User login
Understanding Psychosis in a Veteran With a History of Combat and Multiple Sclerosis (FULL)
A patient with significant combat history and previous diagnoses of multiple sclerosis and unspecified schizophrenia spectrum and other psychotic disorder was admitted with acute psychosis inconsistent with expected clinical presentations.
Multiple sclerosis (MS) is an immune-mediated neurodegenerative disease that affects > 700,000 people in the US.1 The hallmarks of MS pathology are axonal or neuronal loss, demyelination, and astrocytic gliosis. Of these, axonal or neuronal loss is the main underlying mechanism of permanent clinical disability.
MS also has been associated with an increased prevalence of psychiatric illnesses, with mood disorders affecting up to 40% to 60% of the population, and psychosis being reported in 2% to 4% of patients.2 The link between MS and mood disorders, including bipolar disorder and depression, was documented as early as 1926,with mood disorders hypothesized to be manifestations of central nervous system (CNS) inflammation.3 More recently, inflammation-driven microglia have been hypothesized to impair hippocampal connectivity and activate glucocorticoid-insensitive inflammatory cells that then overstimulate the hypothalamic-pituitary-adrenal axis.4,5
Although the prevalence of psychosis in patients with MS is significantly rarer, averaging between 2% and 4%.6 A Canadian study by Patten and colleagues reviewed data from 2.45 million residents of Alberta and found that those who identified as having MS had a 2% to 3% prevalence of psychosis compared with 0.5% to 1% in the general population.7 The connection between psychosis and MS, similar to that between mood disorders and MS, has been described as a common regional demyelination process. Supporting this, MS manifesting as psychosis has been found to present with distinct magnetic resonance imaging (MRI) findings, such as diffuse periventricular lesions.8 Still, no conclusive criteria have been developed to distinguish MS presenting as psychosis from a primary psychiatric illness, such as schizophrenia.
In patients with combat history, it is possible that both neurodegenerative and psychotic symptoms can be explained by autoantibody formation in response to toxin exposure. When soldiers were deployed to Iraq and Afghanistan, they may have been exposed to multiple toxicities, including depleted uranium, dust and fumes, and numerous infectious diseases.9 Gulf War illness (GWI) or chronic multisymptom illness (CMI) encompass a cluster of symptoms, such as chronic pain, chronic fatigue, irritable bowel syndrome, dermatitis, and seizures, as well as mental health issues such as depression and anxiety experienced following exposure to these combat environments.10,11
In light of this diagnostic uncertainty, the authors detail a case of a patient with significant combat history previously diagnosed with MS and unspecified schizophrenia spectrum and other psychotic disorder (USS & OPD) presenting with acute psychosis.
Case Presentation
A 35-year-old male veteran, with a history of MS, USS & OPD, posttraumatic stress disorder, and traumatic brain injuries (TBIs) was admitted to the psychiatric unit after being found by the police lying in the middle of a busy intersection, internally preoccupied. On admission, he reported a week of auditory hallucinations from birds with whom he had been communicating telepathically, and a recurrent visual hallucination of a tall man in white and purple robes. He had discontinued his antipsychotic medication, aripiprazole 10 mg, a few weeks prior for unknown reasons. He was brought to the hospital by ambulance, where he presented with disorganized thinking, tangential thought process, and active auditory and visual hallucinations. The differential diagnoses included USS & OPD, schizophrenia, schizoaffective disorder and ruled out substance-induced psychotic disorder, and psychosis as a manifestation of MS.
The patient had 2 psychotic episodes prior to this presentation. He was hospitalized for his first psychotic break in 2015 at age 32, when he had tailed another car “to come back to reality” and ended up in a motor vehicle accident. During that admission, he reported weeks of thought broadcasting, conspiratorial delusions, and racing thoughts. Two years later, he was admitted to a psychiatric intensive care unit for his second episode of severe psychosis. After several trials of different antipsychotic medications, his most recent pharmacologic regimen was aripiprazole 10 mg once daily.
His medical history was complicated by 2 TBIs, in November 2014 and January 2015, with normal computed tomography (CT) scans. He was diagnosed with MS in December 2017, when he presented with intractable emesis, left facial numbness, right upper extremity ataxia, nystagmus, and imbalance. An MRI scan revealed multifocal bilateral hypodensities in his periventricular, subcortical, and brain stem white matter. Multiple areas of hyperintensity were visualized, including in the right periatrial region and left brachium pontis. More than 5 oligoclonal bands on lumbar puncture confirmed the diagnosis.
He was treated with IV methylprednisolone followed by a 2-week prednisone taper. Within 1 week, he returned to the psychiatric unit with worsening symptoms and received a second dose of IV steroids and plasma exchange treatment. In the following months, he completed a course of rituximab infusions and physical therapy for his dysarthria, gait abnormality, and vision impairment.
His social history was notable for multiple first-degree relatives with schizophrenia. He reported a history of sexual and verbal abuse and attempted suicide once at age 13 years by hanging himself with a bathrobe. He left home at age 18 years to serve in the Marine Corps (2001-2006). His service included deployment to Afghanistan, where he received a purple heart. Upon his return, he received BA and MS degrees. He married and had 2 daughters but became estranged from his wife. By his most recent admission, he was unemployed and living with his half-sister.
On the first day of this most recent psychiatric hospitalization, he was restarted on aripiprazole 10 mg daily, and a medicine consult was sought to evaluate the progression of his MS. No new onset neurologic symptoms were noted, but he had possible residual lower extremity hyperreflexia and tandem gait incoordination. The episodes of psychotic and neurologic symptoms appeared independent, given that his psychiatric history preceded the onset of his MS.
The patient reported no visual hallucinations starting day 2, and he no longer endorsed auditory hallucinations by day 3. However, he continued to appear internally preoccupied and was noticed to be pacing around the unit. On day 4 he presented with newly pressured speech and flights of ideas, while his affect remained euthymic and his sleep stayed consistent. In combination with his ongoing pacing, his newfound symptoms were hypothesized to be possibly akathisia, an adverse effect (AE) of aripiprazole. As such, on day 5 his dose was lowered to 5 mg daily. He continued to report no hallucinations and demonstrated progressively increased emotional range. A MRI scan was done on day 6 in case a new lesion could be identified, suggesting a primary MS flare-up; however, the scan identified no enhancing lesions, indicating no ongoing demyelination. After a neurology consult corroborated this conclusion, he was discharged in stable condition on day 7.
As is the case with the majority of patients with MS-induced psychosis, he continued to have relapsing psychiatric disease even after MS treatment had been started. Unfortunately, because this patient had stopped taking his atypical antipsychotic medication several weeks prior to his hospitalization, we cannot clarify whether his psychosis stems from a primary psychiatric vs MS process.
Discussion
Presently, treatment preferences for MS-related psychosis are divided between atypical antipsychotics and glucocorticoids. Some suggest that the treatment remains similar between MS-related psychosis and primary psychotic disorders in that atypical antipsychotics are the standard of care.12 A variety of atypical antipsychotics have been used successfully in case reports, including zipradisone, risperidone, olanzapine, quetiapine, and aripiprazole.13,14 First-generation antipsychotics and other psychotropic drugs that can precipitate extra-pyramidal AEs are not recommended given their potential additive effect to motor deficits associated with MS.12 Alternatively, several case reports have found that MS-related psychotic symptoms respond to glucocorticoids more effectively, while cautioning that glucocorticoids can precipitate psychosis and depression.15,16 One review article found that 90% of patients who received corticosteroids saw an improvement in their psychotic symptoms.2
Finally, it is possible that our patient’s neuropsychiatric symptoms can be explained by autoantibody formation in response to toxin exposure during his time in Afghanistan. In a pilot study of veterans with GWI, Abou-Donia and colleagues found 2-to-9 fold increase in autoantibody reactivity levels of the following neuronal and glial-specific proteins relative to healthy controls: neurofilament triplet proteins, tubulin, microtubule-associated tau proteins, microtubule-associated protein-2, myelin basic protein, myelin-associated glycoprotein, glial fibrillary acidic protein, and calcium-calmodulin kinase II.17,18 Many of these autoantibodies are longstanding explicit markers for neurodegenerative disorders, given that they target proteins and antigens that support axonal transport and myelination. Still Gulf War veteran status has yet to be explicitly linked to an increased risk of MS,19 making this hypothesis less likely for our patient. Future research should address the clinical and therapeutic implications of different autoantibody levels in combat veterans with psychosis.
Conclusion
For patients with MS, mood disorder and psychotic symptoms should warrant a MRI given the possibility of a psychiatric manifestation of MS relapse. Ultimately, our patient’s presentation was inconsistent with the expected clinical presentations of both a primary psychotic disorder and psychosis as a manifestation of MS. His late age at his first psychotic break is atypical for primary psychotic disease, and the lack of MRI imaging done at his initial psychotic episodes cannot exclude a primary MS diagnosis. Still, his lack of MRI findings at his most recent hospitalization, negative symptomatology, and strong history of schizophrenia make a primary psychotic disorder likely.
Following his future clinical course will be necessary to determine the etiology of his psychotic episodes. Future episodes of psychosis with neurologic symptoms would suggest a primary MS diagnosis and potential benefit of immunosuppressant treatment, whereas repeated psychotic breaks with minimal temporal lobe involvement or demyelination as seen on MRI would be suspicious for separate MS and psychotic disease processes. Further research on treatment regimens for patients experiencing psychosis as a manifestation of MS is still necessary.
1. Wallin MT, Culpepper WJ, Campbell JD, et al. The prevalence of MS in the United States: A population-based estimate using health claims data. Neurology. 2019;92(10):e1029-e1040.
2. Camara-Lemarroy CR, Ibarra-Yruegas BE, Rodriguez-Gutierrez R, Berrios-Morales I, Ionete C, Riskind P. The varieties of psychosis in multiple sclerosis: a systematic review of cases. Mult Scler Relat Disord. 2017;12:9-14.
3. Cottrel SS, Wilson SA. The affective symptomatology of disseminated sclerosis: a study of 100 cases. J Neurol Psychopathology. 1926;7(25):1-30.
4. Johansson V, Lundholm C, Hillert J, et al. Multiple sclerosis and psychiatric disorders: comorbidity and sibling risk in a nationwide Swedish cohort. Mult Scler. 2014;20(14):1881-1891.
5. Rossi S, Studer V, Motta C, et al. Neuroinflammation drives anxiety and depression in relapsing-remitting multiple sclerosis. Neurology. 2017;89(13):1338-1347.
6. Gilberthorpe TG, O’Connell KE, Carolan A, et al. The spectrum of psychosis in multiple sclerosis: a clinical case series. Neuropsychiatric disease and treatment. 2017;13:303.
7. Patten SB, Svenson LW, Metz LM. Psychotic disorders in MS: population-based evidence of an association. Neurology 2005;65(7):1123-1125.
8. Kosmidis MH, Giannakou M, Messinis L, Papathanasopoulos P. Psychotic features associated with multiple sclerosis. Int Rev Psychiatry. 2010; 22(1):55-66.
9. US Department of Veterans Affairs. Public health: military exposures. https://www.publichealth.va.gov/exposures/. Updated April 16, 2019. Accessed May 13, 2019.
10. DeBeer BB, Davidson D, Meyer EC, Kimbrel NA, Gulliver SB, Morissette SB. The association between toxic exposures and chronic multisymptom illness in veterans of the wars of Iraq and Afghanistan. J Occup Environ Med. 2017;59(1):54-60.
11. Kang HK, Li B, Mahan CM, Eisen SA, Engel CC. Health of US veterans of 1991 Gulf War: a follow-up survey in 10 years. J Occup Environ Med. 2009;51(4):401-410.
12. Murphy R, O’Donoghue S, Counihan T, et al. Neuropsychiatric syndromes of multiple sclerosis. J Neurol Neurosurg Psychiatry. 2017;88(8):697-708.
13. Davids E, Hartwig U, Gastpar, M. Antipsychotic treatment of psychosis associated with multiple sclerosis. Prog Neuro Psychopharmacol Biol Psychiatry. 2004;28(4):743-744.
14. Lo Fermo S, Barone R, Patti F, et al. Outcome of psychiatric symptoms presenting at onset of multiple sclerosis: a retrospective study. Mult Scler. 2010;16(6):742-748.
15. Enderami A, Fouladi R, Hosseini HS. First-episode psychosis as the initial presentation of multiple sclerosis: a case report. Int Medical Case Rep J. 2018;11:73-76.
16. Fragoso YD, Frota ER, Lopes JS, et al. Severe depression, suicide attempts, and ideation during the use of interferon beta by patients with multiple sclerosis. Clin Neuropharmacol. 2010;33(6):312-316.
17. Abou-Donia MB, Conboy LA, Kokkotou E, et al. Screening for novel central nervous system biomarkers in veterans with Gulf War Illness. Neurotoxicol Teratol. 2017;61:36-46.
18. Abou-Donia MB, Lieberman A, Curtis L. Neural autoantibodies in patients with neurological symptoms and histories of chemical/mold exposures. Toxicol Ind Health. 2018;34(1):44-53.
19. Wallin MT, Kurtzke JF, Culpepper WJ, et al. Multiple sclerosis in Gulf War era veterans. 2. Military deployment and risk of multiple sclerosis in the first Gulf War. Neuroepidemiology. 2014;42(4):226-234.
A patient with significant combat history and previous diagnoses of multiple sclerosis and unspecified schizophrenia spectrum and other psychotic disorder was admitted with acute psychosis inconsistent with expected clinical presentations.
A patient with significant combat history and previous diagnoses of multiple sclerosis and unspecified schizophrenia spectrum and other psychotic disorder was admitted with acute psychosis inconsistent with expected clinical presentations.
Multiple sclerosis (MS) is an immune-mediated neurodegenerative disease that affects > 700,000 people in the US.1 The hallmarks of MS pathology are axonal or neuronal loss, demyelination, and astrocytic gliosis. Of these, axonal or neuronal loss is the main underlying mechanism of permanent clinical disability.
MS also has been associated with an increased prevalence of psychiatric illnesses, with mood disorders affecting up to 40% to 60% of the population, and psychosis being reported in 2% to 4% of patients.2 The link between MS and mood disorders, including bipolar disorder and depression, was documented as early as 1926,with mood disorders hypothesized to be manifestations of central nervous system (CNS) inflammation.3 More recently, inflammation-driven microglia have been hypothesized to impair hippocampal connectivity and activate glucocorticoid-insensitive inflammatory cells that then overstimulate the hypothalamic-pituitary-adrenal axis.4,5
Although the prevalence of psychosis in patients with MS is significantly rarer, averaging between 2% and 4%.6 A Canadian study by Patten and colleagues reviewed data from 2.45 million residents of Alberta and found that those who identified as having MS had a 2% to 3% prevalence of psychosis compared with 0.5% to 1% in the general population.7 The connection between psychosis and MS, similar to that between mood disorders and MS, has been described as a common regional demyelination process. Supporting this, MS manifesting as psychosis has been found to present with distinct magnetic resonance imaging (MRI) findings, such as diffuse periventricular lesions.8 Still, no conclusive criteria have been developed to distinguish MS presenting as psychosis from a primary psychiatric illness, such as schizophrenia.
In patients with combat history, it is possible that both neurodegenerative and psychotic symptoms can be explained by autoantibody formation in response to toxin exposure. When soldiers were deployed to Iraq and Afghanistan, they may have been exposed to multiple toxicities, including depleted uranium, dust and fumes, and numerous infectious diseases.9 Gulf War illness (GWI) or chronic multisymptom illness (CMI) encompass a cluster of symptoms, such as chronic pain, chronic fatigue, irritable bowel syndrome, dermatitis, and seizures, as well as mental health issues such as depression and anxiety experienced following exposure to these combat environments.10,11
In light of this diagnostic uncertainty, the authors detail a case of a patient with significant combat history previously diagnosed with MS and unspecified schizophrenia spectrum and other psychotic disorder (USS & OPD) presenting with acute psychosis.
Case Presentation
A 35-year-old male veteran, with a history of MS, USS & OPD, posttraumatic stress disorder, and traumatic brain injuries (TBIs) was admitted to the psychiatric unit after being found by the police lying in the middle of a busy intersection, internally preoccupied. On admission, he reported a week of auditory hallucinations from birds with whom he had been communicating telepathically, and a recurrent visual hallucination of a tall man in white and purple robes. He had discontinued his antipsychotic medication, aripiprazole 10 mg, a few weeks prior for unknown reasons. He was brought to the hospital by ambulance, where he presented with disorganized thinking, tangential thought process, and active auditory and visual hallucinations. The differential diagnoses included USS & OPD, schizophrenia, schizoaffective disorder and ruled out substance-induced psychotic disorder, and psychosis as a manifestation of MS.
The patient had 2 psychotic episodes prior to this presentation. He was hospitalized for his first psychotic break in 2015 at age 32, when he had tailed another car “to come back to reality” and ended up in a motor vehicle accident. During that admission, he reported weeks of thought broadcasting, conspiratorial delusions, and racing thoughts. Two years later, he was admitted to a psychiatric intensive care unit for his second episode of severe psychosis. After several trials of different antipsychotic medications, his most recent pharmacologic regimen was aripiprazole 10 mg once daily.
His medical history was complicated by 2 TBIs, in November 2014 and January 2015, with normal computed tomography (CT) scans. He was diagnosed with MS in December 2017, when he presented with intractable emesis, left facial numbness, right upper extremity ataxia, nystagmus, and imbalance. An MRI scan revealed multifocal bilateral hypodensities in his periventricular, subcortical, and brain stem white matter. Multiple areas of hyperintensity were visualized, including in the right periatrial region and left brachium pontis. More than 5 oligoclonal bands on lumbar puncture confirmed the diagnosis.
He was treated with IV methylprednisolone followed by a 2-week prednisone taper. Within 1 week, he returned to the psychiatric unit with worsening symptoms and received a second dose of IV steroids and plasma exchange treatment. In the following months, he completed a course of rituximab infusions and physical therapy for his dysarthria, gait abnormality, and vision impairment.
His social history was notable for multiple first-degree relatives with schizophrenia. He reported a history of sexual and verbal abuse and attempted suicide once at age 13 years by hanging himself with a bathrobe. He left home at age 18 years to serve in the Marine Corps (2001-2006). His service included deployment to Afghanistan, where he received a purple heart. Upon his return, he received BA and MS degrees. He married and had 2 daughters but became estranged from his wife. By his most recent admission, he was unemployed and living with his half-sister.
On the first day of this most recent psychiatric hospitalization, he was restarted on aripiprazole 10 mg daily, and a medicine consult was sought to evaluate the progression of his MS. No new onset neurologic symptoms were noted, but he had possible residual lower extremity hyperreflexia and tandem gait incoordination. The episodes of psychotic and neurologic symptoms appeared independent, given that his psychiatric history preceded the onset of his MS.
The patient reported no visual hallucinations starting day 2, and he no longer endorsed auditory hallucinations by day 3. However, he continued to appear internally preoccupied and was noticed to be pacing around the unit. On day 4 he presented with newly pressured speech and flights of ideas, while his affect remained euthymic and his sleep stayed consistent. In combination with his ongoing pacing, his newfound symptoms were hypothesized to be possibly akathisia, an adverse effect (AE) of aripiprazole. As such, on day 5 his dose was lowered to 5 mg daily. He continued to report no hallucinations and demonstrated progressively increased emotional range. A MRI scan was done on day 6 in case a new lesion could be identified, suggesting a primary MS flare-up; however, the scan identified no enhancing lesions, indicating no ongoing demyelination. After a neurology consult corroborated this conclusion, he was discharged in stable condition on day 7.
As is the case with the majority of patients with MS-induced psychosis, he continued to have relapsing psychiatric disease even after MS treatment had been started. Unfortunately, because this patient had stopped taking his atypical antipsychotic medication several weeks prior to his hospitalization, we cannot clarify whether his psychosis stems from a primary psychiatric vs MS process.
Discussion
Presently, treatment preferences for MS-related psychosis are divided between atypical antipsychotics and glucocorticoids. Some suggest that the treatment remains similar between MS-related psychosis and primary psychotic disorders in that atypical antipsychotics are the standard of care.12 A variety of atypical antipsychotics have been used successfully in case reports, including zipradisone, risperidone, olanzapine, quetiapine, and aripiprazole.13,14 First-generation antipsychotics and other psychotropic drugs that can precipitate extra-pyramidal AEs are not recommended given their potential additive effect to motor deficits associated with MS.12 Alternatively, several case reports have found that MS-related psychotic symptoms respond to glucocorticoids more effectively, while cautioning that glucocorticoids can precipitate psychosis and depression.15,16 One review article found that 90% of patients who received corticosteroids saw an improvement in their psychotic symptoms.2
Finally, it is possible that our patient’s neuropsychiatric symptoms can be explained by autoantibody formation in response to toxin exposure during his time in Afghanistan. In a pilot study of veterans with GWI, Abou-Donia and colleagues found 2-to-9 fold increase in autoantibody reactivity levels of the following neuronal and glial-specific proteins relative to healthy controls: neurofilament triplet proteins, tubulin, microtubule-associated tau proteins, microtubule-associated protein-2, myelin basic protein, myelin-associated glycoprotein, glial fibrillary acidic protein, and calcium-calmodulin kinase II.17,18 Many of these autoantibodies are longstanding explicit markers for neurodegenerative disorders, given that they target proteins and antigens that support axonal transport and myelination. Still Gulf War veteran status has yet to be explicitly linked to an increased risk of MS,19 making this hypothesis less likely for our patient. Future research should address the clinical and therapeutic implications of different autoantibody levels in combat veterans with psychosis.
Conclusion
For patients with MS, mood disorder and psychotic symptoms should warrant a MRI given the possibility of a psychiatric manifestation of MS relapse. Ultimately, our patient’s presentation was inconsistent with the expected clinical presentations of both a primary psychotic disorder and psychosis as a manifestation of MS. His late age at his first psychotic break is atypical for primary psychotic disease, and the lack of MRI imaging done at his initial psychotic episodes cannot exclude a primary MS diagnosis. Still, his lack of MRI findings at his most recent hospitalization, negative symptomatology, and strong history of schizophrenia make a primary psychotic disorder likely.
Following his future clinical course will be necessary to determine the etiology of his psychotic episodes. Future episodes of psychosis with neurologic symptoms would suggest a primary MS diagnosis and potential benefit of immunosuppressant treatment, whereas repeated psychotic breaks with minimal temporal lobe involvement or demyelination as seen on MRI would be suspicious for separate MS and psychotic disease processes. Further research on treatment regimens for patients experiencing psychosis as a manifestation of MS is still necessary.
Multiple sclerosis (MS) is an immune-mediated neurodegenerative disease that affects > 700,000 people in the US.1 The hallmarks of MS pathology are axonal or neuronal loss, demyelination, and astrocytic gliosis. Of these, axonal or neuronal loss is the main underlying mechanism of permanent clinical disability.
MS also has been associated with an increased prevalence of psychiatric illnesses, with mood disorders affecting up to 40% to 60% of the population, and psychosis being reported in 2% to 4% of patients.2 The link between MS and mood disorders, including bipolar disorder and depression, was documented as early as 1926,with mood disorders hypothesized to be manifestations of central nervous system (CNS) inflammation.3 More recently, inflammation-driven microglia have been hypothesized to impair hippocampal connectivity and activate glucocorticoid-insensitive inflammatory cells that then overstimulate the hypothalamic-pituitary-adrenal axis.4,5
Although the prevalence of psychosis in patients with MS is significantly rarer, averaging between 2% and 4%.6 A Canadian study by Patten and colleagues reviewed data from 2.45 million residents of Alberta and found that those who identified as having MS had a 2% to 3% prevalence of psychosis compared with 0.5% to 1% in the general population.7 The connection between psychosis and MS, similar to that between mood disorders and MS, has been described as a common regional demyelination process. Supporting this, MS manifesting as psychosis has been found to present with distinct magnetic resonance imaging (MRI) findings, such as diffuse periventricular lesions.8 Still, no conclusive criteria have been developed to distinguish MS presenting as psychosis from a primary psychiatric illness, such as schizophrenia.
In patients with combat history, it is possible that both neurodegenerative and psychotic symptoms can be explained by autoantibody formation in response to toxin exposure. When soldiers were deployed to Iraq and Afghanistan, they may have been exposed to multiple toxicities, including depleted uranium, dust and fumes, and numerous infectious diseases.9 Gulf War illness (GWI) or chronic multisymptom illness (CMI) encompass a cluster of symptoms, such as chronic pain, chronic fatigue, irritable bowel syndrome, dermatitis, and seizures, as well as mental health issues such as depression and anxiety experienced following exposure to these combat environments.10,11
In light of this diagnostic uncertainty, the authors detail a case of a patient with significant combat history previously diagnosed with MS and unspecified schizophrenia spectrum and other psychotic disorder (USS & OPD) presenting with acute psychosis.
Case Presentation
A 35-year-old male veteran, with a history of MS, USS & OPD, posttraumatic stress disorder, and traumatic brain injuries (TBIs) was admitted to the psychiatric unit after being found by the police lying in the middle of a busy intersection, internally preoccupied. On admission, he reported a week of auditory hallucinations from birds with whom he had been communicating telepathically, and a recurrent visual hallucination of a tall man in white and purple robes. He had discontinued his antipsychotic medication, aripiprazole 10 mg, a few weeks prior for unknown reasons. He was brought to the hospital by ambulance, where he presented with disorganized thinking, tangential thought process, and active auditory and visual hallucinations. The differential diagnoses included USS & OPD, schizophrenia, schizoaffective disorder and ruled out substance-induced psychotic disorder, and psychosis as a manifestation of MS.
The patient had 2 psychotic episodes prior to this presentation. He was hospitalized for his first psychotic break in 2015 at age 32, when he had tailed another car “to come back to reality” and ended up in a motor vehicle accident. During that admission, he reported weeks of thought broadcasting, conspiratorial delusions, and racing thoughts. Two years later, he was admitted to a psychiatric intensive care unit for his second episode of severe psychosis. After several trials of different antipsychotic medications, his most recent pharmacologic regimen was aripiprazole 10 mg once daily.
His medical history was complicated by 2 TBIs, in November 2014 and January 2015, with normal computed tomography (CT) scans. He was diagnosed with MS in December 2017, when he presented with intractable emesis, left facial numbness, right upper extremity ataxia, nystagmus, and imbalance. An MRI scan revealed multifocal bilateral hypodensities in his periventricular, subcortical, and brain stem white matter. Multiple areas of hyperintensity were visualized, including in the right periatrial region and left brachium pontis. More than 5 oligoclonal bands on lumbar puncture confirmed the diagnosis.
He was treated with IV methylprednisolone followed by a 2-week prednisone taper. Within 1 week, he returned to the psychiatric unit with worsening symptoms and received a second dose of IV steroids and plasma exchange treatment. In the following months, he completed a course of rituximab infusions and physical therapy for his dysarthria, gait abnormality, and vision impairment.
His social history was notable for multiple first-degree relatives with schizophrenia. He reported a history of sexual and verbal abuse and attempted suicide once at age 13 years by hanging himself with a bathrobe. He left home at age 18 years to serve in the Marine Corps (2001-2006). His service included deployment to Afghanistan, where he received a purple heart. Upon his return, he received BA and MS degrees. He married and had 2 daughters but became estranged from his wife. By his most recent admission, he was unemployed and living with his half-sister.
On the first day of this most recent psychiatric hospitalization, he was restarted on aripiprazole 10 mg daily, and a medicine consult was sought to evaluate the progression of his MS. No new onset neurologic symptoms were noted, but he had possible residual lower extremity hyperreflexia and tandem gait incoordination. The episodes of psychotic and neurologic symptoms appeared independent, given that his psychiatric history preceded the onset of his MS.
The patient reported no visual hallucinations starting day 2, and he no longer endorsed auditory hallucinations by day 3. However, he continued to appear internally preoccupied and was noticed to be pacing around the unit. On day 4 he presented with newly pressured speech and flights of ideas, while his affect remained euthymic and his sleep stayed consistent. In combination with his ongoing pacing, his newfound symptoms were hypothesized to be possibly akathisia, an adverse effect (AE) of aripiprazole. As such, on day 5 his dose was lowered to 5 mg daily. He continued to report no hallucinations and demonstrated progressively increased emotional range. A MRI scan was done on day 6 in case a new lesion could be identified, suggesting a primary MS flare-up; however, the scan identified no enhancing lesions, indicating no ongoing demyelination. After a neurology consult corroborated this conclusion, he was discharged in stable condition on day 7.
As is the case with the majority of patients with MS-induced psychosis, he continued to have relapsing psychiatric disease even after MS treatment had been started. Unfortunately, because this patient had stopped taking his atypical antipsychotic medication several weeks prior to his hospitalization, we cannot clarify whether his psychosis stems from a primary psychiatric vs MS process.
Discussion
Presently, treatment preferences for MS-related psychosis are divided between atypical antipsychotics and glucocorticoids. Some suggest that the treatment remains similar between MS-related psychosis and primary psychotic disorders in that atypical antipsychotics are the standard of care.12 A variety of atypical antipsychotics have been used successfully in case reports, including zipradisone, risperidone, olanzapine, quetiapine, and aripiprazole.13,14 First-generation antipsychotics and other psychotropic drugs that can precipitate extra-pyramidal AEs are not recommended given their potential additive effect to motor deficits associated with MS.12 Alternatively, several case reports have found that MS-related psychotic symptoms respond to glucocorticoids more effectively, while cautioning that glucocorticoids can precipitate psychosis and depression.15,16 One review article found that 90% of patients who received corticosteroids saw an improvement in their psychotic symptoms.2
Finally, it is possible that our patient’s neuropsychiatric symptoms can be explained by autoantibody formation in response to toxin exposure during his time in Afghanistan. In a pilot study of veterans with GWI, Abou-Donia and colleagues found 2-to-9 fold increase in autoantibody reactivity levels of the following neuronal and glial-specific proteins relative to healthy controls: neurofilament triplet proteins, tubulin, microtubule-associated tau proteins, microtubule-associated protein-2, myelin basic protein, myelin-associated glycoprotein, glial fibrillary acidic protein, and calcium-calmodulin kinase II.17,18 Many of these autoantibodies are longstanding explicit markers for neurodegenerative disorders, given that they target proteins and antigens that support axonal transport and myelination. Still Gulf War veteran status has yet to be explicitly linked to an increased risk of MS,19 making this hypothesis less likely for our patient. Future research should address the clinical and therapeutic implications of different autoantibody levels in combat veterans with psychosis.
Conclusion
For patients with MS, mood disorder and psychotic symptoms should warrant a MRI given the possibility of a psychiatric manifestation of MS relapse. Ultimately, our patient’s presentation was inconsistent with the expected clinical presentations of both a primary psychotic disorder and psychosis as a manifestation of MS. His late age at his first psychotic break is atypical for primary psychotic disease, and the lack of MRI imaging done at his initial psychotic episodes cannot exclude a primary MS diagnosis. Still, his lack of MRI findings at his most recent hospitalization, negative symptomatology, and strong history of schizophrenia make a primary psychotic disorder likely.
Following his future clinical course will be necessary to determine the etiology of his psychotic episodes. Future episodes of psychosis with neurologic symptoms would suggest a primary MS diagnosis and potential benefit of immunosuppressant treatment, whereas repeated psychotic breaks with minimal temporal lobe involvement or demyelination as seen on MRI would be suspicious for separate MS and psychotic disease processes. Further research on treatment regimens for patients experiencing psychosis as a manifestation of MS is still necessary.
1. Wallin MT, Culpepper WJ, Campbell JD, et al. The prevalence of MS in the United States: A population-based estimate using health claims data. Neurology. 2019;92(10):e1029-e1040.
2. Camara-Lemarroy CR, Ibarra-Yruegas BE, Rodriguez-Gutierrez R, Berrios-Morales I, Ionete C, Riskind P. The varieties of psychosis in multiple sclerosis: a systematic review of cases. Mult Scler Relat Disord. 2017;12:9-14.
3. Cottrel SS, Wilson SA. The affective symptomatology of disseminated sclerosis: a study of 100 cases. J Neurol Psychopathology. 1926;7(25):1-30.
4. Johansson V, Lundholm C, Hillert J, et al. Multiple sclerosis and psychiatric disorders: comorbidity and sibling risk in a nationwide Swedish cohort. Mult Scler. 2014;20(14):1881-1891.
5. Rossi S, Studer V, Motta C, et al. Neuroinflammation drives anxiety and depression in relapsing-remitting multiple sclerosis. Neurology. 2017;89(13):1338-1347.
6. Gilberthorpe TG, O’Connell KE, Carolan A, et al. The spectrum of psychosis in multiple sclerosis: a clinical case series. Neuropsychiatric disease and treatment. 2017;13:303.
7. Patten SB, Svenson LW, Metz LM. Psychotic disorders in MS: population-based evidence of an association. Neurology 2005;65(7):1123-1125.
8. Kosmidis MH, Giannakou M, Messinis L, Papathanasopoulos P. Psychotic features associated with multiple sclerosis. Int Rev Psychiatry. 2010; 22(1):55-66.
9. US Department of Veterans Affairs. Public health: military exposures. https://www.publichealth.va.gov/exposures/. Updated April 16, 2019. Accessed May 13, 2019.
10. DeBeer BB, Davidson D, Meyer EC, Kimbrel NA, Gulliver SB, Morissette SB. The association between toxic exposures and chronic multisymptom illness in veterans of the wars of Iraq and Afghanistan. J Occup Environ Med. 2017;59(1):54-60.
11. Kang HK, Li B, Mahan CM, Eisen SA, Engel CC. Health of US veterans of 1991 Gulf War: a follow-up survey in 10 years. J Occup Environ Med. 2009;51(4):401-410.
12. Murphy R, O’Donoghue S, Counihan T, et al. Neuropsychiatric syndromes of multiple sclerosis. J Neurol Neurosurg Psychiatry. 2017;88(8):697-708.
13. Davids E, Hartwig U, Gastpar, M. Antipsychotic treatment of psychosis associated with multiple sclerosis. Prog Neuro Psychopharmacol Biol Psychiatry. 2004;28(4):743-744.
14. Lo Fermo S, Barone R, Patti F, et al. Outcome of psychiatric symptoms presenting at onset of multiple sclerosis: a retrospective study. Mult Scler. 2010;16(6):742-748.
15. Enderami A, Fouladi R, Hosseini HS. First-episode psychosis as the initial presentation of multiple sclerosis: a case report. Int Medical Case Rep J. 2018;11:73-76.
16. Fragoso YD, Frota ER, Lopes JS, et al. Severe depression, suicide attempts, and ideation during the use of interferon beta by patients with multiple sclerosis. Clin Neuropharmacol. 2010;33(6):312-316.
17. Abou-Donia MB, Conboy LA, Kokkotou E, et al. Screening for novel central nervous system biomarkers in veterans with Gulf War Illness. Neurotoxicol Teratol. 2017;61:36-46.
18. Abou-Donia MB, Lieberman A, Curtis L. Neural autoantibodies in patients with neurological symptoms and histories of chemical/mold exposures. Toxicol Ind Health. 2018;34(1):44-53.
19. Wallin MT, Kurtzke JF, Culpepper WJ, et al. Multiple sclerosis in Gulf War era veterans. 2. Military deployment and risk of multiple sclerosis in the first Gulf War. Neuroepidemiology. 2014;42(4):226-234.
1. Wallin MT, Culpepper WJ, Campbell JD, et al. The prevalence of MS in the United States: A population-based estimate using health claims data. Neurology. 2019;92(10):e1029-e1040.
2. Camara-Lemarroy CR, Ibarra-Yruegas BE, Rodriguez-Gutierrez R, Berrios-Morales I, Ionete C, Riskind P. The varieties of psychosis in multiple sclerosis: a systematic review of cases. Mult Scler Relat Disord. 2017;12:9-14.
3. Cottrel SS, Wilson SA. The affective symptomatology of disseminated sclerosis: a study of 100 cases. J Neurol Psychopathology. 1926;7(25):1-30.
4. Johansson V, Lundholm C, Hillert J, et al. Multiple sclerosis and psychiatric disorders: comorbidity and sibling risk in a nationwide Swedish cohort. Mult Scler. 2014;20(14):1881-1891.
5. Rossi S, Studer V, Motta C, et al. Neuroinflammation drives anxiety and depression in relapsing-remitting multiple sclerosis. Neurology. 2017;89(13):1338-1347.
6. Gilberthorpe TG, O’Connell KE, Carolan A, et al. The spectrum of psychosis in multiple sclerosis: a clinical case series. Neuropsychiatric disease and treatment. 2017;13:303.
7. Patten SB, Svenson LW, Metz LM. Psychotic disorders in MS: population-based evidence of an association. Neurology 2005;65(7):1123-1125.
8. Kosmidis MH, Giannakou M, Messinis L, Papathanasopoulos P. Psychotic features associated with multiple sclerosis. Int Rev Psychiatry. 2010; 22(1):55-66.
9. US Department of Veterans Affairs. Public health: military exposures. https://www.publichealth.va.gov/exposures/. Updated April 16, 2019. Accessed May 13, 2019.
10. DeBeer BB, Davidson D, Meyer EC, Kimbrel NA, Gulliver SB, Morissette SB. The association between toxic exposures and chronic multisymptom illness in veterans of the wars of Iraq and Afghanistan. J Occup Environ Med. 2017;59(1):54-60.
11. Kang HK, Li B, Mahan CM, Eisen SA, Engel CC. Health of US veterans of 1991 Gulf War: a follow-up survey in 10 years. J Occup Environ Med. 2009;51(4):401-410.
12. Murphy R, O’Donoghue S, Counihan T, et al. Neuropsychiatric syndromes of multiple sclerosis. J Neurol Neurosurg Psychiatry. 2017;88(8):697-708.
13. Davids E, Hartwig U, Gastpar, M. Antipsychotic treatment of psychosis associated with multiple sclerosis. Prog Neuro Psychopharmacol Biol Psychiatry. 2004;28(4):743-744.
14. Lo Fermo S, Barone R, Patti F, et al. Outcome of psychiatric symptoms presenting at onset of multiple sclerosis: a retrospective study. Mult Scler. 2010;16(6):742-748.
15. Enderami A, Fouladi R, Hosseini HS. First-episode psychosis as the initial presentation of multiple sclerosis: a case report. Int Medical Case Rep J. 2018;11:73-76.
16. Fragoso YD, Frota ER, Lopes JS, et al. Severe depression, suicide attempts, and ideation during the use of interferon beta by patients with multiple sclerosis. Clin Neuropharmacol. 2010;33(6):312-316.
17. Abou-Donia MB, Conboy LA, Kokkotou E, et al. Screening for novel central nervous system biomarkers in veterans with Gulf War Illness. Neurotoxicol Teratol. 2017;61:36-46.
18. Abou-Donia MB, Lieberman A, Curtis L. Neural autoantibodies in patients with neurological symptoms and histories of chemical/mold exposures. Toxicol Ind Health. 2018;34(1):44-53.
19. Wallin MT, Kurtzke JF, Culpepper WJ, et al. Multiple sclerosis in Gulf War era veterans. 2. Military deployment and risk of multiple sclerosis in the first Gulf War. Neuroepidemiology. 2014;42(4):226-234.
Early and Accurate Identification of Parkinson Disease Among US Veterans (FULL)
Parkinson disease (PD) affects about 680,000 in the US, including > 110,000 veterans (Caroline Tanner, MD, PhD, unpublished data).1 In the next 10 years, this number is expected to double, in part because of the aging of the US population.1 Although the classic diagnostic criteria emphasize motor symptoms that include tremor, gait disturbance, and paucity of movement, there is increasing recognition that disease pathology begins decades before the development of motor impairment.2
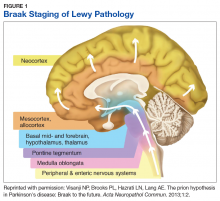
Pathologic studies confirm that by the onset of motor symptoms, at least 30% of nigrostriatal neurons are lost or dysfunctional.3-5 Similarly, the Braak staging hypothesis posits initial deposition of Lewy bodies in the olfactory bulb and the dorsal motor nucleus of the vagus nerve, followed by prion-like spread through the brain stem into the midbrain/substantia nigra, and finally into the cortex (Figure 1).6
The decades-long prodromal or preclinical phase represents a unique opportunity for early identification of those at highest risk for developing the motor symptoms of Parkinson disease.7 Accurate identification, ideally before the onset of manifest motor disability, would not only improve prognostic counseling of veterans and families, but also could allow for early enrollment into trials of potentially disease-modifying therapeutic agents. Thus, early and accurate identification of PD is an important goal of the care of veterans with potential PD.
Prodromal Symptoms
Prodromal PD, as defined by the International Parkinson Disease and Movement Disorders Society (MDS), focuses on nonmotor symptoms that herald the onset of manifest motor PD.8 The most commonly assessed nonmotor features include olfaction, constipation, sleep disturbance, and mood disorders.
Olfaction is impaired in > 90% of patients with motor PD at the time of diagnosis; by contrast, the prevalence of hyposmia in the general population ranges from 20% to 50%, with higher rates in older adults and in smokers.9-11 Thus, olfaction appears to be a relatively sensitive, though nonspecific, prodromal feature. Importantly, subjective report of hyposmia is poorly reliable, so a number of different tests have been developed for objective assessment of olfactory dysfunction.12 The 12-item Brief Smell Identification Test (B-SIT), derived from the longer University of Pennsylvania Smell Identification Test, is a “scratch-and-sniff” forced multiple choice test that can be self-administered by cooperative patients.13,14 The B-SIT has been validated in multiple ethnic and cultural groups and shows high discrimination between PD subjects and controls.13,15 Of note, olfactory impairment appears to be associated with risk of cognitive decline in PD, further emphasizing the need for accurate assessment to guide prognosis.16
Like hyposmia, constipation can be noted long before the diagnosis of manifest motor PD.17 After adjustment for lifestyle factors, constipated individuals have up to 4.5-fold increased odds of developing PD, and those with constipation suffer worsened disease outcomes and health-related quality of life.17-20 Some groups have demonstrated alterations in gut microbiota of those with prodromal PD, which suggests local inflammatory processes and intestinal permeability may contribute to protein misfolding and disease development.21,22 This also raises the intriguing possibility that dietary alterations may be neuroprotective or neurorestorative, although this has yet to be tested in humans.23,24
Like constipation, mood changes can precede the appearance of manifest motor PD.25,26 Case control studies suggest a higher risk of developing PD among individuals who were previously diagnosed with depression or anxiety, particularly in the 1 to 2 years prior to PD diagnosis.27-29 Both apathy and anxiety are associated with striatal dopamine dysfunction, particularly in the right caudate nucleus, which suggests that mood changes are directly related to disease pathology.30,31
Of the prodromal features, rapid eye movement sleep behavior disorder (RBD) is associated with the highest risk of conversion to motor PD.8 Up to 80% of older men with socalled idiopathic RBD develop a parkinsonian syndrome within 20 years; risk is divided about equally between idiopathic PD and dementia with Lewy bodies (DLB).32 Collateral history from a bed-partner is usually sufficient to make the diagnosis, although, this is often confounded by the prevalence of nightmares in those with posttraumatic stress disorder in the veteran population.32 Thus, in suspected cases, obtaining a polysomnogram can aid in distinguishing between idiopathic PC and DLB.33 Given the specificity of RBD as a marker of synuclein deposition and the high risk of progression to a degenerative syndrome, accurate diagnosis and counseling is imperative.
Each of the prodromal nonmotor features of PD are at best moderately sensitive or specific in isolation, but in concert, they can be used to develop a Parkinson risk score. For instance, the MDS prodromal criteria combine individual likelihood ratios into Bayesian analysis to determine a combined probability of PD, which can be further stratified to probable or possible prodromal PD (probability > 80%, > 50%, respectively).8 These criteria have been applied to several independent cohorts and demonstrate high sensitivity and specificity, especially over time.34,35 Applicability in a veteran population has yet to be determined.
Use of Imaging in Diagnosis
Although clinical diagnostic criteria and prodromal features can improve diagnostic accuracy, it can be extremely challenging to distinguish idiopathic PD from nondegenerative parkinsonism or atypical syndromes (see below). Compared with the gold standard of pathologic assessment, the clinical diagnostic accuracy for PD ranges from 73% for nonexperts to 80% for fellowship-trained movement disorders specialists.36 Thus, objective biomarkers are sought to improve diagnostic accuracy both for clinical care as well as for research purposes, such as enrollment into clinical trials.
Multiple potential imaging biomarkers for preclinical PD can aid in early diagnosis and help differentiate PD from related but distinct disorders. While beyond the scope of this review, these techniques have recently been reviewed.7 Of these, the most widely available and accurate is dopamine transporter (DAT) imaging, which uses a radioiodinated ligand that binds to DAT on striatal dopaminergic terminals; binding is detected through single photon emission computed tomography (SPECT) scanning. Thus, a SPECT DaTscan (GE Healthcare Bio-Sciences, Little Chalfont, England) directly assesses the integrity of the presynaptic nigrostriatal system and is well correlated with severity of motor and nonmotor parkinsonism.37,38
In individuals with suspected prodromal PD, abnormal DaTscans are associated with faster progression to manifest motor PD.39 However, it should be noted that a number of medications, several of which are commonly utilized in the veteran population, can affect the outcome of a DaTscan.40 Some of these medications only mildly affect the outcome, so the physician interpreting the scan should be made aware of their use, while others need to be held for days to weeks so as not to invalidate the DaTscan. DaTscan also do not differentiate between PD and atypical degenerative parkinsonisms such as multiple system atrophy (MSA), DLB, progressive supranuclear palsy (PSP), or corticobasal syndrome (CBS). Nevertheless, these scans can be used to distinguish degenerative parkinsonisms from other conditions that can be difficult to distinguish clinically from PD, including essential tremor, normal pressure hydrocephalus, vascular parkinsonism, or druginduced parkinsonism (DIP).
DIP usually is caused by blockade of postsynaptic dopamine receptors by antipsychotic medications, which are prescribed to as many as 1 in 4 older veterans; antiemetic agents such as metoclopramide are also potential offenders if used chronically.41 The risk of DIP appears to be associated with the D2 binding affinity of the drug. Thus, of the newer atypical antipsychotics, clozapine and quetiapine appear to have the lowest risk, while ziprasidone and aripiprazole have the highest binding affinity and therefore the highest risk.42 In many patients, parkinsonism persists even after discontinuation of the offending agent, suggesting that in at least a subset of patients, DIP may be an “unmasking” of latent PD rather than a true adverse effect of the medication. The prodromal features discussed above can be used to distinguish isolated DIP from unmasked latent PD.43 In a study we conducted in veterans at the Michael J. Crescenz VA Medical Center in Philadelphia, Pennsylvania, hyposmia in particular was shown to be highly predictive of an underlying dopaminergic deficit with an odds ratio of 63.44
Other important considerations in the differential diagnosis of PD are the atypical degenerative parkinsonian syndromes, formerly called Parkinson plus syndromes. These may be further divided into the synucleinopathies (MSA, DLB) or the tauopathies (PSP, CBS), depending on the predominant amyloidogenic protein. Early in the disease, the atypical syndromes and idiopathic PD may be clinically indistinguishable, although the atypical syndromes tend to progress more rapidly and often have a less robust response to levodopa.
Radiologic and fluid biomarkers for the atypical syndromes are under active investigation; at present the most accessible study is magnetic resonance imaging (MRI), which may show characteristic features such as degeneration of the pontocerebellar fibers in MSA or midbrain atrophy in PSP.45,46 By contrast, standard MRI sequences in idiopathic PD are usually normal, although high-resolution (7 tesla) imaging can reveal loss of neuromelanin in the substantia nigra.47 MRI also can be useful in the workup of suspected normal pressure hydrocephalus or vascular parkinsonism, which would show disproportionate ventriculomegaly with transependymal flow, or white matter lesions in the basal ganglia, respectively.
Data-Based Identification of Preclinical PD
The integration of clinical motor or prodromal features with biomarker data has led to the development of several large-scale clinical and administrative databases to identify PD. The Parkinson Progression Markers Initiative initially enrolled only de novo clinically identified people with PD, but it expanded to include a prodromal cohort who are being assessed for rates of conversion to PD.48 Similarly, metabolic imaging can be combined with prodromal symptoms, such as hyposmia or RBD, to predict risk for phenoconversion into manifest motor PD.49
The PREDICT-PD study synthesizes mood symptoms, RBD, smell testing, genotyping, and keyboard-tapping tasks to divide individuals into high-, middle-, and low-risk groups; interim analysis at 3 years of follow-up (N = 842) demonstrated a hazard ratio of 4.39 (95% CI, 1.03-18.68) for the diagnosis of PD in the highrisk group compared with the low-risk group.50 Lastly, administrative claims data for prodromal features, such as constipation, RBD, and mood symptoms, is highly predictive of eventual PD diagnosis.51 VA databases accessed through the Corporate Data Warehouse are complementary sources of information to nonveteranspecific Medicare databases; to our knowledge there has not yet been a comprehensive search of VA databases to identify veterans with preclinical PD.
Risk Factors Associated With Military Service
A number of potential environmental risk factors may increase the risk of developing Parkinson disease for veterans. Perhaps the most commonly recognized is pesticide exposure, particularly given the presumptive service connections established by the VA for Parkinson disease and exposure to Agent Orange or contaminated water at Camp Lejeune.52,53 Both dioxin, the toxic ingredient in Agent Orange, and the solvents trichloroethylene and perchloroethylene, found in the water supply at Camp Lejeune, interfere with mitochondrial function leading to oxidative stress and apoptosis of nigrostriatal neurons.54,55 Other potential exposures, which are not necessarily limited to the veteran population, include rotenone, a phytochemical used to kill fish in reservoirs, and paraquat, an herbicide that may directly promote synuclein aggregation.56,57 Veterans who have reported exposure to these or other environmental chemicals in civilian life should be carefully assessed for the presence of motor PD or prodromal features.
Traumatic brain injury (TBI) also may be a risk factor for PD, which may be particularly relevant for veterans who had served in Iraq or Afghanistan. Retrospective claims data suggest a strong association between PD and recent TBI in the 5 to 10 years prior to motor PD diagnosis.58,59 A recent assessment of combat veterans with TBI found that even mild TBI was associated with a 56% increased risk of PD, while moderate-to-severe TBI was associated with an 83% higher risk of PD.60 The pathologic mechanism for this link is unclear, but post-TBI inflammatory processes may lead to the formation of reactive oxygen species and/or glutamatergic excitotoxicity, thus leading to secondary injury in the nigrostriatal pathway.61 As with prodromal symptoms, the risk of PD related to environmental risk factors may be synergistic; repetitive TBI may be more damaging than a single injury, and a combination of TBI and pesticide exposure markedly increases PD risk beyond the risk of TBI or the risk of pesticides alone.62 Recently, parkinsonism, including Parkinson disease, was recognized as a service connected condition for veterans with a servicerelated moderate or severe TBI.63
Conclusion
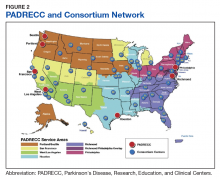
Because of the substantial impact on quality of life and disability-adjusted life years, early and accurate identification and management of veterans at risk for PD is an important priority area for the VA. The 10-year cost of PD-related benefits through the VA was estimated at $3.5 billion in fiscal year 2010, and that number is likely to rise in coming years, due to the aging population as well as synergistic effects of independent risk factors described above.64 In response, the VA has created a network of specialty care sites, known as Parkinson Disease Research, Education, and Clinical Centers (PADRECCs) located in Philadelphia, Pennsylvania; Richmond, Virginia; Houston, Texas; West Los Angeles and San Francisco, California; and Seattle, Washington/ Portland, Oregon (www.parkinsons.va.gov).
The PADRECCs are supplemented by a National VA PD Consortium network of VA physicians trained in PD management (Figure 2). Studies, including one investigating care of veterans with PD, have demonstrated that involvement of specialty care services early in the course of PD leads to improved patient outcomes.65,66 In addition to patient-facing resources such as support groups and specialized physical/occupational/speech therapy, PADRECCs and the consortium sites are national leaders in PD education and clinical trials and provide high-quality, multidisciplinary care for veterans with PD.67 Thus, veterans with significant risk factors or prodromal symptoms of PD should be referred into the PADRECC/Consortium network in order to maximize their quality of care and quality of life.
1. Marras C, Beck JC, Bower JH, et al; Parkinson’s Foundation P4 Group. Prevalence of Parkinson’s disease across North America. NPJ Parkinsons Dis. 2018;4:21.
2. Postuma RB, Berg D, Stern M, et al. MDS clinical diagnostic criteria for Parkinson’s disease. Mov Disord. 2015;30(12):1591-1601.
3. Fearnley JM, Lees AJ. Ageing and Parkinson’s disease: substantia nigra regional selectivity. Brain. 1991;114(pt 5):2283-2301.
4. Greffard S, Verny M, Bonnet A-M, et al. Motor score of the Unified Parkinson Disease Rating Scale as a good predictor of Lewy body-associated neuronal loss in the substantia nigra. Arch Neurol. 2006;63(4):584-588.
5. Hilker R, Schweitzer K, Coburger S, et al. Nonlinear progression of Parkinson disease as determined by serial positron emission tomographic imaging of striatal fluorodopa F 18 activity. Arch Neurol. 2005;62(3):378-382.
6. Braak H, Del Tredici K, Rüb U, de Vos RAI, Jansen Steur ENH, Braak E. Staging of brain pathology related to sporadic Parkinson’s disease. Neurobiol Aging. 2003;24(2):197-211.
7. Mantri S, Morley JF, Siderowf AD. The importance of preclinical diagnostics in Parkinson disease. Parkinsonism Relat Disord. 2018;pii:S1353-8020(18)30396-1. [Epub ahead of print]
8. Berg D, Postuma RB, Adler CH, et al. MDS research criteria for prodromal Parkinson’s disease. Mov Disord. 2015;30(12):1600-1611.
9. Haehner A, Boesveldt S, Berendse HW, et al. Prevalence of smell loss in Parkinson’s disease – a multicenter study. Parkinsonism Relat Disord. 2009;15(7):490-494.
10. Mullol J, Alobid I, Mariño-Sánchez F, et al. Furthering the understanding of olfaction, prevalence of loss of smell and risk factors: a population-based survey (OLFACAT study). BMJ Open. 2012;2(6).pii:e001256.
11. Doty RL, Shaman P, Applebaum SL, Giberson R, Siksorski L, Rosenberg L. Smell identification ability: changes with age. Science. 1984;226(4681):1441-1443.
12. Doty RL. Olfactory dysfunction in Parkinson disease. Nat Rev Neurol. 2012;8(6):329-339.
13. Double KL, Rowe DB, Hayes M, et al. Identifying the pattern of olfactory deficits in Parkinson disease using the brief smell identification test. Arch Neurol. 2003;60(4):545-549.
14. Doty RL, Shaman P, Dann M. Development of the University of Pennsylvania Smell Identification Test: a standardized microencapsulated test of olfactory function. Physiol Behav. 1984;32(3):489-502.
15. Morley JF, Cohen A, Silveira-Moriyama L, et al. Optimizing olfactory testing for the diagnosis of Parkinson’s disease: item analysis of the University of Pennsylvania smell identification test. NPJ Parkinsons Dis. 2018;4:2.
16. Fullard ME, Tran B, Xie SX, et al. Olfactory impairment predicts cognitive decline in early Parkinson’s disease. Parkinsonism Relat Disord. 2016;25:45-51.
17. Savica R, Carlin JM, Grossardt BR, et al. Medical records documentation of constipation preceding Parkinson disease: a case-control study. Neurology. 2009;73(21):1752-1758.
18. Abbott RD, Petrovitch H, White LR, et al. Frequency of bowel movements and the future risk of Parkinson’s disease. Neurology. 2001;57(3):456-462.
19. Stocchi F, Torti M. Constipation in Parkinson’s disease. Int Rev Neurobiol. 2017;134:811-826.
20. Yu QJ, Yu SY, Zuo LJ, et al. Parkinson disease with constipation: clinical features and relevant factors. Sci Rep. 2018;8(1):567.
21. Hill-Burns EM, Debelius JW, Morton JT, et al. Parkinson’s disease and Parkinson’s disease medications have distinct signatures of the gut microbiome. Mov Disord. 2017;32(5):739-749.
22. Mulak A, Bonaz B. Brain-gut-microbiota axis in Parkinson’s disease. World J Gastroenterol. 2015;21(37): 10609-10620.
23. Shah SP, Duda JE. Dietary modifications in Parkinson’s disease: a neuroprotective intervention? Med Hypotheses. 2015;85(6):1002-1005.
24. Perez-Pardo P, de Jong EM, Broersen LM, et al. Promising effects of neurorestorative diets on motor, cognitive, and gastrointestinal dysfunction after symptom development in a mouse model of Parkinson’s disease. Front Aging Neurosci. 2017;9:57.
25. Fang F, Xu Q, Park Y, et al. Depression and the subsequent risk of Parkinson’s disease in the NIH-AARP Diet and Health Study. Mov Disord. 2010;25(9):1157-1162.
26. Leentjens AFG, Van den Akker M, Metsemakers JFM, Lousberg R, Verhey FRJ. Higher incidence of depression preceding the onset of Parkinson’s disease: a register study. Mov Disord. 2003;18(4):414-418.
27. Alonso A, Rodriguez LAG, Logroscino G, Hernán MA. Use of antidepressants and the risk of Parkinson’s disease: a prospective study. J Neurol Neurosurg Psychiatry. 2009;80(6):671-674.
28. Weisskopf MG, Chen H, Schwarzschild MA, Kawachi I, Ascherio A. Prospective study of phobic anxiety and risk of Parkinson’s disease. Mov Disord. 2003;18(6):646-651.
29. Darweesh SK, Verlinden VJ, Stricker BH, Hofman A, Koudstaal PJ, Ikram MA. Trajectories of prediagnostic functioning in Parkinson’s disease. Brain. 2017;140(2):429-441.
30. Santangelo G, Vitale C, Picillo M, et al. Apathy and striatal dopamine transporter levels in de-novo, untreated Parkinson’s disease patients. Parkinsonism Relat Disord. 2015;21(5):489-493.
31. Erro R, Pappatà S, Amboni M, et al. Anxiety is associated with striatal dopamine transporter availability in newly diagnosed untreated Parkinson’s disease patients. Parkinsonism Relat Disord. 2012;18(9):1034-1038.
32. Schenck CH, Boeve BF, Mahowald MW. Delayed emergence of a parkinsonian disorder or dementia in 81% of older men initially diagnosed with idiopathic rapid eye movement sleep behavior disorder: a 16-year update on a previously reported series. Sleep Med. 2013;14(8):
744-748.
33. Melendez J, Hesselbacher S, Sharafkhaneh A, Hirshkowitz M. Assessment of REM sleep behavior disorder in veterans with posttraumatic stress disorder. Chest. 2011;140(4):967A.
34. Pilotto A, Heinzel S, Suenkel U, et al. Application of the movement disorder society prodromal Parkinson’s disease research criteria in 2 independent prospective cohorts. Mov Disord. 2017;32(7):1025-1034.
35. Fereshtehnejad S-M, Montplaisir JY, Pelletier A, Gagnon J-F, Berg D, Postuma RB. Validation of the MDS research criteria for prodromal Parkinson’s disease: Longitudinal assessment in a REM sleep behavior disorder (RBD) cohort. Mov Disord. 2017;32(6):865-873.
36. Rizzo G, Copetti M, Arcuti S, Martino D, Fontana A, Logroscino G. Accuracy of clinical diagnosis of Parkinson disease: a systematic review and meta-analysis. Neurology. 2016;86(6):566-576.
37. Moccia M, Pappatà S, Picillo M, et al. Dopamine transporter availability in motor subtypes of de novo drug-naïve Parkinson’s disease. J Neurol. 2014;261(11):2112-2118.
38. Siepel FJ, Brønnick KS, Booij J, et al. Cognitive executive impairment and dopaminergic deficits in de novo Parkinson’s disease. Mov Disord. 2014;29(14):1802-1808.
39. Iranzo A, Valldeoriola F, Lomeña F, et al. Serial dopamine transporter imaging of nigrostriatal function in patients with idiopathic rapid-eye-movement sleep behaviour disorder: a prospective study. Lancet Neurol. 2011;10(9):797-805.
40. Booij J, Kemp P. Dopamine transporter imaging with [(123)I]FP-CIT SPECT: potential effects of drugs. Eur J Nucl Med Mol Imaging. 2008;35(2):424-438.
41. Gellad WF, Aspinall SL, Handler SM, et al. Use of antipsychotics among older residents in VA nursing homes. Med Care. 2012;50(11):954-960.
42. Mauri MC, Paletta S, Maffini M, et al. Clinical pharmacology of atypical antipsychotics: an update. EXCLI J. 2014;13:1163-1191.
43. Morley JF, Duda JE. Use of hyposmia and other non-motor symptoms to distinguish between drug-induced parkinsonism and Parkinson’s disease. J Parkinsons Dis. 2014;4(2):169-173.
44. Morley JF, Cheng G, Dubroff JG, Wood S, Wilkinson JR, Duda JE. Olfactory impairment predicts underlying dopaminergic deficit in presumed drug-induced parkinsonism. Mov Disord Clin Pract. 2017;4(4):603-606.
45. Whitwell JL, Höglinger GU, Antonini A, et al; Movement Disorder Society-endorsed PSP Study Group. Radiological biomarkers for diagnosis in PSP: where are we and where do we need to be? Mov Disord. 2017;32(7):955-971.
46. Laurens B, Constantinescu R, Freeman R, et al. Fluid biomarkers in multiple system atrophy: A review of the MSA Biomarker Initiative. Neurobiol Dis. 2015;80:29-41.
47. Barber TR, Klein JC, Mackay CE, Hu MTM. Neuroimaging in pre-motor Parkinson’s disease. NeuroImage Clin. 2017;15:215-227.
48. Parkinson Progression Marker Initiative. The Parkinson Progression Marker Initiative (PPMI). Prog Neurobiol. 2011;95(4):629-635.
49. Meles SK, Vadasz D, Renken RJ, et al. FDG PET, dopamine transporter SPECT, and olfaction: combining biomarkers in REM sleep behavior disorder. Mov Disord. 2017;32(10):1482-1486.
50. Noyce AJ, R’Bibo L, Peress L, et al. PREDICT‐PD: an online approach to prospectively identify risk indicators of Parkinson’s disease. Mov Disord. 2017 Feb; 32(2): 219–226.
51. Searles Nielsen S, Warden MN, Camacho-Soto A, Willis AW, Wright BA, Racette BA. A predictive model to identify Parkinson disease from administrative claims data. Neurology. 2017;89(14):1448-1456.
52. Institute of Medicine. Veterans and Agent Orange: Update 2012. National Academies Press: Washington, DC; 2013.
53. Department of Veterans Affairs. Diseases associated with exposure to Contaminants in the Water Supply at Camp Lejeune. Final rule. Fed Regist. 2017;82(9):4173-4185.
54. Goldman SM, Quinlan PJ, Ross GW, et al. Solvent exposures and Parkinson disease risk in twins. Ann Neurol. 2012;71(6):776-784.
55. Liu M, Shin EJ, Dang DK, et al. Trichloroethylene and Parkinson’s disease: risk assessment. Mol Neurobiol. 2018;55(7):6201-6214.
56. Betarbet R, Sherer TB, MacKenzie G, Garcia-Osuna M, Panov AV, Greenamyre JT. Chronic systemic pesticide exposure reproduces features of Parkinson’s disease. Nat Neurosci. 2000;3(12):1301-1306.
57. Manning-Bog AB, McCormack AL, Li J, Uversky VN, Fink AL, Monte DAD. The herbicide paraquat causes up-regulation and aggregation of alpha-synuclein in mice: paraquat and alpha-synuclein. J Biol Chem. 2002;277(3):1641-1644.
58. Camacho-Soto A, Warden MN, Searles Nielsen S, et al. Traumatic brain injury in the prodromal period of Parkinson’s disease: a large epidemiological study using medicare data. Ann Neurol. 2017;82(5):744-754.
59. Gardner RC, Burke JF, Nettiksimmons J, Goldman S, Tanner CM, Yaffe K. Traumatic brain injury in later life increases risk for Parkinson disease. Ann Neurol. 2015;77(6):987-995.
60. Gardner RC, Byers AL, Barnes DE, Li Y, Boscardin J, Yaffe K. Mild TBI and risk of Parkinson disease: a Chronic Effects of Neurotrauma Consortium Study. Neurology. 2018;90(20):e1771-e1779.
61. Cruz-Haces M, Tang J, Acosta G, Fernandez J, Shi R. Pathological correlations between traumatic brain injury and chronic neurodegenerative diseases. Transl Neurodegener. 2017;6:20.
62. Lee PC, Bordelon Y, Bronstein J, Ritz B. Traumatic brain injury, paraquat exposure, and their relationship to Parkinson disease. Neurology. 2012;79(20):2061-2066.
63. Disabilities that are proximately due to, or aggravated by, service-connected disease or injury. 38 CFR §3.310.
64. Diseases Associated With Exposure to Certain Herbicide Agents (Hairy Cell Leukemia and Other Chronic B-Cell Leukemias, Parkinson’s Disease and Ischemic Heart Disease). Federal Regist. 2010;75(173):53202-53216. To be codified at 38 CFR §3.
65. Cheng EM, Swarztrauber K, Siderowf AD, et al. Association of specialist involvement and quality of care for Parkinson’s disease. Mov Disord. 2007;22(4):515-522.
66. Qamar MA, Harington G, Trump S, Johnson J, Roberts F, Frost E. Multidisciplinary care in Parkinson’s disease. Int Rev Neurobiol. 2017;132:511-523.
67. Pogoda TK, Cramer IE, Meterko M, et al. Patient and organizational factors related to education and support use by veterans with Parkinson’s disease. Mov Disord. 2009;24(13):1916-1924.
Parkinson disease (PD) affects about 680,000 in the US, including > 110,000 veterans (Caroline Tanner, MD, PhD, unpublished data).1 In the next 10 years, this number is expected to double, in part because of the aging of the US population.1 Although the classic diagnostic criteria emphasize motor symptoms that include tremor, gait disturbance, and paucity of movement, there is increasing recognition that disease pathology begins decades before the development of motor impairment.2
Pathologic studies confirm that by the onset of motor symptoms, at least 30% of nigrostriatal neurons are lost or dysfunctional.3-5 Similarly, the Braak staging hypothesis posits initial deposition of Lewy bodies in the olfactory bulb and the dorsal motor nucleus of the vagus nerve, followed by prion-like spread through the brain stem into the midbrain/substantia nigra, and finally into the cortex (Figure 1).6
The decades-long prodromal or preclinical phase represents a unique opportunity for early identification of those at highest risk for developing the motor symptoms of Parkinson disease.7 Accurate identification, ideally before the onset of manifest motor disability, would not only improve prognostic counseling of veterans and families, but also could allow for early enrollment into trials of potentially disease-modifying therapeutic agents. Thus, early and accurate identification of PD is an important goal of the care of veterans with potential PD.
Prodromal Symptoms
Prodromal PD, as defined by the International Parkinson Disease and Movement Disorders Society (MDS), focuses on nonmotor symptoms that herald the onset of manifest motor PD.8 The most commonly assessed nonmotor features include olfaction, constipation, sleep disturbance, and mood disorders.
Olfaction is impaired in > 90% of patients with motor PD at the time of diagnosis; by contrast, the prevalence of hyposmia in the general population ranges from 20% to 50%, with higher rates in older adults and in smokers.9-11 Thus, olfaction appears to be a relatively sensitive, though nonspecific, prodromal feature. Importantly, subjective report of hyposmia is poorly reliable, so a number of different tests have been developed for objective assessment of olfactory dysfunction.12 The 12-item Brief Smell Identification Test (B-SIT), derived from the longer University of Pennsylvania Smell Identification Test, is a “scratch-and-sniff” forced multiple choice test that can be self-administered by cooperative patients.13,14 The B-SIT has been validated in multiple ethnic and cultural groups and shows high discrimination between PD subjects and controls.13,15 Of note, olfactory impairment appears to be associated with risk of cognitive decline in PD, further emphasizing the need for accurate assessment to guide prognosis.16
Like hyposmia, constipation can be noted long before the diagnosis of manifest motor PD.17 After adjustment for lifestyle factors, constipated individuals have up to 4.5-fold increased odds of developing PD, and those with constipation suffer worsened disease outcomes and health-related quality of life.17-20 Some groups have demonstrated alterations in gut microbiota of those with prodromal PD, which suggests local inflammatory processes and intestinal permeability may contribute to protein misfolding and disease development.21,22 This also raises the intriguing possibility that dietary alterations may be neuroprotective or neurorestorative, although this has yet to be tested in humans.23,24
Like constipation, mood changes can precede the appearance of manifest motor PD.25,26 Case control studies suggest a higher risk of developing PD among individuals who were previously diagnosed with depression or anxiety, particularly in the 1 to 2 years prior to PD diagnosis.27-29 Both apathy and anxiety are associated with striatal dopamine dysfunction, particularly in the right caudate nucleus, which suggests that mood changes are directly related to disease pathology.30,31
Of the prodromal features, rapid eye movement sleep behavior disorder (RBD) is associated with the highest risk of conversion to motor PD.8 Up to 80% of older men with socalled idiopathic RBD develop a parkinsonian syndrome within 20 years; risk is divided about equally between idiopathic PD and dementia with Lewy bodies (DLB).32 Collateral history from a bed-partner is usually sufficient to make the diagnosis, although, this is often confounded by the prevalence of nightmares in those with posttraumatic stress disorder in the veteran population.32 Thus, in suspected cases, obtaining a polysomnogram can aid in distinguishing between idiopathic PC and DLB.33 Given the specificity of RBD as a marker of synuclein deposition and the high risk of progression to a degenerative syndrome, accurate diagnosis and counseling is imperative.
Each of the prodromal nonmotor features of PD are at best moderately sensitive or specific in isolation, but in concert, they can be used to develop a Parkinson risk score. For instance, the MDS prodromal criteria combine individual likelihood ratios into Bayesian analysis to determine a combined probability of PD, which can be further stratified to probable or possible prodromal PD (probability > 80%, > 50%, respectively).8 These criteria have been applied to several independent cohorts and demonstrate high sensitivity and specificity, especially over time.34,35 Applicability in a veteran population has yet to be determined.
Use of Imaging in Diagnosis
Although clinical diagnostic criteria and prodromal features can improve diagnostic accuracy, it can be extremely challenging to distinguish idiopathic PD from nondegenerative parkinsonism or atypical syndromes (see below). Compared with the gold standard of pathologic assessment, the clinical diagnostic accuracy for PD ranges from 73% for nonexperts to 80% for fellowship-trained movement disorders specialists.36 Thus, objective biomarkers are sought to improve diagnostic accuracy both for clinical care as well as for research purposes, such as enrollment into clinical trials.
Multiple potential imaging biomarkers for preclinical PD can aid in early diagnosis and help differentiate PD from related but distinct disorders. While beyond the scope of this review, these techniques have recently been reviewed.7 Of these, the most widely available and accurate is dopamine transporter (DAT) imaging, which uses a radioiodinated ligand that binds to DAT on striatal dopaminergic terminals; binding is detected through single photon emission computed tomography (SPECT) scanning. Thus, a SPECT DaTscan (GE Healthcare Bio-Sciences, Little Chalfont, England) directly assesses the integrity of the presynaptic nigrostriatal system and is well correlated with severity of motor and nonmotor parkinsonism.37,38
In individuals with suspected prodromal PD, abnormal DaTscans are associated with faster progression to manifest motor PD.39 However, it should be noted that a number of medications, several of which are commonly utilized in the veteran population, can affect the outcome of a DaTscan.40 Some of these medications only mildly affect the outcome, so the physician interpreting the scan should be made aware of their use, while others need to be held for days to weeks so as not to invalidate the DaTscan. DaTscan also do not differentiate between PD and atypical degenerative parkinsonisms such as multiple system atrophy (MSA), DLB, progressive supranuclear palsy (PSP), or corticobasal syndrome (CBS). Nevertheless, these scans can be used to distinguish degenerative parkinsonisms from other conditions that can be difficult to distinguish clinically from PD, including essential tremor, normal pressure hydrocephalus, vascular parkinsonism, or druginduced parkinsonism (DIP).
DIP usually is caused by blockade of postsynaptic dopamine receptors by antipsychotic medications, which are prescribed to as many as 1 in 4 older veterans; antiemetic agents such as metoclopramide are also potential offenders if used chronically.41 The risk of DIP appears to be associated with the D2 binding affinity of the drug. Thus, of the newer atypical antipsychotics, clozapine and quetiapine appear to have the lowest risk, while ziprasidone and aripiprazole have the highest binding affinity and therefore the highest risk.42 In many patients, parkinsonism persists even after discontinuation of the offending agent, suggesting that in at least a subset of patients, DIP may be an “unmasking” of latent PD rather than a true adverse effect of the medication. The prodromal features discussed above can be used to distinguish isolated DIP from unmasked latent PD.43 In a study we conducted in veterans at the Michael J. Crescenz VA Medical Center in Philadelphia, Pennsylvania, hyposmia in particular was shown to be highly predictive of an underlying dopaminergic deficit with an odds ratio of 63.44
Other important considerations in the differential diagnosis of PD are the atypical degenerative parkinsonian syndromes, formerly called Parkinson plus syndromes. These may be further divided into the synucleinopathies (MSA, DLB) or the tauopathies (PSP, CBS), depending on the predominant amyloidogenic protein. Early in the disease, the atypical syndromes and idiopathic PD may be clinically indistinguishable, although the atypical syndromes tend to progress more rapidly and often have a less robust response to levodopa.
Radiologic and fluid biomarkers for the atypical syndromes are under active investigation; at present the most accessible study is magnetic resonance imaging (MRI), which may show characteristic features such as degeneration of the pontocerebellar fibers in MSA or midbrain atrophy in PSP.45,46 By contrast, standard MRI sequences in idiopathic PD are usually normal, although high-resolution (7 tesla) imaging can reveal loss of neuromelanin in the substantia nigra.47 MRI also can be useful in the workup of suspected normal pressure hydrocephalus or vascular parkinsonism, which would show disproportionate ventriculomegaly with transependymal flow, or white matter lesions in the basal ganglia, respectively.
Data-Based Identification of Preclinical PD
The integration of clinical motor or prodromal features with biomarker data has led to the development of several large-scale clinical and administrative databases to identify PD. The Parkinson Progression Markers Initiative initially enrolled only de novo clinically identified people with PD, but it expanded to include a prodromal cohort who are being assessed for rates of conversion to PD.48 Similarly, metabolic imaging can be combined with prodromal symptoms, such as hyposmia or RBD, to predict risk for phenoconversion into manifest motor PD.49
The PREDICT-PD study synthesizes mood symptoms, RBD, smell testing, genotyping, and keyboard-tapping tasks to divide individuals into high-, middle-, and low-risk groups; interim analysis at 3 years of follow-up (N = 842) demonstrated a hazard ratio of 4.39 (95% CI, 1.03-18.68) for the diagnosis of PD in the highrisk group compared with the low-risk group.50 Lastly, administrative claims data for prodromal features, such as constipation, RBD, and mood symptoms, is highly predictive of eventual PD diagnosis.51 VA databases accessed through the Corporate Data Warehouse are complementary sources of information to nonveteranspecific Medicare databases; to our knowledge there has not yet been a comprehensive search of VA databases to identify veterans with preclinical PD.
Risk Factors Associated With Military Service
A number of potential environmental risk factors may increase the risk of developing Parkinson disease for veterans. Perhaps the most commonly recognized is pesticide exposure, particularly given the presumptive service connections established by the VA for Parkinson disease and exposure to Agent Orange or contaminated water at Camp Lejeune.52,53 Both dioxin, the toxic ingredient in Agent Orange, and the solvents trichloroethylene and perchloroethylene, found in the water supply at Camp Lejeune, interfere with mitochondrial function leading to oxidative stress and apoptosis of nigrostriatal neurons.54,55 Other potential exposures, which are not necessarily limited to the veteran population, include rotenone, a phytochemical used to kill fish in reservoirs, and paraquat, an herbicide that may directly promote synuclein aggregation.56,57 Veterans who have reported exposure to these or other environmental chemicals in civilian life should be carefully assessed for the presence of motor PD or prodromal features.
Traumatic brain injury (TBI) also may be a risk factor for PD, which may be particularly relevant for veterans who had served in Iraq or Afghanistan. Retrospective claims data suggest a strong association between PD and recent TBI in the 5 to 10 years prior to motor PD diagnosis.58,59 A recent assessment of combat veterans with TBI found that even mild TBI was associated with a 56% increased risk of PD, while moderate-to-severe TBI was associated with an 83% higher risk of PD.60 The pathologic mechanism for this link is unclear, but post-TBI inflammatory processes may lead to the formation of reactive oxygen species and/or glutamatergic excitotoxicity, thus leading to secondary injury in the nigrostriatal pathway.61 As with prodromal symptoms, the risk of PD related to environmental risk factors may be synergistic; repetitive TBI may be more damaging than a single injury, and a combination of TBI and pesticide exposure markedly increases PD risk beyond the risk of TBI or the risk of pesticides alone.62 Recently, parkinsonism, including Parkinson disease, was recognized as a service connected condition for veterans with a servicerelated moderate or severe TBI.63
Conclusion
Because of the substantial impact on quality of life and disability-adjusted life years, early and accurate identification and management of veterans at risk for PD is an important priority area for the VA. The 10-year cost of PD-related benefits through the VA was estimated at $3.5 billion in fiscal year 2010, and that number is likely to rise in coming years, due to the aging population as well as synergistic effects of independent risk factors described above.64 In response, the VA has created a network of specialty care sites, known as Parkinson Disease Research, Education, and Clinical Centers (PADRECCs) located in Philadelphia, Pennsylvania; Richmond, Virginia; Houston, Texas; West Los Angeles and San Francisco, California; and Seattle, Washington/ Portland, Oregon (www.parkinsons.va.gov).
The PADRECCs are supplemented by a National VA PD Consortium network of VA physicians trained in PD management (Figure 2). Studies, including one investigating care of veterans with PD, have demonstrated that involvement of specialty care services early in the course of PD leads to improved patient outcomes.65,66 In addition to patient-facing resources such as support groups and specialized physical/occupational/speech therapy, PADRECCs and the consortium sites are national leaders in PD education and clinical trials and provide high-quality, multidisciplinary care for veterans with PD.67 Thus, veterans with significant risk factors or prodromal symptoms of PD should be referred into the PADRECC/Consortium network in order to maximize their quality of care and quality of life.
Parkinson disease (PD) affects about 680,000 in the US, including > 110,000 veterans (Caroline Tanner, MD, PhD, unpublished data).1 In the next 10 years, this number is expected to double, in part because of the aging of the US population.1 Although the classic diagnostic criteria emphasize motor symptoms that include tremor, gait disturbance, and paucity of movement, there is increasing recognition that disease pathology begins decades before the development of motor impairment.2
Pathologic studies confirm that by the onset of motor symptoms, at least 30% of nigrostriatal neurons are lost or dysfunctional.3-5 Similarly, the Braak staging hypothesis posits initial deposition of Lewy bodies in the olfactory bulb and the dorsal motor nucleus of the vagus nerve, followed by prion-like spread through the brain stem into the midbrain/substantia nigra, and finally into the cortex (Figure 1).6
The decades-long prodromal or preclinical phase represents a unique opportunity for early identification of those at highest risk for developing the motor symptoms of Parkinson disease.7 Accurate identification, ideally before the onset of manifest motor disability, would not only improve prognostic counseling of veterans and families, but also could allow for early enrollment into trials of potentially disease-modifying therapeutic agents. Thus, early and accurate identification of PD is an important goal of the care of veterans with potential PD.
Prodromal Symptoms
Prodromal PD, as defined by the International Parkinson Disease and Movement Disorders Society (MDS), focuses on nonmotor symptoms that herald the onset of manifest motor PD.8 The most commonly assessed nonmotor features include olfaction, constipation, sleep disturbance, and mood disorders.
Olfaction is impaired in > 90% of patients with motor PD at the time of diagnosis; by contrast, the prevalence of hyposmia in the general population ranges from 20% to 50%, with higher rates in older adults and in smokers.9-11 Thus, olfaction appears to be a relatively sensitive, though nonspecific, prodromal feature. Importantly, subjective report of hyposmia is poorly reliable, so a number of different tests have been developed for objective assessment of olfactory dysfunction.12 The 12-item Brief Smell Identification Test (B-SIT), derived from the longer University of Pennsylvania Smell Identification Test, is a “scratch-and-sniff” forced multiple choice test that can be self-administered by cooperative patients.13,14 The B-SIT has been validated in multiple ethnic and cultural groups and shows high discrimination between PD subjects and controls.13,15 Of note, olfactory impairment appears to be associated with risk of cognitive decline in PD, further emphasizing the need for accurate assessment to guide prognosis.16
Like hyposmia, constipation can be noted long before the diagnosis of manifest motor PD.17 After adjustment for lifestyle factors, constipated individuals have up to 4.5-fold increased odds of developing PD, and those with constipation suffer worsened disease outcomes and health-related quality of life.17-20 Some groups have demonstrated alterations in gut microbiota of those with prodromal PD, which suggests local inflammatory processes and intestinal permeability may contribute to protein misfolding and disease development.21,22 This also raises the intriguing possibility that dietary alterations may be neuroprotective or neurorestorative, although this has yet to be tested in humans.23,24
Like constipation, mood changes can precede the appearance of manifest motor PD.25,26 Case control studies suggest a higher risk of developing PD among individuals who were previously diagnosed with depression or anxiety, particularly in the 1 to 2 years prior to PD diagnosis.27-29 Both apathy and anxiety are associated with striatal dopamine dysfunction, particularly in the right caudate nucleus, which suggests that mood changes are directly related to disease pathology.30,31
Of the prodromal features, rapid eye movement sleep behavior disorder (RBD) is associated with the highest risk of conversion to motor PD.8 Up to 80% of older men with socalled idiopathic RBD develop a parkinsonian syndrome within 20 years; risk is divided about equally between idiopathic PD and dementia with Lewy bodies (DLB).32 Collateral history from a bed-partner is usually sufficient to make the diagnosis, although, this is often confounded by the prevalence of nightmares in those with posttraumatic stress disorder in the veteran population.32 Thus, in suspected cases, obtaining a polysomnogram can aid in distinguishing between idiopathic PC and DLB.33 Given the specificity of RBD as a marker of synuclein deposition and the high risk of progression to a degenerative syndrome, accurate diagnosis and counseling is imperative.
Each of the prodromal nonmotor features of PD are at best moderately sensitive or specific in isolation, but in concert, they can be used to develop a Parkinson risk score. For instance, the MDS prodromal criteria combine individual likelihood ratios into Bayesian analysis to determine a combined probability of PD, which can be further stratified to probable or possible prodromal PD (probability > 80%, > 50%, respectively).8 These criteria have been applied to several independent cohorts and demonstrate high sensitivity and specificity, especially over time.34,35 Applicability in a veteran population has yet to be determined.
Use of Imaging in Diagnosis
Although clinical diagnostic criteria and prodromal features can improve diagnostic accuracy, it can be extremely challenging to distinguish idiopathic PD from nondegenerative parkinsonism or atypical syndromes (see below). Compared with the gold standard of pathologic assessment, the clinical diagnostic accuracy for PD ranges from 73% for nonexperts to 80% for fellowship-trained movement disorders specialists.36 Thus, objective biomarkers are sought to improve diagnostic accuracy both for clinical care as well as for research purposes, such as enrollment into clinical trials.
Multiple potential imaging biomarkers for preclinical PD can aid in early diagnosis and help differentiate PD from related but distinct disorders. While beyond the scope of this review, these techniques have recently been reviewed.7 Of these, the most widely available and accurate is dopamine transporter (DAT) imaging, which uses a radioiodinated ligand that binds to DAT on striatal dopaminergic terminals; binding is detected through single photon emission computed tomography (SPECT) scanning. Thus, a SPECT DaTscan (GE Healthcare Bio-Sciences, Little Chalfont, England) directly assesses the integrity of the presynaptic nigrostriatal system and is well correlated with severity of motor and nonmotor parkinsonism.37,38
In individuals with suspected prodromal PD, abnormal DaTscans are associated with faster progression to manifest motor PD.39 However, it should be noted that a number of medications, several of which are commonly utilized in the veteran population, can affect the outcome of a DaTscan.40 Some of these medications only mildly affect the outcome, so the physician interpreting the scan should be made aware of their use, while others need to be held for days to weeks so as not to invalidate the DaTscan. DaTscan also do not differentiate between PD and atypical degenerative parkinsonisms such as multiple system atrophy (MSA), DLB, progressive supranuclear palsy (PSP), or corticobasal syndrome (CBS). Nevertheless, these scans can be used to distinguish degenerative parkinsonisms from other conditions that can be difficult to distinguish clinically from PD, including essential tremor, normal pressure hydrocephalus, vascular parkinsonism, or druginduced parkinsonism (DIP).
DIP usually is caused by blockade of postsynaptic dopamine receptors by antipsychotic medications, which are prescribed to as many as 1 in 4 older veterans; antiemetic agents such as metoclopramide are also potential offenders if used chronically.41 The risk of DIP appears to be associated with the D2 binding affinity of the drug. Thus, of the newer atypical antipsychotics, clozapine and quetiapine appear to have the lowest risk, while ziprasidone and aripiprazole have the highest binding affinity and therefore the highest risk.42 In many patients, parkinsonism persists even after discontinuation of the offending agent, suggesting that in at least a subset of patients, DIP may be an “unmasking” of latent PD rather than a true adverse effect of the medication. The prodromal features discussed above can be used to distinguish isolated DIP from unmasked latent PD.43 In a study we conducted in veterans at the Michael J. Crescenz VA Medical Center in Philadelphia, Pennsylvania, hyposmia in particular was shown to be highly predictive of an underlying dopaminergic deficit with an odds ratio of 63.44
Other important considerations in the differential diagnosis of PD are the atypical degenerative parkinsonian syndromes, formerly called Parkinson plus syndromes. These may be further divided into the synucleinopathies (MSA, DLB) or the tauopathies (PSP, CBS), depending on the predominant amyloidogenic protein. Early in the disease, the atypical syndromes and idiopathic PD may be clinically indistinguishable, although the atypical syndromes tend to progress more rapidly and often have a less robust response to levodopa.
Radiologic and fluid biomarkers for the atypical syndromes are under active investigation; at present the most accessible study is magnetic resonance imaging (MRI), which may show characteristic features such as degeneration of the pontocerebellar fibers in MSA or midbrain atrophy in PSP.45,46 By contrast, standard MRI sequences in idiopathic PD are usually normal, although high-resolution (7 tesla) imaging can reveal loss of neuromelanin in the substantia nigra.47 MRI also can be useful in the workup of suspected normal pressure hydrocephalus or vascular parkinsonism, which would show disproportionate ventriculomegaly with transependymal flow, or white matter lesions in the basal ganglia, respectively.
Data-Based Identification of Preclinical PD
The integration of clinical motor or prodromal features with biomarker data has led to the development of several large-scale clinical and administrative databases to identify PD. The Parkinson Progression Markers Initiative initially enrolled only de novo clinically identified people with PD, but it expanded to include a prodromal cohort who are being assessed for rates of conversion to PD.48 Similarly, metabolic imaging can be combined with prodromal symptoms, such as hyposmia or RBD, to predict risk for phenoconversion into manifest motor PD.49
The PREDICT-PD study synthesizes mood symptoms, RBD, smell testing, genotyping, and keyboard-tapping tasks to divide individuals into high-, middle-, and low-risk groups; interim analysis at 3 years of follow-up (N = 842) demonstrated a hazard ratio of 4.39 (95% CI, 1.03-18.68) for the diagnosis of PD in the highrisk group compared with the low-risk group.50 Lastly, administrative claims data for prodromal features, such as constipation, RBD, and mood symptoms, is highly predictive of eventual PD diagnosis.51 VA databases accessed through the Corporate Data Warehouse are complementary sources of information to nonveteranspecific Medicare databases; to our knowledge there has not yet been a comprehensive search of VA databases to identify veterans with preclinical PD.
Risk Factors Associated With Military Service
A number of potential environmental risk factors may increase the risk of developing Parkinson disease for veterans. Perhaps the most commonly recognized is pesticide exposure, particularly given the presumptive service connections established by the VA for Parkinson disease and exposure to Agent Orange or contaminated water at Camp Lejeune.52,53 Both dioxin, the toxic ingredient in Agent Orange, and the solvents trichloroethylene and perchloroethylene, found in the water supply at Camp Lejeune, interfere with mitochondrial function leading to oxidative stress and apoptosis of nigrostriatal neurons.54,55 Other potential exposures, which are not necessarily limited to the veteran population, include rotenone, a phytochemical used to kill fish in reservoirs, and paraquat, an herbicide that may directly promote synuclein aggregation.56,57 Veterans who have reported exposure to these or other environmental chemicals in civilian life should be carefully assessed for the presence of motor PD or prodromal features.
Traumatic brain injury (TBI) also may be a risk factor for PD, which may be particularly relevant for veterans who had served in Iraq or Afghanistan. Retrospective claims data suggest a strong association between PD and recent TBI in the 5 to 10 years prior to motor PD diagnosis.58,59 A recent assessment of combat veterans with TBI found that even mild TBI was associated with a 56% increased risk of PD, while moderate-to-severe TBI was associated with an 83% higher risk of PD.60 The pathologic mechanism for this link is unclear, but post-TBI inflammatory processes may lead to the formation of reactive oxygen species and/or glutamatergic excitotoxicity, thus leading to secondary injury in the nigrostriatal pathway.61 As with prodromal symptoms, the risk of PD related to environmental risk factors may be synergistic; repetitive TBI may be more damaging than a single injury, and a combination of TBI and pesticide exposure markedly increases PD risk beyond the risk of TBI or the risk of pesticides alone.62 Recently, parkinsonism, including Parkinson disease, was recognized as a service connected condition for veterans with a servicerelated moderate or severe TBI.63
Conclusion
Because of the substantial impact on quality of life and disability-adjusted life years, early and accurate identification and management of veterans at risk for PD is an important priority area for the VA. The 10-year cost of PD-related benefits through the VA was estimated at $3.5 billion in fiscal year 2010, and that number is likely to rise in coming years, due to the aging population as well as synergistic effects of independent risk factors described above.64 In response, the VA has created a network of specialty care sites, known as Parkinson Disease Research, Education, and Clinical Centers (PADRECCs) located in Philadelphia, Pennsylvania; Richmond, Virginia; Houston, Texas; West Los Angeles and San Francisco, California; and Seattle, Washington/ Portland, Oregon (www.parkinsons.va.gov).
The PADRECCs are supplemented by a National VA PD Consortium network of VA physicians trained in PD management (Figure 2). Studies, including one investigating care of veterans with PD, have demonstrated that involvement of specialty care services early in the course of PD leads to improved patient outcomes.65,66 In addition to patient-facing resources such as support groups and specialized physical/occupational/speech therapy, PADRECCs and the consortium sites are national leaders in PD education and clinical trials and provide high-quality, multidisciplinary care for veterans with PD.67 Thus, veterans with significant risk factors or prodromal symptoms of PD should be referred into the PADRECC/Consortium network in order to maximize their quality of care and quality of life.
1. Marras C, Beck JC, Bower JH, et al; Parkinson’s Foundation P4 Group. Prevalence of Parkinson’s disease across North America. NPJ Parkinsons Dis. 2018;4:21.
2. Postuma RB, Berg D, Stern M, et al. MDS clinical diagnostic criteria for Parkinson’s disease. Mov Disord. 2015;30(12):1591-1601.
3. Fearnley JM, Lees AJ. Ageing and Parkinson’s disease: substantia nigra regional selectivity. Brain. 1991;114(pt 5):2283-2301.
4. Greffard S, Verny M, Bonnet A-M, et al. Motor score of the Unified Parkinson Disease Rating Scale as a good predictor of Lewy body-associated neuronal loss in the substantia nigra. Arch Neurol. 2006;63(4):584-588.
5. Hilker R, Schweitzer K, Coburger S, et al. Nonlinear progression of Parkinson disease as determined by serial positron emission tomographic imaging of striatal fluorodopa F 18 activity. Arch Neurol. 2005;62(3):378-382.
6. Braak H, Del Tredici K, Rüb U, de Vos RAI, Jansen Steur ENH, Braak E. Staging of brain pathology related to sporadic Parkinson’s disease. Neurobiol Aging. 2003;24(2):197-211.
7. Mantri S, Morley JF, Siderowf AD. The importance of preclinical diagnostics in Parkinson disease. Parkinsonism Relat Disord. 2018;pii:S1353-8020(18)30396-1. [Epub ahead of print]
8. Berg D, Postuma RB, Adler CH, et al. MDS research criteria for prodromal Parkinson’s disease. Mov Disord. 2015;30(12):1600-1611.
9. Haehner A, Boesveldt S, Berendse HW, et al. Prevalence of smell loss in Parkinson’s disease – a multicenter study. Parkinsonism Relat Disord. 2009;15(7):490-494.
10. Mullol J, Alobid I, Mariño-Sánchez F, et al. Furthering the understanding of olfaction, prevalence of loss of smell and risk factors: a population-based survey (OLFACAT study). BMJ Open. 2012;2(6).pii:e001256.
11. Doty RL, Shaman P, Applebaum SL, Giberson R, Siksorski L, Rosenberg L. Smell identification ability: changes with age. Science. 1984;226(4681):1441-1443.
12. Doty RL. Olfactory dysfunction in Parkinson disease. Nat Rev Neurol. 2012;8(6):329-339.
13. Double KL, Rowe DB, Hayes M, et al. Identifying the pattern of olfactory deficits in Parkinson disease using the brief smell identification test. Arch Neurol. 2003;60(4):545-549.
14. Doty RL, Shaman P, Dann M. Development of the University of Pennsylvania Smell Identification Test: a standardized microencapsulated test of olfactory function. Physiol Behav. 1984;32(3):489-502.
15. Morley JF, Cohen A, Silveira-Moriyama L, et al. Optimizing olfactory testing for the diagnosis of Parkinson’s disease: item analysis of the University of Pennsylvania smell identification test. NPJ Parkinsons Dis. 2018;4:2.
16. Fullard ME, Tran B, Xie SX, et al. Olfactory impairment predicts cognitive decline in early Parkinson’s disease. Parkinsonism Relat Disord. 2016;25:45-51.
17. Savica R, Carlin JM, Grossardt BR, et al. Medical records documentation of constipation preceding Parkinson disease: a case-control study. Neurology. 2009;73(21):1752-1758.
18. Abbott RD, Petrovitch H, White LR, et al. Frequency of bowel movements and the future risk of Parkinson’s disease. Neurology. 2001;57(3):456-462.
19. Stocchi F, Torti M. Constipation in Parkinson’s disease. Int Rev Neurobiol. 2017;134:811-826.
20. Yu QJ, Yu SY, Zuo LJ, et al. Parkinson disease with constipation: clinical features and relevant factors. Sci Rep. 2018;8(1):567.
21. Hill-Burns EM, Debelius JW, Morton JT, et al. Parkinson’s disease and Parkinson’s disease medications have distinct signatures of the gut microbiome. Mov Disord. 2017;32(5):739-749.
22. Mulak A, Bonaz B. Brain-gut-microbiota axis in Parkinson’s disease. World J Gastroenterol. 2015;21(37): 10609-10620.
23. Shah SP, Duda JE. Dietary modifications in Parkinson’s disease: a neuroprotective intervention? Med Hypotheses. 2015;85(6):1002-1005.
24. Perez-Pardo P, de Jong EM, Broersen LM, et al. Promising effects of neurorestorative diets on motor, cognitive, and gastrointestinal dysfunction after symptom development in a mouse model of Parkinson’s disease. Front Aging Neurosci. 2017;9:57.
25. Fang F, Xu Q, Park Y, et al. Depression and the subsequent risk of Parkinson’s disease in the NIH-AARP Diet and Health Study. Mov Disord. 2010;25(9):1157-1162.
26. Leentjens AFG, Van den Akker M, Metsemakers JFM, Lousberg R, Verhey FRJ. Higher incidence of depression preceding the onset of Parkinson’s disease: a register study. Mov Disord. 2003;18(4):414-418.
27. Alonso A, Rodriguez LAG, Logroscino G, Hernán MA. Use of antidepressants and the risk of Parkinson’s disease: a prospective study. J Neurol Neurosurg Psychiatry. 2009;80(6):671-674.
28. Weisskopf MG, Chen H, Schwarzschild MA, Kawachi I, Ascherio A. Prospective study of phobic anxiety and risk of Parkinson’s disease. Mov Disord. 2003;18(6):646-651.
29. Darweesh SK, Verlinden VJ, Stricker BH, Hofman A, Koudstaal PJ, Ikram MA. Trajectories of prediagnostic functioning in Parkinson’s disease. Brain. 2017;140(2):429-441.
30. Santangelo G, Vitale C, Picillo M, et al. Apathy and striatal dopamine transporter levels in de-novo, untreated Parkinson’s disease patients. Parkinsonism Relat Disord. 2015;21(5):489-493.
31. Erro R, Pappatà S, Amboni M, et al. Anxiety is associated with striatal dopamine transporter availability in newly diagnosed untreated Parkinson’s disease patients. Parkinsonism Relat Disord. 2012;18(9):1034-1038.
32. Schenck CH, Boeve BF, Mahowald MW. Delayed emergence of a parkinsonian disorder or dementia in 81% of older men initially diagnosed with idiopathic rapid eye movement sleep behavior disorder: a 16-year update on a previously reported series. Sleep Med. 2013;14(8):
744-748.
33. Melendez J, Hesselbacher S, Sharafkhaneh A, Hirshkowitz M. Assessment of REM sleep behavior disorder in veterans with posttraumatic stress disorder. Chest. 2011;140(4):967A.
34. Pilotto A, Heinzel S, Suenkel U, et al. Application of the movement disorder society prodromal Parkinson’s disease research criteria in 2 independent prospective cohorts. Mov Disord. 2017;32(7):1025-1034.
35. Fereshtehnejad S-M, Montplaisir JY, Pelletier A, Gagnon J-F, Berg D, Postuma RB. Validation of the MDS research criteria for prodromal Parkinson’s disease: Longitudinal assessment in a REM sleep behavior disorder (RBD) cohort. Mov Disord. 2017;32(6):865-873.
36. Rizzo G, Copetti M, Arcuti S, Martino D, Fontana A, Logroscino G. Accuracy of clinical diagnosis of Parkinson disease: a systematic review and meta-analysis. Neurology. 2016;86(6):566-576.
37. Moccia M, Pappatà S, Picillo M, et al. Dopamine transporter availability in motor subtypes of de novo drug-naïve Parkinson’s disease. J Neurol. 2014;261(11):2112-2118.
38. Siepel FJ, Brønnick KS, Booij J, et al. Cognitive executive impairment and dopaminergic deficits in de novo Parkinson’s disease. Mov Disord. 2014;29(14):1802-1808.
39. Iranzo A, Valldeoriola F, Lomeña F, et al. Serial dopamine transporter imaging of nigrostriatal function in patients with idiopathic rapid-eye-movement sleep behaviour disorder: a prospective study. Lancet Neurol. 2011;10(9):797-805.
40. Booij J, Kemp P. Dopamine transporter imaging with [(123)I]FP-CIT SPECT: potential effects of drugs. Eur J Nucl Med Mol Imaging. 2008;35(2):424-438.
41. Gellad WF, Aspinall SL, Handler SM, et al. Use of antipsychotics among older residents in VA nursing homes. Med Care. 2012;50(11):954-960.
42. Mauri MC, Paletta S, Maffini M, et al. Clinical pharmacology of atypical antipsychotics: an update. EXCLI J. 2014;13:1163-1191.
43. Morley JF, Duda JE. Use of hyposmia and other non-motor symptoms to distinguish between drug-induced parkinsonism and Parkinson’s disease. J Parkinsons Dis. 2014;4(2):169-173.
44. Morley JF, Cheng G, Dubroff JG, Wood S, Wilkinson JR, Duda JE. Olfactory impairment predicts underlying dopaminergic deficit in presumed drug-induced parkinsonism. Mov Disord Clin Pract. 2017;4(4):603-606.
45. Whitwell JL, Höglinger GU, Antonini A, et al; Movement Disorder Society-endorsed PSP Study Group. Radiological biomarkers for diagnosis in PSP: where are we and where do we need to be? Mov Disord. 2017;32(7):955-971.
46. Laurens B, Constantinescu R, Freeman R, et al. Fluid biomarkers in multiple system atrophy: A review of the MSA Biomarker Initiative. Neurobiol Dis. 2015;80:29-41.
47. Barber TR, Klein JC, Mackay CE, Hu MTM. Neuroimaging in pre-motor Parkinson’s disease. NeuroImage Clin. 2017;15:215-227.
48. Parkinson Progression Marker Initiative. The Parkinson Progression Marker Initiative (PPMI). Prog Neurobiol. 2011;95(4):629-635.
49. Meles SK, Vadasz D, Renken RJ, et al. FDG PET, dopamine transporter SPECT, and olfaction: combining biomarkers in REM sleep behavior disorder. Mov Disord. 2017;32(10):1482-1486.
50. Noyce AJ, R’Bibo L, Peress L, et al. PREDICT‐PD: an online approach to prospectively identify risk indicators of Parkinson’s disease. Mov Disord. 2017 Feb; 32(2): 219–226.
51. Searles Nielsen S, Warden MN, Camacho-Soto A, Willis AW, Wright BA, Racette BA. A predictive model to identify Parkinson disease from administrative claims data. Neurology. 2017;89(14):1448-1456.
52. Institute of Medicine. Veterans and Agent Orange: Update 2012. National Academies Press: Washington, DC; 2013.
53. Department of Veterans Affairs. Diseases associated with exposure to Contaminants in the Water Supply at Camp Lejeune. Final rule. Fed Regist. 2017;82(9):4173-4185.
54. Goldman SM, Quinlan PJ, Ross GW, et al. Solvent exposures and Parkinson disease risk in twins. Ann Neurol. 2012;71(6):776-784.
55. Liu M, Shin EJ, Dang DK, et al. Trichloroethylene and Parkinson’s disease: risk assessment. Mol Neurobiol. 2018;55(7):6201-6214.
56. Betarbet R, Sherer TB, MacKenzie G, Garcia-Osuna M, Panov AV, Greenamyre JT. Chronic systemic pesticide exposure reproduces features of Parkinson’s disease. Nat Neurosci. 2000;3(12):1301-1306.
57. Manning-Bog AB, McCormack AL, Li J, Uversky VN, Fink AL, Monte DAD. The herbicide paraquat causes up-regulation and aggregation of alpha-synuclein in mice: paraquat and alpha-synuclein. J Biol Chem. 2002;277(3):1641-1644.
58. Camacho-Soto A, Warden MN, Searles Nielsen S, et al. Traumatic brain injury in the prodromal period of Parkinson’s disease: a large epidemiological study using medicare data. Ann Neurol. 2017;82(5):744-754.
59. Gardner RC, Burke JF, Nettiksimmons J, Goldman S, Tanner CM, Yaffe K. Traumatic brain injury in later life increases risk for Parkinson disease. Ann Neurol. 2015;77(6):987-995.
60. Gardner RC, Byers AL, Barnes DE, Li Y, Boscardin J, Yaffe K. Mild TBI and risk of Parkinson disease: a Chronic Effects of Neurotrauma Consortium Study. Neurology. 2018;90(20):e1771-e1779.
61. Cruz-Haces M, Tang J, Acosta G, Fernandez J, Shi R. Pathological correlations between traumatic brain injury and chronic neurodegenerative diseases. Transl Neurodegener. 2017;6:20.
62. Lee PC, Bordelon Y, Bronstein J, Ritz B. Traumatic brain injury, paraquat exposure, and their relationship to Parkinson disease. Neurology. 2012;79(20):2061-2066.
63. Disabilities that are proximately due to, or aggravated by, service-connected disease or injury. 38 CFR §3.310.
64. Diseases Associated With Exposure to Certain Herbicide Agents (Hairy Cell Leukemia and Other Chronic B-Cell Leukemias, Parkinson’s Disease and Ischemic Heart Disease). Federal Regist. 2010;75(173):53202-53216. To be codified at 38 CFR §3.
65. Cheng EM, Swarztrauber K, Siderowf AD, et al. Association of specialist involvement and quality of care for Parkinson’s disease. Mov Disord. 2007;22(4):515-522.
66. Qamar MA, Harington G, Trump S, Johnson J, Roberts F, Frost E. Multidisciplinary care in Parkinson’s disease. Int Rev Neurobiol. 2017;132:511-523.
67. Pogoda TK, Cramer IE, Meterko M, et al. Patient and organizational factors related to education and support use by veterans with Parkinson’s disease. Mov Disord. 2009;24(13):1916-1924.
1. Marras C, Beck JC, Bower JH, et al; Parkinson’s Foundation P4 Group. Prevalence of Parkinson’s disease across North America. NPJ Parkinsons Dis. 2018;4:21.
2. Postuma RB, Berg D, Stern M, et al. MDS clinical diagnostic criteria for Parkinson’s disease. Mov Disord. 2015;30(12):1591-1601.
3. Fearnley JM, Lees AJ. Ageing and Parkinson’s disease: substantia nigra regional selectivity. Brain. 1991;114(pt 5):2283-2301.
4. Greffard S, Verny M, Bonnet A-M, et al. Motor score of the Unified Parkinson Disease Rating Scale as a good predictor of Lewy body-associated neuronal loss in the substantia nigra. Arch Neurol. 2006;63(4):584-588.
5. Hilker R, Schweitzer K, Coburger S, et al. Nonlinear progression of Parkinson disease as determined by serial positron emission tomographic imaging of striatal fluorodopa F 18 activity. Arch Neurol. 2005;62(3):378-382.
6. Braak H, Del Tredici K, Rüb U, de Vos RAI, Jansen Steur ENH, Braak E. Staging of brain pathology related to sporadic Parkinson’s disease. Neurobiol Aging. 2003;24(2):197-211.
7. Mantri S, Morley JF, Siderowf AD. The importance of preclinical diagnostics in Parkinson disease. Parkinsonism Relat Disord. 2018;pii:S1353-8020(18)30396-1. [Epub ahead of print]
8. Berg D, Postuma RB, Adler CH, et al. MDS research criteria for prodromal Parkinson’s disease. Mov Disord. 2015;30(12):1600-1611.
9. Haehner A, Boesveldt S, Berendse HW, et al. Prevalence of smell loss in Parkinson’s disease – a multicenter study. Parkinsonism Relat Disord. 2009;15(7):490-494.
10. Mullol J, Alobid I, Mariño-Sánchez F, et al. Furthering the understanding of olfaction, prevalence of loss of smell and risk factors: a population-based survey (OLFACAT study). BMJ Open. 2012;2(6).pii:e001256.
11. Doty RL, Shaman P, Applebaum SL, Giberson R, Siksorski L, Rosenberg L. Smell identification ability: changes with age. Science. 1984;226(4681):1441-1443.
12. Doty RL. Olfactory dysfunction in Parkinson disease. Nat Rev Neurol. 2012;8(6):329-339.
13. Double KL, Rowe DB, Hayes M, et al. Identifying the pattern of olfactory deficits in Parkinson disease using the brief smell identification test. Arch Neurol. 2003;60(4):545-549.
14. Doty RL, Shaman P, Dann M. Development of the University of Pennsylvania Smell Identification Test: a standardized microencapsulated test of olfactory function. Physiol Behav. 1984;32(3):489-502.
15. Morley JF, Cohen A, Silveira-Moriyama L, et al. Optimizing olfactory testing for the diagnosis of Parkinson’s disease: item analysis of the University of Pennsylvania smell identification test. NPJ Parkinsons Dis. 2018;4:2.
16. Fullard ME, Tran B, Xie SX, et al. Olfactory impairment predicts cognitive decline in early Parkinson’s disease. Parkinsonism Relat Disord. 2016;25:45-51.
17. Savica R, Carlin JM, Grossardt BR, et al. Medical records documentation of constipation preceding Parkinson disease: a case-control study. Neurology. 2009;73(21):1752-1758.
18. Abbott RD, Petrovitch H, White LR, et al. Frequency of bowel movements and the future risk of Parkinson’s disease. Neurology. 2001;57(3):456-462.
19. Stocchi F, Torti M. Constipation in Parkinson’s disease. Int Rev Neurobiol. 2017;134:811-826.
20. Yu QJ, Yu SY, Zuo LJ, et al. Parkinson disease with constipation: clinical features and relevant factors. Sci Rep. 2018;8(1):567.
21. Hill-Burns EM, Debelius JW, Morton JT, et al. Parkinson’s disease and Parkinson’s disease medications have distinct signatures of the gut microbiome. Mov Disord. 2017;32(5):739-749.
22. Mulak A, Bonaz B. Brain-gut-microbiota axis in Parkinson’s disease. World J Gastroenterol. 2015;21(37): 10609-10620.
23. Shah SP, Duda JE. Dietary modifications in Parkinson’s disease: a neuroprotective intervention? Med Hypotheses. 2015;85(6):1002-1005.
24. Perez-Pardo P, de Jong EM, Broersen LM, et al. Promising effects of neurorestorative diets on motor, cognitive, and gastrointestinal dysfunction after symptom development in a mouse model of Parkinson’s disease. Front Aging Neurosci. 2017;9:57.
25. Fang F, Xu Q, Park Y, et al. Depression and the subsequent risk of Parkinson’s disease in the NIH-AARP Diet and Health Study. Mov Disord. 2010;25(9):1157-1162.
26. Leentjens AFG, Van den Akker M, Metsemakers JFM, Lousberg R, Verhey FRJ. Higher incidence of depression preceding the onset of Parkinson’s disease: a register study. Mov Disord. 2003;18(4):414-418.
27. Alonso A, Rodriguez LAG, Logroscino G, Hernán MA. Use of antidepressants and the risk of Parkinson’s disease: a prospective study. J Neurol Neurosurg Psychiatry. 2009;80(6):671-674.
28. Weisskopf MG, Chen H, Schwarzschild MA, Kawachi I, Ascherio A. Prospective study of phobic anxiety and risk of Parkinson’s disease. Mov Disord. 2003;18(6):646-651.
29. Darweesh SK, Verlinden VJ, Stricker BH, Hofman A, Koudstaal PJ, Ikram MA. Trajectories of prediagnostic functioning in Parkinson’s disease. Brain. 2017;140(2):429-441.
30. Santangelo G, Vitale C, Picillo M, et al. Apathy and striatal dopamine transporter levels in de-novo, untreated Parkinson’s disease patients. Parkinsonism Relat Disord. 2015;21(5):489-493.
31. Erro R, Pappatà S, Amboni M, et al. Anxiety is associated with striatal dopamine transporter availability in newly diagnosed untreated Parkinson’s disease patients. Parkinsonism Relat Disord. 2012;18(9):1034-1038.
32. Schenck CH, Boeve BF, Mahowald MW. Delayed emergence of a parkinsonian disorder or dementia in 81% of older men initially diagnosed with idiopathic rapid eye movement sleep behavior disorder: a 16-year update on a previously reported series. Sleep Med. 2013;14(8):
744-748.
33. Melendez J, Hesselbacher S, Sharafkhaneh A, Hirshkowitz M. Assessment of REM sleep behavior disorder in veterans with posttraumatic stress disorder. Chest. 2011;140(4):967A.
34. Pilotto A, Heinzel S, Suenkel U, et al. Application of the movement disorder society prodromal Parkinson’s disease research criteria in 2 independent prospective cohorts. Mov Disord. 2017;32(7):1025-1034.
35. Fereshtehnejad S-M, Montplaisir JY, Pelletier A, Gagnon J-F, Berg D, Postuma RB. Validation of the MDS research criteria for prodromal Parkinson’s disease: Longitudinal assessment in a REM sleep behavior disorder (RBD) cohort. Mov Disord. 2017;32(6):865-873.
36. Rizzo G, Copetti M, Arcuti S, Martino D, Fontana A, Logroscino G. Accuracy of clinical diagnosis of Parkinson disease: a systematic review and meta-analysis. Neurology. 2016;86(6):566-576.
37. Moccia M, Pappatà S, Picillo M, et al. Dopamine transporter availability in motor subtypes of de novo drug-naïve Parkinson’s disease. J Neurol. 2014;261(11):2112-2118.
38. Siepel FJ, Brønnick KS, Booij J, et al. Cognitive executive impairment and dopaminergic deficits in de novo Parkinson’s disease. Mov Disord. 2014;29(14):1802-1808.
39. Iranzo A, Valldeoriola F, Lomeña F, et al. Serial dopamine transporter imaging of nigrostriatal function in patients with idiopathic rapid-eye-movement sleep behaviour disorder: a prospective study. Lancet Neurol. 2011;10(9):797-805.
40. Booij J, Kemp P. Dopamine transporter imaging with [(123)I]FP-CIT SPECT: potential effects of drugs. Eur J Nucl Med Mol Imaging. 2008;35(2):424-438.
41. Gellad WF, Aspinall SL, Handler SM, et al. Use of antipsychotics among older residents in VA nursing homes. Med Care. 2012;50(11):954-960.
42. Mauri MC, Paletta S, Maffini M, et al. Clinical pharmacology of atypical antipsychotics: an update. EXCLI J. 2014;13:1163-1191.
43. Morley JF, Duda JE. Use of hyposmia and other non-motor symptoms to distinguish between drug-induced parkinsonism and Parkinson’s disease. J Parkinsons Dis. 2014;4(2):169-173.
44. Morley JF, Cheng G, Dubroff JG, Wood S, Wilkinson JR, Duda JE. Olfactory impairment predicts underlying dopaminergic deficit in presumed drug-induced parkinsonism. Mov Disord Clin Pract. 2017;4(4):603-606.
45. Whitwell JL, Höglinger GU, Antonini A, et al; Movement Disorder Society-endorsed PSP Study Group. Radiological biomarkers for diagnosis in PSP: where are we and where do we need to be? Mov Disord. 2017;32(7):955-971.
46. Laurens B, Constantinescu R, Freeman R, et al. Fluid biomarkers in multiple system atrophy: A review of the MSA Biomarker Initiative. Neurobiol Dis. 2015;80:29-41.
47. Barber TR, Klein JC, Mackay CE, Hu MTM. Neuroimaging in pre-motor Parkinson’s disease. NeuroImage Clin. 2017;15:215-227.
48. Parkinson Progression Marker Initiative. The Parkinson Progression Marker Initiative (PPMI). Prog Neurobiol. 2011;95(4):629-635.
49. Meles SK, Vadasz D, Renken RJ, et al. FDG PET, dopamine transporter SPECT, and olfaction: combining biomarkers in REM sleep behavior disorder. Mov Disord. 2017;32(10):1482-1486.
50. Noyce AJ, R’Bibo L, Peress L, et al. PREDICT‐PD: an online approach to prospectively identify risk indicators of Parkinson’s disease. Mov Disord. 2017 Feb; 32(2): 219–226.
51. Searles Nielsen S, Warden MN, Camacho-Soto A, Willis AW, Wright BA, Racette BA. A predictive model to identify Parkinson disease from administrative claims data. Neurology. 2017;89(14):1448-1456.
52. Institute of Medicine. Veterans and Agent Orange: Update 2012. National Academies Press: Washington, DC; 2013.
53. Department of Veterans Affairs. Diseases associated with exposure to Contaminants in the Water Supply at Camp Lejeune. Final rule. Fed Regist. 2017;82(9):4173-4185.
54. Goldman SM, Quinlan PJ, Ross GW, et al. Solvent exposures and Parkinson disease risk in twins. Ann Neurol. 2012;71(6):776-784.
55. Liu M, Shin EJ, Dang DK, et al. Trichloroethylene and Parkinson’s disease: risk assessment. Mol Neurobiol. 2018;55(7):6201-6214.
56. Betarbet R, Sherer TB, MacKenzie G, Garcia-Osuna M, Panov AV, Greenamyre JT. Chronic systemic pesticide exposure reproduces features of Parkinson’s disease. Nat Neurosci. 2000;3(12):1301-1306.
57. Manning-Bog AB, McCormack AL, Li J, Uversky VN, Fink AL, Monte DAD. The herbicide paraquat causes up-regulation and aggregation of alpha-synuclein in mice: paraquat and alpha-synuclein. J Biol Chem. 2002;277(3):1641-1644.
58. Camacho-Soto A, Warden MN, Searles Nielsen S, et al. Traumatic brain injury in the prodromal period of Parkinson’s disease: a large epidemiological study using medicare data. Ann Neurol. 2017;82(5):744-754.
59. Gardner RC, Burke JF, Nettiksimmons J, Goldman S, Tanner CM, Yaffe K. Traumatic brain injury in later life increases risk for Parkinson disease. Ann Neurol. 2015;77(6):987-995.
60. Gardner RC, Byers AL, Barnes DE, Li Y, Boscardin J, Yaffe K. Mild TBI and risk of Parkinson disease: a Chronic Effects of Neurotrauma Consortium Study. Neurology. 2018;90(20):e1771-e1779.
61. Cruz-Haces M, Tang J, Acosta G, Fernandez J, Shi R. Pathological correlations between traumatic brain injury and chronic neurodegenerative diseases. Transl Neurodegener. 2017;6:20.
62. Lee PC, Bordelon Y, Bronstein J, Ritz B. Traumatic brain injury, paraquat exposure, and their relationship to Parkinson disease. Neurology. 2012;79(20):2061-2066.
63. Disabilities that are proximately due to, or aggravated by, service-connected disease or injury. 38 CFR §3.310.
64. Diseases Associated With Exposure to Certain Herbicide Agents (Hairy Cell Leukemia and Other Chronic B-Cell Leukemias, Parkinson’s Disease and Ischemic Heart Disease). Federal Regist. 2010;75(173):53202-53216. To be codified at 38 CFR §3.
65. Cheng EM, Swarztrauber K, Siderowf AD, et al. Association of specialist involvement and quality of care for Parkinson’s disease. Mov Disord. 2007;22(4):515-522.
66. Qamar MA, Harington G, Trump S, Johnson J, Roberts F, Frost E. Multidisciplinary care in Parkinson’s disease. Int Rev Neurobiol. 2017;132:511-523.
67. Pogoda TK, Cramer IE, Meterko M, et al. Patient and organizational factors related to education and support use by veterans with Parkinson’s disease. Mov Disord. 2009;24(13):1916-1924.
Hemolytic Uremic Syndrome With Severe Neurologic Complications in an Adult (FULL)
The case of a female presenting with Shiga toxin-producing Escherichia coli and hemolytic uremic syndrome highlights a severe neurologic complication that canbe associated with these conditions.
Hemolytic uremic syndrome (HUS) is a rare illness that can be acquired through the consumption of food products contaminated with strains of Shiga toxin-producing Escherichia coli (E coli; STEC).1 Between 6% and 15% of individuals infected with STEC develop HUS, with children affected more frequently than adults.2,3 This strain of E coli releases Shiga toxin into the systemic circulation, which causes a thrombotic microangiopathy resulting in the characteristic HUS triad of symptoms: acute renal insufficiency, thrombocytopenia, and hemolytic anemia.4-6
Although neurologic features are common in HUS, they have not been extensively studied, particularly in adults. We report a case of STEC 0157:H7 subtype HUS in an adult with severe neurologic complications. This case highlights the neurological sequelae in an adult with typical STEC-HUS. The use of treatment modalities, such as plasmapheresis and eculizumab, and their use in adult typical STEC-HUS also is explored.
Case
A 53-year-old white woman with no pertinent past medical history presented to the Bay Pines Veterans Affairs Healthcare System Emergency Department with a 2-day history of abdominal pain, vomiting, nausea, diarrhea, and bright bloody stools. She returned from a cruise to the Bahamas 3 days prior, where she ate local foods, including salads. She reported no fever, shortness of breath, chest pain, headache, and cognitive difficulties. She presented with a normal mental status and neurologic exam. Apart from leukocytosis and elevated glucose level, her laboratory results at initial presentation were normal, (Table). A stool sample showed occult blood with white blood cell counts (WBCs) but was negative for Clostridium difficile. She was started on ciprofloxacin 400 mg and metronidazole 500 mg on the day of admission.
Hematuria was found on hospital day 2. On hospital day 4, the patient exhibited word finding difficulties. Blood studies revealed anemia, thrombocytopenia, leukocytosis, and increasing blood urea nitrogen (BUN) and creatinine. A computed tomography scan of the head was normal. Laboratory analysis showed schistocytes in the peripheral blood smear.
The patient’s cognitive functioning deteriorated on hospital day 5. She was not oriented to time or place. Her laboratory results showed complement level C3 at 70 mg/dL (ref: 83-193 mg/dL) complement C4 at 12 mg/dL (ref: 15-57mg/dL). The patient exhibited oliguria and hyponatremia, as well as both metabolic and respiratory acidosis; dialysis was then initiated. Results from the stool sample that was collected on hospital day 1 were received and tested positive for Shiga toxin.
At this point, the patient’s presentation of hemolytic anemia and thrombocytopenia in the setting of acute bloody diarrheal illness with known Shiga toxin, schistocytes on blood smear, and lack of pertinent medical history for other causes of this presentation made STEC-HUS the leading differential diagnosis. Plasmapheresis was ordered and performed on hospital day 6 and 7. Shiga toxin was no longer detected in the stool and antibiotics were stopped on hospital day 7.
The patient’s progressive deterioration in mental status continued on hospital day 8. She was not oriented to time or place, unable to perform simple calculations, and could not spell the word “hand” backwards. Physicians observed repetitive jerking motions of the upper extremities that were worse on the left side. An electroencephalogram (EEG) revealed right hemispheric sharp waves that were thought to be epileptiform (Figure 1). The patient began taking levetiracetam 1500 mg IV with 750 mg bid maintenance for seizure control. Plasmapheresis was discontinued due to her continued neurologic deterioration on this therapy. Consequently, eculizumab 900 mg IV was given along with the Neisseria meningitidis (N meningitidis) vaccine and a 19-day course of azithromycin 250 mg po as prophylaxis for encapsulated bacteria.
The patient continued to seize on hospital days 10 through 13. Oculocephalic maneuvers showed a tendency to keep her eyes deviated to the right. Her pupils continued to react to light. A repeat EEG showed diffuse slowing (5-6 Hz) with no epileptic activity seen (Figure 2). A second dose of eculizumab 900 mg IV was administered on hospital day 15. The patient experienced cardiac arrest on hospital day 16 and was successfully resuscitated. On hospital day 25 (10 days after receiving her second dose of eculizumab), the patient was able to speak and follow simple commands but exhibited difficulty concentrating and poor impulse control.
The patient was alert and oriented to person, place, time, and situation on hospital day 28 (6 days after the third and final dose of eculizumab). A neurologic exam was significant only for a slight intention tremor. She was continued on levetiracetam with a plan to be maintained on the medication for the next 6 months for seizure control. She was discharged on hospital day 30.
Twenty-eight days postdischarge (57 days postadmission), the patient showed marked recovery. She had returned to her previous employment as a business administrator on a part-time basis and exhibited no deficiencies in executive functioning or handling activities of daily living. Although she had been very active prior to this illness, she now experienced decreased physical and mental endurance; however, this gradually improved with physical therapy. She planned on returning to work on a full-time basis when she had regained her stamina. She also noticed difficulties in retaining short term memory since her discharge but believed that these symptoms were remitting. On examination her mental status and neurologic exam was significant for inability to continue serial 7s, left sided 4/5 muscle strength in quadriceps and thumb to 5th metacarpal adduction, bilateral 1+ reflexes in muscle groups tested (triceps, biceps, brachioradialis, patellar, and Achilles), loss of dull pinprick sensation bilaterally at web of hands, deficit in tandem gait while looking away, and slight intention tremor on finger to nose testing bilaterally (with left hand tremor more pronounced than right). Her complete blood count was normal. Her recovery continues to be monitored in an outpatient setting.
Discussion
HUS is characterized by 3 core clinical features: microangiopathic hemolytic anemia, thrombocytopenia, and acute kidney injury.4 Schistocytes are seen on peripheral blood smear and occur due to the passage of red blood cells over the microvascular thrombi induced by the disease. HUS can be classified as typical, atypical, or occurring with a coexisting disease. Typical HUS is associated with STEC 0157:H7 subtype, a bacterium known to be acquired through contaminated food and via human-to-human transmission.6-8 In the case of typical STEC 0157:H7, the bacterium releases a verotoxin that damages the vascular endothelium, thereby leading to activation of the coagulation cascade and eventually the formation of thrombi.4 It has been hypothesized that the Shiga toxin also activates the alternative complement pathway directly, which could contribute to thrombosis.9 This would explain the findings of low complement levels in our patient. Atypical HUS is primarily attributable to mutations in the alternative complement pathway. Causes for the third type of HUS can include Streptococcus pneumoniae, HIV, drug toxicity, and alterations in the metabolism of cobalamin C.
Epidemiologically, 15.3% of children aged < 5 years develop typical HUS after exposure to STEC compared with 1.2% of adults aged 18 to 59 years. The median age of patients who developed HUS from STEC exposure was 4 years compared with 16 years for those who did not develop HUS.2
Neurologic manifestations increase mortality for HUS patients.10 These have been described in the pediatric population as alteration in consciousness (85%), seizures (71%), pyramidal syndrome (52%), and extrapyramidal syndrome with hypertonia (42%).11 Brain imaging in children has demonstrated hemorrhagic lesions involving the pons, basal ganglia, and occipital cortex.11 Blood flow to areas such as the cerebellum, brainstem, and orbitofrontal area can be compromised.10 Adult patients with HUS can present without lesions on cranial magnetic resonance imaging (MRI), but instead with transient symmetric vasogenic edema of the central brain stem.12 Unfortunately in this case, MRI was not performed because it was thought to provide limited aid in diagnosis and to avoid unnecessary testing for the acutely ill patient.
The underlying pathophysiology of neurologic manifestations in patients may be due to a metabolic disturbance, toxin-mediated damage of the vascular endothelium, or toxin-induced cytokine release resulting in death of neural cells and subsequent neuroinflammation. However, the most likely mechanism is parenchymal ischemic changes related to microangiopathy.11,13 Pediatric patients often experience seizures and altered mental status, and their EEGs display delta waves.13 This patient’s diffuse slowing on her second EEG and altered mental status suggests that the neuropathologic mechanisms for typical HUS in adults may be similar to those in children.
HUS Treatment
The treatment and management of adults with typical STEC-HUS is evolving. The patient was first suspected to have an infectious colitis and empiric antibiotics were initiated. Some studies suggest that antibiotic administration may worsen the course of HUS in children as it may lead to release and subsequent absorption of Shiga toxin in the intestine.9,14 However, there is little evidence to suggest harm or efficacy of administration in adults. It is unclear what role antibiotic administration played in the recovery time of HUS given the co-administration of other treatments such as eculizumab and plasmapheresis, but it does appear to have helped with the initial E coli infection.
Plasmapheresis was subsequently administered, due to its documented benefit in the treatment of HUS.15 However, it should be noted that even though plasmapheresis is currently used in patients with CNS involvement, it remains unproven with conflicting information on its efficacy.3,16 The mechanism of action is unclear, but it has been hypothesized that plasmapheresis prevents microangiopathy caused by microthrombi.3,16 For this reason, eculizumab is becoming the mainstay for treatment of STEC-HUS with neurologic complications given the lack of well researched alternative treatments. In this case study, the use of plasmapheresis did not result in clinical improvement, and was abandoned after 2 days of treatment.
Eculizumab is a humanized, recombinant monoclonal IgG antibody that is a terminal complement inhibitor of the alternative complement system at the final step to cleave C5.17 The Shiga toxin may directly activate the complement system via the alternative pathway, which can result in uncontrolled platelet and white blood cell activation and depletion, endothelial cell damage, and hemolysis. The galvanized complement system leads to a series of cascading events that contribute to organ damage and death.9 Eculizumab is FDA approved for use in atypical HUS.18 It also can be used off-label to treat typical-HUS in adults with neurologic complications.
Eculizumab interferes with the immune response against encapsulated bacteria because it inhibits the alternative complement pathway. Thus, vaccination against N meningitides is recommended 2 weeks prior to the administration of eculizumab. However, in situations where the risks of delaying eculizumab for 2 weeks are greater than the risk of developing an N meningitides infection, eculizumab may be given without delay.18 Given the rapid deterioration of our patient’s condition, the vaccine and eculizumab were given together with prophylactic azithromycin. Although penicillin is the standard for prophylaxis in this situation, the patient’s penicillin allergy led to the use of azithromycin 250 mg po once a day. Literature also suggests azithromycin reduces the carriage duration of E coli-induced colitis.19 As such, it is possible that some improvement in the patient’s condition could be attributed to the elimination of the pathogen and toxin.
Conclusion
Three doses of eculizumab were administered at weekly intervals, with the first dose on hospital day 8 and the final dose on hospital day 22. Prior to the first dose, the patient displayed significant decline in mental status with EEG findings of right hemisphere epileptogenic discharges. After her third dose, she was found to have a drastically improved mental status exam and a normal EEG. One week later, she was discharged home. At the time of her 1-month follow-up, she was independent in all activities of daily living and had returned to part-time work. Apart from subtle cognitive changes, the remainder of her neurologic exam was normal.
There is evidence that supports the efficacy of eculizumab in children with HUS with neurologic symptoms on dialysis.20 However, its use in adults is not well established.21 This patient required dialysis and had neurologic symptoms similar to pediatric patients described in the literature, and responded similarly to the eculizumab. The rationale for the use of eculizumab in STEC-HUS also is evidenced by in vitro demonstrations of complement activation in STEC-HUS.22-25 This case report adds to the literature supporting the use of eculizumab in adult patients with typical HUS with neurological complications. Further research is necessary to develop guidelines in the treatment of adult STEC-HUS with regards to neurologic complications.
Acknowledgments
The authors would like to thank Pete DiStaso, REEGT for his work on obtaining the electroencephalograms and Anthony Rinaldi, PsyD; Julie Cessnapalas, PsyD; and Syed Faizan Sagheer for proof-reading the article.
1. Tarr PI, Gordon CA, Chandler WL. Shiga-toxin-producing Escherichia coli and haemolytic uraemic syndrome. Lancet. 2005;365(9464):1073-1086.
2. Gould LH, Demma L, Jones TF, et al. Hemolytic uremic syndrome and death in persons with Escherichia coli O157:H7 infection, foodborne diseases active surveillance network sites, 2000-2006. Clin Infect Dis. 2009;49(10):1480-1485.
3. Boyce TG, Swerdlow DL, Griffin PM. Escherichia coli O157:H7 and the hemolytic-uremic syndrome. N Engl J Med. 1995;333(6):364-368.
4. Rondeau E, Peraldi MN. Escherichia coli and the hemolytic-uremic syndrome. N Engl J Med. 1996;335(9):660-662.
5. Te Loo DM, van Hinsbergh VW, van den Heuvel LP, Monnens LA. Detection of verocytotoxin bound to circulating polymorphonuclear leukocytes of patients with hemolytic uremic syndrome. J Am Soc Nephrol. 2001;12(4):800-806.
6. Tran SL, Jenkins C, Livrelli V, Schüller S. Shiga toxin 2 translocation across intestinal epithelium is linked to virulence of Shiga toxin-producing Escherichia coli in humans. Microbiology. 2018;164(4):509-516.
7. Jokiranta TS. HUS and atypical HUS. Blood. 2017;129(21):2847-2856.
8. Ferens WA, Hovde CJ. Escherichia coli O157:H7: animal reservoir and sources of human infection. Foodborne Pathog Dis. 2011;8(4):465-487.
9. Percheron L, Gramada R, Tellier S, et al. Eculizumab treatment in severe pediatric STEC-HUS: a multicenter retrospective study. Pediatr Nephrol. 2018;33(8):1385-1394.
10. Hosaka T, Nakamagoe K, Tamaoka A. Hemolytic uremic syndrome-associated encephalopathy successfully treated with corticosteroids. Intern Med. 2017;56(21):2937-2941.
11. Nathanson S, Kwon T, Elmaleh M, et al. Acute neurological involvement in diarrhea-associated hemolytic uremic syndrome. Clin J Am Soc Nephrol. 2010;5(7):1218-1228.
12. Wengenroth M, Hoeltje J, Repenthin J, et al. Central nervous system involvement in adults with epidemic hemolytic uremic syndrome. AJNR Am J Neuroradiol. 2013;34(5):1016-1021, S1.
13. Eriksson KJ, Boyd SG, Tasker RC. Acute neurology and neurophysiology of haemolytic-uraemic syndrome. Arch Dis Child. 2001;84(5):434-435.
14. Wong CS, Jelacic S, Habeeb RL, Watkins SL, Tarr PI. The risk of the hemolytic-uremic syndrome after antibiotic treatment of Escherichia coli O157:H7 infections. N Engl J Med. 2000;342(26):1930-1936.
15. Nguyen TC, Kiss JE, Goldman JR, Carcillo JA. The role of plasmapheresis in critical illness. Crit Care Clin. 2012;28(3):453-468, vii.
16. Loos S, Ahlenstiel T, Kranz B, et al. An outbreak of Shiga toxin-producing Escherichia coli O104:H4 hemolytic uremic syndrome in Germany: presentation and short-term outcome in children. Clin Infect Dis. 2012;55(6):753-759.
17. Hossain MA, Cheema A, Kalathil S, et al. Atypical hemolytic uremic syndrome: Laboratory characteristics, complement-amplifying conditions, renal biopsy, and genetic mutations. Saudi J Kidney Dis Transpl. 2018;29(2):276-283.
18. Soliris (eculizumab) [package insert]. Cheshire, CT: Alexion Pharmaceuticals, Inc; 2011.
19. Keenswijk W, Raes A, Vande Walle J. Is eculizumab efficacious in Shigatoxin-associated hemolytic uremic syndrome? A narrative review of current evidence. Eur J Pediatr. 2018;177(3):311-318.
20. Lapeyraque AL, Malina M, Fremeaux-Bacchi V, et al. Eculizumab in severe Shiga-toxin-associated HUS. N Engl J Med. 2011;364(26):2561-2563.
21. Pape L, Hartmann H, Bange FC, Suerbaum S, Bueltmann E, Ahlenstiel-Grunow T. Eculizumab in typical hemolytic uremic syndrome (HUS) with neurological involvement. Medicine (Baltimore). 2015;94(24):e1000.
22. Kim Y, Miller K, Michael AF. Breakdown products of C3 and factor B in hemolytic-uremic syndrome. J Lab Clin Med. 1977;89(4):845-850.
23. Monnens L, Molenaar J, Lambert PH, Proesmans W, van Munster P. The complement system in hemolytic-uremic syndrome in childhood. Clin Nephrol. 1980;13(4):168-171.
24. Thurman JM, Marians R, Emlen W, et al. Alternative pathway of complement in children with diarrhea-associated hemolytic uremic syndrome. Clin J Am Soc Nephrol. 2009;4(12):1920-1924.
25. Ståhl AL, Sartz L, Karpman D. Complement activation on platelet-leukocyte complexes and microparticles in enterohemorrhagic Escherichia coli-induced hemolytic uremic syndrome. Blood. 2011;117(20):5503-5513.
The case of a female presenting with Shiga toxin-producing Escherichia coli and hemolytic uremic syndrome highlights a severe neurologic complication that canbe associated with these conditions.
The case of a female presenting with Shiga toxin-producing Escherichia coli and hemolytic uremic syndrome highlights a severe neurologic complication that canbe associated with these conditions.
Hemolytic uremic syndrome (HUS) is a rare illness that can be acquired through the consumption of food products contaminated with strains of Shiga toxin-producing Escherichia coli (E coli; STEC).1 Between 6% and 15% of individuals infected with STEC develop HUS, with children affected more frequently than adults.2,3 This strain of E coli releases Shiga toxin into the systemic circulation, which causes a thrombotic microangiopathy resulting in the characteristic HUS triad of symptoms: acute renal insufficiency, thrombocytopenia, and hemolytic anemia.4-6
Although neurologic features are common in HUS, they have not been extensively studied, particularly in adults. We report a case of STEC 0157:H7 subtype HUS in an adult with severe neurologic complications. This case highlights the neurological sequelae in an adult with typical STEC-HUS. The use of treatment modalities, such as plasmapheresis and eculizumab, and their use in adult typical STEC-HUS also is explored.
Case
A 53-year-old white woman with no pertinent past medical history presented to the Bay Pines Veterans Affairs Healthcare System Emergency Department with a 2-day history of abdominal pain, vomiting, nausea, diarrhea, and bright bloody stools. She returned from a cruise to the Bahamas 3 days prior, where she ate local foods, including salads. She reported no fever, shortness of breath, chest pain, headache, and cognitive difficulties. She presented with a normal mental status and neurologic exam. Apart from leukocytosis and elevated glucose level, her laboratory results at initial presentation were normal, (Table). A stool sample showed occult blood with white blood cell counts (WBCs) but was negative for Clostridium difficile. She was started on ciprofloxacin 400 mg and metronidazole 500 mg on the day of admission.
Hematuria was found on hospital day 2. On hospital day 4, the patient exhibited word finding difficulties. Blood studies revealed anemia, thrombocytopenia, leukocytosis, and increasing blood urea nitrogen (BUN) and creatinine. A computed tomography scan of the head was normal. Laboratory analysis showed schistocytes in the peripheral blood smear.
The patient’s cognitive functioning deteriorated on hospital day 5. She was not oriented to time or place. Her laboratory results showed complement level C3 at 70 mg/dL (ref: 83-193 mg/dL) complement C4 at 12 mg/dL (ref: 15-57mg/dL). The patient exhibited oliguria and hyponatremia, as well as both metabolic and respiratory acidosis; dialysis was then initiated. Results from the stool sample that was collected on hospital day 1 were received and tested positive for Shiga toxin.
At this point, the patient’s presentation of hemolytic anemia and thrombocytopenia in the setting of acute bloody diarrheal illness with known Shiga toxin, schistocytes on blood smear, and lack of pertinent medical history for other causes of this presentation made STEC-HUS the leading differential diagnosis. Plasmapheresis was ordered and performed on hospital day 6 and 7. Shiga toxin was no longer detected in the stool and antibiotics were stopped on hospital day 7.
The patient’s progressive deterioration in mental status continued on hospital day 8. She was not oriented to time or place, unable to perform simple calculations, and could not spell the word “hand” backwards. Physicians observed repetitive jerking motions of the upper extremities that were worse on the left side. An electroencephalogram (EEG) revealed right hemispheric sharp waves that were thought to be epileptiform (Figure 1). The patient began taking levetiracetam 1500 mg IV with 750 mg bid maintenance for seizure control. Plasmapheresis was discontinued due to her continued neurologic deterioration on this therapy. Consequently, eculizumab 900 mg IV was given along with the Neisseria meningitidis (N meningitidis) vaccine and a 19-day course of azithromycin 250 mg po as prophylaxis for encapsulated bacteria.
The patient continued to seize on hospital days 10 through 13. Oculocephalic maneuvers showed a tendency to keep her eyes deviated to the right. Her pupils continued to react to light. A repeat EEG showed diffuse slowing (5-6 Hz) with no epileptic activity seen (Figure 2). A second dose of eculizumab 900 mg IV was administered on hospital day 15. The patient experienced cardiac arrest on hospital day 16 and was successfully resuscitated. On hospital day 25 (10 days after receiving her second dose of eculizumab), the patient was able to speak and follow simple commands but exhibited difficulty concentrating and poor impulse control.
The patient was alert and oriented to person, place, time, and situation on hospital day 28 (6 days after the third and final dose of eculizumab). A neurologic exam was significant only for a slight intention tremor. She was continued on levetiracetam with a plan to be maintained on the medication for the next 6 months for seizure control. She was discharged on hospital day 30.
Twenty-eight days postdischarge (57 days postadmission), the patient showed marked recovery. She had returned to her previous employment as a business administrator on a part-time basis and exhibited no deficiencies in executive functioning or handling activities of daily living. Although she had been very active prior to this illness, she now experienced decreased physical and mental endurance; however, this gradually improved with physical therapy. She planned on returning to work on a full-time basis when she had regained her stamina. She also noticed difficulties in retaining short term memory since her discharge but believed that these symptoms were remitting. On examination her mental status and neurologic exam was significant for inability to continue serial 7s, left sided 4/5 muscle strength in quadriceps and thumb to 5th metacarpal adduction, bilateral 1+ reflexes in muscle groups tested (triceps, biceps, brachioradialis, patellar, and Achilles), loss of dull pinprick sensation bilaterally at web of hands, deficit in tandem gait while looking away, and slight intention tremor on finger to nose testing bilaterally (with left hand tremor more pronounced than right). Her complete blood count was normal. Her recovery continues to be monitored in an outpatient setting.
Discussion
HUS is characterized by 3 core clinical features: microangiopathic hemolytic anemia, thrombocytopenia, and acute kidney injury.4 Schistocytes are seen on peripheral blood smear and occur due to the passage of red blood cells over the microvascular thrombi induced by the disease. HUS can be classified as typical, atypical, or occurring with a coexisting disease. Typical HUS is associated with STEC 0157:H7 subtype, a bacterium known to be acquired through contaminated food and via human-to-human transmission.6-8 In the case of typical STEC 0157:H7, the bacterium releases a verotoxin that damages the vascular endothelium, thereby leading to activation of the coagulation cascade and eventually the formation of thrombi.4 It has been hypothesized that the Shiga toxin also activates the alternative complement pathway directly, which could contribute to thrombosis.9 This would explain the findings of low complement levels in our patient. Atypical HUS is primarily attributable to mutations in the alternative complement pathway. Causes for the third type of HUS can include Streptococcus pneumoniae, HIV, drug toxicity, and alterations in the metabolism of cobalamin C.
Epidemiologically, 15.3% of children aged < 5 years develop typical HUS after exposure to STEC compared with 1.2% of adults aged 18 to 59 years. The median age of patients who developed HUS from STEC exposure was 4 years compared with 16 years for those who did not develop HUS.2
Neurologic manifestations increase mortality for HUS patients.10 These have been described in the pediatric population as alteration in consciousness (85%), seizures (71%), pyramidal syndrome (52%), and extrapyramidal syndrome with hypertonia (42%).11 Brain imaging in children has demonstrated hemorrhagic lesions involving the pons, basal ganglia, and occipital cortex.11 Blood flow to areas such as the cerebellum, brainstem, and orbitofrontal area can be compromised.10 Adult patients with HUS can present without lesions on cranial magnetic resonance imaging (MRI), but instead with transient symmetric vasogenic edema of the central brain stem.12 Unfortunately in this case, MRI was not performed because it was thought to provide limited aid in diagnosis and to avoid unnecessary testing for the acutely ill patient.
The underlying pathophysiology of neurologic manifestations in patients may be due to a metabolic disturbance, toxin-mediated damage of the vascular endothelium, or toxin-induced cytokine release resulting in death of neural cells and subsequent neuroinflammation. However, the most likely mechanism is parenchymal ischemic changes related to microangiopathy.11,13 Pediatric patients often experience seizures and altered mental status, and their EEGs display delta waves.13 This patient’s diffuse slowing on her second EEG and altered mental status suggests that the neuropathologic mechanisms for typical HUS in adults may be similar to those in children.
HUS Treatment
The treatment and management of adults with typical STEC-HUS is evolving. The patient was first suspected to have an infectious colitis and empiric antibiotics were initiated. Some studies suggest that antibiotic administration may worsen the course of HUS in children as it may lead to release and subsequent absorption of Shiga toxin in the intestine.9,14 However, there is little evidence to suggest harm or efficacy of administration in adults. It is unclear what role antibiotic administration played in the recovery time of HUS given the co-administration of other treatments such as eculizumab and plasmapheresis, but it does appear to have helped with the initial E coli infection.
Plasmapheresis was subsequently administered, due to its documented benefit in the treatment of HUS.15 However, it should be noted that even though plasmapheresis is currently used in patients with CNS involvement, it remains unproven with conflicting information on its efficacy.3,16 The mechanism of action is unclear, but it has been hypothesized that plasmapheresis prevents microangiopathy caused by microthrombi.3,16 For this reason, eculizumab is becoming the mainstay for treatment of STEC-HUS with neurologic complications given the lack of well researched alternative treatments. In this case study, the use of plasmapheresis did not result in clinical improvement, and was abandoned after 2 days of treatment.
Eculizumab is a humanized, recombinant monoclonal IgG antibody that is a terminal complement inhibitor of the alternative complement system at the final step to cleave C5.17 The Shiga toxin may directly activate the complement system via the alternative pathway, which can result in uncontrolled platelet and white blood cell activation and depletion, endothelial cell damage, and hemolysis. The galvanized complement system leads to a series of cascading events that contribute to organ damage and death.9 Eculizumab is FDA approved for use in atypical HUS.18 It also can be used off-label to treat typical-HUS in adults with neurologic complications.
Eculizumab interferes with the immune response against encapsulated bacteria because it inhibits the alternative complement pathway. Thus, vaccination against N meningitides is recommended 2 weeks prior to the administration of eculizumab. However, in situations where the risks of delaying eculizumab for 2 weeks are greater than the risk of developing an N meningitides infection, eculizumab may be given without delay.18 Given the rapid deterioration of our patient’s condition, the vaccine and eculizumab were given together with prophylactic azithromycin. Although penicillin is the standard for prophylaxis in this situation, the patient’s penicillin allergy led to the use of azithromycin 250 mg po once a day. Literature also suggests azithromycin reduces the carriage duration of E coli-induced colitis.19 As such, it is possible that some improvement in the patient’s condition could be attributed to the elimination of the pathogen and toxin.
Conclusion
Three doses of eculizumab were administered at weekly intervals, with the first dose on hospital day 8 and the final dose on hospital day 22. Prior to the first dose, the patient displayed significant decline in mental status with EEG findings of right hemisphere epileptogenic discharges. After her third dose, she was found to have a drastically improved mental status exam and a normal EEG. One week later, she was discharged home. At the time of her 1-month follow-up, she was independent in all activities of daily living and had returned to part-time work. Apart from subtle cognitive changes, the remainder of her neurologic exam was normal.
There is evidence that supports the efficacy of eculizumab in children with HUS with neurologic symptoms on dialysis.20 However, its use in adults is not well established.21 This patient required dialysis and had neurologic symptoms similar to pediatric patients described in the literature, and responded similarly to the eculizumab. The rationale for the use of eculizumab in STEC-HUS also is evidenced by in vitro demonstrations of complement activation in STEC-HUS.22-25 This case report adds to the literature supporting the use of eculizumab in adult patients with typical HUS with neurological complications. Further research is necessary to develop guidelines in the treatment of adult STEC-HUS with regards to neurologic complications.
Acknowledgments
The authors would like to thank Pete DiStaso, REEGT for his work on obtaining the electroencephalograms and Anthony Rinaldi, PsyD; Julie Cessnapalas, PsyD; and Syed Faizan Sagheer for proof-reading the article.
Hemolytic uremic syndrome (HUS) is a rare illness that can be acquired through the consumption of food products contaminated with strains of Shiga toxin-producing Escherichia coli (E coli; STEC).1 Between 6% and 15% of individuals infected with STEC develop HUS, with children affected more frequently than adults.2,3 This strain of E coli releases Shiga toxin into the systemic circulation, which causes a thrombotic microangiopathy resulting in the characteristic HUS triad of symptoms: acute renal insufficiency, thrombocytopenia, and hemolytic anemia.4-6
Although neurologic features are common in HUS, they have not been extensively studied, particularly in adults. We report a case of STEC 0157:H7 subtype HUS in an adult with severe neurologic complications. This case highlights the neurological sequelae in an adult with typical STEC-HUS. The use of treatment modalities, such as plasmapheresis and eculizumab, and their use in adult typical STEC-HUS also is explored.
Case
A 53-year-old white woman with no pertinent past medical history presented to the Bay Pines Veterans Affairs Healthcare System Emergency Department with a 2-day history of abdominal pain, vomiting, nausea, diarrhea, and bright bloody stools. She returned from a cruise to the Bahamas 3 days prior, where she ate local foods, including salads. She reported no fever, shortness of breath, chest pain, headache, and cognitive difficulties. She presented with a normal mental status and neurologic exam. Apart from leukocytosis and elevated glucose level, her laboratory results at initial presentation were normal, (Table). A stool sample showed occult blood with white blood cell counts (WBCs) but was negative for Clostridium difficile. She was started on ciprofloxacin 400 mg and metronidazole 500 mg on the day of admission.
Hematuria was found on hospital day 2. On hospital day 4, the patient exhibited word finding difficulties. Blood studies revealed anemia, thrombocytopenia, leukocytosis, and increasing blood urea nitrogen (BUN) and creatinine. A computed tomography scan of the head was normal. Laboratory analysis showed schistocytes in the peripheral blood smear.
The patient’s cognitive functioning deteriorated on hospital day 5. She was not oriented to time or place. Her laboratory results showed complement level C3 at 70 mg/dL (ref: 83-193 mg/dL) complement C4 at 12 mg/dL (ref: 15-57mg/dL). The patient exhibited oliguria and hyponatremia, as well as both metabolic and respiratory acidosis; dialysis was then initiated. Results from the stool sample that was collected on hospital day 1 were received and tested positive for Shiga toxin.
At this point, the patient’s presentation of hemolytic anemia and thrombocytopenia in the setting of acute bloody diarrheal illness with known Shiga toxin, schistocytes on blood smear, and lack of pertinent medical history for other causes of this presentation made STEC-HUS the leading differential diagnosis. Plasmapheresis was ordered and performed on hospital day 6 and 7. Shiga toxin was no longer detected in the stool and antibiotics were stopped on hospital day 7.
The patient’s progressive deterioration in mental status continued on hospital day 8. She was not oriented to time or place, unable to perform simple calculations, and could not spell the word “hand” backwards. Physicians observed repetitive jerking motions of the upper extremities that were worse on the left side. An electroencephalogram (EEG) revealed right hemispheric sharp waves that were thought to be epileptiform (Figure 1). The patient began taking levetiracetam 1500 mg IV with 750 mg bid maintenance for seizure control. Plasmapheresis was discontinued due to her continued neurologic deterioration on this therapy. Consequently, eculizumab 900 mg IV was given along with the Neisseria meningitidis (N meningitidis) vaccine and a 19-day course of azithromycin 250 mg po as prophylaxis for encapsulated bacteria.
The patient continued to seize on hospital days 10 through 13. Oculocephalic maneuvers showed a tendency to keep her eyes deviated to the right. Her pupils continued to react to light. A repeat EEG showed diffuse slowing (5-6 Hz) with no epileptic activity seen (Figure 2). A second dose of eculizumab 900 mg IV was administered on hospital day 15. The patient experienced cardiac arrest on hospital day 16 and was successfully resuscitated. On hospital day 25 (10 days after receiving her second dose of eculizumab), the patient was able to speak and follow simple commands but exhibited difficulty concentrating and poor impulse control.
The patient was alert and oriented to person, place, time, and situation on hospital day 28 (6 days after the third and final dose of eculizumab). A neurologic exam was significant only for a slight intention tremor. She was continued on levetiracetam with a plan to be maintained on the medication for the next 6 months for seizure control. She was discharged on hospital day 30.
Twenty-eight days postdischarge (57 days postadmission), the patient showed marked recovery. She had returned to her previous employment as a business administrator on a part-time basis and exhibited no deficiencies in executive functioning or handling activities of daily living. Although she had been very active prior to this illness, she now experienced decreased physical and mental endurance; however, this gradually improved with physical therapy. She planned on returning to work on a full-time basis when she had regained her stamina. She also noticed difficulties in retaining short term memory since her discharge but believed that these symptoms were remitting. On examination her mental status and neurologic exam was significant for inability to continue serial 7s, left sided 4/5 muscle strength in quadriceps and thumb to 5th metacarpal adduction, bilateral 1+ reflexes in muscle groups tested (triceps, biceps, brachioradialis, patellar, and Achilles), loss of dull pinprick sensation bilaterally at web of hands, deficit in tandem gait while looking away, and slight intention tremor on finger to nose testing bilaterally (with left hand tremor more pronounced than right). Her complete blood count was normal. Her recovery continues to be monitored in an outpatient setting.
Discussion
HUS is characterized by 3 core clinical features: microangiopathic hemolytic anemia, thrombocytopenia, and acute kidney injury.4 Schistocytes are seen on peripheral blood smear and occur due to the passage of red blood cells over the microvascular thrombi induced by the disease. HUS can be classified as typical, atypical, or occurring with a coexisting disease. Typical HUS is associated with STEC 0157:H7 subtype, a bacterium known to be acquired through contaminated food and via human-to-human transmission.6-8 In the case of typical STEC 0157:H7, the bacterium releases a verotoxin that damages the vascular endothelium, thereby leading to activation of the coagulation cascade and eventually the formation of thrombi.4 It has been hypothesized that the Shiga toxin also activates the alternative complement pathway directly, which could contribute to thrombosis.9 This would explain the findings of low complement levels in our patient. Atypical HUS is primarily attributable to mutations in the alternative complement pathway. Causes for the third type of HUS can include Streptococcus pneumoniae, HIV, drug toxicity, and alterations in the metabolism of cobalamin C.
Epidemiologically, 15.3% of children aged < 5 years develop typical HUS after exposure to STEC compared with 1.2% of adults aged 18 to 59 years. The median age of patients who developed HUS from STEC exposure was 4 years compared with 16 years for those who did not develop HUS.2
Neurologic manifestations increase mortality for HUS patients.10 These have been described in the pediatric population as alteration in consciousness (85%), seizures (71%), pyramidal syndrome (52%), and extrapyramidal syndrome with hypertonia (42%).11 Brain imaging in children has demonstrated hemorrhagic lesions involving the pons, basal ganglia, and occipital cortex.11 Blood flow to areas such as the cerebellum, brainstem, and orbitofrontal area can be compromised.10 Adult patients with HUS can present without lesions on cranial magnetic resonance imaging (MRI), but instead with transient symmetric vasogenic edema of the central brain stem.12 Unfortunately in this case, MRI was not performed because it was thought to provide limited aid in diagnosis and to avoid unnecessary testing for the acutely ill patient.
The underlying pathophysiology of neurologic manifestations in patients may be due to a metabolic disturbance, toxin-mediated damage of the vascular endothelium, or toxin-induced cytokine release resulting in death of neural cells and subsequent neuroinflammation. However, the most likely mechanism is parenchymal ischemic changes related to microangiopathy.11,13 Pediatric patients often experience seizures and altered mental status, and their EEGs display delta waves.13 This patient’s diffuse slowing on her second EEG and altered mental status suggests that the neuropathologic mechanisms for typical HUS in adults may be similar to those in children.
HUS Treatment
The treatment and management of adults with typical STEC-HUS is evolving. The patient was first suspected to have an infectious colitis and empiric antibiotics were initiated. Some studies suggest that antibiotic administration may worsen the course of HUS in children as it may lead to release and subsequent absorption of Shiga toxin in the intestine.9,14 However, there is little evidence to suggest harm or efficacy of administration in adults. It is unclear what role antibiotic administration played in the recovery time of HUS given the co-administration of other treatments such as eculizumab and plasmapheresis, but it does appear to have helped with the initial E coli infection.
Plasmapheresis was subsequently administered, due to its documented benefit in the treatment of HUS.15 However, it should be noted that even though plasmapheresis is currently used in patients with CNS involvement, it remains unproven with conflicting information on its efficacy.3,16 The mechanism of action is unclear, but it has been hypothesized that plasmapheresis prevents microangiopathy caused by microthrombi.3,16 For this reason, eculizumab is becoming the mainstay for treatment of STEC-HUS with neurologic complications given the lack of well researched alternative treatments. In this case study, the use of plasmapheresis did not result in clinical improvement, and was abandoned after 2 days of treatment.
Eculizumab is a humanized, recombinant monoclonal IgG antibody that is a terminal complement inhibitor of the alternative complement system at the final step to cleave C5.17 The Shiga toxin may directly activate the complement system via the alternative pathway, which can result in uncontrolled platelet and white blood cell activation and depletion, endothelial cell damage, and hemolysis. The galvanized complement system leads to a series of cascading events that contribute to organ damage and death.9 Eculizumab is FDA approved for use in atypical HUS.18 It also can be used off-label to treat typical-HUS in adults with neurologic complications.
Eculizumab interferes with the immune response against encapsulated bacteria because it inhibits the alternative complement pathway. Thus, vaccination against N meningitides is recommended 2 weeks prior to the administration of eculizumab. However, in situations where the risks of delaying eculizumab for 2 weeks are greater than the risk of developing an N meningitides infection, eculizumab may be given without delay.18 Given the rapid deterioration of our patient’s condition, the vaccine and eculizumab were given together with prophylactic azithromycin. Although penicillin is the standard for prophylaxis in this situation, the patient’s penicillin allergy led to the use of azithromycin 250 mg po once a day. Literature also suggests azithromycin reduces the carriage duration of E coli-induced colitis.19 As such, it is possible that some improvement in the patient’s condition could be attributed to the elimination of the pathogen and toxin.
Conclusion
Three doses of eculizumab were administered at weekly intervals, with the first dose on hospital day 8 and the final dose on hospital day 22. Prior to the first dose, the patient displayed significant decline in mental status with EEG findings of right hemisphere epileptogenic discharges. After her third dose, she was found to have a drastically improved mental status exam and a normal EEG. One week later, she was discharged home. At the time of her 1-month follow-up, she was independent in all activities of daily living and had returned to part-time work. Apart from subtle cognitive changes, the remainder of her neurologic exam was normal.
There is evidence that supports the efficacy of eculizumab in children with HUS with neurologic symptoms on dialysis.20 However, its use in adults is not well established.21 This patient required dialysis and had neurologic symptoms similar to pediatric patients described in the literature, and responded similarly to the eculizumab. The rationale for the use of eculizumab in STEC-HUS also is evidenced by in vitro demonstrations of complement activation in STEC-HUS.22-25 This case report adds to the literature supporting the use of eculizumab in adult patients with typical HUS with neurological complications. Further research is necessary to develop guidelines in the treatment of adult STEC-HUS with regards to neurologic complications.
Acknowledgments
The authors would like to thank Pete DiStaso, REEGT for his work on obtaining the electroencephalograms and Anthony Rinaldi, PsyD; Julie Cessnapalas, PsyD; and Syed Faizan Sagheer for proof-reading the article.
1. Tarr PI, Gordon CA, Chandler WL. Shiga-toxin-producing Escherichia coli and haemolytic uraemic syndrome. Lancet. 2005;365(9464):1073-1086.
2. Gould LH, Demma L, Jones TF, et al. Hemolytic uremic syndrome and death in persons with Escherichia coli O157:H7 infection, foodborne diseases active surveillance network sites, 2000-2006. Clin Infect Dis. 2009;49(10):1480-1485.
3. Boyce TG, Swerdlow DL, Griffin PM. Escherichia coli O157:H7 and the hemolytic-uremic syndrome. N Engl J Med. 1995;333(6):364-368.
4. Rondeau E, Peraldi MN. Escherichia coli and the hemolytic-uremic syndrome. N Engl J Med. 1996;335(9):660-662.
5. Te Loo DM, van Hinsbergh VW, van den Heuvel LP, Monnens LA. Detection of verocytotoxin bound to circulating polymorphonuclear leukocytes of patients with hemolytic uremic syndrome. J Am Soc Nephrol. 2001;12(4):800-806.
6. Tran SL, Jenkins C, Livrelli V, Schüller S. Shiga toxin 2 translocation across intestinal epithelium is linked to virulence of Shiga toxin-producing Escherichia coli in humans. Microbiology. 2018;164(4):509-516.
7. Jokiranta TS. HUS and atypical HUS. Blood. 2017;129(21):2847-2856.
8. Ferens WA, Hovde CJ. Escherichia coli O157:H7: animal reservoir and sources of human infection. Foodborne Pathog Dis. 2011;8(4):465-487.
9. Percheron L, Gramada R, Tellier S, et al. Eculizumab treatment in severe pediatric STEC-HUS: a multicenter retrospective study. Pediatr Nephrol. 2018;33(8):1385-1394.
10. Hosaka T, Nakamagoe K, Tamaoka A. Hemolytic uremic syndrome-associated encephalopathy successfully treated with corticosteroids. Intern Med. 2017;56(21):2937-2941.
11. Nathanson S, Kwon T, Elmaleh M, et al. Acute neurological involvement in diarrhea-associated hemolytic uremic syndrome. Clin J Am Soc Nephrol. 2010;5(7):1218-1228.
12. Wengenroth M, Hoeltje J, Repenthin J, et al. Central nervous system involvement in adults with epidemic hemolytic uremic syndrome. AJNR Am J Neuroradiol. 2013;34(5):1016-1021, S1.
13. Eriksson KJ, Boyd SG, Tasker RC. Acute neurology and neurophysiology of haemolytic-uraemic syndrome. Arch Dis Child. 2001;84(5):434-435.
14. Wong CS, Jelacic S, Habeeb RL, Watkins SL, Tarr PI. The risk of the hemolytic-uremic syndrome after antibiotic treatment of Escherichia coli O157:H7 infections. N Engl J Med. 2000;342(26):1930-1936.
15. Nguyen TC, Kiss JE, Goldman JR, Carcillo JA. The role of plasmapheresis in critical illness. Crit Care Clin. 2012;28(3):453-468, vii.
16. Loos S, Ahlenstiel T, Kranz B, et al. An outbreak of Shiga toxin-producing Escherichia coli O104:H4 hemolytic uremic syndrome in Germany: presentation and short-term outcome in children. Clin Infect Dis. 2012;55(6):753-759.
17. Hossain MA, Cheema A, Kalathil S, et al. Atypical hemolytic uremic syndrome: Laboratory characteristics, complement-amplifying conditions, renal biopsy, and genetic mutations. Saudi J Kidney Dis Transpl. 2018;29(2):276-283.
18. Soliris (eculizumab) [package insert]. Cheshire, CT: Alexion Pharmaceuticals, Inc; 2011.
19. Keenswijk W, Raes A, Vande Walle J. Is eculizumab efficacious in Shigatoxin-associated hemolytic uremic syndrome? A narrative review of current evidence. Eur J Pediatr. 2018;177(3):311-318.
20. Lapeyraque AL, Malina M, Fremeaux-Bacchi V, et al. Eculizumab in severe Shiga-toxin-associated HUS. N Engl J Med. 2011;364(26):2561-2563.
21. Pape L, Hartmann H, Bange FC, Suerbaum S, Bueltmann E, Ahlenstiel-Grunow T. Eculizumab in typical hemolytic uremic syndrome (HUS) with neurological involvement. Medicine (Baltimore). 2015;94(24):e1000.
22. Kim Y, Miller K, Michael AF. Breakdown products of C3 and factor B in hemolytic-uremic syndrome. J Lab Clin Med. 1977;89(4):845-850.
23. Monnens L, Molenaar J, Lambert PH, Proesmans W, van Munster P. The complement system in hemolytic-uremic syndrome in childhood. Clin Nephrol. 1980;13(4):168-171.
24. Thurman JM, Marians R, Emlen W, et al. Alternative pathway of complement in children with diarrhea-associated hemolytic uremic syndrome. Clin J Am Soc Nephrol. 2009;4(12):1920-1924.
25. Ståhl AL, Sartz L, Karpman D. Complement activation on platelet-leukocyte complexes and microparticles in enterohemorrhagic Escherichia coli-induced hemolytic uremic syndrome. Blood. 2011;117(20):5503-5513.
1. Tarr PI, Gordon CA, Chandler WL. Shiga-toxin-producing Escherichia coli and haemolytic uraemic syndrome. Lancet. 2005;365(9464):1073-1086.
2. Gould LH, Demma L, Jones TF, et al. Hemolytic uremic syndrome and death in persons with Escherichia coli O157:H7 infection, foodborne diseases active surveillance network sites, 2000-2006. Clin Infect Dis. 2009;49(10):1480-1485.
3. Boyce TG, Swerdlow DL, Griffin PM. Escherichia coli O157:H7 and the hemolytic-uremic syndrome. N Engl J Med. 1995;333(6):364-368.
4. Rondeau E, Peraldi MN. Escherichia coli and the hemolytic-uremic syndrome. N Engl J Med. 1996;335(9):660-662.
5. Te Loo DM, van Hinsbergh VW, van den Heuvel LP, Monnens LA. Detection of verocytotoxin bound to circulating polymorphonuclear leukocytes of patients with hemolytic uremic syndrome. J Am Soc Nephrol. 2001;12(4):800-806.
6. Tran SL, Jenkins C, Livrelli V, Schüller S. Shiga toxin 2 translocation across intestinal epithelium is linked to virulence of Shiga toxin-producing Escherichia coli in humans. Microbiology. 2018;164(4):509-516.
7. Jokiranta TS. HUS and atypical HUS. Blood. 2017;129(21):2847-2856.
8. Ferens WA, Hovde CJ. Escherichia coli O157:H7: animal reservoir and sources of human infection. Foodborne Pathog Dis. 2011;8(4):465-487.
9. Percheron L, Gramada R, Tellier S, et al. Eculizumab treatment in severe pediatric STEC-HUS: a multicenter retrospective study. Pediatr Nephrol. 2018;33(8):1385-1394.
10. Hosaka T, Nakamagoe K, Tamaoka A. Hemolytic uremic syndrome-associated encephalopathy successfully treated with corticosteroids. Intern Med. 2017;56(21):2937-2941.
11. Nathanson S, Kwon T, Elmaleh M, et al. Acute neurological involvement in diarrhea-associated hemolytic uremic syndrome. Clin J Am Soc Nephrol. 2010;5(7):1218-1228.
12. Wengenroth M, Hoeltje J, Repenthin J, et al. Central nervous system involvement in adults with epidemic hemolytic uremic syndrome. AJNR Am J Neuroradiol. 2013;34(5):1016-1021, S1.
13. Eriksson KJ, Boyd SG, Tasker RC. Acute neurology and neurophysiology of haemolytic-uraemic syndrome. Arch Dis Child. 2001;84(5):434-435.
14. Wong CS, Jelacic S, Habeeb RL, Watkins SL, Tarr PI. The risk of the hemolytic-uremic syndrome after antibiotic treatment of Escherichia coli O157:H7 infections. N Engl J Med. 2000;342(26):1930-1936.
15. Nguyen TC, Kiss JE, Goldman JR, Carcillo JA. The role of plasmapheresis in critical illness. Crit Care Clin. 2012;28(3):453-468, vii.
16. Loos S, Ahlenstiel T, Kranz B, et al. An outbreak of Shiga toxin-producing Escherichia coli O104:H4 hemolytic uremic syndrome in Germany: presentation and short-term outcome in children. Clin Infect Dis. 2012;55(6):753-759.
17. Hossain MA, Cheema A, Kalathil S, et al. Atypical hemolytic uremic syndrome: Laboratory characteristics, complement-amplifying conditions, renal biopsy, and genetic mutations. Saudi J Kidney Dis Transpl. 2018;29(2):276-283.
18. Soliris (eculizumab) [package insert]. Cheshire, CT: Alexion Pharmaceuticals, Inc; 2011.
19. Keenswijk W, Raes A, Vande Walle J. Is eculizumab efficacious in Shigatoxin-associated hemolytic uremic syndrome? A narrative review of current evidence. Eur J Pediatr. 2018;177(3):311-318.
20. Lapeyraque AL, Malina M, Fremeaux-Bacchi V, et al. Eculizumab in severe Shiga-toxin-associated HUS. N Engl J Med. 2011;364(26):2561-2563.
21. Pape L, Hartmann H, Bange FC, Suerbaum S, Bueltmann E, Ahlenstiel-Grunow T. Eculizumab in typical hemolytic uremic syndrome (HUS) with neurological involvement. Medicine (Baltimore). 2015;94(24):e1000.
22. Kim Y, Miller K, Michael AF. Breakdown products of C3 and factor B in hemolytic-uremic syndrome. J Lab Clin Med. 1977;89(4):845-850.
23. Monnens L, Molenaar J, Lambert PH, Proesmans W, van Munster P. The complement system in hemolytic-uremic syndrome in childhood. Clin Nephrol. 1980;13(4):168-171.
24. Thurman JM, Marians R, Emlen W, et al. Alternative pathway of complement in children with diarrhea-associated hemolytic uremic syndrome. Clin J Am Soc Nephrol. 2009;4(12):1920-1924.
25. Ståhl AL, Sartz L, Karpman D. Complement activation on platelet-leukocyte complexes and microparticles in enterohemorrhagic Escherichia coli-induced hemolytic uremic syndrome. Blood. 2011;117(20):5503-5513.
Nilotinib is safe in moderate and advanced Parkinson’s disease
according to investigators. Nevertheless, other drugs that – like nilotinib – inhibit tyrosine kinase (c-Abl) may have a neuroprotective effect, they added. The study was presented online as part of the American Academy of Neurology’s 2020 Science Highlights.
Research using preclinical models of Parkinson’s disease has indicated that nilotinib offers neuroprotection. Tanya Simuni, MD, the Arthur C. Nielsen Jr., Research Professor of Parkinson’s Disease and Movement Disorders at Northwestern University in Chicago, and colleagues conducted a prospective study to evaluate the safety and tolerability of oral nilotinib in patients with moderate or advanced Parkinson’s disease. The investigators also sought to examine nilotinib’s symptomatic effect, as measured by the Movement Disorder Society–Unified Parkinson’s Disease Rating Scale (MDS-UPDRS) part III. In addition, Dr. Simuni and colleagues analyzed the drug’s effect on progression of disability, as measured by various other Parkinson’s disease scales. The study’s exploratory outcomes included cognitive function, quality of life, pharmacokinetic profile, and a battery of serum and spinal fluid biomarkers.
The researchers conducted their randomized, double-blind, placebo-controlled, parallel-group study at 25 sites in the United States. They randomized 76 patients with Parkinson’s disease in approximately equal groups to a daily dose of placebo, 150 mg of nilotinib, or 300 mg of nilotinib. Safety visits occurred monthly. Patient assessments occurred at 3 months and at 6 months, which was the end of the treatment period. Patients presented off study medication at 1 month and 2 months after the end of the treatment period.
Treatment did not change dopamine levels
Baseline demographics and disease characteristics were balanced between groups. Mean age was about 66 years in the placebo group, 61 years in the 150-mg group, and 67 years in the 300-mg group. The proportion of male participants was 64% in the placebo group, 60% in the 150-mg group, and 81% in the 300-mg group. Disease duration was 9 years in the placebo group, approximately 9 years in the 150-mg group, and approximately 12 years in the 300-mg group. Mean MDS-UPDRS total on score was 46 in the placebo group, 47 in the 150-mg group, and 52 in the 300-mg group.
Tolerability was 84% in the placebo group, 76% in the in the 150-mg group, and 77% in the 300-mg group. The sole treatment-related serious adverse event, arrhythmia, occurred in one patient in the 300-mg group. The rate of any adverse event was 88% in the placebo group, 92% in the 150-mg group, and 88% in the 300-mg group. The rate of any serious adverse event was 8% in the placebo group and 4% in each nilotinib group.
From baseline to 1 month, MDS-UPDRS part III on scores decreased by 0.49 points in the placebo group, increased by 2.08 in the 150-mg group, and increased by 4.67 in the 300-mg group. Differences in other secondary measures (e.g., change in MDS-UPDRS part III on scores from baseline to 6 months and change in MDS-UPDRS part III off score from baseline to 6 months) were not statistically significant.
At 3 months, CSF levels of nilotinib were well below the threshold for c-Abl inhibition (approximately 11 ng/mL). The arithmetic mean levels were 0.91 ng/mL in the 150-mg group and 1.69 ng/mL in the 300-mg group. Nilotinib also failed to alter CSF levels of dopamine or its metabolites at 3 months. Dr. Simuni and colleagues did not see significant differences between treatment groups in the exploratory outcomes of cognitive function and quality of life.
“Nilotinib is not an optimal molecule to assess the therapeutic potential of c-Abl inhibition for Parkinson’s disease,” the investigators concluded.
Nilotinib may be an inappropriate candidate
The data “suggest that the hypothesis wasn’t tested, since the CSF and serum concentration of the drug were insufficient for enzyme inhibition,” said Peter LeWitt, MD, Sastry Foundation Endowed Chair in Neurology and professor of neurology at Wayne State University, Detroit. “A higher dose or a more CNS-penetrant drug would be needed for adequate testing of the hypothesis that c-Abl inhibition could provide disease modification.”
Nilotinib might not be an appropriate drug for this investigation, he continued. “There may be better choices among c-Abl inhibitors for penetration into the CNS, such as dasatinib, or for increased potency of effect, such as imatinib.”
Sun Pharma Advanced Research Company is conducting a clinical trial of KO706, another c-Abl inhibitor, added Dr. LeWitt, who is a researcher in that trial and an editorial adviser to Neurology Reviews. “The studies published recently in JAMA Neurology by Pagan et al. claiming target engagement with nilotinib in Parkinson’s disease patients need to be contrasted with the results of the current investigation. Disease modification with c-Abl inhibition continues to be a promising therapeutic avenue, but both positive and negative study results need careful reassessment and validation.”
The Michael J. Fox Foundation, the Cure Parkinson’s Trust, and Van Andel Research Institute funded the study. Novartis provided the study drug and placebo. The investigators reported no conflicts of interest.
SOURCE: Simuni T et al. AAN 2020. Abstract 43617.
according to investigators. Nevertheless, other drugs that – like nilotinib – inhibit tyrosine kinase (c-Abl) may have a neuroprotective effect, they added. The study was presented online as part of the American Academy of Neurology’s 2020 Science Highlights.
Research using preclinical models of Parkinson’s disease has indicated that nilotinib offers neuroprotection. Tanya Simuni, MD, the Arthur C. Nielsen Jr., Research Professor of Parkinson’s Disease and Movement Disorders at Northwestern University in Chicago, and colleagues conducted a prospective study to evaluate the safety and tolerability of oral nilotinib in patients with moderate or advanced Parkinson’s disease. The investigators also sought to examine nilotinib’s symptomatic effect, as measured by the Movement Disorder Society–Unified Parkinson’s Disease Rating Scale (MDS-UPDRS) part III. In addition, Dr. Simuni and colleagues analyzed the drug’s effect on progression of disability, as measured by various other Parkinson’s disease scales. The study’s exploratory outcomes included cognitive function, quality of life, pharmacokinetic profile, and a battery of serum and spinal fluid biomarkers.
The researchers conducted their randomized, double-blind, placebo-controlled, parallel-group study at 25 sites in the United States. They randomized 76 patients with Parkinson’s disease in approximately equal groups to a daily dose of placebo, 150 mg of nilotinib, or 300 mg of nilotinib. Safety visits occurred monthly. Patient assessments occurred at 3 months and at 6 months, which was the end of the treatment period. Patients presented off study medication at 1 month and 2 months after the end of the treatment period.
Treatment did not change dopamine levels
Baseline demographics and disease characteristics were balanced between groups. Mean age was about 66 years in the placebo group, 61 years in the 150-mg group, and 67 years in the 300-mg group. The proportion of male participants was 64% in the placebo group, 60% in the 150-mg group, and 81% in the 300-mg group. Disease duration was 9 years in the placebo group, approximately 9 years in the 150-mg group, and approximately 12 years in the 300-mg group. Mean MDS-UPDRS total on score was 46 in the placebo group, 47 in the 150-mg group, and 52 in the 300-mg group.
Tolerability was 84% in the placebo group, 76% in the in the 150-mg group, and 77% in the 300-mg group. The sole treatment-related serious adverse event, arrhythmia, occurred in one patient in the 300-mg group. The rate of any adverse event was 88% in the placebo group, 92% in the 150-mg group, and 88% in the 300-mg group. The rate of any serious adverse event was 8% in the placebo group and 4% in each nilotinib group.
From baseline to 1 month, MDS-UPDRS part III on scores decreased by 0.49 points in the placebo group, increased by 2.08 in the 150-mg group, and increased by 4.67 in the 300-mg group. Differences in other secondary measures (e.g., change in MDS-UPDRS part III on scores from baseline to 6 months and change in MDS-UPDRS part III off score from baseline to 6 months) were not statistically significant.
At 3 months, CSF levels of nilotinib were well below the threshold for c-Abl inhibition (approximately 11 ng/mL). The arithmetic mean levels were 0.91 ng/mL in the 150-mg group and 1.69 ng/mL in the 300-mg group. Nilotinib also failed to alter CSF levels of dopamine or its metabolites at 3 months. Dr. Simuni and colleagues did not see significant differences between treatment groups in the exploratory outcomes of cognitive function and quality of life.
“Nilotinib is not an optimal molecule to assess the therapeutic potential of c-Abl inhibition for Parkinson’s disease,” the investigators concluded.
Nilotinib may be an inappropriate candidate
The data “suggest that the hypothesis wasn’t tested, since the CSF and serum concentration of the drug were insufficient for enzyme inhibition,” said Peter LeWitt, MD, Sastry Foundation Endowed Chair in Neurology and professor of neurology at Wayne State University, Detroit. “A higher dose or a more CNS-penetrant drug would be needed for adequate testing of the hypothesis that c-Abl inhibition could provide disease modification.”
Nilotinib might not be an appropriate drug for this investigation, he continued. “There may be better choices among c-Abl inhibitors for penetration into the CNS, such as dasatinib, or for increased potency of effect, such as imatinib.”
Sun Pharma Advanced Research Company is conducting a clinical trial of KO706, another c-Abl inhibitor, added Dr. LeWitt, who is a researcher in that trial and an editorial adviser to Neurology Reviews. “The studies published recently in JAMA Neurology by Pagan et al. claiming target engagement with nilotinib in Parkinson’s disease patients need to be contrasted with the results of the current investigation. Disease modification with c-Abl inhibition continues to be a promising therapeutic avenue, but both positive and negative study results need careful reassessment and validation.”
The Michael J. Fox Foundation, the Cure Parkinson’s Trust, and Van Andel Research Institute funded the study. Novartis provided the study drug and placebo. The investigators reported no conflicts of interest.
SOURCE: Simuni T et al. AAN 2020. Abstract 43617.
according to investigators. Nevertheless, other drugs that – like nilotinib – inhibit tyrosine kinase (c-Abl) may have a neuroprotective effect, they added. The study was presented online as part of the American Academy of Neurology’s 2020 Science Highlights.
Research using preclinical models of Parkinson’s disease has indicated that nilotinib offers neuroprotection. Tanya Simuni, MD, the Arthur C. Nielsen Jr., Research Professor of Parkinson’s Disease and Movement Disorders at Northwestern University in Chicago, and colleagues conducted a prospective study to evaluate the safety and tolerability of oral nilotinib in patients with moderate or advanced Parkinson’s disease. The investigators also sought to examine nilotinib’s symptomatic effect, as measured by the Movement Disorder Society–Unified Parkinson’s Disease Rating Scale (MDS-UPDRS) part III. In addition, Dr. Simuni and colleagues analyzed the drug’s effect on progression of disability, as measured by various other Parkinson’s disease scales. The study’s exploratory outcomes included cognitive function, quality of life, pharmacokinetic profile, and a battery of serum and spinal fluid biomarkers.
The researchers conducted their randomized, double-blind, placebo-controlled, parallel-group study at 25 sites in the United States. They randomized 76 patients with Parkinson’s disease in approximately equal groups to a daily dose of placebo, 150 mg of nilotinib, or 300 mg of nilotinib. Safety visits occurred monthly. Patient assessments occurred at 3 months and at 6 months, which was the end of the treatment period. Patients presented off study medication at 1 month and 2 months after the end of the treatment period.
Treatment did not change dopamine levels
Baseline demographics and disease characteristics were balanced between groups. Mean age was about 66 years in the placebo group, 61 years in the 150-mg group, and 67 years in the 300-mg group. The proportion of male participants was 64% in the placebo group, 60% in the 150-mg group, and 81% in the 300-mg group. Disease duration was 9 years in the placebo group, approximately 9 years in the 150-mg group, and approximately 12 years in the 300-mg group. Mean MDS-UPDRS total on score was 46 in the placebo group, 47 in the 150-mg group, and 52 in the 300-mg group.
Tolerability was 84% in the placebo group, 76% in the in the 150-mg group, and 77% in the 300-mg group. The sole treatment-related serious adverse event, arrhythmia, occurred in one patient in the 300-mg group. The rate of any adverse event was 88% in the placebo group, 92% in the 150-mg group, and 88% in the 300-mg group. The rate of any serious adverse event was 8% in the placebo group and 4% in each nilotinib group.
From baseline to 1 month, MDS-UPDRS part III on scores decreased by 0.49 points in the placebo group, increased by 2.08 in the 150-mg group, and increased by 4.67 in the 300-mg group. Differences in other secondary measures (e.g., change in MDS-UPDRS part III on scores from baseline to 6 months and change in MDS-UPDRS part III off score from baseline to 6 months) were not statistically significant.
At 3 months, CSF levels of nilotinib were well below the threshold for c-Abl inhibition (approximately 11 ng/mL). The arithmetic mean levels were 0.91 ng/mL in the 150-mg group and 1.69 ng/mL in the 300-mg group. Nilotinib also failed to alter CSF levels of dopamine or its metabolites at 3 months. Dr. Simuni and colleagues did not see significant differences between treatment groups in the exploratory outcomes of cognitive function and quality of life.
“Nilotinib is not an optimal molecule to assess the therapeutic potential of c-Abl inhibition for Parkinson’s disease,” the investigators concluded.
Nilotinib may be an inappropriate candidate
The data “suggest that the hypothesis wasn’t tested, since the CSF and serum concentration of the drug were insufficient for enzyme inhibition,” said Peter LeWitt, MD, Sastry Foundation Endowed Chair in Neurology and professor of neurology at Wayne State University, Detroit. “A higher dose or a more CNS-penetrant drug would be needed for adequate testing of the hypothesis that c-Abl inhibition could provide disease modification.”
Nilotinib might not be an appropriate drug for this investigation, he continued. “There may be better choices among c-Abl inhibitors for penetration into the CNS, such as dasatinib, or for increased potency of effect, such as imatinib.”
Sun Pharma Advanced Research Company is conducting a clinical trial of KO706, another c-Abl inhibitor, added Dr. LeWitt, who is a researcher in that trial and an editorial adviser to Neurology Reviews. “The studies published recently in JAMA Neurology by Pagan et al. claiming target engagement with nilotinib in Parkinson’s disease patients need to be contrasted with the results of the current investigation. Disease modification with c-Abl inhibition continues to be a promising therapeutic avenue, but both positive and negative study results need careful reassessment and validation.”
The Michael J. Fox Foundation, the Cure Parkinson’s Trust, and Van Andel Research Institute funded the study. Novartis provided the study drug and placebo. The investigators reported no conflicts of interest.
SOURCE: Simuni T et al. AAN 2020. Abstract 43617.
FROM AAN 2020
Ofatumumab shows high elimination of disease activity in MS
, a new study shows.
The drug, which is already approved for the treatment of chronic lymphocytic leukemia, is currently under review for relapsing MS as a once-per-month self-injected therapy that could offer a convenient alternative to DMTs that require in-office infusion.
The new findings are from a pooled analysis from the phase 3 ASCLEPIOS I/II trials of the use of ofatumumab for patients with relapsing MS. There were 927 patients in the ASCLEPIOS I trial and 955 in the ASCLEPIOS II trial. The trials were conducted in 37 countries and involved patients aged 18-55 years.
The late-breaking research was presented at the virtual meeting of the Consortium of Multiple Sclerosis Centers (CMSC).
The studies compared patients who were treated with subcutaneous ofatumumab 20 mg with patients treated with oral teriflunomide 14 mg once daily for up to 30 months. The average duration of follow-up was 18 months.
NEDA-3, commonly used to determine treatment outcomes for patients with relapsing MS, was defined as a composite of having no worsening of disability over a 6-month period (6mCDW), no confirmed MS relapse, no new/enlarging T2 lesions, and no gadolinium-enhancing T1 lesions.
The pooled results showed that the odds of achieving NEDA-3 during the first 12 months were three times greater with ofatumumab than with teriflunomide (47.0% vs. 24.5%; odds ratio [OR], 3.36; P < .001) and were more than eight times greater from months 12 to 24 (87.8% vs. 48.2%; OR, 8.09; P < .001).
In addition, compared with patients who received teriflunomide, a higher proportion of patients who received ofatumumab were free from 6mCDW over 2 years (91.9% vs. 88.9%), as well as from relapses (82.3% vs 69.2%) and lesion activity (54.1% vs. 27.5%).
There was a significantly greater reduction in annualized relapse rate with ofatumumab compared with teriflunomide at all cumulative time intervals, including months 0 to 3 (P = .011), and at all subsequent time intervals from month 0 to 27 (P < .001).
The pooled findings further showed that ofatumumab reduced the mean number of gadolinium-enhancing T1 lesions per scan by 95.9% compared with teriflunomide (P < .001).
“Ofatumumab increased the probability of achieving NEDA-3 and demonstrated superior efficacy vs teriflunomide in patients with relapsing MS,” said the authors, led by Stephen L. Hauser, MD, of the department of neurology, UCSF Weill Institute for Neurosciences, University of California, San Francisco.
Ofatumumab superior in primary, secondary outcomes
As previously reported, subcutaneous ofatumumab also demonstrated superior efficacy over oral teriflunomide in the primary and secondary endpoints in the ASCLEPIOS I/II trials. The annualized relapse rate was reduced by 0.22 in the teriflunomide group, vs 0.11 in the ofatumumab group (50.5% relative reduction; P < .001) in the ASCLEPIOS I trial, and by 0.25 vs. 0.10 (58.5% relative reduction P < .001) in ASCLEPIOS II.
Ofatumumab also reduced the number of gadolinium-enhancing T1 lesions and new or enlarging T2 lesions compared with teriflunomide (all P < .001). It reduced the risk for disability progression by 34.4% over 3 months and by 32.5% over 6 months.
In the studies, the rate of serious infection with ofatumumab was 2.5%, compared with 1.8% with teriflunomide. Rates of malignancies were 0.5% and 0.3%, respectively.
“Ofatumumab demonstrated superior efficacy versus teriflunomide, with an acceptable safety profile, in patients with relapsing MS,” the authors reported.
Adherence rates with self-injection encouraging
An additional analysis from the two trials presented virtually in a separate abstract at the CMSC showed greater adherence to the self-administered regimen.
The analysis shows that in the ASCLEPIOS I study, 86.0% patients who were randomly assigned to receive ofatumumab and 77.7% who received teriflunomide completed the study on the assigned study drug. The proportion of patients who received ofatumumab and who discontinued treatment was 14.0%, versus 21.2% for those in the teriflunomide group. The most common reasons for discontinuation were patient/guardian decision (ofatumumab, 4.9%; teriflunomide, 8.2%), adverse event (ofatumumab, 5.2%; teriflunomide, 5.0%), and physician decision (ofatumumab, 2.2%; teriflunomide, 6.5%).
In the ASCLEPIOS II study, the rates were similar in all measures.
“In ASCLEPIOS trials, compliance with home-administered subcutaneous ofatumumab was high, and fewer patients discontinued ofatumumab as compared to teriflunomide,” the authors concluded.
Comparator drug a weak choice?
In commenting on the research, Stephen Kamin, MD, professor, vice chair, and chief of service, department of neurology, New Jersey Medical School, in Newark, noted that a limitation of the ASCLEPIOS trials is the comparison with teriflunomide.
“The comparator drug, teriflunomide, is one of the least effective DMTs, and one that some clinicians, including myself, don’t use,” he said.
Previously, when asked in an interview about the choice of teriflunomide as the comparator, Dr. Hauser noted that considerable discussion had gone into the decision. “The rationale was that we wanted to have a comparator that would be present not only against focal disease activity but also potentially against progression, and we were also able to blind the study successfully,” he said at the time.
Dr. Kamin said that ofatumumab will nevertheless likely represent a welcome addition to the tool kit of treatment options for MS. “Any new drug is helpful in adding to our choices as a general rule,” he said. “Subcutaneous injection does have increased convenience.”
It is not likely that the drug will be a game changer, he added, although the treatment’s efficacy compared with other drugs remains to be seen. “It all depends upon the relative efficacy of ofatumumab versus ocrelizumab or siponimod,” Dr. Kamin said.
“There has been another subcutaneous monoclonal for MS, daclizumab, although this was withdrawn from the market due to severe adverse effects not related to route of administration,” he added.
Dr. Hauser has relationships with Alector, Annexon, Bionure, Molecular Stethoscope, Symbiotix, and F. Hoffmann-La Roche. Dr. Kamin has received research support from Biogen, Novartis and CMSC.
A version of this article originally appeared on Medscape.com.
, a new study shows.
The drug, which is already approved for the treatment of chronic lymphocytic leukemia, is currently under review for relapsing MS as a once-per-month self-injected therapy that could offer a convenient alternative to DMTs that require in-office infusion.
The new findings are from a pooled analysis from the phase 3 ASCLEPIOS I/II trials of the use of ofatumumab for patients with relapsing MS. There were 927 patients in the ASCLEPIOS I trial and 955 in the ASCLEPIOS II trial. The trials were conducted in 37 countries and involved patients aged 18-55 years.
The late-breaking research was presented at the virtual meeting of the Consortium of Multiple Sclerosis Centers (CMSC).
The studies compared patients who were treated with subcutaneous ofatumumab 20 mg with patients treated with oral teriflunomide 14 mg once daily for up to 30 months. The average duration of follow-up was 18 months.
NEDA-3, commonly used to determine treatment outcomes for patients with relapsing MS, was defined as a composite of having no worsening of disability over a 6-month period (6mCDW), no confirmed MS relapse, no new/enlarging T2 lesions, and no gadolinium-enhancing T1 lesions.
The pooled results showed that the odds of achieving NEDA-3 during the first 12 months were three times greater with ofatumumab than with teriflunomide (47.0% vs. 24.5%; odds ratio [OR], 3.36; P < .001) and were more than eight times greater from months 12 to 24 (87.8% vs. 48.2%; OR, 8.09; P < .001).
In addition, compared with patients who received teriflunomide, a higher proportion of patients who received ofatumumab were free from 6mCDW over 2 years (91.9% vs. 88.9%), as well as from relapses (82.3% vs 69.2%) and lesion activity (54.1% vs. 27.5%).
There was a significantly greater reduction in annualized relapse rate with ofatumumab compared with teriflunomide at all cumulative time intervals, including months 0 to 3 (P = .011), and at all subsequent time intervals from month 0 to 27 (P < .001).
The pooled findings further showed that ofatumumab reduced the mean number of gadolinium-enhancing T1 lesions per scan by 95.9% compared with teriflunomide (P < .001).
“Ofatumumab increased the probability of achieving NEDA-3 and demonstrated superior efficacy vs teriflunomide in patients with relapsing MS,” said the authors, led by Stephen L. Hauser, MD, of the department of neurology, UCSF Weill Institute for Neurosciences, University of California, San Francisco.
Ofatumumab superior in primary, secondary outcomes
As previously reported, subcutaneous ofatumumab also demonstrated superior efficacy over oral teriflunomide in the primary and secondary endpoints in the ASCLEPIOS I/II trials. The annualized relapse rate was reduced by 0.22 in the teriflunomide group, vs 0.11 in the ofatumumab group (50.5% relative reduction; P < .001) in the ASCLEPIOS I trial, and by 0.25 vs. 0.10 (58.5% relative reduction P < .001) in ASCLEPIOS II.
Ofatumumab also reduced the number of gadolinium-enhancing T1 lesions and new or enlarging T2 lesions compared with teriflunomide (all P < .001). It reduced the risk for disability progression by 34.4% over 3 months and by 32.5% over 6 months.
In the studies, the rate of serious infection with ofatumumab was 2.5%, compared with 1.8% with teriflunomide. Rates of malignancies were 0.5% and 0.3%, respectively.
“Ofatumumab demonstrated superior efficacy versus teriflunomide, with an acceptable safety profile, in patients with relapsing MS,” the authors reported.
Adherence rates with self-injection encouraging
An additional analysis from the two trials presented virtually in a separate abstract at the CMSC showed greater adherence to the self-administered regimen.
The analysis shows that in the ASCLEPIOS I study, 86.0% patients who were randomly assigned to receive ofatumumab and 77.7% who received teriflunomide completed the study on the assigned study drug. The proportion of patients who received ofatumumab and who discontinued treatment was 14.0%, versus 21.2% for those in the teriflunomide group. The most common reasons for discontinuation were patient/guardian decision (ofatumumab, 4.9%; teriflunomide, 8.2%), adverse event (ofatumumab, 5.2%; teriflunomide, 5.0%), and physician decision (ofatumumab, 2.2%; teriflunomide, 6.5%).
In the ASCLEPIOS II study, the rates were similar in all measures.
“In ASCLEPIOS trials, compliance with home-administered subcutaneous ofatumumab was high, and fewer patients discontinued ofatumumab as compared to teriflunomide,” the authors concluded.
Comparator drug a weak choice?
In commenting on the research, Stephen Kamin, MD, professor, vice chair, and chief of service, department of neurology, New Jersey Medical School, in Newark, noted that a limitation of the ASCLEPIOS trials is the comparison with teriflunomide.
“The comparator drug, teriflunomide, is one of the least effective DMTs, and one that some clinicians, including myself, don’t use,” he said.
Previously, when asked in an interview about the choice of teriflunomide as the comparator, Dr. Hauser noted that considerable discussion had gone into the decision. “The rationale was that we wanted to have a comparator that would be present not only against focal disease activity but also potentially against progression, and we were also able to blind the study successfully,” he said at the time.
Dr. Kamin said that ofatumumab will nevertheless likely represent a welcome addition to the tool kit of treatment options for MS. “Any new drug is helpful in adding to our choices as a general rule,” he said. “Subcutaneous injection does have increased convenience.”
It is not likely that the drug will be a game changer, he added, although the treatment’s efficacy compared with other drugs remains to be seen. “It all depends upon the relative efficacy of ofatumumab versus ocrelizumab or siponimod,” Dr. Kamin said.
“There has been another subcutaneous monoclonal for MS, daclizumab, although this was withdrawn from the market due to severe adverse effects not related to route of administration,” he added.
Dr. Hauser has relationships with Alector, Annexon, Bionure, Molecular Stethoscope, Symbiotix, and F. Hoffmann-La Roche. Dr. Kamin has received research support from Biogen, Novartis and CMSC.
A version of this article originally appeared on Medscape.com.
, a new study shows.
The drug, which is already approved for the treatment of chronic lymphocytic leukemia, is currently under review for relapsing MS as a once-per-month self-injected therapy that could offer a convenient alternative to DMTs that require in-office infusion.
The new findings are from a pooled analysis from the phase 3 ASCLEPIOS I/II trials of the use of ofatumumab for patients with relapsing MS. There were 927 patients in the ASCLEPIOS I trial and 955 in the ASCLEPIOS II trial. The trials were conducted in 37 countries and involved patients aged 18-55 years.
The late-breaking research was presented at the virtual meeting of the Consortium of Multiple Sclerosis Centers (CMSC).
The studies compared patients who were treated with subcutaneous ofatumumab 20 mg with patients treated with oral teriflunomide 14 mg once daily for up to 30 months. The average duration of follow-up was 18 months.
NEDA-3, commonly used to determine treatment outcomes for patients with relapsing MS, was defined as a composite of having no worsening of disability over a 6-month period (6mCDW), no confirmed MS relapse, no new/enlarging T2 lesions, and no gadolinium-enhancing T1 lesions.
The pooled results showed that the odds of achieving NEDA-3 during the first 12 months were three times greater with ofatumumab than with teriflunomide (47.0% vs. 24.5%; odds ratio [OR], 3.36; P < .001) and were more than eight times greater from months 12 to 24 (87.8% vs. 48.2%; OR, 8.09; P < .001).
In addition, compared with patients who received teriflunomide, a higher proportion of patients who received ofatumumab were free from 6mCDW over 2 years (91.9% vs. 88.9%), as well as from relapses (82.3% vs 69.2%) and lesion activity (54.1% vs. 27.5%).
There was a significantly greater reduction in annualized relapse rate with ofatumumab compared with teriflunomide at all cumulative time intervals, including months 0 to 3 (P = .011), and at all subsequent time intervals from month 0 to 27 (P < .001).
The pooled findings further showed that ofatumumab reduced the mean number of gadolinium-enhancing T1 lesions per scan by 95.9% compared with teriflunomide (P < .001).
“Ofatumumab increased the probability of achieving NEDA-3 and demonstrated superior efficacy vs teriflunomide in patients with relapsing MS,” said the authors, led by Stephen L. Hauser, MD, of the department of neurology, UCSF Weill Institute for Neurosciences, University of California, San Francisco.
Ofatumumab superior in primary, secondary outcomes
As previously reported, subcutaneous ofatumumab also demonstrated superior efficacy over oral teriflunomide in the primary and secondary endpoints in the ASCLEPIOS I/II trials. The annualized relapse rate was reduced by 0.22 in the teriflunomide group, vs 0.11 in the ofatumumab group (50.5% relative reduction; P < .001) in the ASCLEPIOS I trial, and by 0.25 vs. 0.10 (58.5% relative reduction P < .001) in ASCLEPIOS II.
Ofatumumab also reduced the number of gadolinium-enhancing T1 lesions and new or enlarging T2 lesions compared with teriflunomide (all P < .001). It reduced the risk for disability progression by 34.4% over 3 months and by 32.5% over 6 months.
In the studies, the rate of serious infection with ofatumumab was 2.5%, compared with 1.8% with teriflunomide. Rates of malignancies were 0.5% and 0.3%, respectively.
“Ofatumumab demonstrated superior efficacy versus teriflunomide, with an acceptable safety profile, in patients with relapsing MS,” the authors reported.
Adherence rates with self-injection encouraging
An additional analysis from the two trials presented virtually in a separate abstract at the CMSC showed greater adherence to the self-administered regimen.
The analysis shows that in the ASCLEPIOS I study, 86.0% patients who were randomly assigned to receive ofatumumab and 77.7% who received teriflunomide completed the study on the assigned study drug. The proportion of patients who received ofatumumab and who discontinued treatment was 14.0%, versus 21.2% for those in the teriflunomide group. The most common reasons for discontinuation were patient/guardian decision (ofatumumab, 4.9%; teriflunomide, 8.2%), adverse event (ofatumumab, 5.2%; teriflunomide, 5.0%), and physician decision (ofatumumab, 2.2%; teriflunomide, 6.5%).
In the ASCLEPIOS II study, the rates were similar in all measures.
“In ASCLEPIOS trials, compliance with home-administered subcutaneous ofatumumab was high, and fewer patients discontinued ofatumumab as compared to teriflunomide,” the authors concluded.
Comparator drug a weak choice?
In commenting on the research, Stephen Kamin, MD, professor, vice chair, and chief of service, department of neurology, New Jersey Medical School, in Newark, noted that a limitation of the ASCLEPIOS trials is the comparison with teriflunomide.
“The comparator drug, teriflunomide, is one of the least effective DMTs, and one that some clinicians, including myself, don’t use,” he said.
Previously, when asked in an interview about the choice of teriflunomide as the comparator, Dr. Hauser noted that considerable discussion had gone into the decision. “The rationale was that we wanted to have a comparator that would be present not only against focal disease activity but also potentially against progression, and we were also able to blind the study successfully,” he said at the time.
Dr. Kamin said that ofatumumab will nevertheless likely represent a welcome addition to the tool kit of treatment options for MS. “Any new drug is helpful in adding to our choices as a general rule,” he said. “Subcutaneous injection does have increased convenience.”
It is not likely that the drug will be a game changer, he added, although the treatment’s efficacy compared with other drugs remains to be seen. “It all depends upon the relative efficacy of ofatumumab versus ocrelizumab or siponimod,” Dr. Kamin said.
“There has been another subcutaneous monoclonal for MS, daclizumab, although this was withdrawn from the market due to severe adverse effects not related to route of administration,” he added.
Dr. Hauser has relationships with Alector, Annexon, Bionure, Molecular Stethoscope, Symbiotix, and F. Hoffmann-La Roche. Dr. Kamin has received research support from Biogen, Novartis and CMSC.
A version of this article originally appeared on Medscape.com.
From CMSC 2020
High levels of air pollution linked to increased MS risk
, new research suggests. A large cohort study of almost 550,000 individuals living in Italy showed that participants living in areas with high levels of pollutants had a significantly greater risk of developing MS than those who lived in areas with low levels of pollutants.
The findings further confirm a relationship between exposure to air pollutants and risk for MS that has been shown in previous research, said Roberto Bergamaschi, MD, PhD, director of the Multiple Sclerosis Center, IRCCS Mondino Foundation, Pavia, Italy.
“Countermeasures that cut air pollution can be important for public health, not only to reduce deaths related to cardiac and pulmonary diseases but also the risk of chronic autoimmune diseases such as MS,” Dr. Bergamaschi said.
The findings were presented at the Congress of the European Academy of Neurology (EAN) 2020, which transitioned to a virtual/online meeting because of the COVID-19 pandemic.
Toxic pollutants
Several environmental factors may trigger an abnormal immune response that manifests in MS. The most studied of these are low vitamin D level, cigarette smoking, and an unhealthy diet, Dr. Bergamaschi said. However, “other environmental factors deserve to be studied—pollution included,” he added.
Among the most toxic air pollutants are particulate matter (PM), which is a mixture of fine solid and liquid particles suspended in the earth’s atmosphere. PM may range from 2.5 microns (PM2.5) to 10 microns (PM10) in diameter.
The main sources of such pollutants are household and commercial heating (53%) and industrial activities (17%), followed by road vehicle and non–road vehicle use, agriculture, and electricity production.
The World Health Organization estimates that more than 3.2 million individuals worldwide die prematurely every year because of lung cancer, cardiovascular disease, and other diseases related to air pollutants, said Dr. Bergamaschi.
Epidemiologic research has uncovered a relationship between air pollution and MS. A large American study published in 2008 in Science of the Total Environment showed a significant association between MS prevalence and PM10 levels (P < 0.001). Other studies have shown an increase in the number of clinical relapses of MS that were linked to air pollution.
The current investigators assessed the association between PM2.5 levels and MS prevalence in the northern province of Pavia, which has a population of 547,251 individuals in 188 municipalities.
Peculiar features
Pavia is situated in a flat territory that encompasses the highly industrialized regions of Piedmont, Lombardy, Emilia-Romagna, and Veneto. It has a high level of anthropogenic emissions, or environmental pollutants, originating from human activity, Dr. Bergamaschi reported. The region also has “peculiar” geographical features that “favor the accumulation of pollutants,” such as the natural barrier of the Alps in the north and low wind speed, he said.
The researchers identified 927 individuals with MS (315 male and 612 female) in the province. The overall MS prevalence rate was 169.4 per 100,000 population (95% confidence interval [CI], 158.8 – 180.6), which is 10-fold higher than 50 years ago, Dr. Bergamaschi said. In addition, this MS prevalence is higher than that in the United States, which is about 150 per 100,000 population.
Using sophisticated Bayesian disease mapping, the investigators looked for clusters of MS. They also gathered emission data for PM2.5 from 2010 to 2017 from the European Monitoring and Evaluation Programme database. They then divided the region on the basis of average winter concentrations of PM2.5.
Three distinct lateral areas of air pollution were identified. The more northern region, which includes the large urban center of Milan, had the highest level of air pollution. Concentrations decreased the further south the investigators looked.
After adjusting for age, urbanization (population density), and deprivation index, results showed that living in areas with high levels of pollutants was associated with increased MS risk. When controlling for PM2.5 pollution, participants in urban areas had an increased risk for MS compared with rural dwellers (relative risk [RR], 1.16; 95% CI, 1.04 – 1.30; P = 0.003)
Dr. Bergamaschi said it is unclear whether this risk is higher for certain types of MS. “To my knowledge, no study has analyzed possible relationships between MS phenotypes and air pollution,” he noted.
Vitamin D’s role?
Several mechanisms might help explain the relationship between air pollution and MS risk, he added. These include oxidative stress, which results in cell damage, inflammation, and proinflammatory cytokine release. Vitamin D also likely plays some role, Dr. Bergamaschi said. Upon penetrating the lower strata of the earth’s atmosphere, ultraviolet B radiation is absorbed and scattered by suspended pollutants.
Several studies have highlighted the correlation between living in a polluted area and vitamin D hypovitaminosis; “so air pollution can contribute to increasing the risk of MS by reducing vitamin D synthesis,” he said.
Recent research has also shown that air pollution is associated with a higher risk for other autoimmune disorders, including systemic lupus erythematosus, rheumatoid arthritis, and type 1 diabetes mellitus.
However, pollution alone is only part of the picture. MS prevalence in highly populated and polluted countries such as China and India is low, with no more than 30 to 40 cases per 100,000 population, Dr. Bergamaschi noted. “This discrepancy is explained by different genetic backgrounds. While Caucasians are particularly susceptible to MS, Asians are not,” he said.
Study limitations cited included a possible bias because the analysis did not include other possible contributing risk factors, particularly other pollutants, Dr. Bergamaschi said.
Commenting on the research, Lily Jung Henson, MD, chief of neurology at Piedmont Healthcare in Stockbridge, Georgia, said the findings provide “a fascinating glimpse” into possible causative factors for MS and warrant further investigation.
“This research also suggests other opportunities to look at, such as progression of the degree of air pollution and the incidence of MS over time,” said Dr. Henson, who was not involved with the study.
Drs. Bergamaschi and Dr. Henson have reported no relevant financial relationships.
This article first appeared on Medscape.com.
, new research suggests. A large cohort study of almost 550,000 individuals living in Italy showed that participants living in areas with high levels of pollutants had a significantly greater risk of developing MS than those who lived in areas with low levels of pollutants.
The findings further confirm a relationship between exposure to air pollutants and risk for MS that has been shown in previous research, said Roberto Bergamaschi, MD, PhD, director of the Multiple Sclerosis Center, IRCCS Mondino Foundation, Pavia, Italy.
“Countermeasures that cut air pollution can be important for public health, not only to reduce deaths related to cardiac and pulmonary diseases but also the risk of chronic autoimmune diseases such as MS,” Dr. Bergamaschi said.
The findings were presented at the Congress of the European Academy of Neurology (EAN) 2020, which transitioned to a virtual/online meeting because of the COVID-19 pandemic.
Toxic pollutants
Several environmental factors may trigger an abnormal immune response that manifests in MS. The most studied of these are low vitamin D level, cigarette smoking, and an unhealthy diet, Dr. Bergamaschi said. However, “other environmental factors deserve to be studied—pollution included,” he added.
Among the most toxic air pollutants are particulate matter (PM), which is a mixture of fine solid and liquid particles suspended in the earth’s atmosphere. PM may range from 2.5 microns (PM2.5) to 10 microns (PM10) in diameter.
The main sources of such pollutants are household and commercial heating (53%) and industrial activities (17%), followed by road vehicle and non–road vehicle use, agriculture, and electricity production.
The World Health Organization estimates that more than 3.2 million individuals worldwide die prematurely every year because of lung cancer, cardiovascular disease, and other diseases related to air pollutants, said Dr. Bergamaschi.
Epidemiologic research has uncovered a relationship between air pollution and MS. A large American study published in 2008 in Science of the Total Environment showed a significant association between MS prevalence and PM10 levels (P < 0.001). Other studies have shown an increase in the number of clinical relapses of MS that were linked to air pollution.
The current investigators assessed the association between PM2.5 levels and MS prevalence in the northern province of Pavia, which has a population of 547,251 individuals in 188 municipalities.
Peculiar features
Pavia is situated in a flat territory that encompasses the highly industrialized regions of Piedmont, Lombardy, Emilia-Romagna, and Veneto. It has a high level of anthropogenic emissions, or environmental pollutants, originating from human activity, Dr. Bergamaschi reported. The region also has “peculiar” geographical features that “favor the accumulation of pollutants,” such as the natural barrier of the Alps in the north and low wind speed, he said.
The researchers identified 927 individuals with MS (315 male and 612 female) in the province. The overall MS prevalence rate was 169.4 per 100,000 population (95% confidence interval [CI], 158.8 – 180.6), which is 10-fold higher than 50 years ago, Dr. Bergamaschi said. In addition, this MS prevalence is higher than that in the United States, which is about 150 per 100,000 population.
Using sophisticated Bayesian disease mapping, the investigators looked for clusters of MS. They also gathered emission data for PM2.5 from 2010 to 2017 from the European Monitoring and Evaluation Programme database. They then divided the region on the basis of average winter concentrations of PM2.5.
Three distinct lateral areas of air pollution were identified. The more northern region, which includes the large urban center of Milan, had the highest level of air pollution. Concentrations decreased the further south the investigators looked.
After adjusting for age, urbanization (population density), and deprivation index, results showed that living in areas with high levels of pollutants was associated with increased MS risk. When controlling for PM2.5 pollution, participants in urban areas had an increased risk for MS compared with rural dwellers (relative risk [RR], 1.16; 95% CI, 1.04 – 1.30; P = 0.003)
Dr. Bergamaschi said it is unclear whether this risk is higher for certain types of MS. “To my knowledge, no study has analyzed possible relationships between MS phenotypes and air pollution,” he noted.
Vitamin D’s role?
Several mechanisms might help explain the relationship between air pollution and MS risk, he added. These include oxidative stress, which results in cell damage, inflammation, and proinflammatory cytokine release. Vitamin D also likely plays some role, Dr. Bergamaschi said. Upon penetrating the lower strata of the earth’s atmosphere, ultraviolet B radiation is absorbed and scattered by suspended pollutants.
Several studies have highlighted the correlation between living in a polluted area and vitamin D hypovitaminosis; “so air pollution can contribute to increasing the risk of MS by reducing vitamin D synthesis,” he said.
Recent research has also shown that air pollution is associated with a higher risk for other autoimmune disorders, including systemic lupus erythematosus, rheumatoid arthritis, and type 1 diabetes mellitus.
However, pollution alone is only part of the picture. MS prevalence in highly populated and polluted countries such as China and India is low, with no more than 30 to 40 cases per 100,000 population, Dr. Bergamaschi noted. “This discrepancy is explained by different genetic backgrounds. While Caucasians are particularly susceptible to MS, Asians are not,” he said.
Study limitations cited included a possible bias because the analysis did not include other possible contributing risk factors, particularly other pollutants, Dr. Bergamaschi said.
Commenting on the research, Lily Jung Henson, MD, chief of neurology at Piedmont Healthcare in Stockbridge, Georgia, said the findings provide “a fascinating glimpse” into possible causative factors for MS and warrant further investigation.
“This research also suggests other opportunities to look at, such as progression of the degree of air pollution and the incidence of MS over time,” said Dr. Henson, who was not involved with the study.
Drs. Bergamaschi and Dr. Henson have reported no relevant financial relationships.
This article first appeared on Medscape.com.
, new research suggests. A large cohort study of almost 550,000 individuals living in Italy showed that participants living in areas with high levels of pollutants had a significantly greater risk of developing MS than those who lived in areas with low levels of pollutants.
The findings further confirm a relationship between exposure to air pollutants and risk for MS that has been shown in previous research, said Roberto Bergamaschi, MD, PhD, director of the Multiple Sclerosis Center, IRCCS Mondino Foundation, Pavia, Italy.
“Countermeasures that cut air pollution can be important for public health, not only to reduce deaths related to cardiac and pulmonary diseases but also the risk of chronic autoimmune diseases such as MS,” Dr. Bergamaschi said.
The findings were presented at the Congress of the European Academy of Neurology (EAN) 2020, which transitioned to a virtual/online meeting because of the COVID-19 pandemic.
Toxic pollutants
Several environmental factors may trigger an abnormal immune response that manifests in MS. The most studied of these are low vitamin D level, cigarette smoking, and an unhealthy diet, Dr. Bergamaschi said. However, “other environmental factors deserve to be studied—pollution included,” he added.
Among the most toxic air pollutants are particulate matter (PM), which is a mixture of fine solid and liquid particles suspended in the earth’s atmosphere. PM may range from 2.5 microns (PM2.5) to 10 microns (PM10) in diameter.
The main sources of such pollutants are household and commercial heating (53%) and industrial activities (17%), followed by road vehicle and non–road vehicle use, agriculture, and electricity production.
The World Health Organization estimates that more than 3.2 million individuals worldwide die prematurely every year because of lung cancer, cardiovascular disease, and other diseases related to air pollutants, said Dr. Bergamaschi.
Epidemiologic research has uncovered a relationship between air pollution and MS. A large American study published in 2008 in Science of the Total Environment showed a significant association between MS prevalence and PM10 levels (P < 0.001). Other studies have shown an increase in the number of clinical relapses of MS that were linked to air pollution.
The current investigators assessed the association between PM2.5 levels and MS prevalence in the northern province of Pavia, which has a population of 547,251 individuals in 188 municipalities.
Peculiar features
Pavia is situated in a flat territory that encompasses the highly industrialized regions of Piedmont, Lombardy, Emilia-Romagna, and Veneto. It has a high level of anthropogenic emissions, or environmental pollutants, originating from human activity, Dr. Bergamaschi reported. The region also has “peculiar” geographical features that “favor the accumulation of pollutants,” such as the natural barrier of the Alps in the north and low wind speed, he said.
The researchers identified 927 individuals with MS (315 male and 612 female) in the province. The overall MS prevalence rate was 169.4 per 100,000 population (95% confidence interval [CI], 158.8 – 180.6), which is 10-fold higher than 50 years ago, Dr. Bergamaschi said. In addition, this MS prevalence is higher than that in the United States, which is about 150 per 100,000 population.
Using sophisticated Bayesian disease mapping, the investigators looked for clusters of MS. They also gathered emission data for PM2.5 from 2010 to 2017 from the European Monitoring and Evaluation Programme database. They then divided the region on the basis of average winter concentrations of PM2.5.
Three distinct lateral areas of air pollution were identified. The more northern region, which includes the large urban center of Milan, had the highest level of air pollution. Concentrations decreased the further south the investigators looked.
After adjusting for age, urbanization (population density), and deprivation index, results showed that living in areas with high levels of pollutants was associated with increased MS risk. When controlling for PM2.5 pollution, participants in urban areas had an increased risk for MS compared with rural dwellers (relative risk [RR], 1.16; 95% CI, 1.04 – 1.30; P = 0.003)
Dr. Bergamaschi said it is unclear whether this risk is higher for certain types of MS. “To my knowledge, no study has analyzed possible relationships between MS phenotypes and air pollution,” he noted.
Vitamin D’s role?
Several mechanisms might help explain the relationship between air pollution and MS risk, he added. These include oxidative stress, which results in cell damage, inflammation, and proinflammatory cytokine release. Vitamin D also likely plays some role, Dr. Bergamaschi said. Upon penetrating the lower strata of the earth’s atmosphere, ultraviolet B radiation is absorbed and scattered by suspended pollutants.
Several studies have highlighted the correlation between living in a polluted area and vitamin D hypovitaminosis; “so air pollution can contribute to increasing the risk of MS by reducing vitamin D synthesis,” he said.
Recent research has also shown that air pollution is associated with a higher risk for other autoimmune disorders, including systemic lupus erythematosus, rheumatoid arthritis, and type 1 diabetes mellitus.
However, pollution alone is only part of the picture. MS prevalence in highly populated and polluted countries such as China and India is low, with no more than 30 to 40 cases per 100,000 population, Dr. Bergamaschi noted. “This discrepancy is explained by different genetic backgrounds. While Caucasians are particularly susceptible to MS, Asians are not,” he said.
Study limitations cited included a possible bias because the analysis did not include other possible contributing risk factors, particularly other pollutants, Dr. Bergamaschi said.
Commenting on the research, Lily Jung Henson, MD, chief of neurology at Piedmont Healthcare in Stockbridge, Georgia, said the findings provide “a fascinating glimpse” into possible causative factors for MS and warrant further investigation.
“This research also suggests other opportunities to look at, such as progression of the degree of air pollution and the incidence of MS over time,” said Dr. Henson, who was not involved with the study.
Drs. Bergamaschi and Dr. Henson have reported no relevant financial relationships.
This article first appeared on Medscape.com.
FROM EAN 2020
Mixed results for aducanumab in two phase 3 trials for Alzheimer’s disease
Aducanumab was associated with favorable changes in activities of daily living and in Alzheimer’s disease biomarkers.
The EMERGE and ENGAGE studies compared low-dose and high-dose aducanumab and placebo over 78 weeks. The high-dose EMERGE cohort experienced a 22% improvement in the primary outcome – adjusted mean Clinical Dementia Rating Sum of Box (CDR-SB) scores – compared with baseline.
“We have with EMERGE, in the high-dose group, a positive result,” said lead author Samantha Budd Haeberlein, PhD, who presented this research online as part of the 2020 American Academy of Neurology Science Highlights.
In contrast, the low-dose EMERGE group, as well as the low-dose and high-dose cohorts in the ENGAGE study, experienced no statistically significant change in CDR-SB outcomes.
Clinical benefit was associated with the degree of exposure to aducanumab. For example, a protocol adjustment during the study increased the mean dose of aducanumab, a move associated with better outcomes.
“We believe that the difference between the results was largely due to patients’ greater exposure to the high dose of aducanumab,” Dr. Haerberlein, senior vice president and head of the neurodegeneration development unit at Biogen in Cambridge, Mass., said in an interview.
Although the studies shared an identical design, “because ENGAGE began enrolling first and recruitment remained ahead of EMERGE, more patients in EMERGE were impacted by the protocol amendments, which we believe resulted in a higher number of patients exposed to the highest dose in EMERGE versus ENGAGE,” Dr. Haerberlein added.
The EMERGE and ENGAGE studies were conducted at 348 sites in 20 countries. The research included a total of 3,285 participants with mild cognitive impairment caused by Alzheimer’s disease or mild Alzheimer’s disease dementia.
The mean age was 70 years, about 52% were women, and slightly more than half had a history of taking medication for Alzheimer’s disease. The mean Mini-Mental State Exam (MMSE) score was 26 at baseline.
Key findings
Dr. Haerberlein and colleagues reported that the 22% decrease in CDR-SB scores in the high-dose EMERGE participants was significant (P = .01). No significant difference emerged, however, in the ENGAGE study, where high-dose participants had a 2% decrease at 78 weeks in CDR-SB scores (P = .83).
The high-dose EMERGE regimen was also associated with an 18% improvement in MMSE scores (P < .05). In the ENGAGE study, the high-dose MMSE scores increased a nonsignificant 3% (P = .81).
The researchers reported no significant differences in the low-dose cohorts in both studies regarding CDR-SB or MMSE scores at week 78, compared with baseline.
They also assessed amyloid using PET scans. Levels remained essentially the same throughout both studies in the placebo participants. In contrast, there was a statistically significant, dose- and time-dependent reduction associated with both low- and high-dose aducanumab.
Aducanumab treatment was associated with significant benefits on measures of cognition and function such as memory, orientation, and language, Dr. Haeberlein said. “Patients also experienced benefits on activities of daily living including conducting personal finances; performing household chores such as cleaning, shopping, and doing laundry; and independently traveling out of the home.”
Furthermore, reductions in the CSF biomarker phospho-tau in the high-dose EMERGE and ENGAGE cohorts were statistically significant. In contrast, changes in total tau were not significant.
The proportion of patients who experienced an adverse event during EMERGE was similar across groups – 92% of the high-dose group, 88% of the low-dose group, and 87% of the placebo cohort. Similar rates were reported in the ENGAGE high-dose, 90%; low-dose, 90%; and placebo cohorts, 86%.
Adverse events reported in more than 10% of participants included headache, nasopharyngitis, and two forms of amyloid-related imaging abnormalities (ARIA), one of which related to edema (ARIA-E) and the other to hemosiderosis (ARIA-H).
Future plans
Going forward, the researchers are conducting a redosing study to offer aducanumab to all participants in the clinical trials. Also, Biogen is completing the filing of a Biologics License Application with the Food and Drug Administration and with regulatory agencies in other countries.
Early identification and treatment of Alzheimer’s disease remains a priority, Dr. Haeberlein said, because it offers an opportunity to begin health measures like exercise, mental activity, and social engagement; allows people more time to plan for the future; and gives families and loved ones’ time to prepare and support each other. From a research perspective, early identification of this population can maximize chances of participation in a clinical trial as well.
Unanswered questions
“Briefly, while both [studies] were looking at aducanumab’s effect on rate of decline across a variety of measures, one statistically showed a positive impact in a subset and the other did not,” Richard J. Caselli, MD, said when asked to comment on the EMERGE and ENGAGE findings. “The subset were the mildest affected patients on the highest dose for the longest time.”
The main difference between the two studies was that one was adequately powered for this subanalysis and the other was not. Even the underpowered subanalysis showed a beneficial trend, added Dr. Caselli, a neurologist at the Mayo Clinic in Phoenix, Arizona.
Dr. Caselli said these findings raise a number of unanswered questions. For example, is a subanalysis valid? Is the degree of improvement clinically meaningful or meaningful enough to justify the anticipated cost of the drug itself – “likely to be very expensive” plus the “cost and hassle” of monthly IV infusions? Is there enough provider and infusion center capacity going forward? What will the reimbursement from third party payers be like?
Biogen sponsored the EMERGE and ENGAGE studies. Dr. Haeberlein is a Biogen employee. Dr. Caselli had no relevant disclosures.
SOURCE: Haeberlein SB et al. AAN 2020, Abstract 46977.
Aducanumab was associated with favorable changes in activities of daily living and in Alzheimer’s disease biomarkers.
The EMERGE and ENGAGE studies compared low-dose and high-dose aducanumab and placebo over 78 weeks. The high-dose EMERGE cohort experienced a 22% improvement in the primary outcome – adjusted mean Clinical Dementia Rating Sum of Box (CDR-SB) scores – compared with baseline.
“We have with EMERGE, in the high-dose group, a positive result,” said lead author Samantha Budd Haeberlein, PhD, who presented this research online as part of the 2020 American Academy of Neurology Science Highlights.
In contrast, the low-dose EMERGE group, as well as the low-dose and high-dose cohorts in the ENGAGE study, experienced no statistically significant change in CDR-SB outcomes.
Clinical benefit was associated with the degree of exposure to aducanumab. For example, a protocol adjustment during the study increased the mean dose of aducanumab, a move associated with better outcomes.
“We believe that the difference between the results was largely due to patients’ greater exposure to the high dose of aducanumab,” Dr. Haerberlein, senior vice president and head of the neurodegeneration development unit at Biogen in Cambridge, Mass., said in an interview.
Although the studies shared an identical design, “because ENGAGE began enrolling first and recruitment remained ahead of EMERGE, more patients in EMERGE were impacted by the protocol amendments, which we believe resulted in a higher number of patients exposed to the highest dose in EMERGE versus ENGAGE,” Dr. Haerberlein added.
The EMERGE and ENGAGE studies were conducted at 348 sites in 20 countries. The research included a total of 3,285 participants with mild cognitive impairment caused by Alzheimer’s disease or mild Alzheimer’s disease dementia.
The mean age was 70 years, about 52% were women, and slightly more than half had a history of taking medication for Alzheimer’s disease. The mean Mini-Mental State Exam (MMSE) score was 26 at baseline.
Key findings
Dr. Haerberlein and colleagues reported that the 22% decrease in CDR-SB scores in the high-dose EMERGE participants was significant (P = .01). No significant difference emerged, however, in the ENGAGE study, where high-dose participants had a 2% decrease at 78 weeks in CDR-SB scores (P = .83).
The high-dose EMERGE regimen was also associated with an 18% improvement in MMSE scores (P < .05). In the ENGAGE study, the high-dose MMSE scores increased a nonsignificant 3% (P = .81).
The researchers reported no significant differences in the low-dose cohorts in both studies regarding CDR-SB or MMSE scores at week 78, compared with baseline.
They also assessed amyloid using PET scans. Levels remained essentially the same throughout both studies in the placebo participants. In contrast, there was a statistically significant, dose- and time-dependent reduction associated with both low- and high-dose aducanumab.
Aducanumab treatment was associated with significant benefits on measures of cognition and function such as memory, orientation, and language, Dr. Haeberlein said. “Patients also experienced benefits on activities of daily living including conducting personal finances; performing household chores such as cleaning, shopping, and doing laundry; and independently traveling out of the home.”
Furthermore, reductions in the CSF biomarker phospho-tau in the high-dose EMERGE and ENGAGE cohorts were statistically significant. In contrast, changes in total tau were not significant.
The proportion of patients who experienced an adverse event during EMERGE was similar across groups – 92% of the high-dose group, 88% of the low-dose group, and 87% of the placebo cohort. Similar rates were reported in the ENGAGE high-dose, 90%; low-dose, 90%; and placebo cohorts, 86%.
Adverse events reported in more than 10% of participants included headache, nasopharyngitis, and two forms of amyloid-related imaging abnormalities (ARIA), one of which related to edema (ARIA-E) and the other to hemosiderosis (ARIA-H).
Future plans
Going forward, the researchers are conducting a redosing study to offer aducanumab to all participants in the clinical trials. Also, Biogen is completing the filing of a Biologics License Application with the Food and Drug Administration and with regulatory agencies in other countries.
Early identification and treatment of Alzheimer’s disease remains a priority, Dr. Haeberlein said, because it offers an opportunity to begin health measures like exercise, mental activity, and social engagement; allows people more time to plan for the future; and gives families and loved ones’ time to prepare and support each other. From a research perspective, early identification of this population can maximize chances of participation in a clinical trial as well.
Unanswered questions
“Briefly, while both [studies] were looking at aducanumab’s effect on rate of decline across a variety of measures, one statistically showed a positive impact in a subset and the other did not,” Richard J. Caselli, MD, said when asked to comment on the EMERGE and ENGAGE findings. “The subset were the mildest affected patients on the highest dose for the longest time.”
The main difference between the two studies was that one was adequately powered for this subanalysis and the other was not. Even the underpowered subanalysis showed a beneficial trend, added Dr. Caselli, a neurologist at the Mayo Clinic in Phoenix, Arizona.
Dr. Caselli said these findings raise a number of unanswered questions. For example, is a subanalysis valid? Is the degree of improvement clinically meaningful or meaningful enough to justify the anticipated cost of the drug itself – “likely to be very expensive” plus the “cost and hassle” of monthly IV infusions? Is there enough provider and infusion center capacity going forward? What will the reimbursement from third party payers be like?
Biogen sponsored the EMERGE and ENGAGE studies. Dr. Haeberlein is a Biogen employee. Dr. Caselli had no relevant disclosures.
SOURCE: Haeberlein SB et al. AAN 2020, Abstract 46977.
Aducanumab was associated with favorable changes in activities of daily living and in Alzheimer’s disease biomarkers.
The EMERGE and ENGAGE studies compared low-dose and high-dose aducanumab and placebo over 78 weeks. The high-dose EMERGE cohort experienced a 22% improvement in the primary outcome – adjusted mean Clinical Dementia Rating Sum of Box (CDR-SB) scores – compared with baseline.
“We have with EMERGE, in the high-dose group, a positive result,” said lead author Samantha Budd Haeberlein, PhD, who presented this research online as part of the 2020 American Academy of Neurology Science Highlights.
In contrast, the low-dose EMERGE group, as well as the low-dose and high-dose cohorts in the ENGAGE study, experienced no statistically significant change in CDR-SB outcomes.
Clinical benefit was associated with the degree of exposure to aducanumab. For example, a protocol adjustment during the study increased the mean dose of aducanumab, a move associated with better outcomes.
“We believe that the difference between the results was largely due to patients’ greater exposure to the high dose of aducanumab,” Dr. Haerberlein, senior vice president and head of the neurodegeneration development unit at Biogen in Cambridge, Mass., said in an interview.
Although the studies shared an identical design, “because ENGAGE began enrolling first and recruitment remained ahead of EMERGE, more patients in EMERGE were impacted by the protocol amendments, which we believe resulted in a higher number of patients exposed to the highest dose in EMERGE versus ENGAGE,” Dr. Haerberlein added.
The EMERGE and ENGAGE studies were conducted at 348 sites in 20 countries. The research included a total of 3,285 participants with mild cognitive impairment caused by Alzheimer’s disease or mild Alzheimer’s disease dementia.
The mean age was 70 years, about 52% were women, and slightly more than half had a history of taking medication for Alzheimer’s disease. The mean Mini-Mental State Exam (MMSE) score was 26 at baseline.
Key findings
Dr. Haerberlein and colleagues reported that the 22% decrease in CDR-SB scores in the high-dose EMERGE participants was significant (P = .01). No significant difference emerged, however, in the ENGAGE study, where high-dose participants had a 2% decrease at 78 weeks in CDR-SB scores (P = .83).
The high-dose EMERGE regimen was also associated with an 18% improvement in MMSE scores (P < .05). In the ENGAGE study, the high-dose MMSE scores increased a nonsignificant 3% (P = .81).
The researchers reported no significant differences in the low-dose cohorts in both studies regarding CDR-SB or MMSE scores at week 78, compared with baseline.
They also assessed amyloid using PET scans. Levels remained essentially the same throughout both studies in the placebo participants. In contrast, there was a statistically significant, dose- and time-dependent reduction associated with both low- and high-dose aducanumab.
Aducanumab treatment was associated with significant benefits on measures of cognition and function such as memory, orientation, and language, Dr. Haeberlein said. “Patients also experienced benefits on activities of daily living including conducting personal finances; performing household chores such as cleaning, shopping, and doing laundry; and independently traveling out of the home.”
Furthermore, reductions in the CSF biomarker phospho-tau in the high-dose EMERGE and ENGAGE cohorts were statistically significant. In contrast, changes in total tau were not significant.
The proportion of patients who experienced an adverse event during EMERGE was similar across groups – 92% of the high-dose group, 88% of the low-dose group, and 87% of the placebo cohort. Similar rates were reported in the ENGAGE high-dose, 90%; low-dose, 90%; and placebo cohorts, 86%.
Adverse events reported in more than 10% of participants included headache, nasopharyngitis, and two forms of amyloid-related imaging abnormalities (ARIA), one of which related to edema (ARIA-E) and the other to hemosiderosis (ARIA-H).
Future plans
Going forward, the researchers are conducting a redosing study to offer aducanumab to all participants in the clinical trials. Also, Biogen is completing the filing of a Biologics License Application with the Food and Drug Administration and with regulatory agencies in other countries.
Early identification and treatment of Alzheimer’s disease remains a priority, Dr. Haeberlein said, because it offers an opportunity to begin health measures like exercise, mental activity, and social engagement; allows people more time to plan for the future; and gives families and loved ones’ time to prepare and support each other. From a research perspective, early identification of this population can maximize chances of participation in a clinical trial as well.
Unanswered questions
“Briefly, while both [studies] were looking at aducanumab’s effect on rate of decline across a variety of measures, one statistically showed a positive impact in a subset and the other did not,” Richard J. Caselli, MD, said when asked to comment on the EMERGE and ENGAGE findings. “The subset were the mildest affected patients on the highest dose for the longest time.”
The main difference between the two studies was that one was adequately powered for this subanalysis and the other was not. Even the underpowered subanalysis showed a beneficial trend, added Dr. Caselli, a neurologist at the Mayo Clinic in Phoenix, Arizona.
Dr. Caselli said these findings raise a number of unanswered questions. For example, is a subanalysis valid? Is the degree of improvement clinically meaningful or meaningful enough to justify the anticipated cost of the drug itself – “likely to be very expensive” plus the “cost and hassle” of monthly IV infusions? Is there enough provider and infusion center capacity going forward? What will the reimbursement from third party payers be like?
Biogen sponsored the EMERGE and ENGAGE studies. Dr. Haeberlein is a Biogen employee. Dr. Caselli had no relevant disclosures.
SOURCE: Haeberlein SB et al. AAN 2020, Abstract 46977.
FROM AAN 2020
Galcanezumab looks promising for treatment-resistant migraine
“The patients included in our study had previously tried multiple migraine preventive treatments that didn’t work for them. These patients are left with limited treatment options to help with the debilitating pain of migraine,” said lead author Holland C. Detke, PhD, senior clinical research advisor at Eli Lilly and Company Biomedicines.
Participants who took the drug experienced “a rapid reduction in migraine days starting as early as month 1, and continuing through the 6 months of the study,” Dr. Detke said.
The treatment group reported an average 4.0 fewer monthly migraine days at 3 months, for example, compared with a baseline of 13.4 days, whereas the placebo group decreased an average 1.29 days from a similar baseline of 13.0 migraine days.
Dr. Detke presented these and other results of the open-label phase of the CONQUER phase 3 trial online as part of the 2020 American Academy of Neurology Science Highlights.
The investigators enrolled 462 adults with episodic or chronic migraine. All participants previously failed two to four migraine treatments because of insufficient efficacy or issues around tolerability or safety. At month 0, 232 people were randomly assigned to galcanezumab and another 230 to placebo injections. At 3 months, 449 participants received a galcanezumab injection as part of the open-label treatment phase.
Participants were an average 48 years old, approximately 86% were women, and 82% were white. At baseline, mean Migraine Specific Quality of Life Role Function Restrictive (MSQ RFR) domain score was 45, “indicating significant impairment in functioning,” Dr. Detke said. At the same time, mean Migraine Disability Assessment Test (MIDAS) total score was 51, “indicating quite severe disability.”
Significant outcomes
The decrease in migraine days at 3 months – 4.0 days with treatment versus 1.29 with placebo – was statistically significant (P < .0001). During the open-label phase, participants who switched from placebo “essentially catch up to where the previously treated people were,” Dr. Detke said. At 6 months, the decrease in average monthly headache days was 5.60 in the initial galcanezumab group versus 5.24 in the initial placebo group.
Significant differences at 3 months versus baseline were observed in participants who received galcanezumab when investigators assessed reduction in 50% or more, 75% or more, or 100% of mean monthly migraine days. No such significant decreases were seen in the placebo group.
Treatment-emergent adverse events reported in the open-label phase included nasopharyngitis in 4.2%, injection site pain in 3.8%, and injection site erythema in 2.7%. Five participants discontinued during the open-label phase because of adverse events.
The results of the study suggest galcanezumab “should be considered as a treatment option for patients who have not had success with previous treatments,” Dr. Detke said.
Multiple strengths of study
“It is encouraging that galcanezumab works in patients who have failed prior reduction strategies,” A. Laine Green, MD, a neurologist at Dartmouth-Hitchcock Medical Center in Lebanon, N.H., said when asked to comment.
This study did not look at patients who have failed more than four previous reduction strategies, he added. “Clinically we see many of these patients. To be fair, no one has studied this group using the monoclonal antibodies.”
Dr. Green noted several strengths of the study. The groups were similar, there were few dropouts during the open-label extension, and there were no unexpected side effects or adverse events. “Those who got placebo caught up to those who received active treatment in the double-blind phase,” he said. “It is also nice to see patient reported outcomes improved as headaches improve. This adds consistency to the results.”
One caveat, Dr. Green noted, is “with open-label extensions, there is always the potential for bias because patients know what treatment they are receiving.”
Overall [the study] gives hope that patients who have failed previous reduction strategies may respond to the newer monoclonal antibodies.”
Aligns with previous findings
The results are “the same as any other long-term extension study of a drug for migraine,” Stephen Silberstein, MD, said when asked to comment. “The longer one takes it, the better you get.”
The research also confirms that if you switch patients taking placebo to an active treatment, they get better, added Dr. Silberstein, director of the Headache Center at Jefferson Health in Philadelphia.
Because they are injections, agents such as galcanezumab, other monoclonal antibodies, and botulinum toxin offer better compliance for headache compared with small molecule medications that require daily oral dosing, he added.
Eli Lilly and Company funded the study. Dr. Holland Detke is a Lilly employee. Dr. Green collaborated with Lilly on a poster for the AHS scientific meeting on a similar topic but did not receive compensation. Up until August 2019, he served as a consultant for Lilly, Novartis, Teva and Allergan. Dr. Green is also a member of the Medscape and American Headache Society Migraine Steering Committee. Dr. Silberstein is a member of the advisory board and consultant for Lilly.
Source: Detke HC et al. AAN 2020. Abstract 43625.
“The patients included in our study had previously tried multiple migraine preventive treatments that didn’t work for them. These patients are left with limited treatment options to help with the debilitating pain of migraine,” said lead author Holland C. Detke, PhD, senior clinical research advisor at Eli Lilly and Company Biomedicines.
Participants who took the drug experienced “a rapid reduction in migraine days starting as early as month 1, and continuing through the 6 months of the study,” Dr. Detke said.
The treatment group reported an average 4.0 fewer monthly migraine days at 3 months, for example, compared with a baseline of 13.4 days, whereas the placebo group decreased an average 1.29 days from a similar baseline of 13.0 migraine days.
Dr. Detke presented these and other results of the open-label phase of the CONQUER phase 3 trial online as part of the 2020 American Academy of Neurology Science Highlights.
The investigators enrolled 462 adults with episodic or chronic migraine. All participants previously failed two to four migraine treatments because of insufficient efficacy or issues around tolerability or safety. At month 0, 232 people were randomly assigned to galcanezumab and another 230 to placebo injections. At 3 months, 449 participants received a galcanezumab injection as part of the open-label treatment phase.
Participants were an average 48 years old, approximately 86% were women, and 82% were white. At baseline, mean Migraine Specific Quality of Life Role Function Restrictive (MSQ RFR) domain score was 45, “indicating significant impairment in functioning,” Dr. Detke said. At the same time, mean Migraine Disability Assessment Test (MIDAS) total score was 51, “indicating quite severe disability.”
Significant outcomes
The decrease in migraine days at 3 months – 4.0 days with treatment versus 1.29 with placebo – was statistically significant (P < .0001). During the open-label phase, participants who switched from placebo “essentially catch up to where the previously treated people were,” Dr. Detke said. At 6 months, the decrease in average monthly headache days was 5.60 in the initial galcanezumab group versus 5.24 in the initial placebo group.
Significant differences at 3 months versus baseline were observed in participants who received galcanezumab when investigators assessed reduction in 50% or more, 75% or more, or 100% of mean monthly migraine days. No such significant decreases were seen in the placebo group.
Treatment-emergent adverse events reported in the open-label phase included nasopharyngitis in 4.2%, injection site pain in 3.8%, and injection site erythema in 2.7%. Five participants discontinued during the open-label phase because of adverse events.
The results of the study suggest galcanezumab “should be considered as a treatment option for patients who have not had success with previous treatments,” Dr. Detke said.
Multiple strengths of study
“It is encouraging that galcanezumab works in patients who have failed prior reduction strategies,” A. Laine Green, MD, a neurologist at Dartmouth-Hitchcock Medical Center in Lebanon, N.H., said when asked to comment.
This study did not look at patients who have failed more than four previous reduction strategies, he added. “Clinically we see many of these patients. To be fair, no one has studied this group using the monoclonal antibodies.”
Dr. Green noted several strengths of the study. The groups were similar, there were few dropouts during the open-label extension, and there were no unexpected side effects or adverse events. “Those who got placebo caught up to those who received active treatment in the double-blind phase,” he said. “It is also nice to see patient reported outcomes improved as headaches improve. This adds consistency to the results.”
One caveat, Dr. Green noted, is “with open-label extensions, there is always the potential for bias because patients know what treatment they are receiving.”
Overall [the study] gives hope that patients who have failed previous reduction strategies may respond to the newer monoclonal antibodies.”
Aligns with previous findings
The results are “the same as any other long-term extension study of a drug for migraine,” Stephen Silberstein, MD, said when asked to comment. “The longer one takes it, the better you get.”
The research also confirms that if you switch patients taking placebo to an active treatment, they get better, added Dr. Silberstein, director of the Headache Center at Jefferson Health in Philadelphia.
Because they are injections, agents such as galcanezumab, other monoclonal antibodies, and botulinum toxin offer better compliance for headache compared with small molecule medications that require daily oral dosing, he added.
Eli Lilly and Company funded the study. Dr. Holland Detke is a Lilly employee. Dr. Green collaborated with Lilly on a poster for the AHS scientific meeting on a similar topic but did not receive compensation. Up until August 2019, he served as a consultant for Lilly, Novartis, Teva and Allergan. Dr. Green is also a member of the Medscape and American Headache Society Migraine Steering Committee. Dr. Silberstein is a member of the advisory board and consultant for Lilly.
Source: Detke HC et al. AAN 2020. Abstract 43625.
“The patients included in our study had previously tried multiple migraine preventive treatments that didn’t work for them. These patients are left with limited treatment options to help with the debilitating pain of migraine,” said lead author Holland C. Detke, PhD, senior clinical research advisor at Eli Lilly and Company Biomedicines.
Participants who took the drug experienced “a rapid reduction in migraine days starting as early as month 1, and continuing through the 6 months of the study,” Dr. Detke said.
The treatment group reported an average 4.0 fewer monthly migraine days at 3 months, for example, compared with a baseline of 13.4 days, whereas the placebo group decreased an average 1.29 days from a similar baseline of 13.0 migraine days.
Dr. Detke presented these and other results of the open-label phase of the CONQUER phase 3 trial online as part of the 2020 American Academy of Neurology Science Highlights.
The investigators enrolled 462 adults with episodic or chronic migraine. All participants previously failed two to four migraine treatments because of insufficient efficacy or issues around tolerability or safety. At month 0, 232 people were randomly assigned to galcanezumab and another 230 to placebo injections. At 3 months, 449 participants received a galcanezumab injection as part of the open-label treatment phase.
Participants were an average 48 years old, approximately 86% were women, and 82% were white. At baseline, mean Migraine Specific Quality of Life Role Function Restrictive (MSQ RFR) domain score was 45, “indicating significant impairment in functioning,” Dr. Detke said. At the same time, mean Migraine Disability Assessment Test (MIDAS) total score was 51, “indicating quite severe disability.”
Significant outcomes
The decrease in migraine days at 3 months – 4.0 days with treatment versus 1.29 with placebo – was statistically significant (P < .0001). During the open-label phase, participants who switched from placebo “essentially catch up to where the previously treated people were,” Dr. Detke said. At 6 months, the decrease in average monthly headache days was 5.60 in the initial galcanezumab group versus 5.24 in the initial placebo group.
Significant differences at 3 months versus baseline were observed in participants who received galcanezumab when investigators assessed reduction in 50% or more, 75% or more, or 100% of mean monthly migraine days. No such significant decreases were seen in the placebo group.
Treatment-emergent adverse events reported in the open-label phase included nasopharyngitis in 4.2%, injection site pain in 3.8%, and injection site erythema in 2.7%. Five participants discontinued during the open-label phase because of adverse events.
The results of the study suggest galcanezumab “should be considered as a treatment option for patients who have not had success with previous treatments,” Dr. Detke said.
Multiple strengths of study
“It is encouraging that galcanezumab works in patients who have failed prior reduction strategies,” A. Laine Green, MD, a neurologist at Dartmouth-Hitchcock Medical Center in Lebanon, N.H., said when asked to comment.
This study did not look at patients who have failed more than four previous reduction strategies, he added. “Clinically we see many of these patients. To be fair, no one has studied this group using the monoclonal antibodies.”
Dr. Green noted several strengths of the study. The groups were similar, there were few dropouts during the open-label extension, and there were no unexpected side effects or adverse events. “Those who got placebo caught up to those who received active treatment in the double-blind phase,” he said. “It is also nice to see patient reported outcomes improved as headaches improve. This adds consistency to the results.”
One caveat, Dr. Green noted, is “with open-label extensions, there is always the potential for bias because patients know what treatment they are receiving.”
Overall [the study] gives hope that patients who have failed previous reduction strategies may respond to the newer monoclonal antibodies.”
Aligns with previous findings
The results are “the same as any other long-term extension study of a drug for migraine,” Stephen Silberstein, MD, said when asked to comment. “The longer one takes it, the better you get.”
The research also confirms that if you switch patients taking placebo to an active treatment, they get better, added Dr. Silberstein, director of the Headache Center at Jefferson Health in Philadelphia.
Because they are injections, agents such as galcanezumab, other monoclonal antibodies, and botulinum toxin offer better compliance for headache compared with small molecule medications that require daily oral dosing, he added.
Eli Lilly and Company funded the study. Dr. Holland Detke is a Lilly employee. Dr. Green collaborated with Lilly on a poster for the AHS scientific meeting on a similar topic but did not receive compensation. Up until August 2019, he served as a consultant for Lilly, Novartis, Teva and Allergan. Dr. Green is also a member of the Medscape and American Headache Society Migraine Steering Committee. Dr. Silberstein is a member of the advisory board and consultant for Lilly.
Source: Detke HC et al. AAN 2020. Abstract 43625.
FROM AAN 2020
COVID-19: Psychiatrists assess geriatric harm from social distancing
One of the greatest tragedies of the first wave of the COVID-19 pandemic has been the failure of health policy makers to anticipate and mitigate the enormous havoc the policy of social distancing would wreak on mental health and cognitive function in older persons, speakers agreed at a webinar on COVID-19, social distancing, and its impact on social and mental health in the elderly hosted by the International Psychogeriatric Association in collaboration with INTERDEM.
“Social distancing” is a two-edged sword: It is for now and the foreseeable future the only available effective strategy for protecting against infection in the older population most vulnerable to severe forms of COVID-19. Yet social distancing also has caused many elderly – particularly those in nursing homes and other long-term care facilities – to plunge into a profound experience of loneliness, isolation, distress, feelings of abandonment, anxiety, depression, and accelerated cognitive deterioration. And this needn’t have happened, the mental health professionals asserted.
“When are we going to get rid of the term ‘social distancing?’ ” asked IPA President William E. Reichman, MD. “Many have appreciated – including the World Health Organization – that the real issue is physical distancing to prevent contagion. And physical distancing doesn’t have to mean social distancing.”
Social connectedness between elderly persons and their peers and family members can be maintained and should be emphatically encouraged during the physical distancing required by the pandemic, said Myrra Vernooij-Dassen, PhD, of Radboud University in Nigmegen, the Netherlands, and chair of INTERDEM, a pan-European network of dementia researchers.
This can be achieved using readily available technologies, including the telephone and videoconferencing, as well as by creating opportunities for supervised masked visits between a family member and an elderly loved one in outdoor courtyards or gardens within long-term care facilities. And yet, as the pandemic seized hold in many parts of the world, family members were blocked from entry to these facilities, she observed.
Impact on mental health, cognition
Dr. Vernooij-Dassen noted that studies of previous quarantine periods as well as preliminary findings during the COVID-19 pandemic demonstrate an inverse relationship between social isolation measures and cognitive functioning in the elderly.
“ Conversely, epidemiologic data indicate that a socially integrated lifestyle had a favorable influence on cognitive functioning and could even delay onset of dementia,” she said.
INTERDEM is backing two ongoing studies evaluating the hypothesis that interventions fostering increased social interaction among elderly individuals can delay onset of dementia or favorably affect its course. The proposed mechanism of benefit is stimulation of brain plasticity to enhance cognitive reserve.
“This is a hypothesis of hope. We know that social interaction for humans is like water to plants – we really, really need it,” she explained.
Diego de Leo, MD, PhD, emeritus professor of psychiatry and former director of the Australian Institute for Suicide Research and Prevention at Griffith University in Brisbane, was living in hard-hit Padua, Italy, during the first surge of COVID-19. He described his anecdotal experience.
“What I hear from many Italian colleagues and friends and directors of mental health services is that emergency admissions related to mental disorders declined during the first wave of the COVID pandemic. For example, not many people attended emergency departments due to suicide attempts; there was a very marked decrease in the number of suicide attempts during the worst days of the pandemic,” he said.
People with psychiatric conditions were afraid to go to the hospital because they thought they would contract the infection and die there. That’s changing now, however.
“Now there is an increased number of admissions to mental health units. A new wave. It has been a U-shaped curve. And we’re now witnessing an increasing number of fatal suicides due to persistent fears, due to people imagining that there is no more room for them, and no more future for them from a financial point of view – which is the major negative outcome of this crisis. It will be a disaster for many families,” the psychiatrist continued.
A noteworthy phenomenon in northern Italy was that, when tablets were made available to nursing home residents in an effort to enhance their connectedness to the outside world, those with dementia often became so frustrated and confused by their difficulty in using the devices that they developed a hypokinetic delirium marked by refusal to eat or leave their bed, he reported.
It’s far too early to have reliable data on suicide trends in response to the pandemic, according to Dr. de Leo. But one thing is for sure: The strategy of social distancing employed to curb COVID-19 has increased the prevalence of known risk factors for suicide in older individuals, including loneliness, anxiety, and depression; increased alcohol use; and a perception of being a burden on society. Dr. de Leo directs a foundation dedicated to helping people experiencing traumatic bereavement, and in one recent week, the foundation was contacted by eight families in the province of Padua with a recent death by suicide apparently related to fallout from the COVID-19 pandemic. That’s an unusually high spike in suicide in a province with a population of 1 million.
“People probably preferred to end the agitation, the fear, the extreme anxiety about their destiny by deciding to prematurely truncate their life. That has been reported by nursing staff,” he said.
The Italian government has determined that, to date, 36% of all COVID-related deaths have occurred in people aged 85 years or older, and 84% of deaths were in individuals aged at least 70 years. And in Milan and the surrounding province of Lombardy, it’s estimated that COVID-19 has taken the lives of 25% of all nursing home residents. The North American experience has been uncomfortably similar.
“Almost 80% of COVID deaths in Canada have occurred in congregate settings,” observed Dr. Reichman, professor of psychiatry at the University of Toronto, and president and CEO of Baycrest Health Sciences, a geriatric research center.
“Certainly, the appalling number of deaths in nursing homes is the No. 1 horror of the pandemic,” declared Carmelle Peisah, MBBS, MD, a psychiatrist at the University of New South Wales in Kensington, Australia.
The fire next time
The conventional wisdom holds that COVID-19 has caused all sorts of mayhem in the delivery of elder care. Not so, in Dr. Reichman’s view.
“I would suggest that the pandemic has not caused many of the problems we talk about, it’s actually revealed problems that have always been there under the surface. For example, many older people, even before COVID-19, were socially isolated, socially distant. They had difficulty connecting with their relatives, difficulty accessing transportation to get to the store to buy food and see their doctors, and to interact with other older people,” the psychiatrist said.
“I would say as well that the pandemic didn’t cause the problems we’ve seen in long-term congregate senior care. The pandemic revealed them. We’ve had facilities where older people were severely crowded together, which compromises their quality of life, even when there’s not a pandemic. We’ve had difficulty staffing these kinds of environments with people that are paid an honest wage for the very hard work that they do. In many of these settings they’re inadequately trained, not only in infection prevention and control but in all other aspects of care. And the pandemic has revealed that many of these organizations are not properly funded. The government doesn’t support them well enough across jurisdictions, and they can’t raise enough philanthropic funds to provide the kind of quality of life that residents demand,” Dr. Reichman continued.
Could the pandemic spur improved elder care? His hope is that health care professionals, politicians, and society at large will learn from the devastation left by the first surge of the pandemic and will lobby for the resources necessary for much-needed improvements in geriatric care.
“We need to be better prepared should there be not only a second wave of this pandemic, but for other pandemics to come,” Dr. Reichman concluded.
The speakers indicated they had no financial conflicts regarding their presentations.
One of the greatest tragedies of the first wave of the COVID-19 pandemic has been the failure of health policy makers to anticipate and mitigate the enormous havoc the policy of social distancing would wreak on mental health and cognitive function in older persons, speakers agreed at a webinar on COVID-19, social distancing, and its impact on social and mental health in the elderly hosted by the International Psychogeriatric Association in collaboration with INTERDEM.
“Social distancing” is a two-edged sword: It is for now and the foreseeable future the only available effective strategy for protecting against infection in the older population most vulnerable to severe forms of COVID-19. Yet social distancing also has caused many elderly – particularly those in nursing homes and other long-term care facilities – to plunge into a profound experience of loneliness, isolation, distress, feelings of abandonment, anxiety, depression, and accelerated cognitive deterioration. And this needn’t have happened, the mental health professionals asserted.
“When are we going to get rid of the term ‘social distancing?’ ” asked IPA President William E. Reichman, MD. “Many have appreciated – including the World Health Organization – that the real issue is physical distancing to prevent contagion. And physical distancing doesn’t have to mean social distancing.”
Social connectedness between elderly persons and their peers and family members can be maintained and should be emphatically encouraged during the physical distancing required by the pandemic, said Myrra Vernooij-Dassen, PhD, of Radboud University in Nigmegen, the Netherlands, and chair of INTERDEM, a pan-European network of dementia researchers.
This can be achieved using readily available technologies, including the telephone and videoconferencing, as well as by creating opportunities for supervised masked visits between a family member and an elderly loved one in outdoor courtyards or gardens within long-term care facilities. And yet, as the pandemic seized hold in many parts of the world, family members were blocked from entry to these facilities, she observed.
Impact on mental health, cognition
Dr. Vernooij-Dassen noted that studies of previous quarantine periods as well as preliminary findings during the COVID-19 pandemic demonstrate an inverse relationship between social isolation measures and cognitive functioning in the elderly.
“ Conversely, epidemiologic data indicate that a socially integrated lifestyle had a favorable influence on cognitive functioning and could even delay onset of dementia,” she said.
INTERDEM is backing two ongoing studies evaluating the hypothesis that interventions fostering increased social interaction among elderly individuals can delay onset of dementia or favorably affect its course. The proposed mechanism of benefit is stimulation of brain plasticity to enhance cognitive reserve.
“This is a hypothesis of hope. We know that social interaction for humans is like water to plants – we really, really need it,” she explained.
Diego de Leo, MD, PhD, emeritus professor of psychiatry and former director of the Australian Institute for Suicide Research and Prevention at Griffith University in Brisbane, was living in hard-hit Padua, Italy, during the first surge of COVID-19. He described his anecdotal experience.
“What I hear from many Italian colleagues and friends and directors of mental health services is that emergency admissions related to mental disorders declined during the first wave of the COVID pandemic. For example, not many people attended emergency departments due to suicide attempts; there was a very marked decrease in the number of suicide attempts during the worst days of the pandemic,” he said.
People with psychiatric conditions were afraid to go to the hospital because they thought they would contract the infection and die there. That’s changing now, however.
“Now there is an increased number of admissions to mental health units. A new wave. It has been a U-shaped curve. And we’re now witnessing an increasing number of fatal suicides due to persistent fears, due to people imagining that there is no more room for them, and no more future for them from a financial point of view – which is the major negative outcome of this crisis. It will be a disaster for many families,” the psychiatrist continued.
A noteworthy phenomenon in northern Italy was that, when tablets were made available to nursing home residents in an effort to enhance their connectedness to the outside world, those with dementia often became so frustrated and confused by their difficulty in using the devices that they developed a hypokinetic delirium marked by refusal to eat or leave their bed, he reported.
It’s far too early to have reliable data on suicide trends in response to the pandemic, according to Dr. de Leo. But one thing is for sure: The strategy of social distancing employed to curb COVID-19 has increased the prevalence of known risk factors for suicide in older individuals, including loneliness, anxiety, and depression; increased alcohol use; and a perception of being a burden on society. Dr. de Leo directs a foundation dedicated to helping people experiencing traumatic bereavement, and in one recent week, the foundation was contacted by eight families in the province of Padua with a recent death by suicide apparently related to fallout from the COVID-19 pandemic. That’s an unusually high spike in suicide in a province with a population of 1 million.
“People probably preferred to end the agitation, the fear, the extreme anxiety about their destiny by deciding to prematurely truncate their life. That has been reported by nursing staff,” he said.
The Italian government has determined that, to date, 36% of all COVID-related deaths have occurred in people aged 85 years or older, and 84% of deaths were in individuals aged at least 70 years. And in Milan and the surrounding province of Lombardy, it’s estimated that COVID-19 has taken the lives of 25% of all nursing home residents. The North American experience has been uncomfortably similar.
“Almost 80% of COVID deaths in Canada have occurred in congregate settings,” observed Dr. Reichman, professor of psychiatry at the University of Toronto, and president and CEO of Baycrest Health Sciences, a geriatric research center.
“Certainly, the appalling number of deaths in nursing homes is the No. 1 horror of the pandemic,” declared Carmelle Peisah, MBBS, MD, a psychiatrist at the University of New South Wales in Kensington, Australia.
The fire next time
The conventional wisdom holds that COVID-19 has caused all sorts of mayhem in the delivery of elder care. Not so, in Dr. Reichman’s view.
“I would suggest that the pandemic has not caused many of the problems we talk about, it’s actually revealed problems that have always been there under the surface. For example, many older people, even before COVID-19, were socially isolated, socially distant. They had difficulty connecting with their relatives, difficulty accessing transportation to get to the store to buy food and see their doctors, and to interact with other older people,” the psychiatrist said.
“I would say as well that the pandemic didn’t cause the problems we’ve seen in long-term congregate senior care. The pandemic revealed them. We’ve had facilities where older people were severely crowded together, which compromises their quality of life, even when there’s not a pandemic. We’ve had difficulty staffing these kinds of environments with people that are paid an honest wage for the very hard work that they do. In many of these settings they’re inadequately trained, not only in infection prevention and control but in all other aspects of care. And the pandemic has revealed that many of these organizations are not properly funded. The government doesn’t support them well enough across jurisdictions, and they can’t raise enough philanthropic funds to provide the kind of quality of life that residents demand,” Dr. Reichman continued.
Could the pandemic spur improved elder care? His hope is that health care professionals, politicians, and society at large will learn from the devastation left by the first surge of the pandemic and will lobby for the resources necessary for much-needed improvements in geriatric care.
“We need to be better prepared should there be not only a second wave of this pandemic, but for other pandemics to come,” Dr. Reichman concluded.
The speakers indicated they had no financial conflicts regarding their presentations.
One of the greatest tragedies of the first wave of the COVID-19 pandemic has been the failure of health policy makers to anticipate and mitigate the enormous havoc the policy of social distancing would wreak on mental health and cognitive function in older persons, speakers agreed at a webinar on COVID-19, social distancing, and its impact on social and mental health in the elderly hosted by the International Psychogeriatric Association in collaboration with INTERDEM.
“Social distancing” is a two-edged sword: It is for now and the foreseeable future the only available effective strategy for protecting against infection in the older population most vulnerable to severe forms of COVID-19. Yet social distancing also has caused many elderly – particularly those in nursing homes and other long-term care facilities – to plunge into a profound experience of loneliness, isolation, distress, feelings of abandonment, anxiety, depression, and accelerated cognitive deterioration. And this needn’t have happened, the mental health professionals asserted.
“When are we going to get rid of the term ‘social distancing?’ ” asked IPA President William E. Reichman, MD. “Many have appreciated – including the World Health Organization – that the real issue is physical distancing to prevent contagion. And physical distancing doesn’t have to mean social distancing.”
Social connectedness between elderly persons and their peers and family members can be maintained and should be emphatically encouraged during the physical distancing required by the pandemic, said Myrra Vernooij-Dassen, PhD, of Radboud University in Nigmegen, the Netherlands, and chair of INTERDEM, a pan-European network of dementia researchers.
This can be achieved using readily available technologies, including the telephone and videoconferencing, as well as by creating opportunities for supervised masked visits between a family member and an elderly loved one in outdoor courtyards or gardens within long-term care facilities. And yet, as the pandemic seized hold in many parts of the world, family members were blocked from entry to these facilities, she observed.
Impact on mental health, cognition
Dr. Vernooij-Dassen noted that studies of previous quarantine periods as well as preliminary findings during the COVID-19 pandemic demonstrate an inverse relationship between social isolation measures and cognitive functioning in the elderly.
“ Conversely, epidemiologic data indicate that a socially integrated lifestyle had a favorable influence on cognitive functioning and could even delay onset of dementia,” she said.
INTERDEM is backing two ongoing studies evaluating the hypothesis that interventions fostering increased social interaction among elderly individuals can delay onset of dementia or favorably affect its course. The proposed mechanism of benefit is stimulation of brain plasticity to enhance cognitive reserve.
“This is a hypothesis of hope. We know that social interaction for humans is like water to plants – we really, really need it,” she explained.
Diego de Leo, MD, PhD, emeritus professor of psychiatry and former director of the Australian Institute for Suicide Research and Prevention at Griffith University in Brisbane, was living in hard-hit Padua, Italy, during the first surge of COVID-19. He described his anecdotal experience.
“What I hear from many Italian colleagues and friends and directors of mental health services is that emergency admissions related to mental disorders declined during the first wave of the COVID pandemic. For example, not many people attended emergency departments due to suicide attempts; there was a very marked decrease in the number of suicide attempts during the worst days of the pandemic,” he said.
People with psychiatric conditions were afraid to go to the hospital because they thought they would contract the infection and die there. That’s changing now, however.
“Now there is an increased number of admissions to mental health units. A new wave. It has been a U-shaped curve. And we’re now witnessing an increasing number of fatal suicides due to persistent fears, due to people imagining that there is no more room for them, and no more future for them from a financial point of view – which is the major negative outcome of this crisis. It will be a disaster for many families,” the psychiatrist continued.
A noteworthy phenomenon in northern Italy was that, when tablets were made available to nursing home residents in an effort to enhance their connectedness to the outside world, those with dementia often became so frustrated and confused by their difficulty in using the devices that they developed a hypokinetic delirium marked by refusal to eat or leave their bed, he reported.
It’s far too early to have reliable data on suicide trends in response to the pandemic, according to Dr. de Leo. But one thing is for sure: The strategy of social distancing employed to curb COVID-19 has increased the prevalence of known risk factors for suicide in older individuals, including loneliness, anxiety, and depression; increased alcohol use; and a perception of being a burden on society. Dr. de Leo directs a foundation dedicated to helping people experiencing traumatic bereavement, and in one recent week, the foundation was contacted by eight families in the province of Padua with a recent death by suicide apparently related to fallout from the COVID-19 pandemic. That’s an unusually high spike in suicide in a province with a population of 1 million.
“People probably preferred to end the agitation, the fear, the extreme anxiety about their destiny by deciding to prematurely truncate their life. That has been reported by nursing staff,” he said.
The Italian government has determined that, to date, 36% of all COVID-related deaths have occurred in people aged 85 years or older, and 84% of deaths were in individuals aged at least 70 years. And in Milan and the surrounding province of Lombardy, it’s estimated that COVID-19 has taken the lives of 25% of all nursing home residents. The North American experience has been uncomfortably similar.
“Almost 80% of COVID deaths in Canada have occurred in congregate settings,” observed Dr. Reichman, professor of psychiatry at the University of Toronto, and president and CEO of Baycrest Health Sciences, a geriatric research center.
“Certainly, the appalling number of deaths in nursing homes is the No. 1 horror of the pandemic,” declared Carmelle Peisah, MBBS, MD, a psychiatrist at the University of New South Wales in Kensington, Australia.
The fire next time
The conventional wisdom holds that COVID-19 has caused all sorts of mayhem in the delivery of elder care. Not so, in Dr. Reichman’s view.
“I would suggest that the pandemic has not caused many of the problems we talk about, it’s actually revealed problems that have always been there under the surface. For example, many older people, even before COVID-19, were socially isolated, socially distant. They had difficulty connecting with their relatives, difficulty accessing transportation to get to the store to buy food and see their doctors, and to interact with other older people,” the psychiatrist said.
“I would say as well that the pandemic didn’t cause the problems we’ve seen in long-term congregate senior care. The pandemic revealed them. We’ve had facilities where older people were severely crowded together, which compromises their quality of life, even when there’s not a pandemic. We’ve had difficulty staffing these kinds of environments with people that are paid an honest wage for the very hard work that they do. In many of these settings they’re inadequately trained, not only in infection prevention and control but in all other aspects of care. And the pandemic has revealed that many of these organizations are not properly funded. The government doesn’t support them well enough across jurisdictions, and they can’t raise enough philanthropic funds to provide the kind of quality of life that residents demand,” Dr. Reichman continued.
Could the pandemic spur improved elder care? His hope is that health care professionals, politicians, and society at large will learn from the devastation left by the first surge of the pandemic and will lobby for the resources necessary for much-needed improvements in geriatric care.
“We need to be better prepared should there be not only a second wave of this pandemic, but for other pandemics to come,” Dr. Reichman concluded.
The speakers indicated they had no financial conflicts regarding their presentations.
Social isolation tied to higher risk of cardiovascular events, death
“These results are especially important in the current times of social isolation during the coronavirus crisis,” Janine Gronewold, PhD, University Hospital in Essen, Germany, told a press briefing.
The mechanism by which social isolation may boost risk for stroke, MI, or death is not clear, but other research has shown that loneliness or lack of contact with close friends and family can affect physical health, said Dr. Gronewold.
The findings were presented at the sixth Congress of the European Academy of Neurology (EAN) 2020, which transitioned to a virtual/online meeting because of the COVID-19 pandemic.
For this new study, researchers analyzed data from 4,139 participants, ranging in age from 45 to 75 years (mean 59.1 years), who were recruited into the large community-based Heinz Nixdorf Recall study. The randomly selected study group was representative of an industrial rural area of Germany, said Dr. Gronewold.
Study participants entered the study with no known cardiovascular disease and were followed for a mean of 13.4 years.
Social supports
Investigators collected information on three types of social support: instrumental (getting help with everyday activities such as buying food), emotional (provided with comfort), and financial (receiving monetary assistance when needed). They also looked at social integration (or social isolation) using an index with scores for marital status, number of contacts with family and friends, and membership in political, religious, community, sports, or professional associations.
Of the total, 501 participants reported a lack of instrumental support, 659 a lack of emotional support, and 907 a lack of financial support. A total of 309 lacked social integration, defined by the lowest level on the social integration index.
Participants were asked annually about new cardiovascular events, including stroke and MI. Over the follow-up period, there were 339 such events and 530 deaths.
After adjustment for age, sex, and social support, the analysis showed that social isolation was significantly associated with an increased risk of cardiovascular events (hazard ratio, 1.44; 95% confidence interval, 0.97-2.14) and all-cause mortality (HR, 1.47; 95% CI, 1.09-1.97).
The new research also showed that lack of financial support was significantly associated with increased risk for a cardiovascular event (HR, 1.30; 95% CI, 1.01-1.67).
Direct effect
Additional models that also adjusted for cardiovascular risk factors, health behaviors, depression, and socioeconomic factors, did not significantly change effect estimates.
“Social relationships protect us from cardiovascular events and mortality, not only via good mood, healthy behavior, and lower cardiovascular risk profile,” Dr. Gronewold said. “They seem to have a direct effect on these outcomes.”
Having strong social relationships is as important to cardiovascular health as classic protective factors such as controlling blood pressure and cholesterol levels, and maintaining a normal weight, said Dr. Gronewold.
The new results are worrying and are particularly important during the current COVID-19 pandemic, as social contact has been restricted in many areas, said Dr. Gronewold.
It is not yet clear why people who are socially isolated have such poor health outcomes, she added.
Dr. Gronewold has reported no relevant financial relationships.
This article first appeared on Medscape.com.
“These results are especially important in the current times of social isolation during the coronavirus crisis,” Janine Gronewold, PhD, University Hospital in Essen, Germany, told a press briefing.
The mechanism by which social isolation may boost risk for stroke, MI, or death is not clear, but other research has shown that loneliness or lack of contact with close friends and family can affect physical health, said Dr. Gronewold.
The findings were presented at the sixth Congress of the European Academy of Neurology (EAN) 2020, which transitioned to a virtual/online meeting because of the COVID-19 pandemic.
For this new study, researchers analyzed data from 4,139 participants, ranging in age from 45 to 75 years (mean 59.1 years), who were recruited into the large community-based Heinz Nixdorf Recall study. The randomly selected study group was representative of an industrial rural area of Germany, said Dr. Gronewold.
Study participants entered the study with no known cardiovascular disease and were followed for a mean of 13.4 years.
Social supports
Investigators collected information on three types of social support: instrumental (getting help with everyday activities such as buying food), emotional (provided with comfort), and financial (receiving monetary assistance when needed). They also looked at social integration (or social isolation) using an index with scores for marital status, number of contacts with family and friends, and membership in political, religious, community, sports, or professional associations.
Of the total, 501 participants reported a lack of instrumental support, 659 a lack of emotional support, and 907 a lack of financial support. A total of 309 lacked social integration, defined by the lowest level on the social integration index.
Participants were asked annually about new cardiovascular events, including stroke and MI. Over the follow-up period, there were 339 such events and 530 deaths.
After adjustment for age, sex, and social support, the analysis showed that social isolation was significantly associated with an increased risk of cardiovascular events (hazard ratio, 1.44; 95% confidence interval, 0.97-2.14) and all-cause mortality (HR, 1.47; 95% CI, 1.09-1.97).
The new research also showed that lack of financial support was significantly associated with increased risk for a cardiovascular event (HR, 1.30; 95% CI, 1.01-1.67).
Direct effect
Additional models that also adjusted for cardiovascular risk factors, health behaviors, depression, and socioeconomic factors, did not significantly change effect estimates.
“Social relationships protect us from cardiovascular events and mortality, not only via good mood, healthy behavior, and lower cardiovascular risk profile,” Dr. Gronewold said. “They seem to have a direct effect on these outcomes.”
Having strong social relationships is as important to cardiovascular health as classic protective factors such as controlling blood pressure and cholesterol levels, and maintaining a normal weight, said Dr. Gronewold.
The new results are worrying and are particularly important during the current COVID-19 pandemic, as social contact has been restricted in many areas, said Dr. Gronewold.
It is not yet clear why people who are socially isolated have such poor health outcomes, she added.
Dr. Gronewold has reported no relevant financial relationships.
This article first appeared on Medscape.com.
“These results are especially important in the current times of social isolation during the coronavirus crisis,” Janine Gronewold, PhD, University Hospital in Essen, Germany, told a press briefing.
The mechanism by which social isolation may boost risk for stroke, MI, or death is not clear, but other research has shown that loneliness or lack of contact with close friends and family can affect physical health, said Dr. Gronewold.
The findings were presented at the sixth Congress of the European Academy of Neurology (EAN) 2020, which transitioned to a virtual/online meeting because of the COVID-19 pandemic.
For this new study, researchers analyzed data from 4,139 participants, ranging in age from 45 to 75 years (mean 59.1 years), who were recruited into the large community-based Heinz Nixdorf Recall study. The randomly selected study group was representative of an industrial rural area of Germany, said Dr. Gronewold.
Study participants entered the study with no known cardiovascular disease and were followed for a mean of 13.4 years.
Social supports
Investigators collected information on three types of social support: instrumental (getting help with everyday activities such as buying food), emotional (provided with comfort), and financial (receiving monetary assistance when needed). They also looked at social integration (or social isolation) using an index with scores for marital status, number of contacts with family and friends, and membership in political, religious, community, sports, or professional associations.
Of the total, 501 participants reported a lack of instrumental support, 659 a lack of emotional support, and 907 a lack of financial support. A total of 309 lacked social integration, defined by the lowest level on the social integration index.
Participants were asked annually about new cardiovascular events, including stroke and MI. Over the follow-up period, there were 339 such events and 530 deaths.
After adjustment for age, sex, and social support, the analysis showed that social isolation was significantly associated with an increased risk of cardiovascular events (hazard ratio, 1.44; 95% confidence interval, 0.97-2.14) and all-cause mortality (HR, 1.47; 95% CI, 1.09-1.97).
The new research also showed that lack of financial support was significantly associated with increased risk for a cardiovascular event (HR, 1.30; 95% CI, 1.01-1.67).
Direct effect
Additional models that also adjusted for cardiovascular risk factors, health behaviors, depression, and socioeconomic factors, did not significantly change effect estimates.
“Social relationships protect us from cardiovascular events and mortality, not only via good mood, healthy behavior, and lower cardiovascular risk profile,” Dr. Gronewold said. “They seem to have a direct effect on these outcomes.”
Having strong social relationships is as important to cardiovascular health as classic protective factors such as controlling blood pressure and cholesterol levels, and maintaining a normal weight, said Dr. Gronewold.
The new results are worrying and are particularly important during the current COVID-19 pandemic, as social contact has been restricted in many areas, said Dr. Gronewold.
It is not yet clear why people who are socially isolated have such poor health outcomes, she added.
Dr. Gronewold has reported no relevant financial relationships.
This article first appeared on Medscape.com.
FROM EAN 2020