User login
Unleashing Our Immune Response to Quash Cancer
This article was originally published on February 10 in Eric Topol’s substack “Ground Truths.”
It’s astounding how devious cancer cells and tumor tissue can be. This week in Science we learned how certain lung cancer cells can function like “Catch Me If You Can” — changing their driver mutation and cell identity to escape targeted therapy. This histologic transformation, as seen in an experimental model, is just one of so many cancer tricks that we are learning about.
Recently, as shown by single-cell sequencing, cancer cells can steal the mitochondria from T cells, a double whammy that turbocharges cancer cells with the hijacked fuel supply and, at the same time, dismantles the immune response.
Last week, we saw how tumor cells can release a virus-like protein that unleashes a vicious autoimmune response.
And then there’s the finding that cancer cell spread predominantly is occurring while we sleep.
As I previously reviewed, the ability for cancer cells to hijack neurons and neural circuits is now well established, no less their ability to reprogram neurons to become adrenergic and stimulate tumor progression, and interfere with the immune response. Stay tuned on that for a new Ground Truths podcast with Prof Michelle Monje, a leader in cancer neuroscience, which will post soon.
Add advancing age’s immunosenescence as yet another challenge to the long and growing list of formidable ways that cancer cells, and the tumor microenvironment, evade our immune response.
An Ever-Expanding Armamentarium
Immune Checkpoint Inhibitors
The field of immunotherapies took off with the immune checkpoint inhibitors, first approved by the FDA in 2011, that take the brakes off of T cells, with the programmed death-1 (PD-1), PD-ligand1, and anti-CTLA-4 monoclonal antibodies.
But we’re clearly learning they are not enough to prevail over cancer with common recurrences, only short term success in most patients, with some notable exceptions. Adding other immune response strategies, such as a vaccine, or antibody-drug conjugates, or engineered T cells, are showing improved chances for success.
Therapeutic Cancer Vaccines
There are many therapeutic cancer vaccines in the works, as reviewed in depth here.
Here’s a list of ongoing clinical trials of cancer vaccines. You’ll note most of these are on top of a checkpoint inhibitor and use personalized neoantigens (cancer cell surface proteins) derived from sequencing (whole-exome or whole genome, RNA-sequencing and HLA-profiling) the patient’s tumor.
An example of positive findings is with the combination of an mRNA-nanoparticle vaccine with up to 34 personalized neoantigens and pembrolizumab (Keytruda) vs pembrolizumab alone in advanced melanoma after resection, with improved outcomes at 3-year follow-up, cutting death or relapse rate in half.
Antibody-Drug Conjugates (ADC)
There is considerable excitement about antibody-drug conjugates (ADC) whereby a linker is used to attach a chemotherapy agent to the checkpoint inhibitor antibody, specifically targeting the cancer cell and facilitating entry of the chemotherapy into the cell. Akin to these are bispecific antibodies (BiTEs, binding to a tumor antigen and T cell receptor simultaneously), both of these conjugates acting as “biologic” or “guided” missiles.
A very good example of the potency of an ADC was seen in a “HER2-low” breast cancer randomized trial. The absence or very low expression or amplification of the HER2 receptor is common in breast cancer and successful treatment has been elusive. A randomized trial of an ADC (trastuzumab deruxtecan) compared to physician’s choice therapy demonstrated a marked success for progression-free survival in HER2-low patients, which was characterized as “unheard-of success” by media coverage.
This strategy is being used to target some of the most difficult cancer driver mutations such as TP53 and KRAS.
Oncolytic Viruses
Modifying viruses to infect the tumor and make it more visible to the immune system, potentiating anti-tumor responses, known as oncolytic viruses, have been proposed as a way to rev up the immune response for a long time but without positive Phase 3 clinical trials.
After decades of failure, a recent trial in refractory bladder cancer showed marked success, along with others, summarized here, now providing very encouraging results. It looks like oncolytic viruses are on a comeback path.
Engineering T Cells (Chimeric Antigen Receptor [CAR-T])
As I recently reviewed, there are over 500 ongoing clinical trials to build on the success of the first CAR-T approval for leukemia 7 years ago. I won’t go through that all again here, but to reiterate most of the success to date has been in “liquid” blood (leukemia and lymphoma) cancer tumors. This week in Nature is the discovery of a T cell cancer mutation, a gene fusion CARD11-PIK3R3, from a T cell lymphoma that can potentially be used to augment CAR-T efficacy. It has pronounced and prolonged effects in the experimental model. Instead of 1 million cells needed for treatment, even 20,000 were enough to melt the tumor. This is a noteworthy discovery since CAR-T work to date has largely not exploited such naturally occurring mutations, while instead concentrating on those seen in the patient’s set of key tumor mutations.
As currently conceived, CAR-T, and what is being referred to more broadly as adoptive cell therapies, involves removing T cells from the patient’s body and engineering their activation, then reintroducing them back to the patient. This is laborious, technically difficult, and very expensive. Recently, the idea of achieving all of this via an injection of virus that specifically infects T cells and inserts the genes needed, was advanced by two biotech companies with preclinical results, one in non-human primates.
Gearing up to meet the challenge of solid tumor CAR-T intervention, there’s more work using CRISPR genome editing of T cell receptors. A.I. is increasingly being exploited to process the data from sequencing and identify optimal neoantigens.
Instead of just CAR-T, we’re seeing the emergence of CAR-macrophage and CAR-natural killer (NK) cells strategies, and rapidly expanding potential combinations of all the strategies I’ve mentioned. No less, there’s been maturation of on-off suicide switches programmed in, to limit cytokine release and promote safety of these interventions. Overall, major side effects of immunotherapies are not only cytokine release syndromes, but also include interstitial pneumonitis and neurotoxicity.
Summary
Given the multitude of ways cancer cells and tumor tissue can evade our immune response, durably successful treatment remains a daunting challenge. But the ingenuity of so many different approaches to unleash our immune response, and their combinations, provides considerable hope that we’ll increasingly meet the challenge in the years ahead. We have clearly learned that combining different immunotherapy strategies will be essential for many patients with the most resilient solid tumors.
Of concern, as noted by a recent editorial in The Lancet, entitled “Cancer Research Equity: Innovations For The Many, Not The Few,” is that these individualized, sophisticated strategies are not scalable; they will have limited reach and benefit. The movement towards “off the shelf” CAR-T and inexpensive, orally active checkpoint inhibitors may help mitigate this issue.
Notwithstanding this important concern, we’re seeing an array of diverse and potent immunotherapy strategies that are providing highly encouraging results, engendering more excitement than we’ve seen in this space for some time. These should propel substantial improvements in outcomes for patients in the years ahead. It can’t happen soon enough.
Thanks for reading this edition of Ground Truths. If you found it informative, please share it with your colleagues.
Dr. Topol has disclosed the following relevant financial relationships: Serve(d) as a director, officer, partner, employee, advisor, consultant, or trustee for Dexcom; Illumina; Molecular Stethoscope; Quest Diagnostics; Blue Cross Blue Shield Association. Received research grant from National Institutes of Health.
A version of this article appeared on Medscape.com.
This article was originally published on February 10 in Eric Topol’s substack “Ground Truths.”
It’s astounding how devious cancer cells and tumor tissue can be. This week in Science we learned how certain lung cancer cells can function like “Catch Me If You Can” — changing their driver mutation and cell identity to escape targeted therapy. This histologic transformation, as seen in an experimental model, is just one of so many cancer tricks that we are learning about.
Recently, as shown by single-cell sequencing, cancer cells can steal the mitochondria from T cells, a double whammy that turbocharges cancer cells with the hijacked fuel supply and, at the same time, dismantles the immune response.
Last week, we saw how tumor cells can release a virus-like protein that unleashes a vicious autoimmune response.
And then there’s the finding that cancer cell spread predominantly is occurring while we sleep.
As I previously reviewed, the ability for cancer cells to hijack neurons and neural circuits is now well established, no less their ability to reprogram neurons to become adrenergic and stimulate tumor progression, and interfere with the immune response. Stay tuned on that for a new Ground Truths podcast with Prof Michelle Monje, a leader in cancer neuroscience, which will post soon.
Add advancing age’s immunosenescence as yet another challenge to the long and growing list of formidable ways that cancer cells, and the tumor microenvironment, evade our immune response.
An Ever-Expanding Armamentarium
Immune Checkpoint Inhibitors
The field of immunotherapies took off with the immune checkpoint inhibitors, first approved by the FDA in 2011, that take the brakes off of T cells, with the programmed death-1 (PD-1), PD-ligand1, and anti-CTLA-4 monoclonal antibodies.
But we’re clearly learning they are not enough to prevail over cancer with common recurrences, only short term success in most patients, with some notable exceptions. Adding other immune response strategies, such as a vaccine, or antibody-drug conjugates, or engineered T cells, are showing improved chances for success.
Therapeutic Cancer Vaccines
There are many therapeutic cancer vaccines in the works, as reviewed in depth here.
Here’s a list of ongoing clinical trials of cancer vaccines. You’ll note most of these are on top of a checkpoint inhibitor and use personalized neoantigens (cancer cell surface proteins) derived from sequencing (whole-exome or whole genome, RNA-sequencing and HLA-profiling) the patient’s tumor.
An example of positive findings is with the combination of an mRNA-nanoparticle vaccine with up to 34 personalized neoantigens and pembrolizumab (Keytruda) vs pembrolizumab alone in advanced melanoma after resection, with improved outcomes at 3-year follow-up, cutting death or relapse rate in half.
Antibody-Drug Conjugates (ADC)
There is considerable excitement about antibody-drug conjugates (ADC) whereby a linker is used to attach a chemotherapy agent to the checkpoint inhibitor antibody, specifically targeting the cancer cell and facilitating entry of the chemotherapy into the cell. Akin to these are bispecific antibodies (BiTEs, binding to a tumor antigen and T cell receptor simultaneously), both of these conjugates acting as “biologic” or “guided” missiles.
A very good example of the potency of an ADC was seen in a “HER2-low” breast cancer randomized trial. The absence or very low expression or amplification of the HER2 receptor is common in breast cancer and successful treatment has been elusive. A randomized trial of an ADC (trastuzumab deruxtecan) compared to physician’s choice therapy demonstrated a marked success for progression-free survival in HER2-low patients, which was characterized as “unheard-of success” by media coverage.
This strategy is being used to target some of the most difficult cancer driver mutations such as TP53 and KRAS.
Oncolytic Viruses
Modifying viruses to infect the tumor and make it more visible to the immune system, potentiating anti-tumor responses, known as oncolytic viruses, have been proposed as a way to rev up the immune response for a long time but without positive Phase 3 clinical trials.
After decades of failure, a recent trial in refractory bladder cancer showed marked success, along with others, summarized here, now providing very encouraging results. It looks like oncolytic viruses are on a comeback path.
Engineering T Cells (Chimeric Antigen Receptor [CAR-T])
As I recently reviewed, there are over 500 ongoing clinical trials to build on the success of the first CAR-T approval for leukemia 7 years ago. I won’t go through that all again here, but to reiterate most of the success to date has been in “liquid” blood (leukemia and lymphoma) cancer tumors. This week in Nature is the discovery of a T cell cancer mutation, a gene fusion CARD11-PIK3R3, from a T cell lymphoma that can potentially be used to augment CAR-T efficacy. It has pronounced and prolonged effects in the experimental model. Instead of 1 million cells needed for treatment, even 20,000 were enough to melt the tumor. This is a noteworthy discovery since CAR-T work to date has largely not exploited such naturally occurring mutations, while instead concentrating on those seen in the patient’s set of key tumor mutations.
As currently conceived, CAR-T, and what is being referred to more broadly as adoptive cell therapies, involves removing T cells from the patient’s body and engineering their activation, then reintroducing them back to the patient. This is laborious, technically difficult, and very expensive. Recently, the idea of achieving all of this via an injection of virus that specifically infects T cells and inserts the genes needed, was advanced by two biotech companies with preclinical results, one in non-human primates.
Gearing up to meet the challenge of solid tumor CAR-T intervention, there’s more work using CRISPR genome editing of T cell receptors. A.I. is increasingly being exploited to process the data from sequencing and identify optimal neoantigens.
Instead of just CAR-T, we’re seeing the emergence of CAR-macrophage and CAR-natural killer (NK) cells strategies, and rapidly expanding potential combinations of all the strategies I’ve mentioned. No less, there’s been maturation of on-off suicide switches programmed in, to limit cytokine release and promote safety of these interventions. Overall, major side effects of immunotherapies are not only cytokine release syndromes, but also include interstitial pneumonitis and neurotoxicity.
Summary
Given the multitude of ways cancer cells and tumor tissue can evade our immune response, durably successful treatment remains a daunting challenge. But the ingenuity of so many different approaches to unleash our immune response, and their combinations, provides considerable hope that we’ll increasingly meet the challenge in the years ahead. We have clearly learned that combining different immunotherapy strategies will be essential for many patients with the most resilient solid tumors.
Of concern, as noted by a recent editorial in The Lancet, entitled “Cancer Research Equity: Innovations For The Many, Not The Few,” is that these individualized, sophisticated strategies are not scalable; they will have limited reach and benefit. The movement towards “off the shelf” CAR-T and inexpensive, orally active checkpoint inhibitors may help mitigate this issue.
Notwithstanding this important concern, we’re seeing an array of diverse and potent immunotherapy strategies that are providing highly encouraging results, engendering more excitement than we’ve seen in this space for some time. These should propel substantial improvements in outcomes for patients in the years ahead. It can’t happen soon enough.
Thanks for reading this edition of Ground Truths. If you found it informative, please share it with your colleagues.
Dr. Topol has disclosed the following relevant financial relationships: Serve(d) as a director, officer, partner, employee, advisor, consultant, or trustee for Dexcom; Illumina; Molecular Stethoscope; Quest Diagnostics; Blue Cross Blue Shield Association. Received research grant from National Institutes of Health.
A version of this article appeared on Medscape.com.
This article was originally published on February 10 in Eric Topol’s substack “Ground Truths.”
It’s astounding how devious cancer cells and tumor tissue can be. This week in Science we learned how certain lung cancer cells can function like “Catch Me If You Can” — changing their driver mutation and cell identity to escape targeted therapy. This histologic transformation, as seen in an experimental model, is just one of so many cancer tricks that we are learning about.
Recently, as shown by single-cell sequencing, cancer cells can steal the mitochondria from T cells, a double whammy that turbocharges cancer cells with the hijacked fuel supply and, at the same time, dismantles the immune response.
Last week, we saw how tumor cells can release a virus-like protein that unleashes a vicious autoimmune response.
And then there’s the finding that cancer cell spread predominantly is occurring while we sleep.
As I previously reviewed, the ability for cancer cells to hijack neurons and neural circuits is now well established, no less their ability to reprogram neurons to become adrenergic and stimulate tumor progression, and interfere with the immune response. Stay tuned on that for a new Ground Truths podcast with Prof Michelle Monje, a leader in cancer neuroscience, which will post soon.
Add advancing age’s immunosenescence as yet another challenge to the long and growing list of formidable ways that cancer cells, and the tumor microenvironment, evade our immune response.
An Ever-Expanding Armamentarium
Immune Checkpoint Inhibitors
The field of immunotherapies took off with the immune checkpoint inhibitors, first approved by the FDA in 2011, that take the brakes off of T cells, with the programmed death-1 (PD-1), PD-ligand1, and anti-CTLA-4 monoclonal antibodies.
But we’re clearly learning they are not enough to prevail over cancer with common recurrences, only short term success in most patients, with some notable exceptions. Adding other immune response strategies, such as a vaccine, or antibody-drug conjugates, or engineered T cells, are showing improved chances for success.
Therapeutic Cancer Vaccines
There are many therapeutic cancer vaccines in the works, as reviewed in depth here.
Here’s a list of ongoing clinical trials of cancer vaccines. You’ll note most of these are on top of a checkpoint inhibitor and use personalized neoantigens (cancer cell surface proteins) derived from sequencing (whole-exome or whole genome, RNA-sequencing and HLA-profiling) the patient’s tumor.
An example of positive findings is with the combination of an mRNA-nanoparticle vaccine with up to 34 personalized neoantigens and pembrolizumab (Keytruda) vs pembrolizumab alone in advanced melanoma after resection, with improved outcomes at 3-year follow-up, cutting death or relapse rate in half.
Antibody-Drug Conjugates (ADC)
There is considerable excitement about antibody-drug conjugates (ADC) whereby a linker is used to attach a chemotherapy agent to the checkpoint inhibitor antibody, specifically targeting the cancer cell and facilitating entry of the chemotherapy into the cell. Akin to these are bispecific antibodies (BiTEs, binding to a tumor antigen and T cell receptor simultaneously), both of these conjugates acting as “biologic” or “guided” missiles.
A very good example of the potency of an ADC was seen in a “HER2-low” breast cancer randomized trial. The absence or very low expression or amplification of the HER2 receptor is common in breast cancer and successful treatment has been elusive. A randomized trial of an ADC (trastuzumab deruxtecan) compared to physician’s choice therapy demonstrated a marked success for progression-free survival in HER2-low patients, which was characterized as “unheard-of success” by media coverage.
This strategy is being used to target some of the most difficult cancer driver mutations such as TP53 and KRAS.
Oncolytic Viruses
Modifying viruses to infect the tumor and make it more visible to the immune system, potentiating anti-tumor responses, known as oncolytic viruses, have been proposed as a way to rev up the immune response for a long time but without positive Phase 3 clinical trials.
After decades of failure, a recent trial in refractory bladder cancer showed marked success, along with others, summarized here, now providing very encouraging results. It looks like oncolytic viruses are on a comeback path.
Engineering T Cells (Chimeric Antigen Receptor [CAR-T])
As I recently reviewed, there are over 500 ongoing clinical trials to build on the success of the first CAR-T approval for leukemia 7 years ago. I won’t go through that all again here, but to reiterate most of the success to date has been in “liquid” blood (leukemia and lymphoma) cancer tumors. This week in Nature is the discovery of a T cell cancer mutation, a gene fusion CARD11-PIK3R3, from a T cell lymphoma that can potentially be used to augment CAR-T efficacy. It has pronounced and prolonged effects in the experimental model. Instead of 1 million cells needed for treatment, even 20,000 were enough to melt the tumor. This is a noteworthy discovery since CAR-T work to date has largely not exploited such naturally occurring mutations, while instead concentrating on those seen in the patient’s set of key tumor mutations.
As currently conceived, CAR-T, and what is being referred to more broadly as adoptive cell therapies, involves removing T cells from the patient’s body and engineering their activation, then reintroducing them back to the patient. This is laborious, technically difficult, and very expensive. Recently, the idea of achieving all of this via an injection of virus that specifically infects T cells and inserts the genes needed, was advanced by two biotech companies with preclinical results, one in non-human primates.
Gearing up to meet the challenge of solid tumor CAR-T intervention, there’s more work using CRISPR genome editing of T cell receptors. A.I. is increasingly being exploited to process the data from sequencing and identify optimal neoantigens.
Instead of just CAR-T, we’re seeing the emergence of CAR-macrophage and CAR-natural killer (NK) cells strategies, and rapidly expanding potential combinations of all the strategies I’ve mentioned. No less, there’s been maturation of on-off suicide switches programmed in, to limit cytokine release and promote safety of these interventions. Overall, major side effects of immunotherapies are not only cytokine release syndromes, but also include interstitial pneumonitis and neurotoxicity.
Summary
Given the multitude of ways cancer cells and tumor tissue can evade our immune response, durably successful treatment remains a daunting challenge. But the ingenuity of so many different approaches to unleash our immune response, and their combinations, provides considerable hope that we’ll increasingly meet the challenge in the years ahead. We have clearly learned that combining different immunotherapy strategies will be essential for many patients with the most resilient solid tumors.
Of concern, as noted by a recent editorial in The Lancet, entitled “Cancer Research Equity: Innovations For The Many, Not The Few,” is that these individualized, sophisticated strategies are not scalable; they will have limited reach and benefit. The movement towards “off the shelf” CAR-T and inexpensive, orally active checkpoint inhibitors may help mitigate this issue.
Notwithstanding this important concern, we’re seeing an array of diverse and potent immunotherapy strategies that are providing highly encouraging results, engendering more excitement than we’ve seen in this space for some time. These should propel substantial improvements in outcomes for patients in the years ahead. It can’t happen soon enough.
Thanks for reading this edition of Ground Truths. If you found it informative, please share it with your colleagues.
Dr. Topol has disclosed the following relevant financial relationships: Serve(d) as a director, officer, partner, employee, advisor, consultant, or trustee for Dexcom; Illumina; Molecular Stethoscope; Quest Diagnostics; Blue Cross Blue Shield Association. Received research grant from National Institutes of Health.
A version of this article appeared on Medscape.com.
How the microbiome influences the success of cancer therapy
HAMBURG, Germany — The human microbiome comprises 39 to 44 billion microbes. That is ten times more than the number of cells in our body. Hendrik Poeck, MD, managing senior physician of internal medicine at the University Hospital Regensburg, illustrated this point at the annual meeting of the German Society for Hematology and Medical Oncology. If the gut microbiome falls out of balance, then “intestinal dysbiosis potentially poses a risk for the pathogenesis of local and systemic diseases,” explained Dr. Poeck.
Cancers and their therapies can also be influenced in this way. said Dr. Poeck.
Microbial diversity could be beneficial for cancer therapy, too. The composition of the microbiome varies significantly from host to host and can mutate. These properties make it a target for precision microbiotics, which involves using the gut microbiome as a biomarker to predict various physical reactions and to develop individualized diets.
Microbiome and Pathogenesis
The body’s microbiome fulfills a barrier function, especially where the body is exposed to an external environment: at the epidermis and the internal mucous membranes, in the gastrointestinal tract, and in the lungs, chest, and urogenital system.
Association studies on humans and experimental manipulations on mouse models of cancer showed that certain microorganisms can have either protective or harmful effects on cancer development, on the progression of a malignant disease, and on the response to therapy.
A Master Regulator?
Disruptions of the microbial system in the gut, as occur during antibiotic therapy, can have significant effects on a patient’s response to immunotherapy. Taking antibiotics shortly before or after starting therapy with immune checkpoint inhibitors (ICIs) significantly affected both overall survival (OS) and progression-free survival (PFS), as reported in a recent review and meta-analysis, for example.
Proton pump inhibitors also affect the gut microbiome and reduce the response to immunotherapy; this effect was demonstrated by an analysis of data from more than 2700 cancer patients that was recently presented at the annual meeting of the European Society for Medical Oncology (ESMO).
The extent to which the gut microbiome influences the efficacy of an ICI or predicts said efficacy was examined in a retrospective analysis published in Science in 2018, which Dr. Poeck presented. Resistance to ICI correlated with the relative frequency of the bacteria Akkermansia muciniphila in the gut of patients with cancer. In mouse models, the researchers restored the efficacy of the PD-1 blockade through a stool transplant.
Predicting Immunotherapy Response
If A muciniphila is present, can the composition of the microbiome act as a predictor for an effective ICI therapy?
Laurence Zitvogel, MD, PhD, and her working group at the National Institute of Health and Medical Research in Villejuif, France, performed a prospective study in 338 patients with non–small cell lung cancer and examined the prognostic significance of the fecal bacteria A muciniphila (Akk). The “Akkerman status” (low Akk vs high Akk) in a patient’s stool correlated with an increased objective response rate and a longer OS, independently of PD-L1 expression, antibiotics, and performance status. The OS for low Akk was 13.4 months, vs 18.8 months for high Akk in first-line treatment.
These results are promising, said Dr. Poeck. But there is no one-size-fits-all solution. No conclusions can be drawn from one bacterium on the efficacy of therapies in humans, since “the entirety of the bacteria is decisive,” said Dr. Poeck. In addition to the gut microbiome, the composition of gut metabolites influences the response to immunotherapies, as shown in a study with ICI.
Therapeutic Interventions
One possible therapeutic intervention to restore the gut microbiome is fecal microbiota transplantation (FMT). In a phase 1 study presented by Dr. Poeck, FMT was effective in the treatment of 20 patients with melanoma with ICI in an advanced and treatment-naive stage. Seven days after the patients received FMT, the first cycle with anti-PD-1 immunotherapy was initiated, with a total administration of three to four cycles. After 12 weeks, most patients were in complete or partial remission, as evidenced on imaging.
However, FMT also carries some risks. Two cases of sepsis with multiresistant Escherichia coli occurred, as well as other serious infections. Since then, there has been an FDA condition for extended screening of the donor stool, said Dr. Poeck. Nevertheless, this intervention is promising. A search of the keywords “FMT in cancer/transplant setting” reveals 46 currently clinical studies on clinicaltrials.gov.
Nutritional Interventions
Dr. Poeck advises caution about over-the-counter products. These products usually contain only a few species, such as Lactobacillus and Bifidobacterium. “Over-the-counter probiotics can even delay the reconstitution of the microbiome after antibiotics,” said Dr. Poeck, according to a study. In some studies, the response rates were significantly lower after probiotic intake or led to controversial results, according to Dr. Poeck.
In contrast, Dr. Poeck said prebiotics (that is, a fiber-rich diet with indigestible carbohydrates) were promising. During digestion, prebiotics are split into short-chain fatty acids by bacterial enzymes and promote the growth of certain microbiota.
In this way, just 20 g of extremely fiber-rich food had a significant effect on PFS in 128 patients with melanoma undergoing anti-PD-1 immunotherapy. With 20 g of fiber-rich food per day, the PFS was stable over 60 months. The most significant benefit was observed in patients with a sufficient fiber intake who were not taking probiotics.
What to Recommend?
In summary, Dr. Poeck said that it is important to “budget” well, particularly with antibiotic administration, and to strive for calculated therapy with as narrow a spectrum as possible. For patients who experience complications such as cytokine release syndrome as a reaction to cell therapy, delaying the use of antibiotics is important. However, it is often difficult to differentiate this syndrome from neutropenic fever. The aim should be to avoid high-risk antibiotics, if clinically justifiable. Patients should avoid taking antibiotics for 30 days before starting immunotherapy.
Regarding nutritional interventions, Dr. Poeck referred to the recent Onkopedia recommendation for nutrition after cancer and the 10 nutritional rules of the German Nutrition Society. According to Dr. Poeck, the important aspects of these recommendations are a fiber-rich diet (> 20 g/d) from various plant products and avoiding artificial sweeteners and flavorings, as well as ultraprocessed (convenience) foods. In addition, meat should be consumed only in moderation, and as little processed meat as possible should be consumed. In addition, regular (aerobic and anaerobic) physical activity is important.
“Looking ahead into the future,” said Dr. Poeck, “we need a uniform and functional understanding and we need a randomized prediction for diagnosis.”
This article was translated from the Medscape German edition.
A version of this article appeared on Medscape.com.
HAMBURG, Germany — The human microbiome comprises 39 to 44 billion microbes. That is ten times more than the number of cells in our body. Hendrik Poeck, MD, managing senior physician of internal medicine at the University Hospital Regensburg, illustrated this point at the annual meeting of the German Society for Hematology and Medical Oncology. If the gut microbiome falls out of balance, then “intestinal dysbiosis potentially poses a risk for the pathogenesis of local and systemic diseases,” explained Dr. Poeck.
Cancers and their therapies can also be influenced in this way. said Dr. Poeck.
Microbial diversity could be beneficial for cancer therapy, too. The composition of the microbiome varies significantly from host to host and can mutate. These properties make it a target for precision microbiotics, which involves using the gut microbiome as a biomarker to predict various physical reactions and to develop individualized diets.
Microbiome and Pathogenesis
The body’s microbiome fulfills a barrier function, especially where the body is exposed to an external environment: at the epidermis and the internal mucous membranes, in the gastrointestinal tract, and in the lungs, chest, and urogenital system.
Association studies on humans and experimental manipulations on mouse models of cancer showed that certain microorganisms can have either protective or harmful effects on cancer development, on the progression of a malignant disease, and on the response to therapy.
A Master Regulator?
Disruptions of the microbial system in the gut, as occur during antibiotic therapy, can have significant effects on a patient’s response to immunotherapy. Taking antibiotics shortly before or after starting therapy with immune checkpoint inhibitors (ICIs) significantly affected both overall survival (OS) and progression-free survival (PFS), as reported in a recent review and meta-analysis, for example.
Proton pump inhibitors also affect the gut microbiome and reduce the response to immunotherapy; this effect was demonstrated by an analysis of data from more than 2700 cancer patients that was recently presented at the annual meeting of the European Society for Medical Oncology (ESMO).
The extent to which the gut microbiome influences the efficacy of an ICI or predicts said efficacy was examined in a retrospective analysis published in Science in 2018, which Dr. Poeck presented. Resistance to ICI correlated with the relative frequency of the bacteria Akkermansia muciniphila in the gut of patients with cancer. In mouse models, the researchers restored the efficacy of the PD-1 blockade through a stool transplant.
Predicting Immunotherapy Response
If A muciniphila is present, can the composition of the microbiome act as a predictor for an effective ICI therapy?
Laurence Zitvogel, MD, PhD, and her working group at the National Institute of Health and Medical Research in Villejuif, France, performed a prospective study in 338 patients with non–small cell lung cancer and examined the prognostic significance of the fecal bacteria A muciniphila (Akk). The “Akkerman status” (low Akk vs high Akk) in a patient’s stool correlated with an increased objective response rate and a longer OS, independently of PD-L1 expression, antibiotics, and performance status. The OS for low Akk was 13.4 months, vs 18.8 months for high Akk in first-line treatment.
These results are promising, said Dr. Poeck. But there is no one-size-fits-all solution. No conclusions can be drawn from one bacterium on the efficacy of therapies in humans, since “the entirety of the bacteria is decisive,” said Dr. Poeck. In addition to the gut microbiome, the composition of gut metabolites influences the response to immunotherapies, as shown in a study with ICI.
Therapeutic Interventions
One possible therapeutic intervention to restore the gut microbiome is fecal microbiota transplantation (FMT). In a phase 1 study presented by Dr. Poeck, FMT was effective in the treatment of 20 patients with melanoma with ICI in an advanced and treatment-naive stage. Seven days after the patients received FMT, the first cycle with anti-PD-1 immunotherapy was initiated, with a total administration of three to four cycles. After 12 weeks, most patients were in complete or partial remission, as evidenced on imaging.
However, FMT also carries some risks. Two cases of sepsis with multiresistant Escherichia coli occurred, as well as other serious infections. Since then, there has been an FDA condition for extended screening of the donor stool, said Dr. Poeck. Nevertheless, this intervention is promising. A search of the keywords “FMT in cancer/transplant setting” reveals 46 currently clinical studies on clinicaltrials.gov.
Nutritional Interventions
Dr. Poeck advises caution about over-the-counter products. These products usually contain only a few species, such as Lactobacillus and Bifidobacterium. “Over-the-counter probiotics can even delay the reconstitution of the microbiome after antibiotics,” said Dr. Poeck, according to a study. In some studies, the response rates were significantly lower after probiotic intake or led to controversial results, according to Dr. Poeck.
In contrast, Dr. Poeck said prebiotics (that is, a fiber-rich diet with indigestible carbohydrates) were promising. During digestion, prebiotics are split into short-chain fatty acids by bacterial enzymes and promote the growth of certain microbiota.
In this way, just 20 g of extremely fiber-rich food had a significant effect on PFS in 128 patients with melanoma undergoing anti-PD-1 immunotherapy. With 20 g of fiber-rich food per day, the PFS was stable over 60 months. The most significant benefit was observed in patients with a sufficient fiber intake who were not taking probiotics.
What to Recommend?
In summary, Dr. Poeck said that it is important to “budget” well, particularly with antibiotic administration, and to strive for calculated therapy with as narrow a spectrum as possible. For patients who experience complications such as cytokine release syndrome as a reaction to cell therapy, delaying the use of antibiotics is important. However, it is often difficult to differentiate this syndrome from neutropenic fever. The aim should be to avoid high-risk antibiotics, if clinically justifiable. Patients should avoid taking antibiotics for 30 days before starting immunotherapy.
Regarding nutritional interventions, Dr. Poeck referred to the recent Onkopedia recommendation for nutrition after cancer and the 10 nutritional rules of the German Nutrition Society. According to Dr. Poeck, the important aspects of these recommendations are a fiber-rich diet (> 20 g/d) from various plant products and avoiding artificial sweeteners and flavorings, as well as ultraprocessed (convenience) foods. In addition, meat should be consumed only in moderation, and as little processed meat as possible should be consumed. In addition, regular (aerobic and anaerobic) physical activity is important.
“Looking ahead into the future,” said Dr. Poeck, “we need a uniform and functional understanding and we need a randomized prediction for diagnosis.”
This article was translated from the Medscape German edition.
A version of this article appeared on Medscape.com.
HAMBURG, Germany — The human microbiome comprises 39 to 44 billion microbes. That is ten times more than the number of cells in our body. Hendrik Poeck, MD, managing senior physician of internal medicine at the University Hospital Regensburg, illustrated this point at the annual meeting of the German Society for Hematology and Medical Oncology. If the gut microbiome falls out of balance, then “intestinal dysbiosis potentially poses a risk for the pathogenesis of local and systemic diseases,” explained Dr. Poeck.
Cancers and their therapies can also be influenced in this way. said Dr. Poeck.
Microbial diversity could be beneficial for cancer therapy, too. The composition of the microbiome varies significantly from host to host and can mutate. These properties make it a target for precision microbiotics, which involves using the gut microbiome as a biomarker to predict various physical reactions and to develop individualized diets.
Microbiome and Pathogenesis
The body’s microbiome fulfills a barrier function, especially where the body is exposed to an external environment: at the epidermis and the internal mucous membranes, in the gastrointestinal tract, and in the lungs, chest, and urogenital system.
Association studies on humans and experimental manipulations on mouse models of cancer showed that certain microorganisms can have either protective or harmful effects on cancer development, on the progression of a malignant disease, and on the response to therapy.
A Master Regulator?
Disruptions of the microbial system in the gut, as occur during antibiotic therapy, can have significant effects on a patient’s response to immunotherapy. Taking antibiotics shortly before or after starting therapy with immune checkpoint inhibitors (ICIs) significantly affected both overall survival (OS) and progression-free survival (PFS), as reported in a recent review and meta-analysis, for example.
Proton pump inhibitors also affect the gut microbiome and reduce the response to immunotherapy; this effect was demonstrated by an analysis of data from more than 2700 cancer patients that was recently presented at the annual meeting of the European Society for Medical Oncology (ESMO).
The extent to which the gut microbiome influences the efficacy of an ICI or predicts said efficacy was examined in a retrospective analysis published in Science in 2018, which Dr. Poeck presented. Resistance to ICI correlated with the relative frequency of the bacteria Akkermansia muciniphila in the gut of patients with cancer. In mouse models, the researchers restored the efficacy of the PD-1 blockade through a stool transplant.
Predicting Immunotherapy Response
If A muciniphila is present, can the composition of the microbiome act as a predictor for an effective ICI therapy?
Laurence Zitvogel, MD, PhD, and her working group at the National Institute of Health and Medical Research in Villejuif, France, performed a prospective study in 338 patients with non–small cell lung cancer and examined the prognostic significance of the fecal bacteria A muciniphila (Akk). The “Akkerman status” (low Akk vs high Akk) in a patient’s stool correlated with an increased objective response rate and a longer OS, independently of PD-L1 expression, antibiotics, and performance status. The OS for low Akk was 13.4 months, vs 18.8 months for high Akk in first-line treatment.
These results are promising, said Dr. Poeck. But there is no one-size-fits-all solution. No conclusions can be drawn from one bacterium on the efficacy of therapies in humans, since “the entirety of the bacteria is decisive,” said Dr. Poeck. In addition to the gut microbiome, the composition of gut metabolites influences the response to immunotherapies, as shown in a study with ICI.
Therapeutic Interventions
One possible therapeutic intervention to restore the gut microbiome is fecal microbiota transplantation (FMT). In a phase 1 study presented by Dr. Poeck, FMT was effective in the treatment of 20 patients with melanoma with ICI in an advanced and treatment-naive stage. Seven days after the patients received FMT, the first cycle with anti-PD-1 immunotherapy was initiated, with a total administration of three to four cycles. After 12 weeks, most patients were in complete or partial remission, as evidenced on imaging.
However, FMT also carries some risks. Two cases of sepsis with multiresistant Escherichia coli occurred, as well as other serious infections. Since then, there has been an FDA condition for extended screening of the donor stool, said Dr. Poeck. Nevertheless, this intervention is promising. A search of the keywords “FMT in cancer/transplant setting” reveals 46 currently clinical studies on clinicaltrials.gov.
Nutritional Interventions
Dr. Poeck advises caution about over-the-counter products. These products usually contain only a few species, such as Lactobacillus and Bifidobacterium. “Over-the-counter probiotics can even delay the reconstitution of the microbiome after antibiotics,” said Dr. Poeck, according to a study. In some studies, the response rates were significantly lower after probiotic intake or led to controversial results, according to Dr. Poeck.
In contrast, Dr. Poeck said prebiotics (that is, a fiber-rich diet with indigestible carbohydrates) were promising. During digestion, prebiotics are split into short-chain fatty acids by bacterial enzymes and promote the growth of certain microbiota.
In this way, just 20 g of extremely fiber-rich food had a significant effect on PFS in 128 patients with melanoma undergoing anti-PD-1 immunotherapy. With 20 g of fiber-rich food per day, the PFS was stable over 60 months. The most significant benefit was observed in patients with a sufficient fiber intake who were not taking probiotics.
What to Recommend?
In summary, Dr. Poeck said that it is important to “budget” well, particularly with antibiotic administration, and to strive for calculated therapy with as narrow a spectrum as possible. For patients who experience complications such as cytokine release syndrome as a reaction to cell therapy, delaying the use of antibiotics is important. However, it is often difficult to differentiate this syndrome from neutropenic fever. The aim should be to avoid high-risk antibiotics, if clinically justifiable. Patients should avoid taking antibiotics for 30 days before starting immunotherapy.
Regarding nutritional interventions, Dr. Poeck referred to the recent Onkopedia recommendation for nutrition after cancer and the 10 nutritional rules of the German Nutrition Society. According to Dr. Poeck, the important aspects of these recommendations are a fiber-rich diet (> 20 g/d) from various plant products and avoiding artificial sweeteners and flavorings, as well as ultraprocessed (convenience) foods. In addition, meat should be consumed only in moderation, and as little processed meat as possible should be consumed. In addition, regular (aerobic and anaerobic) physical activity is important.
“Looking ahead into the future,” said Dr. Poeck, “we need a uniform and functional understanding and we need a randomized prediction for diagnosis.”
This article was translated from the Medscape German edition.
A version of this article appeared on Medscape.com.
What We Have Learned About Combining a Ketogenic Diet and Chemoimmunotherapy: A Case Report and Review of Literature
Originally developed for the treatment of refractory epilepsy, the ketogenic diet is distinguished by its high-fat, moderate-protein, and low-carbohydrate food program. Preclinical models provide emerging evidence that a ketogenic diet can have therapeutic potential for a broad range of cancers. The Warburg effect is a condition where cancer cells increase the uptake and fermentation of glucose to produce lactate for their metabolism, which is called aerobic glycolysis. Lactate is the key driver of cancer angiogenesis and proliferation.1,2
The ketogenic diet promotes a metabolic shift from glycolysis to mitochondrial metabolism in normal cells while cancer cells have dysfunction in their mitochondria due to damage in cellular respiration. The ketogenic diet creates a metabolic state whereby blood glucose levels are reduced, and blood ketone bodies (D-β-hydroxybutyrate and acetoacetate) are elevated. In normal cells, the ketogenic diet causes a decrease in glucose intake for glycolysis, which makes them unable to produce enough substrate to enter the tricarboxylic acid (TCA) cycle for adenosine triphosphate (ATP) production. Fatty acid oxidation plays a key role in ketone body synthesis as a “super fuel” that enter the TCA cycle as an alternative pathway to generate ATP. On the other hand, cancer cells are unable to use ketone bodies to produce ATP for energy and metabolism due to mitochondrial defects. Lack of energy subsequently leads to the inhibition of proliferation and survival of cancer cells.3,4
We previously published a safety and feasibility study of the Modified Atkins Diet in metastatic cancer patients after failure of chemotherapy at the US Department of Veterans Affairs (VA) Pittsburgh Healthcare System.1 None of the patients were on chemotherapy at the time of enrollment. The Modified Atkins Diet consists of 60% fat, 30% protein, and 10% carbohydrates and is more tolerable than the ketogenic diet due to higher amounts of protein. Six of 11 patients (54%) had stable disease and partial response on positron emission tomography/computed tomography (PET/CT). Our study showed that patients who lost at least 10% of their body weight had improvement in quality of life (QOL) and cancer response.1 Here we present a case of a veteran with extensive metastatic colon cancer on concurrent ketogenic diet and chemotherapy subsequently followed by concurrent ketogenic diet and immunotherapy at Veterans Affairs Central California Health Care Systems (VACCHCS) in Fresno.
CASE PRESENTATION
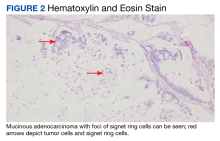
A 69-year-old veteran had iron deficiency anemia (hemoglobin, 6.5 g/dL) about 5 years previously. He underwent a colonoscopy that revealed a near circumferential ulcerated mass measuring 7 cm in the transverse colon. Biopsy results showed mucinous adenocarcinoma of the colon with a foci of signet ring cells (Figure 2).
The patient received adjuvant treatment with FOLFOX (fluorouracil, leucovorin calcium, and oxaliplatin), but within several months he developed pancreatic and worsening omental metastasis seen on PET/CT. He was then started on FOLFIRI (fluorouracil, leucovorin calcium, and irinotecan hydrochloride) plus bevacizumab 16 months after his initial diagnosis. He underwent a pancreatic mastectomy that confirmed adenocarcinoma 9 months later. Afterward, he briefly resumed FOLFIRI and bevacizumab. Next-generation sequencing testing with Foundation One CDx revealed a wild-type (WT) KRAS with a high degree of tumor mutation burden of 37 muts/Mb, BRAF V600E mutation, and high microsatellite instability (MSI-H).
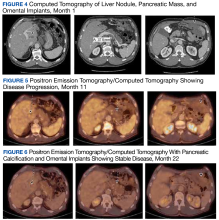
Due to disease progression, the patient’s treatment was changed to encorafenib and cetuximab for 4 months before progressing again with new liver mass and mediastinal lymphadenopathy. He then received pembrolizumab for 4 months until PET/CT showed progression and his carcinoembryonic antigen (CEA) increased from 95 to 1031 ng/mL by January 2021 (Figure 4).
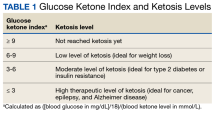
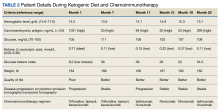
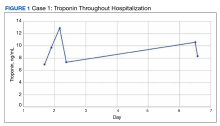
The patient was started on trifluridine/tipiracil, and bevacizumab while concurrently initiating the ketogenic diet in January 2021. Laboratory tests drawn after 1 week of strict dietary ketogenic diet adherence showed low-level ketosis with a glucose ketone index (GKI) of 8.2 (Table 1).
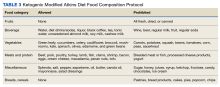
A follow-up PET/CT showed disease progression along with a CEA of 94 ng/mL after 10 months of chemotherapy plus the ketogenic diet (Table 2).
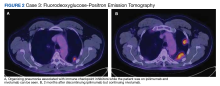
The patient continued to experience excellent QOL based on the QOL Eastern Cooperative Oncology Group (ECOG) core quality of life questionnaire (QLC-C30) forms, which he completed every 3 months. Twenty-two months after starting the ketogenic diet, the patient’s CEA increased to 293 ng/mL although PET/CT continues to show stable disease (Figures 4, 5, and 6).
DISCUSSION
The purpose of this case report is to describe whether a patient receiving active cancer treatment was able to tolerate the ketogenic diet in conjunction with chemotherapy or immunotherapy. Most literature published on the subject evaluated the tolerability and response of the ketogenic diet after the failure of standard therapy. Our patient was diagnosed with stage III mucinous colon adenocarcinoma. He received adjuvant chemotherapy but quickly developed metastatic disease to the pancreas and omentum. We started him on encorafenib and cetuximab based on the BEACON study that showed improvement in response rate and survival when compared with standard chemotherapy for patients with BRAF V600E mutation.5 Unfortunately, his cancer quickly progressed within 4 months and again did not respond to pembrolizumab despite MSI-H, which lasted for another 4 months.
We suggested the ketogenic diet and the patient agreed. He started the diet along with trifluridine/tipiracil, and bevacizumab in January 2021. The patient’s metastatic cancer stabilized for 9 months until his disease progressed again. He was started on doublet immune checkpoint inhibitors ipilimumab and nivolumab based on his MSI-H and high tumor mutation burden with the continuation of the ketogenic diet until now. The CheckMate 142 study revealed that the combination of ipilimumab and nivolumab in patients with MSI-H previously treated for metastatic colon cancer showed some benefit.6
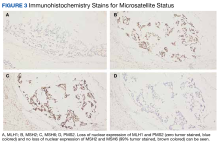
Our patient had the loss of nuclear expression of MLH1 and PMS2 (zero tumor stained) but no evidence of the loss expression of MSH2 and MSH6 genes (99% tumor stained). About 8% to 12% of patients with metastatic colon cancer have BRAF V600E mutations that are usually mucinous type, poorly differentiated, and located in the right side of the colon, which portends to a poor prognosis. Tumor DNA mismatch repair damage results in genetic hypermutability and leads to MSI that is sensitive to treatment with checkpoint inhibitors, as in our patient. Only about 3% of MSI-H tumors are due to germline mutations such as Lynch syndrome (hereditary nonpolyposis colorectal cancer). The presence of both MLH1 hypermethylation and BRAF mutation, as in our patient, is a strong indication of somatic rather than germline mutation.7
GKI, which represents the ratio of glucose to ketone, was developed to evaluate the efficacy of the ketogenic diet. This index measures the degree of metabolic stress on tumor cells through the decrease of glucose levels and increase of ketone bodies. A GKI of ≤ 1.0 has been suggested as the ideal therapeutic goal for cancer management.8 As levels of blood glucose decline, the blood levels of ketone bodies should rise. These 2 lines should eventually intersect at a certain point beyond which one enters the therapeutic zone or therapeutic ketosis zone. This is when tumor growth is expected to slow or cease.9 The patient’s ketone (β-hydroxybutyrate) level was initially high (0.71 mmol/L) with a GKI of 8.2. (low ketotic level), which meant he tolerated a rather strict diet for the first several months. This was also reflected in his 18 lb weight loss (almost 10% of body weight) and cancer stabilization, as in our previous publication.1 Unfortunately, the patient was unable to maintain high ketone and lower GKI levels due to fatigue from depleted carbohydrate intake. He added some carbohydrate snacks in between meals, which improved the fatigue. His ketone level has been < 0.5 mmol/L ever since, albeit his disease continues to be stable. The patient continues his daily work and reports a better QOL, based on the ECOG QLC-C30 form that he completed every 3 months.10 Currently, the patient is still receiving ipilimumab and nivolumab while maintaining the ketogenic diet with stable metastatic disease on PET/CT.
Ketogenic Diet and Cellular Mechanism of Action
PI3K/Akt (phosphatidylinositol-3-kinase) signaling is one of the most important intracellular pathways for tumor cells. It leads to the inhibition of apoptosis and the promotion of cell proliferation, metabolism, and angiogenesis. Deregulation of the PI3K pathway either via amplification of PI3K by tyrosine kinase growth factor receptors or inactivation of the tumor suppressor phosphatase and tensin homolog (PTEN), which is the negative regulator of the PI3K pathway, contributes to the development of cancer cells.11
A study by Goncalves and colleagues revealed an interesting relationship between the PI3K pathway and the benefit of the ketogenic diet to slow tumor growth. PI3K inhibitors inhibit glucose uptake into skeletal muscle and adipose tissue that activate hepatic glycogenolysis. This event results in hyperglycemia due to the pancreas releasing very high levels of insulin into the blood (hyperinsulinemia) that subsequently reactivate PI3K signaling and cause resistance to PI3K inhibitors. The ketogenic diet reportedly minimized the hyperglycemia and hyperinsulinemia induced by the PI3K inhibitor and enhanced the efficacy of PI3K inhibitors in tumor models. Studies combining PI3K inhibitors and ketogenic diet are underway. Hence, combining the ketogenic diet with chemotherapy or other novel treatment should be the focus of ketogenic diet trials.12,13
Ketogenic Diet and Oncology Studies
The impact of the ketogenic diet on the growth of murine pancreatic tumors was evaluated by Yang and colleagues. The ketogenic diet decreased glucose concentration that enters the TCA cycle and increased fatty acid oxidation that produces β-hydroxybutyrate. This event promotes the generation of ATP, although with only modest elevations of NADH with less impact on tumor growth. The combination of ketogenic diet and standard chemotherapy substantially raised tumor NADH and suppressed the growth of murine tumor cells, they noted.14 Furukawa and colleagues compared 10 patients with metastatic colon cancer receiving chemotherapy plus the modified medium-chain triglyceride ketogenic diet for 1 year with 14 patients receiving chemotherapy only. The ketogenic diet group exhibited a response rate of 60% with 5 patients achieving a complete response and a disease control rate of 70%, while the chemotherapy-alone group showed a response rate of only 21% with no complete response and a disease control rate of 64%.15
The ketogenic diet also reportedly stimulates cytokine and CD4+ and CD8+ T-cell production that stimulates T-cell killing activity. The ketogenic diet may overcome several immune escape mechanisms by downregulating the expression of cytotoxic T-lymphocyte-associated protein 4 (CTLA-4) and programmed cell death protein 1 (PD-1) on tumor-infiltrating lymphocytes.16 Our patient tolerated the combination of the ketogenic diet with ipilimumab (CTLA-4 inhibitor) and nivolumab (PD-1 inhibitor) without significant toxicities and stabilization of his disease.
Future Directions
We originally presented the abstract and poster of this case report at the Association of VA Hematology/Oncology annual meeting in San Diego, California, in September 2022.17 Based on our previous experience, we are now using a modified Atkins diet, which is a less strict diet consisting of 60% fat, 30% protein, and 10% carbohydrates combined with chemotherapy and/or immunotherapy. The composition of fat to carbohydrate plus protein in the traditional ketogenic diet is usually 4:1 or 3:1, while in modified Atkins diet the ratio is 1:1 or 2:1. The benefit of the modified Atkins diet is that patients can consume more protein than a strict ketogenic diet and they can be more liberal in carbohydrate allowances. We are about to open a study protocol of combining a modified Atkin diet and chemotherapy and/or immunotherapy as a first-line treatment for veterans with all types of advanced or metastatic solid tumors at VACCHCS. The study protocol was approved by the VA Office of Research and Development and has been submitted to the VACCHCS Institutional Review Board for review. Once approved, we will start patient recruitment.
CONCLUSIONS
Cancer cells have defects in their mitochondria that prevent them from generating energy for metabolism in the absence of glucose. They also depend on the PI3K signaling pathway to survive. The ketogenic diet has the advantage of affecting cancer cell growth by exploiting these mitochondrial defects and blocking hyperglycemia. There is growing evidence that the ketogenic diet is feasible, tolerable, and reportedly inhibits cancer growth. Our case report and previous publications suggest that the ketogenic diet can be added to chemotherapy and/or immunotherapy as an adjunct to standard-of-care cancer treatment while maintaining good QOL. We are planning to open a clinical trial using the modified Atkins diet in conjunction with active cancer treatments as first-line therapy for metastatic solid tumors at the VACCHCS. We are also working closely with researchers from several veteran hospitals to do a diet collaborative study. We believe the ketogenic diet is an important part of cancer treatment and has a promising future. More research should be dedicated to this very interesting field.
Acknowledgments
We previously presented this case report in an abstract and poster at the September 2022 AVAHO meeting in San Diego, California.
1. Tan-Shalaby JL, Carrick J, Edinger K, et al. Modified Atkins diet in advanced malignancies-final results of a safety and feasibility trial within the Veterans Affairs Pittsburgh Healthcare System. Nutr Metab (Lond). 2016;13:52. Published 2016 Aug 12. doi:10.1186/s12986-016-0113-y
2. Talib WH, Mahmod AI, Kamal A, et al. Ketogenic diet in cancer prevention and therapy: molecular targets and therapeutic opportunities. Curr Issues Mol Biol. 2021;43(2):558-589. Published 2021 Jul 3. doi:10.3390/cimb43020042
3. Tan-Shalaby J. Ketogenic diets and cancer: emerging evidence. Fed Pract. 2017;34(suppl 1):37S-42S.
4. Cortez NE, Mackenzie GG. Ketogenic diets in pancreatic cancer and associated cachexia: cellular mechanisms and clinical perspectives. Nutrients. 2021;13(9):3202. Published 2021 Sep 15. doi:10.3390/nu13093202
5. Tabernero J, Grothey A, Van Cutsem E, et al. Encorafenib plus cetuximab as a new standard of care for previously treated BRAF V600E-mutant metastatic colorectal cancer: updated survival results and subgroup analyses from the BEACON study. J Clin Oncol. 2021;39(4):273-284. doi:10.1200/JCO.20.02088
6. André T, Lonardi S, Wong KYM, et al. Nivolumab plus low-dose ipilimumab in previously treated patients with microsatellite instability-high/mismatch repair-deficient metastatic colorectal cancer: 4-year follow-up from CheckMate 142. Ann Oncol. 2022;33(10):1052-1060. doi:10.1016/j.annonc.2022.06.008
7. Grassi E, Corbelli J, Papiani G, Barbera MA, Gazzaneo F, Tamberi S. Current therapeutic strategies in BRAF-mutant metastatic colorectal cancer. Front Oncol. 2021;11:601722. Published 2021 Jun 23. doi:10.3389/fonc.2021.601722
8. Seyfried TN, Mukherjee P, Iyikesici MS, et al. Consideration of ketogenic metabolic therapy as a complementary or alternative approach for managing breast cancer. Front Nutr. 2020;7:21. Published 2020 Mar 11. doi:10.3389/fnut.2020.00021
9. Meidenbauer JJ, Mukherjee P, Seyfried TN. The glucose ketone index calculator: a simple tool to monitor therapeutic efficacy for metabolic management of brain cancer. Nutr Metab (Lond). 2015;12:12. Published 2015 Mar 11. doi:10.1186/s12986-015-0009-2
10. Fayers P, Bottomley A; EORTC Quality of Life Group; Quality of Life Unit. Quality of life research within the EORTC-the EORTC QLQ-C30. European Organisation for Research and Treatment of Cancer. Eur J Cancer. 2002;38(suppl 4):S125-S133. doi:10.1016/s0959-8049(01)00448-8
11. Yang J, Nie J, Ma X, Wei Y, Peng Y, Wei X. Targeting PI3K in cancer: mechanisms and advances in clinical trials. Mol Cancer. 2019;18(1):26. Published 2019 Feb 19. doi:10.1186/s12943-019-0954-x
12. Goncalves MD, Hopkins BD, Cantley LC. Phosphatidylinositol 3-kinase, growth disorders, and cancer. N Engl J Med. 2018;379(21):2052-2062. doi:10.1056/NEJMra1704560
13. Weber DD, Aminzadeh-Gohari S, Tulipan J, Catalano L, Feichtinger RG, Kofler B. Ketogenic diet in the treatment of cancer-where do we stand?. Mol Metab. 2020;33:102-121. doi:10.1016/j.molmet.2019.06.026
14. Yang L, TeSlaa T, Ng S, et al. Ketogenic diet and chemotherapy combine to disrupt pancreatic cancer metabolism and growth. Med. 2022;3(2):119-136. doi:10.1016/j.medj.2021.12.008
15. Furukawa K, Shigematus K, Iwase Y, et al. Clinical effects of one year of chemotherapy with a modified medium-chain triglyceride ketogenic diet on the recurrence of stage IV colon cancer. J Clin Oncol. 2018;36(suppl 15):e15709. doi:10.1200/JCO.2018.36.15_suppl.e15709
16. Zhang X, Li H, Lv X, et al. Impact of diets on response to immune checkpoint inhibitors (ICIs) therapy against tumors. Life (Basel). 2022;12(3):409. Published 2022 Mar 11. doi:10.3390/life12030409
17. Liman, A, Hwang A, Means J, Newson J. Ketogenic diet and cancer: a case report and feasibility study at VA Central California Healthcare System. Fed Pract. 2022;39(suppl 4):S18.
Originally developed for the treatment of refractory epilepsy, the ketogenic diet is distinguished by its high-fat, moderate-protein, and low-carbohydrate food program. Preclinical models provide emerging evidence that a ketogenic diet can have therapeutic potential for a broad range of cancers. The Warburg effect is a condition where cancer cells increase the uptake and fermentation of glucose to produce lactate for their metabolism, which is called aerobic glycolysis. Lactate is the key driver of cancer angiogenesis and proliferation.1,2
The ketogenic diet promotes a metabolic shift from glycolysis to mitochondrial metabolism in normal cells while cancer cells have dysfunction in their mitochondria due to damage in cellular respiration. The ketogenic diet creates a metabolic state whereby blood glucose levels are reduced, and blood ketone bodies (D-β-hydroxybutyrate and acetoacetate) are elevated. In normal cells, the ketogenic diet causes a decrease in glucose intake for glycolysis, which makes them unable to produce enough substrate to enter the tricarboxylic acid (TCA) cycle for adenosine triphosphate (ATP) production. Fatty acid oxidation plays a key role in ketone body synthesis as a “super fuel” that enter the TCA cycle as an alternative pathway to generate ATP. On the other hand, cancer cells are unable to use ketone bodies to produce ATP for energy and metabolism due to mitochondrial defects. Lack of energy subsequently leads to the inhibition of proliferation and survival of cancer cells.3,4
We previously published a safety and feasibility study of the Modified Atkins Diet in metastatic cancer patients after failure of chemotherapy at the US Department of Veterans Affairs (VA) Pittsburgh Healthcare System.1 None of the patients were on chemotherapy at the time of enrollment. The Modified Atkins Diet consists of 60% fat, 30% protein, and 10% carbohydrates and is more tolerable than the ketogenic diet due to higher amounts of protein. Six of 11 patients (54%) had stable disease and partial response on positron emission tomography/computed tomography (PET/CT). Our study showed that patients who lost at least 10% of their body weight had improvement in quality of life (QOL) and cancer response.1 Here we present a case of a veteran with extensive metastatic colon cancer on concurrent ketogenic diet and chemotherapy subsequently followed by concurrent ketogenic diet and immunotherapy at Veterans Affairs Central California Health Care Systems (VACCHCS) in Fresno.
CASE PRESENTATION
A 69-year-old veteran had iron deficiency anemia (hemoglobin, 6.5 g/dL) about 5 years previously. He underwent a colonoscopy that revealed a near circumferential ulcerated mass measuring 7 cm in the transverse colon. Biopsy results showed mucinous adenocarcinoma of the colon with a foci of signet ring cells (Figure 2).
The patient received adjuvant treatment with FOLFOX (fluorouracil, leucovorin calcium, and oxaliplatin), but within several months he developed pancreatic and worsening omental metastasis seen on PET/CT. He was then started on FOLFIRI (fluorouracil, leucovorin calcium, and irinotecan hydrochloride) plus bevacizumab 16 months after his initial diagnosis. He underwent a pancreatic mastectomy that confirmed adenocarcinoma 9 months later. Afterward, he briefly resumed FOLFIRI and bevacizumab. Next-generation sequencing testing with Foundation One CDx revealed a wild-type (WT) KRAS with a high degree of tumor mutation burden of 37 muts/Mb, BRAF V600E mutation, and high microsatellite instability (MSI-H).
Due to disease progression, the patient’s treatment was changed to encorafenib and cetuximab for 4 months before progressing again with new liver mass and mediastinal lymphadenopathy. He then received pembrolizumab for 4 months until PET/CT showed progression and his carcinoembryonic antigen (CEA) increased from 95 to 1031 ng/mL by January 2021 (Figure 4).
The patient was started on trifluridine/tipiracil, and bevacizumab while concurrently initiating the ketogenic diet in January 2021. Laboratory tests drawn after 1 week of strict dietary ketogenic diet adherence showed low-level ketosis with a glucose ketone index (GKI) of 8.2 (Table 1).
A follow-up PET/CT showed disease progression along with a CEA of 94 ng/mL after 10 months of chemotherapy plus the ketogenic diet (Table 2).
The patient continued to experience excellent QOL based on the QOL Eastern Cooperative Oncology Group (ECOG) core quality of life questionnaire (QLC-C30) forms, which he completed every 3 months. Twenty-two months after starting the ketogenic diet, the patient’s CEA increased to 293 ng/mL although PET/CT continues to show stable disease (Figures 4, 5, and 6).
DISCUSSION
The purpose of this case report is to describe whether a patient receiving active cancer treatment was able to tolerate the ketogenic diet in conjunction with chemotherapy or immunotherapy. Most literature published on the subject evaluated the tolerability and response of the ketogenic diet after the failure of standard therapy. Our patient was diagnosed with stage III mucinous colon adenocarcinoma. He received adjuvant chemotherapy but quickly developed metastatic disease to the pancreas and omentum. We started him on encorafenib and cetuximab based on the BEACON study that showed improvement in response rate and survival when compared with standard chemotherapy for patients with BRAF V600E mutation.5 Unfortunately, his cancer quickly progressed within 4 months and again did not respond to pembrolizumab despite MSI-H, which lasted for another 4 months.
We suggested the ketogenic diet and the patient agreed. He started the diet along with trifluridine/tipiracil, and bevacizumab in January 2021. The patient’s metastatic cancer stabilized for 9 months until his disease progressed again. He was started on doublet immune checkpoint inhibitors ipilimumab and nivolumab based on his MSI-H and high tumor mutation burden with the continuation of the ketogenic diet until now. The CheckMate 142 study revealed that the combination of ipilimumab and nivolumab in patients with MSI-H previously treated for metastatic colon cancer showed some benefit.6
Our patient had the loss of nuclear expression of MLH1 and PMS2 (zero tumor stained) but no evidence of the loss expression of MSH2 and MSH6 genes (99% tumor stained). About 8% to 12% of patients with metastatic colon cancer have BRAF V600E mutations that are usually mucinous type, poorly differentiated, and located in the right side of the colon, which portends to a poor prognosis. Tumor DNA mismatch repair damage results in genetic hypermutability and leads to MSI that is sensitive to treatment with checkpoint inhibitors, as in our patient. Only about 3% of MSI-H tumors are due to germline mutations such as Lynch syndrome (hereditary nonpolyposis colorectal cancer). The presence of both MLH1 hypermethylation and BRAF mutation, as in our patient, is a strong indication of somatic rather than germline mutation.7
GKI, which represents the ratio of glucose to ketone, was developed to evaluate the efficacy of the ketogenic diet. This index measures the degree of metabolic stress on tumor cells through the decrease of glucose levels and increase of ketone bodies. A GKI of ≤ 1.0 has been suggested as the ideal therapeutic goal for cancer management.8 As levels of blood glucose decline, the blood levels of ketone bodies should rise. These 2 lines should eventually intersect at a certain point beyond which one enters the therapeutic zone or therapeutic ketosis zone. This is when tumor growth is expected to slow or cease.9 The patient’s ketone (β-hydroxybutyrate) level was initially high (0.71 mmol/L) with a GKI of 8.2. (low ketotic level), which meant he tolerated a rather strict diet for the first several months. This was also reflected in his 18 lb weight loss (almost 10% of body weight) and cancer stabilization, as in our previous publication.1 Unfortunately, the patient was unable to maintain high ketone and lower GKI levels due to fatigue from depleted carbohydrate intake. He added some carbohydrate snacks in between meals, which improved the fatigue. His ketone level has been < 0.5 mmol/L ever since, albeit his disease continues to be stable. The patient continues his daily work and reports a better QOL, based on the ECOG QLC-C30 form that he completed every 3 months.10 Currently, the patient is still receiving ipilimumab and nivolumab while maintaining the ketogenic diet with stable metastatic disease on PET/CT.
Ketogenic Diet and Cellular Mechanism of Action
PI3K/Akt (phosphatidylinositol-3-kinase) signaling is one of the most important intracellular pathways for tumor cells. It leads to the inhibition of apoptosis and the promotion of cell proliferation, metabolism, and angiogenesis. Deregulation of the PI3K pathway either via amplification of PI3K by tyrosine kinase growth factor receptors or inactivation of the tumor suppressor phosphatase and tensin homolog (PTEN), which is the negative regulator of the PI3K pathway, contributes to the development of cancer cells.11
A study by Goncalves and colleagues revealed an interesting relationship between the PI3K pathway and the benefit of the ketogenic diet to slow tumor growth. PI3K inhibitors inhibit glucose uptake into skeletal muscle and adipose tissue that activate hepatic glycogenolysis. This event results in hyperglycemia due to the pancreas releasing very high levels of insulin into the blood (hyperinsulinemia) that subsequently reactivate PI3K signaling and cause resistance to PI3K inhibitors. The ketogenic diet reportedly minimized the hyperglycemia and hyperinsulinemia induced by the PI3K inhibitor and enhanced the efficacy of PI3K inhibitors in tumor models. Studies combining PI3K inhibitors and ketogenic diet are underway. Hence, combining the ketogenic diet with chemotherapy or other novel treatment should be the focus of ketogenic diet trials.12,13
Ketogenic Diet and Oncology Studies
The impact of the ketogenic diet on the growth of murine pancreatic tumors was evaluated by Yang and colleagues. The ketogenic diet decreased glucose concentration that enters the TCA cycle and increased fatty acid oxidation that produces β-hydroxybutyrate. This event promotes the generation of ATP, although with only modest elevations of NADH with less impact on tumor growth. The combination of ketogenic diet and standard chemotherapy substantially raised tumor NADH and suppressed the growth of murine tumor cells, they noted.14 Furukawa and colleagues compared 10 patients with metastatic colon cancer receiving chemotherapy plus the modified medium-chain triglyceride ketogenic diet for 1 year with 14 patients receiving chemotherapy only. The ketogenic diet group exhibited a response rate of 60% with 5 patients achieving a complete response and a disease control rate of 70%, while the chemotherapy-alone group showed a response rate of only 21% with no complete response and a disease control rate of 64%.15
The ketogenic diet also reportedly stimulates cytokine and CD4+ and CD8+ T-cell production that stimulates T-cell killing activity. The ketogenic diet may overcome several immune escape mechanisms by downregulating the expression of cytotoxic T-lymphocyte-associated protein 4 (CTLA-4) and programmed cell death protein 1 (PD-1) on tumor-infiltrating lymphocytes.16 Our patient tolerated the combination of the ketogenic diet with ipilimumab (CTLA-4 inhibitor) and nivolumab (PD-1 inhibitor) without significant toxicities and stabilization of his disease.
Future Directions
We originally presented the abstract and poster of this case report at the Association of VA Hematology/Oncology annual meeting in San Diego, California, in September 2022.17 Based on our previous experience, we are now using a modified Atkins diet, which is a less strict diet consisting of 60% fat, 30% protein, and 10% carbohydrates combined with chemotherapy and/or immunotherapy. The composition of fat to carbohydrate plus protein in the traditional ketogenic diet is usually 4:1 or 3:1, while in modified Atkins diet the ratio is 1:1 or 2:1. The benefit of the modified Atkins diet is that patients can consume more protein than a strict ketogenic diet and they can be more liberal in carbohydrate allowances. We are about to open a study protocol of combining a modified Atkin diet and chemotherapy and/or immunotherapy as a first-line treatment for veterans with all types of advanced or metastatic solid tumors at VACCHCS. The study protocol was approved by the VA Office of Research and Development and has been submitted to the VACCHCS Institutional Review Board for review. Once approved, we will start patient recruitment.
CONCLUSIONS
Cancer cells have defects in their mitochondria that prevent them from generating energy for metabolism in the absence of glucose. They also depend on the PI3K signaling pathway to survive. The ketogenic diet has the advantage of affecting cancer cell growth by exploiting these mitochondrial defects and blocking hyperglycemia. There is growing evidence that the ketogenic diet is feasible, tolerable, and reportedly inhibits cancer growth. Our case report and previous publications suggest that the ketogenic diet can be added to chemotherapy and/or immunotherapy as an adjunct to standard-of-care cancer treatment while maintaining good QOL. We are planning to open a clinical trial using the modified Atkins diet in conjunction with active cancer treatments as first-line therapy for metastatic solid tumors at the VACCHCS. We are also working closely with researchers from several veteran hospitals to do a diet collaborative study. We believe the ketogenic diet is an important part of cancer treatment and has a promising future. More research should be dedicated to this very interesting field.
Acknowledgments
We previously presented this case report in an abstract and poster at the September 2022 AVAHO meeting in San Diego, California.
Originally developed for the treatment of refractory epilepsy, the ketogenic diet is distinguished by its high-fat, moderate-protein, and low-carbohydrate food program. Preclinical models provide emerging evidence that a ketogenic diet can have therapeutic potential for a broad range of cancers. The Warburg effect is a condition where cancer cells increase the uptake and fermentation of glucose to produce lactate for their metabolism, which is called aerobic glycolysis. Lactate is the key driver of cancer angiogenesis and proliferation.1,2
The ketogenic diet promotes a metabolic shift from glycolysis to mitochondrial metabolism in normal cells while cancer cells have dysfunction in their mitochondria due to damage in cellular respiration. The ketogenic diet creates a metabolic state whereby blood glucose levels are reduced, and blood ketone bodies (D-β-hydroxybutyrate and acetoacetate) are elevated. In normal cells, the ketogenic diet causes a decrease in glucose intake for glycolysis, which makes them unable to produce enough substrate to enter the tricarboxylic acid (TCA) cycle for adenosine triphosphate (ATP) production. Fatty acid oxidation plays a key role in ketone body synthesis as a “super fuel” that enter the TCA cycle as an alternative pathway to generate ATP. On the other hand, cancer cells are unable to use ketone bodies to produce ATP for energy and metabolism due to mitochondrial defects. Lack of energy subsequently leads to the inhibition of proliferation and survival of cancer cells.3,4
We previously published a safety and feasibility study of the Modified Atkins Diet in metastatic cancer patients after failure of chemotherapy at the US Department of Veterans Affairs (VA) Pittsburgh Healthcare System.1 None of the patients were on chemotherapy at the time of enrollment. The Modified Atkins Diet consists of 60% fat, 30% protein, and 10% carbohydrates and is more tolerable than the ketogenic diet due to higher amounts of protein. Six of 11 patients (54%) had stable disease and partial response on positron emission tomography/computed tomography (PET/CT). Our study showed that patients who lost at least 10% of their body weight had improvement in quality of life (QOL) and cancer response.1 Here we present a case of a veteran with extensive metastatic colon cancer on concurrent ketogenic diet and chemotherapy subsequently followed by concurrent ketogenic diet and immunotherapy at Veterans Affairs Central California Health Care Systems (VACCHCS) in Fresno.
CASE PRESENTATION
A 69-year-old veteran had iron deficiency anemia (hemoglobin, 6.5 g/dL) about 5 years previously. He underwent a colonoscopy that revealed a near circumferential ulcerated mass measuring 7 cm in the transverse colon. Biopsy results showed mucinous adenocarcinoma of the colon with a foci of signet ring cells (Figure 2).
The patient received adjuvant treatment with FOLFOX (fluorouracil, leucovorin calcium, and oxaliplatin), but within several months he developed pancreatic and worsening omental metastasis seen on PET/CT. He was then started on FOLFIRI (fluorouracil, leucovorin calcium, and irinotecan hydrochloride) plus bevacizumab 16 months after his initial diagnosis. He underwent a pancreatic mastectomy that confirmed adenocarcinoma 9 months later. Afterward, he briefly resumed FOLFIRI and bevacizumab. Next-generation sequencing testing with Foundation One CDx revealed a wild-type (WT) KRAS with a high degree of tumor mutation burden of 37 muts/Mb, BRAF V600E mutation, and high microsatellite instability (MSI-H).
Due to disease progression, the patient’s treatment was changed to encorafenib and cetuximab for 4 months before progressing again with new liver mass and mediastinal lymphadenopathy. He then received pembrolizumab for 4 months until PET/CT showed progression and his carcinoembryonic antigen (CEA) increased from 95 to 1031 ng/mL by January 2021 (Figure 4).
The patient was started on trifluridine/tipiracil, and bevacizumab while concurrently initiating the ketogenic diet in January 2021. Laboratory tests drawn after 1 week of strict dietary ketogenic diet adherence showed low-level ketosis with a glucose ketone index (GKI) of 8.2 (Table 1).
A follow-up PET/CT showed disease progression along with a CEA of 94 ng/mL after 10 months of chemotherapy plus the ketogenic diet (Table 2).
The patient continued to experience excellent QOL based on the QOL Eastern Cooperative Oncology Group (ECOG) core quality of life questionnaire (QLC-C30) forms, which he completed every 3 months. Twenty-two months after starting the ketogenic diet, the patient’s CEA increased to 293 ng/mL although PET/CT continues to show stable disease (Figures 4, 5, and 6).
DISCUSSION
The purpose of this case report is to describe whether a patient receiving active cancer treatment was able to tolerate the ketogenic diet in conjunction with chemotherapy or immunotherapy. Most literature published on the subject evaluated the tolerability and response of the ketogenic diet after the failure of standard therapy. Our patient was diagnosed with stage III mucinous colon adenocarcinoma. He received adjuvant chemotherapy but quickly developed metastatic disease to the pancreas and omentum. We started him on encorafenib and cetuximab based on the BEACON study that showed improvement in response rate and survival when compared with standard chemotherapy for patients with BRAF V600E mutation.5 Unfortunately, his cancer quickly progressed within 4 months and again did not respond to pembrolizumab despite MSI-H, which lasted for another 4 months.
We suggested the ketogenic diet and the patient agreed. He started the diet along with trifluridine/tipiracil, and bevacizumab in January 2021. The patient’s metastatic cancer stabilized for 9 months until his disease progressed again. He was started on doublet immune checkpoint inhibitors ipilimumab and nivolumab based on his MSI-H and high tumor mutation burden with the continuation of the ketogenic diet until now. The CheckMate 142 study revealed that the combination of ipilimumab and nivolumab in patients with MSI-H previously treated for metastatic colon cancer showed some benefit.6
Our patient had the loss of nuclear expression of MLH1 and PMS2 (zero tumor stained) but no evidence of the loss expression of MSH2 and MSH6 genes (99% tumor stained). About 8% to 12% of patients with metastatic colon cancer have BRAF V600E mutations that are usually mucinous type, poorly differentiated, and located in the right side of the colon, which portends to a poor prognosis. Tumor DNA mismatch repair damage results in genetic hypermutability and leads to MSI that is sensitive to treatment with checkpoint inhibitors, as in our patient. Only about 3% of MSI-H tumors are due to germline mutations such as Lynch syndrome (hereditary nonpolyposis colorectal cancer). The presence of both MLH1 hypermethylation and BRAF mutation, as in our patient, is a strong indication of somatic rather than germline mutation.7
GKI, which represents the ratio of glucose to ketone, was developed to evaluate the efficacy of the ketogenic diet. This index measures the degree of metabolic stress on tumor cells through the decrease of glucose levels and increase of ketone bodies. A GKI of ≤ 1.0 has been suggested as the ideal therapeutic goal for cancer management.8 As levels of blood glucose decline, the blood levels of ketone bodies should rise. These 2 lines should eventually intersect at a certain point beyond which one enters the therapeutic zone or therapeutic ketosis zone. This is when tumor growth is expected to slow or cease.9 The patient’s ketone (β-hydroxybutyrate) level was initially high (0.71 mmol/L) with a GKI of 8.2. (low ketotic level), which meant he tolerated a rather strict diet for the first several months. This was also reflected in his 18 lb weight loss (almost 10% of body weight) and cancer stabilization, as in our previous publication.1 Unfortunately, the patient was unable to maintain high ketone and lower GKI levels due to fatigue from depleted carbohydrate intake. He added some carbohydrate snacks in between meals, which improved the fatigue. His ketone level has been < 0.5 mmol/L ever since, albeit his disease continues to be stable. The patient continues his daily work and reports a better QOL, based on the ECOG QLC-C30 form that he completed every 3 months.10 Currently, the patient is still receiving ipilimumab and nivolumab while maintaining the ketogenic diet with stable metastatic disease on PET/CT.
Ketogenic Diet and Cellular Mechanism of Action
PI3K/Akt (phosphatidylinositol-3-kinase) signaling is one of the most important intracellular pathways for tumor cells. It leads to the inhibition of apoptosis and the promotion of cell proliferation, metabolism, and angiogenesis. Deregulation of the PI3K pathway either via amplification of PI3K by tyrosine kinase growth factor receptors or inactivation of the tumor suppressor phosphatase and tensin homolog (PTEN), which is the negative regulator of the PI3K pathway, contributes to the development of cancer cells.11
A study by Goncalves and colleagues revealed an interesting relationship between the PI3K pathway and the benefit of the ketogenic diet to slow tumor growth. PI3K inhibitors inhibit glucose uptake into skeletal muscle and adipose tissue that activate hepatic glycogenolysis. This event results in hyperglycemia due to the pancreas releasing very high levels of insulin into the blood (hyperinsulinemia) that subsequently reactivate PI3K signaling and cause resistance to PI3K inhibitors. The ketogenic diet reportedly minimized the hyperglycemia and hyperinsulinemia induced by the PI3K inhibitor and enhanced the efficacy of PI3K inhibitors in tumor models. Studies combining PI3K inhibitors and ketogenic diet are underway. Hence, combining the ketogenic diet with chemotherapy or other novel treatment should be the focus of ketogenic diet trials.12,13
Ketogenic Diet and Oncology Studies
The impact of the ketogenic diet on the growth of murine pancreatic tumors was evaluated by Yang and colleagues. The ketogenic diet decreased glucose concentration that enters the TCA cycle and increased fatty acid oxidation that produces β-hydroxybutyrate. This event promotes the generation of ATP, although with only modest elevations of NADH with less impact on tumor growth. The combination of ketogenic diet and standard chemotherapy substantially raised tumor NADH and suppressed the growth of murine tumor cells, they noted.14 Furukawa and colleagues compared 10 patients with metastatic colon cancer receiving chemotherapy plus the modified medium-chain triglyceride ketogenic diet for 1 year with 14 patients receiving chemotherapy only. The ketogenic diet group exhibited a response rate of 60% with 5 patients achieving a complete response and a disease control rate of 70%, while the chemotherapy-alone group showed a response rate of only 21% with no complete response and a disease control rate of 64%.15
The ketogenic diet also reportedly stimulates cytokine and CD4+ and CD8+ T-cell production that stimulates T-cell killing activity. The ketogenic diet may overcome several immune escape mechanisms by downregulating the expression of cytotoxic T-lymphocyte-associated protein 4 (CTLA-4) and programmed cell death protein 1 (PD-1) on tumor-infiltrating lymphocytes.16 Our patient tolerated the combination of the ketogenic diet with ipilimumab (CTLA-4 inhibitor) and nivolumab (PD-1 inhibitor) without significant toxicities and stabilization of his disease.
Future Directions
We originally presented the abstract and poster of this case report at the Association of VA Hematology/Oncology annual meeting in San Diego, California, in September 2022.17 Based on our previous experience, we are now using a modified Atkins diet, which is a less strict diet consisting of 60% fat, 30% protein, and 10% carbohydrates combined with chemotherapy and/or immunotherapy. The composition of fat to carbohydrate plus protein in the traditional ketogenic diet is usually 4:1 or 3:1, while in modified Atkins diet the ratio is 1:1 or 2:1. The benefit of the modified Atkins diet is that patients can consume more protein than a strict ketogenic diet and they can be more liberal in carbohydrate allowances. We are about to open a study protocol of combining a modified Atkin diet and chemotherapy and/or immunotherapy as a first-line treatment for veterans with all types of advanced or metastatic solid tumors at VACCHCS. The study protocol was approved by the VA Office of Research and Development and has been submitted to the VACCHCS Institutional Review Board for review. Once approved, we will start patient recruitment.
CONCLUSIONS
Cancer cells have defects in their mitochondria that prevent them from generating energy for metabolism in the absence of glucose. They also depend on the PI3K signaling pathway to survive. The ketogenic diet has the advantage of affecting cancer cell growth by exploiting these mitochondrial defects and blocking hyperglycemia. There is growing evidence that the ketogenic diet is feasible, tolerable, and reportedly inhibits cancer growth. Our case report and previous publications suggest that the ketogenic diet can be added to chemotherapy and/or immunotherapy as an adjunct to standard-of-care cancer treatment while maintaining good QOL. We are planning to open a clinical trial using the modified Atkins diet in conjunction with active cancer treatments as first-line therapy for metastatic solid tumors at the VACCHCS. We are also working closely with researchers from several veteran hospitals to do a diet collaborative study. We believe the ketogenic diet is an important part of cancer treatment and has a promising future. More research should be dedicated to this very interesting field.
Acknowledgments
We previously presented this case report in an abstract and poster at the September 2022 AVAHO meeting in San Diego, California.
1. Tan-Shalaby JL, Carrick J, Edinger K, et al. Modified Atkins diet in advanced malignancies-final results of a safety and feasibility trial within the Veterans Affairs Pittsburgh Healthcare System. Nutr Metab (Lond). 2016;13:52. Published 2016 Aug 12. doi:10.1186/s12986-016-0113-y
2. Talib WH, Mahmod AI, Kamal A, et al. Ketogenic diet in cancer prevention and therapy: molecular targets and therapeutic opportunities. Curr Issues Mol Biol. 2021;43(2):558-589. Published 2021 Jul 3. doi:10.3390/cimb43020042
3. Tan-Shalaby J. Ketogenic diets and cancer: emerging evidence. Fed Pract. 2017;34(suppl 1):37S-42S.
4. Cortez NE, Mackenzie GG. Ketogenic diets in pancreatic cancer and associated cachexia: cellular mechanisms and clinical perspectives. Nutrients. 2021;13(9):3202. Published 2021 Sep 15. doi:10.3390/nu13093202
5. Tabernero J, Grothey A, Van Cutsem E, et al. Encorafenib plus cetuximab as a new standard of care for previously treated BRAF V600E-mutant metastatic colorectal cancer: updated survival results and subgroup analyses from the BEACON study. J Clin Oncol. 2021;39(4):273-284. doi:10.1200/JCO.20.02088
6. André T, Lonardi S, Wong KYM, et al. Nivolumab plus low-dose ipilimumab in previously treated patients with microsatellite instability-high/mismatch repair-deficient metastatic colorectal cancer: 4-year follow-up from CheckMate 142. Ann Oncol. 2022;33(10):1052-1060. doi:10.1016/j.annonc.2022.06.008
7. Grassi E, Corbelli J, Papiani G, Barbera MA, Gazzaneo F, Tamberi S. Current therapeutic strategies in BRAF-mutant metastatic colorectal cancer. Front Oncol. 2021;11:601722. Published 2021 Jun 23. doi:10.3389/fonc.2021.601722
8. Seyfried TN, Mukherjee P, Iyikesici MS, et al. Consideration of ketogenic metabolic therapy as a complementary or alternative approach for managing breast cancer. Front Nutr. 2020;7:21. Published 2020 Mar 11. doi:10.3389/fnut.2020.00021
9. Meidenbauer JJ, Mukherjee P, Seyfried TN. The glucose ketone index calculator: a simple tool to monitor therapeutic efficacy for metabolic management of brain cancer. Nutr Metab (Lond). 2015;12:12. Published 2015 Mar 11. doi:10.1186/s12986-015-0009-2
10. Fayers P, Bottomley A; EORTC Quality of Life Group; Quality of Life Unit. Quality of life research within the EORTC-the EORTC QLQ-C30. European Organisation for Research and Treatment of Cancer. Eur J Cancer. 2002;38(suppl 4):S125-S133. doi:10.1016/s0959-8049(01)00448-8
11. Yang J, Nie J, Ma X, Wei Y, Peng Y, Wei X. Targeting PI3K in cancer: mechanisms and advances in clinical trials. Mol Cancer. 2019;18(1):26. Published 2019 Feb 19. doi:10.1186/s12943-019-0954-x
12. Goncalves MD, Hopkins BD, Cantley LC. Phosphatidylinositol 3-kinase, growth disorders, and cancer. N Engl J Med. 2018;379(21):2052-2062. doi:10.1056/NEJMra1704560
13. Weber DD, Aminzadeh-Gohari S, Tulipan J, Catalano L, Feichtinger RG, Kofler B. Ketogenic diet in the treatment of cancer-where do we stand?. Mol Metab. 2020;33:102-121. doi:10.1016/j.molmet.2019.06.026
14. Yang L, TeSlaa T, Ng S, et al. Ketogenic diet and chemotherapy combine to disrupt pancreatic cancer metabolism and growth. Med. 2022;3(2):119-136. doi:10.1016/j.medj.2021.12.008
15. Furukawa K, Shigematus K, Iwase Y, et al. Clinical effects of one year of chemotherapy with a modified medium-chain triglyceride ketogenic diet on the recurrence of stage IV colon cancer. J Clin Oncol. 2018;36(suppl 15):e15709. doi:10.1200/JCO.2018.36.15_suppl.e15709
16. Zhang X, Li H, Lv X, et al. Impact of diets on response to immune checkpoint inhibitors (ICIs) therapy against tumors. Life (Basel). 2022;12(3):409. Published 2022 Mar 11. doi:10.3390/life12030409
17. Liman, A, Hwang A, Means J, Newson J. Ketogenic diet and cancer: a case report and feasibility study at VA Central California Healthcare System. Fed Pract. 2022;39(suppl 4):S18.
1. Tan-Shalaby JL, Carrick J, Edinger K, et al. Modified Atkins diet in advanced malignancies-final results of a safety and feasibility trial within the Veterans Affairs Pittsburgh Healthcare System. Nutr Metab (Lond). 2016;13:52. Published 2016 Aug 12. doi:10.1186/s12986-016-0113-y
2. Talib WH, Mahmod AI, Kamal A, et al. Ketogenic diet in cancer prevention and therapy: molecular targets and therapeutic opportunities. Curr Issues Mol Biol. 2021;43(2):558-589. Published 2021 Jul 3. doi:10.3390/cimb43020042
3. Tan-Shalaby J. Ketogenic diets and cancer: emerging evidence. Fed Pract. 2017;34(suppl 1):37S-42S.
4. Cortez NE, Mackenzie GG. Ketogenic diets in pancreatic cancer and associated cachexia: cellular mechanisms and clinical perspectives. Nutrients. 2021;13(9):3202. Published 2021 Sep 15. doi:10.3390/nu13093202
5. Tabernero J, Grothey A, Van Cutsem E, et al. Encorafenib plus cetuximab as a new standard of care for previously treated BRAF V600E-mutant metastatic colorectal cancer: updated survival results and subgroup analyses from the BEACON study. J Clin Oncol. 2021;39(4):273-284. doi:10.1200/JCO.20.02088
6. André T, Lonardi S, Wong KYM, et al. Nivolumab plus low-dose ipilimumab in previously treated patients with microsatellite instability-high/mismatch repair-deficient metastatic colorectal cancer: 4-year follow-up from CheckMate 142. Ann Oncol. 2022;33(10):1052-1060. doi:10.1016/j.annonc.2022.06.008
7. Grassi E, Corbelli J, Papiani G, Barbera MA, Gazzaneo F, Tamberi S. Current therapeutic strategies in BRAF-mutant metastatic colorectal cancer. Front Oncol. 2021;11:601722. Published 2021 Jun 23. doi:10.3389/fonc.2021.601722
8. Seyfried TN, Mukherjee P, Iyikesici MS, et al. Consideration of ketogenic metabolic therapy as a complementary or alternative approach for managing breast cancer. Front Nutr. 2020;7:21. Published 2020 Mar 11. doi:10.3389/fnut.2020.00021
9. Meidenbauer JJ, Mukherjee P, Seyfried TN. The glucose ketone index calculator: a simple tool to monitor therapeutic efficacy for metabolic management of brain cancer. Nutr Metab (Lond). 2015;12:12. Published 2015 Mar 11. doi:10.1186/s12986-015-0009-2
10. Fayers P, Bottomley A; EORTC Quality of Life Group; Quality of Life Unit. Quality of life research within the EORTC-the EORTC QLQ-C30. European Organisation for Research and Treatment of Cancer. Eur J Cancer. 2002;38(suppl 4):S125-S133. doi:10.1016/s0959-8049(01)00448-8
11. Yang J, Nie J, Ma X, Wei Y, Peng Y, Wei X. Targeting PI3K in cancer: mechanisms and advances in clinical trials. Mol Cancer. 2019;18(1):26. Published 2019 Feb 19. doi:10.1186/s12943-019-0954-x
12. Goncalves MD, Hopkins BD, Cantley LC. Phosphatidylinositol 3-kinase, growth disorders, and cancer. N Engl J Med. 2018;379(21):2052-2062. doi:10.1056/NEJMra1704560
13. Weber DD, Aminzadeh-Gohari S, Tulipan J, Catalano L, Feichtinger RG, Kofler B. Ketogenic diet in the treatment of cancer-where do we stand?. Mol Metab. 2020;33:102-121. doi:10.1016/j.molmet.2019.06.026
14. Yang L, TeSlaa T, Ng S, et al. Ketogenic diet and chemotherapy combine to disrupt pancreatic cancer metabolism and growth. Med. 2022;3(2):119-136. doi:10.1016/j.medj.2021.12.008
15. Furukawa K, Shigematus K, Iwase Y, et al. Clinical effects of one year of chemotherapy with a modified medium-chain triglyceride ketogenic diet on the recurrence of stage IV colon cancer. J Clin Oncol. 2018;36(suppl 15):e15709. doi:10.1200/JCO.2018.36.15_suppl.e15709
16. Zhang X, Li H, Lv X, et al. Impact of diets on response to immune checkpoint inhibitors (ICIs) therapy against tumors. Life (Basel). 2022;12(3):409. Published 2022 Mar 11. doi:10.3390/life12030409
17. Liman, A, Hwang A, Means J, Newson J. Ketogenic diet and cancer: a case report and feasibility study at VA Central California Healthcare System. Fed Pract. 2022;39(suppl 4):S18.
A Case Series of Rare Immune-Mediated Adverse Reactions at the New Mexico Veterans Affairs Medical Center
Immune checkpoint inhibitors (ICIs), often broadly referred to as immunotherapy, are being prescribed at increasing rates due to their effectiveness in treating a growing number of advanced solid tumors and hematologic malignancies.1 It has been well established that T-cell signaling mechanisms designed to combat foreign pathogens have been involved in the mitigation of tumor proliferation.2 This protective process can be supported or restricted by infection, medication, or mutations.
ICIs support T-cell–mediated destruction of tumor cells by inhibiting the mechanisms designed to limit autoimmunity, specifically the programmed cell death protein 1/programmed cell death ligand 1 (PD-1/PD-L1) and cytotoxic T-lymphocyte–associated antigen 4 (CTLA-4) pathways. The results have been impressive, leading to an expansive number of US Food and Drug Administration (FDA) approvals across a diverse set of malignancies. Consequently, the Nobel Prize in Physiology or Medicine was awarded for such work in 2018.3
BACKGROUND
While altering these pathways has been shown to hinder tumor growth, the lesser restrictions on the immune system can drive unwanted autoimmune inflammation to host tissue. These toxicities are collectively known as immune-mediated adverse reactions (IMARs). Clinically and histologically, IMARs frequently manifest similarly to other autoimmune conditions and may affect any organ, including skin, liver, lungs, heart, intestine (small and large), kidneys, eyes, endocrine glands, and neurologic tissue.4,5 According to recent studies, as many as 20% to 30% of patients receiving a single ICI will experience at least 1 clinically significant IMAR, and about 13% are classified as severe; however, < 10% of patients will have their ICIs discontinued due to these reactions.6
Though infrequent, a thorough understanding of the severity of IMARs to ICIs is critical for the diagnosis and management of these organ-threatening and potentially life-threatening toxicities. With the growing use of these agents and more FDA approvals for dual checkpoint blockage (concurrent use of CTLA-4 and PD-1/PD-L1 inhibitors), the absolute number of IMARs is expected to rise, thereby leading to more exposure of such events to both oncology and nononcology clinicians. Prior literature has clearly described the treatments and outcomes for many common severe toxicities; however, information regarding presentations and outcomes for rare IMARs is lacking.7
A few fascinating cases of rare toxicities have been observed at the New Mexico Veterans Affairs Medical Center (NMVAMC) in Albuquerque despite its relatively small size compared with other US Department of Veterans Affairs medical centers. As such, herein, the diagnostic evaluation, treatments, and outcomes of rare IMARs are reported for each case, and the related literature is reviewed.
Patient Selection
Patients who were required to discontinue or postpone treatment with any ICI blocking the CTLA-4 (ipilimumab), PD-1 (pembrolizumab, nivolumab, cemiplimab), or PD-L1 (atezolizumab, avelumab, durvalumab) pathways between 2015 to 2021 due to toxicity at the NMVAMC were eligible for inclusion. The electronic health record was reviewed for each eligible case, and the patient demographics, disease characteristics, toxicities, and outcomes were documented for each patient. For the 57 patients who received ICIs within the chosen period, 11 required a treatment break or discontinuation. Of these, 3 cases were selected for reporting due to the rare IMARs observed. This study was approved by the NMVAMC Institutional Review Board.
Case 1: Myocarditis
An 84-year-old man receiving a chemoimmunotherapy regimen consisting of carboplatin, pemetrexed, and pembrolizumab for recurrent, stage IV lung adenocarcinoma developed grade 4 cardiomyopathy, as defined by the Common Terminology Criteria for Adverse Events (CTCAE) v5.0, during his treatment.8 He was treated for 2 cycles before he began experiencing an increase in liver enzymes.
The patient’s presentation was concerning for myocarditis, and he was quickly admitted to NMVAMC. Cardiac catheterization did not reveal any signs of coronary occlusive disease. Prednisone 1 mg/kg was administered immediately; however, given continued chest pain and volume overload, he was quickly transitioned to solumedrol 1000 mg IV daily. After the initiation of his treatment, the patient’s transaminitis began to resolve, and troponin levels began to decrease; however, his symptoms continued to worsen, and his troponin rose again. By the fourth day of hospitalization, the patient was treated with infliximab, a tumor necrosis factor-α inhibitor shown to reverse ICI-induced autoimmune inflammation, with only mild improvement of his symptoms. The patient’s condition continued to deteriorate, his troponin levels remained elevated, and his family decided to withhold additional treatment. The patient died shortly thereafter.
Discussion
Cardiotoxicity resulting from ICI therapy is far less common than the other potential severe toxicities associated with ICIs. Nevertheless, many cases of ICI-induced cardiac inflammation have been reported, and it has been widely established that patients treated with ICIs are generally at higher risk for acute coronary syndrome.9-11 Acute cardiotoxicity secondary to autoimmune destruction of cardiac tissue includes myocarditis, pericarditis, and vasculitis, which may manifest with symptoms of heart failure and/or arrhythmia. Grading of ICI-induced cardiomyopathy has been defined by both CTCAE and the American Society of Clinical Oncology (ASCO), with grade 4 representing moderate to severe clinical decompensation requiring IV medications in the setting of life-threatening conditions.
Review articles have described the treatment options for severe cases.7,12 As detailed in prior reports, once ICI-induced cardiomyopathy is suspected, urgent admission and immediate evaluation to rule out acute coronary syndrome should be undertaken. Given the potential for deterioration despite the occasional insidious onset, aggressive cardiac monitoring, and close follow-up to measure response to interventions should be undertaken.
Case 2: Uveitis
A 70-year-old man who received pembrolizumab as a bladder-sparing approach for his superficial bladder cancer refractory to intravesical treatments developed uveitis. Approximately 3 months following the initiation of treatment, the patient reported bilateral itchy eyes, erythema, and tearing. He had a known history of allergic conjunctivitis that predated the ICI therapy, and consequently, it was unclear whether his symptoms were reflective of a more concerning issue. The patient’s symptoms continued to wax and wane for a few months, prompting a referral to ophthalmology colleagues at NMVAMC.
Ophthalmology evaluation identified uveitic glaucoma in the setting of his underlying chronic glaucoma. Pembrolizumab was discontinued, and the patient was counseled on choosing either cystectomy or locoregional therapies if further tumors arose. However, within a few weeks of administering topical steroid drops, his symptoms markedly improved, and he wished to be restarted on pembrolizumab. His uveitis remained in remission, and he has been treated with pembrolizumab for more than 1 year since this episode. He has had no clear findings of superficial bladder cancer recurrence while receiving ICI therapy.
Discussion
Uveitis is a known complication of pembrolizumab, and it has been shown to occur in 1% of patients with this treatment.13,14 It should be noted that most of the studies of this IMAR occurred in patients with metastatic melanoma; therefore the rate of this condition in other patients is less understood. Overall, ocular IMARs secondary to anti-PD-1 and anti-PD-L1 therapies are rare.
The most common IMAR is surface ocular disease, consisting of dry eye disease (DED), conjunctivitis, uveitis, and keratitis. Of these, the most common ocular surface disease is DED, which occurred in 1% to 4% of patients treated with ICI therapy; most of these reactions are mild and self-limiting.15 Atezolizumab has the highest association with ocular inflammation and ipilimumab has the highest association with uveitis, with reported odds ratios of 18.89 and 10.54, respectively.16 Treatment of ICI-induced uveitis generally includes topical steroids and treatment discontinuation or break.17 Oral or IV steroids, infliximab, and procedural involvement may be considered in refractory cases or those initially presenting with marked vision loss. Close communication with ophthalmology colleagues to monitor visual acuity and ocular pressure multiple times weekly during the acute phase is required for treatment titration.
Case 3: Organizing Pneumonia
A man aged 63 years was diagnosed with malignant mesothelioma after incidentally noting a pleural effusion and thickening on routine low-dose computed tomography surveillance of pulmonary nodules. A biopsy was performed and was consistent with mesothelioma, and the patient was started on nivolumab (PD-1 inhibitor) and ipilimumab (CTLA-4 inhibitor). The patient was initiated on dual ICIs, and after 6 months of therapy, he had a promising complete response. However, after 9 months of therapy, he developed a new left upper lobe (LUL) pleural-based lesion (Figure 2A).
A biopsy was performed, and the histopathologic appearance was consistent with organizing pneumonia (OP) (Figure 3).
Discussion
ICIs can uncommonly drive pneumonitis, with the frequency adjusted based on the number of ICIs prescribed and the primary cancer involved. Across all cancers, up to 5% of patients treated with single-agent ICI therapy may experience pneumonitis, though often the findings may simply be radiographic without symptoms. Moreover, up to 10% of patients undergoing treatment for pulmonary cancer or those with dual ICI treatment regimens experience radiographic and/or clinical pneumonitis.18 The clinical manifestations include a broad spectrum of respiratory symptoms. Given the convoluting concerns of cancer progression and infection, a biopsy is often obtained. Histopathologic findings of pneumonitis may include diffuse alveolar damage and/or interstitial lung disease, with OP being a rare variant of ILD.
Among pulmonologists, OP is felt to have polymorphous imaging findings, and biopsy is required to confirm histology; however, histopathology cannot define etiology, and consequently, OP is somewhat of an umbrella diagnosis. The condition can be cryptogenic (idiopathic) or secondary to a multitude of conditions (infection, drug toxicity, or systemic disease). It is classically described as polypoid aggregations of fibroblasts that obstruct the alveolar spaces.19 This histopathologic pattern was demonstrated in our patient’s lung biopsy. Given a prior case description of ICIs, mesothelioma, OP development, and the unremarkable infectious workup, we felt that the patient’s OP was driven by his dual ICI therapy, thereby leading to the ultimate discontinuation of his ICIs and initiation of steroids.20 Thankfully, the patient had already obtained a complete response to his ICIs, and hopefully, he can attain a durable remission with the addition of maintenance chemotherapy.
CONCLUSIONS
ICIs have revolutionized the treatment of a myriad of solid tumors and hematologic malignancies, and their use internationally is expected to increase. With the alteration in immunology pathways, clinicians in all fields will need to be familiarized with IMARs secondary to these agents, including rare subtypes. In addition, the variability in presentations relative to the patients’ treatment course was significant (between 2-9 months), and this highlights that these IMARs can occur at any time point and clinicians should be ever vigilant to spot symptoms in their patients.
It was unexpected for the 3 aforementioned rare toxicities to arise at NMVAMC among only 57 treated patients, and we speculate that these findings may have been observed for 1 of 3 reasons. First, caring for 3 patients with this collection of rare toxicities may have been due to chance. Second, though there is sparse literature studying the topic, the regional environment, including sunlight exposure and air quality, may play a role in the development of one or all of these rare toxicities. Third, rates of these toxicities may be underreported in the literature or attributed to other conditions rather than due to ICIs at other sites, and the uncommon nature of these IMARs may be overstated. Investigations evaluating rates of toxicities, including those traditionally uncommonly seen, based on regional location should be conducted before any further conclusions are drawn.
1. Bagchi S, Yuan R, Engleman EG. Immune checkpoint inhibitors for the treatment of cancer: clinical impact and mechanisms of response and resistance. Published online 2020. doi:10.1146/annurev-pathol-042020
2. Chen DS, Mellman I. Oncology meets immunology: The cancer-immunity cycle. Immunity. 2013;39(1):1-10. doi:10.1016/j.immuni.2013.07.012
3. Smyth MJ, Teng MWL. 2018 Nobel Prize in physiology or medicine. Clin Transl Immunology. 2018;7(10). doi:10.1002/cti2.1041
4. Baxi S, Yang A, Gennarelli RL, et al. Immune-related adverse events for anti-PD-1 and anti-PD-L1 drugs: Systematic review and meta-analysis. BMJ (Online). 2018;360. doi:10.1136/bmj.k793
5. Ellithi M, Elnair R, Chang GV, Abdallah MA. Toxicities of immune checkpoint inhibitors: itis-ending adverse reactions and more. Cureus. Published online February 10, 2020. doi:10.7759/cureus.6935
6. Berti A, Bortolotti R, Dipasquale M, et al. Meta-analysis of immune-related adverse events in phase 3 clinical trials assessing immune checkpoint inhibitors for lung cancer. Crit Rev Oncol Hematol. 2021;162. doi:10.1016/j.critrevonc.2021.103351
7. Davies M, Duffield EA. Safety of checkpoint inhibitors for cancer treatment: strategies for patient monitoring and management of immune-mediated adverse events. Immunotargets Ther. 2017;Volume 6:51-71. doi:10.2147/itt.s141577
8. US Department of Health and Human Services. Common Terminology Criteria for Adverse Events V5.0. Accessed July 17, 2023. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5584920/
9. Johnson DB, Balko JM, Compton ML, et al. Fulminant myocarditis with combination immune checkpoint blockade. N Engl J Med. 2016;375(18):1749-1755. doi:10.1056/nejmoa1609214
10. Mahmood SS, Fradley MG, Cohen J V., et al. Myocarditis in patients treated with immune checkpoint inhibitors. J Am Coll Cardiol. 2018;71(16):1755-1764. doi:10.1016/j.jacc.2018.02.037
11. Wang DY, Salem JE, Cohen JV, et al. Fatal toxic effects associated with immune checkpoint inhibitors: a systematic review and meta-analysis. JAMA Oncol. 2018;4(12):1721-1728. doi:10.1001/jamaoncol.2018.3923
12. Brahmer JR, Lacchetti C, Schneider BJ, et al; National Comprehensive Cancer Network. Management of immune-related adverse events in patients treated with immune checkpoint inhibitor therapy: American Society of Clinical Oncology Clinical Practice Guideline. J Clin Onc. 2018;36(17):1714-1768. doi:10.1200/JCO
13. Ribas A, Hamid O, Daud A, et al. Association of pembrolizumab with tumor response and survival among patients with advanced melanoma. JAMA. 2016;315:1600-1609. doi:10.1001/jama.2016.4059
14. Dalvin LA, Shields CL, Orloff M, Sato T, Shields JA. Checkpoint inhibitor immune therapy: systemic indications and ophthalmic side effects. Retina. 2018;38(6):1063-1078. doi:10.1097/IAE.0000000000002181
15. Park RB, Jain S, Han H, Park J. Ocular surface disease associated with immune checkpoint inhibitor therapy. Ocular Surface. 2021;20:115-129. doi:10.1016/j.jtos.2021.02.004
16. Fang T, Maberley DA, Etminan M. Ocular adverse events with immune checkpoint inhibitors. J Curr Ophthalmol. 2019;31(3):319-322. doi:10.1016/j.joco.2019.05.002
17. Whist E, Symes RJ, Chang JH, et al. Uveitis caused by treatment for malignant melanoma: a case series. Retin Cases Brief Rep. 2021;15(6):718-723. doi:10.1097/ICB.0000000000000876
18. Naidoo J, Wang X, Woo KM, et al. Pneumonitis in patients treated with anti-programmed death-1/programmed death ligand 1 therapy. J Clin Onc. 2017;35(7):709-717. doi:10.1200/JCO.2016.68.2005
19. Yoshikawa A, Bychkov A, Sathirareuangchai S. Other nonneoplastic conditions, acute lung injury, organizing pneumonia. Accessed July 17, 2023. https://www.pathologyoutlines.com/topic/lungnontumorboop.html
20. Kuint R, Lotem M, Neuman T, et al. Organizing pneumonia following treatment with pembrolizumab for metastatic malignant melanoma–a case report. Respir Med Case Rep. 2017;20:95-97. doi:10.1016/j.rmcr.2017.01.003
Immune checkpoint inhibitors (ICIs), often broadly referred to as immunotherapy, are being prescribed at increasing rates due to their effectiveness in treating a growing number of advanced solid tumors and hematologic malignancies.1 It has been well established that T-cell signaling mechanisms designed to combat foreign pathogens have been involved in the mitigation of tumor proliferation.2 This protective process can be supported or restricted by infection, medication, or mutations.
ICIs support T-cell–mediated destruction of tumor cells by inhibiting the mechanisms designed to limit autoimmunity, specifically the programmed cell death protein 1/programmed cell death ligand 1 (PD-1/PD-L1) and cytotoxic T-lymphocyte–associated antigen 4 (CTLA-4) pathways. The results have been impressive, leading to an expansive number of US Food and Drug Administration (FDA) approvals across a diverse set of malignancies. Consequently, the Nobel Prize in Physiology or Medicine was awarded for such work in 2018.3
BACKGROUND
While altering these pathways has been shown to hinder tumor growth, the lesser restrictions on the immune system can drive unwanted autoimmune inflammation to host tissue. These toxicities are collectively known as immune-mediated adverse reactions (IMARs). Clinically and histologically, IMARs frequently manifest similarly to other autoimmune conditions and may affect any organ, including skin, liver, lungs, heart, intestine (small and large), kidneys, eyes, endocrine glands, and neurologic tissue.4,5 According to recent studies, as many as 20% to 30% of patients receiving a single ICI will experience at least 1 clinically significant IMAR, and about 13% are classified as severe; however, < 10% of patients will have their ICIs discontinued due to these reactions.6
Though infrequent, a thorough understanding of the severity of IMARs to ICIs is critical for the diagnosis and management of these organ-threatening and potentially life-threatening toxicities. With the growing use of these agents and more FDA approvals for dual checkpoint blockage (concurrent use of CTLA-4 and PD-1/PD-L1 inhibitors), the absolute number of IMARs is expected to rise, thereby leading to more exposure of such events to both oncology and nononcology clinicians. Prior literature has clearly described the treatments and outcomes for many common severe toxicities; however, information regarding presentations and outcomes for rare IMARs is lacking.7
A few fascinating cases of rare toxicities have been observed at the New Mexico Veterans Affairs Medical Center (NMVAMC) in Albuquerque despite its relatively small size compared with other US Department of Veterans Affairs medical centers. As such, herein, the diagnostic evaluation, treatments, and outcomes of rare IMARs are reported for each case, and the related literature is reviewed.
Patient Selection
Patients who were required to discontinue or postpone treatment with any ICI blocking the CTLA-4 (ipilimumab), PD-1 (pembrolizumab, nivolumab, cemiplimab), or PD-L1 (atezolizumab, avelumab, durvalumab) pathways between 2015 to 2021 due to toxicity at the NMVAMC were eligible for inclusion. The electronic health record was reviewed for each eligible case, and the patient demographics, disease characteristics, toxicities, and outcomes were documented for each patient. For the 57 patients who received ICIs within the chosen period, 11 required a treatment break or discontinuation. Of these, 3 cases were selected for reporting due to the rare IMARs observed. This study was approved by the NMVAMC Institutional Review Board.
Case 1: Myocarditis
An 84-year-old man receiving a chemoimmunotherapy regimen consisting of carboplatin, pemetrexed, and pembrolizumab for recurrent, stage IV lung adenocarcinoma developed grade 4 cardiomyopathy, as defined by the Common Terminology Criteria for Adverse Events (CTCAE) v5.0, during his treatment.8 He was treated for 2 cycles before he began experiencing an increase in liver enzymes.
The patient’s presentation was concerning for myocarditis, and he was quickly admitted to NMVAMC. Cardiac catheterization did not reveal any signs of coronary occlusive disease. Prednisone 1 mg/kg was administered immediately; however, given continued chest pain and volume overload, he was quickly transitioned to solumedrol 1000 mg IV daily. After the initiation of his treatment, the patient’s transaminitis began to resolve, and troponin levels began to decrease; however, his symptoms continued to worsen, and his troponin rose again. By the fourth day of hospitalization, the patient was treated with infliximab, a tumor necrosis factor-α inhibitor shown to reverse ICI-induced autoimmune inflammation, with only mild improvement of his symptoms. The patient’s condition continued to deteriorate, his troponin levels remained elevated, and his family decided to withhold additional treatment. The patient died shortly thereafter.
Discussion
Cardiotoxicity resulting from ICI therapy is far less common than the other potential severe toxicities associated with ICIs. Nevertheless, many cases of ICI-induced cardiac inflammation have been reported, and it has been widely established that patients treated with ICIs are generally at higher risk for acute coronary syndrome.9-11 Acute cardiotoxicity secondary to autoimmune destruction of cardiac tissue includes myocarditis, pericarditis, and vasculitis, which may manifest with symptoms of heart failure and/or arrhythmia. Grading of ICI-induced cardiomyopathy has been defined by both CTCAE and the American Society of Clinical Oncology (ASCO), with grade 4 representing moderate to severe clinical decompensation requiring IV medications in the setting of life-threatening conditions.
Review articles have described the treatment options for severe cases.7,12 As detailed in prior reports, once ICI-induced cardiomyopathy is suspected, urgent admission and immediate evaluation to rule out acute coronary syndrome should be undertaken. Given the potential for deterioration despite the occasional insidious onset, aggressive cardiac monitoring, and close follow-up to measure response to interventions should be undertaken.
Case 2: Uveitis
A 70-year-old man who received pembrolizumab as a bladder-sparing approach for his superficial bladder cancer refractory to intravesical treatments developed uveitis. Approximately 3 months following the initiation of treatment, the patient reported bilateral itchy eyes, erythema, and tearing. He had a known history of allergic conjunctivitis that predated the ICI therapy, and consequently, it was unclear whether his symptoms were reflective of a more concerning issue. The patient’s symptoms continued to wax and wane for a few months, prompting a referral to ophthalmology colleagues at NMVAMC.
Ophthalmology evaluation identified uveitic glaucoma in the setting of his underlying chronic glaucoma. Pembrolizumab was discontinued, and the patient was counseled on choosing either cystectomy or locoregional therapies if further tumors arose. However, within a few weeks of administering topical steroid drops, his symptoms markedly improved, and he wished to be restarted on pembrolizumab. His uveitis remained in remission, and he has been treated with pembrolizumab for more than 1 year since this episode. He has had no clear findings of superficial bladder cancer recurrence while receiving ICI therapy.
Discussion
Uveitis is a known complication of pembrolizumab, and it has been shown to occur in 1% of patients with this treatment.13,14 It should be noted that most of the studies of this IMAR occurred in patients with metastatic melanoma; therefore the rate of this condition in other patients is less understood. Overall, ocular IMARs secondary to anti-PD-1 and anti-PD-L1 therapies are rare.
The most common IMAR is surface ocular disease, consisting of dry eye disease (DED), conjunctivitis, uveitis, and keratitis. Of these, the most common ocular surface disease is DED, which occurred in 1% to 4% of patients treated with ICI therapy; most of these reactions are mild and self-limiting.15 Atezolizumab has the highest association with ocular inflammation and ipilimumab has the highest association with uveitis, with reported odds ratios of 18.89 and 10.54, respectively.16 Treatment of ICI-induced uveitis generally includes topical steroids and treatment discontinuation or break.17 Oral or IV steroids, infliximab, and procedural involvement may be considered in refractory cases or those initially presenting with marked vision loss. Close communication with ophthalmology colleagues to monitor visual acuity and ocular pressure multiple times weekly during the acute phase is required for treatment titration.
Case 3: Organizing Pneumonia
A man aged 63 years was diagnosed with malignant mesothelioma after incidentally noting a pleural effusion and thickening on routine low-dose computed tomography surveillance of pulmonary nodules. A biopsy was performed and was consistent with mesothelioma, and the patient was started on nivolumab (PD-1 inhibitor) and ipilimumab (CTLA-4 inhibitor). The patient was initiated on dual ICIs, and after 6 months of therapy, he had a promising complete response. However, after 9 months of therapy, he developed a new left upper lobe (LUL) pleural-based lesion (Figure 2A).
A biopsy was performed, and the histopathologic appearance was consistent with organizing pneumonia (OP) (Figure 3).
Discussion
ICIs can uncommonly drive pneumonitis, with the frequency adjusted based on the number of ICIs prescribed and the primary cancer involved. Across all cancers, up to 5% of patients treated with single-agent ICI therapy may experience pneumonitis, though often the findings may simply be radiographic without symptoms. Moreover, up to 10% of patients undergoing treatment for pulmonary cancer or those with dual ICI treatment regimens experience radiographic and/or clinical pneumonitis.18 The clinical manifestations include a broad spectrum of respiratory symptoms. Given the convoluting concerns of cancer progression and infection, a biopsy is often obtained. Histopathologic findings of pneumonitis may include diffuse alveolar damage and/or interstitial lung disease, with OP being a rare variant of ILD.
Among pulmonologists, OP is felt to have polymorphous imaging findings, and biopsy is required to confirm histology; however, histopathology cannot define etiology, and consequently, OP is somewhat of an umbrella diagnosis. The condition can be cryptogenic (idiopathic) or secondary to a multitude of conditions (infection, drug toxicity, or systemic disease). It is classically described as polypoid aggregations of fibroblasts that obstruct the alveolar spaces.19 This histopathologic pattern was demonstrated in our patient’s lung biopsy. Given a prior case description of ICIs, mesothelioma, OP development, and the unremarkable infectious workup, we felt that the patient’s OP was driven by his dual ICI therapy, thereby leading to the ultimate discontinuation of his ICIs and initiation of steroids.20 Thankfully, the patient had already obtained a complete response to his ICIs, and hopefully, he can attain a durable remission with the addition of maintenance chemotherapy.
CONCLUSIONS
ICIs have revolutionized the treatment of a myriad of solid tumors and hematologic malignancies, and their use internationally is expected to increase. With the alteration in immunology pathways, clinicians in all fields will need to be familiarized with IMARs secondary to these agents, including rare subtypes. In addition, the variability in presentations relative to the patients’ treatment course was significant (between 2-9 months), and this highlights that these IMARs can occur at any time point and clinicians should be ever vigilant to spot symptoms in their patients.
It was unexpected for the 3 aforementioned rare toxicities to arise at NMVAMC among only 57 treated patients, and we speculate that these findings may have been observed for 1 of 3 reasons. First, caring for 3 patients with this collection of rare toxicities may have been due to chance. Second, though there is sparse literature studying the topic, the regional environment, including sunlight exposure and air quality, may play a role in the development of one or all of these rare toxicities. Third, rates of these toxicities may be underreported in the literature or attributed to other conditions rather than due to ICIs at other sites, and the uncommon nature of these IMARs may be overstated. Investigations evaluating rates of toxicities, including those traditionally uncommonly seen, based on regional location should be conducted before any further conclusions are drawn.
Immune checkpoint inhibitors (ICIs), often broadly referred to as immunotherapy, are being prescribed at increasing rates due to their effectiveness in treating a growing number of advanced solid tumors and hematologic malignancies.1 It has been well established that T-cell signaling mechanisms designed to combat foreign pathogens have been involved in the mitigation of tumor proliferation.2 This protective process can be supported or restricted by infection, medication, or mutations.
ICIs support T-cell–mediated destruction of tumor cells by inhibiting the mechanisms designed to limit autoimmunity, specifically the programmed cell death protein 1/programmed cell death ligand 1 (PD-1/PD-L1) and cytotoxic T-lymphocyte–associated antigen 4 (CTLA-4) pathways. The results have been impressive, leading to an expansive number of US Food and Drug Administration (FDA) approvals across a diverse set of malignancies. Consequently, the Nobel Prize in Physiology or Medicine was awarded for such work in 2018.3
BACKGROUND
While altering these pathways has been shown to hinder tumor growth, the lesser restrictions on the immune system can drive unwanted autoimmune inflammation to host tissue. These toxicities are collectively known as immune-mediated adverse reactions (IMARs). Clinically and histologically, IMARs frequently manifest similarly to other autoimmune conditions and may affect any organ, including skin, liver, lungs, heart, intestine (small and large), kidneys, eyes, endocrine glands, and neurologic tissue.4,5 According to recent studies, as many as 20% to 30% of patients receiving a single ICI will experience at least 1 clinically significant IMAR, and about 13% are classified as severe; however, < 10% of patients will have their ICIs discontinued due to these reactions.6
Though infrequent, a thorough understanding of the severity of IMARs to ICIs is critical for the diagnosis and management of these organ-threatening and potentially life-threatening toxicities. With the growing use of these agents and more FDA approvals for dual checkpoint blockage (concurrent use of CTLA-4 and PD-1/PD-L1 inhibitors), the absolute number of IMARs is expected to rise, thereby leading to more exposure of such events to both oncology and nononcology clinicians. Prior literature has clearly described the treatments and outcomes for many common severe toxicities; however, information regarding presentations and outcomes for rare IMARs is lacking.7
A few fascinating cases of rare toxicities have been observed at the New Mexico Veterans Affairs Medical Center (NMVAMC) in Albuquerque despite its relatively small size compared with other US Department of Veterans Affairs medical centers. As such, herein, the diagnostic evaluation, treatments, and outcomes of rare IMARs are reported for each case, and the related literature is reviewed.
Patient Selection
Patients who were required to discontinue or postpone treatment with any ICI blocking the CTLA-4 (ipilimumab), PD-1 (pembrolizumab, nivolumab, cemiplimab), or PD-L1 (atezolizumab, avelumab, durvalumab) pathways between 2015 to 2021 due to toxicity at the NMVAMC were eligible for inclusion. The electronic health record was reviewed for each eligible case, and the patient demographics, disease characteristics, toxicities, and outcomes were documented for each patient. For the 57 patients who received ICIs within the chosen period, 11 required a treatment break or discontinuation. Of these, 3 cases were selected for reporting due to the rare IMARs observed. This study was approved by the NMVAMC Institutional Review Board.
Case 1: Myocarditis
An 84-year-old man receiving a chemoimmunotherapy regimen consisting of carboplatin, pemetrexed, and pembrolizumab for recurrent, stage IV lung adenocarcinoma developed grade 4 cardiomyopathy, as defined by the Common Terminology Criteria for Adverse Events (CTCAE) v5.0, during his treatment.8 He was treated for 2 cycles before he began experiencing an increase in liver enzymes.
The patient’s presentation was concerning for myocarditis, and he was quickly admitted to NMVAMC. Cardiac catheterization did not reveal any signs of coronary occlusive disease. Prednisone 1 mg/kg was administered immediately; however, given continued chest pain and volume overload, he was quickly transitioned to solumedrol 1000 mg IV daily. After the initiation of his treatment, the patient’s transaminitis began to resolve, and troponin levels began to decrease; however, his symptoms continued to worsen, and his troponin rose again. By the fourth day of hospitalization, the patient was treated with infliximab, a tumor necrosis factor-α inhibitor shown to reverse ICI-induced autoimmune inflammation, with only mild improvement of his symptoms. The patient’s condition continued to deteriorate, his troponin levels remained elevated, and his family decided to withhold additional treatment. The patient died shortly thereafter.
Discussion
Cardiotoxicity resulting from ICI therapy is far less common than the other potential severe toxicities associated with ICIs. Nevertheless, many cases of ICI-induced cardiac inflammation have been reported, and it has been widely established that patients treated with ICIs are generally at higher risk for acute coronary syndrome.9-11 Acute cardiotoxicity secondary to autoimmune destruction of cardiac tissue includes myocarditis, pericarditis, and vasculitis, which may manifest with symptoms of heart failure and/or arrhythmia. Grading of ICI-induced cardiomyopathy has been defined by both CTCAE and the American Society of Clinical Oncology (ASCO), with grade 4 representing moderate to severe clinical decompensation requiring IV medications in the setting of life-threatening conditions.
Review articles have described the treatment options for severe cases.7,12 As detailed in prior reports, once ICI-induced cardiomyopathy is suspected, urgent admission and immediate evaluation to rule out acute coronary syndrome should be undertaken. Given the potential for deterioration despite the occasional insidious onset, aggressive cardiac monitoring, and close follow-up to measure response to interventions should be undertaken.
Case 2: Uveitis
A 70-year-old man who received pembrolizumab as a bladder-sparing approach for his superficial bladder cancer refractory to intravesical treatments developed uveitis. Approximately 3 months following the initiation of treatment, the patient reported bilateral itchy eyes, erythema, and tearing. He had a known history of allergic conjunctivitis that predated the ICI therapy, and consequently, it was unclear whether his symptoms were reflective of a more concerning issue. The patient’s symptoms continued to wax and wane for a few months, prompting a referral to ophthalmology colleagues at NMVAMC.
Ophthalmology evaluation identified uveitic glaucoma in the setting of his underlying chronic glaucoma. Pembrolizumab was discontinued, and the patient was counseled on choosing either cystectomy or locoregional therapies if further tumors arose. However, within a few weeks of administering topical steroid drops, his symptoms markedly improved, and he wished to be restarted on pembrolizumab. His uveitis remained in remission, and he has been treated with pembrolizumab for more than 1 year since this episode. He has had no clear findings of superficial bladder cancer recurrence while receiving ICI therapy.
Discussion
Uveitis is a known complication of pembrolizumab, and it has been shown to occur in 1% of patients with this treatment.13,14 It should be noted that most of the studies of this IMAR occurred in patients with metastatic melanoma; therefore the rate of this condition in other patients is less understood. Overall, ocular IMARs secondary to anti-PD-1 and anti-PD-L1 therapies are rare.
The most common IMAR is surface ocular disease, consisting of dry eye disease (DED), conjunctivitis, uveitis, and keratitis. Of these, the most common ocular surface disease is DED, which occurred in 1% to 4% of patients treated with ICI therapy; most of these reactions are mild and self-limiting.15 Atezolizumab has the highest association with ocular inflammation and ipilimumab has the highest association with uveitis, with reported odds ratios of 18.89 and 10.54, respectively.16 Treatment of ICI-induced uveitis generally includes topical steroids and treatment discontinuation or break.17 Oral or IV steroids, infliximab, and procedural involvement may be considered in refractory cases or those initially presenting with marked vision loss. Close communication with ophthalmology colleagues to monitor visual acuity and ocular pressure multiple times weekly during the acute phase is required for treatment titration.
Case 3: Organizing Pneumonia
A man aged 63 years was diagnosed with malignant mesothelioma after incidentally noting a pleural effusion and thickening on routine low-dose computed tomography surveillance of pulmonary nodules. A biopsy was performed and was consistent with mesothelioma, and the patient was started on nivolumab (PD-1 inhibitor) and ipilimumab (CTLA-4 inhibitor). The patient was initiated on dual ICIs, and after 6 months of therapy, he had a promising complete response. However, after 9 months of therapy, he developed a new left upper lobe (LUL) pleural-based lesion (Figure 2A).
A biopsy was performed, and the histopathologic appearance was consistent with organizing pneumonia (OP) (Figure 3).
Discussion
ICIs can uncommonly drive pneumonitis, with the frequency adjusted based on the number of ICIs prescribed and the primary cancer involved. Across all cancers, up to 5% of patients treated with single-agent ICI therapy may experience pneumonitis, though often the findings may simply be radiographic without symptoms. Moreover, up to 10% of patients undergoing treatment for pulmonary cancer or those with dual ICI treatment regimens experience radiographic and/or clinical pneumonitis.18 The clinical manifestations include a broad spectrum of respiratory symptoms. Given the convoluting concerns of cancer progression and infection, a biopsy is often obtained. Histopathologic findings of pneumonitis may include diffuse alveolar damage and/or interstitial lung disease, with OP being a rare variant of ILD.
Among pulmonologists, OP is felt to have polymorphous imaging findings, and biopsy is required to confirm histology; however, histopathology cannot define etiology, and consequently, OP is somewhat of an umbrella diagnosis. The condition can be cryptogenic (idiopathic) or secondary to a multitude of conditions (infection, drug toxicity, or systemic disease). It is classically described as polypoid aggregations of fibroblasts that obstruct the alveolar spaces.19 This histopathologic pattern was demonstrated in our patient’s lung biopsy. Given a prior case description of ICIs, mesothelioma, OP development, and the unremarkable infectious workup, we felt that the patient’s OP was driven by his dual ICI therapy, thereby leading to the ultimate discontinuation of his ICIs and initiation of steroids.20 Thankfully, the patient had already obtained a complete response to his ICIs, and hopefully, he can attain a durable remission with the addition of maintenance chemotherapy.
CONCLUSIONS
ICIs have revolutionized the treatment of a myriad of solid tumors and hematologic malignancies, and their use internationally is expected to increase. With the alteration in immunology pathways, clinicians in all fields will need to be familiarized with IMARs secondary to these agents, including rare subtypes. In addition, the variability in presentations relative to the patients’ treatment course was significant (between 2-9 months), and this highlights that these IMARs can occur at any time point and clinicians should be ever vigilant to spot symptoms in their patients.
It was unexpected for the 3 aforementioned rare toxicities to arise at NMVAMC among only 57 treated patients, and we speculate that these findings may have been observed for 1 of 3 reasons. First, caring for 3 patients with this collection of rare toxicities may have been due to chance. Second, though there is sparse literature studying the topic, the regional environment, including sunlight exposure and air quality, may play a role in the development of one or all of these rare toxicities. Third, rates of these toxicities may be underreported in the literature or attributed to other conditions rather than due to ICIs at other sites, and the uncommon nature of these IMARs may be overstated. Investigations evaluating rates of toxicities, including those traditionally uncommonly seen, based on regional location should be conducted before any further conclusions are drawn.
1. Bagchi S, Yuan R, Engleman EG. Immune checkpoint inhibitors for the treatment of cancer: clinical impact and mechanisms of response and resistance. Published online 2020. doi:10.1146/annurev-pathol-042020
2. Chen DS, Mellman I. Oncology meets immunology: The cancer-immunity cycle. Immunity. 2013;39(1):1-10. doi:10.1016/j.immuni.2013.07.012
3. Smyth MJ, Teng MWL. 2018 Nobel Prize in physiology or medicine. Clin Transl Immunology. 2018;7(10). doi:10.1002/cti2.1041
4. Baxi S, Yang A, Gennarelli RL, et al. Immune-related adverse events for anti-PD-1 and anti-PD-L1 drugs: Systematic review and meta-analysis. BMJ (Online). 2018;360. doi:10.1136/bmj.k793
5. Ellithi M, Elnair R, Chang GV, Abdallah MA. Toxicities of immune checkpoint inhibitors: itis-ending adverse reactions and more. Cureus. Published online February 10, 2020. doi:10.7759/cureus.6935
6. Berti A, Bortolotti R, Dipasquale M, et al. Meta-analysis of immune-related adverse events in phase 3 clinical trials assessing immune checkpoint inhibitors for lung cancer. Crit Rev Oncol Hematol. 2021;162. doi:10.1016/j.critrevonc.2021.103351
7. Davies M, Duffield EA. Safety of checkpoint inhibitors for cancer treatment: strategies for patient monitoring and management of immune-mediated adverse events. Immunotargets Ther. 2017;Volume 6:51-71. doi:10.2147/itt.s141577
8. US Department of Health and Human Services. Common Terminology Criteria for Adverse Events V5.0. Accessed July 17, 2023. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5584920/
9. Johnson DB, Balko JM, Compton ML, et al. Fulminant myocarditis with combination immune checkpoint blockade. N Engl J Med. 2016;375(18):1749-1755. doi:10.1056/nejmoa1609214
10. Mahmood SS, Fradley MG, Cohen J V., et al. Myocarditis in patients treated with immune checkpoint inhibitors. J Am Coll Cardiol. 2018;71(16):1755-1764. doi:10.1016/j.jacc.2018.02.037
11. Wang DY, Salem JE, Cohen JV, et al. Fatal toxic effects associated with immune checkpoint inhibitors: a systematic review and meta-analysis. JAMA Oncol. 2018;4(12):1721-1728. doi:10.1001/jamaoncol.2018.3923
12. Brahmer JR, Lacchetti C, Schneider BJ, et al; National Comprehensive Cancer Network. Management of immune-related adverse events in patients treated with immune checkpoint inhibitor therapy: American Society of Clinical Oncology Clinical Practice Guideline. J Clin Onc. 2018;36(17):1714-1768. doi:10.1200/JCO
13. Ribas A, Hamid O, Daud A, et al. Association of pembrolizumab with tumor response and survival among patients with advanced melanoma. JAMA. 2016;315:1600-1609. doi:10.1001/jama.2016.4059
14. Dalvin LA, Shields CL, Orloff M, Sato T, Shields JA. Checkpoint inhibitor immune therapy: systemic indications and ophthalmic side effects. Retina. 2018;38(6):1063-1078. doi:10.1097/IAE.0000000000002181
15. Park RB, Jain S, Han H, Park J. Ocular surface disease associated with immune checkpoint inhibitor therapy. Ocular Surface. 2021;20:115-129. doi:10.1016/j.jtos.2021.02.004
16. Fang T, Maberley DA, Etminan M. Ocular adverse events with immune checkpoint inhibitors. J Curr Ophthalmol. 2019;31(3):319-322. doi:10.1016/j.joco.2019.05.002
17. Whist E, Symes RJ, Chang JH, et al. Uveitis caused by treatment for malignant melanoma: a case series. Retin Cases Brief Rep. 2021;15(6):718-723. doi:10.1097/ICB.0000000000000876
18. Naidoo J, Wang X, Woo KM, et al. Pneumonitis in patients treated with anti-programmed death-1/programmed death ligand 1 therapy. J Clin Onc. 2017;35(7):709-717. doi:10.1200/JCO.2016.68.2005
19. Yoshikawa A, Bychkov A, Sathirareuangchai S. Other nonneoplastic conditions, acute lung injury, organizing pneumonia. Accessed July 17, 2023. https://www.pathologyoutlines.com/topic/lungnontumorboop.html
20. Kuint R, Lotem M, Neuman T, et al. Organizing pneumonia following treatment with pembrolizumab for metastatic malignant melanoma–a case report. Respir Med Case Rep. 2017;20:95-97. doi:10.1016/j.rmcr.2017.01.003
1. Bagchi S, Yuan R, Engleman EG. Immune checkpoint inhibitors for the treatment of cancer: clinical impact and mechanisms of response and resistance. Published online 2020. doi:10.1146/annurev-pathol-042020
2. Chen DS, Mellman I. Oncology meets immunology: The cancer-immunity cycle. Immunity. 2013;39(1):1-10. doi:10.1016/j.immuni.2013.07.012
3. Smyth MJ, Teng MWL. 2018 Nobel Prize in physiology or medicine. Clin Transl Immunology. 2018;7(10). doi:10.1002/cti2.1041
4. Baxi S, Yang A, Gennarelli RL, et al. Immune-related adverse events for anti-PD-1 and anti-PD-L1 drugs: Systematic review and meta-analysis. BMJ (Online). 2018;360. doi:10.1136/bmj.k793
5. Ellithi M, Elnair R, Chang GV, Abdallah MA. Toxicities of immune checkpoint inhibitors: itis-ending adverse reactions and more. Cureus. Published online February 10, 2020. doi:10.7759/cureus.6935
6. Berti A, Bortolotti R, Dipasquale M, et al. Meta-analysis of immune-related adverse events in phase 3 clinical trials assessing immune checkpoint inhibitors for lung cancer. Crit Rev Oncol Hematol. 2021;162. doi:10.1016/j.critrevonc.2021.103351
7. Davies M, Duffield EA. Safety of checkpoint inhibitors for cancer treatment: strategies for patient monitoring and management of immune-mediated adverse events. Immunotargets Ther. 2017;Volume 6:51-71. doi:10.2147/itt.s141577
8. US Department of Health and Human Services. Common Terminology Criteria for Adverse Events V5.0. Accessed July 17, 2023. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5584920/
9. Johnson DB, Balko JM, Compton ML, et al. Fulminant myocarditis with combination immune checkpoint blockade. N Engl J Med. 2016;375(18):1749-1755. doi:10.1056/nejmoa1609214
10. Mahmood SS, Fradley MG, Cohen J V., et al. Myocarditis in patients treated with immune checkpoint inhibitors. J Am Coll Cardiol. 2018;71(16):1755-1764. doi:10.1016/j.jacc.2018.02.037
11. Wang DY, Salem JE, Cohen JV, et al. Fatal toxic effects associated with immune checkpoint inhibitors: a systematic review and meta-analysis. JAMA Oncol. 2018;4(12):1721-1728. doi:10.1001/jamaoncol.2018.3923
12. Brahmer JR, Lacchetti C, Schneider BJ, et al; National Comprehensive Cancer Network. Management of immune-related adverse events in patients treated with immune checkpoint inhibitor therapy: American Society of Clinical Oncology Clinical Practice Guideline. J Clin Onc. 2018;36(17):1714-1768. doi:10.1200/JCO
13. Ribas A, Hamid O, Daud A, et al. Association of pembrolizumab with tumor response and survival among patients with advanced melanoma. JAMA. 2016;315:1600-1609. doi:10.1001/jama.2016.4059
14. Dalvin LA, Shields CL, Orloff M, Sato T, Shields JA. Checkpoint inhibitor immune therapy: systemic indications and ophthalmic side effects. Retina. 2018;38(6):1063-1078. doi:10.1097/IAE.0000000000002181
15. Park RB, Jain S, Han H, Park J. Ocular surface disease associated with immune checkpoint inhibitor therapy. Ocular Surface. 2021;20:115-129. doi:10.1016/j.jtos.2021.02.004
16. Fang T, Maberley DA, Etminan M. Ocular adverse events with immune checkpoint inhibitors. J Curr Ophthalmol. 2019;31(3):319-322. doi:10.1016/j.joco.2019.05.002
17. Whist E, Symes RJ, Chang JH, et al. Uveitis caused by treatment for malignant melanoma: a case series. Retin Cases Brief Rep. 2021;15(6):718-723. doi:10.1097/ICB.0000000000000876
18. Naidoo J, Wang X, Woo KM, et al. Pneumonitis in patients treated with anti-programmed death-1/programmed death ligand 1 therapy. J Clin Onc. 2017;35(7):709-717. doi:10.1200/JCO.2016.68.2005
19. Yoshikawa A, Bychkov A, Sathirareuangchai S. Other nonneoplastic conditions, acute lung injury, organizing pneumonia. Accessed July 17, 2023. https://www.pathologyoutlines.com/topic/lungnontumorboop.html
20. Kuint R, Lotem M, Neuman T, et al. Organizing pneumonia following treatment with pembrolizumab for metastatic malignant melanoma–a case report. Respir Med Case Rep. 2017;20:95-97. doi:10.1016/j.rmcr.2017.01.003
Immunotherapy stewardship could save tens of millions a year
Implementing stewardship strategies for immune checkpoint inhibitor (ICI) therapy, including personalized weight-based dosing, dose rounding, and pharmacy-level vial sharing, could generate savings of as much as $74 million each year for the Veterans Health Administration (VHA), a new analysis suggests.
That $74 million in savings would translate to nearly 14% less spent on ICI therapy annually.
first author Alex Bryant, MD, University of Michigan, Ann Arbor, said in an interview.
The study was published in Health Affairs.
ICI therapy is used in about 40 unique cancer indications and, in 2020, accounted for more than $6 billion in Medicare Part B spending.
Two of the most prescribed ICIs – pembrolizumab and nivolumab – initially received their U.S. approval at personalized weight-based doses. But at the request of the manufacturers, the Food and Drug Administration approved “one-size-fits-all” flat doses, despite a lack of data to support this strategy compared with weight-based dosing.
With a fixed dose strategy, “patients with cancer not only tend to get too high a dose of the drug, but costs go up significantly,” Daniel Goldstein, MD, a medical oncologist at the Rabin Medical Center, Petah Tikva, Israel, told this news organization last year. “Why should we give a higher dose with the same efficacy when that dose will cost significantly more and has the potential to increase adverse events?”
To compare the cost of a weight-based vs. fixed-dose strategy, Dr. Bryant and colleagues conducted a simulation analysis under four stewardship scenarios, using data from the VHA and Medicare drug prices. Strategy one looked at weight-based dosing; strategy two combined weight-based dosing and dose rounding but not single-use vial sharing; strategy three used weight-based dosing and single-use vial sharing but not dose rounding; and strategy four, the most aggressive, combined all three.
ICIs in the VHA national formulary included pembrolizumab, nivolumab, atezolizumab, durvalumab, and cemiplimab-rwlc.
Using an algorithm to extract data, the team identified 49,851 administration events in 8,276 unique patients in 2021 – just over half were pembrolizumab, nearly 23% were nivolumab, and the remaining 26% largely included atezolizumab (12.1%) and durvalumab (11.9%).
The team found that the VHA spends roughly $537 million annually on ICIs. But implementing the stewardship measures that combined weight-based dosing, dose rounding, and vial sharing could save the VHA $74 million, or about 14%, annually on ICIs.
Most of the savings came from dosing changes to pembrolizumab and nivolumab, with greater savings achieved by combining more stewardship strategies. For instance, using strategy one (weight-based dosing alone) could lead to annual pembrolizumab savings of $14 million. Adding dose rounding (strategy two) could reduce pembrolizumab spending by $24 million. And using strategy four, with an unlimited window for vial sharing, could mean annual savings of nearly $60 million.
“Our results should prompt cost-conscious systems and payers to ask whether the amounts of drugs they’re providing to patients and how they go about making those doses are the most cost-effective approaches,” said corresponding author Garth W. Strohbehn, MD, of the University of Michigan and the VA Ann Arbor Healthcare System.
Dr. Strohbehn said the prospect of adopting these strategies hinges on several factors, with financial incentives at the prescriber and medical center level likely being the most influential.
“In fee-for-service systems, reimbursement scales with the amount of drug administered, so there can be a financial disincentive to decreasing overall drug usage,” Dr. Strohbehn explained.
“Conversely, integrated systems such as Kaiser Permanente or the VHA and large self-insured employers are incentivized to contain costs and take great care of patients, so they may be more inclined to promote these strategies,” he added.
However, Adam C. Powell, PhD, president, Payer+Provider Syndicate, who wasn’t involved in the analysis, cautioned that such a shift may come with unintended consequences.
The Infrastructure, Investment, and Jobs Act of 2021 let the Centers for Medicare and Medicaid Services seek reimbursement for discarded drugs – in effect, changing the reimbursement model for medications. That led pharmaceutical manufacturers to respond in kind by changing the dosing model, Dr. Powell said.
“Drugs that previously had personalized weight-based dosing were moved to uniform flat dosing, eliminating the potential for the manufacturer to have to issue a reimbursement if the patient’s personalized dose fell short of the amount in the single-use vial,” Dr. Powell added.
If there is a substantial migration to weight-based dosing, “it is possible that pharmaceutical manufacturers will rethink their dosing and pricing models, just as happened previously,” he cautioned.
However, these strategies could also provide relief for another escalating issue: drug shortages. Especially in the current moment, having a stewardship mindset, “might be helpful in navigating drug shortages,” Dr. Strohbehn said.
This research had no commercial funding. Dr. Bryant, Dr. Strohbehn, and Dr. Powell report no relevant financial relationships.
A version of this article appeared on Medscape.com.
Implementing stewardship strategies for immune checkpoint inhibitor (ICI) therapy, including personalized weight-based dosing, dose rounding, and pharmacy-level vial sharing, could generate savings of as much as $74 million each year for the Veterans Health Administration (VHA), a new analysis suggests.
That $74 million in savings would translate to nearly 14% less spent on ICI therapy annually.
first author Alex Bryant, MD, University of Michigan, Ann Arbor, said in an interview.
The study was published in Health Affairs.
ICI therapy is used in about 40 unique cancer indications and, in 2020, accounted for more than $6 billion in Medicare Part B spending.
Two of the most prescribed ICIs – pembrolizumab and nivolumab – initially received their U.S. approval at personalized weight-based doses. But at the request of the manufacturers, the Food and Drug Administration approved “one-size-fits-all” flat doses, despite a lack of data to support this strategy compared with weight-based dosing.
With a fixed dose strategy, “patients with cancer not only tend to get too high a dose of the drug, but costs go up significantly,” Daniel Goldstein, MD, a medical oncologist at the Rabin Medical Center, Petah Tikva, Israel, told this news organization last year. “Why should we give a higher dose with the same efficacy when that dose will cost significantly more and has the potential to increase adverse events?”
To compare the cost of a weight-based vs. fixed-dose strategy, Dr. Bryant and colleagues conducted a simulation analysis under four stewardship scenarios, using data from the VHA and Medicare drug prices. Strategy one looked at weight-based dosing; strategy two combined weight-based dosing and dose rounding but not single-use vial sharing; strategy three used weight-based dosing and single-use vial sharing but not dose rounding; and strategy four, the most aggressive, combined all three.
ICIs in the VHA national formulary included pembrolizumab, nivolumab, atezolizumab, durvalumab, and cemiplimab-rwlc.
Using an algorithm to extract data, the team identified 49,851 administration events in 8,276 unique patients in 2021 – just over half were pembrolizumab, nearly 23% were nivolumab, and the remaining 26% largely included atezolizumab (12.1%) and durvalumab (11.9%).
The team found that the VHA spends roughly $537 million annually on ICIs. But implementing the stewardship measures that combined weight-based dosing, dose rounding, and vial sharing could save the VHA $74 million, or about 14%, annually on ICIs.
Most of the savings came from dosing changes to pembrolizumab and nivolumab, with greater savings achieved by combining more stewardship strategies. For instance, using strategy one (weight-based dosing alone) could lead to annual pembrolizumab savings of $14 million. Adding dose rounding (strategy two) could reduce pembrolizumab spending by $24 million. And using strategy four, with an unlimited window for vial sharing, could mean annual savings of nearly $60 million.
“Our results should prompt cost-conscious systems and payers to ask whether the amounts of drugs they’re providing to patients and how they go about making those doses are the most cost-effective approaches,” said corresponding author Garth W. Strohbehn, MD, of the University of Michigan and the VA Ann Arbor Healthcare System.
Dr. Strohbehn said the prospect of adopting these strategies hinges on several factors, with financial incentives at the prescriber and medical center level likely being the most influential.
“In fee-for-service systems, reimbursement scales with the amount of drug administered, so there can be a financial disincentive to decreasing overall drug usage,” Dr. Strohbehn explained.
“Conversely, integrated systems such as Kaiser Permanente or the VHA and large self-insured employers are incentivized to contain costs and take great care of patients, so they may be more inclined to promote these strategies,” he added.
However, Adam C. Powell, PhD, president, Payer+Provider Syndicate, who wasn’t involved in the analysis, cautioned that such a shift may come with unintended consequences.
The Infrastructure, Investment, and Jobs Act of 2021 let the Centers for Medicare and Medicaid Services seek reimbursement for discarded drugs – in effect, changing the reimbursement model for medications. That led pharmaceutical manufacturers to respond in kind by changing the dosing model, Dr. Powell said.
“Drugs that previously had personalized weight-based dosing were moved to uniform flat dosing, eliminating the potential for the manufacturer to have to issue a reimbursement if the patient’s personalized dose fell short of the amount in the single-use vial,” Dr. Powell added.
If there is a substantial migration to weight-based dosing, “it is possible that pharmaceutical manufacturers will rethink their dosing and pricing models, just as happened previously,” he cautioned.
However, these strategies could also provide relief for another escalating issue: drug shortages. Especially in the current moment, having a stewardship mindset, “might be helpful in navigating drug shortages,” Dr. Strohbehn said.
This research had no commercial funding. Dr. Bryant, Dr. Strohbehn, and Dr. Powell report no relevant financial relationships.
A version of this article appeared on Medscape.com.
Implementing stewardship strategies for immune checkpoint inhibitor (ICI) therapy, including personalized weight-based dosing, dose rounding, and pharmacy-level vial sharing, could generate savings of as much as $74 million each year for the Veterans Health Administration (VHA), a new analysis suggests.
That $74 million in savings would translate to nearly 14% less spent on ICI therapy annually.
first author Alex Bryant, MD, University of Michigan, Ann Arbor, said in an interview.
The study was published in Health Affairs.
ICI therapy is used in about 40 unique cancer indications and, in 2020, accounted for more than $6 billion in Medicare Part B spending.
Two of the most prescribed ICIs – pembrolizumab and nivolumab – initially received their U.S. approval at personalized weight-based doses. But at the request of the manufacturers, the Food and Drug Administration approved “one-size-fits-all” flat doses, despite a lack of data to support this strategy compared with weight-based dosing.
With a fixed dose strategy, “patients with cancer not only tend to get too high a dose of the drug, but costs go up significantly,” Daniel Goldstein, MD, a medical oncologist at the Rabin Medical Center, Petah Tikva, Israel, told this news organization last year. “Why should we give a higher dose with the same efficacy when that dose will cost significantly more and has the potential to increase adverse events?”
To compare the cost of a weight-based vs. fixed-dose strategy, Dr. Bryant and colleagues conducted a simulation analysis under four stewardship scenarios, using data from the VHA and Medicare drug prices. Strategy one looked at weight-based dosing; strategy two combined weight-based dosing and dose rounding but not single-use vial sharing; strategy three used weight-based dosing and single-use vial sharing but not dose rounding; and strategy four, the most aggressive, combined all three.
ICIs in the VHA national formulary included pembrolizumab, nivolumab, atezolizumab, durvalumab, and cemiplimab-rwlc.
Using an algorithm to extract data, the team identified 49,851 administration events in 8,276 unique patients in 2021 – just over half were pembrolizumab, nearly 23% were nivolumab, and the remaining 26% largely included atezolizumab (12.1%) and durvalumab (11.9%).
The team found that the VHA spends roughly $537 million annually on ICIs. But implementing the stewardship measures that combined weight-based dosing, dose rounding, and vial sharing could save the VHA $74 million, or about 14%, annually on ICIs.
Most of the savings came from dosing changes to pembrolizumab and nivolumab, with greater savings achieved by combining more stewardship strategies. For instance, using strategy one (weight-based dosing alone) could lead to annual pembrolizumab savings of $14 million. Adding dose rounding (strategy two) could reduce pembrolizumab spending by $24 million. And using strategy four, with an unlimited window for vial sharing, could mean annual savings of nearly $60 million.
“Our results should prompt cost-conscious systems and payers to ask whether the amounts of drugs they’re providing to patients and how they go about making those doses are the most cost-effective approaches,” said corresponding author Garth W. Strohbehn, MD, of the University of Michigan and the VA Ann Arbor Healthcare System.
Dr. Strohbehn said the prospect of adopting these strategies hinges on several factors, with financial incentives at the prescriber and medical center level likely being the most influential.
“In fee-for-service systems, reimbursement scales with the amount of drug administered, so there can be a financial disincentive to decreasing overall drug usage,” Dr. Strohbehn explained.
“Conversely, integrated systems such as Kaiser Permanente or the VHA and large self-insured employers are incentivized to contain costs and take great care of patients, so they may be more inclined to promote these strategies,” he added.
However, Adam C. Powell, PhD, president, Payer+Provider Syndicate, who wasn’t involved in the analysis, cautioned that such a shift may come with unintended consequences.
The Infrastructure, Investment, and Jobs Act of 2021 let the Centers for Medicare and Medicaid Services seek reimbursement for discarded drugs – in effect, changing the reimbursement model for medications. That led pharmaceutical manufacturers to respond in kind by changing the dosing model, Dr. Powell said.
“Drugs that previously had personalized weight-based dosing were moved to uniform flat dosing, eliminating the potential for the manufacturer to have to issue a reimbursement if the patient’s personalized dose fell short of the amount in the single-use vial,” Dr. Powell added.
If there is a substantial migration to weight-based dosing, “it is possible that pharmaceutical manufacturers will rethink their dosing and pricing models, just as happened previously,” he cautioned.
However, these strategies could also provide relief for another escalating issue: drug shortages. Especially in the current moment, having a stewardship mindset, “might be helpful in navigating drug shortages,” Dr. Strohbehn said.
This research had no commercial funding. Dr. Bryant, Dr. Strohbehn, and Dr. Powell report no relevant financial relationships.
A version of this article appeared on Medscape.com.
FROM HEALTH AFFAIRS
CAR T-cell benefit in lenalidomide-refractory myeloma
New results show that such patients benefit from treatment with the chimeric antigen receptor T-cell (CAR T) construct ciltacabtagene autoleucel (cilta-cel) (Carvykti).
The finding comes from the phase 3 CARTITUDE-4 trial, which was reported at the annual meeting of the American Society of Clinical Oncology (ASCO) and was simultaneously published online in the New England Journal of Medicine.
Patients with lenalidomide-refractory multiple myeloma who received a single infusion of ciltacabtagene autoleucel demonstrated a 74% reduction in the risk for disease progression or death, compared with patients who received the standard of care.
The hazard ratio for death or progression with cilta-cel was 0.26 (P < .001), which “is the best hazard ratio ever reported in this patient population in a randomized clinical setting,” said principal investigator Binod Dhakal, MD, from the Medical College of Wisconsin, Milwaukee.
Dr. Dhakal reported data from the first analysis of the trial. At a median follow-up of 15.9 months, median progression-free survival (PFS), the primary endpoint, had not been reached among 208 patients who received cilta-cel; PFS was 11.8 months for the 211 patients assigned to receive standard of care, which consisted of the physician’s choice of either pomalidomide, bortezomib, and dexamethasone (PVd), or daratumumab, pomalidomide, and dexamethasone (DPd).
Twelve-month PFS rates were 75.9% and 48.6%, respectively, and both the overall response rate (ORR) and the complete response (CR) rate were higher with the CAR T construct than with the standard of care (ORR, 84.6% vs. 67.3%; CR rates, 73.1% and 21.8%, respectively).
“My perspective on Dr. Dakhal and colleague’s data is that myeloma treatment should be revisited in the light of this,” commented invited discussant Asher Chanan-Khan, MD, from the Mayo Clinic Cancer Center in Jacksonville, Fla.
“Early CAR Ts demonstrating efficacy and safety and prior lines of treatment impact survival from CAR T in myeloma. In lymphoma, CAR T is almost replacing, if not already, autotransplant. Can this also be true for multiple myeloma?” he asked.
Dr. Chanan-Khan noted that there are at least four ongoing trials with CAR T targeting either the B-cell maturation antigen (BCMA) alone or in combination with an anti-CD19 CAR T, immune checkpoint inhibitors, or with bortezomib, lenalidomide, and dexamethasone.
Also commenting on the new results, ASCO Expert Oreofe Odejide, MD, of the Dana-Farber Cancer Institute in Boston, said in a statement: “Lenalidomide has become a foundation of care for people with myeloma, but as its use has expanded, so has the number of patients whose disease will no longer respond to the treatment. Ciltacabtagene autoleucel has not only shown that it delivers remarkably effective outcomes, compared with patients’ current options, but also that it can be used safely earlier in the treatment phase.”
Already approved for refractory myeloma
Cilta-cel is a second-generation CAR T that contains two single-domain antibodies that target BCMA. This target was first described in myeloma in 2004 as a mechanism for the growth and survival of malignant plasma cells.
The product is already approved for use in myeloma; it was approved in March 2022 by the U.S. Food and Drug Administration for use in patients with refractory/relapsed multiple myeloma who have already tried four or more therapies. That approval was based on results from phase 1b/2 CARTITUDE-1 trial, which, as previously reported by this news organization, showed that early and deep responses with cilta-cel proved to be durable.
Final results of CARTITUDE-1, reported in a scientific poster at ASCO 2023, showed that almost half of patients (47.5%) who were treated with cilta-cel were free of disease progression at 3 years, and 59.8% had sustained, complete responses. In addition, the median PFS was longer than for any previously reported therapy for heavily pretreated patients with relapsed/refractory multiple myeloma, the authors said.
CARTITUDE-4 details
For the CARTITUDE-4 trial, the investigators enrolled patients aged 18 years or older with lenalidomide-refractory multiple myeloma who had experienced relapse after one to three prior lines of therapy that included a prosteasome inhibitor and immunomodulator. After stratification by the choice of PVd or DPd, Multiple Myeloma International Staging System, and number of prior lines of therapy, patients were randomly assigned to receive either cilta-cel or one of the two standard-of-care regimens previously described.
Patients assigned to cilta-cel received one or more cycles of either PVd or DPd as bridging therapy during the period from apheresis to infusion of the CAR T cells.
As already noted, cilta-cel showed superior PFS and response rates and was associated with a significantly higher rate of minimal residual disease (MRD) negativity, compared with standard of care, in the intention-to-treat population: 60.6% vs. 15.6%, which translates into an odds ratio for achieving MRD negativity with CAR T of 8.7 (P < .0001). Among the subset of patients evaluable for MRD, the respective rates were 87.5% and 32.7%.
Overall survival data were not mature at the time of presentation. In all, 39 patients in the cilta-cel arm and 47 in the standard-of-care arm died during the study.
Grade 3 or 4 adverse events occurred in 97% of patients who received cilta-cel and in 94% of those who received standard-of-care therapies. In the cilta-cel arm, 76.1% of patients had cytokine release syndrome (CRS), although only 1.1% of cases were of grade 3 or 4 in severity, and there were no CRS-associated deaths. Eight patients in this arm had immune effector cell–associated neurotoxicity syndrome, all of grade 1 or 2. One patient had grade 1 movement and neurocognitive symptoms, 16 had grade 2 or 3 cranial nerve palsy, and 5 patients had CAR T–related peripheral neuropathy of grade 1, 2, or 3.
The investigators plan to follow patients to determine the long-term effects of ciltacabtagene autoleucel and are currently performing analyses of health-related quality of life, subgroups, and biomarkers.
The study was funded by Janssen and Legend Biotech, which market ciltacabtagene autoleucel. Dr. Dhakal disclosed consulting, speaker’s bureau participation, and institutional research funding from Janssen and others. Several coauthors are employees of the study funders. Dr. Chanan-Khan’s relevant financial information was not available. Dr. Odejide reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
New results show that such patients benefit from treatment with the chimeric antigen receptor T-cell (CAR T) construct ciltacabtagene autoleucel (cilta-cel) (Carvykti).
The finding comes from the phase 3 CARTITUDE-4 trial, which was reported at the annual meeting of the American Society of Clinical Oncology (ASCO) and was simultaneously published online in the New England Journal of Medicine.
Patients with lenalidomide-refractory multiple myeloma who received a single infusion of ciltacabtagene autoleucel demonstrated a 74% reduction in the risk for disease progression or death, compared with patients who received the standard of care.
The hazard ratio for death or progression with cilta-cel was 0.26 (P < .001), which “is the best hazard ratio ever reported in this patient population in a randomized clinical setting,” said principal investigator Binod Dhakal, MD, from the Medical College of Wisconsin, Milwaukee.
Dr. Dhakal reported data from the first analysis of the trial. At a median follow-up of 15.9 months, median progression-free survival (PFS), the primary endpoint, had not been reached among 208 patients who received cilta-cel; PFS was 11.8 months for the 211 patients assigned to receive standard of care, which consisted of the physician’s choice of either pomalidomide, bortezomib, and dexamethasone (PVd), or daratumumab, pomalidomide, and dexamethasone (DPd).
Twelve-month PFS rates were 75.9% and 48.6%, respectively, and both the overall response rate (ORR) and the complete response (CR) rate were higher with the CAR T construct than with the standard of care (ORR, 84.6% vs. 67.3%; CR rates, 73.1% and 21.8%, respectively).
“My perspective on Dr. Dakhal and colleague’s data is that myeloma treatment should be revisited in the light of this,” commented invited discussant Asher Chanan-Khan, MD, from the Mayo Clinic Cancer Center in Jacksonville, Fla.
“Early CAR Ts demonstrating efficacy and safety and prior lines of treatment impact survival from CAR T in myeloma. In lymphoma, CAR T is almost replacing, if not already, autotransplant. Can this also be true for multiple myeloma?” he asked.
Dr. Chanan-Khan noted that there are at least four ongoing trials with CAR T targeting either the B-cell maturation antigen (BCMA) alone or in combination with an anti-CD19 CAR T, immune checkpoint inhibitors, or with bortezomib, lenalidomide, and dexamethasone.
Also commenting on the new results, ASCO Expert Oreofe Odejide, MD, of the Dana-Farber Cancer Institute in Boston, said in a statement: “Lenalidomide has become a foundation of care for people with myeloma, but as its use has expanded, so has the number of patients whose disease will no longer respond to the treatment. Ciltacabtagene autoleucel has not only shown that it delivers remarkably effective outcomes, compared with patients’ current options, but also that it can be used safely earlier in the treatment phase.”
Already approved for refractory myeloma
Cilta-cel is a second-generation CAR T that contains two single-domain antibodies that target BCMA. This target was first described in myeloma in 2004 as a mechanism for the growth and survival of malignant plasma cells.
The product is already approved for use in myeloma; it was approved in March 2022 by the U.S. Food and Drug Administration for use in patients with refractory/relapsed multiple myeloma who have already tried four or more therapies. That approval was based on results from phase 1b/2 CARTITUDE-1 trial, which, as previously reported by this news organization, showed that early and deep responses with cilta-cel proved to be durable.
Final results of CARTITUDE-1, reported in a scientific poster at ASCO 2023, showed that almost half of patients (47.5%) who were treated with cilta-cel were free of disease progression at 3 years, and 59.8% had sustained, complete responses. In addition, the median PFS was longer than for any previously reported therapy for heavily pretreated patients with relapsed/refractory multiple myeloma, the authors said.
CARTITUDE-4 details
For the CARTITUDE-4 trial, the investigators enrolled patients aged 18 years or older with lenalidomide-refractory multiple myeloma who had experienced relapse after one to three prior lines of therapy that included a prosteasome inhibitor and immunomodulator. After stratification by the choice of PVd or DPd, Multiple Myeloma International Staging System, and number of prior lines of therapy, patients were randomly assigned to receive either cilta-cel or one of the two standard-of-care regimens previously described.
Patients assigned to cilta-cel received one or more cycles of either PVd or DPd as bridging therapy during the period from apheresis to infusion of the CAR T cells.
As already noted, cilta-cel showed superior PFS and response rates and was associated with a significantly higher rate of minimal residual disease (MRD) negativity, compared with standard of care, in the intention-to-treat population: 60.6% vs. 15.6%, which translates into an odds ratio for achieving MRD negativity with CAR T of 8.7 (P < .0001). Among the subset of patients evaluable for MRD, the respective rates were 87.5% and 32.7%.
Overall survival data were not mature at the time of presentation. In all, 39 patients in the cilta-cel arm and 47 in the standard-of-care arm died during the study.
Grade 3 or 4 adverse events occurred in 97% of patients who received cilta-cel and in 94% of those who received standard-of-care therapies. In the cilta-cel arm, 76.1% of patients had cytokine release syndrome (CRS), although only 1.1% of cases were of grade 3 or 4 in severity, and there were no CRS-associated deaths. Eight patients in this arm had immune effector cell–associated neurotoxicity syndrome, all of grade 1 or 2. One patient had grade 1 movement and neurocognitive symptoms, 16 had grade 2 or 3 cranial nerve palsy, and 5 patients had CAR T–related peripheral neuropathy of grade 1, 2, or 3.
The investigators plan to follow patients to determine the long-term effects of ciltacabtagene autoleucel and are currently performing analyses of health-related quality of life, subgroups, and biomarkers.
The study was funded by Janssen and Legend Biotech, which market ciltacabtagene autoleucel. Dr. Dhakal disclosed consulting, speaker’s bureau participation, and institutional research funding from Janssen and others. Several coauthors are employees of the study funders. Dr. Chanan-Khan’s relevant financial information was not available. Dr. Odejide reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
New results show that such patients benefit from treatment with the chimeric antigen receptor T-cell (CAR T) construct ciltacabtagene autoleucel (cilta-cel) (Carvykti).
The finding comes from the phase 3 CARTITUDE-4 trial, which was reported at the annual meeting of the American Society of Clinical Oncology (ASCO) and was simultaneously published online in the New England Journal of Medicine.
Patients with lenalidomide-refractory multiple myeloma who received a single infusion of ciltacabtagene autoleucel demonstrated a 74% reduction in the risk for disease progression or death, compared with patients who received the standard of care.
The hazard ratio for death or progression with cilta-cel was 0.26 (P < .001), which “is the best hazard ratio ever reported in this patient population in a randomized clinical setting,” said principal investigator Binod Dhakal, MD, from the Medical College of Wisconsin, Milwaukee.
Dr. Dhakal reported data from the first analysis of the trial. At a median follow-up of 15.9 months, median progression-free survival (PFS), the primary endpoint, had not been reached among 208 patients who received cilta-cel; PFS was 11.8 months for the 211 patients assigned to receive standard of care, which consisted of the physician’s choice of either pomalidomide, bortezomib, and dexamethasone (PVd), or daratumumab, pomalidomide, and dexamethasone (DPd).
Twelve-month PFS rates were 75.9% and 48.6%, respectively, and both the overall response rate (ORR) and the complete response (CR) rate were higher with the CAR T construct than with the standard of care (ORR, 84.6% vs. 67.3%; CR rates, 73.1% and 21.8%, respectively).
“My perspective on Dr. Dakhal and colleague’s data is that myeloma treatment should be revisited in the light of this,” commented invited discussant Asher Chanan-Khan, MD, from the Mayo Clinic Cancer Center in Jacksonville, Fla.
“Early CAR Ts demonstrating efficacy and safety and prior lines of treatment impact survival from CAR T in myeloma. In lymphoma, CAR T is almost replacing, if not already, autotransplant. Can this also be true for multiple myeloma?” he asked.
Dr. Chanan-Khan noted that there are at least four ongoing trials with CAR T targeting either the B-cell maturation antigen (BCMA) alone or in combination with an anti-CD19 CAR T, immune checkpoint inhibitors, or with bortezomib, lenalidomide, and dexamethasone.
Also commenting on the new results, ASCO Expert Oreofe Odejide, MD, of the Dana-Farber Cancer Institute in Boston, said in a statement: “Lenalidomide has become a foundation of care for people with myeloma, but as its use has expanded, so has the number of patients whose disease will no longer respond to the treatment. Ciltacabtagene autoleucel has not only shown that it delivers remarkably effective outcomes, compared with patients’ current options, but also that it can be used safely earlier in the treatment phase.”
Already approved for refractory myeloma
Cilta-cel is a second-generation CAR T that contains two single-domain antibodies that target BCMA. This target was first described in myeloma in 2004 as a mechanism for the growth and survival of malignant plasma cells.
The product is already approved for use in myeloma; it was approved in March 2022 by the U.S. Food and Drug Administration for use in patients with refractory/relapsed multiple myeloma who have already tried four or more therapies. That approval was based on results from phase 1b/2 CARTITUDE-1 trial, which, as previously reported by this news organization, showed that early and deep responses with cilta-cel proved to be durable.
Final results of CARTITUDE-1, reported in a scientific poster at ASCO 2023, showed that almost half of patients (47.5%) who were treated with cilta-cel were free of disease progression at 3 years, and 59.8% had sustained, complete responses. In addition, the median PFS was longer than for any previously reported therapy for heavily pretreated patients with relapsed/refractory multiple myeloma, the authors said.
CARTITUDE-4 details
For the CARTITUDE-4 trial, the investigators enrolled patients aged 18 years or older with lenalidomide-refractory multiple myeloma who had experienced relapse after one to three prior lines of therapy that included a prosteasome inhibitor and immunomodulator. After stratification by the choice of PVd or DPd, Multiple Myeloma International Staging System, and number of prior lines of therapy, patients were randomly assigned to receive either cilta-cel or one of the two standard-of-care regimens previously described.
Patients assigned to cilta-cel received one or more cycles of either PVd or DPd as bridging therapy during the period from apheresis to infusion of the CAR T cells.
As already noted, cilta-cel showed superior PFS and response rates and was associated with a significantly higher rate of minimal residual disease (MRD) negativity, compared with standard of care, in the intention-to-treat population: 60.6% vs. 15.6%, which translates into an odds ratio for achieving MRD negativity with CAR T of 8.7 (P < .0001). Among the subset of patients evaluable for MRD, the respective rates were 87.5% and 32.7%.
Overall survival data were not mature at the time of presentation. In all, 39 patients in the cilta-cel arm and 47 in the standard-of-care arm died during the study.
Grade 3 or 4 adverse events occurred in 97% of patients who received cilta-cel and in 94% of those who received standard-of-care therapies. In the cilta-cel arm, 76.1% of patients had cytokine release syndrome (CRS), although only 1.1% of cases were of grade 3 or 4 in severity, and there were no CRS-associated deaths. Eight patients in this arm had immune effector cell–associated neurotoxicity syndrome, all of grade 1 or 2. One patient had grade 1 movement and neurocognitive symptoms, 16 had grade 2 or 3 cranial nerve palsy, and 5 patients had CAR T–related peripheral neuropathy of grade 1, 2, or 3.
The investigators plan to follow patients to determine the long-term effects of ciltacabtagene autoleucel and are currently performing analyses of health-related quality of life, subgroups, and biomarkers.
The study was funded by Janssen and Legend Biotech, which market ciltacabtagene autoleucel. Dr. Dhakal disclosed consulting, speaker’s bureau participation, and institutional research funding from Janssen and others. Several coauthors are employees of the study funders. Dr. Chanan-Khan’s relevant financial information was not available. Dr. Odejide reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
AT ASCO 2023
Antibody-drug conjugate changes standard of care for platinum-resistant ovarian cancer
The conclusion of this study marks the first time that a novel therapy has demonstrated an overall survival (OS) improvement in any phase 3 trial in this population, according to lead investigator Kathleen Moore, MD.
“We believe these data are practice changing and position mirvetuximab [soravtansine] as the new standard of care for patients with folate receptor–alpha positive, platinum-resistant ovarian cancer,” said Dr. Moore during a presentation of the study at a special session of the annual meeting of the American Society of Clinical Oncology devoted solely to the MIRASOL study.
New standard of care
Following Dr. Moore’s presentation, Roisin Eilish O’Cearbhaill, MD, served as a discussant, and she confirmed the trial’s importance.
“It has firmly established the role of mirvetuximab [soravtansine] in folate receptor–alpha high-expression, platinum-resistant ovarian cancer,” said Dr. O’Cearbhaill, who is Research director of the gynecologic medical oncology service and clinical director of the solid tumor, cellular therapy service at Memorial Sloan Kettering Cancer Center, New York.
Mirvetuximab soravtansine received accelerated FDA approval in November based on the results of the single-arm SORAYA trial, which demonstrated a progression-free survival (PFS) benefit in platinum-resistant patients who had been previously treated with one to three treatment regimens, at least one of which having included bevacizumab.
The new study compared MIRV with physician choice chemotherapy and found both a PFS and OS benefit in the MIRV arm. The results garnered significant enthusiasm from the audience, and others reacted positively as well.
“The results that she presented are just astounding, with a significant improvement in both progression-free and overall survival. I think certainly the overall survival needs to be highlighted here, because this is a patient population that’s notoriously difficult to treat,” said Ana Valente, MD, a gynecologic oncologist at the Ochsner Health System in New Orleans. Dr. Valente, who did not attend the presentation but was asked to comment on the study, is also a member of the Society of Gynecological Oncologist communications committee.
Unlike SORAYA, MIRASOL was open to patients who had not received bevacizumab, and Dr. Moore and colleagues found similar survival benefits in patients who had not received bevacizumab as in those who had, said Dr. Moore, who is the associate director of clinical research at Stephenson Cancer Center and director of the Oklahoma TSET Phase 1 Program, both in Oklahoma City. This opens the possibility of using MIRV instead of bevacizumab combined with chemotherapy in platinum-resistant patients.
“I think this data really shows you can move right to mirvetuximab [soravtansine] and feel pretty solid about the decision in a biomarker selected [population],” Dr. Moore said, during an interview.
Not just for high expression levels
MIRASOL was restricted to patients with high levels of expression of folate receptor–alpha, which is MIRV’s target on the surface of tumor cells. High expression is defined as at least 75% of viable tumor cells exhibiting a minimum of 2+ level membrane staining intensity by immunohistochemistry. That represents about 35% of patients, according to Dr. Moore, but she said that the drug also shows promise in patients with medium levels of folate receptor–alpha expression.
“I think it’s just going to be now starting to get those label extension studies launched to branch it out. Then you account for 60% of your population which [have] medium to high [expression levels], and that’s really where you see benefit,” said Dr. Moore. Medium expression levels of folate receptor–alpha are defined as 50% to greater than 75% of tumor cells with 2+ level membrane staining intensity.
She also noted that the FORWARD II trial combining mirvetuximab soravtansine with bevacizumab in platinum-resistant ovarian cancer is showing good results.
“We have really beautiful data [from FORWARD II]. If I have a medium expresser, I’m using the doublet [of MIRV and bevacizumab], and it works,” said Dr. Moore, while also pointing out that this remains an off-label use.
It’s possible that the drug could be extended even to low expression levels, defined as 25% to less than 50% of tumor cells with 2+ level membrane staining intensity. “[We are] currently working on that strategy with already available data,” said Dr. Moore.
She speculated that the improved OS may be attributed to the reduced toxicity of MIRV, compared with chemotherapy agents, which leaves patients feeling better and more able to pursue other treatments, which in turn may increase survival odds.
Dr. O’Cearbhaill touted the benefits of ADCs and their ability to target powerful cytotoxic agents while limiting side effects, and she is looking forward to more new therapies on the horizon.
“There are four [ADCs] in late stages of development [for platinum-resistant ovarian cancer], so hopefully there will be other ones coming online as well,” Dr. O’Cearbhaill said in an interview. “Then we’ll have to figure out how to sequence them, which drug will be best in class. Will we be just giving one or will be giving ADC followed by ADC?”
Study methods and results
The study enrolled 453 patients and randomized them to treatment with MIRV or investigator’s choice of chemotherapy, which could be paclitaxel, pegylated liposomal doxorubicin, or topotecan. The MIRV dose was 6 mg/kg adjusted ideal body weight every 3 weeks. The median age was 62 in the chemotherapy arm and 63 years in the MIRV arm. About 63% of the chemotherapy arm had prior bevacizumab exposure, as did 61% of the MIRV arm.
Median PFS was 5.62 months in the MIRV arm and 3.98 months in the chemotherapy arm (hazard ratio, 0.65; P less than .0001). The overall response rate was 42% in the MIRV arm and 16% in the chemotherapy arm (P < .0001).
The safety outcomes also favored MIRV: 42% experienced grade 3 or higher treatment-emergent adverse events (TEAEs) versus 54% in the chemotherapy group. Severe adverse events were also lower in MIRV, 24% versus 33%. Just 9% of patients in the MIRV discontinued because of TEAEs, compared with 16% in the chemotherapy arm.
MIRV was associated with blurred vision (41%), keratopathy (32%), and dry eye (28%), but these issues were generally manageable through collaboration with optometrists or ophthalmologists.
Dr. Moore and Dr. O’Cearbhaill reported receiving honoraria, research funding, and travel expenses from numerous pharmaceutical companies. Dr. O’Cearbhaill has consulted for or advised Aptitude Health, Bayer, Carina Biotech, Fresenius Kabi, GlaxoSmithKline, GOG Foundation, Immunogen, R-Pharm, Regeneron, and Seagen.
The conclusion of this study marks the first time that a novel therapy has demonstrated an overall survival (OS) improvement in any phase 3 trial in this population, according to lead investigator Kathleen Moore, MD.
“We believe these data are practice changing and position mirvetuximab [soravtansine] as the new standard of care for patients with folate receptor–alpha positive, platinum-resistant ovarian cancer,” said Dr. Moore during a presentation of the study at a special session of the annual meeting of the American Society of Clinical Oncology devoted solely to the MIRASOL study.
New standard of care
Following Dr. Moore’s presentation, Roisin Eilish O’Cearbhaill, MD, served as a discussant, and she confirmed the trial’s importance.
“It has firmly established the role of mirvetuximab [soravtansine] in folate receptor–alpha high-expression, platinum-resistant ovarian cancer,” said Dr. O’Cearbhaill, who is Research director of the gynecologic medical oncology service and clinical director of the solid tumor, cellular therapy service at Memorial Sloan Kettering Cancer Center, New York.
Mirvetuximab soravtansine received accelerated FDA approval in November based on the results of the single-arm SORAYA trial, which demonstrated a progression-free survival (PFS) benefit in platinum-resistant patients who had been previously treated with one to three treatment regimens, at least one of which having included bevacizumab.
The new study compared MIRV with physician choice chemotherapy and found both a PFS and OS benefit in the MIRV arm. The results garnered significant enthusiasm from the audience, and others reacted positively as well.
“The results that she presented are just astounding, with a significant improvement in both progression-free and overall survival. I think certainly the overall survival needs to be highlighted here, because this is a patient population that’s notoriously difficult to treat,” said Ana Valente, MD, a gynecologic oncologist at the Ochsner Health System in New Orleans. Dr. Valente, who did not attend the presentation but was asked to comment on the study, is also a member of the Society of Gynecological Oncologist communications committee.
Unlike SORAYA, MIRASOL was open to patients who had not received bevacizumab, and Dr. Moore and colleagues found similar survival benefits in patients who had not received bevacizumab as in those who had, said Dr. Moore, who is the associate director of clinical research at Stephenson Cancer Center and director of the Oklahoma TSET Phase 1 Program, both in Oklahoma City. This opens the possibility of using MIRV instead of bevacizumab combined with chemotherapy in platinum-resistant patients.
“I think this data really shows you can move right to mirvetuximab [soravtansine] and feel pretty solid about the decision in a biomarker selected [population],” Dr. Moore said, during an interview.
Not just for high expression levels
MIRASOL was restricted to patients with high levels of expression of folate receptor–alpha, which is MIRV’s target on the surface of tumor cells. High expression is defined as at least 75% of viable tumor cells exhibiting a minimum of 2+ level membrane staining intensity by immunohistochemistry. That represents about 35% of patients, according to Dr. Moore, but she said that the drug also shows promise in patients with medium levels of folate receptor–alpha expression.
“I think it’s just going to be now starting to get those label extension studies launched to branch it out. Then you account for 60% of your population which [have] medium to high [expression levels], and that’s really where you see benefit,” said Dr. Moore. Medium expression levels of folate receptor–alpha are defined as 50% to greater than 75% of tumor cells with 2+ level membrane staining intensity.
She also noted that the FORWARD II trial combining mirvetuximab soravtansine with bevacizumab in platinum-resistant ovarian cancer is showing good results.
“We have really beautiful data [from FORWARD II]. If I have a medium expresser, I’m using the doublet [of MIRV and bevacizumab], and it works,” said Dr. Moore, while also pointing out that this remains an off-label use.
It’s possible that the drug could be extended even to low expression levels, defined as 25% to less than 50% of tumor cells with 2+ level membrane staining intensity. “[We are] currently working on that strategy with already available data,” said Dr. Moore.
She speculated that the improved OS may be attributed to the reduced toxicity of MIRV, compared with chemotherapy agents, which leaves patients feeling better and more able to pursue other treatments, which in turn may increase survival odds.
Dr. O’Cearbhaill touted the benefits of ADCs and their ability to target powerful cytotoxic agents while limiting side effects, and she is looking forward to more new therapies on the horizon.
“There are four [ADCs] in late stages of development [for platinum-resistant ovarian cancer], so hopefully there will be other ones coming online as well,” Dr. O’Cearbhaill said in an interview. “Then we’ll have to figure out how to sequence them, which drug will be best in class. Will we be just giving one or will be giving ADC followed by ADC?”
Study methods and results
The study enrolled 453 patients and randomized them to treatment with MIRV or investigator’s choice of chemotherapy, which could be paclitaxel, pegylated liposomal doxorubicin, or topotecan. The MIRV dose was 6 mg/kg adjusted ideal body weight every 3 weeks. The median age was 62 in the chemotherapy arm and 63 years in the MIRV arm. About 63% of the chemotherapy arm had prior bevacizumab exposure, as did 61% of the MIRV arm.
Median PFS was 5.62 months in the MIRV arm and 3.98 months in the chemotherapy arm (hazard ratio, 0.65; P less than .0001). The overall response rate was 42% in the MIRV arm and 16% in the chemotherapy arm (P < .0001).
The safety outcomes also favored MIRV: 42% experienced grade 3 or higher treatment-emergent adverse events (TEAEs) versus 54% in the chemotherapy group. Severe adverse events were also lower in MIRV, 24% versus 33%. Just 9% of patients in the MIRV discontinued because of TEAEs, compared with 16% in the chemotherapy arm.
MIRV was associated with blurred vision (41%), keratopathy (32%), and dry eye (28%), but these issues were generally manageable through collaboration with optometrists or ophthalmologists.
Dr. Moore and Dr. O’Cearbhaill reported receiving honoraria, research funding, and travel expenses from numerous pharmaceutical companies. Dr. O’Cearbhaill has consulted for or advised Aptitude Health, Bayer, Carina Biotech, Fresenius Kabi, GlaxoSmithKline, GOG Foundation, Immunogen, R-Pharm, Regeneron, and Seagen.
The conclusion of this study marks the first time that a novel therapy has demonstrated an overall survival (OS) improvement in any phase 3 trial in this population, according to lead investigator Kathleen Moore, MD.
“We believe these data are practice changing and position mirvetuximab [soravtansine] as the new standard of care for patients with folate receptor–alpha positive, platinum-resistant ovarian cancer,” said Dr. Moore during a presentation of the study at a special session of the annual meeting of the American Society of Clinical Oncology devoted solely to the MIRASOL study.
New standard of care
Following Dr. Moore’s presentation, Roisin Eilish O’Cearbhaill, MD, served as a discussant, and she confirmed the trial’s importance.
“It has firmly established the role of mirvetuximab [soravtansine] in folate receptor–alpha high-expression, platinum-resistant ovarian cancer,” said Dr. O’Cearbhaill, who is Research director of the gynecologic medical oncology service and clinical director of the solid tumor, cellular therapy service at Memorial Sloan Kettering Cancer Center, New York.
Mirvetuximab soravtansine received accelerated FDA approval in November based on the results of the single-arm SORAYA trial, which demonstrated a progression-free survival (PFS) benefit in platinum-resistant patients who had been previously treated with one to three treatment regimens, at least one of which having included bevacizumab.
The new study compared MIRV with physician choice chemotherapy and found both a PFS and OS benefit in the MIRV arm. The results garnered significant enthusiasm from the audience, and others reacted positively as well.
“The results that she presented are just astounding, with a significant improvement in both progression-free and overall survival. I think certainly the overall survival needs to be highlighted here, because this is a patient population that’s notoriously difficult to treat,” said Ana Valente, MD, a gynecologic oncologist at the Ochsner Health System in New Orleans. Dr. Valente, who did not attend the presentation but was asked to comment on the study, is also a member of the Society of Gynecological Oncologist communications committee.
Unlike SORAYA, MIRASOL was open to patients who had not received bevacizumab, and Dr. Moore and colleagues found similar survival benefits in patients who had not received bevacizumab as in those who had, said Dr. Moore, who is the associate director of clinical research at Stephenson Cancer Center and director of the Oklahoma TSET Phase 1 Program, both in Oklahoma City. This opens the possibility of using MIRV instead of bevacizumab combined with chemotherapy in platinum-resistant patients.
“I think this data really shows you can move right to mirvetuximab [soravtansine] and feel pretty solid about the decision in a biomarker selected [population],” Dr. Moore said, during an interview.
Not just for high expression levels
MIRASOL was restricted to patients with high levels of expression of folate receptor–alpha, which is MIRV’s target on the surface of tumor cells. High expression is defined as at least 75% of viable tumor cells exhibiting a minimum of 2+ level membrane staining intensity by immunohistochemistry. That represents about 35% of patients, according to Dr. Moore, but she said that the drug also shows promise in patients with medium levels of folate receptor–alpha expression.
“I think it’s just going to be now starting to get those label extension studies launched to branch it out. Then you account for 60% of your population which [have] medium to high [expression levels], and that’s really where you see benefit,” said Dr. Moore. Medium expression levels of folate receptor–alpha are defined as 50% to greater than 75% of tumor cells with 2+ level membrane staining intensity.
She also noted that the FORWARD II trial combining mirvetuximab soravtansine with bevacizumab in platinum-resistant ovarian cancer is showing good results.
“We have really beautiful data [from FORWARD II]. If I have a medium expresser, I’m using the doublet [of MIRV and bevacizumab], and it works,” said Dr. Moore, while also pointing out that this remains an off-label use.
It’s possible that the drug could be extended even to low expression levels, defined as 25% to less than 50% of tumor cells with 2+ level membrane staining intensity. “[We are] currently working on that strategy with already available data,” said Dr. Moore.
She speculated that the improved OS may be attributed to the reduced toxicity of MIRV, compared with chemotherapy agents, which leaves patients feeling better and more able to pursue other treatments, which in turn may increase survival odds.
Dr. O’Cearbhaill touted the benefits of ADCs and their ability to target powerful cytotoxic agents while limiting side effects, and she is looking forward to more new therapies on the horizon.
“There are four [ADCs] in late stages of development [for platinum-resistant ovarian cancer], so hopefully there will be other ones coming online as well,” Dr. O’Cearbhaill said in an interview. “Then we’ll have to figure out how to sequence them, which drug will be best in class. Will we be just giving one or will be giving ADC followed by ADC?”
Study methods and results
The study enrolled 453 patients and randomized them to treatment with MIRV or investigator’s choice of chemotherapy, which could be paclitaxel, pegylated liposomal doxorubicin, or topotecan. The MIRV dose was 6 mg/kg adjusted ideal body weight every 3 weeks. The median age was 62 in the chemotherapy arm and 63 years in the MIRV arm. About 63% of the chemotherapy arm had prior bevacizumab exposure, as did 61% of the MIRV arm.
Median PFS was 5.62 months in the MIRV arm and 3.98 months in the chemotherapy arm (hazard ratio, 0.65; P less than .0001). The overall response rate was 42% in the MIRV arm and 16% in the chemotherapy arm (P < .0001).
The safety outcomes also favored MIRV: 42% experienced grade 3 or higher treatment-emergent adverse events (TEAEs) versus 54% in the chemotherapy group. Severe adverse events were also lower in MIRV, 24% versus 33%. Just 9% of patients in the MIRV discontinued because of TEAEs, compared with 16% in the chemotherapy arm.
MIRV was associated with blurred vision (41%), keratopathy (32%), and dry eye (28%), but these issues were generally manageable through collaboration with optometrists or ophthalmologists.
Dr. Moore and Dr. O’Cearbhaill reported receiving honoraria, research funding, and travel expenses from numerous pharmaceutical companies. Dr. O’Cearbhaill has consulted for or advised Aptitude Health, Bayer, Carina Biotech, Fresenius Kabi, GlaxoSmithKline, GOG Foundation, Immunogen, R-Pharm, Regeneron, and Seagen.
AT ASCO 2023
Up-front pembro plus chemo boost survival in cervical cancer
This is based on final overall survival results from the phase 3, randomized KEYNOTE-826 study, which showed that adding immunotherapy resulted in a 40% reduction in risk of death, compared with chemotherapy alone, for women with advanced cervical cancers expressing programmed death–ligand 1 (PD-L1).
“At this protocol-specified final analysis of KEYNOTE-826, the addition of immune therapy to chemotherapy with or without the antiangiogenic bevacizumab showed substantial and clinically meaningful improvement in survival,” said lead author Bradley J. Monk, MD, from HonorHealth Research Institute, Phoenix.
He was speaking at a media briefing held prior to the annual meeting of the American Society of Clinical Oncology, where the results were presented.
“The results of this study solidify the addition of pembrolizumab to chemotherapy with or without bevacizumab in people with persistent, recurrent, or metastatic cervical cancer as the frontline standard of care for this disease. Survival significantly improved with this approach, regardless of PD-L1 expression, further supporting its use for all patients in this population,” commented ASCO expert Merry Jennifer Markham, MD, from the University of Florida, Gainesville.
At the briefing, Dr. Monk raised the possibility that adding immunotherapy to the standard of care could offer a chance for cure for some patients with advanced or recurrent cervical cancer.
“Is it possible to cure a widely metastatic cancer, a solid tumor? And I think it probably is,” he said. “There’s a tail to this [survival] curve, and I can’t believe that in my lifetime we as a group, as a team, have sort of figured out – and it’s not enough – that we can actually cure some patients, and if not maybe cure, have them at least live a long time, so it’s exciting.”
Briefing comoderater Julie R. Gralow, MD, chief medical officer and executive vice president of ASCO, agreed that the survival benefit “is exciting to see, and in my long career as a breast medical oncologist, I’m pretty sure we cure some metastatic breast cancer. We definitely had patients who lived out their normal life span and died of something else after decades.
“But the definition of cure, sadly, in these situations is that you die of something else without evidence of disease, so we certainly need to do better here and be better able to use the word ‘cure’ in the metastatic setting,” she added.
Promising start
Since 2014, the standard of care for treating patients with recurrent, persistent, or metastatic cervical cancer has been chemotherapy with a platinum compound, paclitaxel, and bevacizumab, based on the results of the GOG 240 study.
Immunotherapy with PD-1 inhibitors had previously shown efficacy as monotherapy in second- or later-line therapy for women with cervical cancer, but KEYNOTE 826 was the first study to show a benefit to promoting immunotherapy to the front ranks.
In the first interim analysis of the trial, reported at the 2021 annual meeting of the European Society for Medical Oncology, after a median follow-up of 22 months, the combination of pembrolizumab and chemotherapy demonstrated significant improvement in progression-free survival (PFS) and overall survival (OS), compared with chemotherapy plus placebo in a biomarker-selected population, which consisted of patients with a combined positive score (CPS) for PD-L1 of 1 or greater.
Pembrolizumab had no apparent efficacy in patients whose tumors did not have detectable PD-L1, however.
Latest results
Now the investigators are reporting the final analysis, conducted after a median follow-up of 39.1 months. The results are those for all comers (308 randomly assigned to receive pembrolizumab plus chemotherapy, and 309 assigned to receive chemotherapy plus placebo), as well as for the biomarker-selected population (consisting of all patients with PD-L1 CPS of 1 or greater) and for the subpopulation of patients with PD-L1 CPS of 10 or greater.
In the all-comers population, the median OS was 26.4 months for patients who received pembrolizumab, compared with 16.8 months for those who received placebo. The 24-month OS rates were 52.1% and 38.7%, respectively. The difference translated into a hazard ratio for death with pembrolizumab of 0.63 (P < .0001).
In the biomarker-selected population (273 assigned to pembrolizumab and 275 assigned to placebo), the respective median OS was 28.6 months versus 16.6 months, with 24-month OS rates of 53.5% versus 39.4%, which translates into an HR for death with pembrolizumab of 0.60 (P < .0001).
Not surprisingly, the best responses to the addition of the PD-1 inhibitor were seen among patients with a PD-L1 CPS of 10 or greater (158 assigned to pembrolizumab and 159 assigned to placebo). In this subgroup, the median OS was 29.6 months with the immune checkpoint inhibitor added to chemotherapy versus 17.4 months for chemotherapy plus placebo. The respective 24-month OS rates were 54.4% and 42.5%, and the HR for overall survival favoring pembrolizumab was 0.58 (P < .0001).
Median PFS 12-month PFS rates also favored pembrolizumab in both the total patient population and the biomarker-selected groups, with median PFS of approximately 10.4 months with pembrolizumab versus approximately 8.2 months with placebo.
The safety profile was manageable, with adverse events as expected from the safety profiles of the individual drugs in the combined regimen. No new safety signals have been seen since the interim analysis, Dr. Monk said.
Regimen details
Patients were randomly assigned in a 1:1 ratio to receive pembrolizumab 200 mg or placebo every 3 weeks for up to 35 cycles plus platinum-based chemotherapy, with bevacizumab added at the investigator’s discretion. Approximately two-thirds of patients in each study arm received bevacizumab.
The dual primary endpoints of PFS and OS were each tested sequentially in patients with a PD-L1 CPS of 1 or greater in both the intention-to-treat or “all-comers” population and in patients with a PD-L1 CPS of 10 or greater.
Patient characteristics were generally well balanced between the treatment groups, except that a slightly higher proportion of patients in the pembrolizumab had tumors of squamous cell histology, compared with the placebo group (76.3% vs. 68.3%).
KEYNOTE-826 was funded by Merck. Dr. Monk has received honoraria and has participated in consulting/advising and speaker’s bureau activity with Merck and other companies. Dr. Gralow has had a consulting or advisory role with Genentech and Roche. Dr. Markham has had a consulting/advisory role for GlaxoSmithKline and has received institutional research funding from Merck and other companies.
A version of this article first appeared on Medscape.com.
This is based on final overall survival results from the phase 3, randomized KEYNOTE-826 study, which showed that adding immunotherapy resulted in a 40% reduction in risk of death, compared with chemotherapy alone, for women with advanced cervical cancers expressing programmed death–ligand 1 (PD-L1).
“At this protocol-specified final analysis of KEYNOTE-826, the addition of immune therapy to chemotherapy with or without the antiangiogenic bevacizumab showed substantial and clinically meaningful improvement in survival,” said lead author Bradley J. Monk, MD, from HonorHealth Research Institute, Phoenix.
He was speaking at a media briefing held prior to the annual meeting of the American Society of Clinical Oncology, where the results were presented.
“The results of this study solidify the addition of pembrolizumab to chemotherapy with or without bevacizumab in people with persistent, recurrent, or metastatic cervical cancer as the frontline standard of care for this disease. Survival significantly improved with this approach, regardless of PD-L1 expression, further supporting its use for all patients in this population,” commented ASCO expert Merry Jennifer Markham, MD, from the University of Florida, Gainesville.
At the briefing, Dr. Monk raised the possibility that adding immunotherapy to the standard of care could offer a chance for cure for some patients with advanced or recurrent cervical cancer.
“Is it possible to cure a widely metastatic cancer, a solid tumor? And I think it probably is,” he said. “There’s a tail to this [survival] curve, and I can’t believe that in my lifetime we as a group, as a team, have sort of figured out – and it’s not enough – that we can actually cure some patients, and if not maybe cure, have them at least live a long time, so it’s exciting.”
Briefing comoderater Julie R. Gralow, MD, chief medical officer and executive vice president of ASCO, agreed that the survival benefit “is exciting to see, and in my long career as a breast medical oncologist, I’m pretty sure we cure some metastatic breast cancer. We definitely had patients who lived out their normal life span and died of something else after decades.
“But the definition of cure, sadly, in these situations is that you die of something else without evidence of disease, so we certainly need to do better here and be better able to use the word ‘cure’ in the metastatic setting,” she added.
Promising start
Since 2014, the standard of care for treating patients with recurrent, persistent, or metastatic cervical cancer has been chemotherapy with a platinum compound, paclitaxel, and bevacizumab, based on the results of the GOG 240 study.
Immunotherapy with PD-1 inhibitors had previously shown efficacy as monotherapy in second- or later-line therapy for women with cervical cancer, but KEYNOTE 826 was the first study to show a benefit to promoting immunotherapy to the front ranks.
In the first interim analysis of the trial, reported at the 2021 annual meeting of the European Society for Medical Oncology, after a median follow-up of 22 months, the combination of pembrolizumab and chemotherapy demonstrated significant improvement in progression-free survival (PFS) and overall survival (OS), compared with chemotherapy plus placebo in a biomarker-selected population, which consisted of patients with a combined positive score (CPS) for PD-L1 of 1 or greater.
Pembrolizumab had no apparent efficacy in patients whose tumors did not have detectable PD-L1, however.
Latest results
Now the investigators are reporting the final analysis, conducted after a median follow-up of 39.1 months. The results are those for all comers (308 randomly assigned to receive pembrolizumab plus chemotherapy, and 309 assigned to receive chemotherapy plus placebo), as well as for the biomarker-selected population (consisting of all patients with PD-L1 CPS of 1 or greater) and for the subpopulation of patients with PD-L1 CPS of 10 or greater.
In the all-comers population, the median OS was 26.4 months for patients who received pembrolizumab, compared with 16.8 months for those who received placebo. The 24-month OS rates were 52.1% and 38.7%, respectively. The difference translated into a hazard ratio for death with pembrolizumab of 0.63 (P < .0001).
In the biomarker-selected population (273 assigned to pembrolizumab and 275 assigned to placebo), the respective median OS was 28.6 months versus 16.6 months, with 24-month OS rates of 53.5% versus 39.4%, which translates into an HR for death with pembrolizumab of 0.60 (P < .0001).
Not surprisingly, the best responses to the addition of the PD-1 inhibitor were seen among patients with a PD-L1 CPS of 10 or greater (158 assigned to pembrolizumab and 159 assigned to placebo). In this subgroup, the median OS was 29.6 months with the immune checkpoint inhibitor added to chemotherapy versus 17.4 months for chemotherapy plus placebo. The respective 24-month OS rates were 54.4% and 42.5%, and the HR for overall survival favoring pembrolizumab was 0.58 (P < .0001).
Median PFS 12-month PFS rates also favored pembrolizumab in both the total patient population and the biomarker-selected groups, with median PFS of approximately 10.4 months with pembrolizumab versus approximately 8.2 months with placebo.
The safety profile was manageable, with adverse events as expected from the safety profiles of the individual drugs in the combined regimen. No new safety signals have been seen since the interim analysis, Dr. Monk said.
Regimen details
Patients were randomly assigned in a 1:1 ratio to receive pembrolizumab 200 mg or placebo every 3 weeks for up to 35 cycles plus platinum-based chemotherapy, with bevacizumab added at the investigator’s discretion. Approximately two-thirds of patients in each study arm received bevacizumab.
The dual primary endpoints of PFS and OS were each tested sequentially in patients with a PD-L1 CPS of 1 or greater in both the intention-to-treat or “all-comers” population and in patients with a PD-L1 CPS of 10 or greater.
Patient characteristics were generally well balanced between the treatment groups, except that a slightly higher proportion of patients in the pembrolizumab had tumors of squamous cell histology, compared with the placebo group (76.3% vs. 68.3%).
KEYNOTE-826 was funded by Merck. Dr. Monk has received honoraria and has participated in consulting/advising and speaker’s bureau activity with Merck and other companies. Dr. Gralow has had a consulting or advisory role with Genentech and Roche. Dr. Markham has had a consulting/advisory role for GlaxoSmithKline and has received institutional research funding from Merck and other companies.
A version of this article first appeared on Medscape.com.
This is based on final overall survival results from the phase 3, randomized KEYNOTE-826 study, which showed that adding immunotherapy resulted in a 40% reduction in risk of death, compared with chemotherapy alone, for women with advanced cervical cancers expressing programmed death–ligand 1 (PD-L1).
“At this protocol-specified final analysis of KEYNOTE-826, the addition of immune therapy to chemotherapy with or without the antiangiogenic bevacizumab showed substantial and clinically meaningful improvement in survival,” said lead author Bradley J. Monk, MD, from HonorHealth Research Institute, Phoenix.
He was speaking at a media briefing held prior to the annual meeting of the American Society of Clinical Oncology, where the results were presented.
“The results of this study solidify the addition of pembrolizumab to chemotherapy with or without bevacizumab in people with persistent, recurrent, or metastatic cervical cancer as the frontline standard of care for this disease. Survival significantly improved with this approach, regardless of PD-L1 expression, further supporting its use for all patients in this population,” commented ASCO expert Merry Jennifer Markham, MD, from the University of Florida, Gainesville.
At the briefing, Dr. Monk raised the possibility that adding immunotherapy to the standard of care could offer a chance for cure for some patients with advanced or recurrent cervical cancer.
“Is it possible to cure a widely metastatic cancer, a solid tumor? And I think it probably is,” he said. “There’s a tail to this [survival] curve, and I can’t believe that in my lifetime we as a group, as a team, have sort of figured out – and it’s not enough – that we can actually cure some patients, and if not maybe cure, have them at least live a long time, so it’s exciting.”
Briefing comoderater Julie R. Gralow, MD, chief medical officer and executive vice president of ASCO, agreed that the survival benefit “is exciting to see, and in my long career as a breast medical oncologist, I’m pretty sure we cure some metastatic breast cancer. We definitely had patients who lived out their normal life span and died of something else after decades.
“But the definition of cure, sadly, in these situations is that you die of something else without evidence of disease, so we certainly need to do better here and be better able to use the word ‘cure’ in the metastatic setting,” she added.
Promising start
Since 2014, the standard of care for treating patients with recurrent, persistent, or metastatic cervical cancer has been chemotherapy with a platinum compound, paclitaxel, and bevacizumab, based on the results of the GOG 240 study.
Immunotherapy with PD-1 inhibitors had previously shown efficacy as monotherapy in second- or later-line therapy for women with cervical cancer, but KEYNOTE 826 was the first study to show a benefit to promoting immunotherapy to the front ranks.
In the first interim analysis of the trial, reported at the 2021 annual meeting of the European Society for Medical Oncology, after a median follow-up of 22 months, the combination of pembrolizumab and chemotherapy demonstrated significant improvement in progression-free survival (PFS) and overall survival (OS), compared with chemotherapy plus placebo in a biomarker-selected population, which consisted of patients with a combined positive score (CPS) for PD-L1 of 1 or greater.
Pembrolizumab had no apparent efficacy in patients whose tumors did not have detectable PD-L1, however.
Latest results
Now the investigators are reporting the final analysis, conducted after a median follow-up of 39.1 months. The results are those for all comers (308 randomly assigned to receive pembrolizumab plus chemotherapy, and 309 assigned to receive chemotherapy plus placebo), as well as for the biomarker-selected population (consisting of all patients with PD-L1 CPS of 1 or greater) and for the subpopulation of patients with PD-L1 CPS of 10 or greater.
In the all-comers population, the median OS was 26.4 months for patients who received pembrolizumab, compared with 16.8 months for those who received placebo. The 24-month OS rates were 52.1% and 38.7%, respectively. The difference translated into a hazard ratio for death with pembrolizumab of 0.63 (P < .0001).
In the biomarker-selected population (273 assigned to pembrolizumab and 275 assigned to placebo), the respective median OS was 28.6 months versus 16.6 months, with 24-month OS rates of 53.5% versus 39.4%, which translates into an HR for death with pembrolizumab of 0.60 (P < .0001).
Not surprisingly, the best responses to the addition of the PD-1 inhibitor were seen among patients with a PD-L1 CPS of 10 or greater (158 assigned to pembrolizumab and 159 assigned to placebo). In this subgroup, the median OS was 29.6 months with the immune checkpoint inhibitor added to chemotherapy versus 17.4 months for chemotherapy plus placebo. The respective 24-month OS rates were 54.4% and 42.5%, and the HR for overall survival favoring pembrolizumab was 0.58 (P < .0001).
Median PFS 12-month PFS rates also favored pembrolizumab in both the total patient population and the biomarker-selected groups, with median PFS of approximately 10.4 months with pembrolizumab versus approximately 8.2 months with placebo.
The safety profile was manageable, with adverse events as expected from the safety profiles of the individual drugs in the combined regimen. No new safety signals have been seen since the interim analysis, Dr. Monk said.
Regimen details
Patients were randomly assigned in a 1:1 ratio to receive pembrolizumab 200 mg or placebo every 3 weeks for up to 35 cycles plus platinum-based chemotherapy, with bevacizumab added at the investigator’s discretion. Approximately two-thirds of patients in each study arm received bevacizumab.
The dual primary endpoints of PFS and OS were each tested sequentially in patients with a PD-L1 CPS of 1 or greater in both the intention-to-treat or “all-comers” population and in patients with a PD-L1 CPS of 10 or greater.
Patient characteristics were generally well balanced between the treatment groups, except that a slightly higher proportion of patients in the pembrolizumab had tumors of squamous cell histology, compared with the placebo group (76.3% vs. 68.3%).
KEYNOTE-826 was funded by Merck. Dr. Monk has received honoraria and has participated in consulting/advising and speaker’s bureau activity with Merck and other companies. Dr. Gralow has had a consulting or advisory role with Genentech and Roche. Dr. Markham has had a consulting/advisory role for GlaxoSmithKline and has received institutional research funding from Merck and other companies.
A version of this article first appeared on Medscape.com.
FROM ASCO 2023
‘Huge step forward’ in advanced ovarian cancer
The results come from the DUO-O trial, in which the poly (ADP-ribose) polymerase (PARP) inhibitor olaparib (Lynparza) and immunotherapy with the anti–PD-L1 antibody durvalumab (Imfinzi) were added on to standard of care with paclitaxel/carboplatin chemotherapy and bevacizumab (Avastin) in patients with newly diagnosed,non–BRCA-mutated advanced ovarian cancer.
A preplanned interim analysis revealed that the addition of durvalumab and olaparib was associated with a 37% improvement of PFS, compared with the standard of care of chemotherapy plus bevacizumab alone.
This improvement increased to 51% in patients who had tumors positive for homologous recombination deficiency (HRD), which indicates the inability to effectively repair double-stranded DNA breaks, a defect that is present in approximately 70% of ovarian cancers.
Coprincipal investigator Carol Aghajanian, MD, chief of the gynecologic medical oncology service at Memorial Sloan Kettering Cancer Center, New York, described the benefit seen with the novel combination therapy as both “statistically significant and clinically meaningful.”
She was speaking at a press briefing held ahead of the annual meeting of the American Society of Clinical Oncology, where the results were presented.
Commenting for ASCO, Merry Jennifer Markham, MD, professor of medicine and chief of the division of hematology and oncology at University of Florida Health, Gainesville, said the results represents a “huge step forward.”
She added the rate of progress it represents may not be “quick enough for our patients with advanced ovarian cancer but every little integral improvement that we can find in studies that are important, like this one, really means so much to that individual patient in that exam room.”
Dr. Markham underlined that around 80% of women with epithelial ovarian cancer are diagnosed at an advanced stage. “They know what they are facing,” she said. “The vast majority” of them will have a recurrence “at some point.”
“So while progression-free survival may not necessarily mean their overall survival, there will be hope it does. And I’m very excited to see where this study heads in that direction.” Dr. Markham added that PFS is “very important to our patients,” and the study does represent progress. “We are chipping away at improving outcomes for advanced ovarian cancer.”
Moreover, “women are often disappointed when their tumor doesn’t have a BRCA mutation because they know that that may limit some of their treatment options,” and so the current study suggests that there are “options for all-comers” and “there is still hope.”
Access to treatment and testing
When asked whether there could be any access issues for patients clinically eligible for the novel combination, Dr. Aghajanian said that all of the drugs have been approved by the Food and Drug Administration for indications that cover this usage.
They are also covered by medical insurance and, for those patients with financial toxicity, “there is access to co-pay assistance programs and the like.”
She said that patients can then “be counseled on their expected benefit,” based on their BRCA and HRD testing.
Dr. Markham, on the other hand, said she is “a little less optimistic” about access, explaining that she practices in the southern United States, and “our populations [and] insurance coverages are a bit different.”
She noted that, at her institution, a “fair number of patients are underinsured,” and they “ran into a lot of issues with people not being able to afford their copays,” which can be “prohibitive.”
“A large portion of my counseling has been and will continue to be around the benefit, but also the financial toxicity, that that individual patient may experience and the need for copay assistance programs or other support mechanisms,” Markham said.
Dr. Aghajanian added that “financial toxicity and the access issue comes even prior to the treatment, in getting those BRCA1/2 tests and the HRD testing done, so patients have the information they need to make informed decisions.”
“We do have disparities with genetic testing and genomic testing that need to be solved,” she said.
Study details
Previous studies, including SOLO1 and PAOLA-1, have shown that maintenance therapy with olaparib and bevacizumab improves outcomes in the first-line treatment of advanced ovarian cancer.
“However, there still remains unmet need, especially in some patient subgroups without a BRCA mutation,” Dr. Aghajanian said.
While the addition of immunotherapy to standard of care has yet to show a clinical benefit in this setting in phase 3 trials, the phase 2 MEDIOLA study indicated that the combination of durvalumab, bevacizumab, and olaparib was active in nongermline, BRCA-mutated, platinum-sensitive relapsed cancer.
The phase 3 DUO-O study therefore set out to determine whether this combination would be beneficial as a maintenance therapy in 1130 patients with newly diagnosed stage III or IV high-grade ovarian cancer without a tumor BRCA1/2 mutation.
Patients were required to have had no prior systemic therapy for ovarian cancer, and be naive to both PARP inhibition and immunotherapy. They also had to have completed up-front primary debulking surgery, or be scheduled to undergo the procedure.
After an initial cycle of paclitaxel/carboplatin chemotherapy, the patients were randomly assigned to one of three regimens:
- Standard of care treatment, comprising chemotherapy plus bevacizumab and durvalumab-placebo, followed by maintenance therapy with bevacizumab, durvalumab-placebo, and olaparib-placebo (arm 1)
- Chemotherapy plus bevacizumab and durvalumab, followed by maintenance therapy with bevacizumab, durvalumab, and olaparib-placebo (arm 2)
- Chemotherapy plus bevacizumab and durvalumab, followed by maintenance therapy with bevacizumab, durvalumab, and olaparib (arm 3)
In the maintenance phase, bevacizumab was to be given for a total of 15 months, while durvalumab and olaparib, or their equivalent placebos, were prescribed for 24 months. Treatment was continued until disease progression, study completion, or another discontinuation criteria was met.
Dr. Aghajanian presented results from a preplanned interim analysis, with a date cutoff of Dec. 5, 2022.
Among HRD-positive patients, those in arm 3 had a significantly longer PFS than those in arm 1, at a median of 37.3 months versus 23 months, or a hazard ratio of 0.49 (P < .0001).
In the intention-to-treat analysis, arm 3 was also associated with a significant improvement in median PFS over arm 1, at 24.2 months versus 19.3 months, or an HR of 0.63 (P < .0001), indicating that the trial met both of its primary endpoints.
While there was a numerical difference in median PFS between arm 2 and arm 1, at a median of 20.6 months versus 19.3 months, this was not significant. This means that relative contribution of adding durvalumab alone is not clear, Dr. Aghajanian commented, and said that this comparison “will be reassessed at the time of the final PFS analysis.”
She added that a “PFS effect was observed across all subgroups for the arm 3 versus arm 1 comparison,” including in the HRD-negative subgroup, at a median of 20.9 months versus 17.4 months, or an HR of 0.68.
The safety and tolerability of the regimens were generally consistent with what is known for the individual agents, she commented.
Serious adverse events were reported in 34%, 43%, and 39% of patients in arms 1, 2, and 3, respectively.
The most common grade 3 or higher adverse events were neutropenia (in 26% of arm 1 patients, 28% of those in arm 2, and 31% of those in arm 3) followed by anemia (in 8%, 8%, and 24%, respectively).
Dose modifications were required in 72% of arm 1 patients, 80% of those in arm 2, and 85% of arm 3 patients. Treatment discontinuation was recorded in 20%, 26%, and 35%, respectively.
Tackling underserved patient populations
Discussing the results, Christina Fotopoulou, MD, PhD, professor of gynecological cancer surgery in the department of surgery and cancer, Imperial College London, said that, while the regimen may seem new, the treatments involved are “veterans,” and that they are nevertheless tackling previously underserved patient populations.
Dr. Fotopoulou, who was not involved in the study, noted that the results were highly anticipated, and the study has delivered a “breakthrough in ovarian cancer.” She nevertheless questioned the choice of the control arm, and pointed out that the hazard ratio in favor of the combination therapy is “relatively modest” considering that it involves three drugs.
Dr. Fotopoulou highlighted, however, that one of the most important results was in the HRD-negative patients, which she characterized as the equivalent of the clinicians going to “the dark side of the moon.” She said that “for the first time, we have a positive study in this patient population,” although she underlined that the results are from an interim analysis.
The key question that remains, Dr. Fotopoulou asked, is “why? What is making the difference?” She noted that, unfortunately, the trial design does not allow the identification of the relative contribution of olaparib and durvalumab.
The study was sponsored by AstraZeneca, and conducted in collaboration with the European Network of Gynaecological Oncological Trial Groups, GOG Foundation, and Myriad Genetic Laboratories. Dr. Aghajanian declared relationships with AstraZeneca, Merck, Eisai, Repare Therapeutics, AbbVie, Clovis Oncology, and Genentech/Roche. Dr. Markham declared relationships with Pfizer, GlaxoSmithKline, Aduro Biotech, Lilly, Tesaro, Novartis, VBL Therapeutics, AstraZeneca, and Merck.
A version of this article first appeared on Medscape.com.
The results come from the DUO-O trial, in which the poly (ADP-ribose) polymerase (PARP) inhibitor olaparib (Lynparza) and immunotherapy with the anti–PD-L1 antibody durvalumab (Imfinzi) were added on to standard of care with paclitaxel/carboplatin chemotherapy and bevacizumab (Avastin) in patients with newly diagnosed,non–BRCA-mutated advanced ovarian cancer.
A preplanned interim analysis revealed that the addition of durvalumab and olaparib was associated with a 37% improvement of PFS, compared with the standard of care of chemotherapy plus bevacizumab alone.
This improvement increased to 51% in patients who had tumors positive for homologous recombination deficiency (HRD), which indicates the inability to effectively repair double-stranded DNA breaks, a defect that is present in approximately 70% of ovarian cancers.
Coprincipal investigator Carol Aghajanian, MD, chief of the gynecologic medical oncology service at Memorial Sloan Kettering Cancer Center, New York, described the benefit seen with the novel combination therapy as both “statistically significant and clinically meaningful.”
She was speaking at a press briefing held ahead of the annual meeting of the American Society of Clinical Oncology, where the results were presented.
Commenting for ASCO, Merry Jennifer Markham, MD, professor of medicine and chief of the division of hematology and oncology at University of Florida Health, Gainesville, said the results represents a “huge step forward.”
She added the rate of progress it represents may not be “quick enough for our patients with advanced ovarian cancer but every little integral improvement that we can find in studies that are important, like this one, really means so much to that individual patient in that exam room.”
Dr. Markham underlined that around 80% of women with epithelial ovarian cancer are diagnosed at an advanced stage. “They know what they are facing,” she said. “The vast majority” of them will have a recurrence “at some point.”
“So while progression-free survival may not necessarily mean their overall survival, there will be hope it does. And I’m very excited to see where this study heads in that direction.” Dr. Markham added that PFS is “very important to our patients,” and the study does represent progress. “We are chipping away at improving outcomes for advanced ovarian cancer.”
Moreover, “women are often disappointed when their tumor doesn’t have a BRCA mutation because they know that that may limit some of their treatment options,” and so the current study suggests that there are “options for all-comers” and “there is still hope.”
Access to treatment and testing
When asked whether there could be any access issues for patients clinically eligible for the novel combination, Dr. Aghajanian said that all of the drugs have been approved by the Food and Drug Administration for indications that cover this usage.
They are also covered by medical insurance and, for those patients with financial toxicity, “there is access to co-pay assistance programs and the like.”
She said that patients can then “be counseled on their expected benefit,” based on their BRCA and HRD testing.
Dr. Markham, on the other hand, said she is “a little less optimistic” about access, explaining that she practices in the southern United States, and “our populations [and] insurance coverages are a bit different.”
She noted that, at her institution, a “fair number of patients are underinsured,” and they “ran into a lot of issues with people not being able to afford their copays,” which can be “prohibitive.”
“A large portion of my counseling has been and will continue to be around the benefit, but also the financial toxicity, that that individual patient may experience and the need for copay assistance programs or other support mechanisms,” Markham said.
Dr. Aghajanian added that “financial toxicity and the access issue comes even prior to the treatment, in getting those BRCA1/2 tests and the HRD testing done, so patients have the information they need to make informed decisions.”
“We do have disparities with genetic testing and genomic testing that need to be solved,” she said.
Study details
Previous studies, including SOLO1 and PAOLA-1, have shown that maintenance therapy with olaparib and bevacizumab improves outcomes in the first-line treatment of advanced ovarian cancer.
“However, there still remains unmet need, especially in some patient subgroups without a BRCA mutation,” Dr. Aghajanian said.
While the addition of immunotherapy to standard of care has yet to show a clinical benefit in this setting in phase 3 trials, the phase 2 MEDIOLA study indicated that the combination of durvalumab, bevacizumab, and olaparib was active in nongermline, BRCA-mutated, platinum-sensitive relapsed cancer.
The phase 3 DUO-O study therefore set out to determine whether this combination would be beneficial as a maintenance therapy in 1130 patients with newly diagnosed stage III or IV high-grade ovarian cancer without a tumor BRCA1/2 mutation.
Patients were required to have had no prior systemic therapy for ovarian cancer, and be naive to both PARP inhibition and immunotherapy. They also had to have completed up-front primary debulking surgery, or be scheduled to undergo the procedure.
After an initial cycle of paclitaxel/carboplatin chemotherapy, the patients were randomly assigned to one of three regimens:
- Standard of care treatment, comprising chemotherapy plus bevacizumab and durvalumab-placebo, followed by maintenance therapy with bevacizumab, durvalumab-placebo, and olaparib-placebo (arm 1)
- Chemotherapy plus bevacizumab and durvalumab, followed by maintenance therapy with bevacizumab, durvalumab, and olaparib-placebo (arm 2)
- Chemotherapy plus bevacizumab and durvalumab, followed by maintenance therapy with bevacizumab, durvalumab, and olaparib (arm 3)
In the maintenance phase, bevacizumab was to be given for a total of 15 months, while durvalumab and olaparib, or their equivalent placebos, were prescribed for 24 months. Treatment was continued until disease progression, study completion, or another discontinuation criteria was met.
Dr. Aghajanian presented results from a preplanned interim analysis, with a date cutoff of Dec. 5, 2022.
Among HRD-positive patients, those in arm 3 had a significantly longer PFS than those in arm 1, at a median of 37.3 months versus 23 months, or a hazard ratio of 0.49 (P < .0001).
In the intention-to-treat analysis, arm 3 was also associated with a significant improvement in median PFS over arm 1, at 24.2 months versus 19.3 months, or an HR of 0.63 (P < .0001), indicating that the trial met both of its primary endpoints.
While there was a numerical difference in median PFS between arm 2 and arm 1, at a median of 20.6 months versus 19.3 months, this was not significant. This means that relative contribution of adding durvalumab alone is not clear, Dr. Aghajanian commented, and said that this comparison “will be reassessed at the time of the final PFS analysis.”
She added that a “PFS effect was observed across all subgroups for the arm 3 versus arm 1 comparison,” including in the HRD-negative subgroup, at a median of 20.9 months versus 17.4 months, or an HR of 0.68.
The safety and tolerability of the regimens were generally consistent with what is known for the individual agents, she commented.
Serious adverse events were reported in 34%, 43%, and 39% of patients in arms 1, 2, and 3, respectively.
The most common grade 3 or higher adverse events were neutropenia (in 26% of arm 1 patients, 28% of those in arm 2, and 31% of those in arm 3) followed by anemia (in 8%, 8%, and 24%, respectively).
Dose modifications were required in 72% of arm 1 patients, 80% of those in arm 2, and 85% of arm 3 patients. Treatment discontinuation was recorded in 20%, 26%, and 35%, respectively.
Tackling underserved patient populations
Discussing the results, Christina Fotopoulou, MD, PhD, professor of gynecological cancer surgery in the department of surgery and cancer, Imperial College London, said that, while the regimen may seem new, the treatments involved are “veterans,” and that they are nevertheless tackling previously underserved patient populations.
Dr. Fotopoulou, who was not involved in the study, noted that the results were highly anticipated, and the study has delivered a “breakthrough in ovarian cancer.” She nevertheless questioned the choice of the control arm, and pointed out that the hazard ratio in favor of the combination therapy is “relatively modest” considering that it involves three drugs.
Dr. Fotopoulou highlighted, however, that one of the most important results was in the HRD-negative patients, which she characterized as the equivalent of the clinicians going to “the dark side of the moon.” She said that “for the first time, we have a positive study in this patient population,” although she underlined that the results are from an interim analysis.
The key question that remains, Dr. Fotopoulou asked, is “why? What is making the difference?” She noted that, unfortunately, the trial design does not allow the identification of the relative contribution of olaparib and durvalumab.
The study was sponsored by AstraZeneca, and conducted in collaboration with the European Network of Gynaecological Oncological Trial Groups, GOG Foundation, and Myriad Genetic Laboratories. Dr. Aghajanian declared relationships with AstraZeneca, Merck, Eisai, Repare Therapeutics, AbbVie, Clovis Oncology, and Genentech/Roche. Dr. Markham declared relationships with Pfizer, GlaxoSmithKline, Aduro Biotech, Lilly, Tesaro, Novartis, VBL Therapeutics, AstraZeneca, and Merck.
A version of this article first appeared on Medscape.com.
The results come from the DUO-O trial, in which the poly (ADP-ribose) polymerase (PARP) inhibitor olaparib (Lynparza) and immunotherapy with the anti–PD-L1 antibody durvalumab (Imfinzi) were added on to standard of care with paclitaxel/carboplatin chemotherapy and bevacizumab (Avastin) in patients with newly diagnosed,non–BRCA-mutated advanced ovarian cancer.
A preplanned interim analysis revealed that the addition of durvalumab and olaparib was associated with a 37% improvement of PFS, compared with the standard of care of chemotherapy plus bevacizumab alone.
This improvement increased to 51% in patients who had tumors positive for homologous recombination deficiency (HRD), which indicates the inability to effectively repair double-stranded DNA breaks, a defect that is present in approximately 70% of ovarian cancers.
Coprincipal investigator Carol Aghajanian, MD, chief of the gynecologic medical oncology service at Memorial Sloan Kettering Cancer Center, New York, described the benefit seen with the novel combination therapy as both “statistically significant and clinically meaningful.”
She was speaking at a press briefing held ahead of the annual meeting of the American Society of Clinical Oncology, where the results were presented.
Commenting for ASCO, Merry Jennifer Markham, MD, professor of medicine and chief of the division of hematology and oncology at University of Florida Health, Gainesville, said the results represents a “huge step forward.”
She added the rate of progress it represents may not be “quick enough for our patients with advanced ovarian cancer but every little integral improvement that we can find in studies that are important, like this one, really means so much to that individual patient in that exam room.”
Dr. Markham underlined that around 80% of women with epithelial ovarian cancer are diagnosed at an advanced stage. “They know what they are facing,” she said. “The vast majority” of them will have a recurrence “at some point.”
“So while progression-free survival may not necessarily mean their overall survival, there will be hope it does. And I’m very excited to see where this study heads in that direction.” Dr. Markham added that PFS is “very important to our patients,” and the study does represent progress. “We are chipping away at improving outcomes for advanced ovarian cancer.”
Moreover, “women are often disappointed when their tumor doesn’t have a BRCA mutation because they know that that may limit some of their treatment options,” and so the current study suggests that there are “options for all-comers” and “there is still hope.”
Access to treatment and testing
When asked whether there could be any access issues for patients clinically eligible for the novel combination, Dr. Aghajanian said that all of the drugs have been approved by the Food and Drug Administration for indications that cover this usage.
They are also covered by medical insurance and, for those patients with financial toxicity, “there is access to co-pay assistance programs and the like.”
She said that patients can then “be counseled on their expected benefit,” based on their BRCA and HRD testing.
Dr. Markham, on the other hand, said she is “a little less optimistic” about access, explaining that she practices in the southern United States, and “our populations [and] insurance coverages are a bit different.”
She noted that, at her institution, a “fair number of patients are underinsured,” and they “ran into a lot of issues with people not being able to afford their copays,” which can be “prohibitive.”
“A large portion of my counseling has been and will continue to be around the benefit, but also the financial toxicity, that that individual patient may experience and the need for copay assistance programs or other support mechanisms,” Markham said.
Dr. Aghajanian added that “financial toxicity and the access issue comes even prior to the treatment, in getting those BRCA1/2 tests and the HRD testing done, so patients have the information they need to make informed decisions.”
“We do have disparities with genetic testing and genomic testing that need to be solved,” she said.
Study details
Previous studies, including SOLO1 and PAOLA-1, have shown that maintenance therapy with olaparib and bevacizumab improves outcomes in the first-line treatment of advanced ovarian cancer.
“However, there still remains unmet need, especially in some patient subgroups without a BRCA mutation,” Dr. Aghajanian said.
While the addition of immunotherapy to standard of care has yet to show a clinical benefit in this setting in phase 3 trials, the phase 2 MEDIOLA study indicated that the combination of durvalumab, bevacizumab, and olaparib was active in nongermline, BRCA-mutated, platinum-sensitive relapsed cancer.
The phase 3 DUO-O study therefore set out to determine whether this combination would be beneficial as a maintenance therapy in 1130 patients with newly diagnosed stage III or IV high-grade ovarian cancer without a tumor BRCA1/2 mutation.
Patients were required to have had no prior systemic therapy for ovarian cancer, and be naive to both PARP inhibition and immunotherapy. They also had to have completed up-front primary debulking surgery, or be scheduled to undergo the procedure.
After an initial cycle of paclitaxel/carboplatin chemotherapy, the patients were randomly assigned to one of three regimens:
- Standard of care treatment, comprising chemotherapy plus bevacizumab and durvalumab-placebo, followed by maintenance therapy with bevacizumab, durvalumab-placebo, and olaparib-placebo (arm 1)
- Chemotherapy plus bevacizumab and durvalumab, followed by maintenance therapy with bevacizumab, durvalumab, and olaparib-placebo (arm 2)
- Chemotherapy plus bevacizumab and durvalumab, followed by maintenance therapy with bevacizumab, durvalumab, and olaparib (arm 3)
In the maintenance phase, bevacizumab was to be given for a total of 15 months, while durvalumab and olaparib, or their equivalent placebos, were prescribed for 24 months. Treatment was continued until disease progression, study completion, or another discontinuation criteria was met.
Dr. Aghajanian presented results from a preplanned interim analysis, with a date cutoff of Dec. 5, 2022.
Among HRD-positive patients, those in arm 3 had a significantly longer PFS than those in arm 1, at a median of 37.3 months versus 23 months, or a hazard ratio of 0.49 (P < .0001).
In the intention-to-treat analysis, arm 3 was also associated with a significant improvement in median PFS over arm 1, at 24.2 months versus 19.3 months, or an HR of 0.63 (P < .0001), indicating that the trial met both of its primary endpoints.
While there was a numerical difference in median PFS between arm 2 and arm 1, at a median of 20.6 months versus 19.3 months, this was not significant. This means that relative contribution of adding durvalumab alone is not clear, Dr. Aghajanian commented, and said that this comparison “will be reassessed at the time of the final PFS analysis.”
She added that a “PFS effect was observed across all subgroups for the arm 3 versus arm 1 comparison,” including in the HRD-negative subgroup, at a median of 20.9 months versus 17.4 months, or an HR of 0.68.
The safety and tolerability of the regimens were generally consistent with what is known for the individual agents, she commented.
Serious adverse events were reported in 34%, 43%, and 39% of patients in arms 1, 2, and 3, respectively.
The most common grade 3 or higher adverse events were neutropenia (in 26% of arm 1 patients, 28% of those in arm 2, and 31% of those in arm 3) followed by anemia (in 8%, 8%, and 24%, respectively).
Dose modifications were required in 72% of arm 1 patients, 80% of those in arm 2, and 85% of arm 3 patients. Treatment discontinuation was recorded in 20%, 26%, and 35%, respectively.
Tackling underserved patient populations
Discussing the results, Christina Fotopoulou, MD, PhD, professor of gynecological cancer surgery in the department of surgery and cancer, Imperial College London, said that, while the regimen may seem new, the treatments involved are “veterans,” and that they are nevertheless tackling previously underserved patient populations.
Dr. Fotopoulou, who was not involved in the study, noted that the results were highly anticipated, and the study has delivered a “breakthrough in ovarian cancer.” She nevertheless questioned the choice of the control arm, and pointed out that the hazard ratio in favor of the combination therapy is “relatively modest” considering that it involves three drugs.
Dr. Fotopoulou highlighted, however, that one of the most important results was in the HRD-negative patients, which she characterized as the equivalent of the clinicians going to “the dark side of the moon.” She said that “for the first time, we have a positive study in this patient population,” although she underlined that the results are from an interim analysis.
The key question that remains, Dr. Fotopoulou asked, is “why? What is making the difference?” She noted that, unfortunately, the trial design does not allow the identification of the relative contribution of olaparib and durvalumab.
The study was sponsored by AstraZeneca, and conducted in collaboration with the European Network of Gynaecological Oncological Trial Groups, GOG Foundation, and Myriad Genetic Laboratories. Dr. Aghajanian declared relationships with AstraZeneca, Merck, Eisai, Repare Therapeutics, AbbVie, Clovis Oncology, and Genentech/Roche. Dr. Markham declared relationships with Pfizer, GlaxoSmithKline, Aduro Biotech, Lilly, Tesaro, Novartis, VBL Therapeutics, AstraZeneca, and Merck.
A version of this article first appeared on Medscape.com.
AT ASCO 2023
SCLC: Bispecific antibody shows phase 1 promise
CHICAGO –
The antibody promotes the destruction of tumor cells by T cells by acting as a bridge between T cells and tumors.
SCLC has largely resisted efforts to identify unique surface markers. DLL3 is an exception: It is rarely expressed in normal cells, and it seems to be important to tumor biology, according to Martin Wermke, MD, who presented the study at the annual meeting of the American Society of Clinical Oncology.
A rare SCLC biomarker
“The problem, I think, is that small cell [lung cancer] with its high mutational burden is a bunch of many different subentities and you will probably not find a single driver mutation as you do in non–small cell lung cancer. So in that [way] it’s different in its biology,” said Dr. Wermke, professor of experimental tumor therapy at the National Center for Tumor Diseases in Dresden, Germany.
Nevertheless, DLL3 is a sensitive biomarker, with over 90% of SCLC tumors positive for the surface marker, according to Dr. Wermke. “It’s one of the first which proved to be a reliable [SCLC] biomarker for therapeutic approaches,” said Dr. Wermke.
This isn’t the first clinical experience with DLL3. An anti-DLL3 antibody was used as part of an antibody-drug conjugate called Rova-T, which failed a phase 3 trial in SCLC in 2021 and was subsequently canceled by AbbVie, but Dr. Wermke believes that the issue was with the drug and linker (a chemical tag that links the cytotoxic drug to the antibody, which is designed to release the drug in an appropriate environment such as the interior of a tumor cell after an antibody-drug conjugate has been internalized by the tumor cell), not DLL3. DLL3 is also being investigated as a component of chimeric antigen receptor T-cell therapy, though no clinical results have been reported, Dr. Wermke said.
Study methods and results
The study included 107 patients. The median age was 60.0 years, and 57% were male. To be included, patients had to have advanced SCLC, large cell neuroendocrine carcinoma, or extrapulmonary neuroendocrine carcinoma, as well as test positive for DLL3 expression.
The drug was well tolerated: 86% of patients experienced at least one treatment-related adverse event: 59% with a grade 1-2 TRAE and 27% with a grade 3-5 TRAE. Cytokine release syndrome (CRS) occurred in 59% of patients, but just 2% were grade 3-5. TRAEs led to discontinuation in 4% of patients. Physicians were able to manage CRS with supportive care, steroids, and anti–interleukin-6 receptor antibodies.
The treatment showed signs of efficacy, with partial responses occurring in 18% of patients, stable disease in 23%, progressive disease in 45%, while 13% were not evaluable.
At doses of 90 mg/kg or above, partial response occurred in 25% of patients, stable disease in 27%, and progressive disease in 31%, while 13% were not evaluable. Similar patterns were seen across three tumor types.
Of 18 responders, 14 continued to be responders at the time of the presentation. The longest response lengths were 13.1 months, 10.7 months, and 9.4 months.
Dr. Wermke said that the responses were encouraging, particularly the duration of some responses.
“Having a small cell [lung cancer] patient responding to something for more than a year is extraordinary. It comes with side effects, which are usually seen during the first [doses]. After that, the drug is pretty well tolerable, and that is also something which distinguishes it from alternative second-line approaches,” he said.
Well tolerated, but take efficacy data with a grain of salt
The study was encouraging but should be treated with caution, according to Vamsidhar Velcheti, MD, who moderated the session where the research was presented.
“The toxicity profile is actually very promising and it’s still very early, but there’s certainly a lot of interest in DLL3-targeted [therapies]. We’ve seen some very exciting data with other assets in this category as well,” said Dr. Velcheti, director of thoracic oncology at NYU Langone Health, New York.
Phase 1 efficacy data can be tantalizing but often fails to hold up to further testing, according to Dr. Velcheti. “We’ve seen signals in phase 1 data before, and we’ve been burned. We saw really promising data with Rova-T, and the confirmatory trials were negative, – so we want to be cautiously optimistic,” said Dr. Velcheti.
He also pointed out that patient selection will be important for such studies, considering that SCLC patients often have a lot of comorbidities and the therapy’s potential for causing CRS.
Both Dr. Wermke and Dr. Velcheti have received funding from numerous pharmaceutical companies. Dr. Wermke has consulted with or advised with Amgen, Bayer, Boehringer Ingelheim, Bristol-Myers Squibb, ImCheck Therapeutics, Immatics, ISA Pharmaceuticals, Lilly, and Novartis.
CHICAGO –
The antibody promotes the destruction of tumor cells by T cells by acting as a bridge between T cells and tumors.
SCLC has largely resisted efforts to identify unique surface markers. DLL3 is an exception: It is rarely expressed in normal cells, and it seems to be important to tumor biology, according to Martin Wermke, MD, who presented the study at the annual meeting of the American Society of Clinical Oncology.
A rare SCLC biomarker
“The problem, I think, is that small cell [lung cancer] with its high mutational burden is a bunch of many different subentities and you will probably not find a single driver mutation as you do in non–small cell lung cancer. So in that [way] it’s different in its biology,” said Dr. Wermke, professor of experimental tumor therapy at the National Center for Tumor Diseases in Dresden, Germany.
Nevertheless, DLL3 is a sensitive biomarker, with over 90% of SCLC tumors positive for the surface marker, according to Dr. Wermke. “It’s one of the first which proved to be a reliable [SCLC] biomarker for therapeutic approaches,” said Dr. Wermke.
This isn’t the first clinical experience with DLL3. An anti-DLL3 antibody was used as part of an antibody-drug conjugate called Rova-T, which failed a phase 3 trial in SCLC in 2021 and was subsequently canceled by AbbVie, but Dr. Wermke believes that the issue was with the drug and linker (a chemical tag that links the cytotoxic drug to the antibody, which is designed to release the drug in an appropriate environment such as the interior of a tumor cell after an antibody-drug conjugate has been internalized by the tumor cell), not DLL3. DLL3 is also being investigated as a component of chimeric antigen receptor T-cell therapy, though no clinical results have been reported, Dr. Wermke said.
Study methods and results
The study included 107 patients. The median age was 60.0 years, and 57% were male. To be included, patients had to have advanced SCLC, large cell neuroendocrine carcinoma, or extrapulmonary neuroendocrine carcinoma, as well as test positive for DLL3 expression.
The drug was well tolerated: 86% of patients experienced at least one treatment-related adverse event: 59% with a grade 1-2 TRAE and 27% with a grade 3-5 TRAE. Cytokine release syndrome (CRS) occurred in 59% of patients, but just 2% were grade 3-5. TRAEs led to discontinuation in 4% of patients. Physicians were able to manage CRS with supportive care, steroids, and anti–interleukin-6 receptor antibodies.
The treatment showed signs of efficacy, with partial responses occurring in 18% of patients, stable disease in 23%, progressive disease in 45%, while 13% were not evaluable.
At doses of 90 mg/kg or above, partial response occurred in 25% of patients, stable disease in 27%, and progressive disease in 31%, while 13% were not evaluable. Similar patterns were seen across three tumor types.
Of 18 responders, 14 continued to be responders at the time of the presentation. The longest response lengths were 13.1 months, 10.7 months, and 9.4 months.
Dr. Wermke said that the responses were encouraging, particularly the duration of some responses.
“Having a small cell [lung cancer] patient responding to something for more than a year is extraordinary. It comes with side effects, which are usually seen during the first [doses]. After that, the drug is pretty well tolerable, and that is also something which distinguishes it from alternative second-line approaches,” he said.
Well tolerated, but take efficacy data with a grain of salt
The study was encouraging but should be treated with caution, according to Vamsidhar Velcheti, MD, who moderated the session where the research was presented.
“The toxicity profile is actually very promising and it’s still very early, but there’s certainly a lot of interest in DLL3-targeted [therapies]. We’ve seen some very exciting data with other assets in this category as well,” said Dr. Velcheti, director of thoracic oncology at NYU Langone Health, New York.
Phase 1 efficacy data can be tantalizing but often fails to hold up to further testing, according to Dr. Velcheti. “We’ve seen signals in phase 1 data before, and we’ve been burned. We saw really promising data with Rova-T, and the confirmatory trials were negative, – so we want to be cautiously optimistic,” said Dr. Velcheti.
He also pointed out that patient selection will be important for such studies, considering that SCLC patients often have a lot of comorbidities and the therapy’s potential for causing CRS.
Both Dr. Wermke and Dr. Velcheti have received funding from numerous pharmaceutical companies. Dr. Wermke has consulted with or advised with Amgen, Bayer, Boehringer Ingelheim, Bristol-Myers Squibb, ImCheck Therapeutics, Immatics, ISA Pharmaceuticals, Lilly, and Novartis.
CHICAGO –
The antibody promotes the destruction of tumor cells by T cells by acting as a bridge between T cells and tumors.
SCLC has largely resisted efforts to identify unique surface markers. DLL3 is an exception: It is rarely expressed in normal cells, and it seems to be important to tumor biology, according to Martin Wermke, MD, who presented the study at the annual meeting of the American Society of Clinical Oncology.
A rare SCLC biomarker
“The problem, I think, is that small cell [lung cancer] with its high mutational burden is a bunch of many different subentities and you will probably not find a single driver mutation as you do in non–small cell lung cancer. So in that [way] it’s different in its biology,” said Dr. Wermke, professor of experimental tumor therapy at the National Center for Tumor Diseases in Dresden, Germany.
Nevertheless, DLL3 is a sensitive biomarker, with over 90% of SCLC tumors positive for the surface marker, according to Dr. Wermke. “It’s one of the first which proved to be a reliable [SCLC] biomarker for therapeutic approaches,” said Dr. Wermke.
This isn’t the first clinical experience with DLL3. An anti-DLL3 antibody was used as part of an antibody-drug conjugate called Rova-T, which failed a phase 3 trial in SCLC in 2021 and was subsequently canceled by AbbVie, but Dr. Wermke believes that the issue was with the drug and linker (a chemical tag that links the cytotoxic drug to the antibody, which is designed to release the drug in an appropriate environment such as the interior of a tumor cell after an antibody-drug conjugate has been internalized by the tumor cell), not DLL3. DLL3 is also being investigated as a component of chimeric antigen receptor T-cell therapy, though no clinical results have been reported, Dr. Wermke said.
Study methods and results
The study included 107 patients. The median age was 60.0 years, and 57% were male. To be included, patients had to have advanced SCLC, large cell neuroendocrine carcinoma, or extrapulmonary neuroendocrine carcinoma, as well as test positive for DLL3 expression.
The drug was well tolerated: 86% of patients experienced at least one treatment-related adverse event: 59% with a grade 1-2 TRAE and 27% with a grade 3-5 TRAE. Cytokine release syndrome (CRS) occurred in 59% of patients, but just 2% were grade 3-5. TRAEs led to discontinuation in 4% of patients. Physicians were able to manage CRS with supportive care, steroids, and anti–interleukin-6 receptor antibodies.
The treatment showed signs of efficacy, with partial responses occurring in 18% of patients, stable disease in 23%, progressive disease in 45%, while 13% were not evaluable.
At doses of 90 mg/kg or above, partial response occurred in 25% of patients, stable disease in 27%, and progressive disease in 31%, while 13% were not evaluable. Similar patterns were seen across three tumor types.
Of 18 responders, 14 continued to be responders at the time of the presentation. The longest response lengths were 13.1 months, 10.7 months, and 9.4 months.
Dr. Wermke said that the responses were encouraging, particularly the duration of some responses.
“Having a small cell [lung cancer] patient responding to something for more than a year is extraordinary. It comes with side effects, which are usually seen during the first [doses]. After that, the drug is pretty well tolerable, and that is also something which distinguishes it from alternative second-line approaches,” he said.
Well tolerated, but take efficacy data with a grain of salt
The study was encouraging but should be treated with caution, according to Vamsidhar Velcheti, MD, who moderated the session where the research was presented.
“The toxicity profile is actually very promising and it’s still very early, but there’s certainly a lot of interest in DLL3-targeted [therapies]. We’ve seen some very exciting data with other assets in this category as well,” said Dr. Velcheti, director of thoracic oncology at NYU Langone Health, New York.
Phase 1 efficacy data can be tantalizing but often fails to hold up to further testing, according to Dr. Velcheti. “We’ve seen signals in phase 1 data before, and we’ve been burned. We saw really promising data with Rova-T, and the confirmatory trials were negative, – so we want to be cautiously optimistic,” said Dr. Velcheti.
He also pointed out that patient selection will be important for such studies, considering that SCLC patients often have a lot of comorbidities and the therapy’s potential for causing CRS.
Both Dr. Wermke and Dr. Velcheti have received funding from numerous pharmaceutical companies. Dr. Wermke has consulted with or advised with Amgen, Bayer, Boehringer Ingelheim, Bristol-Myers Squibb, ImCheck Therapeutics, Immatics, ISA Pharmaceuticals, Lilly, and Novartis.
AT ASCO 2023