User login
Chronic pain patients swapping opioids for medical cannabis
new research shows.
“That patients report substituting cannabis for pain medicines so much really underscores the need for research on the benefits and risks of using cannabis for chronic pain,” lead author Mark C. Bicket, MD, PhD, assistant professor, department of anesthesiology, and director, Opioid Prescribing Engagement Network, University of Michigan, Ann Arbor, said in an interview.
However, he added, the question is whether they’re turning to cannabis and away from other pain treatments. “What’s not clear and one of the gaps that we wanted to address in the study was if medical cannabis use is changing the use of other treatments for chronic pain,” said Dr. Bicket.
The study was published online in JAMA Network Open.
Decreased opioid use
The survey included a representative sample of 1724 American adults aged 18 years or older with chronic noncancer pain living in areas with a medical cannabis program.
Respondents were asked about their use of three categories of pain treatments. This included medical cannabis; pharmacologic treatments including prescription opioids, nonopioid analgesics, and over-the-counter analgesics; and common nonpharmacologic treatments such as physical therapy, meditation, and cognitive-behavioral therapy (CBT).
Just over 96% of respondents completed the full survey. About 57% of the sample was female and the mean age of the study sample was 52.3 years.
Among study participants, 31% (95% CI, 28.2% - 34.1%) reported having ever used cannabis to manage pain; 25.9% (95% confidence interval, 23.2%-28.8%) reported use in the past 12 months, and 23.2% (95% CI, 20.6%-26%) reported use in the past 30 days.
“This translates into a large number of individuals who are using cannabis in an intended medical way” to treat chronic condition such as low back pain, migraine, and fibromyalgia, said Dr. Bicket.
More than half of survey respondents reported their medical cannabis use led to a decrease in prescription opioid use, prescription nonopioid use and use of over-the-counter medications.
Dr. Bicket noted “almost no one” said medical cannabis use led to higher use of these drugs.
As for nonpharmacologic treatments, 38.7% reported their use of cannabis led to decreased use of physical therapy, 19.1% to lower use of meditation, and 26% to less CBT. At the same time, 5.9%, 23.7% and 17.1%, respectively, reported it led to increased use of physical therapy, meditation, and CBT.
Medical cannabis is regulated at a state level. On a federal level, it’s considered a Schedule I substance, which means it’s deemed not to have a therapeutic use, although some groups are trying to change that categorization, said Dr. Bicket.
As a result, cannabis products “are quite variable” in terms of how they’re used (smoked, eaten etc.) and in their composition, including percentage of cannabidiol and tetrahydrocannabinol.
“We really don’t have a good sense of the relative risks and benefits that could come from cannabis as a treatment for chronic pain,” said Dr. Bicket. “As a physician, it’s difficult to have discussions with patients because I’m not able to understand the products they’re using based on this regulatory environment we have.”
He added clinicians “are operating in an area of uncertainty right now.”
What’s needed is research to determine how safe and effective medical cannabis is for chronic pain, he said.
Pain a leading indication
Commenting on the findings, Jason W. Busse, PhD, professor, department of anesthesia, and associate director, Centre for Medicinal Cannabis Research, McMaster University, Hamilton, Ont., said the study reinforces results of some prior research.
“It gives us current information certainly highlighting the high rate of use of medical cannabis among individuals with chronic pain once it becomes legally available.”
In addition, this high rate of use “means we desperately need information about the benefits and harms” of medical marijuana, he said.
Dr. Busse noted the survey didn’t provide information on the types of cannabis being used or the mode of administration. Oil drops and sprays cause less pulmonary harm than smoked versions, he said. It’s also not clear from the survey if participants are taking formulations with high levels of tetrahydrocannabinol that are associated with greater risk of harm.
He noted cannabis may interact with prescription drugs to make them less effective or, in some cases, to augment their adverse effects.
Dr. Busse pointed out some patients could be using fewer opioids because providers are under “enormous pressure” to reduce prescriptions of these drugs in the wake of spikes in opioid overdoses and deaths.
Chronic pain is “absolutely the leading indication” for medical marijuana, said Dr. Busse. U.S. reimbursement data suggest up to 65% of individuals get cannabis to treat a listed indication for chronic pain.
He said he hopes this new study will increase interest in funding new trials “so we can have better evidence to guide practice to help patients make decisions.”
The study received support from the National Institute on Drug Abuse. Dr. Bicket reported receiving personal fees from Axial Healthcare as well as grants from the National Institutes of Health, the Centers for Disease Control and Prevention, Michigan Department of Health and Human Services, Arnold Foundation, and the Patient-Centered Outcomes Research Institute outside the submitted work. Dr. Busse reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
new research shows.
“That patients report substituting cannabis for pain medicines so much really underscores the need for research on the benefits and risks of using cannabis for chronic pain,” lead author Mark C. Bicket, MD, PhD, assistant professor, department of anesthesiology, and director, Opioid Prescribing Engagement Network, University of Michigan, Ann Arbor, said in an interview.
However, he added, the question is whether they’re turning to cannabis and away from other pain treatments. “What’s not clear and one of the gaps that we wanted to address in the study was if medical cannabis use is changing the use of other treatments for chronic pain,” said Dr. Bicket.
The study was published online in JAMA Network Open.
Decreased opioid use
The survey included a representative sample of 1724 American adults aged 18 years or older with chronic noncancer pain living in areas with a medical cannabis program.
Respondents were asked about their use of three categories of pain treatments. This included medical cannabis; pharmacologic treatments including prescription opioids, nonopioid analgesics, and over-the-counter analgesics; and common nonpharmacologic treatments such as physical therapy, meditation, and cognitive-behavioral therapy (CBT).
Just over 96% of respondents completed the full survey. About 57% of the sample was female and the mean age of the study sample was 52.3 years.
Among study participants, 31% (95% CI, 28.2% - 34.1%) reported having ever used cannabis to manage pain; 25.9% (95% confidence interval, 23.2%-28.8%) reported use in the past 12 months, and 23.2% (95% CI, 20.6%-26%) reported use in the past 30 days.
“This translates into a large number of individuals who are using cannabis in an intended medical way” to treat chronic condition such as low back pain, migraine, and fibromyalgia, said Dr. Bicket.
More than half of survey respondents reported their medical cannabis use led to a decrease in prescription opioid use, prescription nonopioid use and use of over-the-counter medications.
Dr. Bicket noted “almost no one” said medical cannabis use led to higher use of these drugs.
As for nonpharmacologic treatments, 38.7% reported their use of cannabis led to decreased use of physical therapy, 19.1% to lower use of meditation, and 26% to less CBT. At the same time, 5.9%, 23.7% and 17.1%, respectively, reported it led to increased use of physical therapy, meditation, and CBT.
Medical cannabis is regulated at a state level. On a federal level, it’s considered a Schedule I substance, which means it’s deemed not to have a therapeutic use, although some groups are trying to change that categorization, said Dr. Bicket.
As a result, cannabis products “are quite variable” in terms of how they’re used (smoked, eaten etc.) and in their composition, including percentage of cannabidiol and tetrahydrocannabinol.
“We really don’t have a good sense of the relative risks and benefits that could come from cannabis as a treatment for chronic pain,” said Dr. Bicket. “As a physician, it’s difficult to have discussions with patients because I’m not able to understand the products they’re using based on this regulatory environment we have.”
He added clinicians “are operating in an area of uncertainty right now.”
What’s needed is research to determine how safe and effective medical cannabis is for chronic pain, he said.
Pain a leading indication
Commenting on the findings, Jason W. Busse, PhD, professor, department of anesthesia, and associate director, Centre for Medicinal Cannabis Research, McMaster University, Hamilton, Ont., said the study reinforces results of some prior research.
“It gives us current information certainly highlighting the high rate of use of medical cannabis among individuals with chronic pain once it becomes legally available.”
In addition, this high rate of use “means we desperately need information about the benefits and harms” of medical marijuana, he said.
Dr. Busse noted the survey didn’t provide information on the types of cannabis being used or the mode of administration. Oil drops and sprays cause less pulmonary harm than smoked versions, he said. It’s also not clear from the survey if participants are taking formulations with high levels of tetrahydrocannabinol that are associated with greater risk of harm.
He noted cannabis may interact with prescription drugs to make them less effective or, in some cases, to augment their adverse effects.
Dr. Busse pointed out some patients could be using fewer opioids because providers are under “enormous pressure” to reduce prescriptions of these drugs in the wake of spikes in opioid overdoses and deaths.
Chronic pain is “absolutely the leading indication” for medical marijuana, said Dr. Busse. U.S. reimbursement data suggest up to 65% of individuals get cannabis to treat a listed indication for chronic pain.
He said he hopes this new study will increase interest in funding new trials “so we can have better evidence to guide practice to help patients make decisions.”
The study received support from the National Institute on Drug Abuse. Dr. Bicket reported receiving personal fees from Axial Healthcare as well as grants from the National Institutes of Health, the Centers for Disease Control and Prevention, Michigan Department of Health and Human Services, Arnold Foundation, and the Patient-Centered Outcomes Research Institute outside the submitted work. Dr. Busse reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
new research shows.
“That patients report substituting cannabis for pain medicines so much really underscores the need for research on the benefits and risks of using cannabis for chronic pain,” lead author Mark C. Bicket, MD, PhD, assistant professor, department of anesthesiology, and director, Opioid Prescribing Engagement Network, University of Michigan, Ann Arbor, said in an interview.
However, he added, the question is whether they’re turning to cannabis and away from other pain treatments. “What’s not clear and one of the gaps that we wanted to address in the study was if medical cannabis use is changing the use of other treatments for chronic pain,” said Dr. Bicket.
The study was published online in JAMA Network Open.
Decreased opioid use
The survey included a representative sample of 1724 American adults aged 18 years or older with chronic noncancer pain living in areas with a medical cannabis program.
Respondents were asked about their use of three categories of pain treatments. This included medical cannabis; pharmacologic treatments including prescription opioids, nonopioid analgesics, and over-the-counter analgesics; and common nonpharmacologic treatments such as physical therapy, meditation, and cognitive-behavioral therapy (CBT).
Just over 96% of respondents completed the full survey. About 57% of the sample was female and the mean age of the study sample was 52.3 years.
Among study participants, 31% (95% CI, 28.2% - 34.1%) reported having ever used cannabis to manage pain; 25.9% (95% confidence interval, 23.2%-28.8%) reported use in the past 12 months, and 23.2% (95% CI, 20.6%-26%) reported use in the past 30 days.
“This translates into a large number of individuals who are using cannabis in an intended medical way” to treat chronic condition such as low back pain, migraine, and fibromyalgia, said Dr. Bicket.
More than half of survey respondents reported their medical cannabis use led to a decrease in prescription opioid use, prescription nonopioid use and use of over-the-counter medications.
Dr. Bicket noted “almost no one” said medical cannabis use led to higher use of these drugs.
As for nonpharmacologic treatments, 38.7% reported their use of cannabis led to decreased use of physical therapy, 19.1% to lower use of meditation, and 26% to less CBT. At the same time, 5.9%, 23.7% and 17.1%, respectively, reported it led to increased use of physical therapy, meditation, and CBT.
Medical cannabis is regulated at a state level. On a federal level, it’s considered a Schedule I substance, which means it’s deemed not to have a therapeutic use, although some groups are trying to change that categorization, said Dr. Bicket.
As a result, cannabis products “are quite variable” in terms of how they’re used (smoked, eaten etc.) and in their composition, including percentage of cannabidiol and tetrahydrocannabinol.
“We really don’t have a good sense of the relative risks and benefits that could come from cannabis as a treatment for chronic pain,” said Dr. Bicket. “As a physician, it’s difficult to have discussions with patients because I’m not able to understand the products they’re using based on this regulatory environment we have.”
He added clinicians “are operating in an area of uncertainty right now.”
What’s needed is research to determine how safe and effective medical cannabis is for chronic pain, he said.
Pain a leading indication
Commenting on the findings, Jason W. Busse, PhD, professor, department of anesthesia, and associate director, Centre for Medicinal Cannabis Research, McMaster University, Hamilton, Ont., said the study reinforces results of some prior research.
“It gives us current information certainly highlighting the high rate of use of medical cannabis among individuals with chronic pain once it becomes legally available.”
In addition, this high rate of use “means we desperately need information about the benefits and harms” of medical marijuana, he said.
Dr. Busse noted the survey didn’t provide information on the types of cannabis being used or the mode of administration. Oil drops and sprays cause less pulmonary harm than smoked versions, he said. It’s also not clear from the survey if participants are taking formulations with high levels of tetrahydrocannabinol that are associated with greater risk of harm.
He noted cannabis may interact with prescription drugs to make them less effective or, in some cases, to augment their adverse effects.
Dr. Busse pointed out some patients could be using fewer opioids because providers are under “enormous pressure” to reduce prescriptions of these drugs in the wake of spikes in opioid overdoses and deaths.
Chronic pain is “absolutely the leading indication” for medical marijuana, said Dr. Busse. U.S. reimbursement data suggest up to 65% of individuals get cannabis to treat a listed indication for chronic pain.
He said he hopes this new study will increase interest in funding new trials “so we can have better evidence to guide practice to help patients make decisions.”
The study received support from the National Institute on Drug Abuse. Dr. Bicket reported receiving personal fees from Axial Healthcare as well as grants from the National Institutes of Health, the Centers for Disease Control and Prevention, Michigan Department of Health and Human Services, Arnold Foundation, and the Patient-Centered Outcomes Research Institute outside the submitted work. Dr. Busse reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM JAMA NETWORK OPEN
Screen all patients for cannabis use before surgery: Guideline
All patients who undergo procedures that require regional or general anesthesia should be asked if, how often, and in what forms they use the drug, according to recommendations from the American Society of Regional Anesthesia and Pain Medicine.
One reason: Patients who regularly use cannabis may experience worse pain and nausea after surgery and may require more opioid analgesia, the group said.
The society’s recommendations – published in Regional Anesthesia and Pain Medicine – are the first guidelines in the United States to cover cannabis use as it relates to surgery, the group said.
Possible interactions
Use of cannabis has increased in recent years, and researchers have been concerned that the drug may interact with anesthesia and complicate pain management. Few studies have evaluated interactions between cannabis and anesthetic agents, however, according to the authors of the new guidelines.
“With the rising prevalence of both medical and recreational cannabis use in the general population, anesthesiologists, surgeons, and perioperative physicians must have an understanding of the effects of cannabis on physiology in order to provide safe perioperative care,” the guideline said.
“Before surgery, anesthesiologists should ask patients if they use cannabis – whether medicinally or recreationally – and be prepared to possibly change the anesthesia plan or delay the procedure in certain situations,” Samer Narouze, MD, PhD, ASRA president and senior author of the guidelines, said in a news release about the recommendations.
Although some patients may use cannabis to relieve pain, research shows that “regular users may have more pain and nausea after surgery, not less, and may need more medications, including opioids, to manage the discomfort,” said Dr. Narouze, chairman of the Center for Pain Medicine at Western Reserve Hospital in Cuyahoga Falls, Ohio.
Risks for vomiting, heart attack
The new recommendations were created by a committee of 13 experts, including anesthesiologists, chronic pain physicians, and a patient advocate. Shalini Shah, MD, vice chair of anesthesiology at the University of California, Irvine, was lead author of the document.
Four of 21 recommendations were classified as grade A, meaning that following them would be expected to provide substantial benefits. Those recommendations are to screen all patients before surgery; postpone elective surgery for patients who have altered mental status or impaired decision-making capacity at the time of surgery; counsel frequent, heavy users about the potential for cannabis use to impair postoperative pain control; and counsel pregnant patients about the risks of cannabis use to unborn children.
The authors cited studies to support their recommendations, including one showing that long-term cannabis use was associated with a 20% increase in the incidence of postoperative nausea and vomiting, a leading complaint of surgery patients. Other research has shown that cannabis use is linked to more pain and use of opioids after surgery.
Other recommendations include delaying elective surgery for at least 2 hours after a patient has smoked cannabis, owing to an increased risk for heart attack, and considering adjustment of ventilation settings during surgery for regular smokers of cannabis. Research has shown that smoking cannabis may be a rare trigger for myocardial infarction and is associated with airway inflammation and self-reported respiratory symptoms.
Nevertheless, doctors should not conduct universal toxicology screening, given a lack of evidence supporting this practice, the guideline stated.
The authors did not have enough information to make recommendations about reducing cannabis use before surgery or adjusting opioid prescriptions after surgery for patients who use cannabis, they said.
Kenneth Finn, MD, president of the American Board of Pain Medicine, welcomed the publication of the new guidelines. Dr. Finn, who practices at Springs Rehabilitation in Colorado Springs, has edited a textbook about cannabis in medicine and founded the International Academy on the Science and Impact of Cannabis.
“The vast majority of medical providers really have no idea about cannabis and what its impacts are on the human body,” Dr. Finn said.
For one, it can interact with numerous other drugs, including warfarin.
Guideline coauthor Eugene R. Viscusi, MD, professor of anesthesiology at the Sidney Kimmel Medical College, Philadelphia, emphasized that, while cannabis may be perceived as “natural,” it should not be considered differently from manufactured drugs.
Cannabis and cannabinoids represent “a class of very potent and pharmacologically active compounds,” Dr. Viscusi said in an interview. While researchers continue to assess possible medically beneficial effects of cannabis compounds, clinicians also need to be aware of the risks.
“The literature continues to emerge, and while we are always hopeful for good news, as physicians, we need to be very well versed on potential risks, especially in a high-risk situation like surgery,” he said.
Dr. Shah has consulted for companies that develop medical devices and drugs. Dr. Finn is the editor of the textbook, “Cannabis in Medicine: An Evidence-Based Approach” (Springer: New York, 2020), for which he receives royalties.
A version of this article first appeared on Medscape.com.
All patients who undergo procedures that require regional or general anesthesia should be asked if, how often, and in what forms they use the drug, according to recommendations from the American Society of Regional Anesthesia and Pain Medicine.
One reason: Patients who regularly use cannabis may experience worse pain and nausea after surgery and may require more opioid analgesia, the group said.
The society’s recommendations – published in Regional Anesthesia and Pain Medicine – are the first guidelines in the United States to cover cannabis use as it relates to surgery, the group said.
Possible interactions
Use of cannabis has increased in recent years, and researchers have been concerned that the drug may interact with anesthesia and complicate pain management. Few studies have evaluated interactions between cannabis and anesthetic agents, however, according to the authors of the new guidelines.
“With the rising prevalence of both medical and recreational cannabis use in the general population, anesthesiologists, surgeons, and perioperative physicians must have an understanding of the effects of cannabis on physiology in order to provide safe perioperative care,” the guideline said.
“Before surgery, anesthesiologists should ask patients if they use cannabis – whether medicinally or recreationally – and be prepared to possibly change the anesthesia plan or delay the procedure in certain situations,” Samer Narouze, MD, PhD, ASRA president and senior author of the guidelines, said in a news release about the recommendations.
Although some patients may use cannabis to relieve pain, research shows that “regular users may have more pain and nausea after surgery, not less, and may need more medications, including opioids, to manage the discomfort,” said Dr. Narouze, chairman of the Center for Pain Medicine at Western Reserve Hospital in Cuyahoga Falls, Ohio.
Risks for vomiting, heart attack
The new recommendations were created by a committee of 13 experts, including anesthesiologists, chronic pain physicians, and a patient advocate. Shalini Shah, MD, vice chair of anesthesiology at the University of California, Irvine, was lead author of the document.
Four of 21 recommendations were classified as grade A, meaning that following them would be expected to provide substantial benefits. Those recommendations are to screen all patients before surgery; postpone elective surgery for patients who have altered mental status or impaired decision-making capacity at the time of surgery; counsel frequent, heavy users about the potential for cannabis use to impair postoperative pain control; and counsel pregnant patients about the risks of cannabis use to unborn children.
The authors cited studies to support their recommendations, including one showing that long-term cannabis use was associated with a 20% increase in the incidence of postoperative nausea and vomiting, a leading complaint of surgery patients. Other research has shown that cannabis use is linked to more pain and use of opioids after surgery.
Other recommendations include delaying elective surgery for at least 2 hours after a patient has smoked cannabis, owing to an increased risk for heart attack, and considering adjustment of ventilation settings during surgery for regular smokers of cannabis. Research has shown that smoking cannabis may be a rare trigger for myocardial infarction and is associated with airway inflammation and self-reported respiratory symptoms.
Nevertheless, doctors should not conduct universal toxicology screening, given a lack of evidence supporting this practice, the guideline stated.
The authors did not have enough information to make recommendations about reducing cannabis use before surgery or adjusting opioid prescriptions after surgery for patients who use cannabis, they said.
Kenneth Finn, MD, president of the American Board of Pain Medicine, welcomed the publication of the new guidelines. Dr. Finn, who practices at Springs Rehabilitation in Colorado Springs, has edited a textbook about cannabis in medicine and founded the International Academy on the Science and Impact of Cannabis.
“The vast majority of medical providers really have no idea about cannabis and what its impacts are on the human body,” Dr. Finn said.
For one, it can interact with numerous other drugs, including warfarin.
Guideline coauthor Eugene R. Viscusi, MD, professor of anesthesiology at the Sidney Kimmel Medical College, Philadelphia, emphasized that, while cannabis may be perceived as “natural,” it should not be considered differently from manufactured drugs.
Cannabis and cannabinoids represent “a class of very potent and pharmacologically active compounds,” Dr. Viscusi said in an interview. While researchers continue to assess possible medically beneficial effects of cannabis compounds, clinicians also need to be aware of the risks.
“The literature continues to emerge, and while we are always hopeful for good news, as physicians, we need to be very well versed on potential risks, especially in a high-risk situation like surgery,” he said.
Dr. Shah has consulted for companies that develop medical devices and drugs. Dr. Finn is the editor of the textbook, “Cannabis in Medicine: An Evidence-Based Approach” (Springer: New York, 2020), for which he receives royalties.
A version of this article first appeared on Medscape.com.
All patients who undergo procedures that require regional or general anesthesia should be asked if, how often, and in what forms they use the drug, according to recommendations from the American Society of Regional Anesthesia and Pain Medicine.
One reason: Patients who regularly use cannabis may experience worse pain and nausea after surgery and may require more opioid analgesia, the group said.
The society’s recommendations – published in Regional Anesthesia and Pain Medicine – are the first guidelines in the United States to cover cannabis use as it relates to surgery, the group said.
Possible interactions
Use of cannabis has increased in recent years, and researchers have been concerned that the drug may interact with anesthesia and complicate pain management. Few studies have evaluated interactions between cannabis and anesthetic agents, however, according to the authors of the new guidelines.
“With the rising prevalence of both medical and recreational cannabis use in the general population, anesthesiologists, surgeons, and perioperative physicians must have an understanding of the effects of cannabis on physiology in order to provide safe perioperative care,” the guideline said.
“Before surgery, anesthesiologists should ask patients if they use cannabis – whether medicinally or recreationally – and be prepared to possibly change the anesthesia plan or delay the procedure in certain situations,” Samer Narouze, MD, PhD, ASRA president and senior author of the guidelines, said in a news release about the recommendations.
Although some patients may use cannabis to relieve pain, research shows that “regular users may have more pain and nausea after surgery, not less, and may need more medications, including opioids, to manage the discomfort,” said Dr. Narouze, chairman of the Center for Pain Medicine at Western Reserve Hospital in Cuyahoga Falls, Ohio.
Risks for vomiting, heart attack
The new recommendations were created by a committee of 13 experts, including anesthesiologists, chronic pain physicians, and a patient advocate. Shalini Shah, MD, vice chair of anesthesiology at the University of California, Irvine, was lead author of the document.
Four of 21 recommendations were classified as grade A, meaning that following them would be expected to provide substantial benefits. Those recommendations are to screen all patients before surgery; postpone elective surgery for patients who have altered mental status or impaired decision-making capacity at the time of surgery; counsel frequent, heavy users about the potential for cannabis use to impair postoperative pain control; and counsel pregnant patients about the risks of cannabis use to unborn children.
The authors cited studies to support their recommendations, including one showing that long-term cannabis use was associated with a 20% increase in the incidence of postoperative nausea and vomiting, a leading complaint of surgery patients. Other research has shown that cannabis use is linked to more pain and use of opioids after surgery.
Other recommendations include delaying elective surgery for at least 2 hours after a patient has smoked cannabis, owing to an increased risk for heart attack, and considering adjustment of ventilation settings during surgery for regular smokers of cannabis. Research has shown that smoking cannabis may be a rare trigger for myocardial infarction and is associated with airway inflammation and self-reported respiratory symptoms.
Nevertheless, doctors should not conduct universal toxicology screening, given a lack of evidence supporting this practice, the guideline stated.
The authors did not have enough information to make recommendations about reducing cannabis use before surgery or adjusting opioid prescriptions after surgery for patients who use cannabis, they said.
Kenneth Finn, MD, president of the American Board of Pain Medicine, welcomed the publication of the new guidelines. Dr. Finn, who practices at Springs Rehabilitation in Colorado Springs, has edited a textbook about cannabis in medicine and founded the International Academy on the Science and Impact of Cannabis.
“The vast majority of medical providers really have no idea about cannabis and what its impacts are on the human body,” Dr. Finn said.
For one, it can interact with numerous other drugs, including warfarin.
Guideline coauthor Eugene R. Viscusi, MD, professor of anesthesiology at the Sidney Kimmel Medical College, Philadelphia, emphasized that, while cannabis may be perceived as “natural,” it should not be considered differently from manufactured drugs.
Cannabis and cannabinoids represent “a class of very potent and pharmacologically active compounds,” Dr. Viscusi said in an interview. While researchers continue to assess possible medically beneficial effects of cannabis compounds, clinicians also need to be aware of the risks.
“The literature continues to emerge, and while we are always hopeful for good news, as physicians, we need to be very well versed on potential risks, especially in a high-risk situation like surgery,” he said.
Dr. Shah has consulted for companies that develop medical devices and drugs. Dr. Finn is the editor of the textbook, “Cannabis in Medicine: An Evidence-Based Approach” (Springer: New York, 2020), for which he receives royalties.
A version of this article first appeared on Medscape.com.
FROM REGIONAL ANETHESIA AND MEDICINE
Two exercise interventions may ease acute, subacute spine pain
Two conservative interventions are effective for treating acute and subacute spine pain, new research suggests.
Results from the SPINE CARE randomized controlled trial showed that 6-8 weeks of an individualized postural therapy (IPT) or a multidisciplinary biopsychosocial intervention known as ICE (identify, coordinate, and enhance) that includes physical therapy were associated with small but statistically significant reductions in pain-related disability at 3 months compared with usual care.
In addition, spine-related health care spending did not differ significantly between ICE and usual care. However, IPT significantly increased spending compared with usual care.
– long after the interventions were over,” lead author Niteesh K. Choudhry, MD, PhD, Brigham and Women’s Hospital and Harvard Medical School, Boston, told this news organization.
The findings were published online in JAMA.
Common complaint
Spine pain is defined as pain that occurs in the neck or back, the investigators noted. It “accounted for more health spending than any other health condition in the U.S. in 2016,” they added.
“Spine pain is an exceptionally common reason for patients to visit their primary care providers,” Dr. Choudhry said.
The SPINE CARE trial enrolled 2,971 adults (60% were women; mean age was 51 years) with back or neck pain that had lasted less than 12 weeks. All were randomly allocated to usual care (no intervention, n = 992) or to the ICE (n = 829) or IPT (n = 1150) interventions.
The ICE care model stratifies patients on the basis of their risk of progression from acute to chronic pain and addresses biopsychosocial contributors to pain. Low-risk patients received one physical therapy (PT) visit and one coaching call, while higher-risk patients received three PT visits, three coaching calls, and one e-consultation.
The IPT intervention, which was delivered in 8 weekly sessions, focuses on postural realignment. IPT also emphasizes self-efficacy and self-management, including daily exercises to improve postural control, coordination, and muscle balance.
Results at 3 months showed that both the ICE and IPT groups improved significantly more in Oswestry Disability Index (ODI) scores than in the usual care group (ICE, 31.2 to 15.4; IPT, 29.3 to 15.4; usual care, 28.9 to 19.5).
At 3 months, the absolute difference in ODI score vs. usual care was −5.8 for ICE (95% confidence interval [CI], −7.7 to −3.9; P < .001) and −4.3 for IPT (95% CI, −5.9 to −2.6; P < .001) for IPT.
Both interventions reduced resource utilization, such as diagnostic imaging, procedures, and specialist visits, Dr. Choudhry reported. “Because of this, both reduced spending unrelated to the interventions themselves,” he added.
When the intervention costs were included, ICE resulted in lower costs overall than those of usual care ($139 less), while overall spending for IPT was higher than for usual care (by $941).
“We tested the interventions in a way that was integrated into primary care, so implementing them in other practice settings should be quite straightforward,” Dr. Choudhry said.
He noted that the ICE model does not currently exist as a complete program – but its components, such as physical therapy or specialist e-consults, do. “And we think that our results justify exploring how to set this up more broadly,” he said.
Dr. Choudhry added that IPT was tested using a specific provider (Egoscue), “which has locations in a variety of places in the U.S. and internationally, and so should also be straightforward to integrate into routine practice.”
However, other important factors, such as insurance coverage, will need to be explored in the future, he said.
Confirmatory evidence?
In an accompanying editorial, Erin Krebs, MD, Minneapolis VA Health Care System, and colleagues, noted that past systematic reviews have concluded that exercise therapies are “generally effective” for chronic back and neck pain, which is usually defined as pain lasting more than 12 weeks, but not for acute pain, defined as pain lasting less than 4-6 weeks.
“The present trial contributes evidence for effectiveness of exercise therapy among patients with a current episode of less than 12 weeks, meaning not yet chronic, but not necessarily acute,” the editorialists wrote.
“Clinicians should more often recommend structured exercise programs for subacute back or neck pain, especially when the pain is recurrent,” they added.
The study was funded by unrestricted philanthropic gifts to Stanford (Calif.) University. Dr. Choudhry received grants from Stanford University during the conduct of the study.
A version of this article first appeared on Medscape.com.
Two conservative interventions are effective for treating acute and subacute spine pain, new research suggests.
Results from the SPINE CARE randomized controlled trial showed that 6-8 weeks of an individualized postural therapy (IPT) or a multidisciplinary biopsychosocial intervention known as ICE (identify, coordinate, and enhance) that includes physical therapy were associated with small but statistically significant reductions in pain-related disability at 3 months compared with usual care.
In addition, spine-related health care spending did not differ significantly between ICE and usual care. However, IPT significantly increased spending compared with usual care.
– long after the interventions were over,” lead author Niteesh K. Choudhry, MD, PhD, Brigham and Women’s Hospital and Harvard Medical School, Boston, told this news organization.
The findings were published online in JAMA.
Common complaint
Spine pain is defined as pain that occurs in the neck or back, the investigators noted. It “accounted for more health spending than any other health condition in the U.S. in 2016,” they added.
“Spine pain is an exceptionally common reason for patients to visit their primary care providers,” Dr. Choudhry said.
The SPINE CARE trial enrolled 2,971 adults (60% were women; mean age was 51 years) with back or neck pain that had lasted less than 12 weeks. All were randomly allocated to usual care (no intervention, n = 992) or to the ICE (n = 829) or IPT (n = 1150) interventions.
The ICE care model stratifies patients on the basis of their risk of progression from acute to chronic pain and addresses biopsychosocial contributors to pain. Low-risk patients received one physical therapy (PT) visit and one coaching call, while higher-risk patients received three PT visits, three coaching calls, and one e-consultation.
The IPT intervention, which was delivered in 8 weekly sessions, focuses on postural realignment. IPT also emphasizes self-efficacy and self-management, including daily exercises to improve postural control, coordination, and muscle balance.
Results at 3 months showed that both the ICE and IPT groups improved significantly more in Oswestry Disability Index (ODI) scores than in the usual care group (ICE, 31.2 to 15.4; IPT, 29.3 to 15.4; usual care, 28.9 to 19.5).
At 3 months, the absolute difference in ODI score vs. usual care was −5.8 for ICE (95% confidence interval [CI], −7.7 to −3.9; P < .001) and −4.3 for IPT (95% CI, −5.9 to −2.6; P < .001) for IPT.
Both interventions reduced resource utilization, such as diagnostic imaging, procedures, and specialist visits, Dr. Choudhry reported. “Because of this, both reduced spending unrelated to the interventions themselves,” he added.
When the intervention costs were included, ICE resulted in lower costs overall than those of usual care ($139 less), while overall spending for IPT was higher than for usual care (by $941).
“We tested the interventions in a way that was integrated into primary care, so implementing them in other practice settings should be quite straightforward,” Dr. Choudhry said.
He noted that the ICE model does not currently exist as a complete program – but its components, such as physical therapy or specialist e-consults, do. “And we think that our results justify exploring how to set this up more broadly,” he said.
Dr. Choudhry added that IPT was tested using a specific provider (Egoscue), “which has locations in a variety of places in the U.S. and internationally, and so should also be straightforward to integrate into routine practice.”
However, other important factors, such as insurance coverage, will need to be explored in the future, he said.
Confirmatory evidence?
In an accompanying editorial, Erin Krebs, MD, Minneapolis VA Health Care System, and colleagues, noted that past systematic reviews have concluded that exercise therapies are “generally effective” for chronic back and neck pain, which is usually defined as pain lasting more than 12 weeks, but not for acute pain, defined as pain lasting less than 4-6 weeks.
“The present trial contributes evidence for effectiveness of exercise therapy among patients with a current episode of less than 12 weeks, meaning not yet chronic, but not necessarily acute,” the editorialists wrote.
“Clinicians should more often recommend structured exercise programs for subacute back or neck pain, especially when the pain is recurrent,” they added.
The study was funded by unrestricted philanthropic gifts to Stanford (Calif.) University. Dr. Choudhry received grants from Stanford University during the conduct of the study.
A version of this article first appeared on Medscape.com.
Two conservative interventions are effective for treating acute and subacute spine pain, new research suggests.
Results from the SPINE CARE randomized controlled trial showed that 6-8 weeks of an individualized postural therapy (IPT) or a multidisciplinary biopsychosocial intervention known as ICE (identify, coordinate, and enhance) that includes physical therapy were associated with small but statistically significant reductions in pain-related disability at 3 months compared with usual care.
In addition, spine-related health care spending did not differ significantly between ICE and usual care. However, IPT significantly increased spending compared with usual care.
– long after the interventions were over,” lead author Niteesh K. Choudhry, MD, PhD, Brigham and Women’s Hospital and Harvard Medical School, Boston, told this news organization.
The findings were published online in JAMA.
Common complaint
Spine pain is defined as pain that occurs in the neck or back, the investigators noted. It “accounted for more health spending than any other health condition in the U.S. in 2016,” they added.
“Spine pain is an exceptionally common reason for patients to visit their primary care providers,” Dr. Choudhry said.
The SPINE CARE trial enrolled 2,971 adults (60% were women; mean age was 51 years) with back or neck pain that had lasted less than 12 weeks. All were randomly allocated to usual care (no intervention, n = 992) or to the ICE (n = 829) or IPT (n = 1150) interventions.
The ICE care model stratifies patients on the basis of their risk of progression from acute to chronic pain and addresses biopsychosocial contributors to pain. Low-risk patients received one physical therapy (PT) visit and one coaching call, while higher-risk patients received three PT visits, three coaching calls, and one e-consultation.
The IPT intervention, which was delivered in 8 weekly sessions, focuses on postural realignment. IPT also emphasizes self-efficacy and self-management, including daily exercises to improve postural control, coordination, and muscle balance.
Results at 3 months showed that both the ICE and IPT groups improved significantly more in Oswestry Disability Index (ODI) scores than in the usual care group (ICE, 31.2 to 15.4; IPT, 29.3 to 15.4; usual care, 28.9 to 19.5).
At 3 months, the absolute difference in ODI score vs. usual care was −5.8 for ICE (95% confidence interval [CI], −7.7 to −3.9; P < .001) and −4.3 for IPT (95% CI, −5.9 to −2.6; P < .001) for IPT.
Both interventions reduced resource utilization, such as diagnostic imaging, procedures, and specialist visits, Dr. Choudhry reported. “Because of this, both reduced spending unrelated to the interventions themselves,” he added.
When the intervention costs were included, ICE resulted in lower costs overall than those of usual care ($139 less), while overall spending for IPT was higher than for usual care (by $941).
“We tested the interventions in a way that was integrated into primary care, so implementing them in other practice settings should be quite straightforward,” Dr. Choudhry said.
He noted that the ICE model does not currently exist as a complete program – but its components, such as physical therapy or specialist e-consults, do. “And we think that our results justify exploring how to set this up more broadly,” he said.
Dr. Choudhry added that IPT was tested using a specific provider (Egoscue), “which has locations in a variety of places in the U.S. and internationally, and so should also be straightforward to integrate into routine practice.”
However, other important factors, such as insurance coverage, will need to be explored in the future, he said.
Confirmatory evidence?
In an accompanying editorial, Erin Krebs, MD, Minneapolis VA Health Care System, and colleagues, noted that past systematic reviews have concluded that exercise therapies are “generally effective” for chronic back and neck pain, which is usually defined as pain lasting more than 12 weeks, but not for acute pain, defined as pain lasting less than 4-6 weeks.
“The present trial contributes evidence for effectiveness of exercise therapy among patients with a current episode of less than 12 weeks, meaning not yet chronic, but not necessarily acute,” the editorialists wrote.
“Clinicians should more often recommend structured exercise programs for subacute back or neck pain, especially when the pain is recurrent,” they added.
The study was funded by unrestricted philanthropic gifts to Stanford (Calif.) University. Dr. Choudhry received grants from Stanford University during the conduct of the study.
A version of this article first appeared on Medscape.com.
FROM JAMA
Cluster headache tied to high risk of mental and neurologic disorders
, leading to significant disability and absenteeism, new research shows.
Results from a Swedish register-based study also showed that patients with cluster headache had a sixfold increased risk for central nervous system disorders and a twofold increased risk for musculoskeletal disorders.
Although cluster headaches are often more prevalent in men, researchers found that multimorbidity rates were significantly higher in women. In addition, rates of external injuries were significantly higher among individuals with cluster headache than among persons without cluster headache.
“The findings very clearly indicate that cluster headache patients suffer from other health issues as well and that they are at risk of having longer periods of times when they cannot work,” said lead investigator Caroline Ran, PhD, a research specialist in the department of neuroscience at the Karolinska Institutet, Stockholm.
“It’s really important for clinicians to look at cluster headache from a broader perspective and make sure that patients are followed up so that they don’t risk ending up in a situation where they have several comorbidities,” Dr. Ran added.
The findings were published online in Neurology.
‘Striking’ finding
Cluster headache is one of the most severe and debilitating types of headache. It causes intense pain behind the eyes, which has been described as being worse than pain associated with childbirth or kidney stones.
Attacks can occur multiple times in a single day and can last up to 3 hours. Cluster headache is rare, occurring in about 1 in 1,000 individuals, and is more common in men. Underdiagnosis is common – especially in women.
The study drew on two Swedish population-based registries and included 3,240 patients with cluster headache aged 16-64 years and 16,200 matched control persons. The analysis covered medical visits from 2001 to 2010.
Results showed that 91.9% of participants with cluster headache had some type of multimorbidity. By comparison, 77.6% of the control group had some type of multimorbidity (odds ratio, 3.26; P < .0001).
Prior studies have shown a higher incidence of mental health and behavioral disorders among patients with cluster headache. However, when the researchers removed those conditions along with external injuries from the dataset, patients with headache were still significantly more likely to have multiple co-occurring illnesses (86.7% vs. 68.8%; OR, 2.95; P < .0001).
The most common comorbid conditions in the overall cluster headache group were diseases of the nervous system (OR, 5.9; 95% CI, 5.46 -6.42); 51.8% of the cluster headache group reported these disorders, compared with just 15.4% of the control group.
Diseases of the eye, the respiratory, gastrointestinal, and musculoskeletal systems, and connective tissue were also significantly more common among patients with cluster headache.
“For each diagnosis that we investigated, we found a higher incidence in the cluster headache group, and we thought this was a very striking finding and worth discussing in the clinical setting that these patients are at risk of general ill health,” Dr. Ran said.
Risky behavior?
Another novel finding was the higher rate of external injuries among the cluster headache group, compared with the control group. The finding seems to back up the theory that patients with cluster headache are more likely to engage in risky behaviors, the researchers noted.
In the cluster headache group, external injuries were reported by 47.1% of men and 41% of women, versus 34.9% and 26.0%, respectively, in the control group.
“Now we can also show that cluster headache patients have more injuries and that is totally unrelated to the biological health of the individuals, so that could also indicate higher risk taking,” Dr. Ran said.
Overall multimorbidity rates and diagnoses in each medical category except external injury were higher among women with cluster headache than men with headaches. In addition, the mean number of days on sick leave and disability pension was higher among women with cluster headache than among men with cluster headache (83.71 days vs. 52.56 days).
Overall, the mean number of sickness absence and disability pension net days in 2010 was nearly twice as high in the cluster headache group as in the control group (63.15 days vs. 34.08 days).
Removing mental and behavioral health disorders from the mix did not lower those numbers.
“Our numbers indicate that the mental health issues that are related to cluster headache might not impact their work situation as much as the other comorbidities,” Dr. Ran said.
Struggle is real
Commenting on the findings, Heidi Schwarz, MD, professor of clinical neurology at the University of Rochester (N.Y.) Medical Center, called the study a “valuable contribution” to the field and to the treatment of cluster headache.
“It’s a good study that addresses factors that really need to be considered as you take care of these patients,” said Dr. Schwarz, who was not involved with the research.
“The most salient features of this is that cluster headache is quite disabling, and if you add a comorbidity to it, it’s even more disabling,” she said.
Dr. Schwarz noted that cluster headache is often misdiagnosed as migraine or is overlooked altogether, especially in women. These data underscore that, although cluster headache is more common in men, it affects women too and could lead to even greater disability.
“This has a direct impact on patient quality of life, and in the end, that really should be what we’re looking to enhance,” Dr. Schwarz said. “When a patient with cluster comes in and they tell you they’re really struggling, believe them because it’s quite real.”
The findings also fill a gap in the literature and offer the kind of data that could not be collected in the United States, she noted. Sweden provides paid sick time for all workers aged 16 and older and offers a disability pension to all workers whose ability to work is temporarily or permanently inhibited because of illness or injury.
“You will never get this kind of data in the United States because this kind of data comes from two datasets that are extremely inclusive and detailed in a society, Sweden, where they have a social support system,” Dr. Schwarz said.
The study was funded by the Swedish Research Council, the Swedish Brain Foundation, and Mellby Gård, Region Stockholm, Märta Lundkvist stiftelse and Karolinska Institutet research funds. Dr. Ran and Dr. Schwarz report no relevant financial relationships.
A version of this article first appeared on Medscape.com.
, leading to significant disability and absenteeism, new research shows.
Results from a Swedish register-based study also showed that patients with cluster headache had a sixfold increased risk for central nervous system disorders and a twofold increased risk for musculoskeletal disorders.
Although cluster headaches are often more prevalent in men, researchers found that multimorbidity rates were significantly higher in women. In addition, rates of external injuries were significantly higher among individuals with cluster headache than among persons without cluster headache.
“The findings very clearly indicate that cluster headache patients suffer from other health issues as well and that they are at risk of having longer periods of times when they cannot work,” said lead investigator Caroline Ran, PhD, a research specialist in the department of neuroscience at the Karolinska Institutet, Stockholm.
“It’s really important for clinicians to look at cluster headache from a broader perspective and make sure that patients are followed up so that they don’t risk ending up in a situation where they have several comorbidities,” Dr. Ran added.
The findings were published online in Neurology.
‘Striking’ finding
Cluster headache is one of the most severe and debilitating types of headache. It causes intense pain behind the eyes, which has been described as being worse than pain associated with childbirth or kidney stones.
Attacks can occur multiple times in a single day and can last up to 3 hours. Cluster headache is rare, occurring in about 1 in 1,000 individuals, and is more common in men. Underdiagnosis is common – especially in women.
The study drew on two Swedish population-based registries and included 3,240 patients with cluster headache aged 16-64 years and 16,200 matched control persons. The analysis covered medical visits from 2001 to 2010.
Results showed that 91.9% of participants with cluster headache had some type of multimorbidity. By comparison, 77.6% of the control group had some type of multimorbidity (odds ratio, 3.26; P < .0001).
Prior studies have shown a higher incidence of mental health and behavioral disorders among patients with cluster headache. However, when the researchers removed those conditions along with external injuries from the dataset, patients with headache were still significantly more likely to have multiple co-occurring illnesses (86.7% vs. 68.8%; OR, 2.95; P < .0001).
The most common comorbid conditions in the overall cluster headache group were diseases of the nervous system (OR, 5.9; 95% CI, 5.46 -6.42); 51.8% of the cluster headache group reported these disorders, compared with just 15.4% of the control group.
Diseases of the eye, the respiratory, gastrointestinal, and musculoskeletal systems, and connective tissue were also significantly more common among patients with cluster headache.
“For each diagnosis that we investigated, we found a higher incidence in the cluster headache group, and we thought this was a very striking finding and worth discussing in the clinical setting that these patients are at risk of general ill health,” Dr. Ran said.
Risky behavior?
Another novel finding was the higher rate of external injuries among the cluster headache group, compared with the control group. The finding seems to back up the theory that patients with cluster headache are more likely to engage in risky behaviors, the researchers noted.
In the cluster headache group, external injuries were reported by 47.1% of men and 41% of women, versus 34.9% and 26.0%, respectively, in the control group.
“Now we can also show that cluster headache patients have more injuries and that is totally unrelated to the biological health of the individuals, so that could also indicate higher risk taking,” Dr. Ran said.
Overall multimorbidity rates and diagnoses in each medical category except external injury were higher among women with cluster headache than men with headaches. In addition, the mean number of days on sick leave and disability pension was higher among women with cluster headache than among men with cluster headache (83.71 days vs. 52.56 days).
Overall, the mean number of sickness absence and disability pension net days in 2010 was nearly twice as high in the cluster headache group as in the control group (63.15 days vs. 34.08 days).
Removing mental and behavioral health disorders from the mix did not lower those numbers.
“Our numbers indicate that the mental health issues that are related to cluster headache might not impact their work situation as much as the other comorbidities,” Dr. Ran said.
Struggle is real
Commenting on the findings, Heidi Schwarz, MD, professor of clinical neurology at the University of Rochester (N.Y.) Medical Center, called the study a “valuable contribution” to the field and to the treatment of cluster headache.
“It’s a good study that addresses factors that really need to be considered as you take care of these patients,” said Dr. Schwarz, who was not involved with the research.
“The most salient features of this is that cluster headache is quite disabling, and if you add a comorbidity to it, it’s even more disabling,” she said.
Dr. Schwarz noted that cluster headache is often misdiagnosed as migraine or is overlooked altogether, especially in women. These data underscore that, although cluster headache is more common in men, it affects women too and could lead to even greater disability.
“This has a direct impact on patient quality of life, and in the end, that really should be what we’re looking to enhance,” Dr. Schwarz said. “When a patient with cluster comes in and they tell you they’re really struggling, believe them because it’s quite real.”
The findings also fill a gap in the literature and offer the kind of data that could not be collected in the United States, she noted. Sweden provides paid sick time for all workers aged 16 and older and offers a disability pension to all workers whose ability to work is temporarily or permanently inhibited because of illness or injury.
“You will never get this kind of data in the United States because this kind of data comes from two datasets that are extremely inclusive and detailed in a society, Sweden, where they have a social support system,” Dr. Schwarz said.
The study was funded by the Swedish Research Council, the Swedish Brain Foundation, and Mellby Gård, Region Stockholm, Märta Lundkvist stiftelse and Karolinska Institutet research funds. Dr. Ran and Dr. Schwarz report no relevant financial relationships.
A version of this article first appeared on Medscape.com.
, leading to significant disability and absenteeism, new research shows.
Results from a Swedish register-based study also showed that patients with cluster headache had a sixfold increased risk for central nervous system disorders and a twofold increased risk for musculoskeletal disorders.
Although cluster headaches are often more prevalent in men, researchers found that multimorbidity rates were significantly higher in women. In addition, rates of external injuries were significantly higher among individuals with cluster headache than among persons without cluster headache.
“The findings very clearly indicate that cluster headache patients suffer from other health issues as well and that they are at risk of having longer periods of times when they cannot work,” said lead investigator Caroline Ran, PhD, a research specialist in the department of neuroscience at the Karolinska Institutet, Stockholm.
“It’s really important for clinicians to look at cluster headache from a broader perspective and make sure that patients are followed up so that they don’t risk ending up in a situation where they have several comorbidities,” Dr. Ran added.
The findings were published online in Neurology.
‘Striking’ finding
Cluster headache is one of the most severe and debilitating types of headache. It causes intense pain behind the eyes, which has been described as being worse than pain associated with childbirth or kidney stones.
Attacks can occur multiple times in a single day and can last up to 3 hours. Cluster headache is rare, occurring in about 1 in 1,000 individuals, and is more common in men. Underdiagnosis is common – especially in women.
The study drew on two Swedish population-based registries and included 3,240 patients with cluster headache aged 16-64 years and 16,200 matched control persons. The analysis covered medical visits from 2001 to 2010.
Results showed that 91.9% of participants with cluster headache had some type of multimorbidity. By comparison, 77.6% of the control group had some type of multimorbidity (odds ratio, 3.26; P < .0001).
Prior studies have shown a higher incidence of mental health and behavioral disorders among patients with cluster headache. However, when the researchers removed those conditions along with external injuries from the dataset, patients with headache were still significantly more likely to have multiple co-occurring illnesses (86.7% vs. 68.8%; OR, 2.95; P < .0001).
The most common comorbid conditions in the overall cluster headache group were diseases of the nervous system (OR, 5.9; 95% CI, 5.46 -6.42); 51.8% of the cluster headache group reported these disorders, compared with just 15.4% of the control group.
Diseases of the eye, the respiratory, gastrointestinal, and musculoskeletal systems, and connective tissue were also significantly more common among patients with cluster headache.
“For each diagnosis that we investigated, we found a higher incidence in the cluster headache group, and we thought this was a very striking finding and worth discussing in the clinical setting that these patients are at risk of general ill health,” Dr. Ran said.
Risky behavior?
Another novel finding was the higher rate of external injuries among the cluster headache group, compared with the control group. The finding seems to back up the theory that patients with cluster headache are more likely to engage in risky behaviors, the researchers noted.
In the cluster headache group, external injuries were reported by 47.1% of men and 41% of women, versus 34.9% and 26.0%, respectively, in the control group.
“Now we can also show that cluster headache patients have more injuries and that is totally unrelated to the biological health of the individuals, so that could also indicate higher risk taking,” Dr. Ran said.
Overall multimorbidity rates and diagnoses in each medical category except external injury were higher among women with cluster headache than men with headaches. In addition, the mean number of days on sick leave and disability pension was higher among women with cluster headache than among men with cluster headache (83.71 days vs. 52.56 days).
Overall, the mean number of sickness absence and disability pension net days in 2010 was nearly twice as high in the cluster headache group as in the control group (63.15 days vs. 34.08 days).
Removing mental and behavioral health disorders from the mix did not lower those numbers.
“Our numbers indicate that the mental health issues that are related to cluster headache might not impact their work situation as much as the other comorbidities,” Dr. Ran said.
Struggle is real
Commenting on the findings, Heidi Schwarz, MD, professor of clinical neurology at the University of Rochester (N.Y.) Medical Center, called the study a “valuable contribution” to the field and to the treatment of cluster headache.
“It’s a good study that addresses factors that really need to be considered as you take care of these patients,” said Dr. Schwarz, who was not involved with the research.
“The most salient features of this is that cluster headache is quite disabling, and if you add a comorbidity to it, it’s even more disabling,” she said.
Dr. Schwarz noted that cluster headache is often misdiagnosed as migraine or is overlooked altogether, especially in women. These data underscore that, although cluster headache is more common in men, it affects women too and could lead to even greater disability.
“This has a direct impact on patient quality of life, and in the end, that really should be what we’re looking to enhance,” Dr. Schwarz said. “When a patient with cluster comes in and they tell you they’re really struggling, believe them because it’s quite real.”
The findings also fill a gap in the literature and offer the kind of data that could not be collected in the United States, she noted. Sweden provides paid sick time for all workers aged 16 and older and offers a disability pension to all workers whose ability to work is temporarily or permanently inhibited because of illness or injury.
“You will never get this kind of data in the United States because this kind of data comes from two datasets that are extremely inclusive and detailed in a society, Sweden, where they have a social support system,” Dr. Schwarz said.
The study was funded by the Swedish Research Council, the Swedish Brain Foundation, and Mellby Gård, Region Stockholm, Märta Lundkvist stiftelse and Karolinska Institutet research funds. Dr. Ran and Dr. Schwarz report no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM NEUROLOGY
Corticosteroid injections may worsen knee OA progression
Injecting hyaluronic acid (HA) instead, or managing the condition without injections, may better preserve knee structure and cartilage, according to results of two related studies presented at the annual meeting of the Radiological Society of North America.
The findings come nonrandomized, observational cohort studies, leading knee OA experts to call for further study in randomized trial settings. In the meantime, shared decision-making between patients and clinicians is advised on the use of these injections.
For knee OA, most patients seek a noninvasive treatment for symptomatic relief. “At least 10% of these patients undergo local treatment with injectable corticosteroids or hyaluronic acid,” the lead author of one of the studies, Upasana Upadhyay Bharadwaj, MD, research fellow in musculoskeletal radiology at the University of California, San Francisco, said in a video press release.
Researchers in both studies used data and images from the Osteoarthritis Initiative (OAI), a multicenter, longitudinal, observational study of 4,796 U.S. patients aged 45-79 years with knee OA. Participants were enrolled from February 2004 to May 2006.
The OAI maintains a natural history database of information regarding participants’ clinical evaluation data, x-rays, MRI scans, and a biospecimen repository. Data are available to researchers worldwide.
Two studies draw similar conclusions
In one study, Dr. Bharadwaj and colleagues found that HA injections appeared to show decreased knee OA progression in bone marrow lesions.
They investigated 8 patients who received one CS injection, 12 who received one HA injection, and 40 control persons who received neither treatment. Participants were propensity-score matched by age, sex, body mass index (BMI), Kellgren-Lawrence (KL) grade, Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC), and Physical Activity Scale for the Elderly (PASE).
The researchers semiquantitatively graded three Tesla MRI scans that had been obtained at baseline, 2 years before the injection, and 2 years after the injection, using whole-organ MRI score (WORMS) for the meniscus, bone marrow lesions, cartilage, joint effusion, and ligaments.
They quantified OA progression using the difference in WORMS between baseline and 2-year follow-up, and they used linear regression models, adjusted for age, sex, BMI, KL grade, WOMAC, and PASE, to identify the link between type of injection and progression of WORMS.
At 2 years, the authors found a significant association between CS injection and postinjection progression of WORMS over 2 years for the knee overall, the lateral meniscus, lateral cartilage, and medial cartilage. There was no significant link between HA injection and postinjection progression of WORMS or between either injection type and progression of pain, as quantified by WOMAC. There was also no significant difference in progression of WORMS over the 2 years prior to injection for CS and HA injections.
“Corticosteroid injections must be administered with caution with respect to long-term effects on osteoarthritis,” Dr. Bharadwaj advised. “Hyaluronic acid injections, on the other hand, may slow down progression of knee osteoarthritis and alleviate long-term effects while offering similar symptomatic relief to corticosteroid injections. Overall, they are perhaps a safer alternative when looking at medium- and long-term disease course of knee osteoarthritis.”
In the second study, lead author Azad Darbandi, MS, a fourth-year medical student at Chicago Medical School, North Chicago, and colleagues found that patients who received CS injections experienced significantly more medial joint space narrowing.
They identified 210 knees with imaging at baseline and at 48 months that received CS injections, and 59 that received HA injections; 6,827 knees served as controls. The investigators matched 50 patients per group on the basis of confounding factors, which included age, sex, BMI, comorbidities, surgery, and semiquantitative imaging outcomes at baseline. They performed ANCOVA testing using 48-month semiquantitative imaging outcomes as dependent variables and confounding variables as covariates.
The researchers analyzed joint space narrowing, KL grade, and tibia/femur medial/lateral compartment osteophyte formation and sclerosis.
At 4 years, the average KL grade in the CS group was 2.79, it was 2.11 in the HA group,;and it was 2.37 in the control group. Intergroup comparisons showed significant differences in KL grade between CS and HA groups and between CS and control groups. Medial compartment joint space narrowing was 1.56 in the CS group, 1.11 in the HA group, and 1.18 in controls. There was a significant difference between the CS and control groups. Other dependent variables were not significant.
“These preliminary results suggest that corticosteroid injections accelerated the radiographic progression of osteoarthritis, specifically medial joint space narrowing and Kellgren-Lawrence grading, whereas hyaluronic acid injections did not,” Mr. Darbandi said in an interview.
“OA radiographic progression does not always correlate with clinical progression, and further research is needed,” he added.
Proper matching of patients at baseline for confounding factors is a strength of the study, Mr. Darbandi said, while the retrospective study design is a weakness.
Experts share their perspectives on the preliminary results
Michael M. Kheir, MD, assistant professor of orthopedic surgery at the University of Michigan Health System, who was not involved in the studies, said he would like to see further related research.
“Perhaps steroid injections are not as benign as they once seemed,” he added. “They should be reserved for patients who already have significant arthritis and are seeking temporary relief prior to surgical reconstruction with a joint replacement, or for patients with recalcitrant pain after having already tried HA injections.”
William A. Jiranek, MD, professor and orthopedic surgeon at Duke Health in Morrisville, N.C., who also was not involved in the studies, was not surprised by the findings.
“It is important to do these studies to learn that steroid injections do not come with zero cost,” he said.
“I am pretty sure that a percentage of these patients had no cartilage loss at all,” he added. “We need to understand which OA phenotypes are not at risk of progressive cartilage loss from steroid injections.”
Annunziato (Ned) Amendola, MD, professor and sports medicine orthopedic surgeon at Duke Health in Durham, N.C., who was also not involved in the studies, said he would like to know how injection effectiveness and activity level are related.
“If the injections were effective at relieving pain, and the patients were more active, that may have predisposed to more joint wear,” he said. “It’s like tires that last longer if you don’t abuse them.”
Shared decision-making and further research recommended
Amanda E. Nelson, MD, associate professor of medicine in the division of rheumatology, allergy, and immunology at the University of North Carolina at Chapel Hill, said: “The lack of randomization introduces potential biases around why certain therapies (CS injection, HA injection, or neither) were selected over others (such as disease severity, preference, comorbid conditions, other contraindications, etc), thus making interpretation of the findings challenging.
“The causal relationship remains in question, and questions around the efficacy of intra-articular HA in particular, and the ideal settings for intra-articular therapy in general, persist,” noted Dr. Nelson, who was also not involved in the studies. “Thus, shared decision-making between patients and their providers is essential when considering these options.”
C. Kent Kwoh, MD, professor of medicine and medical imaging at the University of Arizona and director of the University of Arizona Arthritis Center, both in Tucson, said in an interview that these types of studies are important because CS injections are common treatments for knee OA, they are recommended in treatment guidelines, and other good options are lacking.
But he pointed out that the results of these two studies need to be interpreted with caution and should not be used to decide the course of treatment.
“These data are hypothesis generating. They suggest association, but they do not show causation,” said Dr. Kwoh, who was also not involved in the studies. “Both studies are secondary analyses of data collected from the OAI, which was not specifically designed to answer the questions these studies are posing.
“The OAI was not a treatment study, and participants were seen only once a year or so. They may have had joint injections anytime from only days to around 1 year before their visit, and their levels of activity or pain just prior to or just after their joint injections were not reported,” Dr. Kwoh explained.
The reasons why patients did or did not receive a specific joint injection – including their socioeconomic status, race, access to insurance, and other confounding factors – were not assessed and may have affected the results, he added.
The fact that both studies used the same data and came to the same conclusions gives the conclusions some strength, he said, but “the gold standard to understanding causation would be a randomized, controlled trial.”
Mr. Darbandi’s research received grant support from Boeing, His c-authors, as well as all experts not involved in the studies, reported no relevant financial relationshiips. Dr. Bharadwaj did not provide conflict-of-interest and funding details. Dr. Kwoh reported membership on panels that have developed guidelines for the management of knee OA.
A version of this article first appeared on Medscape.com.
Injecting hyaluronic acid (HA) instead, or managing the condition without injections, may better preserve knee structure and cartilage, according to results of two related studies presented at the annual meeting of the Radiological Society of North America.
The findings come nonrandomized, observational cohort studies, leading knee OA experts to call for further study in randomized trial settings. In the meantime, shared decision-making between patients and clinicians is advised on the use of these injections.
For knee OA, most patients seek a noninvasive treatment for symptomatic relief. “At least 10% of these patients undergo local treatment with injectable corticosteroids or hyaluronic acid,” the lead author of one of the studies, Upasana Upadhyay Bharadwaj, MD, research fellow in musculoskeletal radiology at the University of California, San Francisco, said in a video press release.
Researchers in both studies used data and images from the Osteoarthritis Initiative (OAI), a multicenter, longitudinal, observational study of 4,796 U.S. patients aged 45-79 years with knee OA. Participants were enrolled from February 2004 to May 2006.
The OAI maintains a natural history database of information regarding participants’ clinical evaluation data, x-rays, MRI scans, and a biospecimen repository. Data are available to researchers worldwide.
Two studies draw similar conclusions
In one study, Dr. Bharadwaj and colleagues found that HA injections appeared to show decreased knee OA progression in bone marrow lesions.
They investigated 8 patients who received one CS injection, 12 who received one HA injection, and 40 control persons who received neither treatment. Participants were propensity-score matched by age, sex, body mass index (BMI), Kellgren-Lawrence (KL) grade, Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC), and Physical Activity Scale for the Elderly (PASE).
The researchers semiquantitatively graded three Tesla MRI scans that had been obtained at baseline, 2 years before the injection, and 2 years after the injection, using whole-organ MRI score (WORMS) for the meniscus, bone marrow lesions, cartilage, joint effusion, and ligaments.
They quantified OA progression using the difference in WORMS between baseline and 2-year follow-up, and they used linear regression models, adjusted for age, sex, BMI, KL grade, WOMAC, and PASE, to identify the link between type of injection and progression of WORMS.
At 2 years, the authors found a significant association between CS injection and postinjection progression of WORMS over 2 years for the knee overall, the lateral meniscus, lateral cartilage, and medial cartilage. There was no significant link between HA injection and postinjection progression of WORMS or between either injection type and progression of pain, as quantified by WOMAC. There was also no significant difference in progression of WORMS over the 2 years prior to injection for CS and HA injections.
“Corticosteroid injections must be administered with caution with respect to long-term effects on osteoarthritis,” Dr. Bharadwaj advised. “Hyaluronic acid injections, on the other hand, may slow down progression of knee osteoarthritis and alleviate long-term effects while offering similar symptomatic relief to corticosteroid injections. Overall, they are perhaps a safer alternative when looking at medium- and long-term disease course of knee osteoarthritis.”
In the second study, lead author Azad Darbandi, MS, a fourth-year medical student at Chicago Medical School, North Chicago, and colleagues found that patients who received CS injections experienced significantly more medial joint space narrowing.
They identified 210 knees with imaging at baseline and at 48 months that received CS injections, and 59 that received HA injections; 6,827 knees served as controls. The investigators matched 50 patients per group on the basis of confounding factors, which included age, sex, BMI, comorbidities, surgery, and semiquantitative imaging outcomes at baseline. They performed ANCOVA testing using 48-month semiquantitative imaging outcomes as dependent variables and confounding variables as covariates.
The researchers analyzed joint space narrowing, KL grade, and tibia/femur medial/lateral compartment osteophyte formation and sclerosis.
At 4 years, the average KL grade in the CS group was 2.79, it was 2.11 in the HA group,;and it was 2.37 in the control group. Intergroup comparisons showed significant differences in KL grade between CS and HA groups and between CS and control groups. Medial compartment joint space narrowing was 1.56 in the CS group, 1.11 in the HA group, and 1.18 in controls. There was a significant difference between the CS and control groups. Other dependent variables were not significant.
“These preliminary results suggest that corticosteroid injections accelerated the radiographic progression of osteoarthritis, specifically medial joint space narrowing and Kellgren-Lawrence grading, whereas hyaluronic acid injections did not,” Mr. Darbandi said in an interview.
“OA radiographic progression does not always correlate with clinical progression, and further research is needed,” he added.
Proper matching of patients at baseline for confounding factors is a strength of the study, Mr. Darbandi said, while the retrospective study design is a weakness.
Experts share their perspectives on the preliminary results
Michael M. Kheir, MD, assistant professor of orthopedic surgery at the University of Michigan Health System, who was not involved in the studies, said he would like to see further related research.
“Perhaps steroid injections are not as benign as they once seemed,” he added. “They should be reserved for patients who already have significant arthritis and are seeking temporary relief prior to surgical reconstruction with a joint replacement, or for patients with recalcitrant pain after having already tried HA injections.”
William A. Jiranek, MD, professor and orthopedic surgeon at Duke Health in Morrisville, N.C., who also was not involved in the studies, was not surprised by the findings.
“It is important to do these studies to learn that steroid injections do not come with zero cost,” he said.
“I am pretty sure that a percentage of these patients had no cartilage loss at all,” he added. “We need to understand which OA phenotypes are not at risk of progressive cartilage loss from steroid injections.”
Annunziato (Ned) Amendola, MD, professor and sports medicine orthopedic surgeon at Duke Health in Durham, N.C., who was also not involved in the studies, said he would like to know how injection effectiveness and activity level are related.
“If the injections were effective at relieving pain, and the patients were more active, that may have predisposed to more joint wear,” he said. “It’s like tires that last longer if you don’t abuse them.”
Shared decision-making and further research recommended
Amanda E. Nelson, MD, associate professor of medicine in the division of rheumatology, allergy, and immunology at the University of North Carolina at Chapel Hill, said: “The lack of randomization introduces potential biases around why certain therapies (CS injection, HA injection, or neither) were selected over others (such as disease severity, preference, comorbid conditions, other contraindications, etc), thus making interpretation of the findings challenging.
“The causal relationship remains in question, and questions around the efficacy of intra-articular HA in particular, and the ideal settings for intra-articular therapy in general, persist,” noted Dr. Nelson, who was also not involved in the studies. “Thus, shared decision-making between patients and their providers is essential when considering these options.”
C. Kent Kwoh, MD, professor of medicine and medical imaging at the University of Arizona and director of the University of Arizona Arthritis Center, both in Tucson, said in an interview that these types of studies are important because CS injections are common treatments for knee OA, they are recommended in treatment guidelines, and other good options are lacking.
But he pointed out that the results of these two studies need to be interpreted with caution and should not be used to decide the course of treatment.
“These data are hypothesis generating. They suggest association, but they do not show causation,” said Dr. Kwoh, who was also not involved in the studies. “Both studies are secondary analyses of data collected from the OAI, which was not specifically designed to answer the questions these studies are posing.
“The OAI was not a treatment study, and participants were seen only once a year or so. They may have had joint injections anytime from only days to around 1 year before their visit, and their levels of activity or pain just prior to or just after their joint injections were not reported,” Dr. Kwoh explained.
The reasons why patients did or did not receive a specific joint injection – including their socioeconomic status, race, access to insurance, and other confounding factors – were not assessed and may have affected the results, he added.
The fact that both studies used the same data and came to the same conclusions gives the conclusions some strength, he said, but “the gold standard to understanding causation would be a randomized, controlled trial.”
Mr. Darbandi’s research received grant support from Boeing, His c-authors, as well as all experts not involved in the studies, reported no relevant financial relationshiips. Dr. Bharadwaj did not provide conflict-of-interest and funding details. Dr. Kwoh reported membership on panels that have developed guidelines for the management of knee OA.
A version of this article first appeared on Medscape.com.
Injecting hyaluronic acid (HA) instead, or managing the condition without injections, may better preserve knee structure and cartilage, according to results of two related studies presented at the annual meeting of the Radiological Society of North America.
The findings come nonrandomized, observational cohort studies, leading knee OA experts to call for further study in randomized trial settings. In the meantime, shared decision-making between patients and clinicians is advised on the use of these injections.
For knee OA, most patients seek a noninvasive treatment for symptomatic relief. “At least 10% of these patients undergo local treatment with injectable corticosteroids or hyaluronic acid,” the lead author of one of the studies, Upasana Upadhyay Bharadwaj, MD, research fellow in musculoskeletal radiology at the University of California, San Francisco, said in a video press release.
Researchers in both studies used data and images from the Osteoarthritis Initiative (OAI), a multicenter, longitudinal, observational study of 4,796 U.S. patients aged 45-79 years with knee OA. Participants were enrolled from February 2004 to May 2006.
The OAI maintains a natural history database of information regarding participants’ clinical evaluation data, x-rays, MRI scans, and a biospecimen repository. Data are available to researchers worldwide.
Two studies draw similar conclusions
In one study, Dr. Bharadwaj and colleagues found that HA injections appeared to show decreased knee OA progression in bone marrow lesions.
They investigated 8 patients who received one CS injection, 12 who received one HA injection, and 40 control persons who received neither treatment. Participants were propensity-score matched by age, sex, body mass index (BMI), Kellgren-Lawrence (KL) grade, Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC), and Physical Activity Scale for the Elderly (PASE).
The researchers semiquantitatively graded three Tesla MRI scans that had been obtained at baseline, 2 years before the injection, and 2 years after the injection, using whole-organ MRI score (WORMS) for the meniscus, bone marrow lesions, cartilage, joint effusion, and ligaments.
They quantified OA progression using the difference in WORMS between baseline and 2-year follow-up, and they used linear regression models, adjusted for age, sex, BMI, KL grade, WOMAC, and PASE, to identify the link between type of injection and progression of WORMS.
At 2 years, the authors found a significant association between CS injection and postinjection progression of WORMS over 2 years for the knee overall, the lateral meniscus, lateral cartilage, and medial cartilage. There was no significant link between HA injection and postinjection progression of WORMS or between either injection type and progression of pain, as quantified by WOMAC. There was also no significant difference in progression of WORMS over the 2 years prior to injection for CS and HA injections.
“Corticosteroid injections must be administered with caution with respect to long-term effects on osteoarthritis,” Dr. Bharadwaj advised. “Hyaluronic acid injections, on the other hand, may slow down progression of knee osteoarthritis and alleviate long-term effects while offering similar symptomatic relief to corticosteroid injections. Overall, they are perhaps a safer alternative when looking at medium- and long-term disease course of knee osteoarthritis.”
In the second study, lead author Azad Darbandi, MS, a fourth-year medical student at Chicago Medical School, North Chicago, and colleagues found that patients who received CS injections experienced significantly more medial joint space narrowing.
They identified 210 knees with imaging at baseline and at 48 months that received CS injections, and 59 that received HA injections; 6,827 knees served as controls. The investigators matched 50 patients per group on the basis of confounding factors, which included age, sex, BMI, comorbidities, surgery, and semiquantitative imaging outcomes at baseline. They performed ANCOVA testing using 48-month semiquantitative imaging outcomes as dependent variables and confounding variables as covariates.
The researchers analyzed joint space narrowing, KL grade, and tibia/femur medial/lateral compartment osteophyte formation and sclerosis.
At 4 years, the average KL grade in the CS group was 2.79, it was 2.11 in the HA group,;and it was 2.37 in the control group. Intergroup comparisons showed significant differences in KL grade between CS and HA groups and between CS and control groups. Medial compartment joint space narrowing was 1.56 in the CS group, 1.11 in the HA group, and 1.18 in controls. There was a significant difference between the CS and control groups. Other dependent variables were not significant.
“These preliminary results suggest that corticosteroid injections accelerated the radiographic progression of osteoarthritis, specifically medial joint space narrowing and Kellgren-Lawrence grading, whereas hyaluronic acid injections did not,” Mr. Darbandi said in an interview.
“OA radiographic progression does not always correlate with clinical progression, and further research is needed,” he added.
Proper matching of patients at baseline for confounding factors is a strength of the study, Mr. Darbandi said, while the retrospective study design is a weakness.
Experts share their perspectives on the preliminary results
Michael M. Kheir, MD, assistant professor of orthopedic surgery at the University of Michigan Health System, who was not involved in the studies, said he would like to see further related research.
“Perhaps steroid injections are not as benign as they once seemed,” he added. “They should be reserved for patients who already have significant arthritis and are seeking temporary relief prior to surgical reconstruction with a joint replacement, or for patients with recalcitrant pain after having already tried HA injections.”
William A. Jiranek, MD, professor and orthopedic surgeon at Duke Health in Morrisville, N.C., who also was not involved in the studies, was not surprised by the findings.
“It is important to do these studies to learn that steroid injections do not come with zero cost,” he said.
“I am pretty sure that a percentage of these patients had no cartilage loss at all,” he added. “We need to understand which OA phenotypes are not at risk of progressive cartilage loss from steroid injections.”
Annunziato (Ned) Amendola, MD, professor and sports medicine orthopedic surgeon at Duke Health in Durham, N.C., who was also not involved in the studies, said he would like to know how injection effectiveness and activity level are related.
“If the injections were effective at relieving pain, and the patients were more active, that may have predisposed to more joint wear,” he said. “It’s like tires that last longer if you don’t abuse them.”
Shared decision-making and further research recommended
Amanda E. Nelson, MD, associate professor of medicine in the division of rheumatology, allergy, and immunology at the University of North Carolina at Chapel Hill, said: “The lack of randomization introduces potential biases around why certain therapies (CS injection, HA injection, or neither) were selected over others (such as disease severity, preference, comorbid conditions, other contraindications, etc), thus making interpretation of the findings challenging.
“The causal relationship remains in question, and questions around the efficacy of intra-articular HA in particular, and the ideal settings for intra-articular therapy in general, persist,” noted Dr. Nelson, who was also not involved in the studies. “Thus, shared decision-making between patients and their providers is essential when considering these options.”
C. Kent Kwoh, MD, professor of medicine and medical imaging at the University of Arizona and director of the University of Arizona Arthritis Center, both in Tucson, said in an interview that these types of studies are important because CS injections are common treatments for knee OA, they are recommended in treatment guidelines, and other good options are lacking.
But he pointed out that the results of these two studies need to be interpreted with caution and should not be used to decide the course of treatment.
“These data are hypothesis generating. They suggest association, but they do not show causation,” said Dr. Kwoh, who was also not involved in the studies. “Both studies are secondary analyses of data collected from the OAI, which was not specifically designed to answer the questions these studies are posing.
“The OAI was not a treatment study, and participants were seen only once a year or so. They may have had joint injections anytime from only days to around 1 year before their visit, and their levels of activity or pain just prior to or just after their joint injections were not reported,” Dr. Kwoh explained.
The reasons why patients did or did not receive a specific joint injection – including their socioeconomic status, race, access to insurance, and other confounding factors – were not assessed and may have affected the results, he added.
The fact that both studies used the same data and came to the same conclusions gives the conclusions some strength, he said, but “the gold standard to understanding causation would be a randomized, controlled trial.”
Mr. Darbandi’s research received grant support from Boeing, His c-authors, as well as all experts not involved in the studies, reported no relevant financial relationshiips. Dr. Bharadwaj did not provide conflict-of-interest and funding details. Dr. Kwoh reported membership on panels that have developed guidelines for the management of knee OA.
A version of this article first appeared on Medscape.com.
FROM RSNA 2022
Nitroglycerin’s safety and value examined
He has stable angina, having chest pain with exercise. He uses sublingual nitroglycerin (SL NTG prn) about three times a month. His blood pressure is 140/70 mm Hg. His pulse is 60 beats per minute. His current medications are lisinopril, atorvastatin, aspirin, and SL NTG tablets as needed.
What would you recommend?
A. No sildenafil; refer to urologist for other ED options.
B. Okay to use sildenafil if greater than 6 hours from NTG use.
C. Recommend tadalafil.
Is coprescribing nitrates and phosphodiesterase inhibitors safe?
The FDA warns against the use of phosphodiesterase inhibitors in patients taking nitrates. Combining nitrates with phosphodiesterase type 5 (PDE5) inhibitors is contraindicated because of a synergistic blood pressure lowering effect.1 This warning/contraindication was based on theoretical concerns, as well as concern that of the first 130 deaths reported in patients who took sildenafil, 16 of the patients also were taking nitrates.2
Parker and colleagues studied the safety of giving IV nitroglycerin to patients with coronary artery disease (CAD) who have taken sildenafil.3 The study was a randomized, placebo-controlled, crossover trial. Participants received sildenafil 100 mg or placebo, then received intravenous NTG. Patients who received sildenafil had a 4-6 mm Hg systolic BP drop compared with those who took the placebo. There was no difference in severe events between the sildenafil and placebo groups. The blood levels of nitroglycerin in this study were very likely much higher than the levels that occur with SL NTG.
A recent study by Holt et al. looked at overall cardiovascular outcomes with coprescribing nitrates and phosphodiesterase inhibitors.4 The study was a case crossover design, using a nationwide Danish health registry over the period of 2000-2018. In 2000, the rate of coprescribing of phosphodiesterase inhibitors in ischemic heart disease patients on nitrates was .9 per 100 persons/year and rose to 19.5 prescriptions per 100 persons/year in 2018. During this same time, no statistically significant association was found between the coprescription of nitrates with PDE5 inhibitors and the risk for MI, cardiac arrest, syncope, stroke, or an adverse drug event.
Does nitroglycerin response help determine cause of chest pain?
Nitroglycerin response has long been used as a clinical indicator on whether a patient’s chest pain is cardiac or not. Eric A. Shry, MD, and his colleagues looked at the usefulness of nitroglycerin response in the treatment of chest pain as a predictor of ischemic chest pain in an emergency department setting.5
The study was a retrospective review of 223 patients who presented to the emergency department over a 5-month period with ongoing chest pain. They looked at patients who had ongoing chest pain in the emergency department, received nitroglycerin, and did not receive any therapy other than aspirin within 10 minutes of receiving nitroglycerin. Response to the drug was compared with the final diagnosis of cardiac versus noncardiac chest pain.
Of the patients with a final determination of cardiac chest pain, 88% had a nitroglycerin response, whereas 92% of the patients with noncardiac chest pain had a nitroglycerin response (P = .50).
Deborah B. Diercks, MD, and her colleagues looked at improvement in chest pain scores in the emergency department in patients treated with nitroglycerin and whether it correlated with a cardiac etiology of chest pain.6 The study was a prospective, observational study of 664 patients in an urban tertiary care emergency department over a 16-month period. An 11-point numeric chest pain scale was assessed and recorded by research assistants before and 5 minutes after receiving nitroglycerin. The scale ranged from 0 (no pain) to 10 (worst pain imaginable).
A final diagnosis of a cardiac etiology for chest pain was found in 18% of the patients in the study. Of the patients who had cardiac-related chest pain, 20% had no reduction in pain with nitroglycerin, compared with 19% of the patients without cardiac-related chest pain.
A complete or significant reduction in chest pain occurred with nitroglycerin in 31% of patients with cardiac chest pain and 27% of the patients without cardiac chest pain (P = .76).
Nitroglycerin response does not appear to be helpful in distinguishing cardiac from noncardiac chest pain, but a study by His and colleagues offers an interesting twist.7
The authors of this research studied 118 patients looking to see if the side effect of headache with nitroglycerin was more common in patients who did not have CAD than in those who did. All the patients had a varying degree of relief of chest pain with NTG administration within 10 minutes. In patients with normal coronary arteries or minimal CAD, 73% had headache caused by NTG, whereas in patients with obstructive CAD, only 23% had headache after NTG use.
Take-home messages
- Short acting nitroglycerin may not be a contraindication for phosphodiesterase inhibitor use.
- More data are still needed.
- Nitroglycerin response does not help distinguish chest pain from CAD from noncardiac causes.
Dr. Paauw is professor of medicine in the division of general internal medicine at the University of Washington, Seattle, and he serves as third-year medical student clerkship director at the University of Washington. He is a member of the editorial advisory board of Internal Medicine News. Dr. Paauw has no conflicts to disclose. Contact him at [email protected].
References
1. Schwartz BG, Kloner RA. Drug interactions with phosphodiesterase-5 inhibitors used for the treatment of erectile dysfunction or pulmonary hypertension. Circulation. 2010;122:88-95.
2. Kloner RA, Zusman RM. Cardiovascular effects of sildenafil citrate and recommendations for its use. Am J Cardiol. 1999 Sep 9;84(5B):11N-17N.
3. Parker JD et al. Safety of intravenous nitroglycerin after administration of sildenafil citrate to men with coronary artery disease: A double-blind, placebo-controlled, randomized, crossover trial. Crit Care Med. 2007;35:1863-8.
4. Holt A et al. Adverse events associated with coprescription of phosphodiesterase type inhibitors and oral organic nitrates in male patients with ischemic heart disease. Ann Intern Med. 2022 Jun;175(6):774-82.
5. Shry EA et al. Usefulness of the response to sublingual nitroglycerin as a predictor of ischemic chest pain in the emergency department. Am J Cardiol. 2002 Dec 1;90(11):1264-6.
6. Diercks DB et al. Changes in the numeric descriptive scale for pain after sublingual nitroglycerin do not predict cardiac etiology of chest pain. Ann Emerg Med. 2005 Jun;45(6):581-5.
7. His DH et al. Headache response to glyceryl trinitrate in patients with and without obstructive coronary artery disease. Heart 2005;91:1164-6.
He has stable angina, having chest pain with exercise. He uses sublingual nitroglycerin (SL NTG prn) about three times a month. His blood pressure is 140/70 mm Hg. His pulse is 60 beats per minute. His current medications are lisinopril, atorvastatin, aspirin, and SL NTG tablets as needed.
What would you recommend?
A. No sildenafil; refer to urologist for other ED options.
B. Okay to use sildenafil if greater than 6 hours from NTG use.
C. Recommend tadalafil.
Is coprescribing nitrates and phosphodiesterase inhibitors safe?
The FDA warns against the use of phosphodiesterase inhibitors in patients taking nitrates. Combining nitrates with phosphodiesterase type 5 (PDE5) inhibitors is contraindicated because of a synergistic blood pressure lowering effect.1 This warning/contraindication was based on theoretical concerns, as well as concern that of the first 130 deaths reported in patients who took sildenafil, 16 of the patients also were taking nitrates.2
Parker and colleagues studied the safety of giving IV nitroglycerin to patients with coronary artery disease (CAD) who have taken sildenafil.3 The study was a randomized, placebo-controlled, crossover trial. Participants received sildenafil 100 mg or placebo, then received intravenous NTG. Patients who received sildenafil had a 4-6 mm Hg systolic BP drop compared with those who took the placebo. There was no difference in severe events between the sildenafil and placebo groups. The blood levels of nitroglycerin in this study were very likely much higher than the levels that occur with SL NTG.
A recent study by Holt et al. looked at overall cardiovascular outcomes with coprescribing nitrates and phosphodiesterase inhibitors.4 The study was a case crossover design, using a nationwide Danish health registry over the period of 2000-2018. In 2000, the rate of coprescribing of phosphodiesterase inhibitors in ischemic heart disease patients on nitrates was .9 per 100 persons/year and rose to 19.5 prescriptions per 100 persons/year in 2018. During this same time, no statistically significant association was found between the coprescription of nitrates with PDE5 inhibitors and the risk for MI, cardiac arrest, syncope, stroke, or an adverse drug event.
Does nitroglycerin response help determine cause of chest pain?
Nitroglycerin response has long been used as a clinical indicator on whether a patient’s chest pain is cardiac or not. Eric A. Shry, MD, and his colleagues looked at the usefulness of nitroglycerin response in the treatment of chest pain as a predictor of ischemic chest pain in an emergency department setting.5
The study was a retrospective review of 223 patients who presented to the emergency department over a 5-month period with ongoing chest pain. They looked at patients who had ongoing chest pain in the emergency department, received nitroglycerin, and did not receive any therapy other than aspirin within 10 minutes of receiving nitroglycerin. Response to the drug was compared with the final diagnosis of cardiac versus noncardiac chest pain.
Of the patients with a final determination of cardiac chest pain, 88% had a nitroglycerin response, whereas 92% of the patients with noncardiac chest pain had a nitroglycerin response (P = .50).
Deborah B. Diercks, MD, and her colleagues looked at improvement in chest pain scores in the emergency department in patients treated with nitroglycerin and whether it correlated with a cardiac etiology of chest pain.6 The study was a prospective, observational study of 664 patients in an urban tertiary care emergency department over a 16-month period. An 11-point numeric chest pain scale was assessed and recorded by research assistants before and 5 minutes after receiving nitroglycerin. The scale ranged from 0 (no pain) to 10 (worst pain imaginable).
A final diagnosis of a cardiac etiology for chest pain was found in 18% of the patients in the study. Of the patients who had cardiac-related chest pain, 20% had no reduction in pain with nitroglycerin, compared with 19% of the patients without cardiac-related chest pain.
A complete or significant reduction in chest pain occurred with nitroglycerin in 31% of patients with cardiac chest pain and 27% of the patients without cardiac chest pain (P = .76).
Nitroglycerin response does not appear to be helpful in distinguishing cardiac from noncardiac chest pain, but a study by His and colleagues offers an interesting twist.7
The authors of this research studied 118 patients looking to see if the side effect of headache with nitroglycerin was more common in patients who did not have CAD than in those who did. All the patients had a varying degree of relief of chest pain with NTG administration within 10 minutes. In patients with normal coronary arteries or minimal CAD, 73% had headache caused by NTG, whereas in patients with obstructive CAD, only 23% had headache after NTG use.
Take-home messages
- Short acting nitroglycerin may not be a contraindication for phosphodiesterase inhibitor use.
- More data are still needed.
- Nitroglycerin response does not help distinguish chest pain from CAD from noncardiac causes.
Dr. Paauw is professor of medicine in the division of general internal medicine at the University of Washington, Seattle, and he serves as third-year medical student clerkship director at the University of Washington. He is a member of the editorial advisory board of Internal Medicine News. Dr. Paauw has no conflicts to disclose. Contact him at [email protected].
References
1. Schwartz BG, Kloner RA. Drug interactions with phosphodiesterase-5 inhibitors used for the treatment of erectile dysfunction or pulmonary hypertension. Circulation. 2010;122:88-95.
2. Kloner RA, Zusman RM. Cardiovascular effects of sildenafil citrate and recommendations for its use. Am J Cardiol. 1999 Sep 9;84(5B):11N-17N.
3. Parker JD et al. Safety of intravenous nitroglycerin after administration of sildenafil citrate to men with coronary artery disease: A double-blind, placebo-controlled, randomized, crossover trial. Crit Care Med. 2007;35:1863-8.
4. Holt A et al. Adverse events associated with coprescription of phosphodiesterase type inhibitors and oral organic nitrates in male patients with ischemic heart disease. Ann Intern Med. 2022 Jun;175(6):774-82.
5. Shry EA et al. Usefulness of the response to sublingual nitroglycerin as a predictor of ischemic chest pain in the emergency department. Am J Cardiol. 2002 Dec 1;90(11):1264-6.
6. Diercks DB et al. Changes in the numeric descriptive scale for pain after sublingual nitroglycerin do not predict cardiac etiology of chest pain. Ann Emerg Med. 2005 Jun;45(6):581-5.
7. His DH et al. Headache response to glyceryl trinitrate in patients with and without obstructive coronary artery disease. Heart 2005;91:1164-6.
He has stable angina, having chest pain with exercise. He uses sublingual nitroglycerin (SL NTG prn) about three times a month. His blood pressure is 140/70 mm Hg. His pulse is 60 beats per minute. His current medications are lisinopril, atorvastatin, aspirin, and SL NTG tablets as needed.
What would you recommend?
A. No sildenafil; refer to urologist for other ED options.
B. Okay to use sildenafil if greater than 6 hours from NTG use.
C. Recommend tadalafil.
Is coprescribing nitrates and phosphodiesterase inhibitors safe?
The FDA warns against the use of phosphodiesterase inhibitors in patients taking nitrates. Combining nitrates with phosphodiesterase type 5 (PDE5) inhibitors is contraindicated because of a synergistic blood pressure lowering effect.1 This warning/contraindication was based on theoretical concerns, as well as concern that of the first 130 deaths reported in patients who took sildenafil, 16 of the patients also were taking nitrates.2
Parker and colleagues studied the safety of giving IV nitroglycerin to patients with coronary artery disease (CAD) who have taken sildenafil.3 The study was a randomized, placebo-controlled, crossover trial. Participants received sildenafil 100 mg or placebo, then received intravenous NTG. Patients who received sildenafil had a 4-6 mm Hg systolic BP drop compared with those who took the placebo. There was no difference in severe events between the sildenafil and placebo groups. The blood levels of nitroglycerin in this study were very likely much higher than the levels that occur with SL NTG.
A recent study by Holt et al. looked at overall cardiovascular outcomes with coprescribing nitrates and phosphodiesterase inhibitors.4 The study was a case crossover design, using a nationwide Danish health registry over the period of 2000-2018. In 2000, the rate of coprescribing of phosphodiesterase inhibitors in ischemic heart disease patients on nitrates was .9 per 100 persons/year and rose to 19.5 prescriptions per 100 persons/year in 2018. During this same time, no statistically significant association was found between the coprescription of nitrates with PDE5 inhibitors and the risk for MI, cardiac arrest, syncope, stroke, or an adverse drug event.
Does nitroglycerin response help determine cause of chest pain?
Nitroglycerin response has long been used as a clinical indicator on whether a patient’s chest pain is cardiac or not. Eric A. Shry, MD, and his colleagues looked at the usefulness of nitroglycerin response in the treatment of chest pain as a predictor of ischemic chest pain in an emergency department setting.5
The study was a retrospective review of 223 patients who presented to the emergency department over a 5-month period with ongoing chest pain. They looked at patients who had ongoing chest pain in the emergency department, received nitroglycerin, and did not receive any therapy other than aspirin within 10 minutes of receiving nitroglycerin. Response to the drug was compared with the final diagnosis of cardiac versus noncardiac chest pain.
Of the patients with a final determination of cardiac chest pain, 88% had a nitroglycerin response, whereas 92% of the patients with noncardiac chest pain had a nitroglycerin response (P = .50).
Deborah B. Diercks, MD, and her colleagues looked at improvement in chest pain scores in the emergency department in patients treated with nitroglycerin and whether it correlated with a cardiac etiology of chest pain.6 The study was a prospective, observational study of 664 patients in an urban tertiary care emergency department over a 16-month period. An 11-point numeric chest pain scale was assessed and recorded by research assistants before and 5 minutes after receiving nitroglycerin. The scale ranged from 0 (no pain) to 10 (worst pain imaginable).
A final diagnosis of a cardiac etiology for chest pain was found in 18% of the patients in the study. Of the patients who had cardiac-related chest pain, 20% had no reduction in pain with nitroglycerin, compared with 19% of the patients without cardiac-related chest pain.
A complete or significant reduction in chest pain occurred with nitroglycerin in 31% of patients with cardiac chest pain and 27% of the patients without cardiac chest pain (P = .76).
Nitroglycerin response does not appear to be helpful in distinguishing cardiac from noncardiac chest pain, but a study by His and colleagues offers an interesting twist.7
The authors of this research studied 118 patients looking to see if the side effect of headache with nitroglycerin was more common in patients who did not have CAD than in those who did. All the patients had a varying degree of relief of chest pain with NTG administration within 10 minutes. In patients with normal coronary arteries or minimal CAD, 73% had headache caused by NTG, whereas in patients with obstructive CAD, only 23% had headache after NTG use.
Take-home messages
- Short acting nitroglycerin may not be a contraindication for phosphodiesterase inhibitor use.
- More data are still needed.
- Nitroglycerin response does not help distinguish chest pain from CAD from noncardiac causes.
Dr. Paauw is professor of medicine in the division of general internal medicine at the University of Washington, Seattle, and he serves as third-year medical student clerkship director at the University of Washington. He is a member of the editorial advisory board of Internal Medicine News. Dr. Paauw has no conflicts to disclose. Contact him at [email protected].
References
1. Schwartz BG, Kloner RA. Drug interactions with phosphodiesterase-5 inhibitors used for the treatment of erectile dysfunction or pulmonary hypertension. Circulation. 2010;122:88-95.
2. Kloner RA, Zusman RM. Cardiovascular effects of sildenafil citrate and recommendations for its use. Am J Cardiol. 1999 Sep 9;84(5B):11N-17N.
3. Parker JD et al. Safety of intravenous nitroglycerin after administration of sildenafil citrate to men with coronary artery disease: A double-blind, placebo-controlled, randomized, crossover trial. Crit Care Med. 2007;35:1863-8.
4. Holt A et al. Adverse events associated with coprescription of phosphodiesterase type inhibitors and oral organic nitrates in male patients with ischemic heart disease. Ann Intern Med. 2022 Jun;175(6):774-82.
5. Shry EA et al. Usefulness of the response to sublingual nitroglycerin as a predictor of ischemic chest pain in the emergency department. Am J Cardiol. 2002 Dec 1;90(11):1264-6.
6. Diercks DB et al. Changes in the numeric descriptive scale for pain after sublingual nitroglycerin do not predict cardiac etiology of chest pain. Ann Emerg Med. 2005 Jun;45(6):581-5.
7. His DH et al. Headache response to glyceryl trinitrate in patients with and without obstructive coronary artery disease. Heart 2005;91:1164-6.
Mind the geriatrician gap
These should be the best of times for geriatric medicine.
The baby boom has become a senior surge, bringing in a rapidly growing pool of aging patients for geriatricians to treat. According to the U.S. Census Bureau, more than 56 million adults aged 65 and older live in the United States. They account for about 17% of the nation’s population. That number is expected to hit 73 million by 2030 and 86 million by 2050.
The American Geriatrics Society estimates that 30% of older people require the attention of geriatricians. These clinicians excel in managing complex cases – patients with multiple comorbidities, such as coronary artery disease, dementia, and osteoporosis, who are taking a half dozen, and often more, medications.
. In the 2010s, geriatricians called for “25,000 [such specialists] by 2025.” As of 2021, 7123 certified geriatricians were practicing in the United States, according to the American Board of Medical Specialties.
The Health Resources and Services Administration, a federal agency that addresses medical workforce shortages, estimates that there will be 6,230 geriatricians by 2025, or approximately 1 for every 3,000 older adults requiring geriatric care. HRSA projects a shortage of 27,000 geriatricians by 2025.
The specialty has faced an uphill battle to attract fellows. This year, only 43% of the nation’s 177 geriatrics fellowship slots were filled, according to November’s National Resident Match Program report. Family medicine–based geriatrics achieved only a 32% fill rate, while internal medicine–based programs saw a rate of 45%.
“Our numbers are shrinking so we need another approach to make sure older adults get the care they need and deserve,” said G. Michael Harper, MD, president of the 6,000-member AGS.
But Dr. Harper, who practices at the University of California, San Francisco, and the San Francisco VA Medical Center, added a positive note: “We may be struggling to increase the number of board-certified geriatricians, but the field itself has made a lot of progress in terms of improving clinical care through advancements in science and in the ways we deliver care.”
Dr. Harper cited the Hospital Elder Life Program, a hospital model developed at the Harvard-affiliated Marcus Institute for Aging Research, which uses an interprofessional team and trained volunteers to prevent delirium and functional decline. HELP has been adopted by more than 200 hospitals worldwide and has been successful at returning older adults to their homes or previous living situations with maintained or improved ability to function, he said.
Mark Supiano, MD, professor and chief of geriatrics at the University of Utah, Salt Lake City, said the specialty has been in shortage mode since ABMS recognized it in 1988. He was in the initial cohort of fellowship-trained geriatricians, sitting for the first certifying exam in geriatrics offered that year.
“Back then, the demographic imperative of the aging of our society was on the horizon. We’re living it now. I knew enough to recognize it was coming and saw an opportunity,” Dr. Supiano said in an interview. “There was so much then that we didn’t know about how to understand aging or how to care for older adults that there really was such a knowledge gap.”
Dr. Supiano is an associate editor of Hazzard’s Geriatric Medicine and Gerontology (McGraw-Hill Education), which has more than doubled in pages and word count during his career.
Unfavorable finances
Katherine Thompson, MD, director of the geriatrics fellowship program at the University of Chicago and codirector of UChicago’s Successful Aging and Frailty Evaluation Clinic, said money is a major reason for the struggle. “I think probably the biggest driver is financial,” she said. “A lot of people are graduating medical school with really astronomical amounts of medical school loans.”
Geriatricians, like other doctors, carry a large debt – $200,000, on average, not counting undergraduate debt, according to the Association of American Medical Colleges.
But the typical geriatrician earns less than an internist or family medicine doctor who doesn’t undergo the additional year of training, Dr. Thompson said. “There’s not a lot of financial motivation to do this fellowship,” she said.
The jobs website Zippia reports that geriatricians earned roughly $165,000 per year on average in 2022. The average annual incomes in 2022 were $191,000 for pediatricians, $215,000 for family physicians, and $223,000 for internists, according to the site.
In other words, Dr. Harper said, “geriatrics is one of the few professions where you can actually do additional training and make less money.”
The reason for the pay issue is simple: Geriatricians treat patients covered by Medicare, whose reimbursement schedules lag behind those of commercial insurers. The Kaiser Family Foundation reported in 2020 that private insurance paid 143% of Medicare rates on average for physician services.
Dr. Harper said overall compensation for geriatricians has “not gained a lot of traction,” but they can earn comfortable livings.
Still, representation of the specialty on the American Medical Association’s Relative Value Scale Update Committee has led to approval by the Centers for Medicare & Medicaid Services of billing codes that pay geriatricians “for what they do. Examples include chronic care management, advance care planning, and dementia evaluation,” he said.
But the geriatrician gap goes beyond money.
Ageism, too, may play a role in residents not choosing geriatrics.
“Our culture is ageist. It definitely focuses on youth and looks at aging as being loss rather than just a change in what works well and what doesn’t work well,” said Mary Tinetti, MD, a geriatrician and researcher at Yale University, New Haven, Conn. “Ageism happens among physicians, just because they’re part of the broader society.”
Time for a new goal?
Dr. Tinetti said she’s optimistic that new ideas about geriatricians teaching other primary care clinicians about the tenets of geriatric medicine, which offer a wholistic approach to comorbidities, such as diabetes, atrial fibrillation, dementia, hypertension, hyperlipidemia, and polypharmacy problems faced by this population, especially those 85 and older.
She has called on her profession to abandon the goal of increasing the numbers of board-certified geriatricians – whom she refers to as big “G” geriatricians. She instead wants to develop a “small, elite workforce” that discovers and tests geriatrics principles through research, teaches these principles to all healthcare professions and to the public, and disseminates and implements the policies.
“We need a cadre of geriatricians who train all other clinicians in the care of older adults,” Dr. Tinetti said. “The goal is not more geriatricians but rather the preparation of all clinicians in the care of older adults.”
Dr. Thompson said geriatricians are teaching primary care specialists, nurses, social workers, and other health care providers the principles of age-friendly care. AGS has for the past 20 years led a program called the Geriatrics for Specialists Initiative to increase geriatrics knowledge and expertise of surgical and medical specialists.
Some specialties have taken the cue and have added geriatrics-related hyphens through additional training: geriatric-emergency, geriatric-general surgery, geriatric-hospitalists, and more.
HRSA runs programs to encourage physicians to train as geriatricians and geriatrics faculty, and it encourages the geriatrics interdisciplinary team approach.
Richard Olague, director of public affairs for HRSA, said his agency has invested over $160 million over the past 4 years in the education and training of geriatricians and other health care professionals who care for the elderly through its Geriatrics Workforce Enhancement Program and Geriatrics Academic Career Awards Program. In the academic year 2020-2021, the two programs trained 109 geriatricians; 456 other geriatric/gerontology providers and students; 44,450 other healthcare workforce professionals and students; and served 17,666 patients and 5,409 caregivers.
Dr. Harper, like his fellow geriatricians, tells young doctors that geriatrics is a fulfilling specialty.
“I get to care for the whole person and sometimes their families, too, and in the process form rich and meaningful relationships. And while I’m rarely in the position to cure, I always have the ability to care,” he said. “Sometimes that can mean being an advocate trying to make sure my patients receive the care they need, and other times it might mean protecting them from burdensome care that is unlikely to lead to any meaningful benefit. There is great reward in all of that.”
Dr. Supiano said geriatric patients are being helped by the Age-Friendly Health System initiative of the John A. Hartford Foundation and the Institute for Healthcare Improvement in partnership with the American Hospital Association and the Catholic Health Association of the United States. This is sort of a seal of approval for facilities committed to age-friendly care.
“When you go to your hospital, if they don’t have this age-friendly health system banner on the front door ... you either ask why that is not there, or you vote with your feet and go to another health system that is age friendly,” he said. “Geriatricians are eternal optimists.”
A version of this article first appeared on Medscape.com.
These should be the best of times for geriatric medicine.
The baby boom has become a senior surge, bringing in a rapidly growing pool of aging patients for geriatricians to treat. According to the U.S. Census Bureau, more than 56 million adults aged 65 and older live in the United States. They account for about 17% of the nation’s population. That number is expected to hit 73 million by 2030 and 86 million by 2050.
The American Geriatrics Society estimates that 30% of older people require the attention of geriatricians. These clinicians excel in managing complex cases – patients with multiple comorbidities, such as coronary artery disease, dementia, and osteoporosis, who are taking a half dozen, and often more, medications.
. In the 2010s, geriatricians called for “25,000 [such specialists] by 2025.” As of 2021, 7123 certified geriatricians were practicing in the United States, according to the American Board of Medical Specialties.
The Health Resources and Services Administration, a federal agency that addresses medical workforce shortages, estimates that there will be 6,230 geriatricians by 2025, or approximately 1 for every 3,000 older adults requiring geriatric care. HRSA projects a shortage of 27,000 geriatricians by 2025.
The specialty has faced an uphill battle to attract fellows. This year, only 43% of the nation’s 177 geriatrics fellowship slots were filled, according to November’s National Resident Match Program report. Family medicine–based geriatrics achieved only a 32% fill rate, while internal medicine–based programs saw a rate of 45%.
“Our numbers are shrinking so we need another approach to make sure older adults get the care they need and deserve,” said G. Michael Harper, MD, president of the 6,000-member AGS.
But Dr. Harper, who practices at the University of California, San Francisco, and the San Francisco VA Medical Center, added a positive note: “We may be struggling to increase the number of board-certified geriatricians, but the field itself has made a lot of progress in terms of improving clinical care through advancements in science and in the ways we deliver care.”
Dr. Harper cited the Hospital Elder Life Program, a hospital model developed at the Harvard-affiliated Marcus Institute for Aging Research, which uses an interprofessional team and trained volunteers to prevent delirium and functional decline. HELP has been adopted by more than 200 hospitals worldwide and has been successful at returning older adults to their homes or previous living situations with maintained or improved ability to function, he said.
Mark Supiano, MD, professor and chief of geriatrics at the University of Utah, Salt Lake City, said the specialty has been in shortage mode since ABMS recognized it in 1988. He was in the initial cohort of fellowship-trained geriatricians, sitting for the first certifying exam in geriatrics offered that year.
“Back then, the demographic imperative of the aging of our society was on the horizon. We’re living it now. I knew enough to recognize it was coming and saw an opportunity,” Dr. Supiano said in an interview. “There was so much then that we didn’t know about how to understand aging or how to care for older adults that there really was such a knowledge gap.”
Dr. Supiano is an associate editor of Hazzard’s Geriatric Medicine and Gerontology (McGraw-Hill Education), which has more than doubled in pages and word count during his career.
Unfavorable finances
Katherine Thompson, MD, director of the geriatrics fellowship program at the University of Chicago and codirector of UChicago’s Successful Aging and Frailty Evaluation Clinic, said money is a major reason for the struggle. “I think probably the biggest driver is financial,” she said. “A lot of people are graduating medical school with really astronomical amounts of medical school loans.”
Geriatricians, like other doctors, carry a large debt – $200,000, on average, not counting undergraduate debt, according to the Association of American Medical Colleges.
But the typical geriatrician earns less than an internist or family medicine doctor who doesn’t undergo the additional year of training, Dr. Thompson said. “There’s not a lot of financial motivation to do this fellowship,” she said.
The jobs website Zippia reports that geriatricians earned roughly $165,000 per year on average in 2022. The average annual incomes in 2022 were $191,000 for pediatricians, $215,000 for family physicians, and $223,000 for internists, according to the site.
In other words, Dr. Harper said, “geriatrics is one of the few professions where you can actually do additional training and make less money.”
The reason for the pay issue is simple: Geriatricians treat patients covered by Medicare, whose reimbursement schedules lag behind those of commercial insurers. The Kaiser Family Foundation reported in 2020 that private insurance paid 143% of Medicare rates on average for physician services.
Dr. Harper said overall compensation for geriatricians has “not gained a lot of traction,” but they can earn comfortable livings.
Still, representation of the specialty on the American Medical Association’s Relative Value Scale Update Committee has led to approval by the Centers for Medicare & Medicaid Services of billing codes that pay geriatricians “for what they do. Examples include chronic care management, advance care planning, and dementia evaluation,” he said.
But the geriatrician gap goes beyond money.
Ageism, too, may play a role in residents not choosing geriatrics.
“Our culture is ageist. It definitely focuses on youth and looks at aging as being loss rather than just a change in what works well and what doesn’t work well,” said Mary Tinetti, MD, a geriatrician and researcher at Yale University, New Haven, Conn. “Ageism happens among physicians, just because they’re part of the broader society.”
Time for a new goal?
Dr. Tinetti said she’s optimistic that new ideas about geriatricians teaching other primary care clinicians about the tenets of geriatric medicine, which offer a wholistic approach to comorbidities, such as diabetes, atrial fibrillation, dementia, hypertension, hyperlipidemia, and polypharmacy problems faced by this population, especially those 85 and older.
She has called on her profession to abandon the goal of increasing the numbers of board-certified geriatricians – whom she refers to as big “G” geriatricians. She instead wants to develop a “small, elite workforce” that discovers and tests geriatrics principles through research, teaches these principles to all healthcare professions and to the public, and disseminates and implements the policies.
“We need a cadre of geriatricians who train all other clinicians in the care of older adults,” Dr. Tinetti said. “The goal is not more geriatricians but rather the preparation of all clinicians in the care of older adults.”
Dr. Thompson said geriatricians are teaching primary care specialists, nurses, social workers, and other health care providers the principles of age-friendly care. AGS has for the past 20 years led a program called the Geriatrics for Specialists Initiative to increase geriatrics knowledge and expertise of surgical and medical specialists.
Some specialties have taken the cue and have added geriatrics-related hyphens through additional training: geriatric-emergency, geriatric-general surgery, geriatric-hospitalists, and more.
HRSA runs programs to encourage physicians to train as geriatricians and geriatrics faculty, and it encourages the geriatrics interdisciplinary team approach.
Richard Olague, director of public affairs for HRSA, said his agency has invested over $160 million over the past 4 years in the education and training of geriatricians and other health care professionals who care for the elderly through its Geriatrics Workforce Enhancement Program and Geriatrics Academic Career Awards Program. In the academic year 2020-2021, the two programs trained 109 geriatricians; 456 other geriatric/gerontology providers and students; 44,450 other healthcare workforce professionals and students; and served 17,666 patients and 5,409 caregivers.
Dr. Harper, like his fellow geriatricians, tells young doctors that geriatrics is a fulfilling specialty.
“I get to care for the whole person and sometimes their families, too, and in the process form rich and meaningful relationships. And while I’m rarely in the position to cure, I always have the ability to care,” he said. “Sometimes that can mean being an advocate trying to make sure my patients receive the care they need, and other times it might mean protecting them from burdensome care that is unlikely to lead to any meaningful benefit. There is great reward in all of that.”
Dr. Supiano said geriatric patients are being helped by the Age-Friendly Health System initiative of the John A. Hartford Foundation and the Institute for Healthcare Improvement in partnership with the American Hospital Association and the Catholic Health Association of the United States. This is sort of a seal of approval for facilities committed to age-friendly care.
“When you go to your hospital, if they don’t have this age-friendly health system banner on the front door ... you either ask why that is not there, or you vote with your feet and go to another health system that is age friendly,” he said. “Geriatricians are eternal optimists.”
A version of this article first appeared on Medscape.com.
These should be the best of times for geriatric medicine.
The baby boom has become a senior surge, bringing in a rapidly growing pool of aging patients for geriatricians to treat. According to the U.S. Census Bureau, more than 56 million adults aged 65 and older live in the United States. They account for about 17% of the nation’s population. That number is expected to hit 73 million by 2030 and 86 million by 2050.
The American Geriatrics Society estimates that 30% of older people require the attention of geriatricians. These clinicians excel in managing complex cases – patients with multiple comorbidities, such as coronary artery disease, dementia, and osteoporosis, who are taking a half dozen, and often more, medications.
. In the 2010s, geriatricians called for “25,000 [such specialists] by 2025.” As of 2021, 7123 certified geriatricians were practicing in the United States, according to the American Board of Medical Specialties.
The Health Resources and Services Administration, a federal agency that addresses medical workforce shortages, estimates that there will be 6,230 geriatricians by 2025, or approximately 1 for every 3,000 older adults requiring geriatric care. HRSA projects a shortage of 27,000 geriatricians by 2025.
The specialty has faced an uphill battle to attract fellows. This year, only 43% of the nation’s 177 geriatrics fellowship slots were filled, according to November’s National Resident Match Program report. Family medicine–based geriatrics achieved only a 32% fill rate, while internal medicine–based programs saw a rate of 45%.
“Our numbers are shrinking so we need another approach to make sure older adults get the care they need and deserve,” said G. Michael Harper, MD, president of the 6,000-member AGS.
But Dr. Harper, who practices at the University of California, San Francisco, and the San Francisco VA Medical Center, added a positive note: “We may be struggling to increase the number of board-certified geriatricians, but the field itself has made a lot of progress in terms of improving clinical care through advancements in science and in the ways we deliver care.”
Dr. Harper cited the Hospital Elder Life Program, a hospital model developed at the Harvard-affiliated Marcus Institute for Aging Research, which uses an interprofessional team and trained volunteers to prevent delirium and functional decline. HELP has been adopted by more than 200 hospitals worldwide and has been successful at returning older adults to their homes or previous living situations with maintained or improved ability to function, he said.
Mark Supiano, MD, professor and chief of geriatrics at the University of Utah, Salt Lake City, said the specialty has been in shortage mode since ABMS recognized it in 1988. He was in the initial cohort of fellowship-trained geriatricians, sitting for the first certifying exam in geriatrics offered that year.
“Back then, the demographic imperative of the aging of our society was on the horizon. We’re living it now. I knew enough to recognize it was coming and saw an opportunity,” Dr. Supiano said in an interview. “There was so much then that we didn’t know about how to understand aging or how to care for older adults that there really was such a knowledge gap.”
Dr. Supiano is an associate editor of Hazzard’s Geriatric Medicine and Gerontology (McGraw-Hill Education), which has more than doubled in pages and word count during his career.
Unfavorable finances
Katherine Thompson, MD, director of the geriatrics fellowship program at the University of Chicago and codirector of UChicago’s Successful Aging and Frailty Evaluation Clinic, said money is a major reason for the struggle. “I think probably the biggest driver is financial,” she said. “A lot of people are graduating medical school with really astronomical amounts of medical school loans.”
Geriatricians, like other doctors, carry a large debt – $200,000, on average, not counting undergraduate debt, according to the Association of American Medical Colleges.
But the typical geriatrician earns less than an internist or family medicine doctor who doesn’t undergo the additional year of training, Dr. Thompson said. “There’s not a lot of financial motivation to do this fellowship,” she said.
The jobs website Zippia reports that geriatricians earned roughly $165,000 per year on average in 2022. The average annual incomes in 2022 were $191,000 for pediatricians, $215,000 for family physicians, and $223,000 for internists, according to the site.
In other words, Dr. Harper said, “geriatrics is one of the few professions where you can actually do additional training and make less money.”
The reason for the pay issue is simple: Geriatricians treat patients covered by Medicare, whose reimbursement schedules lag behind those of commercial insurers. The Kaiser Family Foundation reported in 2020 that private insurance paid 143% of Medicare rates on average for physician services.
Dr. Harper said overall compensation for geriatricians has “not gained a lot of traction,” but they can earn comfortable livings.
Still, representation of the specialty on the American Medical Association’s Relative Value Scale Update Committee has led to approval by the Centers for Medicare & Medicaid Services of billing codes that pay geriatricians “for what they do. Examples include chronic care management, advance care planning, and dementia evaluation,” he said.
But the geriatrician gap goes beyond money.
Ageism, too, may play a role in residents not choosing geriatrics.
“Our culture is ageist. It definitely focuses on youth and looks at aging as being loss rather than just a change in what works well and what doesn’t work well,” said Mary Tinetti, MD, a geriatrician and researcher at Yale University, New Haven, Conn. “Ageism happens among physicians, just because they’re part of the broader society.”
Time for a new goal?
Dr. Tinetti said she’s optimistic that new ideas about geriatricians teaching other primary care clinicians about the tenets of geriatric medicine, which offer a wholistic approach to comorbidities, such as diabetes, atrial fibrillation, dementia, hypertension, hyperlipidemia, and polypharmacy problems faced by this population, especially those 85 and older.
She has called on her profession to abandon the goal of increasing the numbers of board-certified geriatricians – whom she refers to as big “G” geriatricians. She instead wants to develop a “small, elite workforce” that discovers and tests geriatrics principles through research, teaches these principles to all healthcare professions and to the public, and disseminates and implements the policies.
“We need a cadre of geriatricians who train all other clinicians in the care of older adults,” Dr. Tinetti said. “The goal is not more geriatricians but rather the preparation of all clinicians in the care of older adults.”
Dr. Thompson said geriatricians are teaching primary care specialists, nurses, social workers, and other health care providers the principles of age-friendly care. AGS has for the past 20 years led a program called the Geriatrics for Specialists Initiative to increase geriatrics knowledge and expertise of surgical and medical specialists.
Some specialties have taken the cue and have added geriatrics-related hyphens through additional training: geriatric-emergency, geriatric-general surgery, geriatric-hospitalists, and more.
HRSA runs programs to encourage physicians to train as geriatricians and geriatrics faculty, and it encourages the geriatrics interdisciplinary team approach.
Richard Olague, director of public affairs for HRSA, said his agency has invested over $160 million over the past 4 years in the education and training of geriatricians and other health care professionals who care for the elderly through its Geriatrics Workforce Enhancement Program and Geriatrics Academic Career Awards Program. In the academic year 2020-2021, the two programs trained 109 geriatricians; 456 other geriatric/gerontology providers and students; 44,450 other healthcare workforce professionals and students; and served 17,666 patients and 5,409 caregivers.
Dr. Harper, like his fellow geriatricians, tells young doctors that geriatrics is a fulfilling specialty.
“I get to care for the whole person and sometimes their families, too, and in the process form rich and meaningful relationships. And while I’m rarely in the position to cure, I always have the ability to care,” he said. “Sometimes that can mean being an advocate trying to make sure my patients receive the care they need, and other times it might mean protecting them from burdensome care that is unlikely to lead to any meaningful benefit. There is great reward in all of that.”
Dr. Supiano said geriatric patients are being helped by the Age-Friendly Health System initiative of the John A. Hartford Foundation and the Institute for Healthcare Improvement in partnership with the American Hospital Association and the Catholic Health Association of the United States. This is sort of a seal of approval for facilities committed to age-friendly care.
“When you go to your hospital, if they don’t have this age-friendly health system banner on the front door ... you either ask why that is not there, or you vote with your feet and go to another health system that is age friendly,” he said. “Geriatricians are eternal optimists.”
A version of this article first appeared on Medscape.com.
Knee lesion that bleeds
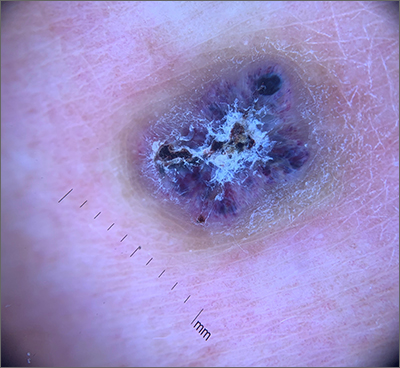
This combination of vascular features with excess keratin fit perfectly with the name of the diagnosis: angiokeratoma. The dark color of the lesion on magnification, or in this case with dermoscopy, showed the lacunar pattern of dilated vessels. The overlying keratin was likely accentuated because it was on an extensor surface; the rim of hyperpigmentation is common for these lesions.
Angiokeratomas result from dilation of the blood vessels underneath the epidermis. There are different inciting events that lead to the 5 different types of angiokeratomas. The overlying epidermal changes are secondary to the underlying process of capillary ectasia.1 This lesion was not part of a cluster, so it was characterized as a solitary angiokeratoma. Smaller lesions are usually less keratinized and are commonly seen on the scrotum and vulva, where there are usually multiple lesions (referred to as angiokeratoma of Fordyce).
Zaballos2 studied the dermoscopic characteristics of 32 solitary angiokeratomas and reported 6 findings in at least half of the solitary lesions. The most common features were dark lacunae in 94% of the lesions, white veil in 91%, and erythema in 69%. Peripheral erythema, red lacunae, and hemorrhagic crusts were all seen at a rate of 53%. The most common location was the lower extremities.
This patient’s previous pathology report from a shave biopsy was found, confirming that the original diagnosis was angiokeratoma. Since the patient’s lesion had not resolved and was symptomatic from minor trauma, he was scheduled to come back in for an elliptical excision to remove the lesion.
Image and text courtesy of Daniel Stulberg, MD, FAAFP, Professor and Chair, Department of Family and Community Medicine, Western Michigan University Homer Stryker, MD School of Medicine, Kalamazoo.
1. Schiller PI, Itin PH. Angiokeratomas: an update. Dermatology. 1996;193:275-282. doi: 10.1159/000246270
2. Zaballos P, Daufí C, Puig S, et al. Dermoscopy of solitary angiokeratomas: a morphological study. Arch Dermatol. 2007;143:318–325. doi:10.1001/archderm.143.3.318
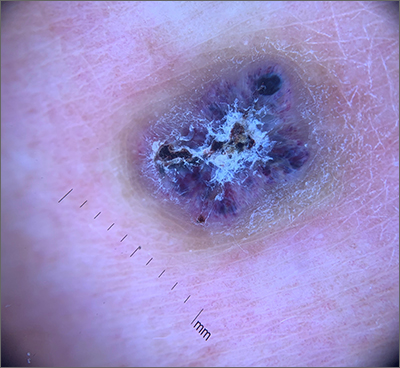
This combination of vascular features with excess keratin fit perfectly with the name of the diagnosis: angiokeratoma. The dark color of the lesion on magnification, or in this case with dermoscopy, showed the lacunar pattern of dilated vessels. The overlying keratin was likely accentuated because it was on an extensor surface; the rim of hyperpigmentation is common for these lesions.
Angiokeratomas result from dilation of the blood vessels underneath the epidermis. There are different inciting events that lead to the 5 different types of angiokeratomas. The overlying epidermal changes are secondary to the underlying process of capillary ectasia.1 This lesion was not part of a cluster, so it was characterized as a solitary angiokeratoma. Smaller lesions are usually less keratinized and are commonly seen on the scrotum and vulva, where there are usually multiple lesions (referred to as angiokeratoma of Fordyce).
Zaballos2 studied the dermoscopic characteristics of 32 solitary angiokeratomas and reported 6 findings in at least half of the solitary lesions. The most common features were dark lacunae in 94% of the lesions, white veil in 91%, and erythema in 69%. Peripheral erythema, red lacunae, and hemorrhagic crusts were all seen at a rate of 53%. The most common location was the lower extremities.
This patient’s previous pathology report from a shave biopsy was found, confirming that the original diagnosis was angiokeratoma. Since the patient’s lesion had not resolved and was symptomatic from minor trauma, he was scheduled to come back in for an elliptical excision to remove the lesion.
Image and text courtesy of Daniel Stulberg, MD, FAAFP, Professor and Chair, Department of Family and Community Medicine, Western Michigan University Homer Stryker, MD School of Medicine, Kalamazoo.
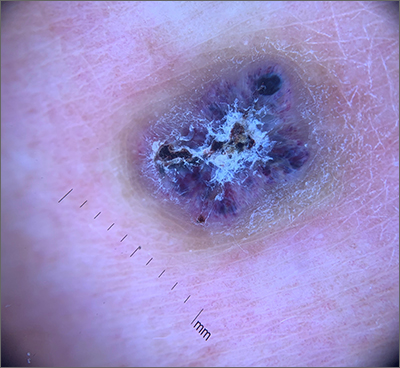
This combination of vascular features with excess keratin fit perfectly with the name of the diagnosis: angiokeratoma. The dark color of the lesion on magnification, or in this case with dermoscopy, showed the lacunar pattern of dilated vessels. The overlying keratin was likely accentuated because it was on an extensor surface; the rim of hyperpigmentation is common for these lesions.
Angiokeratomas result from dilation of the blood vessels underneath the epidermis. There are different inciting events that lead to the 5 different types of angiokeratomas. The overlying epidermal changes are secondary to the underlying process of capillary ectasia.1 This lesion was not part of a cluster, so it was characterized as a solitary angiokeratoma. Smaller lesions are usually less keratinized and are commonly seen on the scrotum and vulva, where there are usually multiple lesions (referred to as angiokeratoma of Fordyce).
Zaballos2 studied the dermoscopic characteristics of 32 solitary angiokeratomas and reported 6 findings in at least half of the solitary lesions. The most common features were dark lacunae in 94% of the lesions, white veil in 91%, and erythema in 69%. Peripheral erythema, red lacunae, and hemorrhagic crusts were all seen at a rate of 53%. The most common location was the lower extremities.
This patient’s previous pathology report from a shave biopsy was found, confirming that the original diagnosis was angiokeratoma. Since the patient’s lesion had not resolved and was symptomatic from minor trauma, he was scheduled to come back in for an elliptical excision to remove the lesion.
Image and text courtesy of Daniel Stulberg, MD, FAAFP, Professor and Chair, Department of Family and Community Medicine, Western Michigan University Homer Stryker, MD School of Medicine, Kalamazoo.
1. Schiller PI, Itin PH. Angiokeratomas: an update. Dermatology. 1996;193:275-282. doi: 10.1159/000246270
2. Zaballos P, Daufí C, Puig S, et al. Dermoscopy of solitary angiokeratomas: a morphological study. Arch Dermatol. 2007;143:318–325. doi:10.1001/archderm.143.3.318
1. Schiller PI, Itin PH. Angiokeratomas: an update. Dermatology. 1996;193:275-282. doi: 10.1159/000246270
2. Zaballos P, Daufí C, Puig S, et al. Dermoscopy of solitary angiokeratomas: a morphological study. Arch Dermatol. 2007;143:318–325. doi:10.1001/archderm.143.3.318
NSAIDs for knee osteoarthritis may worsen pain over time
CHICAGO – Taking NSAIDs for knee osteoarthritis may worsen inflammation and pain over time, suggest new data revealed at the annual meeting of the Radiological Society of North America.
Johanna Luitjens, MD, a postdoctoral scholar in the department of radiology and biomedical Imaging at the University of California, San Francisco, told this news organization that NSAIDs are frequently used to treat OA pain because inflammation is one of the main drivers of OA, but whether they actually help outcomes has been unclear. Her study suggests that they don’t help – and may actually worsen – outcomes.
In particular, this study looked at the impact of NSAIDs on synovitis – the inflammation of the membrane lining the knee joint – by using MRI-based structural biomarkers.
OA, the most common form of arthritis, affects more than 32 million adults in the United States and more than 500 million people worldwide.
No approved therapy to reduce OA progression
Little is known of the long-term effects of NSAIDs on OA progression. Currently, there’s no approved therapy to cure OA or to reduce its advance.
Dr. Luitjens noted, however, that the synovial membrane mediates development and progression of OA and may be a good therapeutic target.
Researchers studied participants from the Osteoarthritis Initiative (OAI) cohort with moderate to severe OA who used NSAIDs regularly for at least 1 year between baseline and 4-year follow-up. All participants had high-quality 3T MRI of the knee at baseline and after 4 years. Images were scored for biomarkers of inflammation, including cartilage thickness and composition.
Dr. Luitjens and associates studied 721 participants who matched the inclusion criteria (129 with and 592 participants without regular NSAID use). The available data did not further specify amounts of NSAIDs used.
At baseline, significantly higher signal intensity in the infrapatellar fat pad (IFP) was seen in patients who used NSAID, compared with controls (adjusted difference in score, 0.26; 95% confidence interval, –0.5 to –0.129; P = .039).
In addition, at the end of the study period, there was a significantly greater increase in signal intensity of IFP (adjusted difference in score, 0.46; 95% CI, 0.2-0.72; P < .001) and higher increase in effusion synovitis (adjusted difference in score, 0.27; 95% CI, 0.06-0.47; P = .01) in NSAID users, compared with controls.
IFP size and synovial proliferation score did not different significantly between groups at the start of the study and showed no significant change over time.
The results showed no long-term benefit of NSAID use. Joint inflammation and cartilage quality were worse at baseline in the participants taking NSAIDs, compared with the control group, and worsened at 4-year follow-up.
Design limits strength
Amanda E. Nelson, MD, associate professor of medicine, division of rheumatology, allergy, and immunology at the University of North Carolina at Chapel Hill, cautioned against assuming causality, pointing out that the OAI is an observational cohort study. (Dr. Nelson was not involved in the OAI or Dr. Luitjens’ analysis.)
“[The OAI is] large and well known, but it wasn’t designed to compare these groups, and this was a small subset,” she said in an interview. Without randomization, it’s hard to judge the results.
“It may be that people on NSAIDs for the duration of the study had more pain and had more disease to begin with, or had more symptoms or had failed other treatments,” she said, adding that the effect sizes were small.
Measures such as the IFP are ranked 0-3, so “the clinical difference of a 0.26 difference on a 0-3 scale is a bit uncertain,” she said.
Dr. Luitjens said that the researchers tried to adjust for potential confounders but agreed that randomized controlled trials are needed to better advise physicians and patients on the benefits or harms of using NSAIDs for OA.
Weighing the risks in older adults
Una Makris, MD, associate professor of internal medicine in the division of rheumatic diseases at the University of Texas Southwestern Medical Center, Dallas, noted that NSAIDs are “not always the safest option.”
“We are still in desperate need of disease-modifying drugs in OA with rigorous randomized trials to show efficacy for outcomes that are most meaningful to patients,” Dr. Makris, who was not involved in the study, told this news organization.
“OA is most common in older adults, those often with multiple comorbidities, so we must always weigh the risks – including known adverse effects which can be amplified in older adults – and benefits with the goal of improved function and less pain,” Dr. Makris said.
NSAID use also should be considered in the context of body mass index, cardiovascular risk, prior trauma or injury, other medication use, and behavioral factors, including physical activity, she said.
Dr. Luitjens, Dr. Nelson, and Dr. Makris reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
CHICAGO – Taking NSAIDs for knee osteoarthritis may worsen inflammation and pain over time, suggest new data revealed at the annual meeting of the Radiological Society of North America.
Johanna Luitjens, MD, a postdoctoral scholar in the department of radiology and biomedical Imaging at the University of California, San Francisco, told this news organization that NSAIDs are frequently used to treat OA pain because inflammation is one of the main drivers of OA, but whether they actually help outcomes has been unclear. Her study suggests that they don’t help – and may actually worsen – outcomes.
In particular, this study looked at the impact of NSAIDs on synovitis – the inflammation of the membrane lining the knee joint – by using MRI-based structural biomarkers.
OA, the most common form of arthritis, affects more than 32 million adults in the United States and more than 500 million people worldwide.
No approved therapy to reduce OA progression
Little is known of the long-term effects of NSAIDs on OA progression. Currently, there’s no approved therapy to cure OA or to reduce its advance.
Dr. Luitjens noted, however, that the synovial membrane mediates development and progression of OA and may be a good therapeutic target.
Researchers studied participants from the Osteoarthritis Initiative (OAI) cohort with moderate to severe OA who used NSAIDs regularly for at least 1 year between baseline and 4-year follow-up. All participants had high-quality 3T MRI of the knee at baseline and after 4 years. Images were scored for biomarkers of inflammation, including cartilage thickness and composition.
Dr. Luitjens and associates studied 721 participants who matched the inclusion criteria (129 with and 592 participants without regular NSAID use). The available data did not further specify amounts of NSAIDs used.
At baseline, significantly higher signal intensity in the infrapatellar fat pad (IFP) was seen in patients who used NSAID, compared with controls (adjusted difference in score, 0.26; 95% confidence interval, –0.5 to –0.129; P = .039).
In addition, at the end of the study period, there was a significantly greater increase in signal intensity of IFP (adjusted difference in score, 0.46; 95% CI, 0.2-0.72; P < .001) and higher increase in effusion synovitis (adjusted difference in score, 0.27; 95% CI, 0.06-0.47; P = .01) in NSAID users, compared with controls.
IFP size and synovial proliferation score did not different significantly between groups at the start of the study and showed no significant change over time.
The results showed no long-term benefit of NSAID use. Joint inflammation and cartilage quality were worse at baseline in the participants taking NSAIDs, compared with the control group, and worsened at 4-year follow-up.
Design limits strength
Amanda E. Nelson, MD, associate professor of medicine, division of rheumatology, allergy, and immunology at the University of North Carolina at Chapel Hill, cautioned against assuming causality, pointing out that the OAI is an observational cohort study. (Dr. Nelson was not involved in the OAI or Dr. Luitjens’ analysis.)
“[The OAI is] large and well known, but it wasn’t designed to compare these groups, and this was a small subset,” she said in an interview. Without randomization, it’s hard to judge the results.
“It may be that people on NSAIDs for the duration of the study had more pain and had more disease to begin with, or had more symptoms or had failed other treatments,” she said, adding that the effect sizes were small.
Measures such as the IFP are ranked 0-3, so “the clinical difference of a 0.26 difference on a 0-3 scale is a bit uncertain,” she said.
Dr. Luitjens said that the researchers tried to adjust for potential confounders but agreed that randomized controlled trials are needed to better advise physicians and patients on the benefits or harms of using NSAIDs for OA.
Weighing the risks in older adults
Una Makris, MD, associate professor of internal medicine in the division of rheumatic diseases at the University of Texas Southwestern Medical Center, Dallas, noted that NSAIDs are “not always the safest option.”
“We are still in desperate need of disease-modifying drugs in OA with rigorous randomized trials to show efficacy for outcomes that are most meaningful to patients,” Dr. Makris, who was not involved in the study, told this news organization.
“OA is most common in older adults, those often with multiple comorbidities, so we must always weigh the risks – including known adverse effects which can be amplified in older adults – and benefits with the goal of improved function and less pain,” Dr. Makris said.
NSAID use also should be considered in the context of body mass index, cardiovascular risk, prior trauma or injury, other medication use, and behavioral factors, including physical activity, she said.
Dr. Luitjens, Dr. Nelson, and Dr. Makris reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
CHICAGO – Taking NSAIDs for knee osteoarthritis may worsen inflammation and pain over time, suggest new data revealed at the annual meeting of the Radiological Society of North America.
Johanna Luitjens, MD, a postdoctoral scholar in the department of radiology and biomedical Imaging at the University of California, San Francisco, told this news organization that NSAIDs are frequently used to treat OA pain because inflammation is one of the main drivers of OA, but whether they actually help outcomes has been unclear. Her study suggests that they don’t help – and may actually worsen – outcomes.
In particular, this study looked at the impact of NSAIDs on synovitis – the inflammation of the membrane lining the knee joint – by using MRI-based structural biomarkers.
OA, the most common form of arthritis, affects more than 32 million adults in the United States and more than 500 million people worldwide.
No approved therapy to reduce OA progression
Little is known of the long-term effects of NSAIDs on OA progression. Currently, there’s no approved therapy to cure OA or to reduce its advance.
Dr. Luitjens noted, however, that the synovial membrane mediates development and progression of OA and may be a good therapeutic target.
Researchers studied participants from the Osteoarthritis Initiative (OAI) cohort with moderate to severe OA who used NSAIDs regularly for at least 1 year between baseline and 4-year follow-up. All participants had high-quality 3T MRI of the knee at baseline and after 4 years. Images were scored for biomarkers of inflammation, including cartilage thickness and composition.
Dr. Luitjens and associates studied 721 participants who matched the inclusion criteria (129 with and 592 participants without regular NSAID use). The available data did not further specify amounts of NSAIDs used.
At baseline, significantly higher signal intensity in the infrapatellar fat pad (IFP) was seen in patients who used NSAID, compared with controls (adjusted difference in score, 0.26; 95% confidence interval, –0.5 to –0.129; P = .039).
In addition, at the end of the study period, there was a significantly greater increase in signal intensity of IFP (adjusted difference in score, 0.46; 95% CI, 0.2-0.72; P < .001) and higher increase in effusion synovitis (adjusted difference in score, 0.27; 95% CI, 0.06-0.47; P = .01) in NSAID users, compared with controls.
IFP size and synovial proliferation score did not different significantly between groups at the start of the study and showed no significant change over time.
The results showed no long-term benefit of NSAID use. Joint inflammation and cartilage quality were worse at baseline in the participants taking NSAIDs, compared with the control group, and worsened at 4-year follow-up.
Design limits strength
Amanda E. Nelson, MD, associate professor of medicine, division of rheumatology, allergy, and immunology at the University of North Carolina at Chapel Hill, cautioned against assuming causality, pointing out that the OAI is an observational cohort study. (Dr. Nelson was not involved in the OAI or Dr. Luitjens’ analysis.)
“[The OAI is] large and well known, but it wasn’t designed to compare these groups, and this was a small subset,” she said in an interview. Without randomization, it’s hard to judge the results.
“It may be that people on NSAIDs for the duration of the study had more pain and had more disease to begin with, or had more symptoms or had failed other treatments,” she said, adding that the effect sizes were small.
Measures such as the IFP are ranked 0-3, so “the clinical difference of a 0.26 difference on a 0-3 scale is a bit uncertain,” she said.
Dr. Luitjens said that the researchers tried to adjust for potential confounders but agreed that randomized controlled trials are needed to better advise physicians and patients on the benefits or harms of using NSAIDs for OA.
Weighing the risks in older adults
Una Makris, MD, associate professor of internal medicine in the division of rheumatic diseases at the University of Texas Southwestern Medical Center, Dallas, noted that NSAIDs are “not always the safest option.”
“We are still in desperate need of disease-modifying drugs in OA with rigorous randomized trials to show efficacy for outcomes that are most meaningful to patients,” Dr. Makris, who was not involved in the study, told this news organization.
“OA is most common in older adults, those often with multiple comorbidities, so we must always weigh the risks – including known adverse effects which can be amplified in older adults – and benefits with the goal of improved function and less pain,” Dr. Makris said.
NSAID use also should be considered in the context of body mass index, cardiovascular risk, prior trauma or injury, other medication use, and behavioral factors, including physical activity, she said.
Dr. Luitjens, Dr. Nelson, and Dr. Makris reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
AT RSNA 2022
Recommending exercise for migraine: Just do it
with high-intensity aerobics coming in second, and both beating top-line migraine medications topiramate and amitriptyline, new research suggests.
The new results should encourage clinicians to recommend patients with migraine engage in strength-training exercise whenever possible, study investigator Yohannes W. Woldeamanuel, MD, a physician-scientist and instructor, department of neurology and neurological sciences, Stanford (Calif.) University, told this news organization.
“Exercise is something patients can do all their lives and use it to prevent migraine attacks instead of taking daily medications or repetitive injections that have several adverse effects.”
The findings were published online in the Journal of Headache and Pain.
Head-to-head comparison
Several clinical trials have shown exercise is effective for migraine management, but to date, there have been no head-to-head comparisons of strength training and aerobic exercise, said Dr. Woldeamanuel.
This new study used a systematic review with network meta-analysis (NMA), which compares multiple interventions and ranks the efficacy of each one.
After a literature search, researchers included 21 clinical trials with an exercise regimen arm and a comparison control arm. All study data reported monthly frequency of migraine at baseline and at the end of the intervention.
The total combined sample size was 1,195 patients with migraine, who were a mean age of 35.5 years, with a female-to-male ratio of 6.7:1. All studies used International Classification of Headache Disorders (ICHD) criteria for migraine diagnosis.
The NMA provided 27 pairwise comparisons and 8 indirect comparisons. The pairwise comparisons provided direct evidence between the different interventions.
Researchers combined strength training, including weightlifting, with resistance training. Both modalities target muscles, while aerobic exercise targets cardiovascular health.
The average number of weeks was 9.3, 9.3, and 10.7, and the average number of hours per session for strength/resistance training, high-intensity aerobic exercise, and moderate-intensity aerobic exercise interventions was 50, 56, and 45.3, respectively.
The analysis showed all exercise interventions were more effective than the placebo groups in reducing the frequency of migraine. In terms of ranking, strength training came out on top, with a mean difference in monthly migraine days of −3.55 (95% confidence interval, −6.15 to −0.95) between the active and placebo groups.
Next was high-intensity aerobic exercise (−3.13; 95% CI, −5.28 to −0.97) and moderate-intensity aerobic exercise (−2.18; 95% CI, −3.25 to −1.11), followed by topiramate, placebo, and then amitriptyline.
Strength/resistance training was superior possibly because it targets muscle strengthening, particularly major muscles in the neck and shoulder area, which can be a source of the pain trigger, said Dr. Woldeamanuel. He added neck pain is highly comorbid with migraine.
Interestingly, patients doing exercises that focus on unaffected muscles – for example, squats – still get the benefits of less migraine burden, said Dr. Woldeamanuel.
Training recommendations
Strength training also increases or preserves lean muscle mass, which is associated with reduced migraine frequency. Research shows preservation of lean body mass combats central sensitization in various pain syndromes, said Dr. Woldeamanuel.
The superior effects of high- versus moderate-intensity aerobic exercise may be due to recruitment of endogenous molecules involved in exercise-mediated hypoalgesia (pain reduction).
The most common pathways are the opioid and endocannabinoid systems, although other systems are also likely involved, said Dr. Woldeamanuel. He noted migraine has been linked to a deficiency of both opioidergic and endocannabinoidergic signaling.
Dr. Woldeamanuel commented on the difficulty of comparing exercise interventions for patients with chronic versus episodic migraine, as many studies include both.
However, the two studies with moderate-intensity aerobic exercise exclusively involving patients with chronic migraine showed large effect sizes (Cohen’s d) of 0.80 and 1.10 in reducing monthly headache frequency.
Based on these new results and their own experience, the researchers recommend strength training start with 50% of repetition maximum (RM) with 2-3 sets of 12-15 repetitions three times a week along with 10 minutes of warm-up, stretching, and cool-down, totaling 45-60 minutes per session. Weight/resistance load can then be increased weekly by 5% of RM if the patient is capable of successfully completing three sets.
They also recommend including active recovery days (low-intensity exercise) between training days. All major muscles, including neck, shoulder, and upper limb muscles, should be trained in a rotation.
For high-intensity aerobic exercise, the authors recommend starting with interval training at 55% VO2max (maximum respiratory capacity), or 50% HRmax (maximal heart rate) for 45-60 minutes per session, including 10 minutes of warm-up and cool-down, three times per week. The intensity can then be increased by 5%-10% each week to reach a maximum target of 80%-90% by week 12.
It is best for patients to start with a trainer for guidance and supervision, but once they master the routines, they can do the exercises independently, said Dr. Woldeamanuel.
Managing flare-ups
Headache flare-ups are normal during exercise, which may be caused by “boom and bust cycles” – exercising excessively when feeling good then completely stopping when feeling bad, said Dr. Woldeamanuel. He noted these flare-ups don’t mean “there’s something wrong with the brain or there’s some injury to muscles.”
The best way to manage such flare-ups is to use a pacing strategy that involves “not going overboard on good days and avoiding excessive rest on bad days,” the investigators note.
Dr. Woldeamanuel noted exercise is a lifestyle-based intervention; it not only helps reduce migraine attacks but also helps control other known comorbidities such as obesity and hypertension.
In a comment, Elizabeth Loder, MD, vice-chair, academic affairs, department of neurology, Brigham and Women’s Hospital, and professor of neurology, Harvard Medical School, both in Boston, said, “It’s useful to collect and summarize all of these studies, and to focus on helping patients and doctors understand the possible value of different kinds of exercise.”
The review was “well done,” said Dr. Loder, adding the researchers “have looked carefully at the quality of included studies.”
The study received support from the National Institute of Neurological Disorders and Stroke of the National Institutes of Health. Dr. Woldeamanuel has reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
with high-intensity aerobics coming in second, and both beating top-line migraine medications topiramate and amitriptyline, new research suggests.
The new results should encourage clinicians to recommend patients with migraine engage in strength-training exercise whenever possible, study investigator Yohannes W. Woldeamanuel, MD, a physician-scientist and instructor, department of neurology and neurological sciences, Stanford (Calif.) University, told this news organization.
“Exercise is something patients can do all their lives and use it to prevent migraine attacks instead of taking daily medications or repetitive injections that have several adverse effects.”
The findings were published online in the Journal of Headache and Pain.
Head-to-head comparison
Several clinical trials have shown exercise is effective for migraine management, but to date, there have been no head-to-head comparisons of strength training and aerobic exercise, said Dr. Woldeamanuel.
This new study used a systematic review with network meta-analysis (NMA), which compares multiple interventions and ranks the efficacy of each one.
After a literature search, researchers included 21 clinical trials with an exercise regimen arm and a comparison control arm. All study data reported monthly frequency of migraine at baseline and at the end of the intervention.
The total combined sample size was 1,195 patients with migraine, who were a mean age of 35.5 years, with a female-to-male ratio of 6.7:1. All studies used International Classification of Headache Disorders (ICHD) criteria for migraine diagnosis.
The NMA provided 27 pairwise comparisons and 8 indirect comparisons. The pairwise comparisons provided direct evidence between the different interventions.
Researchers combined strength training, including weightlifting, with resistance training. Both modalities target muscles, while aerobic exercise targets cardiovascular health.
The average number of weeks was 9.3, 9.3, and 10.7, and the average number of hours per session for strength/resistance training, high-intensity aerobic exercise, and moderate-intensity aerobic exercise interventions was 50, 56, and 45.3, respectively.
The analysis showed all exercise interventions were more effective than the placebo groups in reducing the frequency of migraine. In terms of ranking, strength training came out on top, with a mean difference in monthly migraine days of −3.55 (95% confidence interval, −6.15 to −0.95) between the active and placebo groups.
Next was high-intensity aerobic exercise (−3.13; 95% CI, −5.28 to −0.97) and moderate-intensity aerobic exercise (−2.18; 95% CI, −3.25 to −1.11), followed by topiramate, placebo, and then amitriptyline.
Strength/resistance training was superior possibly because it targets muscle strengthening, particularly major muscles in the neck and shoulder area, which can be a source of the pain trigger, said Dr. Woldeamanuel. He added neck pain is highly comorbid with migraine.
Interestingly, patients doing exercises that focus on unaffected muscles – for example, squats – still get the benefits of less migraine burden, said Dr. Woldeamanuel.
Training recommendations
Strength training also increases or preserves lean muscle mass, which is associated with reduced migraine frequency. Research shows preservation of lean body mass combats central sensitization in various pain syndromes, said Dr. Woldeamanuel.
The superior effects of high- versus moderate-intensity aerobic exercise may be due to recruitment of endogenous molecules involved in exercise-mediated hypoalgesia (pain reduction).
The most common pathways are the opioid and endocannabinoid systems, although other systems are also likely involved, said Dr. Woldeamanuel. He noted migraine has been linked to a deficiency of both opioidergic and endocannabinoidergic signaling.
Dr. Woldeamanuel commented on the difficulty of comparing exercise interventions for patients with chronic versus episodic migraine, as many studies include both.
However, the two studies with moderate-intensity aerobic exercise exclusively involving patients with chronic migraine showed large effect sizes (Cohen’s d) of 0.80 and 1.10 in reducing monthly headache frequency.
Based on these new results and their own experience, the researchers recommend strength training start with 50% of repetition maximum (RM) with 2-3 sets of 12-15 repetitions three times a week along with 10 minutes of warm-up, stretching, and cool-down, totaling 45-60 minutes per session. Weight/resistance load can then be increased weekly by 5% of RM if the patient is capable of successfully completing three sets.
They also recommend including active recovery days (low-intensity exercise) between training days. All major muscles, including neck, shoulder, and upper limb muscles, should be trained in a rotation.
For high-intensity aerobic exercise, the authors recommend starting with interval training at 55% VO2max (maximum respiratory capacity), or 50% HRmax (maximal heart rate) for 45-60 minutes per session, including 10 minutes of warm-up and cool-down, three times per week. The intensity can then be increased by 5%-10% each week to reach a maximum target of 80%-90% by week 12.
It is best for patients to start with a trainer for guidance and supervision, but once they master the routines, they can do the exercises independently, said Dr. Woldeamanuel.
Managing flare-ups
Headache flare-ups are normal during exercise, which may be caused by “boom and bust cycles” – exercising excessively when feeling good then completely stopping when feeling bad, said Dr. Woldeamanuel. He noted these flare-ups don’t mean “there’s something wrong with the brain or there’s some injury to muscles.”
The best way to manage such flare-ups is to use a pacing strategy that involves “not going overboard on good days and avoiding excessive rest on bad days,” the investigators note.
Dr. Woldeamanuel noted exercise is a lifestyle-based intervention; it not only helps reduce migraine attacks but also helps control other known comorbidities such as obesity and hypertension.
In a comment, Elizabeth Loder, MD, vice-chair, academic affairs, department of neurology, Brigham and Women’s Hospital, and professor of neurology, Harvard Medical School, both in Boston, said, “It’s useful to collect and summarize all of these studies, and to focus on helping patients and doctors understand the possible value of different kinds of exercise.”
The review was “well done,” said Dr. Loder, adding the researchers “have looked carefully at the quality of included studies.”
The study received support from the National Institute of Neurological Disorders and Stroke of the National Institutes of Health. Dr. Woldeamanuel has reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
with high-intensity aerobics coming in second, and both beating top-line migraine medications topiramate and amitriptyline, new research suggests.
The new results should encourage clinicians to recommend patients with migraine engage in strength-training exercise whenever possible, study investigator Yohannes W. Woldeamanuel, MD, a physician-scientist and instructor, department of neurology and neurological sciences, Stanford (Calif.) University, told this news organization.
“Exercise is something patients can do all their lives and use it to prevent migraine attacks instead of taking daily medications or repetitive injections that have several adverse effects.”
The findings were published online in the Journal of Headache and Pain.
Head-to-head comparison
Several clinical trials have shown exercise is effective for migraine management, but to date, there have been no head-to-head comparisons of strength training and aerobic exercise, said Dr. Woldeamanuel.
This new study used a systematic review with network meta-analysis (NMA), which compares multiple interventions and ranks the efficacy of each one.
After a literature search, researchers included 21 clinical trials with an exercise regimen arm and a comparison control arm. All study data reported monthly frequency of migraine at baseline and at the end of the intervention.
The total combined sample size was 1,195 patients with migraine, who were a mean age of 35.5 years, with a female-to-male ratio of 6.7:1. All studies used International Classification of Headache Disorders (ICHD) criteria for migraine diagnosis.
The NMA provided 27 pairwise comparisons and 8 indirect comparisons. The pairwise comparisons provided direct evidence between the different interventions.
Researchers combined strength training, including weightlifting, with resistance training. Both modalities target muscles, while aerobic exercise targets cardiovascular health.
The average number of weeks was 9.3, 9.3, and 10.7, and the average number of hours per session for strength/resistance training, high-intensity aerobic exercise, and moderate-intensity aerobic exercise interventions was 50, 56, and 45.3, respectively.
The analysis showed all exercise interventions were more effective than the placebo groups in reducing the frequency of migraine. In terms of ranking, strength training came out on top, with a mean difference in monthly migraine days of −3.55 (95% confidence interval, −6.15 to −0.95) between the active and placebo groups.
Next was high-intensity aerobic exercise (−3.13; 95% CI, −5.28 to −0.97) and moderate-intensity aerobic exercise (−2.18; 95% CI, −3.25 to −1.11), followed by topiramate, placebo, and then amitriptyline.
Strength/resistance training was superior possibly because it targets muscle strengthening, particularly major muscles in the neck and shoulder area, which can be a source of the pain trigger, said Dr. Woldeamanuel. He added neck pain is highly comorbid with migraine.
Interestingly, patients doing exercises that focus on unaffected muscles – for example, squats – still get the benefits of less migraine burden, said Dr. Woldeamanuel.
Training recommendations
Strength training also increases or preserves lean muscle mass, which is associated with reduced migraine frequency. Research shows preservation of lean body mass combats central sensitization in various pain syndromes, said Dr. Woldeamanuel.
The superior effects of high- versus moderate-intensity aerobic exercise may be due to recruitment of endogenous molecules involved in exercise-mediated hypoalgesia (pain reduction).
The most common pathways are the opioid and endocannabinoid systems, although other systems are also likely involved, said Dr. Woldeamanuel. He noted migraine has been linked to a deficiency of both opioidergic and endocannabinoidergic signaling.
Dr. Woldeamanuel commented on the difficulty of comparing exercise interventions for patients with chronic versus episodic migraine, as many studies include both.
However, the two studies with moderate-intensity aerobic exercise exclusively involving patients with chronic migraine showed large effect sizes (Cohen’s d) of 0.80 and 1.10 in reducing monthly headache frequency.
Based on these new results and their own experience, the researchers recommend strength training start with 50% of repetition maximum (RM) with 2-3 sets of 12-15 repetitions three times a week along with 10 minutes of warm-up, stretching, and cool-down, totaling 45-60 minutes per session. Weight/resistance load can then be increased weekly by 5% of RM if the patient is capable of successfully completing three sets.
They also recommend including active recovery days (low-intensity exercise) between training days. All major muscles, including neck, shoulder, and upper limb muscles, should be trained in a rotation.
For high-intensity aerobic exercise, the authors recommend starting with interval training at 55% VO2max (maximum respiratory capacity), or 50% HRmax (maximal heart rate) for 45-60 minutes per session, including 10 minutes of warm-up and cool-down, three times per week. The intensity can then be increased by 5%-10% each week to reach a maximum target of 80%-90% by week 12.
It is best for patients to start with a trainer for guidance and supervision, but once they master the routines, they can do the exercises independently, said Dr. Woldeamanuel.
Managing flare-ups
Headache flare-ups are normal during exercise, which may be caused by “boom and bust cycles” – exercising excessively when feeling good then completely stopping when feeling bad, said Dr. Woldeamanuel. He noted these flare-ups don’t mean “there’s something wrong with the brain or there’s some injury to muscles.”
The best way to manage such flare-ups is to use a pacing strategy that involves “not going overboard on good days and avoiding excessive rest on bad days,” the investigators note.
Dr. Woldeamanuel noted exercise is a lifestyle-based intervention; it not only helps reduce migraine attacks but also helps control other known comorbidities such as obesity and hypertension.
In a comment, Elizabeth Loder, MD, vice-chair, academic affairs, department of neurology, Brigham and Women’s Hospital, and professor of neurology, Harvard Medical School, both in Boston, said, “It’s useful to collect and summarize all of these studies, and to focus on helping patients and doctors understand the possible value of different kinds of exercise.”
The review was “well done,” said Dr. Loder, adding the researchers “have looked carefully at the quality of included studies.”
The study received support from the National Institute of Neurological Disorders and Stroke of the National Institutes of Health. Dr. Woldeamanuel has reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM JOURNAL OF HEADACHE AND PAIN