User login
Almost one-third of ED patients with gout are prescribed opioids
Patients with gout who visit the emergency department are regularly prescribed opioids, based on a review of electronic medical records.
“In addition to regulatory changes, the burden of opioid prescription could be potentially reduced by creating prompts for providers in electronic record systems to avoid prescribing opioids in opioid-naive patients or using lower intensity and shorter duration of prescription,” wrote Deepan S. Dalal, MD, of Brown University, Providence, R.I., and coauthors. The study was published in Arthritis Care & Research.
To determine frequency, dose, and duration of opioid prescription at ED discharge, the researchers reviewed the records of 456 patients with acute gout who were discharged in Rhode Island between March 30, 2015, and Sept. 30, 2017. All data were gathered via electronic medical system records.
Of the 456 discharged patients, 129 (28.3%) were prescribed opioids; 102 (79%) were not on opioids at the time. A full prescription description was available for 119 of the 129 patients; 96 (81%) were prescribed oxycodone or oxycodone combinations. Hydrocodone was prescribed for 9 patients (8%) and tramadol was prescribed for 11 patients (9%).
The median duration of each prescription was 8 days (interquartile range, 5-14 days) and the average daily dose was 37.9 mg of morphine equivalent. Patients who were prescribed opioids tended to be younger and male. After multivariable analysis, diabetes, polyarticular gout attack, and prior opioid use were all associated with a more than 100% higher odds of receiving an opioid prescription.
The authors acknowledged their study’s limitations, including their inability to determine the physicians’ reasoning behind each prescription or the prescribing habits of each provider. In addition, they were only able to assess the prescriptions as being written and not the number of pills actually taken or not taken.
No conflicts of interest were reported.
SOURCE: Dalal DS et al. Arthritis Care Res. 2019 Jul 3. doi: 10.1002/acr.23928.
Patients with gout who visit the emergency department are regularly prescribed opioids, based on a review of electronic medical records.
“In addition to regulatory changes, the burden of opioid prescription could be potentially reduced by creating prompts for providers in electronic record systems to avoid prescribing opioids in opioid-naive patients or using lower intensity and shorter duration of prescription,” wrote Deepan S. Dalal, MD, of Brown University, Providence, R.I., and coauthors. The study was published in Arthritis Care & Research.
To determine frequency, dose, and duration of opioid prescription at ED discharge, the researchers reviewed the records of 456 patients with acute gout who were discharged in Rhode Island between March 30, 2015, and Sept. 30, 2017. All data were gathered via electronic medical system records.
Of the 456 discharged patients, 129 (28.3%) were prescribed opioids; 102 (79%) were not on opioids at the time. A full prescription description was available for 119 of the 129 patients; 96 (81%) were prescribed oxycodone or oxycodone combinations. Hydrocodone was prescribed for 9 patients (8%) and tramadol was prescribed for 11 patients (9%).
The median duration of each prescription was 8 days (interquartile range, 5-14 days) and the average daily dose was 37.9 mg of morphine equivalent. Patients who were prescribed opioids tended to be younger and male. After multivariable analysis, diabetes, polyarticular gout attack, and prior opioid use were all associated with a more than 100% higher odds of receiving an opioid prescription.
The authors acknowledged their study’s limitations, including their inability to determine the physicians’ reasoning behind each prescription or the prescribing habits of each provider. In addition, they were only able to assess the prescriptions as being written and not the number of pills actually taken or not taken.
No conflicts of interest were reported.
SOURCE: Dalal DS et al. Arthritis Care Res. 2019 Jul 3. doi: 10.1002/acr.23928.
Patients with gout who visit the emergency department are regularly prescribed opioids, based on a review of electronic medical records.
“In addition to regulatory changes, the burden of opioid prescription could be potentially reduced by creating prompts for providers in electronic record systems to avoid prescribing opioids in opioid-naive patients or using lower intensity and shorter duration of prescription,” wrote Deepan S. Dalal, MD, of Brown University, Providence, R.I., and coauthors. The study was published in Arthritis Care & Research.
To determine frequency, dose, and duration of opioid prescription at ED discharge, the researchers reviewed the records of 456 patients with acute gout who were discharged in Rhode Island between March 30, 2015, and Sept. 30, 2017. All data were gathered via electronic medical system records.
Of the 456 discharged patients, 129 (28.3%) were prescribed opioids; 102 (79%) were not on opioids at the time. A full prescription description was available for 119 of the 129 patients; 96 (81%) were prescribed oxycodone or oxycodone combinations. Hydrocodone was prescribed for 9 patients (8%) and tramadol was prescribed for 11 patients (9%).
The median duration of each prescription was 8 days (interquartile range, 5-14 days) and the average daily dose was 37.9 mg of morphine equivalent. Patients who were prescribed opioids tended to be younger and male. After multivariable analysis, diabetes, polyarticular gout attack, and prior opioid use were all associated with a more than 100% higher odds of receiving an opioid prescription.
The authors acknowledged their study’s limitations, including their inability to determine the physicians’ reasoning behind each prescription or the prescribing habits of each provider. In addition, they were only able to assess the prescriptions as being written and not the number of pills actually taken or not taken.
No conflicts of interest were reported.
SOURCE: Dalal DS et al. Arthritis Care Res. 2019 Jul 3. doi: 10.1002/acr.23928.
FROM ARTHRITIS CARE & RESEARCH
Key clinical point: Though there are other effective conventional treatments, opioids are often prescribed for patients who present to the ED with gout.
Major finding: After multivariable analysis, diabetes, polyarticular gout attack, and prior opioid use were all associated with a more than 100% higher odds of opioid prescription.
Study details: A retrospective cohort study of 456 patients with acute gout discharged from EDs in Rhode Island.
Disclosures: The authors reported no conflicts of interest.
Source: Dalal DS et al. Arthritis Care Res. 2019 Jul 3. doi: 10.1002/acr.23928.
Unacceptable pain despite inflammation control commonly occurs in PsA patients
MADRID – A considerable number of patients with psoriatic arthritis starting their first biologic treatment report unacceptable pain throughout the first year of treatment, even when their inflammation is controlled, according to Swedish researchers.
“Despite this often efficient therapy, 40% of patients still had unacceptable pain after 1 year, and pain with features indicative of a noninflammatory mechanism accounted for more than 60% of this pain load,” senior study author Tor Olofsson, MD, a rheumatologist and doctoral student at Lund (Sweden) University, said in an interview in advance of his presentation at the European Congress of Rheumatology.
“Within rheumatology, today we are generally very good at treating inflammation in many of the arthritides, but we have a lot of patients with persistent pain despite being well treated for their inflammation,” Dr. Olofsson said. “In psoriatic arthritis patients, this remaining pain seems to be even more frequent than in rheumatoid arthritis with the capturing instruments we use here.”
Dr. Olofsson and his colleagues studied prospectively collected records from 352 psoriatic arthritis patients (48% women) participating in the South Swedish Arthritis Group register who started a first anti–tumor necrosis factor (anti-TNF) therapy during 2004-2010. Participants had a mean age of 47 years and a mean disease duration of 10 years. At the start of anti-TNF therapy, 63% of patients were taking methotrexate, and 68% were taking any conventional disease-modifying antirheumatic drug (DMARD).
Based on the Patient Acceptable Symptom State, unacceptable pain was defined as greater than 40 mm on a 0-100 mm Visual Analog Scale (VAS). Inflammation control was captured through C-reactive protein level less than 10 mg/L in combination with one or no swollen joints. Assessments were performed at baseline, 1.5, 3, 6, and 12 months after the start of the first anti-TNF agent. Analyses were also conducted in relation to European League Against Rheumatism (EULAR)–defined treatment response after 3 months (good, moderate, or no response).
At the start of anti-TNF therapy, 85% of patients reported unacceptable pain, which declined to 43% after 3 months and then remained stable, reaching 39% at 12 months. The fraction of patients who had unacceptable pain despite inflammation control was largely unchanged over the study period (24% at treatment start, 27% at 3 months, and 26% at 12 months). Unacceptable pain at 3 months was strongly related to EULAR 3-month response (24% of good responders vs. 79% of nonresponders; P less than .001). This relationship was less pronounced among patients with unacceptable pain despite inflammation control (19% of good responders vs. 37% of nonresponders; P = .016). Among EULAR good responders, unacceptable pain despite inflammation control constituted 81% of all unacceptable pain at 3 months.
Dr. Olofsson said he was surprised by the high levels of pain despite inflammation control reported by these patients. A similar study he and others conducted in rheumatoid arthritis patients a year ago, soon to be published, found that only 12% had unacceptable pain despite inflammation control 1 year after start of a first anti-TNF agent, “so captured by the same instruments, it looks like this problem might be even bigger among patients with psoriatic arthritis.”
There is a possibility that psoriatic arthritis patients may have ongoing pain from low-grade inflammation, he said, but another hypothesis is that many psoriatic arthritis patients develop a more generalized pain condition in line with fibromyalgia. It could be that, if inflammation isn’t treated quickly enough in the beginning of the disease, it could sensitize the central pain system, he said, and it may not be reversible after it has developed.
Alternative treatment strategies are often needed in affected patients, Dr. Olofsson added. This could include regular painkillers or medicines used for more generalized, noninflammatory pain states, such as amitriptyline or duloxetine, as well as nonpharmacologic treatment options.
“The bottom line here is that, if patients are treated aggressively early enough, we might be able to prevent development of this sensitization process,” Dr. Olofsson said. “If we can also do predictive studies to describe which patients have a higher risk of developing this, then maybe we can be even more focused in the initial management before they become centrally sensitized.”
Dr. Olofsson had no financial conflicts to disclose. Two of his coauthors reported relationships with AbbVie, Eli Lilly, Celgene, Novartis, UCB, and Sandoz.
Mitchel L. Zoler contributed to this report.
SOURCE: Roseman C et al. Ann Rheum Dis. 2019 Jun;78(Suppl 2):129-30. Abstract OP0112, doi: 10.1136/annrheumdis-2019-eular.1839.
MADRID – A considerable number of patients with psoriatic arthritis starting their first biologic treatment report unacceptable pain throughout the first year of treatment, even when their inflammation is controlled, according to Swedish researchers.
“Despite this often efficient therapy, 40% of patients still had unacceptable pain after 1 year, and pain with features indicative of a noninflammatory mechanism accounted for more than 60% of this pain load,” senior study author Tor Olofsson, MD, a rheumatologist and doctoral student at Lund (Sweden) University, said in an interview in advance of his presentation at the European Congress of Rheumatology.
“Within rheumatology, today we are generally very good at treating inflammation in many of the arthritides, but we have a lot of patients with persistent pain despite being well treated for their inflammation,” Dr. Olofsson said. “In psoriatic arthritis patients, this remaining pain seems to be even more frequent than in rheumatoid arthritis with the capturing instruments we use here.”
Dr. Olofsson and his colleagues studied prospectively collected records from 352 psoriatic arthritis patients (48% women) participating in the South Swedish Arthritis Group register who started a first anti–tumor necrosis factor (anti-TNF) therapy during 2004-2010. Participants had a mean age of 47 years and a mean disease duration of 10 years. At the start of anti-TNF therapy, 63% of patients were taking methotrexate, and 68% were taking any conventional disease-modifying antirheumatic drug (DMARD).
Based on the Patient Acceptable Symptom State, unacceptable pain was defined as greater than 40 mm on a 0-100 mm Visual Analog Scale (VAS). Inflammation control was captured through C-reactive protein level less than 10 mg/L in combination with one or no swollen joints. Assessments were performed at baseline, 1.5, 3, 6, and 12 months after the start of the first anti-TNF agent. Analyses were also conducted in relation to European League Against Rheumatism (EULAR)–defined treatment response after 3 months (good, moderate, or no response).
At the start of anti-TNF therapy, 85% of patients reported unacceptable pain, which declined to 43% after 3 months and then remained stable, reaching 39% at 12 months. The fraction of patients who had unacceptable pain despite inflammation control was largely unchanged over the study period (24% at treatment start, 27% at 3 months, and 26% at 12 months). Unacceptable pain at 3 months was strongly related to EULAR 3-month response (24% of good responders vs. 79% of nonresponders; P less than .001). This relationship was less pronounced among patients with unacceptable pain despite inflammation control (19% of good responders vs. 37% of nonresponders; P = .016). Among EULAR good responders, unacceptable pain despite inflammation control constituted 81% of all unacceptable pain at 3 months.
Dr. Olofsson said he was surprised by the high levels of pain despite inflammation control reported by these patients. A similar study he and others conducted in rheumatoid arthritis patients a year ago, soon to be published, found that only 12% had unacceptable pain despite inflammation control 1 year after start of a first anti-TNF agent, “so captured by the same instruments, it looks like this problem might be even bigger among patients with psoriatic arthritis.”
There is a possibility that psoriatic arthritis patients may have ongoing pain from low-grade inflammation, he said, but another hypothesis is that many psoriatic arthritis patients develop a more generalized pain condition in line with fibromyalgia. It could be that, if inflammation isn’t treated quickly enough in the beginning of the disease, it could sensitize the central pain system, he said, and it may not be reversible after it has developed.
Alternative treatment strategies are often needed in affected patients, Dr. Olofsson added. This could include regular painkillers or medicines used for more generalized, noninflammatory pain states, such as amitriptyline or duloxetine, as well as nonpharmacologic treatment options.
“The bottom line here is that, if patients are treated aggressively early enough, we might be able to prevent development of this sensitization process,” Dr. Olofsson said. “If we can also do predictive studies to describe which patients have a higher risk of developing this, then maybe we can be even more focused in the initial management before they become centrally sensitized.”
Dr. Olofsson had no financial conflicts to disclose. Two of his coauthors reported relationships with AbbVie, Eli Lilly, Celgene, Novartis, UCB, and Sandoz.
Mitchel L. Zoler contributed to this report.
SOURCE: Roseman C et al. Ann Rheum Dis. 2019 Jun;78(Suppl 2):129-30. Abstract OP0112, doi: 10.1136/annrheumdis-2019-eular.1839.
MADRID – A considerable number of patients with psoriatic arthritis starting their first biologic treatment report unacceptable pain throughout the first year of treatment, even when their inflammation is controlled, according to Swedish researchers.
“Despite this often efficient therapy, 40% of patients still had unacceptable pain after 1 year, and pain with features indicative of a noninflammatory mechanism accounted for more than 60% of this pain load,” senior study author Tor Olofsson, MD, a rheumatologist and doctoral student at Lund (Sweden) University, said in an interview in advance of his presentation at the European Congress of Rheumatology.
“Within rheumatology, today we are generally very good at treating inflammation in many of the arthritides, but we have a lot of patients with persistent pain despite being well treated for their inflammation,” Dr. Olofsson said. “In psoriatic arthritis patients, this remaining pain seems to be even more frequent than in rheumatoid arthritis with the capturing instruments we use here.”
Dr. Olofsson and his colleagues studied prospectively collected records from 352 psoriatic arthritis patients (48% women) participating in the South Swedish Arthritis Group register who started a first anti–tumor necrosis factor (anti-TNF) therapy during 2004-2010. Participants had a mean age of 47 years and a mean disease duration of 10 years. At the start of anti-TNF therapy, 63% of patients were taking methotrexate, and 68% were taking any conventional disease-modifying antirheumatic drug (DMARD).
Based on the Patient Acceptable Symptom State, unacceptable pain was defined as greater than 40 mm on a 0-100 mm Visual Analog Scale (VAS). Inflammation control was captured through C-reactive protein level less than 10 mg/L in combination with one or no swollen joints. Assessments were performed at baseline, 1.5, 3, 6, and 12 months after the start of the first anti-TNF agent. Analyses were also conducted in relation to European League Against Rheumatism (EULAR)–defined treatment response after 3 months (good, moderate, or no response).
At the start of anti-TNF therapy, 85% of patients reported unacceptable pain, which declined to 43% after 3 months and then remained stable, reaching 39% at 12 months. The fraction of patients who had unacceptable pain despite inflammation control was largely unchanged over the study period (24% at treatment start, 27% at 3 months, and 26% at 12 months). Unacceptable pain at 3 months was strongly related to EULAR 3-month response (24% of good responders vs. 79% of nonresponders; P less than .001). This relationship was less pronounced among patients with unacceptable pain despite inflammation control (19% of good responders vs. 37% of nonresponders; P = .016). Among EULAR good responders, unacceptable pain despite inflammation control constituted 81% of all unacceptable pain at 3 months.
Dr. Olofsson said he was surprised by the high levels of pain despite inflammation control reported by these patients. A similar study he and others conducted in rheumatoid arthritis patients a year ago, soon to be published, found that only 12% had unacceptable pain despite inflammation control 1 year after start of a first anti-TNF agent, “so captured by the same instruments, it looks like this problem might be even bigger among patients with psoriatic arthritis.”
There is a possibility that psoriatic arthritis patients may have ongoing pain from low-grade inflammation, he said, but another hypothesis is that many psoriatic arthritis patients develop a more generalized pain condition in line with fibromyalgia. It could be that, if inflammation isn’t treated quickly enough in the beginning of the disease, it could sensitize the central pain system, he said, and it may not be reversible after it has developed.
Alternative treatment strategies are often needed in affected patients, Dr. Olofsson added. This could include regular painkillers or medicines used for more generalized, noninflammatory pain states, such as amitriptyline or duloxetine, as well as nonpharmacologic treatment options.
“The bottom line here is that, if patients are treated aggressively early enough, we might be able to prevent development of this sensitization process,” Dr. Olofsson said. “If we can also do predictive studies to describe which patients have a higher risk of developing this, then maybe we can be even more focused in the initial management before they become centrally sensitized.”
Dr. Olofsson had no financial conflicts to disclose. Two of his coauthors reported relationships with AbbVie, Eli Lilly, Celgene, Novartis, UCB, and Sandoz.
Mitchel L. Zoler contributed to this report.
SOURCE: Roseman C et al. Ann Rheum Dis. 2019 Jun;78(Suppl 2):129-30. Abstract OP0112, doi: 10.1136/annrheumdis-2019-eular.1839.
REPORTING FROM EULAR 2019 CONGRESS
EULAR keeps csDMARDs as top PsA drugs
MADRID – The draft revision of the European League Against Rheumatism’s recommendations for managing psoriatic arthritis sticks with the group’s already-existing conviction that psoriatic arthritis treatment best starts with an NSAID, and if that fails follow with a conventional synthetic antirheumatic drug such as methotrexate, a position in stark contrast with the 2018 recommendation from the American College of Rheumatology to first treat with a tumor necrosis factor (TNF) inhibitor.
For patients with psoriatic arthritis (PsA) manifesting with polyarthritis, conventional synthetic disease-modifying antirheumatic drugs (csDMARDs) “should be first,” and should “start rapidly” if brief, initial treatment with an NSAID proves inadequate, Laure Gossec, MD, PhD, said while presenting a draft version of an update to the PsA management recommendations from EULAR at the European Congress of Rheumatology.
The EULAR recommendations-revision panel had about the same advice for managing PsA patients with oligoarthritis, monoarthritis, or peripheral arthritis. For oligo- and monoarthritis, “consider a csDMARD after failing NSAIDS, but also consider the patient’s prognostic factors,” like structural damage, and dactylitis. For PsA patients with peripheral arthritis, “it still makes sense to keep csDMARDs as the first line treatment,” said Dr. Gossec, professor of rheumatology at Pitie-Salpétriere Hospital and Sorbonne University, Paris. Once published, the revision will replace existing EULAR recommendations from 2015 (Ann Rheum Dis. 2016 Mar;75[3]:499-510).
The list of csDMARDs she cited included not just methotrexate, still the top csDMARD, but also sulfasalazine and leflunomide as alternatives, she noted, with methotrexate also the preferred csDMARD for patients with skin involvement. When a PsA patient fails at least one csDMARD, then switching to a biologic DMARD is recommended. For a patient with skin involvement, a drug that targets interleukin-17 or IL-12 and -23 is preferred. If skin involvement is not a major issue, then treatment with a TNF inhibitor is equally valid, she said.
The 2018 PsA management guideline from the American College of Rheumatology (ACR) proposed a strikingly different sequence, endorsing initial treatment with a TNF inhibitor first over all other options, including methotrexate and other “oral small molecules” (the ACR term for csDMARD), and also including NSAIDs (Arthritis Rheumatol. 2019 Jan;71[1]:5-32).
This schism between EULAR and the ACR could be seen as predictable, given the different constraints the two societies have set for themselves.
“EULAR recommendations take into account drug costs; the ACR guideline is supposed to be agnostic to costs,” explained Philip J. Mease, MD, a rheumatologist at Swedish Medical Center in Seattle and a member of the ACR panel that wrote the 2018 PsA guideline.
In fact it was a study Dr. Mease recently led and reported results from that provided the most recent and perhaps best assessment of a TNF inhibitor, compared with methotrexate, as initial treatment for PsA, with findings that suggest that, although the advice from the two societies may sharply differ, the viewpoints of both groups are evidence based.
The SEAM-PsA (Study of Etanercept and Methotrexate in Subjects with Psoriatic Arthritis) trial randomized 851 PsA patients receiving their first treatment to methotrexate only, the TNF inhibitor etanercept (Enbrel) only, or both drugs. The study’s two coprimary outcomes, the ACR 20 and minimal disease activity responses after 24 weeks, showed that etanercept monotherapy produced these responses in 61% and 36% of patients, respectively, while methotrexate monotherapy produced response rates of 51% and 23%, respectively. Both these differences between etanercept monotherapy and methotrexate monotherapy were statistically significant. Combining methotrexate with etanercept did not produce a significant improvement over etanercept alone.
Interpreting the meaning of this finding for clinical practice “depends on the lens you look through,” Dr. Mease said in an interview. “A lot of patients respond to methotrexate, which is good when treatment resources are challenged. But when there is no resource challenge, the data support going straight to a TNF inhibitor.”
Dr. Gossec confirmed the importance of the SEAM-PsA findings in the writing panel’s decision during discussion of the draft, replying to a question about consideration of the study’s findings. “We carefully looked at the SEAM-PsA trial results, which provide some of the only data we have on methotrexate” for PsA. “We felt that the results were in favor of methotrexate’s efficacy, and therefore did not go against our proposal to keep a graduated approach starting with a csDMARD.”
Patients who fail to receive adequate relief from a csDMARD could then try a biologic DMARD – a TNF inhibitor, IL-17 inhibitor, or IL-12/23 inhibitor, Dr. Gossec said. When skin involvement is minimal, any of these options are possible, she said. If skin involvement is significant, the panel recommended preferentially using an IL-17 or IL-12/23 inhibitor based on head-to-head trials in patients with psoriasis, she said.
When a biologic DMARD is not appropriate or fails, another option is to then try a targeted synthetic DMARD, such as a Janus kinase inhibitor. When none of these options are appropriate, or they all fail, another option for patients with mild oligo- or monoarthritis or in patients with limited skin involvement is apremilast (Otezla), a phosphodiesterase-4 inhibitor. The draft recommendations also advise clinicians to be sure to distinguish fibromyalgia pain from enthesitis involvement, and they introduce the possibility of, with “great caution,” tapering down DMARD treatment in PsA patients who show sustained remission.
Dr. Gossec and Dr. Mease have both been consultants to and received honoraria from several companies. SEAM-PsA was sponsored by Amgen, the company that markets Enbrel.
MADRID – The draft revision of the European League Against Rheumatism’s recommendations for managing psoriatic arthritis sticks with the group’s already-existing conviction that psoriatic arthritis treatment best starts with an NSAID, and if that fails follow with a conventional synthetic antirheumatic drug such as methotrexate, a position in stark contrast with the 2018 recommendation from the American College of Rheumatology to first treat with a tumor necrosis factor (TNF) inhibitor.
For patients with psoriatic arthritis (PsA) manifesting with polyarthritis, conventional synthetic disease-modifying antirheumatic drugs (csDMARDs) “should be first,” and should “start rapidly” if brief, initial treatment with an NSAID proves inadequate, Laure Gossec, MD, PhD, said while presenting a draft version of an update to the PsA management recommendations from EULAR at the European Congress of Rheumatology.
The EULAR recommendations-revision panel had about the same advice for managing PsA patients with oligoarthritis, monoarthritis, or peripheral arthritis. For oligo- and monoarthritis, “consider a csDMARD after failing NSAIDS, but also consider the patient’s prognostic factors,” like structural damage, and dactylitis. For PsA patients with peripheral arthritis, “it still makes sense to keep csDMARDs as the first line treatment,” said Dr. Gossec, professor of rheumatology at Pitie-Salpétriere Hospital and Sorbonne University, Paris. Once published, the revision will replace existing EULAR recommendations from 2015 (Ann Rheum Dis. 2016 Mar;75[3]:499-510).
The list of csDMARDs she cited included not just methotrexate, still the top csDMARD, but also sulfasalazine and leflunomide as alternatives, she noted, with methotrexate also the preferred csDMARD for patients with skin involvement. When a PsA patient fails at least one csDMARD, then switching to a biologic DMARD is recommended. For a patient with skin involvement, a drug that targets interleukin-17 or IL-12 and -23 is preferred. If skin involvement is not a major issue, then treatment with a TNF inhibitor is equally valid, she said.
The 2018 PsA management guideline from the American College of Rheumatology (ACR) proposed a strikingly different sequence, endorsing initial treatment with a TNF inhibitor first over all other options, including methotrexate and other “oral small molecules” (the ACR term for csDMARD), and also including NSAIDs (Arthritis Rheumatol. 2019 Jan;71[1]:5-32).
This schism between EULAR and the ACR could be seen as predictable, given the different constraints the two societies have set for themselves.
“EULAR recommendations take into account drug costs; the ACR guideline is supposed to be agnostic to costs,” explained Philip J. Mease, MD, a rheumatologist at Swedish Medical Center in Seattle and a member of the ACR panel that wrote the 2018 PsA guideline.
In fact it was a study Dr. Mease recently led and reported results from that provided the most recent and perhaps best assessment of a TNF inhibitor, compared with methotrexate, as initial treatment for PsA, with findings that suggest that, although the advice from the two societies may sharply differ, the viewpoints of both groups are evidence based.
The SEAM-PsA (Study of Etanercept and Methotrexate in Subjects with Psoriatic Arthritis) trial randomized 851 PsA patients receiving their first treatment to methotrexate only, the TNF inhibitor etanercept (Enbrel) only, or both drugs. The study’s two coprimary outcomes, the ACR 20 and minimal disease activity responses after 24 weeks, showed that etanercept monotherapy produced these responses in 61% and 36% of patients, respectively, while methotrexate monotherapy produced response rates of 51% and 23%, respectively. Both these differences between etanercept monotherapy and methotrexate monotherapy were statistically significant. Combining methotrexate with etanercept did not produce a significant improvement over etanercept alone.
Interpreting the meaning of this finding for clinical practice “depends on the lens you look through,” Dr. Mease said in an interview. “A lot of patients respond to methotrexate, which is good when treatment resources are challenged. But when there is no resource challenge, the data support going straight to a TNF inhibitor.”
Dr. Gossec confirmed the importance of the SEAM-PsA findings in the writing panel’s decision during discussion of the draft, replying to a question about consideration of the study’s findings. “We carefully looked at the SEAM-PsA trial results, which provide some of the only data we have on methotrexate” for PsA. “We felt that the results were in favor of methotrexate’s efficacy, and therefore did not go against our proposal to keep a graduated approach starting with a csDMARD.”
Patients who fail to receive adequate relief from a csDMARD could then try a biologic DMARD – a TNF inhibitor, IL-17 inhibitor, or IL-12/23 inhibitor, Dr. Gossec said. When skin involvement is minimal, any of these options are possible, she said. If skin involvement is significant, the panel recommended preferentially using an IL-17 or IL-12/23 inhibitor based on head-to-head trials in patients with psoriasis, she said.
When a biologic DMARD is not appropriate or fails, another option is to then try a targeted synthetic DMARD, such as a Janus kinase inhibitor. When none of these options are appropriate, or they all fail, another option for patients with mild oligo- or monoarthritis or in patients with limited skin involvement is apremilast (Otezla), a phosphodiesterase-4 inhibitor. The draft recommendations also advise clinicians to be sure to distinguish fibromyalgia pain from enthesitis involvement, and they introduce the possibility of, with “great caution,” tapering down DMARD treatment in PsA patients who show sustained remission.
Dr. Gossec and Dr. Mease have both been consultants to and received honoraria from several companies. SEAM-PsA was sponsored by Amgen, the company that markets Enbrel.
MADRID – The draft revision of the European League Against Rheumatism’s recommendations for managing psoriatic arthritis sticks with the group’s already-existing conviction that psoriatic arthritis treatment best starts with an NSAID, and if that fails follow with a conventional synthetic antirheumatic drug such as methotrexate, a position in stark contrast with the 2018 recommendation from the American College of Rheumatology to first treat with a tumor necrosis factor (TNF) inhibitor.
For patients with psoriatic arthritis (PsA) manifesting with polyarthritis, conventional synthetic disease-modifying antirheumatic drugs (csDMARDs) “should be first,” and should “start rapidly” if brief, initial treatment with an NSAID proves inadequate, Laure Gossec, MD, PhD, said while presenting a draft version of an update to the PsA management recommendations from EULAR at the European Congress of Rheumatology.
The EULAR recommendations-revision panel had about the same advice for managing PsA patients with oligoarthritis, monoarthritis, or peripheral arthritis. For oligo- and monoarthritis, “consider a csDMARD after failing NSAIDS, but also consider the patient’s prognostic factors,” like structural damage, and dactylitis. For PsA patients with peripheral arthritis, “it still makes sense to keep csDMARDs as the first line treatment,” said Dr. Gossec, professor of rheumatology at Pitie-Salpétriere Hospital and Sorbonne University, Paris. Once published, the revision will replace existing EULAR recommendations from 2015 (Ann Rheum Dis. 2016 Mar;75[3]:499-510).
The list of csDMARDs she cited included not just methotrexate, still the top csDMARD, but also sulfasalazine and leflunomide as alternatives, she noted, with methotrexate also the preferred csDMARD for patients with skin involvement. When a PsA patient fails at least one csDMARD, then switching to a biologic DMARD is recommended. For a patient with skin involvement, a drug that targets interleukin-17 or IL-12 and -23 is preferred. If skin involvement is not a major issue, then treatment with a TNF inhibitor is equally valid, she said.
The 2018 PsA management guideline from the American College of Rheumatology (ACR) proposed a strikingly different sequence, endorsing initial treatment with a TNF inhibitor first over all other options, including methotrexate and other “oral small molecules” (the ACR term for csDMARD), and also including NSAIDs (Arthritis Rheumatol. 2019 Jan;71[1]:5-32).
This schism between EULAR and the ACR could be seen as predictable, given the different constraints the two societies have set for themselves.
“EULAR recommendations take into account drug costs; the ACR guideline is supposed to be agnostic to costs,” explained Philip J. Mease, MD, a rheumatologist at Swedish Medical Center in Seattle and a member of the ACR panel that wrote the 2018 PsA guideline.
In fact it was a study Dr. Mease recently led and reported results from that provided the most recent and perhaps best assessment of a TNF inhibitor, compared with methotrexate, as initial treatment for PsA, with findings that suggest that, although the advice from the two societies may sharply differ, the viewpoints of both groups are evidence based.
The SEAM-PsA (Study of Etanercept and Methotrexate in Subjects with Psoriatic Arthritis) trial randomized 851 PsA patients receiving their first treatment to methotrexate only, the TNF inhibitor etanercept (Enbrel) only, or both drugs. The study’s two coprimary outcomes, the ACR 20 and minimal disease activity responses after 24 weeks, showed that etanercept monotherapy produced these responses in 61% and 36% of patients, respectively, while methotrexate monotherapy produced response rates of 51% and 23%, respectively. Both these differences between etanercept monotherapy and methotrexate monotherapy were statistically significant. Combining methotrexate with etanercept did not produce a significant improvement over etanercept alone.
Interpreting the meaning of this finding for clinical practice “depends on the lens you look through,” Dr. Mease said in an interview. “A lot of patients respond to methotrexate, which is good when treatment resources are challenged. But when there is no resource challenge, the data support going straight to a TNF inhibitor.”
Dr. Gossec confirmed the importance of the SEAM-PsA findings in the writing panel’s decision during discussion of the draft, replying to a question about consideration of the study’s findings. “We carefully looked at the SEAM-PsA trial results, which provide some of the only data we have on methotrexate” for PsA. “We felt that the results were in favor of methotrexate’s efficacy, and therefore did not go against our proposal to keep a graduated approach starting with a csDMARD.”
Patients who fail to receive adequate relief from a csDMARD could then try a biologic DMARD – a TNF inhibitor, IL-17 inhibitor, or IL-12/23 inhibitor, Dr. Gossec said. When skin involvement is minimal, any of these options are possible, she said. If skin involvement is significant, the panel recommended preferentially using an IL-17 or IL-12/23 inhibitor based on head-to-head trials in patients with psoriasis, she said.
When a biologic DMARD is not appropriate or fails, another option is to then try a targeted synthetic DMARD, such as a Janus kinase inhibitor. When none of these options are appropriate, or they all fail, another option for patients with mild oligo- or monoarthritis or in patients with limited skin involvement is apremilast (Otezla), a phosphodiesterase-4 inhibitor. The draft recommendations also advise clinicians to be sure to distinguish fibromyalgia pain from enthesitis involvement, and they introduce the possibility of, with “great caution,” tapering down DMARD treatment in PsA patients who show sustained remission.
Dr. Gossec and Dr. Mease have both been consultants to and received honoraria from several companies. SEAM-PsA was sponsored by Amgen, the company that markets Enbrel.
REPORTING FROM EULAR 2019 CONGRESS
Giant cell arteritis: An updated review of an old disease
Giant cell arteritis (GCA) is a systemic vasculitis involving medium-sized and large arteries, most commonly the temporal, ophthalmic, occipital, vertebral, posterior ciliary, and proximal vertebral arteries. Moreover, involvement of the ophthalmic artery and its branches results in loss of vision. GCA can also involve the aorta and its proximal branches, especially in the upper extremities.
GCA is the most common systemic vasculitis in adults. It occurs almost exclusively in patients over age 50 and affects women more than men. It is most frequent in populations of northern European ancestry, especially Scandinavian. In a retrospective cohort study in Norway, the average annual cumulative incidence rate of GCA was 16.7 per 100,000 people over age 50.1 Risk factors include older age, history of smoking, current smoking, early menopause, and, possibly, stress-related disorders.2
PATHOGENESIS IS NOT COMPLETELY UNDERSTOOD
The pathogenesis of GCA is not completely understood, but there is evidence of immune activation in the arterial wall leading to activation of macrophages and formation of multinucleated giant cells (which may not always be present in biopsies).
The most relevant cytokines in the ongoing pathogenesis are still being defined, but the presence of interferon gamma and interleukin 6 (IL-6) seem to be critical for the expression of the disease. The primary immunogenic triggers for the elaboration of these cytokines and the arteritis remain elusive.
A SPECTRUM OF PRESENTATIONS
The initial symptoms of GCA may be vague, such as malaise, fever, and night sweats, and are likely due to systemic inflammation. Features of vascular involvement include headache, scalp tenderness, and jaw claudication (cramping pain in the jaw while chewing).
A less common but serious feature associated with GCA is partial or complete vision loss affecting 1 or both eyes.3 Some patients suddenly go completely blind without any visual prodrome.
Overlapping GCA phenotypes exist, with a spectrum of presentations that include classic cranial arteritis, extracranial GCA (also called large-vessel GCA), and polymyalgia rheumatica.2
Cranial GCA, the best-characterized clinical presentation, causes symptoms such as headache or signs such as tenderness of the temporal artery. On examination, the temporal arteries may be tender or nodular, and the pulses may be felt above the zygomatic arch, above and in front of the tragus of the ear. About two-thirds of patients with cranial GCA present with new-onset headache, most often in the temporal area, but possibly anywhere throughout the head.
Visual disturbance, jaw claudication, and tongue pain are less common but, if present, increase the likelihood of this diagnosis.2
Large-vessel involvement in GCA is common and refers to involvement of the aorta and its proximal branches. Imaging methods used in diagnosing large-vessel GCA include color Doppler ultrasonography, computed tomography with angiography, magnetic resonance imaging with angiography, and positron emission tomography. In some centers, such imaging is performed in all patients diagnosed with GCA to survey for large-vessel involvement.
Depending on the imaging study, large-vessel involvement has been found in 30% to 80% of cases of GCA.4,5 It is often associated with nonspecific symptoms such as fever, weight loss, chills, and malaise, but it can also cause more specific symptoms such as unilateral extremity claudication. In contrast to patients with cranial GCA, patients with large-vessel GCA were younger at onset, less likely to have headaches, and more likely to have arm claudication at presentation.6 Aortitis of the ascending aorta can occur with a histopathologic pattern of GCA but without the clinical stigmata of GCA.
The finding of aortitis should prompt the clinician to question the patient about other symptoms of GCA and to order imaging of the whole vascular tree. Ultrasonography and biopsy of the temporal arteries can be considered. Whether idiopathic aortitis is part of the GCA spectrum remains to be seen.
Laboratory tests often show anemia, leukocytosis, and thrombocytosis. Acute-phase reactants such as C-reactive protein and the erythrocyte sedimentation rate are often elevated. The sedimentation rate often exceeds 50 mm/hour and sometimes 100 mm/hour.
In 2 retrospective studies, the number of patients with GCA whose sedimentation rate was less than 50 mm/hour ranged between 5% and 11%.7,8 However, a small percentage of patients with GCA have normal inflammatory markers. Therefore, if the suspicion for GCA is high, treatment should be started and biopsy pursued.9 In patients with paraproteinemia or other causes of a spuriously elevated or low erythrocyte sedimentation rate, C-reactive protein is a more reliable test.
Polymyalgia rheumatica is another rheumatologic condition that can occur independently or in conjunction with GCA. It is characterized by stiffness and pain in the proximal joints such as the hips and shoulders, typically worse in the morning and better with activity. Although the patient may subjectively feel weak, a close neurologic examination will reveal normal muscle strength.
Polymyalgia rheumatica is observed in 40% to 60% of patients with GCA at the time of diagnosis; 16% to 21% of patients with polymyalgia rheumatica may develop GCA, especially if untreated.2,10
Differential diagnosis
Other vasculitides (eg, Takayasu arteritis) can also present with unexplained fever, anemia, and constitutional symptoms.
Infection should be considered if fever is present. An infectious disease accompanied by fever, headache, and elevated inflammatory markers can mimic GCA.
Nonarteritic anterior ischemic optic neuropathy can present with sudden vision loss, prompting concern for underlying GCA. Risk factors include hypertension and diabetes mellitus; other features of GCA, including elevated inflammatory markers, are generally absent.
TEMPORAL ARTERY BIOPSY: THE GOLD STANDARD FOR DIAGNOSIS
Temporal artery biopsy remains the standard to confirm the diagnosis. However, because inflammation in the temporal arteries can affect some segments but not others, biopsy results on conventional hematoxylin and eosin staining can be falsely negative in patients with GCA. In one study,11 the mean sensitivity of unilateral temporal artery biopsy was 86.9%.
Typical positive histologic findings are inflammation with panarteritis, CD4-positive lymphocytes, macrophages, giant cells, and fragmentation of the internal elastic lamina.12
When GCA is suspected, treatment with glucocorticoids should be started immediately and biopsy performed as soon as possible. Delaying biopsy for 14 days or more may not affect the accuracy of biopsy study.13 Treatment should never be withheld while awaiting the results of biopsy study.
Biopsy is usually performed unilaterally, on the same side as the symptoms or abnormal findings on examination. Bilateral temporal artery biopsy is also performed and compared with unilateral biopsy; this approach increases the diagnostic yield by about 5%.14
IMAGING
In patients with suspected GCA, imaging is recommended early to complement the clinical criteria for the diagnosis of GCA.15 Positron emission tomography, computed tomography angiography, magnetic resonance angiography, or Doppler ultrasonography can reveal inflammation of the arteries in the proximal upper or lower limbs or the aorta.2
In patients with suspected cranial GCA, ultrasonography of the temporal and axillary arteries is recommended first. If ultrasonography is not available or is inconclusive, high-resolution magnetic resonance imaging of the cranial arteries can be used as an alternative. Computed tomography and positron emission tomography of the cranial arteries are not recommended.
In patients with suspected large-vessel GCA, ultrasonography, positron emission tomography, computed tomography, and magnetic resonance imaging may be used to screen for vessel wall inflammation, edema, and luminal narrowing in extracranial arteries. Ultrasonography is of limited value in assessing aortitis.
Color duplex ultrasonography can be applied to assess for vascular inflammation of the temporal or large arteries. The typical finding of the “halo” sign, a hypoechoic ring around the arterial lumen, represents the inflammation-induced thickening of the arterial wall. The “compression sign,” the persistence of the “halo” during compression of the vessel lumen by the ultrasound probe, has high specificity for the diagnosis.16
Ultrasonography of suspected GCA has yielded sensitivities of 55% to 100% and specificities of 78% to 100%. However, its sensitivity depends on the user’s level of expertise, so it should be done only in medical centers with a high number of GCA cases and with highly experienced sonographers. High-resolution magnetic resonance imaging is an alternative to ultrasonography and has shown similar sensitivity and specificity.3
TREATMENT WITH GLUCOCORTICOIDS
Glucocorticoids remain the standard for treatment of GCA. The therapeutic effect of glucocorticoids in GCA has been established by years of clinical experience, but has never been proven in a placebo-controlled trial. When started appropriately and expeditiously, glucocorticoids produce exquisite resolution of signs and symptoms and prevent the serious complication of vision loss. Rapid resolution of symptoms is so typical of GCA that if the patient’s symptoms persist more than a few days after starting a glucocorticoid, the diagnosis of GCA should be reconsidered.
In a retrospective study of 245 patients with biopsy-proven GCA treated with glucocorticoids, 34 had permanent loss of sight.17 In 32 (94%) of the 34, the vision loss occurred before glucocorticoids were started. Of the remaining 2 patients, 1 lost vision 8 days into treatment, and the other lost vision 3 years after diagnosis and 1 year after discontinuation of glucocorticoids.
In a series of 144 patients with biopsy-proven GCA, 51 had no vision loss at presentation and no vision loss after starting glucocorticoids, and 93 had vision loss at presentation. In the latter group, symptoms worsened within 5 days of starting glucocorticoids in 9 patients.18 If vision was intact at the time of presentation, prompt initiation of glucocorticoids reduced the risk of vision loss to less than 1%.
High doses, slowly tapered
The European League Against Rheumatism recommends early initiation of high-dose glucocorticoids for patients with large-vessel vasculitis,19 and it also recommends glucocorticoids for patients with polymyalgia rheumatica.20 The optimal initial and tapering dosage has never been formally evaluated, but regimens have been devised on the basis of expert opinion.21
For patients with GCA who do not have vision loss at the time of diagnosis, the initial dose is prednisone 1 mg/kg or its equivalent daily for 2 to 4 weeks, after which it is tapered.21 If the initial dosage is prednisone 60 mg orally daily for 2 to 4 weeks, our practice is to taper it to 50 mg daily for 2 weeks, then 40 mg daily for 2 weeks. Then, it is decreased by 5 mg every 2 weeks until it is 20 mg daily, and then by 2.5 mg every 2 weeks until it is 10 mg orally daily. Thereafter, the dosage is decreased by 1 mg every 2 to 4 weeks.
For patients with GCA who experience transient vision loss or diplopia at the time of diagnosis, intravenous pulse glucocorticoid therapy should be initiated to reduce the risk of vision loss as rapidly as possible.22 A typical pulse regimen is methylprednisolone 1 g intravenously daily for 3 days. Though not rigorously validated in studies, such an approach is used to avoid vision impairment due to GCA, which is rarely reversible.
RELAPSE OF DISEASE
Suspect a relapse of GCA if the patient’s initial symptoms recur, if inflammatory markers become elevated, or if classic symptoms of GCA or polymyalgia rheumatica occur. Elevations in inflammatory markers do not definitely indicate a flare of GCA, but they should trigger close monitoring of the patient’s symptoms.
Relapse is treated by increasing the glucocorticoid dosage as appropriate to the nature of the relapse. If vision is affected or the patient has symptoms of GCA, then increments of 30 to 60 mg of prednisone are warranted, whereas if the patient has symptoms of polymyalgia rheumatica, then increments of 5 to 10 mg of prednisone are usually used.
The incidence of relapses of GCA in multiple tertiary care centers has been reported to vary between 34% and 75%.23,24 Most relapses occur at prednisone dosages of less than 20 mg orally daily and within the first year after diagnosis. The most common symptoms are limb ischemia, jaw claudication, constitutional symptoms, headaches, and polymyalgia rheumatica. In a review of 286 patients,25 213 (74%) had at least 1 relapse. The first relapse occurred in the first year in 50%, by 2 years in 68%, and by 5 years in 79%.
ADVERSE EFFECTS OF GLUCOCORTICOIDS
In high doses, glucocorticoids have well-known adverse effects. In a population-based study of 120 patients, each patient treated with glucocorticoids experienced at least 1 adverse effect (cataract, fracture, infection, osteonecrosis, diabetes, hypertension, weight gain, capillary fragility, or hair loss).26 The effects were related to aging and cumulative dosage of prednisone but not to the initial dosage.
Glucocorticoids can affect many organs and systems:
- Eyes (cataracts, increased intraocular pressure, exophthalmos)
- Heart (premature atherosclerotic disease, hypertension, fluid retention, hyperlipidemia, arrhythmias)
- Gastrointestinal system (ulcer, gastrointestinal bleeding, gastritis, visceral perforation, hepatic steatosis, acute pancreatitis)
- Bone and muscle (osteopenia, osteoporosis, osteonecrosis, myopathy)
- Brain (mood disorder, psychosis, memory impairment)
- Endocrine system (hyperglycemia, hypothalamic-pituitary-adrenal axis suppression)
- Immune system (immunosuppression, leading to infection and leukocytosis).
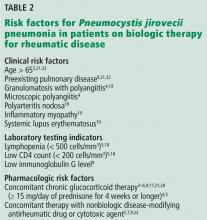
Patients receiving a glucocorticoid dose equivalent to 20 mg or more of prednisone daily for 1 month or more who also have another cause of immunocompromise need prophylaxis against Pneumocystis jirovecii pneumonia.27 They should also receive appropriate immunizations before starting glucocorticoids. Live-virus vaccines should not be given to these patients until they have been off glucocorticoids for 1 month.
Glucocorticoids and bone loss
Glucocorticoids are associated with bone loss and fracture, which can occur within the first few months of use and with dosages as low as 2.5 to 7.5 mg orally daily.28 Therefore, glucocorticoid-induced bone loss has to be treated aggressively, particularly in patients who are older and have a history of fragility fracture.
For patients with GCA who need glucocorticoids in doses greater than 5 mg orally daily for more than 3 months, the following measures are advised to decrease the risk of bone loss:
- Weight-bearing exercise
- Smoking cessation
- Moderation in alcohol intake
- Measures to prevent falls29
- Supplementation with 1,200 mg of calcium and 800 IU of vitamin D.30
Pharmacologic therapy should be initiated in men over age 50 who have established osteoporosis and in postmenopausal women with established osteoporosis or osteopenia. For men over age 50 with established osteopenia, risk assessment with the glucocorticoid-corrected FRAX score (www.sheffield.ac.uk/FRAX) should be performed to identify those at high risk in whom pharmacologic therapy is warranted.31
Bisphosphonates are the first-line therapy for glucocorticoid-induced osteoporosis.32
Teriparatide is the second-line therapy and is used in patients who cannot tolerate bisphosphonates or other osteoporosis therapies, and in those who have severe osteoporosis, with T scores of –3.5 and below if they have not had a fracture, and –2.5 and below if they have had a fragility fracture.33
Denosumab, a monoclonal antibody to an osteoclast differentiating factor, may be beneficial for some patients with glucocorticoid-induced osteoporosis.34
To assess the efficacy of therapy, measuring bone mineral density at baseline and at 1 year of therapy is recommended. If density is stable or improved, then repeating the measurement at 2- to 3-year intervals is suggested.
TOCILIZUMAB: A STEROID-SPARING MEDICATION
Due to the adverse effects of long-term use of glucocorticoids and high rates of relapse, there is a pressing need for medications that are more efficacious and less toxic to treat GCA.
The European League Against Rheumatism, in its 2009 management guidelines for large-vessel vasculitis, recommend using an adjunctive immunosuppressant agent.19 In the case of GCA, they recommend using methotrexate 10 to 15 mg/week, which has shown modest evidence of reducing the relapse rate and lowering the cumulative doses of glucocorticoids needed.35,36
Studies of tumor necrosis factor inhibitors and abatacept have not yielded significant reductions in the relapse rate or decreased cumulative doses of prednisone.37,38
Advances in treatment for GCA have stagnated, but recent trials39,40 have evaluated the IL-6 receptor alpha inhibitor tocilizumab, given the central role of IL-6 in the pathogenesis of GCA. Case reports have revealed rapid induction and maintenance of remission in GCA using tocilizumab.41,42
Villiger et al39 performed a randomized, placebo-controlled trial to study the efficacy and safety of tocilizumab in induction and maintenance of disease remission in 30 patients with newly diagnosed GCA. The primary outcome, complete remission at 12 weeks, was achieved in 85% of patients who received tocilizumab plus tapered prednisolone, compared with 40% of patients who received placebo plus tapering prednisolone. The tocilizumab group also had favorable results in secondary outcomes including relapse-free survival at 52 weeks, time to first relapse after induction of remission, and cumulative dose of prednisolone.
The GiACTA trial. Stone et al40 studied the effect of tocilizumab on rates of relapse during glucocorticoid tapering in 251 GCA patients over the course of 52 weeks. Patients were randomized in a 2:1:1:1 ratio to 4 treatment groups:
- Tocilizumab weekly plus prednisone, with prednisone tapered over 26 weeks
- Tocilizumab every other week plus prednisone tapered over 26 weeks
- Placebo plus prednisone tapered over 26 weeks
- Placebo plus prednisone tapered over 52 weeks.
The primary outcome was the rate of sustained glucocorticoid-free remission at 52 weeks. Secondary outcomes included the remission rate, the cumulative glucocorticoid dose, and safety measures. At 52 weeks, the rates of sustained remission were:
- 56% with tocilizumab weekly
- 53% with tocilizumab every other week
- 14% with placebo plus 26-week prednisone taper
- 18% with placebo plus 52-week taper.
Differences between the active treatment groups and the placebo groups were statistically significant (P < .001).
The cumulative dose of prednisone in tocilizumab recipients was significantly less than in placebo recipients. Rates of adverse events were similar. Ultimately, the study showed that tocilizumab, either weekly or every other week, was more effective than prednisone alone at sustaining glucocorticoid-free remission in patients with GCA.
However, the study also raised questions about tocilizumab’s toxic effect profile and its long-term efficacy, as well as who are the optimal candidates for this therapy. Data on long-term use of tocilizumab are primarily taken from its use in rheumatoid arthritis.43 As of this writing, Stone et al are conducting an open-label trial to help provide long-term safety and efficacy data in patients with GCA. In the meantime, we must extrapolate data from the long-term use of tocilizumab in rheumatoid arthritis.
Tocilizumab and lower gastrointestinal tract perforation
One of the major adverse effects of long-term use of tocilizumab is lower gastrointestinal tract perforation.
Xie et al,44 in 2016, reported that the risk of perforation in patients on tocilizumab for rheumatoid arthritis was more than 2 times higher than in patients taking a tumor necrosis factor inhibitor. However, the absolute rates of perforation were low overall, roughly 1 to 3 per 1,000 patient-years in the tocilizumab group. Risk factors for perforation included older age, history of diverticulitis or other gastrointestinal tract condition, and prednisone doses of 7.5 mg or more a day.
Does tocilizumab prevent blindness?
Another consideration is that tocilizumab may not prevent optic neuropathy. In the GiACTA trial, 1 patient in the group receiving tocilizumab every other week developed optic neuropathy.40 Prednisone had been completely tapered off at the time, and the condition resolved when glucocorticoids were restarted. Thus, it is unknown if tocilizumab would be effective on its own without concomitant use of glucocorticoids.
Vision loss is one of the most severe complications of GCA, and it is still unclear whether tocilizumab can prevent vision loss in GCA. Also, we still have no data on the effect of tocilizumab on histopathologic findings, and whether biopsy yield diminishes over time. We hope future studies will help guide us in this regard.
No guidelines on tocilizumab yet
Clinical guidelines on the appropriate use of tocilizumab in GCA are lacking. The American College of Rheumatology and the European League Against Rheumatism have yet to publish updated guidelines with comments on use of tocilizumab. Therefore, it is unclear if tocilizumab is a first-line treatment in GCA, as its efficacy alone without glucocorticoids and its long-term safety in GCA patients have not been studied.
Treatment with tocilizumab should be individualized; it should be considered in patients who have had adverse effects from glucocorticoids, and in patients who experience a flare or cannot have their glucocorticoid dose lowered to an appropriate range.
The optimal duration of tocilizumab therapy is also unknown. However, using the GiACTA study as a rough guide, we try to limit its use to 1 year until additional data are available.
Patients on IL-6 inhibition may have suppressed C-reactive protein regardless of disease activity.43 Therefore, this laboratory value may not be reliable in determining active disease in patients on tocilizumab.
The GiACTA trial has shown an impressive improvement in the relapse-free remission period in patients with GCA taking tocilizumab. However, much work needs to be done to define the safety of this medication and determine which patients should be started on it. In the meantime, we recommend starting high-dose glucocorticoid therapy as soon as the diagnosis of GCA is suspected. In patients who do not tolerate glucocorticoids or whose disease flares during glucocorticoid taper, we recommend starting treatment with tocilizumab either once a week or every other week for at least 1 year.
- Brekke LK, Diamantopoulos AP, Fevang BT, Aßmus J, Esperø E, Gjesdal CG. Incidence of giant cell arteritis in Western Norway 1972–2012: a retrospective cohort study. Arthritis Res Ther 2017; 19(1):278. doi:10.1186/s13075-017-1479-6
- Dejaco C, Duftner C, Buttgereit F, Matteson EL, Dasgupta B. The spectrum of giant cell arteritis and polymyalgia rheumatica: revisiting the concept of the disease. Rheumatology (Oxford) 2017; 56(4):506–515. doi:10.1093/rheumatology/kew273
- Weyand CM, Goronzy JJ. Giant-cell arteritis and polymyalgia rheumatica. N Engl J Med 2014; 371(17):1653. doi:10.1056/NEJMc1409206
- Ghinoi A, Pipitone N, Nicolini A, et al. Large-vessel involvement in recent-onset giant cell arteritis: a case-control colour-Doppler sonography study. Rheumatology (Oxford) 2012; 51(4):730–734. doi:10.1093/rheumatology/ker329
- Prieto-González S, Depetris M, García-Martínez A, et al. Positron emission tomography assessment of large vessel inflammation in patients with newly diagnosed, biopsy-proven giant cell arteritis: a prospective, case-control study. Ann Rheum Dis 2014; 73(7):1388–1392. doi:10.1136/annrheumdis-2013-204572
- Brack A, Martinez-Taboada V, Stanson A, Goronzy JJ, Weyand CM. Disease pattern in cranial and large-vessel giant cell arteritis. Arthritis Rheum 1999; 42(2):311–317. doi:10.1002/1529-0131(199902)42:2<311::AID-ANR14>3.0.CO;2-F
- Salvarani C, Hunder GG. Giant cell arteritis with low erythrocyte sedimentation rate: frequency of occurence in a population-based study. Arthritis Rheum 2001; 45(2):140–145. doi:10.1002/1529-0131(200104)45:2<140::AID-ANR166>3.0.CO;2-2
- Liozon E, Jauberteau-Marchan MO, Ly K, Loustaud-Ratti V, Soria P, Vidal E. Giant cell arteritis with a low erythrocyte sedimentation rate: comments on the article by Salvarani and Hunder. Arthritis Rheum 2002; 47(6):692–694. doi:10.1002/art.10809
- Yu-Wai-Man P, Dayan MR. Giant cell arteritis with normal inflammatory markers. Acta Ophthalmol Scand 2007; 85(4):460. doi:10.1111/j.1600-0420.2006.00864.x
- Buttgereit F, Dejaco C, Matteson EL, Dasgupta B. Polymyalgia rheumatica and giant cell arteritis: a systematic review. JAMA 2016; 315(22):2442–2458. doi:10.1001/jama.2016.5444
- Niederkohr RD, Levin LA. Management of the patient with suspected temporal arteritis a decision-analytic approach. Ophthalmology 2005; 112(5):744–756. doi:10.1016/j.ophtha.2005.01.031
- Bowling K, Rait J, Atkinson J, Srinivas G. Temporal artery biopsy in the diagnosis of giant cell arteritis: does the end justify the means? Ann Med Surg (Lond) 2017; 20:1–5. doi:10.1016/j.amsu.2017.06.020
- Daily B, Dassow P, Haynes J, Nashelsky J. Giant cell arteritis: biopsy after corticosteroid initiation. Am Fam Physician 2017; 95(2):116–117. pmid:28084703
- Durling B, Toren A, Patel V, Gilberg S, Weis E, Jordan D. Incidence of discordant temporal artery biopsy in the diagnosis of giant cell arteritis. Can J Ophthalmol 2014; 49(2):157–161. doi:10.1016/j.jcjo.2013.12.008
- Dejaco C, Ramiro S, Duftner C, et al. EULAR recommendations for the use of imaging in large vessel vasculitis in clinical practice. Ann Rheum Dis 2018; 77(5):636–643. doi:10.1136/annrheumdis-2017-212649
- Aschwanden M, Imfeld S, Staub D, et al. The ultrasound compression sign to diagnose temporal giant cell arteritis shows an excellent interobserver agreement. Clin Exp Rheumatol 2015; 33(2 suppl 89):S-113–S-115. pmid:26016760
- Aiello PD, Trautmann JC, McPhee TJ, Kunselman AR, Hunder GG. Visual prognosis in giant cell arteritis. Ophthalmology 1993; 100(4):550–555. pmid:8479714
- Hayreh SS, Zimmerman B. Visual deterioration in giant cell arteritis patients while on high doses of corticosteroid therapy. Ophthalmology 2003; 110(6):1204–1215. doi:10.1016/S0161-6420(03)00228-8
- Mukhtyar C, Guillevin L, Cid MC, et al; European Vasculitis Study Group. EULAR recommendations for the management of large vessel vasculitis. Ann Rheum Dis 2009; 68(3):318–323. doi:10.1136/ard.2008.088351
- Dejaco C, Singh YP, Perel P, et al; European League Against Rheumatism; American College of Rheumatology. 2015 recommendations for the management of polymyalgia rheumatica: a European League Against Rheumatism/American College of Rheumatology collaborative initiative. Ann Rheum Dis 2015; 74(10):1799–1807. doi:10.1136/annrheumdis-2015-207492
- Bienvenu B, Ly KH, Lambert M, et al; Groupe d’Étude Français des Artérites des gros Vaisseaux, under the Aegis of the Filière des Maladies Auto-Immunes et Auto-Inflammatoires Rares. Management of giant cell arteritis: recommendations of the French Study Group for Large Vessel Vasculitis (GEFA). Rev Med Interne 2016; 37(3):154–165. doi:10.1016/j.revmed.2015.12.015
- Hayreh SS, Biousse V. Treatment of acute visual loss in giant cell arteritis: should we prescribe high-dose intravenous steroids or just oral steroids? J Neuroophthalmol 2012; 32(3):278–287. doi:10.1097/WNO.0b013e3182688218
- Restuccia G, Boiardi L, Cavazza A, et al. Flares in biopsy-proven giant cell arteritis in Northern Italy: characteristics and predictors in a long-term follow-up study. Medicine (Baltimore) 2016; 95(19):e3524. doi:10.1097/MD.0000000000003524
- Kermani TA, Warrington KJ, Cuthbertson D, et al; Vasculitis Clinical Research Consortium. Disease relapses among patients with giant cell arteritis: a prospective, longitudinal cohort study. J Rheumatol 2015; 42(7):1213–1217. doi:10.3899/jrheum.141347
- Labarca C, Koster MJ, Crowson CS, et al. Predictors of relapse and treatment outcomes in biopsy-proven giant cell arteritis: a retrospective cohort study. Rheumatology (Oxford) 2016; 55(2):347–356. doi:10.1093/rheumatology/kev348
- Proven A, Gabriel SE, Orces C, O’Fallon WM, Hunder GG. Glucocorticoid therapy in giant cell arteritis: duration and adverse outcomes. Arthritis Rheum 2003; 49(5):703–708. doi:10.1002/art.11388
- Sepkowitz KA. Opportunistic infections in patients with and patients without acquired immunodeficiency syndrome. Clin Infect Dis 2002; 34(8):1098–1107. doi:10.1086/339548
- van Staa TP, Leufkens HG, Cooper C. The epidemiology of corticosteroid-induced osteoporosis: a meta-analysis. Osteoporos Int 2002; 13(10):777–787. doi:10.1007/s001980200108
- Heffernan MP, Saag KG, Robinson JK, Callen JP. Prevention of osteoporosis associated with chronic glucocorticoid therapy. JAMA 2006; 295(11):1300–1303. pmid:16541489
- Buckley L, Guyatt G, Fink HA, et al. 2017 American College of Rheumatology guideline for the prevention and treatment of glucocorticoid-induced osteoporosis. Arthritis Care Res (Hoboken) 2017; 69(8):1095–1110. doi:10.1002/acr.23279
- Grossman JM, Gordon R, Ranganath VK, et al. American College of Rheumatology 2010 recommendations for the prevention and treatment of glucocorticoid-induced osteoporosis. Arthritis Care Res 201; 62(11):1515–1526. doi:10.1002/acr.20295
- Allen CS, Yeung JH, Vandermeer B, Homik J. Bisphosphonates for steroid-induced osteoporosis. Cochrane Database Syst Rev 2016; 10:CD001347. doi:10.1002/14651858.CD001347.pub2
- Carpinteri R, Porcelli T, Mejia C, et al. Glucocorticoid-induced osteoporosis and parathyroid hormone. J Endocrinol Invest 2010; 33(suppl 7):16–21. pmid:20938221
- Saag KG, Wagman RB, Geusens P, et al. Denosumab versus risedronate in glucocorticoid-induced osteoporosis: a multicentre, randomised, double-blind, active-controlled, double-dummy, non-inferiority study. Lancet Diabetes Endocrinol 2018; 6(6):445–454. doi:10.1016/S2213-8587(18)30075-5
- Hoffman GS, Cid MC, Hellmann DB, et al; International Network for the Study of Systemic Vasculitides. A multicenter, randomized, double-blind, placebo-controlled trial of adjuvant methotrexate treatment for giant cell arteritis. Arthritis Rheum 2002; 46(5):1309–1318. doi:10.1002/art.10262
- Spiera RF, Mitnick HJ, Kupersmith M, et al. A prospective, double-blind, randomized, placebo controlled trial of methotrexate in the treatment of giant cell arteritis (GCA). Clin Exp Rheumatol 2001; 19(5):495–501. pmid:11579707
- Hoffman GS, Cid MC, Rendt-Zagar KE, et al; Infliximab-GCA Study Group. Infliximab for maintenance of glucocorticosteroid-induced remission of giant cell arteritis: a randomized trial. Ann Intern Med 2007; 146(9):621–630. pmid:17470830
- Langford CA, Cuthbertson D, Ytterberg SR, et al; Vasculitis Clinical Research Consortium. A randomized, double-blind trial of abatacept (CTLA-4Ig) for the treatment of giant cell arteritis. Arthritis Rheumatol 2017; 69(4):837–845. doi:10.1002/art.40044
- Villiger PM, Adler S, Kuchen S, et al. Tocilizumab for induction and maintenance of remission in giant cell arteritis: a phase 2, randomised, double-blind, placebo-controlled trial. Lancet. 2016; 387(10031):1921–1927. doi:10.1016/S0140-6736(16)00560-2
- Stone JH, Tuckwell K, Dimonaco S, et al. Trial of tocilizumab in giant-cell arteritis. N Engl J Med 2017; 377(4):317–328. doi:10.1056/NEJMoa1613849
- Oliveira F, Butendieck RR, Ginsburg WW, Parikh K, Abril A. Tocilizumab, an effective treatment for relapsing giant cell arteritis. Clin Exp Rheumatol 2014; 32(3 suppl 82):S76–S78. pmid:24854376
- Loricera J, Blanco R, Hernández JL, et al. Tocilizumab in giant cell arteritis: multicenter open-label study of 22 patients. Semin Arthritis Rheum 2015; 44(6):717–723. doi:10.1016/j.semarthrit.2014.12.005
- Tamaki H, Hajj-Ali RA. Tocilizumab for giant cell arteritis—a new giant step in an old disease. JAMA Neurol 2018; 75(2):145–146. doi:10.1001/jamaneurol.2017.3811
- Xie F, Yun H, Bernatsky S, Curtis JR. Risk for gastrointestinal perforation among rheumatoid arthritis patients receiving tofacitinib, tocilizumab, or other biologics. Arthritis Rheumatol 2016; 68(11):2612–2617. doi:10.1002/art.39761
Giant cell arteritis (GCA) is a systemic vasculitis involving medium-sized and large arteries, most commonly the temporal, ophthalmic, occipital, vertebral, posterior ciliary, and proximal vertebral arteries. Moreover, involvement of the ophthalmic artery and its branches results in loss of vision. GCA can also involve the aorta and its proximal branches, especially in the upper extremities.
GCA is the most common systemic vasculitis in adults. It occurs almost exclusively in patients over age 50 and affects women more than men. It is most frequent in populations of northern European ancestry, especially Scandinavian. In a retrospective cohort study in Norway, the average annual cumulative incidence rate of GCA was 16.7 per 100,000 people over age 50.1 Risk factors include older age, history of smoking, current smoking, early menopause, and, possibly, stress-related disorders.2
PATHOGENESIS IS NOT COMPLETELY UNDERSTOOD
The pathogenesis of GCA is not completely understood, but there is evidence of immune activation in the arterial wall leading to activation of macrophages and formation of multinucleated giant cells (which may not always be present in biopsies).
The most relevant cytokines in the ongoing pathogenesis are still being defined, but the presence of interferon gamma and interleukin 6 (IL-6) seem to be critical for the expression of the disease. The primary immunogenic triggers for the elaboration of these cytokines and the arteritis remain elusive.
A SPECTRUM OF PRESENTATIONS
The initial symptoms of GCA may be vague, such as malaise, fever, and night sweats, and are likely due to systemic inflammation. Features of vascular involvement include headache, scalp tenderness, and jaw claudication (cramping pain in the jaw while chewing).
A less common but serious feature associated with GCA is partial or complete vision loss affecting 1 or both eyes.3 Some patients suddenly go completely blind without any visual prodrome.
Overlapping GCA phenotypes exist, with a spectrum of presentations that include classic cranial arteritis, extracranial GCA (also called large-vessel GCA), and polymyalgia rheumatica.2
Cranial GCA, the best-characterized clinical presentation, causes symptoms such as headache or signs such as tenderness of the temporal artery. On examination, the temporal arteries may be tender or nodular, and the pulses may be felt above the zygomatic arch, above and in front of the tragus of the ear. About two-thirds of patients with cranial GCA present with new-onset headache, most often in the temporal area, but possibly anywhere throughout the head.
Visual disturbance, jaw claudication, and tongue pain are less common but, if present, increase the likelihood of this diagnosis.2
Large-vessel involvement in GCA is common and refers to involvement of the aorta and its proximal branches. Imaging methods used in diagnosing large-vessel GCA include color Doppler ultrasonography, computed tomography with angiography, magnetic resonance imaging with angiography, and positron emission tomography. In some centers, such imaging is performed in all patients diagnosed with GCA to survey for large-vessel involvement.
Depending on the imaging study, large-vessel involvement has been found in 30% to 80% of cases of GCA.4,5 It is often associated with nonspecific symptoms such as fever, weight loss, chills, and malaise, but it can also cause more specific symptoms such as unilateral extremity claudication. In contrast to patients with cranial GCA, patients with large-vessel GCA were younger at onset, less likely to have headaches, and more likely to have arm claudication at presentation.6 Aortitis of the ascending aorta can occur with a histopathologic pattern of GCA but without the clinical stigmata of GCA.
The finding of aortitis should prompt the clinician to question the patient about other symptoms of GCA and to order imaging of the whole vascular tree. Ultrasonography and biopsy of the temporal arteries can be considered. Whether idiopathic aortitis is part of the GCA spectrum remains to be seen.
Laboratory tests often show anemia, leukocytosis, and thrombocytosis. Acute-phase reactants such as C-reactive protein and the erythrocyte sedimentation rate are often elevated. The sedimentation rate often exceeds 50 mm/hour and sometimes 100 mm/hour.
In 2 retrospective studies, the number of patients with GCA whose sedimentation rate was less than 50 mm/hour ranged between 5% and 11%.7,8 However, a small percentage of patients with GCA have normal inflammatory markers. Therefore, if the suspicion for GCA is high, treatment should be started and biopsy pursued.9 In patients with paraproteinemia or other causes of a spuriously elevated or low erythrocyte sedimentation rate, C-reactive protein is a more reliable test.
Polymyalgia rheumatica is another rheumatologic condition that can occur independently or in conjunction with GCA. It is characterized by stiffness and pain in the proximal joints such as the hips and shoulders, typically worse in the morning and better with activity. Although the patient may subjectively feel weak, a close neurologic examination will reveal normal muscle strength.
Polymyalgia rheumatica is observed in 40% to 60% of patients with GCA at the time of diagnosis; 16% to 21% of patients with polymyalgia rheumatica may develop GCA, especially if untreated.2,10
Differential diagnosis
Other vasculitides (eg, Takayasu arteritis) can also present with unexplained fever, anemia, and constitutional symptoms.
Infection should be considered if fever is present. An infectious disease accompanied by fever, headache, and elevated inflammatory markers can mimic GCA.
Nonarteritic anterior ischemic optic neuropathy can present with sudden vision loss, prompting concern for underlying GCA. Risk factors include hypertension and diabetes mellitus; other features of GCA, including elevated inflammatory markers, are generally absent.
TEMPORAL ARTERY BIOPSY: THE GOLD STANDARD FOR DIAGNOSIS
Temporal artery biopsy remains the standard to confirm the diagnosis. However, because inflammation in the temporal arteries can affect some segments but not others, biopsy results on conventional hematoxylin and eosin staining can be falsely negative in patients with GCA. In one study,11 the mean sensitivity of unilateral temporal artery biopsy was 86.9%.
Typical positive histologic findings are inflammation with panarteritis, CD4-positive lymphocytes, macrophages, giant cells, and fragmentation of the internal elastic lamina.12
When GCA is suspected, treatment with glucocorticoids should be started immediately and biopsy performed as soon as possible. Delaying biopsy for 14 days or more may not affect the accuracy of biopsy study.13 Treatment should never be withheld while awaiting the results of biopsy study.
Biopsy is usually performed unilaterally, on the same side as the symptoms or abnormal findings on examination. Bilateral temporal artery biopsy is also performed and compared with unilateral biopsy; this approach increases the diagnostic yield by about 5%.14
IMAGING
In patients with suspected GCA, imaging is recommended early to complement the clinical criteria for the diagnosis of GCA.15 Positron emission tomography, computed tomography angiography, magnetic resonance angiography, or Doppler ultrasonography can reveal inflammation of the arteries in the proximal upper or lower limbs or the aorta.2
In patients with suspected cranial GCA, ultrasonography of the temporal and axillary arteries is recommended first. If ultrasonography is not available or is inconclusive, high-resolution magnetic resonance imaging of the cranial arteries can be used as an alternative. Computed tomography and positron emission tomography of the cranial arteries are not recommended.
In patients with suspected large-vessel GCA, ultrasonography, positron emission tomography, computed tomography, and magnetic resonance imaging may be used to screen for vessel wall inflammation, edema, and luminal narrowing in extracranial arteries. Ultrasonography is of limited value in assessing aortitis.
Color duplex ultrasonography can be applied to assess for vascular inflammation of the temporal or large arteries. The typical finding of the “halo” sign, a hypoechoic ring around the arterial lumen, represents the inflammation-induced thickening of the arterial wall. The “compression sign,” the persistence of the “halo” during compression of the vessel lumen by the ultrasound probe, has high specificity for the diagnosis.16
Ultrasonography of suspected GCA has yielded sensitivities of 55% to 100% and specificities of 78% to 100%. However, its sensitivity depends on the user’s level of expertise, so it should be done only in medical centers with a high number of GCA cases and with highly experienced sonographers. High-resolution magnetic resonance imaging is an alternative to ultrasonography and has shown similar sensitivity and specificity.3
TREATMENT WITH GLUCOCORTICOIDS
Glucocorticoids remain the standard for treatment of GCA. The therapeutic effect of glucocorticoids in GCA has been established by years of clinical experience, but has never been proven in a placebo-controlled trial. When started appropriately and expeditiously, glucocorticoids produce exquisite resolution of signs and symptoms and prevent the serious complication of vision loss. Rapid resolution of symptoms is so typical of GCA that if the patient’s symptoms persist more than a few days after starting a glucocorticoid, the diagnosis of GCA should be reconsidered.
In a retrospective study of 245 patients with biopsy-proven GCA treated with glucocorticoids, 34 had permanent loss of sight.17 In 32 (94%) of the 34, the vision loss occurred before glucocorticoids were started. Of the remaining 2 patients, 1 lost vision 8 days into treatment, and the other lost vision 3 years after diagnosis and 1 year after discontinuation of glucocorticoids.
In a series of 144 patients with biopsy-proven GCA, 51 had no vision loss at presentation and no vision loss after starting glucocorticoids, and 93 had vision loss at presentation. In the latter group, symptoms worsened within 5 days of starting glucocorticoids in 9 patients.18 If vision was intact at the time of presentation, prompt initiation of glucocorticoids reduced the risk of vision loss to less than 1%.
High doses, slowly tapered
The European League Against Rheumatism recommends early initiation of high-dose glucocorticoids for patients with large-vessel vasculitis,19 and it also recommends glucocorticoids for patients with polymyalgia rheumatica.20 The optimal initial and tapering dosage has never been formally evaluated, but regimens have been devised on the basis of expert opinion.21
For patients with GCA who do not have vision loss at the time of diagnosis, the initial dose is prednisone 1 mg/kg or its equivalent daily for 2 to 4 weeks, after which it is tapered.21 If the initial dosage is prednisone 60 mg orally daily for 2 to 4 weeks, our practice is to taper it to 50 mg daily for 2 weeks, then 40 mg daily for 2 weeks. Then, it is decreased by 5 mg every 2 weeks until it is 20 mg daily, and then by 2.5 mg every 2 weeks until it is 10 mg orally daily. Thereafter, the dosage is decreased by 1 mg every 2 to 4 weeks.
For patients with GCA who experience transient vision loss or diplopia at the time of diagnosis, intravenous pulse glucocorticoid therapy should be initiated to reduce the risk of vision loss as rapidly as possible.22 A typical pulse regimen is methylprednisolone 1 g intravenously daily for 3 days. Though not rigorously validated in studies, such an approach is used to avoid vision impairment due to GCA, which is rarely reversible.
RELAPSE OF DISEASE
Suspect a relapse of GCA if the patient’s initial symptoms recur, if inflammatory markers become elevated, or if classic symptoms of GCA or polymyalgia rheumatica occur. Elevations in inflammatory markers do not definitely indicate a flare of GCA, but they should trigger close monitoring of the patient’s symptoms.
Relapse is treated by increasing the glucocorticoid dosage as appropriate to the nature of the relapse. If vision is affected or the patient has symptoms of GCA, then increments of 30 to 60 mg of prednisone are warranted, whereas if the patient has symptoms of polymyalgia rheumatica, then increments of 5 to 10 mg of prednisone are usually used.
The incidence of relapses of GCA in multiple tertiary care centers has been reported to vary between 34% and 75%.23,24 Most relapses occur at prednisone dosages of less than 20 mg orally daily and within the first year after diagnosis. The most common symptoms are limb ischemia, jaw claudication, constitutional symptoms, headaches, and polymyalgia rheumatica. In a review of 286 patients,25 213 (74%) had at least 1 relapse. The first relapse occurred in the first year in 50%, by 2 years in 68%, and by 5 years in 79%.
ADVERSE EFFECTS OF GLUCOCORTICOIDS
In high doses, glucocorticoids have well-known adverse effects. In a population-based study of 120 patients, each patient treated with glucocorticoids experienced at least 1 adverse effect (cataract, fracture, infection, osteonecrosis, diabetes, hypertension, weight gain, capillary fragility, or hair loss).26 The effects were related to aging and cumulative dosage of prednisone but not to the initial dosage.
Glucocorticoids can affect many organs and systems:
- Eyes (cataracts, increased intraocular pressure, exophthalmos)
- Heart (premature atherosclerotic disease, hypertension, fluid retention, hyperlipidemia, arrhythmias)
- Gastrointestinal system (ulcer, gastrointestinal bleeding, gastritis, visceral perforation, hepatic steatosis, acute pancreatitis)
- Bone and muscle (osteopenia, osteoporosis, osteonecrosis, myopathy)
- Brain (mood disorder, psychosis, memory impairment)
- Endocrine system (hyperglycemia, hypothalamic-pituitary-adrenal axis suppression)
- Immune system (immunosuppression, leading to infection and leukocytosis).
Patients receiving a glucocorticoid dose equivalent to 20 mg or more of prednisone daily for 1 month or more who also have another cause of immunocompromise need prophylaxis against Pneumocystis jirovecii pneumonia.27 They should also receive appropriate immunizations before starting glucocorticoids. Live-virus vaccines should not be given to these patients until they have been off glucocorticoids for 1 month.
Glucocorticoids and bone loss
Glucocorticoids are associated with bone loss and fracture, which can occur within the first few months of use and with dosages as low as 2.5 to 7.5 mg orally daily.28 Therefore, glucocorticoid-induced bone loss has to be treated aggressively, particularly in patients who are older and have a history of fragility fracture.
For patients with GCA who need glucocorticoids in doses greater than 5 mg orally daily for more than 3 months, the following measures are advised to decrease the risk of bone loss:
- Weight-bearing exercise
- Smoking cessation
- Moderation in alcohol intake
- Measures to prevent falls29
- Supplementation with 1,200 mg of calcium and 800 IU of vitamin D.30
Pharmacologic therapy should be initiated in men over age 50 who have established osteoporosis and in postmenopausal women with established osteoporosis or osteopenia. For men over age 50 with established osteopenia, risk assessment with the glucocorticoid-corrected FRAX score (www.sheffield.ac.uk/FRAX) should be performed to identify those at high risk in whom pharmacologic therapy is warranted.31
Bisphosphonates are the first-line therapy for glucocorticoid-induced osteoporosis.32
Teriparatide is the second-line therapy and is used in patients who cannot tolerate bisphosphonates or other osteoporosis therapies, and in those who have severe osteoporosis, with T scores of –3.5 and below if they have not had a fracture, and –2.5 and below if they have had a fragility fracture.33
Denosumab, a monoclonal antibody to an osteoclast differentiating factor, may be beneficial for some patients with glucocorticoid-induced osteoporosis.34
To assess the efficacy of therapy, measuring bone mineral density at baseline and at 1 year of therapy is recommended. If density is stable or improved, then repeating the measurement at 2- to 3-year intervals is suggested.
TOCILIZUMAB: A STEROID-SPARING MEDICATION
Due to the adverse effects of long-term use of glucocorticoids and high rates of relapse, there is a pressing need for medications that are more efficacious and less toxic to treat GCA.
The European League Against Rheumatism, in its 2009 management guidelines for large-vessel vasculitis, recommend using an adjunctive immunosuppressant agent.19 In the case of GCA, they recommend using methotrexate 10 to 15 mg/week, which has shown modest evidence of reducing the relapse rate and lowering the cumulative doses of glucocorticoids needed.35,36
Studies of tumor necrosis factor inhibitors and abatacept have not yielded significant reductions in the relapse rate or decreased cumulative doses of prednisone.37,38
Advances in treatment for GCA have stagnated, but recent trials39,40 have evaluated the IL-6 receptor alpha inhibitor tocilizumab, given the central role of IL-6 in the pathogenesis of GCA. Case reports have revealed rapid induction and maintenance of remission in GCA using tocilizumab.41,42
Villiger et al39 performed a randomized, placebo-controlled trial to study the efficacy and safety of tocilizumab in induction and maintenance of disease remission in 30 patients with newly diagnosed GCA. The primary outcome, complete remission at 12 weeks, was achieved in 85% of patients who received tocilizumab plus tapered prednisolone, compared with 40% of patients who received placebo plus tapering prednisolone. The tocilizumab group also had favorable results in secondary outcomes including relapse-free survival at 52 weeks, time to first relapse after induction of remission, and cumulative dose of prednisolone.
The GiACTA trial. Stone et al40 studied the effect of tocilizumab on rates of relapse during glucocorticoid tapering in 251 GCA patients over the course of 52 weeks. Patients were randomized in a 2:1:1:1 ratio to 4 treatment groups:
- Tocilizumab weekly plus prednisone, with prednisone tapered over 26 weeks
- Tocilizumab every other week plus prednisone tapered over 26 weeks
- Placebo plus prednisone tapered over 26 weeks
- Placebo plus prednisone tapered over 52 weeks.
The primary outcome was the rate of sustained glucocorticoid-free remission at 52 weeks. Secondary outcomes included the remission rate, the cumulative glucocorticoid dose, and safety measures. At 52 weeks, the rates of sustained remission were:
- 56% with tocilizumab weekly
- 53% with tocilizumab every other week
- 14% with placebo plus 26-week prednisone taper
- 18% with placebo plus 52-week taper.
Differences between the active treatment groups and the placebo groups were statistically significant (P < .001).
The cumulative dose of prednisone in tocilizumab recipients was significantly less than in placebo recipients. Rates of adverse events were similar. Ultimately, the study showed that tocilizumab, either weekly or every other week, was more effective than prednisone alone at sustaining glucocorticoid-free remission in patients with GCA.
However, the study also raised questions about tocilizumab’s toxic effect profile and its long-term efficacy, as well as who are the optimal candidates for this therapy. Data on long-term use of tocilizumab are primarily taken from its use in rheumatoid arthritis.43 As of this writing, Stone et al are conducting an open-label trial to help provide long-term safety and efficacy data in patients with GCA. In the meantime, we must extrapolate data from the long-term use of tocilizumab in rheumatoid arthritis.
Tocilizumab and lower gastrointestinal tract perforation
One of the major adverse effects of long-term use of tocilizumab is lower gastrointestinal tract perforation.
Xie et al,44 in 2016, reported that the risk of perforation in patients on tocilizumab for rheumatoid arthritis was more than 2 times higher than in patients taking a tumor necrosis factor inhibitor. However, the absolute rates of perforation were low overall, roughly 1 to 3 per 1,000 patient-years in the tocilizumab group. Risk factors for perforation included older age, history of diverticulitis or other gastrointestinal tract condition, and prednisone doses of 7.5 mg or more a day.
Does tocilizumab prevent blindness?
Another consideration is that tocilizumab may not prevent optic neuropathy. In the GiACTA trial, 1 patient in the group receiving tocilizumab every other week developed optic neuropathy.40 Prednisone had been completely tapered off at the time, and the condition resolved when glucocorticoids were restarted. Thus, it is unknown if tocilizumab would be effective on its own without concomitant use of glucocorticoids.
Vision loss is one of the most severe complications of GCA, and it is still unclear whether tocilizumab can prevent vision loss in GCA. Also, we still have no data on the effect of tocilizumab on histopathologic findings, and whether biopsy yield diminishes over time. We hope future studies will help guide us in this regard.
No guidelines on tocilizumab yet
Clinical guidelines on the appropriate use of tocilizumab in GCA are lacking. The American College of Rheumatology and the European League Against Rheumatism have yet to publish updated guidelines with comments on use of tocilizumab. Therefore, it is unclear if tocilizumab is a first-line treatment in GCA, as its efficacy alone without glucocorticoids and its long-term safety in GCA patients have not been studied.
Treatment with tocilizumab should be individualized; it should be considered in patients who have had adverse effects from glucocorticoids, and in patients who experience a flare or cannot have their glucocorticoid dose lowered to an appropriate range.
The optimal duration of tocilizumab therapy is also unknown. However, using the GiACTA study as a rough guide, we try to limit its use to 1 year until additional data are available.
Patients on IL-6 inhibition may have suppressed C-reactive protein regardless of disease activity.43 Therefore, this laboratory value may not be reliable in determining active disease in patients on tocilizumab.
The GiACTA trial has shown an impressive improvement in the relapse-free remission period in patients with GCA taking tocilizumab. However, much work needs to be done to define the safety of this medication and determine which patients should be started on it. In the meantime, we recommend starting high-dose glucocorticoid therapy as soon as the diagnosis of GCA is suspected. In patients who do not tolerate glucocorticoids or whose disease flares during glucocorticoid taper, we recommend starting treatment with tocilizumab either once a week or every other week for at least 1 year.
Giant cell arteritis (GCA) is a systemic vasculitis involving medium-sized and large arteries, most commonly the temporal, ophthalmic, occipital, vertebral, posterior ciliary, and proximal vertebral arteries. Moreover, involvement of the ophthalmic artery and its branches results in loss of vision. GCA can also involve the aorta and its proximal branches, especially in the upper extremities.
GCA is the most common systemic vasculitis in adults. It occurs almost exclusively in patients over age 50 and affects women more than men. It is most frequent in populations of northern European ancestry, especially Scandinavian. In a retrospective cohort study in Norway, the average annual cumulative incidence rate of GCA was 16.7 per 100,000 people over age 50.1 Risk factors include older age, history of smoking, current smoking, early menopause, and, possibly, stress-related disorders.2
PATHOGENESIS IS NOT COMPLETELY UNDERSTOOD
The pathogenesis of GCA is not completely understood, but there is evidence of immune activation in the arterial wall leading to activation of macrophages and formation of multinucleated giant cells (which may not always be present in biopsies).
The most relevant cytokines in the ongoing pathogenesis are still being defined, but the presence of interferon gamma and interleukin 6 (IL-6) seem to be critical for the expression of the disease. The primary immunogenic triggers for the elaboration of these cytokines and the arteritis remain elusive.
A SPECTRUM OF PRESENTATIONS
The initial symptoms of GCA may be vague, such as malaise, fever, and night sweats, and are likely due to systemic inflammation. Features of vascular involvement include headache, scalp tenderness, and jaw claudication (cramping pain in the jaw while chewing).
A less common but serious feature associated with GCA is partial or complete vision loss affecting 1 or both eyes.3 Some patients suddenly go completely blind without any visual prodrome.
Overlapping GCA phenotypes exist, with a spectrum of presentations that include classic cranial arteritis, extracranial GCA (also called large-vessel GCA), and polymyalgia rheumatica.2
Cranial GCA, the best-characterized clinical presentation, causes symptoms such as headache or signs such as tenderness of the temporal artery. On examination, the temporal arteries may be tender or nodular, and the pulses may be felt above the zygomatic arch, above and in front of the tragus of the ear. About two-thirds of patients with cranial GCA present with new-onset headache, most often in the temporal area, but possibly anywhere throughout the head.
Visual disturbance, jaw claudication, and tongue pain are less common but, if present, increase the likelihood of this diagnosis.2
Large-vessel involvement in GCA is common and refers to involvement of the aorta and its proximal branches. Imaging methods used in diagnosing large-vessel GCA include color Doppler ultrasonography, computed tomography with angiography, magnetic resonance imaging with angiography, and positron emission tomography. In some centers, such imaging is performed in all patients diagnosed with GCA to survey for large-vessel involvement.
Depending on the imaging study, large-vessel involvement has been found in 30% to 80% of cases of GCA.4,5 It is often associated with nonspecific symptoms such as fever, weight loss, chills, and malaise, but it can also cause more specific symptoms such as unilateral extremity claudication. In contrast to patients with cranial GCA, patients with large-vessel GCA were younger at onset, less likely to have headaches, and more likely to have arm claudication at presentation.6 Aortitis of the ascending aorta can occur with a histopathologic pattern of GCA but without the clinical stigmata of GCA.
The finding of aortitis should prompt the clinician to question the patient about other symptoms of GCA and to order imaging of the whole vascular tree. Ultrasonography and biopsy of the temporal arteries can be considered. Whether idiopathic aortitis is part of the GCA spectrum remains to be seen.
Laboratory tests often show anemia, leukocytosis, and thrombocytosis. Acute-phase reactants such as C-reactive protein and the erythrocyte sedimentation rate are often elevated. The sedimentation rate often exceeds 50 mm/hour and sometimes 100 mm/hour.
In 2 retrospective studies, the number of patients with GCA whose sedimentation rate was less than 50 mm/hour ranged between 5% and 11%.7,8 However, a small percentage of patients with GCA have normal inflammatory markers. Therefore, if the suspicion for GCA is high, treatment should be started and biopsy pursued.9 In patients with paraproteinemia or other causes of a spuriously elevated or low erythrocyte sedimentation rate, C-reactive protein is a more reliable test.
Polymyalgia rheumatica is another rheumatologic condition that can occur independently or in conjunction with GCA. It is characterized by stiffness and pain in the proximal joints such as the hips and shoulders, typically worse in the morning and better with activity. Although the patient may subjectively feel weak, a close neurologic examination will reveal normal muscle strength.
Polymyalgia rheumatica is observed in 40% to 60% of patients with GCA at the time of diagnosis; 16% to 21% of patients with polymyalgia rheumatica may develop GCA, especially if untreated.2,10
Differential diagnosis
Other vasculitides (eg, Takayasu arteritis) can also present with unexplained fever, anemia, and constitutional symptoms.
Infection should be considered if fever is present. An infectious disease accompanied by fever, headache, and elevated inflammatory markers can mimic GCA.
Nonarteritic anterior ischemic optic neuropathy can present with sudden vision loss, prompting concern for underlying GCA. Risk factors include hypertension and diabetes mellitus; other features of GCA, including elevated inflammatory markers, are generally absent.
TEMPORAL ARTERY BIOPSY: THE GOLD STANDARD FOR DIAGNOSIS
Temporal artery biopsy remains the standard to confirm the diagnosis. However, because inflammation in the temporal arteries can affect some segments but not others, biopsy results on conventional hematoxylin and eosin staining can be falsely negative in patients with GCA. In one study,11 the mean sensitivity of unilateral temporal artery biopsy was 86.9%.
Typical positive histologic findings are inflammation with panarteritis, CD4-positive lymphocytes, macrophages, giant cells, and fragmentation of the internal elastic lamina.12
When GCA is suspected, treatment with glucocorticoids should be started immediately and biopsy performed as soon as possible. Delaying biopsy for 14 days or more may not affect the accuracy of biopsy study.13 Treatment should never be withheld while awaiting the results of biopsy study.
Biopsy is usually performed unilaterally, on the same side as the symptoms or abnormal findings on examination. Bilateral temporal artery biopsy is also performed and compared with unilateral biopsy; this approach increases the diagnostic yield by about 5%.14
IMAGING
In patients with suspected GCA, imaging is recommended early to complement the clinical criteria for the diagnosis of GCA.15 Positron emission tomography, computed tomography angiography, magnetic resonance angiography, or Doppler ultrasonography can reveal inflammation of the arteries in the proximal upper or lower limbs or the aorta.2
In patients with suspected cranial GCA, ultrasonography of the temporal and axillary arteries is recommended first. If ultrasonography is not available or is inconclusive, high-resolution magnetic resonance imaging of the cranial arteries can be used as an alternative. Computed tomography and positron emission tomography of the cranial arteries are not recommended.
In patients with suspected large-vessel GCA, ultrasonography, positron emission tomography, computed tomography, and magnetic resonance imaging may be used to screen for vessel wall inflammation, edema, and luminal narrowing in extracranial arteries. Ultrasonography is of limited value in assessing aortitis.
Color duplex ultrasonography can be applied to assess for vascular inflammation of the temporal or large arteries. The typical finding of the “halo” sign, a hypoechoic ring around the arterial lumen, represents the inflammation-induced thickening of the arterial wall. The “compression sign,” the persistence of the “halo” during compression of the vessel lumen by the ultrasound probe, has high specificity for the diagnosis.16
Ultrasonography of suspected GCA has yielded sensitivities of 55% to 100% and specificities of 78% to 100%. However, its sensitivity depends on the user’s level of expertise, so it should be done only in medical centers with a high number of GCA cases and with highly experienced sonographers. High-resolution magnetic resonance imaging is an alternative to ultrasonography and has shown similar sensitivity and specificity.3
TREATMENT WITH GLUCOCORTICOIDS
Glucocorticoids remain the standard for treatment of GCA. The therapeutic effect of glucocorticoids in GCA has been established by years of clinical experience, but has never been proven in a placebo-controlled trial. When started appropriately and expeditiously, glucocorticoids produce exquisite resolution of signs and symptoms and prevent the serious complication of vision loss. Rapid resolution of symptoms is so typical of GCA that if the patient’s symptoms persist more than a few days after starting a glucocorticoid, the diagnosis of GCA should be reconsidered.
In a retrospective study of 245 patients with biopsy-proven GCA treated with glucocorticoids, 34 had permanent loss of sight.17 In 32 (94%) of the 34, the vision loss occurred before glucocorticoids were started. Of the remaining 2 patients, 1 lost vision 8 days into treatment, and the other lost vision 3 years after diagnosis and 1 year after discontinuation of glucocorticoids.
In a series of 144 patients with biopsy-proven GCA, 51 had no vision loss at presentation and no vision loss after starting glucocorticoids, and 93 had vision loss at presentation. In the latter group, symptoms worsened within 5 days of starting glucocorticoids in 9 patients.18 If vision was intact at the time of presentation, prompt initiation of glucocorticoids reduced the risk of vision loss to less than 1%.
High doses, slowly tapered
The European League Against Rheumatism recommends early initiation of high-dose glucocorticoids for patients with large-vessel vasculitis,19 and it also recommends glucocorticoids for patients with polymyalgia rheumatica.20 The optimal initial and tapering dosage has never been formally evaluated, but regimens have been devised on the basis of expert opinion.21
For patients with GCA who do not have vision loss at the time of diagnosis, the initial dose is prednisone 1 mg/kg or its equivalent daily for 2 to 4 weeks, after which it is tapered.21 If the initial dosage is prednisone 60 mg orally daily for 2 to 4 weeks, our practice is to taper it to 50 mg daily for 2 weeks, then 40 mg daily for 2 weeks. Then, it is decreased by 5 mg every 2 weeks until it is 20 mg daily, and then by 2.5 mg every 2 weeks until it is 10 mg orally daily. Thereafter, the dosage is decreased by 1 mg every 2 to 4 weeks.
For patients with GCA who experience transient vision loss or diplopia at the time of diagnosis, intravenous pulse glucocorticoid therapy should be initiated to reduce the risk of vision loss as rapidly as possible.22 A typical pulse regimen is methylprednisolone 1 g intravenously daily for 3 days. Though not rigorously validated in studies, such an approach is used to avoid vision impairment due to GCA, which is rarely reversible.
RELAPSE OF DISEASE
Suspect a relapse of GCA if the patient’s initial symptoms recur, if inflammatory markers become elevated, or if classic symptoms of GCA or polymyalgia rheumatica occur. Elevations in inflammatory markers do not definitely indicate a flare of GCA, but they should trigger close monitoring of the patient’s symptoms.
Relapse is treated by increasing the glucocorticoid dosage as appropriate to the nature of the relapse. If vision is affected or the patient has symptoms of GCA, then increments of 30 to 60 mg of prednisone are warranted, whereas if the patient has symptoms of polymyalgia rheumatica, then increments of 5 to 10 mg of prednisone are usually used.
The incidence of relapses of GCA in multiple tertiary care centers has been reported to vary between 34% and 75%.23,24 Most relapses occur at prednisone dosages of less than 20 mg orally daily and within the first year after diagnosis. The most common symptoms are limb ischemia, jaw claudication, constitutional symptoms, headaches, and polymyalgia rheumatica. In a review of 286 patients,25 213 (74%) had at least 1 relapse. The first relapse occurred in the first year in 50%, by 2 years in 68%, and by 5 years in 79%.
ADVERSE EFFECTS OF GLUCOCORTICOIDS
In high doses, glucocorticoids have well-known adverse effects. In a population-based study of 120 patients, each patient treated with glucocorticoids experienced at least 1 adverse effect (cataract, fracture, infection, osteonecrosis, diabetes, hypertension, weight gain, capillary fragility, or hair loss).26 The effects were related to aging and cumulative dosage of prednisone but not to the initial dosage.
Glucocorticoids can affect many organs and systems:
- Eyes (cataracts, increased intraocular pressure, exophthalmos)
- Heart (premature atherosclerotic disease, hypertension, fluid retention, hyperlipidemia, arrhythmias)
- Gastrointestinal system (ulcer, gastrointestinal bleeding, gastritis, visceral perforation, hepatic steatosis, acute pancreatitis)
- Bone and muscle (osteopenia, osteoporosis, osteonecrosis, myopathy)
- Brain (mood disorder, psychosis, memory impairment)
- Endocrine system (hyperglycemia, hypothalamic-pituitary-adrenal axis suppression)
- Immune system (immunosuppression, leading to infection and leukocytosis).
Patients receiving a glucocorticoid dose equivalent to 20 mg or more of prednisone daily for 1 month or more who also have another cause of immunocompromise need prophylaxis against Pneumocystis jirovecii pneumonia.27 They should also receive appropriate immunizations before starting glucocorticoids. Live-virus vaccines should not be given to these patients until they have been off glucocorticoids for 1 month.
Glucocorticoids and bone loss
Glucocorticoids are associated with bone loss and fracture, which can occur within the first few months of use and with dosages as low as 2.5 to 7.5 mg orally daily.28 Therefore, glucocorticoid-induced bone loss has to be treated aggressively, particularly in patients who are older and have a history of fragility fracture.
For patients with GCA who need glucocorticoids in doses greater than 5 mg orally daily for more than 3 months, the following measures are advised to decrease the risk of bone loss:
- Weight-bearing exercise
- Smoking cessation
- Moderation in alcohol intake
- Measures to prevent falls29
- Supplementation with 1,200 mg of calcium and 800 IU of vitamin D.30
Pharmacologic therapy should be initiated in men over age 50 who have established osteoporosis and in postmenopausal women with established osteoporosis or osteopenia. For men over age 50 with established osteopenia, risk assessment with the glucocorticoid-corrected FRAX score (www.sheffield.ac.uk/FRAX) should be performed to identify those at high risk in whom pharmacologic therapy is warranted.31
Bisphosphonates are the first-line therapy for glucocorticoid-induced osteoporosis.32
Teriparatide is the second-line therapy and is used in patients who cannot tolerate bisphosphonates or other osteoporosis therapies, and in those who have severe osteoporosis, with T scores of –3.5 and below if they have not had a fracture, and –2.5 and below if they have had a fragility fracture.33
Denosumab, a monoclonal antibody to an osteoclast differentiating factor, may be beneficial for some patients with glucocorticoid-induced osteoporosis.34
To assess the efficacy of therapy, measuring bone mineral density at baseline and at 1 year of therapy is recommended. If density is stable or improved, then repeating the measurement at 2- to 3-year intervals is suggested.
TOCILIZUMAB: A STEROID-SPARING MEDICATION
Due to the adverse effects of long-term use of glucocorticoids and high rates of relapse, there is a pressing need for medications that are more efficacious and less toxic to treat GCA.
The European League Against Rheumatism, in its 2009 management guidelines for large-vessel vasculitis, recommend using an adjunctive immunosuppressant agent.19 In the case of GCA, they recommend using methotrexate 10 to 15 mg/week, which has shown modest evidence of reducing the relapse rate and lowering the cumulative doses of glucocorticoids needed.35,36
Studies of tumor necrosis factor inhibitors and abatacept have not yielded significant reductions in the relapse rate or decreased cumulative doses of prednisone.37,38
Advances in treatment for GCA have stagnated, but recent trials39,40 have evaluated the IL-6 receptor alpha inhibitor tocilizumab, given the central role of IL-6 in the pathogenesis of GCA. Case reports have revealed rapid induction and maintenance of remission in GCA using tocilizumab.41,42
Villiger et al39 performed a randomized, placebo-controlled trial to study the efficacy and safety of tocilizumab in induction and maintenance of disease remission in 30 patients with newly diagnosed GCA. The primary outcome, complete remission at 12 weeks, was achieved in 85% of patients who received tocilizumab plus tapered prednisolone, compared with 40% of patients who received placebo plus tapering prednisolone. The tocilizumab group also had favorable results in secondary outcomes including relapse-free survival at 52 weeks, time to first relapse after induction of remission, and cumulative dose of prednisolone.
The GiACTA trial. Stone et al40 studied the effect of tocilizumab on rates of relapse during glucocorticoid tapering in 251 GCA patients over the course of 52 weeks. Patients were randomized in a 2:1:1:1 ratio to 4 treatment groups:
- Tocilizumab weekly plus prednisone, with prednisone tapered over 26 weeks
- Tocilizumab every other week plus prednisone tapered over 26 weeks
- Placebo plus prednisone tapered over 26 weeks
- Placebo plus prednisone tapered over 52 weeks.
The primary outcome was the rate of sustained glucocorticoid-free remission at 52 weeks. Secondary outcomes included the remission rate, the cumulative glucocorticoid dose, and safety measures. At 52 weeks, the rates of sustained remission were:
- 56% with tocilizumab weekly
- 53% with tocilizumab every other week
- 14% with placebo plus 26-week prednisone taper
- 18% with placebo plus 52-week taper.
Differences between the active treatment groups and the placebo groups were statistically significant (P < .001).
The cumulative dose of prednisone in tocilizumab recipients was significantly less than in placebo recipients. Rates of adverse events were similar. Ultimately, the study showed that tocilizumab, either weekly or every other week, was more effective than prednisone alone at sustaining glucocorticoid-free remission in patients with GCA.
However, the study also raised questions about tocilizumab’s toxic effect profile and its long-term efficacy, as well as who are the optimal candidates for this therapy. Data on long-term use of tocilizumab are primarily taken from its use in rheumatoid arthritis.43 As of this writing, Stone et al are conducting an open-label trial to help provide long-term safety and efficacy data in patients with GCA. In the meantime, we must extrapolate data from the long-term use of tocilizumab in rheumatoid arthritis.
Tocilizumab and lower gastrointestinal tract perforation
One of the major adverse effects of long-term use of tocilizumab is lower gastrointestinal tract perforation.
Xie et al,44 in 2016, reported that the risk of perforation in patients on tocilizumab for rheumatoid arthritis was more than 2 times higher than in patients taking a tumor necrosis factor inhibitor. However, the absolute rates of perforation were low overall, roughly 1 to 3 per 1,000 patient-years in the tocilizumab group. Risk factors for perforation included older age, history of diverticulitis or other gastrointestinal tract condition, and prednisone doses of 7.5 mg or more a day.
Does tocilizumab prevent blindness?
Another consideration is that tocilizumab may not prevent optic neuropathy. In the GiACTA trial, 1 patient in the group receiving tocilizumab every other week developed optic neuropathy.40 Prednisone had been completely tapered off at the time, and the condition resolved when glucocorticoids were restarted. Thus, it is unknown if tocilizumab would be effective on its own without concomitant use of glucocorticoids.
Vision loss is one of the most severe complications of GCA, and it is still unclear whether tocilizumab can prevent vision loss in GCA. Also, we still have no data on the effect of tocilizumab on histopathologic findings, and whether biopsy yield diminishes over time. We hope future studies will help guide us in this regard.
No guidelines on tocilizumab yet
Clinical guidelines on the appropriate use of tocilizumab in GCA are lacking. The American College of Rheumatology and the European League Against Rheumatism have yet to publish updated guidelines with comments on use of tocilizumab. Therefore, it is unclear if tocilizumab is a first-line treatment in GCA, as its efficacy alone without glucocorticoids and its long-term safety in GCA patients have not been studied.
Treatment with tocilizumab should be individualized; it should be considered in patients who have had adverse effects from glucocorticoids, and in patients who experience a flare or cannot have their glucocorticoid dose lowered to an appropriate range.
The optimal duration of tocilizumab therapy is also unknown. However, using the GiACTA study as a rough guide, we try to limit its use to 1 year until additional data are available.
Patients on IL-6 inhibition may have suppressed C-reactive protein regardless of disease activity.43 Therefore, this laboratory value may not be reliable in determining active disease in patients on tocilizumab.
The GiACTA trial has shown an impressive improvement in the relapse-free remission period in patients with GCA taking tocilizumab. However, much work needs to be done to define the safety of this medication and determine which patients should be started on it. In the meantime, we recommend starting high-dose glucocorticoid therapy as soon as the diagnosis of GCA is suspected. In patients who do not tolerate glucocorticoids or whose disease flares during glucocorticoid taper, we recommend starting treatment with tocilizumab either once a week or every other week for at least 1 year.
- Brekke LK, Diamantopoulos AP, Fevang BT, Aßmus J, Esperø E, Gjesdal CG. Incidence of giant cell arteritis in Western Norway 1972–2012: a retrospective cohort study. Arthritis Res Ther 2017; 19(1):278. doi:10.1186/s13075-017-1479-6
- Dejaco C, Duftner C, Buttgereit F, Matteson EL, Dasgupta B. The spectrum of giant cell arteritis and polymyalgia rheumatica: revisiting the concept of the disease. Rheumatology (Oxford) 2017; 56(4):506–515. doi:10.1093/rheumatology/kew273
- Weyand CM, Goronzy JJ. Giant-cell arteritis and polymyalgia rheumatica. N Engl J Med 2014; 371(17):1653. doi:10.1056/NEJMc1409206
- Ghinoi A, Pipitone N, Nicolini A, et al. Large-vessel involvement in recent-onset giant cell arteritis: a case-control colour-Doppler sonography study. Rheumatology (Oxford) 2012; 51(4):730–734. doi:10.1093/rheumatology/ker329
- Prieto-González S, Depetris M, García-Martínez A, et al. Positron emission tomography assessment of large vessel inflammation in patients with newly diagnosed, biopsy-proven giant cell arteritis: a prospective, case-control study. Ann Rheum Dis 2014; 73(7):1388–1392. doi:10.1136/annrheumdis-2013-204572
- Brack A, Martinez-Taboada V, Stanson A, Goronzy JJ, Weyand CM. Disease pattern in cranial and large-vessel giant cell arteritis. Arthritis Rheum 1999; 42(2):311–317. doi:10.1002/1529-0131(199902)42:2<311::AID-ANR14>3.0.CO;2-F
- Salvarani C, Hunder GG. Giant cell arteritis with low erythrocyte sedimentation rate: frequency of occurence in a population-based study. Arthritis Rheum 2001; 45(2):140–145. doi:10.1002/1529-0131(200104)45:2<140::AID-ANR166>3.0.CO;2-2
- Liozon E, Jauberteau-Marchan MO, Ly K, Loustaud-Ratti V, Soria P, Vidal E. Giant cell arteritis with a low erythrocyte sedimentation rate: comments on the article by Salvarani and Hunder. Arthritis Rheum 2002; 47(6):692–694. doi:10.1002/art.10809
- Yu-Wai-Man P, Dayan MR. Giant cell arteritis with normal inflammatory markers. Acta Ophthalmol Scand 2007; 85(4):460. doi:10.1111/j.1600-0420.2006.00864.x
- Buttgereit F, Dejaco C, Matteson EL, Dasgupta B. Polymyalgia rheumatica and giant cell arteritis: a systematic review. JAMA 2016; 315(22):2442–2458. doi:10.1001/jama.2016.5444
- Niederkohr RD, Levin LA. Management of the patient with suspected temporal arteritis a decision-analytic approach. Ophthalmology 2005; 112(5):744–756. doi:10.1016/j.ophtha.2005.01.031
- Bowling K, Rait J, Atkinson J, Srinivas G. Temporal artery biopsy in the diagnosis of giant cell arteritis: does the end justify the means? Ann Med Surg (Lond) 2017; 20:1–5. doi:10.1016/j.amsu.2017.06.020
- Daily B, Dassow P, Haynes J, Nashelsky J. Giant cell arteritis: biopsy after corticosteroid initiation. Am Fam Physician 2017; 95(2):116–117. pmid:28084703
- Durling B, Toren A, Patel V, Gilberg S, Weis E, Jordan D. Incidence of discordant temporal artery biopsy in the diagnosis of giant cell arteritis. Can J Ophthalmol 2014; 49(2):157–161. doi:10.1016/j.jcjo.2013.12.008
- Dejaco C, Ramiro S, Duftner C, et al. EULAR recommendations for the use of imaging in large vessel vasculitis in clinical practice. Ann Rheum Dis 2018; 77(5):636–643. doi:10.1136/annrheumdis-2017-212649
- Aschwanden M, Imfeld S, Staub D, et al. The ultrasound compression sign to diagnose temporal giant cell arteritis shows an excellent interobserver agreement. Clin Exp Rheumatol 2015; 33(2 suppl 89):S-113–S-115. pmid:26016760
- Aiello PD, Trautmann JC, McPhee TJ, Kunselman AR, Hunder GG. Visual prognosis in giant cell arteritis. Ophthalmology 1993; 100(4):550–555. pmid:8479714
- Hayreh SS, Zimmerman B. Visual deterioration in giant cell arteritis patients while on high doses of corticosteroid therapy. Ophthalmology 2003; 110(6):1204–1215. doi:10.1016/S0161-6420(03)00228-8
- Mukhtyar C, Guillevin L, Cid MC, et al; European Vasculitis Study Group. EULAR recommendations for the management of large vessel vasculitis. Ann Rheum Dis 2009; 68(3):318–323. doi:10.1136/ard.2008.088351
- Dejaco C, Singh YP, Perel P, et al; European League Against Rheumatism; American College of Rheumatology. 2015 recommendations for the management of polymyalgia rheumatica: a European League Against Rheumatism/American College of Rheumatology collaborative initiative. Ann Rheum Dis 2015; 74(10):1799–1807. doi:10.1136/annrheumdis-2015-207492
- Bienvenu B, Ly KH, Lambert M, et al; Groupe d’Étude Français des Artérites des gros Vaisseaux, under the Aegis of the Filière des Maladies Auto-Immunes et Auto-Inflammatoires Rares. Management of giant cell arteritis: recommendations of the French Study Group for Large Vessel Vasculitis (GEFA). Rev Med Interne 2016; 37(3):154–165. doi:10.1016/j.revmed.2015.12.015
- Hayreh SS, Biousse V. Treatment of acute visual loss in giant cell arteritis: should we prescribe high-dose intravenous steroids or just oral steroids? J Neuroophthalmol 2012; 32(3):278–287. doi:10.1097/WNO.0b013e3182688218
- Restuccia G, Boiardi L, Cavazza A, et al. Flares in biopsy-proven giant cell arteritis in Northern Italy: characteristics and predictors in a long-term follow-up study. Medicine (Baltimore) 2016; 95(19):e3524. doi:10.1097/MD.0000000000003524
- Kermani TA, Warrington KJ, Cuthbertson D, et al; Vasculitis Clinical Research Consortium. Disease relapses among patients with giant cell arteritis: a prospective, longitudinal cohort study. J Rheumatol 2015; 42(7):1213–1217. doi:10.3899/jrheum.141347
- Labarca C, Koster MJ, Crowson CS, et al. Predictors of relapse and treatment outcomes in biopsy-proven giant cell arteritis: a retrospective cohort study. Rheumatology (Oxford) 2016; 55(2):347–356. doi:10.1093/rheumatology/kev348
- Proven A, Gabriel SE, Orces C, O’Fallon WM, Hunder GG. Glucocorticoid therapy in giant cell arteritis: duration and adverse outcomes. Arthritis Rheum 2003; 49(5):703–708. doi:10.1002/art.11388
- Sepkowitz KA. Opportunistic infections in patients with and patients without acquired immunodeficiency syndrome. Clin Infect Dis 2002; 34(8):1098–1107. doi:10.1086/339548
- van Staa TP, Leufkens HG, Cooper C. The epidemiology of corticosteroid-induced osteoporosis: a meta-analysis. Osteoporos Int 2002; 13(10):777–787. doi:10.1007/s001980200108
- Heffernan MP, Saag KG, Robinson JK, Callen JP. Prevention of osteoporosis associated with chronic glucocorticoid therapy. JAMA 2006; 295(11):1300–1303. pmid:16541489
- Buckley L, Guyatt G, Fink HA, et al. 2017 American College of Rheumatology guideline for the prevention and treatment of glucocorticoid-induced osteoporosis. Arthritis Care Res (Hoboken) 2017; 69(8):1095–1110. doi:10.1002/acr.23279
- Grossman JM, Gordon R, Ranganath VK, et al. American College of Rheumatology 2010 recommendations for the prevention and treatment of glucocorticoid-induced osteoporosis. Arthritis Care Res 201; 62(11):1515–1526. doi:10.1002/acr.20295
- Allen CS, Yeung JH, Vandermeer B, Homik J. Bisphosphonates for steroid-induced osteoporosis. Cochrane Database Syst Rev 2016; 10:CD001347. doi:10.1002/14651858.CD001347.pub2
- Carpinteri R, Porcelli T, Mejia C, et al. Glucocorticoid-induced osteoporosis and parathyroid hormone. J Endocrinol Invest 2010; 33(suppl 7):16–21. pmid:20938221
- Saag KG, Wagman RB, Geusens P, et al. Denosumab versus risedronate in glucocorticoid-induced osteoporosis: a multicentre, randomised, double-blind, active-controlled, double-dummy, non-inferiority study. Lancet Diabetes Endocrinol 2018; 6(6):445–454. doi:10.1016/S2213-8587(18)30075-5
- Hoffman GS, Cid MC, Hellmann DB, et al; International Network for the Study of Systemic Vasculitides. A multicenter, randomized, double-blind, placebo-controlled trial of adjuvant methotrexate treatment for giant cell arteritis. Arthritis Rheum 2002; 46(5):1309–1318. doi:10.1002/art.10262
- Spiera RF, Mitnick HJ, Kupersmith M, et al. A prospective, double-blind, randomized, placebo controlled trial of methotrexate in the treatment of giant cell arteritis (GCA). Clin Exp Rheumatol 2001; 19(5):495–501. pmid:11579707
- Hoffman GS, Cid MC, Rendt-Zagar KE, et al; Infliximab-GCA Study Group. Infliximab for maintenance of glucocorticosteroid-induced remission of giant cell arteritis: a randomized trial. Ann Intern Med 2007; 146(9):621–630. pmid:17470830
- Langford CA, Cuthbertson D, Ytterberg SR, et al; Vasculitis Clinical Research Consortium. A randomized, double-blind trial of abatacept (CTLA-4Ig) for the treatment of giant cell arteritis. Arthritis Rheumatol 2017; 69(4):837–845. doi:10.1002/art.40044
- Villiger PM, Adler S, Kuchen S, et al. Tocilizumab for induction and maintenance of remission in giant cell arteritis: a phase 2, randomised, double-blind, placebo-controlled trial. Lancet. 2016; 387(10031):1921–1927. doi:10.1016/S0140-6736(16)00560-2
- Stone JH, Tuckwell K, Dimonaco S, et al. Trial of tocilizumab in giant-cell arteritis. N Engl J Med 2017; 377(4):317–328. doi:10.1056/NEJMoa1613849
- Oliveira F, Butendieck RR, Ginsburg WW, Parikh K, Abril A. Tocilizumab, an effective treatment for relapsing giant cell arteritis. Clin Exp Rheumatol 2014; 32(3 suppl 82):S76–S78. pmid:24854376
- Loricera J, Blanco R, Hernández JL, et al. Tocilizumab in giant cell arteritis: multicenter open-label study of 22 patients. Semin Arthritis Rheum 2015; 44(6):717–723. doi:10.1016/j.semarthrit.2014.12.005
- Tamaki H, Hajj-Ali RA. Tocilizumab for giant cell arteritis—a new giant step in an old disease. JAMA Neurol 2018; 75(2):145–146. doi:10.1001/jamaneurol.2017.3811
- Xie F, Yun H, Bernatsky S, Curtis JR. Risk for gastrointestinal perforation among rheumatoid arthritis patients receiving tofacitinib, tocilizumab, or other biologics. Arthritis Rheumatol 2016; 68(11):2612–2617. doi:10.1002/art.39761
- Brekke LK, Diamantopoulos AP, Fevang BT, Aßmus J, Esperø E, Gjesdal CG. Incidence of giant cell arteritis in Western Norway 1972–2012: a retrospective cohort study. Arthritis Res Ther 2017; 19(1):278. doi:10.1186/s13075-017-1479-6
- Dejaco C, Duftner C, Buttgereit F, Matteson EL, Dasgupta B. The spectrum of giant cell arteritis and polymyalgia rheumatica: revisiting the concept of the disease. Rheumatology (Oxford) 2017; 56(4):506–515. doi:10.1093/rheumatology/kew273
- Weyand CM, Goronzy JJ. Giant-cell arteritis and polymyalgia rheumatica. N Engl J Med 2014; 371(17):1653. doi:10.1056/NEJMc1409206
- Ghinoi A, Pipitone N, Nicolini A, et al. Large-vessel involvement in recent-onset giant cell arteritis: a case-control colour-Doppler sonography study. Rheumatology (Oxford) 2012; 51(4):730–734. doi:10.1093/rheumatology/ker329
- Prieto-González S, Depetris M, García-Martínez A, et al. Positron emission tomography assessment of large vessel inflammation in patients with newly diagnosed, biopsy-proven giant cell arteritis: a prospective, case-control study. Ann Rheum Dis 2014; 73(7):1388–1392. doi:10.1136/annrheumdis-2013-204572
- Brack A, Martinez-Taboada V, Stanson A, Goronzy JJ, Weyand CM. Disease pattern in cranial and large-vessel giant cell arteritis. Arthritis Rheum 1999; 42(2):311–317. doi:10.1002/1529-0131(199902)42:2<311::AID-ANR14>3.0.CO;2-F
- Salvarani C, Hunder GG. Giant cell arteritis with low erythrocyte sedimentation rate: frequency of occurence in a population-based study. Arthritis Rheum 2001; 45(2):140–145. doi:10.1002/1529-0131(200104)45:2<140::AID-ANR166>3.0.CO;2-2
- Liozon E, Jauberteau-Marchan MO, Ly K, Loustaud-Ratti V, Soria P, Vidal E. Giant cell arteritis with a low erythrocyte sedimentation rate: comments on the article by Salvarani and Hunder. Arthritis Rheum 2002; 47(6):692–694. doi:10.1002/art.10809
- Yu-Wai-Man P, Dayan MR. Giant cell arteritis with normal inflammatory markers. Acta Ophthalmol Scand 2007; 85(4):460. doi:10.1111/j.1600-0420.2006.00864.x
- Buttgereit F, Dejaco C, Matteson EL, Dasgupta B. Polymyalgia rheumatica and giant cell arteritis: a systematic review. JAMA 2016; 315(22):2442–2458. doi:10.1001/jama.2016.5444
- Niederkohr RD, Levin LA. Management of the patient with suspected temporal arteritis a decision-analytic approach. Ophthalmology 2005; 112(5):744–756. doi:10.1016/j.ophtha.2005.01.031
- Bowling K, Rait J, Atkinson J, Srinivas G. Temporal artery biopsy in the diagnosis of giant cell arteritis: does the end justify the means? Ann Med Surg (Lond) 2017; 20:1–5. doi:10.1016/j.amsu.2017.06.020
- Daily B, Dassow P, Haynes J, Nashelsky J. Giant cell arteritis: biopsy after corticosteroid initiation. Am Fam Physician 2017; 95(2):116–117. pmid:28084703
- Durling B, Toren A, Patel V, Gilberg S, Weis E, Jordan D. Incidence of discordant temporal artery biopsy in the diagnosis of giant cell arteritis. Can J Ophthalmol 2014; 49(2):157–161. doi:10.1016/j.jcjo.2013.12.008
- Dejaco C, Ramiro S, Duftner C, et al. EULAR recommendations for the use of imaging in large vessel vasculitis in clinical practice. Ann Rheum Dis 2018; 77(5):636–643. doi:10.1136/annrheumdis-2017-212649
- Aschwanden M, Imfeld S, Staub D, et al. The ultrasound compression sign to diagnose temporal giant cell arteritis shows an excellent interobserver agreement. Clin Exp Rheumatol 2015; 33(2 suppl 89):S-113–S-115. pmid:26016760
- Aiello PD, Trautmann JC, McPhee TJ, Kunselman AR, Hunder GG. Visual prognosis in giant cell arteritis. Ophthalmology 1993; 100(4):550–555. pmid:8479714
- Hayreh SS, Zimmerman B. Visual deterioration in giant cell arteritis patients while on high doses of corticosteroid therapy. Ophthalmology 2003; 110(6):1204–1215. doi:10.1016/S0161-6420(03)00228-8
- Mukhtyar C, Guillevin L, Cid MC, et al; European Vasculitis Study Group. EULAR recommendations for the management of large vessel vasculitis. Ann Rheum Dis 2009; 68(3):318–323. doi:10.1136/ard.2008.088351
- Dejaco C, Singh YP, Perel P, et al; European League Against Rheumatism; American College of Rheumatology. 2015 recommendations for the management of polymyalgia rheumatica: a European League Against Rheumatism/American College of Rheumatology collaborative initiative. Ann Rheum Dis 2015; 74(10):1799–1807. doi:10.1136/annrheumdis-2015-207492
- Bienvenu B, Ly KH, Lambert M, et al; Groupe d’Étude Français des Artérites des gros Vaisseaux, under the Aegis of the Filière des Maladies Auto-Immunes et Auto-Inflammatoires Rares. Management of giant cell arteritis: recommendations of the French Study Group for Large Vessel Vasculitis (GEFA). Rev Med Interne 2016; 37(3):154–165. doi:10.1016/j.revmed.2015.12.015
- Hayreh SS, Biousse V. Treatment of acute visual loss in giant cell arteritis: should we prescribe high-dose intravenous steroids or just oral steroids? J Neuroophthalmol 2012; 32(3):278–287. doi:10.1097/WNO.0b013e3182688218
- Restuccia G, Boiardi L, Cavazza A, et al. Flares in biopsy-proven giant cell arteritis in Northern Italy: characteristics and predictors in a long-term follow-up study. Medicine (Baltimore) 2016; 95(19):e3524. doi:10.1097/MD.0000000000003524
- Kermani TA, Warrington KJ, Cuthbertson D, et al; Vasculitis Clinical Research Consortium. Disease relapses among patients with giant cell arteritis: a prospective, longitudinal cohort study. J Rheumatol 2015; 42(7):1213–1217. doi:10.3899/jrheum.141347
- Labarca C, Koster MJ, Crowson CS, et al. Predictors of relapse and treatment outcomes in biopsy-proven giant cell arteritis: a retrospective cohort study. Rheumatology (Oxford) 2016; 55(2):347–356. doi:10.1093/rheumatology/kev348
- Proven A, Gabriel SE, Orces C, O’Fallon WM, Hunder GG. Glucocorticoid therapy in giant cell arteritis: duration and adverse outcomes. Arthritis Rheum 2003; 49(5):703–708. doi:10.1002/art.11388
- Sepkowitz KA. Opportunistic infections in patients with and patients without acquired immunodeficiency syndrome. Clin Infect Dis 2002; 34(8):1098–1107. doi:10.1086/339548
- van Staa TP, Leufkens HG, Cooper C. The epidemiology of corticosteroid-induced osteoporosis: a meta-analysis. Osteoporos Int 2002; 13(10):777–787. doi:10.1007/s001980200108
- Heffernan MP, Saag KG, Robinson JK, Callen JP. Prevention of osteoporosis associated with chronic glucocorticoid therapy. JAMA 2006; 295(11):1300–1303. pmid:16541489
- Buckley L, Guyatt G, Fink HA, et al. 2017 American College of Rheumatology guideline for the prevention and treatment of glucocorticoid-induced osteoporosis. Arthritis Care Res (Hoboken) 2017; 69(8):1095–1110. doi:10.1002/acr.23279
- Grossman JM, Gordon R, Ranganath VK, et al. American College of Rheumatology 2010 recommendations for the prevention and treatment of glucocorticoid-induced osteoporosis. Arthritis Care Res 201; 62(11):1515–1526. doi:10.1002/acr.20295
- Allen CS, Yeung JH, Vandermeer B, Homik J. Bisphosphonates for steroid-induced osteoporosis. Cochrane Database Syst Rev 2016; 10:CD001347. doi:10.1002/14651858.CD001347.pub2
- Carpinteri R, Porcelli T, Mejia C, et al. Glucocorticoid-induced osteoporosis and parathyroid hormone. J Endocrinol Invest 2010; 33(suppl 7):16–21. pmid:20938221
- Saag KG, Wagman RB, Geusens P, et al. Denosumab versus risedronate in glucocorticoid-induced osteoporosis: a multicentre, randomised, double-blind, active-controlled, double-dummy, non-inferiority study. Lancet Diabetes Endocrinol 2018; 6(6):445–454. doi:10.1016/S2213-8587(18)30075-5
- Hoffman GS, Cid MC, Hellmann DB, et al; International Network for the Study of Systemic Vasculitides. A multicenter, randomized, double-blind, placebo-controlled trial of adjuvant methotrexate treatment for giant cell arteritis. Arthritis Rheum 2002; 46(5):1309–1318. doi:10.1002/art.10262
- Spiera RF, Mitnick HJ, Kupersmith M, et al. A prospective, double-blind, randomized, placebo controlled trial of methotrexate in the treatment of giant cell arteritis (GCA). Clin Exp Rheumatol 2001; 19(5):495–501. pmid:11579707
- Hoffman GS, Cid MC, Rendt-Zagar KE, et al; Infliximab-GCA Study Group. Infliximab for maintenance of glucocorticosteroid-induced remission of giant cell arteritis: a randomized trial. Ann Intern Med 2007; 146(9):621–630. pmid:17470830
- Langford CA, Cuthbertson D, Ytterberg SR, et al; Vasculitis Clinical Research Consortium. A randomized, double-blind trial of abatacept (CTLA-4Ig) for the treatment of giant cell arteritis. Arthritis Rheumatol 2017; 69(4):837–845. doi:10.1002/art.40044
- Villiger PM, Adler S, Kuchen S, et al. Tocilizumab for induction and maintenance of remission in giant cell arteritis: a phase 2, randomised, double-blind, placebo-controlled trial. Lancet. 2016; 387(10031):1921–1927. doi:10.1016/S0140-6736(16)00560-2
- Stone JH, Tuckwell K, Dimonaco S, et al. Trial of tocilizumab in giant-cell arteritis. N Engl J Med 2017; 377(4):317–328. doi:10.1056/NEJMoa1613849
- Oliveira F, Butendieck RR, Ginsburg WW, Parikh K, Abril A. Tocilizumab, an effective treatment for relapsing giant cell arteritis. Clin Exp Rheumatol 2014; 32(3 suppl 82):S76–S78. pmid:24854376
- Loricera J, Blanco R, Hernández JL, et al. Tocilizumab in giant cell arteritis: multicenter open-label study of 22 patients. Semin Arthritis Rheum 2015; 44(6):717–723. doi:10.1016/j.semarthrit.2014.12.005
- Tamaki H, Hajj-Ali RA. Tocilizumab for giant cell arteritis—a new giant step in an old disease. JAMA Neurol 2018; 75(2):145–146. doi:10.1001/jamaneurol.2017.3811
- Xie F, Yun H, Bernatsky S, Curtis JR. Risk for gastrointestinal perforation among rheumatoid arthritis patients receiving tofacitinib, tocilizumab, or other biologics. Arthritis Rheumatol 2016; 68(11):2612–2617. doi:10.1002/art.39761
KEY POINTS
- Giant cell arteritis can present with cranial symptoms, extracranial large-vessel involvement, or polymyalgia rheumatica.
- Temporal artery biopsy is the standard for diagnosis.
- Adverse effects of glucocorticoid treatment, particularly bone loss, need to be managed.
- In patients treated with glucocorticoids alone, the relapse rate is high when the drugs are tapered; thus, prolonged treatment is required.
Do patients on biologic drugs for rheumatic disease need PCP prophylaxis?
Pneumocystis jirovecii (previously carinii) pneumonia (PCP) is rare in patients taking biologic response modifiers for rheumatic disease.1–10 However, prophylaxis should be considered in patients who have granulomatosis with polyangiitis or underlying pulmonary disease, or who are concomitantly receiving glucocorticoids in high doses. There is some risk of adverse reactions to the prophylactic medicine.1,11–21 Until clear guidelines are available, the decision to initiate PCP prophylaxis and the choice of agent should be individualized.
THE BURDEN OF PCP
In a meta-analysis23 of 867 patients who developed PCP and did not have HIV infection, 20.1% had autoimmune or chronic inflammatory disease and the rest were transplant recipients or had malignancies. The mortality rate was 30.6%.
PHARMACOLOGIC RISK FACTORS FOR PCP
Treatment with glucocorticoids
Treatment with glucocorticoids is an important risk factor for PCP, independent of biologic therapy.
Calero-Bernal et al11 reported on 128 patients with non-HIV PCP, of whom 114 (89%) had received a glucocorticoid for more than 4 weeks, and 98 (76%) were currently receiving one. The mean daily dose was equivalent to 27.73 mg of prednisone per day in those on glucocorticoids only, and 21.34 mg in those receiving glucocorticoids in combination with other immunosuppressants.
Park et al,12 in a retrospective study of Korean patients treated for rheumatic disease with high-dose glucocorticoids (≥ 30 mg/day of prednisone or equivalent for more than 4 weeks), reported an incidence rate of PCP of 2.37 per 100 patient-years in those not on prophylaxis.
Other studies13,14 have also found a prednisone dose greater than 15 to 20 mg per day for more than 4 weeks or concomitant use of 2 or more disease-modifying antirheumatic drugs to be a significant risk factor.13,14
Tumor necrosis factor alpha antagonists
A US Food and Drug Administration review1 of voluntary reports of adverse drug events estimated the incidence of PCP to be 2.3 per 100,000 patient-years with infliximab and 1.6 per 100,000 patient-years with etanercept. In most cases, other immunosuppressants were used concomitantly.1
Postmarketing surveillance2 of 5,000 patients with rheumatoid arthritis showed an incidence of suspected PCP of 0.4% within the first 6 months of starting infliximab therapy.
Komano et al,15 in a case-control study of patients with rheumatoid arthritis treated with infliximab, reported that all 21 patients with PCP were also on methotrexate (median dosage 8 mg per week) and prednisolone (median dosage 7.5 mg per day).
PCP has also been reported after adalimumab use in combination with prednisone, azathioprine, and methotrexate, as well as with certolizumab, golimumab, tocilizumab, abatacept, and rituximab.3–6,24–26
Rituximab
Calero-Bernal et al11 reported that 23% of patients with non-HIV PCP who were receiving immunosuppressant drugs were on rituximab.
Alexandre et al16 performed a retrospective review of 11 cases of PCP complicating rituximab therapy for autoimmune disease, in which 10 (91%) of the patients were also on corticosteroids, with a median dosage of 30 mg of prednisone daily. A literature review of an additional 18 cases revealed similar findings.
PATIENT RISK FACTORS FOR PCP
Pulmonary disease, age, other factors
Komano et al,15 in their study of patients with rheumatoid arthritis treated with infliximab, found that 10 (48%) of 21 patients with PCP had preexisting pulmonary disease, compared with 11 (10.8%) of 102 patients without PCP (P < .001). Patients with PCP were older (mean age 64 vs 54, P < .001), were on higher median doses of prednisolone per day (7.5 vs 5 mg, P = .001), and had lower median serum immunoglobulin G (IgG) levels (944 vs 1,394 mg/dL, P < .001).15
Tadros et al13 performed a case-control study that also showed that patients with autoimmune disease who developed PCP had lower lymphocyte counts than controls on admission. Other risk factors included low CD4 counts and age older than 50.
Li et al17 found that patients with autoimmune or inflammatory disease with PCP were more likely to have low CD3, CD4, and CD8 cell counts, as well as albumin levels less than 28 g/L. They therefore suggested that lymphocyte subtyping may be a useful tool to guide PCP prophylaxis.
Granulomatosis with polyangiitis
Patients with granulomatosis with polyangiitis have a significantly higher incidence of PCP than patients with other connective tissue diseases.
Ward and Donald18 reviewed 223 cases of PCP in patients with connective tissue disease. The highest frequency (89 cases per 10,000 hospitalizations per year) was in patients with granulomatosis with polyangiitis, followed by 65 per 10,000 hospitalizations per year for patients with polyarteritis nodosa. The lowest frequency was in rheumatoid arthritis patients, at 2 per 10,000 hospitalizations per year. In decreasing order, diseases with significant associations with PCP were:
- Polyarteritis nodosa (odds ratio [OR] 10.20, 95% confidence interval [CI] 5.69–18.29)
- Granulomatosis with polyangiitis (OR 7.81, 95% CI 4.71–13.05)
- Inflammatory myopathy (OR 4.44, 95% CI 2.67–7.38)
- Systemic lupus erythematosus (OR 2.52, 95% CI 1.66–3.82).
Vallabhaneni and Chiller,26 in a meta-analysis including rheumatoid arthritis patients on biologics, did not find an increased risk of PCP (OR 1.77, 95% CI 0.42–7.47).
Park et al12 found that the highest incidences of PCP were in patients with granulomatosis with polyangiitis, microscopic polyangiitis, and systemic sclerosis. For systemic sclerosis, the main reason for giving high-dose glucocorticoids was interstitial lung disease.
Other studies19,20,28 also found an association with coexisting pulmonary disease in patients with rheumatoid arthritis.
CURRENT GUIDELINES
There are guidelines for primary and secondary prophylaxis of PCP in HIV-positive patients with CD4 counts less than 200/mm3 or a history of acquired immunodeficiency syndrome (AIDS)-defining illness.27 Additionally, patients with a CD4 cell percentage less than 14% should be considered for prophylaxis.27
Unfortunately, there are no guidelines for prophylaxis in patients taking immunosuppressants for rheumatic disease.
The recommended regimen for PCP prophylaxis in HIV-infected patients is trimethoprim-sulfamethoxazole, 1 double-strength or 1 single-strength tablet daily. Alternative regimens include 1 double-strength tablet 3 times per week, dapsone, aerosolized pentamidine, and atovaquone.27
There are also guidelines for prophylaxis in kidney transplant recipients, as well as for patients with hematologic malignancies and solid-organ malignancies, particularly those on chemotherapeutic agents and the T-cell-depleting agent alemtuzumab.29–31
Italian clinical practice guidelines for the use of tumor necrosis factor antagonists in inflammatory bowel disease recommend consideration of PCP prophylaxis in patients who are also on other immunosuppressants, particularly high-dose glucocorticoids.32
Prophylaxis has been shown to increase life expectancy and quality-adjusted life-years and to reduce cost for patients on immunosuppressive therapy for granulomatosis with polyangiitis.21 The European Society of Clinical Microbiology and Infectious Diseases recently produced consensus statements recommending PCP prophylaxis for patients on rituximab with other concomitant immunosuppressants such as the equivalent of prednisone 20 mg daily for more than 4 weeks.33 Prophylaxis was not recommended for other biologic therapies.34,35
THE RISKS OF PROPHYLAXIS
The risk of PCP should be weighed against the risk of prophylaxis in patients with rheumatic disease. Adverse reactions to sulfonamide antibiotics including disease flares have been reported in patients with systemic lupus erythematosus.36,37 Other studies have found no increased risk of flares in patients taking trimethoprim-sulfamethoxazole for PCP prophylaxis.12,38 A retrospective analysis of patients with vasculitis found no increased risk of combining methotrexate and trimethoprim-sulfamethoxazole.39
KEY POINTS
- PCP is an opportunistic infection with a high risk of death.
- PCP has been reported with biologics used as immunomodulators in rheumatic disease.
- PCP prophylaxis should be considered in patients at high risk of PCP, such as those who have granulomatosis with polyangiitis, underlying pulmonary disease or who are concomitantly taking glucocorticoids.
- US Food and Drug Administration. Safety update on TNF-alpha antagonists: infliximab and etanercept.https://wayback.archive-it.org/7993/20180127041103/https://www.fda.gov/ohrms/dockets/ac/01/briefing/3779b2_01_cber_safety_revision2.htm. Accessed May 3, 2019.
- Takeuchi T, Tatsuki Y, Nogami Y, et al. Postmarketing surveillance of the safety profile of infliximab in 5000 Japanese patients with rheumatoid arthritis. Ann Rheum Dis 2008; 67(2):189–194. doi:10.1136/ard.2007.072967
- Koike T, Harigai M, Ishiguro N, et al. Safety and effectiveness of adalimumab in Japanese rheumatoid arthritis patients: postmarketing surveillance report of the first 3,000 patients. Mod Rheumatol 2012; 22(4):498–508. doi:10.1007/s10165-011-0541-5
- Bykerk V, Cush J, Winthrop K, et al. Update on the safety profile of certolizumab pegol in rheumatoid arthritis: an integrated analysis from clinical trials. Ann Rheum Dis 2015; 74(1):96–103. doi:10.1136/annrheumdis-2013-203660
- Koike T, Harigai M, Inokuma S, et al. Postmarketing surveillance of tocilizumab for rheumatoid arthritis in Japan: interim analysis of 3881 patients. Ann Rheum Dis 2011; 70(12):2148–2151. doi:10.1136/ard.2011.151092
- Harigai M, Ishiguro N, Inokuma S, et al. Postmarketing surveillance of the safety and effectiveness of abatacept in Japanese patients with rheumatoid arthritis. Mod Rheumatol 2016; 26(4):491–498. doi:10.3109/14397595.2015.1123211
- Koike T, Harigai M, Inokuma S, et al. Postmarketing surveillance of the safety and effectiveness of etanercept in Japan. J Rheumatol 2009; 36(5):898–906. doi:10.3899/jrheum.080791
- Grubbs JA, Baddley JW. Pneumocystis jirovecii pneumonia in patients receiving tumor-necrosis-factor-inhibitor therapy: implications for chemoprophylaxis. Curr Rheumatol Rep 2014; 16(10):445. doi:10.1007/s11926-014-0445-4
- US Food and Drug Administration. FDA adverse event reporting system (FAERS) public dashboard. www.fda.gov/Drugs/GuidanceComplianceRegulatoryInformation/Surveillance/AdverseDrugEffects/ucm070093.htm. Accessed May 3, 2019.
- Rutherford AI, Patarata E, Subesinghe S, Hyrich KL, Galloway JB. Opportunistic infections in rheumatoid arthritis patients exposed to biologic therapy: results from the British Society for Rheumatology Biologics Register for Rheumatoid Arthritis. Rheumatology (Oxford) 2018; 57(6):997–1001. doi:10.1093/rheumatology/key023
- Calero-Bernal ML, Martin-Garrido I, Donazar-Ezcurra M, Limper AH, Carmona EM. Intermittent courses of corticosteroids also present a risk for Pneumocystis pneumonia in non-HIV patients. Can Respir J 2016; 2016:2464791. doi:10.1155/2016/2464791
- Park JW, Curtis JR, Moon J, Song YW, Kim S, Lee EB. Prophylactic effect of trimethoprim-sulfamethoxazole for pneumocystis pneumonia in patients with rheumatic diseases exposed to prolonged high-dose glucocorticoids. Ann Rheum Dis 2018; 77(5):644–649. doi:10.1136/annrheumdis-2017-211796
- Tadros S, Teichtahl AJ, Ciciriello S, Wicks IP. Pneumocystis jirovecii pneumonia in systemic autoimmune rheumatic disease: a case-control study. Semin Arthritis Rheum 2017; 46(6):804–809. doi:10.1016/j.semarthrit.2016.09.009
- Demoruelle MK, Kahr A, Verilhac K, Deane K, Fischer A, West S. Recent-onset systemic lupus erythematosus complicated by acute respiratory failure. Arthritis Care Res (Hoboken) 2013; 65(2):314–323. doi:10.1002/acr.21857
- Komano Y, Harigai M, Koike R, et al. Pneumocystis jiroveci pneumonia in patients with rheumatoid arthritis treated with infliximab: a retrospective review and case-control study of 21 patients. Arthritis Rheum 2009; 61(3):305–312. doi:10.1002/art.24283
- Alexandre K, Ingen-Housz-Oro S, Versini M, Sailler L, Benhamou Y. Pneumocystis jirovecii pneumonia in patients treated with rituximab for systemic diseases: report of 11 cases and review of the literature. Eur J Intern Med 2018; 50:e23–e24. doi:10.1016/j.ejim.2017.11.014
- Li Y, Ghannoum M, Deng C, et al. Pneumocystis pneumonia in patients with inflammatory or autoimmune diseases: usefulness of lymphocyte subtyping. Int J Infect Dis 2017; 57:108–115. doi:10.1016/j.ijid.2017.02.010
- Ward MM, Donald F. Pneumocystis carinii pneumonia in patients with connective tissue diseases: the role of hospital experience in diagnosis and mortality. Arthritis Rheum 1999; 42(4):780–789. doi:10.1002/1529-0131(199904)42:4<780::AID-ANR23>3.0.CO;2-M
- Katsuyama T, Saito K, Kubo S, Nawata M, Tanaka Y. Prophylaxis for Pneumocystis pneumonia in patients with rheumatoid arthritis treated with biologics, based on risk factors found in a retrospective study. Arthritis Res Ther 2014; 16(1):R43. doi:10.1186/ar4472
- Tanaka M, Sakai R, Koike R, et al. Pneumocystis jirovecii pneumonia associated with etanercept treatment in patients with rheumatoid arthritis: a retrospective review of 15 cases and analysis of risk factors. Mod Rheumatol 2012; 22(6):849–858. doi:10.1007/s10165-012-0615-z
- Chung JB, Armstrong K, Schwartz JS, Albert D. Cost-effectiveness of prophylaxis against Pneumocystis carinii pneumonia in patients with Wegener’s granulomatosis undergoing immunosuppressive therapy. Arthritis Rheum 2000; 43(8):1841–1848. doi:10.1002/1529-0131(200008)43:8<1841::AID-ANR21>3.0.CO;2-Q
- Selmi C, Generali E, Massarotti M, Bianchi G, Scire CA. New treatments for inflammatory rheumatic disease. Immunol Res 2014; 60(2–3):277–288. doi:10.1007/s12026-014-8565-5
- Liu Y, Su L, Jiang SJ, Qu H. Risk factors for mortality from Pneumocystis carinii pneumonia (PCP) in non-HIV patients: a meta-analysis. Oncotarget 2017; 8(35):59729–59739. doi:10.18632/oncotarget.19927
- Desales AL, Mendez-Navarro J, Méndez-Tovar LJ, et al. Pneumocystosis in a patient with Crohn's disease treated with combination therapy with adalimumab. J Crohns Colitis 2012; 6(4):483–487. doi:10.1016/j.crohns.2011.10.012
- Kalyoncu U, Karadag O, Akdogan A, et al. Pneumocystis carinii pneumonia in a rheumatoid arthritis patient treated with adalimumab. Scand J Infect Dis 2007; 39(5):475–478. doi:10.1080/00365540601071867
- Vallabhaneni S, Chiller TM. Fungal infections and new biologic therapies. Curr Rheumatol Rep 2016; 18(5):29. doi:10.1007/s11926-016-0572-1
- Panel on Opportunistic Infections in HIV-Infected Adults and Adolescents. Guidelines for the prevention and treatment of opportunistic infections in HIV-infected adults and adolescents: recommendations from the Centers for Disease Control and Prevention, the National Institutes of Health, and the HIV Medicine Association of the Infectious Diseases Society of America. www.aidsinfo.nih.gov/contentfiles/lvguidelines/adult_oi.pdf. Accessed May 3, 2019.
- Kourbeti IS, Ziakas PD, Mylonakis E. Biologic therapies in rheumatoid arthritis and the risk of opportunistic infections: a meta-analysis. Clin Infect Dis 2014; 58(12):1649–1657. doi:10.1093/cid/ciu185
- Bia M, Adey DB, Bloom RD, Chan L, Kulkarni S, Tomlanovich S. KDOQI US commentary on the 2009 KDIGO clinical practice guideline for the care of kidney transplant recipients. Am J Kidney Dis 2010; 56(2):189–218. doi:10.1053/j.ajkd.2010.04.010
- Baden LR, Swaminathan S, Angarone M, et al. Prevention and treatment of cancer-related infections, version 2.2016, NCCN clinical practice guidelines in oncology. J Natl Compr Canc Netw 2016; 14(7):882–913. pmid:27407129
- Cooley L, Dendle C, Wolf J, et al. Consensus guidelines for diagnosis, prophylaxis and management of Pneumocystis jirovecii pneumonia in patients with haematological and solid malignancies, 2014. Intern Med J 2014; 44(12b):1350–1363. doi:10.1111/imj.12599
- Orlando A, Armuzzi A, Papi C, et al; Italian Society of Gastroenterology; Italian Group for the study of Inflammatory Bowel Disease. The Italian Society of Gastroenterology (SIGE) and the Italian Group for the study of Inflammatory Bowel Disease (IG-IBD) clinical practice guidelines: the use of tumor necrosis factor-alpha antagonist therapy in inflammatory bowel disease. Dig Liver Dis 2011; 43(1):1–20. doi:10.1016/j.dld.2010.07.010
- Mikulska M, Lanini S, Gudiol C, et al. ESCMID Study Group for Infections in Compromised Hosts (ESGICH) consensus document on the safety of targeted and biological therapies: an infectious diseases perspective (agents targeting lymphoid cells surface antigens [I]: CD19, CD20 and CD52). Clin Microbiol Infect 2018; 24(suppl 2):S71–S82. doi:10.1016/j.cmi.2018.02.003
- Baddley J, Cantini F, Goletti D, et al. ESCMID Study Group for Infections in Compromised Hosts (ESGICH) consensus document on the safety of targeted and biological therapies: an infectious diseases perspective (soluble immune effector molecules [I]: anti-tumor necrosis factor-alpha agents). Clin Microbiol Infect 2018; 24(suppl 2):S10–S20. doi:10.1016/j.cmi.2017.12.025
- Winthrop K, Mariette X, Silva J, et al. ESCMID Study Group for Infections in Compromised Hosts (ESGICH) consensus document on the safety of targeted and biological therapies: an infectious diseases perspective (soluble immune effector molecules [II]: agents targeting interleukins, immunoglobulins and complement factors). Clin Microbiol Infect 2018; 24(suppl 2):S21–S40. doi:10.1016/j.cmi.2018.02.002
- Petri M, Allbritton J. Antibiotic allergy in systemic lupus erythematosus: a case-control study. J Rheumatol 1992; 19(2):265–269. pmid:1629825
- Pope J, Jerome D, Fenlon D, Krizova A, Ouimet J. Frequency of adverse drug reactions in patients with systemic lupus erythematosus. J Rheumatol 2003; 30(3):480–484. pmid:12610805
- Vananuvat P, Suwannalai P, Sungkanuparph S, Limsuwan T, Ngamjanyaporn P, Janwityanujit S. Primary prophylaxis for Pneumocystis jirovecii pneumonia in patients with connective tissue diseases. Semin Arthritis Rheum 2011; 41(3):497–502. doi:10.1016/j.semarthrit.2011.05.004
- Tamaki H, Butler R, Langford C. Abstract Number: 1755: Safety of methotrexate and low-dose trimethoprim-sulfamethoxazole in patients with ANCA-associated vasculitis. www.acrabstracts.org/abstract/safety-of-methotrexate-and-low-dose-trimethoprim-sulfamethoxazole-in-patients-with-anca-associated-vasculitis. Accessed May 3, 2019.
Pneumocystis jirovecii (previously carinii) pneumonia (PCP) is rare in patients taking biologic response modifiers for rheumatic disease.1–10 However, prophylaxis should be considered in patients who have granulomatosis with polyangiitis or underlying pulmonary disease, or who are concomitantly receiving glucocorticoids in high doses. There is some risk of adverse reactions to the prophylactic medicine.1,11–21 Until clear guidelines are available, the decision to initiate PCP prophylaxis and the choice of agent should be individualized.
THE BURDEN OF PCP
In a meta-analysis23 of 867 patients who developed PCP and did not have HIV infection, 20.1% had autoimmune or chronic inflammatory disease and the rest were transplant recipients or had malignancies. The mortality rate was 30.6%.
PHARMACOLOGIC RISK FACTORS FOR PCP
Treatment with glucocorticoids
Treatment with glucocorticoids is an important risk factor for PCP, independent of biologic therapy.
Calero-Bernal et al11 reported on 128 patients with non-HIV PCP, of whom 114 (89%) had received a glucocorticoid for more than 4 weeks, and 98 (76%) were currently receiving one. The mean daily dose was equivalent to 27.73 mg of prednisone per day in those on glucocorticoids only, and 21.34 mg in those receiving glucocorticoids in combination with other immunosuppressants.
Park et al,12 in a retrospective study of Korean patients treated for rheumatic disease with high-dose glucocorticoids (≥ 30 mg/day of prednisone or equivalent for more than 4 weeks), reported an incidence rate of PCP of 2.37 per 100 patient-years in those not on prophylaxis.
Other studies13,14 have also found a prednisone dose greater than 15 to 20 mg per day for more than 4 weeks or concomitant use of 2 or more disease-modifying antirheumatic drugs to be a significant risk factor.13,14
Tumor necrosis factor alpha antagonists
A US Food and Drug Administration review1 of voluntary reports of adverse drug events estimated the incidence of PCP to be 2.3 per 100,000 patient-years with infliximab and 1.6 per 100,000 patient-years with etanercept. In most cases, other immunosuppressants were used concomitantly.1
Postmarketing surveillance2 of 5,000 patients with rheumatoid arthritis showed an incidence of suspected PCP of 0.4% within the first 6 months of starting infliximab therapy.
Komano et al,15 in a case-control study of patients with rheumatoid arthritis treated with infliximab, reported that all 21 patients with PCP were also on methotrexate (median dosage 8 mg per week) and prednisolone (median dosage 7.5 mg per day).
PCP has also been reported after adalimumab use in combination with prednisone, azathioprine, and methotrexate, as well as with certolizumab, golimumab, tocilizumab, abatacept, and rituximab.3–6,24–26
Rituximab
Calero-Bernal et al11 reported that 23% of patients with non-HIV PCP who were receiving immunosuppressant drugs were on rituximab.
Alexandre et al16 performed a retrospective review of 11 cases of PCP complicating rituximab therapy for autoimmune disease, in which 10 (91%) of the patients were also on corticosteroids, with a median dosage of 30 mg of prednisone daily. A literature review of an additional 18 cases revealed similar findings.
PATIENT RISK FACTORS FOR PCP
Pulmonary disease, age, other factors
Komano et al,15 in their study of patients with rheumatoid arthritis treated with infliximab, found that 10 (48%) of 21 patients with PCP had preexisting pulmonary disease, compared with 11 (10.8%) of 102 patients without PCP (P < .001). Patients with PCP were older (mean age 64 vs 54, P < .001), were on higher median doses of prednisolone per day (7.5 vs 5 mg, P = .001), and had lower median serum immunoglobulin G (IgG) levels (944 vs 1,394 mg/dL, P < .001).15
Tadros et al13 performed a case-control study that also showed that patients with autoimmune disease who developed PCP had lower lymphocyte counts than controls on admission. Other risk factors included low CD4 counts and age older than 50.
Li et al17 found that patients with autoimmune or inflammatory disease with PCP were more likely to have low CD3, CD4, and CD8 cell counts, as well as albumin levels less than 28 g/L. They therefore suggested that lymphocyte subtyping may be a useful tool to guide PCP prophylaxis.
Granulomatosis with polyangiitis
Patients with granulomatosis with polyangiitis have a significantly higher incidence of PCP than patients with other connective tissue diseases.
Ward and Donald18 reviewed 223 cases of PCP in patients with connective tissue disease. The highest frequency (89 cases per 10,000 hospitalizations per year) was in patients with granulomatosis with polyangiitis, followed by 65 per 10,000 hospitalizations per year for patients with polyarteritis nodosa. The lowest frequency was in rheumatoid arthritis patients, at 2 per 10,000 hospitalizations per year. In decreasing order, diseases with significant associations with PCP were:
- Polyarteritis nodosa (odds ratio [OR] 10.20, 95% confidence interval [CI] 5.69–18.29)
- Granulomatosis with polyangiitis (OR 7.81, 95% CI 4.71–13.05)
- Inflammatory myopathy (OR 4.44, 95% CI 2.67–7.38)
- Systemic lupus erythematosus (OR 2.52, 95% CI 1.66–3.82).
Vallabhaneni and Chiller,26 in a meta-analysis including rheumatoid arthritis patients on biologics, did not find an increased risk of PCP (OR 1.77, 95% CI 0.42–7.47).
Park et al12 found that the highest incidences of PCP were in patients with granulomatosis with polyangiitis, microscopic polyangiitis, and systemic sclerosis. For systemic sclerosis, the main reason for giving high-dose glucocorticoids was interstitial lung disease.
Other studies19,20,28 also found an association with coexisting pulmonary disease in patients with rheumatoid arthritis.
CURRENT GUIDELINES
There are guidelines for primary and secondary prophylaxis of PCP in HIV-positive patients with CD4 counts less than 200/mm3 or a history of acquired immunodeficiency syndrome (AIDS)-defining illness.27 Additionally, patients with a CD4 cell percentage less than 14% should be considered for prophylaxis.27
Unfortunately, there are no guidelines for prophylaxis in patients taking immunosuppressants for rheumatic disease.
The recommended regimen for PCP prophylaxis in HIV-infected patients is trimethoprim-sulfamethoxazole, 1 double-strength or 1 single-strength tablet daily. Alternative regimens include 1 double-strength tablet 3 times per week, dapsone, aerosolized pentamidine, and atovaquone.27
There are also guidelines for prophylaxis in kidney transplant recipients, as well as for patients with hematologic malignancies and solid-organ malignancies, particularly those on chemotherapeutic agents and the T-cell-depleting agent alemtuzumab.29–31
Italian clinical practice guidelines for the use of tumor necrosis factor antagonists in inflammatory bowel disease recommend consideration of PCP prophylaxis in patients who are also on other immunosuppressants, particularly high-dose glucocorticoids.32
Prophylaxis has been shown to increase life expectancy and quality-adjusted life-years and to reduce cost for patients on immunosuppressive therapy for granulomatosis with polyangiitis.21 The European Society of Clinical Microbiology and Infectious Diseases recently produced consensus statements recommending PCP prophylaxis for patients on rituximab with other concomitant immunosuppressants such as the equivalent of prednisone 20 mg daily for more than 4 weeks.33 Prophylaxis was not recommended for other biologic therapies.34,35
THE RISKS OF PROPHYLAXIS
The risk of PCP should be weighed against the risk of prophylaxis in patients with rheumatic disease. Adverse reactions to sulfonamide antibiotics including disease flares have been reported in patients with systemic lupus erythematosus.36,37 Other studies have found no increased risk of flares in patients taking trimethoprim-sulfamethoxazole for PCP prophylaxis.12,38 A retrospective analysis of patients with vasculitis found no increased risk of combining methotrexate and trimethoprim-sulfamethoxazole.39
KEY POINTS
- PCP is an opportunistic infection with a high risk of death.
- PCP has been reported with biologics used as immunomodulators in rheumatic disease.
- PCP prophylaxis should be considered in patients at high risk of PCP, such as those who have granulomatosis with polyangiitis, underlying pulmonary disease or who are concomitantly taking glucocorticoids.
Pneumocystis jirovecii (previously carinii) pneumonia (PCP) is rare in patients taking biologic response modifiers for rheumatic disease.1–10 However, prophylaxis should be considered in patients who have granulomatosis with polyangiitis or underlying pulmonary disease, or who are concomitantly receiving glucocorticoids in high doses. There is some risk of adverse reactions to the prophylactic medicine.1,11–21 Until clear guidelines are available, the decision to initiate PCP prophylaxis and the choice of agent should be individualized.
THE BURDEN OF PCP
In a meta-analysis23 of 867 patients who developed PCP and did not have HIV infection, 20.1% had autoimmune or chronic inflammatory disease and the rest were transplant recipients or had malignancies. The mortality rate was 30.6%.
PHARMACOLOGIC RISK FACTORS FOR PCP
Treatment with glucocorticoids
Treatment with glucocorticoids is an important risk factor for PCP, independent of biologic therapy.
Calero-Bernal et al11 reported on 128 patients with non-HIV PCP, of whom 114 (89%) had received a glucocorticoid for more than 4 weeks, and 98 (76%) were currently receiving one. The mean daily dose was equivalent to 27.73 mg of prednisone per day in those on glucocorticoids only, and 21.34 mg in those receiving glucocorticoids in combination with other immunosuppressants.
Park et al,12 in a retrospective study of Korean patients treated for rheumatic disease with high-dose glucocorticoids (≥ 30 mg/day of prednisone or equivalent for more than 4 weeks), reported an incidence rate of PCP of 2.37 per 100 patient-years in those not on prophylaxis.
Other studies13,14 have also found a prednisone dose greater than 15 to 20 mg per day for more than 4 weeks or concomitant use of 2 or more disease-modifying antirheumatic drugs to be a significant risk factor.13,14
Tumor necrosis factor alpha antagonists
A US Food and Drug Administration review1 of voluntary reports of adverse drug events estimated the incidence of PCP to be 2.3 per 100,000 patient-years with infliximab and 1.6 per 100,000 patient-years with etanercept. In most cases, other immunosuppressants were used concomitantly.1
Postmarketing surveillance2 of 5,000 patients with rheumatoid arthritis showed an incidence of suspected PCP of 0.4% within the first 6 months of starting infliximab therapy.
Komano et al,15 in a case-control study of patients with rheumatoid arthritis treated with infliximab, reported that all 21 patients with PCP were also on methotrexate (median dosage 8 mg per week) and prednisolone (median dosage 7.5 mg per day).
PCP has also been reported after adalimumab use in combination with prednisone, azathioprine, and methotrexate, as well as with certolizumab, golimumab, tocilizumab, abatacept, and rituximab.3–6,24–26
Rituximab
Calero-Bernal et al11 reported that 23% of patients with non-HIV PCP who were receiving immunosuppressant drugs were on rituximab.
Alexandre et al16 performed a retrospective review of 11 cases of PCP complicating rituximab therapy for autoimmune disease, in which 10 (91%) of the patients were also on corticosteroids, with a median dosage of 30 mg of prednisone daily. A literature review of an additional 18 cases revealed similar findings.
PATIENT RISK FACTORS FOR PCP
Pulmonary disease, age, other factors
Komano et al,15 in their study of patients with rheumatoid arthritis treated with infliximab, found that 10 (48%) of 21 patients with PCP had preexisting pulmonary disease, compared with 11 (10.8%) of 102 patients without PCP (P < .001). Patients with PCP were older (mean age 64 vs 54, P < .001), were on higher median doses of prednisolone per day (7.5 vs 5 mg, P = .001), and had lower median serum immunoglobulin G (IgG) levels (944 vs 1,394 mg/dL, P < .001).15
Tadros et al13 performed a case-control study that also showed that patients with autoimmune disease who developed PCP had lower lymphocyte counts than controls on admission. Other risk factors included low CD4 counts and age older than 50.
Li et al17 found that patients with autoimmune or inflammatory disease with PCP were more likely to have low CD3, CD4, and CD8 cell counts, as well as albumin levels less than 28 g/L. They therefore suggested that lymphocyte subtyping may be a useful tool to guide PCP prophylaxis.
Granulomatosis with polyangiitis
Patients with granulomatosis with polyangiitis have a significantly higher incidence of PCP than patients with other connective tissue diseases.
Ward and Donald18 reviewed 223 cases of PCP in patients with connective tissue disease. The highest frequency (89 cases per 10,000 hospitalizations per year) was in patients with granulomatosis with polyangiitis, followed by 65 per 10,000 hospitalizations per year for patients with polyarteritis nodosa. The lowest frequency was in rheumatoid arthritis patients, at 2 per 10,000 hospitalizations per year. In decreasing order, diseases with significant associations with PCP were:
- Polyarteritis nodosa (odds ratio [OR] 10.20, 95% confidence interval [CI] 5.69–18.29)
- Granulomatosis with polyangiitis (OR 7.81, 95% CI 4.71–13.05)
- Inflammatory myopathy (OR 4.44, 95% CI 2.67–7.38)
- Systemic lupus erythematosus (OR 2.52, 95% CI 1.66–3.82).
Vallabhaneni and Chiller,26 in a meta-analysis including rheumatoid arthritis patients on biologics, did not find an increased risk of PCP (OR 1.77, 95% CI 0.42–7.47).
Park et al12 found that the highest incidences of PCP were in patients with granulomatosis with polyangiitis, microscopic polyangiitis, and systemic sclerosis. For systemic sclerosis, the main reason for giving high-dose glucocorticoids was interstitial lung disease.
Other studies19,20,28 also found an association with coexisting pulmonary disease in patients with rheumatoid arthritis.
CURRENT GUIDELINES
There are guidelines for primary and secondary prophylaxis of PCP in HIV-positive patients with CD4 counts less than 200/mm3 or a history of acquired immunodeficiency syndrome (AIDS)-defining illness.27 Additionally, patients with a CD4 cell percentage less than 14% should be considered for prophylaxis.27
Unfortunately, there are no guidelines for prophylaxis in patients taking immunosuppressants for rheumatic disease.
The recommended regimen for PCP prophylaxis in HIV-infected patients is trimethoprim-sulfamethoxazole, 1 double-strength or 1 single-strength tablet daily. Alternative regimens include 1 double-strength tablet 3 times per week, dapsone, aerosolized pentamidine, and atovaquone.27
There are also guidelines for prophylaxis in kidney transplant recipients, as well as for patients with hematologic malignancies and solid-organ malignancies, particularly those on chemotherapeutic agents and the T-cell-depleting agent alemtuzumab.29–31
Italian clinical practice guidelines for the use of tumor necrosis factor antagonists in inflammatory bowel disease recommend consideration of PCP prophylaxis in patients who are also on other immunosuppressants, particularly high-dose glucocorticoids.32
Prophylaxis has been shown to increase life expectancy and quality-adjusted life-years and to reduce cost for patients on immunosuppressive therapy for granulomatosis with polyangiitis.21 The European Society of Clinical Microbiology and Infectious Diseases recently produced consensus statements recommending PCP prophylaxis for patients on rituximab with other concomitant immunosuppressants such as the equivalent of prednisone 20 mg daily for more than 4 weeks.33 Prophylaxis was not recommended for other biologic therapies.34,35
THE RISKS OF PROPHYLAXIS
The risk of PCP should be weighed against the risk of prophylaxis in patients with rheumatic disease. Adverse reactions to sulfonamide antibiotics including disease flares have been reported in patients with systemic lupus erythematosus.36,37 Other studies have found no increased risk of flares in patients taking trimethoprim-sulfamethoxazole for PCP prophylaxis.12,38 A retrospective analysis of patients with vasculitis found no increased risk of combining methotrexate and trimethoprim-sulfamethoxazole.39
KEY POINTS
- PCP is an opportunistic infection with a high risk of death.
- PCP has been reported with biologics used as immunomodulators in rheumatic disease.
- PCP prophylaxis should be considered in patients at high risk of PCP, such as those who have granulomatosis with polyangiitis, underlying pulmonary disease or who are concomitantly taking glucocorticoids.
- US Food and Drug Administration. Safety update on TNF-alpha antagonists: infliximab and etanercept.https://wayback.archive-it.org/7993/20180127041103/https://www.fda.gov/ohrms/dockets/ac/01/briefing/3779b2_01_cber_safety_revision2.htm. Accessed May 3, 2019.
- Takeuchi T, Tatsuki Y, Nogami Y, et al. Postmarketing surveillance of the safety profile of infliximab in 5000 Japanese patients with rheumatoid arthritis. Ann Rheum Dis 2008; 67(2):189–194. doi:10.1136/ard.2007.072967
- Koike T, Harigai M, Ishiguro N, et al. Safety and effectiveness of adalimumab in Japanese rheumatoid arthritis patients: postmarketing surveillance report of the first 3,000 patients. Mod Rheumatol 2012; 22(4):498–508. doi:10.1007/s10165-011-0541-5
- Bykerk V, Cush J, Winthrop K, et al. Update on the safety profile of certolizumab pegol in rheumatoid arthritis: an integrated analysis from clinical trials. Ann Rheum Dis 2015; 74(1):96–103. doi:10.1136/annrheumdis-2013-203660
- Koike T, Harigai M, Inokuma S, et al. Postmarketing surveillance of tocilizumab for rheumatoid arthritis in Japan: interim analysis of 3881 patients. Ann Rheum Dis 2011; 70(12):2148–2151. doi:10.1136/ard.2011.151092
- Harigai M, Ishiguro N, Inokuma S, et al. Postmarketing surveillance of the safety and effectiveness of abatacept in Japanese patients with rheumatoid arthritis. Mod Rheumatol 2016; 26(4):491–498. doi:10.3109/14397595.2015.1123211
- Koike T, Harigai M, Inokuma S, et al. Postmarketing surveillance of the safety and effectiveness of etanercept in Japan. J Rheumatol 2009; 36(5):898–906. doi:10.3899/jrheum.080791
- Grubbs JA, Baddley JW. Pneumocystis jirovecii pneumonia in patients receiving tumor-necrosis-factor-inhibitor therapy: implications for chemoprophylaxis. Curr Rheumatol Rep 2014; 16(10):445. doi:10.1007/s11926-014-0445-4
- US Food and Drug Administration. FDA adverse event reporting system (FAERS) public dashboard. www.fda.gov/Drugs/GuidanceComplianceRegulatoryInformation/Surveillance/AdverseDrugEffects/ucm070093.htm. Accessed May 3, 2019.
- Rutherford AI, Patarata E, Subesinghe S, Hyrich KL, Galloway JB. Opportunistic infections in rheumatoid arthritis patients exposed to biologic therapy: results from the British Society for Rheumatology Biologics Register for Rheumatoid Arthritis. Rheumatology (Oxford) 2018; 57(6):997–1001. doi:10.1093/rheumatology/key023
- Calero-Bernal ML, Martin-Garrido I, Donazar-Ezcurra M, Limper AH, Carmona EM. Intermittent courses of corticosteroids also present a risk for Pneumocystis pneumonia in non-HIV patients. Can Respir J 2016; 2016:2464791. doi:10.1155/2016/2464791
- Park JW, Curtis JR, Moon J, Song YW, Kim S, Lee EB. Prophylactic effect of trimethoprim-sulfamethoxazole for pneumocystis pneumonia in patients with rheumatic diseases exposed to prolonged high-dose glucocorticoids. Ann Rheum Dis 2018; 77(5):644–649. doi:10.1136/annrheumdis-2017-211796
- Tadros S, Teichtahl AJ, Ciciriello S, Wicks IP. Pneumocystis jirovecii pneumonia in systemic autoimmune rheumatic disease: a case-control study. Semin Arthritis Rheum 2017; 46(6):804–809. doi:10.1016/j.semarthrit.2016.09.009
- Demoruelle MK, Kahr A, Verilhac K, Deane K, Fischer A, West S. Recent-onset systemic lupus erythematosus complicated by acute respiratory failure. Arthritis Care Res (Hoboken) 2013; 65(2):314–323. doi:10.1002/acr.21857
- Komano Y, Harigai M, Koike R, et al. Pneumocystis jiroveci pneumonia in patients with rheumatoid arthritis treated with infliximab: a retrospective review and case-control study of 21 patients. Arthritis Rheum 2009; 61(3):305–312. doi:10.1002/art.24283
- Alexandre K, Ingen-Housz-Oro S, Versini M, Sailler L, Benhamou Y. Pneumocystis jirovecii pneumonia in patients treated with rituximab for systemic diseases: report of 11 cases and review of the literature. Eur J Intern Med 2018; 50:e23–e24. doi:10.1016/j.ejim.2017.11.014
- Li Y, Ghannoum M, Deng C, et al. Pneumocystis pneumonia in patients with inflammatory or autoimmune diseases: usefulness of lymphocyte subtyping. Int J Infect Dis 2017; 57:108–115. doi:10.1016/j.ijid.2017.02.010
- Ward MM, Donald F. Pneumocystis carinii pneumonia in patients with connective tissue diseases: the role of hospital experience in diagnosis and mortality. Arthritis Rheum 1999; 42(4):780–789. doi:10.1002/1529-0131(199904)42:4<780::AID-ANR23>3.0.CO;2-M
- Katsuyama T, Saito K, Kubo S, Nawata M, Tanaka Y. Prophylaxis for Pneumocystis pneumonia in patients with rheumatoid arthritis treated with biologics, based on risk factors found in a retrospective study. Arthritis Res Ther 2014; 16(1):R43. doi:10.1186/ar4472
- Tanaka M, Sakai R, Koike R, et al. Pneumocystis jirovecii pneumonia associated with etanercept treatment in patients with rheumatoid arthritis: a retrospective review of 15 cases and analysis of risk factors. Mod Rheumatol 2012; 22(6):849–858. doi:10.1007/s10165-012-0615-z
- Chung JB, Armstrong K, Schwartz JS, Albert D. Cost-effectiveness of prophylaxis against Pneumocystis carinii pneumonia in patients with Wegener’s granulomatosis undergoing immunosuppressive therapy. Arthritis Rheum 2000; 43(8):1841–1848. doi:10.1002/1529-0131(200008)43:8<1841::AID-ANR21>3.0.CO;2-Q
- Selmi C, Generali E, Massarotti M, Bianchi G, Scire CA. New treatments for inflammatory rheumatic disease. Immunol Res 2014; 60(2–3):277–288. doi:10.1007/s12026-014-8565-5
- Liu Y, Su L, Jiang SJ, Qu H. Risk factors for mortality from Pneumocystis carinii pneumonia (PCP) in non-HIV patients: a meta-analysis. Oncotarget 2017; 8(35):59729–59739. doi:10.18632/oncotarget.19927
- Desales AL, Mendez-Navarro J, Méndez-Tovar LJ, et al. Pneumocystosis in a patient with Crohn's disease treated with combination therapy with adalimumab. J Crohns Colitis 2012; 6(4):483–487. doi:10.1016/j.crohns.2011.10.012
- Kalyoncu U, Karadag O, Akdogan A, et al. Pneumocystis carinii pneumonia in a rheumatoid arthritis patient treated with adalimumab. Scand J Infect Dis 2007; 39(5):475–478. doi:10.1080/00365540601071867
- Vallabhaneni S, Chiller TM. Fungal infections and new biologic therapies. Curr Rheumatol Rep 2016; 18(5):29. doi:10.1007/s11926-016-0572-1
- Panel on Opportunistic Infections in HIV-Infected Adults and Adolescents. Guidelines for the prevention and treatment of opportunistic infections in HIV-infected adults and adolescents: recommendations from the Centers for Disease Control and Prevention, the National Institutes of Health, and the HIV Medicine Association of the Infectious Diseases Society of America. www.aidsinfo.nih.gov/contentfiles/lvguidelines/adult_oi.pdf. Accessed May 3, 2019.
- Kourbeti IS, Ziakas PD, Mylonakis E. Biologic therapies in rheumatoid arthritis and the risk of opportunistic infections: a meta-analysis. Clin Infect Dis 2014; 58(12):1649–1657. doi:10.1093/cid/ciu185
- Bia M, Adey DB, Bloom RD, Chan L, Kulkarni S, Tomlanovich S. KDOQI US commentary on the 2009 KDIGO clinical practice guideline for the care of kidney transplant recipients. Am J Kidney Dis 2010; 56(2):189–218. doi:10.1053/j.ajkd.2010.04.010
- Baden LR, Swaminathan S, Angarone M, et al. Prevention and treatment of cancer-related infections, version 2.2016, NCCN clinical practice guidelines in oncology. J Natl Compr Canc Netw 2016; 14(7):882–913. pmid:27407129
- Cooley L, Dendle C, Wolf J, et al. Consensus guidelines for diagnosis, prophylaxis and management of Pneumocystis jirovecii pneumonia in patients with haematological and solid malignancies, 2014. Intern Med J 2014; 44(12b):1350–1363. doi:10.1111/imj.12599
- Orlando A, Armuzzi A, Papi C, et al; Italian Society of Gastroenterology; Italian Group for the study of Inflammatory Bowel Disease. The Italian Society of Gastroenterology (SIGE) and the Italian Group for the study of Inflammatory Bowel Disease (IG-IBD) clinical practice guidelines: the use of tumor necrosis factor-alpha antagonist therapy in inflammatory bowel disease. Dig Liver Dis 2011; 43(1):1–20. doi:10.1016/j.dld.2010.07.010
- Mikulska M, Lanini S, Gudiol C, et al. ESCMID Study Group for Infections in Compromised Hosts (ESGICH) consensus document on the safety of targeted and biological therapies: an infectious diseases perspective (agents targeting lymphoid cells surface antigens [I]: CD19, CD20 and CD52). Clin Microbiol Infect 2018; 24(suppl 2):S71–S82. doi:10.1016/j.cmi.2018.02.003
- Baddley J, Cantini F, Goletti D, et al. ESCMID Study Group for Infections in Compromised Hosts (ESGICH) consensus document on the safety of targeted and biological therapies: an infectious diseases perspective (soluble immune effector molecules [I]: anti-tumor necrosis factor-alpha agents). Clin Microbiol Infect 2018; 24(suppl 2):S10–S20. doi:10.1016/j.cmi.2017.12.025
- Winthrop K, Mariette X, Silva J, et al. ESCMID Study Group for Infections in Compromised Hosts (ESGICH) consensus document on the safety of targeted and biological therapies: an infectious diseases perspective (soluble immune effector molecules [II]: agents targeting interleukins, immunoglobulins and complement factors). Clin Microbiol Infect 2018; 24(suppl 2):S21–S40. doi:10.1016/j.cmi.2018.02.002
- Petri M, Allbritton J. Antibiotic allergy in systemic lupus erythematosus: a case-control study. J Rheumatol 1992; 19(2):265–269. pmid:1629825
- Pope J, Jerome D, Fenlon D, Krizova A, Ouimet J. Frequency of adverse drug reactions in patients with systemic lupus erythematosus. J Rheumatol 2003; 30(3):480–484. pmid:12610805
- Vananuvat P, Suwannalai P, Sungkanuparph S, Limsuwan T, Ngamjanyaporn P, Janwityanujit S. Primary prophylaxis for Pneumocystis jirovecii pneumonia in patients with connective tissue diseases. Semin Arthritis Rheum 2011; 41(3):497–502. doi:10.1016/j.semarthrit.2011.05.004
- Tamaki H, Butler R, Langford C. Abstract Number: 1755: Safety of methotrexate and low-dose trimethoprim-sulfamethoxazole in patients with ANCA-associated vasculitis. www.acrabstracts.org/abstract/safety-of-methotrexate-and-low-dose-trimethoprim-sulfamethoxazole-in-patients-with-anca-associated-vasculitis. Accessed May 3, 2019.
- US Food and Drug Administration. Safety update on TNF-alpha antagonists: infliximab and etanercept.https://wayback.archive-it.org/7993/20180127041103/https://www.fda.gov/ohrms/dockets/ac/01/briefing/3779b2_01_cber_safety_revision2.htm. Accessed May 3, 2019.
- Takeuchi T, Tatsuki Y, Nogami Y, et al. Postmarketing surveillance of the safety profile of infliximab in 5000 Japanese patients with rheumatoid arthritis. Ann Rheum Dis 2008; 67(2):189–194. doi:10.1136/ard.2007.072967
- Koike T, Harigai M, Ishiguro N, et al. Safety and effectiveness of adalimumab in Japanese rheumatoid arthritis patients: postmarketing surveillance report of the first 3,000 patients. Mod Rheumatol 2012; 22(4):498–508. doi:10.1007/s10165-011-0541-5
- Bykerk V, Cush J, Winthrop K, et al. Update on the safety profile of certolizumab pegol in rheumatoid arthritis: an integrated analysis from clinical trials. Ann Rheum Dis 2015; 74(1):96–103. doi:10.1136/annrheumdis-2013-203660
- Koike T, Harigai M, Inokuma S, et al. Postmarketing surveillance of tocilizumab for rheumatoid arthritis in Japan: interim analysis of 3881 patients. Ann Rheum Dis 2011; 70(12):2148–2151. doi:10.1136/ard.2011.151092
- Harigai M, Ishiguro N, Inokuma S, et al. Postmarketing surveillance of the safety and effectiveness of abatacept in Japanese patients with rheumatoid arthritis. Mod Rheumatol 2016; 26(4):491–498. doi:10.3109/14397595.2015.1123211
- Koike T, Harigai M, Inokuma S, et al. Postmarketing surveillance of the safety and effectiveness of etanercept in Japan. J Rheumatol 2009; 36(5):898–906. doi:10.3899/jrheum.080791
- Grubbs JA, Baddley JW. Pneumocystis jirovecii pneumonia in patients receiving tumor-necrosis-factor-inhibitor therapy: implications for chemoprophylaxis. Curr Rheumatol Rep 2014; 16(10):445. doi:10.1007/s11926-014-0445-4
- US Food and Drug Administration. FDA adverse event reporting system (FAERS) public dashboard. www.fda.gov/Drugs/GuidanceComplianceRegulatoryInformation/Surveillance/AdverseDrugEffects/ucm070093.htm. Accessed May 3, 2019.
- Rutherford AI, Patarata E, Subesinghe S, Hyrich KL, Galloway JB. Opportunistic infections in rheumatoid arthritis patients exposed to biologic therapy: results from the British Society for Rheumatology Biologics Register for Rheumatoid Arthritis. Rheumatology (Oxford) 2018; 57(6):997–1001. doi:10.1093/rheumatology/key023
- Calero-Bernal ML, Martin-Garrido I, Donazar-Ezcurra M, Limper AH, Carmona EM. Intermittent courses of corticosteroids also present a risk for Pneumocystis pneumonia in non-HIV patients. Can Respir J 2016; 2016:2464791. doi:10.1155/2016/2464791
- Park JW, Curtis JR, Moon J, Song YW, Kim S, Lee EB. Prophylactic effect of trimethoprim-sulfamethoxazole for pneumocystis pneumonia in patients with rheumatic diseases exposed to prolonged high-dose glucocorticoids. Ann Rheum Dis 2018; 77(5):644–649. doi:10.1136/annrheumdis-2017-211796
- Tadros S, Teichtahl AJ, Ciciriello S, Wicks IP. Pneumocystis jirovecii pneumonia in systemic autoimmune rheumatic disease: a case-control study. Semin Arthritis Rheum 2017; 46(6):804–809. doi:10.1016/j.semarthrit.2016.09.009
- Demoruelle MK, Kahr A, Verilhac K, Deane K, Fischer A, West S. Recent-onset systemic lupus erythematosus complicated by acute respiratory failure. Arthritis Care Res (Hoboken) 2013; 65(2):314–323. doi:10.1002/acr.21857
- Komano Y, Harigai M, Koike R, et al. Pneumocystis jiroveci pneumonia in patients with rheumatoid arthritis treated with infliximab: a retrospective review and case-control study of 21 patients. Arthritis Rheum 2009; 61(3):305–312. doi:10.1002/art.24283
- Alexandre K, Ingen-Housz-Oro S, Versini M, Sailler L, Benhamou Y. Pneumocystis jirovecii pneumonia in patients treated with rituximab for systemic diseases: report of 11 cases and review of the literature. Eur J Intern Med 2018; 50:e23–e24. doi:10.1016/j.ejim.2017.11.014
- Li Y, Ghannoum M, Deng C, et al. Pneumocystis pneumonia in patients with inflammatory or autoimmune diseases: usefulness of lymphocyte subtyping. Int J Infect Dis 2017; 57:108–115. doi:10.1016/j.ijid.2017.02.010
- Ward MM, Donald F. Pneumocystis carinii pneumonia in patients with connective tissue diseases: the role of hospital experience in diagnosis and mortality. Arthritis Rheum 1999; 42(4):780–789. doi:10.1002/1529-0131(199904)42:4<780::AID-ANR23>3.0.CO;2-M
- Katsuyama T, Saito K, Kubo S, Nawata M, Tanaka Y. Prophylaxis for Pneumocystis pneumonia in patients with rheumatoid arthritis treated with biologics, based on risk factors found in a retrospective study. Arthritis Res Ther 2014; 16(1):R43. doi:10.1186/ar4472
- Tanaka M, Sakai R, Koike R, et al. Pneumocystis jirovecii pneumonia associated with etanercept treatment in patients with rheumatoid arthritis: a retrospective review of 15 cases and analysis of risk factors. Mod Rheumatol 2012; 22(6):849–858. doi:10.1007/s10165-012-0615-z
- Chung JB, Armstrong K, Schwartz JS, Albert D. Cost-effectiveness of prophylaxis against Pneumocystis carinii pneumonia in patients with Wegener’s granulomatosis undergoing immunosuppressive therapy. Arthritis Rheum 2000; 43(8):1841–1848. doi:10.1002/1529-0131(200008)43:8<1841::AID-ANR21>3.0.CO;2-Q
- Selmi C, Generali E, Massarotti M, Bianchi G, Scire CA. New treatments for inflammatory rheumatic disease. Immunol Res 2014; 60(2–3):277–288. doi:10.1007/s12026-014-8565-5
- Liu Y, Su L, Jiang SJ, Qu H. Risk factors for mortality from Pneumocystis carinii pneumonia (PCP) in non-HIV patients: a meta-analysis. Oncotarget 2017; 8(35):59729–59739. doi:10.18632/oncotarget.19927
- Desales AL, Mendez-Navarro J, Méndez-Tovar LJ, et al. Pneumocystosis in a patient with Crohn's disease treated with combination therapy with adalimumab. J Crohns Colitis 2012; 6(4):483–487. doi:10.1016/j.crohns.2011.10.012
- Kalyoncu U, Karadag O, Akdogan A, et al. Pneumocystis carinii pneumonia in a rheumatoid arthritis patient treated with adalimumab. Scand J Infect Dis 2007; 39(5):475–478. doi:10.1080/00365540601071867
- Vallabhaneni S, Chiller TM. Fungal infections and new biologic therapies. Curr Rheumatol Rep 2016; 18(5):29. doi:10.1007/s11926-016-0572-1
- Panel on Opportunistic Infections in HIV-Infected Adults and Adolescents. Guidelines for the prevention and treatment of opportunistic infections in HIV-infected adults and adolescents: recommendations from the Centers for Disease Control and Prevention, the National Institutes of Health, and the HIV Medicine Association of the Infectious Diseases Society of America. www.aidsinfo.nih.gov/contentfiles/lvguidelines/adult_oi.pdf. Accessed May 3, 2019.
- Kourbeti IS, Ziakas PD, Mylonakis E. Biologic therapies in rheumatoid arthritis and the risk of opportunistic infections: a meta-analysis. Clin Infect Dis 2014; 58(12):1649–1657. doi:10.1093/cid/ciu185
- Bia M, Adey DB, Bloom RD, Chan L, Kulkarni S, Tomlanovich S. KDOQI US commentary on the 2009 KDIGO clinical practice guideline for the care of kidney transplant recipients. Am J Kidney Dis 2010; 56(2):189–218. doi:10.1053/j.ajkd.2010.04.010
- Baden LR, Swaminathan S, Angarone M, et al. Prevention and treatment of cancer-related infections, version 2.2016, NCCN clinical practice guidelines in oncology. J Natl Compr Canc Netw 2016; 14(7):882–913. pmid:27407129
- Cooley L, Dendle C, Wolf J, et al. Consensus guidelines for diagnosis, prophylaxis and management of Pneumocystis jirovecii pneumonia in patients with haematological and solid malignancies, 2014. Intern Med J 2014; 44(12b):1350–1363. doi:10.1111/imj.12599
- Orlando A, Armuzzi A, Papi C, et al; Italian Society of Gastroenterology; Italian Group for the study of Inflammatory Bowel Disease. The Italian Society of Gastroenterology (SIGE) and the Italian Group for the study of Inflammatory Bowel Disease (IG-IBD) clinical practice guidelines: the use of tumor necrosis factor-alpha antagonist therapy in inflammatory bowel disease. Dig Liver Dis 2011; 43(1):1–20. doi:10.1016/j.dld.2010.07.010
- Mikulska M, Lanini S, Gudiol C, et al. ESCMID Study Group for Infections in Compromised Hosts (ESGICH) consensus document on the safety of targeted and biological therapies: an infectious diseases perspective (agents targeting lymphoid cells surface antigens [I]: CD19, CD20 and CD52). Clin Microbiol Infect 2018; 24(suppl 2):S71–S82. doi:10.1016/j.cmi.2018.02.003
- Baddley J, Cantini F, Goletti D, et al. ESCMID Study Group for Infections in Compromised Hosts (ESGICH) consensus document on the safety of targeted and biological therapies: an infectious diseases perspective (soluble immune effector molecules [I]: anti-tumor necrosis factor-alpha agents). Clin Microbiol Infect 2018; 24(suppl 2):S10–S20. doi:10.1016/j.cmi.2017.12.025
- Winthrop K, Mariette X, Silva J, et al. ESCMID Study Group for Infections in Compromised Hosts (ESGICH) consensus document on the safety of targeted and biological therapies: an infectious diseases perspective (soluble immune effector molecules [II]: agents targeting interleukins, immunoglobulins and complement factors). Clin Microbiol Infect 2018; 24(suppl 2):S21–S40. doi:10.1016/j.cmi.2018.02.002
- Petri M, Allbritton J. Antibiotic allergy in systemic lupus erythematosus: a case-control study. J Rheumatol 1992; 19(2):265–269. pmid:1629825
- Pope J, Jerome D, Fenlon D, Krizova A, Ouimet J. Frequency of adverse drug reactions in patients with systemic lupus erythematosus. J Rheumatol 2003; 30(3):480–484. pmid:12610805
- Vananuvat P, Suwannalai P, Sungkanuparph S, Limsuwan T, Ngamjanyaporn P, Janwityanujit S. Primary prophylaxis for Pneumocystis jirovecii pneumonia in patients with connective tissue diseases. Semin Arthritis Rheum 2011; 41(3):497–502. doi:10.1016/j.semarthrit.2011.05.004
- Tamaki H, Butler R, Langford C. Abstract Number: 1755: Safety of methotrexate and low-dose trimethoprim-sulfamethoxazole in patients with ANCA-associated vasculitis. www.acrabstracts.org/abstract/safety-of-methotrexate-and-low-dose-trimethoprim-sulfamethoxazole-in-patients-with-anca-associated-vasculitis. Accessed May 3, 2019.
Tanezumab improves osteoarthritis pain, function in phase 3 trial
MADRID – Tanezumab, an investigational monoclonal antibody directed against nerve growth factor that is under development to treat osteoarthritis pain, met most of the coprimary efficacy endpoints set for the drug in a randomized, double-blind, parallel-group, placebo-controlled phase 3 study.
At the end of a 24-week, double-blind treatment period, Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC) pain and WOMAC physical function subscale scores were significantly improved, compared with placebo in the two tanezumab (2.5 mg and 5 mg) dose groups.
The least squares (ls) mean change from baseline in WOMAC pain scores were –2.24 for placebo, –2.70 for tanezumab 2.5 mg, and –2.85 for tanezumab 5 mg (P less than or equal to .01 and P less than or equal to .001 vs. placebo).
The ls mean change from baseline in WOMAC physical function scores were a respective –2.11, –2.70, and –2.82 (P less than or equal to .001 for both vs. placebo).
The coprimary endpoint of patients’ global assessment of OA (PGA-OA) was also significantly improved with tanezumab 5 mg (–0.90; P less than or equal to .05) but not 2.5 mg (–0.82) versus placebo (–0.72).
As the 2.5-mg dose of tanezumab didn’t meet one of the three coprimary endpoints, further hypothesis testing was not possible, but exploratory findings suggested that tanezumab at 2.5 mg or 5 mg yielded higher proportions of patients with reductions from baseline in WOMAC pain scores when compared against placebo. This was the case for reductions of at least 30% (65.6%, 68.7%, 56.6%, respectively), 50% (45.4%, 47.9%, 33.8%), or 70% (21.3%, 23.2%, 17.8%).
“I think that we have now a lot of studies with tanezumab showing a significant effect on hip and knee OA pain and function, so we have the studies in order to have the drug on the market,” study first author Francis Berenbaum, MD, PhD, of Saint-Antoine Hospital, Sorbonne Université in Paris, said in an interview at the European Congress of Rheumatology.
“Of course, because of the safety issue with rapid progressive osteoarthritis (RPOA), what we are discussing now is: ‘For which patients will there be an optimal benefit-to-risk?’ So, it’s now more a discussion around the population of patients who can benefit the most with the drug,” Dr. Berenbaum added.
A possible link between the use of tanezumab and a risk for developing RPOA was first suggested by preclinical and early clinical trial data, prompting the U.S. Food and Drug Administration to place partial holds on its clinical development in 2010, and again in 2012.
However, Dr. Berenbaum noted that a “mitigation plan” had been put in place for the phase 3 program to try to lower the likelihood of RPOA. This included: lowering the dose of the drug used and delivering it subcutaneously rather than intravenously; not prescribing it with NSAIDs and testing its possible effects and safety in a difficult-to-treat population of patients with no known risk factors for the potentially very serious adverse event.
“Based on this mitigation plan, the risk of rapid progressive osteoarthritis has considerably decreased,” Dr. Berenbaum observed. Indeed, in the phase 3 study he presented at the meeting, he said that around 2% of patients developed RPOA, which is “exactly in line with what has already been shown.” RPOA was reported in none of the placebo-treated patients, in 1.4% of those treated with tanezumab 2.5 mg, and in 2.8% in those treated with tanezumab 5 mg.
However, a “striking” finding of the current study was that despite the small increase in RPOA seen, there was no difference between the tanezumab and placebo groups in the number of patients needing total joint replacement (TJR). The percentages of patients undergoing at least one TJR was 6.7% in the placebo group, 7.8% in the tanezumab 2.5-mg group, and 7.0% in the tanezumab 5-mg group.
The joint safety events seen in the study, including TJRs, were adjudicated as being part of the normal progression of OA in the majority (73.4%) of cases. Other joint events of note were one case of subchondral insufficiency fracture occurring in a patient treated with tanezumab 2.5 mg and one case of primary osteonecrosis in a patient treated with tanezumab 5 mg.
During his presentation of the findings in a late-breaking oral abstract session, Dr. Berenbaum noted that this was a difficult-to-treat population of patients. All 849 patients who had been recruited had moderate to severe OA pain of the knee or hip and had a history of insufficient pain relief or intolerance to treatment with acetaminophen, oral NSAIDs, and tramadol and were also not responding to, or unwilling to take, opioid painkillers. Patients had to have no radiographic evidence of specified bone conditions, including RPOA.
Patients had been treated with subcutaneous tanezumab 2.5 mg (n = 283) or 5 mg (n = 284) or placebo (n = 282) at baseline, week 8, and week 16, with the three coprimary efficacy endpoints assessed at week 24.
Discussing the risk-to-benefit ratio of the drug after his presentation, Dr. Berenbaum said: “You have to keep in mind that, first, it was in very difficult-to-treat patients, compared to the other trials in the field of OA symptoms.”
He added: “Second, is that compared to the other trials, this one was able to include patients with Kellgren-Lawrence grade 4, meaning that this is a more serious population,” and third, “when you look at the responders – WOMAC 30%, 50%, 70% – there is a strong difference in terms of responders.”
Dr. Berenbaum and his coauthors noted on the poster that accompanied the late-breaking oral presentation that “an active-controlled study will provide data to further characterize the risk-benefit of tanezumab in patients with OA.”
The study was sponsored by Pfizer and Eli Lilly. Dr. Berenbaum disclosed receiving research funding through his institution from Pfizer and acting as a consultant to, and speaker for, the company as well as multiple other pharmaceutical companies. Coauthors of the study also disclosed research funding or consultancy agreements with Pfizer or Eli Lilly or were employees of the companies.
SOURCE: Berenbaum F et al. Ann Rheum Dis. Jun 2019;78(Suppl 2):262-4. Abstract LB0007, doi: 10.1136/annrheumdis-2019-eular.8660
MADRID – Tanezumab, an investigational monoclonal antibody directed against nerve growth factor that is under development to treat osteoarthritis pain, met most of the coprimary efficacy endpoints set for the drug in a randomized, double-blind, parallel-group, placebo-controlled phase 3 study.
At the end of a 24-week, double-blind treatment period, Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC) pain and WOMAC physical function subscale scores were significantly improved, compared with placebo in the two tanezumab (2.5 mg and 5 mg) dose groups.
The least squares (ls) mean change from baseline in WOMAC pain scores were –2.24 for placebo, –2.70 for tanezumab 2.5 mg, and –2.85 for tanezumab 5 mg (P less than or equal to .01 and P less than or equal to .001 vs. placebo).
The ls mean change from baseline in WOMAC physical function scores were a respective –2.11, –2.70, and –2.82 (P less than or equal to .001 for both vs. placebo).
The coprimary endpoint of patients’ global assessment of OA (PGA-OA) was also significantly improved with tanezumab 5 mg (–0.90; P less than or equal to .05) but not 2.5 mg (–0.82) versus placebo (–0.72).
As the 2.5-mg dose of tanezumab didn’t meet one of the three coprimary endpoints, further hypothesis testing was not possible, but exploratory findings suggested that tanezumab at 2.5 mg or 5 mg yielded higher proportions of patients with reductions from baseline in WOMAC pain scores when compared against placebo. This was the case for reductions of at least 30% (65.6%, 68.7%, 56.6%, respectively), 50% (45.4%, 47.9%, 33.8%), or 70% (21.3%, 23.2%, 17.8%).
“I think that we have now a lot of studies with tanezumab showing a significant effect on hip and knee OA pain and function, so we have the studies in order to have the drug on the market,” study first author Francis Berenbaum, MD, PhD, of Saint-Antoine Hospital, Sorbonne Université in Paris, said in an interview at the European Congress of Rheumatology.
“Of course, because of the safety issue with rapid progressive osteoarthritis (RPOA), what we are discussing now is: ‘For which patients will there be an optimal benefit-to-risk?’ So, it’s now more a discussion around the population of patients who can benefit the most with the drug,” Dr. Berenbaum added.
A possible link between the use of tanezumab and a risk for developing RPOA was first suggested by preclinical and early clinical trial data, prompting the U.S. Food and Drug Administration to place partial holds on its clinical development in 2010, and again in 2012.
However, Dr. Berenbaum noted that a “mitigation plan” had been put in place for the phase 3 program to try to lower the likelihood of RPOA. This included: lowering the dose of the drug used and delivering it subcutaneously rather than intravenously; not prescribing it with NSAIDs and testing its possible effects and safety in a difficult-to-treat population of patients with no known risk factors for the potentially very serious adverse event.
“Based on this mitigation plan, the risk of rapid progressive osteoarthritis has considerably decreased,” Dr. Berenbaum observed. Indeed, in the phase 3 study he presented at the meeting, he said that around 2% of patients developed RPOA, which is “exactly in line with what has already been shown.” RPOA was reported in none of the placebo-treated patients, in 1.4% of those treated with tanezumab 2.5 mg, and in 2.8% in those treated with tanezumab 5 mg.
However, a “striking” finding of the current study was that despite the small increase in RPOA seen, there was no difference between the tanezumab and placebo groups in the number of patients needing total joint replacement (TJR). The percentages of patients undergoing at least one TJR was 6.7% in the placebo group, 7.8% in the tanezumab 2.5-mg group, and 7.0% in the tanezumab 5-mg group.
The joint safety events seen in the study, including TJRs, were adjudicated as being part of the normal progression of OA in the majority (73.4%) of cases. Other joint events of note were one case of subchondral insufficiency fracture occurring in a patient treated with tanezumab 2.5 mg and one case of primary osteonecrosis in a patient treated with tanezumab 5 mg.
During his presentation of the findings in a late-breaking oral abstract session, Dr. Berenbaum noted that this was a difficult-to-treat population of patients. All 849 patients who had been recruited had moderate to severe OA pain of the knee or hip and had a history of insufficient pain relief or intolerance to treatment with acetaminophen, oral NSAIDs, and tramadol and were also not responding to, or unwilling to take, opioid painkillers. Patients had to have no radiographic evidence of specified bone conditions, including RPOA.
Patients had been treated with subcutaneous tanezumab 2.5 mg (n = 283) or 5 mg (n = 284) or placebo (n = 282) at baseline, week 8, and week 16, with the three coprimary efficacy endpoints assessed at week 24.
Discussing the risk-to-benefit ratio of the drug after his presentation, Dr. Berenbaum said: “You have to keep in mind that, first, it was in very difficult-to-treat patients, compared to the other trials in the field of OA symptoms.”
He added: “Second, is that compared to the other trials, this one was able to include patients with Kellgren-Lawrence grade 4, meaning that this is a more serious population,” and third, “when you look at the responders – WOMAC 30%, 50%, 70% – there is a strong difference in terms of responders.”
Dr. Berenbaum and his coauthors noted on the poster that accompanied the late-breaking oral presentation that “an active-controlled study will provide data to further characterize the risk-benefit of tanezumab in patients with OA.”
The study was sponsored by Pfizer and Eli Lilly. Dr. Berenbaum disclosed receiving research funding through his institution from Pfizer and acting as a consultant to, and speaker for, the company as well as multiple other pharmaceutical companies. Coauthors of the study also disclosed research funding or consultancy agreements with Pfizer or Eli Lilly or were employees of the companies.
SOURCE: Berenbaum F et al. Ann Rheum Dis. Jun 2019;78(Suppl 2):262-4. Abstract LB0007, doi: 10.1136/annrheumdis-2019-eular.8660
MADRID – Tanezumab, an investigational monoclonal antibody directed against nerve growth factor that is under development to treat osteoarthritis pain, met most of the coprimary efficacy endpoints set for the drug in a randomized, double-blind, parallel-group, placebo-controlled phase 3 study.
At the end of a 24-week, double-blind treatment period, Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC) pain and WOMAC physical function subscale scores were significantly improved, compared with placebo in the two tanezumab (2.5 mg and 5 mg) dose groups.
The least squares (ls) mean change from baseline in WOMAC pain scores were –2.24 for placebo, –2.70 for tanezumab 2.5 mg, and –2.85 for tanezumab 5 mg (P less than or equal to .01 and P less than or equal to .001 vs. placebo).
The ls mean change from baseline in WOMAC physical function scores were a respective –2.11, –2.70, and –2.82 (P less than or equal to .001 for both vs. placebo).
The coprimary endpoint of patients’ global assessment of OA (PGA-OA) was also significantly improved with tanezumab 5 mg (–0.90; P less than or equal to .05) but not 2.5 mg (–0.82) versus placebo (–0.72).
As the 2.5-mg dose of tanezumab didn’t meet one of the three coprimary endpoints, further hypothesis testing was not possible, but exploratory findings suggested that tanezumab at 2.5 mg or 5 mg yielded higher proportions of patients with reductions from baseline in WOMAC pain scores when compared against placebo. This was the case for reductions of at least 30% (65.6%, 68.7%, 56.6%, respectively), 50% (45.4%, 47.9%, 33.8%), or 70% (21.3%, 23.2%, 17.8%).
“I think that we have now a lot of studies with tanezumab showing a significant effect on hip and knee OA pain and function, so we have the studies in order to have the drug on the market,” study first author Francis Berenbaum, MD, PhD, of Saint-Antoine Hospital, Sorbonne Université in Paris, said in an interview at the European Congress of Rheumatology.
“Of course, because of the safety issue with rapid progressive osteoarthritis (RPOA), what we are discussing now is: ‘For which patients will there be an optimal benefit-to-risk?’ So, it’s now more a discussion around the population of patients who can benefit the most with the drug,” Dr. Berenbaum added.
A possible link between the use of tanezumab and a risk for developing RPOA was first suggested by preclinical and early clinical trial data, prompting the U.S. Food and Drug Administration to place partial holds on its clinical development in 2010, and again in 2012.
However, Dr. Berenbaum noted that a “mitigation plan” had been put in place for the phase 3 program to try to lower the likelihood of RPOA. This included: lowering the dose of the drug used and delivering it subcutaneously rather than intravenously; not prescribing it with NSAIDs and testing its possible effects and safety in a difficult-to-treat population of patients with no known risk factors for the potentially very serious adverse event.
“Based on this mitigation plan, the risk of rapid progressive osteoarthritis has considerably decreased,” Dr. Berenbaum observed. Indeed, in the phase 3 study he presented at the meeting, he said that around 2% of patients developed RPOA, which is “exactly in line with what has already been shown.” RPOA was reported in none of the placebo-treated patients, in 1.4% of those treated with tanezumab 2.5 mg, and in 2.8% in those treated with tanezumab 5 mg.
However, a “striking” finding of the current study was that despite the small increase in RPOA seen, there was no difference between the tanezumab and placebo groups in the number of patients needing total joint replacement (TJR). The percentages of patients undergoing at least one TJR was 6.7% in the placebo group, 7.8% in the tanezumab 2.5-mg group, and 7.0% in the tanezumab 5-mg group.
The joint safety events seen in the study, including TJRs, were adjudicated as being part of the normal progression of OA in the majority (73.4%) of cases. Other joint events of note were one case of subchondral insufficiency fracture occurring in a patient treated with tanezumab 2.5 mg and one case of primary osteonecrosis in a patient treated with tanezumab 5 mg.
During his presentation of the findings in a late-breaking oral abstract session, Dr. Berenbaum noted that this was a difficult-to-treat population of patients. All 849 patients who had been recruited had moderate to severe OA pain of the knee or hip and had a history of insufficient pain relief or intolerance to treatment with acetaminophen, oral NSAIDs, and tramadol and were also not responding to, or unwilling to take, opioid painkillers. Patients had to have no radiographic evidence of specified bone conditions, including RPOA.
Patients had been treated with subcutaneous tanezumab 2.5 mg (n = 283) or 5 mg (n = 284) or placebo (n = 282) at baseline, week 8, and week 16, with the three coprimary efficacy endpoints assessed at week 24.
Discussing the risk-to-benefit ratio of the drug after his presentation, Dr. Berenbaum said: “You have to keep in mind that, first, it was in very difficult-to-treat patients, compared to the other trials in the field of OA symptoms.”
He added: “Second, is that compared to the other trials, this one was able to include patients with Kellgren-Lawrence grade 4, meaning that this is a more serious population,” and third, “when you look at the responders – WOMAC 30%, 50%, 70% – there is a strong difference in terms of responders.”
Dr. Berenbaum and his coauthors noted on the poster that accompanied the late-breaking oral presentation that “an active-controlled study will provide data to further characterize the risk-benefit of tanezumab in patients with OA.”
The study was sponsored by Pfizer and Eli Lilly. Dr. Berenbaum disclosed receiving research funding through his institution from Pfizer and acting as a consultant to, and speaker for, the company as well as multiple other pharmaceutical companies. Coauthors of the study also disclosed research funding or consultancy agreements with Pfizer or Eli Lilly or were employees of the companies.
SOURCE: Berenbaum F et al. Ann Rheum Dis. Jun 2019;78(Suppl 2):262-4. Abstract LB0007, doi: 10.1136/annrheumdis-2019-eular.8660
REPORTING FROM EULAR 2019 CONGRESS
Leflunomide added to glucocorticoids reduces relapse in IgG4-related disease
MADRID – The addition of leflunomide to standard glucocorticoids (GCs) in the treatment of IgG4-related disease increases the median duration of response, reduces the proportion of patients with relapse within 12 months, and permits GCs to be tapered, according to results of a randomized trial presented at the European Congress of Rheumatology.
“The rate of adverse events with the addition of leflunomide was numerically higher, but there were no significant differences in risks of any specific adverse event,” reported Feng Huang, MD, of the department of rheumatology at Chinese People’s Liberation Army General Hospital in Beijing.
GCs are highly effective in IgG4-related disease, which is an autoimmune process driven by elevated concentrations of the antibody IgG4 in the tissue of affected organs and in the serum. It has been described in a broad array of sites, including the heart, lung, kidneys, and meninges. It has been widely recognized only in the last 10 years, according to Dr. Huang. Although most patients respond to GCs, he said the problem is that about 50% of patients relapse within 12 months and more than 90% within 3 years.
This randomized, controlled study was conducted after positive results were observed with leflunomide in a small, uncontrolled pilot study published several years ago (Intern Med J. 2017 Jun;47[6]:680-9. doi: 10.1111/imj.13430). In this randomized trial, the objectives were to confirm that leflunomide extends the relapse-free period and has acceptable safety relative to GC alone.
Patients with confirmed IgG4-related disease were enrolled. Patients randomized to GC were started on 0.5 to 0.8 mg/kg per day. A predefined taper regimen was employed in those with symptom control. Those randomized to the experimental arm received GC in the same dose and schedule plus 20 mg/day of leflunomide.
The 33 patients in each group were well matched at baseline for age, comorbidities, and disease severity.
At the end of 12 months, 50% of those treated with GC alone versus 21.2% of those treated with GC plus leflunomide had relapse. That translated into a significantly higher hazard ratio (HR) for relapse in the GC monotherapy group (HR, 1.75; P = .034).
The mean duration of remission was 7 months on the combination versus 3 months on GC alone. Dr. Huang also reported a significantly higher proportion of complete responses in the group receiving the combination.
In addition, “more patients on the combination therapy were able to adhere to the steroid-tapering schedule without relapse,” Dr. Huang reported. The rate of 54.5% of patients on combination therapy who were able to reach a daily GC dose of 5 mg/day or less proved significantly higher than the 18.2% rate seen with GC alone (P = .002).
Adverse events were reported by 54% of those on the combination versus 42% of those on monotherapy, but this difference did not reach statistical significance. The biggest differences in adverse events were the proportions of patients with infections (18.2% vs. 12.1%) and elevated liver enzymes (12.1% vs. 3.0%), both of which were more common in the combination therapy group. Neither of these differences was statistically significant.
Of patients with relapses, the most common organs involved were the salivary gland, the pancreas, and the bile ducts, each accounting for relapse in five patients. Other organs in which relapse occurred included the lacrimal gland and the skin. There were three cases of relapse characterized by retroperitoneal fibrosis.
Over the course of follow-up, new-onset diabetes mellitus occurred in 21.2% and 27.3% of the combination and GC-only groups, respectively. This difference also did not reach statistical significance.
Although this study was small with an open-label design, Dr. Huang said the data strongly suggest that a combination of leflunomide and GC is superior to GC alone. Based on these results, he said a starting dose of 20 mg/day of leflunomide is a reasonable standard in this setting.
Dr. Huang and colleagues reported no potential conflicts of interest.
SOURCE: Wang Y et al. Ann Rheum Dis. Jun 2019;78(Suppl 2):157. Abstract OPO164, doi: 10.1136/annrheumdis-2019-eular.5717
MADRID – The addition of leflunomide to standard glucocorticoids (GCs) in the treatment of IgG4-related disease increases the median duration of response, reduces the proportion of patients with relapse within 12 months, and permits GCs to be tapered, according to results of a randomized trial presented at the European Congress of Rheumatology.
“The rate of adverse events with the addition of leflunomide was numerically higher, but there were no significant differences in risks of any specific adverse event,” reported Feng Huang, MD, of the department of rheumatology at Chinese People’s Liberation Army General Hospital in Beijing.
GCs are highly effective in IgG4-related disease, which is an autoimmune process driven by elevated concentrations of the antibody IgG4 in the tissue of affected organs and in the serum. It has been described in a broad array of sites, including the heart, lung, kidneys, and meninges. It has been widely recognized only in the last 10 years, according to Dr. Huang. Although most patients respond to GCs, he said the problem is that about 50% of patients relapse within 12 months and more than 90% within 3 years.
This randomized, controlled study was conducted after positive results were observed with leflunomide in a small, uncontrolled pilot study published several years ago (Intern Med J. 2017 Jun;47[6]:680-9. doi: 10.1111/imj.13430). In this randomized trial, the objectives were to confirm that leflunomide extends the relapse-free period and has acceptable safety relative to GC alone.
Patients with confirmed IgG4-related disease were enrolled. Patients randomized to GC were started on 0.5 to 0.8 mg/kg per day. A predefined taper regimen was employed in those with symptom control. Those randomized to the experimental arm received GC in the same dose and schedule plus 20 mg/day of leflunomide.
The 33 patients in each group were well matched at baseline for age, comorbidities, and disease severity.
At the end of 12 months, 50% of those treated with GC alone versus 21.2% of those treated with GC plus leflunomide had relapse. That translated into a significantly higher hazard ratio (HR) for relapse in the GC monotherapy group (HR, 1.75; P = .034).
The mean duration of remission was 7 months on the combination versus 3 months on GC alone. Dr. Huang also reported a significantly higher proportion of complete responses in the group receiving the combination.
In addition, “more patients on the combination therapy were able to adhere to the steroid-tapering schedule without relapse,” Dr. Huang reported. The rate of 54.5% of patients on combination therapy who were able to reach a daily GC dose of 5 mg/day or less proved significantly higher than the 18.2% rate seen with GC alone (P = .002).
Adverse events were reported by 54% of those on the combination versus 42% of those on monotherapy, but this difference did not reach statistical significance. The biggest differences in adverse events were the proportions of patients with infections (18.2% vs. 12.1%) and elevated liver enzymes (12.1% vs. 3.0%), both of which were more common in the combination therapy group. Neither of these differences was statistically significant.
Of patients with relapses, the most common organs involved were the salivary gland, the pancreas, and the bile ducts, each accounting for relapse in five patients. Other organs in which relapse occurred included the lacrimal gland and the skin. There were three cases of relapse characterized by retroperitoneal fibrosis.
Over the course of follow-up, new-onset diabetes mellitus occurred in 21.2% and 27.3% of the combination and GC-only groups, respectively. This difference also did not reach statistical significance.
Although this study was small with an open-label design, Dr. Huang said the data strongly suggest that a combination of leflunomide and GC is superior to GC alone. Based on these results, he said a starting dose of 20 mg/day of leflunomide is a reasonable standard in this setting.
Dr. Huang and colleagues reported no potential conflicts of interest.
SOURCE: Wang Y et al. Ann Rheum Dis. Jun 2019;78(Suppl 2):157. Abstract OPO164, doi: 10.1136/annrheumdis-2019-eular.5717
MADRID – The addition of leflunomide to standard glucocorticoids (GCs) in the treatment of IgG4-related disease increases the median duration of response, reduces the proportion of patients with relapse within 12 months, and permits GCs to be tapered, according to results of a randomized trial presented at the European Congress of Rheumatology.
“The rate of adverse events with the addition of leflunomide was numerically higher, but there were no significant differences in risks of any specific adverse event,” reported Feng Huang, MD, of the department of rheumatology at Chinese People’s Liberation Army General Hospital in Beijing.
GCs are highly effective in IgG4-related disease, which is an autoimmune process driven by elevated concentrations of the antibody IgG4 in the tissue of affected organs and in the serum. It has been described in a broad array of sites, including the heart, lung, kidneys, and meninges. It has been widely recognized only in the last 10 years, according to Dr. Huang. Although most patients respond to GCs, he said the problem is that about 50% of patients relapse within 12 months and more than 90% within 3 years.
This randomized, controlled study was conducted after positive results were observed with leflunomide in a small, uncontrolled pilot study published several years ago (Intern Med J. 2017 Jun;47[6]:680-9. doi: 10.1111/imj.13430). In this randomized trial, the objectives were to confirm that leflunomide extends the relapse-free period and has acceptable safety relative to GC alone.
Patients with confirmed IgG4-related disease were enrolled. Patients randomized to GC were started on 0.5 to 0.8 mg/kg per day. A predefined taper regimen was employed in those with symptom control. Those randomized to the experimental arm received GC in the same dose and schedule plus 20 mg/day of leflunomide.
The 33 patients in each group were well matched at baseline for age, comorbidities, and disease severity.
At the end of 12 months, 50% of those treated with GC alone versus 21.2% of those treated with GC plus leflunomide had relapse. That translated into a significantly higher hazard ratio (HR) for relapse in the GC monotherapy group (HR, 1.75; P = .034).
The mean duration of remission was 7 months on the combination versus 3 months on GC alone. Dr. Huang also reported a significantly higher proportion of complete responses in the group receiving the combination.
In addition, “more patients on the combination therapy were able to adhere to the steroid-tapering schedule without relapse,” Dr. Huang reported. The rate of 54.5% of patients on combination therapy who were able to reach a daily GC dose of 5 mg/day or less proved significantly higher than the 18.2% rate seen with GC alone (P = .002).
Adverse events were reported by 54% of those on the combination versus 42% of those on monotherapy, but this difference did not reach statistical significance. The biggest differences in adverse events were the proportions of patients with infections (18.2% vs. 12.1%) and elevated liver enzymes (12.1% vs. 3.0%), both of which were more common in the combination therapy group. Neither of these differences was statistically significant.
Of patients with relapses, the most common organs involved were the salivary gland, the pancreas, and the bile ducts, each accounting for relapse in five patients. Other organs in which relapse occurred included the lacrimal gland and the skin. There were three cases of relapse characterized by retroperitoneal fibrosis.
Over the course of follow-up, new-onset diabetes mellitus occurred in 21.2% and 27.3% of the combination and GC-only groups, respectively. This difference also did not reach statistical significance.
Although this study was small with an open-label design, Dr. Huang said the data strongly suggest that a combination of leflunomide and GC is superior to GC alone. Based on these results, he said a starting dose of 20 mg/day of leflunomide is a reasonable standard in this setting.
Dr. Huang and colleagues reported no potential conflicts of interest.
SOURCE: Wang Y et al. Ann Rheum Dis. Jun 2019;78(Suppl 2):157. Abstract OPO164, doi: 10.1136/annrheumdis-2019-eular.5717
REPORTING FROM EULAR 2019 CONGRESS
Despite advances, imaging of axSpA remains an adjunctive tool
MADRID – Evidence for always using imaging in an adjunctive role to clinical findings in the diagnosis and assessment of axial spondyloarthritis (axSpA) continues to grow, two experts agreed in a scientific session at the European Congress of Rheumatology.
“Imaging has to be understood in the context of other findings. With the patient history, the physical examination, and the laboratory results, the value of imaging improves substantially. Therefore, before an image is ordered it is important to ask how likely is it that a patient has axial spondylitis,” said Floris A. van Gaalen, MD, PhD, of Leiden (Netherlands) University Medical Center.
As one of the experts who participated in the scientific session, Dr. van Gaalen focused specifically on the value of x-ray and MRI in the diagnosis of axSpA, emphasizing their limited value if interpreted without clinical context. He explained that even highly experienced radiologists are fooled, particularly at early stages of disease.
Although the quality of imaging has been increasing steadily, “there is no cookbook approach with which you can guarantee a diagnosis of spondyloarthritis. Imaging can be valuable, but there is a risk of false positives because features on imaging, such as bone marrow edema, are shared with other sources of back pain,” Dr. van Gaalen said.
Considering the importance of context, Dr. van Gaalen advised clinicians against reading the radiology report without evaluating the images themselves. He said the features on imaging make more sense when they are considered at the same time as the patient’s history, symptoms, and laboratory reports.
Order imaging relevant to treatment decisions
Assigned to discuss the value of imaging for assessing progression, Xenofon Baraliakos, MD, a rheumatologist and clinical researcher at Rheumazentrum Ruhrgebiet, Ruhr-University Bochum, Herne, Germany, offered the same message.
“It is important to consider all of the clinical information available, not just the features on imaging,” Dr. Baraliakos said. Often, MRI findings provide corroboration for other objective measures of disease status, but Dr. Baraliakos advised that imaging should be ordered only when it has the potential to alter therapy.
“What we can learn from imaging might be interesting, but the question to ask is whether it is useful,” Dr. Baraliakos said. Rather than incurring the costs of imaging for reassurance, Dr. Baraliakos recommended ordering these studies with specific objectives relevant to treatment decisions.
Neither Dr. van Gaalen nor Dr. Baraliakos denied the value of imaging, particularly MRI, to increase confidence in the diagnosis of axSpA or to guide therapy. Rather, their point was that imaging should not be considered a reliable stand-alone axSpA assessment strategy.
Clinical and imaging findings better then imaging alone
Data from a blinded radiology study presented during the same scientific session reinforced this conclusion. Led by Dr. Baraliakos and presented separately from his discussion about the adjunctive nature of imaging data in axSpA, the study showed that rheumatologists with access to both clinical and imaging data can detect a greater proportion of axSpA than radiologists working from imaging data alone.
In this study, 300 consecutive patients suspected of axSpA were enrolled. All had chronic back pain of more than 3 months’ duration. While highly experienced radiologists were asked to diagnose or rule out a diagnosis of axSpA on the basis of the MRI blinded to other clinical information, experienced rheumatologists evaluated the patients with access to all clinical, laboratory, and imaging data.
A diagnosis of axSpA was reached in 131 patients by the rheumatologists. The remaining 169 were determined not to have axSpA. Although the radiologists agreed on those with or without axSpA in 86.3% of cases, there were 31 cases (28.1%) in which rheumatologists diagnosed axSpA but radiologists did not.
In an analysis of which MRI features were considered critical by radiologists when there was agreement, they identified bone marrow edema in seven cases (7.2%). In 30 cases (30.9%), the radiologists considered the presence of chronic lesions to be critical to their diagnosis. In the remaining 69.9% of cases, radiologists were confident in their diagnosis only when both bone edema and chronic lesions were present.
Not surprisingly, the presence of chronic lesions and more pronounced bone marrow edema permitted both radiologists and rheumatologists to increase their confidence when discriminating between axSpA and non-axSpA patients.
“The combination of structural changes and bone marrow edema as assessed by MRI performed best in the process of diagnosing or ruling out axSpA in this real-life setting at our center,” Dr. Baraliakos said.
However, when only one or two features are considered, trade-offs of lower sensitivity for higher specificity or higher sensitivity for lower specificity occur. For example, although the specificity for a diagnosis of axSpA reached 99.4% when both bone marrow edema and ankylosis are present, the sensitivity of this finding was only 5.3%, according to data provided by Dr. Baraliakos. Conversely, the presence of sclerosis had a sensitivity of 81.7% but a specificity of only 43.2%.
One lesson from this analysis is that there is “increasing insecurity of only including bone marrow edema of the sacroiliac joint as the major criterion for diagnosing axSpA,” Dr. Baraliakos said. However, the larger point in the context of the earlier expert comments is that MRI findings should be considered important but insufficient for the evaluation of axSpA.
SOURCE: Baraliakos X et al. Ann Rheum Dis. Jun 2019;78(Suppl 2):255-6. Abstract OPO344, doi: 10.1136/annrheumdis-2019-eular.5027
MADRID – Evidence for always using imaging in an adjunctive role to clinical findings in the diagnosis and assessment of axial spondyloarthritis (axSpA) continues to grow, two experts agreed in a scientific session at the European Congress of Rheumatology.
“Imaging has to be understood in the context of other findings. With the patient history, the physical examination, and the laboratory results, the value of imaging improves substantially. Therefore, before an image is ordered it is important to ask how likely is it that a patient has axial spondylitis,” said Floris A. van Gaalen, MD, PhD, of Leiden (Netherlands) University Medical Center.
As one of the experts who participated in the scientific session, Dr. van Gaalen focused specifically on the value of x-ray and MRI in the diagnosis of axSpA, emphasizing their limited value if interpreted without clinical context. He explained that even highly experienced radiologists are fooled, particularly at early stages of disease.
Although the quality of imaging has been increasing steadily, “there is no cookbook approach with which you can guarantee a diagnosis of spondyloarthritis. Imaging can be valuable, but there is a risk of false positives because features on imaging, such as bone marrow edema, are shared with other sources of back pain,” Dr. van Gaalen said.
Considering the importance of context, Dr. van Gaalen advised clinicians against reading the radiology report without evaluating the images themselves. He said the features on imaging make more sense when they are considered at the same time as the patient’s history, symptoms, and laboratory reports.
Order imaging relevant to treatment decisions
Assigned to discuss the value of imaging for assessing progression, Xenofon Baraliakos, MD, a rheumatologist and clinical researcher at Rheumazentrum Ruhrgebiet, Ruhr-University Bochum, Herne, Germany, offered the same message.
“It is important to consider all of the clinical information available, not just the features on imaging,” Dr. Baraliakos said. Often, MRI findings provide corroboration for other objective measures of disease status, but Dr. Baraliakos advised that imaging should be ordered only when it has the potential to alter therapy.
“What we can learn from imaging might be interesting, but the question to ask is whether it is useful,” Dr. Baraliakos said. Rather than incurring the costs of imaging for reassurance, Dr. Baraliakos recommended ordering these studies with specific objectives relevant to treatment decisions.
Neither Dr. van Gaalen nor Dr. Baraliakos denied the value of imaging, particularly MRI, to increase confidence in the diagnosis of axSpA or to guide therapy. Rather, their point was that imaging should not be considered a reliable stand-alone axSpA assessment strategy.
Clinical and imaging findings better then imaging alone
Data from a blinded radiology study presented during the same scientific session reinforced this conclusion. Led by Dr. Baraliakos and presented separately from his discussion about the adjunctive nature of imaging data in axSpA, the study showed that rheumatologists with access to both clinical and imaging data can detect a greater proportion of axSpA than radiologists working from imaging data alone.
In this study, 300 consecutive patients suspected of axSpA were enrolled. All had chronic back pain of more than 3 months’ duration. While highly experienced radiologists were asked to diagnose or rule out a diagnosis of axSpA on the basis of the MRI blinded to other clinical information, experienced rheumatologists evaluated the patients with access to all clinical, laboratory, and imaging data.
A diagnosis of axSpA was reached in 131 patients by the rheumatologists. The remaining 169 were determined not to have axSpA. Although the radiologists agreed on those with or without axSpA in 86.3% of cases, there were 31 cases (28.1%) in which rheumatologists diagnosed axSpA but radiologists did not.
In an analysis of which MRI features were considered critical by radiologists when there was agreement, they identified bone marrow edema in seven cases (7.2%). In 30 cases (30.9%), the radiologists considered the presence of chronic lesions to be critical to their diagnosis. In the remaining 69.9% of cases, radiologists were confident in their diagnosis only when both bone edema and chronic lesions were present.
Not surprisingly, the presence of chronic lesions and more pronounced bone marrow edema permitted both radiologists and rheumatologists to increase their confidence when discriminating between axSpA and non-axSpA patients.
“The combination of structural changes and bone marrow edema as assessed by MRI performed best in the process of diagnosing or ruling out axSpA in this real-life setting at our center,” Dr. Baraliakos said.
However, when only one or two features are considered, trade-offs of lower sensitivity for higher specificity or higher sensitivity for lower specificity occur. For example, although the specificity for a diagnosis of axSpA reached 99.4% when both bone marrow edema and ankylosis are present, the sensitivity of this finding was only 5.3%, according to data provided by Dr. Baraliakos. Conversely, the presence of sclerosis had a sensitivity of 81.7% but a specificity of only 43.2%.
One lesson from this analysis is that there is “increasing insecurity of only including bone marrow edema of the sacroiliac joint as the major criterion for diagnosing axSpA,” Dr. Baraliakos said. However, the larger point in the context of the earlier expert comments is that MRI findings should be considered important but insufficient for the evaluation of axSpA.
SOURCE: Baraliakos X et al. Ann Rheum Dis. Jun 2019;78(Suppl 2):255-6. Abstract OPO344, doi: 10.1136/annrheumdis-2019-eular.5027
MADRID – Evidence for always using imaging in an adjunctive role to clinical findings in the diagnosis and assessment of axial spondyloarthritis (axSpA) continues to grow, two experts agreed in a scientific session at the European Congress of Rheumatology.
“Imaging has to be understood in the context of other findings. With the patient history, the physical examination, and the laboratory results, the value of imaging improves substantially. Therefore, before an image is ordered it is important to ask how likely is it that a patient has axial spondylitis,” said Floris A. van Gaalen, MD, PhD, of Leiden (Netherlands) University Medical Center.
As one of the experts who participated in the scientific session, Dr. van Gaalen focused specifically on the value of x-ray and MRI in the diagnosis of axSpA, emphasizing their limited value if interpreted without clinical context. He explained that even highly experienced radiologists are fooled, particularly at early stages of disease.
Although the quality of imaging has been increasing steadily, “there is no cookbook approach with which you can guarantee a diagnosis of spondyloarthritis. Imaging can be valuable, but there is a risk of false positives because features on imaging, such as bone marrow edema, are shared with other sources of back pain,” Dr. van Gaalen said.
Considering the importance of context, Dr. van Gaalen advised clinicians against reading the radiology report without evaluating the images themselves. He said the features on imaging make more sense when they are considered at the same time as the patient’s history, symptoms, and laboratory reports.
Order imaging relevant to treatment decisions
Assigned to discuss the value of imaging for assessing progression, Xenofon Baraliakos, MD, a rheumatologist and clinical researcher at Rheumazentrum Ruhrgebiet, Ruhr-University Bochum, Herne, Germany, offered the same message.
“It is important to consider all of the clinical information available, not just the features on imaging,” Dr. Baraliakos said. Often, MRI findings provide corroboration for other objective measures of disease status, but Dr. Baraliakos advised that imaging should be ordered only when it has the potential to alter therapy.
“What we can learn from imaging might be interesting, but the question to ask is whether it is useful,” Dr. Baraliakos said. Rather than incurring the costs of imaging for reassurance, Dr. Baraliakos recommended ordering these studies with specific objectives relevant to treatment decisions.
Neither Dr. van Gaalen nor Dr. Baraliakos denied the value of imaging, particularly MRI, to increase confidence in the diagnosis of axSpA or to guide therapy. Rather, their point was that imaging should not be considered a reliable stand-alone axSpA assessment strategy.
Clinical and imaging findings better then imaging alone
Data from a blinded radiology study presented during the same scientific session reinforced this conclusion. Led by Dr. Baraliakos and presented separately from his discussion about the adjunctive nature of imaging data in axSpA, the study showed that rheumatologists with access to both clinical and imaging data can detect a greater proportion of axSpA than radiologists working from imaging data alone.
In this study, 300 consecutive patients suspected of axSpA were enrolled. All had chronic back pain of more than 3 months’ duration. While highly experienced radiologists were asked to diagnose or rule out a diagnosis of axSpA on the basis of the MRI blinded to other clinical information, experienced rheumatologists evaluated the patients with access to all clinical, laboratory, and imaging data.
A diagnosis of axSpA was reached in 131 patients by the rheumatologists. The remaining 169 were determined not to have axSpA. Although the radiologists agreed on those with or without axSpA in 86.3% of cases, there were 31 cases (28.1%) in which rheumatologists diagnosed axSpA but radiologists did not.
In an analysis of which MRI features were considered critical by radiologists when there was agreement, they identified bone marrow edema in seven cases (7.2%). In 30 cases (30.9%), the radiologists considered the presence of chronic lesions to be critical to their diagnosis. In the remaining 69.9% of cases, radiologists were confident in their diagnosis only when both bone edema and chronic lesions were present.
Not surprisingly, the presence of chronic lesions and more pronounced bone marrow edema permitted both radiologists and rheumatologists to increase their confidence when discriminating between axSpA and non-axSpA patients.
“The combination of structural changes and bone marrow edema as assessed by MRI performed best in the process of diagnosing or ruling out axSpA in this real-life setting at our center,” Dr. Baraliakos said.
However, when only one or two features are considered, trade-offs of lower sensitivity for higher specificity or higher sensitivity for lower specificity occur. For example, although the specificity for a diagnosis of axSpA reached 99.4% when both bone marrow edema and ankylosis are present, the sensitivity of this finding was only 5.3%, according to data provided by Dr. Baraliakos. Conversely, the presence of sclerosis had a sensitivity of 81.7% but a specificity of only 43.2%.
One lesson from this analysis is that there is “increasing insecurity of only including bone marrow edema of the sacroiliac joint as the major criterion for diagnosing axSpA,” Dr. Baraliakos said. However, the larger point in the context of the earlier expert comments is that MRI findings should be considered important but insufficient for the evaluation of axSpA.
SOURCE: Baraliakos X et al. Ann Rheum Dis. Jun 2019;78(Suppl 2):255-6. Abstract OPO344, doi: 10.1136/annrheumdis-2019-eular.5027
REPORTING FROM EULAR 2019 CONGRESS
Refractory RA responds to vagus nerve stimulation
MADRID –
A minimal clinically important difference in the 28-joint Disease Activity Score using C-reactive protein (DAS28-CRP) and the Clinical Disease Activity Index (CDAI) at 12 weeks was achieved or exceeded by 5 out of 10 patients; with 2 patients achieving DAS28-CRP–defined remission.
The disease activity scores also were paired with MRI scans and showed, in a handful of individuals, that there was improvement in erosions in those with a clinical response. Greater reductions in proinflammatory cytokines – interleukin (IL)-1-beta, IL-6, IL-17, IL-23, and tumor necrosis factor – were seen with neurostimulation, compared with a sham control group.
“The goal here was to use electrical stimulation to modify or modulate, and improve the treatment of active rheumatoid arthritis,” Mark C. Genovese, MD, said in an interview at the European Congress of Rheumatology.
“The reason for choosing refractory patients is, one, there’s a clear unmet need, but two, because this was a first-in-human study using a novel microregulatory device stimulating the vagus nerve, we thought the benefits-to-risk ratio was most appropriate for its first trial in patients with refractory disease,” explained Dr. Genovese, professor of medicine and director of the rheumatology clinic in the division of immunology and rheumatology at Stanford (Calif.) University.
He added: “Over time, if the device proves successful for modulating disease, one can see it potentially being used earlier in the disease. Whether it is developed as a stand-alone or used as an adjunct on additional therapy will have to be determined based on both its efficacy and its safety.”
Neurostimulation is a novel concept in rheumatology but has been used with success in other areas of medicine – including epilepsy and depression – using electrical pulses instead of drugs. The idea behind it is that it stimulates the inflammatory reflex that modulates multiple the inflammatory pathways. Essentially, it’s thought that electrically stimulating the vagus nerve sends signals to the spleen where T-lymphocytes then signal to other immune cells, such as macrophages and monocytes, to temper their production of proinflammatory cytokines and other mediators.
“Unlike traditional immunosuppressive biologics that may be specifically targeting one inflammatory process, by suppressing the inflammatory reflex we believe we can suppress a variety of inflammatory cytokines in the region of between 30% and 70%,” Dr. Genovese said at a press briefing.
Data from a 12-week, open-label study (Proc Natl Acad Sci U S A. 2016;113:8284-9) have already shown that the approach works in patients with refractory RA (n = 17). Once-daily electrical vagus nerve stimulation using an existing device made for treating epilepsy showed that clinically meaningful changes in DAS28-CRP could be achieved through TNF suppression. The effects on systemic TNF release lasted for around 24-48 hours after stimulation.
For the current study, a much smaller, leadless, investigational neurostimulation device was used. Called a MicroRegulator (SetPoint Medical), it is about 1 inch long, less than 2 cc in total volume, and is surgically implanted by a neurosurgeon at the top of the vagus nerve. When activated through an iPad app by the health care professional, it sends electrical impulses down the vagus nerve. The device’s battery is charged externally and wirelessly a few minutes each week. Dr. Genovese noted that the device needs to be turned on for only 60 seconds at a time to have an effect and that patients may feel a vibration but this was not reported in the study as an adverse event.
Results of the first in-human study with the device were presented by Dr. Genovese during the late-breaking clinical trials session at the meeting. He described how a total of 14 patients had the device implanted, the first 3 of whom received once-daily, open-label neurostimulation. The remaining 11 patients were randomized to either once-daily or four-times-daily neurostimulation via the device, or to receive sham therapy in which the device was implanted but not switched on. The patients had moderate to severe RA, defined as four or more tender joints, four or more swollen joints, and a CDAI score greater than 10, plus they had radiologically active disease and an insufficient response to at least two biologic or targeted synthetic disease-modifying antirheumatic drugs with differing mechanisms of action.
All patients went through the same schedule of device charging and they did not know if they were in the active or sham groups. At the end of the study, patients had the option to continue in a long-term safety extension phase, have the device switched off, or could have it surgically removed.
“This trial was specifically a pilot trial to assess the MicroRegulator from a safety standpoint,” Dr. Genovese noted, but it also was designed to “help understand whether or not there was going to be clinical efficacy and applicability.”
While “there were no device or treatment-related serious adverse events,” there were some “surgical complications associated with the initial procedure.” One patient experienced paralysis of the left vocal cord during implantation that later resolved, and others experienced the following: Horner’s syndrome, tenderness and swelling at the surgical site, acute postoperative pain, and rash and pruritus. That said, there were no withdrawals from the study due to adverse events.
Commenting in a press release issued by the European League Against Rheumatism, Thomas Dörner, MD, of Charité Universitätsmedizin Berlin, said, “This is a really exciting development. For many patients suffering from rheumatoid arthritis, current treatments don’t work, or aren’t tolerated. These results open the door to a novel approach to treating not only rheumatoid arthritis, but other chronic inflammatory diseases. This is certainly an area for further study.”
The study was sponsored by SetPoint Medical. Dr. Genovese disclosed receiving consulting fees from and having contracts with/grants with the company and acting as a consultant to Galvani and Vorso. He has also received research support from and served as a consultant to Sanofi/Genzyme, Genentech/Roche, and R-Pharm. Dr. Dörner was not involved in the study and commented as part of his role as the chairperson of the EULAR Scientific Program Committee.
SOURCE: Genovese M et al. Ann Rheum Dis. Jun 2019; 78(Suppl 2):264. Abstract LB0009, doi: 10.1136/annrheumdis-2019-eular.8716
MADRID –
A minimal clinically important difference in the 28-joint Disease Activity Score using C-reactive protein (DAS28-CRP) and the Clinical Disease Activity Index (CDAI) at 12 weeks was achieved or exceeded by 5 out of 10 patients; with 2 patients achieving DAS28-CRP–defined remission.
The disease activity scores also were paired with MRI scans and showed, in a handful of individuals, that there was improvement in erosions in those with a clinical response. Greater reductions in proinflammatory cytokines – interleukin (IL)-1-beta, IL-6, IL-17, IL-23, and tumor necrosis factor – were seen with neurostimulation, compared with a sham control group.
“The goal here was to use electrical stimulation to modify or modulate, and improve the treatment of active rheumatoid arthritis,” Mark C. Genovese, MD, said in an interview at the European Congress of Rheumatology.
“The reason for choosing refractory patients is, one, there’s a clear unmet need, but two, because this was a first-in-human study using a novel microregulatory device stimulating the vagus nerve, we thought the benefits-to-risk ratio was most appropriate for its first trial in patients with refractory disease,” explained Dr. Genovese, professor of medicine and director of the rheumatology clinic in the division of immunology and rheumatology at Stanford (Calif.) University.
He added: “Over time, if the device proves successful for modulating disease, one can see it potentially being used earlier in the disease. Whether it is developed as a stand-alone or used as an adjunct on additional therapy will have to be determined based on both its efficacy and its safety.”
Neurostimulation is a novel concept in rheumatology but has been used with success in other areas of medicine – including epilepsy and depression – using electrical pulses instead of drugs. The idea behind it is that it stimulates the inflammatory reflex that modulates multiple the inflammatory pathways. Essentially, it’s thought that electrically stimulating the vagus nerve sends signals to the spleen where T-lymphocytes then signal to other immune cells, such as macrophages and monocytes, to temper their production of proinflammatory cytokines and other mediators.
“Unlike traditional immunosuppressive biologics that may be specifically targeting one inflammatory process, by suppressing the inflammatory reflex we believe we can suppress a variety of inflammatory cytokines in the region of between 30% and 70%,” Dr. Genovese said at a press briefing.
Data from a 12-week, open-label study (Proc Natl Acad Sci U S A. 2016;113:8284-9) have already shown that the approach works in patients with refractory RA (n = 17). Once-daily electrical vagus nerve stimulation using an existing device made for treating epilepsy showed that clinically meaningful changes in DAS28-CRP could be achieved through TNF suppression. The effects on systemic TNF release lasted for around 24-48 hours after stimulation.
For the current study, a much smaller, leadless, investigational neurostimulation device was used. Called a MicroRegulator (SetPoint Medical), it is about 1 inch long, less than 2 cc in total volume, and is surgically implanted by a neurosurgeon at the top of the vagus nerve. When activated through an iPad app by the health care professional, it sends electrical impulses down the vagus nerve. The device’s battery is charged externally and wirelessly a few minutes each week. Dr. Genovese noted that the device needs to be turned on for only 60 seconds at a time to have an effect and that patients may feel a vibration but this was not reported in the study as an adverse event.
Results of the first in-human study with the device were presented by Dr. Genovese during the late-breaking clinical trials session at the meeting. He described how a total of 14 patients had the device implanted, the first 3 of whom received once-daily, open-label neurostimulation. The remaining 11 patients were randomized to either once-daily or four-times-daily neurostimulation via the device, or to receive sham therapy in which the device was implanted but not switched on. The patients had moderate to severe RA, defined as four or more tender joints, four or more swollen joints, and a CDAI score greater than 10, plus they had radiologically active disease and an insufficient response to at least two biologic or targeted synthetic disease-modifying antirheumatic drugs with differing mechanisms of action.
All patients went through the same schedule of device charging and they did not know if they were in the active or sham groups. At the end of the study, patients had the option to continue in a long-term safety extension phase, have the device switched off, or could have it surgically removed.
“This trial was specifically a pilot trial to assess the MicroRegulator from a safety standpoint,” Dr. Genovese noted, but it also was designed to “help understand whether or not there was going to be clinical efficacy and applicability.”
While “there were no device or treatment-related serious adverse events,” there were some “surgical complications associated with the initial procedure.” One patient experienced paralysis of the left vocal cord during implantation that later resolved, and others experienced the following: Horner’s syndrome, tenderness and swelling at the surgical site, acute postoperative pain, and rash and pruritus. That said, there were no withdrawals from the study due to adverse events.
Commenting in a press release issued by the European League Against Rheumatism, Thomas Dörner, MD, of Charité Universitätsmedizin Berlin, said, “This is a really exciting development. For many patients suffering from rheumatoid arthritis, current treatments don’t work, or aren’t tolerated. These results open the door to a novel approach to treating not only rheumatoid arthritis, but other chronic inflammatory diseases. This is certainly an area for further study.”
The study was sponsored by SetPoint Medical. Dr. Genovese disclosed receiving consulting fees from and having contracts with/grants with the company and acting as a consultant to Galvani and Vorso. He has also received research support from and served as a consultant to Sanofi/Genzyme, Genentech/Roche, and R-Pharm. Dr. Dörner was not involved in the study and commented as part of his role as the chairperson of the EULAR Scientific Program Committee.
SOURCE: Genovese M et al. Ann Rheum Dis. Jun 2019; 78(Suppl 2):264. Abstract LB0009, doi: 10.1136/annrheumdis-2019-eular.8716
MADRID –
A minimal clinically important difference in the 28-joint Disease Activity Score using C-reactive protein (DAS28-CRP) and the Clinical Disease Activity Index (CDAI) at 12 weeks was achieved or exceeded by 5 out of 10 patients; with 2 patients achieving DAS28-CRP–defined remission.
The disease activity scores also were paired with MRI scans and showed, in a handful of individuals, that there was improvement in erosions in those with a clinical response. Greater reductions in proinflammatory cytokines – interleukin (IL)-1-beta, IL-6, IL-17, IL-23, and tumor necrosis factor – were seen with neurostimulation, compared with a sham control group.
“The goal here was to use electrical stimulation to modify or modulate, and improve the treatment of active rheumatoid arthritis,” Mark C. Genovese, MD, said in an interview at the European Congress of Rheumatology.
“The reason for choosing refractory patients is, one, there’s a clear unmet need, but two, because this was a first-in-human study using a novel microregulatory device stimulating the vagus nerve, we thought the benefits-to-risk ratio was most appropriate for its first trial in patients with refractory disease,” explained Dr. Genovese, professor of medicine and director of the rheumatology clinic in the division of immunology and rheumatology at Stanford (Calif.) University.
He added: “Over time, if the device proves successful for modulating disease, one can see it potentially being used earlier in the disease. Whether it is developed as a stand-alone or used as an adjunct on additional therapy will have to be determined based on both its efficacy and its safety.”
Neurostimulation is a novel concept in rheumatology but has been used with success in other areas of medicine – including epilepsy and depression – using electrical pulses instead of drugs. The idea behind it is that it stimulates the inflammatory reflex that modulates multiple the inflammatory pathways. Essentially, it’s thought that electrically stimulating the vagus nerve sends signals to the spleen where T-lymphocytes then signal to other immune cells, such as macrophages and monocytes, to temper their production of proinflammatory cytokines and other mediators.
“Unlike traditional immunosuppressive biologics that may be specifically targeting one inflammatory process, by suppressing the inflammatory reflex we believe we can suppress a variety of inflammatory cytokines in the region of between 30% and 70%,” Dr. Genovese said at a press briefing.
Data from a 12-week, open-label study (Proc Natl Acad Sci U S A. 2016;113:8284-9) have already shown that the approach works in patients with refractory RA (n = 17). Once-daily electrical vagus nerve stimulation using an existing device made for treating epilepsy showed that clinically meaningful changes in DAS28-CRP could be achieved through TNF suppression. The effects on systemic TNF release lasted for around 24-48 hours after stimulation.
For the current study, a much smaller, leadless, investigational neurostimulation device was used. Called a MicroRegulator (SetPoint Medical), it is about 1 inch long, less than 2 cc in total volume, and is surgically implanted by a neurosurgeon at the top of the vagus nerve. When activated through an iPad app by the health care professional, it sends electrical impulses down the vagus nerve. The device’s battery is charged externally and wirelessly a few minutes each week. Dr. Genovese noted that the device needs to be turned on for only 60 seconds at a time to have an effect and that patients may feel a vibration but this was not reported in the study as an adverse event.
Results of the first in-human study with the device were presented by Dr. Genovese during the late-breaking clinical trials session at the meeting. He described how a total of 14 patients had the device implanted, the first 3 of whom received once-daily, open-label neurostimulation. The remaining 11 patients were randomized to either once-daily or four-times-daily neurostimulation via the device, or to receive sham therapy in which the device was implanted but not switched on. The patients had moderate to severe RA, defined as four or more tender joints, four or more swollen joints, and a CDAI score greater than 10, plus they had radiologically active disease and an insufficient response to at least two biologic or targeted synthetic disease-modifying antirheumatic drugs with differing mechanisms of action.
All patients went through the same schedule of device charging and they did not know if they were in the active or sham groups. At the end of the study, patients had the option to continue in a long-term safety extension phase, have the device switched off, or could have it surgically removed.
“This trial was specifically a pilot trial to assess the MicroRegulator from a safety standpoint,” Dr. Genovese noted, but it also was designed to “help understand whether or not there was going to be clinical efficacy and applicability.”
While “there were no device or treatment-related serious adverse events,” there were some “surgical complications associated with the initial procedure.” One patient experienced paralysis of the left vocal cord during implantation that later resolved, and others experienced the following: Horner’s syndrome, tenderness and swelling at the surgical site, acute postoperative pain, and rash and pruritus. That said, there were no withdrawals from the study due to adverse events.
Commenting in a press release issued by the European League Against Rheumatism, Thomas Dörner, MD, of Charité Universitätsmedizin Berlin, said, “This is a really exciting development. For many patients suffering from rheumatoid arthritis, current treatments don’t work, or aren’t tolerated. These results open the door to a novel approach to treating not only rheumatoid arthritis, but other chronic inflammatory diseases. This is certainly an area for further study.”
The study was sponsored by SetPoint Medical. Dr. Genovese disclosed receiving consulting fees from and having contracts with/grants with the company and acting as a consultant to Galvani and Vorso. He has also received research support from and served as a consultant to Sanofi/Genzyme, Genentech/Roche, and R-Pharm. Dr. Dörner was not involved in the study and commented as part of his role as the chairperson of the EULAR Scientific Program Committee.
SOURCE: Genovese M et al. Ann Rheum Dis. Jun 2019; 78(Suppl 2):264. Abstract LB0009, doi: 10.1136/annrheumdis-2019-eular.8716
REPORTING FROM EULAR 2019 CONGRESS
EULAR revises its RA management recommendations
MADRID – No change to designating methotrexate the first disease-modifying drug to prescribe, before any biologic drug, and no adoption of imaging criteria to determine whether a patient is in remission.
“Imaging with ultrasound or MRI is out” as a remission criterion. “It’s high risk and a waste of resources,” declared Josef S. Smolen, MD, head of the EULAR writing panel, in the most forceful declaration he made while presenting the pending recommendation revision at the European Congress of Rheumatology.
Dr. Smolen’s strong warning against an imaging parameter when treating RA patients toward a remission target was no surprise, as he had already voiced this opinion in an editorial he coauthored earlier this year (JAMA. 2019 Feb 5;321[5]:457-8). The editorial cited data from three independent studies that compared an RA treatment strategy that used an imaging measure of joint inflammation as a treatment target along with clinical assessment against clinical assessment alone. All three studies found no benefit from ultrasound or MRI for defining a treatment goal, and two of the studies showed evidence for harm. “Using imaging to guide therapy led to prescription of potentially harmful medicines without differences in the primary outcomes, but at high costs and potential burden of unnecessary treatment changes and risks for patients,” noted Dr. Smolen and his coauthor in the editorial.
The report that this editorial addressed (JAMA. 2019 Feb 5;321[5]:461-72) also provided some of the most recent evidence for the second omission from the new revision that Dr. Smolen called out: No change to the recommendation to use methotrexate as initial treatment for any RA patient. “We continue to say that methotrexate is the first treatment strategy. There is no new evidence that any biological treatment is better than methotrexate, so there is no change,” said Dr. Smolen, professor of medicine at the Medical University of Vienna, who also led the EULAR writing panel for the immediately preceding set of RA treatment recommendations first unveiled 3 years before (Ann Rheum Dis. 2017 Jun;76[6]:960-77).
Perhaps the most notable changes to the recommendations are the way they handle targeted-synthetic disease-modifying antirheumatic drugs (tsDMARDs), a class that currently is synonymous with the Janus kinase (JAK) inhibitors. “Because of new evidence we have lifted up the tsDMARDs” so that no preference is given to biologic DMARDs over the ts class as happened in the 2016 version, Dr. Smolen said. Another revision to this recommendation was to change the addition of either a biologic or tsDMARD to a patient not fully responsive to a conventional-synthetic (cs) DMARD and with poor prognostic factors from a “should be considered” to a “should be added” recommendation.
Another way in which the pending revision uplifted tsDMARDs was in the wording for the recommendation that deals with patients who do not respond to a first tumor necrosis factor (TNF) inhibitor plus methotrexate or another csDMARD, and now lists as the first option switching to a biologic or tsDMARD with a different mode of action followed by a different TNF inhibitor, a reversal of order from before when a different TNF inhibitor got first mention. This order change was a modest revision that reflected observational evidence that was modestly persuasive that switching to an agent with a different mechanism of action is often the most effective approach, Dr. Smolen said.
The new recommendations also reaffirmed the eleventh recommendation from the 2016 version, which called for tapering of the biologic or tsDMARD from a patient in remission while retaining the csDMARD, usually methotrexate. Dr. Smolen cited new evidence in favor of this approach (Ann Rheum Dis. 2019 Jun;78[6]:746-53), which allowed the writing panel to upgrade the evidence supporting this recommendation to the A level. The concept of tapering down the biologic or tsDMARD for a patient in sustained remission while maintaining the csDMARD was “fully confirmed” in a recent report, he added. The writing panel also upticked its rating of the evidence in favor of cautiously tapering the csDMARD in patients who maintain remission on just a csDMARD.
One final element in the pending revision called out a newly identified safety signal, an increased risk for venous thromboembolism among patients on certain high dosages of JAK inhibitors, especially in patients with increased risk for venous thromboembolism. This new safety concern adds to the already-described increased risk for herpes zoster from JAK inhibitors, especially in Japanese and Korean populations, Dr. Smolen said. In general, more long-term safety data for JAK inhibitors are needed.
The draft update also added one new overarching principle: “Patients require access to multiple drugs with different modes of action to address the heterogeneity of RA, and patients may require multiple, successive treatments throughout life.” Overall, pending changes to the RA recommendations were limited because “the EULAR recommendations have achieved a steady state of the art” for defining whom to treat, treatment targets, and appropriate treatment strategies, Dr. Smolen said.
Dr. Smolen had been a consultant to or a speaker on behalf of several drug companies.
MADRID – No change to designating methotrexate the first disease-modifying drug to prescribe, before any biologic drug, and no adoption of imaging criteria to determine whether a patient is in remission.
“Imaging with ultrasound or MRI is out” as a remission criterion. “It’s high risk and a waste of resources,” declared Josef S. Smolen, MD, head of the EULAR writing panel, in the most forceful declaration he made while presenting the pending recommendation revision at the European Congress of Rheumatology.
Dr. Smolen’s strong warning against an imaging parameter when treating RA patients toward a remission target was no surprise, as he had already voiced this opinion in an editorial he coauthored earlier this year (JAMA. 2019 Feb 5;321[5]:457-8). The editorial cited data from three independent studies that compared an RA treatment strategy that used an imaging measure of joint inflammation as a treatment target along with clinical assessment against clinical assessment alone. All three studies found no benefit from ultrasound or MRI for defining a treatment goal, and two of the studies showed evidence for harm. “Using imaging to guide therapy led to prescription of potentially harmful medicines without differences in the primary outcomes, but at high costs and potential burden of unnecessary treatment changes and risks for patients,” noted Dr. Smolen and his coauthor in the editorial.
The report that this editorial addressed (JAMA. 2019 Feb 5;321[5]:461-72) also provided some of the most recent evidence for the second omission from the new revision that Dr. Smolen called out: No change to the recommendation to use methotrexate as initial treatment for any RA patient. “We continue to say that methotrexate is the first treatment strategy. There is no new evidence that any biological treatment is better than methotrexate, so there is no change,” said Dr. Smolen, professor of medicine at the Medical University of Vienna, who also led the EULAR writing panel for the immediately preceding set of RA treatment recommendations first unveiled 3 years before (Ann Rheum Dis. 2017 Jun;76[6]:960-77).
Perhaps the most notable changes to the recommendations are the way they handle targeted-synthetic disease-modifying antirheumatic drugs (tsDMARDs), a class that currently is synonymous with the Janus kinase (JAK) inhibitors. “Because of new evidence we have lifted up the tsDMARDs” so that no preference is given to biologic DMARDs over the ts class as happened in the 2016 version, Dr. Smolen said. Another revision to this recommendation was to change the addition of either a biologic or tsDMARD to a patient not fully responsive to a conventional-synthetic (cs) DMARD and with poor prognostic factors from a “should be considered” to a “should be added” recommendation.
Another way in which the pending revision uplifted tsDMARDs was in the wording for the recommendation that deals with patients who do not respond to a first tumor necrosis factor (TNF) inhibitor plus methotrexate or another csDMARD, and now lists as the first option switching to a biologic or tsDMARD with a different mode of action followed by a different TNF inhibitor, a reversal of order from before when a different TNF inhibitor got first mention. This order change was a modest revision that reflected observational evidence that was modestly persuasive that switching to an agent with a different mechanism of action is often the most effective approach, Dr. Smolen said.
The new recommendations also reaffirmed the eleventh recommendation from the 2016 version, which called for tapering of the biologic or tsDMARD from a patient in remission while retaining the csDMARD, usually methotrexate. Dr. Smolen cited new evidence in favor of this approach (Ann Rheum Dis. 2019 Jun;78[6]:746-53), which allowed the writing panel to upgrade the evidence supporting this recommendation to the A level. The concept of tapering down the biologic or tsDMARD for a patient in sustained remission while maintaining the csDMARD was “fully confirmed” in a recent report, he added. The writing panel also upticked its rating of the evidence in favor of cautiously tapering the csDMARD in patients who maintain remission on just a csDMARD.
One final element in the pending revision called out a newly identified safety signal, an increased risk for venous thromboembolism among patients on certain high dosages of JAK inhibitors, especially in patients with increased risk for venous thromboembolism. This new safety concern adds to the already-described increased risk for herpes zoster from JAK inhibitors, especially in Japanese and Korean populations, Dr. Smolen said. In general, more long-term safety data for JAK inhibitors are needed.
The draft update also added one new overarching principle: “Patients require access to multiple drugs with different modes of action to address the heterogeneity of RA, and patients may require multiple, successive treatments throughout life.” Overall, pending changes to the RA recommendations were limited because “the EULAR recommendations have achieved a steady state of the art” for defining whom to treat, treatment targets, and appropriate treatment strategies, Dr. Smolen said.
Dr. Smolen had been a consultant to or a speaker on behalf of several drug companies.
MADRID – No change to designating methotrexate the first disease-modifying drug to prescribe, before any biologic drug, and no adoption of imaging criteria to determine whether a patient is in remission.
“Imaging with ultrasound or MRI is out” as a remission criterion. “It’s high risk and a waste of resources,” declared Josef S. Smolen, MD, head of the EULAR writing panel, in the most forceful declaration he made while presenting the pending recommendation revision at the European Congress of Rheumatology.
Dr. Smolen’s strong warning against an imaging parameter when treating RA patients toward a remission target was no surprise, as he had already voiced this opinion in an editorial he coauthored earlier this year (JAMA. 2019 Feb 5;321[5]:457-8). The editorial cited data from three independent studies that compared an RA treatment strategy that used an imaging measure of joint inflammation as a treatment target along with clinical assessment against clinical assessment alone. All three studies found no benefit from ultrasound or MRI for defining a treatment goal, and two of the studies showed evidence for harm. “Using imaging to guide therapy led to prescription of potentially harmful medicines without differences in the primary outcomes, but at high costs and potential burden of unnecessary treatment changes and risks for patients,” noted Dr. Smolen and his coauthor in the editorial.
The report that this editorial addressed (JAMA. 2019 Feb 5;321[5]:461-72) also provided some of the most recent evidence for the second omission from the new revision that Dr. Smolen called out: No change to the recommendation to use methotrexate as initial treatment for any RA patient. “We continue to say that methotrexate is the first treatment strategy. There is no new evidence that any biological treatment is better than methotrexate, so there is no change,” said Dr. Smolen, professor of medicine at the Medical University of Vienna, who also led the EULAR writing panel for the immediately preceding set of RA treatment recommendations first unveiled 3 years before (Ann Rheum Dis. 2017 Jun;76[6]:960-77).
Perhaps the most notable changes to the recommendations are the way they handle targeted-synthetic disease-modifying antirheumatic drugs (tsDMARDs), a class that currently is synonymous with the Janus kinase (JAK) inhibitors. “Because of new evidence we have lifted up the tsDMARDs” so that no preference is given to biologic DMARDs over the ts class as happened in the 2016 version, Dr. Smolen said. Another revision to this recommendation was to change the addition of either a biologic or tsDMARD to a patient not fully responsive to a conventional-synthetic (cs) DMARD and with poor prognostic factors from a “should be considered” to a “should be added” recommendation.
Another way in which the pending revision uplifted tsDMARDs was in the wording for the recommendation that deals with patients who do not respond to a first tumor necrosis factor (TNF) inhibitor plus methotrexate or another csDMARD, and now lists as the first option switching to a biologic or tsDMARD with a different mode of action followed by a different TNF inhibitor, a reversal of order from before when a different TNF inhibitor got first mention. This order change was a modest revision that reflected observational evidence that was modestly persuasive that switching to an agent with a different mechanism of action is often the most effective approach, Dr. Smolen said.
The new recommendations also reaffirmed the eleventh recommendation from the 2016 version, which called for tapering of the biologic or tsDMARD from a patient in remission while retaining the csDMARD, usually methotrexate. Dr. Smolen cited new evidence in favor of this approach (Ann Rheum Dis. 2019 Jun;78[6]:746-53), which allowed the writing panel to upgrade the evidence supporting this recommendation to the A level. The concept of tapering down the biologic or tsDMARD for a patient in sustained remission while maintaining the csDMARD was “fully confirmed” in a recent report, he added. The writing panel also upticked its rating of the evidence in favor of cautiously tapering the csDMARD in patients who maintain remission on just a csDMARD.
One final element in the pending revision called out a newly identified safety signal, an increased risk for venous thromboembolism among patients on certain high dosages of JAK inhibitors, especially in patients with increased risk for venous thromboembolism. This new safety concern adds to the already-described increased risk for herpes zoster from JAK inhibitors, especially in Japanese and Korean populations, Dr. Smolen said. In general, more long-term safety data for JAK inhibitors are needed.
The draft update also added one new overarching principle: “Patients require access to multiple drugs with different modes of action to address the heterogeneity of RA, and patients may require multiple, successive treatments throughout life.” Overall, pending changes to the RA recommendations were limited because “the EULAR recommendations have achieved a steady state of the art” for defining whom to treat, treatment targets, and appropriate treatment strategies, Dr. Smolen said.
Dr. Smolen had been a consultant to or a speaker on behalf of several drug companies.
EXPERT ANALYSIS FROM EULAR 2019 CONGRESS