User login
Could tackling maternal obesity prevent later CVD in offspring?
authors of a thematic literature review concluded.
Maternal obesity has been tied to the development of cardiovascular disease (CVD) and premature death in epidemiologic studies, the authors noted in the review.
One hypothesis, referred to as fetal programming, posits that in utero environmental factors may have adverse metabolic consequences in the offspring. Thus far, however, most evidence supporting this hypothesis has come from animal studies, they cautioned.
Nevertheless, endothelial cell dysfunction is a reversible process, offering a “window of opportunity” for intervention, according to authors Karolien Van De Maele and Inge Gies, MD, of the division of pediatric endocrinology at the University Hospital of Brussels and Roland Devlieger, MD, PhD, head of fetal maternal medicine at the University Hospitals Leuven (Belgium).
“The fundamental solution to break the vicious cycle seems [to be] an intervention before or in early pregnancy,” authors said in the journal Atherosclerosis.
Mary Norine Walsh, MD, immediate past president of the American College of Cardiology, agreed with the review article’s conclusion that more evidence would be needed to show that fetal programming is implicated in the associations between maternal obesity and long-term cardiovascular effects.
“As of right now, we cannot say the offspring of pregnant women have an increased risk of cardiovascular risk in later life due to ‘X’ because those studies haven’t been done yet,” Dr. Walsh said in an interview. “So I think it’s a really good framework to think about based on the animal work that’s been done, but we have yet to identify obesity in pregnant women as an independent risk factor for vascular disease in the offspring – we just have an association.”
On the other hand, it is known that obesity increases the risk of hypertension and diabetes in both pregnant and nonpregnant women, said Dr. Walsh, and that hypertensive disorders are a leading cause of maternal morbidity and mortality.
“I think it’s really important to recognize that maternal obesity puts a woman at significant risk, and we certainly can’t forget that in the process of thinking about the offspring,” said Dr. Walsh, medical director of the heart failure and cardiac transplantation program at St. Vincent Heart Center, Indianapolis.
In the recent review article in Atherosclerosis, Ms. Van De Maele and coauthors cited evidence linking maternal obesity to adverse outcomes in offspring from a 2013 report in the BMJ that included 28,540 women in Scotland and their 37,709 offspring.
In that study, after adjustment for maternal age, socioeconomic status, and other factors, offspring of mothers who had a body mass index greater than 30 kg/m2 had higher all-cause mortality (hazard ratio, 1.35; 95% confidence interval, 1.17-1.55) and increased risk of hospital admission for a cardiovascular event (HR, 1.29; 95% CI, 1.06-1.57), compared with those whose mothers had a healthy BMI.
“Evidence from animal models and emerging data from humans suggest that maternal obesity also creates an adverse in utero environment, with long-term ‘programmed’ detrimental effects for the offspring,” the authors of that BMJ report wrote at the time.
Ms. Van De Maele and her colleagues also cited animal studies, including several looking at offspring of animals fed with a maternal high-fat diet during pregnancy. In those studies, they said, investigators observed impaired endothelial cell relaxation, along with raised thickness of the intimal wall and increased vascular inflammatory marker expression.
“Raised leptin levels, secreted by the adipose tissue, inhibit the in vitro proliferation of smooth muscle cells and could impede the angiogenesis process in vivo, but this assumption needs scientific validation in humans,” they said in their review.
However, human studies are lacking, aside from the epidemiologic reports that “cannot be used to confirm or contradict” the fetal programming hypothesis, they said.
Meanwhile, an increasing body of evidence has suggested that stressors in critical periods of fetal development may lead to epigenetic alterations that could play a role in either up-regulating atherogenic genes or down-regulating enzymatic activities that guard against oxidative stress.
For example, cohort studies have shown differences in DNA methylation among offspring born before and after bariatric surgery in the mother, which has lent credence to the hypothesis that maternal obesity in pregnancy alters methylation patterns for those offspring, Ms. Van De Maele and her colleagues wrote.
Lifestyle changes in obese pregnant women may have an effect on adverse metabolic or cardiovascular outcomes in offspring, although results to date are inconclusive, they added.
Diet, exercise, or both during pregnancy may lower the risk of macrosomia, respiratory distress syndrome, or other neonatal outcomes, particularly in high-risk women, according to the conclusions of a 2015 Cochrane review that Ms. Van De Maele and her coauthors cited.
However, follow-up studies on offspring are scarce and have shown no clear effects on long-term metabolic profiles in offspring, likely because of insufficient follow-up time, they said in their review.
Ms. Van De Maele and her coauthors said they had no conflict of interest disclosures related to their manuscript.
SOURCE: Van De Maele K et al. Atherosclerosis. 2018 Jun. doi: 10.1016/j.atherosclerosis.2018.06.016.
authors of a thematic literature review concluded.
Maternal obesity has been tied to the development of cardiovascular disease (CVD) and premature death in epidemiologic studies, the authors noted in the review.
One hypothesis, referred to as fetal programming, posits that in utero environmental factors may have adverse metabolic consequences in the offspring. Thus far, however, most evidence supporting this hypothesis has come from animal studies, they cautioned.
Nevertheless, endothelial cell dysfunction is a reversible process, offering a “window of opportunity” for intervention, according to authors Karolien Van De Maele and Inge Gies, MD, of the division of pediatric endocrinology at the University Hospital of Brussels and Roland Devlieger, MD, PhD, head of fetal maternal medicine at the University Hospitals Leuven (Belgium).
“The fundamental solution to break the vicious cycle seems [to be] an intervention before or in early pregnancy,” authors said in the journal Atherosclerosis.
Mary Norine Walsh, MD, immediate past president of the American College of Cardiology, agreed with the review article’s conclusion that more evidence would be needed to show that fetal programming is implicated in the associations between maternal obesity and long-term cardiovascular effects.
“As of right now, we cannot say the offspring of pregnant women have an increased risk of cardiovascular risk in later life due to ‘X’ because those studies haven’t been done yet,” Dr. Walsh said in an interview. “So I think it’s a really good framework to think about based on the animal work that’s been done, but we have yet to identify obesity in pregnant women as an independent risk factor for vascular disease in the offspring – we just have an association.”
On the other hand, it is known that obesity increases the risk of hypertension and diabetes in both pregnant and nonpregnant women, said Dr. Walsh, and that hypertensive disorders are a leading cause of maternal morbidity and mortality.
“I think it’s really important to recognize that maternal obesity puts a woman at significant risk, and we certainly can’t forget that in the process of thinking about the offspring,” said Dr. Walsh, medical director of the heart failure and cardiac transplantation program at St. Vincent Heart Center, Indianapolis.
In the recent review article in Atherosclerosis, Ms. Van De Maele and coauthors cited evidence linking maternal obesity to adverse outcomes in offspring from a 2013 report in the BMJ that included 28,540 women in Scotland and their 37,709 offspring.
In that study, after adjustment for maternal age, socioeconomic status, and other factors, offspring of mothers who had a body mass index greater than 30 kg/m2 had higher all-cause mortality (hazard ratio, 1.35; 95% confidence interval, 1.17-1.55) and increased risk of hospital admission for a cardiovascular event (HR, 1.29; 95% CI, 1.06-1.57), compared with those whose mothers had a healthy BMI.
“Evidence from animal models and emerging data from humans suggest that maternal obesity also creates an adverse in utero environment, with long-term ‘programmed’ detrimental effects for the offspring,” the authors of that BMJ report wrote at the time.
Ms. Van De Maele and her colleagues also cited animal studies, including several looking at offspring of animals fed with a maternal high-fat diet during pregnancy. In those studies, they said, investigators observed impaired endothelial cell relaxation, along with raised thickness of the intimal wall and increased vascular inflammatory marker expression.
“Raised leptin levels, secreted by the adipose tissue, inhibit the in vitro proliferation of smooth muscle cells and could impede the angiogenesis process in vivo, but this assumption needs scientific validation in humans,” they said in their review.
However, human studies are lacking, aside from the epidemiologic reports that “cannot be used to confirm or contradict” the fetal programming hypothesis, they said.
Meanwhile, an increasing body of evidence has suggested that stressors in critical periods of fetal development may lead to epigenetic alterations that could play a role in either up-regulating atherogenic genes or down-regulating enzymatic activities that guard against oxidative stress.
For example, cohort studies have shown differences in DNA methylation among offspring born before and after bariatric surgery in the mother, which has lent credence to the hypothesis that maternal obesity in pregnancy alters methylation patterns for those offspring, Ms. Van De Maele and her colleagues wrote.
Lifestyle changes in obese pregnant women may have an effect on adverse metabolic or cardiovascular outcomes in offspring, although results to date are inconclusive, they added.
Diet, exercise, or both during pregnancy may lower the risk of macrosomia, respiratory distress syndrome, or other neonatal outcomes, particularly in high-risk women, according to the conclusions of a 2015 Cochrane review that Ms. Van De Maele and her coauthors cited.
However, follow-up studies on offspring are scarce and have shown no clear effects on long-term metabolic profiles in offspring, likely because of insufficient follow-up time, they said in their review.
Ms. Van De Maele and her coauthors said they had no conflict of interest disclosures related to their manuscript.
SOURCE: Van De Maele K et al. Atherosclerosis. 2018 Jun. doi: 10.1016/j.atherosclerosis.2018.06.016.
authors of a thematic literature review concluded.
Maternal obesity has been tied to the development of cardiovascular disease (CVD) and premature death in epidemiologic studies, the authors noted in the review.
One hypothesis, referred to as fetal programming, posits that in utero environmental factors may have adverse metabolic consequences in the offspring. Thus far, however, most evidence supporting this hypothesis has come from animal studies, they cautioned.
Nevertheless, endothelial cell dysfunction is a reversible process, offering a “window of opportunity” for intervention, according to authors Karolien Van De Maele and Inge Gies, MD, of the division of pediatric endocrinology at the University Hospital of Brussels and Roland Devlieger, MD, PhD, head of fetal maternal medicine at the University Hospitals Leuven (Belgium).
“The fundamental solution to break the vicious cycle seems [to be] an intervention before or in early pregnancy,” authors said in the journal Atherosclerosis.
Mary Norine Walsh, MD, immediate past president of the American College of Cardiology, agreed with the review article’s conclusion that more evidence would be needed to show that fetal programming is implicated in the associations between maternal obesity and long-term cardiovascular effects.
“As of right now, we cannot say the offspring of pregnant women have an increased risk of cardiovascular risk in later life due to ‘X’ because those studies haven’t been done yet,” Dr. Walsh said in an interview. “So I think it’s a really good framework to think about based on the animal work that’s been done, but we have yet to identify obesity in pregnant women as an independent risk factor for vascular disease in the offspring – we just have an association.”
On the other hand, it is known that obesity increases the risk of hypertension and diabetes in both pregnant and nonpregnant women, said Dr. Walsh, and that hypertensive disorders are a leading cause of maternal morbidity and mortality.
“I think it’s really important to recognize that maternal obesity puts a woman at significant risk, and we certainly can’t forget that in the process of thinking about the offspring,” said Dr. Walsh, medical director of the heart failure and cardiac transplantation program at St. Vincent Heart Center, Indianapolis.
In the recent review article in Atherosclerosis, Ms. Van De Maele and coauthors cited evidence linking maternal obesity to adverse outcomes in offspring from a 2013 report in the BMJ that included 28,540 women in Scotland and their 37,709 offspring.
In that study, after adjustment for maternal age, socioeconomic status, and other factors, offspring of mothers who had a body mass index greater than 30 kg/m2 had higher all-cause mortality (hazard ratio, 1.35; 95% confidence interval, 1.17-1.55) and increased risk of hospital admission for a cardiovascular event (HR, 1.29; 95% CI, 1.06-1.57), compared with those whose mothers had a healthy BMI.
“Evidence from animal models and emerging data from humans suggest that maternal obesity also creates an adverse in utero environment, with long-term ‘programmed’ detrimental effects for the offspring,” the authors of that BMJ report wrote at the time.
Ms. Van De Maele and her colleagues also cited animal studies, including several looking at offspring of animals fed with a maternal high-fat diet during pregnancy. In those studies, they said, investigators observed impaired endothelial cell relaxation, along with raised thickness of the intimal wall and increased vascular inflammatory marker expression.
“Raised leptin levels, secreted by the adipose tissue, inhibit the in vitro proliferation of smooth muscle cells and could impede the angiogenesis process in vivo, but this assumption needs scientific validation in humans,” they said in their review.
However, human studies are lacking, aside from the epidemiologic reports that “cannot be used to confirm or contradict” the fetal programming hypothesis, they said.
Meanwhile, an increasing body of evidence has suggested that stressors in critical periods of fetal development may lead to epigenetic alterations that could play a role in either up-regulating atherogenic genes or down-regulating enzymatic activities that guard against oxidative stress.
For example, cohort studies have shown differences in DNA methylation among offspring born before and after bariatric surgery in the mother, which has lent credence to the hypothesis that maternal obesity in pregnancy alters methylation patterns for those offspring, Ms. Van De Maele and her colleagues wrote.
Lifestyle changes in obese pregnant women may have an effect on adverse metabolic or cardiovascular outcomes in offspring, although results to date are inconclusive, they added.
Diet, exercise, or both during pregnancy may lower the risk of macrosomia, respiratory distress syndrome, or other neonatal outcomes, particularly in high-risk women, according to the conclusions of a 2015 Cochrane review that Ms. Van De Maele and her coauthors cited.
However, follow-up studies on offspring are scarce and have shown no clear effects on long-term metabolic profiles in offspring, likely because of insufficient follow-up time, they said in their review.
Ms. Van De Maele and her coauthors said they had no conflict of interest disclosures related to their manuscript.
SOURCE: Van De Maele K et al. Atherosclerosis. 2018 Jun. doi: 10.1016/j.atherosclerosis.2018.06.016.
FROM ATHEROSCLEROSIS
Are we using the right metrics to measure cesarean rates?
St. Joseph Hospital in Orange, California, like most institutions performing deliveries in 2016, started releasing metrics internally before subsequently releasing them to the public. Data for the first 9 months of 2016 were released. As I am often an outlier, I was gratified to see that I ranked 1st in the vaginal birth after cesarean delivery (VBAC) rate at 36.8% and 4th at 15.9% for my cesarean delivery (CD) rate in the low-risk nulliparous term singleton vertex (NTSV) population.
I have been an avid proponent of VBAC since 1984 when one of the fathers of modern obstetric care, Edward J. Quilligan, MD, presented the benefits and safety of VBAC at our institution.
Experiences that may alter a reported rate
I list here a few circumstances of a CD on maternal request:
- A primagravida with a 10-cm nonphysiologic, nonmalignant ovarian cyst at term elects a primary CD with ovarian cystectomy.
- A woman who is concerned about pelvic organ prolapse and urinary incontinence later in life requests a CD. After all, normal babies do not weigh 5 and 6 lb anymore.
- An elderly primagravida with an in vitro fertilization pregnancy requests a CD.
Should these experiences adversely affect a physician’s statistics? Personally, I don’t think so. Is the morbidity and mortality from a CD really all that much higher than a normal spontaneous vaginal delivery (NSVD)? Granted, the cost is more. But are we really helping all our patients by insisting on a NSVD? Thousands of people have medically indicated and elective surgery in the United States each day.
Of course, these data points depend on the denominator (the number of deliveries attributed to each ObGyn). Those with a contradictory opinion will say that this evens out over time. I dispute that claim. This might be closer to being true for the ObGyn with the highest number, say, 134 in the NTSV denominator versus someone with a low number, such as 4. For VBAC, the denominator range at our institution was 1 to 115 cases.
Rethinking my position
Two recent cases have caused me to rethink my position on using VBAC and CD rates to evaluate ObGyns.
Uterine rupture
A 31-year-old G3P1 woman at 39 6/7 weeks’ gestation was admitted in early labor for a VBAC. She had undergone a CD with her first baby because of fetal intolerance to labor. Her prenatal course was complicated by white-coat hypertension, but I monitored her blood pressure at home and it had been normal. She took aspirin 81 mg during the pregnancy. The fetus was not reactive to a nonstress test on the day of admission.
That evening, amniotomy results showed clear fluid. I placed an intrauterine pressure catheter. The patient’s labor progressed well during the night, she received an epidural anesthetic, and labor was augmented with intravenous oxytocin. She progressed to complete dilation. I was notified of severe, prolonged, variable fetal heart-rate decelerations.
The Laborist who evaluated the patient recommended an emergency CD. I came immediately to Labor and Delivery and performed a CD with delivery of a 7 lb 4 oz infant whose Apgars were 2, 5, and 8 at 1, 5, and 10 minutes, respectively. Arterial cord blood gas tests revealed: pH, 6.94; pCO2, 95 mm Hg; pO2, 19.9 mm Hg; HCO3, 19.9 mmol/L; and base excess (BE), –14.4 mmol/L. Venous cord blood gas tests revealed: pH, 7.25; pCO2, 45 mm Hg; pO2, 35 mm Hg; HCO3, 19.2 mmol/L; BE, −8.0 mmol/L. The cord blood gases revealed that the baby was becoming compromised, but was delivered in time to avoid complications.
After advocating and performing many successful VBACs for 33 years, this was my first uterine rupture.
The uterus had ruptured in the lower segment from the mid-portion extending inferolaterally on the right side and was hemorrhaging. I successfully repaired the rupture. Maternal quantitative blood loss was 1,020 mL.
The baby initially was apneic and was limp. He required continuous positive airway pressure (CPAP) and positive pressure ventilation in the operating room. The baby was transferred to the neonatal intensive care unit (NICU), recovered well, and was discharged home with the mother on the 4th day of life.
Commentary: Why should this necessary, emergency CD count against me on my core measure rate? Although I have advocated for VBACs for 33 years, perhaps they aren’t so safe. After this experience, I do not ever want to have to deal with a ruptured uterus, a compromised baby, and maternal hemorrhage again.
Read Dr. Kanofsky’s solution to using this metric.
Depressed baby
A 24-year-old G1P0 woman at 39 weeks’ gestation was admitted for induction of labor because of mild pregnancy-induced hypertension. Her prenatal course was complicated by Class A1 gestational diabetes mellitus, which was untreated due to compliance issues, Group B streptococcus, and cholelithiasis. Clinically, I suspected she was going to have a large (9 lb) baby. An ultrasound to estimate fetal weight at 37 2/7 weeks’ gestation showed the fetus at 3.937 kg. I was concerned, but, because the mother was 5 ft 5 in tall and weighed 282 lbs, I thought it was reasonable for her to attempt a NSVD.
Induction and labor progressed normally. Her labor curve decelerated at an anterior lip, but subsequently stage 2 progressed normally and lasted 2 hrs. Her temperature was elevated in stage 2 to 100.00F. The fetal heart rate tracings were reassuring.
Immediately after delivery of the fetal vertex, a turtleneck sign was seen and shoulder dystocia occurred. A Wood’s maneuver was performed in both directions, the nurse applied suprapubic pressure, and the infant was delivered. A loose nuchal cord x2 was reduced. The infant was apneic and had no tone. She was taken to the warmer, given oxygen, suctioned, and stimulated until the NICU team arrived. Her Apgar scores were 2, 5, and 9 at 1, 5, and 10 minutes, respectively. The birthweight was 9 lb 0 oz.
A depressed baby of this magnitude was certainly not expected from the FHR tracing or the shoulder dystocia. Venous cord gas evaluation revealed pH, 7.16; pCO2, 57 mm Hg; pO2, 17 mm Hg; HCO3, 20.2 mmol/L; and BE, –19.1 mmol/L.
The baby recovered quickly in the labor and delivery recovery room, went to the NICU on CPAP, subsequently transitioned to room air, and was discharged on the 4th day of life with her mother.
Commentary: Did I do the best I could for this mother and baby? In hindsight, I should have performed a CD because of my concerns for a large fetus. The “retrospectoscope” always makes cases more clear! Note that, if I had performed an elective CD for fetal macrosomia, it would have counted against me on this metric. Prior to labor, if I thought an elective CD was the right approach to this patient, and was providing the best care I could for this mother and fetus, why should it count against me?
Is there a solution?
With my newfound concerns, it is my opinion that VBAC and CD/NTSV rates may not be the correct things to use as quality metric measures without some additional qualifying information.
Better metrics of quality and safety that might be more helpful to measure include:
- Prophylactic oxytocin after delivery of the baby’s anterior shoulder
- Since “6 is the new 4,” in order to increase the NTSV rate, we could measure1:
- patients admitted before active labor
- patients receiving an epidural before active labor.
- Since NTSV is a goal, measure the number of patients in an advanced stage of labor whose labor pattern has become dysfunctional, no interventions are taken, and who subsequently deliver by primary CD.
Share your thoughts! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
- Committee on Obstetric Practice, American College of Obstetricians and Gynecologists. Committee Opinion No. 687: Approaches to limit intervention during labor and birth. Obstet Gynecol. 2017;129(2):e20–e28.
St. Joseph Hospital in Orange, California, like most institutions performing deliveries in 2016, started releasing metrics internally before subsequently releasing them to the public. Data for the first 9 months of 2016 were released. As I am often an outlier, I was gratified to see that I ranked 1st in the vaginal birth after cesarean delivery (VBAC) rate at 36.8% and 4th at 15.9% for my cesarean delivery (CD) rate in the low-risk nulliparous term singleton vertex (NTSV) population.
I have been an avid proponent of VBAC since 1984 when one of the fathers of modern obstetric care, Edward J. Quilligan, MD, presented the benefits and safety of VBAC at our institution.
Experiences that may alter a reported rate
I list here a few circumstances of a CD on maternal request:
- A primagravida with a 10-cm nonphysiologic, nonmalignant ovarian cyst at term elects a primary CD with ovarian cystectomy.
- A woman who is concerned about pelvic organ prolapse and urinary incontinence later in life requests a CD. After all, normal babies do not weigh 5 and 6 lb anymore.
- An elderly primagravida with an in vitro fertilization pregnancy requests a CD.
Should these experiences adversely affect a physician’s statistics? Personally, I don’t think so. Is the morbidity and mortality from a CD really all that much higher than a normal spontaneous vaginal delivery (NSVD)? Granted, the cost is more. But are we really helping all our patients by insisting on a NSVD? Thousands of people have medically indicated and elective surgery in the United States each day.
Of course, these data points depend on the denominator (the number of deliveries attributed to each ObGyn). Those with a contradictory opinion will say that this evens out over time. I dispute that claim. This might be closer to being true for the ObGyn with the highest number, say, 134 in the NTSV denominator versus someone with a low number, such as 4. For VBAC, the denominator range at our institution was 1 to 115 cases.
Rethinking my position
Two recent cases have caused me to rethink my position on using VBAC and CD rates to evaluate ObGyns.
Uterine rupture
A 31-year-old G3P1 woman at 39 6/7 weeks’ gestation was admitted in early labor for a VBAC. She had undergone a CD with her first baby because of fetal intolerance to labor. Her prenatal course was complicated by white-coat hypertension, but I monitored her blood pressure at home and it had been normal. She took aspirin 81 mg during the pregnancy. The fetus was not reactive to a nonstress test on the day of admission.
That evening, amniotomy results showed clear fluid. I placed an intrauterine pressure catheter. The patient’s labor progressed well during the night, she received an epidural anesthetic, and labor was augmented with intravenous oxytocin. She progressed to complete dilation. I was notified of severe, prolonged, variable fetal heart-rate decelerations.
The Laborist who evaluated the patient recommended an emergency CD. I came immediately to Labor and Delivery and performed a CD with delivery of a 7 lb 4 oz infant whose Apgars were 2, 5, and 8 at 1, 5, and 10 minutes, respectively. Arterial cord blood gas tests revealed: pH, 6.94; pCO2, 95 mm Hg; pO2, 19.9 mm Hg; HCO3, 19.9 mmol/L; and base excess (BE), –14.4 mmol/L. Venous cord blood gas tests revealed: pH, 7.25; pCO2, 45 mm Hg; pO2, 35 mm Hg; HCO3, 19.2 mmol/L; BE, −8.0 mmol/L. The cord blood gases revealed that the baby was becoming compromised, but was delivered in time to avoid complications.
After advocating and performing many successful VBACs for 33 years, this was my first uterine rupture.
The uterus had ruptured in the lower segment from the mid-portion extending inferolaterally on the right side and was hemorrhaging. I successfully repaired the rupture. Maternal quantitative blood loss was 1,020 mL.
The baby initially was apneic and was limp. He required continuous positive airway pressure (CPAP) and positive pressure ventilation in the operating room. The baby was transferred to the neonatal intensive care unit (NICU), recovered well, and was discharged home with the mother on the 4th day of life.
Commentary: Why should this necessary, emergency CD count against me on my core measure rate? Although I have advocated for VBACs for 33 years, perhaps they aren’t so safe. After this experience, I do not ever want to have to deal with a ruptured uterus, a compromised baby, and maternal hemorrhage again.
Read Dr. Kanofsky’s solution to using this metric.
Depressed baby
A 24-year-old G1P0 woman at 39 weeks’ gestation was admitted for induction of labor because of mild pregnancy-induced hypertension. Her prenatal course was complicated by Class A1 gestational diabetes mellitus, which was untreated due to compliance issues, Group B streptococcus, and cholelithiasis. Clinically, I suspected she was going to have a large (9 lb) baby. An ultrasound to estimate fetal weight at 37 2/7 weeks’ gestation showed the fetus at 3.937 kg. I was concerned, but, because the mother was 5 ft 5 in tall and weighed 282 lbs, I thought it was reasonable for her to attempt a NSVD.
Induction and labor progressed normally. Her labor curve decelerated at an anterior lip, but subsequently stage 2 progressed normally and lasted 2 hrs. Her temperature was elevated in stage 2 to 100.00F. The fetal heart rate tracings were reassuring.
Immediately after delivery of the fetal vertex, a turtleneck sign was seen and shoulder dystocia occurred. A Wood’s maneuver was performed in both directions, the nurse applied suprapubic pressure, and the infant was delivered. A loose nuchal cord x2 was reduced. The infant was apneic and had no tone. She was taken to the warmer, given oxygen, suctioned, and stimulated until the NICU team arrived. Her Apgar scores were 2, 5, and 9 at 1, 5, and 10 minutes, respectively. The birthweight was 9 lb 0 oz.
A depressed baby of this magnitude was certainly not expected from the FHR tracing or the shoulder dystocia. Venous cord gas evaluation revealed pH, 7.16; pCO2, 57 mm Hg; pO2, 17 mm Hg; HCO3, 20.2 mmol/L; and BE, –19.1 mmol/L.
The baby recovered quickly in the labor and delivery recovery room, went to the NICU on CPAP, subsequently transitioned to room air, and was discharged on the 4th day of life with her mother.
Commentary: Did I do the best I could for this mother and baby? In hindsight, I should have performed a CD because of my concerns for a large fetus. The “retrospectoscope” always makes cases more clear! Note that, if I had performed an elective CD for fetal macrosomia, it would have counted against me on this metric. Prior to labor, if I thought an elective CD was the right approach to this patient, and was providing the best care I could for this mother and fetus, why should it count against me?
Is there a solution?
With my newfound concerns, it is my opinion that VBAC and CD/NTSV rates may not be the correct things to use as quality metric measures without some additional qualifying information.
Better metrics of quality and safety that might be more helpful to measure include:
- Prophylactic oxytocin after delivery of the baby’s anterior shoulder
- Since “6 is the new 4,” in order to increase the NTSV rate, we could measure1:
- patients admitted before active labor
- patients receiving an epidural before active labor.
- Since NTSV is a goal, measure the number of patients in an advanced stage of labor whose labor pattern has become dysfunctional, no interventions are taken, and who subsequently deliver by primary CD.
Share your thoughts! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
St. Joseph Hospital in Orange, California, like most institutions performing deliveries in 2016, started releasing metrics internally before subsequently releasing them to the public. Data for the first 9 months of 2016 were released. As I am often an outlier, I was gratified to see that I ranked 1st in the vaginal birth after cesarean delivery (VBAC) rate at 36.8% and 4th at 15.9% for my cesarean delivery (CD) rate in the low-risk nulliparous term singleton vertex (NTSV) population.
I have been an avid proponent of VBAC since 1984 when one of the fathers of modern obstetric care, Edward J. Quilligan, MD, presented the benefits and safety of VBAC at our institution.
Experiences that may alter a reported rate
I list here a few circumstances of a CD on maternal request:
- A primagravida with a 10-cm nonphysiologic, nonmalignant ovarian cyst at term elects a primary CD with ovarian cystectomy.
- A woman who is concerned about pelvic organ prolapse and urinary incontinence later in life requests a CD. After all, normal babies do not weigh 5 and 6 lb anymore.
- An elderly primagravida with an in vitro fertilization pregnancy requests a CD.
Should these experiences adversely affect a physician’s statistics? Personally, I don’t think so. Is the morbidity and mortality from a CD really all that much higher than a normal spontaneous vaginal delivery (NSVD)? Granted, the cost is more. But are we really helping all our patients by insisting on a NSVD? Thousands of people have medically indicated and elective surgery in the United States each day.
Of course, these data points depend on the denominator (the number of deliveries attributed to each ObGyn). Those with a contradictory opinion will say that this evens out over time. I dispute that claim. This might be closer to being true for the ObGyn with the highest number, say, 134 in the NTSV denominator versus someone with a low number, such as 4. For VBAC, the denominator range at our institution was 1 to 115 cases.
Rethinking my position
Two recent cases have caused me to rethink my position on using VBAC and CD rates to evaluate ObGyns.
Uterine rupture
A 31-year-old G3P1 woman at 39 6/7 weeks’ gestation was admitted in early labor for a VBAC. She had undergone a CD with her first baby because of fetal intolerance to labor. Her prenatal course was complicated by white-coat hypertension, but I monitored her blood pressure at home and it had been normal. She took aspirin 81 mg during the pregnancy. The fetus was not reactive to a nonstress test on the day of admission.
That evening, amniotomy results showed clear fluid. I placed an intrauterine pressure catheter. The patient’s labor progressed well during the night, she received an epidural anesthetic, and labor was augmented with intravenous oxytocin. She progressed to complete dilation. I was notified of severe, prolonged, variable fetal heart-rate decelerations.
The Laborist who evaluated the patient recommended an emergency CD. I came immediately to Labor and Delivery and performed a CD with delivery of a 7 lb 4 oz infant whose Apgars were 2, 5, and 8 at 1, 5, and 10 minutes, respectively. Arterial cord blood gas tests revealed: pH, 6.94; pCO2, 95 mm Hg; pO2, 19.9 mm Hg; HCO3, 19.9 mmol/L; and base excess (BE), –14.4 mmol/L. Venous cord blood gas tests revealed: pH, 7.25; pCO2, 45 mm Hg; pO2, 35 mm Hg; HCO3, 19.2 mmol/L; BE, −8.0 mmol/L. The cord blood gases revealed that the baby was becoming compromised, but was delivered in time to avoid complications.
After advocating and performing many successful VBACs for 33 years, this was my first uterine rupture.
The uterus had ruptured in the lower segment from the mid-portion extending inferolaterally on the right side and was hemorrhaging. I successfully repaired the rupture. Maternal quantitative blood loss was 1,020 mL.
The baby initially was apneic and was limp. He required continuous positive airway pressure (CPAP) and positive pressure ventilation in the operating room. The baby was transferred to the neonatal intensive care unit (NICU), recovered well, and was discharged home with the mother on the 4th day of life.
Commentary: Why should this necessary, emergency CD count against me on my core measure rate? Although I have advocated for VBACs for 33 years, perhaps they aren’t so safe. After this experience, I do not ever want to have to deal with a ruptured uterus, a compromised baby, and maternal hemorrhage again.
Read Dr. Kanofsky’s solution to using this metric.
Depressed baby
A 24-year-old G1P0 woman at 39 weeks’ gestation was admitted for induction of labor because of mild pregnancy-induced hypertension. Her prenatal course was complicated by Class A1 gestational diabetes mellitus, which was untreated due to compliance issues, Group B streptococcus, and cholelithiasis. Clinically, I suspected she was going to have a large (9 lb) baby. An ultrasound to estimate fetal weight at 37 2/7 weeks’ gestation showed the fetus at 3.937 kg. I was concerned, but, because the mother was 5 ft 5 in tall and weighed 282 lbs, I thought it was reasonable for her to attempt a NSVD.
Induction and labor progressed normally. Her labor curve decelerated at an anterior lip, but subsequently stage 2 progressed normally and lasted 2 hrs. Her temperature was elevated in stage 2 to 100.00F. The fetal heart rate tracings were reassuring.
Immediately after delivery of the fetal vertex, a turtleneck sign was seen and shoulder dystocia occurred. A Wood’s maneuver was performed in both directions, the nurse applied suprapubic pressure, and the infant was delivered. A loose nuchal cord x2 was reduced. The infant was apneic and had no tone. She was taken to the warmer, given oxygen, suctioned, and stimulated until the NICU team arrived. Her Apgar scores were 2, 5, and 9 at 1, 5, and 10 minutes, respectively. The birthweight was 9 lb 0 oz.
A depressed baby of this magnitude was certainly not expected from the FHR tracing or the shoulder dystocia. Venous cord gas evaluation revealed pH, 7.16; pCO2, 57 mm Hg; pO2, 17 mm Hg; HCO3, 20.2 mmol/L; and BE, –19.1 mmol/L.
The baby recovered quickly in the labor and delivery recovery room, went to the NICU on CPAP, subsequently transitioned to room air, and was discharged on the 4th day of life with her mother.
Commentary: Did I do the best I could for this mother and baby? In hindsight, I should have performed a CD because of my concerns for a large fetus. The “retrospectoscope” always makes cases more clear! Note that, if I had performed an elective CD for fetal macrosomia, it would have counted against me on this metric. Prior to labor, if I thought an elective CD was the right approach to this patient, and was providing the best care I could for this mother and fetus, why should it count against me?
Is there a solution?
With my newfound concerns, it is my opinion that VBAC and CD/NTSV rates may not be the correct things to use as quality metric measures without some additional qualifying information.
Better metrics of quality and safety that might be more helpful to measure include:
- Prophylactic oxytocin after delivery of the baby’s anterior shoulder
- Since “6 is the new 4,” in order to increase the NTSV rate, we could measure1:
- patients admitted before active labor
- patients receiving an epidural before active labor.
- Since NTSV is a goal, measure the number of patients in an advanced stage of labor whose labor pattern has become dysfunctional, no interventions are taken, and who subsequently deliver by primary CD.
Share your thoughts! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
- Committee on Obstetric Practice, American College of Obstetricians and Gynecologists. Committee Opinion No. 687: Approaches to limit intervention during labor and birth. Obstet Gynecol. 2017;129(2):e20–e28.
- Committee on Obstetric Practice, American College of Obstetricians and Gynecologists. Committee Opinion No. 687: Approaches to limit intervention during labor and birth. Obstet Gynecol. 2017;129(2):e20–e28.
Maternal use of pot and tobacco may boost birth defect risk
SAN DIEGO – New research suggests that pregnant users of both cannabis and tobacco may put their unborn children at higher risk of birth defects and small head circumference than if they used either alone.
Researchers also found that 13% of pregnant Medicaid recipients surveyed reported using both cannabis and tobacco within the past month.
, especially if they smoke tobacco, said study lead author Victoria H. Coleman-Cowger, PhD, of the research organization Battelle, in an interview.
In some cases, in fact, pregnant women might think that marijuana is healthier than regular cigarettes, said Dr. Coleman-Cowger. She observed this phenomenon while conducting a smoking intervention study at a prenatal clinic that largely served poor, African American women.
“I learned that many participants were also smoking cannabis and felt that there was lower risk associated with cannabis use than with tobacco use,” she said. “Some women were decreasing their use of tobacco during pregnancy but increasing their use of cannabis.”
Dr. Coleman-Cowger’s observations at the clinic inspired the new study, which reports the findings of a convenience survey of 500 pregnant women.
The mean age in the group was 28, and 71% were black. Two-thirds were employed, and 29% were college graduates.
By comparison, the 45 women in the co-user group – who reported both cannabis and tobacco use in the past month – were 93% black, 42% employed, and 7% college graduates. (An additional 39 women reported tobacco use only, and 60 reported cannabis use only.)
Co-use also was correlated with “never married, being in the first trimester of pregnancy, not wanting to be pregnant when they were, past-month other substance use, and more frequent use of both cannabis and tobacco than either exclusive group,” Dr. Coleman-Cowger said.
In adjusted models, co-users were more likely (odds ratio, 5.7; P = .05) to give birth to babies with small head circumference than nonusers. The risks of giving birth to babies with small head circumference also were more likely among the tobacco-only users (OR, 4.8; P = .05) and cannabis-only users (OR, 2.0; P = .05), compared with nonusers. Birth defects also were more likely in the co-user group.
The study did not allow researchers to speculate on whether co-use may multiply risk vs. cannabis or tobacco use alone.
Dr. Coleman-Cowger said in light of the small sample size, the results should be interpreted with caution. One possible confounder is quantity of use, she said. “We did not assess quantity of use, but given our finding that frequency of use is higher among the co-use group, it could be that the co-use group is simply using more of each substance and thus impacting the health consequences.”
Current clinical practice guidelines do not suggest screening for cannabis use in pregnant women. But Dr. Coleman-Cowger said it’s “particularly important when tobacco use has been identified, though in states where substance use is considered child abuse, professional judgment should be utilized in terms of the legal implications of asking about use.”
More research is planned to better understand issues like quantity of use, and reasons why pregnant women co-use cannabis and tobacco, Dr. Coleman-Cowger said.
The National Institute on Drug Abuse funded the study, which Dr. Coleman-Cowger said is part of a larger project “to compare and validate screeners that assess prescription drug misuse and illicit drug use during pregnancy.” The study authors report no relevant disclosures.
SAN DIEGO – New research suggests that pregnant users of both cannabis and tobacco may put their unborn children at higher risk of birth defects and small head circumference than if they used either alone.
Researchers also found that 13% of pregnant Medicaid recipients surveyed reported using both cannabis and tobacco within the past month.
, especially if they smoke tobacco, said study lead author Victoria H. Coleman-Cowger, PhD, of the research organization Battelle, in an interview.
In some cases, in fact, pregnant women might think that marijuana is healthier than regular cigarettes, said Dr. Coleman-Cowger. She observed this phenomenon while conducting a smoking intervention study at a prenatal clinic that largely served poor, African American women.
“I learned that many participants were also smoking cannabis and felt that there was lower risk associated with cannabis use than with tobacco use,” she said. “Some women were decreasing their use of tobacco during pregnancy but increasing their use of cannabis.”
Dr. Coleman-Cowger’s observations at the clinic inspired the new study, which reports the findings of a convenience survey of 500 pregnant women.
The mean age in the group was 28, and 71% were black. Two-thirds were employed, and 29% were college graduates.
By comparison, the 45 women in the co-user group – who reported both cannabis and tobacco use in the past month – were 93% black, 42% employed, and 7% college graduates. (An additional 39 women reported tobacco use only, and 60 reported cannabis use only.)
Co-use also was correlated with “never married, being in the first trimester of pregnancy, not wanting to be pregnant when they were, past-month other substance use, and more frequent use of both cannabis and tobacco than either exclusive group,” Dr. Coleman-Cowger said.
In adjusted models, co-users were more likely (odds ratio, 5.7; P = .05) to give birth to babies with small head circumference than nonusers. The risks of giving birth to babies with small head circumference also were more likely among the tobacco-only users (OR, 4.8; P = .05) and cannabis-only users (OR, 2.0; P = .05), compared with nonusers. Birth defects also were more likely in the co-user group.
The study did not allow researchers to speculate on whether co-use may multiply risk vs. cannabis or tobacco use alone.
Dr. Coleman-Cowger said in light of the small sample size, the results should be interpreted with caution. One possible confounder is quantity of use, she said. “We did not assess quantity of use, but given our finding that frequency of use is higher among the co-use group, it could be that the co-use group is simply using more of each substance and thus impacting the health consequences.”
Current clinical practice guidelines do not suggest screening for cannabis use in pregnant women. But Dr. Coleman-Cowger said it’s “particularly important when tobacco use has been identified, though in states where substance use is considered child abuse, professional judgment should be utilized in terms of the legal implications of asking about use.”
More research is planned to better understand issues like quantity of use, and reasons why pregnant women co-use cannabis and tobacco, Dr. Coleman-Cowger said.
The National Institute on Drug Abuse funded the study, which Dr. Coleman-Cowger said is part of a larger project “to compare and validate screeners that assess prescription drug misuse and illicit drug use during pregnancy.” The study authors report no relevant disclosures.
SAN DIEGO – New research suggests that pregnant users of both cannabis and tobacco may put their unborn children at higher risk of birth defects and small head circumference than if they used either alone.
Researchers also found that 13% of pregnant Medicaid recipients surveyed reported using both cannabis and tobacco within the past month.
, especially if they smoke tobacco, said study lead author Victoria H. Coleman-Cowger, PhD, of the research organization Battelle, in an interview.
In some cases, in fact, pregnant women might think that marijuana is healthier than regular cigarettes, said Dr. Coleman-Cowger. She observed this phenomenon while conducting a smoking intervention study at a prenatal clinic that largely served poor, African American women.
“I learned that many participants were also smoking cannabis and felt that there was lower risk associated with cannabis use than with tobacco use,” she said. “Some women were decreasing their use of tobacco during pregnancy but increasing their use of cannabis.”
Dr. Coleman-Cowger’s observations at the clinic inspired the new study, which reports the findings of a convenience survey of 500 pregnant women.
The mean age in the group was 28, and 71% were black. Two-thirds were employed, and 29% were college graduates.
By comparison, the 45 women in the co-user group – who reported both cannabis and tobacco use in the past month – were 93% black, 42% employed, and 7% college graduates. (An additional 39 women reported tobacco use only, and 60 reported cannabis use only.)
Co-use also was correlated with “never married, being in the first trimester of pregnancy, not wanting to be pregnant when they were, past-month other substance use, and more frequent use of both cannabis and tobacco than either exclusive group,” Dr. Coleman-Cowger said.
In adjusted models, co-users were more likely (odds ratio, 5.7; P = .05) to give birth to babies with small head circumference than nonusers. The risks of giving birth to babies with small head circumference also were more likely among the tobacco-only users (OR, 4.8; P = .05) and cannabis-only users (OR, 2.0; P = .05), compared with nonusers. Birth defects also were more likely in the co-user group.
The study did not allow researchers to speculate on whether co-use may multiply risk vs. cannabis or tobacco use alone.
Dr. Coleman-Cowger said in light of the small sample size, the results should be interpreted with caution. One possible confounder is quantity of use, she said. “We did not assess quantity of use, but given our finding that frequency of use is higher among the co-use group, it could be that the co-use group is simply using more of each substance and thus impacting the health consequences.”
Current clinical practice guidelines do not suggest screening for cannabis use in pregnant women. But Dr. Coleman-Cowger said it’s “particularly important when tobacco use has been identified, though in states where substance use is considered child abuse, professional judgment should be utilized in terms of the legal implications of asking about use.”
More research is planned to better understand issues like quantity of use, and reasons why pregnant women co-use cannabis and tobacco, Dr. Coleman-Cowger said.
The National Institute on Drug Abuse funded the study, which Dr. Coleman-Cowger said is part of a larger project “to compare and validate screeners that assess prescription drug misuse and illicit drug use during pregnancy.” The study authors report no relevant disclosures.
REPORTING FROM CPDD 2018
Key clinical point: Couse of cannabis and tobacco by pregnant mothers may pose more risk to unborn children than use of either alone.
Major finding: Cousers had a higher risk of giving birth to children with birth detects and small head circumference than tobacco-only or cannabis-only users. In adjusted models, cousers were more likely (odds ratio, 5.7; P = .05) to give birth to babies with small head circumference than nonusers. The risks of giving birth to babies with small head circumference also were more likely among the tobacco-only users (OR, 4.8; P = .05) and cannabis-only users (OR, 2.0; P = .05), compared with nonusers.
Study details: Survey of 500 pregnant Medicaid recipients.
Disclosures: The National Institute on Drug Abuse funded the study. The study authors report no relevant disclosures.
Novel blood test that predicts gestational age, fetal development, could improve prenatal care
Researchers have identified cell-free RNA transcripts obtained from a noninvasive blood test during pregnancy that can predict risk of preterm birth in addition to predicting gestational age with an accuracy similar to ultrasound, which may soon pave the way for a low-cost alternative to ultrasound for prenatal care in developing areas, according to recent results from two pilot studies.
“Our results are thus generally comparable to ultrasound measurements, can be performed throughout pregnancy, and do not require a priori physiological knowledge such as the woman’s last menstrual period,” Stephen Quake, PhD, of Stanford (Calif.) University, and his colleagues wrote in Science.
Dr. Quake and his colleagues recruited 31 women from Denmark who provided weekly blood samples (521 samples) during pregnancy up until they delivered full-term. After analyzing the cell-free RNA (cfRNA) genes, researchers found cfRNA placenta, fetal, and immune genes were highly correlated with one another. They created a random forest model based on nine cfRNA genes (CGA, CAPN6, CGB, ALPP, CSHL1, PLAC4, PSG7, PAPPA, and LGALS14) that corresponded with the placenta. They estimated that those nine genes would predict gestational age and tested the model using 306 samples from 21 women in a training cohort and validated the test using 215 samples from 10 women in a validation cohort. The blood test predicted gestational age within 14 days of delivery in 32% of cases at the second trimester (T2), 23% at the third trimester (3T), and 45% at T2 and T3, compared with a 48% with ultrasound.
In a second pilot study, Dr. Quake and his colleagues created a polymerase chain reaction panel for 38 genes identified from sequencing RNA from patients in Pennsylvania, Alabama, and Denmark, with full-term and preterm deliveries up to 2 months before labor to determine “cfRNA transcripts that might be able to discriminate a spontaneous preterm delivery from a full-term delivery.” The top seven cfRNA transcripts (CLCN3, DAPP1, PPBP, MAP3K7CL, MOB1B, RAB27B, and RGS18), when grouped in “unique combinations” of three genes, predicted 75% of preterm samples and misclassified 1 of 26 samples (4%) from Denmark and Pennsylvania; in a validated cohort of Alabama patients, the test predicted 4 of 5 preterm samples (80%) and misclassified 3 of 18 full-term samples (17%).
“These cfRNA [polymerase chain reaction]–based tests have two advantages over alternatives: broader applicability and lower cost,” Dr. Quake and his colleagues wrote. “They can be applied across the globe as a complement to or substitute for ultrasound, which can be expensive and inaccurate during the second and third trimesters.”
The authors noted a larger sample size and blinded testing on a broader patient population is needed before clinics can apply this blood test in a diagnostic or screening tool for widespread use.
Dr. Quake and three other authors have a patent application submitted by the Chan Zuckerberg Biohub relating to “noninvasive estimates of gestational age, delivery, and preterm birth.” The other authors have no relevant financial disclosures.
SOURCE: Ngo TTM et al. Science. 2018 Jun 7. doi: 10.1126/science.aar3819.
Researchers have identified cell-free RNA transcripts obtained from a noninvasive blood test during pregnancy that can predict risk of preterm birth in addition to predicting gestational age with an accuracy similar to ultrasound, which may soon pave the way for a low-cost alternative to ultrasound for prenatal care in developing areas, according to recent results from two pilot studies.
“Our results are thus generally comparable to ultrasound measurements, can be performed throughout pregnancy, and do not require a priori physiological knowledge such as the woman’s last menstrual period,” Stephen Quake, PhD, of Stanford (Calif.) University, and his colleagues wrote in Science.
Dr. Quake and his colleagues recruited 31 women from Denmark who provided weekly blood samples (521 samples) during pregnancy up until they delivered full-term. After analyzing the cell-free RNA (cfRNA) genes, researchers found cfRNA placenta, fetal, and immune genes were highly correlated with one another. They created a random forest model based on nine cfRNA genes (CGA, CAPN6, CGB, ALPP, CSHL1, PLAC4, PSG7, PAPPA, and LGALS14) that corresponded with the placenta. They estimated that those nine genes would predict gestational age and tested the model using 306 samples from 21 women in a training cohort and validated the test using 215 samples from 10 women in a validation cohort. The blood test predicted gestational age within 14 days of delivery in 32% of cases at the second trimester (T2), 23% at the third trimester (3T), and 45% at T2 and T3, compared with a 48% with ultrasound.
In a second pilot study, Dr. Quake and his colleagues created a polymerase chain reaction panel for 38 genes identified from sequencing RNA from patients in Pennsylvania, Alabama, and Denmark, with full-term and preterm deliveries up to 2 months before labor to determine “cfRNA transcripts that might be able to discriminate a spontaneous preterm delivery from a full-term delivery.” The top seven cfRNA transcripts (CLCN3, DAPP1, PPBP, MAP3K7CL, MOB1B, RAB27B, and RGS18), when grouped in “unique combinations” of three genes, predicted 75% of preterm samples and misclassified 1 of 26 samples (4%) from Denmark and Pennsylvania; in a validated cohort of Alabama patients, the test predicted 4 of 5 preterm samples (80%) and misclassified 3 of 18 full-term samples (17%).
“These cfRNA [polymerase chain reaction]–based tests have two advantages over alternatives: broader applicability and lower cost,” Dr. Quake and his colleagues wrote. “They can be applied across the globe as a complement to or substitute for ultrasound, which can be expensive and inaccurate during the second and third trimesters.”
The authors noted a larger sample size and blinded testing on a broader patient population is needed before clinics can apply this blood test in a diagnostic or screening tool for widespread use.
Dr. Quake and three other authors have a patent application submitted by the Chan Zuckerberg Biohub relating to “noninvasive estimates of gestational age, delivery, and preterm birth.” The other authors have no relevant financial disclosures.
SOURCE: Ngo TTM et al. Science. 2018 Jun 7. doi: 10.1126/science.aar3819.
Researchers have identified cell-free RNA transcripts obtained from a noninvasive blood test during pregnancy that can predict risk of preterm birth in addition to predicting gestational age with an accuracy similar to ultrasound, which may soon pave the way for a low-cost alternative to ultrasound for prenatal care in developing areas, according to recent results from two pilot studies.
“Our results are thus generally comparable to ultrasound measurements, can be performed throughout pregnancy, and do not require a priori physiological knowledge such as the woman’s last menstrual period,” Stephen Quake, PhD, of Stanford (Calif.) University, and his colleagues wrote in Science.
Dr. Quake and his colleagues recruited 31 women from Denmark who provided weekly blood samples (521 samples) during pregnancy up until they delivered full-term. After analyzing the cell-free RNA (cfRNA) genes, researchers found cfRNA placenta, fetal, and immune genes were highly correlated with one another. They created a random forest model based on nine cfRNA genes (CGA, CAPN6, CGB, ALPP, CSHL1, PLAC4, PSG7, PAPPA, and LGALS14) that corresponded with the placenta. They estimated that those nine genes would predict gestational age and tested the model using 306 samples from 21 women in a training cohort and validated the test using 215 samples from 10 women in a validation cohort. The blood test predicted gestational age within 14 days of delivery in 32% of cases at the second trimester (T2), 23% at the third trimester (3T), and 45% at T2 and T3, compared with a 48% with ultrasound.
In a second pilot study, Dr. Quake and his colleagues created a polymerase chain reaction panel for 38 genes identified from sequencing RNA from patients in Pennsylvania, Alabama, and Denmark, with full-term and preterm deliveries up to 2 months before labor to determine “cfRNA transcripts that might be able to discriminate a spontaneous preterm delivery from a full-term delivery.” The top seven cfRNA transcripts (CLCN3, DAPP1, PPBP, MAP3K7CL, MOB1B, RAB27B, and RGS18), when grouped in “unique combinations” of three genes, predicted 75% of preterm samples and misclassified 1 of 26 samples (4%) from Denmark and Pennsylvania; in a validated cohort of Alabama patients, the test predicted 4 of 5 preterm samples (80%) and misclassified 3 of 18 full-term samples (17%).
“These cfRNA [polymerase chain reaction]–based tests have two advantages over alternatives: broader applicability and lower cost,” Dr. Quake and his colleagues wrote. “They can be applied across the globe as a complement to or substitute for ultrasound, which can be expensive and inaccurate during the second and third trimesters.”
The authors noted a larger sample size and blinded testing on a broader patient population is needed before clinics can apply this blood test in a diagnostic or screening tool for widespread use.
Dr. Quake and three other authors have a patent application submitted by the Chan Zuckerberg Biohub relating to “noninvasive estimates of gestational age, delivery, and preterm birth.” The other authors have no relevant financial disclosures.
SOURCE: Ngo TTM et al. Science. 2018 Jun 7. doi: 10.1126/science.aar3819.
FROM SCIENCE
Key clinical point: Cell-free RNA transcripts identified from a single blood sample can reliably predict gestational age similar to ultrasound and can identify risk of preterm birth.
Major finding: Nine cell-free RNA transcripts predicted gestational age at an accuracy similar to ultrasound, while seven cell-free RNA transcripts predicted an increased risk of preterm birth until 2 months prior to delivery.
Study details: A pilot study of 31 pregnant women and a related pilot study of 38 women with full-term or preterm deliveries.
Disclosures: Dr. Quake and three other authors have a patent application submitted by the Chan Zuckerberg Biohub relating to “noninvasive estimates of gestational age, delivery, and preterm birth.” The other authors have no relevant financial disclosures.
Source: Ngo TTM et al. Science. 2018 Jun 7. doi: 10.1126/science.aar3819.
Breastfeeding with the FDA’s novel drugs approved in 2017, and others
The use of only one 2017 novel drug (Benznidazole) during breastfeeding has been reported. No reports describing the use of the other drugs while breastfeeding have been located. Nevertheless, exposure of a nursing infant should be considered if the mother is taking any of these drugs.
During the first 2 days after birth, nearly all drugs will be excreted into milk, but the amounts are very small and will probably have no effect on the nursing infant. After the second day, drugs with molecular weights of less than 1,000 g/mol will be excreted into milk. Some drugs with high molecular weights may also be excreted, but they may be digested in the infant’s gut. If a mother is receiving one of the drugs below and is breastfeeding, her infant should be monitored for the most common adverse effects, shown below, that were observed in nonpregnant adults.
Anti-infectives
Benznidazole (MW 260 g/mol). Abdominal pain, rash, decreased weight, headache, nausea, vomiting, neutropenia, urticaria, pruritus, eosinophilia, decreased appetite.
Delafloxacin (Baxdela) (MW 441 g/mol). Nausea, diarrhea, headache, transaminase elevations, vomiting.
Glecaprevir / Pibrentasvir (Mavyret) (MWs 839, 1,113 g/mol). Headache, fatigue.
Letermovir (Prevymis) (MW 573 g/mol). Nausea, vomiting, diarrhea, peripheral edema, cough, headache, fatigue, abdominal pain.
Meropenem / vaborbactam (Vabomere) (MWs 438, 297 g/mol). Headache, diarrhea.
Ozenoxacin cream (Xepi) (MW 363 g/mol). No relevant adverse reactions.
Sofosbuvir / Velpatasvir / Voxilaprevir (Vosevi) (MWs 529, 883, 869 g/mol). Headache, fatigue, diarrhea, nausea.
Secnidazole (Solosec) (MW 185 g/mol). Headache, nausea, dysgeusia, vomiting, diarrhea, abdominal pain. Manufacturer recommends discontinuing breastfeeding for 96 hours after administration of the drug.
Antineoplastics
[Note: All of the drugs in this category are best avoided, if possible, when breastfeeding.]
Abemaciclib (Verzenio) (MW 507 g/mol). Diarrhea, neutropenia, nausea, vomiting, abdominal pain, infections, fatigue, anemia, leukopenia, decreased appetite, headache, alopecia, thrombocytopenia.
Acalabrutinib (Calquence) (MW 466 g/mol). Anemia, thrombocytopenia, headache, neutropenia, diarrhea, myalgia, bruising.
Avelumab (Bavencio) (MW 147 kg/mol). Fatigue, musculoskeletal pain, diarrhea, nausea, rash, decreased appetite, peripheral edema, urinary tract infection.
Brigatinib (Alunbrig) (MW 584 g/mol). Nausea, fatigue, cough, headache.
Copanlisib (Aliqopa) (MW 480 g/mol). Hyperglycemia, diarrhea, decreased strength and energy, hypertension, leukopenia, neutropenia, nausea, lower respiratory infections, thrombocytopenia.
Durvalumab (Imfinzi) (MW 146 kg/mol). Fatigue, musculoskeletal pain, constipation, decreased appetite, nausea, peripheral edema, urinary tract infections, cough, upper respiratory tract infections, dyspnea, rash.
Enasidenib mesylate (Idhifa) (MW 569 g/mol). Nausea, vomiting, diarrhea, elevated bilirubin, decreased appetite.
Inotuzumab ozogamicin (Besponsa) (MW 160 kg/mol). Thrombocytopenia, neutropenia, anemia, leukopenia, fatigue, hemorrhage, pyrexia, nausea, headache, febrile neutropenia, transaminases increased, abdominal pain, increased gamma-glutamyltransferase, and hyperbilirubinemia.
Midostaurin (Rydapt) (MW 571 g/mol). Febrile neutropenia, nausea, mucositis, vomiting, headache, petechiae, musculoskeletal pain, epistaxis, hyperglycemia, vomiting, diarrhea, edema, pyrexia, dyspnea.
Neratinib (Nerlynx) (MW 557 g/mol). Diarrhea, nausea, vomiting, abdominal pain, fatigue, rash, stomatitis, decreased appetite, muscle spasms, dyspepsia, nail disorder, dry skin, abdominal distention, decreased weight, urinary tract infection.
Niraparib (Zejula) (MW 511 g/mol). Thrombocytopenia, anemia, neutropenia, leukopenia, palpitations, nausea, vomiting, constipation, abdominal pain/distention, mucositis/stomatitis, diarrhea, dry mouth, fatigue/asthenia, decreased appetite, urinary tract infection, myalgia, back pain, arthralgia, headache, dizziness, dysgeusia, insomnia, anxiety, nasopharyngitis, dyspnea, cough, rash, hypertension.
Ribociclib (Kisqali) (MW 553 g/mol). Neutropenia, nausea, fatigue, diarrhea, leukopenia, alopecia, vomiting, constipation, headache, back pain.
Cardiovascular
Angiotensin II (Giapreza) (MW 1,046 g/mol). Thromboembolic events.
Central nervous system
Deutetrabenazine (Austedo) (MW 324 g/mol). Somnolence, diarrhea, dry mouth, fatigue, nasopharyngitis.
Edaravone (Radicava) (MW 174 g/mol). Confusion, gait disturbance, headache.
Naldemedine (Symproic) (MW 743 g/mol). Abdominal pain, diarrhea, nausea, gastroenteritis.
Ocrelizumab (Ocrevus) (MW 145 kg/mol). Upper and lower respiratory tract infections.
Safinamide (Xadago) (MW 399 g/mol). Dyskinesia, fall, nausea, insomnia.
Valbenazine (Ingrezza) (MW 419 g/mol). Somnolence.
Dermatologic
Brodalumab (Siliq) (MW 144 kg/mol). Arthralgia, headache, fatigue, diarrhea, oropharyngeal pain, nausea, myalgia, influenza, neutropenia, tinea infections.
Dupilumab (Dupixent) (MW 146.9 kg/mol). Conjunctivitis, blepharitis, oral herpes, keratitis, eye pruritus, other herpes simplex virus infection, dry eye.
Guselkumab (Tremfya) (MW 143.6 kg/mol). Upper respiratory infections, headache, arthralgia, diarrhea, gastroenteritis, tinea infections, herpes simplex infections.
Endocrine / metabolic
Deflazacort (Emflaza) (MW 442 g/mol). Cushingoid appearance, weight increased, increased appetite, upper respiratory tract infection, cough, pollakiuria, hirsutism, central obesity, nasopharyngitis.
Ertugliflozin (Steglatro) (MW 566 g/mol). Female genital mycotic infections.
Etelcalcetide (Parsabiv) (MW 1,048 g/mol). Blood calcium decreased, muscle spasms, diarrhea, nausea, vomiting, headache, hypocalcemia, paresthesia.
Macimorelin (Macrilen) (MW 535 g/mol). Dysgeusia, dizziness, headache, fatigue, nausea, hunger, diarrhea, upper respiratory tract infection, feeling hot, hyperhidrosis, nasopharyngitis, sinus bradycardia.
Semaglutide (Ozempic) (MW 4,114 g/mol). Nausea, vomiting, diarrhea, abdominal pain, constipation.
Vestronidase alfa (Mepsevii) (MW 72.5 kg/mol). Diarrhea, rash, anaphylaxis, pruritus.
Gastrointestinal
Plecanatide (Trulance) (MW 1.7 kg/mol). Diarrhea.
Telotristat (Xermelo) (MW 574 g/mol). Nausea, headache, increased gamma-glutamyltransferase, depression, flatulence, decreased appetite, peripheral edema, pyrexia.
Hematologic
Betrixaban (Bevyxxa) (MW 568 g/mol). Bleeding.
Emicizumab (Hemlibra) (MW 145.6 kg/mol). Headache, arthralgia.
Immunologic
Sarilumab (Kevzara) (MW 150 kg/mol). Neutropenia, increased ALT, upper respiratory infections, urinary tract infections.
Ophthalmic
Latanoprostene bunod (Vyzulta) (MW 508 g/mol). All related to the eye.
Netarsudil (Rhopressa) (MW 454 g/mol). All related to the eye.
Parathyroid hormone
Abaloparatide (Tymlos) (MW 3.9 kg/mol). Hypercalciuria, dizziness, nausea, headache, palpitations, fatigue, upper abdominal pain, vertigo.
Respiratory
Benralizumab (Fasenra) (MW 150 kg/mol). Headache, pharyngitis.
The use of only one 2017 novel drug (Benznidazole) during breastfeeding has been reported. No reports describing the use of the other drugs while breastfeeding have been located. Nevertheless, exposure of a nursing infant should be considered if the mother is taking any of these drugs.
During the first 2 days after birth, nearly all drugs will be excreted into milk, but the amounts are very small and will probably have no effect on the nursing infant. After the second day, drugs with molecular weights of less than 1,000 g/mol will be excreted into milk. Some drugs with high molecular weights may also be excreted, but they may be digested in the infant’s gut. If a mother is receiving one of the drugs below and is breastfeeding, her infant should be monitored for the most common adverse effects, shown below, that were observed in nonpregnant adults.
Anti-infectives
Benznidazole (MW 260 g/mol). Abdominal pain, rash, decreased weight, headache, nausea, vomiting, neutropenia, urticaria, pruritus, eosinophilia, decreased appetite.
Delafloxacin (Baxdela) (MW 441 g/mol). Nausea, diarrhea, headache, transaminase elevations, vomiting.
Glecaprevir / Pibrentasvir (Mavyret) (MWs 839, 1,113 g/mol). Headache, fatigue.
Letermovir (Prevymis) (MW 573 g/mol). Nausea, vomiting, diarrhea, peripheral edema, cough, headache, fatigue, abdominal pain.
Meropenem / vaborbactam (Vabomere) (MWs 438, 297 g/mol). Headache, diarrhea.
Ozenoxacin cream (Xepi) (MW 363 g/mol). No relevant adverse reactions.
Sofosbuvir / Velpatasvir / Voxilaprevir (Vosevi) (MWs 529, 883, 869 g/mol). Headache, fatigue, diarrhea, nausea.
Secnidazole (Solosec) (MW 185 g/mol). Headache, nausea, dysgeusia, vomiting, diarrhea, abdominal pain. Manufacturer recommends discontinuing breastfeeding for 96 hours after administration of the drug.
Antineoplastics
[Note: All of the drugs in this category are best avoided, if possible, when breastfeeding.]
Abemaciclib (Verzenio) (MW 507 g/mol). Diarrhea, neutropenia, nausea, vomiting, abdominal pain, infections, fatigue, anemia, leukopenia, decreased appetite, headache, alopecia, thrombocytopenia.
Acalabrutinib (Calquence) (MW 466 g/mol). Anemia, thrombocytopenia, headache, neutropenia, diarrhea, myalgia, bruising.
Avelumab (Bavencio) (MW 147 kg/mol). Fatigue, musculoskeletal pain, diarrhea, nausea, rash, decreased appetite, peripheral edema, urinary tract infection.
Brigatinib (Alunbrig) (MW 584 g/mol). Nausea, fatigue, cough, headache.
Copanlisib (Aliqopa) (MW 480 g/mol). Hyperglycemia, diarrhea, decreased strength and energy, hypertension, leukopenia, neutropenia, nausea, lower respiratory infections, thrombocytopenia.
Durvalumab (Imfinzi) (MW 146 kg/mol). Fatigue, musculoskeletal pain, constipation, decreased appetite, nausea, peripheral edema, urinary tract infections, cough, upper respiratory tract infections, dyspnea, rash.
Enasidenib mesylate (Idhifa) (MW 569 g/mol). Nausea, vomiting, diarrhea, elevated bilirubin, decreased appetite.
Inotuzumab ozogamicin (Besponsa) (MW 160 kg/mol). Thrombocytopenia, neutropenia, anemia, leukopenia, fatigue, hemorrhage, pyrexia, nausea, headache, febrile neutropenia, transaminases increased, abdominal pain, increased gamma-glutamyltransferase, and hyperbilirubinemia.
Midostaurin (Rydapt) (MW 571 g/mol). Febrile neutropenia, nausea, mucositis, vomiting, headache, petechiae, musculoskeletal pain, epistaxis, hyperglycemia, vomiting, diarrhea, edema, pyrexia, dyspnea.
Neratinib (Nerlynx) (MW 557 g/mol). Diarrhea, nausea, vomiting, abdominal pain, fatigue, rash, stomatitis, decreased appetite, muscle spasms, dyspepsia, nail disorder, dry skin, abdominal distention, decreased weight, urinary tract infection.
Niraparib (Zejula) (MW 511 g/mol). Thrombocytopenia, anemia, neutropenia, leukopenia, palpitations, nausea, vomiting, constipation, abdominal pain/distention, mucositis/stomatitis, diarrhea, dry mouth, fatigue/asthenia, decreased appetite, urinary tract infection, myalgia, back pain, arthralgia, headache, dizziness, dysgeusia, insomnia, anxiety, nasopharyngitis, dyspnea, cough, rash, hypertension.
Ribociclib (Kisqali) (MW 553 g/mol). Neutropenia, nausea, fatigue, diarrhea, leukopenia, alopecia, vomiting, constipation, headache, back pain.
Cardiovascular
Angiotensin II (Giapreza) (MW 1,046 g/mol). Thromboembolic events.
Central nervous system
Deutetrabenazine (Austedo) (MW 324 g/mol). Somnolence, diarrhea, dry mouth, fatigue, nasopharyngitis.
Edaravone (Radicava) (MW 174 g/mol). Confusion, gait disturbance, headache.
Naldemedine (Symproic) (MW 743 g/mol). Abdominal pain, diarrhea, nausea, gastroenteritis.
Ocrelizumab (Ocrevus) (MW 145 kg/mol). Upper and lower respiratory tract infections.
Safinamide (Xadago) (MW 399 g/mol). Dyskinesia, fall, nausea, insomnia.
Valbenazine (Ingrezza) (MW 419 g/mol). Somnolence.
Dermatologic
Brodalumab (Siliq) (MW 144 kg/mol). Arthralgia, headache, fatigue, diarrhea, oropharyngeal pain, nausea, myalgia, influenza, neutropenia, tinea infections.
Dupilumab (Dupixent) (MW 146.9 kg/mol). Conjunctivitis, blepharitis, oral herpes, keratitis, eye pruritus, other herpes simplex virus infection, dry eye.
Guselkumab (Tremfya) (MW 143.6 kg/mol). Upper respiratory infections, headache, arthralgia, diarrhea, gastroenteritis, tinea infections, herpes simplex infections.
Endocrine / metabolic
Deflazacort (Emflaza) (MW 442 g/mol). Cushingoid appearance, weight increased, increased appetite, upper respiratory tract infection, cough, pollakiuria, hirsutism, central obesity, nasopharyngitis.
Ertugliflozin (Steglatro) (MW 566 g/mol). Female genital mycotic infections.
Etelcalcetide (Parsabiv) (MW 1,048 g/mol). Blood calcium decreased, muscle spasms, diarrhea, nausea, vomiting, headache, hypocalcemia, paresthesia.
Macimorelin (Macrilen) (MW 535 g/mol). Dysgeusia, dizziness, headache, fatigue, nausea, hunger, diarrhea, upper respiratory tract infection, feeling hot, hyperhidrosis, nasopharyngitis, sinus bradycardia.
Semaglutide (Ozempic) (MW 4,114 g/mol). Nausea, vomiting, diarrhea, abdominal pain, constipation.
Vestronidase alfa (Mepsevii) (MW 72.5 kg/mol). Diarrhea, rash, anaphylaxis, pruritus.
Gastrointestinal
Plecanatide (Trulance) (MW 1.7 kg/mol). Diarrhea.
Telotristat (Xermelo) (MW 574 g/mol). Nausea, headache, increased gamma-glutamyltransferase, depression, flatulence, decreased appetite, peripheral edema, pyrexia.
Hematologic
Betrixaban (Bevyxxa) (MW 568 g/mol). Bleeding.
Emicizumab (Hemlibra) (MW 145.6 kg/mol). Headache, arthralgia.
Immunologic
Sarilumab (Kevzara) (MW 150 kg/mol). Neutropenia, increased ALT, upper respiratory infections, urinary tract infections.
Ophthalmic
Latanoprostene bunod (Vyzulta) (MW 508 g/mol). All related to the eye.
Netarsudil (Rhopressa) (MW 454 g/mol). All related to the eye.
Parathyroid hormone
Abaloparatide (Tymlos) (MW 3.9 kg/mol). Hypercalciuria, dizziness, nausea, headache, palpitations, fatigue, upper abdominal pain, vertigo.
Respiratory
Benralizumab (Fasenra) (MW 150 kg/mol). Headache, pharyngitis.
The use of only one 2017 novel drug (Benznidazole) during breastfeeding has been reported. No reports describing the use of the other drugs while breastfeeding have been located. Nevertheless, exposure of a nursing infant should be considered if the mother is taking any of these drugs.
During the first 2 days after birth, nearly all drugs will be excreted into milk, but the amounts are very small and will probably have no effect on the nursing infant. After the second day, drugs with molecular weights of less than 1,000 g/mol will be excreted into milk. Some drugs with high molecular weights may also be excreted, but they may be digested in the infant’s gut. If a mother is receiving one of the drugs below and is breastfeeding, her infant should be monitored for the most common adverse effects, shown below, that were observed in nonpregnant adults.
Anti-infectives
Benznidazole (MW 260 g/mol). Abdominal pain, rash, decreased weight, headache, nausea, vomiting, neutropenia, urticaria, pruritus, eosinophilia, decreased appetite.
Delafloxacin (Baxdela) (MW 441 g/mol). Nausea, diarrhea, headache, transaminase elevations, vomiting.
Glecaprevir / Pibrentasvir (Mavyret) (MWs 839, 1,113 g/mol). Headache, fatigue.
Letermovir (Prevymis) (MW 573 g/mol). Nausea, vomiting, diarrhea, peripheral edema, cough, headache, fatigue, abdominal pain.
Meropenem / vaborbactam (Vabomere) (MWs 438, 297 g/mol). Headache, diarrhea.
Ozenoxacin cream (Xepi) (MW 363 g/mol). No relevant adverse reactions.
Sofosbuvir / Velpatasvir / Voxilaprevir (Vosevi) (MWs 529, 883, 869 g/mol). Headache, fatigue, diarrhea, nausea.
Secnidazole (Solosec) (MW 185 g/mol). Headache, nausea, dysgeusia, vomiting, diarrhea, abdominal pain. Manufacturer recommends discontinuing breastfeeding for 96 hours after administration of the drug.
Antineoplastics
[Note: All of the drugs in this category are best avoided, if possible, when breastfeeding.]
Abemaciclib (Verzenio) (MW 507 g/mol). Diarrhea, neutropenia, nausea, vomiting, abdominal pain, infections, fatigue, anemia, leukopenia, decreased appetite, headache, alopecia, thrombocytopenia.
Acalabrutinib (Calquence) (MW 466 g/mol). Anemia, thrombocytopenia, headache, neutropenia, diarrhea, myalgia, bruising.
Avelumab (Bavencio) (MW 147 kg/mol). Fatigue, musculoskeletal pain, diarrhea, nausea, rash, decreased appetite, peripheral edema, urinary tract infection.
Brigatinib (Alunbrig) (MW 584 g/mol). Nausea, fatigue, cough, headache.
Copanlisib (Aliqopa) (MW 480 g/mol). Hyperglycemia, diarrhea, decreased strength and energy, hypertension, leukopenia, neutropenia, nausea, lower respiratory infections, thrombocytopenia.
Durvalumab (Imfinzi) (MW 146 kg/mol). Fatigue, musculoskeletal pain, constipation, decreased appetite, nausea, peripheral edema, urinary tract infections, cough, upper respiratory tract infections, dyspnea, rash.
Enasidenib mesylate (Idhifa) (MW 569 g/mol). Nausea, vomiting, diarrhea, elevated bilirubin, decreased appetite.
Inotuzumab ozogamicin (Besponsa) (MW 160 kg/mol). Thrombocytopenia, neutropenia, anemia, leukopenia, fatigue, hemorrhage, pyrexia, nausea, headache, febrile neutropenia, transaminases increased, abdominal pain, increased gamma-glutamyltransferase, and hyperbilirubinemia.
Midostaurin (Rydapt) (MW 571 g/mol). Febrile neutropenia, nausea, mucositis, vomiting, headache, petechiae, musculoskeletal pain, epistaxis, hyperglycemia, vomiting, diarrhea, edema, pyrexia, dyspnea.
Neratinib (Nerlynx) (MW 557 g/mol). Diarrhea, nausea, vomiting, abdominal pain, fatigue, rash, stomatitis, decreased appetite, muscle spasms, dyspepsia, nail disorder, dry skin, abdominal distention, decreased weight, urinary tract infection.
Niraparib (Zejula) (MW 511 g/mol). Thrombocytopenia, anemia, neutropenia, leukopenia, palpitations, nausea, vomiting, constipation, abdominal pain/distention, mucositis/stomatitis, diarrhea, dry mouth, fatigue/asthenia, decreased appetite, urinary tract infection, myalgia, back pain, arthralgia, headache, dizziness, dysgeusia, insomnia, anxiety, nasopharyngitis, dyspnea, cough, rash, hypertension.
Ribociclib (Kisqali) (MW 553 g/mol). Neutropenia, nausea, fatigue, diarrhea, leukopenia, alopecia, vomiting, constipation, headache, back pain.
Cardiovascular
Angiotensin II (Giapreza) (MW 1,046 g/mol). Thromboembolic events.
Central nervous system
Deutetrabenazine (Austedo) (MW 324 g/mol). Somnolence, diarrhea, dry mouth, fatigue, nasopharyngitis.
Edaravone (Radicava) (MW 174 g/mol). Confusion, gait disturbance, headache.
Naldemedine (Symproic) (MW 743 g/mol). Abdominal pain, diarrhea, nausea, gastroenteritis.
Ocrelizumab (Ocrevus) (MW 145 kg/mol). Upper and lower respiratory tract infections.
Safinamide (Xadago) (MW 399 g/mol). Dyskinesia, fall, nausea, insomnia.
Valbenazine (Ingrezza) (MW 419 g/mol). Somnolence.
Dermatologic
Brodalumab (Siliq) (MW 144 kg/mol). Arthralgia, headache, fatigue, diarrhea, oropharyngeal pain, nausea, myalgia, influenza, neutropenia, tinea infections.
Dupilumab (Dupixent) (MW 146.9 kg/mol). Conjunctivitis, blepharitis, oral herpes, keratitis, eye pruritus, other herpes simplex virus infection, dry eye.
Guselkumab (Tremfya) (MW 143.6 kg/mol). Upper respiratory infections, headache, arthralgia, diarrhea, gastroenteritis, tinea infections, herpes simplex infections.
Endocrine / metabolic
Deflazacort (Emflaza) (MW 442 g/mol). Cushingoid appearance, weight increased, increased appetite, upper respiratory tract infection, cough, pollakiuria, hirsutism, central obesity, nasopharyngitis.
Ertugliflozin (Steglatro) (MW 566 g/mol). Female genital mycotic infections.
Etelcalcetide (Parsabiv) (MW 1,048 g/mol). Blood calcium decreased, muscle spasms, diarrhea, nausea, vomiting, headache, hypocalcemia, paresthesia.
Macimorelin (Macrilen) (MW 535 g/mol). Dysgeusia, dizziness, headache, fatigue, nausea, hunger, diarrhea, upper respiratory tract infection, feeling hot, hyperhidrosis, nasopharyngitis, sinus bradycardia.
Semaglutide (Ozempic) (MW 4,114 g/mol). Nausea, vomiting, diarrhea, abdominal pain, constipation.
Vestronidase alfa (Mepsevii) (MW 72.5 kg/mol). Diarrhea, rash, anaphylaxis, pruritus.
Gastrointestinal
Plecanatide (Trulance) (MW 1.7 kg/mol). Diarrhea.
Telotristat (Xermelo) (MW 574 g/mol). Nausea, headache, increased gamma-glutamyltransferase, depression, flatulence, decreased appetite, peripheral edema, pyrexia.
Hematologic
Betrixaban (Bevyxxa) (MW 568 g/mol). Bleeding.
Emicizumab (Hemlibra) (MW 145.6 kg/mol). Headache, arthralgia.
Immunologic
Sarilumab (Kevzara) (MW 150 kg/mol). Neutropenia, increased ALT, upper respiratory infections, urinary tract infections.
Ophthalmic
Latanoprostene bunod (Vyzulta) (MW 508 g/mol). All related to the eye.
Netarsudil (Rhopressa) (MW 454 g/mol). All related to the eye.
Parathyroid hormone
Abaloparatide (Tymlos) (MW 3.9 kg/mol). Hypercalciuria, dizziness, nausea, headache, palpitations, fatigue, upper abdominal pain, vertigo.
Respiratory
Benralizumab (Fasenra) (MW 150 kg/mol). Headache, pharyngitis.
How congenital heart disease affects brain development
Congenital heart disease (CHD) is the most common congenital anomaly, with an estimated incidence of 6-12 per 1,000 live births. It is also the congenital anomaly that most often leads to death or significant morbidity. Advances in surgical procedures and operating room care as well as specialized care in the ICU have led to significant improvements in survival over the past 10-20 years – even for the most complex cases of CHD. We now expect the majority of newborns with CHD not only to survive, but to grow up into adulthood.
The focus of clinical research has thus transitioned from survival to issues of long-term morbidity and outcomes, and the more recent literature has clearly shown us that children with CHD are at high risk of learning disabilities and other neurodevelopmental abnormalities. The prevalence of impairment rises with the complexity of CHD, from a prevalence of approximately 20% in mild CHD to as much as 75% in severe CHD. Almost all neonates and infants who undergo palliative surgical procedures have neurodevelopmental impairments.
The neurobehavioral “signature” of CHD includes cognitive defects (usually mild), short attention span, fine and gross motor delays, speech and language delays, visual motor integration, and executive function deficits. Executive function deficits and attention deficits are among the problems that often do not present in children until they reach middle school and beyond, when they are expected to learn more complicated material and handle more complex tasks. Long-term surveillance and care have thus become a major focus at our institution and others throughout the country.
At the same time, evidence has increased in the past 5-10 years that adverse neurodevelopmental outcomes in children with complex CHD may stem from genetic factors as well as compromise to the brain in utero because of altered blood flow, compromise at the time of delivery, and insults during and after corrective or palliative surgery. Surgical strategies and operating room teams have become significantly better at protecting the brain, and new research now is directed toward understanding the neurologic abnormalities that are present in newborns prior to surgical intervention.
Increasingly, researchers are now focused on looking at the in utero origins of brain impairments in children with CHD and trying to understand specific prenatal causes, mechanisms, and potentially modifiable factors. We’re asking what we can do during pregnancy to improve neurodevelopmental outcomes.
Impaired brain growth
The question of how CHD affects blood flow to the fetal brain is an important one. We found some time ago in a study using Doppler ultrasound that 44% of fetuses with CHD had blood flow abnormalities in the middle cerebral artery at some point in the late second or third trimester, suggesting that the blood vessels had dilated to allow more cerebral perfusion. This phenomenon, termed “brain sparing,” is believed to be an autoregulatory mechanism that occurs as a result of diminished oxygen delivery or inadequate blood flow to the brain (Pediatr Cardiol. 2003 Jan;24[5]:436-43).
Subsequent studies have similarly documented abnormal cerebral blood flow in fetuses with various types of congenital heart lesions. What is left to be determined is whether this autoregulatory mechanism is adequate to maintain perfusion in the presence of specific, high-risk CHD.
Abnormalities were more often seen in CHD with obstructed aortic flow, such as hypoplastic left heart syndrome (HLHS) in which the aorta is perfused retrograde through the fetal ductus arteriosus (Circulation. 2010 Jan 4;121:26-33).
Other fetal imaging studies have similarly demonstrated a progressive third-trimester decrease in both cortical gray and white matter and in gyrification (cortical folding) (Cereb Cortex. 2013;23:2932-43), as well as decreased cerebral oxygen delivery and consumption (Circulation. 2015;131:1313-23) in fetuses with severe CHD. It appears that the brain may start out normal in size, but in the third trimester, the accelerated metabolic demands that come with rapid growth and development are not sufficiently met by the fetal cardiovascular circulation in CHD.
In the newborn with CHD, preoperative brain imaging studies have demonstrated structural abnormalities suggesting delayed development (for example, microcephaly and a widened operculum), microstructural abnormalities suggesting abnormal myelination and neuroaxonal development, and lower brain maturity scores (a composite score that combines multiple factors, such as myelination and cortical in-folding, to represent “brain age”).
Moreover, some of the newborn brain imaging studies have correlated brain MRI findings with neonatal neurodevelopmental assessments. For instance, investigators found that full-term newborns with CHD had decreased gray matter brain volume and increased cerebrospinal fluid volume and that these impairments were associated with poor behavioral state regulation and poor visual orienting (J Pediatr. 2014;164:1121-7).
Interestingly, it has been found that the full-term baby with specific complex CHD, including newborns with single ventricle CHD or transposition of the great arteries, is more likely to have a brain maturity score that is equivalent to that of a baby born at 35 weeks’ gestation. This means that, in some infants with CHD, the brain has lagged in growth by about a month, resulting in a pattern of disturbed development and subsequent injury that is similar to that of premature infants.
It also means that infants with CHD and an immature brain are especially vulnerable to brain injury when open-heart surgery is needed. In short, we now appreciate that the brain in patients with CHD is likely more fragile than we previously thought – and that this fragility is prenatal in its origins.
Delivery room planning
Ideally, our goal is to find ways of changing the circulation in utero to improve cerebral oxygenation and blood flow, and, consequently, improve brain development and long-term neurocognitive function. Despite significant efforts in this area, we’re not there yet.
Examples of strategies that are being tested include catheter intervention to open the aortic valve in utero for fetuses with critical aortic stenosis. This procedure currently is being performed to try to prevent progression of the valve abnormality to HLHS, but it has not been determined whether the intervention affects cerebral blood flow. Maternal oxygen therapy has been shown to change cerebral blood flow in the short term for fetuses with HLHS, but its long-term use has not been studied. At the time of birth, to prevent injury in the potentially more fragile brain of the newborn with CHD, what we can do is to identify those fetuses who are more likely to be at risk for hypoxia low cardiac output and hemodynamic compromise in the delivery room, and plan for specialized delivery room and perinatal management beyond standard neonatal care.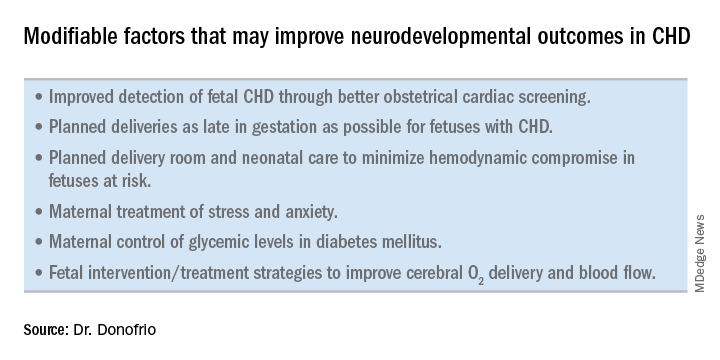
Most newborns with CHD are assigned to Level 1; they have no predicted risk of compromise in the delivery room – or even in the first couple weeks of life – and can deliver at a local hospital with neonatal evaluation and then consult with the pediatric cardiologist. Defects include shunt lesions such as septal defects or mild valve abnormalities.
Patients assigned to Level 2 have minimal risk of compromise in the delivery room but are expected to require postnatal surgery, cardiac catheterization, or another procedure before going home. They can be stabilized by the neonatologist, usually with initiation of a prostaglandin infusion, before transfer to the cardiac center for the planned intervention. Defects include single ventricle CHD and severe Tetralogy of Fallot.
Fetuses assigned to Level 3 and Level 4 are expected to have hemodynamic instability at cord clamping, requiring immediate specialty care in the delivery room that is likely to include urgent cardiac catheterization or surgical intervention. These defects are rare and include diagnoses such as transposition of the great arteries, HLHS with a restrictive or closed foramen ovale, and CHD with associated heart failure and hydrops.
We have found that fetal echocardiography accurately predicts postnatal risk and the need for specialized delivery room care in newborns diagnosed in utero with CHD and that level-of-care protocols ensure safe delivery and optimize fetal outcomes (J Am Soc Echocardiogr. 2015;28:1339-49; Am J Cardiol. 2013;111:737-47).
Such delivery planning, which is coordinated between obstetric, neonatal, cardiology, and surgical services with specialty teams as needed (for example, cardiac intensive care, interventional cardiology, and cardiac surgery), is recommended in a 2014 AHA statement on the diagnosis and treatment of fetal cardiac disease. In recent years it has become the standard of care in many health systems (Circulation. 2014;129[21]:2183-242).
The effect of maternal stress on the in utero environment is also getting increased attention in pediatric cardiology. Alterations in neurocognitive development and fetal and child cardiovascular health are likely to be associated with maternal stress during pregnancy, and studies have shown that maternal stress is high with prenatal diagnoses of CHD. We have to ask: Is stress a modifiable risk factor? There must be ways in which we can do better with prenatal counseling and support after a fetal diagnosis of CHD.
Screening for CHD
Initiating strategies to improve neurodevelopmental outcomes in infants with CHD rests partly on identifying babies with CHD before birth through improved fetal cardiac screening. Research cited in the 2014 AHA statement indicates that nearly all women giving birth to babies with CHD in the United States have obstetric ultrasound examinations in the second or third trimesters, but that only about 30% of the fetuses are diagnosed prenatally.
Current indications for referral for a fetal echocardiogram – in addition to suspicion of a structural heart abnormality on obstetric ultrasound – include maternal factors, such as diabetes mellitus, that raise the risk of CHD above the baseline population risk for low-risk pregnancies.
Women with pregestational diabetes mellitus have a nearly fivefold increase in CHD, compared with the general population (3%-5%), and should be referred for fetal echocardiography. Women with gestational diabetes mellitus have no or minimally increased risk for fetal CHD, but it has been shown that there is an increased risk for cardiac hypertrophy – particularly late in gestation – if glycemic levels are poorly controlled. The 2014 AHA guidelines recommend that fetal echocardiographic evaluation be considered in those who have HbA1c levels greater than 6% in the second half of pregnancy.
Dr. Mary T. Donofrio is a pediatric cardiologist and director of the fetal heart program and critical care delivery program at Children’s National Medical Center, Washington. She reported that she has no disclosures relevant to this article.
Congenital heart disease (CHD) is the most common congenital anomaly, with an estimated incidence of 6-12 per 1,000 live births. It is also the congenital anomaly that most often leads to death or significant morbidity. Advances in surgical procedures and operating room care as well as specialized care in the ICU have led to significant improvements in survival over the past 10-20 years – even for the most complex cases of CHD. We now expect the majority of newborns with CHD not only to survive, but to grow up into adulthood.
The focus of clinical research has thus transitioned from survival to issues of long-term morbidity and outcomes, and the more recent literature has clearly shown us that children with CHD are at high risk of learning disabilities and other neurodevelopmental abnormalities. The prevalence of impairment rises with the complexity of CHD, from a prevalence of approximately 20% in mild CHD to as much as 75% in severe CHD. Almost all neonates and infants who undergo palliative surgical procedures have neurodevelopmental impairments.
The neurobehavioral “signature” of CHD includes cognitive defects (usually mild), short attention span, fine and gross motor delays, speech and language delays, visual motor integration, and executive function deficits. Executive function deficits and attention deficits are among the problems that often do not present in children until they reach middle school and beyond, when they are expected to learn more complicated material and handle more complex tasks. Long-term surveillance and care have thus become a major focus at our institution and others throughout the country.
At the same time, evidence has increased in the past 5-10 years that adverse neurodevelopmental outcomes in children with complex CHD may stem from genetic factors as well as compromise to the brain in utero because of altered blood flow, compromise at the time of delivery, and insults during and after corrective or palliative surgery. Surgical strategies and operating room teams have become significantly better at protecting the brain, and new research now is directed toward understanding the neurologic abnormalities that are present in newborns prior to surgical intervention.
Increasingly, researchers are now focused on looking at the in utero origins of brain impairments in children with CHD and trying to understand specific prenatal causes, mechanisms, and potentially modifiable factors. We’re asking what we can do during pregnancy to improve neurodevelopmental outcomes.
Impaired brain growth
The question of how CHD affects blood flow to the fetal brain is an important one. We found some time ago in a study using Doppler ultrasound that 44% of fetuses with CHD had blood flow abnormalities in the middle cerebral artery at some point in the late second or third trimester, suggesting that the blood vessels had dilated to allow more cerebral perfusion. This phenomenon, termed “brain sparing,” is believed to be an autoregulatory mechanism that occurs as a result of diminished oxygen delivery or inadequate blood flow to the brain (Pediatr Cardiol. 2003 Jan;24[5]:436-43).
Subsequent studies have similarly documented abnormal cerebral blood flow in fetuses with various types of congenital heart lesions. What is left to be determined is whether this autoregulatory mechanism is adequate to maintain perfusion in the presence of specific, high-risk CHD.
Abnormalities were more often seen in CHD with obstructed aortic flow, such as hypoplastic left heart syndrome (HLHS) in which the aorta is perfused retrograde through the fetal ductus arteriosus (Circulation. 2010 Jan 4;121:26-33).
Other fetal imaging studies have similarly demonstrated a progressive third-trimester decrease in both cortical gray and white matter and in gyrification (cortical folding) (Cereb Cortex. 2013;23:2932-43), as well as decreased cerebral oxygen delivery and consumption (Circulation. 2015;131:1313-23) in fetuses with severe CHD. It appears that the brain may start out normal in size, but in the third trimester, the accelerated metabolic demands that come with rapid growth and development are not sufficiently met by the fetal cardiovascular circulation in CHD.
In the newborn with CHD, preoperative brain imaging studies have demonstrated structural abnormalities suggesting delayed development (for example, microcephaly and a widened operculum), microstructural abnormalities suggesting abnormal myelination and neuroaxonal development, and lower brain maturity scores (a composite score that combines multiple factors, such as myelination and cortical in-folding, to represent “brain age”).
Moreover, some of the newborn brain imaging studies have correlated brain MRI findings with neonatal neurodevelopmental assessments. For instance, investigators found that full-term newborns with CHD had decreased gray matter brain volume and increased cerebrospinal fluid volume and that these impairments were associated with poor behavioral state regulation and poor visual orienting (J Pediatr. 2014;164:1121-7).
Interestingly, it has been found that the full-term baby with specific complex CHD, including newborns with single ventricle CHD or transposition of the great arteries, is more likely to have a brain maturity score that is equivalent to that of a baby born at 35 weeks’ gestation. This means that, in some infants with CHD, the brain has lagged in growth by about a month, resulting in a pattern of disturbed development and subsequent injury that is similar to that of premature infants.
It also means that infants with CHD and an immature brain are especially vulnerable to brain injury when open-heart surgery is needed. In short, we now appreciate that the brain in patients with CHD is likely more fragile than we previously thought – and that this fragility is prenatal in its origins.
Delivery room planning
Ideally, our goal is to find ways of changing the circulation in utero to improve cerebral oxygenation and blood flow, and, consequently, improve brain development and long-term neurocognitive function. Despite significant efforts in this area, we’re not there yet.
Examples of strategies that are being tested include catheter intervention to open the aortic valve in utero for fetuses with critical aortic stenosis. This procedure currently is being performed to try to prevent progression of the valve abnormality to HLHS, but it has not been determined whether the intervention affects cerebral blood flow. Maternal oxygen therapy has been shown to change cerebral blood flow in the short term for fetuses with HLHS, but its long-term use has not been studied. At the time of birth, to prevent injury in the potentially more fragile brain of the newborn with CHD, what we can do is to identify those fetuses who are more likely to be at risk for hypoxia low cardiac output and hemodynamic compromise in the delivery room, and plan for specialized delivery room and perinatal management beyond standard neonatal care.
Most newborns with CHD are assigned to Level 1; they have no predicted risk of compromise in the delivery room – or even in the first couple weeks of life – and can deliver at a local hospital with neonatal evaluation and then consult with the pediatric cardiologist. Defects include shunt lesions such as septal defects or mild valve abnormalities.
Patients assigned to Level 2 have minimal risk of compromise in the delivery room but are expected to require postnatal surgery, cardiac catheterization, or another procedure before going home. They can be stabilized by the neonatologist, usually with initiation of a prostaglandin infusion, before transfer to the cardiac center for the planned intervention. Defects include single ventricle CHD and severe Tetralogy of Fallot.
Fetuses assigned to Level 3 and Level 4 are expected to have hemodynamic instability at cord clamping, requiring immediate specialty care in the delivery room that is likely to include urgent cardiac catheterization or surgical intervention. These defects are rare and include diagnoses such as transposition of the great arteries, HLHS with a restrictive or closed foramen ovale, and CHD with associated heart failure and hydrops.
We have found that fetal echocardiography accurately predicts postnatal risk and the need for specialized delivery room care in newborns diagnosed in utero with CHD and that level-of-care protocols ensure safe delivery and optimize fetal outcomes (J Am Soc Echocardiogr. 2015;28:1339-49; Am J Cardiol. 2013;111:737-47).
Such delivery planning, which is coordinated between obstetric, neonatal, cardiology, and surgical services with specialty teams as needed (for example, cardiac intensive care, interventional cardiology, and cardiac surgery), is recommended in a 2014 AHA statement on the diagnosis and treatment of fetal cardiac disease. In recent years it has become the standard of care in many health systems (Circulation. 2014;129[21]:2183-242).
The effect of maternal stress on the in utero environment is also getting increased attention in pediatric cardiology. Alterations in neurocognitive development and fetal and child cardiovascular health are likely to be associated with maternal stress during pregnancy, and studies have shown that maternal stress is high with prenatal diagnoses of CHD. We have to ask: Is stress a modifiable risk factor? There must be ways in which we can do better with prenatal counseling and support after a fetal diagnosis of CHD.
Screening for CHD
Initiating strategies to improve neurodevelopmental outcomes in infants with CHD rests partly on identifying babies with CHD before birth through improved fetal cardiac screening. Research cited in the 2014 AHA statement indicates that nearly all women giving birth to babies with CHD in the United States have obstetric ultrasound examinations in the second or third trimesters, but that only about 30% of the fetuses are diagnosed prenatally.
Current indications for referral for a fetal echocardiogram – in addition to suspicion of a structural heart abnormality on obstetric ultrasound – include maternal factors, such as diabetes mellitus, that raise the risk of CHD above the baseline population risk for low-risk pregnancies.
Women with pregestational diabetes mellitus have a nearly fivefold increase in CHD, compared with the general population (3%-5%), and should be referred for fetal echocardiography. Women with gestational diabetes mellitus have no or minimally increased risk for fetal CHD, but it has been shown that there is an increased risk for cardiac hypertrophy – particularly late in gestation – if glycemic levels are poorly controlled. The 2014 AHA guidelines recommend that fetal echocardiographic evaluation be considered in those who have HbA1c levels greater than 6% in the second half of pregnancy.
Dr. Mary T. Donofrio is a pediatric cardiologist and director of the fetal heart program and critical care delivery program at Children’s National Medical Center, Washington. She reported that she has no disclosures relevant to this article.
Congenital heart disease (CHD) is the most common congenital anomaly, with an estimated incidence of 6-12 per 1,000 live births. It is also the congenital anomaly that most often leads to death or significant morbidity. Advances in surgical procedures and operating room care as well as specialized care in the ICU have led to significant improvements in survival over the past 10-20 years – even for the most complex cases of CHD. We now expect the majority of newborns with CHD not only to survive, but to grow up into adulthood.
The focus of clinical research has thus transitioned from survival to issues of long-term morbidity and outcomes, and the more recent literature has clearly shown us that children with CHD are at high risk of learning disabilities and other neurodevelopmental abnormalities. The prevalence of impairment rises with the complexity of CHD, from a prevalence of approximately 20% in mild CHD to as much as 75% in severe CHD. Almost all neonates and infants who undergo palliative surgical procedures have neurodevelopmental impairments.
The neurobehavioral “signature” of CHD includes cognitive defects (usually mild), short attention span, fine and gross motor delays, speech and language delays, visual motor integration, and executive function deficits. Executive function deficits and attention deficits are among the problems that often do not present in children until they reach middle school and beyond, when they are expected to learn more complicated material and handle more complex tasks. Long-term surveillance and care have thus become a major focus at our institution and others throughout the country.
At the same time, evidence has increased in the past 5-10 years that adverse neurodevelopmental outcomes in children with complex CHD may stem from genetic factors as well as compromise to the brain in utero because of altered blood flow, compromise at the time of delivery, and insults during and after corrective or palliative surgery. Surgical strategies and operating room teams have become significantly better at protecting the brain, and new research now is directed toward understanding the neurologic abnormalities that are present in newborns prior to surgical intervention.
Increasingly, researchers are now focused on looking at the in utero origins of brain impairments in children with CHD and trying to understand specific prenatal causes, mechanisms, and potentially modifiable factors. We’re asking what we can do during pregnancy to improve neurodevelopmental outcomes.
Impaired brain growth
The question of how CHD affects blood flow to the fetal brain is an important one. We found some time ago in a study using Doppler ultrasound that 44% of fetuses with CHD had blood flow abnormalities in the middle cerebral artery at some point in the late second or third trimester, suggesting that the blood vessels had dilated to allow more cerebral perfusion. This phenomenon, termed “brain sparing,” is believed to be an autoregulatory mechanism that occurs as a result of diminished oxygen delivery or inadequate blood flow to the brain (Pediatr Cardiol. 2003 Jan;24[5]:436-43).
Subsequent studies have similarly documented abnormal cerebral blood flow in fetuses with various types of congenital heart lesions. What is left to be determined is whether this autoregulatory mechanism is adequate to maintain perfusion in the presence of specific, high-risk CHD.
Abnormalities were more often seen in CHD with obstructed aortic flow, such as hypoplastic left heart syndrome (HLHS) in which the aorta is perfused retrograde through the fetal ductus arteriosus (Circulation. 2010 Jan 4;121:26-33).
Other fetal imaging studies have similarly demonstrated a progressive third-trimester decrease in both cortical gray and white matter and in gyrification (cortical folding) (Cereb Cortex. 2013;23:2932-43), as well as decreased cerebral oxygen delivery and consumption (Circulation. 2015;131:1313-23) in fetuses with severe CHD. It appears that the brain may start out normal in size, but in the third trimester, the accelerated metabolic demands that come with rapid growth and development are not sufficiently met by the fetal cardiovascular circulation in CHD.
In the newborn with CHD, preoperative brain imaging studies have demonstrated structural abnormalities suggesting delayed development (for example, microcephaly and a widened operculum), microstructural abnormalities suggesting abnormal myelination and neuroaxonal development, and lower brain maturity scores (a composite score that combines multiple factors, such as myelination and cortical in-folding, to represent “brain age”).
Moreover, some of the newborn brain imaging studies have correlated brain MRI findings with neonatal neurodevelopmental assessments. For instance, investigators found that full-term newborns with CHD had decreased gray matter brain volume and increased cerebrospinal fluid volume and that these impairments were associated with poor behavioral state regulation and poor visual orienting (J Pediatr. 2014;164:1121-7).
Interestingly, it has been found that the full-term baby with specific complex CHD, including newborns with single ventricle CHD or transposition of the great arteries, is more likely to have a brain maturity score that is equivalent to that of a baby born at 35 weeks’ gestation. This means that, in some infants with CHD, the brain has lagged in growth by about a month, resulting in a pattern of disturbed development and subsequent injury that is similar to that of premature infants.
It also means that infants with CHD and an immature brain are especially vulnerable to brain injury when open-heart surgery is needed. In short, we now appreciate that the brain in patients with CHD is likely more fragile than we previously thought – and that this fragility is prenatal in its origins.
Delivery room planning
Ideally, our goal is to find ways of changing the circulation in utero to improve cerebral oxygenation and blood flow, and, consequently, improve brain development and long-term neurocognitive function. Despite significant efforts in this area, we’re not there yet.
Examples of strategies that are being tested include catheter intervention to open the aortic valve in utero for fetuses with critical aortic stenosis. This procedure currently is being performed to try to prevent progression of the valve abnormality to HLHS, but it has not been determined whether the intervention affects cerebral blood flow. Maternal oxygen therapy has been shown to change cerebral blood flow in the short term for fetuses with HLHS, but its long-term use has not been studied. At the time of birth, to prevent injury in the potentially more fragile brain of the newborn with CHD, what we can do is to identify those fetuses who are more likely to be at risk for hypoxia low cardiac output and hemodynamic compromise in the delivery room, and plan for specialized delivery room and perinatal management beyond standard neonatal care.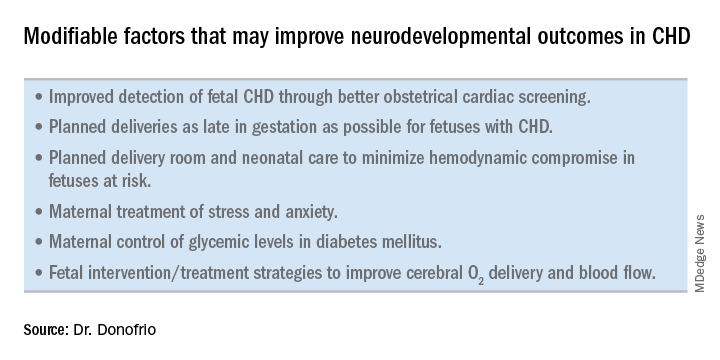
Most newborns with CHD are assigned to Level 1; they have no predicted risk of compromise in the delivery room – or even in the first couple weeks of life – and can deliver at a local hospital with neonatal evaluation and then consult with the pediatric cardiologist. Defects include shunt lesions such as septal defects or mild valve abnormalities.
Patients assigned to Level 2 have minimal risk of compromise in the delivery room but are expected to require postnatal surgery, cardiac catheterization, or another procedure before going home. They can be stabilized by the neonatologist, usually with initiation of a prostaglandin infusion, before transfer to the cardiac center for the planned intervention. Defects include single ventricle CHD and severe Tetralogy of Fallot.
Fetuses assigned to Level 3 and Level 4 are expected to have hemodynamic instability at cord clamping, requiring immediate specialty care in the delivery room that is likely to include urgent cardiac catheterization or surgical intervention. These defects are rare and include diagnoses such as transposition of the great arteries, HLHS with a restrictive or closed foramen ovale, and CHD with associated heart failure and hydrops.
We have found that fetal echocardiography accurately predicts postnatal risk and the need for specialized delivery room care in newborns diagnosed in utero with CHD and that level-of-care protocols ensure safe delivery and optimize fetal outcomes (J Am Soc Echocardiogr. 2015;28:1339-49; Am J Cardiol. 2013;111:737-47).
Such delivery planning, which is coordinated between obstetric, neonatal, cardiology, and surgical services with specialty teams as needed (for example, cardiac intensive care, interventional cardiology, and cardiac surgery), is recommended in a 2014 AHA statement on the diagnosis and treatment of fetal cardiac disease. In recent years it has become the standard of care in many health systems (Circulation. 2014;129[21]:2183-242).
The effect of maternal stress on the in utero environment is also getting increased attention in pediatric cardiology. Alterations in neurocognitive development and fetal and child cardiovascular health are likely to be associated with maternal stress during pregnancy, and studies have shown that maternal stress is high with prenatal diagnoses of CHD. We have to ask: Is stress a modifiable risk factor? There must be ways in which we can do better with prenatal counseling and support after a fetal diagnosis of CHD.
Screening for CHD
Initiating strategies to improve neurodevelopmental outcomes in infants with CHD rests partly on identifying babies with CHD before birth through improved fetal cardiac screening. Research cited in the 2014 AHA statement indicates that nearly all women giving birth to babies with CHD in the United States have obstetric ultrasound examinations in the second or third trimesters, but that only about 30% of the fetuses are diagnosed prenatally.
Current indications for referral for a fetal echocardiogram – in addition to suspicion of a structural heart abnormality on obstetric ultrasound – include maternal factors, such as diabetes mellitus, that raise the risk of CHD above the baseline population risk for low-risk pregnancies.
Women with pregestational diabetes mellitus have a nearly fivefold increase in CHD, compared with the general population (3%-5%), and should be referred for fetal echocardiography. Women with gestational diabetes mellitus have no or minimally increased risk for fetal CHD, but it has been shown that there is an increased risk for cardiac hypertrophy – particularly late in gestation – if glycemic levels are poorly controlled. The 2014 AHA guidelines recommend that fetal echocardiographic evaluation be considered in those who have HbA1c levels greater than 6% in the second half of pregnancy.
Dr. Mary T. Donofrio is a pediatric cardiologist and director of the fetal heart program and critical care delivery program at Children’s National Medical Center, Washington. She reported that she has no disclosures relevant to this article.
How better imaging technology for prenatal diagnoses can improve outcomes
We live during an unprecedented time in the history of ob.gyn. practice. Only a relatively short time ago, the only way ob.gyns. could assess the health of the fetus was through the invasive and risky procedures of the amniocentesis and, later, chorionic villus sampling. A woman who might eventually have had a baby with a congenital abnormality would not have known of her fetus’s defect until after birth, when successful intervention might have been extremely difficult to achieve or even too late. At the time, in utero evaluation could be done only by static, low-resolution sonographic images of the fetus. By today’s standards of imaging technology, these once-revolutionary pictures are almost tantamount to cave paintings.
Therefore, while it is imperative that we employ all available technologies and techniques possible to detect and diagnose potential fetal developmental defects, we must also bear in mind that no test is ever infallible. It is our obligation to provide the very best information based on expert and thorough review.
This month we have invited Mary Donofrio, MD, director of the fetal heart program at Children’s National Medical Center, Washington, to discuss how the latest advances in imaging technology have enabled us to screen for and diagnose congenital heart diseases, and improve outcomes for mother and baby.
Dr. Reece, who specializes in maternal-fetal medicine, is vice president for medical affairs at the University of Maryland, Baltimore, as well as the John Z. and Akiko K. Bowers Distinguished Professor and dean of the school of medicine. Dr. Reece said he had no relevant financial disclosures. He is the medical editor of this column. Contact him at [email protected].
We live during an unprecedented time in the history of ob.gyn. practice. Only a relatively short time ago, the only way ob.gyns. could assess the health of the fetus was through the invasive and risky procedures of the amniocentesis and, later, chorionic villus sampling. A woman who might eventually have had a baby with a congenital abnormality would not have known of her fetus’s defect until after birth, when successful intervention might have been extremely difficult to achieve or even too late. At the time, in utero evaluation could be done only by static, low-resolution sonographic images of the fetus. By today’s standards of imaging technology, these once-revolutionary pictures are almost tantamount to cave paintings.
Therefore, while it is imperative that we employ all available technologies and techniques possible to detect and diagnose potential fetal developmental defects, we must also bear in mind that no test is ever infallible. It is our obligation to provide the very best information based on expert and thorough review.
This month we have invited Mary Donofrio, MD, director of the fetal heart program at Children’s National Medical Center, Washington, to discuss how the latest advances in imaging technology have enabled us to screen for and diagnose congenital heart diseases, and improve outcomes for mother and baby.
Dr. Reece, who specializes in maternal-fetal medicine, is vice president for medical affairs at the University of Maryland, Baltimore, as well as the John Z. and Akiko K. Bowers Distinguished Professor and dean of the school of medicine. Dr. Reece said he had no relevant financial disclosures. He is the medical editor of this column. Contact him at [email protected].
We live during an unprecedented time in the history of ob.gyn. practice. Only a relatively short time ago, the only way ob.gyns. could assess the health of the fetus was through the invasive and risky procedures of the amniocentesis and, later, chorionic villus sampling. A woman who might eventually have had a baby with a congenital abnormality would not have known of her fetus’s defect until after birth, when successful intervention might have been extremely difficult to achieve or even too late. At the time, in utero evaluation could be done only by static, low-resolution sonographic images of the fetus. By today’s standards of imaging technology, these once-revolutionary pictures are almost tantamount to cave paintings.
Therefore, while it is imperative that we employ all available technologies and techniques possible to detect and diagnose potential fetal developmental defects, we must also bear in mind that no test is ever infallible. It is our obligation to provide the very best information based on expert and thorough review.
This month we have invited Mary Donofrio, MD, director of the fetal heart program at Children’s National Medical Center, Washington, to discuss how the latest advances in imaging technology have enabled us to screen for and diagnose congenital heart diseases, and improve outcomes for mother and baby.
Dr. Reece, who specializes in maternal-fetal medicine, is vice president for medical affairs at the University of Maryland, Baltimore, as well as the John Z. and Akiko K. Bowers Distinguished Professor and dean of the school of medicine. Dr. Reece said he had no relevant financial disclosures. He is the medical editor of this column. Contact him at [email protected].
Yale meeting draws cadre of physician-scientists
E. Albert Reece, MD, PhD, MBA, the dean of the University of Maryland School of Medicine, Baltimore, and medical editor of Ob.Gyn. News, has spoken often in the newspaper’s pages about how the fetus has become a visible and intimate patient – one who, “like the mother, can be interrogated, monitored, and sometimes treated before birth.”
Physician-scientists have been instrumental in lifting the cloud of mystery that surrounded the fetus and fetal outcomes. Yet today, in a trend that Dr. Reece and his colleagues call deeply concerning, the number of physician-scientists is declining. “We’re missing out on a workforce that is dedicated to exploring the biologic basis of disease – knowledge that enables the development of targeted therapeutic interventions,” he said in an interview.
Notable Yale physician-scientist alumni have been honored over the years as part of the YOGS meetings, including John C. Hobbins, MD, a former division head of maternal-fetal medicine and a pioneer of ultrasound imaging in the field of obstetrics and gynecology; Roberto Romero, MD, DMedSci, chief of the Perinatology Research Branch at the National Institute of Child Health and Human Development, and editor-in-chief of the American Journal of Obstetrics and Gynecology; and Charles J. Lockwood, MD, dean of the University of South Florida’s Morsani College of Medicine, Tampa, and a former chair of Yale’s ob.gyn. department.
As this year’s honoree, Dr. Reece spoke about the importance of inspiring a new generation of physician-scientists not only within colleges and universities, but also by reaching out to younger students to spark interest in science and research. He recalled being a postdoctoral fellow in perinatology at Yale in the 1980s and being inspired by Dr. Hobbins, whom he credits as his mentor, as well as Dr. Romero, who was finishing his fellowship at Yale while Dr. Reece was beginning his fellowship.
Yale’s department of ob.gyn. and its division of maternal-fetal medicine have had a long history of “firsts” and seminal contributions, including the first ultrasound-guided fetal blood sampling and transfusions in the United States, invention of the fetal heart monitor, the first karyotype in amniotic fluid, the development of postcoital contraception and of methods for early detection of ectopic pregnancies, the discovery of endometrial stem cells and the role that endocrine-disrupting chemicals play in the developmental programming of the uterus, and discovery of the role of cytokines in premature labor and fetal injury.
According to current department chair, Hugh S. Taylor, MD, the 1980s and 1990s were a particularly “exciting time.” Under the tutelage of Dr. Hobbins, who directed both obstetrics and maternal-fetal medicine, obstetrical ultrasound was fast advancing, for instance, and fetoscopy was drawing patients and other physician-scientists from around the world.
“It was an unbelievable time – a magnetic period when many of the things we now take for granted were first being introduced,” said Dr. Reece, who went on after his fellowship to serve as an instructor in ob.gyn. (1982-4), assistant professor (1984-7), and then associate professor (1987-91) at Yale. “It was like going to the symphony and getting to choose the best seat in the house to see the rehearsals all the way through the concert.”
After leaving the Yale faculty and prior to joining the University of Maryland School of Medicine, Dr. Reece served as the chair of obstetrics and gynecology at Temple University School of Medicine, Philadelphia, and then vice chancellor and dean of the University of Arkansas College of Medicine, Little Rock. “Dr. Reece is an incredible bulldog,” said Dr. Hobbins, speaking of the honor given to Dr. Reece at the YOGS meeting. “We could see this right at the beginning at Yale. He latches into something and won’t let it go. He has a work ethic that’s remarkable ... He’s always thinking, ‘How can this be done better?’ ”
Dr. Hobbins, who went on after Yale to a tenure at the University of Colorado at Denver, Aurora, told Ob.Gyn. News that what he remembers “more than anything else, is that we would sit down in a room and just kind of spitball – just brainstorm.”
It is this intellectual curiosity and scientific drive that seems increasingly at risk of being lost, Dr. Hobbins said. “There’s not the same impetus to do a fellowship or to become a physician-scientist or pursue an MD-PhD,” he said. “There just doesn’t seem to be the same oomph to get into the nuts and bolts of how things work, to explore and understand the science. Yes, it has to do with funding. But there’s more to it: We have to somehow stimulate more fire in the belly.”
Dr. Lockwood, who served his fellowship in maternal-fetal medicine at Yale under the guidance of Dr. Hobbins, Dr. Reece, and other faculty, and who later chaired the Yale department of ob.gyn. for 9 years, said that research-rich environments that are “full of inquiry” drive better clinical care.
“The same rigor [gets] applied to the clinical enterprise. Where evidence-based medicine is applicable, it’s done ... and where there are gaps in knowledge, there’s a real spirit of research and inquiry to try to improve care,” Dr. Lockwood said in an interview. “All the great stuff in our health care system is really a direct correlate with the fact that we’ve had this extraordinary research enterprise for so long – most of it funded by the National Institutes of Health, either directly or indirectly.”
The University of Maryland requires all its medical students to take a course in research and critical thinking and to complete a research project. It also runs programs for young students such as a “mini medical school” for underprivileged children who live in nearby neighborhoods. “If you get them excited about science early, and you keep the research continuum going, we believe you’ll have a better chance of recruiting committed physician-scientists into the field,” Dr. Reece said.
The infection has “become an important issue because 10%-20% of women who receive an epidural develop a fever and many of these babies have to have a septic workup and antibiotic treatment,” he said in an e-mail after the meeting. ”Our data indicate that antibiotic administration is not indicated in 40% of cases and the antibiotics currently used do not cover frequent organisms causing infection.”
Dr. Hobbins, who has been using sophisticated imaging techniques to assess subtle changes in fetuses with growth restriction, spoke about the potential value of cardiac size as an indicator of cardiac dysfunction. In utero cardiac dysfunction “sets the tone” for later cardiovascular and neurologic function, he told Ob.Gyn. News. “We think that you can use cardiac size in small babies as a screening tool to tell you whether you need to delve a little further into cardiac function ... Let’s get away from old protocols and rethink other things that are going on in the [small] fetus. Let’s cast a wider net.”
Dr. Lockwood has long been investigating the prevention of recurrent pregnancy loss and preterm delivery, and at the meeting he presented March of Dimes–funded research aimed at identifying mechanisms for dysfunction of the progesterone receptor in premature birth.
Dr. Reece spoke about his research on diabetes in pregnancy and birth defects, and how years of research on diabetes-induced birth defects has shown that maternal hyperglycemia is a teratogen that can trigger a series of developmental fetal defects. “We now have enough information such that we truly have a biomolecular map regarding the precise steps and cascading events which lead to the induction of diabetes-induced birth defects,” said Dr. Reece, who holds a PhD in biochemistry and directs a multimillion-dollar NIH-funded research laboratory at the University of Maryland.
This research began when Dr. Reece asked a question during his fellowship at Yale. “I was struck by the number of birth defects I saw in women with diabetes. I asked Jerry Mahoney, one of the geneticists: Do we know the cause of this? Why is this happening?” he recalled in the interview. “Dr. Mahoney took me to his office, opened his file cabinet and showed me some papers of an [in-vitro rat embryo model], where the rats were made diabetic and the serum seemed to have a way of inducing these birth defects in the embryo. That intrigued me immensely and I thought: I can do this!”
Dr. Reece got his feet wet in an embryology laboratory. As he moved on after his fellowship to join the faculty at Yale, he began directing his own research team – the Diabetes-in-Pregnancy Study Unit.
Dr. Romero said this was the start of “many important contributions to optimize the care of pregnant women with diabetes.” Dr. Reece, he said, has been “able to dissect the role of oxidative stress, program cell death, and lipid metabolism in the genesis of congenital anomalies” in babies of mothers with diabetes.
In other talks at the YOGS meeting, Yale alumnus Ray Bahado-Singh, MD, of Oakwood University, Rochester, Mich., addressed the epigenetics of cardiac dysfunction and the “new frontier” of using epigenetic markers to assess fetal cardiac function. Frank A. Chervenak, MD, of Cornell University, New York, rounded out the meeting by addressing the issue of professionalism and putting the patient first, as well as the professional virtues of self-sacrifice, compassion, and integrity – themes that Dr. Reece frequently cites as integral to both practice and research in ob.gyn.
Clinical care and “the research we’re all doing to assess fetal health both directly and indirectly has to be sitting on a platform of moral, ethical, and solid principles,” said Dr. Reece, who authored a special feature for Ob.Gyn. News – “Obstetrics Moonshots: 50 Years of Discoveries,” on the recent history of obstetrics.
Mary Jane Minkin, MD, a Yale alumna of many levels (medical school through residency) and a longtime Yale faculty member and private-practice ob.gyn. in New Haven, Conn., noted that the YOGS meeting was attended by the 94-year-old Virginia Stuermer, MD, who joined Yale’s ob.gyn. department in 1954 and who is “celebrated within the department” for defying legal barriers to provide patients with contraception and services. “She wanted to come see Dr. Reece,” said Dr. Minkin, who has served as director of YOGS since its inception.
Dr. Stuermer was running the Planned Parenthood clinic in New Haven the day in 1961 when then-department chair Charles Lee Buxton, MD, and Connecticut Planned Parenthood League executive director Estelle Griswold were arrested and jailed. “Everyone knows about the Supreme Court decision, Griswold v. Connecticut [1965], that legalized contraception in the U.S.,” said Dr. Minkin. “But most don’t realize that the doctor who was actually fitting the diaphragms that day was Dr. Stuermer.”
The YOGS reunion preceded a symposium held early in June commemorating the 100-year anniversary of women at Yale Medical School.
E. Albert Reece, MD, PhD, MBA, the dean of the University of Maryland School of Medicine, Baltimore, and medical editor of Ob.Gyn. News, has spoken often in the newspaper’s pages about how the fetus has become a visible and intimate patient – one who, “like the mother, can be interrogated, monitored, and sometimes treated before birth.”
Physician-scientists have been instrumental in lifting the cloud of mystery that surrounded the fetus and fetal outcomes. Yet today, in a trend that Dr. Reece and his colleagues call deeply concerning, the number of physician-scientists is declining. “We’re missing out on a workforce that is dedicated to exploring the biologic basis of disease – knowledge that enables the development of targeted therapeutic interventions,” he said in an interview.
Notable Yale physician-scientist alumni have been honored over the years as part of the YOGS meetings, including John C. Hobbins, MD, a former division head of maternal-fetal medicine and a pioneer of ultrasound imaging in the field of obstetrics and gynecology; Roberto Romero, MD, DMedSci, chief of the Perinatology Research Branch at the National Institute of Child Health and Human Development, and editor-in-chief of the American Journal of Obstetrics and Gynecology; and Charles J. Lockwood, MD, dean of the University of South Florida’s Morsani College of Medicine, Tampa, and a former chair of Yale’s ob.gyn. department.
As this year’s honoree, Dr. Reece spoke about the importance of inspiring a new generation of physician-scientists not only within colleges and universities, but also by reaching out to younger students to spark interest in science and research. He recalled being a postdoctoral fellow in perinatology at Yale in the 1980s and being inspired by Dr. Hobbins, whom he credits as his mentor, as well as Dr. Romero, who was finishing his fellowship at Yale while Dr. Reece was beginning his fellowship.
Yale’s department of ob.gyn. and its division of maternal-fetal medicine have had a long history of “firsts” and seminal contributions, including the first ultrasound-guided fetal blood sampling and transfusions in the United States, invention of the fetal heart monitor, the first karyotype in amniotic fluid, the development of postcoital contraception and of methods for early detection of ectopic pregnancies, the discovery of endometrial stem cells and the role that endocrine-disrupting chemicals play in the developmental programming of the uterus, and discovery of the role of cytokines in premature labor and fetal injury.
According to current department chair, Hugh S. Taylor, MD, the 1980s and 1990s were a particularly “exciting time.” Under the tutelage of Dr. Hobbins, who directed both obstetrics and maternal-fetal medicine, obstetrical ultrasound was fast advancing, for instance, and fetoscopy was drawing patients and other physician-scientists from around the world.
“It was an unbelievable time – a magnetic period when many of the things we now take for granted were first being introduced,” said Dr. Reece, who went on after his fellowship to serve as an instructor in ob.gyn. (1982-4), assistant professor (1984-7), and then associate professor (1987-91) at Yale. “It was like going to the symphony and getting to choose the best seat in the house to see the rehearsals all the way through the concert.”
After leaving the Yale faculty and prior to joining the University of Maryland School of Medicine, Dr. Reece served as the chair of obstetrics and gynecology at Temple University School of Medicine, Philadelphia, and then vice chancellor and dean of the University of Arkansas College of Medicine, Little Rock. “Dr. Reece is an incredible bulldog,” said Dr. Hobbins, speaking of the honor given to Dr. Reece at the YOGS meeting. “We could see this right at the beginning at Yale. He latches into something and won’t let it go. He has a work ethic that’s remarkable ... He’s always thinking, ‘How can this be done better?’ ”
Dr. Hobbins, who went on after Yale to a tenure at the University of Colorado at Denver, Aurora, told Ob.Gyn. News that what he remembers “more than anything else, is that we would sit down in a room and just kind of spitball – just brainstorm.”
It is this intellectual curiosity and scientific drive that seems increasingly at risk of being lost, Dr. Hobbins said. “There’s not the same impetus to do a fellowship or to become a physician-scientist or pursue an MD-PhD,” he said. “There just doesn’t seem to be the same oomph to get into the nuts and bolts of how things work, to explore and understand the science. Yes, it has to do with funding. But there’s more to it: We have to somehow stimulate more fire in the belly.”
Dr. Lockwood, who served his fellowship in maternal-fetal medicine at Yale under the guidance of Dr. Hobbins, Dr. Reece, and other faculty, and who later chaired the Yale department of ob.gyn. for 9 years, said that research-rich environments that are “full of inquiry” drive better clinical care.
“The same rigor [gets] applied to the clinical enterprise. Where evidence-based medicine is applicable, it’s done ... and where there are gaps in knowledge, there’s a real spirit of research and inquiry to try to improve care,” Dr. Lockwood said in an interview. “All the great stuff in our health care system is really a direct correlate with the fact that we’ve had this extraordinary research enterprise for so long – most of it funded by the National Institutes of Health, either directly or indirectly.”
The University of Maryland requires all its medical students to take a course in research and critical thinking and to complete a research project. It also runs programs for young students such as a “mini medical school” for underprivileged children who live in nearby neighborhoods. “If you get them excited about science early, and you keep the research continuum going, we believe you’ll have a better chance of recruiting committed physician-scientists into the field,” Dr. Reece said.
The infection has “become an important issue because 10%-20% of women who receive an epidural develop a fever and many of these babies have to have a septic workup and antibiotic treatment,” he said in an e-mail after the meeting. ”Our data indicate that antibiotic administration is not indicated in 40% of cases and the antibiotics currently used do not cover frequent organisms causing infection.”
Dr. Hobbins, who has been using sophisticated imaging techniques to assess subtle changes in fetuses with growth restriction, spoke about the potential value of cardiac size as an indicator of cardiac dysfunction. In utero cardiac dysfunction “sets the tone” for later cardiovascular and neurologic function, he told Ob.Gyn. News. “We think that you can use cardiac size in small babies as a screening tool to tell you whether you need to delve a little further into cardiac function ... Let’s get away from old protocols and rethink other things that are going on in the [small] fetus. Let’s cast a wider net.”
Dr. Lockwood has long been investigating the prevention of recurrent pregnancy loss and preterm delivery, and at the meeting he presented March of Dimes–funded research aimed at identifying mechanisms for dysfunction of the progesterone receptor in premature birth.
Dr. Reece spoke about his research on diabetes in pregnancy and birth defects, and how years of research on diabetes-induced birth defects has shown that maternal hyperglycemia is a teratogen that can trigger a series of developmental fetal defects. “We now have enough information such that we truly have a biomolecular map regarding the precise steps and cascading events which lead to the induction of diabetes-induced birth defects,” said Dr. Reece, who holds a PhD in biochemistry and directs a multimillion-dollar NIH-funded research laboratory at the University of Maryland.
This research began when Dr. Reece asked a question during his fellowship at Yale. “I was struck by the number of birth defects I saw in women with diabetes. I asked Jerry Mahoney, one of the geneticists: Do we know the cause of this? Why is this happening?” he recalled in the interview. “Dr. Mahoney took me to his office, opened his file cabinet and showed me some papers of an [in-vitro rat embryo model], where the rats were made diabetic and the serum seemed to have a way of inducing these birth defects in the embryo. That intrigued me immensely and I thought: I can do this!”
Dr. Reece got his feet wet in an embryology laboratory. As he moved on after his fellowship to join the faculty at Yale, he began directing his own research team – the Diabetes-in-Pregnancy Study Unit.
Dr. Romero said this was the start of “many important contributions to optimize the care of pregnant women with diabetes.” Dr. Reece, he said, has been “able to dissect the role of oxidative stress, program cell death, and lipid metabolism in the genesis of congenital anomalies” in babies of mothers with diabetes.
In other talks at the YOGS meeting, Yale alumnus Ray Bahado-Singh, MD, of Oakwood University, Rochester, Mich., addressed the epigenetics of cardiac dysfunction and the “new frontier” of using epigenetic markers to assess fetal cardiac function. Frank A. Chervenak, MD, of Cornell University, New York, rounded out the meeting by addressing the issue of professionalism and putting the patient first, as well as the professional virtues of self-sacrifice, compassion, and integrity – themes that Dr. Reece frequently cites as integral to both practice and research in ob.gyn.
Clinical care and “the research we’re all doing to assess fetal health both directly and indirectly has to be sitting on a platform of moral, ethical, and solid principles,” said Dr. Reece, who authored a special feature for Ob.Gyn. News – “Obstetrics Moonshots: 50 Years of Discoveries,” on the recent history of obstetrics.
Mary Jane Minkin, MD, a Yale alumna of many levels (medical school through residency) and a longtime Yale faculty member and private-practice ob.gyn. in New Haven, Conn., noted that the YOGS meeting was attended by the 94-year-old Virginia Stuermer, MD, who joined Yale’s ob.gyn. department in 1954 and who is “celebrated within the department” for defying legal barriers to provide patients with contraception and services. “She wanted to come see Dr. Reece,” said Dr. Minkin, who has served as director of YOGS since its inception.
Dr. Stuermer was running the Planned Parenthood clinic in New Haven the day in 1961 when then-department chair Charles Lee Buxton, MD, and Connecticut Planned Parenthood League executive director Estelle Griswold were arrested and jailed. “Everyone knows about the Supreme Court decision, Griswold v. Connecticut [1965], that legalized contraception in the U.S.,” said Dr. Minkin. “But most don’t realize that the doctor who was actually fitting the diaphragms that day was Dr. Stuermer.”
The YOGS reunion preceded a symposium held early in June commemorating the 100-year anniversary of women at Yale Medical School.
E. Albert Reece, MD, PhD, MBA, the dean of the University of Maryland School of Medicine, Baltimore, and medical editor of Ob.Gyn. News, has spoken often in the newspaper’s pages about how the fetus has become a visible and intimate patient – one who, “like the mother, can be interrogated, monitored, and sometimes treated before birth.”
Physician-scientists have been instrumental in lifting the cloud of mystery that surrounded the fetus and fetal outcomes. Yet today, in a trend that Dr. Reece and his colleagues call deeply concerning, the number of physician-scientists is declining. “We’re missing out on a workforce that is dedicated to exploring the biologic basis of disease – knowledge that enables the development of targeted therapeutic interventions,” he said in an interview.
Notable Yale physician-scientist alumni have been honored over the years as part of the YOGS meetings, including John C. Hobbins, MD, a former division head of maternal-fetal medicine and a pioneer of ultrasound imaging in the field of obstetrics and gynecology; Roberto Romero, MD, DMedSci, chief of the Perinatology Research Branch at the National Institute of Child Health and Human Development, and editor-in-chief of the American Journal of Obstetrics and Gynecology; and Charles J. Lockwood, MD, dean of the University of South Florida’s Morsani College of Medicine, Tampa, and a former chair of Yale’s ob.gyn. department.
As this year’s honoree, Dr. Reece spoke about the importance of inspiring a new generation of physician-scientists not only within colleges and universities, but also by reaching out to younger students to spark interest in science and research. He recalled being a postdoctoral fellow in perinatology at Yale in the 1980s and being inspired by Dr. Hobbins, whom he credits as his mentor, as well as Dr. Romero, who was finishing his fellowship at Yale while Dr. Reece was beginning his fellowship.
Yale’s department of ob.gyn. and its division of maternal-fetal medicine have had a long history of “firsts” and seminal contributions, including the first ultrasound-guided fetal blood sampling and transfusions in the United States, invention of the fetal heart monitor, the first karyotype in amniotic fluid, the development of postcoital contraception and of methods for early detection of ectopic pregnancies, the discovery of endometrial stem cells and the role that endocrine-disrupting chemicals play in the developmental programming of the uterus, and discovery of the role of cytokines in premature labor and fetal injury.
According to current department chair, Hugh S. Taylor, MD, the 1980s and 1990s were a particularly “exciting time.” Under the tutelage of Dr. Hobbins, who directed both obstetrics and maternal-fetal medicine, obstetrical ultrasound was fast advancing, for instance, and fetoscopy was drawing patients and other physician-scientists from around the world.
“It was an unbelievable time – a magnetic period when many of the things we now take for granted were first being introduced,” said Dr. Reece, who went on after his fellowship to serve as an instructor in ob.gyn. (1982-4), assistant professor (1984-7), and then associate professor (1987-91) at Yale. “It was like going to the symphony and getting to choose the best seat in the house to see the rehearsals all the way through the concert.”
After leaving the Yale faculty and prior to joining the University of Maryland School of Medicine, Dr. Reece served as the chair of obstetrics and gynecology at Temple University School of Medicine, Philadelphia, and then vice chancellor and dean of the University of Arkansas College of Medicine, Little Rock. “Dr. Reece is an incredible bulldog,” said Dr. Hobbins, speaking of the honor given to Dr. Reece at the YOGS meeting. “We could see this right at the beginning at Yale. He latches into something and won’t let it go. He has a work ethic that’s remarkable ... He’s always thinking, ‘How can this be done better?’ ”
Dr. Hobbins, who went on after Yale to a tenure at the University of Colorado at Denver, Aurora, told Ob.Gyn. News that what he remembers “more than anything else, is that we would sit down in a room and just kind of spitball – just brainstorm.”
It is this intellectual curiosity and scientific drive that seems increasingly at risk of being lost, Dr. Hobbins said. “There’s not the same impetus to do a fellowship or to become a physician-scientist or pursue an MD-PhD,” he said. “There just doesn’t seem to be the same oomph to get into the nuts and bolts of how things work, to explore and understand the science. Yes, it has to do with funding. But there’s more to it: We have to somehow stimulate more fire in the belly.”
Dr. Lockwood, who served his fellowship in maternal-fetal medicine at Yale under the guidance of Dr. Hobbins, Dr. Reece, and other faculty, and who later chaired the Yale department of ob.gyn. for 9 years, said that research-rich environments that are “full of inquiry” drive better clinical care.
“The same rigor [gets] applied to the clinical enterprise. Where evidence-based medicine is applicable, it’s done ... and where there are gaps in knowledge, there’s a real spirit of research and inquiry to try to improve care,” Dr. Lockwood said in an interview. “All the great stuff in our health care system is really a direct correlate with the fact that we’ve had this extraordinary research enterprise for so long – most of it funded by the National Institutes of Health, either directly or indirectly.”
The University of Maryland requires all its medical students to take a course in research and critical thinking and to complete a research project. It also runs programs for young students such as a “mini medical school” for underprivileged children who live in nearby neighborhoods. “If you get them excited about science early, and you keep the research continuum going, we believe you’ll have a better chance of recruiting committed physician-scientists into the field,” Dr. Reece said.
The infection has “become an important issue because 10%-20% of women who receive an epidural develop a fever and many of these babies have to have a septic workup and antibiotic treatment,” he said in an e-mail after the meeting. ”Our data indicate that antibiotic administration is not indicated in 40% of cases and the antibiotics currently used do not cover frequent organisms causing infection.”
Dr. Hobbins, who has been using sophisticated imaging techniques to assess subtle changes in fetuses with growth restriction, spoke about the potential value of cardiac size as an indicator of cardiac dysfunction. In utero cardiac dysfunction “sets the tone” for later cardiovascular and neurologic function, he told Ob.Gyn. News. “We think that you can use cardiac size in small babies as a screening tool to tell you whether you need to delve a little further into cardiac function ... Let’s get away from old protocols and rethink other things that are going on in the [small] fetus. Let’s cast a wider net.”
Dr. Lockwood has long been investigating the prevention of recurrent pregnancy loss and preterm delivery, and at the meeting he presented March of Dimes–funded research aimed at identifying mechanisms for dysfunction of the progesterone receptor in premature birth.
Dr. Reece spoke about his research on diabetes in pregnancy and birth defects, and how years of research on diabetes-induced birth defects has shown that maternal hyperglycemia is a teratogen that can trigger a series of developmental fetal defects. “We now have enough information such that we truly have a biomolecular map regarding the precise steps and cascading events which lead to the induction of diabetes-induced birth defects,” said Dr. Reece, who holds a PhD in biochemistry and directs a multimillion-dollar NIH-funded research laboratory at the University of Maryland.
This research began when Dr. Reece asked a question during his fellowship at Yale. “I was struck by the number of birth defects I saw in women with diabetes. I asked Jerry Mahoney, one of the geneticists: Do we know the cause of this? Why is this happening?” he recalled in the interview. “Dr. Mahoney took me to his office, opened his file cabinet and showed me some papers of an [in-vitro rat embryo model], where the rats were made diabetic and the serum seemed to have a way of inducing these birth defects in the embryo. That intrigued me immensely and I thought: I can do this!”
Dr. Reece got his feet wet in an embryology laboratory. As he moved on after his fellowship to join the faculty at Yale, he began directing his own research team – the Diabetes-in-Pregnancy Study Unit.
Dr. Romero said this was the start of “many important contributions to optimize the care of pregnant women with diabetes.” Dr. Reece, he said, has been “able to dissect the role of oxidative stress, program cell death, and lipid metabolism in the genesis of congenital anomalies” in babies of mothers with diabetes.
In other talks at the YOGS meeting, Yale alumnus Ray Bahado-Singh, MD, of Oakwood University, Rochester, Mich., addressed the epigenetics of cardiac dysfunction and the “new frontier” of using epigenetic markers to assess fetal cardiac function. Frank A. Chervenak, MD, of Cornell University, New York, rounded out the meeting by addressing the issue of professionalism and putting the patient first, as well as the professional virtues of self-sacrifice, compassion, and integrity – themes that Dr. Reece frequently cites as integral to both practice and research in ob.gyn.
Clinical care and “the research we’re all doing to assess fetal health both directly and indirectly has to be sitting on a platform of moral, ethical, and solid principles,” said Dr. Reece, who authored a special feature for Ob.Gyn. News – “Obstetrics Moonshots: 50 Years of Discoveries,” on the recent history of obstetrics.
Mary Jane Minkin, MD, a Yale alumna of many levels (medical school through residency) and a longtime Yale faculty member and private-practice ob.gyn. in New Haven, Conn., noted that the YOGS meeting was attended by the 94-year-old Virginia Stuermer, MD, who joined Yale’s ob.gyn. department in 1954 and who is “celebrated within the department” for defying legal barriers to provide patients with contraception and services. “She wanted to come see Dr. Reece,” said Dr. Minkin, who has served as director of YOGS since its inception.
Dr. Stuermer was running the Planned Parenthood clinic in New Haven the day in 1961 when then-department chair Charles Lee Buxton, MD, and Connecticut Planned Parenthood League executive director Estelle Griswold were arrested and jailed. “Everyone knows about the Supreme Court decision, Griswold v. Connecticut [1965], that legalized contraception in the U.S.,” said Dr. Minkin. “But most don’t realize that the doctor who was actually fitting the diaphragms that day was Dr. Stuermer.”
The YOGS reunion preceded a symposium held early in June commemorating the 100-year anniversary of women at Yale Medical School.
Thyroid markers linked to risk of gestational diabetes
Thyroid dysfunction early in pregnancy may increase risk of gestational diabetes, results of a longitudinal study suggest.
Increased levels of free triiodothyronine (fT3) and the ratio of fT3 to free thyroxine (fT4) were associated with increased risk of this common metabolic complication of pregnancy, study authors reported in the Journal of Clinical Endocrinology & Metabolism.
“To our knowledge, this is the first study to identify fT3 and the fT3:fT4 ratio measured early in pregnancy as independent risk factors of gestational diabetes,” wrote Shristi Rawal, PhD, of the National Institute of Child Health and Human Development (NICHD) , and her colleagues.
Although routine thyroid function screening during pregnancy remains controversial, Dr. Rawal and colleagues said their results support the “potential benefits” of the practice, particularly in light of other recent evidence suggesting thyroid-related adverse pregnancy outcomes.
The current case control study by Dr. Rawal and her coinvestigators included 107 women with gestational diabetes and 214 nongestational diabetes controls selected from a 12-center pregnancy cohort, which included 2,802 women aged between 18 and 40 years. The thyroid markers fT3, fT4, and thyroid-stimulating hormone (TSH) were measured at four pregnancy visits, including first trimester (weeks 10-14) and second trimester (weeks 15-26).
The fT3:fT4 ratio had the strongest association with gestational diabetes. In the second trimester measurement, women in the highest quartile had an almost 14-fold increase in risk when compared to the lowest quartile, after adjusting for potential confounders including prepregnancy body mass index and diabetes family history (adjusted odds ratio, 13.60; 95% confidence interval, 3.97-46.30), Dr. Rawal and her colleagues reported. The ratio of fT3:fT4 at the first trimester was also associated with increased risk (aOR, 8.63; 95% CI, 2.87-26.00).
Similarly, fT3 was positively associated with gestational diabetes at the first trimester (aOR, 4.25; 95% CI, 1.67-10.80) and second trimester (aOR, 3.89; 95% CI, 1.50-10.10), investigators reported.
By contrast, there was no association between fT4 or TSH and gestational diabetes, they found.
“These findings, in combination with previous evidence of thyroid-related adverse pregnancy outcomes, support the benefits of thyroid screening among pregnant women in early to mid pregnancy,” senior author Cuilin Zhang, MD, MPH, PhD, of the NICHD, said in a press statement.
Thyroid function abnormalities are relatively common in pregnant women and have been associated with obstetric complications such as pregnancy loss and premature delivery, investigators noted.
Previous evidence is sparse regarding a potential link between thyroid dysfunction and gestational diabetes. There are some prospective studies that show women with hypothyroidism have an increased incidence of gestational diabetes, Dr. Rawal and her colleagues wrote. Isolated hypothyroxinema, or normal TSH and low fT4, has also been linked to increased risk in some studies, but not in others, they added.
Support for the study came from NICHD and the American Recovery and Reinvestment Act research grants. The authors reported no conflicts of interest.
SOURCE: Rawal S et al. J Clin Endocrinol Metab. 2018 Jun 7. doi: 10.1210/jc.2017-024421.
Thyroid dysfunction early in pregnancy may increase risk of gestational diabetes, results of a longitudinal study suggest.
Increased levels of free triiodothyronine (fT3) and the ratio of fT3 to free thyroxine (fT4) were associated with increased risk of this common metabolic complication of pregnancy, study authors reported in the Journal of Clinical Endocrinology & Metabolism.
“To our knowledge, this is the first study to identify fT3 and the fT3:fT4 ratio measured early in pregnancy as independent risk factors of gestational diabetes,” wrote Shristi Rawal, PhD, of the National Institute of Child Health and Human Development (NICHD) , and her colleagues.
Although routine thyroid function screening during pregnancy remains controversial, Dr. Rawal and colleagues said their results support the “potential benefits” of the practice, particularly in light of other recent evidence suggesting thyroid-related adverse pregnancy outcomes.
The current case control study by Dr. Rawal and her coinvestigators included 107 women with gestational diabetes and 214 nongestational diabetes controls selected from a 12-center pregnancy cohort, which included 2,802 women aged between 18 and 40 years. The thyroid markers fT3, fT4, and thyroid-stimulating hormone (TSH) were measured at four pregnancy visits, including first trimester (weeks 10-14) and second trimester (weeks 15-26).
The fT3:fT4 ratio had the strongest association with gestational diabetes. In the second trimester measurement, women in the highest quartile had an almost 14-fold increase in risk when compared to the lowest quartile, after adjusting for potential confounders including prepregnancy body mass index and diabetes family history (adjusted odds ratio, 13.60; 95% confidence interval, 3.97-46.30), Dr. Rawal and her colleagues reported. The ratio of fT3:fT4 at the first trimester was also associated with increased risk (aOR, 8.63; 95% CI, 2.87-26.00).
Similarly, fT3 was positively associated with gestational diabetes at the first trimester (aOR, 4.25; 95% CI, 1.67-10.80) and second trimester (aOR, 3.89; 95% CI, 1.50-10.10), investigators reported.
By contrast, there was no association between fT4 or TSH and gestational diabetes, they found.
“These findings, in combination with previous evidence of thyroid-related adverse pregnancy outcomes, support the benefits of thyroid screening among pregnant women in early to mid pregnancy,” senior author Cuilin Zhang, MD, MPH, PhD, of the NICHD, said in a press statement.
Thyroid function abnormalities are relatively common in pregnant women and have been associated with obstetric complications such as pregnancy loss and premature delivery, investigators noted.
Previous evidence is sparse regarding a potential link between thyroid dysfunction and gestational diabetes. There are some prospective studies that show women with hypothyroidism have an increased incidence of gestational diabetes, Dr. Rawal and her colleagues wrote. Isolated hypothyroxinema, or normal TSH and low fT4, has also been linked to increased risk in some studies, but not in others, they added.
Support for the study came from NICHD and the American Recovery and Reinvestment Act research grants. The authors reported no conflicts of interest.
SOURCE: Rawal S et al. J Clin Endocrinol Metab. 2018 Jun 7. doi: 10.1210/jc.2017-024421.
Thyroid dysfunction early in pregnancy may increase risk of gestational diabetes, results of a longitudinal study suggest.
Increased levels of free triiodothyronine (fT3) and the ratio of fT3 to free thyroxine (fT4) were associated with increased risk of this common metabolic complication of pregnancy, study authors reported in the Journal of Clinical Endocrinology & Metabolism.
“To our knowledge, this is the first study to identify fT3 and the fT3:fT4 ratio measured early in pregnancy as independent risk factors of gestational diabetes,” wrote Shristi Rawal, PhD, of the National Institute of Child Health and Human Development (NICHD) , and her colleagues.
Although routine thyroid function screening during pregnancy remains controversial, Dr. Rawal and colleagues said their results support the “potential benefits” of the practice, particularly in light of other recent evidence suggesting thyroid-related adverse pregnancy outcomes.
The current case control study by Dr. Rawal and her coinvestigators included 107 women with gestational diabetes and 214 nongestational diabetes controls selected from a 12-center pregnancy cohort, which included 2,802 women aged between 18 and 40 years. The thyroid markers fT3, fT4, and thyroid-stimulating hormone (TSH) were measured at four pregnancy visits, including first trimester (weeks 10-14) and second trimester (weeks 15-26).
The fT3:fT4 ratio had the strongest association with gestational diabetes. In the second trimester measurement, women in the highest quartile had an almost 14-fold increase in risk when compared to the lowest quartile, after adjusting for potential confounders including prepregnancy body mass index and diabetes family history (adjusted odds ratio, 13.60; 95% confidence interval, 3.97-46.30), Dr. Rawal and her colleagues reported. The ratio of fT3:fT4 at the first trimester was also associated with increased risk (aOR, 8.63; 95% CI, 2.87-26.00).
Similarly, fT3 was positively associated with gestational diabetes at the first trimester (aOR, 4.25; 95% CI, 1.67-10.80) and second trimester (aOR, 3.89; 95% CI, 1.50-10.10), investigators reported.
By contrast, there was no association between fT4 or TSH and gestational diabetes, they found.
“These findings, in combination with previous evidence of thyroid-related adverse pregnancy outcomes, support the benefits of thyroid screening among pregnant women in early to mid pregnancy,” senior author Cuilin Zhang, MD, MPH, PhD, of the NICHD, said in a press statement.
Thyroid function abnormalities are relatively common in pregnant women and have been associated with obstetric complications such as pregnancy loss and premature delivery, investigators noted.
Previous evidence is sparse regarding a potential link between thyroid dysfunction and gestational diabetes. There are some prospective studies that show women with hypothyroidism have an increased incidence of gestational diabetes, Dr. Rawal and her colleagues wrote. Isolated hypothyroxinema, or normal TSH and low fT4, has also been linked to increased risk in some studies, but not in others, they added.
Support for the study came from NICHD and the American Recovery and Reinvestment Act research grants. The authors reported no conflicts of interest.
SOURCE: Rawal S et al. J Clin Endocrinol Metab. 2018 Jun 7. doi: 10.1210/jc.2017-024421.
FROM THE JOURNAL OF CLINICAL ENDOCRINOLOGY & METABOLISM.
Key clinical point: Thyroid dysfunction early in pregnancy may increase risk of gestational diabetes.
Major finding: The triiodothyronine to thyroxine ratio in the second trimester had the strongest association with gestational diabetes (adjusted odds ratio, 13.60; 95% confidence interval, 3.97-46.30).
Study details: A case control study including 107 gestational diabetes cases and 214 nongestational diabetes controls.
Disclosures: The authors had no disclosures. Support for the study came from the National Institute of Child Health and Human Development and the American Recovery and Reinvestment Act research grants.
Source: Rawal S et al. J Clin Endocrinol Metab. 2018 Jun 7. doi: 10.1210/jc.2017-024421.
No link found between fluconazole use and neonatal death risk
Use of oral fluconazole during pregnancy is not associated with an increase in risk of stillbirth or neonatal death, results of a large European cohort study suggest.
The rate of stillbirths was 2.7 per 1,000 fluconazole-exposed pregnancies, versus 3.6 per 1,000 unexposed pregnancies (hazard ratio, 0.76, 95% confidence interval, 0.52-1.10), investigators reported based on an analysis of national registry data including nearly 1.5 million recent pregnancies in Sweden and Norway.
Neonatal deaths occurred in 1.2 per 1,000 exposed pregnancies and 1.7 per 1,000 unexposed pregnancies, investigators added in the report, which appeared in JAMA.
Results were not different for doses of 300 mg or less versus more than 300 mg, said senior researcher Björn Pasternak, MD, PhD, of Karolinska Institutet, Stockholm, and his co-authors.
“Although the data on fluconazole use in pregnancy suggest no increased risk of stillbirth, additional studies should be conducted and the collective body of data scrutinized by drug authorities before recommendations to guide clinical decision making are made, and weighed against the benefits of therapy,” the investigators wrote.
About 4% of pregnant women in the United States take oral fluconazole, even though it is generally discouraged during pregnancy due to concerns that its use may be associated with stillbirth in a previous Danish nationwide register-based study, published in JAMA.
In 2016, investigators similarly found no increased risk of stillbirth in 2,215 fluconazole-exposed women, though they noted the outcome was “relatively rare and the results therefore imprecise.” In a sensitivity analysis, they did find an association between higher doses of fluconazole (i.e., above 300 mg) and stillbirth, with a hazard ratio of 4.10 (95% CI, 1.89-8.90).
The stillbirth analysis in the present study included 10,669 fluconazole-exposed pregnancies from Sweden and Norway, though the number exposed to higher doses was small, Dr. Pasterak and co-authors said in their report.
Although more research and deliberation is needed, this new study does add one novel endpoint to the literature: “The outcome of neonatal death has not been reported previously, to our knowledge.”
Their study was supported by the Thrasher Research Fund, the Magnus Bergvall Foundation, and the Karolinska Institutet Research Foundation. Dr. Pasternak and co-authors reported no conflicts of interest.
SOURCE: Pasternak B, et al. JAMA. 2018 Jun 12;319:22.
Use of oral fluconazole during pregnancy is not associated with an increase in risk of stillbirth or neonatal death, results of a large European cohort study suggest.
The rate of stillbirths was 2.7 per 1,000 fluconazole-exposed pregnancies, versus 3.6 per 1,000 unexposed pregnancies (hazard ratio, 0.76, 95% confidence interval, 0.52-1.10), investigators reported based on an analysis of national registry data including nearly 1.5 million recent pregnancies in Sweden and Norway.
Neonatal deaths occurred in 1.2 per 1,000 exposed pregnancies and 1.7 per 1,000 unexposed pregnancies, investigators added in the report, which appeared in JAMA.
Results were not different for doses of 300 mg or less versus more than 300 mg, said senior researcher Björn Pasternak, MD, PhD, of Karolinska Institutet, Stockholm, and his co-authors.
“Although the data on fluconazole use in pregnancy suggest no increased risk of stillbirth, additional studies should be conducted and the collective body of data scrutinized by drug authorities before recommendations to guide clinical decision making are made, and weighed against the benefits of therapy,” the investigators wrote.
About 4% of pregnant women in the United States take oral fluconazole, even though it is generally discouraged during pregnancy due to concerns that its use may be associated with stillbirth in a previous Danish nationwide register-based study, published in JAMA.
In 2016, investigators similarly found no increased risk of stillbirth in 2,215 fluconazole-exposed women, though they noted the outcome was “relatively rare and the results therefore imprecise.” In a sensitivity analysis, they did find an association between higher doses of fluconazole (i.e., above 300 mg) and stillbirth, with a hazard ratio of 4.10 (95% CI, 1.89-8.90).
The stillbirth analysis in the present study included 10,669 fluconazole-exposed pregnancies from Sweden and Norway, though the number exposed to higher doses was small, Dr. Pasterak and co-authors said in their report.
Although more research and deliberation is needed, this new study does add one novel endpoint to the literature: “The outcome of neonatal death has not been reported previously, to our knowledge.”
Their study was supported by the Thrasher Research Fund, the Magnus Bergvall Foundation, and the Karolinska Institutet Research Foundation. Dr. Pasternak and co-authors reported no conflicts of interest.
SOURCE: Pasternak B, et al. JAMA. 2018 Jun 12;319:22.
Use of oral fluconazole during pregnancy is not associated with an increase in risk of stillbirth or neonatal death, results of a large European cohort study suggest.
The rate of stillbirths was 2.7 per 1,000 fluconazole-exposed pregnancies, versus 3.6 per 1,000 unexposed pregnancies (hazard ratio, 0.76, 95% confidence interval, 0.52-1.10), investigators reported based on an analysis of national registry data including nearly 1.5 million recent pregnancies in Sweden and Norway.
Neonatal deaths occurred in 1.2 per 1,000 exposed pregnancies and 1.7 per 1,000 unexposed pregnancies, investigators added in the report, which appeared in JAMA.
Results were not different for doses of 300 mg or less versus more than 300 mg, said senior researcher Björn Pasternak, MD, PhD, of Karolinska Institutet, Stockholm, and his co-authors.
“Although the data on fluconazole use in pregnancy suggest no increased risk of stillbirth, additional studies should be conducted and the collective body of data scrutinized by drug authorities before recommendations to guide clinical decision making are made, and weighed against the benefits of therapy,” the investigators wrote.
About 4% of pregnant women in the United States take oral fluconazole, even though it is generally discouraged during pregnancy due to concerns that its use may be associated with stillbirth in a previous Danish nationwide register-based study, published in JAMA.
In 2016, investigators similarly found no increased risk of stillbirth in 2,215 fluconazole-exposed women, though they noted the outcome was “relatively rare and the results therefore imprecise.” In a sensitivity analysis, they did find an association between higher doses of fluconazole (i.e., above 300 mg) and stillbirth, with a hazard ratio of 4.10 (95% CI, 1.89-8.90).
The stillbirth analysis in the present study included 10,669 fluconazole-exposed pregnancies from Sweden and Norway, though the number exposed to higher doses was small, Dr. Pasterak and co-authors said in their report.
Although more research and deliberation is needed, this new study does add one novel endpoint to the literature: “The outcome of neonatal death has not been reported previously, to our knowledge.”
Their study was supported by the Thrasher Research Fund, the Magnus Bergvall Foundation, and the Karolinska Institutet Research Foundation. Dr. Pasternak and co-authors reported no conflicts of interest.
SOURCE: Pasternak B, et al. JAMA. 2018 Jun 12;319:22.