User login
Sarilumab effective for polymyalgia rheumatica in phase 3 trial
PHILADELPHIA – Treatment with the interleukin-6 receptor antagonist sarilumab (Kevzara), along with a 14-week taper of glucocorticoids, proved to have significant efficacy in patients with relapsing polymyalgia rheumatica (PMR) who were resistant to glucocorticoids in a phase 3 trial.
No new safety concerns were found with sarilumab in the multicenter, randomized, double-blind, placebo-controlled SAPHYR trial. Sarilumab is approved in the United States for the treatment of moderate to severe active rheumatoid arthritis in adults who have had an inadequate response or intolerance to one or more disease-modifying antirheumatic drugs.
The results, presented at the annual meeting of the American College of Rheumatology by Robert Spiera, MD, director of the Scleroderma, Vasculitis, and Myositis Center at the Hospital for Special Surgery in New York, included clinically meaningful improvement in quality-of-life scores.
The disease, which primarily affects people over age 65, can cause widespread aching and stiffness. It’s one of the most common inflammatory diseases among older adults.
PMR is relatively easy to treat with glucocorticoids, but relapses are common, which means long courses of glucocorticoid therapy and the side effects that come with them.
Need for a steroid-sparing therapy
“We recognize that a steroid-sparing drug in polymyalgia rheumatica seems to be an unmet need,” Dr. Spiera said at the meeting.
The trial, sponsored by Sanofi, included active, refractory PMR patients who flared within 3 months of study entry while on at least 7.5 mg/day of prednisone or the equivalent. They were randomly assigned (1:1) to 52 weeks of treatment with subcutaneous sarilumab 200 mg every 2 weeks plus the rapid 14-week glucocorticoid tapering regimen or were given placebo every 2 weeks plus a more traditional 52-week tapering of glucocorticoids.
COVID hampered recruitment
Recruitment was stopped early because of complications during the COVID-19 pandemic, so between October 2018 and July 2020, 118 of the intended 280 patients were recruited, and 117 were treated (sarilumab = 59, placebo = 58). Median age was 69 years in the treatment group and 70 among those taking placebo.
Of the 117 treated, only 78 patients (67%) completed treatment (sarilumab = 42, placebo = 36). The main reasons for stopping treatment were adverse events – including seven with sarilumab and four with placebo – and lack of efficacy (sarilumab = four, placebo = nine).
The primary outcome was the proportion of patients who reached sustained remission at 52 weeks, defined as disease remission by week 12 and no disease flare, normal C-reactive protein (CRP), and adherence to the glucocorticoid taper during weeks 12-52.
The researchers found that sustained remission was significantly higher in the sarilumab arm versus the control group (28.3% versus 10.3%; P = .0193).
IL-6 inhibitors lower CRP, but if you take CRP out of the definition, Dr. Spiera said, “we still saw this difference: 31.7% of patients treated with sarilumab and 13.8% treated with placebo and a longer taper achieved that endpoint.”
Forty-four percent lower risk of flare with sarilumab
Patients in the sarilumab group also had 44% lower risk of having a flare after achieving clinical remission versus the comparator group (16.7% versus 29.3%; hazard ratio, 0.56; 95% confidence interval, 0.35-0.90; P = .0153).
Patient-reported outcomes, which included physical and mental health scores and disability index results, favored sarilumab.
The incidence of treatment-emergent adverse events (TEAEs) was numerically higher in the sarilumab group, compared with the control group (94.9% versus 84.5%). TEAEs included neutropenia (15.3%) and arthralgia (15.3%) in the sarilumab group and insomnia (15.5%) in the comparator arm.
However, the frequency of serious AEs was higher in the control group, compared with the sarilumab arm (20.7% versus 13.6%). No deaths were reported, and, importantly in this age group treated with concurrent glucocorticoids and an IL-6 inhibitor, Dr. Spiera said, “there were no cases of diverticulitis requiring intervention.”
Dr. Spiera was asked about a seemingly low remission rate. He answered that the bar was very high for remission in this study.
Patients had to achieve remission by week 12 and with the rapid 14-week taper. “That means by week 12 the sarilumab arm patients were only on 2 mg of daily prednisone or its equivalent,” he said.
Patients had to maintain that for another 40 weeks, he noted, adding, “I think especially in the context of quality of life and function indices, these were important results.”
Sebastian E. Sattui, MD, director of the University of Pittsburgh Medical Center vasculitis clinic, told this news organization that prolonged use of glucocorticoids in patients with PMR remains an important concern and the need for other options is critical.
“Around 30% of patients with PMR remain on prednisone 5 years after diagnosis,” he said. “Low-dose glucocorticoids are still associated with significant morbidity. Until recently, there has been a paucity of high-quality data regarding the use of steroid-sparing agents in PMR. “
He noted that the SAPHYR trial data are promising “with sarilumab being successful in achieving remission while minimizing glucocorticoids in patients with relapsing PMR.” The clinically meaningful improvement in patient-reported outcomes was just as important, he added.
The main unanswered question is whether the disease-modifying ability of sarilumab will continue after it is stopped, Dr. Sattui said.
Dr. Spiera is a consultant for Sanofi, which funded the trial. He also disclosed financial relationships with GlaxoSmithKline, Boehringer Ingelheim, Corbus, InflaRx, AbbVie/Abbott, Novartis, Chemocentryx, Roche, and Vera. Dr. Sattui has received research support from AstraZeneca and has done unpaid consulting work for Sanofi.
A version of this article first appeared on Medscape.com.
PHILADELPHIA – Treatment with the interleukin-6 receptor antagonist sarilumab (Kevzara), along with a 14-week taper of glucocorticoids, proved to have significant efficacy in patients with relapsing polymyalgia rheumatica (PMR) who were resistant to glucocorticoids in a phase 3 trial.
No new safety concerns were found with sarilumab in the multicenter, randomized, double-blind, placebo-controlled SAPHYR trial. Sarilumab is approved in the United States for the treatment of moderate to severe active rheumatoid arthritis in adults who have had an inadequate response or intolerance to one or more disease-modifying antirheumatic drugs.
The results, presented at the annual meeting of the American College of Rheumatology by Robert Spiera, MD, director of the Scleroderma, Vasculitis, and Myositis Center at the Hospital for Special Surgery in New York, included clinically meaningful improvement in quality-of-life scores.
The disease, which primarily affects people over age 65, can cause widespread aching and stiffness. It’s one of the most common inflammatory diseases among older adults.
PMR is relatively easy to treat with glucocorticoids, but relapses are common, which means long courses of glucocorticoid therapy and the side effects that come with them.
Need for a steroid-sparing therapy
“We recognize that a steroid-sparing drug in polymyalgia rheumatica seems to be an unmet need,” Dr. Spiera said at the meeting.
The trial, sponsored by Sanofi, included active, refractory PMR patients who flared within 3 months of study entry while on at least 7.5 mg/day of prednisone or the equivalent. They were randomly assigned (1:1) to 52 weeks of treatment with subcutaneous sarilumab 200 mg every 2 weeks plus the rapid 14-week glucocorticoid tapering regimen or were given placebo every 2 weeks plus a more traditional 52-week tapering of glucocorticoids.
COVID hampered recruitment
Recruitment was stopped early because of complications during the COVID-19 pandemic, so between October 2018 and July 2020, 118 of the intended 280 patients were recruited, and 117 were treated (sarilumab = 59, placebo = 58). Median age was 69 years in the treatment group and 70 among those taking placebo.
Of the 117 treated, only 78 patients (67%) completed treatment (sarilumab = 42, placebo = 36). The main reasons for stopping treatment were adverse events – including seven with sarilumab and four with placebo – and lack of efficacy (sarilumab = four, placebo = nine).
The primary outcome was the proportion of patients who reached sustained remission at 52 weeks, defined as disease remission by week 12 and no disease flare, normal C-reactive protein (CRP), and adherence to the glucocorticoid taper during weeks 12-52.
The researchers found that sustained remission was significantly higher in the sarilumab arm versus the control group (28.3% versus 10.3%; P = .0193).
IL-6 inhibitors lower CRP, but if you take CRP out of the definition, Dr. Spiera said, “we still saw this difference: 31.7% of patients treated with sarilumab and 13.8% treated with placebo and a longer taper achieved that endpoint.”
Forty-four percent lower risk of flare with sarilumab
Patients in the sarilumab group also had 44% lower risk of having a flare after achieving clinical remission versus the comparator group (16.7% versus 29.3%; hazard ratio, 0.56; 95% confidence interval, 0.35-0.90; P = .0153).
Patient-reported outcomes, which included physical and mental health scores and disability index results, favored sarilumab.
The incidence of treatment-emergent adverse events (TEAEs) was numerically higher in the sarilumab group, compared with the control group (94.9% versus 84.5%). TEAEs included neutropenia (15.3%) and arthralgia (15.3%) in the sarilumab group and insomnia (15.5%) in the comparator arm.
However, the frequency of serious AEs was higher in the control group, compared with the sarilumab arm (20.7% versus 13.6%). No deaths were reported, and, importantly in this age group treated with concurrent glucocorticoids and an IL-6 inhibitor, Dr. Spiera said, “there were no cases of diverticulitis requiring intervention.”
Dr. Spiera was asked about a seemingly low remission rate. He answered that the bar was very high for remission in this study.
Patients had to achieve remission by week 12 and with the rapid 14-week taper. “That means by week 12 the sarilumab arm patients were only on 2 mg of daily prednisone or its equivalent,” he said.
Patients had to maintain that for another 40 weeks, he noted, adding, “I think especially in the context of quality of life and function indices, these were important results.”
Sebastian E. Sattui, MD, director of the University of Pittsburgh Medical Center vasculitis clinic, told this news organization that prolonged use of glucocorticoids in patients with PMR remains an important concern and the need for other options is critical.
“Around 30% of patients with PMR remain on prednisone 5 years after diagnosis,” he said. “Low-dose glucocorticoids are still associated with significant morbidity. Until recently, there has been a paucity of high-quality data regarding the use of steroid-sparing agents in PMR. “
He noted that the SAPHYR trial data are promising “with sarilumab being successful in achieving remission while minimizing glucocorticoids in patients with relapsing PMR.” The clinically meaningful improvement in patient-reported outcomes was just as important, he added.
The main unanswered question is whether the disease-modifying ability of sarilumab will continue after it is stopped, Dr. Sattui said.
Dr. Spiera is a consultant for Sanofi, which funded the trial. He also disclosed financial relationships with GlaxoSmithKline, Boehringer Ingelheim, Corbus, InflaRx, AbbVie/Abbott, Novartis, Chemocentryx, Roche, and Vera. Dr. Sattui has received research support from AstraZeneca and has done unpaid consulting work for Sanofi.
A version of this article first appeared on Medscape.com.
PHILADELPHIA – Treatment with the interleukin-6 receptor antagonist sarilumab (Kevzara), along with a 14-week taper of glucocorticoids, proved to have significant efficacy in patients with relapsing polymyalgia rheumatica (PMR) who were resistant to glucocorticoids in a phase 3 trial.
No new safety concerns were found with sarilumab in the multicenter, randomized, double-blind, placebo-controlled SAPHYR trial. Sarilumab is approved in the United States for the treatment of moderate to severe active rheumatoid arthritis in adults who have had an inadequate response or intolerance to one or more disease-modifying antirheumatic drugs.
The results, presented at the annual meeting of the American College of Rheumatology by Robert Spiera, MD, director of the Scleroderma, Vasculitis, and Myositis Center at the Hospital for Special Surgery in New York, included clinically meaningful improvement in quality-of-life scores.
The disease, which primarily affects people over age 65, can cause widespread aching and stiffness. It’s one of the most common inflammatory diseases among older adults.
PMR is relatively easy to treat with glucocorticoids, but relapses are common, which means long courses of glucocorticoid therapy and the side effects that come with them.
Need for a steroid-sparing therapy
“We recognize that a steroid-sparing drug in polymyalgia rheumatica seems to be an unmet need,” Dr. Spiera said at the meeting.
The trial, sponsored by Sanofi, included active, refractory PMR patients who flared within 3 months of study entry while on at least 7.5 mg/day of prednisone or the equivalent. They were randomly assigned (1:1) to 52 weeks of treatment with subcutaneous sarilumab 200 mg every 2 weeks plus the rapid 14-week glucocorticoid tapering regimen or were given placebo every 2 weeks plus a more traditional 52-week tapering of glucocorticoids.
COVID hampered recruitment
Recruitment was stopped early because of complications during the COVID-19 pandemic, so between October 2018 and July 2020, 118 of the intended 280 patients were recruited, and 117 were treated (sarilumab = 59, placebo = 58). Median age was 69 years in the treatment group and 70 among those taking placebo.
Of the 117 treated, only 78 patients (67%) completed treatment (sarilumab = 42, placebo = 36). The main reasons for stopping treatment were adverse events – including seven with sarilumab and four with placebo – and lack of efficacy (sarilumab = four, placebo = nine).
The primary outcome was the proportion of patients who reached sustained remission at 52 weeks, defined as disease remission by week 12 and no disease flare, normal C-reactive protein (CRP), and adherence to the glucocorticoid taper during weeks 12-52.
The researchers found that sustained remission was significantly higher in the sarilumab arm versus the control group (28.3% versus 10.3%; P = .0193).
IL-6 inhibitors lower CRP, but if you take CRP out of the definition, Dr. Spiera said, “we still saw this difference: 31.7% of patients treated with sarilumab and 13.8% treated with placebo and a longer taper achieved that endpoint.”
Forty-four percent lower risk of flare with sarilumab
Patients in the sarilumab group also had 44% lower risk of having a flare after achieving clinical remission versus the comparator group (16.7% versus 29.3%; hazard ratio, 0.56; 95% confidence interval, 0.35-0.90; P = .0153).
Patient-reported outcomes, which included physical and mental health scores and disability index results, favored sarilumab.
The incidence of treatment-emergent adverse events (TEAEs) was numerically higher in the sarilumab group, compared with the control group (94.9% versus 84.5%). TEAEs included neutropenia (15.3%) and arthralgia (15.3%) in the sarilumab group and insomnia (15.5%) in the comparator arm.
However, the frequency of serious AEs was higher in the control group, compared with the sarilumab arm (20.7% versus 13.6%). No deaths were reported, and, importantly in this age group treated with concurrent glucocorticoids and an IL-6 inhibitor, Dr. Spiera said, “there were no cases of diverticulitis requiring intervention.”
Dr. Spiera was asked about a seemingly low remission rate. He answered that the bar was very high for remission in this study.
Patients had to achieve remission by week 12 and with the rapid 14-week taper. “That means by week 12 the sarilumab arm patients were only on 2 mg of daily prednisone or its equivalent,” he said.
Patients had to maintain that for another 40 weeks, he noted, adding, “I think especially in the context of quality of life and function indices, these were important results.”
Sebastian E. Sattui, MD, director of the University of Pittsburgh Medical Center vasculitis clinic, told this news organization that prolonged use of glucocorticoids in patients with PMR remains an important concern and the need for other options is critical.
“Around 30% of patients with PMR remain on prednisone 5 years after diagnosis,” he said. “Low-dose glucocorticoids are still associated with significant morbidity. Until recently, there has been a paucity of high-quality data regarding the use of steroid-sparing agents in PMR. “
He noted that the SAPHYR trial data are promising “with sarilumab being successful in achieving remission while minimizing glucocorticoids in patients with relapsing PMR.” The clinically meaningful improvement in patient-reported outcomes was just as important, he added.
The main unanswered question is whether the disease-modifying ability of sarilumab will continue after it is stopped, Dr. Sattui said.
Dr. Spiera is a consultant for Sanofi, which funded the trial. He also disclosed financial relationships with GlaxoSmithKline, Boehringer Ingelheim, Corbus, InflaRx, AbbVie/Abbott, Novartis, Chemocentryx, Roche, and Vera. Dr. Sattui has received research support from AstraZeneca and has done unpaid consulting work for Sanofi.
A version of this article first appeared on Medscape.com.
AT ACR 2022
Fentanyl vaccine a potential ‘game changer’ for opioid crisis
Texas-based researchers have developed a vaccine that blocks the euphoric effects of fentanyl, a potent synthetic opioid that is increasingly involved in opioid overdose deaths in the United States.
In studies in male and female mice, the vaccine generated significant and long-lasting levels of anti-fentanyl antibodies that were highly effective at reducing the antinociceptive, behavioral, and physiological effects of the drug.
“Thus, the individual will not feel the euphoric effects and can ‘get back on the wagon’ to sobriety,” lead investigator Colin Haile, MD, PhD, with University of Houston and founding member of the UH Drug Discovery Institute, said in a news release. The study was published online in the journal Pharmaceutics.
“The anti-fentanyl antibodies were specific to fentanyl and a fentanyl derivative and did not cross-react with other opioids, such as morphine. That means a vaccinated person would still be able to be treated for pain relief with other opioids,” said Dr. Haile.
The vaccine did not cause any adverse effects in the immunized mice. The research team plans to start manufacturing clinical-grade vaccine in the coming months with clinical trials in humans planned soon.
If proven safe and effective in clinical testing, the vaccine could have major implications for the nation’s opioid epidemic by becoming a relapse prevention agent for people trying to quit using opioids, the researchers note.
The United States in 2021 recorded more than 107,000 drug overdose deaths – a record high, according to federal health officials – and fentanyl was involved in most of these deaths.
Senior author Therese Kosten, PhD, director of the UH Developmental, Cognitive & Behavioral Neuroscience program, calls the new fentanyl vaccine a potential “game changer.”
“Fentanyl use and overdose is a particular treatment challenge that is not adequately addressed with current medications because of its pharmacodynamics, and managing acute overdose with the short-acting naloxone [Narcan] is not appropriately effective as multiple doses of naloxone are often needed to reverse fentanyl’s fatal effects,” said Dr. Kosten.
Funding for the study was provided by the Department of Defense through the Alcohol and Substance Abuse Disorders Program managed by RTI International’s Pharmacotherapies for Alcohol and Substance Use Disorders Alliance, which has funded Dr. Haile’s lab for several years to develop the anti-fentanyl vaccine. The authors have no relevant conflicts of interest. A provisional patent has been submitted by the University of Houston on behalf of four of the investigators containing technology related to the fentanyl vaccine.
A version of this article first appeared on Medscape.com.
Texas-based researchers have developed a vaccine that blocks the euphoric effects of fentanyl, a potent synthetic opioid that is increasingly involved in opioid overdose deaths in the United States.
In studies in male and female mice, the vaccine generated significant and long-lasting levels of anti-fentanyl antibodies that were highly effective at reducing the antinociceptive, behavioral, and physiological effects of the drug.
“Thus, the individual will not feel the euphoric effects and can ‘get back on the wagon’ to sobriety,” lead investigator Colin Haile, MD, PhD, with University of Houston and founding member of the UH Drug Discovery Institute, said in a news release. The study was published online in the journal Pharmaceutics.
“The anti-fentanyl antibodies were specific to fentanyl and a fentanyl derivative and did not cross-react with other opioids, such as morphine. That means a vaccinated person would still be able to be treated for pain relief with other opioids,” said Dr. Haile.
The vaccine did not cause any adverse effects in the immunized mice. The research team plans to start manufacturing clinical-grade vaccine in the coming months with clinical trials in humans planned soon.
If proven safe and effective in clinical testing, the vaccine could have major implications for the nation’s opioid epidemic by becoming a relapse prevention agent for people trying to quit using opioids, the researchers note.
The United States in 2021 recorded more than 107,000 drug overdose deaths – a record high, according to federal health officials – and fentanyl was involved in most of these deaths.
Senior author Therese Kosten, PhD, director of the UH Developmental, Cognitive & Behavioral Neuroscience program, calls the new fentanyl vaccine a potential “game changer.”
“Fentanyl use and overdose is a particular treatment challenge that is not adequately addressed with current medications because of its pharmacodynamics, and managing acute overdose with the short-acting naloxone [Narcan] is not appropriately effective as multiple doses of naloxone are often needed to reverse fentanyl’s fatal effects,” said Dr. Kosten.
Funding for the study was provided by the Department of Defense through the Alcohol and Substance Abuse Disorders Program managed by RTI International’s Pharmacotherapies for Alcohol and Substance Use Disorders Alliance, which has funded Dr. Haile’s lab for several years to develop the anti-fentanyl vaccine. The authors have no relevant conflicts of interest. A provisional patent has been submitted by the University of Houston on behalf of four of the investigators containing technology related to the fentanyl vaccine.
A version of this article first appeared on Medscape.com.
Texas-based researchers have developed a vaccine that blocks the euphoric effects of fentanyl, a potent synthetic opioid that is increasingly involved in opioid overdose deaths in the United States.
In studies in male and female mice, the vaccine generated significant and long-lasting levels of anti-fentanyl antibodies that were highly effective at reducing the antinociceptive, behavioral, and physiological effects of the drug.
“Thus, the individual will not feel the euphoric effects and can ‘get back on the wagon’ to sobriety,” lead investigator Colin Haile, MD, PhD, with University of Houston and founding member of the UH Drug Discovery Institute, said in a news release. The study was published online in the journal Pharmaceutics.
“The anti-fentanyl antibodies were specific to fentanyl and a fentanyl derivative and did not cross-react with other opioids, such as morphine. That means a vaccinated person would still be able to be treated for pain relief with other opioids,” said Dr. Haile.
The vaccine did not cause any adverse effects in the immunized mice. The research team plans to start manufacturing clinical-grade vaccine in the coming months with clinical trials in humans planned soon.
If proven safe and effective in clinical testing, the vaccine could have major implications for the nation’s opioid epidemic by becoming a relapse prevention agent for people trying to quit using opioids, the researchers note.
The United States in 2021 recorded more than 107,000 drug overdose deaths – a record high, according to federal health officials – and fentanyl was involved in most of these deaths.
Senior author Therese Kosten, PhD, director of the UH Developmental, Cognitive & Behavioral Neuroscience program, calls the new fentanyl vaccine a potential “game changer.”
“Fentanyl use and overdose is a particular treatment challenge that is not adequately addressed with current medications because of its pharmacodynamics, and managing acute overdose with the short-acting naloxone [Narcan] is not appropriately effective as multiple doses of naloxone are often needed to reverse fentanyl’s fatal effects,” said Dr. Kosten.
Funding for the study was provided by the Department of Defense through the Alcohol and Substance Abuse Disorders Program managed by RTI International’s Pharmacotherapies for Alcohol and Substance Use Disorders Alliance, which has funded Dr. Haile’s lab for several years to develop the anti-fentanyl vaccine. The authors have no relevant conflicts of interest. A provisional patent has been submitted by the University of Houston on behalf of four of the investigators containing technology related to the fentanyl vaccine.
A version of this article first appeared on Medscape.com.
FROM PHARMACEUTICS
‘A huge deal’: Millions have long COVID, and more are expected
with symptoms that have lasted 3 months or longer, according to the latest U.S. government survey done in October. More than a quarter say their condition is severe enough to significantly limit their day-to-day activities – yet the problem is only barely starting to get the attention of employers, the health care system, and policymakers.
With no cure or treatment in sight, long COVID is already burdening not only the health care system, but also the economy – and that burden is set to grow. Many experts worry about the possible long-term ripple effects, from increased spending on medical care costs to lost wages due to not being able to work, as well as the policy implications that come with addressing these issues.
“At this point, anyone who’s looking at this seriously would say this is a huge deal,” says senior Brookings Institution fellow Katie Bach, the author of a study that analyzed long COVID’s impact on the labor market.
“We need a real concerted focus on treating these people, which means both research and the clinical side, and figuring out how to build a labor market that is more inclusive of people with disabilities,” she said.
It’s not only that many people are affected. It’s that they are often affected for months and possibly even years.
The U.S. government figures suggest more than 18 million people could have symptoms of long COVID right now. The latest Household Pulse Survey by the Census Bureau and the National Center for Health Statistics takes data from 41,415 people.
A preprint of a study by researchers from City University of New York, posted on medRxiv in September and based on a similar population survey done between June 30 and July 2, drew comparable results. The study has not been peer reviewed.
More than 7% of all those who answered said they had long COVID at the time of the survey, which the researchers said corresponded to approximately 18.5 million U.S. adults. The same study found that a quarter of those, or an estimated 4.7 million adults, said their daily activities were impacted “a lot.”
This can translate into pain not only for the patients, but for governments and employers, too.
In high-income countries around the world, government surveys and other studies are shedding light on the extent to which post-COVID-19 symptoms – commonly known as long COVID – are affecting populations. While results vary, they generally fall within similar ranges.
The World Health Organization estimates that between 10% and 20% of those with COVID-19 go on to have an array of medium- to long-term post-COVID-19 symptoms that range from mild to debilitating. The U.S. Government Accountability Office puts that estimate at 10% to 30%; one of the latest studies published at the end of October in The Journal of the American Medical Association found that 15% of U.S. adults who had tested positive for COVID-19 reported current long COVID symptoms. Elsewhere, a study from the Netherlands published in The Lancet in August found that one in eight COVID-19 cases, or 12.7%, were likely to become long COVID.
“It’s very clear that the condition is devastating people’s lives and livelihoods,” WHO Director-General Tedros Adhanom Ghebreyesus wrote in an article for The Guardian newspaper in October.
“The world has already lost a significant number of the workforce to illness, death, fatigue, unplanned retirement due to an increase in long-term disability, which not only impacts the health system, but is a hit to the overarching economy … the impact of long COVID for all countries is very serious and needs immediate and sustained action equivalent to its scale.”
Global snapshot: Lasting symptoms, impact on activities
Patients describe a spectrum of persistent issues, with extreme fatigue, brain fog or cognitive problems, and shortness of breath among the most common complaints. Many also have manageable symptoms that worsen significantly after even mild physical or mental exertion.
Women appear almost twice as likely as men to get long COVID. Many patients have other medical conditions and disabilities that make them more vulnerable to the condition. Those who face greater obstacles accessing health care due to discrimination or socioeconomic inequity are at higher risk as well.
While many are older, a large number are also in their prime working age. The Census Bureau data show that people ages 40-49 are more likely than any other group to get long COVID, which has broader implications for labor markets and the global economy. Already, experts have estimated that long COVID is likely to cost the U.S. trillions of dollars and affect multiple industries.
“Whether they’re in the financial world, the medical system, lawyers, they’re telling me they’re sitting at the computer screen and they’re unable to process the data,” said Zachary Schwartz, MD, medical director for Vancouver General Hospital’s Post-COVID-19 Recovery Clinic.
“That is what’s most distressing for people, in that they’re not working, they’re not making money, and they don’t know when, or if, they’re going to get better.”
Nearly a third of respondents in the Census Bureau’s Household Pulse Survey who said they have had COVID-19 reported symptoms that lasted 3 months or longer. People between the ages of 30 and 59 were the most affected, with about 32% reporting symptoms. Across the entire adult U.S. population, the survey found that 1 in 7 adults have had long COVID at some point during the pandemic, with about 1 in 18 saying it limited their activity to some degree, and 1 in 50 saying they have faced “a lot” of limits on their activities. Any way these numbers are dissected, long COVID has impacted a large swath of the population.
Yet research into the causes and possible treatments of long COVID is just getting underway.
“The amount of energy and time devoted to it is way, way less than it should, given how many people are likely affected,” said David Cutler, PhD, professor of economics at Harvard University, Cambridge, Mass., who has written about the economic cost of long COVID. “We’re way, way underdoing it here. And I think that’s really a terrible thing.”
Population surveys and studies from around the world show that long COVID lives up to its name, with people reporting serious symptoms for months on end.
In October, Statistics Canada and the Public Health Agency of Canada published early results from a questionnaire done between spring and summer 2022 that found just under 15% of adults who had a confirmed or suspected case of COVID-19 went on to have new or continuing symptoms 3 or more months later. Nearly half, or 47.3%, dealt with symptoms that lasted a year or more. More than one in five said their symptoms “often or always” limited their day-to-day activities, which included routine tasks such as preparing meals, doing errands and chores, and basic functions such as personal care and moving around in their homes.
Nearly three-quarters of workers or students said they missed an average of 20 days of work or school.
“We haven’t yet been able to determine exactly when symptoms resolve,” said Rainu Kaushal, MD, the senior associate dean for clinical research at Weill Cornell Medicine in New York. She is co-leading a national study on long COVID in adults and children, funded by the National Institutes of Health RECOVER Initiative.
“But there does seem to be, for many of the milder symptoms, resolution at about 4-6 weeks. There seems to be a second point of resolution around 6 months for certain symptoms, and then some symptoms do seem to be permanent, and those tend to be patients who have underlying conditions,” she said.
Reducing the risk
Given all the data so far, experts recommend urgent policy changes to help people with long COVID.
“The population needs to be prepared, that understanding long COVID is going to be a very long and difficult process,” said Alexander Charney, MD, PhD, associate professor and the lead principal investigator of the RECOVER adult cohort at Icahn School of Medicine at Mount Sinai in New York. He said the government can do a great deal to help, including setting up a network of connected clinics treating long COVID, standardizing best practices, and sharing information.
“That would go a long way towards making sure that every person feels like they’re not too far away from a clinic where they can get treated for this particular condition,” he said.
But the only known way to prevent long COVID is to prevent COVID-19 infections in the first place, experts say. That means equitable access to tests, therapeutics, and vaccines.
“I will say that avoiding COVID remains the best treatment in the arsenal right now,” said Dr. Kaushal. This means masking, avoiding crowded places with poor ventilation and high exposure risk, and being up to date on vaccinations, she said.
A number of papers – including a large U.K. study published in May 2022, another one from July, and the JAMA study from October – all suggest that vaccinations can help reduce the risk of long COVID.
“I am absolutely of the belief that vaccination has reduced the incidence and overall amount of long COVID … [and is] still by far the best thing the public can do,” said Dr. Schwartz.
A version of this article first appeared on WebMD.com.
with symptoms that have lasted 3 months or longer, according to the latest U.S. government survey done in October. More than a quarter say their condition is severe enough to significantly limit their day-to-day activities – yet the problem is only barely starting to get the attention of employers, the health care system, and policymakers.
With no cure or treatment in sight, long COVID is already burdening not only the health care system, but also the economy – and that burden is set to grow. Many experts worry about the possible long-term ripple effects, from increased spending on medical care costs to lost wages due to not being able to work, as well as the policy implications that come with addressing these issues.
“At this point, anyone who’s looking at this seriously would say this is a huge deal,” says senior Brookings Institution fellow Katie Bach, the author of a study that analyzed long COVID’s impact on the labor market.
“We need a real concerted focus on treating these people, which means both research and the clinical side, and figuring out how to build a labor market that is more inclusive of people with disabilities,” she said.
It’s not only that many people are affected. It’s that they are often affected for months and possibly even years.
The U.S. government figures suggest more than 18 million people could have symptoms of long COVID right now. The latest Household Pulse Survey by the Census Bureau and the National Center for Health Statistics takes data from 41,415 people.
A preprint of a study by researchers from City University of New York, posted on medRxiv in September and based on a similar population survey done between June 30 and July 2, drew comparable results. The study has not been peer reviewed.
More than 7% of all those who answered said they had long COVID at the time of the survey, which the researchers said corresponded to approximately 18.5 million U.S. adults. The same study found that a quarter of those, or an estimated 4.7 million adults, said their daily activities were impacted “a lot.”
This can translate into pain not only for the patients, but for governments and employers, too.
In high-income countries around the world, government surveys and other studies are shedding light on the extent to which post-COVID-19 symptoms – commonly known as long COVID – are affecting populations. While results vary, they generally fall within similar ranges.
The World Health Organization estimates that between 10% and 20% of those with COVID-19 go on to have an array of medium- to long-term post-COVID-19 symptoms that range from mild to debilitating. The U.S. Government Accountability Office puts that estimate at 10% to 30%; one of the latest studies published at the end of October in The Journal of the American Medical Association found that 15% of U.S. adults who had tested positive for COVID-19 reported current long COVID symptoms. Elsewhere, a study from the Netherlands published in The Lancet in August found that one in eight COVID-19 cases, or 12.7%, were likely to become long COVID.
“It’s very clear that the condition is devastating people’s lives and livelihoods,” WHO Director-General Tedros Adhanom Ghebreyesus wrote in an article for The Guardian newspaper in October.
“The world has already lost a significant number of the workforce to illness, death, fatigue, unplanned retirement due to an increase in long-term disability, which not only impacts the health system, but is a hit to the overarching economy … the impact of long COVID for all countries is very serious and needs immediate and sustained action equivalent to its scale.”
Global snapshot: Lasting symptoms, impact on activities
Patients describe a spectrum of persistent issues, with extreme fatigue, brain fog or cognitive problems, and shortness of breath among the most common complaints. Many also have manageable symptoms that worsen significantly after even mild physical or mental exertion.
Women appear almost twice as likely as men to get long COVID. Many patients have other medical conditions and disabilities that make them more vulnerable to the condition. Those who face greater obstacles accessing health care due to discrimination or socioeconomic inequity are at higher risk as well.
While many are older, a large number are also in their prime working age. The Census Bureau data show that people ages 40-49 are more likely than any other group to get long COVID, which has broader implications for labor markets and the global economy. Already, experts have estimated that long COVID is likely to cost the U.S. trillions of dollars and affect multiple industries.
“Whether they’re in the financial world, the medical system, lawyers, they’re telling me they’re sitting at the computer screen and they’re unable to process the data,” said Zachary Schwartz, MD, medical director for Vancouver General Hospital’s Post-COVID-19 Recovery Clinic.
“That is what’s most distressing for people, in that they’re not working, they’re not making money, and they don’t know when, or if, they’re going to get better.”
Nearly a third of respondents in the Census Bureau’s Household Pulse Survey who said they have had COVID-19 reported symptoms that lasted 3 months or longer. People between the ages of 30 and 59 were the most affected, with about 32% reporting symptoms. Across the entire adult U.S. population, the survey found that 1 in 7 adults have had long COVID at some point during the pandemic, with about 1 in 18 saying it limited their activity to some degree, and 1 in 50 saying they have faced “a lot” of limits on their activities. Any way these numbers are dissected, long COVID has impacted a large swath of the population.
Yet research into the causes and possible treatments of long COVID is just getting underway.
“The amount of energy and time devoted to it is way, way less than it should, given how many people are likely affected,” said David Cutler, PhD, professor of economics at Harvard University, Cambridge, Mass., who has written about the economic cost of long COVID. “We’re way, way underdoing it here. And I think that’s really a terrible thing.”
Population surveys and studies from around the world show that long COVID lives up to its name, with people reporting serious symptoms for months on end.
In October, Statistics Canada and the Public Health Agency of Canada published early results from a questionnaire done between spring and summer 2022 that found just under 15% of adults who had a confirmed or suspected case of COVID-19 went on to have new or continuing symptoms 3 or more months later. Nearly half, or 47.3%, dealt with symptoms that lasted a year or more. More than one in five said their symptoms “often or always” limited their day-to-day activities, which included routine tasks such as preparing meals, doing errands and chores, and basic functions such as personal care and moving around in their homes.
Nearly three-quarters of workers or students said they missed an average of 20 days of work or school.
“We haven’t yet been able to determine exactly when symptoms resolve,” said Rainu Kaushal, MD, the senior associate dean for clinical research at Weill Cornell Medicine in New York. She is co-leading a national study on long COVID in adults and children, funded by the National Institutes of Health RECOVER Initiative.
“But there does seem to be, for many of the milder symptoms, resolution at about 4-6 weeks. There seems to be a second point of resolution around 6 months for certain symptoms, and then some symptoms do seem to be permanent, and those tend to be patients who have underlying conditions,” she said.
Reducing the risk
Given all the data so far, experts recommend urgent policy changes to help people with long COVID.
“The population needs to be prepared, that understanding long COVID is going to be a very long and difficult process,” said Alexander Charney, MD, PhD, associate professor and the lead principal investigator of the RECOVER adult cohort at Icahn School of Medicine at Mount Sinai in New York. He said the government can do a great deal to help, including setting up a network of connected clinics treating long COVID, standardizing best practices, and sharing information.
“That would go a long way towards making sure that every person feels like they’re not too far away from a clinic where they can get treated for this particular condition,” he said.
But the only known way to prevent long COVID is to prevent COVID-19 infections in the first place, experts say. That means equitable access to tests, therapeutics, and vaccines.
“I will say that avoiding COVID remains the best treatment in the arsenal right now,” said Dr. Kaushal. This means masking, avoiding crowded places with poor ventilation and high exposure risk, and being up to date on vaccinations, she said.
A number of papers – including a large U.K. study published in May 2022, another one from July, and the JAMA study from October – all suggest that vaccinations can help reduce the risk of long COVID.
“I am absolutely of the belief that vaccination has reduced the incidence and overall amount of long COVID … [and is] still by far the best thing the public can do,” said Dr. Schwartz.
A version of this article first appeared on WebMD.com.
with symptoms that have lasted 3 months or longer, according to the latest U.S. government survey done in October. More than a quarter say their condition is severe enough to significantly limit their day-to-day activities – yet the problem is only barely starting to get the attention of employers, the health care system, and policymakers.
With no cure or treatment in sight, long COVID is already burdening not only the health care system, but also the economy – and that burden is set to grow. Many experts worry about the possible long-term ripple effects, from increased spending on medical care costs to lost wages due to not being able to work, as well as the policy implications that come with addressing these issues.
“At this point, anyone who’s looking at this seriously would say this is a huge deal,” says senior Brookings Institution fellow Katie Bach, the author of a study that analyzed long COVID’s impact on the labor market.
“We need a real concerted focus on treating these people, which means both research and the clinical side, and figuring out how to build a labor market that is more inclusive of people with disabilities,” she said.
It’s not only that many people are affected. It’s that they are often affected for months and possibly even years.
The U.S. government figures suggest more than 18 million people could have symptoms of long COVID right now. The latest Household Pulse Survey by the Census Bureau and the National Center for Health Statistics takes data from 41,415 people.
A preprint of a study by researchers from City University of New York, posted on medRxiv in September and based on a similar population survey done between June 30 and July 2, drew comparable results. The study has not been peer reviewed.
More than 7% of all those who answered said they had long COVID at the time of the survey, which the researchers said corresponded to approximately 18.5 million U.S. adults. The same study found that a quarter of those, or an estimated 4.7 million adults, said their daily activities were impacted “a lot.”
This can translate into pain not only for the patients, but for governments and employers, too.
In high-income countries around the world, government surveys and other studies are shedding light on the extent to which post-COVID-19 symptoms – commonly known as long COVID – are affecting populations. While results vary, they generally fall within similar ranges.
The World Health Organization estimates that between 10% and 20% of those with COVID-19 go on to have an array of medium- to long-term post-COVID-19 symptoms that range from mild to debilitating. The U.S. Government Accountability Office puts that estimate at 10% to 30%; one of the latest studies published at the end of October in The Journal of the American Medical Association found that 15% of U.S. adults who had tested positive for COVID-19 reported current long COVID symptoms. Elsewhere, a study from the Netherlands published in The Lancet in August found that one in eight COVID-19 cases, or 12.7%, were likely to become long COVID.
“It’s very clear that the condition is devastating people’s lives and livelihoods,” WHO Director-General Tedros Adhanom Ghebreyesus wrote in an article for The Guardian newspaper in October.
“The world has already lost a significant number of the workforce to illness, death, fatigue, unplanned retirement due to an increase in long-term disability, which not only impacts the health system, but is a hit to the overarching economy … the impact of long COVID for all countries is very serious and needs immediate and sustained action equivalent to its scale.”
Global snapshot: Lasting symptoms, impact on activities
Patients describe a spectrum of persistent issues, with extreme fatigue, brain fog or cognitive problems, and shortness of breath among the most common complaints. Many also have manageable symptoms that worsen significantly after even mild physical or mental exertion.
Women appear almost twice as likely as men to get long COVID. Many patients have other medical conditions and disabilities that make them more vulnerable to the condition. Those who face greater obstacles accessing health care due to discrimination or socioeconomic inequity are at higher risk as well.
While many are older, a large number are also in their prime working age. The Census Bureau data show that people ages 40-49 are more likely than any other group to get long COVID, which has broader implications for labor markets and the global economy. Already, experts have estimated that long COVID is likely to cost the U.S. trillions of dollars and affect multiple industries.
“Whether they’re in the financial world, the medical system, lawyers, they’re telling me they’re sitting at the computer screen and they’re unable to process the data,” said Zachary Schwartz, MD, medical director for Vancouver General Hospital’s Post-COVID-19 Recovery Clinic.
“That is what’s most distressing for people, in that they’re not working, they’re not making money, and they don’t know when, or if, they’re going to get better.”
Nearly a third of respondents in the Census Bureau’s Household Pulse Survey who said they have had COVID-19 reported symptoms that lasted 3 months or longer. People between the ages of 30 and 59 were the most affected, with about 32% reporting symptoms. Across the entire adult U.S. population, the survey found that 1 in 7 adults have had long COVID at some point during the pandemic, with about 1 in 18 saying it limited their activity to some degree, and 1 in 50 saying they have faced “a lot” of limits on their activities. Any way these numbers are dissected, long COVID has impacted a large swath of the population.
Yet research into the causes and possible treatments of long COVID is just getting underway.
“The amount of energy and time devoted to it is way, way less than it should, given how many people are likely affected,” said David Cutler, PhD, professor of economics at Harvard University, Cambridge, Mass., who has written about the economic cost of long COVID. “We’re way, way underdoing it here. And I think that’s really a terrible thing.”
Population surveys and studies from around the world show that long COVID lives up to its name, with people reporting serious symptoms for months on end.
In October, Statistics Canada and the Public Health Agency of Canada published early results from a questionnaire done between spring and summer 2022 that found just under 15% of adults who had a confirmed or suspected case of COVID-19 went on to have new or continuing symptoms 3 or more months later. Nearly half, or 47.3%, dealt with symptoms that lasted a year or more. More than one in five said their symptoms “often or always” limited their day-to-day activities, which included routine tasks such as preparing meals, doing errands and chores, and basic functions such as personal care and moving around in their homes.
Nearly three-quarters of workers or students said they missed an average of 20 days of work or school.
“We haven’t yet been able to determine exactly when symptoms resolve,” said Rainu Kaushal, MD, the senior associate dean for clinical research at Weill Cornell Medicine in New York. She is co-leading a national study on long COVID in adults and children, funded by the National Institutes of Health RECOVER Initiative.
“But there does seem to be, for many of the milder symptoms, resolution at about 4-6 weeks. There seems to be a second point of resolution around 6 months for certain symptoms, and then some symptoms do seem to be permanent, and those tend to be patients who have underlying conditions,” she said.
Reducing the risk
Given all the data so far, experts recommend urgent policy changes to help people with long COVID.
“The population needs to be prepared, that understanding long COVID is going to be a very long and difficult process,” said Alexander Charney, MD, PhD, associate professor and the lead principal investigator of the RECOVER adult cohort at Icahn School of Medicine at Mount Sinai in New York. He said the government can do a great deal to help, including setting up a network of connected clinics treating long COVID, standardizing best practices, and sharing information.
“That would go a long way towards making sure that every person feels like they’re not too far away from a clinic where they can get treated for this particular condition,” he said.
But the only known way to prevent long COVID is to prevent COVID-19 infections in the first place, experts say. That means equitable access to tests, therapeutics, and vaccines.
“I will say that avoiding COVID remains the best treatment in the arsenal right now,” said Dr. Kaushal. This means masking, avoiding crowded places with poor ventilation and high exposure risk, and being up to date on vaccinations, she said.
A number of papers – including a large U.K. study published in May 2022, another one from July, and the JAMA study from October – all suggest that vaccinations can help reduce the risk of long COVID.
“I am absolutely of the belief that vaccination has reduced the incidence and overall amount of long COVID … [and is] still by far the best thing the public can do,” said Dr. Schwartz.
A version of this article first appeared on WebMD.com.
Opioids increase risk for all-cause deaths in RA vs. NSAIDs
PHILADELPHIA – For patients with rheumatoid arthritis who are already at increased risk for major adverse cardiovascular events (MACE), NSAIDs may be safer than opioids, results of a new-user active comparator study suggest.
Among 6,866 patients with RA who started on opioids and 13,698 patients who started on NSAIDs for pain, the use of both weak and strong opioids was associated with a 33% increase in risk for all-cause mortality and a trend toward higher rates of venous thromboembolism (VTE), compared with NSAID use, reported Gulsen Ozen, MD, of the University of Nebraska Medical Center, Omaha.
“Pain in RA is a very complex process, and we know that it’s not solely dependent on the disease activity, but there is no evidence that opioids have any benefit in long-term pain management, and it can even cause hyperalgesia. And as we show, it’s not safer than NSAIDs,” she said in an oral abstract session at the annual meeting of the American College of Rheumatology.
She stressed that patients should be assessed for non-RA causes of pain and should use nonpharmacologic methods when possible.
“If a pharmacological treatment is needed and NSAIDs are contraindicated, the lowest possible dose of weak opioids can be used for a very limited time for acute pain only,” she said.
Pain despite disease control
Even when their disease is well controlled, approximately 60% of patients with RA still report pain. NSAIDs are commonly used to treat pain in patients with RA, but they are associated with modest increases in risk for cardiovascular disease (CVD), gastrointestinal bleeding, renal injury, and hypertension.
Some providers are leery of NSAIDs and will instead prescribe either regular or intermittent opioids for pain control in their patients.
Disease-modifying antirheumatic drugs have only minimal pain-relieving benefits, “and even worse, opioids can delay initiation of DMARDs in RA,” Dr. Ozen said.
Opioids have been shown to increase oxidative stress, platelet aggregation, and myocardial fibrosis, as well as hypogonadism, weight gain, and CVD risk factors.
There is little evidence, however, on whether opioids are associated with cardiovascular events in patients with RA. This dearth of data prompted Dr. Ozen and colleagues to study the relative risks for MACE in patients with RA starting on opioids or NSAIDs for pain.
Matched cohorts
They used data from FORWARD, a joint Canadian and U.S. databank for rheumatic diseases, to conduct a new-user active comparator cohort study. The cohort included adults with RA without cancer who participated in FORWARD for a minimum of 1 year between 1998 and 2021.
The patients were followed either from drug initiation until 3 months after the end of treatment, defined as either discontinuation or a switch to a different analgesic, end of study follow-up, or the development of a MACE outcome.
The investigators used propensity score matching to compare each opioid initiator with two NSAID initiators. The participants were matched by age, sex, body mass index, smoking, alcohol, RA duration, disease activity, Health Assessment Questionnaire, visual analog scale for pain, joint surgeries, prior CVD and VTE, hypertension, diabetes, rheumatic diseases comorbidity index, osteoporosis/fractures, thyroid, chronic liver, kidney, lung and mental health diseases, hospitalizations, 36-Item Short Form Health Survey scores, and sleep scores.
The two groups were well matched, except for a slightly higher incidence of VTE in opioid initiators, although incidence rates were low in both groups (0.9% vs. 0.6% of NSAID initiators).
Higher death rate in opioid users
The incidence rate of MACE among opioid initiators was 20.6% versus18.9% among NSAID initiators, a difference that was not statistically significant. There were also no significant differences in incidence rates of the individual components of the MACE composite outcome: myocardial infarction, stroke, heart failure, CVD death, or VTE.
There were, however, significantly more deaths from any cause among patients in the opioid group, with an incidence rate of 13.5% versus 10.8% in the NSAID group.
An analysis of the associaion of drug type with outcomes, adjusted for propensity score weight and prior VTE showed that patients on opioids had a statistically significant hazard ratio for death from any cause of 1.33 (95% confidence interval, 1.06-1.67).
The increased risk for all-cause mortality occurred both in patients starting on weak opioids (hydrocodone, tramadol, codeine, pentazocine, and propoxyphene) and on strong opioids (hydromorphone, dihydromorphinone, oxymorphone, butorphanol, methadone, morphine, oxycodone, meperidine, and fentanyl).
As noted before, there was a trend toward an increased risk for VTE among opioid initiators, but this was not statistically significant.
The increase in risk was higher among patients on strong versus weak opioids, suggesting a dose-dependent relationship, Dr. Ozen said.
A comparison of opioid-associated risk for all-cause mortality vs. NSAIDs according to type (nonselective or selective) showed that most of the increase in risk was relative to selective cycloxygenase-2 inhibitors.
‘Beautiful’ analysis
“This is a beautiful piece of analysis on a really difficult question to address because the confounding is really hard to unpick,” commented James Galloway, MBBS, deputy head of the center for rheumatic diseases at King’s College London and consulting rheumatologist at King’s College Hospital, also in London.
“The headline message is that there didn’t appear to be a clear signal that NSAIDs were worse, which is what I thought the preexisting view might have been. And so, people may have paradoxically prescribed opioids in favor of NSAIDs in a person with cardiovascular risk,” he said in an interview. Dr. Galloway attended the oral abstract session but was not involved in the study.
The study was supported by a grant to Dr. Ozen from the Rheumatology Research Foundation. Dr. Galloway reported having no relevant disclosures.
PHILADELPHIA – For patients with rheumatoid arthritis who are already at increased risk for major adverse cardiovascular events (MACE), NSAIDs may be safer than opioids, results of a new-user active comparator study suggest.
Among 6,866 patients with RA who started on opioids and 13,698 patients who started on NSAIDs for pain, the use of both weak and strong opioids was associated with a 33% increase in risk for all-cause mortality and a trend toward higher rates of venous thromboembolism (VTE), compared with NSAID use, reported Gulsen Ozen, MD, of the University of Nebraska Medical Center, Omaha.
“Pain in RA is a very complex process, and we know that it’s not solely dependent on the disease activity, but there is no evidence that opioids have any benefit in long-term pain management, and it can even cause hyperalgesia. And as we show, it’s not safer than NSAIDs,” she said in an oral abstract session at the annual meeting of the American College of Rheumatology.
She stressed that patients should be assessed for non-RA causes of pain and should use nonpharmacologic methods when possible.
“If a pharmacological treatment is needed and NSAIDs are contraindicated, the lowest possible dose of weak opioids can be used for a very limited time for acute pain only,” she said.
Pain despite disease control
Even when their disease is well controlled, approximately 60% of patients with RA still report pain. NSAIDs are commonly used to treat pain in patients with RA, but they are associated with modest increases in risk for cardiovascular disease (CVD), gastrointestinal bleeding, renal injury, and hypertension.
Some providers are leery of NSAIDs and will instead prescribe either regular or intermittent opioids for pain control in their patients.
Disease-modifying antirheumatic drugs have only minimal pain-relieving benefits, “and even worse, opioids can delay initiation of DMARDs in RA,” Dr. Ozen said.
Opioids have been shown to increase oxidative stress, platelet aggregation, and myocardial fibrosis, as well as hypogonadism, weight gain, and CVD risk factors.
There is little evidence, however, on whether opioids are associated with cardiovascular events in patients with RA. This dearth of data prompted Dr. Ozen and colleagues to study the relative risks for MACE in patients with RA starting on opioids or NSAIDs for pain.
Matched cohorts
They used data from FORWARD, a joint Canadian and U.S. databank for rheumatic diseases, to conduct a new-user active comparator cohort study. The cohort included adults with RA without cancer who participated in FORWARD for a minimum of 1 year between 1998 and 2021.
The patients were followed either from drug initiation until 3 months after the end of treatment, defined as either discontinuation or a switch to a different analgesic, end of study follow-up, or the development of a MACE outcome.
The investigators used propensity score matching to compare each opioid initiator with two NSAID initiators. The participants were matched by age, sex, body mass index, smoking, alcohol, RA duration, disease activity, Health Assessment Questionnaire, visual analog scale for pain, joint surgeries, prior CVD and VTE, hypertension, diabetes, rheumatic diseases comorbidity index, osteoporosis/fractures, thyroid, chronic liver, kidney, lung and mental health diseases, hospitalizations, 36-Item Short Form Health Survey scores, and sleep scores.
The two groups were well matched, except for a slightly higher incidence of VTE in opioid initiators, although incidence rates were low in both groups (0.9% vs. 0.6% of NSAID initiators).
Higher death rate in opioid users
The incidence rate of MACE among opioid initiators was 20.6% versus18.9% among NSAID initiators, a difference that was not statistically significant. There were also no significant differences in incidence rates of the individual components of the MACE composite outcome: myocardial infarction, stroke, heart failure, CVD death, or VTE.
There were, however, significantly more deaths from any cause among patients in the opioid group, with an incidence rate of 13.5% versus 10.8% in the NSAID group.
An analysis of the associaion of drug type with outcomes, adjusted for propensity score weight and prior VTE showed that patients on opioids had a statistically significant hazard ratio for death from any cause of 1.33 (95% confidence interval, 1.06-1.67).
The increased risk for all-cause mortality occurred both in patients starting on weak opioids (hydrocodone, tramadol, codeine, pentazocine, and propoxyphene) and on strong opioids (hydromorphone, dihydromorphinone, oxymorphone, butorphanol, methadone, morphine, oxycodone, meperidine, and fentanyl).
As noted before, there was a trend toward an increased risk for VTE among opioid initiators, but this was not statistically significant.
The increase in risk was higher among patients on strong versus weak opioids, suggesting a dose-dependent relationship, Dr. Ozen said.
A comparison of opioid-associated risk for all-cause mortality vs. NSAIDs according to type (nonselective or selective) showed that most of the increase in risk was relative to selective cycloxygenase-2 inhibitors.
‘Beautiful’ analysis
“This is a beautiful piece of analysis on a really difficult question to address because the confounding is really hard to unpick,” commented James Galloway, MBBS, deputy head of the center for rheumatic diseases at King’s College London and consulting rheumatologist at King’s College Hospital, also in London.
“The headline message is that there didn’t appear to be a clear signal that NSAIDs were worse, which is what I thought the preexisting view might have been. And so, people may have paradoxically prescribed opioids in favor of NSAIDs in a person with cardiovascular risk,” he said in an interview. Dr. Galloway attended the oral abstract session but was not involved in the study.
The study was supported by a grant to Dr. Ozen from the Rheumatology Research Foundation. Dr. Galloway reported having no relevant disclosures.
PHILADELPHIA – For patients with rheumatoid arthritis who are already at increased risk for major adverse cardiovascular events (MACE), NSAIDs may be safer than opioids, results of a new-user active comparator study suggest.
Among 6,866 patients with RA who started on opioids and 13,698 patients who started on NSAIDs for pain, the use of both weak and strong opioids was associated with a 33% increase in risk for all-cause mortality and a trend toward higher rates of venous thromboembolism (VTE), compared with NSAID use, reported Gulsen Ozen, MD, of the University of Nebraska Medical Center, Omaha.
“Pain in RA is a very complex process, and we know that it’s not solely dependent on the disease activity, but there is no evidence that opioids have any benefit in long-term pain management, and it can even cause hyperalgesia. And as we show, it’s not safer than NSAIDs,” she said in an oral abstract session at the annual meeting of the American College of Rheumatology.
She stressed that patients should be assessed for non-RA causes of pain and should use nonpharmacologic methods when possible.
“If a pharmacological treatment is needed and NSAIDs are contraindicated, the lowest possible dose of weak opioids can be used for a very limited time for acute pain only,” she said.
Pain despite disease control
Even when their disease is well controlled, approximately 60% of patients with RA still report pain. NSAIDs are commonly used to treat pain in patients with RA, but they are associated with modest increases in risk for cardiovascular disease (CVD), gastrointestinal bleeding, renal injury, and hypertension.
Some providers are leery of NSAIDs and will instead prescribe either regular or intermittent opioids for pain control in their patients.
Disease-modifying antirheumatic drugs have only minimal pain-relieving benefits, “and even worse, opioids can delay initiation of DMARDs in RA,” Dr. Ozen said.
Opioids have been shown to increase oxidative stress, platelet aggregation, and myocardial fibrosis, as well as hypogonadism, weight gain, and CVD risk factors.
There is little evidence, however, on whether opioids are associated with cardiovascular events in patients with RA. This dearth of data prompted Dr. Ozen and colleagues to study the relative risks for MACE in patients with RA starting on opioids or NSAIDs for pain.
Matched cohorts
They used data from FORWARD, a joint Canadian and U.S. databank for rheumatic diseases, to conduct a new-user active comparator cohort study. The cohort included adults with RA without cancer who participated in FORWARD for a minimum of 1 year between 1998 and 2021.
The patients were followed either from drug initiation until 3 months after the end of treatment, defined as either discontinuation or a switch to a different analgesic, end of study follow-up, or the development of a MACE outcome.
The investigators used propensity score matching to compare each opioid initiator with two NSAID initiators. The participants were matched by age, sex, body mass index, smoking, alcohol, RA duration, disease activity, Health Assessment Questionnaire, visual analog scale for pain, joint surgeries, prior CVD and VTE, hypertension, diabetes, rheumatic diseases comorbidity index, osteoporosis/fractures, thyroid, chronic liver, kidney, lung and mental health diseases, hospitalizations, 36-Item Short Form Health Survey scores, and sleep scores.
The two groups were well matched, except for a slightly higher incidence of VTE in opioid initiators, although incidence rates were low in both groups (0.9% vs. 0.6% of NSAID initiators).
Higher death rate in opioid users
The incidence rate of MACE among opioid initiators was 20.6% versus18.9% among NSAID initiators, a difference that was not statistically significant. There were also no significant differences in incidence rates of the individual components of the MACE composite outcome: myocardial infarction, stroke, heart failure, CVD death, or VTE.
There were, however, significantly more deaths from any cause among patients in the opioid group, with an incidence rate of 13.5% versus 10.8% in the NSAID group.
An analysis of the associaion of drug type with outcomes, adjusted for propensity score weight and prior VTE showed that patients on opioids had a statistically significant hazard ratio for death from any cause of 1.33 (95% confidence interval, 1.06-1.67).
The increased risk for all-cause mortality occurred both in patients starting on weak opioids (hydrocodone, tramadol, codeine, pentazocine, and propoxyphene) and on strong opioids (hydromorphone, dihydromorphinone, oxymorphone, butorphanol, methadone, morphine, oxycodone, meperidine, and fentanyl).
As noted before, there was a trend toward an increased risk for VTE among opioid initiators, but this was not statistically significant.
The increase in risk was higher among patients on strong versus weak opioids, suggesting a dose-dependent relationship, Dr. Ozen said.
A comparison of opioid-associated risk for all-cause mortality vs. NSAIDs according to type (nonselective or selective) showed that most of the increase in risk was relative to selective cycloxygenase-2 inhibitors.
‘Beautiful’ analysis
“This is a beautiful piece of analysis on a really difficult question to address because the confounding is really hard to unpick,” commented James Galloway, MBBS, deputy head of the center for rheumatic diseases at King’s College London and consulting rheumatologist at King’s College Hospital, also in London.
“The headline message is that there didn’t appear to be a clear signal that NSAIDs were worse, which is what I thought the preexisting view might have been. And so, people may have paradoxically prescribed opioids in favor of NSAIDs in a person with cardiovascular risk,” he said in an interview. Dr. Galloway attended the oral abstract session but was not involved in the study.
The study was supported by a grant to Dr. Ozen from the Rheumatology Research Foundation. Dr. Galloway reported having no relevant disclosures.
AT ACR 2022
Prednisone, colchicine equivalent in efficacy for CPP crystal arthritis
PHILADELPHIA – Prednisone appears to have the edge over colchicine for control of pain in patients with acute calcium pyrophosphate (CPP) crystal arthritis, an intensely painful rheumatic disease primarily affecting older patients.
Among 111 patients with acute CPP crystal arthritis randomized to receive either prednisone or colchicine for control of acute pain in a multicenter study, 2 days of therapy with the oral agents provided equivalent pain relief on the second day, and patients generally tolerated each agent well, reported Tristan Pascart, MD, from the Groupement Hospitalier de l’Institut Catholique de Lille (France).
“Almost three-fourths of patients are considered to be good responders to both drugs on day 3, and, maybe, safety is the key issue distinguishing the two treatments: Colchicine was generally well tolerated, but even with this very short time frame of treatment, one patient out of five had diarrhea, which is more of a concern in this elderly population at risk of dehydration,” he said in an oral abstract session at the annual meeting of the American College of Rheumatology.
In contrast, only about 6% of patients assigned to prednisone had diarrhea, and other adverse events that occurred more frequently with the corticosteroid, including hypertension, hyperglycemia, and insomnia all resolved after the therapy was stopped.
Common and acutely painful
Acute CPP crystal arthritis is a common complication that often occurs during hospitalization for primarily nonrheumatologic causes, Dr. Pascart said, and “in the absence of clinical trials, the management relies on expert opinion, which stems from extrapolated data from gap studies” primarily with prednisone or colchicine, Dr. Pascart said.
To fill in the knowledge gap, Dr. Pascart and colleagues conducted the COLCHICORT study to evaluate whether the two drugs were comparable in efficacy and safety for control of acute pain in a vulnerable population.
The multicenter, open-label trial included patients older than age 65 years with an estimated glomerular filtration rate above 30 mL/min per 1.73 m2 who presented with acute CPP deposition arthritis with symptoms occurring within the previous 36 hours. CPP arthritis was defined by the identification of CPP crystals on synovial fluid analysis or typical clinical presentation with evidence of chondrocalcinosis on x-rays or ultrasound.
Patients with a history of gout, cognitive decline that could impair pain assessment, or contraindications to either of the study drugs were excluded.
The participants were randomized to receive either colchicine 1.5 mg (1 mg to start, then 0.5 mg one hour later) at baseline and then 1 mg on day 1, or oral prednisone 30 mg at baseline and on day 1. The patients also received 1 g of systemic acetaminophen, and three 50-mg doses of tramadol during the first 24 hours.
Of the 111 patients randomized, 54 were assigned to receive prednisone, and 57 were assigned to receive colchicine. Baseline characteristics were similar between the groups, with a mean age of about 86 years, body mass index of around 25 kg/m2, and blood pressure in the range of 130/69 mm Hg.
For nearly half of all patients in study each arm the most painful joint was the knee, followed by wrists and ankles.
There was no difference between the groups in the primary efficacy outcome of a change at 24 hours over baseline in visual analog scale (VAS) (0-100 mm) scores, either in a per-protocol analysis or modified intention-to-treat analysis. The mean change in VAS at 24 hours in the colchicine group was –36.6 mm, compared with –37.7 mm in the prednisone group. The investigators had previously determined that any difference between the two drugs of less than 13 mm on pain VAS at 24 hours would meet the definition for equivalent efficacy.
In both groups, a majority of patients had either an improvement greater than 50% in pain VAS scores and/or a pain VAS score less than 40 mm at both 24 and 48 hours.
At 7 days of follow-up, 21.8% of patients assigned to colchicine had diarrhea, compared with 5.6% of those assigned to prednisone. Adverse events occurring more frequently with prednisone included hyperglycemia, hypertension, and insomnia.
Patients who received colchicine and were also on statins had a trend toward a higher risk for diarrhea, but the study was not adequately powered to detect an association, and the trend was not statistically significant, Dr. Pascart said.
“Taken together, safety issues suggest that prednisone should be considered as the first-line therapy in acute CPP crystal arthritis. Future research is warranted to determine factors increasing the risk of colchicine-induced diarrhea,” he concluded.
Both drugs are used
Sara K. Tedeschi, MD, from Brigham & Women’s Hospital in Boston, who attended the session where the data were presented, has a special clinical interest in CPP deposition disease. She applauded Dr. Pascart and colleagues for conducting a rare clinical trial in CPP crystal arthritis.
In an interview, she said that the study suggests “we can keep in mind shorter courses of treatment for acute CPP crystal arthritis; I think that’s one big takeaway from this study.”
Asked whether she would change her practice based on the findings, Dr. Tedeschi replied: “I personally am not sure that I would be moved to use prednisone more than colchicine; I actually take away from this that colchicine is equivalent to prednisone for short-term use for CPP arthritis, but I think it’s also really important to note that this is in the context of quite a lot of acetaminophen and quite a lot of tramadol, and frankly I don’t usually use tramadol with my patients, but I might consider doing that, especially as there were no delirium events in this population.”
Dr. Tedeschi was not involved in the study.
Asked the same question, Michael Toprover, MD, from New York University Langone Medical Center, a moderator of the session who was not involved in the study, said: “I usually use a combination of medications. I generally, in someone who is hospitalized in particular and is in such severe pain, use a combination of colchicine and prednisone, unless I’m worried about infection, in which case I’ll start colchicine until we’ve proven that it’s CPPD, and then I’ll add prednisone.”
The study was funded by PHRC-1 GIRCI Nord Ouest, a clinical research program funded by the Ministry of Health in France. Dr. Pascart, Dr. Tedeschi, and Dr. Toprover all reported having no relevant conflicts of interest.
PHILADELPHIA – Prednisone appears to have the edge over colchicine for control of pain in patients with acute calcium pyrophosphate (CPP) crystal arthritis, an intensely painful rheumatic disease primarily affecting older patients.
Among 111 patients with acute CPP crystal arthritis randomized to receive either prednisone or colchicine for control of acute pain in a multicenter study, 2 days of therapy with the oral agents provided equivalent pain relief on the second day, and patients generally tolerated each agent well, reported Tristan Pascart, MD, from the Groupement Hospitalier de l’Institut Catholique de Lille (France).
“Almost three-fourths of patients are considered to be good responders to both drugs on day 3, and, maybe, safety is the key issue distinguishing the two treatments: Colchicine was generally well tolerated, but even with this very short time frame of treatment, one patient out of five had diarrhea, which is more of a concern in this elderly population at risk of dehydration,” he said in an oral abstract session at the annual meeting of the American College of Rheumatology.
In contrast, only about 6% of patients assigned to prednisone had diarrhea, and other adverse events that occurred more frequently with the corticosteroid, including hypertension, hyperglycemia, and insomnia all resolved after the therapy was stopped.
Common and acutely painful
Acute CPP crystal arthritis is a common complication that often occurs during hospitalization for primarily nonrheumatologic causes, Dr. Pascart said, and “in the absence of clinical trials, the management relies on expert opinion, which stems from extrapolated data from gap studies” primarily with prednisone or colchicine, Dr. Pascart said.
To fill in the knowledge gap, Dr. Pascart and colleagues conducted the COLCHICORT study to evaluate whether the two drugs were comparable in efficacy and safety for control of acute pain in a vulnerable population.
The multicenter, open-label trial included patients older than age 65 years with an estimated glomerular filtration rate above 30 mL/min per 1.73 m2 who presented with acute CPP deposition arthritis with symptoms occurring within the previous 36 hours. CPP arthritis was defined by the identification of CPP crystals on synovial fluid analysis or typical clinical presentation with evidence of chondrocalcinosis on x-rays or ultrasound.
Patients with a history of gout, cognitive decline that could impair pain assessment, or contraindications to either of the study drugs were excluded.
The participants were randomized to receive either colchicine 1.5 mg (1 mg to start, then 0.5 mg one hour later) at baseline and then 1 mg on day 1, or oral prednisone 30 mg at baseline and on day 1. The patients also received 1 g of systemic acetaminophen, and three 50-mg doses of tramadol during the first 24 hours.
Of the 111 patients randomized, 54 were assigned to receive prednisone, and 57 were assigned to receive colchicine. Baseline characteristics were similar between the groups, with a mean age of about 86 years, body mass index of around 25 kg/m2, and blood pressure in the range of 130/69 mm Hg.
For nearly half of all patients in study each arm the most painful joint was the knee, followed by wrists and ankles.
There was no difference between the groups in the primary efficacy outcome of a change at 24 hours over baseline in visual analog scale (VAS) (0-100 mm) scores, either in a per-protocol analysis or modified intention-to-treat analysis. The mean change in VAS at 24 hours in the colchicine group was –36.6 mm, compared with –37.7 mm in the prednisone group. The investigators had previously determined that any difference between the two drugs of less than 13 mm on pain VAS at 24 hours would meet the definition for equivalent efficacy.
In both groups, a majority of patients had either an improvement greater than 50% in pain VAS scores and/or a pain VAS score less than 40 mm at both 24 and 48 hours.
At 7 days of follow-up, 21.8% of patients assigned to colchicine had diarrhea, compared with 5.6% of those assigned to prednisone. Adverse events occurring more frequently with prednisone included hyperglycemia, hypertension, and insomnia.
Patients who received colchicine and were also on statins had a trend toward a higher risk for diarrhea, but the study was not adequately powered to detect an association, and the trend was not statistically significant, Dr. Pascart said.
“Taken together, safety issues suggest that prednisone should be considered as the first-line therapy in acute CPP crystal arthritis. Future research is warranted to determine factors increasing the risk of colchicine-induced diarrhea,” he concluded.
Both drugs are used
Sara K. Tedeschi, MD, from Brigham & Women’s Hospital in Boston, who attended the session where the data were presented, has a special clinical interest in CPP deposition disease. She applauded Dr. Pascart and colleagues for conducting a rare clinical trial in CPP crystal arthritis.
In an interview, she said that the study suggests “we can keep in mind shorter courses of treatment for acute CPP crystal arthritis; I think that’s one big takeaway from this study.”
Asked whether she would change her practice based on the findings, Dr. Tedeschi replied: “I personally am not sure that I would be moved to use prednisone more than colchicine; I actually take away from this that colchicine is equivalent to prednisone for short-term use for CPP arthritis, but I think it’s also really important to note that this is in the context of quite a lot of acetaminophen and quite a lot of tramadol, and frankly I don’t usually use tramadol with my patients, but I might consider doing that, especially as there were no delirium events in this population.”
Dr. Tedeschi was not involved in the study.
Asked the same question, Michael Toprover, MD, from New York University Langone Medical Center, a moderator of the session who was not involved in the study, said: “I usually use a combination of medications. I generally, in someone who is hospitalized in particular and is in such severe pain, use a combination of colchicine and prednisone, unless I’m worried about infection, in which case I’ll start colchicine until we’ve proven that it’s CPPD, and then I’ll add prednisone.”
The study was funded by PHRC-1 GIRCI Nord Ouest, a clinical research program funded by the Ministry of Health in France. Dr. Pascart, Dr. Tedeschi, and Dr. Toprover all reported having no relevant conflicts of interest.
PHILADELPHIA – Prednisone appears to have the edge over colchicine for control of pain in patients with acute calcium pyrophosphate (CPP) crystal arthritis, an intensely painful rheumatic disease primarily affecting older patients.
Among 111 patients with acute CPP crystal arthritis randomized to receive either prednisone or colchicine for control of acute pain in a multicenter study, 2 days of therapy with the oral agents provided equivalent pain relief on the second day, and patients generally tolerated each agent well, reported Tristan Pascart, MD, from the Groupement Hospitalier de l’Institut Catholique de Lille (France).
“Almost three-fourths of patients are considered to be good responders to both drugs on day 3, and, maybe, safety is the key issue distinguishing the two treatments: Colchicine was generally well tolerated, but even with this very short time frame of treatment, one patient out of five had diarrhea, which is more of a concern in this elderly population at risk of dehydration,” he said in an oral abstract session at the annual meeting of the American College of Rheumatology.
In contrast, only about 6% of patients assigned to prednisone had diarrhea, and other adverse events that occurred more frequently with the corticosteroid, including hypertension, hyperglycemia, and insomnia all resolved after the therapy was stopped.
Common and acutely painful
Acute CPP crystal arthritis is a common complication that often occurs during hospitalization for primarily nonrheumatologic causes, Dr. Pascart said, and “in the absence of clinical trials, the management relies on expert opinion, which stems from extrapolated data from gap studies” primarily with prednisone or colchicine, Dr. Pascart said.
To fill in the knowledge gap, Dr. Pascart and colleagues conducted the COLCHICORT study to evaluate whether the two drugs were comparable in efficacy and safety for control of acute pain in a vulnerable population.
The multicenter, open-label trial included patients older than age 65 years with an estimated glomerular filtration rate above 30 mL/min per 1.73 m2 who presented with acute CPP deposition arthritis with symptoms occurring within the previous 36 hours. CPP arthritis was defined by the identification of CPP crystals on synovial fluid analysis or typical clinical presentation with evidence of chondrocalcinosis on x-rays or ultrasound.
Patients with a history of gout, cognitive decline that could impair pain assessment, or contraindications to either of the study drugs were excluded.
The participants were randomized to receive either colchicine 1.5 mg (1 mg to start, then 0.5 mg one hour later) at baseline and then 1 mg on day 1, or oral prednisone 30 mg at baseline and on day 1. The patients also received 1 g of systemic acetaminophen, and three 50-mg doses of tramadol during the first 24 hours.
Of the 111 patients randomized, 54 were assigned to receive prednisone, and 57 were assigned to receive colchicine. Baseline characteristics were similar between the groups, with a mean age of about 86 years, body mass index of around 25 kg/m2, and blood pressure in the range of 130/69 mm Hg.
For nearly half of all patients in study each arm the most painful joint was the knee, followed by wrists and ankles.
There was no difference between the groups in the primary efficacy outcome of a change at 24 hours over baseline in visual analog scale (VAS) (0-100 mm) scores, either in a per-protocol analysis or modified intention-to-treat analysis. The mean change in VAS at 24 hours in the colchicine group was –36.6 mm, compared with –37.7 mm in the prednisone group. The investigators had previously determined that any difference between the two drugs of less than 13 mm on pain VAS at 24 hours would meet the definition for equivalent efficacy.
In both groups, a majority of patients had either an improvement greater than 50% in pain VAS scores and/or a pain VAS score less than 40 mm at both 24 and 48 hours.
At 7 days of follow-up, 21.8% of patients assigned to colchicine had diarrhea, compared with 5.6% of those assigned to prednisone. Adverse events occurring more frequently with prednisone included hyperglycemia, hypertension, and insomnia.
Patients who received colchicine and were also on statins had a trend toward a higher risk for diarrhea, but the study was not adequately powered to detect an association, and the trend was not statistically significant, Dr. Pascart said.
“Taken together, safety issues suggest that prednisone should be considered as the first-line therapy in acute CPP crystal arthritis. Future research is warranted to determine factors increasing the risk of colchicine-induced diarrhea,” he concluded.
Both drugs are used
Sara K. Tedeschi, MD, from Brigham & Women’s Hospital in Boston, who attended the session where the data were presented, has a special clinical interest in CPP deposition disease. She applauded Dr. Pascart and colleagues for conducting a rare clinical trial in CPP crystal arthritis.
In an interview, she said that the study suggests “we can keep in mind shorter courses of treatment for acute CPP crystal arthritis; I think that’s one big takeaway from this study.”
Asked whether she would change her practice based on the findings, Dr. Tedeschi replied: “I personally am not sure that I would be moved to use prednisone more than colchicine; I actually take away from this that colchicine is equivalent to prednisone for short-term use for CPP arthritis, but I think it’s also really important to note that this is in the context of quite a lot of acetaminophen and quite a lot of tramadol, and frankly I don’t usually use tramadol with my patients, but I might consider doing that, especially as there were no delirium events in this population.”
Dr. Tedeschi was not involved in the study.
Asked the same question, Michael Toprover, MD, from New York University Langone Medical Center, a moderator of the session who was not involved in the study, said: “I usually use a combination of medications. I generally, in someone who is hospitalized in particular and is in such severe pain, use a combination of colchicine and prednisone, unless I’m worried about infection, in which case I’ll start colchicine until we’ve proven that it’s CPPD, and then I’ll add prednisone.”
The study was funded by PHRC-1 GIRCI Nord Ouest, a clinical research program funded by the Ministry of Health in France. Dr. Pascart, Dr. Tedeschi, and Dr. Toprover all reported having no relevant conflicts of interest.
AT ACR 2022
Total replacement and fusion yield similar outcomes for ankle osteoarthritis
Ankle osteoarthritis remains a cause of severe pain and disability. Patients are treated nonoperatively if possible, but surgery is often needed for individuals with end-stage disease, wrote Andrew Goldberg, MBBS, of University College London and colleagues in the Annals of Internal Medicine.
“Most patients with ankle arthritis respond to nonoperative treatments, such as weight loss, activity modification, support braces, and analgesia, [but] once the disease has progressed to end-stage osteoarthritis, the main surgical treatments are total ankle re-placement or ankle arthrodesis,” Dr. Goldberg said, in an interview.
In the new study, patients were randomized to receive either a total ankle replacement (TAR) or ankle fusion (AF).
“We showed that, in both treatment groups the clinical scores improved hugely, by more than three times the minimal clinically important difference,” Dr. Goldberg said in an interview.
“Although the ankle replacement arm improved, on average, by more than an extra 4 points over ankle fusion, this was not considered clinically or statistically significant,” he said.
The study is the first randomized trial to show high-quality and robust results, he noted, and findings support data from previous studies.
“Although both TAR and ankle fusion have been shown to be effective, they are very different treatments, with one fusing the bones so that there is no ankle joint movement, and the other replacing the joint with the aim of retaining ankle joint movement. It is difficult for a patient to know which treatment is more suitable for them, with most seeking guidance from their surgeon,” he said.
Generating high-quality evidence
The study, a randomized, multicenter, open-label trial known as TARVA (Total Ankle Replacement Versus Ankle Arthrodesis), aimed to compare the clinical effectiveness of the two existing publicly funded U.K. treatment options, the authors wrote.
Patients were recruited at 17 U.K. centers between March 6, 2015, and Jan. 10, 2019. The study enrolled 303 adults aged 50-85 years with end-stage ankle osteoarthritis. The mean age of the participants was 68 years; 71% were men. A total of 137 TAR patients and 144 ankle fusion patients completed their surgeries with clinical scores available for analysis. Baseline characteristics were mainly similar between the groups.
Blinding was not possible because of the nature of the procedures, but the surgeons who screened the patients were not aware of the randomization allocations, the researchers noted. A total of 33 surgeons participated in the trial, with a median number of seven patients per surgeon during the study period.
For TAR, U.K. surgeons use both two-component, fixed-bearing and three-component, mobile-bearing implants, the authors write. Ankle fusion was done using the surgeon’s usual technique of either arthroscopic-assisted or open ankle fusion.
The primary outcome was the change in the Manchester–Oxford Foot Questionnaire walking/standing (MOXFQ-W/S) domain scores from baseline to 52 weeks after surgery. The MOXFQ-W/S uses a scale of 0-100, with lower scores representing better outcomes. Secondary outcomes included change in the MOXFQ-W/S scores at 26 weeks after surgery, as well as measures of patient quality of life.
No statistically significant difference
Overall, the mean MOXFQ-W/S scores improved significantly from baseline to 52 weeks for both groups, with average improvements of 49.9 in the TAR group and 44.4 points in the AF group. The average scores at 52 weeks were 31.4 in the TAR group and 36.8 in the AF group.
The adjusted difference in score change from baseline was –5.56, showing a slightly greater degree of improvement with TAR, but this difference was not clinically or statistically significant, the researchers noted.
Adverse event numbers were similar for both procedures, with 54% of TAR patients and 53% of AF patients experiencing at least 1 adverse event during the study period. Of those, 18% of TAR patients and 24% of AF patients experienced at least 1 serious adverse event.
However, the TAR patients experienced a higher rate of wound healing complications and nerve injuries, while thromboembolism was higher in the AF patients, the researchers noted.
A prespecified subgroup analysis of patients with osteoarthritis in adjacent joints suggested a greater improvement in TAR, compared with AF, a difference that increased when fixed-bearing TAR was compared with AF, the authors wrote.
“This reinforces previous reports that suggest that the presence of adjacent joint arthritis may be an indication for ankle replacement over AF,” the authors wrote in their discussion.
“Many of these patients did not have any symptoms in the adjacent joints,” they noted.
“The presence of adjacent joint arthritis, meaning the wear and tear of the joints around the ankle joint, seemed to favor ankle replacement,” Dr. Goldberg said. Approximately 30 joints in the foot continue to move after the ankle is fused, and if these adjacent joints are not healthy before surgery [as was the case in 42% of the study patients], the results of fusion were less successful, he explained.
A post hoc analysis between TAR subtypes showed that patients who had fixed-bearing TAR had significantly greater improvements, compared with AF patients, but this difference was not observed in patients who had mobile-bearing TAR, the researchers noted.
Dr. Goldberg said it was surprising “that, in a separate analysis, we found that the fixed-bearing ankle replacement patients [who accounted for half of the implants used] improved by a much greater difference when compared to ankle fusion.”
The study findings were limited by several factors including the short follow-up and study design that allowed surgeons to choose any implant and technique, the researchers noted.
Other limitations include a lack of data on cost-effectiveness and the impact of comorbidities on outcomes, they wrote. However, the study is the first completed multicenter randomized controlled trial to compare TAR and AF procedures for end-stage ankle osteoarthritis and shows that both yield similar clinical improvements, they concluded.
Data can inform treatment discussion
The take-home messages for clinicians are that both ankle replacement and ankle fusion are effective treatments that improve patients’ quality of life, and it is important to establish the health of adjacent joints before making treatment recommendations, Dr. Goldberg said.
“Careful counseling on the relative risks of each procedure should be part of the informed consent process,” he added. Ideally, all patients seeking surgical care for ankle arthritis should have a choice between ankle replacement and ankle fusion, but sometimes there is inequity of provision of the two treatments, he noted.
“We now encourage all surgeons to work in ankle arthritis networks so that every patient, no matter where they live, can have choice about the best treatment for them,” he said.
Researchers met the challenge of surgical RCT
Randomized trials of surgical interventions are challenging to conduct, and therefore limited, wrote Bruce Sangeorzan, MD, of the University of Washington, Seattle, and colleagues in an accompanying editorial. However, the new study was strengthened by the inclusion of 17 centers for heterogeneity of implant type and surgeon experience level, the editorialists said in the Annals of Internal Medicine.
The study is especially important, because ankle arthritis treatment is very understudied, compared with hip and knee arthritis, but it has a similar impact on activity, editorial coauthor Dr. Sangeorzan said in an interview.
“Randomized controlled trials are the gold standard for comparing medical therapies,” he said, “but they are very difficult to do in surgical treatments, particularly when the two treatments can be differentiated, in this case by movement of the ankle.”
In addition, there is a strong placebo effect attached to interventions, Dr. Sangeorzan noted. “Determining best-case treatment relies on prospective research, preferably randomized. Since both ankle fusion and ankle replacement are effective therapies, a prospective randomized trial is the best way to help make treatment decisions,” he said.
The current study findings are not surprising, but they are preliminary, and 1 year of follow-up is not enough to determine effectiveness, Dr. Sangeorzan emphasized. However, “the authors have done the hard work of randomizing the patients and collecting the data, and the patients can now be followed for a longer time,” he said.
“In addition, the trial was designed with multiple secondary outcome measures, so the data can be matched up with larger trials that were not randomized to identify key elements of success for each procedure,” he noted.
The key message for clinicians is that ankle arthritis has a significant impact on patients’ lives, but there are two effective treatments that can reduce the impact of the disease, said Dr. Sangeorzan. “The data suggest that there are differences in implant design and differences in comorbidities that should influence decision-making,” he added.
Additional research is needed in the form of a longer study duration with larger cohorts, said Dr. Sangeorzan. In particular, researchers need to determine what comorbidities might drive patients to one type of care vs. another, he said. “The suggestion that [patients receiving implants with two motion segments have better outcomes than those receiving implants with a one-motion segment] also deserves further study,” he added.
The research was supported by the UK National Institute for Health and Care Research Health Technology Assessment Programme. The trial was sponsored by University College London. Dr. Goldberg disclosed grant support from NIHR HTA, as well as financial relationships with companies including Stryker, Paragon 28, and stock options with Standing CT Company, Elstree Waterfront Outpatients, and X Bolt Orthopedics.
The editorialists had no financial conflicts to disclose.
Ankle osteoarthritis remains a cause of severe pain and disability. Patients are treated nonoperatively if possible, but surgery is often needed for individuals with end-stage disease, wrote Andrew Goldberg, MBBS, of University College London and colleagues in the Annals of Internal Medicine.
“Most patients with ankle arthritis respond to nonoperative treatments, such as weight loss, activity modification, support braces, and analgesia, [but] once the disease has progressed to end-stage osteoarthritis, the main surgical treatments are total ankle re-placement or ankle arthrodesis,” Dr. Goldberg said, in an interview.
In the new study, patients were randomized to receive either a total ankle replacement (TAR) or ankle fusion (AF).
“We showed that, in both treatment groups the clinical scores improved hugely, by more than three times the minimal clinically important difference,” Dr. Goldberg said in an interview.
“Although the ankle replacement arm improved, on average, by more than an extra 4 points over ankle fusion, this was not considered clinically or statistically significant,” he said.
The study is the first randomized trial to show high-quality and robust results, he noted, and findings support data from previous studies.
“Although both TAR and ankle fusion have been shown to be effective, they are very different treatments, with one fusing the bones so that there is no ankle joint movement, and the other replacing the joint with the aim of retaining ankle joint movement. It is difficult for a patient to know which treatment is more suitable for them, with most seeking guidance from their surgeon,” he said.
Generating high-quality evidence
The study, a randomized, multicenter, open-label trial known as TARVA (Total Ankle Replacement Versus Ankle Arthrodesis), aimed to compare the clinical effectiveness of the two existing publicly funded U.K. treatment options, the authors wrote.
Patients were recruited at 17 U.K. centers between March 6, 2015, and Jan. 10, 2019. The study enrolled 303 adults aged 50-85 years with end-stage ankle osteoarthritis. The mean age of the participants was 68 years; 71% were men. A total of 137 TAR patients and 144 ankle fusion patients completed their surgeries with clinical scores available for analysis. Baseline characteristics were mainly similar between the groups.
Blinding was not possible because of the nature of the procedures, but the surgeons who screened the patients were not aware of the randomization allocations, the researchers noted. A total of 33 surgeons participated in the trial, with a median number of seven patients per surgeon during the study period.
For TAR, U.K. surgeons use both two-component, fixed-bearing and three-component, mobile-bearing implants, the authors write. Ankle fusion was done using the surgeon’s usual technique of either arthroscopic-assisted or open ankle fusion.
The primary outcome was the change in the Manchester–Oxford Foot Questionnaire walking/standing (MOXFQ-W/S) domain scores from baseline to 52 weeks after surgery. The MOXFQ-W/S uses a scale of 0-100, with lower scores representing better outcomes. Secondary outcomes included change in the MOXFQ-W/S scores at 26 weeks after surgery, as well as measures of patient quality of life.
No statistically significant difference
Overall, the mean MOXFQ-W/S scores improved significantly from baseline to 52 weeks for both groups, with average improvements of 49.9 in the TAR group and 44.4 points in the AF group. The average scores at 52 weeks were 31.4 in the TAR group and 36.8 in the AF group.
The adjusted difference in score change from baseline was –5.56, showing a slightly greater degree of improvement with TAR, but this difference was not clinically or statistically significant, the researchers noted.
Adverse event numbers were similar for both procedures, with 54% of TAR patients and 53% of AF patients experiencing at least 1 adverse event during the study period. Of those, 18% of TAR patients and 24% of AF patients experienced at least 1 serious adverse event.
However, the TAR patients experienced a higher rate of wound healing complications and nerve injuries, while thromboembolism was higher in the AF patients, the researchers noted.
A prespecified subgroup analysis of patients with osteoarthritis in adjacent joints suggested a greater improvement in TAR, compared with AF, a difference that increased when fixed-bearing TAR was compared with AF, the authors wrote.
“This reinforces previous reports that suggest that the presence of adjacent joint arthritis may be an indication for ankle replacement over AF,” the authors wrote in their discussion.
“Many of these patients did not have any symptoms in the adjacent joints,” they noted.
“The presence of adjacent joint arthritis, meaning the wear and tear of the joints around the ankle joint, seemed to favor ankle replacement,” Dr. Goldberg said. Approximately 30 joints in the foot continue to move after the ankle is fused, and if these adjacent joints are not healthy before surgery [as was the case in 42% of the study patients], the results of fusion were less successful, he explained.
A post hoc analysis between TAR subtypes showed that patients who had fixed-bearing TAR had significantly greater improvements, compared with AF patients, but this difference was not observed in patients who had mobile-bearing TAR, the researchers noted.
Dr. Goldberg said it was surprising “that, in a separate analysis, we found that the fixed-bearing ankle replacement patients [who accounted for half of the implants used] improved by a much greater difference when compared to ankle fusion.”
The study findings were limited by several factors including the short follow-up and study design that allowed surgeons to choose any implant and technique, the researchers noted.
Other limitations include a lack of data on cost-effectiveness and the impact of comorbidities on outcomes, they wrote. However, the study is the first completed multicenter randomized controlled trial to compare TAR and AF procedures for end-stage ankle osteoarthritis and shows that both yield similar clinical improvements, they concluded.
Data can inform treatment discussion
The take-home messages for clinicians are that both ankle replacement and ankle fusion are effective treatments that improve patients’ quality of life, and it is important to establish the health of adjacent joints before making treatment recommendations, Dr. Goldberg said.
“Careful counseling on the relative risks of each procedure should be part of the informed consent process,” he added. Ideally, all patients seeking surgical care for ankle arthritis should have a choice between ankle replacement and ankle fusion, but sometimes there is inequity of provision of the two treatments, he noted.
“We now encourage all surgeons to work in ankle arthritis networks so that every patient, no matter where they live, can have choice about the best treatment for them,” he said.
Researchers met the challenge of surgical RCT
Randomized trials of surgical interventions are challenging to conduct, and therefore limited, wrote Bruce Sangeorzan, MD, of the University of Washington, Seattle, and colleagues in an accompanying editorial. However, the new study was strengthened by the inclusion of 17 centers for heterogeneity of implant type and surgeon experience level, the editorialists said in the Annals of Internal Medicine.
The study is especially important, because ankle arthritis treatment is very understudied, compared with hip and knee arthritis, but it has a similar impact on activity, editorial coauthor Dr. Sangeorzan said in an interview.
“Randomized controlled trials are the gold standard for comparing medical therapies,” he said, “but they are very difficult to do in surgical treatments, particularly when the two treatments can be differentiated, in this case by movement of the ankle.”
In addition, there is a strong placebo effect attached to interventions, Dr. Sangeorzan noted. “Determining best-case treatment relies on prospective research, preferably randomized. Since both ankle fusion and ankle replacement are effective therapies, a prospective randomized trial is the best way to help make treatment decisions,” he said.
The current study findings are not surprising, but they are preliminary, and 1 year of follow-up is not enough to determine effectiveness, Dr. Sangeorzan emphasized. However, “the authors have done the hard work of randomizing the patients and collecting the data, and the patients can now be followed for a longer time,” he said.
“In addition, the trial was designed with multiple secondary outcome measures, so the data can be matched up with larger trials that were not randomized to identify key elements of success for each procedure,” he noted.
The key message for clinicians is that ankle arthritis has a significant impact on patients’ lives, but there are two effective treatments that can reduce the impact of the disease, said Dr. Sangeorzan. “The data suggest that there are differences in implant design and differences in comorbidities that should influence decision-making,” he added.
Additional research is needed in the form of a longer study duration with larger cohorts, said Dr. Sangeorzan. In particular, researchers need to determine what comorbidities might drive patients to one type of care vs. another, he said. “The suggestion that [patients receiving implants with two motion segments have better outcomes than those receiving implants with a one-motion segment] also deserves further study,” he added.
The research was supported by the UK National Institute for Health and Care Research Health Technology Assessment Programme. The trial was sponsored by University College London. Dr. Goldberg disclosed grant support from NIHR HTA, as well as financial relationships with companies including Stryker, Paragon 28, and stock options with Standing CT Company, Elstree Waterfront Outpatients, and X Bolt Orthopedics.
The editorialists had no financial conflicts to disclose.
Ankle osteoarthritis remains a cause of severe pain and disability. Patients are treated nonoperatively if possible, but surgery is often needed for individuals with end-stage disease, wrote Andrew Goldberg, MBBS, of University College London and colleagues in the Annals of Internal Medicine.
“Most patients with ankle arthritis respond to nonoperative treatments, such as weight loss, activity modification, support braces, and analgesia, [but] once the disease has progressed to end-stage osteoarthritis, the main surgical treatments are total ankle re-placement or ankle arthrodesis,” Dr. Goldberg said, in an interview.
In the new study, patients were randomized to receive either a total ankle replacement (TAR) or ankle fusion (AF).
“We showed that, in both treatment groups the clinical scores improved hugely, by more than three times the minimal clinically important difference,” Dr. Goldberg said in an interview.
“Although the ankle replacement arm improved, on average, by more than an extra 4 points over ankle fusion, this was not considered clinically or statistically significant,” he said.
The study is the first randomized trial to show high-quality and robust results, he noted, and findings support data from previous studies.
“Although both TAR and ankle fusion have been shown to be effective, they are very different treatments, with one fusing the bones so that there is no ankle joint movement, and the other replacing the joint with the aim of retaining ankle joint movement. It is difficult for a patient to know which treatment is more suitable for them, with most seeking guidance from their surgeon,” he said.
Generating high-quality evidence
The study, a randomized, multicenter, open-label trial known as TARVA (Total Ankle Replacement Versus Ankle Arthrodesis), aimed to compare the clinical effectiveness of the two existing publicly funded U.K. treatment options, the authors wrote.
Patients were recruited at 17 U.K. centers between March 6, 2015, and Jan. 10, 2019. The study enrolled 303 adults aged 50-85 years with end-stage ankle osteoarthritis. The mean age of the participants was 68 years; 71% were men. A total of 137 TAR patients and 144 ankle fusion patients completed their surgeries with clinical scores available for analysis. Baseline characteristics were mainly similar between the groups.
Blinding was not possible because of the nature of the procedures, but the surgeons who screened the patients were not aware of the randomization allocations, the researchers noted. A total of 33 surgeons participated in the trial, with a median number of seven patients per surgeon during the study period.
For TAR, U.K. surgeons use both two-component, fixed-bearing and three-component, mobile-bearing implants, the authors write. Ankle fusion was done using the surgeon’s usual technique of either arthroscopic-assisted or open ankle fusion.
The primary outcome was the change in the Manchester–Oxford Foot Questionnaire walking/standing (MOXFQ-W/S) domain scores from baseline to 52 weeks after surgery. The MOXFQ-W/S uses a scale of 0-100, with lower scores representing better outcomes. Secondary outcomes included change in the MOXFQ-W/S scores at 26 weeks after surgery, as well as measures of patient quality of life.
No statistically significant difference
Overall, the mean MOXFQ-W/S scores improved significantly from baseline to 52 weeks for both groups, with average improvements of 49.9 in the TAR group and 44.4 points in the AF group. The average scores at 52 weeks were 31.4 in the TAR group and 36.8 in the AF group.
The adjusted difference in score change from baseline was –5.56, showing a slightly greater degree of improvement with TAR, but this difference was not clinically or statistically significant, the researchers noted.
Adverse event numbers were similar for both procedures, with 54% of TAR patients and 53% of AF patients experiencing at least 1 adverse event during the study period. Of those, 18% of TAR patients and 24% of AF patients experienced at least 1 serious adverse event.
However, the TAR patients experienced a higher rate of wound healing complications and nerve injuries, while thromboembolism was higher in the AF patients, the researchers noted.
A prespecified subgroup analysis of patients with osteoarthritis in adjacent joints suggested a greater improvement in TAR, compared with AF, a difference that increased when fixed-bearing TAR was compared with AF, the authors wrote.
“This reinforces previous reports that suggest that the presence of adjacent joint arthritis may be an indication for ankle replacement over AF,” the authors wrote in their discussion.
“Many of these patients did not have any symptoms in the adjacent joints,” they noted.
“The presence of adjacent joint arthritis, meaning the wear and tear of the joints around the ankle joint, seemed to favor ankle replacement,” Dr. Goldberg said. Approximately 30 joints in the foot continue to move after the ankle is fused, and if these adjacent joints are not healthy before surgery [as was the case in 42% of the study patients], the results of fusion were less successful, he explained.
A post hoc analysis between TAR subtypes showed that patients who had fixed-bearing TAR had significantly greater improvements, compared with AF patients, but this difference was not observed in patients who had mobile-bearing TAR, the researchers noted.
Dr. Goldberg said it was surprising “that, in a separate analysis, we found that the fixed-bearing ankle replacement patients [who accounted for half of the implants used] improved by a much greater difference when compared to ankle fusion.”
The study findings were limited by several factors including the short follow-up and study design that allowed surgeons to choose any implant and technique, the researchers noted.
Other limitations include a lack of data on cost-effectiveness and the impact of comorbidities on outcomes, they wrote. However, the study is the first completed multicenter randomized controlled trial to compare TAR and AF procedures for end-stage ankle osteoarthritis and shows that both yield similar clinical improvements, they concluded.
Data can inform treatment discussion
The take-home messages for clinicians are that both ankle replacement and ankle fusion are effective treatments that improve patients’ quality of life, and it is important to establish the health of adjacent joints before making treatment recommendations, Dr. Goldberg said.
“Careful counseling on the relative risks of each procedure should be part of the informed consent process,” he added. Ideally, all patients seeking surgical care for ankle arthritis should have a choice between ankle replacement and ankle fusion, but sometimes there is inequity of provision of the two treatments, he noted.
“We now encourage all surgeons to work in ankle arthritis networks so that every patient, no matter where they live, can have choice about the best treatment for them,” he said.
Researchers met the challenge of surgical RCT
Randomized trials of surgical interventions are challenging to conduct, and therefore limited, wrote Bruce Sangeorzan, MD, of the University of Washington, Seattle, and colleagues in an accompanying editorial. However, the new study was strengthened by the inclusion of 17 centers for heterogeneity of implant type and surgeon experience level, the editorialists said in the Annals of Internal Medicine.
The study is especially important, because ankle arthritis treatment is very understudied, compared with hip and knee arthritis, but it has a similar impact on activity, editorial coauthor Dr. Sangeorzan said in an interview.
“Randomized controlled trials are the gold standard for comparing medical therapies,” he said, “but they are very difficult to do in surgical treatments, particularly when the two treatments can be differentiated, in this case by movement of the ankle.”
In addition, there is a strong placebo effect attached to interventions, Dr. Sangeorzan noted. “Determining best-case treatment relies on prospective research, preferably randomized. Since both ankle fusion and ankle replacement are effective therapies, a prospective randomized trial is the best way to help make treatment decisions,” he said.
The current study findings are not surprising, but they are preliminary, and 1 year of follow-up is not enough to determine effectiveness, Dr. Sangeorzan emphasized. However, “the authors have done the hard work of randomizing the patients and collecting the data, and the patients can now be followed for a longer time,” he said.
“In addition, the trial was designed with multiple secondary outcome measures, so the data can be matched up with larger trials that were not randomized to identify key elements of success for each procedure,” he noted.
The key message for clinicians is that ankle arthritis has a significant impact on patients’ lives, but there are two effective treatments that can reduce the impact of the disease, said Dr. Sangeorzan. “The data suggest that there are differences in implant design and differences in comorbidities that should influence decision-making,” he added.
Additional research is needed in the form of a longer study duration with larger cohorts, said Dr. Sangeorzan. In particular, researchers need to determine what comorbidities might drive patients to one type of care vs. another, he said. “The suggestion that [patients receiving implants with two motion segments have better outcomes than those receiving implants with a one-motion segment] also deserves further study,” he added.
The research was supported by the UK National Institute for Health and Care Research Health Technology Assessment Programme. The trial was sponsored by University College London. Dr. Goldberg disclosed grant support from NIHR HTA, as well as financial relationships with companies including Stryker, Paragon 28, and stock options with Standing CT Company, Elstree Waterfront Outpatients, and X Bolt Orthopedics.
The editorialists had no financial conflicts to disclose.
New CDC guidance on prescribing opioids for pain
The 2022 Clinical Practice Guideline provides guidance on determining whether to initiate opioids for pain; selecting opioids and determining opioid dosages; deciding duration of initial opioid prescription and conducting follow-up; and assessing risk and addressing potential harms of opioid use.
“Patients with pain should receive compassionate, safe, and effective pain care. We want clinicians and patients to have the information they need to weigh the benefits of different approaches to pain care, with the goal of helping people reduce their pain and improve their quality of life,” Christopher M. Jones, PharmD, DrPH, acting director for the CDC’s National Center for Injury Prevention and Control, said in a news release.
How to taper safely
The last guideline on the topic was released by CDC in 2016. Since then, new evidence has emerged regarding the benefits and risks of prescription opioids for acute and chronic pain, comparisons with nonopioid pain treatments, dosing strategies, opioid dose-dependent effects, risk mitigation strategies, and opioid tapering and discontinuation, the CDC says.
A “critical” addition to the 2022 guideline is advice on tapering opioids, Dr. Jones said during a press briefing.
“Practical tips on how to taper in an individualized patient-centered manner have been added to help clinicians if the decision is made to taper opioids, and the guideline explicitly advises against abrupt discontinuation or rapid dose reductions of opioids,” Dr. Jones said.
“That is based on lessons learned over the last several years as well as new science about how we approach tapering and the real harms that can result when patients are abruptly discontinued or rapidly tapered,” he added.
The updated guideline was published online Nov. 3 in the Morbidity and Mortality Weekly Report.
Key recommendations in the 100-page document include the following:
- In determining whether or not to initiate opioids, nonopioid therapies are at least as effective as opioids for many common types of acute pain. Use of nondrug and nonopioid drug therapies should be maximized as appropriate, and opioid therapy should only be considered for acute pain if it is anticipated that benefits outweigh risks to the patient.
- Before starting opioid therapy, providers should discuss with patients the realistic benefits and known risks of opioid therapy.
- Before starting ongoing opioid therapy for patients with subacute pain lasting 1 to 3 months or chronic pain lasting more than 3 months, providers should work with patients to establish treatment goals for pain and function, and consideration should be given as to how opioid therapy will be discontinued if benefits do not outweigh risks.
- Once opioids are started, the lowest effective dose of immediate-release opioids should be prescribed for no longer than needed for the expected duration of pain severe enough to require opioids.
- Within 1 to 4 weeks of starting opioid therapy for subacute or chronic pain, providers should work with patients to evaluate and carefully weigh benefits and risks of continuing opioid therapy; care should be exercised when increasing, continuing, or reducing opioid dosage.
- Before starting and periodically during ongoing opioid therapy, providers should evaluate risk for opioid-related harms and should work with patients to incorporate relevant strategies to mitigate risk, including offering naloxone and reviewing potential interactions with any other prescribed medications or substance used.
- Abrupt discontinuation of opioids should be avoided, especially for patients receiving high doses.
- For treating patients with opioid use disorder, treatment with evidence-based medications should be provided, or arrangements for such treatment should be made.
Dr. Jones emphasized that the guideline is “voluntary and meant to guide shared decision-making between a clinician and patient. It’s not meant to be implemented as absolute limits of policy or practice by clinicians, health systems, insurance companies, governmental entities.”
He also noted that the “current state of the overdose crisis, which is very much driven by illicit synthetic opioids, is not the aim of this guideline.
“The release of this guideline is really about advancing pain care and improving the lives of patients living with pain,” he said.
“We know that at least 1 in 5 people in the country have chronic pain. It’s one of the most common reasons why people present to their health care provider, and the goal here is to advance pain care, function, and quality of life for that patient population, while also reducing misuse, diversion, and consequences of prescription opioid misuse,” Dr. Jones added.
A version of this article first appeared on Medscape.com.
The 2022 Clinical Practice Guideline provides guidance on determining whether to initiate opioids for pain; selecting opioids and determining opioid dosages; deciding duration of initial opioid prescription and conducting follow-up; and assessing risk and addressing potential harms of opioid use.
“Patients with pain should receive compassionate, safe, and effective pain care. We want clinicians and patients to have the information they need to weigh the benefits of different approaches to pain care, with the goal of helping people reduce their pain and improve their quality of life,” Christopher M. Jones, PharmD, DrPH, acting director for the CDC’s National Center for Injury Prevention and Control, said in a news release.
How to taper safely
The last guideline on the topic was released by CDC in 2016. Since then, new evidence has emerged regarding the benefits and risks of prescription opioids for acute and chronic pain, comparisons with nonopioid pain treatments, dosing strategies, opioid dose-dependent effects, risk mitigation strategies, and opioid tapering and discontinuation, the CDC says.
A “critical” addition to the 2022 guideline is advice on tapering opioids, Dr. Jones said during a press briefing.
“Practical tips on how to taper in an individualized patient-centered manner have been added to help clinicians if the decision is made to taper opioids, and the guideline explicitly advises against abrupt discontinuation or rapid dose reductions of opioids,” Dr. Jones said.
“That is based on lessons learned over the last several years as well as new science about how we approach tapering and the real harms that can result when patients are abruptly discontinued or rapidly tapered,” he added.
The updated guideline was published online Nov. 3 in the Morbidity and Mortality Weekly Report.
Key recommendations in the 100-page document include the following:
- In determining whether or not to initiate opioids, nonopioid therapies are at least as effective as opioids for many common types of acute pain. Use of nondrug and nonopioid drug therapies should be maximized as appropriate, and opioid therapy should only be considered for acute pain if it is anticipated that benefits outweigh risks to the patient.
- Before starting opioid therapy, providers should discuss with patients the realistic benefits and known risks of opioid therapy.
- Before starting ongoing opioid therapy for patients with subacute pain lasting 1 to 3 months or chronic pain lasting more than 3 months, providers should work with patients to establish treatment goals for pain and function, and consideration should be given as to how opioid therapy will be discontinued if benefits do not outweigh risks.
- Once opioids are started, the lowest effective dose of immediate-release opioids should be prescribed for no longer than needed for the expected duration of pain severe enough to require opioids.
- Within 1 to 4 weeks of starting opioid therapy for subacute or chronic pain, providers should work with patients to evaluate and carefully weigh benefits and risks of continuing opioid therapy; care should be exercised when increasing, continuing, or reducing opioid dosage.
- Before starting and periodically during ongoing opioid therapy, providers should evaluate risk for opioid-related harms and should work with patients to incorporate relevant strategies to mitigate risk, including offering naloxone and reviewing potential interactions with any other prescribed medications or substance used.
- Abrupt discontinuation of opioids should be avoided, especially for patients receiving high doses.
- For treating patients with opioid use disorder, treatment with evidence-based medications should be provided, or arrangements for such treatment should be made.
Dr. Jones emphasized that the guideline is “voluntary and meant to guide shared decision-making between a clinician and patient. It’s not meant to be implemented as absolute limits of policy or practice by clinicians, health systems, insurance companies, governmental entities.”
He also noted that the “current state of the overdose crisis, which is very much driven by illicit synthetic opioids, is not the aim of this guideline.
“The release of this guideline is really about advancing pain care and improving the lives of patients living with pain,” he said.
“We know that at least 1 in 5 people in the country have chronic pain. It’s one of the most common reasons why people present to their health care provider, and the goal here is to advance pain care, function, and quality of life for that patient population, while also reducing misuse, diversion, and consequences of prescription opioid misuse,” Dr. Jones added.
A version of this article first appeared on Medscape.com.
The 2022 Clinical Practice Guideline provides guidance on determining whether to initiate opioids for pain; selecting opioids and determining opioid dosages; deciding duration of initial opioid prescription and conducting follow-up; and assessing risk and addressing potential harms of opioid use.
“Patients with pain should receive compassionate, safe, and effective pain care. We want clinicians and patients to have the information they need to weigh the benefits of different approaches to pain care, with the goal of helping people reduce their pain and improve their quality of life,” Christopher M. Jones, PharmD, DrPH, acting director for the CDC’s National Center for Injury Prevention and Control, said in a news release.
How to taper safely
The last guideline on the topic was released by CDC in 2016. Since then, new evidence has emerged regarding the benefits and risks of prescription opioids for acute and chronic pain, comparisons with nonopioid pain treatments, dosing strategies, opioid dose-dependent effects, risk mitigation strategies, and opioid tapering and discontinuation, the CDC says.
A “critical” addition to the 2022 guideline is advice on tapering opioids, Dr. Jones said during a press briefing.
“Practical tips on how to taper in an individualized patient-centered manner have been added to help clinicians if the decision is made to taper opioids, and the guideline explicitly advises against abrupt discontinuation or rapid dose reductions of opioids,” Dr. Jones said.
“That is based on lessons learned over the last several years as well as new science about how we approach tapering and the real harms that can result when patients are abruptly discontinued or rapidly tapered,” he added.
The updated guideline was published online Nov. 3 in the Morbidity and Mortality Weekly Report.
Key recommendations in the 100-page document include the following:
- In determining whether or not to initiate opioids, nonopioid therapies are at least as effective as opioids for many common types of acute pain. Use of nondrug and nonopioid drug therapies should be maximized as appropriate, and opioid therapy should only be considered for acute pain if it is anticipated that benefits outweigh risks to the patient.
- Before starting opioid therapy, providers should discuss with patients the realistic benefits and known risks of opioid therapy.
- Before starting ongoing opioid therapy for patients with subacute pain lasting 1 to 3 months or chronic pain lasting more than 3 months, providers should work with patients to establish treatment goals for pain and function, and consideration should be given as to how opioid therapy will be discontinued if benefits do not outweigh risks.
- Once opioids are started, the lowest effective dose of immediate-release opioids should be prescribed for no longer than needed for the expected duration of pain severe enough to require opioids.
- Within 1 to 4 weeks of starting opioid therapy for subacute or chronic pain, providers should work with patients to evaluate and carefully weigh benefits and risks of continuing opioid therapy; care should be exercised when increasing, continuing, or reducing opioid dosage.
- Before starting and periodically during ongoing opioid therapy, providers should evaluate risk for opioid-related harms and should work with patients to incorporate relevant strategies to mitigate risk, including offering naloxone and reviewing potential interactions with any other prescribed medications or substance used.
- Abrupt discontinuation of opioids should be avoided, especially for patients receiving high doses.
- For treating patients with opioid use disorder, treatment with evidence-based medications should be provided, or arrangements for such treatment should be made.
Dr. Jones emphasized that the guideline is “voluntary and meant to guide shared decision-making between a clinician and patient. It’s not meant to be implemented as absolute limits of policy or practice by clinicians, health systems, insurance companies, governmental entities.”
He also noted that the “current state of the overdose crisis, which is very much driven by illicit synthetic opioids, is not the aim of this guideline.
“The release of this guideline is really about advancing pain care and improving the lives of patients living with pain,” he said.
“We know that at least 1 in 5 people in the country have chronic pain. It’s one of the most common reasons why people present to their health care provider, and the goal here is to advance pain care, function, and quality of life for that patient population, while also reducing misuse, diversion, and consequences of prescription opioid misuse,” Dr. Jones added.
A version of this article first appeared on Medscape.com.
Gout too often treated only in emergency department
Only about one in three patients seen in the emergency department of an academic health system for acute gout had a follow-up visit that addressed this condition, Lesley Jackson, MD, of the University of Alabama at Birmingham, reported at the annual research symposium of the Gout, Hyperuricemia, and Crystal Associated Disease Network (G-CAN).
Dr. Jackson presented research done on patients seen within her university’s health system, looking at 72 patients seen in the ED between September 2021 and February 2022. Medications prescribed at discharge from the ED included corticosteroids (46 patients, or 64%), opioids (45 patients, 63%), NSAIDs (31 patients, 43%), and colchicine (23 patients, 32%).
Only 26 patients, or about 36%, had a subsequent outpatient visit in the UAB health system addressing gout, she said. Of 33 patients with any outpatient follow-up visit within the UAB system, 21 were within 1 month after the index ED visit, followed by 3 more prior to 3 months, and 9 more after 3 months.
The limitations of the study includes its collection of data from a single institution. But the results highlight the need for improved quality of care for gout, with too many people being treated for this condition primarily in the ED, she said.
In an email exchange arranged by the Arthritis Foundation, Herbert S. B. Baraf, MD, said he agreed that patients too often limit their treatment for gout to seeking care for acute attacks in the ED.
Because of competing demands, physicians working there are more to take a “Band-Aid” approach and not impress upon patients that gout is a lifelong condition that needs follow-up and monitoring, said Dr. Baraf, clinical professor of medicine at George Washington University, Washington, and an associate clinical professor at the University of Maryland, Baltimore. He retired from private practice in 2022.
“This problem is akin to the patient who has a hip fracture due to osteoporosis who gets a surgical repair but is never referred for osteoporotic management,” wrote Dr. Baraf, who is a former board member of the Arthritis Foundation.
He suggested viewing gout as a form of arthritis that has two components.
“The first, that which brings the patient to seek medical care, is the often exquisitely painful attack of pain and swelling in a joint or joints that comes on acutely,” he wrote. “Calming these attacks are the focus of the patient and the doctor, who does the evaluation as relief of pain and inflammation is the most pressing task at hand.”
But equally important is the second element, addressing the cause of these flare ups of arthritis, he wrote. Elevated uric acid leads to crystalline deposits of urate in the joints, particularly in the feet, ankles, knees, and hands. Over time, these deposits generate seemingly random flare ups of acute joint pain in one or more of these areas.
“Thus, when a patient presents to an emergency room with a first or second attack of gout, pain relief is the primary focus of the visit,” Dr. Baraf wrote. “But if over time that is the only focus, and the elevation of serum uric acid is not addressed, deposits will continue to mount and flare ups will occur with increasing frequency and severity.”
This study was supported by a grant from the National Institute of Arthritis and Musculoskeletal and Skin Diseases. Dr. Jackson has no relevant financial disclosures.
Only about one in three patients seen in the emergency department of an academic health system for acute gout had a follow-up visit that addressed this condition, Lesley Jackson, MD, of the University of Alabama at Birmingham, reported at the annual research symposium of the Gout, Hyperuricemia, and Crystal Associated Disease Network (G-CAN).
Dr. Jackson presented research done on patients seen within her university’s health system, looking at 72 patients seen in the ED between September 2021 and February 2022. Medications prescribed at discharge from the ED included corticosteroids (46 patients, or 64%), opioids (45 patients, 63%), NSAIDs (31 patients, 43%), and colchicine (23 patients, 32%).
Only 26 patients, or about 36%, had a subsequent outpatient visit in the UAB health system addressing gout, she said. Of 33 patients with any outpatient follow-up visit within the UAB system, 21 were within 1 month after the index ED visit, followed by 3 more prior to 3 months, and 9 more after 3 months.
The limitations of the study includes its collection of data from a single institution. But the results highlight the need for improved quality of care for gout, with too many people being treated for this condition primarily in the ED, she said.
In an email exchange arranged by the Arthritis Foundation, Herbert S. B. Baraf, MD, said he agreed that patients too often limit their treatment for gout to seeking care for acute attacks in the ED.
Because of competing demands, physicians working there are more to take a “Band-Aid” approach and not impress upon patients that gout is a lifelong condition that needs follow-up and monitoring, said Dr. Baraf, clinical professor of medicine at George Washington University, Washington, and an associate clinical professor at the University of Maryland, Baltimore. He retired from private practice in 2022.
“This problem is akin to the patient who has a hip fracture due to osteoporosis who gets a surgical repair but is never referred for osteoporotic management,” wrote Dr. Baraf, who is a former board member of the Arthritis Foundation.
He suggested viewing gout as a form of arthritis that has two components.
“The first, that which brings the patient to seek medical care, is the often exquisitely painful attack of pain and swelling in a joint or joints that comes on acutely,” he wrote. “Calming these attacks are the focus of the patient and the doctor, who does the evaluation as relief of pain and inflammation is the most pressing task at hand.”
But equally important is the second element, addressing the cause of these flare ups of arthritis, he wrote. Elevated uric acid leads to crystalline deposits of urate in the joints, particularly in the feet, ankles, knees, and hands. Over time, these deposits generate seemingly random flare ups of acute joint pain in one or more of these areas.
“Thus, when a patient presents to an emergency room with a first or second attack of gout, pain relief is the primary focus of the visit,” Dr. Baraf wrote. “But if over time that is the only focus, and the elevation of serum uric acid is not addressed, deposits will continue to mount and flare ups will occur with increasing frequency and severity.”
This study was supported by a grant from the National Institute of Arthritis and Musculoskeletal and Skin Diseases. Dr. Jackson has no relevant financial disclosures.
Only about one in three patients seen in the emergency department of an academic health system for acute gout had a follow-up visit that addressed this condition, Lesley Jackson, MD, of the University of Alabama at Birmingham, reported at the annual research symposium of the Gout, Hyperuricemia, and Crystal Associated Disease Network (G-CAN).
Dr. Jackson presented research done on patients seen within her university’s health system, looking at 72 patients seen in the ED between September 2021 and February 2022. Medications prescribed at discharge from the ED included corticosteroids (46 patients, or 64%), opioids (45 patients, 63%), NSAIDs (31 patients, 43%), and colchicine (23 patients, 32%).
Only 26 patients, or about 36%, had a subsequent outpatient visit in the UAB health system addressing gout, she said. Of 33 patients with any outpatient follow-up visit within the UAB system, 21 were within 1 month after the index ED visit, followed by 3 more prior to 3 months, and 9 more after 3 months.
The limitations of the study includes its collection of data from a single institution. But the results highlight the need for improved quality of care for gout, with too many people being treated for this condition primarily in the ED, she said.
In an email exchange arranged by the Arthritis Foundation, Herbert S. B. Baraf, MD, said he agreed that patients too often limit their treatment for gout to seeking care for acute attacks in the ED.
Because of competing demands, physicians working there are more to take a “Band-Aid” approach and not impress upon patients that gout is a lifelong condition that needs follow-up and monitoring, said Dr. Baraf, clinical professor of medicine at George Washington University, Washington, and an associate clinical professor at the University of Maryland, Baltimore. He retired from private practice in 2022.
“This problem is akin to the patient who has a hip fracture due to osteoporosis who gets a surgical repair but is never referred for osteoporotic management,” wrote Dr. Baraf, who is a former board member of the Arthritis Foundation.
He suggested viewing gout as a form of arthritis that has two components.
“The first, that which brings the patient to seek medical care, is the often exquisitely painful attack of pain and swelling in a joint or joints that comes on acutely,” he wrote. “Calming these attacks are the focus of the patient and the doctor, who does the evaluation as relief of pain and inflammation is the most pressing task at hand.”
But equally important is the second element, addressing the cause of these flare ups of arthritis, he wrote. Elevated uric acid leads to crystalline deposits of urate in the joints, particularly in the feet, ankles, knees, and hands. Over time, these deposits generate seemingly random flare ups of acute joint pain in one or more of these areas.
“Thus, when a patient presents to an emergency room with a first or second attack of gout, pain relief is the primary focus of the visit,” Dr. Baraf wrote. “But if over time that is the only focus, and the elevation of serum uric acid is not addressed, deposits will continue to mount and flare ups will occur with increasing frequency and severity.”
This study was supported by a grant from the National Institute of Arthritis and Musculoskeletal and Skin Diseases. Dr. Jackson has no relevant financial disclosures.
FROM G-CAN 2022
Pain in Cancer Survivors: Assess, Monitor, and Ask for Help
SAN DIEGO—As patients with cancer live longer, pain is going to become an even bigger challenge for clinicians, a palliative care specialist told cancer specialists in a presentation at the annual meeting of the Association of VA Hematology/Oncology (AVAHO) in September, and decisions about treatment are becoming more complicated amid the opioid epidemic.
Fortunately, guidelines and clinical experience offer helpful insight into the best practices, said hematologist/oncologist Andrea Ruskin, MD, medical director of palliative care at Veterans Administration (VA) Connecticut Healthcare System (VACHS).
As Ruskin pointed out, two-thirds of newly diagnosed cancer patients are living for at least 5 years, “but with this progress comes challenges.” More than one-third (37%) of cancer survivors report cancer pain, 21% have noncancer pain, and 45% have both. About 5% to 8% of VA cancer survivors use opioids for the long term, she said, although there have been few studies in this population.
Among patients with head and neck cancer, specifically, chronic pain affects 45%, and severe pain affects 11%. Subclinical PTSD, depression, anxiety, and low quality of life are common in this population. “We may cure them, but they have a lot of issues going forward.”
One key strategy is to perform a comprehensive pain assessment at the first visit, and then address pain at every subsequent visit. She recommended a physician resource from the American Society of Clinical Oncology, and a template may be useful to provide helpful questions, Ruskin said.
At VACHS certain questions are routine. “Is pain interfering with your function? Sometimes people say it’s always a 10, but it’s not affecting function at all. Ask if the medicine is working. And how are they taking it? Sometimes they say, ‘I’m taking that for sleep,’ and we say ‘No, Mr. Smith, that is not a sleep medication.’”
Be aware that some patients may use nonmedical opioids, she said. And set expectations early on. “Safe opioid use starts with the very first prescription,” she said. “If I have somebody with myeloma or head and neck cancer, I make it very clear that my goal is that we want you off the opioids after the radiation or once the disease is in remission. I really make an effort at the very beginning to make sure that we're all on the same page.”
As you continue to see a patient, consider ordering urine tests, she said, not as a punitive measure but to make sure you’re offering the safest and most effective treatment. “We don’t do it to say ‘no, no, no.’ We do it for safety and to make sure they’re not getting meds elsewhere.”
What are the best practices when pain doesn’t go away? Should they stay on opioids? According to Ruskin, few evidence-based guidelines address the “more nuanced care” that patients need when their pain lasts for months or years.
But there are useful resources. Ruskin highlighted the National Comprehensive Cancer Network’s survivorship guidelines, and she summarized a few of the available painkiller options. “Opioids are great, and adjuvants are so-so. They work in some people, but we definitely have room for improvement.”
What if patients have persistent opioid use after cancer recovery? “I try to taper if I can, and I try to explain why I’m tapering. It could take months or years to taper patients,” she said. And consider transitioning the patient to buprenorphine, a drug that treats both pain and opioid use disorder, if appropriate. “You don’t need a waiver if you use it for pain. It’s definitely something we’re using more of.”
One important step is to bring in colleagues to help. Psychologists, chiropractors, physical therapists, physiatrists, and pain pharmacists can all be helpful, she said. “Learn about your VA resources and who can partner with you to help these complicated patients. They’re all at your fingertips.”
SAN DIEGO—As patients with cancer live longer, pain is going to become an even bigger challenge for clinicians, a palliative care specialist told cancer specialists in a presentation at the annual meeting of the Association of VA Hematology/Oncology (AVAHO) in September, and decisions about treatment are becoming more complicated amid the opioid epidemic.
Fortunately, guidelines and clinical experience offer helpful insight into the best practices, said hematologist/oncologist Andrea Ruskin, MD, medical director of palliative care at Veterans Administration (VA) Connecticut Healthcare System (VACHS).
As Ruskin pointed out, two-thirds of newly diagnosed cancer patients are living for at least 5 years, “but with this progress comes challenges.” More than one-third (37%) of cancer survivors report cancer pain, 21% have noncancer pain, and 45% have both. About 5% to 8% of VA cancer survivors use opioids for the long term, she said, although there have been few studies in this population.
Among patients with head and neck cancer, specifically, chronic pain affects 45%, and severe pain affects 11%. Subclinical PTSD, depression, anxiety, and low quality of life are common in this population. “We may cure them, but they have a lot of issues going forward.”
One key strategy is to perform a comprehensive pain assessment at the first visit, and then address pain at every subsequent visit. She recommended a physician resource from the American Society of Clinical Oncology, and a template may be useful to provide helpful questions, Ruskin said.
At VACHS certain questions are routine. “Is pain interfering with your function? Sometimes people say it’s always a 10, but it’s not affecting function at all. Ask if the medicine is working. And how are they taking it? Sometimes they say, ‘I’m taking that for sleep,’ and we say ‘No, Mr. Smith, that is not a sleep medication.’”
Be aware that some patients may use nonmedical opioids, she said. And set expectations early on. “Safe opioid use starts with the very first prescription,” she said. “If I have somebody with myeloma or head and neck cancer, I make it very clear that my goal is that we want you off the opioids after the radiation or once the disease is in remission. I really make an effort at the very beginning to make sure that we're all on the same page.”
As you continue to see a patient, consider ordering urine tests, she said, not as a punitive measure but to make sure you’re offering the safest and most effective treatment. “We don’t do it to say ‘no, no, no.’ We do it for safety and to make sure they’re not getting meds elsewhere.”
What are the best practices when pain doesn’t go away? Should they stay on opioids? According to Ruskin, few evidence-based guidelines address the “more nuanced care” that patients need when their pain lasts for months or years.
But there are useful resources. Ruskin highlighted the National Comprehensive Cancer Network’s survivorship guidelines, and she summarized a few of the available painkiller options. “Opioids are great, and adjuvants are so-so. They work in some people, but we definitely have room for improvement.”
What if patients have persistent opioid use after cancer recovery? “I try to taper if I can, and I try to explain why I’m tapering. It could take months or years to taper patients,” she said. And consider transitioning the patient to buprenorphine, a drug that treats both pain and opioid use disorder, if appropriate. “You don’t need a waiver if you use it for pain. It’s definitely something we’re using more of.”
One important step is to bring in colleagues to help. Psychologists, chiropractors, physical therapists, physiatrists, and pain pharmacists can all be helpful, she said. “Learn about your VA resources and who can partner with you to help these complicated patients. They’re all at your fingertips.”
SAN DIEGO—As patients with cancer live longer, pain is going to become an even bigger challenge for clinicians, a palliative care specialist told cancer specialists in a presentation at the annual meeting of the Association of VA Hematology/Oncology (AVAHO) in September, and decisions about treatment are becoming more complicated amid the opioid epidemic.
Fortunately, guidelines and clinical experience offer helpful insight into the best practices, said hematologist/oncologist Andrea Ruskin, MD, medical director of palliative care at Veterans Administration (VA) Connecticut Healthcare System (VACHS).
As Ruskin pointed out, two-thirds of newly diagnosed cancer patients are living for at least 5 years, “but with this progress comes challenges.” More than one-third (37%) of cancer survivors report cancer pain, 21% have noncancer pain, and 45% have both. About 5% to 8% of VA cancer survivors use opioids for the long term, she said, although there have been few studies in this population.
Among patients with head and neck cancer, specifically, chronic pain affects 45%, and severe pain affects 11%. Subclinical PTSD, depression, anxiety, and low quality of life are common in this population. “We may cure them, but they have a lot of issues going forward.”
One key strategy is to perform a comprehensive pain assessment at the first visit, and then address pain at every subsequent visit. She recommended a physician resource from the American Society of Clinical Oncology, and a template may be useful to provide helpful questions, Ruskin said.
At VACHS certain questions are routine. “Is pain interfering with your function? Sometimes people say it’s always a 10, but it’s not affecting function at all. Ask if the medicine is working. And how are they taking it? Sometimes they say, ‘I’m taking that for sleep,’ and we say ‘No, Mr. Smith, that is not a sleep medication.’”
Be aware that some patients may use nonmedical opioids, she said. And set expectations early on. “Safe opioid use starts with the very first prescription,” she said. “If I have somebody with myeloma or head and neck cancer, I make it very clear that my goal is that we want you off the opioids after the radiation or once the disease is in remission. I really make an effort at the very beginning to make sure that we're all on the same page.”
As you continue to see a patient, consider ordering urine tests, she said, not as a punitive measure but to make sure you’re offering the safest and most effective treatment. “We don’t do it to say ‘no, no, no.’ We do it for safety and to make sure they’re not getting meds elsewhere.”
What are the best practices when pain doesn’t go away? Should they stay on opioids? According to Ruskin, few evidence-based guidelines address the “more nuanced care” that patients need when their pain lasts for months or years.
But there are useful resources. Ruskin highlighted the National Comprehensive Cancer Network’s survivorship guidelines, and she summarized a few of the available painkiller options. “Opioids are great, and adjuvants are so-so. They work in some people, but we definitely have room for improvement.”
What if patients have persistent opioid use after cancer recovery? “I try to taper if I can, and I try to explain why I’m tapering. It could take months or years to taper patients,” she said. And consider transitioning the patient to buprenorphine, a drug that treats both pain and opioid use disorder, if appropriate. “You don’t need a waiver if you use it for pain. It’s definitely something we’re using more of.”
One important step is to bring in colleagues to help. Psychologists, chiropractors, physical therapists, physiatrists, and pain pharmacists can all be helpful, she said. “Learn about your VA resources and who can partner with you to help these complicated patients. They’re all at your fingertips.”
Psychotropic medications for chronic pain
The opioid crisis presents a need to consider alternative options for treating chronic pain. There is significant overlap in neuroanatomical circuits that process pain, emotions, and motivation. Neurotransmitters modulated by psychotropic medications are also involved in regulating the pain pathways.1,2 In light of this, psychotropics can be considered for treating chronic pain in certain patients. The Table1-3 outlines various uses and adverse effects of select psychotropic medications used to treat pain, as well as their psychiatric uses.
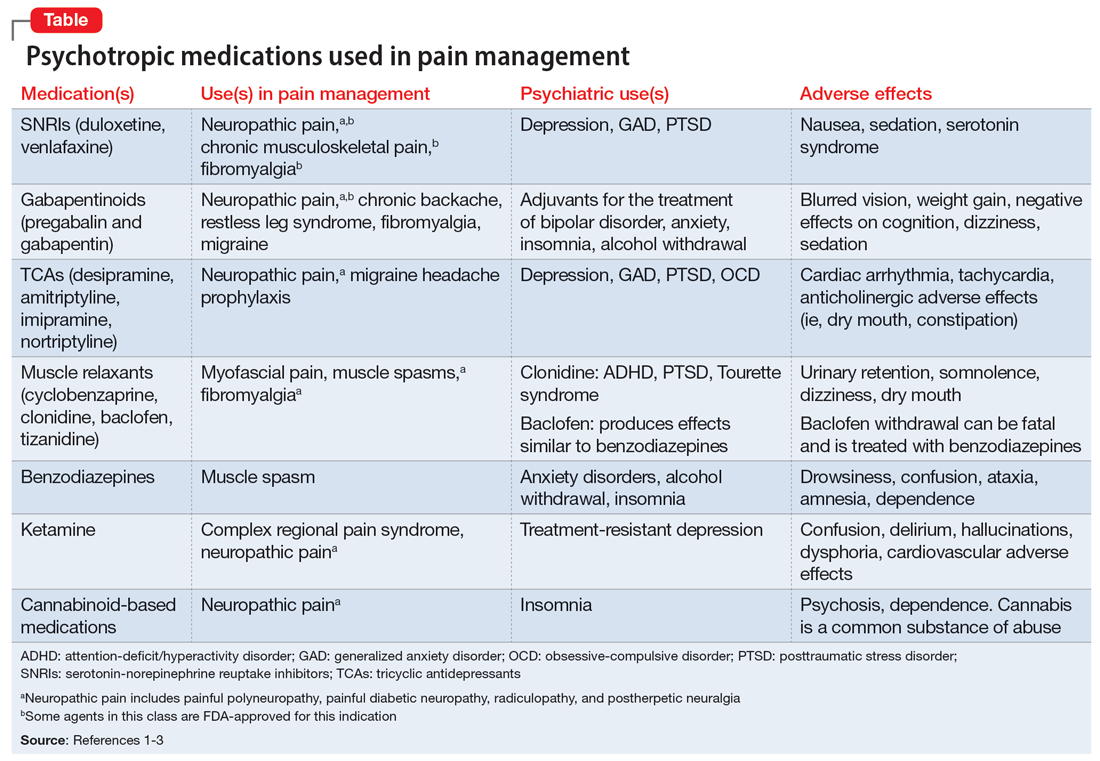
In addition to its psychiatric indications, the serotonin-norepinephrine reuptake inhibitor duloxetine is FDA-approved for treating fibromyalgia and diabetic neuropathic pain. It is often prescribed in the treatment of multiple pain disorders. Tricyclic antidepressants (TCAs) have the largest effect size in the treatment of neuropathic pain.2 Cyclobenzaprine is a TCA used to treat muscle spasms. Gabapentinoids (alpha-2 delta-1 calcium channel inhibition) are FDA-approved for treating postherpetic neuralgia, fibromyalgia, and diabetic neuropathy.1,2
Ketamine is an anesthetic with analgesic and antidepressant properties used as an IV infusion to manage several pain disorders.2 The alpha-2 adrenergic agonists tizanidine and clonidine are muscle relaxants2; the latter is used to treat attention-deficit/hyperactivity disorder and Tourette syndrome. Benzodiazepines (GABA-A agonists) are used for short-term treatment of anxiety disorders, insomnia, and muscle spasms.1,2 Baclofen (GABA-B receptor agonist) is used to treat spasticity.2 Medical cannabis (tetrahydrocannabinol/cannabidiol) is also gaining popularity for treating chronic pain and insomnia.1-3
1. Sutherland AM, Nicholls J, Bao J, et al. Overlaps in pharmacology for the treatment of chronic pain and mental health disorders. Prog Neuropsychopharmacol Biol Psychiatry. 2018;87(Pt B):290-297.
2. Bajwa ZH, Wootton RJ, Warfield CA. Principles and Practice of Pain Medicine. 3rd ed. McGraw Hill; 2016.
3. McDonagh MS, Selph SS, Buckley DI, et al. Nonopioid Pharmacologic Treatments for Chronic Pain. Comparative Effectiveness Review No. 228. Agency for Healthcare Research and Quality; 2020. doi:10.23970/AHRQEPCCER228
The opioid crisis presents a need to consider alternative options for treating chronic pain. There is significant overlap in neuroanatomical circuits that process pain, emotions, and motivation. Neurotransmitters modulated by psychotropic medications are also involved in regulating the pain pathways.1,2 In light of this, psychotropics can be considered for treating chronic pain in certain patients. The Table1-3 outlines various uses and adverse effects of select psychotropic medications used to treat pain, as well as their psychiatric uses.
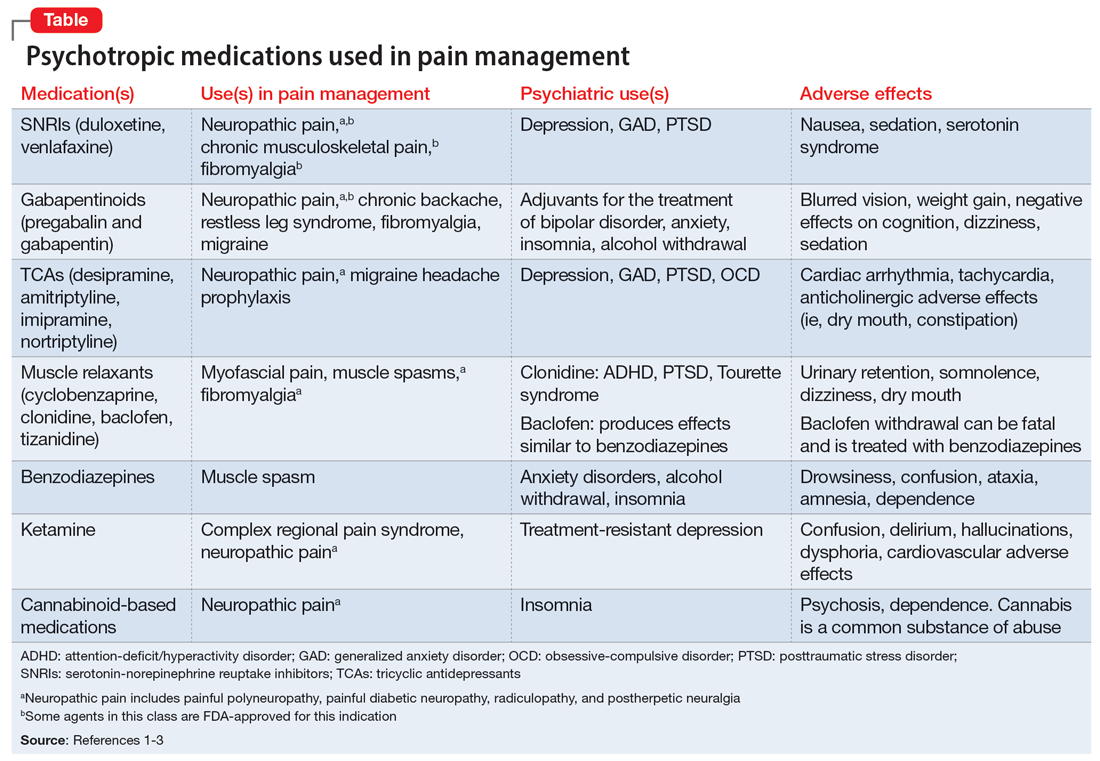
In addition to its psychiatric indications, the serotonin-norepinephrine reuptake inhibitor duloxetine is FDA-approved for treating fibromyalgia and diabetic neuropathic pain. It is often prescribed in the treatment of multiple pain disorders. Tricyclic antidepressants (TCAs) have the largest effect size in the treatment of neuropathic pain.2 Cyclobenzaprine is a TCA used to treat muscle spasms. Gabapentinoids (alpha-2 delta-1 calcium channel inhibition) are FDA-approved for treating postherpetic neuralgia, fibromyalgia, and diabetic neuropathy.1,2
Ketamine is an anesthetic with analgesic and antidepressant properties used as an IV infusion to manage several pain disorders.2 The alpha-2 adrenergic agonists tizanidine and clonidine are muscle relaxants2; the latter is used to treat attention-deficit/hyperactivity disorder and Tourette syndrome. Benzodiazepines (GABA-A agonists) are used for short-term treatment of anxiety disorders, insomnia, and muscle spasms.1,2 Baclofen (GABA-B receptor agonist) is used to treat spasticity.2 Medical cannabis (tetrahydrocannabinol/cannabidiol) is also gaining popularity for treating chronic pain and insomnia.1-3
The opioid crisis presents a need to consider alternative options for treating chronic pain. There is significant overlap in neuroanatomical circuits that process pain, emotions, and motivation. Neurotransmitters modulated by psychotropic medications are also involved in regulating the pain pathways.1,2 In light of this, psychotropics can be considered for treating chronic pain in certain patients. The Table1-3 outlines various uses and adverse effects of select psychotropic medications used to treat pain, as well as their psychiatric uses.
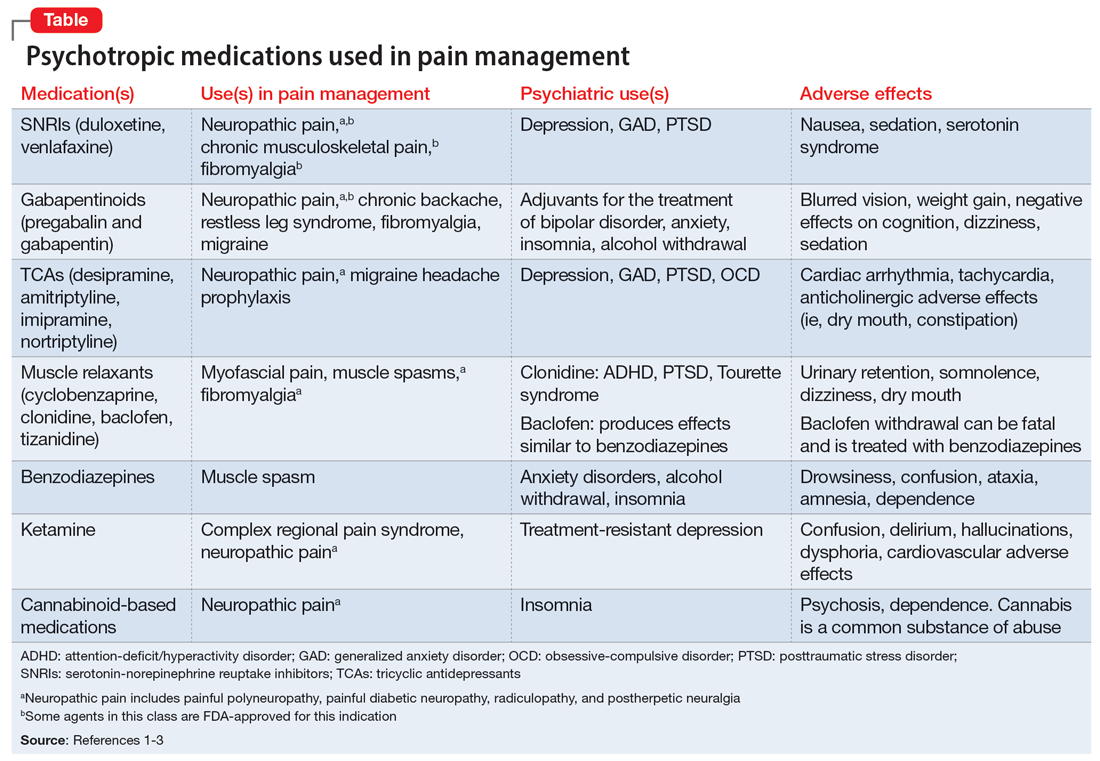
In addition to its psychiatric indications, the serotonin-norepinephrine reuptake inhibitor duloxetine is FDA-approved for treating fibromyalgia and diabetic neuropathic pain. It is often prescribed in the treatment of multiple pain disorders. Tricyclic antidepressants (TCAs) have the largest effect size in the treatment of neuropathic pain.2 Cyclobenzaprine is a TCA used to treat muscle spasms. Gabapentinoids (alpha-2 delta-1 calcium channel inhibition) are FDA-approved for treating postherpetic neuralgia, fibromyalgia, and diabetic neuropathy.1,2
Ketamine is an anesthetic with analgesic and antidepressant properties used as an IV infusion to manage several pain disorders.2 The alpha-2 adrenergic agonists tizanidine and clonidine are muscle relaxants2; the latter is used to treat attention-deficit/hyperactivity disorder and Tourette syndrome. Benzodiazepines (GABA-A agonists) are used for short-term treatment of anxiety disorders, insomnia, and muscle spasms.1,2 Baclofen (GABA-B receptor agonist) is used to treat spasticity.2 Medical cannabis (tetrahydrocannabinol/cannabidiol) is also gaining popularity for treating chronic pain and insomnia.1-3
1. Sutherland AM, Nicholls J, Bao J, et al. Overlaps in pharmacology for the treatment of chronic pain and mental health disorders. Prog Neuropsychopharmacol Biol Psychiatry. 2018;87(Pt B):290-297.
2. Bajwa ZH, Wootton RJ, Warfield CA. Principles and Practice of Pain Medicine. 3rd ed. McGraw Hill; 2016.
3. McDonagh MS, Selph SS, Buckley DI, et al. Nonopioid Pharmacologic Treatments for Chronic Pain. Comparative Effectiveness Review No. 228. Agency for Healthcare Research and Quality; 2020. doi:10.23970/AHRQEPCCER228
1. Sutherland AM, Nicholls J, Bao J, et al. Overlaps in pharmacology for the treatment of chronic pain and mental health disorders. Prog Neuropsychopharmacol Biol Psychiatry. 2018;87(Pt B):290-297.
2. Bajwa ZH, Wootton RJ, Warfield CA. Principles and Practice of Pain Medicine. 3rd ed. McGraw Hill; 2016.
3. McDonagh MS, Selph SS, Buckley DI, et al. Nonopioid Pharmacologic Treatments for Chronic Pain. Comparative Effectiveness Review No. 228. Agency for Healthcare Research and Quality; 2020. doi:10.23970/AHRQEPCCER228







