User login
FDA proposes new breast implant labeling with a boxed warning
Breast implants sold in the United States may soon require a boxed warning in their label, along with other label changes proposed by the Food and Drug Administration aimed at better informing prospective patients and clinicians of the potential risks from breast implants.
Other elements of the proposed labeling changes include creation of a patient-decision checklist, new recommendations for follow-up imaging to monitor for implant rupture, inclusion of detailed and understandable information about materials in the device, and provision of a device card to each patient with details on the specific implant they received.
These labeling changes all stemmed from a breast implant hearing held by the agency’s General and Plastic Surgery Devices Panel in March 2019, according to the draft guidance document officially released by the FDA on Oct. 24.
The proposed labeling changes were generally welcomed by patient advocates and by clinicians as a reasonable response to the concerns discussed at the March hearing. In an earlier move to address issues brought up at the hearing, the FDA in July arranged for a recall for certain Allergan models of textured breast implants because of their link with the development of breast implant–associated anaplastic large cell lymphoma (BIA-ALCL).
The boxed warning proposed by the FDA would highlight four specific facts that patients, physicians, and surgeons should know about breast implants: They are not considered lifetime devices, the chance of developing complications from implants increases over time, some complications require additional surgery, and placement of breast implants has been associated with development of BIA-ALCL and may also be associated with certain systemic symptoms.
The FDA also proposed four other notable labeling changes:
- Creation of a patient-decision checklist to better systematize the informed consent process and make sure that certain aspects of breast implant placement are clearly brought to patients’ attention. The FDA proposed that patients sign their checklist attesting to having read and understood the information and that patients receive a take-home copy for their future reference. Proposed elements of the checklist include situations to not use breast implants; considerations for successful implant recipients; the risks of breast implant surgery; the importance of appropriate physician education, training, and experience; the risk for developing BIA-ALCL or systemic symptoms; and discussion of options other than breast implants.
- A new scheme for systematically and serially using imaging to screen for implant rupture that designates for the first time that ultrasound is an acceptable alternative to MRI and relies on a schedule by which either method initially screens the implant 5-6 years post operatively and then every 2 years thereafter.
- Detailed and understandable information about each material component of the implant with further information on possible adverse health effects of these compounds.
- A device card that patients should receive after their surgery with the implant’s name, serial number, and other identifiers; the boxed warning information; and a web link for accessing more up-to-date information.
The patient group Breast Implant Victim Advocacy praised the draft guidance. “The March Advisory Committee meeting seems to have prompted a shift by the FDA, surgeons, and industry,” said Jamee Cook, cofounder of the group. “We are definitely seeing a change in patient engagement. The FDA has been cooperating with patients and listening to our concerns. We still have a long way to go in raising public awareness of breast implant issues, but progress over the past 1-2 years has been amazing.”
Diana Zuckerman, PhD, president of the National Center for Health Research in Washington, gave the draft guidance a mixed review. “The FDA’s draft includes the types of information that we had proposed to the FDA in recent months in our work with patient advocates and plastic surgeons,” she said. “However, it is not as informative as it should be in describing well-designed studies indicating a risk of systemic illnesses. Patients deserve to make better-informed decisions in the future than most women considering breast implants have been able to make” in the past.
Patricia McGuire, MD, a St. Louis plastic surgeon who specializes in breast surgery and has studied breast implant illness, declared the guidance to be “reasonable.”
“I think the changes address the concerns expressed by patients during the [March] hearing; I agree with everything the FDA proposed in the guidance document,” Dr. McGuire said. “The boxed warning is reasonable and needs to be part of the informed consent process. I also agree with the changes in screening implants postoperatively. Most patients do not get MRI examinations. High-resolution ultrasound is more convenient and cost effective.”
The boxed warning was rated as “reasonably strong” and “the most serious step the FDA can take short of taking a device off the market,” but in the case of breast implants, a wider recall of textured implants than what the FDA arranged last July would be even more appropriate, commented Sidney M. Wolfe, MD, founder and senior adviser to Public Citizen. He also faulted the agency for not taking quicker action in mandating inclusion of the proposed boxed warning.
Issuing the labeling changes as draft guidance “is a ministep forward,” but also a process that “guarantees delay” and “creeps along at a dangerously slow pace,” Dr. Wolfe said. “The FDA is delaying what should be inevitable. The agency could put the boxed warning in place right now if they had the guts to do it.”
Dr. McGuire has been a consultant to Allergan, Establishment Labs, and Hans Biomed. Ms. Cook, Dr. Zuckerman, and Dr. Wolfe reported having no commercial disclosures.
Breast implants sold in the United States may soon require a boxed warning in their label, along with other label changes proposed by the Food and Drug Administration aimed at better informing prospective patients and clinicians of the potential risks from breast implants.
Other elements of the proposed labeling changes include creation of a patient-decision checklist, new recommendations for follow-up imaging to monitor for implant rupture, inclusion of detailed and understandable information about materials in the device, and provision of a device card to each patient with details on the specific implant they received.
These labeling changes all stemmed from a breast implant hearing held by the agency’s General and Plastic Surgery Devices Panel in March 2019, according to the draft guidance document officially released by the FDA on Oct. 24.
The proposed labeling changes were generally welcomed by patient advocates and by clinicians as a reasonable response to the concerns discussed at the March hearing. In an earlier move to address issues brought up at the hearing, the FDA in July arranged for a recall for certain Allergan models of textured breast implants because of their link with the development of breast implant–associated anaplastic large cell lymphoma (BIA-ALCL).
The boxed warning proposed by the FDA would highlight four specific facts that patients, physicians, and surgeons should know about breast implants: They are not considered lifetime devices, the chance of developing complications from implants increases over time, some complications require additional surgery, and placement of breast implants has been associated with development of BIA-ALCL and may also be associated with certain systemic symptoms.
The FDA also proposed four other notable labeling changes:
- Creation of a patient-decision checklist to better systematize the informed consent process and make sure that certain aspects of breast implant placement are clearly brought to patients’ attention. The FDA proposed that patients sign their checklist attesting to having read and understood the information and that patients receive a take-home copy for their future reference. Proposed elements of the checklist include situations to not use breast implants; considerations for successful implant recipients; the risks of breast implant surgery; the importance of appropriate physician education, training, and experience; the risk for developing BIA-ALCL or systemic symptoms; and discussion of options other than breast implants.
- A new scheme for systematically and serially using imaging to screen for implant rupture that designates for the first time that ultrasound is an acceptable alternative to MRI and relies on a schedule by which either method initially screens the implant 5-6 years post operatively and then every 2 years thereafter.
- Detailed and understandable information about each material component of the implant with further information on possible adverse health effects of these compounds.
- A device card that patients should receive after their surgery with the implant’s name, serial number, and other identifiers; the boxed warning information; and a web link for accessing more up-to-date information.
The patient group Breast Implant Victim Advocacy praised the draft guidance. “The March Advisory Committee meeting seems to have prompted a shift by the FDA, surgeons, and industry,” said Jamee Cook, cofounder of the group. “We are definitely seeing a change in patient engagement. The FDA has been cooperating with patients and listening to our concerns. We still have a long way to go in raising public awareness of breast implant issues, but progress over the past 1-2 years has been amazing.”
Diana Zuckerman, PhD, president of the National Center for Health Research in Washington, gave the draft guidance a mixed review. “The FDA’s draft includes the types of information that we had proposed to the FDA in recent months in our work with patient advocates and plastic surgeons,” she said. “However, it is not as informative as it should be in describing well-designed studies indicating a risk of systemic illnesses. Patients deserve to make better-informed decisions in the future than most women considering breast implants have been able to make” in the past.
Patricia McGuire, MD, a St. Louis plastic surgeon who specializes in breast surgery and has studied breast implant illness, declared the guidance to be “reasonable.”
“I think the changes address the concerns expressed by patients during the [March] hearing; I agree with everything the FDA proposed in the guidance document,” Dr. McGuire said. “The boxed warning is reasonable and needs to be part of the informed consent process. I also agree with the changes in screening implants postoperatively. Most patients do not get MRI examinations. High-resolution ultrasound is more convenient and cost effective.”
The boxed warning was rated as “reasonably strong” and “the most serious step the FDA can take short of taking a device off the market,” but in the case of breast implants, a wider recall of textured implants than what the FDA arranged last July would be even more appropriate, commented Sidney M. Wolfe, MD, founder and senior adviser to Public Citizen. He also faulted the agency for not taking quicker action in mandating inclusion of the proposed boxed warning.
Issuing the labeling changes as draft guidance “is a ministep forward,” but also a process that “guarantees delay” and “creeps along at a dangerously slow pace,” Dr. Wolfe said. “The FDA is delaying what should be inevitable. The agency could put the boxed warning in place right now if they had the guts to do it.”
Dr. McGuire has been a consultant to Allergan, Establishment Labs, and Hans Biomed. Ms. Cook, Dr. Zuckerman, and Dr. Wolfe reported having no commercial disclosures.
Breast implants sold in the United States may soon require a boxed warning in their label, along with other label changes proposed by the Food and Drug Administration aimed at better informing prospective patients and clinicians of the potential risks from breast implants.
Other elements of the proposed labeling changes include creation of a patient-decision checklist, new recommendations for follow-up imaging to monitor for implant rupture, inclusion of detailed and understandable information about materials in the device, and provision of a device card to each patient with details on the specific implant they received.
These labeling changes all stemmed from a breast implant hearing held by the agency’s General and Plastic Surgery Devices Panel in March 2019, according to the draft guidance document officially released by the FDA on Oct. 24.
The proposed labeling changes were generally welcomed by patient advocates and by clinicians as a reasonable response to the concerns discussed at the March hearing. In an earlier move to address issues brought up at the hearing, the FDA in July arranged for a recall for certain Allergan models of textured breast implants because of their link with the development of breast implant–associated anaplastic large cell lymphoma (BIA-ALCL).
The boxed warning proposed by the FDA would highlight four specific facts that patients, physicians, and surgeons should know about breast implants: They are not considered lifetime devices, the chance of developing complications from implants increases over time, some complications require additional surgery, and placement of breast implants has been associated with development of BIA-ALCL and may also be associated with certain systemic symptoms.
The FDA also proposed four other notable labeling changes:
- Creation of a patient-decision checklist to better systematize the informed consent process and make sure that certain aspects of breast implant placement are clearly brought to patients’ attention. The FDA proposed that patients sign their checklist attesting to having read and understood the information and that patients receive a take-home copy for their future reference. Proposed elements of the checklist include situations to not use breast implants; considerations for successful implant recipients; the risks of breast implant surgery; the importance of appropriate physician education, training, and experience; the risk for developing BIA-ALCL or systemic symptoms; and discussion of options other than breast implants.
- A new scheme for systematically and serially using imaging to screen for implant rupture that designates for the first time that ultrasound is an acceptable alternative to MRI and relies on a schedule by which either method initially screens the implant 5-6 years post operatively and then every 2 years thereafter.
- Detailed and understandable information about each material component of the implant with further information on possible adverse health effects of these compounds.
- A device card that patients should receive after their surgery with the implant’s name, serial number, and other identifiers; the boxed warning information; and a web link for accessing more up-to-date information.
The patient group Breast Implant Victim Advocacy praised the draft guidance. “The March Advisory Committee meeting seems to have prompted a shift by the FDA, surgeons, and industry,” said Jamee Cook, cofounder of the group. “We are definitely seeing a change in patient engagement. The FDA has been cooperating with patients and listening to our concerns. We still have a long way to go in raising public awareness of breast implant issues, but progress over the past 1-2 years has been amazing.”
Diana Zuckerman, PhD, president of the National Center for Health Research in Washington, gave the draft guidance a mixed review. “The FDA’s draft includes the types of information that we had proposed to the FDA in recent months in our work with patient advocates and plastic surgeons,” she said. “However, it is not as informative as it should be in describing well-designed studies indicating a risk of systemic illnesses. Patients deserve to make better-informed decisions in the future than most women considering breast implants have been able to make” in the past.
Patricia McGuire, MD, a St. Louis plastic surgeon who specializes in breast surgery and has studied breast implant illness, declared the guidance to be “reasonable.”
“I think the changes address the concerns expressed by patients during the [March] hearing; I agree with everything the FDA proposed in the guidance document,” Dr. McGuire said. “The boxed warning is reasonable and needs to be part of the informed consent process. I also agree with the changes in screening implants postoperatively. Most patients do not get MRI examinations. High-resolution ultrasound is more convenient and cost effective.”
The boxed warning was rated as “reasonably strong” and “the most serious step the FDA can take short of taking a device off the market,” but in the case of breast implants, a wider recall of textured implants than what the FDA arranged last July would be even more appropriate, commented Sidney M. Wolfe, MD, founder and senior adviser to Public Citizen. He also faulted the agency for not taking quicker action in mandating inclusion of the proposed boxed warning.
Issuing the labeling changes as draft guidance “is a ministep forward,” but also a process that “guarantees delay” and “creeps along at a dangerously slow pace,” Dr. Wolfe said. “The FDA is delaying what should be inevitable. The agency could put the boxed warning in place right now if they had the guts to do it.”
Dr. McGuire has been a consultant to Allergan, Establishment Labs, and Hans Biomed. Ms. Cook, Dr. Zuckerman, and Dr. Wolfe reported having no commercial disclosures.
ACIP recommends two options for pertussis vaccination
Either the Tdap or Td vaccine is an acceptable option for pertussis vaccination in most situations, recommended the Centers for Disease Control and Prevention’s Advisory Committee on Immunization Practices.
In a unanimous 14-0 vote at the October meeting, based on the immunization schedule for persons aged 7 years and older.
Safety data showed no differences in safety concerns between Tdap and Td, including data from pregnant women, said Fiona Havers, MD, of the CDC’s National Center for Immunization and Respiratory Diseases (NCIRD), Atlanta.
Several of the ACIP members noted that the revised language to include both Tdap and Td reflects the increased use of Tdap and allows for maximum flexibility in clinical settings.
The revised language advises that booster doses of “either Td or Tdap” every 10 years throughout life are recommended for continued protection against tetanus and diphtheria. In addition, either Td or Tdap should be used if a tetanus toxoid–containing vaccine is indicated for prophylaxis in nonpregnant individuals.
For catch-up recommendations, which also apply to pregnant women, the committee approved the following wording for a series of three doses for individuals aged 7-18 years and 19 years and older who have never been vaccinated, that “the preferred schedule is a dose of Tdap (preferably the first dose), followed by either Tdap or Td at least 4 weeks afterward and another dose of either Td or Tdap 6-12 months later.” Individuals in these same age groups who are not fully vaccinated should receive one dose of Tdap, and a dose of either Td or Tdap if additional doses are needed.
The committee also voted unanimously 14-0 to accept the updated wording for pertussis vaccination in the Vaccines for Children program.
The ACIP members had no financial conflicts to disclose.
Either the Tdap or Td vaccine is an acceptable option for pertussis vaccination in most situations, recommended the Centers for Disease Control and Prevention’s Advisory Committee on Immunization Practices.
In a unanimous 14-0 vote at the October meeting, based on the immunization schedule for persons aged 7 years and older.
Safety data showed no differences in safety concerns between Tdap and Td, including data from pregnant women, said Fiona Havers, MD, of the CDC’s National Center for Immunization and Respiratory Diseases (NCIRD), Atlanta.
Several of the ACIP members noted that the revised language to include both Tdap and Td reflects the increased use of Tdap and allows for maximum flexibility in clinical settings.
The revised language advises that booster doses of “either Td or Tdap” every 10 years throughout life are recommended for continued protection against tetanus and diphtheria. In addition, either Td or Tdap should be used if a tetanus toxoid–containing vaccine is indicated for prophylaxis in nonpregnant individuals.
For catch-up recommendations, which also apply to pregnant women, the committee approved the following wording for a series of three doses for individuals aged 7-18 years and 19 years and older who have never been vaccinated, that “the preferred schedule is a dose of Tdap (preferably the first dose), followed by either Tdap or Td at least 4 weeks afterward and another dose of either Td or Tdap 6-12 months later.” Individuals in these same age groups who are not fully vaccinated should receive one dose of Tdap, and a dose of either Td or Tdap if additional doses are needed.
The committee also voted unanimously 14-0 to accept the updated wording for pertussis vaccination in the Vaccines for Children program.
The ACIP members had no financial conflicts to disclose.
Either the Tdap or Td vaccine is an acceptable option for pertussis vaccination in most situations, recommended the Centers for Disease Control and Prevention’s Advisory Committee on Immunization Practices.
In a unanimous 14-0 vote at the October meeting, based on the immunization schedule for persons aged 7 years and older.
Safety data showed no differences in safety concerns between Tdap and Td, including data from pregnant women, said Fiona Havers, MD, of the CDC’s National Center for Immunization and Respiratory Diseases (NCIRD), Atlanta.
Several of the ACIP members noted that the revised language to include both Tdap and Td reflects the increased use of Tdap and allows for maximum flexibility in clinical settings.
The revised language advises that booster doses of “either Td or Tdap” every 10 years throughout life are recommended for continued protection against tetanus and diphtheria. In addition, either Td or Tdap should be used if a tetanus toxoid–containing vaccine is indicated for prophylaxis in nonpregnant individuals.
For catch-up recommendations, which also apply to pregnant women, the committee approved the following wording for a series of three doses for individuals aged 7-18 years and 19 years and older who have never been vaccinated, that “the preferred schedule is a dose of Tdap (preferably the first dose), followed by either Tdap or Td at least 4 weeks afterward and another dose of either Td or Tdap 6-12 months later.” Individuals in these same age groups who are not fully vaccinated should receive one dose of Tdap, and a dose of either Td or Tdap if additional doses are needed.
The committee also voted unanimously 14-0 to accept the updated wording for pertussis vaccination in the Vaccines for Children program.
The ACIP members had no financial conflicts to disclose.
FROM AN ACIP MEETING
Antituberculosis drugs in pregnancy and lactation
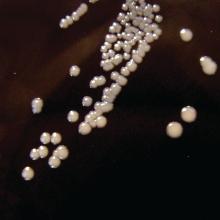
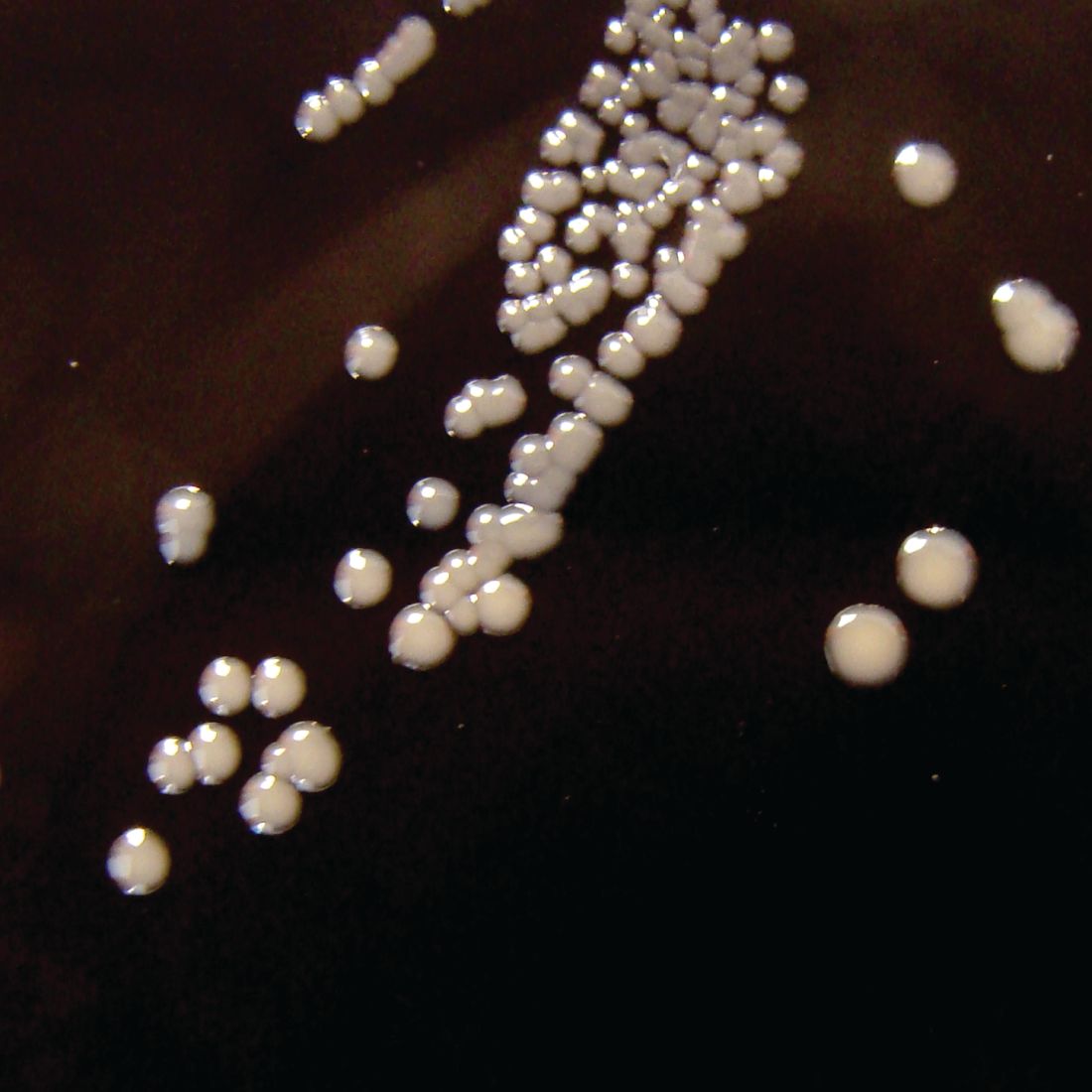
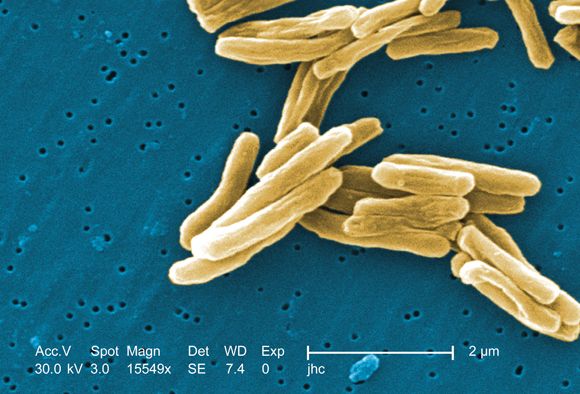
Tuberculosis is one of the top ten causes of death worldwide and the leading cause from a single infectious agent. In the 2012-2017 period, there were more than 9,000 cases of TB each year in the United States. The Centers for Disease Control and Prevention states that untreated TB is a greater hazard to a pregnant woman and her fetus than its treatment.
In the material below, the molecular weights, rounded to the nearest whole number, are shown in parentheses after the drug name. Those less than 1,000 or so suggest that the drug will cross the placenta throughout pregnancy. In the second half of pregnancy, especially in the third trimester, nearly all drugs will cross regardless of their molecular weight.
Para-aminosalicylic acid (Paser) (153) is most frequently used in combination with other agents for the treatment of multidrug-resistant tuberculosis; multidrug-resistant TB (MDR TB) is defined as being caused by TB bacteria that is resistant to at least isoniazid and rifampin, the two most potent TB drugs. The drug has been associated with a marked increased risk of birth defects in some, but not all, studies. Because of this potential risk, the drug is best avoided in the first trimester. The drug is excreted into breast milk, but there are no reports of its use during breastfeeding.
Bedaquiline (Sirturo) (556) is used in combination therapy for patents with multidrug-resistant tuberculosis. One report describing the use of this drug during human pregnancy has been located. Treatment was started in the last 3 weeks of pregnancy and no abnormalities were noted in the child at birth and for 2 years after birth (Emerg Infect Dis. 2017. doi: 10.3201/eid2310.161398). The CDC states that the drug should be used only in a minimum four-drug treatment regimen and administered by direct observation (MMWR Recomm Rep. 2013 Oct 25;62[RR-09]:1-12). The drug probably is excreted into breast milk, but there are no reports of its use during breastfeeding.
Capreomycin (Capastat) (653-669) is a polypeptide antibiotic isolated from Streptomyces capreolus that is given intramuscularly. The human pregnancy data are limited to three reports. The toxicity of capreomycin is similar to aminoglycosides (e.g., cranial nerve VIII and renal) and it should not be used with these agents. The CDC has classified the drug as contraindicated in pregnancy. The drug probably is excreted into breast milk, but there are no reports of its use during breastfeeding.
Cycloserine (Seromycin) (102) is a broad spectrum antibiotic. The human pregnancy data are limited but have not shown embryo-fetal harm. Although the best course is to avoid the drug during gestation, it should not be withheld because of pregnancy if the maternal condition requires the antibiotic. The American Academy of Pediatrics classified cycloserine as compatible with breastfeeding.
Ethambutol (Myambutol) (205) should be used in conjunction with other antituberculosis drugs. The human pregnancy data do not suggest an embryo-fetal risk. A frequently used regimen is ethambutol + isoniazid + rifampin. The American Academy of Pediatrics classified ethambutol as compatible with breastfeeding.
Ethionamide (Trecator) (166) is indicated when Mycobacterium tuberculosis is resistant to isoniazid or rifampin, or when the patient is intolerant to other drugs. Although the animal reproductive data suggest risk, the limited human data suggest that the risk is probably low. If indicated, the drug should not be withheld because of pregnancy. Although the molecular weight suggests that the drug will be excreted into breast milk, no reports describing the amount in milk have been located.
Isoniazid (137) is compatible in pregnancy, even though the molecular weight suggests that it will cross the placenta, because the maternal benefit is much greater than the potential embryo-fetal risk. Although the human data are limited, the molecular weight also suggests that the drug will be excreted into breast milk, but it can be considered probably compatible during breastfeeding. No reports of isoniazid-induced effects in the nursing infant have been located, but the potential for interference with nucleic acid function and for hepatotoxicity may exist.
Pyrazinamide (123) is metabolized to an active metabolite. The molecular weight, low plasma protein binding (10%), and prolonged elimination half-life (9-10 hours) suggest that the drug will cross the placenta throughout pregnancy. The drug has been used in human pregnancy without causing embryo-fetal harm. Similar results, although limited, were reported when the drug was used during breastfeeding.
Rifabutin (Mycobutin) (847) has no reported human pregnancy data, but the animal data suggest low risk. The drug probably crosses the placenta throughout pregnancy. The maternal benefit appears to outweigh the unknown risk to the embryo-fetus, so therapy should not be withheld because of pregnancy. The drug probably is excreted into breast milk.
Rifampin (Rifadin) (823) appears to be compatible in pregnancy. Several reviews and reports have concluded that the drug was not a teratogen and recommended use of the drug with isoniazid and ethambutol. However, prophylactic vitamin K1 has been recommended to prevent drug-induced hemorrhagic disease of the newborn. There are no data regarding its use during breastfeeding, but it is probably compatible.
Rifapentine (Priftin) (877) was toxic and teratogenic in two animal species at doses close to those used in humans. In a 2018 study, however, the rates of fetal loss in pregnancies of less than 20 weeks (8/54, 15%) and congenital anomalies in live births (1/37, 3%) were within the expected background rates (Ann Am Thorac Soc. 2018 May;15[4]:570-80). There are no data regarding its use during breastfeeding, but it is probably compatible.
The CDC classifies four antituberculosis and one class of drugs as contraindicated in pregnancy. In addition to capreomycin mentioned above, they are amikacin, fluoroquinolones (ciprofloxacin, gemifloxacin, levofloxacin, lomefloxacin, moxifloxacin, ofloxacin), kanamycin, and streptomycin. These ten agents are discussed in the 11th edition of my book “Drugs in Pregnancy and Lactation,” (Wolters Kluwer Health: Riverwood, Il., 2017). If they have to be used, checking this source will provide information that has to be discussed with the patient.
Mr. Briggs is clinical professor of pharmacy at the University of California, San Francisco, and adjunct professor of pharmacy at the University of Southern California, Los Angeles, as well as at Washington State University, Spokane. Mr. Briggs had no disclosures, except for his book. Email him at [email protected].
Tuberculosis is one of the top ten causes of death worldwide and the leading cause from a single infectious agent. In the 2012-2017 period, there were more than 9,000 cases of TB each year in the United States. The Centers for Disease Control and Prevention states that untreated TB is a greater hazard to a pregnant woman and her fetus than its treatment.
In the material below, the molecular weights, rounded to the nearest whole number, are shown in parentheses after the drug name. Those less than 1,000 or so suggest that the drug will cross the placenta throughout pregnancy. In the second half of pregnancy, especially in the third trimester, nearly all drugs will cross regardless of their molecular weight.
Para-aminosalicylic acid (Paser) (153) is most frequently used in combination with other agents for the treatment of multidrug-resistant tuberculosis; multidrug-resistant TB (MDR TB) is defined as being caused by TB bacteria that is resistant to at least isoniazid and rifampin, the two most potent TB drugs. The drug has been associated with a marked increased risk of birth defects in some, but not all, studies. Because of this potential risk, the drug is best avoided in the first trimester. The drug is excreted into breast milk, but there are no reports of its use during breastfeeding.
Bedaquiline (Sirturo) (556) is used in combination therapy for patents with multidrug-resistant tuberculosis. One report describing the use of this drug during human pregnancy has been located. Treatment was started in the last 3 weeks of pregnancy and no abnormalities were noted in the child at birth and for 2 years after birth (Emerg Infect Dis. 2017. doi: 10.3201/eid2310.161398). The CDC states that the drug should be used only in a minimum four-drug treatment regimen and administered by direct observation (MMWR Recomm Rep. 2013 Oct 25;62[RR-09]:1-12). The drug probably is excreted into breast milk, but there are no reports of its use during breastfeeding.
Capreomycin (Capastat) (653-669) is a polypeptide antibiotic isolated from Streptomyces capreolus that is given intramuscularly. The human pregnancy data are limited to three reports. The toxicity of capreomycin is similar to aminoglycosides (e.g., cranial nerve VIII and renal) and it should not be used with these agents. The CDC has classified the drug as contraindicated in pregnancy. The drug probably is excreted into breast milk, but there are no reports of its use during breastfeeding.
Cycloserine (Seromycin) (102) is a broad spectrum antibiotic. The human pregnancy data are limited but have not shown embryo-fetal harm. Although the best course is to avoid the drug during gestation, it should not be withheld because of pregnancy if the maternal condition requires the antibiotic. The American Academy of Pediatrics classified cycloserine as compatible with breastfeeding.
Ethambutol (Myambutol) (205) should be used in conjunction with other antituberculosis drugs. The human pregnancy data do not suggest an embryo-fetal risk. A frequently used regimen is ethambutol + isoniazid + rifampin. The American Academy of Pediatrics classified ethambutol as compatible with breastfeeding.
Ethionamide (Trecator) (166) is indicated when Mycobacterium tuberculosis is resistant to isoniazid or rifampin, or when the patient is intolerant to other drugs. Although the animal reproductive data suggest risk, the limited human data suggest that the risk is probably low. If indicated, the drug should not be withheld because of pregnancy. Although the molecular weight suggests that the drug will be excreted into breast milk, no reports describing the amount in milk have been located.
Isoniazid (137) is compatible in pregnancy, even though the molecular weight suggests that it will cross the placenta, because the maternal benefit is much greater than the potential embryo-fetal risk. Although the human data are limited, the molecular weight also suggests that the drug will be excreted into breast milk, but it can be considered probably compatible during breastfeeding. No reports of isoniazid-induced effects in the nursing infant have been located, but the potential for interference with nucleic acid function and for hepatotoxicity may exist.
Pyrazinamide (123) is metabolized to an active metabolite. The molecular weight, low plasma protein binding (10%), and prolonged elimination half-life (9-10 hours) suggest that the drug will cross the placenta throughout pregnancy. The drug has been used in human pregnancy without causing embryo-fetal harm. Similar results, although limited, were reported when the drug was used during breastfeeding.
Rifabutin (Mycobutin) (847) has no reported human pregnancy data, but the animal data suggest low risk. The drug probably crosses the placenta throughout pregnancy. The maternal benefit appears to outweigh the unknown risk to the embryo-fetus, so therapy should not be withheld because of pregnancy. The drug probably is excreted into breast milk.
Rifampin (Rifadin) (823) appears to be compatible in pregnancy. Several reviews and reports have concluded that the drug was not a teratogen and recommended use of the drug with isoniazid and ethambutol. However, prophylactic vitamin K1 has been recommended to prevent drug-induced hemorrhagic disease of the newborn. There are no data regarding its use during breastfeeding, but it is probably compatible.
Rifapentine (Priftin) (877) was toxic and teratogenic in two animal species at doses close to those used in humans. In a 2018 study, however, the rates of fetal loss in pregnancies of less than 20 weeks (8/54, 15%) and congenital anomalies in live births (1/37, 3%) were within the expected background rates (Ann Am Thorac Soc. 2018 May;15[4]:570-80). There are no data regarding its use during breastfeeding, but it is probably compatible.
The CDC classifies four antituberculosis and one class of drugs as contraindicated in pregnancy. In addition to capreomycin mentioned above, they are amikacin, fluoroquinolones (ciprofloxacin, gemifloxacin, levofloxacin, lomefloxacin, moxifloxacin, ofloxacin), kanamycin, and streptomycin. These ten agents are discussed in the 11th edition of my book “Drugs in Pregnancy and Lactation,” (Wolters Kluwer Health: Riverwood, Il., 2017). If they have to be used, checking this source will provide information that has to be discussed with the patient.
Mr. Briggs is clinical professor of pharmacy at the University of California, San Francisco, and adjunct professor of pharmacy at the University of Southern California, Los Angeles, as well as at Washington State University, Spokane. Mr. Briggs had no disclosures, except for his book. Email him at [email protected].
Tuberculosis is one of the top ten causes of death worldwide and the leading cause from a single infectious agent. In the 2012-2017 period, there were more than 9,000 cases of TB each year in the United States. The Centers for Disease Control and Prevention states that untreated TB is a greater hazard to a pregnant woman and her fetus than its treatment.
In the material below, the molecular weights, rounded to the nearest whole number, are shown in parentheses after the drug name. Those less than 1,000 or so suggest that the drug will cross the placenta throughout pregnancy. In the second half of pregnancy, especially in the third trimester, nearly all drugs will cross regardless of their molecular weight.
Para-aminosalicylic acid (Paser) (153) is most frequently used in combination with other agents for the treatment of multidrug-resistant tuberculosis; multidrug-resistant TB (MDR TB) is defined as being caused by TB bacteria that is resistant to at least isoniazid and rifampin, the two most potent TB drugs. The drug has been associated with a marked increased risk of birth defects in some, but not all, studies. Because of this potential risk, the drug is best avoided in the first trimester. The drug is excreted into breast milk, but there are no reports of its use during breastfeeding.
Bedaquiline (Sirturo) (556) is used in combination therapy for patents with multidrug-resistant tuberculosis. One report describing the use of this drug during human pregnancy has been located. Treatment was started in the last 3 weeks of pregnancy and no abnormalities were noted in the child at birth and for 2 years after birth (Emerg Infect Dis. 2017. doi: 10.3201/eid2310.161398). The CDC states that the drug should be used only in a minimum four-drug treatment regimen and administered by direct observation (MMWR Recomm Rep. 2013 Oct 25;62[RR-09]:1-12). The drug probably is excreted into breast milk, but there are no reports of its use during breastfeeding.
Capreomycin (Capastat) (653-669) is a polypeptide antibiotic isolated from Streptomyces capreolus that is given intramuscularly. The human pregnancy data are limited to three reports. The toxicity of capreomycin is similar to aminoglycosides (e.g., cranial nerve VIII and renal) and it should not be used with these agents. The CDC has classified the drug as contraindicated in pregnancy. The drug probably is excreted into breast milk, but there are no reports of its use during breastfeeding.
Cycloserine (Seromycin) (102) is a broad spectrum antibiotic. The human pregnancy data are limited but have not shown embryo-fetal harm. Although the best course is to avoid the drug during gestation, it should not be withheld because of pregnancy if the maternal condition requires the antibiotic. The American Academy of Pediatrics classified cycloserine as compatible with breastfeeding.
Ethambutol (Myambutol) (205) should be used in conjunction with other antituberculosis drugs. The human pregnancy data do not suggest an embryo-fetal risk. A frequently used regimen is ethambutol + isoniazid + rifampin. The American Academy of Pediatrics classified ethambutol as compatible with breastfeeding.
Ethionamide (Trecator) (166) is indicated when Mycobacterium tuberculosis is resistant to isoniazid or rifampin, or when the patient is intolerant to other drugs. Although the animal reproductive data suggest risk, the limited human data suggest that the risk is probably low. If indicated, the drug should not be withheld because of pregnancy. Although the molecular weight suggests that the drug will be excreted into breast milk, no reports describing the amount in milk have been located.
Isoniazid (137) is compatible in pregnancy, even though the molecular weight suggests that it will cross the placenta, because the maternal benefit is much greater than the potential embryo-fetal risk. Although the human data are limited, the molecular weight also suggests that the drug will be excreted into breast milk, but it can be considered probably compatible during breastfeeding. No reports of isoniazid-induced effects in the nursing infant have been located, but the potential for interference with nucleic acid function and for hepatotoxicity may exist.
Pyrazinamide (123) is metabolized to an active metabolite. The molecular weight, low plasma protein binding (10%), and prolonged elimination half-life (9-10 hours) suggest that the drug will cross the placenta throughout pregnancy. The drug has been used in human pregnancy without causing embryo-fetal harm. Similar results, although limited, were reported when the drug was used during breastfeeding.
Rifabutin (Mycobutin) (847) has no reported human pregnancy data, but the animal data suggest low risk. The drug probably crosses the placenta throughout pregnancy. The maternal benefit appears to outweigh the unknown risk to the embryo-fetus, so therapy should not be withheld because of pregnancy. The drug probably is excreted into breast milk.
Rifampin (Rifadin) (823) appears to be compatible in pregnancy. Several reviews and reports have concluded that the drug was not a teratogen and recommended use of the drug with isoniazid and ethambutol. However, prophylactic vitamin K1 has been recommended to prevent drug-induced hemorrhagic disease of the newborn. There are no data regarding its use during breastfeeding, but it is probably compatible.
Rifapentine (Priftin) (877) was toxic and teratogenic in two animal species at doses close to those used in humans. In a 2018 study, however, the rates of fetal loss in pregnancies of less than 20 weeks (8/54, 15%) and congenital anomalies in live births (1/37, 3%) were within the expected background rates (Ann Am Thorac Soc. 2018 May;15[4]:570-80). There are no data regarding its use during breastfeeding, but it is probably compatible.
The CDC classifies four antituberculosis and one class of drugs as contraindicated in pregnancy. In addition to capreomycin mentioned above, they are amikacin, fluoroquinolones (ciprofloxacin, gemifloxacin, levofloxacin, lomefloxacin, moxifloxacin, ofloxacin), kanamycin, and streptomycin. These ten agents are discussed in the 11th edition of my book “Drugs in Pregnancy and Lactation,” (Wolters Kluwer Health: Riverwood, Il., 2017). If they have to be used, checking this source will provide information that has to be discussed with the patient.
Mr. Briggs is clinical professor of pharmacy at the University of California, San Francisco, and adjunct professor of pharmacy at the University of Southern California, Los Angeles, as well as at Washington State University, Spokane. Mr. Briggs had no disclosures, except for his book. Email him at [email protected].
Couples-based cognitive-behavioral therapy curbs postpartum depression
Postpartum women who participated in a couples-based cognitive-behavioral therapy program showed less postpartum depression than did women in a solo program, according to data from 388 couples.
Previous studies have shown that both men and women experience depression up to 1 year after the birth of a child, but “no studies have compared the relative effectiveness of couple-based and women-alone interventions on parental mental health,” wrote F-W Ngai of the Hong Kong Polytechnic University and colleagues.
In a study published in the BJOG: An International Journal of Obstetrics and Gynaecology, the researchers randomized 134 childbearing Chinese couples to a couples-based cognitive-behavioral intervention (CBI), 124 women to a women-only CBI, and 130 controls who did not receive CBI. The CBI consisted of one 3-hour antenatal group session and two 30-mintue postnatal telephone sessions. Depressive symptoms were assessed during pregnancy as a baseline, and at 6 weeks, 6 months, and 12 months post partum and measured using the Edinburgh Postnatal Depression Scale (EPDS). Demographic characteristics were similar among the groups.
Overall, mothers in the couples-based CBI group showed significant improvement in depressive symptoms at 6 weeks post partum, compared with women in the women-only group or the controls (average differences in scores on the EPDS of 1.46 and 1.71, respectively). In addition, the percentage of women who met criteria for postnatal depression with an EPDS score of at least 10 was significantly lower (17.8% difference) in the couples-based CBI group compared with controls at 6 weeks postpartum. However, the differences between the groups were no longer significant at 6 months and 12 months post partum, and no differences in depression scores were seen among fathers at any time point.
“The findings provide evidence for the effectiveness of the couple-based cognitive behavioral intervention in improving postnatal depression among mothers, but not fathers,” and additional research is needed to find interventions that protect new fathers from depression, the researchers said.
The study findings were limited by several factors including the use only of self-reports for postpartum assessment and the homogeneous nature of the study population (all were educated, first-time Chinese parents), the researchers noted. However, the results support those from previous studies and suggest that couples-based CBI is feasible for use in primary care to promote perinatal health, they concluded.
The researchers had no financial conflicts to disclose.
SOURCE: Ngai F-W et al. BJOG. 2019. doi: 10.1111/1471-0528.15862.
Postpartum women who participated in a couples-based cognitive-behavioral therapy program showed less postpartum depression than did women in a solo program, according to data from 388 couples.
Previous studies have shown that both men and women experience depression up to 1 year after the birth of a child, but “no studies have compared the relative effectiveness of couple-based and women-alone interventions on parental mental health,” wrote F-W Ngai of the Hong Kong Polytechnic University and colleagues.
In a study published in the BJOG: An International Journal of Obstetrics and Gynaecology, the researchers randomized 134 childbearing Chinese couples to a couples-based cognitive-behavioral intervention (CBI), 124 women to a women-only CBI, and 130 controls who did not receive CBI. The CBI consisted of one 3-hour antenatal group session and two 30-mintue postnatal telephone sessions. Depressive symptoms were assessed during pregnancy as a baseline, and at 6 weeks, 6 months, and 12 months post partum and measured using the Edinburgh Postnatal Depression Scale (EPDS). Demographic characteristics were similar among the groups.
Overall, mothers in the couples-based CBI group showed significant improvement in depressive symptoms at 6 weeks post partum, compared with women in the women-only group or the controls (average differences in scores on the EPDS of 1.46 and 1.71, respectively). In addition, the percentage of women who met criteria for postnatal depression with an EPDS score of at least 10 was significantly lower (17.8% difference) in the couples-based CBI group compared with controls at 6 weeks postpartum. However, the differences between the groups were no longer significant at 6 months and 12 months post partum, and no differences in depression scores were seen among fathers at any time point.
“The findings provide evidence for the effectiveness of the couple-based cognitive behavioral intervention in improving postnatal depression among mothers, but not fathers,” and additional research is needed to find interventions that protect new fathers from depression, the researchers said.
The study findings were limited by several factors including the use only of self-reports for postpartum assessment and the homogeneous nature of the study population (all were educated, first-time Chinese parents), the researchers noted. However, the results support those from previous studies and suggest that couples-based CBI is feasible for use in primary care to promote perinatal health, they concluded.
The researchers had no financial conflicts to disclose.
SOURCE: Ngai F-W et al. BJOG. 2019. doi: 10.1111/1471-0528.15862.
Postpartum women who participated in a couples-based cognitive-behavioral therapy program showed less postpartum depression than did women in a solo program, according to data from 388 couples.
Previous studies have shown that both men and women experience depression up to 1 year after the birth of a child, but “no studies have compared the relative effectiveness of couple-based and women-alone interventions on parental mental health,” wrote F-W Ngai of the Hong Kong Polytechnic University and colleagues.
In a study published in the BJOG: An International Journal of Obstetrics and Gynaecology, the researchers randomized 134 childbearing Chinese couples to a couples-based cognitive-behavioral intervention (CBI), 124 women to a women-only CBI, and 130 controls who did not receive CBI. The CBI consisted of one 3-hour antenatal group session and two 30-mintue postnatal telephone sessions. Depressive symptoms were assessed during pregnancy as a baseline, and at 6 weeks, 6 months, and 12 months post partum and measured using the Edinburgh Postnatal Depression Scale (EPDS). Demographic characteristics were similar among the groups.
Overall, mothers in the couples-based CBI group showed significant improvement in depressive symptoms at 6 weeks post partum, compared with women in the women-only group or the controls (average differences in scores on the EPDS of 1.46 and 1.71, respectively). In addition, the percentage of women who met criteria for postnatal depression with an EPDS score of at least 10 was significantly lower (17.8% difference) in the couples-based CBI group compared with controls at 6 weeks postpartum. However, the differences between the groups were no longer significant at 6 months and 12 months post partum, and no differences in depression scores were seen among fathers at any time point.
“The findings provide evidence for the effectiveness of the couple-based cognitive behavioral intervention in improving postnatal depression among mothers, but not fathers,” and additional research is needed to find interventions that protect new fathers from depression, the researchers said.
The study findings were limited by several factors including the use only of self-reports for postpartum assessment and the homogeneous nature of the study population (all were educated, first-time Chinese parents), the researchers noted. However, the results support those from previous studies and suggest that couples-based CBI is feasible for use in primary care to promote perinatal health, they concluded.
The researchers had no financial conflicts to disclose.
SOURCE: Ngai F-W et al. BJOG. 2019. doi: 10.1111/1471-0528.15862.
FROM THE BJOG: AN INTERNATIONAL JOURNAL OF OBSTETRICS AND GYNAECOLOGY
Women with PCOS have greater risk of postpartum depression, preeclampsia, eclampsia
PHILADELPHIA – Women with polycystic ovary syndrome (PCOS) are at a higher risk for metabolic and psychiatric comorbidities prior to pregnancy, cardiometabolic complications during pregnancy, and cardiometabolic and psychiatric complications in the postpartum period, according to results from a prize paper at the annual meeting of the American Society for Reproductive Medicine.
“Our findings do support the ACOG [American College of Obstetricians and Gynecologists] recommendations that women with PCOS should be considered a high-risk group, and during the postpartum period should be screened for cardiovascular as well as psychiatric comorbidities,” Anuja Dokras, MD, PhD, director of the Penn Polycystic Ovary Syndrome Center at the University of Pennsylvania, Philadelphia, said in her presentation.
Dr. Dokras and colleagues performed a retrospective cohort study during 2000-2016 of patients aged 18-50 years, in the Optum claims database, which comprised 42,391 women with PCOS and 795,480 women without PCOS in 50 U.S. states. Women were included in the analysis if there were data available for at least 6 months to 1 year before pregnancy and between 6 weeks and 1 year after pregnancy. The researchers looked at risk factors prior to pregnancy, such as depression, hypertension, hyperlipidemia, diabetes, obesity, smoking, and use of assisted reproductive technology. During pregnancy, Dr. Dokras and colleagues analyzed complications such as preterm birth, multiple gestation, cesarean section, gestational hypertension and diabetes, preeclampsia and eclampsia, and depression in addition to outcomes in the postpartum period, such as hypertensive complications, thrombotic disease, peripartum cardiomyopathy, heart failure, arterial complications, perinatal and postpartum depression.
“Realizing that PCOS is underreported in administrative data sets, we looked at not only the diagnosis of PCOS but also tried to combine any menstrual irregularity and hirsutism occurring simultaneously, and then doing a sensitivity analysis and looking at the population,” said Dr. Dokras. “Similarly, knowing that misclassification can be an issue in these datasets, we did the same thing amongst the controls, looking for a single diagnosis of irregular menses and hirsutism.”
Prior to pregnancy, women with PCOS in the dataset tended to have a higher rate of obesity (14.7% vs. 4.7%), hyperlipidemia (11.3% vs. 5.3%), hypertension (6.2% vs. 2.5%), diabetes (5.3% vs. 1.2%), and depression (4.3% vs. 3.1%) and were also more likely to use assisted reproductive technology (5.2% vs. 1.0%) than were patients without PCOS (all P less than .001). During pregnancy, there was a higher rate of gestational diabetes (13.7% vs. 7.7%), preeclampsia (5.0% vs. 2.6%), preterm birth (16.9% vs. 12.2%), multiple gestation (6.6% vs. 2.5%), and cesarean section (45.1% vs. 32.9%) in patients with PCOS, compared with those without PCOS (all P less than .001).
For patients in the postpartum period, women with PCOS were more likely to experience postpartum thrombotic disease (adjusted odds ratio, 1.60; 95% confidence interval, 1.23-2.09; P = .001), hypertensive heart disease (aOR, 1.45; 95% CI, 1.04-2.01; P = .027), eclampsia (aOR, 1.45; 95% CI, 1.14-1.86; P = .003), heart failure (aOR, 1.33; 95% CI, 1.08-1.64; P = .007), preeclampsia (aOR, 1.30; 95% CI, 1.17-1.45; P = than .001), and peripartum cardiomyopathy (aOR, 1.26; 95% CI, 1.03-1.54; P = .027).
With regard to depression, women with PCOS also were at greater risk of developing perinatal (aOR, 1.27; 95% CI, 1.22-1.33) and postpartum (aOR, 1.46; 95% CI, 1.36-1.57) depression, compared with women without PCOS (both P less than .001).
Dr. Dokras acknowledged the limitations of administrative datasets and noted that prospective studies need to be conducted to verify their findings.
This study was funded by a grant from the National Institutes of Health. Dr. Dokras reported being a consultant for Medtronic, AbbVie, and Ferring.
SOURCE: Dokras A, et al. ASRM 2019. Abstract O-93.
PHILADELPHIA – Women with polycystic ovary syndrome (PCOS) are at a higher risk for metabolic and psychiatric comorbidities prior to pregnancy, cardiometabolic complications during pregnancy, and cardiometabolic and psychiatric complications in the postpartum period, according to results from a prize paper at the annual meeting of the American Society for Reproductive Medicine.
“Our findings do support the ACOG [American College of Obstetricians and Gynecologists] recommendations that women with PCOS should be considered a high-risk group, and during the postpartum period should be screened for cardiovascular as well as psychiatric comorbidities,” Anuja Dokras, MD, PhD, director of the Penn Polycystic Ovary Syndrome Center at the University of Pennsylvania, Philadelphia, said in her presentation.
Dr. Dokras and colleagues performed a retrospective cohort study during 2000-2016 of patients aged 18-50 years, in the Optum claims database, which comprised 42,391 women with PCOS and 795,480 women without PCOS in 50 U.S. states. Women were included in the analysis if there were data available for at least 6 months to 1 year before pregnancy and between 6 weeks and 1 year after pregnancy. The researchers looked at risk factors prior to pregnancy, such as depression, hypertension, hyperlipidemia, diabetes, obesity, smoking, and use of assisted reproductive technology. During pregnancy, Dr. Dokras and colleagues analyzed complications such as preterm birth, multiple gestation, cesarean section, gestational hypertension and diabetes, preeclampsia and eclampsia, and depression in addition to outcomes in the postpartum period, such as hypertensive complications, thrombotic disease, peripartum cardiomyopathy, heart failure, arterial complications, perinatal and postpartum depression.
“Realizing that PCOS is underreported in administrative data sets, we looked at not only the diagnosis of PCOS but also tried to combine any menstrual irregularity and hirsutism occurring simultaneously, and then doing a sensitivity analysis and looking at the population,” said Dr. Dokras. “Similarly, knowing that misclassification can be an issue in these datasets, we did the same thing amongst the controls, looking for a single diagnosis of irregular menses and hirsutism.”
Prior to pregnancy, women with PCOS in the dataset tended to have a higher rate of obesity (14.7% vs. 4.7%), hyperlipidemia (11.3% vs. 5.3%), hypertension (6.2% vs. 2.5%), diabetes (5.3% vs. 1.2%), and depression (4.3% vs. 3.1%) and were also more likely to use assisted reproductive technology (5.2% vs. 1.0%) than were patients without PCOS (all P less than .001). During pregnancy, there was a higher rate of gestational diabetes (13.7% vs. 7.7%), preeclampsia (5.0% vs. 2.6%), preterm birth (16.9% vs. 12.2%), multiple gestation (6.6% vs. 2.5%), and cesarean section (45.1% vs. 32.9%) in patients with PCOS, compared with those without PCOS (all P less than .001).
For patients in the postpartum period, women with PCOS were more likely to experience postpartum thrombotic disease (adjusted odds ratio, 1.60; 95% confidence interval, 1.23-2.09; P = .001), hypertensive heart disease (aOR, 1.45; 95% CI, 1.04-2.01; P = .027), eclampsia (aOR, 1.45; 95% CI, 1.14-1.86; P = .003), heart failure (aOR, 1.33; 95% CI, 1.08-1.64; P = .007), preeclampsia (aOR, 1.30; 95% CI, 1.17-1.45; P = than .001), and peripartum cardiomyopathy (aOR, 1.26; 95% CI, 1.03-1.54; P = .027).
With regard to depression, women with PCOS also were at greater risk of developing perinatal (aOR, 1.27; 95% CI, 1.22-1.33) and postpartum (aOR, 1.46; 95% CI, 1.36-1.57) depression, compared with women without PCOS (both P less than .001).
Dr. Dokras acknowledged the limitations of administrative datasets and noted that prospective studies need to be conducted to verify their findings.
This study was funded by a grant from the National Institutes of Health. Dr. Dokras reported being a consultant for Medtronic, AbbVie, and Ferring.
SOURCE: Dokras A, et al. ASRM 2019. Abstract O-93.
PHILADELPHIA – Women with polycystic ovary syndrome (PCOS) are at a higher risk for metabolic and psychiatric comorbidities prior to pregnancy, cardiometabolic complications during pregnancy, and cardiometabolic and psychiatric complications in the postpartum period, according to results from a prize paper at the annual meeting of the American Society for Reproductive Medicine.
“Our findings do support the ACOG [American College of Obstetricians and Gynecologists] recommendations that women with PCOS should be considered a high-risk group, and during the postpartum period should be screened for cardiovascular as well as psychiatric comorbidities,” Anuja Dokras, MD, PhD, director of the Penn Polycystic Ovary Syndrome Center at the University of Pennsylvania, Philadelphia, said in her presentation.
Dr. Dokras and colleagues performed a retrospective cohort study during 2000-2016 of patients aged 18-50 years, in the Optum claims database, which comprised 42,391 women with PCOS and 795,480 women without PCOS in 50 U.S. states. Women were included in the analysis if there were data available for at least 6 months to 1 year before pregnancy and between 6 weeks and 1 year after pregnancy. The researchers looked at risk factors prior to pregnancy, such as depression, hypertension, hyperlipidemia, diabetes, obesity, smoking, and use of assisted reproductive technology. During pregnancy, Dr. Dokras and colleagues analyzed complications such as preterm birth, multiple gestation, cesarean section, gestational hypertension and diabetes, preeclampsia and eclampsia, and depression in addition to outcomes in the postpartum period, such as hypertensive complications, thrombotic disease, peripartum cardiomyopathy, heart failure, arterial complications, perinatal and postpartum depression.
“Realizing that PCOS is underreported in administrative data sets, we looked at not only the diagnosis of PCOS but also tried to combine any menstrual irregularity and hirsutism occurring simultaneously, and then doing a sensitivity analysis and looking at the population,” said Dr. Dokras. “Similarly, knowing that misclassification can be an issue in these datasets, we did the same thing amongst the controls, looking for a single diagnosis of irregular menses and hirsutism.”
Prior to pregnancy, women with PCOS in the dataset tended to have a higher rate of obesity (14.7% vs. 4.7%), hyperlipidemia (11.3% vs. 5.3%), hypertension (6.2% vs. 2.5%), diabetes (5.3% vs. 1.2%), and depression (4.3% vs. 3.1%) and were also more likely to use assisted reproductive technology (5.2% vs. 1.0%) than were patients without PCOS (all P less than .001). During pregnancy, there was a higher rate of gestational diabetes (13.7% vs. 7.7%), preeclampsia (5.0% vs. 2.6%), preterm birth (16.9% vs. 12.2%), multiple gestation (6.6% vs. 2.5%), and cesarean section (45.1% vs. 32.9%) in patients with PCOS, compared with those without PCOS (all P less than .001).
For patients in the postpartum period, women with PCOS were more likely to experience postpartum thrombotic disease (adjusted odds ratio, 1.60; 95% confidence interval, 1.23-2.09; P = .001), hypertensive heart disease (aOR, 1.45; 95% CI, 1.04-2.01; P = .027), eclampsia (aOR, 1.45; 95% CI, 1.14-1.86; P = .003), heart failure (aOR, 1.33; 95% CI, 1.08-1.64; P = .007), preeclampsia (aOR, 1.30; 95% CI, 1.17-1.45; P = than .001), and peripartum cardiomyopathy (aOR, 1.26; 95% CI, 1.03-1.54; P = .027).
With regard to depression, women with PCOS also were at greater risk of developing perinatal (aOR, 1.27; 95% CI, 1.22-1.33) and postpartum (aOR, 1.46; 95% CI, 1.36-1.57) depression, compared with women without PCOS (both P less than .001).
Dr. Dokras acknowledged the limitations of administrative datasets and noted that prospective studies need to be conducted to verify their findings.
This study was funded by a grant from the National Institutes of Health. Dr. Dokras reported being a consultant for Medtronic, AbbVie, and Ferring.
SOURCE: Dokras A, et al. ASRM 2019. Abstract O-93.
REPORTING FROM ASRM 2019
Duloxetine ‘sprinkle’ launches for patients with difficulty swallowing
Drizalma Sprinkle (duloxetine delayed-release capsule) has launched for the treatment of various neuropsychiatric and pain disorders in patients with difficulty swallowing, according to a release from Sun Pharma. It can be swallowed whole, sprinkled on applesauce, or administered via nasogastric tube.
Difficulty swallowing affects approximately 30%-35% of long-term care residents, but the main alternative – crushing tablets – introduces risks of its own to the administration process.
This sprinkle is indicated for the treatment of major depressive disorder in adults, generalized anxiety disorder in patients aged 7 years and older, diabetic peripheral neuropathic pain in adults, and chronic musculoskeletal pain in adults. It was approved by the Food and Drug Administration for these indications July 19, 2019.
It carries a boxed warning for suicidal thoughts and behaviors. The most common adverse reactions (5% or more of treated participants and twice the incidence with placebo) were nausea, dry mouth, somnolence, constipation, decreased appetite, and hyperhidrosis. The full prescribing information can be found on the FDA website.
[email protected]
Drizalma Sprinkle (duloxetine delayed-release capsule) has launched for the treatment of various neuropsychiatric and pain disorders in patients with difficulty swallowing, according to a release from Sun Pharma. It can be swallowed whole, sprinkled on applesauce, or administered via nasogastric tube.
Difficulty swallowing affects approximately 30%-35% of long-term care residents, but the main alternative – crushing tablets – introduces risks of its own to the administration process.
This sprinkle is indicated for the treatment of major depressive disorder in adults, generalized anxiety disorder in patients aged 7 years and older, diabetic peripheral neuropathic pain in adults, and chronic musculoskeletal pain in adults. It was approved by the Food and Drug Administration for these indications July 19, 2019.
It carries a boxed warning for suicidal thoughts and behaviors. The most common adverse reactions (5% or more of treated participants and twice the incidence with placebo) were nausea, dry mouth, somnolence, constipation, decreased appetite, and hyperhidrosis. The full prescribing information can be found on the FDA website.
[email protected]
Drizalma Sprinkle (duloxetine delayed-release capsule) has launched for the treatment of various neuropsychiatric and pain disorders in patients with difficulty swallowing, according to a release from Sun Pharma. It can be swallowed whole, sprinkled on applesauce, or administered via nasogastric tube.
Difficulty swallowing affects approximately 30%-35% of long-term care residents, but the main alternative – crushing tablets – introduces risks of its own to the administration process.
This sprinkle is indicated for the treatment of major depressive disorder in adults, generalized anxiety disorder in patients aged 7 years and older, diabetic peripheral neuropathic pain in adults, and chronic musculoskeletal pain in adults. It was approved by the Food and Drug Administration for these indications July 19, 2019.
It carries a boxed warning for suicidal thoughts and behaviors. The most common adverse reactions (5% or more of treated participants and twice the incidence with placebo) were nausea, dry mouth, somnolence, constipation, decreased appetite, and hyperhidrosis. The full prescribing information can be found on the FDA website.
[email protected]
Study: Half of college women exhibited binge eating symptoms
Approximately half of college-aged women exhibit binge eating symptoms, and these women scored significantly higher on measures of depression, stress, and anxiety than do non–binge eaters, based on data from 154 women at a Palestine Polytechnic University in Hebron.
Previous studies show that binge eating disorder is multifactorial and associated with depression and anxiety, however, “To our knowledge, no study has yet assessed the prevalence of binge eating symptoms among female university students,” wrote Manal M. Badrasawi, PhD, of An-Najah National University, Tulkarm, Palestine, and colleagues.
In a cross-sectional study published in the Journal of Eating Disorders, the researchers interviewed 154 female college students in Palestine using the using BEDS-7 (Binge Eating Disorder Screener-7). The average age of the participants was 20 years.
Overall, 50% of the students showed positive binge eating symptoms, and these individuals had significantly higher scores on measures of depression, stress, and anxiety compared to individuals without binge eating symptoms.
Binge eating also was significantly associated with greater frequency of eating between meals and increased snacking, but no significant association was noted between binge eating and sociodemographic variables, including place of residence, marital status, and years of study. Binge eating was not significantly associated with weight status.
The researchers had no financial conflicts to disclose.
SOURCE: Badrasawi MM et al. J Eat Disord. 2019 Oct 2;7:33. doi: 10.1186/s40337-019-0263-1.2019.
Approximately half of college-aged women exhibit binge eating symptoms, and these women scored significantly higher on measures of depression, stress, and anxiety than do non–binge eaters, based on data from 154 women at a Palestine Polytechnic University in Hebron.
Previous studies show that binge eating disorder is multifactorial and associated with depression and anxiety, however, “To our knowledge, no study has yet assessed the prevalence of binge eating symptoms among female university students,” wrote Manal M. Badrasawi, PhD, of An-Najah National University, Tulkarm, Palestine, and colleagues.
In a cross-sectional study published in the Journal of Eating Disorders, the researchers interviewed 154 female college students in Palestine using the using BEDS-7 (Binge Eating Disorder Screener-7). The average age of the participants was 20 years.
Overall, 50% of the students showed positive binge eating symptoms, and these individuals had significantly higher scores on measures of depression, stress, and anxiety compared to individuals without binge eating symptoms.
Binge eating also was significantly associated with greater frequency of eating between meals and increased snacking, but no significant association was noted between binge eating and sociodemographic variables, including place of residence, marital status, and years of study. Binge eating was not significantly associated with weight status.
The researchers had no financial conflicts to disclose.
SOURCE: Badrasawi MM et al. J Eat Disord. 2019 Oct 2;7:33. doi: 10.1186/s40337-019-0263-1.2019.
Approximately half of college-aged women exhibit binge eating symptoms, and these women scored significantly higher on measures of depression, stress, and anxiety than do non–binge eaters, based on data from 154 women at a Palestine Polytechnic University in Hebron.
Previous studies show that binge eating disorder is multifactorial and associated with depression and anxiety, however, “To our knowledge, no study has yet assessed the prevalence of binge eating symptoms among female university students,” wrote Manal M. Badrasawi, PhD, of An-Najah National University, Tulkarm, Palestine, and colleagues.
In a cross-sectional study published in the Journal of Eating Disorders, the researchers interviewed 154 female college students in Palestine using the using BEDS-7 (Binge Eating Disorder Screener-7). The average age of the participants was 20 years.
Overall, 50% of the students showed positive binge eating symptoms, and these individuals had significantly higher scores on measures of depression, stress, and anxiety compared to individuals without binge eating symptoms.
Binge eating also was significantly associated with greater frequency of eating between meals and increased snacking, but no significant association was noted between binge eating and sociodemographic variables, including place of residence, marital status, and years of study. Binge eating was not significantly associated with weight status.
The researchers had no financial conflicts to disclose.
SOURCE: Badrasawi MM et al. J Eat Disord. 2019 Oct 2;7:33. doi: 10.1186/s40337-019-0263-1.2019.
FROM THE JOURNAL OF EATING DISORDERS
Elagolix with add-back therapy appears efficacious despite uterine and fibroid factors
PHILADELPHIA – according to results presented at the annual meeting of the American Society for Reproductive Medicine.
Ayman Al-Hendy, MD, PhD, director of translational research at the University of Illinois at Chicago, and associates, analyzed a pooled subgroup of 790 patients from the Elaris UF-1 and UF-2 trials who received elagolix twice daily at a dose of 300 mg (199 patients), elagolix 300 mg twice daily with add-back therapy (1 mg of estradiol plus 0.5 mg of norethindrone acetate; 395 patients), and a placebo group (196 patients) for treatment of heavy menstrual bleeding. Patients were premenopausal women aged 18-51 years with more than 80 mL of menstrual blood loss per cycle. The study design included a washout period, followed by a 2.5-month to 3.5-month screening period, and patients were randomized to 6 months of treatment with placebo, elagolix alone, or elagolix with add-back therapy in a 1:1:2 ratio. Researchers evaluated whether patients had less than 80 mL of menstrual blood loss per cycle and a 50% or more reduction in menstrual blood loss per cycle by the end of the study.
In a subgroup analysis, they also analyzed primary fibroid volume, fibroid stage, and uterine volume. The median primary fibroid volume was 36.2 cm3 (range, 1.0-1,081.5 cm3). Fibroid location was classified using the International Federation of Gynecology and Obstetrics (FIGO) staging system, and researchers placed fibroids into FIGO 0-3, FIGO 4, and FIGO 5-8 groups. At baseline, characteristics between groups were similar, but the patients who received elagolix alone had a lower number of fibroids classified as FIGO 0-3 and had a greater percentage of fibroids less than 36.2 cm3. The median uterine volume was 356.5 cm3 (range, 71.6-3,347.9 cm3).
At final follow-up, 81% of patients receiving elagolix alone and 72% of patients receiving elagolix with add-back therapy responded to treatment, compared with placebo (9%).
Patients receiving elagolix plus add-back therapy responded to treatment better than placebo, and there were no significant differences in outcomes in terms of FIGO stage: Response was as follows for patients with FIGO 0-3 classified fibroids (78% of 47 patients vs. 9% of 25 patients), FIGO 4 fibroids (68% of 177 patients vs. 15% of 85 patients) and FIGO 5-8 fibroids (74% of 165 patients vs. 4% of 82 patients). The same was true in terms of both primary fibroid volume and uterine volume in patients who received elagolix plus add-back therapy, compared with those who received placebo: Patients with a primary fibroid volume of less than 36.2 cm3 (74% of 189 patients vs. 15% of 92 patients) responded similarly to elagolix plus add-back therapy as did patients with a primary fibroid volume greater than 36.2 cm3 (70% of 200 patients vs. 5% of 100 patients), and there were no significant differences between the treatment response of patients with a uterine volume less than 365.5 cm3 (75% of 203 patients vs. 15% of 88 patients) and a uterine volume greater than 365.5 cm3 (70% of 192 patients vs. 5% of 108 patients).
“These really are very encouraging results and suggests that, in women with different fibroids, elagolix with add-back therapy would be an effective treatment option despite uterine and fibroid volume and location of fibroids,” said Dr. Al-Hendy.
Dr. Al-Hendy noted there are ongoing studies analyzing elagolix with add-back in women with fibroids, in women with endometriosis, and elagolix in women with polycystic ovary syndrome.
AbbVie recently submitted a new drug application to the Food and Drug Administration for elagolix based on results from these two trials. Elagolix, an oral GnRh receptor antagonist, is an FDA-approved oral medication for the management of endometriosis with associated moderate to severe pain.
This study was funded by AbbVie, and the company was involved in the study design, research, data collection, analysis and interpretation of the data, as well as the writing, reviewing and approving of the study for publication. The authors reported various relationships with industry, pharmaceutical companies, government entities, and other organizations.
SOURCE: Al-Hendy A et al. ASRM 2019, Abstract O-205.
PHILADELPHIA – according to results presented at the annual meeting of the American Society for Reproductive Medicine.
Ayman Al-Hendy, MD, PhD, director of translational research at the University of Illinois at Chicago, and associates, analyzed a pooled subgroup of 790 patients from the Elaris UF-1 and UF-2 trials who received elagolix twice daily at a dose of 300 mg (199 patients), elagolix 300 mg twice daily with add-back therapy (1 mg of estradiol plus 0.5 mg of norethindrone acetate; 395 patients), and a placebo group (196 patients) for treatment of heavy menstrual bleeding. Patients were premenopausal women aged 18-51 years with more than 80 mL of menstrual blood loss per cycle. The study design included a washout period, followed by a 2.5-month to 3.5-month screening period, and patients were randomized to 6 months of treatment with placebo, elagolix alone, or elagolix with add-back therapy in a 1:1:2 ratio. Researchers evaluated whether patients had less than 80 mL of menstrual blood loss per cycle and a 50% or more reduction in menstrual blood loss per cycle by the end of the study.
In a subgroup analysis, they also analyzed primary fibroid volume, fibroid stage, and uterine volume. The median primary fibroid volume was 36.2 cm3 (range, 1.0-1,081.5 cm3). Fibroid location was classified using the International Federation of Gynecology and Obstetrics (FIGO) staging system, and researchers placed fibroids into FIGO 0-3, FIGO 4, and FIGO 5-8 groups. At baseline, characteristics between groups were similar, but the patients who received elagolix alone had a lower number of fibroids classified as FIGO 0-3 and had a greater percentage of fibroids less than 36.2 cm3. The median uterine volume was 356.5 cm3 (range, 71.6-3,347.9 cm3).
At final follow-up, 81% of patients receiving elagolix alone and 72% of patients receiving elagolix with add-back therapy responded to treatment, compared with placebo (9%).
Patients receiving elagolix plus add-back therapy responded to treatment better than placebo, and there were no significant differences in outcomes in terms of FIGO stage: Response was as follows for patients with FIGO 0-3 classified fibroids (78% of 47 patients vs. 9% of 25 patients), FIGO 4 fibroids (68% of 177 patients vs. 15% of 85 patients) and FIGO 5-8 fibroids (74% of 165 patients vs. 4% of 82 patients). The same was true in terms of both primary fibroid volume and uterine volume in patients who received elagolix plus add-back therapy, compared with those who received placebo: Patients with a primary fibroid volume of less than 36.2 cm3 (74% of 189 patients vs. 15% of 92 patients) responded similarly to elagolix plus add-back therapy as did patients with a primary fibroid volume greater than 36.2 cm3 (70% of 200 patients vs. 5% of 100 patients), and there were no significant differences between the treatment response of patients with a uterine volume less than 365.5 cm3 (75% of 203 patients vs. 15% of 88 patients) and a uterine volume greater than 365.5 cm3 (70% of 192 patients vs. 5% of 108 patients).
“These really are very encouraging results and suggests that, in women with different fibroids, elagolix with add-back therapy would be an effective treatment option despite uterine and fibroid volume and location of fibroids,” said Dr. Al-Hendy.
Dr. Al-Hendy noted there are ongoing studies analyzing elagolix with add-back in women with fibroids, in women with endometriosis, and elagolix in women with polycystic ovary syndrome.
AbbVie recently submitted a new drug application to the Food and Drug Administration for elagolix based on results from these two trials. Elagolix, an oral GnRh receptor antagonist, is an FDA-approved oral medication for the management of endometriosis with associated moderate to severe pain.
This study was funded by AbbVie, and the company was involved in the study design, research, data collection, analysis and interpretation of the data, as well as the writing, reviewing and approving of the study for publication. The authors reported various relationships with industry, pharmaceutical companies, government entities, and other organizations.
SOURCE: Al-Hendy A et al. ASRM 2019, Abstract O-205.
PHILADELPHIA – according to results presented at the annual meeting of the American Society for Reproductive Medicine.
Ayman Al-Hendy, MD, PhD, director of translational research at the University of Illinois at Chicago, and associates, analyzed a pooled subgroup of 790 patients from the Elaris UF-1 and UF-2 trials who received elagolix twice daily at a dose of 300 mg (199 patients), elagolix 300 mg twice daily with add-back therapy (1 mg of estradiol plus 0.5 mg of norethindrone acetate; 395 patients), and a placebo group (196 patients) for treatment of heavy menstrual bleeding. Patients were premenopausal women aged 18-51 years with more than 80 mL of menstrual blood loss per cycle. The study design included a washout period, followed by a 2.5-month to 3.5-month screening period, and patients were randomized to 6 months of treatment with placebo, elagolix alone, or elagolix with add-back therapy in a 1:1:2 ratio. Researchers evaluated whether patients had less than 80 mL of menstrual blood loss per cycle and a 50% or more reduction in menstrual blood loss per cycle by the end of the study.
In a subgroup analysis, they also analyzed primary fibroid volume, fibroid stage, and uterine volume. The median primary fibroid volume was 36.2 cm3 (range, 1.0-1,081.5 cm3). Fibroid location was classified using the International Federation of Gynecology and Obstetrics (FIGO) staging system, and researchers placed fibroids into FIGO 0-3, FIGO 4, and FIGO 5-8 groups. At baseline, characteristics between groups were similar, but the patients who received elagolix alone had a lower number of fibroids classified as FIGO 0-3 and had a greater percentage of fibroids less than 36.2 cm3. The median uterine volume was 356.5 cm3 (range, 71.6-3,347.9 cm3).
At final follow-up, 81% of patients receiving elagolix alone and 72% of patients receiving elagolix with add-back therapy responded to treatment, compared with placebo (9%).
Patients receiving elagolix plus add-back therapy responded to treatment better than placebo, and there were no significant differences in outcomes in terms of FIGO stage: Response was as follows for patients with FIGO 0-3 classified fibroids (78% of 47 patients vs. 9% of 25 patients), FIGO 4 fibroids (68% of 177 patients vs. 15% of 85 patients) and FIGO 5-8 fibroids (74% of 165 patients vs. 4% of 82 patients). The same was true in terms of both primary fibroid volume and uterine volume in patients who received elagolix plus add-back therapy, compared with those who received placebo: Patients with a primary fibroid volume of less than 36.2 cm3 (74% of 189 patients vs. 15% of 92 patients) responded similarly to elagolix plus add-back therapy as did patients with a primary fibroid volume greater than 36.2 cm3 (70% of 200 patients vs. 5% of 100 patients), and there were no significant differences between the treatment response of patients with a uterine volume less than 365.5 cm3 (75% of 203 patients vs. 15% of 88 patients) and a uterine volume greater than 365.5 cm3 (70% of 192 patients vs. 5% of 108 patients).
“These really are very encouraging results and suggests that, in women with different fibroids, elagolix with add-back therapy would be an effective treatment option despite uterine and fibroid volume and location of fibroids,” said Dr. Al-Hendy.
Dr. Al-Hendy noted there are ongoing studies analyzing elagolix with add-back in women with fibroids, in women with endometriosis, and elagolix in women with polycystic ovary syndrome.
AbbVie recently submitted a new drug application to the Food and Drug Administration for elagolix based on results from these two trials. Elagolix, an oral GnRh receptor antagonist, is an FDA-approved oral medication for the management of endometriosis with associated moderate to severe pain.
This study was funded by AbbVie, and the company was involved in the study design, research, data collection, analysis and interpretation of the data, as well as the writing, reviewing and approving of the study for publication. The authors reported various relationships with industry, pharmaceutical companies, government entities, and other organizations.
SOURCE: Al-Hendy A et al. ASRM 2019, Abstract O-205.
REPORTING FROM ASRM 2019
Consider treating ovarian torsion with conservative surgery in young women
PHILADELPHIA – Women with ovarian torsion had a lower rate of perioperative complications when treated with conservative surgery, compared with oophorectomy, according to results from a retrospective study presented at the annual meeting of the American Society for Reproductive Medicine.
The effectiveness of laparoscopy and conservative surgery has increased in recent years, but over 75% of women with ovarian torsion in the study were treated with oophorectomy and 60% underwent a laparotomy, said Rachel S. Mandelbaum, MD, of the department of obstetrics & gynecology at the University of Southern California, Los Angeles.
“We believe that conservative surgery should be performed whenever possible in young women with ovarian torsion regardless of the appearance of the ovary intraoperatively,” said Dr. Mandelbaum.
The researchers performed a retrospective, observational study of 89,801 women in the Nationwide Inpatient Sample who were younger than age 50 years, were diagnosed with ovarian torsion during Jan. 2001–Sept. 2015, and were treated with conservative surgery or oophorectomy. Patients were excluded if they had malignancy, were older than 50 years of age, or their surgery information was unavailable. The majority of patients in the study were white (46%), nonobese (91%), without comorbidities, privately insured (59%), and were seen at a large (61%) urban hospital (51% teaching; 38% nonteaching).
Dr. Mandelbaum and colleagues found 78% of patients received a cystectomy, 19% had cyst drainage, 11% had detorsion alone, and 0.5% had an oophoropexy, with less than 10% of patients having a combination of cystectomy, cyst drainage, and oophoropexy. According to a multivariable analysis, patients who were treated with conservative surgery were more likely to be young, have a high income, live in the northeastern United States, be treated with laparoscopy, and be seen at a large hospital or teaching hospital (P less than .001). Oophorectomy was more common in patients with a high number of comorbidities and in patients with morbid obesity (P less than .001).
Between 2001 and 2015, the rate of conservative surgery increased from 19% to 25% (P less than .001); however, the rate of conservative surgery by age was nearly 40% in pediatric patients up to 15 years old, while the rate of conservative surgery declined by almost half until 35 years, followed by a further decline until age 50 years, said Dr. Mandelbaum. Use of laparoscopy also increased from 31% in 2001 to 42% in 2015 (P less than .001).
Overall, 20,643 patients underwent conservative surgery and 69,157 patients received an oophorectomy. Patients in the conservative surgery group were more likely to undergo a conservative surgery with a laparoscopic surgical approach (51%) than a laparotomy (41%), while patients receiving an oophorectomy were more likely to have a laparotomy (67%) than a laparoscopic surgical approach (33%). In 1,663 conservative surgeries (8%), the approach was unknown.
(odds ratio, 0.57; 95% confidence interval, 0.57-0.78; P less than .001), but there was a similar rate of venous thromboembolism (0.3% vs. 0.2%; P equals .568) and sepsis (0.3% vs. 0.3%; P equals .865) in each group.
Dr. Mandelbaum attributed the high rate of oophorectomies in the study to “differential uptake of evidence” in different areas of the United States, fear of complications from leaving an infected ovary in situ, or the surgeon’s belief that the ovary is not viable because of its color intraoperatively. “We know from animal and human studies that the intraoperative appearance of the ovary does not correlate to viability, and that 90% of black or blue ovaries regain function and subsequently appear normal on both transvaginal ultrasound or on a second look grossly,” she said. Oophorectomy rates also vary by surgeon, and gynecologists are more likely to perform conservative surgery, she added.
The researchers said they were unable to obtain data on specific surgical variables such as the size of the mass, time to surgery, intraoperative appearance, laterality, fertility wishes of the patient, and surgeon type. There were also no postdischarge data, or information on the timing of complications.
Dr. Mandelbaum reported no relevant conflicts of interest.
SOURCE: Mandelbaum RS et al. ASRM 2019. Abstract O-96.
PHILADELPHIA – Women with ovarian torsion had a lower rate of perioperative complications when treated with conservative surgery, compared with oophorectomy, according to results from a retrospective study presented at the annual meeting of the American Society for Reproductive Medicine.
The effectiveness of laparoscopy and conservative surgery has increased in recent years, but over 75% of women with ovarian torsion in the study were treated with oophorectomy and 60% underwent a laparotomy, said Rachel S. Mandelbaum, MD, of the department of obstetrics & gynecology at the University of Southern California, Los Angeles.
“We believe that conservative surgery should be performed whenever possible in young women with ovarian torsion regardless of the appearance of the ovary intraoperatively,” said Dr. Mandelbaum.
The researchers performed a retrospective, observational study of 89,801 women in the Nationwide Inpatient Sample who were younger than age 50 years, were diagnosed with ovarian torsion during Jan. 2001–Sept. 2015, and were treated with conservative surgery or oophorectomy. Patients were excluded if they had malignancy, were older than 50 years of age, or their surgery information was unavailable. The majority of patients in the study were white (46%), nonobese (91%), without comorbidities, privately insured (59%), and were seen at a large (61%) urban hospital (51% teaching; 38% nonteaching).
Dr. Mandelbaum and colleagues found 78% of patients received a cystectomy, 19% had cyst drainage, 11% had detorsion alone, and 0.5% had an oophoropexy, with less than 10% of patients having a combination of cystectomy, cyst drainage, and oophoropexy. According to a multivariable analysis, patients who were treated with conservative surgery were more likely to be young, have a high income, live in the northeastern United States, be treated with laparoscopy, and be seen at a large hospital or teaching hospital (P less than .001). Oophorectomy was more common in patients with a high number of comorbidities and in patients with morbid obesity (P less than .001).
Between 2001 and 2015, the rate of conservative surgery increased from 19% to 25% (P less than .001); however, the rate of conservative surgery by age was nearly 40% in pediatric patients up to 15 years old, while the rate of conservative surgery declined by almost half until 35 years, followed by a further decline until age 50 years, said Dr. Mandelbaum. Use of laparoscopy also increased from 31% in 2001 to 42% in 2015 (P less than .001).
Overall, 20,643 patients underwent conservative surgery and 69,157 patients received an oophorectomy. Patients in the conservative surgery group were more likely to undergo a conservative surgery with a laparoscopic surgical approach (51%) than a laparotomy (41%), while patients receiving an oophorectomy were more likely to have a laparotomy (67%) than a laparoscopic surgical approach (33%). In 1,663 conservative surgeries (8%), the approach was unknown.
(odds ratio, 0.57; 95% confidence interval, 0.57-0.78; P less than .001), but there was a similar rate of venous thromboembolism (0.3% vs. 0.2%; P equals .568) and sepsis (0.3% vs. 0.3%; P equals .865) in each group.
Dr. Mandelbaum attributed the high rate of oophorectomies in the study to “differential uptake of evidence” in different areas of the United States, fear of complications from leaving an infected ovary in situ, or the surgeon’s belief that the ovary is not viable because of its color intraoperatively. “We know from animal and human studies that the intraoperative appearance of the ovary does not correlate to viability, and that 90% of black or blue ovaries regain function and subsequently appear normal on both transvaginal ultrasound or on a second look grossly,” she said. Oophorectomy rates also vary by surgeon, and gynecologists are more likely to perform conservative surgery, she added.
The researchers said they were unable to obtain data on specific surgical variables such as the size of the mass, time to surgery, intraoperative appearance, laterality, fertility wishes of the patient, and surgeon type. There were also no postdischarge data, or information on the timing of complications.
Dr. Mandelbaum reported no relevant conflicts of interest.
SOURCE: Mandelbaum RS et al. ASRM 2019. Abstract O-96.
PHILADELPHIA – Women with ovarian torsion had a lower rate of perioperative complications when treated with conservative surgery, compared with oophorectomy, according to results from a retrospective study presented at the annual meeting of the American Society for Reproductive Medicine.
The effectiveness of laparoscopy and conservative surgery has increased in recent years, but over 75% of women with ovarian torsion in the study were treated with oophorectomy and 60% underwent a laparotomy, said Rachel S. Mandelbaum, MD, of the department of obstetrics & gynecology at the University of Southern California, Los Angeles.
“We believe that conservative surgery should be performed whenever possible in young women with ovarian torsion regardless of the appearance of the ovary intraoperatively,” said Dr. Mandelbaum.
The researchers performed a retrospective, observational study of 89,801 women in the Nationwide Inpatient Sample who were younger than age 50 years, were diagnosed with ovarian torsion during Jan. 2001–Sept. 2015, and were treated with conservative surgery or oophorectomy. Patients were excluded if they had malignancy, were older than 50 years of age, or their surgery information was unavailable. The majority of patients in the study were white (46%), nonobese (91%), without comorbidities, privately insured (59%), and were seen at a large (61%) urban hospital (51% teaching; 38% nonteaching).
Dr. Mandelbaum and colleagues found 78% of patients received a cystectomy, 19% had cyst drainage, 11% had detorsion alone, and 0.5% had an oophoropexy, with less than 10% of patients having a combination of cystectomy, cyst drainage, and oophoropexy. According to a multivariable analysis, patients who were treated with conservative surgery were more likely to be young, have a high income, live in the northeastern United States, be treated with laparoscopy, and be seen at a large hospital or teaching hospital (P less than .001). Oophorectomy was more common in patients with a high number of comorbidities and in patients with morbid obesity (P less than .001).
Between 2001 and 2015, the rate of conservative surgery increased from 19% to 25% (P less than .001); however, the rate of conservative surgery by age was nearly 40% in pediatric patients up to 15 years old, while the rate of conservative surgery declined by almost half until 35 years, followed by a further decline until age 50 years, said Dr. Mandelbaum. Use of laparoscopy also increased from 31% in 2001 to 42% in 2015 (P less than .001).
Overall, 20,643 patients underwent conservative surgery and 69,157 patients received an oophorectomy. Patients in the conservative surgery group were more likely to undergo a conservative surgery with a laparoscopic surgical approach (51%) than a laparotomy (41%), while patients receiving an oophorectomy were more likely to have a laparotomy (67%) than a laparoscopic surgical approach (33%). In 1,663 conservative surgeries (8%), the approach was unknown.
(odds ratio, 0.57; 95% confidence interval, 0.57-0.78; P less than .001), but there was a similar rate of venous thromboembolism (0.3% vs. 0.2%; P equals .568) and sepsis (0.3% vs. 0.3%; P equals .865) in each group.
Dr. Mandelbaum attributed the high rate of oophorectomies in the study to “differential uptake of evidence” in different areas of the United States, fear of complications from leaving an infected ovary in situ, or the surgeon’s belief that the ovary is not viable because of its color intraoperatively. “We know from animal and human studies that the intraoperative appearance of the ovary does not correlate to viability, and that 90% of black or blue ovaries regain function and subsequently appear normal on both transvaginal ultrasound or on a second look grossly,” she said. Oophorectomy rates also vary by surgeon, and gynecologists are more likely to perform conservative surgery, she added.
The researchers said they were unable to obtain data on specific surgical variables such as the size of the mass, time to surgery, intraoperative appearance, laterality, fertility wishes of the patient, and surgeon type. There were also no postdischarge data, or information on the timing of complications.
Dr. Mandelbaum reported no relevant conflicts of interest.
SOURCE: Mandelbaum RS et al. ASRM 2019. Abstract O-96.
REPORTING FROM ASRM 2019
In utero Zika exposure can have delayed consequences
WASHINGTON – Evidence continues to mount that infants born to moms infected with Zika virus during pregnancy can have neurodevelopmental abnormalities as they age even if they showed no defects at birth, based on follow-up of 890 Colombian children tracked by epidemiologists from the U.S. Centers for Disease Control and Prevention.
Among the 890 neonates born to mothers apparently infected with Zika during pregnancy and followed for up to 2 years, 40 of the 852 (5%) without a detectable birth defect at delivery went on to show some type of neurodevelopmental sequelae during up to 24 months of age, Margaret Honein, PhD, said at an annual scientific meeting on infectious diseases.
In addition, among the children without birth defects at delivery who received follow-up examinations out to about 2 years, the incidence of “alerts” for possible neurodevelopmental issues was 15%-20% for each of the four domains studied (gross motor, fine motor, hearing and language, and personal and social functions), said Dr. Honein, an epidemiologist and chief of the birth defects branch of the CDC. In contrast, 17 of the 38 children (45%) followed who had identifiable birth defects at delivery also showed neurodevelopmental abnormalities when reexamined as long as 2 years after birth. These possible neurodevelopmental abnormalities, designated as alerts, were identified in comparison with a contemporaneous cohort of children born to uninfected mothers in the same regions of Colombia and assessed by the CDC researchers.
This cohort of children born to mothers who became infected with Zika virus during the 2016 Colombian epidemic will not undergo any planned, additional follow-up beyond the initial 2 years, Dr. Honein noted.
The findings she reported were consistent with observations from a much smaller cohort of 70 infants born to Colombian mothers infected with Zika virus while pregnant who had a normal head circumference and a normal clinical examination at delivery. When assessed once or twice 4-18 months after birth, these 70 infants showed an overall greater than one standard deviation (z-score) drop in their scores on the Warner Initial Developmental Evaluation of Adaptive and Functional Skills (WIDEA) metric by 12 months after birth and continuing out to 18 months, said Sarah B. Mulkey, MD, a fetal-neonatal neurologist at Children’s National Health System in Washington. These deficits were especially pronounced in the mobility and social cognition domains of the four-domain WIDEA metric. The social cognition domain is an important predictor of later problems with executive function and other neurologic disorders, Dr. Mulkey said while reporting her findings in a separate talk at the meeting. She acknowledged that the analysis was flawed by comparing the WIDEA outcomes of the Zika virus–exposed children to healthy children from either inner-city Chicago or Canada. Dr. Mulkey said that she and her associates plan to characterize a population of Zika virus–unexposed children in Colombia to use for future comparisons.
The study reported by Dr. Honein involved an enhanced surveillance program launched by the CDC in 2016 in three regions of Colombia and included 1,190 pregnancies accompanied by Zika symptoms in the mother and with a reported pregnancy outcome, including 1,185 live births. Nearly half of the Zika infections occurred during the first trimester, and 34% occurred during the second trimester. However, fewer than a third of the pregnant women underwent some type of laboratory testing to confirm their infection, either by serology or by a DNA-based assay, and of these 28% had a positive finding. Dr. Honein cautioned that many of the specimens that tested negative for Zika virus may have been false negatives.
The birth defects identified among the infants born from an apparently affected pregnancy included brain abnormalities, eye anomalies, and microcephaly, with 5% of the 1,185 live births showing one or more of these outcomes. The neurodevelopmental deficits identified during follow-up of 890 of the children out to 2 years included seizures; abnormalities of tone, movement, or swallowing; and impairments of vision or hearing.
WASHINGTON – Evidence continues to mount that infants born to moms infected with Zika virus during pregnancy can have neurodevelopmental abnormalities as they age even if they showed no defects at birth, based on follow-up of 890 Colombian children tracked by epidemiologists from the U.S. Centers for Disease Control and Prevention.
Among the 890 neonates born to mothers apparently infected with Zika during pregnancy and followed for up to 2 years, 40 of the 852 (5%) without a detectable birth defect at delivery went on to show some type of neurodevelopmental sequelae during up to 24 months of age, Margaret Honein, PhD, said at an annual scientific meeting on infectious diseases.
In addition, among the children without birth defects at delivery who received follow-up examinations out to about 2 years, the incidence of “alerts” for possible neurodevelopmental issues was 15%-20% for each of the four domains studied (gross motor, fine motor, hearing and language, and personal and social functions), said Dr. Honein, an epidemiologist and chief of the birth defects branch of the CDC. In contrast, 17 of the 38 children (45%) followed who had identifiable birth defects at delivery also showed neurodevelopmental abnormalities when reexamined as long as 2 years after birth. These possible neurodevelopmental abnormalities, designated as alerts, were identified in comparison with a contemporaneous cohort of children born to uninfected mothers in the same regions of Colombia and assessed by the CDC researchers.
This cohort of children born to mothers who became infected with Zika virus during the 2016 Colombian epidemic will not undergo any planned, additional follow-up beyond the initial 2 years, Dr. Honein noted.
The findings she reported were consistent with observations from a much smaller cohort of 70 infants born to Colombian mothers infected with Zika virus while pregnant who had a normal head circumference and a normal clinical examination at delivery. When assessed once or twice 4-18 months after birth, these 70 infants showed an overall greater than one standard deviation (z-score) drop in their scores on the Warner Initial Developmental Evaluation of Adaptive and Functional Skills (WIDEA) metric by 12 months after birth and continuing out to 18 months, said Sarah B. Mulkey, MD, a fetal-neonatal neurologist at Children’s National Health System in Washington. These deficits were especially pronounced in the mobility and social cognition domains of the four-domain WIDEA metric. The social cognition domain is an important predictor of later problems with executive function and other neurologic disorders, Dr. Mulkey said while reporting her findings in a separate talk at the meeting. She acknowledged that the analysis was flawed by comparing the WIDEA outcomes of the Zika virus–exposed children to healthy children from either inner-city Chicago or Canada. Dr. Mulkey said that she and her associates plan to characterize a population of Zika virus–unexposed children in Colombia to use for future comparisons.
The study reported by Dr. Honein involved an enhanced surveillance program launched by the CDC in 2016 in three regions of Colombia and included 1,190 pregnancies accompanied by Zika symptoms in the mother and with a reported pregnancy outcome, including 1,185 live births. Nearly half of the Zika infections occurred during the first trimester, and 34% occurred during the second trimester. However, fewer than a third of the pregnant women underwent some type of laboratory testing to confirm their infection, either by serology or by a DNA-based assay, and of these 28% had a positive finding. Dr. Honein cautioned that many of the specimens that tested negative for Zika virus may have been false negatives.
The birth defects identified among the infants born from an apparently affected pregnancy included brain abnormalities, eye anomalies, and microcephaly, with 5% of the 1,185 live births showing one or more of these outcomes. The neurodevelopmental deficits identified during follow-up of 890 of the children out to 2 years included seizures; abnormalities of tone, movement, or swallowing; and impairments of vision or hearing.
WASHINGTON – Evidence continues to mount that infants born to moms infected with Zika virus during pregnancy can have neurodevelopmental abnormalities as they age even if they showed no defects at birth, based on follow-up of 890 Colombian children tracked by epidemiologists from the U.S. Centers for Disease Control and Prevention.
Among the 890 neonates born to mothers apparently infected with Zika during pregnancy and followed for up to 2 years, 40 of the 852 (5%) without a detectable birth defect at delivery went on to show some type of neurodevelopmental sequelae during up to 24 months of age, Margaret Honein, PhD, said at an annual scientific meeting on infectious diseases.
In addition, among the children without birth defects at delivery who received follow-up examinations out to about 2 years, the incidence of “alerts” for possible neurodevelopmental issues was 15%-20% for each of the four domains studied (gross motor, fine motor, hearing and language, and personal and social functions), said Dr. Honein, an epidemiologist and chief of the birth defects branch of the CDC. In contrast, 17 of the 38 children (45%) followed who had identifiable birth defects at delivery also showed neurodevelopmental abnormalities when reexamined as long as 2 years after birth. These possible neurodevelopmental abnormalities, designated as alerts, were identified in comparison with a contemporaneous cohort of children born to uninfected mothers in the same regions of Colombia and assessed by the CDC researchers.
This cohort of children born to mothers who became infected with Zika virus during the 2016 Colombian epidemic will not undergo any planned, additional follow-up beyond the initial 2 years, Dr. Honein noted.
The findings she reported were consistent with observations from a much smaller cohort of 70 infants born to Colombian mothers infected with Zika virus while pregnant who had a normal head circumference and a normal clinical examination at delivery. When assessed once or twice 4-18 months after birth, these 70 infants showed an overall greater than one standard deviation (z-score) drop in their scores on the Warner Initial Developmental Evaluation of Adaptive and Functional Skills (WIDEA) metric by 12 months after birth and continuing out to 18 months, said Sarah B. Mulkey, MD, a fetal-neonatal neurologist at Children’s National Health System in Washington. These deficits were especially pronounced in the mobility and social cognition domains of the four-domain WIDEA metric. The social cognition domain is an important predictor of later problems with executive function and other neurologic disorders, Dr. Mulkey said while reporting her findings in a separate talk at the meeting. She acknowledged that the analysis was flawed by comparing the WIDEA outcomes of the Zika virus–exposed children to healthy children from either inner-city Chicago or Canada. Dr. Mulkey said that she and her associates plan to characterize a population of Zika virus–unexposed children in Colombia to use for future comparisons.
The study reported by Dr. Honein involved an enhanced surveillance program launched by the CDC in 2016 in three regions of Colombia and included 1,190 pregnancies accompanied by Zika symptoms in the mother and with a reported pregnancy outcome, including 1,185 live births. Nearly half of the Zika infections occurred during the first trimester, and 34% occurred during the second trimester. However, fewer than a third of the pregnant women underwent some type of laboratory testing to confirm their infection, either by serology or by a DNA-based assay, and of these 28% had a positive finding. Dr. Honein cautioned that many of the specimens that tested negative for Zika virus may have been false negatives.
The birth defects identified among the infants born from an apparently affected pregnancy included brain abnormalities, eye anomalies, and microcephaly, with 5% of the 1,185 live births showing one or more of these outcomes. The neurodevelopmental deficits identified during follow-up of 890 of the children out to 2 years included seizures; abnormalities of tone, movement, or swallowing; and impairments of vision or hearing.
REPORTING FROM ID WEEK 2019