User login
Endoscopic obesity treatments offer alternatives to surgery
SAN FRANCISCO – Endoscopic treatments for obesity are under-utilized but represent an opportunity for gastroenterologists to help address the metabolic epidemic that affects up to 40% of people in the United States, according to a presentation reviewing these techniques.
Lifestyle modification is the first intervention, but results in just a 5% average weight loss, according to Allison Schulman, MD, MPH, who discussed these options at the 2022 AGA Tech Summit sponsored by the AGA Center for GI Innovation and Technology. Although surgical interventions induce more weight loss and greater improvement of metabolic outcomes, they come with significant risks and many patients are reluctant to pursue them, she added. In fact, fewer than 1% of obese individuals who qualify for bariatric surgery ultimately undergo it.
Dr. Schulman emphasized another option: Endoscopic bariatric therapies fill this void in between those two extremes, as they are clearly less invasive” said Dr. Schulman, who is an assistant professor of gastroenterology and hepatology at the University of Michigan, Ann Arbor. “They may appeal to those who do not qualify or do not want bariatric surgery. They also could bridge a critical gap in the treatment of obesity, as they reach patients earlier, at BMIs [body mass indexes] where they may not be surgical candidates. Furthermore, these therapies are oftentimes repeatable and commonly can be used in combination [with other weight loss approaches].”
Endoscopic therapies for obesity include devices that occupy space in the stomach, such as intragastric balloons, gastric remodeling procedures like endoscopic sleeve gastroplasty (ESG), and aspiration therapy.
Potential candidates for noninvasive approaches include patients with a BMI over 30 kg/m2 who have not lost sufficient weight through nonsurgical methods or those who do not want to undergo surgery or require a bridge therapy to surgery.
Fluid-filled balloons can be placed and filled to an appropriate volume. One network meta-analysis found that fluid-filled balloons were more likely to lead to weight loss, but also more likely to be removed due to intolerance. She also noted that the Elipse balloon (Allurion Technologies) is designed to be swallowed and thus avoid procedures entirely; it is currently under review by Food and Drug Administration.
Although balloons are linked to 7%-10% weight loss in some studies and reviews, Dr. Schulman said, “we know … that the majority of these lead to much more weight loss in clinical practice, oftentimes closer to 13%-%15.”
One review found that balloons also lead to improvement in obesity-related comorbidities, compared with conventional nonsurgical approaches, and this benefit extends past 1 year. A study of 21 patients with nonalcoholic steatohepatitis (NASH) treated with intragastric balloons found that 90% had an improvement in nonalcoholic fatty liver disease activity score, with a median drop of 3 points, and 80% had a drop of at least 2 points. Of these patients, 50% also had an improvement in fibrosis determined by magnetic resonance elastography.
Balloon therapy should be highly individualized, according to Dr. Schulman.
Dr. Schulman also described ESG, which uses sutures to remodel the stomach and reduce volume by up to 70%. She outlined studies and reviews, such as those from Sharaiha and colleagues and Hedjoudje and colleagues, showing that ESG leads to significant and sustained weight loss. The procedure was also quite safe, with one large, single-center study showing that both fever and significant blood loss each occurred in less than 1% of patients (Gastrointest Endosc. 2019 Jun;89[6]:1132-8), while the systematic review and meta-analysis from Hedjoudje and colleagues found an adverse event frequency of 2.2%.
In a matched control study, laparoscopic sleeve gastrectomy led to more weight loss, but ESG had fewer adverse events (5.2% versus 16.9%; P < .01) and had a greater effect on gastroesophageal reflux disease.
ESG can be effective when repeated, while surgical revisions are associated with much higher morbidity, according to Dr. Schulman.
During her presentation, Dr. Schulman mentioned the AspireAssist device developed by Aspire Bariatrics, which is similar to a percutaneous endoscopic gastrostomy (PEG) tube. It leads to the removal of about 30% of calories consumed during a meal, with patients instructed to aspirate 20-30 minutes after a meal, two to three times a day. It gained Food and Drug Administration approval on the strength of the PATHWAY study, which showed significant weight loss.
“But perhaps more impressive is the overall patient satisfaction and willingness to recommend this device to others,” said Dr. Schulman.
Another approach she described is the transpyloric shuttle (TPS), which leads to faster filling times and delayed gastric emptying, though it must be removed endoscopically at 12 months.
Dr. Schulman also discussed endoscopic bariatric and metabolic therapy. This approach is currently a primary therapy for obesity, and is in development for the treatment of diabetes and non-alcoholic fatty liver disease. The approach is predicated on the idea that obesity is a disorder of energy homeostasis, and that enteric neurons in the small bowel are key players, possibly through reduced production of as yet unknown signaling molecules, leading to insulin resistance. It’s also known that diets high in fat and sugar alter the duodenum, which causes changes in nutrient signaling to the brain.
“It’s thought that this leads to duodenal endocrine hyperactivity and ultimately metabolic disease,” said Dr. Schulman.
Finally, she described small-bowel therapies like endobarrier sleeves, duodenal mucosal resurfacing, and an incisionless anastomosis system designed to improve glycemic control by altering the gut through noninvasive means.
Dr. Schulman has consulted for Apollo Endosurgery, Boston Scientific, Olympus, and MicroTech, and has received research support from GI Dynamics.
SAN FRANCISCO – Endoscopic treatments for obesity are under-utilized but represent an opportunity for gastroenterologists to help address the metabolic epidemic that affects up to 40% of people in the United States, according to a presentation reviewing these techniques.
Lifestyle modification is the first intervention, but results in just a 5% average weight loss, according to Allison Schulman, MD, MPH, who discussed these options at the 2022 AGA Tech Summit sponsored by the AGA Center for GI Innovation and Technology. Although surgical interventions induce more weight loss and greater improvement of metabolic outcomes, they come with significant risks and many patients are reluctant to pursue them, she added. In fact, fewer than 1% of obese individuals who qualify for bariatric surgery ultimately undergo it.
Dr. Schulman emphasized another option: Endoscopic bariatric therapies fill this void in between those two extremes, as they are clearly less invasive” said Dr. Schulman, who is an assistant professor of gastroenterology and hepatology at the University of Michigan, Ann Arbor. “They may appeal to those who do not qualify or do not want bariatric surgery. They also could bridge a critical gap in the treatment of obesity, as they reach patients earlier, at BMIs [body mass indexes] where they may not be surgical candidates. Furthermore, these therapies are oftentimes repeatable and commonly can be used in combination [with other weight loss approaches].”
Endoscopic therapies for obesity include devices that occupy space in the stomach, such as intragastric balloons, gastric remodeling procedures like endoscopic sleeve gastroplasty (ESG), and aspiration therapy.
Potential candidates for noninvasive approaches include patients with a BMI over 30 kg/m2 who have not lost sufficient weight through nonsurgical methods or those who do not want to undergo surgery or require a bridge therapy to surgery.
Fluid-filled balloons can be placed and filled to an appropriate volume. One network meta-analysis found that fluid-filled balloons were more likely to lead to weight loss, but also more likely to be removed due to intolerance. She also noted that the Elipse balloon (Allurion Technologies) is designed to be swallowed and thus avoid procedures entirely; it is currently under review by Food and Drug Administration.
Although balloons are linked to 7%-10% weight loss in some studies and reviews, Dr. Schulman said, “we know … that the majority of these lead to much more weight loss in clinical practice, oftentimes closer to 13%-%15.”
One review found that balloons also lead to improvement in obesity-related comorbidities, compared with conventional nonsurgical approaches, and this benefit extends past 1 year. A study of 21 patients with nonalcoholic steatohepatitis (NASH) treated with intragastric balloons found that 90% had an improvement in nonalcoholic fatty liver disease activity score, with a median drop of 3 points, and 80% had a drop of at least 2 points. Of these patients, 50% also had an improvement in fibrosis determined by magnetic resonance elastography.
Balloon therapy should be highly individualized, according to Dr. Schulman.
Dr. Schulman also described ESG, which uses sutures to remodel the stomach and reduce volume by up to 70%. She outlined studies and reviews, such as those from Sharaiha and colleagues and Hedjoudje and colleagues, showing that ESG leads to significant and sustained weight loss. The procedure was also quite safe, with one large, single-center study showing that both fever and significant blood loss each occurred in less than 1% of patients (Gastrointest Endosc. 2019 Jun;89[6]:1132-8), while the systematic review and meta-analysis from Hedjoudje and colleagues found an adverse event frequency of 2.2%.
In a matched control study, laparoscopic sleeve gastrectomy led to more weight loss, but ESG had fewer adverse events (5.2% versus 16.9%; P < .01) and had a greater effect on gastroesophageal reflux disease.
ESG can be effective when repeated, while surgical revisions are associated with much higher morbidity, according to Dr. Schulman.
During her presentation, Dr. Schulman mentioned the AspireAssist device developed by Aspire Bariatrics, which is similar to a percutaneous endoscopic gastrostomy (PEG) tube. It leads to the removal of about 30% of calories consumed during a meal, with patients instructed to aspirate 20-30 minutes after a meal, two to three times a day. It gained Food and Drug Administration approval on the strength of the PATHWAY study, which showed significant weight loss.
“But perhaps more impressive is the overall patient satisfaction and willingness to recommend this device to others,” said Dr. Schulman.
Another approach she described is the transpyloric shuttle (TPS), which leads to faster filling times and delayed gastric emptying, though it must be removed endoscopically at 12 months.
Dr. Schulman also discussed endoscopic bariatric and metabolic therapy. This approach is currently a primary therapy for obesity, and is in development for the treatment of diabetes and non-alcoholic fatty liver disease. The approach is predicated on the idea that obesity is a disorder of energy homeostasis, and that enteric neurons in the small bowel are key players, possibly through reduced production of as yet unknown signaling molecules, leading to insulin resistance. It’s also known that diets high in fat and sugar alter the duodenum, which causes changes in nutrient signaling to the brain.
“It’s thought that this leads to duodenal endocrine hyperactivity and ultimately metabolic disease,” said Dr. Schulman.
Finally, she described small-bowel therapies like endobarrier sleeves, duodenal mucosal resurfacing, and an incisionless anastomosis system designed to improve glycemic control by altering the gut through noninvasive means.
Dr. Schulman has consulted for Apollo Endosurgery, Boston Scientific, Olympus, and MicroTech, and has received research support from GI Dynamics.
SAN FRANCISCO – Endoscopic treatments for obesity are under-utilized but represent an opportunity for gastroenterologists to help address the metabolic epidemic that affects up to 40% of people in the United States, according to a presentation reviewing these techniques.
Lifestyle modification is the first intervention, but results in just a 5% average weight loss, according to Allison Schulman, MD, MPH, who discussed these options at the 2022 AGA Tech Summit sponsored by the AGA Center for GI Innovation and Technology. Although surgical interventions induce more weight loss and greater improvement of metabolic outcomes, they come with significant risks and many patients are reluctant to pursue them, she added. In fact, fewer than 1% of obese individuals who qualify for bariatric surgery ultimately undergo it.
Dr. Schulman emphasized another option: Endoscopic bariatric therapies fill this void in between those two extremes, as they are clearly less invasive” said Dr. Schulman, who is an assistant professor of gastroenterology and hepatology at the University of Michigan, Ann Arbor. “They may appeal to those who do not qualify or do not want bariatric surgery. They also could bridge a critical gap in the treatment of obesity, as they reach patients earlier, at BMIs [body mass indexes] where they may not be surgical candidates. Furthermore, these therapies are oftentimes repeatable and commonly can be used in combination [with other weight loss approaches].”
Endoscopic therapies for obesity include devices that occupy space in the stomach, such as intragastric balloons, gastric remodeling procedures like endoscopic sleeve gastroplasty (ESG), and aspiration therapy.
Potential candidates for noninvasive approaches include patients with a BMI over 30 kg/m2 who have not lost sufficient weight through nonsurgical methods or those who do not want to undergo surgery or require a bridge therapy to surgery.
Fluid-filled balloons can be placed and filled to an appropriate volume. One network meta-analysis found that fluid-filled balloons were more likely to lead to weight loss, but also more likely to be removed due to intolerance. She also noted that the Elipse balloon (Allurion Technologies) is designed to be swallowed and thus avoid procedures entirely; it is currently under review by Food and Drug Administration.
Although balloons are linked to 7%-10% weight loss in some studies and reviews, Dr. Schulman said, “we know … that the majority of these lead to much more weight loss in clinical practice, oftentimes closer to 13%-%15.”
One review found that balloons also lead to improvement in obesity-related comorbidities, compared with conventional nonsurgical approaches, and this benefit extends past 1 year. A study of 21 patients with nonalcoholic steatohepatitis (NASH) treated with intragastric balloons found that 90% had an improvement in nonalcoholic fatty liver disease activity score, with a median drop of 3 points, and 80% had a drop of at least 2 points. Of these patients, 50% also had an improvement in fibrosis determined by magnetic resonance elastography.
Balloon therapy should be highly individualized, according to Dr. Schulman.
Dr. Schulman also described ESG, which uses sutures to remodel the stomach and reduce volume by up to 70%. She outlined studies and reviews, such as those from Sharaiha and colleagues and Hedjoudje and colleagues, showing that ESG leads to significant and sustained weight loss. The procedure was also quite safe, with one large, single-center study showing that both fever and significant blood loss each occurred in less than 1% of patients (Gastrointest Endosc. 2019 Jun;89[6]:1132-8), while the systematic review and meta-analysis from Hedjoudje and colleagues found an adverse event frequency of 2.2%.
In a matched control study, laparoscopic sleeve gastrectomy led to more weight loss, but ESG had fewer adverse events (5.2% versus 16.9%; P < .01) and had a greater effect on gastroesophageal reflux disease.
ESG can be effective when repeated, while surgical revisions are associated with much higher morbidity, according to Dr. Schulman.
During her presentation, Dr. Schulman mentioned the AspireAssist device developed by Aspire Bariatrics, which is similar to a percutaneous endoscopic gastrostomy (PEG) tube. It leads to the removal of about 30% of calories consumed during a meal, with patients instructed to aspirate 20-30 minutes after a meal, two to three times a day. It gained Food and Drug Administration approval on the strength of the PATHWAY study, which showed significant weight loss.
“But perhaps more impressive is the overall patient satisfaction and willingness to recommend this device to others,” said Dr. Schulman.
Another approach she described is the transpyloric shuttle (TPS), which leads to faster filling times and delayed gastric emptying, though it must be removed endoscopically at 12 months.
Dr. Schulman also discussed endoscopic bariatric and metabolic therapy. This approach is currently a primary therapy for obesity, and is in development for the treatment of diabetes and non-alcoholic fatty liver disease. The approach is predicated on the idea that obesity is a disorder of energy homeostasis, and that enteric neurons in the small bowel are key players, possibly through reduced production of as yet unknown signaling molecules, leading to insulin resistance. It’s also known that diets high in fat and sugar alter the duodenum, which causes changes in nutrient signaling to the brain.
“It’s thought that this leads to duodenal endocrine hyperactivity and ultimately metabolic disease,” said Dr. Schulman.
Finally, she described small-bowel therapies like endobarrier sleeves, duodenal mucosal resurfacing, and an incisionless anastomosis system designed to improve glycemic control by altering the gut through noninvasive means.
Dr. Schulman has consulted for Apollo Endosurgery, Boston Scientific, Olympus, and MicroTech, and has received research support from GI Dynamics.
AT 2022 AGA TECH SUMMIT
Complicated appendicitis during pregnancy: Immediate surgery may be best
Pregnant women who underwent immediate surgery to treat a ruptured or abscessed appendix had lower risk of infectious complications, compared with those whose complicated appendicitis was managed without surgery, according to new research.
Most cases that began with nonoperative management eventually required surgery, and the operative delay was associated with an increased risk of preterm labor, preterm delivery, and abortion.
“Our study findings may help to define the preferred management strategy in complicated appendicitis during pregnancy to be immediate operation,” Kazuhide Matsushima, MD, an assistant professor of clinical surgery at the University of Southern California, Los Angeles, and colleagues wrote.
The retrospective study was published in JAMA Network Open.
While acute appendicitis is relatively rare during pregnancy, it is the most common nonobstetric emergency in pregnant women, Dr. Matsushima said. This condition occurs in an estimated 1 in 700 to 1 in 1,500 pregnancies, and some data suggest that pregnant women are at higher risk for perforation and other forms of complicated appendicitis.
National guidelines support appendectomy as the first-line treatment for pregnant women with acute uncomplicated appendicitis, but there is no clear guidance on the best treatment approach for managing complicated appendicitis in this population, the authors note.
To better understand how surgical and nonoperational interventions affected outcomes, investigators analyzed data from the National Inpatient Sample from January 2003 to September 2015 to identify pregnant women with complicated appendicitis. The condition was defined as “acute appendicitis with generalized peritonitis” and “acute appendicitis with peritoneal abscess.” Patients were excluded if they had complications such as ectopic pregnancy and hydatidiform mole.
Investigators split the patients into three groups: those who underwent immediate operation for complicated appendicitis, those whose appendicitis was successfully managed without surgery, and those in whom nonoperative management of their condition failed, resulting in delayed surgery. Failed nonoperative management was defined as at least 1 day of nonoperative management followed by a laparoscopic or open appendectomy.
Of the 8,087 pregnant women identified during the study with complicated appendicitis, 55.5% underwent immediate appendectomy, 11.8% were successfully treated without surgical intervention, and 32.7% had delayed operations after initial failed nonoperative management. There was no significant difference in preterm delivery, preterm labor, or abortion between the immediate operative and successful nonoperative groups; however, the successful nonoperative group was more than twice as likely to experience premature rupture of membranes (odds ratio, 2.77; P = .03). Patients successfully treated without surgery also were at higher risk for infections such as amniotic infection (OR, 4.35; P < .001), pneumonia (OR, 2.52; P < .001), and sepsis (OR, 1.52; P = .01), compared with patients who underwent immediate operation.
Patients who had delayed surgery were 45% more likely to experience preterm delivery, preterm labor, or abortion (OR, 1.45; P < .001), compared with the immediate surgery group. The delayed surgery group was also at higher risk for antepartum hemorrhage (OR, 1.56; P = .03) and premature rupture of membranes (OR, 3.44; P = .002). They were more than four times as likely to have amniotic infection (OR, 4.74; P < .001), twice as likely to contract pneumonia (OR, 2.01; P < .001), and 58% more likely to develop sepsis (OR, 1.58; P < .001), compared with the immediate surgery group. The researchers calculated that every day surgery was delayed, the risk of preterm delivery, preterm labor, and abortion rose by 23% (OR, 1.23; P < .001).
Delayed surgery and successful nonoperative management were also associated with higher hospital charges and longer hospital stays.
Because this was a retrospective study, there are some limitations to the findings, Dr. Matsushima said, and therefore it should not be used to justify changing standards of care; however, it does give more information on the risks associated with different interventions. “It’s very important to have a discussion with the patient and make a shared decision,” he told this news organization, “because each option has significant risks and benefits.”
Because the data were from a database, he added, the research team was not able to see if outcomes from immediate surgery, nonoperative management, and delayed surgery differed in each trimester.
Kenneth W. Sharp, MD, a professor of surgery at Vanderbilt University Medical Center in Nashville, Tenn., agreed that the study does have limitations, such as lack of information on how complicated appendicitis was identified and diagnosed; however, the study does provide guidance to surgeons in a surgical area with “very sparse literature,” he told this news organization. Dr. Sharp is also a regent from the American College of Surgeons, which arranged the interview.
“Especially with these very complicated patients, it was never clear what to do,” he said. “With the recent studies showing that treatment of appendicitis with antibiotics works for a large number of people, people start extrapolating [those findings] to complicated appendicitis and they start extrapolating it to pregnant women, none of which the studies were meant to show anything about,” he said.
This analysis gives additional information to inform treatment decisions in pregnant women who may be hesitant to undergo this abdominal surgery because of possible complications, like pregnancy loss, he added. “Now, I can say to them that the data would suggest that with your particular complicated appendicitis, we should operate sooner, not later.”
Dr. Matsushima and Dr. Sharp have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Pregnant women who underwent immediate surgery to treat a ruptured or abscessed appendix had lower risk of infectious complications, compared with those whose complicated appendicitis was managed without surgery, according to new research.
Most cases that began with nonoperative management eventually required surgery, and the operative delay was associated with an increased risk of preterm labor, preterm delivery, and abortion.
“Our study findings may help to define the preferred management strategy in complicated appendicitis during pregnancy to be immediate operation,” Kazuhide Matsushima, MD, an assistant professor of clinical surgery at the University of Southern California, Los Angeles, and colleagues wrote.
The retrospective study was published in JAMA Network Open.
While acute appendicitis is relatively rare during pregnancy, it is the most common nonobstetric emergency in pregnant women, Dr. Matsushima said. This condition occurs in an estimated 1 in 700 to 1 in 1,500 pregnancies, and some data suggest that pregnant women are at higher risk for perforation and other forms of complicated appendicitis.
National guidelines support appendectomy as the first-line treatment for pregnant women with acute uncomplicated appendicitis, but there is no clear guidance on the best treatment approach for managing complicated appendicitis in this population, the authors note.
To better understand how surgical and nonoperational interventions affected outcomes, investigators analyzed data from the National Inpatient Sample from January 2003 to September 2015 to identify pregnant women with complicated appendicitis. The condition was defined as “acute appendicitis with generalized peritonitis” and “acute appendicitis with peritoneal abscess.” Patients were excluded if they had complications such as ectopic pregnancy and hydatidiform mole.
Investigators split the patients into three groups: those who underwent immediate operation for complicated appendicitis, those whose appendicitis was successfully managed without surgery, and those in whom nonoperative management of their condition failed, resulting in delayed surgery. Failed nonoperative management was defined as at least 1 day of nonoperative management followed by a laparoscopic or open appendectomy.
Of the 8,087 pregnant women identified during the study with complicated appendicitis, 55.5% underwent immediate appendectomy, 11.8% were successfully treated without surgical intervention, and 32.7% had delayed operations after initial failed nonoperative management. There was no significant difference in preterm delivery, preterm labor, or abortion between the immediate operative and successful nonoperative groups; however, the successful nonoperative group was more than twice as likely to experience premature rupture of membranes (odds ratio, 2.77; P = .03). Patients successfully treated without surgery also were at higher risk for infections such as amniotic infection (OR, 4.35; P < .001), pneumonia (OR, 2.52; P < .001), and sepsis (OR, 1.52; P = .01), compared with patients who underwent immediate operation.
Patients who had delayed surgery were 45% more likely to experience preterm delivery, preterm labor, or abortion (OR, 1.45; P < .001), compared with the immediate surgery group. The delayed surgery group was also at higher risk for antepartum hemorrhage (OR, 1.56; P = .03) and premature rupture of membranes (OR, 3.44; P = .002). They were more than four times as likely to have amniotic infection (OR, 4.74; P < .001), twice as likely to contract pneumonia (OR, 2.01; P < .001), and 58% more likely to develop sepsis (OR, 1.58; P < .001), compared with the immediate surgery group. The researchers calculated that every day surgery was delayed, the risk of preterm delivery, preterm labor, and abortion rose by 23% (OR, 1.23; P < .001).
Delayed surgery and successful nonoperative management were also associated with higher hospital charges and longer hospital stays.
Because this was a retrospective study, there are some limitations to the findings, Dr. Matsushima said, and therefore it should not be used to justify changing standards of care; however, it does give more information on the risks associated with different interventions. “It’s very important to have a discussion with the patient and make a shared decision,” he told this news organization, “because each option has significant risks and benefits.”
Because the data were from a database, he added, the research team was not able to see if outcomes from immediate surgery, nonoperative management, and delayed surgery differed in each trimester.
Kenneth W. Sharp, MD, a professor of surgery at Vanderbilt University Medical Center in Nashville, Tenn., agreed that the study does have limitations, such as lack of information on how complicated appendicitis was identified and diagnosed; however, the study does provide guidance to surgeons in a surgical area with “very sparse literature,” he told this news organization. Dr. Sharp is also a regent from the American College of Surgeons, which arranged the interview.
“Especially with these very complicated patients, it was never clear what to do,” he said. “With the recent studies showing that treatment of appendicitis with antibiotics works for a large number of people, people start extrapolating [those findings] to complicated appendicitis and they start extrapolating it to pregnant women, none of which the studies were meant to show anything about,” he said.
This analysis gives additional information to inform treatment decisions in pregnant women who may be hesitant to undergo this abdominal surgery because of possible complications, like pregnancy loss, he added. “Now, I can say to them that the data would suggest that with your particular complicated appendicitis, we should operate sooner, not later.”
Dr. Matsushima and Dr. Sharp have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Pregnant women who underwent immediate surgery to treat a ruptured or abscessed appendix had lower risk of infectious complications, compared with those whose complicated appendicitis was managed without surgery, according to new research.
Most cases that began with nonoperative management eventually required surgery, and the operative delay was associated with an increased risk of preterm labor, preterm delivery, and abortion.
“Our study findings may help to define the preferred management strategy in complicated appendicitis during pregnancy to be immediate operation,” Kazuhide Matsushima, MD, an assistant professor of clinical surgery at the University of Southern California, Los Angeles, and colleagues wrote.
The retrospective study was published in JAMA Network Open.
While acute appendicitis is relatively rare during pregnancy, it is the most common nonobstetric emergency in pregnant women, Dr. Matsushima said. This condition occurs in an estimated 1 in 700 to 1 in 1,500 pregnancies, and some data suggest that pregnant women are at higher risk for perforation and other forms of complicated appendicitis.
National guidelines support appendectomy as the first-line treatment for pregnant women with acute uncomplicated appendicitis, but there is no clear guidance on the best treatment approach for managing complicated appendicitis in this population, the authors note.
To better understand how surgical and nonoperational interventions affected outcomes, investigators analyzed data from the National Inpatient Sample from January 2003 to September 2015 to identify pregnant women with complicated appendicitis. The condition was defined as “acute appendicitis with generalized peritonitis” and “acute appendicitis with peritoneal abscess.” Patients were excluded if they had complications such as ectopic pregnancy and hydatidiform mole.
Investigators split the patients into three groups: those who underwent immediate operation for complicated appendicitis, those whose appendicitis was successfully managed without surgery, and those in whom nonoperative management of their condition failed, resulting in delayed surgery. Failed nonoperative management was defined as at least 1 day of nonoperative management followed by a laparoscopic or open appendectomy.
Of the 8,087 pregnant women identified during the study with complicated appendicitis, 55.5% underwent immediate appendectomy, 11.8% were successfully treated without surgical intervention, and 32.7% had delayed operations after initial failed nonoperative management. There was no significant difference in preterm delivery, preterm labor, or abortion between the immediate operative and successful nonoperative groups; however, the successful nonoperative group was more than twice as likely to experience premature rupture of membranes (odds ratio, 2.77; P = .03). Patients successfully treated without surgery also were at higher risk for infections such as amniotic infection (OR, 4.35; P < .001), pneumonia (OR, 2.52; P < .001), and sepsis (OR, 1.52; P = .01), compared with patients who underwent immediate operation.
Patients who had delayed surgery were 45% more likely to experience preterm delivery, preterm labor, or abortion (OR, 1.45; P < .001), compared with the immediate surgery group. The delayed surgery group was also at higher risk for antepartum hemorrhage (OR, 1.56; P = .03) and premature rupture of membranes (OR, 3.44; P = .002). They were more than four times as likely to have amniotic infection (OR, 4.74; P < .001), twice as likely to contract pneumonia (OR, 2.01; P < .001), and 58% more likely to develop sepsis (OR, 1.58; P < .001), compared with the immediate surgery group. The researchers calculated that every day surgery was delayed, the risk of preterm delivery, preterm labor, and abortion rose by 23% (OR, 1.23; P < .001).
Delayed surgery and successful nonoperative management were also associated with higher hospital charges and longer hospital stays.
Because this was a retrospective study, there are some limitations to the findings, Dr. Matsushima said, and therefore it should not be used to justify changing standards of care; however, it does give more information on the risks associated with different interventions. “It’s very important to have a discussion with the patient and make a shared decision,” he told this news organization, “because each option has significant risks and benefits.”
Because the data were from a database, he added, the research team was not able to see if outcomes from immediate surgery, nonoperative management, and delayed surgery differed in each trimester.
Kenneth W. Sharp, MD, a professor of surgery at Vanderbilt University Medical Center in Nashville, Tenn., agreed that the study does have limitations, such as lack of information on how complicated appendicitis was identified and diagnosed; however, the study does provide guidance to surgeons in a surgical area with “very sparse literature,” he told this news organization. Dr. Sharp is also a regent from the American College of Surgeons, which arranged the interview.
“Especially with these very complicated patients, it was never clear what to do,” he said. “With the recent studies showing that treatment of appendicitis with antibiotics works for a large number of people, people start extrapolating [those findings] to complicated appendicitis and they start extrapolating it to pregnant women, none of which the studies were meant to show anything about,” he said.
This analysis gives additional information to inform treatment decisions in pregnant women who may be hesitant to undergo this abdominal surgery because of possible complications, like pregnancy loss, he added. “Now, I can say to them that the data would suggest that with your particular complicated appendicitis, we should operate sooner, not later.”
Dr. Matsushima and Dr. Sharp have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM JAMA NETWORK OPEN
TNF inhibitors prior to surgery safe in patients with IBD: Study
Patients with inflammatory bowel disease (IBD) can safely take tumor necrosis factor inhibitors (TNFi) prior to abdominal surgery, a prospective, multicenter, observational study confirms.
The researchers found that exposure to TNFi in the 12 weeks prior to surgery was not associated with an increased risk of either overall infections or surgical site infections (SSI).
The findings should be “very reassuring” for clinicians, lead author Benjamin L. Cohen, MD, Cleveland Clinic Foundation, told this news organization. “In the past, when clinicians were unsure about the safety of using these drugs in the perioperative period, they may have delayed surgeries or stopped medications unnecessarily.”
“For me, the key take-home point of this study is that we need to plan the timing and management of medications around surgery based on factors other than the use of tumor necrosis factor inhibitors in most patients,” Dr. Cohen continued.
Ultimately, “we will help change practice in how we manage patients with IBD having surgery,” he said.
The research was published online in Gastroenterology.
No increased postop infection risk
The Prospective Cohort of Ulcerative Colitis and Crohn’s Disease Patients Undergoing Surgery to Identify Risk Factors for Post-Operative Infection I (PUCCINI) trial enrolled patients with IBD from 17 sites participating in the Crohn’s and Colitis Foundation Clinical Research Alliance between September 2014 and June 2017.
Patients had Crohn’s disease, ulcerative colitis, or indeterminate colitis, as determined by standard criteria, and planned to undergo intra-abdominal surgery or had undergone intra-abdominal surgery in the preceding 4 days.
Among the 947 patients enrolled, 47.8% were women. All were aged 18 years or older. The median disease duration was 10 years; 34.4% of patients had undergone prior bowel resection, and a further 17.5% had undergone other abdominal surgery.
Systemic corticosteroid use within 2 weeks of surgery was reported by 40.9% of patients, and 42.3% had used antibiotics.
TNFi exposure within the 12 weeks prior to surgery was reported by 40.3% of patients. Adalimumab and infliximab were the most commonly used drugs. Among those who had not used TNFi prior to surgery, 23.7% were TNFi-naive, and 36.0% had used them in the past.
The researchers report that there was no significant difference in the rate of postoperative infections between patients who reported using TNFi in the 12 weeks prior to surgery and those who did not (18.1% vs. 20.2%; P = .469). There was also no difference in SSI, as defined using the Centers for Disease Control and Prevention criteria, between the two groups (12.0% vs 12.6%; P = .889).
Multivariate analysis revealed that current TNFi exposure was not associated with any infection, at an odds ratio versus no exposure of 1.050 (P = .80), or with SSI, at an odds ratio of 1.249 (P = .34).
In contrast, preoperative corticosteroid exposure, prior bowel resection, and current smoking were associated with any infection and with SSI.
Approached for comment, Stephen B. Hanauer, MD, medical director of the Digestive Health Center at Northwestern University, Chicago, said that the current findings are consistent with those of previous studies and that their relevance extends beyond abdominal surgery.
In the past, when surgeons were “confronted with a patient on a TNF blocker, even if it’s orthopedic or plastic surgery, they recommended against using a TNF blocker or operating at the end of the cycle when the drug levels are low,” he told this news organization.
Dr. Hanauer said such practice gets clinicians into a “bind because you’ve got a patient, for instance, who’s got a blockage with Crohn’s disease ... but the only way you could manage them when the TNFi was out of their system was with steroids, which is worse” in terms of postoperative infection risk, he explained.
Prospective studies important
The researchers note that up to 50% of patients with IBD are exposed to TNFi prior to their first surgery. They also note that there is concern that preoperative treatment with these and other immunosuppressive medications may increase the risk of postoperative infections.
However, the evidence is inconsistent, they write, so whether to continue or stop the drugs prior to surgery remains controversial.
“A lot of the initial studies in the perioperative population were single-center and retrospective for the most part,” Dr. Cohen said, adding that the studies used different modes of assessment and followed different time frames.
“So, there’s a lot of heterogeneity,” he said.
In addition, early studies of TNFi were often conducted with patients who were very ill and who had started receiving the drug right before surgery, and they sometimes had a complication Dr. Cohen said. “But you don’t know if that’s because of the drug itself or because of many other factors associated with them being very sick, such as being on steroids, being very malnourished, or having other complications of disease.”
It is difficult to control for such risk factors in retrospective analyses because the information is not always available from medical records, he said. “That’s why it’s so important to study clinical questions like this in a prospective manner.”
Dr. Cohen added that it is important that studies such as theirs continue to be undertaken as new drugs become available.
“We’re entering an era of rapidly expanding drug discovery, so we’re going to have new medications available for use in our patients with IBD,” he explained. “It’s important that we continue to build prospective cohorts to look at questions such as the safety of medications in the perioperative period, rather than solely relying on retrospective data.”
The study was funded by a Crohn’s & Colitis Foundation Senior Research Award. Dr. Cohen reports relationships with AbbVie, Celgene, Bristol-Myers Squibb, Pfizer, Sublimity Therapeutics, Target RWE, Janssen, Ferring, AlphaSigma, and Takeda. Other authors report numerous financial relationships. Dr. Hanauer reports relationships with Janssen, AbbVie, Pfizer, Amgen, Genentech, and Merck.
A version of this article first appeared on Medscape.com.
Patients with inflammatory bowel disease (IBD) can safely take tumor necrosis factor inhibitors (TNFi) prior to abdominal surgery, a prospective, multicenter, observational study confirms.
The researchers found that exposure to TNFi in the 12 weeks prior to surgery was not associated with an increased risk of either overall infections or surgical site infections (SSI).
The findings should be “very reassuring” for clinicians, lead author Benjamin L. Cohen, MD, Cleveland Clinic Foundation, told this news organization. “In the past, when clinicians were unsure about the safety of using these drugs in the perioperative period, they may have delayed surgeries or stopped medications unnecessarily.”
“For me, the key take-home point of this study is that we need to plan the timing and management of medications around surgery based on factors other than the use of tumor necrosis factor inhibitors in most patients,” Dr. Cohen continued.
Ultimately, “we will help change practice in how we manage patients with IBD having surgery,” he said.
The research was published online in Gastroenterology.
No increased postop infection risk
The Prospective Cohort of Ulcerative Colitis and Crohn’s Disease Patients Undergoing Surgery to Identify Risk Factors for Post-Operative Infection I (PUCCINI) trial enrolled patients with IBD from 17 sites participating in the Crohn’s and Colitis Foundation Clinical Research Alliance between September 2014 and June 2017.
Patients had Crohn’s disease, ulcerative colitis, or indeterminate colitis, as determined by standard criteria, and planned to undergo intra-abdominal surgery or had undergone intra-abdominal surgery in the preceding 4 days.
Among the 947 patients enrolled, 47.8% were women. All were aged 18 years or older. The median disease duration was 10 years; 34.4% of patients had undergone prior bowel resection, and a further 17.5% had undergone other abdominal surgery.
Systemic corticosteroid use within 2 weeks of surgery was reported by 40.9% of patients, and 42.3% had used antibiotics.
TNFi exposure within the 12 weeks prior to surgery was reported by 40.3% of patients. Adalimumab and infliximab were the most commonly used drugs. Among those who had not used TNFi prior to surgery, 23.7% were TNFi-naive, and 36.0% had used them in the past.
The researchers report that there was no significant difference in the rate of postoperative infections between patients who reported using TNFi in the 12 weeks prior to surgery and those who did not (18.1% vs. 20.2%; P = .469). There was also no difference in SSI, as defined using the Centers for Disease Control and Prevention criteria, between the two groups (12.0% vs 12.6%; P = .889).
Multivariate analysis revealed that current TNFi exposure was not associated with any infection, at an odds ratio versus no exposure of 1.050 (P = .80), or with SSI, at an odds ratio of 1.249 (P = .34).
In contrast, preoperative corticosteroid exposure, prior bowel resection, and current smoking were associated with any infection and with SSI.
Approached for comment, Stephen B. Hanauer, MD, medical director of the Digestive Health Center at Northwestern University, Chicago, said that the current findings are consistent with those of previous studies and that their relevance extends beyond abdominal surgery.
In the past, when surgeons were “confronted with a patient on a TNF blocker, even if it’s orthopedic or plastic surgery, they recommended against using a TNF blocker or operating at the end of the cycle when the drug levels are low,” he told this news organization.
Dr. Hanauer said such practice gets clinicians into a “bind because you’ve got a patient, for instance, who’s got a blockage with Crohn’s disease ... but the only way you could manage them when the TNFi was out of their system was with steroids, which is worse” in terms of postoperative infection risk, he explained.
Prospective studies important
The researchers note that up to 50% of patients with IBD are exposed to TNFi prior to their first surgery. They also note that there is concern that preoperative treatment with these and other immunosuppressive medications may increase the risk of postoperative infections.
However, the evidence is inconsistent, they write, so whether to continue or stop the drugs prior to surgery remains controversial.
“A lot of the initial studies in the perioperative population were single-center and retrospective for the most part,” Dr. Cohen said, adding that the studies used different modes of assessment and followed different time frames.
“So, there’s a lot of heterogeneity,” he said.
In addition, early studies of TNFi were often conducted with patients who were very ill and who had started receiving the drug right before surgery, and they sometimes had a complication Dr. Cohen said. “But you don’t know if that’s because of the drug itself or because of many other factors associated with them being very sick, such as being on steroids, being very malnourished, or having other complications of disease.”
It is difficult to control for such risk factors in retrospective analyses because the information is not always available from medical records, he said. “That’s why it’s so important to study clinical questions like this in a prospective manner.”
Dr. Cohen added that it is important that studies such as theirs continue to be undertaken as new drugs become available.
“We’re entering an era of rapidly expanding drug discovery, so we’re going to have new medications available for use in our patients with IBD,” he explained. “It’s important that we continue to build prospective cohorts to look at questions such as the safety of medications in the perioperative period, rather than solely relying on retrospective data.”
The study was funded by a Crohn’s & Colitis Foundation Senior Research Award. Dr. Cohen reports relationships with AbbVie, Celgene, Bristol-Myers Squibb, Pfizer, Sublimity Therapeutics, Target RWE, Janssen, Ferring, AlphaSigma, and Takeda. Other authors report numerous financial relationships. Dr. Hanauer reports relationships with Janssen, AbbVie, Pfizer, Amgen, Genentech, and Merck.
A version of this article first appeared on Medscape.com.
Patients with inflammatory bowel disease (IBD) can safely take tumor necrosis factor inhibitors (TNFi) prior to abdominal surgery, a prospective, multicenter, observational study confirms.
The researchers found that exposure to TNFi in the 12 weeks prior to surgery was not associated with an increased risk of either overall infections or surgical site infections (SSI).
The findings should be “very reassuring” for clinicians, lead author Benjamin L. Cohen, MD, Cleveland Clinic Foundation, told this news organization. “In the past, when clinicians were unsure about the safety of using these drugs in the perioperative period, they may have delayed surgeries or stopped medications unnecessarily.”
“For me, the key take-home point of this study is that we need to plan the timing and management of medications around surgery based on factors other than the use of tumor necrosis factor inhibitors in most patients,” Dr. Cohen continued.
Ultimately, “we will help change practice in how we manage patients with IBD having surgery,” he said.
The research was published online in Gastroenterology.
No increased postop infection risk
The Prospective Cohort of Ulcerative Colitis and Crohn’s Disease Patients Undergoing Surgery to Identify Risk Factors for Post-Operative Infection I (PUCCINI) trial enrolled patients with IBD from 17 sites participating in the Crohn’s and Colitis Foundation Clinical Research Alliance between September 2014 and June 2017.
Patients had Crohn’s disease, ulcerative colitis, or indeterminate colitis, as determined by standard criteria, and planned to undergo intra-abdominal surgery or had undergone intra-abdominal surgery in the preceding 4 days.
Among the 947 patients enrolled, 47.8% were women. All were aged 18 years or older. The median disease duration was 10 years; 34.4% of patients had undergone prior bowel resection, and a further 17.5% had undergone other abdominal surgery.
Systemic corticosteroid use within 2 weeks of surgery was reported by 40.9% of patients, and 42.3% had used antibiotics.
TNFi exposure within the 12 weeks prior to surgery was reported by 40.3% of patients. Adalimumab and infliximab were the most commonly used drugs. Among those who had not used TNFi prior to surgery, 23.7% were TNFi-naive, and 36.0% had used them in the past.
The researchers report that there was no significant difference in the rate of postoperative infections between patients who reported using TNFi in the 12 weeks prior to surgery and those who did not (18.1% vs. 20.2%; P = .469). There was also no difference in SSI, as defined using the Centers for Disease Control and Prevention criteria, between the two groups (12.0% vs 12.6%; P = .889).
Multivariate analysis revealed that current TNFi exposure was not associated with any infection, at an odds ratio versus no exposure of 1.050 (P = .80), or with SSI, at an odds ratio of 1.249 (P = .34).
In contrast, preoperative corticosteroid exposure, prior bowel resection, and current smoking were associated with any infection and with SSI.
Approached for comment, Stephen B. Hanauer, MD, medical director of the Digestive Health Center at Northwestern University, Chicago, said that the current findings are consistent with those of previous studies and that their relevance extends beyond abdominal surgery.
In the past, when surgeons were “confronted with a patient on a TNF blocker, even if it’s orthopedic or plastic surgery, they recommended against using a TNF blocker or operating at the end of the cycle when the drug levels are low,” he told this news organization.
Dr. Hanauer said such practice gets clinicians into a “bind because you’ve got a patient, for instance, who’s got a blockage with Crohn’s disease ... but the only way you could manage them when the TNFi was out of their system was with steroids, which is worse” in terms of postoperative infection risk, he explained.
Prospective studies important
The researchers note that up to 50% of patients with IBD are exposed to TNFi prior to their first surgery. They also note that there is concern that preoperative treatment with these and other immunosuppressive medications may increase the risk of postoperative infections.
However, the evidence is inconsistent, they write, so whether to continue or stop the drugs prior to surgery remains controversial.
“A lot of the initial studies in the perioperative population were single-center and retrospective for the most part,” Dr. Cohen said, adding that the studies used different modes of assessment and followed different time frames.
“So, there’s a lot of heterogeneity,” he said.
In addition, early studies of TNFi were often conducted with patients who were very ill and who had started receiving the drug right before surgery, and they sometimes had a complication Dr. Cohen said. “But you don’t know if that’s because of the drug itself or because of many other factors associated with them being very sick, such as being on steroids, being very malnourished, or having other complications of disease.”
It is difficult to control for such risk factors in retrospective analyses because the information is not always available from medical records, he said. “That’s why it’s so important to study clinical questions like this in a prospective manner.”
Dr. Cohen added that it is important that studies such as theirs continue to be undertaken as new drugs become available.
“We’re entering an era of rapidly expanding drug discovery, so we’re going to have new medications available for use in our patients with IBD,” he explained. “It’s important that we continue to build prospective cohorts to look at questions such as the safety of medications in the perioperative period, rather than solely relying on retrospective data.”
The study was funded by a Crohn’s & Colitis Foundation Senior Research Award. Dr. Cohen reports relationships with AbbVie, Celgene, Bristol-Myers Squibb, Pfizer, Sublimity Therapeutics, Target RWE, Janssen, Ferring, AlphaSigma, and Takeda. Other authors report numerous financial relationships. Dr. Hanauer reports relationships with Janssen, AbbVie, Pfizer, Amgen, Genentech, and Merck.
A version of this article first appeared on Medscape.com.
FROM GASTROENTEROLOGY
Surgery shows no survival, morbidity benefit for mild hyperparathyroidism
Patients who receive parathyroidectomy for mild primary hyperparathyroidism show no benefits in survival or morbidity, including fractures, cancer, or cardiovascular outcomes over more than 10 years, compared with those not receiving the surgery, results from a randomized, prospective trial show.
“In contrast to existing data showing increased mortality and cardiovascular morbidity in mild primary hyperparathyroidism, we did not find any treatment effect of parathyroidectomy on these important clinical endpoints,” report the authors of the study, published in the Annals of Internal Medicine.
Reason to evaluate and revise current recommendations?
With mild primary hyperparathyroidism becoming the predominant form of hyperparathyroidism, the results suggest rethinking the current recommendations for the condition, the study authors note.
“Over the years, more active management of mild primary hyperparathyroidism has been recommended, with a widening of criteria for parathyroidectomy,” they write.
“With the low number of kidney stones (n = 5) and no effect of parathyroidectomy on fractures, there may be a need to evaluate and potentially revise the current recommendations.”
The authors of an accompanying editorial agree that “the [results] provide a strong rationale for nonoperative management of patients with mild primary hyperparathyroidism.”
“The findings suggest that most patients can be managed nonoperatively, with monitoring of serum calcium levels every 1 to 2 years or if symptoms occur,” write the editorial authors, Mark J. Bolland, PhD, and Andrew Grey, MD, of the department of medicine, University of Auckland, New Zealand.
Although parathyroidectomy is recommended for the treatment in patients with hyperparathyroidism with severe hypercalcemia or overt symptoms, there has been debate on the long-term benefits of surgery among those with milder cases.
Most previous studies that have shown benefits, such as reductions in the risk of fracture with parathyroidectomy, have importantly not distinguished between mild and more severe primary hyperparathyroidism, the authors note.
No significant differences in mortality between surgery, nonsurgery groups
For the Scandinavian Investigation of Primary Hyperparathyroidism (SIPH) trial, first author Mikkel Pretorius, MD, Oslo University Hospital and Faculty of Medicine, University of Oslo, and colleagues enrolled 191 patients between 1998 and 2005 in Sweden, Norway, and Denmark, who were aged 50-80 years and had mild primary hyperparathyroidism, defined as serum calcium levels of 10.42-11.22 mg/dL.
Participants were randomized to receive surgery (n = 95) or nonoperative observation without intervention (n = 96).
After a 10-year follow-up, 129 patients had completed the final visit. The overall death rate was 7.6%, and, with eight deaths in the surgery group and seven in the nonsurgery group, there were no significant differences between groups in terms of mortality (HR, 1.17; P = .76).
During an extended observation period that lasted until 2018, mortality rates increased by 23%, but with a relatively even distribution of 24 deaths in the surgery group and 20 among those with no surgery.
Chronic hypercalcemia related to primary hyperparathyroidism has been debated as being associated with an increased risk of cardiovascular disease or cancer, however, “the absolute numbers for these and the other disease-specific causes of death were nearly identical between groups,” the authors write, with 17 deaths from cardiovascular disease, eight from cancer, and eight from cerebrovascular disease.
In terms of morbidity, including cardiovascular events, cerebrovascular events, cancer, peripheral fractures, and renal stones, there were 101 events overall, with 52 in the parathyroidectomy group and 49 in the nonsurgery group, which again, was not a significant difference.
Sixteen vertebral fractures occurred overall in 14 patients, which were evenly split at seven patients in each group.
The authors note that “the incidence of peripheral fractures for women in our study was around 2,900 per 100,000 person-years, in the same range as for 70-year-old women in a study in Gothenburg, Sweden (about 2,600 per 100,000 person-years).”
There were no between-group differences in terms of time to death or first morbidity event for any of the prespecified events.
Of the 96 patients originally assigned to the nonsurgery group, 17 (18%) had surgery during follow-up, including three for serious hypercalcemia, three by their own choice, two for decreasing bone density, one for kidney stones, and the others for unclear or unrelated reasons.
Study limitations include that only 26 men (13 in each group) were included, and only 16 completed the study. “The external validity for men based on this study is therefore limited,” the authors note.
And although most people with primary hyperparathyroidism are adults, the older age of participants suggests the results should not be generalized to younger patients with benign parathyroid tumors.
The editorialists note that age should be one of the few factors that may, indeed, suggest appropriate candidates for parathyroidectomy.
“Younger patients (aged < 50 years) may have more aggressive disease,” they explain.
In addition, “patients with serum calcium levels above 3 mmol/L (> 12 mg/dL) are at greater risk for symptomatic hypercalcemia, and patients with a recent history of kidney stones may have fewer future stones after surgical cure.”
“Yet, such patients are a small minority of those with primary hyperparathyroidism,” they note.
The study authors underscore that “our data add evidence to guide the decisionmaking process in deliberative dialogue between clinicians and patients.”
The study received funding from Swedish government grants, the Norwegian Research Council, and the South-Eastern Norway Regional Health Authority.
A version of this article first appeared on Medscape.com.
Patients who receive parathyroidectomy for mild primary hyperparathyroidism show no benefits in survival or morbidity, including fractures, cancer, or cardiovascular outcomes over more than 10 years, compared with those not receiving the surgery, results from a randomized, prospective trial show.
“In contrast to existing data showing increased mortality and cardiovascular morbidity in mild primary hyperparathyroidism, we did not find any treatment effect of parathyroidectomy on these important clinical endpoints,” report the authors of the study, published in the Annals of Internal Medicine.
Reason to evaluate and revise current recommendations?
With mild primary hyperparathyroidism becoming the predominant form of hyperparathyroidism, the results suggest rethinking the current recommendations for the condition, the study authors note.
“Over the years, more active management of mild primary hyperparathyroidism has been recommended, with a widening of criteria for parathyroidectomy,” they write.
“With the low number of kidney stones (n = 5) and no effect of parathyroidectomy on fractures, there may be a need to evaluate and potentially revise the current recommendations.”
The authors of an accompanying editorial agree that “the [results] provide a strong rationale for nonoperative management of patients with mild primary hyperparathyroidism.”
“The findings suggest that most patients can be managed nonoperatively, with monitoring of serum calcium levels every 1 to 2 years or if symptoms occur,” write the editorial authors, Mark J. Bolland, PhD, and Andrew Grey, MD, of the department of medicine, University of Auckland, New Zealand.
Although parathyroidectomy is recommended for the treatment in patients with hyperparathyroidism with severe hypercalcemia or overt symptoms, there has been debate on the long-term benefits of surgery among those with milder cases.
Most previous studies that have shown benefits, such as reductions in the risk of fracture with parathyroidectomy, have importantly not distinguished between mild and more severe primary hyperparathyroidism, the authors note.
No significant differences in mortality between surgery, nonsurgery groups
For the Scandinavian Investigation of Primary Hyperparathyroidism (SIPH) trial, first author Mikkel Pretorius, MD, Oslo University Hospital and Faculty of Medicine, University of Oslo, and colleagues enrolled 191 patients between 1998 and 2005 in Sweden, Norway, and Denmark, who were aged 50-80 years and had mild primary hyperparathyroidism, defined as serum calcium levels of 10.42-11.22 mg/dL.
Participants were randomized to receive surgery (n = 95) or nonoperative observation without intervention (n = 96).
After a 10-year follow-up, 129 patients had completed the final visit. The overall death rate was 7.6%, and, with eight deaths in the surgery group and seven in the nonsurgery group, there were no significant differences between groups in terms of mortality (HR, 1.17; P = .76).
During an extended observation period that lasted until 2018, mortality rates increased by 23%, but with a relatively even distribution of 24 deaths in the surgery group and 20 among those with no surgery.
Chronic hypercalcemia related to primary hyperparathyroidism has been debated as being associated with an increased risk of cardiovascular disease or cancer, however, “the absolute numbers for these and the other disease-specific causes of death were nearly identical between groups,” the authors write, with 17 deaths from cardiovascular disease, eight from cancer, and eight from cerebrovascular disease.
In terms of morbidity, including cardiovascular events, cerebrovascular events, cancer, peripheral fractures, and renal stones, there were 101 events overall, with 52 in the parathyroidectomy group and 49 in the nonsurgery group, which again, was not a significant difference.
Sixteen vertebral fractures occurred overall in 14 patients, which were evenly split at seven patients in each group.
The authors note that “the incidence of peripheral fractures for women in our study was around 2,900 per 100,000 person-years, in the same range as for 70-year-old women in a study in Gothenburg, Sweden (about 2,600 per 100,000 person-years).”
There were no between-group differences in terms of time to death or first morbidity event for any of the prespecified events.
Of the 96 patients originally assigned to the nonsurgery group, 17 (18%) had surgery during follow-up, including three for serious hypercalcemia, three by their own choice, two for decreasing bone density, one for kidney stones, and the others for unclear or unrelated reasons.
Study limitations include that only 26 men (13 in each group) were included, and only 16 completed the study. “The external validity for men based on this study is therefore limited,” the authors note.
And although most people with primary hyperparathyroidism are adults, the older age of participants suggests the results should not be generalized to younger patients with benign parathyroid tumors.
The editorialists note that age should be one of the few factors that may, indeed, suggest appropriate candidates for parathyroidectomy.
“Younger patients (aged < 50 years) may have more aggressive disease,” they explain.
In addition, “patients with serum calcium levels above 3 mmol/L (> 12 mg/dL) are at greater risk for symptomatic hypercalcemia, and patients with a recent history of kidney stones may have fewer future stones after surgical cure.”
“Yet, such patients are a small minority of those with primary hyperparathyroidism,” they note.
The study authors underscore that “our data add evidence to guide the decisionmaking process in deliberative dialogue between clinicians and patients.”
The study received funding from Swedish government grants, the Norwegian Research Council, and the South-Eastern Norway Regional Health Authority.
A version of this article first appeared on Medscape.com.
Patients who receive parathyroidectomy for mild primary hyperparathyroidism show no benefits in survival or morbidity, including fractures, cancer, or cardiovascular outcomes over more than 10 years, compared with those not receiving the surgery, results from a randomized, prospective trial show.
“In contrast to existing data showing increased mortality and cardiovascular morbidity in mild primary hyperparathyroidism, we did not find any treatment effect of parathyroidectomy on these important clinical endpoints,” report the authors of the study, published in the Annals of Internal Medicine.
Reason to evaluate and revise current recommendations?
With mild primary hyperparathyroidism becoming the predominant form of hyperparathyroidism, the results suggest rethinking the current recommendations for the condition, the study authors note.
“Over the years, more active management of mild primary hyperparathyroidism has been recommended, with a widening of criteria for parathyroidectomy,” they write.
“With the low number of kidney stones (n = 5) and no effect of parathyroidectomy on fractures, there may be a need to evaluate and potentially revise the current recommendations.”
The authors of an accompanying editorial agree that “the [results] provide a strong rationale for nonoperative management of patients with mild primary hyperparathyroidism.”
“The findings suggest that most patients can be managed nonoperatively, with monitoring of serum calcium levels every 1 to 2 years or if symptoms occur,” write the editorial authors, Mark J. Bolland, PhD, and Andrew Grey, MD, of the department of medicine, University of Auckland, New Zealand.
Although parathyroidectomy is recommended for the treatment in patients with hyperparathyroidism with severe hypercalcemia or overt symptoms, there has been debate on the long-term benefits of surgery among those with milder cases.
Most previous studies that have shown benefits, such as reductions in the risk of fracture with parathyroidectomy, have importantly not distinguished between mild and more severe primary hyperparathyroidism, the authors note.
No significant differences in mortality between surgery, nonsurgery groups
For the Scandinavian Investigation of Primary Hyperparathyroidism (SIPH) trial, first author Mikkel Pretorius, MD, Oslo University Hospital and Faculty of Medicine, University of Oslo, and colleagues enrolled 191 patients between 1998 and 2005 in Sweden, Norway, and Denmark, who were aged 50-80 years and had mild primary hyperparathyroidism, defined as serum calcium levels of 10.42-11.22 mg/dL.
Participants were randomized to receive surgery (n = 95) or nonoperative observation without intervention (n = 96).
After a 10-year follow-up, 129 patients had completed the final visit. The overall death rate was 7.6%, and, with eight deaths in the surgery group and seven in the nonsurgery group, there were no significant differences between groups in terms of mortality (HR, 1.17; P = .76).
During an extended observation period that lasted until 2018, mortality rates increased by 23%, but with a relatively even distribution of 24 deaths in the surgery group and 20 among those with no surgery.
Chronic hypercalcemia related to primary hyperparathyroidism has been debated as being associated with an increased risk of cardiovascular disease or cancer, however, “the absolute numbers for these and the other disease-specific causes of death were nearly identical between groups,” the authors write, with 17 deaths from cardiovascular disease, eight from cancer, and eight from cerebrovascular disease.
In terms of morbidity, including cardiovascular events, cerebrovascular events, cancer, peripheral fractures, and renal stones, there were 101 events overall, with 52 in the parathyroidectomy group and 49 in the nonsurgery group, which again, was not a significant difference.
Sixteen vertebral fractures occurred overall in 14 patients, which were evenly split at seven patients in each group.
The authors note that “the incidence of peripheral fractures for women in our study was around 2,900 per 100,000 person-years, in the same range as for 70-year-old women in a study in Gothenburg, Sweden (about 2,600 per 100,000 person-years).”
There were no between-group differences in terms of time to death or first morbidity event for any of the prespecified events.
Of the 96 patients originally assigned to the nonsurgery group, 17 (18%) had surgery during follow-up, including three for serious hypercalcemia, three by their own choice, two for decreasing bone density, one for kidney stones, and the others for unclear or unrelated reasons.
Study limitations include that only 26 men (13 in each group) were included, and only 16 completed the study. “The external validity for men based on this study is therefore limited,” the authors note.
And although most people with primary hyperparathyroidism are adults, the older age of participants suggests the results should not be generalized to younger patients with benign parathyroid tumors.
The editorialists note that age should be one of the few factors that may, indeed, suggest appropriate candidates for parathyroidectomy.
“Younger patients (aged < 50 years) may have more aggressive disease,” they explain.
In addition, “patients with serum calcium levels above 3 mmol/L (> 12 mg/dL) are at greater risk for symptomatic hypercalcemia, and patients with a recent history of kidney stones may have fewer future stones after surgical cure.”
“Yet, such patients are a small minority of those with primary hyperparathyroidism,” they note.
The study authors underscore that “our data add evidence to guide the decisionmaking process in deliberative dialogue between clinicians and patients.”
The study received funding from Swedish government grants, the Norwegian Research Council, and the South-Eastern Norway Regional Health Authority.
A version of this article first appeared on Medscape.com.
FROM ANNALS OF INTERNAL MEDICINE
POISE-3 backs wider use of tranexamic acid in noncardiac surgery
The antifibrinolytic tranexamic acid (TXA) reduced serious bleeding without a significant effect on major vascular outcomes in patients undergoing noncardiac surgery at risk for these complications in the POISE-3 trial.
TXA cut the primary efficacy outcome of life-threatening, major, and critical organ bleeding at 30 days by 24% compared with placebo (9.1% vs. 11.7%; hazard ratio [HR], 0.76; P < .0001).
The primary safety outcome of myocardial injury after noncardiac surgery (MINS), nonhemorrhagic stroke, peripheral arterial thrombosis, and symptomatic proximal venous thromboembolism (VTE) at 30 days occurred in 14.2% vs.. 13.9% of patients, respectively (HR, 1.023). This failed, however, to meet the study›s threshold to prove TXA noninferior to placebo (one-sided P = .044).
There was no increased risk for death or stroke with TXA, according to results published April 2 in the New England Journal of Medicine.
Principal investigator P.J. Devereaux, MD, PhD, Population Health Research Institute and McMaster University, Hamilton, Ontario, Canada, pointed out that there is only a 4.4% probability that the composite vascular outcome hazard ratio was above the noninferiority margin and that just 10 events separated the two groups (649 vs.. 639).
“Healthcare providers and patients will have to weigh a clear beneficial reduction in the composite bleeding outcome, which is an absolute difference of 2.7%, a result that was highly statistically significant, versus a low probability of a small increase in risk of the composite vascular endpoint, with an absolute difference of 0.3%,” a nonsignificant result, Dr. Devereaux said during the formal presentation of the results at the hybrid annual scientific sessions of the American College of Cardiology.
The findings, he said, should also be put in the context that 300 million adults have a major surgery each year worldwide and most don’t receive TXA. At the same time, there’s an annual global shortage of 30 million blood product units, and surgical bleeding accounts for up to 40% of all transfusions.
“POISE-3 identifies that use of TXA could avoid upwards of 8 million bleeding events resulting in transfusion on an annual basis, indicating potential for large public health and clinical benefit if TXA become standard practice in noncardiac surgery,” Dr. Devereaux said during the late-breaking trial session.
TXA is indicated for heavy menstrual bleeding and hemophilia and has been used in cardiac surgery, but it is increasingly being used in noncardiac surgeries. As previously reported, POISE showed that the beta-blocker metoprolol lowered the risk for myocardial infarction (MI) but increased the risk for severe stroke and overall death, whereas in POISE-2, perioperative low-dose aspirin lowered the risk for MI but was linked to more major bleeding.
The cumulative data have not shown an increased risk for thrombotic events in other settings, Dr. Devereaux told this news organization.
“I’m a cardiologist, and I think that we’ve been guilty at times of always only focusing on the thrombotic side of the equation and ignoring that bleeding is a very important aspect of the circulatory system,” he said. “And I think this shows for the first time clear unequivocal evidence that there’s a cheap, very encouraging, safe way to prevent this.”
“An important point is that if you can give tranexamic acid and prevent bleeding in your cardiac patients having noncardiac surgery, then you can prevent the delay of reinitiating their anticoagulants and their antiplatelets after surgery and getting them back on the medications that are important for them to prevent their cardiovascular event,” Dr. Devereaux added.
Discussant Michael J. Mack, MD, commented that TXA, widely used in cardiac surgery, is an old, inexpensive drug that “should be more widely used in noncardiac surgery.” Dr. Mack, from Baylor Scott & White Health, Dallas, added that he would limit it to major noncardiac surgery.
International trial
PeriOperative ISchemic Evaluation-3 (POISE-3) investigators at 114 hospitals in 22 countries (including countries in North and South America, Europe, and Africa; Russia; India; and Australia) randomly assigned 9,535 patients, aged 45 years or older, with or at risk for cardiovascular and bleeding complications to receive a TXA 1-g intravenous bolus or placebo at the start and end of inpatient noncardiac surgery.
Patients taking at least one long-term antihypertensive medication were also randomly assigned to a perioperative hypotension- or hypertension-avoidance strategy, which differ in the use of antihypertensives on the morning of surgery and the first 2 days after surgery, and in the target mean arterial pressure during surgery. Results from these cohorts will be presented in a separate session on April 4.
The study had planned to enroll 10,000 patients but was stopped early by the steering committee because of financial constraints resulting from slow enrollment during the pandemic. The decision was made without knowledge of the trial results but with knowledge that aggregate composite bleeding and vascular outcomes were higher than originally estimated, Dr. Devereaux noted.
Among all participants, the mean age was 70 years, 56% were male, almost a third had coronary artery disease, 15% had peripheral artery disease, and 8% had a prior stroke. About 80% were undergoing major surgery. Adherence to the study medications was 96.3% in both groups.
Secondary bleeding outcomes were lower in the TXA and placebo groups, including bleeding independently associated with mortality after surgery (8.7% vs. 11.3%), life-threatening bleeding (1.6% vs. 1.7%), major bleeding (7.6% vs. 10.4%), and critical organ bleeding (0.3% vs. 0.4%).
Importantly, the TXA group had significantly lower rates of International Society on Thrombosis and Haemostasis major bleeding (6.6% vs. 8.7%; P = .0001) and the need for transfusion of 1 or more units of packed red blood cells (9.4% vs. 12.0%; P <.0001), Dr. Devereaux noted.
In terms of secondary vascular outcomes, there were no significant differences between the TXA and placebo groups in rates of MINS (12.8% vs. 12.6%), MINS not fulfilling definition of MI (both 11.5%), MI (1.4% vs. 1.1%), and the net risk-benefit outcome (a composite of vascular death and nonfatal life-threatening, major, or critical organ bleeding, MINS, stroke, peripheral arterial thrombosis, and symptomatic proximal VTE; 20.7% vs. 21.9%).
The two groups had similar rates of all-cause (1.1% vs. 1.2%) and vascular (0.5% vs. 0.6%) mortality.
There also were no significant differences in other tertiary outcomes, such as acute kidney injury (14.1% vs. 13.7%), rehospitalization for vascular reasons (1.8% vs. 1.6%), or seizures (0.2% vs. <0.1%). The latter has been a concern, with the risk reported to increase with higher doses.
Subgroup analyses
Preplanned subgroup analyses showed a benefit for TXA over placebo for the primary efficacy outcome in orthopedic and nonorthopedic surgery and in patients with hemoglobin level below 120 g/L or 120 g/L or higher, with an estimated glomerular filtration rate less than 45 mL/min/1.73 m 2 or 45 mL/min/1.73 m 2 or higher, or with an N-terminal pro– B-type natriuretic peptide level below 200 ng/L or 200 ng/L or higher.
For the primary safety outcome, the benefit favored placebo but the interaction was not statistically significant for any of the four subgroups.
A post hoc subgroup analysis also showed similar results across the major categories of surgery, including general, vascular, urologic, and gynecologic, Dr. Devereaux told this news organization.
Although TXA is commonly used in orthopedic procedures, Dr. Devereaux noted, in other types of surgeries, “it’s not used at all.” But because TXA “is so cheap, and we can apply it to a broad population, even at an economic level it looks like it’s a winner to give to almost all patients having noncardiac surgery.”
The team also recently published a risk prediction tool that can help estimate a patient’s baseline risk for bleeding.
“So just using a model, which will bring together the patient’s type of surgery and their risk factors, you can look to see, okay, this is enough risk of bleeding, I’m just going to give tranexamic acid,” he said. “We will also be doing economic analyses because blood is also not cheap.”
The study was funded by the Canadian Institutes of Health Research, National Health and Medical Research Council (Australia), and the Research Grant Council (Hong Kong). Dr. Devereaux reports research/research grants from Abbott Diagnostics, Philips Healthcare, Roche Diagnostics, and Siemens. Dr. Mack reports receiving research grants from Abbott Vascular, Edwards Lifesciences, and Medtronic.
A version of this article first appeared on Medscape.com.
The antifibrinolytic tranexamic acid (TXA) reduced serious bleeding without a significant effect on major vascular outcomes in patients undergoing noncardiac surgery at risk for these complications in the POISE-3 trial.
TXA cut the primary efficacy outcome of life-threatening, major, and critical organ bleeding at 30 days by 24% compared with placebo (9.1% vs. 11.7%; hazard ratio [HR], 0.76; P < .0001).
The primary safety outcome of myocardial injury after noncardiac surgery (MINS), nonhemorrhagic stroke, peripheral arterial thrombosis, and symptomatic proximal venous thromboembolism (VTE) at 30 days occurred in 14.2% vs.. 13.9% of patients, respectively (HR, 1.023). This failed, however, to meet the study›s threshold to prove TXA noninferior to placebo (one-sided P = .044).
There was no increased risk for death or stroke with TXA, according to results published April 2 in the New England Journal of Medicine.
Principal investigator P.J. Devereaux, MD, PhD, Population Health Research Institute and McMaster University, Hamilton, Ontario, Canada, pointed out that there is only a 4.4% probability that the composite vascular outcome hazard ratio was above the noninferiority margin and that just 10 events separated the two groups (649 vs.. 639).
“Healthcare providers and patients will have to weigh a clear beneficial reduction in the composite bleeding outcome, which is an absolute difference of 2.7%, a result that was highly statistically significant, versus a low probability of a small increase in risk of the composite vascular endpoint, with an absolute difference of 0.3%,” a nonsignificant result, Dr. Devereaux said during the formal presentation of the results at the hybrid annual scientific sessions of the American College of Cardiology.
The findings, he said, should also be put in the context that 300 million adults have a major surgery each year worldwide and most don’t receive TXA. At the same time, there’s an annual global shortage of 30 million blood product units, and surgical bleeding accounts for up to 40% of all transfusions.
“POISE-3 identifies that use of TXA could avoid upwards of 8 million bleeding events resulting in transfusion on an annual basis, indicating potential for large public health and clinical benefit if TXA become standard practice in noncardiac surgery,” Dr. Devereaux said during the late-breaking trial session.
TXA is indicated for heavy menstrual bleeding and hemophilia and has been used in cardiac surgery, but it is increasingly being used in noncardiac surgeries. As previously reported, POISE showed that the beta-blocker metoprolol lowered the risk for myocardial infarction (MI) but increased the risk for severe stroke and overall death, whereas in POISE-2, perioperative low-dose aspirin lowered the risk for MI but was linked to more major bleeding.
The cumulative data have not shown an increased risk for thrombotic events in other settings, Dr. Devereaux told this news organization.
“I’m a cardiologist, and I think that we’ve been guilty at times of always only focusing on the thrombotic side of the equation and ignoring that bleeding is a very important aspect of the circulatory system,” he said. “And I think this shows for the first time clear unequivocal evidence that there’s a cheap, very encouraging, safe way to prevent this.”
“An important point is that if you can give tranexamic acid and prevent bleeding in your cardiac patients having noncardiac surgery, then you can prevent the delay of reinitiating their anticoagulants and their antiplatelets after surgery and getting them back on the medications that are important for them to prevent their cardiovascular event,” Dr. Devereaux added.
Discussant Michael J. Mack, MD, commented that TXA, widely used in cardiac surgery, is an old, inexpensive drug that “should be more widely used in noncardiac surgery.” Dr. Mack, from Baylor Scott & White Health, Dallas, added that he would limit it to major noncardiac surgery.
International trial
PeriOperative ISchemic Evaluation-3 (POISE-3) investigators at 114 hospitals in 22 countries (including countries in North and South America, Europe, and Africa; Russia; India; and Australia) randomly assigned 9,535 patients, aged 45 years or older, with or at risk for cardiovascular and bleeding complications to receive a TXA 1-g intravenous bolus or placebo at the start and end of inpatient noncardiac surgery.
Patients taking at least one long-term antihypertensive medication were also randomly assigned to a perioperative hypotension- or hypertension-avoidance strategy, which differ in the use of antihypertensives on the morning of surgery and the first 2 days after surgery, and in the target mean arterial pressure during surgery. Results from these cohorts will be presented in a separate session on April 4.
The study had planned to enroll 10,000 patients but was stopped early by the steering committee because of financial constraints resulting from slow enrollment during the pandemic. The decision was made without knowledge of the trial results but with knowledge that aggregate composite bleeding and vascular outcomes were higher than originally estimated, Dr. Devereaux noted.
Among all participants, the mean age was 70 years, 56% were male, almost a third had coronary artery disease, 15% had peripheral artery disease, and 8% had a prior stroke. About 80% were undergoing major surgery. Adherence to the study medications was 96.3% in both groups.
Secondary bleeding outcomes were lower in the TXA and placebo groups, including bleeding independently associated with mortality after surgery (8.7% vs. 11.3%), life-threatening bleeding (1.6% vs. 1.7%), major bleeding (7.6% vs. 10.4%), and critical organ bleeding (0.3% vs. 0.4%).
Importantly, the TXA group had significantly lower rates of International Society on Thrombosis and Haemostasis major bleeding (6.6% vs. 8.7%; P = .0001) and the need for transfusion of 1 or more units of packed red blood cells (9.4% vs. 12.0%; P <.0001), Dr. Devereaux noted.
In terms of secondary vascular outcomes, there were no significant differences between the TXA and placebo groups in rates of MINS (12.8% vs. 12.6%), MINS not fulfilling definition of MI (both 11.5%), MI (1.4% vs. 1.1%), and the net risk-benefit outcome (a composite of vascular death and nonfatal life-threatening, major, or critical organ bleeding, MINS, stroke, peripheral arterial thrombosis, and symptomatic proximal VTE; 20.7% vs. 21.9%).
The two groups had similar rates of all-cause (1.1% vs. 1.2%) and vascular (0.5% vs. 0.6%) mortality.
There also were no significant differences in other tertiary outcomes, such as acute kidney injury (14.1% vs. 13.7%), rehospitalization for vascular reasons (1.8% vs. 1.6%), or seizures (0.2% vs. <0.1%). The latter has been a concern, with the risk reported to increase with higher doses.
Subgroup analyses
Preplanned subgroup analyses showed a benefit for TXA over placebo for the primary efficacy outcome in orthopedic and nonorthopedic surgery and in patients with hemoglobin level below 120 g/L or 120 g/L or higher, with an estimated glomerular filtration rate less than 45 mL/min/1.73 m 2 or 45 mL/min/1.73 m 2 or higher, or with an N-terminal pro– B-type natriuretic peptide level below 200 ng/L or 200 ng/L or higher.
For the primary safety outcome, the benefit favored placebo but the interaction was not statistically significant for any of the four subgroups.
A post hoc subgroup analysis also showed similar results across the major categories of surgery, including general, vascular, urologic, and gynecologic, Dr. Devereaux told this news organization.
Although TXA is commonly used in orthopedic procedures, Dr. Devereaux noted, in other types of surgeries, “it’s not used at all.” But because TXA “is so cheap, and we can apply it to a broad population, even at an economic level it looks like it’s a winner to give to almost all patients having noncardiac surgery.”
The team also recently published a risk prediction tool that can help estimate a patient’s baseline risk for bleeding.
“So just using a model, which will bring together the patient’s type of surgery and their risk factors, you can look to see, okay, this is enough risk of bleeding, I’m just going to give tranexamic acid,” he said. “We will also be doing economic analyses because blood is also not cheap.”
The study was funded by the Canadian Institutes of Health Research, National Health and Medical Research Council (Australia), and the Research Grant Council (Hong Kong). Dr. Devereaux reports research/research grants from Abbott Diagnostics, Philips Healthcare, Roche Diagnostics, and Siemens. Dr. Mack reports receiving research grants from Abbott Vascular, Edwards Lifesciences, and Medtronic.
A version of this article first appeared on Medscape.com.
The antifibrinolytic tranexamic acid (TXA) reduced serious bleeding without a significant effect on major vascular outcomes in patients undergoing noncardiac surgery at risk for these complications in the POISE-3 trial.
TXA cut the primary efficacy outcome of life-threatening, major, and critical organ bleeding at 30 days by 24% compared with placebo (9.1% vs. 11.7%; hazard ratio [HR], 0.76; P < .0001).
The primary safety outcome of myocardial injury after noncardiac surgery (MINS), nonhemorrhagic stroke, peripheral arterial thrombosis, and symptomatic proximal venous thromboembolism (VTE) at 30 days occurred in 14.2% vs.. 13.9% of patients, respectively (HR, 1.023). This failed, however, to meet the study›s threshold to prove TXA noninferior to placebo (one-sided P = .044).
There was no increased risk for death or stroke with TXA, according to results published April 2 in the New England Journal of Medicine.
Principal investigator P.J. Devereaux, MD, PhD, Population Health Research Institute and McMaster University, Hamilton, Ontario, Canada, pointed out that there is only a 4.4% probability that the composite vascular outcome hazard ratio was above the noninferiority margin and that just 10 events separated the two groups (649 vs.. 639).
“Healthcare providers and patients will have to weigh a clear beneficial reduction in the composite bleeding outcome, which is an absolute difference of 2.7%, a result that was highly statistically significant, versus a low probability of a small increase in risk of the composite vascular endpoint, with an absolute difference of 0.3%,” a nonsignificant result, Dr. Devereaux said during the formal presentation of the results at the hybrid annual scientific sessions of the American College of Cardiology.
The findings, he said, should also be put in the context that 300 million adults have a major surgery each year worldwide and most don’t receive TXA. At the same time, there’s an annual global shortage of 30 million blood product units, and surgical bleeding accounts for up to 40% of all transfusions.
“POISE-3 identifies that use of TXA could avoid upwards of 8 million bleeding events resulting in transfusion on an annual basis, indicating potential for large public health and clinical benefit if TXA become standard practice in noncardiac surgery,” Dr. Devereaux said during the late-breaking trial session.
TXA is indicated for heavy menstrual bleeding and hemophilia and has been used in cardiac surgery, but it is increasingly being used in noncardiac surgeries. As previously reported, POISE showed that the beta-blocker metoprolol lowered the risk for myocardial infarction (MI) but increased the risk for severe stroke and overall death, whereas in POISE-2, perioperative low-dose aspirin lowered the risk for MI but was linked to more major bleeding.
The cumulative data have not shown an increased risk for thrombotic events in other settings, Dr. Devereaux told this news organization.
“I’m a cardiologist, and I think that we’ve been guilty at times of always only focusing on the thrombotic side of the equation and ignoring that bleeding is a very important aspect of the circulatory system,” he said. “And I think this shows for the first time clear unequivocal evidence that there’s a cheap, very encouraging, safe way to prevent this.”
“An important point is that if you can give tranexamic acid and prevent bleeding in your cardiac patients having noncardiac surgery, then you can prevent the delay of reinitiating their anticoagulants and their antiplatelets after surgery and getting them back on the medications that are important for them to prevent their cardiovascular event,” Dr. Devereaux added.
Discussant Michael J. Mack, MD, commented that TXA, widely used in cardiac surgery, is an old, inexpensive drug that “should be more widely used in noncardiac surgery.” Dr. Mack, from Baylor Scott & White Health, Dallas, added that he would limit it to major noncardiac surgery.
International trial
PeriOperative ISchemic Evaluation-3 (POISE-3) investigators at 114 hospitals in 22 countries (including countries in North and South America, Europe, and Africa; Russia; India; and Australia) randomly assigned 9,535 patients, aged 45 years or older, with or at risk for cardiovascular and bleeding complications to receive a TXA 1-g intravenous bolus or placebo at the start and end of inpatient noncardiac surgery.
Patients taking at least one long-term antihypertensive medication were also randomly assigned to a perioperative hypotension- or hypertension-avoidance strategy, which differ in the use of antihypertensives on the morning of surgery and the first 2 days after surgery, and in the target mean arterial pressure during surgery. Results from these cohorts will be presented in a separate session on April 4.
The study had planned to enroll 10,000 patients but was stopped early by the steering committee because of financial constraints resulting from slow enrollment during the pandemic. The decision was made without knowledge of the trial results but with knowledge that aggregate composite bleeding and vascular outcomes were higher than originally estimated, Dr. Devereaux noted.
Among all participants, the mean age was 70 years, 56% were male, almost a third had coronary artery disease, 15% had peripheral artery disease, and 8% had a prior stroke. About 80% were undergoing major surgery. Adherence to the study medications was 96.3% in both groups.
Secondary bleeding outcomes were lower in the TXA and placebo groups, including bleeding independently associated with mortality after surgery (8.7% vs. 11.3%), life-threatening bleeding (1.6% vs. 1.7%), major bleeding (7.6% vs. 10.4%), and critical organ bleeding (0.3% vs. 0.4%).
Importantly, the TXA group had significantly lower rates of International Society on Thrombosis and Haemostasis major bleeding (6.6% vs. 8.7%; P = .0001) and the need for transfusion of 1 or more units of packed red blood cells (9.4% vs. 12.0%; P <.0001), Dr. Devereaux noted.
In terms of secondary vascular outcomes, there were no significant differences between the TXA and placebo groups in rates of MINS (12.8% vs. 12.6%), MINS not fulfilling definition of MI (both 11.5%), MI (1.4% vs. 1.1%), and the net risk-benefit outcome (a composite of vascular death and nonfatal life-threatening, major, or critical organ bleeding, MINS, stroke, peripheral arterial thrombosis, and symptomatic proximal VTE; 20.7% vs. 21.9%).
The two groups had similar rates of all-cause (1.1% vs. 1.2%) and vascular (0.5% vs. 0.6%) mortality.
There also were no significant differences in other tertiary outcomes, such as acute kidney injury (14.1% vs. 13.7%), rehospitalization for vascular reasons (1.8% vs. 1.6%), or seizures (0.2% vs. <0.1%). The latter has been a concern, with the risk reported to increase with higher doses.
Subgroup analyses
Preplanned subgroup analyses showed a benefit for TXA over placebo for the primary efficacy outcome in orthopedic and nonorthopedic surgery and in patients with hemoglobin level below 120 g/L or 120 g/L or higher, with an estimated glomerular filtration rate less than 45 mL/min/1.73 m 2 or 45 mL/min/1.73 m 2 or higher, or with an N-terminal pro– B-type natriuretic peptide level below 200 ng/L or 200 ng/L or higher.
For the primary safety outcome, the benefit favored placebo but the interaction was not statistically significant for any of the four subgroups.
A post hoc subgroup analysis also showed similar results across the major categories of surgery, including general, vascular, urologic, and gynecologic, Dr. Devereaux told this news organization.
Although TXA is commonly used in orthopedic procedures, Dr. Devereaux noted, in other types of surgeries, “it’s not used at all.” But because TXA “is so cheap, and we can apply it to a broad population, even at an economic level it looks like it’s a winner to give to almost all patients having noncardiac surgery.”
The team also recently published a risk prediction tool that can help estimate a patient’s baseline risk for bleeding.
“So just using a model, which will bring together the patient’s type of surgery and their risk factors, you can look to see, okay, this is enough risk of bleeding, I’m just going to give tranexamic acid,” he said. “We will also be doing economic analyses because blood is also not cheap.”
The study was funded by the Canadian Institutes of Health Research, National Health and Medical Research Council (Australia), and the Research Grant Council (Hong Kong). Dr. Devereaux reports research/research grants from Abbott Diagnostics, Philips Healthcare, Roche Diagnostics, and Siemens. Dr. Mack reports receiving research grants from Abbott Vascular, Edwards Lifesciences, and Medtronic.
A version of this article first appeared on Medscape.com.
FROM ACC 2022
Cancer of the appendix on the rise in younger patients with appendicitis
Younger patients with appendicitis appear to be increasingly likely to have cancer of the appendix, a new study suggests.
While acute appendicitis can often be managed with antibiotics instead of surgery, patients who do not have surgery need to be closely followed to avoid missed diagnoses, the authors write.
“The most important finding is that between 2004 and 2017, relative to right-sided colon cancer, the number of appendiceal cancer cases increased,” said Mustafa Raoof, MD, who was not involved in the study. He is a surgical oncologist and an assistant professor of surgical oncology at City of Hope Comprehensive Cancer Center, Duarte, Calif. “Approximately one-fourth of these were carcinoid tumors, and this category saw the greatest increase, particularly in individuals under 50 years of age.”
“There is a push to treat acute appendicitis with only antibiotics to avoid surgery,” Dr. Raoof told this news organization by email. “One underappreciated downside of this strategy is that an appendiceal cancer can be missed if the appendix is not removed.”
As reported in Journal of the American College of Surgeons, lead study author Michelle C. Salazar, MD, MHS, a general surgery resident at Yale School of Medicine in New Haven, Conn., and her colleagues conducted a retrospective analysis of the National Cancer Database (NCDB). The NCDB contains hospital registry data of around 70% of new cancer diagnoses in the United States.
The researchers extracted data on patients aged 18 years and older who were diagnosed with right-sided colon cancer between 2004 and 2017 and who underwent appendectomy. The authors also identified all patients with appendiceal cancer. They divided that group into patients with carcinoid tumors and those with other types of appendiceal cancer. They also investigated trends by age group.
Of 387,867 patients with right-sided colon cancer, 19,570 (5%) had appendiceal cancer, and 5,628 of those patients (29%) had carcinoid tumor. The odds of appendiceal cancer, compared with other right-sided colon cancers, rose over the years studied (odds ratio, 2.56; 95% confidence interval, 2.35-2.79).
This increase in odds occurred in all age groups but was steepest among patients between 40 and 49 years of age, among whom it increased from 10% in 2004 (95% CI, 9-12) to 18% in 2017 (95% CI, 16-20; P < .001).
Odds of appendiceal carcinoid, compared with other appendiceal cancers, also rose during this period (OR, 1.70; 95% CI, 1.40-2.07). The sharpest increase occurred in the likelihood of carcinoid in patients younger than 40, from 24% in 2004 (95% CI, 15-34) to 45% in 2017 (95% CI, 37-53; P < .001).
“The findings in this study are yet another reason to temper excitement about nonoperative management of acute appendicitis in adults,” Richard S. Hoehn, MD, a surgical oncologist at University Hospitals Seidman Cancer Center, Cleveland, said. “The study is important because it reveals a potential risk of deferring appendectomy in adult patients with appendiceal pathology.”
“As our pathologic examinations of appendiceal cancers improve, we are gaining better understanding of these tumors and how to best manage these patients,” Dr. Hoehn, who also was not involved in the study, added in an email. “The findings should make surgeons more suspicious of malignant causes of acute appendicitis in adults, especially those under 40. Colonoscopy and appendectomy are necessary in adult patients with appendicitis.”
Gregory Botta, MD, PhD, a medical oncologist and associate professor of medicine at the University of California San Diego Health, mentioned limitations of the study in an email. They include the NCDB’s omission of around 30% of cases nationally and the study’s omission of patients diagnosed with primary appendiceal tumor, as well as patients who underwent total colectomies and those who did not have surgery.
“Appendiceal tumors are not normally seen during colonoscopies; screening colonoscopies are not recommended to younger patients under 40, and there is less surgical management for appendicitis,” explained Dr. Botta, who also was not involved in the study. “Thus, the cause of the increasing incidence is not due to increased detection on surveillance.
“Gastrointestinal oncologists are seeing an increase in colon cancer in younger patients and a parallel increase in appendix tumors. While carcinoid tumors are usually found localized and [are] therefore curable postsurgical resection, adenocarcinoma or mucinous subtypes tend to be more diffuse, metastatic, and noncurable,” he added. “Although the increase in colon cancer is being found in our younger population, the authors hint at causes not captured by the NCDB, including environmental exposures or each patient’s diet.”
“There is no good answer as to why there is an increase in carcinoids,” Dr. Salazar said in a press release. “It could be due to environmental reasons, or it could be due to better diagnostics technology.”
The researchers and independent experts share concerns that, because surgery provides the only definitive diagnosis of appendiceal cancer, among patients managed nonsurgically, there may be a delay in cancer diagnosis.
“I would counsel patients based on age,” Dr. Salazar added. “If you’re older, you are at less risk for appendiceal cancer and greater risk for complications from surgery. Younger, healthy patients are more likely to be able to tolerate an operation and may want to rule out cancer by undergoing the operation. The characteristics of appendicitis should be considered in the decision.”
Funding information was not provided. The authors, Dr. Raoof, Dr. Hoehn, and Dr. Botta have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Younger patients with appendicitis appear to be increasingly likely to have cancer of the appendix, a new study suggests.
While acute appendicitis can often be managed with antibiotics instead of surgery, patients who do not have surgery need to be closely followed to avoid missed diagnoses, the authors write.
“The most important finding is that between 2004 and 2017, relative to right-sided colon cancer, the number of appendiceal cancer cases increased,” said Mustafa Raoof, MD, who was not involved in the study. He is a surgical oncologist and an assistant professor of surgical oncology at City of Hope Comprehensive Cancer Center, Duarte, Calif. “Approximately one-fourth of these were carcinoid tumors, and this category saw the greatest increase, particularly in individuals under 50 years of age.”
“There is a push to treat acute appendicitis with only antibiotics to avoid surgery,” Dr. Raoof told this news organization by email. “One underappreciated downside of this strategy is that an appendiceal cancer can be missed if the appendix is not removed.”
As reported in Journal of the American College of Surgeons, lead study author Michelle C. Salazar, MD, MHS, a general surgery resident at Yale School of Medicine in New Haven, Conn., and her colleagues conducted a retrospective analysis of the National Cancer Database (NCDB). The NCDB contains hospital registry data of around 70% of new cancer diagnoses in the United States.
The researchers extracted data on patients aged 18 years and older who were diagnosed with right-sided colon cancer between 2004 and 2017 and who underwent appendectomy. The authors also identified all patients with appendiceal cancer. They divided that group into patients with carcinoid tumors and those with other types of appendiceal cancer. They also investigated trends by age group.
Of 387,867 patients with right-sided colon cancer, 19,570 (5%) had appendiceal cancer, and 5,628 of those patients (29%) had carcinoid tumor. The odds of appendiceal cancer, compared with other right-sided colon cancers, rose over the years studied (odds ratio, 2.56; 95% confidence interval, 2.35-2.79).
This increase in odds occurred in all age groups but was steepest among patients between 40 and 49 years of age, among whom it increased from 10% in 2004 (95% CI, 9-12) to 18% in 2017 (95% CI, 16-20; P < .001).
Odds of appendiceal carcinoid, compared with other appendiceal cancers, also rose during this period (OR, 1.70; 95% CI, 1.40-2.07). The sharpest increase occurred in the likelihood of carcinoid in patients younger than 40, from 24% in 2004 (95% CI, 15-34) to 45% in 2017 (95% CI, 37-53; P < .001).
“The findings in this study are yet another reason to temper excitement about nonoperative management of acute appendicitis in adults,” Richard S. Hoehn, MD, a surgical oncologist at University Hospitals Seidman Cancer Center, Cleveland, said. “The study is important because it reveals a potential risk of deferring appendectomy in adult patients with appendiceal pathology.”
“As our pathologic examinations of appendiceal cancers improve, we are gaining better understanding of these tumors and how to best manage these patients,” Dr. Hoehn, who also was not involved in the study, added in an email. “The findings should make surgeons more suspicious of malignant causes of acute appendicitis in adults, especially those under 40. Colonoscopy and appendectomy are necessary in adult patients with appendicitis.”
Gregory Botta, MD, PhD, a medical oncologist and associate professor of medicine at the University of California San Diego Health, mentioned limitations of the study in an email. They include the NCDB’s omission of around 30% of cases nationally and the study’s omission of patients diagnosed with primary appendiceal tumor, as well as patients who underwent total colectomies and those who did not have surgery.
“Appendiceal tumors are not normally seen during colonoscopies; screening colonoscopies are not recommended to younger patients under 40, and there is less surgical management for appendicitis,” explained Dr. Botta, who also was not involved in the study. “Thus, the cause of the increasing incidence is not due to increased detection on surveillance.
“Gastrointestinal oncologists are seeing an increase in colon cancer in younger patients and a parallel increase in appendix tumors. While carcinoid tumors are usually found localized and [are] therefore curable postsurgical resection, adenocarcinoma or mucinous subtypes tend to be more diffuse, metastatic, and noncurable,” he added. “Although the increase in colon cancer is being found in our younger population, the authors hint at causes not captured by the NCDB, including environmental exposures or each patient’s diet.”
“There is no good answer as to why there is an increase in carcinoids,” Dr. Salazar said in a press release. “It could be due to environmental reasons, or it could be due to better diagnostics technology.”
The researchers and independent experts share concerns that, because surgery provides the only definitive diagnosis of appendiceal cancer, among patients managed nonsurgically, there may be a delay in cancer diagnosis.
“I would counsel patients based on age,” Dr. Salazar added. “If you’re older, you are at less risk for appendiceal cancer and greater risk for complications from surgery. Younger, healthy patients are more likely to be able to tolerate an operation and may want to rule out cancer by undergoing the operation. The characteristics of appendicitis should be considered in the decision.”
Funding information was not provided. The authors, Dr. Raoof, Dr. Hoehn, and Dr. Botta have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Younger patients with appendicitis appear to be increasingly likely to have cancer of the appendix, a new study suggests.
While acute appendicitis can often be managed with antibiotics instead of surgery, patients who do not have surgery need to be closely followed to avoid missed diagnoses, the authors write.
“The most important finding is that between 2004 and 2017, relative to right-sided colon cancer, the number of appendiceal cancer cases increased,” said Mustafa Raoof, MD, who was not involved in the study. He is a surgical oncologist and an assistant professor of surgical oncology at City of Hope Comprehensive Cancer Center, Duarte, Calif. “Approximately one-fourth of these were carcinoid tumors, and this category saw the greatest increase, particularly in individuals under 50 years of age.”
“There is a push to treat acute appendicitis with only antibiotics to avoid surgery,” Dr. Raoof told this news organization by email. “One underappreciated downside of this strategy is that an appendiceal cancer can be missed if the appendix is not removed.”
As reported in Journal of the American College of Surgeons, lead study author Michelle C. Salazar, MD, MHS, a general surgery resident at Yale School of Medicine in New Haven, Conn., and her colleagues conducted a retrospective analysis of the National Cancer Database (NCDB). The NCDB contains hospital registry data of around 70% of new cancer diagnoses in the United States.
The researchers extracted data on patients aged 18 years and older who were diagnosed with right-sided colon cancer between 2004 and 2017 and who underwent appendectomy. The authors also identified all patients with appendiceal cancer. They divided that group into patients with carcinoid tumors and those with other types of appendiceal cancer. They also investigated trends by age group.
Of 387,867 patients with right-sided colon cancer, 19,570 (5%) had appendiceal cancer, and 5,628 of those patients (29%) had carcinoid tumor. The odds of appendiceal cancer, compared with other right-sided colon cancers, rose over the years studied (odds ratio, 2.56; 95% confidence interval, 2.35-2.79).
This increase in odds occurred in all age groups but was steepest among patients between 40 and 49 years of age, among whom it increased from 10% in 2004 (95% CI, 9-12) to 18% in 2017 (95% CI, 16-20; P < .001).
Odds of appendiceal carcinoid, compared with other appendiceal cancers, also rose during this period (OR, 1.70; 95% CI, 1.40-2.07). The sharpest increase occurred in the likelihood of carcinoid in patients younger than 40, from 24% in 2004 (95% CI, 15-34) to 45% in 2017 (95% CI, 37-53; P < .001).
“The findings in this study are yet another reason to temper excitement about nonoperative management of acute appendicitis in adults,” Richard S. Hoehn, MD, a surgical oncologist at University Hospitals Seidman Cancer Center, Cleveland, said. “The study is important because it reveals a potential risk of deferring appendectomy in adult patients with appendiceal pathology.”
“As our pathologic examinations of appendiceal cancers improve, we are gaining better understanding of these tumors and how to best manage these patients,” Dr. Hoehn, who also was not involved in the study, added in an email. “The findings should make surgeons more suspicious of malignant causes of acute appendicitis in adults, especially those under 40. Colonoscopy and appendectomy are necessary in adult patients with appendicitis.”
Gregory Botta, MD, PhD, a medical oncologist and associate professor of medicine at the University of California San Diego Health, mentioned limitations of the study in an email. They include the NCDB’s omission of around 30% of cases nationally and the study’s omission of patients diagnosed with primary appendiceal tumor, as well as patients who underwent total colectomies and those who did not have surgery.
“Appendiceal tumors are not normally seen during colonoscopies; screening colonoscopies are not recommended to younger patients under 40, and there is less surgical management for appendicitis,” explained Dr. Botta, who also was not involved in the study. “Thus, the cause of the increasing incidence is not due to increased detection on surveillance.
“Gastrointestinal oncologists are seeing an increase in colon cancer in younger patients and a parallel increase in appendix tumors. While carcinoid tumors are usually found localized and [are] therefore curable postsurgical resection, adenocarcinoma or mucinous subtypes tend to be more diffuse, metastatic, and noncurable,” he added. “Although the increase in colon cancer is being found in our younger population, the authors hint at causes not captured by the NCDB, including environmental exposures or each patient’s diet.”
“There is no good answer as to why there is an increase in carcinoids,” Dr. Salazar said in a press release. “It could be due to environmental reasons, or it could be due to better diagnostics technology.”
The researchers and independent experts share concerns that, because surgery provides the only definitive diagnosis of appendiceal cancer, among patients managed nonsurgically, there may be a delay in cancer diagnosis.
“I would counsel patients based on age,” Dr. Salazar added. “If you’re older, you are at less risk for appendiceal cancer and greater risk for complications from surgery. Younger, healthy patients are more likely to be able to tolerate an operation and may want to rule out cancer by undergoing the operation. The characteristics of appendicitis should be considered in the decision.”
Funding information was not provided. The authors, Dr. Raoof, Dr. Hoehn, and Dr. Botta have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM JOURNAL OF THE AMERICAN COLLEGE OF SURGEONS
Lawsuit: 18-inch sponge left in stomach for 5 years; migrates internally
Carolyn Boerste underwent aortobifemoral bypass surgery at the University of Louisville (Ky.) Hospital in March 2011 to improve circulation in her lower extremities. She had a history of peripheral vascular disease, hypertension, and diabetes, which caused a wound on her toe to become infected and gangrenous, according to court records.
During the surgery, performed by Marvin Morris, MD, the surgical team left a laparotomy sponge in Ms. Boerste’s abdomen. Because of its size, Ms. Boerste’s attorneys characterized the 18-by-18-inch object as “more like a towel,” according to court documents.
During the years that the sponge went undetected, the object eroded via transmural migration from Ms. Boerste’s abdomen into her intestine, causing diarrhea, vomiting, and nausea. In March 2015, Ms. Boerste was transferred by ambulance to an emergency department because of abdominal pain. An emergency physician ordered an abdominal CT scan, which showed the x-ray detectable sponge marker inside Ms. Boerste’s intestine, according to her complaint.
Although the radiologist called the emergency physician to advise him of the sponge marker, the information was not shared with Ms. Boerste and she was discharged from the hospital with a urinary tract infection diagnosis. The emergency physician later testified he had no memory of the call with the radiologist.
The CT scan was faxed to Ms. Boerste’s family physician. She testified that she read the report but did not mention the sponge marker to Ms. Boerste because she believed the issue had been handled by the emergency physician. Thus the sponge remained inside Ms. Boerste for another 20 months.
In November 2016, Ms. Boerste returned to the same emergency department with more intense gastrointestinal issues. Another CT scan was ordered, which revealed the sponge. The object was removed by exploratory laparotomy later that month. In her complaint, Ms. Boerste claimed that the removal surgery resulted in amputation of her leg because of wounds developed on her lower extremities while she was bedridden during recovery.
In 2017, she filed a negligence lawsuit against Dr. Morris, the hospital, and several others involved in her care. On the first day of trial in December 2019, the hospital conceded liability. The trial continued against Dr. Morris and the other defendants as to liability and damages and proceeded against the hospital as to damages.
At trial, evidence showed there was significant confusion among nurses on how to document sponge counts, according to the appellate decision. In general, nurses used a perioperative nursing record to document the surgical procedure, and that record had a place to document some but not all sponge counts required by hospital policy. The nursing record did not have a place to document sponge counts required to be recorded at every break, lunch, and shift change. Nurses also used a worksheet to track sponge counts, but that worksheet was not part of the medical record.
Dr. Morris testified that he relies on nurses regarding sponge counts, but that he also performs a visual and tactile inspection of the abdominal cavity. He acknowledged during trial that the standard of care required him to keep track of the sponges before closing. Dr. Morris also testified that the surgeon and nurses are a team, and “the entire team did not count the sponges correctly when finishing the bypass surgery,” according to the appellate decision.
After a 10-day trial, jurors found Dr. Morris and several other defendants liable. They apportioned 60% liability to the hospital, 10% to Morris, 15% to the family physician, 0% to the emergency physician, and 15% to the rehabilitation center. Ms. Boerste was awarded $9.5 million in damages and an additional $1 million in punitive damages, for a total of $10.5 million.
Dr. Morris and the hospital appealed to the Commonwealth of Kentucky Court of Appeals. As the appeal was pending, Ms. Boerste died, and her son took over the plaintiff’s role.
In their appeal, Dr. Morris and the hospital said they should be granted a new trial for a number of reasons, including that the pain and suffering award was grossly excessive and reflected improper jury sympathy, that the punitive damages award should be vacated because jurors were not properly instructed on the issue, and that the judgment against Dr. Morris should be overturned because there was no evidence he deviated from the standard of care.
The defendants also argued that they were entitled to instructions on “apportionment of fault and mitigation of damages against Boerste.” The mitigation of damages doctrine prevents an injured plaintiff from recovering unreasonable expenses associated with the injury if they could have been avoided through reasonable efforts. Specifically, attorneys for Dr. Morris emphasized that Ms. Boerste failed to follow medical advice for follow-up care, to obtain recommended podiatrist care, and to make necessary efforts to control her diabetes. Had Ms. Boerste taken more proactive steps to manage her health, leg amputation may not have been needed because the sponge may have been found during other treatment, they contended.
In its Jan. 7, 2022, opinion, the appeals court upheld the majority of the jury award. Judges wrote that Dr. Morris’ testimony alone was sufficient for the jury to determine whether he breached the standard of care, and that the defendants are not entitled to a new trial on pain and suffering damages. In addition, judges rejected mitigation of damages.
“The fact that Boerste was a poor patient who failed to properly treat her diabetes is irrelevant,” the panel wrote in their decision. “She was a poor patient prior to the bypass surgery, and Appellants knew Boerste might ultimately need to have her lower leg amputated at the time of the bypass surgery. Therefore, we hold Appellants were not entitled to instructions on apportionment of fault or mitigation of damages.”
The appeals court, however, vacated the $1 million punitive damages award, ruling that the lower court did not give a proper instruction to the jury on punitive damages. The appeals court sent the case back to the lower court for a retrial as it pertains to punitive damages.
Attorneys for Dr. Morris and the hospital did not return messages seeking comment.
Bo Bolus, an attorney for Ms. Boerste’s family, said there will be no retrial on punitive damages, and that the plaintiff is satisfied with the outcome of the case.
“While we are pleased that Carolyn’s family and, equally importantly, her memory, now finally have closure on this extremely trying matter, our pleasure is severely tempered by the loss of Carolyn in November of last year,” Mr. Bolus said. “After having endured all she did, it is, frankly, painful for all concerned that she will not reap the reward of the jury’s verdict.”
A version of this article first appeared on Medscape.com.
Carolyn Boerste underwent aortobifemoral bypass surgery at the University of Louisville (Ky.) Hospital in March 2011 to improve circulation in her lower extremities. She had a history of peripheral vascular disease, hypertension, and diabetes, which caused a wound on her toe to become infected and gangrenous, according to court records.
During the surgery, performed by Marvin Morris, MD, the surgical team left a laparotomy sponge in Ms. Boerste’s abdomen. Because of its size, Ms. Boerste’s attorneys characterized the 18-by-18-inch object as “more like a towel,” according to court documents.
During the years that the sponge went undetected, the object eroded via transmural migration from Ms. Boerste’s abdomen into her intestine, causing diarrhea, vomiting, and nausea. In March 2015, Ms. Boerste was transferred by ambulance to an emergency department because of abdominal pain. An emergency physician ordered an abdominal CT scan, which showed the x-ray detectable sponge marker inside Ms. Boerste’s intestine, according to her complaint.
Although the radiologist called the emergency physician to advise him of the sponge marker, the information was not shared with Ms. Boerste and she was discharged from the hospital with a urinary tract infection diagnosis. The emergency physician later testified he had no memory of the call with the radiologist.
The CT scan was faxed to Ms. Boerste’s family physician. She testified that she read the report but did not mention the sponge marker to Ms. Boerste because she believed the issue had been handled by the emergency physician. Thus the sponge remained inside Ms. Boerste for another 20 months.
In November 2016, Ms. Boerste returned to the same emergency department with more intense gastrointestinal issues. Another CT scan was ordered, which revealed the sponge. The object was removed by exploratory laparotomy later that month. In her complaint, Ms. Boerste claimed that the removal surgery resulted in amputation of her leg because of wounds developed on her lower extremities while she was bedridden during recovery.
In 2017, she filed a negligence lawsuit against Dr. Morris, the hospital, and several others involved in her care. On the first day of trial in December 2019, the hospital conceded liability. The trial continued against Dr. Morris and the other defendants as to liability and damages and proceeded against the hospital as to damages.
At trial, evidence showed there was significant confusion among nurses on how to document sponge counts, according to the appellate decision. In general, nurses used a perioperative nursing record to document the surgical procedure, and that record had a place to document some but not all sponge counts required by hospital policy. The nursing record did not have a place to document sponge counts required to be recorded at every break, lunch, and shift change. Nurses also used a worksheet to track sponge counts, but that worksheet was not part of the medical record.
Dr. Morris testified that he relies on nurses regarding sponge counts, but that he also performs a visual and tactile inspection of the abdominal cavity. He acknowledged during trial that the standard of care required him to keep track of the sponges before closing. Dr. Morris also testified that the surgeon and nurses are a team, and “the entire team did not count the sponges correctly when finishing the bypass surgery,” according to the appellate decision.
After a 10-day trial, jurors found Dr. Morris and several other defendants liable. They apportioned 60% liability to the hospital, 10% to Morris, 15% to the family physician, 0% to the emergency physician, and 15% to the rehabilitation center. Ms. Boerste was awarded $9.5 million in damages and an additional $1 million in punitive damages, for a total of $10.5 million.
Dr. Morris and the hospital appealed to the Commonwealth of Kentucky Court of Appeals. As the appeal was pending, Ms. Boerste died, and her son took over the plaintiff’s role.
In their appeal, Dr. Morris and the hospital said they should be granted a new trial for a number of reasons, including that the pain and suffering award was grossly excessive and reflected improper jury sympathy, that the punitive damages award should be vacated because jurors were not properly instructed on the issue, and that the judgment against Dr. Morris should be overturned because there was no evidence he deviated from the standard of care.
The defendants also argued that they were entitled to instructions on “apportionment of fault and mitigation of damages against Boerste.” The mitigation of damages doctrine prevents an injured plaintiff from recovering unreasonable expenses associated with the injury if they could have been avoided through reasonable efforts. Specifically, attorneys for Dr. Morris emphasized that Ms. Boerste failed to follow medical advice for follow-up care, to obtain recommended podiatrist care, and to make necessary efforts to control her diabetes. Had Ms. Boerste taken more proactive steps to manage her health, leg amputation may not have been needed because the sponge may have been found during other treatment, they contended.
In its Jan. 7, 2022, opinion, the appeals court upheld the majority of the jury award. Judges wrote that Dr. Morris’ testimony alone was sufficient for the jury to determine whether he breached the standard of care, and that the defendants are not entitled to a new trial on pain and suffering damages. In addition, judges rejected mitigation of damages.
“The fact that Boerste was a poor patient who failed to properly treat her diabetes is irrelevant,” the panel wrote in their decision. “She was a poor patient prior to the bypass surgery, and Appellants knew Boerste might ultimately need to have her lower leg amputated at the time of the bypass surgery. Therefore, we hold Appellants were not entitled to instructions on apportionment of fault or mitigation of damages.”
The appeals court, however, vacated the $1 million punitive damages award, ruling that the lower court did not give a proper instruction to the jury on punitive damages. The appeals court sent the case back to the lower court for a retrial as it pertains to punitive damages.
Attorneys for Dr. Morris and the hospital did not return messages seeking comment.
Bo Bolus, an attorney for Ms. Boerste’s family, said there will be no retrial on punitive damages, and that the plaintiff is satisfied with the outcome of the case.
“While we are pleased that Carolyn’s family and, equally importantly, her memory, now finally have closure on this extremely trying matter, our pleasure is severely tempered by the loss of Carolyn in November of last year,” Mr. Bolus said. “After having endured all she did, it is, frankly, painful for all concerned that she will not reap the reward of the jury’s verdict.”
A version of this article first appeared on Medscape.com.
Carolyn Boerste underwent aortobifemoral bypass surgery at the University of Louisville (Ky.) Hospital in March 2011 to improve circulation in her lower extremities. She had a history of peripheral vascular disease, hypertension, and diabetes, which caused a wound on her toe to become infected and gangrenous, according to court records.
During the surgery, performed by Marvin Morris, MD, the surgical team left a laparotomy sponge in Ms. Boerste’s abdomen. Because of its size, Ms. Boerste’s attorneys characterized the 18-by-18-inch object as “more like a towel,” according to court documents.
During the years that the sponge went undetected, the object eroded via transmural migration from Ms. Boerste’s abdomen into her intestine, causing diarrhea, vomiting, and nausea. In March 2015, Ms. Boerste was transferred by ambulance to an emergency department because of abdominal pain. An emergency physician ordered an abdominal CT scan, which showed the x-ray detectable sponge marker inside Ms. Boerste’s intestine, according to her complaint.
Although the radiologist called the emergency physician to advise him of the sponge marker, the information was not shared with Ms. Boerste and she was discharged from the hospital with a urinary tract infection diagnosis. The emergency physician later testified he had no memory of the call with the radiologist.
The CT scan was faxed to Ms. Boerste’s family physician. She testified that she read the report but did not mention the sponge marker to Ms. Boerste because she believed the issue had been handled by the emergency physician. Thus the sponge remained inside Ms. Boerste for another 20 months.
In November 2016, Ms. Boerste returned to the same emergency department with more intense gastrointestinal issues. Another CT scan was ordered, which revealed the sponge. The object was removed by exploratory laparotomy later that month. In her complaint, Ms. Boerste claimed that the removal surgery resulted in amputation of her leg because of wounds developed on her lower extremities while she was bedridden during recovery.
In 2017, she filed a negligence lawsuit against Dr. Morris, the hospital, and several others involved in her care. On the first day of trial in December 2019, the hospital conceded liability. The trial continued against Dr. Morris and the other defendants as to liability and damages and proceeded against the hospital as to damages.
At trial, evidence showed there was significant confusion among nurses on how to document sponge counts, according to the appellate decision. In general, nurses used a perioperative nursing record to document the surgical procedure, and that record had a place to document some but not all sponge counts required by hospital policy. The nursing record did not have a place to document sponge counts required to be recorded at every break, lunch, and shift change. Nurses also used a worksheet to track sponge counts, but that worksheet was not part of the medical record.
Dr. Morris testified that he relies on nurses regarding sponge counts, but that he also performs a visual and tactile inspection of the abdominal cavity. He acknowledged during trial that the standard of care required him to keep track of the sponges before closing. Dr. Morris also testified that the surgeon and nurses are a team, and “the entire team did not count the sponges correctly when finishing the bypass surgery,” according to the appellate decision.
After a 10-day trial, jurors found Dr. Morris and several other defendants liable. They apportioned 60% liability to the hospital, 10% to Morris, 15% to the family physician, 0% to the emergency physician, and 15% to the rehabilitation center. Ms. Boerste was awarded $9.5 million in damages and an additional $1 million in punitive damages, for a total of $10.5 million.
Dr. Morris and the hospital appealed to the Commonwealth of Kentucky Court of Appeals. As the appeal was pending, Ms. Boerste died, and her son took over the plaintiff’s role.
In their appeal, Dr. Morris and the hospital said they should be granted a new trial for a number of reasons, including that the pain and suffering award was grossly excessive and reflected improper jury sympathy, that the punitive damages award should be vacated because jurors were not properly instructed on the issue, and that the judgment against Dr. Morris should be overturned because there was no evidence he deviated from the standard of care.
The defendants also argued that they were entitled to instructions on “apportionment of fault and mitigation of damages against Boerste.” The mitigation of damages doctrine prevents an injured plaintiff from recovering unreasonable expenses associated with the injury if they could have been avoided through reasonable efforts. Specifically, attorneys for Dr. Morris emphasized that Ms. Boerste failed to follow medical advice for follow-up care, to obtain recommended podiatrist care, and to make necessary efforts to control her diabetes. Had Ms. Boerste taken more proactive steps to manage her health, leg amputation may not have been needed because the sponge may have been found during other treatment, they contended.
In its Jan. 7, 2022, opinion, the appeals court upheld the majority of the jury award. Judges wrote that Dr. Morris’ testimony alone was sufficient for the jury to determine whether he breached the standard of care, and that the defendants are not entitled to a new trial on pain and suffering damages. In addition, judges rejected mitigation of damages.
“The fact that Boerste was a poor patient who failed to properly treat her diabetes is irrelevant,” the panel wrote in their decision. “She was a poor patient prior to the bypass surgery, and Appellants knew Boerste might ultimately need to have her lower leg amputated at the time of the bypass surgery. Therefore, we hold Appellants were not entitled to instructions on apportionment of fault or mitigation of damages.”
The appeals court, however, vacated the $1 million punitive damages award, ruling that the lower court did not give a proper instruction to the jury on punitive damages. The appeals court sent the case back to the lower court for a retrial as it pertains to punitive damages.
Attorneys for Dr. Morris and the hospital did not return messages seeking comment.
Bo Bolus, an attorney for Ms. Boerste’s family, said there will be no retrial on punitive damages, and that the plaintiff is satisfied with the outcome of the case.
“While we are pleased that Carolyn’s family and, equally importantly, her memory, now finally have closure on this extremely trying matter, our pleasure is severely tempered by the loss of Carolyn in November of last year,” Mr. Bolus said. “After having endured all she did, it is, frankly, painful for all concerned that she will not reap the reward of the jury’s verdict.”
A version of this article first appeared on Medscape.com.
Hernia recurrence has improved only slightly
, according to a new research letter published March 1 in JAMA. Patients who underwent minimally invasive hernia repair had a higher incidence of reoperation than those who underwent open repairs.
In the United States, surgeons perform more than 1 million hernia repairs each year, according to the U.S. Food and Drug Administration. Despite hernias being such a common condition, it is “not at the forefront of many research agendas,” senior author Dana Telem, MD, an associate professor and section chief of general surgery at University of Michigan Health in Ann Arbor, said in an interview
While many surgical outcomes are measured within 30 days of operation, recurrences generally happen within 2 to 5 years after repair, she said. The last study that looked at reoperations for hernia repair at 10 years was published in 2003 and found that about 20% of patients needed surgery for reoccurrence over a decade. “We don’t really have a good understanding of what happened after these operations,” she explained. “Without knowing that piece, it is hard to go back retrospectively and understand what is the right operation for the right person at the right time.”
To understand rates of reoperation for hernia reoccurrence in today’s U.S. population of older adults, Dr. Telem and colleagues sorted through Medicare claims data to find adult patients who had undergone ventral or incisional and umbilical hernia repair from January 1, 2007 through December 31, 2018. They identified a total of 175,735 patients, 162,292 that underwent ventral or incisional hernia repair and 13,443 that underwent umbilical hernia repair. The average age of patients was 68.9 years and 39.2% were men. Most patients were White (87.2%), 8.1% were Black, 1.9% were Hispanic, and 0.5% were Asian. Median follow-up was 5.3 years.
Over the 10-year study period, 25,061 patients required reoperation for hernia recurrence with an adjusted cumulative incidence of 16.1% (95% CI, 16.1% - 16.2%). Patients who underwent open repair had a lower incidence of recurrence over 10 years than those who underwent minimally invasive repair for all hernia types (Table 1).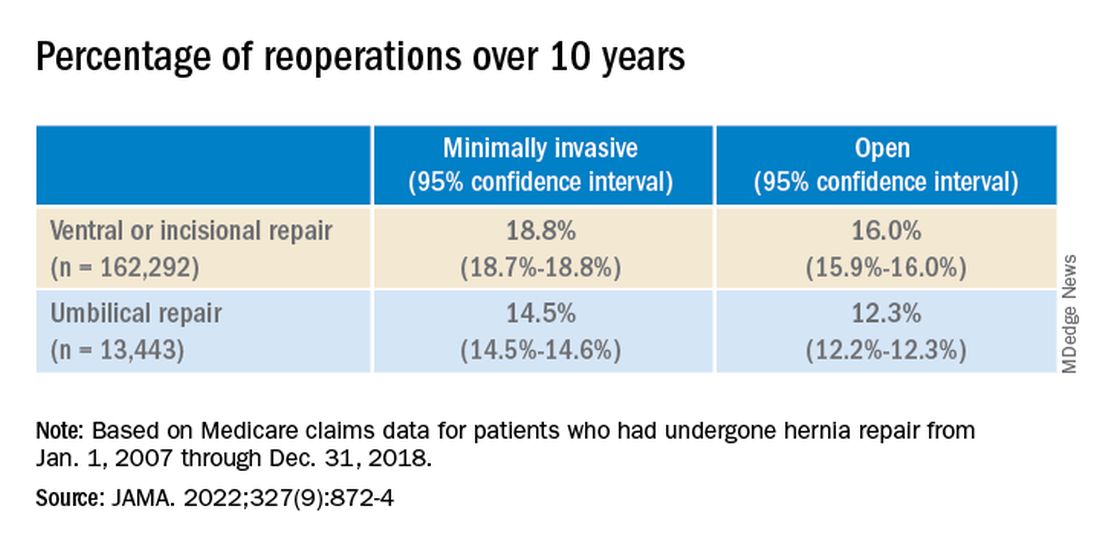
While it appears that hernia recurrence and reoperation have only marginally improved from 2003 to today, Vedra Augenstein, MD, an associate professor of surgery at the Atrium Health General & Complex Abdominal Surgery facility in Charlotte, N.C., suspects there is more to the story. “I think the reason it hasn’t gotten a whole lot better is just because we are operating on much tougher cases than we used to,” she said in an interview. “The way we are fixing hernias has changed and patients are being optimized differently.” Dr. Augenstein was not involved with the research.
To better understand how recurrence has changed over time, there needs to be more data about the comorbidities of patients, the techniques employed, and the meshes used in these surgeries, she said. Those numbers are not available in the published JAMA research letter, but Dr. Telem and colleagues will be submitting an article about this work with greater details.
Dr. Augenstein was also surprised that minimally invasive surgeries had higher incidences of reoperation for recurrence compared to open hernia surgeries. “I would think that patients who had minimally invasive repairs would actually have a lower chance of having postoperative complications because of wound issues,” she said. “Literature has shown that the recurrence rate is lower [in minimally invasive surgeries] because of fewer surgical site infections.”
While Dr. Telem also considers this research letter to be the first step in understanding modern hernia surgery outcomes, it is also a reminder that there is room for improvement in hernia repair surgeries. This includes advising patients on risk factors that may make them more likely to have a hernia recurrence, such as obesity, smoking, and diabetes, she added. “If we know it’s not a perfect science, then we have to do everything that we can upfront to help those numbers.”
Dr. Telem has reported receiving grants from the Agency for Healthcare Research and Quality and consulting fees from Medtronic. Dr. Augenstein has reported consulting for Intuitive Surgical, Medtronic, Allergan, Acelity, Vicarious Surgical, and Bard Pharmaceuticals and has received honoraria for speaking from Medtronic, Allergan, Intuitive Surgical, Acelity, and WL Gore.
A version of this article first appeared on Medscape.com.
, according to a new research letter published March 1 in JAMA. Patients who underwent minimally invasive hernia repair had a higher incidence of reoperation than those who underwent open repairs.
In the United States, surgeons perform more than 1 million hernia repairs each year, according to the U.S. Food and Drug Administration. Despite hernias being such a common condition, it is “not at the forefront of many research agendas,” senior author Dana Telem, MD, an associate professor and section chief of general surgery at University of Michigan Health in Ann Arbor, said in an interview
While many surgical outcomes are measured within 30 days of operation, recurrences generally happen within 2 to 5 years after repair, she said. The last study that looked at reoperations for hernia repair at 10 years was published in 2003 and found that about 20% of patients needed surgery for reoccurrence over a decade. “We don’t really have a good understanding of what happened after these operations,” she explained. “Without knowing that piece, it is hard to go back retrospectively and understand what is the right operation for the right person at the right time.”
To understand rates of reoperation for hernia reoccurrence in today’s U.S. population of older adults, Dr. Telem and colleagues sorted through Medicare claims data to find adult patients who had undergone ventral or incisional and umbilical hernia repair from January 1, 2007 through December 31, 2018. They identified a total of 175,735 patients, 162,292 that underwent ventral or incisional hernia repair and 13,443 that underwent umbilical hernia repair. The average age of patients was 68.9 years and 39.2% were men. Most patients were White (87.2%), 8.1% were Black, 1.9% were Hispanic, and 0.5% were Asian. Median follow-up was 5.3 years.
Over the 10-year study period, 25,061 patients required reoperation for hernia recurrence with an adjusted cumulative incidence of 16.1% (95% CI, 16.1% - 16.2%). Patients who underwent open repair had a lower incidence of recurrence over 10 years than those who underwent minimally invasive repair for all hernia types (Table 1).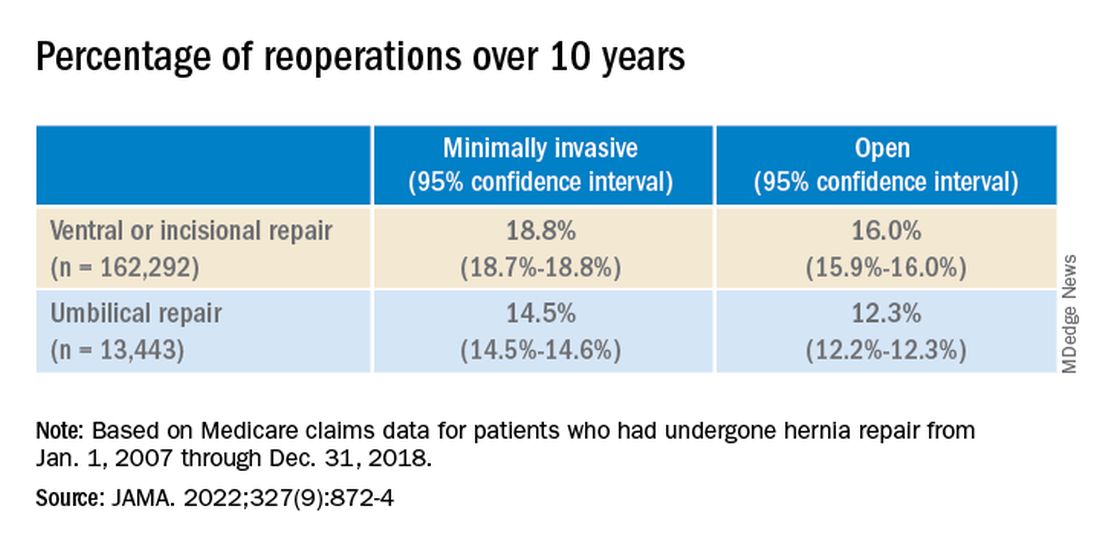
While it appears that hernia recurrence and reoperation have only marginally improved from 2003 to today, Vedra Augenstein, MD, an associate professor of surgery at the Atrium Health General & Complex Abdominal Surgery facility in Charlotte, N.C., suspects there is more to the story. “I think the reason it hasn’t gotten a whole lot better is just because we are operating on much tougher cases than we used to,” she said in an interview. “The way we are fixing hernias has changed and patients are being optimized differently.” Dr. Augenstein was not involved with the research.
To better understand how recurrence has changed over time, there needs to be more data about the comorbidities of patients, the techniques employed, and the meshes used in these surgeries, she said. Those numbers are not available in the published JAMA research letter, but Dr. Telem and colleagues will be submitting an article about this work with greater details.
Dr. Augenstein was also surprised that minimally invasive surgeries had higher incidences of reoperation for recurrence compared to open hernia surgeries. “I would think that patients who had minimally invasive repairs would actually have a lower chance of having postoperative complications because of wound issues,” she said. “Literature has shown that the recurrence rate is lower [in minimally invasive surgeries] because of fewer surgical site infections.”
While Dr. Telem also considers this research letter to be the first step in understanding modern hernia surgery outcomes, it is also a reminder that there is room for improvement in hernia repair surgeries. This includes advising patients on risk factors that may make them more likely to have a hernia recurrence, such as obesity, smoking, and diabetes, she added. “If we know it’s not a perfect science, then we have to do everything that we can upfront to help those numbers.”
Dr. Telem has reported receiving grants from the Agency for Healthcare Research and Quality and consulting fees from Medtronic. Dr. Augenstein has reported consulting for Intuitive Surgical, Medtronic, Allergan, Acelity, Vicarious Surgical, and Bard Pharmaceuticals and has received honoraria for speaking from Medtronic, Allergan, Intuitive Surgical, Acelity, and WL Gore.
A version of this article first appeared on Medscape.com.
, according to a new research letter published March 1 in JAMA. Patients who underwent minimally invasive hernia repair had a higher incidence of reoperation than those who underwent open repairs.
In the United States, surgeons perform more than 1 million hernia repairs each year, according to the U.S. Food and Drug Administration. Despite hernias being such a common condition, it is “not at the forefront of many research agendas,” senior author Dana Telem, MD, an associate professor and section chief of general surgery at University of Michigan Health in Ann Arbor, said in an interview
While many surgical outcomes are measured within 30 days of operation, recurrences generally happen within 2 to 5 years after repair, she said. The last study that looked at reoperations for hernia repair at 10 years was published in 2003 and found that about 20% of patients needed surgery for reoccurrence over a decade. “We don’t really have a good understanding of what happened after these operations,” she explained. “Without knowing that piece, it is hard to go back retrospectively and understand what is the right operation for the right person at the right time.”
To understand rates of reoperation for hernia reoccurrence in today’s U.S. population of older adults, Dr. Telem and colleagues sorted through Medicare claims data to find adult patients who had undergone ventral or incisional and umbilical hernia repair from January 1, 2007 through December 31, 2018. They identified a total of 175,735 patients, 162,292 that underwent ventral or incisional hernia repair and 13,443 that underwent umbilical hernia repair. The average age of patients was 68.9 years and 39.2% were men. Most patients were White (87.2%), 8.1% were Black, 1.9% were Hispanic, and 0.5% were Asian. Median follow-up was 5.3 years.
Over the 10-year study period, 25,061 patients required reoperation for hernia recurrence with an adjusted cumulative incidence of 16.1% (95% CI, 16.1% - 16.2%). Patients who underwent open repair had a lower incidence of recurrence over 10 years than those who underwent minimally invasive repair for all hernia types (Table 1).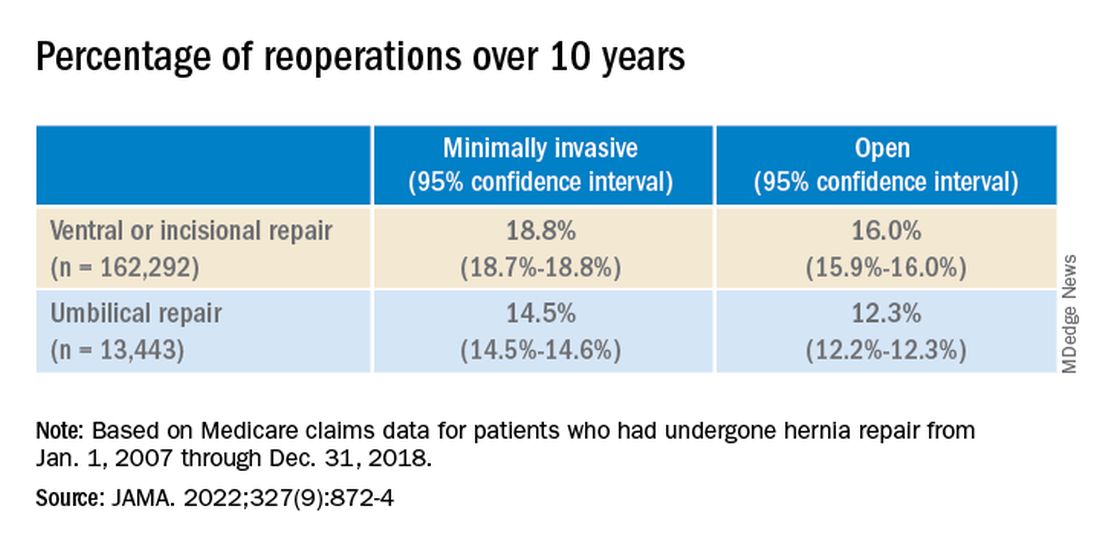
While it appears that hernia recurrence and reoperation have only marginally improved from 2003 to today, Vedra Augenstein, MD, an associate professor of surgery at the Atrium Health General & Complex Abdominal Surgery facility in Charlotte, N.C., suspects there is more to the story. “I think the reason it hasn’t gotten a whole lot better is just because we are operating on much tougher cases than we used to,” she said in an interview. “The way we are fixing hernias has changed and patients are being optimized differently.” Dr. Augenstein was not involved with the research.
To better understand how recurrence has changed over time, there needs to be more data about the comorbidities of patients, the techniques employed, and the meshes used in these surgeries, she said. Those numbers are not available in the published JAMA research letter, but Dr. Telem and colleagues will be submitting an article about this work with greater details.
Dr. Augenstein was also surprised that minimally invasive surgeries had higher incidences of reoperation for recurrence compared to open hernia surgeries. “I would think that patients who had minimally invasive repairs would actually have a lower chance of having postoperative complications because of wound issues,” she said. “Literature has shown that the recurrence rate is lower [in minimally invasive surgeries] because of fewer surgical site infections.”
While Dr. Telem also considers this research letter to be the first step in understanding modern hernia surgery outcomes, it is also a reminder that there is room for improvement in hernia repair surgeries. This includes advising patients on risk factors that may make them more likely to have a hernia recurrence, such as obesity, smoking, and diabetes, she added. “If we know it’s not a perfect science, then we have to do everything that we can upfront to help those numbers.”
Dr. Telem has reported receiving grants from the Agency for Healthcare Research and Quality and consulting fees from Medtronic. Dr. Augenstein has reported consulting for Intuitive Surgical, Medtronic, Allergan, Acelity, Vicarious Surgical, and Bard Pharmaceuticals and has received honoraria for speaking from Medtronic, Allergan, Intuitive Surgical, Acelity, and WL Gore.
A version of this article first appeared on Medscape.com.
FROM JAMA
WPATH draft on gender dysphoria ‘skewed and misses urgent issues’
New draft guidance from the World Professional Association for Transgender Health (WPATH) is raising serious concerns among professionals caring for people with gender dysphoria, prompting claims that WPATH is an organization “captured by activists.”
Experts in adolescent and child psychology, as well as pediatric health, have expressed dismay that the WPATH Standards of Care (SOC) 8 appear to miss some of the most urgent issues in the field of transgender medicine and are considered to express a radical and unreserved leaning towards “gender-affirmation.”
The WPATH SOC 8 document is available for view and comment until Dec. 16 until 11.59 PM EST, after which time revisions will be made and the final version published.
Despite repeated attempts by this news organization to seek clarification on certain aspects of the guidance from members of the WPATH SOC 8 committee, requests were declined “until the guidance is finalized.”
According to the WPATH website, the SOC 8 aims to provide “clinical guidance for health professionals to assist transgender and gender diverse people with safe and effective pathways” to manage their gender dysphoria and potentially transition.
Such pathways may relate to primary care, gynecologic and urologic care, reproductive options, voice and communication therapy, mental health services, and hormonal or surgical treatments, among others.
WPATH adds that it was felt necessary to revise the existing SOC 7 (published in 2012) because of recent “globally unprecedented increase and visibility of transgender and gender-diverse people seeking support and gender-affirming medical treatment.”
Gender-affirming medical treatment means different things at different ages. In the case of kids with gender dysphoria who have not yet entered puberty associated with their birth sex, this might include prescribing so-called “puberty blockers” to delay natural puberty – gonadotrophin-releasing hormone analogs that are licensed for use in precocious puberty in children. Such agents have not been licensed for use in children with gender dysphoria, however, so any use for this purpose is off-label.
Following puberty blockade – or in cases where adolescents have already undergone natural puberty – the next step is to begin cross-sex hormones. So, for a female patient who wants to transition to male (FTM), that would be lifelong testosterone, and for a male who wants to be female (MTF), it involves lifelong estrogen. Again, use of such hormones in transgender individuals is entirely off-label.
Just last month, two of America’s leading experts on transgender medicine, both psychologists – including one who is transgender – told this news organization they were concerned that the quality of the evaluations of youth with gender dysphoria are being stifled by activists who are worried that open discussions will further stigmatize trans individuals.
They subsequently wrote an op-ed on the topic entitled, “The mental health establishment is failing trans kids,” which was finally published in the Washington Post on Nov. 24, after numerous other mainstream U.S. media outlets had rejected it.
New SOC 8 ‘is not evidence based,’ should not be new ‘gold standard’
One expert says the draft SOC 8 lacks balance and does not address certain issues, while paying undue attention to others that detract from real questions facing the field of transgender medicine, both in the United States and around the world.
Julia Mason, MD, is a pediatrician based in Gresham, Oregon, with a special interest in children and adolescents experiencing gender dysphoria. “The SOC 8 shows us that WPATH remains captured by activists,” she asserts.
Dr. Mason questions the integrity of WPATH based on what she has read in the draft SOC 8.
“We need a serious organization to take a sober look at the evidence, and that is why we have established the Society for Evidence-Based Gender Medicine [SEGM],” she noted. “This is what we do – we are looking at all of the evidence.”
Dr. Mason is a clinical advisor to SEGM, an organization set-up to evaluate current interventions and evidence on gender dysphoria.
The pediatrician has particular concerns regarding the child and adolescent chapters in the draft SOC 8. The adolescent chapter states: “Guidelines are meant to provide a gold standard based on the available evidence at this moment of time.”
Dr. Mason disputes this assertion. “This document should not be the new gold standard going forward, primarily because it is not evidence based.”
In an interview, Dr. Mason explained that WPATH say they used the “Delphi consensus process” to determine their recommendations, but “this process is designed for use with a panel of experts when evidence is lacking. I would say they didn’t have a panel of experts. They largely had a panel of activists, with a few experts.”
There is no mention, for example, of England’s National Institute for Health and Care Excellence (NICE) evidence reviews on puberty blockers and cross-sex hormones from earlier this year. These reviews determined that no studies have compared cross-sex hormones or puberty blockers with a control group and all follow-up periods for cross-sex hormones were relatively short.
This disappoints Dr. Mason: “These are significant; they are important documents.”
And much of the evidence quoted comes from the well-known and often-quoted “Dutch-protocol” study of 2011, in which the children studied were much younger at the time of their gender dysphoria, compared with the many adolescents who make up the current surge in presentation at gender clinics worldwide, she adds.
Rapid-onset GD: adolescents presenting late with little history
Dr. Mason also stresses that the SOC 8 does not address the most urgent issues in transgender medicine today, mainly because it does not address rapid-onset gender dysphoria (ROGD): “This is the dilemma of the 21st century; it’s new.”
ROGD – a term first coined in 2018 by researcher Lisa Littman, MD, MPH, now president of the Institute for Comprehensive Gender Dysphoria Research (ICGDR) – refers to the phenomena of adolescents expressing a desire to transition from their birth sex after little or no apparent previous indication.
However, the SOC 8 does make reference to aspects of adolescent development that might impact their decision-making processes around gender identity during teen years. The chapter on adolescents reads: “... adolescence is also often associated with increased risk-taking behaviors. Along with these notable changes ... individuation from parents ... [there is] often a heightened focus on peer relationships, which can be both positive and detrimental.”
The guidance goes on to point out that “it is critical to understand how all of these aspects of development may impact the decision-making for a given young person within their specific cultural context.”
Desistance and detransitioning not adequately addressed
Dr. Mason also says there is little mention “about detransitioning in this SOC [8], and ‘gender dysphoria’ and ‘trans’ are terms that are not defined.”
Likewise, there is no mention of desistance, she highlights, which is when individuals naturally resolve their dysphoria around their birth sex as they grow older.
The most recent published data seen by this news organization relates to a study from March 2021 that showed nearly 88% of boys who struggled with gender identity in childhood (approximate mean age 8 years and follow-up at approximate mean age 20 years) desisted. It reads: “Of the 139 participants, 17 (12.2%) were classified as ‘persisters’ and the remaining 122 (87.8%) were classified as desisters.”
“Most children with gender dysphoria will desist and lose their concept of themselves as being the opposite gender,” Dr. Mason explains. “This is the safest path for a child – desistance.”
“Transition can turn a healthy young person into a lifelong medical patient and has significant health risks,” she emphasizes, stressing that transition has not been shown to decrease the probability of suicide, or attempts at suicide, despite myriad claims saying otherwise.
“Before we were routinely transitioning kids at school, the vast majority of children grew out of their gender dysphoria. This history is not recognized at all in these SOC [8],” she maintains.
Ken Zucker, PhD, CPsych, an author of the study of desistance in boys, says the terms desistence and persistence of gender dysphoria have caused some consternation in certain circles.
An editor of the Archives of Sexual Behavior and professor in the department of psychiatry, University of Toronto, Dr. Zucker has published widely on the topic.
He told this news organization: “The terms persistence and desistance have become verboten among the WPATH cognoscenti. Perhaps the contributors to SOC 8 have come up with alternative descriptors.”
“The term ‘desistance’ is particularly annoying to some of the gender-affirming clinicians, because they don’t believe that desistance is bona fide,” Dr. Zucker points out.
“The desistance resisters are like anti-vaxxers – nothing one can provide as evidence for the efficacy of vaccines is sufficient. There will always be a new objection.”
Other mental health issues, in particular ADHD and autism
It is also widely acknowledged that there is a higher rate of neurodevelopmental and psychiatric diagnoses in individuals with gender dysphoria. For example, one 2020 study found that transgender people were three to six times as likely to be autistic as cisgender people (those whose gender is aligned with their birth sex).
Statement one in the chapter on adolescents in draft WPATH SOC 8 does give a nod to this, pointing out that health professionals working with gender diverse adolescents “should receive training and develop expertise in autism spectrum disorders and other neurodiversity conditions.”
It also notes that in some cases “a more extended assessment process may be useful, such as for youth with more complex presentations (e.g., complicated mental health histories, co-occurring autism spectrum characteristics in particular) and an absence of experienced childhood gender incongruence.”
However, Dr. Mason stresses that underlying mental health issues are central to addressing how to manage a significant number of these patients.
“If a young person has ADHD or autism, they are not ready to make decisions about the rest of their life at age 18. Even a neurotypical young person is still developing their frontal cortex in their early 20s, and it takes longer for those with ADHD or on the autism spectrum.”
She firmly believes that the guidance does not give sufficient consideration to comorbidities in people over the age of 18.
According to their [SOC 8] guidelines, “once someone is 18 they are ready for anything,” says Dr. Mason.
Offering some explanation for the increased prevalence of ADHD and autism in those with gender dysphoria, Dr. Mason notes that children can have “hyperfocus” and those with autism will fixate on a particular area of interest. “If a child is unhappy in their life, and this can be more likely if someone is neuro-atypical, then it is likely that the individual might go online and find this one solution [for example, a transgender identity] that seems to fix everything.”
Perceptions of femininity and masculinity can also be extra challenging for a child with autism, Dr. Mason says. “It is relatively easy for an autistic girl to feel like she should be a boy because the rules of femininity are composed of nonverbal, subtle behaviors that can be difficult to pick up on,” she points out. “An autistic child who isn’t particularly good at nonverbal communication might not pick up on these and thus feel they are not very ‘female.’”
“There’s a whole lot of grass-is-greener-type thinking. Girls think boys have an easier life, and boys think girls have an easier life. I know some detransitioners who have spoken eloquently about realizing their mistake on this,” she adds.
Other parts of the SOC 8 that Dr. Mason disagrees with include the recommendation in the adolescent chapter that 14-year-olds are mature enough to start cross-sex hormones, that is, giving testosterone to a female who wants to transition to male or estrogen to a male who wishes to transition to female. “I think that’s far too young,” she asserts.
And she points out that the document states 17-year-olds are ready for genital reassignment surgery. Again, she believes this is far too young.
“Also, the SOC 8 document does not clarify who is appropriate for surgery. Whenever surgery is discussed, it becomes very vague,” she said.
A version of this article first appeared on Medscape.com.
New draft guidance from the World Professional Association for Transgender Health (WPATH) is raising serious concerns among professionals caring for people with gender dysphoria, prompting claims that WPATH is an organization “captured by activists.”
Experts in adolescent and child psychology, as well as pediatric health, have expressed dismay that the WPATH Standards of Care (SOC) 8 appear to miss some of the most urgent issues in the field of transgender medicine and are considered to express a radical and unreserved leaning towards “gender-affirmation.”
The WPATH SOC 8 document is available for view and comment until Dec. 16 until 11.59 PM EST, after which time revisions will be made and the final version published.
Despite repeated attempts by this news organization to seek clarification on certain aspects of the guidance from members of the WPATH SOC 8 committee, requests were declined “until the guidance is finalized.”
According to the WPATH website, the SOC 8 aims to provide “clinical guidance for health professionals to assist transgender and gender diverse people with safe and effective pathways” to manage their gender dysphoria and potentially transition.
Such pathways may relate to primary care, gynecologic and urologic care, reproductive options, voice and communication therapy, mental health services, and hormonal or surgical treatments, among others.
WPATH adds that it was felt necessary to revise the existing SOC 7 (published in 2012) because of recent “globally unprecedented increase and visibility of transgender and gender-diverse people seeking support and gender-affirming medical treatment.”
Gender-affirming medical treatment means different things at different ages. In the case of kids with gender dysphoria who have not yet entered puberty associated with their birth sex, this might include prescribing so-called “puberty blockers” to delay natural puberty – gonadotrophin-releasing hormone analogs that are licensed for use in precocious puberty in children. Such agents have not been licensed for use in children with gender dysphoria, however, so any use for this purpose is off-label.
Following puberty blockade – or in cases where adolescents have already undergone natural puberty – the next step is to begin cross-sex hormones. So, for a female patient who wants to transition to male (FTM), that would be lifelong testosterone, and for a male who wants to be female (MTF), it involves lifelong estrogen. Again, use of such hormones in transgender individuals is entirely off-label.
Just last month, two of America’s leading experts on transgender medicine, both psychologists – including one who is transgender – told this news organization they were concerned that the quality of the evaluations of youth with gender dysphoria are being stifled by activists who are worried that open discussions will further stigmatize trans individuals.
They subsequently wrote an op-ed on the topic entitled, “The mental health establishment is failing trans kids,” which was finally published in the Washington Post on Nov. 24, after numerous other mainstream U.S. media outlets had rejected it.
New SOC 8 ‘is not evidence based,’ should not be new ‘gold standard’
One expert says the draft SOC 8 lacks balance and does not address certain issues, while paying undue attention to others that detract from real questions facing the field of transgender medicine, both in the United States and around the world.
Julia Mason, MD, is a pediatrician based in Gresham, Oregon, with a special interest in children and adolescents experiencing gender dysphoria. “The SOC 8 shows us that WPATH remains captured by activists,” she asserts.
Dr. Mason questions the integrity of WPATH based on what she has read in the draft SOC 8.
“We need a serious organization to take a sober look at the evidence, and that is why we have established the Society for Evidence-Based Gender Medicine [SEGM],” she noted. “This is what we do – we are looking at all of the evidence.”
Dr. Mason is a clinical advisor to SEGM, an organization set-up to evaluate current interventions and evidence on gender dysphoria.
The pediatrician has particular concerns regarding the child and adolescent chapters in the draft SOC 8. The adolescent chapter states: “Guidelines are meant to provide a gold standard based on the available evidence at this moment of time.”
Dr. Mason disputes this assertion. “This document should not be the new gold standard going forward, primarily because it is not evidence based.”
In an interview, Dr. Mason explained that WPATH say they used the “Delphi consensus process” to determine their recommendations, but “this process is designed for use with a panel of experts when evidence is lacking. I would say they didn’t have a panel of experts. They largely had a panel of activists, with a few experts.”
There is no mention, for example, of England’s National Institute for Health and Care Excellence (NICE) evidence reviews on puberty blockers and cross-sex hormones from earlier this year. These reviews determined that no studies have compared cross-sex hormones or puberty blockers with a control group and all follow-up periods for cross-sex hormones were relatively short.
This disappoints Dr. Mason: “These are significant; they are important documents.”
And much of the evidence quoted comes from the well-known and often-quoted “Dutch-protocol” study of 2011, in which the children studied were much younger at the time of their gender dysphoria, compared with the many adolescents who make up the current surge in presentation at gender clinics worldwide, she adds.
Rapid-onset GD: adolescents presenting late with little history
Dr. Mason also stresses that the SOC 8 does not address the most urgent issues in transgender medicine today, mainly because it does not address rapid-onset gender dysphoria (ROGD): “This is the dilemma of the 21st century; it’s new.”
ROGD – a term first coined in 2018 by researcher Lisa Littman, MD, MPH, now president of the Institute for Comprehensive Gender Dysphoria Research (ICGDR) – refers to the phenomena of adolescents expressing a desire to transition from their birth sex after little or no apparent previous indication.
However, the SOC 8 does make reference to aspects of adolescent development that might impact their decision-making processes around gender identity during teen years. The chapter on adolescents reads: “... adolescence is also often associated with increased risk-taking behaviors. Along with these notable changes ... individuation from parents ... [there is] often a heightened focus on peer relationships, which can be both positive and detrimental.”
The guidance goes on to point out that “it is critical to understand how all of these aspects of development may impact the decision-making for a given young person within their specific cultural context.”
Desistance and detransitioning not adequately addressed
Dr. Mason also says there is little mention “about detransitioning in this SOC [8], and ‘gender dysphoria’ and ‘trans’ are terms that are not defined.”
Likewise, there is no mention of desistance, she highlights, which is when individuals naturally resolve their dysphoria around their birth sex as they grow older.
The most recent published data seen by this news organization relates to a study from March 2021 that showed nearly 88% of boys who struggled with gender identity in childhood (approximate mean age 8 years and follow-up at approximate mean age 20 years) desisted. It reads: “Of the 139 participants, 17 (12.2%) were classified as ‘persisters’ and the remaining 122 (87.8%) were classified as desisters.”
“Most children with gender dysphoria will desist and lose their concept of themselves as being the opposite gender,” Dr. Mason explains. “This is the safest path for a child – desistance.”
“Transition can turn a healthy young person into a lifelong medical patient and has significant health risks,” she emphasizes, stressing that transition has not been shown to decrease the probability of suicide, or attempts at suicide, despite myriad claims saying otherwise.
“Before we were routinely transitioning kids at school, the vast majority of children grew out of their gender dysphoria. This history is not recognized at all in these SOC [8],” she maintains.
Ken Zucker, PhD, CPsych, an author of the study of desistance in boys, says the terms desistence and persistence of gender dysphoria have caused some consternation in certain circles.
An editor of the Archives of Sexual Behavior and professor in the department of psychiatry, University of Toronto, Dr. Zucker has published widely on the topic.
He told this news organization: “The terms persistence and desistance have become verboten among the WPATH cognoscenti. Perhaps the contributors to SOC 8 have come up with alternative descriptors.”
“The term ‘desistance’ is particularly annoying to some of the gender-affirming clinicians, because they don’t believe that desistance is bona fide,” Dr. Zucker points out.
“The desistance resisters are like anti-vaxxers – nothing one can provide as evidence for the efficacy of vaccines is sufficient. There will always be a new objection.”
Other mental health issues, in particular ADHD and autism
It is also widely acknowledged that there is a higher rate of neurodevelopmental and psychiatric diagnoses in individuals with gender dysphoria. For example, one 2020 study found that transgender people were three to six times as likely to be autistic as cisgender people (those whose gender is aligned with their birth sex).
Statement one in the chapter on adolescents in draft WPATH SOC 8 does give a nod to this, pointing out that health professionals working with gender diverse adolescents “should receive training and develop expertise in autism spectrum disorders and other neurodiversity conditions.”
It also notes that in some cases “a more extended assessment process may be useful, such as for youth with more complex presentations (e.g., complicated mental health histories, co-occurring autism spectrum characteristics in particular) and an absence of experienced childhood gender incongruence.”
However, Dr. Mason stresses that underlying mental health issues are central to addressing how to manage a significant number of these patients.
“If a young person has ADHD or autism, they are not ready to make decisions about the rest of their life at age 18. Even a neurotypical young person is still developing their frontal cortex in their early 20s, and it takes longer for those with ADHD or on the autism spectrum.”
She firmly believes that the guidance does not give sufficient consideration to comorbidities in people over the age of 18.
According to their [SOC 8] guidelines, “once someone is 18 they are ready for anything,” says Dr. Mason.
Offering some explanation for the increased prevalence of ADHD and autism in those with gender dysphoria, Dr. Mason notes that children can have “hyperfocus” and those with autism will fixate on a particular area of interest. “If a child is unhappy in their life, and this can be more likely if someone is neuro-atypical, then it is likely that the individual might go online and find this one solution [for example, a transgender identity] that seems to fix everything.”
Perceptions of femininity and masculinity can also be extra challenging for a child with autism, Dr. Mason says. “It is relatively easy for an autistic girl to feel like she should be a boy because the rules of femininity are composed of nonverbal, subtle behaviors that can be difficult to pick up on,” she points out. “An autistic child who isn’t particularly good at nonverbal communication might not pick up on these and thus feel they are not very ‘female.’”
“There’s a whole lot of grass-is-greener-type thinking. Girls think boys have an easier life, and boys think girls have an easier life. I know some detransitioners who have spoken eloquently about realizing their mistake on this,” she adds.
Other parts of the SOC 8 that Dr. Mason disagrees with include the recommendation in the adolescent chapter that 14-year-olds are mature enough to start cross-sex hormones, that is, giving testosterone to a female who wants to transition to male or estrogen to a male who wishes to transition to female. “I think that’s far too young,” she asserts.
And she points out that the document states 17-year-olds are ready for genital reassignment surgery. Again, she believes this is far too young.
“Also, the SOC 8 document does not clarify who is appropriate for surgery. Whenever surgery is discussed, it becomes very vague,” she said.
A version of this article first appeared on Medscape.com.
New draft guidance from the World Professional Association for Transgender Health (WPATH) is raising serious concerns among professionals caring for people with gender dysphoria, prompting claims that WPATH is an organization “captured by activists.”
Experts in adolescent and child psychology, as well as pediatric health, have expressed dismay that the WPATH Standards of Care (SOC) 8 appear to miss some of the most urgent issues in the field of transgender medicine and are considered to express a radical and unreserved leaning towards “gender-affirmation.”
The WPATH SOC 8 document is available for view and comment until Dec. 16 until 11.59 PM EST, after which time revisions will be made and the final version published.
Despite repeated attempts by this news organization to seek clarification on certain aspects of the guidance from members of the WPATH SOC 8 committee, requests were declined “until the guidance is finalized.”
According to the WPATH website, the SOC 8 aims to provide “clinical guidance for health professionals to assist transgender and gender diverse people with safe and effective pathways” to manage their gender dysphoria and potentially transition.
Such pathways may relate to primary care, gynecologic and urologic care, reproductive options, voice and communication therapy, mental health services, and hormonal or surgical treatments, among others.
WPATH adds that it was felt necessary to revise the existing SOC 7 (published in 2012) because of recent “globally unprecedented increase and visibility of transgender and gender-diverse people seeking support and gender-affirming medical treatment.”
Gender-affirming medical treatment means different things at different ages. In the case of kids with gender dysphoria who have not yet entered puberty associated with their birth sex, this might include prescribing so-called “puberty blockers” to delay natural puberty – gonadotrophin-releasing hormone analogs that are licensed for use in precocious puberty in children. Such agents have not been licensed for use in children with gender dysphoria, however, so any use for this purpose is off-label.
Following puberty blockade – or in cases where adolescents have already undergone natural puberty – the next step is to begin cross-sex hormones. So, for a female patient who wants to transition to male (FTM), that would be lifelong testosterone, and for a male who wants to be female (MTF), it involves lifelong estrogen. Again, use of such hormones in transgender individuals is entirely off-label.
Just last month, two of America’s leading experts on transgender medicine, both psychologists – including one who is transgender – told this news organization they were concerned that the quality of the evaluations of youth with gender dysphoria are being stifled by activists who are worried that open discussions will further stigmatize trans individuals.
They subsequently wrote an op-ed on the topic entitled, “The mental health establishment is failing trans kids,” which was finally published in the Washington Post on Nov. 24, after numerous other mainstream U.S. media outlets had rejected it.
New SOC 8 ‘is not evidence based,’ should not be new ‘gold standard’
One expert says the draft SOC 8 lacks balance and does not address certain issues, while paying undue attention to others that detract from real questions facing the field of transgender medicine, both in the United States and around the world.
Julia Mason, MD, is a pediatrician based in Gresham, Oregon, with a special interest in children and adolescents experiencing gender dysphoria. “The SOC 8 shows us that WPATH remains captured by activists,” she asserts.
Dr. Mason questions the integrity of WPATH based on what she has read in the draft SOC 8.
“We need a serious organization to take a sober look at the evidence, and that is why we have established the Society for Evidence-Based Gender Medicine [SEGM],” she noted. “This is what we do – we are looking at all of the evidence.”
Dr. Mason is a clinical advisor to SEGM, an organization set-up to evaluate current interventions and evidence on gender dysphoria.
The pediatrician has particular concerns regarding the child and adolescent chapters in the draft SOC 8. The adolescent chapter states: “Guidelines are meant to provide a gold standard based on the available evidence at this moment of time.”
Dr. Mason disputes this assertion. “This document should not be the new gold standard going forward, primarily because it is not evidence based.”
In an interview, Dr. Mason explained that WPATH say they used the “Delphi consensus process” to determine their recommendations, but “this process is designed for use with a panel of experts when evidence is lacking. I would say they didn’t have a panel of experts. They largely had a panel of activists, with a few experts.”
There is no mention, for example, of England’s National Institute for Health and Care Excellence (NICE) evidence reviews on puberty blockers and cross-sex hormones from earlier this year. These reviews determined that no studies have compared cross-sex hormones or puberty blockers with a control group and all follow-up periods for cross-sex hormones were relatively short.
This disappoints Dr. Mason: “These are significant; they are important documents.”
And much of the evidence quoted comes from the well-known and often-quoted “Dutch-protocol” study of 2011, in which the children studied were much younger at the time of their gender dysphoria, compared with the many adolescents who make up the current surge in presentation at gender clinics worldwide, she adds.
Rapid-onset GD: adolescents presenting late with little history
Dr. Mason also stresses that the SOC 8 does not address the most urgent issues in transgender medicine today, mainly because it does not address rapid-onset gender dysphoria (ROGD): “This is the dilemma of the 21st century; it’s new.”
ROGD – a term first coined in 2018 by researcher Lisa Littman, MD, MPH, now president of the Institute for Comprehensive Gender Dysphoria Research (ICGDR) – refers to the phenomena of adolescents expressing a desire to transition from their birth sex after little or no apparent previous indication.
However, the SOC 8 does make reference to aspects of adolescent development that might impact their decision-making processes around gender identity during teen years. The chapter on adolescents reads: “... adolescence is also often associated with increased risk-taking behaviors. Along with these notable changes ... individuation from parents ... [there is] often a heightened focus on peer relationships, which can be both positive and detrimental.”
The guidance goes on to point out that “it is critical to understand how all of these aspects of development may impact the decision-making for a given young person within their specific cultural context.”
Desistance and detransitioning not adequately addressed
Dr. Mason also says there is little mention “about detransitioning in this SOC [8], and ‘gender dysphoria’ and ‘trans’ are terms that are not defined.”
Likewise, there is no mention of desistance, she highlights, which is when individuals naturally resolve their dysphoria around their birth sex as they grow older.
The most recent published data seen by this news organization relates to a study from March 2021 that showed nearly 88% of boys who struggled with gender identity in childhood (approximate mean age 8 years and follow-up at approximate mean age 20 years) desisted. It reads: “Of the 139 participants, 17 (12.2%) were classified as ‘persisters’ and the remaining 122 (87.8%) were classified as desisters.”
“Most children with gender dysphoria will desist and lose their concept of themselves as being the opposite gender,” Dr. Mason explains. “This is the safest path for a child – desistance.”
“Transition can turn a healthy young person into a lifelong medical patient and has significant health risks,” she emphasizes, stressing that transition has not been shown to decrease the probability of suicide, or attempts at suicide, despite myriad claims saying otherwise.
“Before we were routinely transitioning kids at school, the vast majority of children grew out of their gender dysphoria. This history is not recognized at all in these SOC [8],” she maintains.
Ken Zucker, PhD, CPsych, an author of the study of desistance in boys, says the terms desistence and persistence of gender dysphoria have caused some consternation in certain circles.
An editor of the Archives of Sexual Behavior and professor in the department of psychiatry, University of Toronto, Dr. Zucker has published widely on the topic.
He told this news organization: “The terms persistence and desistance have become verboten among the WPATH cognoscenti. Perhaps the contributors to SOC 8 have come up with alternative descriptors.”
“The term ‘desistance’ is particularly annoying to some of the gender-affirming clinicians, because they don’t believe that desistance is bona fide,” Dr. Zucker points out.
“The desistance resisters are like anti-vaxxers – nothing one can provide as evidence for the efficacy of vaccines is sufficient. There will always be a new objection.”
Other mental health issues, in particular ADHD and autism
It is also widely acknowledged that there is a higher rate of neurodevelopmental and psychiatric diagnoses in individuals with gender dysphoria. For example, one 2020 study found that transgender people were three to six times as likely to be autistic as cisgender people (those whose gender is aligned with their birth sex).
Statement one in the chapter on adolescents in draft WPATH SOC 8 does give a nod to this, pointing out that health professionals working with gender diverse adolescents “should receive training and develop expertise in autism spectrum disorders and other neurodiversity conditions.”
It also notes that in some cases “a more extended assessment process may be useful, such as for youth with more complex presentations (e.g., complicated mental health histories, co-occurring autism spectrum characteristics in particular) and an absence of experienced childhood gender incongruence.”
However, Dr. Mason stresses that underlying mental health issues are central to addressing how to manage a significant number of these patients.
“If a young person has ADHD or autism, they are not ready to make decisions about the rest of their life at age 18. Even a neurotypical young person is still developing their frontal cortex in their early 20s, and it takes longer for those with ADHD or on the autism spectrum.”
She firmly believes that the guidance does not give sufficient consideration to comorbidities in people over the age of 18.
According to their [SOC 8] guidelines, “once someone is 18 they are ready for anything,” says Dr. Mason.
Offering some explanation for the increased prevalence of ADHD and autism in those with gender dysphoria, Dr. Mason notes that children can have “hyperfocus” and those with autism will fixate on a particular area of interest. “If a child is unhappy in their life, and this can be more likely if someone is neuro-atypical, then it is likely that the individual might go online and find this one solution [for example, a transgender identity] that seems to fix everything.”
Perceptions of femininity and masculinity can also be extra challenging for a child with autism, Dr. Mason says. “It is relatively easy for an autistic girl to feel like she should be a boy because the rules of femininity are composed of nonverbal, subtle behaviors that can be difficult to pick up on,” she points out. “An autistic child who isn’t particularly good at nonverbal communication might not pick up on these and thus feel they are not very ‘female.’”
“There’s a whole lot of grass-is-greener-type thinking. Girls think boys have an easier life, and boys think girls have an easier life. I know some detransitioners who have spoken eloquently about realizing their mistake on this,” she adds.
Other parts of the SOC 8 that Dr. Mason disagrees with include the recommendation in the adolescent chapter that 14-year-olds are mature enough to start cross-sex hormones, that is, giving testosterone to a female who wants to transition to male or estrogen to a male who wishes to transition to female. “I think that’s far too young,” she asserts.
And she points out that the document states 17-year-olds are ready for genital reassignment surgery. Again, she believes this is far too young.
“Also, the SOC 8 document does not clarify who is appropriate for surgery. Whenever surgery is discussed, it becomes very vague,” she said.
A version of this article first appeared on Medscape.com.
Appendicitis: Up-front antibiotics OK in select patients
a comprehensive review of the literature suggests.
“I think this is a wonderful thing that we have for our patients now, because think about the patient who had a heart attack yesterday and has appendicitis today – you don’t want to operate on that patient – so this gives us a wonderful option in an environment where sometimes surgery is just bad timing,” Theodore Pappas, MD, professor of surgery, Duke University, Durham, N.C., told this news organization.
“It’s not that every 25-year-old who comes in should get antibiotics instead of surgery. It’s really better to say that this gives us flexibility for patients who we may not want to operate on immediately, and now we have a great option,” he stressed.
The study was published Dec. 14, 2021, in JAMA.
Acute appendicitis is the most common abdominal surgical emergency in the world, as the authors pointed out.
“We think it’s going to be 60%-70% of patients who are good candidates for consideration of antibiotics,” they speculated.
Current evidence
The review summarizes current evidence regarding the diagnosis and management of acute appendicitis based on a total of 71 articles including 10 systematic reviews, 9 meta-analyses, and 11 practice guidelines. “Appendicitis is classified as uncomplicated or complicated,” the authors explained. Uncomplicated appendicitis is acute appendicitis in the absence of clinical or radiographic signs of perforation.
In contrast, complicated appendicitis is when there is appendiceal rupture with subsequent abscess of phlegmon formation, the definitive diagnosis of which can be confirmed by CT scan. “In cases of diagnostic uncertainty imaging should be performed,” investigators cautioned – usually with ultrasound and CT scans.
If uncomplicated appendicitis is confirmed, three different guidelines now support the role of an antibiotics-first approach, including guidelines from the American Association for Surgery of Trauma. For this group of patients, empirical broad-spectrum antibiotic coverage that can be transitioned to outpatient treatment is commonly used. For example, patients may be initially treated with intravenous ertapenem monotherapy or intravenous cephalosporin plus metronidazole, then on discharge put on oral fluoroquinolones plus metronidazole.
Antibiotics that cover streptococci, nonresistant Enterobacteriaceae, and the anaerobes are usually adequate, they added. “The recommended duration of antibiotics is 10 days,” they noted. In most of the clinical trials comparing antibiotics first to surgery, the primary endpoint was treatment failure at 1 year, in other words, recurrence of symptoms during that year-long period. Across a number of clinical trials, that recurrence rate ranged from a low of 15% to a high of 41%.
In contrast, recurrence rarely occurs after surgical appendectomy. Early treatment failure, defined as clinical deterioration or lack of clinical improvement within 24-72 hours following initiation of antibiotics, is much less likely to occur, with a reported rate of between 8% and 12% of patients. The only long-term follow-up of an antibiotics-first approach in uncomplicated appendicitis was done in the Appendicitis Acuta (APPAC) trial, where at 5 years, the recurrence rate of acute appendicitis was 39% (95% confidence interval, 33.1%-45.3%) in patients initially treated with antibiotics alone.
Typically, there have been no differences in the length of hospital stay in most of the clinical trials reviewed. As Dr. Pappas explained, following a standard appendectomy, patients are typically sent home within 24 hours of undergoing surgery. On the other hand, if treated with intravenous antibiotics first, patients are usually admitted overnight then switched to oral antibiotics on discharge – suggesting that there is little difference in the time spent in hospital between the two groups.
However, there are groups of patients who predictably will not do well on antibiotics first, he cautioned. For example, patients who present with a high fever, shaking and chills, and severe abdominal pain do not have a mild case of appendicitis. Neither do patients who may not look sick but on CT scan, they have a hard piece of stool jammed into the end of the appendix that’s causing the blockage: These patients are also more likely to fail antibiotics, Dr. Pappas added.
“There is also a group of patients who have a much more dilated appendix with some fluid around it,” he noted, “and these patients are less likely to be managed with antibiotics successfully as well.” Lastly, though not part of this review and for whom an antibiotics-first protocol has long been in place, there is a subset of patients who have a perforated appendix, and that perforation has been walled off in a pocket of pus.
“These patients are treated with an antibiotic first because if you operate on them, it’s a mess, whereas if patients are reasonably stable, you can drain the abscess and then put them on antibiotics, and then you can decide 6-8 weeks later if you are going to take the appendix out,” Dr. Pappas said, adding: “Most of the time, what should be happening is the surgeon should consult with the patient and then they can weigh in – here are the options and here’s what I recommend.
“But patients will pick what they pick, and surgery is a very compelling argument: It’s laparoscopic surgery, patients are home in 24 hours, and the complication rate [and the recurrence rate] are incredibly low, so you have to think through all sorts of issues and when you come to a certain conclusion, it has to make a lot of sense to the patient,” Dr. Pappas emphasized.
Asked to comment on the findings, Ram Nirula, MD, D. Rees and Eleanor T. Jensen Presidential Chair in Surgery, University of Utah, Salt Lake City, noted that, as with all things in medicine, nothing is 100%.
“There are times where antibiotics for uncomplicated appendicitis may be appropriate, and times where appendectomy is most appropriate,” he said in an interview. Most of the evidence now shows that the risk of treatment failure following nonoperative management for uncomplicated appendicitis is significant, ranging from 15% to 40%, as Dr. Nirula reaffirmed.
A more recent randomized controlled trial from the CODA collaborative found that quality of life was similar for patients who got up-front antibiotics as for those who got surgery at 30 days, but the failure rate was high, particularly for those with appendicolith (what review authors would have classified as complicated appendicitis).
Moreover, when looking at this subset of patients, quality of life and patient satisfaction in the antibiotic treatment group were lower than it was for surgical controls, as Dr. Nirula also pointed out. While length of hospital stay was similar, overall health care resource utilization was higher in the antibiotic group. “So, if it were me, I would want my appendix removed at this stage in my life, however, for those who are poor surgical candidates, I would favor antibiotics,” Dr. Nirula stressed. He added that the presence of an appendicolith makes the argument for surgery more compelling, although he would still try antibiotics in patients with an appendicolith who are poor surgical candidates.
Dr. Pappas reported serving as a paid consultant for Transenterix. Dr. Nirula disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
a comprehensive review of the literature suggests.
“I think this is a wonderful thing that we have for our patients now, because think about the patient who had a heart attack yesterday and has appendicitis today – you don’t want to operate on that patient – so this gives us a wonderful option in an environment where sometimes surgery is just bad timing,” Theodore Pappas, MD, professor of surgery, Duke University, Durham, N.C., told this news organization.
“It’s not that every 25-year-old who comes in should get antibiotics instead of surgery. It’s really better to say that this gives us flexibility for patients who we may not want to operate on immediately, and now we have a great option,” he stressed.
The study was published Dec. 14, 2021, in JAMA.
Acute appendicitis is the most common abdominal surgical emergency in the world, as the authors pointed out.
“We think it’s going to be 60%-70% of patients who are good candidates for consideration of antibiotics,” they speculated.
Current evidence
The review summarizes current evidence regarding the diagnosis and management of acute appendicitis based on a total of 71 articles including 10 systematic reviews, 9 meta-analyses, and 11 practice guidelines. “Appendicitis is classified as uncomplicated or complicated,” the authors explained. Uncomplicated appendicitis is acute appendicitis in the absence of clinical or radiographic signs of perforation.
In contrast, complicated appendicitis is when there is appendiceal rupture with subsequent abscess of phlegmon formation, the definitive diagnosis of which can be confirmed by CT scan. “In cases of diagnostic uncertainty imaging should be performed,” investigators cautioned – usually with ultrasound and CT scans.
If uncomplicated appendicitis is confirmed, three different guidelines now support the role of an antibiotics-first approach, including guidelines from the American Association for Surgery of Trauma. For this group of patients, empirical broad-spectrum antibiotic coverage that can be transitioned to outpatient treatment is commonly used. For example, patients may be initially treated with intravenous ertapenem monotherapy or intravenous cephalosporin plus metronidazole, then on discharge put on oral fluoroquinolones plus metronidazole.
Antibiotics that cover streptococci, nonresistant Enterobacteriaceae, and the anaerobes are usually adequate, they added. “The recommended duration of antibiotics is 10 days,” they noted. In most of the clinical trials comparing antibiotics first to surgery, the primary endpoint was treatment failure at 1 year, in other words, recurrence of symptoms during that year-long period. Across a number of clinical trials, that recurrence rate ranged from a low of 15% to a high of 41%.
In contrast, recurrence rarely occurs after surgical appendectomy. Early treatment failure, defined as clinical deterioration or lack of clinical improvement within 24-72 hours following initiation of antibiotics, is much less likely to occur, with a reported rate of between 8% and 12% of patients. The only long-term follow-up of an antibiotics-first approach in uncomplicated appendicitis was done in the Appendicitis Acuta (APPAC) trial, where at 5 years, the recurrence rate of acute appendicitis was 39% (95% confidence interval, 33.1%-45.3%) in patients initially treated with antibiotics alone.
Typically, there have been no differences in the length of hospital stay in most of the clinical trials reviewed. As Dr. Pappas explained, following a standard appendectomy, patients are typically sent home within 24 hours of undergoing surgery. On the other hand, if treated with intravenous antibiotics first, patients are usually admitted overnight then switched to oral antibiotics on discharge – suggesting that there is little difference in the time spent in hospital between the two groups.
However, there are groups of patients who predictably will not do well on antibiotics first, he cautioned. For example, patients who present with a high fever, shaking and chills, and severe abdominal pain do not have a mild case of appendicitis. Neither do patients who may not look sick but on CT scan, they have a hard piece of stool jammed into the end of the appendix that’s causing the blockage: These patients are also more likely to fail antibiotics, Dr. Pappas added.
“There is also a group of patients who have a much more dilated appendix with some fluid around it,” he noted, “and these patients are less likely to be managed with antibiotics successfully as well.” Lastly, though not part of this review and for whom an antibiotics-first protocol has long been in place, there is a subset of patients who have a perforated appendix, and that perforation has been walled off in a pocket of pus.
“These patients are treated with an antibiotic first because if you operate on them, it’s a mess, whereas if patients are reasonably stable, you can drain the abscess and then put them on antibiotics, and then you can decide 6-8 weeks later if you are going to take the appendix out,” Dr. Pappas said, adding: “Most of the time, what should be happening is the surgeon should consult with the patient and then they can weigh in – here are the options and here’s what I recommend.
“But patients will pick what they pick, and surgery is a very compelling argument: It’s laparoscopic surgery, patients are home in 24 hours, and the complication rate [and the recurrence rate] are incredibly low, so you have to think through all sorts of issues and when you come to a certain conclusion, it has to make a lot of sense to the patient,” Dr. Pappas emphasized.
Asked to comment on the findings, Ram Nirula, MD, D. Rees and Eleanor T. Jensen Presidential Chair in Surgery, University of Utah, Salt Lake City, noted that, as with all things in medicine, nothing is 100%.
“There are times where antibiotics for uncomplicated appendicitis may be appropriate, and times where appendectomy is most appropriate,” he said in an interview. Most of the evidence now shows that the risk of treatment failure following nonoperative management for uncomplicated appendicitis is significant, ranging from 15% to 40%, as Dr. Nirula reaffirmed.
A more recent randomized controlled trial from the CODA collaborative found that quality of life was similar for patients who got up-front antibiotics as for those who got surgery at 30 days, but the failure rate was high, particularly for those with appendicolith (what review authors would have classified as complicated appendicitis).
Moreover, when looking at this subset of patients, quality of life and patient satisfaction in the antibiotic treatment group were lower than it was for surgical controls, as Dr. Nirula also pointed out. While length of hospital stay was similar, overall health care resource utilization was higher in the antibiotic group. “So, if it were me, I would want my appendix removed at this stage in my life, however, for those who are poor surgical candidates, I would favor antibiotics,” Dr. Nirula stressed. He added that the presence of an appendicolith makes the argument for surgery more compelling, although he would still try antibiotics in patients with an appendicolith who are poor surgical candidates.
Dr. Pappas reported serving as a paid consultant for Transenterix. Dr. Nirula disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
a comprehensive review of the literature suggests.
“I think this is a wonderful thing that we have for our patients now, because think about the patient who had a heart attack yesterday and has appendicitis today – you don’t want to operate on that patient – so this gives us a wonderful option in an environment where sometimes surgery is just bad timing,” Theodore Pappas, MD, professor of surgery, Duke University, Durham, N.C., told this news organization.
“It’s not that every 25-year-old who comes in should get antibiotics instead of surgery. It’s really better to say that this gives us flexibility for patients who we may not want to operate on immediately, and now we have a great option,” he stressed.
The study was published Dec. 14, 2021, in JAMA.
Acute appendicitis is the most common abdominal surgical emergency in the world, as the authors pointed out.
“We think it’s going to be 60%-70% of patients who are good candidates for consideration of antibiotics,” they speculated.
Current evidence
The review summarizes current evidence regarding the diagnosis and management of acute appendicitis based on a total of 71 articles including 10 systematic reviews, 9 meta-analyses, and 11 practice guidelines. “Appendicitis is classified as uncomplicated or complicated,” the authors explained. Uncomplicated appendicitis is acute appendicitis in the absence of clinical or radiographic signs of perforation.
In contrast, complicated appendicitis is when there is appendiceal rupture with subsequent abscess of phlegmon formation, the definitive diagnosis of which can be confirmed by CT scan. “In cases of diagnostic uncertainty imaging should be performed,” investigators cautioned – usually with ultrasound and CT scans.
If uncomplicated appendicitis is confirmed, three different guidelines now support the role of an antibiotics-first approach, including guidelines from the American Association for Surgery of Trauma. For this group of patients, empirical broad-spectrum antibiotic coverage that can be transitioned to outpatient treatment is commonly used. For example, patients may be initially treated with intravenous ertapenem monotherapy or intravenous cephalosporin plus metronidazole, then on discharge put on oral fluoroquinolones plus metronidazole.
Antibiotics that cover streptococci, nonresistant Enterobacteriaceae, and the anaerobes are usually adequate, they added. “The recommended duration of antibiotics is 10 days,” they noted. In most of the clinical trials comparing antibiotics first to surgery, the primary endpoint was treatment failure at 1 year, in other words, recurrence of symptoms during that year-long period. Across a number of clinical trials, that recurrence rate ranged from a low of 15% to a high of 41%.
In contrast, recurrence rarely occurs after surgical appendectomy. Early treatment failure, defined as clinical deterioration or lack of clinical improvement within 24-72 hours following initiation of antibiotics, is much less likely to occur, with a reported rate of between 8% and 12% of patients. The only long-term follow-up of an antibiotics-first approach in uncomplicated appendicitis was done in the Appendicitis Acuta (APPAC) trial, where at 5 years, the recurrence rate of acute appendicitis was 39% (95% confidence interval, 33.1%-45.3%) in patients initially treated with antibiotics alone.
Typically, there have been no differences in the length of hospital stay in most of the clinical trials reviewed. As Dr. Pappas explained, following a standard appendectomy, patients are typically sent home within 24 hours of undergoing surgery. On the other hand, if treated with intravenous antibiotics first, patients are usually admitted overnight then switched to oral antibiotics on discharge – suggesting that there is little difference in the time spent in hospital between the two groups.
However, there are groups of patients who predictably will not do well on antibiotics first, he cautioned. For example, patients who present with a high fever, shaking and chills, and severe abdominal pain do not have a mild case of appendicitis. Neither do patients who may not look sick but on CT scan, they have a hard piece of stool jammed into the end of the appendix that’s causing the blockage: These patients are also more likely to fail antibiotics, Dr. Pappas added.
“There is also a group of patients who have a much more dilated appendix with some fluid around it,” he noted, “and these patients are less likely to be managed with antibiotics successfully as well.” Lastly, though not part of this review and for whom an antibiotics-first protocol has long been in place, there is a subset of patients who have a perforated appendix, and that perforation has been walled off in a pocket of pus.
“These patients are treated with an antibiotic first because if you operate on them, it’s a mess, whereas if patients are reasonably stable, you can drain the abscess and then put them on antibiotics, and then you can decide 6-8 weeks later if you are going to take the appendix out,” Dr. Pappas said, adding: “Most of the time, what should be happening is the surgeon should consult with the patient and then they can weigh in – here are the options and here’s what I recommend.
“But patients will pick what they pick, and surgery is a very compelling argument: It’s laparoscopic surgery, patients are home in 24 hours, and the complication rate [and the recurrence rate] are incredibly low, so you have to think through all sorts of issues and when you come to a certain conclusion, it has to make a lot of sense to the patient,” Dr. Pappas emphasized.
Asked to comment on the findings, Ram Nirula, MD, D. Rees and Eleanor T. Jensen Presidential Chair in Surgery, University of Utah, Salt Lake City, noted that, as with all things in medicine, nothing is 100%.
“There are times where antibiotics for uncomplicated appendicitis may be appropriate, and times where appendectomy is most appropriate,” he said in an interview. Most of the evidence now shows that the risk of treatment failure following nonoperative management for uncomplicated appendicitis is significant, ranging from 15% to 40%, as Dr. Nirula reaffirmed.
A more recent randomized controlled trial from the CODA collaborative found that quality of life was similar for patients who got up-front antibiotics as for those who got surgery at 30 days, but the failure rate was high, particularly for those with appendicolith (what review authors would have classified as complicated appendicitis).
Moreover, when looking at this subset of patients, quality of life and patient satisfaction in the antibiotic treatment group were lower than it was for surgical controls, as Dr. Nirula also pointed out. While length of hospital stay was similar, overall health care resource utilization was higher in the antibiotic group. “So, if it were me, I would want my appendix removed at this stage in my life, however, for those who are poor surgical candidates, I would favor antibiotics,” Dr. Nirula stressed. He added that the presence of an appendicolith makes the argument for surgery more compelling, although he would still try antibiotics in patients with an appendicolith who are poor surgical candidates.
Dr. Pappas reported serving as a paid consultant for Transenterix. Dr. Nirula disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM JAMA



