connecting with, the community through ethnic media and trusted community sources, such as primary care doctors, caregivers, and social workers. In line with established American Psychological Association guidelines on caring for individuals of immigrant origin, health care professionals should document the patient’s number of generations in the country, number of years in the country, language fluency, family and community support, educational level, social status changes related to immigration, intimate relationships with people of different backgrounds, and stress related to acculturation. Special attention should be paid to South Asian women. Health care professionals should screen South Asian women for past and current intimate partner violence, provide culturally appropriate intimate partner violence resources, and be prepared to refer them to legal counseling services. Also, South Asian women should be screened for a history of exposure to familial violence and childhood sexual abuse.1
To adequately serve this population, there is a need to build capacity in the provision of culturally appropriate mental health services. Access to mental health care professionals through settings such as shelters for abused women, South Asian community–based organizations, youth centers, college counseling, and senior centers would encourage individuals to seek care without the threat of being stigmatized.
References
1. Hedegaard H et al. Suicide mortality in the United States, 1999–2017. NCHS Data Brief, No. 330. 2018 Nov.
2. Ahmad-Stout DJ and Nath SR. J College Stud Psychother. 2013 Jan 10;27(1):43-61.
3. Li H and Keshavan M. Asian J Psychiatry. 2011;4(1):1.
4. Nagaraj NC et al. J Immigr Minor Health. 2019 Oct;21(5):978-1003.
5. Nagaraj NC et al. J Comm Health. 2018;43(3):543-51.
6. Cao KO. Generations. 2014;30(4):82-5.
7. Hurwitz EJ et al. J Immigr Minor Health. 2006;8(3):251-61.
8. Polanco-Roman L et al. Cultur Divers Ethnic Minor Psychol. 2019 Dec 23. doi: 10.1037/cpd0000313.
9. Erausquin JT et al. J Youth Adolesc. 2019 Sep;48(9):1796-1805.
10. Lane R et al. Asian Am J Psychol. 2016;7(2):120-8.
11. Nath SR et al. Asian Am J Psychol. 2018;9(4):334-343.
12. Robertson HA et al. J Immigr Minor Health. 2016 Jul 31;18(4):921-7.
Mr. Kaleka is a medical student in the class of 2021 at Central Michigan University (CMU) College of Medicine, Mt. Pleasant. He has no disclosures. Mr. Kaleka would like to thank his mentor, Furhut Janssen, DO, for her continued guidance and support in research on mental health in immigrant populations.
Mental health visits account for 19% of ED costs
Emergency department visits for mental and substance use disorders (MUSDs) cost $14.6 billion in 2017, representing 19% of the total for all ED visits that year, according to the Agency for Healthcare Quality and Research.
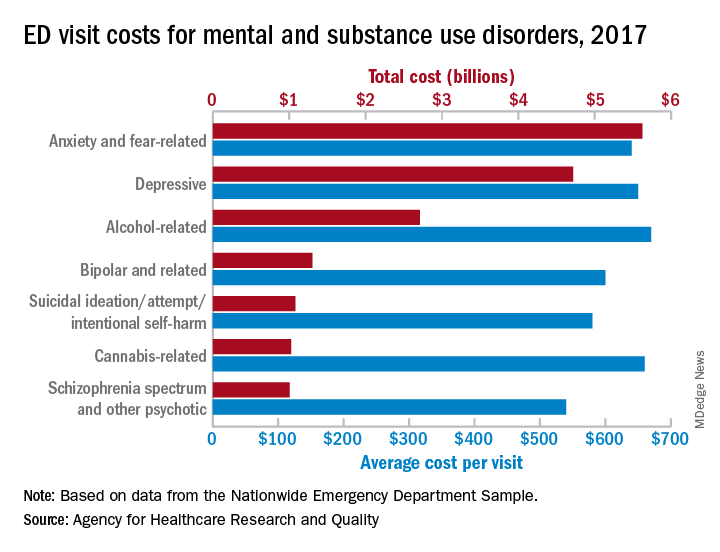
In terms of the total number of visits for MUSDs, 23.1 million, the proportion was slightly lower: 16% of all ED visits for the year, Zeynal Karaca, PhD, a senior economist with AHRQ, and Brian J. Moore, PhD, a senior research leader at IBM Watson Health, said in a recent statistical brief.
Put those figures together and the average visit for an MUSD diagnosis cost $630 and that is 19% higher than the average of $530 for all 145 million ED visits, they reported based on data from the Nationwide Emergency Department Sample.
The most costly MUSD diagnosis in 2017 was anxiety and fear-related disorders, with a total of $5.6 billion for ED visits, followed by depressive disorders at $4.7 billion and alcohol-related disorders at $2.7 billion. Some ED visits may involve more than one MUSD diagnosis, so the sum of all the individual diagnoses does not agree with the total for the entire MUSD category, the researchers noted.
On a per-visit basis, in 2017. [It was not included in the graph because it was 13th.] Other disorders with high per-visit costs were alcohol-related ($670), cannabis-related ($660), and depressive and stimulant-related (both with $650), Dr. Karaca and Dr. Moore said.
Patients with MUSDs who were routinely discharged after an ED visit in 2017 represented a much lower share of the total MUSD cost (68.0%), compared with the overall group of ED visitors (81.4%), but MUSD visits resulting in an inpatient admission made up a larger proportion of costs (19.0%), compared with all visits (9.5%), they said.
Costs between MUSD visits and all ED visits also differed by patient age. Visits by patients aged 0-9 years represented only 0.7% of MUSD-related ED costs but 5.6% of the overall cost, but the respective figures for those aged 45-64 were 36.2% for MUSD costs and 28.5% for the total ED cost, they reported.
SOURCE: Karaca Z and Moore BJ. HCUP Statistical Brief #257. May 12, 2020.
Emergency department visits for mental and substance use disorders (MUSDs) cost $14.6 billion in 2017, representing 19% of the total for all ED visits that year, according to the Agency for Healthcare Quality and Research.
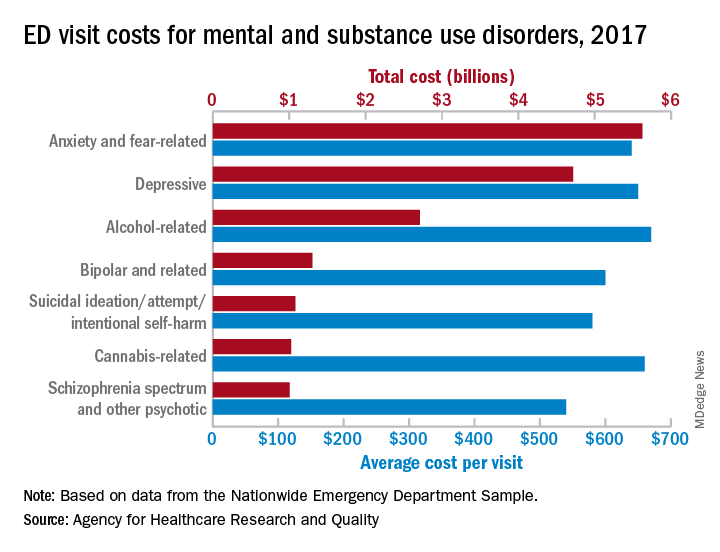
In terms of the total number of visits for MUSDs, 23.1 million, the proportion was slightly lower: 16% of all ED visits for the year, Zeynal Karaca, PhD, a senior economist with AHRQ, and Brian J. Moore, PhD, a senior research leader at IBM Watson Health, said in a recent statistical brief.
Put those figures together and the average visit for an MUSD diagnosis cost $630 and that is 19% higher than the average of $530 for all 145 million ED visits, they reported based on data from the Nationwide Emergency Department Sample.
The most costly MUSD diagnosis in 2017 was anxiety and fear-related disorders, with a total of $5.6 billion for ED visits, followed by depressive disorders at $4.7 billion and alcohol-related disorders at $2.7 billion. Some ED visits may involve more than one MUSD diagnosis, so the sum of all the individual diagnoses does not agree with the total for the entire MUSD category, the researchers noted.
On a per-visit basis, in 2017. [It was not included in the graph because it was 13th.] Other disorders with high per-visit costs were alcohol-related ($670), cannabis-related ($660), and depressive and stimulant-related (both with $650), Dr. Karaca and Dr. Moore said.
Patients with MUSDs who were routinely discharged after an ED visit in 2017 represented a much lower share of the total MUSD cost (68.0%), compared with the overall group of ED visitors (81.4%), but MUSD visits resulting in an inpatient admission made up a larger proportion of costs (19.0%), compared with all visits (9.5%), they said.
Costs between MUSD visits and all ED visits also differed by patient age. Visits by patients aged 0-9 years represented only 0.7% of MUSD-related ED costs but 5.6% of the overall cost, but the respective figures for those aged 45-64 were 36.2% for MUSD costs and 28.5% for the total ED cost, they reported.
SOURCE: Karaca Z and Moore BJ. HCUP Statistical Brief #257. May 12, 2020.
Emergency department visits for mental and substance use disorders (MUSDs) cost $14.6 billion in 2017, representing 19% of the total for all ED visits that year, according to the Agency for Healthcare Quality and Research.
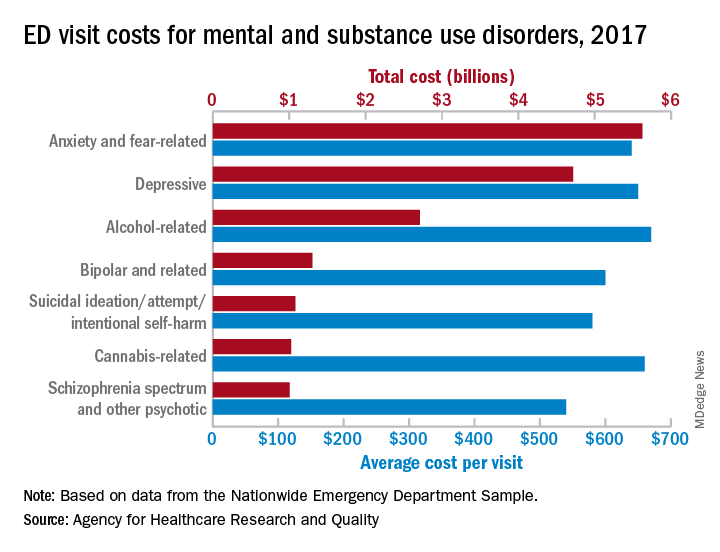
In terms of the total number of visits for MUSDs, 23.1 million, the proportion was slightly lower: 16% of all ED visits for the year, Zeynal Karaca, PhD, a senior economist with AHRQ, and Brian J. Moore, PhD, a senior research leader at IBM Watson Health, said in a recent statistical brief.
Put those figures together and the average visit for an MUSD diagnosis cost $630 and that is 19% higher than the average of $530 for all 145 million ED visits, they reported based on data from the Nationwide Emergency Department Sample.
The most costly MUSD diagnosis in 2017 was anxiety and fear-related disorders, with a total of $5.6 billion for ED visits, followed by depressive disorders at $4.7 billion and alcohol-related disorders at $2.7 billion. Some ED visits may involve more than one MUSD diagnosis, so the sum of all the individual diagnoses does not agree with the total for the entire MUSD category, the researchers noted.
On a per-visit basis, in 2017. [It was not included in the graph because it was 13th.] Other disorders with high per-visit costs were alcohol-related ($670), cannabis-related ($660), and depressive and stimulant-related (both with $650), Dr. Karaca and Dr. Moore said.
Patients with MUSDs who were routinely discharged after an ED visit in 2017 represented a much lower share of the total MUSD cost (68.0%), compared with the overall group of ED visitors (81.4%), but MUSD visits resulting in an inpatient admission made up a larger proportion of costs (19.0%), compared with all visits (9.5%), they said.
Costs between MUSD visits and all ED visits also differed by patient age. Visits by patients aged 0-9 years represented only 0.7% of MUSD-related ED costs but 5.6% of the overall cost, but the respective figures for those aged 45-64 were 36.2% for MUSD costs and 28.5% for the total ED cost, they reported.
SOURCE: Karaca Z and Moore BJ. HCUP Statistical Brief #257. May 12, 2020.
Fracture risk higher for children with anxiety on benzodiazepines
a new study found, which offers further argument for caution with this class of drugs in young patients.
In research published in Pediatrics, Greta A. Bushnell, PhD, of Columbia University in New York and colleagues, looked at private insurance claims data including prescription records from 120,715 children aged 6-17 years diagnosed with an anxiety disorder and from 179,768 young adults aged 18-24 years also diagnosed with anxiety.
The investigators compared fracture incidence within 3 months of treatment initiation between the group prescribed benzodiazepines for anxiety and the group prescribed SSRIs. Subjects prescribed both classes of drugs were excluded from the analysis.
Of patients aged 6-17 years, 11% were prescribed benzodiazepines, with the remainder receiving SSRIs. Children on benzodiazepines saw 33 fractures per 1,000 person-years, compared with 25 of those on SSRIs, with an adjusted incidence rate ratio of 1.53. These were fractures in the upper and lower limbs.
Similar differences in fracture risk were not seen among the young adults in the study, of whom 32% were prescribed benzodiazepines and among whom fracture rates were low overall, 9 per 1,000 person-years in both medication groups.
Several SSRIs have been approved by the Food and Drug Administration to treat anxiety disorders in children, but benzodiazepines are used off label in youth. The drugs most commonly prescribed in the study were alprazolam and lorazepam, and 82% of the group in this study aged 6-17 years did not fill their prescriptions beyond 1 month.
In adults, benzodiazepine treatment has been shown to cause drowsiness, dizziness, and weakness, which can result in injury, and it also is associated with increased risk of car accidents, falls, and fractures. The higher fracture rate among children on benzodiazepine treatment seen in this study is similar to rates reported in studies of older adults, Dr. Bushnell and colleagues noted.
The researchers could not explain why the young adults in the study did not see a higher risk of fractures on benzodiazepines, compared with that among those taking SSRIs. They hypothesized that young adults are less active than children, with fewer opportunities for falls, and there were few fractures among the 18- to 24-year-old cohort in general.
David C. Rettew, MD, from the University of Vermont in Burlington, commented in an interview that, while there are plenty of reasons to be cautious about using benzodiazepines in youth, “fracture risk isn’t usually very prominent among them, so it is a nice reminder to have this on the radar screen.” Most clinicians, he said, already are quite wary of using benzodiazepines in children, which is suggested by the small proportion of children treated with them in this study.
“It seems quite possible that children and adolescents prescribed benzodiazepines are quite different clinically than the group prescribed SSRIs, despite the strong measures the study authors took to control for other variables between the two groups,” Dr. Rettew added. “I’d have to wonder if those clinical differences may be behind some of the fracture rate differences” seen in the study.
Dr. Bushnell and her colleagues acknowledged this among the study’s several limitations. “It is unclear how much unmeasured differences in psychiatric condition severity exist between youth initiating a benzodiazepine versus SSRI and how anxiety severity impacts fracture risk.” The researchers also noted that they could not measure use of the drugs beyond whether and when prescriptions were filled.
Dr. Bushnell and colleagues’ study was funded by the National Institute of Mental Health and by grants from the Agency for Healthcare Research and Quality, the Patient-Centered Outcomes Research Institute, and the National Institutes of Health. One of its coauthors disclosed financial relationships with several pharmaceutical manufacturers. Dr. Rettew said he had no relevant financial disclosures
SOURCE: Bushnell GA et al. Pediatrics. 2020 Jun. doi: 10.1542/peds.2019-3478.
a new study found, which offers further argument for caution with this class of drugs in young patients.
In research published in Pediatrics, Greta A. Bushnell, PhD, of Columbia University in New York and colleagues, looked at private insurance claims data including prescription records from 120,715 children aged 6-17 years diagnosed with an anxiety disorder and from 179,768 young adults aged 18-24 years also diagnosed with anxiety.
The investigators compared fracture incidence within 3 months of treatment initiation between the group prescribed benzodiazepines for anxiety and the group prescribed SSRIs. Subjects prescribed both classes of drugs were excluded from the analysis.
Of patients aged 6-17 years, 11% were prescribed benzodiazepines, with the remainder receiving SSRIs. Children on benzodiazepines saw 33 fractures per 1,000 person-years, compared with 25 of those on SSRIs, with an adjusted incidence rate ratio of 1.53. These were fractures in the upper and lower limbs.
Similar differences in fracture risk were not seen among the young adults in the study, of whom 32% were prescribed benzodiazepines and among whom fracture rates were low overall, 9 per 1,000 person-years in both medication groups.
Several SSRIs have been approved by the Food and Drug Administration to treat anxiety disorders in children, but benzodiazepines are used off label in youth. The drugs most commonly prescribed in the study were alprazolam and lorazepam, and 82% of the group in this study aged 6-17 years did not fill their prescriptions beyond 1 month.
In adults, benzodiazepine treatment has been shown to cause drowsiness, dizziness, and weakness, which can result in injury, and it also is associated with increased risk of car accidents, falls, and fractures. The higher fracture rate among children on benzodiazepine treatment seen in this study is similar to rates reported in studies of older adults, Dr. Bushnell and colleagues noted.
The researchers could not explain why the young adults in the study did not see a higher risk of fractures on benzodiazepines, compared with that among those taking SSRIs. They hypothesized that young adults are less active than children, with fewer opportunities for falls, and there were few fractures among the 18- to 24-year-old cohort in general.
David C. Rettew, MD, from the University of Vermont in Burlington, commented in an interview that, while there are plenty of reasons to be cautious about using benzodiazepines in youth, “fracture risk isn’t usually very prominent among them, so it is a nice reminder to have this on the radar screen.” Most clinicians, he said, already are quite wary of using benzodiazepines in children, which is suggested by the small proportion of children treated with them in this study.
“It seems quite possible that children and adolescents prescribed benzodiazepines are quite different clinically than the group prescribed SSRIs, despite the strong measures the study authors took to control for other variables between the two groups,” Dr. Rettew added. “I’d have to wonder if those clinical differences may be behind some of the fracture rate differences” seen in the study.
Dr. Bushnell and her colleagues acknowledged this among the study’s several limitations. “It is unclear how much unmeasured differences in psychiatric condition severity exist between youth initiating a benzodiazepine versus SSRI and how anxiety severity impacts fracture risk.” The researchers also noted that they could not measure use of the drugs beyond whether and when prescriptions were filled.
Dr. Bushnell and colleagues’ study was funded by the National Institute of Mental Health and by grants from the Agency for Healthcare Research and Quality, the Patient-Centered Outcomes Research Institute, and the National Institutes of Health. One of its coauthors disclosed financial relationships with several pharmaceutical manufacturers. Dr. Rettew said he had no relevant financial disclosures
SOURCE: Bushnell GA et al. Pediatrics. 2020 Jun. doi: 10.1542/peds.2019-3478.
a new study found, which offers further argument for caution with this class of drugs in young patients.
In research published in Pediatrics, Greta A. Bushnell, PhD, of Columbia University in New York and colleagues, looked at private insurance claims data including prescription records from 120,715 children aged 6-17 years diagnosed with an anxiety disorder and from 179,768 young adults aged 18-24 years also diagnosed with anxiety.
The investigators compared fracture incidence within 3 months of treatment initiation between the group prescribed benzodiazepines for anxiety and the group prescribed SSRIs. Subjects prescribed both classes of drugs were excluded from the analysis.
Of patients aged 6-17 years, 11% were prescribed benzodiazepines, with the remainder receiving SSRIs. Children on benzodiazepines saw 33 fractures per 1,000 person-years, compared with 25 of those on SSRIs, with an adjusted incidence rate ratio of 1.53. These were fractures in the upper and lower limbs.
Similar differences in fracture risk were not seen among the young adults in the study, of whom 32% were prescribed benzodiazepines and among whom fracture rates were low overall, 9 per 1,000 person-years in both medication groups.
Several SSRIs have been approved by the Food and Drug Administration to treat anxiety disorders in children, but benzodiazepines are used off label in youth. The drugs most commonly prescribed in the study were alprazolam and lorazepam, and 82% of the group in this study aged 6-17 years did not fill their prescriptions beyond 1 month.
In adults, benzodiazepine treatment has been shown to cause drowsiness, dizziness, and weakness, which can result in injury, and it also is associated with increased risk of car accidents, falls, and fractures. The higher fracture rate among children on benzodiazepine treatment seen in this study is similar to rates reported in studies of older adults, Dr. Bushnell and colleagues noted.
The researchers could not explain why the young adults in the study did not see a higher risk of fractures on benzodiazepines, compared with that among those taking SSRIs. They hypothesized that young adults are less active than children, with fewer opportunities for falls, and there were few fractures among the 18- to 24-year-old cohort in general.
David C. Rettew, MD, from the University of Vermont in Burlington, commented in an interview that, while there are plenty of reasons to be cautious about using benzodiazepines in youth, “fracture risk isn’t usually very prominent among them, so it is a nice reminder to have this on the radar screen.” Most clinicians, he said, already are quite wary of using benzodiazepines in children, which is suggested by the small proportion of children treated with them in this study.
“It seems quite possible that children and adolescents prescribed benzodiazepines are quite different clinically than the group prescribed SSRIs, despite the strong measures the study authors took to control for other variables between the two groups,” Dr. Rettew added. “I’d have to wonder if those clinical differences may be behind some of the fracture rate differences” seen in the study.
Dr. Bushnell and her colleagues acknowledged this among the study’s several limitations. “It is unclear how much unmeasured differences in psychiatric condition severity exist between youth initiating a benzodiazepine versus SSRI and how anxiety severity impacts fracture risk.” The researchers also noted that they could not measure use of the drugs beyond whether and when prescriptions were filled.
Dr. Bushnell and colleagues’ study was funded by the National Institute of Mental Health and by grants from the Agency for Healthcare Research and Quality, the Patient-Centered Outcomes Research Institute, and the National Institutes of Health. One of its coauthors disclosed financial relationships with several pharmaceutical manufacturers. Dr. Rettew said he had no relevant financial disclosures
SOURCE: Bushnell GA et al. Pediatrics. 2020 Jun. doi: 10.1542/peds.2019-3478.
FROM PEDIATRICS
Key clinical point: Children aged 6-17 years prescribed sedatives for anxiety saw a higher risk of fractures, compared with those on SSRIs.
Major finding: Children prescribed benzodiazepines for anxiety had 33 fractures per 1,000 person-years versus 25 among children prescribed SSRIs (adjusted incidence rate ratio, 1.53).
Study details: A retrospective cohort study using commercial insurance claims data from 120,715 children aged 6-17 years and 179,768 young adults ages 18-24 years from 2007 through 2016, all with anxiety diagnoses and prescribed either benzodiazepines or SSRIs.
Disclosures: Dr. Bushnell and colleagues’ study was funded by the National Institute of Mental Health, and grants from the Agency for Healthcare Research and Quality, the Patient-Centered Outcomes Research Institute, and the National Institutes of Health. One of its coauthors disclosed financial relationships with several pharmaceutical manufacturers.
Source: Bushnell GA et al. Pediatrics. 2020 Jun. doi: 10.1542/peds.2019-3478.
Atopic dermatitis in adults, children linked to neuropsychiatric disorders
according to a study presented at the annual meeting of the Society for Investigative Dermatology, held virtually.
“The risk increase ranges from as low as 5% up to 59%, depending on the outcome, with generally greater effects observed among the adults,” Joy Wan, MD, a postdoctoral dermatology fellow at the University of Pennsylvania, Philadelphia, said in her presentation. The risk was independent of other atopic disease, gender, age, and socioeconomic status.
Dr. Wan and colleagues conducted a cohort study of patients with AD in the United Kingdom using data from the Health Improvement Network (THIN) electronic records database, matching AD patients in THIN with up to five patients without AD, similar in age and also registered to general practices. The researchers validated AD disease status using an algorithm that identified patients with a diagnostic code and two therapy codes related to AD. Outcomes of interest included anxiety, depression, bipolar disorder, obsessive-compulsive disorder, ADHD, schizophrenia, and autism. Patients entered into the cohort when they were diagnosed with AD, registered by a practice, or when data from a practice was reported to THIN. The researchers stopped following patients when they developed a neuropsychiatric outcome of interest, left a practice, died, or when the study ended.
“Previous studies have found associations between atopic dermatitis and anxiety, depression, and attention-deficit/hyperactivity disorder. However, many previous studies had been cross-sectional and they were unable to evaluate the directionality of association between atopic dermatitis and neuropsychiatric outcomes, while other previous studies have relied on the self-report of atopic dermatitis and outcomes as well,” Dr. Wan said. “Thus, longitudinal studies, using validated measures of atopic dermatitis, and those that include the entire age span, are really needed.”
Overall, 434,859 children and adolescents under aged 18 with AD in the THIN database were matched to 1,983,589 controls, and 644,802 adults with AD were matched to almost 2,900,000 adults without AD. In the pediatric group, demographics were mostly balanced between children with and without AD: the average age ranged between about 5 and almost 6 years. In pediatric patients with AD, there was a higher rate of allergic rhinitis (6.2% vs. 4%) and asthma (13.5% vs. 9.3%) than in the control group.
For adults, the average age was about 48 years in both groups. Compared with patients who did not have AD, adults with AD also had higher rates of allergic rhinitis (15.2% vs. 9.6%) and asthma (19.9% vs. 12.6%).
After adjusting for age, gender, socioeconomic status, asthma, and allergic rhinitis, Dr. Wan and colleagues found greater rates of bipolar disorder (hazard ratio, 1.34; 95% confidence interval, 1.09-1.65), obsessive-compulsive disorder (HR, 1.30; 95% CI, 1.21-1.41), anxiety (HR, 1.09; 95% CI, 1.07-1.11), and depression (HR, 1.06; 95% CI, 1.04-1.08) among children and adolescents with AD, compared with controls.
In the adult cohort, a diagnosis of AD was associated with an increased risk of autism (HR, 1.53; 95% CI, 1.30-1.80), obsessive-compulsive disorder (HR, 1.49; 95% CI, 1.40-1.59), ADHD (HR, 1.31; 95% CI, 1.13-1.53), anxiety (HR, 1.17; 95% CI, 1.15-1.18), depression (HR, 1.15; 95% CI, 1.14-1.16), and bipolar disorder (HR, 1.12; 95% CI, 1.04-1.21), after adjusting for age, gender, socioeconomic status, asthma, and allergic rhinitis.
One reason for the increased associations among the adults, even for ADHD and autism, which are more characteristically diagnosed in childhood, Dr. Wan said, is that, since they looked at incident outcomes, “many children may already have had these prevalent comorbidities at the time of the entry in the cohort.”
She noted that the study may have observation bias or unknown confounders, but she hopes these results raise awareness of the association between AD and neuropsychiatric disorders, although more research is needed to determine how AD severity affects neuropsychiatric outcomes. “Additional work is needed to really understand the mechanisms that drive these associations, whether it’s mediated through symptoms of atopic dermatitis such as itch and poor sleep, or potentially the stigma of having a chronic skin disease, or perhaps shared pathophysiology between atopic dermatitis and these neuropsychiatric diseases,” she said.
The study was funded by a grant from Pfizer. Dr. Wan reports receiving research funding from Pfizer paid to the University of Pennsylvania.
according to a study presented at the annual meeting of the Society for Investigative Dermatology, held virtually.
“The risk increase ranges from as low as 5% up to 59%, depending on the outcome, with generally greater effects observed among the adults,” Joy Wan, MD, a postdoctoral dermatology fellow at the University of Pennsylvania, Philadelphia, said in her presentation. The risk was independent of other atopic disease, gender, age, and socioeconomic status.
Dr. Wan and colleagues conducted a cohort study of patients with AD in the United Kingdom using data from the Health Improvement Network (THIN) electronic records database, matching AD patients in THIN with up to five patients without AD, similar in age and also registered to general practices. The researchers validated AD disease status using an algorithm that identified patients with a diagnostic code and two therapy codes related to AD. Outcomes of interest included anxiety, depression, bipolar disorder, obsessive-compulsive disorder, ADHD, schizophrenia, and autism. Patients entered into the cohort when they were diagnosed with AD, registered by a practice, or when data from a practice was reported to THIN. The researchers stopped following patients when they developed a neuropsychiatric outcome of interest, left a practice, died, or when the study ended.
“Previous studies have found associations between atopic dermatitis and anxiety, depression, and attention-deficit/hyperactivity disorder. However, many previous studies had been cross-sectional and they were unable to evaluate the directionality of association between atopic dermatitis and neuropsychiatric outcomes, while other previous studies have relied on the self-report of atopic dermatitis and outcomes as well,” Dr. Wan said. “Thus, longitudinal studies, using validated measures of atopic dermatitis, and those that include the entire age span, are really needed.”
Overall, 434,859 children and adolescents under aged 18 with AD in the THIN database were matched to 1,983,589 controls, and 644,802 adults with AD were matched to almost 2,900,000 adults without AD. In the pediatric group, demographics were mostly balanced between children with and without AD: the average age ranged between about 5 and almost 6 years. In pediatric patients with AD, there was a higher rate of allergic rhinitis (6.2% vs. 4%) and asthma (13.5% vs. 9.3%) than in the control group.
For adults, the average age was about 48 years in both groups. Compared with patients who did not have AD, adults with AD also had higher rates of allergic rhinitis (15.2% vs. 9.6%) and asthma (19.9% vs. 12.6%).
After adjusting for age, gender, socioeconomic status, asthma, and allergic rhinitis, Dr. Wan and colleagues found greater rates of bipolar disorder (hazard ratio, 1.34; 95% confidence interval, 1.09-1.65), obsessive-compulsive disorder (HR, 1.30; 95% CI, 1.21-1.41), anxiety (HR, 1.09; 95% CI, 1.07-1.11), and depression (HR, 1.06; 95% CI, 1.04-1.08) among children and adolescents with AD, compared with controls.
In the adult cohort, a diagnosis of AD was associated with an increased risk of autism (HR, 1.53; 95% CI, 1.30-1.80), obsessive-compulsive disorder (HR, 1.49; 95% CI, 1.40-1.59), ADHD (HR, 1.31; 95% CI, 1.13-1.53), anxiety (HR, 1.17; 95% CI, 1.15-1.18), depression (HR, 1.15; 95% CI, 1.14-1.16), and bipolar disorder (HR, 1.12; 95% CI, 1.04-1.21), after adjusting for age, gender, socioeconomic status, asthma, and allergic rhinitis.
One reason for the increased associations among the adults, even for ADHD and autism, which are more characteristically diagnosed in childhood, Dr. Wan said, is that, since they looked at incident outcomes, “many children may already have had these prevalent comorbidities at the time of the entry in the cohort.”
She noted that the study may have observation bias or unknown confounders, but she hopes these results raise awareness of the association between AD and neuropsychiatric disorders, although more research is needed to determine how AD severity affects neuropsychiatric outcomes. “Additional work is needed to really understand the mechanisms that drive these associations, whether it’s mediated through symptoms of atopic dermatitis such as itch and poor sleep, or potentially the stigma of having a chronic skin disease, or perhaps shared pathophysiology between atopic dermatitis and these neuropsychiatric diseases,” she said.
The study was funded by a grant from Pfizer. Dr. Wan reports receiving research funding from Pfizer paid to the University of Pennsylvania.
according to a study presented at the annual meeting of the Society for Investigative Dermatology, held virtually.
“The risk increase ranges from as low as 5% up to 59%, depending on the outcome, with generally greater effects observed among the adults,” Joy Wan, MD, a postdoctoral dermatology fellow at the University of Pennsylvania, Philadelphia, said in her presentation. The risk was independent of other atopic disease, gender, age, and socioeconomic status.
Dr. Wan and colleagues conducted a cohort study of patients with AD in the United Kingdom using data from the Health Improvement Network (THIN) electronic records database, matching AD patients in THIN with up to five patients without AD, similar in age and also registered to general practices. The researchers validated AD disease status using an algorithm that identified patients with a diagnostic code and two therapy codes related to AD. Outcomes of interest included anxiety, depression, bipolar disorder, obsessive-compulsive disorder, ADHD, schizophrenia, and autism. Patients entered into the cohort when they were diagnosed with AD, registered by a practice, or when data from a practice was reported to THIN. The researchers stopped following patients when they developed a neuropsychiatric outcome of interest, left a practice, died, or when the study ended.
“Previous studies have found associations between atopic dermatitis and anxiety, depression, and attention-deficit/hyperactivity disorder. However, many previous studies had been cross-sectional and they were unable to evaluate the directionality of association between atopic dermatitis and neuropsychiatric outcomes, while other previous studies have relied on the self-report of atopic dermatitis and outcomes as well,” Dr. Wan said. “Thus, longitudinal studies, using validated measures of atopic dermatitis, and those that include the entire age span, are really needed.”
Overall, 434,859 children and adolescents under aged 18 with AD in the THIN database were matched to 1,983,589 controls, and 644,802 adults with AD were matched to almost 2,900,000 adults without AD. In the pediatric group, demographics were mostly balanced between children with and without AD: the average age ranged between about 5 and almost 6 years. In pediatric patients with AD, there was a higher rate of allergic rhinitis (6.2% vs. 4%) and asthma (13.5% vs. 9.3%) than in the control group.
For adults, the average age was about 48 years in both groups. Compared with patients who did not have AD, adults with AD also had higher rates of allergic rhinitis (15.2% vs. 9.6%) and asthma (19.9% vs. 12.6%).
After adjusting for age, gender, socioeconomic status, asthma, and allergic rhinitis, Dr. Wan and colleagues found greater rates of bipolar disorder (hazard ratio, 1.34; 95% confidence interval, 1.09-1.65), obsessive-compulsive disorder (HR, 1.30; 95% CI, 1.21-1.41), anxiety (HR, 1.09; 95% CI, 1.07-1.11), and depression (HR, 1.06; 95% CI, 1.04-1.08) among children and adolescents with AD, compared with controls.
In the adult cohort, a diagnosis of AD was associated with an increased risk of autism (HR, 1.53; 95% CI, 1.30-1.80), obsessive-compulsive disorder (HR, 1.49; 95% CI, 1.40-1.59), ADHD (HR, 1.31; 95% CI, 1.13-1.53), anxiety (HR, 1.17; 95% CI, 1.15-1.18), depression (HR, 1.15; 95% CI, 1.14-1.16), and bipolar disorder (HR, 1.12; 95% CI, 1.04-1.21), after adjusting for age, gender, socioeconomic status, asthma, and allergic rhinitis.
One reason for the increased associations among the adults, even for ADHD and autism, which are more characteristically diagnosed in childhood, Dr. Wan said, is that, since they looked at incident outcomes, “many children may already have had these prevalent comorbidities at the time of the entry in the cohort.”
She noted that the study may have observation bias or unknown confounders, but she hopes these results raise awareness of the association between AD and neuropsychiatric disorders, although more research is needed to determine how AD severity affects neuropsychiatric outcomes. “Additional work is needed to really understand the mechanisms that drive these associations, whether it’s mediated through symptoms of atopic dermatitis such as itch and poor sleep, or potentially the stigma of having a chronic skin disease, or perhaps shared pathophysiology between atopic dermatitis and these neuropsychiatric diseases,” she said.
The study was funded by a grant from Pfizer. Dr. Wan reports receiving research funding from Pfizer paid to the University of Pennsylvania.
FROM SID 2020
COVID-19 ravaging the Navajo Nation
The Navajo people have dealt with adversity that has tested our strength and resilience since our creation. In Navajo culture, the Holy People or gods challenged us with Naayee (monsters). We endured and learned from each Naayee, hunger, and death to name a few adversities. The COVID-19 pandemic, or “Big Cough” (Dikos Nitsaa’igii -19 in Navajo language) is a monster confronting the Navajo today. It has had significant impact on our nation and people.
The Navajo have the most cases of the COVID-19 virus of any tribe in the United States, and numbers as of May 31, 2020, are 5,348, with 246 confirmed deaths.1 The Navajo Nation, which once lagged behind New York, has reported the largest per-capita infection rate in the United States.
These devastating numbers, which might be leveling off, are associated with Navajo people having higher-than-average numbers of diabetes, heart disease, and cancer. This is compounded with 30%-40% of homes having no electricity or running water, and a poverty rate of about 38%.2
Geographical and cultural factors also contribute to the inability to gain a foothold in mitigating the number of cases. The Navajo Nation is the largest tribe in the United States, covering 27,000 square miles over an arid, red rock expanse with canyons and mountains. The population is over 250,000,3 and Navajo have traditionally lived in matrilineal clan units throughout the reservation, the size of West Virginia. The family traditional dwelling, called a “hogan,” often is clustered together. Multiple generations live together in these units. The COVID-19 virus inflicted many Navajo and rapidly spread to the elderly in these close-proximity living quarters.
Most Navajo live away from services and grocery stores and travel back and forth for food and water, which contributes to the virus rapidly being transmitted among the community members. Education aimed at curbing travel and spread of the virus was issued with curfews, commands to stay at home and keep social distance, and protect elders. The Navajo leadership and traditional medicine people, meanwhile, advised the people to follow their cultural values by caring for family and community members and providing a safe environment.
Resources are spread out
There are only 13 stores in this expansive reservation,4 so tribal members rely on traveling to border towns, such as Farmington and Gallup, N.M., Families usually travel to these towns on weekends to replenish food and supplies. There has been a cluster of cases in Gallup, N.M., so to reduce the numbers, the town shut itself off from outsiders – including the Navajo people coming to buy food, do laundry, and get water and feed for livestock. This has affected and stressed the Navajo further in attempting to access necessities.
Access to health care is already challenging because of lack of transportation and distance. This has made it more difficult to access COVID-19 testing and more challenging to get the results back. The Indian Health Service has been the designated health care system for the Navajo since 1955. The Treaty of Bosque Redondo, signed by the Navajo in 1868, included the provision of health care, as well as education in exchange for tracts of land, that included the Navajo homeland or Dinetah.5
The Indian Health Service provides care with hospitals and clinics throughout the reservation. Some of the IHS facilities have been taken over by the Navajo, so there are four Navajo tribally controlled hospitals, along with one private hospital. Coordination of care for a pandemic is, therefore, more challenging to coordinate. This contributes to problems with coordination of the health care, establishing alternate care sites, accessing personal protective equipment, and providing testing sites. The Navajo Nation Council is working hard to equitably distribute the $600 million from the CARES Act.6
Dealing with the pandemic is compromised by chronic underfunding from the U.S. government. The treaty obligation of the U.S. government is to provide health care to all federally recognized Native Americans. The IHS, which has been designated to provide that care for a tribal person, gets one-third the Medicare dollars for health care provided for a person in the general population.7 Health factors have led to the public health issues of poorly controlled diabetes, obesity, and coronary artery disease, which is related to this underfunding and the high rate of COVID-19 cases. Parts of the reservation are also exposed to high levels of pollution from oil and gas wells from the coal-fueled power plants. Those exposed to these high levels of pollutions have a higher than average number of cases of COVID-19, higher than in areas where the pollution is markedly lower.8
The Navajo are having to rely on the strength and resilience of traditional Navajo culture and philosophy to confront this monster, Dikos Nitsaa’igii’ 19. We have relied on Western medicine and its limited resources but now need to empower the strength from our traditional ways of knowing. We have used this knowledge in times of adversity for hundreds of years. The Navajo elders and medicine people have reminded us we have dealt with monsters and know how to endure hardship and be resilient. This helps to ameliorate mental health conditions, but there are still issues that remain challenging.
Those having the virus go through times of shortness of breath, which produces anxiety and panic. The risk of death adds further stress, and for a family-oriented culture, the need to isolate from family adds further stress. For the elderly and young people with more serious disease having to go to the hospital alone without family, often far from home, is so challenging. Connecting family by phone or social media with those stricken is essential to decrease anxiety and isolation. Those infected with the virus can learn breathing exercises, which can help the damage from the virus and decrease emotional activation and triggers. Specific breathing techniques can be taught by medical providers. An effective breathing technique to reduce anxiety is coherent breathing, which is done by inhaling 6 seconds and exhaling for 6 seconds without holding your breath. Behavioral health practitioners are available in the tribal and IHS mental health clinics to refer patients to therapy support to manage anxiety and are available by telemedicine. Many of these programs are offering social media informational sessions for the Navajo community. Navajo people often access traditional healing for protection prayers and ceremonies. Some of the tribal and IHS programs provide traditional counselors to talk to. The Navajo access healing that focuses on restoring balance to the body, mind, and spirit.
Taking action against the virus by social distancing, hand washing, and wearing masks can go a long way in reducing anxiety and fear about getting the virus. Resources to help the Navajo Nation are coming from all over the world, from as far as Ireland,9 Doctors Without Borders, 10 and University of San Francisco.11
Two resources that provide relief on the reservation are the Navajo Relief Fund and United Natives.
References
1. Navaho Times. 2020 May 27.
2. Ingalls A et al. BMC Obes. 2019 May 6. doi: 10.1186/s40608-019-0233-9.
3. U.S. Census 2010, as reported by discovernavajo.com.
4. Gould C et al. “Addressing food insecurity on the Navajo reservation through sustainable greenhouses.” 2018 Aug.
5. Native Knowledge 360. Smithsonian Institution. “Bosque Redondo.”
6. Personal communication, Carl Roessel Slater, Navajo Nation Council delegate.
7. IHS Profile Fact Sheet.
8. Wu X et al. medRxiv. 2020 Apr 27.
9. Carroll R. ”Irish support for Native American COVID-19 relief highlights historic bond.” The Guardian. 2020 May 9.
10. Capatides C. “Doctors Without Borders dispatches team to the Navajo Nation” CBS News. 2020 May 11.
11. Weiler N. “UCSF sends second wave of health workers to Navajo Nation.” UCSF.edu. 2020 May 21.
Dr. Roessel is a Navajo board-certified psychiatrist practicing in Santa Fe, N.M., working with the local indigenous population. She has special expertise in cultural psychiatry; her childhood was spent growing up in the Navajo Nation with her grandfather, who was a Navajo medicine man. Her psychiatric practice focuses on integrating indigenous knowledge and principles. Dr. Roessel is a distinguished fellow of the American Psychiatric Association. She has no disclosures.
The Navajo people have dealt with adversity that has tested our strength and resilience since our creation. In Navajo culture, the Holy People or gods challenged us with Naayee (monsters). We endured and learned from each Naayee, hunger, and death to name a few adversities. The COVID-19 pandemic, or “Big Cough” (Dikos Nitsaa’igii -19 in Navajo language) is a monster confronting the Navajo today. It has had significant impact on our nation and people.
The Navajo have the most cases of the COVID-19 virus of any tribe in the United States, and numbers as of May 31, 2020, are 5,348, with 246 confirmed deaths.1 The Navajo Nation, which once lagged behind New York, has reported the largest per-capita infection rate in the United States.
These devastating numbers, which might be leveling off, are associated with Navajo people having higher-than-average numbers of diabetes, heart disease, and cancer. This is compounded with 30%-40% of homes having no electricity or running water, and a poverty rate of about 38%.2
Geographical and cultural factors also contribute to the inability to gain a foothold in mitigating the number of cases. The Navajo Nation is the largest tribe in the United States, covering 27,000 square miles over an arid, red rock expanse with canyons and mountains. The population is over 250,000,3 and Navajo have traditionally lived in matrilineal clan units throughout the reservation, the size of West Virginia. The family traditional dwelling, called a “hogan,” often is clustered together. Multiple generations live together in these units. The COVID-19 virus inflicted many Navajo and rapidly spread to the elderly in these close-proximity living quarters.
Most Navajo live away from services and grocery stores and travel back and forth for food and water, which contributes to the virus rapidly being transmitted among the community members. Education aimed at curbing travel and spread of the virus was issued with curfews, commands to stay at home and keep social distance, and protect elders. The Navajo leadership and traditional medicine people, meanwhile, advised the people to follow their cultural values by caring for family and community members and providing a safe environment.
Resources are spread out
There are only 13 stores in this expansive reservation,4 so tribal members rely on traveling to border towns, such as Farmington and Gallup, N.M., Families usually travel to these towns on weekends to replenish food and supplies. There has been a cluster of cases in Gallup, N.M., so to reduce the numbers, the town shut itself off from outsiders – including the Navajo people coming to buy food, do laundry, and get water and feed for livestock. This has affected and stressed the Navajo further in attempting to access necessities.
Access to health care is already challenging because of lack of transportation and distance. This has made it more difficult to access COVID-19 testing and more challenging to get the results back. The Indian Health Service has been the designated health care system for the Navajo since 1955. The Treaty of Bosque Redondo, signed by the Navajo in 1868, included the provision of health care, as well as education in exchange for tracts of land, that included the Navajo homeland or Dinetah.5
The Indian Health Service provides care with hospitals and clinics throughout the reservation. Some of the IHS facilities have been taken over by the Navajo, so there are four Navajo tribally controlled hospitals, along with one private hospital. Coordination of care for a pandemic is, therefore, more challenging to coordinate. This contributes to problems with coordination of the health care, establishing alternate care sites, accessing personal protective equipment, and providing testing sites. The Navajo Nation Council is working hard to equitably distribute the $600 million from the CARES Act.6
Dealing with the pandemic is compromised by chronic underfunding from the U.S. government. The treaty obligation of the U.S. government is to provide health care to all federally recognized Native Americans. The IHS, which has been designated to provide that care for a tribal person, gets one-third the Medicare dollars for health care provided for a person in the general population.7 Health factors have led to the public health issues of poorly controlled diabetes, obesity, and coronary artery disease, which is related to this underfunding and the high rate of COVID-19 cases. Parts of the reservation are also exposed to high levels of pollution from oil and gas wells from the coal-fueled power plants. Those exposed to these high levels of pollutions have a higher than average number of cases of COVID-19, higher than in areas where the pollution is markedly lower.8
The Navajo are having to rely on the strength and resilience of traditional Navajo culture and philosophy to confront this monster, Dikos Nitsaa’igii’ 19. We have relied on Western medicine and its limited resources but now need to empower the strength from our traditional ways of knowing. We have used this knowledge in times of adversity for hundreds of years. The Navajo elders and medicine people have reminded us we have dealt with monsters and know how to endure hardship and be resilient. This helps to ameliorate mental health conditions, but there are still issues that remain challenging.
Those having the virus go through times of shortness of breath, which produces anxiety and panic. The risk of death adds further stress, and for a family-oriented culture, the need to isolate from family adds further stress. For the elderly and young people with more serious disease having to go to the hospital alone without family, often far from home, is so challenging. Connecting family by phone or social media with those stricken is essential to decrease anxiety and isolation. Those infected with the virus can learn breathing exercises, which can help the damage from the virus and decrease emotional activation and triggers. Specific breathing techniques can be taught by medical providers. An effective breathing technique to reduce anxiety is coherent breathing, which is done by inhaling 6 seconds and exhaling for 6 seconds without holding your breath. Behavioral health practitioners are available in the tribal and IHS mental health clinics to refer patients to therapy support to manage anxiety and are available by telemedicine. Many of these programs are offering social media informational sessions for the Navajo community. Navajo people often access traditional healing for protection prayers and ceremonies. Some of the tribal and IHS programs provide traditional counselors to talk to. The Navajo access healing that focuses on restoring balance to the body, mind, and spirit.
Taking action against the virus by social distancing, hand washing, and wearing masks can go a long way in reducing anxiety and fear about getting the virus. Resources to help the Navajo Nation are coming from all over the world, from as far as Ireland,9 Doctors Without Borders, 10 and University of San Francisco.11
Two resources that provide relief on the reservation are the Navajo Relief Fund and United Natives.
References
1. Navaho Times. 2020 May 27.
2. Ingalls A et al. BMC Obes. 2019 May 6. doi: 10.1186/s40608-019-0233-9.
3. U.S. Census 2010, as reported by discovernavajo.com.
4. Gould C et al. “Addressing food insecurity on the Navajo reservation through sustainable greenhouses.” 2018 Aug.
5. Native Knowledge 360. Smithsonian Institution. “Bosque Redondo.”
6. Personal communication, Carl Roessel Slater, Navajo Nation Council delegate.
7. IHS Profile Fact Sheet.
8. Wu X et al. medRxiv. 2020 Apr 27.
9. Carroll R. ”Irish support for Native American COVID-19 relief highlights historic bond.” The Guardian. 2020 May 9.
10. Capatides C. “Doctors Without Borders dispatches team to the Navajo Nation” CBS News. 2020 May 11.
11. Weiler N. “UCSF sends second wave of health workers to Navajo Nation.” UCSF.edu. 2020 May 21.
Dr. Roessel is a Navajo board-certified psychiatrist practicing in Santa Fe, N.M., working with the local indigenous population. She has special expertise in cultural psychiatry; her childhood was spent growing up in the Navajo Nation with her grandfather, who was a Navajo medicine man. Her psychiatric practice focuses on integrating indigenous knowledge and principles. Dr. Roessel is a distinguished fellow of the American Psychiatric Association. She has no disclosures.
The Navajo people have dealt with adversity that has tested our strength and resilience since our creation. In Navajo culture, the Holy People or gods challenged us with Naayee (monsters). We endured and learned from each Naayee, hunger, and death to name a few adversities. The COVID-19 pandemic, or “Big Cough” (Dikos Nitsaa’igii -19 in Navajo language) is a monster confronting the Navajo today. It has had significant impact on our nation and people.
The Navajo have the most cases of the COVID-19 virus of any tribe in the United States, and numbers as of May 31, 2020, are 5,348, with 246 confirmed deaths.1 The Navajo Nation, which once lagged behind New York, has reported the largest per-capita infection rate in the United States.
These devastating numbers, which might be leveling off, are associated with Navajo people having higher-than-average numbers of diabetes, heart disease, and cancer. This is compounded with 30%-40% of homes having no electricity or running water, and a poverty rate of about 38%.2
Geographical and cultural factors also contribute to the inability to gain a foothold in mitigating the number of cases. The Navajo Nation is the largest tribe in the United States, covering 27,000 square miles over an arid, red rock expanse with canyons and mountains. The population is over 250,000,3 and Navajo have traditionally lived in matrilineal clan units throughout the reservation, the size of West Virginia. The family traditional dwelling, called a “hogan,” often is clustered together. Multiple generations live together in these units. The COVID-19 virus inflicted many Navajo and rapidly spread to the elderly in these close-proximity living quarters.
Most Navajo live away from services and grocery stores and travel back and forth for food and water, which contributes to the virus rapidly being transmitted among the community members. Education aimed at curbing travel and spread of the virus was issued with curfews, commands to stay at home and keep social distance, and protect elders. The Navajo leadership and traditional medicine people, meanwhile, advised the people to follow their cultural values by caring for family and community members and providing a safe environment.
Resources are spread out
There are only 13 stores in this expansive reservation,4 so tribal members rely on traveling to border towns, such as Farmington and Gallup, N.M., Families usually travel to these towns on weekends to replenish food and supplies. There has been a cluster of cases in Gallup, N.M., so to reduce the numbers, the town shut itself off from outsiders – including the Navajo people coming to buy food, do laundry, and get water and feed for livestock. This has affected and stressed the Navajo further in attempting to access necessities.
Access to health care is already challenging because of lack of transportation and distance. This has made it more difficult to access COVID-19 testing and more challenging to get the results back. The Indian Health Service has been the designated health care system for the Navajo since 1955. The Treaty of Bosque Redondo, signed by the Navajo in 1868, included the provision of health care, as well as education in exchange for tracts of land, that included the Navajo homeland or Dinetah.5
The Indian Health Service provides care with hospitals and clinics throughout the reservation. Some of the IHS facilities have been taken over by the Navajo, so there are four Navajo tribally controlled hospitals, along with one private hospital. Coordination of care for a pandemic is, therefore, more challenging to coordinate. This contributes to problems with coordination of the health care, establishing alternate care sites, accessing personal protective equipment, and providing testing sites. The Navajo Nation Council is working hard to equitably distribute the $600 million from the CARES Act.6
Dealing with the pandemic is compromised by chronic underfunding from the U.S. government. The treaty obligation of the U.S. government is to provide health care to all federally recognized Native Americans. The IHS, which has been designated to provide that care for a tribal person, gets one-third the Medicare dollars for health care provided for a person in the general population.7 Health factors have led to the public health issues of poorly controlled diabetes, obesity, and coronary artery disease, which is related to this underfunding and the high rate of COVID-19 cases. Parts of the reservation are also exposed to high levels of pollution from oil and gas wells from the coal-fueled power plants. Those exposed to these high levels of pollutions have a higher than average number of cases of COVID-19, higher than in areas where the pollution is markedly lower.8
The Navajo are having to rely on the strength and resilience of traditional Navajo culture and philosophy to confront this monster, Dikos Nitsaa’igii’ 19. We have relied on Western medicine and its limited resources but now need to empower the strength from our traditional ways of knowing. We have used this knowledge in times of adversity for hundreds of years. The Navajo elders and medicine people have reminded us we have dealt with monsters and know how to endure hardship and be resilient. This helps to ameliorate mental health conditions, but there are still issues that remain challenging.
Those having the virus go through times of shortness of breath, which produces anxiety and panic. The risk of death adds further stress, and for a family-oriented culture, the need to isolate from family adds further stress. For the elderly and young people with more serious disease having to go to the hospital alone without family, often far from home, is so challenging. Connecting family by phone or social media with those stricken is essential to decrease anxiety and isolation. Those infected with the virus can learn breathing exercises, which can help the damage from the virus and decrease emotional activation and triggers. Specific breathing techniques can be taught by medical providers. An effective breathing technique to reduce anxiety is coherent breathing, which is done by inhaling 6 seconds and exhaling for 6 seconds without holding your breath. Behavioral health practitioners are available in the tribal and IHS mental health clinics to refer patients to therapy support to manage anxiety and are available by telemedicine. Many of these programs are offering social media informational sessions for the Navajo community. Navajo people often access traditional healing for protection prayers and ceremonies. Some of the tribal and IHS programs provide traditional counselors to talk to. The Navajo access healing that focuses on restoring balance to the body, mind, and spirit.
Taking action against the virus by social distancing, hand washing, and wearing masks can go a long way in reducing anxiety and fear about getting the virus. Resources to help the Navajo Nation are coming from all over the world, from as far as Ireland,9 Doctors Without Borders, 10 and University of San Francisco.11
Two resources that provide relief on the reservation are the Navajo Relief Fund and United Natives.
References
1. Navaho Times. 2020 May 27.
2. Ingalls A et al. BMC Obes. 2019 May 6. doi: 10.1186/s40608-019-0233-9.
3. U.S. Census 2010, as reported by discovernavajo.com.
4. Gould C et al. “Addressing food insecurity on the Navajo reservation through sustainable greenhouses.” 2018 Aug.
5. Native Knowledge 360. Smithsonian Institution. “Bosque Redondo.”
6. Personal communication, Carl Roessel Slater, Navajo Nation Council delegate.
7. IHS Profile Fact Sheet.
8. Wu X et al. medRxiv. 2020 Apr 27.
9. Carroll R. ”Irish support for Native American COVID-19 relief highlights historic bond.” The Guardian. 2020 May 9.
10. Capatides C. “Doctors Without Borders dispatches team to the Navajo Nation” CBS News. 2020 May 11.
11. Weiler N. “UCSF sends second wave of health workers to Navajo Nation.” UCSF.edu. 2020 May 21.
Dr. Roessel is a Navajo board-certified psychiatrist practicing in Santa Fe, N.M., working with the local indigenous population. She has special expertise in cultural psychiatry; her childhood was spent growing up in the Navajo Nation with her grandfather, who was a Navajo medicine man. Her psychiatric practice focuses on integrating indigenous knowledge and principles. Dr. Roessel is a distinguished fellow of the American Psychiatric Association. She has no disclosures.
‘After Life’ and before good treatment
Portrayal of psychiatry in Netflix series could deter people from getting help
While many across the world who have access to Netflix and other streaming services have been on lockdown, the second season of Ricky Gervais’s dark comedy series, “After Life,” was released. The show will also return for a third season.
The setup of the show is that Lisa, the wife of Gervais’s protagonist, Tony, has died of breast cancer. Knowing that he would need help after, she made him a video guide to life without her, ranging from the mundane of a garbage day or house alarm to feeding their dog Brandy, tidying the house, and constantly reminding him to take care of himself.
When we first see Tony, he is not doing great on self-care, and he has turned his grief into a “super power” allowing himself to do or say whatever he wants to – from pretending to reprimand his dog for calling a man (who had just told him his dog should be on a lead) a “fat hairy nosy !#$%&” to getting into a name-calling exchange with a primary school child. He later (jokingly) threatens this same child with a hammer, so that the child will stop bullying his nephew.
Tony works as the head of features for the Tambury Gazette, the free local paper. The comedy is full of the hometown charm with Tony and the photographer, Lenny, visiting the homes of the interesting personalities who have called into the paper with their small-town newsworthy stories.
Colorful characters abound in his town, including Postman Pat, who pops in and helps himself to a bath. Tony develops an unlikely friendship with a sex worker whom he hires to clean his house – since she said that she would do “anything for 50 quid.”
Tony, in the midst of an existential crisis, visits his wife’s grave frequently. While there, he meets an older widow, Anne, who befriends him and offers good advice. (Anne is played by Penelope Wilton of The Best Exotic Marigold Hotel and Downton Abbey.)
Tony also dutifully visits his father daily at the Autumnal Leaves Care Home. His father has dementia and keeps asking about Lisa, forgetting that she is dead. Tony comments that if his father were a dog, he would euthanize him. In actuality, Tony’s dog, Brandy, stops Tony’s potential suicide throughout the series.
Matt, who is Tony’s brother-in-law (and boss at the paper) describes Tony as “devastated, suicidal.” Tony explains that he can do and say what he wants, and “then when it all gets too much, I can always kill myself.” By season 2, Matt’s wife has left him, and he, too, needs to see the psychiatrist.
The problem is the Tambury psychiatrist (played by Paul Kaye). General psychiatrists in film have been described in various ways by the late Irving Schneider, MD, including Dr. Evil, Dr. Wonderful, and Dr. Dippy types. “Dr. Dippy’s Sanitarium” was a 1906 silent film in which Dr. Dippy is seen lacking in common sense but being harmless overall. Based on the behaviors displayed in and out of therapy, the Tambury psychiatrist could never be described as Dr. Wonderful, leading to the Dr. Evil or the Dr. Dippy options. He is certainly using patients for his own personal gratification (like a Dr. Evil might) and is certainly lacking in common sense and acting “crazier or more foolish than his patients”1 (like a Dr. Dippy). However, this psychiatrist may need a category all to himself.
Tony sought out the psychiatrist at a desperate time in his life. The dark but comical way he expresses himself: “A good day is one where I don’t go around wanting to shoot random strangers in the face and then turn the gun on myself” is not met with compassion, but unfortunately by inappropriate chuckles. Instead of offering solace, the psychiatrist revealed confidential doctor-patient information about other patients. When pressed, the psychiatrist insists, “I didn’t say his name.” The psychiatrist also explains he is telling Tony privileged information to “let you know you’re not … the only mental case out there.” The psychiatrist is also blatantly tweeting on his phone during the session. He tells his patient that it is ridiculous to want a soul mate and explains that other species might rape their sexual conquest. He yawns loudly in a session with Tony. These are just some of the many cringe-worthy behaviors displayed by this (unnamed) fictional embarrassment to our field.
By season 2, the psychiatrist begins seeing Tony’s brother-in-law, Matt, in treatment, the first of his boundary violations with Matt since Matt is Tony’s close friend and relative. The psychiatrist soon makes the crass self-disclosure to Matt that, “I was bleeding from the anus for a month last year, and I never went to the doctor,” implying Matt is a wimp for coming in. The psychiatrist invites him to go out with him and his friends, and gives him a beer in a session. The psychiatrist tells Matt stories of his sex life and complains about why people are bothered about toxic masculinity. When there is no way it can get worse, Tony and Matt run into the psychiatrist and his mates in a pub. The psychiatrist tells his comrades: “That’s the suicidal one with the dead wife I was telling you about.” When asked about confidentiality, he again protests: “I didn’t say your name mate,” Gestures are made, and the patients are mocked and laughed at. Unfathomably, Matt still returns for therapy, but is told by the psychiatrist to “lie, cheat, just be a man,” and about lesbians using dildos. The psychiatrist complains to Matt he is “sick of this @#!&, hearing people winge all day.”
Dr. Dippy or Dr. Evil – or somewhere in between – Tambury’s psychiatrist is not anyone who should be seeing humans, let alone a vulnerable population seeking help. These satirical behaviors and comments perhaps suggest worries of the general population about what happens behind the closed doors of psychotherapy and the concern that there may not be such a thing as a “safe space.” Even though this character is meant to be funny, there is a concern that, in this difficult time, this portrayal could deter even one person from getting the help that they need.
In spite of this unfortunate characterization of psychiatry, “After Life” is a brilliant, dark portrayal of grief after loss, the comfort of pets, grief while losing someone to dementia, and even growth after loss. The theme of grief is especially poignant during this time of collective grief.
The difficulty is the portrayal of psychiatry and therapy – released at a time when in the real world, we are coping with a pandemic and expecting massive mental health fallout. Negative portrayals of psychiatry and therapy in this and other shows could potentially deter people from taking care of their own mental health in this traumatic time in our collective history when we all need to be vigilant about mental health.
Reference
1. Schneider I. Am J Psychiatry. 1987 Aug;144(8):966-1002.
Portrayal of psychiatry in Netflix series could deter people from getting help
Portrayal of psychiatry in Netflix series could deter people from getting help
While many across the world who have access to Netflix and other streaming services have been on lockdown, the second season of Ricky Gervais’s dark comedy series, “After Life,” was released. The show will also return for a third season.
The setup of the show is that Lisa, the wife of Gervais’s protagonist, Tony, has died of breast cancer. Knowing that he would need help after, she made him a video guide to life without her, ranging from the mundane of a garbage day or house alarm to feeding their dog Brandy, tidying the house, and constantly reminding him to take care of himself.
When we first see Tony, he is not doing great on self-care, and he has turned his grief into a “super power” allowing himself to do or say whatever he wants to – from pretending to reprimand his dog for calling a man (who had just told him his dog should be on a lead) a “fat hairy nosy !#$%&” to getting into a name-calling exchange with a primary school child. He later (jokingly) threatens this same child with a hammer, so that the child will stop bullying his nephew.
Tony works as the head of features for the Tambury Gazette, the free local paper. The comedy is full of the hometown charm with Tony and the photographer, Lenny, visiting the homes of the interesting personalities who have called into the paper with their small-town newsworthy stories.
Colorful characters abound in his town, including Postman Pat, who pops in and helps himself to a bath. Tony develops an unlikely friendship with a sex worker whom he hires to clean his house – since she said that she would do “anything for 50 quid.”
Tony, in the midst of an existential crisis, visits his wife’s grave frequently. While there, he meets an older widow, Anne, who befriends him and offers good advice. (Anne is played by Penelope Wilton of The Best Exotic Marigold Hotel and Downton Abbey.)
Tony also dutifully visits his father daily at the Autumnal Leaves Care Home. His father has dementia and keeps asking about Lisa, forgetting that she is dead. Tony comments that if his father were a dog, he would euthanize him. In actuality, Tony’s dog, Brandy, stops Tony’s potential suicide throughout the series.
Matt, who is Tony’s brother-in-law (and boss at the paper) describes Tony as “devastated, suicidal.” Tony explains that he can do and say what he wants, and “then when it all gets too much, I can always kill myself.” By season 2, Matt’s wife has left him, and he, too, needs to see the psychiatrist.
The problem is the Tambury psychiatrist (played by Paul Kaye). General psychiatrists in film have been described in various ways by the late Irving Schneider, MD, including Dr. Evil, Dr. Wonderful, and Dr. Dippy types. “Dr. Dippy’s Sanitarium” was a 1906 silent film in which Dr. Dippy is seen lacking in common sense but being harmless overall. Based on the behaviors displayed in and out of therapy, the Tambury psychiatrist could never be described as Dr. Wonderful, leading to the Dr. Evil or the Dr. Dippy options. He is certainly using patients for his own personal gratification (like a Dr. Evil might) and is certainly lacking in common sense and acting “crazier or more foolish than his patients”1 (like a Dr. Dippy). However, this psychiatrist may need a category all to himself.
Tony sought out the psychiatrist at a desperate time in his life. The dark but comical way he expresses himself: “A good day is one where I don’t go around wanting to shoot random strangers in the face and then turn the gun on myself” is not met with compassion, but unfortunately by inappropriate chuckles. Instead of offering solace, the psychiatrist revealed confidential doctor-patient information about other patients. When pressed, the psychiatrist insists, “I didn’t say his name.” The psychiatrist also explains he is telling Tony privileged information to “let you know you’re not … the only mental case out there.” The psychiatrist is also blatantly tweeting on his phone during the session. He tells his patient that it is ridiculous to want a soul mate and explains that other species might rape their sexual conquest. He yawns loudly in a session with Tony. These are just some of the many cringe-worthy behaviors displayed by this (unnamed) fictional embarrassment to our field.
By season 2, the psychiatrist begins seeing Tony’s brother-in-law, Matt, in treatment, the first of his boundary violations with Matt since Matt is Tony’s close friend and relative. The psychiatrist soon makes the crass self-disclosure to Matt that, “I was bleeding from the anus for a month last year, and I never went to the doctor,” implying Matt is a wimp for coming in. The psychiatrist invites him to go out with him and his friends, and gives him a beer in a session. The psychiatrist tells Matt stories of his sex life and complains about why people are bothered about toxic masculinity. When there is no way it can get worse, Tony and Matt run into the psychiatrist and his mates in a pub. The psychiatrist tells his comrades: “That’s the suicidal one with the dead wife I was telling you about.” When asked about confidentiality, he again protests: “I didn’t say your name mate,” Gestures are made, and the patients are mocked and laughed at. Unfathomably, Matt still returns for therapy, but is told by the psychiatrist to “lie, cheat, just be a man,” and about lesbians using dildos. The psychiatrist complains to Matt he is “sick of this @#!&, hearing people winge all day.”
Dr. Dippy or Dr. Evil – or somewhere in between – Tambury’s psychiatrist is not anyone who should be seeing humans, let alone a vulnerable population seeking help. These satirical behaviors and comments perhaps suggest worries of the general population about what happens behind the closed doors of psychotherapy and the concern that there may not be such a thing as a “safe space.” Even though this character is meant to be funny, there is a concern that, in this difficult time, this portrayal could deter even one person from getting the help that they need.
In spite of this unfortunate characterization of psychiatry, “After Life” is a brilliant, dark portrayal of grief after loss, the comfort of pets, grief while losing someone to dementia, and even growth after loss. The theme of grief is especially poignant during this time of collective grief.
The difficulty is the portrayal of psychiatry and therapy – released at a time when in the real world, we are coping with a pandemic and expecting massive mental health fallout. Negative portrayals of psychiatry and therapy in this and other shows could potentially deter people from taking care of their own mental health in this traumatic time in our collective history when we all need to be vigilant about mental health.
Reference
1. Schneider I. Am J Psychiatry. 1987 Aug;144(8):966-1002.
While many across the world who have access to Netflix and other streaming services have been on lockdown, the second season of Ricky Gervais’s dark comedy series, “After Life,” was released. The show will also return for a third season.
The setup of the show is that Lisa, the wife of Gervais’s protagonist, Tony, has died of breast cancer. Knowing that he would need help after, she made him a video guide to life without her, ranging from the mundane of a garbage day or house alarm to feeding their dog Brandy, tidying the house, and constantly reminding him to take care of himself.
When we first see Tony, he is not doing great on self-care, and he has turned his grief into a “super power” allowing himself to do or say whatever he wants to – from pretending to reprimand his dog for calling a man (who had just told him his dog should be on a lead) a “fat hairy nosy !#$%&” to getting into a name-calling exchange with a primary school child. He later (jokingly) threatens this same child with a hammer, so that the child will stop bullying his nephew.
Tony works as the head of features for the Tambury Gazette, the free local paper. The comedy is full of the hometown charm with Tony and the photographer, Lenny, visiting the homes of the interesting personalities who have called into the paper with their small-town newsworthy stories.
Colorful characters abound in his town, including Postman Pat, who pops in and helps himself to a bath. Tony develops an unlikely friendship with a sex worker whom he hires to clean his house – since she said that she would do “anything for 50 quid.”
Tony, in the midst of an existential crisis, visits his wife’s grave frequently. While there, he meets an older widow, Anne, who befriends him and offers good advice. (Anne is played by Penelope Wilton of The Best Exotic Marigold Hotel and Downton Abbey.)
Tony also dutifully visits his father daily at the Autumnal Leaves Care Home. His father has dementia and keeps asking about Lisa, forgetting that she is dead. Tony comments that if his father were a dog, he would euthanize him. In actuality, Tony’s dog, Brandy, stops Tony’s potential suicide throughout the series.
Matt, who is Tony’s brother-in-law (and boss at the paper) describes Tony as “devastated, suicidal.” Tony explains that he can do and say what he wants, and “then when it all gets too much, I can always kill myself.” By season 2, Matt’s wife has left him, and he, too, needs to see the psychiatrist.
The problem is the Tambury psychiatrist (played by Paul Kaye). General psychiatrists in film have been described in various ways by the late Irving Schneider, MD, including Dr. Evil, Dr. Wonderful, and Dr. Dippy types. “Dr. Dippy’s Sanitarium” was a 1906 silent film in which Dr. Dippy is seen lacking in common sense but being harmless overall. Based on the behaviors displayed in and out of therapy, the Tambury psychiatrist could never be described as Dr. Wonderful, leading to the Dr. Evil or the Dr. Dippy options. He is certainly using patients for his own personal gratification (like a Dr. Evil might) and is certainly lacking in common sense and acting “crazier or more foolish than his patients”1 (like a Dr. Dippy). However, this psychiatrist may need a category all to himself.
Tony sought out the psychiatrist at a desperate time in his life. The dark but comical way he expresses himself: “A good day is one where I don’t go around wanting to shoot random strangers in the face and then turn the gun on myself” is not met with compassion, but unfortunately by inappropriate chuckles. Instead of offering solace, the psychiatrist revealed confidential doctor-patient information about other patients. When pressed, the psychiatrist insists, “I didn’t say his name.” The psychiatrist also explains he is telling Tony privileged information to “let you know you’re not … the only mental case out there.” The psychiatrist is also blatantly tweeting on his phone during the session. He tells his patient that it is ridiculous to want a soul mate and explains that other species might rape their sexual conquest. He yawns loudly in a session with Tony. These are just some of the many cringe-worthy behaviors displayed by this (unnamed) fictional embarrassment to our field.
By season 2, the psychiatrist begins seeing Tony’s brother-in-law, Matt, in treatment, the first of his boundary violations with Matt since Matt is Tony’s close friend and relative. The psychiatrist soon makes the crass self-disclosure to Matt that, “I was bleeding from the anus for a month last year, and I never went to the doctor,” implying Matt is a wimp for coming in. The psychiatrist invites him to go out with him and his friends, and gives him a beer in a session. The psychiatrist tells Matt stories of his sex life and complains about why people are bothered about toxic masculinity. When there is no way it can get worse, Tony and Matt run into the psychiatrist and his mates in a pub. The psychiatrist tells his comrades: “That’s the suicidal one with the dead wife I was telling you about.” When asked about confidentiality, he again protests: “I didn’t say your name mate,” Gestures are made, and the patients are mocked and laughed at. Unfathomably, Matt still returns for therapy, but is told by the psychiatrist to “lie, cheat, just be a man,” and about lesbians using dildos. The psychiatrist complains to Matt he is “sick of this @#!&, hearing people winge all day.”
Dr. Dippy or Dr. Evil – or somewhere in between – Tambury’s psychiatrist is not anyone who should be seeing humans, let alone a vulnerable population seeking help. These satirical behaviors and comments perhaps suggest worries of the general population about what happens behind the closed doors of psychotherapy and the concern that there may not be such a thing as a “safe space.” Even though this character is meant to be funny, there is a concern that, in this difficult time, this portrayal could deter even one person from getting the help that they need.
In spite of this unfortunate characterization of psychiatry, “After Life” is a brilliant, dark portrayal of grief after loss, the comfort of pets, grief while losing someone to dementia, and even growth after loss. The theme of grief is especially poignant during this time of collective grief.
The difficulty is the portrayal of psychiatry and therapy – released at a time when in the real world, we are coping with a pandemic and expecting massive mental health fallout. Negative portrayals of psychiatry and therapy in this and other shows could potentially deter people from taking care of their own mental health in this traumatic time in our collective history when we all need to be vigilant about mental health.
Reference
1. Schneider I. Am J Psychiatry. 1987 Aug;144(8):966-1002.
Domestic violence amid COVID-19: Helping your patients from afar
Roger R., MD, a primary care physician from Philadelphia, set up a telemedicine appointment with a 24-year-old female patient who was experiencing headaches and was worried she might have COVID-19.
During the televisit, Dr. R. noticed that “Tonya” (not her real name) had a purplish bruise under her right eye. When asked how she got the bruise, Tonya said she had bumped into a dresser. The physician suspected abuse. He then heard a man’s voice in the background and thought it might belong to the abuser. “Is this a good time for you to talk?” he asked Tonya.
Tonya hesitated.
“When might be a better time?”
Tonya suggested an alternate time, and the physician called her then. During the visit, she shared that her fiancé, a car salesman who was also sheltering at home, was punching her.
“He always had a bad temper. Once he shoved me, but he’s never hit me before. And when he was upset, we used to go out to eat and he calmed down. Now, we’re stuck inside, we can’t even get away from each other to go to work, and he’s getting scary,” she told the doctor.
The physician asked if she would like to be connected with a domestic violence counselor. When Tonya agreed, he called Jessica DuBois Palardy, a licensed social worker and the program supervisor at STOP Intimate Partner Violence, a Philadelphia-based collaborative project of the Children’s Hospital of Philadelphia and the Lutheran Settlement House’s Bilingual Domestic Violence Program.
A ‘horrifying’ trend
Tonya’s story is not unique. A United Nations report shows that there has been a “horrifying global surge in domestic violence” linked to “lockdowns imposed by the governments responding to the COVID-19 pandemic.” The United States is no exception – 2,345 calls were placed to the National Domestic Violence Hotline during March 16–April 6, 2020.
Carole Warshaw, MD, director of the National Center on Domestic Violence, Trauma, and Mental Health in Chicago, said, “We know that intimate partner violence is increasing among people sheltering at home, and that abuse has become more severe.”
Even in nonabusive situations, being confined together at close quarters, often amid family stress and financial hardship, can be wearing, and tempers can flare. In an abusive relationship, “the main contributor to violence during shelter-in-place restrictions is that the isolation gives abusers more opportunities for controlling their partners, who have fewer options for accessing safety and support,” Dr. Warshaw said.
It is critical to “approach every clinical encounter knowing that domestic violence may be at play,” she emphasized.
Physicians might be the most important lifeline
Physicians are already facing myriad COVID-19–related challenges, and having another concern to keep in mind may be daunting.
“We’re in uncharted territory and we’re all trying to figure out how to navigate this time, how to practice medicine via phone and video conferences, and how to deal with the financial repercussions of the pandemic – not to mention concern for the health of our families,” said Peter F. Cronholm, MD, associate professor of family medicine and community health at the Hospital of the University of Pennsylvania, Philadelphia. “So maintaining vigilance is often difficult. Nevertheless, it’s important not to let this critical issue fall to the wayside.”
Marcella Nyachogo, MSW, a licensed social worker and assistant director of the Bilingual Domestic Violence Program, noted that physicians and other health care providers “may be the only people the patient interacts with, since the abuser may cut the survivor off from family and friends. And because the survivor isn’t leaving the house, he or she doesn’t have an opportunity to interact with coworkers or others – which makes health care providers the most important lifeline.”
COVID-19 as a weapon of abuse
Carey Watson, MD, regional medical director of the Family Violence Prevention Program at Kaiser Permanente in northern California, points to a disturbing trend in COVID-19–related abuse.
“Unfortunately, I’m hearing more and more accounts of how the illness itself can be one more weapon in the abuser’s arsenal,” she said.
Experts say that increasingly, abusers are claiming that their partner, who is employed in an “essential” job outside the home, is carrying the virus, and they are using this as a means of control and manipulation.
This is especially true of abusive partners of health care providers, Dr. Watson noted. She recounted the story of a divorced nurse whose husband did not allow her to have contact with their children, allegedly out of concern that she might have COVID-19, and would threaten her with a gun when she protested.
“It is important to keep this abusive tactic in mind, not only when dealing with patients but also with fellow physicians and health care professionals, and check in to see if everything is okay – especially if they seem particularly stressed out or distant,” Dr. Watson recommended.
Trust your clinical gut
How can you tell if your patients might be experiencing abuse when you’re not seeing them in person?
Pay attention to subtle signals and “trust your clinical gut when something doesn’t feel right,” Ms. Nyachogo advised.
If a patient’s demeanor is jittery or anxious or if someone next to him or her is answering all the questions or interrupting the visit, these could be red flags.
Dr. Cronholm added that telemedicine visits offer a “rare window into a patient’s home life that would not be available in an office visit.” For example, a house in disarray, the presence of broken objects, or the presence of another person hovering in the background suggests the need for further exploration.
“The main thing for all providers to keep in mind is ‘first, do no harm,’ ” Ms. Nyachogo emphasized.
“Our agency has been working for years with medical professionals in how to screen and connect folks with help most effectively and safely, and – although the specific situations posed by COVID are new – the overall approach is the same, which is to proceed with caution in how you approach the subject and how you make referrals,” she said.
Begin by asking if it is a convenient time to talk.
“This question takes the onus off the patient, who may not know how to communicate that she has no privacy or is in the middle of an argument,” explained Elsa Swenson, program manager of Home Free community program, which serves individuals experiencing domestic violence. The program is part of Minnesota-based Missions Inc. Programs, which serves those experiencing domestic abuse and chemical dependency.
If the patient indicates that it isn’t a convenient time to talk, find out when would be a better time. “This might be difficult for busy physicians and may not be what they’re accustomed to when calling a patient at home, but the patient’s circumstances are unknown to you, so it’s essential to organize around their ability to talk,” Ms. Swenson noted.
‘Are you alone?’
Another important piece of information is whether the patient has privacy – which can be tricky if the abuser is standing right there.
“You don’t want to tip the abuser off to your concerns, so you need to frame the question in a neutral way,” Dr. Watson advised.
For example, you might say that HIPAA laws require that you conduct the consultation with no one else present, and find out if there is a location in the house where the patient can have privacy.
It might be easier to talk on the phone than via video, suggests Florence Remes, a New Jersey–based licensed social worker who specializes in domestic violence. Going into another room and playing music or turning on the television might make it less obvious that a call is taking place, and the abuser would be less likely to overhear the caller’s conversation.
Dr. Watson suggested that questions about abuse might be included with other questions and asked in a simple yes/no format. “I’d like to ask you some standard questions I’m asking everyone during the pandemic. Do you have a cough or fever? Do you have any other physical symptoms? Do you have access to hand sanitizer? How is your sleep? Are you experiencing stress? Do you feel safe at home?”
The abuser, if present, will only hear the patient’s “yes” or “no” without knowing the question. If the patient indicates that she is being abused but is unable to talk, a later time can be arranged to further explore the issue.
Technology is a double-edged sword
Modern technologies have been a great boon to patients and physicians during this time of social distancing, allowing ongoing contact and health care when it would not otherwise have been possible. On the other hand, technology is fraught with potential dangers that can jeopardize the patient’s safety and compromise privacy.
Ms. Remes recounted the story of “Susan,” a client with whom she had been conducting teletherapy visits using an approved HIPAA-compliant telemedicine forum. Susan was working from home because of shelter-in-place restrictions. Her husband had been abusive, and Susan was concerned he might be “sabotaging” the household’s WiFi to isolate her from outside sources of support.
At the recommendation of Ms. Remes, Susan continued sessions either via phone calls or by using the WhatsApp program on her cellphone. Many of the requirements governing HIPAA privacy regulations have been temporarily relaxed, and clinicians can use non–encrypted forms of transmission, such as FaceTime, WhatsApp, or Skype, if no other platform is available.
But even cellphones have risks, Dr. Warshaw noted. The patient’s abuser might track texts or look at call logs – especially on unsecured platforms. It’s advisable to ask patients about who has access to their phone and computer and discuss ways to increase security.
Follow the patient’s lead
Proceed slowly and start with nonthreatening questions, Ms. Palardy advised. “I notice you have some injuries; can you tell me how you got them? Did someone hurt you? What does your relationship look like when you argue? Is there anything that makes you feel uncomfortable or unsafe?”
Emphasizing that you are asking these questions because of care and concern is reassuring and helps patients to feel they are not alone, Ms. Nyachogo pointed out.
“As your doctor, I’m worried about your health and (if relevant) your children’s safety. I can help connect you with counseling and support, legal resources, and a shelter, and everything is free and confidential. Would you be interested?” she said.
If the client acknowledges abuse, “follow their lead, but don’t push too hard,” Ms. Nyachogo warned.
“It is the client’s choice whether or not to take action,” she noted. “I’ve met survivors who said that it wasn’t until a doctor or nurse expressed concern about bruises that it even occurred to them that they were being abused. Some lied to the doctor about how they got hurt – but the question planted a seed, even though it might have taken years to follow up on the referral,” she said.
What if the patient doesn’t want to get help?
If a patient is not ready to seek help, you can create a home-safety plan. This might include setting follow-up times. If you don’t hear from him or her, you should then call the police. Or you might create a “code word,” such as “apple pie.” If the patient uses that word during a session, you know her life is in danger, Ms. Remes suggested.
Providing written information about how to get help is important but can be problematic if the abuser finds it.
Ms. Nyachogo recommends e-mailing follow-up materials that cover a variety of topics, such as keeping safe during the COVID-19 pandemic, relaxation, healthy eating, getting exercise while homebound, activities for children, and suggestions for hotlines and other resources if one is feeling suicidal or unsafe.
“If you present these as your ‘standard’ follow-up materials, the abuser is less likely to become suspicious,” Ms. Nyachogo noted.
Resources are available during COVID-19
All of the experts emphasize that resources for victims of domestic violence remain available during the COVID-19 pandemic, although some shelters may be operating at reduced capacity. Some agencies are finding alternatives to group shelters, such as hotels or Airbnb, which carry less risk of catching COVID-19.
Referring a patient to domestic violence resources is a delicate process. “You don’t want referring the patient for help to further endanger their life,” Ms. Nyachogo said.
The more you can take the burden off the patient, the better. If she is interested in getting help, you can call a domestic violence counselor or advocate while she is on the phone.
“This type of ‘warm handoff’ is what Tonya’s physician did,” Ms. Palardy recounted.
A warm handoff requires that physicians be familiar with domestic violence resources, Dr. Warshaw emphasized.
“Don’t wait until you are working with someone who needs help to find out where to refer them. Take the time to proactively research local agencies specializing in domestic violence and have their phone numbers on hand, so you can offer resources immediately if the person is interested,” she advised. The National Domestic Violence Hotline can also assist with safety planning and access to local resources.
‘Thinking on your feet’ critical for physicians
Addressing domestic violence during this unprecedented time requires “thinking on your feet” about novel forms of detection and intervention, Dr. Watson said. This involves a combination of clinical acumen, creativity, and finely honed intuition.
Ms. Nyachogo added, “Keeping an eye on domestic violence can feel like an extra burden, but don’t forget that it is lifesaving work.”
Resources
National Domestic Violence Hotline
- 800-799-SAFE (7233)
- The patient can also text LOVEIS to 22522.
National Center on Domestic Violence, Trauma, and Mental Health
- Provides resources for health care, mental health, and substance use treatment and recovery support providers on responding to domestic violence and other trauma.
- Provides resources for professionals and patients regarding access to substance use and mental health care during the COVID-1 pandemic.
- Provides support for parents, caregivers, and children during the pandemic.
- Provides resources for advocates serving families affected by domestic violence.
- A state-by-state guide to local resources
Children’s Hospital of Philadelphia Research Institute
STOP Intimate Partner Violence (IPV)
New Jersey Coalition for Domestic Violence
American Bar Association COVID-19 resources for communities
- Text HOME to 741741.
National Network to End Domestic Violence (NNEDV) COVID-19 Technology Safety
A version of this article originally appeared on Medscape.com.
Roger R., MD, a primary care physician from Philadelphia, set up a telemedicine appointment with a 24-year-old female patient who was experiencing headaches and was worried she might have COVID-19.
During the televisit, Dr. R. noticed that “Tonya” (not her real name) had a purplish bruise under her right eye. When asked how she got the bruise, Tonya said she had bumped into a dresser. The physician suspected abuse. He then heard a man’s voice in the background and thought it might belong to the abuser. “Is this a good time for you to talk?” he asked Tonya.
Tonya hesitated.
“When might be a better time?”
Tonya suggested an alternate time, and the physician called her then. During the visit, she shared that her fiancé, a car salesman who was also sheltering at home, was punching her.
“He always had a bad temper. Once he shoved me, but he’s never hit me before. And when he was upset, we used to go out to eat and he calmed down. Now, we’re stuck inside, we can’t even get away from each other to go to work, and he’s getting scary,” she told the doctor.
The physician asked if she would like to be connected with a domestic violence counselor. When Tonya agreed, he called Jessica DuBois Palardy, a licensed social worker and the program supervisor at STOP Intimate Partner Violence, a Philadelphia-based collaborative project of the Children’s Hospital of Philadelphia and the Lutheran Settlement House’s Bilingual Domestic Violence Program.
A ‘horrifying’ trend
Tonya’s story is not unique. A United Nations report shows that there has been a “horrifying global surge in domestic violence” linked to “lockdowns imposed by the governments responding to the COVID-19 pandemic.” The United States is no exception – 2,345 calls were placed to the National Domestic Violence Hotline during March 16–April 6, 2020.
Carole Warshaw, MD, director of the National Center on Domestic Violence, Trauma, and Mental Health in Chicago, said, “We know that intimate partner violence is increasing among people sheltering at home, and that abuse has become more severe.”
Even in nonabusive situations, being confined together at close quarters, often amid family stress and financial hardship, can be wearing, and tempers can flare. In an abusive relationship, “the main contributor to violence during shelter-in-place restrictions is that the isolation gives abusers more opportunities for controlling their partners, who have fewer options for accessing safety and support,” Dr. Warshaw said.
It is critical to “approach every clinical encounter knowing that domestic violence may be at play,” she emphasized.
Physicians might be the most important lifeline
Physicians are already facing myriad COVID-19–related challenges, and having another concern to keep in mind may be daunting.
“We’re in uncharted territory and we’re all trying to figure out how to navigate this time, how to practice medicine via phone and video conferences, and how to deal with the financial repercussions of the pandemic – not to mention concern for the health of our families,” said Peter F. Cronholm, MD, associate professor of family medicine and community health at the Hospital of the University of Pennsylvania, Philadelphia. “So maintaining vigilance is often difficult. Nevertheless, it’s important not to let this critical issue fall to the wayside.”
Marcella Nyachogo, MSW, a licensed social worker and assistant director of the Bilingual Domestic Violence Program, noted that physicians and other health care providers “may be the only people the patient interacts with, since the abuser may cut the survivor off from family and friends. And because the survivor isn’t leaving the house, he or she doesn’t have an opportunity to interact with coworkers or others – which makes health care providers the most important lifeline.”
COVID-19 as a weapon of abuse
Carey Watson, MD, regional medical director of the Family Violence Prevention Program at Kaiser Permanente in northern California, points to a disturbing trend in COVID-19–related abuse.
“Unfortunately, I’m hearing more and more accounts of how the illness itself can be one more weapon in the abuser’s arsenal,” she said.
Experts say that increasingly, abusers are claiming that their partner, who is employed in an “essential” job outside the home, is carrying the virus, and they are using this as a means of control and manipulation.
This is especially true of abusive partners of health care providers, Dr. Watson noted. She recounted the story of a divorced nurse whose husband did not allow her to have contact with their children, allegedly out of concern that she might have COVID-19, and would threaten her with a gun when she protested.
“It is important to keep this abusive tactic in mind, not only when dealing with patients but also with fellow physicians and health care professionals, and check in to see if everything is okay – especially if they seem particularly stressed out or distant,” Dr. Watson recommended.
Trust your clinical gut
How can you tell if your patients might be experiencing abuse when you’re not seeing them in person?
Pay attention to subtle signals and “trust your clinical gut when something doesn’t feel right,” Ms. Nyachogo advised.
If a patient’s demeanor is jittery or anxious or if someone next to him or her is answering all the questions or interrupting the visit, these could be red flags.
Dr. Cronholm added that telemedicine visits offer a “rare window into a patient’s home life that would not be available in an office visit.” For example, a house in disarray, the presence of broken objects, or the presence of another person hovering in the background suggests the need for further exploration.
“The main thing for all providers to keep in mind is ‘first, do no harm,’ ” Ms. Nyachogo emphasized.
“Our agency has been working for years with medical professionals in how to screen and connect folks with help most effectively and safely, and – although the specific situations posed by COVID are new – the overall approach is the same, which is to proceed with caution in how you approach the subject and how you make referrals,” she said.
Begin by asking if it is a convenient time to talk.
“This question takes the onus off the patient, who may not know how to communicate that she has no privacy or is in the middle of an argument,” explained Elsa Swenson, program manager of Home Free community program, which serves individuals experiencing domestic violence. The program is part of Minnesota-based Missions Inc. Programs, which serves those experiencing domestic abuse and chemical dependency.
If the patient indicates that it isn’t a convenient time to talk, find out when would be a better time. “This might be difficult for busy physicians and may not be what they’re accustomed to when calling a patient at home, but the patient’s circumstances are unknown to you, so it’s essential to organize around their ability to talk,” Ms. Swenson noted.
‘Are you alone?’
Another important piece of information is whether the patient has privacy – which can be tricky if the abuser is standing right there.
“You don’t want to tip the abuser off to your concerns, so you need to frame the question in a neutral way,” Dr. Watson advised.
For example, you might say that HIPAA laws require that you conduct the consultation with no one else present, and find out if there is a location in the house where the patient can have privacy.
It might be easier to talk on the phone than via video, suggests Florence Remes, a New Jersey–based licensed social worker who specializes in domestic violence. Going into another room and playing music or turning on the television might make it less obvious that a call is taking place, and the abuser would be less likely to overhear the caller’s conversation.
Dr. Watson suggested that questions about abuse might be included with other questions and asked in a simple yes/no format. “I’d like to ask you some standard questions I’m asking everyone during the pandemic. Do you have a cough or fever? Do you have any other physical symptoms? Do you have access to hand sanitizer? How is your sleep? Are you experiencing stress? Do you feel safe at home?”
The abuser, if present, will only hear the patient’s “yes” or “no” without knowing the question. If the patient indicates that she is being abused but is unable to talk, a later time can be arranged to further explore the issue.
Technology is a double-edged sword
Modern technologies have been a great boon to patients and physicians during this time of social distancing, allowing ongoing contact and health care when it would not otherwise have been possible. On the other hand, technology is fraught with potential dangers that can jeopardize the patient’s safety and compromise privacy.
Ms. Remes recounted the story of “Susan,” a client with whom she had been conducting teletherapy visits using an approved HIPAA-compliant telemedicine forum. Susan was working from home because of shelter-in-place restrictions. Her husband had been abusive, and Susan was concerned he might be “sabotaging” the household’s WiFi to isolate her from outside sources of support.
At the recommendation of Ms. Remes, Susan continued sessions either via phone calls or by using the WhatsApp program on her cellphone. Many of the requirements governing HIPAA privacy regulations have been temporarily relaxed, and clinicians can use non–encrypted forms of transmission, such as FaceTime, WhatsApp, or Skype, if no other platform is available.
But even cellphones have risks, Dr. Warshaw noted. The patient’s abuser might track texts or look at call logs – especially on unsecured platforms. It’s advisable to ask patients about who has access to their phone and computer and discuss ways to increase security.
Follow the patient’s lead
Proceed slowly and start with nonthreatening questions, Ms. Palardy advised. “I notice you have some injuries; can you tell me how you got them? Did someone hurt you? What does your relationship look like when you argue? Is there anything that makes you feel uncomfortable or unsafe?”
Emphasizing that you are asking these questions because of care and concern is reassuring and helps patients to feel they are not alone, Ms. Nyachogo pointed out.
“As your doctor, I’m worried about your health and (if relevant) your children’s safety. I can help connect you with counseling and support, legal resources, and a shelter, and everything is free and confidential. Would you be interested?” she said.
If the client acknowledges abuse, “follow their lead, but don’t push too hard,” Ms. Nyachogo warned.
“It is the client’s choice whether or not to take action,” she noted. “I’ve met survivors who said that it wasn’t until a doctor or nurse expressed concern about bruises that it even occurred to them that they were being abused. Some lied to the doctor about how they got hurt – but the question planted a seed, even though it might have taken years to follow up on the referral,” she said.
What if the patient doesn’t want to get help?
If a patient is not ready to seek help, you can create a home-safety plan. This might include setting follow-up times. If you don’t hear from him or her, you should then call the police. Or you might create a “code word,” such as “apple pie.” If the patient uses that word during a session, you know her life is in danger, Ms. Remes suggested.
Providing written information about how to get help is important but can be problematic if the abuser finds it.
Ms. Nyachogo recommends e-mailing follow-up materials that cover a variety of topics, such as keeping safe during the COVID-19 pandemic, relaxation, healthy eating, getting exercise while homebound, activities for children, and suggestions for hotlines and other resources if one is feeling suicidal or unsafe.
“If you present these as your ‘standard’ follow-up materials, the abuser is less likely to become suspicious,” Ms. Nyachogo noted.
Resources are available during COVID-19
All of the experts emphasize that resources for victims of domestic violence remain available during the COVID-19 pandemic, although some shelters may be operating at reduced capacity. Some agencies are finding alternatives to group shelters, such as hotels or Airbnb, which carry less risk of catching COVID-19.
Referring a patient to domestic violence resources is a delicate process. “You don’t want referring the patient for help to further endanger their life,” Ms. Nyachogo said.
The more you can take the burden off the patient, the better. If she is interested in getting help, you can call a domestic violence counselor or advocate while she is on the phone.
“This type of ‘warm handoff’ is what Tonya’s physician did,” Ms. Palardy recounted.
A warm handoff requires that physicians be familiar with domestic violence resources, Dr. Warshaw emphasized.
“Don’t wait until you are working with someone who needs help to find out where to refer them. Take the time to proactively research local agencies specializing in domestic violence and have their phone numbers on hand, so you can offer resources immediately if the person is interested,” she advised. The National Domestic Violence Hotline can also assist with safety planning and access to local resources.
‘Thinking on your feet’ critical for physicians
Addressing domestic violence during this unprecedented time requires “thinking on your feet” about novel forms of detection and intervention, Dr. Watson said. This involves a combination of clinical acumen, creativity, and finely honed intuition.
Ms. Nyachogo added, “Keeping an eye on domestic violence can feel like an extra burden, but don’t forget that it is lifesaving work.”
Resources
National Domestic Violence Hotline
- 800-799-SAFE (7233)
- The patient can also text LOVEIS to 22522.
National Center on Domestic Violence, Trauma, and Mental Health
- Provides resources for health care, mental health, and substance use treatment and recovery support providers on responding to domestic violence and other trauma.
- Provides resources for professionals and patients regarding access to substance use and mental health care during the COVID-1 pandemic.
- Provides support for parents, caregivers, and children during the pandemic.
- Provides resources for advocates serving families affected by domestic violence.
- A state-by-state guide to local resources
Children’s Hospital of Philadelphia Research Institute
STOP Intimate Partner Violence (IPV)
New Jersey Coalition for Domestic Violence
American Bar Association COVID-19 resources for communities
- Text HOME to 741741.
National Network to End Domestic Violence (NNEDV) COVID-19 Technology Safety
A version of this article originally appeared on Medscape.com.
Roger R., MD, a primary care physician from Philadelphia, set up a telemedicine appointment with a 24-year-old female patient who was experiencing headaches and was worried she might have COVID-19.
During the televisit, Dr. R. noticed that “Tonya” (not her real name) had a purplish bruise under her right eye. When asked how she got the bruise, Tonya said she had bumped into a dresser. The physician suspected abuse. He then heard a man’s voice in the background and thought it might belong to the abuser. “Is this a good time for you to talk?” he asked Tonya.
Tonya hesitated.
“When might be a better time?”
Tonya suggested an alternate time, and the physician called her then. During the visit, she shared that her fiancé, a car salesman who was also sheltering at home, was punching her.
“He always had a bad temper. Once he shoved me, but he’s never hit me before. And when he was upset, we used to go out to eat and he calmed down. Now, we’re stuck inside, we can’t even get away from each other to go to work, and he’s getting scary,” she told the doctor.
The physician asked if she would like to be connected with a domestic violence counselor. When Tonya agreed, he called Jessica DuBois Palardy, a licensed social worker and the program supervisor at STOP Intimate Partner Violence, a Philadelphia-based collaborative project of the Children’s Hospital of Philadelphia and the Lutheran Settlement House’s Bilingual Domestic Violence Program.
A ‘horrifying’ trend
Tonya’s story is not unique. A United Nations report shows that there has been a “horrifying global surge in domestic violence” linked to “lockdowns imposed by the governments responding to the COVID-19 pandemic.” The United States is no exception – 2,345 calls were placed to the National Domestic Violence Hotline during March 16–April 6, 2020.
Carole Warshaw, MD, director of the National Center on Domestic Violence, Trauma, and Mental Health in Chicago, said, “We know that intimate partner violence is increasing among people sheltering at home, and that abuse has become more severe.”
Even in nonabusive situations, being confined together at close quarters, often amid family stress and financial hardship, can be wearing, and tempers can flare. In an abusive relationship, “the main contributor to violence during shelter-in-place restrictions is that the isolation gives abusers more opportunities for controlling their partners, who have fewer options for accessing safety and support,” Dr. Warshaw said.
It is critical to “approach every clinical encounter knowing that domestic violence may be at play,” she emphasized.
Physicians might be the most important lifeline
Physicians are already facing myriad COVID-19–related challenges, and having another concern to keep in mind may be daunting.
“We’re in uncharted territory and we’re all trying to figure out how to navigate this time, how to practice medicine via phone and video conferences, and how to deal with the financial repercussions of the pandemic – not to mention concern for the health of our families,” said Peter F. Cronholm, MD, associate professor of family medicine and community health at the Hospital of the University of Pennsylvania, Philadelphia. “So maintaining vigilance is often difficult. Nevertheless, it’s important not to let this critical issue fall to the wayside.”
Marcella Nyachogo, MSW, a licensed social worker and assistant director of the Bilingual Domestic Violence Program, noted that physicians and other health care providers “may be the only people the patient interacts with, since the abuser may cut the survivor off from family and friends. And because the survivor isn’t leaving the house, he or she doesn’t have an opportunity to interact with coworkers or others – which makes health care providers the most important lifeline.”
COVID-19 as a weapon of abuse
Carey Watson, MD, regional medical director of the Family Violence Prevention Program at Kaiser Permanente in northern California, points to a disturbing trend in COVID-19–related abuse.
“Unfortunately, I’m hearing more and more accounts of how the illness itself can be one more weapon in the abuser’s arsenal,” she said.
Experts say that increasingly, abusers are claiming that their partner, who is employed in an “essential” job outside the home, is carrying the virus, and they are using this as a means of control and manipulation.
This is especially true of abusive partners of health care providers, Dr. Watson noted. She recounted the story of a divorced nurse whose husband did not allow her to have contact with their children, allegedly out of concern that she might have COVID-19, and would threaten her with a gun when she protested.
“It is important to keep this abusive tactic in mind, not only when dealing with patients but also with fellow physicians and health care professionals, and check in to see if everything is okay – especially if they seem particularly stressed out or distant,” Dr. Watson recommended.
Trust your clinical gut
How can you tell if your patients might be experiencing abuse when you’re not seeing them in person?
Pay attention to subtle signals and “trust your clinical gut when something doesn’t feel right,” Ms. Nyachogo advised.
If a patient’s demeanor is jittery or anxious or if someone next to him or her is answering all the questions or interrupting the visit, these could be red flags.
Dr. Cronholm added that telemedicine visits offer a “rare window into a patient’s home life that would not be available in an office visit.” For example, a house in disarray, the presence of broken objects, or the presence of another person hovering in the background suggests the need for further exploration.
“The main thing for all providers to keep in mind is ‘first, do no harm,’ ” Ms. Nyachogo emphasized.
“Our agency has been working for years with medical professionals in how to screen and connect folks with help most effectively and safely, and – although the specific situations posed by COVID are new – the overall approach is the same, which is to proceed with caution in how you approach the subject and how you make referrals,” she said.
Begin by asking if it is a convenient time to talk.
“This question takes the onus off the patient, who may not know how to communicate that she has no privacy or is in the middle of an argument,” explained Elsa Swenson, program manager of Home Free community program, which serves individuals experiencing domestic violence. The program is part of Minnesota-based Missions Inc. Programs, which serves those experiencing domestic abuse and chemical dependency.
If the patient indicates that it isn’t a convenient time to talk, find out when would be a better time. “This might be difficult for busy physicians and may not be what they’re accustomed to when calling a patient at home, but the patient’s circumstances are unknown to you, so it’s essential to organize around their ability to talk,” Ms. Swenson noted.
‘Are you alone?’
Another important piece of information is whether the patient has privacy – which can be tricky if the abuser is standing right there.
“You don’t want to tip the abuser off to your concerns, so you need to frame the question in a neutral way,” Dr. Watson advised.
For example, you might say that HIPAA laws require that you conduct the consultation with no one else present, and find out if there is a location in the house where the patient can have privacy.
It might be easier to talk on the phone than via video, suggests Florence Remes, a New Jersey–based licensed social worker who specializes in domestic violence. Going into another room and playing music or turning on the television might make it less obvious that a call is taking place, and the abuser would be less likely to overhear the caller’s conversation.
Dr. Watson suggested that questions about abuse might be included with other questions and asked in a simple yes/no format. “I’d like to ask you some standard questions I’m asking everyone during the pandemic. Do you have a cough or fever? Do you have any other physical symptoms? Do you have access to hand sanitizer? How is your sleep? Are you experiencing stress? Do you feel safe at home?”
The abuser, if present, will only hear the patient’s “yes” or “no” without knowing the question. If the patient indicates that she is being abused but is unable to talk, a later time can be arranged to further explore the issue.
Technology is a double-edged sword
Modern technologies have been a great boon to patients and physicians during this time of social distancing, allowing ongoing contact and health care when it would not otherwise have been possible. On the other hand, technology is fraught with potential dangers that can jeopardize the patient’s safety and compromise privacy.
Ms. Remes recounted the story of “Susan,” a client with whom she had been conducting teletherapy visits using an approved HIPAA-compliant telemedicine forum. Susan was working from home because of shelter-in-place restrictions. Her husband had been abusive, and Susan was concerned he might be “sabotaging” the household’s WiFi to isolate her from outside sources of support.
At the recommendation of Ms. Remes, Susan continued sessions either via phone calls or by using the WhatsApp program on her cellphone. Many of the requirements governing HIPAA privacy regulations have been temporarily relaxed, and clinicians can use non–encrypted forms of transmission, such as FaceTime, WhatsApp, or Skype, if no other platform is available.
But even cellphones have risks, Dr. Warshaw noted. The patient’s abuser might track texts or look at call logs – especially on unsecured platforms. It’s advisable to ask patients about who has access to their phone and computer and discuss ways to increase security.
Follow the patient’s lead
Proceed slowly and start with nonthreatening questions, Ms. Palardy advised. “I notice you have some injuries; can you tell me how you got them? Did someone hurt you? What does your relationship look like when you argue? Is there anything that makes you feel uncomfortable or unsafe?”
Emphasizing that you are asking these questions because of care and concern is reassuring and helps patients to feel they are not alone, Ms. Nyachogo pointed out.
“As your doctor, I’m worried about your health and (if relevant) your children’s safety. I can help connect you with counseling and support, legal resources, and a shelter, and everything is free and confidential. Would you be interested?” she said.
If the client acknowledges abuse, “follow their lead, but don’t push too hard,” Ms. Nyachogo warned.
“It is the client’s choice whether or not to take action,” she noted. “I’ve met survivors who said that it wasn’t until a doctor or nurse expressed concern about bruises that it even occurred to them that they were being abused. Some lied to the doctor about how they got hurt – but the question planted a seed, even though it might have taken years to follow up on the referral,” she said.
What if the patient doesn’t want to get help?
If a patient is not ready to seek help, you can create a home-safety plan. This might include setting follow-up times. If you don’t hear from him or her, you should then call the police. Or you might create a “code word,” such as “apple pie.” If the patient uses that word during a session, you know her life is in danger, Ms. Remes suggested.
Providing written information about how to get help is important but can be problematic if the abuser finds it.
Ms. Nyachogo recommends e-mailing follow-up materials that cover a variety of topics, such as keeping safe during the COVID-19 pandemic, relaxation, healthy eating, getting exercise while homebound, activities for children, and suggestions for hotlines and other resources if one is feeling suicidal or unsafe.
“If you present these as your ‘standard’ follow-up materials, the abuser is less likely to become suspicious,” Ms. Nyachogo noted.
Resources are available during COVID-19
All of the experts emphasize that resources for victims of domestic violence remain available during the COVID-19 pandemic, although some shelters may be operating at reduced capacity. Some agencies are finding alternatives to group shelters, such as hotels or Airbnb, which carry less risk of catching COVID-19.
Referring a patient to domestic violence resources is a delicate process. “You don’t want referring the patient for help to further endanger their life,” Ms. Nyachogo said.
The more you can take the burden off the patient, the better. If she is interested in getting help, you can call a domestic violence counselor or advocate while she is on the phone.
“This type of ‘warm handoff’ is what Tonya’s physician did,” Ms. Palardy recounted.
A warm handoff requires that physicians be familiar with domestic violence resources, Dr. Warshaw emphasized.
“Don’t wait until you are working with someone who needs help to find out where to refer them. Take the time to proactively research local agencies specializing in domestic violence and have their phone numbers on hand, so you can offer resources immediately if the person is interested,” she advised. The National Domestic Violence Hotline can also assist with safety planning and access to local resources.
‘Thinking on your feet’ critical for physicians
Addressing domestic violence during this unprecedented time requires “thinking on your feet” about novel forms of detection and intervention, Dr. Watson said. This involves a combination of clinical acumen, creativity, and finely honed intuition.
Ms. Nyachogo added, “Keeping an eye on domestic violence can feel like an extra burden, but don’t forget that it is lifesaving work.”
Resources
National Domestic Violence Hotline
- 800-799-SAFE (7233)
- The patient can also text LOVEIS to 22522.
National Center on Domestic Violence, Trauma, and Mental Health
- Provides resources for health care, mental health, and substance use treatment and recovery support providers on responding to domestic violence and other trauma.
- Provides resources for professionals and patients regarding access to substance use and mental health care during the COVID-1 pandemic.
- Provides support for parents, caregivers, and children during the pandemic.
- Provides resources for advocates serving families affected by domestic violence.
- A state-by-state guide to local resources
Children’s Hospital of Philadelphia Research Institute
STOP Intimate Partner Violence (IPV)
New Jersey Coalition for Domestic Violence
American Bar Association COVID-19 resources for communities
- Text HOME to 741741.
National Network to End Domestic Violence (NNEDV) COVID-19 Technology Safety
A version of this article originally appeared on Medscape.com.
Domestic abuse linked to cardiac disease, mortality in women
Adult female survivors of domestic abuse were at least one-third more likely to develop cardiovascular disease, type 2 diabetes mellitus, and all-cause mortality over a short follow-up period, although they did not face a higher risk of hypertension, a new British study finds.
The study, published in the Journal of the American Heart Association, provides more evidence of a link between domestic abuse and poor health, even in younger women.
“The prevalence of domestic abuse is vast, so any increased risk in cardiometabolic disease may translate into a large burden of potentially preventable illness in society,” said study lead author Joht Singh Chandan, PhD, MBBS, of the University of Birmingham (England) and University of Warwick in Coventry, England, in an interview.
The researchers retrospectively tracked primary care patients in the United Kingdom from 1995-2017. They compared 18,547 adult female survivors of domestic abuse with a group of 72,231 other women who were matched to them at baseline by age, body mass index, smoking status, and a measure known as the Townsend deprivation score.
The average age of women in the groups was 37 years plus or minus 13 in the domestic abuse group and 37 years plus or minus 12 in the unexposed group. In both groups, 45% of women smoked; women in the domestic abuse group were more likely to drink excessively (10%), compared with those in the unexposed group (4%).
Researchers followed the women in the domestic abuse group for an average of 2 years and the unexposed group for 3 years. Those in the domestic abuse group were more likely to fall out of the study because they transferred to other medical practices.
Over the study period, 181 women in the domestic abuse group and 644 women in the unexposed group developed cardiovascular disease outcomes (adjusted incidence rate ratio, 1.31; 95% confidence interval, 1.11-1.55; P = .001). They were also more likely to develop type 2 diabetes (adjusted IRR, 1.51; 95% CI, 1.30-1.76; P less than .001) and all-cause mortality (adjusted IRR, 1.44; 95% CI, 1.24-1.67; P less than.001). But there was no increased risk of hypertension (adjusted IRR, 0.99; 95% CI, 0.88-1.12; P = 0.873).
Why might exposure to domestic abuse boost cardiovascular risk? “Although our study was not able to answer exactly why this relationship exists, Dr. Chandan said. “These can be broadly put into three categories: adoption of poor lifestyle behaviors due to difficult circumstances (physical inactivity, poor diet, disrupted sleep, substance misuse and smoking); associated development of mental ill health; and the alteration of the immune, metabolic, neuroendocrine, and autonomic nervous system due to the impact of stress on the body.”
It’s not clear why the risk of hypertension may be an outlier among cardiovascular outcomes, Dr. Chandan said. However, he pointed to a similar study whose results hinted that survivors of emotional abuse may be more susceptible to a negative impact on hypertension (Ann Epidemiol. 2012 Aug;22[8]:562-7). The new study does not provide information about the type of abuse suffered by subjects.
Adrienne O’Neil, PhD, a family violence practitioner and cardiovascular epidemiologist at Deakin University in Geelong, Australia, said in an interview that the study is “a very useful contribution to the literature.” However, she cautioned that the study might have missed cases of domestic abuse because it relies on reports from primary care practitioners.
As for the findings, she said they’re surprising because of the divergence of major cardiovascular outcomes such as ischemic heart disease and stroke in groups of women with an average age of 37. “These differential health outcomes were observed over a 2-3 period. You probably wouldn’t expect to see a divergence in cardiovascular outcomes for 5-10 years in this age group.”
Dr. O’Neil said that, moving forward, the research can be helpful to understanding the rise of cardiovascular disease in women aged 35-54, especially in the United States. “The way we assess an individual’s risk of having a heart attack in the future is largely guided by evidence based on men. For a long time, this has neglected female-specific risk factors like polycystic ovary syndrome and hypertensive disorders of pregnancy but also conditions and exposures to which young women are especially vulnerable like depression, anxiety and [domestic abuse],” she said.
“This research is important as it gives us clues about who may be at elevated risk to help us guide prevention efforts. Equally, there is some evidence that chest pain presentation may be a useful predictor of domestic abuse victimization so there could be multiple lines of further inquiry.”
Dr. Chandan, the other study authors, and Dr. O’Neil reported no relevant disclosures.
SOURCE: Chandan JS et al. J Am Heart Assoc. 2020. doi: 10.1161/JAHA.119.014580.
Adult female survivors of domestic abuse were at least one-third more likely to develop cardiovascular disease, type 2 diabetes mellitus, and all-cause mortality over a short follow-up period, although they did not face a higher risk of hypertension, a new British study finds.
The study, published in the Journal of the American Heart Association, provides more evidence of a link between domestic abuse and poor health, even in younger women.
“The prevalence of domestic abuse is vast, so any increased risk in cardiometabolic disease may translate into a large burden of potentially preventable illness in society,” said study lead author Joht Singh Chandan, PhD, MBBS, of the University of Birmingham (England) and University of Warwick in Coventry, England, in an interview.
The researchers retrospectively tracked primary care patients in the United Kingdom from 1995-2017. They compared 18,547 adult female survivors of domestic abuse with a group of 72,231 other women who were matched to them at baseline by age, body mass index, smoking status, and a measure known as the Townsend deprivation score.
The average age of women in the groups was 37 years plus or minus 13 in the domestic abuse group and 37 years plus or minus 12 in the unexposed group. In both groups, 45% of women smoked; women in the domestic abuse group were more likely to drink excessively (10%), compared with those in the unexposed group (4%).
Researchers followed the women in the domestic abuse group for an average of 2 years and the unexposed group for 3 years. Those in the domestic abuse group were more likely to fall out of the study because they transferred to other medical practices.
Over the study period, 181 women in the domestic abuse group and 644 women in the unexposed group developed cardiovascular disease outcomes (adjusted incidence rate ratio, 1.31; 95% confidence interval, 1.11-1.55; P = .001). They were also more likely to develop type 2 diabetes (adjusted IRR, 1.51; 95% CI, 1.30-1.76; P less than .001) and all-cause mortality (adjusted IRR, 1.44; 95% CI, 1.24-1.67; P less than.001). But there was no increased risk of hypertension (adjusted IRR, 0.99; 95% CI, 0.88-1.12; P = 0.873).
Why might exposure to domestic abuse boost cardiovascular risk? “Although our study was not able to answer exactly why this relationship exists, Dr. Chandan said. “These can be broadly put into three categories: adoption of poor lifestyle behaviors due to difficult circumstances (physical inactivity, poor diet, disrupted sleep, substance misuse and smoking); associated development of mental ill health; and the alteration of the immune, metabolic, neuroendocrine, and autonomic nervous system due to the impact of stress on the body.”
It’s not clear why the risk of hypertension may be an outlier among cardiovascular outcomes, Dr. Chandan said. However, he pointed to a similar study whose results hinted that survivors of emotional abuse may be more susceptible to a negative impact on hypertension (Ann Epidemiol. 2012 Aug;22[8]:562-7). The new study does not provide information about the type of abuse suffered by subjects.
Adrienne O’Neil, PhD, a family violence practitioner and cardiovascular epidemiologist at Deakin University in Geelong, Australia, said in an interview that the study is “a very useful contribution to the literature.” However, she cautioned that the study might have missed cases of domestic abuse because it relies on reports from primary care practitioners.
As for the findings, she said they’re surprising because of the divergence of major cardiovascular outcomes such as ischemic heart disease and stroke in groups of women with an average age of 37. “These differential health outcomes were observed over a 2-3 period. You probably wouldn’t expect to see a divergence in cardiovascular outcomes for 5-10 years in this age group.”
Dr. O’Neil said that, moving forward, the research can be helpful to understanding the rise of cardiovascular disease in women aged 35-54, especially in the United States. “The way we assess an individual’s risk of having a heart attack in the future is largely guided by evidence based on men. For a long time, this has neglected female-specific risk factors like polycystic ovary syndrome and hypertensive disorders of pregnancy but also conditions and exposures to which young women are especially vulnerable like depression, anxiety and [domestic abuse],” she said.
“This research is important as it gives us clues about who may be at elevated risk to help us guide prevention efforts. Equally, there is some evidence that chest pain presentation may be a useful predictor of domestic abuse victimization so there could be multiple lines of further inquiry.”
Dr. Chandan, the other study authors, and Dr. O’Neil reported no relevant disclosures.
SOURCE: Chandan JS et al. J Am Heart Assoc. 2020. doi: 10.1161/JAHA.119.014580.
Adult female survivors of domestic abuse were at least one-third more likely to develop cardiovascular disease, type 2 diabetes mellitus, and all-cause mortality over a short follow-up period, although they did not face a higher risk of hypertension, a new British study finds.
The study, published in the Journal of the American Heart Association, provides more evidence of a link between domestic abuse and poor health, even in younger women.
“The prevalence of domestic abuse is vast, so any increased risk in cardiometabolic disease may translate into a large burden of potentially preventable illness in society,” said study lead author Joht Singh Chandan, PhD, MBBS, of the University of Birmingham (England) and University of Warwick in Coventry, England, in an interview.
The researchers retrospectively tracked primary care patients in the United Kingdom from 1995-2017. They compared 18,547 adult female survivors of domestic abuse with a group of 72,231 other women who were matched to them at baseline by age, body mass index, smoking status, and a measure known as the Townsend deprivation score.
The average age of women in the groups was 37 years plus or minus 13 in the domestic abuse group and 37 years plus or minus 12 in the unexposed group. In both groups, 45% of women smoked; women in the domestic abuse group were more likely to drink excessively (10%), compared with those in the unexposed group (4%).
Researchers followed the women in the domestic abuse group for an average of 2 years and the unexposed group for 3 years. Those in the domestic abuse group were more likely to fall out of the study because they transferred to other medical practices.
Over the study period, 181 women in the domestic abuse group and 644 women in the unexposed group developed cardiovascular disease outcomes (adjusted incidence rate ratio, 1.31; 95% confidence interval, 1.11-1.55; P = .001). They were also more likely to develop type 2 diabetes (adjusted IRR, 1.51; 95% CI, 1.30-1.76; P less than .001) and all-cause mortality (adjusted IRR, 1.44; 95% CI, 1.24-1.67; P less than.001). But there was no increased risk of hypertension (adjusted IRR, 0.99; 95% CI, 0.88-1.12; P = 0.873).
Why might exposure to domestic abuse boost cardiovascular risk? “Although our study was not able to answer exactly why this relationship exists, Dr. Chandan said. “These can be broadly put into three categories: adoption of poor lifestyle behaviors due to difficult circumstances (physical inactivity, poor diet, disrupted sleep, substance misuse and smoking); associated development of mental ill health; and the alteration of the immune, metabolic, neuroendocrine, and autonomic nervous system due to the impact of stress on the body.”
It’s not clear why the risk of hypertension may be an outlier among cardiovascular outcomes, Dr. Chandan said. However, he pointed to a similar study whose results hinted that survivors of emotional abuse may be more susceptible to a negative impact on hypertension (Ann Epidemiol. 2012 Aug;22[8]:562-7). The new study does not provide information about the type of abuse suffered by subjects.
Adrienne O’Neil, PhD, a family violence practitioner and cardiovascular epidemiologist at Deakin University in Geelong, Australia, said in an interview that the study is “a very useful contribution to the literature.” However, she cautioned that the study might have missed cases of domestic abuse because it relies on reports from primary care practitioners.
As for the findings, she said they’re surprising because of the divergence of major cardiovascular outcomes such as ischemic heart disease and stroke in groups of women with an average age of 37. “These differential health outcomes were observed over a 2-3 period. You probably wouldn’t expect to see a divergence in cardiovascular outcomes for 5-10 years in this age group.”
Dr. O’Neil said that, moving forward, the research can be helpful to understanding the rise of cardiovascular disease in women aged 35-54, especially in the United States. “The way we assess an individual’s risk of having a heart attack in the future is largely guided by evidence based on men. For a long time, this has neglected female-specific risk factors like polycystic ovary syndrome and hypertensive disorders of pregnancy but also conditions and exposures to which young women are especially vulnerable like depression, anxiety and [domestic abuse],” she said.
“This research is important as it gives us clues about who may be at elevated risk to help us guide prevention efforts. Equally, there is some evidence that chest pain presentation may be a useful predictor of domestic abuse victimization so there could be multiple lines of further inquiry.”
Dr. Chandan, the other study authors, and Dr. O’Neil reported no relevant disclosures.
SOURCE: Chandan JS et al. J Am Heart Assoc. 2020. doi: 10.1161/JAHA.119.014580.
FROM THE JOURNAL OF THE AMERICAN HEART ASSOCIATION
COVID-19: Psychiatrists assess geriatric harm from social distancing
One of the greatest tragedies of the first wave of the COVID-19 pandemic has been the failure of health policy makers to anticipate and mitigate the enormous havoc the policy of social distancing would wreak on mental health and cognitive function in older persons, speakers agreed at a webinar on COVID-19, social distancing, and its impact on social and mental health in the elderly hosted by the International Psychogeriatric Association in collaboration with INTERDEM.
“Social distancing” is a two-edged sword: It is for now and the foreseeable future the only available effective strategy for protecting against infection in the older population most vulnerable to severe forms of COVID-19. Yet social distancing also has caused many elderly – particularly those in nursing homes and other long-term care facilities – to plunge into a profound experience of loneliness, isolation, distress, feelings of abandonment, anxiety, depression, and accelerated cognitive deterioration. And this needn’t have happened, the mental health professionals asserted.
“When are we going to get rid of the term ‘social distancing?’ ” asked IPA President William E. Reichman, MD. “Many have appreciated – including the World Health Organization – that the real issue is physical distancing to prevent contagion. And physical distancing doesn’t have to mean social distancing.”
Social connectedness between elderly persons and their peers and family members can be maintained and should be emphatically encouraged during the physical distancing required by the pandemic, said Myrra Vernooij-Dassen, PhD, of Radboud University in Nigmegen, the Netherlands, and chair of INTERDEM, a pan-European network of dementia researchers.
This can be achieved using readily available technologies, including the telephone and videoconferencing, as well as by creating opportunities for supervised masked visits between a family member and an elderly loved one in outdoor courtyards or gardens within long-term care facilities. And yet, as the pandemic seized hold in many parts of the world, family members were blocked from entry to these facilities, she observed.
Impact on mental health, cognition
Dr. Vernooij-Dassen noted that studies of previous quarantine periods as well as preliminary findings during the COVID-19 pandemic demonstrate an inverse relationship between social isolation measures and cognitive functioning in the elderly.
“ Conversely, epidemiologic data indicate that a socially integrated lifestyle had a favorable influence on cognitive functioning and could even delay onset of dementia,” she said.
INTERDEM is backing two ongoing studies evaluating the hypothesis that interventions fostering increased social interaction among elderly individuals can delay onset of dementia or favorably affect its course. The proposed mechanism of benefit is stimulation of brain plasticity to enhance cognitive reserve.
“This is a hypothesis of hope. We know that social interaction for humans is like water to plants – we really, really need it,” she explained.
Diego de Leo, MD, PhD, emeritus professor of psychiatry and former director of the Australian Institute for Suicide Research and Prevention at Griffith University in Brisbane, was living in hard-hit Padua, Italy, during the first surge of COVID-19. He described his anecdotal experience.
“What I hear from many Italian colleagues and friends and directors of mental health services is that emergency admissions related to mental disorders declined during the first wave of the COVID pandemic. For example, not many people attended emergency departments due to suicide attempts; there was a very marked decrease in the number of suicide attempts during the worst days of the pandemic,” he said.
People with psychiatric conditions were afraid to go to the hospital because they thought they would contract the infection and die there. That’s changing now, however.
“Now there is an increased number of admissions to mental health units. A new wave. It has been a U-shaped curve. And we’re now witnessing an increasing number of fatal suicides due to persistent fears, due to people imagining that there is no more room for them, and no more future for them from a financial point of view – which is the major negative outcome of this crisis. It will be a disaster for many families,” the psychiatrist continued.
A noteworthy phenomenon in northern Italy was that, when tablets were made available to nursing home residents in an effort to enhance their connectedness to the outside world, those with dementia often became so frustrated and confused by their difficulty in using the devices that they developed a hypokinetic delirium marked by refusal to eat or leave their bed, he reported.
It’s far too early to have reliable data on suicide trends in response to the pandemic, according to Dr. de Leo. But one thing is for sure: The strategy of social distancing employed to curb COVID-19 has increased the prevalence of known risk factors for suicide in older individuals, including loneliness, anxiety, and depression; increased alcohol use; and a perception of being a burden on society. Dr. de Leo directs a foundation dedicated to helping people experiencing traumatic bereavement, and in one recent week, the foundation was contacted by eight families in the province of Padua with a recent death by suicide apparently related to fallout from the COVID-19 pandemic. That’s an unusually high spike in suicide in a province with a population of 1 million.
“People probably preferred to end the agitation, the fear, the extreme anxiety about their destiny by deciding to prematurely truncate their life. That has been reported by nursing staff,” he said.
The Italian government has determined that, to date, 36% of all COVID-related deaths have occurred in people aged 85 years or older, and 84% of deaths were in individuals aged at least 70 years. And in Milan and the surrounding province of Lombardy, it’s estimated that COVID-19 has taken the lives of 25% of all nursing home residents. The North American experience has been uncomfortably similar.
“Almost 80% of COVID deaths in Canada have occurred in congregate settings,” observed Dr. Reichman, professor of psychiatry at the University of Toronto, and president and CEO of Baycrest Health Sciences, a geriatric research center.
“Certainly, the appalling number of deaths in nursing homes is the No. 1 horror of the pandemic,” declared Carmelle Peisah, MBBS, MD, a psychiatrist at the University of New South Wales in Kensington, Australia.
The fire next time
The conventional wisdom holds that COVID-19 has caused all sorts of mayhem in the delivery of elder care. Not so, in Dr. Reichman’s view.
“I would suggest that the pandemic has not caused many of the problems we talk about, it’s actually revealed problems that have always been there under the surface. For example, many older people, even before COVID-19, were socially isolated, socially distant. They had difficulty connecting with their relatives, difficulty accessing transportation to get to the store to buy food and see their doctors, and to interact with other older people,” the psychiatrist said.
“I would say as well that the pandemic didn’t cause the problems we’ve seen in long-term congregate senior care. The pandemic revealed them. We’ve had facilities where older people were severely crowded together, which compromises their quality of life, even when there’s not a pandemic. We’ve had difficulty staffing these kinds of environments with people that are paid an honest wage for the very hard work that they do. In many of these settings they’re inadequately trained, not only in infection prevention and control but in all other aspects of care. And the pandemic has revealed that many of these organizations are not properly funded. The government doesn’t support them well enough across jurisdictions, and they can’t raise enough philanthropic funds to provide the kind of quality of life that residents demand,” Dr. Reichman continued.
Could the pandemic spur improved elder care? His hope is that health care professionals, politicians, and society at large will learn from the devastation left by the first surge of the pandemic and will lobby for the resources necessary for much-needed improvements in geriatric care.
“We need to be better prepared should there be not only a second wave of this pandemic, but for other pandemics to come,” Dr. Reichman concluded.
The speakers indicated they had no financial conflicts regarding their presentations.
One of the greatest tragedies of the first wave of the COVID-19 pandemic has been the failure of health policy makers to anticipate and mitigate the enormous havoc the policy of social distancing would wreak on mental health and cognitive function in older persons, speakers agreed at a webinar on COVID-19, social distancing, and its impact on social and mental health in the elderly hosted by the International Psychogeriatric Association in collaboration with INTERDEM.
“Social distancing” is a two-edged sword: It is for now and the foreseeable future the only available effective strategy for protecting against infection in the older population most vulnerable to severe forms of COVID-19. Yet social distancing also has caused many elderly – particularly those in nursing homes and other long-term care facilities – to plunge into a profound experience of loneliness, isolation, distress, feelings of abandonment, anxiety, depression, and accelerated cognitive deterioration. And this needn’t have happened, the mental health professionals asserted.
“When are we going to get rid of the term ‘social distancing?’ ” asked IPA President William E. Reichman, MD. “Many have appreciated – including the World Health Organization – that the real issue is physical distancing to prevent contagion. And physical distancing doesn’t have to mean social distancing.”
Social connectedness between elderly persons and their peers and family members can be maintained and should be emphatically encouraged during the physical distancing required by the pandemic, said Myrra Vernooij-Dassen, PhD, of Radboud University in Nigmegen, the Netherlands, and chair of INTERDEM, a pan-European network of dementia researchers.
This can be achieved using readily available technologies, including the telephone and videoconferencing, as well as by creating opportunities for supervised masked visits between a family member and an elderly loved one in outdoor courtyards or gardens within long-term care facilities. And yet, as the pandemic seized hold in many parts of the world, family members were blocked from entry to these facilities, she observed.
Impact on mental health, cognition
Dr. Vernooij-Dassen noted that studies of previous quarantine periods as well as preliminary findings during the COVID-19 pandemic demonstrate an inverse relationship between social isolation measures and cognitive functioning in the elderly.
“ Conversely, epidemiologic data indicate that a socially integrated lifestyle had a favorable influence on cognitive functioning and could even delay onset of dementia,” she said.
INTERDEM is backing two ongoing studies evaluating the hypothesis that interventions fostering increased social interaction among elderly individuals can delay onset of dementia or favorably affect its course. The proposed mechanism of benefit is stimulation of brain plasticity to enhance cognitive reserve.
“This is a hypothesis of hope. We know that social interaction for humans is like water to plants – we really, really need it,” she explained.
Diego de Leo, MD, PhD, emeritus professor of psychiatry and former director of the Australian Institute for Suicide Research and Prevention at Griffith University in Brisbane, was living in hard-hit Padua, Italy, during the first surge of COVID-19. He described his anecdotal experience.
“What I hear from many Italian colleagues and friends and directors of mental health services is that emergency admissions related to mental disorders declined during the first wave of the COVID pandemic. For example, not many people attended emergency departments due to suicide attempts; there was a very marked decrease in the number of suicide attempts during the worst days of the pandemic,” he said.
People with psychiatric conditions were afraid to go to the hospital because they thought they would contract the infection and die there. That’s changing now, however.
“Now there is an increased number of admissions to mental health units. A new wave. It has been a U-shaped curve. And we’re now witnessing an increasing number of fatal suicides due to persistent fears, due to people imagining that there is no more room for them, and no more future for them from a financial point of view – which is the major negative outcome of this crisis. It will be a disaster for many families,” the psychiatrist continued.
A noteworthy phenomenon in northern Italy was that, when tablets were made available to nursing home residents in an effort to enhance their connectedness to the outside world, those with dementia often became so frustrated and confused by their difficulty in using the devices that they developed a hypokinetic delirium marked by refusal to eat or leave their bed, he reported.
It’s far too early to have reliable data on suicide trends in response to the pandemic, according to Dr. de Leo. But one thing is for sure: The strategy of social distancing employed to curb COVID-19 has increased the prevalence of known risk factors for suicide in older individuals, including loneliness, anxiety, and depression; increased alcohol use; and a perception of being a burden on society. Dr. de Leo directs a foundation dedicated to helping people experiencing traumatic bereavement, and in one recent week, the foundation was contacted by eight families in the province of Padua with a recent death by suicide apparently related to fallout from the COVID-19 pandemic. That’s an unusually high spike in suicide in a province with a population of 1 million.
“People probably preferred to end the agitation, the fear, the extreme anxiety about their destiny by deciding to prematurely truncate their life. That has been reported by nursing staff,” he said.
The Italian government has determined that, to date, 36% of all COVID-related deaths have occurred in people aged 85 years or older, and 84% of deaths were in individuals aged at least 70 years. And in Milan and the surrounding province of Lombardy, it’s estimated that COVID-19 has taken the lives of 25% of all nursing home residents. The North American experience has been uncomfortably similar.
“Almost 80% of COVID deaths in Canada have occurred in congregate settings,” observed Dr. Reichman, professor of psychiatry at the University of Toronto, and president and CEO of Baycrest Health Sciences, a geriatric research center.
“Certainly, the appalling number of deaths in nursing homes is the No. 1 horror of the pandemic,” declared Carmelle Peisah, MBBS, MD, a psychiatrist at the University of New South Wales in Kensington, Australia.
The fire next time
The conventional wisdom holds that COVID-19 has caused all sorts of mayhem in the delivery of elder care. Not so, in Dr. Reichman’s view.
“I would suggest that the pandemic has not caused many of the problems we talk about, it’s actually revealed problems that have always been there under the surface. For example, many older people, even before COVID-19, were socially isolated, socially distant. They had difficulty connecting with their relatives, difficulty accessing transportation to get to the store to buy food and see their doctors, and to interact with other older people,” the psychiatrist said.
“I would say as well that the pandemic didn’t cause the problems we’ve seen in long-term congregate senior care. The pandemic revealed them. We’ve had facilities where older people were severely crowded together, which compromises their quality of life, even when there’s not a pandemic. We’ve had difficulty staffing these kinds of environments with people that are paid an honest wage for the very hard work that they do. In many of these settings they’re inadequately trained, not only in infection prevention and control but in all other aspects of care. And the pandemic has revealed that many of these organizations are not properly funded. The government doesn’t support them well enough across jurisdictions, and they can’t raise enough philanthropic funds to provide the kind of quality of life that residents demand,” Dr. Reichman continued.
Could the pandemic spur improved elder care? His hope is that health care professionals, politicians, and society at large will learn from the devastation left by the first surge of the pandemic and will lobby for the resources necessary for much-needed improvements in geriatric care.
“We need to be better prepared should there be not only a second wave of this pandemic, but for other pandemics to come,” Dr. Reichman concluded.
The speakers indicated they had no financial conflicts regarding their presentations.
One of the greatest tragedies of the first wave of the COVID-19 pandemic has been the failure of health policy makers to anticipate and mitigate the enormous havoc the policy of social distancing would wreak on mental health and cognitive function in older persons, speakers agreed at a webinar on COVID-19, social distancing, and its impact on social and mental health in the elderly hosted by the International Psychogeriatric Association in collaboration with INTERDEM.
“Social distancing” is a two-edged sword: It is for now and the foreseeable future the only available effective strategy for protecting against infection in the older population most vulnerable to severe forms of COVID-19. Yet social distancing also has caused many elderly – particularly those in nursing homes and other long-term care facilities – to plunge into a profound experience of loneliness, isolation, distress, feelings of abandonment, anxiety, depression, and accelerated cognitive deterioration. And this needn’t have happened, the mental health professionals asserted.
“When are we going to get rid of the term ‘social distancing?’ ” asked IPA President William E. Reichman, MD. “Many have appreciated – including the World Health Organization – that the real issue is physical distancing to prevent contagion. And physical distancing doesn’t have to mean social distancing.”
Social connectedness between elderly persons and their peers and family members can be maintained and should be emphatically encouraged during the physical distancing required by the pandemic, said Myrra Vernooij-Dassen, PhD, of Radboud University in Nigmegen, the Netherlands, and chair of INTERDEM, a pan-European network of dementia researchers.
This can be achieved using readily available technologies, including the telephone and videoconferencing, as well as by creating opportunities for supervised masked visits between a family member and an elderly loved one in outdoor courtyards or gardens within long-term care facilities. And yet, as the pandemic seized hold in many parts of the world, family members were blocked from entry to these facilities, she observed.
Impact on mental health, cognition
Dr. Vernooij-Dassen noted that studies of previous quarantine periods as well as preliminary findings during the COVID-19 pandemic demonstrate an inverse relationship between social isolation measures and cognitive functioning in the elderly.
“ Conversely, epidemiologic data indicate that a socially integrated lifestyle had a favorable influence on cognitive functioning and could even delay onset of dementia,” she said.
INTERDEM is backing two ongoing studies evaluating the hypothesis that interventions fostering increased social interaction among elderly individuals can delay onset of dementia or favorably affect its course. The proposed mechanism of benefit is stimulation of brain plasticity to enhance cognitive reserve.
“This is a hypothesis of hope. We know that social interaction for humans is like water to plants – we really, really need it,” she explained.
Diego de Leo, MD, PhD, emeritus professor of psychiatry and former director of the Australian Institute for Suicide Research and Prevention at Griffith University in Brisbane, was living in hard-hit Padua, Italy, during the first surge of COVID-19. He described his anecdotal experience.
“What I hear from many Italian colleagues and friends and directors of mental health services is that emergency admissions related to mental disorders declined during the first wave of the COVID pandemic. For example, not many people attended emergency departments due to suicide attempts; there was a very marked decrease in the number of suicide attempts during the worst days of the pandemic,” he said.
People with psychiatric conditions were afraid to go to the hospital because they thought they would contract the infection and die there. That’s changing now, however.
“Now there is an increased number of admissions to mental health units. A new wave. It has been a U-shaped curve. And we’re now witnessing an increasing number of fatal suicides due to persistent fears, due to people imagining that there is no more room for them, and no more future for them from a financial point of view – which is the major negative outcome of this crisis. It will be a disaster for many families,” the psychiatrist continued.
A noteworthy phenomenon in northern Italy was that, when tablets were made available to nursing home residents in an effort to enhance their connectedness to the outside world, those with dementia often became so frustrated and confused by their difficulty in using the devices that they developed a hypokinetic delirium marked by refusal to eat or leave their bed, he reported.
It’s far too early to have reliable data on suicide trends in response to the pandemic, according to Dr. de Leo. But one thing is for sure: The strategy of social distancing employed to curb COVID-19 has increased the prevalence of known risk factors for suicide in older individuals, including loneliness, anxiety, and depression; increased alcohol use; and a perception of being a burden on society. Dr. de Leo directs a foundation dedicated to helping people experiencing traumatic bereavement, and in one recent week, the foundation was contacted by eight families in the province of Padua with a recent death by suicide apparently related to fallout from the COVID-19 pandemic. That’s an unusually high spike in suicide in a province with a population of 1 million.
“People probably preferred to end the agitation, the fear, the extreme anxiety about their destiny by deciding to prematurely truncate their life. That has been reported by nursing staff,” he said.
The Italian government has determined that, to date, 36% of all COVID-related deaths have occurred in people aged 85 years or older, and 84% of deaths were in individuals aged at least 70 years. And in Milan and the surrounding province of Lombardy, it’s estimated that COVID-19 has taken the lives of 25% of all nursing home residents. The North American experience has been uncomfortably similar.
“Almost 80% of COVID deaths in Canada have occurred in congregate settings,” observed Dr. Reichman, professor of psychiatry at the University of Toronto, and president and CEO of Baycrest Health Sciences, a geriatric research center.
“Certainly, the appalling number of deaths in nursing homes is the No. 1 horror of the pandemic,” declared Carmelle Peisah, MBBS, MD, a psychiatrist at the University of New South Wales in Kensington, Australia.
The fire next time
The conventional wisdom holds that COVID-19 has caused all sorts of mayhem in the delivery of elder care. Not so, in Dr. Reichman’s view.
“I would suggest that the pandemic has not caused many of the problems we talk about, it’s actually revealed problems that have always been there under the surface. For example, many older people, even before COVID-19, were socially isolated, socially distant. They had difficulty connecting with their relatives, difficulty accessing transportation to get to the store to buy food and see their doctors, and to interact with other older people,” the psychiatrist said.
“I would say as well that the pandemic didn’t cause the problems we’ve seen in long-term congregate senior care. The pandemic revealed them. We’ve had facilities where older people were severely crowded together, which compromises their quality of life, even when there’s not a pandemic. We’ve had difficulty staffing these kinds of environments with people that are paid an honest wage for the very hard work that they do. In many of these settings they’re inadequately trained, not only in infection prevention and control but in all other aspects of care. And the pandemic has revealed that many of these organizations are not properly funded. The government doesn’t support them well enough across jurisdictions, and they can’t raise enough philanthropic funds to provide the kind of quality of life that residents demand,” Dr. Reichman continued.
Could the pandemic spur improved elder care? His hope is that health care professionals, politicians, and society at large will learn from the devastation left by the first surge of the pandemic and will lobby for the resources necessary for much-needed improvements in geriatric care.
“We need to be better prepared should there be not only a second wave of this pandemic, but for other pandemics to come,” Dr. Reichman concluded.
The speakers indicated they had no financial conflicts regarding their presentations.










