User login
Shift in approach is encouraged in assessing chronic pain
In many cases, dietary interventions can lead to less inflammation
SAN DIEGO – When clinicians ask patients to quantify their level of chronic pain on a scale of 1-10, and they rate it as a 7, what does that really mean?
Robert A. Bonakdar, MD, said posing such a question as the main determinator of the treatment approach during a pain assessment “depersonalizes medicine to the point where you’re making a patient a number.” Dr. Bonakdar spoke at Natural Supplements: An Evidence-Based Update, presented by Scripps Center for Integrative Medicine.
“It considers areas that are often overlooked, such as the role of the gut microbiome, mood, and epigenetics.”
Over the past two decades, the number of American adults suffering from pain has increased from 120 million to 178 million, or to 41% of the adult population, said Dr. Bonakdar, a family physician who is director of pain management at the Scripps Center for Integrative Medicine. Data from the National Institutes of Health estimate that Americans spend more than $600 billion each year on the treatment of pain, which surpasses monies spent on cancer, heart disease, and diabetes. According to a 2016 report from the United States Bone and Joint Initiative, arthritis and rheumatologic conditions resulted in an estimated 6.7 million annual hospitalizations, and the average annual cost per person for treatment of a musculoskeletal condition is $7,800.
“If we continue on our current trajectory, we are choosing to accept more prevalence and incidence of these disorders, spiraling costs, restricted access to needed services, and less success in alleviating pain and suffering – a high cost,” Edward H. Yelin, PhD, cochair of the report’s steering committee, and professor of medicine and health policy at the University of California, San Francisco, said in a prepared statement in 2016. That same year, Brian F. Mandell, MD, PhD, editor of the Cleveland Clinic Journal of Medicine, penned an editorial in which he stated that “The time has come to move past using a one-size-fits-all fifth vital sign . . . and reflexively prescribing an opioid when pain is characterized as severe” (Clev Clin J Med. 2016. Jun;83[6]:400-1). A decade earlier, authors of a cross-sectional review at a single Department of Veterans Affairs medical center set out to assess the impact of the VA’s “Pain as the 5th Vital Sign” initiative on the quality of pain management (J Gen Intern Med. 2006;21[6]:607–12). They found that patients with substantial pain documented by the fifth vital sign often had inadequate pain management. The preponderance of existing evidence suggests that a different approach is needed to prescribing opioids, Dr. Bonakdar said. “It’s coming from every voice in pain care: that what we are doing is not working,” he said. “It’s not only not working; it’s dangerous. That’s the consequence of depersonalized medicine. What’s the consequence of depersonalized nutrition? It’s the same industrialized approach.”
The typical American diet, he continued, is rife with processed foods and lacks an adequate proportion of plant-based products. “It’s basically a setup for inflammation,” Dr. Bonakdar said. “Most people who come into our clinic are eating 63% processed foods, 25% animal foods, and 12% plant foods. When we are eating, we’re oversizing it because that’s the American thing to do. At the end of the day, this process is not only killing us from heart disease and stroke as causes of death, but it’s also killing us as far as pain. The same diet that’s causing heart disease is the same diet that’s increasing pain.”
Dr. Bonakdar said that the ingestion of ultra-processed foods over time jumpstarts the process of dysbiosis, which increases gut permeability. “When gut permeability happens, and you have high levels of polysaccharides and inflammatory markers such as zonulin and lipopolysaccharide (LPS), it not only goes on to affect adipose tissue and insulin resistance, it can affect the muscle and joints,” he explained. “That is a setup for sarcopenia, or muscle loss, which then makes it harder for patients to be fully functional and active. It goes on to cause joint problems as well.”
He likened an increase in gut permeability to “a bomb going off in the gut.” Routine consumption of highly processed foods “creates this wave of inflammation that goes throughout your body affecting joints and muscles, and causes an increased amount of pain. Over time, patients make the connection but it’s much easier to say, ‘take this NSAID’ or ‘take this Cox-2 inhibitor’ to suppress the pain. But if all you’re doing is suppressing, you’re not going to the source of the pain.”
Dr. Bonakdar cited several recent articles that help to make the connection between dysbiosis and pain, including a review that concluded that dysbiosis of gut microbiota can influence the onset and progression of chronic degenerative diseases (Nutrients. 2019;11[8]:1707). Authors of a separate review concluded that human microbiome studies strongly suggest an incriminating role of microbes in the pathophysiology and progression of RA. Lastly, several studies have noted that pain conditions such as fibromyalgia may have microbiome “signatures” related to dysbiosis, which may pave the way for interventions, such as dietary shifting and probiotics that target individuals with microbiome abnormalities (Pain. 2019 Nov;160[11]:2589-602 and EBioMedicine. 2019 Aug 1;46:499-511).
Clinicians can begin to help patients who present with pain complaints “by listening to what their current pattern is: strategies that have worked, and those that haven’t,” he said. “If we’re not understanding the person and we’re just ordering genetic studies or microbiome studies and going off of the assessment, we sometime miss what interventions to start. In many cases, a simple intervention like a dietary shift is all that’s required.”
A survey of more than 1 million individuals found that BMI and daily pain are positively correlated in the United States (Obesity 2012;20[7]:1491-5). “This is increased more significantly for women and the elderly,” said Dr. Bonakdar, who was not affiliated with the study. “If we can change the diet that person is taking, that’s going to begin the process of reversing this to the point where they’re having less pain from inflammation that’s affecting the adipose tissue and adipokines traveling to their joints, which can cause less dysbiosis. It is very much a vicious cycle that patients follow, but if you begin to unwind it, it’s going to help multiple areas.”
In the Intensive Diet and Exercise for Arthritis (IDEA) trial, researchers randomized 450 patients with osteoarthritis to intensive dietary restriction only, exercise only, or a combination of both (BMC Musculoskelet Disord. 2009;10:93). They found that a 5% weight loss over the course of 18 months led to a 30% reduction in pain and a 24% improvement in function.
Inspired by the IDEA trial design, Dr. Bonakdar and his colleagues completed an unpublished 12-week pilot program with 12 patients with a BMI of 27 kg/m2 or greater plus comorbidities. The program consisted of weekly group meetings, including a lecture by team clinicians, dietician, and fitness staff; group support sessions with a behavioral counselor; and a group exercise session. It also included weekly 1:1 personal training sessions and biweekly 1:1 dietitian meetings. The researchers also evaluated several deficiencies linked to pain, including magnesium, vitamin D, vitamins B1, B2, and B12, folate, calcium, amino acids, omega 3s, zinc, coenzyme Q10, carnitine, and vitamin C. The goal was a weight reduction of 5%.
The intervention consisted of a 28-day detox/protein shake consumed 1-3 times per day, which contained 17 g of protein per serving. Nutritional supplementation was added based on results of individual diagnostics.
According to preliminary results from the trial, the intended weight goal was achieved. “More importantly, there were significant improvements in markers of dysbiosis, including zonulin and lipopolysaccharide, as well as the adipokine leptin, which appeared to be associated with improvement in quality of life measures and pain,” Dr. Bonakdar said.
He concluded his presentation by highlighting a pilot study conducted in an Australian tertiary pain clinic. It found that a personalized dietitian-delivered dietary intervention can improve pain scores, quality of life, and dietary intake of people experiencing chronic pain (Nutrients. 2019 Jan 16;11[1] pii: E181). “This is another piece of the puzzle showing that these dietary interventions can be done in multiple settings, including tertiary centers with nutrition staff, and that this important step can improve pain and quality of life,” he said.
Dr. Bonakdar disclosed that he receives royalties from Oxford University Press, Lippincott, and Elsevier. He is also a consultant to Standard Process.
In many cases, dietary interventions can lead to less inflammation
In many cases, dietary interventions can lead to less inflammation
SAN DIEGO – When clinicians ask patients to quantify their level of chronic pain on a scale of 1-10, and they rate it as a 7, what does that really mean?
Robert A. Bonakdar, MD, said posing such a question as the main determinator of the treatment approach during a pain assessment “depersonalizes medicine to the point where you’re making a patient a number.” Dr. Bonakdar spoke at Natural Supplements: An Evidence-Based Update, presented by Scripps Center for Integrative Medicine.
“It considers areas that are often overlooked, such as the role of the gut microbiome, mood, and epigenetics.”
Over the past two decades, the number of American adults suffering from pain has increased from 120 million to 178 million, or to 41% of the adult population, said Dr. Bonakdar, a family physician who is director of pain management at the Scripps Center for Integrative Medicine. Data from the National Institutes of Health estimate that Americans spend more than $600 billion each year on the treatment of pain, which surpasses monies spent on cancer, heart disease, and diabetes. According to a 2016 report from the United States Bone and Joint Initiative, arthritis and rheumatologic conditions resulted in an estimated 6.7 million annual hospitalizations, and the average annual cost per person for treatment of a musculoskeletal condition is $7,800.
“If we continue on our current trajectory, we are choosing to accept more prevalence and incidence of these disorders, spiraling costs, restricted access to needed services, and less success in alleviating pain and suffering – a high cost,” Edward H. Yelin, PhD, cochair of the report’s steering committee, and professor of medicine and health policy at the University of California, San Francisco, said in a prepared statement in 2016. That same year, Brian F. Mandell, MD, PhD, editor of the Cleveland Clinic Journal of Medicine, penned an editorial in which he stated that “The time has come to move past using a one-size-fits-all fifth vital sign . . . and reflexively prescribing an opioid when pain is characterized as severe” (Clev Clin J Med. 2016. Jun;83[6]:400-1). A decade earlier, authors of a cross-sectional review at a single Department of Veterans Affairs medical center set out to assess the impact of the VA’s “Pain as the 5th Vital Sign” initiative on the quality of pain management (J Gen Intern Med. 2006;21[6]:607–12). They found that patients with substantial pain documented by the fifth vital sign often had inadequate pain management. The preponderance of existing evidence suggests that a different approach is needed to prescribing opioids, Dr. Bonakdar said. “It’s coming from every voice in pain care: that what we are doing is not working,” he said. “It’s not only not working; it’s dangerous. That’s the consequence of depersonalized medicine. What’s the consequence of depersonalized nutrition? It’s the same industrialized approach.”
The typical American diet, he continued, is rife with processed foods and lacks an adequate proportion of plant-based products. “It’s basically a setup for inflammation,” Dr. Bonakdar said. “Most people who come into our clinic are eating 63% processed foods, 25% animal foods, and 12% plant foods. When we are eating, we’re oversizing it because that’s the American thing to do. At the end of the day, this process is not only killing us from heart disease and stroke as causes of death, but it’s also killing us as far as pain. The same diet that’s causing heart disease is the same diet that’s increasing pain.”
Dr. Bonakdar said that the ingestion of ultra-processed foods over time jumpstarts the process of dysbiosis, which increases gut permeability. “When gut permeability happens, and you have high levels of polysaccharides and inflammatory markers such as zonulin and lipopolysaccharide (LPS), it not only goes on to affect adipose tissue and insulin resistance, it can affect the muscle and joints,” he explained. “That is a setup for sarcopenia, or muscle loss, which then makes it harder for patients to be fully functional and active. It goes on to cause joint problems as well.”
He likened an increase in gut permeability to “a bomb going off in the gut.” Routine consumption of highly processed foods “creates this wave of inflammation that goes throughout your body affecting joints and muscles, and causes an increased amount of pain. Over time, patients make the connection but it’s much easier to say, ‘take this NSAID’ or ‘take this Cox-2 inhibitor’ to suppress the pain. But if all you’re doing is suppressing, you’re not going to the source of the pain.”
Dr. Bonakdar cited several recent articles that help to make the connection between dysbiosis and pain, including a review that concluded that dysbiosis of gut microbiota can influence the onset and progression of chronic degenerative diseases (Nutrients. 2019;11[8]:1707). Authors of a separate review concluded that human microbiome studies strongly suggest an incriminating role of microbes in the pathophysiology and progression of RA. Lastly, several studies have noted that pain conditions such as fibromyalgia may have microbiome “signatures” related to dysbiosis, which may pave the way for interventions, such as dietary shifting and probiotics that target individuals with microbiome abnormalities (Pain. 2019 Nov;160[11]:2589-602 and EBioMedicine. 2019 Aug 1;46:499-511).
Clinicians can begin to help patients who present with pain complaints “by listening to what their current pattern is: strategies that have worked, and those that haven’t,” he said. “If we’re not understanding the person and we’re just ordering genetic studies or microbiome studies and going off of the assessment, we sometime miss what interventions to start. In many cases, a simple intervention like a dietary shift is all that’s required.”
A survey of more than 1 million individuals found that BMI and daily pain are positively correlated in the United States (Obesity 2012;20[7]:1491-5). “This is increased more significantly for women and the elderly,” said Dr. Bonakdar, who was not affiliated with the study. “If we can change the diet that person is taking, that’s going to begin the process of reversing this to the point where they’re having less pain from inflammation that’s affecting the adipose tissue and adipokines traveling to their joints, which can cause less dysbiosis. It is very much a vicious cycle that patients follow, but if you begin to unwind it, it’s going to help multiple areas.”
In the Intensive Diet and Exercise for Arthritis (IDEA) trial, researchers randomized 450 patients with osteoarthritis to intensive dietary restriction only, exercise only, or a combination of both (BMC Musculoskelet Disord. 2009;10:93). They found that a 5% weight loss over the course of 18 months led to a 30% reduction in pain and a 24% improvement in function.
Inspired by the IDEA trial design, Dr. Bonakdar and his colleagues completed an unpublished 12-week pilot program with 12 patients with a BMI of 27 kg/m2 or greater plus comorbidities. The program consisted of weekly group meetings, including a lecture by team clinicians, dietician, and fitness staff; group support sessions with a behavioral counselor; and a group exercise session. It also included weekly 1:1 personal training sessions and biweekly 1:1 dietitian meetings. The researchers also evaluated several deficiencies linked to pain, including magnesium, vitamin D, vitamins B1, B2, and B12, folate, calcium, amino acids, omega 3s, zinc, coenzyme Q10, carnitine, and vitamin C. The goal was a weight reduction of 5%.
The intervention consisted of a 28-day detox/protein shake consumed 1-3 times per day, which contained 17 g of protein per serving. Nutritional supplementation was added based on results of individual diagnostics.
According to preliminary results from the trial, the intended weight goal was achieved. “More importantly, there were significant improvements in markers of dysbiosis, including zonulin and lipopolysaccharide, as well as the adipokine leptin, which appeared to be associated with improvement in quality of life measures and pain,” Dr. Bonakdar said.
He concluded his presentation by highlighting a pilot study conducted in an Australian tertiary pain clinic. It found that a personalized dietitian-delivered dietary intervention can improve pain scores, quality of life, and dietary intake of people experiencing chronic pain (Nutrients. 2019 Jan 16;11[1] pii: E181). “This is another piece of the puzzle showing that these dietary interventions can be done in multiple settings, including tertiary centers with nutrition staff, and that this important step can improve pain and quality of life,” he said.
Dr. Bonakdar disclosed that he receives royalties from Oxford University Press, Lippincott, and Elsevier. He is also a consultant to Standard Process.
SAN DIEGO – When clinicians ask patients to quantify their level of chronic pain on a scale of 1-10, and they rate it as a 7, what does that really mean?
Robert A. Bonakdar, MD, said posing such a question as the main determinator of the treatment approach during a pain assessment “depersonalizes medicine to the point where you’re making a patient a number.” Dr. Bonakdar spoke at Natural Supplements: An Evidence-Based Update, presented by Scripps Center for Integrative Medicine.
“It considers areas that are often overlooked, such as the role of the gut microbiome, mood, and epigenetics.”
Over the past two decades, the number of American adults suffering from pain has increased from 120 million to 178 million, or to 41% of the adult population, said Dr. Bonakdar, a family physician who is director of pain management at the Scripps Center for Integrative Medicine. Data from the National Institutes of Health estimate that Americans spend more than $600 billion each year on the treatment of pain, which surpasses monies spent on cancer, heart disease, and diabetes. According to a 2016 report from the United States Bone and Joint Initiative, arthritis and rheumatologic conditions resulted in an estimated 6.7 million annual hospitalizations, and the average annual cost per person for treatment of a musculoskeletal condition is $7,800.
“If we continue on our current trajectory, we are choosing to accept more prevalence and incidence of these disorders, spiraling costs, restricted access to needed services, and less success in alleviating pain and suffering – a high cost,” Edward H. Yelin, PhD, cochair of the report’s steering committee, and professor of medicine and health policy at the University of California, San Francisco, said in a prepared statement in 2016. That same year, Brian F. Mandell, MD, PhD, editor of the Cleveland Clinic Journal of Medicine, penned an editorial in which he stated that “The time has come to move past using a one-size-fits-all fifth vital sign . . . and reflexively prescribing an opioid when pain is characterized as severe” (Clev Clin J Med. 2016. Jun;83[6]:400-1). A decade earlier, authors of a cross-sectional review at a single Department of Veterans Affairs medical center set out to assess the impact of the VA’s “Pain as the 5th Vital Sign” initiative on the quality of pain management (J Gen Intern Med. 2006;21[6]:607–12). They found that patients with substantial pain documented by the fifth vital sign often had inadequate pain management. The preponderance of existing evidence suggests that a different approach is needed to prescribing opioids, Dr. Bonakdar said. “It’s coming from every voice in pain care: that what we are doing is not working,” he said. “It’s not only not working; it’s dangerous. That’s the consequence of depersonalized medicine. What’s the consequence of depersonalized nutrition? It’s the same industrialized approach.”
The typical American diet, he continued, is rife with processed foods and lacks an adequate proportion of plant-based products. “It’s basically a setup for inflammation,” Dr. Bonakdar said. “Most people who come into our clinic are eating 63% processed foods, 25% animal foods, and 12% plant foods. When we are eating, we’re oversizing it because that’s the American thing to do. At the end of the day, this process is not only killing us from heart disease and stroke as causes of death, but it’s also killing us as far as pain. The same diet that’s causing heart disease is the same diet that’s increasing pain.”
Dr. Bonakdar said that the ingestion of ultra-processed foods over time jumpstarts the process of dysbiosis, which increases gut permeability. “When gut permeability happens, and you have high levels of polysaccharides and inflammatory markers such as zonulin and lipopolysaccharide (LPS), it not only goes on to affect adipose tissue and insulin resistance, it can affect the muscle and joints,” he explained. “That is a setup for sarcopenia, or muscle loss, which then makes it harder for patients to be fully functional and active. It goes on to cause joint problems as well.”
He likened an increase in gut permeability to “a bomb going off in the gut.” Routine consumption of highly processed foods “creates this wave of inflammation that goes throughout your body affecting joints and muscles, and causes an increased amount of pain. Over time, patients make the connection but it’s much easier to say, ‘take this NSAID’ or ‘take this Cox-2 inhibitor’ to suppress the pain. But if all you’re doing is suppressing, you’re not going to the source of the pain.”
Dr. Bonakdar cited several recent articles that help to make the connection between dysbiosis and pain, including a review that concluded that dysbiosis of gut microbiota can influence the onset and progression of chronic degenerative diseases (Nutrients. 2019;11[8]:1707). Authors of a separate review concluded that human microbiome studies strongly suggest an incriminating role of microbes in the pathophysiology and progression of RA. Lastly, several studies have noted that pain conditions such as fibromyalgia may have microbiome “signatures” related to dysbiosis, which may pave the way for interventions, such as dietary shifting and probiotics that target individuals with microbiome abnormalities (Pain. 2019 Nov;160[11]:2589-602 and EBioMedicine. 2019 Aug 1;46:499-511).
Clinicians can begin to help patients who present with pain complaints “by listening to what their current pattern is: strategies that have worked, and those that haven’t,” he said. “If we’re not understanding the person and we’re just ordering genetic studies or microbiome studies and going off of the assessment, we sometime miss what interventions to start. In many cases, a simple intervention like a dietary shift is all that’s required.”
A survey of more than 1 million individuals found that BMI and daily pain are positively correlated in the United States (Obesity 2012;20[7]:1491-5). “This is increased more significantly for women and the elderly,” said Dr. Bonakdar, who was not affiliated with the study. “If we can change the diet that person is taking, that’s going to begin the process of reversing this to the point where they’re having less pain from inflammation that’s affecting the adipose tissue and adipokines traveling to their joints, which can cause less dysbiosis. It is very much a vicious cycle that patients follow, but if you begin to unwind it, it’s going to help multiple areas.”
In the Intensive Diet and Exercise for Arthritis (IDEA) trial, researchers randomized 450 patients with osteoarthritis to intensive dietary restriction only, exercise only, or a combination of both (BMC Musculoskelet Disord. 2009;10:93). They found that a 5% weight loss over the course of 18 months led to a 30% reduction in pain and a 24% improvement in function.
Inspired by the IDEA trial design, Dr. Bonakdar and his colleagues completed an unpublished 12-week pilot program with 12 patients with a BMI of 27 kg/m2 or greater plus comorbidities. The program consisted of weekly group meetings, including a lecture by team clinicians, dietician, and fitness staff; group support sessions with a behavioral counselor; and a group exercise session. It also included weekly 1:1 personal training sessions and biweekly 1:1 dietitian meetings. The researchers also evaluated several deficiencies linked to pain, including magnesium, vitamin D, vitamins B1, B2, and B12, folate, calcium, amino acids, omega 3s, zinc, coenzyme Q10, carnitine, and vitamin C. The goal was a weight reduction of 5%.
The intervention consisted of a 28-day detox/protein shake consumed 1-3 times per day, which contained 17 g of protein per serving. Nutritional supplementation was added based on results of individual diagnostics.
According to preliminary results from the trial, the intended weight goal was achieved. “More importantly, there were significant improvements in markers of dysbiosis, including zonulin and lipopolysaccharide, as well as the adipokine leptin, which appeared to be associated with improvement in quality of life measures and pain,” Dr. Bonakdar said.
He concluded his presentation by highlighting a pilot study conducted in an Australian tertiary pain clinic. It found that a personalized dietitian-delivered dietary intervention can improve pain scores, quality of life, and dietary intake of people experiencing chronic pain (Nutrients. 2019 Jan 16;11[1] pii: E181). “This is another piece of the puzzle showing that these dietary interventions can be done in multiple settings, including tertiary centers with nutrition staff, and that this important step can improve pain and quality of life,” he said.
Dr. Bonakdar disclosed that he receives royalties from Oxford University Press, Lippincott, and Elsevier. He is also a consultant to Standard Process.
REPORTING FROM A NATURAL SUPPLEMENTS UPDATE
EEG abnormalities may indicate increased risk for epilepsy in patients with autism
BALTIMORE – , according to research presented at the annual meeting of the American Epilepsy Society. In addition, a positive family history of febrile seizures also is associated with an increased risk of epilepsy in this population.
The literature suggests that the prevalence of epilepsy in patients with ASD ranges from 5% to 40%. This broad range may result from the heterogeneity of epilepsy risk factors among patients with ASD. These risk factors include intellectual disability, age, and syndromic forms of ASD such as tuberous sclerosis complex. Regardless of whether they have epilepsy, approximately 60% of patients with ASD have EEG abnormalities. The prognostic implications of these abnormalities are uncertain.
Investigators reviewed patients’ charts retrospectively
Divya Nadkarni, MD, a neurologist at Ronald Reagan UCLA Medical Center in Los Angeles, and colleagues sought to clarify the relationship between risk factors such as EEG abnormalities and subsequent epilepsy in patients with ASD. They retrospectively identified patients who were followed jointly at UCLA and at Pediatric Minds, a neurodevelopmental clinic in Torrance, Calif. Eligible patients had a diagnosis of ASD, based on criteria from DSM-IV, DSM-5, or the Autism Diagnostic Observation Schedule. In addition, patients had overnight, continuous video EEG evaluation and a minimum follow-up of 1 week after EEG. Patients with a history of epilepsy before the initial EEG evaluation were excluded. Dr. Nadkarni and colleagues collected clinical and electrographic data by chart review.
The study’s primary outcome was time to onset of epilepsy. Among the variables that the investigators analyzed were EEG abnormalities, which they defined as focal slowing or generalized or focal epileptiform discharges. The other variables were history of febrile seizures, family history of epilepsy, family history of febrile seizures, and family history of ASD. Dr. Nadkarni and colleagues analyzed the data using the Kaplan–Meier method and Cox proportional hazards models.
In all, 164 patients met the study’s inclusion criteria. The population’s median age at the initial EEG evaluation was 4.5 years. The median follow-up after this evaluation was 2.4 years. The investigators found 63 patients (38.4%) with abnormal EEGs, and 18 patients (11%) subsequently developed epilepsy after a median of 1.9 years.
Family history of febrile seizures was associated with time to epilepsy onset
The time to epilepsy onset was associated with abnormalities on the initial overnight continuous EEG. The hazard ratio of epilepsy among patients with EEG abnormalities was 8.0. Approximately one-third of patients with EEG abnormalities developed subsequent epilepsy, compared with approximately 5% of patients without EEG abnormalities, said Dr. Nadkarni.
In addition, time to epilepsy onset was independently associated with a positive family history of febrile seizures. This finding was unexpected, said Dr. Nadkarni. The hazard ratio of epilepsy among patients with a positive family history of febrile seizures was 12.6.
The patient’s own history of febrile seizures was not associated with time to epilepsy onset. One potential explanation for this result is that it is difficult to distinguish between febrile seizure and seizure with fever in the general pediatric population. Making this distinction in children with ASD, who may have atypical febrile seizures, might be still more difficult, said Dr. Nadkarni.
Time for guideline updates?
“Statements from the Centers for Disease Control and Prevention, the American Academy of Pediatrics, the American Academy of Neurology, and the Child Neurology Society do not currently recommend routine EEG screening for all children with ASD,” said Dr. Nadkarni. Investigators are suggesting that the guidelines should be reevaluated, however. “Research shows that EEG abnormalities, particularly epileptiform abnormalities, are associated with worse outcome, in terms of developmental and adaptive functioning. EEG endophenotypes in ASD are starting to be elucidated ... That’s one reason to consider EEG screening.” Furthermore, preliminary connectivity research suggests that EEG screening of high-risk siblings of children with ASD may predict the development of ASD.
The small cohort and retrospective design were among the study’s limitations, said Dr. Nadkarni. Some patients were lost to follow-up, and some data were missing from patients’ charts.
“In our opinion, further study – ideally, a prospective, observational cohort study – might be warranted to determine whether overnight continuous EEG monitoring might be useful as a screening tool for epilepsy in patients with ASD,” Dr. Nadkarni concluded.
The study was conducted without external funding, and the investigators had no disclosures.
SOURCE: Nadkarni D et al. AES 2019. Abstract 1.29.
BALTIMORE – , according to research presented at the annual meeting of the American Epilepsy Society. In addition, a positive family history of febrile seizures also is associated with an increased risk of epilepsy in this population.
The literature suggests that the prevalence of epilepsy in patients with ASD ranges from 5% to 40%. This broad range may result from the heterogeneity of epilepsy risk factors among patients with ASD. These risk factors include intellectual disability, age, and syndromic forms of ASD such as tuberous sclerosis complex. Regardless of whether they have epilepsy, approximately 60% of patients with ASD have EEG abnormalities. The prognostic implications of these abnormalities are uncertain.
Investigators reviewed patients’ charts retrospectively
Divya Nadkarni, MD, a neurologist at Ronald Reagan UCLA Medical Center in Los Angeles, and colleagues sought to clarify the relationship between risk factors such as EEG abnormalities and subsequent epilepsy in patients with ASD. They retrospectively identified patients who were followed jointly at UCLA and at Pediatric Minds, a neurodevelopmental clinic in Torrance, Calif. Eligible patients had a diagnosis of ASD, based on criteria from DSM-IV, DSM-5, or the Autism Diagnostic Observation Schedule. In addition, patients had overnight, continuous video EEG evaluation and a minimum follow-up of 1 week after EEG. Patients with a history of epilepsy before the initial EEG evaluation were excluded. Dr. Nadkarni and colleagues collected clinical and electrographic data by chart review.
The study’s primary outcome was time to onset of epilepsy. Among the variables that the investigators analyzed were EEG abnormalities, which they defined as focal slowing or generalized or focal epileptiform discharges. The other variables were history of febrile seizures, family history of epilepsy, family history of febrile seizures, and family history of ASD. Dr. Nadkarni and colleagues analyzed the data using the Kaplan–Meier method and Cox proportional hazards models.
In all, 164 patients met the study’s inclusion criteria. The population’s median age at the initial EEG evaluation was 4.5 years. The median follow-up after this evaluation was 2.4 years. The investigators found 63 patients (38.4%) with abnormal EEGs, and 18 patients (11%) subsequently developed epilepsy after a median of 1.9 years.
Family history of febrile seizures was associated with time to epilepsy onset
The time to epilepsy onset was associated with abnormalities on the initial overnight continuous EEG. The hazard ratio of epilepsy among patients with EEG abnormalities was 8.0. Approximately one-third of patients with EEG abnormalities developed subsequent epilepsy, compared with approximately 5% of patients without EEG abnormalities, said Dr. Nadkarni.
In addition, time to epilepsy onset was independently associated with a positive family history of febrile seizures. This finding was unexpected, said Dr. Nadkarni. The hazard ratio of epilepsy among patients with a positive family history of febrile seizures was 12.6.
The patient’s own history of febrile seizures was not associated with time to epilepsy onset. One potential explanation for this result is that it is difficult to distinguish between febrile seizure and seizure with fever in the general pediatric population. Making this distinction in children with ASD, who may have atypical febrile seizures, might be still more difficult, said Dr. Nadkarni.
Time for guideline updates?
“Statements from the Centers for Disease Control and Prevention, the American Academy of Pediatrics, the American Academy of Neurology, and the Child Neurology Society do not currently recommend routine EEG screening for all children with ASD,” said Dr. Nadkarni. Investigators are suggesting that the guidelines should be reevaluated, however. “Research shows that EEG abnormalities, particularly epileptiform abnormalities, are associated with worse outcome, in terms of developmental and adaptive functioning. EEG endophenotypes in ASD are starting to be elucidated ... That’s one reason to consider EEG screening.” Furthermore, preliminary connectivity research suggests that EEG screening of high-risk siblings of children with ASD may predict the development of ASD.
The small cohort and retrospective design were among the study’s limitations, said Dr. Nadkarni. Some patients were lost to follow-up, and some data were missing from patients’ charts.
“In our opinion, further study – ideally, a prospective, observational cohort study – might be warranted to determine whether overnight continuous EEG monitoring might be useful as a screening tool for epilepsy in patients with ASD,” Dr. Nadkarni concluded.
The study was conducted without external funding, and the investigators had no disclosures.
SOURCE: Nadkarni D et al. AES 2019. Abstract 1.29.
BALTIMORE – , according to research presented at the annual meeting of the American Epilepsy Society. In addition, a positive family history of febrile seizures also is associated with an increased risk of epilepsy in this population.
The literature suggests that the prevalence of epilepsy in patients with ASD ranges from 5% to 40%. This broad range may result from the heterogeneity of epilepsy risk factors among patients with ASD. These risk factors include intellectual disability, age, and syndromic forms of ASD such as tuberous sclerosis complex. Regardless of whether they have epilepsy, approximately 60% of patients with ASD have EEG abnormalities. The prognostic implications of these abnormalities are uncertain.
Investigators reviewed patients’ charts retrospectively
Divya Nadkarni, MD, a neurologist at Ronald Reagan UCLA Medical Center in Los Angeles, and colleagues sought to clarify the relationship between risk factors such as EEG abnormalities and subsequent epilepsy in patients with ASD. They retrospectively identified patients who were followed jointly at UCLA and at Pediatric Minds, a neurodevelopmental clinic in Torrance, Calif. Eligible patients had a diagnosis of ASD, based on criteria from DSM-IV, DSM-5, or the Autism Diagnostic Observation Schedule. In addition, patients had overnight, continuous video EEG evaluation and a minimum follow-up of 1 week after EEG. Patients with a history of epilepsy before the initial EEG evaluation were excluded. Dr. Nadkarni and colleagues collected clinical and electrographic data by chart review.
The study’s primary outcome was time to onset of epilepsy. Among the variables that the investigators analyzed were EEG abnormalities, which they defined as focal slowing or generalized or focal epileptiform discharges. The other variables were history of febrile seizures, family history of epilepsy, family history of febrile seizures, and family history of ASD. Dr. Nadkarni and colleagues analyzed the data using the Kaplan–Meier method and Cox proportional hazards models.
In all, 164 patients met the study’s inclusion criteria. The population’s median age at the initial EEG evaluation was 4.5 years. The median follow-up after this evaluation was 2.4 years. The investigators found 63 patients (38.4%) with abnormal EEGs, and 18 patients (11%) subsequently developed epilepsy after a median of 1.9 years.
Family history of febrile seizures was associated with time to epilepsy onset
The time to epilepsy onset was associated with abnormalities on the initial overnight continuous EEG. The hazard ratio of epilepsy among patients with EEG abnormalities was 8.0. Approximately one-third of patients with EEG abnormalities developed subsequent epilepsy, compared with approximately 5% of patients without EEG abnormalities, said Dr. Nadkarni.
In addition, time to epilepsy onset was independently associated with a positive family history of febrile seizures. This finding was unexpected, said Dr. Nadkarni. The hazard ratio of epilepsy among patients with a positive family history of febrile seizures was 12.6.
The patient’s own history of febrile seizures was not associated with time to epilepsy onset. One potential explanation for this result is that it is difficult to distinguish between febrile seizure and seizure with fever in the general pediatric population. Making this distinction in children with ASD, who may have atypical febrile seizures, might be still more difficult, said Dr. Nadkarni.
Time for guideline updates?
“Statements from the Centers for Disease Control and Prevention, the American Academy of Pediatrics, the American Academy of Neurology, and the Child Neurology Society do not currently recommend routine EEG screening for all children with ASD,” said Dr. Nadkarni. Investigators are suggesting that the guidelines should be reevaluated, however. “Research shows that EEG abnormalities, particularly epileptiform abnormalities, are associated with worse outcome, in terms of developmental and adaptive functioning. EEG endophenotypes in ASD are starting to be elucidated ... That’s one reason to consider EEG screening.” Furthermore, preliminary connectivity research suggests that EEG screening of high-risk siblings of children with ASD may predict the development of ASD.
The small cohort and retrospective design were among the study’s limitations, said Dr. Nadkarni. Some patients were lost to follow-up, and some data were missing from patients’ charts.
“In our opinion, further study – ideally, a prospective, observational cohort study – might be warranted to determine whether overnight continuous EEG monitoring might be useful as a screening tool for epilepsy in patients with ASD,” Dr. Nadkarni concluded.
The study was conducted without external funding, and the investigators had no disclosures.
SOURCE: Nadkarni D et al. AES 2019. Abstract 1.29.
REPORTING FROM AES 2019
Serum levels of neurofilament light are increased before clinical onset of MS
(MS), according to research published in the January issue of JAMA Neurology. These results lend weight to the idea that MS has a prodromal phase, and this phase appears to be associated with neurodegeneration, according to the authors.
Patients often have CNS lesions of various stages of development at the time of their first demyelinating event, and this finding was one basis for neurologists’ hypothesis of a prodromal phase of MS. The finding that one-third of patients with radiologically isolated syndrome develop MS within 5 years also lends credence to this idea. Diagnosing MS early would enable early treatment that could prevent demyelination and the progression of neurodegeneration.
Researchers compared presymptomatic and symptomatic samples
With this idea in mind, Kjetil Bjornevik, MD, PhD, a member of the neuroepidemiology research group at Harvard TH Chan School of Public Health in Boston, and colleagues evaluated whether serum levels of NfL, a marker of ongoing neuroaxonal degeneration, were increased in the years before and around the time of clinical onset of MS. For their study population, the investigators chose active-duty U.S. military personnel who have at least one serum sample stored in the U.S. Department of Defense Serum Repository. Samples are collected after routine HIV type 1 antibody testing.
Within this population, Dr. Bjornevik and colleagues identified patients with MS who had at least one presymptomatic serum sample. The date of clinical MS onset was defined as the date of the first neurologic symptoms attributable to MS documented in the medical record. The investigators randomly selected two control individuals from the population and matched them to each case by age, sex, race or ethnicity, and dates of sample collection. Eligible controls were on active duty on the date of onset of the matched case.
Dr. Bjornevik and colleagues identified 245 patients with MS. Among this sample, the researchers selected two groups that each included 30 cases and 30 controls. The first group included patients who had provided at least one serum sample before MS onset and one sample within 2 years after MS onset. The second group included cases with at least two presymptomatic serum samples, one of which was collected more than 5 years before MS diagnosis, and the other of which was collected between 2 and 5 years before diagnosis. The investigators handled pairs of serum samples in the same way and assayed them in the same batch. The order of the samples in each pair was arranged at random.
Levels were higher in cases than in controls
About 77% of the population was male. Sixty percent of participants were white, 28% were black, and 6.7% were Hispanic. The population’s mean age at first sample collection was approximately 27 years. Mean age at MS onset was approximately 31 years.
For patients who provided samples before and after the clinical onset of MS, serum NfL levels were higher than in matched controls at both points. Most patients who passed from the presymptomatic stage to the symptomatic stage had a significant increase in serum NfL level (i.e., from a median of 25.0 pg/mL to a median of 45.1 pg/mL). Serum NfL levels at the two time points in controls did not differ significantly. For any given patient, an increase in serum NfL level from the presymptomatic measurement to the symptomatic measurement was associated with an increased risk of MS.
In patients with two presymptomatic samples, serum NfL levels were significantly higher in both samples than in the corresponding samples from matched controls. In cases, the earlier sample was collected at a median of 6 years before clinical onset of MS, and the later sample was collected at a median of 1 year before clinical onset. The serum NfL levels increased significantly between the two points for cases (i.e., a median increase of 1.3 pg/mL per year), but there was no significant difference in serum NfL level between the two samples in controls. A within-patient increase in presymptomatic serum NfL level was associated with an increased risk of MS.
Population included few women
“Our study differs from previous studies on the prodromal phase of MS because these have used indirect markers of this phase, which included unspecific symptoms or disturbances occurring before the clinical onset, compared with a marker of neurodegeneration,” wrote Dr. Bjornevik and colleagues. Initiation of treatment with disease-modifying therapy is associated with reductions in serum NfL levels, and this association could explain why some patients in the current study had higher NfL levels before MS onset than afterward. Furthermore, serum NfL levels are highly associated with levels of NfL in cerebrospinal fluid. “Thus, our findings of a presymptomatic increase in serum NfL not only suggest the presence of a prodromal phase in MS, but also that this phase is associated with neurodegeneration,” wrote the investigators.
The study’s well-defined population helped to minimize selection bias, and the blinded, randomized method of analyzing the serum samples eliminated artifactual differences in serum NfL concentrations. But the small sample size precluded analyses that could have influenced clinical practice, wrote Dr. Bjornevik and colleagues. For example, the researchers could not evaluate distinct cutoffs in serum NfL level that could mark the beginning of the prodromal phase of MS. Nor could they determine whether presymptomatic serum NfL levels varied with age at clinical onset, sex, or race. The small number of women in the sample was another limitation of the study.
The Swiss National Research Foundation and the National Institute of Neurologic Disorders and Stroke funded the study. Several of the investigators received fees from various drug companies that were unrelated to the study, and one researcher received grants from the National Institutes of Health during the study.
SOURCE: Bjornevik K et al. JAMA Neurol. 2020;77(1):58-64.
(MS), according to research published in the January issue of JAMA Neurology. These results lend weight to the idea that MS has a prodromal phase, and this phase appears to be associated with neurodegeneration, according to the authors.
Patients often have CNS lesions of various stages of development at the time of their first demyelinating event, and this finding was one basis for neurologists’ hypothesis of a prodromal phase of MS. The finding that one-third of patients with radiologically isolated syndrome develop MS within 5 years also lends credence to this idea. Diagnosing MS early would enable early treatment that could prevent demyelination and the progression of neurodegeneration.
Researchers compared presymptomatic and symptomatic samples
With this idea in mind, Kjetil Bjornevik, MD, PhD, a member of the neuroepidemiology research group at Harvard TH Chan School of Public Health in Boston, and colleagues evaluated whether serum levels of NfL, a marker of ongoing neuroaxonal degeneration, were increased in the years before and around the time of clinical onset of MS. For their study population, the investigators chose active-duty U.S. military personnel who have at least one serum sample stored in the U.S. Department of Defense Serum Repository. Samples are collected after routine HIV type 1 antibody testing.
Within this population, Dr. Bjornevik and colleagues identified patients with MS who had at least one presymptomatic serum sample. The date of clinical MS onset was defined as the date of the first neurologic symptoms attributable to MS documented in the medical record. The investigators randomly selected two control individuals from the population and matched them to each case by age, sex, race or ethnicity, and dates of sample collection. Eligible controls were on active duty on the date of onset of the matched case.
Dr. Bjornevik and colleagues identified 245 patients with MS. Among this sample, the researchers selected two groups that each included 30 cases and 30 controls. The first group included patients who had provided at least one serum sample before MS onset and one sample within 2 years after MS onset. The second group included cases with at least two presymptomatic serum samples, one of which was collected more than 5 years before MS diagnosis, and the other of which was collected between 2 and 5 years before diagnosis. The investigators handled pairs of serum samples in the same way and assayed them in the same batch. The order of the samples in each pair was arranged at random.
Levels were higher in cases than in controls
About 77% of the population was male. Sixty percent of participants were white, 28% were black, and 6.7% were Hispanic. The population’s mean age at first sample collection was approximately 27 years. Mean age at MS onset was approximately 31 years.
For patients who provided samples before and after the clinical onset of MS, serum NfL levels were higher than in matched controls at both points. Most patients who passed from the presymptomatic stage to the symptomatic stage had a significant increase in serum NfL level (i.e., from a median of 25.0 pg/mL to a median of 45.1 pg/mL). Serum NfL levels at the two time points in controls did not differ significantly. For any given patient, an increase in serum NfL level from the presymptomatic measurement to the symptomatic measurement was associated with an increased risk of MS.
In patients with two presymptomatic samples, serum NfL levels were significantly higher in both samples than in the corresponding samples from matched controls. In cases, the earlier sample was collected at a median of 6 years before clinical onset of MS, and the later sample was collected at a median of 1 year before clinical onset. The serum NfL levels increased significantly between the two points for cases (i.e., a median increase of 1.3 pg/mL per year), but there was no significant difference in serum NfL level between the two samples in controls. A within-patient increase in presymptomatic serum NfL level was associated with an increased risk of MS.
Population included few women
“Our study differs from previous studies on the prodromal phase of MS because these have used indirect markers of this phase, which included unspecific symptoms or disturbances occurring before the clinical onset, compared with a marker of neurodegeneration,” wrote Dr. Bjornevik and colleagues. Initiation of treatment with disease-modifying therapy is associated with reductions in serum NfL levels, and this association could explain why some patients in the current study had higher NfL levels before MS onset than afterward. Furthermore, serum NfL levels are highly associated with levels of NfL in cerebrospinal fluid. “Thus, our findings of a presymptomatic increase in serum NfL not only suggest the presence of a prodromal phase in MS, but also that this phase is associated with neurodegeneration,” wrote the investigators.
The study’s well-defined population helped to minimize selection bias, and the blinded, randomized method of analyzing the serum samples eliminated artifactual differences in serum NfL concentrations. But the small sample size precluded analyses that could have influenced clinical practice, wrote Dr. Bjornevik and colleagues. For example, the researchers could not evaluate distinct cutoffs in serum NfL level that could mark the beginning of the prodromal phase of MS. Nor could they determine whether presymptomatic serum NfL levels varied with age at clinical onset, sex, or race. The small number of women in the sample was another limitation of the study.
The Swiss National Research Foundation and the National Institute of Neurologic Disorders and Stroke funded the study. Several of the investigators received fees from various drug companies that were unrelated to the study, and one researcher received grants from the National Institutes of Health during the study.
SOURCE: Bjornevik K et al. JAMA Neurol. 2020;77(1):58-64.
(MS), according to research published in the January issue of JAMA Neurology. These results lend weight to the idea that MS has a prodromal phase, and this phase appears to be associated with neurodegeneration, according to the authors.
Patients often have CNS lesions of various stages of development at the time of their first demyelinating event, and this finding was one basis for neurologists’ hypothesis of a prodromal phase of MS. The finding that one-third of patients with radiologically isolated syndrome develop MS within 5 years also lends credence to this idea. Diagnosing MS early would enable early treatment that could prevent demyelination and the progression of neurodegeneration.
Researchers compared presymptomatic and symptomatic samples
With this idea in mind, Kjetil Bjornevik, MD, PhD, a member of the neuroepidemiology research group at Harvard TH Chan School of Public Health in Boston, and colleagues evaluated whether serum levels of NfL, a marker of ongoing neuroaxonal degeneration, were increased in the years before and around the time of clinical onset of MS. For their study population, the investigators chose active-duty U.S. military personnel who have at least one serum sample stored in the U.S. Department of Defense Serum Repository. Samples are collected after routine HIV type 1 antibody testing.
Within this population, Dr. Bjornevik and colleagues identified patients with MS who had at least one presymptomatic serum sample. The date of clinical MS onset was defined as the date of the first neurologic symptoms attributable to MS documented in the medical record. The investigators randomly selected two control individuals from the population and matched them to each case by age, sex, race or ethnicity, and dates of sample collection. Eligible controls were on active duty on the date of onset of the matched case.
Dr. Bjornevik and colleagues identified 245 patients with MS. Among this sample, the researchers selected two groups that each included 30 cases and 30 controls. The first group included patients who had provided at least one serum sample before MS onset and one sample within 2 years after MS onset. The second group included cases with at least two presymptomatic serum samples, one of which was collected more than 5 years before MS diagnosis, and the other of which was collected between 2 and 5 years before diagnosis. The investigators handled pairs of serum samples in the same way and assayed them in the same batch. The order of the samples in each pair was arranged at random.
Levels were higher in cases than in controls
About 77% of the population was male. Sixty percent of participants were white, 28% were black, and 6.7% were Hispanic. The population’s mean age at first sample collection was approximately 27 years. Mean age at MS onset was approximately 31 years.
For patients who provided samples before and after the clinical onset of MS, serum NfL levels were higher than in matched controls at both points. Most patients who passed from the presymptomatic stage to the symptomatic stage had a significant increase in serum NfL level (i.e., from a median of 25.0 pg/mL to a median of 45.1 pg/mL). Serum NfL levels at the two time points in controls did not differ significantly. For any given patient, an increase in serum NfL level from the presymptomatic measurement to the symptomatic measurement was associated with an increased risk of MS.
In patients with two presymptomatic samples, serum NfL levels were significantly higher in both samples than in the corresponding samples from matched controls. In cases, the earlier sample was collected at a median of 6 years before clinical onset of MS, and the later sample was collected at a median of 1 year before clinical onset. The serum NfL levels increased significantly between the two points for cases (i.e., a median increase of 1.3 pg/mL per year), but there was no significant difference in serum NfL level between the two samples in controls. A within-patient increase in presymptomatic serum NfL level was associated with an increased risk of MS.
Population included few women
“Our study differs from previous studies on the prodromal phase of MS because these have used indirect markers of this phase, which included unspecific symptoms or disturbances occurring before the clinical onset, compared with a marker of neurodegeneration,” wrote Dr. Bjornevik and colleagues. Initiation of treatment with disease-modifying therapy is associated with reductions in serum NfL levels, and this association could explain why some patients in the current study had higher NfL levels before MS onset than afterward. Furthermore, serum NfL levels are highly associated with levels of NfL in cerebrospinal fluid. “Thus, our findings of a presymptomatic increase in serum NfL not only suggest the presence of a prodromal phase in MS, but also that this phase is associated with neurodegeneration,” wrote the investigators.
The study’s well-defined population helped to minimize selection bias, and the blinded, randomized method of analyzing the serum samples eliminated artifactual differences in serum NfL concentrations. But the small sample size precluded analyses that could have influenced clinical practice, wrote Dr. Bjornevik and colleagues. For example, the researchers could not evaluate distinct cutoffs in serum NfL level that could mark the beginning of the prodromal phase of MS. Nor could they determine whether presymptomatic serum NfL levels varied with age at clinical onset, sex, or race. The small number of women in the sample was another limitation of the study.
The Swiss National Research Foundation and the National Institute of Neurologic Disorders and Stroke funded the study. Several of the investigators received fees from various drug companies that were unrelated to the study, and one researcher received grants from the National Institutes of Health during the study.
SOURCE: Bjornevik K et al. JAMA Neurol. 2020;77(1):58-64.
FROM JAMA NEUROLOGY
Rate of suicide is higher in people with neurologic disorders
The absolute risk difference is small, but statistically significant. “These findings do not necessarily warrant changing the management of treatment for individual patients,” wrote Annette Erlangsen, PhD, a researcher at the Danish Research Institute for Suicide Prevention in Hellerup, and colleagues. “As with all patients, physicians should be aware of the potential for depression, demoralization, and suicide.”
In addition, dementia, Alzheimer’s disease, and intellectual disabilities may be associated with lower suicide rates, according to the study, which was published in JAMA.
“Plausible mechanisms” could underlie the association between neurologic disease and suicide, the authors wrote. A neurologic diagnosis “may constitute a distressing life event,” and the diseases may have psychological, physical, and psychiatric effects. Patients may see themselves as a burden or have less financial security. In addition, the diseases may entail “communication difficulties, poor sleep, and pain.” Neurologic diseases may alter brain circuitry and functioning and influence aggression and impulsivity. “People with neurologic disorders may also have easier access to toxic medication,” they added.
More than a dozen conditions examined
Prior studies have found associations between neurologic conditions and rates of suicide, but data have been inconclusive or inconsistent for some of the disorders. To examine whether people with neurologic disorders have higher suicide rates, relative to people without these disorders, the researchers conducted a retrospective study. They analyzed data from more than 7.3 million people aged 15 years or older who lived in Denmark between 1980 and 2016. The cohort included more than 1.2 million people with neurologic disorders. The investigators identified neurologic disorders using ICD codes for head injury, stroke, epilepsy, polyneuropathy, diseases of the myoneural junction, Parkinson’s disease, multiple sclerosis, CNS infections, meningitis, encephalitis, amyotrophic lateral sclerosis, Huntington’s disease, dementia, intellectual disability, and other brain disorders. They compared incidence rates using a Poisson regression model and adjusted for time period, sex, age, region, socioeconomic status, comorbidity, self-harm or psychiatric hospitalization prior to a neurologic diagnosis, and whether a person lived alone.
In all, 35,483 people in the cohort died by suicide at an average age of about 52 years; 77.4% were male. About 15% of those who died by suicide had a neurologic disorder. The suicide incidence rate among people with a neurologic disorder was 44.0 per 100,000 person-years, whereas the rate among people without a neurologic disorder was 20.1 per 100,000 person-years.
The adjusted incidence rate ratio for people with a neurologic disorder was 1.8. The rate ratio was highest during the 3 months after diagnosis, at 3.1. Huntington’s disease and amyotrophic lateral sclerosis were associated with “the largest excess adjusted [incidence rate ratios] of suicide mortality,” with a rate ratio of 4.9 for each condition, the researchers reported. The adjusted incidence rate ratio was 1.7 for head injury, 1.3 for stroke, 1.7 for epilepsy, 1.4 for intracerebral hemorrhage, 1.3 for cerebral infarction, 1.3 for subarachnoid hemorrhage, 1.7 for polyneuropathy and peripheral neuropathy, 2.2 for Guillain-Barré syndrome, 1.9 for diseases of myoneural junction and muscle, 1.8 for other brain disorders, 1.7 for Parkinson’s disease, 2.2 for multiple sclerosis, and 1.6 for CNS infection.
Compared with people without a neurologic condition, people with dementia, Alzheimer’s disease, and intellectual disabilities had lower suicide rates, with adjusted incidence rate ratios of 0.8, 0.2, and 0.6, respectively. “However, the adjusted [incidence rate ratio] for people with dementia during the first month after diagnosis was 3.0,” the researchers wrote.
In addition, the suicide rate increased with an increasing cumulative number of hospital contacts for neurologic conditions.
Overall incidence rates declined
“Over the study period, the suicide incidence rate for people with neurological disorders decreased from 78.6 per 100,000 person-years during the 1980-1999 years to 27.3 per 100,000 person-years during the 2000-2016 years,” wrote Dr. Erlangsen and colleagues. “The suicide incidence rate for those without a disorder decreased from 26.3 to 12.7 during the same time spans. ... The decline in the overall suicide rate over time did not affect the relative risk pattern.”
The decline in the general suicide rate in Denmark “has largely been attributed to means restriction, such as efforts to limit availability of firearms and particularly toxic medication,” the authors added.
In those time spans, the adjusted incidence rate ratio for suicide among those with dementia decreased from 2.4 to 1.0, and among those with multiple sclerosis from 2.0 to 1.0. “It is possible that the improvements observed for dementia and multiple sclerosis may be related to improvements in treatment and intensified community-based support,” Dr. Erlangsen and coauthors wrote.
When the researchers used people with rheumatoid arthritis as a reference group, those with a neurologic disorder had a higher suicide rate per 100,000 person-years, 30.2 versus 18.4. The adjusted incidence rate ratio for that comparison was 1.4.
In patients with Huntington’s disease, depression mediated by hyperactivity in the hypothalamic-pituitary-adrenal axis may contribute to the risk of suicide. “Witnessing the course of the disease in one’s parent” also may contribute the risk, the researchers wrote.
The analysis may have missed people with neurologic disorders diagnosed before 1977 if they did not have subsequent contact with a hospital, the investigators noted. In addition, diagnoses given in primary care were not included, suicide deaths may be underrecorded, and “adjusting for preexisting mental disorders could be viewed as overadjusting,” they wrote.
The study was supported by a grant from the Psychiatric Research Foundation in Denmark. The authors reported that they had no disclosures.
SOURCE: Erlangsen A et al. JAMA. 2020 Feb 4. doi: 10.1001/jama.2019.21834.
The absolute risk difference is small, but statistically significant. “These findings do not necessarily warrant changing the management of treatment for individual patients,” wrote Annette Erlangsen, PhD, a researcher at the Danish Research Institute for Suicide Prevention in Hellerup, and colleagues. “As with all patients, physicians should be aware of the potential for depression, demoralization, and suicide.”
In addition, dementia, Alzheimer’s disease, and intellectual disabilities may be associated with lower suicide rates, according to the study, which was published in JAMA.
“Plausible mechanisms” could underlie the association between neurologic disease and suicide, the authors wrote. A neurologic diagnosis “may constitute a distressing life event,” and the diseases may have psychological, physical, and psychiatric effects. Patients may see themselves as a burden or have less financial security. In addition, the diseases may entail “communication difficulties, poor sleep, and pain.” Neurologic diseases may alter brain circuitry and functioning and influence aggression and impulsivity. “People with neurologic disorders may also have easier access to toxic medication,” they added.
More than a dozen conditions examined
Prior studies have found associations between neurologic conditions and rates of suicide, but data have been inconclusive or inconsistent for some of the disorders. To examine whether people with neurologic disorders have higher suicide rates, relative to people without these disorders, the researchers conducted a retrospective study. They analyzed data from more than 7.3 million people aged 15 years or older who lived in Denmark between 1980 and 2016. The cohort included more than 1.2 million people with neurologic disorders. The investigators identified neurologic disorders using ICD codes for head injury, stroke, epilepsy, polyneuropathy, diseases of the myoneural junction, Parkinson’s disease, multiple sclerosis, CNS infections, meningitis, encephalitis, amyotrophic lateral sclerosis, Huntington’s disease, dementia, intellectual disability, and other brain disorders. They compared incidence rates using a Poisson regression model and adjusted for time period, sex, age, region, socioeconomic status, comorbidity, self-harm or psychiatric hospitalization prior to a neurologic diagnosis, and whether a person lived alone.
In all, 35,483 people in the cohort died by suicide at an average age of about 52 years; 77.4% were male. About 15% of those who died by suicide had a neurologic disorder. The suicide incidence rate among people with a neurologic disorder was 44.0 per 100,000 person-years, whereas the rate among people without a neurologic disorder was 20.1 per 100,000 person-years.
The adjusted incidence rate ratio for people with a neurologic disorder was 1.8. The rate ratio was highest during the 3 months after diagnosis, at 3.1. Huntington’s disease and amyotrophic lateral sclerosis were associated with “the largest excess adjusted [incidence rate ratios] of suicide mortality,” with a rate ratio of 4.9 for each condition, the researchers reported. The adjusted incidence rate ratio was 1.7 for head injury, 1.3 for stroke, 1.7 for epilepsy, 1.4 for intracerebral hemorrhage, 1.3 for cerebral infarction, 1.3 for subarachnoid hemorrhage, 1.7 for polyneuropathy and peripheral neuropathy, 2.2 for Guillain-Barré syndrome, 1.9 for diseases of myoneural junction and muscle, 1.8 for other brain disorders, 1.7 for Parkinson’s disease, 2.2 for multiple sclerosis, and 1.6 for CNS infection.
Compared with people without a neurologic condition, people with dementia, Alzheimer’s disease, and intellectual disabilities had lower suicide rates, with adjusted incidence rate ratios of 0.8, 0.2, and 0.6, respectively. “However, the adjusted [incidence rate ratio] for people with dementia during the first month after diagnosis was 3.0,” the researchers wrote.
In addition, the suicide rate increased with an increasing cumulative number of hospital contacts for neurologic conditions.
Overall incidence rates declined
“Over the study period, the suicide incidence rate for people with neurological disorders decreased from 78.6 per 100,000 person-years during the 1980-1999 years to 27.3 per 100,000 person-years during the 2000-2016 years,” wrote Dr. Erlangsen and colleagues. “The suicide incidence rate for those without a disorder decreased from 26.3 to 12.7 during the same time spans. ... The decline in the overall suicide rate over time did not affect the relative risk pattern.”
The decline in the general suicide rate in Denmark “has largely been attributed to means restriction, such as efforts to limit availability of firearms and particularly toxic medication,” the authors added.
In those time spans, the adjusted incidence rate ratio for suicide among those with dementia decreased from 2.4 to 1.0, and among those with multiple sclerosis from 2.0 to 1.0. “It is possible that the improvements observed for dementia and multiple sclerosis may be related to improvements in treatment and intensified community-based support,” Dr. Erlangsen and coauthors wrote.
When the researchers used people with rheumatoid arthritis as a reference group, those with a neurologic disorder had a higher suicide rate per 100,000 person-years, 30.2 versus 18.4. The adjusted incidence rate ratio for that comparison was 1.4.
In patients with Huntington’s disease, depression mediated by hyperactivity in the hypothalamic-pituitary-adrenal axis may contribute to the risk of suicide. “Witnessing the course of the disease in one’s parent” also may contribute the risk, the researchers wrote.
The analysis may have missed people with neurologic disorders diagnosed before 1977 if they did not have subsequent contact with a hospital, the investigators noted. In addition, diagnoses given in primary care were not included, suicide deaths may be underrecorded, and “adjusting for preexisting mental disorders could be viewed as overadjusting,” they wrote.
The study was supported by a grant from the Psychiatric Research Foundation in Denmark. The authors reported that they had no disclosures.
SOURCE: Erlangsen A et al. JAMA. 2020 Feb 4. doi: 10.1001/jama.2019.21834.
The absolute risk difference is small, but statistically significant. “These findings do not necessarily warrant changing the management of treatment for individual patients,” wrote Annette Erlangsen, PhD, a researcher at the Danish Research Institute for Suicide Prevention in Hellerup, and colleagues. “As with all patients, physicians should be aware of the potential for depression, demoralization, and suicide.”
In addition, dementia, Alzheimer’s disease, and intellectual disabilities may be associated with lower suicide rates, according to the study, which was published in JAMA.
“Plausible mechanisms” could underlie the association between neurologic disease and suicide, the authors wrote. A neurologic diagnosis “may constitute a distressing life event,” and the diseases may have psychological, physical, and psychiatric effects. Patients may see themselves as a burden or have less financial security. In addition, the diseases may entail “communication difficulties, poor sleep, and pain.” Neurologic diseases may alter brain circuitry and functioning and influence aggression and impulsivity. “People with neurologic disorders may also have easier access to toxic medication,” they added.
More than a dozen conditions examined
Prior studies have found associations between neurologic conditions and rates of suicide, but data have been inconclusive or inconsistent for some of the disorders. To examine whether people with neurologic disorders have higher suicide rates, relative to people without these disorders, the researchers conducted a retrospective study. They analyzed data from more than 7.3 million people aged 15 years or older who lived in Denmark between 1980 and 2016. The cohort included more than 1.2 million people with neurologic disorders. The investigators identified neurologic disorders using ICD codes for head injury, stroke, epilepsy, polyneuropathy, diseases of the myoneural junction, Parkinson’s disease, multiple sclerosis, CNS infections, meningitis, encephalitis, amyotrophic lateral sclerosis, Huntington’s disease, dementia, intellectual disability, and other brain disorders. They compared incidence rates using a Poisson regression model and adjusted for time period, sex, age, region, socioeconomic status, comorbidity, self-harm or psychiatric hospitalization prior to a neurologic diagnosis, and whether a person lived alone.
In all, 35,483 people in the cohort died by suicide at an average age of about 52 years; 77.4% were male. About 15% of those who died by suicide had a neurologic disorder. The suicide incidence rate among people with a neurologic disorder was 44.0 per 100,000 person-years, whereas the rate among people without a neurologic disorder was 20.1 per 100,000 person-years.
The adjusted incidence rate ratio for people with a neurologic disorder was 1.8. The rate ratio was highest during the 3 months after diagnosis, at 3.1. Huntington’s disease and amyotrophic lateral sclerosis were associated with “the largest excess adjusted [incidence rate ratios] of suicide mortality,” with a rate ratio of 4.9 for each condition, the researchers reported. The adjusted incidence rate ratio was 1.7 for head injury, 1.3 for stroke, 1.7 for epilepsy, 1.4 for intracerebral hemorrhage, 1.3 for cerebral infarction, 1.3 for subarachnoid hemorrhage, 1.7 for polyneuropathy and peripheral neuropathy, 2.2 for Guillain-Barré syndrome, 1.9 for diseases of myoneural junction and muscle, 1.8 for other brain disorders, 1.7 for Parkinson’s disease, 2.2 for multiple sclerosis, and 1.6 for CNS infection.
Compared with people without a neurologic condition, people with dementia, Alzheimer’s disease, and intellectual disabilities had lower suicide rates, with adjusted incidence rate ratios of 0.8, 0.2, and 0.6, respectively. “However, the adjusted [incidence rate ratio] for people with dementia during the first month after diagnosis was 3.0,” the researchers wrote.
In addition, the suicide rate increased with an increasing cumulative number of hospital contacts for neurologic conditions.
Overall incidence rates declined
“Over the study period, the suicide incidence rate for people with neurological disorders decreased from 78.6 per 100,000 person-years during the 1980-1999 years to 27.3 per 100,000 person-years during the 2000-2016 years,” wrote Dr. Erlangsen and colleagues. “The suicide incidence rate for those without a disorder decreased from 26.3 to 12.7 during the same time spans. ... The decline in the overall suicide rate over time did not affect the relative risk pattern.”
The decline in the general suicide rate in Denmark “has largely been attributed to means restriction, such as efforts to limit availability of firearms and particularly toxic medication,” the authors added.
In those time spans, the adjusted incidence rate ratio for suicide among those with dementia decreased from 2.4 to 1.0, and among those with multiple sclerosis from 2.0 to 1.0. “It is possible that the improvements observed for dementia and multiple sclerosis may be related to improvements in treatment and intensified community-based support,” Dr. Erlangsen and coauthors wrote.
When the researchers used people with rheumatoid arthritis as a reference group, those with a neurologic disorder had a higher suicide rate per 100,000 person-years, 30.2 versus 18.4. The adjusted incidence rate ratio for that comparison was 1.4.
In patients with Huntington’s disease, depression mediated by hyperactivity in the hypothalamic-pituitary-adrenal axis may contribute to the risk of suicide. “Witnessing the course of the disease in one’s parent” also may contribute the risk, the researchers wrote.
The analysis may have missed people with neurologic disorders diagnosed before 1977 if they did not have subsequent contact with a hospital, the investigators noted. In addition, diagnoses given in primary care were not included, suicide deaths may be underrecorded, and “adjusting for preexisting mental disorders could be viewed as overadjusting,” they wrote.
The study was supported by a grant from the Psychiatric Research Foundation in Denmark. The authors reported that they had no disclosures.
SOURCE: Erlangsen A et al. JAMA. 2020 Feb 4. doi: 10.1001/jama.2019.21834.
FROM JAMA
Opioid use disorder in adolescents: An overview
Ms. L, age 17, seeks treatment because she has an ongoing struggle with multiple substances, including benzodiazepines, heroin, alcohol, cannabis, and prescription opioids.
She reports that she was 13 when she first used a prescription opioid that was not prescribed for her. She also reports engaging in unsafe sexual practices while using these substances, and has been diagnosed and treated for a sexually transmitted disease. She dropped out of school and is estranged from her family. She says that for a long time she has felt depressed and that she uses drugs to “self-medicate my emotions.” She endorses high anxiety and lack of motivation. Ms. L also reports having several criminal charges for theft, assault, and exchanging sex for drugs. She has undergone 3 admissions for detoxification, but promptly resumed using drugs, primarily heroin and oxycodone, immediately after discharge. Ms. L meets DSM-5 criteria for opioid use disorder (OUD).
Ms. L’s case illustrates a disturbing trend in the current opioid epidemic in the United States. Nearly 11.8 million individuals age ≥12 reported misuse of opioids in the last year.1 Adolescents who misuse prescription or illicit opioids are more likely to be involved with the legal system due to truancy, running away from home, physical altercations, prostitution, exchanging sex for drugs, robbery, and gang involvement. Adolescents who use opioids may also struggle with academic decline, drop out of school early, be unable to maintain a job, and have relationship difficulties, especially with family members.
In this article, I describe the scope of OUD among adolescents, including epidemiology, clinical manifestations, screening tools, and treatment approaches.
Scope of the problem
According to the most recent Monitoring the Future survey of more than 42,500 8th, 10th, and 12th grade students, 2.7% of 12th graders reported prescription opioid misuse (reported in the survey as “narcotics other than heroin”) in the past year.2 In addition, 0.4% of 12th graders reported heroin use over the same period.2 Although the prevalence of opioid use among adolescents has been declining over the past 5 years,2 it still represents a serious health crisis.
Part of the issue may relate to easier access to more potent opioids. For example, heroin available today can be >4 times purer than it was in the past. In 2002, t
Between 1997 and 2012, the annual incidence of youth (age 15 to 19) hospitalizations for prescription opioid poisoning increased >170%.5 Approximately 6% to 9% of youth involved in risky opioid use develop OUD 6 to 12 months after s
Continue to: In recent years...
In recent years, deaths from drug overdose have increased for all age groups; however, limited data is available regarding adolescent overdose deaths. According to the Centers for Disease Control and Prevention (CDC), from 2015 to 2016, drug overdose death rates for persons age 15 to 24 increased to 28%.9
How opioids work
Opioids activate specific transmembrane neurotransmitter receptors, including mu, kappa, and delta, in the CNS and peripheral nervous system (PNS). This leads to activation of G protein–mediated intracellular signal transduction. Mainly it is activation of endogenous mu opioid receptors that mediates the reward, withdrawal, and analgesic effects of opioids. These effects depend on the location of mu receptors. In the CNS, activation of mu opioid receptors may cause miosis, respiratory depression, euphoria, and analgesia.10
Different opioids vary in terms of their half-life; for most opioids, the half-life ranges from 2 to 4 hours.10 Heroin has a half-life of 30 minutes, but due to active metabolites its duration of action is 4 to 5 hours. Opioid metabolites can be detected in urine toxicology within approximately 1 to 2 days since last use.10
Chronic opioid use is associated with neurologic effects that change the function of areas of the brain that control pleasure/reward, stress, decision-making, and more. This leads to cravings, continued substance use, and dependence.11 After continued long-term use, patients report decreased euphoria, but typically they continue to use opioids to avoid withdrawal symptoms or worsening mood.
Criteria for opioid use disorder
In DSM-5, substance use disorders (SUDs)are no longer categorized as abuse or dependence.12 For opioids, the diagnosis is OUD. The Table12 outlines the DSM-5 criteria for OUD. Craving opioids is included for the first time in the OUD diagnosis. Having problems with the legal system is no longer considered a diagnostic criterion for OUD.
Continue to: A vulnerable population
A vulnerable population
As defined by Erik Erikson’s psychosocial stages of development, adolescents struggle between establishing their own identity vs role confusion.13 In an attempt to relate to peers or give in to peer pressure, some adolescents start by experimenting with nicotine, alcohol, and/or marijuana; however, some may move on to using other illicit drugs.14 Risk factors for the development of SUDs include early onset of substance use and a rapid progression through stages of substance use from experimentation to regular use, risky use, and dependence.15 In our case study, Ms. L’s substance use followed a similar pattern. Further, the comorbidity of SUDs and other psychiatric disorders may add a layer of complexity when caring for adolescents. Box 116-20 describes the relationship between comorbid psychiatric disorders and SUDs in adolescents.
Box 1
Disruptive behavior disorders are the most common coexisting psychiatric disorders in an adolescent with a substance use disorder (SUD), including opioid use disorder. These individuals typically present with aggression and other conduct disorder symptoms, and have early involvement with the legal system. Conversely, patients with conduct disorder are at high risk of early initiation of illicit substance use, including opioids. Early onset of substance use is a strong risk factor for developing an SUD.16
Mood disorders, particularly depression, can either precede or occur as a result of heavy and prolonged substance use.17 The estimated prevalence of major depressive disorder in individuals with an SUD is 24% to 50%. Among adolescents, an SUD is also a risk factor for suicidal ideation, suicide attempts, and completed suicide.18-20
Anxiety disorders, especially social phobia, and posttraumatic stress disorder are common in individuals with SUD.
Adolescents with SUD should be carefully evaluated for comorbid psychiatric disorders and treated accordingly.
Clinical manifestations
Common clinical manifestations of opioid use vary depending on when the patient is seen. An individual with OUD may appear acutely intoxicated, be in withdrawal, or show no effects. Chronic/prolonged use can lead to tolerance, such that a user needs to ingest larger amounts of the opioid to produce the same effects.
Acute intoxication can cause sedation, slurring of speech, and pinpoint pupils. Fresh injection sites may be visible on physical examination of IV users. The effects of acute intoxication usually depend on the half-life of the specific opioid and the individual’s tolerance.10 Tolerance to heroin can occur in 10 days and withdrawal can manifest in 3 to 7 hours after last use, depending on dose and purity.3 Tolerance can lead to unintentional overdose and death.
Withdrawal. Individuals experiencing withdrawal from opioids present with flu-like physical symptoms, including generalized body ache, rhinorrhea, diarrhea, goose bumps, lacrimation, and vomiting. Individuals also may experience irritability, restlessness, insomnia, anxiety, and depression during withdrawal.
Other manifestations. Excessive and chronic/prolonged opioid use can adversely impact socio-occupational functioning and cause academic decline in adolescents and youth. Personal relationships are significantly affected. Opioid users may have legal difficulties as a result of committing crimes such as theft, prostitution, or robbery in order to obtain opioids.
Continue to: Screening for OUD
Screening for OUD
Several screening tools are available to assess adolescents for SUDs, including OUD.
CRAFFT is a 6-item, clinician-administered screening tool that has been approved by American Academy of Pediatrics’ Committee on Substance Abuse for adolescents and young adults age <21.21-23 This commonly used tool can assess for alcohol, cannabis, and other drug use. A score ≥2 is considered positive for drug use, indicating that the individual would require further evaluation and assessment22,23 (Figure). There is also a self-administered CRAFFT questionnaire that can be completed by the patient.
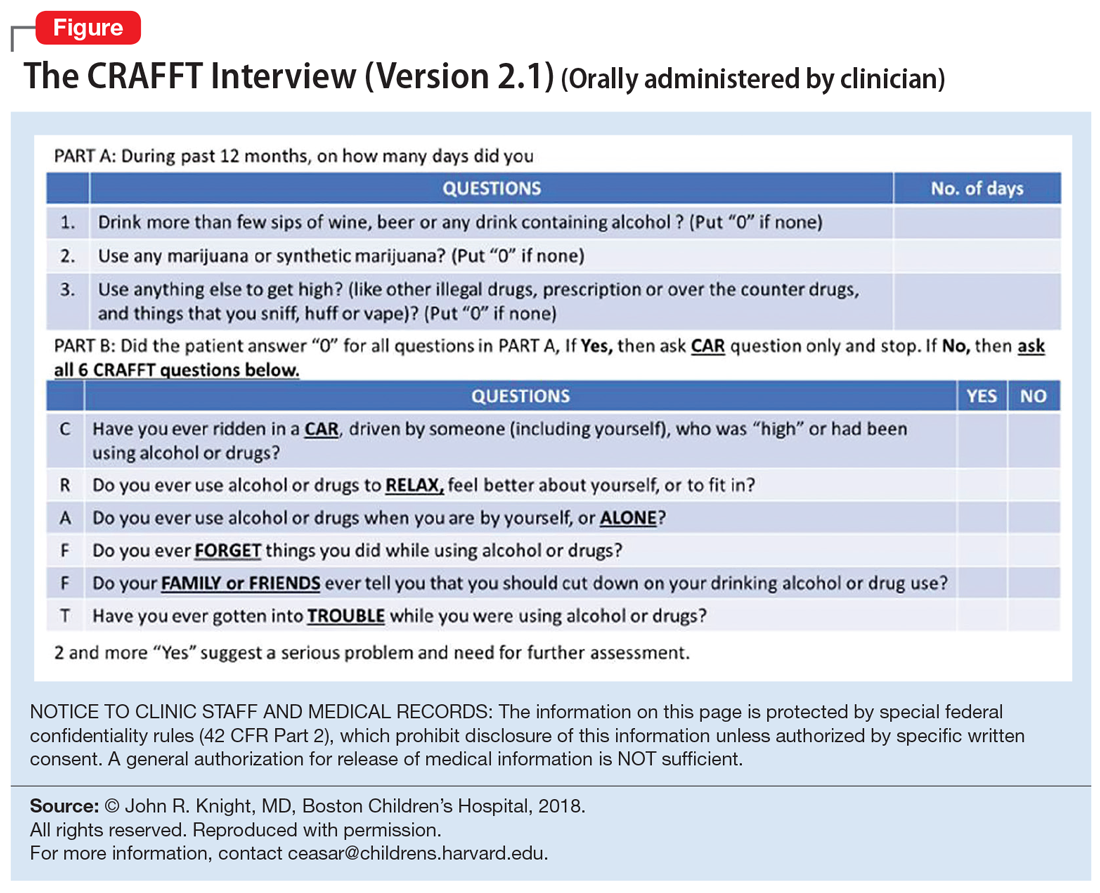
NIDA-modified ASSIST. The American Psychiatric Association has adapted the National Institute on Drug Abuse (NIDA)-modified ASSIST. One version is designated for parents/guardians to administer to their children (age 6 to 17), and one is designated for adolescents (age 11 to 17) to self-administer.24,25 Each screening tool has 2 levels: Level 1 screens for substance use and other mental health symptoms, and Level 2 is more specific for substance use alone.
Drug Use Screening Inventory (DUSI) is a self-report questionnaire that has 149 items that assess the use of numerous drugs. It is designed to quantify the severity of consequences associated with drug and alcohol use.26,27
Problem-Oriented Screening Instrument for Teenagers (PO
Continue to: Personal Experience Screening Questionnaire (PESQ)...
Personal Experience Screening Questionnaire (PESQ) is a brief, 40-item, cost-effective, self-report questionnaire that can help identify adolescents (age 12 to 18) who should be referred for further evaluation.30
Addressing treatment expectations
For an adolescent with OUD, treatment should begin in the least restrictive environment that is perceived as safe for the patient. An adolescent’s readiness and motivation to achieve and maintain abstinence are crucial. Treatment planning should include the adolescent as well as his/her family to ensure they are able to verbalize their expectations. Start with a definitive treatment plan that addresses an individual’s needs. The plan should provide structure and an understanding of treatment expectations. The treatment team should clarify the realistic plan and goals based on empirical and clinical evidence. Treatment goals should include interventions to strengthen interpersonal relationships and assist with rehabilitation, such as establishing academic and/or vocational goals. Addressing readiness and working on a patient’s motivation is extremely important for most of these interventions.
In order for any intervention to be successful, clinicians need to establish and foster rapport with the adolescent. By law, substance use or behaviors related to substance use are not allowed to be shared outside the patient-clinician relationship, unless the adolescent gives consent or there are concerns that such behaviors might put the patient or others at risk. It is important to prime the adolescent and help them understand that any information pertaining to their safety or the safety of others may need to be shared outside the patient-clinician relationship.
Choosing an intervention
Less than 50% of a nationally representative sample of 345 addiction treatment programs serving adolescents and adults offer medications for treating OUD.31 Even in programs that offer pharmacotherapy, medications are significantly underutilized. Fewer than 30% of patients in addiction treatment programs receive medication, compared with 74% of patients receiving treatment for other mental health disorders.31 A
Psychotherapy may be used to treat OUD in adolescents. Several family therapies have been studied and are considered as critical psychotherapeutic interventions for treating SUDs, including structural family treatment and functional family therapy approaches.34 An integrated behavioral and family therapy model is also recommended for adolescent patients with SUDs. Cognitive distortions and use of self-deprecatory statements are common among adolescents.35 Therefore, using approaches of cognitive-behavioral therapy (CBT), or CBT plus motivational enhancement therapy, also might be effective for this population.36 The adolescent community reinforcement approach (A-CRA) is a behavioral treatment designed to help adolescents and their families learn how to lead a healthy and happy life without the use of drugs or alcohol by increasing access to social, familial, and educational/vocational reinforcers. Support groups and peer and family support should be encouraged as adjuncts to other interventions. In some areas, sober housing options for adolescents are also available.
Continue to: Harm-reduction strategies
Harm-reduction strategies. Although the primary goal of treatment for adolescents with OUD is to achieve and maintain abstinence from opioid use, implicit and explicit goals can be set. Short-term implicit goals may include harm-reduction strategies that emphasize decreasing the duration, frequency, and amount of substance use and limiting the chances of adverse effects, while the long-term explicit goal should be abstinence from opioid use.
Naloxone nasal spray is used as a harm-reduction strategy. It is an FDA-approved formulation that can reverse the effects of unintentional opioid overdoses and potentially prevent death from respiratory depression.37 Other harm-reduction strategies include needle exchange programs, which provide sterile needles to individuals who inject drugs in an effort to prevent or reduce the transmission of human immunodeficiency virus and other bloodborne viruses that can be spread via shared injection equipment. Fentanyl testing strips allow opioid users to test for the presence fentanyl and fentanyl analogs in the unregulated “street” opioid supply.
Pharmacologic interventions. Because there is limited empirical evidence on the efficacy of medication-assisted treatment (MAT) for adolescents with OUD, clinicians need to rely on evidence from research and experience with adults. Unfortunately, MAT is offered to adolescents considerably less often than it is to adults. Feder et al38 reported that only 2.4% of adolescents received MAT for heroin use and only 0.4% of adolescents received MAT for prescription opioid use, compared with 26.3% and 12% of adults, respectively.
Detoxification. Medications available for detoxification from opioids include opiates (such as methadone or buprenorphine) and clonidine (a central sympathomimetic). If the patient has used heroin for a short period (<1 year) and has no history of detoxification, consider a detoxification strategy with a longer-term taper (90 to 180 days) to allow for stabilization.
Maintenance treatment. Consider maintenance treatment for adolescents with a history of long-term opioid use and at least 2 prior short-term detoxification attempts or nonpharmacotherapy-based treatment within 12 months. Be sure to receive consent from a legal guardian and the patient. Maintenance treatment is usually recommended to continue for 1 to 6 years. Maintenance programs with longer durations have shown higher rates of abstinence, improved engagement, and retention in treatment.39
Continue to: According to guidelines from...
According to guidelines from the American Society of Addiction Medicine (ASAM), adolescents age >16 should be offered MAT; the first-line treatment is buprenorphine.40 To avoid risks of abuse and diversion, a combination of buprenorphine/naloxone may be administered.
Maintenance with buprenorphine
In order to prescribe and dispense buprenorphine, clinicians need to obtain a waiver from the Substance Abuse and Mental Health Services Administration. Before initiating buprenorphine, consider the type of opioid the individual used (short- or long-acting), the severity of the OUD, and the last reported use. The 3 phases of buprenorphine treatment are41:
- Induction phase. Buprenorphine can be initiated at 2 to 4 mg/d. Some patients may require up to 8 mg/d on the first day, which can be administered in divided doses.42 Evaluate and monitor patients carefully during the first few hours after the first dose. Patients should be in early withdrawal; otherwise, the buprenorphine might precipitate withdrawal. The induction phase can be completed in 2 to 4 days by titrating the dose so that the signs and symptoms of opioid withdrawal are minimal, and the patient is able to continue treatment. It may be helpful to have the patient’s legal guardian nearby in case the patient does not tolerate the medication or experiences withdrawal. The initial target dose for buprenorphine is approximately 12 to 16 mg/d.
- Stabilization phase. Patients no longer experience withdrawal symptoms and no longer have cravings. This phase can last 6 to 8 weeks. During this phase, patients should be seen weekly and doses should be adjusted if necessary. As a partial mu agonist, buprenorphine does not activate mu receptors fully and reaches a ceiling effect. Hence, doses >24 mg/d have limited added agonist properties.
- Maintenance phase. Because discontinuation of buprenorphine is associated with high relapse rates, patients may need to be maintained long-term on their stabilization dose, and for some patients, the length of time could be indefinite.39 During this phase, patients continue to undergo follow-up, but do so less frequently.
Methadone maintenance is generally not recommended for individuals age <18.
Preventing opioid diversion
Prescription medications that are kept in the home are a substantial source of opioids for adolescents. In 2014, 56% of 12th graders who did not need medications for medical purposes were able to acquire them from their friends or relatives; 36% of 12th graders used their own prescriptions.21 Limiting adolescents’ access to prescription opioids is the first line of prevention. Box 2 describes interventions and strategies to limit adolescents’ access to opioids.
Box 2
Many adolescents obtain opioids for recreational use from medications that were legitimately prescribed to family or friends. Both clinicians and parents/ guardians can take steps to reduce or prevent this type of diversion
Health care facilities. Regulating the number of pills dispensed to patients is crucial. It is highly recommended to prescribe only the minimal number of opioids necessary. In most cases, 3 to 7 days’ worth of opioids at a time might be sufficient, especially after surgical procedures.
Home. Families can limit adolescents’ access to prescription opioids in the home by keeping all medications in a lock box.
Proper disposal. Various entities offer locations for patients to drop off their unused opioids and other medications for safe disposal. These include police or fire departments and retail pharmacies. The US Drug Enforcement Administration sponsors a National Prescription Drug Take Back Day; see https://www.deadiversion.usdoj.gov/drug_disposal/takeback/index.html. The FDA also offers information on where and how to dispose of unused medicines at https://www.fda.gov/consumers/consumer-updates/where-and-how-dispose-unused-medicines.
CASE CONTINUED
Ms. L is initially prescribed, clonidine, 0.1 mg every 6 hours, to address opioid withdrawal. Clonidine is then tapered and maintained at 0.1 mg twice a day for irritability and impulse control. She is also prescribed sertraline, 100 mg/d, for depression and anxiety, and trazodone, 75 mg as needed at night, to assist with sleep.
Continue to: Following inpatient hospitalization...
Following inpatient hospitalization, during 12 weeks of partial hospital treatment, Ms. L participates in individual psychotherapy sessions 5 days/week; family therapy sessions once a week; and experiential therapy along with group sessions with other peers. She undergoes medication evaluations and adjustments on a weekly basis. Ms. L is now working at a store and is pursuing a high school equivalency certificate. She manages to avoid high-risk behaviors, although she reports having occasional cravings. Ms. L is actively involved in Narcotics Anonymous and has a sponsor. She has reconciled with her mother and moved back home, so she can stay away from her former acquaintances who are still using.
Bottom Line
Adolescents with opioid use disorder can benefit from an individualized treatment plan that includes psychosocial interventions, pharmacotherapy, or a combination of the two. Treatment planning should include the adolescent and his/her family to ensure they are able to verbalize their expectations. Treatment should focus on interventions that strengthen interpersonal relationships and assist with rehabilitation. Ongoing follow-up care is necessary for maintaining abstinence.
Related Resource
- Patkar AA, Weisler RH. Opioid abuse and overdose: Keep your patients safe. Current Psychiatry. 2017;16(8):8-12,14-16.
Drug Brand Names
Buprenorphine • Subutex, Sublocade
Buprenorphine/naloxone • Suboxone
Clonidine • Clorpres
Methadone • Methadose
Naloxone • Narcan
Oxycodone • OxyContin
Sertraline • Zoloft
Tramadol • Ultram
Trazodone • Desyrel, Oleptro
1. Davis JP, Prindle JJ, Eddie D, et al. Addressing the opioid epidemic with behavioral interventions for adolescents and young adults: a quasi-experimental design. J Consult Clin Psychol. 2019;87(10):941-951.
2. National Institute on Drug Abuse; National Institutes of Health; U.S. Department of Health and Human Services. Monitoring the Future Survey: High School and Youth Trends. https://www.drugabuse.gov/publications/drugfacts/monitoring-future-survey-high-school-youth-trends. Updated December 2019. Accessed January 13, 2020.
3. Hopfer CJ, Khuri E, Crowley TJ. Treating adolescent heroin use. J Am Acad Child Adolesc Psychiatry. 2003;42(5):609-611.
4. US Department of Justice, Drug Enforcement Agency, Diversion Control Division. https://www.deadiversion.usdoj.gov/. Accessed January 21, 2020.
5. Gaither JR, Leventhal JM, Ryan SA, et al. National trends in hospitalizations for opioid poisonings among children and adolescents, 1997-2012. JAMA Pediatr. 2016;170(12):1195-1201.
6. Parker MA, Anthony JC. Epidemiological evidence on extra-medical use of prescription pain relievers: transitions from newly incident use to dependence among 12-21 year olds in United States using meta-analysis, 2002-13. Peer J. 2015;3:e1340. doi: 10.7717/peerj.1340. eCollection 2015.
7. Subramaniam GA, Fishman MJ, Woody G. Treatment of opioid-dependent adolescents and young adults with buprenorphine. Curr Psychiatry Rep. 2009;11(5):360-363.
8. Borodovsky JT, Levy S, Fishman M. Buprenorphine treatment for adolescents and young adults with opioid use disorders: a narrative review. J Addict Med. 2018;12(3):170-183.
9. Centers for Disease Control and Prevention: National Center for Health Statistics. Drug overdose deaths in the United States, 1999-2016. https://www.cdc.gov/nchs/products/databriefs/db294.htm. Published December 2017. Accessed January 15, 2020.
10. Strain E. Opioid use disorder: epidemiology, pharmacology, clinical manifestation, course, screening, assessment, diagnosis. https://www.uptodate.com/contents/opioid-use-disorder-epidemiology-pharmacology-clinical-manifestations-course-screening-assessment-and-diagnosis. Updated August 15, 2019. Accessed January 21, 2020.
11. American Academy of Pediatrics Committee on Substance Use and Prevention. Policy statement: medication-assisted treatment of adolescents with opioid use disorder. Pediatrics. 2016;138(3):e20161893. doi: https://doi.org/10.1542/peds.2016-1893.
12. Diagnostic and Statistical Manual of Mental Disorders, 5th ed. Washington, DC: American Psychiatric Association; 2013:514.
13. Sadock BJ, Sadock VA. Chapter 6: Theories of personality and psychopathology. In: Sadock BJ, Sadock VA, eds. Kaplan and Sadock’s synopsis of psychiatry: behavioral sciences/clinical. 10th ed. Philadelphia, PA: Lippincott Williams & Wilkins; 2007:209.
14. Kandel DB. Stages and pathways of drug involvement: examining the gateway hypothesis. Cambridge, United Kingdom: Cambridge University Press; 2002.
15. Robins LN, McEvoy L. Conduct problems as predictors of substance abuse. In: Robins LN, Rutter M, eds. Straight and devious pathways from childhood to adulthood. Cambridge, United Kingdom: Cambridge University Press; 1990;182-204.
16. Hopfer C, Salomonsen-Sautel S, Mikulich-Gilbertson S, et al. Conduct disorder and initiation of substance use: a prospective longitudinal study. J Am Acad Child Adolesc Psychiatry. 2013;52(5):511-518.e4.
17. Armstrong TD, Costello EJ. Community studies on adolescent substance use, abuse, or dependence and psychiatric comorbidity. J Consult Clin Psychol. 2002;70(6):1224-1239.
18. Crumley FE. Substance abuse and adolescent suicidal behavior. JAMA. 1990;263(22):3051-3056.
19. Lewinsohn PM, Rohde P, Seeley JR. Adolescent suicidal ideation and attempts: prevalence, risk factors, and clinical implications. Clinical Psychology: Science and Practice. 1996;3(1):25-46.
20. Kendler KS, Bulik CM, Silberg J, et al. Childhood sexual abuse and adult psychiatric and substance use disorder in women: an epidemiological and cotwin control analysis. Arch Gen Psychiatry. 2000;57(10):953-959.
21. Yule AM, Wilens TE, Rausch PK. The opioid epidemic: what a child psychiatrist is to do? J Am Acad Child Adolesc Psychiatry. 2017;56(7);541-543.
22. CRAFFT. https://crafft.org. Accessed January 21, 2020.
23. Knight JR, Sherritt L, Harris SK, et al. Validity of brief alcohol screening tests among adolescents: a comparison of the AUDIT, POSIT, CAGE, and CRAFFT. Alcohol Clin Exp Res. 2003;27(1):67-73.
24. American Psychiatric Association. Online assessment measures. https://www.psychiatry.org/psychiatrists/practice/dsm/educational-resources/assessment-measures. Accessed January 15, 2020.
25. National Institute of Drug Abuse. American Psychiatric Association adapted NIDA modified ASSIST tools. https://www.drugabuse.gov/nidamed-medical-health-professionals/tool-resources-your-practice/screening-assessment-drug-testing-resources/american-psychiatric-association-adapted-nida. Updated November 15, 2015. Accessed January 21, 2020.
26. Canada’s Mental Health & Addiction Network. Drug Use Screening Inventory (DUSI). https://www.porticonetwork.ca/web/knowledgex-archive/amh-specialists/screening-for-cd-in-youth/screening-both-mh-sud/dusi. Published 2009. Accessed January 21, 2020.
27. Tarter RE. Evaluation and treatment of adolescent substance abuse: a decision tree method. Am J Drug Alcohol Abuse. 1990;16(1-2):1-46.
28. Klitzner M, Gruenwald PJ, Taff GA, et al. The adolescent assessment referral system-final report. National Institute on Drug Abuse; Rockville, MD: 1993. NIDA Contract No. 271-89-8252.
29. Slesnick N, Tonigan JS. Assessment of alcohol and other drug use by runaway youths: a test-retest study of the Form 90. Alcohol Treat Q. 2004;22(2):21-34.
30. Winters KC, Kaminer Y. Screening and assessing adolescent substance use disorders in clinical populations. J Am Acad Child Adolesc Psychiatry. 2008;47(7):740-744.
31. Knudsen HK, Abraham AJ, Roman PM. Adoption and implementation of medications in addiction treatment programs. J Addict Med. 2011;5(1):21-27.
32. Deas D, Thomas SE. An overview of controlled study of adolescent substance abuse treatment. Am J Addiction. 2001;10(2):178-189.
33. William RJ, Chang, SY. A comprehensive and comparative review of adolescent substance abuse treatment outcome. Clinical Psychology: Science and Practice. 2000;7(2):138-166.
34. Bukstein OG, Work Group on Quality Issues. Practice parameters for the assessment and treatment of children and adolescents with substance use disorders. J Am Acad Child Adolesc Psychiatry. 2005;44(6):609-621.
35. Van Hasselt VB, Null JA, Kempton T, et al. Social skills and depression in adolescent substance abusers. Addict Behav. 1993;18(1):9-18.
36. Dennis M, Godley SH, Diamond G, et al. The Cannabis Youth Treatment (CYT) study: main findings from two randomized trials. J Subst Abuse Treat. 2004;27(3):197-213.
37. US Food and Drug Administration. Information about naloxone. https://www.fda.gov/drugs/postmarket-drug-safety-information-patients-and-providers/information-about-naloxone. Updated December 19, 2019. Accessed January 21, 2020.
38. Feder KA, Krawcyzk N, Saloner, B. Medication-assisted treatment for adolescents in specialty treatment for opioid use disorder. J Adolesc Health. 2018;60(6):747-750.
39. Woody GE, Poole SA, Subramaniam G, et al. Extended vs short-term buprenorphine-naloxone for treatment of opioid-addicted youth: a randomized trial. JAMA. 2008;300(17):2003-2011.
40. US Department of Health and Human Services. Substance Abuse and Mental Health Ser-vices Administration. Medication-assisted treatment for opioid addiction in opioid treatment programs: a treatment improvement protocol TIP 43. https://www.asam.org/docs/advocacy/samhsa_tip43_matforopioidaddiction.pdf?sfvrsn=0. Published 2005. Accessed January 15, 2020.
41. US Department of Health and Human Services. Substance Abuse and Mental Health Services Administration. Medication-assisted treatment (MAT). https://www.samhsa.gov/medication-assisted-treatment. Updated September 9, 2019. Accessed January 21, 2020.
42. Johnson RE, Strain EC, Amass L. Buprenorphine: how to use it right. Drug Alcohol Depend. 2003;70(suppl 2):S59-S77.
Ms. L, age 17, seeks treatment because she has an ongoing struggle with multiple substances, including benzodiazepines, heroin, alcohol, cannabis, and prescription opioids.
She reports that she was 13 when she first used a prescription opioid that was not prescribed for her. She also reports engaging in unsafe sexual practices while using these substances, and has been diagnosed and treated for a sexually transmitted disease. She dropped out of school and is estranged from her family. She says that for a long time she has felt depressed and that she uses drugs to “self-medicate my emotions.” She endorses high anxiety and lack of motivation. Ms. L also reports having several criminal charges for theft, assault, and exchanging sex for drugs. She has undergone 3 admissions for detoxification, but promptly resumed using drugs, primarily heroin and oxycodone, immediately after discharge. Ms. L meets DSM-5 criteria for opioid use disorder (OUD).
Ms. L’s case illustrates a disturbing trend in the current opioid epidemic in the United States. Nearly 11.8 million individuals age ≥12 reported misuse of opioids in the last year.1 Adolescents who misuse prescription or illicit opioids are more likely to be involved with the legal system due to truancy, running away from home, physical altercations, prostitution, exchanging sex for drugs, robbery, and gang involvement. Adolescents who use opioids may also struggle with academic decline, drop out of school early, be unable to maintain a job, and have relationship difficulties, especially with family members.
In this article, I describe the scope of OUD among adolescents, including epidemiology, clinical manifestations, screening tools, and treatment approaches.
Scope of the problem
According to the most recent Monitoring the Future survey of more than 42,500 8th, 10th, and 12th grade students, 2.7% of 12th graders reported prescription opioid misuse (reported in the survey as “narcotics other than heroin”) in the past year.2 In addition, 0.4% of 12th graders reported heroin use over the same period.2 Although the prevalence of opioid use among adolescents has been declining over the past 5 years,2 it still represents a serious health crisis.
Part of the issue may relate to easier access to more potent opioids. For example, heroin available today can be >4 times purer than it was in the past. In 2002, t
Between 1997 and 2012, the annual incidence of youth (age 15 to 19) hospitalizations for prescription opioid poisoning increased >170%.5 Approximately 6% to 9% of youth involved in risky opioid use develop OUD 6 to 12 months after s
Continue to: In recent years...
In recent years, deaths from drug overdose have increased for all age groups; however, limited data is available regarding adolescent overdose deaths. According to the Centers for Disease Control and Prevention (CDC), from 2015 to 2016, drug overdose death rates for persons age 15 to 24 increased to 28%.9
How opioids work
Opioids activate specific transmembrane neurotransmitter receptors, including mu, kappa, and delta, in the CNS and peripheral nervous system (PNS). This leads to activation of G protein–mediated intracellular signal transduction. Mainly it is activation of endogenous mu opioid receptors that mediates the reward, withdrawal, and analgesic effects of opioids. These effects depend on the location of mu receptors. In the CNS, activation of mu opioid receptors may cause miosis, respiratory depression, euphoria, and analgesia.10
Different opioids vary in terms of their half-life; for most opioids, the half-life ranges from 2 to 4 hours.10 Heroin has a half-life of 30 minutes, but due to active metabolites its duration of action is 4 to 5 hours. Opioid metabolites can be detected in urine toxicology within approximately 1 to 2 days since last use.10
Chronic opioid use is associated with neurologic effects that change the function of areas of the brain that control pleasure/reward, stress, decision-making, and more. This leads to cravings, continued substance use, and dependence.11 After continued long-term use, patients report decreased euphoria, but typically they continue to use opioids to avoid withdrawal symptoms or worsening mood.
Criteria for opioid use disorder
In DSM-5, substance use disorders (SUDs)are no longer categorized as abuse or dependence.12 For opioids, the diagnosis is OUD. The Table12 outlines the DSM-5 criteria for OUD. Craving opioids is included for the first time in the OUD diagnosis. Having problems with the legal system is no longer considered a diagnostic criterion for OUD.
Continue to: A vulnerable population
A vulnerable population
As defined by Erik Erikson’s psychosocial stages of development, adolescents struggle between establishing their own identity vs role confusion.13 In an attempt to relate to peers or give in to peer pressure, some adolescents start by experimenting with nicotine, alcohol, and/or marijuana; however, some may move on to using other illicit drugs.14 Risk factors for the development of SUDs include early onset of substance use and a rapid progression through stages of substance use from experimentation to regular use, risky use, and dependence.15 In our case study, Ms. L’s substance use followed a similar pattern. Further, the comorbidity of SUDs and other psychiatric disorders may add a layer of complexity when caring for adolescents. Box 116-20 describes the relationship between comorbid psychiatric disorders and SUDs in adolescents.
Box 1
Disruptive behavior disorders are the most common coexisting psychiatric disorders in an adolescent with a substance use disorder (SUD), including opioid use disorder. These individuals typically present with aggression and other conduct disorder symptoms, and have early involvement with the legal system. Conversely, patients with conduct disorder are at high risk of early initiation of illicit substance use, including opioids. Early onset of substance use is a strong risk factor for developing an SUD.16
Mood disorders, particularly depression, can either precede or occur as a result of heavy and prolonged substance use.17 The estimated prevalence of major depressive disorder in individuals with an SUD is 24% to 50%. Among adolescents, an SUD is also a risk factor for suicidal ideation, suicide attempts, and completed suicide.18-20
Anxiety disorders, especially social phobia, and posttraumatic stress disorder are common in individuals with SUD.
Adolescents with SUD should be carefully evaluated for comorbid psychiatric disorders and treated accordingly.
Clinical manifestations
Common clinical manifestations of opioid use vary depending on when the patient is seen. An individual with OUD may appear acutely intoxicated, be in withdrawal, or show no effects. Chronic/prolonged use can lead to tolerance, such that a user needs to ingest larger amounts of the opioid to produce the same effects.
Acute intoxication can cause sedation, slurring of speech, and pinpoint pupils. Fresh injection sites may be visible on physical examination of IV users. The effects of acute intoxication usually depend on the half-life of the specific opioid and the individual’s tolerance.10 Tolerance to heroin can occur in 10 days and withdrawal can manifest in 3 to 7 hours after last use, depending on dose and purity.3 Tolerance can lead to unintentional overdose and death.
Withdrawal. Individuals experiencing withdrawal from opioids present with flu-like physical symptoms, including generalized body ache, rhinorrhea, diarrhea, goose bumps, lacrimation, and vomiting. Individuals also may experience irritability, restlessness, insomnia, anxiety, and depression during withdrawal.
Other manifestations. Excessive and chronic/prolonged opioid use can adversely impact socio-occupational functioning and cause academic decline in adolescents and youth. Personal relationships are significantly affected. Opioid users may have legal difficulties as a result of committing crimes such as theft, prostitution, or robbery in order to obtain opioids.
Continue to: Screening for OUD
Screening for OUD
Several screening tools are available to assess adolescents for SUDs, including OUD.
CRAFFT is a 6-item, clinician-administered screening tool that has been approved by American Academy of Pediatrics’ Committee on Substance Abuse for adolescents and young adults age <21.21-23 This commonly used tool can assess for alcohol, cannabis, and other drug use. A score ≥2 is considered positive for drug use, indicating that the individual would require further evaluation and assessment22,23 (Figure). There is also a self-administered CRAFFT questionnaire that can be completed by the patient.
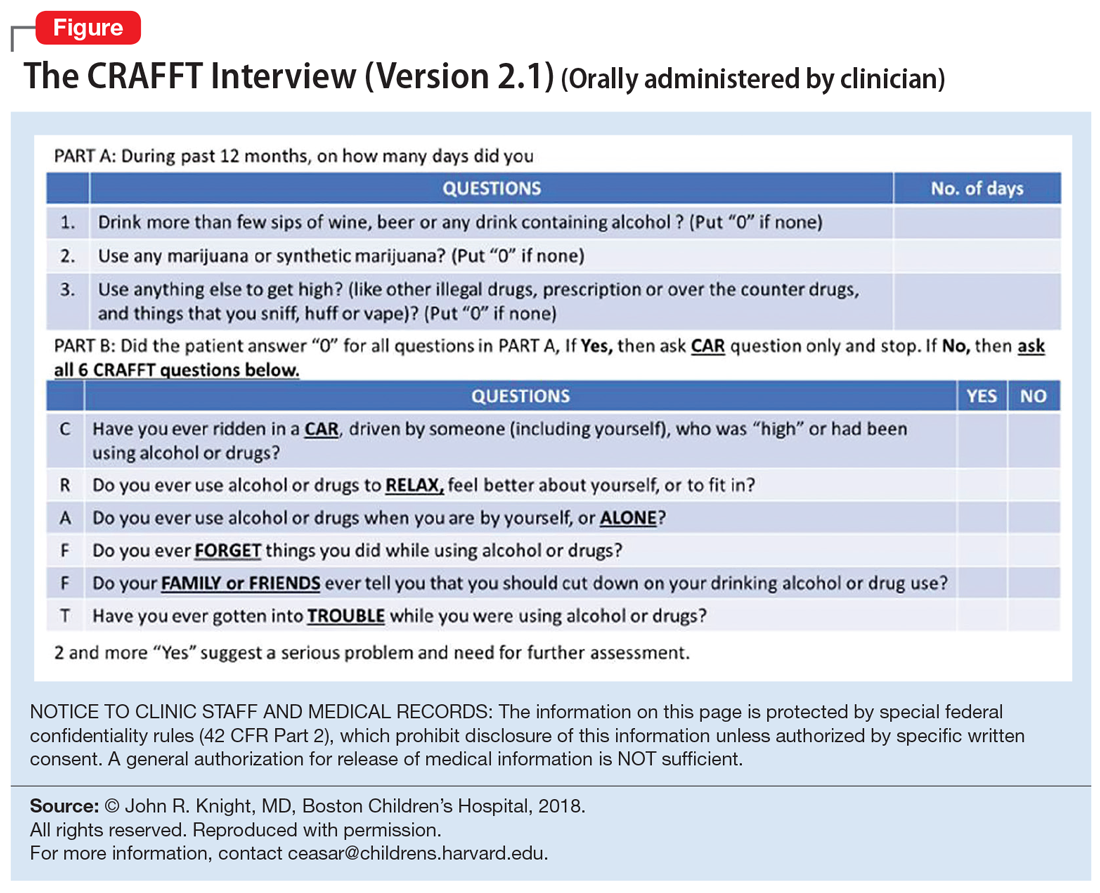
NIDA-modified ASSIST. The American Psychiatric Association has adapted the National Institute on Drug Abuse (NIDA)-modified ASSIST. One version is designated for parents/guardians to administer to their children (age 6 to 17), and one is designated for adolescents (age 11 to 17) to self-administer.24,25 Each screening tool has 2 levels: Level 1 screens for substance use and other mental health symptoms, and Level 2 is more specific for substance use alone.
Drug Use Screening Inventory (DUSI) is a self-report questionnaire that has 149 items that assess the use of numerous drugs. It is designed to quantify the severity of consequences associated with drug and alcohol use.26,27
Problem-Oriented Screening Instrument for Teenagers (PO
Continue to: Personal Experience Screening Questionnaire (PESQ)...
Personal Experience Screening Questionnaire (PESQ) is a brief, 40-item, cost-effective, self-report questionnaire that can help identify adolescents (age 12 to 18) who should be referred for further evaluation.30
Addressing treatment expectations
For an adolescent with OUD, treatment should begin in the least restrictive environment that is perceived as safe for the patient. An adolescent’s readiness and motivation to achieve and maintain abstinence are crucial. Treatment planning should include the adolescent as well as his/her family to ensure they are able to verbalize their expectations. Start with a definitive treatment plan that addresses an individual’s needs. The plan should provide structure and an understanding of treatment expectations. The treatment team should clarify the realistic plan and goals based on empirical and clinical evidence. Treatment goals should include interventions to strengthen interpersonal relationships and assist with rehabilitation, such as establishing academic and/or vocational goals. Addressing readiness and working on a patient’s motivation is extremely important for most of these interventions.
In order for any intervention to be successful, clinicians need to establish and foster rapport with the adolescent. By law, substance use or behaviors related to substance use are not allowed to be shared outside the patient-clinician relationship, unless the adolescent gives consent or there are concerns that such behaviors might put the patient or others at risk. It is important to prime the adolescent and help them understand that any information pertaining to their safety or the safety of others may need to be shared outside the patient-clinician relationship.
Choosing an intervention
Less than 50% of a nationally representative sample of 345 addiction treatment programs serving adolescents and adults offer medications for treating OUD.31 Even in programs that offer pharmacotherapy, medications are significantly underutilized. Fewer than 30% of patients in addiction treatment programs receive medication, compared with 74% of patients receiving treatment for other mental health disorders.31 A
Psychotherapy may be used to treat OUD in adolescents. Several family therapies have been studied and are considered as critical psychotherapeutic interventions for treating SUDs, including structural family treatment and functional family therapy approaches.34 An integrated behavioral and family therapy model is also recommended for adolescent patients with SUDs. Cognitive distortions and use of self-deprecatory statements are common among adolescents.35 Therefore, using approaches of cognitive-behavioral therapy (CBT), or CBT plus motivational enhancement therapy, also might be effective for this population.36 The adolescent community reinforcement approach (A-CRA) is a behavioral treatment designed to help adolescents and their families learn how to lead a healthy and happy life without the use of drugs or alcohol by increasing access to social, familial, and educational/vocational reinforcers. Support groups and peer and family support should be encouraged as adjuncts to other interventions. In some areas, sober housing options for adolescents are also available.
Continue to: Harm-reduction strategies
Harm-reduction strategies. Although the primary goal of treatment for adolescents with OUD is to achieve and maintain abstinence from opioid use, implicit and explicit goals can be set. Short-term implicit goals may include harm-reduction strategies that emphasize decreasing the duration, frequency, and amount of substance use and limiting the chances of adverse effects, while the long-term explicit goal should be abstinence from opioid use.
Naloxone nasal spray is used as a harm-reduction strategy. It is an FDA-approved formulation that can reverse the effects of unintentional opioid overdoses and potentially prevent death from respiratory depression.37 Other harm-reduction strategies include needle exchange programs, which provide sterile needles to individuals who inject drugs in an effort to prevent or reduce the transmission of human immunodeficiency virus and other bloodborne viruses that can be spread via shared injection equipment. Fentanyl testing strips allow opioid users to test for the presence fentanyl and fentanyl analogs in the unregulated “street” opioid supply.
Pharmacologic interventions. Because there is limited empirical evidence on the efficacy of medication-assisted treatment (MAT) for adolescents with OUD, clinicians need to rely on evidence from research and experience with adults. Unfortunately, MAT is offered to adolescents considerably less often than it is to adults. Feder et al38 reported that only 2.4% of adolescents received MAT for heroin use and only 0.4% of adolescents received MAT for prescription opioid use, compared with 26.3% and 12% of adults, respectively.
Detoxification. Medications available for detoxification from opioids include opiates (such as methadone or buprenorphine) and clonidine (a central sympathomimetic). If the patient has used heroin for a short period (<1 year) and has no history of detoxification, consider a detoxification strategy with a longer-term taper (90 to 180 days) to allow for stabilization.
Maintenance treatment. Consider maintenance treatment for adolescents with a history of long-term opioid use and at least 2 prior short-term detoxification attempts or nonpharmacotherapy-based treatment within 12 months. Be sure to receive consent from a legal guardian and the patient. Maintenance treatment is usually recommended to continue for 1 to 6 years. Maintenance programs with longer durations have shown higher rates of abstinence, improved engagement, and retention in treatment.39
Continue to: According to guidelines from...
According to guidelines from the American Society of Addiction Medicine (ASAM), adolescents age >16 should be offered MAT; the first-line treatment is buprenorphine.40 To avoid risks of abuse and diversion, a combination of buprenorphine/naloxone may be administered.
Maintenance with buprenorphine
In order to prescribe and dispense buprenorphine, clinicians need to obtain a waiver from the Substance Abuse and Mental Health Services Administration. Before initiating buprenorphine, consider the type of opioid the individual used (short- or long-acting), the severity of the OUD, and the last reported use. The 3 phases of buprenorphine treatment are41:
- Induction phase. Buprenorphine can be initiated at 2 to 4 mg/d. Some patients may require up to 8 mg/d on the first day, which can be administered in divided doses.42 Evaluate and monitor patients carefully during the first few hours after the first dose. Patients should be in early withdrawal; otherwise, the buprenorphine might precipitate withdrawal. The induction phase can be completed in 2 to 4 days by titrating the dose so that the signs and symptoms of opioid withdrawal are minimal, and the patient is able to continue treatment. It may be helpful to have the patient’s legal guardian nearby in case the patient does not tolerate the medication or experiences withdrawal. The initial target dose for buprenorphine is approximately 12 to 16 mg/d.
- Stabilization phase. Patients no longer experience withdrawal symptoms and no longer have cravings. This phase can last 6 to 8 weeks. During this phase, patients should be seen weekly and doses should be adjusted if necessary. As a partial mu agonist, buprenorphine does not activate mu receptors fully and reaches a ceiling effect. Hence, doses >24 mg/d have limited added agonist properties.
- Maintenance phase. Because discontinuation of buprenorphine is associated with high relapse rates, patients may need to be maintained long-term on their stabilization dose, and for some patients, the length of time could be indefinite.39 During this phase, patients continue to undergo follow-up, but do so less frequently.
Methadone maintenance is generally not recommended for individuals age <18.
Preventing opioid diversion
Prescription medications that are kept in the home are a substantial source of opioids for adolescents. In 2014, 56% of 12th graders who did not need medications for medical purposes were able to acquire them from their friends or relatives; 36% of 12th graders used their own prescriptions.21 Limiting adolescents’ access to prescription opioids is the first line of prevention. Box 2 describes interventions and strategies to limit adolescents’ access to opioids.
Box 2
Many adolescents obtain opioids for recreational use from medications that were legitimately prescribed to family or friends. Both clinicians and parents/ guardians can take steps to reduce or prevent this type of diversion
Health care facilities. Regulating the number of pills dispensed to patients is crucial. It is highly recommended to prescribe only the minimal number of opioids necessary. In most cases, 3 to 7 days’ worth of opioids at a time might be sufficient, especially after surgical procedures.
Home. Families can limit adolescents’ access to prescription opioids in the home by keeping all medications in a lock box.
Proper disposal. Various entities offer locations for patients to drop off their unused opioids and other medications for safe disposal. These include police or fire departments and retail pharmacies. The US Drug Enforcement Administration sponsors a National Prescription Drug Take Back Day; see https://www.deadiversion.usdoj.gov/drug_disposal/takeback/index.html. The FDA also offers information on where and how to dispose of unused medicines at https://www.fda.gov/consumers/consumer-updates/where-and-how-dispose-unused-medicines.
CASE CONTINUED
Ms. L is initially prescribed, clonidine, 0.1 mg every 6 hours, to address opioid withdrawal. Clonidine is then tapered and maintained at 0.1 mg twice a day for irritability and impulse control. She is also prescribed sertraline, 100 mg/d, for depression and anxiety, and trazodone, 75 mg as needed at night, to assist with sleep.
Continue to: Following inpatient hospitalization...
Following inpatient hospitalization, during 12 weeks of partial hospital treatment, Ms. L participates in individual psychotherapy sessions 5 days/week; family therapy sessions once a week; and experiential therapy along with group sessions with other peers. She undergoes medication evaluations and adjustments on a weekly basis. Ms. L is now working at a store and is pursuing a high school equivalency certificate. She manages to avoid high-risk behaviors, although she reports having occasional cravings. Ms. L is actively involved in Narcotics Anonymous and has a sponsor. She has reconciled with her mother and moved back home, so she can stay away from her former acquaintances who are still using.
Bottom Line
Adolescents with opioid use disorder can benefit from an individualized treatment plan that includes psychosocial interventions, pharmacotherapy, or a combination of the two. Treatment planning should include the adolescent and his/her family to ensure they are able to verbalize their expectations. Treatment should focus on interventions that strengthen interpersonal relationships and assist with rehabilitation. Ongoing follow-up care is necessary for maintaining abstinence.
Related Resource
- Patkar AA, Weisler RH. Opioid abuse and overdose: Keep your patients safe. Current Psychiatry. 2017;16(8):8-12,14-16.
Drug Brand Names
Buprenorphine • Subutex, Sublocade
Buprenorphine/naloxone • Suboxone
Clonidine • Clorpres
Methadone • Methadose
Naloxone • Narcan
Oxycodone • OxyContin
Sertraline • Zoloft
Tramadol • Ultram
Trazodone • Desyrel, Oleptro
Ms. L, age 17, seeks treatment because she has an ongoing struggle with multiple substances, including benzodiazepines, heroin, alcohol, cannabis, and prescription opioids.
She reports that she was 13 when she first used a prescription opioid that was not prescribed for her. She also reports engaging in unsafe sexual practices while using these substances, and has been diagnosed and treated for a sexually transmitted disease. She dropped out of school and is estranged from her family. She says that for a long time she has felt depressed and that she uses drugs to “self-medicate my emotions.” She endorses high anxiety and lack of motivation. Ms. L also reports having several criminal charges for theft, assault, and exchanging sex for drugs. She has undergone 3 admissions for detoxification, but promptly resumed using drugs, primarily heroin and oxycodone, immediately after discharge. Ms. L meets DSM-5 criteria for opioid use disorder (OUD).
Ms. L’s case illustrates a disturbing trend in the current opioid epidemic in the United States. Nearly 11.8 million individuals age ≥12 reported misuse of opioids in the last year.1 Adolescents who misuse prescription or illicit opioids are more likely to be involved with the legal system due to truancy, running away from home, physical altercations, prostitution, exchanging sex for drugs, robbery, and gang involvement. Adolescents who use opioids may also struggle with academic decline, drop out of school early, be unable to maintain a job, and have relationship difficulties, especially with family members.
In this article, I describe the scope of OUD among adolescents, including epidemiology, clinical manifestations, screening tools, and treatment approaches.
Scope of the problem
According to the most recent Monitoring the Future survey of more than 42,500 8th, 10th, and 12th grade students, 2.7% of 12th graders reported prescription opioid misuse (reported in the survey as “narcotics other than heroin”) in the past year.2 In addition, 0.4% of 12th graders reported heroin use over the same period.2 Although the prevalence of opioid use among adolescents has been declining over the past 5 years,2 it still represents a serious health crisis.
Part of the issue may relate to easier access to more potent opioids. For example, heroin available today can be >4 times purer than it was in the past. In 2002, t
Between 1997 and 2012, the annual incidence of youth (age 15 to 19) hospitalizations for prescription opioid poisoning increased >170%.5 Approximately 6% to 9% of youth involved in risky opioid use develop OUD 6 to 12 months after s
Continue to: In recent years...
In recent years, deaths from drug overdose have increased for all age groups; however, limited data is available regarding adolescent overdose deaths. According to the Centers for Disease Control and Prevention (CDC), from 2015 to 2016, drug overdose death rates for persons age 15 to 24 increased to 28%.9
How opioids work
Opioids activate specific transmembrane neurotransmitter receptors, including mu, kappa, and delta, in the CNS and peripheral nervous system (PNS). This leads to activation of G protein–mediated intracellular signal transduction. Mainly it is activation of endogenous mu opioid receptors that mediates the reward, withdrawal, and analgesic effects of opioids. These effects depend on the location of mu receptors. In the CNS, activation of mu opioid receptors may cause miosis, respiratory depression, euphoria, and analgesia.10
Different opioids vary in terms of their half-life; for most opioids, the half-life ranges from 2 to 4 hours.10 Heroin has a half-life of 30 minutes, but due to active metabolites its duration of action is 4 to 5 hours. Opioid metabolites can be detected in urine toxicology within approximately 1 to 2 days since last use.10
Chronic opioid use is associated with neurologic effects that change the function of areas of the brain that control pleasure/reward, stress, decision-making, and more. This leads to cravings, continued substance use, and dependence.11 After continued long-term use, patients report decreased euphoria, but typically they continue to use opioids to avoid withdrawal symptoms or worsening mood.
Criteria for opioid use disorder
In DSM-5, substance use disorders (SUDs)are no longer categorized as abuse or dependence.12 For opioids, the diagnosis is OUD. The Table12 outlines the DSM-5 criteria for OUD. Craving opioids is included for the first time in the OUD diagnosis. Having problems with the legal system is no longer considered a diagnostic criterion for OUD.
Continue to: A vulnerable population
A vulnerable population
As defined by Erik Erikson’s psychosocial stages of development, adolescents struggle between establishing their own identity vs role confusion.13 In an attempt to relate to peers or give in to peer pressure, some adolescents start by experimenting with nicotine, alcohol, and/or marijuana; however, some may move on to using other illicit drugs.14 Risk factors for the development of SUDs include early onset of substance use and a rapid progression through stages of substance use from experimentation to regular use, risky use, and dependence.15 In our case study, Ms. L’s substance use followed a similar pattern. Further, the comorbidity of SUDs and other psychiatric disorders may add a layer of complexity when caring for adolescents. Box 116-20 describes the relationship between comorbid psychiatric disorders and SUDs in adolescents.
Box 1
Disruptive behavior disorders are the most common coexisting psychiatric disorders in an adolescent with a substance use disorder (SUD), including opioid use disorder. These individuals typically present with aggression and other conduct disorder symptoms, and have early involvement with the legal system. Conversely, patients with conduct disorder are at high risk of early initiation of illicit substance use, including opioids. Early onset of substance use is a strong risk factor for developing an SUD.16
Mood disorders, particularly depression, can either precede or occur as a result of heavy and prolonged substance use.17 The estimated prevalence of major depressive disorder in individuals with an SUD is 24% to 50%. Among adolescents, an SUD is also a risk factor for suicidal ideation, suicide attempts, and completed suicide.18-20
Anxiety disorders, especially social phobia, and posttraumatic stress disorder are common in individuals with SUD.
Adolescents with SUD should be carefully evaluated for comorbid psychiatric disorders and treated accordingly.
Clinical manifestations
Common clinical manifestations of opioid use vary depending on when the patient is seen. An individual with OUD may appear acutely intoxicated, be in withdrawal, or show no effects. Chronic/prolonged use can lead to tolerance, such that a user needs to ingest larger amounts of the opioid to produce the same effects.
Acute intoxication can cause sedation, slurring of speech, and pinpoint pupils. Fresh injection sites may be visible on physical examination of IV users. The effects of acute intoxication usually depend on the half-life of the specific opioid and the individual’s tolerance.10 Tolerance to heroin can occur in 10 days and withdrawal can manifest in 3 to 7 hours after last use, depending on dose and purity.3 Tolerance can lead to unintentional overdose and death.
Withdrawal. Individuals experiencing withdrawal from opioids present with flu-like physical symptoms, including generalized body ache, rhinorrhea, diarrhea, goose bumps, lacrimation, and vomiting. Individuals also may experience irritability, restlessness, insomnia, anxiety, and depression during withdrawal.
Other manifestations. Excessive and chronic/prolonged opioid use can adversely impact socio-occupational functioning and cause academic decline in adolescents and youth. Personal relationships are significantly affected. Opioid users may have legal difficulties as a result of committing crimes such as theft, prostitution, or robbery in order to obtain opioids.
Continue to: Screening for OUD
Screening for OUD
Several screening tools are available to assess adolescents for SUDs, including OUD.
CRAFFT is a 6-item, clinician-administered screening tool that has been approved by American Academy of Pediatrics’ Committee on Substance Abuse for adolescents and young adults age <21.21-23 This commonly used tool can assess for alcohol, cannabis, and other drug use. A score ≥2 is considered positive for drug use, indicating that the individual would require further evaluation and assessment22,23 (Figure). There is also a self-administered CRAFFT questionnaire that can be completed by the patient.
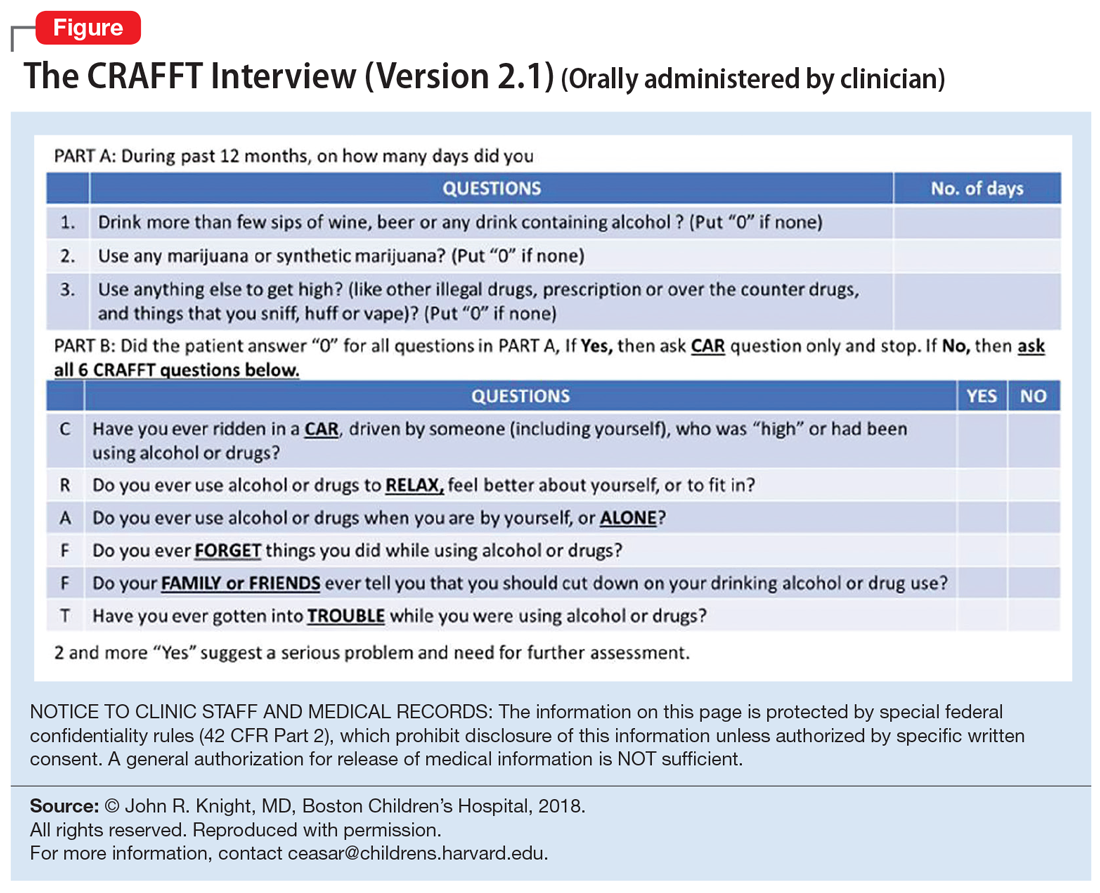
NIDA-modified ASSIST. The American Psychiatric Association has adapted the National Institute on Drug Abuse (NIDA)-modified ASSIST. One version is designated for parents/guardians to administer to their children (age 6 to 17), and one is designated for adolescents (age 11 to 17) to self-administer.24,25 Each screening tool has 2 levels: Level 1 screens for substance use and other mental health symptoms, and Level 2 is more specific for substance use alone.
Drug Use Screening Inventory (DUSI) is a self-report questionnaire that has 149 items that assess the use of numerous drugs. It is designed to quantify the severity of consequences associated with drug and alcohol use.26,27
Problem-Oriented Screening Instrument for Teenagers (PO
Continue to: Personal Experience Screening Questionnaire (PESQ)...
Personal Experience Screening Questionnaire (PESQ) is a brief, 40-item, cost-effective, self-report questionnaire that can help identify adolescents (age 12 to 18) who should be referred for further evaluation.30
Addressing treatment expectations
For an adolescent with OUD, treatment should begin in the least restrictive environment that is perceived as safe for the patient. An adolescent’s readiness and motivation to achieve and maintain abstinence are crucial. Treatment planning should include the adolescent as well as his/her family to ensure they are able to verbalize their expectations. Start with a definitive treatment plan that addresses an individual’s needs. The plan should provide structure and an understanding of treatment expectations. The treatment team should clarify the realistic plan and goals based on empirical and clinical evidence. Treatment goals should include interventions to strengthen interpersonal relationships and assist with rehabilitation, such as establishing academic and/or vocational goals. Addressing readiness and working on a patient’s motivation is extremely important for most of these interventions.
In order for any intervention to be successful, clinicians need to establish and foster rapport with the adolescent. By law, substance use or behaviors related to substance use are not allowed to be shared outside the patient-clinician relationship, unless the adolescent gives consent or there are concerns that such behaviors might put the patient or others at risk. It is important to prime the adolescent and help them understand that any information pertaining to their safety or the safety of others may need to be shared outside the patient-clinician relationship.
Choosing an intervention
Less than 50% of a nationally representative sample of 345 addiction treatment programs serving adolescents and adults offer medications for treating OUD.31 Even in programs that offer pharmacotherapy, medications are significantly underutilized. Fewer than 30% of patients in addiction treatment programs receive medication, compared with 74% of patients receiving treatment for other mental health disorders.31 A
Psychotherapy may be used to treat OUD in adolescents. Several family therapies have been studied and are considered as critical psychotherapeutic interventions for treating SUDs, including structural family treatment and functional family therapy approaches.34 An integrated behavioral and family therapy model is also recommended for adolescent patients with SUDs. Cognitive distortions and use of self-deprecatory statements are common among adolescents.35 Therefore, using approaches of cognitive-behavioral therapy (CBT), or CBT plus motivational enhancement therapy, also might be effective for this population.36 The adolescent community reinforcement approach (A-CRA) is a behavioral treatment designed to help adolescents and their families learn how to lead a healthy and happy life without the use of drugs or alcohol by increasing access to social, familial, and educational/vocational reinforcers. Support groups and peer and family support should be encouraged as adjuncts to other interventions. In some areas, sober housing options for adolescents are also available.
Continue to: Harm-reduction strategies
Harm-reduction strategies. Although the primary goal of treatment for adolescents with OUD is to achieve and maintain abstinence from opioid use, implicit and explicit goals can be set. Short-term implicit goals may include harm-reduction strategies that emphasize decreasing the duration, frequency, and amount of substance use and limiting the chances of adverse effects, while the long-term explicit goal should be abstinence from opioid use.
Naloxone nasal spray is used as a harm-reduction strategy. It is an FDA-approved formulation that can reverse the effects of unintentional opioid overdoses and potentially prevent death from respiratory depression.37 Other harm-reduction strategies include needle exchange programs, which provide sterile needles to individuals who inject drugs in an effort to prevent or reduce the transmission of human immunodeficiency virus and other bloodborne viruses that can be spread via shared injection equipment. Fentanyl testing strips allow opioid users to test for the presence fentanyl and fentanyl analogs in the unregulated “street” opioid supply.
Pharmacologic interventions. Because there is limited empirical evidence on the efficacy of medication-assisted treatment (MAT) for adolescents with OUD, clinicians need to rely on evidence from research and experience with adults. Unfortunately, MAT is offered to adolescents considerably less often than it is to adults. Feder et al38 reported that only 2.4% of adolescents received MAT for heroin use and only 0.4% of adolescents received MAT for prescription opioid use, compared with 26.3% and 12% of adults, respectively.
Detoxification. Medications available for detoxification from opioids include opiates (such as methadone or buprenorphine) and clonidine (a central sympathomimetic). If the patient has used heroin for a short period (<1 year) and has no history of detoxification, consider a detoxification strategy with a longer-term taper (90 to 180 days) to allow for stabilization.
Maintenance treatment. Consider maintenance treatment for adolescents with a history of long-term opioid use and at least 2 prior short-term detoxification attempts or nonpharmacotherapy-based treatment within 12 months. Be sure to receive consent from a legal guardian and the patient. Maintenance treatment is usually recommended to continue for 1 to 6 years. Maintenance programs with longer durations have shown higher rates of abstinence, improved engagement, and retention in treatment.39
Continue to: According to guidelines from...
According to guidelines from the American Society of Addiction Medicine (ASAM), adolescents age >16 should be offered MAT; the first-line treatment is buprenorphine.40 To avoid risks of abuse and diversion, a combination of buprenorphine/naloxone may be administered.
Maintenance with buprenorphine
In order to prescribe and dispense buprenorphine, clinicians need to obtain a waiver from the Substance Abuse and Mental Health Services Administration. Before initiating buprenorphine, consider the type of opioid the individual used (short- or long-acting), the severity of the OUD, and the last reported use. The 3 phases of buprenorphine treatment are41:
- Induction phase. Buprenorphine can be initiated at 2 to 4 mg/d. Some patients may require up to 8 mg/d on the first day, which can be administered in divided doses.42 Evaluate and monitor patients carefully during the first few hours after the first dose. Patients should be in early withdrawal; otherwise, the buprenorphine might precipitate withdrawal. The induction phase can be completed in 2 to 4 days by titrating the dose so that the signs and symptoms of opioid withdrawal are minimal, and the patient is able to continue treatment. It may be helpful to have the patient’s legal guardian nearby in case the patient does not tolerate the medication or experiences withdrawal. The initial target dose for buprenorphine is approximately 12 to 16 mg/d.
- Stabilization phase. Patients no longer experience withdrawal symptoms and no longer have cravings. This phase can last 6 to 8 weeks. During this phase, patients should be seen weekly and doses should be adjusted if necessary. As a partial mu agonist, buprenorphine does not activate mu receptors fully and reaches a ceiling effect. Hence, doses >24 mg/d have limited added agonist properties.
- Maintenance phase. Because discontinuation of buprenorphine is associated with high relapse rates, patients may need to be maintained long-term on their stabilization dose, and for some patients, the length of time could be indefinite.39 During this phase, patients continue to undergo follow-up, but do so less frequently.
Methadone maintenance is generally not recommended for individuals age <18.
Preventing opioid diversion
Prescription medications that are kept in the home are a substantial source of opioids for adolescents. In 2014, 56% of 12th graders who did not need medications for medical purposes were able to acquire them from their friends or relatives; 36% of 12th graders used their own prescriptions.21 Limiting adolescents’ access to prescription opioids is the first line of prevention. Box 2 describes interventions and strategies to limit adolescents’ access to opioids.
Box 2
Many adolescents obtain opioids for recreational use from medications that were legitimately prescribed to family or friends. Both clinicians and parents/ guardians can take steps to reduce or prevent this type of diversion
Health care facilities. Regulating the number of pills dispensed to patients is crucial. It is highly recommended to prescribe only the minimal number of opioids necessary. In most cases, 3 to 7 days’ worth of opioids at a time might be sufficient, especially after surgical procedures.
Home. Families can limit adolescents’ access to prescription opioids in the home by keeping all medications in a lock box.
Proper disposal. Various entities offer locations for patients to drop off their unused opioids and other medications for safe disposal. These include police or fire departments and retail pharmacies. The US Drug Enforcement Administration sponsors a National Prescription Drug Take Back Day; see https://www.deadiversion.usdoj.gov/drug_disposal/takeback/index.html. The FDA also offers information on where and how to dispose of unused medicines at https://www.fda.gov/consumers/consumer-updates/where-and-how-dispose-unused-medicines.
CASE CONTINUED
Ms. L is initially prescribed, clonidine, 0.1 mg every 6 hours, to address opioid withdrawal. Clonidine is then tapered and maintained at 0.1 mg twice a day for irritability and impulse control. She is also prescribed sertraline, 100 mg/d, for depression and anxiety, and trazodone, 75 mg as needed at night, to assist with sleep.
Continue to: Following inpatient hospitalization...
Following inpatient hospitalization, during 12 weeks of partial hospital treatment, Ms. L participates in individual psychotherapy sessions 5 days/week; family therapy sessions once a week; and experiential therapy along with group sessions with other peers. She undergoes medication evaluations and adjustments on a weekly basis. Ms. L is now working at a store and is pursuing a high school equivalency certificate. She manages to avoid high-risk behaviors, although she reports having occasional cravings. Ms. L is actively involved in Narcotics Anonymous and has a sponsor. She has reconciled with her mother and moved back home, so she can stay away from her former acquaintances who are still using.
Bottom Line
Adolescents with opioid use disorder can benefit from an individualized treatment plan that includes psychosocial interventions, pharmacotherapy, or a combination of the two. Treatment planning should include the adolescent and his/her family to ensure they are able to verbalize their expectations. Treatment should focus on interventions that strengthen interpersonal relationships and assist with rehabilitation. Ongoing follow-up care is necessary for maintaining abstinence.
Related Resource
- Patkar AA, Weisler RH. Opioid abuse and overdose: Keep your patients safe. Current Psychiatry. 2017;16(8):8-12,14-16.
Drug Brand Names
Buprenorphine • Subutex, Sublocade
Buprenorphine/naloxone • Suboxone
Clonidine • Clorpres
Methadone • Methadose
Naloxone • Narcan
Oxycodone • OxyContin
Sertraline • Zoloft
Tramadol • Ultram
Trazodone • Desyrel, Oleptro
1. Davis JP, Prindle JJ, Eddie D, et al. Addressing the opioid epidemic with behavioral interventions for adolescents and young adults: a quasi-experimental design. J Consult Clin Psychol. 2019;87(10):941-951.
2. National Institute on Drug Abuse; National Institutes of Health; U.S. Department of Health and Human Services. Monitoring the Future Survey: High School and Youth Trends. https://www.drugabuse.gov/publications/drugfacts/monitoring-future-survey-high-school-youth-trends. Updated December 2019. Accessed January 13, 2020.
3. Hopfer CJ, Khuri E, Crowley TJ. Treating adolescent heroin use. J Am Acad Child Adolesc Psychiatry. 2003;42(5):609-611.
4. US Department of Justice, Drug Enforcement Agency, Diversion Control Division. https://www.deadiversion.usdoj.gov/. Accessed January 21, 2020.
5. Gaither JR, Leventhal JM, Ryan SA, et al. National trends in hospitalizations for opioid poisonings among children and adolescents, 1997-2012. JAMA Pediatr. 2016;170(12):1195-1201.
6. Parker MA, Anthony JC. Epidemiological evidence on extra-medical use of prescription pain relievers: transitions from newly incident use to dependence among 12-21 year olds in United States using meta-analysis, 2002-13. Peer J. 2015;3:e1340. doi: 10.7717/peerj.1340. eCollection 2015.
7. Subramaniam GA, Fishman MJ, Woody G. Treatment of opioid-dependent adolescents and young adults with buprenorphine. Curr Psychiatry Rep. 2009;11(5):360-363.
8. Borodovsky JT, Levy S, Fishman M. Buprenorphine treatment for adolescents and young adults with opioid use disorders: a narrative review. J Addict Med. 2018;12(3):170-183.
9. Centers for Disease Control and Prevention: National Center for Health Statistics. Drug overdose deaths in the United States, 1999-2016. https://www.cdc.gov/nchs/products/databriefs/db294.htm. Published December 2017. Accessed January 15, 2020.
10. Strain E. Opioid use disorder: epidemiology, pharmacology, clinical manifestation, course, screening, assessment, diagnosis. https://www.uptodate.com/contents/opioid-use-disorder-epidemiology-pharmacology-clinical-manifestations-course-screening-assessment-and-diagnosis. Updated August 15, 2019. Accessed January 21, 2020.
11. American Academy of Pediatrics Committee on Substance Use and Prevention. Policy statement: medication-assisted treatment of adolescents with opioid use disorder. Pediatrics. 2016;138(3):e20161893. doi: https://doi.org/10.1542/peds.2016-1893.
12. Diagnostic and Statistical Manual of Mental Disorders, 5th ed. Washington, DC: American Psychiatric Association; 2013:514.
13. Sadock BJ, Sadock VA. Chapter 6: Theories of personality and psychopathology. In: Sadock BJ, Sadock VA, eds. Kaplan and Sadock’s synopsis of psychiatry: behavioral sciences/clinical. 10th ed. Philadelphia, PA: Lippincott Williams & Wilkins; 2007:209.
14. Kandel DB. Stages and pathways of drug involvement: examining the gateway hypothesis. Cambridge, United Kingdom: Cambridge University Press; 2002.
15. Robins LN, McEvoy L. Conduct problems as predictors of substance abuse. In: Robins LN, Rutter M, eds. Straight and devious pathways from childhood to adulthood. Cambridge, United Kingdom: Cambridge University Press; 1990;182-204.
16. Hopfer C, Salomonsen-Sautel S, Mikulich-Gilbertson S, et al. Conduct disorder and initiation of substance use: a prospective longitudinal study. J Am Acad Child Adolesc Psychiatry. 2013;52(5):511-518.e4.
17. Armstrong TD, Costello EJ. Community studies on adolescent substance use, abuse, or dependence and psychiatric comorbidity. J Consult Clin Psychol. 2002;70(6):1224-1239.
18. Crumley FE. Substance abuse and adolescent suicidal behavior. JAMA. 1990;263(22):3051-3056.
19. Lewinsohn PM, Rohde P, Seeley JR. Adolescent suicidal ideation and attempts: prevalence, risk factors, and clinical implications. Clinical Psychology: Science and Practice. 1996;3(1):25-46.
20. Kendler KS, Bulik CM, Silberg J, et al. Childhood sexual abuse and adult psychiatric and substance use disorder in women: an epidemiological and cotwin control analysis. Arch Gen Psychiatry. 2000;57(10):953-959.
21. Yule AM, Wilens TE, Rausch PK. The opioid epidemic: what a child psychiatrist is to do? J Am Acad Child Adolesc Psychiatry. 2017;56(7);541-543.
22. CRAFFT. https://crafft.org. Accessed January 21, 2020.
23. Knight JR, Sherritt L, Harris SK, et al. Validity of brief alcohol screening tests among adolescents: a comparison of the AUDIT, POSIT, CAGE, and CRAFFT. Alcohol Clin Exp Res. 2003;27(1):67-73.
24. American Psychiatric Association. Online assessment measures. https://www.psychiatry.org/psychiatrists/practice/dsm/educational-resources/assessment-measures. Accessed January 15, 2020.
25. National Institute of Drug Abuse. American Psychiatric Association adapted NIDA modified ASSIST tools. https://www.drugabuse.gov/nidamed-medical-health-professionals/tool-resources-your-practice/screening-assessment-drug-testing-resources/american-psychiatric-association-adapted-nida. Updated November 15, 2015. Accessed January 21, 2020.
26. Canada’s Mental Health & Addiction Network. Drug Use Screening Inventory (DUSI). https://www.porticonetwork.ca/web/knowledgex-archive/amh-specialists/screening-for-cd-in-youth/screening-both-mh-sud/dusi. Published 2009. Accessed January 21, 2020.
27. Tarter RE. Evaluation and treatment of adolescent substance abuse: a decision tree method. Am J Drug Alcohol Abuse. 1990;16(1-2):1-46.
28. Klitzner M, Gruenwald PJ, Taff GA, et al. The adolescent assessment referral system-final report. National Institute on Drug Abuse; Rockville, MD: 1993. NIDA Contract No. 271-89-8252.
29. Slesnick N, Tonigan JS. Assessment of alcohol and other drug use by runaway youths: a test-retest study of the Form 90. Alcohol Treat Q. 2004;22(2):21-34.
30. Winters KC, Kaminer Y. Screening and assessing adolescent substance use disorders in clinical populations. J Am Acad Child Adolesc Psychiatry. 2008;47(7):740-744.
31. Knudsen HK, Abraham AJ, Roman PM. Adoption and implementation of medications in addiction treatment programs. J Addict Med. 2011;5(1):21-27.
32. Deas D, Thomas SE. An overview of controlled study of adolescent substance abuse treatment. Am J Addiction. 2001;10(2):178-189.
33. William RJ, Chang, SY. A comprehensive and comparative review of adolescent substance abuse treatment outcome. Clinical Psychology: Science and Practice. 2000;7(2):138-166.
34. Bukstein OG, Work Group on Quality Issues. Practice parameters for the assessment and treatment of children and adolescents with substance use disorders. J Am Acad Child Adolesc Psychiatry. 2005;44(6):609-621.
35. Van Hasselt VB, Null JA, Kempton T, et al. Social skills and depression in adolescent substance abusers. Addict Behav. 1993;18(1):9-18.
36. Dennis M, Godley SH, Diamond G, et al. The Cannabis Youth Treatment (CYT) study: main findings from two randomized trials. J Subst Abuse Treat. 2004;27(3):197-213.
37. US Food and Drug Administration. Information about naloxone. https://www.fda.gov/drugs/postmarket-drug-safety-information-patients-and-providers/information-about-naloxone. Updated December 19, 2019. Accessed January 21, 2020.
38. Feder KA, Krawcyzk N, Saloner, B. Medication-assisted treatment for adolescents in specialty treatment for opioid use disorder. J Adolesc Health. 2018;60(6):747-750.
39. Woody GE, Poole SA, Subramaniam G, et al. Extended vs short-term buprenorphine-naloxone for treatment of opioid-addicted youth: a randomized trial. JAMA. 2008;300(17):2003-2011.
40. US Department of Health and Human Services. Substance Abuse and Mental Health Ser-vices Administration. Medication-assisted treatment for opioid addiction in opioid treatment programs: a treatment improvement protocol TIP 43. https://www.asam.org/docs/advocacy/samhsa_tip43_matforopioidaddiction.pdf?sfvrsn=0. Published 2005. Accessed January 15, 2020.
41. US Department of Health and Human Services. Substance Abuse and Mental Health Services Administration. Medication-assisted treatment (MAT). https://www.samhsa.gov/medication-assisted-treatment. Updated September 9, 2019. Accessed January 21, 2020.
42. Johnson RE, Strain EC, Amass L. Buprenorphine: how to use it right. Drug Alcohol Depend. 2003;70(suppl 2):S59-S77.
1. Davis JP, Prindle JJ, Eddie D, et al. Addressing the opioid epidemic with behavioral interventions for adolescents and young adults: a quasi-experimental design. J Consult Clin Psychol. 2019;87(10):941-951.
2. National Institute on Drug Abuse; National Institutes of Health; U.S. Department of Health and Human Services. Monitoring the Future Survey: High School and Youth Trends. https://www.drugabuse.gov/publications/drugfacts/monitoring-future-survey-high-school-youth-trends. Updated December 2019. Accessed January 13, 2020.
3. Hopfer CJ, Khuri E, Crowley TJ. Treating adolescent heroin use. J Am Acad Child Adolesc Psychiatry. 2003;42(5):609-611.
4. US Department of Justice, Drug Enforcement Agency, Diversion Control Division. https://www.deadiversion.usdoj.gov/. Accessed January 21, 2020.
5. Gaither JR, Leventhal JM, Ryan SA, et al. National trends in hospitalizations for opioid poisonings among children and adolescents, 1997-2012. JAMA Pediatr. 2016;170(12):1195-1201.
6. Parker MA, Anthony JC. Epidemiological evidence on extra-medical use of prescription pain relievers: transitions from newly incident use to dependence among 12-21 year olds in United States using meta-analysis, 2002-13. Peer J. 2015;3:e1340. doi: 10.7717/peerj.1340. eCollection 2015.
7. Subramaniam GA, Fishman MJ, Woody G. Treatment of opioid-dependent adolescents and young adults with buprenorphine. Curr Psychiatry Rep. 2009;11(5):360-363.
8. Borodovsky JT, Levy S, Fishman M. Buprenorphine treatment for adolescents and young adults with opioid use disorders: a narrative review. J Addict Med. 2018;12(3):170-183.
9. Centers for Disease Control and Prevention: National Center for Health Statistics. Drug overdose deaths in the United States, 1999-2016. https://www.cdc.gov/nchs/products/databriefs/db294.htm. Published December 2017. Accessed January 15, 2020.
10. Strain E. Opioid use disorder: epidemiology, pharmacology, clinical manifestation, course, screening, assessment, diagnosis. https://www.uptodate.com/contents/opioid-use-disorder-epidemiology-pharmacology-clinical-manifestations-course-screening-assessment-and-diagnosis. Updated August 15, 2019. Accessed January 21, 2020.
11. American Academy of Pediatrics Committee on Substance Use and Prevention. Policy statement: medication-assisted treatment of adolescents with opioid use disorder. Pediatrics. 2016;138(3):e20161893. doi: https://doi.org/10.1542/peds.2016-1893.
12. Diagnostic and Statistical Manual of Mental Disorders, 5th ed. Washington, DC: American Psychiatric Association; 2013:514.
13. Sadock BJ, Sadock VA. Chapter 6: Theories of personality and psychopathology. In: Sadock BJ, Sadock VA, eds. Kaplan and Sadock’s synopsis of psychiatry: behavioral sciences/clinical. 10th ed. Philadelphia, PA: Lippincott Williams & Wilkins; 2007:209.
14. Kandel DB. Stages and pathways of drug involvement: examining the gateway hypothesis. Cambridge, United Kingdom: Cambridge University Press; 2002.
15. Robins LN, McEvoy L. Conduct problems as predictors of substance abuse. In: Robins LN, Rutter M, eds. Straight and devious pathways from childhood to adulthood. Cambridge, United Kingdom: Cambridge University Press; 1990;182-204.
16. Hopfer C, Salomonsen-Sautel S, Mikulich-Gilbertson S, et al. Conduct disorder and initiation of substance use: a prospective longitudinal study. J Am Acad Child Adolesc Psychiatry. 2013;52(5):511-518.e4.
17. Armstrong TD, Costello EJ. Community studies on adolescent substance use, abuse, or dependence and psychiatric comorbidity. J Consult Clin Psychol. 2002;70(6):1224-1239.
18. Crumley FE. Substance abuse and adolescent suicidal behavior. JAMA. 1990;263(22):3051-3056.
19. Lewinsohn PM, Rohde P, Seeley JR. Adolescent suicidal ideation and attempts: prevalence, risk factors, and clinical implications. Clinical Psychology: Science and Practice. 1996;3(1):25-46.
20. Kendler KS, Bulik CM, Silberg J, et al. Childhood sexual abuse and adult psychiatric and substance use disorder in women: an epidemiological and cotwin control analysis. Arch Gen Psychiatry. 2000;57(10):953-959.
21. Yule AM, Wilens TE, Rausch PK. The opioid epidemic: what a child psychiatrist is to do? J Am Acad Child Adolesc Psychiatry. 2017;56(7);541-543.
22. CRAFFT. https://crafft.org. Accessed January 21, 2020.
23. Knight JR, Sherritt L, Harris SK, et al. Validity of brief alcohol screening tests among adolescents: a comparison of the AUDIT, POSIT, CAGE, and CRAFFT. Alcohol Clin Exp Res. 2003;27(1):67-73.
24. American Psychiatric Association. Online assessment measures. https://www.psychiatry.org/psychiatrists/practice/dsm/educational-resources/assessment-measures. Accessed January 15, 2020.
25. National Institute of Drug Abuse. American Psychiatric Association adapted NIDA modified ASSIST tools. https://www.drugabuse.gov/nidamed-medical-health-professionals/tool-resources-your-practice/screening-assessment-drug-testing-resources/american-psychiatric-association-adapted-nida. Updated November 15, 2015. Accessed January 21, 2020.
26. Canada’s Mental Health & Addiction Network. Drug Use Screening Inventory (DUSI). https://www.porticonetwork.ca/web/knowledgex-archive/amh-specialists/screening-for-cd-in-youth/screening-both-mh-sud/dusi. Published 2009. Accessed January 21, 2020.
27. Tarter RE. Evaluation and treatment of adolescent substance abuse: a decision tree method. Am J Drug Alcohol Abuse. 1990;16(1-2):1-46.
28. Klitzner M, Gruenwald PJ, Taff GA, et al. The adolescent assessment referral system-final report. National Institute on Drug Abuse; Rockville, MD: 1993. NIDA Contract No. 271-89-8252.
29. Slesnick N, Tonigan JS. Assessment of alcohol and other drug use by runaway youths: a test-retest study of the Form 90. Alcohol Treat Q. 2004;22(2):21-34.
30. Winters KC, Kaminer Y. Screening and assessing adolescent substance use disorders in clinical populations. J Am Acad Child Adolesc Psychiatry. 2008;47(7):740-744.
31. Knudsen HK, Abraham AJ, Roman PM. Adoption and implementation of medications in addiction treatment programs. J Addict Med. 2011;5(1):21-27.
32. Deas D, Thomas SE. An overview of controlled study of adolescent substance abuse treatment. Am J Addiction. 2001;10(2):178-189.
33. William RJ, Chang, SY. A comprehensive and comparative review of adolescent substance abuse treatment outcome. Clinical Psychology: Science and Practice. 2000;7(2):138-166.
34. Bukstein OG, Work Group on Quality Issues. Practice parameters for the assessment and treatment of children and adolescents with substance use disorders. J Am Acad Child Adolesc Psychiatry. 2005;44(6):609-621.
35. Van Hasselt VB, Null JA, Kempton T, et al. Social skills and depression in adolescent substance abusers. Addict Behav. 1993;18(1):9-18.
36. Dennis M, Godley SH, Diamond G, et al. The Cannabis Youth Treatment (CYT) study: main findings from two randomized trials. J Subst Abuse Treat. 2004;27(3):197-213.
37. US Food and Drug Administration. Information about naloxone. https://www.fda.gov/drugs/postmarket-drug-safety-information-patients-and-providers/information-about-naloxone. Updated December 19, 2019. Accessed January 21, 2020.
38. Feder KA, Krawcyzk N, Saloner, B. Medication-assisted treatment for adolescents in specialty treatment for opioid use disorder. J Adolesc Health. 2018;60(6):747-750.
39. Woody GE, Poole SA, Subramaniam G, et al. Extended vs short-term buprenorphine-naloxone for treatment of opioid-addicted youth: a randomized trial. JAMA. 2008;300(17):2003-2011.
40. US Department of Health and Human Services. Substance Abuse and Mental Health Ser-vices Administration. Medication-assisted treatment for opioid addiction in opioid treatment programs: a treatment improvement protocol TIP 43. https://www.asam.org/docs/advocacy/samhsa_tip43_matforopioidaddiction.pdf?sfvrsn=0. Published 2005. Accessed January 15, 2020.
41. US Department of Health and Human Services. Substance Abuse and Mental Health Services Administration. Medication-assisted treatment (MAT). https://www.samhsa.gov/medication-assisted-treatment. Updated September 9, 2019. Accessed January 21, 2020.
42. Johnson RE, Strain EC, Amass L. Buprenorphine: how to use it right. Drug Alcohol Depend. 2003;70(suppl 2):S59-S77.
Collaborative Dementia Care via Telephone and Internet Improves Quality of Life and Reduces Caregiver Burden
Study Overview
Objective. To examine the effectiveness of a hub site–based care delivery system in delivering a dementia care management program to persons with dementia and their caregivers.
Design. Randomized pragmatic clinical trial enrolling dyads of persons with dementia and their caregiver. Study participants were randomly assigned to the dementia care management program and usual care in a 2:1 ratio.
Setting and participants. The study was conducted from 2 hub sites: the University of California, San Francisco, and the University of Nebraska Medical Center in Omaha. Each hub-site team served persons with dementia and their caregivers in California, Nebraska, and Iowa in both urban and rural areas. Participants were recruited through referral by treating providers or self-referral in response to advertising presented through a community outreach event, in the news, or on the internet. Eligibility requirements included: having a dementia diagnosis made by a treating provider; age older than 45 years; Medicare or Medicaid enrollment or eligibility; presence of a caregiver willing to enroll in the study; fluency in English, Spanish, or Cantonese; and residence in California, Nebraska, or Iowa. Exclusion criteria included residence in a nursing home. Out of 2585 referred dyads of persons with dementia and caregivers, 780 met inclusion criteria and were enrolled. A 2:1 randomization yielded 512 dyads in the intervention group and 268 dyads in the control group.
Intervention. The dementia care management program was implemented through the Care Ecosystem, a telephone- and internet-based supportive care intervention delivered by care team navigators. The navigators were unlicensed but trained dementia care guides working under the supervision of an advanced practice nurse, social worker, and pharmacist. The intervention consisted of telephone calls, monthly or at a frequency determined by needs and preferences, placed by navigators over a 12-month period; the content of the calls included response to immediate needs of persons with dementia and their caregiver, screening for common problems, and provision of support and education using care plan protocols. Caregivers and persons with dementia were encouraged to initiate contact through email, mail, or telephone for dementia-related questions. Additional support was provided by an advanced practice nurse, social worker, or pharmacist, as needed, and these health care professionals conducted further communication with the persons with dementia, caregiver, or outside professionals, such as physicians, for the persons with dementia, as needed. The average number of telephone calls over the 12-month period was 15.3 (standard deviation, 11.3). Participants assigned to usual care were offered contact information on dementia and aging-related organizations, including the Alzheimer’s Association and the Area Agencies on Aging, and also were sent a quarterly newsletter with general information about dementia.
Main outcome measures. The primary outcome measure was the Quality of Life in Alzheimer’s Disease score obtained by caregiver interview. This quality of life measure includes the following aspects, each rated on an ordinal scale of 1 to 4: physical health, energy level, mood, living situation, memory, family, closest relationship, friends, self, ability to do things for fun, finances, and life as a whole. The scores range from 13 to 52, with a higher score indicating better quality of life for persons with dementia. Other outcomes included frequency of emergency room visits, hospital use, and ambulance use; caregiver depression score from the Patient Health Questionnaire scale; caregiver burden score using the 12-item Zarit Burden Interview; caregiver self-efficacy; and caregiver satisfaction.
Main results. The study found that the quality of life for persons with dementia declined more in the usual care group than in the intervention group during the 12-month study period (difference of 0.53; 95% confidence interval, 0.25-1.3; P = 0.04). Persons with dementia also had fewer emergency room visits, with a number needed to treat to prevent 1 emergency room visit of 5. The intervention did not reduce ambulance use or hospital use. Caregivers in the intervention group had a greater decline in depression when compared to usual care; the frequency of moderate to severe depression decreased from 13.4% at baseline to 7.9% at 12 months (P = 0.004). Caregiver burden declined more in the intervention group than in the control group at 12 months (P = 0.046). In terms of caregiver satisfaction, 97% of caregivers surveyed in the intervention group said they would recommend the intervention to another caregiver; 45% indicated they were very satisfied, and 33% that they were satisfied.
Conclusion. Delivering dementia care via telephone and internet through a collaborative program with care navigators can improve caregiver burden and well-being and improve quality of life, emergency room utilization, and depression for persons with dementia. In addition, the program was well received.
Commentary
Dementia, including Alzheimer’s disease, primarily affects older adults and is characterized by declines in memory and cognitive function. It is often accompanied by neuropsychological symptoms such as agitation, wandering, and physical and verbal outbursts, which are debilitating for persons living with dementia and difficult to cope with for caregivers.1 These symptoms are often the source of caregiver stress, potentially leading to caregiver depression and eventual need for long-term institution-based care, such as nursing home placement.2
Prior literature has established the potential effect of support in improving caregiver outcomes, including caregiver stress and burden, through interventions such as enhancing resources for caregivers, teaching coping strategies to caregivers, and teaching caregivers how to manage support for their loved ones.3,4 However, wider adoption of these interventions may be limited if the interventions involve in-person meetings or activities that take caregivers away from caregiving; the scalability of these programs is also limited by their ability to reach persons with dementia and their caregivers. These barriers are particularly important for older adults living in rural areas, where the availability of resources and distance from access to quality care may be particularly limiting.5 Leveraging advances in technology and telecommunication, this study examined the effects of providing dementia care support via telephone and internet using a trained, unlicensed care navigator as the main point of contact. The results showed improved quality of life for persons with dementia, reduced need for emergency room visits, and reduced caregiver burden and depression. The intervention is promising as a scalable intervention that may impact dementia care nationwide.
Despite the promising results, there are several issues regarding the intervention’s applicability and impact that future studies may help to further clarify. Although the improvement in quality of life in persons with dementia is important to document, it is unclear whether this difference is clinically significant. Also, it may be important to examine whether the 12-month program has sustained impact beyond the study period, although the intervention could be conceived as a long-term care solution. If the intervention is sustained beyond 12 months, future studies may look at other clinical outcomes, such as incidence of institutionalization and perhaps time to institutionalization. The study population consisted of persons with dementia of various stages, half of whom had mild disease. Future studies may further clarify at which stage of dementia the intervention is most useful. Other changes that occurred during the study period, such as change in the use of paid home-based support services and referrals to other relevant evaluations and treatment, may provide further clues about how the dementia care intervention achieved its beneficial effects.
Applications for Clinical Practice
From the health systems perspective, dementia care accounts for significant resources, and these costs are expected to grow as the population ages and dementia prevalence increases. Identifying potentially scalable interventions that yield clinical benefits and are sustainable from a cost perspective is an important step forward in improving care for persons with dementia and their caregivers across the nation. The use of centralized hubs to deliver this intervention and the novel use of telecommunications advances make this intervention applicable across large areas. Policy makers should explore how an intervention such as this could be established and sustained in our health care system.
–William W. Hung, MD, MPH
1. Mega MS, Cummings JL, Fiorello T, Gornbein J. The spectrum of behavioral changes in Alzheimer’s disease. Neurology. 1996;46:130-135.
2. Gallagher-Thompson D, Brooks JO 3rd, Bliwise D, et al. The relations among caregiver stress, “sundowning” symptoms, and cognitive decline in Alzheimer’s disease. J Am Geriatr Soc. 1992;40:807-810.
3. Livingston G, Barber J, Rapaport P, et al. Clinical effectiveness of a manual based coping strategy programme (START, STrAtegies for RelaTives) in promoting the mental health of carers of family members with dementia: pragmatic randomised controlled trial. BMJ. 2013;347:f6276.
4. Belle SH, Burgio L, Burns R, et al; Resources for Enhancing Alzheimer’s Caregiver Health (REACH) II Investigators. Enhancing the quality of life of dementia caregivers from different ethnic or racial groups: a randomized, controlled trial. Ann Intern Med. 2006;145:727-738.
5. Goins RT, Williams KA, Carter MW, et al. Perceived barriers to health care access among rural older adults: a qualitative study. J Rural Health. 2005;21:206-213.
Study Overview
Objective. To examine the effectiveness of a hub site–based care delivery system in delivering a dementia care management program to persons with dementia and their caregivers.
Design. Randomized pragmatic clinical trial enrolling dyads of persons with dementia and their caregiver. Study participants were randomly assigned to the dementia care management program and usual care in a 2:1 ratio.
Setting and participants. The study was conducted from 2 hub sites: the University of California, San Francisco, and the University of Nebraska Medical Center in Omaha. Each hub-site team served persons with dementia and their caregivers in California, Nebraska, and Iowa in both urban and rural areas. Participants were recruited through referral by treating providers or self-referral in response to advertising presented through a community outreach event, in the news, or on the internet. Eligibility requirements included: having a dementia diagnosis made by a treating provider; age older than 45 years; Medicare or Medicaid enrollment or eligibility; presence of a caregiver willing to enroll in the study; fluency in English, Spanish, or Cantonese; and residence in California, Nebraska, or Iowa. Exclusion criteria included residence in a nursing home. Out of 2585 referred dyads of persons with dementia and caregivers, 780 met inclusion criteria and were enrolled. A 2:1 randomization yielded 512 dyads in the intervention group and 268 dyads in the control group.
Intervention. The dementia care management program was implemented through the Care Ecosystem, a telephone- and internet-based supportive care intervention delivered by care team navigators. The navigators were unlicensed but trained dementia care guides working under the supervision of an advanced practice nurse, social worker, and pharmacist. The intervention consisted of telephone calls, monthly or at a frequency determined by needs and preferences, placed by navigators over a 12-month period; the content of the calls included response to immediate needs of persons with dementia and their caregiver, screening for common problems, and provision of support and education using care plan protocols. Caregivers and persons with dementia were encouraged to initiate contact through email, mail, or telephone for dementia-related questions. Additional support was provided by an advanced practice nurse, social worker, or pharmacist, as needed, and these health care professionals conducted further communication with the persons with dementia, caregiver, or outside professionals, such as physicians, for the persons with dementia, as needed. The average number of telephone calls over the 12-month period was 15.3 (standard deviation, 11.3). Participants assigned to usual care were offered contact information on dementia and aging-related organizations, including the Alzheimer’s Association and the Area Agencies on Aging, and also were sent a quarterly newsletter with general information about dementia.
Main outcome measures. The primary outcome measure was the Quality of Life in Alzheimer’s Disease score obtained by caregiver interview. This quality of life measure includes the following aspects, each rated on an ordinal scale of 1 to 4: physical health, energy level, mood, living situation, memory, family, closest relationship, friends, self, ability to do things for fun, finances, and life as a whole. The scores range from 13 to 52, with a higher score indicating better quality of life for persons with dementia. Other outcomes included frequency of emergency room visits, hospital use, and ambulance use; caregiver depression score from the Patient Health Questionnaire scale; caregiver burden score using the 12-item Zarit Burden Interview; caregiver self-efficacy; and caregiver satisfaction.
Main results. The study found that the quality of life for persons with dementia declined more in the usual care group than in the intervention group during the 12-month study period (difference of 0.53; 95% confidence interval, 0.25-1.3; P = 0.04). Persons with dementia also had fewer emergency room visits, with a number needed to treat to prevent 1 emergency room visit of 5. The intervention did not reduce ambulance use or hospital use. Caregivers in the intervention group had a greater decline in depression when compared to usual care; the frequency of moderate to severe depression decreased from 13.4% at baseline to 7.9% at 12 months (P = 0.004). Caregiver burden declined more in the intervention group than in the control group at 12 months (P = 0.046). In terms of caregiver satisfaction, 97% of caregivers surveyed in the intervention group said they would recommend the intervention to another caregiver; 45% indicated they were very satisfied, and 33% that they were satisfied.
Conclusion. Delivering dementia care via telephone and internet through a collaborative program with care navigators can improve caregiver burden and well-being and improve quality of life, emergency room utilization, and depression for persons with dementia. In addition, the program was well received.
Commentary
Dementia, including Alzheimer’s disease, primarily affects older adults and is characterized by declines in memory and cognitive function. It is often accompanied by neuropsychological symptoms such as agitation, wandering, and physical and verbal outbursts, which are debilitating for persons living with dementia and difficult to cope with for caregivers.1 These symptoms are often the source of caregiver stress, potentially leading to caregiver depression and eventual need for long-term institution-based care, such as nursing home placement.2
Prior literature has established the potential effect of support in improving caregiver outcomes, including caregiver stress and burden, through interventions such as enhancing resources for caregivers, teaching coping strategies to caregivers, and teaching caregivers how to manage support for their loved ones.3,4 However, wider adoption of these interventions may be limited if the interventions involve in-person meetings or activities that take caregivers away from caregiving; the scalability of these programs is also limited by their ability to reach persons with dementia and their caregivers. These barriers are particularly important for older adults living in rural areas, where the availability of resources and distance from access to quality care may be particularly limiting.5 Leveraging advances in technology and telecommunication, this study examined the effects of providing dementia care support via telephone and internet using a trained, unlicensed care navigator as the main point of contact. The results showed improved quality of life for persons with dementia, reduced need for emergency room visits, and reduced caregiver burden and depression. The intervention is promising as a scalable intervention that may impact dementia care nationwide.
Despite the promising results, there are several issues regarding the intervention’s applicability and impact that future studies may help to further clarify. Although the improvement in quality of life in persons with dementia is important to document, it is unclear whether this difference is clinically significant. Also, it may be important to examine whether the 12-month program has sustained impact beyond the study period, although the intervention could be conceived as a long-term care solution. If the intervention is sustained beyond 12 months, future studies may look at other clinical outcomes, such as incidence of institutionalization and perhaps time to institutionalization. The study population consisted of persons with dementia of various stages, half of whom had mild disease. Future studies may further clarify at which stage of dementia the intervention is most useful. Other changes that occurred during the study period, such as change in the use of paid home-based support services and referrals to other relevant evaluations and treatment, may provide further clues about how the dementia care intervention achieved its beneficial effects.
Applications for Clinical Practice
From the health systems perspective, dementia care accounts for significant resources, and these costs are expected to grow as the population ages and dementia prevalence increases. Identifying potentially scalable interventions that yield clinical benefits and are sustainable from a cost perspective is an important step forward in improving care for persons with dementia and their caregivers across the nation. The use of centralized hubs to deliver this intervention and the novel use of telecommunications advances make this intervention applicable across large areas. Policy makers should explore how an intervention such as this could be established and sustained in our health care system.
–William W. Hung, MD, MPH
Study Overview
Objective. To examine the effectiveness of a hub site–based care delivery system in delivering a dementia care management program to persons with dementia and their caregivers.
Design. Randomized pragmatic clinical trial enrolling dyads of persons with dementia and their caregiver. Study participants were randomly assigned to the dementia care management program and usual care in a 2:1 ratio.
Setting and participants. The study was conducted from 2 hub sites: the University of California, San Francisco, and the University of Nebraska Medical Center in Omaha. Each hub-site team served persons with dementia and their caregivers in California, Nebraska, and Iowa in both urban and rural areas. Participants were recruited through referral by treating providers or self-referral in response to advertising presented through a community outreach event, in the news, or on the internet. Eligibility requirements included: having a dementia diagnosis made by a treating provider; age older than 45 years; Medicare or Medicaid enrollment or eligibility; presence of a caregiver willing to enroll in the study; fluency in English, Spanish, or Cantonese; and residence in California, Nebraska, or Iowa. Exclusion criteria included residence in a nursing home. Out of 2585 referred dyads of persons with dementia and caregivers, 780 met inclusion criteria and were enrolled. A 2:1 randomization yielded 512 dyads in the intervention group and 268 dyads in the control group.
Intervention. The dementia care management program was implemented through the Care Ecosystem, a telephone- and internet-based supportive care intervention delivered by care team navigators. The navigators were unlicensed but trained dementia care guides working under the supervision of an advanced practice nurse, social worker, and pharmacist. The intervention consisted of telephone calls, monthly or at a frequency determined by needs and preferences, placed by navigators over a 12-month period; the content of the calls included response to immediate needs of persons with dementia and their caregiver, screening for common problems, and provision of support and education using care plan protocols. Caregivers and persons with dementia were encouraged to initiate contact through email, mail, or telephone for dementia-related questions. Additional support was provided by an advanced practice nurse, social worker, or pharmacist, as needed, and these health care professionals conducted further communication with the persons with dementia, caregiver, or outside professionals, such as physicians, for the persons with dementia, as needed. The average number of telephone calls over the 12-month period was 15.3 (standard deviation, 11.3). Participants assigned to usual care were offered contact information on dementia and aging-related organizations, including the Alzheimer’s Association and the Area Agencies on Aging, and also were sent a quarterly newsletter with general information about dementia.
Main outcome measures. The primary outcome measure was the Quality of Life in Alzheimer’s Disease score obtained by caregiver interview. This quality of life measure includes the following aspects, each rated on an ordinal scale of 1 to 4: physical health, energy level, mood, living situation, memory, family, closest relationship, friends, self, ability to do things for fun, finances, and life as a whole. The scores range from 13 to 52, with a higher score indicating better quality of life for persons with dementia. Other outcomes included frequency of emergency room visits, hospital use, and ambulance use; caregiver depression score from the Patient Health Questionnaire scale; caregiver burden score using the 12-item Zarit Burden Interview; caregiver self-efficacy; and caregiver satisfaction.
Main results. The study found that the quality of life for persons with dementia declined more in the usual care group than in the intervention group during the 12-month study period (difference of 0.53; 95% confidence interval, 0.25-1.3; P = 0.04). Persons with dementia also had fewer emergency room visits, with a number needed to treat to prevent 1 emergency room visit of 5. The intervention did not reduce ambulance use or hospital use. Caregivers in the intervention group had a greater decline in depression when compared to usual care; the frequency of moderate to severe depression decreased from 13.4% at baseline to 7.9% at 12 months (P = 0.004). Caregiver burden declined more in the intervention group than in the control group at 12 months (P = 0.046). In terms of caregiver satisfaction, 97% of caregivers surveyed in the intervention group said they would recommend the intervention to another caregiver; 45% indicated they were very satisfied, and 33% that they were satisfied.
Conclusion. Delivering dementia care via telephone and internet through a collaborative program with care navigators can improve caregiver burden and well-being and improve quality of life, emergency room utilization, and depression for persons with dementia. In addition, the program was well received.
Commentary
Dementia, including Alzheimer’s disease, primarily affects older adults and is characterized by declines in memory and cognitive function. It is often accompanied by neuropsychological symptoms such as agitation, wandering, and physical and verbal outbursts, which are debilitating for persons living with dementia and difficult to cope with for caregivers.1 These symptoms are often the source of caregiver stress, potentially leading to caregiver depression and eventual need for long-term institution-based care, such as nursing home placement.2
Prior literature has established the potential effect of support in improving caregiver outcomes, including caregiver stress and burden, through interventions such as enhancing resources for caregivers, teaching coping strategies to caregivers, and teaching caregivers how to manage support for their loved ones.3,4 However, wider adoption of these interventions may be limited if the interventions involve in-person meetings or activities that take caregivers away from caregiving; the scalability of these programs is also limited by their ability to reach persons with dementia and their caregivers. These barriers are particularly important for older adults living in rural areas, where the availability of resources and distance from access to quality care may be particularly limiting.5 Leveraging advances in technology and telecommunication, this study examined the effects of providing dementia care support via telephone and internet using a trained, unlicensed care navigator as the main point of contact. The results showed improved quality of life for persons with dementia, reduced need for emergency room visits, and reduced caregiver burden and depression. The intervention is promising as a scalable intervention that may impact dementia care nationwide.
Despite the promising results, there are several issues regarding the intervention’s applicability and impact that future studies may help to further clarify. Although the improvement in quality of life in persons with dementia is important to document, it is unclear whether this difference is clinically significant. Also, it may be important to examine whether the 12-month program has sustained impact beyond the study period, although the intervention could be conceived as a long-term care solution. If the intervention is sustained beyond 12 months, future studies may look at other clinical outcomes, such as incidence of institutionalization and perhaps time to institutionalization. The study population consisted of persons with dementia of various stages, half of whom had mild disease. Future studies may further clarify at which stage of dementia the intervention is most useful. Other changes that occurred during the study period, such as change in the use of paid home-based support services and referrals to other relevant evaluations and treatment, may provide further clues about how the dementia care intervention achieved its beneficial effects.
Applications for Clinical Practice
From the health systems perspective, dementia care accounts for significant resources, and these costs are expected to grow as the population ages and dementia prevalence increases. Identifying potentially scalable interventions that yield clinical benefits and are sustainable from a cost perspective is an important step forward in improving care for persons with dementia and their caregivers across the nation. The use of centralized hubs to deliver this intervention and the novel use of telecommunications advances make this intervention applicable across large areas. Policy makers should explore how an intervention such as this could be established and sustained in our health care system.
–William W. Hung, MD, MPH
1. Mega MS, Cummings JL, Fiorello T, Gornbein J. The spectrum of behavioral changes in Alzheimer’s disease. Neurology. 1996;46:130-135.
2. Gallagher-Thompson D, Brooks JO 3rd, Bliwise D, et al. The relations among caregiver stress, “sundowning” symptoms, and cognitive decline in Alzheimer’s disease. J Am Geriatr Soc. 1992;40:807-810.
3. Livingston G, Barber J, Rapaport P, et al. Clinical effectiveness of a manual based coping strategy programme (START, STrAtegies for RelaTives) in promoting the mental health of carers of family members with dementia: pragmatic randomised controlled trial. BMJ. 2013;347:f6276.
4. Belle SH, Burgio L, Burns R, et al; Resources for Enhancing Alzheimer’s Caregiver Health (REACH) II Investigators. Enhancing the quality of life of dementia caregivers from different ethnic or racial groups: a randomized, controlled trial. Ann Intern Med. 2006;145:727-738.
5. Goins RT, Williams KA, Carter MW, et al. Perceived barriers to health care access among rural older adults: a qualitative study. J Rural Health. 2005;21:206-213.
1. Mega MS, Cummings JL, Fiorello T, Gornbein J. The spectrum of behavioral changes in Alzheimer’s disease. Neurology. 1996;46:130-135.
2. Gallagher-Thompson D, Brooks JO 3rd, Bliwise D, et al. The relations among caregiver stress, “sundowning” symptoms, and cognitive decline in Alzheimer’s disease. J Am Geriatr Soc. 1992;40:807-810.
3. Livingston G, Barber J, Rapaport P, et al. Clinical effectiveness of a manual based coping strategy programme (START, STrAtegies for RelaTives) in promoting the mental health of carers of family members with dementia: pragmatic randomised controlled trial. BMJ. 2013;347:f6276.
4. Belle SH, Burgio L, Burns R, et al; Resources for Enhancing Alzheimer’s Caregiver Health (REACH) II Investigators. Enhancing the quality of life of dementia caregivers from different ethnic or racial groups: a randomized, controlled trial. Ann Intern Med. 2006;145:727-738.
5. Goins RT, Williams KA, Carter MW, et al. Perceived barriers to health care access among rural older adults: a qualitative study. J Rural Health. 2005;21:206-213.
Staged hemispheric embolization: How to treat hemimegalencephaly within days of birth
BALTIMORE – About one in 4,000 children are born with hemimegalencephaly, meaning one brain hemisphere is abnormally formed and larger than the other.
The abnormal hemisphere causes seizures, and when they become intractable, the standard of care is to remove it as soon as possible; the longer the abnormal hemisphere is left in, the worse children do developmentally, and the less likely hemispherectomy will stop the seizures.
A problem comes up, however, when children become intractable before they’re 3 months old: “Neurosurgeons won’t touch them,” said Taeun Chang, MD, a neonatal neurointensivist at Children’s National Medical Center in Washington.
Newborns’ coagulation systems aren’t fully developed, and the risk of fatal hemorrhage is too high, she explained.
Out of what she said was a sense of “desperation” to address the situation, Dr. Chang has spearheaded a new approach for newborns at Children’s National, serial glue embolization to induce targeted strokes in the affected hemisphere. She reported on the first five cases at the American Epilepsy Society annual meeting.
At this point, “I feel like we’ve pretty much figured out the technique in terms of minimizing the complications. There’s no reason to wait anymore” for surgery as newborns get worse and worse, she said.
The technique
In two or three stages over several days, the major branches of the affected hemisphere’s anterior, middle, and posterior cerebral arteries are embolized. “You have to glue a long area and put in a lot of glue and glue up the secondary branches because [newborns] are so good at forming collaterals,” Dr. Chang said.
Fresh frozen plasma is given before and after each embolization session to boost coagulation proteins. Nicardipine is given during the procedure to prevent vasospasms. The one death in the series, case four, was in an 11-day old girl who vasospasmed, ruptured an artery over the tip of the guidewire, and hemorrhaged.
After the procedure, body temperature is kept at 36° C to prevent fever; sodium is kept high, and ins and outs are matched, to reduce brain edema; and blood pressure is tightly controlled. Children are kept on EEG during embolization and for days afterwards, and seizures, if any, are treated. The next embolization comes after peak swelling has passed in about 48-72 hours.
“The reason we can get away with this without herniation is that newborns’ skulls are soft, and their sutures are open,” so cerebral edema is manageable, Dr. Chang said.
Learning curve and outcomes
“What we learned in the first two cases” – a 23-day-old boy and 49-day-old girl – “was to create effective strokes. That’s not something any of us are taught to do,” she said.
“We were not trying to destroy the whole hemisphere, just the area that was seizing on EEG.” That was a mistake, she said: Adjacent areas began seizing and both children went on to anatomical hemispherectomies and needed shunts.
They are 5 years old now, and both on four seizure medications. The boy is in a wheelchair, fed by a G-tube, and has fewer than 20 words. The girl has a gait trainer, is fed mostly by G-tube, and has more than 50 words.
The third patient had her middle and posterior cerebral arteries embolized beginning when she was 43 days old. She was seizure free when she left the NICU, but eventually had a functional hemispherectomy. She’s 2 years old now, eating by mouth, in a gait trainer, and speaks in one- or two-word sentences. She’s on three seizure medications.
Outcomes have been best for patient five. Her posterior, middle, and anterior cerebral arteries were embolized starting at 14 days. She’s 1 year old now, seizure free on three medications, eating by G-tube and mouth, and has three-five words.
Dr. Chang said that newborns with hemimegalencephaly at Children’s National aren’t lingering as long on failing drug regimens these days. “We go to intervention now that we have this option” after they fail just two or three medications.
Given that the fifth patient, treated at 2 weeks old, is the only one who has been seizure free, she suspects it’s probably best to do embolization sooner rather than later, just as with anatomical hemispherectomy in older children. “We’ve got the sense that even a couple of weeks makes a difference. People need to come to us sooner,” Dr. Chang said.
It’s possible embolization could be a sound alternative to surgery even after 3 months of age. Focal embolization might also be a viable alternative to surgery to knock out epileptogenic lesions in children with tuberous sclerosis. Dr. Chang and her colleagues are interested in those and other possibilities, and plan to continue to develop the approach, she said.
There was no funding, and the investigators didn’t have any relevant disclosures.
SOURCE: Chang T et al. AES 2019, Abstract 1.225.
BALTIMORE – About one in 4,000 children are born with hemimegalencephaly, meaning one brain hemisphere is abnormally formed and larger than the other.
The abnormal hemisphere causes seizures, and when they become intractable, the standard of care is to remove it as soon as possible; the longer the abnormal hemisphere is left in, the worse children do developmentally, and the less likely hemispherectomy will stop the seizures.
A problem comes up, however, when children become intractable before they’re 3 months old: “Neurosurgeons won’t touch them,” said Taeun Chang, MD, a neonatal neurointensivist at Children’s National Medical Center in Washington.
Newborns’ coagulation systems aren’t fully developed, and the risk of fatal hemorrhage is too high, she explained.
Out of what she said was a sense of “desperation” to address the situation, Dr. Chang has spearheaded a new approach for newborns at Children’s National, serial glue embolization to induce targeted strokes in the affected hemisphere. She reported on the first five cases at the American Epilepsy Society annual meeting.
At this point, “I feel like we’ve pretty much figured out the technique in terms of minimizing the complications. There’s no reason to wait anymore” for surgery as newborns get worse and worse, she said.
The technique
In two or three stages over several days, the major branches of the affected hemisphere’s anterior, middle, and posterior cerebral arteries are embolized. “You have to glue a long area and put in a lot of glue and glue up the secondary branches because [newborns] are so good at forming collaterals,” Dr. Chang said.
Fresh frozen plasma is given before and after each embolization session to boost coagulation proteins. Nicardipine is given during the procedure to prevent vasospasms. The one death in the series, case four, was in an 11-day old girl who vasospasmed, ruptured an artery over the tip of the guidewire, and hemorrhaged.
After the procedure, body temperature is kept at 36° C to prevent fever; sodium is kept high, and ins and outs are matched, to reduce brain edema; and blood pressure is tightly controlled. Children are kept on EEG during embolization and for days afterwards, and seizures, if any, are treated. The next embolization comes after peak swelling has passed in about 48-72 hours.
“The reason we can get away with this without herniation is that newborns’ skulls are soft, and their sutures are open,” so cerebral edema is manageable, Dr. Chang said.
Learning curve and outcomes
“What we learned in the first two cases” – a 23-day-old boy and 49-day-old girl – “was to create effective strokes. That’s not something any of us are taught to do,” she said.
“We were not trying to destroy the whole hemisphere, just the area that was seizing on EEG.” That was a mistake, she said: Adjacent areas began seizing and both children went on to anatomical hemispherectomies and needed shunts.
They are 5 years old now, and both on four seizure medications. The boy is in a wheelchair, fed by a G-tube, and has fewer than 20 words. The girl has a gait trainer, is fed mostly by G-tube, and has more than 50 words.
The third patient had her middle and posterior cerebral arteries embolized beginning when she was 43 days old. She was seizure free when she left the NICU, but eventually had a functional hemispherectomy. She’s 2 years old now, eating by mouth, in a gait trainer, and speaks in one- or two-word sentences. She’s on three seizure medications.
Outcomes have been best for patient five. Her posterior, middle, and anterior cerebral arteries were embolized starting at 14 days. She’s 1 year old now, seizure free on three medications, eating by G-tube and mouth, and has three-five words.
Dr. Chang said that newborns with hemimegalencephaly at Children’s National aren’t lingering as long on failing drug regimens these days. “We go to intervention now that we have this option” after they fail just two or three medications.
Given that the fifth patient, treated at 2 weeks old, is the only one who has been seizure free, she suspects it’s probably best to do embolization sooner rather than later, just as with anatomical hemispherectomy in older children. “We’ve got the sense that even a couple of weeks makes a difference. People need to come to us sooner,” Dr. Chang said.
It’s possible embolization could be a sound alternative to surgery even after 3 months of age. Focal embolization might also be a viable alternative to surgery to knock out epileptogenic lesions in children with tuberous sclerosis. Dr. Chang and her colleagues are interested in those and other possibilities, and plan to continue to develop the approach, she said.
There was no funding, and the investigators didn’t have any relevant disclosures.
SOURCE: Chang T et al. AES 2019, Abstract 1.225.
BALTIMORE – About one in 4,000 children are born with hemimegalencephaly, meaning one brain hemisphere is abnormally formed and larger than the other.
The abnormal hemisphere causes seizures, and when they become intractable, the standard of care is to remove it as soon as possible; the longer the abnormal hemisphere is left in, the worse children do developmentally, and the less likely hemispherectomy will stop the seizures.
A problem comes up, however, when children become intractable before they’re 3 months old: “Neurosurgeons won’t touch them,” said Taeun Chang, MD, a neonatal neurointensivist at Children’s National Medical Center in Washington.
Newborns’ coagulation systems aren’t fully developed, and the risk of fatal hemorrhage is too high, she explained.
Out of what she said was a sense of “desperation” to address the situation, Dr. Chang has spearheaded a new approach for newborns at Children’s National, serial glue embolization to induce targeted strokes in the affected hemisphere. She reported on the first five cases at the American Epilepsy Society annual meeting.
At this point, “I feel like we’ve pretty much figured out the technique in terms of minimizing the complications. There’s no reason to wait anymore” for surgery as newborns get worse and worse, she said.
The technique
In two or three stages over several days, the major branches of the affected hemisphere’s anterior, middle, and posterior cerebral arteries are embolized. “You have to glue a long area and put in a lot of glue and glue up the secondary branches because [newborns] are so good at forming collaterals,” Dr. Chang said.
Fresh frozen plasma is given before and after each embolization session to boost coagulation proteins. Nicardipine is given during the procedure to prevent vasospasms. The one death in the series, case four, was in an 11-day old girl who vasospasmed, ruptured an artery over the tip of the guidewire, and hemorrhaged.
After the procedure, body temperature is kept at 36° C to prevent fever; sodium is kept high, and ins and outs are matched, to reduce brain edema; and blood pressure is tightly controlled. Children are kept on EEG during embolization and for days afterwards, and seizures, if any, are treated. The next embolization comes after peak swelling has passed in about 48-72 hours.
“The reason we can get away with this without herniation is that newborns’ skulls are soft, and their sutures are open,” so cerebral edema is manageable, Dr. Chang said.
Learning curve and outcomes
“What we learned in the first two cases” – a 23-day-old boy and 49-day-old girl – “was to create effective strokes. That’s not something any of us are taught to do,” she said.
“We were not trying to destroy the whole hemisphere, just the area that was seizing on EEG.” That was a mistake, she said: Adjacent areas began seizing and both children went on to anatomical hemispherectomies and needed shunts.
They are 5 years old now, and both on four seizure medications. The boy is in a wheelchair, fed by a G-tube, and has fewer than 20 words. The girl has a gait trainer, is fed mostly by G-tube, and has more than 50 words.
The third patient had her middle and posterior cerebral arteries embolized beginning when she was 43 days old. She was seizure free when she left the NICU, but eventually had a functional hemispherectomy. She’s 2 years old now, eating by mouth, in a gait trainer, and speaks in one- or two-word sentences. She’s on three seizure medications.
Outcomes have been best for patient five. Her posterior, middle, and anterior cerebral arteries were embolized starting at 14 days. She’s 1 year old now, seizure free on three medications, eating by G-tube and mouth, and has three-five words.
Dr. Chang said that newborns with hemimegalencephaly at Children’s National aren’t lingering as long on failing drug regimens these days. “We go to intervention now that we have this option” after they fail just two or three medications.
Given that the fifth patient, treated at 2 weeks old, is the only one who has been seizure free, she suspects it’s probably best to do embolization sooner rather than later, just as with anatomical hemispherectomy in older children. “We’ve got the sense that even a couple of weeks makes a difference. People need to come to us sooner,” Dr. Chang said.
It’s possible embolization could be a sound alternative to surgery even after 3 months of age. Focal embolization might also be a viable alternative to surgery to knock out epileptogenic lesions in children with tuberous sclerosis. Dr. Chang and her colleagues are interested in those and other possibilities, and plan to continue to develop the approach, she said.
There was no funding, and the investigators didn’t have any relevant disclosures.
SOURCE: Chang T et al. AES 2019, Abstract 1.225.
REPORTING FROM AES 2019
Dependent trait in chronic migraine may predict nonresponse to onabotulinumtoxin A
according to research published in the January issue of Headache. The research may be the first to show that personality traits predict response to onabotulinumtoxin A in this population.
“These findings point out that conducting an evaluation of personality traits in patients with chronic migraine might be helpful in the prediction of the course and election of the treatment, as well as identifying patients who might benefit from a multidisciplinary approach,” wrote Alicia Gonzalez-Martinez, MD, of the Hospital Universitario de La Princesa and Instituto de Investigación Sanitaria de La Princesa in Madrid and colleagues. “Categorical questionnaires such as the Salamanca screening test seem to be useful for this purpose.”
Researchers used ICD-10 personality criteria
Personality patterns in patients with migraine and other primary headaches have been the subject of decades of research. Munoz et al. found that certain personality traits are associated with migraine and chronic migraine, and this association may influence clinical management and treatment. The effect of personality traits on response to treatment, however, had not been studied previously.
Dr. Gonzalez-Martinez and colleagues hypothesized that cluster C traits (e.g., obsessive-compulsive, dependent, and anxious), as defined by ICD-10, are associated with nonresponse to onabotulinumtoxin A. To test this hypothesis, they conducted a case-control observational study in a cohort of patients with chronic migraine. Eligible patients presented to one of two headache units of a tertiary hospital between January and May 2018. The investigators obtained a complete headache history and demographic information from each patient. Patients had at least two treatment cycles of onabotulinumtoxin A. Dr. Gonzalez-Martinez and colleagues defined treatment response as a reduction in the number of monthly migraine days of at least 50% after at least two treatment cycles.
The investigators assessed participants’ personality traits by administering the Salamanca test, a brief categorical inventory that examines 11 personality traits using 22 questions. Patients completed the test at the beginning of the study period and before they were classified as responders or nonresponders.
Medication overuse was a potential confounder
The study population included 112 patients with chronic migraine. One hundred patients (89%) were women. Participants’ mean age at initiation of onabotulinumtoxin A treatment was 43 years. The population’s mean duration of chronic migraine was 29 months. Eighty-three patients (74.1%) had medication overuse, and 96 (85.7%) responded to onabotulinumtoxin A.
Cluster A traits in the population included paranoid (prevalence, 10.7%), schizoid (38.4%), and schizotypal (7.1%). Cluster B traits included histrionic (50%), antisocial (1.8%), narcissistic (9.8%), emotional instability subtype impulsive (27.7%), and emotional instability subtype limit (EISL, 24.1%). Cluster C traits were anxious (58.9%) anancastic (i.e., obsessive-compulsive, 54.5%), and dependent (32.1%).
The investigators found no differences in demographics between responders and nonresponders. In a univariate analysis, dependent traits (e.g., passivity and emotional overdependence on others) and EISL traits (e.g., impulsivity and disturbed self-image) were significantly more common among nonresponders. In a multivariate analysis, dependent traits remained significantly associated with nonresponse to onabotulinumtoxin A.
Medication overuse was a potential confounder in the study, according to Dr. Gonzalez-Martinez and colleagues. One of the study’s limitations was its absence of a healthy control group. Another was the fact that the psychometrics of the Salamanca screening test have not been published in a peer-reviewed journal and may need further examination.
Dependent personality “may also be part of the proposed chronic pain sufferer personality,” wrote the investigators. “Early detection of personality traits could improve management and outcome of chronic migraine patients. Additionally, the possibility to predict the effectiveness of onabotulinumtoxin A therapy may reduce costs and latency time of effect in patients with improbable effectiveness.”
The study had no outside funding, and the authors reported no conflicts of interest.
SOURCE: Gonzalez-Martinez A et al. Headache. 2020;60(1):153-61.
according to research published in the January issue of Headache. The research may be the first to show that personality traits predict response to onabotulinumtoxin A in this population.
“These findings point out that conducting an evaluation of personality traits in patients with chronic migraine might be helpful in the prediction of the course and election of the treatment, as well as identifying patients who might benefit from a multidisciplinary approach,” wrote Alicia Gonzalez-Martinez, MD, of the Hospital Universitario de La Princesa and Instituto de Investigación Sanitaria de La Princesa in Madrid and colleagues. “Categorical questionnaires such as the Salamanca screening test seem to be useful for this purpose.”
Researchers used ICD-10 personality criteria
Personality patterns in patients with migraine and other primary headaches have been the subject of decades of research. Munoz et al. found that certain personality traits are associated with migraine and chronic migraine, and this association may influence clinical management and treatment. The effect of personality traits on response to treatment, however, had not been studied previously.
Dr. Gonzalez-Martinez and colleagues hypothesized that cluster C traits (e.g., obsessive-compulsive, dependent, and anxious), as defined by ICD-10, are associated with nonresponse to onabotulinumtoxin A. To test this hypothesis, they conducted a case-control observational study in a cohort of patients with chronic migraine. Eligible patients presented to one of two headache units of a tertiary hospital between January and May 2018. The investigators obtained a complete headache history and demographic information from each patient. Patients had at least two treatment cycles of onabotulinumtoxin A. Dr. Gonzalez-Martinez and colleagues defined treatment response as a reduction in the number of monthly migraine days of at least 50% after at least two treatment cycles.
The investigators assessed participants’ personality traits by administering the Salamanca test, a brief categorical inventory that examines 11 personality traits using 22 questions. Patients completed the test at the beginning of the study period and before they were classified as responders or nonresponders.
Medication overuse was a potential confounder
The study population included 112 patients with chronic migraine. One hundred patients (89%) were women. Participants’ mean age at initiation of onabotulinumtoxin A treatment was 43 years. The population’s mean duration of chronic migraine was 29 months. Eighty-three patients (74.1%) had medication overuse, and 96 (85.7%) responded to onabotulinumtoxin A.
Cluster A traits in the population included paranoid (prevalence, 10.7%), schizoid (38.4%), and schizotypal (7.1%). Cluster B traits included histrionic (50%), antisocial (1.8%), narcissistic (9.8%), emotional instability subtype impulsive (27.7%), and emotional instability subtype limit (EISL, 24.1%). Cluster C traits were anxious (58.9%) anancastic (i.e., obsessive-compulsive, 54.5%), and dependent (32.1%).
The investigators found no differences in demographics between responders and nonresponders. In a univariate analysis, dependent traits (e.g., passivity and emotional overdependence on others) and EISL traits (e.g., impulsivity and disturbed self-image) were significantly more common among nonresponders. In a multivariate analysis, dependent traits remained significantly associated with nonresponse to onabotulinumtoxin A.
Medication overuse was a potential confounder in the study, according to Dr. Gonzalez-Martinez and colleagues. One of the study’s limitations was its absence of a healthy control group. Another was the fact that the psychometrics of the Salamanca screening test have not been published in a peer-reviewed journal and may need further examination.
Dependent personality “may also be part of the proposed chronic pain sufferer personality,” wrote the investigators. “Early detection of personality traits could improve management and outcome of chronic migraine patients. Additionally, the possibility to predict the effectiveness of onabotulinumtoxin A therapy may reduce costs and latency time of effect in patients with improbable effectiveness.”
The study had no outside funding, and the authors reported no conflicts of interest.
SOURCE: Gonzalez-Martinez A et al. Headache. 2020;60(1):153-61.
according to research published in the January issue of Headache. The research may be the first to show that personality traits predict response to onabotulinumtoxin A in this population.
“These findings point out that conducting an evaluation of personality traits in patients with chronic migraine might be helpful in the prediction of the course and election of the treatment, as well as identifying patients who might benefit from a multidisciplinary approach,” wrote Alicia Gonzalez-Martinez, MD, of the Hospital Universitario de La Princesa and Instituto de Investigación Sanitaria de La Princesa in Madrid and colleagues. “Categorical questionnaires such as the Salamanca screening test seem to be useful for this purpose.”
Researchers used ICD-10 personality criteria
Personality patterns in patients with migraine and other primary headaches have been the subject of decades of research. Munoz et al. found that certain personality traits are associated with migraine and chronic migraine, and this association may influence clinical management and treatment. The effect of personality traits on response to treatment, however, had not been studied previously.
Dr. Gonzalez-Martinez and colleagues hypothesized that cluster C traits (e.g., obsessive-compulsive, dependent, and anxious), as defined by ICD-10, are associated with nonresponse to onabotulinumtoxin A. To test this hypothesis, they conducted a case-control observational study in a cohort of patients with chronic migraine. Eligible patients presented to one of two headache units of a tertiary hospital between January and May 2018. The investigators obtained a complete headache history and demographic information from each patient. Patients had at least two treatment cycles of onabotulinumtoxin A. Dr. Gonzalez-Martinez and colleagues defined treatment response as a reduction in the number of monthly migraine days of at least 50% after at least two treatment cycles.
The investigators assessed participants’ personality traits by administering the Salamanca test, a brief categorical inventory that examines 11 personality traits using 22 questions. Patients completed the test at the beginning of the study period and before they were classified as responders or nonresponders.
Medication overuse was a potential confounder
The study population included 112 patients with chronic migraine. One hundred patients (89%) were women. Participants’ mean age at initiation of onabotulinumtoxin A treatment was 43 years. The population’s mean duration of chronic migraine was 29 months. Eighty-three patients (74.1%) had medication overuse, and 96 (85.7%) responded to onabotulinumtoxin A.
Cluster A traits in the population included paranoid (prevalence, 10.7%), schizoid (38.4%), and schizotypal (7.1%). Cluster B traits included histrionic (50%), antisocial (1.8%), narcissistic (9.8%), emotional instability subtype impulsive (27.7%), and emotional instability subtype limit (EISL, 24.1%). Cluster C traits were anxious (58.9%) anancastic (i.e., obsessive-compulsive, 54.5%), and dependent (32.1%).
The investigators found no differences in demographics between responders and nonresponders. In a univariate analysis, dependent traits (e.g., passivity and emotional overdependence on others) and EISL traits (e.g., impulsivity and disturbed self-image) were significantly more common among nonresponders. In a multivariate analysis, dependent traits remained significantly associated with nonresponse to onabotulinumtoxin A.
Medication overuse was a potential confounder in the study, according to Dr. Gonzalez-Martinez and colleagues. One of the study’s limitations was its absence of a healthy control group. Another was the fact that the psychometrics of the Salamanca screening test have not been published in a peer-reviewed journal and may need further examination.
Dependent personality “may also be part of the proposed chronic pain sufferer personality,” wrote the investigators. “Early detection of personality traits could improve management and outcome of chronic migraine patients. Additionally, the possibility to predict the effectiveness of onabotulinumtoxin A therapy may reduce costs and latency time of effect in patients with improbable effectiveness.”
The study had no outside funding, and the authors reported no conflicts of interest.
SOURCE: Gonzalez-Martinez A et al. Headache. 2020;60(1):153-61.
FROM HEADACHE
CDC: Opioid prescribing and use rates down since 2010
Trends in opioid prescribing and use from 2010 to 2016 offer some encouragement, but opioid-attributable deaths continued to increase over that period, according to the Centers for Disease Control and Prevention.
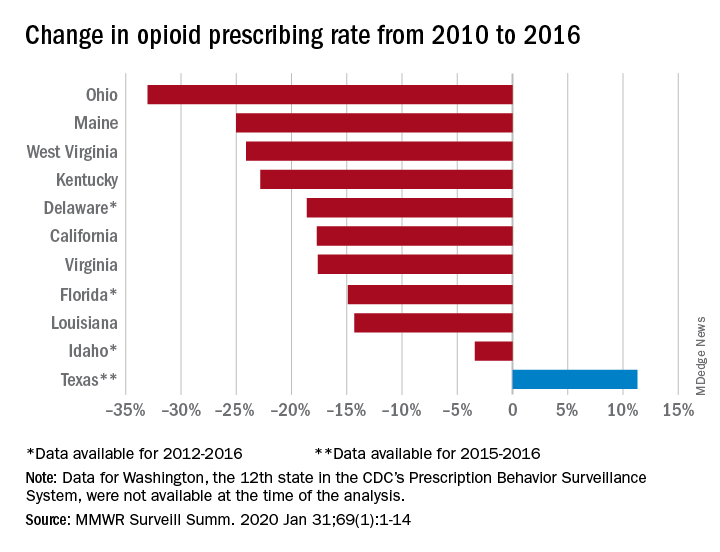
Prescribing rates dropped during that period, as did daily opioid dosage rates and the percentage of patients with high daily opioid dosages, Gail K. Strickler, PhD, of the Institute for Behavioral Health at Brandeis University in Waltham, Mass., and associates wrote in MMWR Surveillance Summaries.
Their analysis involved 11 of the 12 states (Washington was unable to provide data for the analysis) participating in the CDC’s Prescription Behavior Surveillance System, which uses data from the states’ prescription drug monitoring programs. The 11 states represented about 38% of the U.S. population in 2016.
The opioid prescribing rate fell in 10 of those 11 states, with declines varying from 3.4% in Idaho to 33.0% in Ohio. Prescribing went up in Texas by 11.3%, but the state only had data available for 2015 and 2016. Three other states – Delaware, Florida, and Idaho – were limited to data from 2012 to 2016, the investigators noted.
As for the other measures, all states showed declines for the mean daily opioid dosage. Texas had the smallest drop at 2.9% and Florida saw the largest, at 27.4%. All states also had reductions in the percentage of patients with high daily opioid dosage, with decreases varying from 5.7% in Idaho to 43.9% in Louisiana, Dr. Strickler and associates reported. A high daily dosage was defined as at least 90 morphine milligram equivalents for all class II-V opioid drugs.
“Despite these favorable trends ... opioid overdose deaths attributable to the most commonly prescribed opioids, the natural and semisynthetics (e.g., morphine and oxycodone), increased during 2010-2016,” they said.
It is possible that a change in mortality is lagging “behind changes in prescribing behaviors” or that “the trend in deaths related to these types of opioids has been driven by factors other than prescription opioid misuse rates, such as increasing mortality from heroin, which is frequently classified as morphine or found concomitantly with morphine postmortem, and a spike in deaths involving illicitly manufactured fentanyl combined with heroin and prescribed opioids since 2013,” the investigators suggested.
SOURCE: Strickler GK et al. MMWR Surveill Summ. 2020 Jan 31;69(1):1-14.
Trends in opioid prescribing and use from 2010 to 2016 offer some encouragement, but opioid-attributable deaths continued to increase over that period, according to the Centers for Disease Control and Prevention.
Prescribing rates dropped during that period, as did daily opioid dosage rates and the percentage of patients with high daily opioid dosages, Gail K. Strickler, PhD, of the Institute for Behavioral Health at Brandeis University in Waltham, Mass., and associates wrote in MMWR Surveillance Summaries.
Their analysis involved 11 of the 12 states (Washington was unable to provide data for the analysis) participating in the CDC’s Prescription Behavior Surveillance System, which uses data from the states’ prescription drug monitoring programs. The 11 states represented about 38% of the U.S. population in 2016.
The opioid prescribing rate fell in 10 of those 11 states, with declines varying from 3.4% in Idaho to 33.0% in Ohio. Prescribing went up in Texas by 11.3%, but the state only had data available for 2015 and 2016. Three other states – Delaware, Florida, and Idaho – were limited to data from 2012 to 2016, the investigators noted.
As for the other measures, all states showed declines for the mean daily opioid dosage. Texas had the smallest drop at 2.9% and Florida saw the largest, at 27.4%. All states also had reductions in the percentage of patients with high daily opioid dosage, with decreases varying from 5.7% in Idaho to 43.9% in Louisiana, Dr. Strickler and associates reported. A high daily dosage was defined as at least 90 morphine milligram equivalents for all class II-V opioid drugs.
“Despite these favorable trends ... opioid overdose deaths attributable to the most commonly prescribed opioids, the natural and semisynthetics (e.g., morphine and oxycodone), increased during 2010-2016,” they said.
It is possible that a change in mortality is lagging “behind changes in prescribing behaviors” or that “the trend in deaths related to these types of opioids has been driven by factors other than prescription opioid misuse rates, such as increasing mortality from heroin, which is frequently classified as morphine or found concomitantly with morphine postmortem, and a spike in deaths involving illicitly manufactured fentanyl combined with heroin and prescribed opioids since 2013,” the investigators suggested.
SOURCE: Strickler GK et al. MMWR Surveill Summ. 2020 Jan 31;69(1):1-14.
Trends in opioid prescribing and use from 2010 to 2016 offer some encouragement, but opioid-attributable deaths continued to increase over that period, according to the Centers for Disease Control and Prevention.
Prescribing rates dropped during that period, as did daily opioid dosage rates and the percentage of patients with high daily opioid dosages, Gail K. Strickler, PhD, of the Institute for Behavioral Health at Brandeis University in Waltham, Mass., and associates wrote in MMWR Surveillance Summaries.
Their analysis involved 11 of the 12 states (Washington was unable to provide data for the analysis) participating in the CDC’s Prescription Behavior Surveillance System, which uses data from the states’ prescription drug monitoring programs. The 11 states represented about 38% of the U.S. population in 2016.
The opioid prescribing rate fell in 10 of those 11 states, with declines varying from 3.4% in Idaho to 33.0% in Ohio. Prescribing went up in Texas by 11.3%, but the state only had data available for 2015 and 2016. Three other states – Delaware, Florida, and Idaho – were limited to data from 2012 to 2016, the investigators noted.
As for the other measures, all states showed declines for the mean daily opioid dosage. Texas had the smallest drop at 2.9% and Florida saw the largest, at 27.4%. All states also had reductions in the percentage of patients with high daily opioid dosage, with decreases varying from 5.7% in Idaho to 43.9% in Louisiana, Dr. Strickler and associates reported. A high daily dosage was defined as at least 90 morphine milligram equivalents for all class II-V opioid drugs.
“Despite these favorable trends ... opioid overdose deaths attributable to the most commonly prescribed opioids, the natural and semisynthetics (e.g., morphine and oxycodone), increased during 2010-2016,” they said.
It is possible that a change in mortality is lagging “behind changes in prescribing behaviors” or that “the trend in deaths related to these types of opioids has been driven by factors other than prescription opioid misuse rates, such as increasing mortality from heroin, which is frequently classified as morphine or found concomitantly with morphine postmortem, and a spike in deaths involving illicitly manufactured fentanyl combined with heroin and prescribed opioids since 2013,” the investigators suggested.
SOURCE: Strickler GK et al. MMWR Surveill Summ. 2020 Jan 31;69(1):1-14.
FROM MMWR SURVEILLANCE SUMMARIES
Acknowledging Disparities in Dementia Care for Increasingly Diverse Ethnoracial Patient Populations
Alzheimer disease and related dementias are a global health concern, affecting nearly 47 million people worldwide. Alzheimer disease and related dementias were among the top 10 causes of death worldwide in 2015 and are expected to increase by 10 million cases annually.1 Despite the ethnic diversity of the US, there are considerable gaps in the literature regarding dementia and how it is diagnosed and treated among many ethnic and racial groups.
In 2012, President Barack Obama signed a declaration with the intention of decreasing ethnoracial disparities in Alzheimer disease research and treatment by increasing clinical care, research, and services targeted to racial and ethnic minorities.2 Despite that declaration, in the US there are gaps in access to care for the geriatric population in general. The American Geriatrics Society estimates that the US has fewer than half the needed number of practicing geriatricians. In 2016, there was 1 geriatrician for every 1,924 Americans aged ≥ 65 years.3 Furthermore, health care providers (HCPs) are often not of the same ethnicity or adequately trained to assess and build relationships with ethnically and racially diverse populations.2 Given the projected growth in the numbers of individuals worldwide with dementia, we have a responsibility to continue to develop strategies to provide more inclusive care.
By 2060, minority populations aged ≥ 65 years are expected to represent 45% of the US population, up from 22% in 2014.4 The growth of racial and ethnic minority groups are expected to exceed the growth of the non-Hispanic white population in the next few decades. By 2060, it is estimated that the US population will increase by 75% for non-Hispanic whites, 172% for African Americans, 270% for Asian and Pacific Islanders, 274% for American Indian and Alaska Natives, and 391% for Hispanics.4
A growing body of evidence suggests that Alzheimer disease and related dementias may disproportionately afflict minority groups in the US, which will become quite significant in the years ahead. The Alzheimer’s Association estimates that the prevalence of Alzheimer disease and other dementias among those aged > 65 years, is about twice the rate in African Americans and about 1.5 times the rate in Hispanics when compared with non-Hispanic whites.5 While increases in the incidence of Alzheimer disease and related dementias in non-Hispanic whites is expected to plateau around 2050, its incidence in ethnic and racial minority groups will continue to grow, especially among Hispanics.4 This stark realization provides additional compelling reasons for the US to develop preventative interventions or treatment options that may help delay the onset of the disease and to improve the quality of life of those with the disease or caregiving for those afflicted with it. Culturally competent care of these individuals is paramount.
Diagnosis
Early and accurate diagnosis of individuals with dementia confers many benefits, including early treatment; clinical trial participation; management of comorbid conditions; training, education, and support for patients and families; and legal, financial, and end of life care planning.3 Beyond the logistical concerns (such as HCP shortages), one of the challenges of assessing minority groups is finding staff who are culturally competent or speak the language necessary to accurately communicate and interact with these subgroups. Hispanics and African Americans often receive delayed or inadequate health care services or are diagnosed in an emergency department or other nontraditional setting.5
Even those individuals seeking or receiving care in primary care settings are not always forthcoming about their cognitive status. Only 56% of respondents in a recent survey of patients who had experienced subjective cognitive decline reported that they had discussed it with their HCP.4 This reticence is thought to be influenced by multiple factors, including distrust of the medical establishment, religious or spiritual beliefs, cultural or family beliefs and expectations about geriatric care, and lack of understanding about normal aging vs cognitive disorders. Furthermore, the sensitivity and specificity of current diagnostic tests for dementia have been questioned for nonwhite populations given the clinical presentation of dementia can vary across ethnoracial groups.5
As Luria noted, cognitive assessment tools developed and validated for use with one culture frequently results in experimental failures and are not valid for use with other cultural groups.1 Cognitive testing results are influenced by educational and cultural factors, and this is one of the challenges in correctly diagnosing those of differing ethnoracial backgrounds. Individuals in racial and ethnic minorities may have limited formal education and/or high illiteracy rates and/or cultural nuances to problem solving, thinking, and memory that may not be reflected in current assessment tools.1
There is hope that testing bias could be altered or eliminated using neuroimaging or biomarkers. However, the Alzheimer’s Disease Neuroimaging Initiative study of patients in the US and Canada included < 5% African American or Hispanic participants in its total sample. Few studies have systematically examined ethnoracial differences in amyloid positron emission tomography, and none have been published to date in ethnoracially diverse groups that assess the more recently developed tau imaging agents.1
Diversity Among Caregivers
The research community must make greater efforts to improve recruitment of more diverse populations into clinical trials. Recent efforts by the National Institute on Aging in conjunction with the Alzheimer’s Association include developing a national strategy for clinical research recruitment and retention with an emphasis on local and diverse populations. This strategy should include various training modules, webinars, and similar educational opportunities for researchers and clinical HCPs, including HCPs from diverse ethnoracial backgrounds, to implement culturally appropriate research methodologies across these diverse groups. It is important that these educational materials be disseminated to caregivers in a way they can comprehend, as the impact on caregivers of those with Alzheimer disease and related dementias is considerable.
The US currently has 7 unpaid caregivers for every adult in the high-risk group of patients aged ≥ 65 years, but this will decline to a ratio of 4:1 by 2030.4 More than two-thirds of caregivers are non-Hispanic white, while 10% are African American, 8% are Hispanic, and 5% are Asian.3 About 34% of caregivers are themselves aged ≥ 65 years and are at risk for declines in their own health given the time and financial requirements of caring for someone else.3 In 2017, the 16.1 million family and other unpaid caregivers of people with dementia provided an estimated 18.4 billion hours of unpaid care, often resulting in considerable financial strain for these individuals. More than half of the caregivers report providing ≥ 21 hours of care per week; and 42% reported providing an average of 9 hours of care per day for people with dementia.
Caregivers report increased stress, sleep deprivation, depression and anxiety, and uncertainty in their ability to provide quality care to the individual with Alzheimer or a related dementia.3 The disproportionate prevalence of Alzheimer disease and other dementias in racially and ethnically diverse populations could further magnify already existing socioeconomic and other disparities and potentially lead to worsening of health outcomes in these groups.4 Given that minority populations tend to cluster geographically, community partnerships with local churches, senior centers, community centers, and other nontraditional settings may offer better opportunities for connecting with caregivers.
Conclusions
The growth and increasing diversity of the US older adult population in the coming decades require us as HCPs, researchers, and educators to dedicate more resources to ethnoracially diverse populations. There are still a great many unknowns about Alzheimer disease and dementia, most especially among nonwhites. Research, clinical care, and education must focus on outreach to marginalized groups so we may better be able to diagnose and treat the fastest growing older adult populations in the US. A complex combination of educational, cultural, social, and environmental factors likely contribute to delayed diagnosis and care of these groups, as well as lack of access to medical care, research venues, and trust issues between minority groups and the medical establishment. We all have an obligation to acknowledge these disparities and elicit the support of our colleagues and workplaces to raise awareness and dedicate necessary resources to this growing concern.
1. Babulal GM, Quiroz YT, Albensi BC, et al; International Society to Advance Alzheimer’s Research and Treatment, Alzheimer’s Association. Perspectives on ethnic and racial disparities in Alzheimer’s disease and related dementias: update and areas of immediate need. Alzheimers Dement. 2019;15(2):292-312.
2. Brewster P, Barnes L, Haan M, et al. Progress and future challenges in aging and diversity research in the United States. Alzheimers Dement. 2019;15(7):995-1003.
3. Alzheimer’s Association. 2019 Alzheimer’s disease facts and figures. Alzheimers Dement. 2019;15(3):321-387.
4. Matthews KA, Xu W, Gaglioti AH, et al. Racial and ethnic estimates of Alzheimer’s disease and related dementias in the United States (2015-2060) in adults aged ≥65 years. Alzheimers Dement. 2019;15(1):17-24.
5. Chin AL, Negash S, Hamilton R. Diversity and disparity in dementia: the impact of ethnoracial differences in Alzheimer disease. Alzheimer Dis Assoc Disord. 2011;25(3):187-195.
Alzheimer disease and related dementias are a global health concern, affecting nearly 47 million people worldwide. Alzheimer disease and related dementias were among the top 10 causes of death worldwide in 2015 and are expected to increase by 10 million cases annually.1 Despite the ethnic diversity of the US, there are considerable gaps in the literature regarding dementia and how it is diagnosed and treated among many ethnic and racial groups.
In 2012, President Barack Obama signed a declaration with the intention of decreasing ethnoracial disparities in Alzheimer disease research and treatment by increasing clinical care, research, and services targeted to racial and ethnic minorities.2 Despite that declaration, in the US there are gaps in access to care for the geriatric population in general. The American Geriatrics Society estimates that the US has fewer than half the needed number of practicing geriatricians. In 2016, there was 1 geriatrician for every 1,924 Americans aged ≥ 65 years.3 Furthermore, health care providers (HCPs) are often not of the same ethnicity or adequately trained to assess and build relationships with ethnically and racially diverse populations.2 Given the projected growth in the numbers of individuals worldwide with dementia, we have a responsibility to continue to develop strategies to provide more inclusive care.
By 2060, minority populations aged ≥ 65 years are expected to represent 45% of the US population, up from 22% in 2014.4 The growth of racial and ethnic minority groups are expected to exceed the growth of the non-Hispanic white population in the next few decades. By 2060, it is estimated that the US population will increase by 75% for non-Hispanic whites, 172% for African Americans, 270% for Asian and Pacific Islanders, 274% for American Indian and Alaska Natives, and 391% for Hispanics.4
A growing body of evidence suggests that Alzheimer disease and related dementias may disproportionately afflict minority groups in the US, which will become quite significant in the years ahead. The Alzheimer’s Association estimates that the prevalence of Alzheimer disease and other dementias among those aged > 65 years, is about twice the rate in African Americans and about 1.5 times the rate in Hispanics when compared with non-Hispanic whites.5 While increases in the incidence of Alzheimer disease and related dementias in non-Hispanic whites is expected to plateau around 2050, its incidence in ethnic and racial minority groups will continue to grow, especially among Hispanics.4 This stark realization provides additional compelling reasons for the US to develop preventative interventions or treatment options that may help delay the onset of the disease and to improve the quality of life of those with the disease or caregiving for those afflicted with it. Culturally competent care of these individuals is paramount.
Diagnosis
Early and accurate diagnosis of individuals with dementia confers many benefits, including early treatment; clinical trial participation; management of comorbid conditions; training, education, and support for patients and families; and legal, financial, and end of life care planning.3 Beyond the logistical concerns (such as HCP shortages), one of the challenges of assessing minority groups is finding staff who are culturally competent or speak the language necessary to accurately communicate and interact with these subgroups. Hispanics and African Americans often receive delayed or inadequate health care services or are diagnosed in an emergency department or other nontraditional setting.5
Even those individuals seeking or receiving care in primary care settings are not always forthcoming about their cognitive status. Only 56% of respondents in a recent survey of patients who had experienced subjective cognitive decline reported that they had discussed it with their HCP.4 This reticence is thought to be influenced by multiple factors, including distrust of the medical establishment, religious or spiritual beliefs, cultural or family beliefs and expectations about geriatric care, and lack of understanding about normal aging vs cognitive disorders. Furthermore, the sensitivity and specificity of current diagnostic tests for dementia have been questioned for nonwhite populations given the clinical presentation of dementia can vary across ethnoracial groups.5
As Luria noted, cognitive assessment tools developed and validated for use with one culture frequently results in experimental failures and are not valid for use with other cultural groups.1 Cognitive testing results are influenced by educational and cultural factors, and this is one of the challenges in correctly diagnosing those of differing ethnoracial backgrounds. Individuals in racial and ethnic minorities may have limited formal education and/or high illiteracy rates and/or cultural nuances to problem solving, thinking, and memory that may not be reflected in current assessment tools.1
There is hope that testing bias could be altered or eliminated using neuroimaging or biomarkers. However, the Alzheimer’s Disease Neuroimaging Initiative study of patients in the US and Canada included < 5% African American or Hispanic participants in its total sample. Few studies have systematically examined ethnoracial differences in amyloid positron emission tomography, and none have been published to date in ethnoracially diverse groups that assess the more recently developed tau imaging agents.1
Diversity Among Caregivers
The research community must make greater efforts to improve recruitment of more diverse populations into clinical trials. Recent efforts by the National Institute on Aging in conjunction with the Alzheimer’s Association include developing a national strategy for clinical research recruitment and retention with an emphasis on local and diverse populations. This strategy should include various training modules, webinars, and similar educational opportunities for researchers and clinical HCPs, including HCPs from diverse ethnoracial backgrounds, to implement culturally appropriate research methodologies across these diverse groups. It is important that these educational materials be disseminated to caregivers in a way they can comprehend, as the impact on caregivers of those with Alzheimer disease and related dementias is considerable.
The US currently has 7 unpaid caregivers for every adult in the high-risk group of patients aged ≥ 65 years, but this will decline to a ratio of 4:1 by 2030.4 More than two-thirds of caregivers are non-Hispanic white, while 10% are African American, 8% are Hispanic, and 5% are Asian.3 About 34% of caregivers are themselves aged ≥ 65 years and are at risk for declines in their own health given the time and financial requirements of caring for someone else.3 In 2017, the 16.1 million family and other unpaid caregivers of people with dementia provided an estimated 18.4 billion hours of unpaid care, often resulting in considerable financial strain for these individuals. More than half of the caregivers report providing ≥ 21 hours of care per week; and 42% reported providing an average of 9 hours of care per day for people with dementia.
Caregivers report increased stress, sleep deprivation, depression and anxiety, and uncertainty in their ability to provide quality care to the individual with Alzheimer or a related dementia.3 The disproportionate prevalence of Alzheimer disease and other dementias in racially and ethnically diverse populations could further magnify already existing socioeconomic and other disparities and potentially lead to worsening of health outcomes in these groups.4 Given that minority populations tend to cluster geographically, community partnerships with local churches, senior centers, community centers, and other nontraditional settings may offer better opportunities for connecting with caregivers.
Conclusions
The growth and increasing diversity of the US older adult population in the coming decades require us as HCPs, researchers, and educators to dedicate more resources to ethnoracially diverse populations. There are still a great many unknowns about Alzheimer disease and dementia, most especially among nonwhites. Research, clinical care, and education must focus on outreach to marginalized groups so we may better be able to diagnose and treat the fastest growing older adult populations in the US. A complex combination of educational, cultural, social, and environmental factors likely contribute to delayed diagnosis and care of these groups, as well as lack of access to medical care, research venues, and trust issues between minority groups and the medical establishment. We all have an obligation to acknowledge these disparities and elicit the support of our colleagues and workplaces to raise awareness and dedicate necessary resources to this growing concern.
Alzheimer disease and related dementias are a global health concern, affecting nearly 47 million people worldwide. Alzheimer disease and related dementias were among the top 10 causes of death worldwide in 2015 and are expected to increase by 10 million cases annually.1 Despite the ethnic diversity of the US, there are considerable gaps in the literature regarding dementia and how it is diagnosed and treated among many ethnic and racial groups.
In 2012, President Barack Obama signed a declaration with the intention of decreasing ethnoracial disparities in Alzheimer disease research and treatment by increasing clinical care, research, and services targeted to racial and ethnic minorities.2 Despite that declaration, in the US there are gaps in access to care for the geriatric population in general. The American Geriatrics Society estimates that the US has fewer than half the needed number of practicing geriatricians. In 2016, there was 1 geriatrician for every 1,924 Americans aged ≥ 65 years.3 Furthermore, health care providers (HCPs) are often not of the same ethnicity or adequately trained to assess and build relationships with ethnically and racially diverse populations.2 Given the projected growth in the numbers of individuals worldwide with dementia, we have a responsibility to continue to develop strategies to provide more inclusive care.
By 2060, minority populations aged ≥ 65 years are expected to represent 45% of the US population, up from 22% in 2014.4 The growth of racial and ethnic minority groups are expected to exceed the growth of the non-Hispanic white population in the next few decades. By 2060, it is estimated that the US population will increase by 75% for non-Hispanic whites, 172% for African Americans, 270% for Asian and Pacific Islanders, 274% for American Indian and Alaska Natives, and 391% for Hispanics.4
A growing body of evidence suggests that Alzheimer disease and related dementias may disproportionately afflict minority groups in the US, which will become quite significant in the years ahead. The Alzheimer’s Association estimates that the prevalence of Alzheimer disease and other dementias among those aged > 65 years, is about twice the rate in African Americans and about 1.5 times the rate in Hispanics when compared with non-Hispanic whites.5 While increases in the incidence of Alzheimer disease and related dementias in non-Hispanic whites is expected to plateau around 2050, its incidence in ethnic and racial minority groups will continue to grow, especially among Hispanics.4 This stark realization provides additional compelling reasons for the US to develop preventative interventions or treatment options that may help delay the onset of the disease and to improve the quality of life of those with the disease or caregiving for those afflicted with it. Culturally competent care of these individuals is paramount.
Diagnosis
Early and accurate diagnosis of individuals with dementia confers many benefits, including early treatment; clinical trial participation; management of comorbid conditions; training, education, and support for patients and families; and legal, financial, and end of life care planning.3 Beyond the logistical concerns (such as HCP shortages), one of the challenges of assessing minority groups is finding staff who are culturally competent or speak the language necessary to accurately communicate and interact with these subgroups. Hispanics and African Americans often receive delayed or inadequate health care services or are diagnosed in an emergency department or other nontraditional setting.5
Even those individuals seeking or receiving care in primary care settings are not always forthcoming about their cognitive status. Only 56% of respondents in a recent survey of patients who had experienced subjective cognitive decline reported that they had discussed it with their HCP.4 This reticence is thought to be influenced by multiple factors, including distrust of the medical establishment, religious or spiritual beliefs, cultural or family beliefs and expectations about geriatric care, and lack of understanding about normal aging vs cognitive disorders. Furthermore, the sensitivity and specificity of current diagnostic tests for dementia have been questioned for nonwhite populations given the clinical presentation of dementia can vary across ethnoracial groups.5
As Luria noted, cognitive assessment tools developed and validated for use with one culture frequently results in experimental failures and are not valid for use with other cultural groups.1 Cognitive testing results are influenced by educational and cultural factors, and this is one of the challenges in correctly diagnosing those of differing ethnoracial backgrounds. Individuals in racial and ethnic minorities may have limited formal education and/or high illiteracy rates and/or cultural nuances to problem solving, thinking, and memory that may not be reflected in current assessment tools.1
There is hope that testing bias could be altered or eliminated using neuroimaging or biomarkers. However, the Alzheimer’s Disease Neuroimaging Initiative study of patients in the US and Canada included < 5% African American or Hispanic participants in its total sample. Few studies have systematically examined ethnoracial differences in amyloid positron emission tomography, and none have been published to date in ethnoracially diverse groups that assess the more recently developed tau imaging agents.1
Diversity Among Caregivers
The research community must make greater efforts to improve recruitment of more diverse populations into clinical trials. Recent efforts by the National Institute on Aging in conjunction with the Alzheimer’s Association include developing a national strategy for clinical research recruitment and retention with an emphasis on local and diverse populations. This strategy should include various training modules, webinars, and similar educational opportunities for researchers and clinical HCPs, including HCPs from diverse ethnoracial backgrounds, to implement culturally appropriate research methodologies across these diverse groups. It is important that these educational materials be disseminated to caregivers in a way they can comprehend, as the impact on caregivers of those with Alzheimer disease and related dementias is considerable.
The US currently has 7 unpaid caregivers for every adult in the high-risk group of patients aged ≥ 65 years, but this will decline to a ratio of 4:1 by 2030.4 More than two-thirds of caregivers are non-Hispanic white, while 10% are African American, 8% are Hispanic, and 5% are Asian.3 About 34% of caregivers are themselves aged ≥ 65 years and are at risk for declines in their own health given the time and financial requirements of caring for someone else.3 In 2017, the 16.1 million family and other unpaid caregivers of people with dementia provided an estimated 18.4 billion hours of unpaid care, often resulting in considerable financial strain for these individuals. More than half of the caregivers report providing ≥ 21 hours of care per week; and 42% reported providing an average of 9 hours of care per day for people with dementia.
Caregivers report increased stress, sleep deprivation, depression and anxiety, and uncertainty in their ability to provide quality care to the individual with Alzheimer or a related dementia.3 The disproportionate prevalence of Alzheimer disease and other dementias in racially and ethnically diverse populations could further magnify already existing socioeconomic and other disparities and potentially lead to worsening of health outcomes in these groups.4 Given that minority populations tend to cluster geographically, community partnerships with local churches, senior centers, community centers, and other nontraditional settings may offer better opportunities for connecting with caregivers.
Conclusions
The growth and increasing diversity of the US older adult population in the coming decades require us as HCPs, researchers, and educators to dedicate more resources to ethnoracially diverse populations. There are still a great many unknowns about Alzheimer disease and dementia, most especially among nonwhites. Research, clinical care, and education must focus on outreach to marginalized groups so we may better be able to diagnose and treat the fastest growing older adult populations in the US. A complex combination of educational, cultural, social, and environmental factors likely contribute to delayed diagnosis and care of these groups, as well as lack of access to medical care, research venues, and trust issues between minority groups and the medical establishment. We all have an obligation to acknowledge these disparities and elicit the support of our colleagues and workplaces to raise awareness and dedicate necessary resources to this growing concern.
1. Babulal GM, Quiroz YT, Albensi BC, et al; International Society to Advance Alzheimer’s Research and Treatment, Alzheimer’s Association. Perspectives on ethnic and racial disparities in Alzheimer’s disease and related dementias: update and areas of immediate need. Alzheimers Dement. 2019;15(2):292-312.
2. Brewster P, Barnes L, Haan M, et al. Progress and future challenges in aging and diversity research in the United States. Alzheimers Dement. 2019;15(7):995-1003.
3. Alzheimer’s Association. 2019 Alzheimer’s disease facts and figures. Alzheimers Dement. 2019;15(3):321-387.
4. Matthews KA, Xu W, Gaglioti AH, et al. Racial and ethnic estimates of Alzheimer’s disease and related dementias in the United States (2015-2060) in adults aged ≥65 years. Alzheimers Dement. 2019;15(1):17-24.
5. Chin AL, Negash S, Hamilton R. Diversity and disparity in dementia: the impact of ethnoracial differences in Alzheimer disease. Alzheimer Dis Assoc Disord. 2011;25(3):187-195.
1. Babulal GM, Quiroz YT, Albensi BC, et al; International Society to Advance Alzheimer’s Research and Treatment, Alzheimer’s Association. Perspectives on ethnic and racial disparities in Alzheimer’s disease and related dementias: update and areas of immediate need. Alzheimers Dement. 2019;15(2):292-312.
2. Brewster P, Barnes L, Haan M, et al. Progress and future challenges in aging and diversity research in the United States. Alzheimers Dement. 2019;15(7):995-1003.
3. Alzheimer’s Association. 2019 Alzheimer’s disease facts and figures. Alzheimers Dement. 2019;15(3):321-387.
4. Matthews KA, Xu W, Gaglioti AH, et al. Racial and ethnic estimates of Alzheimer’s disease and related dementias in the United States (2015-2060) in adults aged ≥65 years. Alzheimers Dement. 2019;15(1):17-24.
5. Chin AL, Negash S, Hamilton R. Diversity and disparity in dementia: the impact of ethnoracial differences in Alzheimer disease. Alzheimer Dis Assoc Disord. 2011;25(3):187-195.