User login
Better bone builder: High-intensity exercise vs. Pilates
An 8-month high-intensity resistance and impact training program (HiRIT, Onero) led to greater gains in lumbar spine bone mineral density (BMD) and leg/back strength than a low-intensity Pilates-based program (Buff Bones).
These findings are from the Medication and Exercise for Osteoporosis (MEDEX-OP) trial, which included 115 postmenopausal women with low bone mass. Patients were randomly assigned to attend either the HiRIT or Pilates-based exercise program. The participants attended supervised 45-min sessions twice weekly.
HiRIT was better than the low-intensity Pilates-based exercise program for enhancing bone mass, muscle strength, functional performance, and stature, the researchers reported. The low-intensity program did improve function, but to a lesser extent
Of the 115 participants, most (86) were not taking osteoporosis medicine. For the 29 women who were receiving it, the medication appeared to enhance the effect of exercise.
Melanie Fischbacher, PhD candidate, Griffith University, Gold Coast, Australia, presented these findings in an oral session at the annual meeting of the American Society for Bone and Mineral Research; the study was also published in the Journal of Bone and Mineral Research.
The study’s senior author, Belinda R. Beck, PhD, director of the Bone Clinic in Brisbane, Australia, developed the Onero HiRIT program and has licensed it to others in Australia.
“It is a very effective program and we have shown it can be undertaken safely, but it must be supervised because of the heavy weights and high-risk clientele,” Beck stressed to this news organization.
“This is not a program you should just hand to a patient and tell them to do in a gym,” she said.
“Both forms of exercise in our study were beneficial for functional outcomes but Onero improved back extensor strength, mobility and stature considerably more than Buff Bones,” Ms. Fischbacher said in an interview.
Nevertheless, “the contribution of functional capacity to risk of falling and fracture cannot be overstated, and bone medications do not address function,” she noted.
“More trials combining bone medication and bone-targeted exercise are needed,” the researchers concluded.
Compliance stands out, study supports high-intensity exercise
Kristen M. Beavers, PhD, MPH, RD, who was not involved with this research, told this news organization that participant compliance in the study really stands out.
“Compliance to an 8-month, 2 day/week high-intensity resistance training program among older women with low bone mass was quite good in this study [>80%], with very few adverse events reported,” said Dr. Beavers, of the department of health and exercise science, Wake Forest University, Winston Salem, N.C.
“A lot of individuals wouldn’t even consider recommending this type/intensity of exercise to this population, because they are worried it is too risky and/or the uptake will be low,” she said.
Although the benefit in BMD and strength wasn’t seen universally across all bone/muscle outcomes assessed, the findings do reinforce the idea that high-intensity exercise is more efficacious for bone health than low-intensity exercise, she noted.
“The possible additive effect of high-intensity exercise when combined with medication is worth confirming in larger, adequately designed/powered studies,” according to Dr. Beavers.
“The general consensus in the field is that higher-intensity exercise is more osteogenic than low-intensity exercise, but improving muscle mass, quality, and function (including balance) are also important to reduce the risk of falls, which is a major contributor to incident fracture,” she noted.
Exercise, even low-intensity exercise, reduces the risk for falls, as shown in a recent meta-analysis, she added. This is something antiresorptive medications don’t do.
Building on the LIFTMOR and LIFTMOR-M Trials
Previously, the Australian group showed that HiRIT is efficacious and safe for bone formation in individuals with low to very low bone mass – in postmenopausal women in the LIFTMOR study (J Bone Miner Res. 2017 Oct 4 .doi: 10.1002/jbmr.3284), and in men in the LIFTMOR-M study.
The current study compared two exercise programs. The researchers randomly assigned 86 women who were not taking antiresorptive medication to the high-intensity (42) or low-intensity (44) exercise program. They also assigned 29 women who were receiving antiresorptive medication to the high-intensity (15) or low-intensity (14) exercise program.
In the high-intensity exercise plus medication subgroup, the women were taking denosumab (12), risedronate (2) or alendronate (1). In the low-intensity exercise plus medication subgroup, the women were taking denosumab (9), risedronate (1), alendronate (3), or zoledronic acid (1).
The mean age of the women was 64-68 years. The mean lumbar spine T score was –1.5 to –2.3, and the mean femoral neck T score was –1.7 to –2.0 (determined by dual-energy x-ray absorptiometry) .
The HiRIT training program consisted of three free-weight resistance training exercises (deadlift, back squat, overhead press), one high-impact exercise (jump drop), and two balance exercises. The exercises varied each session.
The low-intensity training consisted of bone-specific Pilates-based exercises performed on the mat; standing weight-bearing exercise with 1-kg dumbbells; and impact exercises, such as heel drops and stomping.
At 8 months, compared with women in the low-intensity exercise program, those in the HiRIT program demonstrated greater improvement in lumbar spine BMD (1.9% vs. 0.1%) and stature (0.2 cm vs. 0.0 cm), muscle strength, and functional performance.
Functional performance improved with both exercise programs, but the HiRIT program led to greater leg and back muscle strength and better results in the five times sit-to-stand test (P < .05).
HiRIT plus bone medication improved BMD at the femoral neck and total hip, whereas HiRIT alone did not. Low-intensity exercise plus bone medication improved BMD at the lumbar spine and total hip, whereas low-intensity exercise alone did not.
The retention rate was 90%. The rate of exercise compliance was 83% in the high-intensity group and 82% in the low-intensity group.
Thirty falls were reported by 24 participants (21%). One fracture occurred in each exercise group. Three adverse events occurred in the low-intensity group, and four occurred in the high-intensity group.
Dr. Beck owns the Bone Clinic and sells licenses to the Onero program. The other researchers disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
An 8-month high-intensity resistance and impact training program (HiRIT, Onero) led to greater gains in lumbar spine bone mineral density (BMD) and leg/back strength than a low-intensity Pilates-based program (Buff Bones).
These findings are from the Medication and Exercise for Osteoporosis (MEDEX-OP) trial, which included 115 postmenopausal women with low bone mass. Patients were randomly assigned to attend either the HiRIT or Pilates-based exercise program. The participants attended supervised 45-min sessions twice weekly.
HiRIT was better than the low-intensity Pilates-based exercise program for enhancing bone mass, muscle strength, functional performance, and stature, the researchers reported. The low-intensity program did improve function, but to a lesser extent
Of the 115 participants, most (86) were not taking osteoporosis medicine. For the 29 women who were receiving it, the medication appeared to enhance the effect of exercise.
Melanie Fischbacher, PhD candidate, Griffith University, Gold Coast, Australia, presented these findings in an oral session at the annual meeting of the American Society for Bone and Mineral Research; the study was also published in the Journal of Bone and Mineral Research.
The study’s senior author, Belinda R. Beck, PhD, director of the Bone Clinic in Brisbane, Australia, developed the Onero HiRIT program and has licensed it to others in Australia.
“It is a very effective program and we have shown it can be undertaken safely, but it must be supervised because of the heavy weights and high-risk clientele,” Beck stressed to this news organization.
“This is not a program you should just hand to a patient and tell them to do in a gym,” she said.
“Both forms of exercise in our study were beneficial for functional outcomes but Onero improved back extensor strength, mobility and stature considerably more than Buff Bones,” Ms. Fischbacher said in an interview.
Nevertheless, “the contribution of functional capacity to risk of falling and fracture cannot be overstated, and bone medications do not address function,” she noted.
“More trials combining bone medication and bone-targeted exercise are needed,” the researchers concluded.
Compliance stands out, study supports high-intensity exercise
Kristen M. Beavers, PhD, MPH, RD, who was not involved with this research, told this news organization that participant compliance in the study really stands out.
“Compliance to an 8-month, 2 day/week high-intensity resistance training program among older women with low bone mass was quite good in this study [>80%], with very few adverse events reported,” said Dr. Beavers, of the department of health and exercise science, Wake Forest University, Winston Salem, N.C.
“A lot of individuals wouldn’t even consider recommending this type/intensity of exercise to this population, because they are worried it is too risky and/or the uptake will be low,” she said.
Although the benefit in BMD and strength wasn’t seen universally across all bone/muscle outcomes assessed, the findings do reinforce the idea that high-intensity exercise is more efficacious for bone health than low-intensity exercise, she noted.
“The possible additive effect of high-intensity exercise when combined with medication is worth confirming in larger, adequately designed/powered studies,” according to Dr. Beavers.
“The general consensus in the field is that higher-intensity exercise is more osteogenic than low-intensity exercise, but improving muscle mass, quality, and function (including balance) are also important to reduce the risk of falls, which is a major contributor to incident fracture,” she noted.
Exercise, even low-intensity exercise, reduces the risk for falls, as shown in a recent meta-analysis, she added. This is something antiresorptive medications don’t do.
Building on the LIFTMOR and LIFTMOR-M Trials
Previously, the Australian group showed that HiRIT is efficacious and safe for bone formation in individuals with low to very low bone mass – in postmenopausal women in the LIFTMOR study (J Bone Miner Res. 2017 Oct 4 .doi: 10.1002/jbmr.3284), and in men in the LIFTMOR-M study.
The current study compared two exercise programs. The researchers randomly assigned 86 women who were not taking antiresorptive medication to the high-intensity (42) or low-intensity (44) exercise program. They also assigned 29 women who were receiving antiresorptive medication to the high-intensity (15) or low-intensity (14) exercise program.
In the high-intensity exercise plus medication subgroup, the women were taking denosumab (12), risedronate (2) or alendronate (1). In the low-intensity exercise plus medication subgroup, the women were taking denosumab (9), risedronate (1), alendronate (3), or zoledronic acid (1).
The mean age of the women was 64-68 years. The mean lumbar spine T score was –1.5 to –2.3, and the mean femoral neck T score was –1.7 to –2.0 (determined by dual-energy x-ray absorptiometry) .
The HiRIT training program consisted of three free-weight resistance training exercises (deadlift, back squat, overhead press), one high-impact exercise (jump drop), and two balance exercises. The exercises varied each session.
The low-intensity training consisted of bone-specific Pilates-based exercises performed on the mat; standing weight-bearing exercise with 1-kg dumbbells; and impact exercises, such as heel drops and stomping.
At 8 months, compared with women in the low-intensity exercise program, those in the HiRIT program demonstrated greater improvement in lumbar spine BMD (1.9% vs. 0.1%) and stature (0.2 cm vs. 0.0 cm), muscle strength, and functional performance.
Functional performance improved with both exercise programs, but the HiRIT program led to greater leg and back muscle strength and better results in the five times sit-to-stand test (P < .05).
HiRIT plus bone medication improved BMD at the femoral neck and total hip, whereas HiRIT alone did not. Low-intensity exercise plus bone medication improved BMD at the lumbar spine and total hip, whereas low-intensity exercise alone did not.
The retention rate was 90%. The rate of exercise compliance was 83% in the high-intensity group and 82% in the low-intensity group.
Thirty falls were reported by 24 participants (21%). One fracture occurred in each exercise group. Three adverse events occurred in the low-intensity group, and four occurred in the high-intensity group.
Dr. Beck owns the Bone Clinic and sells licenses to the Onero program. The other researchers disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
An 8-month high-intensity resistance and impact training program (HiRIT, Onero) led to greater gains in lumbar spine bone mineral density (BMD) and leg/back strength than a low-intensity Pilates-based program (Buff Bones).
These findings are from the Medication and Exercise for Osteoporosis (MEDEX-OP) trial, which included 115 postmenopausal women with low bone mass. Patients were randomly assigned to attend either the HiRIT or Pilates-based exercise program. The participants attended supervised 45-min sessions twice weekly.
HiRIT was better than the low-intensity Pilates-based exercise program for enhancing bone mass, muscle strength, functional performance, and stature, the researchers reported. The low-intensity program did improve function, but to a lesser extent
Of the 115 participants, most (86) were not taking osteoporosis medicine. For the 29 women who were receiving it, the medication appeared to enhance the effect of exercise.
Melanie Fischbacher, PhD candidate, Griffith University, Gold Coast, Australia, presented these findings in an oral session at the annual meeting of the American Society for Bone and Mineral Research; the study was also published in the Journal of Bone and Mineral Research.
The study’s senior author, Belinda R. Beck, PhD, director of the Bone Clinic in Brisbane, Australia, developed the Onero HiRIT program and has licensed it to others in Australia.
“It is a very effective program and we have shown it can be undertaken safely, but it must be supervised because of the heavy weights and high-risk clientele,” Beck stressed to this news organization.
“This is not a program you should just hand to a patient and tell them to do in a gym,” she said.
“Both forms of exercise in our study were beneficial for functional outcomes but Onero improved back extensor strength, mobility and stature considerably more than Buff Bones,” Ms. Fischbacher said in an interview.
Nevertheless, “the contribution of functional capacity to risk of falling and fracture cannot be overstated, and bone medications do not address function,” she noted.
“More trials combining bone medication and bone-targeted exercise are needed,” the researchers concluded.
Compliance stands out, study supports high-intensity exercise
Kristen M. Beavers, PhD, MPH, RD, who was not involved with this research, told this news organization that participant compliance in the study really stands out.
“Compliance to an 8-month, 2 day/week high-intensity resistance training program among older women with low bone mass was quite good in this study [>80%], with very few adverse events reported,” said Dr. Beavers, of the department of health and exercise science, Wake Forest University, Winston Salem, N.C.
“A lot of individuals wouldn’t even consider recommending this type/intensity of exercise to this population, because they are worried it is too risky and/or the uptake will be low,” she said.
Although the benefit in BMD and strength wasn’t seen universally across all bone/muscle outcomes assessed, the findings do reinforce the idea that high-intensity exercise is more efficacious for bone health than low-intensity exercise, she noted.
“The possible additive effect of high-intensity exercise when combined with medication is worth confirming in larger, adequately designed/powered studies,” according to Dr. Beavers.
“The general consensus in the field is that higher-intensity exercise is more osteogenic than low-intensity exercise, but improving muscle mass, quality, and function (including balance) are also important to reduce the risk of falls, which is a major contributor to incident fracture,” she noted.
Exercise, even low-intensity exercise, reduces the risk for falls, as shown in a recent meta-analysis, she added. This is something antiresorptive medications don’t do.
Building on the LIFTMOR and LIFTMOR-M Trials
Previously, the Australian group showed that HiRIT is efficacious and safe for bone formation in individuals with low to very low bone mass – in postmenopausal women in the LIFTMOR study (J Bone Miner Res. 2017 Oct 4 .doi: 10.1002/jbmr.3284), and in men in the LIFTMOR-M study.
The current study compared two exercise programs. The researchers randomly assigned 86 women who were not taking antiresorptive medication to the high-intensity (42) or low-intensity (44) exercise program. They also assigned 29 women who were receiving antiresorptive medication to the high-intensity (15) or low-intensity (14) exercise program.
In the high-intensity exercise plus medication subgroup, the women were taking denosumab (12), risedronate (2) or alendronate (1). In the low-intensity exercise plus medication subgroup, the women were taking denosumab (9), risedronate (1), alendronate (3), or zoledronic acid (1).
The mean age of the women was 64-68 years. The mean lumbar spine T score was –1.5 to –2.3, and the mean femoral neck T score was –1.7 to –2.0 (determined by dual-energy x-ray absorptiometry) .
The HiRIT training program consisted of three free-weight resistance training exercises (deadlift, back squat, overhead press), one high-impact exercise (jump drop), and two balance exercises. The exercises varied each session.
The low-intensity training consisted of bone-specific Pilates-based exercises performed on the mat; standing weight-bearing exercise with 1-kg dumbbells; and impact exercises, such as heel drops and stomping.
At 8 months, compared with women in the low-intensity exercise program, those in the HiRIT program demonstrated greater improvement in lumbar spine BMD (1.9% vs. 0.1%) and stature (0.2 cm vs. 0.0 cm), muscle strength, and functional performance.
Functional performance improved with both exercise programs, but the HiRIT program led to greater leg and back muscle strength and better results in the five times sit-to-stand test (P < .05).
HiRIT plus bone medication improved BMD at the femoral neck and total hip, whereas HiRIT alone did not. Low-intensity exercise plus bone medication improved BMD at the lumbar spine and total hip, whereas low-intensity exercise alone did not.
The retention rate was 90%. The rate of exercise compliance was 83% in the high-intensity group and 82% in the low-intensity group.
Thirty falls were reported by 24 participants (21%). One fracture occurred in each exercise group. Three adverse events occurred in the low-intensity group, and four occurred in the high-intensity group.
Dr. Beck owns the Bone Clinic and sells licenses to the Onero program. The other researchers disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Lumbar epidural steroid jab lowers bone formation in older women
Among postmenopausal women who received an epidural steroid injection (ESI) in the lumbar spine to treat back and leg pain arising from a compressed nerve in the spine, levels of bone formation biomarkers were decreased. The decrease in levels persisted more than 12 weeks, results from a new study show.
In addition, serum cortisol levels decreased by 50% at week 1 after the ESI, indicating systemic absorption of the steroid.
“The extent and duration of these effects suggest that patients who receive multiple [ESIs in the lumbar spine] may be at particular risk for harmful skeletal consequences,” Shannon Clare reported in an oral presentation at the annual meeting of the American Society for Bone and Mineral Research.
Further studies are needed of the relationship between these short-term changes in bone turnover and bone loss and the risk for fracture among the burgeoning population treated with ESIs, added Ms. Clare, of the Hospital for Special Surgery, New York.
The researchers examined changes in serum levels of bone formation and resorption markers and other analytes in 24 women who received a lumbar ESI for radicular back pain and in 8 other women from the hospital population who served as control persons.
Among the women who received ESI, 1 week after the injection, serum levels of two bone formation biomarkers – total procollagen type 1 N-terminal peptide (P1NP) and osteocalcin – were about 27% lower than at baseline. The suppression persisted beyond 12 weeks.
Serum levels of the bone resorption biomarker C-terminal telopeptide of type I collagen (CTX) did not differ significantly after ESI.
“Our results are notable because we found that the duration of suppression of bone formation extended beyond 12 weeks, a far longer duration than seen previously with intra-articular injections” of glucocorticoids, said Ms. Clare and senior author Emily M. Stein, MD, director of research for the Metabolic Bone Service and an endocrinologist at the Hospital for Special Surgery and is associate professor of medicine at Weill Cornell Medicine, both in New York.
The findings suggest that patients should not receive multiple doses within a 12-week period, they told this news organization in a joint email response.
Women are not typically screened for osteopenia or osteoporosis before ESI. However, “our results suggest that physicians should consider screening women for osteoporosis who receive ESI, particularly those who are treated with multiple doses,” said Ms. Clare and Dr. Stein. “Steroid exposure should be minimized as much as possible by having patients space injections as far as they can tolerate.”
Systemic absorption, negative impact on bone turnover markers
“The hypothesis that [ESIs] interfere with the vertebral osseous microenvironment and increase the risk of vertebral fractures has been supported with evidence in the literature,” Mohamad Bydon, MD, professor of neurosurgery, orthopedic surgery, and health services research at the Mayo Clinic, Rochester, Minn., said in an interview.
Prior studies have demonstrated a decrease in bone mineral density (BMD) and an increase in vertebral fractures following ESI, added Dr. Bydon, senior author of a 2018 review of the effect of ESI on BMD and vertebral fracture risk that was published in Pain Medicine. He was not involved with the current study.
“The article by Clare et al. provides evidence on the systemic absorption of glucocorticoids by demonstrating a drop in serum cortisol following ESI,” he noted. “The measurement of bone metabolism biomarkers offers molecular confirmation of clinical and radiological observations of previous studies” showing that ESI affects the vertebrae.
More than 9 million ESIs each year
Each year, more than 9 million ESIs are administered to patients in the United States to relieve radicular back and leg pain that may be caused by a herniated disc or spinal stenosis (a gradual narrowing of the open spaces in the spinal column, which is common in older adults), the researchers explained.
Some patients experience sufficient pain relief with ESIs. Others may not be eligible for surgery and may receive multiple ESIs annually for many years because they provide pain relief.
It is well established that oral and intravenous glucocorticoids profoundly suppress bone formation and transiently increase bone resorption, causing substantial bone loss and increased fracture risk within 3 months of administration, Ms. Clare explained in the session.
Long-term use of high-dose inhaled glucocorticoids has been associated with bone loss and fractures. However, the effect of ESIs on bone has been less well studied.
The researchers hypothesized that ESIs are systemically absorbed and cause suppression of bone formation without a compensatory decrease in bone resorption.
They enrolled 24 patients who had undergone lumbar ESIs and 8 control patients. The mean age of the patients in the two groups was 63 years and 68 years, respectively. Most patients were White (88% and 100%, respectively). The mean body mass index was 27 kg/m2 and 28 kg/m2, respectively. On average, the patients had entered menopause 12 and 16 years earlier, respectively.
In the group that received steroid injections, almost two-thirds (15 patients, 63%) received triamcinolone. The rest received dexamethasone (six patients, 25%) or betamethasone (three patients, 12%) at doses that were equivalent to 80 mg triamcinolone.
The patients’ baseline serum levels of 25-hydroxy vitamin D, parathyroid hormone, cortisol, P1NP, osteocalcin, and CTX were within the reference ranges and were similar in the two groups.
The researchers also determined serum levels of cortisol (to assess suppression of endogenous glucocorticoids), osteocalcin, P1NP, and CTX in the patients and control persons at 1, 4, 12, 26, and 52 weeks after patients had received the ESI.
The researchers acknowledged that the small sample is a study limitation. In addition, the first serum samples were taken 1 week after the injection, and so any earlier changes in analyte levels were not captured. The patients also received different types of steroids, although the doses were similar when converted to triamcinolone equivalents.
The study was supported by a Spine Service grant from the Hospital for Special Surgery. The authors disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Among postmenopausal women who received an epidural steroid injection (ESI) in the lumbar spine to treat back and leg pain arising from a compressed nerve in the spine, levels of bone formation biomarkers were decreased. The decrease in levels persisted more than 12 weeks, results from a new study show.
In addition, serum cortisol levels decreased by 50% at week 1 after the ESI, indicating systemic absorption of the steroid.
“The extent and duration of these effects suggest that patients who receive multiple [ESIs in the lumbar spine] may be at particular risk for harmful skeletal consequences,” Shannon Clare reported in an oral presentation at the annual meeting of the American Society for Bone and Mineral Research.
Further studies are needed of the relationship between these short-term changes in bone turnover and bone loss and the risk for fracture among the burgeoning population treated with ESIs, added Ms. Clare, of the Hospital for Special Surgery, New York.
The researchers examined changes in serum levels of bone formation and resorption markers and other analytes in 24 women who received a lumbar ESI for radicular back pain and in 8 other women from the hospital population who served as control persons.
Among the women who received ESI, 1 week after the injection, serum levels of two bone formation biomarkers – total procollagen type 1 N-terminal peptide (P1NP) and osteocalcin – were about 27% lower than at baseline. The suppression persisted beyond 12 weeks.
Serum levels of the bone resorption biomarker C-terminal telopeptide of type I collagen (CTX) did not differ significantly after ESI.
“Our results are notable because we found that the duration of suppression of bone formation extended beyond 12 weeks, a far longer duration than seen previously with intra-articular injections” of glucocorticoids, said Ms. Clare and senior author Emily M. Stein, MD, director of research for the Metabolic Bone Service and an endocrinologist at the Hospital for Special Surgery and is associate professor of medicine at Weill Cornell Medicine, both in New York.
The findings suggest that patients should not receive multiple doses within a 12-week period, they told this news organization in a joint email response.
Women are not typically screened for osteopenia or osteoporosis before ESI. However, “our results suggest that physicians should consider screening women for osteoporosis who receive ESI, particularly those who are treated with multiple doses,” said Ms. Clare and Dr. Stein. “Steroid exposure should be minimized as much as possible by having patients space injections as far as they can tolerate.”
Systemic absorption, negative impact on bone turnover markers
“The hypothesis that [ESIs] interfere with the vertebral osseous microenvironment and increase the risk of vertebral fractures has been supported with evidence in the literature,” Mohamad Bydon, MD, professor of neurosurgery, orthopedic surgery, and health services research at the Mayo Clinic, Rochester, Minn., said in an interview.
Prior studies have demonstrated a decrease in bone mineral density (BMD) and an increase in vertebral fractures following ESI, added Dr. Bydon, senior author of a 2018 review of the effect of ESI on BMD and vertebral fracture risk that was published in Pain Medicine. He was not involved with the current study.
“The article by Clare et al. provides evidence on the systemic absorption of glucocorticoids by demonstrating a drop in serum cortisol following ESI,” he noted. “The measurement of bone metabolism biomarkers offers molecular confirmation of clinical and radiological observations of previous studies” showing that ESI affects the vertebrae.
More than 9 million ESIs each year
Each year, more than 9 million ESIs are administered to patients in the United States to relieve radicular back and leg pain that may be caused by a herniated disc or spinal stenosis (a gradual narrowing of the open spaces in the spinal column, which is common in older adults), the researchers explained.
Some patients experience sufficient pain relief with ESIs. Others may not be eligible for surgery and may receive multiple ESIs annually for many years because they provide pain relief.
It is well established that oral and intravenous glucocorticoids profoundly suppress bone formation and transiently increase bone resorption, causing substantial bone loss and increased fracture risk within 3 months of administration, Ms. Clare explained in the session.
Long-term use of high-dose inhaled glucocorticoids has been associated with bone loss and fractures. However, the effect of ESIs on bone has been less well studied.
The researchers hypothesized that ESIs are systemically absorbed and cause suppression of bone formation without a compensatory decrease in bone resorption.
They enrolled 24 patients who had undergone lumbar ESIs and 8 control patients. The mean age of the patients in the two groups was 63 years and 68 years, respectively. Most patients were White (88% and 100%, respectively). The mean body mass index was 27 kg/m2 and 28 kg/m2, respectively. On average, the patients had entered menopause 12 and 16 years earlier, respectively.
In the group that received steroid injections, almost two-thirds (15 patients, 63%) received triamcinolone. The rest received dexamethasone (six patients, 25%) or betamethasone (three patients, 12%) at doses that were equivalent to 80 mg triamcinolone.
The patients’ baseline serum levels of 25-hydroxy vitamin D, parathyroid hormone, cortisol, P1NP, osteocalcin, and CTX were within the reference ranges and were similar in the two groups.
The researchers also determined serum levels of cortisol (to assess suppression of endogenous glucocorticoids), osteocalcin, P1NP, and CTX in the patients and control persons at 1, 4, 12, 26, and 52 weeks after patients had received the ESI.
The researchers acknowledged that the small sample is a study limitation. In addition, the first serum samples were taken 1 week after the injection, and so any earlier changes in analyte levels were not captured. The patients also received different types of steroids, although the doses were similar when converted to triamcinolone equivalents.
The study was supported by a Spine Service grant from the Hospital for Special Surgery. The authors disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Among postmenopausal women who received an epidural steroid injection (ESI) in the lumbar spine to treat back and leg pain arising from a compressed nerve in the spine, levels of bone formation biomarkers were decreased. The decrease in levels persisted more than 12 weeks, results from a new study show.
In addition, serum cortisol levels decreased by 50% at week 1 after the ESI, indicating systemic absorption of the steroid.
“The extent and duration of these effects suggest that patients who receive multiple [ESIs in the lumbar spine] may be at particular risk for harmful skeletal consequences,” Shannon Clare reported in an oral presentation at the annual meeting of the American Society for Bone and Mineral Research.
Further studies are needed of the relationship between these short-term changes in bone turnover and bone loss and the risk for fracture among the burgeoning population treated with ESIs, added Ms. Clare, of the Hospital for Special Surgery, New York.
The researchers examined changes in serum levels of bone formation and resorption markers and other analytes in 24 women who received a lumbar ESI for radicular back pain and in 8 other women from the hospital population who served as control persons.
Among the women who received ESI, 1 week after the injection, serum levels of two bone formation biomarkers – total procollagen type 1 N-terminal peptide (P1NP) and osteocalcin – were about 27% lower than at baseline. The suppression persisted beyond 12 weeks.
Serum levels of the bone resorption biomarker C-terminal telopeptide of type I collagen (CTX) did not differ significantly after ESI.
“Our results are notable because we found that the duration of suppression of bone formation extended beyond 12 weeks, a far longer duration than seen previously with intra-articular injections” of glucocorticoids, said Ms. Clare and senior author Emily M. Stein, MD, director of research for the Metabolic Bone Service and an endocrinologist at the Hospital for Special Surgery and is associate professor of medicine at Weill Cornell Medicine, both in New York.
The findings suggest that patients should not receive multiple doses within a 12-week period, they told this news organization in a joint email response.
Women are not typically screened for osteopenia or osteoporosis before ESI. However, “our results suggest that physicians should consider screening women for osteoporosis who receive ESI, particularly those who are treated with multiple doses,” said Ms. Clare and Dr. Stein. “Steroid exposure should be minimized as much as possible by having patients space injections as far as they can tolerate.”
Systemic absorption, negative impact on bone turnover markers
“The hypothesis that [ESIs] interfere with the vertebral osseous microenvironment and increase the risk of vertebral fractures has been supported with evidence in the literature,” Mohamad Bydon, MD, professor of neurosurgery, orthopedic surgery, and health services research at the Mayo Clinic, Rochester, Minn., said in an interview.
Prior studies have demonstrated a decrease in bone mineral density (BMD) and an increase in vertebral fractures following ESI, added Dr. Bydon, senior author of a 2018 review of the effect of ESI on BMD and vertebral fracture risk that was published in Pain Medicine. He was not involved with the current study.
“The article by Clare et al. provides evidence on the systemic absorption of glucocorticoids by demonstrating a drop in serum cortisol following ESI,” he noted. “The measurement of bone metabolism biomarkers offers molecular confirmation of clinical and radiological observations of previous studies” showing that ESI affects the vertebrae.
More than 9 million ESIs each year
Each year, more than 9 million ESIs are administered to patients in the United States to relieve radicular back and leg pain that may be caused by a herniated disc or spinal stenosis (a gradual narrowing of the open spaces in the spinal column, which is common in older adults), the researchers explained.
Some patients experience sufficient pain relief with ESIs. Others may not be eligible for surgery and may receive multiple ESIs annually for many years because they provide pain relief.
It is well established that oral and intravenous glucocorticoids profoundly suppress bone formation and transiently increase bone resorption, causing substantial bone loss and increased fracture risk within 3 months of administration, Ms. Clare explained in the session.
Long-term use of high-dose inhaled glucocorticoids has been associated with bone loss and fractures. However, the effect of ESIs on bone has been less well studied.
The researchers hypothesized that ESIs are systemically absorbed and cause suppression of bone formation without a compensatory decrease in bone resorption.
They enrolled 24 patients who had undergone lumbar ESIs and 8 control patients. The mean age of the patients in the two groups was 63 years and 68 years, respectively. Most patients were White (88% and 100%, respectively). The mean body mass index was 27 kg/m2 and 28 kg/m2, respectively. On average, the patients had entered menopause 12 and 16 years earlier, respectively.
In the group that received steroid injections, almost two-thirds (15 patients, 63%) received triamcinolone. The rest received dexamethasone (six patients, 25%) or betamethasone (three patients, 12%) at doses that were equivalent to 80 mg triamcinolone.
The patients’ baseline serum levels of 25-hydroxy vitamin D, parathyroid hormone, cortisol, P1NP, osteocalcin, and CTX were within the reference ranges and were similar in the two groups.
The researchers also determined serum levels of cortisol (to assess suppression of endogenous glucocorticoids), osteocalcin, P1NP, and CTX in the patients and control persons at 1, 4, 12, 26, and 52 weeks after patients had received the ESI.
The researchers acknowledged that the small sample is a study limitation. In addition, the first serum samples were taken 1 week after the injection, and so any earlier changes in analyte levels were not captured. The patients also received different types of steroids, although the doses were similar when converted to triamcinolone equivalents.
The study was supported by a Spine Service grant from the Hospital for Special Surgery. The authors disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
HHS okays first U.S. pilot to mandate coverage of gender-affirming care
The approval means transgender-related care must be included as part of the essential benefits offered on the state’s Affordable Care Act marketplace, which includes private individual and small group insurance plans. The coverage will start Jan. 1, 2023. Colorado is the first state in the United States to require such coverage.
The HHS notes that gender-affirming treatments to be covered include eye and lid modifications, face tightening, facial bone remodeling for facial feminization, breast/chest construction and reductions, and laser hair removal.
“I am proud to stand with Colorado to remove barriers that have historically made it difficult for transgender people to access health coverage and medical care,” said HHS Secretary Xavier Becerra in a statement.
“Colorado’s expansion of their essential health benefits to include gender-affirming surgery and other treatments is a model for other states to follow, and we invite other states to follow suit,” said Centers for Medicare & Medicaid Services Administrator Chiquita Brooks-LaSure in the statement.
Medicaid already covers comprehensive transgender care in Colorado.
The LGBTQ+ advocacy group One Colorado estimated that, thanks to the Affordable Care Act, only 5% of the state’s LGBTQ+ community was uninsured in 2019, compared to 10% in 2011.
However, 34% of transgender respondents to a One Colorado poll in 2018 said they had been denied coverage for an LGBTQ-specific medical service, such as gender-affirming care. Sixty-two percent said that a lack of insurance or limited insurance was a barrier to care; 84% said another barrier was the lack of adequately trained mental and behavioral health professionals.
Mental health also covered
The Colorado plan requires individual and small group plans to cover an annual 45- to 60-minute mental health wellness exam with a qualified mental health care practitioner. The visit can include behavioral health screening, education and consultation about healthy lifestyle changes, referrals to mental health treatment, and discussion of potential medication options.
The plans also must cover an additional 15 medications as alternatives to opioids and up to six acupuncture visits annually.
“This plan expands access to mental health services for Coloradans while helping those fighting substance abuse to overcome their addiction,” said Governor Jared Polis in a statement.
“This improves care for Coloradans and ensures that even more Coloradans have access to help when they need it,” he said.
A version of this article first appeared on Medscape.com.
The approval means transgender-related care must be included as part of the essential benefits offered on the state’s Affordable Care Act marketplace, which includes private individual and small group insurance plans. The coverage will start Jan. 1, 2023. Colorado is the first state in the United States to require such coverage.
The HHS notes that gender-affirming treatments to be covered include eye and lid modifications, face tightening, facial bone remodeling for facial feminization, breast/chest construction and reductions, and laser hair removal.
“I am proud to stand with Colorado to remove barriers that have historically made it difficult for transgender people to access health coverage and medical care,” said HHS Secretary Xavier Becerra in a statement.
“Colorado’s expansion of their essential health benefits to include gender-affirming surgery and other treatments is a model for other states to follow, and we invite other states to follow suit,” said Centers for Medicare & Medicaid Services Administrator Chiquita Brooks-LaSure in the statement.
Medicaid already covers comprehensive transgender care in Colorado.
The LGBTQ+ advocacy group One Colorado estimated that, thanks to the Affordable Care Act, only 5% of the state’s LGBTQ+ community was uninsured in 2019, compared to 10% in 2011.
However, 34% of transgender respondents to a One Colorado poll in 2018 said they had been denied coverage for an LGBTQ-specific medical service, such as gender-affirming care. Sixty-two percent said that a lack of insurance or limited insurance was a barrier to care; 84% said another barrier was the lack of adequately trained mental and behavioral health professionals.
Mental health also covered
The Colorado plan requires individual and small group plans to cover an annual 45- to 60-minute mental health wellness exam with a qualified mental health care practitioner. The visit can include behavioral health screening, education and consultation about healthy lifestyle changes, referrals to mental health treatment, and discussion of potential medication options.
The plans also must cover an additional 15 medications as alternatives to opioids and up to six acupuncture visits annually.
“This plan expands access to mental health services for Coloradans while helping those fighting substance abuse to overcome their addiction,” said Governor Jared Polis in a statement.
“This improves care for Coloradans and ensures that even more Coloradans have access to help when they need it,” he said.
A version of this article first appeared on Medscape.com.
The approval means transgender-related care must be included as part of the essential benefits offered on the state’s Affordable Care Act marketplace, which includes private individual and small group insurance plans. The coverage will start Jan. 1, 2023. Colorado is the first state in the United States to require such coverage.
The HHS notes that gender-affirming treatments to be covered include eye and lid modifications, face tightening, facial bone remodeling for facial feminization, breast/chest construction and reductions, and laser hair removal.
“I am proud to stand with Colorado to remove barriers that have historically made it difficult for transgender people to access health coverage and medical care,” said HHS Secretary Xavier Becerra in a statement.
“Colorado’s expansion of their essential health benefits to include gender-affirming surgery and other treatments is a model for other states to follow, and we invite other states to follow suit,” said Centers for Medicare & Medicaid Services Administrator Chiquita Brooks-LaSure in the statement.
Medicaid already covers comprehensive transgender care in Colorado.
The LGBTQ+ advocacy group One Colorado estimated that, thanks to the Affordable Care Act, only 5% of the state’s LGBTQ+ community was uninsured in 2019, compared to 10% in 2011.
However, 34% of transgender respondents to a One Colorado poll in 2018 said they had been denied coverage for an LGBTQ-specific medical service, such as gender-affirming care. Sixty-two percent said that a lack of insurance or limited insurance was a barrier to care; 84% said another barrier was the lack of adequately trained mental and behavioral health professionals.
Mental health also covered
The Colorado plan requires individual and small group plans to cover an annual 45- to 60-minute mental health wellness exam with a qualified mental health care practitioner. The visit can include behavioral health screening, education and consultation about healthy lifestyle changes, referrals to mental health treatment, and discussion of potential medication options.
The plans also must cover an additional 15 medications as alternatives to opioids and up to six acupuncture visits annually.
“This plan expands access to mental health services for Coloradans while helping those fighting substance abuse to overcome their addiction,” said Governor Jared Polis in a statement.
“This improves care for Coloradans and ensures that even more Coloradans have access to help when they need it,” he said.
A version of this article first appeared on Medscape.com.
Synthetic chemical in consumer products linked to early death, study says
Daily exposure to phthalates, which are synthetic chemicals founds in many consumer products, may lead to hundreds of thousands of early deaths each year among older adults in the United States, according to a new study published Oct. 12, 2021, in the peer-reviewed journal Environmental Pollution.
The chemicals are found in hundreds of types of products, including children’s toys, food storage containers, makeup, perfume, and shampoo. In the study, those with the highest levels of phthalates had a greater risk of death from any cause, especially heart disease.
“This study adds to the growing database on the impact of plastics on the human body and bolsters public health and business cases for reducing or eliminating the use of plastics,” Leonardo Trasande, MD, the lead author and a professor of environmental medicine and population health at New York University Langone Health, told CNN.
Dr. Trasande and colleagues measured the urine concentration of phthalates in more than 5,000 adults aged 55-64 and compared the levels with the risk of early death over an average of 10 years. The research team controlled for preexisting heart diseases, diabetes, cancer, poor eating habits, physical activity, body mass, and other known hormone disruptors such as bisphenol A, or BPA, an industrial chemical that’s been used since the 1950s to make certain plastics and resins, according to the Mayo Clinic
The research team found that phthalates could contribute to 91,000-107,000 premature deaths per year in the United States. These early deaths could cost the nation $40 billion to $47 billion each year in lost economic productivity.
Phthalates interrupt the body’s endocrine system and hormone production. Previous studies have found that the chemicals are linked with developmental, reproductive, and immune system problems, according to NYU Langone Health. They’ve also been linked with asthma, childhood obesity, heart issues, and cancer.
“These chemicals have a rap sheet,” Dr. Trasande told CNN. “And the fact of the matter is that when you look at the entire body of evidence, it provides a haunting pattern of concern.”
Phthalates are often called “everywhere chemicals” because they are so common, CNN reported. Also called “plasticizers,” they are added to products to make them more durable, including PVC plumbing, vinyl flooring, medical tubing, garden hoses, food packaging, detergents, clothing, furniture, and automotive materials.
People are often exposed when they breathe contaminated air or consume food that comes into contact with the chemical, according to the Centers for Disease Control and Prevention. Children may be exposed by touching plastic items and putting their hands in their mouth.
Dr. Trasande told CNN that it’s possible to lessen exposure to phthalates and other endocrine disruptors such as BPA by using unscented lotions, laundry detergents, and cleaning supplies, as well as substituting glass, stainless steel, ceramic, and wood for plastic food storage.
“First, avoid plastics as much as you can. Never put plastic containers in the microwave or dishwasher, where the heat can break down the linings so they might be absorbed more readily,” he said. “In addition, cooking at home and reducing your use of processed foods can reduce the levels of the chemical exposures you come in contact with.”
A version of this article first appeared on WebMD.com.
Daily exposure to phthalates, which are synthetic chemicals founds in many consumer products, may lead to hundreds of thousands of early deaths each year among older adults in the United States, according to a new study published Oct. 12, 2021, in the peer-reviewed journal Environmental Pollution.
The chemicals are found in hundreds of types of products, including children’s toys, food storage containers, makeup, perfume, and shampoo. In the study, those with the highest levels of phthalates had a greater risk of death from any cause, especially heart disease.
“This study adds to the growing database on the impact of plastics on the human body and bolsters public health and business cases for reducing or eliminating the use of plastics,” Leonardo Trasande, MD, the lead author and a professor of environmental medicine and population health at New York University Langone Health, told CNN.
Dr. Trasande and colleagues measured the urine concentration of phthalates in more than 5,000 adults aged 55-64 and compared the levels with the risk of early death over an average of 10 years. The research team controlled for preexisting heart diseases, diabetes, cancer, poor eating habits, physical activity, body mass, and other known hormone disruptors such as bisphenol A, or BPA, an industrial chemical that’s been used since the 1950s to make certain plastics and resins, according to the Mayo Clinic
The research team found that phthalates could contribute to 91,000-107,000 premature deaths per year in the United States. These early deaths could cost the nation $40 billion to $47 billion each year in lost economic productivity.
Phthalates interrupt the body’s endocrine system and hormone production. Previous studies have found that the chemicals are linked with developmental, reproductive, and immune system problems, according to NYU Langone Health. They’ve also been linked with asthma, childhood obesity, heart issues, and cancer.
“These chemicals have a rap sheet,” Dr. Trasande told CNN. “And the fact of the matter is that when you look at the entire body of evidence, it provides a haunting pattern of concern.”
Phthalates are often called “everywhere chemicals” because they are so common, CNN reported. Also called “plasticizers,” they are added to products to make them more durable, including PVC plumbing, vinyl flooring, medical tubing, garden hoses, food packaging, detergents, clothing, furniture, and automotive materials.
People are often exposed when they breathe contaminated air or consume food that comes into contact with the chemical, according to the Centers for Disease Control and Prevention. Children may be exposed by touching plastic items and putting their hands in their mouth.
Dr. Trasande told CNN that it’s possible to lessen exposure to phthalates and other endocrine disruptors such as BPA by using unscented lotions, laundry detergents, and cleaning supplies, as well as substituting glass, stainless steel, ceramic, and wood for plastic food storage.
“First, avoid plastics as much as you can. Never put plastic containers in the microwave or dishwasher, where the heat can break down the linings so they might be absorbed more readily,” he said. “In addition, cooking at home and reducing your use of processed foods can reduce the levels of the chemical exposures you come in contact with.”
A version of this article first appeared on WebMD.com.
Daily exposure to phthalates, which are synthetic chemicals founds in many consumer products, may lead to hundreds of thousands of early deaths each year among older adults in the United States, according to a new study published Oct. 12, 2021, in the peer-reviewed journal Environmental Pollution.
The chemicals are found in hundreds of types of products, including children’s toys, food storage containers, makeup, perfume, and shampoo. In the study, those with the highest levels of phthalates had a greater risk of death from any cause, especially heart disease.
“This study adds to the growing database on the impact of plastics on the human body and bolsters public health and business cases for reducing or eliminating the use of plastics,” Leonardo Trasande, MD, the lead author and a professor of environmental medicine and population health at New York University Langone Health, told CNN.
Dr. Trasande and colleagues measured the urine concentration of phthalates in more than 5,000 adults aged 55-64 and compared the levels with the risk of early death over an average of 10 years. The research team controlled for preexisting heart diseases, diabetes, cancer, poor eating habits, physical activity, body mass, and other known hormone disruptors such as bisphenol A, or BPA, an industrial chemical that’s been used since the 1950s to make certain plastics and resins, according to the Mayo Clinic
The research team found that phthalates could contribute to 91,000-107,000 premature deaths per year in the United States. These early deaths could cost the nation $40 billion to $47 billion each year in lost economic productivity.
Phthalates interrupt the body’s endocrine system and hormone production. Previous studies have found that the chemicals are linked with developmental, reproductive, and immune system problems, according to NYU Langone Health. They’ve also been linked with asthma, childhood obesity, heart issues, and cancer.
“These chemicals have a rap sheet,” Dr. Trasande told CNN. “And the fact of the matter is that when you look at the entire body of evidence, it provides a haunting pattern of concern.”
Phthalates are often called “everywhere chemicals” because they are so common, CNN reported. Also called “plasticizers,” they are added to products to make them more durable, including PVC plumbing, vinyl flooring, medical tubing, garden hoses, food packaging, detergents, clothing, furniture, and automotive materials.
People are often exposed when they breathe contaminated air or consume food that comes into contact with the chemical, according to the Centers for Disease Control and Prevention. Children may be exposed by touching plastic items and putting their hands in their mouth.
Dr. Trasande told CNN that it’s possible to lessen exposure to phthalates and other endocrine disruptors such as BPA by using unscented lotions, laundry detergents, and cleaning supplies, as well as substituting glass, stainless steel, ceramic, and wood for plastic food storage.
“First, avoid plastics as much as you can. Never put plastic containers in the microwave or dishwasher, where the heat can break down the linings so they might be absorbed more readily,” he said. “In addition, cooking at home and reducing your use of processed foods can reduce the levels of the chemical exposures you come in contact with.”
A version of this article first appeared on WebMD.com.
Adding statins to steroids in thyroid eye disease improves outcomes
Treatment of Graves’ orbitopathy with statins in combination with glucocorticoids shows benefits among people with – and even without – high cholesterol, results from a new randomized clinical trial show.
“Our results [indicate] that adding atorvastatin to intravenous glucocorticoids seems to potentiate the effects of glucocorticoids,” senior author Michelle Marino, MD, associate professor of endocrinology in the department of clinical and experimental medicine at the University of Pisa, Italy, told this news organization.
“At least in hypercholesterolemic patients with moderate to severe and active Graves’ orbitopathy, atorvastatin should be considered in addition to intravenous glucocorticoids,” Dr. Marino said.
The study was presented by first author Giulia Lanzolla, MD, also of the University of Pisa and University Hospital of Pisa, at the virtual annual meeting of the American Thyroid Association.
Hypercholesterolemia, well known to promote systemic inflammation, has been previously linked to Graves’ orbitopathy, and the use of statins has also been shown to possibly provide a protective effect in the risk of developing the thyroid eye disease.
Furthermore, patients with Graves’ orbitopathy and high cholesterol levels, compared with those with normal cholesterol, have been shown to have poorer responses to treatment with glucocorticoids, which have long been the first line of treatment.
Asked for comment on the findings, Marius Stan, MD, a consultant in the division of endocrinology, diabetes, metabolism, and nutrition, Mayo Clinic, Rochester, Minn., said he didn’t think the outcome measure used – a composite of a variety of measures of thyroid eye disease – was best to truly understand the benefits.
Statins for Graves’ orbitopathy (STAGO) study details
For a better understanding of the effects with and without the addition of statins in a randomized trial, Dr. Lanzolla and colleagues enrolled 88 patients with high cholesterol and moderate to severe active Graves’ orbitopathy in the phase 2 STAGO trial.
Patients were randomized to two groups of 44 patients each to receive treatment either with intravenous (IV) methylprednisolone at 500 mg per week for 6 weeks, followed by 250 mg per week for another 6 weeks, in combination with atorvastatin 20 mg daily for 12 weeks, or methylprednisolone alone for 12 weeks.
The primary endpoint was a composite of Graves orbitopathy outcomes and included measures of exophthalmos, clinical activity score, eyelid aperture, diplopia, and visual acuity, as assessed in the modified intention-to-treat population.
The trial met the primary composite endpoint, with 51.2% of those treated with statins achieving the outcome (21 of 41) versus 28.2% (11 of 39) of those treated with glucocorticoids alone (odds ratio, 2.76; P = .03).
The study also achieved secondary outcomes, with 43.9% in the statin group having a response to treatment at 12 weeks versus 23% in the glucocorticoid group (OR 2.60; P = .05). The statin group also had a greater improvement in quality of life measures (P = .03).
The glucocorticoid-only group meanwhile had a significantly greater rate of Graves orbitopathy relapse at 24 weeks, with six relapses versus none in the statin group (15.3% vs. 0.0%; OR 0.06; P = .01).
There were no significant differences in low-density lipoprotein (LDL) cholesterol between those who did and did not respond to treatment in the statin group.
The most likely explanation for those findings is that “atorvastatin acts through its pleiotropic action, resulting in an anti-inflammatory effect,” Dr. Marino said.
“In addition, the effect may be related to the capability of statins to inhibit fibroblast proliferation,” Dr. Marino added.
“Total cholesterol had a behavior similar to LDL cholesterol, [while] HDL cholesterol did not change across the study.”
There were no major adverse events related to atorvastatin, with one patient in each group requiring treatment discontinuation.
In the rapidly evolving landscape of treatments for Graves’ orbitopathy, including the recent Food and Drug Administration approval for teprotumumab in thyroid eye disease, the potential role of statins remains to be seen, Dr. Marino noted.
“Graves’ orbitopathy is a rather complex disease, and in its mild to moderate forms it is very rare for a patient to require only a single treatment,” Dr. Marino explained. “Rehabilitative surgery is needed quite often once the disease is inactive.”
The authors noted that a composite overall Graves’ orbitopathy outcome was used as the primary endpoint because the alternative of a change in single eye features may not reflect a true modification of Graves’ orbitopathy and could be affected by a number of unrelated factors.
“By contrast, the composite evaluation offers a more realistic picture,” the authors wrote in the article, which was published in The Lancet Diabetes and Endocrinology.
Composite outcome not best way of assessing effects of statins
Dr. Stan extrapolated on his criticism of the trial.
“The study has interesting results but fails to show that any particular eye feature is benefited by the combination therapy, showing only the composite outcome to be improved,” he told this news organization.
“Unfortunately, that is hard to extrapolate to patient care, where one or another of Graves’ orbitopathy features are present and are the intended target of therapy,” he said.
Dr. Stan added that IV glucocorticoids are meanwhile also changing the landscape of treatment of thyroid eye disease.
“This ... current plan is to recommend a more individualized approach, depending on what is the main problem for that thyroid eye disease case,” he explained.
Dr. Marino noted that the authors are planning a double-blind, placebo-controlled phase 3 clinical trial of the statin/glucocorticoid combination to include patients regardless of their cholesterol levels.
The study received funding from Associazione Allievi Endocrinologia Pisana. The authors have reported no relevant financial relationships. Dr. Stan is on the advisory board for Horizon Pharma/Immunovant and provides general consulting for VasaraGen/Septerna and ValenzaBio/Medicxi.
A version of this article first appeared on Medscape.com.
Treatment of Graves’ orbitopathy with statins in combination with glucocorticoids shows benefits among people with – and even without – high cholesterol, results from a new randomized clinical trial show.
“Our results [indicate] that adding atorvastatin to intravenous glucocorticoids seems to potentiate the effects of glucocorticoids,” senior author Michelle Marino, MD, associate professor of endocrinology in the department of clinical and experimental medicine at the University of Pisa, Italy, told this news organization.
“At least in hypercholesterolemic patients with moderate to severe and active Graves’ orbitopathy, atorvastatin should be considered in addition to intravenous glucocorticoids,” Dr. Marino said.
The study was presented by first author Giulia Lanzolla, MD, also of the University of Pisa and University Hospital of Pisa, at the virtual annual meeting of the American Thyroid Association.
Hypercholesterolemia, well known to promote systemic inflammation, has been previously linked to Graves’ orbitopathy, and the use of statins has also been shown to possibly provide a protective effect in the risk of developing the thyroid eye disease.
Furthermore, patients with Graves’ orbitopathy and high cholesterol levels, compared with those with normal cholesterol, have been shown to have poorer responses to treatment with glucocorticoids, which have long been the first line of treatment.
Asked for comment on the findings, Marius Stan, MD, a consultant in the division of endocrinology, diabetes, metabolism, and nutrition, Mayo Clinic, Rochester, Minn., said he didn’t think the outcome measure used – a composite of a variety of measures of thyroid eye disease – was best to truly understand the benefits.
Statins for Graves’ orbitopathy (STAGO) study details
For a better understanding of the effects with and without the addition of statins in a randomized trial, Dr. Lanzolla and colleagues enrolled 88 patients with high cholesterol and moderate to severe active Graves’ orbitopathy in the phase 2 STAGO trial.
Patients were randomized to two groups of 44 patients each to receive treatment either with intravenous (IV) methylprednisolone at 500 mg per week for 6 weeks, followed by 250 mg per week for another 6 weeks, in combination with atorvastatin 20 mg daily for 12 weeks, or methylprednisolone alone for 12 weeks.
The primary endpoint was a composite of Graves orbitopathy outcomes and included measures of exophthalmos, clinical activity score, eyelid aperture, diplopia, and visual acuity, as assessed in the modified intention-to-treat population.
The trial met the primary composite endpoint, with 51.2% of those treated with statins achieving the outcome (21 of 41) versus 28.2% (11 of 39) of those treated with glucocorticoids alone (odds ratio, 2.76; P = .03).
The study also achieved secondary outcomes, with 43.9% in the statin group having a response to treatment at 12 weeks versus 23% in the glucocorticoid group (OR 2.60; P = .05). The statin group also had a greater improvement in quality of life measures (P = .03).
The glucocorticoid-only group meanwhile had a significantly greater rate of Graves orbitopathy relapse at 24 weeks, with six relapses versus none in the statin group (15.3% vs. 0.0%; OR 0.06; P = .01).
There were no significant differences in low-density lipoprotein (LDL) cholesterol between those who did and did not respond to treatment in the statin group.
The most likely explanation for those findings is that “atorvastatin acts through its pleiotropic action, resulting in an anti-inflammatory effect,” Dr. Marino said.
“In addition, the effect may be related to the capability of statins to inhibit fibroblast proliferation,” Dr. Marino added.
“Total cholesterol had a behavior similar to LDL cholesterol, [while] HDL cholesterol did not change across the study.”
There were no major adverse events related to atorvastatin, with one patient in each group requiring treatment discontinuation.
In the rapidly evolving landscape of treatments for Graves’ orbitopathy, including the recent Food and Drug Administration approval for teprotumumab in thyroid eye disease, the potential role of statins remains to be seen, Dr. Marino noted.
“Graves’ orbitopathy is a rather complex disease, and in its mild to moderate forms it is very rare for a patient to require only a single treatment,” Dr. Marino explained. “Rehabilitative surgery is needed quite often once the disease is inactive.”
The authors noted that a composite overall Graves’ orbitopathy outcome was used as the primary endpoint because the alternative of a change in single eye features may not reflect a true modification of Graves’ orbitopathy and could be affected by a number of unrelated factors.
“By contrast, the composite evaluation offers a more realistic picture,” the authors wrote in the article, which was published in The Lancet Diabetes and Endocrinology.
Composite outcome not best way of assessing effects of statins
Dr. Stan extrapolated on his criticism of the trial.
“The study has interesting results but fails to show that any particular eye feature is benefited by the combination therapy, showing only the composite outcome to be improved,” he told this news organization.
“Unfortunately, that is hard to extrapolate to patient care, where one or another of Graves’ orbitopathy features are present and are the intended target of therapy,” he said.
Dr. Stan added that IV glucocorticoids are meanwhile also changing the landscape of treatment of thyroid eye disease.
“This ... current plan is to recommend a more individualized approach, depending on what is the main problem for that thyroid eye disease case,” he explained.
Dr. Marino noted that the authors are planning a double-blind, placebo-controlled phase 3 clinical trial of the statin/glucocorticoid combination to include patients regardless of their cholesterol levels.
The study received funding from Associazione Allievi Endocrinologia Pisana. The authors have reported no relevant financial relationships. Dr. Stan is on the advisory board for Horizon Pharma/Immunovant and provides general consulting for VasaraGen/Septerna and ValenzaBio/Medicxi.
A version of this article first appeared on Medscape.com.
Treatment of Graves’ orbitopathy with statins in combination with glucocorticoids shows benefits among people with – and even without – high cholesterol, results from a new randomized clinical trial show.
“Our results [indicate] that adding atorvastatin to intravenous glucocorticoids seems to potentiate the effects of glucocorticoids,” senior author Michelle Marino, MD, associate professor of endocrinology in the department of clinical and experimental medicine at the University of Pisa, Italy, told this news organization.
“At least in hypercholesterolemic patients with moderate to severe and active Graves’ orbitopathy, atorvastatin should be considered in addition to intravenous glucocorticoids,” Dr. Marino said.
The study was presented by first author Giulia Lanzolla, MD, also of the University of Pisa and University Hospital of Pisa, at the virtual annual meeting of the American Thyroid Association.
Hypercholesterolemia, well known to promote systemic inflammation, has been previously linked to Graves’ orbitopathy, and the use of statins has also been shown to possibly provide a protective effect in the risk of developing the thyroid eye disease.
Furthermore, patients with Graves’ orbitopathy and high cholesterol levels, compared with those with normal cholesterol, have been shown to have poorer responses to treatment with glucocorticoids, which have long been the first line of treatment.
Asked for comment on the findings, Marius Stan, MD, a consultant in the division of endocrinology, diabetes, metabolism, and nutrition, Mayo Clinic, Rochester, Minn., said he didn’t think the outcome measure used – a composite of a variety of measures of thyroid eye disease – was best to truly understand the benefits.
Statins for Graves’ orbitopathy (STAGO) study details
For a better understanding of the effects with and without the addition of statins in a randomized trial, Dr. Lanzolla and colleagues enrolled 88 patients with high cholesterol and moderate to severe active Graves’ orbitopathy in the phase 2 STAGO trial.
Patients were randomized to two groups of 44 patients each to receive treatment either with intravenous (IV) methylprednisolone at 500 mg per week for 6 weeks, followed by 250 mg per week for another 6 weeks, in combination with atorvastatin 20 mg daily for 12 weeks, or methylprednisolone alone for 12 weeks.
The primary endpoint was a composite of Graves orbitopathy outcomes and included measures of exophthalmos, clinical activity score, eyelid aperture, diplopia, and visual acuity, as assessed in the modified intention-to-treat population.
The trial met the primary composite endpoint, with 51.2% of those treated with statins achieving the outcome (21 of 41) versus 28.2% (11 of 39) of those treated with glucocorticoids alone (odds ratio, 2.76; P = .03).
The study also achieved secondary outcomes, with 43.9% in the statin group having a response to treatment at 12 weeks versus 23% in the glucocorticoid group (OR 2.60; P = .05). The statin group also had a greater improvement in quality of life measures (P = .03).
The glucocorticoid-only group meanwhile had a significantly greater rate of Graves orbitopathy relapse at 24 weeks, with six relapses versus none in the statin group (15.3% vs. 0.0%; OR 0.06; P = .01).
There were no significant differences in low-density lipoprotein (LDL) cholesterol between those who did and did not respond to treatment in the statin group.
The most likely explanation for those findings is that “atorvastatin acts through its pleiotropic action, resulting in an anti-inflammatory effect,” Dr. Marino said.
“In addition, the effect may be related to the capability of statins to inhibit fibroblast proliferation,” Dr. Marino added.
“Total cholesterol had a behavior similar to LDL cholesterol, [while] HDL cholesterol did not change across the study.”
There were no major adverse events related to atorvastatin, with one patient in each group requiring treatment discontinuation.
In the rapidly evolving landscape of treatments for Graves’ orbitopathy, including the recent Food and Drug Administration approval for teprotumumab in thyroid eye disease, the potential role of statins remains to be seen, Dr. Marino noted.
“Graves’ orbitopathy is a rather complex disease, and in its mild to moderate forms it is very rare for a patient to require only a single treatment,” Dr. Marino explained. “Rehabilitative surgery is needed quite often once the disease is inactive.”
The authors noted that a composite overall Graves’ orbitopathy outcome was used as the primary endpoint because the alternative of a change in single eye features may not reflect a true modification of Graves’ orbitopathy and could be affected by a number of unrelated factors.
“By contrast, the composite evaluation offers a more realistic picture,” the authors wrote in the article, which was published in The Lancet Diabetes and Endocrinology.
Composite outcome not best way of assessing effects of statins
Dr. Stan extrapolated on his criticism of the trial.
“The study has interesting results but fails to show that any particular eye feature is benefited by the combination therapy, showing only the composite outcome to be improved,” he told this news organization.
“Unfortunately, that is hard to extrapolate to patient care, where one or another of Graves’ orbitopathy features are present and are the intended target of therapy,” he said.
Dr. Stan added that IV glucocorticoids are meanwhile also changing the landscape of treatment of thyroid eye disease.
“This ... current plan is to recommend a more individualized approach, depending on what is the main problem for that thyroid eye disease case,” he explained.
Dr. Marino noted that the authors are planning a double-blind, placebo-controlled phase 3 clinical trial of the statin/glucocorticoid combination to include patients regardless of their cholesterol levels.
The study received funding from Associazione Allievi Endocrinologia Pisana. The authors have reported no relevant financial relationships. Dr. Stan is on the advisory board for Horizon Pharma/Immunovant and provides general consulting for VasaraGen/Septerna and ValenzaBio/Medicxi.
A version of this article first appeared on Medscape.com.
FROM ATA 2021
Abaloparatide significantly reduced fractures, increased BMD in women at high fracture risk
Postmenopausal women at high or very high risk of fracture gained significantly more bone mineral density and were significantly less likely to experience a fracture when taking abaloparatide for 18 months, according to new research presented at the hybrid annual meeting of the North American Menopause Society.
“The findings showed that abaloparatide was better than teriparatide in a number of parameters important in osteoporosis treatment, and similar in others, in high-risk and very-high-risk postmenopausal women with osteoporosis,” Bart Clarke, MD, a professor of medicine at Mayo Clinic in Rochester, Minn., said in an interview. “Abaloparatide is safe and effective for use in high-risk or very-high-risk postmenopausal women,” as defined by the new American Association of Clinical Endocrinology/American College of Endocrinology osteoporosis guidelines.
Ricardo R. Correa, MD, of the department of endocrinology and director of diversity for graduate medical education at the University of Arizona, Phoenix, said that the study demonstrates that abaloparatide and teriparatide have a very similar effect with abaloparatide providing a slightly better absolute risk reduction in fracture. Dr. Correa was not involved in the research.
“What will drive my decision in what to prescribe will be the cost and insurance coverage,” Dr. Correa said. “At the Veterans Administration hospital, the option that we have is abaloparatide, so this is the option that we use.”
Among women at least 65 years old who have already had one fracture, 1 in 10 will experience another fracture within the next year, and 30% will have another fracture within the next 5 years, the authors noted in their background material. Since phase 3 ACTIVE study data in 2016 showed that abaloparatide reduces fracture risk while increasing bone mineral density, compared with placebo, the researchers reanalyzed that data to assess the drug’s efficacy in patients at high or very high risk for fracture.
The study involved 2,463 postmenopausal women with osteoporosis who received one of three interventions: 80 mcg abaloparatide daily, placebo, or 20 mcg subcutaneous teriparatide daily. Only the abaloparatide and placebo groups were double blinded.
“Teriparatide was used as the comparator drug because teriparatide was previously approved as the first anabolic drug for osteoporosis,” Dr. Clarke said in an interview. “The hope was to show that abaloparatide was a better anabolic drug.”
Women were considered at high or very high risk of fracture if they met at least one of the following four criteria from the 2020 American Association of Clinical Endocrinology guidelines:
- Fracture within the past 12 months or prevalent vertebral fracture.
- Very low T-score (less than –3.0) at baseline at any site.
- Multiple fractures at baseline since age 45.
- Very high fracture risk based on the Fracture Risk Assessment Tool (FRAX) (at least 30% for major osteoporotic fracture or at least 4.5% for hip fracture).
Among the 2,026 patients who met at least one of these criteria, 664 received abaloparatide, 685 received teriparatide, and 677 received placebo. Both the abaloparatide and teriparatide significantly reduced new vertebral fracture risk, compared with placebo. In the abaloparatide group, 0.72% of women had a new vertebral fracture, compared with 0.99% in the teriparatide group and 4.77% in the placebo group (P < .0001).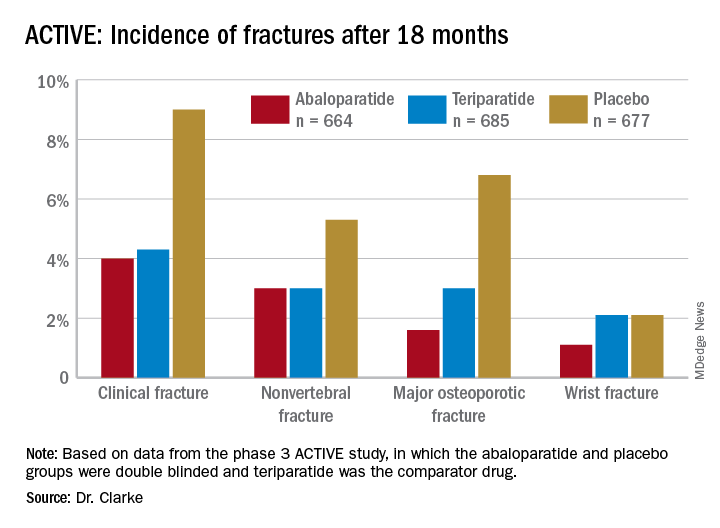
Abaloparatide and teriparatide also led to significant increases in lumbar spine, total hip, and femoral neck bone mineral density, compared with placebo (P < .0001).
The study was limited by its duration of 18 months and the Food and Drug Administration’s restriction on using abaloparatide for more than 2 years because of the theoretical risk of increasing osteosarcoma, although that risk has never been demonstrated in humans, Dr. Correa said. ”We need more data with abaloparitide in more than 2 years,” he added.
In determining which medication clinicians should first prescribe to manage osteoporosis, Dr. Correa said practitioners should consider the type of osteoporosis women have, their preferences, and their labs on kidney function.
With mild to moderate osteoporosis, bisphosphonates will be the first option while denosumab will be preferred for moderate to severe osteoporosis. Teriparatide and abaloparitide are the first-line options for severe osteoporosis, he said.
“If the glomerular filtration rate is low, we cannot use bisphosphonate and we will have to limit our use to denosumab,” he said. Route and frequency of delivery plays a role in patient preferences.
“If the patient prefers an infusion once a year or a pill, then bisphosphonate,” he said, but “if the patient is fine with an injection every 6 months, then denosumab.” Patients who need and can do an injection every day can take abaloparitide or teriparatide.
Failure of previous treatments also guide clinical decisions, he added. ”If the patient has been on one medication and has a fracture or the bone mineral density decreases, then we need to switch to another medication, usually teriparatide or abaloparitide, to build new bone.”
Contraindications for abaloparatide include a high serum calcium before therapy or prior allergic reactions to components in abaloparatide, Dr. Clarke said. No new safety signals showed up in the data analysis.
The research was funded by Radius Health. Dr. Clarke is an advisory board member of Amgen, and another author consults and speaks for Amgen and is a Radius Health Advisory Board member. Two other authors are Radius Health employees who own stock in the company. Dr Correa has no disclosures.
Postmenopausal women at high or very high risk of fracture gained significantly more bone mineral density and were significantly less likely to experience a fracture when taking abaloparatide for 18 months, according to new research presented at the hybrid annual meeting of the North American Menopause Society.
“The findings showed that abaloparatide was better than teriparatide in a number of parameters important in osteoporosis treatment, and similar in others, in high-risk and very-high-risk postmenopausal women with osteoporosis,” Bart Clarke, MD, a professor of medicine at Mayo Clinic in Rochester, Minn., said in an interview. “Abaloparatide is safe and effective for use in high-risk or very-high-risk postmenopausal women,” as defined by the new American Association of Clinical Endocrinology/American College of Endocrinology osteoporosis guidelines.
Ricardo R. Correa, MD, of the department of endocrinology and director of diversity for graduate medical education at the University of Arizona, Phoenix, said that the study demonstrates that abaloparatide and teriparatide have a very similar effect with abaloparatide providing a slightly better absolute risk reduction in fracture. Dr. Correa was not involved in the research.
“What will drive my decision in what to prescribe will be the cost and insurance coverage,” Dr. Correa said. “At the Veterans Administration hospital, the option that we have is abaloparatide, so this is the option that we use.”
Among women at least 65 years old who have already had one fracture, 1 in 10 will experience another fracture within the next year, and 30% will have another fracture within the next 5 years, the authors noted in their background material. Since phase 3 ACTIVE study data in 2016 showed that abaloparatide reduces fracture risk while increasing bone mineral density, compared with placebo, the researchers reanalyzed that data to assess the drug’s efficacy in patients at high or very high risk for fracture.
The study involved 2,463 postmenopausal women with osteoporosis who received one of three interventions: 80 mcg abaloparatide daily, placebo, or 20 mcg subcutaneous teriparatide daily. Only the abaloparatide and placebo groups were double blinded.
“Teriparatide was used as the comparator drug because teriparatide was previously approved as the first anabolic drug for osteoporosis,” Dr. Clarke said in an interview. “The hope was to show that abaloparatide was a better anabolic drug.”
Women were considered at high or very high risk of fracture if they met at least one of the following four criteria from the 2020 American Association of Clinical Endocrinology guidelines:
- Fracture within the past 12 months or prevalent vertebral fracture.
- Very low T-score (less than –3.0) at baseline at any site.
- Multiple fractures at baseline since age 45.
- Very high fracture risk based on the Fracture Risk Assessment Tool (FRAX) (at least 30% for major osteoporotic fracture or at least 4.5% for hip fracture).
Among the 2,026 patients who met at least one of these criteria, 664 received abaloparatide, 685 received teriparatide, and 677 received placebo. Both the abaloparatide and teriparatide significantly reduced new vertebral fracture risk, compared with placebo. In the abaloparatide group, 0.72% of women had a new vertebral fracture, compared with 0.99% in the teriparatide group and 4.77% in the placebo group (P < .0001).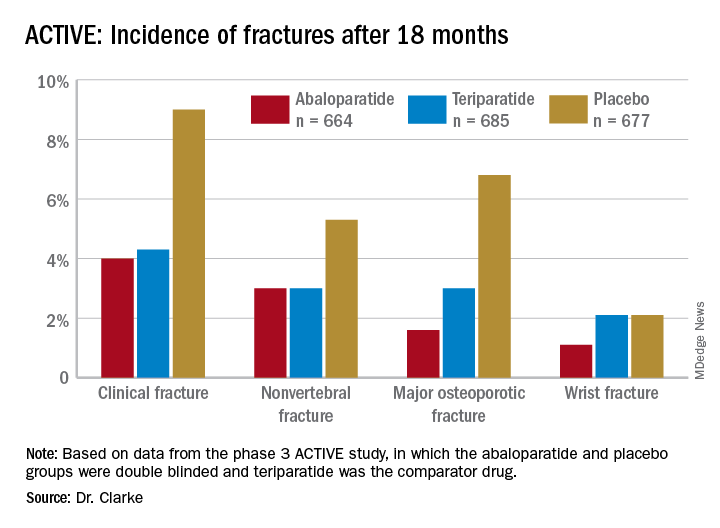
Abaloparatide and teriparatide also led to significant increases in lumbar spine, total hip, and femoral neck bone mineral density, compared with placebo (P < .0001).
The study was limited by its duration of 18 months and the Food and Drug Administration’s restriction on using abaloparatide for more than 2 years because of the theoretical risk of increasing osteosarcoma, although that risk has never been demonstrated in humans, Dr. Correa said. ”We need more data with abaloparitide in more than 2 years,” he added.
In determining which medication clinicians should first prescribe to manage osteoporosis, Dr. Correa said practitioners should consider the type of osteoporosis women have, their preferences, and their labs on kidney function.
With mild to moderate osteoporosis, bisphosphonates will be the first option while denosumab will be preferred for moderate to severe osteoporosis. Teriparatide and abaloparitide are the first-line options for severe osteoporosis, he said.
“If the glomerular filtration rate is low, we cannot use bisphosphonate and we will have to limit our use to denosumab,” he said. Route and frequency of delivery plays a role in patient preferences.
“If the patient prefers an infusion once a year or a pill, then bisphosphonate,” he said, but “if the patient is fine with an injection every 6 months, then denosumab.” Patients who need and can do an injection every day can take abaloparitide or teriparatide.
Failure of previous treatments also guide clinical decisions, he added. ”If the patient has been on one medication and has a fracture or the bone mineral density decreases, then we need to switch to another medication, usually teriparatide or abaloparitide, to build new bone.”
Contraindications for abaloparatide include a high serum calcium before therapy or prior allergic reactions to components in abaloparatide, Dr. Clarke said. No new safety signals showed up in the data analysis.
The research was funded by Radius Health. Dr. Clarke is an advisory board member of Amgen, and another author consults and speaks for Amgen and is a Radius Health Advisory Board member. Two other authors are Radius Health employees who own stock in the company. Dr Correa has no disclosures.
Postmenopausal women at high or very high risk of fracture gained significantly more bone mineral density and were significantly less likely to experience a fracture when taking abaloparatide for 18 months, according to new research presented at the hybrid annual meeting of the North American Menopause Society.
“The findings showed that abaloparatide was better than teriparatide in a number of parameters important in osteoporosis treatment, and similar in others, in high-risk and very-high-risk postmenopausal women with osteoporosis,” Bart Clarke, MD, a professor of medicine at Mayo Clinic in Rochester, Minn., said in an interview. “Abaloparatide is safe and effective for use in high-risk or very-high-risk postmenopausal women,” as defined by the new American Association of Clinical Endocrinology/American College of Endocrinology osteoporosis guidelines.
Ricardo R. Correa, MD, of the department of endocrinology and director of diversity for graduate medical education at the University of Arizona, Phoenix, said that the study demonstrates that abaloparatide and teriparatide have a very similar effect with abaloparatide providing a slightly better absolute risk reduction in fracture. Dr. Correa was not involved in the research.
“What will drive my decision in what to prescribe will be the cost and insurance coverage,” Dr. Correa said. “At the Veterans Administration hospital, the option that we have is abaloparatide, so this is the option that we use.”
Among women at least 65 years old who have already had one fracture, 1 in 10 will experience another fracture within the next year, and 30% will have another fracture within the next 5 years, the authors noted in their background material. Since phase 3 ACTIVE study data in 2016 showed that abaloparatide reduces fracture risk while increasing bone mineral density, compared with placebo, the researchers reanalyzed that data to assess the drug’s efficacy in patients at high or very high risk for fracture.
The study involved 2,463 postmenopausal women with osteoporosis who received one of three interventions: 80 mcg abaloparatide daily, placebo, or 20 mcg subcutaneous teriparatide daily. Only the abaloparatide and placebo groups were double blinded.
“Teriparatide was used as the comparator drug because teriparatide was previously approved as the first anabolic drug for osteoporosis,” Dr. Clarke said in an interview. “The hope was to show that abaloparatide was a better anabolic drug.”
Women were considered at high or very high risk of fracture if they met at least one of the following four criteria from the 2020 American Association of Clinical Endocrinology guidelines:
- Fracture within the past 12 months or prevalent vertebral fracture.
- Very low T-score (less than –3.0) at baseline at any site.
- Multiple fractures at baseline since age 45.
- Very high fracture risk based on the Fracture Risk Assessment Tool (FRAX) (at least 30% for major osteoporotic fracture or at least 4.5% for hip fracture).
Among the 2,026 patients who met at least one of these criteria, 664 received abaloparatide, 685 received teriparatide, and 677 received placebo. Both the abaloparatide and teriparatide significantly reduced new vertebral fracture risk, compared with placebo. In the abaloparatide group, 0.72% of women had a new vertebral fracture, compared with 0.99% in the teriparatide group and 4.77% in the placebo group (P < .0001).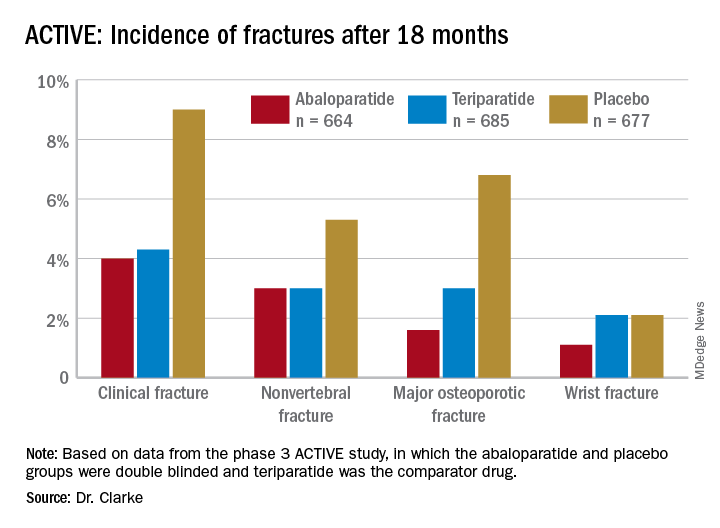
Abaloparatide and teriparatide also led to significant increases in lumbar spine, total hip, and femoral neck bone mineral density, compared with placebo (P < .0001).
The study was limited by its duration of 18 months and the Food and Drug Administration’s restriction on using abaloparatide for more than 2 years because of the theoretical risk of increasing osteosarcoma, although that risk has never been demonstrated in humans, Dr. Correa said. ”We need more data with abaloparitide in more than 2 years,” he added.
In determining which medication clinicians should first prescribe to manage osteoporosis, Dr. Correa said practitioners should consider the type of osteoporosis women have, their preferences, and their labs on kidney function.
With mild to moderate osteoporosis, bisphosphonates will be the first option while denosumab will be preferred for moderate to severe osteoporosis. Teriparatide and abaloparitide are the first-line options for severe osteoporosis, he said.
“If the glomerular filtration rate is low, we cannot use bisphosphonate and we will have to limit our use to denosumab,” he said. Route and frequency of delivery plays a role in patient preferences.
“If the patient prefers an infusion once a year or a pill, then bisphosphonate,” he said, but “if the patient is fine with an injection every 6 months, then denosumab.” Patients who need and can do an injection every day can take abaloparitide or teriparatide.
Failure of previous treatments also guide clinical decisions, he added. ”If the patient has been on one medication and has a fracture or the bone mineral density decreases, then we need to switch to another medication, usually teriparatide or abaloparitide, to build new bone.”
Contraindications for abaloparatide include a high serum calcium before therapy or prior allergic reactions to components in abaloparatide, Dr. Clarke said. No new safety signals showed up in the data analysis.
The research was funded by Radius Health. Dr. Clarke is an advisory board member of Amgen, and another author consults and speaks for Amgen and is a Radius Health Advisory Board member. Two other authors are Radius Health employees who own stock in the company. Dr Correa has no disclosures.
FROM NAMS 2021
New nonhormonal therapies for hot flashes on the horizon
Hot flashes affect three out of four women and can last 7-10 years, but the current standard of care treatment isn’t necessarily appropriate for all women who experience vasomotor symptoms, according to Stephanie Faubion, MD, MBA, director of the Mayo Clinic Women’s Health Clinic in Jacksonville, Fla.
For the majority of women under age 60 who are within 10 years of menopause, hormone therapy currently remains the most effective management option for hot flashes where the benefits outweigh the risks, Dr. Faubion told attendees Sept. 25 during a plenary at the annual meeting of the North American Menopause Society. “But really, individualizing treatment is the goal, and there are some women who are going to need some other options.”
Contraindications for hormone therapy include having a history of breast cancer, coronary heart disease, active liver disease, unexplained vaginal bleeding, high-risk endometrial cancer, transient ischemic attack, and a previous venous thromboembolic event or stroke.
“Fortunately, we have things in development,” Dr. Faubion said. She reviewed a wide range of therapies that are not currently Food and Drug Administration approved for vasomotor symptoms but are either available off label or are in clinical trials.
One of these is oxybutynin, an antimuscarinic, anticholinergic agent currently used to treat overactive bladder and overactive sweating. In a 2016 trial, 73% of women taking 15 mg extended-release oxybutynin once daily rated their symptoms as “much better,” compared with 26% who received placebo. The women experienced reduced frequency and severity of hot flashes and better sleep.
Subsequent research found a 60% reduction in hot flash frequency with 2.5 mg twice a day and a 77% reduction with 5 mg twice a day, compared with a 27% reduction with placebo. The only reported side effect that occurred more often with oxybutynin was dry mouth, but there were no significant differences in reasons for discontinuation between the treatment and placebo groups.
There are, however, some potential long-term cognitive effects from oxybutynin, Dr. Faubion said. Some research has shown an increased risk of dementia from oxybutynin and from an overall higher cumulative use of anticholinergics.
“There’s some concern about that for long-term use,” she said, but it’s effective, it’s “probably not harmful [when] used short term in women with significant, bothersome hot flashes who are unwilling or unable to use hormone therapy, and the adverse effects are tolerable for most women.” Women with bladder symptoms would be especially ideal candidates since the drug already treats those.
Dr. Faubion then discussed a new estrogen called estetrol (E4), a naturally occurring estrogen with selection action in tissues that is produced by the fetal liver and crosses the placenta. It has a long half-life of 28-32 hours, and its potential mechanism may give it a different safety profile than estradiol (E2). “There may be a lower risk of drug-drug interactions; lower breast stimulation, pain or carcinogenic impact; lower impact on triglycerides; and a neutral impact on markers of coagulation,” she said.
Though estetrol was recently approved as an oral contraceptive under the name Estelle, it’s also under investigation as a postmenopausal regimen. Preliminary findings suggest it reduces vasomotor symptom severity by 44%, compared with 30% with placebo, at 15 mg, the apparent minimum effective dose. The safety profile showed no endometrial hyperplasia and no unexpected adverse events. In those taking 15 mg of estetrol, mean endometrial thickness increased from 2 to 6 mm but returned to baseline after progestin therapy.
“The 15-mg dose also positively influenced markers of bone turnover, increased HDL [cholesterol], improved glucose tolerance,” and had no effects on coagulation parameters or triglycerides, Dr. Faubion added.
Another group of potential agents being studied for hot flashes are NK3 antagonists, which aim to exploit the recent discovery that kisspeptin, neurokinin B, and dynorphin (KNDy) neurons may play an important role in the etiology of vasomotor symptoms. Development of one of these, MLE 4901, was halted despite a 45% reduction in hot flashes because 3 of 28 women developed transiently elevated liver function tests, about four to six times the upper limit of normal.
Two others, fezolinetant and NT-814, are in phase 2 trials and have shown a significant reduction in symptoms, compared with placebo. The most commonly reported adverse effect in the phase 2a trial was gastrointestinal effects, but none of the participants stopped the drug because of these, and no elevated liver tests occurred. In the larger phase 2b trial, the most commonly reported treatment-emergent adverse events included nausea, diarrhea, fatigue, urinary tract infection, sinusitis, upper respiratory infection, headache, and cough. Five women discontinued the drug because of elevated liver enzymes.
“Overall, NK3 inhibitors appear to be generally well tolerated,” Dr. Faubion said. “There does seem to be mild transaminase elevation,” though it’s not yet known if this is an effect from this class of drugs as a whole. She noted that follicle-stimulating hormone does not significantly increase, which is important because elevated FSH is associated with poor bone health, nor does estradiol significantly increase, which is clinically relevant for women at high risk of breast cancer.
“We don’t know the effects on the heart, the brain, the bone, mood, weight, or sexual health, so there’s a lot that is still not known,” Dr. Faubion said. “We still don’t know about long-term safety and efficacy with these chemical compounds,” but clinical trials of them are ongoing.
They “would be a welcome alternative to hormone therapy for those who can’t or prefer not to use a hormonal option,” Dr. Faubion said. “However, we may need broad education of clinicians to caution against widespread abandonment of hormone therapy, particularly in women with premature or early menopause.”
Donna Klassen, LCSW, the cofounder of Let’s Talk Menopause, asked whether any of these new therapies were being tested in women with breast cancer and whether anything was known about taking oxybutynin at the same time as letrozole.
“I suspect that most women with chronic diseases would have been excluded from these initial studies, but I can’t speak to that,” Dr. Faubion said, and she wasn’t aware of any data related to taking oxybutynin and letrozole concurrently.
James Simon, MD, medical director and founder of IntimMedicine and one of those who led the research on oxybutynin, responded that his trials excluded breast cancer survivors and anyone taking aromatase inhibitors.
“It will be unlikely that, in the very near future, that data will be available because all the clinical developments on these NK3s or KNDy neuron-modulating drugs exclude cancer patients,” Dr. Simon said.
However, another attendee, Lisa Larkin, MD, of Cincinnati, introduced herself as a breast cancer survivor who takes tamoxifen and said she feels “completely comfortable” prescribing oxybutynin to breast cancer survivors.
“In terms of side effects and effectiveness in patients on tamoxifen and aromatase inhibitors, I’ve had incredibly good luck with it, and I think it’s underutilized,” Dr. Larkin said. “The clinical pearl I would tell you is you can start really low, and the dry mouth really seems to improve with time.” She added that patients should be informed that it takes 2 weeks before it begins working, but the side effects eventually go away. “It becomes very tolerable, so I just encourage all of you to consider it as another great option.”
Dr. Faubion had no disclosures. Disclosure information was unavailable for Dr. Simon, Dr. Larkin, and Ms. Klassen.
Hot flashes affect three out of four women and can last 7-10 years, but the current standard of care treatment isn’t necessarily appropriate for all women who experience vasomotor symptoms, according to Stephanie Faubion, MD, MBA, director of the Mayo Clinic Women’s Health Clinic in Jacksonville, Fla.
For the majority of women under age 60 who are within 10 years of menopause, hormone therapy currently remains the most effective management option for hot flashes where the benefits outweigh the risks, Dr. Faubion told attendees Sept. 25 during a plenary at the annual meeting of the North American Menopause Society. “But really, individualizing treatment is the goal, and there are some women who are going to need some other options.”
Contraindications for hormone therapy include having a history of breast cancer, coronary heart disease, active liver disease, unexplained vaginal bleeding, high-risk endometrial cancer, transient ischemic attack, and a previous venous thromboembolic event or stroke.
“Fortunately, we have things in development,” Dr. Faubion said. She reviewed a wide range of therapies that are not currently Food and Drug Administration approved for vasomotor symptoms but are either available off label or are in clinical trials.
One of these is oxybutynin, an antimuscarinic, anticholinergic agent currently used to treat overactive bladder and overactive sweating. In a 2016 trial, 73% of women taking 15 mg extended-release oxybutynin once daily rated their symptoms as “much better,” compared with 26% who received placebo. The women experienced reduced frequency and severity of hot flashes and better sleep.
Subsequent research found a 60% reduction in hot flash frequency with 2.5 mg twice a day and a 77% reduction with 5 mg twice a day, compared with a 27% reduction with placebo. The only reported side effect that occurred more often with oxybutynin was dry mouth, but there were no significant differences in reasons for discontinuation between the treatment and placebo groups.
There are, however, some potential long-term cognitive effects from oxybutynin, Dr. Faubion said. Some research has shown an increased risk of dementia from oxybutynin and from an overall higher cumulative use of anticholinergics.
“There’s some concern about that for long-term use,” she said, but it’s effective, it’s “probably not harmful [when] used short term in women with significant, bothersome hot flashes who are unwilling or unable to use hormone therapy, and the adverse effects are tolerable for most women.” Women with bladder symptoms would be especially ideal candidates since the drug already treats those.
Dr. Faubion then discussed a new estrogen called estetrol (E4), a naturally occurring estrogen with selection action in tissues that is produced by the fetal liver and crosses the placenta. It has a long half-life of 28-32 hours, and its potential mechanism may give it a different safety profile than estradiol (E2). “There may be a lower risk of drug-drug interactions; lower breast stimulation, pain or carcinogenic impact; lower impact on triglycerides; and a neutral impact on markers of coagulation,” she said.
Though estetrol was recently approved as an oral contraceptive under the name Estelle, it’s also under investigation as a postmenopausal regimen. Preliminary findings suggest it reduces vasomotor symptom severity by 44%, compared with 30% with placebo, at 15 mg, the apparent minimum effective dose. The safety profile showed no endometrial hyperplasia and no unexpected adverse events. In those taking 15 mg of estetrol, mean endometrial thickness increased from 2 to 6 mm but returned to baseline after progestin therapy.
“The 15-mg dose also positively influenced markers of bone turnover, increased HDL [cholesterol], improved glucose tolerance,” and had no effects on coagulation parameters or triglycerides, Dr. Faubion added.
Another group of potential agents being studied for hot flashes are NK3 antagonists, which aim to exploit the recent discovery that kisspeptin, neurokinin B, and dynorphin (KNDy) neurons may play an important role in the etiology of vasomotor symptoms. Development of one of these, MLE 4901, was halted despite a 45% reduction in hot flashes because 3 of 28 women developed transiently elevated liver function tests, about four to six times the upper limit of normal.
Two others, fezolinetant and NT-814, are in phase 2 trials and have shown a significant reduction in symptoms, compared with placebo. The most commonly reported adverse effect in the phase 2a trial was gastrointestinal effects, but none of the participants stopped the drug because of these, and no elevated liver tests occurred. In the larger phase 2b trial, the most commonly reported treatment-emergent adverse events included nausea, diarrhea, fatigue, urinary tract infection, sinusitis, upper respiratory infection, headache, and cough. Five women discontinued the drug because of elevated liver enzymes.
“Overall, NK3 inhibitors appear to be generally well tolerated,” Dr. Faubion said. “There does seem to be mild transaminase elevation,” though it’s not yet known if this is an effect from this class of drugs as a whole. She noted that follicle-stimulating hormone does not significantly increase, which is important because elevated FSH is associated with poor bone health, nor does estradiol significantly increase, which is clinically relevant for women at high risk of breast cancer.
“We don’t know the effects on the heart, the brain, the bone, mood, weight, or sexual health, so there’s a lot that is still not known,” Dr. Faubion said. “We still don’t know about long-term safety and efficacy with these chemical compounds,” but clinical trials of them are ongoing.
They “would be a welcome alternative to hormone therapy for those who can’t or prefer not to use a hormonal option,” Dr. Faubion said. “However, we may need broad education of clinicians to caution against widespread abandonment of hormone therapy, particularly in women with premature or early menopause.”
Donna Klassen, LCSW, the cofounder of Let’s Talk Menopause, asked whether any of these new therapies were being tested in women with breast cancer and whether anything was known about taking oxybutynin at the same time as letrozole.
“I suspect that most women with chronic diseases would have been excluded from these initial studies, but I can’t speak to that,” Dr. Faubion said, and she wasn’t aware of any data related to taking oxybutynin and letrozole concurrently.
James Simon, MD, medical director and founder of IntimMedicine and one of those who led the research on oxybutynin, responded that his trials excluded breast cancer survivors and anyone taking aromatase inhibitors.
“It will be unlikely that, in the very near future, that data will be available because all the clinical developments on these NK3s or KNDy neuron-modulating drugs exclude cancer patients,” Dr. Simon said.
However, another attendee, Lisa Larkin, MD, of Cincinnati, introduced herself as a breast cancer survivor who takes tamoxifen and said she feels “completely comfortable” prescribing oxybutynin to breast cancer survivors.
“In terms of side effects and effectiveness in patients on tamoxifen and aromatase inhibitors, I’ve had incredibly good luck with it, and I think it’s underutilized,” Dr. Larkin said. “The clinical pearl I would tell you is you can start really low, and the dry mouth really seems to improve with time.” She added that patients should be informed that it takes 2 weeks before it begins working, but the side effects eventually go away. “It becomes very tolerable, so I just encourage all of you to consider it as another great option.”
Dr. Faubion had no disclosures. Disclosure information was unavailable for Dr. Simon, Dr. Larkin, and Ms. Klassen.
Hot flashes affect three out of four women and can last 7-10 years, but the current standard of care treatment isn’t necessarily appropriate for all women who experience vasomotor symptoms, according to Stephanie Faubion, MD, MBA, director of the Mayo Clinic Women’s Health Clinic in Jacksonville, Fla.
For the majority of women under age 60 who are within 10 years of menopause, hormone therapy currently remains the most effective management option for hot flashes where the benefits outweigh the risks, Dr. Faubion told attendees Sept. 25 during a plenary at the annual meeting of the North American Menopause Society. “But really, individualizing treatment is the goal, and there are some women who are going to need some other options.”
Contraindications for hormone therapy include having a history of breast cancer, coronary heart disease, active liver disease, unexplained vaginal bleeding, high-risk endometrial cancer, transient ischemic attack, and a previous venous thromboembolic event or stroke.
“Fortunately, we have things in development,” Dr. Faubion said. She reviewed a wide range of therapies that are not currently Food and Drug Administration approved for vasomotor symptoms but are either available off label or are in clinical trials.
One of these is oxybutynin, an antimuscarinic, anticholinergic agent currently used to treat overactive bladder and overactive sweating. In a 2016 trial, 73% of women taking 15 mg extended-release oxybutynin once daily rated their symptoms as “much better,” compared with 26% who received placebo. The women experienced reduced frequency and severity of hot flashes and better sleep.
Subsequent research found a 60% reduction in hot flash frequency with 2.5 mg twice a day and a 77% reduction with 5 mg twice a day, compared with a 27% reduction with placebo. The only reported side effect that occurred more often with oxybutynin was dry mouth, but there were no significant differences in reasons for discontinuation between the treatment and placebo groups.
There are, however, some potential long-term cognitive effects from oxybutynin, Dr. Faubion said. Some research has shown an increased risk of dementia from oxybutynin and from an overall higher cumulative use of anticholinergics.
“There’s some concern about that for long-term use,” she said, but it’s effective, it’s “probably not harmful [when] used short term in women with significant, bothersome hot flashes who are unwilling or unable to use hormone therapy, and the adverse effects are tolerable for most women.” Women with bladder symptoms would be especially ideal candidates since the drug already treats those.
Dr. Faubion then discussed a new estrogen called estetrol (E4), a naturally occurring estrogen with selection action in tissues that is produced by the fetal liver and crosses the placenta. It has a long half-life of 28-32 hours, and its potential mechanism may give it a different safety profile than estradiol (E2). “There may be a lower risk of drug-drug interactions; lower breast stimulation, pain or carcinogenic impact; lower impact on triglycerides; and a neutral impact on markers of coagulation,” she said.
Though estetrol was recently approved as an oral contraceptive under the name Estelle, it’s also under investigation as a postmenopausal regimen. Preliminary findings suggest it reduces vasomotor symptom severity by 44%, compared with 30% with placebo, at 15 mg, the apparent minimum effective dose. The safety profile showed no endometrial hyperplasia and no unexpected adverse events. In those taking 15 mg of estetrol, mean endometrial thickness increased from 2 to 6 mm but returned to baseline after progestin therapy.
“The 15-mg dose also positively influenced markers of bone turnover, increased HDL [cholesterol], improved glucose tolerance,” and had no effects on coagulation parameters or triglycerides, Dr. Faubion added.
Another group of potential agents being studied for hot flashes are NK3 antagonists, which aim to exploit the recent discovery that kisspeptin, neurokinin B, and dynorphin (KNDy) neurons may play an important role in the etiology of vasomotor symptoms. Development of one of these, MLE 4901, was halted despite a 45% reduction in hot flashes because 3 of 28 women developed transiently elevated liver function tests, about four to six times the upper limit of normal.
Two others, fezolinetant and NT-814, are in phase 2 trials and have shown a significant reduction in symptoms, compared with placebo. The most commonly reported adverse effect in the phase 2a trial was gastrointestinal effects, but none of the participants stopped the drug because of these, and no elevated liver tests occurred. In the larger phase 2b trial, the most commonly reported treatment-emergent adverse events included nausea, diarrhea, fatigue, urinary tract infection, sinusitis, upper respiratory infection, headache, and cough. Five women discontinued the drug because of elevated liver enzymes.
“Overall, NK3 inhibitors appear to be generally well tolerated,” Dr. Faubion said. “There does seem to be mild transaminase elevation,” though it’s not yet known if this is an effect from this class of drugs as a whole. She noted that follicle-stimulating hormone does not significantly increase, which is important because elevated FSH is associated with poor bone health, nor does estradiol significantly increase, which is clinically relevant for women at high risk of breast cancer.
“We don’t know the effects on the heart, the brain, the bone, mood, weight, or sexual health, so there’s a lot that is still not known,” Dr. Faubion said. “We still don’t know about long-term safety and efficacy with these chemical compounds,” but clinical trials of them are ongoing.
They “would be a welcome alternative to hormone therapy for those who can’t or prefer not to use a hormonal option,” Dr. Faubion said. “However, we may need broad education of clinicians to caution against widespread abandonment of hormone therapy, particularly in women with premature or early menopause.”
Donna Klassen, LCSW, the cofounder of Let’s Talk Menopause, asked whether any of these new therapies were being tested in women with breast cancer and whether anything was known about taking oxybutynin at the same time as letrozole.
“I suspect that most women with chronic diseases would have been excluded from these initial studies, but I can’t speak to that,” Dr. Faubion said, and she wasn’t aware of any data related to taking oxybutynin and letrozole concurrently.
James Simon, MD, medical director and founder of IntimMedicine and one of those who led the research on oxybutynin, responded that his trials excluded breast cancer survivors and anyone taking aromatase inhibitors.
“It will be unlikely that, in the very near future, that data will be available because all the clinical developments on these NK3s or KNDy neuron-modulating drugs exclude cancer patients,” Dr. Simon said.
However, another attendee, Lisa Larkin, MD, of Cincinnati, introduced herself as a breast cancer survivor who takes tamoxifen and said she feels “completely comfortable” prescribing oxybutynin to breast cancer survivors.
“In terms of side effects and effectiveness in patients on tamoxifen and aromatase inhibitors, I’ve had incredibly good luck with it, and I think it’s underutilized,” Dr. Larkin said. “The clinical pearl I would tell you is you can start really low, and the dry mouth really seems to improve with time.” She added that patients should be informed that it takes 2 weeks before it begins working, but the side effects eventually go away. “It becomes very tolerable, so I just encourage all of you to consider it as another great option.”
Dr. Faubion had no disclosures. Disclosure information was unavailable for Dr. Simon, Dr. Larkin, and Ms. Klassen.
FROM NAMS 2021
Cut risedronate drug holiday to under 2 years in older patients
Any pause in taking the osteoporosis drug risedronate (Actonel) should last no longer than 2 years rather than the 2-3 years currently recommended for bisphosphonates, new research suggests.
In a cohort of patients aged 66 and older in Ontario, Canada, those who had been taking risedronate had a 34% greater risk of a hip fracture during year 2 to year 3 of a pause in taking the drug – a drug holiday – compared with those who had been taking alendronate (Fosamax).
The study showed that “risedronate, which has a shorter half-life, confers relatively less hip fracture protection than alendronate during drug holidays longer than 2 years and careful monitoring and follow-up after 2 years is likely warranted,” Kaley (Kaleen) N. Hayes, Pharm D, PhD, summarized in an oral presentation at the annual meeting of the American Society for Bone and Mineral Research. Dr. Hayes is an assistant professor in the department of health services, policy, and practice at Brown University School of Public Health, Providence, R.I.
“Although alendronate and risedronate have similar effectiveness for preventing fractures on treatment, our findings suggest that older patients on a risedronate drug holiday may benefit from assessment to consider resuming therapy after 2 years to prevent hip fractures,” she elaborated in an email.
Juliet Compston, MD, identified this study as one of the meeting’s clinical science highlights.
“This is the first study to directly compare fracture incidence during a drug holiday after treatment with the two most commonly prescribed oral bisphosphonates, alendronate and risedronate,” she told this news organization in an email.
The difference in fracture incidence during the 3-year drug holiday is “consistent with the known difference in pharmacokinetic properties of the two drugs,” noted Dr. Compston, professor of bone medicine and honorary consultant physician at the University of Cambridge (England) School of Clinical Medicine.
Since the increased risk of fracture after stopping risedronate vs. alendronate was seen by 2 years, “reevaluation of risk in risedronate-treated patients should therefore be considered earlier than the recommended period of 2-3 years after discontinuation,” she said.
“The study does not provide information about the optimal duration of drug holiday for either risedronate or alendronate, but it supports a shorter duration for the former of up to 2 years,” according to Dr. Compston.
Study rationale and findings
“The question of whether people treated for osteoporosis with oral bisphosphonates should have drug holidays is controversial,” Dr. Compston noted, “but many guidelines recommend that in lower-risk individuals who have received bisphosphonates for 5 years, a break from treatment of 2-3 years should be considered.”
Five or more years of bisphosphonate treatment for osteoporosis has been associated with rare adverse effects such as atypical femoral fractures, and these drugs appear to have fracture protection effects that linger for a while, so a drug holiday is recommended for most patients, Dr. Hayes added.
Guidelines such as the 2016 ASBMR task force report on long-term bisphosphonates for osteoporosis, she continued, “acknowledge that evidence for this recommendation comes primarily from the extension trial for alendronate, and patients undergoing a risedronate drug holiday may need to be reassessed earlier because of risedronate’s shorter half-life.”
Compared with alendronate, risedronate accumulates less in the bone and is eliminated more quickly from the body, so its fracture protection during drug holidays may be shorter.
The researchers aimed to estimate the 3-year fracture risk after discontinuing long-term (3 or more years) risedronate vs. alendronate therapy among older adults in Ontario.
From health care administrative data, they identified 120,368 patients aged 66 years and older who had started taking risedronate or alendronate as initial therapy for osteoporosis during the period 2000-2016. They had taken the therapy for 3 or more years (with at least 80% adherence) before stopping it for 120 days or longer.
The researchers found that 45% of patients were taking risedronate and 55% were taking alendronate, which are the main bisphosphonates used in Ontario, Dr. Hayes noted. Etidronate (Didronel) is recommended as second-line therapy and accounts for less than 2% of patients starting oral bisphosphonate therapy.
In an earlier study, the researchers identified a shift toward greater use of risedronate than alendronate since 2008, likely related to newer formulations (for example, monthly and weekly delayed-release formulations of risedronate vs. only weekly alendronate formulations).
The researchers matched 25,077 patients taking alendronate with 25,077 patients taking risedronate, based on fracture risk–related characteristics, including demographics, diagnoses, medication use, and health care use.
The patients had a mean age of 74 when they started taking an oral bisphosphonate; 82% were women and most were White.
Most patients (78%) had received a prescription from a general practitioner and, on average, they took the bisphosphonate therapy for 5.9 years before the drug holiday.
The primary outcome of incident hip fracture during a 3-year drug holiday occurred in 915 patients. There were 12.4 events per 1,000 patients in the risedronate group vs. 10.6 events per 1,000 patients in the alendronate group (hazard ratio, 1.18; 95% confidence interval, 1.04-1.34).
The risks were not significantly higher during year 1 or year 2 of the drug holiday, but the curves began to diverge after 2 years, coauthor Suzanne Cadarette, PhD, of the Leslie Dan Faculty of Pharmacy at the University of Toronto, explained when replying to a question after the presentation. Dr. Cadarette supervised this PhD dissertation research by Dr. Hayes.
The researchers acknowledged that the limitations of their study include a lack of information about race or bone mineral density, and the findings may not apply to a younger, more racially diverse population.
The research was supported by the University of Toronto Dalla Lana School of Public Health and the Leslie Dan Faculty of Pharmacy, a Canadian Institutes of Health Research grant, and a doctoral research award. The authors have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Any pause in taking the osteoporosis drug risedronate (Actonel) should last no longer than 2 years rather than the 2-3 years currently recommended for bisphosphonates, new research suggests.
In a cohort of patients aged 66 and older in Ontario, Canada, those who had been taking risedronate had a 34% greater risk of a hip fracture during year 2 to year 3 of a pause in taking the drug – a drug holiday – compared with those who had been taking alendronate (Fosamax).
The study showed that “risedronate, which has a shorter half-life, confers relatively less hip fracture protection than alendronate during drug holidays longer than 2 years and careful monitoring and follow-up after 2 years is likely warranted,” Kaley (Kaleen) N. Hayes, Pharm D, PhD, summarized in an oral presentation at the annual meeting of the American Society for Bone and Mineral Research. Dr. Hayes is an assistant professor in the department of health services, policy, and practice at Brown University School of Public Health, Providence, R.I.
“Although alendronate and risedronate have similar effectiveness for preventing fractures on treatment, our findings suggest that older patients on a risedronate drug holiday may benefit from assessment to consider resuming therapy after 2 years to prevent hip fractures,” she elaborated in an email.
Juliet Compston, MD, identified this study as one of the meeting’s clinical science highlights.
“This is the first study to directly compare fracture incidence during a drug holiday after treatment with the two most commonly prescribed oral bisphosphonates, alendronate and risedronate,” she told this news organization in an email.
The difference in fracture incidence during the 3-year drug holiday is “consistent with the known difference in pharmacokinetic properties of the two drugs,” noted Dr. Compston, professor of bone medicine and honorary consultant physician at the University of Cambridge (England) School of Clinical Medicine.
Since the increased risk of fracture after stopping risedronate vs. alendronate was seen by 2 years, “reevaluation of risk in risedronate-treated patients should therefore be considered earlier than the recommended period of 2-3 years after discontinuation,” she said.
“The study does not provide information about the optimal duration of drug holiday for either risedronate or alendronate, but it supports a shorter duration for the former of up to 2 years,” according to Dr. Compston.
Study rationale and findings
“The question of whether people treated for osteoporosis with oral bisphosphonates should have drug holidays is controversial,” Dr. Compston noted, “but many guidelines recommend that in lower-risk individuals who have received bisphosphonates for 5 years, a break from treatment of 2-3 years should be considered.”
Five or more years of bisphosphonate treatment for osteoporosis has been associated with rare adverse effects such as atypical femoral fractures, and these drugs appear to have fracture protection effects that linger for a while, so a drug holiday is recommended for most patients, Dr. Hayes added.
Guidelines such as the 2016 ASBMR task force report on long-term bisphosphonates for osteoporosis, she continued, “acknowledge that evidence for this recommendation comes primarily from the extension trial for alendronate, and patients undergoing a risedronate drug holiday may need to be reassessed earlier because of risedronate’s shorter half-life.”
Compared with alendronate, risedronate accumulates less in the bone and is eliminated more quickly from the body, so its fracture protection during drug holidays may be shorter.
The researchers aimed to estimate the 3-year fracture risk after discontinuing long-term (3 or more years) risedronate vs. alendronate therapy among older adults in Ontario.
From health care administrative data, they identified 120,368 patients aged 66 years and older who had started taking risedronate or alendronate as initial therapy for osteoporosis during the period 2000-2016. They had taken the therapy for 3 or more years (with at least 80% adherence) before stopping it for 120 days or longer.
The researchers found that 45% of patients were taking risedronate and 55% were taking alendronate, which are the main bisphosphonates used in Ontario, Dr. Hayes noted. Etidronate (Didronel) is recommended as second-line therapy and accounts for less than 2% of patients starting oral bisphosphonate therapy.
In an earlier study, the researchers identified a shift toward greater use of risedronate than alendronate since 2008, likely related to newer formulations (for example, monthly and weekly delayed-release formulations of risedronate vs. only weekly alendronate formulations).
The researchers matched 25,077 patients taking alendronate with 25,077 patients taking risedronate, based on fracture risk–related characteristics, including demographics, diagnoses, medication use, and health care use.
The patients had a mean age of 74 when they started taking an oral bisphosphonate; 82% were women and most were White.
Most patients (78%) had received a prescription from a general practitioner and, on average, they took the bisphosphonate therapy for 5.9 years before the drug holiday.
The primary outcome of incident hip fracture during a 3-year drug holiday occurred in 915 patients. There were 12.4 events per 1,000 patients in the risedronate group vs. 10.6 events per 1,000 patients in the alendronate group (hazard ratio, 1.18; 95% confidence interval, 1.04-1.34).
The risks were not significantly higher during year 1 or year 2 of the drug holiday, but the curves began to diverge after 2 years, coauthor Suzanne Cadarette, PhD, of the Leslie Dan Faculty of Pharmacy at the University of Toronto, explained when replying to a question after the presentation. Dr. Cadarette supervised this PhD dissertation research by Dr. Hayes.
The researchers acknowledged that the limitations of their study include a lack of information about race or bone mineral density, and the findings may not apply to a younger, more racially diverse population.
The research was supported by the University of Toronto Dalla Lana School of Public Health and the Leslie Dan Faculty of Pharmacy, a Canadian Institutes of Health Research grant, and a doctoral research award. The authors have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Any pause in taking the osteoporosis drug risedronate (Actonel) should last no longer than 2 years rather than the 2-3 years currently recommended for bisphosphonates, new research suggests.
In a cohort of patients aged 66 and older in Ontario, Canada, those who had been taking risedronate had a 34% greater risk of a hip fracture during year 2 to year 3 of a pause in taking the drug – a drug holiday – compared with those who had been taking alendronate (Fosamax).
The study showed that “risedronate, which has a shorter half-life, confers relatively less hip fracture protection than alendronate during drug holidays longer than 2 years and careful monitoring and follow-up after 2 years is likely warranted,” Kaley (Kaleen) N. Hayes, Pharm D, PhD, summarized in an oral presentation at the annual meeting of the American Society for Bone and Mineral Research. Dr. Hayes is an assistant professor in the department of health services, policy, and practice at Brown University School of Public Health, Providence, R.I.
“Although alendronate and risedronate have similar effectiveness for preventing fractures on treatment, our findings suggest that older patients on a risedronate drug holiday may benefit from assessment to consider resuming therapy after 2 years to prevent hip fractures,” she elaborated in an email.
Juliet Compston, MD, identified this study as one of the meeting’s clinical science highlights.
“This is the first study to directly compare fracture incidence during a drug holiday after treatment with the two most commonly prescribed oral bisphosphonates, alendronate and risedronate,” she told this news organization in an email.
The difference in fracture incidence during the 3-year drug holiday is “consistent with the known difference in pharmacokinetic properties of the two drugs,” noted Dr. Compston, professor of bone medicine and honorary consultant physician at the University of Cambridge (England) School of Clinical Medicine.
Since the increased risk of fracture after stopping risedronate vs. alendronate was seen by 2 years, “reevaluation of risk in risedronate-treated patients should therefore be considered earlier than the recommended period of 2-3 years after discontinuation,” she said.
“The study does not provide information about the optimal duration of drug holiday for either risedronate or alendronate, but it supports a shorter duration for the former of up to 2 years,” according to Dr. Compston.
Study rationale and findings
“The question of whether people treated for osteoporosis with oral bisphosphonates should have drug holidays is controversial,” Dr. Compston noted, “but many guidelines recommend that in lower-risk individuals who have received bisphosphonates for 5 years, a break from treatment of 2-3 years should be considered.”
Five or more years of bisphosphonate treatment for osteoporosis has been associated with rare adverse effects such as atypical femoral fractures, and these drugs appear to have fracture protection effects that linger for a while, so a drug holiday is recommended for most patients, Dr. Hayes added.
Guidelines such as the 2016 ASBMR task force report on long-term bisphosphonates for osteoporosis, she continued, “acknowledge that evidence for this recommendation comes primarily from the extension trial for alendronate, and patients undergoing a risedronate drug holiday may need to be reassessed earlier because of risedronate’s shorter half-life.”
Compared with alendronate, risedronate accumulates less in the bone and is eliminated more quickly from the body, so its fracture protection during drug holidays may be shorter.
The researchers aimed to estimate the 3-year fracture risk after discontinuing long-term (3 or more years) risedronate vs. alendronate therapy among older adults in Ontario.
From health care administrative data, they identified 120,368 patients aged 66 years and older who had started taking risedronate or alendronate as initial therapy for osteoporosis during the period 2000-2016. They had taken the therapy for 3 or more years (with at least 80% adherence) before stopping it for 120 days or longer.
The researchers found that 45% of patients were taking risedronate and 55% were taking alendronate, which are the main bisphosphonates used in Ontario, Dr. Hayes noted. Etidronate (Didronel) is recommended as second-line therapy and accounts for less than 2% of patients starting oral bisphosphonate therapy.
In an earlier study, the researchers identified a shift toward greater use of risedronate than alendronate since 2008, likely related to newer formulations (for example, monthly and weekly delayed-release formulations of risedronate vs. only weekly alendronate formulations).
The researchers matched 25,077 patients taking alendronate with 25,077 patients taking risedronate, based on fracture risk–related characteristics, including demographics, diagnoses, medication use, and health care use.
The patients had a mean age of 74 when they started taking an oral bisphosphonate; 82% were women and most were White.
Most patients (78%) had received a prescription from a general practitioner and, on average, they took the bisphosphonate therapy for 5.9 years before the drug holiday.
The primary outcome of incident hip fracture during a 3-year drug holiday occurred in 915 patients. There were 12.4 events per 1,000 patients in the risedronate group vs. 10.6 events per 1,000 patients in the alendronate group (hazard ratio, 1.18; 95% confidence interval, 1.04-1.34).
The risks were not significantly higher during year 1 or year 2 of the drug holiday, but the curves began to diverge after 2 years, coauthor Suzanne Cadarette, PhD, of the Leslie Dan Faculty of Pharmacy at the University of Toronto, explained when replying to a question after the presentation. Dr. Cadarette supervised this PhD dissertation research by Dr. Hayes.
The researchers acknowledged that the limitations of their study include a lack of information about race or bone mineral density, and the findings may not apply to a younger, more racially diverse population.
The research was supported by the University of Toronto Dalla Lana School of Public Health and the Leslie Dan Faculty of Pharmacy, a Canadian Institutes of Health Research grant, and a doctoral research award. The authors have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM ASBMR 2021
Exercise appears to improve bone structure, not density
“Postmenopausal women with low bone mass should obtain adequate calcium and vitamin D and participate in bone-loading exercises,” researchers noted in a recent study published in Osteoporosis International.
“Additional use of bisphosphonates will increase bone mineral density (BMD), especially at the spine,” wrote Nancy Waltman, PhD, College of Nursing, University of Nebraska Medical Center, Omaha, and colleagues.
The findings are partial results from the Heartland Osteoporosis Prevention Study (HOPS), which randomized women who had entered menopause within the previous 6 months and had osteopenia (low bone mass, T score –1.0 to –2.49) to receive one of three treatments for 12 months:
- Bone-loading and resistance exercise plus calcium and vitamin D supplements.
- Risedronate plus calcium and vitamin D supplements.
- Calcium and vitamin D supplements alone (control).
At 1 year, “risedronate significantly increased BMD at the spine, compared to exercise and control, and serum biomarkers of bone turnover also significantly reduced in the risedronate group,” Laura Bilek, PT, PhD, said during an oral presentation of the research at the annual meeting of the American Society for Bone and Mineral Research.
However, the results also showed that, importantly, “in postmenopausal women, exercise appears to improve strength at the hip through changes in structure, not BMD,” stressed Dr. Bilek, of the College of Allied Health Professionals, University of Nebraska Medical Center.
Bone health is about more than just bone mineral density
“The key takeaway for clinicians is that bone health is about more than just density!” she noted in an email.
Current guidelines don’t recommend prescribing risedronate until a woman has overt osteoporosis, she said.
On the other hand, many studies have shown that, to be most effective, bone-loading exercises should be a lifelong habit and women should begin to do them at least during menopause and should not wait until bone loss occurs.
Other studies have shown that exercise changes bone structure (size or geometry), which improves bone strength. The current study supports both prior observations.
And exercise also improves muscle strength and decreases the risk of falls and fractures, Dr. Bilek noted.
Invited to comment, Pauline M. Camacho, MD, cochair of the task force for the American Association of Clinical Endocrinologists (AACE) guidelines for osteoporosis, noted that all three measures – pharmacotherapy, exercise, and calcium/vitamin D – are important in the successful management of osteoporosis.
This study showed that risedronate is superior to calcium/vitamin D supplementation as well as exercise for BMD and for bone turnover in these women with osteopenia, said Dr. Camacho, professor of medicine and director of the Osteoporosis and Metabolic Bone Disease Center, Loyola University Medical Center, Chicago.
“Most women with osteopenia do not receive pharmacologic therapy,” she noted, and receive it only “if there is a history of fractures or they have other features that change that diagnosis to osteoporosis.
“There is no downside to exercise, and this needs to be advised to all patients,” she said. “The other aspect of exercise that was not assessed in this study is its effect on balance. Patients who exercise will have improved balance, which should translate into fewer falls, and thus fewer fractures.”
How can women with osteopenia maintain bone health?
In their article, Dr. Waltman and colleagues say the Lifting Intervention for Training Muscle and Osteoporosis Rehabilitation (LIFTMOR) clinical trial is one of the first to address clinician concerns about the safety and effectiveness of exercise to improve bone health.
In that trial of 101 postmenopausal women with low bone mass, 8 months of 30-minute, twice-weekly, supervised high-intensity resistance and impact training was safe and BMD increased by 2.9% at the lumbar spine and 0.3% at the femoral neck.
“Our [HOPS] study,” Dr. Waltman and colleagues explained, “builds on the LIFTMOR clinical trial and adds further data to inform whether postmenopausal women with low bone mass can effectively maintain or even improve BMD with bone-loading exercises prior to prescriptions for medication.
“Our long-term goal is to contribute to the development of clinical practice guidelines for the prevention of fractures in postmenopausal women with low bone mass,” they said.
They randomized 276 postmenopausal women who were a mean age of 54 (range, 44-63); most were White (78%) or Hispanic (6%).
Women were excluded from the study if they had a diagnosis of osteoporosis (T-score < −2.5); had an increased risk of a major fracture or hip fracture; had been on bisphosphonates within the last 6 months; were currently on estrogen, tamoxifen, or aromatase inhibitors; had a serum vitamin D level < 10 mg/mL or > 100 mg/mL; had any conditions that prohibited prescriptions for calcium and vitamin D supplements, risedronate, or exercise; or weighed more than 300 pounds.
All women received 1,200 mg/day of calcium (from supplements or diet) and 1,000-3,000 IU/day of vitamin D supplements, based on their serum 25(OH) vitamin D levels.
The exercise program consisted of visiting a gym three times a week for 45 minutes of bone-loading exercise – jogging with a weighted vest – and resistance exercises, which were supervised by a trainer for the first 2 weeks.
Women in the risedronate group received a 150-mg tablet of risedronate every 4 weeks.
At baseline, 6 months, and 12 months, the women had DXA scans to determine BMD and hip structure, and had blood tests to determine levels of serum markers for bone formation (bone specific alkaline phosphatase [Alkphase B]) and bone resorption (N-terminal telopeptide [NTx]).
Compared with baseline, at 12 months, the women had the following changes in BMD at the following sites:
- Spine: +1.9%, +0.9%, and –0.4%, in the risedronate, exercise, and control groups.
- Total hip: +0.9%, +0.5%, and +0.5%, in the risedronate, exercise, and control groups.
- Femoral neck: +0.09%, –0.4%, and –0.5%, in the risedronate, exercise, and control groups.
These improvements in BMD were significantly greater in the risedronate group than in the exercise or control groups (P < .01 for both).
The decreases in serum levels of NtX and Alkphase B were also greater with risedronate than in the exercise or control groups (P < .01 for all).
The most frequent adverse effect with the calcium supplement was constipation (n = 4). Some women taking risedronate had gastrointestinal disturbances (n = 4), muscle or joint pain (n = 11), or chest pain and dizziness (n = 2). None of the women had adverse effects from vitamin D. A few women had muscle soreness from exercise that went away after the exercises were adapted. None of the women had a serious injury or fracture from exercise.
More women in the exercise group withdrew from the study (n = 20), with most citing lack of time as the reason; 13 women withdrew from the risedronate group, and 16 withdrew from the control group.
Of the 276 participants who completed the 12-month study, treatment adherence was 92% for calcium, 94% for vitamin D, 75% for risedronate, and 59% for exercise.
Exercise was associated with positive changes in intertrochanter hip structural analysis measures, which will be described in an upcoming study, Dr. Bilek said.
The study was funded by the National Institute of Nursing Research of the National Institutes of Health. The researchers have reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
“Postmenopausal women with low bone mass should obtain adequate calcium and vitamin D and participate in bone-loading exercises,” researchers noted in a recent study published in Osteoporosis International.
“Additional use of bisphosphonates will increase bone mineral density (BMD), especially at the spine,” wrote Nancy Waltman, PhD, College of Nursing, University of Nebraska Medical Center, Omaha, and colleagues.
The findings are partial results from the Heartland Osteoporosis Prevention Study (HOPS), which randomized women who had entered menopause within the previous 6 months and had osteopenia (low bone mass, T score –1.0 to –2.49) to receive one of three treatments for 12 months:
- Bone-loading and resistance exercise plus calcium and vitamin D supplements.
- Risedronate plus calcium and vitamin D supplements.
- Calcium and vitamin D supplements alone (control).
At 1 year, “risedronate significantly increased BMD at the spine, compared to exercise and control, and serum biomarkers of bone turnover also significantly reduced in the risedronate group,” Laura Bilek, PT, PhD, said during an oral presentation of the research at the annual meeting of the American Society for Bone and Mineral Research.
However, the results also showed that, importantly, “in postmenopausal women, exercise appears to improve strength at the hip through changes in structure, not BMD,” stressed Dr. Bilek, of the College of Allied Health Professionals, University of Nebraska Medical Center.
Bone health is about more than just bone mineral density
“The key takeaway for clinicians is that bone health is about more than just density!” she noted in an email.
Current guidelines don’t recommend prescribing risedronate until a woman has overt osteoporosis, she said.
On the other hand, many studies have shown that, to be most effective, bone-loading exercises should be a lifelong habit and women should begin to do them at least during menopause and should not wait until bone loss occurs.
Other studies have shown that exercise changes bone structure (size or geometry), which improves bone strength. The current study supports both prior observations.
And exercise also improves muscle strength and decreases the risk of falls and fractures, Dr. Bilek noted.
Invited to comment, Pauline M. Camacho, MD, cochair of the task force for the American Association of Clinical Endocrinologists (AACE) guidelines for osteoporosis, noted that all three measures – pharmacotherapy, exercise, and calcium/vitamin D – are important in the successful management of osteoporosis.
This study showed that risedronate is superior to calcium/vitamin D supplementation as well as exercise for BMD and for bone turnover in these women with osteopenia, said Dr. Camacho, professor of medicine and director of the Osteoporosis and Metabolic Bone Disease Center, Loyola University Medical Center, Chicago.
“Most women with osteopenia do not receive pharmacologic therapy,” she noted, and receive it only “if there is a history of fractures or they have other features that change that diagnosis to osteoporosis.
“There is no downside to exercise, and this needs to be advised to all patients,” she said. “The other aspect of exercise that was not assessed in this study is its effect on balance. Patients who exercise will have improved balance, which should translate into fewer falls, and thus fewer fractures.”
How can women with osteopenia maintain bone health?
In their article, Dr. Waltman and colleagues say the Lifting Intervention for Training Muscle and Osteoporosis Rehabilitation (LIFTMOR) clinical trial is one of the first to address clinician concerns about the safety and effectiveness of exercise to improve bone health.
In that trial of 101 postmenopausal women with low bone mass, 8 months of 30-minute, twice-weekly, supervised high-intensity resistance and impact training was safe and BMD increased by 2.9% at the lumbar spine and 0.3% at the femoral neck.
“Our [HOPS] study,” Dr. Waltman and colleagues explained, “builds on the LIFTMOR clinical trial and adds further data to inform whether postmenopausal women with low bone mass can effectively maintain or even improve BMD with bone-loading exercises prior to prescriptions for medication.
“Our long-term goal is to contribute to the development of clinical practice guidelines for the prevention of fractures in postmenopausal women with low bone mass,” they said.
They randomized 276 postmenopausal women who were a mean age of 54 (range, 44-63); most were White (78%) or Hispanic (6%).
Women were excluded from the study if they had a diagnosis of osteoporosis (T-score < −2.5); had an increased risk of a major fracture or hip fracture; had been on bisphosphonates within the last 6 months; were currently on estrogen, tamoxifen, or aromatase inhibitors; had a serum vitamin D level < 10 mg/mL or > 100 mg/mL; had any conditions that prohibited prescriptions for calcium and vitamin D supplements, risedronate, or exercise; or weighed more than 300 pounds.
All women received 1,200 mg/day of calcium (from supplements or diet) and 1,000-3,000 IU/day of vitamin D supplements, based on their serum 25(OH) vitamin D levels.
The exercise program consisted of visiting a gym three times a week for 45 minutes of bone-loading exercise – jogging with a weighted vest – and resistance exercises, which were supervised by a trainer for the first 2 weeks.
Women in the risedronate group received a 150-mg tablet of risedronate every 4 weeks.
At baseline, 6 months, and 12 months, the women had DXA scans to determine BMD and hip structure, and had blood tests to determine levels of serum markers for bone formation (bone specific alkaline phosphatase [Alkphase B]) and bone resorption (N-terminal telopeptide [NTx]).
Compared with baseline, at 12 months, the women had the following changes in BMD at the following sites:
- Spine: +1.9%, +0.9%, and –0.4%, in the risedronate, exercise, and control groups.
- Total hip: +0.9%, +0.5%, and +0.5%, in the risedronate, exercise, and control groups.
- Femoral neck: +0.09%, –0.4%, and –0.5%, in the risedronate, exercise, and control groups.
These improvements in BMD were significantly greater in the risedronate group than in the exercise or control groups (P < .01 for both).
The decreases in serum levels of NtX and Alkphase B were also greater with risedronate than in the exercise or control groups (P < .01 for all).
The most frequent adverse effect with the calcium supplement was constipation (n = 4). Some women taking risedronate had gastrointestinal disturbances (n = 4), muscle or joint pain (n = 11), or chest pain and dizziness (n = 2). None of the women had adverse effects from vitamin D. A few women had muscle soreness from exercise that went away after the exercises were adapted. None of the women had a serious injury or fracture from exercise.
More women in the exercise group withdrew from the study (n = 20), with most citing lack of time as the reason; 13 women withdrew from the risedronate group, and 16 withdrew from the control group.
Of the 276 participants who completed the 12-month study, treatment adherence was 92% for calcium, 94% for vitamin D, 75% for risedronate, and 59% for exercise.
Exercise was associated with positive changes in intertrochanter hip structural analysis measures, which will be described in an upcoming study, Dr. Bilek said.
The study was funded by the National Institute of Nursing Research of the National Institutes of Health. The researchers have reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
“Postmenopausal women with low bone mass should obtain adequate calcium and vitamin D and participate in bone-loading exercises,” researchers noted in a recent study published in Osteoporosis International.
“Additional use of bisphosphonates will increase bone mineral density (BMD), especially at the spine,” wrote Nancy Waltman, PhD, College of Nursing, University of Nebraska Medical Center, Omaha, and colleagues.
The findings are partial results from the Heartland Osteoporosis Prevention Study (HOPS), which randomized women who had entered menopause within the previous 6 months and had osteopenia (low bone mass, T score –1.0 to –2.49) to receive one of three treatments for 12 months:
- Bone-loading and resistance exercise plus calcium and vitamin D supplements.
- Risedronate plus calcium and vitamin D supplements.
- Calcium and vitamin D supplements alone (control).
At 1 year, “risedronate significantly increased BMD at the spine, compared to exercise and control, and serum biomarkers of bone turnover also significantly reduced in the risedronate group,” Laura Bilek, PT, PhD, said during an oral presentation of the research at the annual meeting of the American Society for Bone and Mineral Research.
However, the results also showed that, importantly, “in postmenopausal women, exercise appears to improve strength at the hip through changes in structure, not BMD,” stressed Dr. Bilek, of the College of Allied Health Professionals, University of Nebraska Medical Center.
Bone health is about more than just bone mineral density
“The key takeaway for clinicians is that bone health is about more than just density!” she noted in an email.
Current guidelines don’t recommend prescribing risedronate until a woman has overt osteoporosis, she said.
On the other hand, many studies have shown that, to be most effective, bone-loading exercises should be a lifelong habit and women should begin to do them at least during menopause and should not wait until bone loss occurs.
Other studies have shown that exercise changes bone structure (size or geometry), which improves bone strength. The current study supports both prior observations.
And exercise also improves muscle strength and decreases the risk of falls and fractures, Dr. Bilek noted.
Invited to comment, Pauline M. Camacho, MD, cochair of the task force for the American Association of Clinical Endocrinologists (AACE) guidelines for osteoporosis, noted that all three measures – pharmacotherapy, exercise, and calcium/vitamin D – are important in the successful management of osteoporosis.
This study showed that risedronate is superior to calcium/vitamin D supplementation as well as exercise for BMD and for bone turnover in these women with osteopenia, said Dr. Camacho, professor of medicine and director of the Osteoporosis and Metabolic Bone Disease Center, Loyola University Medical Center, Chicago.
“Most women with osteopenia do not receive pharmacologic therapy,” she noted, and receive it only “if there is a history of fractures or they have other features that change that diagnosis to osteoporosis.
“There is no downside to exercise, and this needs to be advised to all patients,” she said. “The other aspect of exercise that was not assessed in this study is its effect on balance. Patients who exercise will have improved balance, which should translate into fewer falls, and thus fewer fractures.”
How can women with osteopenia maintain bone health?
In their article, Dr. Waltman and colleagues say the Lifting Intervention for Training Muscle and Osteoporosis Rehabilitation (LIFTMOR) clinical trial is one of the first to address clinician concerns about the safety and effectiveness of exercise to improve bone health.
In that trial of 101 postmenopausal women with low bone mass, 8 months of 30-minute, twice-weekly, supervised high-intensity resistance and impact training was safe and BMD increased by 2.9% at the lumbar spine and 0.3% at the femoral neck.
“Our [HOPS] study,” Dr. Waltman and colleagues explained, “builds on the LIFTMOR clinical trial and adds further data to inform whether postmenopausal women with low bone mass can effectively maintain or even improve BMD with bone-loading exercises prior to prescriptions for medication.
“Our long-term goal is to contribute to the development of clinical practice guidelines for the prevention of fractures in postmenopausal women with low bone mass,” they said.
They randomized 276 postmenopausal women who were a mean age of 54 (range, 44-63); most were White (78%) or Hispanic (6%).
Women were excluded from the study if they had a diagnosis of osteoporosis (T-score < −2.5); had an increased risk of a major fracture or hip fracture; had been on bisphosphonates within the last 6 months; were currently on estrogen, tamoxifen, or aromatase inhibitors; had a serum vitamin D level < 10 mg/mL or > 100 mg/mL; had any conditions that prohibited prescriptions for calcium and vitamin D supplements, risedronate, or exercise; or weighed more than 300 pounds.
All women received 1,200 mg/day of calcium (from supplements or diet) and 1,000-3,000 IU/day of vitamin D supplements, based on their serum 25(OH) vitamin D levels.
The exercise program consisted of visiting a gym three times a week for 45 minutes of bone-loading exercise – jogging with a weighted vest – and resistance exercises, which were supervised by a trainer for the first 2 weeks.
Women in the risedronate group received a 150-mg tablet of risedronate every 4 weeks.
At baseline, 6 months, and 12 months, the women had DXA scans to determine BMD and hip structure, and had blood tests to determine levels of serum markers for bone formation (bone specific alkaline phosphatase [Alkphase B]) and bone resorption (N-terminal telopeptide [NTx]).
Compared with baseline, at 12 months, the women had the following changes in BMD at the following sites:
- Spine: +1.9%, +0.9%, and –0.4%, in the risedronate, exercise, and control groups.
- Total hip: +0.9%, +0.5%, and +0.5%, in the risedronate, exercise, and control groups.
- Femoral neck: +0.09%, –0.4%, and –0.5%, in the risedronate, exercise, and control groups.
These improvements in BMD were significantly greater in the risedronate group than in the exercise or control groups (P < .01 for both).
The decreases in serum levels of NtX and Alkphase B were also greater with risedronate than in the exercise or control groups (P < .01 for all).
The most frequent adverse effect with the calcium supplement was constipation (n = 4). Some women taking risedronate had gastrointestinal disturbances (n = 4), muscle or joint pain (n = 11), or chest pain and dizziness (n = 2). None of the women had adverse effects from vitamin D. A few women had muscle soreness from exercise that went away after the exercises were adapted. None of the women had a serious injury or fracture from exercise.
More women in the exercise group withdrew from the study (n = 20), with most citing lack of time as the reason; 13 women withdrew from the risedronate group, and 16 withdrew from the control group.
Of the 276 participants who completed the 12-month study, treatment adherence was 92% for calcium, 94% for vitamin D, 75% for risedronate, and 59% for exercise.
Exercise was associated with positive changes in intertrochanter hip structural analysis measures, which will be described in an upcoming study, Dr. Bilek said.
The study was funded by the National Institute of Nursing Research of the National Institutes of Health. The researchers have reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM ASBMR 2021
Statins tied to diabetes progression
Statin use is associated with increased likelihood of diabetes progression, according to a new matched cohort analysis of data from the Department of Veteran Affairs.
Patients with diabetes who were on statins were more likely to begin taking insulin, become hyperglycemic, and to develop acute glycemic complications, and they were also more likely to be prescribed medications from more glucose-lowering drug classes.
Although previous observational and randomized, controlled trials suggested a link between statin use and diabetes progression, they typically relied on measures like insulin resistance, hemoglobin A1c, or fasting blood glucose levels. The new work, however, outlines changes in glycemic control.
The differences between fasting glucose levels and A1c levels were generally smaller than the differences in insulin sensitivity. But A1c and fasting glucose may underestimate a potential effect of statins, since physicians may escalate antidiabetes therapy in response to changes.
Insulin sensitivity is also rarely measured in real-world settings. “This study translated findings reported on academic studies of increased insulin resistance associated with statin use in research papers into everyday language of patient care. That is, patients on statins may need to escalate their antidiabetes therapy and there may have higher occurrences of uncontrolled diabetes events,” lead author Ishak Mansi, MD, said in an interview.
The study was published online in JAMA Internal Medicine.
Dr. Mansi, who is staff internist at the VA North Texas Health System and a professor of medicine and data and population science at the University of Texas, both in Dallas, cautioned about overinterpretation of the findings. “This is an observational study; therefore, it can establish association, but not causation.”
No reason to turn down statins
Dr. Mansi noted that it’s important to distinguish between those being prescribed statins as a primary preventive measurement against cardiovascular disease, and those starting statins with preexisting cardiovascular disease for secondary prevention. Statins are a key therapeutic class for secondary prevention. “Their benefits are tremendous, and we should emphasize that no patient should stop taking their statins based on our study – rather, they should talk to their doctors,” said Dr. Mansi.
The study is one of few to look at statin use and diabetes progression in patients who already have diabetes, and the first with a propensity-matched design, according to Om Ganda, MD, who was asked for comment. The results should not deter physicians from prescribing and patients from accepting statins. “Statins should not be withheld in people with high risk of cardiovascular disease, even for primary prevention, as the risk of progression of glucose levels is relatively much smaller and manageable, rather than risking cardiovascular events by stopping or not initiating when indicated by current guidelines,” said Dr. Ganda, who is the medical director of the Lipid Clinic at the Joslin Diabetes Center and an associate professor of medicine at Harvard Medical School, both in Boston.
It’s possible that statins could increase risk of diabetes progression through promoting insulin resistance, and they may also reduce beta-cell function, which could in turn reduce insulin secretion, according to Dr. Ganda.
The study group included 83,022 pairs of statin users and matched controls, of whom 95% were men; 68.2% were White; 22% were Black; 2.1% were Native American, Pacific Islander, or Alaska Native; and 0.8% were Asian. The mean age was 60 years.
Some 56% of statin users experienced diabetes progression, compared with 48% of control patients (odds ratio, 1.37; P < .001). Progression was defined as intensification of diabetes therapy through new use of insulin or increase in the number of medication classes, new onset chronic hyperglycemia, or acute complications from hyperglycemia.
The association was seen in the component measures, including an increased number of glucose-lowering medication classes (OR, 1.41; P < .001), the frequency of new insulin use (OR, 1.16; P < .001), persistent glycemia (OR, 1.13; P < .001), and a new diagnosis of ketoacidosis or uncontrolled diabetes (OR, 1.24; P < .001).
There was also a dose-response relationship between the intensity of LDL cholesterol–lowering medication and diabetes progression.
More research needed
The findings don’t necessarily have a strong clinical impact, but the researchers hope it pushes toward greater personalization of statin treatment. The benefits of statins have been well studied, but their potential harms have not received the same attention. Dr. Mansi hopes to learn more about which populations stand to gain the most for primary cardiovascular disease prevention, such as older versus younger populations, healthier or sicker patients, and those with well-controlled versus uncontrolled diabetes. “Answering these questions [would] impact hundreds of millions of patients and cannot be postponed,” said Dr. Mansi. He also called for dedicated funding for research into the adverse events of frequently used medications.
Dr. Mansi and Dr. Ganda have no relevant financial disclosures.
Statin use is associated with increased likelihood of diabetes progression, according to a new matched cohort analysis of data from the Department of Veteran Affairs.
Patients with diabetes who were on statins were more likely to begin taking insulin, become hyperglycemic, and to develop acute glycemic complications, and they were also more likely to be prescribed medications from more glucose-lowering drug classes.
Although previous observational and randomized, controlled trials suggested a link between statin use and diabetes progression, they typically relied on measures like insulin resistance, hemoglobin A1c, or fasting blood glucose levels. The new work, however, outlines changes in glycemic control.
The differences between fasting glucose levels and A1c levels were generally smaller than the differences in insulin sensitivity. But A1c and fasting glucose may underestimate a potential effect of statins, since physicians may escalate antidiabetes therapy in response to changes.
Insulin sensitivity is also rarely measured in real-world settings. “This study translated findings reported on academic studies of increased insulin resistance associated with statin use in research papers into everyday language of patient care. That is, patients on statins may need to escalate their antidiabetes therapy and there may have higher occurrences of uncontrolled diabetes events,” lead author Ishak Mansi, MD, said in an interview.
The study was published online in JAMA Internal Medicine.
Dr. Mansi, who is staff internist at the VA North Texas Health System and a professor of medicine and data and population science at the University of Texas, both in Dallas, cautioned about overinterpretation of the findings. “This is an observational study; therefore, it can establish association, but not causation.”
No reason to turn down statins
Dr. Mansi noted that it’s important to distinguish between those being prescribed statins as a primary preventive measurement against cardiovascular disease, and those starting statins with preexisting cardiovascular disease for secondary prevention. Statins are a key therapeutic class for secondary prevention. “Their benefits are tremendous, and we should emphasize that no patient should stop taking their statins based on our study – rather, they should talk to their doctors,” said Dr. Mansi.
The study is one of few to look at statin use and diabetes progression in patients who already have diabetes, and the first with a propensity-matched design, according to Om Ganda, MD, who was asked for comment. The results should not deter physicians from prescribing and patients from accepting statins. “Statins should not be withheld in people with high risk of cardiovascular disease, even for primary prevention, as the risk of progression of glucose levels is relatively much smaller and manageable, rather than risking cardiovascular events by stopping or not initiating when indicated by current guidelines,” said Dr. Ganda, who is the medical director of the Lipid Clinic at the Joslin Diabetes Center and an associate professor of medicine at Harvard Medical School, both in Boston.
It’s possible that statins could increase risk of diabetes progression through promoting insulin resistance, and they may also reduce beta-cell function, which could in turn reduce insulin secretion, according to Dr. Ganda.
The study group included 83,022 pairs of statin users and matched controls, of whom 95% were men; 68.2% were White; 22% were Black; 2.1% were Native American, Pacific Islander, or Alaska Native; and 0.8% were Asian. The mean age was 60 years.
Some 56% of statin users experienced diabetes progression, compared with 48% of control patients (odds ratio, 1.37; P < .001). Progression was defined as intensification of diabetes therapy through new use of insulin or increase in the number of medication classes, new onset chronic hyperglycemia, or acute complications from hyperglycemia.
The association was seen in the component measures, including an increased number of glucose-lowering medication classes (OR, 1.41; P < .001), the frequency of new insulin use (OR, 1.16; P < .001), persistent glycemia (OR, 1.13; P < .001), and a new diagnosis of ketoacidosis or uncontrolled diabetes (OR, 1.24; P < .001).
There was also a dose-response relationship between the intensity of LDL cholesterol–lowering medication and diabetes progression.
More research needed
The findings don’t necessarily have a strong clinical impact, but the researchers hope it pushes toward greater personalization of statin treatment. The benefits of statins have been well studied, but their potential harms have not received the same attention. Dr. Mansi hopes to learn more about which populations stand to gain the most for primary cardiovascular disease prevention, such as older versus younger populations, healthier or sicker patients, and those with well-controlled versus uncontrolled diabetes. “Answering these questions [would] impact hundreds of millions of patients and cannot be postponed,” said Dr. Mansi. He also called for dedicated funding for research into the adverse events of frequently used medications.
Dr. Mansi and Dr. Ganda have no relevant financial disclosures.
Statin use is associated with increased likelihood of diabetes progression, according to a new matched cohort analysis of data from the Department of Veteran Affairs.
Patients with diabetes who were on statins were more likely to begin taking insulin, become hyperglycemic, and to develop acute glycemic complications, and they were also more likely to be prescribed medications from more glucose-lowering drug classes.
Although previous observational and randomized, controlled trials suggested a link between statin use and diabetes progression, they typically relied on measures like insulin resistance, hemoglobin A1c, or fasting blood glucose levels. The new work, however, outlines changes in glycemic control.
The differences between fasting glucose levels and A1c levels were generally smaller than the differences in insulin sensitivity. But A1c and fasting glucose may underestimate a potential effect of statins, since physicians may escalate antidiabetes therapy in response to changes.
Insulin sensitivity is also rarely measured in real-world settings. “This study translated findings reported on academic studies of increased insulin resistance associated with statin use in research papers into everyday language of patient care. That is, patients on statins may need to escalate their antidiabetes therapy and there may have higher occurrences of uncontrolled diabetes events,” lead author Ishak Mansi, MD, said in an interview.
The study was published online in JAMA Internal Medicine.
Dr. Mansi, who is staff internist at the VA North Texas Health System and a professor of medicine and data and population science at the University of Texas, both in Dallas, cautioned about overinterpretation of the findings. “This is an observational study; therefore, it can establish association, but not causation.”
No reason to turn down statins
Dr. Mansi noted that it’s important to distinguish between those being prescribed statins as a primary preventive measurement against cardiovascular disease, and those starting statins with preexisting cardiovascular disease for secondary prevention. Statins are a key therapeutic class for secondary prevention. “Their benefits are tremendous, and we should emphasize that no patient should stop taking their statins based on our study – rather, they should talk to their doctors,” said Dr. Mansi.
The study is one of few to look at statin use and diabetes progression in patients who already have diabetes, and the first with a propensity-matched design, according to Om Ganda, MD, who was asked for comment. The results should not deter physicians from prescribing and patients from accepting statins. “Statins should not be withheld in people with high risk of cardiovascular disease, even for primary prevention, as the risk of progression of glucose levels is relatively much smaller and manageable, rather than risking cardiovascular events by stopping or not initiating when indicated by current guidelines,” said Dr. Ganda, who is the medical director of the Lipid Clinic at the Joslin Diabetes Center and an associate professor of medicine at Harvard Medical School, both in Boston.
It’s possible that statins could increase risk of diabetes progression through promoting insulin resistance, and they may also reduce beta-cell function, which could in turn reduce insulin secretion, according to Dr. Ganda.
The study group included 83,022 pairs of statin users and matched controls, of whom 95% were men; 68.2% were White; 22% were Black; 2.1% were Native American, Pacific Islander, or Alaska Native; and 0.8% were Asian. The mean age was 60 years.
Some 56% of statin users experienced diabetes progression, compared with 48% of control patients (odds ratio, 1.37; P < .001). Progression was defined as intensification of diabetes therapy through new use of insulin or increase in the number of medication classes, new onset chronic hyperglycemia, or acute complications from hyperglycemia.
The association was seen in the component measures, including an increased number of glucose-lowering medication classes (OR, 1.41; P < .001), the frequency of new insulin use (OR, 1.16; P < .001), persistent glycemia (OR, 1.13; P < .001), and a new diagnosis of ketoacidosis or uncontrolled diabetes (OR, 1.24; P < .001).
There was also a dose-response relationship between the intensity of LDL cholesterol–lowering medication and diabetes progression.
More research needed
The findings don’t necessarily have a strong clinical impact, but the researchers hope it pushes toward greater personalization of statin treatment. The benefits of statins have been well studied, but their potential harms have not received the same attention. Dr. Mansi hopes to learn more about which populations stand to gain the most for primary cardiovascular disease prevention, such as older versus younger populations, healthier or sicker patients, and those with well-controlled versus uncontrolled diabetes. “Answering these questions [would] impact hundreds of millions of patients and cannot be postponed,” said Dr. Mansi. He also called for dedicated funding for research into the adverse events of frequently used medications.
Dr. Mansi and Dr. Ganda have no relevant financial disclosures.
FROM JAMA INTERNAL MEDICINE