User login
Botanical over-the-counter regimen reduces acne lesions
An over-the-counter botanical acne regimen outperformed a conventional acne regimen, with improved skin appearance and fewer lesions after 12 weeks of treatment, in a double-blind randomized controlled trial.
Eighty individuals aged 12 years and older with mild to moderate acne were randomized either to a three-step botanical-based acne treatment regimen (Receutics) consisting of a skin cleanser, breakout treatment, and tone and complexion corrector twice daily, or the currently marketed acne treatment kit, Proactiv (Guthy-Renker).
The botanical-based acne treatment contains a range of botanical ingredients, including algae and lentil seed extracts; cranberry seed, grape seed, and pumpkin seed oils; and allantoin; with 3.4% benzoyl peroxide as the active ingredient. The active ingredient in the cleanser is 2% salicylic acid, and niacinamide is the active ingredient in the tone and complexion corrector; both also contain botanical ingredients.
In the study, published in December, the investigator, Dr. Zoe Diana Draelos, reported that the botanical regimen achieved a significantly greater reduction in lesion count, in terms of closed comedones and inflammatory lesions, by week four, compared with the control treatment (J Drugs Dermatol. 2015 Dec; 14 [12]:1418-21).
This effect persisted at 12 weeks, with fewer closed comedones (P = .006). The botanical regimen also achieved greater reductions in pus, erythema, lesion height, and inflammation at weeks 2 and 4; although this difference disappeared by week 12. By week four and onwards, the botanical regimen also outperformed the conventional treatment on all blinded, investigator-assessed cosmetic appearance parameters, including skin tone, blemishes, erythema, and overall appearance.
While both treatments were effective at improving acne, Dr. Draelos, of Dermatology Consulting Services, High Point, N.C., said the botanical three-step regimen had the advantage of cosmetic ingredients such as emollients, anti-inflammatory/antioxidants, and “sensitive skin modulators.”
“This study demonstrates the value of combining monographed acne ingredients with advanced cosmeceutical technology,” she wrote.
The author received a grant from manufacturer Receutics to conduct the study.
An over-the-counter botanical acne regimen outperformed a conventional acne regimen, with improved skin appearance and fewer lesions after 12 weeks of treatment, in a double-blind randomized controlled trial.
Eighty individuals aged 12 years and older with mild to moderate acne were randomized either to a three-step botanical-based acne treatment regimen (Receutics) consisting of a skin cleanser, breakout treatment, and tone and complexion corrector twice daily, or the currently marketed acne treatment kit, Proactiv (Guthy-Renker).
The botanical-based acne treatment contains a range of botanical ingredients, including algae and lentil seed extracts; cranberry seed, grape seed, and pumpkin seed oils; and allantoin; with 3.4% benzoyl peroxide as the active ingredient. The active ingredient in the cleanser is 2% salicylic acid, and niacinamide is the active ingredient in the tone and complexion corrector; both also contain botanical ingredients.
In the study, published in December, the investigator, Dr. Zoe Diana Draelos, reported that the botanical regimen achieved a significantly greater reduction in lesion count, in terms of closed comedones and inflammatory lesions, by week four, compared with the control treatment (J Drugs Dermatol. 2015 Dec; 14 [12]:1418-21).
This effect persisted at 12 weeks, with fewer closed comedones (P = .006). The botanical regimen also achieved greater reductions in pus, erythema, lesion height, and inflammation at weeks 2 and 4; although this difference disappeared by week 12. By week four and onwards, the botanical regimen also outperformed the conventional treatment on all blinded, investigator-assessed cosmetic appearance parameters, including skin tone, blemishes, erythema, and overall appearance.
While both treatments were effective at improving acne, Dr. Draelos, of Dermatology Consulting Services, High Point, N.C., said the botanical three-step regimen had the advantage of cosmetic ingredients such as emollients, anti-inflammatory/antioxidants, and “sensitive skin modulators.”
“This study demonstrates the value of combining monographed acne ingredients with advanced cosmeceutical technology,” she wrote.
The author received a grant from manufacturer Receutics to conduct the study.
An over-the-counter botanical acne regimen outperformed a conventional acne regimen, with improved skin appearance and fewer lesions after 12 weeks of treatment, in a double-blind randomized controlled trial.
Eighty individuals aged 12 years and older with mild to moderate acne were randomized either to a three-step botanical-based acne treatment regimen (Receutics) consisting of a skin cleanser, breakout treatment, and tone and complexion corrector twice daily, or the currently marketed acne treatment kit, Proactiv (Guthy-Renker).
The botanical-based acne treatment contains a range of botanical ingredients, including algae and lentil seed extracts; cranberry seed, grape seed, and pumpkin seed oils; and allantoin; with 3.4% benzoyl peroxide as the active ingredient. The active ingredient in the cleanser is 2% salicylic acid, and niacinamide is the active ingredient in the tone and complexion corrector; both also contain botanical ingredients.
In the study, published in December, the investigator, Dr. Zoe Diana Draelos, reported that the botanical regimen achieved a significantly greater reduction in lesion count, in terms of closed comedones and inflammatory lesions, by week four, compared with the control treatment (J Drugs Dermatol. 2015 Dec; 14 [12]:1418-21).
This effect persisted at 12 weeks, with fewer closed comedones (P = .006). The botanical regimen also achieved greater reductions in pus, erythema, lesion height, and inflammation at weeks 2 and 4; although this difference disappeared by week 12. By week four and onwards, the botanical regimen also outperformed the conventional treatment on all blinded, investigator-assessed cosmetic appearance parameters, including skin tone, blemishes, erythema, and overall appearance.
While both treatments were effective at improving acne, Dr. Draelos, of Dermatology Consulting Services, High Point, N.C., said the botanical three-step regimen had the advantage of cosmetic ingredients such as emollients, anti-inflammatory/antioxidants, and “sensitive skin modulators.”
“This study demonstrates the value of combining monographed acne ingredients with advanced cosmeceutical technology,” she wrote.
The author received a grant from manufacturer Receutics to conduct the study.
FROM THE JOURNAL OF DRUGS IN DERMATOLOGY
Key clinical point: A botanical over-the-counter acne regimen achieved greater reductions in lesions than a currently marketed acne treatment.
Major finding: A three-step botanical-based acne regimen achieved significantly greater reduction in lesion counts and improvements in skin appearance than a conventional acne treatment.
Data source: A randomized, double-blind, controlled trial of 80 patients with mild to moderate acne.
Disclosures: The author received a grant from treatment manufacturer Receutics to conduct the study.
Meta-analysis backs SPRINT findings, argues for lower BP targets
In high-risk patients, blood pressure lowering is associated with significant reductions in vascular events for a range of comorbidities and baseline blood pressures, said the authors of a meta-analysis of 123 randomized controlled trials published in the last 50 years.
Each 10–mm Hg reduction in systolic blood pressure was associated with a 20% reduction in major cardiovascular disease events (95% confidence interval, 0.77-0.83), a 17% reduction in coronary heart disease (95% CI, 0.78-0.88), a 27% reduction in stroke (95% CI, 0.68-0.77), and a 28% reduction in heart failure (95% CI, 0.67-0.78), based on the meta-analysis published Dec. 23 by the Lancet.
The exception was a lack of overall benefit of blood pressure lowering for renal failure events, a finding consistent with a previous meta-analysis of moderate versus intensive blood pressure reduction.
“Lowering of blood pressure into what has been regarded the normotensive range should therefore be routinely considered for the prevention of cardiovascular disease among those deemed to be of sufficient absolute risk,” wrote Dena Ettehad of the George Institute for Global Health, Oxford, and coauthors.
“Revision is urgently needed to recent blood pressure lowering guidelines that have relaxed the blood pressure lowering thresholds,” they added.
The researchers conducted a meta-analysis of blood pressure lowering treatment, involving a total of 613,815 participants and a minimum of 1,000 patient-years of follow-up in each study arm.
The analysis indicated that a 10–mm Hg reduction in systolic blood pressure achieved an overall 13% reduction in all-cause mortality (95% CI, 0.84-0.91) but had no significant impact on the risk of renal failure events.
These effects remained similar even when the effects were compared between strata of mean baseline systolic blood pressure, baseline coronary heart disease, or baseline cardiovascular disease (Lancet 2015 Dec 23. doi: 10.1016/S0140-6736(15)01225-8).
“In stratified analyses, we saw no strong evidence that proportional effects were diminished in trials that included people with lower baseline systolic blood pressure (less than 130 mm Hg), and major cardiovascular events were clearly reduced in high-risk patients with various baseline comorbidities,” the investigators wrote.
“Both of these major findings – the efficacy of blood pressure lowering below 130 mm Hg and the similar proportional effects in high-risk populations – are consistent with and extend the findings of the SPRINT trial,” they said.
The authors did note greater proportional reductions in the risk of stroke in populations without a history of cerebrovascular disease, compared with those with a history.
Populations without diabetes had significantly greater proportional reductions in risk, compared with those with diabetes, while populations without chronic kidney disease had greater proportional reductions in the risk of major cardiovascular disease events, compared with those with chronic kidney disease.
The five classes of antihypertensives were generally as effective as each other in reducing the risk of major outcomes.
The authors noted that, while there were small but significant differences between drug classes for outcomes, these effects may have been the result of differences in control regimens or the concurrent use of multiple drug classes in many trials.
Two authors were supported by the National Institute of Health Research, one by the Clarendon Fund, and one by the Rhodes Trust. The George Institute is supported by the Oxford Martin School. Two authors declared grants from Servier, and one also declared investments for the development of a polypill. No other conflicts of interest were declared.
The finding from this meta-analysis that there is no increased risk of any outcome with systolic blood pressure lowering shows that a J-shaped relationship could not be substantiated and that the treatment effects were unlikely to be attenuated in trials that included participants with low systolic blood pressures at baseline, particularly those with less than 130 mm Hg.
Since data are accumulating against the J-shaped relationship, and because energetic lowering of blood pressure seems safe and beneficial to patients, there is no reason not to apply this approach to high-risk patients.
Dr. Stéphane Laurent and Dr. Pierre Boutouyrie are with the department of pharmacology at European Georges Pompidou Hospital, Paris. These comments were taken from an accompanying editorial (Lancet 2015 Dec 23. doi: 10.1016/S0140-6736(15)01344-6). Dr. Boutouyrie declared grants and personal fees from Servier. Dr. Laurent had no conflicts of interest to declare.
The finding from this meta-analysis that there is no increased risk of any outcome with systolic blood pressure lowering shows that a J-shaped relationship could not be substantiated and that the treatment effects were unlikely to be attenuated in trials that included participants with low systolic blood pressures at baseline, particularly those with less than 130 mm Hg.
Since data are accumulating against the J-shaped relationship, and because energetic lowering of blood pressure seems safe and beneficial to patients, there is no reason not to apply this approach to high-risk patients.
Dr. Stéphane Laurent and Dr. Pierre Boutouyrie are with the department of pharmacology at European Georges Pompidou Hospital, Paris. These comments were taken from an accompanying editorial (Lancet 2015 Dec 23. doi: 10.1016/S0140-6736(15)01344-6). Dr. Boutouyrie declared grants and personal fees from Servier. Dr. Laurent had no conflicts of interest to declare.
The finding from this meta-analysis that there is no increased risk of any outcome with systolic blood pressure lowering shows that a J-shaped relationship could not be substantiated and that the treatment effects were unlikely to be attenuated in trials that included participants with low systolic blood pressures at baseline, particularly those with less than 130 mm Hg.
Since data are accumulating against the J-shaped relationship, and because energetic lowering of blood pressure seems safe and beneficial to patients, there is no reason not to apply this approach to high-risk patients.
Dr. Stéphane Laurent and Dr. Pierre Boutouyrie are with the department of pharmacology at European Georges Pompidou Hospital, Paris. These comments were taken from an accompanying editorial (Lancet 2015 Dec 23. doi: 10.1016/S0140-6736(15)01344-6). Dr. Boutouyrie declared grants and personal fees from Servier. Dr. Laurent had no conflicts of interest to declare.
In high-risk patients, blood pressure lowering is associated with significant reductions in vascular events for a range of comorbidities and baseline blood pressures, said the authors of a meta-analysis of 123 randomized controlled trials published in the last 50 years.
Each 10–mm Hg reduction in systolic blood pressure was associated with a 20% reduction in major cardiovascular disease events (95% confidence interval, 0.77-0.83), a 17% reduction in coronary heart disease (95% CI, 0.78-0.88), a 27% reduction in stroke (95% CI, 0.68-0.77), and a 28% reduction in heart failure (95% CI, 0.67-0.78), based on the meta-analysis published Dec. 23 by the Lancet.
The exception was a lack of overall benefit of blood pressure lowering for renal failure events, a finding consistent with a previous meta-analysis of moderate versus intensive blood pressure reduction.
“Lowering of blood pressure into what has been regarded the normotensive range should therefore be routinely considered for the prevention of cardiovascular disease among those deemed to be of sufficient absolute risk,” wrote Dena Ettehad of the George Institute for Global Health, Oxford, and coauthors.
“Revision is urgently needed to recent blood pressure lowering guidelines that have relaxed the blood pressure lowering thresholds,” they added.
The researchers conducted a meta-analysis of blood pressure lowering treatment, involving a total of 613,815 participants and a minimum of 1,000 patient-years of follow-up in each study arm.
The analysis indicated that a 10–mm Hg reduction in systolic blood pressure achieved an overall 13% reduction in all-cause mortality (95% CI, 0.84-0.91) but had no significant impact on the risk of renal failure events.
These effects remained similar even when the effects were compared between strata of mean baseline systolic blood pressure, baseline coronary heart disease, or baseline cardiovascular disease (Lancet 2015 Dec 23. doi: 10.1016/S0140-6736(15)01225-8).
“In stratified analyses, we saw no strong evidence that proportional effects were diminished in trials that included people with lower baseline systolic blood pressure (less than 130 mm Hg), and major cardiovascular events were clearly reduced in high-risk patients with various baseline comorbidities,” the investigators wrote.
“Both of these major findings – the efficacy of blood pressure lowering below 130 mm Hg and the similar proportional effects in high-risk populations – are consistent with and extend the findings of the SPRINT trial,” they said.
The authors did note greater proportional reductions in the risk of stroke in populations without a history of cerebrovascular disease, compared with those with a history.
Populations without diabetes had significantly greater proportional reductions in risk, compared with those with diabetes, while populations without chronic kidney disease had greater proportional reductions in the risk of major cardiovascular disease events, compared with those with chronic kidney disease.
The five classes of antihypertensives were generally as effective as each other in reducing the risk of major outcomes.
The authors noted that, while there were small but significant differences between drug classes for outcomes, these effects may have been the result of differences in control regimens or the concurrent use of multiple drug classes in many trials.
Two authors were supported by the National Institute of Health Research, one by the Clarendon Fund, and one by the Rhodes Trust. The George Institute is supported by the Oxford Martin School. Two authors declared grants from Servier, and one also declared investments for the development of a polypill. No other conflicts of interest were declared.
In high-risk patients, blood pressure lowering is associated with significant reductions in vascular events for a range of comorbidities and baseline blood pressures, said the authors of a meta-analysis of 123 randomized controlled trials published in the last 50 years.
Each 10–mm Hg reduction in systolic blood pressure was associated with a 20% reduction in major cardiovascular disease events (95% confidence interval, 0.77-0.83), a 17% reduction in coronary heart disease (95% CI, 0.78-0.88), a 27% reduction in stroke (95% CI, 0.68-0.77), and a 28% reduction in heart failure (95% CI, 0.67-0.78), based on the meta-analysis published Dec. 23 by the Lancet.
The exception was a lack of overall benefit of blood pressure lowering for renal failure events, a finding consistent with a previous meta-analysis of moderate versus intensive blood pressure reduction.
“Lowering of blood pressure into what has been regarded the normotensive range should therefore be routinely considered for the prevention of cardiovascular disease among those deemed to be of sufficient absolute risk,” wrote Dena Ettehad of the George Institute for Global Health, Oxford, and coauthors.
“Revision is urgently needed to recent blood pressure lowering guidelines that have relaxed the blood pressure lowering thresholds,” they added.
The researchers conducted a meta-analysis of blood pressure lowering treatment, involving a total of 613,815 participants and a minimum of 1,000 patient-years of follow-up in each study arm.
The analysis indicated that a 10–mm Hg reduction in systolic blood pressure achieved an overall 13% reduction in all-cause mortality (95% CI, 0.84-0.91) but had no significant impact on the risk of renal failure events.
These effects remained similar even when the effects were compared between strata of mean baseline systolic blood pressure, baseline coronary heart disease, or baseline cardiovascular disease (Lancet 2015 Dec 23. doi: 10.1016/S0140-6736(15)01225-8).
“In stratified analyses, we saw no strong evidence that proportional effects were diminished in trials that included people with lower baseline systolic blood pressure (less than 130 mm Hg), and major cardiovascular events were clearly reduced in high-risk patients with various baseline comorbidities,” the investigators wrote.
“Both of these major findings – the efficacy of blood pressure lowering below 130 mm Hg and the similar proportional effects in high-risk populations – are consistent with and extend the findings of the SPRINT trial,” they said.
The authors did note greater proportional reductions in the risk of stroke in populations without a history of cerebrovascular disease, compared with those with a history.
Populations without diabetes had significantly greater proportional reductions in risk, compared with those with diabetes, while populations without chronic kidney disease had greater proportional reductions in the risk of major cardiovascular disease events, compared with those with chronic kidney disease.
The five classes of antihypertensives were generally as effective as each other in reducing the risk of major outcomes.
The authors noted that, while there were small but significant differences between drug classes for outcomes, these effects may have been the result of differences in control regimens or the concurrent use of multiple drug classes in many trials.
Two authors were supported by the National Institute of Health Research, one by the Clarendon Fund, and one by the Rhodes Trust. The George Institute is supported by the Oxford Martin School. Two authors declared grants from Servier, and one also declared investments for the development of a polypill. No other conflicts of interest were declared.
FROM THE LANCET
Key clinical point: Blood pressure lowering is associated with significant reductions in vascular events in patients with a range of comorbidities and baseline blood pressures.
Major finding: Each 10–mm Hg reduction in systolic blood pressure is associated with a 20% reduction in major cardiovascular disease events.
Data source: A meta-analysis of 123 randomized controlled trials of blood pressure lowering treatment, involving a total of 613,815 participants.
Disclosures: Two authors were supported by the National Institute of Health Research, one by the Clarendon Fund, and one by the Rhodes Trust. The George Institute is supported by the Oxford Martin School. Two authors declared grants from Servier, and one also declared investments for the development of a polypill. No other conflicts of interest were declared.
Hepatitis C linked to Parkinson’s disease
Hepatitis C infection may increase the risk of Parkinson’s disease, according to a nationwide population-based study.
Researchers analyzed 10 years of data from the Taiwan National Health Insurance Research Database, which included 49,967 patients with viral hepatitis – 35,619 with hepatitis B infection, 10,286 with hepatitis C, and 4,062 with both – and 199,868 noninfected controls.
According to a paper published online Dec. 23 in Neurology, individuals with hepatitis C infection had a 29% greater incidence of Parkinson’s disease after adjustment for confounders such as sex, age, heart disease, stroke, and head injury (hazard ratio, 1.29; 95% confidence interval, 1.06-1.56).
There were no significant associations between hepatitis B or coinfection, and Parkinson’s disease risk (Neurology. 2016;86:1-7).
Age was the most common risk factor for Parkinson’s disease across all cohorts, and in the control group comorbidities such as hyperlipidemia, hypertension, ischemic heart disease, diabetes, and head injury all were associated with a significant increase in the risk of Parkinson’s disease.
Among individuals with hepatitis C infection, however, only ischemic heart disease and head injury remained significantly associated with Parkinson’s disease risk.
The possibility of an association between hepatitis C infection and Parkinson’s disease has emerged recently with evidence showing that the virus is neurotropic and can replicate in the central nervous system, reported Dr. Hsin-Hsi Tsai of the National Taiwan University Hospital, Taipei, and coauthors.
“Parkinsonism is rarely a described feature in patients with HCV. However, a recent study has discovered that HCV can induce dopaminergic neuron death, suggesting a possible association between HCV infection and” Parkinson’s disease, the authors wrote.
The study also showed that the association between hepatitis C infection and Parkinson’s disease was even more significant in individuals younger than 65 years old, who had a 61% greater risk of developing the neurodegenerative disease.
“Some of the risk factors for HCV infection, such as illicit drug use and associated behaviors, may be confounding factors in this age group,” the authors wrote, although they pointed out that, in Taiwan, use of intravenous drugs was not known to be a risk factor for infection. Commenting on a possible mechanism for the association between hepatitis C infection and Parkinson’s disease, Dr. Tsai and associates suggested the hepatitis C virus could be a possible viral candidate for triggering the neuroinflammation that is a characteristic feature of the disease.
“An earlier imaging study that involved using magnetic resonance spectroscopy to investigate the cerebral effect of HCV showed that chronic HCV infection was associated with elevated choline/creatinine ratios, a biomarker indicating inflammatory and infective conditions, in the basal ganglia and white matter,” they wrote.
The study was supported by the Taiwan Ministry of Health and Welfare Clinical Trial and Research Center of Excellence, China Medical University Hospital, Academia Sinica Taiwan Biobank, Stroke Biosignature Project, NRPB Stroke Clinical Trial Consortium, the Tseng-Lien Lin Foundation, the Taiwan Brain Disease Foundation, the Katsuzo and Kiyo Aoshima Memorial Funds, and CMU under the Aim for Top University Plan of the Ministry of Education. There were no conflicts of interest declared.
Hepatitis C infection may increase the risk of Parkinson’s disease, according to a nationwide population-based study.
Researchers analyzed 10 years of data from the Taiwan National Health Insurance Research Database, which included 49,967 patients with viral hepatitis – 35,619 with hepatitis B infection, 10,286 with hepatitis C, and 4,062 with both – and 199,868 noninfected controls.
According to a paper published online Dec. 23 in Neurology, individuals with hepatitis C infection had a 29% greater incidence of Parkinson’s disease after adjustment for confounders such as sex, age, heart disease, stroke, and head injury (hazard ratio, 1.29; 95% confidence interval, 1.06-1.56).
There were no significant associations between hepatitis B or coinfection, and Parkinson’s disease risk (Neurology. 2016;86:1-7).
Age was the most common risk factor for Parkinson’s disease across all cohorts, and in the control group comorbidities such as hyperlipidemia, hypertension, ischemic heart disease, diabetes, and head injury all were associated with a significant increase in the risk of Parkinson’s disease.
Among individuals with hepatitis C infection, however, only ischemic heart disease and head injury remained significantly associated with Parkinson’s disease risk.
The possibility of an association between hepatitis C infection and Parkinson’s disease has emerged recently with evidence showing that the virus is neurotropic and can replicate in the central nervous system, reported Dr. Hsin-Hsi Tsai of the National Taiwan University Hospital, Taipei, and coauthors.
“Parkinsonism is rarely a described feature in patients with HCV. However, a recent study has discovered that HCV can induce dopaminergic neuron death, suggesting a possible association between HCV infection and” Parkinson’s disease, the authors wrote.
The study also showed that the association between hepatitis C infection and Parkinson’s disease was even more significant in individuals younger than 65 years old, who had a 61% greater risk of developing the neurodegenerative disease.
“Some of the risk factors for HCV infection, such as illicit drug use and associated behaviors, may be confounding factors in this age group,” the authors wrote, although they pointed out that, in Taiwan, use of intravenous drugs was not known to be a risk factor for infection. Commenting on a possible mechanism for the association between hepatitis C infection and Parkinson’s disease, Dr. Tsai and associates suggested the hepatitis C virus could be a possible viral candidate for triggering the neuroinflammation that is a characteristic feature of the disease.
“An earlier imaging study that involved using magnetic resonance spectroscopy to investigate the cerebral effect of HCV showed that chronic HCV infection was associated with elevated choline/creatinine ratios, a biomarker indicating inflammatory and infective conditions, in the basal ganglia and white matter,” they wrote.
The study was supported by the Taiwan Ministry of Health and Welfare Clinical Trial and Research Center of Excellence, China Medical University Hospital, Academia Sinica Taiwan Biobank, Stroke Biosignature Project, NRPB Stroke Clinical Trial Consortium, the Tseng-Lien Lin Foundation, the Taiwan Brain Disease Foundation, the Katsuzo and Kiyo Aoshima Memorial Funds, and CMU under the Aim for Top University Plan of the Ministry of Education. There were no conflicts of interest declared.
Hepatitis C infection may increase the risk of Parkinson’s disease, according to a nationwide population-based study.
Researchers analyzed 10 years of data from the Taiwan National Health Insurance Research Database, which included 49,967 patients with viral hepatitis – 35,619 with hepatitis B infection, 10,286 with hepatitis C, and 4,062 with both – and 199,868 noninfected controls.
According to a paper published online Dec. 23 in Neurology, individuals with hepatitis C infection had a 29% greater incidence of Parkinson’s disease after adjustment for confounders such as sex, age, heart disease, stroke, and head injury (hazard ratio, 1.29; 95% confidence interval, 1.06-1.56).
There were no significant associations between hepatitis B or coinfection, and Parkinson’s disease risk (Neurology. 2016;86:1-7).
Age was the most common risk factor for Parkinson’s disease across all cohorts, and in the control group comorbidities such as hyperlipidemia, hypertension, ischemic heart disease, diabetes, and head injury all were associated with a significant increase in the risk of Parkinson’s disease.
Among individuals with hepatitis C infection, however, only ischemic heart disease and head injury remained significantly associated with Parkinson’s disease risk.
The possibility of an association between hepatitis C infection and Parkinson’s disease has emerged recently with evidence showing that the virus is neurotropic and can replicate in the central nervous system, reported Dr. Hsin-Hsi Tsai of the National Taiwan University Hospital, Taipei, and coauthors.
“Parkinsonism is rarely a described feature in patients with HCV. However, a recent study has discovered that HCV can induce dopaminergic neuron death, suggesting a possible association between HCV infection and” Parkinson’s disease, the authors wrote.
The study also showed that the association between hepatitis C infection and Parkinson’s disease was even more significant in individuals younger than 65 years old, who had a 61% greater risk of developing the neurodegenerative disease.
“Some of the risk factors for HCV infection, such as illicit drug use and associated behaviors, may be confounding factors in this age group,” the authors wrote, although they pointed out that, in Taiwan, use of intravenous drugs was not known to be a risk factor for infection. Commenting on a possible mechanism for the association between hepatitis C infection and Parkinson’s disease, Dr. Tsai and associates suggested the hepatitis C virus could be a possible viral candidate for triggering the neuroinflammation that is a characteristic feature of the disease.
“An earlier imaging study that involved using magnetic resonance spectroscopy to investigate the cerebral effect of HCV showed that chronic HCV infection was associated with elevated choline/creatinine ratios, a biomarker indicating inflammatory and infective conditions, in the basal ganglia and white matter,” they wrote.
The study was supported by the Taiwan Ministry of Health and Welfare Clinical Trial and Research Center of Excellence, China Medical University Hospital, Academia Sinica Taiwan Biobank, Stroke Biosignature Project, NRPB Stroke Clinical Trial Consortium, the Tseng-Lien Lin Foundation, the Taiwan Brain Disease Foundation, the Katsuzo and Kiyo Aoshima Memorial Funds, and CMU under the Aim for Top University Plan of the Ministry of Education. There were no conflicts of interest declared.
FROM NEUROLOGY
Key clinical point: Hepatitis C infection is associated with an increased risk of Parkinson’s disease.
Major finding: Individuals with hepatitis C infection had a 29% greater incidence of Parkinson’s disease.
Data source: Analysis of data from the Taiwan National Health Insurance Research Database, including 49,967 patients with viral hepatitis and 199,868 noninfected controls.
Disclosures: The study was supported by the Taiwan Ministry of Health and Welfare Clinical Trial and Research Center of Excellence, China Medical University Hospital, Academia Sinica Taiwan Biobank, Stroke Biosignature Project, NRPB Stroke Clinical Trial Consortium, the Tseng-Lien Lin Foundation, the Taiwan Brain Disease Foundation, the Katsuzo and Kiyo Aoshima Memorial Funds, and CMU under the Aim for Top University Plan of the Ministry of Education. There were no conflicts of interest declared.
HIV-positive patients may be at greater risk of atherosclerosis
HIV-infected individuals without any traditional cardiovascular disease risk factors still show signs of vascular thickening, compared with HIV-negative controls, researchers reported in a British study.
A team led by Dr. Kathleen A.M. Rose of the cardiovascular biomedical research unit at London’s Royal Brompton Hospital performed carotid cardiovascular magnetic resonance imaging on 33 HIV-infected patients and 35 HIV-negative controls, with both groups being at low cardiovascular risk. The study showed HIV infection was associated with a significantly greater ratio of carotid wall to outer wall thickness (36.7% vs. 32.5%, P less than .0001) – an indicator of carotid intima-media thickening that has been shown in HIV-negative populations to be predictive of future cardiovascular events.
Women with HIV had an even greater increase in carotid intima-media thickening, compared with men with HIV, according to the study results (JAIDS. 2015 Nov 16. doi: 10.1097/QAI.0000000000000900)
While there were no significant differences between the cases and controls in total carotid lumen volume, carotid artery volume, and carotid wall volume, total wall volume was higher in HIV-infected individuals, and there was a nonsignificant decrease in carotid artery distensibility in the HIV-infected group.
“Although traditional cardiovascular risk factors are highly prevalent and accepted to play a role in HIV-associated cardiovascular disease, the role of long-term cART [combination antiretroviral therapy] and HIV infection itself remains controversial,” wrote Dr. Rose and her coauthors.
The researchers cited earlier studies linking the antiretroviral agents indinavir, abacavir, and lopinavir with increased cardiovascular risk, although they pointed out there was conflicting evidence of a link with type of antiretroviral therapy.
The HIV-infected participants were all stable on combination antiretroviral therapy for a median duration of 7 years (2-21 years), and all had a plasma HIV-1 RNA viral load below 50 copies/mL.
Years of antiretroviral therapy and use of nonnucleoside reverse transcriptase inhibitors or protease inhibitors did not significantly impact carotid intima-media thickness, although patients taking abacavir – which is associated with increased cardiovascular risk – had a lower wall/outer wall ratio than those on zidovudine.
“This result may also reflect a channeling bias whereby clinicians only use abacavir in subjects they consider to have very low cardiovascular risk,” the authors wrote.
Other parameters such as age, ethnicity, CD4 cell count, nadir CD4 cell count, and years since HIV diagnosis did not impact atherosclerosis in HIV-positive subjects.
“Although our study has not followed up patients or controls longitudinally, the diverging lines between the groups with increasing age suggests that HIV infection and/or its treatment may be associated with progression of vascular wall thickening beyond that normally seen with age,” the authors reported.
“As increasing C-IMT [carotid intima-media thickness] has been found to be independently predictive of future stroke and myocardial infarction in HIV-uninfected populations, the findings of this study suggest that the rate of vascular events is likely to remain elevated in HIV-patients despite aggressive treatment of cardiovascular risk factors, highlighting the need for improved patient and health care provider education to detect and manage aggressively early signs of cardiovascular disease.”
The study was supported by the National Institute of Health Research cardiovascular biomedical research unit at Royal Brompton and Harefield NHS Foundation Trust, and Imperial College London. Three authors declared honoraria, grants, sponsorship, and consultancies from the pharmaceutical industry.
HIV-infected individuals without any traditional cardiovascular disease risk factors still show signs of vascular thickening, compared with HIV-negative controls, researchers reported in a British study.
A team led by Dr. Kathleen A.M. Rose of the cardiovascular biomedical research unit at London’s Royal Brompton Hospital performed carotid cardiovascular magnetic resonance imaging on 33 HIV-infected patients and 35 HIV-negative controls, with both groups being at low cardiovascular risk. The study showed HIV infection was associated with a significantly greater ratio of carotid wall to outer wall thickness (36.7% vs. 32.5%, P less than .0001) – an indicator of carotid intima-media thickening that has been shown in HIV-negative populations to be predictive of future cardiovascular events.
Women with HIV had an even greater increase in carotid intima-media thickening, compared with men with HIV, according to the study results (JAIDS. 2015 Nov 16. doi: 10.1097/QAI.0000000000000900)
While there were no significant differences between the cases and controls in total carotid lumen volume, carotid artery volume, and carotid wall volume, total wall volume was higher in HIV-infected individuals, and there was a nonsignificant decrease in carotid artery distensibility in the HIV-infected group.
“Although traditional cardiovascular risk factors are highly prevalent and accepted to play a role in HIV-associated cardiovascular disease, the role of long-term cART [combination antiretroviral therapy] and HIV infection itself remains controversial,” wrote Dr. Rose and her coauthors.
The researchers cited earlier studies linking the antiretroviral agents indinavir, abacavir, and lopinavir with increased cardiovascular risk, although they pointed out there was conflicting evidence of a link with type of antiretroviral therapy.
The HIV-infected participants were all stable on combination antiretroviral therapy for a median duration of 7 years (2-21 years), and all had a plasma HIV-1 RNA viral load below 50 copies/mL.
Years of antiretroviral therapy and use of nonnucleoside reverse transcriptase inhibitors or protease inhibitors did not significantly impact carotid intima-media thickness, although patients taking abacavir – which is associated with increased cardiovascular risk – had a lower wall/outer wall ratio than those on zidovudine.
“This result may also reflect a channeling bias whereby clinicians only use abacavir in subjects they consider to have very low cardiovascular risk,” the authors wrote.
Other parameters such as age, ethnicity, CD4 cell count, nadir CD4 cell count, and years since HIV diagnosis did not impact atherosclerosis in HIV-positive subjects.
“Although our study has not followed up patients or controls longitudinally, the diverging lines between the groups with increasing age suggests that HIV infection and/or its treatment may be associated with progression of vascular wall thickening beyond that normally seen with age,” the authors reported.
“As increasing C-IMT [carotid intima-media thickness] has been found to be independently predictive of future stroke and myocardial infarction in HIV-uninfected populations, the findings of this study suggest that the rate of vascular events is likely to remain elevated in HIV-patients despite aggressive treatment of cardiovascular risk factors, highlighting the need for improved patient and health care provider education to detect and manage aggressively early signs of cardiovascular disease.”
The study was supported by the National Institute of Health Research cardiovascular biomedical research unit at Royal Brompton and Harefield NHS Foundation Trust, and Imperial College London. Three authors declared honoraria, grants, sponsorship, and consultancies from the pharmaceutical industry.
HIV-infected individuals without any traditional cardiovascular disease risk factors still show signs of vascular thickening, compared with HIV-negative controls, researchers reported in a British study.
A team led by Dr. Kathleen A.M. Rose of the cardiovascular biomedical research unit at London’s Royal Brompton Hospital performed carotid cardiovascular magnetic resonance imaging on 33 HIV-infected patients and 35 HIV-negative controls, with both groups being at low cardiovascular risk. The study showed HIV infection was associated with a significantly greater ratio of carotid wall to outer wall thickness (36.7% vs. 32.5%, P less than .0001) – an indicator of carotid intima-media thickening that has been shown in HIV-negative populations to be predictive of future cardiovascular events.
Women with HIV had an even greater increase in carotid intima-media thickening, compared with men with HIV, according to the study results (JAIDS. 2015 Nov 16. doi: 10.1097/QAI.0000000000000900)
While there were no significant differences between the cases and controls in total carotid lumen volume, carotid artery volume, and carotid wall volume, total wall volume was higher in HIV-infected individuals, and there was a nonsignificant decrease in carotid artery distensibility in the HIV-infected group.
“Although traditional cardiovascular risk factors are highly prevalent and accepted to play a role in HIV-associated cardiovascular disease, the role of long-term cART [combination antiretroviral therapy] and HIV infection itself remains controversial,” wrote Dr. Rose and her coauthors.
The researchers cited earlier studies linking the antiretroviral agents indinavir, abacavir, and lopinavir with increased cardiovascular risk, although they pointed out there was conflicting evidence of a link with type of antiretroviral therapy.
The HIV-infected participants were all stable on combination antiretroviral therapy for a median duration of 7 years (2-21 years), and all had a plasma HIV-1 RNA viral load below 50 copies/mL.
Years of antiretroviral therapy and use of nonnucleoside reverse transcriptase inhibitors or protease inhibitors did not significantly impact carotid intima-media thickness, although patients taking abacavir – which is associated with increased cardiovascular risk – had a lower wall/outer wall ratio than those on zidovudine.
“This result may also reflect a channeling bias whereby clinicians only use abacavir in subjects they consider to have very low cardiovascular risk,” the authors wrote.
Other parameters such as age, ethnicity, CD4 cell count, nadir CD4 cell count, and years since HIV diagnosis did not impact atherosclerosis in HIV-positive subjects.
“Although our study has not followed up patients or controls longitudinally, the diverging lines between the groups with increasing age suggests that HIV infection and/or its treatment may be associated with progression of vascular wall thickening beyond that normally seen with age,” the authors reported.
“As increasing C-IMT [carotid intima-media thickness] has been found to be independently predictive of future stroke and myocardial infarction in HIV-uninfected populations, the findings of this study suggest that the rate of vascular events is likely to remain elevated in HIV-patients despite aggressive treatment of cardiovascular risk factors, highlighting the need for improved patient and health care provider education to detect and manage aggressively early signs of cardiovascular disease.”
The study was supported by the National Institute of Health Research cardiovascular biomedical research unit at Royal Brompton and Harefield NHS Foundation Trust, and Imperial College London. Three authors declared honoraria, grants, sponsorship, and consultancies from the pharmaceutical industry.
Key clinical point: HIV infection and/or treatment are associated with significantly greater vascular thickening, even in the absence of other cardiovascular risk factors.
Major finding: HIV-infected patients had a significantly greater ratio of carotid wall to outer wall thickness, compared with HIV-negative controls.
Data source: An observational study of 33 HIV-infected patients and 35 HIV-negative controls.
Disclosures: The study was supported by the National Institute of Health Research cardiovascular biomedical research unit at Royal Brompton and Harefield NHS Foundation Trust, and Imperial College London. Three authors declared honoraria, grants, sponsorship, and consultancies from the pharmaceutical industry.
Few teen females prescribed teratogenic meds get contraceptive advice, Rx
Fewer than one-third of adolescent females prescribed a teratogenic medication were counseled about, prescribed, or referred for contraception, according to a retrospective review of data from a single academic pediatric medical center.
The records from 1,694 female patients aged 14-25 years, who received 4,506 medications of Food and Drug Administration pregnancy risk category D or X – mostly commonly topiramate, methotrexate, diazepam, isotretinoin, or enalapril – showed that contraceptive counseling, prescription, or referral occurred in 29% of visits, according to a paper published online Dec. 16 in Pediatrics.
White females were 61% more likely to receive contraceptive provision than were nonwhites, and girls aged 16 years or older were 20% more likely to receive it than were girls aged 14-15 years (Pediatrics 2016, Jan. doi: 10.1542/peds.2015-1454).
Teratogens with a federal surveillance system, such as iPLEDGE or REMS, were associated with twofold increase in the rate of contraceptive provision, but a much lower likelihood of documentation of menstrual and sexual histories.
“This finding was unexpected given that the focus of these systems is to proactively reduce the risk of unplanned pregnancy during drug treatment,” wrote Stephani L. Stancil of Children’s Mercy Hospital, Kansas City, Mo., and coauthors.
“Opportunity exists in these adolescents to increase rates of contraceptive counsel, the prescription of contraception if appropriate, or referral for such care when it becomes necessary to use a medication with known teratogenic potential,” they said.
Children’s Mercy Hospital supported the study. No conflicts of interest were declared.
“Even if a provider does not think it is within his or her scope of care to provide a contraceptive method, asking the questions to assess whether a contraceptive method might be needed from another provider is essential.
“In addition, all providers should be aware of the newer recommendation that all adolescents should be offered the option of a long-acting reversible contraceptive method to prevent pregnancy.
The fact that the Affordable Care Act allows us to provide 18 different contraceptive methods without any cost sharing to the patient should also make adolescent pregnancy prevention easier than ever.”
Erica J. Gibson, M.D., is an expert in adolescent medicine in the department of pediatrics at the University of Vermont Children’s Hospital, Burlington. Her remarks are excerpted from an article published in Pediatrics (2016, Jan. doi:10.1542/peds.2015-3826). She disclosed no conflicts of interest.
“Even if a provider does not think it is within his or her scope of care to provide a contraceptive method, asking the questions to assess whether a contraceptive method might be needed from another provider is essential.
“In addition, all providers should be aware of the newer recommendation that all adolescents should be offered the option of a long-acting reversible contraceptive method to prevent pregnancy.
The fact that the Affordable Care Act allows us to provide 18 different contraceptive methods without any cost sharing to the patient should also make adolescent pregnancy prevention easier than ever.”
Erica J. Gibson, M.D., is an expert in adolescent medicine in the department of pediatrics at the University of Vermont Children’s Hospital, Burlington. Her remarks are excerpted from an article published in Pediatrics (2016, Jan. doi:10.1542/peds.2015-3826). She disclosed no conflicts of interest.
“Even if a provider does not think it is within his or her scope of care to provide a contraceptive method, asking the questions to assess whether a contraceptive method might be needed from another provider is essential.
“In addition, all providers should be aware of the newer recommendation that all adolescents should be offered the option of a long-acting reversible contraceptive method to prevent pregnancy.
The fact that the Affordable Care Act allows us to provide 18 different contraceptive methods without any cost sharing to the patient should also make adolescent pregnancy prevention easier than ever.”
Erica J. Gibson, M.D., is an expert in adolescent medicine in the department of pediatrics at the University of Vermont Children’s Hospital, Burlington. Her remarks are excerpted from an article published in Pediatrics (2016, Jan. doi:10.1542/peds.2015-3826). She disclosed no conflicts of interest.
Fewer than one-third of adolescent females prescribed a teratogenic medication were counseled about, prescribed, or referred for contraception, according to a retrospective review of data from a single academic pediatric medical center.
The records from 1,694 female patients aged 14-25 years, who received 4,506 medications of Food and Drug Administration pregnancy risk category D or X – mostly commonly topiramate, methotrexate, diazepam, isotretinoin, or enalapril – showed that contraceptive counseling, prescription, or referral occurred in 29% of visits, according to a paper published online Dec. 16 in Pediatrics.
White females were 61% more likely to receive contraceptive provision than were nonwhites, and girls aged 16 years or older were 20% more likely to receive it than were girls aged 14-15 years (Pediatrics 2016, Jan. doi: 10.1542/peds.2015-1454).
Teratogens with a federal surveillance system, such as iPLEDGE or REMS, were associated with twofold increase in the rate of contraceptive provision, but a much lower likelihood of documentation of menstrual and sexual histories.
“This finding was unexpected given that the focus of these systems is to proactively reduce the risk of unplanned pregnancy during drug treatment,” wrote Stephani L. Stancil of Children’s Mercy Hospital, Kansas City, Mo., and coauthors.
“Opportunity exists in these adolescents to increase rates of contraceptive counsel, the prescription of contraception if appropriate, or referral for such care when it becomes necessary to use a medication with known teratogenic potential,” they said.
Children’s Mercy Hospital supported the study. No conflicts of interest were declared.
Fewer than one-third of adolescent females prescribed a teratogenic medication were counseled about, prescribed, or referred for contraception, according to a retrospective review of data from a single academic pediatric medical center.
The records from 1,694 female patients aged 14-25 years, who received 4,506 medications of Food and Drug Administration pregnancy risk category D or X – mostly commonly topiramate, methotrexate, diazepam, isotretinoin, or enalapril – showed that contraceptive counseling, prescription, or referral occurred in 29% of visits, according to a paper published online Dec. 16 in Pediatrics.
White females were 61% more likely to receive contraceptive provision than were nonwhites, and girls aged 16 years or older were 20% more likely to receive it than were girls aged 14-15 years (Pediatrics 2016, Jan. doi: 10.1542/peds.2015-1454).
Teratogens with a federal surveillance system, such as iPLEDGE or REMS, were associated with twofold increase in the rate of contraceptive provision, but a much lower likelihood of documentation of menstrual and sexual histories.
“This finding was unexpected given that the focus of these systems is to proactively reduce the risk of unplanned pregnancy during drug treatment,” wrote Stephani L. Stancil of Children’s Mercy Hospital, Kansas City, Mo., and coauthors.
“Opportunity exists in these adolescents to increase rates of contraceptive counsel, the prescription of contraception if appropriate, or referral for such care when it becomes necessary to use a medication with known teratogenic potential,” they said.
Children’s Mercy Hospital supported the study. No conflicts of interest were declared.
FROM PEDIATRICS
Key clinical point: Fewer than one-third of adolescent females prescribed a teratogenic medication also receive contraception provision.
Major finding: Among adolescent females prescribed a known teratogen, contraception provision occurred in 29% of visits.
Data source: A single-center, retrospective study of 1,694 female patients aged 14-25 years, prescribed a medication of FDA pregnancy risk category D or X.
Disclosures: Children’s Mercy Hospital, Kansas City, supported the study. No conflicts of interest were declared.
Memantine reduces frequency of migraine without aura
The Alzheimer’s disease drug memantine may help reduce the frequency of migraines, say the authors of a study showing that memantine prophylaxis significantly reduced the incidence of migraines without aura.
Results of a randomized, double-blind, placebo-controlled trial in 52 patients who experienced two or more migraines without aura a month showed that those treated with 10 mg/day of memantine experienced at least two fewer migraines each month, compared with the placebo group (mean difference, 2.3; 95% confidence interval, 1.1-3.5).
Treatment with the glutamate N-methyl-D-aspartate receptor antagonist was associated with an average 62% reduction in monthly attack frequency, compared with a 17% reduction in the placebo group, and a significantly greater reduction in the mean number of migraine days and headache severity, compared with placebo.
The study, published online Dec. 6 in Headache, also found greater reductions in Migraine Disability Assessment Scale (MIDAS) score in the memantine group; decreasing by at least two categories in 44% of patients on memantine, compared with 11% of patients on placebo.
Dr. Rezvan Noruzzadeh of the Tehran University of Medical Sciences and coauthors wrote that there is growing interest in the role of glutamate in migraine pathophysiology.
“Glutamate levels are elevated in cerebrospinal fluid of patients with chronic migraine, suggesting an excess of this neurotransmitter in the brains of patients,” the authors reported (Headache. 2015 Dec 6. doi: 10.1111/head.12732).
Memantine showed a favorable side effect profile, with three patients in the intervention arm and two patients in the placebo arm reporting sedation, mild vertigo, nausea, or drowsiness.
“Other prophylactic antimigraine agents are often associated with considerable side effects; [the] significant hair loss and weight gain of valproate are particularly undesirable for women, who are the main sufferers of migraine headaches,” the authors wrote.
They also pointed out that unlike other migraine prophylactic treatments, memantine is suitable for use in pregnancy.
The study was supported by the Tehran University of Medical Sciences. No conflicts of interest were declared.
The Alzheimer’s disease drug memantine may help reduce the frequency of migraines, say the authors of a study showing that memantine prophylaxis significantly reduced the incidence of migraines without aura.
Results of a randomized, double-blind, placebo-controlled trial in 52 patients who experienced two or more migraines without aura a month showed that those treated with 10 mg/day of memantine experienced at least two fewer migraines each month, compared with the placebo group (mean difference, 2.3; 95% confidence interval, 1.1-3.5).
Treatment with the glutamate N-methyl-D-aspartate receptor antagonist was associated with an average 62% reduction in monthly attack frequency, compared with a 17% reduction in the placebo group, and a significantly greater reduction in the mean number of migraine days and headache severity, compared with placebo.
The study, published online Dec. 6 in Headache, also found greater reductions in Migraine Disability Assessment Scale (MIDAS) score in the memantine group; decreasing by at least two categories in 44% of patients on memantine, compared with 11% of patients on placebo.
Dr. Rezvan Noruzzadeh of the Tehran University of Medical Sciences and coauthors wrote that there is growing interest in the role of glutamate in migraine pathophysiology.
“Glutamate levels are elevated in cerebrospinal fluid of patients with chronic migraine, suggesting an excess of this neurotransmitter in the brains of patients,” the authors reported (Headache. 2015 Dec 6. doi: 10.1111/head.12732).
Memantine showed a favorable side effect profile, with three patients in the intervention arm and two patients in the placebo arm reporting sedation, mild vertigo, nausea, or drowsiness.
“Other prophylactic antimigraine agents are often associated with considerable side effects; [the] significant hair loss and weight gain of valproate are particularly undesirable for women, who are the main sufferers of migraine headaches,” the authors wrote.
They also pointed out that unlike other migraine prophylactic treatments, memantine is suitable for use in pregnancy.
The study was supported by the Tehran University of Medical Sciences. No conflicts of interest were declared.
The Alzheimer’s disease drug memantine may help reduce the frequency of migraines, say the authors of a study showing that memantine prophylaxis significantly reduced the incidence of migraines without aura.
Results of a randomized, double-blind, placebo-controlled trial in 52 patients who experienced two or more migraines without aura a month showed that those treated with 10 mg/day of memantine experienced at least two fewer migraines each month, compared with the placebo group (mean difference, 2.3; 95% confidence interval, 1.1-3.5).
Treatment with the glutamate N-methyl-D-aspartate receptor antagonist was associated with an average 62% reduction in monthly attack frequency, compared with a 17% reduction in the placebo group, and a significantly greater reduction in the mean number of migraine days and headache severity, compared with placebo.
The study, published online Dec. 6 in Headache, also found greater reductions in Migraine Disability Assessment Scale (MIDAS) score in the memantine group; decreasing by at least two categories in 44% of patients on memantine, compared with 11% of patients on placebo.
Dr. Rezvan Noruzzadeh of the Tehran University of Medical Sciences and coauthors wrote that there is growing interest in the role of glutamate in migraine pathophysiology.
“Glutamate levels are elevated in cerebrospinal fluid of patients with chronic migraine, suggesting an excess of this neurotransmitter in the brains of patients,” the authors reported (Headache. 2015 Dec 6. doi: 10.1111/head.12732).
Memantine showed a favorable side effect profile, with three patients in the intervention arm and two patients in the placebo arm reporting sedation, mild vertigo, nausea, or drowsiness.
“Other prophylactic antimigraine agents are often associated with considerable side effects; [the] significant hair loss and weight gain of valproate are particularly undesirable for women, who are the main sufferers of migraine headaches,” the authors wrote.
They also pointed out that unlike other migraine prophylactic treatments, memantine is suitable for use in pregnancy.
The study was supported by the Tehran University of Medical Sciences. No conflicts of interest were declared.
FROM HEADACHE
Key clinical point: Memantine may help reduce the frequency of migraines without aura.
Major finding: Treatment with memantine was associated with an average 62% reduction in monthly attack frequency, compared with 17% reduction with placebo.
Data source: A randomized, double-blind, placebo-controlled trial in 52 patients who experienced regular migraines without aura.
Disclosures: The study was supported by the Tehran University of Medical Sciences. No conflicts of interest were declared.
Lifestyle risk index score predicts all-cause mortality
An index score incorporating lifestyle risk factors such as sedentary behavior, smoking, alcohol consumption, diet, and too little or too much sleep shows a strong relationship with all-cause mortality.
Researchers linked mortality records with the results of lifestyle questionnaires from a 6-year Australian cohort study in 231,048 individuals aged over 45 years, and used this data to develop a lifestyle risk index score based on six health behaviors, with a minimum score of zero and maximum of six, according to Dr. Ding Ding of Prevention Research Collaboration, Sydney School of Public Health and the Charles Perkins Centre, both at the University of Sydney in Camperdown, New South Wales, Australia, and associates.
Compared with individuals with a score of zero, representing no lifestyle risk factors, the all-cause mortality hazard ratios for scores of one, two, three, four, five, and six were 1.27, 1.73, 2.45, 3.06, 4.61, and 5.38, respectively, even after adjusting for factors such as body mass index, cardiovascular or metabolic disease, and total number of chronic diseases.
The relationship between the lifestyle risk index score and mortality was even more significant among women, individuals with lower educational attainment, normal weight/underweight, or without a cancer diagnosis in the previous 10 years, according to a paper published online December 8 in PLoS Medicine.
Of the six risk behaviors, smoking and physical inactivity showed the strongest association with mortality, followed by prolonged sitting, excess or not enough sleep and poor diet, although there was no significant association between high alcohol intake and mortality (PLoS Med. 2015 Dec 8. [doi: 10.1371/journal.pmed.1001917]).
“This reinforces an important message for public health and clinical practice that adherence to low-risk lifestyles is likely to be protective for all,” the investigators wrote.
The study was funded by the National Health and Medical Research Council. No conflicts of interest were declared.
An index score incorporating lifestyle risk factors such as sedentary behavior, smoking, alcohol consumption, diet, and too little or too much sleep shows a strong relationship with all-cause mortality.
Researchers linked mortality records with the results of lifestyle questionnaires from a 6-year Australian cohort study in 231,048 individuals aged over 45 years, and used this data to develop a lifestyle risk index score based on six health behaviors, with a minimum score of zero and maximum of six, according to Dr. Ding Ding of Prevention Research Collaboration, Sydney School of Public Health and the Charles Perkins Centre, both at the University of Sydney in Camperdown, New South Wales, Australia, and associates.
Compared with individuals with a score of zero, representing no lifestyle risk factors, the all-cause mortality hazard ratios for scores of one, two, three, four, five, and six were 1.27, 1.73, 2.45, 3.06, 4.61, and 5.38, respectively, even after adjusting for factors such as body mass index, cardiovascular or metabolic disease, and total number of chronic diseases.
The relationship between the lifestyle risk index score and mortality was even more significant among women, individuals with lower educational attainment, normal weight/underweight, or without a cancer diagnosis in the previous 10 years, according to a paper published online December 8 in PLoS Medicine.
Of the six risk behaviors, smoking and physical inactivity showed the strongest association with mortality, followed by prolonged sitting, excess or not enough sleep and poor diet, although there was no significant association between high alcohol intake and mortality (PLoS Med. 2015 Dec 8. [doi: 10.1371/journal.pmed.1001917]).
“This reinforces an important message for public health and clinical practice that adherence to low-risk lifestyles is likely to be protective for all,” the investigators wrote.
The study was funded by the National Health and Medical Research Council. No conflicts of interest were declared.
An index score incorporating lifestyle risk factors such as sedentary behavior, smoking, alcohol consumption, diet, and too little or too much sleep shows a strong relationship with all-cause mortality.
Researchers linked mortality records with the results of lifestyle questionnaires from a 6-year Australian cohort study in 231,048 individuals aged over 45 years, and used this data to develop a lifestyle risk index score based on six health behaviors, with a minimum score of zero and maximum of six, according to Dr. Ding Ding of Prevention Research Collaboration, Sydney School of Public Health and the Charles Perkins Centre, both at the University of Sydney in Camperdown, New South Wales, Australia, and associates.
Compared with individuals with a score of zero, representing no lifestyle risk factors, the all-cause mortality hazard ratios for scores of one, two, three, four, five, and six were 1.27, 1.73, 2.45, 3.06, 4.61, and 5.38, respectively, even after adjusting for factors such as body mass index, cardiovascular or metabolic disease, and total number of chronic diseases.
The relationship between the lifestyle risk index score and mortality was even more significant among women, individuals with lower educational attainment, normal weight/underweight, or without a cancer diagnosis in the previous 10 years, according to a paper published online December 8 in PLoS Medicine.
Of the six risk behaviors, smoking and physical inactivity showed the strongest association with mortality, followed by prolonged sitting, excess or not enough sleep and poor diet, although there was no significant association between high alcohol intake and mortality (PLoS Med. 2015 Dec 8. [doi: 10.1371/journal.pmed.1001917]).
“This reinforces an important message for public health and clinical practice that adherence to low-risk lifestyles is likely to be protective for all,” the investigators wrote.
The study was funded by the National Health and Medical Research Council. No conflicts of interest were declared.
FROM PLOS MEDICINE
Key clinical point: A lifestyle risk index score is a strong predictor of all-cause mortality.
Major finding: Individuals with the highest lifestyle index risk score of six have a fivefold greater risk of all-cause mortality than those with a score of zero.
Data source: A 6-year Australian cohort study in 231,048 individuals aged over 45 years.
Disclosures: The study was funded by the National Health and Medical Research Council. No conflicts of interest were declared.
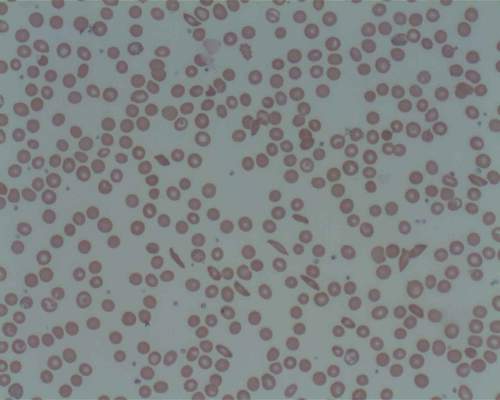
ASH: Prasugrel does not reduce vaso-occlusive crises in sickle cell anemia
Platelet inhibitor prasugrel has failed to show a significant reduction in the rate of vaso-occlusive crises events in children and adolescents with sickle cell anemia, according to data presented Dec. 8 at the annual meeting of the American Society of Hematology.
The phase III randomized placebo-controlled trial of 341 children and adolescents (aged 2-17 years), known as the Determining Effects of Platelet Inhibition on Vaso-Occlusive Events (DOVE) trial – simultaneously published in the New England Journal of Medicine – showed the rate of vaso-occlusive crises was 2.30 per person-year in the prasugrel group and 2.77 in the placebo group (rate ratio 0.83, 95% confidence interval 0.66-1.05, P = 0.12), with a slightly greater but still nonsignificant reduction among the older patients aged 12-17 years.
Treatment with prasugrel did not achieve any significant reductions in secondary outcomes of hospitalizations for vaso-occlusive crises, red-cell transfusions, pain rate or intensity, analgesic use, or school absences, compared with placebo. Platelet reactivity, however, was significantly lower in the prasugrel group (N Engl J Med. 2015, Dec 8. doi: 10.1056/NEJMoa1512021).
“Sickle cell anemia is a heterogeneous and complex disease in which platelet activation is only one of several mechanisms of vascular injury, which perhaps explains why prasugrel was ineffective,” wrote Dr. Matthew M. Heeney of Dana-Farber/Boston Children’s Cancer and Blood Disorders Center, and his coauthors.
“However, the nonsignificant effect of prasugrel in the oldest age group may suggest that platelet activation is relatively more important in these older patients, a hypothesis that is consistent with the fact that endothelial dysfunction in sickle cell disease is progressive.”
Daiichi Sankyo and Eli Lilly funded the study. Several authors disclosed ties with Eli Lilly or other pharmaceutical companies. Three authors were employees of Eli Lilly, and one was an employee of Daiichi Sankyo.
Platelet inhibitor prasugrel has failed to show a significant reduction in the rate of vaso-occlusive crises events in children and adolescents with sickle cell anemia, according to data presented Dec. 8 at the annual meeting of the American Society of Hematology.
The phase III randomized placebo-controlled trial of 341 children and adolescents (aged 2-17 years), known as the Determining Effects of Platelet Inhibition on Vaso-Occlusive Events (DOVE) trial – simultaneously published in the New England Journal of Medicine – showed the rate of vaso-occlusive crises was 2.30 per person-year in the prasugrel group and 2.77 in the placebo group (rate ratio 0.83, 95% confidence interval 0.66-1.05, P = 0.12), with a slightly greater but still nonsignificant reduction among the older patients aged 12-17 years.
Treatment with prasugrel did not achieve any significant reductions in secondary outcomes of hospitalizations for vaso-occlusive crises, red-cell transfusions, pain rate or intensity, analgesic use, or school absences, compared with placebo. Platelet reactivity, however, was significantly lower in the prasugrel group (N Engl J Med. 2015, Dec 8. doi: 10.1056/NEJMoa1512021).
“Sickle cell anemia is a heterogeneous and complex disease in which platelet activation is only one of several mechanisms of vascular injury, which perhaps explains why prasugrel was ineffective,” wrote Dr. Matthew M. Heeney of Dana-Farber/Boston Children’s Cancer and Blood Disorders Center, and his coauthors.
“However, the nonsignificant effect of prasugrel in the oldest age group may suggest that platelet activation is relatively more important in these older patients, a hypothesis that is consistent with the fact that endothelial dysfunction in sickle cell disease is progressive.”
Daiichi Sankyo and Eli Lilly funded the study. Several authors disclosed ties with Eli Lilly or other pharmaceutical companies. Three authors were employees of Eli Lilly, and one was an employee of Daiichi Sankyo.
Platelet inhibitor prasugrel has failed to show a significant reduction in the rate of vaso-occlusive crises events in children and adolescents with sickle cell anemia, according to data presented Dec. 8 at the annual meeting of the American Society of Hematology.
The phase III randomized placebo-controlled trial of 341 children and adolescents (aged 2-17 years), known as the Determining Effects of Platelet Inhibition on Vaso-Occlusive Events (DOVE) trial – simultaneously published in the New England Journal of Medicine – showed the rate of vaso-occlusive crises was 2.30 per person-year in the prasugrel group and 2.77 in the placebo group (rate ratio 0.83, 95% confidence interval 0.66-1.05, P = 0.12), with a slightly greater but still nonsignificant reduction among the older patients aged 12-17 years.
Treatment with prasugrel did not achieve any significant reductions in secondary outcomes of hospitalizations for vaso-occlusive crises, red-cell transfusions, pain rate or intensity, analgesic use, or school absences, compared with placebo. Platelet reactivity, however, was significantly lower in the prasugrel group (N Engl J Med. 2015, Dec 8. doi: 10.1056/NEJMoa1512021).
“Sickle cell anemia is a heterogeneous and complex disease in which platelet activation is only one of several mechanisms of vascular injury, which perhaps explains why prasugrel was ineffective,” wrote Dr. Matthew M. Heeney of Dana-Farber/Boston Children’s Cancer and Blood Disorders Center, and his coauthors.
“However, the nonsignificant effect of prasugrel in the oldest age group may suggest that platelet activation is relatively more important in these older patients, a hypothesis that is consistent with the fact that endothelial dysfunction in sickle cell disease is progressive.”
Daiichi Sankyo and Eli Lilly funded the study. Several authors disclosed ties with Eli Lilly or other pharmaceutical companies. Three authors were employees of Eli Lilly, and one was an employee of Daiichi Sankyo.
FROM ASH 2015
Key clinical point: Platelet inhibitor prasugrel does not reduce the rate of vaso-occlusive crises events in young patients with sickle cell anemia.
Major finding: Prasugrel did not achieve a significant reduction in vaso-occlusive crises, compared with placebo.
Data source: A phase III randomized placebo-controlled trial of 341 children and adolescents with sickle cell anemia.
Disclosures: Daiichi Sankyo and Eli Lilly funded the study. Several authors disclosed ties with Eli Lilly or other pharmaceutical companies. Three authors were employees of Eli Lilly, and one was an employee of Daiichi Sankyo.
Diabetes raises the cardiovascular risk higher in women than men
Women with type 2 diabetes mellitus have a twofold greater risk of developing coronary heart disease, compared with men with type 2 diabetes, according to a scientific statement from the American Heart Association.
In outlining the many sex differences in the impact of diabetes on cardiovascular disease risk, the authors of the statement have also called for more research into why there are these sex differences and how to treat them.
Around 1 in 10 adult Americans are estimated to have diabetes, and among those individuals, cardiovascular disease alone accounts for more than three-quarters of hospitalizations and half of all deaths.
“Although nondiabetic women have fewer cardiovascular events than nondiabetic men of the same age, this advantage appears to be lost in the context of [type 2 diabetes],” wrote American Heart Association Diabetes Committee Cochair Dr. Judith G. Regensteiner, director of the Center for Women’s Health Research at the University of Colorado at Denver, Aurora, and her coauthors.
Women with type 2 diabetes experience myocardial infarctions earlier in life than do men and are more likely to die from them, yet the rates of revascularization are lower in women with diabetes, compared with men, according to a statement published in the December 7 online issue of Circulation.
Women with diabetes also have more impaired endothelium-dependent vasodilation, worse atherogenic dyslipidemia, prothrombotic coagulation profile and higher metabolic syndrome prevalence than men with diabetes (Circulation. 2015 Dec 7. doi: 10.1161/CIR.0000000000000343).
Diabetes is also associated with a greater risk of incident heart failure and is a stronger risk factor for stroke in women than in men, although men with stroke are more likely to have diabetes.
Black and Hispanic women with type 2 diabetes also experience a disproportionately larger impact of the disease on their coronary artery disease and stroke risk, compared with men.
The authors of the statement also observed that, compared with men with diabetes, women are less likely to be taking statins, aspirin, ACE inhibitors, or beta-blockers, with the suggestion of lower medication adherence in women.
While the overall prevalence of diabetes is similar in men and women, there are sex-specific conditions such as gestational diabetes and polycystic ovary syndrome that contribute to women’s risk of the disease.
Research is needed to explore the full extent of sex differences between men and women, as this may have therapeutic implications, Dr. Regensteiner said in an interview.
“There really isn’t too much a clinician can do differently at this point because we don’t have information to guide changes in therapy,” she said, noting that any potential heart problems should be subject to the same level of scrutiny in women as in men.
The authors of the statement pointed out that observational evidence suggested women with diabetes may benefit from a higher frequency and intensity of physical activity than men with diabetes, and women with type 1 diabetes may experience greater improvements in hemoglobin A1c with exercise, compared with men.
The American Heart Association issued the statement. Several authors declared research grants or consultancies from the pharmaceutical industry or ownership interests in private companies.
Women with type 2 diabetes mellitus have a twofold greater risk of developing coronary heart disease, compared with men with type 2 diabetes, according to a scientific statement from the American Heart Association.
In outlining the many sex differences in the impact of diabetes on cardiovascular disease risk, the authors of the statement have also called for more research into why there are these sex differences and how to treat them.
Around 1 in 10 adult Americans are estimated to have diabetes, and among those individuals, cardiovascular disease alone accounts for more than three-quarters of hospitalizations and half of all deaths.
“Although nondiabetic women have fewer cardiovascular events than nondiabetic men of the same age, this advantage appears to be lost in the context of [type 2 diabetes],” wrote American Heart Association Diabetes Committee Cochair Dr. Judith G. Regensteiner, director of the Center for Women’s Health Research at the University of Colorado at Denver, Aurora, and her coauthors.
Women with type 2 diabetes experience myocardial infarctions earlier in life than do men and are more likely to die from them, yet the rates of revascularization are lower in women with diabetes, compared with men, according to a statement published in the December 7 online issue of Circulation.
Women with diabetes also have more impaired endothelium-dependent vasodilation, worse atherogenic dyslipidemia, prothrombotic coagulation profile and higher metabolic syndrome prevalence than men with diabetes (Circulation. 2015 Dec 7. doi: 10.1161/CIR.0000000000000343).
Diabetes is also associated with a greater risk of incident heart failure and is a stronger risk factor for stroke in women than in men, although men with stroke are more likely to have diabetes.
Black and Hispanic women with type 2 diabetes also experience a disproportionately larger impact of the disease on their coronary artery disease and stroke risk, compared with men.
The authors of the statement also observed that, compared with men with diabetes, women are less likely to be taking statins, aspirin, ACE inhibitors, or beta-blockers, with the suggestion of lower medication adherence in women.
While the overall prevalence of diabetes is similar in men and women, there are sex-specific conditions such as gestational diabetes and polycystic ovary syndrome that contribute to women’s risk of the disease.
Research is needed to explore the full extent of sex differences between men and women, as this may have therapeutic implications, Dr. Regensteiner said in an interview.
“There really isn’t too much a clinician can do differently at this point because we don’t have information to guide changes in therapy,” she said, noting that any potential heart problems should be subject to the same level of scrutiny in women as in men.
The authors of the statement pointed out that observational evidence suggested women with diabetes may benefit from a higher frequency and intensity of physical activity than men with diabetes, and women with type 1 diabetes may experience greater improvements in hemoglobin A1c with exercise, compared with men.
The American Heart Association issued the statement. Several authors declared research grants or consultancies from the pharmaceutical industry or ownership interests in private companies.
Women with type 2 diabetes mellitus have a twofold greater risk of developing coronary heart disease, compared with men with type 2 diabetes, according to a scientific statement from the American Heart Association.
In outlining the many sex differences in the impact of diabetes on cardiovascular disease risk, the authors of the statement have also called for more research into why there are these sex differences and how to treat them.
Around 1 in 10 adult Americans are estimated to have diabetes, and among those individuals, cardiovascular disease alone accounts for more than three-quarters of hospitalizations and half of all deaths.
“Although nondiabetic women have fewer cardiovascular events than nondiabetic men of the same age, this advantage appears to be lost in the context of [type 2 diabetes],” wrote American Heart Association Diabetes Committee Cochair Dr. Judith G. Regensteiner, director of the Center for Women’s Health Research at the University of Colorado at Denver, Aurora, and her coauthors.
Women with type 2 diabetes experience myocardial infarctions earlier in life than do men and are more likely to die from them, yet the rates of revascularization are lower in women with diabetes, compared with men, according to a statement published in the December 7 online issue of Circulation.
Women with diabetes also have more impaired endothelium-dependent vasodilation, worse atherogenic dyslipidemia, prothrombotic coagulation profile and higher metabolic syndrome prevalence than men with diabetes (Circulation. 2015 Dec 7. doi: 10.1161/CIR.0000000000000343).
Diabetes is also associated with a greater risk of incident heart failure and is a stronger risk factor for stroke in women than in men, although men with stroke are more likely to have diabetes.
Black and Hispanic women with type 2 diabetes also experience a disproportionately larger impact of the disease on their coronary artery disease and stroke risk, compared with men.
The authors of the statement also observed that, compared with men with diabetes, women are less likely to be taking statins, aspirin, ACE inhibitors, or beta-blockers, with the suggestion of lower medication adherence in women.
While the overall prevalence of diabetes is similar in men and women, there are sex-specific conditions such as gestational diabetes and polycystic ovary syndrome that contribute to women’s risk of the disease.
Research is needed to explore the full extent of sex differences between men and women, as this may have therapeutic implications, Dr. Regensteiner said in an interview.
“There really isn’t too much a clinician can do differently at this point because we don’t have information to guide changes in therapy,” she said, noting that any potential heart problems should be subject to the same level of scrutiny in women as in men.
The authors of the statement pointed out that observational evidence suggested women with diabetes may benefit from a higher frequency and intensity of physical activity than men with diabetes, and women with type 1 diabetes may experience greater improvements in hemoglobin A1c with exercise, compared with men.
The American Heart Association issued the statement. Several authors declared research grants or consultancies from the pharmaceutical industry or ownership interests in private companies.
FROM CIRCULATION
Key clinical point: There are significant sex differences in the impact of diabetes on cardiovascular risk.
Major finding: Women with diabetes have a greater than twofold risk of coronary artery disease, compared with men with diabetes.
Data source: Scientific statement from the American Heart Association.
Disclosures: The statement is produced by the American Heart Association. Several authors declared research grants or consultancies from the pharmaceutical industry or ownership interests in private companies.
Type 1 diabetes linked to excess weight gain before age 1
Extra weight gain during the first year of life is associated with an increased risk of type 1 diabetes, according to research that points to early environmental origins for the disease.
An analysis of data from two population-based cohorts – representing a total of 99,832 children from Norway and Denmark – showed each 1–standard deviation increase in weight from birth to 1 year of age was associated with a 24% increase in the risk of type 1 diabetes, even after adjustment for potential confounding factors such as birth weight, sex, maternal body mass index, maternal diabetes, and breastfeeding duration.
However, the study did not find an association between increase in the baby’s length from birth to 1 year and type 1 diabetes risk.
The association between growth rate and type 1 diabetes risk was significant only for the first half-year of life, and the data did not find a significant relationship between peak weight velocity and type 1 diabetes risk (JAMA Pediatrics 2015 Dec 7. doi: 10.1001/jamapediatrics.2015.3759).
The authors said the evidence did not support a strong role for genetic and epigenetic factors, and they also accounted for other potential environmental factors such as infant feeding.
“A general mechanism that may plausibly explain our findings is that rapid growth increases the demand on beta cells to secrete insulin, and it has been shown that beta cells actively secreting insulin are more susceptible to cytokine damage in vitro,” wrote Maria C. Magnus, Ph.D., of the Norwegian Institute of Public Health, and her coauthors.
The cohort studies were supported by the National Institutes of Health and the Norwegian Research Council March of Dimes Birth Defects Foundation, the Danish Heart Association, the Danish National Research Foundation, the Danish Pharmaceutical Association, the Ministry of Health, and the National Board of Health. No other conflicts of interest were declared.
Extra weight gain during the first year of life is associated with an increased risk of type 1 diabetes, according to research that points to early environmental origins for the disease.
An analysis of data from two population-based cohorts – representing a total of 99,832 children from Norway and Denmark – showed each 1–standard deviation increase in weight from birth to 1 year of age was associated with a 24% increase in the risk of type 1 diabetes, even after adjustment for potential confounding factors such as birth weight, sex, maternal body mass index, maternal diabetes, and breastfeeding duration.
However, the study did not find an association between increase in the baby’s length from birth to 1 year and type 1 diabetes risk.
The association between growth rate and type 1 diabetes risk was significant only for the first half-year of life, and the data did not find a significant relationship between peak weight velocity and type 1 diabetes risk (JAMA Pediatrics 2015 Dec 7. doi: 10.1001/jamapediatrics.2015.3759).
The authors said the evidence did not support a strong role for genetic and epigenetic factors, and they also accounted for other potential environmental factors such as infant feeding.
“A general mechanism that may plausibly explain our findings is that rapid growth increases the demand on beta cells to secrete insulin, and it has been shown that beta cells actively secreting insulin are more susceptible to cytokine damage in vitro,” wrote Maria C. Magnus, Ph.D., of the Norwegian Institute of Public Health, and her coauthors.
The cohort studies were supported by the National Institutes of Health and the Norwegian Research Council March of Dimes Birth Defects Foundation, the Danish Heart Association, the Danish National Research Foundation, the Danish Pharmaceutical Association, the Ministry of Health, and the National Board of Health. No other conflicts of interest were declared.
Extra weight gain during the first year of life is associated with an increased risk of type 1 diabetes, according to research that points to early environmental origins for the disease.
An analysis of data from two population-based cohorts – representing a total of 99,832 children from Norway and Denmark – showed each 1–standard deviation increase in weight from birth to 1 year of age was associated with a 24% increase in the risk of type 1 diabetes, even after adjustment for potential confounding factors such as birth weight, sex, maternal body mass index, maternal diabetes, and breastfeeding duration.
However, the study did not find an association between increase in the baby’s length from birth to 1 year and type 1 diabetes risk.
The association between growth rate and type 1 diabetes risk was significant only for the first half-year of life, and the data did not find a significant relationship between peak weight velocity and type 1 diabetes risk (JAMA Pediatrics 2015 Dec 7. doi: 10.1001/jamapediatrics.2015.3759).
The authors said the evidence did not support a strong role for genetic and epigenetic factors, and they also accounted for other potential environmental factors such as infant feeding.
“A general mechanism that may plausibly explain our findings is that rapid growth increases the demand on beta cells to secrete insulin, and it has been shown that beta cells actively secreting insulin are more susceptible to cytokine damage in vitro,” wrote Maria C. Magnus, Ph.D., of the Norwegian Institute of Public Health, and her coauthors.
The cohort studies were supported by the National Institutes of Health and the Norwegian Research Council March of Dimes Birth Defects Foundation, the Danish Heart Association, the Danish National Research Foundation, the Danish Pharmaceutical Association, the Ministry of Health, and the National Board of Health. No other conflicts of interest were declared.
FROM JAMA PEDIATRICS
Key clinical point: Extra weight gain during the first year of life is associated with an increased risk of type 1 diabetes.
Major finding: Each 1–standard deviation increase in weight from birth to 1 year of age was associated with a 24% increase in the risk of type 1 diabetes.
Data source: An analysis of data from two population-based cohorts, representing a total of 99,832 children.
Disclosures: The cohort studies were supported by the National Institutes of Health and the Norwegian Research Council March of Dimes Birth Defects Foundation, the Danish Heart Association, the Danish National Research Foundation, the Danish Pharmaceutical Association, the Ministry of Health, and the National Board of Health. No other conflicts of interest were declared.