User login
Vitamin D deficiency linked to early cognitive impairment in MS
according to new research that adds to the known adverse relationship between low vitamin D and MS.
“We confirmed that low vitamin D may affect not only early disability but also cognition in newly MS diagnosed patients,” said lead author Eleonora Virgilio, MD, of the MS Center, neurology unit, at the University of Eastern Piedmont, Novara, Italy.
“The possible effects of vitamin D on both cognition (in particular, information processing speed) and early disability in newly diagnosed MS patients needs to be further investigated because this association might represent a marker of future disability, supporting the need for prompt supplementation,” she said.
The findings were presented at the meeting held by the Americas Committee for Treatment and Research in Multiple Sclerosis.
Low vitamin D and MS
Previous studies have linked insufficient serum vitamin D with everything from the development of MS to activity and disease progression, but less has been reported on a specific link to the impairment of cognitive function, an important complication of MS.
“Cognitive impairment, and, in particular, slowed information processing speed, is very frequent in the MS population from the early stages of disease, and frequently underestimated,” Dr. Virgilio noted. “It has yet to be completely elucidated what the exact underlying mechanisms are.”
To evaluate the relationship, Dr. Virgilio and colleagues enrolled 60 patients in Italy with MS who were newly diagnosed and had serum vitamin D levels collected upon diagnosis. The participants were also tested at diagnosis with the Symbol Digit Modalities Test (SDMT) for information processing speed, which is a hallmark of the cognitive impairment that can occur in MS and is typically the first cognitive domain to show effects of the disease.
Among the patients, 40 were female and the mean age at diagnosis was 39.5 years; 90% had relapsing remitting MS at baseline and 10% had progressive MS. Their median Expanded Disability Status Scale score at diagnosis was 1.5.
At baseline, as many as 85% of the participants (51) had low serum vitamin D levels, defined as below 30 ng/mL, which Dr. Virgilio noted is consistent with other rates reported among people with MS in the Lombardy region of Italy, where the study was conducted.
The patients had a mean vitamin D level of 21.17 ng/mL (± 10.02), with 51.7% considered to have a deficiency (less than 20 ng/mL) and 33.3% with an insufficiency (20-30 ng/mL).
Of the patients, 16 (27%) had cognitive impairment, defined as a z score of 1.5 or less. Their mean raw SDMT score was 46.50 (± 14.73) and mean z score was –0.62 (± 1.29).
Importantly, those with cognitive impairment were significantly more likely to have severe hypovitaminosis D, compared with those with sufficient vitamin D levels, none of whom showed cognitive impairment (P = .02).
Furthermore, vitamin D levels positively correlated with SDMT raw values (P = .001) and z score (P = .008).
Over a mean follow-up of 2 years, a significant correlation was observed between serum vitamin D levels at diagnosis and early disability on the MS severity score (MSSS; P = .02) and a weak correlation with age-related MSSS (ARMSS; P = .08) at the last clinical follow-up.
Dr. Virgilio noted that factors including disease treatment effects or other factors could have played a role in the weaker results. “It is possible that the linear correlation we found was not as strong as expected [because of] an effect of treatment with disease-modifying therapies or vitamin D supplementation, or because of the short follow-up available at the moment for our population – only for a mean period of 2 years after MS diagnosis.”
The mechanisms for vitamin D deficiency in the MS population are likely multifactorial, with genetic as well as environmental links, she noted.
“The immunomodulatory effects of vitamin D are well known,” Dr. Virgilio said.
“Vitamin D was already linked to cognitive function in other neurodegenerative diseases, [including] Alzheimer’s disease, but more importantly, also in other autoimmune diseases, such as systemic lupus erythematosus,” she explained.
Vitamin D also linked to long-term cognitive function
The study adds to recent research showing longer-term effects of vitamin D deficiency and cognitive impairment in MS: In the longitudinal BENEFIT trial published in 2020, researchers following 278 patients with MS over the course of 11 years found that a 50 ng/L higher mean vitamin D level in the first 2 years of the study was associated with a 65% lower odds of a poor performance on Paced Auditory Serial Addition Test scores at the 11-year follow-up.
That study also looked at neurofilament light chain concentrations, which are associated with MS disease activity, and found they were 20% lower among those with higher vitamin D at baseline. Smokers also had lower cognitive scores.
“Lower vitamin D and smoking after clinical onset predicted worse long-term cognitive function and neuronal integrity in patients with MS,” the authors concluded.
The authors disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
according to new research that adds to the known adverse relationship between low vitamin D and MS.
“We confirmed that low vitamin D may affect not only early disability but also cognition in newly MS diagnosed patients,” said lead author Eleonora Virgilio, MD, of the MS Center, neurology unit, at the University of Eastern Piedmont, Novara, Italy.
“The possible effects of vitamin D on both cognition (in particular, information processing speed) and early disability in newly diagnosed MS patients needs to be further investigated because this association might represent a marker of future disability, supporting the need for prompt supplementation,” she said.
The findings were presented at the meeting held by the Americas Committee for Treatment and Research in Multiple Sclerosis.
Low vitamin D and MS
Previous studies have linked insufficient serum vitamin D with everything from the development of MS to activity and disease progression, but less has been reported on a specific link to the impairment of cognitive function, an important complication of MS.
“Cognitive impairment, and, in particular, slowed information processing speed, is very frequent in the MS population from the early stages of disease, and frequently underestimated,” Dr. Virgilio noted. “It has yet to be completely elucidated what the exact underlying mechanisms are.”
To evaluate the relationship, Dr. Virgilio and colleagues enrolled 60 patients in Italy with MS who were newly diagnosed and had serum vitamin D levels collected upon diagnosis. The participants were also tested at diagnosis with the Symbol Digit Modalities Test (SDMT) for information processing speed, which is a hallmark of the cognitive impairment that can occur in MS and is typically the first cognitive domain to show effects of the disease.
Among the patients, 40 were female and the mean age at diagnosis was 39.5 years; 90% had relapsing remitting MS at baseline and 10% had progressive MS. Their median Expanded Disability Status Scale score at diagnosis was 1.5.
At baseline, as many as 85% of the participants (51) had low serum vitamin D levels, defined as below 30 ng/mL, which Dr. Virgilio noted is consistent with other rates reported among people with MS in the Lombardy region of Italy, where the study was conducted.
The patients had a mean vitamin D level of 21.17 ng/mL (± 10.02), with 51.7% considered to have a deficiency (less than 20 ng/mL) and 33.3% with an insufficiency (20-30 ng/mL).
Of the patients, 16 (27%) had cognitive impairment, defined as a z score of 1.5 or less. Their mean raw SDMT score was 46.50 (± 14.73) and mean z score was –0.62 (± 1.29).
Importantly, those with cognitive impairment were significantly more likely to have severe hypovitaminosis D, compared with those with sufficient vitamin D levels, none of whom showed cognitive impairment (P = .02).
Furthermore, vitamin D levels positively correlated with SDMT raw values (P = .001) and z score (P = .008).
Over a mean follow-up of 2 years, a significant correlation was observed between serum vitamin D levels at diagnosis and early disability on the MS severity score (MSSS; P = .02) and a weak correlation with age-related MSSS (ARMSS; P = .08) at the last clinical follow-up.
Dr. Virgilio noted that factors including disease treatment effects or other factors could have played a role in the weaker results. “It is possible that the linear correlation we found was not as strong as expected [because of] an effect of treatment with disease-modifying therapies or vitamin D supplementation, or because of the short follow-up available at the moment for our population – only for a mean period of 2 years after MS diagnosis.”
The mechanisms for vitamin D deficiency in the MS population are likely multifactorial, with genetic as well as environmental links, she noted.
“The immunomodulatory effects of vitamin D are well known,” Dr. Virgilio said.
“Vitamin D was already linked to cognitive function in other neurodegenerative diseases, [including] Alzheimer’s disease, but more importantly, also in other autoimmune diseases, such as systemic lupus erythematosus,” she explained.
Vitamin D also linked to long-term cognitive function
The study adds to recent research showing longer-term effects of vitamin D deficiency and cognitive impairment in MS: In the longitudinal BENEFIT trial published in 2020, researchers following 278 patients with MS over the course of 11 years found that a 50 ng/L higher mean vitamin D level in the first 2 years of the study was associated with a 65% lower odds of a poor performance on Paced Auditory Serial Addition Test scores at the 11-year follow-up.
That study also looked at neurofilament light chain concentrations, which are associated with MS disease activity, and found they were 20% lower among those with higher vitamin D at baseline. Smokers also had lower cognitive scores.
“Lower vitamin D and smoking after clinical onset predicted worse long-term cognitive function and neuronal integrity in patients with MS,” the authors concluded.
The authors disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
according to new research that adds to the known adverse relationship between low vitamin D and MS.
“We confirmed that low vitamin D may affect not only early disability but also cognition in newly MS diagnosed patients,” said lead author Eleonora Virgilio, MD, of the MS Center, neurology unit, at the University of Eastern Piedmont, Novara, Italy.
“The possible effects of vitamin D on both cognition (in particular, information processing speed) and early disability in newly diagnosed MS patients needs to be further investigated because this association might represent a marker of future disability, supporting the need for prompt supplementation,” she said.
The findings were presented at the meeting held by the Americas Committee for Treatment and Research in Multiple Sclerosis.
Low vitamin D and MS
Previous studies have linked insufficient serum vitamin D with everything from the development of MS to activity and disease progression, but less has been reported on a specific link to the impairment of cognitive function, an important complication of MS.
“Cognitive impairment, and, in particular, slowed information processing speed, is very frequent in the MS population from the early stages of disease, and frequently underestimated,” Dr. Virgilio noted. “It has yet to be completely elucidated what the exact underlying mechanisms are.”
To evaluate the relationship, Dr. Virgilio and colleagues enrolled 60 patients in Italy with MS who were newly diagnosed and had serum vitamin D levels collected upon diagnosis. The participants were also tested at diagnosis with the Symbol Digit Modalities Test (SDMT) for information processing speed, which is a hallmark of the cognitive impairment that can occur in MS and is typically the first cognitive domain to show effects of the disease.
Among the patients, 40 were female and the mean age at diagnosis was 39.5 years; 90% had relapsing remitting MS at baseline and 10% had progressive MS. Their median Expanded Disability Status Scale score at diagnosis was 1.5.
At baseline, as many as 85% of the participants (51) had low serum vitamin D levels, defined as below 30 ng/mL, which Dr. Virgilio noted is consistent with other rates reported among people with MS in the Lombardy region of Italy, where the study was conducted.
The patients had a mean vitamin D level of 21.17 ng/mL (± 10.02), with 51.7% considered to have a deficiency (less than 20 ng/mL) and 33.3% with an insufficiency (20-30 ng/mL).
Of the patients, 16 (27%) had cognitive impairment, defined as a z score of 1.5 or less. Their mean raw SDMT score was 46.50 (± 14.73) and mean z score was –0.62 (± 1.29).
Importantly, those with cognitive impairment were significantly more likely to have severe hypovitaminosis D, compared with those with sufficient vitamin D levels, none of whom showed cognitive impairment (P = .02).
Furthermore, vitamin D levels positively correlated with SDMT raw values (P = .001) and z score (P = .008).
Over a mean follow-up of 2 years, a significant correlation was observed between serum vitamin D levels at diagnosis and early disability on the MS severity score (MSSS; P = .02) and a weak correlation with age-related MSSS (ARMSS; P = .08) at the last clinical follow-up.
Dr. Virgilio noted that factors including disease treatment effects or other factors could have played a role in the weaker results. “It is possible that the linear correlation we found was not as strong as expected [because of] an effect of treatment with disease-modifying therapies or vitamin D supplementation, or because of the short follow-up available at the moment for our population – only for a mean period of 2 years after MS diagnosis.”
The mechanisms for vitamin D deficiency in the MS population are likely multifactorial, with genetic as well as environmental links, she noted.
“The immunomodulatory effects of vitamin D are well known,” Dr. Virgilio said.
“Vitamin D was already linked to cognitive function in other neurodegenerative diseases, [including] Alzheimer’s disease, but more importantly, also in other autoimmune diseases, such as systemic lupus erythematosus,” she explained.
Vitamin D also linked to long-term cognitive function
The study adds to recent research showing longer-term effects of vitamin D deficiency and cognitive impairment in MS: In the longitudinal BENEFIT trial published in 2020, researchers following 278 patients with MS over the course of 11 years found that a 50 ng/L higher mean vitamin D level in the first 2 years of the study was associated with a 65% lower odds of a poor performance on Paced Auditory Serial Addition Test scores at the 11-year follow-up.
That study also looked at neurofilament light chain concentrations, which are associated with MS disease activity, and found they were 20% lower among those with higher vitamin D at baseline. Smokers also had lower cognitive scores.
“Lower vitamin D and smoking after clinical onset predicted worse long-term cognitive function and neuronal integrity in patients with MS,” the authors concluded.
The authors disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM ACTRIMS FORUM 2021
Opioid use common for pain in multiple sclerosis
, new research shows.
“This high level of opioid use supports that better pain management treatment options, including nonpharmacological options, are needed for people with MS and pain,” wrote the authors of the study, which was presented at ACTRIMS Forum 2021, held by the Americas Committee for Treatment and Research in Multiple Sclerosis.
Previous research has shown that more than 50% of people with MS report chronic pain that is serious enough to interfere with daily activities, employment, and quality of life. Many with MS report that pain is one of their worst symptoms, the authors noted.
With surprisingly few studies evaluating opioid use in the MS population, Cinda L. Hugos, PT, associate professor of neurology with the VA Portland Health Care System and the department of neurology, Oregon Health and Science University, Portland, and colleagues investigated the issue in a sample of patients participating in a U.S. multisite MS fatigue management trial conducted between 2013 and 2014.
Of the 281 participants with MS in the study, 58 patients (20.6%) reported using prescription opioids. Among them, most – 44 (76%) – reported regular daily use, 10 (17%) reported using the drugs only as needed, 3 (5%) reported only short-term use, including after recent injury or dental surgery, and 1 provided incomplete information.
Those who reported opioid use had significantly worse fatigue scores on the Modified Fatigue Impact Scale (P = .015) and worse pain scores (P < .0001).
There were no significant differences in terms of age (mean age, 53 years), gender (69% were female), or race (in both groups, about 76% were White). No significant differences were seen in disability or depression scores in the opioid users versus nonusers.
“In this sample of people with multiple sclerosis who self-reported fatigue and volunteered to join an MS fatigue management research study, more than one in five reported using prescription opioids and nearly one in six used opioids daily,” the authors wrote. “Opioid users had more pain and fatigue than nonusers.”
Commenting on the study, Jeffrey Cohen, MD, president of ACTRIMS, said that the findings are consistent with his observations that “in the general population, opioids often are used to treat chronic pain in people with MS.”
But they’re not getting the drugs from his clinic. “We do not prescribe opioids in our clinic, referring such patients to a chronic pain program,” Dr. Cohen said. “However, there clearly is need for better treatment options.”
A previous study on opioid use by people with MS, published in 2015, found even higher rates – 42% reported having ever used opioids, and 38% reported currently using opioids.
Although reports of opioid use by patients with MS have been lacking, more has been published on the emerging use of cannabis-related products. One recent study showed that nearly half of people with MS reported using a cannabis-based therapy for nerve-based pain and sleep disturbances.
Although cannabis is considered safer than opioids, the authors noted that it has its own significant drawback – a “paucity of provider guidance.”
“The range of perceived benefits and potential differential effects of THC and cannabinoid highlight the need for personalized, evidence-based guidelines regarding cannabinoid use,” they wrote.
Stretching program for spasticity shows benefits
With spasticity representing a key contributor to MS pain and affecting more than 80% of people with MS, Ms. Hugos and colleagues are developing an alternative to medication – a nonpharmacologic stretching regimen called Spasticity: Take Control” (STC).
Based on evidence-based strategies for the treatment of spasticity in MS, the program involves exercises with daily routines of 15-20 minutes over 6 months.
In a pilot study of 66 patients, also presented at the ACTRIMS meeting, the investigators reported that the program showed significant reductions in pain severity and interference, measured with the Brief Pain Inventory–Short Form, compared with a control consisting of range of motion instruction over 6 months.
The study also offered insights on the specific areas of pain. Among those who reported chronic pain (42% in the STC group and 63.3% in the range-of-motion group), the pain was most frequently reported in the lower back (74.3%), legs (68.6%), or lower back and legs (88.6%).
Ms. Hugos noted that the findings suggest a potentially important nonpharmacologic alternative to spasticity-related pain in MS.
“Stretching is the cornerstone treatment for spasticity from all causes, but there is very little information on stretching exercises in MS or any other conditions,” Ms. Hugos said. “[Our] pilot study is the first and only study using a standardized, daily stretching exercise program to treat MS spasticity,” she said.
“A fully powered study is needed to better understand the impact of different types of exercise on pain severity and interference in multiple sclerosis,” she noted.
Ms. Hugos has received consulting fees from Greenwich Biosciences, Evidera, and Techspert.io. Dr. Cohen has received personal compensation for consulting for Adamas, Atara, Bristol-Myers Squibb, Convelo, MedDay, and Mylan.
A version of this article first appeared on Medscape.com.
, new research shows.
“This high level of opioid use supports that better pain management treatment options, including nonpharmacological options, are needed for people with MS and pain,” wrote the authors of the study, which was presented at ACTRIMS Forum 2021, held by the Americas Committee for Treatment and Research in Multiple Sclerosis.
Previous research has shown that more than 50% of people with MS report chronic pain that is serious enough to interfere with daily activities, employment, and quality of life. Many with MS report that pain is one of their worst symptoms, the authors noted.
With surprisingly few studies evaluating opioid use in the MS population, Cinda L. Hugos, PT, associate professor of neurology with the VA Portland Health Care System and the department of neurology, Oregon Health and Science University, Portland, and colleagues investigated the issue in a sample of patients participating in a U.S. multisite MS fatigue management trial conducted between 2013 and 2014.
Of the 281 participants with MS in the study, 58 patients (20.6%) reported using prescription opioids. Among them, most – 44 (76%) – reported regular daily use, 10 (17%) reported using the drugs only as needed, 3 (5%) reported only short-term use, including after recent injury or dental surgery, and 1 provided incomplete information.
Those who reported opioid use had significantly worse fatigue scores on the Modified Fatigue Impact Scale (P = .015) and worse pain scores (P < .0001).
There were no significant differences in terms of age (mean age, 53 years), gender (69% were female), or race (in both groups, about 76% were White). No significant differences were seen in disability or depression scores in the opioid users versus nonusers.
“In this sample of people with multiple sclerosis who self-reported fatigue and volunteered to join an MS fatigue management research study, more than one in five reported using prescription opioids and nearly one in six used opioids daily,” the authors wrote. “Opioid users had more pain and fatigue than nonusers.”
Commenting on the study, Jeffrey Cohen, MD, president of ACTRIMS, said that the findings are consistent with his observations that “in the general population, opioids often are used to treat chronic pain in people with MS.”
But they’re not getting the drugs from his clinic. “We do not prescribe opioids in our clinic, referring such patients to a chronic pain program,” Dr. Cohen said. “However, there clearly is need for better treatment options.”
A previous study on opioid use by people with MS, published in 2015, found even higher rates – 42% reported having ever used opioids, and 38% reported currently using opioids.
Although reports of opioid use by patients with MS have been lacking, more has been published on the emerging use of cannabis-related products. One recent study showed that nearly half of people with MS reported using a cannabis-based therapy for nerve-based pain and sleep disturbances.
Although cannabis is considered safer than opioids, the authors noted that it has its own significant drawback – a “paucity of provider guidance.”
“The range of perceived benefits and potential differential effects of THC and cannabinoid highlight the need for personalized, evidence-based guidelines regarding cannabinoid use,” they wrote.
Stretching program for spasticity shows benefits
With spasticity representing a key contributor to MS pain and affecting more than 80% of people with MS, Ms. Hugos and colleagues are developing an alternative to medication – a nonpharmacologic stretching regimen called Spasticity: Take Control” (STC).
Based on evidence-based strategies for the treatment of spasticity in MS, the program involves exercises with daily routines of 15-20 minutes over 6 months.
In a pilot study of 66 patients, also presented at the ACTRIMS meeting, the investigators reported that the program showed significant reductions in pain severity and interference, measured with the Brief Pain Inventory–Short Form, compared with a control consisting of range of motion instruction over 6 months.
The study also offered insights on the specific areas of pain. Among those who reported chronic pain (42% in the STC group and 63.3% in the range-of-motion group), the pain was most frequently reported in the lower back (74.3%), legs (68.6%), or lower back and legs (88.6%).
Ms. Hugos noted that the findings suggest a potentially important nonpharmacologic alternative to spasticity-related pain in MS.
“Stretching is the cornerstone treatment for spasticity from all causes, but there is very little information on stretching exercises in MS or any other conditions,” Ms. Hugos said. “[Our] pilot study is the first and only study using a standardized, daily stretching exercise program to treat MS spasticity,” she said.
“A fully powered study is needed to better understand the impact of different types of exercise on pain severity and interference in multiple sclerosis,” she noted.
Ms. Hugos has received consulting fees from Greenwich Biosciences, Evidera, and Techspert.io. Dr. Cohen has received personal compensation for consulting for Adamas, Atara, Bristol-Myers Squibb, Convelo, MedDay, and Mylan.
A version of this article first appeared on Medscape.com.
, new research shows.
“This high level of opioid use supports that better pain management treatment options, including nonpharmacological options, are needed for people with MS and pain,” wrote the authors of the study, which was presented at ACTRIMS Forum 2021, held by the Americas Committee for Treatment and Research in Multiple Sclerosis.
Previous research has shown that more than 50% of people with MS report chronic pain that is serious enough to interfere with daily activities, employment, and quality of life. Many with MS report that pain is one of their worst symptoms, the authors noted.
With surprisingly few studies evaluating opioid use in the MS population, Cinda L. Hugos, PT, associate professor of neurology with the VA Portland Health Care System and the department of neurology, Oregon Health and Science University, Portland, and colleagues investigated the issue in a sample of patients participating in a U.S. multisite MS fatigue management trial conducted between 2013 and 2014.
Of the 281 participants with MS in the study, 58 patients (20.6%) reported using prescription opioids. Among them, most – 44 (76%) – reported regular daily use, 10 (17%) reported using the drugs only as needed, 3 (5%) reported only short-term use, including after recent injury or dental surgery, and 1 provided incomplete information.
Those who reported opioid use had significantly worse fatigue scores on the Modified Fatigue Impact Scale (P = .015) and worse pain scores (P < .0001).
There were no significant differences in terms of age (mean age, 53 years), gender (69% were female), or race (in both groups, about 76% were White). No significant differences were seen in disability or depression scores in the opioid users versus nonusers.
“In this sample of people with multiple sclerosis who self-reported fatigue and volunteered to join an MS fatigue management research study, more than one in five reported using prescription opioids and nearly one in six used opioids daily,” the authors wrote. “Opioid users had more pain and fatigue than nonusers.”
Commenting on the study, Jeffrey Cohen, MD, president of ACTRIMS, said that the findings are consistent with his observations that “in the general population, opioids often are used to treat chronic pain in people with MS.”
But they’re not getting the drugs from his clinic. “We do not prescribe opioids in our clinic, referring such patients to a chronic pain program,” Dr. Cohen said. “However, there clearly is need for better treatment options.”
A previous study on opioid use by people with MS, published in 2015, found even higher rates – 42% reported having ever used opioids, and 38% reported currently using opioids.
Although reports of opioid use by patients with MS have been lacking, more has been published on the emerging use of cannabis-related products. One recent study showed that nearly half of people with MS reported using a cannabis-based therapy for nerve-based pain and sleep disturbances.
Although cannabis is considered safer than opioids, the authors noted that it has its own significant drawback – a “paucity of provider guidance.”
“The range of perceived benefits and potential differential effects of THC and cannabinoid highlight the need for personalized, evidence-based guidelines regarding cannabinoid use,” they wrote.
Stretching program for spasticity shows benefits
With spasticity representing a key contributor to MS pain and affecting more than 80% of people with MS, Ms. Hugos and colleagues are developing an alternative to medication – a nonpharmacologic stretching regimen called Spasticity: Take Control” (STC).
Based on evidence-based strategies for the treatment of spasticity in MS, the program involves exercises with daily routines of 15-20 minutes over 6 months.
In a pilot study of 66 patients, also presented at the ACTRIMS meeting, the investigators reported that the program showed significant reductions in pain severity and interference, measured with the Brief Pain Inventory–Short Form, compared with a control consisting of range of motion instruction over 6 months.
The study also offered insights on the specific areas of pain. Among those who reported chronic pain (42% in the STC group and 63.3% in the range-of-motion group), the pain was most frequently reported in the lower back (74.3%), legs (68.6%), or lower back and legs (88.6%).
Ms. Hugos noted that the findings suggest a potentially important nonpharmacologic alternative to spasticity-related pain in MS.
“Stretching is the cornerstone treatment for spasticity from all causes, but there is very little information on stretching exercises in MS or any other conditions,” Ms. Hugos said. “[Our] pilot study is the first and only study using a standardized, daily stretching exercise program to treat MS spasticity,” she said.
“A fully powered study is needed to better understand the impact of different types of exercise on pain severity and interference in multiple sclerosis,” she noted.
Ms. Hugos has received consulting fees from Greenwich Biosciences, Evidera, and Techspert.io. Dr. Cohen has received personal compensation for consulting for Adamas, Atara, Bristol-Myers Squibb, Convelo, MedDay, and Mylan.
A version of this article first appeared on Medscape.com.
FROM ACTRIMS FORUM 2021
Neurologic disorders ubiquitous and rising in the U.S.
, according to new findings derived from the 2017 Global Burden of Disease study.
The authors of the analysis, led by Valery Feigin, MD, PhD, of New Zealand’s National Institute for Stroke and Applied Neurosciences, and published in the February 2021 issue of JAMA Neurology, looked at prevalence, incidence, mortality, and disability-adjusted life years for 14 neurological disorders across 50 states between 1990 and 2017. The diseases included in the analysis were stroke, Alzheimer’s disease and other dementias, Parkinson’s disease, epilepsy, multiple sclerosis, motor neuron disease, headaches, traumatic brain injury, spinal cord injuries, brain and other nervous system cancers, meningitis, encephalitis, and tetanus.
Tracking the burden of neurologic diseases
Dr. Feigin and colleagues estimated that a full 60% of the U.S. population lives with one or more of these disorders, a figure much greater than previous estimates for neurological disease burden nationwide. Tension-type headache and migraine were the most prevalent in the analysis by Dr. Feigin and colleagues. During the study period, they found, prevalence, incidence, and disability burden of nearly all the included disorders increased, with the exception of brain and spinal cord injuries, meningitis, and encephalitis.
The researchers attributed most of the rise in noncommunicable neurological diseases to population aging. An age-standardized analysis found trends for stroke and Alzheimer’s disease and other dementias to be declining or flat. Age-standardized stroke incidence dropped by 16% from 1990 to 2017, while stroke mortality declined by nearly a third, and stroke disability by a quarter. Age-standardized incidence of Alzheimer’s disease and other dementias dropped by 12%, and their prevalence by 13%, during the study period, though dementia mortality and disability were seen increasing.
The authors surmised that the age-standardized declines in stroke and dementias could reflect that “primary prevention of these disorders are beginning to show an influence.” With dementia, which is linked to cognitive reserve and education, “improving educational levels of cohort reaching the age groups at greatest risk of disease may also be contributing to a modest decline over time,” Dr. Feigin and his colleagues wrote.
Parkinson’s disease and multiple sclerosis, meanwhile, were both seen rising in incidence, prevalence, and disability adjusted life years (DALYs) even with age-standardized figures. The United States saw comparatively more disability in 2017 from dementias, Parkinson’s disease, epilepsy, multiple sclerosis, motor neuron disease, and headache disorders, which together comprised 6.7% of DALYs, compared with 4.4% globally; these also accounted for a higher share of mortality in the U.S. than worldwide. The authors attributed at least some of the difference to better case ascertainment in the U.S.
Regional variations
The researchers also reported variations in disease burden by state and region. While previous studies have identified a “stroke belt” concentrated in North Carolina, South Carolina, and Georgia, the new findings point to stroke disability highest in Alabama, Arkansas, and Mississippi, and mortality highest in Alabama, Mississippi, and South Carolina. The researchers noted increases in dementia mortality in these states, “likely attributable to the reciprocal association between stroke and dementia.”
Northern states saw higher burdens of multiple sclerosis compared with the rest of the country, while eastern states had higher rates of Parkinson’s disease.
Such regional and state-by state variations, Dr. Feigin and colleagues wrote in their analysis, “may be associated with differences in the case ascertainment, as well as access to health care; racial/ethnic, genetic, and socioeconomic diversity; quality and comprehensiveness of preventive strategies; and risk factor distribution.”
The researchers noted as a limitation of their study that the 14 diseases captured were not an exhaustive list of neurological conditions; chronic lower back pain, a condition included in a previous major study of the burden of neurological disease in the United States, was omitted, as were restless legs syndrome and peripheral neuropathy. The researchers cited changes to coding practice in the U.S. and accuracy of medical claims data as potential limitations of their analysis. The Global Burden of Disease study is funded by the Bill and Melinda Gates Foundation, and several of Dr. Feigin’s coauthors reported financial relationships with industry.
Time to adjust the stroke belt?
Amelia Boehme, PhD, a stroke epidemiologist at Columbia University Mailman School of Public Health in New York, said in an interview that the current study added to recent findings showing surprising local variability in stroke prevalence, incidence, and mortality. “What we had always conceptually thought of as the ‘stroke belt’ isn’t necessarily the case,” Dr. Boehme said, but is rather subject to local, county-by-county variations. “Looking at the data here in conjunction with what previous authors have found, it raises some questions as to whether or not state-level data is giving a completely accurate picture, and whether we need to start looking at the county level and adjust for populations and age.” Importantly, Dr. Boehme said, data collected in the Global Burden of Disease study tends to be exceptionally rigorous and systematic, adding weight to Dr. Feigin and colleagues’ suggestions that prevention efforts may be making a dent in stroke and dementia.
“More data is always needed before we start to say we’re seeing things change,” Dr. Boehme noted. “But any glimmer of optimism is welcome, especially with regard to interventions that have been put in place, to allow us to build on those interventions.”
Dr. Boehme disclosed no financial conflicts of interest.
, according to new findings derived from the 2017 Global Burden of Disease study.
The authors of the analysis, led by Valery Feigin, MD, PhD, of New Zealand’s National Institute for Stroke and Applied Neurosciences, and published in the February 2021 issue of JAMA Neurology, looked at prevalence, incidence, mortality, and disability-adjusted life years for 14 neurological disorders across 50 states between 1990 and 2017. The diseases included in the analysis were stroke, Alzheimer’s disease and other dementias, Parkinson’s disease, epilepsy, multiple sclerosis, motor neuron disease, headaches, traumatic brain injury, spinal cord injuries, brain and other nervous system cancers, meningitis, encephalitis, and tetanus.
Tracking the burden of neurologic diseases
Dr. Feigin and colleagues estimated that a full 60% of the U.S. population lives with one or more of these disorders, a figure much greater than previous estimates for neurological disease burden nationwide. Tension-type headache and migraine were the most prevalent in the analysis by Dr. Feigin and colleagues. During the study period, they found, prevalence, incidence, and disability burden of nearly all the included disorders increased, with the exception of brain and spinal cord injuries, meningitis, and encephalitis.
The researchers attributed most of the rise in noncommunicable neurological diseases to population aging. An age-standardized analysis found trends for stroke and Alzheimer’s disease and other dementias to be declining or flat. Age-standardized stroke incidence dropped by 16% from 1990 to 2017, while stroke mortality declined by nearly a third, and stroke disability by a quarter. Age-standardized incidence of Alzheimer’s disease and other dementias dropped by 12%, and their prevalence by 13%, during the study period, though dementia mortality and disability were seen increasing.
The authors surmised that the age-standardized declines in stroke and dementias could reflect that “primary prevention of these disorders are beginning to show an influence.” With dementia, which is linked to cognitive reserve and education, “improving educational levels of cohort reaching the age groups at greatest risk of disease may also be contributing to a modest decline over time,” Dr. Feigin and his colleagues wrote.
Parkinson’s disease and multiple sclerosis, meanwhile, were both seen rising in incidence, prevalence, and disability adjusted life years (DALYs) even with age-standardized figures. The United States saw comparatively more disability in 2017 from dementias, Parkinson’s disease, epilepsy, multiple sclerosis, motor neuron disease, and headache disorders, which together comprised 6.7% of DALYs, compared with 4.4% globally; these also accounted for a higher share of mortality in the U.S. than worldwide. The authors attributed at least some of the difference to better case ascertainment in the U.S.
Regional variations
The researchers also reported variations in disease burden by state and region. While previous studies have identified a “stroke belt” concentrated in North Carolina, South Carolina, and Georgia, the new findings point to stroke disability highest in Alabama, Arkansas, and Mississippi, and mortality highest in Alabama, Mississippi, and South Carolina. The researchers noted increases in dementia mortality in these states, “likely attributable to the reciprocal association between stroke and dementia.”
Northern states saw higher burdens of multiple sclerosis compared with the rest of the country, while eastern states had higher rates of Parkinson’s disease.
Such regional and state-by state variations, Dr. Feigin and colleagues wrote in their analysis, “may be associated with differences in the case ascertainment, as well as access to health care; racial/ethnic, genetic, and socioeconomic diversity; quality and comprehensiveness of preventive strategies; and risk factor distribution.”
The researchers noted as a limitation of their study that the 14 diseases captured were not an exhaustive list of neurological conditions; chronic lower back pain, a condition included in a previous major study of the burden of neurological disease in the United States, was omitted, as were restless legs syndrome and peripheral neuropathy. The researchers cited changes to coding practice in the U.S. and accuracy of medical claims data as potential limitations of their analysis. The Global Burden of Disease study is funded by the Bill and Melinda Gates Foundation, and several of Dr. Feigin’s coauthors reported financial relationships with industry.
Time to adjust the stroke belt?
Amelia Boehme, PhD, a stroke epidemiologist at Columbia University Mailman School of Public Health in New York, said in an interview that the current study added to recent findings showing surprising local variability in stroke prevalence, incidence, and mortality. “What we had always conceptually thought of as the ‘stroke belt’ isn’t necessarily the case,” Dr. Boehme said, but is rather subject to local, county-by-county variations. “Looking at the data here in conjunction with what previous authors have found, it raises some questions as to whether or not state-level data is giving a completely accurate picture, and whether we need to start looking at the county level and adjust for populations and age.” Importantly, Dr. Boehme said, data collected in the Global Burden of Disease study tends to be exceptionally rigorous and systematic, adding weight to Dr. Feigin and colleagues’ suggestions that prevention efforts may be making a dent in stroke and dementia.
“More data is always needed before we start to say we’re seeing things change,” Dr. Boehme noted. “But any glimmer of optimism is welcome, especially with regard to interventions that have been put in place, to allow us to build on those interventions.”
Dr. Boehme disclosed no financial conflicts of interest.
, according to new findings derived from the 2017 Global Burden of Disease study.
The authors of the analysis, led by Valery Feigin, MD, PhD, of New Zealand’s National Institute for Stroke and Applied Neurosciences, and published in the February 2021 issue of JAMA Neurology, looked at prevalence, incidence, mortality, and disability-adjusted life years for 14 neurological disorders across 50 states between 1990 and 2017. The diseases included in the analysis were stroke, Alzheimer’s disease and other dementias, Parkinson’s disease, epilepsy, multiple sclerosis, motor neuron disease, headaches, traumatic brain injury, spinal cord injuries, brain and other nervous system cancers, meningitis, encephalitis, and tetanus.
Tracking the burden of neurologic diseases
Dr. Feigin and colleagues estimated that a full 60% of the U.S. population lives with one or more of these disorders, a figure much greater than previous estimates for neurological disease burden nationwide. Tension-type headache and migraine were the most prevalent in the analysis by Dr. Feigin and colleagues. During the study period, they found, prevalence, incidence, and disability burden of nearly all the included disorders increased, with the exception of brain and spinal cord injuries, meningitis, and encephalitis.
The researchers attributed most of the rise in noncommunicable neurological diseases to population aging. An age-standardized analysis found trends for stroke and Alzheimer’s disease and other dementias to be declining or flat. Age-standardized stroke incidence dropped by 16% from 1990 to 2017, while stroke mortality declined by nearly a third, and stroke disability by a quarter. Age-standardized incidence of Alzheimer’s disease and other dementias dropped by 12%, and their prevalence by 13%, during the study period, though dementia mortality and disability were seen increasing.
The authors surmised that the age-standardized declines in stroke and dementias could reflect that “primary prevention of these disorders are beginning to show an influence.” With dementia, which is linked to cognitive reserve and education, “improving educational levels of cohort reaching the age groups at greatest risk of disease may also be contributing to a modest decline over time,” Dr. Feigin and his colleagues wrote.
Parkinson’s disease and multiple sclerosis, meanwhile, were both seen rising in incidence, prevalence, and disability adjusted life years (DALYs) even with age-standardized figures. The United States saw comparatively more disability in 2017 from dementias, Parkinson’s disease, epilepsy, multiple sclerosis, motor neuron disease, and headache disorders, which together comprised 6.7% of DALYs, compared with 4.4% globally; these also accounted for a higher share of mortality in the U.S. than worldwide. The authors attributed at least some of the difference to better case ascertainment in the U.S.
Regional variations
The researchers also reported variations in disease burden by state and region. While previous studies have identified a “stroke belt” concentrated in North Carolina, South Carolina, and Georgia, the new findings point to stroke disability highest in Alabama, Arkansas, and Mississippi, and mortality highest in Alabama, Mississippi, and South Carolina. The researchers noted increases in dementia mortality in these states, “likely attributable to the reciprocal association between stroke and dementia.”
Northern states saw higher burdens of multiple sclerosis compared with the rest of the country, while eastern states had higher rates of Parkinson’s disease.
Such regional and state-by state variations, Dr. Feigin and colleagues wrote in their analysis, “may be associated with differences in the case ascertainment, as well as access to health care; racial/ethnic, genetic, and socioeconomic diversity; quality and comprehensiveness of preventive strategies; and risk factor distribution.”
The researchers noted as a limitation of their study that the 14 diseases captured were not an exhaustive list of neurological conditions; chronic lower back pain, a condition included in a previous major study of the burden of neurological disease in the United States, was omitted, as were restless legs syndrome and peripheral neuropathy. The researchers cited changes to coding practice in the U.S. and accuracy of medical claims data as potential limitations of their analysis. The Global Burden of Disease study is funded by the Bill and Melinda Gates Foundation, and several of Dr. Feigin’s coauthors reported financial relationships with industry.
Time to adjust the stroke belt?
Amelia Boehme, PhD, a stroke epidemiologist at Columbia University Mailman School of Public Health in New York, said in an interview that the current study added to recent findings showing surprising local variability in stroke prevalence, incidence, and mortality. “What we had always conceptually thought of as the ‘stroke belt’ isn’t necessarily the case,” Dr. Boehme said, but is rather subject to local, county-by-county variations. “Looking at the data here in conjunction with what previous authors have found, it raises some questions as to whether or not state-level data is giving a completely accurate picture, and whether we need to start looking at the county level and adjust for populations and age.” Importantly, Dr. Boehme said, data collected in the Global Burden of Disease study tends to be exceptionally rigorous and systematic, adding weight to Dr. Feigin and colleagues’ suggestions that prevention efforts may be making a dent in stroke and dementia.
“More data is always needed before we start to say we’re seeing things change,” Dr. Boehme noted. “But any glimmer of optimism is welcome, especially with regard to interventions that have been put in place, to allow us to build on those interventions.”
Dr. Boehme disclosed no financial conflicts of interest.
FROM JAMA NEUROLOGY
'Living brain implants' may restore stroke mobility
Researchers behind the ongoing Cortimo trial successfully performed a procedure on a patient 2 years removed from a stroke, in which microelectrode arrays were implanted into his brain to decode signals driving motor function. These signals then allowed him to operate a powered brace worn on his paralyzed arm.
This news organization spoke with the trial’s principal investigator, Mijail D. Serruya, MD, PhD, an assistant professor of neurology at Thomas Jefferson University Hospital, Philadelphia, about the trial’s initial findings, what this technology may ultimately look like, and the implications for stroke patients in knowing that restorative interventions may be on the horizon.
How did you first get involved with implanting electrodes to help stroke patients with recovery?
I was involved in the first human application of a microelectrode array in a young man who had quadriplegia because of a spinal cord injury. We showed that we could record signal directly from his motor cortex and use it to move a cursor on the screen, and open and close a prosthetic hand and arm.
I was naive and thought that this would soon be a widely available clinical medical device. Now it’s nearly 15 years later, and while it certainly has been safely used in multiple labs to record signals from people with spinal cord injury, amyotrophic lateral sclerosis (ALS), or locked-in syndrome from a brain stem stroke, it still requires a team of technicians and a percutaneous connector. It really has not gotten out of the university.
A few years ago I spoke with Robert Rosenwasser, MD, chairman of the department of neurosurgery at Thomas Jefferson, who runs a very busy stroke center and performed the surgery in this trial. We put our heads together and said: “Maybe the time is now to see whether we can move this technology to this much more prevalent condition of a hemispheric stroke.” And that’s what we did.
How did the idea of using computer brain electrode interfaces begin?
Around 20 years ago, if you had someone who had severe paralysis and you wanted to restore movement, the question was, where can you get a good control signal from? Obviously, if someone can talk, they can use a voice-actuated system with speech recognition and maybe you can track their eye gaze. But if they’re trying to move their limbs, you want a motor control signal.
In someone who has end-stage ALS or a brain stem stroke, you can’t even record residual muscle activity; you have almost nothing to work with. The only thing left is to try to record directly from the brain itself.
It’s important to clarify that brain-computer interfaces are not necessarily stimulating the brain to inject the signal. They’re just recording the endogenous activity that the brain makes. In comparison, a deep brain stimulator is usually not recording anything; it’s just delivering energy to the brain and hoping for the best.
But what we’re doing is asking, if the person is trying to move the paralyzed limb but can’t, can we get to the source of the signal and then do something with it?
What’s the process for measuring that in, for example, someone who has a localized lesion in the motor cortex?
The first step is a scan. People have been doing functional MRI on patients who have had a stroke as long as we’ve had fMRI. We know that people can actually activate on MRI areas of their brain around the stroke, but obviously not in the stroke because it’s been lesioned. However, we do know that the circuit adjacent to it and other regions do appear able to be modulated.
So by having a person either imagine trying to do what they want to do or doing what they can do, if they have some tiny residual movement, you can then identify a kind of hot spot on the fMRI where the brain gobbles up all the oxygen because it’s so active. Then that gives you an anatomical target for the surgeon to place the electrode arrays.
The Cortimo trial’s enticing findings
What are the most striking results that you’ve seen so far with the device?
The first thing is that we were able to get such recordings at all. We knew from fMRIs that there were fluctuations in oxygen changing when the person was trying to do something they couldn’t do. But nobody knew that you would see this whole population of individual neurons chattering away when you place these electrode arrays in the motor cortex right next to the stroke, and make sense of what we’re recording.
Obviously, that’s very encouraging and gives us hope that many months or years after a stroke, people’s brains are able to maintain this representation of all these different movements and plans. It’s almost like it’s trapped on the other side of the stroke and some of the signals can’t get out.
The other discovery we’re pleased with is that we can actually decode signals in real time and the person can use it to do something, such as trigger the brain to open and close the hand. That’s very different from all the prior research with brain array interfaces.
Furthermore, the gentleman who participated actually had strokes in other parts of his brain affecting his vision; he had homonymous hemianopia. That raised the question of what happens if you affect parts of the brain that have to do with attention and visual processing. Could a system like this work? And again, the answer appears to be yes.
What are the next steps for this technology before it can potentially become available in the clinic?
For this to work, the system clearly has to be fully implantable. What we used was percutaneous. The risk-benefit may be acceptable for someone who has quadriplegia because of, for example, spinal cord injury or end-stage ALS who may already have a tracheostomy and a percutaneous endoscopic gastrostomy. But for someone who is hemiparetic and ambulatory, that may not be acceptable. And a fully implantable system would also have much better patient compliance.
Also, when you’re recording from lots and lots of individual brain cells at many, many samples a second on many, many channels, it’s certainly an engineering challenge. It’s not just a single channel that you occasionally query; it’s hundreds of thousands of channels of this complicated data stream.
But these are solvable challenges. People have been making a lot of progress. It’s really a matter of funding and the engineering expertise, rather than some sort of fundamental scientific breakthrough.
With that said, I think it could be within the next 5-10 years that we could actually have a product that expands the toolbox of what can be done for patients who’ve had a stroke, if they’re motivated and there’s no real contraindication.
Creating a novel device
On that point, are you partnering with engineering and technology companies?
The hope is that we and other groups working on this can do for the interface sort of what Celera Genomics did for the Human Genome Project. By having enough interest and investment, you may be able to propel the field forward to widespread use rather than just a purely academic, lab-science type of project.
We are in discussion with different companies to see how we can move ahead with this, and we would be pleased to work with whomever is interested. It may be that different companies have different pieces of the puzzle – a better sensor or a better wireless transmitter.
The plan is to move as quickly as we can to a fully implantable system. And then the benchmark for any kind of clinical advancement is to do a prospective trial. With devices, if you can get a big enough effect size, then you sometimes don’t need quite as many patients to prove it. If paralysis is striking enough and you can reverse that, then you can convince the Food and Drug Administration of its safety and efficacy, and the various insurance companies, that it’s actually reasonable and necessary.
How long will an implantable device last?
That’s a key question and concern. If you have someone like our participant, who’s in his early 40s, will it keep working 10, 20, 30, 40 years? For the rest of his life? Deep brain stimulators and cochlear implants do function for those long durations, but their designs are quite different. There’s a macroelectrode that’s just delivering current, which is very different from listening in on this microscopic scale. There are different technical considerations.
One possible solution is to make the device out of living tissue, which is something I just wrote about with my colleague D. Kacy Cullen. Living electrodes and amplifiers may seem a bit like science fiction, but on the other hand, we have over a century of plastic surgeons, neurosurgeons, and orthopedic surgeons doing all kinds of complicated modifications of the body, moving nerves and vessels around. It makes you realize that, in a sense, they’ve already done living electrodes by doing a nerve transfer. So the question becomes whether we can refine that living electrode technology, which could then open up more possibilities.
Are there any final messages you’d like to share with clinician audience of this news organization?
Regardless of our specialty, we’re always telling our patients about the benefits of things like eating healthy, exercise, and sleep. Now we can point to the fact that, 2 years after stroke, all of these brain areas are still active, and devices that can potentially reverse and unparalyze your limbs may be available in the coming 5- or 10-plus years. That gives clinicians more justification to tell their patients to really stay on top of those things so that they can be in as optimal brain-mind health as possible to someday benefit from them.
Patients and their families need to be part of the conversation of where this is all going. That’s one thing that’s totally different for brain devices versus other devices, where a person’s psychological state doesn’t necessarily matter. But with a brain device, your mental state, psychosocial situation, exercise, sleep – the way you think about and approach it – actually changes to the structure of the brain pretty dramatically.
I don’t want to cause unreasonable hope that we’re going to snap our fingers and it’s going to be cured. But I do think it’s fair to raise a possibility as a way to say that keeping oneself really healthy is justified.
A version of this article first appeared on Medscape.com.
Researchers behind the ongoing Cortimo trial successfully performed a procedure on a patient 2 years removed from a stroke, in which microelectrode arrays were implanted into his brain to decode signals driving motor function. These signals then allowed him to operate a powered brace worn on his paralyzed arm.
This news organization spoke with the trial’s principal investigator, Mijail D. Serruya, MD, PhD, an assistant professor of neurology at Thomas Jefferson University Hospital, Philadelphia, about the trial’s initial findings, what this technology may ultimately look like, and the implications for stroke patients in knowing that restorative interventions may be on the horizon.
How did you first get involved with implanting electrodes to help stroke patients with recovery?
I was involved in the first human application of a microelectrode array in a young man who had quadriplegia because of a spinal cord injury. We showed that we could record signal directly from his motor cortex and use it to move a cursor on the screen, and open and close a prosthetic hand and arm.
I was naive and thought that this would soon be a widely available clinical medical device. Now it’s nearly 15 years later, and while it certainly has been safely used in multiple labs to record signals from people with spinal cord injury, amyotrophic lateral sclerosis (ALS), or locked-in syndrome from a brain stem stroke, it still requires a team of technicians and a percutaneous connector. It really has not gotten out of the university.
A few years ago I spoke with Robert Rosenwasser, MD, chairman of the department of neurosurgery at Thomas Jefferson, who runs a very busy stroke center and performed the surgery in this trial. We put our heads together and said: “Maybe the time is now to see whether we can move this technology to this much more prevalent condition of a hemispheric stroke.” And that’s what we did.
How did the idea of using computer brain electrode interfaces begin?
Around 20 years ago, if you had someone who had severe paralysis and you wanted to restore movement, the question was, where can you get a good control signal from? Obviously, if someone can talk, they can use a voice-actuated system with speech recognition and maybe you can track their eye gaze. But if they’re trying to move their limbs, you want a motor control signal.
In someone who has end-stage ALS or a brain stem stroke, you can’t even record residual muscle activity; you have almost nothing to work with. The only thing left is to try to record directly from the brain itself.
It’s important to clarify that brain-computer interfaces are not necessarily stimulating the brain to inject the signal. They’re just recording the endogenous activity that the brain makes. In comparison, a deep brain stimulator is usually not recording anything; it’s just delivering energy to the brain and hoping for the best.
But what we’re doing is asking, if the person is trying to move the paralyzed limb but can’t, can we get to the source of the signal and then do something with it?
What’s the process for measuring that in, for example, someone who has a localized lesion in the motor cortex?
The first step is a scan. People have been doing functional MRI on patients who have had a stroke as long as we’ve had fMRI. We know that people can actually activate on MRI areas of their brain around the stroke, but obviously not in the stroke because it’s been lesioned. However, we do know that the circuit adjacent to it and other regions do appear able to be modulated.
So by having a person either imagine trying to do what they want to do or doing what they can do, if they have some tiny residual movement, you can then identify a kind of hot spot on the fMRI where the brain gobbles up all the oxygen because it’s so active. Then that gives you an anatomical target for the surgeon to place the electrode arrays.
The Cortimo trial’s enticing findings
What are the most striking results that you’ve seen so far with the device?
The first thing is that we were able to get such recordings at all. We knew from fMRIs that there were fluctuations in oxygen changing when the person was trying to do something they couldn’t do. But nobody knew that you would see this whole population of individual neurons chattering away when you place these electrode arrays in the motor cortex right next to the stroke, and make sense of what we’re recording.
Obviously, that’s very encouraging and gives us hope that many months or years after a stroke, people’s brains are able to maintain this representation of all these different movements and plans. It’s almost like it’s trapped on the other side of the stroke and some of the signals can’t get out.
The other discovery we’re pleased with is that we can actually decode signals in real time and the person can use it to do something, such as trigger the brain to open and close the hand. That’s very different from all the prior research with brain array interfaces.
Furthermore, the gentleman who participated actually had strokes in other parts of his brain affecting his vision; he had homonymous hemianopia. That raised the question of what happens if you affect parts of the brain that have to do with attention and visual processing. Could a system like this work? And again, the answer appears to be yes.
What are the next steps for this technology before it can potentially become available in the clinic?
For this to work, the system clearly has to be fully implantable. What we used was percutaneous. The risk-benefit may be acceptable for someone who has quadriplegia because of, for example, spinal cord injury or end-stage ALS who may already have a tracheostomy and a percutaneous endoscopic gastrostomy. But for someone who is hemiparetic and ambulatory, that may not be acceptable. And a fully implantable system would also have much better patient compliance.
Also, when you’re recording from lots and lots of individual brain cells at many, many samples a second on many, many channels, it’s certainly an engineering challenge. It’s not just a single channel that you occasionally query; it’s hundreds of thousands of channels of this complicated data stream.
But these are solvable challenges. People have been making a lot of progress. It’s really a matter of funding and the engineering expertise, rather than some sort of fundamental scientific breakthrough.
With that said, I think it could be within the next 5-10 years that we could actually have a product that expands the toolbox of what can be done for patients who’ve had a stroke, if they’re motivated and there’s no real contraindication.
Creating a novel device
On that point, are you partnering with engineering and technology companies?
The hope is that we and other groups working on this can do for the interface sort of what Celera Genomics did for the Human Genome Project. By having enough interest and investment, you may be able to propel the field forward to widespread use rather than just a purely academic, lab-science type of project.
We are in discussion with different companies to see how we can move ahead with this, and we would be pleased to work with whomever is interested. It may be that different companies have different pieces of the puzzle – a better sensor or a better wireless transmitter.
The plan is to move as quickly as we can to a fully implantable system. And then the benchmark for any kind of clinical advancement is to do a prospective trial. With devices, if you can get a big enough effect size, then you sometimes don’t need quite as many patients to prove it. If paralysis is striking enough and you can reverse that, then you can convince the Food and Drug Administration of its safety and efficacy, and the various insurance companies, that it’s actually reasonable and necessary.
How long will an implantable device last?
That’s a key question and concern. If you have someone like our participant, who’s in his early 40s, will it keep working 10, 20, 30, 40 years? For the rest of his life? Deep brain stimulators and cochlear implants do function for those long durations, but their designs are quite different. There’s a macroelectrode that’s just delivering current, which is very different from listening in on this microscopic scale. There are different technical considerations.
One possible solution is to make the device out of living tissue, which is something I just wrote about with my colleague D. Kacy Cullen. Living electrodes and amplifiers may seem a bit like science fiction, but on the other hand, we have over a century of plastic surgeons, neurosurgeons, and orthopedic surgeons doing all kinds of complicated modifications of the body, moving nerves and vessels around. It makes you realize that, in a sense, they’ve already done living electrodes by doing a nerve transfer. So the question becomes whether we can refine that living electrode technology, which could then open up more possibilities.
Are there any final messages you’d like to share with clinician audience of this news organization?
Regardless of our specialty, we’re always telling our patients about the benefits of things like eating healthy, exercise, and sleep. Now we can point to the fact that, 2 years after stroke, all of these brain areas are still active, and devices that can potentially reverse and unparalyze your limbs may be available in the coming 5- or 10-plus years. That gives clinicians more justification to tell their patients to really stay on top of those things so that they can be in as optimal brain-mind health as possible to someday benefit from them.
Patients and their families need to be part of the conversation of where this is all going. That’s one thing that’s totally different for brain devices versus other devices, where a person’s psychological state doesn’t necessarily matter. But with a brain device, your mental state, psychosocial situation, exercise, sleep – the way you think about and approach it – actually changes to the structure of the brain pretty dramatically.
I don’t want to cause unreasonable hope that we’re going to snap our fingers and it’s going to be cured. But I do think it’s fair to raise a possibility as a way to say that keeping oneself really healthy is justified.
A version of this article first appeared on Medscape.com.
Researchers behind the ongoing Cortimo trial successfully performed a procedure on a patient 2 years removed from a stroke, in which microelectrode arrays were implanted into his brain to decode signals driving motor function. These signals then allowed him to operate a powered brace worn on his paralyzed arm.
This news organization spoke with the trial’s principal investigator, Mijail D. Serruya, MD, PhD, an assistant professor of neurology at Thomas Jefferson University Hospital, Philadelphia, about the trial’s initial findings, what this technology may ultimately look like, and the implications for stroke patients in knowing that restorative interventions may be on the horizon.
How did you first get involved with implanting electrodes to help stroke patients with recovery?
I was involved in the first human application of a microelectrode array in a young man who had quadriplegia because of a spinal cord injury. We showed that we could record signal directly from his motor cortex and use it to move a cursor on the screen, and open and close a prosthetic hand and arm.
I was naive and thought that this would soon be a widely available clinical medical device. Now it’s nearly 15 years later, and while it certainly has been safely used in multiple labs to record signals from people with spinal cord injury, amyotrophic lateral sclerosis (ALS), or locked-in syndrome from a brain stem stroke, it still requires a team of technicians and a percutaneous connector. It really has not gotten out of the university.
A few years ago I spoke with Robert Rosenwasser, MD, chairman of the department of neurosurgery at Thomas Jefferson, who runs a very busy stroke center and performed the surgery in this trial. We put our heads together and said: “Maybe the time is now to see whether we can move this technology to this much more prevalent condition of a hemispheric stroke.” And that’s what we did.
How did the idea of using computer brain electrode interfaces begin?
Around 20 years ago, if you had someone who had severe paralysis and you wanted to restore movement, the question was, where can you get a good control signal from? Obviously, if someone can talk, they can use a voice-actuated system with speech recognition and maybe you can track their eye gaze. But if they’re trying to move their limbs, you want a motor control signal.
In someone who has end-stage ALS or a brain stem stroke, you can’t even record residual muscle activity; you have almost nothing to work with. The only thing left is to try to record directly from the brain itself.
It’s important to clarify that brain-computer interfaces are not necessarily stimulating the brain to inject the signal. They’re just recording the endogenous activity that the brain makes. In comparison, a deep brain stimulator is usually not recording anything; it’s just delivering energy to the brain and hoping for the best.
But what we’re doing is asking, if the person is trying to move the paralyzed limb but can’t, can we get to the source of the signal and then do something with it?
What’s the process for measuring that in, for example, someone who has a localized lesion in the motor cortex?
The first step is a scan. People have been doing functional MRI on patients who have had a stroke as long as we’ve had fMRI. We know that people can actually activate on MRI areas of their brain around the stroke, but obviously not in the stroke because it’s been lesioned. However, we do know that the circuit adjacent to it and other regions do appear able to be modulated.
So by having a person either imagine trying to do what they want to do or doing what they can do, if they have some tiny residual movement, you can then identify a kind of hot spot on the fMRI where the brain gobbles up all the oxygen because it’s so active. Then that gives you an anatomical target for the surgeon to place the electrode arrays.
The Cortimo trial’s enticing findings
What are the most striking results that you’ve seen so far with the device?
The first thing is that we were able to get such recordings at all. We knew from fMRIs that there were fluctuations in oxygen changing when the person was trying to do something they couldn’t do. But nobody knew that you would see this whole population of individual neurons chattering away when you place these electrode arrays in the motor cortex right next to the stroke, and make sense of what we’re recording.
Obviously, that’s very encouraging and gives us hope that many months or years after a stroke, people’s brains are able to maintain this representation of all these different movements and plans. It’s almost like it’s trapped on the other side of the stroke and some of the signals can’t get out.
The other discovery we’re pleased with is that we can actually decode signals in real time and the person can use it to do something, such as trigger the brain to open and close the hand. That’s very different from all the prior research with brain array interfaces.
Furthermore, the gentleman who participated actually had strokes in other parts of his brain affecting his vision; he had homonymous hemianopia. That raised the question of what happens if you affect parts of the brain that have to do with attention and visual processing. Could a system like this work? And again, the answer appears to be yes.
What are the next steps for this technology before it can potentially become available in the clinic?
For this to work, the system clearly has to be fully implantable. What we used was percutaneous. The risk-benefit may be acceptable for someone who has quadriplegia because of, for example, spinal cord injury or end-stage ALS who may already have a tracheostomy and a percutaneous endoscopic gastrostomy. But for someone who is hemiparetic and ambulatory, that may not be acceptable. And a fully implantable system would also have much better patient compliance.
Also, when you’re recording from lots and lots of individual brain cells at many, many samples a second on many, many channels, it’s certainly an engineering challenge. It’s not just a single channel that you occasionally query; it’s hundreds of thousands of channels of this complicated data stream.
But these are solvable challenges. People have been making a lot of progress. It’s really a matter of funding and the engineering expertise, rather than some sort of fundamental scientific breakthrough.
With that said, I think it could be within the next 5-10 years that we could actually have a product that expands the toolbox of what can be done for patients who’ve had a stroke, if they’re motivated and there’s no real contraindication.
Creating a novel device
On that point, are you partnering with engineering and technology companies?
The hope is that we and other groups working on this can do for the interface sort of what Celera Genomics did for the Human Genome Project. By having enough interest and investment, you may be able to propel the field forward to widespread use rather than just a purely academic, lab-science type of project.
We are in discussion with different companies to see how we can move ahead with this, and we would be pleased to work with whomever is interested. It may be that different companies have different pieces of the puzzle – a better sensor or a better wireless transmitter.
The plan is to move as quickly as we can to a fully implantable system. And then the benchmark for any kind of clinical advancement is to do a prospective trial. With devices, if you can get a big enough effect size, then you sometimes don’t need quite as many patients to prove it. If paralysis is striking enough and you can reverse that, then you can convince the Food and Drug Administration of its safety and efficacy, and the various insurance companies, that it’s actually reasonable and necessary.
How long will an implantable device last?
That’s a key question and concern. If you have someone like our participant, who’s in his early 40s, will it keep working 10, 20, 30, 40 years? For the rest of his life? Deep brain stimulators and cochlear implants do function for those long durations, but their designs are quite different. There’s a macroelectrode that’s just delivering current, which is very different from listening in on this microscopic scale. There are different technical considerations.
One possible solution is to make the device out of living tissue, which is something I just wrote about with my colleague D. Kacy Cullen. Living electrodes and amplifiers may seem a bit like science fiction, but on the other hand, we have over a century of plastic surgeons, neurosurgeons, and orthopedic surgeons doing all kinds of complicated modifications of the body, moving nerves and vessels around. It makes you realize that, in a sense, they’ve already done living electrodes by doing a nerve transfer. So the question becomes whether we can refine that living electrode technology, which could then open up more possibilities.
Are there any final messages you’d like to share with clinician audience of this news organization?
Regardless of our specialty, we’re always telling our patients about the benefits of things like eating healthy, exercise, and sleep. Now we can point to the fact that, 2 years after stroke, all of these brain areas are still active, and devices that can potentially reverse and unparalyze your limbs may be available in the coming 5- or 10-plus years. That gives clinicians more justification to tell their patients to really stay on top of those things so that they can be in as optimal brain-mind health as possible to someday benefit from them.
Patients and their families need to be part of the conversation of where this is all going. That’s one thing that’s totally different for brain devices versus other devices, where a person’s psychological state doesn’t necessarily matter. But with a brain device, your mental state, psychosocial situation, exercise, sleep – the way you think about and approach it – actually changes to the structure of the brain pretty dramatically.
I don’t want to cause unreasonable hope that we’re going to snap our fingers and it’s going to be cured. But I do think it’s fair to raise a possibility as a way to say that keeping oneself really healthy is justified.
A version of this article first appeared on Medscape.com.
FDA approves first targeted treatment for rare DMD mutation
, the agency has announced.
This particular mutation of the DMD gene “is amenable to exon 45 skipping,” the FDA noted in a press release. The agency added that this is its first approval of a targeted treatment for patients with the mutation.
“Developing drugs designed for patients with specific mutations is a critical part of personalized medicine,” Eric Bastings, MD, deputy director of the Office of Neuroscience at the FDA’s Center for Drug Evaluation and Research, said in a statement.
The approval was based on results from a 43-person randomized controlled trial. Patients who received casimersen had a greater increase in production of the muscle-fiber protein dystrophin compared with their counterparts who received placebo.
Approved – with cautions
The FDA noted that DMD prevalence worldwide is about 1 in 3,600 boys – although it can also affect girls in rare cases. Symptoms of the disorder are commonly first observed around age 3 years but worsen steadily over time. DMD gene mutations lead to a decrease in dystrophin.
As reported by Medscape Medical News in August, the FDA approved viltolarsen (Viltepso, NS Pharma) for the treatment of DMD in patients with a confirmed mutation amenable to exon 53 skipping, following approval of golodirsen injection (Vyondys 53, Sarepta Therapeutics) for the same indication in December 2019.
The DMD gene mutation that is amenable to exon 45 skipping is present in about 8% of patients with DMD.
The trial that carried weight with the FDA included 43 male participants with DMD aged 7-20 years. All were confirmed to have the exon 45-skipping gene mutation and all were randomly assigned 2:1 to received IV casimersen 30 mg/kg or matching placebo.
Results showed that, between baseline and 48 weeks post treatment, the casimersen group showed a significantly higher increase in levels of dystrophin protein than in the placebo group.
Upper respiratory tract infections, fever, joint and throat pain, headache, and cough were the most common adverse events experienced by the active-treatment group.
Although the clinical studies assessing casimersen did not show any reports of kidney toxicity, the adverse event was observed in some nonclinical studies. Therefore, clinicians should monitor kidney function in any patient receiving this treatment, the FDA recommended.
Overall, “the FDA has concluded that the data submitted by the applicant demonstrated an increase in dystrophin production that is reasonably likely to predict clinical benefit” in this patient population, the agency said in its press release.
However, it noted that definitive clinical benefits such as improved motor function were not “established.”
“In making this decision, the FDA considered the potential risks associated with the drug, the life-threatening and debilitating nature of the disease, and the lack of [other] available therapy,” the agency said.
It added that the manufacturer is currently conducting a multicenter study focused on the safety and efficacy of the drug in ambulatory patients with DMD.
The FDA approved casimersen using its Accelerated Approval pathway, granted Fast Track and Priority Review designations to its applications, and gave the treatment Orphan Drug designation.
A version of this article first appeared on Medscape.com.
, the agency has announced.
This particular mutation of the DMD gene “is amenable to exon 45 skipping,” the FDA noted in a press release. The agency added that this is its first approval of a targeted treatment for patients with the mutation.
“Developing drugs designed for patients with specific mutations is a critical part of personalized medicine,” Eric Bastings, MD, deputy director of the Office of Neuroscience at the FDA’s Center for Drug Evaluation and Research, said in a statement.
The approval was based on results from a 43-person randomized controlled trial. Patients who received casimersen had a greater increase in production of the muscle-fiber protein dystrophin compared with their counterparts who received placebo.
Approved – with cautions
The FDA noted that DMD prevalence worldwide is about 1 in 3,600 boys – although it can also affect girls in rare cases. Symptoms of the disorder are commonly first observed around age 3 years but worsen steadily over time. DMD gene mutations lead to a decrease in dystrophin.
As reported by Medscape Medical News in August, the FDA approved viltolarsen (Viltepso, NS Pharma) for the treatment of DMD in patients with a confirmed mutation amenable to exon 53 skipping, following approval of golodirsen injection (Vyondys 53, Sarepta Therapeutics) for the same indication in December 2019.
The DMD gene mutation that is amenable to exon 45 skipping is present in about 8% of patients with DMD.
The trial that carried weight with the FDA included 43 male participants with DMD aged 7-20 years. All were confirmed to have the exon 45-skipping gene mutation and all were randomly assigned 2:1 to received IV casimersen 30 mg/kg or matching placebo.
Results showed that, between baseline and 48 weeks post treatment, the casimersen group showed a significantly higher increase in levels of dystrophin protein than in the placebo group.
Upper respiratory tract infections, fever, joint and throat pain, headache, and cough were the most common adverse events experienced by the active-treatment group.
Although the clinical studies assessing casimersen did not show any reports of kidney toxicity, the adverse event was observed in some nonclinical studies. Therefore, clinicians should monitor kidney function in any patient receiving this treatment, the FDA recommended.
Overall, “the FDA has concluded that the data submitted by the applicant demonstrated an increase in dystrophin production that is reasonably likely to predict clinical benefit” in this patient population, the agency said in its press release.
However, it noted that definitive clinical benefits such as improved motor function were not “established.”
“In making this decision, the FDA considered the potential risks associated with the drug, the life-threatening and debilitating nature of the disease, and the lack of [other] available therapy,” the agency said.
It added that the manufacturer is currently conducting a multicenter study focused on the safety and efficacy of the drug in ambulatory patients with DMD.
The FDA approved casimersen using its Accelerated Approval pathway, granted Fast Track and Priority Review designations to its applications, and gave the treatment Orphan Drug designation.
A version of this article first appeared on Medscape.com.
, the agency has announced.
This particular mutation of the DMD gene “is amenable to exon 45 skipping,” the FDA noted in a press release. The agency added that this is its first approval of a targeted treatment for patients with the mutation.
“Developing drugs designed for patients with specific mutations is a critical part of personalized medicine,” Eric Bastings, MD, deputy director of the Office of Neuroscience at the FDA’s Center for Drug Evaluation and Research, said in a statement.
The approval was based on results from a 43-person randomized controlled trial. Patients who received casimersen had a greater increase in production of the muscle-fiber protein dystrophin compared with their counterparts who received placebo.
Approved – with cautions
The FDA noted that DMD prevalence worldwide is about 1 in 3,600 boys – although it can also affect girls in rare cases. Symptoms of the disorder are commonly first observed around age 3 years but worsen steadily over time. DMD gene mutations lead to a decrease in dystrophin.
As reported by Medscape Medical News in August, the FDA approved viltolarsen (Viltepso, NS Pharma) for the treatment of DMD in patients with a confirmed mutation amenable to exon 53 skipping, following approval of golodirsen injection (Vyondys 53, Sarepta Therapeutics) for the same indication in December 2019.
The DMD gene mutation that is amenable to exon 45 skipping is present in about 8% of patients with DMD.
The trial that carried weight with the FDA included 43 male participants with DMD aged 7-20 years. All were confirmed to have the exon 45-skipping gene mutation and all were randomly assigned 2:1 to received IV casimersen 30 mg/kg or matching placebo.
Results showed that, between baseline and 48 weeks post treatment, the casimersen group showed a significantly higher increase in levels of dystrophin protein than in the placebo group.
Upper respiratory tract infections, fever, joint and throat pain, headache, and cough were the most common adverse events experienced by the active-treatment group.
Although the clinical studies assessing casimersen did not show any reports of kidney toxicity, the adverse event was observed in some nonclinical studies. Therefore, clinicians should monitor kidney function in any patient receiving this treatment, the FDA recommended.
Overall, “the FDA has concluded that the data submitted by the applicant demonstrated an increase in dystrophin production that is reasonably likely to predict clinical benefit” in this patient population, the agency said in its press release.
However, it noted that definitive clinical benefits such as improved motor function were not “established.”
“In making this decision, the FDA considered the potential risks associated with the drug, the life-threatening and debilitating nature of the disease, and the lack of [other] available therapy,” the agency said.
It added that the manufacturer is currently conducting a multicenter study focused on the safety and efficacy of the drug in ambulatory patients with DMD.
The FDA approved casimersen using its Accelerated Approval pathway, granted Fast Track and Priority Review designations to its applications, and gave the treatment Orphan Drug designation.
A version of this article first appeared on Medscape.com.
Study: Central sleep apnea is common in ticagrelor users post ACS
The prevalence of asymptomatic central sleep apnea after acute coronary syndrome is high and may be associated with the use of ticagrelor, a new study finds.
Prior studies have suggested that ticagrelor is associated with an increased likelihood of central sleep apnea. The drug’s label notes that two respiratory conditions – central sleep apnea and Cheyne-Stokes respiration – are adverse reactions that were identified after the drug’s approval in the United States in 2011. “Because these reactions are reported voluntarily from a population of an unknown size, it is not always possible to reliably estimate their frequency or establish a causal relationship to drug exposure,” the label says.
Among 80 patients receiving ticagrelor, 24 had central sleep apnea hypopnea syndrome (CSAHS), whereas of 41 patients not taking ticagrelor, 3 had this condition (30% vs. 7.3%, P = .004), in the new study published online Jan. 20, 2021, in Sleep Medicine. A multivariable analysis included in the paper found that age and ticagrelor administration were the only two factors associated with the occurrence of CSAHS.
Findings are ‘striking’
The different rates of central sleep apnea in the study are striking, but it is not clear that asymptomatic central sleep apnea in patients taking ticagrelor is a concern, Ofer Jacobowitz, MD, PhD, associate professor of otolaryngology at Hofstra University, Hempstead, N.Y, said in an interview.
“Whether this particular drug-induced central sleep apnea is consequential” is an open question, noted Dr. Jacobowitz. “There is no evidence that shows that this is definitely harmful.”
“The different types of central sleep apnea are caused by different mechanisms and this one, we don’t know,” Dr. Jacobwitz added.
Study author continues to prescribe ticagrelor
One of the study authors, Philippe Meurin, MD, said that he continues to prescribe ticagrelor every day and that the side effect is not necessarily important.
It is possible that central sleep apnea may resolve, although further studies would need to examine central sleep apnea over time to establish the duration of the condition, he added. Nevertheless, awareness of the association could have implications for clinical practice, Dr. Meurin said.
Central sleep apnea is rare, and if doctors detect it during a sleep study, they may perform extensive tests to assess for possible neurologic diseases, for example, when the cause may be attributed to the medication, he said. In addition, if a patient who is taking ticagrelor has dyspnea, the presence of central sleep apnea may suggest that dyspnea could be related to the drug, although this possibility needs further study, he noted.
Study included patients with ACS history, but no heart failure
Dr. Meurin, of Centre de Réadaptation Cardiaque de La Brie, Les Grands Prés, Villeneuve-Saint-Denis, France, and colleagues included in their study patients between 1 week and 1 year after acute coronary syndrome who did not have heart failure or a history of sleep apnea.
After an overnight sleep study, they classified patients as normal, as having CSAHS (i.e., an apnea-hypopnea index of 15 or greater, mostly with central sleep apneas), or as having obstructive sleep apnea hypopnea syndrome (OSAHS; i.e., an apnea-hypopnea index of 15 or greater, mostly with obstructive sleep apneas).
The prospective study included 121 consecutive patients between January 2018 and March 2020. Patients had a mean age of 56.8, and 88% were men.
Switching to another P2Y12 inhibitor ‘does not seem appropriate’
“CSAHS could be promoted by the use of ticagrelor, a relatively new drug that modifies the apneic threshold,” the study authors wrote. “Regarding underlying mechanisms, the most probable explanation seems to be increased chemosensitivity to hypercapnia by a direct P2Y12 inhibitory effect on the central nervous system.”
Doctors should not overestimate the severity of the adverse reaction or consider it the same way they do OSASH, they added.
Among patients with acute coronary syndrome in the PLATO study, ticagrelor, compared with clopidogrel, “significantly reduced the rate of death from vascular causes, myocardial infarction, or stroke,” Dr. Meurin and colleagues said. “Because in this study more than 9,000 patients received ticagrelor for 12 months, CSAHS (even if it seems frequent in our study) did not seem to impair the good efficacy/tolerance balance of the drug. Therefore, in asymptomatic CSAHS patients, switching from ticagrelor to another P2Y12 inhibitor does not seem appropriate.”
A recent analysis of data from randomized, controlled trials with ticagrelor did not find excess cases of sleep apnea with the drug. But an asymptomatic adverse event such as central sleep apnea “cannot emerge from a post hoc analysis,” Dr. Meurin and colleagues said.
The analysis of randomized trial data was conducted by Marc S. Sabatine, MD, MPH, chairman of the Thrombolysis in Myocardial Infarction (TIMI) Study Group at Brigham and Women’s Hospital, and coauthors. It was published in JACC: Cardiovascular Interventions in April 2020.
They “used the gold standard for medical evidence (randomized, placebo-controlled trials) and found 158 cases of sleep apnea reported, with absolutely no difference between ticagrelor and placebo,” Dr. Sabatine said in an interview. Their analysis examined clinically overt apnea, he noted.
“It is quite clear that when looking at large numbers in placebo-controlled trials, there is no excess,” Dr. Sabatine said. “Meurin et al. are examining a different outcome: the results of a lab test in what may be entirely asymptomatic patients.”
A randomized trial could confirm the association, he said.
“The association may be real, but also may be play of chance or confounded,” said Dr. Sabatine. “To convince the medical community, the next step would be for the investigators to do a randomized trial and test whether ticagrelor increases the risk of central sleep apnea.”
Dr. Meurin and the study coauthors had no disclosures. The analysis of randomized, controlled trial data by Dr. Sabatine and colleagues was funded by AstraZeneca, which distributes ticagrelor under the trade name Brilinta. Dr. Sabatine has been a consultant for AstraZeneca and received research grants through Brigham and Women’s Hospital from AstraZeneca. He has consulted for and received grants through the hospital from other companies as well. Dr. Jacobowitz had no relevant disclosures.
[email protected]
The prevalence of asymptomatic central sleep apnea after acute coronary syndrome is high and may be associated with the use of ticagrelor, a new study finds.
Prior studies have suggested that ticagrelor is associated with an increased likelihood of central sleep apnea. The drug’s label notes that two respiratory conditions – central sleep apnea and Cheyne-Stokes respiration – are adverse reactions that were identified after the drug’s approval in the United States in 2011. “Because these reactions are reported voluntarily from a population of an unknown size, it is not always possible to reliably estimate their frequency or establish a causal relationship to drug exposure,” the label says.
Among 80 patients receiving ticagrelor, 24 had central sleep apnea hypopnea syndrome (CSAHS), whereas of 41 patients not taking ticagrelor, 3 had this condition (30% vs. 7.3%, P = .004), in the new study published online Jan. 20, 2021, in Sleep Medicine. A multivariable analysis included in the paper found that age and ticagrelor administration were the only two factors associated with the occurrence of CSAHS.
Findings are ‘striking’
The different rates of central sleep apnea in the study are striking, but it is not clear that asymptomatic central sleep apnea in patients taking ticagrelor is a concern, Ofer Jacobowitz, MD, PhD, associate professor of otolaryngology at Hofstra University, Hempstead, N.Y, said in an interview.
“Whether this particular drug-induced central sleep apnea is consequential” is an open question, noted Dr. Jacobowitz. “There is no evidence that shows that this is definitely harmful.”
“The different types of central sleep apnea are caused by different mechanisms and this one, we don’t know,” Dr. Jacobwitz added.
Study author continues to prescribe ticagrelor
One of the study authors, Philippe Meurin, MD, said that he continues to prescribe ticagrelor every day and that the side effect is not necessarily important.
It is possible that central sleep apnea may resolve, although further studies would need to examine central sleep apnea over time to establish the duration of the condition, he added. Nevertheless, awareness of the association could have implications for clinical practice, Dr. Meurin said.
Central sleep apnea is rare, and if doctors detect it during a sleep study, they may perform extensive tests to assess for possible neurologic diseases, for example, when the cause may be attributed to the medication, he said. In addition, if a patient who is taking ticagrelor has dyspnea, the presence of central sleep apnea may suggest that dyspnea could be related to the drug, although this possibility needs further study, he noted.
Study included patients with ACS history, but no heart failure
Dr. Meurin, of Centre de Réadaptation Cardiaque de La Brie, Les Grands Prés, Villeneuve-Saint-Denis, France, and colleagues included in their study patients between 1 week and 1 year after acute coronary syndrome who did not have heart failure or a history of sleep apnea.
After an overnight sleep study, they classified patients as normal, as having CSAHS (i.e., an apnea-hypopnea index of 15 or greater, mostly with central sleep apneas), or as having obstructive sleep apnea hypopnea syndrome (OSAHS; i.e., an apnea-hypopnea index of 15 or greater, mostly with obstructive sleep apneas).
The prospective study included 121 consecutive patients between January 2018 and March 2020. Patients had a mean age of 56.8, and 88% were men.
Switching to another P2Y12 inhibitor ‘does not seem appropriate’
“CSAHS could be promoted by the use of ticagrelor, a relatively new drug that modifies the apneic threshold,” the study authors wrote. “Regarding underlying mechanisms, the most probable explanation seems to be increased chemosensitivity to hypercapnia by a direct P2Y12 inhibitory effect on the central nervous system.”
Doctors should not overestimate the severity of the adverse reaction or consider it the same way they do OSASH, they added.
Among patients with acute coronary syndrome in the PLATO study, ticagrelor, compared with clopidogrel, “significantly reduced the rate of death from vascular causes, myocardial infarction, or stroke,” Dr. Meurin and colleagues said. “Because in this study more than 9,000 patients received ticagrelor for 12 months, CSAHS (even if it seems frequent in our study) did not seem to impair the good efficacy/tolerance balance of the drug. Therefore, in asymptomatic CSAHS patients, switching from ticagrelor to another P2Y12 inhibitor does not seem appropriate.”
A recent analysis of data from randomized, controlled trials with ticagrelor did not find excess cases of sleep apnea with the drug. But an asymptomatic adverse event such as central sleep apnea “cannot emerge from a post hoc analysis,” Dr. Meurin and colleagues said.
The analysis of randomized trial data was conducted by Marc S. Sabatine, MD, MPH, chairman of the Thrombolysis in Myocardial Infarction (TIMI) Study Group at Brigham and Women’s Hospital, and coauthors. It was published in JACC: Cardiovascular Interventions in April 2020.
They “used the gold standard for medical evidence (randomized, placebo-controlled trials) and found 158 cases of sleep apnea reported, with absolutely no difference between ticagrelor and placebo,” Dr. Sabatine said in an interview. Their analysis examined clinically overt apnea, he noted.
“It is quite clear that when looking at large numbers in placebo-controlled trials, there is no excess,” Dr. Sabatine said. “Meurin et al. are examining a different outcome: the results of a lab test in what may be entirely asymptomatic patients.”
A randomized trial could confirm the association, he said.
“The association may be real, but also may be play of chance or confounded,” said Dr. Sabatine. “To convince the medical community, the next step would be for the investigators to do a randomized trial and test whether ticagrelor increases the risk of central sleep apnea.”
Dr. Meurin and the study coauthors had no disclosures. The analysis of randomized, controlled trial data by Dr. Sabatine and colleagues was funded by AstraZeneca, which distributes ticagrelor under the trade name Brilinta. Dr. Sabatine has been a consultant for AstraZeneca and received research grants through Brigham and Women’s Hospital from AstraZeneca. He has consulted for and received grants through the hospital from other companies as well. Dr. Jacobowitz had no relevant disclosures.
[email protected]
The prevalence of asymptomatic central sleep apnea after acute coronary syndrome is high and may be associated with the use of ticagrelor, a new study finds.
Prior studies have suggested that ticagrelor is associated with an increased likelihood of central sleep apnea. The drug’s label notes that two respiratory conditions – central sleep apnea and Cheyne-Stokes respiration – are adverse reactions that were identified after the drug’s approval in the United States in 2011. “Because these reactions are reported voluntarily from a population of an unknown size, it is not always possible to reliably estimate their frequency or establish a causal relationship to drug exposure,” the label says.
Among 80 patients receiving ticagrelor, 24 had central sleep apnea hypopnea syndrome (CSAHS), whereas of 41 patients not taking ticagrelor, 3 had this condition (30% vs. 7.3%, P = .004), in the new study published online Jan. 20, 2021, in Sleep Medicine. A multivariable analysis included in the paper found that age and ticagrelor administration were the only two factors associated with the occurrence of CSAHS.
Findings are ‘striking’
The different rates of central sleep apnea in the study are striking, but it is not clear that asymptomatic central sleep apnea in patients taking ticagrelor is a concern, Ofer Jacobowitz, MD, PhD, associate professor of otolaryngology at Hofstra University, Hempstead, N.Y, said in an interview.
“Whether this particular drug-induced central sleep apnea is consequential” is an open question, noted Dr. Jacobowitz. “There is no evidence that shows that this is definitely harmful.”
“The different types of central sleep apnea are caused by different mechanisms and this one, we don’t know,” Dr. Jacobwitz added.
Study author continues to prescribe ticagrelor
One of the study authors, Philippe Meurin, MD, said that he continues to prescribe ticagrelor every day and that the side effect is not necessarily important.
It is possible that central sleep apnea may resolve, although further studies would need to examine central sleep apnea over time to establish the duration of the condition, he added. Nevertheless, awareness of the association could have implications for clinical practice, Dr. Meurin said.
Central sleep apnea is rare, and if doctors detect it during a sleep study, they may perform extensive tests to assess for possible neurologic diseases, for example, when the cause may be attributed to the medication, he said. In addition, if a patient who is taking ticagrelor has dyspnea, the presence of central sleep apnea may suggest that dyspnea could be related to the drug, although this possibility needs further study, he noted.
Study included patients with ACS history, but no heart failure
Dr. Meurin, of Centre de Réadaptation Cardiaque de La Brie, Les Grands Prés, Villeneuve-Saint-Denis, France, and colleagues included in their study patients between 1 week and 1 year after acute coronary syndrome who did not have heart failure or a history of sleep apnea.
After an overnight sleep study, they classified patients as normal, as having CSAHS (i.e., an apnea-hypopnea index of 15 or greater, mostly with central sleep apneas), or as having obstructive sleep apnea hypopnea syndrome (OSAHS; i.e., an apnea-hypopnea index of 15 or greater, mostly with obstructive sleep apneas).
The prospective study included 121 consecutive patients between January 2018 and March 2020. Patients had a mean age of 56.8, and 88% were men.
Switching to another P2Y12 inhibitor ‘does not seem appropriate’
“CSAHS could be promoted by the use of ticagrelor, a relatively new drug that modifies the apneic threshold,” the study authors wrote. “Regarding underlying mechanisms, the most probable explanation seems to be increased chemosensitivity to hypercapnia by a direct P2Y12 inhibitory effect on the central nervous system.”
Doctors should not overestimate the severity of the adverse reaction or consider it the same way they do OSASH, they added.
Among patients with acute coronary syndrome in the PLATO study, ticagrelor, compared with clopidogrel, “significantly reduced the rate of death from vascular causes, myocardial infarction, or stroke,” Dr. Meurin and colleagues said. “Because in this study more than 9,000 patients received ticagrelor for 12 months, CSAHS (even if it seems frequent in our study) did not seem to impair the good efficacy/tolerance balance of the drug. Therefore, in asymptomatic CSAHS patients, switching from ticagrelor to another P2Y12 inhibitor does not seem appropriate.”
A recent analysis of data from randomized, controlled trials with ticagrelor did not find excess cases of sleep apnea with the drug. But an asymptomatic adverse event such as central sleep apnea “cannot emerge from a post hoc analysis,” Dr. Meurin and colleagues said.
The analysis of randomized trial data was conducted by Marc S. Sabatine, MD, MPH, chairman of the Thrombolysis in Myocardial Infarction (TIMI) Study Group at Brigham and Women’s Hospital, and coauthors. It was published in JACC: Cardiovascular Interventions in April 2020.
They “used the gold standard for medical evidence (randomized, placebo-controlled trials) and found 158 cases of sleep apnea reported, with absolutely no difference between ticagrelor and placebo,” Dr. Sabatine said in an interview. Their analysis examined clinically overt apnea, he noted.
“It is quite clear that when looking at large numbers in placebo-controlled trials, there is no excess,” Dr. Sabatine said. “Meurin et al. are examining a different outcome: the results of a lab test in what may be entirely asymptomatic patients.”
A randomized trial could confirm the association, he said.
“The association may be real, but also may be play of chance or confounded,” said Dr. Sabatine. “To convince the medical community, the next step would be for the investigators to do a randomized trial and test whether ticagrelor increases the risk of central sleep apnea.”
Dr. Meurin and the study coauthors had no disclosures. The analysis of randomized, controlled trial data by Dr. Sabatine and colleagues was funded by AstraZeneca, which distributes ticagrelor under the trade name Brilinta. Dr. Sabatine has been a consultant for AstraZeneca and received research grants through Brigham and Women’s Hospital from AstraZeneca. He has consulted for and received grants through the hospital from other companies as well. Dr. Jacobowitz had no relevant disclosures.
[email protected]
FROM SLEEP MEDICINE
New data may help intercept head injuries in college football
Novel research from the Concussion Assessment, Research and Education (CARE) Consortium sheds new light on how to effectively reduce the incidence of concussion and head injury exposure in college football.
The study, led by neurotrauma experts Michael McCrea, PhD, and Brian Stemper, PhD, professors of neurosurgery at the Medical College of Wisconsin in Milwaukee, reports data from hundreds of college football players across five seasons and shows
The research also reveals that such injuries occur more often during practices than games.
“We think that with the findings from this paper, there’s a role for everybody to play in reducing injury,” Dr. McCrea said. “We hope these data help inform broad-based policy about practice and preseason training policies in collegiate football. We also think there’s a role for athletic administrators, coaches, and even athletes themselves.”
The study was published online Feb. 1 in JAMA Neurology.
More injuries in preseason
Concussion is one of the most common injuries in football. Beyond these harms are growing concerns that repetitive HIE may increase the risk of long-term neurologic health problems including chronic traumatic encephalopathy (CTE).
The CARE Consortium, which has been conducting research with college athletes across 26 sports and military cadets since 2014, has been interested in multiple facets of concussion and brain trauma.
“We’ve enrolled more than 50,000 athletes and service academy cadets into the consortium over the last 6 years to research all involved aspects including the clinical core, the imaging core, the blood biomarker core, and the genetic core, and we have a head impact measurement core.”
To investigate the pattern of concussion incidence across the football season in college players, the investigators used impact measurement technology across six Division I NCAA football programs participating in the CARE Consortium from 2015 to 2019.
A total of 658 players – all male, mean age 19 years – were fitted with the Head Impact Telemetry System (HITS) sensor arrays in their helmets to measure head impact frequency, location, and magnitude during play.
“This particular study had built-in algorithms that weeded out impacts that were below 10G of linear magnitude, because those have been determined not likely to be real impacts,” Dr. McCrea said.
Across the five seasons studied, 528,684 head impacts recorded met the quality standards for analysis. Players sustained a median of 415 (interquartile range [IQR], 190-727) impacts per season.
Of those, 68 players sustained a diagnosed concussion. In total, 48.5% of concussions occurred during preseason training, despite preseason representing only 20.8% of the football season. Total head injury exposure in the preseason occurred at twice the proportion of the regular season (324.9 vs. 162.4 impacts per team per day; mean difference, 162.6 impacts; 95% confidence interval, 110.9-214.3; P < .001).
“Preseason training often has a much higher intensity to it, in terms of the total hours, the actual training, and the heavy emphasis on full-contact drills like tackling and blocking,” said Dr. McCrea. “Even the volume of players that are participating is greater.”
Results also showed that in each of the five seasons, head injury exposure per athlete was highest in August (preseason) (median, 146.0 impacts; IQR, 63.0-247.8) and lowest in November (median, 80.0 impacts; IQR, 35.0-148.0). In the studied period, 72% of concussions and 66.9% of head injury exposure occurred in practice. Even within the regular season, total head injury exposure in practices was 84.2% higher than in games.
“This incredible dataset we have on head impact measurement also gives us the opportunity to compare it with our other research looking at the correlation between a single head impact and changes in brain structure and function on MRI, on blood biomarkers, giving us the ability to look at the connection between mechanism of effect of injury and recovery from injury,” said Dr. McCrea.
These findings also provide an opportunity to modify approaches to preseason training and football practices to keep players safer, said Dr. McCrea, noting that about half of the variance in head injury exposure is at the level of the individual athlete.
“With this large body of athletes we’ve instrumented, we can look at, for instance, all of the running backs and understand the athlete and what his head injury exposure looks like compared to all other running backs. If we find out that an athlete has a rate of head injury exposure that’s 300% higher than most other players that play the same position, we can take that data directly to the athlete to work on their technique and approach to the game.
“Every researcher wishes that their basic science or their clinical research findings will have some impact on the health and well-being of the population they’re studying. By modifying practices and preseason training, football teams could greatly reduce the risk of injury and exposure for their players, while still maintaining the competitive nature of game play,” he added.
Through a combination of policy and education, similar strategies could be implemented to help prevent concussion and HIE in high school and youth football too, said Dr. McCrea.
‘Shocking’ findings
In an accompanying editorial, Christopher J. Nowinski, PhD, of the Concussion Legacy Foundation, Boston, and Robert C. Cantu, MD, department of neurosurgery, Emerson Hospital, Concord, Massachusetts, said the findings could have significant policy implications and offer a valuable expansion of prior research.
“From 2005 to 2010, studies on college football revealed that about two-thirds of head impacts occurred in practice,” they noted. “We cited this data in 2010 when we proposed to the NFL Players Association that the most effective way to reduce the risks of negative neurological outcomes was to reduce hitting in practice. They agreed, and in 2011 collectively bargained for severe contact limits in practice, with 14 full-contact practices allowed during the 17-week season. Since that rule was implemented, only 18% of NFL concussions have occurred in practice.”
“Against this backdrop, the results of the study by McCrea et al. are shocking,” they added. “It reveals that college football players still experience 72% of their concussions and 67% of their total head injury exposure in practice.”
Even more shocking, noted Dr. Nowinski and Dr. Cantu, is that these numbers are almost certainly an underestimate of the dangers of practice.
“As a former college football player and a former team physician, respectively, we find this situation inexcusable. Concussions in games are inevitable, but concussions in practice are preventable,” they wrote.
“Laudably,” they added “the investigators call on the NCAA and football conferences to explore policy and rule changes to reduce concussion incidence and HIE and to create robust educational offerings to encourage change from coaches and college administrators.”
A version of this article first appeared on Medscape.com.
Novel research from the Concussion Assessment, Research and Education (CARE) Consortium sheds new light on how to effectively reduce the incidence of concussion and head injury exposure in college football.
The study, led by neurotrauma experts Michael McCrea, PhD, and Brian Stemper, PhD, professors of neurosurgery at the Medical College of Wisconsin in Milwaukee, reports data from hundreds of college football players across five seasons and shows
The research also reveals that such injuries occur more often during practices than games.
“We think that with the findings from this paper, there’s a role for everybody to play in reducing injury,” Dr. McCrea said. “We hope these data help inform broad-based policy about practice and preseason training policies in collegiate football. We also think there’s a role for athletic administrators, coaches, and even athletes themselves.”
The study was published online Feb. 1 in JAMA Neurology.
More injuries in preseason
Concussion is one of the most common injuries in football. Beyond these harms are growing concerns that repetitive HIE may increase the risk of long-term neurologic health problems including chronic traumatic encephalopathy (CTE).
The CARE Consortium, which has been conducting research with college athletes across 26 sports and military cadets since 2014, has been interested in multiple facets of concussion and brain trauma.
“We’ve enrolled more than 50,000 athletes and service academy cadets into the consortium over the last 6 years to research all involved aspects including the clinical core, the imaging core, the blood biomarker core, and the genetic core, and we have a head impact measurement core.”
To investigate the pattern of concussion incidence across the football season in college players, the investigators used impact measurement technology across six Division I NCAA football programs participating in the CARE Consortium from 2015 to 2019.
A total of 658 players – all male, mean age 19 years – were fitted with the Head Impact Telemetry System (HITS) sensor arrays in their helmets to measure head impact frequency, location, and magnitude during play.
“This particular study had built-in algorithms that weeded out impacts that were below 10G of linear magnitude, because those have been determined not likely to be real impacts,” Dr. McCrea said.
Across the five seasons studied, 528,684 head impacts recorded met the quality standards for analysis. Players sustained a median of 415 (interquartile range [IQR], 190-727) impacts per season.
Of those, 68 players sustained a diagnosed concussion. In total, 48.5% of concussions occurred during preseason training, despite preseason representing only 20.8% of the football season. Total head injury exposure in the preseason occurred at twice the proportion of the regular season (324.9 vs. 162.4 impacts per team per day; mean difference, 162.6 impacts; 95% confidence interval, 110.9-214.3; P < .001).
“Preseason training often has a much higher intensity to it, in terms of the total hours, the actual training, and the heavy emphasis on full-contact drills like tackling and blocking,” said Dr. McCrea. “Even the volume of players that are participating is greater.”
Results also showed that in each of the five seasons, head injury exposure per athlete was highest in August (preseason) (median, 146.0 impacts; IQR, 63.0-247.8) and lowest in November (median, 80.0 impacts; IQR, 35.0-148.0). In the studied period, 72% of concussions and 66.9% of head injury exposure occurred in practice. Even within the regular season, total head injury exposure in practices was 84.2% higher than in games.
“This incredible dataset we have on head impact measurement also gives us the opportunity to compare it with our other research looking at the correlation between a single head impact and changes in brain structure and function on MRI, on blood biomarkers, giving us the ability to look at the connection between mechanism of effect of injury and recovery from injury,” said Dr. McCrea.
These findings also provide an opportunity to modify approaches to preseason training and football practices to keep players safer, said Dr. McCrea, noting that about half of the variance in head injury exposure is at the level of the individual athlete.
“With this large body of athletes we’ve instrumented, we can look at, for instance, all of the running backs and understand the athlete and what his head injury exposure looks like compared to all other running backs. If we find out that an athlete has a rate of head injury exposure that’s 300% higher than most other players that play the same position, we can take that data directly to the athlete to work on their technique and approach to the game.
“Every researcher wishes that their basic science or their clinical research findings will have some impact on the health and well-being of the population they’re studying. By modifying practices and preseason training, football teams could greatly reduce the risk of injury and exposure for their players, while still maintaining the competitive nature of game play,” he added.
Through a combination of policy and education, similar strategies could be implemented to help prevent concussion and HIE in high school and youth football too, said Dr. McCrea.
‘Shocking’ findings
In an accompanying editorial, Christopher J. Nowinski, PhD, of the Concussion Legacy Foundation, Boston, and Robert C. Cantu, MD, department of neurosurgery, Emerson Hospital, Concord, Massachusetts, said the findings could have significant policy implications and offer a valuable expansion of prior research.
“From 2005 to 2010, studies on college football revealed that about two-thirds of head impacts occurred in practice,” they noted. “We cited this data in 2010 when we proposed to the NFL Players Association that the most effective way to reduce the risks of negative neurological outcomes was to reduce hitting in practice. They agreed, and in 2011 collectively bargained for severe contact limits in practice, with 14 full-contact practices allowed during the 17-week season. Since that rule was implemented, only 18% of NFL concussions have occurred in practice.”
“Against this backdrop, the results of the study by McCrea et al. are shocking,” they added. “It reveals that college football players still experience 72% of their concussions and 67% of their total head injury exposure in practice.”
Even more shocking, noted Dr. Nowinski and Dr. Cantu, is that these numbers are almost certainly an underestimate of the dangers of practice.
“As a former college football player and a former team physician, respectively, we find this situation inexcusable. Concussions in games are inevitable, but concussions in practice are preventable,” they wrote.
“Laudably,” they added “the investigators call on the NCAA and football conferences to explore policy and rule changes to reduce concussion incidence and HIE and to create robust educational offerings to encourage change from coaches and college administrators.”
A version of this article first appeared on Medscape.com.
Novel research from the Concussion Assessment, Research and Education (CARE) Consortium sheds new light on how to effectively reduce the incidence of concussion and head injury exposure in college football.
The study, led by neurotrauma experts Michael McCrea, PhD, and Brian Stemper, PhD, professors of neurosurgery at the Medical College of Wisconsin in Milwaukee, reports data from hundreds of college football players across five seasons and shows
The research also reveals that such injuries occur more often during practices than games.
“We think that with the findings from this paper, there’s a role for everybody to play in reducing injury,” Dr. McCrea said. “We hope these data help inform broad-based policy about practice and preseason training policies in collegiate football. We also think there’s a role for athletic administrators, coaches, and even athletes themselves.”
The study was published online Feb. 1 in JAMA Neurology.
More injuries in preseason
Concussion is one of the most common injuries in football. Beyond these harms are growing concerns that repetitive HIE may increase the risk of long-term neurologic health problems including chronic traumatic encephalopathy (CTE).
The CARE Consortium, which has been conducting research with college athletes across 26 sports and military cadets since 2014, has been interested in multiple facets of concussion and brain trauma.
“We’ve enrolled more than 50,000 athletes and service academy cadets into the consortium over the last 6 years to research all involved aspects including the clinical core, the imaging core, the blood biomarker core, and the genetic core, and we have a head impact measurement core.”
To investigate the pattern of concussion incidence across the football season in college players, the investigators used impact measurement technology across six Division I NCAA football programs participating in the CARE Consortium from 2015 to 2019.
A total of 658 players – all male, mean age 19 years – were fitted with the Head Impact Telemetry System (HITS) sensor arrays in their helmets to measure head impact frequency, location, and magnitude during play.
“This particular study had built-in algorithms that weeded out impacts that were below 10G of linear magnitude, because those have been determined not likely to be real impacts,” Dr. McCrea said.
Across the five seasons studied, 528,684 head impacts recorded met the quality standards for analysis. Players sustained a median of 415 (interquartile range [IQR], 190-727) impacts per season.
Of those, 68 players sustained a diagnosed concussion. In total, 48.5% of concussions occurred during preseason training, despite preseason representing only 20.8% of the football season. Total head injury exposure in the preseason occurred at twice the proportion of the regular season (324.9 vs. 162.4 impacts per team per day; mean difference, 162.6 impacts; 95% confidence interval, 110.9-214.3; P < .001).
“Preseason training often has a much higher intensity to it, in terms of the total hours, the actual training, and the heavy emphasis on full-contact drills like tackling and blocking,” said Dr. McCrea. “Even the volume of players that are participating is greater.”
Results also showed that in each of the five seasons, head injury exposure per athlete was highest in August (preseason) (median, 146.0 impacts; IQR, 63.0-247.8) and lowest in November (median, 80.0 impacts; IQR, 35.0-148.0). In the studied period, 72% of concussions and 66.9% of head injury exposure occurred in practice. Even within the regular season, total head injury exposure in practices was 84.2% higher than in games.
“This incredible dataset we have on head impact measurement also gives us the opportunity to compare it with our other research looking at the correlation between a single head impact and changes in brain structure and function on MRI, on blood biomarkers, giving us the ability to look at the connection between mechanism of effect of injury and recovery from injury,” said Dr. McCrea.
These findings also provide an opportunity to modify approaches to preseason training and football practices to keep players safer, said Dr. McCrea, noting that about half of the variance in head injury exposure is at the level of the individual athlete.
“With this large body of athletes we’ve instrumented, we can look at, for instance, all of the running backs and understand the athlete and what his head injury exposure looks like compared to all other running backs. If we find out that an athlete has a rate of head injury exposure that’s 300% higher than most other players that play the same position, we can take that data directly to the athlete to work on their technique and approach to the game.
“Every researcher wishes that their basic science or their clinical research findings will have some impact on the health and well-being of the population they’re studying. By modifying practices and preseason training, football teams could greatly reduce the risk of injury and exposure for their players, while still maintaining the competitive nature of game play,” he added.
Through a combination of policy and education, similar strategies could be implemented to help prevent concussion and HIE in high school and youth football too, said Dr. McCrea.
‘Shocking’ findings
In an accompanying editorial, Christopher J. Nowinski, PhD, of the Concussion Legacy Foundation, Boston, and Robert C. Cantu, MD, department of neurosurgery, Emerson Hospital, Concord, Massachusetts, said the findings could have significant policy implications and offer a valuable expansion of prior research.
“From 2005 to 2010, studies on college football revealed that about two-thirds of head impacts occurred in practice,” they noted. “We cited this data in 2010 when we proposed to the NFL Players Association that the most effective way to reduce the risks of negative neurological outcomes was to reduce hitting in practice. They agreed, and in 2011 collectively bargained for severe contact limits in practice, with 14 full-contact practices allowed during the 17-week season. Since that rule was implemented, only 18% of NFL concussions have occurred in practice.”
“Against this backdrop, the results of the study by McCrea et al. are shocking,” they added. “It reveals that college football players still experience 72% of their concussions and 67% of their total head injury exposure in practice.”
Even more shocking, noted Dr. Nowinski and Dr. Cantu, is that these numbers are almost certainly an underestimate of the dangers of practice.
“As a former college football player and a former team physician, respectively, we find this situation inexcusable. Concussions in games are inevitable, but concussions in practice are preventable,” they wrote.
“Laudably,” they added “the investigators call on the NCAA and football conferences to explore policy and rule changes to reduce concussion incidence and HIE and to create robust educational offerings to encourage change from coaches and college administrators.”
A version of this article first appeared on Medscape.com.
FROM JAMA NEUROLOGY
Loss of smell lingers post COVID-19
The findings illustrate that olfactory problems are common not only during the acute COVID-19 phase but also “in the long run” and that these problems should be “taken into consideration” when following up these patients, study investigator Johannes Frasnelli, MD, professor, department of anatomy, Université du Québec à Trois-Rivières, said in an interview.
Loss of the sense of smell can affect quality of life because it affects eating and drinking, and may even be dangerous, said Dr. Frasnelli. “If your sense of smell is impaired, you may unknowingly eat spoiled food, or you may not smell smoke or gas in your home,” he said. In addition, Dr. Frasnelli noted that an impaired sense of smell is associated with higher rates of depression. The findings will be presented at the annual meeting of the American Academy of Neurology in April.
‘Striking’ finding
Research shows that about 60% of patients with COVID-19 lose their sense of smell to some degree during the acute phase of the disease. “But we wanted to go further and look at the longer-term effects of loss of smell and taste,” said Dr. Frasnelli.
The analysis included 813 health care workers in the province of Quebec. For all the patients, SARS-CoV-2 infection was confirmed through testing with a nasopharyngeal viral swab.
Participants completed a 64-item online questionnaire that asked about three senses: olfactory; gustatory, which includes tastes such as sweet, sour, bitter, salty, savory and umami; and trigeminal, which includes sensations such as spiciness of hot peppers and “coolness” of mint.
They were asked to rate these on a scale of 0 (no perception) to 10 (very strong perception) before the infection, during the infection, and currently. They were also asked about other symptoms, including fatigue.
Most respondents had been infected in the first wave of the virus in March and April of 2020 and responded to the questionnaire an average of 5 months later.
The vast majority of respondents (84.1%) were women, which Dr. Frasnelli said was not surprising because women predominate in the health care field.
The analysis showed that average smell ratings were 8.98 before infection, 2.85 during the acute phase, and 7.41 when respondents answered the questionnaire. The sense of taste was less affected and recovered faster than did the sense of smell. Results for taste were 9.20 before infection, 3.59 during the acute phase, and 8.05 after COVID-19.
Among 580 respondents who indicated a compromised sense of smell during the acute phase, the average smell rating when answering the questionnaire was 6.89, compared to 9.03 before the infection. More than half (51.2%) reported not regaining full olfactory function.
The fact that the sense of smell had not returned to normal for half the participants so long after being infected is “novel and quite striking,” said Dr. Frasnelli.
However, he noted, this doesn’t necessarily mean all those with a compromised sense of smell “have huge problems.” In some cases, he said, the problem “is more subtle.”
Not a CNS problem?
Respondents also completed a chemosensory dysfunction home test (CD-HT). They were asked to prepare common household food items, such as peanut butter, sugar, salt, and vinegar, in a particular way – for example, to add sugar or salt to water – and provide feedback on how they smell and taste.
For this CD-HT analysis, 18.4% of respondents reported having persistent loss of smell. This, Dr. Frasnelli said, adds to evidence from self-reported responses and suggests that in some cases, the problem is more than senses not returning to normal.
“From the questionnaires, roughly 50% said their sense of smell is still not back to normal, and when we look at the CD home test, we see that almost 20% of subjects indeed have pretty strong impairment of their sense of smell,” he said.
The results showed no sex differences, although Dr. Frasnelli noted that most of the sample were women. “It’s tricky to look at the data with regard to sex because it’s a bit skewed,” he said.
Male respondents were older than female participants, but there was no difference in impairment between age groups. Dr. Frasnelli said this was “quite interesting,” inasmuch as older people usually lose some sense of smell.
The researchers have not yet examined whether the results differ by type of health care worker.
They also have not examined in detail whether infection severity affects the risk for extended olfactory impairment. Although some research suggests that the problem with smell is more common in less severe cases, Dr. Frasnelli noted this could be because loss of smell is not a huge problem for patients battling grave health problems.
As for other symptoms, many respondents reported lingering fatigue; some reported debilitating fatigue, said Dr. Frasnelli. However, he cautioned that this is difficult to interpret, because the participants were health care workers, many of whom returned to work during the pandemic and perhaps had not fully rested.
He also noted that he and his colleagues have not “made the link” between impaired smell and the degree of fatigue.
The COVID-19 virus appears to attack supporting sustentacular cells in the olfactory epithelium, not nerve cells.
“Right now, it seems that the smell problem is not a central nervous system problem but a peripheral problem,” said Dr. Frasnelli. “But we don’t know for sure; it may be that the virus somehow gets into the brain and some symptoms are caused by the effects of the infection on the brain.”
The researchers will extend their research with another questionnaire to assess senses 10-12 months after COVID-19.
Limitations of the study include the subjective nature of the smell and taste ratings and the single time point at which data were collected.
Confirmatory findings
Commenting on the research in an interview, Thomas Hummel, MD, professor, smell and taste clinic, department of otorhinolaryngology, Technische Universität Dresden (Germany), said the new results regarding loss of smell after COVID-19 are “very congruent” with what he and his colleagues have observed.
Research shows that up to one in five of those infected with SARS-CoV-2 experience olfactory loss. “While the numbers may vary a bit from study to study or lab to lab, I think 5% to 20% of post–COVID-19 patients exhibit long-term olfactory loss,” Dr. Hummel said.
His group has observed that “many more are not back to normal,” which conforms with what Dr. Frasnelli’s study reveals, said Dr. Hummel.
Also commenting on the research, Kenneth L. Tyler, MD, professor of neurology, University of Colorado at Denver, Aurora, and a fellow of the American Academy of Neurology, said the study was relatively large and the results “interesting.”
Although it “provides more evidence there’s a subset of patients with symptoms even well past the acute phase” of COVID-19, the results are “mostly confirmatory” and include “nothing super surprising,” Dr. Tyler said in an interview.
However, the investigators did attempt to make the study “a little more quantitative” and “to confirm the self-reporting with their validated CD home test,” he said.
Dr. Tyler wondered how representative the sample was and whether the study drew more participants with impaired senses. “If I had a loss of smell or taste, maybe I would be more likely to respond to such a survey,” he said.
He also noted the difficulty of separating loss of smell from loss of taste.
“If you lose your sense of smell, things don’t taste right, so it can be confounding as to how to separate out those two,” he noted.
The study was supported by the Foundation of the Université du Québec à Trois-Rivières and the Province of Quebec. Dr. Frasnelli has received royalties from Styriabooks in Austria for a book on olfaction published in 2019 and has received honoraria for speaking engagements. Dr. Hummel and Dr. Tyler have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
The findings illustrate that olfactory problems are common not only during the acute COVID-19 phase but also “in the long run” and that these problems should be “taken into consideration” when following up these patients, study investigator Johannes Frasnelli, MD, professor, department of anatomy, Université du Québec à Trois-Rivières, said in an interview.
Loss of the sense of smell can affect quality of life because it affects eating and drinking, and may even be dangerous, said Dr. Frasnelli. “If your sense of smell is impaired, you may unknowingly eat spoiled food, or you may not smell smoke or gas in your home,” he said. In addition, Dr. Frasnelli noted that an impaired sense of smell is associated with higher rates of depression. The findings will be presented at the annual meeting of the American Academy of Neurology in April.
‘Striking’ finding
Research shows that about 60% of patients with COVID-19 lose their sense of smell to some degree during the acute phase of the disease. “But we wanted to go further and look at the longer-term effects of loss of smell and taste,” said Dr. Frasnelli.
The analysis included 813 health care workers in the province of Quebec. For all the patients, SARS-CoV-2 infection was confirmed through testing with a nasopharyngeal viral swab.
Participants completed a 64-item online questionnaire that asked about three senses: olfactory; gustatory, which includes tastes such as sweet, sour, bitter, salty, savory and umami; and trigeminal, which includes sensations such as spiciness of hot peppers and “coolness” of mint.
They were asked to rate these on a scale of 0 (no perception) to 10 (very strong perception) before the infection, during the infection, and currently. They were also asked about other symptoms, including fatigue.
Most respondents had been infected in the first wave of the virus in March and April of 2020 and responded to the questionnaire an average of 5 months later.
The vast majority of respondents (84.1%) were women, which Dr. Frasnelli said was not surprising because women predominate in the health care field.
The analysis showed that average smell ratings were 8.98 before infection, 2.85 during the acute phase, and 7.41 when respondents answered the questionnaire. The sense of taste was less affected and recovered faster than did the sense of smell. Results for taste were 9.20 before infection, 3.59 during the acute phase, and 8.05 after COVID-19.
Among 580 respondents who indicated a compromised sense of smell during the acute phase, the average smell rating when answering the questionnaire was 6.89, compared to 9.03 before the infection. More than half (51.2%) reported not regaining full olfactory function.
The fact that the sense of smell had not returned to normal for half the participants so long after being infected is “novel and quite striking,” said Dr. Frasnelli.
However, he noted, this doesn’t necessarily mean all those with a compromised sense of smell “have huge problems.” In some cases, he said, the problem “is more subtle.”
Not a CNS problem?
Respondents also completed a chemosensory dysfunction home test (CD-HT). They were asked to prepare common household food items, such as peanut butter, sugar, salt, and vinegar, in a particular way – for example, to add sugar or salt to water – and provide feedback on how they smell and taste.
For this CD-HT analysis, 18.4% of respondents reported having persistent loss of smell. This, Dr. Frasnelli said, adds to evidence from self-reported responses and suggests that in some cases, the problem is more than senses not returning to normal.
“From the questionnaires, roughly 50% said their sense of smell is still not back to normal, and when we look at the CD home test, we see that almost 20% of subjects indeed have pretty strong impairment of their sense of smell,” he said.
The results showed no sex differences, although Dr. Frasnelli noted that most of the sample were women. “It’s tricky to look at the data with regard to sex because it’s a bit skewed,” he said.
Male respondents were older than female participants, but there was no difference in impairment between age groups. Dr. Frasnelli said this was “quite interesting,” inasmuch as older people usually lose some sense of smell.
The researchers have not yet examined whether the results differ by type of health care worker.
They also have not examined in detail whether infection severity affects the risk for extended olfactory impairment. Although some research suggests that the problem with smell is more common in less severe cases, Dr. Frasnelli noted this could be because loss of smell is not a huge problem for patients battling grave health problems.
As for other symptoms, many respondents reported lingering fatigue; some reported debilitating fatigue, said Dr. Frasnelli. However, he cautioned that this is difficult to interpret, because the participants were health care workers, many of whom returned to work during the pandemic and perhaps had not fully rested.
He also noted that he and his colleagues have not “made the link” between impaired smell and the degree of fatigue.
The COVID-19 virus appears to attack supporting sustentacular cells in the olfactory epithelium, not nerve cells.
“Right now, it seems that the smell problem is not a central nervous system problem but a peripheral problem,” said Dr. Frasnelli. “But we don’t know for sure; it may be that the virus somehow gets into the brain and some symptoms are caused by the effects of the infection on the brain.”
The researchers will extend their research with another questionnaire to assess senses 10-12 months after COVID-19.
Limitations of the study include the subjective nature of the smell and taste ratings and the single time point at which data were collected.
Confirmatory findings
Commenting on the research in an interview, Thomas Hummel, MD, professor, smell and taste clinic, department of otorhinolaryngology, Technische Universität Dresden (Germany), said the new results regarding loss of smell after COVID-19 are “very congruent” with what he and his colleagues have observed.
Research shows that up to one in five of those infected with SARS-CoV-2 experience olfactory loss. “While the numbers may vary a bit from study to study or lab to lab, I think 5% to 20% of post–COVID-19 patients exhibit long-term olfactory loss,” Dr. Hummel said.
His group has observed that “many more are not back to normal,” which conforms with what Dr. Frasnelli’s study reveals, said Dr. Hummel.
Also commenting on the research, Kenneth L. Tyler, MD, professor of neurology, University of Colorado at Denver, Aurora, and a fellow of the American Academy of Neurology, said the study was relatively large and the results “interesting.”
Although it “provides more evidence there’s a subset of patients with symptoms even well past the acute phase” of COVID-19, the results are “mostly confirmatory” and include “nothing super surprising,” Dr. Tyler said in an interview.
However, the investigators did attempt to make the study “a little more quantitative” and “to confirm the self-reporting with their validated CD home test,” he said.
Dr. Tyler wondered how representative the sample was and whether the study drew more participants with impaired senses. “If I had a loss of smell or taste, maybe I would be more likely to respond to such a survey,” he said.
He also noted the difficulty of separating loss of smell from loss of taste.
“If you lose your sense of smell, things don’t taste right, so it can be confounding as to how to separate out those two,” he noted.
The study was supported by the Foundation of the Université du Québec à Trois-Rivières and the Province of Quebec. Dr. Frasnelli has received royalties from Styriabooks in Austria for a book on olfaction published in 2019 and has received honoraria for speaking engagements. Dr. Hummel and Dr. Tyler have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
The findings illustrate that olfactory problems are common not only during the acute COVID-19 phase but also “in the long run” and that these problems should be “taken into consideration” when following up these patients, study investigator Johannes Frasnelli, MD, professor, department of anatomy, Université du Québec à Trois-Rivières, said in an interview.
Loss of the sense of smell can affect quality of life because it affects eating and drinking, and may even be dangerous, said Dr. Frasnelli. “If your sense of smell is impaired, you may unknowingly eat spoiled food, or you may not smell smoke or gas in your home,” he said. In addition, Dr. Frasnelli noted that an impaired sense of smell is associated with higher rates of depression. The findings will be presented at the annual meeting of the American Academy of Neurology in April.
‘Striking’ finding
Research shows that about 60% of patients with COVID-19 lose their sense of smell to some degree during the acute phase of the disease. “But we wanted to go further and look at the longer-term effects of loss of smell and taste,” said Dr. Frasnelli.
The analysis included 813 health care workers in the province of Quebec. For all the patients, SARS-CoV-2 infection was confirmed through testing with a nasopharyngeal viral swab.
Participants completed a 64-item online questionnaire that asked about three senses: olfactory; gustatory, which includes tastes such as sweet, sour, bitter, salty, savory and umami; and trigeminal, which includes sensations such as spiciness of hot peppers and “coolness” of mint.
They were asked to rate these on a scale of 0 (no perception) to 10 (very strong perception) before the infection, during the infection, and currently. They were also asked about other symptoms, including fatigue.
Most respondents had been infected in the first wave of the virus in March and April of 2020 and responded to the questionnaire an average of 5 months later.
The vast majority of respondents (84.1%) were women, which Dr. Frasnelli said was not surprising because women predominate in the health care field.
The analysis showed that average smell ratings were 8.98 before infection, 2.85 during the acute phase, and 7.41 when respondents answered the questionnaire. The sense of taste was less affected and recovered faster than did the sense of smell. Results for taste were 9.20 before infection, 3.59 during the acute phase, and 8.05 after COVID-19.
Among 580 respondents who indicated a compromised sense of smell during the acute phase, the average smell rating when answering the questionnaire was 6.89, compared to 9.03 before the infection. More than half (51.2%) reported not regaining full olfactory function.
The fact that the sense of smell had not returned to normal for half the participants so long after being infected is “novel and quite striking,” said Dr. Frasnelli.
However, he noted, this doesn’t necessarily mean all those with a compromised sense of smell “have huge problems.” In some cases, he said, the problem “is more subtle.”
Not a CNS problem?
Respondents also completed a chemosensory dysfunction home test (CD-HT). They were asked to prepare common household food items, such as peanut butter, sugar, salt, and vinegar, in a particular way – for example, to add sugar or salt to water – and provide feedback on how they smell and taste.
For this CD-HT analysis, 18.4% of respondents reported having persistent loss of smell. This, Dr. Frasnelli said, adds to evidence from self-reported responses and suggests that in some cases, the problem is more than senses not returning to normal.
“From the questionnaires, roughly 50% said their sense of smell is still not back to normal, and when we look at the CD home test, we see that almost 20% of subjects indeed have pretty strong impairment of their sense of smell,” he said.
The results showed no sex differences, although Dr. Frasnelli noted that most of the sample were women. “It’s tricky to look at the data with regard to sex because it’s a bit skewed,” he said.
Male respondents were older than female participants, but there was no difference in impairment between age groups. Dr. Frasnelli said this was “quite interesting,” inasmuch as older people usually lose some sense of smell.
The researchers have not yet examined whether the results differ by type of health care worker.
They also have not examined in detail whether infection severity affects the risk for extended olfactory impairment. Although some research suggests that the problem with smell is more common in less severe cases, Dr. Frasnelli noted this could be because loss of smell is not a huge problem for patients battling grave health problems.
As for other symptoms, many respondents reported lingering fatigue; some reported debilitating fatigue, said Dr. Frasnelli. However, he cautioned that this is difficult to interpret, because the participants were health care workers, many of whom returned to work during the pandemic and perhaps had not fully rested.
He also noted that he and his colleagues have not “made the link” between impaired smell and the degree of fatigue.
The COVID-19 virus appears to attack supporting sustentacular cells in the olfactory epithelium, not nerve cells.
“Right now, it seems that the smell problem is not a central nervous system problem but a peripheral problem,” said Dr. Frasnelli. “But we don’t know for sure; it may be that the virus somehow gets into the brain and some symptoms are caused by the effects of the infection on the brain.”
The researchers will extend their research with another questionnaire to assess senses 10-12 months after COVID-19.
Limitations of the study include the subjective nature of the smell and taste ratings and the single time point at which data were collected.
Confirmatory findings
Commenting on the research in an interview, Thomas Hummel, MD, professor, smell and taste clinic, department of otorhinolaryngology, Technische Universität Dresden (Germany), said the new results regarding loss of smell after COVID-19 are “very congruent” with what he and his colleagues have observed.
Research shows that up to one in five of those infected with SARS-CoV-2 experience olfactory loss. “While the numbers may vary a bit from study to study or lab to lab, I think 5% to 20% of post–COVID-19 patients exhibit long-term olfactory loss,” Dr. Hummel said.
His group has observed that “many more are not back to normal,” which conforms with what Dr. Frasnelli’s study reveals, said Dr. Hummel.
Also commenting on the research, Kenneth L. Tyler, MD, professor of neurology, University of Colorado at Denver, Aurora, and a fellow of the American Academy of Neurology, said the study was relatively large and the results “interesting.”
Although it “provides more evidence there’s a subset of patients with symptoms even well past the acute phase” of COVID-19, the results are “mostly confirmatory” and include “nothing super surprising,” Dr. Tyler said in an interview.
However, the investigators did attempt to make the study “a little more quantitative” and “to confirm the self-reporting with their validated CD home test,” he said.
Dr. Tyler wondered how representative the sample was and whether the study drew more participants with impaired senses. “If I had a loss of smell or taste, maybe I would be more likely to respond to such a survey,” he said.
He also noted the difficulty of separating loss of smell from loss of taste.
“If you lose your sense of smell, things don’t taste right, so it can be confounding as to how to separate out those two,” he noted.
The study was supported by the Foundation of the Université du Québec à Trois-Rivières and the Province of Quebec. Dr. Frasnelli has received royalties from Styriabooks in Austria for a book on olfaction published in 2019 and has received honoraria for speaking engagements. Dr. Hummel and Dr. Tyler have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Strep A and tic worsening: Final word?
Exposure to Group A streptococcus (GAS) does not appear to worsen symptoms of Tourette syndrome and other chronic tic disorders (CTDs) in children and adolescents, new research suggests.
Investigators studied over 700 children and teenagers with CTDs, one-third of whom also had attention deficit hyperactivity disorder and one-third who had obsessive-compulsive disorder (OCD).
The youngsters were followed for an average of 16 months and evaluated at 4-month intervals to see if they were infected with GAS. Tic severity was monitored through telephone interviews, in-person visits, and parental reports.
A little less than half the children experienced worsening of tics during the study period, but the researchers found no association between these exacerbations and GAS exposure.
There was also no link between GAS and worsening OCD. However, researchers did find an association between GAS exposure and an increase in hyperactivity and impulsivity in patients with ADHD.
“This study does not support GAS exposures as contributing factors for tic exacerbations in children with CTD,” the authors note.
“Specific work-up or active management of GAS infections is unlikely to help modifying the course of tics in CTD and is therefore not recommended,” they conclude.
The study was published online in Neurology.
‘Intense debate’
The association between GAS and CTD stems from the description of Pediatric Autoimmune Neuropsychiatric Disorders Associated with Streptococcal infection (PANDAS) – a condition that is now incorporated in the pediatric acute neuropsychiatric syndromes (PANS), the authors note. Tics constitute an “accompanying feature” of this condition.
However, neither population-based nor longitudinal clinical studies “could definitely establish if tic exacerbations in CTD are associated with GAS infections,” they note.
“The link between streptococcus and tics in children is still a matter of intense debate,” said study author Davide Martino, MD, PhD, director of the Movement Disorders Program at the University of Calgary (Alta.), in a press release.
“We wanted to look at that question, as well as a possible link between strep and behavioral symptoms like obsessive-compulsive disorder and attention deficit hyperactivity disorder,” he said.
The researchers followed 715 children with CTD (mean age 10.7 years, 76.8% male) who were drawn from 16 specialist clinics in nine countries. Almost all (90.8%) had a diagnosis of Tourette syndrome (TS); 31.7% had OCD, and 36.1% had ADHD.
Participants received a throat swab at baseline, and of these, 8.4% tested positive for GAS.
Participants were evaluated over a 16- to 18-month period, consisting of:
- Face-to-face interviews and collection of throat swabs and serum at 4-month intervals.
- Telephone interviews at 4-month intervals, which took place at 2 months between study visit.
- Weekly diaries: Parents were asked to indicate any worsening of tics and focus on detecting the earliest possible tic exacerbation.
Beyond the regularly scheduled visits, parents were instructed to report, by phone or email, any noticeable increase in tic severity and then attend an in-person visit.
Tic exacerbations were defined as an increase of greater than or equal to 6 points on the Yale Global Tic Severity Scale-Total Tic Severity Score (YGTSS-TTS), compared with the previous assessment.
OCD and ADHD symptoms were assessed according to the Yale-Brown Obsessive-Compulsive Scale and the parent-reported Swanson, Nolan, and Pelham-IV (SNAP-IV) questionnaire.
The researchers divided GAS exposures into four categories: new definite exposure; new possible exposure; ongoing definite exposure; and ongoing possible exposure.
Unlikely trigger
During the follow-up period, 43.1% (n = 308) of participants experienced tic exacerbations. Of these, 218 participants experienced one exacerbation, while 90 participants experienced two, three, or four exacerbations.
The researchers did not find a significant association between GAS exposure status and tic exacerbation.
Participants who did develop a GAS-associated exacerbation (n = 49) were younger at study exit (9.63 vs. 11.4 years, P < .0001) and were more likely to be male (46/49 vs. 210/259, Fisher’s = .035), compared with participants who developed a non-GAS-associated tic exacerbation (n = 259).
Additional analyses were adjusted for sex, age at onset, exposure to psychotropic medications, exposures to antibiotics, geographical regions, and number of visits in the time interval of interest. These analyses continued to yield no significant association between new or ongoing concurrent GAS exposure episodes and tic exacerbation events.
Of the children in the study, 103 had a positive throat swab, indicating a new definite GAS exposure, whereas 46 had a positive throat swab indicating an ongoing definite exposure (n = 149 visits). Of these visits, only 20 corresponded to tic exacerbations.
There was also no association between GAS exposure and OCD symptom severity. However, it was associated with longitudinal changes (between 17% and 21%, depending on GAS exposure definition) in the severity of hyperactivity-impulsivity symptoms in children with ADHD.
“It is known that immune activation may concur with tic severity in youth with CTDs and that psychosocial stress levels may predict short-term future tic severity in these patients,” the authors write.
“Our findings suggest that GAS is unlikely to be the main trigger for immune activation in these patients,” they add.
Brick or cornerstone?
Commenting on the study for this news organization, Margo Thienemann, MD, clinical professor of psychiatry, Stanford (Calif.) University, said that in the clinic population they treat, GAS, other pathogens, and other stresses can “each be associated with PANS symptom exacerbations.”
However, these “would not be likely to cause PANS symptoms exacerbations in the vast majority of individuals, only individuals with genetic backgrounds and immunologic dysfunctions creating susceptibility,” said Dr. Thienemann, who also directs the Pediatric Acute-Onset Neuropsychiatric Syndrome (PANS) Clinic at Stanford Children’s Health. She was not involved with the study.
In an accompanying editorial, Andrea Cavanna, MD, PhD, honorary reader in neuropsychiatry, Birmingham (England) Medical School and Keith Coffman, MD, director, Tourette Syndrome Center of Excellence, Children’s Mercy Hospital, Kansas City, Mo., suggest that perhaps the “interaction of psychosocial stress and GAS infections contributes more to tic exacerbation than psychosocial stress alone.”
“Time will tell whether this study stands as another brick – a cornerstone? – in the wall that separates streptococcus from tics,” they write.
The study was supported by the European Union’s Seventh Framework Program. Dr. Martino has received honoraria for lecturing from the Movement Disorders Society, Tourette Syndrome Association of America, and Dystonia Medical Research Foundation Canada; research funding support from Dystonia Medical Research Foundation Canada, the University of Calgary (Alta.), the Michael P. Smith Family, the Owerko Foundation, Ipsen Corporate, the Parkinson Association of Alberta, and the Canadian Institutes for Health Research; and royalties from Springer-Verlag. The other authors’ disclosures are listed in the original article. Dr. Cavanna, Dr. Coffman, and Dr. Thienemann have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Exposure to Group A streptococcus (GAS) does not appear to worsen symptoms of Tourette syndrome and other chronic tic disorders (CTDs) in children and adolescents, new research suggests.
Investigators studied over 700 children and teenagers with CTDs, one-third of whom also had attention deficit hyperactivity disorder and one-third who had obsessive-compulsive disorder (OCD).
The youngsters were followed for an average of 16 months and evaluated at 4-month intervals to see if they were infected with GAS. Tic severity was monitored through telephone interviews, in-person visits, and parental reports.
A little less than half the children experienced worsening of tics during the study period, but the researchers found no association between these exacerbations and GAS exposure.
There was also no link between GAS and worsening OCD. However, researchers did find an association between GAS exposure and an increase in hyperactivity and impulsivity in patients with ADHD.
“This study does not support GAS exposures as contributing factors for tic exacerbations in children with CTD,” the authors note.
“Specific work-up or active management of GAS infections is unlikely to help modifying the course of tics in CTD and is therefore not recommended,” they conclude.
The study was published online in Neurology.
‘Intense debate’
The association between GAS and CTD stems from the description of Pediatric Autoimmune Neuropsychiatric Disorders Associated with Streptococcal infection (PANDAS) – a condition that is now incorporated in the pediatric acute neuropsychiatric syndromes (PANS), the authors note. Tics constitute an “accompanying feature” of this condition.
However, neither population-based nor longitudinal clinical studies “could definitely establish if tic exacerbations in CTD are associated with GAS infections,” they note.
“The link between streptococcus and tics in children is still a matter of intense debate,” said study author Davide Martino, MD, PhD, director of the Movement Disorders Program at the University of Calgary (Alta.), in a press release.
“We wanted to look at that question, as well as a possible link between strep and behavioral symptoms like obsessive-compulsive disorder and attention deficit hyperactivity disorder,” he said.
The researchers followed 715 children with CTD (mean age 10.7 years, 76.8% male) who were drawn from 16 specialist clinics in nine countries. Almost all (90.8%) had a diagnosis of Tourette syndrome (TS); 31.7% had OCD, and 36.1% had ADHD.
Participants received a throat swab at baseline, and of these, 8.4% tested positive for GAS.
Participants were evaluated over a 16- to 18-month period, consisting of:
- Face-to-face interviews and collection of throat swabs and serum at 4-month intervals.
- Telephone interviews at 4-month intervals, which took place at 2 months between study visit.
- Weekly diaries: Parents were asked to indicate any worsening of tics and focus on detecting the earliest possible tic exacerbation.
Beyond the regularly scheduled visits, parents were instructed to report, by phone or email, any noticeable increase in tic severity and then attend an in-person visit.
Tic exacerbations were defined as an increase of greater than or equal to 6 points on the Yale Global Tic Severity Scale-Total Tic Severity Score (YGTSS-TTS), compared with the previous assessment.
OCD and ADHD symptoms were assessed according to the Yale-Brown Obsessive-Compulsive Scale and the parent-reported Swanson, Nolan, and Pelham-IV (SNAP-IV) questionnaire.
The researchers divided GAS exposures into four categories: new definite exposure; new possible exposure; ongoing definite exposure; and ongoing possible exposure.
Unlikely trigger
During the follow-up period, 43.1% (n = 308) of participants experienced tic exacerbations. Of these, 218 participants experienced one exacerbation, while 90 participants experienced two, three, or four exacerbations.
The researchers did not find a significant association between GAS exposure status and tic exacerbation.
Participants who did develop a GAS-associated exacerbation (n = 49) were younger at study exit (9.63 vs. 11.4 years, P < .0001) and were more likely to be male (46/49 vs. 210/259, Fisher’s = .035), compared with participants who developed a non-GAS-associated tic exacerbation (n = 259).
Additional analyses were adjusted for sex, age at onset, exposure to psychotropic medications, exposures to antibiotics, geographical regions, and number of visits in the time interval of interest. These analyses continued to yield no significant association between new or ongoing concurrent GAS exposure episodes and tic exacerbation events.
Of the children in the study, 103 had a positive throat swab, indicating a new definite GAS exposure, whereas 46 had a positive throat swab indicating an ongoing definite exposure (n = 149 visits). Of these visits, only 20 corresponded to tic exacerbations.
There was also no association between GAS exposure and OCD symptom severity. However, it was associated with longitudinal changes (between 17% and 21%, depending on GAS exposure definition) in the severity of hyperactivity-impulsivity symptoms in children with ADHD.
“It is known that immune activation may concur with tic severity in youth with CTDs and that psychosocial stress levels may predict short-term future tic severity in these patients,” the authors write.
“Our findings suggest that GAS is unlikely to be the main trigger for immune activation in these patients,” they add.
Brick or cornerstone?
Commenting on the study for this news organization, Margo Thienemann, MD, clinical professor of psychiatry, Stanford (Calif.) University, said that in the clinic population they treat, GAS, other pathogens, and other stresses can “each be associated with PANS symptom exacerbations.”
However, these “would not be likely to cause PANS symptoms exacerbations in the vast majority of individuals, only individuals with genetic backgrounds and immunologic dysfunctions creating susceptibility,” said Dr. Thienemann, who also directs the Pediatric Acute-Onset Neuropsychiatric Syndrome (PANS) Clinic at Stanford Children’s Health. She was not involved with the study.
In an accompanying editorial, Andrea Cavanna, MD, PhD, honorary reader in neuropsychiatry, Birmingham (England) Medical School and Keith Coffman, MD, director, Tourette Syndrome Center of Excellence, Children’s Mercy Hospital, Kansas City, Mo., suggest that perhaps the “interaction of psychosocial stress and GAS infections contributes more to tic exacerbation than psychosocial stress alone.”
“Time will tell whether this study stands as another brick – a cornerstone? – in the wall that separates streptococcus from tics,” they write.
The study was supported by the European Union’s Seventh Framework Program. Dr. Martino has received honoraria for lecturing from the Movement Disorders Society, Tourette Syndrome Association of America, and Dystonia Medical Research Foundation Canada; research funding support from Dystonia Medical Research Foundation Canada, the University of Calgary (Alta.), the Michael P. Smith Family, the Owerko Foundation, Ipsen Corporate, the Parkinson Association of Alberta, and the Canadian Institutes for Health Research; and royalties from Springer-Verlag. The other authors’ disclosures are listed in the original article. Dr. Cavanna, Dr. Coffman, and Dr. Thienemann have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Exposure to Group A streptococcus (GAS) does not appear to worsen symptoms of Tourette syndrome and other chronic tic disorders (CTDs) in children and adolescents, new research suggests.
Investigators studied over 700 children and teenagers with CTDs, one-third of whom also had attention deficit hyperactivity disorder and one-third who had obsessive-compulsive disorder (OCD).
The youngsters were followed for an average of 16 months and evaluated at 4-month intervals to see if they were infected with GAS. Tic severity was monitored through telephone interviews, in-person visits, and parental reports.
A little less than half the children experienced worsening of tics during the study period, but the researchers found no association between these exacerbations and GAS exposure.
There was also no link between GAS and worsening OCD. However, researchers did find an association between GAS exposure and an increase in hyperactivity and impulsivity in patients with ADHD.
“This study does not support GAS exposures as contributing factors for tic exacerbations in children with CTD,” the authors note.
“Specific work-up or active management of GAS infections is unlikely to help modifying the course of tics in CTD and is therefore not recommended,” they conclude.
The study was published online in Neurology.
‘Intense debate’
The association between GAS and CTD stems from the description of Pediatric Autoimmune Neuropsychiatric Disorders Associated with Streptococcal infection (PANDAS) – a condition that is now incorporated in the pediatric acute neuropsychiatric syndromes (PANS), the authors note. Tics constitute an “accompanying feature” of this condition.
However, neither population-based nor longitudinal clinical studies “could definitely establish if tic exacerbations in CTD are associated with GAS infections,” they note.
“The link between streptococcus and tics in children is still a matter of intense debate,” said study author Davide Martino, MD, PhD, director of the Movement Disorders Program at the University of Calgary (Alta.), in a press release.
“We wanted to look at that question, as well as a possible link between strep and behavioral symptoms like obsessive-compulsive disorder and attention deficit hyperactivity disorder,” he said.
The researchers followed 715 children with CTD (mean age 10.7 years, 76.8% male) who were drawn from 16 specialist clinics in nine countries. Almost all (90.8%) had a diagnosis of Tourette syndrome (TS); 31.7% had OCD, and 36.1% had ADHD.
Participants received a throat swab at baseline, and of these, 8.4% tested positive for GAS.
Participants were evaluated over a 16- to 18-month period, consisting of:
- Face-to-face interviews and collection of throat swabs and serum at 4-month intervals.
- Telephone interviews at 4-month intervals, which took place at 2 months between study visit.
- Weekly diaries: Parents were asked to indicate any worsening of tics and focus on detecting the earliest possible tic exacerbation.
Beyond the regularly scheduled visits, parents were instructed to report, by phone or email, any noticeable increase in tic severity and then attend an in-person visit.
Tic exacerbations were defined as an increase of greater than or equal to 6 points on the Yale Global Tic Severity Scale-Total Tic Severity Score (YGTSS-TTS), compared with the previous assessment.
OCD and ADHD symptoms were assessed according to the Yale-Brown Obsessive-Compulsive Scale and the parent-reported Swanson, Nolan, and Pelham-IV (SNAP-IV) questionnaire.
The researchers divided GAS exposures into four categories: new definite exposure; new possible exposure; ongoing definite exposure; and ongoing possible exposure.
Unlikely trigger
During the follow-up period, 43.1% (n = 308) of participants experienced tic exacerbations. Of these, 218 participants experienced one exacerbation, while 90 participants experienced two, three, or four exacerbations.
The researchers did not find a significant association between GAS exposure status and tic exacerbation.
Participants who did develop a GAS-associated exacerbation (n = 49) were younger at study exit (9.63 vs. 11.4 years, P < .0001) and were more likely to be male (46/49 vs. 210/259, Fisher’s = .035), compared with participants who developed a non-GAS-associated tic exacerbation (n = 259).
Additional analyses were adjusted for sex, age at onset, exposure to psychotropic medications, exposures to antibiotics, geographical regions, and number of visits in the time interval of interest. These analyses continued to yield no significant association between new or ongoing concurrent GAS exposure episodes and tic exacerbation events.
Of the children in the study, 103 had a positive throat swab, indicating a new definite GAS exposure, whereas 46 had a positive throat swab indicating an ongoing definite exposure (n = 149 visits). Of these visits, only 20 corresponded to tic exacerbations.
There was also no association between GAS exposure and OCD symptom severity. However, it was associated with longitudinal changes (between 17% and 21%, depending on GAS exposure definition) in the severity of hyperactivity-impulsivity symptoms in children with ADHD.
“It is known that immune activation may concur with tic severity in youth with CTDs and that psychosocial stress levels may predict short-term future tic severity in these patients,” the authors write.
“Our findings suggest that GAS is unlikely to be the main trigger for immune activation in these patients,” they add.
Brick or cornerstone?
Commenting on the study for this news organization, Margo Thienemann, MD, clinical professor of psychiatry, Stanford (Calif.) University, said that in the clinic population they treat, GAS, other pathogens, and other stresses can “each be associated with PANS symptom exacerbations.”
However, these “would not be likely to cause PANS symptoms exacerbations in the vast majority of individuals, only individuals with genetic backgrounds and immunologic dysfunctions creating susceptibility,” said Dr. Thienemann, who also directs the Pediatric Acute-Onset Neuropsychiatric Syndrome (PANS) Clinic at Stanford Children’s Health. She was not involved with the study.
In an accompanying editorial, Andrea Cavanna, MD, PhD, honorary reader in neuropsychiatry, Birmingham (England) Medical School and Keith Coffman, MD, director, Tourette Syndrome Center of Excellence, Children’s Mercy Hospital, Kansas City, Mo., suggest that perhaps the “interaction of psychosocial stress and GAS infections contributes more to tic exacerbation than psychosocial stress alone.”
“Time will tell whether this study stands as another brick – a cornerstone? – in the wall that separates streptococcus from tics,” they write.
The study was supported by the European Union’s Seventh Framework Program. Dr. Martino has received honoraria for lecturing from the Movement Disorders Society, Tourette Syndrome Association of America, and Dystonia Medical Research Foundation Canada; research funding support from Dystonia Medical Research Foundation Canada, the University of Calgary (Alta.), the Michael P. Smith Family, the Owerko Foundation, Ipsen Corporate, the Parkinson Association of Alberta, and the Canadian Institutes for Health Research; and royalties from Springer-Verlag. The other authors’ disclosures are listed in the original article. Dr. Cavanna, Dr. Coffman, and Dr. Thienemann have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Short sleep predicts incident dementia and all-cause mortality
More evidence has emerged linking sleep deficiency, dementia, and mortality.
“Sleep disturbance and insufficiency have been shown to be associated with both the development and progression of Alzheimer’s disease and with all-cause mortality,” wrote Rebecca S. Robbins, PhD, of Brigham and Women’s Hospital, Boston, and colleagues. However, research on this topic has yielded conflicting results, and “few studies have included a comprehensive set of sleep characteristics in a single examination of incident dementia and all-cause mortality.”
In a study published in Aging, the researchers identified 2,812 adults aged 65 years and older from the National Health and Aging Trends Study (NHATS), a nationally representative longitudinal study of Medicare beneficiaries aged 65 years and older in the United States.
Participants completed surveys about sleep disturbance and duration in 2013 (1,575 individuals) and in 2014 (1,237 individuals), and the researchers examined the relationship between sleep disturbance and deficiency and incident dementia and all-cause mortality over the next 5 years. The average age of the study participants was 76.9 years, 60% were women, and 72% were White.
Overall, approximately 60% of the participants reported never or rarely having problems with alertness, approximately half said that they rarely or never napped, and more than half said they fell asleep in 15 minutes or less. Approximately 70% rated their sleep quality as good or very good, and more than 90% said they rarely or never snored.
The researchers examined the relationships between sleep characteristics and the development of incident dementia over 5 years. In a fully adjusted Cox multivariate analysis, individuals who slept 5 hours or less per night had approximately twice the risk for incident dementia as those who slept longer (hazard ratio, 2.04); risk of dementia also was higher among those who took 30 minutes or longer to fall asleep (HR, 1.45).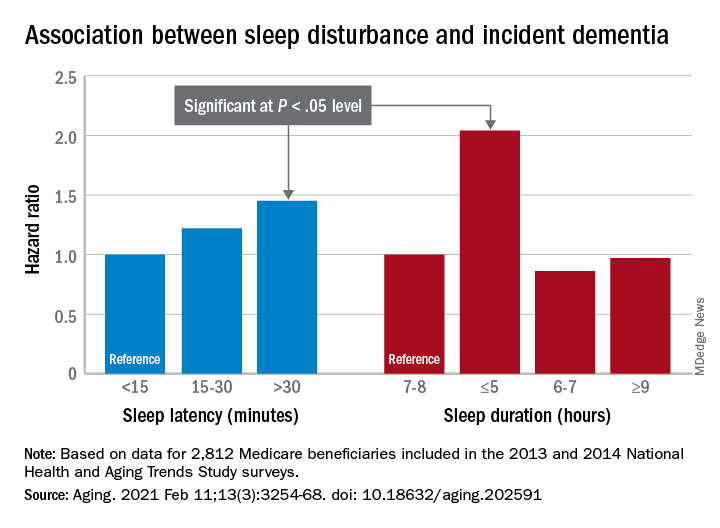
In addition, the risk of all-cause mortality was significantly higher among individuals who reported difficulty maintaining alertness some days or most days/every day (HR, 1.49 and HR, 1.65, respectively), routinely napping some days or most days/every day (HR, 1.38 and HR, 1.73, respectively), poor or very poor sleep quality (HR, 1.75), and sleeping 5 hours or less each night (HR, 2.38).
The study findings were limited by several factors including a population representing only one-quarter of the NHATS cohort, which prevented nationally representative estimates, the availability of only 2 years of sleep data, and small sample size for certain response categories, the researchers noted.
However, “our study offers a contribution to the literature on sleep among aging populations in its assessment of incident dementia and all-cause mortality and a range of sleep characteristics among older adults,” they said. In particular, “short sleep duration was a strong predictor of both incident dementia and all-cause mortality, suggesting this may be a sleep characteristic that is important – over and above the other predictors – of adverse outcomes among older adults,” and future areas for research include the development of novel behavioral interventions to improve sleep in this population.
The study was supported in part by the National Institute for Occupational Safety and Health; the National Heart, Lung, and Blood Institute; the National Institute on Aging; and the Brigham Research Institute Fund to Sustain Research Excellence. Lead author Dr. Robbins disclosed fees from Denihan Hospitality, Rituals Cosmetics, Dagmejan, Asystem, and SleepCycle. Several coauthors disclosed relationships with multiple pharmaceutical companies, and support from various philanthropic organizations.
More evidence has emerged linking sleep deficiency, dementia, and mortality.
“Sleep disturbance and insufficiency have been shown to be associated with both the development and progression of Alzheimer’s disease and with all-cause mortality,” wrote Rebecca S. Robbins, PhD, of Brigham and Women’s Hospital, Boston, and colleagues. However, research on this topic has yielded conflicting results, and “few studies have included a comprehensive set of sleep characteristics in a single examination of incident dementia and all-cause mortality.”
In a study published in Aging, the researchers identified 2,812 adults aged 65 years and older from the National Health and Aging Trends Study (NHATS), a nationally representative longitudinal study of Medicare beneficiaries aged 65 years and older in the United States.
Participants completed surveys about sleep disturbance and duration in 2013 (1,575 individuals) and in 2014 (1,237 individuals), and the researchers examined the relationship between sleep disturbance and deficiency and incident dementia and all-cause mortality over the next 5 years. The average age of the study participants was 76.9 years, 60% were women, and 72% were White.
Overall, approximately 60% of the participants reported never or rarely having problems with alertness, approximately half said that they rarely or never napped, and more than half said they fell asleep in 15 minutes or less. Approximately 70% rated their sleep quality as good or very good, and more than 90% said they rarely or never snored.
The researchers examined the relationships between sleep characteristics and the development of incident dementia over 5 years. In a fully adjusted Cox multivariate analysis, individuals who slept 5 hours or less per night had approximately twice the risk for incident dementia as those who slept longer (hazard ratio, 2.04); risk of dementia also was higher among those who took 30 minutes or longer to fall asleep (HR, 1.45).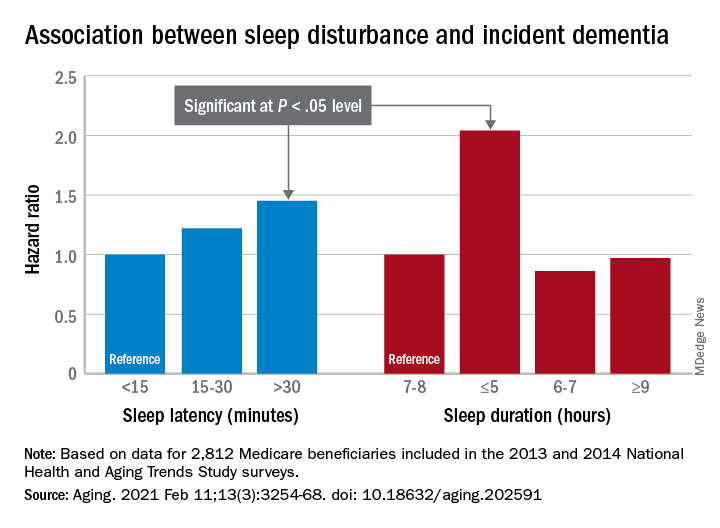
In addition, the risk of all-cause mortality was significantly higher among individuals who reported difficulty maintaining alertness some days or most days/every day (HR, 1.49 and HR, 1.65, respectively), routinely napping some days or most days/every day (HR, 1.38 and HR, 1.73, respectively), poor or very poor sleep quality (HR, 1.75), and sleeping 5 hours or less each night (HR, 2.38).
The study findings were limited by several factors including a population representing only one-quarter of the NHATS cohort, which prevented nationally representative estimates, the availability of only 2 years of sleep data, and small sample size for certain response categories, the researchers noted.
However, “our study offers a contribution to the literature on sleep among aging populations in its assessment of incident dementia and all-cause mortality and a range of sleep characteristics among older adults,” they said. In particular, “short sleep duration was a strong predictor of both incident dementia and all-cause mortality, suggesting this may be a sleep characteristic that is important – over and above the other predictors – of adverse outcomes among older adults,” and future areas for research include the development of novel behavioral interventions to improve sleep in this population.
The study was supported in part by the National Institute for Occupational Safety and Health; the National Heart, Lung, and Blood Institute; the National Institute on Aging; and the Brigham Research Institute Fund to Sustain Research Excellence. Lead author Dr. Robbins disclosed fees from Denihan Hospitality, Rituals Cosmetics, Dagmejan, Asystem, and SleepCycle. Several coauthors disclosed relationships with multiple pharmaceutical companies, and support from various philanthropic organizations.
More evidence has emerged linking sleep deficiency, dementia, and mortality.
“Sleep disturbance and insufficiency have been shown to be associated with both the development and progression of Alzheimer’s disease and with all-cause mortality,” wrote Rebecca S. Robbins, PhD, of Brigham and Women’s Hospital, Boston, and colleagues. However, research on this topic has yielded conflicting results, and “few studies have included a comprehensive set of sleep characteristics in a single examination of incident dementia and all-cause mortality.”
In a study published in Aging, the researchers identified 2,812 adults aged 65 years and older from the National Health and Aging Trends Study (NHATS), a nationally representative longitudinal study of Medicare beneficiaries aged 65 years and older in the United States.
Participants completed surveys about sleep disturbance and duration in 2013 (1,575 individuals) and in 2014 (1,237 individuals), and the researchers examined the relationship between sleep disturbance and deficiency and incident dementia and all-cause mortality over the next 5 years. The average age of the study participants was 76.9 years, 60% were women, and 72% were White.
Overall, approximately 60% of the participants reported never or rarely having problems with alertness, approximately half said that they rarely or never napped, and more than half said they fell asleep in 15 minutes or less. Approximately 70% rated their sleep quality as good or very good, and more than 90% said they rarely or never snored.
The researchers examined the relationships between sleep characteristics and the development of incident dementia over 5 years. In a fully adjusted Cox multivariate analysis, individuals who slept 5 hours or less per night had approximately twice the risk for incident dementia as those who slept longer (hazard ratio, 2.04); risk of dementia also was higher among those who took 30 minutes or longer to fall asleep (HR, 1.45).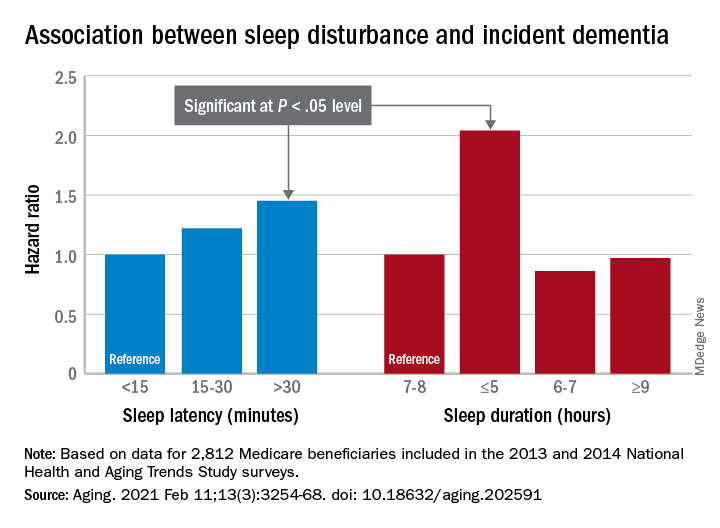
In addition, the risk of all-cause mortality was significantly higher among individuals who reported difficulty maintaining alertness some days or most days/every day (HR, 1.49 and HR, 1.65, respectively), routinely napping some days or most days/every day (HR, 1.38 and HR, 1.73, respectively), poor or very poor sleep quality (HR, 1.75), and sleeping 5 hours or less each night (HR, 2.38).
The study findings were limited by several factors including a population representing only one-quarter of the NHATS cohort, which prevented nationally representative estimates, the availability of only 2 years of sleep data, and small sample size for certain response categories, the researchers noted.
However, “our study offers a contribution to the literature on sleep among aging populations in its assessment of incident dementia and all-cause mortality and a range of sleep characteristics among older adults,” they said. In particular, “short sleep duration was a strong predictor of both incident dementia and all-cause mortality, suggesting this may be a sleep characteristic that is important – over and above the other predictors – of adverse outcomes among older adults,” and future areas for research include the development of novel behavioral interventions to improve sleep in this population.
The study was supported in part by the National Institute for Occupational Safety and Health; the National Heart, Lung, and Blood Institute; the National Institute on Aging; and the Brigham Research Institute Fund to Sustain Research Excellence. Lead author Dr. Robbins disclosed fees from Denihan Hospitality, Rituals Cosmetics, Dagmejan, Asystem, and SleepCycle. Several coauthors disclosed relationships with multiple pharmaceutical companies, and support from various philanthropic organizations.
FROM AGING











