User login
Spikes out: A COVID mystery
Welcome to Impact Factor, your weekly dose of commentary on a new medical study. I’m Dr. F. Perry Wilson of the Yale School of Medicine.
To date, it has been a mystery, like “Glass Onion.” And in the spirit of all the great mysteries, to get to the bottom of this, we’ll need to round up the usual suspects.
Appearing in Circulation, a new study does a great job of systematically evaluating multiple hypotheses linking vaccination to myocarditis, and eliminating them, Poirot-style, one by one until only one remains. We’ll get there.
But first, let’s review the suspects. Why do the mRNA vaccines cause myocarditis in a small subset of people?
There are a few leading candidates.
Number one: antibody responses. There are two flavors here. The quantitative hypothesis suggests that some people simply generate too many antibodies to the vaccine, leading to increased inflammation and heart damage.
The qualitative hypothesis suggests that maybe it’s the nature of the antibodies generated rather than the amount; they might cross-react with some protein on the surface of heart cells for instance.
Or maybe it is driven by T-cell responses, which, of course, are independent of antibody levels.
There’s the idea that myocarditis is due to excessive cytokine release – sort of like what we see in the multisystem inflammatory syndrome in children.
Or it could be due to the viral antigens themselves – the spike protein the mRNA codes for that is generated after vaccination.
To tease all these possibilities apart, researchers led by Lael Yonker at Mass General performed a case-control study. Sixteen children with postvaccine myocarditis were matched by age to 45 control children who had been vaccinated without complications.
The matching was OK, but as you can see here, there were more boys in the myocarditis group, and the time from vaccination was a bit shorter in that group as well. We’ll keep that in mind as we go through the results.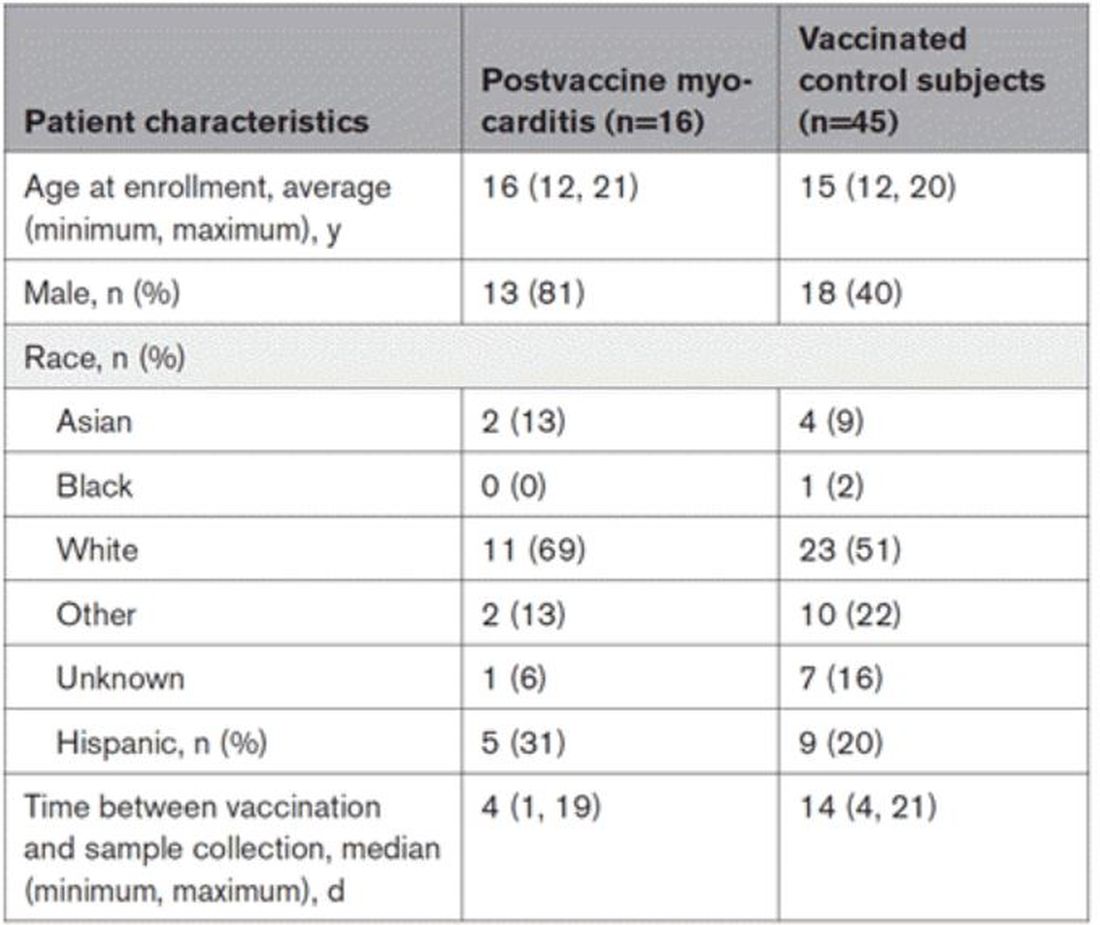
OK, let’s start eliminating suspects.
First, quantitative antibodies. Seems unlikely. Absolute antibody titers were really no different in the myocarditis vs. the control group.
What about the quality of the antibodies? Would the kids with myocarditis have more self-recognizing antibodies present? It doesn’t appear so. Autoantibody levels were similar in the two groups.
Take antibodies off the list.
T-cell responses come next, and, again, no major differences here, save for one specific T-cell subtype that was moderately elevated in the myocarditis group. Not what I would call a smoking gun, frankly.
Cytokines give us a bit more to chew on. Levels of interleukin (IL)-8, IL-6, tumor necrosis factor (TNF)-alpha, and IL-10 were all substantially higher in the kids with myocarditis.
But the thing about cytokines is that they are not particularly specific. OK, kids with myocarditis have more systemic inflammation than kids without; that’s not really surprising. It still leaves us with the question of what is causing all this inflammation? Who is the arch-villain? The kingpin? The don?
It’s the analyses of antigens – the protein products of vaccination – that may hold the key here.
In 12 out of 16 kids with myocarditis, the researchers were able to measure free spike protein in the blood – that is to say spike protein, not bound by antispike antibodies.
These free spikes were present in – wait for it – zero of the 45 control patients. That makes spike protein itself our prime suspect. J’accuse free spike protein!
Of course, all good detectives need to wrap up the case with a good story: How was it all done?
And here’s where we could use Agatha Christie’s help. How could this all work? The vaccine gets injected; mRNA is taken up into cells, where spike protein is generated and released, generating antibody and T-cell responses all the while. Those responses rapidly clear that spike protein from the system – this has been demonstrated in multiple studies – in adults, at least. But in some small number of people, apparently, spike protein is not cleared. Why? It makes no damn sense. Compels me, though. Some have suggested that inadvertent intravenous injection of vaccine, compared with the appropriate intramuscular route, might distribute the vaccine to sites with less immune surveillance. But that is definitely not proven yet.
We are on the path for sure, but this is, as Benoit Blanc would say, a twisted web – and we are not finished untangling it. Not yet.
F. Perry Wilson, MD, MSCE, is an associate professor of medicine and director of Yale’s Clinical and Translational Research Accelerator. His science communication work can be found in the Huffington Post, on NPR, and here. He tweets @fperrywilson and his new book, “How Medicine Works and When It Doesn’t,” is available for preorder now. He reports no conflicts of interest.
A version of this article first appeared on Medscape.com.
Welcome to Impact Factor, your weekly dose of commentary on a new medical study. I’m Dr. F. Perry Wilson of the Yale School of Medicine.
To date, it has been a mystery, like “Glass Onion.” And in the spirit of all the great mysteries, to get to the bottom of this, we’ll need to round up the usual suspects.
Appearing in Circulation, a new study does a great job of systematically evaluating multiple hypotheses linking vaccination to myocarditis, and eliminating them, Poirot-style, one by one until only one remains. We’ll get there.
But first, let’s review the suspects. Why do the mRNA vaccines cause myocarditis in a small subset of people?
There are a few leading candidates.
Number one: antibody responses. There are two flavors here. The quantitative hypothesis suggests that some people simply generate too many antibodies to the vaccine, leading to increased inflammation and heart damage.
The qualitative hypothesis suggests that maybe it’s the nature of the antibodies generated rather than the amount; they might cross-react with some protein on the surface of heart cells for instance.
Or maybe it is driven by T-cell responses, which, of course, are independent of antibody levels.
There’s the idea that myocarditis is due to excessive cytokine release – sort of like what we see in the multisystem inflammatory syndrome in children.
Or it could be due to the viral antigens themselves – the spike protein the mRNA codes for that is generated after vaccination.
To tease all these possibilities apart, researchers led by Lael Yonker at Mass General performed a case-control study. Sixteen children with postvaccine myocarditis were matched by age to 45 control children who had been vaccinated without complications.
The matching was OK, but as you can see here, there were more boys in the myocarditis group, and the time from vaccination was a bit shorter in that group as well. We’ll keep that in mind as we go through the results.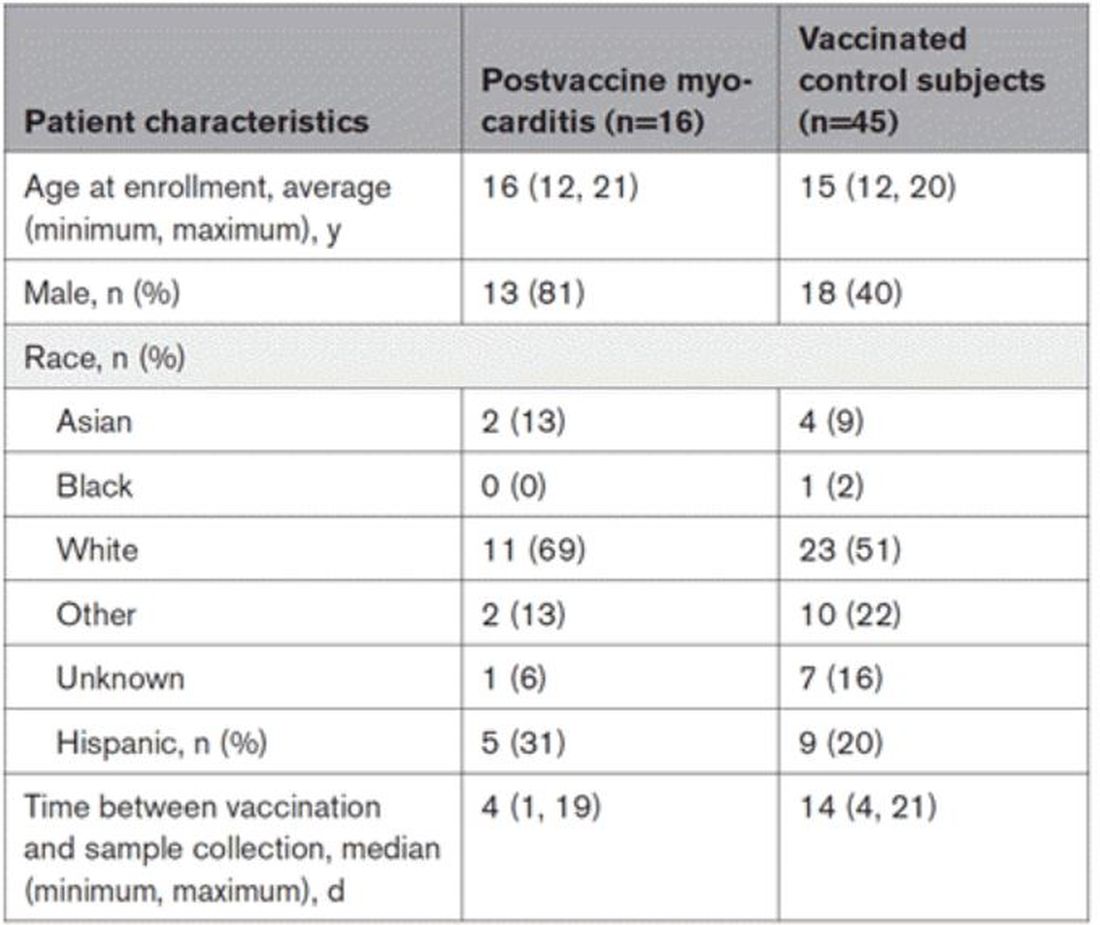
OK, let’s start eliminating suspects.
First, quantitative antibodies. Seems unlikely. Absolute antibody titers were really no different in the myocarditis vs. the control group.
What about the quality of the antibodies? Would the kids with myocarditis have more self-recognizing antibodies present? It doesn’t appear so. Autoantibody levels were similar in the two groups.
Take antibodies off the list.
T-cell responses come next, and, again, no major differences here, save for one specific T-cell subtype that was moderately elevated in the myocarditis group. Not what I would call a smoking gun, frankly.
Cytokines give us a bit more to chew on. Levels of interleukin (IL)-8, IL-6, tumor necrosis factor (TNF)-alpha, and IL-10 were all substantially higher in the kids with myocarditis.
But the thing about cytokines is that they are not particularly specific. OK, kids with myocarditis have more systemic inflammation than kids without; that’s not really surprising. It still leaves us with the question of what is causing all this inflammation? Who is the arch-villain? The kingpin? The don?
It’s the analyses of antigens – the protein products of vaccination – that may hold the key here.
In 12 out of 16 kids with myocarditis, the researchers were able to measure free spike protein in the blood – that is to say spike protein, not bound by antispike antibodies.
These free spikes were present in – wait for it – zero of the 45 control patients. That makes spike protein itself our prime suspect. J’accuse free spike protein!
Of course, all good detectives need to wrap up the case with a good story: How was it all done?
And here’s where we could use Agatha Christie’s help. How could this all work? The vaccine gets injected; mRNA is taken up into cells, where spike protein is generated and released, generating antibody and T-cell responses all the while. Those responses rapidly clear that spike protein from the system – this has been demonstrated in multiple studies – in adults, at least. But in some small number of people, apparently, spike protein is not cleared. Why? It makes no damn sense. Compels me, though. Some have suggested that inadvertent intravenous injection of vaccine, compared with the appropriate intramuscular route, might distribute the vaccine to sites with less immune surveillance. But that is definitely not proven yet.
We are on the path for sure, but this is, as Benoit Blanc would say, a twisted web – and we are not finished untangling it. Not yet.
F. Perry Wilson, MD, MSCE, is an associate professor of medicine and director of Yale’s Clinical and Translational Research Accelerator. His science communication work can be found in the Huffington Post, on NPR, and here. He tweets @fperrywilson and his new book, “How Medicine Works and When It Doesn’t,” is available for preorder now. He reports no conflicts of interest.
A version of this article first appeared on Medscape.com.
Welcome to Impact Factor, your weekly dose of commentary on a new medical study. I’m Dr. F. Perry Wilson of the Yale School of Medicine.
To date, it has been a mystery, like “Glass Onion.” And in the spirit of all the great mysteries, to get to the bottom of this, we’ll need to round up the usual suspects.
Appearing in Circulation, a new study does a great job of systematically evaluating multiple hypotheses linking vaccination to myocarditis, and eliminating them, Poirot-style, one by one until only one remains. We’ll get there.
But first, let’s review the suspects. Why do the mRNA vaccines cause myocarditis in a small subset of people?
There are a few leading candidates.
Number one: antibody responses. There are two flavors here. The quantitative hypothesis suggests that some people simply generate too many antibodies to the vaccine, leading to increased inflammation and heart damage.
The qualitative hypothesis suggests that maybe it’s the nature of the antibodies generated rather than the amount; they might cross-react with some protein on the surface of heart cells for instance.
Or maybe it is driven by T-cell responses, which, of course, are independent of antibody levels.
There’s the idea that myocarditis is due to excessive cytokine release – sort of like what we see in the multisystem inflammatory syndrome in children.
Or it could be due to the viral antigens themselves – the spike protein the mRNA codes for that is generated after vaccination.
To tease all these possibilities apart, researchers led by Lael Yonker at Mass General performed a case-control study. Sixteen children with postvaccine myocarditis were matched by age to 45 control children who had been vaccinated without complications.
The matching was OK, but as you can see here, there were more boys in the myocarditis group, and the time from vaccination was a bit shorter in that group as well. We’ll keep that in mind as we go through the results.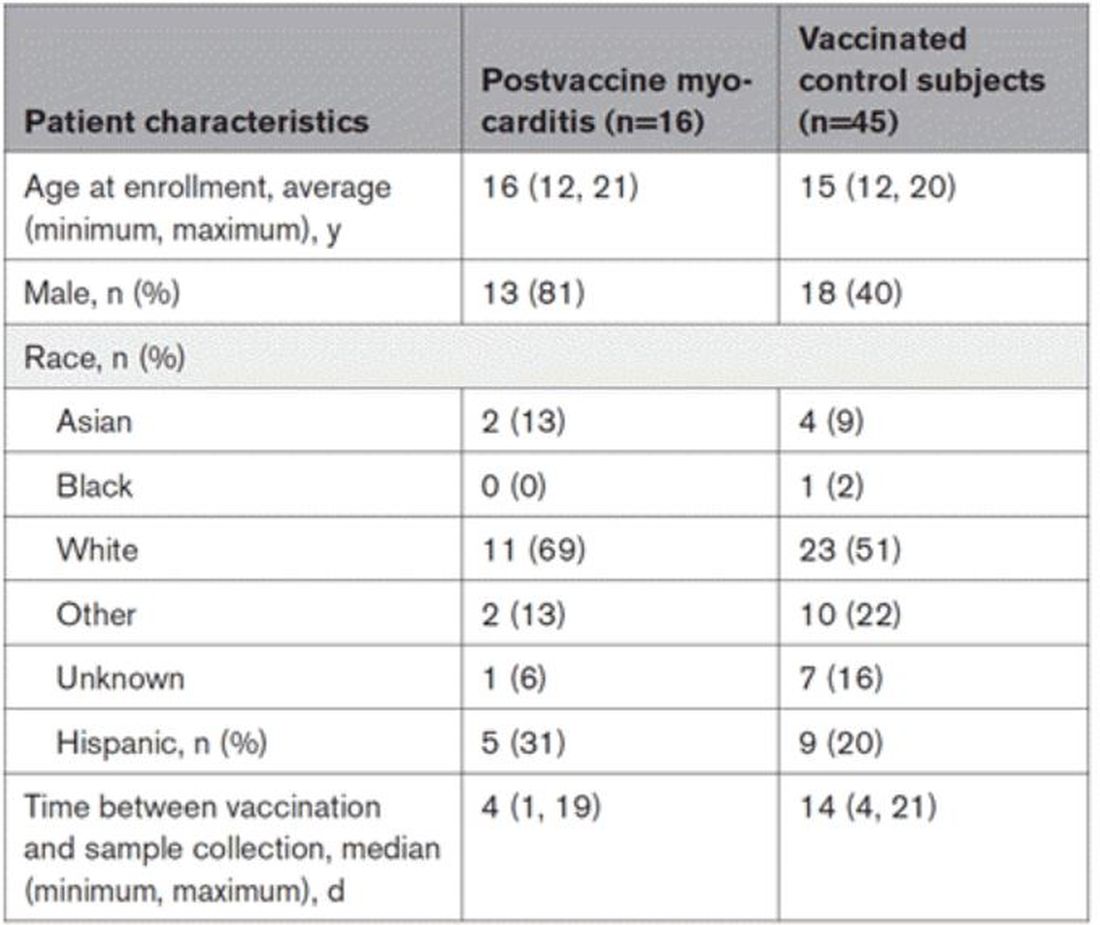
OK, let’s start eliminating suspects.
First, quantitative antibodies. Seems unlikely. Absolute antibody titers were really no different in the myocarditis vs. the control group.
What about the quality of the antibodies? Would the kids with myocarditis have more self-recognizing antibodies present? It doesn’t appear so. Autoantibody levels were similar in the two groups.
Take antibodies off the list.
T-cell responses come next, and, again, no major differences here, save for one specific T-cell subtype that was moderately elevated in the myocarditis group. Not what I would call a smoking gun, frankly.
Cytokines give us a bit more to chew on. Levels of interleukin (IL)-8, IL-6, tumor necrosis factor (TNF)-alpha, and IL-10 were all substantially higher in the kids with myocarditis.
But the thing about cytokines is that they are not particularly specific. OK, kids with myocarditis have more systemic inflammation than kids without; that’s not really surprising. It still leaves us with the question of what is causing all this inflammation? Who is the arch-villain? The kingpin? The don?
It’s the analyses of antigens – the protein products of vaccination – that may hold the key here.
In 12 out of 16 kids with myocarditis, the researchers were able to measure free spike protein in the blood – that is to say spike protein, not bound by antispike antibodies.
These free spikes were present in – wait for it – zero of the 45 control patients. That makes spike protein itself our prime suspect. J’accuse free spike protein!
Of course, all good detectives need to wrap up the case with a good story: How was it all done?
And here’s where we could use Agatha Christie’s help. How could this all work? The vaccine gets injected; mRNA is taken up into cells, where spike protein is generated and released, generating antibody and T-cell responses all the while. Those responses rapidly clear that spike protein from the system – this has been demonstrated in multiple studies – in adults, at least. But in some small number of people, apparently, spike protein is not cleared. Why? It makes no damn sense. Compels me, though. Some have suggested that inadvertent intravenous injection of vaccine, compared with the appropriate intramuscular route, might distribute the vaccine to sites with less immune surveillance. But that is definitely not proven yet.
We are on the path for sure, but this is, as Benoit Blanc would say, a twisted web – and we are not finished untangling it. Not yet.
F. Perry Wilson, MD, MSCE, is an associate professor of medicine and director of Yale’s Clinical and Translational Research Accelerator. His science communication work can be found in the Huffington Post, on NPR, and here. He tweets @fperrywilson and his new book, “How Medicine Works and When It Doesn’t,” is available for preorder now. He reports no conflicts of interest.
A version of this article first appeared on Medscape.com.
Debating the clinical trial upending colonoscopy practices
This transcript has been edited for clarity.
F. Perry Wilson, MD, MSCE: Hello, and thank you for joining us today for what promises to be a lively discussion about screening for colon cancer.
My name is Perry Wilson. I’m an associate professor of medicine and director of the Clinical and Translational Research Accelerator at the Yale School of Medicine. My new book, “How Medicine Works and When It Doesn’t: Learning Who to Trust to Get and Stay Healthy,” is available for pre-order now anywhere that books are sold.
I’m joined by two wonderful experts. Dr. David Johnson is a professor of medicine and the chief of gastroenterology at the Eastern Virginia School of Medicine. He is the past president of the American College of Gastroenterology. And I’m very encouraged to see that he’s won a Distinguished Educator Award for his efforts in gastroenterology.
I’m also joined by Dr Kenny Lin. He’s a frequent contributor to Medscape and WebMD. He’s a family physician and public health consultant from Lancaster, Pa., and deputy editor of the American Family Physician journal. He’s also a teacher of residents and students at Lancaster General Health and the Penn Medicine Family Medicine Residency program.
So, we have two great educators with us today to hopefully help teach us something about colon cancer and colon cancer screening. Thank you for joining me today.
David A. Johnson, MD: Thanks for having us.
Kenneth W. Lin, MD, MPH: Good to be here.
Dr. Wilson: Colon cancer is the second leading cause of cancer mortality in the United States. A little over 50,000 people die every year in the United States due to colon cancer.
A month ago, I would have said that there was a pretty broad consensus, at least from my perspective, that people should be getting colonoscopies. That’s certainly what we tell our patients.
Then a paper came out in the New England Journal of Medicine, a very prestigious journal, that has caused a lot of consternation online and led to my receiving a lot questions from patients and their family members. Today,
Dr Johnson, can you give us a brief overview of what this trial was about?
Dr. Johnson: This was a randomized trial looking at screening colonoscopy versus no screening test whatsoever. They looked at the outcomes of prevention of cancer and the prevention of colon cancer–related death.
The short answer was that it was disappointing as it relates to colonoscopy. The study looked at patients from four European countries, with data from three of them (Norway, Poland, and Sweden) ultimately analyzed in this report in NEJM. It got a lot of attention because it surprised a lot of people by saying maybe colonoscopy wasn’t quite as good as we thought it was.
They tried to correct that by only looking at the numbers of patients who got their colonoscopy screening, which still showed value, but it was less than that we’ve seen before. There’s lots of reasons for that, which we’ll discuss shortly.
An invitation to a screening
Dr. Wilson: This was a bit of an interesting trial design. I think I’m correct, Dr Lin, that this was the first randomized trial of screening colonoscopy. But they didn’t really randomize people to get a colonoscopy versus not get a colonoscopy. Can you tell us why this differed from that study design, which I’d have thought would be simpler way of assessing this?
Dr. Lin: It’s definitely an important point to highlight about the study. What investigators did was randomize patients to receive an invitation to get a screening colonoscopy. When the trial was set up, they randomized people before they were asked whether they wanted to participate in the study. If you did it the other way around, by first asking them whether they wanted to be in the study and then randomizing them, you would have been assured that more of them probably would have gotten the colonoscopy.
But in this case, they were more interested in figuring out the real-life results of having a national program that invited patients to receive screening colonoscopy. Because we know that everyone that you recommend to get a colonoscopy doesn’t necessarily want to do that, forgets to do it, or something happens that prevents their actually getting it.
When it comes to measuring the effectiveness of the colonoscopy, it perhaps wasn’t the greatest type of study to do that. But I think it did provide some information about what would happen if you invited people to get colonoscopy, in terms of how many would do it and the results overall for that population.
Lower participation numbers than expected
Dr. Wilson: Dr. Johnson, the data show that 42% of people who were in that invitation arm followed through and got their colonoscopy. You’re a gastroenterologist. Does that seem low or about right? Do about half of people who should get a colonoscopy end up getting one?
Dr. Johnson: No, it’s low. In the United States, those numbers are probably in the 70% range. Certainly, the test doesn’t work for people who don’t get the test performed. So, if 42% of those randomized to receive an invitation to get the colonoscopy got one, that really means the majority of patients never got the test.
Dr. Wilson: Certainly, we wouldn’t expect impressive results if they don’t get the test. But on the other hand, I imagine that people who choose to get the test when they’re invited are sort of a different breed. Perhaps they’re more health conscious or living in other healthy ways. Is that something we should worry about when we look at these results?
Dr. Johnson: I don’t think you can stratify based on this study. Factors like ethnicities and diet weren’t really explained. The key element that will hopefully have the major take-home impact is quality. It’s not just the test. It’s how the test is done.
The key results
Dr. Wilson: Let’s start with the big picture. This was a study looking at everyone invited; not the subgroup of people who got the colonoscopy, but the real randomized study population.
Dr. Lin, the study did show that the invited group had a lower risk of colon cancer over the next 10 years. That’s a good thing, I imagine.
Dr. Lin: I think that’s a significant benefit. Initially in the first few years, they had more colon cancers diagnosed. But that’s probably because those were cancers that were already existing and couldn’t be prevented by the test.
But then over the years the curves crossed, and by the end of the average follow-up of 10 years, there was a significantly lower rate of colon cancers being detected. That’s as you would expect, because you’re finding polyps and removing them before they became colon cancer.
Dr. Wilson: Dr. Johnson, is that the natural history of colon cancer? It starts out as a polyp that maybe can be easily removed and doesn’t require more therapy. Is that why screening colonoscopy is helpful?
Dr. Johnson: The ultimate goal of screening is prevention of cancer, rather than detection of cancer. That occurs by identification and complete removal of the polyps that we find that are precancerous. The key is, first, detection, and second, resection. Adequate resection comes down to some very significant issues of quality, which are questions that I’d raised about this study, and we can talk about momentarily.
Dr. Wilson: Absolutely. Let me first go through the two other big findings in this study.
The fact that there were fewer cases of colon cancer over 10 years seems good. But colon cancer mortality was not significantly different in the two groups. Now, of course, we know that not everyone got a colonoscopy. I would have expected though, if you had less colon cancer, you’d have less death from colon cancer.
Dr. Lin, what might explain this disconnect?
Dr. Lin: I think there are a couple of possible explanations.
One explanation is that they just didn’t follow the people long enough. Colon cancer takes a long time to go from an adenoma to cancer, and from cancer to something that would cause the patient’s death. You may need to follow them for longer than the 10 years that most of these patients were followed to see that benefit. I think there probably will be benefit after a while, because if you are removing colon cancers that otherwise would have progressed and metastasized, you often see a benefit.
We also have to consider the other possibility that not all the polyps removed necessarily were going to progress to advanced cancer. Therefore, you weren’t seeing the death benefit because not every polyp that was removed was necessarily going to cause health consequences.
In colonoscopy, quality is key to success
Dr. Wilson: You’re removing things and have no way of knowing in advance which are the bad ones and which aren’t.
Dr. Johnson, you’ve mentioned several times now that the quality of colonoscopy matters here. So, I’m intuiting that it’s not one-size-fits-all, that it’s not all the same. What do you mean by quality of colonoscopy, and what was it in the NEJM study?
Dr. Johnson: Quality colonoscopy is the quality of the whole process. It starts with the warm-up, if you will, and the clean out for the procedure. That allows the colonoscopist to be able to identify precancerous polyps, which we call adenomas (there are other precancerous polyps called sessile serrated lesions).
The identification of adenomas is extremely important. Even a small increase in the detection of those precancerous polyps has benefits. Well-performed studies looking at large databases show that a small, 1% increase in the adenoma detection leads to a 3% decrease in colon cancer and a 5% decrease in colon cancer–related death. There’s a huge array of effect when we talk about small increases in the adenoma detection rate.
Now, let’s go back to this study in NEJM.
If we base quality on the physician performing the colonoscopy, and say that the colonoscopy is achieving the act of getting all the way around the colon, but not all physicians in the study were able to do that, it starts to raise the question about quality, because adenoma detection is so important. Earlier reports from this group [Nordic-European Initiative on Colorectal Cancer Study Group] have shown that the adenoma detection rates have been way below the national thresholds. So, this raises the question of whether they found the polyp, and then whether they resected the polyp. They also don’t tell us where these cancers were. It is about the colonoscopy quality. It’s not the instrument. It’s the process.
An overview of other screening tools
Dr. Wilson: Dr. Lin, colonoscopy, which requires prep and anesthesia, is not the only colon cancer screening method we have. In fact, there are a bunch. I think we’re on board saying it’s probably better to detect colon cancer early than not detect it. But what are our other options aside from colonoscopy that can allow for early detection of colon cancer?
Dr. Lin: For most of my career, there were three options that I presented patients with. The first was the fecal test, which used to be in the form of initial hemoccult tests. These have been mostly replaced by fecal immunochemical testing. But they’re both just basically looking for the presence of blood in the stool. Anyone who has a positive test would be referred for a diagnostic colonoscopy.
The other test besides colonoscopy, which has been largely phased out in the United States, although it is still very much used in Canada and much of Europe, is flexible sigmoidoscopy. Until this study, the tests supported by randomized controlled trials were the fecal tests and flexible sigmoidoscopy.
Interestingly, there was a recent systematic review of flexible sigmoidoscopy looking at four trials and their effects over 15 years. They showed not only a reduction in colon cancer, but also a reduction in colon cancer mortality, and even a small reduction in all-cause mortality.
I believe three out of the four trials were done where the patients were consented and then randomized, so they had a higher uptake of the procedure.
But when you compare this with the colonoscopy trial, it really isn’t that impressive. You would expect a much larger benefit, because obviously you’re looking at the entire colon. But you really didn’t see that. It was, at best, maybe equivalent to sigmoidoscopy, but not a whole lot better.
Dr. Johnson: Perry, you mentioned sedation. It’s important to understand that this particular cohort of patients are from Norway, Sweden, and Poland, where it’s very much the norm to not get sedation for your colonoscopy. Any of the [audience] who have had colonoscopy will tell you that they are not ones to say, “Don’t give me sedation.” The rate of sedation is around 11% in Norway, maybe 23% in Sweden, and around 45% in Poland. So, the examiner and the patient were never really super comfortable.
I’ve done 50,000 colonoscopies in my career, and many nonsedated. We know that taking time increases the finding of polyps and the adequate identification and resection. So, that ability to perform at a high quality is very much impacted when the patients aren’t comfortable.
Dr. Wilson: Dr. Johnson, we brought up flexible sigmoidoscopy. For the patients watching whose doctors are talking to them about screening colonoscopy, what’s the difference?
Dr. Johnson: Flexible sigmoidoscopy is just a short scope examination, in which you see about one-third of the colon. I’ve been in the field for 45 years, and during that time we’ve seen that there’s a progressive increase in the development of cancers above that bottom third of the colon to the higher end, the two-thirds of the colon that you would miss without doing a full colonoscopy. Also, flexible sigmoidoscopy typically does not get covered for sedation.
Again, if you do the exam and find something, then you’re going to have to come back and do an adequate resection with a colonoscopy. So, one-stop-shopping colon cancer screening is not about detection of cancer, it’s about prevention of cancer, and that’s what colonoscopy does.
Patients want convenience, but at what cost?
Dr. Wilson: Dr. Lin, how are your patients in your family practice handling this study? Have conversations changed around colon cancer screening? What are people asking about these days?
Dr. Lin: I don’t think the conversations have changed in my practice that much. When patients ask about this study, we do discuss the limitations, that it wasn’t designed to assess the maximum benefit of getting a colonoscopy because the majority of people assigned to that group didn’t get colonoscopy.
But I think it is an opportunity in primary care to consider the way we present the options to patients. Because I would guess that a majority of primary care physicians, when they present the options, would say colonoscopy is the gold standard and recommend their patients get it. And they only offer fecal testing to patients who don’t want the colonoscopy or really refuse.
That hasn’t been my practice. I’m usually more agnostic, because there are both harms and benefits. If you get a fecal test, the chance of you having a complication from colonoscopy is automatically lower because most of those people will not get colonoscopy. Now obviously, the complications with colonoscopy are pretty rare and usually self-limited, but they do exist. If you’re doing lots and lots of these, eventually you’ll see them. Probably all primary care physicians have patients who’ve had a complication from colonoscopy and may or may not have regretted it depending on how information was presented.
But I feel like this study reinforces my feeling that we ought to be presenting these, and not saying one is superior or inferior to the other. Instead, I’d base it on what the patient’s priorities are. But I feel like this study reinforces my feeling that we ought to be presenting these, and not saying one is superior or inferior to the other. Instead, I’d base it on what the patient’s priorities are. Is your priority finding every single cancer? Do you want to know exactly what the benefit is? I think with colonoscopy, we’re still trying to figure out exactly what the benefit is. Whereas we can say it pretty confidently for fecal tests because we have those randomized trials.
Dr. Wilson: Dr. Johnson, I think patients who are watching need to know, first of all, that if they do the fecal test route, a positive fecal test does lead to colonoscopy. In some sense, all roads lead to colonoscopy once you have a positive screening test. So, I can certainly see the value of just sort of skipping to that point. But what about this risk-versus-benefit relationship? Colonoscopy, albeit a relatively safe procedure, is still a procedure. There is some risk associated with it. If we can get the same benefit from yearly fecal immunochemical testing, is that a better choice potentially, at least for patients at average risk?
Dr. Johnson: The stool-based testing is really more effective for detection of cancer. That’s not screening, where the entire goal is the prevention of cancer. The fecal-based testing, including the stool-based DNA testing, misses the majority of precancerous polyps. And the fecal immunochemical tests, which Dr. Lin just mentioned, misses virtually all of them. We really want to get to the prevention of cancer, meaning identification and removal of polyps, not just screening for cancer.
Dr. Wilson: Do you see anything on the horizon that could unseat colonoscopy as, to quote Dr. Lin, the potential gold standard for screening for colon cancer?
Dr. Johnson: I think not on the horizon for identification and removal of polyps. That’s really the gold standard. Technology continues to advance. We’ll see what happens. But on the short and intermediate horizon, colonoscopy is going to be needed.
We are finding that some patients are starting to acquiesce to stool-based testing because they can do it at home. Maybe they don’t have to do a prep. We’re talking about screening only here, not about the follow-up of patients who have a family history, patients who have colitis, patients who have had colon polyps, or other reasons. Stool-based testing is not an option for the follow-up of those patients.
Convenience testing, in the face of COVID, also has thrown a wrench into things. Patients may have wanted to stay home and do these tests. Again, we need to be proactive, not reactive. We want to prevent cancer, not detect it.
Changing advice in the face of younger screening thresholds
Dr. Wilson: Dr. Lin, I’m 42 years old. I don’t believe I’m at any increased risk of colon cancer based on my family history or other risk factors. I’m 3 years away from when the U.S. Preventive Services Task Force tells me I should potentially consider starting to screen for colon cancer. That recommendation has recently been moved down from 50 years old to 45 years old. So, it’s on my mind as I approach that age. What do you advise younger patients approaching 45 right now in terms of screening for colon cancer?
Dr. Lin: For patients with the risk factors that Dr. Johnson mentioned, I would recommend screening colonoscopy as the initial test.
Assuming you don’t have those risk factors, I present it as we have a couple of different fecal tests. There’s the traditional one that just looks for blood. Then there’s the newer one that also adds DNA, which is more sensitive for colorectal cancer, but a little less specific, which is a problem just because there are more false positives.
But you need to compare that with colonoscopy, which you only need to get done ideally every 10 years if there are no findings. That is more complete. And theoretically, as we’ve been talking about, it would also prevent as well as detect early cancers.
So, I think it’s really down to your preference in terms of how the various factors that come into play, such as convenience of the test and your level of concern about cancer. I do tell patients that family history of cancer is not terribly predictive of whether you get it or not. A lot of people unfortunately who develop colorectal cancer have no previous family history. Diet will come into play to some extent. There are some things that point to increased risk for colorectal cancer if you have a diet high in red meat and things like that. But ultimately, it really is up to the patient. I lay out the options, and whatever they choose, I’m happy to pursue.
But the most important thing is that they do some test, because doing no test is not going to help anyone. I do agree with the notion that the best test is the test that gets done.
Dr. Wilson: Absolutely. I think the NEJM study supports that, even when we’re talking about colonoscopy.
Dr. Johnson, you’ve had some criticisms about the NEJM study, and I think they make sense. At the same time, as this is the first randomized trial of colonoscopy, it’s kind of the only data we have. Are we going to get better data? Are there other studies going on out there that might help shed some light on what’s turning out to be a complicated issue?
Dr. Johnson: Yes, there are ongoing studies. They’re not taking place within the United States, because you couldn’t get through a no-screening option trial. There are comparative studies that are probably still 5 years away looking at stool-based testing.
But again, we have to recognize that if you do these alternative tests that were eloquently discussed by Dr. Lin, and not the colonoscopy, which would be every 10 years with high-quality performance, that you have to annualize or do them in sequence. It’s important that you follow up on those with regularity. It’s not just a one-time test every 10 years for these individual tests.
And any of the time that those tests are ordered, the patient should be instructed that if it’s positive you need a colonoscopy. We’re seeing a lot of slippage on that front for the stool-based testing. Convenience is not the answer. It’s getting the job done.
Dr. Wilson: Would you agree, Dr. Johnson, that for patients that really don’t want to do the colonoscopy for one reason or another, and you’ve done your best in explaining what you think the risks and benefits are, that you’d rather have them get something than nothing?
Dr. Johnson: Absolutely. It comes down to what I recommend and then what you decide. But I still make the point explicit: If we’ve gone through those checkpoints and it’s positive, we agree that you understand that colonoscopy is the next step.
Final take-home messages
Dr. Wilson: Dr. Lin, I’ll turn the last word over to you, as the person who is probably discussing the choice of screening modalities more than any of us, before someone would get referred to someone like Dr. Johnson. What’s your final take-home message about the NEJM study and the state of colon cancer screening in the United States?
Dr. Lin: My take-home points about the study are that there were some limitations, but it is good to finally have a randomized trial of colonoscopy screening 2 decades after we really started doing that in the United States. It won’t immediately change – nor do I think it should – the way we practice and discuss different options. I think that some of Dr. Johnson’s points about making sure that whoever’s doing the colonoscopies for your practices is doing it in a high-quality way are really important. Just as it’s important, if you’re doing the fecal tests, to make sure that all patients who have positives get expeditiously referred for colonoscopy.
Dr. Johnson: Perry, I’d like to make one concluding comment as the gastroenterology expert in this discussion. I’ve had countless questions about this study from my patients and my peers. I tell them the following: Don’t let the headlines mislead you.
When you look at this study, the instrument is not so much the question. We know that getting the test is the first step in colon cancer screening. But we also know that getting the test done, with the highest-quality providers and the best-quality performance, is really the key to optimizing the true value of colonoscopy for colon cancer prevention.
So please don’t lose sight of this when reading the headlines in the media around this study. We really need to analyze the true characteristics of what we call a quality performance, because that’s what drives success and that’s what prevents colon cancer.
Dr. Wilson: Dr. Johnson and Dr. Lin, thank you very much. I appreciate you spending time with me here today and wish you all the best.
I guess I’ll sum up by saying that if you’re getting a colonoscopy, make sure it’s a good one. But do get screened.
This video originally appeared on WebMD. A transcript appeared on Medscape.com.
This transcript has been edited for clarity.
F. Perry Wilson, MD, MSCE: Hello, and thank you for joining us today for what promises to be a lively discussion about screening for colon cancer.
My name is Perry Wilson. I’m an associate professor of medicine and director of the Clinical and Translational Research Accelerator at the Yale School of Medicine. My new book, “How Medicine Works and When It Doesn’t: Learning Who to Trust to Get and Stay Healthy,” is available for pre-order now anywhere that books are sold.
I’m joined by two wonderful experts. Dr. David Johnson is a professor of medicine and the chief of gastroenterology at the Eastern Virginia School of Medicine. He is the past president of the American College of Gastroenterology. And I’m very encouraged to see that he’s won a Distinguished Educator Award for his efforts in gastroenterology.
I’m also joined by Dr Kenny Lin. He’s a frequent contributor to Medscape and WebMD. He’s a family physician and public health consultant from Lancaster, Pa., and deputy editor of the American Family Physician journal. He’s also a teacher of residents and students at Lancaster General Health and the Penn Medicine Family Medicine Residency program.
So, we have two great educators with us today to hopefully help teach us something about colon cancer and colon cancer screening. Thank you for joining me today.
David A. Johnson, MD: Thanks for having us.
Kenneth W. Lin, MD, MPH: Good to be here.
Dr. Wilson: Colon cancer is the second leading cause of cancer mortality in the United States. A little over 50,000 people die every year in the United States due to colon cancer.
A month ago, I would have said that there was a pretty broad consensus, at least from my perspective, that people should be getting colonoscopies. That’s certainly what we tell our patients.
Then a paper came out in the New England Journal of Medicine, a very prestigious journal, that has caused a lot of consternation online and led to my receiving a lot questions from patients and their family members. Today,
Dr Johnson, can you give us a brief overview of what this trial was about?
Dr. Johnson: This was a randomized trial looking at screening colonoscopy versus no screening test whatsoever. They looked at the outcomes of prevention of cancer and the prevention of colon cancer–related death.
The short answer was that it was disappointing as it relates to colonoscopy. The study looked at patients from four European countries, with data from three of them (Norway, Poland, and Sweden) ultimately analyzed in this report in NEJM. It got a lot of attention because it surprised a lot of people by saying maybe colonoscopy wasn’t quite as good as we thought it was.
They tried to correct that by only looking at the numbers of patients who got their colonoscopy screening, which still showed value, but it was less than that we’ve seen before. There’s lots of reasons for that, which we’ll discuss shortly.
An invitation to a screening
Dr. Wilson: This was a bit of an interesting trial design. I think I’m correct, Dr Lin, that this was the first randomized trial of screening colonoscopy. But they didn’t really randomize people to get a colonoscopy versus not get a colonoscopy. Can you tell us why this differed from that study design, which I’d have thought would be simpler way of assessing this?
Dr. Lin: It’s definitely an important point to highlight about the study. What investigators did was randomize patients to receive an invitation to get a screening colonoscopy. When the trial was set up, they randomized people before they were asked whether they wanted to participate in the study. If you did it the other way around, by first asking them whether they wanted to be in the study and then randomizing them, you would have been assured that more of them probably would have gotten the colonoscopy.
But in this case, they were more interested in figuring out the real-life results of having a national program that invited patients to receive screening colonoscopy. Because we know that everyone that you recommend to get a colonoscopy doesn’t necessarily want to do that, forgets to do it, or something happens that prevents their actually getting it.
When it comes to measuring the effectiveness of the colonoscopy, it perhaps wasn’t the greatest type of study to do that. But I think it did provide some information about what would happen if you invited people to get colonoscopy, in terms of how many would do it and the results overall for that population.
Lower participation numbers than expected
Dr. Wilson: Dr. Johnson, the data show that 42% of people who were in that invitation arm followed through and got their colonoscopy. You’re a gastroenterologist. Does that seem low or about right? Do about half of people who should get a colonoscopy end up getting one?
Dr. Johnson: No, it’s low. In the United States, those numbers are probably in the 70% range. Certainly, the test doesn’t work for people who don’t get the test performed. So, if 42% of those randomized to receive an invitation to get the colonoscopy got one, that really means the majority of patients never got the test.
Dr. Wilson: Certainly, we wouldn’t expect impressive results if they don’t get the test. But on the other hand, I imagine that people who choose to get the test when they’re invited are sort of a different breed. Perhaps they’re more health conscious or living in other healthy ways. Is that something we should worry about when we look at these results?
Dr. Johnson: I don’t think you can stratify based on this study. Factors like ethnicities and diet weren’t really explained. The key element that will hopefully have the major take-home impact is quality. It’s not just the test. It’s how the test is done.
The key results
Dr. Wilson: Let’s start with the big picture. This was a study looking at everyone invited; not the subgroup of people who got the colonoscopy, but the real randomized study population.
Dr. Lin, the study did show that the invited group had a lower risk of colon cancer over the next 10 years. That’s a good thing, I imagine.
Dr. Lin: I think that’s a significant benefit. Initially in the first few years, they had more colon cancers diagnosed. But that’s probably because those were cancers that were already existing and couldn’t be prevented by the test.
But then over the years the curves crossed, and by the end of the average follow-up of 10 years, there was a significantly lower rate of colon cancers being detected. That’s as you would expect, because you’re finding polyps and removing them before they became colon cancer.
Dr. Wilson: Dr. Johnson, is that the natural history of colon cancer? It starts out as a polyp that maybe can be easily removed and doesn’t require more therapy. Is that why screening colonoscopy is helpful?
Dr. Johnson: The ultimate goal of screening is prevention of cancer, rather than detection of cancer. That occurs by identification and complete removal of the polyps that we find that are precancerous. The key is, first, detection, and second, resection. Adequate resection comes down to some very significant issues of quality, which are questions that I’d raised about this study, and we can talk about momentarily.
Dr. Wilson: Absolutely. Let me first go through the two other big findings in this study.
The fact that there were fewer cases of colon cancer over 10 years seems good. But colon cancer mortality was not significantly different in the two groups. Now, of course, we know that not everyone got a colonoscopy. I would have expected though, if you had less colon cancer, you’d have less death from colon cancer.
Dr. Lin, what might explain this disconnect?
Dr. Lin: I think there are a couple of possible explanations.
One explanation is that they just didn’t follow the people long enough. Colon cancer takes a long time to go from an adenoma to cancer, and from cancer to something that would cause the patient’s death. You may need to follow them for longer than the 10 years that most of these patients were followed to see that benefit. I think there probably will be benefit after a while, because if you are removing colon cancers that otherwise would have progressed and metastasized, you often see a benefit.
We also have to consider the other possibility that not all the polyps removed necessarily were going to progress to advanced cancer. Therefore, you weren’t seeing the death benefit because not every polyp that was removed was necessarily going to cause health consequences.
In colonoscopy, quality is key to success
Dr. Wilson: You’re removing things and have no way of knowing in advance which are the bad ones and which aren’t.
Dr. Johnson, you’ve mentioned several times now that the quality of colonoscopy matters here. So, I’m intuiting that it’s not one-size-fits-all, that it’s not all the same. What do you mean by quality of colonoscopy, and what was it in the NEJM study?
Dr. Johnson: Quality colonoscopy is the quality of the whole process. It starts with the warm-up, if you will, and the clean out for the procedure. That allows the colonoscopist to be able to identify precancerous polyps, which we call adenomas (there are other precancerous polyps called sessile serrated lesions).
The identification of adenomas is extremely important. Even a small increase in the detection of those precancerous polyps has benefits. Well-performed studies looking at large databases show that a small, 1% increase in the adenoma detection leads to a 3% decrease in colon cancer and a 5% decrease in colon cancer–related death. There’s a huge array of effect when we talk about small increases in the adenoma detection rate.
Now, let’s go back to this study in NEJM.
If we base quality on the physician performing the colonoscopy, and say that the colonoscopy is achieving the act of getting all the way around the colon, but not all physicians in the study were able to do that, it starts to raise the question about quality, because adenoma detection is so important. Earlier reports from this group [Nordic-European Initiative on Colorectal Cancer Study Group] have shown that the adenoma detection rates have been way below the national thresholds. So, this raises the question of whether they found the polyp, and then whether they resected the polyp. They also don’t tell us where these cancers were. It is about the colonoscopy quality. It’s not the instrument. It’s the process.
An overview of other screening tools
Dr. Wilson: Dr. Lin, colonoscopy, which requires prep and anesthesia, is not the only colon cancer screening method we have. In fact, there are a bunch. I think we’re on board saying it’s probably better to detect colon cancer early than not detect it. But what are our other options aside from colonoscopy that can allow for early detection of colon cancer?
Dr. Lin: For most of my career, there were three options that I presented patients with. The first was the fecal test, which used to be in the form of initial hemoccult tests. These have been mostly replaced by fecal immunochemical testing. But they’re both just basically looking for the presence of blood in the stool. Anyone who has a positive test would be referred for a diagnostic colonoscopy.
The other test besides colonoscopy, which has been largely phased out in the United States, although it is still very much used in Canada and much of Europe, is flexible sigmoidoscopy. Until this study, the tests supported by randomized controlled trials were the fecal tests and flexible sigmoidoscopy.
Interestingly, there was a recent systematic review of flexible sigmoidoscopy looking at four trials and their effects over 15 years. They showed not only a reduction in colon cancer, but also a reduction in colon cancer mortality, and even a small reduction in all-cause mortality.
I believe three out of the four trials were done where the patients were consented and then randomized, so they had a higher uptake of the procedure.
But when you compare this with the colonoscopy trial, it really isn’t that impressive. You would expect a much larger benefit, because obviously you’re looking at the entire colon. But you really didn’t see that. It was, at best, maybe equivalent to sigmoidoscopy, but not a whole lot better.
Dr. Johnson: Perry, you mentioned sedation. It’s important to understand that this particular cohort of patients are from Norway, Sweden, and Poland, where it’s very much the norm to not get sedation for your colonoscopy. Any of the [audience] who have had colonoscopy will tell you that they are not ones to say, “Don’t give me sedation.” The rate of sedation is around 11% in Norway, maybe 23% in Sweden, and around 45% in Poland. So, the examiner and the patient were never really super comfortable.
I’ve done 50,000 colonoscopies in my career, and many nonsedated. We know that taking time increases the finding of polyps and the adequate identification and resection. So, that ability to perform at a high quality is very much impacted when the patients aren’t comfortable.
Dr. Wilson: Dr. Johnson, we brought up flexible sigmoidoscopy. For the patients watching whose doctors are talking to them about screening colonoscopy, what’s the difference?
Dr. Johnson: Flexible sigmoidoscopy is just a short scope examination, in which you see about one-third of the colon. I’ve been in the field for 45 years, and during that time we’ve seen that there’s a progressive increase in the development of cancers above that bottom third of the colon to the higher end, the two-thirds of the colon that you would miss without doing a full colonoscopy. Also, flexible sigmoidoscopy typically does not get covered for sedation.
Again, if you do the exam and find something, then you’re going to have to come back and do an adequate resection with a colonoscopy. So, one-stop-shopping colon cancer screening is not about detection of cancer, it’s about prevention of cancer, and that’s what colonoscopy does.
Patients want convenience, but at what cost?
Dr. Wilson: Dr. Lin, how are your patients in your family practice handling this study? Have conversations changed around colon cancer screening? What are people asking about these days?
Dr. Lin: I don’t think the conversations have changed in my practice that much. When patients ask about this study, we do discuss the limitations, that it wasn’t designed to assess the maximum benefit of getting a colonoscopy because the majority of people assigned to that group didn’t get colonoscopy.
But I think it is an opportunity in primary care to consider the way we present the options to patients. Because I would guess that a majority of primary care physicians, when they present the options, would say colonoscopy is the gold standard and recommend their patients get it. And they only offer fecal testing to patients who don’t want the colonoscopy or really refuse.
That hasn’t been my practice. I’m usually more agnostic, because there are both harms and benefits. If you get a fecal test, the chance of you having a complication from colonoscopy is automatically lower because most of those people will not get colonoscopy. Now obviously, the complications with colonoscopy are pretty rare and usually self-limited, but they do exist. If you’re doing lots and lots of these, eventually you’ll see them. Probably all primary care physicians have patients who’ve had a complication from colonoscopy and may or may not have regretted it depending on how information was presented.
But I feel like this study reinforces my feeling that we ought to be presenting these, and not saying one is superior or inferior to the other. Instead, I’d base it on what the patient’s priorities are. But I feel like this study reinforces my feeling that we ought to be presenting these, and not saying one is superior or inferior to the other. Instead, I’d base it on what the patient’s priorities are. Is your priority finding every single cancer? Do you want to know exactly what the benefit is? I think with colonoscopy, we’re still trying to figure out exactly what the benefit is. Whereas we can say it pretty confidently for fecal tests because we have those randomized trials.
Dr. Wilson: Dr. Johnson, I think patients who are watching need to know, first of all, that if they do the fecal test route, a positive fecal test does lead to colonoscopy. In some sense, all roads lead to colonoscopy once you have a positive screening test. So, I can certainly see the value of just sort of skipping to that point. But what about this risk-versus-benefit relationship? Colonoscopy, albeit a relatively safe procedure, is still a procedure. There is some risk associated with it. If we can get the same benefit from yearly fecal immunochemical testing, is that a better choice potentially, at least for patients at average risk?
Dr. Johnson: The stool-based testing is really more effective for detection of cancer. That’s not screening, where the entire goal is the prevention of cancer. The fecal-based testing, including the stool-based DNA testing, misses the majority of precancerous polyps. And the fecal immunochemical tests, which Dr. Lin just mentioned, misses virtually all of them. We really want to get to the prevention of cancer, meaning identification and removal of polyps, not just screening for cancer.
Dr. Wilson: Do you see anything on the horizon that could unseat colonoscopy as, to quote Dr. Lin, the potential gold standard for screening for colon cancer?
Dr. Johnson: I think not on the horizon for identification and removal of polyps. That’s really the gold standard. Technology continues to advance. We’ll see what happens. But on the short and intermediate horizon, colonoscopy is going to be needed.
We are finding that some patients are starting to acquiesce to stool-based testing because they can do it at home. Maybe they don’t have to do a prep. We’re talking about screening only here, not about the follow-up of patients who have a family history, patients who have colitis, patients who have had colon polyps, or other reasons. Stool-based testing is not an option for the follow-up of those patients.
Convenience testing, in the face of COVID, also has thrown a wrench into things. Patients may have wanted to stay home and do these tests. Again, we need to be proactive, not reactive. We want to prevent cancer, not detect it.
Changing advice in the face of younger screening thresholds
Dr. Wilson: Dr. Lin, I’m 42 years old. I don’t believe I’m at any increased risk of colon cancer based on my family history or other risk factors. I’m 3 years away from when the U.S. Preventive Services Task Force tells me I should potentially consider starting to screen for colon cancer. That recommendation has recently been moved down from 50 years old to 45 years old. So, it’s on my mind as I approach that age. What do you advise younger patients approaching 45 right now in terms of screening for colon cancer?
Dr. Lin: For patients with the risk factors that Dr. Johnson mentioned, I would recommend screening colonoscopy as the initial test.
Assuming you don’t have those risk factors, I present it as we have a couple of different fecal tests. There’s the traditional one that just looks for blood. Then there’s the newer one that also adds DNA, which is more sensitive for colorectal cancer, but a little less specific, which is a problem just because there are more false positives.
But you need to compare that with colonoscopy, which you only need to get done ideally every 10 years if there are no findings. That is more complete. And theoretically, as we’ve been talking about, it would also prevent as well as detect early cancers.
So, I think it’s really down to your preference in terms of how the various factors that come into play, such as convenience of the test and your level of concern about cancer. I do tell patients that family history of cancer is not terribly predictive of whether you get it or not. A lot of people unfortunately who develop colorectal cancer have no previous family history. Diet will come into play to some extent. There are some things that point to increased risk for colorectal cancer if you have a diet high in red meat and things like that. But ultimately, it really is up to the patient. I lay out the options, and whatever they choose, I’m happy to pursue.
But the most important thing is that they do some test, because doing no test is not going to help anyone. I do agree with the notion that the best test is the test that gets done.
Dr. Wilson: Absolutely. I think the NEJM study supports that, even when we’re talking about colonoscopy.
Dr. Johnson, you’ve had some criticisms about the NEJM study, and I think they make sense. At the same time, as this is the first randomized trial of colonoscopy, it’s kind of the only data we have. Are we going to get better data? Are there other studies going on out there that might help shed some light on what’s turning out to be a complicated issue?
Dr. Johnson: Yes, there are ongoing studies. They’re not taking place within the United States, because you couldn’t get through a no-screening option trial. There are comparative studies that are probably still 5 years away looking at stool-based testing.
But again, we have to recognize that if you do these alternative tests that were eloquently discussed by Dr. Lin, and not the colonoscopy, which would be every 10 years with high-quality performance, that you have to annualize or do them in sequence. It’s important that you follow up on those with regularity. It’s not just a one-time test every 10 years for these individual tests.
And any of the time that those tests are ordered, the patient should be instructed that if it’s positive you need a colonoscopy. We’re seeing a lot of slippage on that front for the stool-based testing. Convenience is not the answer. It’s getting the job done.
Dr. Wilson: Would you agree, Dr. Johnson, that for patients that really don’t want to do the colonoscopy for one reason or another, and you’ve done your best in explaining what you think the risks and benefits are, that you’d rather have them get something than nothing?
Dr. Johnson: Absolutely. It comes down to what I recommend and then what you decide. But I still make the point explicit: If we’ve gone through those checkpoints and it’s positive, we agree that you understand that colonoscopy is the next step.
Final take-home messages
Dr. Wilson: Dr. Lin, I’ll turn the last word over to you, as the person who is probably discussing the choice of screening modalities more than any of us, before someone would get referred to someone like Dr. Johnson. What’s your final take-home message about the NEJM study and the state of colon cancer screening in the United States?
Dr. Lin: My take-home points about the study are that there were some limitations, but it is good to finally have a randomized trial of colonoscopy screening 2 decades after we really started doing that in the United States. It won’t immediately change – nor do I think it should – the way we practice and discuss different options. I think that some of Dr. Johnson’s points about making sure that whoever’s doing the colonoscopies for your practices is doing it in a high-quality way are really important. Just as it’s important, if you’re doing the fecal tests, to make sure that all patients who have positives get expeditiously referred for colonoscopy.
Dr. Johnson: Perry, I’d like to make one concluding comment as the gastroenterology expert in this discussion. I’ve had countless questions about this study from my patients and my peers. I tell them the following: Don’t let the headlines mislead you.
When you look at this study, the instrument is not so much the question. We know that getting the test is the first step in colon cancer screening. But we also know that getting the test done, with the highest-quality providers and the best-quality performance, is really the key to optimizing the true value of colonoscopy for colon cancer prevention.
So please don’t lose sight of this when reading the headlines in the media around this study. We really need to analyze the true characteristics of what we call a quality performance, because that’s what drives success and that’s what prevents colon cancer.
Dr. Wilson: Dr. Johnson and Dr. Lin, thank you very much. I appreciate you spending time with me here today and wish you all the best.
I guess I’ll sum up by saying that if you’re getting a colonoscopy, make sure it’s a good one. But do get screened.
This video originally appeared on WebMD. A transcript appeared on Medscape.com.
This transcript has been edited for clarity.
F. Perry Wilson, MD, MSCE: Hello, and thank you for joining us today for what promises to be a lively discussion about screening for colon cancer.
My name is Perry Wilson. I’m an associate professor of medicine and director of the Clinical and Translational Research Accelerator at the Yale School of Medicine. My new book, “How Medicine Works and When It Doesn’t: Learning Who to Trust to Get and Stay Healthy,” is available for pre-order now anywhere that books are sold.
I’m joined by two wonderful experts. Dr. David Johnson is a professor of medicine and the chief of gastroenterology at the Eastern Virginia School of Medicine. He is the past president of the American College of Gastroenterology. And I’m very encouraged to see that he’s won a Distinguished Educator Award for his efforts in gastroenterology.
I’m also joined by Dr Kenny Lin. He’s a frequent contributor to Medscape and WebMD. He’s a family physician and public health consultant from Lancaster, Pa., and deputy editor of the American Family Physician journal. He’s also a teacher of residents and students at Lancaster General Health and the Penn Medicine Family Medicine Residency program.
So, we have two great educators with us today to hopefully help teach us something about colon cancer and colon cancer screening. Thank you for joining me today.
David A. Johnson, MD: Thanks for having us.
Kenneth W. Lin, MD, MPH: Good to be here.
Dr. Wilson: Colon cancer is the second leading cause of cancer mortality in the United States. A little over 50,000 people die every year in the United States due to colon cancer.
A month ago, I would have said that there was a pretty broad consensus, at least from my perspective, that people should be getting colonoscopies. That’s certainly what we tell our patients.
Then a paper came out in the New England Journal of Medicine, a very prestigious journal, that has caused a lot of consternation online and led to my receiving a lot questions from patients and their family members. Today,
Dr Johnson, can you give us a brief overview of what this trial was about?
Dr. Johnson: This was a randomized trial looking at screening colonoscopy versus no screening test whatsoever. They looked at the outcomes of prevention of cancer and the prevention of colon cancer–related death.
The short answer was that it was disappointing as it relates to colonoscopy. The study looked at patients from four European countries, with data from three of them (Norway, Poland, and Sweden) ultimately analyzed in this report in NEJM. It got a lot of attention because it surprised a lot of people by saying maybe colonoscopy wasn’t quite as good as we thought it was.
They tried to correct that by only looking at the numbers of patients who got their colonoscopy screening, which still showed value, but it was less than that we’ve seen before. There’s lots of reasons for that, which we’ll discuss shortly.
An invitation to a screening
Dr. Wilson: This was a bit of an interesting trial design. I think I’m correct, Dr Lin, that this was the first randomized trial of screening colonoscopy. But they didn’t really randomize people to get a colonoscopy versus not get a colonoscopy. Can you tell us why this differed from that study design, which I’d have thought would be simpler way of assessing this?
Dr. Lin: It’s definitely an important point to highlight about the study. What investigators did was randomize patients to receive an invitation to get a screening colonoscopy. When the trial was set up, they randomized people before they were asked whether they wanted to participate in the study. If you did it the other way around, by first asking them whether they wanted to be in the study and then randomizing them, you would have been assured that more of them probably would have gotten the colonoscopy.
But in this case, they were more interested in figuring out the real-life results of having a national program that invited patients to receive screening colonoscopy. Because we know that everyone that you recommend to get a colonoscopy doesn’t necessarily want to do that, forgets to do it, or something happens that prevents their actually getting it.
When it comes to measuring the effectiveness of the colonoscopy, it perhaps wasn’t the greatest type of study to do that. But I think it did provide some information about what would happen if you invited people to get colonoscopy, in terms of how many would do it and the results overall for that population.
Lower participation numbers than expected
Dr. Wilson: Dr. Johnson, the data show that 42% of people who were in that invitation arm followed through and got their colonoscopy. You’re a gastroenterologist. Does that seem low or about right? Do about half of people who should get a colonoscopy end up getting one?
Dr. Johnson: No, it’s low. In the United States, those numbers are probably in the 70% range. Certainly, the test doesn’t work for people who don’t get the test performed. So, if 42% of those randomized to receive an invitation to get the colonoscopy got one, that really means the majority of patients never got the test.
Dr. Wilson: Certainly, we wouldn’t expect impressive results if they don’t get the test. But on the other hand, I imagine that people who choose to get the test when they’re invited are sort of a different breed. Perhaps they’re more health conscious or living in other healthy ways. Is that something we should worry about when we look at these results?
Dr. Johnson: I don’t think you can stratify based on this study. Factors like ethnicities and diet weren’t really explained. The key element that will hopefully have the major take-home impact is quality. It’s not just the test. It’s how the test is done.
The key results
Dr. Wilson: Let’s start with the big picture. This was a study looking at everyone invited; not the subgroup of people who got the colonoscopy, but the real randomized study population.
Dr. Lin, the study did show that the invited group had a lower risk of colon cancer over the next 10 years. That’s a good thing, I imagine.
Dr. Lin: I think that’s a significant benefit. Initially in the first few years, they had more colon cancers diagnosed. But that’s probably because those were cancers that were already existing and couldn’t be prevented by the test.
But then over the years the curves crossed, and by the end of the average follow-up of 10 years, there was a significantly lower rate of colon cancers being detected. That’s as you would expect, because you’re finding polyps and removing them before they became colon cancer.
Dr. Wilson: Dr. Johnson, is that the natural history of colon cancer? It starts out as a polyp that maybe can be easily removed and doesn’t require more therapy. Is that why screening colonoscopy is helpful?
Dr. Johnson: The ultimate goal of screening is prevention of cancer, rather than detection of cancer. That occurs by identification and complete removal of the polyps that we find that are precancerous. The key is, first, detection, and second, resection. Adequate resection comes down to some very significant issues of quality, which are questions that I’d raised about this study, and we can talk about momentarily.
Dr. Wilson: Absolutely. Let me first go through the two other big findings in this study.
The fact that there were fewer cases of colon cancer over 10 years seems good. But colon cancer mortality was not significantly different in the two groups. Now, of course, we know that not everyone got a colonoscopy. I would have expected though, if you had less colon cancer, you’d have less death from colon cancer.
Dr. Lin, what might explain this disconnect?
Dr. Lin: I think there are a couple of possible explanations.
One explanation is that they just didn’t follow the people long enough. Colon cancer takes a long time to go from an adenoma to cancer, and from cancer to something that would cause the patient’s death. You may need to follow them for longer than the 10 years that most of these patients were followed to see that benefit. I think there probably will be benefit after a while, because if you are removing colon cancers that otherwise would have progressed and metastasized, you often see a benefit.
We also have to consider the other possibility that not all the polyps removed necessarily were going to progress to advanced cancer. Therefore, you weren’t seeing the death benefit because not every polyp that was removed was necessarily going to cause health consequences.
In colonoscopy, quality is key to success
Dr. Wilson: You’re removing things and have no way of knowing in advance which are the bad ones and which aren’t.
Dr. Johnson, you’ve mentioned several times now that the quality of colonoscopy matters here. So, I’m intuiting that it’s not one-size-fits-all, that it’s not all the same. What do you mean by quality of colonoscopy, and what was it in the NEJM study?
Dr. Johnson: Quality colonoscopy is the quality of the whole process. It starts with the warm-up, if you will, and the clean out for the procedure. That allows the colonoscopist to be able to identify precancerous polyps, which we call adenomas (there are other precancerous polyps called sessile serrated lesions).
The identification of adenomas is extremely important. Even a small increase in the detection of those precancerous polyps has benefits. Well-performed studies looking at large databases show that a small, 1% increase in the adenoma detection leads to a 3% decrease in colon cancer and a 5% decrease in colon cancer–related death. There’s a huge array of effect when we talk about small increases in the adenoma detection rate.
Now, let’s go back to this study in NEJM.
If we base quality on the physician performing the colonoscopy, and say that the colonoscopy is achieving the act of getting all the way around the colon, but not all physicians in the study were able to do that, it starts to raise the question about quality, because adenoma detection is so important. Earlier reports from this group [Nordic-European Initiative on Colorectal Cancer Study Group] have shown that the adenoma detection rates have been way below the national thresholds. So, this raises the question of whether they found the polyp, and then whether they resected the polyp. They also don’t tell us where these cancers were. It is about the colonoscopy quality. It’s not the instrument. It’s the process.
An overview of other screening tools
Dr. Wilson: Dr. Lin, colonoscopy, which requires prep and anesthesia, is not the only colon cancer screening method we have. In fact, there are a bunch. I think we’re on board saying it’s probably better to detect colon cancer early than not detect it. But what are our other options aside from colonoscopy that can allow for early detection of colon cancer?
Dr. Lin: For most of my career, there were three options that I presented patients with. The first was the fecal test, which used to be in the form of initial hemoccult tests. These have been mostly replaced by fecal immunochemical testing. But they’re both just basically looking for the presence of blood in the stool. Anyone who has a positive test would be referred for a diagnostic colonoscopy.
The other test besides colonoscopy, which has been largely phased out in the United States, although it is still very much used in Canada and much of Europe, is flexible sigmoidoscopy. Until this study, the tests supported by randomized controlled trials were the fecal tests and flexible sigmoidoscopy.
Interestingly, there was a recent systematic review of flexible sigmoidoscopy looking at four trials and their effects over 15 years. They showed not only a reduction in colon cancer, but also a reduction in colon cancer mortality, and even a small reduction in all-cause mortality.
I believe three out of the four trials were done where the patients were consented and then randomized, so they had a higher uptake of the procedure.
But when you compare this with the colonoscopy trial, it really isn’t that impressive. You would expect a much larger benefit, because obviously you’re looking at the entire colon. But you really didn’t see that. It was, at best, maybe equivalent to sigmoidoscopy, but not a whole lot better.
Dr. Johnson: Perry, you mentioned sedation. It’s important to understand that this particular cohort of patients are from Norway, Sweden, and Poland, where it’s very much the norm to not get sedation for your colonoscopy. Any of the [audience] who have had colonoscopy will tell you that they are not ones to say, “Don’t give me sedation.” The rate of sedation is around 11% in Norway, maybe 23% in Sweden, and around 45% in Poland. So, the examiner and the patient were never really super comfortable.
I’ve done 50,000 colonoscopies in my career, and many nonsedated. We know that taking time increases the finding of polyps and the adequate identification and resection. So, that ability to perform at a high quality is very much impacted when the patients aren’t comfortable.
Dr. Wilson: Dr. Johnson, we brought up flexible sigmoidoscopy. For the patients watching whose doctors are talking to them about screening colonoscopy, what’s the difference?
Dr. Johnson: Flexible sigmoidoscopy is just a short scope examination, in which you see about one-third of the colon. I’ve been in the field for 45 years, and during that time we’ve seen that there’s a progressive increase in the development of cancers above that bottom third of the colon to the higher end, the two-thirds of the colon that you would miss without doing a full colonoscopy. Also, flexible sigmoidoscopy typically does not get covered for sedation.
Again, if you do the exam and find something, then you’re going to have to come back and do an adequate resection with a colonoscopy. So, one-stop-shopping colon cancer screening is not about detection of cancer, it’s about prevention of cancer, and that’s what colonoscopy does.
Patients want convenience, but at what cost?
Dr. Wilson: Dr. Lin, how are your patients in your family practice handling this study? Have conversations changed around colon cancer screening? What are people asking about these days?
Dr. Lin: I don’t think the conversations have changed in my practice that much. When patients ask about this study, we do discuss the limitations, that it wasn’t designed to assess the maximum benefit of getting a colonoscopy because the majority of people assigned to that group didn’t get colonoscopy.
But I think it is an opportunity in primary care to consider the way we present the options to patients. Because I would guess that a majority of primary care physicians, when they present the options, would say colonoscopy is the gold standard and recommend their patients get it. And they only offer fecal testing to patients who don’t want the colonoscopy or really refuse.
That hasn’t been my practice. I’m usually more agnostic, because there are both harms and benefits. If you get a fecal test, the chance of you having a complication from colonoscopy is automatically lower because most of those people will not get colonoscopy. Now obviously, the complications with colonoscopy are pretty rare and usually self-limited, but they do exist. If you’re doing lots and lots of these, eventually you’ll see them. Probably all primary care physicians have patients who’ve had a complication from colonoscopy and may or may not have regretted it depending on how information was presented.
But I feel like this study reinforces my feeling that we ought to be presenting these, and not saying one is superior or inferior to the other. Instead, I’d base it on what the patient’s priorities are. But I feel like this study reinforces my feeling that we ought to be presenting these, and not saying one is superior or inferior to the other. Instead, I’d base it on what the patient’s priorities are. Is your priority finding every single cancer? Do you want to know exactly what the benefit is? I think with colonoscopy, we’re still trying to figure out exactly what the benefit is. Whereas we can say it pretty confidently for fecal tests because we have those randomized trials.
Dr. Wilson: Dr. Johnson, I think patients who are watching need to know, first of all, that if they do the fecal test route, a positive fecal test does lead to colonoscopy. In some sense, all roads lead to colonoscopy once you have a positive screening test. So, I can certainly see the value of just sort of skipping to that point. But what about this risk-versus-benefit relationship? Colonoscopy, albeit a relatively safe procedure, is still a procedure. There is some risk associated with it. If we can get the same benefit from yearly fecal immunochemical testing, is that a better choice potentially, at least for patients at average risk?
Dr. Johnson: The stool-based testing is really more effective for detection of cancer. That’s not screening, where the entire goal is the prevention of cancer. The fecal-based testing, including the stool-based DNA testing, misses the majority of precancerous polyps. And the fecal immunochemical tests, which Dr. Lin just mentioned, misses virtually all of them. We really want to get to the prevention of cancer, meaning identification and removal of polyps, not just screening for cancer.
Dr. Wilson: Do you see anything on the horizon that could unseat colonoscopy as, to quote Dr. Lin, the potential gold standard for screening for colon cancer?
Dr. Johnson: I think not on the horizon for identification and removal of polyps. That’s really the gold standard. Technology continues to advance. We’ll see what happens. But on the short and intermediate horizon, colonoscopy is going to be needed.
We are finding that some patients are starting to acquiesce to stool-based testing because they can do it at home. Maybe they don’t have to do a prep. We’re talking about screening only here, not about the follow-up of patients who have a family history, patients who have colitis, patients who have had colon polyps, or other reasons. Stool-based testing is not an option for the follow-up of those patients.
Convenience testing, in the face of COVID, also has thrown a wrench into things. Patients may have wanted to stay home and do these tests. Again, we need to be proactive, not reactive. We want to prevent cancer, not detect it.
Changing advice in the face of younger screening thresholds
Dr. Wilson: Dr. Lin, I’m 42 years old. I don’t believe I’m at any increased risk of colon cancer based on my family history or other risk factors. I’m 3 years away from when the U.S. Preventive Services Task Force tells me I should potentially consider starting to screen for colon cancer. That recommendation has recently been moved down from 50 years old to 45 years old. So, it’s on my mind as I approach that age. What do you advise younger patients approaching 45 right now in terms of screening for colon cancer?
Dr. Lin: For patients with the risk factors that Dr. Johnson mentioned, I would recommend screening colonoscopy as the initial test.
Assuming you don’t have those risk factors, I present it as we have a couple of different fecal tests. There’s the traditional one that just looks for blood. Then there’s the newer one that also adds DNA, which is more sensitive for colorectal cancer, but a little less specific, which is a problem just because there are more false positives.
But you need to compare that with colonoscopy, which you only need to get done ideally every 10 years if there are no findings. That is more complete. And theoretically, as we’ve been talking about, it would also prevent as well as detect early cancers.
So, I think it’s really down to your preference in terms of how the various factors that come into play, such as convenience of the test and your level of concern about cancer. I do tell patients that family history of cancer is not terribly predictive of whether you get it or not. A lot of people unfortunately who develop colorectal cancer have no previous family history. Diet will come into play to some extent. There are some things that point to increased risk for colorectal cancer if you have a diet high in red meat and things like that. But ultimately, it really is up to the patient. I lay out the options, and whatever they choose, I’m happy to pursue.
But the most important thing is that they do some test, because doing no test is not going to help anyone. I do agree with the notion that the best test is the test that gets done.
Dr. Wilson: Absolutely. I think the NEJM study supports that, even when we’re talking about colonoscopy.
Dr. Johnson, you’ve had some criticisms about the NEJM study, and I think they make sense. At the same time, as this is the first randomized trial of colonoscopy, it’s kind of the only data we have. Are we going to get better data? Are there other studies going on out there that might help shed some light on what’s turning out to be a complicated issue?
Dr. Johnson: Yes, there are ongoing studies. They’re not taking place within the United States, because you couldn’t get through a no-screening option trial. There are comparative studies that are probably still 5 years away looking at stool-based testing.
But again, we have to recognize that if you do these alternative tests that were eloquently discussed by Dr. Lin, and not the colonoscopy, which would be every 10 years with high-quality performance, that you have to annualize or do them in sequence. It’s important that you follow up on those with regularity. It’s not just a one-time test every 10 years for these individual tests.
And any of the time that those tests are ordered, the patient should be instructed that if it’s positive you need a colonoscopy. We’re seeing a lot of slippage on that front for the stool-based testing. Convenience is not the answer. It’s getting the job done.
Dr. Wilson: Would you agree, Dr. Johnson, that for patients that really don’t want to do the colonoscopy for one reason or another, and you’ve done your best in explaining what you think the risks and benefits are, that you’d rather have them get something than nothing?
Dr. Johnson: Absolutely. It comes down to what I recommend and then what you decide. But I still make the point explicit: If we’ve gone through those checkpoints and it’s positive, we agree that you understand that colonoscopy is the next step.
Final take-home messages
Dr. Wilson: Dr. Lin, I’ll turn the last word over to you, as the person who is probably discussing the choice of screening modalities more than any of us, before someone would get referred to someone like Dr. Johnson. What’s your final take-home message about the NEJM study and the state of colon cancer screening in the United States?
Dr. Lin: My take-home points about the study are that there were some limitations, but it is good to finally have a randomized trial of colonoscopy screening 2 decades after we really started doing that in the United States. It won’t immediately change – nor do I think it should – the way we practice and discuss different options. I think that some of Dr. Johnson’s points about making sure that whoever’s doing the colonoscopies for your practices is doing it in a high-quality way are really important. Just as it’s important, if you’re doing the fecal tests, to make sure that all patients who have positives get expeditiously referred for colonoscopy.
Dr. Johnson: Perry, I’d like to make one concluding comment as the gastroenterology expert in this discussion. I’ve had countless questions about this study from my patients and my peers. I tell them the following: Don’t let the headlines mislead you.
When you look at this study, the instrument is not so much the question. We know that getting the test is the first step in colon cancer screening. But we also know that getting the test done, with the highest-quality providers and the best-quality performance, is really the key to optimizing the true value of colonoscopy for colon cancer prevention.
So please don’t lose sight of this when reading the headlines in the media around this study. We really need to analyze the true characteristics of what we call a quality performance, because that’s what drives success and that’s what prevents colon cancer.
Dr. Wilson: Dr. Johnson and Dr. Lin, thank you very much. I appreciate you spending time with me here today and wish you all the best.
I guess I’ll sum up by saying that if you’re getting a colonoscopy, make sure it’s a good one. But do get screened.
This video originally appeared on WebMD. A transcript appeared on Medscape.com.
Mindfulness, exercise strike out in memory trial
Welcome to Impact Factor, your weekly dose of commentary on a new medical study. I’m Dr. F. Perry Wilson of the Yale School of Medicine.
We are coming to the end of the year, which always makes me think about getting older. Much like the search for the fountain of youth, many promising leads have ultimately led to dead ends. And yet, I had high hopes for a trial that focused on two cornerstones of wellness – exercise and mindfulness – to address the subjective loss of memory that comes with aging. Alas, meditation and exercise do not appear to be the fountain of youth.
I’m talking about this study, appearing in JAMA, known as the MEDEX trial.
It’s a clever design: a 2 x 2 factorial randomized trial where participants could be randomized to a mindfulness intervention, an exercise intervention, both, or neither.
In this manner, you can test multiple hypotheses exploiting a shared control group. Or as a mentor of mine used to say, you get two trials for the price of one and a half.
The participants were older adults, aged 65-84, living in the community. They had to be relatively sedentary at baseline and not engaging in mindfulness practices. They had to subjectively report some memory or concentration issues but had to be cognitively intact, based on a standard dementia screening test. In other words, these are your average older people who are worried that they aren’t as sharp as they used to be.
The interventions themselves were fairly intense. The exercise group had instructor-led sessions for 90 minutes twice a week for the first 6 months of the study, once a week thereafter. And participants were encouraged to exercise at home such that they had a total of 300 minutes of weekly exercise.
The mindfulness program was characterized by eight weekly classes of 2.5 hours each as well as a half-day retreat to teach the tenets of mindfulness and meditation, with monthly refreshers thereafter. Participants were instructed to meditate for 60 minutes a day in addition to the classes.
For the 144 people who were randomized to both meditation and exercise, this trial amounted to something of a part-time job. So you might think that adherence to the interventions was low, but apparently that’s not the case. Attendance to the mindfulness classes was over 90%, and over 80% for the exercise classes. And diary-based reporting of home efforts was also pretty good.
The control group wasn’t left to their own devices. Recognizing that the community aspect of exercise or mindfulness classes might convey a benefit independent of the actual exercise or mindfulness, the control group met on a similar schedule to discuss health education, but no mention of exercise or mindfulness occurred in that setting.
The primary outcome was change in memory and executive function scores across a battery of neuropsychologic testing, but the story is told in just a few pictures.
Memory scores improved in all three groups – mindfulness, exercise, and health education – over time. Cognitive composite score improved in all three groups similarly. There was no synergistic effect of mindfulness and exercise either. Basically, everyone got a bit better.
But the study did way more than look at scores on tests. Researchers used MRI to measure brain anatomic outcomes as well. And the surprising thing is that virtually none of these outcomes were different between the groups either.
Hippocampal volume decreased a bit in all the groups. Dorsolateral prefrontal cortex volume was flat. There was no change in scores measuring tasks of daily living.
When you see negative results like this, right away you worry that the intervention wasn’t properly delivered. Were these people really exercising and meditating? Well, the authors showed that individuals randomized to exercise, at least, had less sleep latency, greater aerobic fitness, and greater strength. So we know something was happening.
They then asked, would the people in the exercise group with the greatest changes in those physiologic parameters show some improvement in cognitive parameters? In other words, we know you were exercising because you got stronger and are sleeping better; is your memory better? The answer? Surprisingly, still no. Even in that honestly somewhat cherry-picked group, the interventions had no effect.
Could it be that the control was inappropriate, that the “health education” intervention was actually so helpful that it obscured the benefits of exercise and meditation? After all, cognitive scores did improve in all groups. The authors doubt it. They say they think the improvement in cognitive scores reflects the fact that patients had learned a bit about how to take the tests. This is pretty common in the neuropsychiatric literature.
So here we are and I just want to say, well, shoot. This is not the result I wanted. And I think the reason I’m so disappointed is because aging and the loss of cognitive faculties that comes with aging are just sort of scary. We are all looking for some control over that fear, and how nice it would be to be able to tell ourselves not to worry – that we won’t have those problems as we get older because we exercise, or meditate, or drink red wine, or don’t drink wine, or whatever. And while I have no doubt that staying healthier physically will keep you healthier mentally, it may take more than one simple thing to move the needle.
Dr. Wilson is associate professor, department of medicine, and director of the Clinical and Translational Research Accelerator at Yale University, New Haven, Conn. He reported no conflicts of interest.
A version of this article first appeared on Medscape.com.
Welcome to Impact Factor, your weekly dose of commentary on a new medical study. I’m Dr. F. Perry Wilson of the Yale School of Medicine.
We are coming to the end of the year, which always makes me think about getting older. Much like the search for the fountain of youth, many promising leads have ultimately led to dead ends. And yet, I had high hopes for a trial that focused on two cornerstones of wellness – exercise and mindfulness – to address the subjective loss of memory that comes with aging. Alas, meditation and exercise do not appear to be the fountain of youth.
I’m talking about this study, appearing in JAMA, known as the MEDEX trial.
It’s a clever design: a 2 x 2 factorial randomized trial where participants could be randomized to a mindfulness intervention, an exercise intervention, both, or neither.
In this manner, you can test multiple hypotheses exploiting a shared control group. Or as a mentor of mine used to say, you get two trials for the price of one and a half.
The participants were older adults, aged 65-84, living in the community. They had to be relatively sedentary at baseline and not engaging in mindfulness practices. They had to subjectively report some memory or concentration issues but had to be cognitively intact, based on a standard dementia screening test. In other words, these are your average older people who are worried that they aren’t as sharp as they used to be.
The interventions themselves were fairly intense. The exercise group had instructor-led sessions for 90 minutes twice a week for the first 6 months of the study, once a week thereafter. And participants were encouraged to exercise at home such that they had a total of 300 minutes of weekly exercise.
The mindfulness program was characterized by eight weekly classes of 2.5 hours each as well as a half-day retreat to teach the tenets of mindfulness and meditation, with monthly refreshers thereafter. Participants were instructed to meditate for 60 minutes a day in addition to the classes.
For the 144 people who were randomized to both meditation and exercise, this trial amounted to something of a part-time job. So you might think that adherence to the interventions was low, but apparently that’s not the case. Attendance to the mindfulness classes was over 90%, and over 80% for the exercise classes. And diary-based reporting of home efforts was also pretty good.
The control group wasn’t left to their own devices. Recognizing that the community aspect of exercise or mindfulness classes might convey a benefit independent of the actual exercise or mindfulness, the control group met on a similar schedule to discuss health education, but no mention of exercise or mindfulness occurred in that setting.
The primary outcome was change in memory and executive function scores across a battery of neuropsychologic testing, but the story is told in just a few pictures.
Memory scores improved in all three groups – mindfulness, exercise, and health education – over time. Cognitive composite score improved in all three groups similarly. There was no synergistic effect of mindfulness and exercise either. Basically, everyone got a bit better.
But the study did way more than look at scores on tests. Researchers used MRI to measure brain anatomic outcomes as well. And the surprising thing is that virtually none of these outcomes were different between the groups either.
Hippocampal volume decreased a bit in all the groups. Dorsolateral prefrontal cortex volume was flat. There was no change in scores measuring tasks of daily living.
When you see negative results like this, right away you worry that the intervention wasn’t properly delivered. Were these people really exercising and meditating? Well, the authors showed that individuals randomized to exercise, at least, had less sleep latency, greater aerobic fitness, and greater strength. So we know something was happening.
They then asked, would the people in the exercise group with the greatest changes in those physiologic parameters show some improvement in cognitive parameters? In other words, we know you were exercising because you got stronger and are sleeping better; is your memory better? The answer? Surprisingly, still no. Even in that honestly somewhat cherry-picked group, the interventions had no effect.
Could it be that the control was inappropriate, that the “health education” intervention was actually so helpful that it obscured the benefits of exercise and meditation? After all, cognitive scores did improve in all groups. The authors doubt it. They say they think the improvement in cognitive scores reflects the fact that patients had learned a bit about how to take the tests. This is pretty common in the neuropsychiatric literature.
So here we are and I just want to say, well, shoot. This is not the result I wanted. And I think the reason I’m so disappointed is because aging and the loss of cognitive faculties that comes with aging are just sort of scary. We are all looking for some control over that fear, and how nice it would be to be able to tell ourselves not to worry – that we won’t have those problems as we get older because we exercise, or meditate, or drink red wine, or don’t drink wine, or whatever. And while I have no doubt that staying healthier physically will keep you healthier mentally, it may take more than one simple thing to move the needle.
Dr. Wilson is associate professor, department of medicine, and director of the Clinical and Translational Research Accelerator at Yale University, New Haven, Conn. He reported no conflicts of interest.
A version of this article first appeared on Medscape.com.
Welcome to Impact Factor, your weekly dose of commentary on a new medical study. I’m Dr. F. Perry Wilson of the Yale School of Medicine.
We are coming to the end of the year, which always makes me think about getting older. Much like the search for the fountain of youth, many promising leads have ultimately led to dead ends. And yet, I had high hopes for a trial that focused on two cornerstones of wellness – exercise and mindfulness – to address the subjective loss of memory that comes with aging. Alas, meditation and exercise do not appear to be the fountain of youth.
I’m talking about this study, appearing in JAMA, known as the MEDEX trial.
It’s a clever design: a 2 x 2 factorial randomized trial where participants could be randomized to a mindfulness intervention, an exercise intervention, both, or neither.
In this manner, you can test multiple hypotheses exploiting a shared control group. Or as a mentor of mine used to say, you get two trials for the price of one and a half.
The participants were older adults, aged 65-84, living in the community. They had to be relatively sedentary at baseline and not engaging in mindfulness practices. They had to subjectively report some memory or concentration issues but had to be cognitively intact, based on a standard dementia screening test. In other words, these are your average older people who are worried that they aren’t as sharp as they used to be.
The interventions themselves were fairly intense. The exercise group had instructor-led sessions for 90 minutes twice a week for the first 6 months of the study, once a week thereafter. And participants were encouraged to exercise at home such that they had a total of 300 minutes of weekly exercise.
The mindfulness program was characterized by eight weekly classes of 2.5 hours each as well as a half-day retreat to teach the tenets of mindfulness and meditation, with monthly refreshers thereafter. Participants were instructed to meditate for 60 minutes a day in addition to the classes.
For the 144 people who were randomized to both meditation and exercise, this trial amounted to something of a part-time job. So you might think that adherence to the interventions was low, but apparently that’s not the case. Attendance to the mindfulness classes was over 90%, and over 80% for the exercise classes. And diary-based reporting of home efforts was also pretty good.
The control group wasn’t left to their own devices. Recognizing that the community aspect of exercise or mindfulness classes might convey a benefit independent of the actual exercise or mindfulness, the control group met on a similar schedule to discuss health education, but no mention of exercise or mindfulness occurred in that setting.
The primary outcome was change in memory and executive function scores across a battery of neuropsychologic testing, but the story is told in just a few pictures.
Memory scores improved in all three groups – mindfulness, exercise, and health education – over time. Cognitive composite score improved in all three groups similarly. There was no synergistic effect of mindfulness and exercise either. Basically, everyone got a bit better.
But the study did way more than look at scores on tests. Researchers used MRI to measure brain anatomic outcomes as well. And the surprising thing is that virtually none of these outcomes were different between the groups either.
Hippocampal volume decreased a bit in all the groups. Dorsolateral prefrontal cortex volume was flat. There was no change in scores measuring tasks of daily living.
When you see negative results like this, right away you worry that the intervention wasn’t properly delivered. Were these people really exercising and meditating? Well, the authors showed that individuals randomized to exercise, at least, had less sleep latency, greater aerobic fitness, and greater strength. So we know something was happening.
They then asked, would the people in the exercise group with the greatest changes in those physiologic parameters show some improvement in cognitive parameters? In other words, we know you were exercising because you got stronger and are sleeping better; is your memory better? The answer? Surprisingly, still no. Even in that honestly somewhat cherry-picked group, the interventions had no effect.
Could it be that the control was inappropriate, that the “health education” intervention was actually so helpful that it obscured the benefits of exercise and meditation? After all, cognitive scores did improve in all groups. The authors doubt it. They say they think the improvement in cognitive scores reflects the fact that patients had learned a bit about how to take the tests. This is pretty common in the neuropsychiatric literature.
So here we are and I just want to say, well, shoot. This is not the result I wanted. And I think the reason I’m so disappointed is because aging and the loss of cognitive faculties that comes with aging are just sort of scary. We are all looking for some control over that fear, and how nice it would be to be able to tell ourselves not to worry – that we won’t have those problems as we get older because we exercise, or meditate, or drink red wine, or don’t drink wine, or whatever. And while I have no doubt that staying healthier physically will keep you healthier mentally, it may take more than one simple thing to move the needle.
Dr. Wilson is associate professor, department of medicine, and director of the Clinical and Translational Research Accelerator at Yale University, New Haven, Conn. He reported no conflicts of interest.
A version of this article first appeared on Medscape.com.
How a cheap liver drug may be the key to preventing COVID
Welcome to Impact Factor, your weekly dose of commentary on a new medical study. I’m Dr F. Perry Wilson of the Yale School of Medicine.
As soon as the pandemic started, the search was on for a medication that could stave off infection, or at least the worst consequences of infection.
One that would be cheap to make, safe, easy to distribute, and, ideally, was already available. The search had a quest-like quality, like something from a fairy tale. Society, poisoned by COVID, would find the antidote out there, somewhere, if we looked hard enough.
You know the story. There were some pretty dramatic failures: hydroxychloroquine, ivermectin. There were some successes, like dexamethasone.
I’m not here today to tell you that the antidote has been found – no, it takes large randomized trials to figure that out. But
How do you make a case that an existing drug – UDCA, in this case – might be useful to prevent or treat COVID? In contrast to prior basic-science studies, like the original ivermectin study, which essentially took a bunch of cells and virus in a tube filled with varying concentrations of the antiparasitic agent, the authors of this paper appearing in Nature give us multiple, complementary lines of evidence. Let me walk you through it.
All good science starts with a biologically plausible hypothesis. In this case, the authors recognized that SARS-CoV-2, in all its variants, requires the presence of the ACE2 receptor on the surface of cells to bind.
That is the doorway to infection. Vaccines and antibodies block the key to this door, the spike protein and its receptor binding domain. But what if you could get rid of the doors altogether?
The authors first showed that ACE2 expression is controlled by a certain transcription factor known as the farnesoid X receptor, or FXR. Reducing the binding of FXR should therefore reduce ACE2 expression.
As luck would have it, UDCA – Actigall – reduces the levels of FXR and thus the expression of ACE2 in cells.
Okay. So we have a drug that can reduce ACE2, and we know that ACE2 is necessary for the virus to infect cells. Would UDCA prevent viral infection?
They started with test tubes, showing that cells were less likely to be infected by SARS-CoV-2 in the presence of UDCA at concentrations similar to what humans achieve in their blood after standard dosing. The red staining here is spike protein; you can see that it is markedly lower in the cells exposed to UDCA.
So far, so good. But test tubes aren’t people. So they moved up to mice and Syrian golden hamsters. These cute fellows are quite susceptible to human COVID and have been a model organism in countless studies
Mice and hamsters treated with UDCA in the presence of littermates with COVID infections were less likely to become infected themselves compared with mice not so treated. They also showed that mice and hamsters treated with UDCA had lower levels of ACE2 in their nasal passages.
Of course, mice aren’t humans either. So the researchers didn’t stop there.
To determine the effects of UDCA on human tissue, they utilized perfused human lungs that had been declined for transplantation. The lungs were perfused with a special fluid to keep them viable, and were mechanically ventilated. One lung was exposed to UDCA and the other served as a control. The authors were able to show that ACE2 levels went down in the exposed lung. And, importantly, when samples of tissue from both lungs were exposed to SARS-CoV-2, the lung tissue exposed to UDCA had lower levels of viral infection.
They didn’t stop there.
Eight human volunteers were recruited to take UDCA for 5 days. ACE2 levels in the nasal passages went down over the course of treatment. They confirmed those results from a proteomics dataset with several hundred people who had received UDCA for clinical reasons. Treated individuals had lower ACE2 levels.
Finally, they looked at the epidemiologic effect. They examined a dataset that contained information on over 1,000 patients with liver disease who had contracted COVID-19, 31 of whom had been receiving UDCA. Even after adjustment for baseline differences, those receiving UDCA were less likely to be hospitalized, require an ICU, or die.
Okay, we’ll stop there. Reading this study, all I could think was, Yes! This is how you generate evidence that you have a drug that might work – step by careful step.
But let’s be careful as well. Does this study show that taking Actigall will prevent COVID? Of course not. It doesn’t show that it will treat COVID either. But I bring it up because the rigor of this study stands in contrast to those that generated huge enthusiasm earlier in the pandemic only to let us down in randomized trials. If there has been a drug out there this whole time which will prevent or treat COVID, this is how we’ll find it. The next step? Test it in a randomized trial.
For Medscape, I’m Perry Wilson.
F. Perry Wilson, MD, MSCE, is an associate professor of medicine and director of Yale’s Clinical and Translational Research Accelerator. He disclosed no relevant financial relationships.
A version of this video transcript first appeared on Medscape.com.
Welcome to Impact Factor, your weekly dose of commentary on a new medical study. I’m Dr F. Perry Wilson of the Yale School of Medicine.
As soon as the pandemic started, the search was on for a medication that could stave off infection, or at least the worst consequences of infection.
One that would be cheap to make, safe, easy to distribute, and, ideally, was already available. The search had a quest-like quality, like something from a fairy tale. Society, poisoned by COVID, would find the antidote out there, somewhere, if we looked hard enough.
You know the story. There were some pretty dramatic failures: hydroxychloroquine, ivermectin. There were some successes, like dexamethasone.
I’m not here today to tell you that the antidote has been found – no, it takes large randomized trials to figure that out. But
How do you make a case that an existing drug – UDCA, in this case – might be useful to prevent or treat COVID? In contrast to prior basic-science studies, like the original ivermectin study, which essentially took a bunch of cells and virus in a tube filled with varying concentrations of the antiparasitic agent, the authors of this paper appearing in Nature give us multiple, complementary lines of evidence. Let me walk you through it.
All good science starts with a biologically plausible hypothesis. In this case, the authors recognized that SARS-CoV-2, in all its variants, requires the presence of the ACE2 receptor on the surface of cells to bind.
That is the doorway to infection. Vaccines and antibodies block the key to this door, the spike protein and its receptor binding domain. But what if you could get rid of the doors altogether?
The authors first showed that ACE2 expression is controlled by a certain transcription factor known as the farnesoid X receptor, or FXR. Reducing the binding of FXR should therefore reduce ACE2 expression.
As luck would have it, UDCA – Actigall – reduces the levels of FXR and thus the expression of ACE2 in cells.
Okay. So we have a drug that can reduce ACE2, and we know that ACE2 is necessary for the virus to infect cells. Would UDCA prevent viral infection?
They started with test tubes, showing that cells were less likely to be infected by SARS-CoV-2 in the presence of UDCA at concentrations similar to what humans achieve in their blood after standard dosing. The red staining here is spike protein; you can see that it is markedly lower in the cells exposed to UDCA.
So far, so good. But test tubes aren’t people. So they moved up to mice and Syrian golden hamsters. These cute fellows are quite susceptible to human COVID and have been a model organism in countless studies
Mice and hamsters treated with UDCA in the presence of littermates with COVID infections were less likely to become infected themselves compared with mice not so treated. They also showed that mice and hamsters treated with UDCA had lower levels of ACE2 in their nasal passages.
Of course, mice aren’t humans either. So the researchers didn’t stop there.
To determine the effects of UDCA on human tissue, they utilized perfused human lungs that had been declined for transplantation. The lungs were perfused with a special fluid to keep them viable, and were mechanically ventilated. One lung was exposed to UDCA and the other served as a control. The authors were able to show that ACE2 levels went down in the exposed lung. And, importantly, when samples of tissue from both lungs were exposed to SARS-CoV-2, the lung tissue exposed to UDCA had lower levels of viral infection.
They didn’t stop there.
Eight human volunteers were recruited to take UDCA for 5 days. ACE2 levels in the nasal passages went down over the course of treatment. They confirmed those results from a proteomics dataset with several hundred people who had received UDCA for clinical reasons. Treated individuals had lower ACE2 levels.
Finally, they looked at the epidemiologic effect. They examined a dataset that contained information on over 1,000 patients with liver disease who had contracted COVID-19, 31 of whom had been receiving UDCA. Even after adjustment for baseline differences, those receiving UDCA were less likely to be hospitalized, require an ICU, or die.
Okay, we’ll stop there. Reading this study, all I could think was, Yes! This is how you generate evidence that you have a drug that might work – step by careful step.
But let’s be careful as well. Does this study show that taking Actigall will prevent COVID? Of course not. It doesn’t show that it will treat COVID either. But I bring it up because the rigor of this study stands in contrast to those that generated huge enthusiasm earlier in the pandemic only to let us down in randomized trials. If there has been a drug out there this whole time which will prevent or treat COVID, this is how we’ll find it. The next step? Test it in a randomized trial.
For Medscape, I’m Perry Wilson.
F. Perry Wilson, MD, MSCE, is an associate professor of medicine and director of Yale’s Clinical and Translational Research Accelerator. He disclosed no relevant financial relationships.
A version of this video transcript first appeared on Medscape.com.
Welcome to Impact Factor, your weekly dose of commentary on a new medical study. I’m Dr F. Perry Wilson of the Yale School of Medicine.
As soon as the pandemic started, the search was on for a medication that could stave off infection, or at least the worst consequences of infection.
One that would be cheap to make, safe, easy to distribute, and, ideally, was already available. The search had a quest-like quality, like something from a fairy tale. Society, poisoned by COVID, would find the antidote out there, somewhere, if we looked hard enough.
You know the story. There were some pretty dramatic failures: hydroxychloroquine, ivermectin. There were some successes, like dexamethasone.
I’m not here today to tell you that the antidote has been found – no, it takes large randomized trials to figure that out. But
How do you make a case that an existing drug – UDCA, in this case – might be useful to prevent or treat COVID? In contrast to prior basic-science studies, like the original ivermectin study, which essentially took a bunch of cells and virus in a tube filled with varying concentrations of the antiparasitic agent, the authors of this paper appearing in Nature give us multiple, complementary lines of evidence. Let me walk you through it.
All good science starts with a biologically plausible hypothesis. In this case, the authors recognized that SARS-CoV-2, in all its variants, requires the presence of the ACE2 receptor on the surface of cells to bind.
That is the doorway to infection. Vaccines and antibodies block the key to this door, the spike protein and its receptor binding domain. But what if you could get rid of the doors altogether?
The authors first showed that ACE2 expression is controlled by a certain transcription factor known as the farnesoid X receptor, or FXR. Reducing the binding of FXR should therefore reduce ACE2 expression.
As luck would have it, UDCA – Actigall – reduces the levels of FXR and thus the expression of ACE2 in cells.
Okay. So we have a drug that can reduce ACE2, and we know that ACE2 is necessary for the virus to infect cells. Would UDCA prevent viral infection?
They started with test tubes, showing that cells were less likely to be infected by SARS-CoV-2 in the presence of UDCA at concentrations similar to what humans achieve in their blood after standard dosing. The red staining here is spike protein; you can see that it is markedly lower in the cells exposed to UDCA.
So far, so good. But test tubes aren’t people. So they moved up to mice and Syrian golden hamsters. These cute fellows are quite susceptible to human COVID and have been a model organism in countless studies
Mice and hamsters treated with UDCA in the presence of littermates with COVID infections were less likely to become infected themselves compared with mice not so treated. They also showed that mice and hamsters treated with UDCA had lower levels of ACE2 in their nasal passages.
Of course, mice aren’t humans either. So the researchers didn’t stop there.
To determine the effects of UDCA on human tissue, they utilized perfused human lungs that had been declined for transplantation. The lungs were perfused with a special fluid to keep them viable, and were mechanically ventilated. One lung was exposed to UDCA and the other served as a control. The authors were able to show that ACE2 levels went down in the exposed lung. And, importantly, when samples of tissue from both lungs were exposed to SARS-CoV-2, the lung tissue exposed to UDCA had lower levels of viral infection.
They didn’t stop there.
Eight human volunteers were recruited to take UDCA for 5 days. ACE2 levels in the nasal passages went down over the course of treatment. They confirmed those results from a proteomics dataset with several hundred people who had received UDCA for clinical reasons. Treated individuals had lower ACE2 levels.
Finally, they looked at the epidemiologic effect. They examined a dataset that contained information on over 1,000 patients with liver disease who had contracted COVID-19, 31 of whom had been receiving UDCA. Even after adjustment for baseline differences, those receiving UDCA were less likely to be hospitalized, require an ICU, or die.
Okay, we’ll stop there. Reading this study, all I could think was, Yes! This is how you generate evidence that you have a drug that might work – step by careful step.
But let’s be careful as well. Does this study show that taking Actigall will prevent COVID? Of course not. It doesn’t show that it will treat COVID either. But I bring it up because the rigor of this study stands in contrast to those that generated huge enthusiasm earlier in the pandemic only to let us down in randomized trials. If there has been a drug out there this whole time which will prevent or treat COVID, this is how we’ll find it. The next step? Test it in a randomized trial.
For Medscape, I’m Perry Wilson.
F. Perry Wilson, MD, MSCE, is an associate professor of medicine and director of Yale’s Clinical and Translational Research Accelerator. He disclosed no relevant financial relationships.
A version of this video transcript first appeared on Medscape.com.
The surprising failure of vitamin D in deficient kids
Welcome to Impact Factor, your weekly dose of commentary on a new medical study. I’m Dr F. Perry Wilson of the Yale School of Medicine.
My basic gripe is that you’ve got all these observational studies linking lower levels of vitamin D to everything from dementia to falls to cancer to COVID infection, and then you do a big randomized trial of supplementation and don’t see an effect.
And the explanation is that vitamin D is not necessarily the thing causing these bad outcomes; it’s a bystander – a canary in the coal mine. Your vitamin D level is a marker of your lifestyle; it’s higher in people who eat healthier foods, who exercise, and who spend more time out in the sun.
And yet ... if you were to ask me whether supplementing vitamin D in children with vitamin D deficiency would help them grow better and be healthier, I probably would have been on board for the idea.
And, it looks like, I would have been wrong.
Yes, it’s another negative randomized trial of vitamin D supplementation to add to the seemingly ever-growing body of literature suggesting that your money is better spent on a day at the park rather than buying D3 from your local GNC.
We are talking about this study, appearing in JAMA Pediatrics.
Briefly, 8,851 children from around Ulaanbaatar, Mongolia, were randomized to receive 14,000 international units of vitamin D3 or placebo every week for 3 years.
Before we get into the results of the study, I need to point out that this part of Mongolia has a high rate of vitamin D deficiency. Beyond that, a prior observational study by these authors had shown that lower vitamin D levels were linked to the risk of acquiring latent tuberculosis infection in this area. Other studies have linked vitamin D deficiency with poorer growth metrics in children. Given the global scourge that is TB (around 2 million deaths a year) and childhood malnutrition (around 10% of children around the world), vitamin D supplementation is incredibly attractive as a public health intervention. It is relatively low on side effects and, importantly, it is cheap – and thus scalable.
Back to the study. These kids had pretty poor vitamin D levels at baseline; 95% of them were deficient, based on the accepted standard of levels less than 20 ng/mL. Over 30% were severely deficient, with levels less than 10 ng/mL.
The initial purpose of this study was to see if supplementation would prevent TB, but that analysis, which was published a few months ago, was negative. Vitamin D levels went up dramatically in the intervention group – they were taking their pills – but there was no difference in the rate of latent TB infection, active TB, other respiratory infections, or even serum interferon gamma levels.
Nothing.
But to be fair, the TB seroconversion rate was lower than expected, potentially leading to an underpowered study.
Which brings us to the just-published analysis which moves away from infectious disease to something where vitamin D should have some stronger footing: growth.
Would the kids who were randomized to vitamin D, those same kids who got their vitamin D levels into the normal range over 3 years of supplementation, grow more or grow better than the kids who didn’t?
And, unfortunately, the answer is still no.
At the end of follow-up, height z scores were not different between the groups. BMI z scores were not different between the groups. Pubertal development was not different between the groups. This was true not only overall, but across various subgroups, including analyses of those kids who had vitamin D levels less than 10 ng/mL to start with.
So, what’s going on? There are two very broad possibilities we can endorse. First, there’s the idea that vitamin D supplementation simply doesn’t do much for health. This is supported, now, by a long string of large clinical trials that show no effect across a variety of disease states and predisease states. In other words, the observational data linking low vitamin D to bad outcomes is correlation, not causation.
Or we can take the tack of some vitamin D apologists and decide that this trial just got it wrong. Perhaps the dose wasn’t given correctly, or 3 years isn’t long enough to see a real difference, or the growth metrics were wrong, or vitamin D needs to be given alongside something else to really work and so on. This is fine; no study is perfect and there is always something to criticize, believe me. But we need to be careful not to fall into the baby-and-bathwater fallacy. Just because we think a study could have done something better, or differently, doesn’t mean we can ignore all the results. And as each new randomized trial of vitamin D supplementation comes out, it’s getting harder and harder to believe that these trialists keep getting their methods wrong. Maybe they are just testing something that doesn’t work.
What to do? Well, it should be obvious. If low vitamin D levels are linked to TB rates and poor growth but supplementation doesn’t fix the problem, then we have to fix what is upstream of the problem. We need to boost vitamin D levels not through supplements, but through nutrition, exercise, activity, and getting outside. That’s a randomized trial you can sign me up for any day.
Dr. Wilson is associate professor, department of medicine, Yale University, New Haven, Conn. He reported no relevant conflicts of interest.
A version of this video transcript first appeared on Medscape.com.
Welcome to Impact Factor, your weekly dose of commentary on a new medical study. I’m Dr F. Perry Wilson of the Yale School of Medicine.
My basic gripe is that you’ve got all these observational studies linking lower levels of vitamin D to everything from dementia to falls to cancer to COVID infection, and then you do a big randomized trial of supplementation and don’t see an effect.
And the explanation is that vitamin D is not necessarily the thing causing these bad outcomes; it’s a bystander – a canary in the coal mine. Your vitamin D level is a marker of your lifestyle; it’s higher in people who eat healthier foods, who exercise, and who spend more time out in the sun.
And yet ... if you were to ask me whether supplementing vitamin D in children with vitamin D deficiency would help them grow better and be healthier, I probably would have been on board for the idea.
And, it looks like, I would have been wrong.
Yes, it’s another negative randomized trial of vitamin D supplementation to add to the seemingly ever-growing body of literature suggesting that your money is better spent on a day at the park rather than buying D3 from your local GNC.
We are talking about this study, appearing in JAMA Pediatrics.
Briefly, 8,851 children from around Ulaanbaatar, Mongolia, were randomized to receive 14,000 international units of vitamin D3 or placebo every week for 3 years.
Before we get into the results of the study, I need to point out that this part of Mongolia has a high rate of vitamin D deficiency. Beyond that, a prior observational study by these authors had shown that lower vitamin D levels were linked to the risk of acquiring latent tuberculosis infection in this area. Other studies have linked vitamin D deficiency with poorer growth metrics in children. Given the global scourge that is TB (around 2 million deaths a year) and childhood malnutrition (around 10% of children around the world), vitamin D supplementation is incredibly attractive as a public health intervention. It is relatively low on side effects and, importantly, it is cheap – and thus scalable.
Back to the study. These kids had pretty poor vitamin D levels at baseline; 95% of them were deficient, based on the accepted standard of levels less than 20 ng/mL. Over 30% were severely deficient, with levels less than 10 ng/mL.
The initial purpose of this study was to see if supplementation would prevent TB, but that analysis, which was published a few months ago, was negative. Vitamin D levels went up dramatically in the intervention group – they were taking their pills – but there was no difference in the rate of latent TB infection, active TB, other respiratory infections, or even serum interferon gamma levels.
Nothing.
But to be fair, the TB seroconversion rate was lower than expected, potentially leading to an underpowered study.
Which brings us to the just-published analysis which moves away from infectious disease to something where vitamin D should have some stronger footing: growth.
Would the kids who were randomized to vitamin D, those same kids who got their vitamin D levels into the normal range over 3 years of supplementation, grow more or grow better than the kids who didn’t?
And, unfortunately, the answer is still no.
At the end of follow-up, height z scores were not different between the groups. BMI z scores were not different between the groups. Pubertal development was not different between the groups. This was true not only overall, but across various subgroups, including analyses of those kids who had vitamin D levels less than 10 ng/mL to start with.
So, what’s going on? There are two very broad possibilities we can endorse. First, there’s the idea that vitamin D supplementation simply doesn’t do much for health. This is supported, now, by a long string of large clinical trials that show no effect across a variety of disease states and predisease states. In other words, the observational data linking low vitamin D to bad outcomes is correlation, not causation.
Or we can take the tack of some vitamin D apologists and decide that this trial just got it wrong. Perhaps the dose wasn’t given correctly, or 3 years isn’t long enough to see a real difference, or the growth metrics were wrong, or vitamin D needs to be given alongside something else to really work and so on. This is fine; no study is perfect and there is always something to criticize, believe me. But we need to be careful not to fall into the baby-and-bathwater fallacy. Just because we think a study could have done something better, or differently, doesn’t mean we can ignore all the results. And as each new randomized trial of vitamin D supplementation comes out, it’s getting harder and harder to believe that these trialists keep getting their methods wrong. Maybe they are just testing something that doesn’t work.
What to do? Well, it should be obvious. If low vitamin D levels are linked to TB rates and poor growth but supplementation doesn’t fix the problem, then we have to fix what is upstream of the problem. We need to boost vitamin D levels not through supplements, but through nutrition, exercise, activity, and getting outside. That’s a randomized trial you can sign me up for any day.
Dr. Wilson is associate professor, department of medicine, Yale University, New Haven, Conn. He reported no relevant conflicts of interest.
A version of this video transcript first appeared on Medscape.com.
Welcome to Impact Factor, your weekly dose of commentary on a new medical study. I’m Dr F. Perry Wilson of the Yale School of Medicine.
My basic gripe is that you’ve got all these observational studies linking lower levels of vitamin D to everything from dementia to falls to cancer to COVID infection, and then you do a big randomized trial of supplementation and don’t see an effect.
And the explanation is that vitamin D is not necessarily the thing causing these bad outcomes; it’s a bystander – a canary in the coal mine. Your vitamin D level is a marker of your lifestyle; it’s higher in people who eat healthier foods, who exercise, and who spend more time out in the sun.
And yet ... if you were to ask me whether supplementing vitamin D in children with vitamin D deficiency would help them grow better and be healthier, I probably would have been on board for the idea.
And, it looks like, I would have been wrong.
Yes, it’s another negative randomized trial of vitamin D supplementation to add to the seemingly ever-growing body of literature suggesting that your money is better spent on a day at the park rather than buying D3 from your local GNC.
We are talking about this study, appearing in JAMA Pediatrics.
Briefly, 8,851 children from around Ulaanbaatar, Mongolia, were randomized to receive 14,000 international units of vitamin D3 or placebo every week for 3 years.
Before we get into the results of the study, I need to point out that this part of Mongolia has a high rate of vitamin D deficiency. Beyond that, a prior observational study by these authors had shown that lower vitamin D levels were linked to the risk of acquiring latent tuberculosis infection in this area. Other studies have linked vitamin D deficiency with poorer growth metrics in children. Given the global scourge that is TB (around 2 million deaths a year) and childhood malnutrition (around 10% of children around the world), vitamin D supplementation is incredibly attractive as a public health intervention. It is relatively low on side effects and, importantly, it is cheap – and thus scalable.
Back to the study. These kids had pretty poor vitamin D levels at baseline; 95% of them were deficient, based on the accepted standard of levels less than 20 ng/mL. Over 30% were severely deficient, with levels less than 10 ng/mL.
The initial purpose of this study was to see if supplementation would prevent TB, but that analysis, which was published a few months ago, was negative. Vitamin D levels went up dramatically in the intervention group – they were taking their pills – but there was no difference in the rate of latent TB infection, active TB, other respiratory infections, or even serum interferon gamma levels.
Nothing.
But to be fair, the TB seroconversion rate was lower than expected, potentially leading to an underpowered study.
Which brings us to the just-published analysis which moves away from infectious disease to something where vitamin D should have some stronger footing: growth.
Would the kids who were randomized to vitamin D, those same kids who got their vitamin D levels into the normal range over 3 years of supplementation, grow more or grow better than the kids who didn’t?
And, unfortunately, the answer is still no.
At the end of follow-up, height z scores were not different between the groups. BMI z scores were not different between the groups. Pubertal development was not different between the groups. This was true not only overall, but across various subgroups, including analyses of those kids who had vitamin D levels less than 10 ng/mL to start with.
So, what’s going on? There are two very broad possibilities we can endorse. First, there’s the idea that vitamin D supplementation simply doesn’t do much for health. This is supported, now, by a long string of large clinical trials that show no effect across a variety of disease states and predisease states. In other words, the observational data linking low vitamin D to bad outcomes is correlation, not causation.
Or we can take the tack of some vitamin D apologists and decide that this trial just got it wrong. Perhaps the dose wasn’t given correctly, or 3 years isn’t long enough to see a real difference, or the growth metrics were wrong, or vitamin D needs to be given alongside something else to really work and so on. This is fine; no study is perfect and there is always something to criticize, believe me. But we need to be careful not to fall into the baby-and-bathwater fallacy. Just because we think a study could have done something better, or differently, doesn’t mean we can ignore all the results. And as each new randomized trial of vitamin D supplementation comes out, it’s getting harder and harder to believe that these trialists keep getting their methods wrong. Maybe they are just testing something that doesn’t work.
What to do? Well, it should be obvious. If low vitamin D levels are linked to TB rates and poor growth but supplementation doesn’t fix the problem, then we have to fix what is upstream of the problem. We need to boost vitamin D levels not through supplements, but through nutrition, exercise, activity, and getting outside. That’s a randomized trial you can sign me up for any day.
Dr. Wilson is associate professor, department of medicine, Yale University, New Haven, Conn. He reported no relevant conflicts of interest.
A version of this video transcript first appeared on Medscape.com.
Love them or hate them, masks in schools work
This transcript has been edited for clarity.
Welcome to Impact Factor, your weekly dose of commentary on a new medical study. I’m Dr. F. Perry Wilson of the Yale School of Medicine.
On March 26, 2022, Hawaii became the last state in the United States to lift its indoor mask mandate. By the time the current school year started, there were essentially no public school mask mandates either.
Whether you viewed the mask as an emblem of stalwart defiance against a rampaging virus, or a scarlet letter emblematic of the overreaches of public policy, you probably aren’t seeing them much anymore.
And yet, the debate about masks still rages. Who was right, who was wrong? Who trusted science, and what does the science even say? If we brought our country into marriage counseling, would we be told it is time to move on? To look forward, not backward? To plan for our bright future together?
Perhaps. But this question isn’t really moot just because masks have largely disappeared in the United States. Variants may emerge that lead to more infection waves – and other pandemics may occur in the future. And so I think it is important to discuss a study that, with quite rigorous analysis, attempts to answer the following question: Did masking in schools lower students’ and teachers’ risk of COVID?
We are talking about this study, appearing in the New England Journal of Medicine. The short version goes like this.
Researchers had access to two important sources of data. One – an accounting of all the teachers and students (more than 300,000 of them) in 79 public, noncharter school districts in Eastern Massachusetts who tested positive for COVID every week. Two – the date that each of those school districts lifted their mask mandates or (in the case of two districts) didn’t.
Right away, I’m sure you’re thinking of potential issues. Districts that kept masks even when the statewide ban was lifted are likely quite a bit different from districts that dropped masks right away. You’re right, of course – hold on to that thought; we’ll get there.
But first – the big question – would districts that kept their masks on longer do better when it comes to the rate of COVID infection?
When everyone was masking, COVID case rates were pretty similar. Statewide mandates are lifted in late February – and most school districts remove their mandates within a few weeks – the black line are the two districts (Boston and Chelsea) where mask mandates remained in place.
Prior to the mask mandate lifting, you see very similar COVID rates in districts that would eventually remove the mandate and those that would not, with a bit of noise around the initial Omicron wave which saw just a huge amount of people get infected.
And then, after the mandate was lifted, separation. Districts that held on to masks longer had lower rates of COVID infection.
In all, over the 15-weeks of the study, there were roughly 12,000 extra cases of COVID in the mask-free school districts, which corresponds to about 35% of the total COVID burden during that time. And, yes, kids do well with COVID – on average. But 12,000 extra cases is enough to translate into a significant number of important clinical outcomes – think hospitalizations and post-COVID syndromes. And of course, maybe most importantly, missed school days. Positive kids were not allowed in class no matter what district they were in.
Okay – I promised we’d address confounders. This was not a cluster-randomized trial, where some school districts had their mandates removed based on the vicissitudes of a virtual coin flip, as much as many of us would have been interested to see that. The decision to remove masks was up to the various school boards – and they had a lot of pressure on them from many different directions. But all we need to worry about is whether any of those things that pressure a school board to keep masks on would ALSO lead to fewer COVID cases. That’s how confounders work, and how you can get false results in a study like this.
And yes – districts that kept the masks on longer were different than those who took them right off. But check out how they were different.
The districts that kept masks on longer had more low-income students. More Black and Latino students. More students per classroom. These are all risk factors that increase the risk of COVID infection. In other words, the confounding here goes in the opposite direction of the results. If anything, these factors should make you more certain that masking works.
The authors also adjusted for other factors – the community transmission of COVID-19, vaccination rates, school district sizes, and so on. No major change in the results.
One concern I addressed to Dr. Ellie Murray, the biostatistician on the study – could districts that removed masks simply have been testing more to compensate, leading to increased capturing of cases?
If anything, the schools that kept masks on were testing more than the schools that took them off – again that would tend to imply that the results are even stronger than what was reported.
Is this a perfect study? Of course not – it’s one study, it’s from one state. And the relatively large effects from keeping masks on for one or 2 weeks require us to really embrace the concept of exponential growth of infections, but, if COVID has taught us anything, it is that small changes in initial conditions can have pretty big effects.
My daughter, who goes to a public school here in Connecticut, unmasked, was home with COVID this past week. She’s fine. But you know what? She missed a week of school. I worked from home to be with her – though I didn’t test positive. And that is a real cost to both of us that I think we need to consider when we consider the value of masks. Yes, they’re annoying – but if they keep kids in school, might they be worth it? Perhaps not for now, as cases aren’t surging. But in the future, be it a particularly concerning variant, or a whole new pandemic, we should not discount the simple, cheap, and apparently beneficial act of wearing masks to decrease transmission.
Dr. Perry Wilson is an associate professor of medicine and director of the Clinical and Translational Research Accelerator at Yale University, New Haven, Conn. He disclosed no relevant conflicts of interest.
A version of this article first appeared on Medscape.com.
This transcript has been edited for clarity.
Welcome to Impact Factor, your weekly dose of commentary on a new medical study. I’m Dr. F. Perry Wilson of the Yale School of Medicine.
On March 26, 2022, Hawaii became the last state in the United States to lift its indoor mask mandate. By the time the current school year started, there were essentially no public school mask mandates either.
Whether you viewed the mask as an emblem of stalwart defiance against a rampaging virus, or a scarlet letter emblematic of the overreaches of public policy, you probably aren’t seeing them much anymore.
And yet, the debate about masks still rages. Who was right, who was wrong? Who trusted science, and what does the science even say? If we brought our country into marriage counseling, would we be told it is time to move on? To look forward, not backward? To plan for our bright future together?
Perhaps. But this question isn’t really moot just because masks have largely disappeared in the United States. Variants may emerge that lead to more infection waves – and other pandemics may occur in the future. And so I think it is important to discuss a study that, with quite rigorous analysis, attempts to answer the following question: Did masking in schools lower students’ and teachers’ risk of COVID?
We are talking about this study, appearing in the New England Journal of Medicine. The short version goes like this.
Researchers had access to two important sources of data. One – an accounting of all the teachers and students (more than 300,000 of them) in 79 public, noncharter school districts in Eastern Massachusetts who tested positive for COVID every week. Two – the date that each of those school districts lifted their mask mandates or (in the case of two districts) didn’t.
Right away, I’m sure you’re thinking of potential issues. Districts that kept masks even when the statewide ban was lifted are likely quite a bit different from districts that dropped masks right away. You’re right, of course – hold on to that thought; we’ll get there.
But first – the big question – would districts that kept their masks on longer do better when it comes to the rate of COVID infection?
When everyone was masking, COVID case rates were pretty similar. Statewide mandates are lifted in late February – and most school districts remove their mandates within a few weeks – the black line are the two districts (Boston and Chelsea) where mask mandates remained in place.
Prior to the mask mandate lifting, you see very similar COVID rates in districts that would eventually remove the mandate and those that would not, with a bit of noise around the initial Omicron wave which saw just a huge amount of people get infected.
And then, after the mandate was lifted, separation. Districts that held on to masks longer had lower rates of COVID infection.
In all, over the 15-weeks of the study, there were roughly 12,000 extra cases of COVID in the mask-free school districts, which corresponds to about 35% of the total COVID burden during that time. And, yes, kids do well with COVID – on average. But 12,000 extra cases is enough to translate into a significant number of important clinical outcomes – think hospitalizations and post-COVID syndromes. And of course, maybe most importantly, missed school days. Positive kids were not allowed in class no matter what district they were in.
Okay – I promised we’d address confounders. This was not a cluster-randomized trial, where some school districts had their mandates removed based on the vicissitudes of a virtual coin flip, as much as many of us would have been interested to see that. The decision to remove masks was up to the various school boards – and they had a lot of pressure on them from many different directions. But all we need to worry about is whether any of those things that pressure a school board to keep masks on would ALSO lead to fewer COVID cases. That’s how confounders work, and how you can get false results in a study like this.
And yes – districts that kept the masks on longer were different than those who took them right off. But check out how they were different.
The districts that kept masks on longer had more low-income students. More Black and Latino students. More students per classroom. These are all risk factors that increase the risk of COVID infection. In other words, the confounding here goes in the opposite direction of the results. If anything, these factors should make you more certain that masking works.
The authors also adjusted for other factors – the community transmission of COVID-19, vaccination rates, school district sizes, and so on. No major change in the results.
One concern I addressed to Dr. Ellie Murray, the biostatistician on the study – could districts that removed masks simply have been testing more to compensate, leading to increased capturing of cases?
If anything, the schools that kept masks on were testing more than the schools that took them off – again that would tend to imply that the results are even stronger than what was reported.
Is this a perfect study? Of course not – it’s one study, it’s from one state. And the relatively large effects from keeping masks on for one or 2 weeks require us to really embrace the concept of exponential growth of infections, but, if COVID has taught us anything, it is that small changes in initial conditions can have pretty big effects.
My daughter, who goes to a public school here in Connecticut, unmasked, was home with COVID this past week. She’s fine. But you know what? She missed a week of school. I worked from home to be with her – though I didn’t test positive. And that is a real cost to both of us that I think we need to consider when we consider the value of masks. Yes, they’re annoying – but if they keep kids in school, might they be worth it? Perhaps not for now, as cases aren’t surging. But in the future, be it a particularly concerning variant, or a whole new pandemic, we should not discount the simple, cheap, and apparently beneficial act of wearing masks to decrease transmission.
Dr. Perry Wilson is an associate professor of medicine and director of the Clinical and Translational Research Accelerator at Yale University, New Haven, Conn. He disclosed no relevant conflicts of interest.
A version of this article first appeared on Medscape.com.
This transcript has been edited for clarity.
Welcome to Impact Factor, your weekly dose of commentary on a new medical study. I’m Dr. F. Perry Wilson of the Yale School of Medicine.
On March 26, 2022, Hawaii became the last state in the United States to lift its indoor mask mandate. By the time the current school year started, there were essentially no public school mask mandates either.
Whether you viewed the mask as an emblem of stalwart defiance against a rampaging virus, or a scarlet letter emblematic of the overreaches of public policy, you probably aren’t seeing them much anymore.
And yet, the debate about masks still rages. Who was right, who was wrong? Who trusted science, and what does the science even say? If we brought our country into marriage counseling, would we be told it is time to move on? To look forward, not backward? To plan for our bright future together?
Perhaps. But this question isn’t really moot just because masks have largely disappeared in the United States. Variants may emerge that lead to more infection waves – and other pandemics may occur in the future. And so I think it is important to discuss a study that, with quite rigorous analysis, attempts to answer the following question: Did masking in schools lower students’ and teachers’ risk of COVID?
We are talking about this study, appearing in the New England Journal of Medicine. The short version goes like this.
Researchers had access to two important sources of data. One – an accounting of all the teachers and students (more than 300,000 of them) in 79 public, noncharter school districts in Eastern Massachusetts who tested positive for COVID every week. Two – the date that each of those school districts lifted their mask mandates or (in the case of two districts) didn’t.
Right away, I’m sure you’re thinking of potential issues. Districts that kept masks even when the statewide ban was lifted are likely quite a bit different from districts that dropped masks right away. You’re right, of course – hold on to that thought; we’ll get there.
But first – the big question – would districts that kept their masks on longer do better when it comes to the rate of COVID infection?
When everyone was masking, COVID case rates were pretty similar. Statewide mandates are lifted in late February – and most school districts remove their mandates within a few weeks – the black line are the two districts (Boston and Chelsea) where mask mandates remained in place.
Prior to the mask mandate lifting, you see very similar COVID rates in districts that would eventually remove the mandate and those that would not, with a bit of noise around the initial Omicron wave which saw just a huge amount of people get infected.
And then, after the mandate was lifted, separation. Districts that held on to masks longer had lower rates of COVID infection.
In all, over the 15-weeks of the study, there were roughly 12,000 extra cases of COVID in the mask-free school districts, which corresponds to about 35% of the total COVID burden during that time. And, yes, kids do well with COVID – on average. But 12,000 extra cases is enough to translate into a significant number of important clinical outcomes – think hospitalizations and post-COVID syndromes. And of course, maybe most importantly, missed school days. Positive kids were not allowed in class no matter what district they were in.
Okay – I promised we’d address confounders. This was not a cluster-randomized trial, where some school districts had their mandates removed based on the vicissitudes of a virtual coin flip, as much as many of us would have been interested to see that. The decision to remove masks was up to the various school boards – and they had a lot of pressure on them from many different directions. But all we need to worry about is whether any of those things that pressure a school board to keep masks on would ALSO lead to fewer COVID cases. That’s how confounders work, and how you can get false results in a study like this.
And yes – districts that kept the masks on longer were different than those who took them right off. But check out how they were different.
The districts that kept masks on longer had more low-income students. More Black and Latino students. More students per classroom. These are all risk factors that increase the risk of COVID infection. In other words, the confounding here goes in the opposite direction of the results. If anything, these factors should make you more certain that masking works.
The authors also adjusted for other factors – the community transmission of COVID-19, vaccination rates, school district sizes, and so on. No major change in the results.
One concern I addressed to Dr. Ellie Murray, the biostatistician on the study – could districts that removed masks simply have been testing more to compensate, leading to increased capturing of cases?
If anything, the schools that kept masks on were testing more than the schools that took them off – again that would tend to imply that the results are even stronger than what was reported.
Is this a perfect study? Of course not – it’s one study, it’s from one state. And the relatively large effects from keeping masks on for one or 2 weeks require us to really embrace the concept of exponential growth of infections, but, if COVID has taught us anything, it is that small changes in initial conditions can have pretty big effects.
My daughter, who goes to a public school here in Connecticut, unmasked, was home with COVID this past week. She’s fine. But you know what? She missed a week of school. I worked from home to be with her – though I didn’t test positive. And that is a real cost to both of us that I think we need to consider when we consider the value of masks. Yes, they’re annoying – but if they keep kids in school, might they be worth it? Perhaps not for now, as cases aren’t surging. But in the future, be it a particularly concerning variant, or a whole new pandemic, we should not discount the simple, cheap, and apparently beneficial act of wearing masks to decrease transmission.
Dr. Perry Wilson is an associate professor of medicine and director of the Clinical and Translational Research Accelerator at Yale University, New Haven, Conn. He disclosed no relevant conflicts of interest.
A version of this article first appeared on Medscape.com.
Ivermectin for COVID-19: Final nail in the coffin
Welcome to Impact Factor, your weekly dose of commentary on a new medical study. I’m Dr F. Perry Wilson of the Yale School of Medicine.
It began in a petri dish.
Ivermectin, a widely available, cheap, and well-tolerated drug on the WHO’s list of essential medicines for its critical role in treating river blindness, was shown to dramatically reduce the proliferation of SARS-CoV-2 virus in cell culture.
You know the rest of the story. Despite the fact that the median inhibitory concentration in cell culture is about 100-fold higher than what one can achieve with oral dosing in humans, anecdotal reports of miraculous cures proliferated.
Cohort studies suggested that people who got ivermectin did very well in terms of COVID outcomes.
A narrative started to develop online – one that is still quite present today – that authorities were suppressing the good news about ivermectin in order to line their own pockets and those of the execs at Big Pharma. The official Twitter account of the Food and Drug Administration clapped back, reminding the populace that we are not horses or cows.
And every time a study came out that seemed like the nail in the coffin for the so-called horse paste, it rose again, vampire-like, feasting on the blood of social media outrage.
The truth is that, while excitement for ivermectin mounted online, it crashed quite quickly in scientific circles. Most randomized trials showed no effect of the drug. A couple of larger trials which seemed to show dramatic effects were subsequently shown to be fraudulent.
Then the TOGETHER trial was published. The 1,400-patient study from Brazil, which treated outpatients with COVID-19, found no significant difference in hospitalization or ER visits – the primary outcome – between those randomized to ivermectin vs. placebo or another therapy.
But still, Brazil. Different population than the United States. Different health systems. And very different rates of Strongyloides infections (this is a parasite that may be incidentally treated by ivermectin, leading to improvement independent of the drug’s effect on COVID). We all wanted a U.S. trial.
And now we have it. ACTIV-6 was published Oct. 21 in JAMA, a study randomizing outpatients with COVID-19 from 93 sites around the United States to ivermectin or placebo.
A total of 1,591 individuals – median age 47, 60% female – with confirmed symptomatic COVID-19 were randomized from June 2021 to February 2022. About half had been vaccinated.
The primary outcome was straightforward: time to clinical recovery. The time to recovery, defined as having three symptom-free days, was 12 days in the ivermectin group and 13 days in the placebo group – that’s within the margin of error.
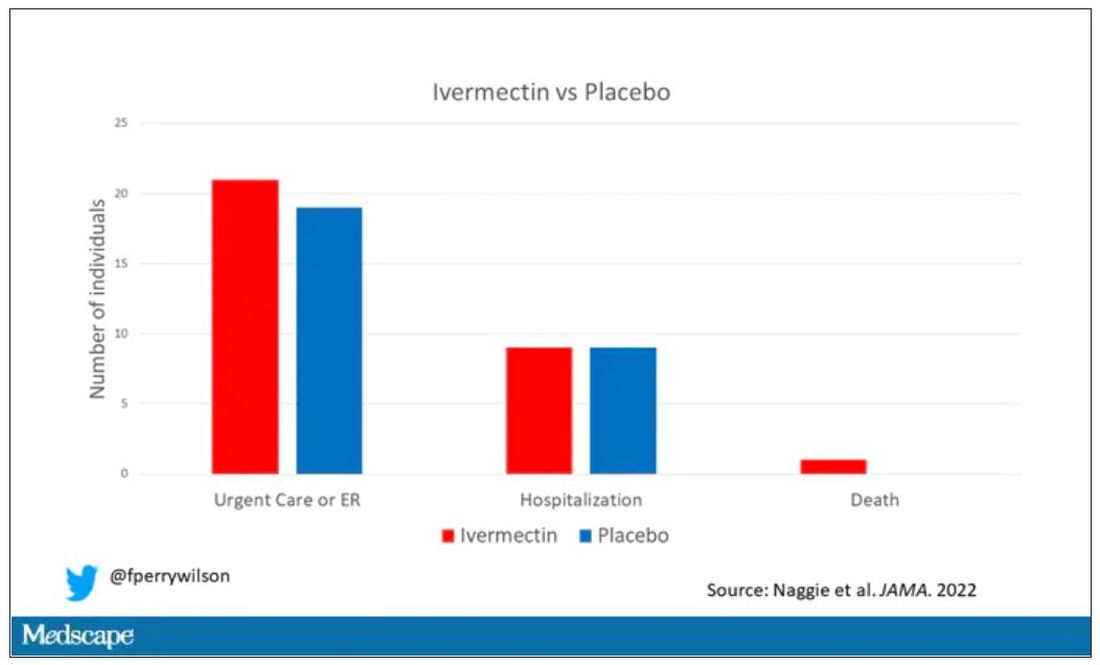
But overall, everyone in the trial did fairly well. Serious outcomes, like death, hospitalization, urgent care, or ER visits, occurred in 32 people in the ivermectin group and 28 in the placebo group. Death itself was rare – just one occurred in the trial, in someone receiving ivermectin.OK, are we done with this drug yet? Is this nice U.S. randomized trial enough to convince people that results from a petri dish don’t always transfer to humans, regardless of the presence or absence of an evil pharmaceutical cabal?
No, of course not. At this point, I can predict the responses. The dose wasn’t high enough. It wasn’t given early enough. The patients weren’t sick enough, or they were too sick. This is motivated reasoning, plain and simple. It’s not to say that there isn’t a chance that this drug has some off-target effects on COVID that we haven’t adequately measured, but studies like ACTIV-6 effectively rule out the idea that it’s a miracle cure. And you know what? That’s OK. Miracle cures are vanishingly rare. Most things that work in medicine work OK; they make us a little better, and we learn why they do that and improve on them, and try again and again. It’s not flashy; it doesn’t have that allure of secret knowledge. But it’s what separates science from magic.
F. Perry Wilson, MD, MSCE, is an associate professor of medicine and director of Yale’s Clinical and Translational Research Accelerator; his science communication work can be found in the Huffington Post, on NPR, and on Medscape.
A version of this article first appeared on Medscape.com.
Welcome to Impact Factor, your weekly dose of commentary on a new medical study. I’m Dr F. Perry Wilson of the Yale School of Medicine.
It began in a petri dish.
Ivermectin, a widely available, cheap, and well-tolerated drug on the WHO’s list of essential medicines for its critical role in treating river blindness, was shown to dramatically reduce the proliferation of SARS-CoV-2 virus in cell culture.
You know the rest of the story. Despite the fact that the median inhibitory concentration in cell culture is about 100-fold higher than what one can achieve with oral dosing in humans, anecdotal reports of miraculous cures proliferated.
Cohort studies suggested that people who got ivermectin did very well in terms of COVID outcomes.
A narrative started to develop online – one that is still quite present today – that authorities were suppressing the good news about ivermectin in order to line their own pockets and those of the execs at Big Pharma. The official Twitter account of the Food and Drug Administration clapped back, reminding the populace that we are not horses or cows.
And every time a study came out that seemed like the nail in the coffin for the so-called horse paste, it rose again, vampire-like, feasting on the blood of social media outrage.
The truth is that, while excitement for ivermectin mounted online, it crashed quite quickly in scientific circles. Most randomized trials showed no effect of the drug. A couple of larger trials which seemed to show dramatic effects were subsequently shown to be fraudulent.
Then the TOGETHER trial was published. The 1,400-patient study from Brazil, which treated outpatients with COVID-19, found no significant difference in hospitalization or ER visits – the primary outcome – between those randomized to ivermectin vs. placebo or another therapy.
But still, Brazil. Different population than the United States. Different health systems. And very different rates of Strongyloides infections (this is a parasite that may be incidentally treated by ivermectin, leading to improvement independent of the drug’s effect on COVID). We all wanted a U.S. trial.
And now we have it. ACTIV-6 was published Oct. 21 in JAMA, a study randomizing outpatients with COVID-19 from 93 sites around the United States to ivermectin or placebo.
A total of 1,591 individuals – median age 47, 60% female – with confirmed symptomatic COVID-19 were randomized from June 2021 to February 2022. About half had been vaccinated.
The primary outcome was straightforward: time to clinical recovery. The time to recovery, defined as having three symptom-free days, was 12 days in the ivermectin group and 13 days in the placebo group – that’s within the margin of error.
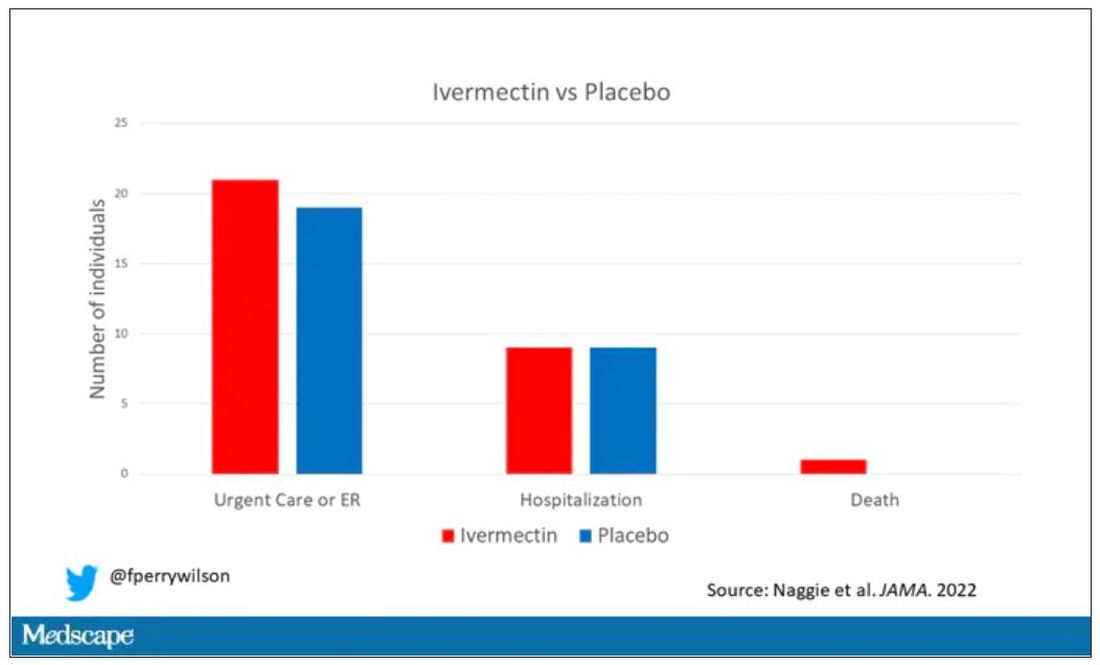
But overall, everyone in the trial did fairly well. Serious outcomes, like death, hospitalization, urgent care, or ER visits, occurred in 32 people in the ivermectin group and 28 in the placebo group. Death itself was rare – just one occurred in the trial, in someone receiving ivermectin.OK, are we done with this drug yet? Is this nice U.S. randomized trial enough to convince people that results from a petri dish don’t always transfer to humans, regardless of the presence or absence of an evil pharmaceutical cabal?
No, of course not. At this point, I can predict the responses. The dose wasn’t high enough. It wasn’t given early enough. The patients weren’t sick enough, or they were too sick. This is motivated reasoning, plain and simple. It’s not to say that there isn’t a chance that this drug has some off-target effects on COVID that we haven’t adequately measured, but studies like ACTIV-6 effectively rule out the idea that it’s a miracle cure. And you know what? That’s OK. Miracle cures are vanishingly rare. Most things that work in medicine work OK; they make us a little better, and we learn why they do that and improve on them, and try again and again. It’s not flashy; it doesn’t have that allure of secret knowledge. But it’s what separates science from magic.
F. Perry Wilson, MD, MSCE, is an associate professor of medicine and director of Yale’s Clinical and Translational Research Accelerator; his science communication work can be found in the Huffington Post, on NPR, and on Medscape.
A version of this article first appeared on Medscape.com.
Welcome to Impact Factor, your weekly dose of commentary on a new medical study. I’m Dr F. Perry Wilson of the Yale School of Medicine.
It began in a petri dish.
Ivermectin, a widely available, cheap, and well-tolerated drug on the WHO’s list of essential medicines for its critical role in treating river blindness, was shown to dramatically reduce the proliferation of SARS-CoV-2 virus in cell culture.
You know the rest of the story. Despite the fact that the median inhibitory concentration in cell culture is about 100-fold higher than what one can achieve with oral dosing in humans, anecdotal reports of miraculous cures proliferated.
Cohort studies suggested that people who got ivermectin did very well in terms of COVID outcomes.
A narrative started to develop online – one that is still quite present today – that authorities were suppressing the good news about ivermectin in order to line their own pockets and those of the execs at Big Pharma. The official Twitter account of the Food and Drug Administration clapped back, reminding the populace that we are not horses or cows.
And every time a study came out that seemed like the nail in the coffin for the so-called horse paste, it rose again, vampire-like, feasting on the blood of social media outrage.
The truth is that, while excitement for ivermectin mounted online, it crashed quite quickly in scientific circles. Most randomized trials showed no effect of the drug. A couple of larger trials which seemed to show dramatic effects were subsequently shown to be fraudulent.
Then the TOGETHER trial was published. The 1,400-patient study from Brazil, which treated outpatients with COVID-19, found no significant difference in hospitalization or ER visits – the primary outcome – between those randomized to ivermectin vs. placebo or another therapy.
But still, Brazil. Different population than the United States. Different health systems. And very different rates of Strongyloides infections (this is a parasite that may be incidentally treated by ivermectin, leading to improvement independent of the drug’s effect on COVID). We all wanted a U.S. trial.
And now we have it. ACTIV-6 was published Oct. 21 in JAMA, a study randomizing outpatients with COVID-19 from 93 sites around the United States to ivermectin or placebo.
A total of 1,591 individuals – median age 47, 60% female – with confirmed symptomatic COVID-19 were randomized from June 2021 to February 2022. About half had been vaccinated.
The primary outcome was straightforward: time to clinical recovery. The time to recovery, defined as having three symptom-free days, was 12 days in the ivermectin group and 13 days in the placebo group – that’s within the margin of error.
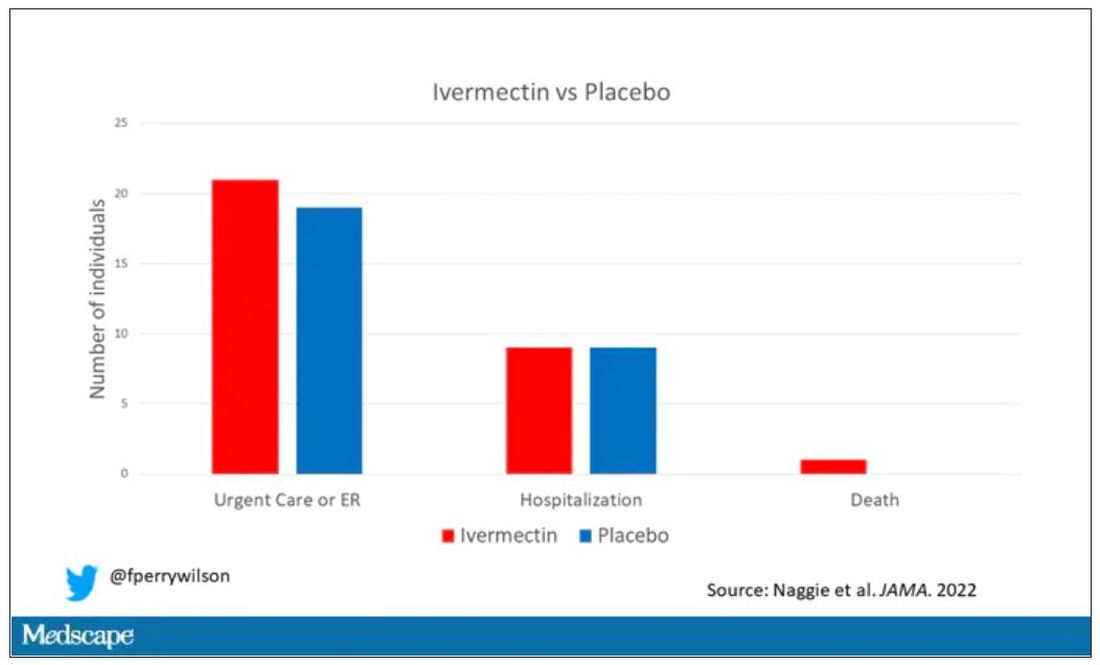
But overall, everyone in the trial did fairly well. Serious outcomes, like death, hospitalization, urgent care, or ER visits, occurred in 32 people in the ivermectin group and 28 in the placebo group. Death itself was rare – just one occurred in the trial, in someone receiving ivermectin.OK, are we done with this drug yet? Is this nice U.S. randomized trial enough to convince people that results from a petri dish don’t always transfer to humans, regardless of the presence or absence of an evil pharmaceutical cabal?
No, of course not. At this point, I can predict the responses. The dose wasn’t high enough. It wasn’t given early enough. The patients weren’t sick enough, or they were too sick. This is motivated reasoning, plain and simple. It’s not to say that there isn’t a chance that this drug has some off-target effects on COVID that we haven’t adequately measured, but studies like ACTIV-6 effectively rule out the idea that it’s a miracle cure. And you know what? That’s OK. Miracle cures are vanishingly rare. Most things that work in medicine work OK; they make us a little better, and we learn why they do that and improve on them, and try again and again. It’s not flashy; it doesn’t have that allure of secret knowledge. But it’s what separates science from magic.
F. Perry Wilson, MD, MSCE, is an associate professor of medicine and director of Yale’s Clinical and Translational Research Accelerator; his science communication work can be found in the Huffington Post, on NPR, and on Medscape.
A version of this article first appeared on Medscape.com.
Why the 5-day isolation period for COVID makes no sense
Welcome to Impact Factor, your weekly dose of commentary on a new medical study. I’m Dr. F. Perry Wilson of the Yale School of Medicine.
One of the more baffling decisions the CDC made during this pandemic was when they reduced the duration of isolation after a positive COVID test from 10 days to 5 days and did not require a negative antigen test to end isolation.
Multiple studies had suggested, after all, that positive antigen tests, while not perfect, were a decent proxy for infectivity. And if the purpose of isolation is to keep other community members safe, why not use a readily available test to know when it might be safe to go out in public again?
Also, 5 days just wasn’t that much time. Many individuals are symptomatic long after that point. Many people test positive long after that point. What exactly is the point of the 5-day isolation period?
We got some hard numbers this week to show just how good (or bad) an arbitrary-seeming 5-day isolation period is, thanks to this study from JAMA Network Open, which gives us a low-end estimate for the proportion of people who remain positive on antigen tests, which is to say infectious, after an isolation period.
This study estimates the low end of postisolation infectivity because of the study population: student athletes at an NCAA Division I school, which may or may not be Stanford. These athletes tested positive for COVID after having at least one dose of vaccine from January to May 2022. School protocol was to put the students in isolation for 7 days, at which time they could “test out” with a negative antigen test.
Put simply, these were healthy people. They were young. They were athletes. They were vaccinated. If anyone is going to have a brief, easy COVID course, it would be them. And they are doing at least a week of isolation, not 5 days.
So – isolation for 7 days. Antigen testing on day 7. How many still tested positive? Of 248 individuals tested, 67 (27%) tested positive. One in four.
More than half of those positive on day 7 tested positive on day 8, and more than half of those tested positive again on day 9. By day 10, they were released from isolation without further testing.
So, right there .
There were some predictors of prolonged positivity.
Symptomatic athletes were much more likely to test positive than asymptomatic athletes.
And the particular variant seemed to matter as well. In this time period, BA.1 and BA.2 were dominant, and it was pretty clear that BA.2 persisted longer than BA.1.
This brings me back to my original question: What is the point of the 5-day isolation period? On the basis of this study, you could imagine a guideline based on symptoms: Stay home until you feel better. You could imagine a guideline based on testing: Stay home until you test negative. A guideline based on time alone just doesn’t comport with the data. The benefit of policies based on symptoms or testing are obvious; some people would be out of isolation even before 5 days. But the downside, of course, is that some people would be stuck in isolation for much longer.
Maybe we should just say it. At this point, you could even imagine there being no recommendation at all – no isolation period. Like, you just stay home if you feel like you should stay home. I’m not entirely sure that such a policy would necessarily result in a greater number of infectious people out in the community.
In any case, as the arbitrariness of this particular 5-day isolation policy becomes more clear, the policy itself may be living on borrowed time.
F. Perry Wilson, MD, MSCE, is an associate professor of medicine and director of Yale’s Clinical and Translational Research Accelerator. His science communication work can be found in the Huffington Post, on NPR, and on Medscape. He tweets @fperrywilson and hosts a repository of his communication work at www.methodsman.com. He disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Welcome to Impact Factor, your weekly dose of commentary on a new medical study. I’m Dr. F. Perry Wilson of the Yale School of Medicine.
One of the more baffling decisions the CDC made during this pandemic was when they reduced the duration of isolation after a positive COVID test from 10 days to 5 days and did not require a negative antigen test to end isolation.
Multiple studies had suggested, after all, that positive antigen tests, while not perfect, were a decent proxy for infectivity. And if the purpose of isolation is to keep other community members safe, why not use a readily available test to know when it might be safe to go out in public again?
Also, 5 days just wasn’t that much time. Many individuals are symptomatic long after that point. Many people test positive long after that point. What exactly is the point of the 5-day isolation period?
We got some hard numbers this week to show just how good (or bad) an arbitrary-seeming 5-day isolation period is, thanks to this study from JAMA Network Open, which gives us a low-end estimate for the proportion of people who remain positive on antigen tests, which is to say infectious, after an isolation period.
This study estimates the low end of postisolation infectivity because of the study population: student athletes at an NCAA Division I school, which may or may not be Stanford. These athletes tested positive for COVID after having at least one dose of vaccine from January to May 2022. School protocol was to put the students in isolation for 7 days, at which time they could “test out” with a negative antigen test.
Put simply, these were healthy people. They were young. They were athletes. They were vaccinated. If anyone is going to have a brief, easy COVID course, it would be them. And they are doing at least a week of isolation, not 5 days.
So – isolation for 7 days. Antigen testing on day 7. How many still tested positive? Of 248 individuals tested, 67 (27%) tested positive. One in four.
More than half of those positive on day 7 tested positive on day 8, and more than half of those tested positive again on day 9. By day 10, they were released from isolation without further testing.
So, right there .
There were some predictors of prolonged positivity.
Symptomatic athletes were much more likely to test positive than asymptomatic athletes.
And the particular variant seemed to matter as well. In this time period, BA.1 and BA.2 were dominant, and it was pretty clear that BA.2 persisted longer than BA.1.
This brings me back to my original question: What is the point of the 5-day isolation period? On the basis of this study, you could imagine a guideline based on symptoms: Stay home until you feel better. You could imagine a guideline based on testing: Stay home until you test negative. A guideline based on time alone just doesn’t comport with the data. The benefit of policies based on symptoms or testing are obvious; some people would be out of isolation even before 5 days. But the downside, of course, is that some people would be stuck in isolation for much longer.
Maybe we should just say it. At this point, you could even imagine there being no recommendation at all – no isolation period. Like, you just stay home if you feel like you should stay home. I’m not entirely sure that such a policy would necessarily result in a greater number of infectious people out in the community.
In any case, as the arbitrariness of this particular 5-day isolation policy becomes more clear, the policy itself may be living on borrowed time.
F. Perry Wilson, MD, MSCE, is an associate professor of medicine and director of Yale’s Clinical and Translational Research Accelerator. His science communication work can be found in the Huffington Post, on NPR, and on Medscape. He tweets @fperrywilson and hosts a repository of his communication work at www.methodsman.com. He disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Welcome to Impact Factor, your weekly dose of commentary on a new medical study. I’m Dr. F. Perry Wilson of the Yale School of Medicine.
One of the more baffling decisions the CDC made during this pandemic was when they reduced the duration of isolation after a positive COVID test from 10 days to 5 days and did not require a negative antigen test to end isolation.
Multiple studies had suggested, after all, that positive antigen tests, while not perfect, were a decent proxy for infectivity. And if the purpose of isolation is to keep other community members safe, why not use a readily available test to know when it might be safe to go out in public again?
Also, 5 days just wasn’t that much time. Many individuals are symptomatic long after that point. Many people test positive long after that point. What exactly is the point of the 5-day isolation period?
We got some hard numbers this week to show just how good (or bad) an arbitrary-seeming 5-day isolation period is, thanks to this study from JAMA Network Open, which gives us a low-end estimate for the proportion of people who remain positive on antigen tests, which is to say infectious, after an isolation period.
This study estimates the low end of postisolation infectivity because of the study population: student athletes at an NCAA Division I school, which may or may not be Stanford. These athletes tested positive for COVID after having at least one dose of vaccine from January to May 2022. School protocol was to put the students in isolation for 7 days, at which time they could “test out” with a negative antigen test.
Put simply, these were healthy people. They were young. They were athletes. They were vaccinated. If anyone is going to have a brief, easy COVID course, it would be them. And they are doing at least a week of isolation, not 5 days.
So – isolation for 7 days. Antigen testing on day 7. How many still tested positive? Of 248 individuals tested, 67 (27%) tested positive. One in four.
More than half of those positive on day 7 tested positive on day 8, and more than half of those tested positive again on day 9. By day 10, they were released from isolation without further testing.
So, right there .
There were some predictors of prolonged positivity.
Symptomatic athletes were much more likely to test positive than asymptomatic athletes.
And the particular variant seemed to matter as well. In this time period, BA.1 and BA.2 were dominant, and it was pretty clear that BA.2 persisted longer than BA.1.
This brings me back to my original question: What is the point of the 5-day isolation period? On the basis of this study, you could imagine a guideline based on symptoms: Stay home until you feel better. You could imagine a guideline based on testing: Stay home until you test negative. A guideline based on time alone just doesn’t comport with the data. The benefit of policies based on symptoms or testing are obvious; some people would be out of isolation even before 5 days. But the downside, of course, is that some people would be stuck in isolation for much longer.
Maybe we should just say it. At this point, you could even imagine there being no recommendation at all – no isolation period. Like, you just stay home if you feel like you should stay home. I’m not entirely sure that such a policy would necessarily result in a greater number of infectious people out in the community.
In any case, as the arbitrariness of this particular 5-day isolation policy becomes more clear, the policy itself may be living on borrowed time.
F. Perry Wilson, MD, MSCE, is an associate professor of medicine and director of Yale’s Clinical and Translational Research Accelerator. His science communication work can be found in the Huffington Post, on NPR, and on Medscape. He tweets @fperrywilson and hosts a repository of his communication work at www.methodsman.com. He disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Why people lie about COVID
This transcript has been edited for clarity.
Welcome to Impact Factor, your weekly dose of commentary on a new medical study. I’m Dr. F. Perry Wilson of the Yale School of Medicine.
Have you ever lied about COVID-19?
Before you get upset, before the “how dare you,” I want you to think carefully.
Did you have COVID-19 (or think you did) and not mention it to someone you were going to be with? Did you tell someone you were taking more COVID precautions than you really were? Did you tell someone you were vaccinated when you weren’t? Have you avoided getting a COVID test even though you knew you should have?
Researchers appreciated the fact that public health interventions in COVID are important but are only as good as the percentage of people who actually abide by them. So, they designed a survey to ask the questions that many people don’t want to hear the answer to.
A total of 1,733 participants – 80% of those invited – responded to the survey. By design, approximately one-third of respondents (477) had already had COVID, one-third (499) were vaccinated and not yet infected, and one-third (509) were unvaccinated and not yet infected.
Of those surveyed, 41.6% admitted that they lied about COVID or didn’t adhere to COVID guidelines - a conservative estimate, if you ask me.
Breaking down some of the results, about 20% of people who previously were infected with COVID said they didn’t mention it when meeting with someone. A similar number said they didn’t tell anyone when they were entering a public place. A bit more concerning to me, roughly 20% reported not disclosing their COVID-positive status when going to a health care provider’s office.
About 10% of those who had not been vaccinated reported lying about their vaccination status. That’s actually less than the 15% of vaccinated people who lied and told someone they weren’t vaccinated.
About 17% of people lied about the need to quarantine, and many more broke quarantine rules.
The authors tried to see if certain personal characteristics predicted people who were more likely to lie about COVID-19–related issues. Turns out there was only one thing that predicted honesty: age.
Older people were more honest about their COVID status and COVID habits. Other factors – gender, education, race, political affiliation, COVID-19 conspiracy beliefs, and where you got your COVID information – did not seem to make much of a difference. Why are older people more honest? Because older people take COVID more seriously. And they should; COVID is more severe in older people.
The problem arises, of course, because people who are at lower risk for COVID complications interact with people at higher risk – and in those situations, honesty matters more.
On the other hand, isn’t lying about COVID stuff inevitable? If you know that a positive test means you can’t go to work, and not going to work means you won’t get paid, might you not be more likely to lie about the test? Or not get the test at all?
The authors explored the reasons for dishonesty and they are fairly broad, ranging from the desire for life to feel normal (more than half of people who lied) to not believing that COVID was real (a whopping 30%). Some of the reasons for lying included:
- Wanted life to feel normal (50%).
- Freedom (45%).
- It’s no one’s business (40%).
- COVID isn’t real (30%).
In the end, though, we need to realize that public health recommendations are not going to be universally followed, and people may tell us they are following them when, in fact, they are not.
What this adds is another data point to a trend we’ve seen across the course of the pandemic, a shift from collective to individual responsibility. If you can’t be sure what others are doing in regard to COVID, you need to focus on protecting yourself. Perhaps that shift was inevitable. Doesn’t mean we have to like it.
A version of this article first appeared on Medscape.com.
F. Perry Wilson, MD, MSCE, is an associate professor of medicine and director of Yale’s Clinical and Translational Research Accelerator. His science communication work can be found in the Huffington Post, on NPR, and here on Medscape. He tweets @fperrywilson and hosts a repository of his communication work at www.methodsman.com.
This transcript has been edited for clarity.
Welcome to Impact Factor, your weekly dose of commentary on a new medical study. I’m Dr. F. Perry Wilson of the Yale School of Medicine.
Have you ever lied about COVID-19?
Before you get upset, before the “how dare you,” I want you to think carefully.
Did you have COVID-19 (or think you did) and not mention it to someone you were going to be with? Did you tell someone you were taking more COVID precautions than you really were? Did you tell someone you were vaccinated when you weren’t? Have you avoided getting a COVID test even though you knew you should have?
Researchers appreciated the fact that public health interventions in COVID are important but are only as good as the percentage of people who actually abide by them. So, they designed a survey to ask the questions that many people don’t want to hear the answer to.
A total of 1,733 participants – 80% of those invited – responded to the survey. By design, approximately one-third of respondents (477) had already had COVID, one-third (499) were vaccinated and not yet infected, and one-third (509) were unvaccinated and not yet infected.
Of those surveyed, 41.6% admitted that they lied about COVID or didn’t adhere to COVID guidelines - a conservative estimate, if you ask me.
Breaking down some of the results, about 20% of people who previously were infected with COVID said they didn’t mention it when meeting with someone. A similar number said they didn’t tell anyone when they were entering a public place. A bit more concerning to me, roughly 20% reported not disclosing their COVID-positive status when going to a health care provider’s office.
About 10% of those who had not been vaccinated reported lying about their vaccination status. That’s actually less than the 15% of vaccinated people who lied and told someone they weren’t vaccinated.
About 17% of people lied about the need to quarantine, and many more broke quarantine rules.
The authors tried to see if certain personal characteristics predicted people who were more likely to lie about COVID-19–related issues. Turns out there was only one thing that predicted honesty: age.
Older people were more honest about their COVID status and COVID habits. Other factors – gender, education, race, political affiliation, COVID-19 conspiracy beliefs, and where you got your COVID information – did not seem to make much of a difference. Why are older people more honest? Because older people take COVID more seriously. And they should; COVID is more severe in older people.
The problem arises, of course, because people who are at lower risk for COVID complications interact with people at higher risk – and in those situations, honesty matters more.
On the other hand, isn’t lying about COVID stuff inevitable? If you know that a positive test means you can’t go to work, and not going to work means you won’t get paid, might you not be more likely to lie about the test? Or not get the test at all?
The authors explored the reasons for dishonesty and they are fairly broad, ranging from the desire for life to feel normal (more than half of people who lied) to not believing that COVID was real (a whopping 30%). Some of the reasons for lying included:
- Wanted life to feel normal (50%).
- Freedom (45%).
- It’s no one’s business (40%).
- COVID isn’t real (30%).
In the end, though, we need to realize that public health recommendations are not going to be universally followed, and people may tell us they are following them when, in fact, they are not.
What this adds is another data point to a trend we’ve seen across the course of the pandemic, a shift from collective to individual responsibility. If you can’t be sure what others are doing in regard to COVID, you need to focus on protecting yourself. Perhaps that shift was inevitable. Doesn’t mean we have to like it.
A version of this article first appeared on Medscape.com.
F. Perry Wilson, MD, MSCE, is an associate professor of medicine and director of Yale’s Clinical and Translational Research Accelerator. His science communication work can be found in the Huffington Post, on NPR, and here on Medscape. He tweets @fperrywilson and hosts a repository of his communication work at www.methodsman.com.
This transcript has been edited for clarity.
Welcome to Impact Factor, your weekly dose of commentary on a new medical study. I’m Dr. F. Perry Wilson of the Yale School of Medicine.
Have you ever lied about COVID-19?
Before you get upset, before the “how dare you,” I want you to think carefully.
Did you have COVID-19 (or think you did) and not mention it to someone you were going to be with? Did you tell someone you were taking more COVID precautions than you really were? Did you tell someone you were vaccinated when you weren’t? Have you avoided getting a COVID test even though you knew you should have?
Researchers appreciated the fact that public health interventions in COVID are important but are only as good as the percentage of people who actually abide by them. So, they designed a survey to ask the questions that many people don’t want to hear the answer to.
A total of 1,733 participants – 80% of those invited – responded to the survey. By design, approximately one-third of respondents (477) had already had COVID, one-third (499) were vaccinated and not yet infected, and one-third (509) were unvaccinated and not yet infected.
Of those surveyed, 41.6% admitted that they lied about COVID or didn’t adhere to COVID guidelines - a conservative estimate, if you ask me.
Breaking down some of the results, about 20% of people who previously were infected with COVID said they didn’t mention it when meeting with someone. A similar number said they didn’t tell anyone when they were entering a public place. A bit more concerning to me, roughly 20% reported not disclosing their COVID-positive status when going to a health care provider’s office.
About 10% of those who had not been vaccinated reported lying about their vaccination status. That’s actually less than the 15% of vaccinated people who lied and told someone they weren’t vaccinated.
About 17% of people lied about the need to quarantine, and many more broke quarantine rules.
The authors tried to see if certain personal characteristics predicted people who were more likely to lie about COVID-19–related issues. Turns out there was only one thing that predicted honesty: age.
Older people were more honest about their COVID status and COVID habits. Other factors – gender, education, race, political affiliation, COVID-19 conspiracy beliefs, and where you got your COVID information – did not seem to make much of a difference. Why are older people more honest? Because older people take COVID more seriously. And they should; COVID is more severe in older people.
The problem arises, of course, because people who are at lower risk for COVID complications interact with people at higher risk – and in those situations, honesty matters more.
On the other hand, isn’t lying about COVID stuff inevitable? If you know that a positive test means you can’t go to work, and not going to work means you won’t get paid, might you not be more likely to lie about the test? Or not get the test at all?
The authors explored the reasons for dishonesty and they are fairly broad, ranging from the desire for life to feel normal (more than half of people who lied) to not believing that COVID was real (a whopping 30%). Some of the reasons for lying included:
- Wanted life to feel normal (50%).
- Freedom (45%).
- It’s no one’s business (40%).
- COVID isn’t real (30%).
In the end, though, we need to realize that public health recommendations are not going to be universally followed, and people may tell us they are following them when, in fact, they are not.
What this adds is another data point to a trend we’ve seen across the course of the pandemic, a shift from collective to individual responsibility. If you can’t be sure what others are doing in regard to COVID, you need to focus on protecting yourself. Perhaps that shift was inevitable. Doesn’t mean we have to like it.
A version of this article first appeared on Medscape.com.
F. Perry Wilson, MD, MSCE, is an associate professor of medicine and director of Yale’s Clinical and Translational Research Accelerator. His science communication work can be found in the Huffington Post, on NPR, and here on Medscape. He tweets @fperrywilson and hosts a repository of his communication work at www.methodsman.com.
The bionic pancreas triumphs in pivotal trial
This transcript of Impact Factor with F. Perry Wilson has been edited for clarity.
It was 100 years ago when Leonard Thompson, age 13, received a reprieve from a death sentence. Young master Thompson had type 1 diabetes, a disease that was uniformly fatal within months of diagnosis. But he received a new treatment, insulin, from a canine pancreas. He would live 13 more years before dying at age 26 of pneumonia.
The history of type 1 diabetes since that time has been a battle on two fronts: First, the search for a cause of and cure for the disease; second, the effort to make the administration of insulin safer, more reliable, and easier.
The past 2 decades have seen a technological revolution in type 1 diabetes care, with continuous glucose monitors decreasing the need for painful finger sticks, and insulin pumps allowing for more precise titration of doses.
The dream, of course, has been to combine those two technologies, continuous glucose monitoring and insulin pumps, to create so-called closed-loop systems – basically an artificial pancreas – that would obviate the need for any intervention on the part of the patient, save the occasional refilling of an insulin reservoir.
We aren’t there yet, but we are closer than ever.
Closed-loop systems for insulin delivery, like the Tandem Control IQ system, are a marvel of technology, but they are not exactly hands-free. Users need to dial in settings for their insulin usage, count carbohydrates at meals, and inform the system that they are about to eat those meals to allow the algorithm to administer an appropriate insulin dose.
The perceived complexity of these systems may be responsible for why there are substantial disparities in the prescription of closed-loop systems. Kids of lower socioeconomic status are dramatically less likely to receive these advanced technologies. Providers may feel that patients with lower health literacy or social supports are not “ideal” for these technologies, even though they lead to demonstrably better outcomes.
That means that easier might be better. And a “bionic pancreas,” as reported in an article from The New England Journal of Medicine, is exactly that.
Broadly, it’s another closed-loop system. The bionic pancreas integrates with a continuous glucose monitor and administers insulin when needed. But the algorithm appears to be a bit smarter than what we have in existing devices. For example, patients do not need to provide any information about their usual insulin doses – just their body weight. They don’t need to count carbohydrates at meals – just to inform the device when they are eating, and whether the meal is the usual amount they eat, more, or less. The algorithm learns and adapts as it is used. Easy.
And in this randomized trial, easy does it.
A total of 219 participants were randomized in a 2:1 ratio to the bionic pancreas or usual diabetes care, though it was required that control participants use a continuous glucose monitor. Participants were as young as 6 years old and up to 79 years old; the majority were White and had a relatively high household income. The mean A1c was around 7.8% at baseline.
By the end of the study, the A1c was significantly improved in the bionic pancreas group, with a mean of 7.3% vs. 7.7% in the usual-care group.
This effect was most pronounced in those with a higher A1c at baseline.
People randomized to the bionic pancreas also spent more time in the target glucose range of 70-180 mg/dL.
All in all, the technology that makes it easy to manage your blood sugar, well, made it easy to manage your blood sugar.
But new technology is never without its hiccups. Those randomized to the bionic pancreas had a markedly higher rate of adverse events (244 events in 126 people compared with 10 events in 8 people in the usual-care group.)
This is actually a little misleading, though. The vast majority of these events were hyperglycemic episodes due to infusion set failures, which were reportable only in the bionic pancreas group. In other words, the patients in the control group who had an infusion set failure (assuming they were using an insulin pump at all) would have just called their regular doctor to get things sorted and not reported it to the study team.
Nevertheless, these adverse events – not serious, but common – highlight the fact that good software is not the only key to solving the closed-loop problem. We need good hardware too, hardware that can withstand the very active lives that children with type 1 diabetes deserve to live.
In short, the dream of a functional cure to type 1 diabetes, a true artificial pancreas, is closer than ever, but it’s still just a dream. With iterative advances like this, though, the reality may be here before you know it.
Dr. Wilson is associate professor of medicine and director of Yale University’s Clinical and Translational Research Accelerator. His science communication work can be found in the Huffington Post, on NPR, and on Medscape. He tweets @fperrywilson and hosts a repository of his communication work at www.methodsman.com. A version of this article first appeared on Medscape.com.
This transcript of Impact Factor with F. Perry Wilson has been edited for clarity.
It was 100 years ago when Leonard Thompson, age 13, received a reprieve from a death sentence. Young master Thompson had type 1 diabetes, a disease that was uniformly fatal within months of diagnosis. But he received a new treatment, insulin, from a canine pancreas. He would live 13 more years before dying at age 26 of pneumonia.
The history of type 1 diabetes since that time has been a battle on two fronts: First, the search for a cause of and cure for the disease; second, the effort to make the administration of insulin safer, more reliable, and easier.
The past 2 decades have seen a technological revolution in type 1 diabetes care, with continuous glucose monitors decreasing the need for painful finger sticks, and insulin pumps allowing for more precise titration of doses.
The dream, of course, has been to combine those two technologies, continuous glucose monitoring and insulin pumps, to create so-called closed-loop systems – basically an artificial pancreas – that would obviate the need for any intervention on the part of the patient, save the occasional refilling of an insulin reservoir.
We aren’t there yet, but we are closer than ever.
Closed-loop systems for insulin delivery, like the Tandem Control IQ system, are a marvel of technology, but they are not exactly hands-free. Users need to dial in settings for their insulin usage, count carbohydrates at meals, and inform the system that they are about to eat those meals to allow the algorithm to administer an appropriate insulin dose.
The perceived complexity of these systems may be responsible for why there are substantial disparities in the prescription of closed-loop systems. Kids of lower socioeconomic status are dramatically less likely to receive these advanced technologies. Providers may feel that patients with lower health literacy or social supports are not “ideal” for these technologies, even though they lead to demonstrably better outcomes.
That means that easier might be better. And a “bionic pancreas,” as reported in an article from The New England Journal of Medicine, is exactly that.
Broadly, it’s another closed-loop system. The bionic pancreas integrates with a continuous glucose monitor and administers insulin when needed. But the algorithm appears to be a bit smarter than what we have in existing devices. For example, patients do not need to provide any information about their usual insulin doses – just their body weight. They don’t need to count carbohydrates at meals – just to inform the device when they are eating, and whether the meal is the usual amount they eat, more, or less. The algorithm learns and adapts as it is used. Easy.
And in this randomized trial, easy does it.
A total of 219 participants were randomized in a 2:1 ratio to the bionic pancreas or usual diabetes care, though it was required that control participants use a continuous glucose monitor. Participants were as young as 6 years old and up to 79 years old; the majority were White and had a relatively high household income. The mean A1c was around 7.8% at baseline.
By the end of the study, the A1c was significantly improved in the bionic pancreas group, with a mean of 7.3% vs. 7.7% in the usual-care group.
This effect was most pronounced in those with a higher A1c at baseline.
People randomized to the bionic pancreas also spent more time in the target glucose range of 70-180 mg/dL.
All in all, the technology that makes it easy to manage your blood sugar, well, made it easy to manage your blood sugar.
But new technology is never without its hiccups. Those randomized to the bionic pancreas had a markedly higher rate of adverse events (244 events in 126 people compared with 10 events in 8 people in the usual-care group.)
This is actually a little misleading, though. The vast majority of these events were hyperglycemic episodes due to infusion set failures, which were reportable only in the bionic pancreas group. In other words, the patients in the control group who had an infusion set failure (assuming they were using an insulin pump at all) would have just called their regular doctor to get things sorted and not reported it to the study team.
Nevertheless, these adverse events – not serious, but common – highlight the fact that good software is not the only key to solving the closed-loop problem. We need good hardware too, hardware that can withstand the very active lives that children with type 1 diabetes deserve to live.
In short, the dream of a functional cure to type 1 diabetes, a true artificial pancreas, is closer than ever, but it’s still just a dream. With iterative advances like this, though, the reality may be here before you know it.
Dr. Wilson is associate professor of medicine and director of Yale University’s Clinical and Translational Research Accelerator. His science communication work can be found in the Huffington Post, on NPR, and on Medscape. He tweets @fperrywilson and hosts a repository of his communication work at www.methodsman.com. A version of this article first appeared on Medscape.com.
This transcript of Impact Factor with F. Perry Wilson has been edited for clarity.
It was 100 years ago when Leonard Thompson, age 13, received a reprieve from a death sentence. Young master Thompson had type 1 diabetes, a disease that was uniformly fatal within months of diagnosis. But he received a new treatment, insulin, from a canine pancreas. He would live 13 more years before dying at age 26 of pneumonia.
The history of type 1 diabetes since that time has been a battle on two fronts: First, the search for a cause of and cure for the disease; second, the effort to make the administration of insulin safer, more reliable, and easier.
The past 2 decades have seen a technological revolution in type 1 diabetes care, with continuous glucose monitors decreasing the need for painful finger sticks, and insulin pumps allowing for more precise titration of doses.
The dream, of course, has been to combine those two technologies, continuous glucose monitoring and insulin pumps, to create so-called closed-loop systems – basically an artificial pancreas – that would obviate the need for any intervention on the part of the patient, save the occasional refilling of an insulin reservoir.
We aren’t there yet, but we are closer than ever.
Closed-loop systems for insulin delivery, like the Tandem Control IQ system, are a marvel of technology, but they are not exactly hands-free. Users need to dial in settings for their insulin usage, count carbohydrates at meals, and inform the system that they are about to eat those meals to allow the algorithm to administer an appropriate insulin dose.
The perceived complexity of these systems may be responsible for why there are substantial disparities in the prescription of closed-loop systems. Kids of lower socioeconomic status are dramatically less likely to receive these advanced technologies. Providers may feel that patients with lower health literacy or social supports are not “ideal” for these technologies, even though they lead to demonstrably better outcomes.
That means that easier might be better. And a “bionic pancreas,” as reported in an article from The New England Journal of Medicine, is exactly that.
Broadly, it’s another closed-loop system. The bionic pancreas integrates with a continuous glucose monitor and administers insulin when needed. But the algorithm appears to be a bit smarter than what we have in existing devices. For example, patients do not need to provide any information about their usual insulin doses – just their body weight. They don’t need to count carbohydrates at meals – just to inform the device when they are eating, and whether the meal is the usual amount they eat, more, or less. The algorithm learns and adapts as it is used. Easy.
And in this randomized trial, easy does it.
A total of 219 participants were randomized in a 2:1 ratio to the bionic pancreas or usual diabetes care, though it was required that control participants use a continuous glucose monitor. Participants were as young as 6 years old and up to 79 years old; the majority were White and had a relatively high household income. The mean A1c was around 7.8% at baseline.
By the end of the study, the A1c was significantly improved in the bionic pancreas group, with a mean of 7.3% vs. 7.7% in the usual-care group.
This effect was most pronounced in those with a higher A1c at baseline.
People randomized to the bionic pancreas also spent more time in the target glucose range of 70-180 mg/dL.
All in all, the technology that makes it easy to manage your blood sugar, well, made it easy to manage your blood sugar.
But new technology is never without its hiccups. Those randomized to the bionic pancreas had a markedly higher rate of adverse events (244 events in 126 people compared with 10 events in 8 people in the usual-care group.)
This is actually a little misleading, though. The vast majority of these events were hyperglycemic episodes due to infusion set failures, which were reportable only in the bionic pancreas group. In other words, the patients in the control group who had an infusion set failure (assuming they were using an insulin pump at all) would have just called their regular doctor to get things sorted and not reported it to the study team.
Nevertheless, these adverse events – not serious, but common – highlight the fact that good software is not the only key to solving the closed-loop problem. We need good hardware too, hardware that can withstand the very active lives that children with type 1 diabetes deserve to live.
In short, the dream of a functional cure to type 1 diabetes, a true artificial pancreas, is closer than ever, but it’s still just a dream. With iterative advances like this, though, the reality may be here before you know it.
Dr. Wilson is associate professor of medicine and director of Yale University’s Clinical and Translational Research Accelerator. His science communication work can be found in the Huffington Post, on NPR, and on Medscape. He tweets @fperrywilson and hosts a repository of his communication work at www.methodsman.com. A version of this article first appeared on Medscape.com.