User login
FDA panel leans toward more robust breast implant surveillance
SILVER SPRING, MD. – A mandatory, comprehensive approach to collecting adverse event data from breast implant recipients was favored during a March 25 hearing by a Food and Drug Administration advisory panel that oversees surgical devices.
This additional data could offer more complete information during the informed consent process for breast implants and potentially validate a new, autoimmune-like syndrome – breast implant illness (BII).
On the first day of a scheduled 2-day hearing, the advisory panel held no votes and took no formal actions. After a day of expert presentations and comments from more than 40 members of the public – mostly personal stories from affected patients and from plastic surgeons who place breast implants, panel members discussed a handful of questions from the FDA about relevant data to collect to better define the risks posed to breast implant recipients from breast-implant associated anaplastic large cell lymphoma (BIA-ALCL) and BII.
The advisory panel meeting took place as reports recently appeared documenting the scope of BIA-ALCL (Plast Reconstr Surg. 2019 March;143[3S]:65S-73S) and how to diagnose and manage BIA-ALCL (Aesthetic Surg J. 2019 March;39[S1}:S3-S13), and the existence of BII (Plast Reconstr Surg. 2019 March;143[3S]:74S-81S).
During the day’s two public comment periods, the panel heard from several women who gave brief accounts of developing and dealing with BIA-ALCL or BII.
“We think it’s important that all breast implant patients be aware of the risk for BIA-ALCL,” said Binita Ashar, MD, director of the FDAs Division of Surgical Devices. The FDA “is asking the panel what further steps need to be taken to understand the BIA-ALCL risk,” said Dr. Ashar as she opened the meeting of the General and Plastic Surgery Devices Panel of the Medical Devices Advisory Committee.
While the agency, as well as the plastic surgery community, have acknowledged the existence of BIA-ALCL since 2011, only recently have good data emerged on the scope of the complication. During the hearing, Mark W. Clemens, MD, a plastic surgeon at MD Anderson Cancer Center in Houston, reported on his analysis of 457 unique cases of BIA-ALCL reported to the FDA since 2011. He found that the vast majority of cases had occurred in women who had received textured implants while a relatively small minority were linked with the placement of smooth implants.
Further scrutiny of the reported details of each case showed that none of the lymphomas were linked with a confirmed instance of “pure” smooth implant exposure. He also estimated the U.S. incidence of BIA-ALCL as roughly one case for every 20,000 implants. Complete, en bloc removal of the implant seems to be the most effective way to treat the cancer; most explanted patients have a good prognosis, he said.
Despite the apparent link between textured implants specifically and onset of BIA-ALCL, some panel members did not see a ban on textured implants as the answer.
Texturing the implant helps to stabilize the implant in position. Without texturing “we would need to use something else to stabilize the implant, or there would be a tsunami of reoperations,” said panel member Mary H. McGrath, MD, professor of surgery at the University of California, San Francisco. The main alternative to texturing for stabilizing implants is to wrap them in place using surgical mesh, but that approach may also cause problems.
“Instead of just taking textured implants off the market, we need to also look at their advantages. A critical issue is informed consent,” said panel member Marc E. Lippman, MD, a professor of medicine at Georgetown University, Washington. Banning smooth implants based on what’s known so far “would be an extraordinary over reaction,” he said during the first day’s session.
Current U.S. anecdotal experience suggests that a ban may not even be necessary because “plastic surgeons are more and more walking away from textured implants” because of the apparent link to BIA-ALCL, Dr. McGrath said.
BII has been a more recent and more controversial complication of breast implants. As recently as September 2018, Dr. Ashar said in a written statement that “the agency continues to believe that the weight of the currently available scientific evidence does not conclusively demonstrate an association between breast implants and connective tissue diseases,” the types of symptoms that characterize BII.
While the panel heard no new, conclusive evidence of a causal link between breast implants and the range of symptoms that some implant recipients report and is now collectively known as BII, several participants seemed convinced that the syndrome was real and needed better surveillance and study.
“It’s in the same family as chronic fatigue syndrome and fibromyalgia. It’s not a diagnosis, but a set of symptoms.” said Benjamin O. Anderson, MD, a surgical oncologist and professor of surgery at the University of Washington in Seattle and a panel member. “It’s a giant challenge. BII is a constellation of difficult symptoms. We need to think about how we ask patients, what are your symptoms?”
Frank R. Lewis Jr., MD, committee chair, said a more standardized measure of the most common BII symptoms is needed. “That may be exceedingly difficult, with as many as a hundred reported symptoms,” said Dr. Lewis, executive director, emeritus, of the American Board of Surgery in Philadelphia.
The hearing featured results from some of the most research projects aimed at fleshing out an understanding of BII.
Diana Zuckerman, PhD, president of the National Center for Health Research, reported data she and her associates collected in an online survey completed in late 2018 and early 2019 by 449 women who had approached the Center for help in getting health insurance coverage for medically-necessary explantation of their breast implants.
Their most common symptoms included joint, muscle or back pain, weakness or stiffness; fatigue; “brain fog;” and anxiety and depression. More than two-thirds of the respondents had a family history and 3% had a personal history of an autoimmune disease, and 61% said their symptoms improved after their implants were removed, Dr. Zuckerman reported during her presentation to the panel.
During the discussion, panel members seemed intent on expanding mandatory, routine surveillance to all breast implants placed in U.S. practice.
Andrea L. Pusic, MD, president of the Plastic Surgery Foundation, summarized the recent launch of the National Breast Implant Registry by the Foundation and its parent organization, the American Society of Plastic Surgeons. These organizations, and plastic surgeons in general, would be amenable to collecting the data the FDA deemed necessary to better track BIA-ALCL and BII, said Dr. Pusic, professor of surgery at Harvard Medical School and chief of plastic and reconstructive surgery at Brigham and Women’s Hospital in Boston.
“Plastic surgeons are willing to enter these data because we know they are important,” she told the FDA panel.
Dr. Ashar, Dr. Clemens, Dr. McGrath, Dr. Lippman, Dr. Anderson, Dr. Lewis, Dr. Zuckerman, and Dr. Pusic reported having no relevant commercial disclosures.
SILVER SPRING, MD. – A mandatory, comprehensive approach to collecting adverse event data from breast implant recipients was favored during a March 25 hearing by a Food and Drug Administration advisory panel that oversees surgical devices.
This additional data could offer more complete information during the informed consent process for breast implants and potentially validate a new, autoimmune-like syndrome – breast implant illness (BII).
On the first day of a scheduled 2-day hearing, the advisory panel held no votes and took no formal actions. After a day of expert presentations and comments from more than 40 members of the public – mostly personal stories from affected patients and from plastic surgeons who place breast implants, panel members discussed a handful of questions from the FDA about relevant data to collect to better define the risks posed to breast implant recipients from breast-implant associated anaplastic large cell lymphoma (BIA-ALCL) and BII.
The advisory panel meeting took place as reports recently appeared documenting the scope of BIA-ALCL (Plast Reconstr Surg. 2019 March;143[3S]:65S-73S) and how to diagnose and manage BIA-ALCL (Aesthetic Surg J. 2019 March;39[S1}:S3-S13), and the existence of BII (Plast Reconstr Surg. 2019 March;143[3S]:74S-81S).
During the day’s two public comment periods, the panel heard from several women who gave brief accounts of developing and dealing with BIA-ALCL or BII.
“We think it’s important that all breast implant patients be aware of the risk for BIA-ALCL,” said Binita Ashar, MD, director of the FDAs Division of Surgical Devices. The FDA “is asking the panel what further steps need to be taken to understand the BIA-ALCL risk,” said Dr. Ashar as she opened the meeting of the General and Plastic Surgery Devices Panel of the Medical Devices Advisory Committee.
While the agency, as well as the plastic surgery community, have acknowledged the existence of BIA-ALCL since 2011, only recently have good data emerged on the scope of the complication. During the hearing, Mark W. Clemens, MD, a plastic surgeon at MD Anderson Cancer Center in Houston, reported on his analysis of 457 unique cases of BIA-ALCL reported to the FDA since 2011. He found that the vast majority of cases had occurred in women who had received textured implants while a relatively small minority were linked with the placement of smooth implants.
Further scrutiny of the reported details of each case showed that none of the lymphomas were linked with a confirmed instance of “pure” smooth implant exposure. He also estimated the U.S. incidence of BIA-ALCL as roughly one case for every 20,000 implants. Complete, en bloc removal of the implant seems to be the most effective way to treat the cancer; most explanted patients have a good prognosis, he said.
Despite the apparent link between textured implants specifically and onset of BIA-ALCL, some panel members did not see a ban on textured implants as the answer.
Texturing the implant helps to stabilize the implant in position. Without texturing “we would need to use something else to stabilize the implant, or there would be a tsunami of reoperations,” said panel member Mary H. McGrath, MD, professor of surgery at the University of California, San Francisco. The main alternative to texturing for stabilizing implants is to wrap them in place using surgical mesh, but that approach may also cause problems.
“Instead of just taking textured implants off the market, we need to also look at their advantages. A critical issue is informed consent,” said panel member Marc E. Lippman, MD, a professor of medicine at Georgetown University, Washington. Banning smooth implants based on what’s known so far “would be an extraordinary over reaction,” he said during the first day’s session.
Current U.S. anecdotal experience suggests that a ban may not even be necessary because “plastic surgeons are more and more walking away from textured implants” because of the apparent link to BIA-ALCL, Dr. McGrath said.
BII has been a more recent and more controversial complication of breast implants. As recently as September 2018, Dr. Ashar said in a written statement that “the agency continues to believe that the weight of the currently available scientific evidence does not conclusively demonstrate an association between breast implants and connective tissue diseases,” the types of symptoms that characterize BII.
While the panel heard no new, conclusive evidence of a causal link between breast implants and the range of symptoms that some implant recipients report and is now collectively known as BII, several participants seemed convinced that the syndrome was real and needed better surveillance and study.
“It’s in the same family as chronic fatigue syndrome and fibromyalgia. It’s not a diagnosis, but a set of symptoms.” said Benjamin O. Anderson, MD, a surgical oncologist and professor of surgery at the University of Washington in Seattle and a panel member. “It’s a giant challenge. BII is a constellation of difficult symptoms. We need to think about how we ask patients, what are your symptoms?”
Frank R. Lewis Jr., MD, committee chair, said a more standardized measure of the most common BII symptoms is needed. “That may be exceedingly difficult, with as many as a hundred reported symptoms,” said Dr. Lewis, executive director, emeritus, of the American Board of Surgery in Philadelphia.
The hearing featured results from some of the most research projects aimed at fleshing out an understanding of BII.
Diana Zuckerman, PhD, president of the National Center for Health Research, reported data she and her associates collected in an online survey completed in late 2018 and early 2019 by 449 women who had approached the Center for help in getting health insurance coverage for medically-necessary explantation of their breast implants.
Their most common symptoms included joint, muscle or back pain, weakness or stiffness; fatigue; “brain fog;” and anxiety and depression. More than two-thirds of the respondents had a family history and 3% had a personal history of an autoimmune disease, and 61% said their symptoms improved after their implants were removed, Dr. Zuckerman reported during her presentation to the panel.
During the discussion, panel members seemed intent on expanding mandatory, routine surveillance to all breast implants placed in U.S. practice.
Andrea L. Pusic, MD, president of the Plastic Surgery Foundation, summarized the recent launch of the National Breast Implant Registry by the Foundation and its parent organization, the American Society of Plastic Surgeons. These organizations, and plastic surgeons in general, would be amenable to collecting the data the FDA deemed necessary to better track BIA-ALCL and BII, said Dr. Pusic, professor of surgery at Harvard Medical School and chief of plastic and reconstructive surgery at Brigham and Women’s Hospital in Boston.
“Plastic surgeons are willing to enter these data because we know they are important,” she told the FDA panel.
Dr. Ashar, Dr. Clemens, Dr. McGrath, Dr. Lippman, Dr. Anderson, Dr. Lewis, Dr. Zuckerman, and Dr. Pusic reported having no relevant commercial disclosures.
SILVER SPRING, MD. – A mandatory, comprehensive approach to collecting adverse event data from breast implant recipients was favored during a March 25 hearing by a Food and Drug Administration advisory panel that oversees surgical devices.
This additional data could offer more complete information during the informed consent process for breast implants and potentially validate a new, autoimmune-like syndrome – breast implant illness (BII).
On the first day of a scheduled 2-day hearing, the advisory panel held no votes and took no formal actions. After a day of expert presentations and comments from more than 40 members of the public – mostly personal stories from affected patients and from plastic surgeons who place breast implants, panel members discussed a handful of questions from the FDA about relevant data to collect to better define the risks posed to breast implant recipients from breast-implant associated anaplastic large cell lymphoma (BIA-ALCL) and BII.
The advisory panel meeting took place as reports recently appeared documenting the scope of BIA-ALCL (Plast Reconstr Surg. 2019 March;143[3S]:65S-73S) and how to diagnose and manage BIA-ALCL (Aesthetic Surg J. 2019 March;39[S1}:S3-S13), and the existence of BII (Plast Reconstr Surg. 2019 March;143[3S]:74S-81S).
During the day’s two public comment periods, the panel heard from several women who gave brief accounts of developing and dealing with BIA-ALCL or BII.
“We think it’s important that all breast implant patients be aware of the risk for BIA-ALCL,” said Binita Ashar, MD, director of the FDAs Division of Surgical Devices. The FDA “is asking the panel what further steps need to be taken to understand the BIA-ALCL risk,” said Dr. Ashar as she opened the meeting of the General and Plastic Surgery Devices Panel of the Medical Devices Advisory Committee.
While the agency, as well as the plastic surgery community, have acknowledged the existence of BIA-ALCL since 2011, only recently have good data emerged on the scope of the complication. During the hearing, Mark W. Clemens, MD, a plastic surgeon at MD Anderson Cancer Center in Houston, reported on his analysis of 457 unique cases of BIA-ALCL reported to the FDA since 2011. He found that the vast majority of cases had occurred in women who had received textured implants while a relatively small minority were linked with the placement of smooth implants.
Further scrutiny of the reported details of each case showed that none of the lymphomas were linked with a confirmed instance of “pure” smooth implant exposure. He also estimated the U.S. incidence of BIA-ALCL as roughly one case for every 20,000 implants. Complete, en bloc removal of the implant seems to be the most effective way to treat the cancer; most explanted patients have a good prognosis, he said.
Despite the apparent link between textured implants specifically and onset of BIA-ALCL, some panel members did not see a ban on textured implants as the answer.
Texturing the implant helps to stabilize the implant in position. Without texturing “we would need to use something else to stabilize the implant, or there would be a tsunami of reoperations,” said panel member Mary H. McGrath, MD, professor of surgery at the University of California, San Francisco. The main alternative to texturing for stabilizing implants is to wrap them in place using surgical mesh, but that approach may also cause problems.
“Instead of just taking textured implants off the market, we need to also look at their advantages. A critical issue is informed consent,” said panel member Marc E. Lippman, MD, a professor of medicine at Georgetown University, Washington. Banning smooth implants based on what’s known so far “would be an extraordinary over reaction,” he said during the first day’s session.
Current U.S. anecdotal experience suggests that a ban may not even be necessary because “plastic surgeons are more and more walking away from textured implants” because of the apparent link to BIA-ALCL, Dr. McGrath said.
BII has been a more recent and more controversial complication of breast implants. As recently as September 2018, Dr. Ashar said in a written statement that “the agency continues to believe that the weight of the currently available scientific evidence does not conclusively demonstrate an association between breast implants and connective tissue diseases,” the types of symptoms that characterize BII.
While the panel heard no new, conclusive evidence of a causal link between breast implants and the range of symptoms that some implant recipients report and is now collectively known as BII, several participants seemed convinced that the syndrome was real and needed better surveillance and study.
“It’s in the same family as chronic fatigue syndrome and fibromyalgia. It’s not a diagnosis, but a set of symptoms.” said Benjamin O. Anderson, MD, a surgical oncologist and professor of surgery at the University of Washington in Seattle and a panel member. “It’s a giant challenge. BII is a constellation of difficult symptoms. We need to think about how we ask patients, what are your symptoms?”
Frank R. Lewis Jr., MD, committee chair, said a more standardized measure of the most common BII symptoms is needed. “That may be exceedingly difficult, with as many as a hundred reported symptoms,” said Dr. Lewis, executive director, emeritus, of the American Board of Surgery in Philadelphia.
The hearing featured results from some of the most research projects aimed at fleshing out an understanding of BII.
Diana Zuckerman, PhD, president of the National Center for Health Research, reported data she and her associates collected in an online survey completed in late 2018 and early 2019 by 449 women who had approached the Center for help in getting health insurance coverage for medically-necessary explantation of their breast implants.
Their most common symptoms included joint, muscle or back pain, weakness or stiffness; fatigue; “brain fog;” and anxiety and depression. More than two-thirds of the respondents had a family history and 3% had a personal history of an autoimmune disease, and 61% said their symptoms improved after their implants were removed, Dr. Zuckerman reported during her presentation to the panel.
During the discussion, panel members seemed intent on expanding mandatory, routine surveillance to all breast implants placed in U.S. practice.
Andrea L. Pusic, MD, president of the Plastic Surgery Foundation, summarized the recent launch of the National Breast Implant Registry by the Foundation and its parent organization, the American Society of Plastic Surgeons. These organizations, and plastic surgeons in general, would be amenable to collecting the data the FDA deemed necessary to better track BIA-ALCL and BII, said Dr. Pusic, professor of surgery at Harvard Medical School and chief of plastic and reconstructive surgery at Brigham and Women’s Hospital in Boston.
“Plastic surgeons are willing to enter these data because we know they are important,” she told the FDA panel.
Dr. Ashar, Dr. Clemens, Dr. McGrath, Dr. Lippman, Dr. Anderson, Dr. Lewis, Dr. Zuckerman, and Dr. Pusic reported having no relevant commercial disclosures.
REPORTING FROM AN FDA ADVISORY COMMITTEE MEETING
Brachytherapy access may mediate poor cervical cancer survival in blacks
HONOLULU – , according to a speaker at the Society of Gynecologic Oncology’s Annual Meeting on Women’s Cancer.
Stephanie Alimena, MD, of Brigham and Women’s Hospital in Boston, presented a large, retrospective study showing that use of brachytherapy mediated survival differences by race.
In the absence of brachytherapy, black patients had a significantly higher risk of death than did non-black patients (P = .013). However, when brachytherapy was used, black and non-black patients had a similar risk of death (P = .83).
“[W]e know that use of a brachytherapy boost is associated with improved patient outcomes, including improved cancer-specific and overall survival,” Dr. Alimena said. “We also know that African-American women have one of the highest incidences of cervical cancer in the United States and also have worse mortality from cervical cancer.”
“Studies have reached varying conclusions about the impact of race on brachytherapy utilization, with several smaller studies suggesting that minority women may be less likely to receive brachytherapy services compared to white women. No studies have specifically examined the interaction between race, radiation, and survival.”
Dr. Alimena and her colleagues decided to examine the interaction using data from the National Cancer Database. The researchers evaluated 15,411 women diagnosed with cervical cancer from 2004 to 2014. The patients had stage IB2 to IVA disease, their mean age was 54 years (range, 19-90), 58% had received brachytherapy, and 19% were black.
“Race was defined as black or non-black race, given that previous data had shown similar and even increased survival rates for Hispanic and Asian-American women compared to white patients diagnosed with cervical cancer,” Dr. Alimena noted.
Differences by race
The researchers found that black patients were significantly less likely to receive brachytherapy than were non-black patients: 52.5% vs. 59.0%, respectively (P less than .001).
Black patients were significantly more likely to have stage III disease (42.7% vs. 37.6%; P less than .001) and less likely to have stage IVA disease (6.8% vs. 7.3%; P less than .001).
Black patients were significantly more likely to have government insurance (57.0% vs. 49.1%; P less than .001) and less likely to have private insurance (27.6% vs. 36.7%; P less than .001).
And black patients were significantly more likely to have annual incomes below $38,000 (49.4% vs. 22.6%; P less than .001).
Factors associated with brachytherapy
In a multivariate analysis, black race was significantly associated with a reduced likelihood of receiving brachytherapy. The odds ratio (OR) was 0.86 (P = .003).
Other factors significantly associated with a reduced likelihood of receiving brachytherapy were:
- Being older than 70 years (OR = 0.59; P less than .001)
- Having government insurance (OR = 0.89; P = .008) or no insurance/unknown insurance status (OR = 0.75; P less than .001)
- Having stage III disease (OR = 0.47; P less than .001) or stage IVA disease (OR = 0.20; P less than .001)
- Being treated in southern states (OR = 0.67; P less than .001) or western states (OR = 0.86; P = .02)
- Having a Charlson/Deyo score of 2 or more (OR = 0.73; P less than .001).
Race, brachytherapy, and survival
“Consistent with prior data, we found that black patients had a significant decrease in overall survival, compared to non-black women,” Dr. Alimena said. “Furthermore, we found survival differences by race were mediated by brachytherapy use.”
The median overall survival was 52.5 months among black patients and 65.3 months among non-black patients (P less than .001).
Among patients who did not receive brachytherapy, black patients had a significantly higher risk of death than non-black patients (adjusted hazard ratio = 1.11; P = .013).
However, among patients who did receive brachytherapy, black and non-black patients had a similar risk of death (adjusted hazard ratio = 1.01; P = .83). The interaction term comparing these survival curves was statistically significant (P = .043).
“This is the first study, to our knowledge, to show such an interaction between race and survival being mediated by one particular treatment modality,” Dr. Alimena said.
“While not directly tested in this study, the most likely hypothesis why black patients may be less likely to receive brachytherapy is having poor access to brachytherapy services. This suggests that reducing racial disparities in survival is possible by increasing access to brachytherapy for black patients.”
Dr. Alimena had no financial disclosures.
SOURCE: Alimena S et al. SGO 2019. Abstract 11.
HONOLULU – , according to a speaker at the Society of Gynecologic Oncology’s Annual Meeting on Women’s Cancer.
Stephanie Alimena, MD, of Brigham and Women’s Hospital in Boston, presented a large, retrospective study showing that use of brachytherapy mediated survival differences by race.
In the absence of brachytherapy, black patients had a significantly higher risk of death than did non-black patients (P = .013). However, when brachytherapy was used, black and non-black patients had a similar risk of death (P = .83).
“[W]e know that use of a brachytherapy boost is associated with improved patient outcomes, including improved cancer-specific and overall survival,” Dr. Alimena said. “We also know that African-American women have one of the highest incidences of cervical cancer in the United States and also have worse mortality from cervical cancer.”
“Studies have reached varying conclusions about the impact of race on brachytherapy utilization, with several smaller studies suggesting that minority women may be less likely to receive brachytherapy services compared to white women. No studies have specifically examined the interaction between race, radiation, and survival.”
Dr. Alimena and her colleagues decided to examine the interaction using data from the National Cancer Database. The researchers evaluated 15,411 women diagnosed with cervical cancer from 2004 to 2014. The patients had stage IB2 to IVA disease, their mean age was 54 years (range, 19-90), 58% had received brachytherapy, and 19% were black.
“Race was defined as black or non-black race, given that previous data had shown similar and even increased survival rates for Hispanic and Asian-American women compared to white patients diagnosed with cervical cancer,” Dr. Alimena noted.
Differences by race
The researchers found that black patients were significantly less likely to receive brachytherapy than were non-black patients: 52.5% vs. 59.0%, respectively (P less than .001).
Black patients were significantly more likely to have stage III disease (42.7% vs. 37.6%; P less than .001) and less likely to have stage IVA disease (6.8% vs. 7.3%; P less than .001).
Black patients were significantly more likely to have government insurance (57.0% vs. 49.1%; P less than .001) and less likely to have private insurance (27.6% vs. 36.7%; P less than .001).
And black patients were significantly more likely to have annual incomes below $38,000 (49.4% vs. 22.6%; P less than .001).
Factors associated with brachytherapy
In a multivariate analysis, black race was significantly associated with a reduced likelihood of receiving brachytherapy. The odds ratio (OR) was 0.86 (P = .003).
Other factors significantly associated with a reduced likelihood of receiving brachytherapy were:
- Being older than 70 years (OR = 0.59; P less than .001)
- Having government insurance (OR = 0.89; P = .008) or no insurance/unknown insurance status (OR = 0.75; P less than .001)
- Having stage III disease (OR = 0.47; P less than .001) or stage IVA disease (OR = 0.20; P less than .001)
- Being treated in southern states (OR = 0.67; P less than .001) or western states (OR = 0.86; P = .02)
- Having a Charlson/Deyo score of 2 or more (OR = 0.73; P less than .001).
Race, brachytherapy, and survival
“Consistent with prior data, we found that black patients had a significant decrease in overall survival, compared to non-black women,” Dr. Alimena said. “Furthermore, we found survival differences by race were mediated by brachytherapy use.”
The median overall survival was 52.5 months among black patients and 65.3 months among non-black patients (P less than .001).
Among patients who did not receive brachytherapy, black patients had a significantly higher risk of death than non-black patients (adjusted hazard ratio = 1.11; P = .013).
However, among patients who did receive brachytherapy, black and non-black patients had a similar risk of death (adjusted hazard ratio = 1.01; P = .83). The interaction term comparing these survival curves was statistically significant (P = .043).
“This is the first study, to our knowledge, to show such an interaction between race and survival being mediated by one particular treatment modality,” Dr. Alimena said.
“While not directly tested in this study, the most likely hypothesis why black patients may be less likely to receive brachytherapy is having poor access to brachytherapy services. This suggests that reducing racial disparities in survival is possible by increasing access to brachytherapy for black patients.”
Dr. Alimena had no financial disclosures.
SOURCE: Alimena S et al. SGO 2019. Abstract 11.
HONOLULU – , according to a speaker at the Society of Gynecologic Oncology’s Annual Meeting on Women’s Cancer.
Stephanie Alimena, MD, of Brigham and Women’s Hospital in Boston, presented a large, retrospective study showing that use of brachytherapy mediated survival differences by race.
In the absence of brachytherapy, black patients had a significantly higher risk of death than did non-black patients (P = .013). However, when brachytherapy was used, black and non-black patients had a similar risk of death (P = .83).
“[W]e know that use of a brachytherapy boost is associated with improved patient outcomes, including improved cancer-specific and overall survival,” Dr. Alimena said. “We also know that African-American women have one of the highest incidences of cervical cancer in the United States and also have worse mortality from cervical cancer.”
“Studies have reached varying conclusions about the impact of race on brachytherapy utilization, with several smaller studies suggesting that minority women may be less likely to receive brachytherapy services compared to white women. No studies have specifically examined the interaction between race, radiation, and survival.”
Dr. Alimena and her colleagues decided to examine the interaction using data from the National Cancer Database. The researchers evaluated 15,411 women diagnosed with cervical cancer from 2004 to 2014. The patients had stage IB2 to IVA disease, their mean age was 54 years (range, 19-90), 58% had received brachytherapy, and 19% were black.
“Race was defined as black or non-black race, given that previous data had shown similar and even increased survival rates for Hispanic and Asian-American women compared to white patients diagnosed with cervical cancer,” Dr. Alimena noted.
Differences by race
The researchers found that black patients were significantly less likely to receive brachytherapy than were non-black patients: 52.5% vs. 59.0%, respectively (P less than .001).
Black patients were significantly more likely to have stage III disease (42.7% vs. 37.6%; P less than .001) and less likely to have stage IVA disease (6.8% vs. 7.3%; P less than .001).
Black patients were significantly more likely to have government insurance (57.0% vs. 49.1%; P less than .001) and less likely to have private insurance (27.6% vs. 36.7%; P less than .001).
And black patients were significantly more likely to have annual incomes below $38,000 (49.4% vs. 22.6%; P less than .001).
Factors associated with brachytherapy
In a multivariate analysis, black race was significantly associated with a reduced likelihood of receiving brachytherapy. The odds ratio (OR) was 0.86 (P = .003).
Other factors significantly associated with a reduced likelihood of receiving brachytherapy were:
- Being older than 70 years (OR = 0.59; P less than .001)
- Having government insurance (OR = 0.89; P = .008) or no insurance/unknown insurance status (OR = 0.75; P less than .001)
- Having stage III disease (OR = 0.47; P less than .001) or stage IVA disease (OR = 0.20; P less than .001)
- Being treated in southern states (OR = 0.67; P less than .001) or western states (OR = 0.86; P = .02)
- Having a Charlson/Deyo score of 2 or more (OR = 0.73; P less than .001).
Race, brachytherapy, and survival
“Consistent with prior data, we found that black patients had a significant decrease in overall survival, compared to non-black women,” Dr. Alimena said. “Furthermore, we found survival differences by race were mediated by brachytherapy use.”
The median overall survival was 52.5 months among black patients and 65.3 months among non-black patients (P less than .001).
Among patients who did not receive brachytherapy, black patients had a significantly higher risk of death than non-black patients (adjusted hazard ratio = 1.11; P = .013).
However, among patients who did receive brachytherapy, black and non-black patients had a similar risk of death (adjusted hazard ratio = 1.01; P = .83). The interaction term comparing these survival curves was statistically significant (P = .043).
“This is the first study, to our knowledge, to show such an interaction between race and survival being mediated by one particular treatment modality,” Dr. Alimena said.
“While not directly tested in this study, the most likely hypothesis why black patients may be less likely to receive brachytherapy is having poor access to brachytherapy services. This suggests that reducing racial disparities in survival is possible by increasing access to brachytherapy for black patients.”
Dr. Alimena had no financial disclosures.
SOURCE: Alimena S et al. SGO 2019. Abstract 11.
REPORTING FROM SGO 2019
No birth rate gains from levothyroxine in pregnancy
Treatment with levothyroxine does not improve the live birth rate in women with thyroid peroxidase antibodies before conception, according to data presented at the annual meeting of the Endocrine Society.
Until now, the evidence for the use of levothyroxine in pregnant women with thyroid peroxidase antibodies but normal thyroid function has been inconclusive, Rima K. Dhillon-Smith, MBChB, PhD, of the University of Birmingham (England), and her coauthors said in a paper published simultaneously with the meeting presentation March 23 in the New England Journal of Medicine.
Previous studies have shown that women with thyroid peroxidase antibodies but normal thyroid function have a nearly fourfold higher risk of miscarriage and twofold higher risk of preterm birth, compared with women who don’t have the antibodies.
In the new double-blind study, 952 women with thyroid peroxidase antibodies, normal thyroid function, and a history of miscarriage or infertility were randomized either to daily 50 mcg levothyroxine or placebo, taken from conception to the end of pregnancy.
The rate of pregnancy was similar in the levothyroxine and placebo groups (56.6% vs. 58.3%, respectively), as was the live birth rate (37.4% vs. 37.9%), despite the observation that the levothyroxine group had consistently lower serum thyrotropin and higher free T4 concentrations than did the placebo group.
There were also no significant differences between the two groups in secondary outcomes of miscarriage, preterm birth, or neonatal outcomes such as birth weight.
Researchers also saw no statistically significant differences in the rate of serious adverse events or in the number of women who showed abnormal results on thyroid function tests.
The authors noted that the dosage of levothyroxine used in the study was fixed, leaving the possibility that “the dose may need to be adjusted depending on the participant’s body weight, thyroid peroxidase antibody level, or thyrotropin concentration.”
Existing guidelines from the American Thyroid Association acknowledge the lack of evidence in favor of levothyroxine decreasing the risk of pregnancy loss. However, the guidelines also state that it can be considered in antibody-positive, euthyroid women with a history of loss, “given its potential benefits in comparison with its minimal risk.”
The study was supported by the National Institute for Health Research. No conflicts of interest were declared.
SOURCE: Dhillon-Smith R et al. N Engl J Med. 2019 March 23. doi: 10.1056/NEJMoa1812537
Treatment with levothyroxine does not improve the live birth rate in women with thyroid peroxidase antibodies before conception, according to data presented at the annual meeting of the Endocrine Society.
Until now, the evidence for the use of levothyroxine in pregnant women with thyroid peroxidase antibodies but normal thyroid function has been inconclusive, Rima K. Dhillon-Smith, MBChB, PhD, of the University of Birmingham (England), and her coauthors said in a paper published simultaneously with the meeting presentation March 23 in the New England Journal of Medicine.
Previous studies have shown that women with thyroid peroxidase antibodies but normal thyroid function have a nearly fourfold higher risk of miscarriage and twofold higher risk of preterm birth, compared with women who don’t have the antibodies.
In the new double-blind study, 952 women with thyroid peroxidase antibodies, normal thyroid function, and a history of miscarriage or infertility were randomized either to daily 50 mcg levothyroxine or placebo, taken from conception to the end of pregnancy.
The rate of pregnancy was similar in the levothyroxine and placebo groups (56.6% vs. 58.3%, respectively), as was the live birth rate (37.4% vs. 37.9%), despite the observation that the levothyroxine group had consistently lower serum thyrotropin and higher free T4 concentrations than did the placebo group.
There were also no significant differences between the two groups in secondary outcomes of miscarriage, preterm birth, or neonatal outcomes such as birth weight.
Researchers also saw no statistically significant differences in the rate of serious adverse events or in the number of women who showed abnormal results on thyroid function tests.
The authors noted that the dosage of levothyroxine used in the study was fixed, leaving the possibility that “the dose may need to be adjusted depending on the participant’s body weight, thyroid peroxidase antibody level, or thyrotropin concentration.”
Existing guidelines from the American Thyroid Association acknowledge the lack of evidence in favor of levothyroxine decreasing the risk of pregnancy loss. However, the guidelines also state that it can be considered in antibody-positive, euthyroid women with a history of loss, “given its potential benefits in comparison with its minimal risk.”
The study was supported by the National Institute for Health Research. No conflicts of interest were declared.
SOURCE: Dhillon-Smith R et al. N Engl J Med. 2019 March 23. doi: 10.1056/NEJMoa1812537
Treatment with levothyroxine does not improve the live birth rate in women with thyroid peroxidase antibodies before conception, according to data presented at the annual meeting of the Endocrine Society.
Until now, the evidence for the use of levothyroxine in pregnant women with thyroid peroxidase antibodies but normal thyroid function has been inconclusive, Rima K. Dhillon-Smith, MBChB, PhD, of the University of Birmingham (England), and her coauthors said in a paper published simultaneously with the meeting presentation March 23 in the New England Journal of Medicine.
Previous studies have shown that women with thyroid peroxidase antibodies but normal thyroid function have a nearly fourfold higher risk of miscarriage and twofold higher risk of preterm birth, compared with women who don’t have the antibodies.
In the new double-blind study, 952 women with thyroid peroxidase antibodies, normal thyroid function, and a history of miscarriage or infertility were randomized either to daily 50 mcg levothyroxine or placebo, taken from conception to the end of pregnancy.
The rate of pregnancy was similar in the levothyroxine and placebo groups (56.6% vs. 58.3%, respectively), as was the live birth rate (37.4% vs. 37.9%), despite the observation that the levothyroxine group had consistently lower serum thyrotropin and higher free T4 concentrations than did the placebo group.
There were also no significant differences between the two groups in secondary outcomes of miscarriage, preterm birth, or neonatal outcomes such as birth weight.
Researchers also saw no statistically significant differences in the rate of serious adverse events or in the number of women who showed abnormal results on thyroid function tests.
The authors noted that the dosage of levothyroxine used in the study was fixed, leaving the possibility that “the dose may need to be adjusted depending on the participant’s body weight, thyroid peroxidase antibody level, or thyrotropin concentration.”
Existing guidelines from the American Thyroid Association acknowledge the lack of evidence in favor of levothyroxine decreasing the risk of pregnancy loss. However, the guidelines also state that it can be considered in antibody-positive, euthyroid women with a history of loss, “given its potential benefits in comparison with its minimal risk.”
The study was supported by the National Institute for Health Research. No conflicts of interest were declared.
SOURCE: Dhillon-Smith R et al. N Engl J Med. 2019 March 23. doi: 10.1056/NEJMoa1812537
FROM ENDO 2019
Key clinical point:
Major finding: Pregnancy rates and outcomes were similar in women treated with levothyroxine and those treated with placebo.
Study details: Double-blind, randomized, placebo-controlled trial in 952 women.
Disclosures: The study was supported by the National Institute for Health Research. No conflicts of interest were declared.
Source: Dhillon-Smith R et al. N Engl J Med. 2019 March 23. doi: 10.1056/NEJMoa1812537
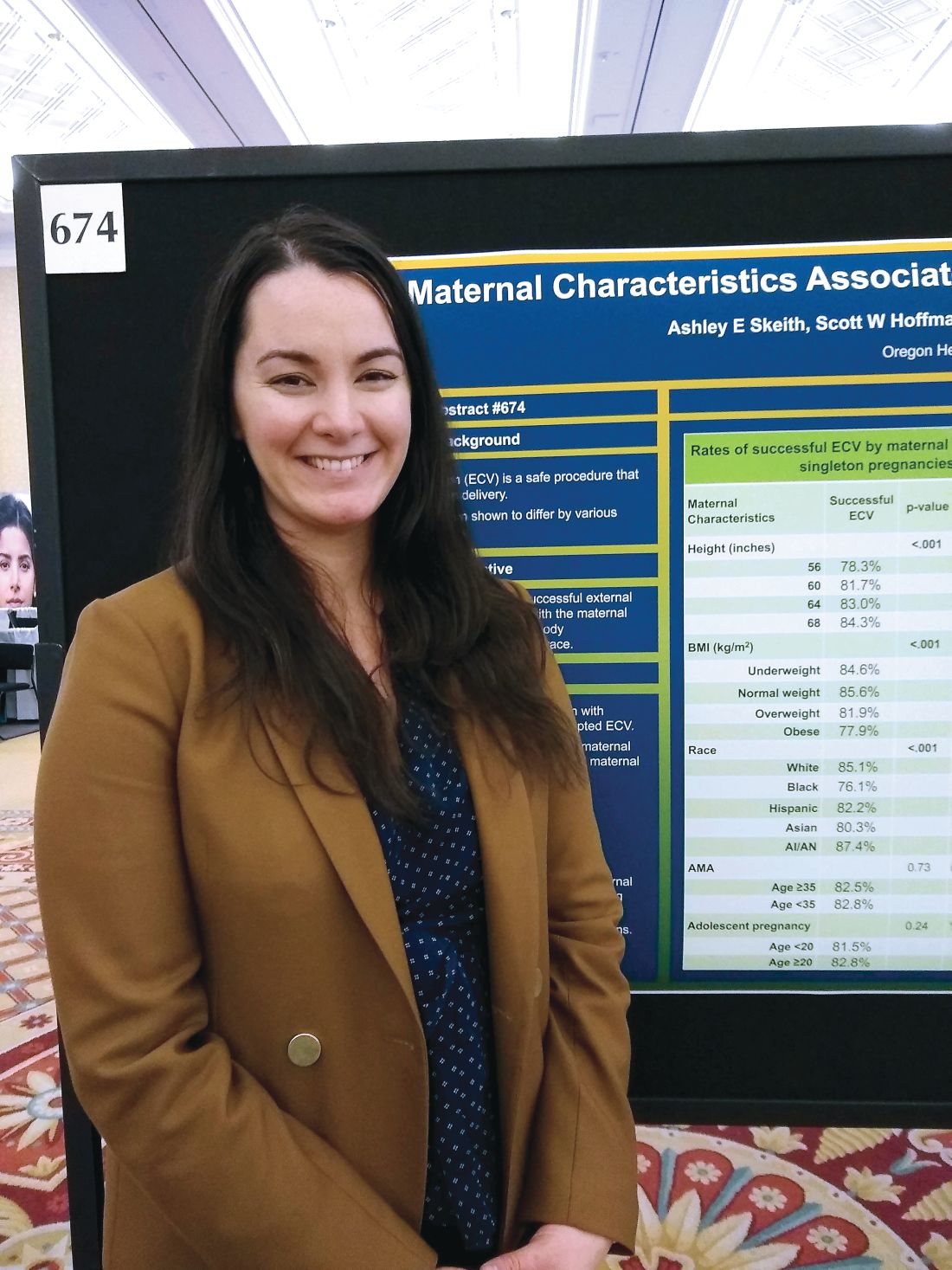
Successful external cephalic version more likely in taller, leaner women
LAS VEGAS – according to data shared in a poster session at the meeting sponsored by the Society for Maternal-Fetal Medicine.
Race/ethnicity also had an impact on the likelihood that external cephalic version (ECV) would be successful.
In an interview, first author Ashley E. Skeith, a medical student at Oregon Health and Sciences University, Portland, said that various characteristics of a pregnancy may affect the success of ECV, but it wasn’t known which maternal characteristics might be associated with greater success of the maneuver.
She and her collaborators found that rates of success were high overall, but that 84% of women 68 inches or taller had successful ECVs, compared with 78% of women less than 60 inches tall. Rates were 82% and 83% for women 60-64 inches and 64-68 inches tall, respectively (adjusted odds ratio, 1.03; P less than .001).
The retrospective cohort study used data from 18,896 women who had singleton, breech, term gestations for whom ECV was attempted. Variables extracted from the medical record included maternal age, height, race, and prepregnancy body mass index (BMI).
For analysis, maternal BMI was grouped into four categories: underweight (BMI, less than 18.5 kg/m2), normal weight (BMI, 18.5-24.9 kg/m2), overweight (BMI, 25-29 kg/m2), and obese (BMI, greater than 30 kg/m2).
Women who were normal weight had the highest likelihood of a successful ECV, at 86%, followed by underweight women at 85%. Women who were overweight and obese had lower success rates, at 82% and 78%, respectively (aOR, 0.86; P less than .001).
Compared with white women, black women had an aOR of 0.60 for successful ECV (P less than .001). The aOR for successful ECV for Asian women was 0.71; for Hispanic women, the aOR was 0.82. American Indian and Alaska Native women were slightly more likely to have successful ECV than white women, but the difference was not significant after statistical adjustment.
Neither advanced maternal age (greater than 35 years) nor adolescent pregnancy were associated with decreased likelihood of successful ECV.
Potential confounders included maternal education level and insurance status, how much weight was gained during pregnancy, whether an epidural was administered, and whether the mother had diabetes. Multivariable regression analysis adjusted for these variables, said Ms. Skeith.
“External cephalic version is a safe procedure that reduces risk of cesarean delivery,” wrote Ms. Skeith and her colleagues. “Though fetal positioning and analgesia have been considered in the prediction of ECV success, [these] data [suggest] that maternal stature and race/ethnicity could be incorporated into potential prediction tools.”
Ms. Skeith reported no outside sources of funding or conflicts of interest.
SOURCE: Skeith AE et al. Am J Obstet Gynecol. 2019 Jan;220(1):S445-7, Abstract 674.
LAS VEGAS – according to data shared in a poster session at the meeting sponsored by the Society for Maternal-Fetal Medicine.
Race/ethnicity also had an impact on the likelihood that external cephalic version (ECV) would be successful.
In an interview, first author Ashley E. Skeith, a medical student at Oregon Health and Sciences University, Portland, said that various characteristics of a pregnancy may affect the success of ECV, but it wasn’t known which maternal characteristics might be associated with greater success of the maneuver.
She and her collaborators found that rates of success were high overall, but that 84% of women 68 inches or taller had successful ECVs, compared with 78% of women less than 60 inches tall. Rates were 82% and 83% for women 60-64 inches and 64-68 inches tall, respectively (adjusted odds ratio, 1.03; P less than .001).
The retrospective cohort study used data from 18,896 women who had singleton, breech, term gestations for whom ECV was attempted. Variables extracted from the medical record included maternal age, height, race, and prepregnancy body mass index (BMI).
For analysis, maternal BMI was grouped into four categories: underweight (BMI, less than 18.5 kg/m2), normal weight (BMI, 18.5-24.9 kg/m2), overweight (BMI, 25-29 kg/m2), and obese (BMI, greater than 30 kg/m2).
Women who were normal weight had the highest likelihood of a successful ECV, at 86%, followed by underweight women at 85%. Women who were overweight and obese had lower success rates, at 82% and 78%, respectively (aOR, 0.86; P less than .001).
Compared with white women, black women had an aOR of 0.60 for successful ECV (P less than .001). The aOR for successful ECV for Asian women was 0.71; for Hispanic women, the aOR was 0.82. American Indian and Alaska Native women were slightly more likely to have successful ECV than white women, but the difference was not significant after statistical adjustment.
Neither advanced maternal age (greater than 35 years) nor adolescent pregnancy were associated with decreased likelihood of successful ECV.
Potential confounders included maternal education level and insurance status, how much weight was gained during pregnancy, whether an epidural was administered, and whether the mother had diabetes. Multivariable regression analysis adjusted for these variables, said Ms. Skeith.
“External cephalic version is a safe procedure that reduces risk of cesarean delivery,” wrote Ms. Skeith and her colleagues. “Though fetal positioning and analgesia have been considered in the prediction of ECV success, [these] data [suggest] that maternal stature and race/ethnicity could be incorporated into potential prediction tools.”
Ms. Skeith reported no outside sources of funding or conflicts of interest.
SOURCE: Skeith AE et al. Am J Obstet Gynecol. 2019 Jan;220(1):S445-7, Abstract 674.
LAS VEGAS – according to data shared in a poster session at the meeting sponsored by the Society for Maternal-Fetal Medicine.
Race/ethnicity also had an impact on the likelihood that external cephalic version (ECV) would be successful.
In an interview, first author Ashley E. Skeith, a medical student at Oregon Health and Sciences University, Portland, said that various characteristics of a pregnancy may affect the success of ECV, but it wasn’t known which maternal characteristics might be associated with greater success of the maneuver.
She and her collaborators found that rates of success were high overall, but that 84% of women 68 inches or taller had successful ECVs, compared with 78% of women less than 60 inches tall. Rates were 82% and 83% for women 60-64 inches and 64-68 inches tall, respectively (adjusted odds ratio, 1.03; P less than .001).
The retrospective cohort study used data from 18,896 women who had singleton, breech, term gestations for whom ECV was attempted. Variables extracted from the medical record included maternal age, height, race, and prepregnancy body mass index (BMI).
For analysis, maternal BMI was grouped into four categories: underweight (BMI, less than 18.5 kg/m2), normal weight (BMI, 18.5-24.9 kg/m2), overweight (BMI, 25-29 kg/m2), and obese (BMI, greater than 30 kg/m2).
Women who were normal weight had the highest likelihood of a successful ECV, at 86%, followed by underweight women at 85%. Women who were overweight and obese had lower success rates, at 82% and 78%, respectively (aOR, 0.86; P less than .001).
Compared with white women, black women had an aOR of 0.60 for successful ECV (P less than .001). The aOR for successful ECV for Asian women was 0.71; for Hispanic women, the aOR was 0.82. American Indian and Alaska Native women were slightly more likely to have successful ECV than white women, but the difference was not significant after statistical adjustment.
Neither advanced maternal age (greater than 35 years) nor adolescent pregnancy were associated with decreased likelihood of successful ECV.
Potential confounders included maternal education level and insurance status, how much weight was gained during pregnancy, whether an epidural was administered, and whether the mother had diabetes. Multivariable regression analysis adjusted for these variables, said Ms. Skeith.
“External cephalic version is a safe procedure that reduces risk of cesarean delivery,” wrote Ms. Skeith and her colleagues. “Though fetal positioning and analgesia have been considered in the prediction of ECV success, [these] data [suggest] that maternal stature and race/ethnicity could be incorporated into potential prediction tools.”
Ms. Skeith reported no outside sources of funding or conflicts of interest.
SOURCE: Skeith AE et al. Am J Obstet Gynecol. 2019 Jan;220(1):S445-7, Abstract 674.
REPORTING FROM THE PREGNANCY MEETING
Knotless, absorbable sutures best staples for postcesarean skin closure
LAS VEGAS – compared with staples, in a single-site, retrospective study.
For women whose skin incisions were closed with knotless sutures, mean surgical time was 38 minutes; for women who received a staple closure, mean surgical time was 44 minutes (P less than .001). Also, fewer women whose incisions were closed with knotless sutures experienced surgical bleeding greater than 1,000 mL, compared with those who received staples (0.3% vs. 3.0%; P less than .001).
Two previous randomized, controlled trials comparing knotless sutures with staples for skin closure after cesarean delivery were small and had methodological limitations, Inna Bleicher, MD, said in an interview during a poster session at the meeting sponsored by the Society for Maternal-Fetal Medicine.
Dr. Bleicher and her colleagues reviewed records from 2,173 elective cesarean deliveries over a period of 4 years. Absorbable, antibacterial, knotless sutures were used for closure for 1,172 women, while staples were used for the remaining 1,001 women.
Over the study period, Dr. Bleicher noted that there was a gradual transition from the use of staples to absorbable, knotless sutures, which also were increasingly used for the hysterotomy closure. She added that, in conversation with peers at Bnai-Zion Medical Center, Haifa, Israel, where she practices as an ob.gyn, she’s found that physicians find the sutures easy and quick to use, because the sutures are double ended, allowing the possibility for two operators to work together in wound closure.
The study’s primary outcome measure was the rate of postoperative infection, defined as postoperative white blood count greater than 18,000 per microliter and antimicrobial treatment. Secondary outcome measures included C-reactive protein levels, hospital readmission for infection related to the delivery, duration of surgery, and surgical blood loss estimated at 1,000 mL or more.
A higher proportion of women in the staple closure group than the knotless suture group required postsurgical antibiotic treatment (11% vs. 10%), but this difference didn’t reach statistical significance (P = .243).
There were no significant differences in the groups in terms of maternal age (about 32 years), or gestational age at delivery (about 39 weeks).
“Our results suggest that cesarean scar skin closure with antibacterial knotless sutures did not increase, and may even reduce, the rates of postoperative infection, morbidity, surgical blood loss, and may shorten operation time,” wrote Dr. Bleicher and her colleagues.
Dr. Bleicher reported no outside sources of funding and no conflicts of interest.
SOURCE: Bleicher I et al. Am J Obstet Gynecol. 2019 Jan. 220;1:S622, Abstract 966.
LAS VEGAS – compared with staples, in a single-site, retrospective study.
For women whose skin incisions were closed with knotless sutures, mean surgical time was 38 minutes; for women who received a staple closure, mean surgical time was 44 minutes (P less than .001). Also, fewer women whose incisions were closed with knotless sutures experienced surgical bleeding greater than 1,000 mL, compared with those who received staples (0.3% vs. 3.0%; P less than .001).
Two previous randomized, controlled trials comparing knotless sutures with staples for skin closure after cesarean delivery were small and had methodological limitations, Inna Bleicher, MD, said in an interview during a poster session at the meeting sponsored by the Society for Maternal-Fetal Medicine.
Dr. Bleicher and her colleagues reviewed records from 2,173 elective cesarean deliveries over a period of 4 years. Absorbable, antibacterial, knotless sutures were used for closure for 1,172 women, while staples were used for the remaining 1,001 women.
Over the study period, Dr. Bleicher noted that there was a gradual transition from the use of staples to absorbable, knotless sutures, which also were increasingly used for the hysterotomy closure. She added that, in conversation with peers at Bnai-Zion Medical Center, Haifa, Israel, where she practices as an ob.gyn, she’s found that physicians find the sutures easy and quick to use, because the sutures are double ended, allowing the possibility for two operators to work together in wound closure.
The study’s primary outcome measure was the rate of postoperative infection, defined as postoperative white blood count greater than 18,000 per microliter and antimicrobial treatment. Secondary outcome measures included C-reactive protein levels, hospital readmission for infection related to the delivery, duration of surgery, and surgical blood loss estimated at 1,000 mL or more.
A higher proportion of women in the staple closure group than the knotless suture group required postsurgical antibiotic treatment (11% vs. 10%), but this difference didn’t reach statistical significance (P = .243).
There were no significant differences in the groups in terms of maternal age (about 32 years), or gestational age at delivery (about 39 weeks).
“Our results suggest that cesarean scar skin closure with antibacterial knotless sutures did not increase, and may even reduce, the rates of postoperative infection, morbidity, surgical blood loss, and may shorten operation time,” wrote Dr. Bleicher and her colleagues.
Dr. Bleicher reported no outside sources of funding and no conflicts of interest.
SOURCE: Bleicher I et al. Am J Obstet Gynecol. 2019 Jan. 220;1:S622, Abstract 966.
LAS VEGAS – compared with staples, in a single-site, retrospective study.
For women whose skin incisions were closed with knotless sutures, mean surgical time was 38 minutes; for women who received a staple closure, mean surgical time was 44 minutes (P less than .001). Also, fewer women whose incisions were closed with knotless sutures experienced surgical bleeding greater than 1,000 mL, compared with those who received staples (0.3% vs. 3.0%; P less than .001).
Two previous randomized, controlled trials comparing knotless sutures with staples for skin closure after cesarean delivery were small and had methodological limitations, Inna Bleicher, MD, said in an interview during a poster session at the meeting sponsored by the Society for Maternal-Fetal Medicine.
Dr. Bleicher and her colleagues reviewed records from 2,173 elective cesarean deliveries over a period of 4 years. Absorbable, antibacterial, knotless sutures were used for closure for 1,172 women, while staples were used for the remaining 1,001 women.
Over the study period, Dr. Bleicher noted that there was a gradual transition from the use of staples to absorbable, knotless sutures, which also were increasingly used for the hysterotomy closure. She added that, in conversation with peers at Bnai-Zion Medical Center, Haifa, Israel, where she practices as an ob.gyn, she’s found that physicians find the sutures easy and quick to use, because the sutures are double ended, allowing the possibility for two operators to work together in wound closure.
The study’s primary outcome measure was the rate of postoperative infection, defined as postoperative white blood count greater than 18,000 per microliter and antimicrobial treatment. Secondary outcome measures included C-reactive protein levels, hospital readmission for infection related to the delivery, duration of surgery, and surgical blood loss estimated at 1,000 mL or more.
A higher proportion of women in the staple closure group than the knotless suture group required postsurgical antibiotic treatment (11% vs. 10%), but this difference didn’t reach statistical significance (P = .243).
There were no significant differences in the groups in terms of maternal age (about 32 years), or gestational age at delivery (about 39 weeks).
“Our results suggest that cesarean scar skin closure with antibacterial knotless sutures did not increase, and may even reduce, the rates of postoperative infection, morbidity, surgical blood loss, and may shorten operation time,” wrote Dr. Bleicher and her colleagues.
Dr. Bleicher reported no outside sources of funding and no conflicts of interest.
SOURCE: Bleicher I et al. Am J Obstet Gynecol. 2019 Jan. 220;1:S622, Abstract 966.
REPORTING FROM THE PREGNANCY MEETING
Rapid preeclampsia urine test is simple, noninvasive
according to a research letter in EClinicalMedicine.
The research team, led by Kara M. Rood, MD, of the department of obstetrics and gynecology at the Ohio State University, Columbus, said that their pragmatic study in 346 consecutive pregnant patients demonstrated that the test is not only inexpensive, but also easy to use and well received by the nursing staff. A positive Congo Red Dot Rapid Paper Test had 80% sensitivity, 89% specificity, 92% negative predictive value and 87% accuracy to correctly diagnose preeclampsia.
The patients were recruited from the labor and delivery triage unit at the Ohio State University Wexner Medical Center. Certain misfolded proteins typically are found in the urine of women with preeclampsia, so in prior research, the researchers had hypothesized that a urine test that could detect these proteins would carry “diagnostic and prognostic potential for” preeclampsia. The researchers were able to show that this was possible with a laboratory test that used Congo Red dye because those misfolded proteins bind with it. This current study explored the accuracy of a 3-minute, point-of-care urine test that uses a dot of Congo Red dye on a piece of paper.
Other serum and urine tests, which often have been more complicated or time intensive, have failed to gain traction in real-world practice, as well as in low-resource countries where mortality and morbidity from preeclampsia are highest, the authors noted. By contrast, the researchers hope the rapid paper test they studied in the current research will fulfill that unmet need.
The study was funded by the Saving Lives at Birth grant and a grant from the Eunice Kennedy Shriver National Institute of Child Health and Human Development.
SOURCE: Rood KM et al. EClinicalMedicine. 2019. doi: 10.1016/j.eclinm.2019.02.004.
according to a research letter in EClinicalMedicine.
The research team, led by Kara M. Rood, MD, of the department of obstetrics and gynecology at the Ohio State University, Columbus, said that their pragmatic study in 346 consecutive pregnant patients demonstrated that the test is not only inexpensive, but also easy to use and well received by the nursing staff. A positive Congo Red Dot Rapid Paper Test had 80% sensitivity, 89% specificity, 92% negative predictive value and 87% accuracy to correctly diagnose preeclampsia.
The patients were recruited from the labor and delivery triage unit at the Ohio State University Wexner Medical Center. Certain misfolded proteins typically are found in the urine of women with preeclampsia, so in prior research, the researchers had hypothesized that a urine test that could detect these proteins would carry “diagnostic and prognostic potential for” preeclampsia. The researchers were able to show that this was possible with a laboratory test that used Congo Red dye because those misfolded proteins bind with it. This current study explored the accuracy of a 3-minute, point-of-care urine test that uses a dot of Congo Red dye on a piece of paper.
Other serum and urine tests, which often have been more complicated or time intensive, have failed to gain traction in real-world practice, as well as in low-resource countries where mortality and morbidity from preeclampsia are highest, the authors noted. By contrast, the researchers hope the rapid paper test they studied in the current research will fulfill that unmet need.
The study was funded by the Saving Lives at Birth grant and a grant from the Eunice Kennedy Shriver National Institute of Child Health and Human Development.
SOURCE: Rood KM et al. EClinicalMedicine. 2019. doi: 10.1016/j.eclinm.2019.02.004.
according to a research letter in EClinicalMedicine.
The research team, led by Kara M. Rood, MD, of the department of obstetrics and gynecology at the Ohio State University, Columbus, said that their pragmatic study in 346 consecutive pregnant patients demonstrated that the test is not only inexpensive, but also easy to use and well received by the nursing staff. A positive Congo Red Dot Rapid Paper Test had 80% sensitivity, 89% specificity, 92% negative predictive value and 87% accuracy to correctly diagnose preeclampsia.
The patients were recruited from the labor and delivery triage unit at the Ohio State University Wexner Medical Center. Certain misfolded proteins typically are found in the urine of women with preeclampsia, so in prior research, the researchers had hypothesized that a urine test that could detect these proteins would carry “diagnostic and prognostic potential for” preeclampsia. The researchers were able to show that this was possible with a laboratory test that used Congo Red dye because those misfolded proteins bind with it. This current study explored the accuracy of a 3-minute, point-of-care urine test that uses a dot of Congo Red dye on a piece of paper.
Other serum and urine tests, which often have been more complicated or time intensive, have failed to gain traction in real-world practice, as well as in low-resource countries where mortality and morbidity from preeclampsia are highest, the authors noted. By contrast, the researchers hope the rapid paper test they studied in the current research will fulfill that unmet need.
The study was funded by the Saving Lives at Birth grant and a grant from the Eunice Kennedy Shriver National Institute of Child Health and Human Development.
SOURCE: Rood KM et al. EClinicalMedicine. 2019. doi: 10.1016/j.eclinm.2019.02.004.
FROM ECLINICALMEDICINE
Sex differences in MS: It’s the chromosomes, not just the hormones
DALLAS – Hormonal differences are not the only reason that multiple sclerosis (MS) disease progression and severity differ between the sexes, according to Rhonda Voskuhl, MD, who delivered the Kenneth P. Johnson Memorial Lecture at a meeting of the Americas Committee for Treatment and Research in Multiple Sclerosis.
“Sex differences in disease are widely prevalent across immunological and neurological diseases. For example, lupus affects women 9:1 more frequently, rheumatoid arthritis is about 3:1, and MS is 3:1,” said Dr. Voskuhl, director of the MS program and Jack H. Skirball Chair of Multiple Sclerosis Research at the University of California, Los Angeles.
However, although women are more likely to experience these diseases, men are often more severely affected by them, Dr. Voskuhl said. “Sometimes in neurodegenerative diseases like MS, we’re seeing that the men, although they get it less frequently, they do worse. ... So these are actually two very important sex differences in disease, one affecting susceptibility and frequency, and the other affecting how they do over the long run with respect to their progression and severity.”
This clinically apparent observation, known for decades, prompted Dr. Voskuhl and others to parse why sex differences exist in this gamut of diseases.
A novel animal model – the four-core genotype mouse model – has allowed Dr. Voskuhl and others to discern the contributions of hormonal versus chromosomal influences on disease susceptibility and progression. The model separates the sex chromosome complement (XX or XY) from gonadal influences, and it’s been extremely helpful in revealing the surprising influence that sex chromosomes play in MS and similar diseases, said Dr. Voskuhl in an interview.
Dr. Voskuhl is also the president-elect of the Organization for the Study of Sex Differences.
DALLAS – Hormonal differences are not the only reason that multiple sclerosis (MS) disease progression and severity differ between the sexes, according to Rhonda Voskuhl, MD, who delivered the Kenneth P. Johnson Memorial Lecture at a meeting of the Americas Committee for Treatment and Research in Multiple Sclerosis.
“Sex differences in disease are widely prevalent across immunological and neurological diseases. For example, lupus affects women 9:1 more frequently, rheumatoid arthritis is about 3:1, and MS is 3:1,” said Dr. Voskuhl, director of the MS program and Jack H. Skirball Chair of Multiple Sclerosis Research at the University of California, Los Angeles.
However, although women are more likely to experience these diseases, men are often more severely affected by them, Dr. Voskuhl said. “Sometimes in neurodegenerative diseases like MS, we’re seeing that the men, although they get it less frequently, they do worse. ... So these are actually two very important sex differences in disease, one affecting susceptibility and frequency, and the other affecting how they do over the long run with respect to their progression and severity.”
This clinically apparent observation, known for decades, prompted Dr. Voskuhl and others to parse why sex differences exist in this gamut of diseases.
A novel animal model – the four-core genotype mouse model – has allowed Dr. Voskuhl and others to discern the contributions of hormonal versus chromosomal influences on disease susceptibility and progression. The model separates the sex chromosome complement (XX or XY) from gonadal influences, and it’s been extremely helpful in revealing the surprising influence that sex chromosomes play in MS and similar diseases, said Dr. Voskuhl in an interview.
Dr. Voskuhl is also the president-elect of the Organization for the Study of Sex Differences.
DALLAS – Hormonal differences are not the only reason that multiple sclerosis (MS) disease progression and severity differ between the sexes, according to Rhonda Voskuhl, MD, who delivered the Kenneth P. Johnson Memorial Lecture at a meeting of the Americas Committee for Treatment and Research in Multiple Sclerosis.
“Sex differences in disease are widely prevalent across immunological and neurological diseases. For example, lupus affects women 9:1 more frequently, rheumatoid arthritis is about 3:1, and MS is 3:1,” said Dr. Voskuhl, director of the MS program and Jack H. Skirball Chair of Multiple Sclerosis Research at the University of California, Los Angeles.
However, although women are more likely to experience these diseases, men are often more severely affected by them, Dr. Voskuhl said. “Sometimes in neurodegenerative diseases like MS, we’re seeing that the men, although they get it less frequently, they do worse. ... So these are actually two very important sex differences in disease, one affecting susceptibility and frequency, and the other affecting how they do over the long run with respect to their progression and severity.”
This clinically apparent observation, known for decades, prompted Dr. Voskuhl and others to parse why sex differences exist in this gamut of diseases.
A novel animal model – the four-core genotype mouse model – has allowed Dr. Voskuhl and others to discern the contributions of hormonal versus chromosomal influences on disease susceptibility and progression. The model separates the sex chromosome complement (XX or XY) from gonadal influences, and it’s been extremely helpful in revealing the surprising influence that sex chromosomes play in MS and similar diseases, said Dr. Voskuhl in an interview.
Dr. Voskuhl is also the president-elect of the Organization for the Study of Sex Differences.
REPORTING FROM ACTRIMS FORUM 2019
Financial toxicity may be common in gynecologic cancer patients
HONOLULU – Financial toxicity may be common among gynecologic cancer patients starting a new line of treatment, based on the results of a survey presented at the Society of Gynecologic Oncology’s Annual Meeting on Women’s Cancer.
More than half of the 121 patients surveyed reported mild, moderate, or severe financial toxicity, Margaret Liang, MD, of University of Alabama at Birmingham, said in presenting the findings.
Younger age and lower income were both risk factors for financial toxicity, and having insurance did not protect patients from financial toxicity. Dr. Liang noted that insurance coverage “was not protective for financial toxicity, as the majority of those who screened positive for financial toxicity were insured.” Specifically, 89% of patients with financial toxicity and 98% of patients without it were insured (P = .07).
“This finding supports financial toxicity screening regardless of insurance status and may favor universal screening,” Dr. Liang said.
She and her colleagues conducted the survey of 121 gynecologic cancer patients who had started a new line of systemic therapy in the previous 8 weeks.
The patients’ mean age was 59 years (range, 33-80), and 58% were starting their first line of systemic therapy. Half of the patients had a household income below $40,000, and about one-third of the patients were employed. Most had private (74%) or public (20%) insurance, and 7% of patients were uninsured.
To assess financial toxicity, the researchers used the Comprehensive Score for Financial Toxicity (COST). A score of less than 26 was used as a threshold of financial toxicity. The severity of financial toxicity was graded on a scale of 1 to 4, with a lower score indicating worse toxicity.
Patients were most concerned about having enough money to cover the cost of treatment. Patients reported the lowest mean score—0.97—in response to the statement, “I know that I have enough money in savings, retirement, or assets to cover the costs of my treatment.”
Patients were least concerned about losing their job or income. They reported the highest mean score—3.29—in response to the statement, “I am concerned about keeping my job and income, including working at home.” However, as Dr. Liang pointed out, only one-third of patients were employed at baseline.
In all, 54% of patients reported financial toxicity—37% mild, 16% moderate, and 1% severe.
Dr. Liang and her colleagues found that younger age and lower income were associated with an increased risk for financial toxicity. The mean age was 57 years in patients with financial toxicity and 62 years in patients without it (P = .02). Household incomes were below $40,000 in 63% of patients with financial toxicity and 34% of those without it (P less than .01).
The researchers also found that patients with financial toxicity were significantly more likely to say their cancer diagnosis resulted in lost wages, borrowed money, altered spending habits, the need to sacrifice other things, and not paying bills on time (P less than .01 for all).
On the other hand, patients with financial toxicity were not significantly more likely to become unemployed, file for bankruptcy, sell their house, or get a second job due to their cancer diagnosis.
However, it’s important to note that these data were collected within 8 weeks of patients starting their new line of therapy. The final survey results will include follow-up at 3 months and 6 months.
Dr. Liang said the fact that more than half of patients reported financial toxicity within 8 weeks of starting a new line of therapy suggests early interventions are needed to prevent or reduce financial toxicity. This may include counseling patients on anticipated costs of care, screening for financial toxicity, and linking patients to available financial resources.
Dr. Liang had no financial disclosures.
SOURCE: Liang M et al. SGO 2019. Abstract 8.
HONOLULU – Financial toxicity may be common among gynecologic cancer patients starting a new line of treatment, based on the results of a survey presented at the Society of Gynecologic Oncology’s Annual Meeting on Women’s Cancer.
More than half of the 121 patients surveyed reported mild, moderate, or severe financial toxicity, Margaret Liang, MD, of University of Alabama at Birmingham, said in presenting the findings.
Younger age and lower income were both risk factors for financial toxicity, and having insurance did not protect patients from financial toxicity. Dr. Liang noted that insurance coverage “was not protective for financial toxicity, as the majority of those who screened positive for financial toxicity were insured.” Specifically, 89% of patients with financial toxicity and 98% of patients without it were insured (P = .07).
“This finding supports financial toxicity screening regardless of insurance status and may favor universal screening,” Dr. Liang said.
She and her colleagues conducted the survey of 121 gynecologic cancer patients who had started a new line of systemic therapy in the previous 8 weeks.
The patients’ mean age was 59 years (range, 33-80), and 58% were starting their first line of systemic therapy. Half of the patients had a household income below $40,000, and about one-third of the patients were employed. Most had private (74%) or public (20%) insurance, and 7% of patients were uninsured.
To assess financial toxicity, the researchers used the Comprehensive Score for Financial Toxicity (COST). A score of less than 26 was used as a threshold of financial toxicity. The severity of financial toxicity was graded on a scale of 1 to 4, with a lower score indicating worse toxicity.
Patients were most concerned about having enough money to cover the cost of treatment. Patients reported the lowest mean score—0.97—in response to the statement, “I know that I have enough money in savings, retirement, or assets to cover the costs of my treatment.”
Patients were least concerned about losing their job or income. They reported the highest mean score—3.29—in response to the statement, “I am concerned about keeping my job and income, including working at home.” However, as Dr. Liang pointed out, only one-third of patients were employed at baseline.
In all, 54% of patients reported financial toxicity—37% mild, 16% moderate, and 1% severe.
Dr. Liang and her colleagues found that younger age and lower income were associated with an increased risk for financial toxicity. The mean age was 57 years in patients with financial toxicity and 62 years in patients without it (P = .02). Household incomes were below $40,000 in 63% of patients with financial toxicity and 34% of those without it (P less than .01).
The researchers also found that patients with financial toxicity were significantly more likely to say their cancer diagnosis resulted in lost wages, borrowed money, altered spending habits, the need to sacrifice other things, and not paying bills on time (P less than .01 for all).
On the other hand, patients with financial toxicity were not significantly more likely to become unemployed, file for bankruptcy, sell their house, or get a second job due to their cancer diagnosis.
However, it’s important to note that these data were collected within 8 weeks of patients starting their new line of therapy. The final survey results will include follow-up at 3 months and 6 months.
Dr. Liang said the fact that more than half of patients reported financial toxicity within 8 weeks of starting a new line of therapy suggests early interventions are needed to prevent or reduce financial toxicity. This may include counseling patients on anticipated costs of care, screening for financial toxicity, and linking patients to available financial resources.
Dr. Liang had no financial disclosures.
SOURCE: Liang M et al. SGO 2019. Abstract 8.
HONOLULU – Financial toxicity may be common among gynecologic cancer patients starting a new line of treatment, based on the results of a survey presented at the Society of Gynecologic Oncology’s Annual Meeting on Women’s Cancer.
More than half of the 121 patients surveyed reported mild, moderate, or severe financial toxicity, Margaret Liang, MD, of University of Alabama at Birmingham, said in presenting the findings.
Younger age and lower income were both risk factors for financial toxicity, and having insurance did not protect patients from financial toxicity. Dr. Liang noted that insurance coverage “was not protective for financial toxicity, as the majority of those who screened positive for financial toxicity were insured.” Specifically, 89% of patients with financial toxicity and 98% of patients without it were insured (P = .07).
“This finding supports financial toxicity screening regardless of insurance status and may favor universal screening,” Dr. Liang said.
She and her colleagues conducted the survey of 121 gynecologic cancer patients who had started a new line of systemic therapy in the previous 8 weeks.
The patients’ mean age was 59 years (range, 33-80), and 58% were starting their first line of systemic therapy. Half of the patients had a household income below $40,000, and about one-third of the patients were employed. Most had private (74%) or public (20%) insurance, and 7% of patients were uninsured.
To assess financial toxicity, the researchers used the Comprehensive Score for Financial Toxicity (COST). A score of less than 26 was used as a threshold of financial toxicity. The severity of financial toxicity was graded on a scale of 1 to 4, with a lower score indicating worse toxicity.
Patients were most concerned about having enough money to cover the cost of treatment. Patients reported the lowest mean score—0.97—in response to the statement, “I know that I have enough money in savings, retirement, or assets to cover the costs of my treatment.”
Patients were least concerned about losing their job or income. They reported the highest mean score—3.29—in response to the statement, “I am concerned about keeping my job and income, including working at home.” However, as Dr. Liang pointed out, only one-third of patients were employed at baseline.
In all, 54% of patients reported financial toxicity—37% mild, 16% moderate, and 1% severe.
Dr. Liang and her colleagues found that younger age and lower income were associated with an increased risk for financial toxicity. The mean age was 57 years in patients with financial toxicity and 62 years in patients without it (P = .02). Household incomes were below $40,000 in 63% of patients with financial toxicity and 34% of those without it (P less than .01).
The researchers also found that patients with financial toxicity were significantly more likely to say their cancer diagnosis resulted in lost wages, borrowed money, altered spending habits, the need to sacrifice other things, and not paying bills on time (P less than .01 for all).
On the other hand, patients with financial toxicity were not significantly more likely to become unemployed, file for bankruptcy, sell their house, or get a second job due to their cancer diagnosis.
However, it’s important to note that these data were collected within 8 weeks of patients starting their new line of therapy. The final survey results will include follow-up at 3 months and 6 months.
Dr. Liang said the fact that more than half of patients reported financial toxicity within 8 weeks of starting a new line of therapy suggests early interventions are needed to prevent or reduce financial toxicity. This may include counseling patients on anticipated costs of care, screening for financial toxicity, and linking patients to available financial resources.
Dr. Liang had no financial disclosures.
SOURCE: Liang M et al. SGO 2019. Abstract 8.
REPORTING FROM SGO 2019
Light physical activity lowers CVD risk in older women
Even light physical activity can significantly reduce the risks of acquiring coronary heart disease specifically and the broad range of cardiovascular diseases in older women, new data suggests.
A paper published in JAMA Network Open reported the outcome of a prospective cohort study in 5,861 women, with a mean age of 78.5 years, who wore accelerometers for 7 days to measure physical activity.
than those in the lowest quartile of activity, who engaged in less than 3.9 hours per day, after adjusting for factors such as comorbidities, lifestyle, and cardiovascular risk.
Similarly, those in the highest quartile had an 18% lower risk of cardiovascular disease than those in the lowest quartile, after adjusting for potential confounders.
Researchers saw a significant dose-dependent decrease in the risk for incident coronary heart disease and cardiovascular disease with increasing light physical activity, such that each 1-hour increment of activity was associated with a 20% decrease in coronary heart disease risk and 10% decrease in cardiovascular disease risk.
Andrea Z. LaCroix, PhD, from the University of California, San Diego, and her coauthors noted that physical activity guidelines for aerobic activity suggest 75 minutes of vigorous physical activity or 150 minutes of moderate activity each day, but only around 25% of U.S. women aged over 75 years are estimated to meet this requirement.
“These guidelines may have discouraged PA [physical activity] when perceived to be unattainable by large segments of the population,” they wrote.
While the majority of active time in older adults is spent doing light physical activity, little is known about the cardiovascular effects of participating in this level of activity. “A major barrier has been that self-reported questionnaires measuring leisure-time PA do not adequately capture light PA that is acquired throughout the day in activities of daily living,” they wrote.
The study also looked at the impact of moderate to vigorous physical activity, finding a significant 46% reduction between the highest to lowest quartiles of activity in coronary heart disease risk and a 31% reduction in cardiovascular disease risk.
Even after adjusting for the use of lipid-lowering medication, antihypertensive medication or healthy eating scores, the results remained unchanged. The researchers also saw no change when women with angina and heart failure at baseline were excluded or when they excluded cardiovascular events that occurred during the first 6 months of follow-up.
The study was supported by the National Heart, Lung, and Blood Institute; the National Institutes of Health; and the Department of Health & Human Services. Six authors reported receiving funding from the study supporters and other research institutions, and one reported membership on the advisory committee for physical activity guidelines. No other conflicts of interest were reported.
SOURCE: LaCroix AZ et al. JAMA Netw Open. 2019 Mar 15. doi: 10.1001/jamanetworkopen.2019.0419.
Older women do not get enough physical activity, so this finding that light physical activity is associated with improved coronary heart disease and cardiovascular disease outcomes supports the recent scientific report by the 2018 Physical Activity Guidelines Advisory Committee. It is also helpful in extending the evidence about the benefits of physical activity in reducing incident coronary heart disease to older women, as previous studies on this topic showed such benefits in men.
These findings should remind health care professionals, systems, and agencies to promote the 2018 Physical Activity Guidelines for Americans to all patients. Otherwise, the future health and well-being of older women is likely to suffer from the consequences of sedentary behavior and inadequate physical activity.
Gregory W. Heath, DHSc, MPH, is from the department of health and human performance at the University of Tennessee, Chattanooga. These comments are adapted from an accompanying editorial (JAMA Netw Open. 2019 Mar 15. doi: 10.1001/jamanetworkopen.2019.0405). No conflicts of interest were reported.
Older women do not get enough physical activity, so this finding that light physical activity is associated with improved coronary heart disease and cardiovascular disease outcomes supports the recent scientific report by the 2018 Physical Activity Guidelines Advisory Committee. It is also helpful in extending the evidence about the benefits of physical activity in reducing incident coronary heart disease to older women, as previous studies on this topic showed such benefits in men.
These findings should remind health care professionals, systems, and agencies to promote the 2018 Physical Activity Guidelines for Americans to all patients. Otherwise, the future health and well-being of older women is likely to suffer from the consequences of sedentary behavior and inadequate physical activity.
Gregory W. Heath, DHSc, MPH, is from the department of health and human performance at the University of Tennessee, Chattanooga. These comments are adapted from an accompanying editorial (JAMA Netw Open. 2019 Mar 15. doi: 10.1001/jamanetworkopen.2019.0405). No conflicts of interest were reported.
Older women do not get enough physical activity, so this finding that light physical activity is associated with improved coronary heart disease and cardiovascular disease outcomes supports the recent scientific report by the 2018 Physical Activity Guidelines Advisory Committee. It is also helpful in extending the evidence about the benefits of physical activity in reducing incident coronary heart disease to older women, as previous studies on this topic showed such benefits in men.
These findings should remind health care professionals, systems, and agencies to promote the 2018 Physical Activity Guidelines for Americans to all patients. Otherwise, the future health and well-being of older women is likely to suffer from the consequences of sedentary behavior and inadequate physical activity.
Gregory W. Heath, DHSc, MPH, is from the department of health and human performance at the University of Tennessee, Chattanooga. These comments are adapted from an accompanying editorial (JAMA Netw Open. 2019 Mar 15. doi: 10.1001/jamanetworkopen.2019.0405). No conflicts of interest were reported.
Even light physical activity can significantly reduce the risks of acquiring coronary heart disease specifically and the broad range of cardiovascular diseases in older women, new data suggests.
A paper published in JAMA Network Open reported the outcome of a prospective cohort study in 5,861 women, with a mean age of 78.5 years, who wore accelerometers for 7 days to measure physical activity.
than those in the lowest quartile of activity, who engaged in less than 3.9 hours per day, after adjusting for factors such as comorbidities, lifestyle, and cardiovascular risk.
Similarly, those in the highest quartile had an 18% lower risk of cardiovascular disease than those in the lowest quartile, after adjusting for potential confounders.
Researchers saw a significant dose-dependent decrease in the risk for incident coronary heart disease and cardiovascular disease with increasing light physical activity, such that each 1-hour increment of activity was associated with a 20% decrease in coronary heart disease risk and 10% decrease in cardiovascular disease risk.
Andrea Z. LaCroix, PhD, from the University of California, San Diego, and her coauthors noted that physical activity guidelines for aerobic activity suggest 75 minutes of vigorous physical activity or 150 minutes of moderate activity each day, but only around 25% of U.S. women aged over 75 years are estimated to meet this requirement.
“These guidelines may have discouraged PA [physical activity] when perceived to be unattainable by large segments of the population,” they wrote.
While the majority of active time in older adults is spent doing light physical activity, little is known about the cardiovascular effects of participating in this level of activity. “A major barrier has been that self-reported questionnaires measuring leisure-time PA do not adequately capture light PA that is acquired throughout the day in activities of daily living,” they wrote.
The study also looked at the impact of moderate to vigorous physical activity, finding a significant 46% reduction between the highest to lowest quartiles of activity in coronary heart disease risk and a 31% reduction in cardiovascular disease risk.
Even after adjusting for the use of lipid-lowering medication, antihypertensive medication or healthy eating scores, the results remained unchanged. The researchers also saw no change when women with angina and heart failure at baseline were excluded or when they excluded cardiovascular events that occurred during the first 6 months of follow-up.
The study was supported by the National Heart, Lung, and Blood Institute; the National Institutes of Health; and the Department of Health & Human Services. Six authors reported receiving funding from the study supporters and other research institutions, and one reported membership on the advisory committee for physical activity guidelines. No other conflicts of interest were reported.
SOURCE: LaCroix AZ et al. JAMA Netw Open. 2019 Mar 15. doi: 10.1001/jamanetworkopen.2019.0419.
Even light physical activity can significantly reduce the risks of acquiring coronary heart disease specifically and the broad range of cardiovascular diseases in older women, new data suggests.
A paper published in JAMA Network Open reported the outcome of a prospective cohort study in 5,861 women, with a mean age of 78.5 years, who wore accelerometers for 7 days to measure physical activity.
than those in the lowest quartile of activity, who engaged in less than 3.9 hours per day, after adjusting for factors such as comorbidities, lifestyle, and cardiovascular risk.
Similarly, those in the highest quartile had an 18% lower risk of cardiovascular disease than those in the lowest quartile, after adjusting for potential confounders.
Researchers saw a significant dose-dependent decrease in the risk for incident coronary heart disease and cardiovascular disease with increasing light physical activity, such that each 1-hour increment of activity was associated with a 20% decrease in coronary heart disease risk and 10% decrease in cardiovascular disease risk.
Andrea Z. LaCroix, PhD, from the University of California, San Diego, and her coauthors noted that physical activity guidelines for aerobic activity suggest 75 minutes of vigorous physical activity or 150 minutes of moderate activity each day, but only around 25% of U.S. women aged over 75 years are estimated to meet this requirement.
“These guidelines may have discouraged PA [physical activity] when perceived to be unattainable by large segments of the population,” they wrote.
While the majority of active time in older adults is spent doing light physical activity, little is known about the cardiovascular effects of participating in this level of activity. “A major barrier has been that self-reported questionnaires measuring leisure-time PA do not adequately capture light PA that is acquired throughout the day in activities of daily living,” they wrote.
The study also looked at the impact of moderate to vigorous physical activity, finding a significant 46% reduction between the highest to lowest quartiles of activity in coronary heart disease risk and a 31% reduction in cardiovascular disease risk.
Even after adjusting for the use of lipid-lowering medication, antihypertensive medication or healthy eating scores, the results remained unchanged. The researchers also saw no change when women with angina and heart failure at baseline were excluded or when they excluded cardiovascular events that occurred during the first 6 months of follow-up.
The study was supported by the National Heart, Lung, and Blood Institute; the National Institutes of Health; and the Department of Health & Human Services. Six authors reported receiving funding from the study supporters and other research institutions, and one reported membership on the advisory committee for physical activity guidelines. No other conflicts of interest were reported.
SOURCE: LaCroix AZ et al. JAMA Netw Open. 2019 Mar 15. doi: 10.1001/jamanetworkopen.2019.0419.
FROM JAMA NETWORK OPEN
‘The birth of a mother is a complex process’
Softening the blow to women and families of severe perinatal, postpartum psychiatric disorders
Editor’s Note: Alison M. Heru, MD, the Families in Psychiatry columnist, invited Dr. Reinstein to address this topic.
“But this was not what I expected!” That’s a statement I have heard from countless new mothers.
Women often envision pregnancy and the postpartum period as a time of pure joy. The glow of an expectant woman and the excitement of the arrival of a new baby masks the reality that many women struggle emotionally when transitioning to motherhood. Like the birth of a child, the birth of a mother is a complex process. Upholding the myth that all women seamlessly transform into mothers can have devastating effects and hinder access to mental health care.
As a psychiatrist working on a women’s inpatient unit with a perinatal program, I treat women at times of crisis. What may have begun as mild anxiety or depression sometimes quickly spirals into severe psychiatric illness. The sheer force of these severe perinatal and postpartum psychiatric disorders often leaves women and families shocked and confused, wondering what happened to their crumbled dreams of early motherhood.
What must general psychiatrists know about perinatal and postpartum psychiatric disorders? Why is maternal mental health so important? What are the barriers to treatment for these women? How can general psychiatrists best support and treat these new mothers and their families?
What data show
Maternal depression is now known to be one of the most common complications of pregnancy. Studies have suggested that about 11% of women experience depression during pregnancy1 and approximately 17% of women are depressed in the postpartum period.2 Perinatal generalized anxiety disorder has been shown to have a prevalence of 8.5%-10.5% during pregnancy with a wider variance post partum.3 Approximately 3% of women in the general community develop PTSD symptoms following childbirth.4 Research suggests that about 2% of women develop obsessive-compulsive disorder symptoms in the postpartum period.5 Postpartum psychosis, a rare but potentially devastating illness, occurs after 0.1%-0.2% of births.6
Importance of maternal mental health
There is a growing body of literature supporting both obstetric and pediatric adverse outcomes related to untreated psychiatric illness. Untreated maternal depression has been associated with obstetric complications, such as preterm delivery, preeclampsia, low birth weight, as well as the child’s developing cognitive function.7 Anxiety during pregnancy has been associated with both a shorter gestational period and adverse implications for fetal neurodevelopment.
These adverse effects were found to be even more potent in “pregnancy anxiety,” or anxiety specifically focused on the pregnancy, the birth experience, and the transition to motherhood.8 The psychotic symptoms occurring during postpartum psychosis can jeopardize the lives of both a woman and her child and carries a 4% risk of infanticide.9 Although there are limited data about the long-term effects of postpartum obsessive-compulsive disorders and PTSD, it is reasonable to assume that they might carry negative long-term implications for the mother and possibly her child.
Barriers to treatment
Despite the significant rates of mental illness, pregnant and new mothers often face barriers to receiving treatment. Many psychiatrists are hesitant to prescribe psychiatric medication to pregnant women because of concerns about teratogenic potential of psychiatric medications; similar concerns exist for newborn babies when prescribing medications to lactating mothers. In addition, the field of reproductive psychiatry is evolving at a rapid pace, making it difficult for busy psychiatrists to keep up with the ever-growing literature.
Also, it is hard to imagine a population that has more barriers to attending outpatient appointments. For many new mothers, the exhaustion and all-consuming work involved with taking care of a newborn are insurmountable barriers to obtaining mental health care. In addition, despite the awareness that new mothers often are more emotional, families can be slow to recognize the developing severity of a psychiatric illness during the peripartum and postpartum periods.
Supporting and treating new mothers
As general psychiatrists, there are several ways to directly help these women.
1. Expect the expected. Even in women with no prior psychiatric history, a significant percentage of expectant and postpartum women will develop acute psychiatric symptoms. Learn about the different presentations and treatments of perinatal and postpartum psychiatric disorders. For example, a woman might have thoughts of harming her baby in both postpartum psychosis and obsessive-compulsive disorder. However, the acuity and treatment of these two conditions drastically differ.
2. Learn more about psychiatric medications. Several apps and websites are available to psychiatrists to learn about the safety profile of psychiatric medications, such as Reprotox.org, mothertobaby.org, lactmed, and womensmentalhealth.org. Many medications are considered to be relatively safe during pregnancy and breastfeeding. It is important for psychiatrists to appreciate the risks when choosing not to prescribe to pregnant and postpartum women. Sometimes a known risk of a specific medication may be preferable to the unknown risk of leaving a woman susceptible to a severe psychiatric decompensation.
3. Involve all members of the family. A mother’s mental health has significant implications for the entire family. Psychoeducation for the family as well as frequent family sessions are key tools when treating this population. In addition, prescribing to pregnant women provides the opportunity for a psychiatrist to refine skills in joint decision making; it is crucial to involve both a patient and her spouse when discussing psychiatric medications.
4. Provide ready access and collaborate care. It is important to understand the potential rapid onset of psychiatric symptoms during the pregnancy and postpartum period. Psychiatrists should be prepared to collaborate care with other specialties. It is important to establish relationships with community psychotherapists specializing in maternal mental health, pediatricians, as well as obstetricians.
5. Learn when to seek a higher level of care. Although many women with perinatal and postpartum psychiatric symptoms can be managed as outpatients, women at times need a higher level of care. Similar to general psychiatry, women who are acutely suicidal or homicidal or have a sudden onset of psychotic and manic symptoms all should be evaluated immediately for inpatient hospitalization. Women with less severe symptoms but who require a higher level of care than typically offered in standard outpatient treatment should be candidates for partial hospitalization programs.
General intensive programs usually can accommodate these women, but it is ideal to refer this population to perinatal intensive programs. Postpartum Support International (postpartum.net) lists the nationwide inpatient and partial perinatal programs as well as regional and local services. An example of inpatient perinatal care is the women’s unit at Zucker Hillside Hospital (Northwell Health System, Glen Oaks, N.Y.), which houses an inpatient perinatal program. As a psychiatrist on the unit, I treat acute symptoms such as depression, anxiety, psychosis, mania, and catatonia that occur during the perinatal and postpartum periods. Given the severity of symptoms, I use a wide range of psychiatric medications with the possibility of electroconvulsive therapy when indicated. Psychotherapy staff on the unit offer specialized perinatal, mothers, and dialectical behavioral therapy groups. Breast pumps are available for women who wish to breastfeed. Accommodations are made for babies and children to visit their mother when clinically appropriate. Once discharged, women often are referred to Zucker Hillside’s own perinatal outpatient clinic for continued treatment. Similar models exist in select inpatient units as well as an increasing number of partial programs across the United States.
Conclusion
Psychiatric care for pregnant and new mothers can be challenging, but it is also immensely rewarding. Restoring a mother’s mental health usually leads to increased emotional stability for her entire family. Given the prevalence of maternal mental health disorders, psychiatrists in nearly every setting will encounter this population of women. With dedicated time devoted to reviewing the literature and learning about local resources, psychiatrists can feel comfortable treating women throughout the childbearing experience.
References
1. J Affect Disord. 2017 Sep;219:86-92.
2. J Psychiatr Res. 2018 Sep;104:235-48.
3. J Womens Health. (Larchmt). 2015 Sep;24(9):762-70.
4. Clin Psychol Rev. 2014 Jul;34(5):389-401.
5. Compr Psychiatry. 2009 Nov-Dec;50(6):503-9.
6. Int Rev Psychiatry. 2003 Aug;15(3):231-42.
7. Clin Obstet Gynecol. 2018 Sep;61(3):533-43.
8. Curr Opinion Psychiatry. 2012 Mar;25(2):141-8.
9. Am J Psychiatry. 2009 Apr;166(4):405-8.
Dr. Reinstein is a psychiatry attending at Zucker Hillside Hospital. Her clinical interests include reproductive psychiatry and family therapy, with a specific focus on maternal mental health. Dr. Reinstein completed her adult psychiatry residency training at Montefiore Hospital/Albert Einstein College of Medicine, New York, after graduating from the Albert Einstein College of Medicine and Yeshiva University, New York, with a BA in biology. She is one of the recipients of the 4th Annual Resident Recognition Award for Excellence in Family Oriented Care.
Softening the blow to women and families of severe perinatal, postpartum psychiatric disorders
Softening the blow to women and families of severe perinatal, postpartum psychiatric disorders
Editor’s Note: Alison M. Heru, MD, the Families in Psychiatry columnist, invited Dr. Reinstein to address this topic.
“But this was not what I expected!” That’s a statement I have heard from countless new mothers.
Women often envision pregnancy and the postpartum period as a time of pure joy. The glow of an expectant woman and the excitement of the arrival of a new baby masks the reality that many women struggle emotionally when transitioning to motherhood. Like the birth of a child, the birth of a mother is a complex process. Upholding the myth that all women seamlessly transform into mothers can have devastating effects and hinder access to mental health care.
As a psychiatrist working on a women’s inpatient unit with a perinatal program, I treat women at times of crisis. What may have begun as mild anxiety or depression sometimes quickly spirals into severe psychiatric illness. The sheer force of these severe perinatal and postpartum psychiatric disorders often leaves women and families shocked and confused, wondering what happened to their crumbled dreams of early motherhood.
What must general psychiatrists know about perinatal and postpartum psychiatric disorders? Why is maternal mental health so important? What are the barriers to treatment for these women? How can general psychiatrists best support and treat these new mothers and their families?
What data show
Maternal depression is now known to be one of the most common complications of pregnancy. Studies have suggested that about 11% of women experience depression during pregnancy1 and approximately 17% of women are depressed in the postpartum period.2 Perinatal generalized anxiety disorder has been shown to have a prevalence of 8.5%-10.5% during pregnancy with a wider variance post partum.3 Approximately 3% of women in the general community develop PTSD symptoms following childbirth.4 Research suggests that about 2% of women develop obsessive-compulsive disorder symptoms in the postpartum period.5 Postpartum psychosis, a rare but potentially devastating illness, occurs after 0.1%-0.2% of births.6
Importance of maternal mental health
There is a growing body of literature supporting both obstetric and pediatric adverse outcomes related to untreated psychiatric illness. Untreated maternal depression has been associated with obstetric complications, such as preterm delivery, preeclampsia, low birth weight, as well as the child’s developing cognitive function.7 Anxiety during pregnancy has been associated with both a shorter gestational period and adverse implications for fetal neurodevelopment.
These adverse effects were found to be even more potent in “pregnancy anxiety,” or anxiety specifically focused on the pregnancy, the birth experience, and the transition to motherhood.8 The psychotic symptoms occurring during postpartum psychosis can jeopardize the lives of both a woman and her child and carries a 4% risk of infanticide.9 Although there are limited data about the long-term effects of postpartum obsessive-compulsive disorders and PTSD, it is reasonable to assume that they might carry negative long-term implications for the mother and possibly her child.
Barriers to treatment
Despite the significant rates of mental illness, pregnant and new mothers often face barriers to receiving treatment. Many psychiatrists are hesitant to prescribe psychiatric medication to pregnant women because of concerns about teratogenic potential of psychiatric medications; similar concerns exist for newborn babies when prescribing medications to lactating mothers. In addition, the field of reproductive psychiatry is evolving at a rapid pace, making it difficult for busy psychiatrists to keep up with the ever-growing literature.
Also, it is hard to imagine a population that has more barriers to attending outpatient appointments. For many new mothers, the exhaustion and all-consuming work involved with taking care of a newborn are insurmountable barriers to obtaining mental health care. In addition, despite the awareness that new mothers often are more emotional, families can be slow to recognize the developing severity of a psychiatric illness during the peripartum and postpartum periods.
Supporting and treating new mothers
As general psychiatrists, there are several ways to directly help these women.
1. Expect the expected. Even in women with no prior psychiatric history, a significant percentage of expectant and postpartum women will develop acute psychiatric symptoms. Learn about the different presentations and treatments of perinatal and postpartum psychiatric disorders. For example, a woman might have thoughts of harming her baby in both postpartum psychosis and obsessive-compulsive disorder. However, the acuity and treatment of these two conditions drastically differ.
2. Learn more about psychiatric medications. Several apps and websites are available to psychiatrists to learn about the safety profile of psychiatric medications, such as Reprotox.org, mothertobaby.org, lactmed, and womensmentalhealth.org. Many medications are considered to be relatively safe during pregnancy and breastfeeding. It is important for psychiatrists to appreciate the risks when choosing not to prescribe to pregnant and postpartum women. Sometimes a known risk of a specific medication may be preferable to the unknown risk of leaving a woman susceptible to a severe psychiatric decompensation.
3. Involve all members of the family. A mother’s mental health has significant implications for the entire family. Psychoeducation for the family as well as frequent family sessions are key tools when treating this population. In addition, prescribing to pregnant women provides the opportunity for a psychiatrist to refine skills in joint decision making; it is crucial to involve both a patient and her spouse when discussing psychiatric medications.
4. Provide ready access and collaborate care. It is important to understand the potential rapid onset of psychiatric symptoms during the pregnancy and postpartum period. Psychiatrists should be prepared to collaborate care with other specialties. It is important to establish relationships with community psychotherapists specializing in maternal mental health, pediatricians, as well as obstetricians.
5. Learn when to seek a higher level of care. Although many women with perinatal and postpartum psychiatric symptoms can be managed as outpatients, women at times need a higher level of care. Similar to general psychiatry, women who are acutely suicidal or homicidal or have a sudden onset of psychotic and manic symptoms all should be evaluated immediately for inpatient hospitalization. Women with less severe symptoms but who require a higher level of care than typically offered in standard outpatient treatment should be candidates for partial hospitalization programs.
General intensive programs usually can accommodate these women, but it is ideal to refer this population to perinatal intensive programs. Postpartum Support International (postpartum.net) lists the nationwide inpatient and partial perinatal programs as well as regional and local services. An example of inpatient perinatal care is the women’s unit at Zucker Hillside Hospital (Northwell Health System, Glen Oaks, N.Y.), which houses an inpatient perinatal program. As a psychiatrist on the unit, I treat acute symptoms such as depression, anxiety, psychosis, mania, and catatonia that occur during the perinatal and postpartum periods. Given the severity of symptoms, I use a wide range of psychiatric medications with the possibility of electroconvulsive therapy when indicated. Psychotherapy staff on the unit offer specialized perinatal, mothers, and dialectical behavioral therapy groups. Breast pumps are available for women who wish to breastfeed. Accommodations are made for babies and children to visit their mother when clinically appropriate. Once discharged, women often are referred to Zucker Hillside’s own perinatal outpatient clinic for continued treatment. Similar models exist in select inpatient units as well as an increasing number of partial programs across the United States.
Conclusion
Psychiatric care for pregnant and new mothers can be challenging, but it is also immensely rewarding. Restoring a mother’s mental health usually leads to increased emotional stability for her entire family. Given the prevalence of maternal mental health disorders, psychiatrists in nearly every setting will encounter this population of women. With dedicated time devoted to reviewing the literature and learning about local resources, psychiatrists can feel comfortable treating women throughout the childbearing experience.
References
1. J Affect Disord. 2017 Sep;219:86-92.
2. J Psychiatr Res. 2018 Sep;104:235-48.
3. J Womens Health. (Larchmt). 2015 Sep;24(9):762-70.
4. Clin Psychol Rev. 2014 Jul;34(5):389-401.
5. Compr Psychiatry. 2009 Nov-Dec;50(6):503-9.
6. Int Rev Psychiatry. 2003 Aug;15(3):231-42.
7. Clin Obstet Gynecol. 2018 Sep;61(3):533-43.
8. Curr Opinion Psychiatry. 2012 Mar;25(2):141-8.
9. Am J Psychiatry. 2009 Apr;166(4):405-8.
Dr. Reinstein is a psychiatry attending at Zucker Hillside Hospital. Her clinical interests include reproductive psychiatry and family therapy, with a specific focus on maternal mental health. Dr. Reinstein completed her adult psychiatry residency training at Montefiore Hospital/Albert Einstein College of Medicine, New York, after graduating from the Albert Einstein College of Medicine and Yeshiva University, New York, with a BA in biology. She is one of the recipients of the 4th Annual Resident Recognition Award for Excellence in Family Oriented Care.
Editor’s Note: Alison M. Heru, MD, the Families in Psychiatry columnist, invited Dr. Reinstein to address this topic.
“But this was not what I expected!” That’s a statement I have heard from countless new mothers.
Women often envision pregnancy and the postpartum period as a time of pure joy. The glow of an expectant woman and the excitement of the arrival of a new baby masks the reality that many women struggle emotionally when transitioning to motherhood. Like the birth of a child, the birth of a mother is a complex process. Upholding the myth that all women seamlessly transform into mothers can have devastating effects and hinder access to mental health care.
As a psychiatrist working on a women’s inpatient unit with a perinatal program, I treat women at times of crisis. What may have begun as mild anxiety or depression sometimes quickly spirals into severe psychiatric illness. The sheer force of these severe perinatal and postpartum psychiatric disorders often leaves women and families shocked and confused, wondering what happened to their crumbled dreams of early motherhood.
What must general psychiatrists know about perinatal and postpartum psychiatric disorders? Why is maternal mental health so important? What are the barriers to treatment for these women? How can general psychiatrists best support and treat these new mothers and their families?
What data show
Maternal depression is now known to be one of the most common complications of pregnancy. Studies have suggested that about 11% of women experience depression during pregnancy1 and approximately 17% of women are depressed in the postpartum period.2 Perinatal generalized anxiety disorder has been shown to have a prevalence of 8.5%-10.5% during pregnancy with a wider variance post partum.3 Approximately 3% of women in the general community develop PTSD symptoms following childbirth.4 Research suggests that about 2% of women develop obsessive-compulsive disorder symptoms in the postpartum period.5 Postpartum psychosis, a rare but potentially devastating illness, occurs after 0.1%-0.2% of births.6
Importance of maternal mental health
There is a growing body of literature supporting both obstetric and pediatric adverse outcomes related to untreated psychiatric illness. Untreated maternal depression has been associated with obstetric complications, such as preterm delivery, preeclampsia, low birth weight, as well as the child’s developing cognitive function.7 Anxiety during pregnancy has been associated with both a shorter gestational period and adverse implications for fetal neurodevelopment.
These adverse effects were found to be even more potent in “pregnancy anxiety,” or anxiety specifically focused on the pregnancy, the birth experience, and the transition to motherhood.8 The psychotic symptoms occurring during postpartum psychosis can jeopardize the lives of both a woman and her child and carries a 4% risk of infanticide.9 Although there are limited data about the long-term effects of postpartum obsessive-compulsive disorders and PTSD, it is reasonable to assume that they might carry negative long-term implications for the mother and possibly her child.
Barriers to treatment
Despite the significant rates of mental illness, pregnant and new mothers often face barriers to receiving treatment. Many psychiatrists are hesitant to prescribe psychiatric medication to pregnant women because of concerns about teratogenic potential of psychiatric medications; similar concerns exist for newborn babies when prescribing medications to lactating mothers. In addition, the field of reproductive psychiatry is evolving at a rapid pace, making it difficult for busy psychiatrists to keep up with the ever-growing literature.
Also, it is hard to imagine a population that has more barriers to attending outpatient appointments. For many new mothers, the exhaustion and all-consuming work involved with taking care of a newborn are insurmountable barriers to obtaining mental health care. In addition, despite the awareness that new mothers often are more emotional, families can be slow to recognize the developing severity of a psychiatric illness during the peripartum and postpartum periods.
Supporting and treating new mothers
As general psychiatrists, there are several ways to directly help these women.
1. Expect the expected. Even in women with no prior psychiatric history, a significant percentage of expectant and postpartum women will develop acute psychiatric symptoms. Learn about the different presentations and treatments of perinatal and postpartum psychiatric disorders. For example, a woman might have thoughts of harming her baby in both postpartum psychosis and obsessive-compulsive disorder. However, the acuity and treatment of these two conditions drastically differ.
2. Learn more about psychiatric medications. Several apps and websites are available to psychiatrists to learn about the safety profile of psychiatric medications, such as Reprotox.org, mothertobaby.org, lactmed, and womensmentalhealth.org. Many medications are considered to be relatively safe during pregnancy and breastfeeding. It is important for psychiatrists to appreciate the risks when choosing not to prescribe to pregnant and postpartum women. Sometimes a known risk of a specific medication may be preferable to the unknown risk of leaving a woman susceptible to a severe psychiatric decompensation.
3. Involve all members of the family. A mother’s mental health has significant implications for the entire family. Psychoeducation for the family as well as frequent family sessions are key tools when treating this population. In addition, prescribing to pregnant women provides the opportunity for a psychiatrist to refine skills in joint decision making; it is crucial to involve both a patient and her spouse when discussing psychiatric medications.
4. Provide ready access and collaborate care. It is important to understand the potential rapid onset of psychiatric symptoms during the pregnancy and postpartum period. Psychiatrists should be prepared to collaborate care with other specialties. It is important to establish relationships with community psychotherapists specializing in maternal mental health, pediatricians, as well as obstetricians.
5. Learn when to seek a higher level of care. Although many women with perinatal and postpartum psychiatric symptoms can be managed as outpatients, women at times need a higher level of care. Similar to general psychiatry, women who are acutely suicidal or homicidal or have a sudden onset of psychotic and manic symptoms all should be evaluated immediately for inpatient hospitalization. Women with less severe symptoms but who require a higher level of care than typically offered in standard outpatient treatment should be candidates for partial hospitalization programs.
General intensive programs usually can accommodate these women, but it is ideal to refer this population to perinatal intensive programs. Postpartum Support International (postpartum.net) lists the nationwide inpatient and partial perinatal programs as well as regional and local services. An example of inpatient perinatal care is the women’s unit at Zucker Hillside Hospital (Northwell Health System, Glen Oaks, N.Y.), which houses an inpatient perinatal program. As a psychiatrist on the unit, I treat acute symptoms such as depression, anxiety, psychosis, mania, and catatonia that occur during the perinatal and postpartum periods. Given the severity of symptoms, I use a wide range of psychiatric medications with the possibility of electroconvulsive therapy when indicated. Psychotherapy staff on the unit offer specialized perinatal, mothers, and dialectical behavioral therapy groups. Breast pumps are available for women who wish to breastfeed. Accommodations are made for babies and children to visit their mother when clinically appropriate. Once discharged, women often are referred to Zucker Hillside’s own perinatal outpatient clinic for continued treatment. Similar models exist in select inpatient units as well as an increasing number of partial programs across the United States.
Conclusion
Psychiatric care for pregnant and new mothers can be challenging, but it is also immensely rewarding. Restoring a mother’s mental health usually leads to increased emotional stability for her entire family. Given the prevalence of maternal mental health disorders, psychiatrists in nearly every setting will encounter this population of women. With dedicated time devoted to reviewing the literature and learning about local resources, psychiatrists can feel comfortable treating women throughout the childbearing experience.
References
1. J Affect Disord. 2017 Sep;219:86-92.
2. J Psychiatr Res. 2018 Sep;104:235-48.
3. J Womens Health. (Larchmt). 2015 Sep;24(9):762-70.
4. Clin Psychol Rev. 2014 Jul;34(5):389-401.
5. Compr Psychiatry. 2009 Nov-Dec;50(6):503-9.
6. Int Rev Psychiatry. 2003 Aug;15(3):231-42.
7. Clin Obstet Gynecol. 2018 Sep;61(3):533-43.
8. Curr Opinion Psychiatry. 2012 Mar;25(2):141-8.
9. Am J Psychiatry. 2009 Apr;166(4):405-8.
Dr. Reinstein is a psychiatry attending at Zucker Hillside Hospital. Her clinical interests include reproductive psychiatry and family therapy, with a specific focus on maternal mental health. Dr. Reinstein completed her adult psychiatry residency training at Montefiore Hospital/Albert Einstein College of Medicine, New York, after graduating from the Albert Einstein College of Medicine and Yeshiva University, New York, with a BA in biology. She is one of the recipients of the 4th Annual Resident Recognition Award for Excellence in Family Oriented Care.