User login
Despite PCV, pediatric asthma patients face pneumococcal risks
Even on-time pneumococcal vaccines don’t completely protect children with asthma from developing invasive pneumococcal disease, a meta-analysis has determined.
Despite receiving pneumococcal valent 7, 10, or 13, children with asthma were still almost twice as likely to develop the disease as were children without asthma, Jose A. Castro-Rodriguez, MD, PhD, and colleagues reported in Pediatrics (2020 Jan. doi: 10.1542/peds.2019-1200). None of the studies included rates for those who received the pneumococcal polysaccharide vaccine (PPSV23).
“For the first time, this meta-analysis reveals 90% increased odds of invasive pneumococcal disease (IPD) among [vaccinated] children with asthma,” said Dr. Castro-Rodriguez, of Pontificia Universidad Católica de Chile, Santiago, and colleagues. “If confirmed, these findings will bear clinical and public health importance,” they noted, because guidelines now recommend PPSV23 after age 2 in children with asthma only if they’re treated with prolonged high-dose oral corticosteroids.
However, because the analysis comprised only four studies, the authors cautioned that the results aren’t enough to justify changes to practice recommendations.
Asthma treatment with inhaled corticosteroids (ICS) may be driving the increased risk, Dr. Castro-Rodriguez and his coauthors suggested. ICS deposition in the oropharynx could boost oropharyngeal candidiasis risk by weakening the mucosal immune response, the researchers noted. And that same process may be at work with Streptococcus pneumoniae.
A prior study found that children with asthma who received ICS for at least 1 month were almost four times more likely to have oropharyngeal colonization by S. pneumoniae as were those who didn’t get the drugs. Thus, a higher carrier rate of S. pneumoniae in the oropharynx, along with asthma’s impaired airway clearance, might increase the risk of pneumococcal diseases, the investigators explained.
Dr. Castro-Rodriguez and colleagues analyzed four studies with more than 4,000 cases and controls, and about 26 million person-years of follow-up.
Rates and risks of IPD in the four studies were as follows:
- Among those with IPD, 27% had asthma, with 18% of those without, an adjusted odds ratio (aOR) of 1.8.
- In a European of patients who received at least 3 doses of PCV7, IPD rates per 100,000 person-years for 5-year-olds were 11.6 for children with asthma and 7.3 for those without. For 5- to 17-year-olds with and without asthma, the rates were 2.3 and 1.6, respectively.
- In 2001, a Korean found an aOR of 2.08 for IPD in children with asthma, compared with those without. In 2010, the aOR was 3.26. No vaccine types were reported in the study.
- of IPD were 3.7 per 100,000 person-years for children with asthma, compared with 2.5 for healthy controls – an adjusted relative risk of 1.5.
The pooled estimate of the four studies revealed an aOR of 1.9 for IPD among children with asthma, compared with those without, Dr. Castro-Rodriguez and his team concluded.
None of the studies reported hospital admissions, mortality, length of hospital stay, intensive care admission, invasive respiratory support, or additional medication use.
One, however, did find asthma severity was significantly associated with increasing IPD treatment costs per 100,000 person-years: $72,581 for healthy controls, compared with $100,020 for children with mild asthma, $172,002 for moderate asthma, and $638,452 for severe asthma.
In addition, treating all-cause pneumonia was more expensive in children with asthma. For all-cause pneumonia, the researchers found that estimated costs per 100,000 person-years for mild, moderate, and severe asthma were $7.5 million, $14.6 million, and $46.8 million, respectively, compared with $1.7 million for healthy controls.
The authors had no relevant financial disclosures.
SOURCE: Castro-Rodriguez J et al. Pediatrics. 2020 Jan. doi: 10.1542/peds.2019-1200.
The meta-analysis contains some important lessons for pediatricians, Tina Q. Tan, MD, wrote in an accompanying editorial.
“First, asthma remains a risk factor for invasive pneumococcal disease and pneumococcal pneumonia, even in the era of widespread use of PCV,” Dr. Tan noted. “Second, it is important that all patients, especially those with asthma, are receiving their vaccinations on time and, most notably, are up to date on their pneumococcal vaccinations. This will provide the best protection against pneumococcal infections and their complications for pediatric patients with asthma.”
Pneumococcal conjugate vaccines (PCV) have impressively decreased rates of invasive pneumococcal disease (IPD) and pneumonia in children in the United States, Dr. Tan explained. Overall, incidence dropped from 95 cases per 100,000 person-years in 1998 to only 9 cases per 100,000 in 2016.
In addition, the incidence of IPD caused by 13-valent PCV serotypes fell, from 88 cases per 100,000 in 1998 to 2 cases per 100,000 in 2016.
The threat is not over, however.
“IPD still remains a leading cause of morbidity and mortality in the United States and worldwide,” Dr. Tan cautioned. “In 2017, the CDC’s Active Bacterial Core surveillance network reported that there were 31,000 cases of IPD (meningitis, bacteremia, and bacteremic pneumonia) and 3,590 deaths, of which 147 cases and 9 deaths occurred in children younger than 5 years of age.”
Dr. Tan is a professor of pediatrics at Northwestern University, Chicago. Her comments appear in Pediatrics 2020 Jan. doi: 10.1542/peds.2019-3360 .
The meta-analysis contains some important lessons for pediatricians, Tina Q. Tan, MD, wrote in an accompanying editorial.
“First, asthma remains a risk factor for invasive pneumococcal disease and pneumococcal pneumonia, even in the era of widespread use of PCV,” Dr. Tan noted. “Second, it is important that all patients, especially those with asthma, are receiving their vaccinations on time and, most notably, are up to date on their pneumococcal vaccinations. This will provide the best protection against pneumococcal infections and their complications for pediatric patients with asthma.”
Pneumococcal conjugate vaccines (PCV) have impressively decreased rates of invasive pneumococcal disease (IPD) and pneumonia in children in the United States, Dr. Tan explained. Overall, incidence dropped from 95 cases per 100,000 person-years in 1998 to only 9 cases per 100,000 in 2016.
In addition, the incidence of IPD caused by 13-valent PCV serotypes fell, from 88 cases per 100,000 in 1998 to 2 cases per 100,000 in 2016.
The threat is not over, however.
“IPD still remains a leading cause of morbidity and mortality in the United States and worldwide,” Dr. Tan cautioned. “In 2017, the CDC’s Active Bacterial Core surveillance network reported that there were 31,000 cases of IPD (meningitis, bacteremia, and bacteremic pneumonia) and 3,590 deaths, of which 147 cases and 9 deaths occurred in children younger than 5 years of age.”
Dr. Tan is a professor of pediatrics at Northwestern University, Chicago. Her comments appear in Pediatrics 2020 Jan. doi: 10.1542/peds.2019-3360 .
The meta-analysis contains some important lessons for pediatricians, Tina Q. Tan, MD, wrote in an accompanying editorial.
“First, asthma remains a risk factor for invasive pneumococcal disease and pneumococcal pneumonia, even in the era of widespread use of PCV,” Dr. Tan noted. “Second, it is important that all patients, especially those with asthma, are receiving their vaccinations on time and, most notably, are up to date on their pneumococcal vaccinations. This will provide the best protection against pneumococcal infections and their complications for pediatric patients with asthma.”
Pneumococcal conjugate vaccines (PCV) have impressively decreased rates of invasive pneumococcal disease (IPD) and pneumonia in children in the United States, Dr. Tan explained. Overall, incidence dropped from 95 cases per 100,000 person-years in 1998 to only 9 cases per 100,000 in 2016.
In addition, the incidence of IPD caused by 13-valent PCV serotypes fell, from 88 cases per 100,000 in 1998 to 2 cases per 100,000 in 2016.
The threat is not over, however.
“IPD still remains a leading cause of morbidity and mortality in the United States and worldwide,” Dr. Tan cautioned. “In 2017, the CDC’s Active Bacterial Core surveillance network reported that there were 31,000 cases of IPD (meningitis, bacteremia, and bacteremic pneumonia) and 3,590 deaths, of which 147 cases and 9 deaths occurred in children younger than 5 years of age.”
Dr. Tan is a professor of pediatrics at Northwestern University, Chicago. Her comments appear in Pediatrics 2020 Jan. doi: 10.1542/peds.2019-3360 .
Even on-time pneumococcal vaccines don’t completely protect children with asthma from developing invasive pneumococcal disease, a meta-analysis has determined.
Despite receiving pneumococcal valent 7, 10, or 13, children with asthma were still almost twice as likely to develop the disease as were children without asthma, Jose A. Castro-Rodriguez, MD, PhD, and colleagues reported in Pediatrics (2020 Jan. doi: 10.1542/peds.2019-1200). None of the studies included rates for those who received the pneumococcal polysaccharide vaccine (PPSV23).
“For the first time, this meta-analysis reveals 90% increased odds of invasive pneumococcal disease (IPD) among [vaccinated] children with asthma,” said Dr. Castro-Rodriguez, of Pontificia Universidad Católica de Chile, Santiago, and colleagues. “If confirmed, these findings will bear clinical and public health importance,” they noted, because guidelines now recommend PPSV23 after age 2 in children with asthma only if they’re treated with prolonged high-dose oral corticosteroids.
However, because the analysis comprised only four studies, the authors cautioned that the results aren’t enough to justify changes to practice recommendations.
Asthma treatment with inhaled corticosteroids (ICS) may be driving the increased risk, Dr. Castro-Rodriguez and his coauthors suggested. ICS deposition in the oropharynx could boost oropharyngeal candidiasis risk by weakening the mucosal immune response, the researchers noted. And that same process may be at work with Streptococcus pneumoniae.
A prior study found that children with asthma who received ICS for at least 1 month were almost four times more likely to have oropharyngeal colonization by S. pneumoniae as were those who didn’t get the drugs. Thus, a higher carrier rate of S. pneumoniae in the oropharynx, along with asthma’s impaired airway clearance, might increase the risk of pneumococcal diseases, the investigators explained.
Dr. Castro-Rodriguez and colleagues analyzed four studies with more than 4,000 cases and controls, and about 26 million person-years of follow-up.
Rates and risks of IPD in the four studies were as follows:
- Among those with IPD, 27% had asthma, with 18% of those without, an adjusted odds ratio (aOR) of 1.8.
- In a European of patients who received at least 3 doses of PCV7, IPD rates per 100,000 person-years for 5-year-olds were 11.6 for children with asthma and 7.3 for those without. For 5- to 17-year-olds with and without asthma, the rates were 2.3 and 1.6, respectively.
- In 2001, a Korean found an aOR of 2.08 for IPD in children with asthma, compared with those without. In 2010, the aOR was 3.26. No vaccine types were reported in the study.
- of IPD were 3.7 per 100,000 person-years for children with asthma, compared with 2.5 for healthy controls – an adjusted relative risk of 1.5.
The pooled estimate of the four studies revealed an aOR of 1.9 for IPD among children with asthma, compared with those without, Dr. Castro-Rodriguez and his team concluded.
None of the studies reported hospital admissions, mortality, length of hospital stay, intensive care admission, invasive respiratory support, or additional medication use.
One, however, did find asthma severity was significantly associated with increasing IPD treatment costs per 100,000 person-years: $72,581 for healthy controls, compared with $100,020 for children with mild asthma, $172,002 for moderate asthma, and $638,452 for severe asthma.
In addition, treating all-cause pneumonia was more expensive in children with asthma. For all-cause pneumonia, the researchers found that estimated costs per 100,000 person-years for mild, moderate, and severe asthma were $7.5 million, $14.6 million, and $46.8 million, respectively, compared with $1.7 million for healthy controls.
The authors had no relevant financial disclosures.
SOURCE: Castro-Rodriguez J et al. Pediatrics. 2020 Jan. doi: 10.1542/peds.2019-1200.
Even on-time pneumococcal vaccines don’t completely protect children with asthma from developing invasive pneumococcal disease, a meta-analysis has determined.
Despite receiving pneumococcal valent 7, 10, or 13, children with asthma were still almost twice as likely to develop the disease as were children without asthma, Jose A. Castro-Rodriguez, MD, PhD, and colleagues reported in Pediatrics (2020 Jan. doi: 10.1542/peds.2019-1200). None of the studies included rates for those who received the pneumococcal polysaccharide vaccine (PPSV23).
“For the first time, this meta-analysis reveals 90% increased odds of invasive pneumococcal disease (IPD) among [vaccinated] children with asthma,” said Dr. Castro-Rodriguez, of Pontificia Universidad Católica de Chile, Santiago, and colleagues. “If confirmed, these findings will bear clinical and public health importance,” they noted, because guidelines now recommend PPSV23 after age 2 in children with asthma only if they’re treated with prolonged high-dose oral corticosteroids.
However, because the analysis comprised only four studies, the authors cautioned that the results aren’t enough to justify changes to practice recommendations.
Asthma treatment with inhaled corticosteroids (ICS) may be driving the increased risk, Dr. Castro-Rodriguez and his coauthors suggested. ICS deposition in the oropharynx could boost oropharyngeal candidiasis risk by weakening the mucosal immune response, the researchers noted. And that same process may be at work with Streptococcus pneumoniae.
A prior study found that children with asthma who received ICS for at least 1 month were almost four times more likely to have oropharyngeal colonization by S. pneumoniae as were those who didn’t get the drugs. Thus, a higher carrier rate of S. pneumoniae in the oropharynx, along with asthma’s impaired airway clearance, might increase the risk of pneumococcal diseases, the investigators explained.
Dr. Castro-Rodriguez and colleagues analyzed four studies with more than 4,000 cases and controls, and about 26 million person-years of follow-up.
Rates and risks of IPD in the four studies were as follows:
- Among those with IPD, 27% had asthma, with 18% of those without, an adjusted odds ratio (aOR) of 1.8.
- In a European of patients who received at least 3 doses of PCV7, IPD rates per 100,000 person-years for 5-year-olds were 11.6 for children with asthma and 7.3 for those without. For 5- to 17-year-olds with and without asthma, the rates were 2.3 and 1.6, respectively.
- In 2001, a Korean found an aOR of 2.08 for IPD in children with asthma, compared with those without. In 2010, the aOR was 3.26. No vaccine types were reported in the study.
- of IPD were 3.7 per 100,000 person-years for children with asthma, compared with 2.5 for healthy controls – an adjusted relative risk of 1.5.
The pooled estimate of the four studies revealed an aOR of 1.9 for IPD among children with asthma, compared with those without, Dr. Castro-Rodriguez and his team concluded.
None of the studies reported hospital admissions, mortality, length of hospital stay, intensive care admission, invasive respiratory support, or additional medication use.
One, however, did find asthma severity was significantly associated with increasing IPD treatment costs per 100,000 person-years: $72,581 for healthy controls, compared with $100,020 for children with mild asthma, $172,002 for moderate asthma, and $638,452 for severe asthma.
In addition, treating all-cause pneumonia was more expensive in children with asthma. For all-cause pneumonia, the researchers found that estimated costs per 100,000 person-years for mild, moderate, and severe asthma were $7.5 million, $14.6 million, and $46.8 million, respectively, compared with $1.7 million for healthy controls.
The authors had no relevant financial disclosures.
SOURCE: Castro-Rodriguez J et al. Pediatrics. 2020 Jan. doi: 10.1542/peds.2019-1200.
FROM PEDIATRICS
EEG surveillance, preseizure treatment prevents TSC epilepsy, cognitive loss
BALTIMORE – Monitoring children who have tuberous sclerosis with EEG and treating them with vigabatrin (Sabril) at the first sign of preseizure abnormalities, rather than the usual practice of no surveillance and waiting until they have seizures, prevents epilepsy and cognitive decline, according to European investigators.
Early surveillance is recommended and standard practice in Europe. That’s not the case in the United States, but might be someday pending the results of the PREVENT trial (Preventing Epilepsy Using Vigabatrin In Infants With Tuberous Sclerosis Complex), an ongoing, National Institute of Neurological Disorders and Stroke–funded study to confirm the European findings.
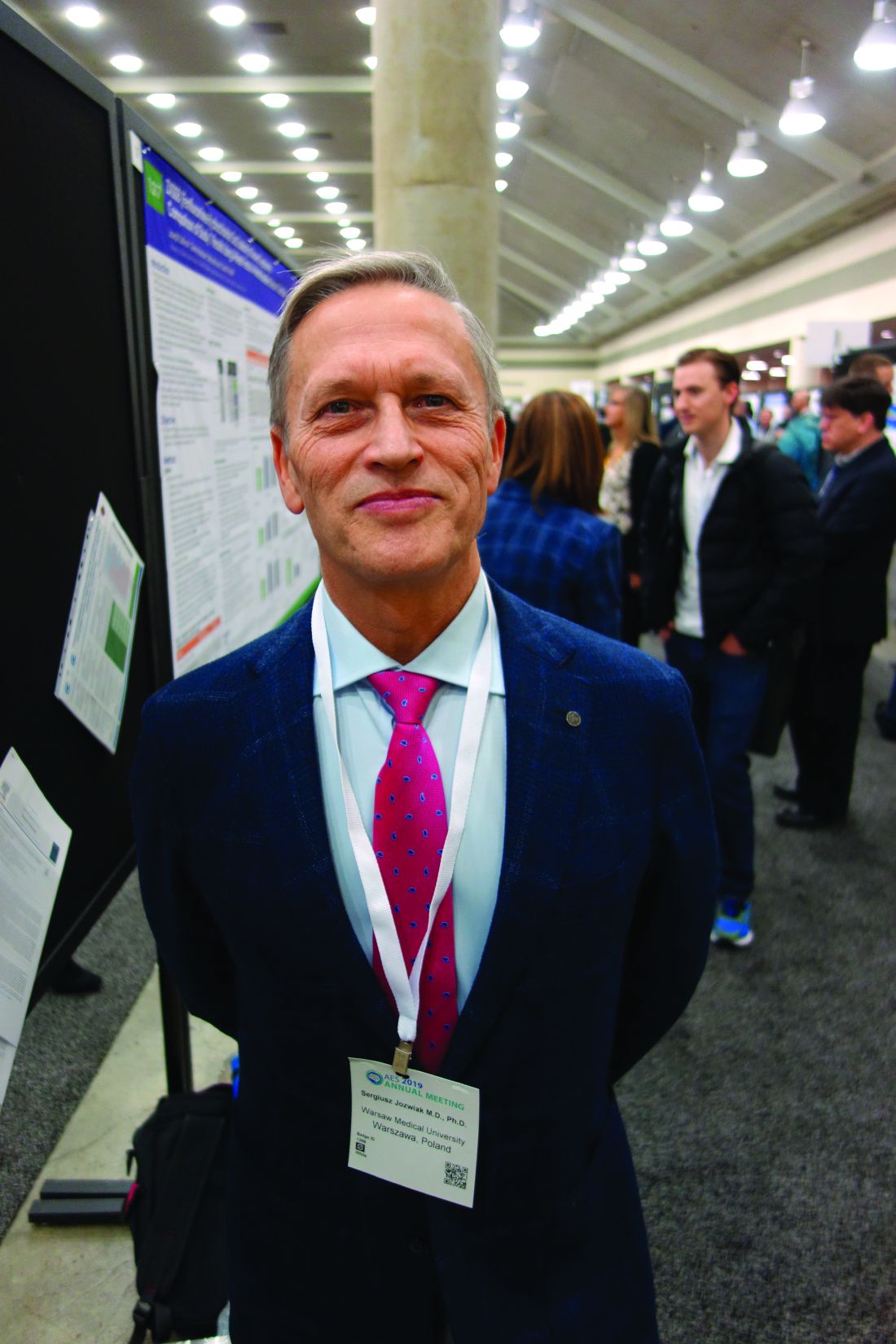
“We are trying to convince doctors” in the United States and other “countries to do this. If you are not convinced to do early treatment,” at least “do surveillance with EEG. You will diagnose epilepsy earlier, and treat earlier, and children will do much better,” said Sergiusz Jozwiak, MD, PhD, head of pediatric neurology at Warsaw Medical University and recipient of an award from the U.S. Tuberous Sclerosis Alliance for his pioneering work.
Some U.S. physicians are already doing preventive treatment, but it’s hit and miss. “We are talking about monitoring children below the age of 2 years,” when seizures are associated with cognitive decline, he noted at the annual meeting of the American Epilepsy Society.
Dr. Jozwiak presented a follow-up at the meeting to his 2011 investigation, the first prevention study in tuberous sclerosis. Fourteen infants diagnosed within 2 months of birth underwent video-EEG monitoring every 4-6 weeks until age 2 years and were treated with vigabatrin 100-150 mg/kg per day when multifocal epileptiform discharges – a sign of impending seizures – were detected. Outcomes were compared with infants treated traditionally, with no EEG monitoring and vigabatrin only after they seized.
The children are about 9 years old now; the median IQ in the prevention arm is 94 versus 46 in the control group (P less than .03). Seven of the 14 prevention children (50%) never had a clinical seizure, while all but 1 of 25 (96%) in the control arm did (P = .001). Six of 11 prevention children (55%) versus 4 of 24 in the control group (17%), were able to come off antiepileptic drugs altogether, with no seizures (P less than .03). The work was published shortly before the epilepsy meeting.
The original 2011 report, which had similarly favorable outcomes when the children were 2 years old, led directly to the EpiStop trial, conducted at 16 mostly European centers and also reported at the meeting. Dr. Jozwiak was the senior investigator.
The design was different; all of the infants had EEG monitoring every 4 weeks until month 6, then every 6 weeks until age 12 months, then every 2 months until age 2 years. At the first detection of multifocal epileptiform discharges, infants were randomized 1:1 to vigabatrin or to the control group, with further monitoring followed by vigabatrin at the first seizure on EEG or first clinical seizure. An additional group of children – the open-label arm – also had EEG monitoring, but when to start vigabatrin was left up to the study site.
Only 50 of the original 94 children completed the trial to the full 2 years; tuberous sclerosis comorbidities drove many of them out, said lead investigator Katarzyna Kotulska-Jozwiak, MD, PhD, head of neurology at Children’s Memorial Health Institute, Warsaw.
Even so, the 25 children treated preventively in the randomized and open-label cohorts were more than three times as likely to be seizure free at 2 years (P = .01), and 74% less likely to develop drug-resistant epilepsy (P = .013). None of the prevention children developed infantile spasms versus 10 controls (40%) treated at first clinical or EEG seizure.
The incidence of neurodevelopmental delay was 34%, and autism 33%, at 24 months, and did not differ between prevention and control subjects. It’s probably because even children in the control group benefited from EEG surveillance and early treatment, the investigators said.
Historically, the rate of intellectual disability with usual treatment is around 60%, Dr. Kotulska-Jozwiak noted.
Overall, Dr. Jozwiak said that European physicians are more comfortable using vigabatrin than U.S. doctors, where the drug hasn’t been on the market as long and carries a Food and Drug Administration boxed warning of visual impairment. Its indications in the United States include infantile spasms in children 1-24 months old.
Levetiracetam (Keppra) is another option, but it’s not as effective in tuberous sclerosis. The PREVENT trial is using vigabatrin, and some U.S. doctors “are changing their minds, but it takes time,” Dr. Jozwiak said.
He noted that TSC is increasingly being diagnosed in utero, which gives a leg up on early diagnosis and prevention. The giveaways are heart tumors on ECG and cortical tubers on fetal MRI.
Dr. Jozwiak thinks the prevention approach might also help in other early seizure disorders, such as Sturge-Weber syndrome.
The work was funded by the European Commission and Polish government. Dr. Jozwiak and Dr. Kotulska-Jozwiak didn’t have any disclosures.
SOURCES: Jozwiak S et al. AES 2019, Abstract 1.218; Kotulska-Jozwiak K et al. AES 2019, Abstract 2.121.
BALTIMORE – Monitoring children who have tuberous sclerosis with EEG and treating them with vigabatrin (Sabril) at the first sign of preseizure abnormalities, rather than the usual practice of no surveillance and waiting until they have seizures, prevents epilepsy and cognitive decline, according to European investigators.
Early surveillance is recommended and standard practice in Europe. That’s not the case in the United States, but might be someday pending the results of the PREVENT trial (Preventing Epilepsy Using Vigabatrin In Infants With Tuberous Sclerosis Complex), an ongoing, National Institute of Neurological Disorders and Stroke–funded study to confirm the European findings.
“We are trying to convince doctors” in the United States and other “countries to do this. If you are not convinced to do early treatment,” at least “do surveillance with EEG. You will diagnose epilepsy earlier, and treat earlier, and children will do much better,” said Sergiusz Jozwiak, MD, PhD, head of pediatric neurology at Warsaw Medical University and recipient of an award from the U.S. Tuberous Sclerosis Alliance for his pioneering work.
Some U.S. physicians are already doing preventive treatment, but it’s hit and miss. “We are talking about monitoring children below the age of 2 years,” when seizures are associated with cognitive decline, he noted at the annual meeting of the American Epilepsy Society.
Dr. Jozwiak presented a follow-up at the meeting to his 2011 investigation, the first prevention study in tuberous sclerosis. Fourteen infants diagnosed within 2 months of birth underwent video-EEG monitoring every 4-6 weeks until age 2 years and were treated with vigabatrin 100-150 mg/kg per day when multifocal epileptiform discharges – a sign of impending seizures – were detected. Outcomes were compared with infants treated traditionally, with no EEG monitoring and vigabatrin only after they seized.
The children are about 9 years old now; the median IQ in the prevention arm is 94 versus 46 in the control group (P less than .03). Seven of the 14 prevention children (50%) never had a clinical seizure, while all but 1 of 25 (96%) in the control arm did (P = .001). Six of 11 prevention children (55%) versus 4 of 24 in the control group (17%), were able to come off antiepileptic drugs altogether, with no seizures (P less than .03). The work was published shortly before the epilepsy meeting.
The original 2011 report, which had similarly favorable outcomes when the children were 2 years old, led directly to the EpiStop trial, conducted at 16 mostly European centers and also reported at the meeting. Dr. Jozwiak was the senior investigator.
The design was different; all of the infants had EEG monitoring every 4 weeks until month 6, then every 6 weeks until age 12 months, then every 2 months until age 2 years. At the first detection of multifocal epileptiform discharges, infants were randomized 1:1 to vigabatrin or to the control group, with further monitoring followed by vigabatrin at the first seizure on EEG or first clinical seizure. An additional group of children – the open-label arm – also had EEG monitoring, but when to start vigabatrin was left up to the study site.
Only 50 of the original 94 children completed the trial to the full 2 years; tuberous sclerosis comorbidities drove many of them out, said lead investigator Katarzyna Kotulska-Jozwiak, MD, PhD, head of neurology at Children’s Memorial Health Institute, Warsaw.
Even so, the 25 children treated preventively in the randomized and open-label cohorts were more than three times as likely to be seizure free at 2 years (P = .01), and 74% less likely to develop drug-resistant epilepsy (P = .013). None of the prevention children developed infantile spasms versus 10 controls (40%) treated at first clinical or EEG seizure.
The incidence of neurodevelopmental delay was 34%, and autism 33%, at 24 months, and did not differ between prevention and control subjects. It’s probably because even children in the control group benefited from EEG surveillance and early treatment, the investigators said.
Historically, the rate of intellectual disability with usual treatment is around 60%, Dr. Kotulska-Jozwiak noted.
Overall, Dr. Jozwiak said that European physicians are more comfortable using vigabatrin than U.S. doctors, where the drug hasn’t been on the market as long and carries a Food and Drug Administration boxed warning of visual impairment. Its indications in the United States include infantile spasms in children 1-24 months old.
Levetiracetam (Keppra) is another option, but it’s not as effective in tuberous sclerosis. The PREVENT trial is using vigabatrin, and some U.S. doctors “are changing their minds, but it takes time,” Dr. Jozwiak said.
He noted that TSC is increasingly being diagnosed in utero, which gives a leg up on early diagnosis and prevention. The giveaways are heart tumors on ECG and cortical tubers on fetal MRI.
Dr. Jozwiak thinks the prevention approach might also help in other early seizure disorders, such as Sturge-Weber syndrome.
The work was funded by the European Commission and Polish government. Dr. Jozwiak and Dr. Kotulska-Jozwiak didn’t have any disclosures.
SOURCES: Jozwiak S et al. AES 2019, Abstract 1.218; Kotulska-Jozwiak K et al. AES 2019, Abstract 2.121.
BALTIMORE – Monitoring children who have tuberous sclerosis with EEG and treating them with vigabatrin (Sabril) at the first sign of preseizure abnormalities, rather than the usual practice of no surveillance and waiting until they have seizures, prevents epilepsy and cognitive decline, according to European investigators.
Early surveillance is recommended and standard practice in Europe. That’s not the case in the United States, but might be someday pending the results of the PREVENT trial (Preventing Epilepsy Using Vigabatrin In Infants With Tuberous Sclerosis Complex), an ongoing, National Institute of Neurological Disorders and Stroke–funded study to confirm the European findings.
“We are trying to convince doctors” in the United States and other “countries to do this. If you are not convinced to do early treatment,” at least “do surveillance with EEG. You will diagnose epilepsy earlier, and treat earlier, and children will do much better,” said Sergiusz Jozwiak, MD, PhD, head of pediatric neurology at Warsaw Medical University and recipient of an award from the U.S. Tuberous Sclerosis Alliance for his pioneering work.
Some U.S. physicians are already doing preventive treatment, but it’s hit and miss. “We are talking about monitoring children below the age of 2 years,” when seizures are associated with cognitive decline, he noted at the annual meeting of the American Epilepsy Society.
Dr. Jozwiak presented a follow-up at the meeting to his 2011 investigation, the first prevention study in tuberous sclerosis. Fourteen infants diagnosed within 2 months of birth underwent video-EEG monitoring every 4-6 weeks until age 2 years and were treated with vigabatrin 100-150 mg/kg per day when multifocal epileptiform discharges – a sign of impending seizures – were detected. Outcomes were compared with infants treated traditionally, with no EEG monitoring and vigabatrin only after they seized.
The children are about 9 years old now; the median IQ in the prevention arm is 94 versus 46 in the control group (P less than .03). Seven of the 14 prevention children (50%) never had a clinical seizure, while all but 1 of 25 (96%) in the control arm did (P = .001). Six of 11 prevention children (55%) versus 4 of 24 in the control group (17%), were able to come off antiepileptic drugs altogether, with no seizures (P less than .03). The work was published shortly before the epilepsy meeting.
The original 2011 report, which had similarly favorable outcomes when the children were 2 years old, led directly to the EpiStop trial, conducted at 16 mostly European centers and also reported at the meeting. Dr. Jozwiak was the senior investigator.
The design was different; all of the infants had EEG monitoring every 4 weeks until month 6, then every 6 weeks until age 12 months, then every 2 months until age 2 years. At the first detection of multifocal epileptiform discharges, infants were randomized 1:1 to vigabatrin or to the control group, with further monitoring followed by vigabatrin at the first seizure on EEG or first clinical seizure. An additional group of children – the open-label arm – also had EEG monitoring, but when to start vigabatrin was left up to the study site.
Only 50 of the original 94 children completed the trial to the full 2 years; tuberous sclerosis comorbidities drove many of them out, said lead investigator Katarzyna Kotulska-Jozwiak, MD, PhD, head of neurology at Children’s Memorial Health Institute, Warsaw.
Even so, the 25 children treated preventively in the randomized and open-label cohorts were more than three times as likely to be seizure free at 2 years (P = .01), and 74% less likely to develop drug-resistant epilepsy (P = .013). None of the prevention children developed infantile spasms versus 10 controls (40%) treated at first clinical or EEG seizure.
The incidence of neurodevelopmental delay was 34%, and autism 33%, at 24 months, and did not differ between prevention and control subjects. It’s probably because even children in the control group benefited from EEG surveillance and early treatment, the investigators said.
Historically, the rate of intellectual disability with usual treatment is around 60%, Dr. Kotulska-Jozwiak noted.
Overall, Dr. Jozwiak said that European physicians are more comfortable using vigabatrin than U.S. doctors, where the drug hasn’t been on the market as long and carries a Food and Drug Administration boxed warning of visual impairment. Its indications in the United States include infantile spasms in children 1-24 months old.
Levetiracetam (Keppra) is another option, but it’s not as effective in tuberous sclerosis. The PREVENT trial is using vigabatrin, and some U.S. doctors “are changing their minds, but it takes time,” Dr. Jozwiak said.
He noted that TSC is increasingly being diagnosed in utero, which gives a leg up on early diagnosis and prevention. The giveaways are heart tumors on ECG and cortical tubers on fetal MRI.
Dr. Jozwiak thinks the prevention approach might also help in other early seizure disorders, such as Sturge-Weber syndrome.
The work was funded by the European Commission and Polish government. Dr. Jozwiak and Dr. Kotulska-Jozwiak didn’t have any disclosures.
SOURCES: Jozwiak S et al. AES 2019, Abstract 1.218; Kotulska-Jozwiak K et al. AES 2019, Abstract 2.121.
REPORTING FROM AES 2019
Experts call to revise the Uniform Determination of Death Act
, according to an editorial published online Dec. 24, 2019, in Annals of Internal Medicine. Proposed revisions would identify the standards for determining death by neurologic criteria and address the question of whether consent is required to make this determination. If accepted, the revisions would enhance public trust in the determination of death by neurologic criteria, the authors said.
“There is a disconnect between the medical and legal standards for brain death,” said Ariane K. Lewis, MD, associate professor of neurology and neurosurgery at New York University and lead author of the editorial. The discrepancy must be remedied because it has led to lawsuits and has proved to be problematic from a societal standpoint, she added.
“We defend changing the law to match medical practice, rather than changing medical practice to match the law,” said Thaddeus Mason Pope, JD, PhD, director of the Health Law Institute at Mitchell Hamline School of Law in Saint Paul, Minnesota, and an author of the editorial.
Accepted medical standards are unclear
The UDDA was drafted in 1981 to establish a uniform legal standard for death by neurologic criteria. A person with “irreversible cessation of all functions of the entire brain, including the brainstem,” is dead, according to the statute. A determination of death, it adds, “must be made in accordance with accepted medical standards.”
But the medical standards used to determine death by neurologic cause have not been uniform. In 2015, the Supreme Court of Nevada ruled that it was not clear that the standard published by the American Academy of Neurology (AAN), which had been used in the case at issue, was the “accepted medical standard.” An AAN summit later affirmed that the accepted medical standards for determination of death by neurologic cause are the 2010 AAN standard for determination of brain death in adults and the 2011 Society of Critical Care Medicine (SCCM), American Academy of Pediatrics (AAP), and Child Neurology Society (CNS) standard for determination of brain death in children. The Nevada legislature amended the state UDDA to identify these standards as the accepted standards. A revised UDDA also should identify these standards and grant an administrative agency (i.e., the board of medicine) the power to review and update the accepted medical standards as needed, according to the editorial.
To the extent that hospitals are not following the AAN or SCCM/AAP/CNS standards for determining death by neurologic cause, “enshrining” these standards in a revised UDDA “should increase uniformity and consistency” in hospitals’ policies on brain death, Dr. Pope said.
The question of hormonal function
Lawsuits in California and Nevada raised the question of whether the pituitary gland and hypothalamus are parts of the brain. If so, then the accepted medical standards for death by neurologic cause are not consistent with the statutory requirements for the determination of death, since the former do not test for cessation of hormonal function.
The current edition of the adult standards for determining death by neurologic cause were published in 2010. “Whenever we measure brain death, we’re not measuring the cessation of all functions of the entire brain,” Dr. Pope said. “That’s not a new thing; that’s been the case for a long time.”
To address the discrepancy between medical practice and the legal statute, Dr. Lewis and colleagues proposed that the UDDA’s reference to “irreversible cessation of functions of the entire brain” be followed by the following clause: “including the brainstem, leading to unresponsive coma with loss of capacity for consciousness, brainstem areflexia, and the inability to breathe spontaneously.” An alternative revision would be to add the briefer phrase “... with the exception of hormonal function.”
Authors say consent is not required for testing
Other complications have arisen from the UDDA’s failure to specify whether consent is required for a determination of death by neurologic cause. Court rulings on this question have not been consistent. Dr. Lewis and colleagues propose adding the following text to the UDDA: “Reasonable efforts should be made to notify a patient’s legally authorized decision-maker before performing a determination of death by neurologic criteria, but consent is not required to initiate such an evaluation.”
The proposed revisions to the UDDA “might give [clinicians] more confidence to proceed with brain death testing, because it would clarify that they don’t need the parents’ [or the patient’s legally authorized decision-maker] consent to do the tests,” said Dr. Pope. “If anything, they might even have a duty to do the tests.”
The final problem with the UDDA that Dr. Lewis and colleagues cited is that it does not provide clear guidance about how to respond to religious objections to discontinuation of organ support after a determination of death by neurologic cause. “Because the issue is rather complicated, we have not advocated for a singular position related to this [question] in our revised UDDA,” Dr. Lewis said. “Rather, we recommended the need for a multidisciplinary group to come together to determine what is the best approach. In an ideal world, this [approach] would be universal throughout the country.”
Although a revised UDDA would provide greater clarity to physicians and promote uniformity of practice, it would not resolve ongoing theological and philosophical debates about whether brain death is biological death, Dr. Pope said. “The key thing is that it would give clinicians a green light or certainty and clarity that they may proceed to do the test in the first place. If the tests are positive and the patient really is dead, then they could proceed to organ procurement or to move to the morgue.”
Dr. Lewis is a member of various AAN committees and working groups but receives no compensation for her role. A coauthor received personal fees from the AAN that were unrelated to the editorial.
SOURCE: Lewis A et al. Ann Intern Med. 2019 Dec 24. doi: 10.7326/M19-2731.
, according to an editorial published online Dec. 24, 2019, in Annals of Internal Medicine. Proposed revisions would identify the standards for determining death by neurologic criteria and address the question of whether consent is required to make this determination. If accepted, the revisions would enhance public trust in the determination of death by neurologic criteria, the authors said.
“There is a disconnect between the medical and legal standards for brain death,” said Ariane K. Lewis, MD, associate professor of neurology and neurosurgery at New York University and lead author of the editorial. The discrepancy must be remedied because it has led to lawsuits and has proved to be problematic from a societal standpoint, she added.
“We defend changing the law to match medical practice, rather than changing medical practice to match the law,” said Thaddeus Mason Pope, JD, PhD, director of the Health Law Institute at Mitchell Hamline School of Law in Saint Paul, Minnesota, and an author of the editorial.
Accepted medical standards are unclear
The UDDA was drafted in 1981 to establish a uniform legal standard for death by neurologic criteria. A person with “irreversible cessation of all functions of the entire brain, including the brainstem,” is dead, according to the statute. A determination of death, it adds, “must be made in accordance with accepted medical standards.”
But the medical standards used to determine death by neurologic cause have not been uniform. In 2015, the Supreme Court of Nevada ruled that it was not clear that the standard published by the American Academy of Neurology (AAN), which had been used in the case at issue, was the “accepted medical standard.” An AAN summit later affirmed that the accepted medical standards for determination of death by neurologic cause are the 2010 AAN standard for determination of brain death in adults and the 2011 Society of Critical Care Medicine (SCCM), American Academy of Pediatrics (AAP), and Child Neurology Society (CNS) standard for determination of brain death in children. The Nevada legislature amended the state UDDA to identify these standards as the accepted standards. A revised UDDA also should identify these standards and grant an administrative agency (i.e., the board of medicine) the power to review and update the accepted medical standards as needed, according to the editorial.
To the extent that hospitals are not following the AAN or SCCM/AAP/CNS standards for determining death by neurologic cause, “enshrining” these standards in a revised UDDA “should increase uniformity and consistency” in hospitals’ policies on brain death, Dr. Pope said.
The question of hormonal function
Lawsuits in California and Nevada raised the question of whether the pituitary gland and hypothalamus are parts of the brain. If so, then the accepted medical standards for death by neurologic cause are not consistent with the statutory requirements for the determination of death, since the former do not test for cessation of hormonal function.
The current edition of the adult standards for determining death by neurologic cause were published in 2010. “Whenever we measure brain death, we’re not measuring the cessation of all functions of the entire brain,” Dr. Pope said. “That’s not a new thing; that’s been the case for a long time.”
To address the discrepancy between medical practice and the legal statute, Dr. Lewis and colleagues proposed that the UDDA’s reference to “irreversible cessation of functions of the entire brain” be followed by the following clause: “including the brainstem, leading to unresponsive coma with loss of capacity for consciousness, brainstem areflexia, and the inability to breathe spontaneously.” An alternative revision would be to add the briefer phrase “... with the exception of hormonal function.”
Authors say consent is not required for testing
Other complications have arisen from the UDDA’s failure to specify whether consent is required for a determination of death by neurologic cause. Court rulings on this question have not been consistent. Dr. Lewis and colleagues propose adding the following text to the UDDA: “Reasonable efforts should be made to notify a patient’s legally authorized decision-maker before performing a determination of death by neurologic criteria, but consent is not required to initiate such an evaluation.”
The proposed revisions to the UDDA “might give [clinicians] more confidence to proceed with brain death testing, because it would clarify that they don’t need the parents’ [or the patient’s legally authorized decision-maker] consent to do the tests,” said Dr. Pope. “If anything, they might even have a duty to do the tests.”
The final problem with the UDDA that Dr. Lewis and colleagues cited is that it does not provide clear guidance about how to respond to religious objections to discontinuation of organ support after a determination of death by neurologic cause. “Because the issue is rather complicated, we have not advocated for a singular position related to this [question] in our revised UDDA,” Dr. Lewis said. “Rather, we recommended the need for a multidisciplinary group to come together to determine what is the best approach. In an ideal world, this [approach] would be universal throughout the country.”
Although a revised UDDA would provide greater clarity to physicians and promote uniformity of practice, it would not resolve ongoing theological and philosophical debates about whether brain death is biological death, Dr. Pope said. “The key thing is that it would give clinicians a green light or certainty and clarity that they may proceed to do the test in the first place. If the tests are positive and the patient really is dead, then they could proceed to organ procurement or to move to the morgue.”
Dr. Lewis is a member of various AAN committees and working groups but receives no compensation for her role. A coauthor received personal fees from the AAN that were unrelated to the editorial.
SOURCE: Lewis A et al. Ann Intern Med. 2019 Dec 24. doi: 10.7326/M19-2731.
, according to an editorial published online Dec. 24, 2019, in Annals of Internal Medicine. Proposed revisions would identify the standards for determining death by neurologic criteria and address the question of whether consent is required to make this determination. If accepted, the revisions would enhance public trust in the determination of death by neurologic criteria, the authors said.
“There is a disconnect between the medical and legal standards for brain death,” said Ariane K. Lewis, MD, associate professor of neurology and neurosurgery at New York University and lead author of the editorial. The discrepancy must be remedied because it has led to lawsuits and has proved to be problematic from a societal standpoint, she added.
“We defend changing the law to match medical practice, rather than changing medical practice to match the law,” said Thaddeus Mason Pope, JD, PhD, director of the Health Law Institute at Mitchell Hamline School of Law in Saint Paul, Minnesota, and an author of the editorial.
Accepted medical standards are unclear
The UDDA was drafted in 1981 to establish a uniform legal standard for death by neurologic criteria. A person with “irreversible cessation of all functions of the entire brain, including the brainstem,” is dead, according to the statute. A determination of death, it adds, “must be made in accordance with accepted medical standards.”
But the medical standards used to determine death by neurologic cause have not been uniform. In 2015, the Supreme Court of Nevada ruled that it was not clear that the standard published by the American Academy of Neurology (AAN), which had been used in the case at issue, was the “accepted medical standard.” An AAN summit later affirmed that the accepted medical standards for determination of death by neurologic cause are the 2010 AAN standard for determination of brain death in adults and the 2011 Society of Critical Care Medicine (SCCM), American Academy of Pediatrics (AAP), and Child Neurology Society (CNS) standard for determination of brain death in children. The Nevada legislature amended the state UDDA to identify these standards as the accepted standards. A revised UDDA also should identify these standards and grant an administrative agency (i.e., the board of medicine) the power to review and update the accepted medical standards as needed, according to the editorial.
To the extent that hospitals are not following the AAN or SCCM/AAP/CNS standards for determining death by neurologic cause, “enshrining” these standards in a revised UDDA “should increase uniformity and consistency” in hospitals’ policies on brain death, Dr. Pope said.
The question of hormonal function
Lawsuits in California and Nevada raised the question of whether the pituitary gland and hypothalamus are parts of the brain. If so, then the accepted medical standards for death by neurologic cause are not consistent with the statutory requirements for the determination of death, since the former do not test for cessation of hormonal function.
The current edition of the adult standards for determining death by neurologic cause were published in 2010. “Whenever we measure brain death, we’re not measuring the cessation of all functions of the entire brain,” Dr. Pope said. “That’s not a new thing; that’s been the case for a long time.”
To address the discrepancy between medical practice and the legal statute, Dr. Lewis and colleagues proposed that the UDDA’s reference to “irreversible cessation of functions of the entire brain” be followed by the following clause: “including the brainstem, leading to unresponsive coma with loss of capacity for consciousness, brainstem areflexia, and the inability to breathe spontaneously.” An alternative revision would be to add the briefer phrase “... with the exception of hormonal function.”
Authors say consent is not required for testing
Other complications have arisen from the UDDA’s failure to specify whether consent is required for a determination of death by neurologic cause. Court rulings on this question have not been consistent. Dr. Lewis and colleagues propose adding the following text to the UDDA: “Reasonable efforts should be made to notify a patient’s legally authorized decision-maker before performing a determination of death by neurologic criteria, but consent is not required to initiate such an evaluation.”
The proposed revisions to the UDDA “might give [clinicians] more confidence to proceed with brain death testing, because it would clarify that they don’t need the parents’ [or the patient’s legally authorized decision-maker] consent to do the tests,” said Dr. Pope. “If anything, they might even have a duty to do the tests.”
The final problem with the UDDA that Dr. Lewis and colleagues cited is that it does not provide clear guidance about how to respond to religious objections to discontinuation of organ support after a determination of death by neurologic cause. “Because the issue is rather complicated, we have not advocated for a singular position related to this [question] in our revised UDDA,” Dr. Lewis said. “Rather, we recommended the need for a multidisciplinary group to come together to determine what is the best approach. In an ideal world, this [approach] would be universal throughout the country.”
Although a revised UDDA would provide greater clarity to physicians and promote uniformity of practice, it would not resolve ongoing theological and philosophical debates about whether brain death is biological death, Dr. Pope said. “The key thing is that it would give clinicians a green light or certainty and clarity that they may proceed to do the test in the first place. If the tests are positive and the patient really is dead, then they could proceed to organ procurement or to move to the morgue.”
Dr. Lewis is a member of various AAN committees and working groups but receives no compensation for her role. A coauthor received personal fees from the AAN that were unrelated to the editorial.
SOURCE: Lewis A et al. Ann Intern Med. 2019 Dec 24. doi: 10.7326/M19-2731.
FROM ANNALS OF INTERNAL MEDICINE
FDA targets flavored cartridge-based e-cigarettes, but says it is not a ‘ban’
but states it is not a “ban.”
On Jan. 2, the agency issued enforcement guidance alerting companies that manufacture, distribute, and sell unauthorized flavored cartridge-based e-cigarettes within the next 30 days will risk FDA enforcement action.
FDA has had the authority to require premarket authorization of all e-cigarettes and other electronic nicotine delivery systems (ENDS) since August 2016, but thus far has exercised enforcement discretion regarding the need for premarket authorization for these types of products.
“By prioritizing enforcement against the products that are most widely used by children, our action today seeks to strike the right public health balance by maintaining e-cigarettes as a potential off-ramp for adults using combustible tobacco while ensuring these products don’t provide an on-ramp to nicotine addiction for our youth,” Department of Health & Human Services Secretary Alex Azar said in a statement.
The action comes in the wake of more than 2,500 vaping-related injuries being reported, including more than 50 deaths associated with vaping reported by the Centers for Disease Control and Prevention (although many are related to the use of tetrahydrocannabinol [THC] within vaping products) and a continued rise in youth use of e-cigarettes noted in government surveys.
The agency noted in a Jan. 2 statement announcing the enforcement action that, to date, no ENDS products have received a premarket authorization, “meaning that all ENDS products currently on the market are considered illegally marketed and are subject to enforcement, at any time, in the FDA’s discretion.”
FDA said it is prioritizing enforcement in 30 days against:
- Any flavored, cartridge-based ENDS product, other than those with a tobacco or menthol flavoring.
- All other ENDS products for which manufacturers are failing to take adequate measures to prevent access by minors.
- Any ENDS product that is targeted to minors or is likely to promote use by minors.
In the last category, this might include labeling or advertising resembling “kid-friendly food and drinks such as juice boxes or kid-friendly cereal; products marketed directly to minors by promoting ease of concealing the product or disguising it as another product; and products marketed with characters designed to appeal to youth,” according to the FDA statement.
As of May 12, FDA also will prioritize enforcement against any ENDS product for which the manufacturer has not submitted a premarket application. The agency will continue to exercise enforcement discretion for up to 1 year on these products if an application has been submitted, pending the review of that application.
“By not prioritizing enforcement against other flavored ENDS products in the same way as flavored cartridge-based ENDS products, the FDA has attempted to balance the public health concerns related to youth use of ENDS products with consideration regarding addicted adult cigarette smokers who may try to use ENDS products to transition away from combustible tobacco products,” the agency stated, adding that cartridge-based ENDS products are most commonly used among youth.
The FDA statement noted that the enforcement priorities outlined in the guidance document were not a “ban” on flavored or cartridge-based ENDS, noting the agency “has already accepted and begun review of several premarket applications for flavored ENDS products through the pathway that Congress established in the Tobacco Control Act. ... If a company can demonstrate to the FDA that a specific product meets the applicable standard set forth by Congress, including considering how the marketing of the product may affect youth initiation and use, then the FDA could authorize that product for sale.”
“Coupled with the recently signed legislation increasing the minimum age of sale of tobacco to 21, we believe this policy balances the urgency with which we must address the public health threat of youth use of e-cigarette products with the potential role that e-cigarettes may play in helping adult smokers transition completely away from combustible tobacco to a potentially less risky form of nicotine delivery,” FDA Commissioner Stephen Hahn, MD, said in a statement. “While we expect that responsible members of industry will comply with premarket requirements, we’re ready to take action against any unauthorized e-cigarette products as outlined in our priorities. We’ll also closely monitor the use rates of all e-cigarette products and take additional steps to address youth use as necessary.”
The American Medical Association criticized the action as not going far enough, even though it was a step in the right direction.
“The AMA is disappointed that menthol flavors, one of the most popular, will still be allowed, and that flavored e-liquids will remain on the market, leaving young people with easy access to alternative flavored e-cigarette products,” AMA President Patrice A. Harris, MD, said in a statement. “If we are serious about tackling this epidemic and keeping these harmful products out of the hands of young people, a total ban on all flavored e-cigarettes, in all forms and at all locations, is prudent and urgently needed. We are pleased the administration committed today to closely monitoring the situation and trends in e-cigarette use among young people, and to taking further action if needed.”
but states it is not a “ban.”
On Jan. 2, the agency issued enforcement guidance alerting companies that manufacture, distribute, and sell unauthorized flavored cartridge-based e-cigarettes within the next 30 days will risk FDA enforcement action.
FDA has had the authority to require premarket authorization of all e-cigarettes and other electronic nicotine delivery systems (ENDS) since August 2016, but thus far has exercised enforcement discretion regarding the need for premarket authorization for these types of products.
“By prioritizing enforcement against the products that are most widely used by children, our action today seeks to strike the right public health balance by maintaining e-cigarettes as a potential off-ramp for adults using combustible tobacco while ensuring these products don’t provide an on-ramp to nicotine addiction for our youth,” Department of Health & Human Services Secretary Alex Azar said in a statement.
The action comes in the wake of more than 2,500 vaping-related injuries being reported, including more than 50 deaths associated with vaping reported by the Centers for Disease Control and Prevention (although many are related to the use of tetrahydrocannabinol [THC] within vaping products) and a continued rise in youth use of e-cigarettes noted in government surveys.
The agency noted in a Jan. 2 statement announcing the enforcement action that, to date, no ENDS products have received a premarket authorization, “meaning that all ENDS products currently on the market are considered illegally marketed and are subject to enforcement, at any time, in the FDA’s discretion.”
FDA said it is prioritizing enforcement in 30 days against:
- Any flavored, cartridge-based ENDS product, other than those with a tobacco or menthol flavoring.
- All other ENDS products for which manufacturers are failing to take adequate measures to prevent access by minors.
- Any ENDS product that is targeted to minors or is likely to promote use by minors.
In the last category, this might include labeling or advertising resembling “kid-friendly food and drinks such as juice boxes or kid-friendly cereal; products marketed directly to minors by promoting ease of concealing the product or disguising it as another product; and products marketed with characters designed to appeal to youth,” according to the FDA statement.
As of May 12, FDA also will prioritize enforcement against any ENDS product for which the manufacturer has not submitted a premarket application. The agency will continue to exercise enforcement discretion for up to 1 year on these products if an application has been submitted, pending the review of that application.
“By not prioritizing enforcement against other flavored ENDS products in the same way as flavored cartridge-based ENDS products, the FDA has attempted to balance the public health concerns related to youth use of ENDS products with consideration regarding addicted adult cigarette smokers who may try to use ENDS products to transition away from combustible tobacco products,” the agency stated, adding that cartridge-based ENDS products are most commonly used among youth.
The FDA statement noted that the enforcement priorities outlined in the guidance document were not a “ban” on flavored or cartridge-based ENDS, noting the agency “has already accepted and begun review of several premarket applications for flavored ENDS products through the pathway that Congress established in the Tobacco Control Act. ... If a company can demonstrate to the FDA that a specific product meets the applicable standard set forth by Congress, including considering how the marketing of the product may affect youth initiation and use, then the FDA could authorize that product for sale.”
“Coupled with the recently signed legislation increasing the minimum age of sale of tobacco to 21, we believe this policy balances the urgency with which we must address the public health threat of youth use of e-cigarette products with the potential role that e-cigarettes may play in helping adult smokers transition completely away from combustible tobacco to a potentially less risky form of nicotine delivery,” FDA Commissioner Stephen Hahn, MD, said in a statement. “While we expect that responsible members of industry will comply with premarket requirements, we’re ready to take action against any unauthorized e-cigarette products as outlined in our priorities. We’ll also closely monitor the use rates of all e-cigarette products and take additional steps to address youth use as necessary.”
The American Medical Association criticized the action as not going far enough, even though it was a step in the right direction.
“The AMA is disappointed that menthol flavors, one of the most popular, will still be allowed, and that flavored e-liquids will remain on the market, leaving young people with easy access to alternative flavored e-cigarette products,” AMA President Patrice A. Harris, MD, said in a statement. “If we are serious about tackling this epidemic and keeping these harmful products out of the hands of young people, a total ban on all flavored e-cigarettes, in all forms and at all locations, is prudent and urgently needed. We are pleased the administration committed today to closely monitoring the situation and trends in e-cigarette use among young people, and to taking further action if needed.”
but states it is not a “ban.”
On Jan. 2, the agency issued enforcement guidance alerting companies that manufacture, distribute, and sell unauthorized flavored cartridge-based e-cigarettes within the next 30 days will risk FDA enforcement action.
FDA has had the authority to require premarket authorization of all e-cigarettes and other electronic nicotine delivery systems (ENDS) since August 2016, but thus far has exercised enforcement discretion regarding the need for premarket authorization for these types of products.
“By prioritizing enforcement against the products that are most widely used by children, our action today seeks to strike the right public health balance by maintaining e-cigarettes as a potential off-ramp for adults using combustible tobacco while ensuring these products don’t provide an on-ramp to nicotine addiction for our youth,” Department of Health & Human Services Secretary Alex Azar said in a statement.
The action comes in the wake of more than 2,500 vaping-related injuries being reported, including more than 50 deaths associated with vaping reported by the Centers for Disease Control and Prevention (although many are related to the use of tetrahydrocannabinol [THC] within vaping products) and a continued rise in youth use of e-cigarettes noted in government surveys.
The agency noted in a Jan. 2 statement announcing the enforcement action that, to date, no ENDS products have received a premarket authorization, “meaning that all ENDS products currently on the market are considered illegally marketed and are subject to enforcement, at any time, in the FDA’s discretion.”
FDA said it is prioritizing enforcement in 30 days against:
- Any flavored, cartridge-based ENDS product, other than those with a tobacco or menthol flavoring.
- All other ENDS products for which manufacturers are failing to take adequate measures to prevent access by minors.
- Any ENDS product that is targeted to minors or is likely to promote use by minors.
In the last category, this might include labeling or advertising resembling “kid-friendly food and drinks such as juice boxes or kid-friendly cereal; products marketed directly to minors by promoting ease of concealing the product or disguising it as another product; and products marketed with characters designed to appeal to youth,” according to the FDA statement.
As of May 12, FDA also will prioritize enforcement against any ENDS product for which the manufacturer has not submitted a premarket application. The agency will continue to exercise enforcement discretion for up to 1 year on these products if an application has been submitted, pending the review of that application.
“By not prioritizing enforcement against other flavored ENDS products in the same way as flavored cartridge-based ENDS products, the FDA has attempted to balance the public health concerns related to youth use of ENDS products with consideration regarding addicted adult cigarette smokers who may try to use ENDS products to transition away from combustible tobacco products,” the agency stated, adding that cartridge-based ENDS products are most commonly used among youth.
The FDA statement noted that the enforcement priorities outlined in the guidance document were not a “ban” on flavored or cartridge-based ENDS, noting the agency “has already accepted and begun review of several premarket applications for flavored ENDS products through the pathway that Congress established in the Tobacco Control Act. ... If a company can demonstrate to the FDA that a specific product meets the applicable standard set forth by Congress, including considering how the marketing of the product may affect youth initiation and use, then the FDA could authorize that product for sale.”
“Coupled with the recently signed legislation increasing the minimum age of sale of tobacco to 21, we believe this policy balances the urgency with which we must address the public health threat of youth use of e-cigarette products with the potential role that e-cigarettes may play in helping adult smokers transition completely away from combustible tobacco to a potentially less risky form of nicotine delivery,” FDA Commissioner Stephen Hahn, MD, said in a statement. “While we expect that responsible members of industry will comply with premarket requirements, we’re ready to take action against any unauthorized e-cigarette products as outlined in our priorities. We’ll also closely monitor the use rates of all e-cigarette products and take additional steps to address youth use as necessary.”
The American Medical Association criticized the action as not going far enough, even though it was a step in the right direction.
“The AMA is disappointed that menthol flavors, one of the most popular, will still be allowed, and that flavored e-liquids will remain on the market, leaving young people with easy access to alternative flavored e-cigarette products,” AMA President Patrice A. Harris, MD, said in a statement. “If we are serious about tackling this epidemic and keeping these harmful products out of the hands of young people, a total ban on all flavored e-cigarettes, in all forms and at all locations, is prudent and urgently needed. We are pleased the administration committed today to closely monitoring the situation and trends in e-cigarette use among young people, and to taking further action if needed.”
Down syndrome arthritis: Distinct from JIA and missed in the clinic
ATLANTA – Pediatric Down syndrome arthritis is more aggressive and severe than juvenile idiopathic arthritis (JIA), but it’s underrecognized and undertreated, according to reports at the annual meeting of the American College of Rheumatology.
“The vast majority of parents don’t know their kids are at risk for arthritis,” and a lot of doctors don’t realize it, either. Meanwhile, children show up in the clinic a year or more into the process with irreversible joint damage, said pediatric rheumatologist Jordan Jones, DO, an assistant professor at the University of Missouri, Kansas City, and the lead investigator on a review of 36 children with Down syndrome (DS) in the national Childhood Arthritis and Rheumatology Research Alliance (CARRA) registry.
One solution is to add routine musculoskeletal exams to American Academy of Pediatrics DS guidelines, something Dr. Jones said he and his colleagues are hoping to do.
Part of the problem is that children with DS have a hard time articulating and localizing pain, and it’s easy to attribute functional issues to DS itself. Charlene Foley, MD, PhD, from the National Centre for Paediatric Rheumatology in Dublin, said she’s seen “loads of cases” in which parents were told that their children were acting up, probably because of the DS, when they didn’t want to walk down stairs anymore or hold their parent’s hand.
She was the lead investigator on an Irish program that screened 503 DS children, about one-third of the country’s pediatric DS population, for arthritis; 33 cases were identified, including 18 new ones. Most of the children had polyarticular, rheumatoid factor–negative arthritis, and all of them were antinuclear antibody negative.
A key take-home from the work is that DS arthritis preferentially attacks the hands and wrists and was present exclusively in the hands and wrists of about one-third of the Irish cohort. “So, if you only have a second to examine a child or you can’t get them to sit still, just go straight for the hands, and have a low threshold for imaging,” Dr. Foley said.
DS arthritis is often considered a subtype of JIA, but findings from the studies call that into question and suggest the need for novel therapeutic targets, the investigators said.
The Irish team found that 42% of their subjects (14 of 33) had joint erosions, far more than the 14% of JIA children (3 of 21) who served as controls, and Dr. Foley and colleagues didn’t think that was solely because of delayed diagnosis. Also, at about 20 cases per 1,000, they estimated that arthritis was far more prevalent in DS than was JIA in the general pediatrics population.
Disease onset was at a mean of 7.1 years in Dr. Jones’ CARRA registry review, and mean delay to diagnosis was 11.5 months. The 36 children presented with an average of four affected joints. Only 22% (8 of 36) had elevated inflammatory markers; just one-third were positive for antinuclear antibody, and 17% for human leukocyte antigen B27. It means that “these kids can present with normal labs, even with very aggressive disease. The threshold of concern for arthritis has to be very high when you evaluate these children,” Dr. Jones said.
Treatment was initiated with disease-modifying antirheumatic drugs (DMARDs) in two-thirds of the registry children, often with a concomitant biologic, most commonly etanercept. Over half had at least one switch during a mean follow-up of 4.5 years; methotrexate was a leading culprit, frequently discontinued because of nausea and other problems, and biologics were changed for lack of effect. Active joint counts and physician assessments improved, but there were no significant changes in limited joint counts and health assessments.
In short, “the current therapies for JIA appear to be poorly tolerated, more toxic, and less effective in patients with Down syndrome. These kids don’t respond the same. They have a very high disease burden despite being treated aggressively,” Dr. Jones said.
That finding adds additional weight to the idea that DS arthritis is a distinct disease entity, with unique therapeutic targets. “Down syndrome has a lot of immunologic issues associated with it; maybe that’s it. I think in the next few years, we will be able to show that this is a different disease,” Dr. Jones said.
There was a boost in that direction from benchwork, also led and presented by Dr. Foley, that found significant immunologic, histologic, and genetic differences between JIA and DS arthritis, including lower CD19- and CD20-positive B-cell counts in DS arthritis and higher interferon-gamma and tumor necrosis factor–alpha production, greater synovial lining hyperplasia, and different minor allele frequencies.
There was no industry funding for the studies, and the investigators didn’t have any industry disclosures.
SOURCES: Jones J et al. Arthritis Rheumatol. 2019;71(suppl 10), Abstract 2722; Foley C et al. Arthritis Rheumatol. 2019;71(suppl 10), Abstract 1817; and Foley C et al. Arthritis Rheumatol. 2019;71(suppl 10), Abstract 781
ATLANTA – Pediatric Down syndrome arthritis is more aggressive and severe than juvenile idiopathic arthritis (JIA), but it’s underrecognized and undertreated, according to reports at the annual meeting of the American College of Rheumatology.
“The vast majority of parents don’t know their kids are at risk for arthritis,” and a lot of doctors don’t realize it, either. Meanwhile, children show up in the clinic a year or more into the process with irreversible joint damage, said pediatric rheumatologist Jordan Jones, DO, an assistant professor at the University of Missouri, Kansas City, and the lead investigator on a review of 36 children with Down syndrome (DS) in the national Childhood Arthritis and Rheumatology Research Alliance (CARRA) registry.
One solution is to add routine musculoskeletal exams to American Academy of Pediatrics DS guidelines, something Dr. Jones said he and his colleagues are hoping to do.
Part of the problem is that children with DS have a hard time articulating and localizing pain, and it’s easy to attribute functional issues to DS itself. Charlene Foley, MD, PhD, from the National Centre for Paediatric Rheumatology in Dublin, said she’s seen “loads of cases” in which parents were told that their children were acting up, probably because of the DS, when they didn’t want to walk down stairs anymore or hold their parent’s hand.
She was the lead investigator on an Irish program that screened 503 DS children, about one-third of the country’s pediatric DS population, for arthritis; 33 cases were identified, including 18 new ones. Most of the children had polyarticular, rheumatoid factor–negative arthritis, and all of them were antinuclear antibody negative.
A key take-home from the work is that DS arthritis preferentially attacks the hands and wrists and was present exclusively in the hands and wrists of about one-third of the Irish cohort. “So, if you only have a second to examine a child or you can’t get them to sit still, just go straight for the hands, and have a low threshold for imaging,” Dr. Foley said.
DS arthritis is often considered a subtype of JIA, but findings from the studies call that into question and suggest the need for novel therapeutic targets, the investigators said.
The Irish team found that 42% of their subjects (14 of 33) had joint erosions, far more than the 14% of JIA children (3 of 21) who served as controls, and Dr. Foley and colleagues didn’t think that was solely because of delayed diagnosis. Also, at about 20 cases per 1,000, they estimated that arthritis was far more prevalent in DS than was JIA in the general pediatrics population.
Disease onset was at a mean of 7.1 years in Dr. Jones’ CARRA registry review, and mean delay to diagnosis was 11.5 months. The 36 children presented with an average of four affected joints. Only 22% (8 of 36) had elevated inflammatory markers; just one-third were positive for antinuclear antibody, and 17% for human leukocyte antigen B27. It means that “these kids can present with normal labs, even with very aggressive disease. The threshold of concern for arthritis has to be very high when you evaluate these children,” Dr. Jones said.
Treatment was initiated with disease-modifying antirheumatic drugs (DMARDs) in two-thirds of the registry children, often with a concomitant biologic, most commonly etanercept. Over half had at least one switch during a mean follow-up of 4.5 years; methotrexate was a leading culprit, frequently discontinued because of nausea and other problems, and biologics were changed for lack of effect. Active joint counts and physician assessments improved, but there were no significant changes in limited joint counts and health assessments.
In short, “the current therapies for JIA appear to be poorly tolerated, more toxic, and less effective in patients with Down syndrome. These kids don’t respond the same. They have a very high disease burden despite being treated aggressively,” Dr. Jones said.
That finding adds additional weight to the idea that DS arthritis is a distinct disease entity, with unique therapeutic targets. “Down syndrome has a lot of immunologic issues associated with it; maybe that’s it. I think in the next few years, we will be able to show that this is a different disease,” Dr. Jones said.
There was a boost in that direction from benchwork, also led and presented by Dr. Foley, that found significant immunologic, histologic, and genetic differences between JIA and DS arthritis, including lower CD19- and CD20-positive B-cell counts in DS arthritis and higher interferon-gamma and tumor necrosis factor–alpha production, greater synovial lining hyperplasia, and different minor allele frequencies.
There was no industry funding for the studies, and the investigators didn’t have any industry disclosures.
SOURCES: Jones J et al. Arthritis Rheumatol. 2019;71(suppl 10), Abstract 2722; Foley C et al. Arthritis Rheumatol. 2019;71(suppl 10), Abstract 1817; and Foley C et al. Arthritis Rheumatol. 2019;71(suppl 10), Abstract 781
ATLANTA – Pediatric Down syndrome arthritis is more aggressive and severe than juvenile idiopathic arthritis (JIA), but it’s underrecognized and undertreated, according to reports at the annual meeting of the American College of Rheumatology.
“The vast majority of parents don’t know their kids are at risk for arthritis,” and a lot of doctors don’t realize it, either. Meanwhile, children show up in the clinic a year or more into the process with irreversible joint damage, said pediatric rheumatologist Jordan Jones, DO, an assistant professor at the University of Missouri, Kansas City, and the lead investigator on a review of 36 children with Down syndrome (DS) in the national Childhood Arthritis and Rheumatology Research Alliance (CARRA) registry.
One solution is to add routine musculoskeletal exams to American Academy of Pediatrics DS guidelines, something Dr. Jones said he and his colleagues are hoping to do.
Part of the problem is that children with DS have a hard time articulating and localizing pain, and it’s easy to attribute functional issues to DS itself. Charlene Foley, MD, PhD, from the National Centre for Paediatric Rheumatology in Dublin, said she’s seen “loads of cases” in which parents were told that their children were acting up, probably because of the DS, when they didn’t want to walk down stairs anymore or hold their parent’s hand.
She was the lead investigator on an Irish program that screened 503 DS children, about one-third of the country’s pediatric DS population, for arthritis; 33 cases were identified, including 18 new ones. Most of the children had polyarticular, rheumatoid factor–negative arthritis, and all of them were antinuclear antibody negative.
A key take-home from the work is that DS arthritis preferentially attacks the hands and wrists and was present exclusively in the hands and wrists of about one-third of the Irish cohort. “So, if you only have a second to examine a child or you can’t get them to sit still, just go straight for the hands, and have a low threshold for imaging,” Dr. Foley said.
DS arthritis is often considered a subtype of JIA, but findings from the studies call that into question and suggest the need for novel therapeutic targets, the investigators said.
The Irish team found that 42% of their subjects (14 of 33) had joint erosions, far more than the 14% of JIA children (3 of 21) who served as controls, and Dr. Foley and colleagues didn’t think that was solely because of delayed diagnosis. Also, at about 20 cases per 1,000, they estimated that arthritis was far more prevalent in DS than was JIA in the general pediatrics population.
Disease onset was at a mean of 7.1 years in Dr. Jones’ CARRA registry review, and mean delay to diagnosis was 11.5 months. The 36 children presented with an average of four affected joints. Only 22% (8 of 36) had elevated inflammatory markers; just one-third were positive for antinuclear antibody, and 17% for human leukocyte antigen B27. It means that “these kids can present with normal labs, even with very aggressive disease. The threshold of concern for arthritis has to be very high when you evaluate these children,” Dr. Jones said.
Treatment was initiated with disease-modifying antirheumatic drugs (DMARDs) in two-thirds of the registry children, often with a concomitant biologic, most commonly etanercept. Over half had at least one switch during a mean follow-up of 4.5 years; methotrexate was a leading culprit, frequently discontinued because of nausea and other problems, and biologics were changed for lack of effect. Active joint counts and physician assessments improved, but there were no significant changes in limited joint counts and health assessments.
In short, “the current therapies for JIA appear to be poorly tolerated, more toxic, and less effective in patients with Down syndrome. These kids don’t respond the same. They have a very high disease burden despite being treated aggressively,” Dr. Jones said.
That finding adds additional weight to the idea that DS arthritis is a distinct disease entity, with unique therapeutic targets. “Down syndrome has a lot of immunologic issues associated with it; maybe that’s it. I think in the next few years, we will be able to show that this is a different disease,” Dr. Jones said.
There was a boost in that direction from benchwork, also led and presented by Dr. Foley, that found significant immunologic, histologic, and genetic differences between JIA and DS arthritis, including lower CD19- and CD20-positive B-cell counts in DS arthritis and higher interferon-gamma and tumor necrosis factor–alpha production, greater synovial lining hyperplasia, and different minor allele frequencies.
There was no industry funding for the studies, and the investigators didn’t have any industry disclosures.
SOURCES: Jones J et al. Arthritis Rheumatol. 2019;71(suppl 10), Abstract 2722; Foley C et al. Arthritis Rheumatol. 2019;71(suppl 10), Abstract 1817; and Foley C et al. Arthritis Rheumatol. 2019;71(suppl 10), Abstract 781
REPORTING FROM ACR 2019
John Bowlby and Heinz Kohut, meet Karl Friston
Attachment theory and object relations theory, meet neuroscience
The bonding process between individuals is essential to human life as we know it. The depth and strength of emotional bonds that we develop with other individuals are among the cardinal aspects of being human.
The strengths of the bonds that we form with others often are the most enduring aspects of our lives and can stretch back in time to include family members and friends who are no longer alive. The brain processes and neurochemicals involved in the bonding process are related to psychological processes using Bayesian theory. Abnormalities in attachment are described in terms of abnormal predictive models.
John Bowlby MD, and colleagues developed a psychological theory of early childhood attachment that shows the impact of different childhood experiences.1 Over many decades, they conducted painstaking observations, trials, and retrials that elucidated specific types of attachment that reflect the child’s internal representations of the parent.
Dr. Bowlby described the mental representations of attachment as “the internal working models of expectations” about the maternal-child relationship. This internal model guides the child’s behaviors, attitudes, and expectations, and is constantly being revised and expanded as the child matures in order to adapt to increasingly complex relationships. More current research has shown that adults who have experienced extreme early childhood adversity develop odd or deficient descriptions of primary attachment relationships, now refined into a low-coherence CC category.2 These children experience attachments that are characterized by feelings of emptiness, inconsistency, and fragmentation.
Object relations theory was created by Heinz Kohut, MD, to explain our internal models of others in psychoanalytic language.3 Dr. Kohut expands the concept of transference describing three new transferential relationships: mirroring, idealized, and twinship transferences. A mirroring transference describes the psychological mechanism whereby “the other” serves as a mirror that reflects back to the person a sense of self-worth and value. A mirroring transference uses the affirming and positive responses of others so that a person then can see positive traits within themselves. The idealizing transference refers to a person’s need for “another” who will make them feel calm and comfortable. The other is idealized as somebody who is calm and soothing when the person cannot provide that on their own. The twinship/alter ego transference occurs when a person feels a sense of likeness with “an other.” These advances in psychoanalytic theory advance our understanding of how we internalize aspects of other people and use these internalizations in our own development.
The neuroscience of attachment was revealed in the study of the children abandoned in Romanian orphanages before the 1989 revolution. These children were placed in orphanages that lacked adequate staff, and they were subjected to profound psychosocial neglect. In the Bucharest Early Intervention Project, the effects of neglect were seen in children aged less than 30-96 months, in EEG data.4 Abnormalities were found in two aberrantly connected brain networks: a hyperconnected parieto-occipital network and a hypoconnected network between left temporal and distributed bilateral regions. This study provides the first evidence of the adverse effects of early psychosocial neglect on the wiring of the developing brain.
Neurochemistry has suggested the impact of oxytocin on the promotion of attachment. Oxytocin has been called the “cuddle hormone,” as it is stimulated in mothers to promote bonding with their infant. Many studies have examined the introduction of intranasal oxytocin increases bonding and trust with others, but recent meta-analyses challenge those findings.5,6 Nevertheless, the process of bonding and attachment is thought to engage the mesocorticolimbic, nigrostriatal dopaminergic, and oxytocinergic systems. Tops and colleagues proposed that oxytocin facilitates a shift from ventral striatal “novelty processing” toward dorsal striatal “familiarity processing.”7 This shift to familiarity is thought to create secure internal working models. In addition, brain activity in specific regions, such as the right caudate, is correlated with romantic love.8 In summary, specific pathways and neurotransmitters underlie the emotional process of bonding and attachment.
However, it is Karl Friston, MD, who suggests a model of brain functioning that describes how we actually process our experiences of the world.9 Dr. Friston uses Bayesian modeling to describe how we interact and understand our world, describing the way we process information. Dr. Friston states that the process of inference that we use to discern our world is a process that uses Bayes’ theorem to update the probability for a specific hypothesis about our world. As more evidence or information becomes available, we update our internal models of the world. Predictive modeling is the term used in Bayesian terms to describe this process of continuous revision of our internal model of the world. Any new sensory input is compared to our current internal model, and if they do not match, our internal model of the world is updated and revised. Dr. Friston states: “As surprise is resolved, Bayesian model evidence is increased. This means that every living organism behaves as if it is a little statistician, analyzing its sensory data in exactly the same way that scientists evaluate the evidence for their hypotheses about how experimental data were caused. In this view, minimizing surprise is, literally, the search for evidence for one’s own existence.” This process of predictive modeling also can be applied to our internal models of other people, meaning that our internal model of another person is an iterative process that changes as the other person changes.
When our experience of the world and others fall into predictive patterns, we expect the “usual” responses from our world and from the people in it. This predictive processing makes it easier for us to understand our world, so that we do not have to continually analyze and reanalyze each event as a new experience. For example, a young child examines the waves as they crash on the shore. For a while, he will watch the waves but soon begins to recognize that there is a predictable pattern. With each ocean he visits, he will examine wave action and soon develop an internal model of what happens when the water reaches the shore. Similarly, when a young child has a secure and loving parent, he will expect security and love in his future relationships. On the other hand, the child who has been subjected to abuse and neglect has an internal working model of the other as nonreciprocal and perhaps irrelevant to their well-being. They will, therefore, have extreme difficulty in understanding the purpose or value of relationships. Their predictive model of the other reflects a lack of input in the case of neglect, or perverted input in the case of abuse. Their internal predictive model will require a great deal of therapeutic healthy inputs to be able to evolve to allow a healthy relationship with the other. This is the work of therapy.
When thinking about relationships, predictive processing makes clinical sense. In a committed partnership, each partner has a predictive model of their partner’s response to events/speech utterances/emotional displays. The prediction of the partner’s response is based on prior experience. This predictive model reduces the need to repeatedly reinterpret the partner’s actions. The partner is understood through an internal predictive model. When one partner changes their behavior, the other partner experiences the world/environment as disrupted or different. The couple, through an iterative process, can incorporate change and grow together. If the patient has an internalized model of a loving relationship, then they are more likely to find a partner who resonates with this internalized model. Using predictive modeling, we can understand how two people with their own internal models of each other interact. As one person approaches the other person, each internal model of the other person finds a “fit” with the behaviors of the other person. When a child with emotional deprivation approaches the other, the child perceives the other person in a way that fits with their prior experience of deprivation. It is an easy fit that requires little internal work, and the patient falls into a familiar relational pattern. This model of predictive processing explains why people repeatedly fall into similar familiar relationships: They recognize the relationship patterns. There is less predictive processing required, less emotional and cognitive work, and therefore less adjustment.
Psychotherapy helps patients by improving their understanding of the link between prior and current experience. Each piece of behavior is analyzed and compared with the patient’s internal model of the event. What neuroscience now provides is a deeper scientific understanding of this process.
In summary, the processes of attachment and bonding occur through oxytocin-mediated caudate–dorsal striatum pathways. Bayesian predictive modeling describes the processes by which our internal models of others are shaped and refined, and underscores the work of our psychotherapies. Neuroscience is beginning to delineate the “where” and “how” of attachment and bonding, thus advancing our understanding of the attachment process and giving us a new language to describe the work of psychotherapy.
References
1. Bowlby J. “A Secure Base: Parent-Child Attachment and Healthy Human Development.” New York: Basic Books, 1988.
2. Speranza AM et al. Attach Hum Dev. 2017 Dec;19(6):613-34.
3. Kohut H. “How Does Analysis Cure?” Chicago: University of Chicago Press, 1984.
4. Stamoulis C et al. J Neurophysiol. 2017 Oct 1;118(4):2275-88.
5. Leng G and Ludwig M.Biol Psychiatry. 2016 Feb 1;79(3):243-50.
6. Leppanen J et al. Neurosci Biobehav Rev. 2017 Jul;78:125-44.
7. Tops M et al. Pharmacol Biochem Behav. 2014 Apr;119:39-48.
8. Acevedo BP et al. Soc Cogn Affect Neurosci. 2012 Feb;7(2):145-59.
9. Friston K. Entropy (Basel). 2012 Nov;14(11):2100-21.
Attachment theory and object relations theory, meet neuroscience
Attachment theory and object relations theory, meet neuroscience
The bonding process between individuals is essential to human life as we know it. The depth and strength of emotional bonds that we develop with other individuals are among the cardinal aspects of being human.
The strengths of the bonds that we form with others often are the most enduring aspects of our lives and can stretch back in time to include family members and friends who are no longer alive. The brain processes and neurochemicals involved in the bonding process are related to psychological processes using Bayesian theory. Abnormalities in attachment are described in terms of abnormal predictive models.
John Bowlby MD, and colleagues developed a psychological theory of early childhood attachment that shows the impact of different childhood experiences.1 Over many decades, they conducted painstaking observations, trials, and retrials that elucidated specific types of attachment that reflect the child’s internal representations of the parent.
Dr. Bowlby described the mental representations of attachment as “the internal working models of expectations” about the maternal-child relationship. This internal model guides the child’s behaviors, attitudes, and expectations, and is constantly being revised and expanded as the child matures in order to adapt to increasingly complex relationships. More current research has shown that adults who have experienced extreme early childhood adversity develop odd or deficient descriptions of primary attachment relationships, now refined into a low-coherence CC category.2 These children experience attachments that are characterized by feelings of emptiness, inconsistency, and fragmentation.
Object relations theory was created by Heinz Kohut, MD, to explain our internal models of others in psychoanalytic language.3 Dr. Kohut expands the concept of transference describing three new transferential relationships: mirroring, idealized, and twinship transferences. A mirroring transference describes the psychological mechanism whereby “the other” serves as a mirror that reflects back to the person a sense of self-worth and value. A mirroring transference uses the affirming and positive responses of others so that a person then can see positive traits within themselves. The idealizing transference refers to a person’s need for “another” who will make them feel calm and comfortable. The other is idealized as somebody who is calm and soothing when the person cannot provide that on their own. The twinship/alter ego transference occurs when a person feels a sense of likeness with “an other.” These advances in psychoanalytic theory advance our understanding of how we internalize aspects of other people and use these internalizations in our own development.
The neuroscience of attachment was revealed in the study of the children abandoned in Romanian orphanages before the 1989 revolution. These children were placed in orphanages that lacked adequate staff, and they were subjected to profound psychosocial neglect. In the Bucharest Early Intervention Project, the effects of neglect were seen in children aged less than 30-96 months, in EEG data.4 Abnormalities were found in two aberrantly connected brain networks: a hyperconnected parieto-occipital network and a hypoconnected network between left temporal and distributed bilateral regions. This study provides the first evidence of the adverse effects of early psychosocial neglect on the wiring of the developing brain.
Neurochemistry has suggested the impact of oxytocin on the promotion of attachment. Oxytocin has been called the “cuddle hormone,” as it is stimulated in mothers to promote bonding with their infant. Many studies have examined the introduction of intranasal oxytocin increases bonding and trust with others, but recent meta-analyses challenge those findings.5,6 Nevertheless, the process of bonding and attachment is thought to engage the mesocorticolimbic, nigrostriatal dopaminergic, and oxytocinergic systems. Tops and colleagues proposed that oxytocin facilitates a shift from ventral striatal “novelty processing” toward dorsal striatal “familiarity processing.”7 This shift to familiarity is thought to create secure internal working models. In addition, brain activity in specific regions, such as the right caudate, is correlated with romantic love.8 In summary, specific pathways and neurotransmitters underlie the emotional process of bonding and attachment.
However, it is Karl Friston, MD, who suggests a model of brain functioning that describes how we actually process our experiences of the world.9 Dr. Friston uses Bayesian modeling to describe how we interact and understand our world, describing the way we process information. Dr. Friston states that the process of inference that we use to discern our world is a process that uses Bayes’ theorem to update the probability for a specific hypothesis about our world. As more evidence or information becomes available, we update our internal models of the world. Predictive modeling is the term used in Bayesian terms to describe this process of continuous revision of our internal model of the world. Any new sensory input is compared to our current internal model, and if they do not match, our internal model of the world is updated and revised. Dr. Friston states: “As surprise is resolved, Bayesian model evidence is increased. This means that every living organism behaves as if it is a little statistician, analyzing its sensory data in exactly the same way that scientists evaluate the evidence for their hypotheses about how experimental data were caused. In this view, minimizing surprise is, literally, the search for evidence for one’s own existence.” This process of predictive modeling also can be applied to our internal models of other people, meaning that our internal model of another person is an iterative process that changes as the other person changes.
When our experience of the world and others fall into predictive patterns, we expect the “usual” responses from our world and from the people in it. This predictive processing makes it easier for us to understand our world, so that we do not have to continually analyze and reanalyze each event as a new experience. For example, a young child examines the waves as they crash on the shore. For a while, he will watch the waves but soon begins to recognize that there is a predictable pattern. With each ocean he visits, he will examine wave action and soon develop an internal model of what happens when the water reaches the shore. Similarly, when a young child has a secure and loving parent, he will expect security and love in his future relationships. On the other hand, the child who has been subjected to abuse and neglect has an internal working model of the other as nonreciprocal and perhaps irrelevant to their well-being. They will, therefore, have extreme difficulty in understanding the purpose or value of relationships. Their predictive model of the other reflects a lack of input in the case of neglect, or perverted input in the case of abuse. Their internal predictive model will require a great deal of therapeutic healthy inputs to be able to evolve to allow a healthy relationship with the other. This is the work of therapy.
When thinking about relationships, predictive processing makes clinical sense. In a committed partnership, each partner has a predictive model of their partner’s response to events/speech utterances/emotional displays. The prediction of the partner’s response is based on prior experience. This predictive model reduces the need to repeatedly reinterpret the partner’s actions. The partner is understood through an internal predictive model. When one partner changes their behavior, the other partner experiences the world/environment as disrupted or different. The couple, through an iterative process, can incorporate change and grow together. If the patient has an internalized model of a loving relationship, then they are more likely to find a partner who resonates with this internalized model. Using predictive modeling, we can understand how two people with their own internal models of each other interact. As one person approaches the other person, each internal model of the other person finds a “fit” with the behaviors of the other person. When a child with emotional deprivation approaches the other, the child perceives the other person in a way that fits with their prior experience of deprivation. It is an easy fit that requires little internal work, and the patient falls into a familiar relational pattern. This model of predictive processing explains why people repeatedly fall into similar familiar relationships: They recognize the relationship patterns. There is less predictive processing required, less emotional and cognitive work, and therefore less adjustment.
Psychotherapy helps patients by improving their understanding of the link between prior and current experience. Each piece of behavior is analyzed and compared with the patient’s internal model of the event. What neuroscience now provides is a deeper scientific understanding of this process.
In summary, the processes of attachment and bonding occur through oxytocin-mediated caudate–dorsal striatum pathways. Bayesian predictive modeling describes the processes by which our internal models of others are shaped and refined, and underscores the work of our psychotherapies. Neuroscience is beginning to delineate the “where” and “how” of attachment and bonding, thus advancing our understanding of the attachment process and giving us a new language to describe the work of psychotherapy.
References
1. Bowlby J. “A Secure Base: Parent-Child Attachment and Healthy Human Development.” New York: Basic Books, 1988.
2. Speranza AM et al. Attach Hum Dev. 2017 Dec;19(6):613-34.
3. Kohut H. “How Does Analysis Cure?” Chicago: University of Chicago Press, 1984.
4. Stamoulis C et al. J Neurophysiol. 2017 Oct 1;118(4):2275-88.
5. Leng G and Ludwig M.Biol Psychiatry. 2016 Feb 1;79(3):243-50.
6. Leppanen J et al. Neurosci Biobehav Rev. 2017 Jul;78:125-44.
7. Tops M et al. Pharmacol Biochem Behav. 2014 Apr;119:39-48.
8. Acevedo BP et al. Soc Cogn Affect Neurosci. 2012 Feb;7(2):145-59.
9. Friston K. Entropy (Basel). 2012 Nov;14(11):2100-21.
The bonding process between individuals is essential to human life as we know it. The depth and strength of emotional bonds that we develop with other individuals are among the cardinal aspects of being human.
The strengths of the bonds that we form with others often are the most enduring aspects of our lives and can stretch back in time to include family members and friends who are no longer alive. The brain processes and neurochemicals involved in the bonding process are related to psychological processes using Bayesian theory. Abnormalities in attachment are described in terms of abnormal predictive models.
John Bowlby MD, and colleagues developed a psychological theory of early childhood attachment that shows the impact of different childhood experiences.1 Over many decades, they conducted painstaking observations, trials, and retrials that elucidated specific types of attachment that reflect the child’s internal representations of the parent.
Dr. Bowlby described the mental representations of attachment as “the internal working models of expectations” about the maternal-child relationship. This internal model guides the child’s behaviors, attitudes, and expectations, and is constantly being revised and expanded as the child matures in order to adapt to increasingly complex relationships. More current research has shown that adults who have experienced extreme early childhood adversity develop odd or deficient descriptions of primary attachment relationships, now refined into a low-coherence CC category.2 These children experience attachments that are characterized by feelings of emptiness, inconsistency, and fragmentation.
Object relations theory was created by Heinz Kohut, MD, to explain our internal models of others in psychoanalytic language.3 Dr. Kohut expands the concept of transference describing three new transferential relationships: mirroring, idealized, and twinship transferences. A mirroring transference describes the psychological mechanism whereby “the other” serves as a mirror that reflects back to the person a sense of self-worth and value. A mirroring transference uses the affirming and positive responses of others so that a person then can see positive traits within themselves. The idealizing transference refers to a person’s need for “another” who will make them feel calm and comfortable. The other is idealized as somebody who is calm and soothing when the person cannot provide that on their own. The twinship/alter ego transference occurs when a person feels a sense of likeness with “an other.” These advances in psychoanalytic theory advance our understanding of how we internalize aspects of other people and use these internalizations in our own development.
The neuroscience of attachment was revealed in the study of the children abandoned in Romanian orphanages before the 1989 revolution. These children were placed in orphanages that lacked adequate staff, and they were subjected to profound psychosocial neglect. In the Bucharest Early Intervention Project, the effects of neglect were seen in children aged less than 30-96 months, in EEG data.4 Abnormalities were found in two aberrantly connected brain networks: a hyperconnected parieto-occipital network and a hypoconnected network between left temporal and distributed bilateral regions. This study provides the first evidence of the adverse effects of early psychosocial neglect on the wiring of the developing brain.
Neurochemistry has suggested the impact of oxytocin on the promotion of attachment. Oxytocin has been called the “cuddle hormone,” as it is stimulated in mothers to promote bonding with their infant. Many studies have examined the introduction of intranasal oxytocin increases bonding and trust with others, but recent meta-analyses challenge those findings.5,6 Nevertheless, the process of bonding and attachment is thought to engage the mesocorticolimbic, nigrostriatal dopaminergic, and oxytocinergic systems. Tops and colleagues proposed that oxytocin facilitates a shift from ventral striatal “novelty processing” toward dorsal striatal “familiarity processing.”7 This shift to familiarity is thought to create secure internal working models. In addition, brain activity in specific regions, such as the right caudate, is correlated with romantic love.8 In summary, specific pathways and neurotransmitters underlie the emotional process of bonding and attachment.
However, it is Karl Friston, MD, who suggests a model of brain functioning that describes how we actually process our experiences of the world.9 Dr. Friston uses Bayesian modeling to describe how we interact and understand our world, describing the way we process information. Dr. Friston states that the process of inference that we use to discern our world is a process that uses Bayes’ theorem to update the probability for a specific hypothesis about our world. As more evidence or information becomes available, we update our internal models of the world. Predictive modeling is the term used in Bayesian terms to describe this process of continuous revision of our internal model of the world. Any new sensory input is compared to our current internal model, and if they do not match, our internal model of the world is updated and revised. Dr. Friston states: “As surprise is resolved, Bayesian model evidence is increased. This means that every living organism behaves as if it is a little statistician, analyzing its sensory data in exactly the same way that scientists evaluate the evidence for their hypotheses about how experimental data were caused. In this view, minimizing surprise is, literally, the search for evidence for one’s own existence.” This process of predictive modeling also can be applied to our internal models of other people, meaning that our internal model of another person is an iterative process that changes as the other person changes.
When our experience of the world and others fall into predictive patterns, we expect the “usual” responses from our world and from the people in it. This predictive processing makes it easier for us to understand our world, so that we do not have to continually analyze and reanalyze each event as a new experience. For example, a young child examines the waves as they crash on the shore. For a while, he will watch the waves but soon begins to recognize that there is a predictable pattern. With each ocean he visits, he will examine wave action and soon develop an internal model of what happens when the water reaches the shore. Similarly, when a young child has a secure and loving parent, he will expect security and love in his future relationships. On the other hand, the child who has been subjected to abuse and neglect has an internal working model of the other as nonreciprocal and perhaps irrelevant to their well-being. They will, therefore, have extreme difficulty in understanding the purpose or value of relationships. Their predictive model of the other reflects a lack of input in the case of neglect, or perverted input in the case of abuse. Their internal predictive model will require a great deal of therapeutic healthy inputs to be able to evolve to allow a healthy relationship with the other. This is the work of therapy.
When thinking about relationships, predictive processing makes clinical sense. In a committed partnership, each partner has a predictive model of their partner’s response to events/speech utterances/emotional displays. The prediction of the partner’s response is based on prior experience. This predictive model reduces the need to repeatedly reinterpret the partner’s actions. The partner is understood through an internal predictive model. When one partner changes their behavior, the other partner experiences the world/environment as disrupted or different. The couple, through an iterative process, can incorporate change and grow together. If the patient has an internalized model of a loving relationship, then they are more likely to find a partner who resonates with this internalized model. Using predictive modeling, we can understand how two people with their own internal models of each other interact. As one person approaches the other person, each internal model of the other person finds a “fit” with the behaviors of the other person. When a child with emotional deprivation approaches the other, the child perceives the other person in a way that fits with their prior experience of deprivation. It is an easy fit that requires little internal work, and the patient falls into a familiar relational pattern. This model of predictive processing explains why people repeatedly fall into similar familiar relationships: They recognize the relationship patterns. There is less predictive processing required, less emotional and cognitive work, and therefore less adjustment.
Psychotherapy helps patients by improving their understanding of the link between prior and current experience. Each piece of behavior is analyzed and compared with the patient’s internal model of the event. What neuroscience now provides is a deeper scientific understanding of this process.
In summary, the processes of attachment and bonding occur through oxytocin-mediated caudate–dorsal striatum pathways. Bayesian predictive modeling describes the processes by which our internal models of others are shaped and refined, and underscores the work of our psychotherapies. Neuroscience is beginning to delineate the “where” and “how” of attachment and bonding, thus advancing our understanding of the attachment process and giving us a new language to describe the work of psychotherapy.
References
1. Bowlby J. “A Secure Base: Parent-Child Attachment and Healthy Human Development.” New York: Basic Books, 1988.
2. Speranza AM et al. Attach Hum Dev. 2017 Dec;19(6):613-34.
3. Kohut H. “How Does Analysis Cure?” Chicago: University of Chicago Press, 1984.
4. Stamoulis C et al. J Neurophysiol. 2017 Oct 1;118(4):2275-88.
5. Leng G and Ludwig M.Biol Psychiatry. 2016 Feb 1;79(3):243-50.
6. Leppanen J et al. Neurosci Biobehav Rev. 2017 Jul;78:125-44.
7. Tops M et al. Pharmacol Biochem Behav. 2014 Apr;119:39-48.
8. Acevedo BP et al. Soc Cogn Affect Neurosci. 2012 Feb;7(2):145-59.
9. Friston K. Entropy (Basel). 2012 Nov;14(11):2100-21.
Early increase in flu activity shows no signs of slowing
An important measure of U.S. flu activity for the 2019-2020 season has already surpassed last season’s high, and more than half the states are experiencing high levels of activity, according to the Centers for Disease Control and Prevention.
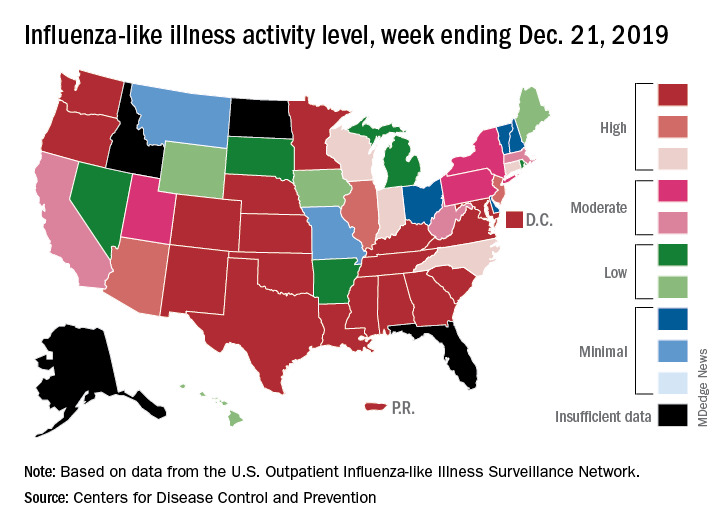
reported Dec. 27.
The last time the outpatient visit rate was higher than that was in February of the 2017-2018 season, when it peaked at 7.5%. The peak month of flu activity occurs most often – about once every 3 years – in February, and the odds of a December peak are about one in five, the CDC has said.
Outpatient illness activity also increased at the state level during the week ending Dec. 21. There were 20 jurisdictions – 18 states, the District of Columbia, and Puerto Rico – at level 10 on the CDC’s 1-10 scale of activity, compared with 13 the previous week, and the number of jurisdictions in the “high” range (levels 8-10) jumped from 21 to 28, the CDC data show.
The influenza division estimated that there have been 4.6 million flu illnesses so far this season, nearly a million more than the total after last week, along with 39,000 hospitalizations. The overall hospitalization rate for the season is up to 6.6 per 100,000 population, which is about average at this point. The proportion of deaths attributed to pneumonia and influenza increased to 5.7%, which is below the epidemic threshold, the CDC said.
Three pediatric deaths related to influenza-like illness were reported during the week ending Dec. 21, two of which occurred in an earlier week. For the 2019-2020 season so far, a total of 22 pediatric deaths have been reported to the CDC.
An important measure of U.S. flu activity for the 2019-2020 season has already surpassed last season’s high, and more than half the states are experiencing high levels of activity, according to the Centers for Disease Control and Prevention.
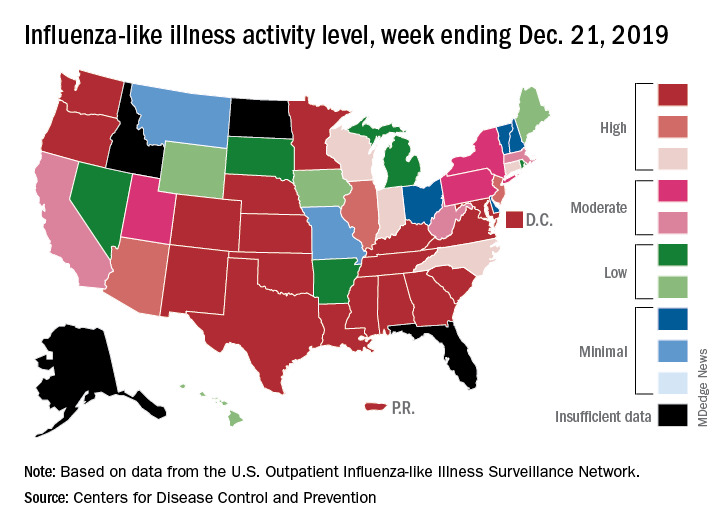
reported Dec. 27.
The last time the outpatient visit rate was higher than that was in February of the 2017-2018 season, when it peaked at 7.5%. The peak month of flu activity occurs most often – about once every 3 years – in February, and the odds of a December peak are about one in five, the CDC has said.
Outpatient illness activity also increased at the state level during the week ending Dec. 21. There were 20 jurisdictions – 18 states, the District of Columbia, and Puerto Rico – at level 10 on the CDC’s 1-10 scale of activity, compared with 13 the previous week, and the number of jurisdictions in the “high” range (levels 8-10) jumped from 21 to 28, the CDC data show.
The influenza division estimated that there have been 4.6 million flu illnesses so far this season, nearly a million more than the total after last week, along with 39,000 hospitalizations. The overall hospitalization rate for the season is up to 6.6 per 100,000 population, which is about average at this point. The proportion of deaths attributed to pneumonia and influenza increased to 5.7%, which is below the epidemic threshold, the CDC said.
Three pediatric deaths related to influenza-like illness were reported during the week ending Dec. 21, two of which occurred in an earlier week. For the 2019-2020 season so far, a total of 22 pediatric deaths have been reported to the CDC.
An important measure of U.S. flu activity for the 2019-2020 season has already surpassed last season’s high, and more than half the states are experiencing high levels of activity, according to the Centers for Disease Control and Prevention.
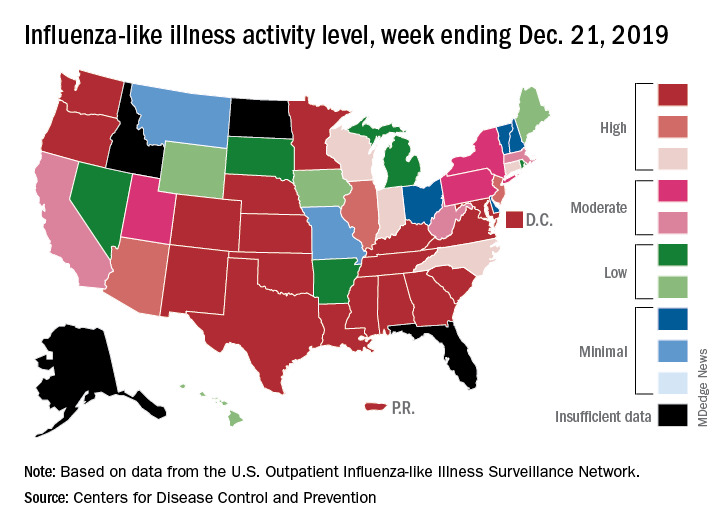
reported Dec. 27.
The last time the outpatient visit rate was higher than that was in February of the 2017-2018 season, when it peaked at 7.5%. The peak month of flu activity occurs most often – about once every 3 years – in February, and the odds of a December peak are about one in five, the CDC has said.
Outpatient illness activity also increased at the state level during the week ending Dec. 21. There were 20 jurisdictions – 18 states, the District of Columbia, and Puerto Rico – at level 10 on the CDC’s 1-10 scale of activity, compared with 13 the previous week, and the number of jurisdictions in the “high” range (levels 8-10) jumped from 21 to 28, the CDC data show.
The influenza division estimated that there have been 4.6 million flu illnesses so far this season, nearly a million more than the total after last week, along with 39,000 hospitalizations. The overall hospitalization rate for the season is up to 6.6 per 100,000 population, which is about average at this point. The proportion of deaths attributed to pneumonia and influenza increased to 5.7%, which is below the epidemic threshold, the CDC said.
Three pediatric deaths related to influenza-like illness were reported during the week ending Dec. 21, two of which occurred in an earlier week. For the 2019-2020 season so far, a total of 22 pediatric deaths have been reported to the CDC.
The measles comeback of 2019
Measles made a comeback in 2019.
The Centers for Disease Control and Prevention reported that, as of Dec. 5, 2019, 1,276 individual cases of measles of measles were confirmed in 31 states, the largest number since 1992. This number is a major uptick in cases, compared with previous years since 2000 when the CDC declared measles eliminated from the United States. No deaths have been reported for 2019.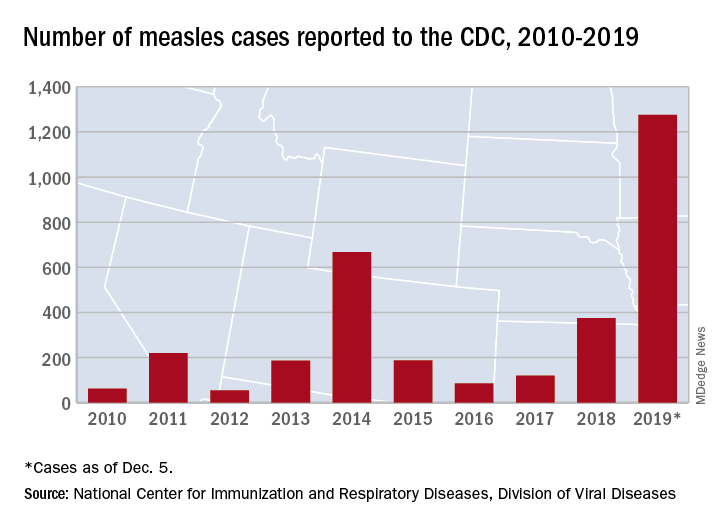
Three-quarters of these cases in 2019 were linked to recent outbreaks in New York and occurred in primarily in underimmunized, close-knit communities and in patients with links to international travel. A total of 124 of the people who got measles this year were hospitalized, and 61 reported having complications, including pneumonia and encephalitis. The overall median patient age was 6 years (31% aged 1-4 years, 27% aged 5-17 years, and 29% aged at least 18 years).
The good news is that most of these cases occurred in unvaccinated patients. The national vaccination rate for the almost 4 million kindergartners reported as enrolled in 2018-2019 was 94.7% for two doses of the MMR vaccine, falling just short of the CDC recommended 95% vaccination rate threshold. The CDC reported an approximate 2.5% rate of vaccination exemptions among school-age children.
The bad news is that, despite the high rate of MMR vaccination rates among U.S. children, there are gaps in measles protection in the U.S. population because of factors leaving patients immunocompromised and antivaccination sentiment that has led some parents to defer or refuse the MMR.
In addition, adults who were vaccinated prior to 1968 with either inactivated measles vaccine or measles vaccine of unknown type may have limited immunity. The inactivated measles vaccine, which was available in 1963-1967, did not achieve effective measles protection.
A global measles surge
While antivaccination sentiment contributed to the 2019 measles cases, a more significant factor may be the global surge of measles. More than 140,000 people worldwide died from measles in 2018, according to the World Health Organization and the CDC.
“[Recent data on measles] indicates that during the first 6 months of the year there have been more measles cases reported worldwide than in any year since 2006. From Jan. 1 to July 31, 2019, 182 countries reported 364,808 measles cases to the WHO. This surpasses the 129,239 reported during the same time period in 2018. WHO regions with the biggest increases in cases include the African region (900%), the Western Pacific region (230%), and the European region (150%),” according to a CDC report.
Studies on hospitalization and complications linked to measles in the United States are scarce, but two outbreaks in Minnesota (2011 and 2017) provided some data on what to expect if the measles surge continues into 2020. The investigators found that poor feeding was a primary reason for admission (97%); additional complications included otitis media (42%), pneumonia (30%), and tracheitis (6%). Three-quarters received antibiotics, 30% required oxygen, and 21% received vitamin A. Median length of stay was 3.7 days (range, 1.1-26.2 days) (Pediatr Infect Dis J. 2019 Jun;38[6]:547-52. doi: 10.1097/INF.0000000000002221).
‘Immunological amnesia’
Infection with the measles virus appears to reduce immunity to other pathogens, according to a paper published in Science (2019 Nov 1;366[6465]599-606).
The hypothesis that the measles virus could cause “immunological amnesia” by impairing immune memory is supported by early research showing children with measles had negative cutaneous tuberculin reactions after having previously tested positive.
“Subsequent studies have shown decreased interferon signaling, skewed cytokine responses, lymphopenia, and suppression of lymphocyte proliferation shortly after infection,” wrote Michael Mina, MD, from Brigham and Women’s Hospital in Boston, and coauthors.
“Given the variation in the degree of immune repertoire modulation we observed, we anticipate that future risk of morbidity and mortality after measles would not be homogeneous but would be skewed toward individuals with the most severe elimination of immunological memory,” they wrote. “These findings underscore the crucial need for continued widespread vaccination.”
In this study, researchers compared the levels of around 400 pathogen-specific antibodies in blood samples from 77 unvaccinated children, taken before and 2 months after natural measles infection, with 5 unvaccinated children who did not contract measles. A total of 34 children experienced mild measles, and 43 had severe measles.
They found that the samples taken after measles infection showed “substantial” reductions in the number of pathogen epitopes, compared with the samples from children who did not get infected with measles.
This amounted to approximately a 20% mean reduction in overall diversity or size of the antibody repertoire. However, in children who experienced severe measles, there was a median loss of 40% (range, 11%-62%) of antibody repertoire, compared with a median of 33% (range, 12%-73%) range in children who experienced mild infection. Meanwhile, the control subjects retained approximately 90% of their antibody repertoire over a similar or longer time period. Some children lost up to 70% of antibodies for specific pathogens.
Maternal-acquired immunity fades
In another study of measles immunity, maternal antibodies were found to be insufficient to provide immunity to infants after 6 months.
The study of 196 infants showed that maternal measles antibodies had dropped below the protective threshold by 3 months of age – well before the recommended age of 12-15 months for the first dose of MMR vaccine.
The odds of inadequate protection doubled for each additional month of age, Michelle Science, MD, of the University of Toronto and associates reported in Pediatrics (2019 Dec 1. doi 10.1542/peds.2019-0630).
“The widening gap between loss of maternal antibodies and measles vaccination described in our study leaves infants vulnerable to measles for much of their infancy and highlights the need for further research to support public health policy,” Dr. Science and colleagues wrote.
The researchers randomly selected 25 samples for each of eight different age groups: up to 30 days old; 1 month (31-60 days), 2 months (61-89 days), 3 months (90-119 days), 4 months, 5 months, 6-9 months, and 9-11 months.
Just over half the babies (56%) were male, and 35% had an underlying condition, but none had conditions that might affect antibody levels. The conditions were primarily a developmental delay or otherwise affecting the central nervous system, liver, or gastrointestinal function. Mean maternal age was 32 years.
To ensure high test sensitivity, the researchers used the plaque-reduction neutralization test to test for measles-neutralizing antibodies instead of using enzyme-linked immunosorbent assay, because “ELISA sensitivity decreases as antibody titers decrease,” Dr. Science and colleagues wrote. They used a neutralization titer of less than 192 mIU/mL as the threshold for protection against measles.
When the researchers calculated the predicted standardized mean antibody titer for infants with a mother aged 32 years, they determined their mean to be 541 mIU/mL at 1 month, 142 mIU/mL at 3 months (below the measles threshold of susceptibility of 192 mIU/mL), and 64 mIU/mL at 6 months. None of the infants had measles antibodies above the protective threshold at 6 months old, the authors noted.
Children’s odds of susceptibility to measles doubled for each additional month of age, after adjustment for infant sex and maternal age (odds ratio, 2.13). Children’s likelihood of susceptibility to measles modestly increased as maternal age increased in 5-year increments from 25 to 40 years.
Children with an underlying conditions had greater susceptibility to measles (83%), compared with those without a comorbidity (68%, P = .03). No difference in susceptibility existed between males and females or based on gestational age at birth (ranging from 37 to 41 weeks).
The Advisory Committee on Immunization Practices permits measles vaccination “as early as 6 months for infants who plan to travel internationally, infants with ongoing risk for exposure during measles outbreaks and as postexposure prophylaxis,” Huong Q. McLean, PhD, of Marshfield (Wisc.) Clinic Research Institute, and Walter A. Orenstein, MD, of Emory University, Atlanta, noted in an editorial.
The research was funded by the Public Health Ontario Project Initiation Fund. The authors had no relevant financial disclosures.
Bianca Nogrady and Tara Haelle contributed to this story.
Measles made a comeback in 2019.
The Centers for Disease Control and Prevention reported that, as of Dec. 5, 2019, 1,276 individual cases of measles of measles were confirmed in 31 states, the largest number since 1992. This number is a major uptick in cases, compared with previous years since 2000 when the CDC declared measles eliminated from the United States. No deaths have been reported for 2019.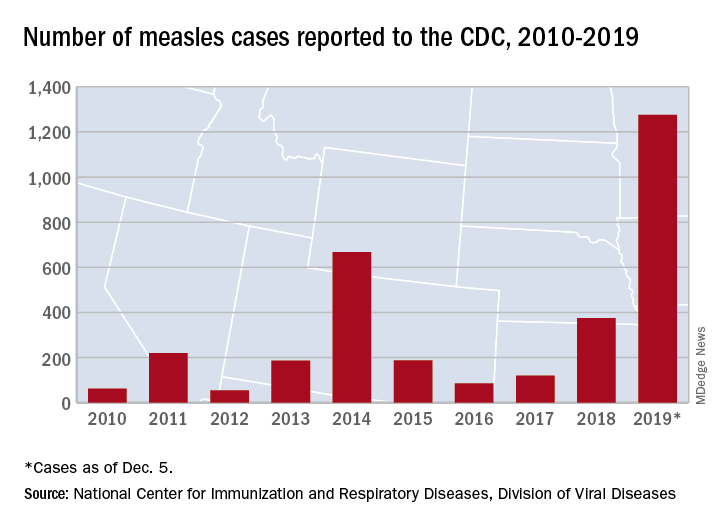
Three-quarters of these cases in 2019 were linked to recent outbreaks in New York and occurred in primarily in underimmunized, close-knit communities and in patients with links to international travel. A total of 124 of the people who got measles this year were hospitalized, and 61 reported having complications, including pneumonia and encephalitis. The overall median patient age was 6 years (31% aged 1-4 years, 27% aged 5-17 years, and 29% aged at least 18 years).
The good news is that most of these cases occurred in unvaccinated patients. The national vaccination rate for the almost 4 million kindergartners reported as enrolled in 2018-2019 was 94.7% for two doses of the MMR vaccine, falling just short of the CDC recommended 95% vaccination rate threshold. The CDC reported an approximate 2.5% rate of vaccination exemptions among school-age children.
The bad news is that, despite the high rate of MMR vaccination rates among U.S. children, there are gaps in measles protection in the U.S. population because of factors leaving patients immunocompromised and antivaccination sentiment that has led some parents to defer or refuse the MMR.
In addition, adults who were vaccinated prior to 1968 with either inactivated measles vaccine or measles vaccine of unknown type may have limited immunity. The inactivated measles vaccine, which was available in 1963-1967, did not achieve effective measles protection.
A global measles surge
While antivaccination sentiment contributed to the 2019 measles cases, a more significant factor may be the global surge of measles. More than 140,000 people worldwide died from measles in 2018, according to the World Health Organization and the CDC.
“[Recent data on measles] indicates that during the first 6 months of the year there have been more measles cases reported worldwide than in any year since 2006. From Jan. 1 to July 31, 2019, 182 countries reported 364,808 measles cases to the WHO. This surpasses the 129,239 reported during the same time period in 2018. WHO regions with the biggest increases in cases include the African region (900%), the Western Pacific region (230%), and the European region (150%),” according to a CDC report.
Studies on hospitalization and complications linked to measles in the United States are scarce, but two outbreaks in Minnesota (2011 and 2017) provided some data on what to expect if the measles surge continues into 2020. The investigators found that poor feeding was a primary reason for admission (97%); additional complications included otitis media (42%), pneumonia (30%), and tracheitis (6%). Three-quarters received antibiotics, 30% required oxygen, and 21% received vitamin A. Median length of stay was 3.7 days (range, 1.1-26.2 days) (Pediatr Infect Dis J. 2019 Jun;38[6]:547-52. doi: 10.1097/INF.0000000000002221).
‘Immunological amnesia’
Infection with the measles virus appears to reduce immunity to other pathogens, according to a paper published in Science (2019 Nov 1;366[6465]599-606).
The hypothesis that the measles virus could cause “immunological amnesia” by impairing immune memory is supported by early research showing children with measles had negative cutaneous tuberculin reactions after having previously tested positive.
“Subsequent studies have shown decreased interferon signaling, skewed cytokine responses, lymphopenia, and suppression of lymphocyte proliferation shortly after infection,” wrote Michael Mina, MD, from Brigham and Women’s Hospital in Boston, and coauthors.
“Given the variation in the degree of immune repertoire modulation we observed, we anticipate that future risk of morbidity and mortality after measles would not be homogeneous but would be skewed toward individuals with the most severe elimination of immunological memory,” they wrote. “These findings underscore the crucial need for continued widespread vaccination.”
In this study, researchers compared the levels of around 400 pathogen-specific antibodies in blood samples from 77 unvaccinated children, taken before and 2 months after natural measles infection, with 5 unvaccinated children who did not contract measles. A total of 34 children experienced mild measles, and 43 had severe measles.
They found that the samples taken after measles infection showed “substantial” reductions in the number of pathogen epitopes, compared with the samples from children who did not get infected with measles.
This amounted to approximately a 20% mean reduction in overall diversity or size of the antibody repertoire. However, in children who experienced severe measles, there was a median loss of 40% (range, 11%-62%) of antibody repertoire, compared with a median of 33% (range, 12%-73%) range in children who experienced mild infection. Meanwhile, the control subjects retained approximately 90% of their antibody repertoire over a similar or longer time period. Some children lost up to 70% of antibodies for specific pathogens.
Maternal-acquired immunity fades
In another study of measles immunity, maternal antibodies were found to be insufficient to provide immunity to infants after 6 months.
The study of 196 infants showed that maternal measles antibodies had dropped below the protective threshold by 3 months of age – well before the recommended age of 12-15 months for the first dose of MMR vaccine.
The odds of inadequate protection doubled for each additional month of age, Michelle Science, MD, of the University of Toronto and associates reported in Pediatrics (2019 Dec 1. doi 10.1542/peds.2019-0630).
“The widening gap between loss of maternal antibodies and measles vaccination described in our study leaves infants vulnerable to measles for much of their infancy and highlights the need for further research to support public health policy,” Dr. Science and colleagues wrote.
The researchers randomly selected 25 samples for each of eight different age groups: up to 30 days old; 1 month (31-60 days), 2 months (61-89 days), 3 months (90-119 days), 4 months, 5 months, 6-9 months, and 9-11 months.
Just over half the babies (56%) were male, and 35% had an underlying condition, but none had conditions that might affect antibody levels. The conditions were primarily a developmental delay or otherwise affecting the central nervous system, liver, or gastrointestinal function. Mean maternal age was 32 years.
To ensure high test sensitivity, the researchers used the plaque-reduction neutralization test to test for measles-neutralizing antibodies instead of using enzyme-linked immunosorbent assay, because “ELISA sensitivity decreases as antibody titers decrease,” Dr. Science and colleagues wrote. They used a neutralization titer of less than 192 mIU/mL as the threshold for protection against measles.
When the researchers calculated the predicted standardized mean antibody titer for infants with a mother aged 32 years, they determined their mean to be 541 mIU/mL at 1 month, 142 mIU/mL at 3 months (below the measles threshold of susceptibility of 192 mIU/mL), and 64 mIU/mL at 6 months. None of the infants had measles antibodies above the protective threshold at 6 months old, the authors noted.
Children’s odds of susceptibility to measles doubled for each additional month of age, after adjustment for infant sex and maternal age (odds ratio, 2.13). Children’s likelihood of susceptibility to measles modestly increased as maternal age increased in 5-year increments from 25 to 40 years.
Children with an underlying conditions had greater susceptibility to measles (83%), compared with those without a comorbidity (68%, P = .03). No difference in susceptibility existed between males and females or based on gestational age at birth (ranging from 37 to 41 weeks).
The Advisory Committee on Immunization Practices permits measles vaccination “as early as 6 months for infants who plan to travel internationally, infants with ongoing risk for exposure during measles outbreaks and as postexposure prophylaxis,” Huong Q. McLean, PhD, of Marshfield (Wisc.) Clinic Research Institute, and Walter A. Orenstein, MD, of Emory University, Atlanta, noted in an editorial.
The research was funded by the Public Health Ontario Project Initiation Fund. The authors had no relevant financial disclosures.
Bianca Nogrady and Tara Haelle contributed to this story.
Measles made a comeback in 2019.
The Centers for Disease Control and Prevention reported that, as of Dec. 5, 2019, 1,276 individual cases of measles of measles were confirmed in 31 states, the largest number since 1992. This number is a major uptick in cases, compared with previous years since 2000 when the CDC declared measles eliminated from the United States. No deaths have been reported for 2019.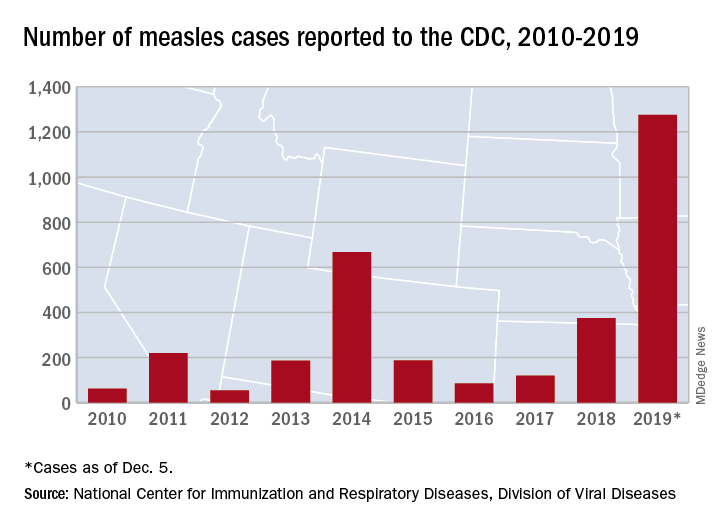
Three-quarters of these cases in 2019 were linked to recent outbreaks in New York and occurred in primarily in underimmunized, close-knit communities and in patients with links to international travel. A total of 124 of the people who got measles this year were hospitalized, and 61 reported having complications, including pneumonia and encephalitis. The overall median patient age was 6 years (31% aged 1-4 years, 27% aged 5-17 years, and 29% aged at least 18 years).
The good news is that most of these cases occurred in unvaccinated patients. The national vaccination rate for the almost 4 million kindergartners reported as enrolled in 2018-2019 was 94.7% for two doses of the MMR vaccine, falling just short of the CDC recommended 95% vaccination rate threshold. The CDC reported an approximate 2.5% rate of vaccination exemptions among school-age children.
The bad news is that, despite the high rate of MMR vaccination rates among U.S. children, there are gaps in measles protection in the U.S. population because of factors leaving patients immunocompromised and antivaccination sentiment that has led some parents to defer or refuse the MMR.
In addition, adults who were vaccinated prior to 1968 with either inactivated measles vaccine or measles vaccine of unknown type may have limited immunity. The inactivated measles vaccine, which was available in 1963-1967, did not achieve effective measles protection.
A global measles surge
While antivaccination sentiment contributed to the 2019 measles cases, a more significant factor may be the global surge of measles. More than 140,000 people worldwide died from measles in 2018, according to the World Health Organization and the CDC.
“[Recent data on measles] indicates that during the first 6 months of the year there have been more measles cases reported worldwide than in any year since 2006. From Jan. 1 to July 31, 2019, 182 countries reported 364,808 measles cases to the WHO. This surpasses the 129,239 reported during the same time period in 2018. WHO regions with the biggest increases in cases include the African region (900%), the Western Pacific region (230%), and the European region (150%),” according to a CDC report.
Studies on hospitalization and complications linked to measles in the United States are scarce, but two outbreaks in Minnesota (2011 and 2017) provided some data on what to expect if the measles surge continues into 2020. The investigators found that poor feeding was a primary reason for admission (97%); additional complications included otitis media (42%), pneumonia (30%), and tracheitis (6%). Three-quarters received antibiotics, 30% required oxygen, and 21% received vitamin A. Median length of stay was 3.7 days (range, 1.1-26.2 days) (Pediatr Infect Dis J. 2019 Jun;38[6]:547-52. doi: 10.1097/INF.0000000000002221).
‘Immunological amnesia’
Infection with the measles virus appears to reduce immunity to other pathogens, according to a paper published in Science (2019 Nov 1;366[6465]599-606).
The hypothesis that the measles virus could cause “immunological amnesia” by impairing immune memory is supported by early research showing children with measles had negative cutaneous tuberculin reactions after having previously tested positive.
“Subsequent studies have shown decreased interferon signaling, skewed cytokine responses, lymphopenia, and suppression of lymphocyte proliferation shortly after infection,” wrote Michael Mina, MD, from Brigham and Women’s Hospital in Boston, and coauthors.
“Given the variation in the degree of immune repertoire modulation we observed, we anticipate that future risk of morbidity and mortality after measles would not be homogeneous but would be skewed toward individuals with the most severe elimination of immunological memory,” they wrote. “These findings underscore the crucial need for continued widespread vaccination.”
In this study, researchers compared the levels of around 400 pathogen-specific antibodies in blood samples from 77 unvaccinated children, taken before and 2 months after natural measles infection, with 5 unvaccinated children who did not contract measles. A total of 34 children experienced mild measles, and 43 had severe measles.
They found that the samples taken after measles infection showed “substantial” reductions in the number of pathogen epitopes, compared with the samples from children who did not get infected with measles.
This amounted to approximately a 20% mean reduction in overall diversity or size of the antibody repertoire. However, in children who experienced severe measles, there was a median loss of 40% (range, 11%-62%) of antibody repertoire, compared with a median of 33% (range, 12%-73%) range in children who experienced mild infection. Meanwhile, the control subjects retained approximately 90% of their antibody repertoire over a similar or longer time period. Some children lost up to 70% of antibodies for specific pathogens.
Maternal-acquired immunity fades
In another study of measles immunity, maternal antibodies were found to be insufficient to provide immunity to infants after 6 months.
The study of 196 infants showed that maternal measles antibodies had dropped below the protective threshold by 3 months of age – well before the recommended age of 12-15 months for the first dose of MMR vaccine.
The odds of inadequate protection doubled for each additional month of age, Michelle Science, MD, of the University of Toronto and associates reported in Pediatrics (2019 Dec 1. doi 10.1542/peds.2019-0630).
“The widening gap between loss of maternal antibodies and measles vaccination described in our study leaves infants vulnerable to measles for much of their infancy and highlights the need for further research to support public health policy,” Dr. Science and colleagues wrote.
The researchers randomly selected 25 samples for each of eight different age groups: up to 30 days old; 1 month (31-60 days), 2 months (61-89 days), 3 months (90-119 days), 4 months, 5 months, 6-9 months, and 9-11 months.
Just over half the babies (56%) were male, and 35% had an underlying condition, but none had conditions that might affect antibody levels. The conditions were primarily a developmental delay or otherwise affecting the central nervous system, liver, or gastrointestinal function. Mean maternal age was 32 years.
To ensure high test sensitivity, the researchers used the plaque-reduction neutralization test to test for measles-neutralizing antibodies instead of using enzyme-linked immunosorbent assay, because “ELISA sensitivity decreases as antibody titers decrease,” Dr. Science and colleagues wrote. They used a neutralization titer of less than 192 mIU/mL as the threshold for protection against measles.
When the researchers calculated the predicted standardized mean antibody titer for infants with a mother aged 32 years, they determined their mean to be 541 mIU/mL at 1 month, 142 mIU/mL at 3 months (below the measles threshold of susceptibility of 192 mIU/mL), and 64 mIU/mL at 6 months. None of the infants had measles antibodies above the protective threshold at 6 months old, the authors noted.
Children’s odds of susceptibility to measles doubled for each additional month of age, after adjustment for infant sex and maternal age (odds ratio, 2.13). Children’s likelihood of susceptibility to measles modestly increased as maternal age increased in 5-year increments from 25 to 40 years.
Children with an underlying conditions had greater susceptibility to measles (83%), compared with those without a comorbidity (68%, P = .03). No difference in susceptibility existed between males and females or based on gestational age at birth (ranging from 37 to 41 weeks).
The Advisory Committee on Immunization Practices permits measles vaccination “as early as 6 months for infants who plan to travel internationally, infants with ongoing risk for exposure during measles outbreaks and as postexposure prophylaxis,” Huong Q. McLean, PhD, of Marshfield (Wisc.) Clinic Research Institute, and Walter A. Orenstein, MD, of Emory University, Atlanta, noted in an editorial.
The research was funded by the Public Health Ontario Project Initiation Fund. The authors had no relevant financial disclosures.
Bianca Nogrady and Tara Haelle contributed to this story.
Which children are at greatest risk for atopic dermatitis?
MADRID – A parental history of asthma or allergic rhinitis significantly increases the risk that a child will develop atopic dermatitis, and that risk doubles if a parent has a history of atopic dermatitis rather than another atopic disease, Nina H. Ravn reported at a meeting of the European Task Force on Atopic Dermatitis held in conjunction with the annual congress of the European Academy of Dermatology and Venereology.
She presented a comprehensive meta-analysis of 149 published studies addressing the risk of developing atopic dermatitis according to parental history of atopic disease. The studies included more than 656,000 participants. The picture that emerged from the meta-analysis was one of a stepwise increase in the risk of pediatric atopic dermatitis according to the type and number of parental atopic diseases present.
“This is something that hopefully can be useful when you talk with parents or parents-to-be with atopic diseases and they want to know how their disease might affect their child,” explained Ms. Ravn of the University of Copenhagen.
It’s also information that clinicians will find helpful in appropriately targeting primary prevention interventions if and when methods of proven efficacy become available. That’s a likely prospect, as this is now an extremely active field of research, she noted.
The meta-analysis showed that a parental history of atopic dermatitis was associated with a 3.3-fold greater risk of atopic dermatitis in the offspring than in families without a parental history of atopy. A parental history of asthma was associated with a 1.56-fold increased risk, while allergic rhinitis in a parent was linked to a 1.68-fold increased risk.
“It does matter what type of atopic disease the parents have,” she observed. “Those with a parental history of asthma or allergic rhinitis can be considered as being at more of an intermediate risk level, while those with a parental history of atopic dermatitis are a particularly high risk group.”
Of note, the risk of pediatric atopic dermatitis was the same regardless of whether the father or mother was the one with a history of atopic disease. If one parent had a history of an atopic disease, the pediatric risk was increased 1.3-fold compared to when the parental history was negative. If both parents had a history of atopic illness, the risk jumped to 2.08-fold. And if one parent had a history of more than one form of atopic disease, the pediatric risk of atopic dermatitis was increased 2.32-fold.
“An interesting result that was new to me what that fathers’ and mothers’ contribution to risk is equal,” said session cochair Andreas Wollenberg, MD, professor of dermatology at Ludwig Maximilian University of Munich. “For the past 2 decades we were always taught that the mother would have a greater impact on that risk.”
“I was also surprised by our findings,” Ms. Ravn replied. “But when we pooled all the data there really was no difference, nor in any of our subanalyses.”
She reported having no financial conflicts regarding her study.
SOURCE: Ravn NH. THE EADV CONGRESS.
MADRID – A parental history of asthma or allergic rhinitis significantly increases the risk that a child will develop atopic dermatitis, and that risk doubles if a parent has a history of atopic dermatitis rather than another atopic disease, Nina H. Ravn reported at a meeting of the European Task Force on Atopic Dermatitis held in conjunction with the annual congress of the European Academy of Dermatology and Venereology.
She presented a comprehensive meta-analysis of 149 published studies addressing the risk of developing atopic dermatitis according to parental history of atopic disease. The studies included more than 656,000 participants. The picture that emerged from the meta-analysis was one of a stepwise increase in the risk of pediatric atopic dermatitis according to the type and number of parental atopic diseases present.
“This is something that hopefully can be useful when you talk with parents or parents-to-be with atopic diseases and they want to know how their disease might affect their child,” explained Ms. Ravn of the University of Copenhagen.
It’s also information that clinicians will find helpful in appropriately targeting primary prevention interventions if and when methods of proven efficacy become available. That’s a likely prospect, as this is now an extremely active field of research, she noted.
The meta-analysis showed that a parental history of atopic dermatitis was associated with a 3.3-fold greater risk of atopic dermatitis in the offspring than in families without a parental history of atopy. A parental history of asthma was associated with a 1.56-fold increased risk, while allergic rhinitis in a parent was linked to a 1.68-fold increased risk.
“It does matter what type of atopic disease the parents have,” she observed. “Those with a parental history of asthma or allergic rhinitis can be considered as being at more of an intermediate risk level, while those with a parental history of atopic dermatitis are a particularly high risk group.”
Of note, the risk of pediatric atopic dermatitis was the same regardless of whether the father or mother was the one with a history of atopic disease. If one parent had a history of an atopic disease, the pediatric risk was increased 1.3-fold compared to when the parental history was negative. If both parents had a history of atopic illness, the risk jumped to 2.08-fold. And if one parent had a history of more than one form of atopic disease, the pediatric risk of atopic dermatitis was increased 2.32-fold.
“An interesting result that was new to me what that fathers’ and mothers’ contribution to risk is equal,” said session cochair Andreas Wollenberg, MD, professor of dermatology at Ludwig Maximilian University of Munich. “For the past 2 decades we were always taught that the mother would have a greater impact on that risk.”
“I was also surprised by our findings,” Ms. Ravn replied. “But when we pooled all the data there really was no difference, nor in any of our subanalyses.”
She reported having no financial conflicts regarding her study.
SOURCE: Ravn NH. THE EADV CONGRESS.
MADRID – A parental history of asthma or allergic rhinitis significantly increases the risk that a child will develop atopic dermatitis, and that risk doubles if a parent has a history of atopic dermatitis rather than another atopic disease, Nina H. Ravn reported at a meeting of the European Task Force on Atopic Dermatitis held in conjunction with the annual congress of the European Academy of Dermatology and Venereology.
She presented a comprehensive meta-analysis of 149 published studies addressing the risk of developing atopic dermatitis according to parental history of atopic disease. The studies included more than 656,000 participants. The picture that emerged from the meta-analysis was one of a stepwise increase in the risk of pediatric atopic dermatitis according to the type and number of parental atopic diseases present.
“This is something that hopefully can be useful when you talk with parents or parents-to-be with atopic diseases and they want to know how their disease might affect their child,” explained Ms. Ravn of the University of Copenhagen.
It’s also information that clinicians will find helpful in appropriately targeting primary prevention interventions if and when methods of proven efficacy become available. That’s a likely prospect, as this is now an extremely active field of research, she noted.
The meta-analysis showed that a parental history of atopic dermatitis was associated with a 3.3-fold greater risk of atopic dermatitis in the offspring than in families without a parental history of atopy. A parental history of asthma was associated with a 1.56-fold increased risk, while allergic rhinitis in a parent was linked to a 1.68-fold increased risk.
“It does matter what type of atopic disease the parents have,” she observed. “Those with a parental history of asthma or allergic rhinitis can be considered as being at more of an intermediate risk level, while those with a parental history of atopic dermatitis are a particularly high risk group.”
Of note, the risk of pediatric atopic dermatitis was the same regardless of whether the father or mother was the one with a history of atopic disease. If one parent had a history of an atopic disease, the pediatric risk was increased 1.3-fold compared to when the parental history was negative. If both parents had a history of atopic illness, the risk jumped to 2.08-fold. And if one parent had a history of more than one form of atopic disease, the pediatric risk of atopic dermatitis was increased 2.32-fold.
“An interesting result that was new to me what that fathers’ and mothers’ contribution to risk is equal,” said session cochair Andreas Wollenberg, MD, professor of dermatology at Ludwig Maximilian University of Munich. “For the past 2 decades we were always taught that the mother would have a greater impact on that risk.”
“I was also surprised by our findings,” Ms. Ravn replied. “But when we pooled all the data there really was no difference, nor in any of our subanalyses.”
She reported having no financial conflicts regarding her study.
SOURCE: Ravn NH. THE EADV CONGRESS.
REPORTING FROM The EADV CONGRESS
Key clinical point: Pediatric atopic dermatitis risk varies according to type of parental history of atopic disease.
Major finding: A parental history of atopic dermatitis is associated with a 3.3-fold increased risk of atopic dermatitis in the child, twice the risk associated with parental asthma or allergic rhinitis.
Study details: This was a systematic review and meta-analysis of 149 published studies with 656,711 participants.
Disclosures: The presenter reported having no financial conflicts regarding the study, conducted free of commercial support.
Source: Ravn NH. The EADV Congress.
Influenza activity continues to be unusually high
The 2019-2020 flu season continues its unusually early rise in activity, with the Centers for Disease Control and Prevention estimating that 3.7 million cases have occurred through Dec. 14.
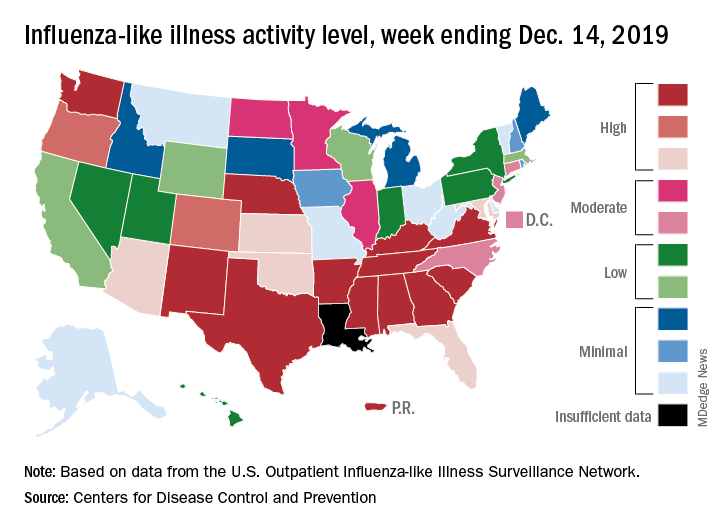
which is up from 3.2% the previous week and is the sixth consecutive week that the United States has been at or above the national baseline of 2.4%, the CDC reported Dec. 20. This year’s 3.9% is the highest mid-December rate recorded since 2003, when it reached almost 7.4%.
Most of the influenza activity so far this season is being driven by influenza B/Victoria viruses. Nationwide testing puts influenza B prevalence at 68.5% of all positive specimens, exactly the same as last week, but A(H1N1) viruses “are increasing in proportion relative to other influenza viruses in some regions,” the CDC’s influenza division said.
A look at this week’s activity map shows that 21 states, compared with 12 last week, were in the “high” range of activity – that’s levels 8-10 on the CDC’s 1-10 scale. Twelve of those states, along with Puerto Rico, were at level 10, which was up from nine a week earlier, the CDC said.
The overall hospitalization rate through the week of Dec. 8-14 (5.5 per 100,000 population) “is similar to what has been seen at this time during recent seasons,” the CDC noted. The highest rates are occurring among adults over age 65 years (12.7 per 100,000) and children aged 0-4 years (10.9 per 100,000).
Three ILI-related deaths among children that occurred last week were reported, which brings the total for the 2019-2020 season to 19, the CDC said.
The 2019-2020 flu season continues its unusually early rise in activity, with the Centers for Disease Control and Prevention estimating that 3.7 million cases have occurred through Dec. 14.
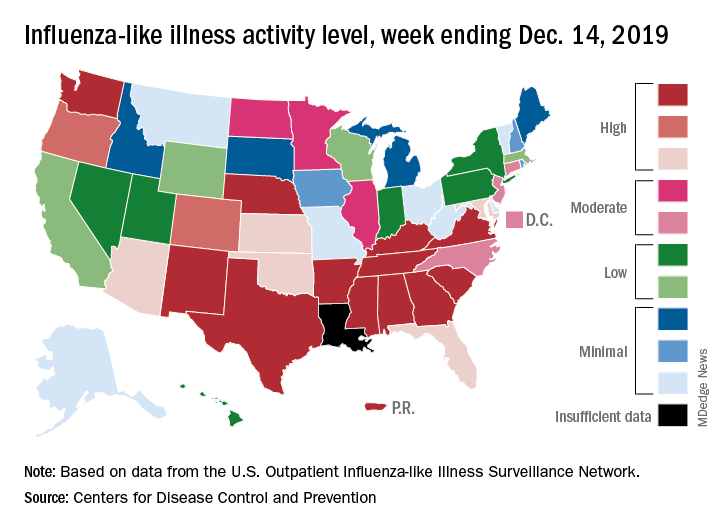
which is up from 3.2% the previous week and is the sixth consecutive week that the United States has been at or above the national baseline of 2.4%, the CDC reported Dec. 20. This year’s 3.9% is the highest mid-December rate recorded since 2003, when it reached almost 7.4%.
Most of the influenza activity so far this season is being driven by influenza B/Victoria viruses. Nationwide testing puts influenza B prevalence at 68.5% of all positive specimens, exactly the same as last week, but A(H1N1) viruses “are increasing in proportion relative to other influenza viruses in some regions,” the CDC’s influenza division said.
A look at this week’s activity map shows that 21 states, compared with 12 last week, were in the “high” range of activity – that’s levels 8-10 on the CDC’s 1-10 scale. Twelve of those states, along with Puerto Rico, were at level 10, which was up from nine a week earlier, the CDC said.
The overall hospitalization rate through the week of Dec. 8-14 (5.5 per 100,000 population) “is similar to what has been seen at this time during recent seasons,” the CDC noted. The highest rates are occurring among adults over age 65 years (12.7 per 100,000) and children aged 0-4 years (10.9 per 100,000).
Three ILI-related deaths among children that occurred last week were reported, which brings the total for the 2019-2020 season to 19, the CDC said.
The 2019-2020 flu season continues its unusually early rise in activity, with the Centers for Disease Control and Prevention estimating that 3.7 million cases have occurred through Dec. 14.
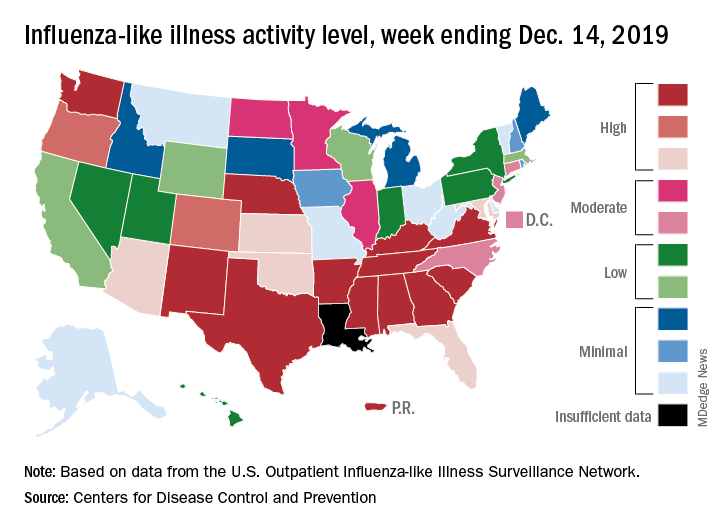
which is up from 3.2% the previous week and is the sixth consecutive week that the United States has been at or above the national baseline of 2.4%, the CDC reported Dec. 20. This year’s 3.9% is the highest mid-December rate recorded since 2003, when it reached almost 7.4%.
Most of the influenza activity so far this season is being driven by influenza B/Victoria viruses. Nationwide testing puts influenza B prevalence at 68.5% of all positive specimens, exactly the same as last week, but A(H1N1) viruses “are increasing in proportion relative to other influenza viruses in some regions,” the CDC’s influenza division said.
A look at this week’s activity map shows that 21 states, compared with 12 last week, were in the “high” range of activity – that’s levels 8-10 on the CDC’s 1-10 scale. Twelve of those states, along with Puerto Rico, were at level 10, which was up from nine a week earlier, the CDC said.
The overall hospitalization rate through the week of Dec. 8-14 (5.5 per 100,000 population) “is similar to what has been seen at this time during recent seasons,” the CDC noted. The highest rates are occurring among adults over age 65 years (12.7 per 100,000) and children aged 0-4 years (10.9 per 100,000).
Three ILI-related deaths among children that occurred last week were reported, which brings the total for the 2019-2020 season to 19, the CDC said.