User login
Big geographic access gaps for oncofertility services in U.S.
TOPLINE:
, a study shows.
METHODOLOGY:
- In this cross-sectional analysis, researchers identified 370 fertility centers in the United States (361 in the continental U.S.) that provide oncofertility services and that met criteria for an oncofertility center.
- Clinics were considered oncofertility centers if they offered oocyte cryopreservation, had performed at least one fertility preservation cycle in 2018, reported serving people without partners, and had an embryology laboratory that was accredited per Centers for Disease Control and Prevention guidelines.
- Researchers then quantified the number of young women potentially eligible for oncofertility services who lived farther than 2 hours from an oncofertility center.
- In a secondary analysis, the team assessed the association between geographic access and state fertility preservation insurance mandates.
TAKEAWAY:
- Overall, 3.63 million (5.7%) young women of reproductive age in the United States (aged 15-4) live more than 2 hours from an oncofertility center.
- The greatest gaps in access are in the Mountain West, West North Central, and Southwest regions; for instance, in Montana, North Dakota, and Wyoming fewer than half of the at-risk population has geographic access to an oncofertility center.
- Among the 11 states with fertility preservation insurance mandates, 98.5% of at-risk women have geographic access to an oncofertility center; in the 17 states without fertility preservation legislation, 79.6% of at-risk women have access to an oncofertility center.
IN PRACTICE:
Just over 3.6 million “reproductive-age female individuals lack geographic access to oncofertility services, especially in the Mountain West and West North Central regions,” the authors concluded. “Significant geographic disparities in access to fertility preservation in the U.S. require strategic expansion of care, especially given the growing demand for oncofertility services.”
SOURCE:
The study, led by Benjamin Peipert, MD, with Duke University, Durham, N.C., was published online in JAMA Oncology.
LIMITATIONS:
The authors relied on clinic data reported to the CDC, made assumptions about reasonable travel time, and may have underestimated access in some areas.
DISCLOSURES:
The study had no commercial funding. The authors have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
TOPLINE:
, a study shows.
METHODOLOGY:
- In this cross-sectional analysis, researchers identified 370 fertility centers in the United States (361 in the continental U.S.) that provide oncofertility services and that met criteria for an oncofertility center.
- Clinics were considered oncofertility centers if they offered oocyte cryopreservation, had performed at least one fertility preservation cycle in 2018, reported serving people without partners, and had an embryology laboratory that was accredited per Centers for Disease Control and Prevention guidelines.
- Researchers then quantified the number of young women potentially eligible for oncofertility services who lived farther than 2 hours from an oncofertility center.
- In a secondary analysis, the team assessed the association between geographic access and state fertility preservation insurance mandates.
TAKEAWAY:
- Overall, 3.63 million (5.7%) young women of reproductive age in the United States (aged 15-4) live more than 2 hours from an oncofertility center.
- The greatest gaps in access are in the Mountain West, West North Central, and Southwest regions; for instance, in Montana, North Dakota, and Wyoming fewer than half of the at-risk population has geographic access to an oncofertility center.
- Among the 11 states with fertility preservation insurance mandates, 98.5% of at-risk women have geographic access to an oncofertility center; in the 17 states without fertility preservation legislation, 79.6% of at-risk women have access to an oncofertility center.
IN PRACTICE:
Just over 3.6 million “reproductive-age female individuals lack geographic access to oncofertility services, especially in the Mountain West and West North Central regions,” the authors concluded. “Significant geographic disparities in access to fertility preservation in the U.S. require strategic expansion of care, especially given the growing demand for oncofertility services.”
SOURCE:
The study, led by Benjamin Peipert, MD, with Duke University, Durham, N.C., was published online in JAMA Oncology.
LIMITATIONS:
The authors relied on clinic data reported to the CDC, made assumptions about reasonable travel time, and may have underestimated access in some areas.
DISCLOSURES:
The study had no commercial funding. The authors have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
TOPLINE:
, a study shows.
METHODOLOGY:
- In this cross-sectional analysis, researchers identified 370 fertility centers in the United States (361 in the continental U.S.) that provide oncofertility services and that met criteria for an oncofertility center.
- Clinics were considered oncofertility centers if they offered oocyte cryopreservation, had performed at least one fertility preservation cycle in 2018, reported serving people without partners, and had an embryology laboratory that was accredited per Centers for Disease Control and Prevention guidelines.
- Researchers then quantified the number of young women potentially eligible for oncofertility services who lived farther than 2 hours from an oncofertility center.
- In a secondary analysis, the team assessed the association between geographic access and state fertility preservation insurance mandates.
TAKEAWAY:
- Overall, 3.63 million (5.7%) young women of reproductive age in the United States (aged 15-4) live more than 2 hours from an oncofertility center.
- The greatest gaps in access are in the Mountain West, West North Central, and Southwest regions; for instance, in Montana, North Dakota, and Wyoming fewer than half of the at-risk population has geographic access to an oncofertility center.
- Among the 11 states with fertility preservation insurance mandates, 98.5% of at-risk women have geographic access to an oncofertility center; in the 17 states without fertility preservation legislation, 79.6% of at-risk women have access to an oncofertility center.
IN PRACTICE:
Just over 3.6 million “reproductive-age female individuals lack geographic access to oncofertility services, especially in the Mountain West and West North Central regions,” the authors concluded. “Significant geographic disparities in access to fertility preservation in the U.S. require strategic expansion of care, especially given the growing demand for oncofertility services.”
SOURCE:
The study, led by Benjamin Peipert, MD, with Duke University, Durham, N.C., was published online in JAMA Oncology.
LIMITATIONS:
The authors relied on clinic data reported to the CDC, made assumptions about reasonable travel time, and may have underestimated access in some areas.
DISCLOSURES:
The study had no commercial funding. The authors have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM JAMA ONCOLOGY
The fertile future of fertility technology
Fifth pregnancy, first baby.
After four pregnancies resulted in losses – and doing things as natural as possible and leaving it up to the birds, bees, and fate – my husband and I decided to explore in vitro fertilization (IVF).
Drugs to direct my follicles to produce more eggs, an egg retrieval procedure, genetic testing of our embryos, a quick procedure to remove a residual uterine septum from my uterus, drugs to thicken my endometrial lining to prepare my body to receive an embryo, an embryo transfer, steroids to suppress my immune system so my body would accept the pregnancy, blood thinner shots to promote blood flow to the baby, and 10 weeks of progesterone in oil shots later and we’re days away from welcoming our first baby into our lives.
In short, there’s more than one way to define “miracle baby.”
Global estimates say 48 million couples and 186 million individuals struggle with infertility. On average, 2 million infants born in the United States each year are conceived through assisted reproductive technology and the demand for treatments like IVF have doubled in the last decade.
Now the need for treatments outweighs clinician availability. “We have about 1,250 practicing fertility physicians in the U.S. to serve the whole country, which is highly inadequate,” said Eduardo Hariton, MD, a reproductive endocrinology physician in San Francisco and managing director of the U.S. Fertility Innovation Fund. “We have people that want to get care waiting 1 to 3 months to be seen.”
Dr. Hariton explains that U.S. IVF clinics are performing around 250,000 to 300,000 IVF cycles per year and need to be doing a million-plus to meet demand. This, plus the cost of fertility treatments – an average IVF cycle runs $23,500 and the majority of patients need multiple cycles to conceive – keeps the barrier to entry high.
Enter technology: New advances are on the way to help the assisted fertility process to run smoother and be less costly. “The field is really coming into an age of great progress and innovation,” added S. Zev Williams, MD, PhD, chief of the division of reproductive endocrinology and Infertility at Columbia University Irving Medical Center, New York City.
I’m personally grateful that such technology exists.
AI will help, of course
Fertility treatments involve endless analysis, diagnosis, and recommendations – dozens if not hundreds of decisions from each physician for each patient. Human action and reaction can affect this process, Dr. Hariton explained.
For example, if he hyperstimulated a woman during the follicle growing stage of her egg retrieval and ended up with eggs too large to retrieve, Dr. Hariton said he may subconsciously be more inclined to be extra cautious with his patients the week after, and vice versa.
This is where AI can help. “Rather than me making decisions from a couple of thousands of cycles of experience, I get to leverage hundreds of thousands of cycles from different providers over different people,” said Dr. Hariton. “I get to use all the data from that patient today – her age, her weight, what happened last cycle, how she’s doing – and make a very objective decision about the optimal time to give that woman or that couple the best outcome possible.”
AI can also assist with tasks like embryo grading. “Once our embryos are made in the lab, we usually have an embryologist looking at those embryos, grading them on a three-variable scale, and then picking the nicest one for transfer,” said Dr. Hariton. Machine learning computer vision software can help doctors select the best embryo.
Many of these AI products are in trials in the United States and some AI-based technology is already being used in fertility labs, especially in other countries. “ALife recently launched a suite of products to help with their decisions during stimulation that can help with the quality KPIs [key performance indicators] in the lab,” said Dr. Hariton. “There’s also a company that does AI-based predictions of success to give patients a better estimate called Univfy.” More AI products are still in development or awaiting Food and Drug Administration clearance.
Robots lend a hand
Like artificial intelligence, robots can be a big help in the IVF lab. Columbia University Fertility Center recently became the first to use an articulated (ART) robot to handle precise and highly repetitive work.
“IVF, from the initial point, involves creating these special plates where embryos can grow, and you do that by making little droplets,” said Dr. Williams. “It’s very time-consuming to create tons of these little droplets for the embryos to grow.” Thus, the lab created a robot to help squirt drops of the media substance required to sustain embryos in a way that is 10 times more precise than that of a trained embryologist.
“It’s a win-win because you allow the robots to do things better than a human can and this allows the humans to do things that a robot just can’t do,” explained Dr. Williams. He and his team began using this technology in the beginning of November 2022.
Dr. Williams sees ART robots being used in many more parts of the fertility treatment journey along the way, like preparing eggs after they are retrieved and performing intracytoplasmic sperm injection (ICSI), with the robot injecting the sperm into the egg.
Launching with the plate making, said Dr. Williams, is a low stakes entry point for robotic technology in the lab. “It allows us to introduce robotics to automate and optimize each step along the way, but to do so in the safest possible way.”
Dr. Williams estimates that robots will have their hands on actual eggs and sperm in 5 years.
Updates in genetic testing
Currently, if a couple wants to have their embryos genetically tested, also known as preimplantation genetic testing, each embryo must be frozen, then a biopsy of that embryo is performed and sent to the lab.
“It takes time to get the results,” said Dr. Williams. “The whole time you’re waiting, you don’t know if you’re going to have any embryos that are transferable or if next month you’re going to have to do another IVF cycle.”
Columbia researchers recently developed a new in-house test that can determine if a fetus or embryo has the right number of chromosomes. This STORK (Short-read Transpore Rapid Karyotyping) can be performed without freezing embryos and sending them out, which Dr. Williams said can save couples money and time, as they won’t necessarily need to do a separate embryo transfer cycle and can transfer an embryo in the same cycle. “You can test in the morning and transfer in the afternoon,” said Dr. Williams.
The test is currently awaiting approval and will first be used to test miscarriage samples to see if embryos were genetically normal or not, which he said should cost around $200 vs. the $2,000 to $4,000 it can cost to have fetal tissue sent to the lab – and insurance doesn’t cover the procedure until after a second or third miscarriage.
This, said Dr. Williams, should be in the field in less than a year, and he estimates that the test will be used for fresh embryos in about a year and a half.
Sperm collection made simpler
Typically, a man delivers a sperm sample in a room at an IVF clinic or by collecting a sample at home and rushing it to the clinic before it degrades, which Dr. Williams said can happen in as little as 15 minutes.
In 2020, Dr. Williams and his team began using a custom at-home sperm collection box that houses sperm in a recyclable foam container that holds a sample cup, which is filled with special sperm-supporting media, at an angle that prevents evaporation and maintains temperature and pH. This allows patients to collect samples in the comfort of their homes and increases the clock to 3 hours.
“It’s great for the patients because it’s much more comfortable,” said Dr. Williams, who notes that having to “perform” on site can be stressful for men. Studies the team has conducted have shown sperm collected in this manner have a better success rate than those collected in the lab, and 90% of Columbia’s Fertility Center patients are now providing sperm samples this way.
Similar innovations to deliver sperm, like Protex, are now on the market, while companies like myLabBox and Legacy are offering at-home sperm testing kits to mail in for a full semen analysis.
At-home monitoring: More and better
Wearable reproductive health devices are also helping more women get pregnant. “I am very excited about biometric data harnessed in wearables to predict periods, ovulation, and fertility,” said Amander Clark, PhD, director of the UCLA Center for Reproductive Science, Health, and Education, Los Angeles.
The Tempdrop Fertility and Ovulation Tracker, for instance, is a wearable sensor with an accompanying charting app that helps a woman identify her most fertile days to conceive. The Bellabeat Ivy is a women’s health smart bracelet with a strong focus on tracking a woman’s cycle and fertility, pregnancy, and postnatal symptoms. And Mirvie, which is currently in development, is a blood test that will be able to predict pregnancy complications earlier.
Physicians are also looking to move as much of the lab experience as they can into a patient’s home, which streamlines processes while offering privacy and comfort. For example, Dr. Hariton, who runs a strategic venture capital fund for physicians, said his team is currently working with a company that does remote ultrasounds.
And Mira, an at-home hormone monitor, uses patented AI algorithms to accurately measure the levels of major reproductive health hormones (E3G, LH, PdG, FSH) in urine, said Meir Olcha, MD, chief medical officer at Sama Fertility. The product recently completed a clinical trial, which showed it was a viable alternative to blood serum for patients undergoing IVF.
Stem cells could make eggs ageless
Research shows that a woman’s egg quality decreases gradually but significantly starting at age 32 and more rapidly after 37. Sperm quality may also decrease with age. A possible workaround: Scientists are actively researching how to create eggs and sperm from stem cells.
“I think getting eggs from stem cells will happen in the future,” said Dr. Hariton, who notes that this type of technology would be a game changer in his clinic. “It will make some of the hardest diagnoses that I have – which is on a daily basis, ‘I’m so sorry, you’re in premature menopause’ or ‘I don’t think we’re going to be successful getting you pregnant with your own eggs; here are some other options like donor eggs’ – much better,” he added. And stem cells are currently being used to research causes of infertility.
Clinics like UCLA have already been making strides. “We are using stem cells to identify new genes required for reproduction and to define the role of these genes in human fertility and infertility,” said Dr. Clark, a member of the Eli and Edythe Broad Center of Regenerative Medicine and Stem Cell Research at UCLA, who recently led a study in this arena. “In vitro gametogenesis (IVG), another stem cell technology, is currently used in the research lab to understand causes of infertility.”
These stem cell-based embryo models, she said, can help researchers understand the first few days of embryo development after an embryo implants and be used to provide critical information on causes of early pregnancy loss or birth defects.
A version of this article appeared on Medscape.com.
Fifth pregnancy, first baby.
After four pregnancies resulted in losses – and doing things as natural as possible and leaving it up to the birds, bees, and fate – my husband and I decided to explore in vitro fertilization (IVF).
Drugs to direct my follicles to produce more eggs, an egg retrieval procedure, genetic testing of our embryos, a quick procedure to remove a residual uterine septum from my uterus, drugs to thicken my endometrial lining to prepare my body to receive an embryo, an embryo transfer, steroids to suppress my immune system so my body would accept the pregnancy, blood thinner shots to promote blood flow to the baby, and 10 weeks of progesterone in oil shots later and we’re days away from welcoming our first baby into our lives.
In short, there’s more than one way to define “miracle baby.”
Global estimates say 48 million couples and 186 million individuals struggle with infertility. On average, 2 million infants born in the United States each year are conceived through assisted reproductive technology and the demand for treatments like IVF have doubled in the last decade.
Now the need for treatments outweighs clinician availability. “We have about 1,250 practicing fertility physicians in the U.S. to serve the whole country, which is highly inadequate,” said Eduardo Hariton, MD, a reproductive endocrinology physician in San Francisco and managing director of the U.S. Fertility Innovation Fund. “We have people that want to get care waiting 1 to 3 months to be seen.”
Dr. Hariton explains that U.S. IVF clinics are performing around 250,000 to 300,000 IVF cycles per year and need to be doing a million-plus to meet demand. This, plus the cost of fertility treatments – an average IVF cycle runs $23,500 and the majority of patients need multiple cycles to conceive – keeps the barrier to entry high.
Enter technology: New advances are on the way to help the assisted fertility process to run smoother and be less costly. “The field is really coming into an age of great progress and innovation,” added S. Zev Williams, MD, PhD, chief of the division of reproductive endocrinology and Infertility at Columbia University Irving Medical Center, New York City.
I’m personally grateful that such technology exists.
AI will help, of course
Fertility treatments involve endless analysis, diagnosis, and recommendations – dozens if not hundreds of decisions from each physician for each patient. Human action and reaction can affect this process, Dr. Hariton explained.
For example, if he hyperstimulated a woman during the follicle growing stage of her egg retrieval and ended up with eggs too large to retrieve, Dr. Hariton said he may subconsciously be more inclined to be extra cautious with his patients the week after, and vice versa.
This is where AI can help. “Rather than me making decisions from a couple of thousands of cycles of experience, I get to leverage hundreds of thousands of cycles from different providers over different people,” said Dr. Hariton. “I get to use all the data from that patient today – her age, her weight, what happened last cycle, how she’s doing – and make a very objective decision about the optimal time to give that woman or that couple the best outcome possible.”
AI can also assist with tasks like embryo grading. “Once our embryos are made in the lab, we usually have an embryologist looking at those embryos, grading them on a three-variable scale, and then picking the nicest one for transfer,” said Dr. Hariton. Machine learning computer vision software can help doctors select the best embryo.
Many of these AI products are in trials in the United States and some AI-based technology is already being used in fertility labs, especially in other countries. “ALife recently launched a suite of products to help with their decisions during stimulation that can help with the quality KPIs [key performance indicators] in the lab,” said Dr. Hariton. “There’s also a company that does AI-based predictions of success to give patients a better estimate called Univfy.” More AI products are still in development or awaiting Food and Drug Administration clearance.
Robots lend a hand
Like artificial intelligence, robots can be a big help in the IVF lab. Columbia University Fertility Center recently became the first to use an articulated (ART) robot to handle precise and highly repetitive work.
“IVF, from the initial point, involves creating these special plates where embryos can grow, and you do that by making little droplets,” said Dr. Williams. “It’s very time-consuming to create tons of these little droplets for the embryos to grow.” Thus, the lab created a robot to help squirt drops of the media substance required to sustain embryos in a way that is 10 times more precise than that of a trained embryologist.
“It’s a win-win because you allow the robots to do things better than a human can and this allows the humans to do things that a robot just can’t do,” explained Dr. Williams. He and his team began using this technology in the beginning of November 2022.
Dr. Williams sees ART robots being used in many more parts of the fertility treatment journey along the way, like preparing eggs after they are retrieved and performing intracytoplasmic sperm injection (ICSI), with the robot injecting the sperm into the egg.
Launching with the plate making, said Dr. Williams, is a low stakes entry point for robotic technology in the lab. “It allows us to introduce robotics to automate and optimize each step along the way, but to do so in the safest possible way.”
Dr. Williams estimates that robots will have their hands on actual eggs and sperm in 5 years.
Updates in genetic testing
Currently, if a couple wants to have their embryos genetically tested, also known as preimplantation genetic testing, each embryo must be frozen, then a biopsy of that embryo is performed and sent to the lab.
“It takes time to get the results,” said Dr. Williams. “The whole time you’re waiting, you don’t know if you’re going to have any embryos that are transferable or if next month you’re going to have to do another IVF cycle.”
Columbia researchers recently developed a new in-house test that can determine if a fetus or embryo has the right number of chromosomes. This STORK (Short-read Transpore Rapid Karyotyping) can be performed without freezing embryos and sending them out, which Dr. Williams said can save couples money and time, as they won’t necessarily need to do a separate embryo transfer cycle and can transfer an embryo in the same cycle. “You can test in the morning and transfer in the afternoon,” said Dr. Williams.
The test is currently awaiting approval and will first be used to test miscarriage samples to see if embryos were genetically normal or not, which he said should cost around $200 vs. the $2,000 to $4,000 it can cost to have fetal tissue sent to the lab – and insurance doesn’t cover the procedure until after a second or third miscarriage.
This, said Dr. Williams, should be in the field in less than a year, and he estimates that the test will be used for fresh embryos in about a year and a half.
Sperm collection made simpler
Typically, a man delivers a sperm sample in a room at an IVF clinic or by collecting a sample at home and rushing it to the clinic before it degrades, which Dr. Williams said can happen in as little as 15 minutes.
In 2020, Dr. Williams and his team began using a custom at-home sperm collection box that houses sperm in a recyclable foam container that holds a sample cup, which is filled with special sperm-supporting media, at an angle that prevents evaporation and maintains temperature and pH. This allows patients to collect samples in the comfort of their homes and increases the clock to 3 hours.
“It’s great for the patients because it’s much more comfortable,” said Dr. Williams, who notes that having to “perform” on site can be stressful for men. Studies the team has conducted have shown sperm collected in this manner have a better success rate than those collected in the lab, and 90% of Columbia’s Fertility Center patients are now providing sperm samples this way.
Similar innovations to deliver sperm, like Protex, are now on the market, while companies like myLabBox and Legacy are offering at-home sperm testing kits to mail in for a full semen analysis.
At-home monitoring: More and better
Wearable reproductive health devices are also helping more women get pregnant. “I am very excited about biometric data harnessed in wearables to predict periods, ovulation, and fertility,” said Amander Clark, PhD, director of the UCLA Center for Reproductive Science, Health, and Education, Los Angeles.
The Tempdrop Fertility and Ovulation Tracker, for instance, is a wearable sensor with an accompanying charting app that helps a woman identify her most fertile days to conceive. The Bellabeat Ivy is a women’s health smart bracelet with a strong focus on tracking a woman’s cycle and fertility, pregnancy, and postnatal symptoms. And Mirvie, which is currently in development, is a blood test that will be able to predict pregnancy complications earlier.
Physicians are also looking to move as much of the lab experience as they can into a patient’s home, which streamlines processes while offering privacy and comfort. For example, Dr. Hariton, who runs a strategic venture capital fund for physicians, said his team is currently working with a company that does remote ultrasounds.
And Mira, an at-home hormone monitor, uses patented AI algorithms to accurately measure the levels of major reproductive health hormones (E3G, LH, PdG, FSH) in urine, said Meir Olcha, MD, chief medical officer at Sama Fertility. The product recently completed a clinical trial, which showed it was a viable alternative to blood serum for patients undergoing IVF.
Stem cells could make eggs ageless
Research shows that a woman’s egg quality decreases gradually but significantly starting at age 32 and more rapidly after 37. Sperm quality may also decrease with age. A possible workaround: Scientists are actively researching how to create eggs and sperm from stem cells.
“I think getting eggs from stem cells will happen in the future,” said Dr. Hariton, who notes that this type of technology would be a game changer in his clinic. “It will make some of the hardest diagnoses that I have – which is on a daily basis, ‘I’m so sorry, you’re in premature menopause’ or ‘I don’t think we’re going to be successful getting you pregnant with your own eggs; here are some other options like donor eggs’ – much better,” he added. And stem cells are currently being used to research causes of infertility.
Clinics like UCLA have already been making strides. “We are using stem cells to identify new genes required for reproduction and to define the role of these genes in human fertility and infertility,” said Dr. Clark, a member of the Eli and Edythe Broad Center of Regenerative Medicine and Stem Cell Research at UCLA, who recently led a study in this arena. “In vitro gametogenesis (IVG), another stem cell technology, is currently used in the research lab to understand causes of infertility.”
These stem cell-based embryo models, she said, can help researchers understand the first few days of embryo development after an embryo implants and be used to provide critical information on causes of early pregnancy loss or birth defects.
A version of this article appeared on Medscape.com.
Fifth pregnancy, first baby.
After four pregnancies resulted in losses – and doing things as natural as possible and leaving it up to the birds, bees, and fate – my husband and I decided to explore in vitro fertilization (IVF).
Drugs to direct my follicles to produce more eggs, an egg retrieval procedure, genetic testing of our embryos, a quick procedure to remove a residual uterine septum from my uterus, drugs to thicken my endometrial lining to prepare my body to receive an embryo, an embryo transfer, steroids to suppress my immune system so my body would accept the pregnancy, blood thinner shots to promote blood flow to the baby, and 10 weeks of progesterone in oil shots later and we’re days away from welcoming our first baby into our lives.
In short, there’s more than one way to define “miracle baby.”
Global estimates say 48 million couples and 186 million individuals struggle with infertility. On average, 2 million infants born in the United States each year are conceived through assisted reproductive technology and the demand for treatments like IVF have doubled in the last decade.
Now the need for treatments outweighs clinician availability. “We have about 1,250 practicing fertility physicians in the U.S. to serve the whole country, which is highly inadequate,” said Eduardo Hariton, MD, a reproductive endocrinology physician in San Francisco and managing director of the U.S. Fertility Innovation Fund. “We have people that want to get care waiting 1 to 3 months to be seen.”
Dr. Hariton explains that U.S. IVF clinics are performing around 250,000 to 300,000 IVF cycles per year and need to be doing a million-plus to meet demand. This, plus the cost of fertility treatments – an average IVF cycle runs $23,500 and the majority of patients need multiple cycles to conceive – keeps the barrier to entry high.
Enter technology: New advances are on the way to help the assisted fertility process to run smoother and be less costly. “The field is really coming into an age of great progress and innovation,” added S. Zev Williams, MD, PhD, chief of the division of reproductive endocrinology and Infertility at Columbia University Irving Medical Center, New York City.
I’m personally grateful that such technology exists.
AI will help, of course
Fertility treatments involve endless analysis, diagnosis, and recommendations – dozens if not hundreds of decisions from each physician for each patient. Human action and reaction can affect this process, Dr. Hariton explained.
For example, if he hyperstimulated a woman during the follicle growing stage of her egg retrieval and ended up with eggs too large to retrieve, Dr. Hariton said he may subconsciously be more inclined to be extra cautious with his patients the week after, and vice versa.
This is where AI can help. “Rather than me making decisions from a couple of thousands of cycles of experience, I get to leverage hundreds of thousands of cycles from different providers over different people,” said Dr. Hariton. “I get to use all the data from that patient today – her age, her weight, what happened last cycle, how she’s doing – and make a very objective decision about the optimal time to give that woman or that couple the best outcome possible.”
AI can also assist with tasks like embryo grading. “Once our embryos are made in the lab, we usually have an embryologist looking at those embryos, grading them on a three-variable scale, and then picking the nicest one for transfer,” said Dr. Hariton. Machine learning computer vision software can help doctors select the best embryo.
Many of these AI products are in trials in the United States and some AI-based technology is already being used in fertility labs, especially in other countries. “ALife recently launched a suite of products to help with their decisions during stimulation that can help with the quality KPIs [key performance indicators] in the lab,” said Dr. Hariton. “There’s also a company that does AI-based predictions of success to give patients a better estimate called Univfy.” More AI products are still in development or awaiting Food and Drug Administration clearance.
Robots lend a hand
Like artificial intelligence, robots can be a big help in the IVF lab. Columbia University Fertility Center recently became the first to use an articulated (ART) robot to handle precise and highly repetitive work.
“IVF, from the initial point, involves creating these special plates where embryos can grow, and you do that by making little droplets,” said Dr. Williams. “It’s very time-consuming to create tons of these little droplets for the embryos to grow.” Thus, the lab created a robot to help squirt drops of the media substance required to sustain embryos in a way that is 10 times more precise than that of a trained embryologist.
“It’s a win-win because you allow the robots to do things better than a human can and this allows the humans to do things that a robot just can’t do,” explained Dr. Williams. He and his team began using this technology in the beginning of November 2022.
Dr. Williams sees ART robots being used in many more parts of the fertility treatment journey along the way, like preparing eggs after they are retrieved and performing intracytoplasmic sperm injection (ICSI), with the robot injecting the sperm into the egg.
Launching with the plate making, said Dr. Williams, is a low stakes entry point for robotic technology in the lab. “It allows us to introduce robotics to automate and optimize each step along the way, but to do so in the safest possible way.”
Dr. Williams estimates that robots will have their hands on actual eggs and sperm in 5 years.
Updates in genetic testing
Currently, if a couple wants to have their embryos genetically tested, also known as preimplantation genetic testing, each embryo must be frozen, then a biopsy of that embryo is performed and sent to the lab.
“It takes time to get the results,” said Dr. Williams. “The whole time you’re waiting, you don’t know if you’re going to have any embryos that are transferable or if next month you’re going to have to do another IVF cycle.”
Columbia researchers recently developed a new in-house test that can determine if a fetus or embryo has the right number of chromosomes. This STORK (Short-read Transpore Rapid Karyotyping) can be performed without freezing embryos and sending them out, which Dr. Williams said can save couples money and time, as they won’t necessarily need to do a separate embryo transfer cycle and can transfer an embryo in the same cycle. “You can test in the morning and transfer in the afternoon,” said Dr. Williams.
The test is currently awaiting approval and will first be used to test miscarriage samples to see if embryos were genetically normal or not, which he said should cost around $200 vs. the $2,000 to $4,000 it can cost to have fetal tissue sent to the lab – and insurance doesn’t cover the procedure until after a second or third miscarriage.
This, said Dr. Williams, should be in the field in less than a year, and he estimates that the test will be used for fresh embryos in about a year and a half.
Sperm collection made simpler
Typically, a man delivers a sperm sample in a room at an IVF clinic or by collecting a sample at home and rushing it to the clinic before it degrades, which Dr. Williams said can happen in as little as 15 minutes.
In 2020, Dr. Williams and his team began using a custom at-home sperm collection box that houses sperm in a recyclable foam container that holds a sample cup, which is filled with special sperm-supporting media, at an angle that prevents evaporation and maintains temperature and pH. This allows patients to collect samples in the comfort of their homes and increases the clock to 3 hours.
“It’s great for the patients because it’s much more comfortable,” said Dr. Williams, who notes that having to “perform” on site can be stressful for men. Studies the team has conducted have shown sperm collected in this manner have a better success rate than those collected in the lab, and 90% of Columbia’s Fertility Center patients are now providing sperm samples this way.
Similar innovations to deliver sperm, like Protex, are now on the market, while companies like myLabBox and Legacy are offering at-home sperm testing kits to mail in for a full semen analysis.
At-home monitoring: More and better
Wearable reproductive health devices are also helping more women get pregnant. “I am very excited about biometric data harnessed in wearables to predict periods, ovulation, and fertility,” said Amander Clark, PhD, director of the UCLA Center for Reproductive Science, Health, and Education, Los Angeles.
The Tempdrop Fertility and Ovulation Tracker, for instance, is a wearable sensor with an accompanying charting app that helps a woman identify her most fertile days to conceive. The Bellabeat Ivy is a women’s health smart bracelet with a strong focus on tracking a woman’s cycle and fertility, pregnancy, and postnatal symptoms. And Mirvie, which is currently in development, is a blood test that will be able to predict pregnancy complications earlier.
Physicians are also looking to move as much of the lab experience as they can into a patient’s home, which streamlines processes while offering privacy and comfort. For example, Dr. Hariton, who runs a strategic venture capital fund for physicians, said his team is currently working with a company that does remote ultrasounds.
And Mira, an at-home hormone monitor, uses patented AI algorithms to accurately measure the levels of major reproductive health hormones (E3G, LH, PdG, FSH) in urine, said Meir Olcha, MD, chief medical officer at Sama Fertility. The product recently completed a clinical trial, which showed it was a viable alternative to blood serum for patients undergoing IVF.
Stem cells could make eggs ageless
Research shows that a woman’s egg quality decreases gradually but significantly starting at age 32 and more rapidly after 37. Sperm quality may also decrease with age. A possible workaround: Scientists are actively researching how to create eggs and sperm from stem cells.
“I think getting eggs from stem cells will happen in the future,” said Dr. Hariton, who notes that this type of technology would be a game changer in his clinic. “It will make some of the hardest diagnoses that I have – which is on a daily basis, ‘I’m so sorry, you’re in premature menopause’ or ‘I don’t think we’re going to be successful getting you pregnant with your own eggs; here are some other options like donor eggs’ – much better,” he added. And stem cells are currently being used to research causes of infertility.
Clinics like UCLA have already been making strides. “We are using stem cells to identify new genes required for reproduction and to define the role of these genes in human fertility and infertility,” said Dr. Clark, a member of the Eli and Edythe Broad Center of Regenerative Medicine and Stem Cell Research at UCLA, who recently led a study in this arena. “In vitro gametogenesis (IVG), another stem cell technology, is currently used in the research lab to understand causes of infertility.”
These stem cell-based embryo models, she said, can help researchers understand the first few days of embryo development after an embryo implants and be used to provide critical information on causes of early pregnancy loss or birth defects.
A version of this article appeared on Medscape.com.
Affordable IVF – Are we there yet?
The price for an in vitro fertilization (IVF) cycle continues to increase annually by many clinics, particularly because of “add-ons” of dubious value.
The initial application of IVF was for tubal factor infertility. Over the decades since 1981, the year of the first successful live birth in the United States, indications for IVF have dramatically expanded – ovulation dysfunction, unexplained infertility, male factor, advanced stage endometriosis, unexplained infertility, embryo testing to avoid an inherited genetic disease from the intended parents carrying the same mutation, and family balancing for gender, along with fertility preservation, including before potentially gonadotoxic treatment and “elective” planned oocyte cryopreservation.
From RESOLVE.org, the National Infertility Association: “As of June 2022, 20 states have passed fertility insurance coverage laws, 14 of those laws include IVF coverage, and 12 states have fertility preservation laws for iatrogenic (medically induced) infertility.” Consequently, “affordable IVF” is paramount to providing equal access for patients.
I spoke with the past president of The Society for Assisted Reproductive Technology (SART.org), Kevin Doody, MD, HCLD, to discuss current IVF treatment options for couples that may decrease their financial burden, particularly by applying a novel approach – called INVOcell – that involves using the woman’s vagina as the embryo “incubator.” Dr. Doody is director of CARE Fertility in Bedford, Tex., and clinical professor at UT Southwestern Medical Center, Dallas.
How does limiting the dosage of gonadotropins in IVF cycles, known as “minimal stimulation,” affect pregnancy outcomes?
IVF medications are often costly, so it is logical to try and minimize expenses by using them judiciously. “Minimal stimulation” generally is not the best approach, as having more eggs usually leads to better pregnancy rates. High egg yield increases short-term success and provides additional embryos for future attempts.
However, extremely high gonadotropin doses do not necessarily yield more eggs or successful pregnancies. The dose response to gonadotropins follows a sigmoid curve, and typically doses beyond 225-300 IU per day do not offer additional benefits, except for women with an elevated body weight. Yet, some physicians continue to use higher doses in women with low ovarian reserve, which is often not beneficial and can add unnecessary costs.
Is “natural cycle” IVF cost-effective with acceptable pregnancy success rates?
Although the first-ever IVF baby was conceived through a natural cycle, this approach has very low success rates. Even with advancements in IVF laboratory technologies, the outcomes of natural cycle IVF have remained disappointingly low and are generally considered unacceptable.
Are there other cost-saving alternatives for IVF that still maintain reasonable success rates?
Some patients can undergo a more simplified ovarian stimulation protocol that reduces the number of monitoring visits, thus reducing costs. In couples without a severe male factor, the application and additional expense of intracytoplasmic sperm injection (ICSI) is unnecessary. Pre-implantation genetic testing for embryo aneuploidy, another “add-on” procedure, has specific indications and medical evidence does not support its use in all patient cycles.
How can the cost of a standard IVF cycle be reduced, especially in areas without mandated infertility insurance coverage?
Addressing this issue involves considering principles of justice in medical ethics, which emphasize equal health care access for all individuals. Infertility is a medical condition and IVF is expensive, so lack of insurance coverage often restricts access. Our clinic offers a more affordable option called “effortless IVF” using an intravaginal culture system (INVOcell), which minimizes the monitoring process while maintaining satisfactory success rates and reducing the risks associated with ovarian hyperstimulation syndrome.
What is INVOcell, and how successful is it in terms of live birth rates?
INVOcell is an innovative approach to IVF, where an intravaginal culture system is used as an “embryo incubator whereby freshly harvested eggs along with sperm are immediately added to a small chamber device that is placed in the woman’s vagina for up to 5 days to allow for fertilization and embryo development.” The woman, typically, has no discomfort from the device. For appropriately selected patients, the literature has shown live birth rates are comparable to those achieved using conventional laboratory incubation systems.
As an early participant in INVOcell research, can you share insights on the ideal candidates for this procedure and any contraindications?
The INVOcell system is best suited for straightforward cases. It is not recommended for severe male factor infertility requiring ICSI, since this will delay application of the chamber device and increase cost. Further, cases involving preimplantation genetic testing are not recommended because the embryos may not develop synchronously within the device to the embryo stage needed for a biopsy.
What training is required for embryologists and physicians to use INVOcell?
Embryologists require training for a few hours to learn the basics of INVOcell. They must master loading eggs into and retrieving embryos from the device. Practicing on discarded eggs and embryos, embryologists can accelerate the acquisition of the proper technique needed for INVOcell. Physicians find the training easier; they mainly need to learn the correct placement and removal of the device in the vagina.
Is INVOcell gaining acceptance among patients and IVF centers?
Acceptance varies. In our practice, INVOcell has largely replaced superovulation and intrauterine insemination treatments. However, some clinics still need to determine how this tool fits within their practice.
Have IVF success rates plateaued as affordable options increase?
IVF success rates grew substantially in the 1980s and 1990s, fostered by improved embryo culture systems and higher numbers of embryos transferred, the latter at the expense of a multiple gestation. While the rate of improvement has slowed, coinciding with the increasing use of single embryo transfer, advancements in IVF continue toward the goal of improving the singleton live birth rate per IVF cycle. There is still room for enhancement in success rates alongside cost reduction. Continued innovation is needed, especially for patients with challenging underlying biological issues.
Can you provide insight into the next potential breakthrough in IVF that may reduce costs, be less invasive, and maintain optimal pregnancy rates?
I am very excited about recent breakthroughs in in vitro maturation (IVM) of oocytes. The bottleneck in IVF clinics (and significant expense) primarily relates to the need to stimulate the ovaries to get mature and competent eggs. The technology of IVM has existed for decades but has yet to be fully embraced by clinics because of the poor competency of oocytes matured in the laboratory.
Immature eggs resume meiosis immediately upon removal from the ovary. Nuclear maturation of eggs in the lab is easy. In fact, it happens too quickly, thereby not allowing for the maturation of the egg cytoplasm. This has previously led to poor development of embryos following fertilization and low success rates.
Recently, a new laboratory strategy has resulted in a significant improvement in success. This improved culture system uses a peptide that prevents the resumption of meiosis for the initial culture time frame. Substances, including follicle stimulating hormone, can be added to the media to promote oocyte cytoplasmic maturation. Following this, the eggs are placed in a media without the meiosis inhibitor to allow for nuclear maturation. This results in a significantly higher proportion of competent mature eggs.
Dr. Trolice is director of The IVF Center in Winter Park, Fla., and professor of obstetrics and gynecology at the University of Central Florida, Orlando.
The price for an in vitro fertilization (IVF) cycle continues to increase annually by many clinics, particularly because of “add-ons” of dubious value.
The initial application of IVF was for tubal factor infertility. Over the decades since 1981, the year of the first successful live birth in the United States, indications for IVF have dramatically expanded – ovulation dysfunction, unexplained infertility, male factor, advanced stage endometriosis, unexplained infertility, embryo testing to avoid an inherited genetic disease from the intended parents carrying the same mutation, and family balancing for gender, along with fertility preservation, including before potentially gonadotoxic treatment and “elective” planned oocyte cryopreservation.
From RESOLVE.org, the National Infertility Association: “As of June 2022, 20 states have passed fertility insurance coverage laws, 14 of those laws include IVF coverage, and 12 states have fertility preservation laws for iatrogenic (medically induced) infertility.” Consequently, “affordable IVF” is paramount to providing equal access for patients.
I spoke with the past president of The Society for Assisted Reproductive Technology (SART.org), Kevin Doody, MD, HCLD, to discuss current IVF treatment options for couples that may decrease their financial burden, particularly by applying a novel approach – called INVOcell – that involves using the woman’s vagina as the embryo “incubator.” Dr. Doody is director of CARE Fertility in Bedford, Tex., and clinical professor at UT Southwestern Medical Center, Dallas.
How does limiting the dosage of gonadotropins in IVF cycles, known as “minimal stimulation,” affect pregnancy outcomes?
IVF medications are often costly, so it is logical to try and minimize expenses by using them judiciously. “Minimal stimulation” generally is not the best approach, as having more eggs usually leads to better pregnancy rates. High egg yield increases short-term success and provides additional embryos for future attempts.
However, extremely high gonadotropin doses do not necessarily yield more eggs or successful pregnancies. The dose response to gonadotropins follows a sigmoid curve, and typically doses beyond 225-300 IU per day do not offer additional benefits, except for women with an elevated body weight. Yet, some physicians continue to use higher doses in women with low ovarian reserve, which is often not beneficial and can add unnecessary costs.
Is “natural cycle” IVF cost-effective with acceptable pregnancy success rates?
Although the first-ever IVF baby was conceived through a natural cycle, this approach has very low success rates. Even with advancements in IVF laboratory technologies, the outcomes of natural cycle IVF have remained disappointingly low and are generally considered unacceptable.
Are there other cost-saving alternatives for IVF that still maintain reasonable success rates?
Some patients can undergo a more simplified ovarian stimulation protocol that reduces the number of monitoring visits, thus reducing costs. In couples without a severe male factor, the application and additional expense of intracytoplasmic sperm injection (ICSI) is unnecessary. Pre-implantation genetic testing for embryo aneuploidy, another “add-on” procedure, has specific indications and medical evidence does not support its use in all patient cycles.
How can the cost of a standard IVF cycle be reduced, especially in areas without mandated infertility insurance coverage?
Addressing this issue involves considering principles of justice in medical ethics, which emphasize equal health care access for all individuals. Infertility is a medical condition and IVF is expensive, so lack of insurance coverage often restricts access. Our clinic offers a more affordable option called “effortless IVF” using an intravaginal culture system (INVOcell), which minimizes the monitoring process while maintaining satisfactory success rates and reducing the risks associated with ovarian hyperstimulation syndrome.
What is INVOcell, and how successful is it in terms of live birth rates?
INVOcell is an innovative approach to IVF, where an intravaginal culture system is used as an “embryo incubator whereby freshly harvested eggs along with sperm are immediately added to a small chamber device that is placed in the woman’s vagina for up to 5 days to allow for fertilization and embryo development.” The woman, typically, has no discomfort from the device. For appropriately selected patients, the literature has shown live birth rates are comparable to those achieved using conventional laboratory incubation systems.
As an early participant in INVOcell research, can you share insights on the ideal candidates for this procedure and any contraindications?
The INVOcell system is best suited for straightforward cases. It is not recommended for severe male factor infertility requiring ICSI, since this will delay application of the chamber device and increase cost. Further, cases involving preimplantation genetic testing are not recommended because the embryos may not develop synchronously within the device to the embryo stage needed for a biopsy.
What training is required for embryologists and physicians to use INVOcell?
Embryologists require training for a few hours to learn the basics of INVOcell. They must master loading eggs into and retrieving embryos from the device. Practicing on discarded eggs and embryos, embryologists can accelerate the acquisition of the proper technique needed for INVOcell. Physicians find the training easier; they mainly need to learn the correct placement and removal of the device in the vagina.
Is INVOcell gaining acceptance among patients and IVF centers?
Acceptance varies. In our practice, INVOcell has largely replaced superovulation and intrauterine insemination treatments. However, some clinics still need to determine how this tool fits within their practice.
Have IVF success rates plateaued as affordable options increase?
IVF success rates grew substantially in the 1980s and 1990s, fostered by improved embryo culture systems and higher numbers of embryos transferred, the latter at the expense of a multiple gestation. While the rate of improvement has slowed, coinciding with the increasing use of single embryo transfer, advancements in IVF continue toward the goal of improving the singleton live birth rate per IVF cycle. There is still room for enhancement in success rates alongside cost reduction. Continued innovation is needed, especially for patients with challenging underlying biological issues.
Can you provide insight into the next potential breakthrough in IVF that may reduce costs, be less invasive, and maintain optimal pregnancy rates?
I am very excited about recent breakthroughs in in vitro maturation (IVM) of oocytes. The bottleneck in IVF clinics (and significant expense) primarily relates to the need to stimulate the ovaries to get mature and competent eggs. The technology of IVM has existed for decades but has yet to be fully embraced by clinics because of the poor competency of oocytes matured in the laboratory.
Immature eggs resume meiosis immediately upon removal from the ovary. Nuclear maturation of eggs in the lab is easy. In fact, it happens too quickly, thereby not allowing for the maturation of the egg cytoplasm. This has previously led to poor development of embryos following fertilization and low success rates.
Recently, a new laboratory strategy has resulted in a significant improvement in success. This improved culture system uses a peptide that prevents the resumption of meiosis for the initial culture time frame. Substances, including follicle stimulating hormone, can be added to the media to promote oocyte cytoplasmic maturation. Following this, the eggs are placed in a media without the meiosis inhibitor to allow for nuclear maturation. This results in a significantly higher proportion of competent mature eggs.
Dr. Trolice is director of The IVF Center in Winter Park, Fla., and professor of obstetrics and gynecology at the University of Central Florida, Orlando.
The price for an in vitro fertilization (IVF) cycle continues to increase annually by many clinics, particularly because of “add-ons” of dubious value.
The initial application of IVF was for tubal factor infertility. Over the decades since 1981, the year of the first successful live birth in the United States, indications for IVF have dramatically expanded – ovulation dysfunction, unexplained infertility, male factor, advanced stage endometriosis, unexplained infertility, embryo testing to avoid an inherited genetic disease from the intended parents carrying the same mutation, and family balancing for gender, along with fertility preservation, including before potentially gonadotoxic treatment and “elective” planned oocyte cryopreservation.
From RESOLVE.org, the National Infertility Association: “As of June 2022, 20 states have passed fertility insurance coverage laws, 14 of those laws include IVF coverage, and 12 states have fertility preservation laws for iatrogenic (medically induced) infertility.” Consequently, “affordable IVF” is paramount to providing equal access for patients.
I spoke with the past president of The Society for Assisted Reproductive Technology (SART.org), Kevin Doody, MD, HCLD, to discuss current IVF treatment options for couples that may decrease their financial burden, particularly by applying a novel approach – called INVOcell – that involves using the woman’s vagina as the embryo “incubator.” Dr. Doody is director of CARE Fertility in Bedford, Tex., and clinical professor at UT Southwestern Medical Center, Dallas.
How does limiting the dosage of gonadotropins in IVF cycles, known as “minimal stimulation,” affect pregnancy outcomes?
IVF medications are often costly, so it is logical to try and minimize expenses by using them judiciously. “Minimal stimulation” generally is not the best approach, as having more eggs usually leads to better pregnancy rates. High egg yield increases short-term success and provides additional embryos for future attempts.
However, extremely high gonadotropin doses do not necessarily yield more eggs or successful pregnancies. The dose response to gonadotropins follows a sigmoid curve, and typically doses beyond 225-300 IU per day do not offer additional benefits, except for women with an elevated body weight. Yet, some physicians continue to use higher doses in women with low ovarian reserve, which is often not beneficial and can add unnecessary costs.
Is “natural cycle” IVF cost-effective with acceptable pregnancy success rates?
Although the first-ever IVF baby was conceived through a natural cycle, this approach has very low success rates. Even with advancements in IVF laboratory technologies, the outcomes of natural cycle IVF have remained disappointingly low and are generally considered unacceptable.
Are there other cost-saving alternatives for IVF that still maintain reasonable success rates?
Some patients can undergo a more simplified ovarian stimulation protocol that reduces the number of monitoring visits, thus reducing costs. In couples without a severe male factor, the application and additional expense of intracytoplasmic sperm injection (ICSI) is unnecessary. Pre-implantation genetic testing for embryo aneuploidy, another “add-on” procedure, has specific indications and medical evidence does not support its use in all patient cycles.
How can the cost of a standard IVF cycle be reduced, especially in areas without mandated infertility insurance coverage?
Addressing this issue involves considering principles of justice in medical ethics, which emphasize equal health care access for all individuals. Infertility is a medical condition and IVF is expensive, so lack of insurance coverage often restricts access. Our clinic offers a more affordable option called “effortless IVF” using an intravaginal culture system (INVOcell), which minimizes the monitoring process while maintaining satisfactory success rates and reducing the risks associated with ovarian hyperstimulation syndrome.
What is INVOcell, and how successful is it in terms of live birth rates?
INVOcell is an innovative approach to IVF, where an intravaginal culture system is used as an “embryo incubator whereby freshly harvested eggs along with sperm are immediately added to a small chamber device that is placed in the woman’s vagina for up to 5 days to allow for fertilization and embryo development.” The woman, typically, has no discomfort from the device. For appropriately selected patients, the literature has shown live birth rates are comparable to those achieved using conventional laboratory incubation systems.
As an early participant in INVOcell research, can you share insights on the ideal candidates for this procedure and any contraindications?
The INVOcell system is best suited for straightforward cases. It is not recommended for severe male factor infertility requiring ICSI, since this will delay application of the chamber device and increase cost. Further, cases involving preimplantation genetic testing are not recommended because the embryos may not develop synchronously within the device to the embryo stage needed for a biopsy.
What training is required for embryologists and physicians to use INVOcell?
Embryologists require training for a few hours to learn the basics of INVOcell. They must master loading eggs into and retrieving embryos from the device. Practicing on discarded eggs and embryos, embryologists can accelerate the acquisition of the proper technique needed for INVOcell. Physicians find the training easier; they mainly need to learn the correct placement and removal of the device in the vagina.
Is INVOcell gaining acceptance among patients and IVF centers?
Acceptance varies. In our practice, INVOcell has largely replaced superovulation and intrauterine insemination treatments. However, some clinics still need to determine how this tool fits within their practice.
Have IVF success rates plateaued as affordable options increase?
IVF success rates grew substantially in the 1980s and 1990s, fostered by improved embryo culture systems and higher numbers of embryos transferred, the latter at the expense of a multiple gestation. While the rate of improvement has slowed, coinciding with the increasing use of single embryo transfer, advancements in IVF continue toward the goal of improving the singleton live birth rate per IVF cycle. There is still room for enhancement in success rates alongside cost reduction. Continued innovation is needed, especially for patients with challenging underlying biological issues.
Can you provide insight into the next potential breakthrough in IVF that may reduce costs, be less invasive, and maintain optimal pregnancy rates?
I am very excited about recent breakthroughs in in vitro maturation (IVM) of oocytes. The bottleneck in IVF clinics (and significant expense) primarily relates to the need to stimulate the ovaries to get mature and competent eggs. The technology of IVM has existed for decades but has yet to be fully embraced by clinics because of the poor competency of oocytes matured in the laboratory.
Immature eggs resume meiosis immediately upon removal from the ovary. Nuclear maturation of eggs in the lab is easy. In fact, it happens too quickly, thereby not allowing for the maturation of the egg cytoplasm. This has previously led to poor development of embryos following fertilization and low success rates.
Recently, a new laboratory strategy has resulted in a significant improvement in success. This improved culture system uses a peptide that prevents the resumption of meiosis for the initial culture time frame. Substances, including follicle stimulating hormone, can be added to the media to promote oocyte cytoplasmic maturation. Following this, the eggs are placed in a media without the meiosis inhibitor to allow for nuclear maturation. This results in a significantly higher proportion of competent mature eggs.
Dr. Trolice is director of The IVF Center in Winter Park, Fla., and professor of obstetrics and gynecology at the University of Central Florida, Orlando.
FDA approves first over-the-counter birth control pill
The Food and Drug Administration’s approval today of the first birth control pill for women to be available without a prescription is being hailed by many as a long-needed development, but there remain questions to be resolved, including how much the drug will cost and how it will be used.
The drug, Opill, is expected to be available early next year, and its maker has yet to reveal a retail price. It is the same birth control pill that has been available by prescription for 50 years. But for the first time, women will be able to buy the contraception at a local pharmacy, other retail locations, or online without having to see a doctor first.
Likely to drive debate
Contraception in the United States is not without controversy. The FDA’s approval spurred reactions both for and against making hormonal birth control for women available without a prescription.
“It’s an exciting time, especially right now when reproductive rights are being curtailed in a lot of states. Giving people an additional option for contraception will change people’s lives,” said Beverly Gray, MD, division director of Women’s Community and Population Health at Duke University Medical Center in Durham, N.C.
“It’s a huge win for patients who need better access to contraception,” said Dr. Gray, who is also a spokesperson for the American College of Obstetricians and Gynecologists.
Women who want hormonal birth control but live in areas without convenient access to a doctor, women who cannot easily take time off of work to see a doctor and get a prescription filled, and women without insurance are examples of people who will benefit, she said.
The Catholic Medical Association, in contrast, expressed “deep concern and disappointment” after an FDA advisory committee’s unanimous vote on May 11 recommending the drug be available over the counter. In a statement after the vote, the group cited “extensive medical studies demonstrating the risks and adverse effects of hormonal contraceptives,” adding that “the social impact of [full approval] would be dramatic.”
But doctors largely disagreed.
“It is definitely a huge win for reproductive autonomy. I’m glad that the FDA is prioritizing patient safety and well-being over politics,” said Catherine Cansino, MD, MPH, an ob.gyn. and clinical professor in the University of California Davis department of obstetrics and gynecology. She said the FDA approved the over-the-counter version because the medication is safe.
While opponents like the Catholic Medical Association cite safety concerns and believe doctors should screen all women before prescribing hormonal contraception, Dr. Gray disagreed. “There’s a lot of evidence that patients can figure out if a progestin-only pill is right for them and safe for them. Medical professionals don’t have to be the gatekeepers for contraception,” she said.
Pricing unknown
Whether insurance companies will pay for Opill now that it will be available without a prescription remains unknown. For some medications, paying a copay through insurance can be less expensive than buying at a retail price.
“Although pricing issues will be relevant, the FDA’s decision will enhance women’s access to hormonal birth control,” said Andrew M. Kaunitz, MD, a professor and associate chairman in the department of obstetrics and gynecology at the University of Florida College of Medicine in Jacksonville.
The drugmaker, Perrigo, based in Ireland, has not yet announced how much the pill will cost. The price tag could affect how widely available this form of birth control is. The drug has been shown to be as much as 93% effective for pregnancy prevention. Perrigo says it plans to make the pill available at low or no cost to some women.
Caveats to consider
There are some women for whom hormonal contraceptives have always carried greater risks. For example, women who have breast cancer or a history of breast cancer should not use hormonal contraceptives, the FDA said in a news release announcing the approval. Women with other types of cancer should check with their doctors first, the agency noted.
Women who smoke, who take some medications to lower blood pressure, or who have migraines should also take caution, Dr. Cansino said. “People with migraines may not be suitable for over-the-counter oral contraceptives. But a simple screening through a provider can identify whether you are truly eligible or not.”
Irregular bleeding, headaches, dizziness, nausea, increased appetite, belly pain, cramps, or bloating are the most common side effects of Opill, the FDA said.
The Opill is a progestin-only birth control pill. Similar pills have been available in the United Kingdiom for about 2 years, often referred to as “mini pills” because they contain a single hormone. In contrast, prescription birth control pills in the United States and elsewhere contain more than one hormone, estrogen and progestin, to prevent pregnancy.
Prescription pill packs for combination contraception often feature a week of placebo pills without an active ingredient. While skipping a placebo pill might not make a difference in pregnancy prevention, Opill is different. Every pill in the packet will contain medication, Gray said. “So it’s important to take the pill the same time every day for it to be most effective.”
Even though this may mean one less visit to your doctor, Dr. Kaunitz hopes women will stay up to date on their other medical checkups. “One of our challenges as providers of care to women will be to encourage them to continue to receive important services, including cancer screening and vaccinations, even while they can initiate and continue hormonal contraception without contact with a provider.”
Just the beginning?
The American Medical Association hopes this approval signals more to come.
“While we applaud this move, the AMA continues to urge the FDA and HHS to consider a variety of oral contraceptive options for over-the-counter use,” the association, which has more than 250,000 doctor members, said in a statement. “It is important patients have options when choosing which type of birth control works best for them,”
The American College of Obstetricians and Gynecologists said the FDA’s decision will help many women. “We are glad that more patients will now be empowered to choose when and where they obtain a safe method of contraception without having to wait for a medical appointment or for a prescription to be filled,” Verda J. Hicks, MD, the group’s president, and Christopher M. Zahn, MD, interim chief executive officer, said in a statement.
“Allowing individuals to access birth control at their local pharmacy or drug store will eliminate some barriers,” they said.
A version of this article first appeared on WebMD.com.
This article was updated 7/13/23.
The Food and Drug Administration’s approval today of the first birth control pill for women to be available without a prescription is being hailed by many as a long-needed development, but there remain questions to be resolved, including how much the drug will cost and how it will be used.
The drug, Opill, is expected to be available early next year, and its maker has yet to reveal a retail price. It is the same birth control pill that has been available by prescription for 50 years. But for the first time, women will be able to buy the contraception at a local pharmacy, other retail locations, or online without having to see a doctor first.
Likely to drive debate
Contraception in the United States is not without controversy. The FDA’s approval spurred reactions both for and against making hormonal birth control for women available without a prescription.
“It’s an exciting time, especially right now when reproductive rights are being curtailed in a lot of states. Giving people an additional option for contraception will change people’s lives,” said Beverly Gray, MD, division director of Women’s Community and Population Health at Duke University Medical Center in Durham, N.C.
“It’s a huge win for patients who need better access to contraception,” said Dr. Gray, who is also a spokesperson for the American College of Obstetricians and Gynecologists.
Women who want hormonal birth control but live in areas without convenient access to a doctor, women who cannot easily take time off of work to see a doctor and get a prescription filled, and women without insurance are examples of people who will benefit, she said.
The Catholic Medical Association, in contrast, expressed “deep concern and disappointment” after an FDA advisory committee’s unanimous vote on May 11 recommending the drug be available over the counter. In a statement after the vote, the group cited “extensive medical studies demonstrating the risks and adverse effects of hormonal contraceptives,” adding that “the social impact of [full approval] would be dramatic.”
But doctors largely disagreed.
“It is definitely a huge win for reproductive autonomy. I’m glad that the FDA is prioritizing patient safety and well-being over politics,” said Catherine Cansino, MD, MPH, an ob.gyn. and clinical professor in the University of California Davis department of obstetrics and gynecology. She said the FDA approved the over-the-counter version because the medication is safe.
While opponents like the Catholic Medical Association cite safety concerns and believe doctors should screen all women before prescribing hormonal contraception, Dr. Gray disagreed. “There’s a lot of evidence that patients can figure out if a progestin-only pill is right for them and safe for them. Medical professionals don’t have to be the gatekeepers for contraception,” she said.
Pricing unknown
Whether insurance companies will pay for Opill now that it will be available without a prescription remains unknown. For some medications, paying a copay through insurance can be less expensive than buying at a retail price.
“Although pricing issues will be relevant, the FDA’s decision will enhance women’s access to hormonal birth control,” said Andrew M. Kaunitz, MD, a professor and associate chairman in the department of obstetrics and gynecology at the University of Florida College of Medicine in Jacksonville.
The drugmaker, Perrigo, based in Ireland, has not yet announced how much the pill will cost. The price tag could affect how widely available this form of birth control is. The drug has been shown to be as much as 93% effective for pregnancy prevention. Perrigo says it plans to make the pill available at low or no cost to some women.
Caveats to consider
There are some women for whom hormonal contraceptives have always carried greater risks. For example, women who have breast cancer or a history of breast cancer should not use hormonal contraceptives, the FDA said in a news release announcing the approval. Women with other types of cancer should check with their doctors first, the agency noted.
Women who smoke, who take some medications to lower blood pressure, or who have migraines should also take caution, Dr. Cansino said. “People with migraines may not be suitable for over-the-counter oral contraceptives. But a simple screening through a provider can identify whether you are truly eligible or not.”
Irregular bleeding, headaches, dizziness, nausea, increased appetite, belly pain, cramps, or bloating are the most common side effects of Opill, the FDA said.
The Opill is a progestin-only birth control pill. Similar pills have been available in the United Kingdiom for about 2 years, often referred to as “mini pills” because they contain a single hormone. In contrast, prescription birth control pills in the United States and elsewhere contain more than one hormone, estrogen and progestin, to prevent pregnancy.
Prescription pill packs for combination contraception often feature a week of placebo pills without an active ingredient. While skipping a placebo pill might not make a difference in pregnancy prevention, Opill is different. Every pill in the packet will contain medication, Gray said. “So it’s important to take the pill the same time every day for it to be most effective.”
Even though this may mean one less visit to your doctor, Dr. Kaunitz hopes women will stay up to date on their other medical checkups. “One of our challenges as providers of care to women will be to encourage them to continue to receive important services, including cancer screening and vaccinations, even while they can initiate and continue hormonal contraception without contact with a provider.”
Just the beginning?
The American Medical Association hopes this approval signals more to come.
“While we applaud this move, the AMA continues to urge the FDA and HHS to consider a variety of oral contraceptive options for over-the-counter use,” the association, which has more than 250,000 doctor members, said in a statement. “It is important patients have options when choosing which type of birth control works best for them,”
The American College of Obstetricians and Gynecologists said the FDA’s decision will help many women. “We are glad that more patients will now be empowered to choose when and where they obtain a safe method of contraception without having to wait for a medical appointment or for a prescription to be filled,” Verda J. Hicks, MD, the group’s president, and Christopher M. Zahn, MD, interim chief executive officer, said in a statement.
“Allowing individuals to access birth control at their local pharmacy or drug store will eliminate some barriers,” they said.
A version of this article first appeared on WebMD.com.
This article was updated 7/13/23.
The Food and Drug Administration’s approval today of the first birth control pill for women to be available without a prescription is being hailed by many as a long-needed development, but there remain questions to be resolved, including how much the drug will cost and how it will be used.
The drug, Opill, is expected to be available early next year, and its maker has yet to reveal a retail price. It is the same birth control pill that has been available by prescription for 50 years. But for the first time, women will be able to buy the contraception at a local pharmacy, other retail locations, or online without having to see a doctor first.
Likely to drive debate
Contraception in the United States is not without controversy. The FDA’s approval spurred reactions both for and against making hormonal birth control for women available without a prescription.
“It’s an exciting time, especially right now when reproductive rights are being curtailed in a lot of states. Giving people an additional option for contraception will change people’s lives,” said Beverly Gray, MD, division director of Women’s Community and Population Health at Duke University Medical Center in Durham, N.C.
“It’s a huge win for patients who need better access to contraception,” said Dr. Gray, who is also a spokesperson for the American College of Obstetricians and Gynecologists.
Women who want hormonal birth control but live in areas without convenient access to a doctor, women who cannot easily take time off of work to see a doctor and get a prescription filled, and women without insurance are examples of people who will benefit, she said.
The Catholic Medical Association, in contrast, expressed “deep concern and disappointment” after an FDA advisory committee’s unanimous vote on May 11 recommending the drug be available over the counter. In a statement after the vote, the group cited “extensive medical studies demonstrating the risks and adverse effects of hormonal contraceptives,” adding that “the social impact of [full approval] would be dramatic.”
But doctors largely disagreed.
“It is definitely a huge win for reproductive autonomy. I’m glad that the FDA is prioritizing patient safety and well-being over politics,” said Catherine Cansino, MD, MPH, an ob.gyn. and clinical professor in the University of California Davis department of obstetrics and gynecology. She said the FDA approved the over-the-counter version because the medication is safe.
While opponents like the Catholic Medical Association cite safety concerns and believe doctors should screen all women before prescribing hormonal contraception, Dr. Gray disagreed. “There’s a lot of evidence that patients can figure out if a progestin-only pill is right for them and safe for them. Medical professionals don’t have to be the gatekeepers for contraception,” she said.
Pricing unknown
Whether insurance companies will pay for Opill now that it will be available without a prescription remains unknown. For some medications, paying a copay through insurance can be less expensive than buying at a retail price.
“Although pricing issues will be relevant, the FDA’s decision will enhance women’s access to hormonal birth control,” said Andrew M. Kaunitz, MD, a professor and associate chairman in the department of obstetrics and gynecology at the University of Florida College of Medicine in Jacksonville.
The drugmaker, Perrigo, based in Ireland, has not yet announced how much the pill will cost. The price tag could affect how widely available this form of birth control is. The drug has been shown to be as much as 93% effective for pregnancy prevention. Perrigo says it plans to make the pill available at low or no cost to some women.
Caveats to consider
There are some women for whom hormonal contraceptives have always carried greater risks. For example, women who have breast cancer or a history of breast cancer should not use hormonal contraceptives, the FDA said in a news release announcing the approval. Women with other types of cancer should check with their doctors first, the agency noted.
Women who smoke, who take some medications to lower blood pressure, or who have migraines should also take caution, Dr. Cansino said. “People with migraines may not be suitable for over-the-counter oral contraceptives. But a simple screening through a provider can identify whether you are truly eligible or not.”
Irregular bleeding, headaches, dizziness, nausea, increased appetite, belly pain, cramps, or bloating are the most common side effects of Opill, the FDA said.
The Opill is a progestin-only birth control pill. Similar pills have been available in the United Kingdiom for about 2 years, often referred to as “mini pills” because they contain a single hormone. In contrast, prescription birth control pills in the United States and elsewhere contain more than one hormone, estrogen and progestin, to prevent pregnancy.
Prescription pill packs for combination contraception often feature a week of placebo pills without an active ingredient. While skipping a placebo pill might not make a difference in pregnancy prevention, Opill is different. Every pill in the packet will contain medication, Gray said. “So it’s important to take the pill the same time every day for it to be most effective.”
Even though this may mean one less visit to your doctor, Dr. Kaunitz hopes women will stay up to date on their other medical checkups. “One of our challenges as providers of care to women will be to encourage them to continue to receive important services, including cancer screening and vaccinations, even while they can initiate and continue hormonal contraception without contact with a provider.”
Just the beginning?
The American Medical Association hopes this approval signals more to come.
“While we applaud this move, the AMA continues to urge the FDA and HHS to consider a variety of oral contraceptive options for over-the-counter use,” the association, which has more than 250,000 doctor members, said in a statement. “It is important patients have options when choosing which type of birth control works best for them,”
The American College of Obstetricians and Gynecologists said the FDA’s decision will help many women. “We are glad that more patients will now be empowered to choose when and where they obtain a safe method of contraception without having to wait for a medical appointment or for a prescription to be filled,” Verda J. Hicks, MD, the group’s president, and Christopher M. Zahn, MD, interim chief executive officer, said in a statement.
“Allowing individuals to access birth control at their local pharmacy or drug store will eliminate some barriers,” they said.
A version of this article first appeared on WebMD.com.
This article was updated 7/13/23.
Do oral contraceptives increase depression risk?
In addition, OC use in adolescence has been tied to an increased risk for depression later in life. However, some experts believe the study’s methodology may be flawed.
The investigators tracked more than 250,000 women from birth to menopause, gathering information about their use of combined contraceptive pills (progesterone and estrogen), the timing of the initial depression diagnosis, and the onset of depressive symptoms that were not formally diagnosed.
Women who began using these OCs before or at the age of 20 experienced a 130% higher incidence of depressive symptoms, whereas adult users saw a 92% increase. But the higher occurrence of depression tended to decline after the first 2 years of use, except in teenagers, who maintained an increased incidence of depression even after discontinuation.
This effect remained, even after analysis of potential familial confounding.
“Our findings suggest that the use of OCs, particularly during the first 2 years, increases the risk of depression. Additionally, OC use during adolescence might increase the risk of depression later in life,” Therese Johansson, of the department of immunology, genetics, and pathology, Science for Life Laboratory, Uppsala (Sweden) University, and colleagues wrote.
The study was published online in Epidemiology and Psychiatric Sciences.
Inconsistent findings
Previous studies suggest an association between adolescent use of hormonal contraceptives (HCs) and increased depression risk, but it’s “less clear” whether these effects are similar in adults, the authors wrote. Randomized clinical trials have “shown little or no effect” of HCs on mood. However, most of these studies didn’t consider previous use of HC.
The researchers wanted to estimate the incidence rate of depression associated with first initiation of OC use as well as the lifetime risk associated with use.
They studied 264,557 female participants in the UK Biobank (aged 37-71 years), collecting data from questionnaires, interviews, physical health measures, biological samples, imaging, and linked health records.
Most participants taking OCs had initiated use during the 1970s/early 1980s when second-generation OCs were predominantly used, consisting of levonorgestrel and ethinyl estradiol.
The researchers conducted a secondary outcome analysis on women who completed the UK Biobank Mental Health Questionnaire (MHQ) to evaluate depressive symptoms.
They estimated the associated risk for depression within 2 years after starting OCs in all women, as well as in groups stratified by age at initiation: before age 20 (adolescents) and age 20 and older (adults). In addition, the investigators estimated the lifetime risk for depression.
Time-dependent analysis compared the effect of OC use at initiation to the effect during the remaining years of use in recent and previous users.
They analyzed a subcohort of female siblings, utilizing “inference about causation from examination of familial confounding,” defined by the authors as a “regression-based approach for determining causality through the use of paired observational data collected from related individuals.”
Adolescents at highest risk
Of the participants, 80.6% had used OCs at some point.
The first 2 years of use were associated with a higher rate of depression among users, compared with never-users (hazard ration, 1.79; 95% confidence interval, 1.63-1.96). Although the risk became less pronounced after that, ever-use was still associated with increased lifetime risk for depression (HR, 1.05; 95% CI, 1.01-1.09).
Adolescents and adult OC users both experienced higher rates of depression during the first 2 years, with a more marked effect in adolescents than in adults (HR, 1.95; 95% CI, 1.64-2.32; and HR, 1.74; 95% CI, 1.54-1.95, respectively).
Previous users of OCs had a higher lifetime risk for depression, compared with never-users (HR, 1.05; 95% CI, 1.01-1.09).
Of the subcohort of women who completed the MHQ (n = 82,232), about half reported experiencing at least one of the core depressive symptoms.
OC initiation was associated with an increased risk for depressive symptoms during the first 2 years in ever- versus never-users (HR, 2.00; 95% CI, 1.91-2.10).
Those who began using OCs during adolescence had a dramatically higher rate of depressive symptoms, compared with never-users (HR, 2.30; 95% CI, 2.11-2.51), as did adult initiators (HR, 1.92; 95% CI, 2.11-2.51).
In the analysis of 7,354 first-degree sister pairs, 81% had initiated OCs. A sibling’s OC use was positively associated with a depression diagnosis, and the cosibling’s OC use was also associated with the sibling’s depression diagnosis. “These results support the hypothesis of a causal relationship between OC use and depression, such that OC use increases the risk of depression,” the authors wrote.
The main limitation is the potential for recall bias in the self-reported data, and that the UK Biobank sample consists of a healthier population than the overall U.K. population, which “hampers the generalizability” of the findings, the authors stated.
Flawed study
In a comment, Natalie Rasgon, MD, founder and director of the Stanford (Calif.) Center for Neuroscience in Women’s Health, said the study was “well researched” and “well written” but had “methodological issues.”
She questioned the sibling component, “which the researchers regard as confirming causality.” The effect may be “important but not causative.” Causality in people who are recalling retrospectively “is highly questionable by any adept researcher because it’s subject to memory. Different siblings may have different recall.”
The authors also didn’t study the indication for OC use. Several medical conditions are treated with OCs, including premenstrual dysphoric disorder, the “number one mood disorder among women of reproductive age.” Including this “could have made a huge difference in outcome data,” said Dr. Rasgon, who was not involved with the study.
Anne-Marie Amies Oelschlager, MD, professor of obstetrics and gynecology, University of Washington, Seattle, noted participants were asked to recall depressive symptoms and OC use as far back as 20-30 years ago, which lends itself to inaccurate recall.
And the researchers didn’t ascertain whether the contraceptives had been used continuously or had been started, stopped, and restarted. Nor did they look at different formulations and doses. And the observational nature of the study “limits the ability to infer causation,” continued Dr. Oelschlager, chair of the American College of Obstetrics and Gynecology Clinical Consensus Gynecology Committee. She was not involved with the study.
“This study is too flawed to use meaningfully in clinical practice,” Dr. Oelschlager concluded.
The study was primarily funded by the Swedish Research Council, the Swedish Brain Foundation, and the Uppsala University Center for Women ‘s Mental Health during the Reproductive Lifespan. The authors, Dr. Rasgon, and Dr. Oelschlager declared no relevant financial relationships.
A version of this article first appeared on Medscape.com.
In addition, OC use in adolescence has been tied to an increased risk for depression later in life. However, some experts believe the study’s methodology may be flawed.
The investigators tracked more than 250,000 women from birth to menopause, gathering information about their use of combined contraceptive pills (progesterone and estrogen), the timing of the initial depression diagnosis, and the onset of depressive symptoms that were not formally diagnosed.
Women who began using these OCs before or at the age of 20 experienced a 130% higher incidence of depressive symptoms, whereas adult users saw a 92% increase. But the higher occurrence of depression tended to decline after the first 2 years of use, except in teenagers, who maintained an increased incidence of depression even after discontinuation.
This effect remained, even after analysis of potential familial confounding.
“Our findings suggest that the use of OCs, particularly during the first 2 years, increases the risk of depression. Additionally, OC use during adolescence might increase the risk of depression later in life,” Therese Johansson, of the department of immunology, genetics, and pathology, Science for Life Laboratory, Uppsala (Sweden) University, and colleagues wrote.
The study was published online in Epidemiology and Psychiatric Sciences.
Inconsistent findings
Previous studies suggest an association between adolescent use of hormonal contraceptives (HCs) and increased depression risk, but it’s “less clear” whether these effects are similar in adults, the authors wrote. Randomized clinical trials have “shown little or no effect” of HCs on mood. However, most of these studies didn’t consider previous use of HC.
The researchers wanted to estimate the incidence rate of depression associated with first initiation of OC use as well as the lifetime risk associated with use.
They studied 264,557 female participants in the UK Biobank (aged 37-71 years), collecting data from questionnaires, interviews, physical health measures, biological samples, imaging, and linked health records.
Most participants taking OCs had initiated use during the 1970s/early 1980s when second-generation OCs were predominantly used, consisting of levonorgestrel and ethinyl estradiol.
The researchers conducted a secondary outcome analysis on women who completed the UK Biobank Mental Health Questionnaire (MHQ) to evaluate depressive symptoms.
They estimated the associated risk for depression within 2 years after starting OCs in all women, as well as in groups stratified by age at initiation: before age 20 (adolescents) and age 20 and older (adults). In addition, the investigators estimated the lifetime risk for depression.
Time-dependent analysis compared the effect of OC use at initiation to the effect during the remaining years of use in recent and previous users.
They analyzed a subcohort of female siblings, utilizing “inference about causation from examination of familial confounding,” defined by the authors as a “regression-based approach for determining causality through the use of paired observational data collected from related individuals.”
Adolescents at highest risk
Of the participants, 80.6% had used OCs at some point.
The first 2 years of use were associated with a higher rate of depression among users, compared with never-users (hazard ration, 1.79; 95% confidence interval, 1.63-1.96). Although the risk became less pronounced after that, ever-use was still associated with increased lifetime risk for depression (HR, 1.05; 95% CI, 1.01-1.09).
Adolescents and adult OC users both experienced higher rates of depression during the first 2 years, with a more marked effect in adolescents than in adults (HR, 1.95; 95% CI, 1.64-2.32; and HR, 1.74; 95% CI, 1.54-1.95, respectively).
Previous users of OCs had a higher lifetime risk for depression, compared with never-users (HR, 1.05; 95% CI, 1.01-1.09).
Of the subcohort of women who completed the MHQ (n = 82,232), about half reported experiencing at least one of the core depressive symptoms.
OC initiation was associated with an increased risk for depressive symptoms during the first 2 years in ever- versus never-users (HR, 2.00; 95% CI, 1.91-2.10).
Those who began using OCs during adolescence had a dramatically higher rate of depressive symptoms, compared with never-users (HR, 2.30; 95% CI, 2.11-2.51), as did adult initiators (HR, 1.92; 95% CI, 2.11-2.51).
In the analysis of 7,354 first-degree sister pairs, 81% had initiated OCs. A sibling’s OC use was positively associated with a depression diagnosis, and the cosibling’s OC use was also associated with the sibling’s depression diagnosis. “These results support the hypothesis of a causal relationship between OC use and depression, such that OC use increases the risk of depression,” the authors wrote.
The main limitation is the potential for recall bias in the self-reported data, and that the UK Biobank sample consists of a healthier population than the overall U.K. population, which “hampers the generalizability” of the findings, the authors stated.
Flawed study
In a comment, Natalie Rasgon, MD, founder and director of the Stanford (Calif.) Center for Neuroscience in Women’s Health, said the study was “well researched” and “well written” but had “methodological issues.”
She questioned the sibling component, “which the researchers regard as confirming causality.” The effect may be “important but not causative.” Causality in people who are recalling retrospectively “is highly questionable by any adept researcher because it’s subject to memory. Different siblings may have different recall.”
The authors also didn’t study the indication for OC use. Several medical conditions are treated with OCs, including premenstrual dysphoric disorder, the “number one mood disorder among women of reproductive age.” Including this “could have made a huge difference in outcome data,” said Dr. Rasgon, who was not involved with the study.
Anne-Marie Amies Oelschlager, MD, professor of obstetrics and gynecology, University of Washington, Seattle, noted participants were asked to recall depressive symptoms and OC use as far back as 20-30 years ago, which lends itself to inaccurate recall.
And the researchers didn’t ascertain whether the contraceptives had been used continuously or had been started, stopped, and restarted. Nor did they look at different formulations and doses. And the observational nature of the study “limits the ability to infer causation,” continued Dr. Oelschlager, chair of the American College of Obstetrics and Gynecology Clinical Consensus Gynecology Committee. She was not involved with the study.
“This study is too flawed to use meaningfully in clinical practice,” Dr. Oelschlager concluded.
The study was primarily funded by the Swedish Research Council, the Swedish Brain Foundation, and the Uppsala University Center for Women ‘s Mental Health during the Reproductive Lifespan. The authors, Dr. Rasgon, and Dr. Oelschlager declared no relevant financial relationships.
A version of this article first appeared on Medscape.com.
In addition, OC use in adolescence has been tied to an increased risk for depression later in life. However, some experts believe the study’s methodology may be flawed.
The investigators tracked more than 250,000 women from birth to menopause, gathering information about their use of combined contraceptive pills (progesterone and estrogen), the timing of the initial depression diagnosis, and the onset of depressive symptoms that were not formally diagnosed.
Women who began using these OCs before or at the age of 20 experienced a 130% higher incidence of depressive symptoms, whereas adult users saw a 92% increase. But the higher occurrence of depression tended to decline after the first 2 years of use, except in teenagers, who maintained an increased incidence of depression even after discontinuation.
This effect remained, even after analysis of potential familial confounding.
“Our findings suggest that the use of OCs, particularly during the first 2 years, increases the risk of depression. Additionally, OC use during adolescence might increase the risk of depression later in life,” Therese Johansson, of the department of immunology, genetics, and pathology, Science for Life Laboratory, Uppsala (Sweden) University, and colleagues wrote.
The study was published online in Epidemiology and Psychiatric Sciences.
Inconsistent findings
Previous studies suggest an association between adolescent use of hormonal contraceptives (HCs) and increased depression risk, but it’s “less clear” whether these effects are similar in adults, the authors wrote. Randomized clinical trials have “shown little or no effect” of HCs on mood. However, most of these studies didn’t consider previous use of HC.
The researchers wanted to estimate the incidence rate of depression associated with first initiation of OC use as well as the lifetime risk associated with use.
They studied 264,557 female participants in the UK Biobank (aged 37-71 years), collecting data from questionnaires, interviews, physical health measures, biological samples, imaging, and linked health records.
Most participants taking OCs had initiated use during the 1970s/early 1980s when second-generation OCs were predominantly used, consisting of levonorgestrel and ethinyl estradiol.
The researchers conducted a secondary outcome analysis on women who completed the UK Biobank Mental Health Questionnaire (MHQ) to evaluate depressive symptoms.
They estimated the associated risk for depression within 2 years after starting OCs in all women, as well as in groups stratified by age at initiation: before age 20 (adolescents) and age 20 and older (adults). In addition, the investigators estimated the lifetime risk for depression.
Time-dependent analysis compared the effect of OC use at initiation to the effect during the remaining years of use in recent and previous users.
They analyzed a subcohort of female siblings, utilizing “inference about causation from examination of familial confounding,” defined by the authors as a “regression-based approach for determining causality through the use of paired observational data collected from related individuals.”
Adolescents at highest risk
Of the participants, 80.6% had used OCs at some point.
The first 2 years of use were associated with a higher rate of depression among users, compared with never-users (hazard ration, 1.79; 95% confidence interval, 1.63-1.96). Although the risk became less pronounced after that, ever-use was still associated with increased lifetime risk for depression (HR, 1.05; 95% CI, 1.01-1.09).
Adolescents and adult OC users both experienced higher rates of depression during the first 2 years, with a more marked effect in adolescents than in adults (HR, 1.95; 95% CI, 1.64-2.32; and HR, 1.74; 95% CI, 1.54-1.95, respectively).
Previous users of OCs had a higher lifetime risk for depression, compared with never-users (HR, 1.05; 95% CI, 1.01-1.09).
Of the subcohort of women who completed the MHQ (n = 82,232), about half reported experiencing at least one of the core depressive symptoms.
OC initiation was associated with an increased risk for depressive symptoms during the first 2 years in ever- versus never-users (HR, 2.00; 95% CI, 1.91-2.10).
Those who began using OCs during adolescence had a dramatically higher rate of depressive symptoms, compared with never-users (HR, 2.30; 95% CI, 2.11-2.51), as did adult initiators (HR, 1.92; 95% CI, 2.11-2.51).
In the analysis of 7,354 first-degree sister pairs, 81% had initiated OCs. A sibling’s OC use was positively associated with a depression diagnosis, and the cosibling’s OC use was also associated with the sibling’s depression diagnosis. “These results support the hypothesis of a causal relationship between OC use and depression, such that OC use increases the risk of depression,” the authors wrote.
The main limitation is the potential for recall bias in the self-reported data, and that the UK Biobank sample consists of a healthier population than the overall U.K. population, which “hampers the generalizability” of the findings, the authors stated.
Flawed study
In a comment, Natalie Rasgon, MD, founder and director of the Stanford (Calif.) Center for Neuroscience in Women’s Health, said the study was “well researched” and “well written” but had “methodological issues.”
She questioned the sibling component, “which the researchers regard as confirming causality.” The effect may be “important but not causative.” Causality in people who are recalling retrospectively “is highly questionable by any adept researcher because it’s subject to memory. Different siblings may have different recall.”
The authors also didn’t study the indication for OC use. Several medical conditions are treated with OCs, including premenstrual dysphoric disorder, the “number one mood disorder among women of reproductive age.” Including this “could have made a huge difference in outcome data,” said Dr. Rasgon, who was not involved with the study.
Anne-Marie Amies Oelschlager, MD, professor of obstetrics and gynecology, University of Washington, Seattle, noted participants were asked to recall depressive symptoms and OC use as far back as 20-30 years ago, which lends itself to inaccurate recall.
And the researchers didn’t ascertain whether the contraceptives had been used continuously or had been started, stopped, and restarted. Nor did they look at different formulations and doses. And the observational nature of the study “limits the ability to infer causation,” continued Dr. Oelschlager, chair of the American College of Obstetrics and Gynecology Clinical Consensus Gynecology Committee. She was not involved with the study.
“This study is too flawed to use meaningfully in clinical practice,” Dr. Oelschlager concluded.
The study was primarily funded by the Swedish Research Council, the Swedish Brain Foundation, and the Uppsala University Center for Women ‘s Mental Health during the Reproductive Lifespan. The authors, Dr. Rasgon, and Dr. Oelschlager declared no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM EPIDEMIOLOGY AND PSYCHIATRIC SCIENCES
PCOS associated with shorter lifespan
CHICAGO –
In the study, involving nearly 10,000 women with PCOS and matched controls from Finland, women with PCOS died on average a year earlier than their age-matched counterparts, primarily from diseases of the circulatory system, cancer, and diabetes.
PCOS is the most common endocrine disorder of reproductive-age women, of whom about 50%-70% also have obesity.
“I think we need to acknowledge that this is a health burden and not just a reproductive problem. In many cases we deal with the reproductive problem, and then these women are left alone. … So I think the message is we need to look beyond the reproductive outcomes, which are … really good. We can manage that,” said Terhi T. Piltonen, MD, PhD, during a press briefing held June 15 at the annual meeting of the Endocrine Society.
“I think the difficult part is [managing] the lifelong health for these women and supporting them to achieve the best health they can get. We need a multidisciplinary effort and to put more resources into the research,” added Dr. Piltonen, professor in the departments of ob.gyn. and reproductive endocrinology at the University of Oulu, Finland.
Indeed, Punith Kempegowda, MD, PhD, of the University of Birmingham (England) observed: “In our medical schools in the U.K., over 5 years, students get 45 minutes [of education] on PCOS, and they’re expected to learn about it.”
And over the last 20 years, funding for research into the condition has totaled less than a half percent of overall medical funding. “And we’re talking about 10% of all women. …We need to acknowledge it and educate people more. We need more published studies to understand more about it,” he noted.
Asked to comment, Greg Dodell, MD, owner and president of Central Park Endocrinology, New York, said: “PCOS is about a lot more than fertility, and that may not be the goal or on the mind of a woman at the time they start having symptoms of PCOS or get the diagnosis.”
“PCOS is largely a metabolic condition rooted in insulin resistance, and therefore, the potential clinical outcomes, including mortality, are important to recognize.”
Dr. Dodell, who has a special interest in PCOS, advised that, for women with the condition, “focus on reducing insulin resistance with health-promoting behaviors and medications as needed. Data demonstrate that improving fitness, irrespective of a change in weight, can improve metabolic markers.” And, he advised that these women be routinely screened for mental health issues.
He also noted, “PCOS occurs across the size spectrum, but those patients in larger bodies may face weight stigma which has negative health consequences. These patients may avoid going to doctors for routine health screenings, so it is an important issue to continue to address.”
Women with PCOS lose a year of life
The new data come from 9,839 women with PCOS and 70,705 age- and region-matched controls from the Finnish Care Register for Health Care. The group with PCOS had been diagnosed at a mean age of 27 years.
The mean follow-up time was 13.1 years in both groups, during which 1,003 controls and 177 women with PCOS died. The mean age at death was 51.4 years for the PCOS group versus 52.6 years for the control women, a significant difference (P < .001).
Causes of death that were significantly higher among the women with PCOS versus controls after adjustments were cancer (hazard ratio, 1.39), and diseases of the circulatory system (1.68).
In more specific subcategories, after adjustment for education, the women with PCOS had increased mortality from nonischemic diseases, such as hypertensive heart disease, pulmonary embolism, etc. (HR, 2.06), and diabetes (HR, 2.85).
One study limitation was the inability to adjust for body mass index, Dr. Piltonen noted.
Dr. Piltonen, Dr. Kempegowda, and Dr. Dodell have no disclosures.
CHICAGO –
In the study, involving nearly 10,000 women with PCOS and matched controls from Finland, women with PCOS died on average a year earlier than their age-matched counterparts, primarily from diseases of the circulatory system, cancer, and diabetes.
PCOS is the most common endocrine disorder of reproductive-age women, of whom about 50%-70% also have obesity.
“I think we need to acknowledge that this is a health burden and not just a reproductive problem. In many cases we deal with the reproductive problem, and then these women are left alone. … So I think the message is we need to look beyond the reproductive outcomes, which are … really good. We can manage that,” said Terhi T. Piltonen, MD, PhD, during a press briefing held June 15 at the annual meeting of the Endocrine Society.
“I think the difficult part is [managing] the lifelong health for these women and supporting them to achieve the best health they can get. We need a multidisciplinary effort and to put more resources into the research,” added Dr. Piltonen, professor in the departments of ob.gyn. and reproductive endocrinology at the University of Oulu, Finland.
Indeed, Punith Kempegowda, MD, PhD, of the University of Birmingham (England) observed: “In our medical schools in the U.K., over 5 years, students get 45 minutes [of education] on PCOS, and they’re expected to learn about it.”
And over the last 20 years, funding for research into the condition has totaled less than a half percent of overall medical funding. “And we’re talking about 10% of all women. …We need to acknowledge it and educate people more. We need more published studies to understand more about it,” he noted.
Asked to comment, Greg Dodell, MD, owner and president of Central Park Endocrinology, New York, said: “PCOS is about a lot more than fertility, and that may not be the goal or on the mind of a woman at the time they start having symptoms of PCOS or get the diagnosis.”
“PCOS is largely a metabolic condition rooted in insulin resistance, and therefore, the potential clinical outcomes, including mortality, are important to recognize.”
Dr. Dodell, who has a special interest in PCOS, advised that, for women with the condition, “focus on reducing insulin resistance with health-promoting behaviors and medications as needed. Data demonstrate that improving fitness, irrespective of a change in weight, can improve metabolic markers.” And, he advised that these women be routinely screened for mental health issues.
He also noted, “PCOS occurs across the size spectrum, but those patients in larger bodies may face weight stigma which has negative health consequences. These patients may avoid going to doctors for routine health screenings, so it is an important issue to continue to address.”
Women with PCOS lose a year of life
The new data come from 9,839 women with PCOS and 70,705 age- and region-matched controls from the Finnish Care Register for Health Care. The group with PCOS had been diagnosed at a mean age of 27 years.
The mean follow-up time was 13.1 years in both groups, during which 1,003 controls and 177 women with PCOS died. The mean age at death was 51.4 years for the PCOS group versus 52.6 years for the control women, a significant difference (P < .001).
Causes of death that were significantly higher among the women with PCOS versus controls after adjustments were cancer (hazard ratio, 1.39), and diseases of the circulatory system (1.68).
In more specific subcategories, after adjustment for education, the women with PCOS had increased mortality from nonischemic diseases, such as hypertensive heart disease, pulmonary embolism, etc. (HR, 2.06), and diabetes (HR, 2.85).
One study limitation was the inability to adjust for body mass index, Dr. Piltonen noted.
Dr. Piltonen, Dr. Kempegowda, and Dr. Dodell have no disclosures.
CHICAGO –
In the study, involving nearly 10,000 women with PCOS and matched controls from Finland, women with PCOS died on average a year earlier than their age-matched counterparts, primarily from diseases of the circulatory system, cancer, and diabetes.
PCOS is the most common endocrine disorder of reproductive-age women, of whom about 50%-70% also have obesity.
“I think we need to acknowledge that this is a health burden and not just a reproductive problem. In many cases we deal with the reproductive problem, and then these women are left alone. … So I think the message is we need to look beyond the reproductive outcomes, which are … really good. We can manage that,” said Terhi T. Piltonen, MD, PhD, during a press briefing held June 15 at the annual meeting of the Endocrine Society.
“I think the difficult part is [managing] the lifelong health for these women and supporting them to achieve the best health they can get. We need a multidisciplinary effort and to put more resources into the research,” added Dr. Piltonen, professor in the departments of ob.gyn. and reproductive endocrinology at the University of Oulu, Finland.
Indeed, Punith Kempegowda, MD, PhD, of the University of Birmingham (England) observed: “In our medical schools in the U.K., over 5 years, students get 45 minutes [of education] on PCOS, and they’re expected to learn about it.”
And over the last 20 years, funding for research into the condition has totaled less than a half percent of overall medical funding. “And we’re talking about 10% of all women. …We need to acknowledge it and educate people more. We need more published studies to understand more about it,” he noted.
Asked to comment, Greg Dodell, MD, owner and president of Central Park Endocrinology, New York, said: “PCOS is about a lot more than fertility, and that may not be the goal or on the mind of a woman at the time they start having symptoms of PCOS or get the diagnosis.”
“PCOS is largely a metabolic condition rooted in insulin resistance, and therefore, the potential clinical outcomes, including mortality, are important to recognize.”
Dr. Dodell, who has a special interest in PCOS, advised that, for women with the condition, “focus on reducing insulin resistance with health-promoting behaviors and medications as needed. Data demonstrate that improving fitness, irrespective of a change in weight, can improve metabolic markers.” And, he advised that these women be routinely screened for mental health issues.
He also noted, “PCOS occurs across the size spectrum, but those patients in larger bodies may face weight stigma which has negative health consequences. These patients may avoid going to doctors for routine health screenings, so it is an important issue to continue to address.”
Women with PCOS lose a year of life
The new data come from 9,839 women with PCOS and 70,705 age- and region-matched controls from the Finnish Care Register for Health Care. The group with PCOS had been diagnosed at a mean age of 27 years.
The mean follow-up time was 13.1 years in both groups, during which 1,003 controls and 177 women with PCOS died. The mean age at death was 51.4 years for the PCOS group versus 52.6 years for the control women, a significant difference (P < .001).
Causes of death that were significantly higher among the women with PCOS versus controls after adjustments were cancer (hazard ratio, 1.39), and diseases of the circulatory system (1.68).
In more specific subcategories, after adjustment for education, the women with PCOS had increased mortality from nonischemic diseases, such as hypertensive heart disease, pulmonary embolism, etc. (HR, 2.06), and diabetes (HR, 2.85).
One study limitation was the inability to adjust for body mass index, Dr. Piltonen noted.
Dr. Piltonen, Dr. Kempegowda, and Dr. Dodell have no disclosures.
AT ENDO 2023
Applications of office hysteroscopy for the infertility patient
What role does diagnostic office hysteroscopy play in an infertility evaluation?
.1
More specifically, hysteroscopy is the gold standard for assessing the uterine cavity. The sensitivity, specificity, and positive predictive and negative predictive values of hysterosalpingography (HSG) in evaluating uterine cavity abnormalities were 44.83%; 86.67%; 56.52%; and 80.25%, respectively.2 Given the poor sensitivity of HSG, a diagnosis of endometrial polyps and/or chronic endometritis is more likely to be missed.
Our crossover trial comparing HSG to office hysteroscopy for tubal patency showed that women were 110 times more likely to have the maximum level of pain with HSG than diagnostic hysteroscopy when using a 2.8-mm flexible hysteroscope.3 Further, infection rates and vasovagal events were far lower with hysteroscopy.1
Finally, compared with HSG, we showed 98%-100% sensitivity and 84% specificity for tubal occlusion with hysteroscopy by air-infused saline. Conversely, HSG typically is associated with 76%-96% sensitivity and 67%-100% specificity.4 Additionally, we can often perform diagnostic hysteroscopies for approximately $35 per procedure for total fixed and disposable equipment costs.
How should physicians perform office hysteroscopy to minimize patient discomfort?
The classic paradigm has been to focus on paracervical blocks, anxiolytics, and a supportive environment (such as mood music). However, those are far more important when your hysteroscope is larger than the natural cervical lumen. If you can use small hysteroscopes (< 3 mm for the nulliparous cervix, < 4 mm for the parous cervix), most women will not require cervical dilation, which further enhances the patient experience.
Using a flexible hysteroscope for suspected pathology, making sure not to overdistend the uterus (particularly in high-risk patients such as those with tubal occlusion and cervical stenosis), and vaginoscopy can all minimize patient discomfort. We have published data showing that by using a 2.8-mm flexible diagnostic hysteroscope in a group of mostly nulliparous women, greater than 50% have no discomfort, and more than 90% will have mild to no discomfort.3
What operative hysteroscopy procedures can be performed safely in a physician’s office, and what equipment is required?
Though highly dependent on experience and resources, reproductive endocrinology and infertility specialists (REIs) arguably have the easiest transition to operative office hysteroscopy by utilizing the analgesia and procedure room that is standard for oocyte retrieval and simply adding hysteroscopic procedures. The accompanying table stratifies general hysteroscopic procedures by difficulty.
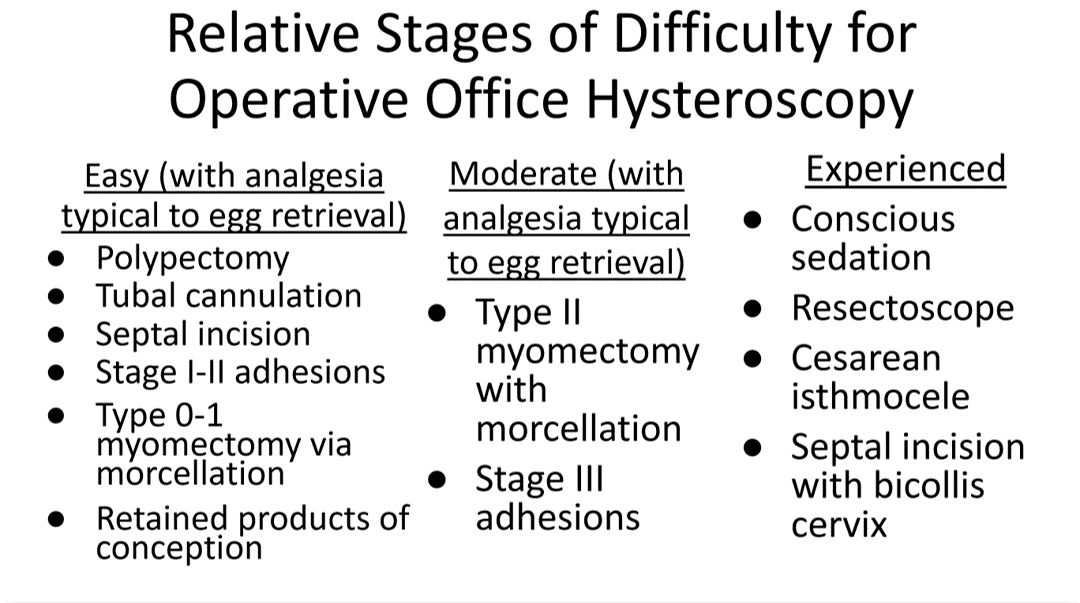
If one can use propofol or a similar level of sedation (which is routinely utilized for oocyte aspiration), there are few hysteroscopies that cannot be accomplished in the office. However, the less sedation and analgesia, the more judicious one must be in patient selection. Moreover, there are trade-offs between visualization, comfort, and instrumentation.
The greater the uterine distention and diameter of the hysteroscope, the more patients experience pain. One-third of patients (especially nulliparous) will discontinue a procedure with a 5-mm hysteroscope because of discomfort.5 However, as one drops to 4.5 mm and smaller operative hysteroscopes, instruments often occupy the inflow channel, limiting distention and visualization, which also can affect completion rates and safety.
When is operative hysteroscopy best suited for the OR?
In addition to physician experience and clinical resources, the critical factors guiding our choices for selecting the OR rather than the office, include:
- Loss of landmarks. Though Dr. Parry now does most severe intrauterine adhesion cases in the office with ultrasound guidance, when neither ostia can be visualized there is meaningful risk for perforation. Preoperative estrogen, development of planes with the diagnostic hysteroscope prior, and preparing the patient for a possible multistage procedure are all important.
- Use of energy. There are many excellent hysteroscopic surgeons who use the resectoscope well in the office. However, with possible patient movement and potential perforation with energy leading to a bowel injury, there can be greater risk when using energy relative to other methods (such as forceps, scissors, and mechanical morcellation).
- Deeper fibroids. Fibroids displace rather than invade the myometrium, and one can sonographically visualize the myometrium reapproximate over a fibroid as it herniates more into the uterine cavity. Nevertheless, the closer a fibroid comes to the serosa, the more mindful one should be of risks and balances for hysteroscopic removal.
In a patient with a severely stenotic cervix or tortuous endocervical canal, what preprocedure methods do you find helpful, and do you utilize abdominal ultrasound guidance?
If using a 2.8-mm flexible diagnostic hysteroscope, we find 99.8%-99.9% of cervices can be successfully cannulated in the office, with rare exception, that is, following cryotherapy or chlamydia cervicitis. This is the equivalent of your dilator having a camera on the tip and fully articulating to adjust to the cervical path.
Transvaginal sonography prior to hysteroscopy where one maps the cervical lumen helps anticipate problems (along with being familiar with the patient’s history). For the rare dilation under anesthesia, concurrent sonography with a 2.8-mm flexible hysteroscope and intermittent dilator use has been sufficient for our exceptions without the need for lacrimal dilators, vasopressin, misoprostol, and other adjuncts. Of note, we use a 1080p flexible endoscope, as lower resolution would make this more challenging.
In patients with recurrent implantation failure following IVF, is hysteroscopy superior to 3D saline infusion sonogram?
At an American Society of Reproductive Medicine 2021 session, Ilan Tur-Kaspa, MD, and Dr. Parry debated the topic of 2D ultrasound combined with hysteroscopy vs. 3D saline infusion sonography. Core areas of agreement were that expert hands for any approach are better than nonexpert, and high-resolution technology is better than lower resolution. There was also agreement that extrauterine and myometrial disease, such as intramural fibroids and adenomyosis, are contributory factors.
So, sonography will always have a role. However, existing and forthcoming data show hysteroscopy to improve live birth rates for patients with recurrent implantation failure after IVF. Dr. Parry finds diagnostic hysteroscopy easier for identifying endometritis, sessile and cornual polyps, retained products of conception (which are often isoechogenic with the endometrium) and lateral adhesions.
The reality is that there is variability among physicians and midlevel providers in both sonographic and diagnostic hysteroscopic skill. If one wants to verify findings with another team member, acknowledging that there can be nuances to identifying these pathologies by sonography, it is easier to share and discuss findings through hysteroscopic video than sonographic records.
When is endometrial biopsy indicated during office hysteroscopy?
The patients of an REI are very unlikely to have endometrial cancer (or even hyperplasia) outside of polyps (or arguably hypervascular areas of overgrowth), so the focus is on resecting visualized pathology relative to random biopsy.
However, the threshold for biopsy should be adjusted to the patient population, as well as to individual findings and risk. RVUs are greatly increased (11.1 > 41.57) with biopsy, helping sustainability. Additionally, if one places the hysteroscope on endometrium and applies suction through the inflow channel, one can obtain a sample with small-caliber diagnostic hysteroscopes and without having to use forceps.
What is your threshold for fluid deficit in hysteroscopy?
We follow AAGL guidelines, which for operative hysteroscopy are 2,500 mL of isotonic fluids or 1,000 mL of hypotonic fluids in low-risk patients. This should be further reduced to 500 mL of isotonic fluids in the elderly and even 300 mL in those with cardiovascular compromise.6
For patients who request sedation for office hysteroscopy, which option do you recommend – paracervical block alone, nitrous oxide, or the combination?
For diagnostic, greater than 95% of our patients do not require even over-the-counter analgesic medications. For operative, we consider all permissible resources that allow for a safe combination that is appropriate to the pathology and clinical setting, such as paracervical blocks, nitrous oxide, NSAIDs such as ketorolac, anxiolytics, and more.
The goal is to optimize the patient experience. However, the top three criteria that influence successful operative office hysteroscopy for a conscious patient are a parous cervix, judicious patient selection, and pre- and intraoperative verbal analgesia. Informed consent and engagement improve the experience of both the patient and physician.
Dr. Parry is the founder of Positive Steps Fertility in Madison, Miss. Dr. Trolice is director of The IVF Center in Winter Park, Fla., and professor of obstetrics and gynecology at the University of Central Florida, Orlando.
References
1. Parry JP et al. J Minim Invasive Gynecol. 2017 May-Jun. doi: 10.1016/j.jmig.2017.02.010.
2. Wadhwa L et al. 2017 Apr-Jun. doi: 10.4103/jhrs.JHRS_123_16.
3. Parry JP et al. Fertil Steril. 2017 Oct. doi: 10.1016/j.fertnstert.2017.07.1159.
4. Penzias A et al. Fertil Steril. 2021 Nov. doi: 10.1016/j.fertnstert.2021.08.038.
5. Campo R et al. Hum Reprod. 2005 Jan;20(1):258-63. doi: 10.1093/humrep/deh559.
6. AAGL AAGL practice report: Practice guidelines for the management of hysteroscopic distending media. J Minim Invasive Gynecol. 2013 Mar-Apr. doi: 10.1016/j.jmig.2012.12.002.
What role does diagnostic office hysteroscopy play in an infertility evaluation?
.1
More specifically, hysteroscopy is the gold standard for assessing the uterine cavity. The sensitivity, specificity, and positive predictive and negative predictive values of hysterosalpingography (HSG) in evaluating uterine cavity abnormalities were 44.83%; 86.67%; 56.52%; and 80.25%, respectively.2 Given the poor sensitivity of HSG, a diagnosis of endometrial polyps and/or chronic endometritis is more likely to be missed.
Our crossover trial comparing HSG to office hysteroscopy for tubal patency showed that women were 110 times more likely to have the maximum level of pain with HSG than diagnostic hysteroscopy when using a 2.8-mm flexible hysteroscope.3 Further, infection rates and vasovagal events were far lower with hysteroscopy.1
Finally, compared with HSG, we showed 98%-100% sensitivity and 84% specificity for tubal occlusion with hysteroscopy by air-infused saline. Conversely, HSG typically is associated with 76%-96% sensitivity and 67%-100% specificity.4 Additionally, we can often perform diagnostic hysteroscopies for approximately $35 per procedure for total fixed and disposable equipment costs.
How should physicians perform office hysteroscopy to minimize patient discomfort?
The classic paradigm has been to focus on paracervical blocks, anxiolytics, and a supportive environment (such as mood music). However, those are far more important when your hysteroscope is larger than the natural cervical lumen. If you can use small hysteroscopes (< 3 mm for the nulliparous cervix, < 4 mm for the parous cervix), most women will not require cervical dilation, which further enhances the patient experience.
Using a flexible hysteroscope for suspected pathology, making sure not to overdistend the uterus (particularly in high-risk patients such as those with tubal occlusion and cervical stenosis), and vaginoscopy can all minimize patient discomfort. We have published data showing that by using a 2.8-mm flexible diagnostic hysteroscope in a group of mostly nulliparous women, greater than 50% have no discomfort, and more than 90% will have mild to no discomfort.3
What operative hysteroscopy procedures can be performed safely in a physician’s office, and what equipment is required?
Though highly dependent on experience and resources, reproductive endocrinology and infertility specialists (REIs) arguably have the easiest transition to operative office hysteroscopy by utilizing the analgesia and procedure room that is standard for oocyte retrieval and simply adding hysteroscopic procedures. The accompanying table stratifies general hysteroscopic procedures by difficulty.
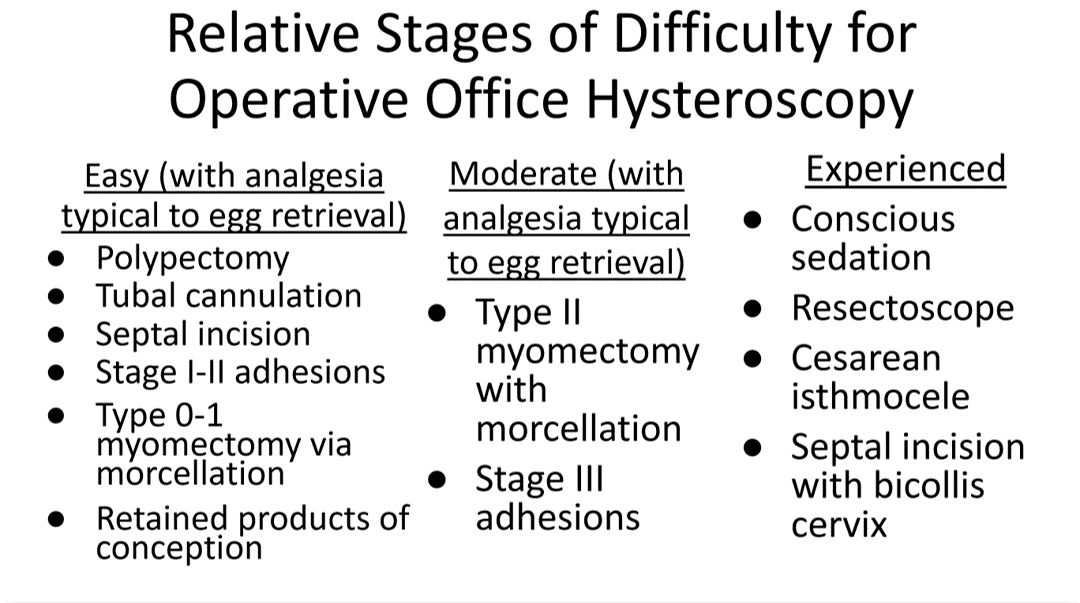
If one can use propofol or a similar level of sedation (which is routinely utilized for oocyte aspiration), there are few hysteroscopies that cannot be accomplished in the office. However, the less sedation and analgesia, the more judicious one must be in patient selection. Moreover, there are trade-offs between visualization, comfort, and instrumentation.
The greater the uterine distention and diameter of the hysteroscope, the more patients experience pain. One-third of patients (especially nulliparous) will discontinue a procedure with a 5-mm hysteroscope because of discomfort.5 However, as one drops to 4.5 mm and smaller operative hysteroscopes, instruments often occupy the inflow channel, limiting distention and visualization, which also can affect completion rates and safety.
When is operative hysteroscopy best suited for the OR?
In addition to physician experience and clinical resources, the critical factors guiding our choices for selecting the OR rather than the office, include:
- Loss of landmarks. Though Dr. Parry now does most severe intrauterine adhesion cases in the office with ultrasound guidance, when neither ostia can be visualized there is meaningful risk for perforation. Preoperative estrogen, development of planes with the diagnostic hysteroscope prior, and preparing the patient for a possible multistage procedure are all important.
- Use of energy. There are many excellent hysteroscopic surgeons who use the resectoscope well in the office. However, with possible patient movement and potential perforation with energy leading to a bowel injury, there can be greater risk when using energy relative to other methods (such as forceps, scissors, and mechanical morcellation).
- Deeper fibroids. Fibroids displace rather than invade the myometrium, and one can sonographically visualize the myometrium reapproximate over a fibroid as it herniates more into the uterine cavity. Nevertheless, the closer a fibroid comes to the serosa, the more mindful one should be of risks and balances for hysteroscopic removal.
In a patient with a severely stenotic cervix or tortuous endocervical canal, what preprocedure methods do you find helpful, and do you utilize abdominal ultrasound guidance?
If using a 2.8-mm flexible diagnostic hysteroscope, we find 99.8%-99.9% of cervices can be successfully cannulated in the office, with rare exception, that is, following cryotherapy or chlamydia cervicitis. This is the equivalent of your dilator having a camera on the tip and fully articulating to adjust to the cervical path.
Transvaginal sonography prior to hysteroscopy where one maps the cervical lumen helps anticipate problems (along with being familiar with the patient’s history). For the rare dilation under anesthesia, concurrent sonography with a 2.8-mm flexible hysteroscope and intermittent dilator use has been sufficient for our exceptions without the need for lacrimal dilators, vasopressin, misoprostol, and other adjuncts. Of note, we use a 1080p flexible endoscope, as lower resolution would make this more challenging.
In patients with recurrent implantation failure following IVF, is hysteroscopy superior to 3D saline infusion sonogram?
At an American Society of Reproductive Medicine 2021 session, Ilan Tur-Kaspa, MD, and Dr. Parry debated the topic of 2D ultrasound combined with hysteroscopy vs. 3D saline infusion sonography. Core areas of agreement were that expert hands for any approach are better than nonexpert, and high-resolution technology is better than lower resolution. There was also agreement that extrauterine and myometrial disease, such as intramural fibroids and adenomyosis, are contributory factors.
So, sonography will always have a role. However, existing and forthcoming data show hysteroscopy to improve live birth rates for patients with recurrent implantation failure after IVF. Dr. Parry finds diagnostic hysteroscopy easier for identifying endometritis, sessile and cornual polyps, retained products of conception (which are often isoechogenic with the endometrium) and lateral adhesions.
The reality is that there is variability among physicians and midlevel providers in both sonographic and diagnostic hysteroscopic skill. If one wants to verify findings with another team member, acknowledging that there can be nuances to identifying these pathologies by sonography, it is easier to share and discuss findings through hysteroscopic video than sonographic records.
When is endometrial biopsy indicated during office hysteroscopy?
The patients of an REI are very unlikely to have endometrial cancer (or even hyperplasia) outside of polyps (or arguably hypervascular areas of overgrowth), so the focus is on resecting visualized pathology relative to random biopsy.
However, the threshold for biopsy should be adjusted to the patient population, as well as to individual findings and risk. RVUs are greatly increased (11.1 > 41.57) with biopsy, helping sustainability. Additionally, if one places the hysteroscope on endometrium and applies suction through the inflow channel, one can obtain a sample with small-caliber diagnostic hysteroscopes and without having to use forceps.
What is your threshold for fluid deficit in hysteroscopy?
We follow AAGL guidelines, which for operative hysteroscopy are 2,500 mL of isotonic fluids or 1,000 mL of hypotonic fluids in low-risk patients. This should be further reduced to 500 mL of isotonic fluids in the elderly and even 300 mL in those with cardiovascular compromise.6
For patients who request sedation for office hysteroscopy, which option do you recommend – paracervical block alone, nitrous oxide, or the combination?
For diagnostic, greater than 95% of our patients do not require even over-the-counter analgesic medications. For operative, we consider all permissible resources that allow for a safe combination that is appropriate to the pathology and clinical setting, such as paracervical blocks, nitrous oxide, NSAIDs such as ketorolac, anxiolytics, and more.
The goal is to optimize the patient experience. However, the top three criteria that influence successful operative office hysteroscopy for a conscious patient are a parous cervix, judicious patient selection, and pre- and intraoperative verbal analgesia. Informed consent and engagement improve the experience of both the patient and physician.
Dr. Parry is the founder of Positive Steps Fertility in Madison, Miss. Dr. Trolice is director of The IVF Center in Winter Park, Fla., and professor of obstetrics and gynecology at the University of Central Florida, Orlando.
References
1. Parry JP et al. J Minim Invasive Gynecol. 2017 May-Jun. doi: 10.1016/j.jmig.2017.02.010.
2. Wadhwa L et al. 2017 Apr-Jun. doi: 10.4103/jhrs.JHRS_123_16.
3. Parry JP et al. Fertil Steril. 2017 Oct. doi: 10.1016/j.fertnstert.2017.07.1159.
4. Penzias A et al. Fertil Steril. 2021 Nov. doi: 10.1016/j.fertnstert.2021.08.038.
5. Campo R et al. Hum Reprod. 2005 Jan;20(1):258-63. doi: 10.1093/humrep/deh559.
6. AAGL AAGL practice report: Practice guidelines for the management of hysteroscopic distending media. J Minim Invasive Gynecol. 2013 Mar-Apr. doi: 10.1016/j.jmig.2012.12.002.
What role does diagnostic office hysteroscopy play in an infertility evaluation?
.1
More specifically, hysteroscopy is the gold standard for assessing the uterine cavity. The sensitivity, specificity, and positive predictive and negative predictive values of hysterosalpingography (HSG) in evaluating uterine cavity abnormalities were 44.83%; 86.67%; 56.52%; and 80.25%, respectively.2 Given the poor sensitivity of HSG, a diagnosis of endometrial polyps and/or chronic endometritis is more likely to be missed.
Our crossover trial comparing HSG to office hysteroscopy for tubal patency showed that women were 110 times more likely to have the maximum level of pain with HSG than diagnostic hysteroscopy when using a 2.8-mm flexible hysteroscope.3 Further, infection rates and vasovagal events were far lower with hysteroscopy.1
Finally, compared with HSG, we showed 98%-100% sensitivity and 84% specificity for tubal occlusion with hysteroscopy by air-infused saline. Conversely, HSG typically is associated with 76%-96% sensitivity and 67%-100% specificity.4 Additionally, we can often perform diagnostic hysteroscopies for approximately $35 per procedure for total fixed and disposable equipment costs.
How should physicians perform office hysteroscopy to minimize patient discomfort?
The classic paradigm has been to focus on paracervical blocks, anxiolytics, and a supportive environment (such as mood music). However, those are far more important when your hysteroscope is larger than the natural cervical lumen. If you can use small hysteroscopes (< 3 mm for the nulliparous cervix, < 4 mm for the parous cervix), most women will not require cervical dilation, which further enhances the patient experience.
Using a flexible hysteroscope for suspected pathology, making sure not to overdistend the uterus (particularly in high-risk patients such as those with tubal occlusion and cervical stenosis), and vaginoscopy can all minimize patient discomfort. We have published data showing that by using a 2.8-mm flexible diagnostic hysteroscope in a group of mostly nulliparous women, greater than 50% have no discomfort, and more than 90% will have mild to no discomfort.3
What operative hysteroscopy procedures can be performed safely in a physician’s office, and what equipment is required?
Though highly dependent on experience and resources, reproductive endocrinology and infertility specialists (REIs) arguably have the easiest transition to operative office hysteroscopy by utilizing the analgesia and procedure room that is standard for oocyte retrieval and simply adding hysteroscopic procedures. The accompanying table stratifies general hysteroscopic procedures by difficulty.
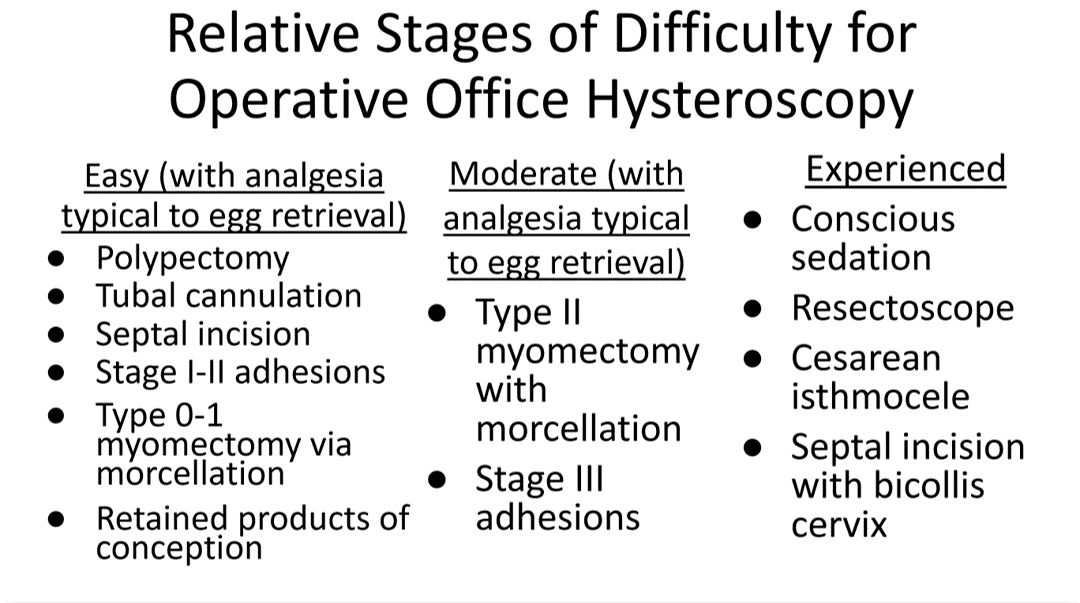
If one can use propofol or a similar level of sedation (which is routinely utilized for oocyte aspiration), there are few hysteroscopies that cannot be accomplished in the office. However, the less sedation and analgesia, the more judicious one must be in patient selection. Moreover, there are trade-offs between visualization, comfort, and instrumentation.
The greater the uterine distention and diameter of the hysteroscope, the more patients experience pain. One-third of patients (especially nulliparous) will discontinue a procedure with a 5-mm hysteroscope because of discomfort.5 However, as one drops to 4.5 mm and smaller operative hysteroscopes, instruments often occupy the inflow channel, limiting distention and visualization, which also can affect completion rates and safety.
When is operative hysteroscopy best suited for the OR?
In addition to physician experience and clinical resources, the critical factors guiding our choices for selecting the OR rather than the office, include:
- Loss of landmarks. Though Dr. Parry now does most severe intrauterine adhesion cases in the office with ultrasound guidance, when neither ostia can be visualized there is meaningful risk for perforation. Preoperative estrogen, development of planes with the diagnostic hysteroscope prior, and preparing the patient for a possible multistage procedure are all important.
- Use of energy. There are many excellent hysteroscopic surgeons who use the resectoscope well in the office. However, with possible patient movement and potential perforation with energy leading to a bowel injury, there can be greater risk when using energy relative to other methods (such as forceps, scissors, and mechanical morcellation).
- Deeper fibroids. Fibroids displace rather than invade the myometrium, and one can sonographically visualize the myometrium reapproximate over a fibroid as it herniates more into the uterine cavity. Nevertheless, the closer a fibroid comes to the serosa, the more mindful one should be of risks and balances for hysteroscopic removal.
In a patient with a severely stenotic cervix or tortuous endocervical canal, what preprocedure methods do you find helpful, and do you utilize abdominal ultrasound guidance?
If using a 2.8-mm flexible diagnostic hysteroscope, we find 99.8%-99.9% of cervices can be successfully cannulated in the office, with rare exception, that is, following cryotherapy or chlamydia cervicitis. This is the equivalent of your dilator having a camera on the tip and fully articulating to adjust to the cervical path.
Transvaginal sonography prior to hysteroscopy where one maps the cervical lumen helps anticipate problems (along with being familiar with the patient’s history). For the rare dilation under anesthesia, concurrent sonography with a 2.8-mm flexible hysteroscope and intermittent dilator use has been sufficient for our exceptions without the need for lacrimal dilators, vasopressin, misoprostol, and other adjuncts. Of note, we use a 1080p flexible endoscope, as lower resolution would make this more challenging.
In patients with recurrent implantation failure following IVF, is hysteroscopy superior to 3D saline infusion sonogram?
At an American Society of Reproductive Medicine 2021 session, Ilan Tur-Kaspa, MD, and Dr. Parry debated the topic of 2D ultrasound combined with hysteroscopy vs. 3D saline infusion sonography. Core areas of agreement were that expert hands for any approach are better than nonexpert, and high-resolution technology is better than lower resolution. There was also agreement that extrauterine and myometrial disease, such as intramural fibroids and adenomyosis, are contributory factors.
So, sonography will always have a role. However, existing and forthcoming data show hysteroscopy to improve live birth rates for patients with recurrent implantation failure after IVF. Dr. Parry finds diagnostic hysteroscopy easier for identifying endometritis, sessile and cornual polyps, retained products of conception (which are often isoechogenic with the endometrium) and lateral adhesions.
The reality is that there is variability among physicians and midlevel providers in both sonographic and diagnostic hysteroscopic skill. If one wants to verify findings with another team member, acknowledging that there can be nuances to identifying these pathologies by sonography, it is easier to share and discuss findings through hysteroscopic video than sonographic records.
When is endometrial biopsy indicated during office hysteroscopy?
The patients of an REI are very unlikely to have endometrial cancer (or even hyperplasia) outside of polyps (or arguably hypervascular areas of overgrowth), so the focus is on resecting visualized pathology relative to random biopsy.
However, the threshold for biopsy should be adjusted to the patient population, as well as to individual findings and risk. RVUs are greatly increased (11.1 > 41.57) with biopsy, helping sustainability. Additionally, if one places the hysteroscope on endometrium and applies suction through the inflow channel, one can obtain a sample with small-caliber diagnostic hysteroscopes and without having to use forceps.
What is your threshold for fluid deficit in hysteroscopy?
We follow AAGL guidelines, which for operative hysteroscopy are 2,500 mL of isotonic fluids or 1,000 mL of hypotonic fluids in low-risk patients. This should be further reduced to 500 mL of isotonic fluids in the elderly and even 300 mL in those with cardiovascular compromise.6
For patients who request sedation for office hysteroscopy, which option do you recommend – paracervical block alone, nitrous oxide, or the combination?
For diagnostic, greater than 95% of our patients do not require even over-the-counter analgesic medications. For operative, we consider all permissible resources that allow for a safe combination that is appropriate to the pathology and clinical setting, such as paracervical blocks, nitrous oxide, NSAIDs such as ketorolac, anxiolytics, and more.
The goal is to optimize the patient experience. However, the top three criteria that influence successful operative office hysteroscopy for a conscious patient are a parous cervix, judicious patient selection, and pre- and intraoperative verbal analgesia. Informed consent and engagement improve the experience of both the patient and physician.
Dr. Parry is the founder of Positive Steps Fertility in Madison, Miss. Dr. Trolice is director of The IVF Center in Winter Park, Fla., and professor of obstetrics and gynecology at the University of Central Florida, Orlando.
References
1. Parry JP et al. J Minim Invasive Gynecol. 2017 May-Jun. doi: 10.1016/j.jmig.2017.02.010.
2. Wadhwa L et al. 2017 Apr-Jun. doi: 10.4103/jhrs.JHRS_123_16.
3. Parry JP et al. Fertil Steril. 2017 Oct. doi: 10.1016/j.fertnstert.2017.07.1159.
4. Penzias A et al. Fertil Steril. 2021 Nov. doi: 10.1016/j.fertnstert.2021.08.038.
5. Campo R et al. Hum Reprod. 2005 Jan;20(1):258-63. doi: 10.1093/humrep/deh559.
6. AAGL AAGL practice report: Practice guidelines for the management of hysteroscopic distending media. J Minim Invasive Gynecol. 2013 Mar-Apr. doi: 10.1016/j.jmig.2012.12.002.
Over half of pregnant patients not properly screened for thyroid disease
BALTIMORE – Less than half of the pregnant patients who met the criteria for thyroid screening were actually screened by their clinician, according to a retrospective cohort study presented at the annual clinical and scientific meeting of the American College of Obstetricians and Gynecologists in Baltimore. Those who met criteria and did receive screening had higher live birth rates and lower miscarriage rates than those who met the criteria but did not undergo screening, the study found.
“These results suggest that improving thyroid screening adherence may lead to improved pregnancy outcomes,” lead author Allan Dong, MD, of Advocate Lutheran General Hospital in Des Plaines, Ill., told attendees. “However, following targeted screening guidelines can be difficult for clinicians. In practice, universal screening for diabetes and pregnancy may provide more comprehensive screening coverage and potentially lead to improved outcomes.”
Instead of universal screening for thyroid disease, ACOG and the American Thyroid Association recommend targeted screening of high-risk patients, though ATA’s criteria are substantially broader than ACOG’s. But, Dr. Dong told attendees, “guidelines are only beneficial if they are followed appropriately,” and Ob.Gyns. have limited time to screen for risk factors in the midst of other clinical priorities. So he aimed to learn whether Ob.Gyns. were following the guidelines of either organization in screening people at higher risk for thyroid disease.
Dr. Dong and his coauthor, Melisa Lott, DO, reviewed the charts of all 1,025 patients who presented at their institution for new obstetrical visits in 2020 to determine which ones had risk factors that would qualify them for screening under ATA or ACOG guidelines. ACOG’s screening criteria included having a personal or family history of thyroid disease or type 1 diabetes, or there being clinical suspicion for thyroid disease. ATA’s screening criteria included the following:
- Personal or family history of thyroid disease.
- History of head or neck radiation.
- History of a prior thyroid surgery.
- Over age 30.
- Any autoimmune disease.
- A body mass index greater than 40 kg/m2.
- History of pregnancy loss, preterm delivery, or infertility.
- Recently used amiodarone lithium or iodine-based contrast.
- Lived in an area of known iodine deficiency.
- Clinical suspicion of thyroid disease.
ATA screening criteria identified four times as many patients requiring screening than did ACOG criteria, Dr. Dong noted. Of the 198 patients who met ACOG’s criteria, 43.9% were screened with thyroid function testing. Meanwhile, 826 patients – including all those who met ACOG’s criteria – met ATA’s criteria for screening, but only 13.1% of them underwent thyroid function testing.
Live birth rates were significantly higher among patients who met ATA criteria and were screened (92.6%) than among patients who met ATA criteria but were not screened (83.3%, P = .006). Similarly, the miscarriage rate was 4.6% in patients who met ATA criteria and were screened, compared to 12.4% in patients who met the criteria but did not undergo thyroid function testing (P = .009).
“A similar difference, although not statistically significant, was noted when comparing patients who were screened appropriately per ACOG criteria with those who met criteria for screening but were not screened,” Dr. Dong told attendees. “However, our study was underpowered to detect this difference due to the lower number of patients who meet criteria for screening under ACOG guidelines.”
The researchers did not find any significant difference in preterm delivery rates.
Anna Whelan, MD, of Women & Infants Hospital of Brown University, Providence, R.I., was not involved in the study but viewed the poster and pointed out that many of the patients, if seen by a primary care provider prior to pregnancy, would likely have been screened by their PCP. The rate of underscreening therefore suggests that patients “are not getting good, consistent primary care because there’s a lack of primary care physicians,” Dr. Whelan said in an interview.
In addition, she added, “maybe not all obstetricians and those providing care, such as midwives and other providers, are aware of the [ATA] guidelines on who should be screened.” She added that additional education about thyroid screening guidelines might be helpful for providers.
Dr. Dong reported being a stock shareholder in 3M, AbbVie, General Electric, Johnson & Johnson, Medtronic, Pfizer, and Viking Therapeutics. Dr. Whelan had no disclosures.
BALTIMORE – Less than half of the pregnant patients who met the criteria for thyroid screening were actually screened by their clinician, according to a retrospective cohort study presented at the annual clinical and scientific meeting of the American College of Obstetricians and Gynecologists in Baltimore. Those who met criteria and did receive screening had higher live birth rates and lower miscarriage rates than those who met the criteria but did not undergo screening, the study found.
“These results suggest that improving thyroid screening adherence may lead to improved pregnancy outcomes,” lead author Allan Dong, MD, of Advocate Lutheran General Hospital in Des Plaines, Ill., told attendees. “However, following targeted screening guidelines can be difficult for clinicians. In practice, universal screening for diabetes and pregnancy may provide more comprehensive screening coverage and potentially lead to improved outcomes.”
Instead of universal screening for thyroid disease, ACOG and the American Thyroid Association recommend targeted screening of high-risk patients, though ATA’s criteria are substantially broader than ACOG’s. But, Dr. Dong told attendees, “guidelines are only beneficial if they are followed appropriately,” and Ob.Gyns. have limited time to screen for risk factors in the midst of other clinical priorities. So he aimed to learn whether Ob.Gyns. were following the guidelines of either organization in screening people at higher risk for thyroid disease.
Dr. Dong and his coauthor, Melisa Lott, DO, reviewed the charts of all 1,025 patients who presented at their institution for new obstetrical visits in 2020 to determine which ones had risk factors that would qualify them for screening under ATA or ACOG guidelines. ACOG’s screening criteria included having a personal or family history of thyroid disease or type 1 diabetes, or there being clinical suspicion for thyroid disease. ATA’s screening criteria included the following:
- Personal or family history of thyroid disease.
- History of head or neck radiation.
- History of a prior thyroid surgery.
- Over age 30.
- Any autoimmune disease.
- A body mass index greater than 40 kg/m2.
- History of pregnancy loss, preterm delivery, or infertility.
- Recently used amiodarone lithium or iodine-based contrast.
- Lived in an area of known iodine deficiency.
- Clinical suspicion of thyroid disease.
ATA screening criteria identified four times as many patients requiring screening than did ACOG criteria, Dr. Dong noted. Of the 198 patients who met ACOG’s criteria, 43.9% were screened with thyroid function testing. Meanwhile, 826 patients – including all those who met ACOG’s criteria – met ATA’s criteria for screening, but only 13.1% of them underwent thyroid function testing.
Live birth rates were significantly higher among patients who met ATA criteria and were screened (92.6%) than among patients who met ATA criteria but were not screened (83.3%, P = .006). Similarly, the miscarriage rate was 4.6% in patients who met ATA criteria and were screened, compared to 12.4% in patients who met the criteria but did not undergo thyroid function testing (P = .009).
“A similar difference, although not statistically significant, was noted when comparing patients who were screened appropriately per ACOG criteria with those who met criteria for screening but were not screened,” Dr. Dong told attendees. “However, our study was underpowered to detect this difference due to the lower number of patients who meet criteria for screening under ACOG guidelines.”
The researchers did not find any significant difference in preterm delivery rates.
Anna Whelan, MD, of Women & Infants Hospital of Brown University, Providence, R.I., was not involved in the study but viewed the poster and pointed out that many of the patients, if seen by a primary care provider prior to pregnancy, would likely have been screened by their PCP. The rate of underscreening therefore suggests that patients “are not getting good, consistent primary care because there’s a lack of primary care physicians,” Dr. Whelan said in an interview.
In addition, she added, “maybe not all obstetricians and those providing care, such as midwives and other providers, are aware of the [ATA] guidelines on who should be screened.” She added that additional education about thyroid screening guidelines might be helpful for providers.
Dr. Dong reported being a stock shareholder in 3M, AbbVie, General Electric, Johnson & Johnson, Medtronic, Pfizer, and Viking Therapeutics. Dr. Whelan had no disclosures.
BALTIMORE – Less than half of the pregnant patients who met the criteria for thyroid screening were actually screened by their clinician, according to a retrospective cohort study presented at the annual clinical and scientific meeting of the American College of Obstetricians and Gynecologists in Baltimore. Those who met criteria and did receive screening had higher live birth rates and lower miscarriage rates than those who met the criteria but did not undergo screening, the study found.
“These results suggest that improving thyroid screening adherence may lead to improved pregnancy outcomes,” lead author Allan Dong, MD, of Advocate Lutheran General Hospital in Des Plaines, Ill., told attendees. “However, following targeted screening guidelines can be difficult for clinicians. In practice, universal screening for diabetes and pregnancy may provide more comprehensive screening coverage and potentially lead to improved outcomes.”
Instead of universal screening for thyroid disease, ACOG and the American Thyroid Association recommend targeted screening of high-risk patients, though ATA’s criteria are substantially broader than ACOG’s. But, Dr. Dong told attendees, “guidelines are only beneficial if they are followed appropriately,” and Ob.Gyns. have limited time to screen for risk factors in the midst of other clinical priorities. So he aimed to learn whether Ob.Gyns. were following the guidelines of either organization in screening people at higher risk for thyroid disease.
Dr. Dong and his coauthor, Melisa Lott, DO, reviewed the charts of all 1,025 patients who presented at their institution for new obstetrical visits in 2020 to determine which ones had risk factors that would qualify them for screening under ATA or ACOG guidelines. ACOG’s screening criteria included having a personal or family history of thyroid disease or type 1 diabetes, or there being clinical suspicion for thyroid disease. ATA’s screening criteria included the following:
- Personal or family history of thyroid disease.
- History of head or neck radiation.
- History of a prior thyroid surgery.
- Over age 30.
- Any autoimmune disease.
- A body mass index greater than 40 kg/m2.
- History of pregnancy loss, preterm delivery, or infertility.
- Recently used amiodarone lithium or iodine-based contrast.
- Lived in an area of known iodine deficiency.
- Clinical suspicion of thyroid disease.
ATA screening criteria identified four times as many patients requiring screening than did ACOG criteria, Dr. Dong noted. Of the 198 patients who met ACOG’s criteria, 43.9% were screened with thyroid function testing. Meanwhile, 826 patients – including all those who met ACOG’s criteria – met ATA’s criteria for screening, but only 13.1% of them underwent thyroid function testing.
Live birth rates were significantly higher among patients who met ATA criteria and were screened (92.6%) than among patients who met ATA criteria but were not screened (83.3%, P = .006). Similarly, the miscarriage rate was 4.6% in patients who met ATA criteria and were screened, compared to 12.4% in patients who met the criteria but did not undergo thyroid function testing (P = .009).
“A similar difference, although not statistically significant, was noted when comparing patients who were screened appropriately per ACOG criteria with those who met criteria for screening but were not screened,” Dr. Dong told attendees. “However, our study was underpowered to detect this difference due to the lower number of patients who meet criteria for screening under ACOG guidelines.”
The researchers did not find any significant difference in preterm delivery rates.
Anna Whelan, MD, of Women & Infants Hospital of Brown University, Providence, R.I., was not involved in the study but viewed the poster and pointed out that many of the patients, if seen by a primary care provider prior to pregnancy, would likely have been screened by their PCP. The rate of underscreening therefore suggests that patients “are not getting good, consistent primary care because there’s a lack of primary care physicians,” Dr. Whelan said in an interview.
In addition, she added, “maybe not all obstetricians and those providing care, such as midwives and other providers, are aware of the [ATA] guidelines on who should be screened.” She added that additional education about thyroid screening guidelines might be helpful for providers.
Dr. Dong reported being a stock shareholder in 3M, AbbVie, General Electric, Johnson & Johnson, Medtronic, Pfizer, and Viking Therapeutics. Dr. Whelan had no disclosures.
FROM ACOG 2023
Understanding clinic-reported IVF success rates
The field of assisted reproductive technologies (ART) continues to evolve from its first successful birth in 1978 in England, and then in 1981 in the United States. Over the last 6 years, the total number of cycles in the U.S. has increased by 44% to nearly 370,000.
SART membership consists of more than 350 clinics throughout the United States, representing 80% of ART clinics. Over 95% of ART cycles in 2021 in the United States were performed in SART-member clinics.
SART is an invaluable resource for both patients and physicians. Their website includes a “Predict My Success” calculator that allows patients and physicians to enter individualized data to calculate the chance of having a baby over one or more complete cycles of IVF. To help us understand the pregnancy outcome data from ART – cycles per clinic along with national results – I posed the questions below to Amy Sparks, PhD, HCLD, director of the IVF and Andrology Laboratories and the Center for Advanced Reproductive Care at University of Iowa Hospitals and Clinics, Iowa City. Dr. Sparks is past president of SART and former chairperson of the SART Registry committee when the current Clinic Summary Report format was initially released.
Question: The Fertility Clinic Success Rate and Certification Act (FCSRCA) of 1992 mandated that all ART clinics report success rate data to the federal government, through the Centers for Disease Control and Prevention, in a standardized manner. As ART is the only field in medicine to be required to annually report their patient outcomes, that is, all initiated cycles and live births, why do you believe this law was enacted and is limited to reproductive medicine?
Answer: The FCSRCA of 1992 was enacted in response to the lack of open and reliable pregnancy success rate information for patients seeking infertility care using assisted reproductive technologies. Success rates of 25%-50% were being advertised by independent clinics when, nationally, fewer than 15% of ART procedures led to live births. The Federal Trade Commission said such claims were deceptive and filed charges against five clinics, saying they misrepresented their success in helping women become pregnant. The government won one case by court order and the other four cases were settled out of court.
This field of medicine was in the spotlight as the majority of patients lacked insurance coverage for their ART cycles, and there was a strong desire to protect consumers paying out of pocket for relatively low success. Recognizing that the FTC’s mission is to ensure truth in advertising and not regulate medical care, Congress passed the FCSRCA, mandating that all centers providing ART services report all initiated cycles and their outcomes. The CDC was appointed as the agency responsible for collecting cycle data and reporting outcomes. Centers not reporting their cycles are listed as nonreporting centers.
This act also established standards for accreditation of embryology laboratories including personnel and traditional clinical laboratory management requirements. These standards serve as the foundation for embryology laboratory accrediting agencies.
Q: Why have live-birth rates on SART appeared to be focused on “per IVF cycle” as opposed to the CDC reporting of live births “per embryo transfer?”
A: An ART cycle “start” is defined as the initiation of ovarian stimulation with medication that may or may not include administration of exogenous gonadotropins, followed by oocyte retrieval and embryo transfer. Not every patient beginning a cycle will undergo an oocyte retrieval and not all patients who undergo oocyte retrieval have an embryo transfer. The live-birth rates (LBR) for each of these steps of progression in the ART process are available in the SART and CDC reports.
In 2016, SART recognized that practices were foregoing fresh embryo transfer after oocyte retrieval, opting to cryopreserve all embryos to either accommodate genetic testing of the embryos prior to transfer or to avoid embryo transfer to an unfavorable uterine environment. In response to changes in practice and in an effort to deemphasize live birth per transfer, thereby alleviating a potential motivator or pressure for practitioners to transfer multiple embryos, SART moved to a report that displays the cumulative live-birth rate per cycle start for oocyte retrieval. The cumulative live-birth rate per cycle start for oocyte retrieval is the chance of live birth from transfers of embryos derived from the oocyte retrieval and performed within 1 year of the oocyte retrieval.
This change in reporting further reduced the pressure to transfer multiple embryos and encouraged elective, single-embryo transfer. The outcome per transfer is no longer the report’s primary focus.
Q: The latest pregnancy outcomes statistics are from the year 2020 and are finalized by the CDC. Why does the SART website have this same year labeled “preliminary” outcomes?
A: Shortly after the 2016 SART report change, the CDC made similar changes to their report. The difference is that SART provides a “preliminary” report of outcomes within the year of the cycle start for oocyte retrieval. The cumulative outcome is not “finalized” until the following year as transfers may be performed as late as 12 months after the oocyte retrieval.
SART has opted to report both the “preliminary” or interim outcome and the “final” outcome a year later. The CDC has opted to limit their report to “final” outcomes. I’m happy to report that SART recently released the final report for 2021 cycles.
Q: Have national success rates in the United States continued to rise or have they plateaued?
A: It appears that success rates have plateaued; however, we find ourselves at another point where practice patterns and patients’ approach to using ART for family building have changed.
Recognizing the impact of maternal aging on reproductive potential, patients are opting to undergo multiple ART cycles to cryopreserve embryos for family building before they attempt to get pregnant. This family-building path reduces the value of measuring the LBR per cycle start as we may not know the outcome for many years. SART leaders are deliberating intently as to how to best represent this growing patient population in outcome reporting.
Q: Can you comment on the reduction of multiple gestations with the increasing use of single-embryo transfer?
A: The reduction in emphasis on live births per transfer, emphasis on singleton live-birth rates in both the SART and CDC reports, and American Society for Reproductive Medicine practice committee guidelines strongly supporting single embryo transfer have significantly reduced the rate of multiple gestations.
A decade ago, only a third of the transfers were single-embryo transfers and over 25% of live births resulted in a multiple birth. Today, the majority of embryo transfers are elective, single-embryo transfers, and the multiple birth rate has been reduced by nearly 80%. In 2020, 93% of live births from IVF were singletons.
Q: SART offers an online IVF calculator so both patients and physicians can plug in data for an approximate cumulative success rate for up to three IVF cycles. The calculator pools data from all U.S.-reporting IVF centers. Can you explain what an “IVF cycle” is and what patient information is required? Why do success rates increase over time?
A: Each “IVF cycle” is a cycle start for an oocyte retrieval and all transfers of embryos from that cycle within a year of the oocyte retrieval. If the first cycle and subsequent transfers do not lead to a live birth, patients still have a chance to achieve a live birth with a second or third cycle. The success rate increases over time as it reflects the chance of success for a population of patients, with some achieving a live birth after the first cycle and additional patients who achieve success following their third cycle.
Q: The SART IVF calculator can be used with no prior IVF cycles or following an unsuccessful cycle. Are there data to support an estimation of outcome following two or even more unsuccessful cycles?
A: The variables in the SART IVF calculator are based upon the cycle-specific data from patients seeking care at SART member clinics. The current predictor was built with data from cycles performed in 2015-2016. SART is adjusting the predictor and developing a calculator that will be routinely updated, accordingly.
Q: Only approximately 40% of states have some form of infertility coverage law in place; however the number of IVF cycles in the United States continues to increase on an annual basis. What do you think are the driving factors behind this?
A: Advocacy efforts to improve patients’ access to infertility care have included giving patients tools to encourage their employers to include infertility care in their health care benefits package. More recently, the “Great Resignation” has led to the “Great Recruitment” and employers are recognizing that the addition of infertility care to health care benefits is a powerful recruitment tool.
Dr. Trolice is director of The IVF Center in Winter Park, Fla., and professor of obstetrics and gynecology at the University of Central Florida, Orlando.
The field of assisted reproductive technologies (ART) continues to evolve from its first successful birth in 1978 in England, and then in 1981 in the United States. Over the last 6 years, the total number of cycles in the U.S. has increased by 44% to nearly 370,000.
SART membership consists of more than 350 clinics throughout the United States, representing 80% of ART clinics. Over 95% of ART cycles in 2021 in the United States were performed in SART-member clinics.
SART is an invaluable resource for both patients and physicians. Their website includes a “Predict My Success” calculator that allows patients and physicians to enter individualized data to calculate the chance of having a baby over one or more complete cycles of IVF. To help us understand the pregnancy outcome data from ART – cycles per clinic along with national results – I posed the questions below to Amy Sparks, PhD, HCLD, director of the IVF and Andrology Laboratories and the Center for Advanced Reproductive Care at University of Iowa Hospitals and Clinics, Iowa City. Dr. Sparks is past president of SART and former chairperson of the SART Registry committee when the current Clinic Summary Report format was initially released.
Question: The Fertility Clinic Success Rate and Certification Act (FCSRCA) of 1992 mandated that all ART clinics report success rate data to the federal government, through the Centers for Disease Control and Prevention, in a standardized manner. As ART is the only field in medicine to be required to annually report their patient outcomes, that is, all initiated cycles and live births, why do you believe this law was enacted and is limited to reproductive medicine?
Answer: The FCSRCA of 1992 was enacted in response to the lack of open and reliable pregnancy success rate information for patients seeking infertility care using assisted reproductive technologies. Success rates of 25%-50% were being advertised by independent clinics when, nationally, fewer than 15% of ART procedures led to live births. The Federal Trade Commission said such claims were deceptive and filed charges against five clinics, saying they misrepresented their success in helping women become pregnant. The government won one case by court order and the other four cases were settled out of court.
This field of medicine was in the spotlight as the majority of patients lacked insurance coverage for their ART cycles, and there was a strong desire to protect consumers paying out of pocket for relatively low success. Recognizing that the FTC’s mission is to ensure truth in advertising and not regulate medical care, Congress passed the FCSRCA, mandating that all centers providing ART services report all initiated cycles and their outcomes. The CDC was appointed as the agency responsible for collecting cycle data and reporting outcomes. Centers not reporting their cycles are listed as nonreporting centers.
This act also established standards for accreditation of embryology laboratories including personnel and traditional clinical laboratory management requirements. These standards serve as the foundation for embryology laboratory accrediting agencies.
Q: Why have live-birth rates on SART appeared to be focused on “per IVF cycle” as opposed to the CDC reporting of live births “per embryo transfer?”
A: An ART cycle “start” is defined as the initiation of ovarian stimulation with medication that may or may not include administration of exogenous gonadotropins, followed by oocyte retrieval and embryo transfer. Not every patient beginning a cycle will undergo an oocyte retrieval and not all patients who undergo oocyte retrieval have an embryo transfer. The live-birth rates (LBR) for each of these steps of progression in the ART process are available in the SART and CDC reports.
In 2016, SART recognized that practices were foregoing fresh embryo transfer after oocyte retrieval, opting to cryopreserve all embryos to either accommodate genetic testing of the embryos prior to transfer or to avoid embryo transfer to an unfavorable uterine environment. In response to changes in practice and in an effort to deemphasize live birth per transfer, thereby alleviating a potential motivator or pressure for practitioners to transfer multiple embryos, SART moved to a report that displays the cumulative live-birth rate per cycle start for oocyte retrieval. The cumulative live-birth rate per cycle start for oocyte retrieval is the chance of live birth from transfers of embryos derived from the oocyte retrieval and performed within 1 year of the oocyte retrieval.
This change in reporting further reduced the pressure to transfer multiple embryos and encouraged elective, single-embryo transfer. The outcome per transfer is no longer the report’s primary focus.
Q: The latest pregnancy outcomes statistics are from the year 2020 and are finalized by the CDC. Why does the SART website have this same year labeled “preliminary” outcomes?
A: Shortly after the 2016 SART report change, the CDC made similar changes to their report. The difference is that SART provides a “preliminary” report of outcomes within the year of the cycle start for oocyte retrieval. The cumulative outcome is not “finalized” until the following year as transfers may be performed as late as 12 months after the oocyte retrieval.
SART has opted to report both the “preliminary” or interim outcome and the “final” outcome a year later. The CDC has opted to limit their report to “final” outcomes. I’m happy to report that SART recently released the final report for 2021 cycles.
Q: Have national success rates in the United States continued to rise or have they plateaued?
A: It appears that success rates have plateaued; however, we find ourselves at another point where practice patterns and patients’ approach to using ART for family building have changed.
Recognizing the impact of maternal aging on reproductive potential, patients are opting to undergo multiple ART cycles to cryopreserve embryos for family building before they attempt to get pregnant. This family-building path reduces the value of measuring the LBR per cycle start as we may not know the outcome for many years. SART leaders are deliberating intently as to how to best represent this growing patient population in outcome reporting.
Q: Can you comment on the reduction of multiple gestations with the increasing use of single-embryo transfer?
A: The reduction in emphasis on live births per transfer, emphasis on singleton live-birth rates in both the SART and CDC reports, and American Society for Reproductive Medicine practice committee guidelines strongly supporting single embryo transfer have significantly reduced the rate of multiple gestations.
A decade ago, only a third of the transfers were single-embryo transfers and over 25% of live births resulted in a multiple birth. Today, the majority of embryo transfers are elective, single-embryo transfers, and the multiple birth rate has been reduced by nearly 80%. In 2020, 93% of live births from IVF were singletons.
Q: SART offers an online IVF calculator so both patients and physicians can plug in data for an approximate cumulative success rate for up to three IVF cycles. The calculator pools data from all U.S.-reporting IVF centers. Can you explain what an “IVF cycle” is and what patient information is required? Why do success rates increase over time?
A: Each “IVF cycle” is a cycle start for an oocyte retrieval and all transfers of embryos from that cycle within a year of the oocyte retrieval. If the first cycle and subsequent transfers do not lead to a live birth, patients still have a chance to achieve a live birth with a second or third cycle. The success rate increases over time as it reflects the chance of success for a population of patients, with some achieving a live birth after the first cycle and additional patients who achieve success following their third cycle.
Q: The SART IVF calculator can be used with no prior IVF cycles or following an unsuccessful cycle. Are there data to support an estimation of outcome following two or even more unsuccessful cycles?
A: The variables in the SART IVF calculator are based upon the cycle-specific data from patients seeking care at SART member clinics. The current predictor was built with data from cycles performed in 2015-2016. SART is adjusting the predictor and developing a calculator that will be routinely updated, accordingly.
Q: Only approximately 40% of states have some form of infertility coverage law in place; however the number of IVF cycles in the United States continues to increase on an annual basis. What do you think are the driving factors behind this?
A: Advocacy efforts to improve patients’ access to infertility care have included giving patients tools to encourage their employers to include infertility care in their health care benefits package. More recently, the “Great Resignation” has led to the “Great Recruitment” and employers are recognizing that the addition of infertility care to health care benefits is a powerful recruitment tool.
Dr. Trolice is director of The IVF Center in Winter Park, Fla., and professor of obstetrics and gynecology at the University of Central Florida, Orlando.
The field of assisted reproductive technologies (ART) continues to evolve from its first successful birth in 1978 in England, and then in 1981 in the United States. Over the last 6 years, the total number of cycles in the U.S. has increased by 44% to nearly 370,000.
SART membership consists of more than 350 clinics throughout the United States, representing 80% of ART clinics. Over 95% of ART cycles in 2021 in the United States were performed in SART-member clinics.
SART is an invaluable resource for both patients and physicians. Their website includes a “Predict My Success” calculator that allows patients and physicians to enter individualized data to calculate the chance of having a baby over one or more complete cycles of IVF. To help us understand the pregnancy outcome data from ART – cycles per clinic along with national results – I posed the questions below to Amy Sparks, PhD, HCLD, director of the IVF and Andrology Laboratories and the Center for Advanced Reproductive Care at University of Iowa Hospitals and Clinics, Iowa City. Dr. Sparks is past president of SART and former chairperson of the SART Registry committee when the current Clinic Summary Report format was initially released.
Question: The Fertility Clinic Success Rate and Certification Act (FCSRCA) of 1992 mandated that all ART clinics report success rate data to the federal government, through the Centers for Disease Control and Prevention, in a standardized manner. As ART is the only field in medicine to be required to annually report their patient outcomes, that is, all initiated cycles and live births, why do you believe this law was enacted and is limited to reproductive medicine?
Answer: The FCSRCA of 1992 was enacted in response to the lack of open and reliable pregnancy success rate information for patients seeking infertility care using assisted reproductive technologies. Success rates of 25%-50% were being advertised by independent clinics when, nationally, fewer than 15% of ART procedures led to live births. The Federal Trade Commission said such claims were deceptive and filed charges against five clinics, saying they misrepresented their success in helping women become pregnant. The government won one case by court order and the other four cases were settled out of court.
This field of medicine was in the spotlight as the majority of patients lacked insurance coverage for their ART cycles, and there was a strong desire to protect consumers paying out of pocket for relatively low success. Recognizing that the FTC’s mission is to ensure truth in advertising and not regulate medical care, Congress passed the FCSRCA, mandating that all centers providing ART services report all initiated cycles and their outcomes. The CDC was appointed as the agency responsible for collecting cycle data and reporting outcomes. Centers not reporting their cycles are listed as nonreporting centers.
This act also established standards for accreditation of embryology laboratories including personnel and traditional clinical laboratory management requirements. These standards serve as the foundation for embryology laboratory accrediting agencies.
Q: Why have live-birth rates on SART appeared to be focused on “per IVF cycle” as opposed to the CDC reporting of live births “per embryo transfer?”
A: An ART cycle “start” is defined as the initiation of ovarian stimulation with medication that may or may not include administration of exogenous gonadotropins, followed by oocyte retrieval and embryo transfer. Not every patient beginning a cycle will undergo an oocyte retrieval and not all patients who undergo oocyte retrieval have an embryo transfer. The live-birth rates (LBR) for each of these steps of progression in the ART process are available in the SART and CDC reports.
In 2016, SART recognized that practices were foregoing fresh embryo transfer after oocyte retrieval, opting to cryopreserve all embryos to either accommodate genetic testing of the embryos prior to transfer or to avoid embryo transfer to an unfavorable uterine environment. In response to changes in practice and in an effort to deemphasize live birth per transfer, thereby alleviating a potential motivator or pressure for practitioners to transfer multiple embryos, SART moved to a report that displays the cumulative live-birth rate per cycle start for oocyte retrieval. The cumulative live-birth rate per cycle start for oocyte retrieval is the chance of live birth from transfers of embryos derived from the oocyte retrieval and performed within 1 year of the oocyte retrieval.
This change in reporting further reduced the pressure to transfer multiple embryos and encouraged elective, single-embryo transfer. The outcome per transfer is no longer the report’s primary focus.
Q: The latest pregnancy outcomes statistics are from the year 2020 and are finalized by the CDC. Why does the SART website have this same year labeled “preliminary” outcomes?
A: Shortly after the 2016 SART report change, the CDC made similar changes to their report. The difference is that SART provides a “preliminary” report of outcomes within the year of the cycle start for oocyte retrieval. The cumulative outcome is not “finalized” until the following year as transfers may be performed as late as 12 months after the oocyte retrieval.
SART has opted to report both the “preliminary” or interim outcome and the “final” outcome a year later. The CDC has opted to limit their report to “final” outcomes. I’m happy to report that SART recently released the final report for 2021 cycles.
Q: Have national success rates in the United States continued to rise or have they plateaued?
A: It appears that success rates have plateaued; however, we find ourselves at another point where practice patterns and patients’ approach to using ART for family building have changed.
Recognizing the impact of maternal aging on reproductive potential, patients are opting to undergo multiple ART cycles to cryopreserve embryos for family building before they attempt to get pregnant. This family-building path reduces the value of measuring the LBR per cycle start as we may not know the outcome for many years. SART leaders are deliberating intently as to how to best represent this growing patient population in outcome reporting.
Q: Can you comment on the reduction of multiple gestations with the increasing use of single-embryo transfer?
A: The reduction in emphasis on live births per transfer, emphasis on singleton live-birth rates in both the SART and CDC reports, and American Society for Reproductive Medicine practice committee guidelines strongly supporting single embryo transfer have significantly reduced the rate of multiple gestations.
A decade ago, only a third of the transfers were single-embryo transfers and over 25% of live births resulted in a multiple birth. Today, the majority of embryo transfers are elective, single-embryo transfers, and the multiple birth rate has been reduced by nearly 80%. In 2020, 93% of live births from IVF were singletons.
Q: SART offers an online IVF calculator so both patients and physicians can plug in data for an approximate cumulative success rate for up to three IVF cycles. The calculator pools data from all U.S.-reporting IVF centers. Can you explain what an “IVF cycle” is and what patient information is required? Why do success rates increase over time?
A: Each “IVF cycle” is a cycle start for an oocyte retrieval and all transfers of embryos from that cycle within a year of the oocyte retrieval. If the first cycle and subsequent transfers do not lead to a live birth, patients still have a chance to achieve a live birth with a second or third cycle. The success rate increases over time as it reflects the chance of success for a population of patients, with some achieving a live birth after the first cycle and additional patients who achieve success following their third cycle.
Q: The SART IVF calculator can be used with no prior IVF cycles or following an unsuccessful cycle. Are there data to support an estimation of outcome following two or even more unsuccessful cycles?
A: The variables in the SART IVF calculator are based upon the cycle-specific data from patients seeking care at SART member clinics. The current predictor was built with data from cycles performed in 2015-2016. SART is adjusting the predictor and developing a calculator that will be routinely updated, accordingly.
Q: Only approximately 40% of states have some form of infertility coverage law in place; however the number of IVF cycles in the United States continues to increase on an annual basis. What do you think are the driving factors behind this?
A: Advocacy efforts to improve patients’ access to infertility care have included giving patients tools to encourage their employers to include infertility care in their health care benefits package. More recently, the “Great Resignation” has led to the “Great Recruitment” and employers are recognizing that the addition of infertility care to health care benefits is a powerful recruitment tool.
Dr. Trolice is director of The IVF Center in Winter Park, Fla., and professor of obstetrics and gynecology at the University of Central Florida, Orlando.
Liver disease does not worsen IVF outcomes
Having chronic liver disease does not affect outcomes for women who undergo in vitro fertilization (IVF), new research suggests.
The study, published online in the American Journal of Gastroenterology, compared women with and those without chronic liver disease who had normal ovarian reserve and who underwent assisted reproductive technology (ART) treatment in a high-volume fertility practice from 2002 to 2021.
“IVF treatment and pregnancy outcomes were not significantly different compared to controls,” the researchers wrote.
Women with liver disease may experience impaired fertility. For example, women with chronic liver disease, such as hepatitis C virus infection, may have premature ovarian insufficiency, while women with advanced liver disease, cirrhosis, and hepatic decompensation are known to have abnormally low gonadotropin levels.
leading to “an immediate need for the clinical assessment of reproductive potential in women with chronic liver disease,” the authors wrote.
The literature about ART treatment outcomes for women with liver disease was limited and may not reflect current therapy protocols, researchers found.
“To the best of our knowledge, this study is the largest to date to evaluate IVF efficacy in women with liver disease,” they wrote.
Similar outcomes
Researchers identified 295 women with liver disease (mean age, 37.8 ± 5.2 years) who underwent 1,033 contemporary, standard ART treatment cycles. Six patients (2%) had cirrhosis, eight (2.7%) had undergone liver transplantation, and 281 (95.3%) had chronic liver disease, of which viral hepatitis B and C infections were the most prevalent. The final study population consisted of 115 women who underwent 186 IVF cycles, as well as embryo biopsy for genetic testing.
The control group consisted of all the women at the treatment center without liver disease who received contemporary, standard ART treatment because of male factor infertility, which served as an indication that the women had normal ovarian reserve and were considered fertile. These 624 patients underwent 868 IVF cycles with embryo biopsy.
The mean age of the patients with liver disease was significantly higher than that of the control participants. Mean body mass index was also significantly higher for the patients with liver disease, and there were differences in baseline levels of selected hormones, compared with control participants. In addition, among those with liver disease, the number of oocytes retrieved was significantly lower (12.3 ± 7.6 vs. 16.5 ± 8.2; P < .05), as were the number of mature oocytes (9.1 ± 6.2 vs. 12.6 ± 6.7; P < .05), the number of fertilized embryos (7.0 ± 5.2 vs. 9.9 ± 5.9; P < .05), the number of embryos for which biopsy was performed (3.4 ± 2.2 vs. 5.1 ± 3.5; P < .05), and the number of euploid embryos (1.6 ± 1.4 vs. 2.7 ± 2.4; P < .05), compared with control participants.
Among the two groups, there were no statistically significant differences in mature oocyte rate (an indicator of response to controlled ovarian stimulation), fertilization per mature oocyte rate (an indicator of oocyte quality and ability to be fertilized), or embryo ploidy rate (an indicator of genetically normal embryos), as determined by embryo biopsy, the researchers write.
A subanalysis of women who went on to have a single thawed euploid (chromosomally normal) embryo transfer to achieve pregnancy found no statistically significant differences in rates of clinical pregnancy, clinical pregnancy loss, or live births between the liver disease group and the control group.
“Overall, women with chronic liver disease can be counseled that IVF treatment will not significantly differ in response to controlled ovarian stimulation, embryo fertilization rate, or ploidy outcome compared to women without liver disease,” the researchers wrote.
Data for patient counseling
The results could change the current common thinking among clinicians that IVF should not be conducted until liver disease is under optimal control, first author Jessica Lee, BS, a student at Icahn School of Medicine at Mount Sinai, New York, said.
“There was a knowledge gap for studies in the United States, and we hope this study will not only help patients with liver disease but also providers with counseling,” she said.
The findings suggest that “even if you have chronic liver disease and it’s not fully optimized, that should not interfere with pursuing IVF,” said principal investigator Tatyana Kushner, MD, an associate professor of medicine in liver diseases at the Icahn School.
Women with liver disease whose fertility is impaired should receive counseling about fertility preservation options earlier to help access fertility care, the researchers write.
The study’s findings are “encouraging,” said Monika Sarkar, MD, associate professor of medicine in gastroenterology at the University of California, San Francisco.
“With rising numbers of young adults with liver disease, it is encouraging to see dedicated studies that address a topic of importance to our patients – namely, their reproductive health,” she said. “The current study nicely expands beyond previous data to include a control population without liver disease.”
Differences in oocyte numbers
Although there were no differences in the success rate of embryo transfer, the researchers did see differences in the number of oocytes. Only 37 mature oocytes made it to transfer in the liver disease group, compared with 609 in the control group, noted Dr. Sarkar, who was not involved with the study.
“The challenge of ART is less at the level of embryo transfer, which is very successful once a euploid embryo is achieved, but rather at the earlier step of retrieval of mature oocytes,” Dr. Sarkar said. “Here, the authors found that patients with liver disease had a significantly lower number of oocytes retrieved, number of mature oocytes, and lower number of fertilized embryos.”
The data suggest that fewer eggs are retrieved per cycle from patients with liver disease, “which ultimately will lower the success per cycle,” Dr. Sarkar said.
“This suggests that referring women with chronic liver disease to ART sooner may help to optimize outcomes,” she added. “Larger data evaluating ability to achieve mature oocytes and subsequent fertilization will also be key for determining whether ART success differs by presence, severity, and type of liver disease.”
As more research on ART outcomes in women with liver disease is conducted, subspecialists in gastrointestinal and liver disease may gain confidence in counseling patients, Dr. Sarkar said.
Ms. Lee, Dr. Kushner, and Dr. Sarkar report no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Having chronic liver disease does not affect outcomes for women who undergo in vitro fertilization (IVF), new research suggests.
The study, published online in the American Journal of Gastroenterology, compared women with and those without chronic liver disease who had normal ovarian reserve and who underwent assisted reproductive technology (ART) treatment in a high-volume fertility practice from 2002 to 2021.
“IVF treatment and pregnancy outcomes were not significantly different compared to controls,” the researchers wrote.
Women with liver disease may experience impaired fertility. For example, women with chronic liver disease, such as hepatitis C virus infection, may have premature ovarian insufficiency, while women with advanced liver disease, cirrhosis, and hepatic decompensation are known to have abnormally low gonadotropin levels.
leading to “an immediate need for the clinical assessment of reproductive potential in women with chronic liver disease,” the authors wrote.
The literature about ART treatment outcomes for women with liver disease was limited and may not reflect current therapy protocols, researchers found.
“To the best of our knowledge, this study is the largest to date to evaluate IVF efficacy in women with liver disease,” they wrote.
Similar outcomes
Researchers identified 295 women with liver disease (mean age, 37.8 ± 5.2 years) who underwent 1,033 contemporary, standard ART treatment cycles. Six patients (2%) had cirrhosis, eight (2.7%) had undergone liver transplantation, and 281 (95.3%) had chronic liver disease, of which viral hepatitis B and C infections were the most prevalent. The final study population consisted of 115 women who underwent 186 IVF cycles, as well as embryo biopsy for genetic testing.
The control group consisted of all the women at the treatment center without liver disease who received contemporary, standard ART treatment because of male factor infertility, which served as an indication that the women had normal ovarian reserve and were considered fertile. These 624 patients underwent 868 IVF cycles with embryo biopsy.
The mean age of the patients with liver disease was significantly higher than that of the control participants. Mean body mass index was also significantly higher for the patients with liver disease, and there were differences in baseline levels of selected hormones, compared with control participants. In addition, among those with liver disease, the number of oocytes retrieved was significantly lower (12.3 ± 7.6 vs. 16.5 ± 8.2; P < .05), as were the number of mature oocytes (9.1 ± 6.2 vs. 12.6 ± 6.7; P < .05), the number of fertilized embryos (7.0 ± 5.2 vs. 9.9 ± 5.9; P < .05), the number of embryos for which biopsy was performed (3.4 ± 2.2 vs. 5.1 ± 3.5; P < .05), and the number of euploid embryos (1.6 ± 1.4 vs. 2.7 ± 2.4; P < .05), compared with control participants.
Among the two groups, there were no statistically significant differences in mature oocyte rate (an indicator of response to controlled ovarian stimulation), fertilization per mature oocyte rate (an indicator of oocyte quality and ability to be fertilized), or embryo ploidy rate (an indicator of genetically normal embryos), as determined by embryo biopsy, the researchers write.
A subanalysis of women who went on to have a single thawed euploid (chromosomally normal) embryo transfer to achieve pregnancy found no statistically significant differences in rates of clinical pregnancy, clinical pregnancy loss, or live births between the liver disease group and the control group.
“Overall, women with chronic liver disease can be counseled that IVF treatment will not significantly differ in response to controlled ovarian stimulation, embryo fertilization rate, or ploidy outcome compared to women without liver disease,” the researchers wrote.
Data for patient counseling
The results could change the current common thinking among clinicians that IVF should not be conducted until liver disease is under optimal control, first author Jessica Lee, BS, a student at Icahn School of Medicine at Mount Sinai, New York, said.
“There was a knowledge gap for studies in the United States, and we hope this study will not only help patients with liver disease but also providers with counseling,” she said.
The findings suggest that “even if you have chronic liver disease and it’s not fully optimized, that should not interfere with pursuing IVF,” said principal investigator Tatyana Kushner, MD, an associate professor of medicine in liver diseases at the Icahn School.
Women with liver disease whose fertility is impaired should receive counseling about fertility preservation options earlier to help access fertility care, the researchers write.
The study’s findings are “encouraging,” said Monika Sarkar, MD, associate professor of medicine in gastroenterology at the University of California, San Francisco.
“With rising numbers of young adults with liver disease, it is encouraging to see dedicated studies that address a topic of importance to our patients – namely, their reproductive health,” she said. “The current study nicely expands beyond previous data to include a control population without liver disease.”
Differences in oocyte numbers
Although there were no differences in the success rate of embryo transfer, the researchers did see differences in the number of oocytes. Only 37 mature oocytes made it to transfer in the liver disease group, compared with 609 in the control group, noted Dr. Sarkar, who was not involved with the study.
“The challenge of ART is less at the level of embryo transfer, which is very successful once a euploid embryo is achieved, but rather at the earlier step of retrieval of mature oocytes,” Dr. Sarkar said. “Here, the authors found that patients with liver disease had a significantly lower number of oocytes retrieved, number of mature oocytes, and lower number of fertilized embryos.”
The data suggest that fewer eggs are retrieved per cycle from patients with liver disease, “which ultimately will lower the success per cycle,” Dr. Sarkar said.
“This suggests that referring women with chronic liver disease to ART sooner may help to optimize outcomes,” she added. “Larger data evaluating ability to achieve mature oocytes and subsequent fertilization will also be key for determining whether ART success differs by presence, severity, and type of liver disease.”
As more research on ART outcomes in women with liver disease is conducted, subspecialists in gastrointestinal and liver disease may gain confidence in counseling patients, Dr. Sarkar said.
Ms. Lee, Dr. Kushner, and Dr. Sarkar report no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Having chronic liver disease does not affect outcomes for women who undergo in vitro fertilization (IVF), new research suggests.
The study, published online in the American Journal of Gastroenterology, compared women with and those without chronic liver disease who had normal ovarian reserve and who underwent assisted reproductive technology (ART) treatment in a high-volume fertility practice from 2002 to 2021.
“IVF treatment and pregnancy outcomes were not significantly different compared to controls,” the researchers wrote.
Women with liver disease may experience impaired fertility. For example, women with chronic liver disease, such as hepatitis C virus infection, may have premature ovarian insufficiency, while women with advanced liver disease, cirrhosis, and hepatic decompensation are known to have abnormally low gonadotropin levels.
leading to “an immediate need for the clinical assessment of reproductive potential in women with chronic liver disease,” the authors wrote.
The literature about ART treatment outcomes for women with liver disease was limited and may not reflect current therapy protocols, researchers found.
“To the best of our knowledge, this study is the largest to date to evaluate IVF efficacy in women with liver disease,” they wrote.
Similar outcomes
Researchers identified 295 women with liver disease (mean age, 37.8 ± 5.2 years) who underwent 1,033 contemporary, standard ART treatment cycles. Six patients (2%) had cirrhosis, eight (2.7%) had undergone liver transplantation, and 281 (95.3%) had chronic liver disease, of which viral hepatitis B and C infections were the most prevalent. The final study population consisted of 115 women who underwent 186 IVF cycles, as well as embryo biopsy for genetic testing.
The control group consisted of all the women at the treatment center without liver disease who received contemporary, standard ART treatment because of male factor infertility, which served as an indication that the women had normal ovarian reserve and were considered fertile. These 624 patients underwent 868 IVF cycles with embryo biopsy.
The mean age of the patients with liver disease was significantly higher than that of the control participants. Mean body mass index was also significantly higher for the patients with liver disease, and there were differences in baseline levels of selected hormones, compared with control participants. In addition, among those with liver disease, the number of oocytes retrieved was significantly lower (12.3 ± 7.6 vs. 16.5 ± 8.2; P < .05), as were the number of mature oocytes (9.1 ± 6.2 vs. 12.6 ± 6.7; P < .05), the number of fertilized embryos (7.0 ± 5.2 vs. 9.9 ± 5.9; P < .05), the number of embryos for which biopsy was performed (3.4 ± 2.2 vs. 5.1 ± 3.5; P < .05), and the number of euploid embryos (1.6 ± 1.4 vs. 2.7 ± 2.4; P < .05), compared with control participants.
Among the two groups, there were no statistically significant differences in mature oocyte rate (an indicator of response to controlled ovarian stimulation), fertilization per mature oocyte rate (an indicator of oocyte quality and ability to be fertilized), or embryo ploidy rate (an indicator of genetically normal embryos), as determined by embryo biopsy, the researchers write.
A subanalysis of women who went on to have a single thawed euploid (chromosomally normal) embryo transfer to achieve pregnancy found no statistically significant differences in rates of clinical pregnancy, clinical pregnancy loss, or live births between the liver disease group and the control group.
“Overall, women with chronic liver disease can be counseled that IVF treatment will not significantly differ in response to controlled ovarian stimulation, embryo fertilization rate, or ploidy outcome compared to women without liver disease,” the researchers wrote.
Data for patient counseling
The results could change the current common thinking among clinicians that IVF should not be conducted until liver disease is under optimal control, first author Jessica Lee, BS, a student at Icahn School of Medicine at Mount Sinai, New York, said.
“There was a knowledge gap for studies in the United States, and we hope this study will not only help patients with liver disease but also providers with counseling,” she said.
The findings suggest that “even if you have chronic liver disease and it’s not fully optimized, that should not interfere with pursuing IVF,” said principal investigator Tatyana Kushner, MD, an associate professor of medicine in liver diseases at the Icahn School.
Women with liver disease whose fertility is impaired should receive counseling about fertility preservation options earlier to help access fertility care, the researchers write.
The study’s findings are “encouraging,” said Monika Sarkar, MD, associate professor of medicine in gastroenterology at the University of California, San Francisco.
“With rising numbers of young adults with liver disease, it is encouraging to see dedicated studies that address a topic of importance to our patients – namely, their reproductive health,” she said. “The current study nicely expands beyond previous data to include a control population without liver disease.”
Differences in oocyte numbers
Although there were no differences in the success rate of embryo transfer, the researchers did see differences in the number of oocytes. Only 37 mature oocytes made it to transfer in the liver disease group, compared with 609 in the control group, noted Dr. Sarkar, who was not involved with the study.
“The challenge of ART is less at the level of embryo transfer, which is very successful once a euploid embryo is achieved, but rather at the earlier step of retrieval of mature oocytes,” Dr. Sarkar said. “Here, the authors found that patients with liver disease had a significantly lower number of oocytes retrieved, number of mature oocytes, and lower number of fertilized embryos.”
The data suggest that fewer eggs are retrieved per cycle from patients with liver disease, “which ultimately will lower the success per cycle,” Dr. Sarkar said.
“This suggests that referring women with chronic liver disease to ART sooner may help to optimize outcomes,” she added. “Larger data evaluating ability to achieve mature oocytes and subsequent fertilization will also be key for determining whether ART success differs by presence, severity, and type of liver disease.”
As more research on ART outcomes in women with liver disease is conducted, subspecialists in gastrointestinal and liver disease may gain confidence in counseling patients, Dr. Sarkar said.
Ms. Lee, Dr. Kushner, and Dr. Sarkar report no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM THE AMERICAN JOURNAL OF GASTROENTEROLOGY









