User login
FDA clears app for FreeStyle Libre 2 glucose monitor
The Food and Drug Administration has cleared the FreeStyle Libre 2 iOS application for use with compatible iPhones.
The new app works with the FreeStyle Libre 2 with optional glucose alarms, which was approved in the United States in June 2020 for people with diabetes aged 4 years and older.
Until now, it was only a reader device with no app compatibility. The older FreeStyle Libre 14-day, available in the United States since July 2018, has both a reader and an app, but not optional alarms.
The new app, which will soon be available for download from the App Store, enables users to view glucose readings on their iPhones and allows for caregivers or other individuals to remotely monitor the patient’s glucose levels and receive real-time alarms via the LibreLinkUp app.
Worn for 14 days before replacement is needed, the FreeStyle Libre 2 is the longest-lasting integrated continuous glucose monitoring (iCGM) sensor currently on the market. The first iCGM, the Dexcom G6, is worn for 10 days.
The Libre 2 is available at pharmacies, typically at a lower cost than other CGM systems based on a list price comparison. The actual cost for patients varies depending on insurance coverage.
Abbott has secured partial or full reimbursement for the FreeStyle Libre system in 38 countries, including Canada, France, Germany, Japan, the United Kingdom, and the United States.
The FreeStyle Libre 3 is approved for use in the European Union.
A version of this article first appeared on Medscape.com.
The Food and Drug Administration has cleared the FreeStyle Libre 2 iOS application for use with compatible iPhones.
The new app works with the FreeStyle Libre 2 with optional glucose alarms, which was approved in the United States in June 2020 for people with diabetes aged 4 years and older.
Until now, it was only a reader device with no app compatibility. The older FreeStyle Libre 14-day, available in the United States since July 2018, has both a reader and an app, but not optional alarms.
The new app, which will soon be available for download from the App Store, enables users to view glucose readings on their iPhones and allows for caregivers or other individuals to remotely monitor the patient’s glucose levels and receive real-time alarms via the LibreLinkUp app.
Worn for 14 days before replacement is needed, the FreeStyle Libre 2 is the longest-lasting integrated continuous glucose monitoring (iCGM) sensor currently on the market. The first iCGM, the Dexcom G6, is worn for 10 days.
The Libre 2 is available at pharmacies, typically at a lower cost than other CGM systems based on a list price comparison. The actual cost for patients varies depending on insurance coverage.
Abbott has secured partial or full reimbursement for the FreeStyle Libre system in 38 countries, including Canada, France, Germany, Japan, the United Kingdom, and the United States.
The FreeStyle Libre 3 is approved for use in the European Union.
A version of this article first appeared on Medscape.com.
The Food and Drug Administration has cleared the FreeStyle Libre 2 iOS application for use with compatible iPhones.
The new app works with the FreeStyle Libre 2 with optional glucose alarms, which was approved in the United States in June 2020 for people with diabetes aged 4 years and older.
Until now, it was only a reader device with no app compatibility. The older FreeStyle Libre 14-day, available in the United States since July 2018, has both a reader and an app, but not optional alarms.
The new app, which will soon be available for download from the App Store, enables users to view glucose readings on their iPhones and allows for caregivers or other individuals to remotely monitor the patient’s glucose levels and receive real-time alarms via the LibreLinkUp app.
Worn for 14 days before replacement is needed, the FreeStyle Libre 2 is the longest-lasting integrated continuous glucose monitoring (iCGM) sensor currently on the market. The first iCGM, the Dexcom G6, is worn for 10 days.
The Libre 2 is available at pharmacies, typically at a lower cost than other CGM systems based on a list price comparison. The actual cost for patients varies depending on insurance coverage.
Abbott has secured partial or full reimbursement for the FreeStyle Libre system in 38 countries, including Canada, France, Germany, Japan, the United Kingdom, and the United States.
The FreeStyle Libre 3 is approved for use in the European Union.
A version of this article first appeared on Medscape.com.
Modest calorie reduction plus exercise linked with improved vascular health
Finding applies to seniors with obesity, who were part of a new study
The authors of the paper, published in Circulation, found a link between greater vascular benefits and exercise with modest – rather than intense – calorie restriction (CR) in elderly individuals with obesity.
“The finding that higher-intensity calorie restriction may not be necessary or advised has important implications for weight loss recommendations,” noted Tina E. Brinkley, Ph.D., lead author of the study and associate professor of gerontology and geriatric medicine at the Sticht Center for Healthy Aging and Alzheimer’s Prevention at Wake Forest University in Winston-Salem, N.C.
It’s “not entirely clear” why greater calorie restriction did not translate to greater vascular benefit, but it “could be related in part to potentially adverse effects of severe CR on vascular function,” she noted. “These findings have important implications for reducing cardiovascular risk with nonpharmacological interventions in high-risk populations.”
Methods and findings
The study included 160 men and women aged 65-79 years, with a body mass index (BMI) of 30 to 45 kg/m2. The subjects were randomized to one of three groups for 20 weeks of aerobic exercise only, aerobic exercise plus moderate CR, or aerobic exercise plus more intensive CR. Their exercise regimen involved 30 minutes of supervised treadmill walking for 4 days per week at 65%-70% of heart rate reserve.
Subjects in the moderate CR group decreased caloric intake by 250 kcals a day, while the intense calorie reduction group cut 600 kcals per day. Their meals contained less than 30% of calories from fat and at least 0.8 g of protein per kg of ideal body weight. They were also provided with supplemental calcium (1,200 mg/day) and vitamin D (800 IU/day).
Cardiovascular magnetic resonance imaging was used to assess various aspects of aortic structure and function, including aortic arch pulse wave velocity, aortic distensibility and dimensions, and periaortic fat.
Weight loss was greater among subjects with CR plus exercise, compared with that of patients in the exercise-only group. The degree of weight loss was not significantly different between those with moderate versus intense CR ( 8.02 kg vs. 8.98 kg).
Among the exercise-only group, researchers observed no changes in aortic stiffness. However, adding moderate CR significantly improved this measure, while intense CR did not.
Specifically, subjects in the moderate-CR group had a “robust” 21% increase in distensibility in the descending aorta (DA), and an 8% decrease in aortic arch pulse wave velocity, whereas there were no significant vascular changes in the intense-CR group.
Bests results seen in exercise plus modest CR group
“Collectively, these data suggest that combining exercise with modest CR (as opposed to more intensive CR or no CR) provides the greatest benefit for proximal aortic stiffness, while also optimizing weight loss and improvements in body composition and body fat distribution,” noted the authors in their paper.
“Our data support the growing number of studies indicating that intentional weight loss can be safe for older adults with obesity and extend our previous findings, suggesting that obesity may blunt the beneficial effects of exercise for not only cardiorespiratory fitness, but likely vascular health as well.”
William E. Kraus, MD, professor in the Department of Medicine, Division of Cardiology at Duke University Medical Center, in Durham, NC, described the study as important and interesting for several reasons.
“First, it demonstrates one can change aortic vascular function with a combined diet and exercise program, even in older, obese Americans. This implies it is never too late to make meaningful lifestyle changes that will benefit cardiovascular health,” he said. “Second, it is among an increasing number of studies demonstrating that more is not always better than less in exercise and diet lifestyle changes - and in fact the converse is true.”
“This gives hope that more people can benefit from modest lifestyle changes - in this case following guidelines for physical activity and only a modest reduction of 250 kilocalories per day resulted in benefit,” Dr. Kraus added.
The authors of the paper and Dr. Kraus disclosed no conflicts of interest.
Finding applies to seniors with obesity, who were part of a new study
Finding applies to seniors with obesity, who were part of a new study
The authors of the paper, published in Circulation, found a link between greater vascular benefits and exercise with modest – rather than intense – calorie restriction (CR) in elderly individuals with obesity.
“The finding that higher-intensity calorie restriction may not be necessary or advised has important implications for weight loss recommendations,” noted Tina E. Brinkley, Ph.D., lead author of the study and associate professor of gerontology and geriatric medicine at the Sticht Center for Healthy Aging and Alzheimer’s Prevention at Wake Forest University in Winston-Salem, N.C.
It’s “not entirely clear” why greater calorie restriction did not translate to greater vascular benefit, but it “could be related in part to potentially adverse effects of severe CR on vascular function,” she noted. “These findings have important implications for reducing cardiovascular risk with nonpharmacological interventions in high-risk populations.”
Methods and findings
The study included 160 men and women aged 65-79 years, with a body mass index (BMI) of 30 to 45 kg/m2. The subjects were randomized to one of three groups for 20 weeks of aerobic exercise only, aerobic exercise plus moderate CR, or aerobic exercise plus more intensive CR. Their exercise regimen involved 30 minutes of supervised treadmill walking for 4 days per week at 65%-70% of heart rate reserve.
Subjects in the moderate CR group decreased caloric intake by 250 kcals a day, while the intense calorie reduction group cut 600 kcals per day. Their meals contained less than 30% of calories from fat and at least 0.8 g of protein per kg of ideal body weight. They were also provided with supplemental calcium (1,200 mg/day) and vitamin D (800 IU/day).
Cardiovascular magnetic resonance imaging was used to assess various aspects of aortic structure and function, including aortic arch pulse wave velocity, aortic distensibility and dimensions, and periaortic fat.
Weight loss was greater among subjects with CR plus exercise, compared with that of patients in the exercise-only group. The degree of weight loss was not significantly different between those with moderate versus intense CR ( 8.02 kg vs. 8.98 kg).
Among the exercise-only group, researchers observed no changes in aortic stiffness. However, adding moderate CR significantly improved this measure, while intense CR did not.
Specifically, subjects in the moderate-CR group had a “robust” 21% increase in distensibility in the descending aorta (DA), and an 8% decrease in aortic arch pulse wave velocity, whereas there were no significant vascular changes in the intense-CR group.
Bests results seen in exercise plus modest CR group
“Collectively, these data suggest that combining exercise with modest CR (as opposed to more intensive CR or no CR) provides the greatest benefit for proximal aortic stiffness, while also optimizing weight loss and improvements in body composition and body fat distribution,” noted the authors in their paper.
“Our data support the growing number of studies indicating that intentional weight loss can be safe for older adults with obesity and extend our previous findings, suggesting that obesity may blunt the beneficial effects of exercise for not only cardiorespiratory fitness, but likely vascular health as well.”
William E. Kraus, MD, professor in the Department of Medicine, Division of Cardiology at Duke University Medical Center, in Durham, NC, described the study as important and interesting for several reasons.
“First, it demonstrates one can change aortic vascular function with a combined diet and exercise program, even in older, obese Americans. This implies it is never too late to make meaningful lifestyle changes that will benefit cardiovascular health,” he said. “Second, it is among an increasing number of studies demonstrating that more is not always better than less in exercise and diet lifestyle changes - and in fact the converse is true.”
“This gives hope that more people can benefit from modest lifestyle changes - in this case following guidelines for physical activity and only a modest reduction of 250 kilocalories per day resulted in benefit,” Dr. Kraus added.
The authors of the paper and Dr. Kraus disclosed no conflicts of interest.
The authors of the paper, published in Circulation, found a link between greater vascular benefits and exercise with modest – rather than intense – calorie restriction (CR) in elderly individuals with obesity.
“The finding that higher-intensity calorie restriction may not be necessary or advised has important implications for weight loss recommendations,” noted Tina E. Brinkley, Ph.D., lead author of the study and associate professor of gerontology and geriatric medicine at the Sticht Center for Healthy Aging and Alzheimer’s Prevention at Wake Forest University in Winston-Salem, N.C.
It’s “not entirely clear” why greater calorie restriction did not translate to greater vascular benefit, but it “could be related in part to potentially adverse effects of severe CR on vascular function,” she noted. “These findings have important implications for reducing cardiovascular risk with nonpharmacological interventions in high-risk populations.”
Methods and findings
The study included 160 men and women aged 65-79 years, with a body mass index (BMI) of 30 to 45 kg/m2. The subjects were randomized to one of three groups for 20 weeks of aerobic exercise only, aerobic exercise plus moderate CR, or aerobic exercise plus more intensive CR. Their exercise regimen involved 30 minutes of supervised treadmill walking for 4 days per week at 65%-70% of heart rate reserve.
Subjects in the moderate CR group decreased caloric intake by 250 kcals a day, while the intense calorie reduction group cut 600 kcals per day. Their meals contained less than 30% of calories from fat and at least 0.8 g of protein per kg of ideal body weight. They were also provided with supplemental calcium (1,200 mg/day) and vitamin D (800 IU/day).
Cardiovascular magnetic resonance imaging was used to assess various aspects of aortic structure and function, including aortic arch pulse wave velocity, aortic distensibility and dimensions, and periaortic fat.
Weight loss was greater among subjects with CR plus exercise, compared with that of patients in the exercise-only group. The degree of weight loss was not significantly different between those with moderate versus intense CR ( 8.02 kg vs. 8.98 kg).
Among the exercise-only group, researchers observed no changes in aortic stiffness. However, adding moderate CR significantly improved this measure, while intense CR did not.
Specifically, subjects in the moderate-CR group had a “robust” 21% increase in distensibility in the descending aorta (DA), and an 8% decrease in aortic arch pulse wave velocity, whereas there were no significant vascular changes in the intense-CR group.
Bests results seen in exercise plus modest CR group
“Collectively, these data suggest that combining exercise with modest CR (as opposed to more intensive CR or no CR) provides the greatest benefit for proximal aortic stiffness, while also optimizing weight loss and improvements in body composition and body fat distribution,” noted the authors in their paper.
“Our data support the growing number of studies indicating that intentional weight loss can be safe for older adults with obesity and extend our previous findings, suggesting that obesity may blunt the beneficial effects of exercise for not only cardiorespiratory fitness, but likely vascular health as well.”
William E. Kraus, MD, professor in the Department of Medicine, Division of Cardiology at Duke University Medical Center, in Durham, NC, described the study as important and interesting for several reasons.
“First, it demonstrates one can change aortic vascular function with a combined diet and exercise program, even in older, obese Americans. This implies it is never too late to make meaningful lifestyle changes that will benefit cardiovascular health,” he said. “Second, it is among an increasing number of studies demonstrating that more is not always better than less in exercise and diet lifestyle changes - and in fact the converse is true.”
“This gives hope that more people can benefit from modest lifestyle changes - in this case following guidelines for physical activity and only a modest reduction of 250 kilocalories per day resulted in benefit,” Dr. Kraus added.
The authors of the paper and Dr. Kraus disclosed no conflicts of interest.
FROM CIRCULATION
ESC heart failure guideline to integrate bounty of new meds
Today there are so many evidence-based drug therapies for heart failure with reduced ejection fraction (HFrEF) that physicians treating HF patients almost don’t know what to do them.
It’s an exciting new age that way, but to many vexingly unclear how best to merge the shiny new options with mainstay regimens based on time-honored renin-angiotensin system (RAS) inhibitors and beta-blockers.
To impart some clarity, the authors of a new HF guideline document recently took center stage at the Heart Failure Association of the European Society of Cardiology (ESC-HFA) annual meeting to preview their updated recommendations, with novel twists based on recent major trials, for the new age of HF pharmacotherapeutics.
The guideline committee considered the evidence base that existed “up until the end of March of this year,” Theresa A. McDonagh, MD, King’s College London, said during the presentation. The document “is now finalized, it’s with the publishers, and it will be presented in full with simultaneous publication at the ESC meeting” that starts August 27.
It describes a game plan, already followed by some clinicians in practice without official guidance, for initiating drugs from each of four classes in virtually all patients with HFrEF.
New indicated drugs, new perspective for HFrEF
Three of the drug categories are old acquaintances. Among them are the RAS inhibitors, which include angiotensin-receptor/neprilysin inhibitors, beta-blockers, and the mineralocorticoid receptor antagonists. The latter drugs are gaining new respect after having been underplayed in HF prescribing despite longstanding evidence of efficacy.
Completing the quartet of first-line HFrEF drug classes is a recent arrival to the HF arena, the sodium-glucose cotransporter 2 inhibitors.
“We now have new data and a simplified treatment algorithm for heart failure with reduced ejection fraction based on the early administration of the four major classes of drugs,” said Marco Metra, MD, University of Brescia (Italy), previewing the medical-therapy portions of the new guideline at the ESC-HFA sessions, which launched virtually and live in Florence, Italy, on July 29.
The new game plan offers a simple answer to a once-common but complex question: How and in what order are the different drug classes initiated in patients with HFrEF? In the new document, the stated goal is to get them all on board expeditiously and safely, by any means possible.
The guideline writers did not specify a sequence, preferring to leave that decision to physicians, said Dr. Metra, who stated only two guiding principles. The first is to consider the patient’s unique circumstances. The order in which the drugs are introduced might vary, depending on, for example, whether the patient has low or high blood pressure or renal dysfunction.
Second, “it is very important that we try to give all four classes of drugs to the patient in the shortest time possible, because this saves lives,” he said.
That there is no recommendation on sequencing the drugs has led some to the wrong interpretation that all should be started at once, observed coauthor Javed Butler, MD, MPH, University of Mississippi, Jackson, as a panelist during the presentation. Far from it, he said. “The doctor with the patient in front of you can make the best decision. The idea here is to get all the therapies on as soon as possible, as safely as possible.”
“The order in which they are introduced is not really important,” agreed Vijay Chopra, MD, Max Super Specialty Hospital Saket, New Delhi, another coauthor on the panel. “The important thing is that at least some dose of all the four drugs needs to be introduced in the first 4-6 weeks, and then up-titrated.”
Other medical therapy can be more tailored, Dr. Metra noted, such as loop diuretics for patients with congestion, iron for those with iron deficiency, and other drugs depending on whether there is, for example, atrial fibrillation or coronary disease.
Adoption of emerging definitions
The document adopts the emerging characterization of HFrEF by a left ventricular ejection fraction (LVEF) up to 40%.
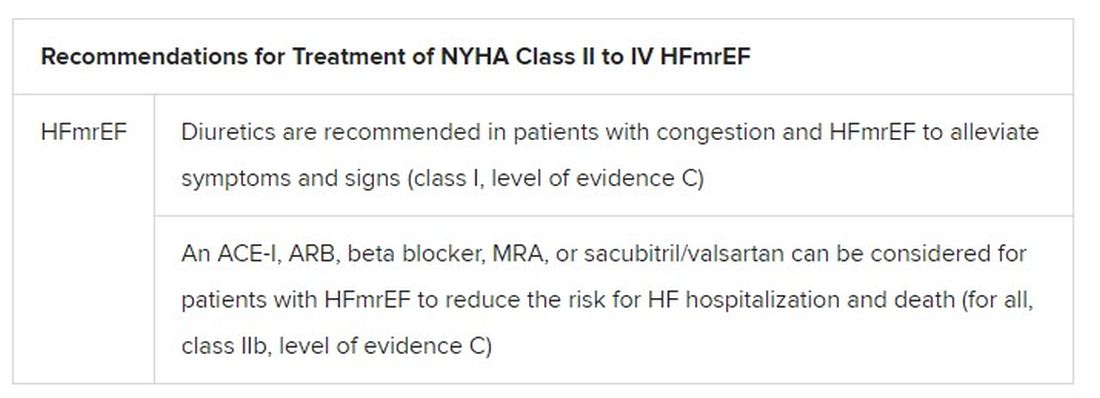
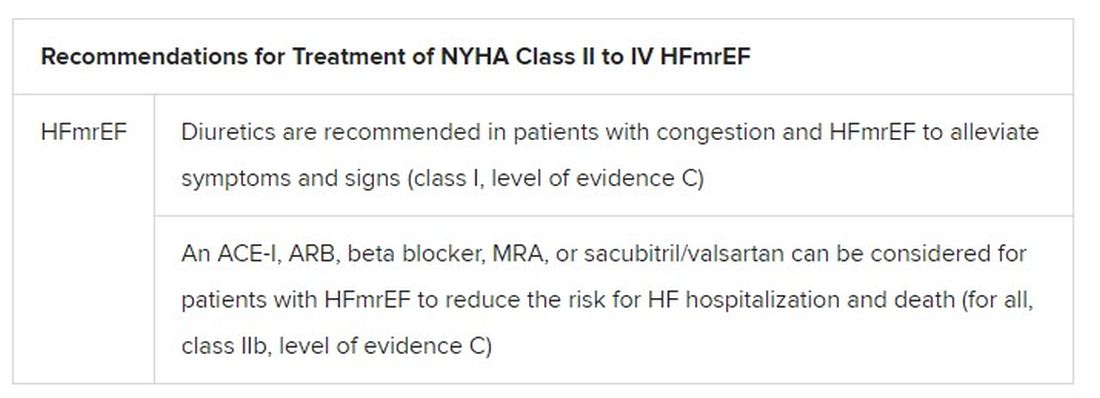
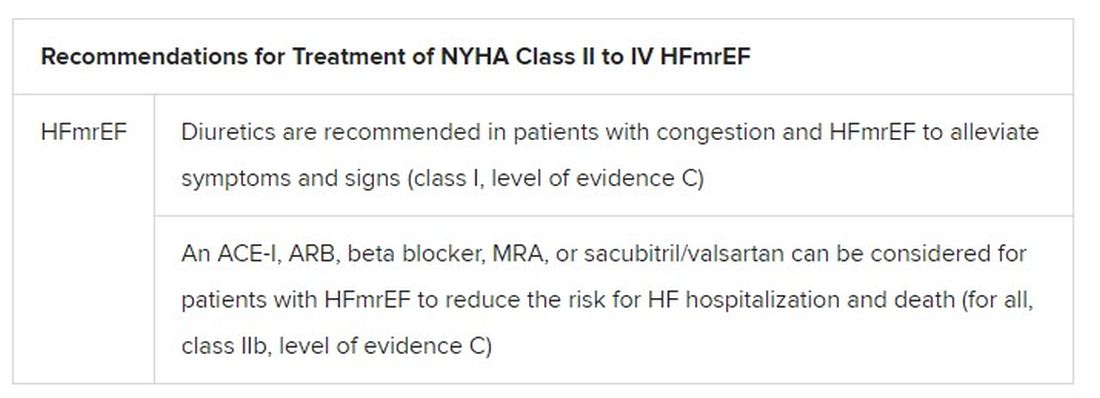
And it will leverage an expanding evidence base for medication in a segment of patients once said to have HF with preserved ejection fraction (HFpEF), who had therefore lacked specific, guideline-directed medical therapies. Now, patients with an LVEF of 41%-49% will be said to have HF with mildly reduced ejection fraction (HFmrEF), a tweak to the recently introduced HF with “mid-range” LVEF that is designed to assert its nature as something to treat. The new document’s HFmrEF recommendations come with various class and level-of-evidence ratings.
That leaves HFpEF to be characterized by an LVEF of 50% in combination with structural or functional abnormalities associated with LV diastolic dysfunction or raised LV filling pressures, including raised natriuretic peptide levels.
The definitions are consistent with those proposed internationally by the ESC-HFA, the Heart Failure Society of America, and other groups in a statement published in March.
Expanded HFrEF med landscape
Since the 2016 ESC guideline on HF therapy, Dr. McDonagh said, “there’s been no substantial change in the evidence for many of the classical drugs that we use in heart failure. However, we had a lot of new and exciting evidence to consider,” especially in support of the SGLT2 inhibitors as one of the core medications in HFrEF.
The new data came from two controlled trials in particular. In DAPA-HF, patients with HFrEF who were initially without diabetes and who went on dapagliflozin (Farxiga, AstraZeneca) showed a 27% drop in cardiovascular (CV) death or worsening-HF events over a median of 18 months.
“That was followed up with very concordant results with empagliflozin [Jardiance, Boehringer Ingelheim/Eli Lilly] in HFrEF in the EMPEROR-Reduced trial,” Dr. McDonagh said. In that trial, comparable patients who took empagliflozin showed a 25% drop in a primary endpoint similar to that in DAPA-HF over the median 16-month follow-up.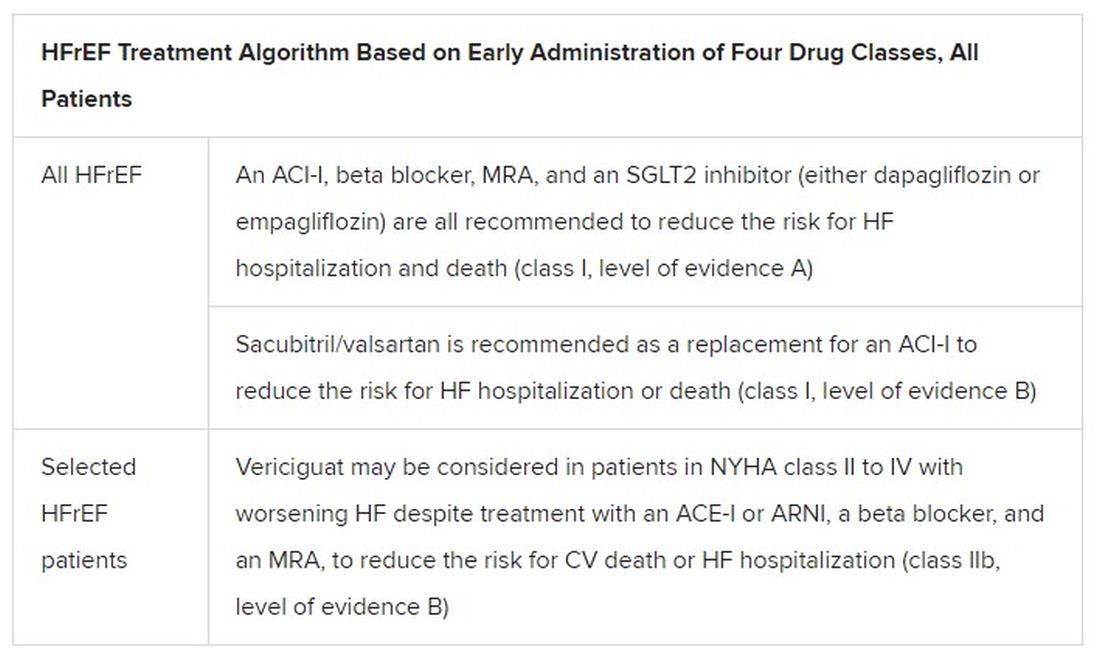
Other HFrEF recommendations are for selected patients. They include ivabradine, already in the guidelines, for patients in sinus rhythm with an elevated resting heart rate who can’t take beta-blockers for whatever reason. But, Dr. McDonagh noted, “we had some new classes of drugs to consider as well.”
In particular, the oral soluble guanylate-cyclase receptor stimulator vericiguat (Verquvo) emerged about a year ago from the VICTORIA trial as a modest success for patients with HFrEF and a previous HF hospitalization. In the trial with more than 5,000 patients, treatment with vericiguat atop standard drug and device therapy was followed by a significant 10% drop in risk for CV death or HF hospitalization.
Available now or likely to be available in the United States, the European Union, Japan, and other countries, vericiguat is recommended in the new guideline for VICTORIA-like patients who don’t adequately respond to other indicated medications.
Little for HFpEF as newly defined
“Almost nothing is new” in the guidelines for HFpEF, Dr. Metra said. The document recommends screening for and treatment of any underlying disorder and comorbidities, plus diuretics for any congestion. “That’s what we have to date.”
But that evidence base might soon change. The new HFpEF recommendations could possibly be up-staged at the ESC sessions by the August 27 scheduled presentation of EMPEROR-Preserved, a randomized test of empagliflozin in HFpEF and – it could be said – HFmrEF. The trial entered patients with chronic HF and an LVEF greater than 40%.
Eli Lilly and Boehringer Ingelheim offered the world a peek at the results, which suggest the SGLT2 inhibitor had a positive impact on the primary endpoint of CV death or HF hospitalization. They announced the cursory top-line outcomes in early July as part of its regulatory obligations, noting that the trial had “met” its primary endpoint.
But many unknowns remain, including the degree of benefit and whether it varied among subgroups, and especially whether outcomes were different for HFmrEF than for HFpEF.
Upgrades for familiar agents
Still, HFmrEF gets noteworthy attention in the document. “For the first time, we have recommendations for these patients,” Dr. Metra said. “We already knew that diuretics are indicated for the treatment of congestion. But now, ACE inhibitors, ARBs, beta-blockers, mineralocorticoid antagonists, as well as sacubitril/valsartan, may be considered to improve outcomes in these patients.” Their upgrades in the new guidelines were based on review of trials in the CHARM program and of TOPCAT and PARAGON-HF, among others, he said.
The new document also includes “treatment algorithms based on phenotypes”; that is, comorbidities and less common HF precipitants. For example, “assessment of iron status is now mandated in all patients with heart failure,” Dr. Metra said.
AFFIRM-HF is the key trial in this arena, with its more than 1,100 iron-deficient patients with LVEF less than 50% who had been recently hospitalized for HF. A year of treatment with ferric carboxymaltose (Ferinject/Injectafer, Vifor) led to a 26% drop in risk for HF hospitalization, but without affecting mortality.
For those who are iron deficient, Dr. Metra said, “ferric carboxymaltose intravenously should be considered not only in patients with low ejection fraction and outpatients, but also in patients recently hospitalized for acute heart failure.”
The SGLT2 inhibitors are recommended in HFrEF patients with type 2 diabetes. And treatment with tafamidis (Vyndaqel, Pfizer) in patients with genetic or wild-type transthyretin cardiac amyloidosis gets a class I recommendation based on survival gains seen in the ATTR-ACT trial.
Also recommended is a full CV assessment for patients with cancer who are on cardiotoxic agents or otherwise might be at risk for chemotherapy cardiotoxicity. “Beta-blockers and ACE inhibitors should be considered in those who develop left ventricular systolic dysfunction after anticancer therapy,” Dr. Metra said.
The ongoing pandemic made its mark on the document’s genesis, as it has with most everything else. “For better or worse, we were a ‘COVID guideline,’ ” Dr. McDonagh said. The writing committee consisted of “a large task force of 31 individuals, including two patients,” and there were “only two face-to-face meetings prior to the first wave of COVID hitting Europe.”
The committee voted on each of the recommendations, “and we had to have agreement of more than 75% of the task force to assign a class of recommendation or level of evidence,” she said. “I think we did the best we could in the circumstances. We had the benefit of many discussions over Zoom, and I think at the end of the day we have achieved a consensus.”
With such a large body of participants and the 75% threshold for agreement, “you end up with perhaps a conservative guideline. But that’s not a bad thing for clinical practice, for guidelines to be conservative,” Dr. McDonagh said. “They’re mainly concerned with looking at evidence and safety.”
A version of this article first appeared on Medscape.com.
Today there are so many evidence-based drug therapies for heart failure with reduced ejection fraction (HFrEF) that physicians treating HF patients almost don’t know what to do them.
It’s an exciting new age that way, but to many vexingly unclear how best to merge the shiny new options with mainstay regimens based on time-honored renin-angiotensin system (RAS) inhibitors and beta-blockers.
To impart some clarity, the authors of a new HF guideline document recently took center stage at the Heart Failure Association of the European Society of Cardiology (ESC-HFA) annual meeting to preview their updated recommendations, with novel twists based on recent major trials, for the new age of HF pharmacotherapeutics.
The guideline committee considered the evidence base that existed “up until the end of March of this year,” Theresa A. McDonagh, MD, King’s College London, said during the presentation. The document “is now finalized, it’s with the publishers, and it will be presented in full with simultaneous publication at the ESC meeting” that starts August 27.
It describes a game plan, already followed by some clinicians in practice without official guidance, for initiating drugs from each of four classes in virtually all patients with HFrEF.
New indicated drugs, new perspective for HFrEF
Three of the drug categories are old acquaintances. Among them are the RAS inhibitors, which include angiotensin-receptor/neprilysin inhibitors, beta-blockers, and the mineralocorticoid receptor antagonists. The latter drugs are gaining new respect after having been underplayed in HF prescribing despite longstanding evidence of efficacy.
Completing the quartet of first-line HFrEF drug classes is a recent arrival to the HF arena, the sodium-glucose cotransporter 2 inhibitors.
“We now have new data and a simplified treatment algorithm for heart failure with reduced ejection fraction based on the early administration of the four major classes of drugs,” said Marco Metra, MD, University of Brescia (Italy), previewing the medical-therapy portions of the new guideline at the ESC-HFA sessions, which launched virtually and live in Florence, Italy, on July 29.
The new game plan offers a simple answer to a once-common but complex question: How and in what order are the different drug classes initiated in patients with HFrEF? In the new document, the stated goal is to get them all on board expeditiously and safely, by any means possible.
The guideline writers did not specify a sequence, preferring to leave that decision to physicians, said Dr. Metra, who stated only two guiding principles. The first is to consider the patient’s unique circumstances. The order in which the drugs are introduced might vary, depending on, for example, whether the patient has low or high blood pressure or renal dysfunction.
Second, “it is very important that we try to give all four classes of drugs to the patient in the shortest time possible, because this saves lives,” he said.
That there is no recommendation on sequencing the drugs has led some to the wrong interpretation that all should be started at once, observed coauthor Javed Butler, MD, MPH, University of Mississippi, Jackson, as a panelist during the presentation. Far from it, he said. “The doctor with the patient in front of you can make the best decision. The idea here is to get all the therapies on as soon as possible, as safely as possible.”
“The order in which they are introduced is not really important,” agreed Vijay Chopra, MD, Max Super Specialty Hospital Saket, New Delhi, another coauthor on the panel. “The important thing is that at least some dose of all the four drugs needs to be introduced in the first 4-6 weeks, and then up-titrated.”
Other medical therapy can be more tailored, Dr. Metra noted, such as loop diuretics for patients with congestion, iron for those with iron deficiency, and other drugs depending on whether there is, for example, atrial fibrillation or coronary disease.
Adoption of emerging definitions
The document adopts the emerging characterization of HFrEF by a left ventricular ejection fraction (LVEF) up to 40%.
And it will leverage an expanding evidence base for medication in a segment of patients once said to have HF with preserved ejection fraction (HFpEF), who had therefore lacked specific, guideline-directed medical therapies. Now, patients with an LVEF of 41%-49% will be said to have HF with mildly reduced ejection fraction (HFmrEF), a tweak to the recently introduced HF with “mid-range” LVEF that is designed to assert its nature as something to treat. The new document’s HFmrEF recommendations come with various class and level-of-evidence ratings.
That leaves HFpEF to be characterized by an LVEF of 50% in combination with structural or functional abnormalities associated with LV diastolic dysfunction or raised LV filling pressures, including raised natriuretic peptide levels.
The definitions are consistent with those proposed internationally by the ESC-HFA, the Heart Failure Society of America, and other groups in a statement published in March.
Expanded HFrEF med landscape
Since the 2016 ESC guideline on HF therapy, Dr. McDonagh said, “there’s been no substantial change in the evidence for many of the classical drugs that we use in heart failure. However, we had a lot of new and exciting evidence to consider,” especially in support of the SGLT2 inhibitors as one of the core medications in HFrEF.
The new data came from two controlled trials in particular. In DAPA-HF, patients with HFrEF who were initially without diabetes and who went on dapagliflozin (Farxiga, AstraZeneca) showed a 27% drop in cardiovascular (CV) death or worsening-HF events over a median of 18 months.
“That was followed up with very concordant results with empagliflozin [Jardiance, Boehringer Ingelheim/Eli Lilly] in HFrEF in the EMPEROR-Reduced trial,” Dr. McDonagh said. In that trial, comparable patients who took empagliflozin showed a 25% drop in a primary endpoint similar to that in DAPA-HF over the median 16-month follow-up.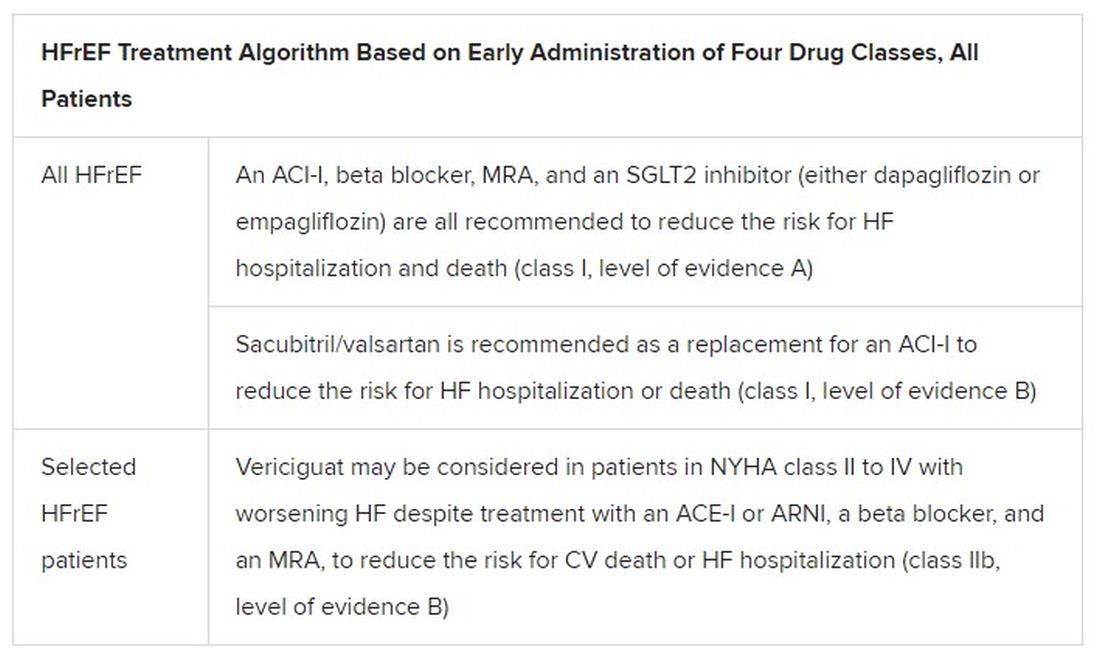
Other HFrEF recommendations are for selected patients. They include ivabradine, already in the guidelines, for patients in sinus rhythm with an elevated resting heart rate who can’t take beta-blockers for whatever reason. But, Dr. McDonagh noted, “we had some new classes of drugs to consider as well.”
In particular, the oral soluble guanylate-cyclase receptor stimulator vericiguat (Verquvo) emerged about a year ago from the VICTORIA trial as a modest success for patients with HFrEF and a previous HF hospitalization. In the trial with more than 5,000 patients, treatment with vericiguat atop standard drug and device therapy was followed by a significant 10% drop in risk for CV death or HF hospitalization.
Available now or likely to be available in the United States, the European Union, Japan, and other countries, vericiguat is recommended in the new guideline for VICTORIA-like patients who don’t adequately respond to other indicated medications.
Little for HFpEF as newly defined
“Almost nothing is new” in the guidelines for HFpEF, Dr. Metra said. The document recommends screening for and treatment of any underlying disorder and comorbidities, plus diuretics for any congestion. “That’s what we have to date.”
But that evidence base might soon change. The new HFpEF recommendations could possibly be up-staged at the ESC sessions by the August 27 scheduled presentation of EMPEROR-Preserved, a randomized test of empagliflozin in HFpEF and – it could be said – HFmrEF. The trial entered patients with chronic HF and an LVEF greater than 40%.
Eli Lilly and Boehringer Ingelheim offered the world a peek at the results, which suggest the SGLT2 inhibitor had a positive impact on the primary endpoint of CV death or HF hospitalization. They announced the cursory top-line outcomes in early July as part of its regulatory obligations, noting that the trial had “met” its primary endpoint.
But many unknowns remain, including the degree of benefit and whether it varied among subgroups, and especially whether outcomes were different for HFmrEF than for HFpEF.
Upgrades for familiar agents
Still, HFmrEF gets noteworthy attention in the document. “For the first time, we have recommendations for these patients,” Dr. Metra said. “We already knew that diuretics are indicated for the treatment of congestion. But now, ACE inhibitors, ARBs, beta-blockers, mineralocorticoid antagonists, as well as sacubitril/valsartan, may be considered to improve outcomes in these patients.” Their upgrades in the new guidelines were based on review of trials in the CHARM program and of TOPCAT and PARAGON-HF, among others, he said.
The new document also includes “treatment algorithms based on phenotypes”; that is, comorbidities and less common HF precipitants. For example, “assessment of iron status is now mandated in all patients with heart failure,” Dr. Metra said.
AFFIRM-HF is the key trial in this arena, with its more than 1,100 iron-deficient patients with LVEF less than 50% who had been recently hospitalized for HF. A year of treatment with ferric carboxymaltose (Ferinject/Injectafer, Vifor) led to a 26% drop in risk for HF hospitalization, but without affecting mortality.
For those who are iron deficient, Dr. Metra said, “ferric carboxymaltose intravenously should be considered not only in patients with low ejection fraction and outpatients, but also in patients recently hospitalized for acute heart failure.”
The SGLT2 inhibitors are recommended in HFrEF patients with type 2 diabetes. And treatment with tafamidis (Vyndaqel, Pfizer) in patients with genetic or wild-type transthyretin cardiac amyloidosis gets a class I recommendation based on survival gains seen in the ATTR-ACT trial.
Also recommended is a full CV assessment for patients with cancer who are on cardiotoxic agents or otherwise might be at risk for chemotherapy cardiotoxicity. “Beta-blockers and ACE inhibitors should be considered in those who develop left ventricular systolic dysfunction after anticancer therapy,” Dr. Metra said.
The ongoing pandemic made its mark on the document’s genesis, as it has with most everything else. “For better or worse, we were a ‘COVID guideline,’ ” Dr. McDonagh said. The writing committee consisted of “a large task force of 31 individuals, including two patients,” and there were “only two face-to-face meetings prior to the first wave of COVID hitting Europe.”
The committee voted on each of the recommendations, “and we had to have agreement of more than 75% of the task force to assign a class of recommendation or level of evidence,” she said. “I think we did the best we could in the circumstances. We had the benefit of many discussions over Zoom, and I think at the end of the day we have achieved a consensus.”
With such a large body of participants and the 75% threshold for agreement, “you end up with perhaps a conservative guideline. But that’s not a bad thing for clinical practice, for guidelines to be conservative,” Dr. McDonagh said. “They’re mainly concerned with looking at evidence and safety.”
A version of this article first appeared on Medscape.com.
Today there are so many evidence-based drug therapies for heart failure with reduced ejection fraction (HFrEF) that physicians treating HF patients almost don’t know what to do them.
It’s an exciting new age that way, but to many vexingly unclear how best to merge the shiny new options with mainstay regimens based on time-honored renin-angiotensin system (RAS) inhibitors and beta-blockers.
To impart some clarity, the authors of a new HF guideline document recently took center stage at the Heart Failure Association of the European Society of Cardiology (ESC-HFA) annual meeting to preview their updated recommendations, with novel twists based on recent major trials, for the new age of HF pharmacotherapeutics.
The guideline committee considered the evidence base that existed “up until the end of March of this year,” Theresa A. McDonagh, MD, King’s College London, said during the presentation. The document “is now finalized, it’s with the publishers, and it will be presented in full with simultaneous publication at the ESC meeting” that starts August 27.
It describes a game plan, already followed by some clinicians in practice without official guidance, for initiating drugs from each of four classes in virtually all patients with HFrEF.
New indicated drugs, new perspective for HFrEF
Three of the drug categories are old acquaintances. Among them are the RAS inhibitors, which include angiotensin-receptor/neprilysin inhibitors, beta-blockers, and the mineralocorticoid receptor antagonists. The latter drugs are gaining new respect after having been underplayed in HF prescribing despite longstanding evidence of efficacy.
Completing the quartet of first-line HFrEF drug classes is a recent arrival to the HF arena, the sodium-glucose cotransporter 2 inhibitors.
“We now have new data and a simplified treatment algorithm for heart failure with reduced ejection fraction based on the early administration of the four major classes of drugs,” said Marco Metra, MD, University of Brescia (Italy), previewing the medical-therapy portions of the new guideline at the ESC-HFA sessions, which launched virtually and live in Florence, Italy, on July 29.
The new game plan offers a simple answer to a once-common but complex question: How and in what order are the different drug classes initiated in patients with HFrEF? In the new document, the stated goal is to get them all on board expeditiously and safely, by any means possible.
The guideline writers did not specify a sequence, preferring to leave that decision to physicians, said Dr. Metra, who stated only two guiding principles. The first is to consider the patient’s unique circumstances. The order in which the drugs are introduced might vary, depending on, for example, whether the patient has low or high blood pressure or renal dysfunction.
Second, “it is very important that we try to give all four classes of drugs to the patient in the shortest time possible, because this saves lives,” he said.
That there is no recommendation on sequencing the drugs has led some to the wrong interpretation that all should be started at once, observed coauthor Javed Butler, MD, MPH, University of Mississippi, Jackson, as a panelist during the presentation. Far from it, he said. “The doctor with the patient in front of you can make the best decision. The idea here is to get all the therapies on as soon as possible, as safely as possible.”
“The order in which they are introduced is not really important,” agreed Vijay Chopra, MD, Max Super Specialty Hospital Saket, New Delhi, another coauthor on the panel. “The important thing is that at least some dose of all the four drugs needs to be introduced in the first 4-6 weeks, and then up-titrated.”
Other medical therapy can be more tailored, Dr. Metra noted, such as loop diuretics for patients with congestion, iron for those with iron deficiency, and other drugs depending on whether there is, for example, atrial fibrillation or coronary disease.
Adoption of emerging definitions
The document adopts the emerging characterization of HFrEF by a left ventricular ejection fraction (LVEF) up to 40%.
And it will leverage an expanding evidence base for medication in a segment of patients once said to have HF with preserved ejection fraction (HFpEF), who had therefore lacked specific, guideline-directed medical therapies. Now, patients with an LVEF of 41%-49% will be said to have HF with mildly reduced ejection fraction (HFmrEF), a tweak to the recently introduced HF with “mid-range” LVEF that is designed to assert its nature as something to treat. The new document’s HFmrEF recommendations come with various class and level-of-evidence ratings.
That leaves HFpEF to be characterized by an LVEF of 50% in combination with structural or functional abnormalities associated with LV diastolic dysfunction or raised LV filling pressures, including raised natriuretic peptide levels.
The definitions are consistent with those proposed internationally by the ESC-HFA, the Heart Failure Society of America, and other groups in a statement published in March.
Expanded HFrEF med landscape
Since the 2016 ESC guideline on HF therapy, Dr. McDonagh said, “there’s been no substantial change in the evidence for many of the classical drugs that we use in heart failure. However, we had a lot of new and exciting evidence to consider,” especially in support of the SGLT2 inhibitors as one of the core medications in HFrEF.
The new data came from two controlled trials in particular. In DAPA-HF, patients with HFrEF who were initially without diabetes and who went on dapagliflozin (Farxiga, AstraZeneca) showed a 27% drop in cardiovascular (CV) death or worsening-HF events over a median of 18 months.
“That was followed up with very concordant results with empagliflozin [Jardiance, Boehringer Ingelheim/Eli Lilly] in HFrEF in the EMPEROR-Reduced trial,” Dr. McDonagh said. In that trial, comparable patients who took empagliflozin showed a 25% drop in a primary endpoint similar to that in DAPA-HF over the median 16-month follow-up.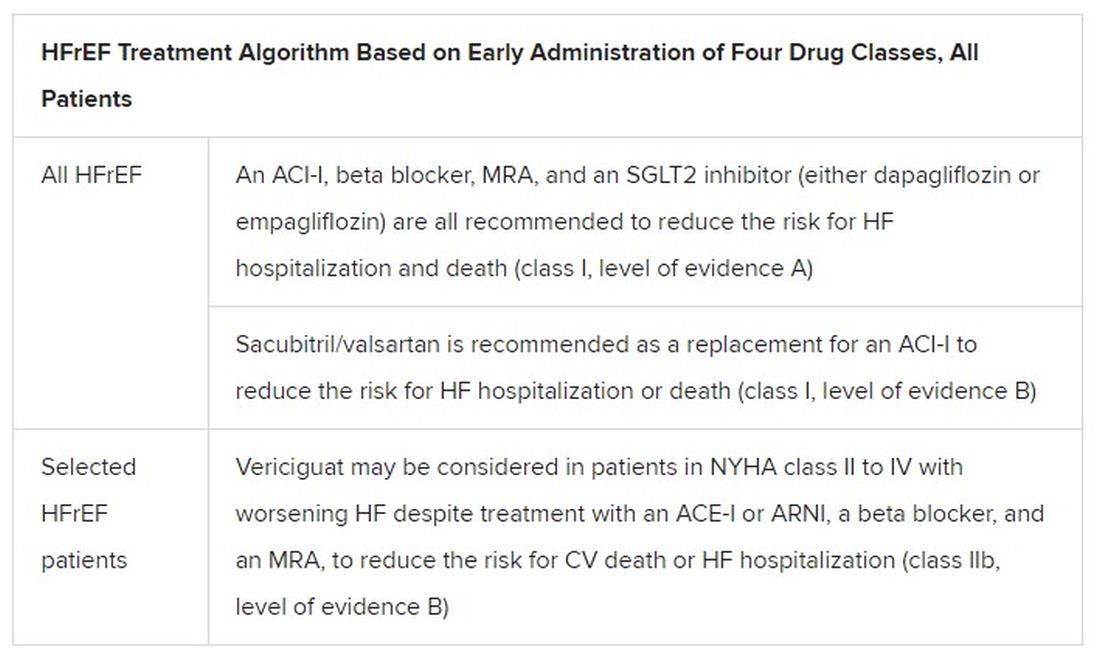
Other HFrEF recommendations are for selected patients. They include ivabradine, already in the guidelines, for patients in sinus rhythm with an elevated resting heart rate who can’t take beta-blockers for whatever reason. But, Dr. McDonagh noted, “we had some new classes of drugs to consider as well.”
In particular, the oral soluble guanylate-cyclase receptor stimulator vericiguat (Verquvo) emerged about a year ago from the VICTORIA trial as a modest success for patients with HFrEF and a previous HF hospitalization. In the trial with more than 5,000 patients, treatment with vericiguat atop standard drug and device therapy was followed by a significant 10% drop in risk for CV death or HF hospitalization.
Available now or likely to be available in the United States, the European Union, Japan, and other countries, vericiguat is recommended in the new guideline for VICTORIA-like patients who don’t adequately respond to other indicated medications.
Little for HFpEF as newly defined
“Almost nothing is new” in the guidelines for HFpEF, Dr. Metra said. The document recommends screening for and treatment of any underlying disorder and comorbidities, plus diuretics for any congestion. “That’s what we have to date.”
But that evidence base might soon change. The new HFpEF recommendations could possibly be up-staged at the ESC sessions by the August 27 scheduled presentation of EMPEROR-Preserved, a randomized test of empagliflozin in HFpEF and – it could be said – HFmrEF. The trial entered patients with chronic HF and an LVEF greater than 40%.
Eli Lilly and Boehringer Ingelheim offered the world a peek at the results, which suggest the SGLT2 inhibitor had a positive impact on the primary endpoint of CV death or HF hospitalization. They announced the cursory top-line outcomes in early July as part of its regulatory obligations, noting that the trial had “met” its primary endpoint.
But many unknowns remain, including the degree of benefit and whether it varied among subgroups, and especially whether outcomes were different for HFmrEF than for HFpEF.
Upgrades for familiar agents
Still, HFmrEF gets noteworthy attention in the document. “For the first time, we have recommendations for these patients,” Dr. Metra said. “We already knew that diuretics are indicated for the treatment of congestion. But now, ACE inhibitors, ARBs, beta-blockers, mineralocorticoid antagonists, as well as sacubitril/valsartan, may be considered to improve outcomes in these patients.” Their upgrades in the new guidelines were based on review of trials in the CHARM program and of TOPCAT and PARAGON-HF, among others, he said.
The new document also includes “treatment algorithms based on phenotypes”; that is, comorbidities and less common HF precipitants. For example, “assessment of iron status is now mandated in all patients with heart failure,” Dr. Metra said.
AFFIRM-HF is the key trial in this arena, with its more than 1,100 iron-deficient patients with LVEF less than 50% who had been recently hospitalized for HF. A year of treatment with ferric carboxymaltose (Ferinject/Injectafer, Vifor) led to a 26% drop in risk for HF hospitalization, but without affecting mortality.
For those who are iron deficient, Dr. Metra said, “ferric carboxymaltose intravenously should be considered not only in patients with low ejection fraction and outpatients, but also in patients recently hospitalized for acute heart failure.”
The SGLT2 inhibitors are recommended in HFrEF patients with type 2 diabetes. And treatment with tafamidis (Vyndaqel, Pfizer) in patients with genetic or wild-type transthyretin cardiac amyloidosis gets a class I recommendation based on survival gains seen in the ATTR-ACT trial.
Also recommended is a full CV assessment for patients with cancer who are on cardiotoxic agents or otherwise might be at risk for chemotherapy cardiotoxicity. “Beta-blockers and ACE inhibitors should be considered in those who develop left ventricular systolic dysfunction after anticancer therapy,” Dr. Metra said.
The ongoing pandemic made its mark on the document’s genesis, as it has with most everything else. “For better or worse, we were a ‘COVID guideline,’ ” Dr. McDonagh said. The writing committee consisted of “a large task force of 31 individuals, including two patients,” and there were “only two face-to-face meetings prior to the first wave of COVID hitting Europe.”
The committee voted on each of the recommendations, “and we had to have agreement of more than 75% of the task force to assign a class of recommendation or level of evidence,” she said. “I think we did the best we could in the circumstances. We had the benefit of many discussions over Zoom, and I think at the end of the day we have achieved a consensus.”
With such a large body of participants and the 75% threshold for agreement, “you end up with perhaps a conservative guideline. But that’s not a bad thing for clinical practice, for guidelines to be conservative,” Dr. McDonagh said. “They’re mainly concerned with looking at evidence and safety.”
A version of this article first appeared on Medscape.com.
PCPs lag on albuminuria tests in patients with type 2 diabetes
U.S. primary care physicians are not properly checking patients with type 2 diabetes for chronic kidney disease (CKD) nearly as often as they should, meaning many of these patients miss getting a timely diagnosis.
Inadequate measurement of urinary albumin-to-creatinine ratio (uACR) is the issue.
Review of data from more than half a million U.S. primary care patients with type 2 diabetes seen at any of 1,164 practice sites run by any of 24 health care organizations during 2016-2019 showed that barely more than half, 52%, had both their uACR and estimated glomerular filtration rate (eGFR) checked annually as recommended by several U.S. medical societies, and just 73% had both values checked during a 3-year period, Nikita Stempniewicz, MSc, and associates reported in Diabetes Care.
More detailed data showed that measurement of eGFR was reasonably robust, measured at a 90% rate annually and in 97% of patients at least once every 3 years. But recording uACR values lagged, with a 53% annual rate and a 74% rate of measurement at least once every 3 years, reported Mr. Stempniewicz, director of research and analytics for the American Medical Group Association, a trade association based in Alexandria, Va. The 24 health care organizations that supplied the study’s data are all members of this association.
Prevailing recommendations from various medical societies call for annual monitoring of urinary albumin in patients with type 2 diabetes and specify the uACR, such as in the Standards of Medical Care in Diabetes from the American Diabetes Association, as well as in recommendations promoted by the National Kidney Foundation.
Missing half the CKD patients with eGFR only
“Half the patients with type 2 diabetes and chronic kidney disease have elevated albuminuria without decreased eGFR and would not be detected with eGFR testing alone,” Mr. Stempniewicz noted in an interview.
“Many patients who present for nephrology care are incompletely assessed with only low eGFR but no urine testing. Missing albuminuria testing and uACR values means patients with high levels of albuminuria but normal kidney function go undetected and thus are not able to benefit from evidenced-based interventions, including nephrology services,” said Joseph A. Vassalotti, MD, a nephrologist, chief medical officer for the National Kidney Foundation, and a coauthor of the report.
Not testing patients with type 2 diabetes regularly for their uACR “is a missed opportunity to identify the highest-risk patients and treat them,” added Josef Coresh, MD, PhD, a professor of clinical epidemiology at Johns Hopkins University, Baltimore, and senior author on the study. Measurement of albuminuria is especially important for these patients because medications from the sodium-glucose cotransporter 2 inhibitor class have been proven to slow progression of CKD in patients with type 2 diabetes, but these drugs are expensive, and in some cases have labeling that specifies the presence of albuminuria.
“I have no doubt that improving albuminuria testing is a critical step to identify patients with diabetes at highest risk who should get the best treatment possible, including SGLT2 inhibitors,” Dr. Coresh said in an interview.
The new report is not the first to document inadequate assessment of albuminuria and uACR among primary care physicians (PCPs), but it came from the largest reported U.S. study to date. “eGFR is commonly collected in a routine laboratory blood panel, but collecting urine requires additional work flow,” noted Cara B. Litvin, MD, a general internal medicine researcher at the Medical University of South Carolina, Charleston, who has tested interventions aimed at boosting CKD assessment by PCPs and was not involved in the new study.
“There have also been conflicting guidelines,” such as a “now-inactive guideline from the American College of Physicians that recommended against routine urine albumin screening in patients with diabetes and already on treatment with an angiotensin converting enzyme inhibitor or an angiotensin receptor blocker,” she said.
New renal drugs change the stakes
The availability of newer drugs for slowing CKD progression such as the SGLT2 inhibitors will help trigger greater support for routine albuminuria testing, Dr. Litvin predicted in an interview. “Now that we have more medications that can reduce albuminuria and improve outcomes, I see screening for albuminuria increasing.” Finerenone (Kerendia) is another new agent from a new class that recently received Food and Drug Administration approval for treating CKD in patients with type 2 diabetes.
Other drivers of increased uACR testing she expects include revised clinical practice guidelines, and new quality measures of clinical care.
“Undertesting of albuminuria means that [nephrologists] have incomplete data to detect and completely risk stratify the CKD population. That in turn results in a reduced ability to match population health interventions to the severity of the condition or the risk stratification based on eGFR and uACR,” Dr. Vassalotti said in an interview.
“We are missing opportunities to prevent or delay kidney failure and reduce the risk of cardiovascular events and cardiovascular death in these patients, particularly now that we have a number of medications that offer kidney and cardiovascular protection such as SGLT2 inhibitors,” he added. “Leaders in nephrology are beginning to understand the consequences of undertesting, and are working to innovate to improve risk stratification, CKD detection, and apply interventions to give Americans living with CKD better outcomes.”
Strategies proven to boost albuminuria testing
Mr. Stempniewicz and coauthors cited in their report potential strategies for improving albuminuria testing, including benchmarking to identify best-performing sites for albumin testing within a health system and encouraging replication of identified best practices at lower-performing sites, and implementation of clinical-decision support tools in the EHR such as pop-up test reminders.
These were among the tools tested in two studies led by Dr. Litvin. One study, with results reported in 2016, involved 12 small U.S. primary care practices with a total of more than 30,000 patients and compared performance in a series of clinical quality measures at baseline with performance after 2 years of receiving various interventions designed to boost awareness for albuminuria testing.
The second study, with findings reported in 2019, involved 21 U.S. primary care practices that collectively cared for more than 100,000 patients and randomized the practices to either undergo interventions aimed at boosting testing awareness or to serve as controls.
Results from both studies showed significant and substantial increases in serial testing for albuminuria in patients with diabetes or hypertension when practices received the interventions.
“We showed that [using a] clinical-decision support tool, along with standing orders to automatically collect urine specimens, dramatically increased screening for urinary albumin in primary care practices,” Dr. Litvin said. “However, perhaps because of conflicting guidelines and clinical inertia there hasn’t been a major impetus for primary care practices in general to improve screening.” She hopes that will quickly change.
“As we have shown, adoption of EHR-based reminders along with standing orders can very quickly improve screening for albuminuria in primary care.”
Variation in testing rates among sites ‘tremendous’
One finding of the new study gives Mr. Stempniewicz hope for greater future testing: The large variance that the researchers saw in albuminuria testing rates within individual health systems.
“The paper shows that higher rates of testing are completely achievable within each system. Some clinics do very well, and the other units can learn from these local successes,” he said. At least half the organizations in the study had individual sites that fell into the top 10% for testing rates across all the greater than 1,000 sites included, and those same organizations also had at least one site that fell into the bottom 10% for testing.
“The variation is tremendous, and highlights an opportunity for improvement,” declared Mr. Stempniewicz.
“For routine testing, you need systems that help people. Clinicians shouldn’t have to think about doing routine testing. It should just happen,” said Dr. Coresh.
The study was funded in part by Janssen. Mr. Stempniewicz and Dr. Litvin had no disclosures. Dr. Coresh is an adviser to Healthy.io, a company that markets a home albuminuria testing kit to patients. Dr. Vassalotti has received personal fees from Renalytix.
U.S. primary care physicians are not properly checking patients with type 2 diabetes for chronic kidney disease (CKD) nearly as often as they should, meaning many of these patients miss getting a timely diagnosis.
Inadequate measurement of urinary albumin-to-creatinine ratio (uACR) is the issue.
Review of data from more than half a million U.S. primary care patients with type 2 diabetes seen at any of 1,164 practice sites run by any of 24 health care organizations during 2016-2019 showed that barely more than half, 52%, had both their uACR and estimated glomerular filtration rate (eGFR) checked annually as recommended by several U.S. medical societies, and just 73% had both values checked during a 3-year period, Nikita Stempniewicz, MSc, and associates reported in Diabetes Care.
More detailed data showed that measurement of eGFR was reasonably robust, measured at a 90% rate annually and in 97% of patients at least once every 3 years. But recording uACR values lagged, with a 53% annual rate and a 74% rate of measurement at least once every 3 years, reported Mr. Stempniewicz, director of research and analytics for the American Medical Group Association, a trade association based in Alexandria, Va. The 24 health care organizations that supplied the study’s data are all members of this association.
Prevailing recommendations from various medical societies call for annual monitoring of urinary albumin in patients with type 2 diabetes and specify the uACR, such as in the Standards of Medical Care in Diabetes from the American Diabetes Association, as well as in recommendations promoted by the National Kidney Foundation.
Missing half the CKD patients with eGFR only
“Half the patients with type 2 diabetes and chronic kidney disease have elevated albuminuria without decreased eGFR and would not be detected with eGFR testing alone,” Mr. Stempniewicz noted in an interview.
“Many patients who present for nephrology care are incompletely assessed with only low eGFR but no urine testing. Missing albuminuria testing and uACR values means patients with high levels of albuminuria but normal kidney function go undetected and thus are not able to benefit from evidenced-based interventions, including nephrology services,” said Joseph A. Vassalotti, MD, a nephrologist, chief medical officer for the National Kidney Foundation, and a coauthor of the report.
Not testing patients with type 2 diabetes regularly for their uACR “is a missed opportunity to identify the highest-risk patients and treat them,” added Josef Coresh, MD, PhD, a professor of clinical epidemiology at Johns Hopkins University, Baltimore, and senior author on the study. Measurement of albuminuria is especially important for these patients because medications from the sodium-glucose cotransporter 2 inhibitor class have been proven to slow progression of CKD in patients with type 2 diabetes, but these drugs are expensive, and in some cases have labeling that specifies the presence of albuminuria.
“I have no doubt that improving albuminuria testing is a critical step to identify patients with diabetes at highest risk who should get the best treatment possible, including SGLT2 inhibitors,” Dr. Coresh said in an interview.
The new report is not the first to document inadequate assessment of albuminuria and uACR among primary care physicians (PCPs), but it came from the largest reported U.S. study to date. “eGFR is commonly collected in a routine laboratory blood panel, but collecting urine requires additional work flow,” noted Cara B. Litvin, MD, a general internal medicine researcher at the Medical University of South Carolina, Charleston, who has tested interventions aimed at boosting CKD assessment by PCPs and was not involved in the new study.
“There have also been conflicting guidelines,” such as a “now-inactive guideline from the American College of Physicians that recommended against routine urine albumin screening in patients with diabetes and already on treatment with an angiotensin converting enzyme inhibitor or an angiotensin receptor blocker,” she said.
New renal drugs change the stakes
The availability of newer drugs for slowing CKD progression such as the SGLT2 inhibitors will help trigger greater support for routine albuminuria testing, Dr. Litvin predicted in an interview. “Now that we have more medications that can reduce albuminuria and improve outcomes, I see screening for albuminuria increasing.” Finerenone (Kerendia) is another new agent from a new class that recently received Food and Drug Administration approval for treating CKD in patients with type 2 diabetes.
Other drivers of increased uACR testing she expects include revised clinical practice guidelines, and new quality measures of clinical care.
“Undertesting of albuminuria means that [nephrologists] have incomplete data to detect and completely risk stratify the CKD population. That in turn results in a reduced ability to match population health interventions to the severity of the condition or the risk stratification based on eGFR and uACR,” Dr. Vassalotti said in an interview.
“We are missing opportunities to prevent or delay kidney failure and reduce the risk of cardiovascular events and cardiovascular death in these patients, particularly now that we have a number of medications that offer kidney and cardiovascular protection such as SGLT2 inhibitors,” he added. “Leaders in nephrology are beginning to understand the consequences of undertesting, and are working to innovate to improve risk stratification, CKD detection, and apply interventions to give Americans living with CKD better outcomes.”
Strategies proven to boost albuminuria testing
Mr. Stempniewicz and coauthors cited in their report potential strategies for improving albuminuria testing, including benchmarking to identify best-performing sites for albumin testing within a health system and encouraging replication of identified best practices at lower-performing sites, and implementation of clinical-decision support tools in the EHR such as pop-up test reminders.
These were among the tools tested in two studies led by Dr. Litvin. One study, with results reported in 2016, involved 12 small U.S. primary care practices with a total of more than 30,000 patients and compared performance in a series of clinical quality measures at baseline with performance after 2 years of receiving various interventions designed to boost awareness for albuminuria testing.
The second study, with findings reported in 2019, involved 21 U.S. primary care practices that collectively cared for more than 100,000 patients and randomized the practices to either undergo interventions aimed at boosting testing awareness or to serve as controls.
Results from both studies showed significant and substantial increases in serial testing for albuminuria in patients with diabetes or hypertension when practices received the interventions.
“We showed that [using a] clinical-decision support tool, along with standing orders to automatically collect urine specimens, dramatically increased screening for urinary albumin in primary care practices,” Dr. Litvin said. “However, perhaps because of conflicting guidelines and clinical inertia there hasn’t been a major impetus for primary care practices in general to improve screening.” She hopes that will quickly change.
“As we have shown, adoption of EHR-based reminders along with standing orders can very quickly improve screening for albuminuria in primary care.”
Variation in testing rates among sites ‘tremendous’
One finding of the new study gives Mr. Stempniewicz hope for greater future testing: The large variance that the researchers saw in albuminuria testing rates within individual health systems.
“The paper shows that higher rates of testing are completely achievable within each system. Some clinics do very well, and the other units can learn from these local successes,” he said. At least half the organizations in the study had individual sites that fell into the top 10% for testing rates across all the greater than 1,000 sites included, and those same organizations also had at least one site that fell into the bottom 10% for testing.
“The variation is tremendous, and highlights an opportunity for improvement,” declared Mr. Stempniewicz.
“For routine testing, you need systems that help people. Clinicians shouldn’t have to think about doing routine testing. It should just happen,” said Dr. Coresh.
The study was funded in part by Janssen. Mr. Stempniewicz and Dr. Litvin had no disclosures. Dr. Coresh is an adviser to Healthy.io, a company that markets a home albuminuria testing kit to patients. Dr. Vassalotti has received personal fees from Renalytix.
U.S. primary care physicians are not properly checking patients with type 2 diabetes for chronic kidney disease (CKD) nearly as often as they should, meaning many of these patients miss getting a timely diagnosis.
Inadequate measurement of urinary albumin-to-creatinine ratio (uACR) is the issue.
Review of data from more than half a million U.S. primary care patients with type 2 diabetes seen at any of 1,164 practice sites run by any of 24 health care organizations during 2016-2019 showed that barely more than half, 52%, had both their uACR and estimated glomerular filtration rate (eGFR) checked annually as recommended by several U.S. medical societies, and just 73% had both values checked during a 3-year period, Nikita Stempniewicz, MSc, and associates reported in Diabetes Care.
More detailed data showed that measurement of eGFR was reasonably robust, measured at a 90% rate annually and in 97% of patients at least once every 3 years. But recording uACR values lagged, with a 53% annual rate and a 74% rate of measurement at least once every 3 years, reported Mr. Stempniewicz, director of research and analytics for the American Medical Group Association, a trade association based in Alexandria, Va. The 24 health care organizations that supplied the study’s data are all members of this association.
Prevailing recommendations from various medical societies call for annual monitoring of urinary albumin in patients with type 2 diabetes and specify the uACR, such as in the Standards of Medical Care in Diabetes from the American Diabetes Association, as well as in recommendations promoted by the National Kidney Foundation.
Missing half the CKD patients with eGFR only
“Half the patients with type 2 diabetes and chronic kidney disease have elevated albuminuria without decreased eGFR and would not be detected with eGFR testing alone,” Mr. Stempniewicz noted in an interview.
“Many patients who present for nephrology care are incompletely assessed with only low eGFR but no urine testing. Missing albuminuria testing and uACR values means patients with high levels of albuminuria but normal kidney function go undetected and thus are not able to benefit from evidenced-based interventions, including nephrology services,” said Joseph A. Vassalotti, MD, a nephrologist, chief medical officer for the National Kidney Foundation, and a coauthor of the report.
Not testing patients with type 2 diabetes regularly for their uACR “is a missed opportunity to identify the highest-risk patients and treat them,” added Josef Coresh, MD, PhD, a professor of clinical epidemiology at Johns Hopkins University, Baltimore, and senior author on the study. Measurement of albuminuria is especially important for these patients because medications from the sodium-glucose cotransporter 2 inhibitor class have been proven to slow progression of CKD in patients with type 2 diabetes, but these drugs are expensive, and in some cases have labeling that specifies the presence of albuminuria.
“I have no doubt that improving albuminuria testing is a critical step to identify patients with diabetes at highest risk who should get the best treatment possible, including SGLT2 inhibitors,” Dr. Coresh said in an interview.
The new report is not the first to document inadequate assessment of albuminuria and uACR among primary care physicians (PCPs), but it came from the largest reported U.S. study to date. “eGFR is commonly collected in a routine laboratory blood panel, but collecting urine requires additional work flow,” noted Cara B. Litvin, MD, a general internal medicine researcher at the Medical University of South Carolina, Charleston, who has tested interventions aimed at boosting CKD assessment by PCPs and was not involved in the new study.
“There have also been conflicting guidelines,” such as a “now-inactive guideline from the American College of Physicians that recommended against routine urine albumin screening in patients with diabetes and already on treatment with an angiotensin converting enzyme inhibitor or an angiotensin receptor blocker,” she said.
New renal drugs change the stakes
The availability of newer drugs for slowing CKD progression such as the SGLT2 inhibitors will help trigger greater support for routine albuminuria testing, Dr. Litvin predicted in an interview. “Now that we have more medications that can reduce albuminuria and improve outcomes, I see screening for albuminuria increasing.” Finerenone (Kerendia) is another new agent from a new class that recently received Food and Drug Administration approval for treating CKD in patients with type 2 diabetes.
Other drivers of increased uACR testing she expects include revised clinical practice guidelines, and new quality measures of clinical care.
“Undertesting of albuminuria means that [nephrologists] have incomplete data to detect and completely risk stratify the CKD population. That in turn results in a reduced ability to match population health interventions to the severity of the condition or the risk stratification based on eGFR and uACR,” Dr. Vassalotti said in an interview.
“We are missing opportunities to prevent or delay kidney failure and reduce the risk of cardiovascular events and cardiovascular death in these patients, particularly now that we have a number of medications that offer kidney and cardiovascular protection such as SGLT2 inhibitors,” he added. “Leaders in nephrology are beginning to understand the consequences of undertesting, and are working to innovate to improve risk stratification, CKD detection, and apply interventions to give Americans living with CKD better outcomes.”
Strategies proven to boost albuminuria testing
Mr. Stempniewicz and coauthors cited in their report potential strategies for improving albuminuria testing, including benchmarking to identify best-performing sites for albumin testing within a health system and encouraging replication of identified best practices at lower-performing sites, and implementation of clinical-decision support tools in the EHR such as pop-up test reminders.
These were among the tools tested in two studies led by Dr. Litvin. One study, with results reported in 2016, involved 12 small U.S. primary care practices with a total of more than 30,000 patients and compared performance in a series of clinical quality measures at baseline with performance after 2 years of receiving various interventions designed to boost awareness for albuminuria testing.
The second study, with findings reported in 2019, involved 21 U.S. primary care practices that collectively cared for more than 100,000 patients and randomized the practices to either undergo interventions aimed at boosting testing awareness or to serve as controls.
Results from both studies showed significant and substantial increases in serial testing for albuminuria in patients with diabetes or hypertension when practices received the interventions.
“We showed that [using a] clinical-decision support tool, along with standing orders to automatically collect urine specimens, dramatically increased screening for urinary albumin in primary care practices,” Dr. Litvin said. “However, perhaps because of conflicting guidelines and clinical inertia there hasn’t been a major impetus for primary care practices in general to improve screening.” She hopes that will quickly change.
“As we have shown, adoption of EHR-based reminders along with standing orders can very quickly improve screening for albuminuria in primary care.”
Variation in testing rates among sites ‘tremendous’
One finding of the new study gives Mr. Stempniewicz hope for greater future testing: The large variance that the researchers saw in albuminuria testing rates within individual health systems.
“The paper shows that higher rates of testing are completely achievable within each system. Some clinics do very well, and the other units can learn from these local successes,” he said. At least half the organizations in the study had individual sites that fell into the top 10% for testing rates across all the greater than 1,000 sites included, and those same organizations also had at least one site that fell into the bottom 10% for testing.
“The variation is tremendous, and highlights an opportunity for improvement,” declared Mr. Stempniewicz.
“For routine testing, you need systems that help people. Clinicians shouldn’t have to think about doing routine testing. It should just happen,” said Dr. Coresh.
The study was funded in part by Janssen. Mr. Stempniewicz and Dr. Litvin had no disclosures. Dr. Coresh is an adviser to Healthy.io, a company that markets a home albuminuria testing kit to patients. Dr. Vassalotti has received personal fees from Renalytix.
FROM DIABETES CARE
Obesity treatment in mental illness: Is semaglutide a game changer?
It’s probably fair to say that most people would like to be thinner. More than 42% of Americans have obesity and another 30% are classified as being overweight, according to the latest statistics from the CDC.
Excess body weight is associated with many illnesses and plays a role in mental health; being heavy can take a toll on self-esteem. Many people worry that carrying excess weight makes them less attractive to potential romantic partners, and both physicians and employers treat those with obesity differently. Furthermore, in psychiatry, many of the medications we prescribe lead to weight gain.
In my clinical practice, I have listened as patients blamed themselves for their body habitus; many won’t consider biological treatments as they feel that would be “cheating” or taking an easy way out. They often point to periods in their life when they did lose weight and believe that they should be able to do it again, even if the weight loss took tremendous effort, was not sustained, and occurred decades ago.
That said, we psychiatrists often find ourselves in the position of managing obesity in our patients. I have been known to give patients who gain weight on antipsychotics either stimulants or metformin, or to add naltrexone to their Wellbutrin (bupropion) to effectively mimic a weight-loss medicine called Contrave.
Obesity a treatable medical condition
It wasn’t until 2013 that the American Medical Association recognized obesity as a medical condition.
In a New Yorker article that same year, “Diet Drugs Work: Why Won’t Doctors Prescribe Them?” Suzanne Koven wrote: “Several obesity experts told me they’ve encountered doctors who confide that they just didn’t like fat people and don’t enjoy taking care of them. Even doctors who treat obese patients feel stigmatized: ‘diet doctor’ is not a flattering term.”
Eat less, exercise more – with a blame-the-patient attitude – is still what people see as the “right” way to lose weight.
On June 4, 2021, the FDA approved semaglutide, a glucagonlike peptide–1 receptor agonist, previously used for the treatment of diabetes, for use as a weight loss agent for patients with obesity, or for those with a body mass index over 27 kg/m2 if they also have a weight-related comorbidity.
Semaglutide has three trade names, all manufactured by Novo Nordisk. The pill version is called Rybelsus and comes in 7-mg and 14-mg tablets. Ozempic is available in 0.5-mg and 1.0-mg doses and is administered weekly by subcutaneous injection for diabetes. The new, higher-dose preparation for weight loss, Wegovy, 2.4 mg, also comes as a weekly subcutaneous dose and is now available for the hefty price of $1,400 per month.
In STEP 1 trials, the higher-dose Wegovy was associated with an average 14.9% weight loss (15.3 kg) over 68 weeks, more than any other single-agent weight loss medication on the market.
GLP-1 receptor agonists work in the brain to decrease appetite, slow gastric emptying, increase insulin secretion, and stimulate brown adipose tissue thermogenesis.
Psych drugs lead to weight gain
Elaine Weiner, MD, is the medical director in the outpatient research program of the Maryland Psychiatric Research Center in Catonsville, where she treats patients with schizophrenia.
“Nearly all of our patients gain 20 pounds or more on the combinations of medications we use, mostly atypical antipsychotics,” she said. “Weight management is difficult for people who don’t have problems with motivation, but in our patients, lack of motivation is a core part of their illness, so asking them to adhere to diet and exercise regimens is of limited utility.
“Then, add to that the fact that they sometimes don’t have primary care doctors, and these issues of weight gain and metabolic syndrome come back to the psychiatrist. It is a really bad problem and we need more treatments.”
Fatima Cody Stanford, MD, MPH, MPA, is a fellowship-trained obesity medicine physician-scientist at the Massachusetts General Hospital Weight Center and Harvard Medical School, both in Boston. She has treated thousands of patients with obesity, speaks internationally on the topic of weight loss medicine, and has published over 100 peer-reviewed articles on obesity.
We spoke at length about recent changes in the field of obesity medicine and the introduction of the new GLP-1 receptor agonists.
“We as physicians have learned so little,” Dr. Stanford said. “This mantra of ‘calories in, calories out’ is not working; this is inaccurate and our focus on this has led to a rise in obesity. All calories are not created the same, and I think we are finally starting to see obesity medicine take off.”
Dr. Stanford is quick to note that obesity is a complex problem. Several different hormones are involved in regulating both appetite and satiety, processed foods promote weight gain, sleep is crucial to weight loss, and exercise helps maintain weight loss but is not usually effective in promoting it. “There are many contributors to energy storage,” she said.
The stimulant phentermine was approved in 1959. Addiction was a concern, and then in the 1990s, it was used in combination with fenfluramine to promote weight loss, a combination known as phen-fen. Fenfluramine was pulled from the market in 1997 when it was found to be associated with pulmonary hypertension and then heart valve abnormalities.
“This frightened quite a few physicians,” Dr. Stanford noted. Phentermine is still used for weight loss, either alone or together with topiramate, as a combination medication called Qsymia, nicknamed phen-top.
“Phen-top is the next best thing we have to semaglutide, and there is an average weight loss of 8%-9% of body weight. Semaglutide is going to be really significant for those people who are responders, and this has been quite well tolerated, the most common side effect being nausea,” she said.
However, she is quick to note that not everyone responds to every medication. “I use each patient’s clinical profile to determine what strategies and which medications to use.”
Cardiologists getting in the game
Michael Miller, MD, is a cardiologist at the University of Maryland, Baltimore, and author of “Heal Your Heart” (Emmaus, Pa.: Rodale, 2014). He is very enthusiastic about the approval of semaglutide.
“We are so excited because you finally can use these medicines without having to be diabetic,” Dr. Miller said. “We’re waiting on the results of the SELECT [Semaglutide Effects on Heart Disease and Stroke in Patients With Overweight or Obesity] trials looking at people who are not diabetic or who are prediabetic, to see the 5-year outcomes with regard to cardiac events.
“Usually endocrinologists prescribe these medications, but cardiologists have started to get into the game since GLP-1 receptor agonists reduce cardiovascular events.” Dr. Miller is hopeful that this medication may neutralize the weight gain caused by psychotropic medications.
Wegovy is administered via weekly injection and, like insulin, is a subcutaneous medication that patients self-administer. Will patients be amenable to injecting a medication for weight loss? Dr. Stanford said that roughly 20%-30% of her patients are hesitant when she suggests that they use liraglutide, another GLP-1 receptor agonist that is approved for weight loss, and some are very fearful of needles.
However, she also noted that during the COVID-19 pandemic, many more patients have sought treatment from obesity medicine physicians because of the association between obesity and mortality from COVID-19. Patients have been willing to consider treatments that they were not previously open to pursuing.
So if people are willing to take Wegovy and doctors are willing to prescribe it, will insurers pay for it? As of this writing, the medication is not yet available, but Ozempic, the lower-dose agent for diabetes, costs $850-$900 for a 4-week supply, according to the GoodRx website.
Liraglutide (Saxenda), the GLP-1 receptor agonist that is currently available for weight loss as a daily injectable, costs $1,300-$1,400 per month.
These medications are not covered by Medicare or Medicaid, and Dr. Stanford, who is well versed as to exactly which private insurers in Massachusetts will and will not reimburse specific medications, said her patients with insurance coverage have been known to delay retirement so that they can remain on the more expensive medications.
“For the past 8 years,” she said, “the Treat and Reduce Obesity Act has had bipartisan support in Congress but has not passed. We are still hopeful that insurers will be required to cover medical and behavioral treatments for obesity.”
As our society struggles to destigmatize so many disorders, obesity remains a highly stigmatized condition, one that our patients cannot hide and one that leads to so many other comorbid illnesses. As new treatments are approved, there will be more for physicians to offer. Semaglutide, if it becomes available to those who need it most, could be a game changer. For patients who have not had success with traditional weight-loss methods, it’s encouraging to have another option available, one that may be reasonable to try before resorting to bariatric surgery.
For decades, psychiatrists have been comfortable prescribing treatments that lead to weight gain. Now, maybe it’s time they also prescribe those that prevent it.
A version of this article first appeared on Medscape.com.
It’s probably fair to say that most people would like to be thinner. More than 42% of Americans have obesity and another 30% are classified as being overweight, according to the latest statistics from the CDC.
Excess body weight is associated with many illnesses and plays a role in mental health; being heavy can take a toll on self-esteem. Many people worry that carrying excess weight makes them less attractive to potential romantic partners, and both physicians and employers treat those with obesity differently. Furthermore, in psychiatry, many of the medications we prescribe lead to weight gain.
In my clinical practice, I have listened as patients blamed themselves for their body habitus; many won’t consider biological treatments as they feel that would be “cheating” or taking an easy way out. They often point to periods in their life when they did lose weight and believe that they should be able to do it again, even if the weight loss took tremendous effort, was not sustained, and occurred decades ago.
That said, we psychiatrists often find ourselves in the position of managing obesity in our patients. I have been known to give patients who gain weight on antipsychotics either stimulants or metformin, or to add naltrexone to their Wellbutrin (bupropion) to effectively mimic a weight-loss medicine called Contrave.
Obesity a treatable medical condition
It wasn’t until 2013 that the American Medical Association recognized obesity as a medical condition.
In a New Yorker article that same year, “Diet Drugs Work: Why Won’t Doctors Prescribe Them?” Suzanne Koven wrote: “Several obesity experts told me they’ve encountered doctors who confide that they just didn’t like fat people and don’t enjoy taking care of them. Even doctors who treat obese patients feel stigmatized: ‘diet doctor’ is not a flattering term.”
Eat less, exercise more – with a blame-the-patient attitude – is still what people see as the “right” way to lose weight.
On June 4, 2021, the FDA approved semaglutide, a glucagonlike peptide–1 receptor agonist, previously used for the treatment of diabetes, for use as a weight loss agent for patients with obesity, or for those with a body mass index over 27 kg/m2 if they also have a weight-related comorbidity.
Semaglutide has three trade names, all manufactured by Novo Nordisk. The pill version is called Rybelsus and comes in 7-mg and 14-mg tablets. Ozempic is available in 0.5-mg and 1.0-mg doses and is administered weekly by subcutaneous injection for diabetes. The new, higher-dose preparation for weight loss, Wegovy, 2.4 mg, also comes as a weekly subcutaneous dose and is now available for the hefty price of $1,400 per month.
In STEP 1 trials, the higher-dose Wegovy was associated with an average 14.9% weight loss (15.3 kg) over 68 weeks, more than any other single-agent weight loss medication on the market.
GLP-1 receptor agonists work in the brain to decrease appetite, slow gastric emptying, increase insulin secretion, and stimulate brown adipose tissue thermogenesis.
Psych drugs lead to weight gain
Elaine Weiner, MD, is the medical director in the outpatient research program of the Maryland Psychiatric Research Center in Catonsville, where she treats patients with schizophrenia.
“Nearly all of our patients gain 20 pounds or more on the combinations of medications we use, mostly atypical antipsychotics,” she said. “Weight management is difficult for people who don’t have problems with motivation, but in our patients, lack of motivation is a core part of their illness, so asking them to adhere to diet and exercise regimens is of limited utility.
“Then, add to that the fact that they sometimes don’t have primary care doctors, and these issues of weight gain and metabolic syndrome come back to the psychiatrist. It is a really bad problem and we need more treatments.”
Fatima Cody Stanford, MD, MPH, MPA, is a fellowship-trained obesity medicine physician-scientist at the Massachusetts General Hospital Weight Center and Harvard Medical School, both in Boston. She has treated thousands of patients with obesity, speaks internationally on the topic of weight loss medicine, and has published over 100 peer-reviewed articles on obesity.
We spoke at length about recent changes in the field of obesity medicine and the introduction of the new GLP-1 receptor agonists.
“We as physicians have learned so little,” Dr. Stanford said. “This mantra of ‘calories in, calories out’ is not working; this is inaccurate and our focus on this has led to a rise in obesity. All calories are not created the same, and I think we are finally starting to see obesity medicine take off.”
Dr. Stanford is quick to note that obesity is a complex problem. Several different hormones are involved in regulating both appetite and satiety, processed foods promote weight gain, sleep is crucial to weight loss, and exercise helps maintain weight loss but is not usually effective in promoting it. “There are many contributors to energy storage,” she said.
The stimulant phentermine was approved in 1959. Addiction was a concern, and then in the 1990s, it was used in combination with fenfluramine to promote weight loss, a combination known as phen-fen. Fenfluramine was pulled from the market in 1997 when it was found to be associated with pulmonary hypertension and then heart valve abnormalities.
“This frightened quite a few physicians,” Dr. Stanford noted. Phentermine is still used for weight loss, either alone or together with topiramate, as a combination medication called Qsymia, nicknamed phen-top.
“Phen-top is the next best thing we have to semaglutide, and there is an average weight loss of 8%-9% of body weight. Semaglutide is going to be really significant for those people who are responders, and this has been quite well tolerated, the most common side effect being nausea,” she said.
However, she is quick to note that not everyone responds to every medication. “I use each patient’s clinical profile to determine what strategies and which medications to use.”
Cardiologists getting in the game
Michael Miller, MD, is a cardiologist at the University of Maryland, Baltimore, and author of “Heal Your Heart” (Emmaus, Pa.: Rodale, 2014). He is very enthusiastic about the approval of semaglutide.
“We are so excited because you finally can use these medicines without having to be diabetic,” Dr. Miller said. “We’re waiting on the results of the SELECT [Semaglutide Effects on Heart Disease and Stroke in Patients With Overweight or Obesity] trials looking at people who are not diabetic or who are prediabetic, to see the 5-year outcomes with regard to cardiac events.
“Usually endocrinologists prescribe these medications, but cardiologists have started to get into the game since GLP-1 receptor agonists reduce cardiovascular events.” Dr. Miller is hopeful that this medication may neutralize the weight gain caused by psychotropic medications.
Wegovy is administered via weekly injection and, like insulin, is a subcutaneous medication that patients self-administer. Will patients be amenable to injecting a medication for weight loss? Dr. Stanford said that roughly 20%-30% of her patients are hesitant when she suggests that they use liraglutide, another GLP-1 receptor agonist that is approved for weight loss, and some are very fearful of needles.
However, she also noted that during the COVID-19 pandemic, many more patients have sought treatment from obesity medicine physicians because of the association between obesity and mortality from COVID-19. Patients have been willing to consider treatments that they were not previously open to pursuing.
So if people are willing to take Wegovy and doctors are willing to prescribe it, will insurers pay for it? As of this writing, the medication is not yet available, but Ozempic, the lower-dose agent for diabetes, costs $850-$900 for a 4-week supply, according to the GoodRx website.
Liraglutide (Saxenda), the GLP-1 receptor agonist that is currently available for weight loss as a daily injectable, costs $1,300-$1,400 per month.
These medications are not covered by Medicare or Medicaid, and Dr. Stanford, who is well versed as to exactly which private insurers in Massachusetts will and will not reimburse specific medications, said her patients with insurance coverage have been known to delay retirement so that they can remain on the more expensive medications.
“For the past 8 years,” she said, “the Treat and Reduce Obesity Act has had bipartisan support in Congress but has not passed. We are still hopeful that insurers will be required to cover medical and behavioral treatments for obesity.”
As our society struggles to destigmatize so many disorders, obesity remains a highly stigmatized condition, one that our patients cannot hide and one that leads to so many other comorbid illnesses. As new treatments are approved, there will be more for physicians to offer. Semaglutide, if it becomes available to those who need it most, could be a game changer. For patients who have not had success with traditional weight-loss methods, it’s encouraging to have another option available, one that may be reasonable to try before resorting to bariatric surgery.
For decades, psychiatrists have been comfortable prescribing treatments that lead to weight gain. Now, maybe it’s time they also prescribe those that prevent it.
A version of this article first appeared on Medscape.com.
It’s probably fair to say that most people would like to be thinner. More than 42% of Americans have obesity and another 30% are classified as being overweight, according to the latest statistics from the CDC.
Excess body weight is associated with many illnesses and plays a role in mental health; being heavy can take a toll on self-esteem. Many people worry that carrying excess weight makes them less attractive to potential romantic partners, and both physicians and employers treat those with obesity differently. Furthermore, in psychiatry, many of the medications we prescribe lead to weight gain.
In my clinical practice, I have listened as patients blamed themselves for their body habitus; many won’t consider biological treatments as they feel that would be “cheating” or taking an easy way out. They often point to periods in their life when they did lose weight and believe that they should be able to do it again, even if the weight loss took tremendous effort, was not sustained, and occurred decades ago.
That said, we psychiatrists often find ourselves in the position of managing obesity in our patients. I have been known to give patients who gain weight on antipsychotics either stimulants or metformin, or to add naltrexone to their Wellbutrin (bupropion) to effectively mimic a weight-loss medicine called Contrave.
Obesity a treatable medical condition
It wasn’t until 2013 that the American Medical Association recognized obesity as a medical condition.
In a New Yorker article that same year, “Diet Drugs Work: Why Won’t Doctors Prescribe Them?” Suzanne Koven wrote: “Several obesity experts told me they’ve encountered doctors who confide that they just didn’t like fat people and don’t enjoy taking care of them. Even doctors who treat obese patients feel stigmatized: ‘diet doctor’ is not a flattering term.”
Eat less, exercise more – with a blame-the-patient attitude – is still what people see as the “right” way to lose weight.
On June 4, 2021, the FDA approved semaglutide, a glucagonlike peptide–1 receptor agonist, previously used for the treatment of diabetes, for use as a weight loss agent for patients with obesity, or for those with a body mass index over 27 kg/m2 if they also have a weight-related comorbidity.
Semaglutide has three trade names, all manufactured by Novo Nordisk. The pill version is called Rybelsus and comes in 7-mg and 14-mg tablets. Ozempic is available in 0.5-mg and 1.0-mg doses and is administered weekly by subcutaneous injection for diabetes. The new, higher-dose preparation for weight loss, Wegovy, 2.4 mg, also comes as a weekly subcutaneous dose and is now available for the hefty price of $1,400 per month.
In STEP 1 trials, the higher-dose Wegovy was associated with an average 14.9% weight loss (15.3 kg) over 68 weeks, more than any other single-agent weight loss medication on the market.
GLP-1 receptor agonists work in the brain to decrease appetite, slow gastric emptying, increase insulin secretion, and stimulate brown adipose tissue thermogenesis.
Psych drugs lead to weight gain
Elaine Weiner, MD, is the medical director in the outpatient research program of the Maryland Psychiatric Research Center in Catonsville, where she treats patients with schizophrenia.
“Nearly all of our patients gain 20 pounds or more on the combinations of medications we use, mostly atypical antipsychotics,” she said. “Weight management is difficult for people who don’t have problems with motivation, but in our patients, lack of motivation is a core part of their illness, so asking them to adhere to diet and exercise regimens is of limited utility.
“Then, add to that the fact that they sometimes don’t have primary care doctors, and these issues of weight gain and metabolic syndrome come back to the psychiatrist. It is a really bad problem and we need more treatments.”
Fatima Cody Stanford, MD, MPH, MPA, is a fellowship-trained obesity medicine physician-scientist at the Massachusetts General Hospital Weight Center and Harvard Medical School, both in Boston. She has treated thousands of patients with obesity, speaks internationally on the topic of weight loss medicine, and has published over 100 peer-reviewed articles on obesity.
We spoke at length about recent changes in the field of obesity medicine and the introduction of the new GLP-1 receptor agonists.
“We as physicians have learned so little,” Dr. Stanford said. “This mantra of ‘calories in, calories out’ is not working; this is inaccurate and our focus on this has led to a rise in obesity. All calories are not created the same, and I think we are finally starting to see obesity medicine take off.”
Dr. Stanford is quick to note that obesity is a complex problem. Several different hormones are involved in regulating both appetite and satiety, processed foods promote weight gain, sleep is crucial to weight loss, and exercise helps maintain weight loss but is not usually effective in promoting it. “There are many contributors to energy storage,” she said.
The stimulant phentermine was approved in 1959. Addiction was a concern, and then in the 1990s, it was used in combination with fenfluramine to promote weight loss, a combination known as phen-fen. Fenfluramine was pulled from the market in 1997 when it was found to be associated with pulmonary hypertension and then heart valve abnormalities.
“This frightened quite a few physicians,” Dr. Stanford noted. Phentermine is still used for weight loss, either alone or together with topiramate, as a combination medication called Qsymia, nicknamed phen-top.
“Phen-top is the next best thing we have to semaglutide, and there is an average weight loss of 8%-9% of body weight. Semaglutide is going to be really significant for those people who are responders, and this has been quite well tolerated, the most common side effect being nausea,” she said.
However, she is quick to note that not everyone responds to every medication. “I use each patient’s clinical profile to determine what strategies and which medications to use.”
Cardiologists getting in the game
Michael Miller, MD, is a cardiologist at the University of Maryland, Baltimore, and author of “Heal Your Heart” (Emmaus, Pa.: Rodale, 2014). He is very enthusiastic about the approval of semaglutide.
“We are so excited because you finally can use these medicines without having to be diabetic,” Dr. Miller said. “We’re waiting on the results of the SELECT [Semaglutide Effects on Heart Disease and Stroke in Patients With Overweight or Obesity] trials looking at people who are not diabetic or who are prediabetic, to see the 5-year outcomes with regard to cardiac events.
“Usually endocrinologists prescribe these medications, but cardiologists have started to get into the game since GLP-1 receptor agonists reduce cardiovascular events.” Dr. Miller is hopeful that this medication may neutralize the weight gain caused by psychotropic medications.
Wegovy is administered via weekly injection and, like insulin, is a subcutaneous medication that patients self-administer. Will patients be amenable to injecting a medication for weight loss? Dr. Stanford said that roughly 20%-30% of her patients are hesitant when she suggests that they use liraglutide, another GLP-1 receptor agonist that is approved for weight loss, and some are very fearful of needles.
However, she also noted that during the COVID-19 pandemic, many more patients have sought treatment from obesity medicine physicians because of the association between obesity and mortality from COVID-19. Patients have been willing to consider treatments that they were not previously open to pursuing.
So if people are willing to take Wegovy and doctors are willing to prescribe it, will insurers pay for it? As of this writing, the medication is not yet available, but Ozempic, the lower-dose agent for diabetes, costs $850-$900 for a 4-week supply, according to the GoodRx website.
Liraglutide (Saxenda), the GLP-1 receptor agonist that is currently available for weight loss as a daily injectable, costs $1,300-$1,400 per month.
These medications are not covered by Medicare or Medicaid, and Dr. Stanford, who is well versed as to exactly which private insurers in Massachusetts will and will not reimburse specific medications, said her patients with insurance coverage have been known to delay retirement so that they can remain on the more expensive medications.
“For the past 8 years,” she said, “the Treat and Reduce Obesity Act has had bipartisan support in Congress but has not passed. We are still hopeful that insurers will be required to cover medical and behavioral treatments for obesity.”
As our society struggles to destigmatize so many disorders, obesity remains a highly stigmatized condition, one that our patients cannot hide and one that leads to so many other comorbid illnesses. As new treatments are approved, there will be more for physicians to offer. Semaglutide, if it becomes available to those who need it most, could be a game changer. For patients who have not had success with traditional weight-loss methods, it’s encouraging to have another option available, one that may be reasonable to try before resorting to bariatric surgery.
For decades, psychiatrists have been comfortable prescribing treatments that lead to weight gain. Now, maybe it’s time they also prescribe those that prevent it.
A version of this article first appeared on Medscape.com.
ACC issues decision pathway for hypertriglyceridemia management
A new decision pathway for the management of hypertriglyceridemia, prompted by a large and growing body of evidence that elevated triglycerides to a targetable risk factor for atherosclerotic cardiovascular disease (ASCVD), has been issued by the American College of Cardiology.
According to the chairman of the writing committee, Salim S. Virani, MD, PhD, the recommendations amplify and update more than alter the hypertriglyceridemia treatment recommendations in the 2018 joint multisociety blood cholesterol guidelines issued in 2018.
This decision pathway, however, is focused on triglycerides alone.
“The previous guidelines included a section on strategies for addressing hypertriglyceridemia to reduce ASCVD risk, but this new decision pathway builds on the recommendations with more details and with additional information,” explained Dr. Virani, professor of medicine in the section of cardiovascular research, Baylor College of Medicine, Houston.
Within this newly published document, the definitions of hypertriglyceridemia and rationale for treatment are followed by detailed algorithms for four specific patient groups with varying triglyceride levels:
- Adults with ASCVD.
- Adults at least 40 years of age with diabetes but no ASCVD.
- Adults at least 20 years of age with no ASCVD or diabetes.
- Adults at least 20 years of age with severe hypertriglyceridemia.
“In the design of these algorithms, we made an active effort to make them suitable for use by primary care physicians as well as specialists,” said Dr. Virani. Despite “lots of boxes and arrows,” the flowcharts for each of these patient groups permit clinicians to follow the decision pathway without having to reread the text.
The common emphasis in all four algorithms is to begin by evaluating patients for secondary causes of hypertriglyceridemia, such as multifactorial chylomicronemia syndrome and other diseases associated with elevated triglycerides. The next steps, also common to all algorithms, are to optimize diet and lifestyle changes that lower triglycerides, optimize glycemic control, and optimize statin therapy.
“Although commonly recognized for their impact on LDL-C, statins also provide a 10%-30% dose-dependent reduction in triglycerides in patients with elevated levels,” the guidelines state. Statins are considered a fundamental step to secondary prevention of ASCVD regardless of triglyceride levels.
Once treatable causes or contributors to hypertriglyceridemia have been addressed, lifestyle interventions and statin therapy have been optimized, pharmacologic therapy directed specifically at control of hypertriglyceridemia “can be considered” in those at highest risk of ASCVD events, but Dr. Virani explained that this is never an early or first step in control of elevated triglycerides.
“The entire working group agreed that lifestyle interventions should be highlighted front and center before considering any other intervention,” Dr. Virani explained.
Pharmacologic therapy for hypertriglyceridemia is not ignored. Prescription omega-3 fatty acid products are preferred over nonprescription dietary supplements, which may vary in quality and purity. But these products, rather than a standalone solution, are best applied within the context of efforts to improve diet, lower body weight, and increase physical activity.
Several trials have associated ethyl ester and carboxylic acid preparations with meaningful reductions in triglycerides, but these drugs, including icosapent ethyl (IPE), are not without adverse events. In the pivotal REDUCE-IT trial, IPE was linked with an increased risk of atrial fibrillation relative to placebo.
IPE is “the best option” and the only therapy with an indication for reduction in ASCVD risk, according to Dr. Virani, but he explained that safety concerns led the authors of the new decision pathway to employ cautious language in regard to its use, suggesting that it be “considered” in high-risk patients after other methods of lowering triglycerides have been optimized.
In the algorithm for the four different risk groups, the decision pathways follow stratifications for different levels of hypertriglyceridemia (defined under fasting and nonfasting conditions) and also for specific levels of LDL cholesterol. ASCVD risk assessment is also a factor in determining the next steps along the decision pathway.
According to Michael Davidson, MD, director of the lipid clinic at the University of Chicago, the emphasis on lifestyle changes for hypertriglyceridemia and the prudent language in regard to pharmacologic therapy is appropriate.
“In light of the controversies regarding the REDUCE-IT trial, the writing committee has done a nice job with providing useful guidance regarding the utilization of icosapent ethyl in higher risk patients,” Dr. Davidson said.
Calling the ACC decision pathway “a welcome enhancement of the 2018 ACC/AHA cholesterol guidelines,” Dr. Davidson praised the way in which the limitations of the evidence regarding pharmacologic therapies were explained.
“Most importantly, this decision pathway helps clinicians appreciate that hypertriglyceridemia can be best managed with lifestyle changes and addressing potential secondary causes,” Dr. Davidson said.
Dr. Virani reports no potential conflicts of interest. Dr. Davidson reports financial relationships with multiple pharmaceutical companies including those making or pursuing therapies for control of hypertriglyceridemia.
A new decision pathway for the management of hypertriglyceridemia, prompted by a large and growing body of evidence that elevated triglycerides to a targetable risk factor for atherosclerotic cardiovascular disease (ASCVD), has been issued by the American College of Cardiology.
According to the chairman of the writing committee, Salim S. Virani, MD, PhD, the recommendations amplify and update more than alter the hypertriglyceridemia treatment recommendations in the 2018 joint multisociety blood cholesterol guidelines issued in 2018.
This decision pathway, however, is focused on triglycerides alone.
“The previous guidelines included a section on strategies for addressing hypertriglyceridemia to reduce ASCVD risk, but this new decision pathway builds on the recommendations with more details and with additional information,” explained Dr. Virani, professor of medicine in the section of cardiovascular research, Baylor College of Medicine, Houston.
Within this newly published document, the definitions of hypertriglyceridemia and rationale for treatment are followed by detailed algorithms for four specific patient groups with varying triglyceride levels:
- Adults with ASCVD.
- Adults at least 40 years of age with diabetes but no ASCVD.
- Adults at least 20 years of age with no ASCVD or diabetes.
- Adults at least 20 years of age with severe hypertriglyceridemia.
“In the design of these algorithms, we made an active effort to make them suitable for use by primary care physicians as well as specialists,” said Dr. Virani. Despite “lots of boxes and arrows,” the flowcharts for each of these patient groups permit clinicians to follow the decision pathway without having to reread the text.
The common emphasis in all four algorithms is to begin by evaluating patients for secondary causes of hypertriglyceridemia, such as multifactorial chylomicronemia syndrome and other diseases associated with elevated triglycerides. The next steps, also common to all algorithms, are to optimize diet and lifestyle changes that lower triglycerides, optimize glycemic control, and optimize statin therapy.
“Although commonly recognized for their impact on LDL-C, statins also provide a 10%-30% dose-dependent reduction in triglycerides in patients with elevated levels,” the guidelines state. Statins are considered a fundamental step to secondary prevention of ASCVD regardless of triglyceride levels.
Once treatable causes or contributors to hypertriglyceridemia have been addressed, lifestyle interventions and statin therapy have been optimized, pharmacologic therapy directed specifically at control of hypertriglyceridemia “can be considered” in those at highest risk of ASCVD events, but Dr. Virani explained that this is never an early or first step in control of elevated triglycerides.
“The entire working group agreed that lifestyle interventions should be highlighted front and center before considering any other intervention,” Dr. Virani explained.
Pharmacologic therapy for hypertriglyceridemia is not ignored. Prescription omega-3 fatty acid products are preferred over nonprescription dietary supplements, which may vary in quality and purity. But these products, rather than a standalone solution, are best applied within the context of efforts to improve diet, lower body weight, and increase physical activity.
Several trials have associated ethyl ester and carboxylic acid preparations with meaningful reductions in triglycerides, but these drugs, including icosapent ethyl (IPE), are not without adverse events. In the pivotal REDUCE-IT trial, IPE was linked with an increased risk of atrial fibrillation relative to placebo.
IPE is “the best option” and the only therapy with an indication for reduction in ASCVD risk, according to Dr. Virani, but he explained that safety concerns led the authors of the new decision pathway to employ cautious language in regard to its use, suggesting that it be “considered” in high-risk patients after other methods of lowering triglycerides have been optimized.
In the algorithm for the four different risk groups, the decision pathways follow stratifications for different levels of hypertriglyceridemia (defined under fasting and nonfasting conditions) and also for specific levels of LDL cholesterol. ASCVD risk assessment is also a factor in determining the next steps along the decision pathway.
According to Michael Davidson, MD, director of the lipid clinic at the University of Chicago, the emphasis on lifestyle changes for hypertriglyceridemia and the prudent language in regard to pharmacologic therapy is appropriate.
“In light of the controversies regarding the REDUCE-IT trial, the writing committee has done a nice job with providing useful guidance regarding the utilization of icosapent ethyl in higher risk patients,” Dr. Davidson said.
Calling the ACC decision pathway “a welcome enhancement of the 2018 ACC/AHA cholesterol guidelines,” Dr. Davidson praised the way in which the limitations of the evidence regarding pharmacologic therapies were explained.
“Most importantly, this decision pathway helps clinicians appreciate that hypertriglyceridemia can be best managed with lifestyle changes and addressing potential secondary causes,” Dr. Davidson said.
Dr. Virani reports no potential conflicts of interest. Dr. Davidson reports financial relationships with multiple pharmaceutical companies including those making or pursuing therapies for control of hypertriglyceridemia.
A new decision pathway for the management of hypertriglyceridemia, prompted by a large and growing body of evidence that elevated triglycerides to a targetable risk factor for atherosclerotic cardiovascular disease (ASCVD), has been issued by the American College of Cardiology.
According to the chairman of the writing committee, Salim S. Virani, MD, PhD, the recommendations amplify and update more than alter the hypertriglyceridemia treatment recommendations in the 2018 joint multisociety blood cholesterol guidelines issued in 2018.
This decision pathway, however, is focused on triglycerides alone.
“The previous guidelines included a section on strategies for addressing hypertriglyceridemia to reduce ASCVD risk, but this new decision pathway builds on the recommendations with more details and with additional information,” explained Dr. Virani, professor of medicine in the section of cardiovascular research, Baylor College of Medicine, Houston.
Within this newly published document, the definitions of hypertriglyceridemia and rationale for treatment are followed by detailed algorithms for four specific patient groups with varying triglyceride levels:
- Adults with ASCVD.
- Adults at least 40 years of age with diabetes but no ASCVD.
- Adults at least 20 years of age with no ASCVD or diabetes.
- Adults at least 20 years of age with severe hypertriglyceridemia.
“In the design of these algorithms, we made an active effort to make them suitable for use by primary care physicians as well as specialists,” said Dr. Virani. Despite “lots of boxes and arrows,” the flowcharts for each of these patient groups permit clinicians to follow the decision pathway without having to reread the text.
The common emphasis in all four algorithms is to begin by evaluating patients for secondary causes of hypertriglyceridemia, such as multifactorial chylomicronemia syndrome and other diseases associated with elevated triglycerides. The next steps, also common to all algorithms, are to optimize diet and lifestyle changes that lower triglycerides, optimize glycemic control, and optimize statin therapy.
“Although commonly recognized for their impact on LDL-C, statins also provide a 10%-30% dose-dependent reduction in triglycerides in patients with elevated levels,” the guidelines state. Statins are considered a fundamental step to secondary prevention of ASCVD regardless of triglyceride levels.
Once treatable causes or contributors to hypertriglyceridemia have been addressed, lifestyle interventions and statin therapy have been optimized, pharmacologic therapy directed specifically at control of hypertriglyceridemia “can be considered” in those at highest risk of ASCVD events, but Dr. Virani explained that this is never an early or first step in control of elevated triglycerides.
“The entire working group agreed that lifestyle interventions should be highlighted front and center before considering any other intervention,” Dr. Virani explained.
Pharmacologic therapy for hypertriglyceridemia is not ignored. Prescription omega-3 fatty acid products are preferred over nonprescription dietary supplements, which may vary in quality and purity. But these products, rather than a standalone solution, are best applied within the context of efforts to improve diet, lower body weight, and increase physical activity.
Several trials have associated ethyl ester and carboxylic acid preparations with meaningful reductions in triglycerides, but these drugs, including icosapent ethyl (IPE), are not without adverse events. In the pivotal REDUCE-IT trial, IPE was linked with an increased risk of atrial fibrillation relative to placebo.
IPE is “the best option” and the only therapy with an indication for reduction in ASCVD risk, according to Dr. Virani, but he explained that safety concerns led the authors of the new decision pathway to employ cautious language in regard to its use, suggesting that it be “considered” in high-risk patients after other methods of lowering triglycerides have been optimized.
In the algorithm for the four different risk groups, the decision pathways follow stratifications for different levels of hypertriglyceridemia (defined under fasting and nonfasting conditions) and also for specific levels of LDL cholesterol. ASCVD risk assessment is also a factor in determining the next steps along the decision pathway.
According to Michael Davidson, MD, director of the lipid clinic at the University of Chicago, the emphasis on lifestyle changes for hypertriglyceridemia and the prudent language in regard to pharmacologic therapy is appropriate.
“In light of the controversies regarding the REDUCE-IT trial, the writing committee has done a nice job with providing useful guidance regarding the utilization of icosapent ethyl in higher risk patients,” Dr. Davidson said.
Calling the ACC decision pathway “a welcome enhancement of the 2018 ACC/AHA cholesterol guidelines,” Dr. Davidson praised the way in which the limitations of the evidence regarding pharmacologic therapies were explained.
“Most importantly, this decision pathway helps clinicians appreciate that hypertriglyceridemia can be best managed with lifestyle changes and addressing potential secondary causes,” Dr. Davidson said.
Dr. Virani reports no potential conflicts of interest. Dr. Davidson reports financial relationships with multiple pharmaceutical companies including those making or pursuing therapies for control of hypertriglyceridemia.
FROM THE JOURNAL OF THE AMERICAN COLLEGE OF CARDIOLOGY
ARBs equal ACE inhibitors for hypertension, and better tolerated
In the largest comparison of angiotensin receptor blockers (ARBs) and ACE inhibitors to date, a study of nearly 2.3 million patients starting the drugs as monotherapy shows no significant differences between the two in the long-term prevention of hypertension-related cardiovascular events.
However, side effects were notably lower with ARBs.
“This is a very large, well-executed observational study that confirms that ARBs appear to have fewer side effects than ACE inhibitors, and no unexpected ARB side effects were detected,” senior author George Hripcsak, MD, professor and chair of biomedical informatics at Columbia University, New York, told this news organization.
“Despite being equally guideline-recommended first-line therapies for hypertension, these results support preferentially starting ARBs rather than ACE inhibitors when initiating treatment for hypertension for physicians and patients considering renin-angiotensin system (RAS) inhibition,” the authors added in the study, published online July 26, 2021, in the journal Hypertension.
They noted that both drug classes have been on the market a long time, with proven efficacy in hypertension and “a wide availability of inexpensive generic forms.”
They also stressed that their findings only apply to patients with hypertension for whom a RAS inhibitor would be the best choice of therapy.
Commenting on the research, George Bakris, MD, of the American Heart Association’s Comprehensive Hypertension Center at the University of Chicago, said the findings were consistent with his experience in prescribing as well as researching the two drug classes.
“I have been in practice for over 30 years and studied both classes, including head-to-head prospective trials to assess blood pressure, and found in many cases better blood pressure lowering by some ARBs and always better tolerability,” he told this news organization. “I think this study confirms and extends my thoughts between the two classes of blood pressure–lowering agents.”
Head-to-head comparisons of ACE inhibitors and ARBs limited to date
ACE inhibitors and ARBs each have extensive evidence supporting their roles as first-line medications in the treatment of hypertension, and each have the strongest recommendations in international guidelines.
However, ACE inhibitors are prescribed more commonly than ARBs as the first-line drug for lowering blood pressure, and head-to-head comparisons of the two are limited, with conflicting results.
For the study, Dr. Hripcsak and colleagues evaluated data on almost 3 million patients starting monotherapy with an ACE inhibitor or ARB for the first time between 1996 and 2018 in the United States, Germany, and South Korea, who had no history of heart disease or stroke.
They identified a total of 2,297,881 patients initiating ACE inhibitors and 673,938 starting ARBs. Among new users of ACE inhibitors, most received lisinopril (80%), followed by ramipril and enalapril, while most patients prescribed ARBs received losartan (45%), followed by valsartan and olmesartan.
With follow-up times ranging from about 4 months to more than 18 months, the data show no statistically significant differences between ACE inhibitors versus ARBs in the primary outcomes of acute myocardial infarction (hazard ratio, 1.11), heart failure (HR, 1.03), stroke (HR, 1.07), or composite cardiovascular events (HR, 1.06).
For secondary and safety outcomes, including an analysis of 51 possible side effects, ACE inhibitors, compared with ARBs, were associated with a significantly higher risk of angioedema (HR, 3.31; P < .01), cough (HR, 1.32; P < .01), acute pancreatitis (HR, 1.32; P = .02), gastrointestinal bleeding (HR, 1.18; P = .04), and abnormal weight loss (HR, 1.18; P = .04).
While the link between ACE inhibitors and pancreatitis has been previously reported, the association with GI bleeding may be a novel finding, with no prior studies comparing those effects in the two drug classes, the authors noted.
Despite most patients taking just a couple of drugs in either class, Dr. Hripcsak said, “we don’t expect that other drugs from those classes will have fewer differences. It is possible, of course, but that is not our expectation.”
Results only applicable to those starting therapy with RAS inhibitors
First author RuiJun Chen, MD, added that, importantly, the results may not apply to patients switching therapies or adding on therapy, “such as for the patient whose hypertension is not effectively controlled with one drug and requires the addition of a second medication,” he said in an interview.
“Also, the suggestion of preferentially prescribing ARBs only applies to those patients and providers intending to control blood pressure through RAS inhibition,” said Dr. Chen, an assistant professor in translational data science and informatics at Geisinger Medical Center in Danville, Pa., who was a National Library of Medicine postdoctoral fellow at Columbia University at the time of the study.
Hence, he stressed the results do not extend to other classes of recommended first-line blood pressure medications.
“Essentially, since this is an ACE inhibitor versus ARB study, we would not claim that ARBs are preferred over all other types of hypertension medications which were not studied here,” the researchers emphasize.
In addition to ARBs and ACE inhibitors, other medications recommended by the AHA/American College of Cardiology in the 2017 “Guideline for the Prevention, Detection, Evaluation and Management of High Blood Pressure in Adults” for the primary treatment of hypertension include thiazide diuretics and calcium channel blockers.
The study received support from the National Library of Medicine and the National Institute of Allergy and Infectious Diseases of the National Institutes of Health; the National Science Foundation; and the Ministries of Health & Welfare and of Trade, Industry & Energy of the Republic of Korea. Dr. Hripcsak reported receiving grants from the National Library of Medicine during the study and grants from Janssen Research outside the submitted work. Dr. Bakris reported being a consultant for Merck, KBP Biosciences, and Ionis.
A version of this article first appeared on Medscape.com.
In the largest comparison of angiotensin receptor blockers (ARBs) and ACE inhibitors to date, a study of nearly 2.3 million patients starting the drugs as monotherapy shows no significant differences between the two in the long-term prevention of hypertension-related cardiovascular events.
However, side effects were notably lower with ARBs.
“This is a very large, well-executed observational study that confirms that ARBs appear to have fewer side effects than ACE inhibitors, and no unexpected ARB side effects were detected,” senior author George Hripcsak, MD, professor and chair of biomedical informatics at Columbia University, New York, told this news organization.
“Despite being equally guideline-recommended first-line therapies for hypertension, these results support preferentially starting ARBs rather than ACE inhibitors when initiating treatment for hypertension for physicians and patients considering renin-angiotensin system (RAS) inhibition,” the authors added in the study, published online July 26, 2021, in the journal Hypertension.
They noted that both drug classes have been on the market a long time, with proven efficacy in hypertension and “a wide availability of inexpensive generic forms.”
They also stressed that their findings only apply to patients with hypertension for whom a RAS inhibitor would be the best choice of therapy.
Commenting on the research, George Bakris, MD, of the American Heart Association’s Comprehensive Hypertension Center at the University of Chicago, said the findings were consistent with his experience in prescribing as well as researching the two drug classes.
“I have been in practice for over 30 years and studied both classes, including head-to-head prospective trials to assess blood pressure, and found in many cases better blood pressure lowering by some ARBs and always better tolerability,” he told this news organization. “I think this study confirms and extends my thoughts between the two classes of blood pressure–lowering agents.”
Head-to-head comparisons of ACE inhibitors and ARBs limited to date
ACE inhibitors and ARBs each have extensive evidence supporting their roles as first-line medications in the treatment of hypertension, and each have the strongest recommendations in international guidelines.
However, ACE inhibitors are prescribed more commonly than ARBs as the first-line drug for lowering blood pressure, and head-to-head comparisons of the two are limited, with conflicting results.
For the study, Dr. Hripcsak and colleagues evaluated data on almost 3 million patients starting monotherapy with an ACE inhibitor or ARB for the first time between 1996 and 2018 in the United States, Germany, and South Korea, who had no history of heart disease or stroke.
They identified a total of 2,297,881 patients initiating ACE inhibitors and 673,938 starting ARBs. Among new users of ACE inhibitors, most received lisinopril (80%), followed by ramipril and enalapril, while most patients prescribed ARBs received losartan (45%), followed by valsartan and olmesartan.
With follow-up times ranging from about 4 months to more than 18 months, the data show no statistically significant differences between ACE inhibitors versus ARBs in the primary outcomes of acute myocardial infarction (hazard ratio, 1.11), heart failure (HR, 1.03), stroke (HR, 1.07), or composite cardiovascular events (HR, 1.06).
For secondary and safety outcomes, including an analysis of 51 possible side effects, ACE inhibitors, compared with ARBs, were associated with a significantly higher risk of angioedema (HR, 3.31; P < .01), cough (HR, 1.32; P < .01), acute pancreatitis (HR, 1.32; P = .02), gastrointestinal bleeding (HR, 1.18; P = .04), and abnormal weight loss (HR, 1.18; P = .04).
While the link between ACE inhibitors and pancreatitis has been previously reported, the association with GI bleeding may be a novel finding, with no prior studies comparing those effects in the two drug classes, the authors noted.
Despite most patients taking just a couple of drugs in either class, Dr. Hripcsak said, “we don’t expect that other drugs from those classes will have fewer differences. It is possible, of course, but that is not our expectation.”
Results only applicable to those starting therapy with RAS inhibitors
First author RuiJun Chen, MD, added that, importantly, the results may not apply to patients switching therapies or adding on therapy, “such as for the patient whose hypertension is not effectively controlled with one drug and requires the addition of a second medication,” he said in an interview.
“Also, the suggestion of preferentially prescribing ARBs only applies to those patients and providers intending to control blood pressure through RAS inhibition,” said Dr. Chen, an assistant professor in translational data science and informatics at Geisinger Medical Center in Danville, Pa., who was a National Library of Medicine postdoctoral fellow at Columbia University at the time of the study.
Hence, he stressed the results do not extend to other classes of recommended first-line blood pressure medications.
“Essentially, since this is an ACE inhibitor versus ARB study, we would not claim that ARBs are preferred over all other types of hypertension medications which were not studied here,” the researchers emphasize.
In addition to ARBs and ACE inhibitors, other medications recommended by the AHA/American College of Cardiology in the 2017 “Guideline for the Prevention, Detection, Evaluation and Management of High Blood Pressure in Adults” for the primary treatment of hypertension include thiazide diuretics and calcium channel blockers.
The study received support from the National Library of Medicine and the National Institute of Allergy and Infectious Diseases of the National Institutes of Health; the National Science Foundation; and the Ministries of Health & Welfare and of Trade, Industry & Energy of the Republic of Korea. Dr. Hripcsak reported receiving grants from the National Library of Medicine during the study and grants from Janssen Research outside the submitted work. Dr. Bakris reported being a consultant for Merck, KBP Biosciences, and Ionis.
A version of this article first appeared on Medscape.com.
In the largest comparison of angiotensin receptor blockers (ARBs) and ACE inhibitors to date, a study of nearly 2.3 million patients starting the drugs as monotherapy shows no significant differences between the two in the long-term prevention of hypertension-related cardiovascular events.
However, side effects were notably lower with ARBs.
“This is a very large, well-executed observational study that confirms that ARBs appear to have fewer side effects than ACE inhibitors, and no unexpected ARB side effects were detected,” senior author George Hripcsak, MD, professor and chair of biomedical informatics at Columbia University, New York, told this news organization.
“Despite being equally guideline-recommended first-line therapies for hypertension, these results support preferentially starting ARBs rather than ACE inhibitors when initiating treatment for hypertension for physicians and patients considering renin-angiotensin system (RAS) inhibition,” the authors added in the study, published online July 26, 2021, in the journal Hypertension.
They noted that both drug classes have been on the market a long time, with proven efficacy in hypertension and “a wide availability of inexpensive generic forms.”
They also stressed that their findings only apply to patients with hypertension for whom a RAS inhibitor would be the best choice of therapy.
Commenting on the research, George Bakris, MD, of the American Heart Association’s Comprehensive Hypertension Center at the University of Chicago, said the findings were consistent with his experience in prescribing as well as researching the two drug classes.
“I have been in practice for over 30 years and studied both classes, including head-to-head prospective trials to assess blood pressure, and found in many cases better blood pressure lowering by some ARBs and always better tolerability,” he told this news organization. “I think this study confirms and extends my thoughts between the two classes of blood pressure–lowering agents.”
Head-to-head comparisons of ACE inhibitors and ARBs limited to date
ACE inhibitors and ARBs each have extensive evidence supporting their roles as first-line medications in the treatment of hypertension, and each have the strongest recommendations in international guidelines.
However, ACE inhibitors are prescribed more commonly than ARBs as the first-line drug for lowering blood pressure, and head-to-head comparisons of the two are limited, with conflicting results.
For the study, Dr. Hripcsak and colleagues evaluated data on almost 3 million patients starting monotherapy with an ACE inhibitor or ARB for the first time between 1996 and 2018 in the United States, Germany, and South Korea, who had no history of heart disease or stroke.
They identified a total of 2,297,881 patients initiating ACE inhibitors and 673,938 starting ARBs. Among new users of ACE inhibitors, most received lisinopril (80%), followed by ramipril and enalapril, while most patients prescribed ARBs received losartan (45%), followed by valsartan and olmesartan.
With follow-up times ranging from about 4 months to more than 18 months, the data show no statistically significant differences between ACE inhibitors versus ARBs in the primary outcomes of acute myocardial infarction (hazard ratio, 1.11), heart failure (HR, 1.03), stroke (HR, 1.07), or composite cardiovascular events (HR, 1.06).
For secondary and safety outcomes, including an analysis of 51 possible side effects, ACE inhibitors, compared with ARBs, were associated with a significantly higher risk of angioedema (HR, 3.31; P < .01), cough (HR, 1.32; P < .01), acute pancreatitis (HR, 1.32; P = .02), gastrointestinal bleeding (HR, 1.18; P = .04), and abnormal weight loss (HR, 1.18; P = .04).
While the link between ACE inhibitors and pancreatitis has been previously reported, the association with GI bleeding may be a novel finding, with no prior studies comparing those effects in the two drug classes, the authors noted.
Despite most patients taking just a couple of drugs in either class, Dr. Hripcsak said, “we don’t expect that other drugs from those classes will have fewer differences. It is possible, of course, but that is not our expectation.”
Results only applicable to those starting therapy with RAS inhibitors
First author RuiJun Chen, MD, added that, importantly, the results may not apply to patients switching therapies or adding on therapy, “such as for the patient whose hypertension is not effectively controlled with one drug and requires the addition of a second medication,” he said in an interview.
“Also, the suggestion of preferentially prescribing ARBs only applies to those patients and providers intending to control blood pressure through RAS inhibition,” said Dr. Chen, an assistant professor in translational data science and informatics at Geisinger Medical Center in Danville, Pa., who was a National Library of Medicine postdoctoral fellow at Columbia University at the time of the study.
Hence, he stressed the results do not extend to other classes of recommended first-line blood pressure medications.
“Essentially, since this is an ACE inhibitor versus ARB study, we would not claim that ARBs are preferred over all other types of hypertension medications which were not studied here,” the researchers emphasize.
In addition to ARBs and ACE inhibitors, other medications recommended by the AHA/American College of Cardiology in the 2017 “Guideline for the Prevention, Detection, Evaluation and Management of High Blood Pressure in Adults” for the primary treatment of hypertension include thiazide diuretics and calcium channel blockers.
The study received support from the National Library of Medicine and the National Institute of Allergy and Infectious Diseases of the National Institutes of Health; the National Science Foundation; and the Ministries of Health & Welfare and of Trade, Industry & Energy of the Republic of Korea. Dr. Hripcsak reported receiving grants from the National Library of Medicine during the study and grants from Janssen Research outside the submitted work. Dr. Bakris reported being a consultant for Merck, KBP Biosciences, and Ionis.
A version of this article first appeared on Medscape.com.
Diabetes duration linked to increasing heart failure risk
In a multivariable analysis the rate of incident heart failure increased steadily and significantly as diabetes duration increased. Among the 168 study subjects (2% of the total study group) who had diabetes for at least 15 years, the subsequent incidence of heart failure was nearly threefold higher than among the 4,802 subjects (49%) who never had diabetes or prediabetes, reported Justin B. Echouffo-Tcheugui, MD, PhD, and coauthors in an article published in JACC Heart Failure.
People with prediabetes (32% of the study population) had a significant but modest increased rate of incident heart failure that was 16% higher than in control subjects who never developed diabetes. People with diabetes for durations of 0-4.9 years, 5.0-9.9 years, or 10-14.9 years, had steadily increasing relative incident heart failure rates of 29%, 97%, and 210%, respectively, compared with controls, reported Dr. Echouffo-Tcheugui, an endocrinologist at Johns Hopkins Medicine in Baltimore.
Similar rates of HFrEF and HFpEF
Among all 1,841 people in the dataset with diabetes for any length of time each additional 5 years of the disorder linked with a significant, relative 17% increase in the rate of incident heart failure. Incidence of heart failure rose even more sharply with added duration among those with a hemoglobin A1c of 7% or greater, compared with those with better glycemic control. And the rate of incident heart failure with reduced ejection fraction (HFrEF) roughly matched the rate of incident heart failure with preserved ejection fraction (HFpEF).
The study dataset included 9,734 adults enrolled into the Atherosclerosis Risk in Communities (ARIC) study, and during a median follow-up of 22.5 years they had nearly 2,000 episodes of either hospitalization or death secondary to incident heart failure. This included 617 (31%) events involving HFpEF, 495 events (25%) involving HFrEF, and 876 unclassified heart failure events.
The cohort averaged 63 years of age; 58% were women, 23% were Black, and 77% were White (the study design excluded people with other racial and ethnic backgrounds). The study design also excluded people with a history of heart failure or coronary artery disease, as well as those diagnosed with diabetes prior to age 18 resulting in a study group that presumably mostly had type 2 diabetes when diabetes was present. The report provided no data on the specific numbers of patients with type 1 or type 2 diabetes.
“It’s not surprising that a longer duration of diabetes is associated with heart failure, but the etiology remains problematic,” commented Robert H. Eckel, MD, an endocrinologist at the University of Colorado at Denver, Aurora. “The impact of diabetes on incident heart failure is not well know, particularly duration of diabetes,” although disorders often found in patients with diabetes, such as hypertension and diabetic cardiomyopathy, likely have roles in causing heart failure, he said.
Diabetes duration may signal need for an SGLT2 inhibitor
“With emerging novel treatments like the SGLT2 [sodium-glucose cotransporter 2] inhibitors for preventing heart failure hospitalizations and deaths in patients with type 2 diabetes, this is a timely analysis,” Dr. Eckel said in an interview.
“There is no question that with increased duration of type 2 diabetes” the need for an agent from the SGLT2-inhibitor class increases. Although, because of the proven protection these drugs give against heart failure events and progression of chronic kidney disease, treatment with this drug class should start early in patients with type 2 diabetes, he added.
Dr. Echouffo-Tcheugui and his coauthors agreed, citing two important clinical take-aways from their findings:
First, interventions that delay the onset of diabetes may potentially reduce incident heart failure; second, patients with diabetes might benefit from cardioprotective treatments such as SGLT2 inhibitors, the report said.
“Our observations suggest the potential prognostic relevance of diabetes duration in assessing heart failure,” the authors wrote. Integrating diabetes duration into heart failure risk estimation in people with diabetes “could help refine the selection of high-risk individuals who may derive the greatest absolute benefit from aggressive cardioprotective therapies such as SGLT2 inhibitors.”
The analysis also identified several other demographic and clinical factors that influenced the relative effect of diabetes duration. Longer duration was linked with higher rates of incident heart failure in women compared with men, in Blacks compared with Whites, in people younger than 65 compared with older people, in people with an A1c of 7% or higher, and in those with a body mass index of 30 kg/m2 or greater.
The ARIC study and the analyses run by Dr. Echouffo-Tcheugui and his coauthors received no commercial funding. Dr. Echouffo-Tcheugui and Dr. Eckel had no relevant disclosures.
In a multivariable analysis the rate of incident heart failure increased steadily and significantly as diabetes duration increased. Among the 168 study subjects (2% of the total study group) who had diabetes for at least 15 years, the subsequent incidence of heart failure was nearly threefold higher than among the 4,802 subjects (49%) who never had diabetes or prediabetes, reported Justin B. Echouffo-Tcheugui, MD, PhD, and coauthors in an article published in JACC Heart Failure.
People with prediabetes (32% of the study population) had a significant but modest increased rate of incident heart failure that was 16% higher than in control subjects who never developed diabetes. People with diabetes for durations of 0-4.9 years, 5.0-9.9 years, or 10-14.9 years, had steadily increasing relative incident heart failure rates of 29%, 97%, and 210%, respectively, compared with controls, reported Dr. Echouffo-Tcheugui, an endocrinologist at Johns Hopkins Medicine in Baltimore.
Similar rates of HFrEF and HFpEF
Among all 1,841 people in the dataset with diabetes for any length of time each additional 5 years of the disorder linked with a significant, relative 17% increase in the rate of incident heart failure. Incidence of heart failure rose even more sharply with added duration among those with a hemoglobin A1c of 7% or greater, compared with those with better glycemic control. And the rate of incident heart failure with reduced ejection fraction (HFrEF) roughly matched the rate of incident heart failure with preserved ejection fraction (HFpEF).
The study dataset included 9,734 adults enrolled into the Atherosclerosis Risk in Communities (ARIC) study, and during a median follow-up of 22.5 years they had nearly 2,000 episodes of either hospitalization or death secondary to incident heart failure. This included 617 (31%) events involving HFpEF, 495 events (25%) involving HFrEF, and 876 unclassified heart failure events.
The cohort averaged 63 years of age; 58% were women, 23% were Black, and 77% were White (the study design excluded people with other racial and ethnic backgrounds). The study design also excluded people with a history of heart failure or coronary artery disease, as well as those diagnosed with diabetes prior to age 18 resulting in a study group that presumably mostly had type 2 diabetes when diabetes was present. The report provided no data on the specific numbers of patients with type 1 or type 2 diabetes.
“It’s not surprising that a longer duration of diabetes is associated with heart failure, but the etiology remains problematic,” commented Robert H. Eckel, MD, an endocrinologist at the University of Colorado at Denver, Aurora. “The impact of diabetes on incident heart failure is not well know, particularly duration of diabetes,” although disorders often found in patients with diabetes, such as hypertension and diabetic cardiomyopathy, likely have roles in causing heart failure, he said.
Diabetes duration may signal need for an SGLT2 inhibitor
“With emerging novel treatments like the SGLT2 [sodium-glucose cotransporter 2] inhibitors for preventing heart failure hospitalizations and deaths in patients with type 2 diabetes, this is a timely analysis,” Dr. Eckel said in an interview.
“There is no question that with increased duration of type 2 diabetes” the need for an agent from the SGLT2-inhibitor class increases. Although, because of the proven protection these drugs give against heart failure events and progression of chronic kidney disease, treatment with this drug class should start early in patients with type 2 diabetes, he added.
Dr. Echouffo-Tcheugui and his coauthors agreed, citing two important clinical take-aways from their findings:
First, interventions that delay the onset of diabetes may potentially reduce incident heart failure; second, patients with diabetes might benefit from cardioprotective treatments such as SGLT2 inhibitors, the report said.
“Our observations suggest the potential prognostic relevance of diabetes duration in assessing heart failure,” the authors wrote. Integrating diabetes duration into heart failure risk estimation in people with diabetes “could help refine the selection of high-risk individuals who may derive the greatest absolute benefit from aggressive cardioprotective therapies such as SGLT2 inhibitors.”
The analysis also identified several other demographic and clinical factors that influenced the relative effect of diabetes duration. Longer duration was linked with higher rates of incident heart failure in women compared with men, in Blacks compared with Whites, in people younger than 65 compared with older people, in people with an A1c of 7% or higher, and in those with a body mass index of 30 kg/m2 or greater.
The ARIC study and the analyses run by Dr. Echouffo-Tcheugui and his coauthors received no commercial funding. Dr. Echouffo-Tcheugui and Dr. Eckel had no relevant disclosures.
In a multivariable analysis the rate of incident heart failure increased steadily and significantly as diabetes duration increased. Among the 168 study subjects (2% of the total study group) who had diabetes for at least 15 years, the subsequent incidence of heart failure was nearly threefold higher than among the 4,802 subjects (49%) who never had diabetes or prediabetes, reported Justin B. Echouffo-Tcheugui, MD, PhD, and coauthors in an article published in JACC Heart Failure.
People with prediabetes (32% of the study population) had a significant but modest increased rate of incident heart failure that was 16% higher than in control subjects who never developed diabetes. People with diabetes for durations of 0-4.9 years, 5.0-9.9 years, or 10-14.9 years, had steadily increasing relative incident heart failure rates of 29%, 97%, and 210%, respectively, compared with controls, reported Dr. Echouffo-Tcheugui, an endocrinologist at Johns Hopkins Medicine in Baltimore.
Similar rates of HFrEF and HFpEF
Among all 1,841 people in the dataset with diabetes for any length of time each additional 5 years of the disorder linked with a significant, relative 17% increase in the rate of incident heart failure. Incidence of heart failure rose even more sharply with added duration among those with a hemoglobin A1c of 7% or greater, compared with those with better glycemic control. And the rate of incident heart failure with reduced ejection fraction (HFrEF) roughly matched the rate of incident heart failure with preserved ejection fraction (HFpEF).
The study dataset included 9,734 adults enrolled into the Atherosclerosis Risk in Communities (ARIC) study, and during a median follow-up of 22.5 years they had nearly 2,000 episodes of either hospitalization or death secondary to incident heart failure. This included 617 (31%) events involving HFpEF, 495 events (25%) involving HFrEF, and 876 unclassified heart failure events.
The cohort averaged 63 years of age; 58% were women, 23% were Black, and 77% were White (the study design excluded people with other racial and ethnic backgrounds). The study design also excluded people with a history of heart failure or coronary artery disease, as well as those diagnosed with diabetes prior to age 18 resulting in a study group that presumably mostly had type 2 diabetes when diabetes was present. The report provided no data on the specific numbers of patients with type 1 or type 2 diabetes.
“It’s not surprising that a longer duration of diabetes is associated with heart failure, but the etiology remains problematic,” commented Robert H. Eckel, MD, an endocrinologist at the University of Colorado at Denver, Aurora. “The impact of diabetes on incident heart failure is not well know, particularly duration of diabetes,” although disorders often found in patients with diabetes, such as hypertension and diabetic cardiomyopathy, likely have roles in causing heart failure, he said.
Diabetes duration may signal need for an SGLT2 inhibitor
“With emerging novel treatments like the SGLT2 [sodium-glucose cotransporter 2] inhibitors for preventing heart failure hospitalizations and deaths in patients with type 2 diabetes, this is a timely analysis,” Dr. Eckel said in an interview.
“There is no question that with increased duration of type 2 diabetes” the need for an agent from the SGLT2-inhibitor class increases. Although, because of the proven protection these drugs give against heart failure events and progression of chronic kidney disease, treatment with this drug class should start early in patients with type 2 diabetes, he added.
Dr. Echouffo-Tcheugui and his coauthors agreed, citing two important clinical take-aways from their findings:
First, interventions that delay the onset of diabetes may potentially reduce incident heart failure; second, patients with diabetes might benefit from cardioprotective treatments such as SGLT2 inhibitors, the report said.
“Our observations suggest the potential prognostic relevance of diabetes duration in assessing heart failure,” the authors wrote. Integrating diabetes duration into heart failure risk estimation in people with diabetes “could help refine the selection of high-risk individuals who may derive the greatest absolute benefit from aggressive cardioprotective therapies such as SGLT2 inhibitors.”
The analysis also identified several other demographic and clinical factors that influenced the relative effect of diabetes duration. Longer duration was linked with higher rates of incident heart failure in women compared with men, in Blacks compared with Whites, in people younger than 65 compared with older people, in people with an A1c of 7% or higher, and in those with a body mass index of 30 kg/m2 or greater.
The ARIC study and the analyses run by Dr. Echouffo-Tcheugui and his coauthors received no commercial funding. Dr. Echouffo-Tcheugui and Dr. Eckel had no relevant disclosures.
FROM JACC HEART FAILURE
Dapagliflozin safe, protective in advanced kidney disease
Patients with stage 4 chronic kidney disease (CKD) who were in the DAPA-CKD trial had cardiorenal benefits from dapagliflozin that were similar to those of patients in the overall trial, with no added safety signal.
DAPA-CKD (Dapagliflozin and Prevention of Adverse Outcomes in Chronic Kidney Disease) was a landmark study of more than 4,000 patients with CKD, with an estimated glomerular filtration rate (eGFR) of 25-75 mL/min per 1.73 m2 and albuminuria with/without type 2 diabetes.
The primary results showed that patients who received the sodium-glucose cotransporter 2 (SGLT2) inhibitor dapagliflozin for a median of 2.4 years were significantly less likely to have worsening kidney disease or die from all causes than were patients who received placebo.
“This prespecified subanalysis of people with an eGFR < 30 mL/min/1.73 m2 [stage 4 CKD] in the DAPA-CKD study shows first, that in this very vulnerable population, use of the SGLT2 inhibitor is safe,” said Chantal Mathieu, MD, PhD.
Furthermore, there was no signal whatsoever of more adverse events and even a trend to fewer events, she said in an email to this news organization.
The analysis also showed that “although now in small numbers (around 300 each in the treated group vs. placebo group), there is no suggestion that the protective effect of dapagliflozin on the renal and cardiovascular front would not happen in this group” with advanced CKD. The efficacy findings just missed statistical significance, noted Dr. Mathieu, of Catholic University, Leuven, Belgium, who was not involved in the study.
Although dapagliflozin is now approved for treating patients with CKD who are at risk of kidney disease progression (on the basis of the DAPA-CKD results), guidelines have not yet been updated to reflect this, lead investigator Glenn M. Chertow, MD, MPH, of Stanford (Calif.) University, told this news organization in an email.
“For clinicians,” Dr. Mathieu said, “this is now the absolute reassurance that we do not have to stop an SGLT2 inhibitor in people with eGFR < 30 mL/min for safety reasons and that we should maintain them at these values for renal and cardiovascular protection!
“I absolutely hope labels will change soon to reflect these observations (and indeed movement on that front is happening),” she continued.
“The American Diabetes Association/European Association for the Study of Diabetes consensus on glucose-lowering therapies in type 2 diabetes already advocated keeping these agents until eGFR 30 mL/min (on the basis of evidence in 2019),” Dr. Mathieu added, “but this study will probably push the statements even further.”
“Of note,” she pointed out, “at these low eGFRs, the glucose-lowering potential of the SGLT2 inhibitor is negligible.”
Dapagliflozin risks and benefits in advanced CKD
Based on the DAPA-CKD study, published in the New England Journal of Medicine Oct. 8, 2020, the Food and Drug Administration expanded the indication for dapagliflozin (Farxiga, AstraZeneca) in April of 2021.
However, relatively little is known about the safety and efficacy of SGLT2 inhibitors in patients with advanced CKD, who are particularly vulnerable to cardiovascular events and progressive kidney failure, Dr. Chertow and colleagues wrote.
The DAPA-CKD trial randomized 4,304 patients with CKD 1:1 to dapagliflozin 10 mg/day or placebo, including 624 patients (14%) who had eGFR < 30 mL/min per 1.73 m2 and albuminuria at baseline.
Patients in the subgroup with advanced CKD had a mean age of 62 years, and 37% were female. About two-thirds had type 2 diabetes and about one-third had cardiovascular disease.
A total of 293 patients received dapagliflozin and 331 patients received placebo.
During a median follow-up of 2.4 years, patients who received dapagliflozin as opposed to placebo had a lower risk of the primary efficacy outcome – a composite of a 50% or greater sustained decline in eGFR, end-stage kidney disease, or death from cardiovascular or renal causes (hazard ratio, 0.73; 95% confidence interval, 0.53-1.02).
In secondary efficacy outcomes, patients who received dapagliflozin as opposed to placebo also had a lower risk of the following:
- A renal composite outcome – a ≥ 50% sustained decline in eGFR, end-stage kidney disease, or death from renal causes (HR, 0.71; 95% CI, 0.49-1.02).
- A cardiovascular composite outcome comprising cardiovascular death or hospitalization for heart failure (HR, 0.83; 95% CI, 0.45-1.53).
- All-cause mortality (HR, 0.68; 95% CI, 0.39 to 1.21).
The eGFR slope declined by 2.15 mL/min per 1.73 m2 per year and by 3.38 mL/min per 1.73 m2 per year in the dapagliflozin and placebo groups, respectively (P = .005).
“The trial was not powered to detect a statistically significant difference in the primary and key secondary endpoints in modest-sized subgroups,” the researchers noted.
The researchers limited their safety analysis to serious adverse events or symptoms of volume depletion, kidney-related events, major hypoglycemia, bone fractures, amputations, and potential diabetic ketoacidosis.
There was no evidence of increased risk of these adverse events in patients who received dapagliflozin.
The subanalysis of the DAPA-CKD trial was published July 16 in the Journal of the American Society of Nephrology.
The study was funded by AstraZeneca. Dr. Chertow has received fees from AstraZeneca for the DAPA-CKD trial steering committee. The disclosures of the other authors are listed in the article. Dr. Mathieu has served on the advisory panel/speakers bureau for AstraZeneca. Dr. Chertow and Dr. Mathieu also have financial relationships with many other pharmaceutical companies.
Patients with stage 4 chronic kidney disease (CKD) who were in the DAPA-CKD trial had cardiorenal benefits from dapagliflozin that were similar to those of patients in the overall trial, with no added safety signal.
DAPA-CKD (Dapagliflozin and Prevention of Adverse Outcomes in Chronic Kidney Disease) was a landmark study of more than 4,000 patients with CKD, with an estimated glomerular filtration rate (eGFR) of 25-75 mL/min per 1.73 m2 and albuminuria with/without type 2 diabetes.
The primary results showed that patients who received the sodium-glucose cotransporter 2 (SGLT2) inhibitor dapagliflozin for a median of 2.4 years were significantly less likely to have worsening kidney disease or die from all causes than were patients who received placebo.
“This prespecified subanalysis of people with an eGFR < 30 mL/min/1.73 m2 [stage 4 CKD] in the DAPA-CKD study shows first, that in this very vulnerable population, use of the SGLT2 inhibitor is safe,” said Chantal Mathieu, MD, PhD.
Furthermore, there was no signal whatsoever of more adverse events and even a trend to fewer events, she said in an email to this news organization.
The analysis also showed that “although now in small numbers (around 300 each in the treated group vs. placebo group), there is no suggestion that the protective effect of dapagliflozin on the renal and cardiovascular front would not happen in this group” with advanced CKD. The efficacy findings just missed statistical significance, noted Dr. Mathieu, of Catholic University, Leuven, Belgium, who was not involved in the study.
Although dapagliflozin is now approved for treating patients with CKD who are at risk of kidney disease progression (on the basis of the DAPA-CKD results), guidelines have not yet been updated to reflect this, lead investigator Glenn M. Chertow, MD, MPH, of Stanford (Calif.) University, told this news organization in an email.
“For clinicians,” Dr. Mathieu said, “this is now the absolute reassurance that we do not have to stop an SGLT2 inhibitor in people with eGFR < 30 mL/min for safety reasons and that we should maintain them at these values for renal and cardiovascular protection!
“I absolutely hope labels will change soon to reflect these observations (and indeed movement on that front is happening),” she continued.
“The American Diabetes Association/European Association for the Study of Diabetes consensus on glucose-lowering therapies in type 2 diabetes already advocated keeping these agents until eGFR 30 mL/min (on the basis of evidence in 2019),” Dr. Mathieu added, “but this study will probably push the statements even further.”
“Of note,” she pointed out, “at these low eGFRs, the glucose-lowering potential of the SGLT2 inhibitor is negligible.”
Dapagliflozin risks and benefits in advanced CKD
Based on the DAPA-CKD study, published in the New England Journal of Medicine Oct. 8, 2020, the Food and Drug Administration expanded the indication for dapagliflozin (Farxiga, AstraZeneca) in April of 2021.
However, relatively little is known about the safety and efficacy of SGLT2 inhibitors in patients with advanced CKD, who are particularly vulnerable to cardiovascular events and progressive kidney failure, Dr. Chertow and colleagues wrote.
The DAPA-CKD trial randomized 4,304 patients with CKD 1:1 to dapagliflozin 10 mg/day or placebo, including 624 patients (14%) who had eGFR < 30 mL/min per 1.73 m2 and albuminuria at baseline.
Patients in the subgroup with advanced CKD had a mean age of 62 years, and 37% were female. About two-thirds had type 2 diabetes and about one-third had cardiovascular disease.
A total of 293 patients received dapagliflozin and 331 patients received placebo.
During a median follow-up of 2.4 years, patients who received dapagliflozin as opposed to placebo had a lower risk of the primary efficacy outcome – a composite of a 50% or greater sustained decline in eGFR, end-stage kidney disease, or death from cardiovascular or renal causes (hazard ratio, 0.73; 95% confidence interval, 0.53-1.02).
In secondary efficacy outcomes, patients who received dapagliflozin as opposed to placebo also had a lower risk of the following:
- A renal composite outcome – a ≥ 50% sustained decline in eGFR, end-stage kidney disease, or death from renal causes (HR, 0.71; 95% CI, 0.49-1.02).
- A cardiovascular composite outcome comprising cardiovascular death or hospitalization for heart failure (HR, 0.83; 95% CI, 0.45-1.53).
- All-cause mortality (HR, 0.68; 95% CI, 0.39 to 1.21).
The eGFR slope declined by 2.15 mL/min per 1.73 m2 per year and by 3.38 mL/min per 1.73 m2 per year in the dapagliflozin and placebo groups, respectively (P = .005).
“The trial was not powered to detect a statistically significant difference in the primary and key secondary endpoints in modest-sized subgroups,” the researchers noted.
The researchers limited their safety analysis to serious adverse events or symptoms of volume depletion, kidney-related events, major hypoglycemia, bone fractures, amputations, and potential diabetic ketoacidosis.
There was no evidence of increased risk of these adverse events in patients who received dapagliflozin.
The subanalysis of the DAPA-CKD trial was published July 16 in the Journal of the American Society of Nephrology.
The study was funded by AstraZeneca. Dr. Chertow has received fees from AstraZeneca for the DAPA-CKD trial steering committee. The disclosures of the other authors are listed in the article. Dr. Mathieu has served on the advisory panel/speakers bureau for AstraZeneca. Dr. Chertow and Dr. Mathieu also have financial relationships with many other pharmaceutical companies.
Patients with stage 4 chronic kidney disease (CKD) who were in the DAPA-CKD trial had cardiorenal benefits from dapagliflozin that were similar to those of patients in the overall trial, with no added safety signal.
DAPA-CKD (Dapagliflozin and Prevention of Adverse Outcomes in Chronic Kidney Disease) was a landmark study of more than 4,000 patients with CKD, with an estimated glomerular filtration rate (eGFR) of 25-75 mL/min per 1.73 m2 and albuminuria with/without type 2 diabetes.
The primary results showed that patients who received the sodium-glucose cotransporter 2 (SGLT2) inhibitor dapagliflozin for a median of 2.4 years were significantly less likely to have worsening kidney disease or die from all causes than were patients who received placebo.
“This prespecified subanalysis of people with an eGFR < 30 mL/min/1.73 m2 [stage 4 CKD] in the DAPA-CKD study shows first, that in this very vulnerable population, use of the SGLT2 inhibitor is safe,” said Chantal Mathieu, MD, PhD.
Furthermore, there was no signal whatsoever of more adverse events and even a trend to fewer events, she said in an email to this news organization.
The analysis also showed that “although now in small numbers (around 300 each in the treated group vs. placebo group), there is no suggestion that the protective effect of dapagliflozin on the renal and cardiovascular front would not happen in this group” with advanced CKD. The efficacy findings just missed statistical significance, noted Dr. Mathieu, of Catholic University, Leuven, Belgium, who was not involved in the study.
Although dapagliflozin is now approved for treating patients with CKD who are at risk of kidney disease progression (on the basis of the DAPA-CKD results), guidelines have not yet been updated to reflect this, lead investigator Glenn M. Chertow, MD, MPH, of Stanford (Calif.) University, told this news organization in an email.
“For clinicians,” Dr. Mathieu said, “this is now the absolute reassurance that we do not have to stop an SGLT2 inhibitor in people with eGFR < 30 mL/min for safety reasons and that we should maintain them at these values for renal and cardiovascular protection!
“I absolutely hope labels will change soon to reflect these observations (and indeed movement on that front is happening),” she continued.
“The American Diabetes Association/European Association for the Study of Diabetes consensus on glucose-lowering therapies in type 2 diabetes already advocated keeping these agents until eGFR 30 mL/min (on the basis of evidence in 2019),” Dr. Mathieu added, “but this study will probably push the statements even further.”
“Of note,” she pointed out, “at these low eGFRs, the glucose-lowering potential of the SGLT2 inhibitor is negligible.”
Dapagliflozin risks and benefits in advanced CKD
Based on the DAPA-CKD study, published in the New England Journal of Medicine Oct. 8, 2020, the Food and Drug Administration expanded the indication for dapagliflozin (Farxiga, AstraZeneca) in April of 2021.
However, relatively little is known about the safety and efficacy of SGLT2 inhibitors in patients with advanced CKD, who are particularly vulnerable to cardiovascular events and progressive kidney failure, Dr. Chertow and colleagues wrote.
The DAPA-CKD trial randomized 4,304 patients with CKD 1:1 to dapagliflozin 10 mg/day or placebo, including 624 patients (14%) who had eGFR < 30 mL/min per 1.73 m2 and albuminuria at baseline.
Patients in the subgroup with advanced CKD had a mean age of 62 years, and 37% were female. About two-thirds had type 2 diabetes and about one-third had cardiovascular disease.
A total of 293 patients received dapagliflozin and 331 patients received placebo.
During a median follow-up of 2.4 years, patients who received dapagliflozin as opposed to placebo had a lower risk of the primary efficacy outcome – a composite of a 50% or greater sustained decline in eGFR, end-stage kidney disease, or death from cardiovascular or renal causes (hazard ratio, 0.73; 95% confidence interval, 0.53-1.02).
In secondary efficacy outcomes, patients who received dapagliflozin as opposed to placebo also had a lower risk of the following:
- A renal composite outcome – a ≥ 50% sustained decline in eGFR, end-stage kidney disease, or death from renal causes (HR, 0.71; 95% CI, 0.49-1.02).
- A cardiovascular composite outcome comprising cardiovascular death or hospitalization for heart failure (HR, 0.83; 95% CI, 0.45-1.53).
- All-cause mortality (HR, 0.68; 95% CI, 0.39 to 1.21).
The eGFR slope declined by 2.15 mL/min per 1.73 m2 per year and by 3.38 mL/min per 1.73 m2 per year in the dapagliflozin and placebo groups, respectively (P = .005).
“The trial was not powered to detect a statistically significant difference in the primary and key secondary endpoints in modest-sized subgroups,” the researchers noted.
The researchers limited their safety analysis to serious adverse events or symptoms of volume depletion, kidney-related events, major hypoglycemia, bone fractures, amputations, and potential diabetic ketoacidosis.
There was no evidence of increased risk of these adverse events in patients who received dapagliflozin.
The subanalysis of the DAPA-CKD trial was published July 16 in the Journal of the American Society of Nephrology.
The study was funded by AstraZeneca. Dr. Chertow has received fees from AstraZeneca for the DAPA-CKD trial steering committee. The disclosures of the other authors are listed in the article. Dr. Mathieu has served on the advisory panel/speakers bureau for AstraZeneca. Dr. Chertow and Dr. Mathieu also have financial relationships with many other pharmaceutical companies.
FROM THE JOURNAL OF THE AMERICAN SOCIETY OF NEPHROLOGY
Statins again linked to lower COVID-19 mortality
Among patients hospitalized for COVID-19, those who had been taking statins had a substantially lower risk of death in a new large observational study.
Results showed that use of statins prior to admission was linked to a greater than 40% reduction in mortality and a greater than 25% reduction in risk of developing a severe outcome.
The findings come an analysis of data from the American Heart Association’s COVID-19 Cardiovascular Disease Registry on more than 10,000 patients hospitalized with COVID-19 at 104 hospitals across the United States published in PLoS One.
While several other studies have suggested benefits of statins in COVID-19, this is by far the largest study so far on this topic.
“I would say this is the most reliable study on statins in COVID-19 to date, with the results adjusted for many confounders, including socioeconomic factors and insurance type,” lead author Lori B. Daniels, MD, told this news organization. “However, it still an observational study and therefore falls short of a randomized study. But I would think a randomized study of statins in COVID-19 is probably not feasible, so this study provides excellent data at an observational level.”
After propensity matching for cardiovascular disease, results showed that most of the benefit of statins occurred in patients with known cardiovascular disease.
“While most patients taking statins will have cardiovascular disease, there are also many patients who take these drugs who don’t have heart disease but do have cardiovascular risk factors, such as those with raised cholesterol, or a family history of cardiovascular disease. For [such patients], the effect of statins was also in the same direction but it was not significant. This doesn’t exclude an effect,” noted Dr. Daniels, who is professor of medicine and director of cardiovascular intensive care at the University of California, San Diego.
“We are not saying that everyone should rush out and take a statin if they do not have risk factors for cardiovascular in order to lower their risk of dying from COVID. But if individuals do have an indication for a statin and are not taking one of these dugs this is another good reason to start taking them now,” she added.
The investigators embarked on the study because, although previous observational studies have found that statins may reduce the severity of COVID-19 infection, these studies have been limited in size with mostly single-center or regional studies, and some results have been conflicting. They therefore conducted the current, much larger analysis, in the AHA COVID-19 CVD Registry which systematically collected hospitalized patient–level data in a broad and diverse hospital and patient population across the United States.
For the analysis, the researchers analyzed data from 10,541 patients hospitalized with COVID-19 through September 2020 at 104 U.S. hospitals enrolled in the AHA registry to evaluate the associations between statin use and outcomes.
Most patients (71%) had either cardiovascular disease, hypertension, or both. Prior to admission, 42% of subjects used statins, with 7% being on statins alone and 35% on statins plus antihypertensives. Death (or discharge to hospice) occurred in 2,212 subjects (21%).
Results showed that outpatient use of statins, either alone or with antihypertensives, was associated with a 41% reduced risk of death (odds ratio, 0.59; 95% confidence interval, 0.50-0.69), after adjusting for demographic characteristics, underlying conditions, insurance status, hospital site, and concurrent medications. Statin use was also associated with a roughly 25% lower adjusted odds of developing severe disease.
Noting that patients on statins are also likely to be on antihypertensive medication, the researchers found that the statin benefit on mortality was seen in both patients taking a statin alone (OR, 0.54) and in those taking statins with an antihypertensive medication (OR, 0.60).
Use of antihypertensive drugs was associated with a smaller, albeit still substantial, 27% lower odds of death (OR, 0.73; 95% CI, 0.62-0.87).
In propensity-matched analyses, use of statins and/or antihypertensives was tied to a 32% reduced risk of death among those with a history of CVD and/or hypertension (OR, 0.68; 95% CI, 0.58-0.81). An observed 16% reduction in odds of death with statins and/or antihypertensive drugs among those without cardiovascular disease and/or hypertension was not statistically significant (OR, 0.84; 95% CI, 0.58-1.22).
Stabilizing the underlying disease
The researchers pointed out that the results of the propensity matching analysis are consistent with the hypothesis that the major benefit of these medications accrues from treating and/or stabilizing underlying disease.
“Although it is well known that statins improve long-term outcomes among patients with or at elevated risk for cardiovascular disease, the association with a large short-term benefit which accrues in the setting of hospitalization for COVID-19 is a new and intriguing finding,” they said.
They cited several “plausible mechanisms whereby statins could directly mitigate outcomes in COVID-19 beyond treating underlying disease conditions,” including anti-inflammatory effects and a direct inhibitory effect on the SARS-CoV-2 virus.
Dr. Daniels elaborated more on the potential mechanism at play in an interview: “I think what is happening is that the statin is stabilizing the coronary disease so patients are less likely to die from MI or stroke, and this gives them more time and strength to recover from COVID-19.”
She added: “Statins may also have some direct anti-COVID effects such as an anti-inflammatory actions, but I would guess that this is probably not the primary effect behind what we’re seeing here.”
‘Important clinical implications’
The authors say their findings have “important clinical implications.”
They noted that early in the pandemic there was speculation that certain medications, including statins, and the ACE inhibitor/angiotensin receptor blocker (ARB) classes of antihypertensives may confer an increased susceptibility to COVID-19 positivity and/or severity.
“Our study reinforces the AHA and others’ recommendations that not only is it safe to remain on these medications, but they may substantially reduce risk of severe COVID-19 and especially death from COVID-19, particularly statins, and particularly among those with associated underlying conditions,” the authors stressed.
Dr. Daniels added that, although statins are very safe drugs, there are always some patients who prefer not to take medication even if indicated, and others who may have borderline indications and decide not to take a statin at present.
“This study may persuade these patients that taking a statin is the right thing to do. It may give those patients on the cusp of thinking about taking one of these drugs a reason to go ahead,” she said.
‘Provocative but not definitive’
Commenting on the study, Robert Harrington, MD, professor of medicine and chair of the department of medicine at Stanford (Calif.) University, said: “These are interesting observational data but as such have all the limitations of nonrandomized comparisons despite the best attempts to adjust for a variety of potential confounders. For example, is this an effect of statins (perhaps through some anti-inflammatory mechanism) or is it more an effect that can be attributed to the patients who are prescribed and taking a statin, compared with those who are not?”
He added: “The primary clinical benefit of statins, based on many large randomized clinical trials, seems to be derived from their LDL lowering effect. Observational studies have suggested potential benefits from anti-inflammatory effects of statins, but the randomized trials have not confirmed these observations. So, the current data are interesting, even provocative, but ultimately hypothesis generating rather than definitive.”
Also commenting on the study, Steven Nissen, MD, professor of medicine at the Cleveland Clinic, said: “While statins have many established benefits, their role in preventing COVID-19 complications is very speculative. Like all observational studies, the current study must be viewed as hypothesis generating, not definitive evidence of benefit. There are many potential confounders. I’m skeptical.”
The authors of this study received no specific funding for this work and report no competing interests. Dr. Harrington was AHA president when the COVID registry was created and he is still a member of the AHA board, which has oversight over the project.
Among patients hospitalized for COVID-19, those who had been taking statins had a substantially lower risk of death in a new large observational study.
Results showed that use of statins prior to admission was linked to a greater than 40% reduction in mortality and a greater than 25% reduction in risk of developing a severe outcome.
The findings come an analysis of data from the American Heart Association’s COVID-19 Cardiovascular Disease Registry on more than 10,000 patients hospitalized with COVID-19 at 104 hospitals across the United States published in PLoS One.
While several other studies have suggested benefits of statins in COVID-19, this is by far the largest study so far on this topic.
“I would say this is the most reliable study on statins in COVID-19 to date, with the results adjusted for many confounders, including socioeconomic factors and insurance type,” lead author Lori B. Daniels, MD, told this news organization. “However, it still an observational study and therefore falls short of a randomized study. But I would think a randomized study of statins in COVID-19 is probably not feasible, so this study provides excellent data at an observational level.”
After propensity matching for cardiovascular disease, results showed that most of the benefit of statins occurred in patients with known cardiovascular disease.
“While most patients taking statins will have cardiovascular disease, there are also many patients who take these drugs who don’t have heart disease but do have cardiovascular risk factors, such as those with raised cholesterol, or a family history of cardiovascular disease. For [such patients], the effect of statins was also in the same direction but it was not significant. This doesn’t exclude an effect,” noted Dr. Daniels, who is professor of medicine and director of cardiovascular intensive care at the University of California, San Diego.
“We are not saying that everyone should rush out and take a statin if they do not have risk factors for cardiovascular in order to lower their risk of dying from COVID. But if individuals do have an indication for a statin and are not taking one of these dugs this is another good reason to start taking them now,” she added.
The investigators embarked on the study because, although previous observational studies have found that statins may reduce the severity of COVID-19 infection, these studies have been limited in size with mostly single-center or regional studies, and some results have been conflicting. They therefore conducted the current, much larger analysis, in the AHA COVID-19 CVD Registry which systematically collected hospitalized patient–level data in a broad and diverse hospital and patient population across the United States.
For the analysis, the researchers analyzed data from 10,541 patients hospitalized with COVID-19 through September 2020 at 104 U.S. hospitals enrolled in the AHA registry to evaluate the associations between statin use and outcomes.
Most patients (71%) had either cardiovascular disease, hypertension, or both. Prior to admission, 42% of subjects used statins, with 7% being on statins alone and 35% on statins plus antihypertensives. Death (or discharge to hospice) occurred in 2,212 subjects (21%).
Results showed that outpatient use of statins, either alone or with antihypertensives, was associated with a 41% reduced risk of death (odds ratio, 0.59; 95% confidence interval, 0.50-0.69), after adjusting for demographic characteristics, underlying conditions, insurance status, hospital site, and concurrent medications. Statin use was also associated with a roughly 25% lower adjusted odds of developing severe disease.
Noting that patients on statins are also likely to be on antihypertensive medication, the researchers found that the statin benefit on mortality was seen in both patients taking a statin alone (OR, 0.54) and in those taking statins with an antihypertensive medication (OR, 0.60).
Use of antihypertensive drugs was associated with a smaller, albeit still substantial, 27% lower odds of death (OR, 0.73; 95% CI, 0.62-0.87).
In propensity-matched analyses, use of statins and/or antihypertensives was tied to a 32% reduced risk of death among those with a history of CVD and/or hypertension (OR, 0.68; 95% CI, 0.58-0.81). An observed 16% reduction in odds of death with statins and/or antihypertensive drugs among those without cardiovascular disease and/or hypertension was not statistically significant (OR, 0.84; 95% CI, 0.58-1.22).
Stabilizing the underlying disease
The researchers pointed out that the results of the propensity matching analysis are consistent with the hypothesis that the major benefit of these medications accrues from treating and/or stabilizing underlying disease.
“Although it is well known that statins improve long-term outcomes among patients with or at elevated risk for cardiovascular disease, the association with a large short-term benefit which accrues in the setting of hospitalization for COVID-19 is a new and intriguing finding,” they said.
They cited several “plausible mechanisms whereby statins could directly mitigate outcomes in COVID-19 beyond treating underlying disease conditions,” including anti-inflammatory effects and a direct inhibitory effect on the SARS-CoV-2 virus.
Dr. Daniels elaborated more on the potential mechanism at play in an interview: “I think what is happening is that the statin is stabilizing the coronary disease so patients are less likely to die from MI or stroke, and this gives them more time and strength to recover from COVID-19.”
She added: “Statins may also have some direct anti-COVID effects such as an anti-inflammatory actions, but I would guess that this is probably not the primary effect behind what we’re seeing here.”
‘Important clinical implications’
The authors say their findings have “important clinical implications.”
They noted that early in the pandemic there was speculation that certain medications, including statins, and the ACE inhibitor/angiotensin receptor blocker (ARB) classes of antihypertensives may confer an increased susceptibility to COVID-19 positivity and/or severity.
“Our study reinforces the AHA and others’ recommendations that not only is it safe to remain on these medications, but they may substantially reduce risk of severe COVID-19 and especially death from COVID-19, particularly statins, and particularly among those with associated underlying conditions,” the authors stressed.
Dr. Daniels added that, although statins are very safe drugs, there are always some patients who prefer not to take medication even if indicated, and others who may have borderline indications and decide not to take a statin at present.
“This study may persuade these patients that taking a statin is the right thing to do. It may give those patients on the cusp of thinking about taking one of these drugs a reason to go ahead,” she said.
‘Provocative but not definitive’
Commenting on the study, Robert Harrington, MD, professor of medicine and chair of the department of medicine at Stanford (Calif.) University, said: “These are interesting observational data but as such have all the limitations of nonrandomized comparisons despite the best attempts to adjust for a variety of potential confounders. For example, is this an effect of statins (perhaps through some anti-inflammatory mechanism) or is it more an effect that can be attributed to the patients who are prescribed and taking a statin, compared with those who are not?”
He added: “The primary clinical benefit of statins, based on many large randomized clinical trials, seems to be derived from their LDL lowering effect. Observational studies have suggested potential benefits from anti-inflammatory effects of statins, but the randomized trials have not confirmed these observations. So, the current data are interesting, even provocative, but ultimately hypothesis generating rather than definitive.”
Also commenting on the study, Steven Nissen, MD, professor of medicine at the Cleveland Clinic, said: “While statins have many established benefits, their role in preventing COVID-19 complications is very speculative. Like all observational studies, the current study must be viewed as hypothesis generating, not definitive evidence of benefit. There are many potential confounders. I’m skeptical.”
The authors of this study received no specific funding for this work and report no competing interests. Dr. Harrington was AHA president when the COVID registry was created and he is still a member of the AHA board, which has oversight over the project.
Among patients hospitalized for COVID-19, those who had been taking statins had a substantially lower risk of death in a new large observational study.
Results showed that use of statins prior to admission was linked to a greater than 40% reduction in mortality and a greater than 25% reduction in risk of developing a severe outcome.
The findings come an analysis of data from the American Heart Association’s COVID-19 Cardiovascular Disease Registry on more than 10,000 patients hospitalized with COVID-19 at 104 hospitals across the United States published in PLoS One.
While several other studies have suggested benefits of statins in COVID-19, this is by far the largest study so far on this topic.
“I would say this is the most reliable study on statins in COVID-19 to date, with the results adjusted for many confounders, including socioeconomic factors and insurance type,” lead author Lori B. Daniels, MD, told this news organization. “However, it still an observational study and therefore falls short of a randomized study. But I would think a randomized study of statins in COVID-19 is probably not feasible, so this study provides excellent data at an observational level.”
After propensity matching for cardiovascular disease, results showed that most of the benefit of statins occurred in patients with known cardiovascular disease.
“While most patients taking statins will have cardiovascular disease, there are also many patients who take these drugs who don’t have heart disease but do have cardiovascular risk factors, such as those with raised cholesterol, or a family history of cardiovascular disease. For [such patients], the effect of statins was also in the same direction but it was not significant. This doesn’t exclude an effect,” noted Dr. Daniels, who is professor of medicine and director of cardiovascular intensive care at the University of California, San Diego.
“We are not saying that everyone should rush out and take a statin if they do not have risk factors for cardiovascular in order to lower their risk of dying from COVID. But if individuals do have an indication for a statin and are not taking one of these dugs this is another good reason to start taking them now,” she added.
The investigators embarked on the study because, although previous observational studies have found that statins may reduce the severity of COVID-19 infection, these studies have been limited in size with mostly single-center or regional studies, and some results have been conflicting. They therefore conducted the current, much larger analysis, in the AHA COVID-19 CVD Registry which systematically collected hospitalized patient–level data in a broad and diverse hospital and patient population across the United States.
For the analysis, the researchers analyzed data from 10,541 patients hospitalized with COVID-19 through September 2020 at 104 U.S. hospitals enrolled in the AHA registry to evaluate the associations between statin use and outcomes.
Most patients (71%) had either cardiovascular disease, hypertension, or both. Prior to admission, 42% of subjects used statins, with 7% being on statins alone and 35% on statins plus antihypertensives. Death (or discharge to hospice) occurred in 2,212 subjects (21%).
Results showed that outpatient use of statins, either alone or with antihypertensives, was associated with a 41% reduced risk of death (odds ratio, 0.59; 95% confidence interval, 0.50-0.69), after adjusting for demographic characteristics, underlying conditions, insurance status, hospital site, and concurrent medications. Statin use was also associated with a roughly 25% lower adjusted odds of developing severe disease.
Noting that patients on statins are also likely to be on antihypertensive medication, the researchers found that the statin benefit on mortality was seen in both patients taking a statin alone (OR, 0.54) and in those taking statins with an antihypertensive medication (OR, 0.60).
Use of antihypertensive drugs was associated with a smaller, albeit still substantial, 27% lower odds of death (OR, 0.73; 95% CI, 0.62-0.87).
In propensity-matched analyses, use of statins and/or antihypertensives was tied to a 32% reduced risk of death among those with a history of CVD and/or hypertension (OR, 0.68; 95% CI, 0.58-0.81). An observed 16% reduction in odds of death with statins and/or antihypertensive drugs among those without cardiovascular disease and/or hypertension was not statistically significant (OR, 0.84; 95% CI, 0.58-1.22).
Stabilizing the underlying disease
The researchers pointed out that the results of the propensity matching analysis are consistent with the hypothesis that the major benefit of these medications accrues from treating and/or stabilizing underlying disease.
“Although it is well known that statins improve long-term outcomes among patients with or at elevated risk for cardiovascular disease, the association with a large short-term benefit which accrues in the setting of hospitalization for COVID-19 is a new and intriguing finding,” they said.
They cited several “plausible mechanisms whereby statins could directly mitigate outcomes in COVID-19 beyond treating underlying disease conditions,” including anti-inflammatory effects and a direct inhibitory effect on the SARS-CoV-2 virus.
Dr. Daniels elaborated more on the potential mechanism at play in an interview: “I think what is happening is that the statin is stabilizing the coronary disease so patients are less likely to die from MI or stroke, and this gives them more time and strength to recover from COVID-19.”
She added: “Statins may also have some direct anti-COVID effects such as an anti-inflammatory actions, but I would guess that this is probably not the primary effect behind what we’re seeing here.”
‘Important clinical implications’
The authors say their findings have “important clinical implications.”
They noted that early in the pandemic there was speculation that certain medications, including statins, and the ACE inhibitor/angiotensin receptor blocker (ARB) classes of antihypertensives may confer an increased susceptibility to COVID-19 positivity and/or severity.
“Our study reinforces the AHA and others’ recommendations that not only is it safe to remain on these medications, but they may substantially reduce risk of severe COVID-19 and especially death from COVID-19, particularly statins, and particularly among those with associated underlying conditions,” the authors stressed.
Dr. Daniels added that, although statins are very safe drugs, there are always some patients who prefer not to take medication even if indicated, and others who may have borderline indications and decide not to take a statin at present.
“This study may persuade these patients that taking a statin is the right thing to do. It may give those patients on the cusp of thinking about taking one of these drugs a reason to go ahead,” she said.
‘Provocative but not definitive’
Commenting on the study, Robert Harrington, MD, professor of medicine and chair of the department of medicine at Stanford (Calif.) University, said: “These are interesting observational data but as such have all the limitations of nonrandomized comparisons despite the best attempts to adjust for a variety of potential confounders. For example, is this an effect of statins (perhaps through some anti-inflammatory mechanism) or is it more an effect that can be attributed to the patients who are prescribed and taking a statin, compared with those who are not?”
He added: “The primary clinical benefit of statins, based on many large randomized clinical trials, seems to be derived from their LDL lowering effect. Observational studies have suggested potential benefits from anti-inflammatory effects of statins, but the randomized trials have not confirmed these observations. So, the current data are interesting, even provocative, but ultimately hypothesis generating rather than definitive.”
Also commenting on the study, Steven Nissen, MD, professor of medicine at the Cleveland Clinic, said: “While statins have many established benefits, their role in preventing COVID-19 complications is very speculative. Like all observational studies, the current study must be viewed as hypothesis generating, not definitive evidence of benefit. There are many potential confounders. I’m skeptical.”
The authors of this study received no specific funding for this work and report no competing interests. Dr. Harrington was AHA president when the COVID registry was created and he is still a member of the AHA board, which has oversight over the project.
FROM PLOS ONE





















