User login
Bringing you the latest news, research and reviews, exclusive interviews, podcasts, quizzes, and more.
One weird trick to fight burnout
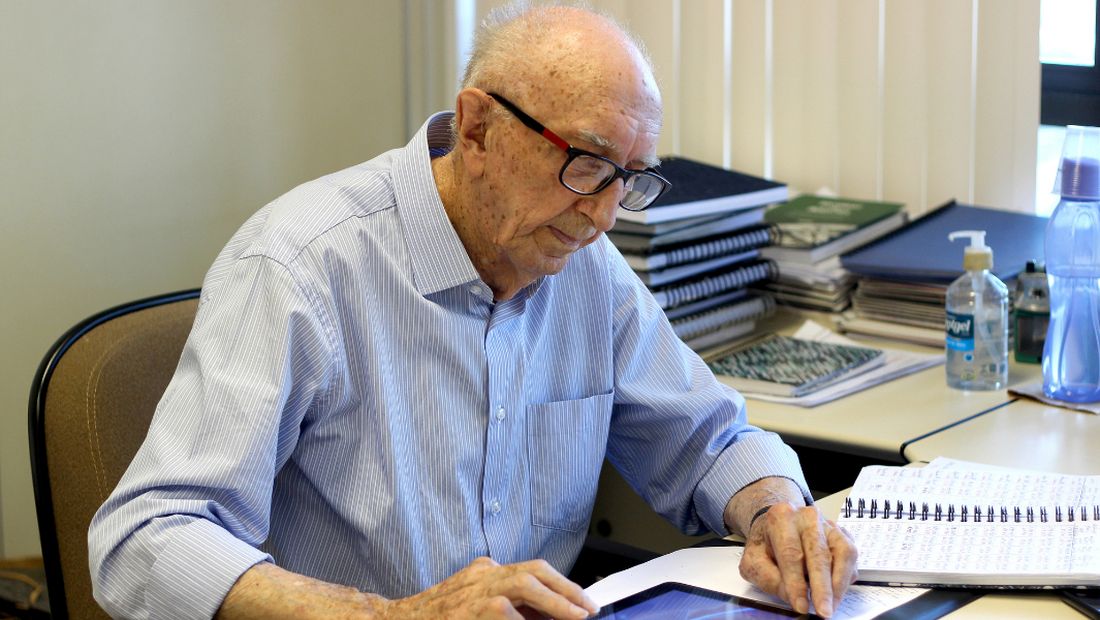
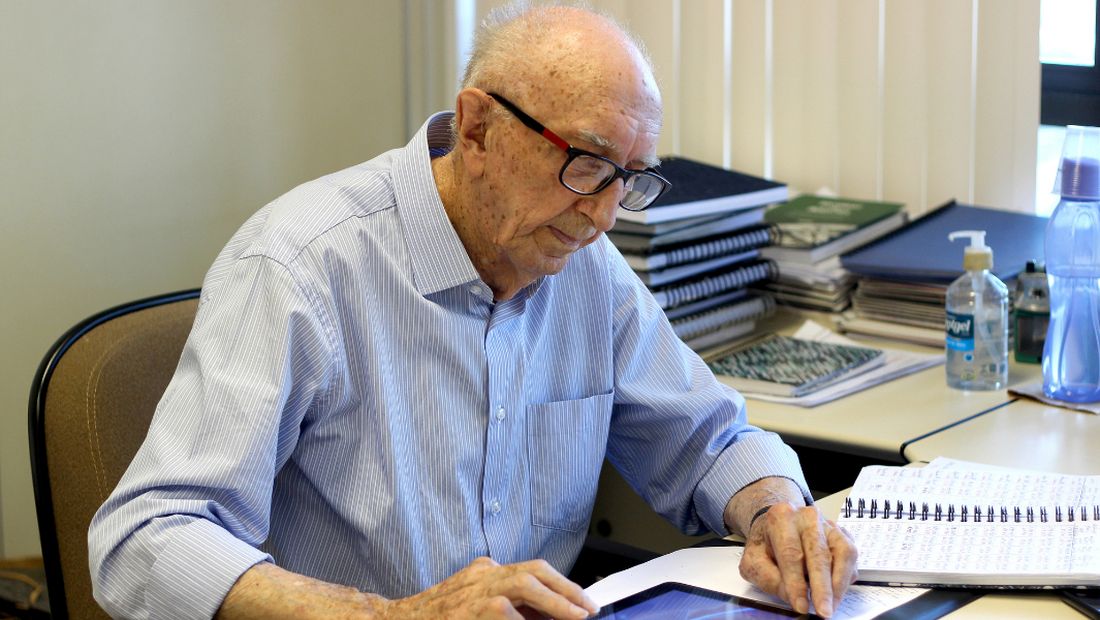
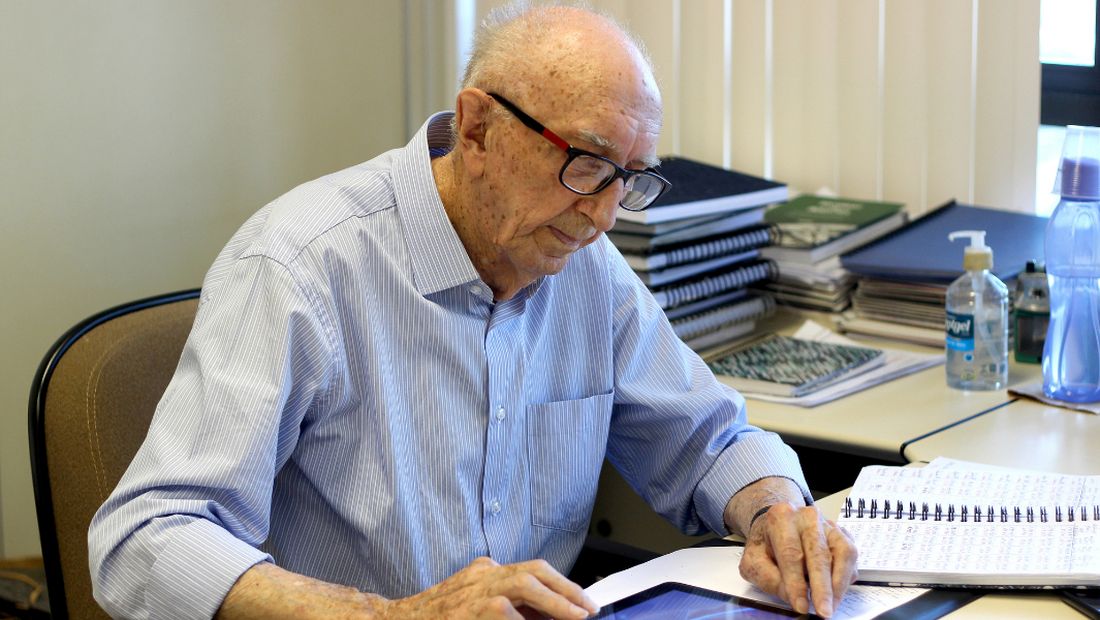
“Here and now is what counts. So, let’s go to work!” –Walter Orthmann, 100 years old
How long before you retire? If you know the answer in exact years, months, and days, you aren’t alone. For many good reasons, we doctors are more likely to be counting down the years until we retire rather than counting up the years since we started working. For me, if I’m to break the Guinness World Record, I have 69 more years, 3 months and 6 days left to go. That would surpass the current achievement for the longest career at one company, Mr. Walter Orthmann, who has been sitting at the same desk for 84 years. At 100 years old, Mr. Orthmann still shows up every Monday morning, as bright eyed and bushy tailed as a young squirrel. I’ll be 119 when I break his streak, which would also put me past Anthony Mancinelli, a New York barber who at 107 years of age was still brushing off his chair for the next customer. Unbelievable, I know! I wonder, what’s the one weird trick these guys are doing that keeps them going?
Of course, the job itself matters. Some jobs, like being a police officer, aren’t suitable for old people. Or are they? Officer L.C. “Buckshot” Smith was still keeping streets safe from his patrol car at 91 years old. After a bit of searching, I found pretty much any job you can think of has a very long-lasting Energizer Bunny story: A female surgeon who was operating at 90 years old, a 100-year-old rheumatologist who was still teaching at University of California, San Francisco, and a 105-year-old Japanese physician who was still seeing patients. There are plenty of geriatric lawyers, nurses, land surveyors, accountants, judges, you name it. So it seems it’s not the work, but the worker that matters. Why do some older workers recharge daily and carry on while many younger ones say the daily grind is burning them out? What makes the Greatest Generation so great?
We all know colleagues who hung up their white coats early. In my medical group, it’s often financially feasible to retire at 58 and many have chosen that option. Yet, we have loads of Partner Emeritus docs in their 70’s who still log on to EPIC and pitch in everyday.
“So, how do you keep going?” I asked my 105-year-old patient who still walks and manages his affairs. “Just stay healthy,” he advised. A circular argument, yet he’s right. You must both be lucky and also choose to be active mentally and physically. Mr. Mancinelli, who was barbering full time at 107 years old, had no aches and pains and all his teeth. He pruned his own bushes. The data are crystal clear that physical activity adds not only years of life, but also improves cognitive capabilities during those years.
As for beating burnout, it seems the one trick that these ultraworkers do is to focus only on the present. Mr. Orthmann’s pithy advice as quoted by NPR is, “You need to get busy with the present, not the past or the future.” These centenarian employees also frame their work not as stressful but rather as their daily series of problems to be solved.
When I asked my super-geriatric patient how he sleeps so well, he said, “I never worry when I get into bed, I just shut my eyes and sleep. I’ll think about tomorrow when I wake up.” Now if I can do that about 25,000 more times, I’ll have the record.
Dr. Jeff Benabio is director of Healthcare Transformation and chief of dermatology at Kaiser Permanente San Diego. The opinions expressed in this column are his own and do not represent those of Kaiser Permanente. Dr. Benabio is @Dermdoc on Twitter. Write to him at [email protected]
“Here and now is what counts. So, let’s go to work!” –Walter Orthmann, 100 years old
How long before you retire? If you know the answer in exact years, months, and days, you aren’t alone. For many good reasons, we doctors are more likely to be counting down the years until we retire rather than counting up the years since we started working. For me, if I’m to break the Guinness World Record, I have 69 more years, 3 months and 6 days left to go. That would surpass the current achievement for the longest career at one company, Mr. Walter Orthmann, who has been sitting at the same desk for 84 years. At 100 years old, Mr. Orthmann still shows up every Monday morning, as bright eyed and bushy tailed as a young squirrel. I’ll be 119 when I break his streak, which would also put me past Anthony Mancinelli, a New York barber who at 107 years of age was still brushing off his chair for the next customer. Unbelievable, I know! I wonder, what’s the one weird trick these guys are doing that keeps them going?
Of course, the job itself matters. Some jobs, like being a police officer, aren’t suitable for old people. Or are they? Officer L.C. “Buckshot” Smith was still keeping streets safe from his patrol car at 91 years old. After a bit of searching, I found pretty much any job you can think of has a very long-lasting Energizer Bunny story: A female surgeon who was operating at 90 years old, a 100-year-old rheumatologist who was still teaching at University of California, San Francisco, and a 105-year-old Japanese physician who was still seeing patients. There are plenty of geriatric lawyers, nurses, land surveyors, accountants, judges, you name it. So it seems it’s not the work, but the worker that matters. Why do some older workers recharge daily and carry on while many younger ones say the daily grind is burning them out? What makes the Greatest Generation so great?
We all know colleagues who hung up their white coats early. In my medical group, it’s often financially feasible to retire at 58 and many have chosen that option. Yet, we have loads of Partner Emeritus docs in their 70’s who still log on to EPIC and pitch in everyday.
“So, how do you keep going?” I asked my 105-year-old patient who still walks and manages his affairs. “Just stay healthy,” he advised. A circular argument, yet he’s right. You must both be lucky and also choose to be active mentally and physically. Mr. Mancinelli, who was barbering full time at 107 years old, had no aches and pains and all his teeth. He pruned his own bushes. The data are crystal clear that physical activity adds not only years of life, but also improves cognitive capabilities during those years.
As for beating burnout, it seems the one trick that these ultraworkers do is to focus only on the present. Mr. Orthmann’s pithy advice as quoted by NPR is, “You need to get busy with the present, not the past or the future.” These centenarian employees also frame their work not as stressful but rather as their daily series of problems to be solved.
When I asked my super-geriatric patient how he sleeps so well, he said, “I never worry when I get into bed, I just shut my eyes and sleep. I’ll think about tomorrow when I wake up.” Now if I can do that about 25,000 more times, I’ll have the record.
Dr. Jeff Benabio is director of Healthcare Transformation and chief of dermatology at Kaiser Permanente San Diego. The opinions expressed in this column are his own and do not represent those of Kaiser Permanente. Dr. Benabio is @Dermdoc on Twitter. Write to him at [email protected]
“Here and now is what counts. So, let’s go to work!” –Walter Orthmann, 100 years old
How long before you retire? If you know the answer in exact years, months, and days, you aren’t alone. For many good reasons, we doctors are more likely to be counting down the years until we retire rather than counting up the years since we started working. For me, if I’m to break the Guinness World Record, I have 69 more years, 3 months and 6 days left to go. That would surpass the current achievement for the longest career at one company, Mr. Walter Orthmann, who has been sitting at the same desk for 84 years. At 100 years old, Mr. Orthmann still shows up every Monday morning, as bright eyed and bushy tailed as a young squirrel. I’ll be 119 when I break his streak, which would also put me past Anthony Mancinelli, a New York barber who at 107 years of age was still brushing off his chair for the next customer. Unbelievable, I know! I wonder, what’s the one weird trick these guys are doing that keeps them going?
Of course, the job itself matters. Some jobs, like being a police officer, aren’t suitable for old people. Or are they? Officer L.C. “Buckshot” Smith was still keeping streets safe from his patrol car at 91 years old. After a bit of searching, I found pretty much any job you can think of has a very long-lasting Energizer Bunny story: A female surgeon who was operating at 90 years old, a 100-year-old rheumatologist who was still teaching at University of California, San Francisco, and a 105-year-old Japanese physician who was still seeing patients. There are plenty of geriatric lawyers, nurses, land surveyors, accountants, judges, you name it. So it seems it’s not the work, but the worker that matters. Why do some older workers recharge daily and carry on while many younger ones say the daily grind is burning them out? What makes the Greatest Generation so great?
We all know colleagues who hung up their white coats early. In my medical group, it’s often financially feasible to retire at 58 and many have chosen that option. Yet, we have loads of Partner Emeritus docs in their 70’s who still log on to EPIC and pitch in everyday.
“So, how do you keep going?” I asked my 105-year-old patient who still walks and manages his affairs. “Just stay healthy,” he advised. A circular argument, yet he’s right. You must both be lucky and also choose to be active mentally and physically. Mr. Mancinelli, who was barbering full time at 107 years old, had no aches and pains and all his teeth. He pruned his own bushes. The data are crystal clear that physical activity adds not only years of life, but also improves cognitive capabilities during those years.
As for beating burnout, it seems the one trick that these ultraworkers do is to focus only on the present. Mr. Orthmann’s pithy advice as quoted by NPR is, “You need to get busy with the present, not the past or the future.” These centenarian employees also frame their work not as stressful but rather as their daily series of problems to be solved.
When I asked my super-geriatric patient how he sleeps so well, he said, “I never worry when I get into bed, I just shut my eyes and sleep. I’ll think about tomorrow when I wake up.” Now if I can do that about 25,000 more times, I’ll have the record.
Dr. Jeff Benabio is director of Healthcare Transformation and chief of dermatology at Kaiser Permanente San Diego. The opinions expressed in this column are his own and do not represent those of Kaiser Permanente. Dr. Benabio is @Dermdoc on Twitter. Write to him at [email protected]
Merging small practices
Difficult economic times and the unpredictable consequences of health care reform are making an increasing number of solo practitioners and small private groups very nervous. Yet, many balk at the prospect of selling to private equity companies.
Merging offers many benefits: Better overall management, centralized and efficient billing and collection, group purchasing discounts, and reduced overhead, among others; but careful planning, and a written agreement, are essential. If you are considering such an option, here are some things to think about.
You should begin with an evaluation and comparison of the separate groups’ respective finances. This should include a history of production, collections, overhead, and liabilities. Basically, you want to locate and identify all assets and liabilities that will be combined into the new group. One area of immediate importance is Medicare participation. Which members now currently participate and which do not? Since the new group will need to have a single position, all of the physicians must agree on that issue.
Who will be in charge? Not every physician is a qualified manager. The manager should be the physician who is willing to spend the time it takes to sign checks, interact with the administrator, and ensure that other matters such as filing tax returns and approving minor purchases arc carried out properly.
What is the compensation formula? Compensation arrangements should be based on each physician’s current financial data and the goals of the practice. Will everyone be paid only for what they do individually, or will revenue be shared equally? I favor a combination, so productivity is rewarded but your income doesn’t drop to zero when you take time off.
Which practices have a retirement plan and which do not? Will you keep your retirement plans separate, or combine them? If the latter, you will have to agree on the terms of the new plan, which can be the same or different from any of the existing plans. You’ll probably need some legal guidance to insure that assets from existing plans can be transferred into a new plan without tax issues. You may also have to address the problem of physicians who currently do not have a plan who, for whatever reason, may not want to be forced into making retirement plan contributions.
The often-problematic issue of employees and their salaries needs to be addressed, to decide which employees will be needed in the new group, and to determine a salary structure. Each practice’s policies related to vacation, sick leave, and other such issues should be reviewed, and an overall policy for the new group developed.
Other common sticking points are issues related to facilities. If the practices intend to consolidate into one location, the physicians must decide which of the specific assets of each practice will be contributed to the new entity. Ideally, each party brings an equal amount of assets to the table, but in the real world that is hardly ever the case. Physicians whose assets are to be used generally want to be compensated, and those who have to dispose of or store assets are in a quandary. The solution to this predicament will vary depending on the circumstances of each merger. One alternative is to agree that any inequalities will be compensated at the other end, in the form of buyout value; that is, physicians contributing more assets will receive larger buyouts when they leave or retire than those contributing less.
Buyouts should be addressed in advance as well. You must decide when a buyout would occur – usually in the event of retirement, death, disability, or withdrawal (voluntary or involuntary) – how the buyout amount will be calculated, and how it will be paid. Then, you must agree on how a buyout amount will be valued. Remember that any buyout calculated at “appraised value” is a problem, because the buyout amount remains a mystery until an appraisal is performed. If the appraised value ends up being too high, the remaining owners may refuse to pay it. I suggest having an actuary create a formula, so that the buyout figure can be calculated at any time. This area, especially, is where you need experienced, competent legal advice.
Noncompete provisions are always a difficult issue, mostly because they are so hard (and expensive) to enforce. An increasingly popular alternative is, once again, to deal with it at the other end, with a buyout penalty. An unhappy partner can leave, and compete, but at the cost of a substantially reduced buyout. This permits competition, but discourages it; and it compensates the remaining partners.
These are only some of the pivotal business and legal issues that must be settled in advance. A little planning and negotiation can prevent a lot of grief, regret, and legal expenses in the future. I’ll discuss some other, more complicated merger options in my next column.
Dr. Eastern practices dermatology and dermatologic surgery in Belleville, N.J. He is the author of numerous articles and textbook chapters, and is a longtime monthly columnist for Dermatology News. Write to him at [email protected].
Difficult economic times and the unpredictable consequences of health care reform are making an increasing number of solo practitioners and small private groups very nervous. Yet, many balk at the prospect of selling to private equity companies.
Merging offers many benefits: Better overall management, centralized and efficient billing and collection, group purchasing discounts, and reduced overhead, among others; but careful planning, and a written agreement, are essential. If you are considering such an option, here are some things to think about.
You should begin with an evaluation and comparison of the separate groups’ respective finances. This should include a history of production, collections, overhead, and liabilities. Basically, you want to locate and identify all assets and liabilities that will be combined into the new group. One area of immediate importance is Medicare participation. Which members now currently participate and which do not? Since the new group will need to have a single position, all of the physicians must agree on that issue.
Who will be in charge? Not every physician is a qualified manager. The manager should be the physician who is willing to spend the time it takes to sign checks, interact with the administrator, and ensure that other matters such as filing tax returns and approving minor purchases arc carried out properly.
What is the compensation formula? Compensation arrangements should be based on each physician’s current financial data and the goals of the practice. Will everyone be paid only for what they do individually, or will revenue be shared equally? I favor a combination, so productivity is rewarded but your income doesn’t drop to zero when you take time off.
Which practices have a retirement plan and which do not? Will you keep your retirement plans separate, or combine them? If the latter, you will have to agree on the terms of the new plan, which can be the same or different from any of the existing plans. You’ll probably need some legal guidance to insure that assets from existing plans can be transferred into a new plan without tax issues. You may also have to address the problem of physicians who currently do not have a plan who, for whatever reason, may not want to be forced into making retirement plan contributions.
The often-problematic issue of employees and their salaries needs to be addressed, to decide which employees will be needed in the new group, and to determine a salary structure. Each practice’s policies related to vacation, sick leave, and other such issues should be reviewed, and an overall policy for the new group developed.
Other common sticking points are issues related to facilities. If the practices intend to consolidate into one location, the physicians must decide which of the specific assets of each practice will be contributed to the new entity. Ideally, each party brings an equal amount of assets to the table, but in the real world that is hardly ever the case. Physicians whose assets are to be used generally want to be compensated, and those who have to dispose of or store assets are in a quandary. The solution to this predicament will vary depending on the circumstances of each merger. One alternative is to agree that any inequalities will be compensated at the other end, in the form of buyout value; that is, physicians contributing more assets will receive larger buyouts when they leave or retire than those contributing less.
Buyouts should be addressed in advance as well. You must decide when a buyout would occur – usually in the event of retirement, death, disability, or withdrawal (voluntary or involuntary) – how the buyout amount will be calculated, and how it will be paid. Then, you must agree on how a buyout amount will be valued. Remember that any buyout calculated at “appraised value” is a problem, because the buyout amount remains a mystery until an appraisal is performed. If the appraised value ends up being too high, the remaining owners may refuse to pay it. I suggest having an actuary create a formula, so that the buyout figure can be calculated at any time. This area, especially, is where you need experienced, competent legal advice.
Noncompete provisions are always a difficult issue, mostly because they are so hard (and expensive) to enforce. An increasingly popular alternative is, once again, to deal with it at the other end, with a buyout penalty. An unhappy partner can leave, and compete, but at the cost of a substantially reduced buyout. This permits competition, but discourages it; and it compensates the remaining partners.
These are only some of the pivotal business and legal issues that must be settled in advance. A little planning and negotiation can prevent a lot of grief, regret, and legal expenses in the future. I’ll discuss some other, more complicated merger options in my next column.
Dr. Eastern practices dermatology and dermatologic surgery in Belleville, N.J. He is the author of numerous articles and textbook chapters, and is a longtime monthly columnist for Dermatology News. Write to him at [email protected].
Difficult economic times and the unpredictable consequences of health care reform are making an increasing number of solo practitioners and small private groups very nervous. Yet, many balk at the prospect of selling to private equity companies.
Merging offers many benefits: Better overall management, centralized and efficient billing and collection, group purchasing discounts, and reduced overhead, among others; but careful planning, and a written agreement, are essential. If you are considering such an option, here are some things to think about.
You should begin with an evaluation and comparison of the separate groups’ respective finances. This should include a history of production, collections, overhead, and liabilities. Basically, you want to locate and identify all assets and liabilities that will be combined into the new group. One area of immediate importance is Medicare participation. Which members now currently participate and which do not? Since the new group will need to have a single position, all of the physicians must agree on that issue.
Who will be in charge? Not every physician is a qualified manager. The manager should be the physician who is willing to spend the time it takes to sign checks, interact with the administrator, and ensure that other matters such as filing tax returns and approving minor purchases arc carried out properly.
What is the compensation formula? Compensation arrangements should be based on each physician’s current financial data and the goals of the practice. Will everyone be paid only for what they do individually, or will revenue be shared equally? I favor a combination, so productivity is rewarded but your income doesn’t drop to zero when you take time off.
Which practices have a retirement plan and which do not? Will you keep your retirement plans separate, or combine them? If the latter, you will have to agree on the terms of the new plan, which can be the same or different from any of the existing plans. You’ll probably need some legal guidance to insure that assets from existing plans can be transferred into a new plan without tax issues. You may also have to address the problem of physicians who currently do not have a plan who, for whatever reason, may not want to be forced into making retirement plan contributions.
The often-problematic issue of employees and their salaries needs to be addressed, to decide which employees will be needed in the new group, and to determine a salary structure. Each practice’s policies related to vacation, sick leave, and other such issues should be reviewed, and an overall policy for the new group developed.
Other common sticking points are issues related to facilities. If the practices intend to consolidate into one location, the physicians must decide which of the specific assets of each practice will be contributed to the new entity. Ideally, each party brings an equal amount of assets to the table, but in the real world that is hardly ever the case. Physicians whose assets are to be used generally want to be compensated, and those who have to dispose of or store assets are in a quandary. The solution to this predicament will vary depending on the circumstances of each merger. One alternative is to agree that any inequalities will be compensated at the other end, in the form of buyout value; that is, physicians contributing more assets will receive larger buyouts when they leave or retire than those contributing less.
Buyouts should be addressed in advance as well. You must decide when a buyout would occur – usually in the event of retirement, death, disability, or withdrawal (voluntary or involuntary) – how the buyout amount will be calculated, and how it will be paid. Then, you must agree on how a buyout amount will be valued. Remember that any buyout calculated at “appraised value” is a problem, because the buyout amount remains a mystery until an appraisal is performed. If the appraised value ends up being too high, the remaining owners may refuse to pay it. I suggest having an actuary create a formula, so that the buyout figure can be calculated at any time. This area, especially, is where you need experienced, competent legal advice.
Noncompete provisions are always a difficult issue, mostly because they are so hard (and expensive) to enforce. An increasingly popular alternative is, once again, to deal with it at the other end, with a buyout penalty. An unhappy partner can leave, and compete, but at the cost of a substantially reduced buyout. This permits competition, but discourages it; and it compensates the remaining partners.
These are only some of the pivotal business and legal issues that must be settled in advance. A little planning and negotiation can prevent a lot of grief, regret, and legal expenses in the future. I’ll discuss some other, more complicated merger options in my next column.
Dr. Eastern practices dermatology and dermatologic surgery in Belleville, N.J. He is the author of numerous articles and textbook chapters, and is a longtime monthly columnist for Dermatology News. Write to him at [email protected].
The work after work
Across the country, taxes unite us. Not that we all share the same, rather that we all have to do them. It was recently tax weekend in our house: The Saturday and Sunday that cap off weeks of hunting and gathering faded receipts and sorting through reams of credit card bills to find all the dollars we spent on work. The task is more tedious than all the Wednesdays of taking out trash bins combined, and equally as exciting. But wait, that’s not all.
This weekend I’ve been chatting with bots from a solar company trying to solve our drop in energy production and sat on terminal hold with apparently one person who answers the phone for Amazon. There’s also an homeowner’s association meeting to prepare for and research to be done on ceiling fans.
“Life admin” is a crisp phrase coined by Elizabeth Emens, JD, PhD, that captures the never-ending to-do list that comes with running a household. An accomplished law professor at Columbia University, New York, Dr. Emens noticed the negative impact this life admin has on our quality of life. Reading her book, “Life Admin: How I Learned to Do Less, Do Better, and Live More” (New York: HarperOne, 2019), your eyes widen as she magically makes salient all this hidden work that is stealing our time. Life admin, kidmin, mom and dadmin, just rattling them off feels like donning x-ray glasses allowing us to see how much work we do outside of our work. As doctors, I would add “family house calls,” as a contributing factor: Random family and friends who want to talk for a minute about their knee replacement or what drug the ICU should give Uncle Larry who is fighting COVID. (I only know ivermectin, but it would only help if he just had scabies).
By all accounts, the amount of life admin is growing insidiously, worsened by the great pandemic. There are events to plan and reply to, more DIY customer service to fix your own problems, more work to find a VRBO for a weekend getaway at the beach. (There are none on the entire coast of California this summer, so I just saved you time there. You’re welcome.)
There is no good time to do this work and combined with the heavy burden of our responsibilities as physicians, it can feel like fuel feeding the burnout fire.
Dr. Emens has some top tips to help. First up, know your admin type. Are you a super doer, reluctant doer, admin denier, or admin avoider? I’m mostly in the avoider quadrant, dropping into reluctant doer when consequences loom. Next, choose strategies that fit you. Instead of avoiding, there are some things I might deflect. For example, When your aunt in Peoria asks where she can get a COVID test, you can use LMGTFY.com to generate a link that will show them how to use Google to help with their question. Dr. Emens is joking, but the point rang true. We can lighten the load a bit if we delegate or push back the excessive or undue requests. For some tasks, we’d be better off paying someone to take it over. Last tip here, try doing life admin with a partner, be it spouse, friend, or colleague. This is particularly useful when your partner is a super doer, as mine is. Not only can they make the work lighter, but also less dreary.
We physicians are focused on fixing physician burnout. Maybe we should also be looking at what happens in the “second shift” at home. Tax season is over, but will be back soon.
Dr. Benabio is director of Healthcare Transformation and chief of dermatology at Kaiser Permanente San Diego. The opinions expressed in this column are his own and do not represent those of Kaiser Permanente. Dr. Benabio is @Dermdoc on Twitter. Write to him at [email protected]
Across the country, taxes unite us. Not that we all share the same, rather that we all have to do them. It was recently tax weekend in our house: The Saturday and Sunday that cap off weeks of hunting and gathering faded receipts and sorting through reams of credit card bills to find all the dollars we spent on work. The task is more tedious than all the Wednesdays of taking out trash bins combined, and equally as exciting. But wait, that’s not all.
This weekend I’ve been chatting with bots from a solar company trying to solve our drop in energy production and sat on terminal hold with apparently one person who answers the phone for Amazon. There’s also an homeowner’s association meeting to prepare for and research to be done on ceiling fans.
“Life admin” is a crisp phrase coined by Elizabeth Emens, JD, PhD, that captures the never-ending to-do list that comes with running a household. An accomplished law professor at Columbia University, New York, Dr. Emens noticed the negative impact this life admin has on our quality of life. Reading her book, “Life Admin: How I Learned to Do Less, Do Better, and Live More” (New York: HarperOne, 2019), your eyes widen as she magically makes salient all this hidden work that is stealing our time. Life admin, kidmin, mom and dadmin, just rattling them off feels like donning x-ray glasses allowing us to see how much work we do outside of our work. As doctors, I would add “family house calls,” as a contributing factor: Random family and friends who want to talk for a minute about their knee replacement or what drug the ICU should give Uncle Larry who is fighting COVID. (I only know ivermectin, but it would only help if he just had scabies).
By all accounts, the amount of life admin is growing insidiously, worsened by the great pandemic. There are events to plan and reply to, more DIY customer service to fix your own problems, more work to find a VRBO for a weekend getaway at the beach. (There are none on the entire coast of California this summer, so I just saved you time there. You’re welcome.)
There is no good time to do this work and combined with the heavy burden of our responsibilities as physicians, it can feel like fuel feeding the burnout fire.
Dr. Emens has some top tips to help. First up, know your admin type. Are you a super doer, reluctant doer, admin denier, or admin avoider? I’m mostly in the avoider quadrant, dropping into reluctant doer when consequences loom. Next, choose strategies that fit you. Instead of avoiding, there are some things I might deflect. For example, When your aunt in Peoria asks where she can get a COVID test, you can use LMGTFY.com to generate a link that will show them how to use Google to help with their question. Dr. Emens is joking, but the point rang true. We can lighten the load a bit if we delegate or push back the excessive or undue requests. For some tasks, we’d be better off paying someone to take it over. Last tip here, try doing life admin with a partner, be it spouse, friend, or colleague. This is particularly useful when your partner is a super doer, as mine is. Not only can they make the work lighter, but also less dreary.
We physicians are focused on fixing physician burnout. Maybe we should also be looking at what happens in the “second shift” at home. Tax season is over, but will be back soon.
Dr. Benabio is director of Healthcare Transformation and chief of dermatology at Kaiser Permanente San Diego. The opinions expressed in this column are his own and do not represent those of Kaiser Permanente. Dr. Benabio is @Dermdoc on Twitter. Write to him at [email protected]
Across the country, taxes unite us. Not that we all share the same, rather that we all have to do them. It was recently tax weekend in our house: The Saturday and Sunday that cap off weeks of hunting and gathering faded receipts and sorting through reams of credit card bills to find all the dollars we spent on work. The task is more tedious than all the Wednesdays of taking out trash bins combined, and equally as exciting. But wait, that’s not all.
This weekend I’ve been chatting with bots from a solar company trying to solve our drop in energy production and sat on terminal hold with apparently one person who answers the phone for Amazon. There’s also an homeowner’s association meeting to prepare for and research to be done on ceiling fans.
“Life admin” is a crisp phrase coined by Elizabeth Emens, JD, PhD, that captures the never-ending to-do list that comes with running a household. An accomplished law professor at Columbia University, New York, Dr. Emens noticed the negative impact this life admin has on our quality of life. Reading her book, “Life Admin: How I Learned to Do Less, Do Better, and Live More” (New York: HarperOne, 2019), your eyes widen as she magically makes salient all this hidden work that is stealing our time. Life admin, kidmin, mom and dadmin, just rattling them off feels like donning x-ray glasses allowing us to see how much work we do outside of our work. As doctors, I would add “family house calls,” as a contributing factor: Random family and friends who want to talk for a minute about their knee replacement or what drug the ICU should give Uncle Larry who is fighting COVID. (I only know ivermectin, but it would only help if he just had scabies).
By all accounts, the amount of life admin is growing insidiously, worsened by the great pandemic. There are events to plan and reply to, more DIY customer service to fix your own problems, more work to find a VRBO for a weekend getaway at the beach. (There are none on the entire coast of California this summer, so I just saved you time there. You’re welcome.)
There is no good time to do this work and combined with the heavy burden of our responsibilities as physicians, it can feel like fuel feeding the burnout fire.
Dr. Emens has some top tips to help. First up, know your admin type. Are you a super doer, reluctant doer, admin denier, or admin avoider? I’m mostly in the avoider quadrant, dropping into reluctant doer when consequences loom. Next, choose strategies that fit you. Instead of avoiding, there are some things I might deflect. For example, When your aunt in Peoria asks where she can get a COVID test, you can use LMGTFY.com to generate a link that will show them how to use Google to help with their question. Dr. Emens is joking, but the point rang true. We can lighten the load a bit if we delegate or push back the excessive or undue requests. For some tasks, we’d be better off paying someone to take it over. Last tip here, try doing life admin with a partner, be it spouse, friend, or colleague. This is particularly useful when your partner is a super doer, as mine is. Not only can they make the work lighter, but also less dreary.
We physicians are focused on fixing physician burnout. Maybe we should also be looking at what happens in the “second shift” at home. Tax season is over, but will be back soon.
Dr. Benabio is director of Healthcare Transformation and chief of dermatology at Kaiser Permanente San Diego. The opinions expressed in this column are his own and do not represent those of Kaiser Permanente. Dr. Benabio is @Dermdoc on Twitter. Write to him at [email protected]
More medical schools build training in transgender care
Klay Noto wants to be the kind of doctor he never had when he began to question his gender identity.
A second-year student at Tulane University in New Orleans, he wants to listen compassionately to patients’ concerns and recognize the hurt when they question who they are. He will be the kind of doctor who knows that a breast exam can be traumatizing if someone has been breast binding or that instructing a patient to take everything off and put on a gown can be triggering for someone with gender dysphoria.
Being in the room for hard conversations is part of why he pursued med school. “There aren’t many LGBT people in medicine and as I started to understand all the dynamics that go into it, I started to see that I could do it and I could be that different kind of doctor,” he told this news organization.
Mr. Noto, who transitioned after college, wants to see more transgender people like himself teaching gender medicine, and for all medical students to be trained in what it means to be transgender and how to give compassionate and comprehensive care to all patients.
Gains have been made in providing curriculum in transgender care that trains medical students in such concepts as how to approach gender identity with sensitivity and how to manage hormone therapy and surgery for transitioning patients who request that, according to those interviewed for this story.
But they agree there’s a long way to go to having widespread medical school integration of the health care needs of about 1.4 million transgender people in the United States.
According to the Association of American Medical Colleges (AAMC) Curriculum Inventory data collected from 131 U.S. medical schools, more than 65% offered some form of transgender-related education in 2018, and more than 80% of those provided such curriculum in required courses.
Lack of transgender, nonbinary faculty
Jason Klein, MD, is a pediatric endocrinologist and medical director of the Transgender Youth Health Program at New York (N.Y.) University.
He said in an interview that the number of programs nationally that have gender medicine as a structured part of their curriculum has increased over the last 5-10 years, but that education is not standardized from program to program.
The program at NYU includes lecture-style learning, case presentations, real-world conversations with people in the community, group discussions, and patient care, Dr. Klein said. There are formal lectures as part of adolescent medicine where students learn the differences between gender and sexual identity, and education on medical treatment of transgender and nonbinary adolescents, starting with puberty blockers and moving into affirming hormones.
Doctors also learn to know their limits and decide when to refer patients to a specialist.
“The focus is really about empathic and supportive care,” said Dr. Klein, assistant professor in the department of pediatrics at Hassenfeld Children’s Hospital at NYU Langone Health. “It’s about communication and understanding and the language we use and how to deliver affirming care in a health care setting in general.”
Imagine the potential stressors, he said, of a transgender person entering a typical health care setting. The electronic health record may only have room for the legal name of a person and not the name a person may currently be using. The intake form typically asks patients to check either male or female. The bathrooms give the same two choices.
“Every physician should know how to speak with, treat, emote with, and empathize with care for the trans and nonbinary individual,” Dr. Klein said.
Dr. Klein noted there is a glaring shortage of trans and nonbinary physicians to lead efforts to expand education on integrating the medical, psychological, and psychosocial care that patients will receive.
Currently, gender medicine is not included on board exams for adolescent medicine or endocrinology, he said.
“Adding formal training in gender medicine to board exams would really help solidify the importance of this arena of medicine,” he noted.
First AAMC standards
In 2014, the AAMC released the first standards to guide curricula across medical school and residency to support training doctors to be competent in caring for transgender patients.
The standards include recommending that all doctors be able to communicate with patients related to their gender identity and understand how to deliver high-quality care to transgender and gender-diverse patients within their specialty, Kristen L. Eckstrand, MD, a coauthor of the guidelines, told this news organization.
“Many medical schools have developed their own curricula to meet these standards,” said Dr. Eckstrand, medical director for LGBTQIA+ Health at the University of Pittsburgh Medical Center.
Norma Poll-Hunter, PhD, AAMC’s senior director for workforce diversity, noted that the organization recently released its diversity, equity, and inclusion competencies that guide the medical education of students, residents, and faculty.
Dr. Poll-Hunter told this news organization that AAMC partners with the Building the Next Generation of Academic Physicians LGBT Health Workforce Conference “to support safe spaces for scholarly efforts and mentorship to advance this area of work.”
Team approach at Rutgers
Among the medical schools that incorporate comprehensive transgender care into the curriculum is Rutgers University’s Robert Wood Johnson Medical School in New Brunswick, N.J.
Gloria Bachmann, MD, is professor of obstetrics and gynecology at the school and medical director of its partner, the PROUD Gender Center of New Jersey. PROUD stands for “Promoting Respect, Outreach, Understanding, and Dignity,” and the center provides comprehensive care for transgender and nonbinary patients in one location.
Dr. Bachmann said Rutgers takes a team approach with both instructors and learners teaching medical students about transgender care. The teachers are not only professors in traditional classroom lectures, but patient navigators and nurses at the PROUD center, established as part of the medical school in 2020. Students learn from the navigators, for instance, how to help patients through the spectrum of inpatient and outpatient care.
“All of our learners do get to care for individuals who identify as transgender,” said Dr. Bachmann.
Among the improvements in educating students on transgender care over the years, she said, is the emphasis on social determinants of health. In the transgender population, initial questions may include whether the person is able to access care through insurance as laws vary widely on what care and procedures are covered.
As another example, Dr. Bachmann cites: “If they are seen on an emergency basis and are sent home with medication and follow-up, can they afford it?”
Another consideration is whether there is a home to which they can return.
“Many individuals who are transgender may not have a home. Their family may not be accepting of them. Therefore, it’s the social determinants of health as well as their transgender identity that have to be put into the equation of best care,” she said.
Giving back to the trans community
Mr. Noto doesn’t know whether he will specialize in gender medicine, but he is committed to serving the transgender community in whatever physician path he chooses.
He said he realizes he is fortunate to have strong family support and good insurance and that he can afford fees, such as the copay to see transgender care specialists. Many in the community do not have those resources and are likely to get care “only if they have to.”
At Tulane, training in transgender care starts during orientation week and continues on different levels, with different options, throughout medical school and residency, he added.
Mr. Noto said he would like to see more mandatory learning such as a “queer-centered exam, where you have to give an organ inventory and you have to ask patients if it’s OK to talk about X, Y, and Z.” He’d also like more opportunities for clinical interaction with transgender patients, such as queer-centered rotations.
When physicians aren’t well trained in transgender care, you have patients educating the doctors, which, Mr. Noto said, should not be acceptable.
“People come to you on their worst day. And to not be informed about them in my mind is negligent. In what other population can you choose not to learn about someone just because you don’t want to?” he said.
A version of this article first appeared on Medscape.com.
Klay Noto wants to be the kind of doctor he never had when he began to question his gender identity.
A second-year student at Tulane University in New Orleans, he wants to listen compassionately to patients’ concerns and recognize the hurt when they question who they are. He will be the kind of doctor who knows that a breast exam can be traumatizing if someone has been breast binding or that instructing a patient to take everything off and put on a gown can be triggering for someone with gender dysphoria.
Being in the room for hard conversations is part of why he pursued med school. “There aren’t many LGBT people in medicine and as I started to understand all the dynamics that go into it, I started to see that I could do it and I could be that different kind of doctor,” he told this news organization.
Mr. Noto, who transitioned after college, wants to see more transgender people like himself teaching gender medicine, and for all medical students to be trained in what it means to be transgender and how to give compassionate and comprehensive care to all patients.
Gains have been made in providing curriculum in transgender care that trains medical students in such concepts as how to approach gender identity with sensitivity and how to manage hormone therapy and surgery for transitioning patients who request that, according to those interviewed for this story.
But they agree there’s a long way to go to having widespread medical school integration of the health care needs of about 1.4 million transgender people in the United States.
According to the Association of American Medical Colleges (AAMC) Curriculum Inventory data collected from 131 U.S. medical schools, more than 65% offered some form of transgender-related education in 2018, and more than 80% of those provided such curriculum in required courses.
Lack of transgender, nonbinary faculty
Jason Klein, MD, is a pediatric endocrinologist and medical director of the Transgender Youth Health Program at New York (N.Y.) University.
He said in an interview that the number of programs nationally that have gender medicine as a structured part of their curriculum has increased over the last 5-10 years, but that education is not standardized from program to program.
The program at NYU includes lecture-style learning, case presentations, real-world conversations with people in the community, group discussions, and patient care, Dr. Klein said. There are formal lectures as part of adolescent medicine where students learn the differences between gender and sexual identity, and education on medical treatment of transgender and nonbinary adolescents, starting with puberty blockers and moving into affirming hormones.
Doctors also learn to know their limits and decide when to refer patients to a specialist.
“The focus is really about empathic and supportive care,” said Dr. Klein, assistant professor in the department of pediatrics at Hassenfeld Children’s Hospital at NYU Langone Health. “It’s about communication and understanding and the language we use and how to deliver affirming care in a health care setting in general.”
Imagine the potential stressors, he said, of a transgender person entering a typical health care setting. The electronic health record may only have room for the legal name of a person and not the name a person may currently be using. The intake form typically asks patients to check either male or female. The bathrooms give the same two choices.
“Every physician should know how to speak with, treat, emote with, and empathize with care for the trans and nonbinary individual,” Dr. Klein said.
Dr. Klein noted there is a glaring shortage of trans and nonbinary physicians to lead efforts to expand education on integrating the medical, psychological, and psychosocial care that patients will receive.
Currently, gender medicine is not included on board exams for adolescent medicine or endocrinology, he said.
“Adding formal training in gender medicine to board exams would really help solidify the importance of this arena of medicine,” he noted.
First AAMC standards
In 2014, the AAMC released the first standards to guide curricula across medical school and residency to support training doctors to be competent in caring for transgender patients.
The standards include recommending that all doctors be able to communicate with patients related to their gender identity and understand how to deliver high-quality care to transgender and gender-diverse patients within their specialty, Kristen L. Eckstrand, MD, a coauthor of the guidelines, told this news organization.
“Many medical schools have developed their own curricula to meet these standards,” said Dr. Eckstrand, medical director for LGBTQIA+ Health at the University of Pittsburgh Medical Center.
Norma Poll-Hunter, PhD, AAMC’s senior director for workforce diversity, noted that the organization recently released its diversity, equity, and inclusion competencies that guide the medical education of students, residents, and faculty.
Dr. Poll-Hunter told this news organization that AAMC partners with the Building the Next Generation of Academic Physicians LGBT Health Workforce Conference “to support safe spaces for scholarly efforts and mentorship to advance this area of work.”
Team approach at Rutgers
Among the medical schools that incorporate comprehensive transgender care into the curriculum is Rutgers University’s Robert Wood Johnson Medical School in New Brunswick, N.J.
Gloria Bachmann, MD, is professor of obstetrics and gynecology at the school and medical director of its partner, the PROUD Gender Center of New Jersey. PROUD stands for “Promoting Respect, Outreach, Understanding, and Dignity,” and the center provides comprehensive care for transgender and nonbinary patients in one location.
Dr. Bachmann said Rutgers takes a team approach with both instructors and learners teaching medical students about transgender care. The teachers are not only professors in traditional classroom lectures, but patient navigators and nurses at the PROUD center, established as part of the medical school in 2020. Students learn from the navigators, for instance, how to help patients through the spectrum of inpatient and outpatient care.
“All of our learners do get to care for individuals who identify as transgender,” said Dr. Bachmann.
Among the improvements in educating students on transgender care over the years, she said, is the emphasis on social determinants of health. In the transgender population, initial questions may include whether the person is able to access care through insurance as laws vary widely on what care and procedures are covered.
As another example, Dr. Bachmann cites: “If they are seen on an emergency basis and are sent home with medication and follow-up, can they afford it?”
Another consideration is whether there is a home to which they can return.
“Many individuals who are transgender may not have a home. Their family may not be accepting of them. Therefore, it’s the social determinants of health as well as their transgender identity that have to be put into the equation of best care,” she said.
Giving back to the trans community
Mr. Noto doesn’t know whether he will specialize in gender medicine, but he is committed to serving the transgender community in whatever physician path he chooses.
He said he realizes he is fortunate to have strong family support and good insurance and that he can afford fees, such as the copay to see transgender care specialists. Many in the community do not have those resources and are likely to get care “only if they have to.”
At Tulane, training in transgender care starts during orientation week and continues on different levels, with different options, throughout medical school and residency, he added.
Mr. Noto said he would like to see more mandatory learning such as a “queer-centered exam, where you have to give an organ inventory and you have to ask patients if it’s OK to talk about X, Y, and Z.” He’d also like more opportunities for clinical interaction with transgender patients, such as queer-centered rotations.
When physicians aren’t well trained in transgender care, you have patients educating the doctors, which, Mr. Noto said, should not be acceptable.
“People come to you on their worst day. And to not be informed about them in my mind is negligent. In what other population can you choose not to learn about someone just because you don’t want to?” he said.
A version of this article first appeared on Medscape.com.
Klay Noto wants to be the kind of doctor he never had when he began to question his gender identity.
A second-year student at Tulane University in New Orleans, he wants to listen compassionately to patients’ concerns and recognize the hurt when they question who they are. He will be the kind of doctor who knows that a breast exam can be traumatizing if someone has been breast binding or that instructing a patient to take everything off and put on a gown can be triggering for someone with gender dysphoria.
Being in the room for hard conversations is part of why he pursued med school. “There aren’t many LGBT people in medicine and as I started to understand all the dynamics that go into it, I started to see that I could do it and I could be that different kind of doctor,” he told this news organization.
Mr. Noto, who transitioned after college, wants to see more transgender people like himself teaching gender medicine, and for all medical students to be trained in what it means to be transgender and how to give compassionate and comprehensive care to all patients.
Gains have been made in providing curriculum in transgender care that trains medical students in such concepts as how to approach gender identity with sensitivity and how to manage hormone therapy and surgery for transitioning patients who request that, according to those interviewed for this story.
But they agree there’s a long way to go to having widespread medical school integration of the health care needs of about 1.4 million transgender people in the United States.
According to the Association of American Medical Colleges (AAMC) Curriculum Inventory data collected from 131 U.S. medical schools, more than 65% offered some form of transgender-related education in 2018, and more than 80% of those provided such curriculum in required courses.
Lack of transgender, nonbinary faculty
Jason Klein, MD, is a pediatric endocrinologist and medical director of the Transgender Youth Health Program at New York (N.Y.) University.
He said in an interview that the number of programs nationally that have gender medicine as a structured part of their curriculum has increased over the last 5-10 years, but that education is not standardized from program to program.
The program at NYU includes lecture-style learning, case presentations, real-world conversations with people in the community, group discussions, and patient care, Dr. Klein said. There are formal lectures as part of adolescent medicine where students learn the differences between gender and sexual identity, and education on medical treatment of transgender and nonbinary adolescents, starting with puberty blockers and moving into affirming hormones.
Doctors also learn to know their limits and decide when to refer patients to a specialist.
“The focus is really about empathic and supportive care,” said Dr. Klein, assistant professor in the department of pediatrics at Hassenfeld Children’s Hospital at NYU Langone Health. “It’s about communication and understanding and the language we use and how to deliver affirming care in a health care setting in general.”
Imagine the potential stressors, he said, of a transgender person entering a typical health care setting. The electronic health record may only have room for the legal name of a person and not the name a person may currently be using. The intake form typically asks patients to check either male or female. The bathrooms give the same two choices.
“Every physician should know how to speak with, treat, emote with, and empathize with care for the trans and nonbinary individual,” Dr. Klein said.
Dr. Klein noted there is a glaring shortage of trans and nonbinary physicians to lead efforts to expand education on integrating the medical, psychological, and psychosocial care that patients will receive.
Currently, gender medicine is not included on board exams for adolescent medicine or endocrinology, he said.
“Adding formal training in gender medicine to board exams would really help solidify the importance of this arena of medicine,” he noted.
First AAMC standards
In 2014, the AAMC released the first standards to guide curricula across medical school and residency to support training doctors to be competent in caring for transgender patients.
The standards include recommending that all doctors be able to communicate with patients related to their gender identity and understand how to deliver high-quality care to transgender and gender-diverse patients within their specialty, Kristen L. Eckstrand, MD, a coauthor of the guidelines, told this news organization.
“Many medical schools have developed their own curricula to meet these standards,” said Dr. Eckstrand, medical director for LGBTQIA+ Health at the University of Pittsburgh Medical Center.
Norma Poll-Hunter, PhD, AAMC’s senior director for workforce diversity, noted that the organization recently released its diversity, equity, and inclusion competencies that guide the medical education of students, residents, and faculty.
Dr. Poll-Hunter told this news organization that AAMC partners with the Building the Next Generation of Academic Physicians LGBT Health Workforce Conference “to support safe spaces for scholarly efforts and mentorship to advance this area of work.”
Team approach at Rutgers
Among the medical schools that incorporate comprehensive transgender care into the curriculum is Rutgers University’s Robert Wood Johnson Medical School in New Brunswick, N.J.
Gloria Bachmann, MD, is professor of obstetrics and gynecology at the school and medical director of its partner, the PROUD Gender Center of New Jersey. PROUD stands for “Promoting Respect, Outreach, Understanding, and Dignity,” and the center provides comprehensive care for transgender and nonbinary patients in one location.
Dr. Bachmann said Rutgers takes a team approach with both instructors and learners teaching medical students about transgender care. The teachers are not only professors in traditional classroom lectures, but patient navigators and nurses at the PROUD center, established as part of the medical school in 2020. Students learn from the navigators, for instance, how to help patients through the spectrum of inpatient and outpatient care.
“All of our learners do get to care for individuals who identify as transgender,” said Dr. Bachmann.
Among the improvements in educating students on transgender care over the years, she said, is the emphasis on social determinants of health. In the transgender population, initial questions may include whether the person is able to access care through insurance as laws vary widely on what care and procedures are covered.
As another example, Dr. Bachmann cites: “If they are seen on an emergency basis and are sent home with medication and follow-up, can they afford it?”
Another consideration is whether there is a home to which they can return.
“Many individuals who are transgender may not have a home. Their family may not be accepting of them. Therefore, it’s the social determinants of health as well as their transgender identity that have to be put into the equation of best care,” she said.
Giving back to the trans community
Mr. Noto doesn’t know whether he will specialize in gender medicine, but he is committed to serving the transgender community in whatever physician path he chooses.
He said he realizes he is fortunate to have strong family support and good insurance and that he can afford fees, such as the copay to see transgender care specialists. Many in the community do not have those resources and are likely to get care “only if they have to.”
At Tulane, training in transgender care starts during orientation week and continues on different levels, with different options, throughout medical school and residency, he added.
Mr. Noto said he would like to see more mandatory learning such as a “queer-centered exam, where you have to give an organ inventory and you have to ask patients if it’s OK to talk about X, Y, and Z.” He’d also like more opportunities for clinical interaction with transgender patients, such as queer-centered rotations.
When physicians aren’t well trained in transgender care, you have patients educating the doctors, which, Mr. Noto said, should not be acceptable.
“People come to you on their worst day. And to not be informed about them in my mind is negligent. In what other population can you choose not to learn about someone just because you don’t want to?” he said.
A version of this article first appeared on Medscape.com.
Abnormal growth of the amygdala in infants tied to autism
A new study suggests that overgrowth of the amygdala in infants during the first 6-12 months of life is tied to a later diagnosis of autism spectrum disorder (ASD).
“The faster the amygdala grew in infancy, the more social difficulties the child showed when diagnosed with autism a year later,” first author Mark Shen, PhD, assistant professor of psychiatry and neuroscience, University of North Carolina, Chapel Hill, told this news organization.
The study was published online in the American Journal of Psychiatry.
Unique to autism
The amygdala plays a key role in processing memory, emotional responses, and decisionmaking.
It’s long been known that the amygdala is abnormally large in school-aged children with ASD, but until now, it was not known precisely when aberrant amygdala growth happens, what the clinical consequences may be, and whether amygdala overgrowth is unique to autism.
To investigate, Dr. Shen and colleagues evaluated 1,099 longitudinal MRI scans obtained during natural sleep at 6, 12, and 24 months of age in 408 infants in the Infant Brain Imaging Study (IBIS) Network.
The cohort included 58 infants at high likelihood of developing ASD who were later diagnosed with the disorder, 212 infants at high likelihood of ASD who did not develop ASD, 109 typically-developing control infants, and 29 infants with fragile X syndrome.
At 6 months, infants who developed ASD had typically sized amygdala volumes but showed significantly faster amygdala growth between 6 and 24 months, such that by 12 months the ASD group had significantly larger amygdala volume (Cohen’s d = 0.56), compared with all other groups.
Amygdala growth rate between 6 and 12 months was significantly associated with greater social deficits at 24 months when the children were diagnosed with ASD.
“We found that the amygdala grows too rapidly between 6 and 12 months of age, during a presymptomatic period in autism, prior to when the diagnostic symptoms of autism (social difficulties and repetitive behaviors) are evident and lead to the later diagnosis of autism,” Dr. Shen said in an interview.
This brain growth pattern appears to be unique to autism, as babies with the genetic disorder fragile X syndrome – another neurodevelopmental condition – showed a markedly different brain growth pattern: no differences in amygdala growth but enlargement of a different brain structure, the caudate, which was linked to increased repetitive behaviors, the investigators found.
Earlier intervention
Prior research has shown that children who are later diagnosed with ASD often display problems in infancy with how they attend to visual stimuli in their surroundings.
These early problems with processing visual and sensory information may put increased stress on the amygdala, potentially leading to amygdala hyperactivity, deficits in pruning dendritic connections, and overgrowth, Dr. Shen and colleagues hypothesize.
Amygdala overgrowth has also been linked to chronic stress in studies of other psychiatric conditions, such as depression and anxiety, and may provide a clue to understanding this observation in infants who later develop autism.
“This research suggests that an optimal time to begin supports for children who are at the highest likelihood of developing autism may be during the first year of life: to improve early precursors to social development, such as sensory processing, in babies even before social difficulties arise,” Dr. Shen said.
Cyrus A. Raji, MD, PhD, assistant professor of radiology and neurology, Washington University, St. Louis, said, “What makes this study important is the finding of abnormally increased amygdala growth rate in autism using a longitudinal design that focuses on earlier development.”
“While we are typically used to understanding brain structure as abnormally decreasing over time in certain disorders like Alzheimer’s disease, this study challenges us to understand that too much brain volume growth can also be abnormal in specific conditions,” Dr. Raji added.
This research was supported by grants from the Eunice Kennedy Shriver National Institute of Child Health and Human Development, National Institute of Environmental Health Sciences, and National Institute of Mental Health, along with Autism Speaks and the Simons Foundation. Dr. Shen and Dr. Raji have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
A new study suggests that overgrowth of the amygdala in infants during the first 6-12 months of life is tied to a later diagnosis of autism spectrum disorder (ASD).
“The faster the amygdala grew in infancy, the more social difficulties the child showed when diagnosed with autism a year later,” first author Mark Shen, PhD, assistant professor of psychiatry and neuroscience, University of North Carolina, Chapel Hill, told this news organization.
The study was published online in the American Journal of Psychiatry.
Unique to autism
The amygdala plays a key role in processing memory, emotional responses, and decisionmaking.
It’s long been known that the amygdala is abnormally large in school-aged children with ASD, but until now, it was not known precisely when aberrant amygdala growth happens, what the clinical consequences may be, and whether amygdala overgrowth is unique to autism.
To investigate, Dr. Shen and colleagues evaluated 1,099 longitudinal MRI scans obtained during natural sleep at 6, 12, and 24 months of age in 408 infants in the Infant Brain Imaging Study (IBIS) Network.
The cohort included 58 infants at high likelihood of developing ASD who were later diagnosed with the disorder, 212 infants at high likelihood of ASD who did not develop ASD, 109 typically-developing control infants, and 29 infants with fragile X syndrome.
At 6 months, infants who developed ASD had typically sized amygdala volumes but showed significantly faster amygdala growth between 6 and 24 months, such that by 12 months the ASD group had significantly larger amygdala volume (Cohen’s d = 0.56), compared with all other groups.
Amygdala growth rate between 6 and 12 months was significantly associated with greater social deficits at 24 months when the children were diagnosed with ASD.
“We found that the amygdala grows too rapidly between 6 and 12 months of age, during a presymptomatic period in autism, prior to when the diagnostic symptoms of autism (social difficulties and repetitive behaviors) are evident and lead to the later diagnosis of autism,” Dr. Shen said in an interview.
This brain growth pattern appears to be unique to autism, as babies with the genetic disorder fragile X syndrome – another neurodevelopmental condition – showed a markedly different brain growth pattern: no differences in amygdala growth but enlargement of a different brain structure, the caudate, which was linked to increased repetitive behaviors, the investigators found.
Earlier intervention
Prior research has shown that children who are later diagnosed with ASD often display problems in infancy with how they attend to visual stimuli in their surroundings.
These early problems with processing visual and sensory information may put increased stress on the amygdala, potentially leading to amygdala hyperactivity, deficits in pruning dendritic connections, and overgrowth, Dr. Shen and colleagues hypothesize.
Amygdala overgrowth has also been linked to chronic stress in studies of other psychiatric conditions, such as depression and anxiety, and may provide a clue to understanding this observation in infants who later develop autism.
“This research suggests that an optimal time to begin supports for children who are at the highest likelihood of developing autism may be during the first year of life: to improve early precursors to social development, such as sensory processing, in babies even before social difficulties arise,” Dr. Shen said.
Cyrus A. Raji, MD, PhD, assistant professor of radiology and neurology, Washington University, St. Louis, said, “What makes this study important is the finding of abnormally increased amygdala growth rate in autism using a longitudinal design that focuses on earlier development.”
“While we are typically used to understanding brain structure as abnormally decreasing over time in certain disorders like Alzheimer’s disease, this study challenges us to understand that too much brain volume growth can also be abnormal in specific conditions,” Dr. Raji added.
This research was supported by grants from the Eunice Kennedy Shriver National Institute of Child Health and Human Development, National Institute of Environmental Health Sciences, and National Institute of Mental Health, along with Autism Speaks and the Simons Foundation. Dr. Shen and Dr. Raji have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
A new study suggests that overgrowth of the amygdala in infants during the first 6-12 months of life is tied to a later diagnosis of autism spectrum disorder (ASD).
“The faster the amygdala grew in infancy, the more social difficulties the child showed when diagnosed with autism a year later,” first author Mark Shen, PhD, assistant professor of psychiatry and neuroscience, University of North Carolina, Chapel Hill, told this news organization.
The study was published online in the American Journal of Psychiatry.
Unique to autism
The amygdala plays a key role in processing memory, emotional responses, and decisionmaking.
It’s long been known that the amygdala is abnormally large in school-aged children with ASD, but until now, it was not known precisely when aberrant amygdala growth happens, what the clinical consequences may be, and whether amygdala overgrowth is unique to autism.
To investigate, Dr. Shen and colleagues evaluated 1,099 longitudinal MRI scans obtained during natural sleep at 6, 12, and 24 months of age in 408 infants in the Infant Brain Imaging Study (IBIS) Network.
The cohort included 58 infants at high likelihood of developing ASD who were later diagnosed with the disorder, 212 infants at high likelihood of ASD who did not develop ASD, 109 typically-developing control infants, and 29 infants with fragile X syndrome.
At 6 months, infants who developed ASD had typically sized amygdala volumes but showed significantly faster amygdala growth between 6 and 24 months, such that by 12 months the ASD group had significantly larger amygdala volume (Cohen’s d = 0.56), compared with all other groups.
Amygdala growth rate between 6 and 12 months was significantly associated with greater social deficits at 24 months when the children were diagnosed with ASD.
“We found that the amygdala grows too rapidly between 6 and 12 months of age, during a presymptomatic period in autism, prior to when the diagnostic symptoms of autism (social difficulties and repetitive behaviors) are evident and lead to the later diagnosis of autism,” Dr. Shen said in an interview.
This brain growth pattern appears to be unique to autism, as babies with the genetic disorder fragile X syndrome – another neurodevelopmental condition – showed a markedly different brain growth pattern: no differences in amygdala growth but enlargement of a different brain structure, the caudate, which was linked to increased repetitive behaviors, the investigators found.
Earlier intervention
Prior research has shown that children who are later diagnosed with ASD often display problems in infancy with how they attend to visual stimuli in their surroundings.
These early problems with processing visual and sensory information may put increased stress on the amygdala, potentially leading to amygdala hyperactivity, deficits in pruning dendritic connections, and overgrowth, Dr. Shen and colleagues hypothesize.
Amygdala overgrowth has also been linked to chronic stress in studies of other psychiatric conditions, such as depression and anxiety, and may provide a clue to understanding this observation in infants who later develop autism.
“This research suggests that an optimal time to begin supports for children who are at the highest likelihood of developing autism may be during the first year of life: to improve early precursors to social development, such as sensory processing, in babies even before social difficulties arise,” Dr. Shen said.
Cyrus A. Raji, MD, PhD, assistant professor of radiology and neurology, Washington University, St. Louis, said, “What makes this study important is the finding of abnormally increased amygdala growth rate in autism using a longitudinal design that focuses on earlier development.”
“While we are typically used to understanding brain structure as abnormally decreasing over time in certain disorders like Alzheimer’s disease, this study challenges us to understand that too much brain volume growth can also be abnormal in specific conditions,” Dr. Raji added.
This research was supported by grants from the Eunice Kennedy Shriver National Institute of Child Health and Human Development, National Institute of Environmental Health Sciences, and National Institute of Mental Health, along with Autism Speaks and the Simons Foundation. Dr. Shen and Dr. Raji have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Skin reactions to first COVID-19 vaccine don’t justify forgoing second dose
BOSTON – Requests for a according to an analysis of several large sets of data presented at the annual meeting of the American Academy of Dermatology.
According to the data, “there are no serious adverse consequences from these cutaneous reactions,” said Esther Freeman, MD, PhD, director of Global Health Dermatology, Massachusetts General Hospital, Boston.
This is important because the risk of vaccine hesitancy goes up dramatically in patients who experience reactions to the first vaccine dose, according to follow-up of more than 50,000 employees vaccinated in the Mass General Brigham Healthcare System (MGBHS). According to Dr. Freeman, there was almost a fourfold increase in the rate of second-dose refusals for those with cutaneous reactions and a more than fourfold increase in those who developed angioedema.
Before the data were available, skin reactions were a source of concern among dermatologists and others involved in monitoring vaccine-related adverse events. Injection site reactions (ISRs) are associated with essentially every injectable vaccine, so these were expected, but a small proportion of patients developed large red plaques in the injection arm 7-8 days after the inoculation.
“These delayed reactions caused a lot of initial panic,” said Dr. Freeman, who counted herself among those alarmed about what the reactions might signify. “Was this cellulitis? Would the next dose cause anaphylaxis? We were concerned.”
This concern dissipated with the availability of more data. In a global registry that has so far captured more than 1,000 cutaneous reactions from 52 participating countries, it appears that about 2% of patients have a cutaneous reaction other than an ISR after the first dose. All resolve with minimal skin care or no treatment.
After the second dose, the proportion is lower. If there is a reaction, it typically occurs earlier and resolves more quickly.
“What we have learned is that fewer than half of patients who had a reaction to the first dose have a reaction to the second, and those who did have a reaction had a milder course,” said Dr. Freeman.
These data are “incredibly reassuring” on many levels, she explained. In addition, it allows clinicians to confidently explain to patients that there are no serious sequelae from the rashes, whether immediate or delayed, from the available COVID-19 vaccines.
“Every skin reaction I have seen is something we can treat through,” she added, noting that most reactions resolve with little or no supportive care. Following skin reactions, particularly the delayed lesions, it is not uncommon for patients to refuse a second shot. Some request a medical waiver to avoid further vaccine exposure. According to Dr. Freeman, this is unwarranted.
“I have granted exactly zero waivers,” she said. She explains to patients that these reactions have not been predictive of serious events, such as anaphylaxis. Although the trigger of the hypersensitivity reaction remains unknown, there is no evidence of serious consequences.
Delayed skin reactions are more commonly associated with the Moderna than the Pfizer vaccine. One notable difference between these vaccines is the greater content of mRNA in the Moderna formulation, but Freeman said that this is only one potential hypothesis for higher frequency of reactions to this version of the vaccine.
Patients with a history of allergic disease are more likely to develop a reaction but not significantly more likely to have a reaction that is more difficult to manage, according to Kimberly G. Blumenthal, MD, quality and safety officer for allergy, and codirector of the clinical epidemiology program in the division of rheumatology, allergy, and immunology at Mass General.
Anaphylaxis has been associated with COVD-19 vaccines just as it has with essentially every injectable vaccine, Dr. Blumenthal said during the same session. But the risk is very low, and it stays low even among those with a history of severe hypersensitivity reactions in the past.
Among the data collected from more than 52,000 vaccinated MGBHS employees, 0.9% had a history of severe allergic reaction to a prior vaccine. Of these, 11.6% had an allergic reaction to the COVID-19 vaccine. This was more than twice the 4.6% rate of allergic reactions among employees without a history of allergic reactions, but serious consequences were rare in both groups.
Of those with a reaction to the first dose, all but 2.4% took a subsequent dose. Again, serious reactions were exceedingly rare. These serious reactions did include anaphylaxis and hospitalization in 3% of patients, but there were no fatalities and all resolved.
The absence of serious sequelae from a reaction to a COVID-19 vaccine must be considered within the context of the benefit, which includes protection from death and hospitalization from the virus, according to Dr. Blumenthal. Citing the evidence that first-shot reactions are a source of vaccine hesitancy, she agreed that it is important to educate patients about relative risks.
“Even in our own cohort of MGBHS employees, we have people, including those who had been provaccine in the past, become hesitant,” commented Dr. Blumenthal, who said there are data from the Kaiser Permanente System showing similar vaccine reluctance following a first-shot reaction.
After more than 500 million doses of the Moderna and Pfizer vaccines had been administered worldwide, there was not a single reported death from anaphylaxis. Although Dr. Blumenthal said that an unconfirmed death of this type had been recently reported, she emphasized that this single death, if valid, is dwarfed by the lives saved with vaccination.
Asked about her strategy for counseling patients with vaccine hesitancy, Dr. Freeman said the body of safety data is large and compelling. There is overwhelming evidence of a favorable benefit-to-risk ratio overall and among those with a first-shot reaction.
“I can reassure them on the basis of the data,” Dr. Freeman said in an interview. “Less than half will have a reaction to the second shot and even if they do have a reaction, it is likely to be less severe.”
Although the main message is that vaccination is potentially lifesaving and far outweighs any risks, Freeman specifically gives this message to those hesitant to take a second shot after a first-shot reaction: “I can get you through it.”
Dr. Freeman encouraged health care professionals to report cases of COVID-19 vaccine–related dermatologic side effects to the American Academy of Dermatology / International League of Dermatologic Societies COVID-19 dermatology registry. Dermatologic manifestations of COVID-19 can also be reported to the registry.
Dr. Freeman disclosed receiving grants/research funding from the International League of Dermatologic Societies and from the National Institutes of Health. Dr. Blumenthal disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
BOSTON – Requests for a according to an analysis of several large sets of data presented at the annual meeting of the American Academy of Dermatology.
According to the data, “there are no serious adverse consequences from these cutaneous reactions,” said Esther Freeman, MD, PhD, director of Global Health Dermatology, Massachusetts General Hospital, Boston.
This is important because the risk of vaccine hesitancy goes up dramatically in patients who experience reactions to the first vaccine dose, according to follow-up of more than 50,000 employees vaccinated in the Mass General Brigham Healthcare System (MGBHS). According to Dr. Freeman, there was almost a fourfold increase in the rate of second-dose refusals for those with cutaneous reactions and a more than fourfold increase in those who developed angioedema.
Before the data were available, skin reactions were a source of concern among dermatologists and others involved in monitoring vaccine-related adverse events. Injection site reactions (ISRs) are associated with essentially every injectable vaccine, so these were expected, but a small proportion of patients developed large red plaques in the injection arm 7-8 days after the inoculation.
“These delayed reactions caused a lot of initial panic,” said Dr. Freeman, who counted herself among those alarmed about what the reactions might signify. “Was this cellulitis? Would the next dose cause anaphylaxis? We were concerned.”
This concern dissipated with the availability of more data. In a global registry that has so far captured more than 1,000 cutaneous reactions from 52 participating countries, it appears that about 2% of patients have a cutaneous reaction other than an ISR after the first dose. All resolve with minimal skin care or no treatment.
After the second dose, the proportion is lower. If there is a reaction, it typically occurs earlier and resolves more quickly.
“What we have learned is that fewer than half of patients who had a reaction to the first dose have a reaction to the second, and those who did have a reaction had a milder course,” said Dr. Freeman.
These data are “incredibly reassuring” on many levels, she explained. In addition, it allows clinicians to confidently explain to patients that there are no serious sequelae from the rashes, whether immediate or delayed, from the available COVID-19 vaccines.
“Every skin reaction I have seen is something we can treat through,” she added, noting that most reactions resolve with little or no supportive care. Following skin reactions, particularly the delayed lesions, it is not uncommon for patients to refuse a second shot. Some request a medical waiver to avoid further vaccine exposure. According to Dr. Freeman, this is unwarranted.
“I have granted exactly zero waivers,” she said. She explains to patients that these reactions have not been predictive of serious events, such as anaphylaxis. Although the trigger of the hypersensitivity reaction remains unknown, there is no evidence of serious consequences.
Delayed skin reactions are more commonly associated with the Moderna than the Pfizer vaccine. One notable difference between these vaccines is the greater content of mRNA in the Moderna formulation, but Freeman said that this is only one potential hypothesis for higher frequency of reactions to this version of the vaccine.
Patients with a history of allergic disease are more likely to develop a reaction but not significantly more likely to have a reaction that is more difficult to manage, according to Kimberly G. Blumenthal, MD, quality and safety officer for allergy, and codirector of the clinical epidemiology program in the division of rheumatology, allergy, and immunology at Mass General.
Anaphylaxis has been associated with COVD-19 vaccines just as it has with essentially every injectable vaccine, Dr. Blumenthal said during the same session. But the risk is very low, and it stays low even among those with a history of severe hypersensitivity reactions in the past.
Among the data collected from more than 52,000 vaccinated MGBHS employees, 0.9% had a history of severe allergic reaction to a prior vaccine. Of these, 11.6% had an allergic reaction to the COVID-19 vaccine. This was more than twice the 4.6% rate of allergic reactions among employees without a history of allergic reactions, but serious consequences were rare in both groups.
Of those with a reaction to the first dose, all but 2.4% took a subsequent dose. Again, serious reactions were exceedingly rare. These serious reactions did include anaphylaxis and hospitalization in 3% of patients, but there were no fatalities and all resolved.
The absence of serious sequelae from a reaction to a COVID-19 vaccine must be considered within the context of the benefit, which includes protection from death and hospitalization from the virus, according to Dr. Blumenthal. Citing the evidence that first-shot reactions are a source of vaccine hesitancy, she agreed that it is important to educate patients about relative risks.
“Even in our own cohort of MGBHS employees, we have people, including those who had been provaccine in the past, become hesitant,” commented Dr. Blumenthal, who said there are data from the Kaiser Permanente System showing similar vaccine reluctance following a first-shot reaction.
After more than 500 million doses of the Moderna and Pfizer vaccines had been administered worldwide, there was not a single reported death from anaphylaxis. Although Dr. Blumenthal said that an unconfirmed death of this type had been recently reported, she emphasized that this single death, if valid, is dwarfed by the lives saved with vaccination.
Asked about her strategy for counseling patients with vaccine hesitancy, Dr. Freeman said the body of safety data is large and compelling. There is overwhelming evidence of a favorable benefit-to-risk ratio overall and among those with a first-shot reaction.
“I can reassure them on the basis of the data,” Dr. Freeman said in an interview. “Less than half will have a reaction to the second shot and even if they do have a reaction, it is likely to be less severe.”
Although the main message is that vaccination is potentially lifesaving and far outweighs any risks, Freeman specifically gives this message to those hesitant to take a second shot after a first-shot reaction: “I can get you through it.”
Dr. Freeman encouraged health care professionals to report cases of COVID-19 vaccine–related dermatologic side effects to the American Academy of Dermatology / International League of Dermatologic Societies COVID-19 dermatology registry. Dermatologic manifestations of COVID-19 can also be reported to the registry.
Dr. Freeman disclosed receiving grants/research funding from the International League of Dermatologic Societies and from the National Institutes of Health. Dr. Blumenthal disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
BOSTON – Requests for a according to an analysis of several large sets of data presented at the annual meeting of the American Academy of Dermatology.
According to the data, “there are no serious adverse consequences from these cutaneous reactions,” said Esther Freeman, MD, PhD, director of Global Health Dermatology, Massachusetts General Hospital, Boston.
This is important because the risk of vaccine hesitancy goes up dramatically in patients who experience reactions to the first vaccine dose, according to follow-up of more than 50,000 employees vaccinated in the Mass General Brigham Healthcare System (MGBHS). According to Dr. Freeman, there was almost a fourfold increase in the rate of second-dose refusals for those with cutaneous reactions and a more than fourfold increase in those who developed angioedema.
Before the data were available, skin reactions were a source of concern among dermatologists and others involved in monitoring vaccine-related adverse events. Injection site reactions (ISRs) are associated with essentially every injectable vaccine, so these were expected, but a small proportion of patients developed large red plaques in the injection arm 7-8 days after the inoculation.
“These delayed reactions caused a lot of initial panic,” said Dr. Freeman, who counted herself among those alarmed about what the reactions might signify. “Was this cellulitis? Would the next dose cause anaphylaxis? We were concerned.”
This concern dissipated with the availability of more data. In a global registry that has so far captured more than 1,000 cutaneous reactions from 52 participating countries, it appears that about 2% of patients have a cutaneous reaction other than an ISR after the first dose. All resolve with minimal skin care or no treatment.
After the second dose, the proportion is lower. If there is a reaction, it typically occurs earlier and resolves more quickly.
“What we have learned is that fewer than half of patients who had a reaction to the first dose have a reaction to the second, and those who did have a reaction had a milder course,” said Dr. Freeman.
These data are “incredibly reassuring” on many levels, she explained. In addition, it allows clinicians to confidently explain to patients that there are no serious sequelae from the rashes, whether immediate or delayed, from the available COVID-19 vaccines.
“Every skin reaction I have seen is something we can treat through,” she added, noting that most reactions resolve with little or no supportive care. Following skin reactions, particularly the delayed lesions, it is not uncommon for patients to refuse a second shot. Some request a medical waiver to avoid further vaccine exposure. According to Dr. Freeman, this is unwarranted.
“I have granted exactly zero waivers,” she said. She explains to patients that these reactions have not been predictive of serious events, such as anaphylaxis. Although the trigger of the hypersensitivity reaction remains unknown, there is no evidence of serious consequences.
Delayed skin reactions are more commonly associated with the Moderna than the Pfizer vaccine. One notable difference between these vaccines is the greater content of mRNA in the Moderna formulation, but Freeman said that this is only one potential hypothesis for higher frequency of reactions to this version of the vaccine.
Patients with a history of allergic disease are more likely to develop a reaction but not significantly more likely to have a reaction that is more difficult to manage, according to Kimberly G. Blumenthal, MD, quality and safety officer for allergy, and codirector of the clinical epidemiology program in the division of rheumatology, allergy, and immunology at Mass General.
Anaphylaxis has been associated with COVD-19 vaccines just as it has with essentially every injectable vaccine, Dr. Blumenthal said during the same session. But the risk is very low, and it stays low even among those with a history of severe hypersensitivity reactions in the past.
Among the data collected from more than 52,000 vaccinated MGBHS employees, 0.9% had a history of severe allergic reaction to a prior vaccine. Of these, 11.6% had an allergic reaction to the COVID-19 vaccine. This was more than twice the 4.6% rate of allergic reactions among employees without a history of allergic reactions, but serious consequences were rare in both groups.
Of those with a reaction to the first dose, all but 2.4% took a subsequent dose. Again, serious reactions were exceedingly rare. These serious reactions did include anaphylaxis and hospitalization in 3% of patients, but there were no fatalities and all resolved.
The absence of serious sequelae from a reaction to a COVID-19 vaccine must be considered within the context of the benefit, which includes protection from death and hospitalization from the virus, according to Dr. Blumenthal. Citing the evidence that first-shot reactions are a source of vaccine hesitancy, she agreed that it is important to educate patients about relative risks.
“Even in our own cohort of MGBHS employees, we have people, including those who had been provaccine in the past, become hesitant,” commented Dr. Blumenthal, who said there are data from the Kaiser Permanente System showing similar vaccine reluctance following a first-shot reaction.
After more than 500 million doses of the Moderna and Pfizer vaccines had been administered worldwide, there was not a single reported death from anaphylaxis. Although Dr. Blumenthal said that an unconfirmed death of this type had been recently reported, she emphasized that this single death, if valid, is dwarfed by the lives saved with vaccination.
Asked about her strategy for counseling patients with vaccine hesitancy, Dr. Freeman said the body of safety data is large and compelling. There is overwhelming evidence of a favorable benefit-to-risk ratio overall and among those with a first-shot reaction.
“I can reassure them on the basis of the data,” Dr. Freeman said in an interview. “Less than half will have a reaction to the second shot and even if they do have a reaction, it is likely to be less severe.”
Although the main message is that vaccination is potentially lifesaving and far outweighs any risks, Freeman specifically gives this message to those hesitant to take a second shot after a first-shot reaction: “I can get you through it.”
Dr. Freeman encouraged health care professionals to report cases of COVID-19 vaccine–related dermatologic side effects to the American Academy of Dermatology / International League of Dermatologic Societies COVID-19 dermatology registry. Dermatologic manifestations of COVID-19 can also be reported to the registry.
Dr. Freeman disclosed receiving grants/research funding from the International League of Dermatologic Societies and from the National Institutes of Health. Dr. Blumenthal disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
AT AAD 2022
Doctors treat osteoporosis with hormone therapy against guidelines
This type of hormone therapy (HT) can be given as estrogen or a combination of hormones including estrogen. The physicians interviewed for this piece who prescribe HT for osteoporosis suggest the benefits outweigh the downsides to its use for some of their patients. But such doctors may be a minority group, suggests Michael R. McClung, MD, founding director of the Oregon Osteoporosis Center, Portland.
According to Dr. McClung, HT is now rarely prescribed as treatment – as opposed to prevention – for osteoporosis in the absence of additional benefits such as reducing vasomotor symptoms.
Researchers’ findings on HT use in women with osteoporosis are complex. While HT is approved for menopausal prevention of osteoporosis, it is not indicated as a treatment for the disease by the Food and Drug Administration. See the prescribing information for Premarin tablets, which contain a mixture of estrogen hormones, for an example of the FDA’s indications and usage for the type of HT addressed in this article.
Women’s Health Initiative findings
The Women’s Health Initiative (WHI) hormone therapy trials showed that HT reduces the incidence of all osteoporosis-related fractures in postmenopausal women, even those at low risk of fracture, but osteoporosis-related fractures was not a study endpoint. These trials also revealed that HT was associated with increased risks of cardiovascular and cerebrovascular events, an increased risk of breast cancer, and other adverse health outcomes.
The release of the interim results of the WHI trials in 2002 led to a fair amount of fear and confusion about the use of HT after menopause. After the WHI findings were published, estrogen use dropped dramatically, but for everything, including for vasomotor symptoms and the prevention and treatment of osteoporosis.
Prior to the WHI study, it was very common for hormone therapy to be prescribed as women neared or entered menopause, said Risa Kagan MD, clinical professor of obstetrics, gynecology, and reproductive sciences, University of California, San Francisco.
“When a woman turned 50, that was one of the first things we did – was to put her on hormone therapy. All that changed with the WHI, but now we are coming full circle,” noted Dr. Kagan, who currently prescribes HT as first line treatment for osteoporosis to some women.
Hormone therapy’s complex history
HT’s ability to reduce bone loss in postmenopausal women is well-documented in many papers, including one published March 8, 2018, in Osteoporosis International, by Dr. Kagan and colleagues. This reduced bone loss has been shown to significantly reduce fractures in patients with low bone mass and osteoporosis.
While a growing number of therapies are now available to treat osteoporosis, HT was traditionally viewed as a standard method of preventing fractures in this population. It was also widely used to prevent other types of symptoms associated with the menopause, such as hot flashes, night sweats, and sleep disturbances, and multiple observational studies had demonstrated that its use appeared to reduce the incidence of cardiovascular disease (CVD) in symptomatic menopausal women who initiated HT in early menopause.
Even though the WHI studies were the largest randomized trials ever performed in postmenopausal women, they had notable limitations, according to Dr. Kagan.
“The women were older – the average age was 63 years,” she said. “And they only investigated one route and one dose of estrogen.”
Since then, many different formulations and routes of administration with more favorable safety profiles than what was used in the WHI have become available.
It’s both scientifically and clinically unsound to extrapolate the unfavorable risk-benefit profile of HT seen in the WHI trials to all women regardless of age, HT dosage or formulation, or the length of time they’re on it, she added.
Today’s use of HT in women with osteoporosis
Re-analyses and follow-up studies from the WHI trials, along with data from other studies, have suggested that the benefit-risk profiles of HT are affected by a variety of factors. These include the timing of use in relation to menopause and chronological age and the type of hormone regimen.
“Clinically, many advocate for [hormone therapy] use, especially in the newer younger postmenopausal women to prevent bone loss, but also in younger women who are diagnosed with osteoporosis and then as they get older transition to more bone specific agents,” noted Dr. Kagan.
“Some advocate preserving bone mass and preventing osteoporosis and even treating the younger newly postmenopausal women who have no contraindications with hormone therapy initially, and then gradually transitioning them to a bone specific agent as they get older and at risk for fracture.
“If a woman is already fractured and/or has very low bone density with no other obvious secondary metabolic reason, we also often advocate anabolic agents for 1-2 years then consider estrogen for maintenance – again, if [there is] no contraindication to using HT,” she added.
Thus, an individualized approach is recommended to determine a woman’s risk-benefit ratio of HT use based on the absolute risk of adverse effects, Dr. Kagan noted.
“Transdermal and low/ultra-low doses of HT, have a favorable risk profile, and are effective in preserving bone mineral density and bone quality in many women,” she said.
According to Dr. McClung, HT “is most often used for treatment in women in whom hormone therapy was begun for hot flashes and then, when osteoporosis was found later, was simply continued.
“Society guidelines are cautious about recommending hormone therapy for osteoporosis treatment since estrogen is not approved for treatment, despite the clear fracture protection benefit observed in the WHI study,” he said. “Since [women in the WHI trials] were not recruited as having osteoporosis, those results do not meet the FDA requirement for treatment approval, namely the reduction in fracture risk in patients with osteoporosis. However, knowing what we know about the salutary skeletal effects of estrogen, many of us do use them in our patients with osteoporosis – although not prescribed for that purpose.”
Additional scenarios when doctors may advise HT
“I often recommend – and I think colleagues do as well – that women with recent menopause and menopausal symptoms who also have low bone mineral density or even scores showing osteoporosis see their gynecologist to discuss HT for a few years, perhaps until age 60 if no contraindications, and if it is well tolerated,” said Ethel S. Siris, MD, professor of medicine at Columbia University Medical Center in New York.
“Once they stop it we can then give one of our other bone drugs, but it delays the need to start them since on adequate estrogen the bone density should remain stable while they take it,” added Dr. Siris, an endocrinologist and internist, and director of the Toni Stabile Osteoporosis Center in New York. “They may need a bisphosphonate or another bone drug to further protect them from bone loss and future fracture [after stopping HT].”
Victor L. Roberts, MD, founder of Endocrine Associates of Florida, Lake Mary, pointed out that women now have many options for treatment of osteoporosis.
“If a woman is in early menopause and is having other symptoms, then estrogen is warranted,” he said. “If she has osteoporosis, then it’s a bonus.”
“We have better agents that are bone specific,” for a patient who presents with osteoporosis and no other symptoms, he said.
“If a woman is intolerant of alendronate or other similar drugs, or chooses not to have an injectable, then estrogen or a SERM [selective estrogen receptor modulator] would be an option.”
Dr. Roberts added that HT would be more of a niche drug.
“It has a role and documented benefit and works,” he said. “There is good scientific data for the use of estrogen.”
Dr. Kagan is a consultant for Pfizer, Therapeutics MD, Amgen, on the Medical and Scientific Advisory Board of American Bone Health. The other experts interviewed for this piece reported no conflicts.
This type of hormone therapy (HT) can be given as estrogen or a combination of hormones including estrogen. The physicians interviewed for this piece who prescribe HT for osteoporosis suggest the benefits outweigh the downsides to its use for some of their patients. But such doctors may be a minority group, suggests Michael R. McClung, MD, founding director of the Oregon Osteoporosis Center, Portland.
According to Dr. McClung, HT is now rarely prescribed as treatment – as opposed to prevention – for osteoporosis in the absence of additional benefits such as reducing vasomotor symptoms.
Researchers’ findings on HT use in women with osteoporosis are complex. While HT is approved for menopausal prevention of osteoporosis, it is not indicated as a treatment for the disease by the Food and Drug Administration. See the prescribing information for Premarin tablets, which contain a mixture of estrogen hormones, for an example of the FDA’s indications and usage for the type of HT addressed in this article.
Women’s Health Initiative findings
The Women’s Health Initiative (WHI) hormone therapy trials showed that HT reduces the incidence of all osteoporosis-related fractures in postmenopausal women, even those at low risk of fracture, but osteoporosis-related fractures was not a study endpoint. These trials also revealed that HT was associated with increased risks of cardiovascular and cerebrovascular events, an increased risk of breast cancer, and other adverse health outcomes.
The release of the interim results of the WHI trials in 2002 led to a fair amount of fear and confusion about the use of HT after menopause. After the WHI findings were published, estrogen use dropped dramatically, but for everything, including for vasomotor symptoms and the prevention and treatment of osteoporosis.
Prior to the WHI study, it was very common for hormone therapy to be prescribed as women neared or entered menopause, said Risa Kagan MD, clinical professor of obstetrics, gynecology, and reproductive sciences, University of California, San Francisco.
“When a woman turned 50, that was one of the first things we did – was to put her on hormone therapy. All that changed with the WHI, but now we are coming full circle,” noted Dr. Kagan, who currently prescribes HT as first line treatment for osteoporosis to some women.
Hormone therapy’s complex history
HT’s ability to reduce bone loss in postmenopausal women is well-documented in many papers, including one published March 8, 2018, in Osteoporosis International, by Dr. Kagan and colleagues. This reduced bone loss has been shown to significantly reduce fractures in patients with low bone mass and osteoporosis.
While a growing number of therapies are now available to treat osteoporosis, HT was traditionally viewed as a standard method of preventing fractures in this population. It was also widely used to prevent other types of symptoms associated with the menopause, such as hot flashes, night sweats, and sleep disturbances, and multiple observational studies had demonstrated that its use appeared to reduce the incidence of cardiovascular disease (CVD) in symptomatic menopausal women who initiated HT in early menopause.
Even though the WHI studies were the largest randomized trials ever performed in postmenopausal women, they had notable limitations, according to Dr. Kagan.
“The women were older – the average age was 63 years,” she said. “And they only investigated one route and one dose of estrogen.”
Since then, many different formulations and routes of administration with more favorable safety profiles than what was used in the WHI have become available.
It’s both scientifically and clinically unsound to extrapolate the unfavorable risk-benefit profile of HT seen in the WHI trials to all women regardless of age, HT dosage or formulation, or the length of time they’re on it, she added.
Today’s use of HT in women with osteoporosis
Re-analyses and follow-up studies from the WHI trials, along with data from other studies, have suggested that the benefit-risk profiles of HT are affected by a variety of factors. These include the timing of use in relation to menopause and chronological age and the type of hormone regimen.
“Clinically, many advocate for [hormone therapy] use, especially in the newer younger postmenopausal women to prevent bone loss, but also in younger women who are diagnosed with osteoporosis and then as they get older transition to more bone specific agents,” noted Dr. Kagan.
“Some advocate preserving bone mass and preventing osteoporosis and even treating the younger newly postmenopausal women who have no contraindications with hormone therapy initially, and then gradually transitioning them to a bone specific agent as they get older and at risk for fracture.
“If a woman is already fractured and/or has very low bone density with no other obvious secondary metabolic reason, we also often advocate anabolic agents for 1-2 years then consider estrogen for maintenance – again, if [there is] no contraindication to using HT,” she added.
Thus, an individualized approach is recommended to determine a woman’s risk-benefit ratio of HT use based on the absolute risk of adverse effects, Dr. Kagan noted.
“Transdermal and low/ultra-low doses of HT, have a favorable risk profile, and are effective in preserving bone mineral density and bone quality in many women,” she said.
According to Dr. McClung, HT “is most often used for treatment in women in whom hormone therapy was begun for hot flashes and then, when osteoporosis was found later, was simply continued.
“Society guidelines are cautious about recommending hormone therapy for osteoporosis treatment since estrogen is not approved for treatment, despite the clear fracture protection benefit observed in the WHI study,” he said. “Since [women in the WHI trials] were not recruited as having osteoporosis, those results do not meet the FDA requirement for treatment approval, namely the reduction in fracture risk in patients with osteoporosis. However, knowing what we know about the salutary skeletal effects of estrogen, many of us do use them in our patients with osteoporosis – although not prescribed for that purpose.”
Additional scenarios when doctors may advise HT
“I often recommend – and I think colleagues do as well – that women with recent menopause and menopausal symptoms who also have low bone mineral density or even scores showing osteoporosis see their gynecologist to discuss HT for a few years, perhaps until age 60 if no contraindications, and if it is well tolerated,” said Ethel S. Siris, MD, professor of medicine at Columbia University Medical Center in New York.
“Once they stop it we can then give one of our other bone drugs, but it delays the need to start them since on adequate estrogen the bone density should remain stable while they take it,” added Dr. Siris, an endocrinologist and internist, and director of the Toni Stabile Osteoporosis Center in New York. “They may need a bisphosphonate or another bone drug to further protect them from bone loss and future fracture [after stopping HT].”
Victor L. Roberts, MD, founder of Endocrine Associates of Florida, Lake Mary, pointed out that women now have many options for treatment of osteoporosis.
“If a woman is in early menopause and is having other symptoms, then estrogen is warranted,” he said. “If she has osteoporosis, then it’s a bonus.”
“We have better agents that are bone specific,” for a patient who presents with osteoporosis and no other symptoms, he said.
“If a woman is intolerant of alendronate or other similar drugs, or chooses not to have an injectable, then estrogen or a SERM [selective estrogen receptor modulator] would be an option.”
Dr. Roberts added that HT would be more of a niche drug.
“It has a role and documented benefit and works,” he said. “There is good scientific data for the use of estrogen.”
Dr. Kagan is a consultant for Pfizer, Therapeutics MD, Amgen, on the Medical and Scientific Advisory Board of American Bone Health. The other experts interviewed for this piece reported no conflicts.
This type of hormone therapy (HT) can be given as estrogen or a combination of hormones including estrogen. The physicians interviewed for this piece who prescribe HT for osteoporosis suggest the benefits outweigh the downsides to its use for some of their patients. But such doctors may be a minority group, suggests Michael R. McClung, MD, founding director of the Oregon Osteoporosis Center, Portland.
According to Dr. McClung, HT is now rarely prescribed as treatment – as opposed to prevention – for osteoporosis in the absence of additional benefits such as reducing vasomotor symptoms.
Researchers’ findings on HT use in women with osteoporosis are complex. While HT is approved for menopausal prevention of osteoporosis, it is not indicated as a treatment for the disease by the Food and Drug Administration. See the prescribing information for Premarin tablets, which contain a mixture of estrogen hormones, for an example of the FDA’s indications and usage for the type of HT addressed in this article.
Women’s Health Initiative findings
The Women’s Health Initiative (WHI) hormone therapy trials showed that HT reduces the incidence of all osteoporosis-related fractures in postmenopausal women, even those at low risk of fracture, but osteoporosis-related fractures was not a study endpoint. These trials also revealed that HT was associated with increased risks of cardiovascular and cerebrovascular events, an increased risk of breast cancer, and other adverse health outcomes.
The release of the interim results of the WHI trials in 2002 led to a fair amount of fear and confusion about the use of HT after menopause. After the WHI findings were published, estrogen use dropped dramatically, but for everything, including for vasomotor symptoms and the prevention and treatment of osteoporosis.
Prior to the WHI study, it was very common for hormone therapy to be prescribed as women neared or entered menopause, said Risa Kagan MD, clinical professor of obstetrics, gynecology, and reproductive sciences, University of California, San Francisco.
“When a woman turned 50, that was one of the first things we did – was to put her on hormone therapy. All that changed with the WHI, but now we are coming full circle,” noted Dr. Kagan, who currently prescribes HT as first line treatment for osteoporosis to some women.
Hormone therapy’s complex history
HT’s ability to reduce bone loss in postmenopausal women is well-documented in many papers, including one published March 8, 2018, in Osteoporosis International, by Dr. Kagan and colleagues. This reduced bone loss has been shown to significantly reduce fractures in patients with low bone mass and osteoporosis.
While a growing number of therapies are now available to treat osteoporosis, HT was traditionally viewed as a standard method of preventing fractures in this population. It was also widely used to prevent other types of symptoms associated with the menopause, such as hot flashes, night sweats, and sleep disturbances, and multiple observational studies had demonstrated that its use appeared to reduce the incidence of cardiovascular disease (CVD) in symptomatic menopausal women who initiated HT in early menopause.
Even though the WHI studies were the largest randomized trials ever performed in postmenopausal women, they had notable limitations, according to Dr. Kagan.
“The women were older – the average age was 63 years,” she said. “And they only investigated one route and one dose of estrogen.”
Since then, many different formulations and routes of administration with more favorable safety profiles than what was used in the WHI have become available.
It’s both scientifically and clinically unsound to extrapolate the unfavorable risk-benefit profile of HT seen in the WHI trials to all women regardless of age, HT dosage or formulation, or the length of time they’re on it, she added.
Today’s use of HT in women with osteoporosis
Re-analyses and follow-up studies from the WHI trials, along with data from other studies, have suggested that the benefit-risk profiles of HT are affected by a variety of factors. These include the timing of use in relation to menopause and chronological age and the type of hormone regimen.
“Clinically, many advocate for [hormone therapy] use, especially in the newer younger postmenopausal women to prevent bone loss, but also in younger women who are diagnosed with osteoporosis and then as they get older transition to more bone specific agents,” noted Dr. Kagan.
“Some advocate preserving bone mass and preventing osteoporosis and even treating the younger newly postmenopausal women who have no contraindications with hormone therapy initially, and then gradually transitioning them to a bone specific agent as they get older and at risk for fracture.
“If a woman is already fractured and/or has very low bone density with no other obvious secondary metabolic reason, we also often advocate anabolic agents for 1-2 years then consider estrogen for maintenance – again, if [there is] no contraindication to using HT,” she added.
Thus, an individualized approach is recommended to determine a woman’s risk-benefit ratio of HT use based on the absolute risk of adverse effects, Dr. Kagan noted.
“Transdermal and low/ultra-low doses of HT, have a favorable risk profile, and are effective in preserving bone mineral density and bone quality in many women,” she said.
According to Dr. McClung, HT “is most often used for treatment in women in whom hormone therapy was begun for hot flashes and then, when osteoporosis was found later, was simply continued.
“Society guidelines are cautious about recommending hormone therapy for osteoporosis treatment since estrogen is not approved for treatment, despite the clear fracture protection benefit observed in the WHI study,” he said. “Since [women in the WHI trials] were not recruited as having osteoporosis, those results do not meet the FDA requirement for treatment approval, namely the reduction in fracture risk in patients with osteoporosis. However, knowing what we know about the salutary skeletal effects of estrogen, many of us do use them in our patients with osteoporosis – although not prescribed for that purpose.”
Additional scenarios when doctors may advise HT
“I often recommend – and I think colleagues do as well – that women with recent menopause and menopausal symptoms who also have low bone mineral density or even scores showing osteoporosis see their gynecologist to discuss HT for a few years, perhaps until age 60 if no contraindications, and if it is well tolerated,” said Ethel S. Siris, MD, professor of medicine at Columbia University Medical Center in New York.
“Once they stop it we can then give one of our other bone drugs, but it delays the need to start them since on adequate estrogen the bone density should remain stable while they take it,” added Dr. Siris, an endocrinologist and internist, and director of the Toni Stabile Osteoporosis Center in New York. “They may need a bisphosphonate or another bone drug to further protect them from bone loss and future fracture [after stopping HT].”
Victor L. Roberts, MD, founder of Endocrine Associates of Florida, Lake Mary, pointed out that women now have many options for treatment of osteoporosis.
“If a woman is in early menopause and is having other symptoms, then estrogen is warranted,” he said. “If she has osteoporosis, then it’s a bonus.”
“We have better agents that are bone specific,” for a patient who presents with osteoporosis and no other symptoms, he said.
“If a woman is intolerant of alendronate or other similar drugs, or chooses not to have an injectable, then estrogen or a SERM [selective estrogen receptor modulator] would be an option.”
Dr. Roberts added that HT would be more of a niche drug.
“It has a role and documented benefit and works,” he said. “There is good scientific data for the use of estrogen.”
Dr. Kagan is a consultant for Pfizer, Therapeutics MD, Amgen, on the Medical and Scientific Advisory Board of American Bone Health. The other experts interviewed for this piece reported no conflicts.
Surveillance program highly predictive for early autism
A population-based developmental surveillance program showed high diagnostic accuracy in identifying autism in a community-based sample of infants, toddlers, and preschoolers, according to new data published online in JAMA Network Open.
Researchers, led by Josephine Barbaro, PhD, of Olga Tennison Autism Research Centre at La Trobe University, Bundoora, Australia, said their findings indicate the benefit of using early autism developmental surveillance from infancy to the preschool period rather than one-time screening.
For the study, maternal and child health nurses in Melbourne were trained to use the Social Attention and Communication Surveillance–Revised (SACS-R) and SACS-Preschool (SACS-PR) tools during well-child checkups at 11-30 months of age and at follow-up (42 months of age). Dr. Barbaro helped develop the SACS tools.
Children identified as being at high likelihood for autism (1-2 years of age: n = 327; 42 months of age: n = 168) and at low likelihood for autism plus concerns (42 months of age: n = 28) were referred by their nurse for diagnostic assessment by the researchers.
Diagnostic accuracy of the SACS-R and SACS-PR was determined by comparing likelihood for autism with children’s diagnostic outcome using clinical judgment based on standard autism assessments.
Researchers included 13,511 children ages 11 months to 42 months. Results indicated the SACS-R with SACS-PR (SACS-R+PR) had very high diagnostic accuracy for early autism detection.
According to the paper, SACS-R showed 83% positive predictive value (95% confidence interval, 0.77-0.87) and 99% estimated negative predictive value (95% CI, 0.01-0.02). Specificity (99.6%; 95% CI, 0.99-1.00) was high, with modest sensitivity (62%; 95% CI, 0.57-0.66). When the SACS-PR 42-month assessment was added, estimated sensitivity grew to 96% (95% CI, 0.94-0.98).
“Its greater accuracy, compared with psychometrics of commonly used autism screening tools when used in community-based samples, suggests that the SACS-R+PR can be used universally for the early identification of autism,” the authors wrote.
According to La Trobe University, the tool is used in 10 other countries around the world – among them China, Singapore, Poland, Japan, New Zealand, Nepal, and Bangladesh.
Early identification is crucial for children on the autism spectrum and their families because it facilitates early diagnosis and can help families get access to supports and services.
About 2% of the world’s population is on the autism spectrum. Some studies report prevalence of 4% or higher, the authors noted.
The authors called attention to a systematic review of universal autism screening in primary care, including the Infant-Toddler Checklist and the Modified Checklist for Autism in Toddlers and various versions. The authors of the review noted that few studies had enough participants to establish population sensitivity, specificity, and positive predictive value. Also, psychometric properties reported were modest and/or wide ranging, putting into question the diagnostic accuracy of the tools.
Dr. Barbaro and colleagues highlighted an advantage the current study offers. “A critical difference in this study was the use of a community-based sample rather than a clinical or high-likelihood sibling sample, which may not be representative of the general population of children on the autism spectrum because child outcomes, cognition, and autism prevalence vary by ascertainment strategy and multiplex or simplex status.”
The authors explained that, in the United States, The U.S. Preventive Services Task Force has said there is not enough evidence to recommend universal autism screening and instead recommends routine general developmental surveillance. The American Academy of Pediatrics recommends developmental surveillance between 9 and 30 months and autism-specific screening at 18 and 24 months because of the benefits of early supports and services.
Karen Pierce, PhD, codirector of the Autism Center of Excellence at University of California, San Diego, said in an interview that she was pleased to see that the researchers were able to identify a high percentage of children on the autism spectrum.
She said, however, that the system proposed in this paper involves a substantial amount of time for training the nurses.
The authors acknowledged that, saying, “there may be instances in which this could be impractical.”
Dr. Pierce said that, in the United States, parent questionnaires are combined with clinical judgment to decide which kids are at risk.
“It doesn’t take very much time to fill out these questionnaires,” she said. “That’s the sticking point. I’m not saying necessarily that it shouldn’t be adopted. It would be very hard, I think, to incorporate into current pediatric practice.”
She said a benefit of the SACS program is more hands-on observation of the child, beyond the parent report, which sometimes can reflect more emotionally how the parent is feeling about the child.
She pointed out it was impressive that the Australian team found virtually no false positives.
The researchers also identified an additional 168 children using the preschool version at 42 months who had actually passed at the earlier checkpoint, using the regular SACS-R.
“This underscores a supercritical point,” Dr. Pierce said. “Just because your child may have gotten screened at 12, 18, 24 months and they pass and everything’s looking great, it doesn’t necessarily mean at some point early in development around age 3 that there [wouldn’t] be some clearer signs of autism.”
She said in her own study, published in JAMA Pediatrics, 24% of their sample tested fine at first but were later identified as having autism.
“It underscores the need for repeat screening,” Dr. Pierce said. “That was a striking finding in this study.”
She also pointed out that the authors talk about the “false dichotomy” between screening and surveillance. “They are saying it doesn’t have to be that way. It can be a combined effort. We can have parents filling out screening tools and we can have more observational sessions with kids during checkups. It doesn’t have to be this rigid line between screening and surveillance. I would completely agree with that.”
Dr. Barbaro reported receiving grants from the Sir Robert Menzies Foundation and the Cooperative Research Centre for Living with Autism (Autism CRC) during the study. Funds are partially distributed to Dr. Barbaro for the background intellectual property. One coauthor reported grants from the Menzies Foundation and Autism CRC during the study. Another coauthor reported receiving salary from Autism CRC during the study. No other disclosures were reported. This work was supported by an Allied Health Sciences start-up grant from the Menzies Foundation and the Cooperative Research Centre for Living with Autism, established and supported under the Australian Government’s Cooperative Research Centres Program. Dr. Pierce reports no relevant financial relationships.
A population-based developmental surveillance program showed high diagnostic accuracy in identifying autism in a community-based sample of infants, toddlers, and preschoolers, according to new data published online in JAMA Network Open.
Researchers, led by Josephine Barbaro, PhD, of Olga Tennison Autism Research Centre at La Trobe University, Bundoora, Australia, said their findings indicate the benefit of using early autism developmental surveillance from infancy to the preschool period rather than one-time screening.
For the study, maternal and child health nurses in Melbourne were trained to use the Social Attention and Communication Surveillance–Revised (SACS-R) and SACS-Preschool (SACS-PR) tools during well-child checkups at 11-30 months of age and at follow-up (42 months of age). Dr. Barbaro helped develop the SACS tools.
Children identified as being at high likelihood for autism (1-2 years of age: n = 327; 42 months of age: n = 168) and at low likelihood for autism plus concerns (42 months of age: n = 28) were referred by their nurse for diagnostic assessment by the researchers.
Diagnostic accuracy of the SACS-R and SACS-PR was determined by comparing likelihood for autism with children’s diagnostic outcome using clinical judgment based on standard autism assessments.
Researchers included 13,511 children ages 11 months to 42 months. Results indicated the SACS-R with SACS-PR (SACS-R+PR) had very high diagnostic accuracy for early autism detection.
According to the paper, SACS-R showed 83% positive predictive value (95% confidence interval, 0.77-0.87) and 99% estimated negative predictive value (95% CI, 0.01-0.02). Specificity (99.6%; 95% CI, 0.99-1.00) was high, with modest sensitivity (62%; 95% CI, 0.57-0.66). When the SACS-PR 42-month assessment was added, estimated sensitivity grew to 96% (95% CI, 0.94-0.98).
“Its greater accuracy, compared with psychometrics of commonly used autism screening tools when used in community-based samples, suggests that the SACS-R+PR can be used universally for the early identification of autism,” the authors wrote.
According to La Trobe University, the tool is used in 10 other countries around the world – among them China, Singapore, Poland, Japan, New Zealand, Nepal, and Bangladesh.
Early identification is crucial for children on the autism spectrum and their families because it facilitates early diagnosis and can help families get access to supports and services.
About 2% of the world’s population is on the autism spectrum. Some studies report prevalence of 4% or higher, the authors noted.
The authors called attention to a systematic review of universal autism screening in primary care, including the Infant-Toddler Checklist and the Modified Checklist for Autism in Toddlers and various versions. The authors of the review noted that few studies had enough participants to establish population sensitivity, specificity, and positive predictive value. Also, psychometric properties reported were modest and/or wide ranging, putting into question the diagnostic accuracy of the tools.
Dr. Barbaro and colleagues highlighted an advantage the current study offers. “A critical difference in this study was the use of a community-based sample rather than a clinical or high-likelihood sibling sample, which may not be representative of the general population of children on the autism spectrum because child outcomes, cognition, and autism prevalence vary by ascertainment strategy and multiplex or simplex status.”
The authors explained that, in the United States, The U.S. Preventive Services Task Force has said there is not enough evidence to recommend universal autism screening and instead recommends routine general developmental surveillance. The American Academy of Pediatrics recommends developmental surveillance between 9 and 30 months and autism-specific screening at 18 and 24 months because of the benefits of early supports and services.
Karen Pierce, PhD, codirector of the Autism Center of Excellence at University of California, San Diego, said in an interview that she was pleased to see that the researchers were able to identify a high percentage of children on the autism spectrum.
She said, however, that the system proposed in this paper involves a substantial amount of time for training the nurses.
The authors acknowledged that, saying, “there may be instances in which this could be impractical.”
Dr. Pierce said that, in the United States, parent questionnaires are combined with clinical judgment to decide which kids are at risk.
“It doesn’t take very much time to fill out these questionnaires,” she said. “That’s the sticking point. I’m not saying necessarily that it shouldn’t be adopted. It would be very hard, I think, to incorporate into current pediatric practice.”
She said a benefit of the SACS program is more hands-on observation of the child, beyond the parent report, which sometimes can reflect more emotionally how the parent is feeling about the child.
She pointed out it was impressive that the Australian team found virtually no false positives.
The researchers also identified an additional 168 children using the preschool version at 42 months who had actually passed at the earlier checkpoint, using the regular SACS-R.
“This underscores a supercritical point,” Dr. Pierce said. “Just because your child may have gotten screened at 12, 18, 24 months and they pass and everything’s looking great, it doesn’t necessarily mean at some point early in development around age 3 that there [wouldn’t] be some clearer signs of autism.”
She said in her own study, published in JAMA Pediatrics, 24% of their sample tested fine at first but were later identified as having autism.
“It underscores the need for repeat screening,” Dr. Pierce said. “That was a striking finding in this study.”
She also pointed out that the authors talk about the “false dichotomy” between screening and surveillance. “They are saying it doesn’t have to be that way. It can be a combined effort. We can have parents filling out screening tools and we can have more observational sessions with kids during checkups. It doesn’t have to be this rigid line between screening and surveillance. I would completely agree with that.”
Dr. Barbaro reported receiving grants from the Sir Robert Menzies Foundation and the Cooperative Research Centre for Living with Autism (Autism CRC) during the study. Funds are partially distributed to Dr. Barbaro for the background intellectual property. One coauthor reported grants from the Menzies Foundation and Autism CRC during the study. Another coauthor reported receiving salary from Autism CRC during the study. No other disclosures were reported. This work was supported by an Allied Health Sciences start-up grant from the Menzies Foundation and the Cooperative Research Centre for Living with Autism, established and supported under the Australian Government’s Cooperative Research Centres Program. Dr. Pierce reports no relevant financial relationships.
A population-based developmental surveillance program showed high diagnostic accuracy in identifying autism in a community-based sample of infants, toddlers, and preschoolers, according to new data published online in JAMA Network Open.
Researchers, led by Josephine Barbaro, PhD, of Olga Tennison Autism Research Centre at La Trobe University, Bundoora, Australia, said their findings indicate the benefit of using early autism developmental surveillance from infancy to the preschool period rather than one-time screening.
For the study, maternal and child health nurses in Melbourne were trained to use the Social Attention and Communication Surveillance–Revised (SACS-R) and SACS-Preschool (SACS-PR) tools during well-child checkups at 11-30 months of age and at follow-up (42 months of age). Dr. Barbaro helped develop the SACS tools.
Children identified as being at high likelihood for autism (1-2 years of age: n = 327; 42 months of age: n = 168) and at low likelihood for autism plus concerns (42 months of age: n = 28) were referred by their nurse for diagnostic assessment by the researchers.
Diagnostic accuracy of the SACS-R and SACS-PR was determined by comparing likelihood for autism with children’s diagnostic outcome using clinical judgment based on standard autism assessments.
Researchers included 13,511 children ages 11 months to 42 months. Results indicated the SACS-R with SACS-PR (SACS-R+PR) had very high diagnostic accuracy for early autism detection.
According to the paper, SACS-R showed 83% positive predictive value (95% confidence interval, 0.77-0.87) and 99% estimated negative predictive value (95% CI, 0.01-0.02). Specificity (99.6%; 95% CI, 0.99-1.00) was high, with modest sensitivity (62%; 95% CI, 0.57-0.66). When the SACS-PR 42-month assessment was added, estimated sensitivity grew to 96% (95% CI, 0.94-0.98).
“Its greater accuracy, compared with psychometrics of commonly used autism screening tools when used in community-based samples, suggests that the SACS-R+PR can be used universally for the early identification of autism,” the authors wrote.
According to La Trobe University, the tool is used in 10 other countries around the world – among them China, Singapore, Poland, Japan, New Zealand, Nepal, and Bangladesh.
Early identification is crucial for children on the autism spectrum and their families because it facilitates early diagnosis and can help families get access to supports and services.
About 2% of the world’s population is on the autism spectrum. Some studies report prevalence of 4% or higher, the authors noted.
The authors called attention to a systematic review of universal autism screening in primary care, including the Infant-Toddler Checklist and the Modified Checklist for Autism in Toddlers and various versions. The authors of the review noted that few studies had enough participants to establish population sensitivity, specificity, and positive predictive value. Also, psychometric properties reported were modest and/or wide ranging, putting into question the diagnostic accuracy of the tools.
Dr. Barbaro and colleagues highlighted an advantage the current study offers. “A critical difference in this study was the use of a community-based sample rather than a clinical or high-likelihood sibling sample, which may not be representative of the general population of children on the autism spectrum because child outcomes, cognition, and autism prevalence vary by ascertainment strategy and multiplex or simplex status.”
The authors explained that, in the United States, The U.S. Preventive Services Task Force has said there is not enough evidence to recommend universal autism screening and instead recommends routine general developmental surveillance. The American Academy of Pediatrics recommends developmental surveillance between 9 and 30 months and autism-specific screening at 18 and 24 months because of the benefits of early supports and services.
Karen Pierce, PhD, codirector of the Autism Center of Excellence at University of California, San Diego, said in an interview that she was pleased to see that the researchers were able to identify a high percentage of children on the autism spectrum.
She said, however, that the system proposed in this paper involves a substantial amount of time for training the nurses.
The authors acknowledged that, saying, “there may be instances in which this could be impractical.”
Dr. Pierce said that, in the United States, parent questionnaires are combined with clinical judgment to decide which kids are at risk.
“It doesn’t take very much time to fill out these questionnaires,” she said. “That’s the sticking point. I’m not saying necessarily that it shouldn’t be adopted. It would be very hard, I think, to incorporate into current pediatric practice.”
She said a benefit of the SACS program is more hands-on observation of the child, beyond the parent report, which sometimes can reflect more emotionally how the parent is feeling about the child.
She pointed out it was impressive that the Australian team found virtually no false positives.
The researchers also identified an additional 168 children using the preschool version at 42 months who had actually passed at the earlier checkpoint, using the regular SACS-R.
“This underscores a supercritical point,” Dr. Pierce said. “Just because your child may have gotten screened at 12, 18, 24 months and they pass and everything’s looking great, it doesn’t necessarily mean at some point early in development around age 3 that there [wouldn’t] be some clearer signs of autism.”
She said in her own study, published in JAMA Pediatrics, 24% of their sample tested fine at first but were later identified as having autism.
“It underscores the need for repeat screening,” Dr. Pierce said. “That was a striking finding in this study.”
She also pointed out that the authors talk about the “false dichotomy” between screening and surveillance. “They are saying it doesn’t have to be that way. It can be a combined effort. We can have parents filling out screening tools and we can have more observational sessions with kids during checkups. It doesn’t have to be this rigid line between screening and surveillance. I would completely agree with that.”
Dr. Barbaro reported receiving grants from the Sir Robert Menzies Foundation and the Cooperative Research Centre for Living with Autism (Autism CRC) during the study. Funds are partially distributed to Dr. Barbaro for the background intellectual property. One coauthor reported grants from the Menzies Foundation and Autism CRC during the study. Another coauthor reported receiving salary from Autism CRC during the study. No other disclosures were reported. This work was supported by an Allied Health Sciences start-up grant from the Menzies Foundation and the Cooperative Research Centre for Living with Autism, established and supported under the Australian Government’s Cooperative Research Centres Program. Dr. Pierce reports no relevant financial relationships.
FROM JAMA NETWORK OPEN
Selling your practice
My previous column on practice valuation prompted a number of questions on the mechanics of selling a private practice. As usual, I cannot hope to cover this complex topic comprehensively in only 750 words, but here are the basics.
A generation ago, the sale of a medical practice was much like the sale of any other business: A retiring physician would sell his or her practice to a young doctor and the practice would continue on as before. Occasionally, that still happens, but changes in the business of medicine – most significantly the growth of managed care – have had a big impact on the way medical practices are bought and sold.
For one thing, there are far fewer solo practitioners these days, and polls indicate that most young physicians intend to continue that trend. .
For another, because the rules governing such sales have become so numbingly complex, the services of expert (and expensive) third parties are essential.
While these issues may complicate matters, there is still a market for the sale of medical practices. However, you must do everything possible to ensure you identify the best possible buyer and structure the best deal.
The first hurdle is the accurate valuation of your practice, which was covered in some detail in my last column. Briefly, for the protection of both parties, it is important that the appraisal be done by an experienced and neutral financial consultant, that all techniques used in the valuation be divulged and explained, and that documentation be supplied to support the conclusions reached.
Keep in mind that the valuation will not necessarily equal the purchase price; other factors may need to be considered before a final price can be agreed upon. Keep in mind, too, that there may be legal constraints on the purchase price. For example, if the buyer is a nonprofit corporation such as a hospital or HMO, by law it cannot pay in excess of fair market value for the practice – which may rule out any valuation of “good will.” In some states, the purchase of private practices by hospitals is prohibited altogether – so you might need to consider a long-term lease rather than a sale.
Once a value has been agreed upon, you must consider how the transaction will be structured. The most popular structures include purchase of assets, purchase of corporate stock, and merger.
Many buyers prefer to purchase assets, because it allows them to pick and choose only those items that have value to them. This can leave you with a bunch of “odd lot” assets to dispose of. But depending on the circumstances, an asset sale may still be to your advantage.
Sellers typically prefer to sell stock, because it allows them to sell their entire practice, which is often worth more than the sum of its parts, and often provides tax advantages.
The third option, merger, continues to grow in popularity and is a column subject in itself, and I will address it separately next month.
Tax issues must always be considered. Most private practices are corporations, and the sale of corporate stock will result in a long-term capital gain that will be taxed – currently at 15%-20%. As the saying goes, it’s not what you earn, it’s what you keep. So it may benefit you to accept a slightly lower price if the sale can be structured to provide significantly lower tax treatment. However, any gain that does not qualify as a long-term capital gain will be taxed as regular income – currently in the 32%-37% percent range – plus a Social Security tax of about 15%.
Payment in installments is a popular way to defer taxes, since they are incurred on each installment as it is paid; but such payments may be mistaken by the IRS for payments for referrals, which is illegal. And there is always the problem of making certain all payments are eventually made.
You may wish to continue working at the practice as an employee for an agreed-upon period of time, and this is often to the buyer’s advantage as well. Transitioning to new ownership in stages often maximizes the value of the business by improving patient retention, and allows patients to become accustomed to the transition. However, care must be taken, with the aid of good legal advice, to structure such an arrangement in a way that minimizes concerns of fraud and abuse.
Dr. Eastern practices dermatology and dermatologic surgery in Belleville, N.J. He is the author of numerous articles and textbook chapters, and is a longtime monthly columnist for Dermatology News. Write to him at [email protected].
My previous column on practice valuation prompted a number of questions on the mechanics of selling a private practice. As usual, I cannot hope to cover this complex topic comprehensively in only 750 words, but here are the basics.
A generation ago, the sale of a medical practice was much like the sale of any other business: A retiring physician would sell his or her practice to a young doctor and the practice would continue on as before. Occasionally, that still happens, but changes in the business of medicine – most significantly the growth of managed care – have had a big impact on the way medical practices are bought and sold.
For one thing, there are far fewer solo practitioners these days, and polls indicate that most young physicians intend to continue that trend. .
For another, because the rules governing such sales have become so numbingly complex, the services of expert (and expensive) third parties are essential.
While these issues may complicate matters, there is still a market for the sale of medical practices. However, you must do everything possible to ensure you identify the best possible buyer and structure the best deal.
The first hurdle is the accurate valuation of your practice, which was covered in some detail in my last column. Briefly, for the protection of both parties, it is important that the appraisal be done by an experienced and neutral financial consultant, that all techniques used in the valuation be divulged and explained, and that documentation be supplied to support the conclusions reached.
Keep in mind that the valuation will not necessarily equal the purchase price; other factors may need to be considered before a final price can be agreed upon. Keep in mind, too, that there may be legal constraints on the purchase price. For example, if the buyer is a nonprofit corporation such as a hospital or HMO, by law it cannot pay in excess of fair market value for the practice – which may rule out any valuation of “good will.” In some states, the purchase of private practices by hospitals is prohibited altogether – so you might need to consider a long-term lease rather than a sale.
Once a value has been agreed upon, you must consider how the transaction will be structured. The most popular structures include purchase of assets, purchase of corporate stock, and merger.
Many buyers prefer to purchase assets, because it allows them to pick and choose only those items that have value to them. This can leave you with a bunch of “odd lot” assets to dispose of. But depending on the circumstances, an asset sale may still be to your advantage.
Sellers typically prefer to sell stock, because it allows them to sell their entire practice, which is often worth more than the sum of its parts, and often provides tax advantages.
The third option, merger, continues to grow in popularity and is a column subject in itself, and I will address it separately next month.
Tax issues must always be considered. Most private practices are corporations, and the sale of corporate stock will result in a long-term capital gain that will be taxed – currently at 15%-20%. As the saying goes, it’s not what you earn, it’s what you keep. So it may benefit you to accept a slightly lower price if the sale can be structured to provide significantly lower tax treatment. However, any gain that does not qualify as a long-term capital gain will be taxed as regular income – currently in the 32%-37% percent range – plus a Social Security tax of about 15%.
Payment in installments is a popular way to defer taxes, since they are incurred on each installment as it is paid; but such payments may be mistaken by the IRS for payments for referrals, which is illegal. And there is always the problem of making certain all payments are eventually made.
You may wish to continue working at the practice as an employee for an agreed-upon period of time, and this is often to the buyer’s advantage as well. Transitioning to new ownership in stages often maximizes the value of the business by improving patient retention, and allows patients to become accustomed to the transition. However, care must be taken, with the aid of good legal advice, to structure such an arrangement in a way that minimizes concerns of fraud and abuse.
Dr. Eastern practices dermatology and dermatologic surgery in Belleville, N.J. He is the author of numerous articles and textbook chapters, and is a longtime monthly columnist for Dermatology News. Write to him at [email protected].
My previous column on practice valuation prompted a number of questions on the mechanics of selling a private practice. As usual, I cannot hope to cover this complex topic comprehensively in only 750 words, but here are the basics.
A generation ago, the sale of a medical practice was much like the sale of any other business: A retiring physician would sell his or her practice to a young doctor and the practice would continue on as before. Occasionally, that still happens, but changes in the business of medicine – most significantly the growth of managed care – have had a big impact on the way medical practices are bought and sold.
For one thing, there are far fewer solo practitioners these days, and polls indicate that most young physicians intend to continue that trend. .
For another, because the rules governing such sales have become so numbingly complex, the services of expert (and expensive) third parties are essential.
While these issues may complicate matters, there is still a market for the sale of medical practices. However, you must do everything possible to ensure you identify the best possible buyer and structure the best deal.
The first hurdle is the accurate valuation of your practice, which was covered in some detail in my last column. Briefly, for the protection of both parties, it is important that the appraisal be done by an experienced and neutral financial consultant, that all techniques used in the valuation be divulged and explained, and that documentation be supplied to support the conclusions reached.
Keep in mind that the valuation will not necessarily equal the purchase price; other factors may need to be considered before a final price can be agreed upon. Keep in mind, too, that there may be legal constraints on the purchase price. For example, if the buyer is a nonprofit corporation such as a hospital or HMO, by law it cannot pay in excess of fair market value for the practice – which may rule out any valuation of “good will.” In some states, the purchase of private practices by hospitals is prohibited altogether – so you might need to consider a long-term lease rather than a sale.
Once a value has been agreed upon, you must consider how the transaction will be structured. The most popular structures include purchase of assets, purchase of corporate stock, and merger.
Many buyers prefer to purchase assets, because it allows them to pick and choose only those items that have value to them. This can leave you with a bunch of “odd lot” assets to dispose of. But depending on the circumstances, an asset sale may still be to your advantage.
Sellers typically prefer to sell stock, because it allows them to sell their entire practice, which is often worth more than the sum of its parts, and often provides tax advantages.
The third option, merger, continues to grow in popularity and is a column subject in itself, and I will address it separately next month.
Tax issues must always be considered. Most private practices are corporations, and the sale of corporate stock will result in a long-term capital gain that will be taxed – currently at 15%-20%. As the saying goes, it’s not what you earn, it’s what you keep. So it may benefit you to accept a slightly lower price if the sale can be structured to provide significantly lower tax treatment. However, any gain that does not qualify as a long-term capital gain will be taxed as regular income – currently in the 32%-37% percent range – plus a Social Security tax of about 15%.
Payment in installments is a popular way to defer taxes, since they are incurred on each installment as it is paid; but such payments may be mistaken by the IRS for payments for referrals, which is illegal. And there is always the problem of making certain all payments are eventually made.
You may wish to continue working at the practice as an employee for an agreed-upon period of time, and this is often to the buyer’s advantage as well. Transitioning to new ownership in stages often maximizes the value of the business by improving patient retention, and allows patients to become accustomed to the transition. However, care must be taken, with the aid of good legal advice, to structure such an arrangement in a way that minimizes concerns of fraud and abuse.
Dr. Eastern practices dermatology and dermatologic surgery in Belleville, N.J. He is the author of numerous articles and textbook chapters, and is a longtime monthly columnist for Dermatology News. Write to him at [email protected].
Screen time in first year may raise autism risk at age 3
Boys exposed to at least 2 hours a day of screen time by 1 year of age were significantly more likely to have an autism spectrum disorder (ASD) diagnosis at 3 years, based on data from more than 80,000 children.
The World Health Organization and the American Academy of Pediatrics recommend against any screen time for infants up to 1 year of age and 18 months of age, respectively, wrote Megumi Kushima, MA, of the University of Yamanashi (Japan), and colleagues on behalf of the Japan Environment and Children’s Study Group.
The extent to which screen time duration in infancy is associated with subsequent ASD diagnosis remains unclear, the researchers said. The ongoing COVID-19 pandemic has increased screen time among children worldwide, which makes an examination of the impact of screen time on children’s health an important public health issue.
In a study published in JAMA Pediatrics, the researchers recruited pregnant women between 2011 and 2014; data were analyzed in December 2020. The final study population included 84,030 mother-child pairs. The primary exposure of screen time at 1 year of age was assessed by questionnaire, in which mothers were asked to report their number of hours they let their child watch TV or DVDs daily. Responses were none (no screen time), less than 1 hour, 1 hour or more but less than 2 hours, 2 hours or more but less than 4 hours, and 4 hours or more.
The primary outcome was ASD diagnosis at 3 years of age, and mothers were asked via questionnaire whether their 3-year-old had been diagnosed with ASD from age 2.
The study was conducted by the Japan Environment and Children’s Study Group at 15 regional centers across Japan.
Overall, 330 children had received an ASD diagnosis at age 3 years, a prevalence of 0.4%. Of these, 251 (76%) were boys, and 79 (24%) were girls. Independent of ASD, the most common response for screen time was less than 1 hour, which was reported by 27,707 mothers. The proportion of children with ASD at age 3 increased as screen time at age 1 increased, the percentages were 5.8%, 22.3%, 30.2%, and 31.7% for children with no screen time, less than 1 hour, 1 to less than 2 hours, and 2 to less than 4 hours, respectively. The percentage of children with ASD diagnoses who had 4 hours or more of daily screen time was 10%.
Logistic regression analysis showed that longer screen time at age 1 year was significantly associated with higher odds of ASD at 3 years in boys, but not in girls. The researchers controlled for variables including maternal maltreatment and children’s predisposition to ASD. Among boys, the adjusted odds ratios for screen times of less than 1 hour, 1 hour to less than 2 hours, 2 hours to less than 4 hours, and more than 4 hours were 1.38, 2.16, 3.48, and 3.02, respectively.
Screen time at age 3 years was not associated with ASD diagnosis at age 3 years, potentially “because the association with environmental factors on brain development varies with age,” the researchers noted.
The study findings were limited by several factors including the reliance on parental reports of screen time and potential for reporting bias, the researchers noted. Other limitations included the possible missed diagnoses of mild ASD cases at 3 years, and the inability to consider variables such as childcare environment, living conditions, diseases, genetics, and disabilities.
However, the results were strengthened by the large study population and examination of screen time in early childhood, they said. More research is needed to examine other factors that contribute to the association between ASD and screen time, but given the rapid increase in device use in children, “it is necessary to review its health effects on infants and control excessive screen time.”
Strong study, but some gaps appear
The study is strong in many respects, Karalyn Kinsella, MD, a pediatrician in private practice in Cheshire, Conn., said in an interview.
However, “what I am not sure they addressed is that children on the spectrum are often not entertained by basic toys and may be hard to manage behaviorally,” Dr. Kinsella said. Consequently, parents may be more inclined to offer screen time as a way to pacify children with behavioral difficulties. “Parents also may see that their children are happier interacting with devices, so they may be more apt to let them continue with screen time.We know screen time is not good for the developing brain, however; I worry that the message from this study is that screen time causes autism in boys.
“What I would have liked to know from the parents who allowed more screen time was why they were offering it,” Dr. Kinsella said. “Was it because their child was difficult behaviorally or because that is the one place that they seemed to have satisfaction? To me, that would indicate the reverse hypothesis.” That said, the study findings “remind us to counsel families about screen time, especially in the age of COVID-19. Kids are home much longer than usual, which ultimately leads to more screen time.”
The study was funded by the Japanese Ministry of Environment. The researchers had no financial conflicts to disclose. Dr. Kinsella had no financial conflicts to disclose, but serves as a member of the Pediatric News editorial advisory board.
Boys exposed to at least 2 hours a day of screen time by 1 year of age were significantly more likely to have an autism spectrum disorder (ASD) diagnosis at 3 years, based on data from more than 80,000 children.
The World Health Organization and the American Academy of Pediatrics recommend against any screen time for infants up to 1 year of age and 18 months of age, respectively, wrote Megumi Kushima, MA, of the University of Yamanashi (Japan), and colleagues on behalf of the Japan Environment and Children’s Study Group.
The extent to which screen time duration in infancy is associated with subsequent ASD diagnosis remains unclear, the researchers said. The ongoing COVID-19 pandemic has increased screen time among children worldwide, which makes an examination of the impact of screen time on children’s health an important public health issue.
In a study published in JAMA Pediatrics, the researchers recruited pregnant women between 2011 and 2014; data were analyzed in December 2020. The final study population included 84,030 mother-child pairs. The primary exposure of screen time at 1 year of age was assessed by questionnaire, in which mothers were asked to report their number of hours they let their child watch TV or DVDs daily. Responses were none (no screen time), less than 1 hour, 1 hour or more but less than 2 hours, 2 hours or more but less than 4 hours, and 4 hours or more.
The primary outcome was ASD diagnosis at 3 years of age, and mothers were asked via questionnaire whether their 3-year-old had been diagnosed with ASD from age 2.
The study was conducted by the Japan Environment and Children’s Study Group at 15 regional centers across Japan.
Overall, 330 children had received an ASD diagnosis at age 3 years, a prevalence of 0.4%. Of these, 251 (76%) were boys, and 79 (24%) were girls. Independent of ASD, the most common response for screen time was less than 1 hour, which was reported by 27,707 mothers. The proportion of children with ASD at age 3 increased as screen time at age 1 increased, the percentages were 5.8%, 22.3%, 30.2%, and 31.7% for children with no screen time, less than 1 hour, 1 to less than 2 hours, and 2 to less than 4 hours, respectively. The percentage of children with ASD diagnoses who had 4 hours or more of daily screen time was 10%.
Logistic regression analysis showed that longer screen time at age 1 year was significantly associated with higher odds of ASD at 3 years in boys, but not in girls. The researchers controlled for variables including maternal maltreatment and children’s predisposition to ASD. Among boys, the adjusted odds ratios for screen times of less than 1 hour, 1 hour to less than 2 hours, 2 hours to less than 4 hours, and more than 4 hours were 1.38, 2.16, 3.48, and 3.02, respectively.
Screen time at age 3 years was not associated with ASD diagnosis at age 3 years, potentially “because the association with environmental factors on brain development varies with age,” the researchers noted.
The study findings were limited by several factors including the reliance on parental reports of screen time and potential for reporting bias, the researchers noted. Other limitations included the possible missed diagnoses of mild ASD cases at 3 years, and the inability to consider variables such as childcare environment, living conditions, diseases, genetics, and disabilities.
However, the results were strengthened by the large study population and examination of screen time in early childhood, they said. More research is needed to examine other factors that contribute to the association between ASD and screen time, but given the rapid increase in device use in children, “it is necessary to review its health effects on infants and control excessive screen time.”
Strong study, but some gaps appear
The study is strong in many respects, Karalyn Kinsella, MD, a pediatrician in private practice in Cheshire, Conn., said in an interview.
However, “what I am not sure they addressed is that children on the spectrum are often not entertained by basic toys and may be hard to manage behaviorally,” Dr. Kinsella said. Consequently, parents may be more inclined to offer screen time as a way to pacify children with behavioral difficulties. “Parents also may see that their children are happier interacting with devices, so they may be more apt to let them continue with screen time.We know screen time is not good for the developing brain, however; I worry that the message from this study is that screen time causes autism in boys.
“What I would have liked to know from the parents who allowed more screen time was why they were offering it,” Dr. Kinsella said. “Was it because their child was difficult behaviorally or because that is the one place that they seemed to have satisfaction? To me, that would indicate the reverse hypothesis.” That said, the study findings “remind us to counsel families about screen time, especially in the age of COVID-19. Kids are home much longer than usual, which ultimately leads to more screen time.”
The study was funded by the Japanese Ministry of Environment. The researchers had no financial conflicts to disclose. Dr. Kinsella had no financial conflicts to disclose, but serves as a member of the Pediatric News editorial advisory board.
Boys exposed to at least 2 hours a day of screen time by 1 year of age were significantly more likely to have an autism spectrum disorder (ASD) diagnosis at 3 years, based on data from more than 80,000 children.
The World Health Organization and the American Academy of Pediatrics recommend against any screen time for infants up to 1 year of age and 18 months of age, respectively, wrote Megumi Kushima, MA, of the University of Yamanashi (Japan), and colleagues on behalf of the Japan Environment and Children’s Study Group.
The extent to which screen time duration in infancy is associated with subsequent ASD diagnosis remains unclear, the researchers said. The ongoing COVID-19 pandemic has increased screen time among children worldwide, which makes an examination of the impact of screen time on children’s health an important public health issue.
In a study published in JAMA Pediatrics, the researchers recruited pregnant women between 2011 and 2014; data were analyzed in December 2020. The final study population included 84,030 mother-child pairs. The primary exposure of screen time at 1 year of age was assessed by questionnaire, in which mothers were asked to report their number of hours they let their child watch TV or DVDs daily. Responses were none (no screen time), less than 1 hour, 1 hour or more but less than 2 hours, 2 hours or more but less than 4 hours, and 4 hours or more.
The primary outcome was ASD diagnosis at 3 years of age, and mothers were asked via questionnaire whether their 3-year-old had been diagnosed with ASD from age 2.
The study was conducted by the Japan Environment and Children’s Study Group at 15 regional centers across Japan.
Overall, 330 children had received an ASD diagnosis at age 3 years, a prevalence of 0.4%. Of these, 251 (76%) were boys, and 79 (24%) were girls. Independent of ASD, the most common response for screen time was less than 1 hour, which was reported by 27,707 mothers. The proportion of children with ASD at age 3 increased as screen time at age 1 increased, the percentages were 5.8%, 22.3%, 30.2%, and 31.7% for children with no screen time, less than 1 hour, 1 to less than 2 hours, and 2 to less than 4 hours, respectively. The percentage of children with ASD diagnoses who had 4 hours or more of daily screen time was 10%.
Logistic regression analysis showed that longer screen time at age 1 year was significantly associated with higher odds of ASD at 3 years in boys, but not in girls. The researchers controlled for variables including maternal maltreatment and children’s predisposition to ASD. Among boys, the adjusted odds ratios for screen times of less than 1 hour, 1 hour to less than 2 hours, 2 hours to less than 4 hours, and more than 4 hours were 1.38, 2.16, 3.48, and 3.02, respectively.
Screen time at age 3 years was not associated with ASD diagnosis at age 3 years, potentially “because the association with environmental factors on brain development varies with age,” the researchers noted.
The study findings were limited by several factors including the reliance on parental reports of screen time and potential for reporting bias, the researchers noted. Other limitations included the possible missed diagnoses of mild ASD cases at 3 years, and the inability to consider variables such as childcare environment, living conditions, diseases, genetics, and disabilities.
However, the results were strengthened by the large study population and examination of screen time in early childhood, they said. More research is needed to examine other factors that contribute to the association between ASD and screen time, but given the rapid increase in device use in children, “it is necessary to review its health effects on infants and control excessive screen time.”
Strong study, but some gaps appear
The study is strong in many respects, Karalyn Kinsella, MD, a pediatrician in private practice in Cheshire, Conn., said in an interview.
However, “what I am not sure they addressed is that children on the spectrum are often not entertained by basic toys and may be hard to manage behaviorally,” Dr. Kinsella said. Consequently, parents may be more inclined to offer screen time as a way to pacify children with behavioral difficulties. “Parents also may see that their children are happier interacting with devices, so they may be more apt to let them continue with screen time.We know screen time is not good for the developing brain, however; I worry that the message from this study is that screen time causes autism in boys.
“What I would have liked to know from the parents who allowed more screen time was why they were offering it,” Dr. Kinsella said. “Was it because their child was difficult behaviorally or because that is the one place that they seemed to have satisfaction? To me, that would indicate the reverse hypothesis.” That said, the study findings “remind us to counsel families about screen time, especially in the age of COVID-19. Kids are home much longer than usual, which ultimately leads to more screen time.”
The study was funded by the Japanese Ministry of Environment. The researchers had no financial conflicts to disclose. Dr. Kinsella had no financial conflicts to disclose, but serves as a member of the Pediatric News editorial advisory board.
FROM JAMA PEDIATRICS















