User login
Obesity Etiology
Editor's Note: This article was created using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication.
Editor's Note: This article was created using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication.
Editor's Note: This article was created using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication.
Type 2 Diabetes: Insulin-Free for 24 Months After Novel Endoscopic Procedure
TOPLINE:
VIENNA, AUSTRIA —
METHODOLOGY:
- ReCET technology, manufactured by Endogenex, uses a specialized catheter that ablates the duodenal mucosa with electroporation, enhancing sensitivity to endogenous insulin.
- In the first-in-human study, a total of 14 participants (aged 28-75 years; body mass index, 24-40) underwent the ReCET procedure. They then followed a 2-week isocaloric liquid diet, after which they were initiated on semaglutide and gradually titrated up to 1 mg/wk.
- Patients were followed for a total of 24 months.
TAKEAWAY:
- Of the 14 participants, 12 (86%) no longer required insulin at the 6- and 12-month follow-ups.
- At the 24-month follow-up, 11 patients were still insulin-free while maintaining A1c levels below 7.5%. (One patient withdrew consent at 18 months.)
- Semaglutide at the maximum dose was well-tolerated by 93% of participants. One patient experienced nausea that limited titration to the maximum dose. There were no serious adverse events to the ReCET procedure.
- Researchers have started the EMINENT-2 trial that will compare the use of ReCET with a sham procedure. All patients will still receive semaglutide.
IN PRACTICE:
- “These findings are very encouraging, suggesting that ReCET is a safe and feasible procedure that, when combined with semaglutide, can effectively eliminate the need for insulin therapy,” said the study’s lead author.
- It’s a novel way of treating type 2 diabetes using a single endoscopic procedure instead of repeated insulin injections, Busch explained. “But we do need to consider whether repeat treatment will be necessary because I don’t believe this will be forever.”
SOURCE:
This study was led by Celine Busch, MBBS, a PhD candidate in gastroenterology at Amsterdam University Medical Center, Amsterdam, the Netherlands, and was presented (abstract OP049) at the United European Gastroenterology (UEG) Week 2024 in Vienna, Austria, on October 14, 2024.
LIMITATIONS:
Limitations included the small sample size, uncontrolled nature, and bias due to combination therapy.
DISCLOSURES:
This study received an unrestricted research grant from Endogenex. No other relevant disclosures were declared.
A version of this article first appeared on Medscape.com.
TOPLINE:
VIENNA, AUSTRIA —
METHODOLOGY:
- ReCET technology, manufactured by Endogenex, uses a specialized catheter that ablates the duodenal mucosa with electroporation, enhancing sensitivity to endogenous insulin.
- In the first-in-human study, a total of 14 participants (aged 28-75 years; body mass index, 24-40) underwent the ReCET procedure. They then followed a 2-week isocaloric liquid diet, after which they were initiated on semaglutide and gradually titrated up to 1 mg/wk.
- Patients were followed for a total of 24 months.
TAKEAWAY:
- Of the 14 participants, 12 (86%) no longer required insulin at the 6- and 12-month follow-ups.
- At the 24-month follow-up, 11 patients were still insulin-free while maintaining A1c levels below 7.5%. (One patient withdrew consent at 18 months.)
- Semaglutide at the maximum dose was well-tolerated by 93% of participants. One patient experienced nausea that limited titration to the maximum dose. There were no serious adverse events to the ReCET procedure.
- Researchers have started the EMINENT-2 trial that will compare the use of ReCET with a sham procedure. All patients will still receive semaglutide.
IN PRACTICE:
- “These findings are very encouraging, suggesting that ReCET is a safe and feasible procedure that, when combined with semaglutide, can effectively eliminate the need for insulin therapy,” said the study’s lead author.
- It’s a novel way of treating type 2 diabetes using a single endoscopic procedure instead of repeated insulin injections, Busch explained. “But we do need to consider whether repeat treatment will be necessary because I don’t believe this will be forever.”
SOURCE:
This study was led by Celine Busch, MBBS, a PhD candidate in gastroenterology at Amsterdam University Medical Center, Amsterdam, the Netherlands, and was presented (abstract OP049) at the United European Gastroenterology (UEG) Week 2024 in Vienna, Austria, on October 14, 2024.
LIMITATIONS:
Limitations included the small sample size, uncontrolled nature, and bias due to combination therapy.
DISCLOSURES:
This study received an unrestricted research grant from Endogenex. No other relevant disclosures were declared.
A version of this article first appeared on Medscape.com.
TOPLINE:
VIENNA, AUSTRIA —
METHODOLOGY:
- ReCET technology, manufactured by Endogenex, uses a specialized catheter that ablates the duodenal mucosa with electroporation, enhancing sensitivity to endogenous insulin.
- In the first-in-human study, a total of 14 participants (aged 28-75 years; body mass index, 24-40) underwent the ReCET procedure. They then followed a 2-week isocaloric liquid diet, after which they were initiated on semaglutide and gradually titrated up to 1 mg/wk.
- Patients were followed for a total of 24 months.
TAKEAWAY:
- Of the 14 participants, 12 (86%) no longer required insulin at the 6- and 12-month follow-ups.
- At the 24-month follow-up, 11 patients were still insulin-free while maintaining A1c levels below 7.5%. (One patient withdrew consent at 18 months.)
- Semaglutide at the maximum dose was well-tolerated by 93% of participants. One patient experienced nausea that limited titration to the maximum dose. There were no serious adverse events to the ReCET procedure.
- Researchers have started the EMINENT-2 trial that will compare the use of ReCET with a sham procedure. All patients will still receive semaglutide.
IN PRACTICE:
- “These findings are very encouraging, suggesting that ReCET is a safe and feasible procedure that, when combined with semaglutide, can effectively eliminate the need for insulin therapy,” said the study’s lead author.
- It’s a novel way of treating type 2 diabetes using a single endoscopic procedure instead of repeated insulin injections, Busch explained. “But we do need to consider whether repeat treatment will be necessary because I don’t believe this will be forever.”
SOURCE:
This study was led by Celine Busch, MBBS, a PhD candidate in gastroenterology at Amsterdam University Medical Center, Amsterdam, the Netherlands, and was presented (abstract OP049) at the United European Gastroenterology (UEG) Week 2024 in Vienna, Austria, on October 14, 2024.
LIMITATIONS:
Limitations included the small sample size, uncontrolled nature, and bias due to combination therapy.
DISCLOSURES:
This study received an unrestricted research grant from Endogenex. No other relevant disclosures were declared.
A version of this article first appeared on Medscape.com.
Eggs: A Weighty Matter for Postmenopausal Women?
TOPLINE:
such as processed and red meat, French fries, sweets, and deserts. Genetic predisposition for a high body mass index (BMI) also influences weight gain with higher egg intake.
METHODOLOGY:
- Egg consumption and elevated body weight are each linked to an increased risk for serious chronic diseases; however, whether elevated body weight mediates the association between egg intake and an elevated risk for serious chronic diseases needs further assessment.
- To investigate the association between eating eggs and weight gain, as well as the role of genetic susceptibility to an elevated BMI, researchers conducted a prospective study including 4439 postmenopausal women of European descent from the Women’s Health Initiative (WHI).
- They measured the participants’ consumption of egg and egg nutrients using a self-administered food frequency questionnaire.
- Changes in the consumption of eggs and egg nutrients such as cholesterol, choline, and betaine were assessed between baseline and follow-up visits at 1, 3, 6, and 9 years.
- The primary outcome was the change in body weight between baseline and each follow-up visit. Furthermore, an exploratory analysis evaluated how eating Western foods and genetic predisposition for a high BMI (assessed through a polygenic score) influenced weight change.
TAKEAWAY:
- An increased consumption of eggs was associated with weight gain, showing a positive linear trend at 1, 2, 3, and 6 years. By the third year, women whose egg consumption had increased by two eggs per week gained 0.70 kg more weight (P = .0002) than women whose egg consumption was reduced by 2.4 eggs per week (P-linear < .0001).
- An increase in the consumption of nutrients obtained from eggs, including cholesterol (P-linear < .0001) and choline (P-linear < .02), was positively associated with weight gain.
- Women with a higher consumption of Western foods showed significant associations between changes in egg, cholesterol, and choline intake and weight gain.
- A significant association was found between the BMI polygenic score and changes in body weight, with women most genetically predisposed to a higher BMI showing greater weight gain when their egg consumption increased by an average of 3.5 eggs per week.
IN PRACTICE:
“These results suggest that even relatively small increases or decreases in egg consumption could cause increases or decreases, respectively, in body weight among postmenopausal women, unless there are adequate compensating changes in factors such as dietary energy intake or physical activity,” the authors wrote. “Our results require confirmation,” they added.
SOURCE:
This study, led by James A. Greenberg, Department of Health and Nutrition Sciences, Brooklyn College, The City University of New York, was published online in Clinical Nutrition.
LIMITATIONS:
This observational study was susceptible to residual confounding, which suggests that the observed associations may not have established causality. Additionally, the results were according to data from a group of postmenopausal American women of European descent, which limited the generalizability to other populations.
DISCLOSURES:
The WHI program was funded by the National Heart, Lung, and Blood Institute, National Institutes of Health, Department of Health & Human Services. The authors declared no conflicts of interest.
This article was created using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication. A version of this article first appeared on Medscape.com.
TOPLINE:
such as processed and red meat, French fries, sweets, and deserts. Genetic predisposition for a high body mass index (BMI) also influences weight gain with higher egg intake.
METHODOLOGY:
- Egg consumption and elevated body weight are each linked to an increased risk for serious chronic diseases; however, whether elevated body weight mediates the association between egg intake and an elevated risk for serious chronic diseases needs further assessment.
- To investigate the association between eating eggs and weight gain, as well as the role of genetic susceptibility to an elevated BMI, researchers conducted a prospective study including 4439 postmenopausal women of European descent from the Women’s Health Initiative (WHI).
- They measured the participants’ consumption of egg and egg nutrients using a self-administered food frequency questionnaire.
- Changes in the consumption of eggs and egg nutrients such as cholesterol, choline, and betaine were assessed between baseline and follow-up visits at 1, 3, 6, and 9 years.
- The primary outcome was the change in body weight between baseline and each follow-up visit. Furthermore, an exploratory analysis evaluated how eating Western foods and genetic predisposition for a high BMI (assessed through a polygenic score) influenced weight change.
TAKEAWAY:
- An increased consumption of eggs was associated with weight gain, showing a positive linear trend at 1, 2, 3, and 6 years. By the third year, women whose egg consumption had increased by two eggs per week gained 0.70 kg more weight (P = .0002) than women whose egg consumption was reduced by 2.4 eggs per week (P-linear < .0001).
- An increase in the consumption of nutrients obtained from eggs, including cholesterol (P-linear < .0001) and choline (P-linear < .02), was positively associated with weight gain.
- Women with a higher consumption of Western foods showed significant associations between changes in egg, cholesterol, and choline intake and weight gain.
- A significant association was found between the BMI polygenic score and changes in body weight, with women most genetically predisposed to a higher BMI showing greater weight gain when their egg consumption increased by an average of 3.5 eggs per week.
IN PRACTICE:
“These results suggest that even relatively small increases or decreases in egg consumption could cause increases or decreases, respectively, in body weight among postmenopausal women, unless there are adequate compensating changes in factors such as dietary energy intake or physical activity,” the authors wrote. “Our results require confirmation,” they added.
SOURCE:
This study, led by James A. Greenberg, Department of Health and Nutrition Sciences, Brooklyn College, The City University of New York, was published online in Clinical Nutrition.
LIMITATIONS:
This observational study was susceptible to residual confounding, which suggests that the observed associations may not have established causality. Additionally, the results were according to data from a group of postmenopausal American women of European descent, which limited the generalizability to other populations.
DISCLOSURES:
The WHI program was funded by the National Heart, Lung, and Blood Institute, National Institutes of Health, Department of Health & Human Services. The authors declared no conflicts of interest.
This article was created using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication. A version of this article first appeared on Medscape.com.
TOPLINE:
such as processed and red meat, French fries, sweets, and deserts. Genetic predisposition for a high body mass index (BMI) also influences weight gain with higher egg intake.
METHODOLOGY:
- Egg consumption and elevated body weight are each linked to an increased risk for serious chronic diseases; however, whether elevated body weight mediates the association between egg intake and an elevated risk for serious chronic diseases needs further assessment.
- To investigate the association between eating eggs and weight gain, as well as the role of genetic susceptibility to an elevated BMI, researchers conducted a prospective study including 4439 postmenopausal women of European descent from the Women’s Health Initiative (WHI).
- They measured the participants’ consumption of egg and egg nutrients using a self-administered food frequency questionnaire.
- Changes in the consumption of eggs and egg nutrients such as cholesterol, choline, and betaine were assessed between baseline and follow-up visits at 1, 3, 6, and 9 years.
- The primary outcome was the change in body weight between baseline and each follow-up visit. Furthermore, an exploratory analysis evaluated how eating Western foods and genetic predisposition for a high BMI (assessed through a polygenic score) influenced weight change.
TAKEAWAY:
- An increased consumption of eggs was associated with weight gain, showing a positive linear trend at 1, 2, 3, and 6 years. By the third year, women whose egg consumption had increased by two eggs per week gained 0.70 kg more weight (P = .0002) than women whose egg consumption was reduced by 2.4 eggs per week (P-linear < .0001).
- An increase in the consumption of nutrients obtained from eggs, including cholesterol (P-linear < .0001) and choline (P-linear < .02), was positively associated with weight gain.
- Women with a higher consumption of Western foods showed significant associations between changes in egg, cholesterol, and choline intake and weight gain.
- A significant association was found between the BMI polygenic score and changes in body weight, with women most genetically predisposed to a higher BMI showing greater weight gain when their egg consumption increased by an average of 3.5 eggs per week.
IN PRACTICE:
“These results suggest that even relatively small increases or decreases in egg consumption could cause increases or decreases, respectively, in body weight among postmenopausal women, unless there are adequate compensating changes in factors such as dietary energy intake or physical activity,” the authors wrote. “Our results require confirmation,” they added.
SOURCE:
This study, led by James A. Greenberg, Department of Health and Nutrition Sciences, Brooklyn College, The City University of New York, was published online in Clinical Nutrition.
LIMITATIONS:
This observational study was susceptible to residual confounding, which suggests that the observed associations may not have established causality. Additionally, the results were according to data from a group of postmenopausal American women of European descent, which limited the generalizability to other populations.
DISCLOSURES:
The WHI program was funded by the National Heart, Lung, and Blood Institute, National Institutes of Health, Department of Health & Human Services. The authors declared no conflicts of interest.
This article was created using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication. A version of this article first appeared on Medscape.com.
Excess Body Weight Tied to Increased Risk for Second Cancers
TOPLINE:
Cancer survivors who had overweight or obesity at the time of their initial cancer diagnosis have a higher risk for a second primary cancer, particularly an obesity-related cancer, a new analysis found.
METHODOLOGY:
- Cancer survivors have an increased risk for another primary cancer. Studies suggest that lifestyle factors, such as excess body weight, may contribute to the risk for a second cancer; however, prospective long-term data on this association remain limited.
- Researchers evaluated 26,894 participants (mean age at first cancer diagnosis, 72.2 years; 97.6% White) from the Cancer Prevention Study II Nutrition cohort, who were diagnosed with a first nonmetastatic primary cancer between 1992 and 2015.
- Body mass index (BMI) was calculated from self-reported data at the time of the first primary cancer diagnosis; 10,713 participants had a normal BMI (18.5 to < 25.0), 11,497 had overweight (25.0 to < 30.0), and 4684 had obesity (≥ 30.0). Participants were followed through 2017.
- The study outcomes were the incidences of any second primary cancer and obesity-related second cancers.
- The most common first primary cancers were prostate (35.0%), breast (19.1%), and colorectal (9.5%) cancers; almost 40% of all first primary cancers were related to obesity.
TAKEAWAY:
- Overall, 13.9% participants (3749 of 26,894) were diagnosed with a second cancer over a median of 7.9 years; 33.2% of these cancers were related to obesity.
- Compared with participants with a normal BMI, those who had overweight had a 15% higher risk for any second cancer (adjusted hazard ratio [aHR], 1.15) and a 40% higher risk for an obesity-related second cancer (aHR, 1.40). Additionally, those with obesity had a 34% higher risk for any second cancer and a 78% higher risk for an obesity-related second cancer.
- For every 5-unit increase in BMI, the risk for an obesity-related cancer (aHR, 1.28) was considerably higher than the risk for any second cancer (aHR, 1.13).
- Among all survivors, every 5-unit increase in BMI was associated with a 42% increased risk for colorectal cancer as a second cancer (aHR, 1.42) and a 70% higher risk for kidney cancer as a second cancer (aHR, 1.70).
IN PRACTICE:
“In this cohort study of older survivors of nonmetastatic cancer, those who had overweight or obesity at the time of their first cancer diagnosis were at higher risk of developing a second cancer, especially obesity-related cancers,” the authors wrote. “These findings have important public health implications and may inform evidence-based survivorship guidelines to reduce the risk of second primary cancers among cancer survivors.”
SOURCE:
This study, led by Clara Bodelon, PhD, MS, American Cancer Society, Atlanta, was published online in JAMA Network Open.
LIMITATIONS:
The exclusion of multiple primary cancers in the same site could have underestimated the magnitude of the association of excess body weight with the risk for second primary cancers. BMI was used as a measure of excess body fat in this study, which does not differentiate between fat and lean mass. Unmeasured or residual confounding factors might be present.
DISCLOSURES:
The study was supported by grants from the Centers for Disease Control and Prevention’s National Program of Cancer Registries and cancer registries supported by the National Cancer Institute’s Surveillance, Epidemiology, and End Results Program. No relevant conflicts of interest were disclosed by the authors.
This article was created using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication. A version of this article first appeared on Medscape.com.
TOPLINE:
Cancer survivors who had overweight or obesity at the time of their initial cancer diagnosis have a higher risk for a second primary cancer, particularly an obesity-related cancer, a new analysis found.
METHODOLOGY:
- Cancer survivors have an increased risk for another primary cancer. Studies suggest that lifestyle factors, such as excess body weight, may contribute to the risk for a second cancer; however, prospective long-term data on this association remain limited.
- Researchers evaluated 26,894 participants (mean age at first cancer diagnosis, 72.2 years; 97.6% White) from the Cancer Prevention Study II Nutrition cohort, who were diagnosed with a first nonmetastatic primary cancer between 1992 and 2015.
- Body mass index (BMI) was calculated from self-reported data at the time of the first primary cancer diagnosis; 10,713 participants had a normal BMI (18.5 to < 25.0), 11,497 had overweight (25.0 to < 30.0), and 4684 had obesity (≥ 30.0). Participants were followed through 2017.
- The study outcomes were the incidences of any second primary cancer and obesity-related second cancers.
- The most common first primary cancers were prostate (35.0%), breast (19.1%), and colorectal (9.5%) cancers; almost 40% of all first primary cancers were related to obesity.
TAKEAWAY:
- Overall, 13.9% participants (3749 of 26,894) were diagnosed with a second cancer over a median of 7.9 years; 33.2% of these cancers were related to obesity.
- Compared with participants with a normal BMI, those who had overweight had a 15% higher risk for any second cancer (adjusted hazard ratio [aHR], 1.15) and a 40% higher risk for an obesity-related second cancer (aHR, 1.40). Additionally, those with obesity had a 34% higher risk for any second cancer and a 78% higher risk for an obesity-related second cancer.
- For every 5-unit increase in BMI, the risk for an obesity-related cancer (aHR, 1.28) was considerably higher than the risk for any second cancer (aHR, 1.13).
- Among all survivors, every 5-unit increase in BMI was associated with a 42% increased risk for colorectal cancer as a second cancer (aHR, 1.42) and a 70% higher risk for kidney cancer as a second cancer (aHR, 1.70).
IN PRACTICE:
“In this cohort study of older survivors of nonmetastatic cancer, those who had overweight or obesity at the time of their first cancer diagnosis were at higher risk of developing a second cancer, especially obesity-related cancers,” the authors wrote. “These findings have important public health implications and may inform evidence-based survivorship guidelines to reduce the risk of second primary cancers among cancer survivors.”
SOURCE:
This study, led by Clara Bodelon, PhD, MS, American Cancer Society, Atlanta, was published online in JAMA Network Open.
LIMITATIONS:
The exclusion of multiple primary cancers in the same site could have underestimated the magnitude of the association of excess body weight with the risk for second primary cancers. BMI was used as a measure of excess body fat in this study, which does not differentiate between fat and lean mass. Unmeasured or residual confounding factors might be present.
DISCLOSURES:
The study was supported by grants from the Centers for Disease Control and Prevention’s National Program of Cancer Registries and cancer registries supported by the National Cancer Institute’s Surveillance, Epidemiology, and End Results Program. No relevant conflicts of interest were disclosed by the authors.
This article was created using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication. A version of this article first appeared on Medscape.com.
TOPLINE:
Cancer survivors who had overweight or obesity at the time of their initial cancer diagnosis have a higher risk for a second primary cancer, particularly an obesity-related cancer, a new analysis found.
METHODOLOGY:
- Cancer survivors have an increased risk for another primary cancer. Studies suggest that lifestyle factors, such as excess body weight, may contribute to the risk for a second cancer; however, prospective long-term data on this association remain limited.
- Researchers evaluated 26,894 participants (mean age at first cancer diagnosis, 72.2 years; 97.6% White) from the Cancer Prevention Study II Nutrition cohort, who were diagnosed with a first nonmetastatic primary cancer between 1992 and 2015.
- Body mass index (BMI) was calculated from self-reported data at the time of the first primary cancer diagnosis; 10,713 participants had a normal BMI (18.5 to < 25.0), 11,497 had overweight (25.0 to < 30.0), and 4684 had obesity (≥ 30.0). Participants were followed through 2017.
- The study outcomes were the incidences of any second primary cancer and obesity-related second cancers.
- The most common first primary cancers were prostate (35.0%), breast (19.1%), and colorectal (9.5%) cancers; almost 40% of all first primary cancers were related to obesity.
TAKEAWAY:
- Overall, 13.9% participants (3749 of 26,894) were diagnosed with a second cancer over a median of 7.9 years; 33.2% of these cancers were related to obesity.
- Compared with participants with a normal BMI, those who had overweight had a 15% higher risk for any second cancer (adjusted hazard ratio [aHR], 1.15) and a 40% higher risk for an obesity-related second cancer (aHR, 1.40). Additionally, those with obesity had a 34% higher risk for any second cancer and a 78% higher risk for an obesity-related second cancer.
- For every 5-unit increase in BMI, the risk for an obesity-related cancer (aHR, 1.28) was considerably higher than the risk for any second cancer (aHR, 1.13).
- Among all survivors, every 5-unit increase in BMI was associated with a 42% increased risk for colorectal cancer as a second cancer (aHR, 1.42) and a 70% higher risk for kidney cancer as a second cancer (aHR, 1.70).
IN PRACTICE:
“In this cohort study of older survivors of nonmetastatic cancer, those who had overweight or obesity at the time of their first cancer diagnosis were at higher risk of developing a second cancer, especially obesity-related cancers,” the authors wrote. “These findings have important public health implications and may inform evidence-based survivorship guidelines to reduce the risk of second primary cancers among cancer survivors.”
SOURCE:
This study, led by Clara Bodelon, PhD, MS, American Cancer Society, Atlanta, was published online in JAMA Network Open.
LIMITATIONS:
The exclusion of multiple primary cancers in the same site could have underestimated the magnitude of the association of excess body weight with the risk for second primary cancers. BMI was used as a measure of excess body fat in this study, which does not differentiate between fat and lean mass. Unmeasured or residual confounding factors might be present.
DISCLOSURES:
The study was supported by grants from the Centers for Disease Control and Prevention’s National Program of Cancer Registries and cancer registries supported by the National Cancer Institute’s Surveillance, Epidemiology, and End Results Program. No relevant conflicts of interest were disclosed by the authors.
This article was created using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication. A version of this article first appeared on Medscape.com.
Swollen elbow and knee joints
Obesity is a chronic disease affecting more than 20% of adults in the United States. In 2022, prevalence was 20.5% among those aged 18 to 24 and 39.9% among those aged 45 to 54 years. This patient meets criteria for obesity (BMI ≥ 30), and it is likely that her obesity contributed to development of T2D, hypertension, osteoarthritis, and joint edema (as shown in the image).
Patients with obesity are at high risk of developing cardiometabolic disease and osteoarthritis. Obesity is a key driver of T2D and cardiovascular disease development through its influence on insulin and lipid metabolism and proinflammatory changes. Factors associated with obesity that foster arthritis development include the erosive effects of adiponectin and leptin on cartilage and direct inflammation in joint tissues.
It is important for patients with obesity and comorbid T2D and hypertension to receive multidisciplinary care designed to address all aspects of their health and minimize their risk for progression. The primary goal for this patient should be to promote weight loss safely while also improving her glycemic control and blood pressure. For patients with obesity and comorbid T2D, the American Diabetes Association recommends glucagon-like peptide-1 receptor agonists (GLP-1 RAs; semaglutide or liraglutide) or the dual gastric inhibitory polypeptide (GIP)/GLP-1 RA tirzepatide. The GLP-1 RA drugs reduce the risk for major cardiovascular events for patients with T2D while also providing substantial reductions in glucose levels without increasing hypoglycemia risk. They are available in higher doses (semaglutide 2.4 mg weekly, liraglutide 3.0 mg daily) for patients with obesity. These drugs also have salubrious effects on cardiorenal health and reduce progression of kidney disease. Tirzepatide produced greater reductions in A1c vs semaglutide in patients with T2D in the SURPASS-2 trial. It also has been shown to reduce atherosclerotic cardiovascular events in patients with overweight or obesity (without diabetes) in a post hoc analysis of the SURMOUNT-1 trial. Its effect on a broad set of cardiac, renal, and metabolic outcomes is being studied in the ongoing SURMOUNT-MMO trial. The American Gastroenterological Association and other organizations recommend treatment with antiobesity medications along with lifestyle modifications for patients with obesity (BMI ≥ 30) and weight-related complications (BMI > 27).
Pharmacologic interventions for osteoarthritis include nonsteroidal anti-inflammatory drugs, including ibuprofen, naproxen, meloxicam, diclofenac, or celecoxib. These may be used with regular follow-up to assess cardiovascular and gastrointestinal health. Topical nonsteroidal anti-inflammatory drugs also may be useful. For more intractable joint pain, options include injecting corticosteroid or sodium hyaluronate into the affected joints or joint replacement.
In addition, comprehensive care includes lifestyle modifications designed to promote weight loss, reduce sodium, and increase exercise and intake of healthy foods. While maintaining intensive lifestyle modifications can be challenging, achieving weight loss of ≥ 5% can improve cardiometabolic risk factors in patients with obesity and T2D. Greater benefit is seen with greater reductions in body weight. Other interventions include behavioral modification and encouragement of increased physical activity to the extent of the patient's ability. Achieving substantial weight loss also could help relieve stress on the patient's joints, improve physical function, and mitigate osteoarthritis-related pain. The patient also may benefit from nonpharmacologic approaches to joint pain, including hot or cold compresses, physical therapy, and strength and resistance training to improve the strength of muscles supporting the joints.
Carolyn Newberry, MD, Assistant Professor of Medicine, Director of GI Nutrition, Innovative Center for Health and Nutrition in Gastroenterology (ICHANGE), Division of Gastroenterology, Weill Cornell Medical Center, New York, NY.
Disclosure: Carolyn Newberry, MD, has disclosed the following relevant financial relationships:
Serve(d) as a speaker or a member of a speakers bureau for: Baster International; InBody.
Image Quizzes are fictional or fictionalized clinical scenarios intended to provide evidence-based educational takeaways.
Obesity is a chronic disease affecting more than 20% of adults in the United States. In 2022, prevalence was 20.5% among those aged 18 to 24 and 39.9% among those aged 45 to 54 years. This patient meets criteria for obesity (BMI ≥ 30), and it is likely that her obesity contributed to development of T2D, hypertension, osteoarthritis, and joint edema (as shown in the image).
Patients with obesity are at high risk of developing cardiometabolic disease and osteoarthritis. Obesity is a key driver of T2D and cardiovascular disease development through its influence on insulin and lipid metabolism and proinflammatory changes. Factors associated with obesity that foster arthritis development include the erosive effects of adiponectin and leptin on cartilage and direct inflammation in joint tissues.
It is important for patients with obesity and comorbid T2D and hypertension to receive multidisciplinary care designed to address all aspects of their health and minimize their risk for progression. The primary goal for this patient should be to promote weight loss safely while also improving her glycemic control and blood pressure. For patients with obesity and comorbid T2D, the American Diabetes Association recommends glucagon-like peptide-1 receptor agonists (GLP-1 RAs; semaglutide or liraglutide) or the dual gastric inhibitory polypeptide (GIP)/GLP-1 RA tirzepatide. The GLP-1 RA drugs reduce the risk for major cardiovascular events for patients with T2D while also providing substantial reductions in glucose levels without increasing hypoglycemia risk. They are available in higher doses (semaglutide 2.4 mg weekly, liraglutide 3.0 mg daily) for patients with obesity. These drugs also have salubrious effects on cardiorenal health and reduce progression of kidney disease. Tirzepatide produced greater reductions in A1c vs semaglutide in patients with T2D in the SURPASS-2 trial. It also has been shown to reduce atherosclerotic cardiovascular events in patients with overweight or obesity (without diabetes) in a post hoc analysis of the SURMOUNT-1 trial. Its effect on a broad set of cardiac, renal, and metabolic outcomes is being studied in the ongoing SURMOUNT-MMO trial. The American Gastroenterological Association and other organizations recommend treatment with antiobesity medications along with lifestyle modifications for patients with obesity (BMI ≥ 30) and weight-related complications (BMI > 27).
Pharmacologic interventions for osteoarthritis include nonsteroidal anti-inflammatory drugs, including ibuprofen, naproxen, meloxicam, diclofenac, or celecoxib. These may be used with regular follow-up to assess cardiovascular and gastrointestinal health. Topical nonsteroidal anti-inflammatory drugs also may be useful. For more intractable joint pain, options include injecting corticosteroid or sodium hyaluronate into the affected joints or joint replacement.
In addition, comprehensive care includes lifestyle modifications designed to promote weight loss, reduce sodium, and increase exercise and intake of healthy foods. While maintaining intensive lifestyle modifications can be challenging, achieving weight loss of ≥ 5% can improve cardiometabolic risk factors in patients with obesity and T2D. Greater benefit is seen with greater reductions in body weight. Other interventions include behavioral modification and encouragement of increased physical activity to the extent of the patient's ability. Achieving substantial weight loss also could help relieve stress on the patient's joints, improve physical function, and mitigate osteoarthritis-related pain. The patient also may benefit from nonpharmacologic approaches to joint pain, including hot or cold compresses, physical therapy, and strength and resistance training to improve the strength of muscles supporting the joints.
Carolyn Newberry, MD, Assistant Professor of Medicine, Director of GI Nutrition, Innovative Center for Health and Nutrition in Gastroenterology (ICHANGE), Division of Gastroenterology, Weill Cornell Medical Center, New York, NY.
Disclosure: Carolyn Newberry, MD, has disclosed the following relevant financial relationships:
Serve(d) as a speaker or a member of a speakers bureau for: Baster International; InBody.
Image Quizzes are fictional or fictionalized clinical scenarios intended to provide evidence-based educational takeaways.
Obesity is a chronic disease affecting more than 20% of adults in the United States. In 2022, prevalence was 20.5% among those aged 18 to 24 and 39.9% among those aged 45 to 54 years. This patient meets criteria for obesity (BMI ≥ 30), and it is likely that her obesity contributed to development of T2D, hypertension, osteoarthritis, and joint edema (as shown in the image).
Patients with obesity are at high risk of developing cardiometabolic disease and osteoarthritis. Obesity is a key driver of T2D and cardiovascular disease development through its influence on insulin and lipid metabolism and proinflammatory changes. Factors associated with obesity that foster arthritis development include the erosive effects of adiponectin and leptin on cartilage and direct inflammation in joint tissues.
It is important for patients with obesity and comorbid T2D and hypertension to receive multidisciplinary care designed to address all aspects of their health and minimize their risk for progression. The primary goal for this patient should be to promote weight loss safely while also improving her glycemic control and blood pressure. For patients with obesity and comorbid T2D, the American Diabetes Association recommends glucagon-like peptide-1 receptor agonists (GLP-1 RAs; semaglutide or liraglutide) or the dual gastric inhibitory polypeptide (GIP)/GLP-1 RA tirzepatide. The GLP-1 RA drugs reduce the risk for major cardiovascular events for patients with T2D while also providing substantial reductions in glucose levels without increasing hypoglycemia risk. They are available in higher doses (semaglutide 2.4 mg weekly, liraglutide 3.0 mg daily) for patients with obesity. These drugs also have salubrious effects on cardiorenal health and reduce progression of kidney disease. Tirzepatide produced greater reductions in A1c vs semaglutide in patients with T2D in the SURPASS-2 trial. It also has been shown to reduce atherosclerotic cardiovascular events in patients with overweight or obesity (without diabetes) in a post hoc analysis of the SURMOUNT-1 trial. Its effect on a broad set of cardiac, renal, and metabolic outcomes is being studied in the ongoing SURMOUNT-MMO trial. The American Gastroenterological Association and other organizations recommend treatment with antiobesity medications along with lifestyle modifications for patients with obesity (BMI ≥ 30) and weight-related complications (BMI > 27).
Pharmacologic interventions for osteoarthritis include nonsteroidal anti-inflammatory drugs, including ibuprofen, naproxen, meloxicam, diclofenac, or celecoxib. These may be used with regular follow-up to assess cardiovascular and gastrointestinal health. Topical nonsteroidal anti-inflammatory drugs also may be useful. For more intractable joint pain, options include injecting corticosteroid or sodium hyaluronate into the affected joints or joint replacement.
In addition, comprehensive care includes lifestyle modifications designed to promote weight loss, reduce sodium, and increase exercise and intake of healthy foods. While maintaining intensive lifestyle modifications can be challenging, achieving weight loss of ≥ 5% can improve cardiometabolic risk factors in patients with obesity and T2D. Greater benefit is seen with greater reductions in body weight. Other interventions include behavioral modification and encouragement of increased physical activity to the extent of the patient's ability. Achieving substantial weight loss also could help relieve stress on the patient's joints, improve physical function, and mitigate osteoarthritis-related pain. The patient also may benefit from nonpharmacologic approaches to joint pain, including hot or cold compresses, physical therapy, and strength and resistance training to improve the strength of muscles supporting the joints.
Carolyn Newberry, MD, Assistant Professor of Medicine, Director of GI Nutrition, Innovative Center for Health and Nutrition in Gastroenterology (ICHANGE), Division of Gastroenterology, Weill Cornell Medical Center, New York, NY.
Disclosure: Carolyn Newberry, MD, has disclosed the following relevant financial relationships:
Serve(d) as a speaker or a member of a speakers bureau for: Baster International; InBody.
Image Quizzes are fictional or fictionalized clinical scenarios intended to provide evidence-based educational takeaways.
A 24-year-old woman presents for swollen and painful elbow and knee joints. The patient is 5 ft 7 in tall and weighs 235 lb (BMI 36.8). The patient says she has been overweight since her preteen years and has never been involved in sports or exercise activities. She has gained a significant amount of weight in the past 2 years since beginning work in an insurance office. She has lived at home with her parents since graduating from college.
Her elbows are tender to the touch; further examination reveals tender joints at her wrists, knees, and hips as well. Extremities are thick because of obesity.
Medical history includes diagnosis of type 2 diabetes (T2D) at age 22. In the office, her blood pressure is elevated (150/85 mm Hg), heart rate is 110 beats/min, and respiratory rate is 18 breaths/min. Lab results indicate A1c = 8.5%, low-density lipoprotein cholesterol = 145 mg/dL, and estimated glomerular filtration rate = 90 mL/min/1.73 m2; all other results are within normal range. Her only current medication is metformin 1000 mg daily.
In-office radiography reveals no obvious bone or joint damage.
Ghost Fat: The Unseen Consequences of Weight Loss
Many people who lose weight, whether through diet and lifestyle changes, medication, or bariatric surgery, recognize their body has changed. While they also experience improvements in quality of life and psychosocial areas, that’s not true for everyone. Some patients don’t “see” they’ve lost weight — a phenomenon referred to as “phantom fat,” “ghost fat,” or “vestigial body image.”
“Most people are happy with their appearance, or at least their body shape, after weight loss — although some are unhappy with the loose, sagging skin that can follow weight loss and seek plastic surgery to remedy that,” David B. Sarwer, PhD, director of the Center for Obesity Research and Education and professor of social and behavioral sciences, Temple University College of Public Health, Philadelphia, told this news organization. “There’s a subset of people who remain dissatisfied with their body image, including their shape.”
This body dissatisfaction of people who lose weight may be long-standing, predating the weight loss, or may be new because weight loss has catalyzed a host of previously unaddressed psychosocial issues. Some may show up at assessments on treatment onset, while others may be detected by monitoring changes during or after weight loss. “Mental health counseling after bariatric surgery is greatly underutilized,” Dr. Sarwer observed.
Ghost Fat
Research has corroborated the lingering self-perception of being “obese” vs “ex-obese.” In one study, patients who had undergone bariatric surgery reported being unable to see the difference in their size and shape 18-30 months following their procedure, despite substantial weight loss.
Some research suggests that rapid weight loss (eg, through bariatric surgery) is more likely to generate the perception of “phantom fat,” but additional research is needed to investigate whether the mode and speed of weight loss affect subsequent body image.
Being habituated to one’s former appearance may play a role, Dr. Sarwer suggested. “We see this not only with weight loss but with other body-altering procedures. It takes the brain time to catch up to the new appearance. In rhinoplasty, for example, it may take patients a while before they become accustomed to looking at their new face in the mirror after decades of looking at a more prominent nose.”
Years of Social Stigma
It may also take time for people to overcome years of enduring the stigma of obesity.
There are “pervasive” negative attitudes implying that individuals who are overweight and/or obese are “lazy, weak-willed, lacking in self-discipline and willpower” — a problem compounded by social media and media in general, which present unrealistic, glorified body images and disparaging messages about those with weight problems.
“Body image is a construct, rather than what you see in the mirror,” Sheethal Reddy, PhD, a psychologist at the Emory Bariatric Center, Emory University Hospital Midtown, Atlanta, told this news organization. “It’s the mental construct of our physical selves.”
According to Dr. Reddy, body image develops “within a broader societal context and is influenced by the person’s ethnic, racial, and cultural heritage.”
Adolescents are particularly vulnerable to body dissatisfaction. This is compounded in those with obesity, who often experience weight-based victimization and internalized weight-based stigma, compared with adolescents with lower weights. Weight stigma often takes the form of teasing and bullying.
“Appearance-related bullying and teasing during childhood and adolescence can reverberate into adulthood and persist throughout the lifespan,” Dr. Sarwer said. “When we see these patients and ask if they’ve ever been teased or bullied, not only do many say yes but it takes them back to those moments, to that origin story, and they remember someone saying something mean, cruel, and hurtful.”
Stigmatizing experiences can affect subjective body image, even after the weight has been lost and the person’s body is objectively thinner. Research comparing individuals who were overweight and lost weight to individuals who are currently overweight and haven’t lost weight and individuals who were never overweight suggests that “vestigial” body disparagement may persist following weight loss — especially in those with early-onset obesity.
The Role of Genetics
Genetics may contribute to people’s self-perception and body dissatisfaction, both before and after weight loss. A study of 827 community-based adolescents examined the association between polygenic risk scores (PRS) for body mass index (BMI) and type 2 diabetes and symptoms of body dissatisfaction and depression.
“Given the significant genetic role in BMI, we wanted to explore whether genetic risk for BMI might also predict body dissatisfaction,” lead author Krista Ekberg, MS, a doctoral candidate in clinical psychology, Rosalind Franklin University of Medicine and Science, North Chicago, Illinois, told this news organization.
Genetic influences on BMI, as measured by PRS, were significantly associated with both phenotypic BMI and body dissatisfaction. “The association between PRS and body dissatisfaction was largely explained by BMI, suggesting that BMI itself accounts for much of the link between genetic risk and body dissatisfaction.”
Psychiatric History and Trauma
Adverse experiences, particularly sexual or physical abuse, may also account for body dissatisfaction after weight loss. “When some people with a history of this type of abuse lose a large amount of weight — typically after bariatric surgery — they often go through a period of emotional turbulence,” Dr. Sarwer said.
Childhood maltreatment can also be associated with body image disturbances in adulthood, according to a meta-analysis of 12 studies, encompassing 15,481 participants. Sexual abuse is “surprisingly common” among patients with obesity, according to Dr. Sarwer. A chart review of 131 patients revealed that 60% of those who reported a history of rape or sexual molestation were ≥ 50 pounds overweight vs only 28% of age- and sex-matched controls without a history of abuse. Other studies have corroborated these findings.
Excess weight can serve an “adaptive function,” Dr. Sarwer noted. It can be a self-protective mechanism that “insulates” them from sexual advances by potential romantic partners or abusers. Some may find that, after weight loss, repressed memories of a sexual assault surface as a result of the newer, more “attractive” appearance. Feeling vulnerable in their thinner bodies, they may need to regard themselves as overweight to maintain that feeling of “protection.” Weight loss may also trigger memories, flashbacks, or nightmares, as people return to a weight at which they were abused.
Dissociation is another mechanism linking trauma with post–weight loss body dysmorphia, Supatra Tovar, PsyD, RD, a clinical psychologist and registered dietitian with a practice in California, told this news organization. Dissociation from the body is often a coping mechanism for dealing with an overwhelming traumatic experience.
Individuals with a history of depression, anxiety, or posttraumatic stress disorder have higher levels of body dysmorphia, both before and after weight loss. One study found that patients undergoing bariatric surgery who had some type of psychopathology and other psychological risk factors were significantly more likely to report body image concerns 3 months after the surgery. Body image concerns were also more common in patients with preoperative depression, current psychotropic medication use, and a history of outpatient therapy or psychotropic medication use.
“Depression, anxiety, and trauma play a role in how you see yourself and how you carry yourself,” Dr. Reddy said. “This is wrapped up in any type of psychopathology. Being depressed is like looking at yourself through a cloud. It’s the opposite of ‘rose-colored glasses’ and instead, looking at yourself through a negative lens.”
Diagnosis and Interventions
Some helpful tools to assess the presence and extent of weight dissatisfaction and body dysmorphia include the Eating Disorder Inventory — Body Dissatisfaction Subscale and the Body Shape Questionnaire. It’s also important to take into account “the extent to which people are invested in their appearance psychologically,” Dr. Sarwer advised. The AO subscale of the Multidimensional Body-Self Relations Questionnaire generally assesses this. The Body Image Quality of Life Inventory assesses how and to what extent the perceived body image affects the person’s quality of life.
Experts recommend cognitive behavioral therapy (CBT) as an evidence-based intervention for body image issues, including those following weight loss.
“There’s an extensive CBT body image therapy program specifically tailored to the needs of overweight and obese individuals,” Dr. Sarwer said. “We don’t ignore historical variables that may have contributed to the problem, like early bullying, but we encourage people to think about what’s going on in their day-to-day life today. We drill down not only into the maladaptive behaviors but also the cognition and beliefs that may be erroneous but underlie these behaviors.”
The aim of CBT is to “modify irrational and dysfunctional thoughts, emotions, and behaviors through techniques such as self-monitoring, cognitive structuring, psychoeducation, desensitization, and exposure and response prevention.” The program laid out in Cash’s body image workbook includes eight steps. (Figure).
Weight Loss Doesn’t Automatically Equate With Happiness
Another realistic expectation runs counter to a common misperception that becoming thin will automatically translate into becoming happier. That’s not always the case, according to Dr. Tovar.
“If you haven’t worked deeply on addressing self-compassion and understanding that who you are at the core has nothing to do with your physical appearance, you can have an empty feeling once you’ve reached this point,” she said. “You still don’t know who you are and what you’re contributing to the world [because] you’ve been so focused on losing weight.”
Weight loss can also “unmask” questions about self-worth, even when receiving compliments about one’s “improved” appearance. “Praise and compliments after weight loss can be a double-edged sword,” Dr. Tovar observed. “You might think, ‘I wasn’t accepted or praised when I was overweight. The only way to be acceptable or validated is by losing weight, so I have to continue losing weight.’ ” This fuels fear of regaining the weight and can lead to continuing to see oneself as overweight, perhaps as a way to stay motivated to continue with weight loss. “Feeling that one’s value depends on remaining thin hampers body satisfaction,” she said.
Dr. Tovar, author of the book Deprogram Diet Culture: Rethink Your Relationship with Food, Heal Your Mind, and Live a Diet-Free Life, encourages people to shift the emphasis from weight loss to a holistic focus on self-worth and to explore obstacles to those feelings both before and after weight loss.
Endocrinologists and other medical professionals can help by not engaging in “weight and body shaming,” Dr. Tovar said.
She recommends physicians “encourage patients to tune in to their own bodies, helping them become more aware of how different foods affect their physical and emotional well-being.”
Set realistic expectations through “open, nonjudgmental conversations about the complexities of metabolism, weight, and health.”
Dr. Tovar advises rather than focusing on weight loss as the primary goal, physicians should focus on health markers such as blood glucose, energy levels, mental well-being, and physical fitness.
Prioritize “listening over lecturing.” Begin with empathy, asking questions such as “How do you feel about your health right now? What changes have you noticed in your body lately?” Doing this “creates space for the patient to express their concerns without feeling judged or shamed.”
Refer patients to a mental health professional when a patient exhibits signs of disordered eating or poor body image or when emotional factors are playing a significant role in the relationship with food and weight. “If a patient is caught in a cycle of dieting and weight gain, struggles with binge eating, or displays symptoms of depression or anxiety related to body, then psychological help is crucial.”
Ultimately, the goal of treatment “should be to provide a safe, supportive environment where patients can heal — not just physically but also emotionally and mentally,” Dr. Tovar added.
Dr. Tovar, Ms. Ekberg, and Dr. Reddy reported no relevant financial relationships. Dr. Sarwer received grant funding from the National Institute of Dental and Craniofacial Research and National Institute of Diabetes and Digestive and Kidney Diseases. He has consulting relationships with Novo Nordisk and Twenty30 Health. He is an associate editor for Obesity Surgery and editor in chief of Obesity Science & Practice.
A version of this article first appeared on Medscape.com.
Many people who lose weight, whether through diet and lifestyle changes, medication, or bariatric surgery, recognize their body has changed. While they also experience improvements in quality of life and psychosocial areas, that’s not true for everyone. Some patients don’t “see” they’ve lost weight — a phenomenon referred to as “phantom fat,” “ghost fat,” or “vestigial body image.”
“Most people are happy with their appearance, or at least their body shape, after weight loss — although some are unhappy with the loose, sagging skin that can follow weight loss and seek plastic surgery to remedy that,” David B. Sarwer, PhD, director of the Center for Obesity Research and Education and professor of social and behavioral sciences, Temple University College of Public Health, Philadelphia, told this news organization. “There’s a subset of people who remain dissatisfied with their body image, including their shape.”
This body dissatisfaction of people who lose weight may be long-standing, predating the weight loss, or may be new because weight loss has catalyzed a host of previously unaddressed psychosocial issues. Some may show up at assessments on treatment onset, while others may be detected by monitoring changes during or after weight loss. “Mental health counseling after bariatric surgery is greatly underutilized,” Dr. Sarwer observed.
Ghost Fat
Research has corroborated the lingering self-perception of being “obese” vs “ex-obese.” In one study, patients who had undergone bariatric surgery reported being unable to see the difference in their size and shape 18-30 months following their procedure, despite substantial weight loss.
Some research suggests that rapid weight loss (eg, through bariatric surgery) is more likely to generate the perception of “phantom fat,” but additional research is needed to investigate whether the mode and speed of weight loss affect subsequent body image.
Being habituated to one’s former appearance may play a role, Dr. Sarwer suggested. “We see this not only with weight loss but with other body-altering procedures. It takes the brain time to catch up to the new appearance. In rhinoplasty, for example, it may take patients a while before they become accustomed to looking at their new face in the mirror after decades of looking at a more prominent nose.”
Years of Social Stigma
It may also take time for people to overcome years of enduring the stigma of obesity.
There are “pervasive” negative attitudes implying that individuals who are overweight and/or obese are “lazy, weak-willed, lacking in self-discipline and willpower” — a problem compounded by social media and media in general, which present unrealistic, glorified body images and disparaging messages about those with weight problems.
“Body image is a construct, rather than what you see in the mirror,” Sheethal Reddy, PhD, a psychologist at the Emory Bariatric Center, Emory University Hospital Midtown, Atlanta, told this news organization. “It’s the mental construct of our physical selves.”
According to Dr. Reddy, body image develops “within a broader societal context and is influenced by the person’s ethnic, racial, and cultural heritage.”
Adolescents are particularly vulnerable to body dissatisfaction. This is compounded in those with obesity, who often experience weight-based victimization and internalized weight-based stigma, compared with adolescents with lower weights. Weight stigma often takes the form of teasing and bullying.
“Appearance-related bullying and teasing during childhood and adolescence can reverberate into adulthood and persist throughout the lifespan,” Dr. Sarwer said. “When we see these patients and ask if they’ve ever been teased or bullied, not only do many say yes but it takes them back to those moments, to that origin story, and they remember someone saying something mean, cruel, and hurtful.”
Stigmatizing experiences can affect subjective body image, even after the weight has been lost and the person’s body is objectively thinner. Research comparing individuals who were overweight and lost weight to individuals who are currently overweight and haven’t lost weight and individuals who were never overweight suggests that “vestigial” body disparagement may persist following weight loss — especially in those with early-onset obesity.
The Role of Genetics
Genetics may contribute to people’s self-perception and body dissatisfaction, both before and after weight loss. A study of 827 community-based adolescents examined the association between polygenic risk scores (PRS) for body mass index (BMI) and type 2 diabetes and symptoms of body dissatisfaction and depression.
“Given the significant genetic role in BMI, we wanted to explore whether genetic risk for BMI might also predict body dissatisfaction,” lead author Krista Ekberg, MS, a doctoral candidate in clinical psychology, Rosalind Franklin University of Medicine and Science, North Chicago, Illinois, told this news organization.
Genetic influences on BMI, as measured by PRS, were significantly associated with both phenotypic BMI and body dissatisfaction. “The association between PRS and body dissatisfaction was largely explained by BMI, suggesting that BMI itself accounts for much of the link between genetic risk and body dissatisfaction.”
Psychiatric History and Trauma
Adverse experiences, particularly sexual or physical abuse, may also account for body dissatisfaction after weight loss. “When some people with a history of this type of abuse lose a large amount of weight — typically after bariatric surgery — they often go through a period of emotional turbulence,” Dr. Sarwer said.
Childhood maltreatment can also be associated with body image disturbances in adulthood, according to a meta-analysis of 12 studies, encompassing 15,481 participants. Sexual abuse is “surprisingly common” among patients with obesity, according to Dr. Sarwer. A chart review of 131 patients revealed that 60% of those who reported a history of rape or sexual molestation were ≥ 50 pounds overweight vs only 28% of age- and sex-matched controls without a history of abuse. Other studies have corroborated these findings.
Excess weight can serve an “adaptive function,” Dr. Sarwer noted. It can be a self-protective mechanism that “insulates” them from sexual advances by potential romantic partners or abusers. Some may find that, after weight loss, repressed memories of a sexual assault surface as a result of the newer, more “attractive” appearance. Feeling vulnerable in their thinner bodies, they may need to regard themselves as overweight to maintain that feeling of “protection.” Weight loss may also trigger memories, flashbacks, or nightmares, as people return to a weight at which they were abused.
Dissociation is another mechanism linking trauma with post–weight loss body dysmorphia, Supatra Tovar, PsyD, RD, a clinical psychologist and registered dietitian with a practice in California, told this news organization. Dissociation from the body is often a coping mechanism for dealing with an overwhelming traumatic experience.
Individuals with a history of depression, anxiety, or posttraumatic stress disorder have higher levels of body dysmorphia, both before and after weight loss. One study found that patients undergoing bariatric surgery who had some type of psychopathology and other psychological risk factors were significantly more likely to report body image concerns 3 months after the surgery. Body image concerns were also more common in patients with preoperative depression, current psychotropic medication use, and a history of outpatient therapy or psychotropic medication use.
“Depression, anxiety, and trauma play a role in how you see yourself and how you carry yourself,” Dr. Reddy said. “This is wrapped up in any type of psychopathology. Being depressed is like looking at yourself through a cloud. It’s the opposite of ‘rose-colored glasses’ and instead, looking at yourself through a negative lens.”
Diagnosis and Interventions
Some helpful tools to assess the presence and extent of weight dissatisfaction and body dysmorphia include the Eating Disorder Inventory — Body Dissatisfaction Subscale and the Body Shape Questionnaire. It’s also important to take into account “the extent to which people are invested in their appearance psychologically,” Dr. Sarwer advised. The AO subscale of the Multidimensional Body-Self Relations Questionnaire generally assesses this. The Body Image Quality of Life Inventory assesses how and to what extent the perceived body image affects the person’s quality of life.
Experts recommend cognitive behavioral therapy (CBT) as an evidence-based intervention for body image issues, including those following weight loss.
“There’s an extensive CBT body image therapy program specifically tailored to the needs of overweight and obese individuals,” Dr. Sarwer said. “We don’t ignore historical variables that may have contributed to the problem, like early bullying, but we encourage people to think about what’s going on in their day-to-day life today. We drill down not only into the maladaptive behaviors but also the cognition and beliefs that may be erroneous but underlie these behaviors.”
The aim of CBT is to “modify irrational and dysfunctional thoughts, emotions, and behaviors through techniques such as self-monitoring, cognitive structuring, psychoeducation, desensitization, and exposure and response prevention.” The program laid out in Cash’s body image workbook includes eight steps. (Figure).
Weight Loss Doesn’t Automatically Equate With Happiness
Another realistic expectation runs counter to a common misperception that becoming thin will automatically translate into becoming happier. That’s not always the case, according to Dr. Tovar.
“If you haven’t worked deeply on addressing self-compassion and understanding that who you are at the core has nothing to do with your physical appearance, you can have an empty feeling once you’ve reached this point,” she said. “You still don’t know who you are and what you’re contributing to the world [because] you’ve been so focused on losing weight.”
Weight loss can also “unmask” questions about self-worth, even when receiving compliments about one’s “improved” appearance. “Praise and compliments after weight loss can be a double-edged sword,” Dr. Tovar observed. “You might think, ‘I wasn’t accepted or praised when I was overweight. The only way to be acceptable or validated is by losing weight, so I have to continue losing weight.’ ” This fuels fear of regaining the weight and can lead to continuing to see oneself as overweight, perhaps as a way to stay motivated to continue with weight loss. “Feeling that one’s value depends on remaining thin hampers body satisfaction,” she said.
Dr. Tovar, author of the book Deprogram Diet Culture: Rethink Your Relationship with Food, Heal Your Mind, and Live a Diet-Free Life, encourages people to shift the emphasis from weight loss to a holistic focus on self-worth and to explore obstacles to those feelings both before and after weight loss.
Endocrinologists and other medical professionals can help by not engaging in “weight and body shaming,” Dr. Tovar said.
She recommends physicians “encourage patients to tune in to their own bodies, helping them become more aware of how different foods affect their physical and emotional well-being.”
Set realistic expectations through “open, nonjudgmental conversations about the complexities of metabolism, weight, and health.”
Dr. Tovar advises rather than focusing on weight loss as the primary goal, physicians should focus on health markers such as blood glucose, energy levels, mental well-being, and physical fitness.
Prioritize “listening over lecturing.” Begin with empathy, asking questions such as “How do you feel about your health right now? What changes have you noticed in your body lately?” Doing this “creates space for the patient to express their concerns without feeling judged or shamed.”
Refer patients to a mental health professional when a patient exhibits signs of disordered eating or poor body image or when emotional factors are playing a significant role in the relationship with food and weight. “If a patient is caught in a cycle of dieting and weight gain, struggles with binge eating, or displays symptoms of depression or anxiety related to body, then psychological help is crucial.”
Ultimately, the goal of treatment “should be to provide a safe, supportive environment where patients can heal — not just physically but also emotionally and mentally,” Dr. Tovar added.
Dr. Tovar, Ms. Ekberg, and Dr. Reddy reported no relevant financial relationships. Dr. Sarwer received grant funding from the National Institute of Dental and Craniofacial Research and National Institute of Diabetes and Digestive and Kidney Diseases. He has consulting relationships with Novo Nordisk and Twenty30 Health. He is an associate editor for Obesity Surgery and editor in chief of Obesity Science & Practice.
A version of this article first appeared on Medscape.com.
Many people who lose weight, whether through diet and lifestyle changes, medication, or bariatric surgery, recognize their body has changed. While they also experience improvements in quality of life and psychosocial areas, that’s not true for everyone. Some patients don’t “see” they’ve lost weight — a phenomenon referred to as “phantom fat,” “ghost fat,” or “vestigial body image.”
“Most people are happy with their appearance, or at least their body shape, after weight loss — although some are unhappy with the loose, sagging skin that can follow weight loss and seek plastic surgery to remedy that,” David B. Sarwer, PhD, director of the Center for Obesity Research and Education and professor of social and behavioral sciences, Temple University College of Public Health, Philadelphia, told this news organization. “There’s a subset of people who remain dissatisfied with their body image, including their shape.”
This body dissatisfaction of people who lose weight may be long-standing, predating the weight loss, or may be new because weight loss has catalyzed a host of previously unaddressed psychosocial issues. Some may show up at assessments on treatment onset, while others may be detected by monitoring changes during or after weight loss. “Mental health counseling after bariatric surgery is greatly underutilized,” Dr. Sarwer observed.
Ghost Fat
Research has corroborated the lingering self-perception of being “obese” vs “ex-obese.” In one study, patients who had undergone bariatric surgery reported being unable to see the difference in their size and shape 18-30 months following their procedure, despite substantial weight loss.
Some research suggests that rapid weight loss (eg, through bariatric surgery) is more likely to generate the perception of “phantom fat,” but additional research is needed to investigate whether the mode and speed of weight loss affect subsequent body image.
Being habituated to one’s former appearance may play a role, Dr. Sarwer suggested. “We see this not only with weight loss but with other body-altering procedures. It takes the brain time to catch up to the new appearance. In rhinoplasty, for example, it may take patients a while before they become accustomed to looking at their new face in the mirror after decades of looking at a more prominent nose.”
Years of Social Stigma
It may also take time for people to overcome years of enduring the stigma of obesity.
There are “pervasive” negative attitudes implying that individuals who are overweight and/or obese are “lazy, weak-willed, lacking in self-discipline and willpower” — a problem compounded by social media and media in general, which present unrealistic, glorified body images and disparaging messages about those with weight problems.
“Body image is a construct, rather than what you see in the mirror,” Sheethal Reddy, PhD, a psychologist at the Emory Bariatric Center, Emory University Hospital Midtown, Atlanta, told this news organization. “It’s the mental construct of our physical selves.”
According to Dr. Reddy, body image develops “within a broader societal context and is influenced by the person’s ethnic, racial, and cultural heritage.”
Adolescents are particularly vulnerable to body dissatisfaction. This is compounded in those with obesity, who often experience weight-based victimization and internalized weight-based stigma, compared with adolescents with lower weights. Weight stigma often takes the form of teasing and bullying.
“Appearance-related bullying and teasing during childhood and adolescence can reverberate into adulthood and persist throughout the lifespan,” Dr. Sarwer said. “When we see these patients and ask if they’ve ever been teased or bullied, not only do many say yes but it takes them back to those moments, to that origin story, and they remember someone saying something mean, cruel, and hurtful.”
Stigmatizing experiences can affect subjective body image, even after the weight has been lost and the person’s body is objectively thinner. Research comparing individuals who were overweight and lost weight to individuals who are currently overweight and haven’t lost weight and individuals who were never overweight suggests that “vestigial” body disparagement may persist following weight loss — especially in those with early-onset obesity.
The Role of Genetics
Genetics may contribute to people’s self-perception and body dissatisfaction, both before and after weight loss. A study of 827 community-based adolescents examined the association between polygenic risk scores (PRS) for body mass index (BMI) and type 2 diabetes and symptoms of body dissatisfaction and depression.
“Given the significant genetic role in BMI, we wanted to explore whether genetic risk for BMI might also predict body dissatisfaction,” lead author Krista Ekberg, MS, a doctoral candidate in clinical psychology, Rosalind Franklin University of Medicine and Science, North Chicago, Illinois, told this news organization.
Genetic influences on BMI, as measured by PRS, were significantly associated with both phenotypic BMI and body dissatisfaction. “The association between PRS and body dissatisfaction was largely explained by BMI, suggesting that BMI itself accounts for much of the link between genetic risk and body dissatisfaction.”
Psychiatric History and Trauma
Adverse experiences, particularly sexual or physical abuse, may also account for body dissatisfaction after weight loss. “When some people with a history of this type of abuse lose a large amount of weight — typically after bariatric surgery — they often go through a period of emotional turbulence,” Dr. Sarwer said.
Childhood maltreatment can also be associated with body image disturbances in adulthood, according to a meta-analysis of 12 studies, encompassing 15,481 participants. Sexual abuse is “surprisingly common” among patients with obesity, according to Dr. Sarwer. A chart review of 131 patients revealed that 60% of those who reported a history of rape or sexual molestation were ≥ 50 pounds overweight vs only 28% of age- and sex-matched controls without a history of abuse. Other studies have corroborated these findings.
Excess weight can serve an “adaptive function,” Dr. Sarwer noted. It can be a self-protective mechanism that “insulates” them from sexual advances by potential romantic partners or abusers. Some may find that, after weight loss, repressed memories of a sexual assault surface as a result of the newer, more “attractive” appearance. Feeling vulnerable in their thinner bodies, they may need to regard themselves as overweight to maintain that feeling of “protection.” Weight loss may also trigger memories, flashbacks, or nightmares, as people return to a weight at which they were abused.
Dissociation is another mechanism linking trauma with post–weight loss body dysmorphia, Supatra Tovar, PsyD, RD, a clinical psychologist and registered dietitian with a practice in California, told this news organization. Dissociation from the body is often a coping mechanism for dealing with an overwhelming traumatic experience.
Individuals with a history of depression, anxiety, or posttraumatic stress disorder have higher levels of body dysmorphia, both before and after weight loss. One study found that patients undergoing bariatric surgery who had some type of psychopathology and other psychological risk factors were significantly more likely to report body image concerns 3 months after the surgery. Body image concerns were also more common in patients with preoperative depression, current psychotropic medication use, and a history of outpatient therapy or psychotropic medication use.
“Depression, anxiety, and trauma play a role in how you see yourself and how you carry yourself,” Dr. Reddy said. “This is wrapped up in any type of psychopathology. Being depressed is like looking at yourself through a cloud. It’s the opposite of ‘rose-colored glasses’ and instead, looking at yourself through a negative lens.”
Diagnosis and Interventions
Some helpful tools to assess the presence and extent of weight dissatisfaction and body dysmorphia include the Eating Disorder Inventory — Body Dissatisfaction Subscale and the Body Shape Questionnaire. It’s also important to take into account “the extent to which people are invested in their appearance psychologically,” Dr. Sarwer advised. The AO subscale of the Multidimensional Body-Self Relations Questionnaire generally assesses this. The Body Image Quality of Life Inventory assesses how and to what extent the perceived body image affects the person’s quality of life.
Experts recommend cognitive behavioral therapy (CBT) as an evidence-based intervention for body image issues, including those following weight loss.
“There’s an extensive CBT body image therapy program specifically tailored to the needs of overweight and obese individuals,” Dr. Sarwer said. “We don’t ignore historical variables that may have contributed to the problem, like early bullying, but we encourage people to think about what’s going on in their day-to-day life today. We drill down not only into the maladaptive behaviors but also the cognition and beliefs that may be erroneous but underlie these behaviors.”
The aim of CBT is to “modify irrational and dysfunctional thoughts, emotions, and behaviors through techniques such as self-monitoring, cognitive structuring, psychoeducation, desensitization, and exposure and response prevention.” The program laid out in Cash’s body image workbook includes eight steps. (Figure).
Weight Loss Doesn’t Automatically Equate With Happiness
Another realistic expectation runs counter to a common misperception that becoming thin will automatically translate into becoming happier. That’s not always the case, according to Dr. Tovar.
“If you haven’t worked deeply on addressing self-compassion and understanding that who you are at the core has nothing to do with your physical appearance, you can have an empty feeling once you’ve reached this point,” she said. “You still don’t know who you are and what you’re contributing to the world [because] you’ve been so focused on losing weight.”
Weight loss can also “unmask” questions about self-worth, even when receiving compliments about one’s “improved” appearance. “Praise and compliments after weight loss can be a double-edged sword,” Dr. Tovar observed. “You might think, ‘I wasn’t accepted or praised when I was overweight. The only way to be acceptable or validated is by losing weight, so I have to continue losing weight.’ ” This fuels fear of regaining the weight and can lead to continuing to see oneself as overweight, perhaps as a way to stay motivated to continue with weight loss. “Feeling that one’s value depends on remaining thin hampers body satisfaction,” she said.
Dr. Tovar, author of the book Deprogram Diet Culture: Rethink Your Relationship with Food, Heal Your Mind, and Live a Diet-Free Life, encourages people to shift the emphasis from weight loss to a holistic focus on self-worth and to explore obstacles to those feelings both before and after weight loss.
Endocrinologists and other medical professionals can help by not engaging in “weight and body shaming,” Dr. Tovar said.
She recommends physicians “encourage patients to tune in to their own bodies, helping them become more aware of how different foods affect their physical and emotional well-being.”
Set realistic expectations through “open, nonjudgmental conversations about the complexities of metabolism, weight, and health.”
Dr. Tovar advises rather than focusing on weight loss as the primary goal, physicians should focus on health markers such as blood glucose, energy levels, mental well-being, and physical fitness.
Prioritize “listening over lecturing.” Begin with empathy, asking questions such as “How do you feel about your health right now? What changes have you noticed in your body lately?” Doing this “creates space for the patient to express their concerns without feeling judged or shamed.”
Refer patients to a mental health professional when a patient exhibits signs of disordered eating or poor body image or when emotional factors are playing a significant role in the relationship with food and weight. “If a patient is caught in a cycle of dieting and weight gain, struggles with binge eating, or displays symptoms of depression or anxiety related to body, then psychological help is crucial.”
Ultimately, the goal of treatment “should be to provide a safe, supportive environment where patients can heal — not just physically but also emotionally and mentally,” Dr. Tovar added.
Dr. Tovar, Ms. Ekberg, and Dr. Reddy reported no relevant financial relationships. Dr. Sarwer received grant funding from the National Institute of Dental and Craniofacial Research and National Institute of Diabetes and Digestive and Kidney Diseases. He has consulting relationships with Novo Nordisk and Twenty30 Health. He is an associate editor for Obesity Surgery and editor in chief of Obesity Science & Practice.
A version of this article first appeared on Medscape.com.
Tirzepatide Shortage Resolved? FDA Says Yes, Compounders No
The agency wrote in a clarification aimed at compounders that Lilly said it can meet the “present and projected national demand” and that compounders are restricted from making the products.
Nevertheless, patients and prescribers may still see “intermittent localized supply disruptions as the products move through the supply chain,” the FDA noted.
The Alliance for Pharmacy Compounding (APC) responded swiftly, alerting its members and the public to the resolved shortage and stating that compounders “must immediately cease preparing and dispensing compounded copies” of the two drugs.
However, APC CEO Scott Brunner added it often takes a long time for FDA-approved versions of the drug to become widely available to wholesalers, hospitals, and clinics. Even after Lilly announced greater availability for the drugs, including in a new vial format for low doses, “for most pharmacies, they’re lucky to get two or three boxes of Zepbound a day from their wholesaler — for a patient waiting list that can number in the hundreds.”
“We have already heard this morning from APC members that they are unable to fill orders for their patients,” he said.
Furthermore, he contended, “I suspect plenty of patients taking compounded tirzepatide are going to be caught flat-footed by this. They are being cut off cold turkey, their prescription no longer fillable. They’ll need to get in to see their provider to get a new prescription, and that will take some time. It’s possible that so many patients presently taking compounded GLP-1s [glucagon-like peptide 1] will be eventually switched to the FDA-approved versions — if they can afford them, of course — that it will push tirzepatide injection back into shortage.”
Commenting on the shortage resolution, endocrinologist Beverly Tchang, MD, DABOM, an assistant professor of clinical medicine at Weill Cornell Medicine in New York City told this news organization, “we are not yet experiencing relief from the shortages, but I hope this resolves at least one barrier to access for our patients.”
“I don’t think it will create confusion,” she said. “Fortunately or unfortunately, patients and clinicians are adept by now with therapeutic transitions because we’ve been forced to do so whenever insurance withdraws coverage or a shortage recurs or a coupon expires. It’s obviously not ideal but patients are motivated and clinicians don’t give up.”
This news organization has previously reported on the impact of the shortages and how endocrinologists and obesity medicine specialists were handling them, in light of concerns about compounding pharmacies that may or may not be well founded.
Dr. Tchang declared that she is an adviser to Novo Nordisk.
A version of this article appeared on Medscape.com.
The agency wrote in a clarification aimed at compounders that Lilly said it can meet the “present and projected national demand” and that compounders are restricted from making the products.
Nevertheless, patients and prescribers may still see “intermittent localized supply disruptions as the products move through the supply chain,” the FDA noted.
The Alliance for Pharmacy Compounding (APC) responded swiftly, alerting its members and the public to the resolved shortage and stating that compounders “must immediately cease preparing and dispensing compounded copies” of the two drugs.
However, APC CEO Scott Brunner added it often takes a long time for FDA-approved versions of the drug to become widely available to wholesalers, hospitals, and clinics. Even after Lilly announced greater availability for the drugs, including in a new vial format for low doses, “for most pharmacies, they’re lucky to get two or three boxes of Zepbound a day from their wholesaler — for a patient waiting list that can number in the hundreds.”
“We have already heard this morning from APC members that they are unable to fill orders for their patients,” he said.
Furthermore, he contended, “I suspect plenty of patients taking compounded tirzepatide are going to be caught flat-footed by this. They are being cut off cold turkey, their prescription no longer fillable. They’ll need to get in to see their provider to get a new prescription, and that will take some time. It’s possible that so many patients presently taking compounded GLP-1s [glucagon-like peptide 1] will be eventually switched to the FDA-approved versions — if they can afford them, of course — that it will push tirzepatide injection back into shortage.”
Commenting on the shortage resolution, endocrinologist Beverly Tchang, MD, DABOM, an assistant professor of clinical medicine at Weill Cornell Medicine in New York City told this news organization, “we are not yet experiencing relief from the shortages, but I hope this resolves at least one barrier to access for our patients.”
“I don’t think it will create confusion,” she said. “Fortunately or unfortunately, patients and clinicians are adept by now with therapeutic transitions because we’ve been forced to do so whenever insurance withdraws coverage or a shortage recurs or a coupon expires. It’s obviously not ideal but patients are motivated and clinicians don’t give up.”
This news organization has previously reported on the impact of the shortages and how endocrinologists and obesity medicine specialists were handling them, in light of concerns about compounding pharmacies that may or may not be well founded.
Dr. Tchang declared that she is an adviser to Novo Nordisk.
A version of this article appeared on Medscape.com.
The agency wrote in a clarification aimed at compounders that Lilly said it can meet the “present and projected national demand” and that compounders are restricted from making the products.
Nevertheless, patients and prescribers may still see “intermittent localized supply disruptions as the products move through the supply chain,” the FDA noted.
The Alliance for Pharmacy Compounding (APC) responded swiftly, alerting its members and the public to the resolved shortage and stating that compounders “must immediately cease preparing and dispensing compounded copies” of the two drugs.
However, APC CEO Scott Brunner added it often takes a long time for FDA-approved versions of the drug to become widely available to wholesalers, hospitals, and clinics. Even after Lilly announced greater availability for the drugs, including in a new vial format for low doses, “for most pharmacies, they’re lucky to get two or three boxes of Zepbound a day from their wholesaler — for a patient waiting list that can number in the hundreds.”
“We have already heard this morning from APC members that they are unable to fill orders for their patients,” he said.
Furthermore, he contended, “I suspect plenty of patients taking compounded tirzepatide are going to be caught flat-footed by this. They are being cut off cold turkey, their prescription no longer fillable. They’ll need to get in to see their provider to get a new prescription, and that will take some time. It’s possible that so many patients presently taking compounded GLP-1s [glucagon-like peptide 1] will be eventually switched to the FDA-approved versions — if they can afford them, of course — that it will push tirzepatide injection back into shortage.”
Commenting on the shortage resolution, endocrinologist Beverly Tchang, MD, DABOM, an assistant professor of clinical medicine at Weill Cornell Medicine in New York City told this news organization, “we are not yet experiencing relief from the shortages, but I hope this resolves at least one barrier to access for our patients.”
“I don’t think it will create confusion,” she said. “Fortunately or unfortunately, patients and clinicians are adept by now with therapeutic transitions because we’ve been forced to do so whenever insurance withdraws coverage or a shortage recurs or a coupon expires. It’s obviously not ideal but patients are motivated and clinicians don’t give up.”
This news organization has previously reported on the impact of the shortages and how endocrinologists and obesity medicine specialists were handling them, in light of concerns about compounding pharmacies that may or may not be well founded.
Dr. Tchang declared that she is an adviser to Novo Nordisk.
A version of this article appeared on Medscape.com.
Weight Loss After Anti-Obesity Medications Linked to Reduced Gout Risk
TOPLINE:
A higher rate of weight loss within 1 year of initiating orlistat is associated with lower risks for incident gout and recurrent gout flares in individuals with body mass index (BMI) > 25, particularly if they have obesity or high baseline serum urate levels.
METHODOLOGY:
- Researchers conducted a population-based cohort study using data from The Health Improvement Network in the United Kingdom to examine the association between weight loss rates after the initiation of anti-obesity medication (orlistat) and the risk for incident gout and recurrent gout flares in patients with overweight or obesity.
- The risk for incident gout was analyzed in 131,000 patients with overweight or obesity (mean age, 45 years; 77.3% women; mean BMI, 37.2) who did not have gout before initiating orlistat.
- The risk for recurrent gout flares was evaluated in 3847 individuals with overweight or obesity (mean age, 56.6 years; 29.4% women; mean BMI, 38.5), who had gout before initiating orlistat.
- Participants were divided into four groups based on their rate of weight loss during the first year of orlistat use: Weight gain or stable (< 2%), slow (2% to < 5%), moderate (5% to < 10%), and fast (≥ 10%).
- The primary outcome was incident gout, and the secondary outcome was the rate of recurrent gout flares during the 5-year follow-up period after initiating orlistat.
TAKEAWAY:
- The 5-year risk for incident gout was the lowest among patients in the fast weight loss group (1.2%) and highest among those in the weight gain or stable weight group (1.6%).
- The risk for incident gout was lower in the fast (hazard ratio [HR], 0.73; 95% CI, 0.62-0.86) and moderate (HR, 0.82; 95% CI, 0.72-0.92) weight loss groups than in the weight gain or stable weight group.
- Similarly, faster weight loss rates were linked to lower rates of recurrent gout flares, with risk ratios of 0.71 (95% CI, 0.60-0.84) and 0.83 (95% CI, 0.71-0.96) in the fast and moderate weight loss groups, respectively.
- This study found that .
IN PRACTICE:
“Pharmacologic treatments, such as orlistat, present an alternative strategy for managing overweight and obesity. Our study provides empirical evidence of a dose-response effect of weight loss after initiating orlistat within 1 year lowers the risk of incident gout and recurrent gout flares,” the authors wrote.
SOURCE:
This study was led by Jie Wei, PhD, Department of Orthopaedics, Xiangya Hospital, Central South University, Changsha, China, and was published online on September 19, 2024, in Arthritis & Rheumatology.
LIMITATIONS:
Despite adjustment for many variables, factors such as disease severity, exercise levels, and diet were not fully captured, which might have influenced the results. The lack of hospitalization data could have resulted in recurrent gout flares being underreported. The current study may have been subjected to bias due to potential exposure misclassification resulting from the timing of weight measurements and missing updated weight data.
DISCLOSURES:
This study was supported by the National Key Research and Development Plan, the National Natural Science Foundation of China, the Project Program of National Clinical Research Center for Geriatric Disorders, and other sources. No disclosures of interest were reported by the authors.
This article was created using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication. A version of this article first appeared on Medscape.com.
TOPLINE:
A higher rate of weight loss within 1 year of initiating orlistat is associated with lower risks for incident gout and recurrent gout flares in individuals with body mass index (BMI) > 25, particularly if they have obesity or high baseline serum urate levels.
METHODOLOGY:
- Researchers conducted a population-based cohort study using data from The Health Improvement Network in the United Kingdom to examine the association between weight loss rates after the initiation of anti-obesity medication (orlistat) and the risk for incident gout and recurrent gout flares in patients with overweight or obesity.
- The risk for incident gout was analyzed in 131,000 patients with overweight or obesity (mean age, 45 years; 77.3% women; mean BMI, 37.2) who did not have gout before initiating orlistat.
- The risk for recurrent gout flares was evaluated in 3847 individuals with overweight or obesity (mean age, 56.6 years; 29.4% women; mean BMI, 38.5), who had gout before initiating orlistat.
- Participants were divided into four groups based on their rate of weight loss during the first year of orlistat use: Weight gain or stable (< 2%), slow (2% to < 5%), moderate (5% to < 10%), and fast (≥ 10%).
- The primary outcome was incident gout, and the secondary outcome was the rate of recurrent gout flares during the 5-year follow-up period after initiating orlistat.
TAKEAWAY:
- The 5-year risk for incident gout was the lowest among patients in the fast weight loss group (1.2%) and highest among those in the weight gain or stable weight group (1.6%).
- The risk for incident gout was lower in the fast (hazard ratio [HR], 0.73; 95% CI, 0.62-0.86) and moderate (HR, 0.82; 95% CI, 0.72-0.92) weight loss groups than in the weight gain or stable weight group.
- Similarly, faster weight loss rates were linked to lower rates of recurrent gout flares, with risk ratios of 0.71 (95% CI, 0.60-0.84) and 0.83 (95% CI, 0.71-0.96) in the fast and moderate weight loss groups, respectively.
- This study found that .
IN PRACTICE:
“Pharmacologic treatments, such as orlistat, present an alternative strategy for managing overweight and obesity. Our study provides empirical evidence of a dose-response effect of weight loss after initiating orlistat within 1 year lowers the risk of incident gout and recurrent gout flares,” the authors wrote.
SOURCE:
This study was led by Jie Wei, PhD, Department of Orthopaedics, Xiangya Hospital, Central South University, Changsha, China, and was published online on September 19, 2024, in Arthritis & Rheumatology.
LIMITATIONS:
Despite adjustment for many variables, factors such as disease severity, exercise levels, and diet were not fully captured, which might have influenced the results. The lack of hospitalization data could have resulted in recurrent gout flares being underreported. The current study may have been subjected to bias due to potential exposure misclassification resulting from the timing of weight measurements and missing updated weight data.
DISCLOSURES:
This study was supported by the National Key Research and Development Plan, the National Natural Science Foundation of China, the Project Program of National Clinical Research Center for Geriatric Disorders, and other sources. No disclosures of interest were reported by the authors.
This article was created using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication. A version of this article first appeared on Medscape.com.
TOPLINE:
A higher rate of weight loss within 1 year of initiating orlistat is associated with lower risks for incident gout and recurrent gout flares in individuals with body mass index (BMI) > 25, particularly if they have obesity or high baseline serum urate levels.
METHODOLOGY:
- Researchers conducted a population-based cohort study using data from The Health Improvement Network in the United Kingdom to examine the association between weight loss rates after the initiation of anti-obesity medication (orlistat) and the risk for incident gout and recurrent gout flares in patients with overweight or obesity.
- The risk for incident gout was analyzed in 131,000 patients with overweight or obesity (mean age, 45 years; 77.3% women; mean BMI, 37.2) who did not have gout before initiating orlistat.
- The risk for recurrent gout flares was evaluated in 3847 individuals with overweight or obesity (mean age, 56.6 years; 29.4% women; mean BMI, 38.5), who had gout before initiating orlistat.
- Participants were divided into four groups based on their rate of weight loss during the first year of orlistat use: Weight gain or stable (< 2%), slow (2% to < 5%), moderate (5% to < 10%), and fast (≥ 10%).
- The primary outcome was incident gout, and the secondary outcome was the rate of recurrent gout flares during the 5-year follow-up period after initiating orlistat.
TAKEAWAY:
- The 5-year risk for incident gout was the lowest among patients in the fast weight loss group (1.2%) and highest among those in the weight gain or stable weight group (1.6%).
- The risk for incident gout was lower in the fast (hazard ratio [HR], 0.73; 95% CI, 0.62-0.86) and moderate (HR, 0.82; 95% CI, 0.72-0.92) weight loss groups than in the weight gain or stable weight group.
- Similarly, faster weight loss rates were linked to lower rates of recurrent gout flares, with risk ratios of 0.71 (95% CI, 0.60-0.84) and 0.83 (95% CI, 0.71-0.96) in the fast and moderate weight loss groups, respectively.
- This study found that .
IN PRACTICE:
“Pharmacologic treatments, such as orlistat, present an alternative strategy for managing overweight and obesity. Our study provides empirical evidence of a dose-response effect of weight loss after initiating orlistat within 1 year lowers the risk of incident gout and recurrent gout flares,” the authors wrote.
SOURCE:
This study was led by Jie Wei, PhD, Department of Orthopaedics, Xiangya Hospital, Central South University, Changsha, China, and was published online on September 19, 2024, in Arthritis & Rheumatology.
LIMITATIONS:
Despite adjustment for many variables, factors such as disease severity, exercise levels, and diet were not fully captured, which might have influenced the results. The lack of hospitalization data could have resulted in recurrent gout flares being underreported. The current study may have been subjected to bias due to potential exposure misclassification resulting from the timing of weight measurements and missing updated weight data.
DISCLOSURES:
This study was supported by the National Key Research and Development Plan, the National Natural Science Foundation of China, the Project Program of National Clinical Research Center for Geriatric Disorders, and other sources. No disclosures of interest were reported by the authors.
This article was created using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication. A version of this article first appeared on Medscape.com.
Time-Restricted Eating Is Not a Metabolic Magic Bullet
This transcript has been edited for clarity.
One out of three American adults — about 100 million people in this country — have the metabolic syndrome. I’m showing you the official criteria here, but essentially this is a syndrome of insulin resistance and visceral adiposity that predisposes us to a host of chronic diseases such as diabetes, heart disease, and even dementia.
The metabolic syndrome is, fundamentally, a lifestyle disease. There is a direct line between our dietary habits and the wide availability of carbohydrate-rich, highly processed foods, and the rise in the syndrome in the population.
A saying I learned from one of my epidemiology teachers comes to mind: “Lifestyle diseases require lifestyle reinterventions.” But you know what? I’m not so sure anymore.
I’ve been around long enough to see multiple dietary fads come and go with varying efficacy. I grew up in the low-fat era, probably the most detrimental time to our national health as food manufacturers started replacing fats with carbohydrates, driving much of the problem we’re faced with today.
But I was also around for the Atkins diet and the low-carb craze — a healthier approach, all things being equal. And I’ve seen variants of these: the paleo diet (essentially a low-carb, high-protein diet based on minimally processed foods) and the Mediterranean diet, which sought to replace some percentage of fats with healthier fats.
And, of course, there is time-restricted eating.
Time-restricted eating, a variant of intermittent fasting, has the advantage of being very simple. No cookbooks, no recipes. Eat what you want — but limit it to certain hours in the day, ideally a window of less than 10 hours, such as 8 a.m. to 6 p.m.
When it comes to weight loss, the diets that work tend to work because they reduce calorie intake. I know, people will get angry about this, but thermodynamics is not just a good idea, it’s the law.
But weight loss is not the only reason we need to eat healthier. What we eat can impact our health in multiple ways; certain foods lead to more atherosclerosis, more inflammation, increased strain on the kidney and liver, and can affect our glucose homeostasis.
So I was really interested when I saw this article, “Time-Restricted Eating in Adults With Metabolic Syndrome,” appearing in Annals of Internal Medicine October 1, which examined the effect of time-restricted eating on the metabolic syndrome itself. Could this lifestyle intervention cure this lifestyle disease?
In the study, 108 individuals, all of whom had the metabolic syndrome but not full-blown diabetes, were randomized to usual care — basically, nutrition education — vs time-restricted eating. In that group, participants were instructed to reduce their window of eating by at least 4 hours to achieve an 8- to 10-hour eating window. The groups were followed for 3 months.
Now, before we get to the results, it’s important to remember that the success of a lifestyle intervention trial is quite dependent on how well people adhere to the lifestyle intervention. Time-restricted eating is not as easy as taking a pill once a day.
The researchers had participants log their consumption using a smartphone app to confirm whether they were adhering to that restricted eating window.
Broadly speaking, they did. At baseline, both groups had an eating window of about 14 hours a day — think 7 a.m. to 9 p.m. The intervention group reduced that to just under 10 hours, with 10% of days falling outside of the target window.
Lifestyle change achieved, the primary outcome was the change in hemoglobin A1c at 3 months. A1c integrates the serum glucose over time and is thus a good indicator of the success of the intervention in terms of insulin resistance. But the effect was, honestly, disappointing.
Technically, the time-restricted-eating group had a greater A1c change than the control group — by 0.1 percentage points. On average, they went from a baseline A1c of 5.87 to a 3-month A1c of 5.75.
Other metabolic syndrome markers were equally lackluster: no difference in fasting glucose, mean glucose, or fasting insulin.
There was some weight change. The control group, which got that dietary education, lost 1.5% of body weight over the 3 months. The time-restricted-eating group lost 3.3% — about 7 pounds, which is reasonable.
With that weight loss came statistically significant, albeit modest improvements in BMI, body fat percentage, and LDL cholesterol.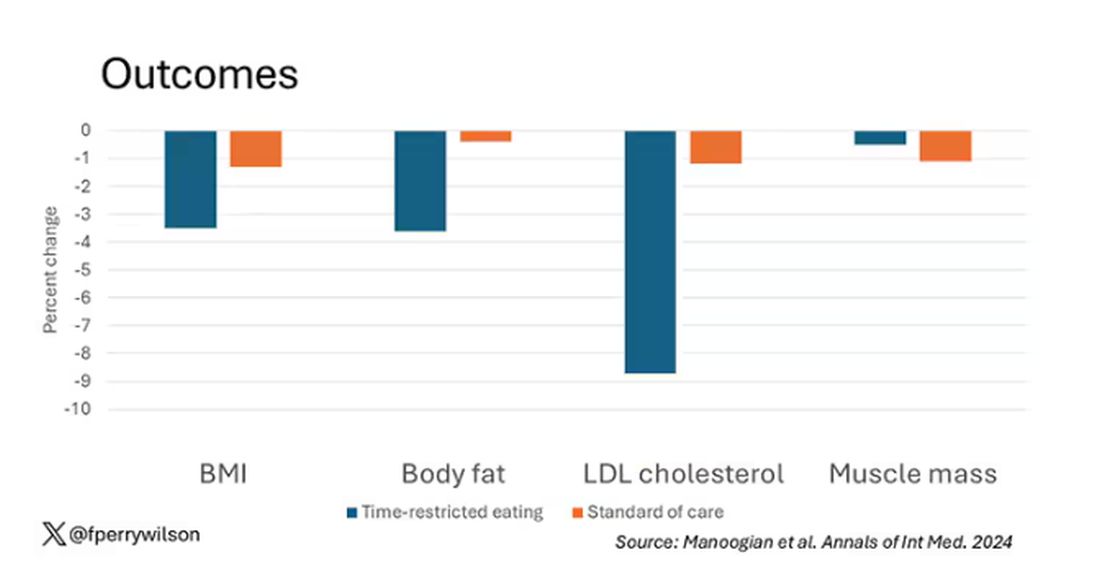
Of interest, despite the larger weight loss in the intermittent-fasting group, there was no difference in muscle mass loss, which is encouraging.
Taken together, we can say that, yes, it seems like time-restricted eating can help people lose some weight. This is essentially due to the fact that people eat fewer calories when they do time-restricted eating, as you can see here.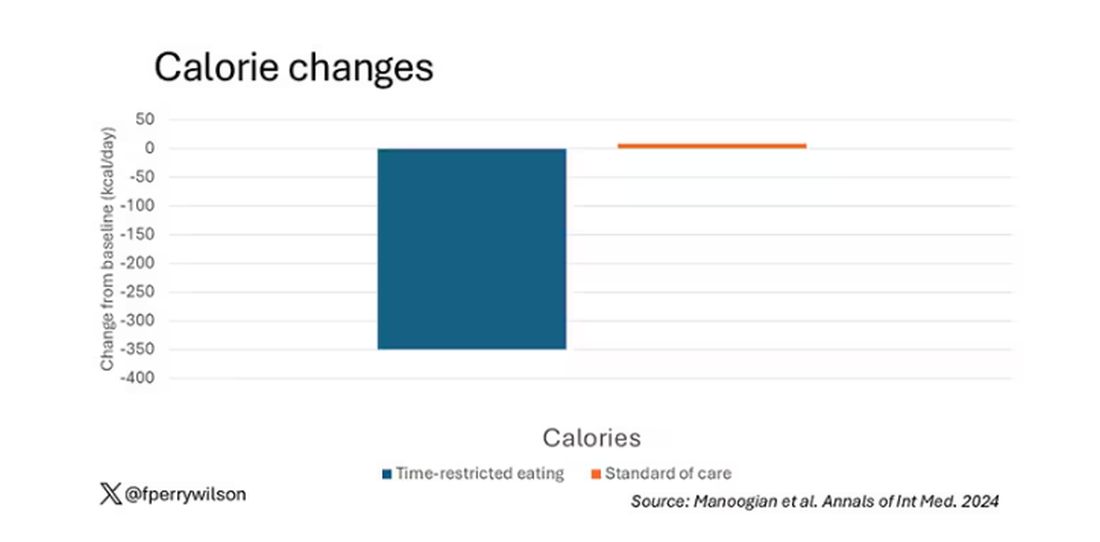
But, in the end, this trial examined whether this relatively straightforward lifestyle intervention would move the needle in terms of metabolic syndrome, and the data are not very compelling for that.
This graph shows how many of those five factors for metabolic syndrome the individuals in this trial had from the start to the end. You see that, over the 3 months, seven people in the time-restricted-eating group moved from having three criteria to two or one — being “cured” of metabolic syndrome, if you will. Nine people in the standard group were cured by that definition. Remember, they had to have at least three to have the syndrome and thus be eligible for the trial. 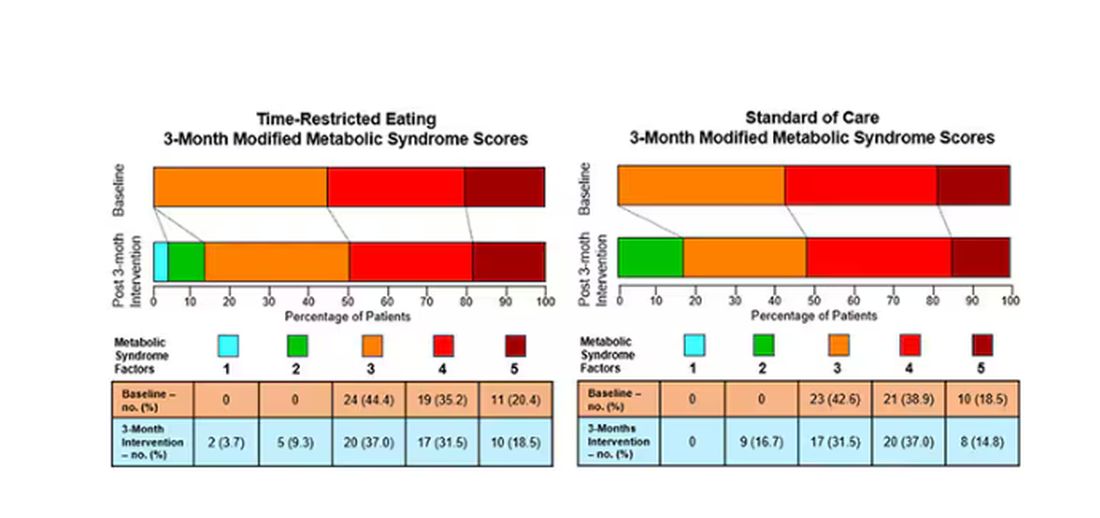
So If it just leads to weight loss by forcing people to consume less calories, then we need to acknowledge that we probably have better methods to achieve this same end. Ten years ago, I would have said that lifestyle change is the only way to end the epidemic of the metabolic syndrome in this country. Today, well, we live in a world of GLP-1 weight loss drugs. It is simply a different world now. Yes, they are expensive. Yes, they have side effects. But we need to evaluate them against the comparison. And so far, lifestyle changes alone are really no comparison.
Dr. Wilson is associate professor of medicine and public health and director of the Clinical and Translational Research Accelerator at Yale University, New Haven, Conn. He has disclosed no relevant financial relationships.
A version of this article appeared on Medscape.com.
This transcript has been edited for clarity.
One out of three American adults — about 100 million people in this country — have the metabolic syndrome. I’m showing you the official criteria here, but essentially this is a syndrome of insulin resistance and visceral adiposity that predisposes us to a host of chronic diseases such as diabetes, heart disease, and even dementia.
The metabolic syndrome is, fundamentally, a lifestyle disease. There is a direct line between our dietary habits and the wide availability of carbohydrate-rich, highly processed foods, and the rise in the syndrome in the population.
A saying I learned from one of my epidemiology teachers comes to mind: “Lifestyle diseases require lifestyle reinterventions.” But you know what? I’m not so sure anymore.
I’ve been around long enough to see multiple dietary fads come and go with varying efficacy. I grew up in the low-fat era, probably the most detrimental time to our national health as food manufacturers started replacing fats with carbohydrates, driving much of the problem we’re faced with today.
But I was also around for the Atkins diet and the low-carb craze — a healthier approach, all things being equal. And I’ve seen variants of these: the paleo diet (essentially a low-carb, high-protein diet based on minimally processed foods) and the Mediterranean diet, which sought to replace some percentage of fats with healthier fats.
And, of course, there is time-restricted eating.
Time-restricted eating, a variant of intermittent fasting, has the advantage of being very simple. No cookbooks, no recipes. Eat what you want — but limit it to certain hours in the day, ideally a window of less than 10 hours, such as 8 a.m. to 6 p.m.
When it comes to weight loss, the diets that work tend to work because they reduce calorie intake. I know, people will get angry about this, but thermodynamics is not just a good idea, it’s the law.
But weight loss is not the only reason we need to eat healthier. What we eat can impact our health in multiple ways; certain foods lead to more atherosclerosis, more inflammation, increased strain on the kidney and liver, and can affect our glucose homeostasis.
So I was really interested when I saw this article, “Time-Restricted Eating in Adults With Metabolic Syndrome,” appearing in Annals of Internal Medicine October 1, which examined the effect of time-restricted eating on the metabolic syndrome itself. Could this lifestyle intervention cure this lifestyle disease?
In the study, 108 individuals, all of whom had the metabolic syndrome but not full-blown diabetes, were randomized to usual care — basically, nutrition education — vs time-restricted eating. In that group, participants were instructed to reduce their window of eating by at least 4 hours to achieve an 8- to 10-hour eating window. The groups were followed for 3 months.
Now, before we get to the results, it’s important to remember that the success of a lifestyle intervention trial is quite dependent on how well people adhere to the lifestyle intervention. Time-restricted eating is not as easy as taking a pill once a day.
The researchers had participants log their consumption using a smartphone app to confirm whether they were adhering to that restricted eating window.
Broadly speaking, they did. At baseline, both groups had an eating window of about 14 hours a day — think 7 a.m. to 9 p.m. The intervention group reduced that to just under 10 hours, with 10% of days falling outside of the target window.
Lifestyle change achieved, the primary outcome was the change in hemoglobin A1c at 3 months. A1c integrates the serum glucose over time and is thus a good indicator of the success of the intervention in terms of insulin resistance. But the effect was, honestly, disappointing.
Technically, the time-restricted-eating group had a greater A1c change than the control group — by 0.1 percentage points. On average, they went from a baseline A1c of 5.87 to a 3-month A1c of 5.75.
Other metabolic syndrome markers were equally lackluster: no difference in fasting glucose, mean glucose, or fasting insulin.
There was some weight change. The control group, which got that dietary education, lost 1.5% of body weight over the 3 months. The time-restricted-eating group lost 3.3% — about 7 pounds, which is reasonable.
With that weight loss came statistically significant, albeit modest improvements in BMI, body fat percentage, and LDL cholesterol.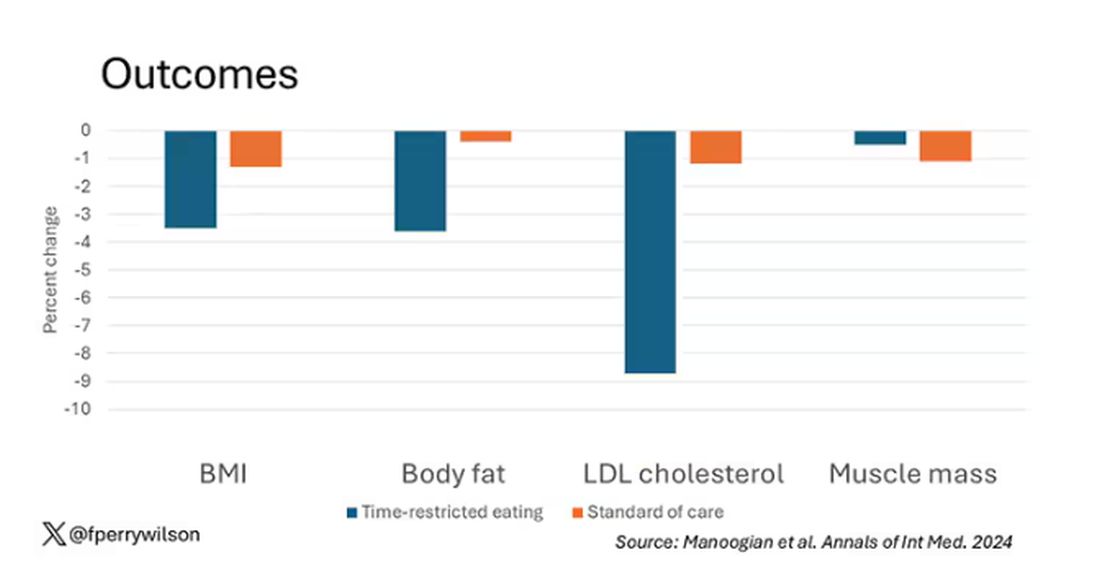
Of interest, despite the larger weight loss in the intermittent-fasting group, there was no difference in muscle mass loss, which is encouraging.
Taken together, we can say that, yes, it seems like time-restricted eating can help people lose some weight. This is essentially due to the fact that people eat fewer calories when they do time-restricted eating, as you can see here.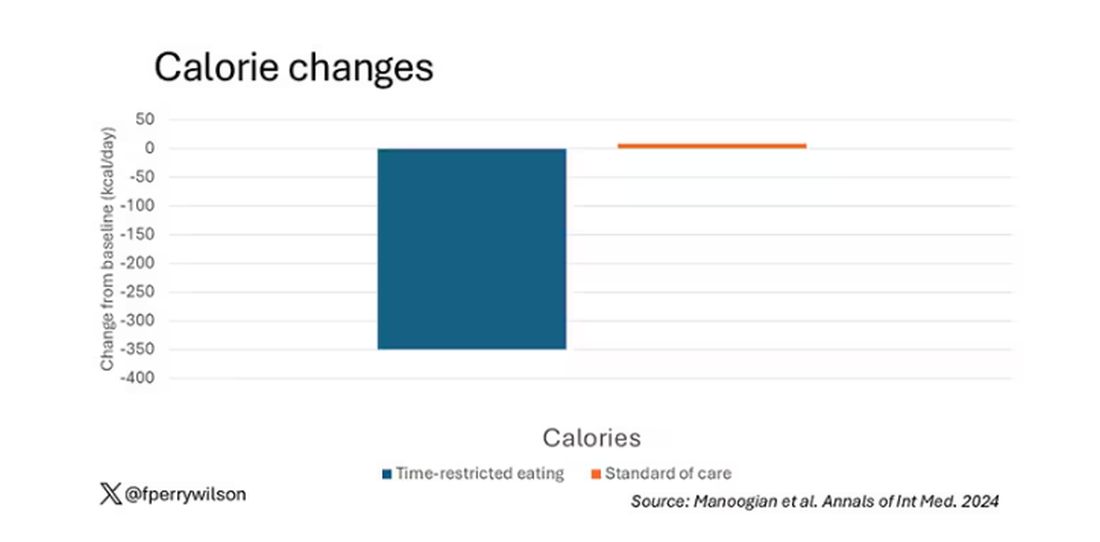
But, in the end, this trial examined whether this relatively straightforward lifestyle intervention would move the needle in terms of metabolic syndrome, and the data are not very compelling for that.
This graph shows how many of those five factors for metabolic syndrome the individuals in this trial had from the start to the end. You see that, over the 3 months, seven people in the time-restricted-eating group moved from having three criteria to two or one — being “cured” of metabolic syndrome, if you will. Nine people in the standard group were cured by that definition. Remember, they had to have at least three to have the syndrome and thus be eligible for the trial. 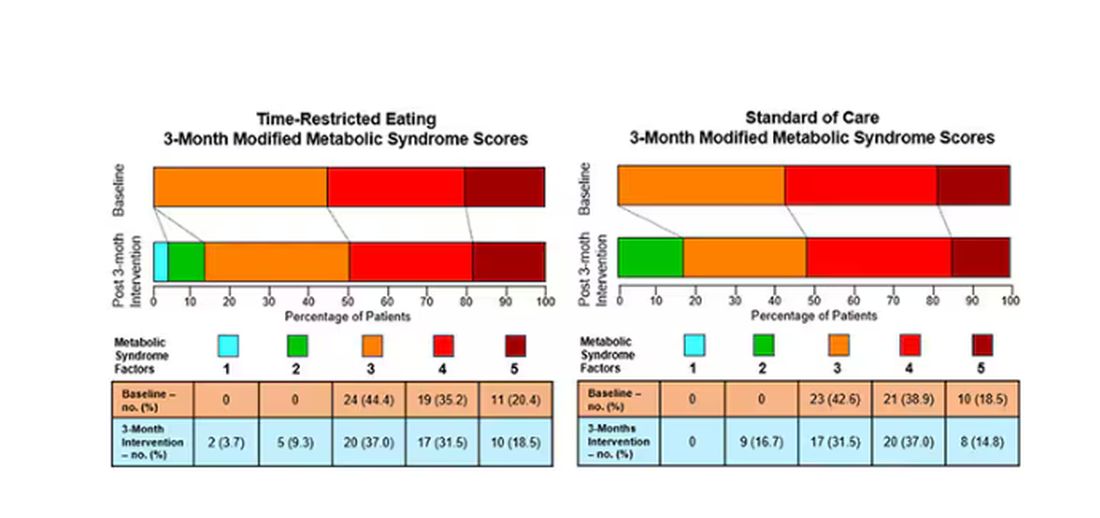
So If it just leads to weight loss by forcing people to consume less calories, then we need to acknowledge that we probably have better methods to achieve this same end. Ten years ago, I would have said that lifestyle change is the only way to end the epidemic of the metabolic syndrome in this country. Today, well, we live in a world of GLP-1 weight loss drugs. It is simply a different world now. Yes, they are expensive. Yes, they have side effects. But we need to evaluate them against the comparison. And so far, lifestyle changes alone are really no comparison.
Dr. Wilson is associate professor of medicine and public health and director of the Clinical and Translational Research Accelerator at Yale University, New Haven, Conn. He has disclosed no relevant financial relationships.
A version of this article appeared on Medscape.com.
This transcript has been edited for clarity.
One out of three American adults — about 100 million people in this country — have the metabolic syndrome. I’m showing you the official criteria here, but essentially this is a syndrome of insulin resistance and visceral adiposity that predisposes us to a host of chronic diseases such as diabetes, heart disease, and even dementia.
The metabolic syndrome is, fundamentally, a lifestyle disease. There is a direct line between our dietary habits and the wide availability of carbohydrate-rich, highly processed foods, and the rise in the syndrome in the population.
A saying I learned from one of my epidemiology teachers comes to mind: “Lifestyle diseases require lifestyle reinterventions.” But you know what? I’m not so sure anymore.
I’ve been around long enough to see multiple dietary fads come and go with varying efficacy. I grew up in the low-fat era, probably the most detrimental time to our national health as food manufacturers started replacing fats with carbohydrates, driving much of the problem we’re faced with today.
But I was also around for the Atkins diet and the low-carb craze — a healthier approach, all things being equal. And I’ve seen variants of these: the paleo diet (essentially a low-carb, high-protein diet based on minimally processed foods) and the Mediterranean diet, which sought to replace some percentage of fats with healthier fats.
And, of course, there is time-restricted eating.
Time-restricted eating, a variant of intermittent fasting, has the advantage of being very simple. No cookbooks, no recipes. Eat what you want — but limit it to certain hours in the day, ideally a window of less than 10 hours, such as 8 a.m. to 6 p.m.
When it comes to weight loss, the diets that work tend to work because they reduce calorie intake. I know, people will get angry about this, but thermodynamics is not just a good idea, it’s the law.
But weight loss is not the only reason we need to eat healthier. What we eat can impact our health in multiple ways; certain foods lead to more atherosclerosis, more inflammation, increased strain on the kidney and liver, and can affect our glucose homeostasis.
So I was really interested when I saw this article, “Time-Restricted Eating in Adults With Metabolic Syndrome,” appearing in Annals of Internal Medicine October 1, which examined the effect of time-restricted eating on the metabolic syndrome itself. Could this lifestyle intervention cure this lifestyle disease?
In the study, 108 individuals, all of whom had the metabolic syndrome but not full-blown diabetes, were randomized to usual care — basically, nutrition education — vs time-restricted eating. In that group, participants were instructed to reduce their window of eating by at least 4 hours to achieve an 8- to 10-hour eating window. The groups were followed for 3 months.
Now, before we get to the results, it’s important to remember that the success of a lifestyle intervention trial is quite dependent on how well people adhere to the lifestyle intervention. Time-restricted eating is not as easy as taking a pill once a day.
The researchers had participants log their consumption using a smartphone app to confirm whether they were adhering to that restricted eating window.
Broadly speaking, they did. At baseline, both groups had an eating window of about 14 hours a day — think 7 a.m. to 9 p.m. The intervention group reduced that to just under 10 hours, with 10% of days falling outside of the target window.
Lifestyle change achieved, the primary outcome was the change in hemoglobin A1c at 3 months. A1c integrates the serum glucose over time and is thus a good indicator of the success of the intervention in terms of insulin resistance. But the effect was, honestly, disappointing.
Technically, the time-restricted-eating group had a greater A1c change than the control group — by 0.1 percentage points. On average, they went from a baseline A1c of 5.87 to a 3-month A1c of 5.75.
Other metabolic syndrome markers were equally lackluster: no difference in fasting glucose, mean glucose, or fasting insulin.
There was some weight change. The control group, which got that dietary education, lost 1.5% of body weight over the 3 months. The time-restricted-eating group lost 3.3% — about 7 pounds, which is reasonable.
With that weight loss came statistically significant, albeit modest improvements in BMI, body fat percentage, and LDL cholesterol.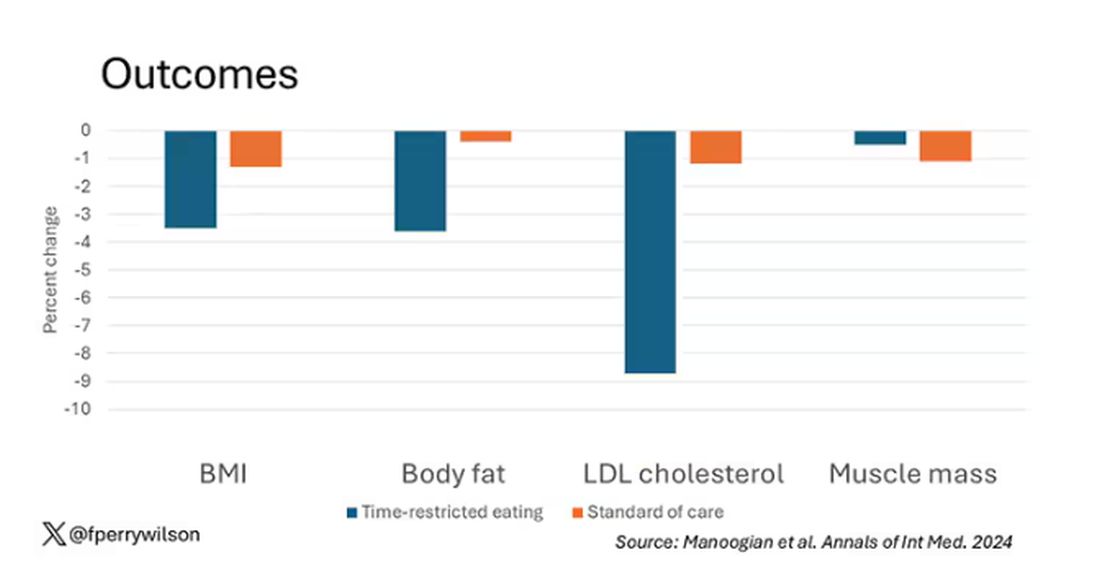
Of interest, despite the larger weight loss in the intermittent-fasting group, there was no difference in muscle mass loss, which is encouraging.
Taken together, we can say that, yes, it seems like time-restricted eating can help people lose some weight. This is essentially due to the fact that people eat fewer calories when they do time-restricted eating, as you can see here.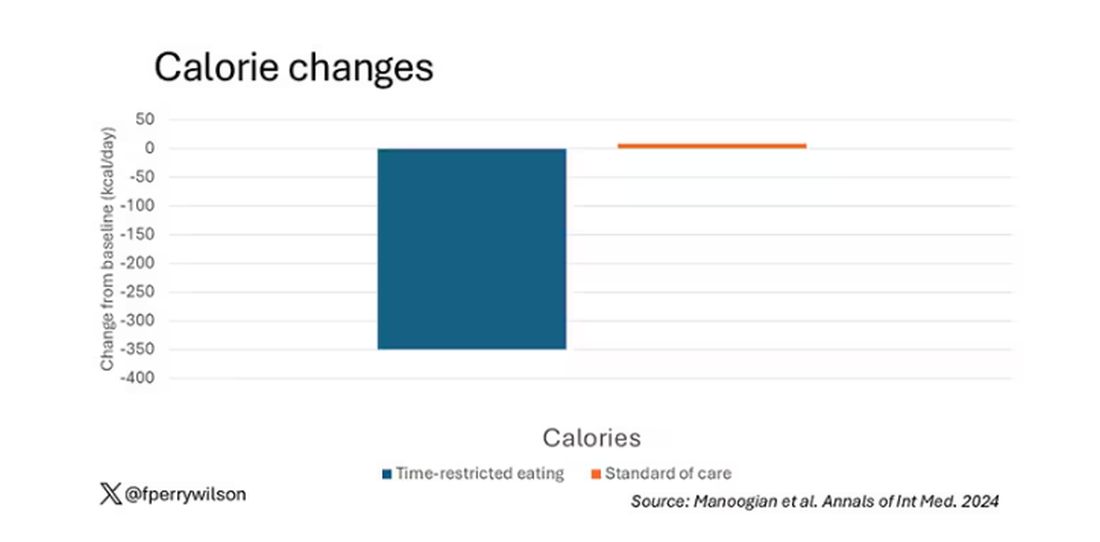
But, in the end, this trial examined whether this relatively straightforward lifestyle intervention would move the needle in terms of metabolic syndrome, and the data are not very compelling for that.
This graph shows how many of those five factors for metabolic syndrome the individuals in this trial had from the start to the end. You see that, over the 3 months, seven people in the time-restricted-eating group moved from having three criteria to two or one — being “cured” of metabolic syndrome, if you will. Nine people in the standard group were cured by that definition. Remember, they had to have at least three to have the syndrome and thus be eligible for the trial. 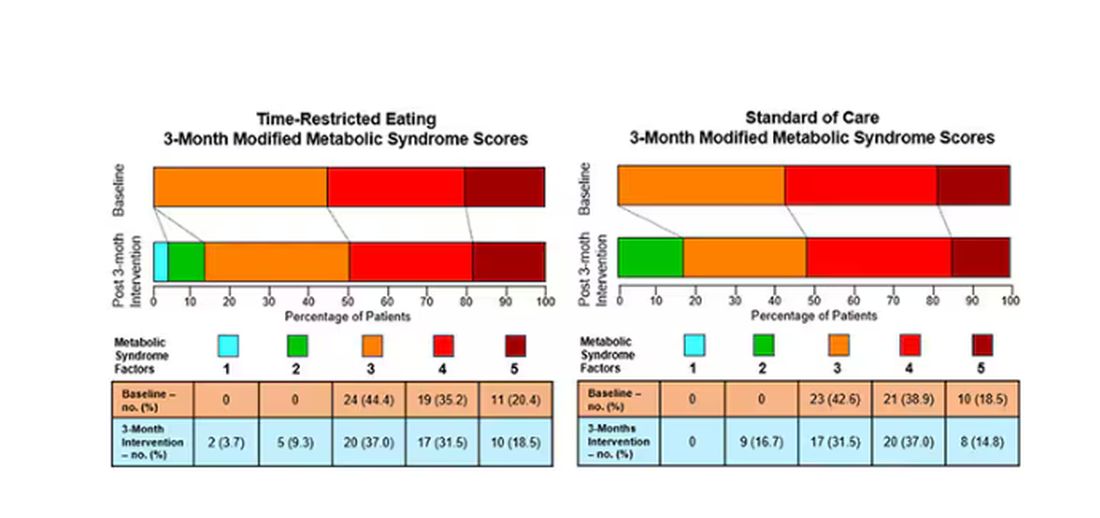
So If it just leads to weight loss by forcing people to consume less calories, then we need to acknowledge that we probably have better methods to achieve this same end. Ten years ago, I would have said that lifestyle change is the only way to end the epidemic of the metabolic syndrome in this country. Today, well, we live in a world of GLP-1 weight loss drugs. It is simply a different world now. Yes, they are expensive. Yes, they have side effects. But we need to evaluate them against the comparison. And so far, lifestyle changes alone are really no comparison.
Dr. Wilson is associate professor of medicine and public health and director of the Clinical and Translational Research Accelerator at Yale University, New Haven, Conn. He has disclosed no relevant financial relationships.
A version of this article appeared on Medscape.com.
New Guidelines Emphasize Liver Care in T2D, Obesity
MADRID — Individuals with type 2 diabetes and/or obesity plus one or more metabolic risk factors are at a higher risk for metabolic dysfunction–associated steatotic liver disease (MASLD) with fibrosis and progression to more severe liver disease, stated new European guidelines that provide recommendations for diagnosis and management.
“The availability of improved treatment options underlines the need to identify at-risk individuals with MASLD early, as we now possess the tools to positively influence the course of the diseases, which is expected to prevent relevant clinical events,” stated the clinical practice guidelines, updated for the first time since 2016.
“Now we have guidelines that tell clinicians how to monitor the liver,” said Amalia Gastaldelli, PhD, research director at the Institute of Clinical Physiology of the National Research Council in Pisa, Italy, and a member of the panel that developed the guidelines.
Dr. Gastaldelli moderated a session focused on the guidelines at the annual meeting of the European Association for the Study of Diabetes (EASD). In an interview after the session, Dr. Gastaldelli, who leads a cardiometabolic risk research group, stressed the importance of the liver’s role in the body and the need for diabetes specialists to start paying more attention to this vital organ.
“It’s an important organ for monitoring because liver disease is silent, and the patient doesn’t feel unwell until disease is severe,” she said. “Diabetologists already monitor the eye, the heart, the kidney, and so on, but the liver is often neglected,” she said. A 2024 study found that the global pooled prevalence of MASLD among patients with type 2 diabetes was 65.33%.
Dr. Gastaldelli noted the importance of liver status in diabetes care. The liver makes triglycerides and very-low-density lipoprotein cholesterol, which are all major risk factors for atherosclerosis and cardiovascular disease (CVD), she said, as well as producing glucose, which in excess can lead to hyperglycemia.
The guidelines were jointly written by EASD, the European Association for the Study of the Liver, and the European Association for the Study of Obesity, and published in Diabetologia, The Journal of Hepatology, and Obesity Facts.
A Metabolic Condition
In the EASD meeting session, Dr. Gastaldelli discussed the reasons for, and implications of, shifting the name from nonalcoholic fatty liver disease (NAFLD) to MASLD.
“The name change focuses on the fact that this is a metabolic disease, while NAFLD had no mention of this and was considered stigmatizing by patients, especially in relation to the words ‘fatty’ and ‘nonalcoholic,’” she said.
According to the guidelines, MASLD is defined as liver steatosis in the presence of one or more cardiometabolic risk factor(s) and the absence of excess alcohol intake.
MASLD has become the most common chronic liver disease and includes isolated steatosis, metabolic dysfunction-associated steatohepatitis (MASH, previously NASH), MASH-related fibrosis, and cirrhosis.
In the overarching group of steatotic liver disease, a totally new intermediate category has been added: MASLD with moderate (increased) alcohol intake (MetALD), which represents MASLD in people who consume greater amounts of alcohol per week (140-350 g/week and 210-420 g/week for women and men, respectively).
The change in the nomenclature has been incremental and regional, Dr. Gastaldelli said. “The definition first changed from NAFLD to MAFLD, which recognizes the importance of metabolism in the pathophysiology of this disease but does not take into account alcohol intake. MAFLD is still used in Asia, Australasia, and North Africa, while Europe and the Americas have endorsed MASLD.”
Case-Finding and Diagnosis
Identifying MASLD cases in people at risk remains incidental, largely because it is a silent disease and is symptom-free until it becomes severe, said Dr. Gastaldelli.
The guideline recognizes that individuals with type 2 diabetes or obesity with additional metabolic risk factor(s) are at a higher risk for MASLD with fibrosis and progression to MASH.
Assessment strategies for severe liver fibrosis in MASLD include the use of noninvasive tests in people who have cardiometabolic risk factors, abnormal liver enzymes, and/or radiological signs of hepatic steatosis, particularly in the presence of type 2 diabetes or obesity or in the presence of one or more metabolic risk factors.
Dr. Gastaldelli noted that type 2 diabetes, metabolic syndrome, and obesity, including abdominal obesity identified by large waist circumference, are the major risk factors and should be warning signs.
“We need to consider abdominal obesity too — we’ve published data in relatively lean people, body mass index < 25, with MASH but without diabetes. Most of the patients accumulated fat viscerally and in the liver and had hypertriglyceridemia and hypercholesterolemia,” she said.
“The guidelines reflect this because the definition of MASLD includes steatosis plus at least one metabolic factor — waist circumference, for example, which is related to visceral fat, hyperlipidemia, or hyperglycemia. Of note, in both pharmacological and diet-induced weight loss, the decrease in liver fat was associated with the decrease in visceral fat.”
The noninvasive biomarker test, Fibrosis-4 (FIB-4) may be used to assess the risk for liver fibrosis. The FIB-4 index is calculated using a patient’s age and results of three blood tests — aspartate aminotransferase, alanine aminotransferase, and platelet count.
Advanced fibrosis (grade F3-F4) “is a major risk factor for severe outcomes,” said Dr. Gastaldelli. A FIB-4 test result below 1.3 indicates low risk for advanced liver fibrosis, 1.30-2.67 indicates intermediate risk, and above 2.67 indicates high risk.
“When fibrosis increases, then liver enzymes increase and the platelets decrease,” said Dr. Gastaldelli. “It is not a perfect tool, and we need to add in age because at a young age, it is prone to false negatives and when very old — false positives. It’s important to take a global view, especially if the patient has persistent high liver enzymes, but FIB-4 is low.”
“And if they have more than one metabolic risk factor, proceed with more tests, for example, transient elastography,” she advised. Imaging techniques such as transient elastography may rule out or rule in advanced fibrosis, which is predictive of liver-related outcomes.
“However, imaging techniques only diagnose steatosis and fibrosis, and right now, MASH can only be diagnosed with liver biopsy because we do not have any markers of liver inflammation and ballooning. In the future, noninvasive tests based on imaging and blood tests will be used to identify patients with MASH,” she added.
Management of MASLD — Lifestyle and Treatment
“Pharmacological treatments are designed for [patients] with MASH and fibrosis grade F2 or F3, but not MASLD,” Dr. Gastaldelli said. As such, lifestyle interventions are the mainstay of management — including weight loss, dietary changes, physical exercise, and low to no alcohol consumption. “Eating good-quality food and reducing calories are both important because the metabolism responds differently to different nutrients,” Dr. Gastaldelli said.
“In particular, the guidelines advise dietary management because some foods carry liver toxicity, for example, sugary foods with sucrose/fructose especially,” she said, adding that, “complex carbohydrates are less harmful than refined carbohydrates. Processed foods should be avoided if possible because they contain sugars, [as well as] saturated fats and hydrogenated fat, which is particularly bad for the liver. Olive oil is better than butter or margarine, which are rich in saturated fat, and fish and white meat are preferable.”
She added that a diet to help manage type 2 diabetes was not so dissimilar because sugar again needs to be reduced.
If a patient has severe obesity (and MASLD), data show that bariatric surgery is beneficial. “It not only helps weight loss, but it improves liver histology and has been shown to improve or resolve type 2 diabetes and reduce CVD risk. Importantly, regarding fibrosis, nutritional management after the bariatric surgery is the most important thing,” said Dr. Gastaldelli.
Optimal management of comorbidities — including the use of incretin-based therapies such as semaglutide or tirzepatide for type 2 diabetes or obesity, if indicated — is advised, according to the guidelines.
Glucagon-like peptide 1 receptor agonists (GLP-1 RAs) have been shown to have a beneficial effect on MASH, said Dr. Gastaldelli. “They have not shown effectiveness in the resolution of fibrosis, but this might take longer to manifest. However, if the medication is started early enough, it may prevent severe fibrosis. Significant weight loss, both with lifestyle and pharmacological treatment, should lead to an improvement in the liver too.”
There are currently no drugs available in Europe for the treatment of noncirrhotic MASH and severe fibrosis (stage ≥ 2). Resmetirom is the first approved MASH-targeted treatment in noncirrhotic MASH and significant liver fibrosis, with histological effectiveness on steatohepatitis and fibrosis, together with an acceptable safety and tolerability profile, but, for the moment, this agent is only available in United States.
Finally, turning to MASH-related cirrhosis, the guidelines advise adaptations of metabolic drugs, nutritional counseling, and surveillance for portal hypertension and hepatocellular carcinoma, as well as liver transplantation in decompensated cirrhosis.
After the session, this news organization spoke to Tushy Kailayanathan, MBBS BSc, medical director of the liver MRI company, Perspectum, who reviewed the limitations of the FIB-4 test. The FIB-4 test identifies those with advanced fibrosis in the liver, for example, patients with hepatitis C, she noted; however, “it performs worse in type 2 diabetic patients and in the elderly. There is little clinical guidance on the adjustment of FIB-4 thresholds needed for these high cardiometabolic risk groups. The priority patients are missed by FIB-4 because those individuals with early and active disease may not yet have progressed to advanced disease detected by FIB-4.”
These individuals are exactly those amenable to primary care prevention strategies, said Dr. Kailayanathan. Because of the nature of early and active liver disease in patients with high cardiometabolic risk, it would make sense to shift some diagnostic protocols into primary care.
“These individuals are exactly those amenable to primary care prevention strategies at annual diabetic review because they are likely to have modifiable cardiometabolic risk factors such as metabolic syndrome and would benefit from lifestyle and therapeutic intervention, including GLP-1 RAs and SGLT2is [sodium-glucose cotransporter-2 inhibitors],” she said. “Case-finding and detection of early-stage MASLD is a priority in diabetics, and there is an unmet need for accurate biomarkers to measure liver fat and inflammation early.”
Dr. Gastaldelli has been on the advisory board or consulting for Boehringer Ingelheim, Novo Nordisk, Eli Lilly, Fractyl, Pfizer, Merck-MSD, MetaDeq and a speaker for Eli Lilly, Novo Nordisk, and Pfizer. Dr. Kailayanathan is medical director at Perspectum, a UK-based company involved in liver imaging technology.
A version of this article first appeared on Medscape.com.
MADRID — Individuals with type 2 diabetes and/or obesity plus one or more metabolic risk factors are at a higher risk for metabolic dysfunction–associated steatotic liver disease (MASLD) with fibrosis and progression to more severe liver disease, stated new European guidelines that provide recommendations for diagnosis and management.
“The availability of improved treatment options underlines the need to identify at-risk individuals with MASLD early, as we now possess the tools to positively influence the course of the diseases, which is expected to prevent relevant clinical events,” stated the clinical practice guidelines, updated for the first time since 2016.
“Now we have guidelines that tell clinicians how to monitor the liver,” said Amalia Gastaldelli, PhD, research director at the Institute of Clinical Physiology of the National Research Council in Pisa, Italy, and a member of the panel that developed the guidelines.
Dr. Gastaldelli moderated a session focused on the guidelines at the annual meeting of the European Association for the Study of Diabetes (EASD). In an interview after the session, Dr. Gastaldelli, who leads a cardiometabolic risk research group, stressed the importance of the liver’s role in the body and the need for diabetes specialists to start paying more attention to this vital organ.
“It’s an important organ for monitoring because liver disease is silent, and the patient doesn’t feel unwell until disease is severe,” she said. “Diabetologists already monitor the eye, the heart, the kidney, and so on, but the liver is often neglected,” she said. A 2024 study found that the global pooled prevalence of MASLD among patients with type 2 diabetes was 65.33%.
Dr. Gastaldelli noted the importance of liver status in diabetes care. The liver makes triglycerides and very-low-density lipoprotein cholesterol, which are all major risk factors for atherosclerosis and cardiovascular disease (CVD), she said, as well as producing glucose, which in excess can lead to hyperglycemia.
The guidelines were jointly written by EASD, the European Association for the Study of the Liver, and the European Association for the Study of Obesity, and published in Diabetologia, The Journal of Hepatology, and Obesity Facts.
A Metabolic Condition
In the EASD meeting session, Dr. Gastaldelli discussed the reasons for, and implications of, shifting the name from nonalcoholic fatty liver disease (NAFLD) to MASLD.
“The name change focuses on the fact that this is a metabolic disease, while NAFLD had no mention of this and was considered stigmatizing by patients, especially in relation to the words ‘fatty’ and ‘nonalcoholic,’” she said.
According to the guidelines, MASLD is defined as liver steatosis in the presence of one or more cardiometabolic risk factor(s) and the absence of excess alcohol intake.
MASLD has become the most common chronic liver disease and includes isolated steatosis, metabolic dysfunction-associated steatohepatitis (MASH, previously NASH), MASH-related fibrosis, and cirrhosis.
In the overarching group of steatotic liver disease, a totally new intermediate category has been added: MASLD with moderate (increased) alcohol intake (MetALD), which represents MASLD in people who consume greater amounts of alcohol per week (140-350 g/week and 210-420 g/week for women and men, respectively).
The change in the nomenclature has been incremental and regional, Dr. Gastaldelli said. “The definition first changed from NAFLD to MAFLD, which recognizes the importance of metabolism in the pathophysiology of this disease but does not take into account alcohol intake. MAFLD is still used in Asia, Australasia, and North Africa, while Europe and the Americas have endorsed MASLD.”
Case-Finding and Diagnosis
Identifying MASLD cases in people at risk remains incidental, largely because it is a silent disease and is symptom-free until it becomes severe, said Dr. Gastaldelli.
The guideline recognizes that individuals with type 2 diabetes or obesity with additional metabolic risk factor(s) are at a higher risk for MASLD with fibrosis and progression to MASH.
Assessment strategies for severe liver fibrosis in MASLD include the use of noninvasive tests in people who have cardiometabolic risk factors, abnormal liver enzymes, and/or radiological signs of hepatic steatosis, particularly in the presence of type 2 diabetes or obesity or in the presence of one or more metabolic risk factors.
Dr. Gastaldelli noted that type 2 diabetes, metabolic syndrome, and obesity, including abdominal obesity identified by large waist circumference, are the major risk factors and should be warning signs.
“We need to consider abdominal obesity too — we’ve published data in relatively lean people, body mass index < 25, with MASH but without diabetes. Most of the patients accumulated fat viscerally and in the liver and had hypertriglyceridemia and hypercholesterolemia,” she said.
“The guidelines reflect this because the definition of MASLD includes steatosis plus at least one metabolic factor — waist circumference, for example, which is related to visceral fat, hyperlipidemia, or hyperglycemia. Of note, in both pharmacological and diet-induced weight loss, the decrease in liver fat was associated with the decrease in visceral fat.”
The noninvasive biomarker test, Fibrosis-4 (FIB-4) may be used to assess the risk for liver fibrosis. The FIB-4 index is calculated using a patient’s age and results of three blood tests — aspartate aminotransferase, alanine aminotransferase, and platelet count.
Advanced fibrosis (grade F3-F4) “is a major risk factor for severe outcomes,” said Dr. Gastaldelli. A FIB-4 test result below 1.3 indicates low risk for advanced liver fibrosis, 1.30-2.67 indicates intermediate risk, and above 2.67 indicates high risk.
“When fibrosis increases, then liver enzymes increase and the platelets decrease,” said Dr. Gastaldelli. “It is not a perfect tool, and we need to add in age because at a young age, it is prone to false negatives and when very old — false positives. It’s important to take a global view, especially if the patient has persistent high liver enzymes, but FIB-4 is low.”
“And if they have more than one metabolic risk factor, proceed with more tests, for example, transient elastography,” she advised. Imaging techniques such as transient elastography may rule out or rule in advanced fibrosis, which is predictive of liver-related outcomes.
“However, imaging techniques only diagnose steatosis and fibrosis, and right now, MASH can only be diagnosed with liver biopsy because we do not have any markers of liver inflammation and ballooning. In the future, noninvasive tests based on imaging and blood tests will be used to identify patients with MASH,” she added.
Management of MASLD — Lifestyle and Treatment
“Pharmacological treatments are designed for [patients] with MASH and fibrosis grade F2 or F3, but not MASLD,” Dr. Gastaldelli said. As such, lifestyle interventions are the mainstay of management — including weight loss, dietary changes, physical exercise, and low to no alcohol consumption. “Eating good-quality food and reducing calories are both important because the metabolism responds differently to different nutrients,” Dr. Gastaldelli said.
“In particular, the guidelines advise dietary management because some foods carry liver toxicity, for example, sugary foods with sucrose/fructose especially,” she said, adding that, “complex carbohydrates are less harmful than refined carbohydrates. Processed foods should be avoided if possible because they contain sugars, [as well as] saturated fats and hydrogenated fat, which is particularly bad for the liver. Olive oil is better than butter or margarine, which are rich in saturated fat, and fish and white meat are preferable.”
She added that a diet to help manage type 2 diabetes was not so dissimilar because sugar again needs to be reduced.
If a patient has severe obesity (and MASLD), data show that bariatric surgery is beneficial. “It not only helps weight loss, but it improves liver histology and has been shown to improve or resolve type 2 diabetes and reduce CVD risk. Importantly, regarding fibrosis, nutritional management after the bariatric surgery is the most important thing,” said Dr. Gastaldelli.
Optimal management of comorbidities — including the use of incretin-based therapies such as semaglutide or tirzepatide for type 2 diabetes or obesity, if indicated — is advised, according to the guidelines.
Glucagon-like peptide 1 receptor agonists (GLP-1 RAs) have been shown to have a beneficial effect on MASH, said Dr. Gastaldelli. “They have not shown effectiveness in the resolution of fibrosis, but this might take longer to manifest. However, if the medication is started early enough, it may prevent severe fibrosis. Significant weight loss, both with lifestyle and pharmacological treatment, should lead to an improvement in the liver too.”
There are currently no drugs available in Europe for the treatment of noncirrhotic MASH and severe fibrosis (stage ≥ 2). Resmetirom is the first approved MASH-targeted treatment in noncirrhotic MASH and significant liver fibrosis, with histological effectiveness on steatohepatitis and fibrosis, together with an acceptable safety and tolerability profile, but, for the moment, this agent is only available in United States.
Finally, turning to MASH-related cirrhosis, the guidelines advise adaptations of metabolic drugs, nutritional counseling, and surveillance for portal hypertension and hepatocellular carcinoma, as well as liver transplantation in decompensated cirrhosis.
After the session, this news organization spoke to Tushy Kailayanathan, MBBS BSc, medical director of the liver MRI company, Perspectum, who reviewed the limitations of the FIB-4 test. The FIB-4 test identifies those with advanced fibrosis in the liver, for example, patients with hepatitis C, she noted; however, “it performs worse in type 2 diabetic patients and in the elderly. There is little clinical guidance on the adjustment of FIB-4 thresholds needed for these high cardiometabolic risk groups. The priority patients are missed by FIB-4 because those individuals with early and active disease may not yet have progressed to advanced disease detected by FIB-4.”
These individuals are exactly those amenable to primary care prevention strategies, said Dr. Kailayanathan. Because of the nature of early and active liver disease in patients with high cardiometabolic risk, it would make sense to shift some diagnostic protocols into primary care.
“These individuals are exactly those amenable to primary care prevention strategies at annual diabetic review because they are likely to have modifiable cardiometabolic risk factors such as metabolic syndrome and would benefit from lifestyle and therapeutic intervention, including GLP-1 RAs and SGLT2is [sodium-glucose cotransporter-2 inhibitors],” she said. “Case-finding and detection of early-stage MASLD is a priority in diabetics, and there is an unmet need for accurate biomarkers to measure liver fat and inflammation early.”
Dr. Gastaldelli has been on the advisory board or consulting for Boehringer Ingelheim, Novo Nordisk, Eli Lilly, Fractyl, Pfizer, Merck-MSD, MetaDeq and a speaker for Eli Lilly, Novo Nordisk, and Pfizer. Dr. Kailayanathan is medical director at Perspectum, a UK-based company involved in liver imaging technology.
A version of this article first appeared on Medscape.com.
MADRID — Individuals with type 2 diabetes and/or obesity plus one or more metabolic risk factors are at a higher risk for metabolic dysfunction–associated steatotic liver disease (MASLD) with fibrosis and progression to more severe liver disease, stated new European guidelines that provide recommendations for diagnosis and management.
“The availability of improved treatment options underlines the need to identify at-risk individuals with MASLD early, as we now possess the tools to positively influence the course of the diseases, which is expected to prevent relevant clinical events,” stated the clinical practice guidelines, updated for the first time since 2016.
“Now we have guidelines that tell clinicians how to monitor the liver,” said Amalia Gastaldelli, PhD, research director at the Institute of Clinical Physiology of the National Research Council in Pisa, Italy, and a member of the panel that developed the guidelines.
Dr. Gastaldelli moderated a session focused on the guidelines at the annual meeting of the European Association for the Study of Diabetes (EASD). In an interview after the session, Dr. Gastaldelli, who leads a cardiometabolic risk research group, stressed the importance of the liver’s role in the body and the need for diabetes specialists to start paying more attention to this vital organ.
“It’s an important organ for monitoring because liver disease is silent, and the patient doesn’t feel unwell until disease is severe,” she said. “Diabetologists already monitor the eye, the heart, the kidney, and so on, but the liver is often neglected,” she said. A 2024 study found that the global pooled prevalence of MASLD among patients with type 2 diabetes was 65.33%.
Dr. Gastaldelli noted the importance of liver status in diabetes care. The liver makes triglycerides and very-low-density lipoprotein cholesterol, which are all major risk factors for atherosclerosis and cardiovascular disease (CVD), she said, as well as producing glucose, which in excess can lead to hyperglycemia.
The guidelines were jointly written by EASD, the European Association for the Study of the Liver, and the European Association for the Study of Obesity, and published in Diabetologia, The Journal of Hepatology, and Obesity Facts.
A Metabolic Condition
In the EASD meeting session, Dr. Gastaldelli discussed the reasons for, and implications of, shifting the name from nonalcoholic fatty liver disease (NAFLD) to MASLD.
“The name change focuses on the fact that this is a metabolic disease, while NAFLD had no mention of this and was considered stigmatizing by patients, especially in relation to the words ‘fatty’ and ‘nonalcoholic,’” she said.
According to the guidelines, MASLD is defined as liver steatosis in the presence of one or more cardiometabolic risk factor(s) and the absence of excess alcohol intake.
MASLD has become the most common chronic liver disease and includes isolated steatosis, metabolic dysfunction-associated steatohepatitis (MASH, previously NASH), MASH-related fibrosis, and cirrhosis.
In the overarching group of steatotic liver disease, a totally new intermediate category has been added: MASLD with moderate (increased) alcohol intake (MetALD), which represents MASLD in people who consume greater amounts of alcohol per week (140-350 g/week and 210-420 g/week for women and men, respectively).
The change in the nomenclature has been incremental and regional, Dr. Gastaldelli said. “The definition first changed from NAFLD to MAFLD, which recognizes the importance of metabolism in the pathophysiology of this disease but does not take into account alcohol intake. MAFLD is still used in Asia, Australasia, and North Africa, while Europe and the Americas have endorsed MASLD.”
Case-Finding and Diagnosis
Identifying MASLD cases in people at risk remains incidental, largely because it is a silent disease and is symptom-free until it becomes severe, said Dr. Gastaldelli.
The guideline recognizes that individuals with type 2 diabetes or obesity with additional metabolic risk factor(s) are at a higher risk for MASLD with fibrosis and progression to MASH.
Assessment strategies for severe liver fibrosis in MASLD include the use of noninvasive tests in people who have cardiometabolic risk factors, abnormal liver enzymes, and/or radiological signs of hepatic steatosis, particularly in the presence of type 2 diabetes or obesity or in the presence of one or more metabolic risk factors.
Dr. Gastaldelli noted that type 2 diabetes, metabolic syndrome, and obesity, including abdominal obesity identified by large waist circumference, are the major risk factors and should be warning signs.
“We need to consider abdominal obesity too — we’ve published data in relatively lean people, body mass index < 25, with MASH but without diabetes. Most of the patients accumulated fat viscerally and in the liver and had hypertriglyceridemia and hypercholesterolemia,” she said.
“The guidelines reflect this because the definition of MASLD includes steatosis plus at least one metabolic factor — waist circumference, for example, which is related to visceral fat, hyperlipidemia, or hyperglycemia. Of note, in both pharmacological and diet-induced weight loss, the decrease in liver fat was associated with the decrease in visceral fat.”
The noninvasive biomarker test, Fibrosis-4 (FIB-4) may be used to assess the risk for liver fibrosis. The FIB-4 index is calculated using a patient’s age and results of three blood tests — aspartate aminotransferase, alanine aminotransferase, and platelet count.
Advanced fibrosis (grade F3-F4) “is a major risk factor for severe outcomes,” said Dr. Gastaldelli. A FIB-4 test result below 1.3 indicates low risk for advanced liver fibrosis, 1.30-2.67 indicates intermediate risk, and above 2.67 indicates high risk.
“When fibrosis increases, then liver enzymes increase and the platelets decrease,” said Dr. Gastaldelli. “It is not a perfect tool, and we need to add in age because at a young age, it is prone to false negatives and when very old — false positives. It’s important to take a global view, especially if the patient has persistent high liver enzymes, but FIB-4 is low.”
“And if they have more than one metabolic risk factor, proceed with more tests, for example, transient elastography,” she advised. Imaging techniques such as transient elastography may rule out or rule in advanced fibrosis, which is predictive of liver-related outcomes.
“However, imaging techniques only diagnose steatosis and fibrosis, and right now, MASH can only be diagnosed with liver biopsy because we do not have any markers of liver inflammation and ballooning. In the future, noninvasive tests based on imaging and blood tests will be used to identify patients with MASH,” she added.
Management of MASLD — Lifestyle and Treatment
“Pharmacological treatments are designed for [patients] with MASH and fibrosis grade F2 or F3, but not MASLD,” Dr. Gastaldelli said. As such, lifestyle interventions are the mainstay of management — including weight loss, dietary changes, physical exercise, and low to no alcohol consumption. “Eating good-quality food and reducing calories are both important because the metabolism responds differently to different nutrients,” Dr. Gastaldelli said.
“In particular, the guidelines advise dietary management because some foods carry liver toxicity, for example, sugary foods with sucrose/fructose especially,” she said, adding that, “complex carbohydrates are less harmful than refined carbohydrates. Processed foods should be avoided if possible because they contain sugars, [as well as] saturated fats and hydrogenated fat, which is particularly bad for the liver. Olive oil is better than butter or margarine, which are rich in saturated fat, and fish and white meat are preferable.”
She added that a diet to help manage type 2 diabetes was not so dissimilar because sugar again needs to be reduced.
If a patient has severe obesity (and MASLD), data show that bariatric surgery is beneficial. “It not only helps weight loss, but it improves liver histology and has been shown to improve or resolve type 2 diabetes and reduce CVD risk. Importantly, regarding fibrosis, nutritional management after the bariatric surgery is the most important thing,” said Dr. Gastaldelli.
Optimal management of comorbidities — including the use of incretin-based therapies such as semaglutide or tirzepatide for type 2 diabetes or obesity, if indicated — is advised, according to the guidelines.
Glucagon-like peptide 1 receptor agonists (GLP-1 RAs) have been shown to have a beneficial effect on MASH, said Dr. Gastaldelli. “They have not shown effectiveness in the resolution of fibrosis, but this might take longer to manifest. However, if the medication is started early enough, it may prevent severe fibrosis. Significant weight loss, both with lifestyle and pharmacological treatment, should lead to an improvement in the liver too.”
There are currently no drugs available in Europe for the treatment of noncirrhotic MASH and severe fibrosis (stage ≥ 2). Resmetirom is the first approved MASH-targeted treatment in noncirrhotic MASH and significant liver fibrosis, with histological effectiveness on steatohepatitis and fibrosis, together with an acceptable safety and tolerability profile, but, for the moment, this agent is only available in United States.
Finally, turning to MASH-related cirrhosis, the guidelines advise adaptations of metabolic drugs, nutritional counseling, and surveillance for portal hypertension and hepatocellular carcinoma, as well as liver transplantation in decompensated cirrhosis.
After the session, this news organization spoke to Tushy Kailayanathan, MBBS BSc, medical director of the liver MRI company, Perspectum, who reviewed the limitations of the FIB-4 test. The FIB-4 test identifies those with advanced fibrosis in the liver, for example, patients with hepatitis C, she noted; however, “it performs worse in type 2 diabetic patients and in the elderly. There is little clinical guidance on the adjustment of FIB-4 thresholds needed for these high cardiometabolic risk groups. The priority patients are missed by FIB-4 because those individuals with early and active disease may not yet have progressed to advanced disease detected by FIB-4.”
These individuals are exactly those amenable to primary care prevention strategies, said Dr. Kailayanathan. Because of the nature of early and active liver disease in patients with high cardiometabolic risk, it would make sense to shift some diagnostic protocols into primary care.
“These individuals are exactly those amenable to primary care prevention strategies at annual diabetic review because they are likely to have modifiable cardiometabolic risk factors such as metabolic syndrome and would benefit from lifestyle and therapeutic intervention, including GLP-1 RAs and SGLT2is [sodium-glucose cotransporter-2 inhibitors],” she said. “Case-finding and detection of early-stage MASLD is a priority in diabetics, and there is an unmet need for accurate biomarkers to measure liver fat and inflammation early.”
Dr. Gastaldelli has been on the advisory board or consulting for Boehringer Ingelheim, Novo Nordisk, Eli Lilly, Fractyl, Pfizer, Merck-MSD, MetaDeq and a speaker for Eli Lilly, Novo Nordisk, and Pfizer. Dr. Kailayanathan is medical director at Perspectum, a UK-based company involved in liver imaging technology.
A version of this article first appeared on Medscape.com.
FROM EASD 2024