User login
No staff COVID-19 diagnoses after plan at Chinese cancer center
Short-term results
No staff members or patients were diagnosed with COVID-19 after “strict protective measures” for screening and managing patients were implemented at the National Cancer Center/Cancer Hospital, Chinese Academy of Sciences, in Beijing, according to a report published online April 1 in JAMA Oncology.
However, the time period for the analysis, which included nearly 3000 patients, was short — only about 3 weeks (February 12 to March 3). Also, Beijing is more than 1100 kilometers from Wuhan, the center of the Chinese outbreak of COVID-19.
The Beijing cancer hospital implemented a multipronged safety plan in February in order to “avoid COVID-19 related nosocomial cross-infection between patients and medical staff,” explain the authors, led by medical oncologist Zhijie Wang, MD.
Notably, “all of the measures taken in China are actively being implemented and used in major oncology centers in the United States,” Robert Carlson, MD, chief executive officer, National Comprehensive Cancer Network (NCCN), told Medscape Medical News.
John Greene, MD, section chief, Infectious Disease and Tropical Medicine, Moffitt Cancer Center, Tampa, Florida, pointed out that the Chinese safety plan, which is full of “good measures,” is being largely used at his center. However, he observed that one tool — doing a temperature check at the hospital front door — is not well supported by most of the literature. “It gives good optics and looks like you are doing the most you possibly can, but scientifically it may not be as effective [as other screening measures],” he said.
The Chinese plan consists of four broad elements
First, the above-mentioned on-site temperature tests are performed at the entrances of the hospital, outpatient clinic, and wards. Contact and travel histories related to the Wuhan epidemic area are also established and recorded.
Second, an outpatient appointment scheduling system allows both online scheduling and on-site registration. Online consultation channels are open daily, featuring instruction on medication taking and cancer-related symptom management. These “substantially reduced the flow of people in the hospital,” write the authors. On-site patients must wear a mask and have their own disinfectant.
Third, for patients with cancer preparing to be admitted to hospital, symptoms associated with COVID-19, such as fever and cough, are recorded. Mandatory blood tests and CT scans of the lungs are performed. COVID-19 virus nucleic acid tests are performed for patients with suspected pneumonia on imaging.
Fourth, some anticancer drugs conventionally administered by infusion have been changed to oral administration, such as etoposide and vinorelbine. For adjuvant or maintenance chemotherapy, the infusion intervals were appropriately prolonged depending on patients’ conditions.
Eight out of 2,900 patients had imaging suspicious for infection
The Chinese authors report that a total of 2,944 patients with cancer were seen for clinic consultation and treatment in the wards (2795 outpatients and 149 inpatients).
Patients with cancer are believed to have a higher probability of severe illness and increased mortality compared with the healthy population once infected with COVID-19, point out the authors.
Under the new “strict screening strategy,” 27 patients showed radiologic manifestations of inflammatory changes or multiple-site exudative pneumonia in the lungs, including eight suspected of having COVID-19 infection. “Fortunately, negative results from nucleic acid testing ultimately excluded COVID-19 infection in all these patients,” the authors report.
However, two of these patients “presented with recovered pneumonia after symptomatic treatment.” Commenting on this finding, Moffitt’s Greene said that may mean these two patients were tested and found to be positive but were early in the infection and not yet shedding the virus, or they were infected after the initial negative result.
Greene said his center has implemented some measures not mentioned in the Chinese plan. For example, the Florida center no longer allows inpatient visitation. Also, one third of staff now work from home, resulting in less social interaction. Social distancing in meetings, the cafeteria, and hallways is being observed “aggressively,” and most meetings are now on Zoom, he said.
Moffitt has not been hard hit with COVID-19 and is at level one preparedness, the lowest rung. The center has performed 60 tests to date, with only one positive for the virus (< 2%), Greene told Medscape Medical News.
Currently, in the larger Tampa Bay community setting, about 12% of tests are positive.
The low percentage found among the Moffitt patients “tells you that a lot of cancer patients have fever and respiratory symptoms due to other viruses and, more importantly, other reasons, whether it’s their immunotherapy or chemotherapy or their cancer,” said Greene.
NCCN’s Carlson said the publication of the Chinese data was a good sign in terms of international science.
“This is a strong example of how the global oncology community rapidly shares information and experience whenever it makes a difference in patient care,” he commented.
The authors, as well as Carlson and Greene, have reported no relevant financial relationships.
This article first appeared on Medscape.com.
Short-term results
Short-term results
No staff members or patients were diagnosed with COVID-19 after “strict protective measures” for screening and managing patients were implemented at the National Cancer Center/Cancer Hospital, Chinese Academy of Sciences, in Beijing, according to a report published online April 1 in JAMA Oncology.
However, the time period for the analysis, which included nearly 3000 patients, was short — only about 3 weeks (February 12 to March 3). Also, Beijing is more than 1100 kilometers from Wuhan, the center of the Chinese outbreak of COVID-19.
The Beijing cancer hospital implemented a multipronged safety plan in February in order to “avoid COVID-19 related nosocomial cross-infection between patients and medical staff,” explain the authors, led by medical oncologist Zhijie Wang, MD.
Notably, “all of the measures taken in China are actively being implemented and used in major oncology centers in the United States,” Robert Carlson, MD, chief executive officer, National Comprehensive Cancer Network (NCCN), told Medscape Medical News.
John Greene, MD, section chief, Infectious Disease and Tropical Medicine, Moffitt Cancer Center, Tampa, Florida, pointed out that the Chinese safety plan, which is full of “good measures,” is being largely used at his center. However, he observed that one tool — doing a temperature check at the hospital front door — is not well supported by most of the literature. “It gives good optics and looks like you are doing the most you possibly can, but scientifically it may not be as effective [as other screening measures],” he said.
The Chinese plan consists of four broad elements
First, the above-mentioned on-site temperature tests are performed at the entrances of the hospital, outpatient clinic, and wards. Contact and travel histories related to the Wuhan epidemic area are also established and recorded.
Second, an outpatient appointment scheduling system allows both online scheduling and on-site registration. Online consultation channels are open daily, featuring instruction on medication taking and cancer-related symptom management. These “substantially reduced the flow of people in the hospital,” write the authors. On-site patients must wear a mask and have their own disinfectant.
Third, for patients with cancer preparing to be admitted to hospital, symptoms associated with COVID-19, such as fever and cough, are recorded. Mandatory blood tests and CT scans of the lungs are performed. COVID-19 virus nucleic acid tests are performed for patients with suspected pneumonia on imaging.
Fourth, some anticancer drugs conventionally administered by infusion have been changed to oral administration, such as etoposide and vinorelbine. For adjuvant or maintenance chemotherapy, the infusion intervals were appropriately prolonged depending on patients’ conditions.
Eight out of 2,900 patients had imaging suspicious for infection
The Chinese authors report that a total of 2,944 patients with cancer were seen for clinic consultation and treatment in the wards (2795 outpatients and 149 inpatients).
Patients with cancer are believed to have a higher probability of severe illness and increased mortality compared with the healthy population once infected with COVID-19, point out the authors.
Under the new “strict screening strategy,” 27 patients showed radiologic manifestations of inflammatory changes or multiple-site exudative pneumonia in the lungs, including eight suspected of having COVID-19 infection. “Fortunately, negative results from nucleic acid testing ultimately excluded COVID-19 infection in all these patients,” the authors report.
However, two of these patients “presented with recovered pneumonia after symptomatic treatment.” Commenting on this finding, Moffitt’s Greene said that may mean these two patients were tested and found to be positive but were early in the infection and not yet shedding the virus, or they were infected after the initial negative result.
Greene said his center has implemented some measures not mentioned in the Chinese plan. For example, the Florida center no longer allows inpatient visitation. Also, one third of staff now work from home, resulting in less social interaction. Social distancing in meetings, the cafeteria, and hallways is being observed “aggressively,” and most meetings are now on Zoom, he said.
Moffitt has not been hard hit with COVID-19 and is at level one preparedness, the lowest rung. The center has performed 60 tests to date, with only one positive for the virus (< 2%), Greene told Medscape Medical News.
Currently, in the larger Tampa Bay community setting, about 12% of tests are positive.
The low percentage found among the Moffitt patients “tells you that a lot of cancer patients have fever and respiratory symptoms due to other viruses and, more importantly, other reasons, whether it’s their immunotherapy or chemotherapy or their cancer,” said Greene.
NCCN’s Carlson said the publication of the Chinese data was a good sign in terms of international science.
“This is a strong example of how the global oncology community rapidly shares information and experience whenever it makes a difference in patient care,” he commented.
The authors, as well as Carlson and Greene, have reported no relevant financial relationships.
This article first appeared on Medscape.com.
No staff members or patients were diagnosed with COVID-19 after “strict protective measures” for screening and managing patients were implemented at the National Cancer Center/Cancer Hospital, Chinese Academy of Sciences, in Beijing, according to a report published online April 1 in JAMA Oncology.
However, the time period for the analysis, which included nearly 3000 patients, was short — only about 3 weeks (February 12 to March 3). Also, Beijing is more than 1100 kilometers from Wuhan, the center of the Chinese outbreak of COVID-19.
The Beijing cancer hospital implemented a multipronged safety plan in February in order to “avoid COVID-19 related nosocomial cross-infection between patients and medical staff,” explain the authors, led by medical oncologist Zhijie Wang, MD.
Notably, “all of the measures taken in China are actively being implemented and used in major oncology centers in the United States,” Robert Carlson, MD, chief executive officer, National Comprehensive Cancer Network (NCCN), told Medscape Medical News.
John Greene, MD, section chief, Infectious Disease and Tropical Medicine, Moffitt Cancer Center, Tampa, Florida, pointed out that the Chinese safety plan, which is full of “good measures,” is being largely used at his center. However, he observed that one tool — doing a temperature check at the hospital front door — is not well supported by most of the literature. “It gives good optics and looks like you are doing the most you possibly can, but scientifically it may not be as effective [as other screening measures],” he said.
The Chinese plan consists of four broad elements
First, the above-mentioned on-site temperature tests are performed at the entrances of the hospital, outpatient clinic, and wards. Contact and travel histories related to the Wuhan epidemic area are also established and recorded.
Second, an outpatient appointment scheduling system allows both online scheduling and on-site registration. Online consultation channels are open daily, featuring instruction on medication taking and cancer-related symptom management. These “substantially reduced the flow of people in the hospital,” write the authors. On-site patients must wear a mask and have their own disinfectant.
Third, for patients with cancer preparing to be admitted to hospital, symptoms associated with COVID-19, such as fever and cough, are recorded. Mandatory blood tests and CT scans of the lungs are performed. COVID-19 virus nucleic acid tests are performed for patients with suspected pneumonia on imaging.
Fourth, some anticancer drugs conventionally administered by infusion have been changed to oral administration, such as etoposide and vinorelbine. For adjuvant or maintenance chemotherapy, the infusion intervals were appropriately prolonged depending on patients’ conditions.
Eight out of 2,900 patients had imaging suspicious for infection
The Chinese authors report that a total of 2,944 patients with cancer were seen for clinic consultation and treatment in the wards (2795 outpatients and 149 inpatients).
Patients with cancer are believed to have a higher probability of severe illness and increased mortality compared with the healthy population once infected with COVID-19, point out the authors.
Under the new “strict screening strategy,” 27 patients showed radiologic manifestations of inflammatory changes or multiple-site exudative pneumonia in the lungs, including eight suspected of having COVID-19 infection. “Fortunately, negative results from nucleic acid testing ultimately excluded COVID-19 infection in all these patients,” the authors report.
However, two of these patients “presented with recovered pneumonia after symptomatic treatment.” Commenting on this finding, Moffitt’s Greene said that may mean these two patients were tested and found to be positive but were early in the infection and not yet shedding the virus, or they were infected after the initial negative result.
Greene said his center has implemented some measures not mentioned in the Chinese plan. For example, the Florida center no longer allows inpatient visitation. Also, one third of staff now work from home, resulting in less social interaction. Social distancing in meetings, the cafeteria, and hallways is being observed “aggressively,” and most meetings are now on Zoom, he said.
Moffitt has not been hard hit with COVID-19 and is at level one preparedness, the lowest rung. The center has performed 60 tests to date, with only one positive for the virus (< 2%), Greene told Medscape Medical News.
Currently, in the larger Tampa Bay community setting, about 12% of tests are positive.
The low percentage found among the Moffitt patients “tells you that a lot of cancer patients have fever and respiratory symptoms due to other viruses and, more importantly, other reasons, whether it’s their immunotherapy or chemotherapy or their cancer,” said Greene.
NCCN’s Carlson said the publication of the Chinese data was a good sign in terms of international science.
“This is a strong example of how the global oncology community rapidly shares information and experience whenever it makes a difference in patient care,” he commented.
The authors, as well as Carlson and Greene, have reported no relevant financial relationships.
This article first appeared on Medscape.com.
Maintaining cancer care in the face of COVID-19
Medical oncologist Anne Chiang, MD, PhD, is scrambling to maintain cancer care in New Haven, Connecticut, while COVID-19 advances unrelentingly. As deputy chief medical officer of the Smilow Cancer Network, the largest cancer care delivery system in Connecticut and Rhode Island, she has no illusions about dodging what’s unfolding just 2 hours down the road in New York City.
“They’re trying their best to continue active cancer treatment but it’s getting harder,” she says of her colleagues in the thick of the pandemic. “We have to be prepared for it here.”
In anticipation of what’s coming, her team has just emptied the top three floors of the Smilow Cancer Hospital, moving 60 patients by ambulance and other medical transport to a different hospital nearby.
The move frees the Smilow Cancer hospital’s negative-pressure wards for the anticipated wave of COVID-19 patients. It will keep the virus sealed off from the rest of the hospital. But in other locations it’s harder to shield patients with cancer from the infection.
Around the state, Smilow Cancer Network’s affiliated hospitals are already treating a growing number of COVID-19 patients, especially at Greenwich Hospital, right on the border with New York state.
To protect patients with cancer, who are among the most vulnerable to the virus, oncologists are embracing telemedicine to allow most patients to stay home.
“We’re really concentrating on decreasing the risk to these patients, with a widespread massive-scale conversion to telehealth,” said Chiang. “This is something that, in the space of about a week, has transformed the care of our patients — it’s a really amazing transformation.”
If anything good comes out of the COVID-19 pandemic, it will be this global adoption of virtual healthcare.
Across the US border in Canada, the medical director of Toronto’s Princess Margaret Cancer Centre is directing a similar transformation.
“We have converted probably about 70% to 80% of our clinic visits to virtual visits,” says radiation oncologist Mary Gospodarowicz, MD.
“We have three priorities: number one, to keep our patients safe; number two, to keep our staff safe, because if staff are sick we won’t be treating anybody; and number three, to treat as many patients with cancer as possible.”
Gospodarowicz woke up last week to a local headline about a woman whose mastectomy had been canceled “because of the coronavirus.” The story exposed the many layers of the COVID-19 crisis. “A lot of hospitals have canceled elective surgeries,” she acknowledged. “For patients who have treatment or surgery deferred, we have a database and we’ll make sure we look after those patients eventually. We have a priority system, so low-risk prostate cancer, very low-risk breast cancer patients are waiting. All the urgent head and neck, breast, and other higher priority surgeries are still being done, but it just depends how it goes. The situation changes every day.”
It’s similar in Los Angeles, at the University of Southern California, says Elizabeth David, MD, a cardiothoracic surgeon with Keck Medicine.
“For thoracic, we just had a conference call with about 30 surgeons around the country going through really nitty-gritty specifics to help with our decision making about what could wait without detriment to the patient – hopefully – and what should be done now,” she told Medscape Medical News.
“There are some hospitals where they are not doing anything but life and death emergency operations, whereas we are still doing our emergent cancer operations in our institution, but we all know – and patients know – that could change from one day to the next. They may think they’re having surgery tomorrow but may get a call saying we can’t do it,” David said.
Many of David’s patients have non–small cell lung cancer, putting them at particular risk with a pulmonary infection like COVID-19. For now, she says delivery of postsurgical chemotherapy and radiotherapy has not been impacted in her area, but her videoconference discussions with patients are much longer – and harder – these days.
“I’ve been in practice a while now and I’ve had numerous conversations with patients this week that I never trained for, and I’ve never known anyone else who has. It’s really hard as a provider to know what to say,” she said.
In cardiothoracic surgery, David said guidance on clinical decision making is coming from the American College of Surgeons, Society of Thoracic Surgery, and American Association of Thoracic Surgeons. Yet, she says each patient is being assessed – and reassessed – individually.
“You have to balance the risk of delaying the intervention with supply issues, hospital exposure issues, the danger to the patient of being in the hospital environment – there’s just so many factors. We’re spending so much time talking through cases, and a lot of times we’re talking about cases we already talked about, but we’re just making sure that based on today’s numbers we should still be moving forward,” she commented.
In Connecticut, Chiang said treatment decisions are also mostly on a case-by-case basis at the moment, although more standardized guidelines are being worked out.
“Our disease teams have been really proactive in terms of offering alternative solutions to patients, creative ways to basically keep them out of the hospital and also reduce the immunosuppressive regimens that we give them,” she said.
Examples include offering endocrine therapy to patients who can’t get breast cancer surgery, or offering alternative drug regimens and dosing schedules. “At this point we haven’t needed to ration actual treatment – patients are continuing to get active therapy if that’s appropriate – it’s more about how can we protect them,” she said. “It’s a complex puzzle of moving pieces.”
In Toronto, Gospodarowicz says newly published medical and radiation oncology guidelines from France are the backbone of her hospital’s policy discussions about treating cancer and protecting patients from COVID-19.
While patients’ concerns are understandable, she says even in the current hot spots of infection, it’s encouraging to know that cancer patients are not being forgotten.
“I recently had email communication with a radiation oncologist in Brescia, one of the worst-affected areas in Italy, and he told me the radiotherapy department has been 60% to 70% capacity, so they still treat 70% these patients, just taking precautions and separating the COVID-positive and negative ones. When we read the stats it looks horrible, but life still goes on and people are still being treated,” she said.
Although telemedicine offers meaningful solutions to the COVID-19 crisis in North America, it may not be possible in other parts of the world.
Web consultations were only just approved in Brazil this week. “We are still discussing how to make it official and reimbursed,” says Rachel Riechelmann, MD, head of clinical oncology at AC Camargo Cancer Center in São Paulo.
To minimize infection risk for patients, Riechelmann says her hospital is doing the following: postponing surgeries in cases where there is good evidence of neoadjuvant treatment, such as total neoadjuvant therapy for rectal cancer; avoiding adjuvant chemo for stage 2 colon cancer; moving to hypofractionated radiotherapy if possible; adopting watchful waiting in grade 1 nonfunctional neuroendocrine tumors; and postponing follow-up visits.
“We do our best,” she wrote in an email. “We keep treating cancer if treatment cannot wait.”
Riechelmann’s center has just launched a trial of hydroxychloroquine and tocilizumab therapy in patients with cancer who have severe COVID-19 and acute respiratory distress syndrome (ARDS).
Meanwhile in New Haven, Chiang says for patients with cancer who are infected with COVID-19, her team is also prognosticating about the fair allocation of limited resources such as ventilators.
“If it ever gets to the point where somebody has to choose between a cancer patient and a noncancer patient in providing life support, it’s really important that people understand that cancer patients are doing very well nowadays and even with a diagnosis of cancer they can potentially live for many years, so that shouldn’t necessarily be a decision-point,” she emphasized.
This article first appeared on Medscape.com.
Medical oncologist Anne Chiang, MD, PhD, is scrambling to maintain cancer care in New Haven, Connecticut, while COVID-19 advances unrelentingly. As deputy chief medical officer of the Smilow Cancer Network, the largest cancer care delivery system in Connecticut and Rhode Island, she has no illusions about dodging what’s unfolding just 2 hours down the road in New York City.
“They’re trying their best to continue active cancer treatment but it’s getting harder,” she says of her colleagues in the thick of the pandemic. “We have to be prepared for it here.”
In anticipation of what’s coming, her team has just emptied the top three floors of the Smilow Cancer Hospital, moving 60 patients by ambulance and other medical transport to a different hospital nearby.
The move frees the Smilow Cancer hospital’s negative-pressure wards for the anticipated wave of COVID-19 patients. It will keep the virus sealed off from the rest of the hospital. But in other locations it’s harder to shield patients with cancer from the infection.
Around the state, Smilow Cancer Network’s affiliated hospitals are already treating a growing number of COVID-19 patients, especially at Greenwich Hospital, right on the border with New York state.
To protect patients with cancer, who are among the most vulnerable to the virus, oncologists are embracing telemedicine to allow most patients to stay home.
“We’re really concentrating on decreasing the risk to these patients, with a widespread massive-scale conversion to telehealth,” said Chiang. “This is something that, in the space of about a week, has transformed the care of our patients — it’s a really amazing transformation.”
If anything good comes out of the COVID-19 pandemic, it will be this global adoption of virtual healthcare.
Across the US border in Canada, the medical director of Toronto’s Princess Margaret Cancer Centre is directing a similar transformation.
“We have converted probably about 70% to 80% of our clinic visits to virtual visits,” says radiation oncologist Mary Gospodarowicz, MD.
“We have three priorities: number one, to keep our patients safe; number two, to keep our staff safe, because if staff are sick we won’t be treating anybody; and number three, to treat as many patients with cancer as possible.”
Gospodarowicz woke up last week to a local headline about a woman whose mastectomy had been canceled “because of the coronavirus.” The story exposed the many layers of the COVID-19 crisis. “A lot of hospitals have canceled elective surgeries,” she acknowledged. “For patients who have treatment or surgery deferred, we have a database and we’ll make sure we look after those patients eventually. We have a priority system, so low-risk prostate cancer, very low-risk breast cancer patients are waiting. All the urgent head and neck, breast, and other higher priority surgeries are still being done, but it just depends how it goes. The situation changes every day.”
It’s similar in Los Angeles, at the University of Southern California, says Elizabeth David, MD, a cardiothoracic surgeon with Keck Medicine.
“For thoracic, we just had a conference call with about 30 surgeons around the country going through really nitty-gritty specifics to help with our decision making about what could wait without detriment to the patient – hopefully – and what should be done now,” she told Medscape Medical News.
“There are some hospitals where they are not doing anything but life and death emergency operations, whereas we are still doing our emergent cancer operations in our institution, but we all know – and patients know – that could change from one day to the next. They may think they’re having surgery tomorrow but may get a call saying we can’t do it,” David said.
Many of David’s patients have non–small cell lung cancer, putting them at particular risk with a pulmonary infection like COVID-19. For now, she says delivery of postsurgical chemotherapy and radiotherapy has not been impacted in her area, but her videoconference discussions with patients are much longer – and harder – these days.
“I’ve been in practice a while now and I’ve had numerous conversations with patients this week that I never trained for, and I’ve never known anyone else who has. It’s really hard as a provider to know what to say,” she said.
In cardiothoracic surgery, David said guidance on clinical decision making is coming from the American College of Surgeons, Society of Thoracic Surgery, and American Association of Thoracic Surgeons. Yet, she says each patient is being assessed – and reassessed – individually.
“You have to balance the risk of delaying the intervention with supply issues, hospital exposure issues, the danger to the patient of being in the hospital environment – there’s just so many factors. We’re spending so much time talking through cases, and a lot of times we’re talking about cases we already talked about, but we’re just making sure that based on today’s numbers we should still be moving forward,” she commented.
In Connecticut, Chiang said treatment decisions are also mostly on a case-by-case basis at the moment, although more standardized guidelines are being worked out.
“Our disease teams have been really proactive in terms of offering alternative solutions to patients, creative ways to basically keep them out of the hospital and also reduce the immunosuppressive regimens that we give them,” she said.
Examples include offering endocrine therapy to patients who can’t get breast cancer surgery, or offering alternative drug regimens and dosing schedules. “At this point we haven’t needed to ration actual treatment – patients are continuing to get active therapy if that’s appropriate – it’s more about how can we protect them,” she said. “It’s a complex puzzle of moving pieces.”
In Toronto, Gospodarowicz says newly published medical and radiation oncology guidelines from France are the backbone of her hospital’s policy discussions about treating cancer and protecting patients from COVID-19.
While patients’ concerns are understandable, she says even in the current hot spots of infection, it’s encouraging to know that cancer patients are not being forgotten.
“I recently had email communication with a radiation oncologist in Brescia, one of the worst-affected areas in Italy, and he told me the radiotherapy department has been 60% to 70% capacity, so they still treat 70% these patients, just taking precautions and separating the COVID-positive and negative ones. When we read the stats it looks horrible, but life still goes on and people are still being treated,” she said.
Although telemedicine offers meaningful solutions to the COVID-19 crisis in North America, it may not be possible in other parts of the world.
Web consultations were only just approved in Brazil this week. “We are still discussing how to make it official and reimbursed,” says Rachel Riechelmann, MD, head of clinical oncology at AC Camargo Cancer Center in São Paulo.
To minimize infection risk for patients, Riechelmann says her hospital is doing the following: postponing surgeries in cases where there is good evidence of neoadjuvant treatment, such as total neoadjuvant therapy for rectal cancer; avoiding adjuvant chemo for stage 2 colon cancer; moving to hypofractionated radiotherapy if possible; adopting watchful waiting in grade 1 nonfunctional neuroendocrine tumors; and postponing follow-up visits.
“We do our best,” she wrote in an email. “We keep treating cancer if treatment cannot wait.”
Riechelmann’s center has just launched a trial of hydroxychloroquine and tocilizumab therapy in patients with cancer who have severe COVID-19 and acute respiratory distress syndrome (ARDS).
Meanwhile in New Haven, Chiang says for patients with cancer who are infected with COVID-19, her team is also prognosticating about the fair allocation of limited resources such as ventilators.
“If it ever gets to the point where somebody has to choose between a cancer patient and a noncancer patient in providing life support, it’s really important that people understand that cancer patients are doing very well nowadays and even with a diagnosis of cancer they can potentially live for many years, so that shouldn’t necessarily be a decision-point,” she emphasized.
This article first appeared on Medscape.com.
Medical oncologist Anne Chiang, MD, PhD, is scrambling to maintain cancer care in New Haven, Connecticut, while COVID-19 advances unrelentingly. As deputy chief medical officer of the Smilow Cancer Network, the largest cancer care delivery system in Connecticut and Rhode Island, she has no illusions about dodging what’s unfolding just 2 hours down the road in New York City.
“They’re trying their best to continue active cancer treatment but it’s getting harder,” she says of her colleagues in the thick of the pandemic. “We have to be prepared for it here.”
In anticipation of what’s coming, her team has just emptied the top three floors of the Smilow Cancer Hospital, moving 60 patients by ambulance and other medical transport to a different hospital nearby.
The move frees the Smilow Cancer hospital’s negative-pressure wards for the anticipated wave of COVID-19 patients. It will keep the virus sealed off from the rest of the hospital. But in other locations it’s harder to shield patients with cancer from the infection.
Around the state, Smilow Cancer Network’s affiliated hospitals are already treating a growing number of COVID-19 patients, especially at Greenwich Hospital, right on the border with New York state.
To protect patients with cancer, who are among the most vulnerable to the virus, oncologists are embracing telemedicine to allow most patients to stay home.
“We’re really concentrating on decreasing the risk to these patients, with a widespread massive-scale conversion to telehealth,” said Chiang. “This is something that, in the space of about a week, has transformed the care of our patients — it’s a really amazing transformation.”
If anything good comes out of the COVID-19 pandemic, it will be this global adoption of virtual healthcare.
Across the US border in Canada, the medical director of Toronto’s Princess Margaret Cancer Centre is directing a similar transformation.
“We have converted probably about 70% to 80% of our clinic visits to virtual visits,” says radiation oncologist Mary Gospodarowicz, MD.
“We have three priorities: number one, to keep our patients safe; number two, to keep our staff safe, because if staff are sick we won’t be treating anybody; and number three, to treat as many patients with cancer as possible.”
Gospodarowicz woke up last week to a local headline about a woman whose mastectomy had been canceled “because of the coronavirus.” The story exposed the many layers of the COVID-19 crisis. “A lot of hospitals have canceled elective surgeries,” she acknowledged. “For patients who have treatment or surgery deferred, we have a database and we’ll make sure we look after those patients eventually. We have a priority system, so low-risk prostate cancer, very low-risk breast cancer patients are waiting. All the urgent head and neck, breast, and other higher priority surgeries are still being done, but it just depends how it goes. The situation changes every day.”
It’s similar in Los Angeles, at the University of Southern California, says Elizabeth David, MD, a cardiothoracic surgeon with Keck Medicine.
“For thoracic, we just had a conference call with about 30 surgeons around the country going through really nitty-gritty specifics to help with our decision making about what could wait without detriment to the patient – hopefully – and what should be done now,” she told Medscape Medical News.
“There are some hospitals where they are not doing anything but life and death emergency operations, whereas we are still doing our emergent cancer operations in our institution, but we all know – and patients know – that could change from one day to the next. They may think they’re having surgery tomorrow but may get a call saying we can’t do it,” David said.
Many of David’s patients have non–small cell lung cancer, putting them at particular risk with a pulmonary infection like COVID-19. For now, she says delivery of postsurgical chemotherapy and radiotherapy has not been impacted in her area, but her videoconference discussions with patients are much longer – and harder – these days.
“I’ve been in practice a while now and I’ve had numerous conversations with patients this week that I never trained for, and I’ve never known anyone else who has. It’s really hard as a provider to know what to say,” she said.
In cardiothoracic surgery, David said guidance on clinical decision making is coming from the American College of Surgeons, Society of Thoracic Surgery, and American Association of Thoracic Surgeons. Yet, she says each patient is being assessed – and reassessed – individually.
“You have to balance the risk of delaying the intervention with supply issues, hospital exposure issues, the danger to the patient of being in the hospital environment – there’s just so many factors. We’re spending so much time talking through cases, and a lot of times we’re talking about cases we already talked about, but we’re just making sure that based on today’s numbers we should still be moving forward,” she commented.
In Connecticut, Chiang said treatment decisions are also mostly on a case-by-case basis at the moment, although more standardized guidelines are being worked out.
“Our disease teams have been really proactive in terms of offering alternative solutions to patients, creative ways to basically keep them out of the hospital and also reduce the immunosuppressive regimens that we give them,” she said.
Examples include offering endocrine therapy to patients who can’t get breast cancer surgery, or offering alternative drug regimens and dosing schedules. “At this point we haven’t needed to ration actual treatment – patients are continuing to get active therapy if that’s appropriate – it’s more about how can we protect them,” she said. “It’s a complex puzzle of moving pieces.”
In Toronto, Gospodarowicz says newly published medical and radiation oncology guidelines from France are the backbone of her hospital’s policy discussions about treating cancer and protecting patients from COVID-19.
While patients’ concerns are understandable, she says even in the current hot spots of infection, it’s encouraging to know that cancer patients are not being forgotten.
“I recently had email communication with a radiation oncologist in Brescia, one of the worst-affected areas in Italy, and he told me the radiotherapy department has been 60% to 70% capacity, so they still treat 70% these patients, just taking precautions and separating the COVID-positive and negative ones. When we read the stats it looks horrible, but life still goes on and people are still being treated,” she said.
Although telemedicine offers meaningful solutions to the COVID-19 crisis in North America, it may not be possible in other parts of the world.
Web consultations were only just approved in Brazil this week. “We are still discussing how to make it official and reimbursed,” says Rachel Riechelmann, MD, head of clinical oncology at AC Camargo Cancer Center in São Paulo.
To minimize infection risk for patients, Riechelmann says her hospital is doing the following: postponing surgeries in cases where there is good evidence of neoadjuvant treatment, such as total neoadjuvant therapy for rectal cancer; avoiding adjuvant chemo for stage 2 colon cancer; moving to hypofractionated radiotherapy if possible; adopting watchful waiting in grade 1 nonfunctional neuroendocrine tumors; and postponing follow-up visits.
“We do our best,” she wrote in an email. “We keep treating cancer if treatment cannot wait.”
Riechelmann’s center has just launched a trial of hydroxychloroquine and tocilizumab therapy in patients with cancer who have severe COVID-19 and acute respiratory distress syndrome (ARDS).
Meanwhile in New Haven, Chiang says for patients with cancer who are infected with COVID-19, her team is also prognosticating about the fair allocation of limited resources such as ventilators.
“If it ever gets to the point where somebody has to choose between a cancer patient and a noncancer patient in providing life support, it’s really important that people understand that cancer patients are doing very well nowadays and even with a diagnosis of cancer they can potentially live for many years, so that shouldn’t necessarily be a decision-point,” she emphasized.
This article first appeared on Medscape.com.
Perspective from the heartland: Cancer care and research during a public health crisis
I have no knowledge of, or experience with, managing a cancer patient during a pandemic. However, from the published and otherwise shared experience of others, we should not allow ourselves to underestimate the voracity of the coronavirus pandemic on our patients, communities, and health care systems.
Data from China suggest cancer patients infected with SARS-CoV-2 face a 3.5 times higher risk of mechanical ventilation, intensive care unit admission, or death, compared with infected patients without cancer (Lancet Oncol 2020;21:335-7).
Health care workers in Seattle have also shared their experiences battling coronavirus infections in cancer patients (J Natl Compr Canc Netw. 2020 Mar 20. doi: 10.6004/jnccn.2020.7560). Masumi Ueda, MD, of Seattle Cancer Care Alliance, and colleagues reviewed their decisions in multiple domains over a 7-week period, during which the state of Washington went from a single case of SARS-CoV-2 infection to nearly 650 cases and 40 deaths.
Making tough treatment decisions
Dr. Ueda and colleagues contrasted their customary resource-rich, innovation-oriented, cancer-combatting environment with their current circumstance, in which they must prioritize treatment for patients for whom the risk-reward balance has tilted substantially toward “risk.”
The authors noted that their most difficult decisions were those regarding delay of cancer treatment. They suggested that plans for potentially curative adjuvant therapy should likely proceed, but, for patients with metastatic disease, the equation is more nuanced.
In some cases, treatment should be delayed or interrupted with recognition of how that could result in worsening performance status and admission for symptom palliation, further stressing inpatient resources.
The authors suggested scenarios for prioritizing cancer surgery. For example, several months of systemic therapy (ideally, low-risk systemic therapy such as hormone therapy for breast or prostate cancer) and surgical delay may be worthwhile, without compromising patient care.
Patients with aggressive hematologic malignancy requiring urgent systemic treatment (potentially stem cell transplantation and cellular immunotherapies) should be treated promptly. However, even in those cases, opportunities should be sought to lessen immunosuppression and transition care as quickly as possible to the outpatient clinic, according to guidelines from the American Society of Transplantation and Cellular Therapy.
See one, do one, teach one
Rendering patient care during a pandemic would be unique for me. However, I, like all physicians, am familiar with feelings of inadequacy at times of professional challenge. On countless occasions, I have started my day or walked into a patient’s room wondering whether I will have the fortitude, knowledge, creativity, or help I need to get through that day or make that patient “better” by any definition of that word.
We all know the formula: “Work hard. Make evidence-based, personalized decisions for those who have entrusted their care to us. Learn from those encounters. Teach from our knowledge and experience – that is, ‘See one, do one, teach one.’ ”
The Seattle oncologists are living the lives of first responders and deserve our admiration for putting pen to paper so we can learn from their considerable, relevant experience.
Similar admiration is due to Giuseppe Curigliano, MD, of the European Institute of Oncology in Milan. In the ASCO Daily News, Dr. Curigliano described an epidemic that, within 3 weeks, overloaded the health care system across northern Italy.
Hospitalization was needed for over 60% of infected patients, and nearly 15% of those patients needed intensive care unit services for respiratory distress. The Italians centralized oncology care in specialized hubs, with spokes of institutions working in parallel to provide cancer-specific care in a COVID-free environment.
To build upon cancer-specific information from Italy and other areas hard-hit by COVID-19, more than 30 cancer centers have joined together to form the COVID-19 and Cancer Consortium. The consortium’s website hosts a survey designed to “capture details related to cancer patients presumed to have COVID-19.”
Calculating deaths and long-term consequences for cancer care delivery
It is proper that the authors from China, Italy, and Seattle did not focus attention on the case fatality rate from the COVID-19 pandemic among cancer patients. To say the least, it would be complicated to tally the direct mortality – either overall or in clinically important subsets of patients, including country-specific cohorts.
What we know from published reports is that, in Italy, cancer patients account for about 20% of deaths from coronavirus. In China, the case-fatality rate for patients with cancer was 5.6% (JAMA. 2020 Feb 24. doi: 10.1001/jama.2020.2648).
However, we know nothing about the indirect death toll from malignancy (without coronavirus infection) that was untreated or managed less than optimally because of personnel and physical resources that were diverted to COVID-19–associated cases.
Similarly, we cannot begin to estimate indirect consequences of the pandemic to oncology practices, such as accelerated burnout and posttraumatic stress disorder, as well as the long-range effects of economic turmoil on patients, health care workers, and provider organizations.
What happens to cancer trials?
From China, Italy, and Seattle, thus far, there is little information about how the pandemic will affect the vital clinical research endeavor. The Seattle physicians did say they plan to enroll patients on clinical trials only when the trial offers a high chance of benefiting the patient over standard therapy alone.
Fortunately, the National Institutes of Health and Food and Drug Administration have released guidance documents related to clinical trials.
The National Cancer Institute (NCI) has also released guidance documents (March 13 guidance; March 23 guidance) for patients on clinical trials supported by the NCI Cancer Therapy Evaluation Program (CTEP) and the NCI Community Oncology Research Program (NCORP).
CTEP and NCORP are making reasonable accommodations to suspend monitoring visits and audits, allow tele–follow-up visits for patients, and permit local physicians to provide care for patients on study. In addition, with appropriate procedural adherence and documentation, CTEP and NCORP will allow oral investigational medicines to be mailed directly to patients’ homes.
Planned NCI National Clinical Trials Network meetings will be conducted via remote access webinars, conference calls, and similar technology. These adjustments – and probably many more to come – are geared toward facilitating ongoing care to proceed safely and with minimal risk for patients currently receiving investigational therapies and for the sites and investigators engaged in those studies.
Each of us has probably faced a personal “defining professional moment,” when we had to utilize every skill in our arsenal and examine the motivations that led us to a career in oncology. However, it is clear from the forgoing clinical and research processes and guidelines that the COVID-19 pandemic is such a defining professional moment for each of us, in every community we serve.
Critical junctures like this cause more rapid behavior change and innovation than the slow-moving pace that characterizes our idealized preferences. As oncologists who embrace new data and behavioral change, we stand to learn processes that will facilitate more perfected systems of care than the one that preceded this unprecedented crisis, promote more efficient sharing of high-quality information, and improve the outcome for our future patients.
Dr. Lyss was an oncologist and researcher for more than 35 years before his recent retirement. His clinical and research interests were focused on breast and lung cancers, as well as expanding clinical trial access to medically underserved populations. He is based in St. Louis. He has no conflicts of interest.
I have no knowledge of, or experience with, managing a cancer patient during a pandemic. However, from the published and otherwise shared experience of others, we should not allow ourselves to underestimate the voracity of the coronavirus pandemic on our patients, communities, and health care systems.
Data from China suggest cancer patients infected with SARS-CoV-2 face a 3.5 times higher risk of mechanical ventilation, intensive care unit admission, or death, compared with infected patients without cancer (Lancet Oncol 2020;21:335-7).
Health care workers in Seattle have also shared their experiences battling coronavirus infections in cancer patients (J Natl Compr Canc Netw. 2020 Mar 20. doi: 10.6004/jnccn.2020.7560). Masumi Ueda, MD, of Seattle Cancer Care Alliance, and colleagues reviewed their decisions in multiple domains over a 7-week period, during which the state of Washington went from a single case of SARS-CoV-2 infection to nearly 650 cases and 40 deaths.
Making tough treatment decisions
Dr. Ueda and colleagues contrasted their customary resource-rich, innovation-oriented, cancer-combatting environment with their current circumstance, in which they must prioritize treatment for patients for whom the risk-reward balance has tilted substantially toward “risk.”
The authors noted that their most difficult decisions were those regarding delay of cancer treatment. They suggested that plans for potentially curative adjuvant therapy should likely proceed, but, for patients with metastatic disease, the equation is more nuanced.
In some cases, treatment should be delayed or interrupted with recognition of how that could result in worsening performance status and admission for symptom palliation, further stressing inpatient resources.
The authors suggested scenarios for prioritizing cancer surgery. For example, several months of systemic therapy (ideally, low-risk systemic therapy such as hormone therapy for breast or prostate cancer) and surgical delay may be worthwhile, without compromising patient care.
Patients with aggressive hematologic malignancy requiring urgent systemic treatment (potentially stem cell transplantation and cellular immunotherapies) should be treated promptly. However, even in those cases, opportunities should be sought to lessen immunosuppression and transition care as quickly as possible to the outpatient clinic, according to guidelines from the American Society of Transplantation and Cellular Therapy.
See one, do one, teach one
Rendering patient care during a pandemic would be unique for me. However, I, like all physicians, am familiar with feelings of inadequacy at times of professional challenge. On countless occasions, I have started my day or walked into a patient’s room wondering whether I will have the fortitude, knowledge, creativity, or help I need to get through that day or make that patient “better” by any definition of that word.
We all know the formula: “Work hard. Make evidence-based, personalized decisions for those who have entrusted their care to us. Learn from those encounters. Teach from our knowledge and experience – that is, ‘See one, do one, teach one.’ ”
The Seattle oncologists are living the lives of first responders and deserve our admiration for putting pen to paper so we can learn from their considerable, relevant experience.
Similar admiration is due to Giuseppe Curigliano, MD, of the European Institute of Oncology in Milan. In the ASCO Daily News, Dr. Curigliano described an epidemic that, within 3 weeks, overloaded the health care system across northern Italy.
Hospitalization was needed for over 60% of infected patients, and nearly 15% of those patients needed intensive care unit services for respiratory distress. The Italians centralized oncology care in specialized hubs, with spokes of institutions working in parallel to provide cancer-specific care in a COVID-free environment.
To build upon cancer-specific information from Italy and other areas hard-hit by COVID-19, more than 30 cancer centers have joined together to form the COVID-19 and Cancer Consortium. The consortium’s website hosts a survey designed to “capture details related to cancer patients presumed to have COVID-19.”
Calculating deaths and long-term consequences for cancer care delivery
It is proper that the authors from China, Italy, and Seattle did not focus attention on the case fatality rate from the COVID-19 pandemic among cancer patients. To say the least, it would be complicated to tally the direct mortality – either overall or in clinically important subsets of patients, including country-specific cohorts.
What we know from published reports is that, in Italy, cancer patients account for about 20% of deaths from coronavirus. In China, the case-fatality rate for patients with cancer was 5.6% (JAMA. 2020 Feb 24. doi: 10.1001/jama.2020.2648).
However, we know nothing about the indirect death toll from malignancy (without coronavirus infection) that was untreated or managed less than optimally because of personnel and physical resources that were diverted to COVID-19–associated cases.
Similarly, we cannot begin to estimate indirect consequences of the pandemic to oncology practices, such as accelerated burnout and posttraumatic stress disorder, as well as the long-range effects of economic turmoil on patients, health care workers, and provider organizations.
What happens to cancer trials?
From China, Italy, and Seattle, thus far, there is little information about how the pandemic will affect the vital clinical research endeavor. The Seattle physicians did say they plan to enroll patients on clinical trials only when the trial offers a high chance of benefiting the patient over standard therapy alone.
Fortunately, the National Institutes of Health and Food and Drug Administration have released guidance documents related to clinical trials.
The National Cancer Institute (NCI) has also released guidance documents (March 13 guidance; March 23 guidance) for patients on clinical trials supported by the NCI Cancer Therapy Evaluation Program (CTEP) and the NCI Community Oncology Research Program (NCORP).
CTEP and NCORP are making reasonable accommodations to suspend monitoring visits and audits, allow tele–follow-up visits for patients, and permit local physicians to provide care for patients on study. In addition, with appropriate procedural adherence and documentation, CTEP and NCORP will allow oral investigational medicines to be mailed directly to patients’ homes.
Planned NCI National Clinical Trials Network meetings will be conducted via remote access webinars, conference calls, and similar technology. These adjustments – and probably many more to come – are geared toward facilitating ongoing care to proceed safely and with minimal risk for patients currently receiving investigational therapies and for the sites and investigators engaged in those studies.
Each of us has probably faced a personal “defining professional moment,” when we had to utilize every skill in our arsenal and examine the motivations that led us to a career in oncology. However, it is clear from the forgoing clinical and research processes and guidelines that the COVID-19 pandemic is such a defining professional moment for each of us, in every community we serve.
Critical junctures like this cause more rapid behavior change and innovation than the slow-moving pace that characterizes our idealized preferences. As oncologists who embrace new data and behavioral change, we stand to learn processes that will facilitate more perfected systems of care than the one that preceded this unprecedented crisis, promote more efficient sharing of high-quality information, and improve the outcome for our future patients.
Dr. Lyss was an oncologist and researcher for more than 35 years before his recent retirement. His clinical and research interests were focused on breast and lung cancers, as well as expanding clinical trial access to medically underserved populations. He is based in St. Louis. He has no conflicts of interest.
I have no knowledge of, or experience with, managing a cancer patient during a pandemic. However, from the published and otherwise shared experience of others, we should not allow ourselves to underestimate the voracity of the coronavirus pandemic on our patients, communities, and health care systems.
Data from China suggest cancer patients infected with SARS-CoV-2 face a 3.5 times higher risk of mechanical ventilation, intensive care unit admission, or death, compared with infected patients without cancer (Lancet Oncol 2020;21:335-7).
Health care workers in Seattle have also shared their experiences battling coronavirus infections in cancer patients (J Natl Compr Canc Netw. 2020 Mar 20. doi: 10.6004/jnccn.2020.7560). Masumi Ueda, MD, of Seattle Cancer Care Alliance, and colleagues reviewed their decisions in multiple domains over a 7-week period, during which the state of Washington went from a single case of SARS-CoV-2 infection to nearly 650 cases and 40 deaths.
Making tough treatment decisions
Dr. Ueda and colleagues contrasted their customary resource-rich, innovation-oriented, cancer-combatting environment with their current circumstance, in which they must prioritize treatment for patients for whom the risk-reward balance has tilted substantially toward “risk.”
The authors noted that their most difficult decisions were those regarding delay of cancer treatment. They suggested that plans for potentially curative adjuvant therapy should likely proceed, but, for patients with metastatic disease, the equation is more nuanced.
In some cases, treatment should be delayed or interrupted with recognition of how that could result in worsening performance status and admission for symptom palliation, further stressing inpatient resources.
The authors suggested scenarios for prioritizing cancer surgery. For example, several months of systemic therapy (ideally, low-risk systemic therapy such as hormone therapy for breast or prostate cancer) and surgical delay may be worthwhile, without compromising patient care.
Patients with aggressive hematologic malignancy requiring urgent systemic treatment (potentially stem cell transplantation and cellular immunotherapies) should be treated promptly. However, even in those cases, opportunities should be sought to lessen immunosuppression and transition care as quickly as possible to the outpatient clinic, according to guidelines from the American Society of Transplantation and Cellular Therapy.
See one, do one, teach one
Rendering patient care during a pandemic would be unique for me. However, I, like all physicians, am familiar with feelings of inadequacy at times of professional challenge. On countless occasions, I have started my day or walked into a patient’s room wondering whether I will have the fortitude, knowledge, creativity, or help I need to get through that day or make that patient “better” by any definition of that word.
We all know the formula: “Work hard. Make evidence-based, personalized decisions for those who have entrusted their care to us. Learn from those encounters. Teach from our knowledge and experience – that is, ‘See one, do one, teach one.’ ”
The Seattle oncologists are living the lives of first responders and deserve our admiration for putting pen to paper so we can learn from their considerable, relevant experience.
Similar admiration is due to Giuseppe Curigliano, MD, of the European Institute of Oncology in Milan. In the ASCO Daily News, Dr. Curigliano described an epidemic that, within 3 weeks, overloaded the health care system across northern Italy.
Hospitalization was needed for over 60% of infected patients, and nearly 15% of those patients needed intensive care unit services for respiratory distress. The Italians centralized oncology care in specialized hubs, with spokes of institutions working in parallel to provide cancer-specific care in a COVID-free environment.
To build upon cancer-specific information from Italy and other areas hard-hit by COVID-19, more than 30 cancer centers have joined together to form the COVID-19 and Cancer Consortium. The consortium’s website hosts a survey designed to “capture details related to cancer patients presumed to have COVID-19.”
Calculating deaths and long-term consequences for cancer care delivery
It is proper that the authors from China, Italy, and Seattle did not focus attention on the case fatality rate from the COVID-19 pandemic among cancer patients. To say the least, it would be complicated to tally the direct mortality – either overall or in clinically important subsets of patients, including country-specific cohorts.
What we know from published reports is that, in Italy, cancer patients account for about 20% of deaths from coronavirus. In China, the case-fatality rate for patients with cancer was 5.6% (JAMA. 2020 Feb 24. doi: 10.1001/jama.2020.2648).
However, we know nothing about the indirect death toll from malignancy (without coronavirus infection) that was untreated or managed less than optimally because of personnel and physical resources that were diverted to COVID-19–associated cases.
Similarly, we cannot begin to estimate indirect consequences of the pandemic to oncology practices, such as accelerated burnout and posttraumatic stress disorder, as well as the long-range effects of economic turmoil on patients, health care workers, and provider organizations.
What happens to cancer trials?
From China, Italy, and Seattle, thus far, there is little information about how the pandemic will affect the vital clinical research endeavor. The Seattle physicians did say they plan to enroll patients on clinical trials only when the trial offers a high chance of benefiting the patient over standard therapy alone.
Fortunately, the National Institutes of Health and Food and Drug Administration have released guidance documents related to clinical trials.
The National Cancer Institute (NCI) has also released guidance documents (March 13 guidance; March 23 guidance) for patients on clinical trials supported by the NCI Cancer Therapy Evaluation Program (CTEP) and the NCI Community Oncology Research Program (NCORP).
CTEP and NCORP are making reasonable accommodations to suspend monitoring visits and audits, allow tele–follow-up visits for patients, and permit local physicians to provide care for patients on study. In addition, with appropriate procedural adherence and documentation, CTEP and NCORP will allow oral investigational medicines to be mailed directly to patients’ homes.
Planned NCI National Clinical Trials Network meetings will be conducted via remote access webinars, conference calls, and similar technology. These adjustments – and probably many more to come – are geared toward facilitating ongoing care to proceed safely and with minimal risk for patients currently receiving investigational therapies and for the sites and investigators engaged in those studies.
Each of us has probably faced a personal “defining professional moment,” when we had to utilize every skill in our arsenal and examine the motivations that led us to a career in oncology. However, it is clear from the forgoing clinical and research processes and guidelines that the COVID-19 pandemic is such a defining professional moment for each of us, in every community we serve.
Critical junctures like this cause more rapid behavior change and innovation than the slow-moving pace that characterizes our idealized preferences. As oncologists who embrace new data and behavioral change, we stand to learn processes that will facilitate more perfected systems of care than the one that preceded this unprecedented crisis, promote more efficient sharing of high-quality information, and improve the outcome for our future patients.
Dr. Lyss was an oncologist and researcher for more than 35 years before his recent retirement. His clinical and research interests were focused on breast and lung cancers, as well as expanding clinical trial access to medically underserved populations. He is based in St. Louis. He has no conflicts of interest.
Cancer care and COVID-19 in Seattle, the first U.S. epicenter
Two months after the first patient with COVID-19 was identified in China, the first case was reported in the United States in the Seattle, Washington, metropolitan area.
Seattle rapidly became the first US epicenter for COVID-19, and local experts are now offering their expertise and advice on how to provide optimal cancer care during the pandemic in a special feature published online March 20 in the Journal of the National Comprehensive Cancer Network.
“We began implementing measures in early March, including infection control and screening of visitors, staff, and patients at the door,” said lead author Masumi Ueda, MD, who holds positions at the Seattle Cancer Care Alliance, the University of Washington, and the Fred Hutchinson Research Center.
“A lot of changes have been implemented, and it changes on a daily basis. We are responding to the growing rate of COVID-19 infection in the community,” she told Medscape Medical News.
Ueda notes that as a result of the quick implementation of new procedures, so far, very few cancer patients at their facilities have been infected by the virus. “It has not hit our cancer population hard, which is a good thing,” she said.
Create “Incident Command Structure”
In sharing their experience, the authors emphasize the importance of keeping channels of communication open between all stakeholders ― administrators and staff, patients, caregivers, and the general public. They also recommend that each facility create an “incident command structure” that can provide early coordination of institution-wide efforts and that can rapidly respond to changing information.
Ueda noted that their command structure was set up very early on, “so we could get communication set up and start building an infrastructure for response.”
Several areas of care that required new strategies were addressed, both to protect patients and to work around staff shortages caused by possible exposure and/or school closings, as well as projected shortages of supplies and hospital resources.
First and foremost was to identify patients and visitors who had respiratory symptoms and to provide them with masks. Although this is always routine practice during the respiratory virus season, screening has now been initiated at entry points throughout the system.
“We were lucky in Seattle and Washington state in that the University of Washington virology lab developed PCR [polymerase chain reaction] testing early on for COVID-19, which subsequently got FDA approval,” said Ueda. “So we were able to have local testing and didn’t have to rely on the state lab. Testing has also been rapidly scaled up.”
Initiating a comprehensive policy for testing staff, tracking results and exposures for persons under investigation, and defining when it is possible to return to work are essential elements for maintaining a stable workforce. In addition, reinforcing a strict “stay at home when ill” policy and providing access to testing for symptomatic staff have been key to limiting exposures.
“What is unique to our region is that we had testing early on, and we are turning it around in 24 hours,” she pointed out. “This is important for staff to be able to return to work.” Currently, staff, patients, and visitors are being tested only if they show the cardinal symptoms associated with COVID-19: fever, shortness of breath, and cough, although muscle aches have recently been added to their testing protocol.
“I think if we had unlimited capacity, we might consider testing people who are asymptomatic,” Ueda noted, “although if you don’t have symptoms, you may not have the viral load needed for an accurate test.”
Educational materials explaining infection control were also needed for patients and families, along with signs and a website to provide COVID-19 education. These were quickly developed.
In addition, a telephone triage line was established for patients with mild symptoms in order to minimize exposures in clinics and to lessen the number of patients presenting at emergency departments.
Outpatient Care
Because theirs is a referral center, many cancer patients come from out of town, and so there is concern about exposing nonlocal patients to COVID-19 as the virus spreads in the Seattle area. In addition, staffing shortages due to factors such as illness, exposure, and school closures are anticipated.
To address these problems, an initial priority was to establish a “multilayer” coverage system for the clinics in the event that practitioners had to be quarantined on short notice, the authors explain.
One decision was to reschedule all wellness visits for current patients or to use telemedicine. Capacity for that option expanded quickly, which was greatly helped by the recent decision by the Centers for Medicare & Medicaid Services to lift Medicare restrictions on the use of certain telemedicine services.
Another approach is to defer all consultations for second opinions for patients who were already undergoing treatment and to increase clinic hours of operations and capabilities for acute evaluations. This helps reserve emergency departments and hospital resources for patients who require higher-level care, the authors comment.
Treatment Decisions
Treatment decisions were more challenging to make, the authors note. One decision was that, despite the risk for COVID-19 for patients with solid tumors, adjuvant therapy with curative intent should proceed, they note. Similarly, patients with metastatic disease might lose the window of opportunity for treatment if it is delayed.
Treatment for aggressive hematologic malignancies is usually urgent, and stem cell transplant and cellular immunotherapies that provide curative treatments cannot be delayed in many cases.
Enrollment in clinical trials will most likely be limited to those trials that are most likely to benefit the patient.
Ueda noted that, because their patients come from all over the country, they are now conducting consultations for stem cell transplant by telephone so that nonlocal patients do not have to travel to Seattle. “If there is some way we can delay the treatment, we have taken that approach,” Ueda told Medscape Medical News. “If we can divert a patient to an area that is not as heavily affected, that’s another option we are taking.”
Although cancer surgery is not considered elective, surgical intervention needs to be prioritized, the authors comment. In the Seattle system, there is currently a 2-week ban on elective surgery in the healthcare system, owing to limited availability of personal protective equipment (PPE), staffing, and beds.
The oncology teams are currently reviewing treatment regimens to determine which treatments might lessen immunosuppression and which treatment options can be moved from the inpatient to the outpatient setting or can be delayed.
Inpatient Care
For hospitalized patients, several issues are being addressed. The priority is to prepare for an upcoming shortage of beds and resources because of the surge of patients with COVID-19 that is predicted. For both clinic and hospitalized patients, shortages of blood products have necessitated stricter adherence to thresholds for transfusion, and consideration is being given to lowering those thresholds.
Another important problem is the need to conserve PPE, which includes masks, gowns, gloves, and other products. The Seattle teams have implemented solutions such as favoring handwashing with soap and water over the use of hand gel for standard-precaution rooms, limiting the number of personnel entering patient rooms (so as to use less PPE), and reducing nursing procedures that require PPE, such as measuring urine output, unless they are necessary.
In addition, a no-visitor policy has been adopted in inpatient units to conserve PPE, with the exception of end-of-life situations.
The Future
The future trajectory of the COVID-19 pandemic is uncertain, Ueda commented. She emphasized that “we must continue to prepare for its widespread impact. The unknown is what we are looking at. We are expecting it to evolve, and the number of infections cannot go down.”
Ueda and coauthors end their article on a positive note. “To many of us, this has become the health care challenge of our generation, one that modern cancer therapy has never had to face. We will prevail, and when the pandemic ends, we will all be proud of what we did for our patients and each other in this critical moment for humanity.”
Two months after the first patient with COVID-19 was identified in China, the first case was reported in the United States in the Seattle, Washington, metropolitan area.
Seattle rapidly became the first US epicenter for COVID-19, and local experts are now offering their expertise and advice on how to provide optimal cancer care during the pandemic in a special feature published online March 20 in the Journal of the National Comprehensive Cancer Network.
“We began implementing measures in early March, including infection control and screening of visitors, staff, and patients at the door,” said lead author Masumi Ueda, MD, who holds positions at the Seattle Cancer Care Alliance, the University of Washington, and the Fred Hutchinson Research Center.
“A lot of changes have been implemented, and it changes on a daily basis. We are responding to the growing rate of COVID-19 infection in the community,” she told Medscape Medical News.
Ueda notes that as a result of the quick implementation of new procedures, so far, very few cancer patients at their facilities have been infected by the virus. “It has not hit our cancer population hard, which is a good thing,” she said.
Create “Incident Command Structure”
In sharing their experience, the authors emphasize the importance of keeping channels of communication open between all stakeholders ― administrators and staff, patients, caregivers, and the general public. They also recommend that each facility create an “incident command structure” that can provide early coordination of institution-wide efforts and that can rapidly respond to changing information.
Ueda noted that their command structure was set up very early on, “so we could get communication set up and start building an infrastructure for response.”
Several areas of care that required new strategies were addressed, both to protect patients and to work around staff shortages caused by possible exposure and/or school closings, as well as projected shortages of supplies and hospital resources.
First and foremost was to identify patients and visitors who had respiratory symptoms and to provide them with masks. Although this is always routine practice during the respiratory virus season, screening has now been initiated at entry points throughout the system.
“We were lucky in Seattle and Washington state in that the University of Washington virology lab developed PCR [polymerase chain reaction] testing early on for COVID-19, which subsequently got FDA approval,” said Ueda. “So we were able to have local testing and didn’t have to rely on the state lab. Testing has also been rapidly scaled up.”
Initiating a comprehensive policy for testing staff, tracking results and exposures for persons under investigation, and defining when it is possible to return to work are essential elements for maintaining a stable workforce. In addition, reinforcing a strict “stay at home when ill” policy and providing access to testing for symptomatic staff have been key to limiting exposures.
“What is unique to our region is that we had testing early on, and we are turning it around in 24 hours,” she pointed out. “This is important for staff to be able to return to work.” Currently, staff, patients, and visitors are being tested only if they show the cardinal symptoms associated with COVID-19: fever, shortness of breath, and cough, although muscle aches have recently been added to their testing protocol.
“I think if we had unlimited capacity, we might consider testing people who are asymptomatic,” Ueda noted, “although if you don’t have symptoms, you may not have the viral load needed for an accurate test.”
Educational materials explaining infection control were also needed for patients and families, along with signs and a website to provide COVID-19 education. These were quickly developed.
In addition, a telephone triage line was established for patients with mild symptoms in order to minimize exposures in clinics and to lessen the number of patients presenting at emergency departments.
Outpatient Care
Because theirs is a referral center, many cancer patients come from out of town, and so there is concern about exposing nonlocal patients to COVID-19 as the virus spreads in the Seattle area. In addition, staffing shortages due to factors such as illness, exposure, and school closures are anticipated.
To address these problems, an initial priority was to establish a “multilayer” coverage system for the clinics in the event that practitioners had to be quarantined on short notice, the authors explain.
One decision was to reschedule all wellness visits for current patients or to use telemedicine. Capacity for that option expanded quickly, which was greatly helped by the recent decision by the Centers for Medicare & Medicaid Services to lift Medicare restrictions on the use of certain telemedicine services.
Another approach is to defer all consultations for second opinions for patients who were already undergoing treatment and to increase clinic hours of operations and capabilities for acute evaluations. This helps reserve emergency departments and hospital resources for patients who require higher-level care, the authors comment.
Treatment Decisions
Treatment decisions were more challenging to make, the authors note. One decision was that, despite the risk for COVID-19 for patients with solid tumors, adjuvant therapy with curative intent should proceed, they note. Similarly, patients with metastatic disease might lose the window of opportunity for treatment if it is delayed.
Treatment for aggressive hematologic malignancies is usually urgent, and stem cell transplant and cellular immunotherapies that provide curative treatments cannot be delayed in many cases.
Enrollment in clinical trials will most likely be limited to those trials that are most likely to benefit the patient.
Ueda noted that, because their patients come from all over the country, they are now conducting consultations for stem cell transplant by telephone so that nonlocal patients do not have to travel to Seattle. “If there is some way we can delay the treatment, we have taken that approach,” Ueda told Medscape Medical News. “If we can divert a patient to an area that is not as heavily affected, that’s another option we are taking.”
Although cancer surgery is not considered elective, surgical intervention needs to be prioritized, the authors comment. In the Seattle system, there is currently a 2-week ban on elective surgery in the healthcare system, owing to limited availability of personal protective equipment (PPE), staffing, and beds.
The oncology teams are currently reviewing treatment regimens to determine which treatments might lessen immunosuppression and which treatment options can be moved from the inpatient to the outpatient setting or can be delayed.
Inpatient Care
For hospitalized patients, several issues are being addressed. The priority is to prepare for an upcoming shortage of beds and resources because of the surge of patients with COVID-19 that is predicted. For both clinic and hospitalized patients, shortages of blood products have necessitated stricter adherence to thresholds for transfusion, and consideration is being given to lowering those thresholds.
Another important problem is the need to conserve PPE, which includes masks, gowns, gloves, and other products. The Seattle teams have implemented solutions such as favoring handwashing with soap and water over the use of hand gel for standard-precaution rooms, limiting the number of personnel entering patient rooms (so as to use less PPE), and reducing nursing procedures that require PPE, such as measuring urine output, unless they are necessary.
In addition, a no-visitor policy has been adopted in inpatient units to conserve PPE, with the exception of end-of-life situations.
The Future
The future trajectory of the COVID-19 pandemic is uncertain, Ueda commented. She emphasized that “we must continue to prepare for its widespread impact. The unknown is what we are looking at. We are expecting it to evolve, and the number of infections cannot go down.”
Ueda and coauthors end their article on a positive note. “To many of us, this has become the health care challenge of our generation, one that modern cancer therapy has never had to face. We will prevail, and when the pandemic ends, we will all be proud of what we did for our patients and each other in this critical moment for humanity.”
Two months after the first patient with COVID-19 was identified in China, the first case was reported in the United States in the Seattle, Washington, metropolitan area.
Seattle rapidly became the first US epicenter for COVID-19, and local experts are now offering their expertise and advice on how to provide optimal cancer care during the pandemic in a special feature published online March 20 in the Journal of the National Comprehensive Cancer Network.
“We began implementing measures in early March, including infection control and screening of visitors, staff, and patients at the door,” said lead author Masumi Ueda, MD, who holds positions at the Seattle Cancer Care Alliance, the University of Washington, and the Fred Hutchinson Research Center.
“A lot of changes have been implemented, and it changes on a daily basis. We are responding to the growing rate of COVID-19 infection in the community,” she told Medscape Medical News.
Ueda notes that as a result of the quick implementation of new procedures, so far, very few cancer patients at their facilities have been infected by the virus. “It has not hit our cancer population hard, which is a good thing,” she said.
Create “Incident Command Structure”
In sharing their experience, the authors emphasize the importance of keeping channels of communication open between all stakeholders ― administrators and staff, patients, caregivers, and the general public. They also recommend that each facility create an “incident command structure” that can provide early coordination of institution-wide efforts and that can rapidly respond to changing information.
Ueda noted that their command structure was set up very early on, “so we could get communication set up and start building an infrastructure for response.”
Several areas of care that required new strategies were addressed, both to protect patients and to work around staff shortages caused by possible exposure and/or school closings, as well as projected shortages of supplies and hospital resources.
First and foremost was to identify patients and visitors who had respiratory symptoms and to provide them with masks. Although this is always routine practice during the respiratory virus season, screening has now been initiated at entry points throughout the system.
“We were lucky in Seattle and Washington state in that the University of Washington virology lab developed PCR [polymerase chain reaction] testing early on for COVID-19, which subsequently got FDA approval,” said Ueda. “So we were able to have local testing and didn’t have to rely on the state lab. Testing has also been rapidly scaled up.”
Initiating a comprehensive policy for testing staff, tracking results and exposures for persons under investigation, and defining when it is possible to return to work are essential elements for maintaining a stable workforce. In addition, reinforcing a strict “stay at home when ill” policy and providing access to testing for symptomatic staff have been key to limiting exposures.
“What is unique to our region is that we had testing early on, and we are turning it around in 24 hours,” she pointed out. “This is important for staff to be able to return to work.” Currently, staff, patients, and visitors are being tested only if they show the cardinal symptoms associated with COVID-19: fever, shortness of breath, and cough, although muscle aches have recently been added to their testing protocol.
“I think if we had unlimited capacity, we might consider testing people who are asymptomatic,” Ueda noted, “although if you don’t have symptoms, you may not have the viral load needed for an accurate test.”
Educational materials explaining infection control were also needed for patients and families, along with signs and a website to provide COVID-19 education. These were quickly developed.
In addition, a telephone triage line was established for patients with mild symptoms in order to minimize exposures in clinics and to lessen the number of patients presenting at emergency departments.
Outpatient Care
Because theirs is a referral center, many cancer patients come from out of town, and so there is concern about exposing nonlocal patients to COVID-19 as the virus spreads in the Seattle area. In addition, staffing shortages due to factors such as illness, exposure, and school closures are anticipated.
To address these problems, an initial priority was to establish a “multilayer” coverage system for the clinics in the event that practitioners had to be quarantined on short notice, the authors explain.
One decision was to reschedule all wellness visits for current patients or to use telemedicine. Capacity for that option expanded quickly, which was greatly helped by the recent decision by the Centers for Medicare & Medicaid Services to lift Medicare restrictions on the use of certain telemedicine services.
Another approach is to defer all consultations for second opinions for patients who were already undergoing treatment and to increase clinic hours of operations and capabilities for acute evaluations. This helps reserve emergency departments and hospital resources for patients who require higher-level care, the authors comment.
Treatment Decisions
Treatment decisions were more challenging to make, the authors note. One decision was that, despite the risk for COVID-19 for patients with solid tumors, adjuvant therapy with curative intent should proceed, they note. Similarly, patients with metastatic disease might lose the window of opportunity for treatment if it is delayed.
Treatment for aggressive hematologic malignancies is usually urgent, and stem cell transplant and cellular immunotherapies that provide curative treatments cannot be delayed in many cases.
Enrollment in clinical trials will most likely be limited to those trials that are most likely to benefit the patient.
Ueda noted that, because their patients come from all over the country, they are now conducting consultations for stem cell transplant by telephone so that nonlocal patients do not have to travel to Seattle. “If there is some way we can delay the treatment, we have taken that approach,” Ueda told Medscape Medical News. “If we can divert a patient to an area that is not as heavily affected, that’s another option we are taking.”
Although cancer surgery is not considered elective, surgical intervention needs to be prioritized, the authors comment. In the Seattle system, there is currently a 2-week ban on elective surgery in the healthcare system, owing to limited availability of personal protective equipment (PPE), staffing, and beds.
The oncology teams are currently reviewing treatment regimens to determine which treatments might lessen immunosuppression and which treatment options can be moved from the inpatient to the outpatient setting or can be delayed.
Inpatient Care
For hospitalized patients, several issues are being addressed. The priority is to prepare for an upcoming shortage of beds and resources because of the surge of patients with COVID-19 that is predicted. For both clinic and hospitalized patients, shortages of blood products have necessitated stricter adherence to thresholds for transfusion, and consideration is being given to lowering those thresholds.
Another important problem is the need to conserve PPE, which includes masks, gowns, gloves, and other products. The Seattle teams have implemented solutions such as favoring handwashing with soap and water over the use of hand gel for standard-precaution rooms, limiting the number of personnel entering patient rooms (so as to use less PPE), and reducing nursing procedures that require PPE, such as measuring urine output, unless they are necessary.
In addition, a no-visitor policy has been adopted in inpatient units to conserve PPE, with the exception of end-of-life situations.
The Future
The future trajectory of the COVID-19 pandemic is uncertain, Ueda commented. She emphasized that “we must continue to prepare for its widespread impact. The unknown is what we are looking at. We are expecting it to evolve, and the number of infections cannot go down.”
Ueda and coauthors end their article on a positive note. “To many of us, this has become the health care challenge of our generation, one that modern cancer therapy has never had to face. We will prevail, and when the pandemic ends, we will all be proud of what we did for our patients and each other in this critical moment for humanity.”
How is oncology adapting to COVID-19?
As the coronavirus pandemic escalates in the United States, Medscape Oncology reached out to a group of our contributors and asked them to provide their perspective on how their oncology departments and centers are preparing. Here are their responses to a number of issues facing oncologists in the US and around the world.
Have you shifted nonurgent follow-up visits to telemedicine, either via video or phone?
Kathy Miller, MD, Associate Director of Indiana University Simon Cancer Center: We are reviewing our clinic schedules and identifying “routine” follow-up patients who can be rescheduled. When patients are contacted to reschedule, they are asked if they have any urgent, immediate concerns that need to be addressed before the new appointment. If yes, they are offered a virtual visit.
Don Dizon, MD, Director of Women’s Cancers, Lifespan Cancer Institute; Director of Medical Oncology, Rhode Island Hospital: We have started to do this in preparation for a surge of people with COVID-19. Patients who are in long-term follow-up (no evidence of disease at 3 years or longer, being seen annually) or those in routine surveillance after curative treatment (that is, seen every 3 months) as well as those being seen for supportive care–type visits, like sexual health or survivorship, are all being contacted and visits are being moved to telehealth.
Jeffrey S. Weber, MD, PhD, Deputy Director of the Laura and Isaac Perlmutter Cancer Center at NYU Langone Medical Center: Yes. Any follow-up, nontreatment visits are done by phone or video if the patient agrees. (They all have).
Have you delayed or canceled cancer surgeries?
Ravi B. Parikh, MD, MPP, Medical oncologist at the University of Pennsylvania and the Philadelphia VA Medical Center: The University of Pennsylvania has taken this seriously. We’ve canceled all elective surgeries, have ramped up our telemedicine (video and phone) capabilities significantly, are limiting our appointments mostly to on-treatment visits, and have been asked to reconsider regular scans and reviews.
Dizon: We have not done this. There are apparently differences in interpretation in what institutions might mean as “elective surgeries.” At our institution, surgery for invasive malignancies is not elective. However, this may (or will) change if resources become an issue.
Lidia Schapira, MD, Associate Professor of Medicine and Director of Cancer Survivorship at the Stanford Comprehensive Cancer Institute: Delaying elective surgery is something that hospitals here have already implemented, and I imagine that this trend will spread. But it may be difficult to decide in situations that are not exactly “life-saving” but where an earlier intervention could preserve function or improve quality of life.
Mark A. Lewis, MD, Director of Gastrointestinal Oncology at Intermountain Healthcare in Utah: Cancer surgeries have not been deemed elective or delayed.
Have you delayed or altered the delivery of potentially immune-comprising treatments?
David Kerr, MD, Professor of Cancer Medicine at the University of Oxford in England: We are considering delaying initiation of our adjuvant colorectal cancer treatments, as we have data from our own QUASAR trials suggesting that patients who commence chemotherapy between 2 and 6 weeks do equally as well as those who begin 6-12 weeks after surgery.
Parikh: I personally haven’t delayed giving chemotherapy to avoid immune compromise, but I believe some others may have. It’s a delicate balance between wanting to ensure cancer control and making sure we are flattening the curve. As an example, though, I delayed three on-treatment visits for my clinic last Monday, and I converted 70% of my visits to telemedicine. However, I’m a genitourinary cancer specialist and the treatments I give are very different from others.
Lewis: The most difficult calculus is around adjuvant therapy. For metastatic patients, I am trying to use the least immunosuppressive regimen possible that will still control their disease. As you can imagine, it’s an assessment of competing risks.
Schapira: Patients who need essential anticancer therapy should still get it, but attempts to deintensify therapy should continue—for example, holding or postponing treatment without harm (based on evidence, not opinion). This may be possible for patients considering hormonal therapies for breast or prostate cancer.
Patients who need radiation should discuss the timing with their radiation oncologist. In some cases, it may be possible to delay treatment without affecting outcomes, but these decisions should be made carefully. Alternatively, shorter courses of radiation may be appropriate.
Have you advised your own patients differently given the high risk to cancer patients?
Kerr: We have factored potential infection with the virus into discussions where the benefits of chemotherapy are very marginal. This could tip the balance toward the patient deciding not to pursue chemotherapy.
Dizon: The data from China are not entirely crystal-clear. While they noted that people with active cancer and those who had a history of cancer are at increased risk for more severe infections and worse outcomes, the Chinese cohort was small, and compared with people without cancer, it tended to be much older and to be smokers (former or current). Having said this, we are counseling everyone about the importance of social distancing, washing hands, and not touching your face.
Lewis: If I have a complete blood count with a differential that includes lymphocytes, I can advise my lymphopenic patients (who are particularly vulnerable to viral infection) to take special precautions regarding social distancing in their own families.
Have any of your hospitalized patients been affected by policy changes to prepare beds/departments for the expected increase in COVID-19–positive patients?
Weber: Not yet.
Dizon: No, not at the moment.
Have you been asked to assist with other services or COVID-19 task forces?
Dizon: I am keenly involved in the preparations and modifications to procedures, including staffing decisions in outpatient, movement to telehealth, and work-from-home policies.
Lewis: I am engaged in system-wide COVID-19 efforts around oncology.
Kerr: Perhaps oddest of all, I am learning with some of our junior doctors to care for ventilated patients. I still consider myself enough of a general physician that I would hope to be able to contribute to the truly sick, but I accept that I do need an appropriate refresher course.
Bishal Gyawali, MD, PhD, medical oncologist at Queen’s University Cancer Research Institute: Queen’s Hospital medical students are now volunteering to help with daycare, groceries, and other tasks for staff who are working in the hospital.
Are you experiencing any shortages in personal protective equipment (PPE) at your center?
Miller: Some supplies are running short, though none are frankly out at this point. However, rationing and controls are in place to stretch the supplies as far as possible, including reusing some PPE.
Dizon: We are rationing face masks and N95 respirators, eye shields, and even surgical scrubs. We are talking about postponing elective surgery to save PPE but are not yet to that point. We’re asking that face masks be reused for at least 2 days, maybe longer. PPEs are one per day. Scrubs are kept secure.
Lewis: We are being very careful not to overuse PPE but currently have an adequate inventory. We have had to move gloves and masks to areas where they are not accessible to the general public, as otherwise they were being stolen (this started weeks ago).
Kerr: Our National Health System has an adequate supply of PPE equipment centrally, but there seems to be a problem with distribution, as some hospitals are reporting shortages.
Weber: Masks are in short supply, so they are being used for several days if not wet. We are short of plastic gowns and are using paper chemo gowns. Similar story at many places.
This article first appeared on Medscape.com.
As the coronavirus pandemic escalates in the United States, Medscape Oncology reached out to a group of our contributors and asked them to provide their perspective on how their oncology departments and centers are preparing. Here are their responses to a number of issues facing oncologists in the US and around the world.
Have you shifted nonurgent follow-up visits to telemedicine, either via video or phone?
Kathy Miller, MD, Associate Director of Indiana University Simon Cancer Center: We are reviewing our clinic schedules and identifying “routine” follow-up patients who can be rescheduled. When patients are contacted to reschedule, they are asked if they have any urgent, immediate concerns that need to be addressed before the new appointment. If yes, they are offered a virtual visit.
Don Dizon, MD, Director of Women’s Cancers, Lifespan Cancer Institute; Director of Medical Oncology, Rhode Island Hospital: We have started to do this in preparation for a surge of people with COVID-19. Patients who are in long-term follow-up (no evidence of disease at 3 years or longer, being seen annually) or those in routine surveillance after curative treatment (that is, seen every 3 months) as well as those being seen for supportive care–type visits, like sexual health or survivorship, are all being contacted and visits are being moved to telehealth.
Jeffrey S. Weber, MD, PhD, Deputy Director of the Laura and Isaac Perlmutter Cancer Center at NYU Langone Medical Center: Yes. Any follow-up, nontreatment visits are done by phone or video if the patient agrees. (They all have).
Have you delayed or canceled cancer surgeries?
Ravi B. Parikh, MD, MPP, Medical oncologist at the University of Pennsylvania and the Philadelphia VA Medical Center: The University of Pennsylvania has taken this seriously. We’ve canceled all elective surgeries, have ramped up our telemedicine (video and phone) capabilities significantly, are limiting our appointments mostly to on-treatment visits, and have been asked to reconsider regular scans and reviews.
Dizon: We have not done this. There are apparently differences in interpretation in what institutions might mean as “elective surgeries.” At our institution, surgery for invasive malignancies is not elective. However, this may (or will) change if resources become an issue.
Lidia Schapira, MD, Associate Professor of Medicine and Director of Cancer Survivorship at the Stanford Comprehensive Cancer Institute: Delaying elective surgery is something that hospitals here have already implemented, and I imagine that this trend will spread. But it may be difficult to decide in situations that are not exactly “life-saving” but where an earlier intervention could preserve function or improve quality of life.
Mark A. Lewis, MD, Director of Gastrointestinal Oncology at Intermountain Healthcare in Utah: Cancer surgeries have not been deemed elective or delayed.
Have you delayed or altered the delivery of potentially immune-comprising treatments?
David Kerr, MD, Professor of Cancer Medicine at the University of Oxford in England: We are considering delaying initiation of our adjuvant colorectal cancer treatments, as we have data from our own QUASAR trials suggesting that patients who commence chemotherapy between 2 and 6 weeks do equally as well as those who begin 6-12 weeks after surgery.
Parikh: I personally haven’t delayed giving chemotherapy to avoid immune compromise, but I believe some others may have. It’s a delicate balance between wanting to ensure cancer control and making sure we are flattening the curve. As an example, though, I delayed three on-treatment visits for my clinic last Monday, and I converted 70% of my visits to telemedicine. However, I’m a genitourinary cancer specialist and the treatments I give are very different from others.
Lewis: The most difficult calculus is around adjuvant therapy. For metastatic patients, I am trying to use the least immunosuppressive regimen possible that will still control their disease. As you can imagine, it’s an assessment of competing risks.
Schapira: Patients who need essential anticancer therapy should still get it, but attempts to deintensify therapy should continue—for example, holding or postponing treatment without harm (based on evidence, not opinion). This may be possible for patients considering hormonal therapies for breast or prostate cancer.
Patients who need radiation should discuss the timing with their radiation oncologist. In some cases, it may be possible to delay treatment without affecting outcomes, but these decisions should be made carefully. Alternatively, shorter courses of radiation may be appropriate.
Have you advised your own patients differently given the high risk to cancer patients?
Kerr: We have factored potential infection with the virus into discussions where the benefits of chemotherapy are very marginal. This could tip the balance toward the patient deciding not to pursue chemotherapy.
Dizon: The data from China are not entirely crystal-clear. While they noted that people with active cancer and those who had a history of cancer are at increased risk for more severe infections and worse outcomes, the Chinese cohort was small, and compared with people without cancer, it tended to be much older and to be smokers (former or current). Having said this, we are counseling everyone about the importance of social distancing, washing hands, and not touching your face.
Lewis: If I have a complete blood count with a differential that includes lymphocytes, I can advise my lymphopenic patients (who are particularly vulnerable to viral infection) to take special precautions regarding social distancing in their own families.
Have any of your hospitalized patients been affected by policy changes to prepare beds/departments for the expected increase in COVID-19–positive patients?
Weber: Not yet.
Dizon: No, not at the moment.
Have you been asked to assist with other services or COVID-19 task forces?
Dizon: I am keenly involved in the preparations and modifications to procedures, including staffing decisions in outpatient, movement to telehealth, and work-from-home policies.
Lewis: I am engaged in system-wide COVID-19 efforts around oncology.
Kerr: Perhaps oddest of all, I am learning with some of our junior doctors to care for ventilated patients. I still consider myself enough of a general physician that I would hope to be able to contribute to the truly sick, but I accept that I do need an appropriate refresher course.
Bishal Gyawali, MD, PhD, medical oncologist at Queen’s University Cancer Research Institute: Queen’s Hospital medical students are now volunteering to help with daycare, groceries, and other tasks for staff who are working in the hospital.
Are you experiencing any shortages in personal protective equipment (PPE) at your center?
Miller: Some supplies are running short, though none are frankly out at this point. However, rationing and controls are in place to stretch the supplies as far as possible, including reusing some PPE.
Dizon: We are rationing face masks and N95 respirators, eye shields, and even surgical scrubs. We are talking about postponing elective surgery to save PPE but are not yet to that point. We’re asking that face masks be reused for at least 2 days, maybe longer. PPEs are one per day. Scrubs are kept secure.
Lewis: We are being very careful not to overuse PPE but currently have an adequate inventory. We have had to move gloves and masks to areas where they are not accessible to the general public, as otherwise they were being stolen (this started weeks ago).
Kerr: Our National Health System has an adequate supply of PPE equipment centrally, but there seems to be a problem with distribution, as some hospitals are reporting shortages.
Weber: Masks are in short supply, so they are being used for several days if not wet. We are short of plastic gowns and are using paper chemo gowns. Similar story at many places.
This article first appeared on Medscape.com.
As the coronavirus pandemic escalates in the United States, Medscape Oncology reached out to a group of our contributors and asked them to provide their perspective on how their oncology departments and centers are preparing. Here are their responses to a number of issues facing oncologists in the US and around the world.
Have you shifted nonurgent follow-up visits to telemedicine, either via video or phone?
Kathy Miller, MD, Associate Director of Indiana University Simon Cancer Center: We are reviewing our clinic schedules and identifying “routine” follow-up patients who can be rescheduled. When patients are contacted to reschedule, they are asked if they have any urgent, immediate concerns that need to be addressed before the new appointment. If yes, they are offered a virtual visit.
Don Dizon, MD, Director of Women’s Cancers, Lifespan Cancer Institute; Director of Medical Oncology, Rhode Island Hospital: We have started to do this in preparation for a surge of people with COVID-19. Patients who are in long-term follow-up (no evidence of disease at 3 years or longer, being seen annually) or those in routine surveillance after curative treatment (that is, seen every 3 months) as well as those being seen for supportive care–type visits, like sexual health or survivorship, are all being contacted and visits are being moved to telehealth.
Jeffrey S. Weber, MD, PhD, Deputy Director of the Laura and Isaac Perlmutter Cancer Center at NYU Langone Medical Center: Yes. Any follow-up, nontreatment visits are done by phone or video if the patient agrees. (They all have).
Have you delayed or canceled cancer surgeries?
Ravi B. Parikh, MD, MPP, Medical oncologist at the University of Pennsylvania and the Philadelphia VA Medical Center: The University of Pennsylvania has taken this seriously. We’ve canceled all elective surgeries, have ramped up our telemedicine (video and phone) capabilities significantly, are limiting our appointments mostly to on-treatment visits, and have been asked to reconsider regular scans and reviews.
Dizon: We have not done this. There are apparently differences in interpretation in what institutions might mean as “elective surgeries.” At our institution, surgery for invasive malignancies is not elective. However, this may (or will) change if resources become an issue.
Lidia Schapira, MD, Associate Professor of Medicine and Director of Cancer Survivorship at the Stanford Comprehensive Cancer Institute: Delaying elective surgery is something that hospitals here have already implemented, and I imagine that this trend will spread. But it may be difficult to decide in situations that are not exactly “life-saving” but where an earlier intervention could preserve function or improve quality of life.
Mark A. Lewis, MD, Director of Gastrointestinal Oncology at Intermountain Healthcare in Utah: Cancer surgeries have not been deemed elective or delayed.
Have you delayed or altered the delivery of potentially immune-comprising treatments?
David Kerr, MD, Professor of Cancer Medicine at the University of Oxford in England: We are considering delaying initiation of our adjuvant colorectal cancer treatments, as we have data from our own QUASAR trials suggesting that patients who commence chemotherapy between 2 and 6 weeks do equally as well as those who begin 6-12 weeks after surgery.
Parikh: I personally haven’t delayed giving chemotherapy to avoid immune compromise, but I believe some others may have. It’s a delicate balance between wanting to ensure cancer control and making sure we are flattening the curve. As an example, though, I delayed three on-treatment visits for my clinic last Monday, and I converted 70% of my visits to telemedicine. However, I’m a genitourinary cancer specialist and the treatments I give are very different from others.
Lewis: The most difficult calculus is around adjuvant therapy. For metastatic patients, I am trying to use the least immunosuppressive regimen possible that will still control their disease. As you can imagine, it’s an assessment of competing risks.
Schapira: Patients who need essential anticancer therapy should still get it, but attempts to deintensify therapy should continue—for example, holding or postponing treatment without harm (based on evidence, not opinion). This may be possible for patients considering hormonal therapies for breast or prostate cancer.
Patients who need radiation should discuss the timing with their radiation oncologist. In some cases, it may be possible to delay treatment without affecting outcomes, but these decisions should be made carefully. Alternatively, shorter courses of radiation may be appropriate.
Have you advised your own patients differently given the high risk to cancer patients?
Kerr: We have factored potential infection with the virus into discussions where the benefits of chemotherapy are very marginal. This could tip the balance toward the patient deciding not to pursue chemotherapy.
Dizon: The data from China are not entirely crystal-clear. While they noted that people with active cancer and those who had a history of cancer are at increased risk for more severe infections and worse outcomes, the Chinese cohort was small, and compared with people without cancer, it tended to be much older and to be smokers (former or current). Having said this, we are counseling everyone about the importance of social distancing, washing hands, and not touching your face.
Lewis: If I have a complete blood count with a differential that includes lymphocytes, I can advise my lymphopenic patients (who are particularly vulnerable to viral infection) to take special precautions regarding social distancing in their own families.
Have any of your hospitalized patients been affected by policy changes to prepare beds/departments for the expected increase in COVID-19–positive patients?
Weber: Not yet.
Dizon: No, not at the moment.
Have you been asked to assist with other services or COVID-19 task forces?
Dizon: I am keenly involved in the preparations and modifications to procedures, including staffing decisions in outpatient, movement to telehealth, and work-from-home policies.
Lewis: I am engaged in system-wide COVID-19 efforts around oncology.
Kerr: Perhaps oddest of all, I am learning with some of our junior doctors to care for ventilated patients. I still consider myself enough of a general physician that I would hope to be able to contribute to the truly sick, but I accept that I do need an appropriate refresher course.
Bishal Gyawali, MD, PhD, medical oncologist at Queen’s University Cancer Research Institute: Queen’s Hospital medical students are now volunteering to help with daycare, groceries, and other tasks for staff who are working in the hospital.
Are you experiencing any shortages in personal protective equipment (PPE) at your center?
Miller: Some supplies are running short, though none are frankly out at this point. However, rationing and controls are in place to stretch the supplies as far as possible, including reusing some PPE.
Dizon: We are rationing face masks and N95 respirators, eye shields, and even surgical scrubs. We are talking about postponing elective surgery to save PPE but are not yet to that point. We’re asking that face masks be reused for at least 2 days, maybe longer. PPEs are one per day. Scrubs are kept secure.
Lewis: We are being very careful not to overuse PPE but currently have an adequate inventory. We have had to move gloves and masks to areas where they are not accessible to the general public, as otherwise they were being stolen (this started weeks ago).
Kerr: Our National Health System has an adequate supply of PPE equipment centrally, but there seems to be a problem with distribution, as some hospitals are reporting shortages.
Weber: Masks are in short supply, so they are being used for several days if not wet. We are short of plastic gowns and are using paper chemo gowns. Similar story at many places.
This article first appeared on Medscape.com.
Disruptions in cancer care in the era of COVID-19
Editor’s note: Find the latest COVID-19 news and guidance in Medscape’s Coronavirus Resource Center.
Even in the midst of the COVID-19 pandemic, cancer care must go on, but changes may need to be made in the way some care is delivered.
“We’re headed for a time when there will be significant disruptions in the care of patients with cancer,” said Len Lichtenfeld, MD, deputy chief medical officer of the American Cancer Society (ACS), in a statement. “For some it may be as straightforward as a delay in having elective surgery. For others it may be delaying preventive care or adjuvant chemotherapy that’s meant to keep cancer from returning or rescheduling appointments.”
Lichtenfeld emphasized that cancer care teams are going to do the best they can to deliver care to those most in need. However, even in those circumstances, it won’t be life as usual. “It will require patience on everyone’s part as we go through this pandemic,” he said.
“The way we treat cancer over the next few months will change enormously,” writes a British oncologist in an article published in the Guardian.
“As oncologists, we will have to find a tenuous balance between undertreating people with cancer, resulting in more deaths from the disease in the medium to long term, and increasing deaths from COVID-19 in a vulnerable patient population. Alongside our patients we will have to make difficult decisions regarding treatments, with only low-quality evidence to guide us,” writes Lucy Gossage, MD, consultant oncologist at Nottingham University Hospital, UK.
The evidence to date (from reports from China in Lancet Oncology) suggests that people with cancer have a significantly higher risk of severe illness resulting in intensive care admissions or death when infected with COVID-19, particularly if they recently had chemotherapy or surgery.
“Many of the oncology treatments we currently use, especially those given after surgery to reduce risk of cancer recurrence, have relatively small benefits,” she writes.
“In the current climate, the balance of offering these treatments may shift; a small reduction in risk of cancer recurrence over the next 5 years may be outweighed by the potential for a short-term increase in risk of death from COVID-19. In the long term, more people’s cancer will return if we aren’t able to offer these treatments,” she adds.
Postpone Routine Screening
One thing that can go on the back burner for now is routine cancer screening, which can be postponed for now in order to conserve health system resources and reduce contact with healthcare facilities, says the ACS.
“Patients seeking routine cancer screenings should delay those until further notice,” said Lichtenfeld. “While timely screening is important, the need to prevent the spread of coronavirus and to reduce the strain on the medical system is more important right now.”
But as soon as restrictions to slow the spread of COVID-19 are lifted and routine visits to health facilities are safe, regular screening tests should be rescheduled.
Guidance From ASCO
The American Society of Clinical Oncology (ASCO) has issued new guidance on caring for patients with cancer during the COVID-19 outbreak.
First and foremost, ASCO encourages providers, facilities, and anyone caring for patients with cancer to follow the existing guidelines from the Center for Disease Control and Prevention when possible.
ASCO highlights the CDC’s general recommendation for healthcare facilities that suggests “elective surgeries” at inpatient facilities be rescheduled if possible, which has also been recommended by the American College of Surgeons.
However, in many cases, cancer surgery is not elective but essential, it points out. So this is largely an individual determination that clinicians and patients will need to make, taking into account the potential harms of delaying needed cancer-related surgery.
Systemic treatments, including chemotherapy and immunotherapy, leave cancer patients vulnerable to infection, but ASCO says there is no direct evidence to support changes in regimens during the pandemic. Therefore, routinely stopping anticancer or immunosuppressive therapy is not recommended, as the balance of potential harms that may result from delaying or interrupting treatment versus the potential benefits of possibly preventing or delaying COVID-19 infection remains very unclear.
Clinical decisions must be individualized, ASCO emphasized, and suggested the following practice points be considered:
- For patients already in deep remission who are receiving maintenance therapy, stopping treatment may be an option.
- Some patients may be able to switch from IV to oral therapies, which would decrease the frequency of clinic visits.
- Decisions on modifying or withholding chemotherapy need to consider both the indication and goals of care, as well as where the patient is in the treatment regimen and tolerance to the therapy. As an example, the risk–benefit assessment for proceeding with chemotherapy in patients with untreated extensive small-cell lung cancer is quite different than proceeding with maintenance pemetrexed for metastatic non–small cell lung cancer.
- If local coronavirus transmission is an issue at a particular cancer center, reasonable options may include taking a 2-week treatment break or arranging treatment at a different facility.
- Evaluate if home infusion is medically and logistically feasible.
- In some settings, delaying or modifying adjuvant treatment presents a higher risk of compromised disease control and long-term survival than in others, but in cases where the absolute benefit of adjuvant chemotherapy may be quite small and other options are available, the risk of COVID-19 may be considered an additional factor when evaluating care.
Delay Stem Cell Transplants
For patients who are candidates for allogeneic stem cell transplantation, a delay may be reasonable if the patient is currently well controlled with conventional treatment, ASCO comments. It also directs clinicians to follow the recommendations provided by the American Society of Transplantation and Cellular Therapy and from the European Society for Blood and Marrow Transplantation regarding this issue.
Finally, there is also the question of prophylactic antiviral therapy: Should it be considered for cancer patients undergoing active therapy?
The answer to that question is currently unknown, says ASCO, but “this is an active area of research and evidence may be available at any time.”
This article first appeared on Medscape.com.
Editor’s note: Find the latest COVID-19 news and guidance in Medscape’s Coronavirus Resource Center.
Even in the midst of the COVID-19 pandemic, cancer care must go on, but changes may need to be made in the way some care is delivered.
“We’re headed for a time when there will be significant disruptions in the care of patients with cancer,” said Len Lichtenfeld, MD, deputy chief medical officer of the American Cancer Society (ACS), in a statement. “For some it may be as straightforward as a delay in having elective surgery. For others it may be delaying preventive care or adjuvant chemotherapy that’s meant to keep cancer from returning or rescheduling appointments.”
Lichtenfeld emphasized that cancer care teams are going to do the best they can to deliver care to those most in need. However, even in those circumstances, it won’t be life as usual. “It will require patience on everyone’s part as we go through this pandemic,” he said.
“The way we treat cancer over the next few months will change enormously,” writes a British oncologist in an article published in the Guardian.
“As oncologists, we will have to find a tenuous balance between undertreating people with cancer, resulting in more deaths from the disease in the medium to long term, and increasing deaths from COVID-19 in a vulnerable patient population. Alongside our patients we will have to make difficult decisions regarding treatments, with only low-quality evidence to guide us,” writes Lucy Gossage, MD, consultant oncologist at Nottingham University Hospital, UK.
The evidence to date (from reports from China in Lancet Oncology) suggests that people with cancer have a significantly higher risk of severe illness resulting in intensive care admissions or death when infected with COVID-19, particularly if they recently had chemotherapy or surgery.
“Many of the oncology treatments we currently use, especially those given after surgery to reduce risk of cancer recurrence, have relatively small benefits,” she writes.
“In the current climate, the balance of offering these treatments may shift; a small reduction in risk of cancer recurrence over the next 5 years may be outweighed by the potential for a short-term increase in risk of death from COVID-19. In the long term, more people’s cancer will return if we aren’t able to offer these treatments,” she adds.
Postpone Routine Screening
One thing that can go on the back burner for now is routine cancer screening, which can be postponed for now in order to conserve health system resources and reduce contact with healthcare facilities, says the ACS.
“Patients seeking routine cancer screenings should delay those until further notice,” said Lichtenfeld. “While timely screening is important, the need to prevent the spread of coronavirus and to reduce the strain on the medical system is more important right now.”
But as soon as restrictions to slow the spread of COVID-19 are lifted and routine visits to health facilities are safe, regular screening tests should be rescheduled.
Guidance From ASCO
The American Society of Clinical Oncology (ASCO) has issued new guidance on caring for patients with cancer during the COVID-19 outbreak.
First and foremost, ASCO encourages providers, facilities, and anyone caring for patients with cancer to follow the existing guidelines from the Center for Disease Control and Prevention when possible.
ASCO highlights the CDC’s general recommendation for healthcare facilities that suggests “elective surgeries” at inpatient facilities be rescheduled if possible, which has also been recommended by the American College of Surgeons.
However, in many cases, cancer surgery is not elective but essential, it points out. So this is largely an individual determination that clinicians and patients will need to make, taking into account the potential harms of delaying needed cancer-related surgery.
Systemic treatments, including chemotherapy and immunotherapy, leave cancer patients vulnerable to infection, but ASCO says there is no direct evidence to support changes in regimens during the pandemic. Therefore, routinely stopping anticancer or immunosuppressive therapy is not recommended, as the balance of potential harms that may result from delaying or interrupting treatment versus the potential benefits of possibly preventing or delaying COVID-19 infection remains very unclear.
Clinical decisions must be individualized, ASCO emphasized, and suggested the following practice points be considered:
- For patients already in deep remission who are receiving maintenance therapy, stopping treatment may be an option.
- Some patients may be able to switch from IV to oral therapies, which would decrease the frequency of clinic visits.
- Decisions on modifying or withholding chemotherapy need to consider both the indication and goals of care, as well as where the patient is in the treatment regimen and tolerance to the therapy. As an example, the risk–benefit assessment for proceeding with chemotherapy in patients with untreated extensive small-cell lung cancer is quite different than proceeding with maintenance pemetrexed for metastatic non–small cell lung cancer.
- If local coronavirus transmission is an issue at a particular cancer center, reasonable options may include taking a 2-week treatment break or arranging treatment at a different facility.
- Evaluate if home infusion is medically and logistically feasible.
- In some settings, delaying or modifying adjuvant treatment presents a higher risk of compromised disease control and long-term survival than in others, but in cases where the absolute benefit of adjuvant chemotherapy may be quite small and other options are available, the risk of COVID-19 may be considered an additional factor when evaluating care.
Delay Stem Cell Transplants
For patients who are candidates for allogeneic stem cell transplantation, a delay may be reasonable if the patient is currently well controlled with conventional treatment, ASCO comments. It also directs clinicians to follow the recommendations provided by the American Society of Transplantation and Cellular Therapy and from the European Society for Blood and Marrow Transplantation regarding this issue.
Finally, there is also the question of prophylactic antiviral therapy: Should it be considered for cancer patients undergoing active therapy?
The answer to that question is currently unknown, says ASCO, but “this is an active area of research and evidence may be available at any time.”
This article first appeared on Medscape.com.
Editor’s note: Find the latest COVID-19 news and guidance in Medscape’s Coronavirus Resource Center.
Even in the midst of the COVID-19 pandemic, cancer care must go on, but changes may need to be made in the way some care is delivered.
“We’re headed for a time when there will be significant disruptions in the care of patients with cancer,” said Len Lichtenfeld, MD, deputy chief medical officer of the American Cancer Society (ACS), in a statement. “For some it may be as straightforward as a delay in having elective surgery. For others it may be delaying preventive care or adjuvant chemotherapy that’s meant to keep cancer from returning or rescheduling appointments.”
Lichtenfeld emphasized that cancer care teams are going to do the best they can to deliver care to those most in need. However, even in those circumstances, it won’t be life as usual. “It will require patience on everyone’s part as we go through this pandemic,” he said.
“The way we treat cancer over the next few months will change enormously,” writes a British oncologist in an article published in the Guardian.
“As oncologists, we will have to find a tenuous balance between undertreating people with cancer, resulting in more deaths from the disease in the medium to long term, and increasing deaths from COVID-19 in a vulnerable patient population. Alongside our patients we will have to make difficult decisions regarding treatments, with only low-quality evidence to guide us,” writes Lucy Gossage, MD, consultant oncologist at Nottingham University Hospital, UK.
The evidence to date (from reports from China in Lancet Oncology) suggests that people with cancer have a significantly higher risk of severe illness resulting in intensive care admissions or death when infected with COVID-19, particularly if they recently had chemotherapy or surgery.
“Many of the oncology treatments we currently use, especially those given after surgery to reduce risk of cancer recurrence, have relatively small benefits,” she writes.
“In the current climate, the balance of offering these treatments may shift; a small reduction in risk of cancer recurrence over the next 5 years may be outweighed by the potential for a short-term increase in risk of death from COVID-19. In the long term, more people’s cancer will return if we aren’t able to offer these treatments,” she adds.
Postpone Routine Screening
One thing that can go on the back burner for now is routine cancer screening, which can be postponed for now in order to conserve health system resources and reduce contact with healthcare facilities, says the ACS.
“Patients seeking routine cancer screenings should delay those until further notice,” said Lichtenfeld. “While timely screening is important, the need to prevent the spread of coronavirus and to reduce the strain on the medical system is more important right now.”
But as soon as restrictions to slow the spread of COVID-19 are lifted and routine visits to health facilities are safe, regular screening tests should be rescheduled.
Guidance From ASCO
The American Society of Clinical Oncology (ASCO) has issued new guidance on caring for patients with cancer during the COVID-19 outbreak.
First and foremost, ASCO encourages providers, facilities, and anyone caring for patients with cancer to follow the existing guidelines from the Center for Disease Control and Prevention when possible.
ASCO highlights the CDC’s general recommendation for healthcare facilities that suggests “elective surgeries” at inpatient facilities be rescheduled if possible, which has also been recommended by the American College of Surgeons.
However, in many cases, cancer surgery is not elective but essential, it points out. So this is largely an individual determination that clinicians and patients will need to make, taking into account the potential harms of delaying needed cancer-related surgery.
Systemic treatments, including chemotherapy and immunotherapy, leave cancer patients vulnerable to infection, but ASCO says there is no direct evidence to support changes in regimens during the pandemic. Therefore, routinely stopping anticancer or immunosuppressive therapy is not recommended, as the balance of potential harms that may result from delaying or interrupting treatment versus the potential benefits of possibly preventing or delaying COVID-19 infection remains very unclear.
Clinical decisions must be individualized, ASCO emphasized, and suggested the following practice points be considered:
- For patients already in deep remission who are receiving maintenance therapy, stopping treatment may be an option.
- Some patients may be able to switch from IV to oral therapies, which would decrease the frequency of clinic visits.
- Decisions on modifying or withholding chemotherapy need to consider both the indication and goals of care, as well as where the patient is in the treatment regimen and tolerance to the therapy. As an example, the risk–benefit assessment for proceeding with chemotherapy in patients with untreated extensive small-cell lung cancer is quite different than proceeding with maintenance pemetrexed for metastatic non–small cell lung cancer.
- If local coronavirus transmission is an issue at a particular cancer center, reasonable options may include taking a 2-week treatment break or arranging treatment at a different facility.
- Evaluate if home infusion is medically and logistically feasible.
- In some settings, delaying or modifying adjuvant treatment presents a higher risk of compromised disease control and long-term survival than in others, but in cases where the absolute benefit of adjuvant chemotherapy may be quite small and other options are available, the risk of COVID-19 may be considered an additional factor when evaluating care.
Delay Stem Cell Transplants
For patients who are candidates for allogeneic stem cell transplantation, a delay may be reasonable if the patient is currently well controlled with conventional treatment, ASCO comments. It also directs clinicians to follow the recommendations provided by the American Society of Transplantation and Cellular Therapy and from the European Society for Blood and Marrow Transplantation regarding this issue.
Finally, there is also the question of prophylactic antiviral therapy: Should it be considered for cancer patients undergoing active therapy?
The answer to that question is currently unknown, says ASCO, but “this is an active area of research and evidence may be available at any time.”
This article first appeared on Medscape.com.
New melanoma treatments linked to mortality decline
Recent advances in treatment appear to have reversed the course of melanoma mortality since 2013, according to data published in the American Journal of Public Health.
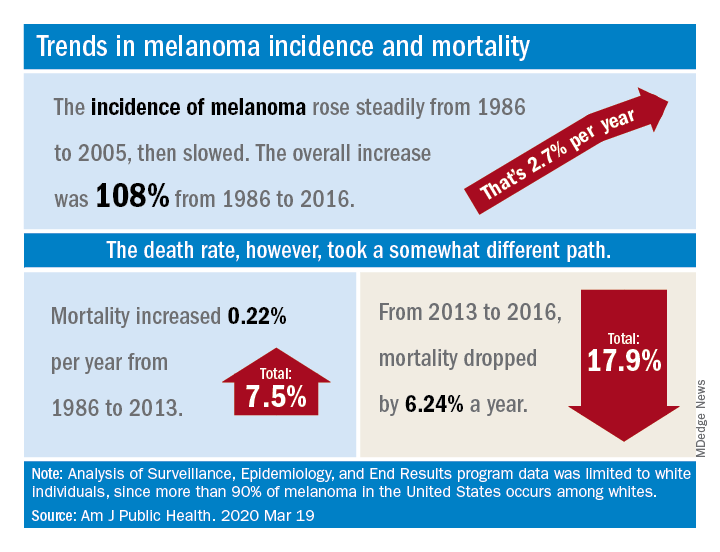
The U.S. death rate for melanoma, which had been rising at a rate of 0.22% a year for more than 2 decades, dropped by 17.9%, or 6.24% per year, during 2013-2016. That decline “coincides with the introduction of multiple new and efficacious treatments for metastatic melanoma,” such as BRAF inhibitors and immune checkpoint inhibitors, study author Juliana Berk-Krauss, MD, of the State University of New York Downstate Medical Center in Brooklyn and colleagues wrote.
The other possible explanation for the decline in deaths, “education and early detection resulting in migration toward earlier stage melanomas with a greater chance of surgical cure,” is unlikely, according to the investigators. That’s because the small decrease in median tumor thickness that occurred during 1989-2009 “is not associated with changes in prognosis.”
The investigators’ analysis encompassed data from the Surveillance, Epidemiology, and End Results registry recorded during 1986-2016. Nine registry areas were included (Atlanta, Connecticut, Detroit, Hawaii, Iowa, New Mexico, San Francisco-Oakland, Seattle-Puget Sound, and Utah), which covered about 9.4% of the U.S. population. The analysis was limited to the white population, which accounts for more than 90% of melanoma cases in the United States.
The data showed a slight decline in annual percent change in melanoma incidence, from 3.24% for 1986-2005 to 1.72% for 2006-2016. However, over the whole period studied (1986-2016), melanoma incidence increased by 108%, or about 2.7% per year.
“Given the increased incidence of melanoma throughout this period and the lack of stage migration, these data strongly suggest that the mortality decline is due to the extended survival associated with these [newer] treatments,” the investigators wrote.
This study was funded by NYU Langone. Two investigators disclosed potential conflicts of interest, including relationships with Bio-Rad Laboratories, Novartis, Merck, and several other companies.
SOURCE: Berk-Krauss J et al. Am J Public Health. 2020 Mar 19. doi: 10.2105/AJPH.2020.305567.
Recent advances in treatment appear to have reversed the course of melanoma mortality since 2013, according to data published in the American Journal of Public Health.
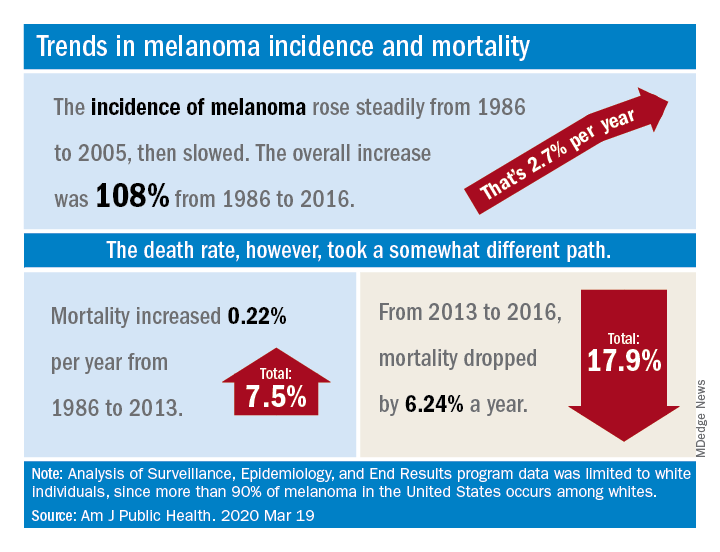
The U.S. death rate for melanoma, which had been rising at a rate of 0.22% a year for more than 2 decades, dropped by 17.9%, or 6.24% per year, during 2013-2016. That decline “coincides with the introduction of multiple new and efficacious treatments for metastatic melanoma,” such as BRAF inhibitors and immune checkpoint inhibitors, study author Juliana Berk-Krauss, MD, of the State University of New York Downstate Medical Center in Brooklyn and colleagues wrote.
The other possible explanation for the decline in deaths, “education and early detection resulting in migration toward earlier stage melanomas with a greater chance of surgical cure,” is unlikely, according to the investigators. That’s because the small decrease in median tumor thickness that occurred during 1989-2009 “is not associated with changes in prognosis.”
The investigators’ analysis encompassed data from the Surveillance, Epidemiology, and End Results registry recorded during 1986-2016. Nine registry areas were included (Atlanta, Connecticut, Detroit, Hawaii, Iowa, New Mexico, San Francisco-Oakland, Seattle-Puget Sound, and Utah), which covered about 9.4% of the U.S. population. The analysis was limited to the white population, which accounts for more than 90% of melanoma cases in the United States.
The data showed a slight decline in annual percent change in melanoma incidence, from 3.24% for 1986-2005 to 1.72% for 2006-2016. However, over the whole period studied (1986-2016), melanoma incidence increased by 108%, or about 2.7% per year.
“Given the increased incidence of melanoma throughout this period and the lack of stage migration, these data strongly suggest that the mortality decline is due to the extended survival associated with these [newer] treatments,” the investigators wrote.
This study was funded by NYU Langone. Two investigators disclosed potential conflicts of interest, including relationships with Bio-Rad Laboratories, Novartis, Merck, and several other companies.
SOURCE: Berk-Krauss J et al. Am J Public Health. 2020 Mar 19. doi: 10.2105/AJPH.2020.305567.
Recent advances in treatment appear to have reversed the course of melanoma mortality since 2013, according to data published in the American Journal of Public Health.
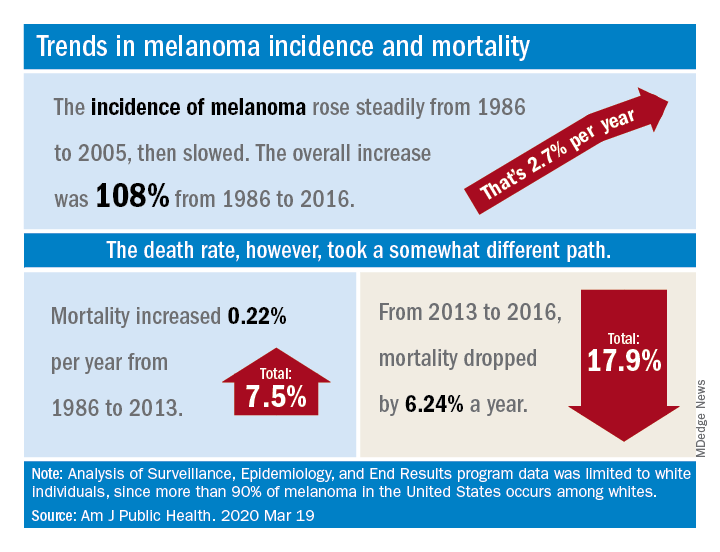
The U.S. death rate for melanoma, which had been rising at a rate of 0.22% a year for more than 2 decades, dropped by 17.9%, or 6.24% per year, during 2013-2016. That decline “coincides with the introduction of multiple new and efficacious treatments for metastatic melanoma,” such as BRAF inhibitors and immune checkpoint inhibitors, study author Juliana Berk-Krauss, MD, of the State University of New York Downstate Medical Center in Brooklyn and colleagues wrote.
The other possible explanation for the decline in deaths, “education and early detection resulting in migration toward earlier stage melanomas with a greater chance of surgical cure,” is unlikely, according to the investigators. That’s because the small decrease in median tumor thickness that occurred during 1989-2009 “is not associated with changes in prognosis.”
The investigators’ analysis encompassed data from the Surveillance, Epidemiology, and End Results registry recorded during 1986-2016. Nine registry areas were included (Atlanta, Connecticut, Detroit, Hawaii, Iowa, New Mexico, San Francisco-Oakland, Seattle-Puget Sound, and Utah), which covered about 9.4% of the U.S. population. The analysis was limited to the white population, which accounts for more than 90% of melanoma cases in the United States.
The data showed a slight decline in annual percent change in melanoma incidence, from 3.24% for 1986-2005 to 1.72% for 2006-2016. However, over the whole period studied (1986-2016), melanoma incidence increased by 108%, or about 2.7% per year.
“Given the increased incidence of melanoma throughout this period and the lack of stage migration, these data strongly suggest that the mortality decline is due to the extended survival associated with these [newer] treatments,” the investigators wrote.
This study was funded by NYU Langone. Two investigators disclosed potential conflicts of interest, including relationships with Bio-Rad Laboratories, Novartis, Merck, and several other companies.
SOURCE: Berk-Krauss J et al. Am J Public Health. 2020 Mar 19. doi: 10.2105/AJPH.2020.305567.
FROM THE AMERICAN JOURNAL OF PUBLIC HEALTH
Teledermoscopy using smartphones fails to boost skin cancer detection
Skin cancer detection does not improve when patients use a dermatoscope for smartphones to capture and send photos of lesions for diagnosis, according to the Australian SKIN Project trial.
“Mobile health applications are increasingly used in cancer prevention and early detection but rarely tested stringently for their value with regard to patient care,” noted trial investigators, who were led by Monika Janda, PhD, of the University of Queensland in Brisbane, Australia. The trial was published in Lancet Digital Health.
The investigators studied 234 adults at high risk for skin cancer, asking them to perform whole-body skin self-exams in their homes at baseline, 1 month, and 2 months.
Half of patients were randomized to perform standard naked-eye exams, note suspicious lesions on a body chart, and submit the chart by email. The other half were randomized to supplement their exams with mobile dermoscopy, and they were provided with a dermatoscope (FotoFinder) that interfaces with smartphones to capture and submit photos of suspicious lesions to a dermatologist for telediagnosis.
Both groups received Web-based instructions on how to complete whole-body skin self-exams and were examined in person within 3 months of their last self-exam to provide a reference standard.
In comparing the two approaches for early detection of skin cancer, the investigators determined that teledermoscopy-enhanced exams would have to show 20% greater sensitivity to establish their superiority.
The median number of lesions submitted was six per person in both the group using adjunctive teledermoscopy and the group performing only naked-eye exams.
At the lesion level, teledermoscopy-enhanced exams had lower sensitivity than naked-eye exams in detecting suspected skin cancers or precursor lesions (75% vs. 88%; P = .04) and similar specificity (87% vs. 89%; P = .42). At the patient level, the two approaches had statistically indistinguishable sensitivity (87% vs. 97%; P = .26) and specificity (95% vs. 96%; P = .96).
At the same time, telediagnosis showed good overall diagnostic concordance with in-person clinical skin examination (88%).
“For the early detection of skin cancer, naked-eye skin self-examination should continue to be recommended by cancer agencies,” Dr. Janda and colleagues concluded. “Further improvements to the instructions for participants on the relevance of nonpigmented skin lesions, training for partners, and the integration of automatic algorithms that rule out clearly benign skin lesions at the time of photographing might increase sensitivity of teledermoscopy in the future.”
This trial was funded by the National Health and Medical Research Council. The authors disclosed relationships with e-derm-consult, SciBase, Canfield Scientific, and other companies.
SOURCE: Janda M et al. Lancet Digit Health. 2020 March; 2(3):e129-e137.
Skin cancer detection does not improve when patients use a dermatoscope for smartphones to capture and send photos of lesions for diagnosis, according to the Australian SKIN Project trial.
“Mobile health applications are increasingly used in cancer prevention and early detection but rarely tested stringently for their value with regard to patient care,” noted trial investigators, who were led by Monika Janda, PhD, of the University of Queensland in Brisbane, Australia. The trial was published in Lancet Digital Health.
The investigators studied 234 adults at high risk for skin cancer, asking them to perform whole-body skin self-exams in their homes at baseline, 1 month, and 2 months.
Half of patients were randomized to perform standard naked-eye exams, note suspicious lesions on a body chart, and submit the chart by email. The other half were randomized to supplement their exams with mobile dermoscopy, and they were provided with a dermatoscope (FotoFinder) that interfaces with smartphones to capture and submit photos of suspicious lesions to a dermatologist for telediagnosis.
Both groups received Web-based instructions on how to complete whole-body skin self-exams and were examined in person within 3 months of their last self-exam to provide a reference standard.
In comparing the two approaches for early detection of skin cancer, the investigators determined that teledermoscopy-enhanced exams would have to show 20% greater sensitivity to establish their superiority.
The median number of lesions submitted was six per person in both the group using adjunctive teledermoscopy and the group performing only naked-eye exams.
At the lesion level, teledermoscopy-enhanced exams had lower sensitivity than naked-eye exams in detecting suspected skin cancers or precursor lesions (75% vs. 88%; P = .04) and similar specificity (87% vs. 89%; P = .42). At the patient level, the two approaches had statistically indistinguishable sensitivity (87% vs. 97%; P = .26) and specificity (95% vs. 96%; P = .96).
At the same time, telediagnosis showed good overall diagnostic concordance with in-person clinical skin examination (88%).
“For the early detection of skin cancer, naked-eye skin self-examination should continue to be recommended by cancer agencies,” Dr. Janda and colleagues concluded. “Further improvements to the instructions for participants on the relevance of nonpigmented skin lesions, training for partners, and the integration of automatic algorithms that rule out clearly benign skin lesions at the time of photographing might increase sensitivity of teledermoscopy in the future.”
This trial was funded by the National Health and Medical Research Council. The authors disclosed relationships with e-derm-consult, SciBase, Canfield Scientific, and other companies.
SOURCE: Janda M et al. Lancet Digit Health. 2020 March; 2(3):e129-e137.
Skin cancer detection does not improve when patients use a dermatoscope for smartphones to capture and send photos of lesions for diagnosis, according to the Australian SKIN Project trial.
“Mobile health applications are increasingly used in cancer prevention and early detection but rarely tested stringently for their value with regard to patient care,” noted trial investigators, who were led by Monika Janda, PhD, of the University of Queensland in Brisbane, Australia. The trial was published in Lancet Digital Health.
The investigators studied 234 adults at high risk for skin cancer, asking them to perform whole-body skin self-exams in their homes at baseline, 1 month, and 2 months.
Half of patients were randomized to perform standard naked-eye exams, note suspicious lesions on a body chart, and submit the chart by email. The other half were randomized to supplement their exams with mobile dermoscopy, and they were provided with a dermatoscope (FotoFinder) that interfaces with smartphones to capture and submit photos of suspicious lesions to a dermatologist for telediagnosis.
Both groups received Web-based instructions on how to complete whole-body skin self-exams and were examined in person within 3 months of their last self-exam to provide a reference standard.
In comparing the two approaches for early detection of skin cancer, the investigators determined that teledermoscopy-enhanced exams would have to show 20% greater sensitivity to establish their superiority.
The median number of lesions submitted was six per person in both the group using adjunctive teledermoscopy and the group performing only naked-eye exams.
At the lesion level, teledermoscopy-enhanced exams had lower sensitivity than naked-eye exams in detecting suspected skin cancers or precursor lesions (75% vs. 88%; P = .04) and similar specificity (87% vs. 89%; P = .42). At the patient level, the two approaches had statistically indistinguishable sensitivity (87% vs. 97%; P = .26) and specificity (95% vs. 96%; P = .96).
At the same time, telediagnosis showed good overall diagnostic concordance with in-person clinical skin examination (88%).
“For the early detection of skin cancer, naked-eye skin self-examination should continue to be recommended by cancer agencies,” Dr. Janda and colleagues concluded. “Further improvements to the instructions for participants on the relevance of nonpigmented skin lesions, training for partners, and the integration of automatic algorithms that rule out clearly benign skin lesions at the time of photographing might increase sensitivity of teledermoscopy in the future.”
This trial was funded by the National Health and Medical Research Council. The authors disclosed relationships with e-derm-consult, SciBase, Canfield Scientific, and other companies.
SOURCE: Janda M et al. Lancet Digit Health. 2020 March; 2(3):e129-e137.
FROM LANCET DIGITAL HEALTH
Patients accept artificial intelligence in skin cancer screening
In a small survey, 75% of dermatology patients said they would recommend the use of artificial intelligence (AI) for skin cancer screening to friends and family members, but 94% emphasized the need for symbiosis between doctors, patients, and AI.
AI under investigation in dermatology includes both direct-to-patient and clinician decision-support AI tools for skin cancer screening, but patients’ perceptions of AI in health care remains unclear, Caroline A. Nelson, MD, of Yale University in New Haven, Conn., and colleagues wrote in JAMA Dermatology.
“We sought to elucidate perceived benefits and risks, strengths and weaknesses, implementation, response to conflict between human and AI clinical decision making, and recommendation for or against AI,” the researchers wrote.
They identified 48 patients seen from May 6, 2019, to July 8, 2019, at general dermatology clinics and melanoma clinics. This included 16 patients with a history of melanoma, 16 with a history of nonmelanoma skin cancer, and 16 with no history of skin cancer. The average age of the patients was 53.3 years, 54% were women, and 94% were white.
The researchers interviewed 24 patients about a direct-to-patient AI tool and 24 patients about a clinician decision-support AI tool.
Overall, 36 patients (75%) said they would recommend the AI tool to family and friends, with 17 patients (71%) saying they would recommend the direct-to-patient tool and 19 (79%) saying they would recommend the clinician decision-support tool. Another nine patients (19%) were ambivalent about the AI tools, and three patients (6%) said they would not recommend the tools.
Diagnostic speed and health care access were the most common perceived benefits of AI (by 60% of patients for each), and increased patient anxiety was the most common perceived risk (by 40% of patients). In addition, 69% of patients perceived more accurate diagnosis to be the greatest strength of an AI tool, and 85% perceived less accurate diagnosis to be the greatest weakness.
The study findings were limited by several factors, including the small sample size, qualitative design, use of a hypothetical rather than real-world situation, and a homogeneous study population, the researchers noted. However, the results merit more studies to obtain perspectives from diverse populations, they said.
“This expansion is particularly important in light of concerns raised that AI tools may exacerbate health care disparities in dermatology,” the researchers wrote.
From the patient perspective, the use of AI “may improve health care quality but should be implemented in a manner that preserves the integrity of the human physician-patient relationship,” the authors concluded.
“Although AI technology has not been widely implemented in dermatology yet, it is the pivotal time to assess patients’ views on the subject to understand their knowledge base, as well as values, preferences, and concerns regarding AI,” wrote Carrie L. Kovarik, MD, of the University of Pennsylvania in Philadelphia, in an accompanying editorial.
“Vulnerable patients, including racial and ethnic minorities, the underinsured or uninsured, economically disadvantaged, and those with chronic health conditions, may be at risk for improper consent for or use of AI,” she wrote.
Dr. Kovarik cited the position statement on augmented intelligence from the American Academy of Dermatology, which states that, for both patients and clinicians, “there should be transparency and choice on how their medical information is gathered, utilized, and stored and when, what, and how augmented intelligence technologies are utilized in their care process. There should be clarity in the symbiotic and synergistic roles of augmented intelligence and human judgment so that it is clear to the patient and provider when and how this technology is utilized to augment human judgment and interpretation.”
Clinicians will need to understand the perspectives on AI from patients of a range of backgrounds to achieve this goal, Dr. Kovarik said.
Dr. Nelson had no financial conflicts to disclose, but her colleagues disclosed relationships with pharmaceutical companies, government agencies, and nonprofit organizations. Dr. Kovarik disclosed serving on the artificial intelligence task force for the American Academy of Dermatology.
SOURCES: Nelson CA et al. JAMA Dermatol. 2020 Mar 11. doi: 10.1001/jamadermatol.2019.5014; Kovarik CL. JAMA Dermatol. 2020 Mar 11. doi: 10.1001/jamadermatol.2019.5013.
In a small survey, 75% of dermatology patients said they would recommend the use of artificial intelligence (AI) for skin cancer screening to friends and family members, but 94% emphasized the need for symbiosis between doctors, patients, and AI.
AI under investigation in dermatology includes both direct-to-patient and clinician decision-support AI tools for skin cancer screening, but patients’ perceptions of AI in health care remains unclear, Caroline A. Nelson, MD, of Yale University in New Haven, Conn., and colleagues wrote in JAMA Dermatology.
“We sought to elucidate perceived benefits and risks, strengths and weaknesses, implementation, response to conflict between human and AI clinical decision making, and recommendation for or against AI,” the researchers wrote.
They identified 48 patients seen from May 6, 2019, to July 8, 2019, at general dermatology clinics and melanoma clinics. This included 16 patients with a history of melanoma, 16 with a history of nonmelanoma skin cancer, and 16 with no history of skin cancer. The average age of the patients was 53.3 years, 54% were women, and 94% were white.
The researchers interviewed 24 patients about a direct-to-patient AI tool and 24 patients about a clinician decision-support AI tool.
Overall, 36 patients (75%) said they would recommend the AI tool to family and friends, with 17 patients (71%) saying they would recommend the direct-to-patient tool and 19 (79%) saying they would recommend the clinician decision-support tool. Another nine patients (19%) were ambivalent about the AI tools, and three patients (6%) said they would not recommend the tools.
Diagnostic speed and health care access were the most common perceived benefits of AI (by 60% of patients for each), and increased patient anxiety was the most common perceived risk (by 40% of patients). In addition, 69% of patients perceived more accurate diagnosis to be the greatest strength of an AI tool, and 85% perceived less accurate diagnosis to be the greatest weakness.
The study findings were limited by several factors, including the small sample size, qualitative design, use of a hypothetical rather than real-world situation, and a homogeneous study population, the researchers noted. However, the results merit more studies to obtain perspectives from diverse populations, they said.
“This expansion is particularly important in light of concerns raised that AI tools may exacerbate health care disparities in dermatology,” the researchers wrote.
From the patient perspective, the use of AI “may improve health care quality but should be implemented in a manner that preserves the integrity of the human physician-patient relationship,” the authors concluded.
“Although AI technology has not been widely implemented in dermatology yet, it is the pivotal time to assess patients’ views on the subject to understand their knowledge base, as well as values, preferences, and concerns regarding AI,” wrote Carrie L. Kovarik, MD, of the University of Pennsylvania in Philadelphia, in an accompanying editorial.
“Vulnerable patients, including racial and ethnic minorities, the underinsured or uninsured, economically disadvantaged, and those with chronic health conditions, may be at risk for improper consent for or use of AI,” she wrote.
Dr. Kovarik cited the position statement on augmented intelligence from the American Academy of Dermatology, which states that, for both patients and clinicians, “there should be transparency and choice on how their medical information is gathered, utilized, and stored and when, what, and how augmented intelligence technologies are utilized in their care process. There should be clarity in the symbiotic and synergistic roles of augmented intelligence and human judgment so that it is clear to the patient and provider when and how this technology is utilized to augment human judgment and interpretation.”
Clinicians will need to understand the perspectives on AI from patients of a range of backgrounds to achieve this goal, Dr. Kovarik said.
Dr. Nelson had no financial conflicts to disclose, but her colleagues disclosed relationships with pharmaceutical companies, government agencies, and nonprofit organizations. Dr. Kovarik disclosed serving on the artificial intelligence task force for the American Academy of Dermatology.
SOURCES: Nelson CA et al. JAMA Dermatol. 2020 Mar 11. doi: 10.1001/jamadermatol.2019.5014; Kovarik CL. JAMA Dermatol. 2020 Mar 11. doi: 10.1001/jamadermatol.2019.5013.
In a small survey, 75% of dermatology patients said they would recommend the use of artificial intelligence (AI) for skin cancer screening to friends and family members, but 94% emphasized the need for symbiosis between doctors, patients, and AI.
AI under investigation in dermatology includes both direct-to-patient and clinician decision-support AI tools for skin cancer screening, but patients’ perceptions of AI in health care remains unclear, Caroline A. Nelson, MD, of Yale University in New Haven, Conn., and colleagues wrote in JAMA Dermatology.
“We sought to elucidate perceived benefits and risks, strengths and weaknesses, implementation, response to conflict between human and AI clinical decision making, and recommendation for or against AI,” the researchers wrote.
They identified 48 patients seen from May 6, 2019, to July 8, 2019, at general dermatology clinics and melanoma clinics. This included 16 patients with a history of melanoma, 16 with a history of nonmelanoma skin cancer, and 16 with no history of skin cancer. The average age of the patients was 53.3 years, 54% were women, and 94% were white.
The researchers interviewed 24 patients about a direct-to-patient AI tool and 24 patients about a clinician decision-support AI tool.
Overall, 36 patients (75%) said they would recommend the AI tool to family and friends, with 17 patients (71%) saying they would recommend the direct-to-patient tool and 19 (79%) saying they would recommend the clinician decision-support tool. Another nine patients (19%) were ambivalent about the AI tools, and three patients (6%) said they would not recommend the tools.
Diagnostic speed and health care access were the most common perceived benefits of AI (by 60% of patients for each), and increased patient anxiety was the most common perceived risk (by 40% of patients). In addition, 69% of patients perceived more accurate diagnosis to be the greatest strength of an AI tool, and 85% perceived less accurate diagnosis to be the greatest weakness.
The study findings were limited by several factors, including the small sample size, qualitative design, use of a hypothetical rather than real-world situation, and a homogeneous study population, the researchers noted. However, the results merit more studies to obtain perspectives from diverse populations, they said.
“This expansion is particularly important in light of concerns raised that AI tools may exacerbate health care disparities in dermatology,” the researchers wrote.
From the patient perspective, the use of AI “may improve health care quality but should be implemented in a manner that preserves the integrity of the human physician-patient relationship,” the authors concluded.
“Although AI technology has not been widely implemented in dermatology yet, it is the pivotal time to assess patients’ views on the subject to understand their knowledge base, as well as values, preferences, and concerns regarding AI,” wrote Carrie L. Kovarik, MD, of the University of Pennsylvania in Philadelphia, in an accompanying editorial.
“Vulnerable patients, including racial and ethnic minorities, the underinsured or uninsured, economically disadvantaged, and those with chronic health conditions, may be at risk for improper consent for or use of AI,” she wrote.
Dr. Kovarik cited the position statement on augmented intelligence from the American Academy of Dermatology, which states that, for both patients and clinicians, “there should be transparency and choice on how their medical information is gathered, utilized, and stored and when, what, and how augmented intelligence technologies are utilized in their care process. There should be clarity in the symbiotic and synergistic roles of augmented intelligence and human judgment so that it is clear to the patient and provider when and how this technology is utilized to augment human judgment and interpretation.”
Clinicians will need to understand the perspectives on AI from patients of a range of backgrounds to achieve this goal, Dr. Kovarik said.
Dr. Nelson had no financial conflicts to disclose, but her colleagues disclosed relationships with pharmaceutical companies, government agencies, and nonprofit organizations. Dr. Kovarik disclosed serving on the artificial intelligence task force for the American Academy of Dermatology.
SOURCES: Nelson CA et al. JAMA Dermatol. 2020 Mar 11. doi: 10.1001/jamadermatol.2019.5014; Kovarik CL. JAMA Dermatol. 2020 Mar 11. doi: 10.1001/jamadermatol.2019.5013.
FROM JAMA DERMATOLOGY
Largest meeting on cancer research canceled: AACR
The biggest cancer research meeting of the year has been canceled as a reaction to the novel coronavirus (COVID-19) outbreak, which has also led to many other medical conferences being canceled or postponed.
The annual meeting of the American Association for Cancer Research (AACR) was due to take place April 24-29 in San Diego, California. More than 24,000 delegates from 80 countries and more than 500 exhibitors were expected to attend.
There are plans to reschedule it for later this year.
This has been a “difficult decision,” said the AACR board of directors, but “we believe that the decision to postpone the meeting is absolutely the correct one to safeguard our meeting participants from further potential exposure to the coronavirus.”
The board goes on to explain that “this evidence-based decision was made after a thorough review and discussion of all factors impacting the annual meeting, including the US government’s enforcement of restrictions on international travelers to enter the US; the imposition of travel restrictions issued by US government agencies, cancer centers, academic institutions, and pharmaceutical and biotech companies; and the counsel of infectious disease experts. It is clear that all of these elements significantly affect the ability of delegates, speakers, presenters of proffered papers, and exhibitors to participate fully in the annual meeting.”
Other cancer conferences that were planned for March and that have been canceled include the following:
- European Breast Cancer Conference (EBCC), Barcelona, Spain, which was to have taken place March 18-20. This conference has been postponed and will now take place September 30 to October 2 at the same venue. Abstracts that have been accepted for the initial conference will remain in the program, and organizers will reopen abstract submissions in May.
- National Comprehensive Cancer Network (NCCN), Orlando, Florida, was scheduled for March 19-22. This conference has been postponed. No new dates have been provided, but the society notes that “NCCN staff is working as quickly as possible to notify all conference registrants about the postponement and further information regarding the refund process.”
- European Association of Urology (EAU), Amsterdam, the Netherlands, at which there is always new research presented on prostate, kidney, and bladder cancer, was due to take place March 20-24. This conference has been postponed to July 2020.
- Society of Gynecologic Oncology (SGO), in Toronto, Canada, which was scheduled for March 28-31. SGO is “exploring alternatives for delivering the science and education.”
Overall, the move to cancel medical conferences over the next few months is a good idea, commented F. Perry Wilson, MD, MSCE, associate professor of medicine and director of Yale’s Program of Applied Translational Research, in a Medscape Medical News commentary.
“There’s a pretty straightforward case here,” he argued. “Medical professionals are at higher risk for exposure to coronavirus because we come into contact with lots and lots of patients. Gathering a large group of medical professionals in a single place increases the risk for exposure further. Factor in airplane flights to and from the conferences, and the chance that infection is spread is significant.”
This article first appeared on Medscape.com.
The biggest cancer research meeting of the year has been canceled as a reaction to the novel coronavirus (COVID-19) outbreak, which has also led to many other medical conferences being canceled or postponed.
The annual meeting of the American Association for Cancer Research (AACR) was due to take place April 24-29 in San Diego, California. More than 24,000 delegates from 80 countries and more than 500 exhibitors were expected to attend.
There are plans to reschedule it for later this year.
This has been a “difficult decision,” said the AACR board of directors, but “we believe that the decision to postpone the meeting is absolutely the correct one to safeguard our meeting participants from further potential exposure to the coronavirus.”
The board goes on to explain that “this evidence-based decision was made after a thorough review and discussion of all factors impacting the annual meeting, including the US government’s enforcement of restrictions on international travelers to enter the US; the imposition of travel restrictions issued by US government agencies, cancer centers, academic institutions, and pharmaceutical and biotech companies; and the counsel of infectious disease experts. It is clear that all of these elements significantly affect the ability of delegates, speakers, presenters of proffered papers, and exhibitors to participate fully in the annual meeting.”
Other cancer conferences that were planned for March and that have been canceled include the following:
- European Breast Cancer Conference (EBCC), Barcelona, Spain, which was to have taken place March 18-20. This conference has been postponed and will now take place September 30 to October 2 at the same venue. Abstracts that have been accepted for the initial conference will remain in the program, and organizers will reopen abstract submissions in May.
- National Comprehensive Cancer Network (NCCN), Orlando, Florida, was scheduled for March 19-22. This conference has been postponed. No new dates have been provided, but the society notes that “NCCN staff is working as quickly as possible to notify all conference registrants about the postponement and further information regarding the refund process.”
- European Association of Urology (EAU), Amsterdam, the Netherlands, at which there is always new research presented on prostate, kidney, and bladder cancer, was due to take place March 20-24. This conference has been postponed to July 2020.
- Society of Gynecologic Oncology (SGO), in Toronto, Canada, which was scheduled for March 28-31. SGO is “exploring alternatives for delivering the science and education.”
Overall, the move to cancel medical conferences over the next few months is a good idea, commented F. Perry Wilson, MD, MSCE, associate professor of medicine and director of Yale’s Program of Applied Translational Research, in a Medscape Medical News commentary.
“There’s a pretty straightforward case here,” he argued. “Medical professionals are at higher risk for exposure to coronavirus because we come into contact with lots and lots of patients. Gathering a large group of medical professionals in a single place increases the risk for exposure further. Factor in airplane flights to and from the conferences, and the chance that infection is spread is significant.”
This article first appeared on Medscape.com.
The biggest cancer research meeting of the year has been canceled as a reaction to the novel coronavirus (COVID-19) outbreak, which has also led to many other medical conferences being canceled or postponed.
The annual meeting of the American Association for Cancer Research (AACR) was due to take place April 24-29 in San Diego, California. More than 24,000 delegates from 80 countries and more than 500 exhibitors were expected to attend.
There are plans to reschedule it for later this year.
This has been a “difficult decision,” said the AACR board of directors, but “we believe that the decision to postpone the meeting is absolutely the correct one to safeguard our meeting participants from further potential exposure to the coronavirus.”
The board goes on to explain that “this evidence-based decision was made after a thorough review and discussion of all factors impacting the annual meeting, including the US government’s enforcement of restrictions on international travelers to enter the US; the imposition of travel restrictions issued by US government agencies, cancer centers, academic institutions, and pharmaceutical and biotech companies; and the counsel of infectious disease experts. It is clear that all of these elements significantly affect the ability of delegates, speakers, presenters of proffered papers, and exhibitors to participate fully in the annual meeting.”
Other cancer conferences that were planned for March and that have been canceled include the following:
- European Breast Cancer Conference (EBCC), Barcelona, Spain, which was to have taken place March 18-20. This conference has been postponed and will now take place September 30 to October 2 at the same venue. Abstracts that have been accepted for the initial conference will remain in the program, and organizers will reopen abstract submissions in May.
- National Comprehensive Cancer Network (NCCN), Orlando, Florida, was scheduled for March 19-22. This conference has been postponed. No new dates have been provided, but the society notes that “NCCN staff is working as quickly as possible to notify all conference registrants about the postponement and further information regarding the refund process.”
- European Association of Urology (EAU), Amsterdam, the Netherlands, at which there is always new research presented on prostate, kidney, and bladder cancer, was due to take place March 20-24. This conference has been postponed to July 2020.
- Society of Gynecologic Oncology (SGO), in Toronto, Canada, which was scheduled for March 28-31. SGO is “exploring alternatives for delivering the science and education.”
Overall, the move to cancel medical conferences over the next few months is a good idea, commented F. Perry Wilson, MD, MSCE, associate professor of medicine and director of Yale’s Program of Applied Translational Research, in a Medscape Medical News commentary.
“There’s a pretty straightforward case here,” he argued. “Medical professionals are at higher risk for exposure to coronavirus because we come into contact with lots and lots of patients. Gathering a large group of medical professionals in a single place increases the risk for exposure further. Factor in airplane flights to and from the conferences, and the chance that infection is spread is significant.”
This article first appeared on Medscape.com.



