User login
New data on IV ketamine for resistant depression in the elderly
NEW ORLEANS –
“These were patients with depression who had not responded even to intensive therapies or procedures, and we found that after a 6-week ketamine infusion regimen, there was no difference in the response to the treatment between the treatment-resistant geriatric and nongeriatric patients,” study investigator Jonathan Kim, of Emory University, Atlanta, the first author of one of two studies presented as part of the American Association for Geriatric Psychiatry annual meeting, said in an interview.
The findings are important because research on the effects of IV ketamine have not been well documented in geriatric patients, who have high rates of depression and TRD.
“There is a lack of data on IV ketamine in older adults with treatment-resistant depression, and there are some safety and tolerability concerns which may lead some older adults and their clinicians to be reluctant to pursue IV ketamine treatment,” study coinvestigator Hanadi Ajam Oughli, MD, a health sciences assistant clinical professor in the department of psychiatry and biobehavioral sciences, University of California, Los Angeles, told this news organization.
Nasal vs. IV administration
Ketamine has traditionally been used as an anesthetic that blocks N-methyl-D-aspartate (NMDA) glutamate receptors, Dr. Oughli and colleagues note.
In the treatment of TRD, an infusion of 0.5 mg/kg is typically administered over 40 minutes, producing a rapid antidepressant response. Recent research shows the drug reduces suicidality and improves mood and quality of life.
A more recent intranasal formulation of ketamine, esketamine, was approved by the U.S. Food and Drug Administration for TRD in 2019, and some experts questioned its path to approval. In addition, the drug’s high cost and poor bioavailability in comparison with IV ketamine remains an issue, said Dr. Oughli.
In the previous TRANSFORM-3 study, a placebo-controlled randomized trial, there was no difference between esketamine, used in conjunction with an antidepressant, and placebo for geriatric patients.
To better understand the effects of IV ketamine in this patient population, Mr. Kim’s team conducted a retrospective chart review of 91 older patients with TRD who received IV ketamine treatment between October 2016 and August 2022.
Patients were divided into two groups – those older than 60 years (n = 36; 44% women; mean age, 68.86) and those younger than 60 (n = 55; 49% women; mean age, 41.05). Participants in each age group received six ketamine infusions over 6 weeks.
Results showed that with regard to depression severity, as assessed using Beck Depression Inventory (BDI-II) scores, 27.8% of patients in the geriatric group had a 50% or greater improvement, vs. 25.4% of those younger than 60.
The average BDI-II scores represented a significant improvement for both groups (P < .01), and the difference in scores between the groups was not statistically significant (P = .973).
“It is important to note that our study was conducted in a real-world clinical setting with a treatment-resistant population; other clinical studies may not have such sick patients in their trials. Additional studies are therefore warranted to establish further treatment guidelines in this area,” Mr. Kim said.
Open-label trial results
In the second study, Dr. Oughli and colleagues evaluated additional key outcomes in geriatric patients treated with IV ketamine as part of a larger open-label late-life trial on TRD.
The secondary analysis of the trial focused on 23 patients (mean age, 71.5 years) who had been initially treated with twice-a-week IV ketamine for 4 weeks.
After the first 4 weeks, patients who had experienced a partial response received an additional 4 weeks of once-weekly IV ketamine.
Overall, 48% of participants achieved a response, and 24% achieved remission of depressive symptoms following the first 4 weeks of twice-weekly treatment. This effect was maintained during the continuation phase of the study.
These findings are consistent with research in younger adults and demonstrate that twice-weekly infusions yield a more sustained antidepressant response than once-weekly infusions, the authors note.
The analysis also showed important increases in psychological well-being scores on the Scale for Suicidal Ideation, improved sleep quality as measured by the Pittsburgh Sleep Quality Index, and overall psychological well-being as shown on the NIH Toolbox Positive Affect on happiness/contentment and the NIH Toolbox General Life Satisfaction scales.
In a previous analysis, published in The American Journal of Geriatric Psychiatry, the researchers also evaluated cognitive function using the NIH Cognitive Battery, which showed that geriatric patients with TRD had significant improvements in a composite of executive functioning and fluid cognition during the 4-week acute treatment period of twice-weekly IV ketamine infusions (Cohen’s d = 0.61) and that those improvements were sustained in the continuation phase of once-weekly infusions for 4 more weeks.
Those results are consistent with ketamine’s known potential procognitive effects in TRD, due to a putative antidepressant mechanism that rescues prefrontal circuit dysfunction through synaptogenesis, the researchers note.
Dr. Oughli said that in both analyses, patients tolerated ketamine well, and there were no serious adverse events.
“Adverse events, including hypertension, dissociated effects, and cravings, were rare and did not prevent the continued use of IV ketamine by older adults. We were able to use clonidine to help manage blood pressure changes seen during the infusions,” she noted.
“These findings are very promising and will need to be confirmed and extended in a larger randomized controlled trial.”
Unsettling for some older patients
George T. Grossberg, MD, director, geriatric psychiatry, Saint Louis University, noted that in his experience, IV ketamine treatment can be unsettling for some older geriatric patients, such as those in their 80s.
“Particularly with some of my older patients, the kind of psychotomimetic properties of ketamine and the out-of-body experiences [with the initial treatment] can be frightening,” he said. “They may be willing to try, but I’ve had more than one patient quit after one treatment because they became so frightened.”
However, the dire nature of TRD and failure to respond to multiple medications and combinations and other strategies may prompt patients to try ketamine as a measure with at least some potential, he noted.
“But there is a high bar for acceptance, especially on the part of older adults and their families, more than for younger people,” he said.
The investigators have disclosed no relevant financial relationships. Dr. Grossberg has received consulting fees from Acadia, Avanir, Biogen, BioXcel, Genentech, Karuna, Lundbeck, Otsuka, Roche, and Takeda.
A version of this article first appeared on Medscape.com.
NEW ORLEANS –
“These were patients with depression who had not responded even to intensive therapies or procedures, and we found that after a 6-week ketamine infusion regimen, there was no difference in the response to the treatment between the treatment-resistant geriatric and nongeriatric patients,” study investigator Jonathan Kim, of Emory University, Atlanta, the first author of one of two studies presented as part of the American Association for Geriatric Psychiatry annual meeting, said in an interview.
The findings are important because research on the effects of IV ketamine have not been well documented in geriatric patients, who have high rates of depression and TRD.
“There is a lack of data on IV ketamine in older adults with treatment-resistant depression, and there are some safety and tolerability concerns which may lead some older adults and their clinicians to be reluctant to pursue IV ketamine treatment,” study coinvestigator Hanadi Ajam Oughli, MD, a health sciences assistant clinical professor in the department of psychiatry and biobehavioral sciences, University of California, Los Angeles, told this news organization.
Nasal vs. IV administration
Ketamine has traditionally been used as an anesthetic that blocks N-methyl-D-aspartate (NMDA) glutamate receptors, Dr. Oughli and colleagues note.
In the treatment of TRD, an infusion of 0.5 mg/kg is typically administered over 40 minutes, producing a rapid antidepressant response. Recent research shows the drug reduces suicidality and improves mood and quality of life.
A more recent intranasal formulation of ketamine, esketamine, was approved by the U.S. Food and Drug Administration for TRD in 2019, and some experts questioned its path to approval. In addition, the drug’s high cost and poor bioavailability in comparison with IV ketamine remains an issue, said Dr. Oughli.
In the previous TRANSFORM-3 study, a placebo-controlled randomized trial, there was no difference between esketamine, used in conjunction with an antidepressant, and placebo for geriatric patients.
To better understand the effects of IV ketamine in this patient population, Mr. Kim’s team conducted a retrospective chart review of 91 older patients with TRD who received IV ketamine treatment between October 2016 and August 2022.
Patients were divided into two groups – those older than 60 years (n = 36; 44% women; mean age, 68.86) and those younger than 60 (n = 55; 49% women; mean age, 41.05). Participants in each age group received six ketamine infusions over 6 weeks.
Results showed that with regard to depression severity, as assessed using Beck Depression Inventory (BDI-II) scores, 27.8% of patients in the geriatric group had a 50% or greater improvement, vs. 25.4% of those younger than 60.
The average BDI-II scores represented a significant improvement for both groups (P < .01), and the difference in scores between the groups was not statistically significant (P = .973).
“It is important to note that our study was conducted in a real-world clinical setting with a treatment-resistant population; other clinical studies may not have such sick patients in their trials. Additional studies are therefore warranted to establish further treatment guidelines in this area,” Mr. Kim said.
Open-label trial results
In the second study, Dr. Oughli and colleagues evaluated additional key outcomes in geriatric patients treated with IV ketamine as part of a larger open-label late-life trial on TRD.
The secondary analysis of the trial focused on 23 patients (mean age, 71.5 years) who had been initially treated with twice-a-week IV ketamine for 4 weeks.
After the first 4 weeks, patients who had experienced a partial response received an additional 4 weeks of once-weekly IV ketamine.
Overall, 48% of participants achieved a response, and 24% achieved remission of depressive symptoms following the first 4 weeks of twice-weekly treatment. This effect was maintained during the continuation phase of the study.
These findings are consistent with research in younger adults and demonstrate that twice-weekly infusions yield a more sustained antidepressant response than once-weekly infusions, the authors note.
The analysis also showed important increases in psychological well-being scores on the Scale for Suicidal Ideation, improved sleep quality as measured by the Pittsburgh Sleep Quality Index, and overall psychological well-being as shown on the NIH Toolbox Positive Affect on happiness/contentment and the NIH Toolbox General Life Satisfaction scales.
In a previous analysis, published in The American Journal of Geriatric Psychiatry, the researchers also evaluated cognitive function using the NIH Cognitive Battery, which showed that geriatric patients with TRD had significant improvements in a composite of executive functioning and fluid cognition during the 4-week acute treatment period of twice-weekly IV ketamine infusions (Cohen’s d = 0.61) and that those improvements were sustained in the continuation phase of once-weekly infusions for 4 more weeks.
Those results are consistent with ketamine’s known potential procognitive effects in TRD, due to a putative antidepressant mechanism that rescues prefrontal circuit dysfunction through synaptogenesis, the researchers note.
Dr. Oughli said that in both analyses, patients tolerated ketamine well, and there were no serious adverse events.
“Adverse events, including hypertension, dissociated effects, and cravings, were rare and did not prevent the continued use of IV ketamine by older adults. We were able to use clonidine to help manage blood pressure changes seen during the infusions,” she noted.
“These findings are very promising and will need to be confirmed and extended in a larger randomized controlled trial.”
Unsettling for some older patients
George T. Grossberg, MD, director, geriatric psychiatry, Saint Louis University, noted that in his experience, IV ketamine treatment can be unsettling for some older geriatric patients, such as those in their 80s.
“Particularly with some of my older patients, the kind of psychotomimetic properties of ketamine and the out-of-body experiences [with the initial treatment] can be frightening,” he said. “They may be willing to try, but I’ve had more than one patient quit after one treatment because they became so frightened.”
However, the dire nature of TRD and failure to respond to multiple medications and combinations and other strategies may prompt patients to try ketamine as a measure with at least some potential, he noted.
“But there is a high bar for acceptance, especially on the part of older adults and their families, more than for younger people,” he said.
The investigators have disclosed no relevant financial relationships. Dr. Grossberg has received consulting fees from Acadia, Avanir, Biogen, BioXcel, Genentech, Karuna, Lundbeck, Otsuka, Roche, and Takeda.
A version of this article first appeared on Medscape.com.
NEW ORLEANS –
“These were patients with depression who had not responded even to intensive therapies or procedures, and we found that after a 6-week ketamine infusion regimen, there was no difference in the response to the treatment between the treatment-resistant geriatric and nongeriatric patients,” study investigator Jonathan Kim, of Emory University, Atlanta, the first author of one of two studies presented as part of the American Association for Geriatric Psychiatry annual meeting, said in an interview.
The findings are important because research on the effects of IV ketamine have not been well documented in geriatric patients, who have high rates of depression and TRD.
“There is a lack of data on IV ketamine in older adults with treatment-resistant depression, and there are some safety and tolerability concerns which may lead some older adults and their clinicians to be reluctant to pursue IV ketamine treatment,” study coinvestigator Hanadi Ajam Oughli, MD, a health sciences assistant clinical professor in the department of psychiatry and biobehavioral sciences, University of California, Los Angeles, told this news organization.
Nasal vs. IV administration
Ketamine has traditionally been used as an anesthetic that blocks N-methyl-D-aspartate (NMDA) glutamate receptors, Dr. Oughli and colleagues note.
In the treatment of TRD, an infusion of 0.5 mg/kg is typically administered over 40 minutes, producing a rapid antidepressant response. Recent research shows the drug reduces suicidality and improves mood and quality of life.
A more recent intranasal formulation of ketamine, esketamine, was approved by the U.S. Food and Drug Administration for TRD in 2019, and some experts questioned its path to approval. In addition, the drug’s high cost and poor bioavailability in comparison with IV ketamine remains an issue, said Dr. Oughli.
In the previous TRANSFORM-3 study, a placebo-controlled randomized trial, there was no difference between esketamine, used in conjunction with an antidepressant, and placebo for geriatric patients.
To better understand the effects of IV ketamine in this patient population, Mr. Kim’s team conducted a retrospective chart review of 91 older patients with TRD who received IV ketamine treatment between October 2016 and August 2022.
Patients were divided into two groups – those older than 60 years (n = 36; 44% women; mean age, 68.86) and those younger than 60 (n = 55; 49% women; mean age, 41.05). Participants in each age group received six ketamine infusions over 6 weeks.
Results showed that with regard to depression severity, as assessed using Beck Depression Inventory (BDI-II) scores, 27.8% of patients in the geriatric group had a 50% or greater improvement, vs. 25.4% of those younger than 60.
The average BDI-II scores represented a significant improvement for both groups (P < .01), and the difference in scores between the groups was not statistically significant (P = .973).
“It is important to note that our study was conducted in a real-world clinical setting with a treatment-resistant population; other clinical studies may not have such sick patients in their trials. Additional studies are therefore warranted to establish further treatment guidelines in this area,” Mr. Kim said.
Open-label trial results
In the second study, Dr. Oughli and colleagues evaluated additional key outcomes in geriatric patients treated with IV ketamine as part of a larger open-label late-life trial on TRD.
The secondary analysis of the trial focused on 23 patients (mean age, 71.5 years) who had been initially treated with twice-a-week IV ketamine for 4 weeks.
After the first 4 weeks, patients who had experienced a partial response received an additional 4 weeks of once-weekly IV ketamine.
Overall, 48% of participants achieved a response, and 24% achieved remission of depressive symptoms following the first 4 weeks of twice-weekly treatment. This effect was maintained during the continuation phase of the study.
These findings are consistent with research in younger adults and demonstrate that twice-weekly infusions yield a more sustained antidepressant response than once-weekly infusions, the authors note.
The analysis also showed important increases in psychological well-being scores on the Scale for Suicidal Ideation, improved sleep quality as measured by the Pittsburgh Sleep Quality Index, and overall psychological well-being as shown on the NIH Toolbox Positive Affect on happiness/contentment and the NIH Toolbox General Life Satisfaction scales.
In a previous analysis, published in The American Journal of Geriatric Psychiatry, the researchers also evaluated cognitive function using the NIH Cognitive Battery, which showed that geriatric patients with TRD had significant improvements in a composite of executive functioning and fluid cognition during the 4-week acute treatment period of twice-weekly IV ketamine infusions (Cohen’s d = 0.61) and that those improvements were sustained in the continuation phase of once-weekly infusions for 4 more weeks.
Those results are consistent with ketamine’s known potential procognitive effects in TRD, due to a putative antidepressant mechanism that rescues prefrontal circuit dysfunction through synaptogenesis, the researchers note.
Dr. Oughli said that in both analyses, patients tolerated ketamine well, and there were no serious adverse events.
“Adverse events, including hypertension, dissociated effects, and cravings, were rare and did not prevent the continued use of IV ketamine by older adults. We were able to use clonidine to help manage blood pressure changes seen during the infusions,” she noted.
“These findings are very promising and will need to be confirmed and extended in a larger randomized controlled trial.”
Unsettling for some older patients
George T. Grossberg, MD, director, geriatric psychiatry, Saint Louis University, noted that in his experience, IV ketamine treatment can be unsettling for some older geriatric patients, such as those in their 80s.
“Particularly with some of my older patients, the kind of psychotomimetic properties of ketamine and the out-of-body experiences [with the initial treatment] can be frightening,” he said. “They may be willing to try, but I’ve had more than one patient quit after one treatment because they became so frightened.”
However, the dire nature of TRD and failure to respond to multiple medications and combinations and other strategies may prompt patients to try ketamine as a measure with at least some potential, he noted.
“But there is a high bar for acceptance, especially on the part of older adults and their families, more than for younger people,” he said.
The investigators have disclosed no relevant financial relationships. Dr. Grossberg has received consulting fees from Acadia, Avanir, Biogen, BioXcel, Genentech, Karuna, Lundbeck, Otsuka, Roche, and Takeda.
A version of this article first appeared on Medscape.com.
AT AAGP 2023
Add-on antipsychotic beats switching meds in older adults with resistant depression
NEW ORLEANS –
“We found that adding aripiprazole led to higher rates of depression remission and greater improvements in psychological well-being – which means how positive and satisfied patients felt – and this is good news,” study investigator Eric J. Lenze, MD, of the department of psychiatry, Washington University, St. Louis, said in a press statement.
“However, even that approach helped only about 30% of people in the study with treatment-resistant depression, underscoring the need to find and develop more effective treatments that can help more people,” he added.
The findings were presented here as part of the American Association for Geriatric Psychiatry annual meeting, and published concurrently in the New England Journal of Medicine.
Need for safe treatment options
Treatment-resistant depression is common in older patients, but switching medications or adding other agents can be challenging. With higher rates of comorbidity and polypharmacy, treatment decisions in this patient population are more complex compared with those involving younger patients.
To compare the benefits of augmentation vs. drug-switching strategies, the researchers conducted a multicenter, two-step trial involving 619 patients with an average baseline age of 69 who had failed to respond to two courses of selective serotonin reuptake inhibitors (SSRIs).
Patients were randomly assigned to one of three groups. These included augmentation of existing antidepressant medication with either aripiprazole (n = 211) or the dopamine and norepinephrine–reuptake inhibitor bupropion (Wellbutrin, Zyban) (n = 206), or to taper off of their current antidepressant and switch to bupropion (n = 202).
After 10 weeks, patients’ psychological well-being was assessed via the National Institutes of Health Toolbox Positive Affect and General Life Satisfaction subscales. The researchers found patients in the aripiprazole and bupropion add-on groups improved by 4.83 points and 4.33 points, respectively. The bupropion switch group had a change of 2.04 points.
The difference between the aripiprazole augmentation group and the switch to bupropion group was significant (difference 2.79 points; P = .014). Other between-group differences were not significantly different.
Remission rates were similar in the aripiprazole and bupropion groups at 28.9% and 28.2%, respectively. The remission rate in the bupropion switch group was 19.3%.
The study results showed patients who received adjunctive bupropion had the highest fall rate at 0.55 falls per patient, vs. 0.33 falls per patient in the aripiprazole group, suggesting that among the three treatment options, adjunctive aripiprazole may be the best choice because of its superior efficacy and lower fall risk.
A total of 248 patients enrolled in the study showed no improvement and were further randomly assigned to receive adjunctive lithium (n = 127) or switch from current therapy to nortriptyline (n = 121).
Well-being scores in the lithium group improved by 3.17 points and 2.18 points in the nortriptyline group. Remission occurred in 18.9% of patients in the lithium group and 21.5% in the nortriptyline group. Fall rates were similar among the two groups.
Overall, “this large, randomized study demonstrated that adding aripiprazole was a superior option for older adults with treatment-resistant depression,” Dr. Lenze told this news organization.
“Since neither lithium nor nortriptyline were promising against treatment-resistant depression in older adults, those medications are unlikely to be helpful in most cases,” he added.
Practice changing?
In an accompanying editorial, Gemma Lewis, PhD, and Glyn Lewis, PhD, division of psychiatry, University of College London, noted the findings “support aripiprazole augmentation as a strategy for treatment-resistant depression in older persons, largely because of the lower risk of falls than with bupropion augmentation.”
However, “in clinical practice, [it] would be important to tailor treatment in light of potential adverse effects and the preferences of the patient,” they added.
Akathisia, for instance, is a common side effect of aripiprazole, shown in one recent trial to affect 11% of the patients. In addition, weight gain, though typically lower than seen with other antipsychotics, is a consideration with aripiprazole.
With respect to fall risk, they noted that bupropion was largely used in relatively high doses of 300 mg and 450 mg, despite some recent research showing little clinical benefit from increasing antidepressant doses above minimum recommendations.
“It is possible that smaller doses of bupropion than those used in the current trial would retain effectiveness while minimizing adverse effects such as falls,” the editorialists noted.
Commenting on the study, Jennifer R. Gatchel, MD, PhD, assistant psychiatrist at Massachusetts General Hospital/McLean Hospital and assistant professor of psychiatry at Harvard Medical School, Boston, said the findings have high clinical significance in the treatment of geriatric depression.
“These results are of great impact for clinicians managing older adults with treatment-resistant depression. They provide some of the first evidence of safety and efficacy of augmentation with aripiprazole as a strategy in clinical management of older adults who fail to initially respond to treatment,” said Dr. Gatchel, who was not associated with this research.
“Of particular significance, efficacy here is based on patient-centered outcomes and psychological well-being as a primary effectiveness outcome, which could translate into strengthened physician-patient alliance.”
While adjunctive aripiprazole is not necessarily a first-line strategy when older adults fail to respond to antidepressants, there is a lack of data on the risks and benefits of any other antipsychotic medications, she noted.
“Thus, this is evidence that will impact clinical practice and hopefully contribute to reduced societal burden of depression in older adults and the morbidity and mortality associated with it,” Dr. Gatchel said.
The study received support from a Patient-Centered Outcomes Research Institute (PCORI) Award (TRD-1511-33321). Dr. Lenze received additional support from the Taylor Family Institute for Innovative Psychiatric Research at Washington University School of Medicine, as well as the Washington University Institute of Clinical and Translational Sciences grant (UL1TR002345) from the National Center for Advancing Translational Sciences of the National Institutes of Health. Dr. Gatchel reports no relevant financial relationships.
A version of this article first appeared on Medscape.com.
NEW ORLEANS –
“We found that adding aripiprazole led to higher rates of depression remission and greater improvements in psychological well-being – which means how positive and satisfied patients felt – and this is good news,” study investigator Eric J. Lenze, MD, of the department of psychiatry, Washington University, St. Louis, said in a press statement.
“However, even that approach helped only about 30% of people in the study with treatment-resistant depression, underscoring the need to find and develop more effective treatments that can help more people,” he added.
The findings were presented here as part of the American Association for Geriatric Psychiatry annual meeting, and published concurrently in the New England Journal of Medicine.
Need for safe treatment options
Treatment-resistant depression is common in older patients, but switching medications or adding other agents can be challenging. With higher rates of comorbidity and polypharmacy, treatment decisions in this patient population are more complex compared with those involving younger patients.
To compare the benefits of augmentation vs. drug-switching strategies, the researchers conducted a multicenter, two-step trial involving 619 patients with an average baseline age of 69 who had failed to respond to two courses of selective serotonin reuptake inhibitors (SSRIs).
Patients were randomly assigned to one of three groups. These included augmentation of existing antidepressant medication with either aripiprazole (n = 211) or the dopamine and norepinephrine–reuptake inhibitor bupropion (Wellbutrin, Zyban) (n = 206), or to taper off of their current antidepressant and switch to bupropion (n = 202).
After 10 weeks, patients’ psychological well-being was assessed via the National Institutes of Health Toolbox Positive Affect and General Life Satisfaction subscales. The researchers found patients in the aripiprazole and bupropion add-on groups improved by 4.83 points and 4.33 points, respectively. The bupropion switch group had a change of 2.04 points.
The difference between the aripiprazole augmentation group and the switch to bupropion group was significant (difference 2.79 points; P = .014). Other between-group differences were not significantly different.
Remission rates were similar in the aripiprazole and bupropion groups at 28.9% and 28.2%, respectively. The remission rate in the bupropion switch group was 19.3%.
The study results showed patients who received adjunctive bupropion had the highest fall rate at 0.55 falls per patient, vs. 0.33 falls per patient in the aripiprazole group, suggesting that among the three treatment options, adjunctive aripiprazole may be the best choice because of its superior efficacy and lower fall risk.
A total of 248 patients enrolled in the study showed no improvement and were further randomly assigned to receive adjunctive lithium (n = 127) or switch from current therapy to nortriptyline (n = 121).
Well-being scores in the lithium group improved by 3.17 points and 2.18 points in the nortriptyline group. Remission occurred in 18.9% of patients in the lithium group and 21.5% in the nortriptyline group. Fall rates were similar among the two groups.
Overall, “this large, randomized study demonstrated that adding aripiprazole was a superior option for older adults with treatment-resistant depression,” Dr. Lenze told this news organization.
“Since neither lithium nor nortriptyline were promising against treatment-resistant depression in older adults, those medications are unlikely to be helpful in most cases,” he added.
Practice changing?
In an accompanying editorial, Gemma Lewis, PhD, and Glyn Lewis, PhD, division of psychiatry, University of College London, noted the findings “support aripiprazole augmentation as a strategy for treatment-resistant depression in older persons, largely because of the lower risk of falls than with bupropion augmentation.”
However, “in clinical practice, [it] would be important to tailor treatment in light of potential adverse effects and the preferences of the patient,” they added.
Akathisia, for instance, is a common side effect of aripiprazole, shown in one recent trial to affect 11% of the patients. In addition, weight gain, though typically lower than seen with other antipsychotics, is a consideration with aripiprazole.
With respect to fall risk, they noted that bupropion was largely used in relatively high doses of 300 mg and 450 mg, despite some recent research showing little clinical benefit from increasing antidepressant doses above minimum recommendations.
“It is possible that smaller doses of bupropion than those used in the current trial would retain effectiveness while minimizing adverse effects such as falls,” the editorialists noted.
Commenting on the study, Jennifer R. Gatchel, MD, PhD, assistant psychiatrist at Massachusetts General Hospital/McLean Hospital and assistant professor of psychiatry at Harvard Medical School, Boston, said the findings have high clinical significance in the treatment of geriatric depression.
“These results are of great impact for clinicians managing older adults with treatment-resistant depression. They provide some of the first evidence of safety and efficacy of augmentation with aripiprazole as a strategy in clinical management of older adults who fail to initially respond to treatment,” said Dr. Gatchel, who was not associated with this research.
“Of particular significance, efficacy here is based on patient-centered outcomes and psychological well-being as a primary effectiveness outcome, which could translate into strengthened physician-patient alliance.”
While adjunctive aripiprazole is not necessarily a first-line strategy when older adults fail to respond to antidepressants, there is a lack of data on the risks and benefits of any other antipsychotic medications, she noted.
“Thus, this is evidence that will impact clinical practice and hopefully contribute to reduced societal burden of depression in older adults and the morbidity and mortality associated with it,” Dr. Gatchel said.
The study received support from a Patient-Centered Outcomes Research Institute (PCORI) Award (TRD-1511-33321). Dr. Lenze received additional support from the Taylor Family Institute for Innovative Psychiatric Research at Washington University School of Medicine, as well as the Washington University Institute of Clinical and Translational Sciences grant (UL1TR002345) from the National Center for Advancing Translational Sciences of the National Institutes of Health. Dr. Gatchel reports no relevant financial relationships.
A version of this article first appeared on Medscape.com.
NEW ORLEANS –
“We found that adding aripiprazole led to higher rates of depression remission and greater improvements in psychological well-being – which means how positive and satisfied patients felt – and this is good news,” study investigator Eric J. Lenze, MD, of the department of psychiatry, Washington University, St. Louis, said in a press statement.
“However, even that approach helped only about 30% of people in the study with treatment-resistant depression, underscoring the need to find and develop more effective treatments that can help more people,” he added.
The findings were presented here as part of the American Association for Geriatric Psychiatry annual meeting, and published concurrently in the New England Journal of Medicine.
Need for safe treatment options
Treatment-resistant depression is common in older patients, but switching medications or adding other agents can be challenging. With higher rates of comorbidity and polypharmacy, treatment decisions in this patient population are more complex compared with those involving younger patients.
To compare the benefits of augmentation vs. drug-switching strategies, the researchers conducted a multicenter, two-step trial involving 619 patients with an average baseline age of 69 who had failed to respond to two courses of selective serotonin reuptake inhibitors (SSRIs).
Patients were randomly assigned to one of three groups. These included augmentation of existing antidepressant medication with either aripiprazole (n = 211) or the dopamine and norepinephrine–reuptake inhibitor bupropion (Wellbutrin, Zyban) (n = 206), or to taper off of their current antidepressant and switch to bupropion (n = 202).
After 10 weeks, patients’ psychological well-being was assessed via the National Institutes of Health Toolbox Positive Affect and General Life Satisfaction subscales. The researchers found patients in the aripiprazole and bupropion add-on groups improved by 4.83 points and 4.33 points, respectively. The bupropion switch group had a change of 2.04 points.
The difference between the aripiprazole augmentation group and the switch to bupropion group was significant (difference 2.79 points; P = .014). Other between-group differences were not significantly different.
Remission rates were similar in the aripiprazole and bupropion groups at 28.9% and 28.2%, respectively. The remission rate in the bupropion switch group was 19.3%.
The study results showed patients who received adjunctive bupropion had the highest fall rate at 0.55 falls per patient, vs. 0.33 falls per patient in the aripiprazole group, suggesting that among the three treatment options, adjunctive aripiprazole may be the best choice because of its superior efficacy and lower fall risk.
A total of 248 patients enrolled in the study showed no improvement and were further randomly assigned to receive adjunctive lithium (n = 127) or switch from current therapy to nortriptyline (n = 121).
Well-being scores in the lithium group improved by 3.17 points and 2.18 points in the nortriptyline group. Remission occurred in 18.9% of patients in the lithium group and 21.5% in the nortriptyline group. Fall rates were similar among the two groups.
Overall, “this large, randomized study demonstrated that adding aripiprazole was a superior option for older adults with treatment-resistant depression,” Dr. Lenze told this news organization.
“Since neither lithium nor nortriptyline were promising against treatment-resistant depression in older adults, those medications are unlikely to be helpful in most cases,” he added.
Practice changing?
In an accompanying editorial, Gemma Lewis, PhD, and Glyn Lewis, PhD, division of psychiatry, University of College London, noted the findings “support aripiprazole augmentation as a strategy for treatment-resistant depression in older persons, largely because of the lower risk of falls than with bupropion augmentation.”
However, “in clinical practice, [it] would be important to tailor treatment in light of potential adverse effects and the preferences of the patient,” they added.
Akathisia, for instance, is a common side effect of aripiprazole, shown in one recent trial to affect 11% of the patients. In addition, weight gain, though typically lower than seen with other antipsychotics, is a consideration with aripiprazole.
With respect to fall risk, they noted that bupropion was largely used in relatively high doses of 300 mg and 450 mg, despite some recent research showing little clinical benefit from increasing antidepressant doses above minimum recommendations.
“It is possible that smaller doses of bupropion than those used in the current trial would retain effectiveness while minimizing adverse effects such as falls,” the editorialists noted.
Commenting on the study, Jennifer R. Gatchel, MD, PhD, assistant psychiatrist at Massachusetts General Hospital/McLean Hospital and assistant professor of psychiatry at Harvard Medical School, Boston, said the findings have high clinical significance in the treatment of geriatric depression.
“These results are of great impact for clinicians managing older adults with treatment-resistant depression. They provide some of the first evidence of safety and efficacy of augmentation with aripiprazole as a strategy in clinical management of older adults who fail to initially respond to treatment,” said Dr. Gatchel, who was not associated with this research.
“Of particular significance, efficacy here is based on patient-centered outcomes and psychological well-being as a primary effectiveness outcome, which could translate into strengthened physician-patient alliance.”
While adjunctive aripiprazole is not necessarily a first-line strategy when older adults fail to respond to antidepressants, there is a lack of data on the risks and benefits of any other antipsychotic medications, she noted.
“Thus, this is evidence that will impact clinical practice and hopefully contribute to reduced societal burden of depression in older adults and the morbidity and mortality associated with it,” Dr. Gatchel said.
The study received support from a Patient-Centered Outcomes Research Institute (PCORI) Award (TRD-1511-33321). Dr. Lenze received additional support from the Taylor Family Institute for Innovative Psychiatric Research at Washington University School of Medicine, as well as the Washington University Institute of Clinical and Translational Sciences grant (UL1TR002345) from the National Center for Advancing Translational Sciences of the National Institutes of Health. Dr. Gatchel reports no relevant financial relationships.
A version of this article first appeared on Medscape.com.
AT AAGP 2023
No Wrong Floor on the Elevator: A Vision for the VA as an Age-Friendly Health System
One morning I stepped into the elevator in the lobby of the US Department of Veterans Affairs (VA) medical center where I work, holding a cup of coffee, joining another staffer, a middle-aged man, wearing a veteran’s pin on his employee badge. An older veteran slowly approached the elevator doors, shuffling with each step, and since he was at the front of the elevator, he cheerfully bellowed “Which floor?” as he offered to push the button for us.
“What’s on 12?” he asked in a jovial voice. I smiled. “Aging research,” referring to the Geriatrics Research Education and Clinical Center where I work.1
“I definitely need that—I forgot where I’m going!” he joked, his fingers hovering over the elevator buttons.
As we reached his floor, the doors opened, he waved with a smile and unsteadily made his way out of the elevator and down the hall to his appointment. As the elevator doors closed behind him, the other staffer turned to me and said with a shrug, “That’ll be me one day,” as he got off at the next floor.
When I got off the elevator and walked toward my office, I reflected on the care that I as a geriatrician and we at the VA hope to provide to aging veterans, now and in the future: Age-Friendly care. Age-Friendly means the compassionate care that we want for those who have served our country, for our loved ones, and for ourselves as we age. Age-Friendly means person-centered, evidence-based care that as we grow older will help us to address challenges that may come with older age, such as falls, cognitive impairment, and polypharmacy. Too often the health care system remains focused on the chief concern or on a clinician’s specialty and may not focus on those important areas where we can potentially intervene to support aging veterans.
The VA has set a goal to become the largest Age-Friendly Health System (AFHS) in the country.2 Led by the Institute for Healthcare Improvement and funded by the John A. Hartford Foundation, the Age-Friendly Health Systems Initiative aims to help clinicians and care settings “follow an essential set of evidence-based practices; cause no harm; and align with what matters to the older adult and their family caregivers.”3 An AFHS cares for older adults with attention to the 4Ms—What Matters, Mobility, Mentation, and Medications.4 Specifically, in an AFHS, older adults are asked what matters to them so we can align their health care with their goals; clinicians evaluate veterans for safe mobility and fall risk reduction, cognitive impairment and mood disorders, and identify and avoid high-risk medications.5 In an AFHS, the 4Ms are practiced as a set, reliably, across settings, so that there should be no wrong door or wrong floor for an older veteran to receive Age-Friendly care within the VA health care system.6
I thought of the veteran with the sense of humor getting off the elevator and wondered whether the clinician seeing him would have training in some of the many VA resources available for delivering Age-Friendly care (Table).
Too often our health care system and health professions education have left clinicians unprepared to care for older adults using an Age-Friendly framework; rather, we have been trained in problem-based or disease-based care that can miss the forest for the trees in an older adult living with multiple chronic conditions and/or frailty. We may focus on providing evidence-based care for individual medical conditions while neglecting the often practical interventions that can help an older person age in place by focusing on what matters, supporting safe mobility, addressing cognition and mood, and optimizing medications.18
The vision of the VA as the largest AFHS in America is urgently needed; nearly half of the veteran population is aged 65 ≥ years, compared with 16% of the general population.19 Building on the VA’s legacy of creativity and innovation in geriatrics, and the VA’s goal of being a high reliability organization, becoming an AFHS will ensure that for that older veteran stepping off that elevator there is no wrong floor, and no wrong door to receive the Age-Friendly care he deserves and that we all hope for as we age.1,5,19,20
Acknowledgments
This material is the result of work supported with resources and the use of facilities at the Veterans Affairs Boston Healthcare System and the New England Geriatric Research Education and Clinical Center.
1. Supiano MA, Alessi C, Chernoff R, Goldberg A, Morley JE, Schmader KE, Shay K; GRECC Directors Association. Department of Veterans Affairs Geriatric Research, Education and Clinical Centers: translating aging research into clinical geriatrics. J Am Geriatr Soc. 2012;60(7):1347-1356. doi:10.1111/j.1532-5415.2012.04004.x
2. US Department of Veterans Affairs. VA geriatrics and extended care: the Age-Friendly Health Systems Initiative. Updated July 29, 2022. Accessed February 8, 2023. https://www.va.gov/geriatrics/pages/VA_Age_Friendly_Health_Systems_Initiative.asp
3. What is an age-friendly health system? Accessed November 15, 2022. https://www.ihi.org/Engage/Initiatives/Age-Friendly-Health-Systems/Pages/default.aspx
4. Mate KS, Berman A, Laderman M, Kabcenell A, Fulmer T. Creating age-friendly health systems - a vision for better care of older adults. Healthc (Amst). 2018;6(1):4-6. doi:10.1016/j.hjdsi.2017.05.005
5. Church K, Munro S, Shaughnessy M, Clancy C. Age-friendly health systems: improving care for older adults in the Veterans Health Administration. Health Serv Res. Published online December 7, 2022. doi:10.1111/1475-6773.14110
6. Emery-Tiburcio EE, Berg-Weger M, Husser EK, et al. The geriatrics education and care revolution: diverse implementation of age-friendly health systems. J Am Geriatr Soc. Published online October 8, 2021. doi:10.1111/jgs.17497
7. James K, Schwartz AW, Orkaby AR. Mobility assessment in older adults. N Engl J Med. 2021;385(8):e22. doi:10.1056/NEJMvcm2009406
8. Harris R, Bean J. The Llive Long Walk Strong clinical rehabilitation program. Arch Phys Med Rehabil. 2019;100(12):e205. doi:10.1016/j.arrct.2022.100205
9. Morey MC, Lee CC, Castle S, et al. Should structured exercise be promoted as a model of care? Dissemination of the Department of Veterans Affairs Gerofit program. J Am Geriatr Soc. 2018;66(5):1009-1016. doi:10.1111/jgs.15276
10. McCarten JR, Anderson P, Kuskowski MA, McPherson SE, Borson S. Screening for cognitive impairment in an elderly veteran population: acceptability and results using different versions of the Mini-Cog. J Am Geriatr Soc. 2011;59(2):309-313. doi:10.1111/j.1532-5415.2010.03249.x
11. American Geriatrics Society Beers Criteria Update Expert Panel. American Geriatrics Society 2019 Updated AGS Beers Criteria for Potentially Inappropriate Medication Use in Older Adults. J Am Geriatr Soc. 2019;67(4):674-694. doi:10.1111/jgs.15767
12. Linsky A, Gellad WF, Linder JA, Friedberg MW. Advancing the science of deprescribing: a novel comprehensive conceptual framework. J Am Geriatr Soc. 2019;67(10):2018-2022. doi:10.1111/jgs.16136
13. Battar S, Watson Dickerson KR, Sedgwick C, Cmelik T. Understanding principles of high reliability organizations through the eyes of VIONE: a clinical program to improve patient safety by deprescribing potentially inappropriate medications and reducing polypharmacy. Fed Pract. 2019;36(12):564-568.
14. Tinetti ME, Naik AD, Dindo L, et al. Association of patient priorities-aligned decision-making with patient outcomes and ambulatory health care burden among older adults with multiple chronic conditions: a nonrandomized clinical trial. JAMA Intern Med. 2019;179(12):1688. doi:10.1001/jamainternmed.2019.4235
15. Levy C, Ersek M, Scott W, et al. Life-sustaining treatment decisions initiative: early implementation results of a national Veterans Affairs program to honor veterans’ care preferences. J Gen Intern Med. 2020;35(6):1803-1812. doi:10.1007/s11606-020-05697-2
16. Nathan S, Fiore LL, Saunders S, et al. My life, my story: teaching patient centered care competencies for older adults through life story work. Gerontol Geriatr Educ. 2022;43(2):225-238. doi:10.1080/02701960.2019.1665038
17. Reddy KP, Schult TM, Whitehead AM, Bokhour BG. Veterans Health Administration’s whole health system of care: supporting the health, well-being, and resiliency of employees. Glob Adv Health Med. 2021;10:21649561211022696. doi:10.1177/21649561211022698
18. Aronson L. Necessary steps: how health care fails older patients, and how it can be done better. Health Aff (Millwood). 2015;34(3):528-532. doi:10.1377/hlthaff.2014.1238
19. Farrell TW, Volden TA, Butler JM, et al. Age-friendly care in the Veterans Health Administration: past, present, and future. J Am Geriatr Soc. 2023;71(1):18-25. doi:10.1111/jgs.18070
20. Burke RE, Brown RT, Kinosian B. Selecting implementation strategies to drive age-friendly health system adoption. J Am Geriatr Soc. 2022;70(1):313-318. doi:10.1111/jgs.17489
21. Centers for Disease Control and Prevention. STEADI- older adult fall prevention. July 26,2021. Updated July 26, 2021. Accessed February 6, 2023. https://www.cdc.gov/steadi/index.html
22. Exercise and physical activity. National Institute on Aging. Accessed February 6, 2023. https://www.nia.nih.gov/health/topics/exercise-and-physical-activity
23. Hastings SN, Sloane R, Morey MC, Pavon JM, Hoenig H. Assisted early mobility for hospitalized older veterans: preliminary data from the STRIDE program. J Am Geriatr Soc. 2014;62(11):2180-2184.
24. Ashcroft T, Middleton A, Driver JA, Ruopp M, Harris R, Bean JF. An innovative rehabilitation program for the Veterans Affairs post-acute skilled nursing setting: preliminary results. J Am Geriatr Soc. 2023;10.1111/jgs.18214. doi:10.1111/jgs.18214
25. AGS CoCare. Accessed February 6, 2023. https://www.americangeriatrics.org/programs/ags-cocarer
26. Jedele JM, Curyto K, Ludwin BM, Karel MJ. Addressing behavioral symptoms of dementia through STAR-VA implementation: do outcomes vary by behavior type? Am J Alzheimers Dis Other Demen. 2020;35:1533317520911577.
27. Phung E, Triantafylidis L, Zhang H, Yeh IM. New Media, Part 5: Online Deprescribing Tools. J Palliat Med. 2018;21(2):269-270.
28. Freytag J, Dindo L, Catic A, et al. Feasibility of clinicians aligning health care with patient priorities in geriatrics ambulatory care. J Am Geriatr Soc. 2020;68(9):2112-2116.
29. The Conversation Project. Accessed February 22, 2023. https://theconversationproject.org
30. Daubman BR, Bernacki R, Stoltenberg M, Wilson E, Jacobsen J. Best practices for teaching clinicians to use a serious illness conversation guide. Palliat Med Rep. 2020;1(1):135-142. Published 2020 Jul 28. doi:10.1089/pmr.2020.0066
31. Freytag J, Street RL Jr, Barnes DE, et al. Empowering older adults to discuss advance care planning during clinical visits: The PREPARE Randomized Trial. J Am Geriatr Soc. 2020;68(6):1210-1217. doi:10.1111/jgs.16405
One morning I stepped into the elevator in the lobby of the US Department of Veterans Affairs (VA) medical center where I work, holding a cup of coffee, joining another staffer, a middle-aged man, wearing a veteran’s pin on his employee badge. An older veteran slowly approached the elevator doors, shuffling with each step, and since he was at the front of the elevator, he cheerfully bellowed “Which floor?” as he offered to push the button for us.
“What’s on 12?” he asked in a jovial voice. I smiled. “Aging research,” referring to the Geriatrics Research Education and Clinical Center where I work.1
“I definitely need that—I forgot where I’m going!” he joked, his fingers hovering over the elevator buttons.
As we reached his floor, the doors opened, he waved with a smile and unsteadily made his way out of the elevator and down the hall to his appointment. As the elevator doors closed behind him, the other staffer turned to me and said with a shrug, “That’ll be me one day,” as he got off at the next floor.
When I got off the elevator and walked toward my office, I reflected on the care that I as a geriatrician and we at the VA hope to provide to aging veterans, now and in the future: Age-Friendly care. Age-Friendly means the compassionate care that we want for those who have served our country, for our loved ones, and for ourselves as we age. Age-Friendly means person-centered, evidence-based care that as we grow older will help us to address challenges that may come with older age, such as falls, cognitive impairment, and polypharmacy. Too often the health care system remains focused on the chief concern or on a clinician’s specialty and may not focus on those important areas where we can potentially intervene to support aging veterans.
The VA has set a goal to become the largest Age-Friendly Health System (AFHS) in the country.2 Led by the Institute for Healthcare Improvement and funded by the John A. Hartford Foundation, the Age-Friendly Health Systems Initiative aims to help clinicians and care settings “follow an essential set of evidence-based practices; cause no harm; and align with what matters to the older adult and their family caregivers.”3 An AFHS cares for older adults with attention to the 4Ms—What Matters, Mobility, Mentation, and Medications.4 Specifically, in an AFHS, older adults are asked what matters to them so we can align their health care with their goals; clinicians evaluate veterans for safe mobility and fall risk reduction, cognitive impairment and mood disorders, and identify and avoid high-risk medications.5 In an AFHS, the 4Ms are practiced as a set, reliably, across settings, so that there should be no wrong door or wrong floor for an older veteran to receive Age-Friendly care within the VA health care system.6
I thought of the veteran with the sense of humor getting off the elevator and wondered whether the clinician seeing him would have training in some of the many VA resources available for delivering Age-Friendly care (Table).
Too often our health care system and health professions education have left clinicians unprepared to care for older adults using an Age-Friendly framework; rather, we have been trained in problem-based or disease-based care that can miss the forest for the trees in an older adult living with multiple chronic conditions and/or frailty. We may focus on providing evidence-based care for individual medical conditions while neglecting the often practical interventions that can help an older person age in place by focusing on what matters, supporting safe mobility, addressing cognition and mood, and optimizing medications.18
The vision of the VA as the largest AFHS in America is urgently needed; nearly half of the veteran population is aged 65 ≥ years, compared with 16% of the general population.19 Building on the VA’s legacy of creativity and innovation in geriatrics, and the VA’s goal of being a high reliability organization, becoming an AFHS will ensure that for that older veteran stepping off that elevator there is no wrong floor, and no wrong door to receive the Age-Friendly care he deserves and that we all hope for as we age.1,5,19,20
Acknowledgments
This material is the result of work supported with resources and the use of facilities at the Veterans Affairs Boston Healthcare System and the New England Geriatric Research Education and Clinical Center.
One morning I stepped into the elevator in the lobby of the US Department of Veterans Affairs (VA) medical center where I work, holding a cup of coffee, joining another staffer, a middle-aged man, wearing a veteran’s pin on his employee badge. An older veteran slowly approached the elevator doors, shuffling with each step, and since he was at the front of the elevator, he cheerfully bellowed “Which floor?” as he offered to push the button for us.
“What’s on 12?” he asked in a jovial voice. I smiled. “Aging research,” referring to the Geriatrics Research Education and Clinical Center where I work.1
“I definitely need that—I forgot where I’m going!” he joked, his fingers hovering over the elevator buttons.
As we reached his floor, the doors opened, he waved with a smile and unsteadily made his way out of the elevator and down the hall to his appointment. As the elevator doors closed behind him, the other staffer turned to me and said with a shrug, “That’ll be me one day,” as he got off at the next floor.
When I got off the elevator and walked toward my office, I reflected on the care that I as a geriatrician and we at the VA hope to provide to aging veterans, now and in the future: Age-Friendly care. Age-Friendly means the compassionate care that we want for those who have served our country, for our loved ones, and for ourselves as we age. Age-Friendly means person-centered, evidence-based care that as we grow older will help us to address challenges that may come with older age, such as falls, cognitive impairment, and polypharmacy. Too often the health care system remains focused on the chief concern or on a clinician’s specialty and may not focus on those important areas where we can potentially intervene to support aging veterans.
The VA has set a goal to become the largest Age-Friendly Health System (AFHS) in the country.2 Led by the Institute for Healthcare Improvement and funded by the John A. Hartford Foundation, the Age-Friendly Health Systems Initiative aims to help clinicians and care settings “follow an essential set of evidence-based practices; cause no harm; and align with what matters to the older adult and their family caregivers.”3 An AFHS cares for older adults with attention to the 4Ms—What Matters, Mobility, Mentation, and Medications.4 Specifically, in an AFHS, older adults are asked what matters to them so we can align their health care with their goals; clinicians evaluate veterans for safe mobility and fall risk reduction, cognitive impairment and mood disorders, and identify and avoid high-risk medications.5 In an AFHS, the 4Ms are practiced as a set, reliably, across settings, so that there should be no wrong door or wrong floor for an older veteran to receive Age-Friendly care within the VA health care system.6
I thought of the veteran with the sense of humor getting off the elevator and wondered whether the clinician seeing him would have training in some of the many VA resources available for delivering Age-Friendly care (Table).
Too often our health care system and health professions education have left clinicians unprepared to care for older adults using an Age-Friendly framework; rather, we have been trained in problem-based or disease-based care that can miss the forest for the trees in an older adult living with multiple chronic conditions and/or frailty. We may focus on providing evidence-based care for individual medical conditions while neglecting the often practical interventions that can help an older person age in place by focusing on what matters, supporting safe mobility, addressing cognition and mood, and optimizing medications.18
The vision of the VA as the largest AFHS in America is urgently needed; nearly half of the veteran population is aged 65 ≥ years, compared with 16% of the general population.19 Building on the VA’s legacy of creativity and innovation in geriatrics, and the VA’s goal of being a high reliability organization, becoming an AFHS will ensure that for that older veteran stepping off that elevator there is no wrong floor, and no wrong door to receive the Age-Friendly care he deserves and that we all hope for as we age.1,5,19,20
Acknowledgments
This material is the result of work supported with resources and the use of facilities at the Veterans Affairs Boston Healthcare System and the New England Geriatric Research Education and Clinical Center.
1. Supiano MA, Alessi C, Chernoff R, Goldberg A, Morley JE, Schmader KE, Shay K; GRECC Directors Association. Department of Veterans Affairs Geriatric Research, Education and Clinical Centers: translating aging research into clinical geriatrics. J Am Geriatr Soc. 2012;60(7):1347-1356. doi:10.1111/j.1532-5415.2012.04004.x
2. US Department of Veterans Affairs. VA geriatrics and extended care: the Age-Friendly Health Systems Initiative. Updated July 29, 2022. Accessed February 8, 2023. https://www.va.gov/geriatrics/pages/VA_Age_Friendly_Health_Systems_Initiative.asp
3. What is an age-friendly health system? Accessed November 15, 2022. https://www.ihi.org/Engage/Initiatives/Age-Friendly-Health-Systems/Pages/default.aspx
4. Mate KS, Berman A, Laderman M, Kabcenell A, Fulmer T. Creating age-friendly health systems - a vision for better care of older adults. Healthc (Amst). 2018;6(1):4-6. doi:10.1016/j.hjdsi.2017.05.005
5. Church K, Munro S, Shaughnessy M, Clancy C. Age-friendly health systems: improving care for older adults in the Veterans Health Administration. Health Serv Res. Published online December 7, 2022. doi:10.1111/1475-6773.14110
6. Emery-Tiburcio EE, Berg-Weger M, Husser EK, et al. The geriatrics education and care revolution: diverse implementation of age-friendly health systems. J Am Geriatr Soc. Published online October 8, 2021. doi:10.1111/jgs.17497
7. James K, Schwartz AW, Orkaby AR. Mobility assessment in older adults. N Engl J Med. 2021;385(8):e22. doi:10.1056/NEJMvcm2009406
8. Harris R, Bean J. The Llive Long Walk Strong clinical rehabilitation program. Arch Phys Med Rehabil. 2019;100(12):e205. doi:10.1016/j.arrct.2022.100205
9. Morey MC, Lee CC, Castle S, et al. Should structured exercise be promoted as a model of care? Dissemination of the Department of Veterans Affairs Gerofit program. J Am Geriatr Soc. 2018;66(5):1009-1016. doi:10.1111/jgs.15276
10. McCarten JR, Anderson P, Kuskowski MA, McPherson SE, Borson S. Screening for cognitive impairment in an elderly veteran population: acceptability and results using different versions of the Mini-Cog. J Am Geriatr Soc. 2011;59(2):309-313. doi:10.1111/j.1532-5415.2010.03249.x
11. American Geriatrics Society Beers Criteria Update Expert Panel. American Geriatrics Society 2019 Updated AGS Beers Criteria for Potentially Inappropriate Medication Use in Older Adults. J Am Geriatr Soc. 2019;67(4):674-694. doi:10.1111/jgs.15767
12. Linsky A, Gellad WF, Linder JA, Friedberg MW. Advancing the science of deprescribing: a novel comprehensive conceptual framework. J Am Geriatr Soc. 2019;67(10):2018-2022. doi:10.1111/jgs.16136
13. Battar S, Watson Dickerson KR, Sedgwick C, Cmelik T. Understanding principles of high reliability organizations through the eyes of VIONE: a clinical program to improve patient safety by deprescribing potentially inappropriate medications and reducing polypharmacy. Fed Pract. 2019;36(12):564-568.
14. Tinetti ME, Naik AD, Dindo L, et al. Association of patient priorities-aligned decision-making with patient outcomes and ambulatory health care burden among older adults with multiple chronic conditions: a nonrandomized clinical trial. JAMA Intern Med. 2019;179(12):1688. doi:10.1001/jamainternmed.2019.4235
15. Levy C, Ersek M, Scott W, et al. Life-sustaining treatment decisions initiative: early implementation results of a national Veterans Affairs program to honor veterans’ care preferences. J Gen Intern Med. 2020;35(6):1803-1812. doi:10.1007/s11606-020-05697-2
16. Nathan S, Fiore LL, Saunders S, et al. My life, my story: teaching patient centered care competencies for older adults through life story work. Gerontol Geriatr Educ. 2022;43(2):225-238. doi:10.1080/02701960.2019.1665038
17. Reddy KP, Schult TM, Whitehead AM, Bokhour BG. Veterans Health Administration’s whole health system of care: supporting the health, well-being, and resiliency of employees. Glob Adv Health Med. 2021;10:21649561211022696. doi:10.1177/21649561211022698
18. Aronson L. Necessary steps: how health care fails older patients, and how it can be done better. Health Aff (Millwood). 2015;34(3):528-532. doi:10.1377/hlthaff.2014.1238
19. Farrell TW, Volden TA, Butler JM, et al. Age-friendly care in the Veterans Health Administration: past, present, and future. J Am Geriatr Soc. 2023;71(1):18-25. doi:10.1111/jgs.18070
20. Burke RE, Brown RT, Kinosian B. Selecting implementation strategies to drive age-friendly health system adoption. J Am Geriatr Soc. 2022;70(1):313-318. doi:10.1111/jgs.17489
21. Centers for Disease Control and Prevention. STEADI- older adult fall prevention. July 26,2021. Updated July 26, 2021. Accessed February 6, 2023. https://www.cdc.gov/steadi/index.html
22. Exercise and physical activity. National Institute on Aging. Accessed February 6, 2023. https://www.nia.nih.gov/health/topics/exercise-and-physical-activity
23. Hastings SN, Sloane R, Morey MC, Pavon JM, Hoenig H. Assisted early mobility for hospitalized older veterans: preliminary data from the STRIDE program. J Am Geriatr Soc. 2014;62(11):2180-2184.
24. Ashcroft T, Middleton A, Driver JA, Ruopp M, Harris R, Bean JF. An innovative rehabilitation program for the Veterans Affairs post-acute skilled nursing setting: preliminary results. J Am Geriatr Soc. 2023;10.1111/jgs.18214. doi:10.1111/jgs.18214
25. AGS CoCare. Accessed February 6, 2023. https://www.americangeriatrics.org/programs/ags-cocarer
26. Jedele JM, Curyto K, Ludwin BM, Karel MJ. Addressing behavioral symptoms of dementia through STAR-VA implementation: do outcomes vary by behavior type? Am J Alzheimers Dis Other Demen. 2020;35:1533317520911577.
27. Phung E, Triantafylidis L, Zhang H, Yeh IM. New Media, Part 5: Online Deprescribing Tools. J Palliat Med. 2018;21(2):269-270.
28. Freytag J, Dindo L, Catic A, et al. Feasibility of clinicians aligning health care with patient priorities in geriatrics ambulatory care. J Am Geriatr Soc. 2020;68(9):2112-2116.
29. The Conversation Project. Accessed February 22, 2023. https://theconversationproject.org
30. Daubman BR, Bernacki R, Stoltenberg M, Wilson E, Jacobsen J. Best practices for teaching clinicians to use a serious illness conversation guide. Palliat Med Rep. 2020;1(1):135-142. Published 2020 Jul 28. doi:10.1089/pmr.2020.0066
31. Freytag J, Street RL Jr, Barnes DE, et al. Empowering older adults to discuss advance care planning during clinical visits: The PREPARE Randomized Trial. J Am Geriatr Soc. 2020;68(6):1210-1217. doi:10.1111/jgs.16405
1. Supiano MA, Alessi C, Chernoff R, Goldberg A, Morley JE, Schmader KE, Shay K; GRECC Directors Association. Department of Veterans Affairs Geriatric Research, Education and Clinical Centers: translating aging research into clinical geriatrics. J Am Geriatr Soc. 2012;60(7):1347-1356. doi:10.1111/j.1532-5415.2012.04004.x
2. US Department of Veterans Affairs. VA geriatrics and extended care: the Age-Friendly Health Systems Initiative. Updated July 29, 2022. Accessed February 8, 2023. https://www.va.gov/geriatrics/pages/VA_Age_Friendly_Health_Systems_Initiative.asp
3. What is an age-friendly health system? Accessed November 15, 2022. https://www.ihi.org/Engage/Initiatives/Age-Friendly-Health-Systems/Pages/default.aspx
4. Mate KS, Berman A, Laderman M, Kabcenell A, Fulmer T. Creating age-friendly health systems - a vision for better care of older adults. Healthc (Amst). 2018;6(1):4-6. doi:10.1016/j.hjdsi.2017.05.005
5. Church K, Munro S, Shaughnessy M, Clancy C. Age-friendly health systems: improving care for older adults in the Veterans Health Administration. Health Serv Res. Published online December 7, 2022. doi:10.1111/1475-6773.14110
6. Emery-Tiburcio EE, Berg-Weger M, Husser EK, et al. The geriatrics education and care revolution: diverse implementation of age-friendly health systems. J Am Geriatr Soc. Published online October 8, 2021. doi:10.1111/jgs.17497
7. James K, Schwartz AW, Orkaby AR. Mobility assessment in older adults. N Engl J Med. 2021;385(8):e22. doi:10.1056/NEJMvcm2009406
8. Harris R, Bean J. The Llive Long Walk Strong clinical rehabilitation program. Arch Phys Med Rehabil. 2019;100(12):e205. doi:10.1016/j.arrct.2022.100205
9. Morey MC, Lee CC, Castle S, et al. Should structured exercise be promoted as a model of care? Dissemination of the Department of Veterans Affairs Gerofit program. J Am Geriatr Soc. 2018;66(5):1009-1016. doi:10.1111/jgs.15276
10. McCarten JR, Anderson P, Kuskowski MA, McPherson SE, Borson S. Screening for cognitive impairment in an elderly veteran population: acceptability and results using different versions of the Mini-Cog. J Am Geriatr Soc. 2011;59(2):309-313. doi:10.1111/j.1532-5415.2010.03249.x
11. American Geriatrics Society Beers Criteria Update Expert Panel. American Geriatrics Society 2019 Updated AGS Beers Criteria for Potentially Inappropriate Medication Use in Older Adults. J Am Geriatr Soc. 2019;67(4):674-694. doi:10.1111/jgs.15767
12. Linsky A, Gellad WF, Linder JA, Friedberg MW. Advancing the science of deprescribing: a novel comprehensive conceptual framework. J Am Geriatr Soc. 2019;67(10):2018-2022. doi:10.1111/jgs.16136
13. Battar S, Watson Dickerson KR, Sedgwick C, Cmelik T. Understanding principles of high reliability organizations through the eyes of VIONE: a clinical program to improve patient safety by deprescribing potentially inappropriate medications and reducing polypharmacy. Fed Pract. 2019;36(12):564-568.
14. Tinetti ME, Naik AD, Dindo L, et al. Association of patient priorities-aligned decision-making with patient outcomes and ambulatory health care burden among older adults with multiple chronic conditions: a nonrandomized clinical trial. JAMA Intern Med. 2019;179(12):1688. doi:10.1001/jamainternmed.2019.4235
15. Levy C, Ersek M, Scott W, et al. Life-sustaining treatment decisions initiative: early implementation results of a national Veterans Affairs program to honor veterans’ care preferences. J Gen Intern Med. 2020;35(6):1803-1812. doi:10.1007/s11606-020-05697-2
16. Nathan S, Fiore LL, Saunders S, et al. My life, my story: teaching patient centered care competencies for older adults through life story work. Gerontol Geriatr Educ. 2022;43(2):225-238. doi:10.1080/02701960.2019.1665038
17. Reddy KP, Schult TM, Whitehead AM, Bokhour BG. Veterans Health Administration’s whole health system of care: supporting the health, well-being, and resiliency of employees. Glob Adv Health Med. 2021;10:21649561211022696. doi:10.1177/21649561211022698
18. Aronson L. Necessary steps: how health care fails older patients, and how it can be done better. Health Aff (Millwood). 2015;34(3):528-532. doi:10.1377/hlthaff.2014.1238
19. Farrell TW, Volden TA, Butler JM, et al. Age-friendly care in the Veterans Health Administration: past, present, and future. J Am Geriatr Soc. 2023;71(1):18-25. doi:10.1111/jgs.18070
20. Burke RE, Brown RT, Kinosian B. Selecting implementation strategies to drive age-friendly health system adoption. J Am Geriatr Soc. 2022;70(1):313-318. doi:10.1111/jgs.17489
21. Centers for Disease Control and Prevention. STEADI- older adult fall prevention. July 26,2021. Updated July 26, 2021. Accessed February 6, 2023. https://www.cdc.gov/steadi/index.html
22. Exercise and physical activity. National Institute on Aging. Accessed February 6, 2023. https://www.nia.nih.gov/health/topics/exercise-and-physical-activity
23. Hastings SN, Sloane R, Morey MC, Pavon JM, Hoenig H. Assisted early mobility for hospitalized older veterans: preliminary data from the STRIDE program. J Am Geriatr Soc. 2014;62(11):2180-2184.
24. Ashcroft T, Middleton A, Driver JA, Ruopp M, Harris R, Bean JF. An innovative rehabilitation program for the Veterans Affairs post-acute skilled nursing setting: preliminary results. J Am Geriatr Soc. 2023;10.1111/jgs.18214. doi:10.1111/jgs.18214
25. AGS CoCare. Accessed February 6, 2023. https://www.americangeriatrics.org/programs/ags-cocarer
26. Jedele JM, Curyto K, Ludwin BM, Karel MJ. Addressing behavioral symptoms of dementia through STAR-VA implementation: do outcomes vary by behavior type? Am J Alzheimers Dis Other Demen. 2020;35:1533317520911577.
27. Phung E, Triantafylidis L, Zhang H, Yeh IM. New Media, Part 5: Online Deprescribing Tools. J Palliat Med. 2018;21(2):269-270.
28. Freytag J, Dindo L, Catic A, et al. Feasibility of clinicians aligning health care with patient priorities in geriatrics ambulatory care. J Am Geriatr Soc. 2020;68(9):2112-2116.
29. The Conversation Project. Accessed February 22, 2023. https://theconversationproject.org
30. Daubman BR, Bernacki R, Stoltenberg M, Wilson E, Jacobsen J. Best practices for teaching clinicians to use a serious illness conversation guide. Palliat Med Rep. 2020;1(1):135-142. Published 2020 Jul 28. doi:10.1089/pmr.2020.0066
31. Freytag J, Street RL Jr, Barnes DE, et al. Empowering older adults to discuss advance care planning during clinical visits: The PREPARE Randomized Trial. J Am Geriatr Soc. 2020;68(6):1210-1217. doi:10.1111/jgs.16405
Yoga linked with improved gait speed, lower extremity strength in older adults
“Up to 50% of adults aged 80 years or older are estimated to be frail, and the global prevalence is expected to rise given the aging of our population,” therefore more interventions are needed to help with frailty, corresponding author Julia Loewenthal, MD, said in an interview.
Yoga integrates across multiple body systems including the musculoskeletal system, nervous system, and others, said Dr. Loewenthal of Brigham and Women’s Hospital, Boston. Previous research has shown that yoga has a positive effect on cardiovascular risk factors, mood, and quality of life, but the effects of yoga on frailty have not been well studied.
“We wanted to evaluate whether [yoga] might help with frailty, since it touches on so many systems, as frailty does,” she noted.
In a systematic review published in Annals of Internal Medicine, the researchers identified 33 randomized, controlled trials of yoga-based interventions including 2,384 adults aged 65 years and older. The studies mainly involved Iyengar or chair-based yoga methods. The study population included community-dwelling seniors, nursing home residents, and individuals with chronic diseases.
The studies assessed the effect of a range of yoga practices on frailty markers including gait speed, handgrip strength, balance, lower extremity strength and endurance, and multicomponent measures of physical performance.
Overall, individuals who were randomized to engage in a yoga practice showed improved gait speed and lower extremity strength, compared with controls who were inactive or received an education intervention, with moderate-certainty evidence. The researchers also found low-certainty evidence in favor of yoga for improved balance and for a composite measure of physical function, and low-certainty evidence in favor of yoga for improved handgrip strength.
The findings were limited by several factors, mainly the heterogenous study designs, populations, and yoga styles, the researchers noted. Other limitations included the small sample sizes, variation in descriptions of the studies’ randomizations, and a lack of data on race and ethnicity of the participants.
Yoga’s role in healthy aging
“Overall, we were not surprised by the results since we have seen similar findings from other mind-body practices such as tai chi,” Dr. Loewenthal said in an interview. “We were surprised by the degree of improvement many of the participants had with gait speed.
“Yoga practices usually include a mix of poses in the standing, seated, and lying-down positions,” Dr. Loewenthal said. Some of the studies in the review also involved chair-based methods with few standing poses, and some involved gentle or slow-paced practices. “We know that many of the practices helped with leg strength, and perhaps they are also helping with coordination between the brain and body for walking.”
The findings suggest that clinicians can view yoga practice in general as part of a strategy to support healthy aging, Dr. Loewenthal said. “While our work looked at frailty markers and not overall frailty, I think it would be reasonable to offer yoga as a strategy along with already-established interventions such as resistance training and the Mediterranean diet, and if older adults are already practicing yoga, this could help them understand how the practice is impacting the aging process.”
There are many styles of yoga that overlap and are related to one another, so it is hard to make recommendations about a single type, said Dr. Loewenthal. Many of the studies in the review involved Iyengar yoga, named for yoga master B.K.S. Iyengar, which focuses on precise alignment and breath and seems to be conducive for older populations. Iyengar yoga also involves use of props such as blocks, bolsters, straps, and chairs, which makes it well suited for older individuals who may have a chronic condition or other limitations.
“Some styles of yoga are very physical and may reach energy expenditure and cardiovascular effects similar to aerobic exercise, but this is generally not the case for most styles of yoga,” she added.
As for additional research, “I think it is important that trials use a validated definition of frailty as an outcome; all of the trials in our study used markers of frailty but did not look at overall frailty,” said Dr. Loewenthal. In addition, it is important to understand how yoga affects people who have different levels of frailty, since previous research shows that those who are the most frail benefit most from physical activity interventions.
Yoga as an entry point for physical activity
With the increasing population of older adults in the United States and around the world, frailty is a major health concern because its association with significant declines in health and potential loss of independence, Amanda Paluch, PhD, said in an interview.
“Therefore, it is important to identify programs that can prevent frailty to support longevity and living independently for older adults. Yoga can be a feasible solution to promote movement and prevent frailty,” said Dr. Paluch, of the University of Massachusetts, Amherst, an assistant professor in the department of kinesiology and Institute for Applied Life Sciences.
“Other studies have demonstrated that light-intensity movement, as in yoga, may be particularly beneficial for older adults,” Dr. Paluch said. “Additionally, research has demonstrated that balance training activities are important to maintain physical function, prevent falls, and maintain their independence for older adults, so it makes sense that yoga was associated with lower likelihood of frailty.”
Although there may be additional benefits with higher intensity activity, “yoga could be a great place to start for older adults who are starting at low activity levels,” she said.
The takeaway for clinicians is to consider encouraging more physical activity for their patients to support healthy aging, including reducing the risk factors for frailty, said Dr. Paluch. “Particularly for older adults, physical activity may not need to be of high intensity for benefits. Activities such as yoga that focus on flexibility, balance, and movement at lower intensities can support healthy aging, and yoga may be a particularly good option for older adults who are least active.”
The study received no outside funding. The researchers and Dr. Paluch had no financial conflicts to disclose.
“Up to 50% of adults aged 80 years or older are estimated to be frail, and the global prevalence is expected to rise given the aging of our population,” therefore more interventions are needed to help with frailty, corresponding author Julia Loewenthal, MD, said in an interview.
Yoga integrates across multiple body systems including the musculoskeletal system, nervous system, and others, said Dr. Loewenthal of Brigham and Women’s Hospital, Boston. Previous research has shown that yoga has a positive effect on cardiovascular risk factors, mood, and quality of life, but the effects of yoga on frailty have not been well studied.
“We wanted to evaluate whether [yoga] might help with frailty, since it touches on so many systems, as frailty does,” she noted.
In a systematic review published in Annals of Internal Medicine, the researchers identified 33 randomized, controlled trials of yoga-based interventions including 2,384 adults aged 65 years and older. The studies mainly involved Iyengar or chair-based yoga methods. The study population included community-dwelling seniors, nursing home residents, and individuals with chronic diseases.
The studies assessed the effect of a range of yoga practices on frailty markers including gait speed, handgrip strength, balance, lower extremity strength and endurance, and multicomponent measures of physical performance.
Overall, individuals who were randomized to engage in a yoga practice showed improved gait speed and lower extremity strength, compared with controls who were inactive or received an education intervention, with moderate-certainty evidence. The researchers also found low-certainty evidence in favor of yoga for improved balance and for a composite measure of physical function, and low-certainty evidence in favor of yoga for improved handgrip strength.
The findings were limited by several factors, mainly the heterogenous study designs, populations, and yoga styles, the researchers noted. Other limitations included the small sample sizes, variation in descriptions of the studies’ randomizations, and a lack of data on race and ethnicity of the participants.
Yoga’s role in healthy aging
“Overall, we were not surprised by the results since we have seen similar findings from other mind-body practices such as tai chi,” Dr. Loewenthal said in an interview. “We were surprised by the degree of improvement many of the participants had with gait speed.
“Yoga practices usually include a mix of poses in the standing, seated, and lying-down positions,” Dr. Loewenthal said. Some of the studies in the review also involved chair-based methods with few standing poses, and some involved gentle or slow-paced practices. “We know that many of the practices helped with leg strength, and perhaps they are also helping with coordination between the brain and body for walking.”
The findings suggest that clinicians can view yoga practice in general as part of a strategy to support healthy aging, Dr. Loewenthal said. “While our work looked at frailty markers and not overall frailty, I think it would be reasonable to offer yoga as a strategy along with already-established interventions such as resistance training and the Mediterranean diet, and if older adults are already practicing yoga, this could help them understand how the practice is impacting the aging process.”
There are many styles of yoga that overlap and are related to one another, so it is hard to make recommendations about a single type, said Dr. Loewenthal. Many of the studies in the review involved Iyengar yoga, named for yoga master B.K.S. Iyengar, which focuses on precise alignment and breath and seems to be conducive for older populations. Iyengar yoga also involves use of props such as blocks, bolsters, straps, and chairs, which makes it well suited for older individuals who may have a chronic condition or other limitations.
“Some styles of yoga are very physical and may reach energy expenditure and cardiovascular effects similar to aerobic exercise, but this is generally not the case for most styles of yoga,” she added.
As for additional research, “I think it is important that trials use a validated definition of frailty as an outcome; all of the trials in our study used markers of frailty but did not look at overall frailty,” said Dr. Loewenthal. In addition, it is important to understand how yoga affects people who have different levels of frailty, since previous research shows that those who are the most frail benefit most from physical activity interventions.
Yoga as an entry point for physical activity
With the increasing population of older adults in the United States and around the world, frailty is a major health concern because its association with significant declines in health and potential loss of independence, Amanda Paluch, PhD, said in an interview.
“Therefore, it is important to identify programs that can prevent frailty to support longevity and living independently for older adults. Yoga can be a feasible solution to promote movement and prevent frailty,” said Dr. Paluch, of the University of Massachusetts, Amherst, an assistant professor in the department of kinesiology and Institute for Applied Life Sciences.
“Other studies have demonstrated that light-intensity movement, as in yoga, may be particularly beneficial for older adults,” Dr. Paluch said. “Additionally, research has demonstrated that balance training activities are important to maintain physical function, prevent falls, and maintain their independence for older adults, so it makes sense that yoga was associated with lower likelihood of frailty.”
Although there may be additional benefits with higher intensity activity, “yoga could be a great place to start for older adults who are starting at low activity levels,” she said.
The takeaway for clinicians is to consider encouraging more physical activity for their patients to support healthy aging, including reducing the risk factors for frailty, said Dr. Paluch. “Particularly for older adults, physical activity may not need to be of high intensity for benefits. Activities such as yoga that focus on flexibility, balance, and movement at lower intensities can support healthy aging, and yoga may be a particularly good option for older adults who are least active.”
The study received no outside funding. The researchers and Dr. Paluch had no financial conflicts to disclose.
“Up to 50% of adults aged 80 years or older are estimated to be frail, and the global prevalence is expected to rise given the aging of our population,” therefore more interventions are needed to help with frailty, corresponding author Julia Loewenthal, MD, said in an interview.
Yoga integrates across multiple body systems including the musculoskeletal system, nervous system, and others, said Dr. Loewenthal of Brigham and Women’s Hospital, Boston. Previous research has shown that yoga has a positive effect on cardiovascular risk factors, mood, and quality of life, but the effects of yoga on frailty have not been well studied.
“We wanted to evaluate whether [yoga] might help with frailty, since it touches on so many systems, as frailty does,” she noted.
In a systematic review published in Annals of Internal Medicine, the researchers identified 33 randomized, controlled trials of yoga-based interventions including 2,384 adults aged 65 years and older. The studies mainly involved Iyengar or chair-based yoga methods. The study population included community-dwelling seniors, nursing home residents, and individuals with chronic diseases.
The studies assessed the effect of a range of yoga practices on frailty markers including gait speed, handgrip strength, balance, lower extremity strength and endurance, and multicomponent measures of physical performance.
Overall, individuals who were randomized to engage in a yoga practice showed improved gait speed and lower extremity strength, compared with controls who were inactive or received an education intervention, with moderate-certainty evidence. The researchers also found low-certainty evidence in favor of yoga for improved balance and for a composite measure of physical function, and low-certainty evidence in favor of yoga for improved handgrip strength.
The findings were limited by several factors, mainly the heterogenous study designs, populations, and yoga styles, the researchers noted. Other limitations included the small sample sizes, variation in descriptions of the studies’ randomizations, and a lack of data on race and ethnicity of the participants.
Yoga’s role in healthy aging
“Overall, we were not surprised by the results since we have seen similar findings from other mind-body practices such as tai chi,” Dr. Loewenthal said in an interview. “We were surprised by the degree of improvement many of the participants had with gait speed.
“Yoga practices usually include a mix of poses in the standing, seated, and lying-down positions,” Dr. Loewenthal said. Some of the studies in the review also involved chair-based methods with few standing poses, and some involved gentle or slow-paced practices. “We know that many of the practices helped with leg strength, and perhaps they are also helping with coordination between the brain and body for walking.”
The findings suggest that clinicians can view yoga practice in general as part of a strategy to support healthy aging, Dr. Loewenthal said. “While our work looked at frailty markers and not overall frailty, I think it would be reasonable to offer yoga as a strategy along with already-established interventions such as resistance training and the Mediterranean diet, and if older adults are already practicing yoga, this could help them understand how the practice is impacting the aging process.”
There are many styles of yoga that overlap and are related to one another, so it is hard to make recommendations about a single type, said Dr. Loewenthal. Many of the studies in the review involved Iyengar yoga, named for yoga master B.K.S. Iyengar, which focuses on precise alignment and breath and seems to be conducive for older populations. Iyengar yoga also involves use of props such as blocks, bolsters, straps, and chairs, which makes it well suited for older individuals who may have a chronic condition or other limitations.
“Some styles of yoga are very physical and may reach energy expenditure and cardiovascular effects similar to aerobic exercise, but this is generally not the case for most styles of yoga,” she added.
As for additional research, “I think it is important that trials use a validated definition of frailty as an outcome; all of the trials in our study used markers of frailty but did not look at overall frailty,” said Dr. Loewenthal. In addition, it is important to understand how yoga affects people who have different levels of frailty, since previous research shows that those who are the most frail benefit most from physical activity interventions.
Yoga as an entry point for physical activity
With the increasing population of older adults in the United States and around the world, frailty is a major health concern because its association with significant declines in health and potential loss of independence, Amanda Paluch, PhD, said in an interview.
“Therefore, it is important to identify programs that can prevent frailty to support longevity and living independently for older adults. Yoga can be a feasible solution to promote movement and prevent frailty,” said Dr. Paluch, of the University of Massachusetts, Amherst, an assistant professor in the department of kinesiology and Institute for Applied Life Sciences.
“Other studies have demonstrated that light-intensity movement, as in yoga, may be particularly beneficial for older adults,” Dr. Paluch said. “Additionally, research has demonstrated that balance training activities are important to maintain physical function, prevent falls, and maintain their independence for older adults, so it makes sense that yoga was associated with lower likelihood of frailty.”
Although there may be additional benefits with higher intensity activity, “yoga could be a great place to start for older adults who are starting at low activity levels,” she said.
The takeaway for clinicians is to consider encouraging more physical activity for their patients to support healthy aging, including reducing the risk factors for frailty, said Dr. Paluch. “Particularly for older adults, physical activity may not need to be of high intensity for benefits. Activities such as yoga that focus on flexibility, balance, and movement at lower intensities can support healthy aging, and yoga may be a particularly good option for older adults who are least active.”
The study received no outside funding. The researchers and Dr. Paluch had no financial conflicts to disclose.
FROM ANNALS OF INTERNAL MEDICINE
Antipsychotic cuts Alzheimer’s-related agitation
results of a phase 3 study suggest.
“In this phase 3 trial of patients with agitation in Alzheimer’s dementia, treatment with brexpiprazole 2 or 3 mg/day resulted in statistically significantly greater improvements in agitation versus placebo on the primary and key secondary endpoints,” said study investigator George Grossberg, MD, professor and director of the division of geriatric psychiatry, department of psychiatry & behavioral neuroscience, Saint Louis University.
Dr. Grossberg presented the findings as part of the annual meeting of the American Association for Geriatric Psychiatry.
Agitation common, distressing
With two previous studies also showing efficacy of brexpiprazole in AD-related agitation, Dr. Grossberg speculated that brexpiprazole will become the first drug to be approved for agitation in AD.
Agitation is one of the most common AD symptoms and is arguably the most distressing for patients and caregivers alike, Dr. Grossberg noted.
The drug was approved by the Food and Drug Administration in 2015 as an adjunctive therapy to antidepressants for adults with major depressive disorder and for adults with schizophrenia.
To investigate the drug at effective doses for AD-related agitation, the researchers conducted a phase 3 multicenter trial that included 345 patients with AD who met criteria for agitation and aggression.
Study participants had a mean Mini-Mental State Examination (MMSE) score between 5 and 22 at screening and baseline and a mean Cohen-Mansfield Agitation Inventory (CMAI) total score of about 79. A score above 45 is considered clinically significant agitation. Use of AD medications were permitted.
Patients had a mean age of 74 years and were randomly assigned in a 2:1 ratio to receive treatment with brexpiprazole 2 mg (n = 75) or 3 mg (n = 153) per day, or placebo (n = 117).
The study’s primary endpoint was improvement as assessed by the CMAI. Over 12 weeks, participants in the brexpiprazole group experienced greater improvement in agitation, with a mean change of –22.6 with brexpiprazole vs. –17.3 with placebo (P = .0026).
Brexpiprazole was also associated with significantly greater improvement in the secondary outcome of change from baseline to week 12 in agitation severity, as assessed using the Clinical Global Impression-Severity of Illness (CGI-S) score (mean change, –1.20 with brexpiprazole vs. –0.93 with placebo; P = .0078).
Specifically, treatment with the drug resulted in improvements in three key subscales of agitation, including aggressive behavior, such as physically striking out (P < .01 vs. placebo); physically nonaggressive; and verbally agitated, such as screaming or cursing (both P < .05).
Treatment-emergent adverse events (TEAEs) associated with brexpiprazole vs. placebo included somnolence (3.5% vs. 0.9%), nasopharyngitis (3.1% vs. 1.7%), dizziness (2.7% vs. 1.7%), diarrhea (2.2% vs. 0.9%), urinary tract infection (2.2% vs. 0.9%), and asthenia (2.2% vs. 0.0%).
“Aside from headache, no other TEAEs had an incidence of more than 5% in the brexpiprazole (2 or 3 mg) group, or in either dose group,” Dr. Grossberg said. “Cognition also remained stable,” he added.
Boxed warnings
Adverse events commonly associated with brexpiprazole include weight change, extrapyramidal events, falls, cardiovascular events, and sedation. In the study, all occurred at an incidence of less than 2% in both study groups, he noted.
Compared with the antipsychotic aripiprazole, brexpiprazole is associated with lower weight gain and akathisia, or motor restlessness.
One death occurred in the brexpiprazole 3 mg group in a patient who had heart failure, pneumonia, and cachexia. At autopsy, it was found the patient had cerebral and coronary atherosclerosis. The death was considered to be unrelated to brexpiprazole, said Dr. Grossberg.
This finding is notable because a caveat is that brexpiprazole, like aripiprazole and other typical and atypical antipsychotics, carries an FDA boxed warning related to an increased risk for death in older patients when used for dementia-related psychosis.
Noting that a black box warning about mortality risk is not a minor issue, Dr. Grossberg added that the risks are relatively low, whereas the risks associated with agitation in dementia can be high.
“If it’s an emergency situation, you have to treat the patient because otherwise they may harm someone else, or harm the staff, or harm their loved ones or themselves, and in those cases, we want to treat the patient first, get them under control, and then we worry about the black box,” he said.
In addition, “the No. 1 reason for getting kicked out of a nursing home is agitation or severe behaviors in the context of a dementia or a major neurocognitive disorder that the facility cannot control,” Dr. Grossberg added.
In such cases, patients may wind up in an emergency department and may not be welcome back at the nursing home.
“There’s always a risk/benefit ratio, and I have that discussion with patients and their families, but I can tell you that I’ve never had a family ask me not to use a medication because of the black box warning, because they see how miserable and how out of control their loved one is and they’re miserable because they see the suffering and will ask that we do anything that we can to get this behavior under control,” Dr. Grossberg said.
Caution still warranted
Commenting on the study, Rajesh R. Tampi, MD, professor and chairman of the department of psychiatry and the Bhatia Family Endowed Chair in Psychiatry at Creighton University, Omaha, Neb., underscored that, owing to the concerns behind the FDA warnings, “nonpharmacologic management is the cornerstone of treating agitation in Alzheimer’s dementia.”
He noted that the lack of an FDA-approved drug for agitation with AD is the result of “the overall benefits of any of the drug classes or drugs trialed to treat agitation in Alzheimer’s dementia vs. their adverse effect profile,” he said.
Therefore, he continued, “any medication or medication class should be used with caution among these individuals who often have polymorbidity.”
Dr. Tampi agreed that “the use of each drug for agitation in AD should be on a case-by-case basis with a clear and documented risk/benefit discussion with the patient and their families.”
“These medications should only be used for refractory symptoms or emergency situations where the agitation is not managed adequately with nonpharmacologic techniques and with a clear and documented risk/benefit discussion with patients and their families,” Dr. Tampi said.
The study was supported by Otsuka Pharmaceutical Development & Commercialization and H. Lundbeck. Dr. Grossberg has received consulting fees from Acadia, Avanir, Biogen, BioXcel, Genentech, Karuna, Lundbeck, Otsuka, Roche, and Takeda. Dr. Tampi had no disclosures to report.
A version of this article first appeared on Medscape.com.
This article was updated 3/14/23.
results of a phase 3 study suggest.
“In this phase 3 trial of patients with agitation in Alzheimer’s dementia, treatment with brexpiprazole 2 or 3 mg/day resulted in statistically significantly greater improvements in agitation versus placebo on the primary and key secondary endpoints,” said study investigator George Grossberg, MD, professor and director of the division of geriatric psychiatry, department of psychiatry & behavioral neuroscience, Saint Louis University.
Dr. Grossberg presented the findings as part of the annual meeting of the American Association for Geriatric Psychiatry.
Agitation common, distressing
With two previous studies also showing efficacy of brexpiprazole in AD-related agitation, Dr. Grossberg speculated that brexpiprazole will become the first drug to be approved for agitation in AD.
Agitation is one of the most common AD symptoms and is arguably the most distressing for patients and caregivers alike, Dr. Grossberg noted.
The drug was approved by the Food and Drug Administration in 2015 as an adjunctive therapy to antidepressants for adults with major depressive disorder and for adults with schizophrenia.
To investigate the drug at effective doses for AD-related agitation, the researchers conducted a phase 3 multicenter trial that included 345 patients with AD who met criteria for agitation and aggression.
Study participants had a mean Mini-Mental State Examination (MMSE) score between 5 and 22 at screening and baseline and a mean Cohen-Mansfield Agitation Inventory (CMAI) total score of about 79. A score above 45 is considered clinically significant agitation. Use of AD medications were permitted.
Patients had a mean age of 74 years and were randomly assigned in a 2:1 ratio to receive treatment with brexpiprazole 2 mg (n = 75) or 3 mg (n = 153) per day, or placebo (n = 117).
The study’s primary endpoint was improvement as assessed by the CMAI. Over 12 weeks, participants in the brexpiprazole group experienced greater improvement in agitation, with a mean change of –22.6 with brexpiprazole vs. –17.3 with placebo (P = .0026).
Brexpiprazole was also associated with significantly greater improvement in the secondary outcome of change from baseline to week 12 in agitation severity, as assessed using the Clinical Global Impression-Severity of Illness (CGI-S) score (mean change, –1.20 with brexpiprazole vs. –0.93 with placebo; P = .0078).
Specifically, treatment with the drug resulted in improvements in three key subscales of agitation, including aggressive behavior, such as physically striking out (P < .01 vs. placebo); physically nonaggressive; and verbally agitated, such as screaming or cursing (both P < .05).
Treatment-emergent adverse events (TEAEs) associated with brexpiprazole vs. placebo included somnolence (3.5% vs. 0.9%), nasopharyngitis (3.1% vs. 1.7%), dizziness (2.7% vs. 1.7%), diarrhea (2.2% vs. 0.9%), urinary tract infection (2.2% vs. 0.9%), and asthenia (2.2% vs. 0.0%).
“Aside from headache, no other TEAEs had an incidence of more than 5% in the brexpiprazole (2 or 3 mg) group, or in either dose group,” Dr. Grossberg said. “Cognition also remained stable,” he added.
Boxed warnings
Adverse events commonly associated with brexpiprazole include weight change, extrapyramidal events, falls, cardiovascular events, and sedation. In the study, all occurred at an incidence of less than 2% in both study groups, he noted.
Compared with the antipsychotic aripiprazole, brexpiprazole is associated with lower weight gain and akathisia, or motor restlessness.
One death occurred in the brexpiprazole 3 mg group in a patient who had heart failure, pneumonia, and cachexia. At autopsy, it was found the patient had cerebral and coronary atherosclerosis. The death was considered to be unrelated to brexpiprazole, said Dr. Grossberg.
This finding is notable because a caveat is that brexpiprazole, like aripiprazole and other typical and atypical antipsychotics, carries an FDA boxed warning related to an increased risk for death in older patients when used for dementia-related psychosis.
Noting that a black box warning about mortality risk is not a minor issue, Dr. Grossberg added that the risks are relatively low, whereas the risks associated with agitation in dementia can be high.
“If it’s an emergency situation, you have to treat the patient because otherwise they may harm someone else, or harm the staff, or harm their loved ones or themselves, and in those cases, we want to treat the patient first, get them under control, and then we worry about the black box,” he said.
In addition, “the No. 1 reason for getting kicked out of a nursing home is agitation or severe behaviors in the context of a dementia or a major neurocognitive disorder that the facility cannot control,” Dr. Grossberg added.
In such cases, patients may wind up in an emergency department and may not be welcome back at the nursing home.
“There’s always a risk/benefit ratio, and I have that discussion with patients and their families, but I can tell you that I’ve never had a family ask me not to use a medication because of the black box warning, because they see how miserable and how out of control their loved one is and they’re miserable because they see the suffering and will ask that we do anything that we can to get this behavior under control,” Dr. Grossberg said.
Caution still warranted
Commenting on the study, Rajesh R. Tampi, MD, professor and chairman of the department of psychiatry and the Bhatia Family Endowed Chair in Psychiatry at Creighton University, Omaha, Neb., underscored that, owing to the concerns behind the FDA warnings, “nonpharmacologic management is the cornerstone of treating agitation in Alzheimer’s dementia.”
He noted that the lack of an FDA-approved drug for agitation with AD is the result of “the overall benefits of any of the drug classes or drugs trialed to treat agitation in Alzheimer’s dementia vs. their adverse effect profile,” he said.
Therefore, he continued, “any medication or medication class should be used with caution among these individuals who often have polymorbidity.”
Dr. Tampi agreed that “the use of each drug for agitation in AD should be on a case-by-case basis with a clear and documented risk/benefit discussion with the patient and their families.”
“These medications should only be used for refractory symptoms or emergency situations where the agitation is not managed adequately with nonpharmacologic techniques and with a clear and documented risk/benefit discussion with patients and their families,” Dr. Tampi said.
The study was supported by Otsuka Pharmaceutical Development & Commercialization and H. Lundbeck. Dr. Grossberg has received consulting fees from Acadia, Avanir, Biogen, BioXcel, Genentech, Karuna, Lundbeck, Otsuka, Roche, and Takeda. Dr. Tampi had no disclosures to report.
A version of this article first appeared on Medscape.com.
This article was updated 3/14/23.
results of a phase 3 study suggest.
“In this phase 3 trial of patients with agitation in Alzheimer’s dementia, treatment with brexpiprazole 2 or 3 mg/day resulted in statistically significantly greater improvements in agitation versus placebo on the primary and key secondary endpoints,” said study investigator George Grossberg, MD, professor and director of the division of geriatric psychiatry, department of psychiatry & behavioral neuroscience, Saint Louis University.
Dr. Grossberg presented the findings as part of the annual meeting of the American Association for Geriatric Psychiatry.
Agitation common, distressing
With two previous studies also showing efficacy of brexpiprazole in AD-related agitation, Dr. Grossberg speculated that brexpiprazole will become the first drug to be approved for agitation in AD.
Agitation is one of the most common AD symptoms and is arguably the most distressing for patients and caregivers alike, Dr. Grossberg noted.
The drug was approved by the Food and Drug Administration in 2015 as an adjunctive therapy to antidepressants for adults with major depressive disorder and for adults with schizophrenia.
To investigate the drug at effective doses for AD-related agitation, the researchers conducted a phase 3 multicenter trial that included 345 patients with AD who met criteria for agitation and aggression.
Study participants had a mean Mini-Mental State Examination (MMSE) score between 5 and 22 at screening and baseline and a mean Cohen-Mansfield Agitation Inventory (CMAI) total score of about 79. A score above 45 is considered clinically significant agitation. Use of AD medications were permitted.
Patients had a mean age of 74 years and were randomly assigned in a 2:1 ratio to receive treatment with brexpiprazole 2 mg (n = 75) or 3 mg (n = 153) per day, or placebo (n = 117).
The study’s primary endpoint was improvement as assessed by the CMAI. Over 12 weeks, participants in the brexpiprazole group experienced greater improvement in agitation, with a mean change of –22.6 with brexpiprazole vs. –17.3 with placebo (P = .0026).
Brexpiprazole was also associated with significantly greater improvement in the secondary outcome of change from baseline to week 12 in agitation severity, as assessed using the Clinical Global Impression-Severity of Illness (CGI-S) score (mean change, –1.20 with brexpiprazole vs. –0.93 with placebo; P = .0078).
Specifically, treatment with the drug resulted in improvements in three key subscales of agitation, including aggressive behavior, such as physically striking out (P < .01 vs. placebo); physically nonaggressive; and verbally agitated, such as screaming or cursing (both P < .05).
Treatment-emergent adverse events (TEAEs) associated with brexpiprazole vs. placebo included somnolence (3.5% vs. 0.9%), nasopharyngitis (3.1% vs. 1.7%), dizziness (2.7% vs. 1.7%), diarrhea (2.2% vs. 0.9%), urinary tract infection (2.2% vs. 0.9%), and asthenia (2.2% vs. 0.0%).
“Aside from headache, no other TEAEs had an incidence of more than 5% in the brexpiprazole (2 or 3 mg) group, or in either dose group,” Dr. Grossberg said. “Cognition also remained stable,” he added.
Boxed warnings
Adverse events commonly associated with brexpiprazole include weight change, extrapyramidal events, falls, cardiovascular events, and sedation. In the study, all occurred at an incidence of less than 2% in both study groups, he noted.
Compared with the antipsychotic aripiprazole, brexpiprazole is associated with lower weight gain and akathisia, or motor restlessness.
One death occurred in the brexpiprazole 3 mg group in a patient who had heart failure, pneumonia, and cachexia. At autopsy, it was found the patient had cerebral and coronary atherosclerosis. The death was considered to be unrelated to brexpiprazole, said Dr. Grossberg.
This finding is notable because a caveat is that brexpiprazole, like aripiprazole and other typical and atypical antipsychotics, carries an FDA boxed warning related to an increased risk for death in older patients when used for dementia-related psychosis.
Noting that a black box warning about mortality risk is not a minor issue, Dr. Grossberg added that the risks are relatively low, whereas the risks associated with agitation in dementia can be high.
“If it’s an emergency situation, you have to treat the patient because otherwise they may harm someone else, or harm the staff, or harm their loved ones or themselves, and in those cases, we want to treat the patient first, get them under control, and then we worry about the black box,” he said.
In addition, “the No. 1 reason for getting kicked out of a nursing home is agitation or severe behaviors in the context of a dementia or a major neurocognitive disorder that the facility cannot control,” Dr. Grossberg added.
In such cases, patients may wind up in an emergency department and may not be welcome back at the nursing home.
“There’s always a risk/benefit ratio, and I have that discussion with patients and their families, but I can tell you that I’ve never had a family ask me not to use a medication because of the black box warning, because they see how miserable and how out of control their loved one is and they’re miserable because they see the suffering and will ask that we do anything that we can to get this behavior under control,” Dr. Grossberg said.
Caution still warranted
Commenting on the study, Rajesh R. Tampi, MD, professor and chairman of the department of psychiatry and the Bhatia Family Endowed Chair in Psychiatry at Creighton University, Omaha, Neb., underscored that, owing to the concerns behind the FDA warnings, “nonpharmacologic management is the cornerstone of treating agitation in Alzheimer’s dementia.”
He noted that the lack of an FDA-approved drug for agitation with AD is the result of “the overall benefits of any of the drug classes or drugs trialed to treat agitation in Alzheimer’s dementia vs. their adverse effect profile,” he said.
Therefore, he continued, “any medication or medication class should be used with caution among these individuals who often have polymorbidity.”
Dr. Tampi agreed that “the use of each drug for agitation in AD should be on a case-by-case basis with a clear and documented risk/benefit discussion with the patient and their families.”
“These medications should only be used for refractory symptoms or emergency situations where the agitation is not managed adequately with nonpharmacologic techniques and with a clear and documented risk/benefit discussion with patients and their families,” Dr. Tampi said.
The study was supported by Otsuka Pharmaceutical Development & Commercialization and H. Lundbeck. Dr. Grossberg has received consulting fees from Acadia, Avanir, Biogen, BioXcel, Genentech, Karuna, Lundbeck, Otsuka, Roche, and Takeda. Dr. Tampi had no disclosures to report.
A version of this article first appeared on Medscape.com.
This article was updated 3/14/23.
AT AAGP 2023
Childhood nightmares a prelude to cognitive problems, Parkinson’s?
new research shows.
Compared with children who never had distressing dreams between ages 7 and 11 years, those who had persistent distressing dreams were 76% more likely to develop cognitive impairment and roughly seven times more likely to develop PD by age 50 years.
It’s been shown previously that sleep problems in adulthood, including distressing dreams, can precede the onset of neurodegenerative diseases such as Alzheimer’s disease (AD) or PD by several years, and in some cases decades, study investigator Abidemi Otaiku, BMBS, University of Birmingham (England), told this news organization.
However, no studies have investigated whether distressing dreams during childhood might also be associated with increased risk for cognitive decline or PD.
“As such, these findings provide evidence for the first time that certain sleep problems in childhood (having regular distressing dreams) could be an early indicator of increased dementia and PD risk,” Dr. Otaiku said.
He noted that the findings build on previous studies which showed that regular nightmares in childhood could be an early indicator for psychiatric problems in adolescence, such as borderline personality disorder, attention-deficit/hyperactivity disorder, and psychosis.
The study was published online February 26 in The Lancet journal eClinicalMedicine.
Statistically significant
The prospective, longitudinal analysis used data from the 1958 British Birth Cohort Study, a prospective birth cohort which included all people born in Britain during a single week in 1958.
At age 7 years (in 1965) and 11 years (in 1969), mothers were asked to report whether their child experienced “bad dreams or night terrors” in the past 3 months, and cognitive impairment and PD were determined at age 50 (2008).
Among a total of 6,991 children (51% girls), 78.2% never had distressing dreams, 17.9% had transient distressing dreams (either at ages 7 or 11 years), and 3.8% had persistent distressing dreams (at both ages 7 and 11 years).
By age 50, 262 participants had developed cognitive impairment, and five had been diagnosed with PD.
After adjusting for all covariates, having more regular distressing dreams during childhood was “linearly and statistically significantly” associated with higher risk of developing cognitive impairment or PD by age 50 years (P = .037). This was the case in both boys and girls.
Compared with children who never had bad dreams, peers who had persistent distressing dreams (at ages 7 and 11 years) had an 85% increased risk for cognitive impairment or PD by age 50 (adjusted odds ratio, 1.85; 95% confidence interval, 1.10-3.11; P = .019).
The associations remained when incident cognitive impairment and incident PD were analyzed separately.
Compared with children who never had distressing dreams, children who had persistent distressing dreams were 76% more likely to develop cognitive impairment by age 50 years (aOR, 1.76; 95% CI, 1.03-2.99; P = .037), and were about seven times more likely to be diagnosed with PD by age 50 years (aOR, 7.35; 95% CI, 1.03-52.73; P = .047).
The linear association was statistically significant for PD (P = .050) and had a trend toward statistical significance for cognitive impairment (P = .074).
Mechanism unclear
“Early-life nightmares might be causally associated with cognitive impairment and PD, noncausally associated with cognitive impairment and PD, or both. At this stage it remains unclear which of the three options is correct. Therefore, further research on mechanisms is needed,” Dr. Otaiku told this news organization.
“One plausible noncausal explanation is that there are shared genetic factors which predispose individuals to having frequent nightmares in childhood, and to developing neurodegenerative diseases such as AD or PD in adulthood,” he added.
It’s also plausible that having regular nightmares throughout childhood could be a causal risk factor for cognitive impairment and PD by causing chronic sleep disruption, he noted.
“Chronic sleep disruption due to nightmares might lead to impaired glymphatic clearance during sleep – and thus greater accumulation of pathological proteins in the brain, such as amyloid-beta and alpha-synuclein,” Dr. Otaiku said.
Disrupted sleep throughout childhood might also impair normal brain development, which could make children’s brains less resilient to neuropathologic damage, he said.
Clinical implications?
There are established treatments for childhood nightmares, including nonpharmacologic approaches.
“For children who have regular nightmares that lead to impaired daytime functioning, it may well be a good idea for them to see a sleep physician to discuss whether treatment may be needed,” Dr. Otaiku said.
But should doctors treat children with persistent nightmares for the purpose of preventing neurodegenerative diseases in adulthood or psychiatric problems in adolescence?
“It’s an interesting possibility. However, more research is needed to confirm these epidemiological associations and to determine whether or not nightmares are a causal risk factor for these conditions,” Dr. Otaiku concluded.
The study received no external funding. Dr. Otaiku reports no relevant disclosures.
A version of this article first appeared on Medscape.com.
new research shows.
Compared with children who never had distressing dreams between ages 7 and 11 years, those who had persistent distressing dreams were 76% more likely to develop cognitive impairment and roughly seven times more likely to develop PD by age 50 years.
It’s been shown previously that sleep problems in adulthood, including distressing dreams, can precede the onset of neurodegenerative diseases such as Alzheimer’s disease (AD) or PD by several years, and in some cases decades, study investigator Abidemi Otaiku, BMBS, University of Birmingham (England), told this news organization.
However, no studies have investigated whether distressing dreams during childhood might also be associated with increased risk for cognitive decline or PD.
“As such, these findings provide evidence for the first time that certain sleep problems in childhood (having regular distressing dreams) could be an early indicator of increased dementia and PD risk,” Dr. Otaiku said.
He noted that the findings build on previous studies which showed that regular nightmares in childhood could be an early indicator for psychiatric problems in adolescence, such as borderline personality disorder, attention-deficit/hyperactivity disorder, and psychosis.
The study was published online February 26 in The Lancet journal eClinicalMedicine.
Statistically significant
The prospective, longitudinal analysis used data from the 1958 British Birth Cohort Study, a prospective birth cohort which included all people born in Britain during a single week in 1958.
At age 7 years (in 1965) and 11 years (in 1969), mothers were asked to report whether their child experienced “bad dreams or night terrors” in the past 3 months, and cognitive impairment and PD were determined at age 50 (2008).
Among a total of 6,991 children (51% girls), 78.2% never had distressing dreams, 17.9% had transient distressing dreams (either at ages 7 or 11 years), and 3.8% had persistent distressing dreams (at both ages 7 and 11 years).
By age 50, 262 participants had developed cognitive impairment, and five had been diagnosed with PD.
After adjusting for all covariates, having more regular distressing dreams during childhood was “linearly and statistically significantly” associated with higher risk of developing cognitive impairment or PD by age 50 years (P = .037). This was the case in both boys and girls.
Compared with children who never had bad dreams, peers who had persistent distressing dreams (at ages 7 and 11 years) had an 85% increased risk for cognitive impairment or PD by age 50 (adjusted odds ratio, 1.85; 95% confidence interval, 1.10-3.11; P = .019).
The associations remained when incident cognitive impairment and incident PD were analyzed separately.
Compared with children who never had distressing dreams, children who had persistent distressing dreams were 76% more likely to develop cognitive impairment by age 50 years (aOR, 1.76; 95% CI, 1.03-2.99; P = .037), and were about seven times more likely to be diagnosed with PD by age 50 years (aOR, 7.35; 95% CI, 1.03-52.73; P = .047).
The linear association was statistically significant for PD (P = .050) and had a trend toward statistical significance for cognitive impairment (P = .074).
Mechanism unclear
“Early-life nightmares might be causally associated with cognitive impairment and PD, noncausally associated with cognitive impairment and PD, or both. At this stage it remains unclear which of the three options is correct. Therefore, further research on mechanisms is needed,” Dr. Otaiku told this news organization.
“One plausible noncausal explanation is that there are shared genetic factors which predispose individuals to having frequent nightmares in childhood, and to developing neurodegenerative diseases such as AD or PD in adulthood,” he added.
It’s also plausible that having regular nightmares throughout childhood could be a causal risk factor for cognitive impairment and PD by causing chronic sleep disruption, he noted.
“Chronic sleep disruption due to nightmares might lead to impaired glymphatic clearance during sleep – and thus greater accumulation of pathological proteins in the brain, such as amyloid-beta and alpha-synuclein,” Dr. Otaiku said.
Disrupted sleep throughout childhood might also impair normal brain development, which could make children’s brains less resilient to neuropathologic damage, he said.
Clinical implications?
There are established treatments for childhood nightmares, including nonpharmacologic approaches.
“For children who have regular nightmares that lead to impaired daytime functioning, it may well be a good idea for them to see a sleep physician to discuss whether treatment may be needed,” Dr. Otaiku said.
But should doctors treat children with persistent nightmares for the purpose of preventing neurodegenerative diseases in adulthood or psychiatric problems in adolescence?
“It’s an interesting possibility. However, more research is needed to confirm these epidemiological associations and to determine whether or not nightmares are a causal risk factor for these conditions,” Dr. Otaiku concluded.
The study received no external funding. Dr. Otaiku reports no relevant disclosures.
A version of this article first appeared on Medscape.com.
new research shows.
Compared with children who never had distressing dreams between ages 7 and 11 years, those who had persistent distressing dreams were 76% more likely to develop cognitive impairment and roughly seven times more likely to develop PD by age 50 years.
It’s been shown previously that sleep problems in adulthood, including distressing dreams, can precede the onset of neurodegenerative diseases such as Alzheimer’s disease (AD) or PD by several years, and in some cases decades, study investigator Abidemi Otaiku, BMBS, University of Birmingham (England), told this news organization.
However, no studies have investigated whether distressing dreams during childhood might also be associated with increased risk for cognitive decline or PD.
“As such, these findings provide evidence for the first time that certain sleep problems in childhood (having regular distressing dreams) could be an early indicator of increased dementia and PD risk,” Dr. Otaiku said.
He noted that the findings build on previous studies which showed that regular nightmares in childhood could be an early indicator for psychiatric problems in adolescence, such as borderline personality disorder, attention-deficit/hyperactivity disorder, and psychosis.
The study was published online February 26 in The Lancet journal eClinicalMedicine.
Statistically significant
The prospective, longitudinal analysis used data from the 1958 British Birth Cohort Study, a prospective birth cohort which included all people born in Britain during a single week in 1958.
At age 7 years (in 1965) and 11 years (in 1969), mothers were asked to report whether their child experienced “bad dreams or night terrors” in the past 3 months, and cognitive impairment and PD were determined at age 50 (2008).
Among a total of 6,991 children (51% girls), 78.2% never had distressing dreams, 17.9% had transient distressing dreams (either at ages 7 or 11 years), and 3.8% had persistent distressing dreams (at both ages 7 and 11 years).
By age 50, 262 participants had developed cognitive impairment, and five had been diagnosed with PD.
After adjusting for all covariates, having more regular distressing dreams during childhood was “linearly and statistically significantly” associated with higher risk of developing cognitive impairment or PD by age 50 years (P = .037). This was the case in both boys and girls.
Compared with children who never had bad dreams, peers who had persistent distressing dreams (at ages 7 and 11 years) had an 85% increased risk for cognitive impairment or PD by age 50 (adjusted odds ratio, 1.85; 95% confidence interval, 1.10-3.11; P = .019).
The associations remained when incident cognitive impairment and incident PD were analyzed separately.
Compared with children who never had distressing dreams, children who had persistent distressing dreams were 76% more likely to develop cognitive impairment by age 50 years (aOR, 1.76; 95% CI, 1.03-2.99; P = .037), and were about seven times more likely to be diagnosed with PD by age 50 years (aOR, 7.35; 95% CI, 1.03-52.73; P = .047).
The linear association was statistically significant for PD (P = .050) and had a trend toward statistical significance for cognitive impairment (P = .074).
Mechanism unclear
“Early-life nightmares might be causally associated with cognitive impairment and PD, noncausally associated with cognitive impairment and PD, or both. At this stage it remains unclear which of the three options is correct. Therefore, further research on mechanisms is needed,” Dr. Otaiku told this news organization.
“One plausible noncausal explanation is that there are shared genetic factors which predispose individuals to having frequent nightmares in childhood, and to developing neurodegenerative diseases such as AD or PD in adulthood,” he added.
It’s also plausible that having regular nightmares throughout childhood could be a causal risk factor for cognitive impairment and PD by causing chronic sleep disruption, he noted.
“Chronic sleep disruption due to nightmares might lead to impaired glymphatic clearance during sleep – and thus greater accumulation of pathological proteins in the brain, such as amyloid-beta and alpha-synuclein,” Dr. Otaiku said.
Disrupted sleep throughout childhood might also impair normal brain development, which could make children’s brains less resilient to neuropathologic damage, he said.
Clinical implications?
There are established treatments for childhood nightmares, including nonpharmacologic approaches.
“For children who have regular nightmares that lead to impaired daytime functioning, it may well be a good idea for them to see a sleep physician to discuss whether treatment may be needed,” Dr. Otaiku said.
But should doctors treat children with persistent nightmares for the purpose of preventing neurodegenerative diseases in adulthood or psychiatric problems in adolescence?
“It’s an interesting possibility. However, more research is needed to confirm these epidemiological associations and to determine whether or not nightmares are a causal risk factor for these conditions,” Dr. Otaiku concluded.
The study received no external funding. Dr. Otaiku reports no relevant disclosures.
A version of this article first appeared on Medscape.com.
FROM ECLINICALMEDICINE
Daily socialization may extend lifespan in elderly
Sometimes more is more.
Correlations between socializing and survival were detected regardless of baseline health status, suggesting that physicians should be recommending daily socialization for all elderly patients, lead author Ziqiong Wang, MD, of Sichuan University West China Hospital, Chengdu, China, and colleagues reported.
These findings align with an array of prior studies reporting physical and mental health benefits from socialization, and negative impacts from isolation, the investigators wrote in the Journal of Epidemiology & Community Health. Not all studies have yielded the same picture, however, and most research has been conducted in Western countries, leading to uncertainty about whether different outcomes would be seen in populations in other parts of the world. Furthermore, the authors added that few studies have explored the amount of socialization needed to derive a positive benefit.
To address this knowledge gap, the investigators analyzed survival data from 28,563 participants in the Chinese Longitudinal Healthy Longevity Survey with a median age of 89 years at baseline.
“[This analysis] is from a highly respected ongoing longitudinal study of aging in China, which includes a large number of subjects and employs very strong research design and statistical analytical methods, so it has credibility,” John W. Rowe, MD, Julius B. Richmond Professor of Health Policy and Aging at Columbia University, New York, said in a written comment.
The investigators stratified frequency of socialization into five tiers: never, not monthly but sometimes, not weekly but at least once per month, not daily but at least once per week, and almost every day.
Survival proportions were calculated using the Kaplan-Meier method after accounting for a range of individual characteristics, including age, sex, household income, smoking status, diabetes, self-rated health, and others. Comparative findings were described in terms of time ratios using multivariable parametric accelerated failure time (AFT) models.
“The AFT model estimates the time ratio (TR), which is interpreted as the expected time to events in one category relative to the reference group,” the investigators wrote. “Unlike the interpretation of proportional hazard model results where hazard ratios larger than 1 are equal to higher risk, a TR of greater than 1 is considered to have a longer time to events, compared with the reference group.”
From baseline to 5 years, each socialization tier was significantly associated with prolonged survival, suggesting a general benefit. Compared with no socialization, socializing sometimes but not monthly was associated with 42% longer survival, at least monthly socialization was associated with 48% longer survival, at least weekly was associated with 110% longer survival, and socializing almost every day was associated with 87% longer survival.
The outsized benefit of daily socialization became clear in a long-term survival analysis, which spanned 5 years through the end of follow-up. Compared with no socialization, daily socialization tripled survival (TR, 3.04; P < .001), compared with prolongations ranging from 5% to 64% for less socialization, with just one of these lower tiers achieving statistical significance (P = .046).
Of note, the benefit of daily socialization was detected regardless of a person’s health status at baseline.
“No matter if elderly participants had chronic diseases or not, [and] no matter if older people had good self-rated health or not, the survival benefits of frequently participating in social activity were the same,” said principal author Sen He, MD, of Sichuan University, in a written comment.
“Socializing almost every day seems to be the most beneficial for a long life,” Dr. Sen added, noting that more research is needed to determine if there is an optimal type of social activity.
Dr. Rowe pointed out two key findings from the study. The first was that it confirmed “prior studies that have identified a beneficial effect of social activity on life expectancy.
“We have known that engagement is essential for successful aging and that isolation is toxic. While this finding is not novel, it is nice to see this confirmation of what we thought we knew,” he wrote.
Secondly, the study has identified “a threshold effect”, which is that “the long-term benefit on life expectancy was only seen in the presence of fairly intense social interactions, essentially daily,” he said.
According to Preeti Malani, MD, professor of medicine and geriatrician at the University of Michigan, Ann Arbor, the findings are also helpful because they offer data from another part of the world, adding confidence in findings from Western countries.
“This [study] happens to focus on older adults in China, which is helpful since aging is not the same everywhere in the world,” Dr. Malani said. “While the numbers here may not be precise, it’s fair to say that socialization is good for your health – for everyone but especially for older adults.”
Considering the body of evidence now spanning a range of populations, Dr. Malani said physicians should be screening for, and recommending, socialization for all elderly patients, particularly because many aren’t getting enough of it.
“Work that my colleagues and I have done (with the National Poll on Healthy Aging) suggests that there is a portion of older adults that have very little to no social contact,” Dr. Malani said. “A physician may not know this unless they are asking routinely about socialization the way we might ask about diet and exercise. How much is enough? No one knows, but anything is better than nothing and likely more is better.”
She also suggested that personalization is key.
“Physical and emotional health may limit the ability to socialize, so not everyone can engage all the time,” Dr. Malani said. “Also, socialization can look different for different people. Technology allows for socialization even if an individual has trouble leaving their home. I especially worry about this issue for older adults that are also caregivers. Those individuals also need time for themselves” and on way to fulfill that need is by socializing with others.
The study was supported by Sichuan (China) Science and Technology Program, the National Key R&D Program of China, and the National Natural Science Foundation of China. The investigators, Dr. Rowe, and Dr. Malani disclosed no relevant conflicts of interest.
Sometimes more is more.
Correlations between socializing and survival were detected regardless of baseline health status, suggesting that physicians should be recommending daily socialization for all elderly patients, lead author Ziqiong Wang, MD, of Sichuan University West China Hospital, Chengdu, China, and colleagues reported.
These findings align with an array of prior studies reporting physical and mental health benefits from socialization, and negative impacts from isolation, the investigators wrote in the Journal of Epidemiology & Community Health. Not all studies have yielded the same picture, however, and most research has been conducted in Western countries, leading to uncertainty about whether different outcomes would be seen in populations in other parts of the world. Furthermore, the authors added that few studies have explored the amount of socialization needed to derive a positive benefit.
To address this knowledge gap, the investigators analyzed survival data from 28,563 participants in the Chinese Longitudinal Healthy Longevity Survey with a median age of 89 years at baseline.
“[This analysis] is from a highly respected ongoing longitudinal study of aging in China, which includes a large number of subjects and employs very strong research design and statistical analytical methods, so it has credibility,” John W. Rowe, MD, Julius B. Richmond Professor of Health Policy and Aging at Columbia University, New York, said in a written comment.
The investigators stratified frequency of socialization into five tiers: never, not monthly but sometimes, not weekly but at least once per month, not daily but at least once per week, and almost every day.
Survival proportions were calculated using the Kaplan-Meier method after accounting for a range of individual characteristics, including age, sex, household income, smoking status, diabetes, self-rated health, and others. Comparative findings were described in terms of time ratios using multivariable parametric accelerated failure time (AFT) models.
“The AFT model estimates the time ratio (TR), which is interpreted as the expected time to events in one category relative to the reference group,” the investigators wrote. “Unlike the interpretation of proportional hazard model results where hazard ratios larger than 1 are equal to higher risk, a TR of greater than 1 is considered to have a longer time to events, compared with the reference group.”
From baseline to 5 years, each socialization tier was significantly associated with prolonged survival, suggesting a general benefit. Compared with no socialization, socializing sometimes but not monthly was associated with 42% longer survival, at least monthly socialization was associated with 48% longer survival, at least weekly was associated with 110% longer survival, and socializing almost every day was associated with 87% longer survival.
The outsized benefit of daily socialization became clear in a long-term survival analysis, which spanned 5 years through the end of follow-up. Compared with no socialization, daily socialization tripled survival (TR, 3.04; P < .001), compared with prolongations ranging from 5% to 64% for less socialization, with just one of these lower tiers achieving statistical significance (P = .046).
Of note, the benefit of daily socialization was detected regardless of a person’s health status at baseline.
“No matter if elderly participants had chronic diseases or not, [and] no matter if older people had good self-rated health or not, the survival benefits of frequently participating in social activity were the same,” said principal author Sen He, MD, of Sichuan University, in a written comment.
“Socializing almost every day seems to be the most beneficial for a long life,” Dr. Sen added, noting that more research is needed to determine if there is an optimal type of social activity.
Dr. Rowe pointed out two key findings from the study. The first was that it confirmed “prior studies that have identified a beneficial effect of social activity on life expectancy.
“We have known that engagement is essential for successful aging and that isolation is toxic. While this finding is not novel, it is nice to see this confirmation of what we thought we knew,” he wrote.
Secondly, the study has identified “a threshold effect”, which is that “the long-term benefit on life expectancy was only seen in the presence of fairly intense social interactions, essentially daily,” he said.
According to Preeti Malani, MD, professor of medicine and geriatrician at the University of Michigan, Ann Arbor, the findings are also helpful because they offer data from another part of the world, adding confidence in findings from Western countries.
“This [study] happens to focus on older adults in China, which is helpful since aging is not the same everywhere in the world,” Dr. Malani said. “While the numbers here may not be precise, it’s fair to say that socialization is good for your health – for everyone but especially for older adults.”
Considering the body of evidence now spanning a range of populations, Dr. Malani said physicians should be screening for, and recommending, socialization for all elderly patients, particularly because many aren’t getting enough of it.
“Work that my colleagues and I have done (with the National Poll on Healthy Aging) suggests that there is a portion of older adults that have very little to no social contact,” Dr. Malani said. “A physician may not know this unless they are asking routinely about socialization the way we might ask about diet and exercise. How much is enough? No one knows, but anything is better than nothing and likely more is better.”
She also suggested that personalization is key.
“Physical and emotional health may limit the ability to socialize, so not everyone can engage all the time,” Dr. Malani said. “Also, socialization can look different for different people. Technology allows for socialization even if an individual has trouble leaving their home. I especially worry about this issue for older adults that are also caregivers. Those individuals also need time for themselves” and on way to fulfill that need is by socializing with others.
The study was supported by Sichuan (China) Science and Technology Program, the National Key R&D Program of China, and the National Natural Science Foundation of China. The investigators, Dr. Rowe, and Dr. Malani disclosed no relevant conflicts of interest.
Sometimes more is more.
Correlations between socializing and survival were detected regardless of baseline health status, suggesting that physicians should be recommending daily socialization for all elderly patients, lead author Ziqiong Wang, MD, of Sichuan University West China Hospital, Chengdu, China, and colleagues reported.
These findings align with an array of prior studies reporting physical and mental health benefits from socialization, and negative impacts from isolation, the investigators wrote in the Journal of Epidemiology & Community Health. Not all studies have yielded the same picture, however, and most research has been conducted in Western countries, leading to uncertainty about whether different outcomes would be seen in populations in other parts of the world. Furthermore, the authors added that few studies have explored the amount of socialization needed to derive a positive benefit.
To address this knowledge gap, the investigators analyzed survival data from 28,563 participants in the Chinese Longitudinal Healthy Longevity Survey with a median age of 89 years at baseline.
“[This analysis] is from a highly respected ongoing longitudinal study of aging in China, which includes a large number of subjects and employs very strong research design and statistical analytical methods, so it has credibility,” John W. Rowe, MD, Julius B. Richmond Professor of Health Policy and Aging at Columbia University, New York, said in a written comment.
The investigators stratified frequency of socialization into five tiers: never, not monthly but sometimes, not weekly but at least once per month, not daily but at least once per week, and almost every day.
Survival proportions were calculated using the Kaplan-Meier method after accounting for a range of individual characteristics, including age, sex, household income, smoking status, diabetes, self-rated health, and others. Comparative findings were described in terms of time ratios using multivariable parametric accelerated failure time (AFT) models.
“The AFT model estimates the time ratio (TR), which is interpreted as the expected time to events in one category relative to the reference group,” the investigators wrote. “Unlike the interpretation of proportional hazard model results where hazard ratios larger than 1 are equal to higher risk, a TR of greater than 1 is considered to have a longer time to events, compared with the reference group.”
From baseline to 5 years, each socialization tier was significantly associated with prolonged survival, suggesting a general benefit. Compared with no socialization, socializing sometimes but not monthly was associated with 42% longer survival, at least monthly socialization was associated with 48% longer survival, at least weekly was associated with 110% longer survival, and socializing almost every day was associated with 87% longer survival.
The outsized benefit of daily socialization became clear in a long-term survival analysis, which spanned 5 years through the end of follow-up. Compared with no socialization, daily socialization tripled survival (TR, 3.04; P < .001), compared with prolongations ranging from 5% to 64% for less socialization, with just one of these lower tiers achieving statistical significance (P = .046).
Of note, the benefit of daily socialization was detected regardless of a person’s health status at baseline.
“No matter if elderly participants had chronic diseases or not, [and] no matter if older people had good self-rated health or not, the survival benefits of frequently participating in social activity were the same,” said principal author Sen He, MD, of Sichuan University, in a written comment.
“Socializing almost every day seems to be the most beneficial for a long life,” Dr. Sen added, noting that more research is needed to determine if there is an optimal type of social activity.
Dr. Rowe pointed out two key findings from the study. The first was that it confirmed “prior studies that have identified a beneficial effect of social activity on life expectancy.
“We have known that engagement is essential for successful aging and that isolation is toxic. While this finding is not novel, it is nice to see this confirmation of what we thought we knew,” he wrote.
Secondly, the study has identified “a threshold effect”, which is that “the long-term benefit on life expectancy was only seen in the presence of fairly intense social interactions, essentially daily,” he said.
According to Preeti Malani, MD, professor of medicine and geriatrician at the University of Michigan, Ann Arbor, the findings are also helpful because they offer data from another part of the world, adding confidence in findings from Western countries.
“This [study] happens to focus on older adults in China, which is helpful since aging is not the same everywhere in the world,” Dr. Malani said. “While the numbers here may not be precise, it’s fair to say that socialization is good for your health – for everyone but especially for older adults.”
Considering the body of evidence now spanning a range of populations, Dr. Malani said physicians should be screening for, and recommending, socialization for all elderly patients, particularly because many aren’t getting enough of it.
“Work that my colleagues and I have done (with the National Poll on Healthy Aging) suggests that there is a portion of older adults that have very little to no social contact,” Dr. Malani said. “A physician may not know this unless they are asking routinely about socialization the way we might ask about diet and exercise. How much is enough? No one knows, but anything is better than nothing and likely more is better.”
She also suggested that personalization is key.
“Physical and emotional health may limit the ability to socialize, so not everyone can engage all the time,” Dr. Malani said. “Also, socialization can look different for different people. Technology allows for socialization even if an individual has trouble leaving their home. I especially worry about this issue for older adults that are also caregivers. Those individuals also need time for themselves” and on way to fulfill that need is by socializing with others.
The study was supported by Sichuan (China) Science and Technology Program, the National Key R&D Program of China, and the National Natural Science Foundation of China. The investigators, Dr. Rowe, and Dr. Malani disclosed no relevant conflicts of interest.
FROM THE JOURNAL OF EPIDEMIOLOGY & COMMUNITY HEALTH
Distinct suicidal thought patterns flag those at highest risk
Long-term assessment of suicide risk and ideation in older adults may help identify distinct ideation patterns and predict potential future suicidal behavior, new research suggests.
Investigators studied over 300 older adults, assessing suicidal ideation and behavior for up to 14 years at least once annually. They then identified four suicidal ideation profiles.
They found that In turn, fast-remitting ideators were at higher risk in comparison to low/nonideators with no attempts or suicide.
Chronic severe ideators also showed the most severe levels of dysfunction across personality, social characteristics, and impulsivity measures, while highly variable and fast-remitting ideators displayed more specific deficits.
“We identified longitudinal ideation profiles that convey differential risk of future suicidal behavior to help clinicians recognize high suicide risk patients for preventing suicide,” said lead author Hanga Galfalvy, PhD, associate professor, department of psychiatry, Columbia University Irving Medical Center, New York.
“Clinicians should repeatedly assess suicidal ideation and ask not only about current ideation but also about the worst ideation since the last visit [because] similar levels of ideation during a single assessment can belong to very different risk profiles,” said Dr. Galfalvy, also a professor of biostatistics and a coinvestigator in the Conte Center for Suicide Prevention at Columbia University.
The study was published online in the Journal of Clinical Psychiatry.
Vulnerable population
“Older adults in most countries, including the U.S., are at the highest risk of dying of suicide out of all age groups,” said Dr. Galfalvy. “A significant number of depressed older adults experience thoughts of killing themselves, but fortunately, only a few transition from suicidal thoughts to behavior.”
Senior author Katalin Szanto, MD, professor of psychiatry, University of Pittsburgh, said in an interview that currently established clinical and psychosocial suicide risk factors have “low predictive value and provide little insight into the high suicide rate in the elderly.”
These traditional risk factors “poorly distinguish between suicide ideators and suicide attempters and do not take into consideration the heterogeneity of suicidal behavior,” said Dr. Szanto, principal investigator at the University of Pittsburgh’s Longitudinal research Program in Late-Life Suicide, where the study was conducted.
“Suicidal ideation measured at one time point – current or lifetime – may not be enough to accurately predict suicide risk,” the investigators wrote.
The current study, a collaboration between investigators from the Longitudinal Research Program in Late-Life Suicide and the Conte Center for Suicide Prevention, investigates “profiles of suicidal thoughts and behavior in patients with late-life depression over a longer period of time,” Dr. Galfalvy said.
The researchers used latent profile analysis (LPA) in a cohort of adults with nonpsychotic unipolar depression (aged 50-93 years; n = 337; mean age, 65.12 years) to “identify distinct ideation profiles and their clinical correlates” and to “test the profiles’ association with the risk of suicidal behavior before and during follow-up.”
LPA is “a data-driven method of grouping individuals into subgroups, based on quantitative characteristics,” Dr. Galfalvy explained.
The LPA yielded four profiles of ideation.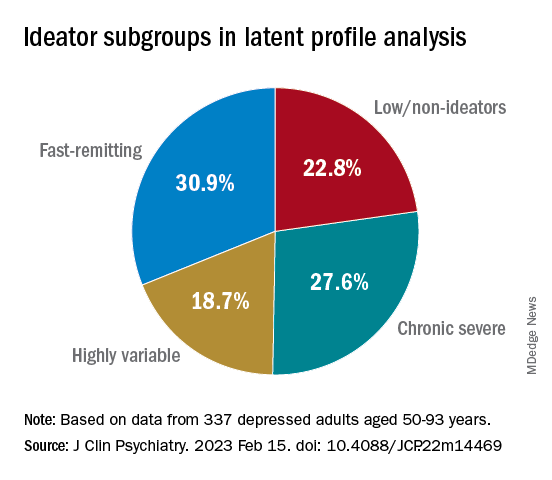
At baseline, the researchers assessed the presence or absence of suicidal behavior history and the number and lethality of attempts. They prospectively assessed suicidal ideation and attempts at least once annually thereafter over a period ranging from 3 months to 14 years (median, 3 years; IQR, 1.6-4 years).
At baseline and at follow-ups, they assessed ideation severity.
They also assessed depression severity, impulsivity, and personality measures, as well as perception of social support, social problem solving, cognitive performance, and physical comorbidities.
Personalized prevention
Of the original cohort, 92 patients died during the follow-up period, with 13 dying of suicide (or suspected suicide).
Over half (60%) of the chronic severe as well as the highly variable groups and almost half (48%) of the fast-remitting group had a history of past suicide attempt – all significantly higher than the low-nonideators (0%).
Despite comparable current ideation severity at baseline, the risk of suicide attempt/death was greater for chronic severe ideators versus fast-remitting ideators, but not greater than for highly variable ideators. On the other hand, highly variable ideators were at greater risk, compared with fast-remitting ideators.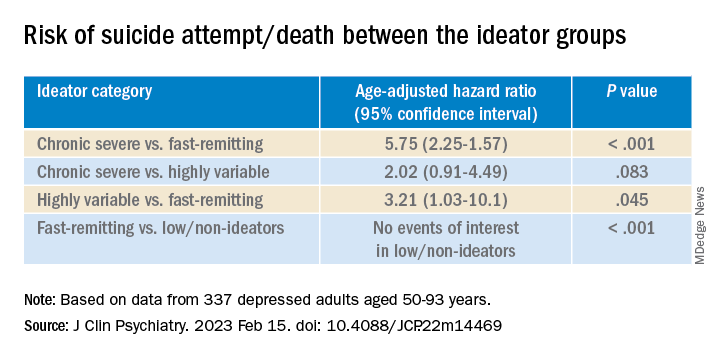
Cognitive factors “did not significantly discriminate between the ideation profiles, although ... lower global cognitive performance predicted suicidal behavior during follow-up,” the authors wrote.
This finding “aligns with prior studies indicating that late-life suicidal behavior but not ideation may be related to cognition ... and instead, ideation and cognition may act as independent risk factors for suicidal behavior,” they added.
“Patients in the fluctuating ideator group generally had moderate or high levels of worst suicidal ideation between visits, but not when asked about current ideation levels at the time of the follow-up assessment,” Dr. Galfalvy noted. “For them, the time frame of the question made a difference as to the level of ideation reported.”
The study “identified several clinical differences among these subgroups which could lead to more personalized suicide prevention efforts and further research into the heterogeneity of suicidal behavior,” she suggested.
New insight
Commenting on the study, Ari Cuperfain, MD, of the University of Toronto said the study “adds to the nuanced understanding of how changes in suicidal ideation over time can lead to suicidal actions and behavior.”
The study “sheds light on the notion of how older adults who die by suicide can demonstrate a greater degree of premeditated intent relative to younger cohorts, with chronic severe ideators portending the highest risk for suicide in this sample,” added Dr. Cuperfain, who was not involved with the current research.
“Overall, the paper highlights the importance of both screening for current levels of suicidal ideation in addition to the evolution of suicidal ideation in developing a risk assessment and in finding interventions to reduce this risk when it is most prominent,” he stated.
The research was supported by the National Institutes of Health. The authors and Dr. Cuperfain disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Long-term assessment of suicide risk and ideation in older adults may help identify distinct ideation patterns and predict potential future suicidal behavior, new research suggests.
Investigators studied over 300 older adults, assessing suicidal ideation and behavior for up to 14 years at least once annually. They then identified four suicidal ideation profiles.
They found that In turn, fast-remitting ideators were at higher risk in comparison to low/nonideators with no attempts or suicide.
Chronic severe ideators also showed the most severe levels of dysfunction across personality, social characteristics, and impulsivity measures, while highly variable and fast-remitting ideators displayed more specific deficits.
“We identified longitudinal ideation profiles that convey differential risk of future suicidal behavior to help clinicians recognize high suicide risk patients for preventing suicide,” said lead author Hanga Galfalvy, PhD, associate professor, department of psychiatry, Columbia University Irving Medical Center, New York.
“Clinicians should repeatedly assess suicidal ideation and ask not only about current ideation but also about the worst ideation since the last visit [because] similar levels of ideation during a single assessment can belong to very different risk profiles,” said Dr. Galfalvy, also a professor of biostatistics and a coinvestigator in the Conte Center for Suicide Prevention at Columbia University.
The study was published online in the Journal of Clinical Psychiatry.
Vulnerable population
“Older adults in most countries, including the U.S., are at the highest risk of dying of suicide out of all age groups,” said Dr. Galfalvy. “A significant number of depressed older adults experience thoughts of killing themselves, but fortunately, only a few transition from suicidal thoughts to behavior.”
Senior author Katalin Szanto, MD, professor of psychiatry, University of Pittsburgh, said in an interview that currently established clinical and psychosocial suicide risk factors have “low predictive value and provide little insight into the high suicide rate in the elderly.”
These traditional risk factors “poorly distinguish between suicide ideators and suicide attempters and do not take into consideration the heterogeneity of suicidal behavior,” said Dr. Szanto, principal investigator at the University of Pittsburgh’s Longitudinal research Program in Late-Life Suicide, where the study was conducted.
“Suicidal ideation measured at one time point – current or lifetime – may not be enough to accurately predict suicide risk,” the investigators wrote.
The current study, a collaboration between investigators from the Longitudinal Research Program in Late-Life Suicide and the Conte Center for Suicide Prevention, investigates “profiles of suicidal thoughts and behavior in patients with late-life depression over a longer period of time,” Dr. Galfalvy said.
The researchers used latent profile analysis (LPA) in a cohort of adults with nonpsychotic unipolar depression (aged 50-93 years; n = 337; mean age, 65.12 years) to “identify distinct ideation profiles and their clinical correlates” and to “test the profiles’ association with the risk of suicidal behavior before and during follow-up.”
LPA is “a data-driven method of grouping individuals into subgroups, based on quantitative characteristics,” Dr. Galfalvy explained.
The LPA yielded four profiles of ideation.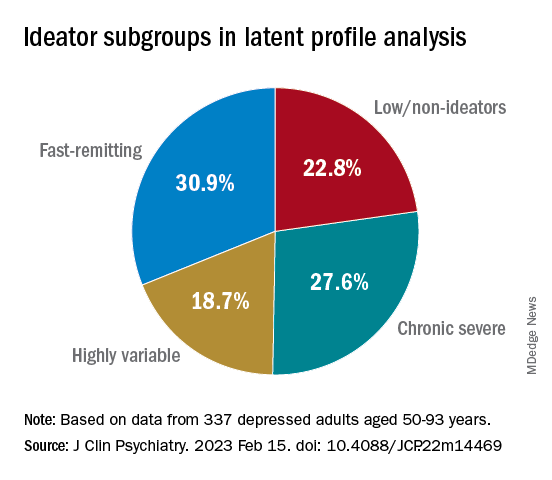
At baseline, the researchers assessed the presence or absence of suicidal behavior history and the number and lethality of attempts. They prospectively assessed suicidal ideation and attempts at least once annually thereafter over a period ranging from 3 months to 14 years (median, 3 years; IQR, 1.6-4 years).
At baseline and at follow-ups, they assessed ideation severity.
They also assessed depression severity, impulsivity, and personality measures, as well as perception of social support, social problem solving, cognitive performance, and physical comorbidities.
Personalized prevention
Of the original cohort, 92 patients died during the follow-up period, with 13 dying of suicide (or suspected suicide).
Over half (60%) of the chronic severe as well as the highly variable groups and almost half (48%) of the fast-remitting group had a history of past suicide attempt – all significantly higher than the low-nonideators (0%).
Despite comparable current ideation severity at baseline, the risk of suicide attempt/death was greater for chronic severe ideators versus fast-remitting ideators, but not greater than for highly variable ideators. On the other hand, highly variable ideators were at greater risk, compared with fast-remitting ideators.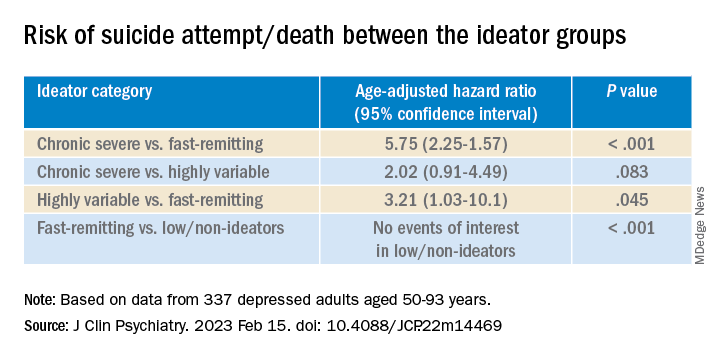
Cognitive factors “did not significantly discriminate between the ideation profiles, although ... lower global cognitive performance predicted suicidal behavior during follow-up,” the authors wrote.
This finding “aligns with prior studies indicating that late-life suicidal behavior but not ideation may be related to cognition ... and instead, ideation and cognition may act as independent risk factors for suicidal behavior,” they added.
“Patients in the fluctuating ideator group generally had moderate or high levels of worst suicidal ideation between visits, but not when asked about current ideation levels at the time of the follow-up assessment,” Dr. Galfalvy noted. “For them, the time frame of the question made a difference as to the level of ideation reported.”
The study “identified several clinical differences among these subgroups which could lead to more personalized suicide prevention efforts and further research into the heterogeneity of suicidal behavior,” she suggested.
New insight
Commenting on the study, Ari Cuperfain, MD, of the University of Toronto said the study “adds to the nuanced understanding of how changes in suicidal ideation over time can lead to suicidal actions and behavior.”
The study “sheds light on the notion of how older adults who die by suicide can demonstrate a greater degree of premeditated intent relative to younger cohorts, with chronic severe ideators portending the highest risk for suicide in this sample,” added Dr. Cuperfain, who was not involved with the current research.
“Overall, the paper highlights the importance of both screening for current levels of suicidal ideation in addition to the evolution of suicidal ideation in developing a risk assessment and in finding interventions to reduce this risk when it is most prominent,” he stated.
The research was supported by the National Institutes of Health. The authors and Dr. Cuperfain disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Long-term assessment of suicide risk and ideation in older adults may help identify distinct ideation patterns and predict potential future suicidal behavior, new research suggests.
Investigators studied over 300 older adults, assessing suicidal ideation and behavior for up to 14 years at least once annually. They then identified four suicidal ideation profiles.
They found that In turn, fast-remitting ideators were at higher risk in comparison to low/nonideators with no attempts or suicide.
Chronic severe ideators also showed the most severe levels of dysfunction across personality, social characteristics, and impulsivity measures, while highly variable and fast-remitting ideators displayed more specific deficits.
“We identified longitudinal ideation profiles that convey differential risk of future suicidal behavior to help clinicians recognize high suicide risk patients for preventing suicide,” said lead author Hanga Galfalvy, PhD, associate professor, department of psychiatry, Columbia University Irving Medical Center, New York.
“Clinicians should repeatedly assess suicidal ideation and ask not only about current ideation but also about the worst ideation since the last visit [because] similar levels of ideation during a single assessment can belong to very different risk profiles,” said Dr. Galfalvy, also a professor of biostatistics and a coinvestigator in the Conte Center for Suicide Prevention at Columbia University.
The study was published online in the Journal of Clinical Psychiatry.
Vulnerable population
“Older adults in most countries, including the U.S., are at the highest risk of dying of suicide out of all age groups,” said Dr. Galfalvy. “A significant number of depressed older adults experience thoughts of killing themselves, but fortunately, only a few transition from suicidal thoughts to behavior.”
Senior author Katalin Szanto, MD, professor of psychiatry, University of Pittsburgh, said in an interview that currently established clinical and psychosocial suicide risk factors have “low predictive value and provide little insight into the high suicide rate in the elderly.”
These traditional risk factors “poorly distinguish between suicide ideators and suicide attempters and do not take into consideration the heterogeneity of suicidal behavior,” said Dr. Szanto, principal investigator at the University of Pittsburgh’s Longitudinal research Program in Late-Life Suicide, where the study was conducted.
“Suicidal ideation measured at one time point – current or lifetime – may not be enough to accurately predict suicide risk,” the investigators wrote.
The current study, a collaboration between investigators from the Longitudinal Research Program in Late-Life Suicide and the Conte Center for Suicide Prevention, investigates “profiles of suicidal thoughts and behavior in patients with late-life depression over a longer period of time,” Dr. Galfalvy said.
The researchers used latent profile analysis (LPA) in a cohort of adults with nonpsychotic unipolar depression (aged 50-93 years; n = 337; mean age, 65.12 years) to “identify distinct ideation profiles and their clinical correlates” and to “test the profiles’ association with the risk of suicidal behavior before and during follow-up.”
LPA is “a data-driven method of grouping individuals into subgroups, based on quantitative characteristics,” Dr. Galfalvy explained.
The LPA yielded four profiles of ideation.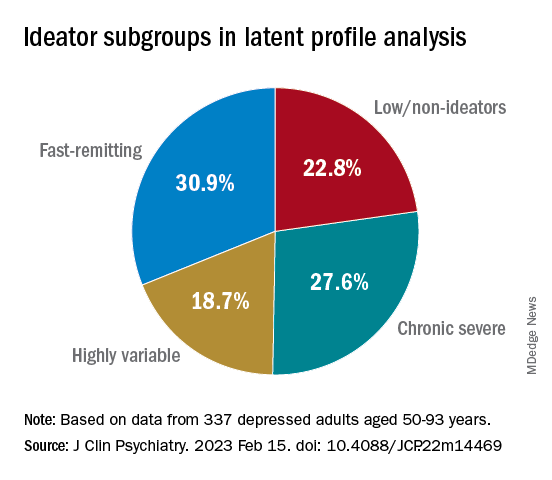
At baseline, the researchers assessed the presence or absence of suicidal behavior history and the number and lethality of attempts. They prospectively assessed suicidal ideation and attempts at least once annually thereafter over a period ranging from 3 months to 14 years (median, 3 years; IQR, 1.6-4 years).
At baseline and at follow-ups, they assessed ideation severity.
They also assessed depression severity, impulsivity, and personality measures, as well as perception of social support, social problem solving, cognitive performance, and physical comorbidities.
Personalized prevention
Of the original cohort, 92 patients died during the follow-up period, with 13 dying of suicide (or suspected suicide).
Over half (60%) of the chronic severe as well as the highly variable groups and almost half (48%) of the fast-remitting group had a history of past suicide attempt – all significantly higher than the low-nonideators (0%).
Despite comparable current ideation severity at baseline, the risk of suicide attempt/death was greater for chronic severe ideators versus fast-remitting ideators, but not greater than for highly variable ideators. On the other hand, highly variable ideators were at greater risk, compared with fast-remitting ideators.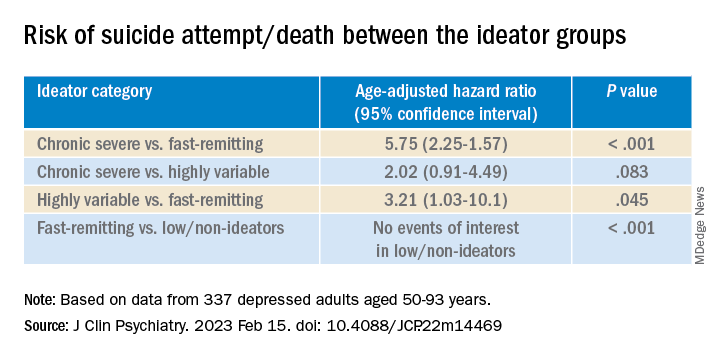
Cognitive factors “did not significantly discriminate between the ideation profiles, although ... lower global cognitive performance predicted suicidal behavior during follow-up,” the authors wrote.
This finding “aligns with prior studies indicating that late-life suicidal behavior but not ideation may be related to cognition ... and instead, ideation and cognition may act as independent risk factors for suicidal behavior,” they added.
“Patients in the fluctuating ideator group generally had moderate or high levels of worst suicidal ideation between visits, but not when asked about current ideation levels at the time of the follow-up assessment,” Dr. Galfalvy noted. “For them, the time frame of the question made a difference as to the level of ideation reported.”
The study “identified several clinical differences among these subgroups which could lead to more personalized suicide prevention efforts and further research into the heterogeneity of suicidal behavior,” she suggested.
New insight
Commenting on the study, Ari Cuperfain, MD, of the University of Toronto said the study “adds to the nuanced understanding of how changes in suicidal ideation over time can lead to suicidal actions and behavior.”
The study “sheds light on the notion of how older adults who die by suicide can demonstrate a greater degree of premeditated intent relative to younger cohorts, with chronic severe ideators portending the highest risk for suicide in this sample,” added Dr. Cuperfain, who was not involved with the current research.
“Overall, the paper highlights the importance of both screening for current levels of suicidal ideation in addition to the evolution of suicidal ideation in developing a risk assessment and in finding interventions to reduce this risk when it is most prominent,” he stated.
The research was supported by the National Institutes of Health. The authors and Dr. Cuperfain disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM THE JOURNAL OF CLINICAL PSYCHIATRY
Childhood trauma tied to increased Parkinson’s disease severity
new research shows.
Results of the first study to evaluate the relationship between childhood trauma and PD investigators found that the relationship appears to be dose dependent. Patients with PD who reported more than one ACE all experienced a statistically significant decrease in QOL, and for each additional ACE, there was significant worsening of motor symptoms.
This study supports a recent-call to-action paper in JAMA Neurology encouraging adoption of “trauma-informed neurology,” study investigator Indu Subramanian, MD, clinical professor, department of neurology, University of California, Los Angeles, said in an interview.
“We need to start asking about ACEs in everyone. It should be part of our medical intake,” said Dr. Subramanian, who is also the director of the Southwest Parkinson’s Disease Research, Education, and Clinical Center, West Los Angeles Veterans Affairs Medical Center.
The study was published online in Neurology: Clinical Practice.
Hard on the mind and body
A robust body of literature has clearly established a connection between ACEs, which include physical and emotional abuse, neglect, and household dysfunction, and negative physical health outcomes across the lifespan. These include stroke, dementia, diabetes, cancer, cardiovascular disease, autoimmune disorders, hypertension, and premature death as well as psychosocial health outcomes such as anxiety, depression, substance use, and suicide.
However, until now, the effects of childhood trauma have not been evaluated in a PD population.
As part of the MVP study, 712 adults with PD responded to an online survey asking about childhood trauma.
As anticipated, patients with the least reported childhood trauma reported the highest current QOL and lowest patient-reported motor and nonmotor symptom burden compared with peers with higher reported childhood trauma, the researchers reported.
PD symptom burden increased and QOL decreased as the number of ACEs increased.
Patients with ACE scores of 4 or higher reported greater PD symptom severity for 45% of the variables assessed, including apathy, muscle pain, daytime sleepiness, restless leg syndrome, depression, fatigue, comprehension, and anxiety (P < .05), compared with peers with trauma scores of 0.
Limitations of the study included the cross-sectional nature, which prevents making any causal determinations. Also, the ACE questionnaire, because it is self-reported and a retrospective collection of data, introduces the risk for recall bias. In addition, 65% of respondents were women, and racial and ethnic minority groups were not well represented.
Looking ahead, Dr. Subramanian and coauthors believe future research should “attempt to include more diverse populations, attempt improve the response rate of these sensitive questions and, most importantly, determine whether the adverse outcomes associated with childhood trauma can be mitigated with lifestyle modification, psychosocial support, and intervention in adulthood.”
“As a trauma-informed approach, something sorely lacking yet needed in the field of movement disorders, clinicians can proactively screen for ACEs while being mindful to avoid retraumatization,” they suggested. “They can begin to identify how ACEs may physiologically contribute to PD symptom and focus on targeting appropriate interventions that may improve outcomes.”
Life experiences matter
In a comment, Michael S. Okun, MD, medical advisor, Parkinson’s Foundation, and director of the Norman Fixel Institute for Neurological Diseases, University of Florida Health, Gainesville, said that “the idea that childhood trauma could be associated with a mild increase in severity of Parkinson’s symptoms such as apathy, pain, sleepiness and depression is fascinating.”
“We should however temper our enthusiasm for the results of this study because they were obtained through a direct patient survey, and not collected from large well characterized medical database,” Dr. Okun said.
He added” “If the data on childhood trauma and Parkinson’s can be replicated, we must ask why this could be?
“For Parkinson clinicians this as a reminder of how important obtaining a complete life history can be when strategizing on a plan to reduce motor and nonmotor Parkinson symptoms. Life experiences matter and can impact symptoms,” Dr. Okun said.
The MVP study was initiated with support of the National Center for Complementary and Integrative Health. The ongoing data collection has been supported by a donation from Sondra and Bill Fondren. Dr. Subramanian and Dr. Okun disclosed no potential conflicts of interest.
A version of this article first appeared on Medscape.com.
new research shows.
Results of the first study to evaluate the relationship between childhood trauma and PD investigators found that the relationship appears to be dose dependent. Patients with PD who reported more than one ACE all experienced a statistically significant decrease in QOL, and for each additional ACE, there was significant worsening of motor symptoms.
This study supports a recent-call to-action paper in JAMA Neurology encouraging adoption of “trauma-informed neurology,” study investigator Indu Subramanian, MD, clinical professor, department of neurology, University of California, Los Angeles, said in an interview.
“We need to start asking about ACEs in everyone. It should be part of our medical intake,” said Dr. Subramanian, who is also the director of the Southwest Parkinson’s Disease Research, Education, and Clinical Center, West Los Angeles Veterans Affairs Medical Center.
The study was published online in Neurology: Clinical Practice.
Hard on the mind and body
A robust body of literature has clearly established a connection between ACEs, which include physical and emotional abuse, neglect, and household dysfunction, and negative physical health outcomes across the lifespan. These include stroke, dementia, diabetes, cancer, cardiovascular disease, autoimmune disorders, hypertension, and premature death as well as psychosocial health outcomes such as anxiety, depression, substance use, and suicide.
However, until now, the effects of childhood trauma have not been evaluated in a PD population.
As part of the MVP study, 712 adults with PD responded to an online survey asking about childhood trauma.
As anticipated, patients with the least reported childhood trauma reported the highest current QOL and lowest patient-reported motor and nonmotor symptom burden compared with peers with higher reported childhood trauma, the researchers reported.
PD symptom burden increased and QOL decreased as the number of ACEs increased.
Patients with ACE scores of 4 or higher reported greater PD symptom severity for 45% of the variables assessed, including apathy, muscle pain, daytime sleepiness, restless leg syndrome, depression, fatigue, comprehension, and anxiety (P < .05), compared with peers with trauma scores of 0.
Limitations of the study included the cross-sectional nature, which prevents making any causal determinations. Also, the ACE questionnaire, because it is self-reported and a retrospective collection of data, introduces the risk for recall bias. In addition, 65% of respondents were women, and racial and ethnic minority groups were not well represented.
Looking ahead, Dr. Subramanian and coauthors believe future research should “attempt to include more diverse populations, attempt improve the response rate of these sensitive questions and, most importantly, determine whether the adverse outcomes associated with childhood trauma can be mitigated with lifestyle modification, psychosocial support, and intervention in adulthood.”
“As a trauma-informed approach, something sorely lacking yet needed in the field of movement disorders, clinicians can proactively screen for ACEs while being mindful to avoid retraumatization,” they suggested. “They can begin to identify how ACEs may physiologically contribute to PD symptom and focus on targeting appropriate interventions that may improve outcomes.”
Life experiences matter
In a comment, Michael S. Okun, MD, medical advisor, Parkinson’s Foundation, and director of the Norman Fixel Institute for Neurological Diseases, University of Florida Health, Gainesville, said that “the idea that childhood trauma could be associated with a mild increase in severity of Parkinson’s symptoms such as apathy, pain, sleepiness and depression is fascinating.”
“We should however temper our enthusiasm for the results of this study because they were obtained through a direct patient survey, and not collected from large well characterized medical database,” Dr. Okun said.
He added” “If the data on childhood trauma and Parkinson’s can be replicated, we must ask why this could be?
“For Parkinson clinicians this as a reminder of how important obtaining a complete life history can be when strategizing on a plan to reduce motor and nonmotor Parkinson symptoms. Life experiences matter and can impact symptoms,” Dr. Okun said.
The MVP study was initiated with support of the National Center for Complementary and Integrative Health. The ongoing data collection has been supported by a donation from Sondra and Bill Fondren. Dr. Subramanian and Dr. Okun disclosed no potential conflicts of interest.
A version of this article first appeared on Medscape.com.
new research shows.
Results of the first study to evaluate the relationship between childhood trauma and PD investigators found that the relationship appears to be dose dependent. Patients with PD who reported more than one ACE all experienced a statistically significant decrease in QOL, and for each additional ACE, there was significant worsening of motor symptoms.
This study supports a recent-call to-action paper in JAMA Neurology encouraging adoption of “trauma-informed neurology,” study investigator Indu Subramanian, MD, clinical professor, department of neurology, University of California, Los Angeles, said in an interview.
“We need to start asking about ACEs in everyone. It should be part of our medical intake,” said Dr. Subramanian, who is also the director of the Southwest Parkinson’s Disease Research, Education, and Clinical Center, West Los Angeles Veterans Affairs Medical Center.
The study was published online in Neurology: Clinical Practice.
Hard on the mind and body
A robust body of literature has clearly established a connection between ACEs, which include physical and emotional abuse, neglect, and household dysfunction, and negative physical health outcomes across the lifespan. These include stroke, dementia, diabetes, cancer, cardiovascular disease, autoimmune disorders, hypertension, and premature death as well as psychosocial health outcomes such as anxiety, depression, substance use, and suicide.
However, until now, the effects of childhood trauma have not been evaluated in a PD population.
As part of the MVP study, 712 adults with PD responded to an online survey asking about childhood trauma.
As anticipated, patients with the least reported childhood trauma reported the highest current QOL and lowest patient-reported motor and nonmotor symptom burden compared with peers with higher reported childhood trauma, the researchers reported.
PD symptom burden increased and QOL decreased as the number of ACEs increased.
Patients with ACE scores of 4 or higher reported greater PD symptom severity for 45% of the variables assessed, including apathy, muscle pain, daytime sleepiness, restless leg syndrome, depression, fatigue, comprehension, and anxiety (P < .05), compared with peers with trauma scores of 0.
Limitations of the study included the cross-sectional nature, which prevents making any causal determinations. Also, the ACE questionnaire, because it is self-reported and a retrospective collection of data, introduces the risk for recall bias. In addition, 65% of respondents were women, and racial and ethnic minority groups were not well represented.
Looking ahead, Dr. Subramanian and coauthors believe future research should “attempt to include more diverse populations, attempt improve the response rate of these sensitive questions and, most importantly, determine whether the adverse outcomes associated with childhood trauma can be mitigated with lifestyle modification, psychosocial support, and intervention in adulthood.”
“As a trauma-informed approach, something sorely lacking yet needed in the field of movement disorders, clinicians can proactively screen for ACEs while being mindful to avoid retraumatization,” they suggested. “They can begin to identify how ACEs may physiologically contribute to PD symptom and focus on targeting appropriate interventions that may improve outcomes.”
Life experiences matter
In a comment, Michael S. Okun, MD, medical advisor, Parkinson’s Foundation, and director of the Norman Fixel Institute for Neurological Diseases, University of Florida Health, Gainesville, said that “the idea that childhood trauma could be associated with a mild increase in severity of Parkinson’s symptoms such as apathy, pain, sleepiness and depression is fascinating.”
“We should however temper our enthusiasm for the results of this study because they were obtained through a direct patient survey, and not collected from large well characterized medical database,” Dr. Okun said.
He added” “If the data on childhood trauma and Parkinson’s can be replicated, we must ask why this could be?
“For Parkinson clinicians this as a reminder of how important obtaining a complete life history can be when strategizing on a plan to reduce motor and nonmotor Parkinson symptoms. Life experiences matter and can impact symptoms,” Dr. Okun said.
The MVP study was initiated with support of the National Center for Complementary and Integrative Health. The ongoing data collection has been supported by a donation from Sondra and Bill Fondren. Dr. Subramanian and Dr. Okun disclosed no potential conflicts of interest.
A version of this article first appeared on Medscape.com.
FROM NEUROLOGY: CLINICAL PRACTICE
Any level of physical activity tied to better later-life memory
new research suggests.
A prospective study of 1,400 participants showed that those who exercised to any extent in adulthood had significantly better cognitive scores later in life, compared with their peers who were physically inactive.
Maintaining an exercise routine throughout adulthood showed the strongest link to subsequent mental acuity.
Although these associations lessened when investigators controlled for childhood cognitive ability, socioeconomic background, and education, they remained statistically significant.
“Our findings support recommendations for greater participation in physical activity across adulthood,” lead investigator Sarah-Naomi James, PhD, research fellow at the Medical Research Council Unit for Lifelong Health and Ageing at the University College London, told this news organization.
“We provide evidence to encourage inactive adults to be active even to a small extent … at any point during adulthood,” which can improve cognition and memory later in life, Dr. James said.
The findings were published online in the Journal of Neurology, Neurosurgery & Psychiatry.
Exercise timing
Previous studies have established a link between fitness training and cognitive benefit later in life, but the researchers wanted to explore whether the timing or type of exercise influenced cognitive outcomes in later life.
The investigators asked more than 1,400 participants in the 1946 British birth cohort how much they had exercised at ages 36, 43, 60, and 69 years.
The questions changed slightly for each assessment period, but in general, participants were asked whether in the past month they had exercised or participated in such activities as badminton, swimming, fitness exercises, yoga, dancing, football, mountain climbing, jogging, or brisk walks for 30 minutes or more; and if so, how many times they participated per month.
Prior research showed that when the participants were aged 60 years, the most commonly reported activities were walking (71%), swimming (33%), floor exercises (24%), and cycling (15%).
When they turned 69, researchers tested participants’ cognitive performance using the Addenbrooke’s Cognitive Examination–III, which measures attention and orientation, verbal fluency, memory, language, and visuospatial function. In this study sample, 53% were women, and all were White.
Physical activity levels were classified as inactive, moderately active (one to four times per month), and most active (five or more times per month). In addition, they were summed across all five assessments to create a total score ranging from 0 (inactive at all ages) to 5 (active at all ages).
Overall, 11% of participants were physically inactive at all five time points; 17% were active at one time point; 20% were active at two and three time points; 17% were active at four time points; and 15% were active at all five time points.
‘Cradle to grave’ study?
Results showed that being physically active at all study time points was significantly associated with higher cognitive performance, verbal memory, and processing speed when participants were aged 69 (P < .01).
Those who exercised to any extent in adulthood – even just once a month during one of the time periods, fared better cognitively in later life, compared with physically inactive participants. (P < .01).
Study limitations cited include a lack of diversity among participants and a disproportionately high attrition rate among those who were socially disadvantaged.
“Our findings show that being active during every decade from their 30s on was associated with better cognition at around 70. Indeed, those who were active for longer had the highest cognitive function,” Dr. James said.
“However, it is also never too late to start. People in our study who only started being active in their 50s or 60s still had higher cognitive scores at age 70, compared to people of the same age who had never been active,” she added.
Dr. James intends to continue following the study sample to determine whether physical activity is linked to preserved cognitive aging “and buffers the effects of cognitive deterioration in the presence of disease markers that cause dementia, ultimately delaying dementia onset.
“We hope the cohort we study will be the first ‘cradle to grave’ study in the world, where we have followed people for their entire lives,” she said.
Encouraging finding
In a comment, Joel Hughes, PhD, professor of psychology and director of clinical training at Kent (Ohio) State University, said the study contributes to the idea that “accumulation of physical activity over one’s lifetime fits the data better than a ‘sensitive period’ – which suggests that it’s never too late to start exercising.”
Dr. Hughes, who was not involved in the research, noted that “exercise can improve cerebral blood flow and hemodynamic function, as well as greater activation of relevant brain regions such as the frontal lobes.”
While observing that the effects of exercise on cognition are likely complex from a mechanistic point of view, the finding that “exercise preserves or improves cognition later in life is encouraging,” he said.
The study received funding from the UK Medical Research Council and Alzheimer’s Research UK. The investigators and Dr. Hughes report no relevant financial relationships.
A version of this article first appeared on Medscape.com.
new research suggests.
A prospective study of 1,400 participants showed that those who exercised to any extent in adulthood had significantly better cognitive scores later in life, compared with their peers who were physically inactive.
Maintaining an exercise routine throughout adulthood showed the strongest link to subsequent mental acuity.
Although these associations lessened when investigators controlled for childhood cognitive ability, socioeconomic background, and education, they remained statistically significant.
“Our findings support recommendations for greater participation in physical activity across adulthood,” lead investigator Sarah-Naomi James, PhD, research fellow at the Medical Research Council Unit for Lifelong Health and Ageing at the University College London, told this news organization.
“We provide evidence to encourage inactive adults to be active even to a small extent … at any point during adulthood,” which can improve cognition and memory later in life, Dr. James said.
The findings were published online in the Journal of Neurology, Neurosurgery & Psychiatry.
Exercise timing
Previous studies have established a link between fitness training and cognitive benefit later in life, but the researchers wanted to explore whether the timing or type of exercise influenced cognitive outcomes in later life.
The investigators asked more than 1,400 participants in the 1946 British birth cohort how much they had exercised at ages 36, 43, 60, and 69 years.
The questions changed slightly for each assessment period, but in general, participants were asked whether in the past month they had exercised or participated in such activities as badminton, swimming, fitness exercises, yoga, dancing, football, mountain climbing, jogging, or brisk walks for 30 minutes or more; and if so, how many times they participated per month.
Prior research showed that when the participants were aged 60 years, the most commonly reported activities were walking (71%), swimming (33%), floor exercises (24%), and cycling (15%).
When they turned 69, researchers tested participants’ cognitive performance using the Addenbrooke’s Cognitive Examination–III, which measures attention and orientation, verbal fluency, memory, language, and visuospatial function. In this study sample, 53% were women, and all were White.
Physical activity levels were classified as inactive, moderately active (one to four times per month), and most active (five or more times per month). In addition, they were summed across all five assessments to create a total score ranging from 0 (inactive at all ages) to 5 (active at all ages).
Overall, 11% of participants were physically inactive at all five time points; 17% were active at one time point; 20% were active at two and three time points; 17% were active at four time points; and 15% were active at all five time points.
‘Cradle to grave’ study?
Results showed that being physically active at all study time points was significantly associated with higher cognitive performance, verbal memory, and processing speed when participants were aged 69 (P < .01).
Those who exercised to any extent in adulthood – even just once a month during one of the time periods, fared better cognitively in later life, compared with physically inactive participants. (P < .01).
Study limitations cited include a lack of diversity among participants and a disproportionately high attrition rate among those who were socially disadvantaged.
“Our findings show that being active during every decade from their 30s on was associated with better cognition at around 70. Indeed, those who were active for longer had the highest cognitive function,” Dr. James said.
“However, it is also never too late to start. People in our study who only started being active in their 50s or 60s still had higher cognitive scores at age 70, compared to people of the same age who had never been active,” she added.
Dr. James intends to continue following the study sample to determine whether physical activity is linked to preserved cognitive aging “and buffers the effects of cognitive deterioration in the presence of disease markers that cause dementia, ultimately delaying dementia onset.
“We hope the cohort we study will be the first ‘cradle to grave’ study in the world, where we have followed people for their entire lives,” she said.
Encouraging finding
In a comment, Joel Hughes, PhD, professor of psychology and director of clinical training at Kent (Ohio) State University, said the study contributes to the idea that “accumulation of physical activity over one’s lifetime fits the data better than a ‘sensitive period’ – which suggests that it’s never too late to start exercising.”
Dr. Hughes, who was not involved in the research, noted that “exercise can improve cerebral blood flow and hemodynamic function, as well as greater activation of relevant brain regions such as the frontal lobes.”
While observing that the effects of exercise on cognition are likely complex from a mechanistic point of view, the finding that “exercise preserves or improves cognition later in life is encouraging,” he said.
The study received funding from the UK Medical Research Council and Alzheimer’s Research UK. The investigators and Dr. Hughes report no relevant financial relationships.
A version of this article first appeared on Medscape.com.
new research suggests.
A prospective study of 1,400 participants showed that those who exercised to any extent in adulthood had significantly better cognitive scores later in life, compared with their peers who were physically inactive.
Maintaining an exercise routine throughout adulthood showed the strongest link to subsequent mental acuity.
Although these associations lessened when investigators controlled for childhood cognitive ability, socioeconomic background, and education, they remained statistically significant.
“Our findings support recommendations for greater participation in physical activity across adulthood,” lead investigator Sarah-Naomi James, PhD, research fellow at the Medical Research Council Unit for Lifelong Health and Ageing at the University College London, told this news organization.
“We provide evidence to encourage inactive adults to be active even to a small extent … at any point during adulthood,” which can improve cognition and memory later in life, Dr. James said.
The findings were published online in the Journal of Neurology, Neurosurgery & Psychiatry.
Exercise timing
Previous studies have established a link between fitness training and cognitive benefit later in life, but the researchers wanted to explore whether the timing or type of exercise influenced cognitive outcomes in later life.
The investigators asked more than 1,400 participants in the 1946 British birth cohort how much they had exercised at ages 36, 43, 60, and 69 years.
The questions changed slightly for each assessment period, but in general, participants were asked whether in the past month they had exercised or participated in such activities as badminton, swimming, fitness exercises, yoga, dancing, football, mountain climbing, jogging, or brisk walks for 30 minutes or more; and if so, how many times they participated per month.
Prior research showed that when the participants were aged 60 years, the most commonly reported activities were walking (71%), swimming (33%), floor exercises (24%), and cycling (15%).
When they turned 69, researchers tested participants’ cognitive performance using the Addenbrooke’s Cognitive Examination–III, which measures attention and orientation, verbal fluency, memory, language, and visuospatial function. In this study sample, 53% were women, and all were White.
Physical activity levels were classified as inactive, moderately active (one to four times per month), and most active (five or more times per month). In addition, they were summed across all five assessments to create a total score ranging from 0 (inactive at all ages) to 5 (active at all ages).
Overall, 11% of participants were physically inactive at all five time points; 17% were active at one time point; 20% were active at two and three time points; 17% were active at four time points; and 15% were active at all five time points.
‘Cradle to grave’ study?
Results showed that being physically active at all study time points was significantly associated with higher cognitive performance, verbal memory, and processing speed when participants were aged 69 (P < .01).
Those who exercised to any extent in adulthood – even just once a month during one of the time periods, fared better cognitively in later life, compared with physically inactive participants. (P < .01).
Study limitations cited include a lack of diversity among participants and a disproportionately high attrition rate among those who were socially disadvantaged.
“Our findings show that being active during every decade from their 30s on was associated with better cognition at around 70. Indeed, those who were active for longer had the highest cognitive function,” Dr. James said.
“However, it is also never too late to start. People in our study who only started being active in their 50s or 60s still had higher cognitive scores at age 70, compared to people of the same age who had never been active,” she added.
Dr. James intends to continue following the study sample to determine whether physical activity is linked to preserved cognitive aging “and buffers the effects of cognitive deterioration in the presence of disease markers that cause dementia, ultimately delaying dementia onset.
“We hope the cohort we study will be the first ‘cradle to grave’ study in the world, where we have followed people for their entire lives,” she said.
Encouraging finding
In a comment, Joel Hughes, PhD, professor of psychology and director of clinical training at Kent (Ohio) State University, said the study contributes to the idea that “accumulation of physical activity over one’s lifetime fits the data better than a ‘sensitive period’ – which suggests that it’s never too late to start exercising.”
Dr. Hughes, who was not involved in the research, noted that “exercise can improve cerebral blood flow and hemodynamic function, as well as greater activation of relevant brain regions such as the frontal lobes.”
While observing that the effects of exercise on cognition are likely complex from a mechanistic point of view, the finding that “exercise preserves or improves cognition later in life is encouraging,” he said.
The study received funding from the UK Medical Research Council and Alzheimer’s Research UK. The investigators and Dr. Hughes report no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM THE JOURNAL OF NEUROLOGY, NEUROSURGERY & PSYCHIATRY