User login
Clinical Psychiatry News is the online destination and multimedia properties of Clinica Psychiatry News, the independent news publication for psychiatrists. Since 1971, Clinical Psychiatry News has been the leading source of news and commentary about clinical developments in psychiatry as well as health care policy and regulations that affect the physician's practice.
Dear Drupal User: You're seeing this because you're logged in to Drupal, and not redirected to MDedge.com/psychiatry.
Depression
adolescent depression
adolescent major depressive disorder
adolescent schizophrenia
adolescent with major depressive disorder
animals
autism
baby
brexpiprazole
child
child bipolar
child depression
child schizophrenia
children with bipolar disorder
children with depression
children with major depressive disorder
compulsive behaviors
cure
elderly bipolar
elderly depression
elderly major depressive disorder
elderly schizophrenia
elderly with dementia
first break
first episode
gambling
gaming
geriatric depression
geriatric major depressive disorder
geriatric schizophrenia
infant
ketamine
kid
major depressive disorder
major depressive disorder in adolescents
major depressive disorder in children
parenting
pediatric
pediatric bipolar
pediatric depression
pediatric major depressive disorder
pediatric schizophrenia
pregnancy
pregnant
rexulti
skin care
suicide
teen
wine
section[contains(@class, 'nav-hidden')]
footer[@id='footer']
div[contains(@class, 'pane-pub-article-cpn')]
div[contains(@class, 'pane-pub-home-cpn')]
div[contains(@class, 'pane-pub-topic-cpn')]
div[contains(@class, 'panel-panel-inner')]
div[contains(@class, 'pane-node-field-article-topics')]
section[contains(@class, 'footer-nav-section-wrapper')]
COVID pandemic associated with anorexia in Canadian youth
, data suggest.
Preliminary results of the Canadian Paediatric Surveillance Program (CPSP) indicate that the pandemic has been a precipitating factor in the development of anorexia nervosa in almost half of children and adolescents studied. The pandemic also has precipitated hospitalizations for anorexia in more than one-third of cases.
“Data globally, and certainly our data here in Canada, have shown a real increase in health care utilization with the onset of the COVID-19 pandemic,” study author Debra Katzman, MD, professor of pediatrics at the Hospital for Sick Children in Toronto and the University of Toronto, said in an interview. “And when I talk about health care utilization, I’m talking about hospitalizations for eating disorders.”
The data were included in the 2021 results of the CPSP.
Focus on appearance
CPSP is a collaboration between the Public Health Agency of Canada and the Canadian Pediatric Society that consists of a network of 2,800 pediatricians and pediatric subspecialists across Canada. The latest results include surveillance studies on 14 diseases and conditions, with data collected during various periods.
From April 2020 to May 2021, researchers identified 1,800 COVID-19 cases in children and collected detailed information on 1,456 of them, including 405 cases hospitalized with pediatric inflammatory multisystem syndrome (PIMS). The median age of hospitalized cases was 3.2 years for SARS-CoV-2 infection and 5.4 years for PIMS.
Dr. Katzman and colleagues observed 118 first-time hospitalizations for anorexia nervosa between Sept. 1 and Dec. 31, 2021. More than 90% of reported cases were female, with 66% of verified cases in teens aged 14-17 years and the remainder in adolescents aged 11-13 years.
In 49% of cases, the reporting physician identified the COVID-19 pandemic as a precipitating factor in the development of anorexia nervosa. In 37% of cases, the reporting physician identified the pandemic as having precipitated the anorexia-related hospitalization.
Last year, a cross-sectional analysis of children in Canada reported that monthly hospitalizations for anorexia nervosa increased from 7.5 to 20 from March through November 2020. The monthly rate in the CPSP study was closer to 30 for first-time hospitalizations.
Dr. Katzman said that the findings about anorexia nervosa didn’t surprise her. “There was so much disruption and [so many] restrictions to young peoples’ daily routines – closures of schools and recreational activities – they lost regular connection with their peers, and they lost extracurricular and social activities,” she said. “That led to heightened anxiety and depression and really a lack of control.”
Adolescents and teens were also spending more time on social media than they were before the pandemic, she noted. “They were looking at themselves all the time, so they were getting preoccupied with their body image. There was a heightened focus on appearance, and I think that things like public-health mitigation strategies – things like hand washing, social distancing, mask wearing – may have impacted the psychological well-being of young people.”
The closure of outpatient facilities, long waiting lists to get into facilities that were opened, and “coronaphobia” about going to physicians’ offices and emergency departments compounded the problem, Dr. Katzman added.
The long-term effects of COVID and eating disorders in children are unknown, Dr. Katzman said. “This is sort of a wake-up call for the health care system that during times of stress or pandemics or crises, these kinds of things can happen, and we need to be prepared to provide the resources for vulnerable populations moving forward,” she said.
Heightened anxiety
Commenting on the data, Margaret Thew, APNP, director of the eating disorders program at Children’s Wisconsin in Milwaukee, said that isolation due to school closures and negative social media messages created the “perfect storm” for eating disorders in adolescents and teenagers because of higher rates of anxiety and depression. Ms. Thew was not involved in the research.
The storm is not over yet, she said. “What everyone needs to keep in mind is that we still have this very heightened state of anxiety and depression ... for adolescents, teenagers, and preteens alike,” Ms. Thew said in an interview, “and we know that many of them are not coping with their anxiety very well.”
In her experience, since the start of the pandemic, the average age of pediatric patients with eating disorders declined from 16 to 15 years, and the youngest age declined from 12 to 11 years.
Overall, the CPSP results show that children are affected by mental health issues at an earlier age than before the pandemic, said Ms. Thew. “Years ago, we wouldn’t have thought that an 8-year-old needed to be screened for some of these risk factors, but now we’re definitely getting more younger children who are struggling, and I think it’s taking too long for them to get the care they need because it’s being overlooked,” she said.
The report was funded by the Public Health Agency of Canada, Health Canada, Alberta Children’s Hospital Research Institute, Bethanys Hope Foundation, CHEO Research Institute, and Children’s Hospital Research Institute of Manitoba. Dr. Katzman and Ms. Thew have no relevant disclosures.
A version of this article first appeared on Medscape.com.
, data suggest.
Preliminary results of the Canadian Paediatric Surveillance Program (CPSP) indicate that the pandemic has been a precipitating factor in the development of anorexia nervosa in almost half of children and adolescents studied. The pandemic also has precipitated hospitalizations for anorexia in more than one-third of cases.
“Data globally, and certainly our data here in Canada, have shown a real increase in health care utilization with the onset of the COVID-19 pandemic,” study author Debra Katzman, MD, professor of pediatrics at the Hospital for Sick Children in Toronto and the University of Toronto, said in an interview. “And when I talk about health care utilization, I’m talking about hospitalizations for eating disorders.”
The data were included in the 2021 results of the CPSP.
Focus on appearance
CPSP is a collaboration between the Public Health Agency of Canada and the Canadian Pediatric Society that consists of a network of 2,800 pediatricians and pediatric subspecialists across Canada. The latest results include surveillance studies on 14 diseases and conditions, with data collected during various periods.
From April 2020 to May 2021, researchers identified 1,800 COVID-19 cases in children and collected detailed information on 1,456 of them, including 405 cases hospitalized with pediatric inflammatory multisystem syndrome (PIMS). The median age of hospitalized cases was 3.2 years for SARS-CoV-2 infection and 5.4 years for PIMS.
Dr. Katzman and colleagues observed 118 first-time hospitalizations for anorexia nervosa between Sept. 1 and Dec. 31, 2021. More than 90% of reported cases were female, with 66% of verified cases in teens aged 14-17 years and the remainder in adolescents aged 11-13 years.
In 49% of cases, the reporting physician identified the COVID-19 pandemic as a precipitating factor in the development of anorexia nervosa. In 37% of cases, the reporting physician identified the pandemic as having precipitated the anorexia-related hospitalization.
Last year, a cross-sectional analysis of children in Canada reported that monthly hospitalizations for anorexia nervosa increased from 7.5 to 20 from March through November 2020. The monthly rate in the CPSP study was closer to 30 for first-time hospitalizations.
Dr. Katzman said that the findings about anorexia nervosa didn’t surprise her. “There was so much disruption and [so many] restrictions to young peoples’ daily routines – closures of schools and recreational activities – they lost regular connection with their peers, and they lost extracurricular and social activities,” she said. “That led to heightened anxiety and depression and really a lack of control.”
Adolescents and teens were also spending more time on social media than they were before the pandemic, she noted. “They were looking at themselves all the time, so they were getting preoccupied with their body image. There was a heightened focus on appearance, and I think that things like public-health mitigation strategies – things like hand washing, social distancing, mask wearing – may have impacted the psychological well-being of young people.”
The closure of outpatient facilities, long waiting lists to get into facilities that were opened, and “coronaphobia” about going to physicians’ offices and emergency departments compounded the problem, Dr. Katzman added.
The long-term effects of COVID and eating disorders in children are unknown, Dr. Katzman said. “This is sort of a wake-up call for the health care system that during times of stress or pandemics or crises, these kinds of things can happen, and we need to be prepared to provide the resources for vulnerable populations moving forward,” she said.
Heightened anxiety
Commenting on the data, Margaret Thew, APNP, director of the eating disorders program at Children’s Wisconsin in Milwaukee, said that isolation due to school closures and negative social media messages created the “perfect storm” for eating disorders in adolescents and teenagers because of higher rates of anxiety and depression. Ms. Thew was not involved in the research.
The storm is not over yet, she said. “What everyone needs to keep in mind is that we still have this very heightened state of anxiety and depression ... for adolescents, teenagers, and preteens alike,” Ms. Thew said in an interview, “and we know that many of them are not coping with their anxiety very well.”
In her experience, since the start of the pandemic, the average age of pediatric patients with eating disorders declined from 16 to 15 years, and the youngest age declined from 12 to 11 years.
Overall, the CPSP results show that children are affected by mental health issues at an earlier age than before the pandemic, said Ms. Thew. “Years ago, we wouldn’t have thought that an 8-year-old needed to be screened for some of these risk factors, but now we’re definitely getting more younger children who are struggling, and I think it’s taking too long for them to get the care they need because it’s being overlooked,” she said.
The report was funded by the Public Health Agency of Canada, Health Canada, Alberta Children’s Hospital Research Institute, Bethanys Hope Foundation, CHEO Research Institute, and Children’s Hospital Research Institute of Manitoba. Dr. Katzman and Ms. Thew have no relevant disclosures.
A version of this article first appeared on Medscape.com.
, data suggest.
Preliminary results of the Canadian Paediatric Surveillance Program (CPSP) indicate that the pandemic has been a precipitating factor in the development of anorexia nervosa in almost half of children and adolescents studied. The pandemic also has precipitated hospitalizations for anorexia in more than one-third of cases.
“Data globally, and certainly our data here in Canada, have shown a real increase in health care utilization with the onset of the COVID-19 pandemic,” study author Debra Katzman, MD, professor of pediatrics at the Hospital for Sick Children in Toronto and the University of Toronto, said in an interview. “And when I talk about health care utilization, I’m talking about hospitalizations for eating disorders.”
The data were included in the 2021 results of the CPSP.
Focus on appearance
CPSP is a collaboration between the Public Health Agency of Canada and the Canadian Pediatric Society that consists of a network of 2,800 pediatricians and pediatric subspecialists across Canada. The latest results include surveillance studies on 14 diseases and conditions, with data collected during various periods.
From April 2020 to May 2021, researchers identified 1,800 COVID-19 cases in children and collected detailed information on 1,456 of them, including 405 cases hospitalized with pediatric inflammatory multisystem syndrome (PIMS). The median age of hospitalized cases was 3.2 years for SARS-CoV-2 infection and 5.4 years for PIMS.
Dr. Katzman and colleagues observed 118 first-time hospitalizations for anorexia nervosa between Sept. 1 and Dec. 31, 2021. More than 90% of reported cases were female, with 66% of verified cases in teens aged 14-17 years and the remainder in adolescents aged 11-13 years.
In 49% of cases, the reporting physician identified the COVID-19 pandemic as a precipitating factor in the development of anorexia nervosa. In 37% of cases, the reporting physician identified the pandemic as having precipitated the anorexia-related hospitalization.
Last year, a cross-sectional analysis of children in Canada reported that monthly hospitalizations for anorexia nervosa increased from 7.5 to 20 from March through November 2020. The monthly rate in the CPSP study was closer to 30 for first-time hospitalizations.
Dr. Katzman said that the findings about anorexia nervosa didn’t surprise her. “There was so much disruption and [so many] restrictions to young peoples’ daily routines – closures of schools and recreational activities – they lost regular connection with their peers, and they lost extracurricular and social activities,” she said. “That led to heightened anxiety and depression and really a lack of control.”
Adolescents and teens were also spending more time on social media than they were before the pandemic, she noted. “They were looking at themselves all the time, so they were getting preoccupied with their body image. There was a heightened focus on appearance, and I think that things like public-health mitigation strategies – things like hand washing, social distancing, mask wearing – may have impacted the psychological well-being of young people.”
The closure of outpatient facilities, long waiting lists to get into facilities that were opened, and “coronaphobia” about going to physicians’ offices and emergency departments compounded the problem, Dr. Katzman added.
The long-term effects of COVID and eating disorders in children are unknown, Dr. Katzman said. “This is sort of a wake-up call for the health care system that during times of stress or pandemics or crises, these kinds of things can happen, and we need to be prepared to provide the resources for vulnerable populations moving forward,” she said.
Heightened anxiety
Commenting on the data, Margaret Thew, APNP, director of the eating disorders program at Children’s Wisconsin in Milwaukee, said that isolation due to school closures and negative social media messages created the “perfect storm” for eating disorders in adolescents and teenagers because of higher rates of anxiety and depression. Ms. Thew was not involved in the research.
The storm is not over yet, she said. “What everyone needs to keep in mind is that we still have this very heightened state of anxiety and depression ... for adolescents, teenagers, and preteens alike,” Ms. Thew said in an interview, “and we know that many of them are not coping with their anxiety very well.”
In her experience, since the start of the pandemic, the average age of pediatric patients with eating disorders declined from 16 to 15 years, and the youngest age declined from 12 to 11 years.
Overall, the CPSP results show that children are affected by mental health issues at an earlier age than before the pandemic, said Ms. Thew. “Years ago, we wouldn’t have thought that an 8-year-old needed to be screened for some of these risk factors, but now we’re definitely getting more younger children who are struggling, and I think it’s taking too long for them to get the care they need because it’s being overlooked,” she said.
The report was funded by the Public Health Agency of Canada, Health Canada, Alberta Children’s Hospital Research Institute, Bethanys Hope Foundation, CHEO Research Institute, and Children’s Hospital Research Institute of Manitoba. Dr. Katzman and Ms. Thew have no relevant disclosures.
A version of this article first appeared on Medscape.com.
Positive top-line phase 3 data for lecanemab in early Alzheimer’s
compared with placebo and decreased amyloid levels in the brain of adults enrolled in a phase 3 trial.
The Clarity AD trial included 1,795 adults with early AD and confirmed amyloid pathology in the brain. Treatment consisted of lecanemab 10 mg/kg biweekly or matching placebo.
Treatment with lecanemab met the primary endpoint, reducing clinical decline on the global cognitive and functional scale, the Clinical Dementia Rating–Sum of Boxes (CDR-SB), at 18 months by 27%, compared with placebo, with a treatment difference in the score change of –0.45 (P = .00005), the companies reported.
Starting as early as 6 months, across all time points, treatment with lecanemab yielded highly statistically significant changes in CDR-SB from baseline, compared with placebo (all P < .01).
The study also met all key secondary endpoints with highly statistically significant results, compared with placebo (P < .01).
Key secondary endpoints, in comparison with placebo, were change from baseline at 18 months in amyloid levels in the brain measured by amyloid PET, the AD Assessment Scale–cognitive subscale14 (ADAS-cog14), the AD Composite Score (ADCOMS), and the AD Cooperative Study–Activities of Daily Living Scale for Mild Cognitive Impairment (ADCS MCI-ADL).
Imaging abnormalities within expectations
Overall, rates of amyloid-related imaging abnormalities (ARIA) related to lecanemab were “within expectations,” the companies said.
The incidence of ARIA related to edema (ARIA-E) was 12.5% in the lecanemab group and 1.7% in the placebo group.
The incidence of symptomatic ARIA-E was 2.8% and 0.0%, respectively, and the rate of cerebral hemorrhage (ARIA-H) was 17.0% and 8.7%. The total incidence of ARIA (ARIA-E and/or ARIA-H) was 21.3% in the lecanemab group and 9.3% in the placebo group.
Full results of the Clarity AD trial will be presented in November at the Clinical Trials on Alzheimer’s Congress.
Incremental benefit
Responding to the findings, the Alzheimer’s Association said in a statement that it “enthusiastically welcomes” the positive findings. It noted that these are “the most encouraging results in clinical trials treating the underlying causes of Alzheimer’s to date.
“For people in the earliest stages of Alzheimer’s, this treatment has the potential to change the course of the disease in a clinically meaningful way. These results indicate lecanemab may give people more time at or near their full abilities to participate in daily life, remain independent and make future health care decisions,” the Alzheimer’s Association added.
Also weighing in, Howard Fillit, MD, cofounder and chief science officer at the Alzheimer’s Drug Discovery Foundation, said in a release that “the combination of the biomarker change – reduced amyloid – plus slowing of cognitive decline in this study is encouraging news for the 57 million patients around the world living with Alzheimer’s.
“However, amyloid-clearing drugs will provide an incremental benefit at best, and there is still a pressing need for the next generation of drugs focused on other targets based on our knowledge of the biology of aging,” Dr. Fillit cautioned.
“We are optimistic about the future as many of these drugs are in development, with 75% of drugs in the pipeline now targeting nonamyloid pathways of neurodegeneration,” he added.
In July 2022, the Food and Drug Administration accepted Eisai’s biologics license application for lecanemab under the accelerated approval pathway and granted priority review. Lecanemab has a prescription Drugs User Fee Act action date of Jan. 6, 2023.
A version of this article first appeared on Medscape.com.
compared with placebo and decreased amyloid levels in the brain of adults enrolled in a phase 3 trial.
The Clarity AD trial included 1,795 adults with early AD and confirmed amyloid pathology in the brain. Treatment consisted of lecanemab 10 mg/kg biweekly or matching placebo.
Treatment with lecanemab met the primary endpoint, reducing clinical decline on the global cognitive and functional scale, the Clinical Dementia Rating–Sum of Boxes (CDR-SB), at 18 months by 27%, compared with placebo, with a treatment difference in the score change of –0.45 (P = .00005), the companies reported.
Starting as early as 6 months, across all time points, treatment with lecanemab yielded highly statistically significant changes in CDR-SB from baseline, compared with placebo (all P < .01).
The study also met all key secondary endpoints with highly statistically significant results, compared with placebo (P < .01).
Key secondary endpoints, in comparison with placebo, were change from baseline at 18 months in amyloid levels in the brain measured by amyloid PET, the AD Assessment Scale–cognitive subscale14 (ADAS-cog14), the AD Composite Score (ADCOMS), and the AD Cooperative Study–Activities of Daily Living Scale for Mild Cognitive Impairment (ADCS MCI-ADL).
Imaging abnormalities within expectations
Overall, rates of amyloid-related imaging abnormalities (ARIA) related to lecanemab were “within expectations,” the companies said.
The incidence of ARIA related to edema (ARIA-E) was 12.5% in the lecanemab group and 1.7% in the placebo group.
The incidence of symptomatic ARIA-E was 2.8% and 0.0%, respectively, and the rate of cerebral hemorrhage (ARIA-H) was 17.0% and 8.7%. The total incidence of ARIA (ARIA-E and/or ARIA-H) was 21.3% in the lecanemab group and 9.3% in the placebo group.
Full results of the Clarity AD trial will be presented in November at the Clinical Trials on Alzheimer’s Congress.
Incremental benefit
Responding to the findings, the Alzheimer’s Association said in a statement that it “enthusiastically welcomes” the positive findings. It noted that these are “the most encouraging results in clinical trials treating the underlying causes of Alzheimer’s to date.
“For people in the earliest stages of Alzheimer’s, this treatment has the potential to change the course of the disease in a clinically meaningful way. These results indicate lecanemab may give people more time at or near their full abilities to participate in daily life, remain independent and make future health care decisions,” the Alzheimer’s Association added.
Also weighing in, Howard Fillit, MD, cofounder and chief science officer at the Alzheimer’s Drug Discovery Foundation, said in a release that “the combination of the biomarker change – reduced amyloid – plus slowing of cognitive decline in this study is encouraging news for the 57 million patients around the world living with Alzheimer’s.
“However, amyloid-clearing drugs will provide an incremental benefit at best, and there is still a pressing need for the next generation of drugs focused on other targets based on our knowledge of the biology of aging,” Dr. Fillit cautioned.
“We are optimistic about the future as many of these drugs are in development, with 75% of drugs in the pipeline now targeting nonamyloid pathways of neurodegeneration,” he added.
In July 2022, the Food and Drug Administration accepted Eisai’s biologics license application for lecanemab under the accelerated approval pathway and granted priority review. Lecanemab has a prescription Drugs User Fee Act action date of Jan. 6, 2023.
A version of this article first appeared on Medscape.com.
compared with placebo and decreased amyloid levels in the brain of adults enrolled in a phase 3 trial.
The Clarity AD trial included 1,795 adults with early AD and confirmed amyloid pathology in the brain. Treatment consisted of lecanemab 10 mg/kg biweekly or matching placebo.
Treatment with lecanemab met the primary endpoint, reducing clinical decline on the global cognitive and functional scale, the Clinical Dementia Rating–Sum of Boxes (CDR-SB), at 18 months by 27%, compared with placebo, with a treatment difference in the score change of –0.45 (P = .00005), the companies reported.
Starting as early as 6 months, across all time points, treatment with lecanemab yielded highly statistically significant changes in CDR-SB from baseline, compared with placebo (all P < .01).
The study also met all key secondary endpoints with highly statistically significant results, compared with placebo (P < .01).
Key secondary endpoints, in comparison with placebo, were change from baseline at 18 months in amyloid levels in the brain measured by amyloid PET, the AD Assessment Scale–cognitive subscale14 (ADAS-cog14), the AD Composite Score (ADCOMS), and the AD Cooperative Study–Activities of Daily Living Scale for Mild Cognitive Impairment (ADCS MCI-ADL).
Imaging abnormalities within expectations
Overall, rates of amyloid-related imaging abnormalities (ARIA) related to lecanemab were “within expectations,” the companies said.
The incidence of ARIA related to edema (ARIA-E) was 12.5% in the lecanemab group and 1.7% in the placebo group.
The incidence of symptomatic ARIA-E was 2.8% and 0.0%, respectively, and the rate of cerebral hemorrhage (ARIA-H) was 17.0% and 8.7%. The total incidence of ARIA (ARIA-E and/or ARIA-H) was 21.3% in the lecanemab group and 9.3% in the placebo group.
Full results of the Clarity AD trial will be presented in November at the Clinical Trials on Alzheimer’s Congress.
Incremental benefit
Responding to the findings, the Alzheimer’s Association said in a statement that it “enthusiastically welcomes” the positive findings. It noted that these are “the most encouraging results in clinical trials treating the underlying causes of Alzheimer’s to date.
“For people in the earliest stages of Alzheimer’s, this treatment has the potential to change the course of the disease in a clinically meaningful way. These results indicate lecanemab may give people more time at or near their full abilities to participate in daily life, remain independent and make future health care decisions,” the Alzheimer’s Association added.
Also weighing in, Howard Fillit, MD, cofounder and chief science officer at the Alzheimer’s Drug Discovery Foundation, said in a release that “the combination of the biomarker change – reduced amyloid – plus slowing of cognitive decline in this study is encouraging news for the 57 million patients around the world living with Alzheimer’s.
“However, amyloid-clearing drugs will provide an incremental benefit at best, and there is still a pressing need for the next generation of drugs focused on other targets based on our knowledge of the biology of aging,” Dr. Fillit cautioned.
“We are optimistic about the future as many of these drugs are in development, with 75% of drugs in the pipeline now targeting nonamyloid pathways of neurodegeneration,” he added.
In July 2022, the Food and Drug Administration accepted Eisai’s biologics license application for lecanemab under the accelerated approval pathway and granted priority review. Lecanemab has a prescription Drugs User Fee Act action date of Jan. 6, 2023.
A version of this article first appeared on Medscape.com.
Understanding of developmental language disorder in children
Developmental language disorder (DLD) is characterized by receptive or expressive language difficulties or both. Children with the neurodevelopmental condition “struggle to comprehend and use their native language for no obvious reason,” said the authors of a new study. This leads to problems with grammar, vocabulary, and holding conversations, and in turn an increased risk of “difficulties when learning to read, underachieving academically, being unemployed, and facing social and mental health challenges.”
The condition is common and estimated to affect 7% of children – approximately two in every classroom – but is “underrecognized” said the authors.
Saloni Krishnan, PhD, reader at Royal Holloway, University of London, who led the study as a research fellow at the University of Oxford, England, explained: “DLD is a relatively unknown and understudied condition, unlike better known neurodevelopmental conditions such as ADHD, dyslexia, or autism.”
It is suspected that children with DLD may have differences in areas of the brain involved with learning habits and rules. “Although we know that DLD does not result from gross neural lesions, we still do not have a clear picture of how brain anatomy differs in children with DLD,” the authors highlighted.
Language learning difficulties linked to brain differences
For their study, published in eLife, researchers used an MRI technique called multiparameter mapping (MPM) to investigate microstructural neural differences in children with DLD. The technique measures the properties of brain tissue and is particularly useful for measuring the amounts of myelin.
“Understanding the neural basis of DLD is particularly challenging given the developmental nature of the disorder, as well as the lack of animal models for understanding language,” explained the authors. However, they pointed out that MPM allows an “unparalleled in vivo method” to investigate microstructural neural changes in children with DLD.
Kate Watkins, PhD, professor of cognitive neuroscience at the University of Oxford and senior author, said: “This type of scan tells us more about the makeup or composition of the brain tissue in different areas.”
As part of the Oxford Brain Organisation in Language Development (OxBOLD) study, the researchers recruited and tested 175 children between the ages of 10 and 15 years. Subsequently, 56 children with typical language development and 33 children with DLD were scanned using MPM.
The researchers compared the two groups and found that children with DLD have less myelin in parts of the brain responsible for speaking, listening, and learning rules and habits.
Specifically, maps of magnetization transfer saturation (MTsat) – which index myelin – in children with DLD showed reductions in MTsat values in the caudate nucleus bilaterally, and in the left ventral sensorimotor cortex and Heschl’s gyrus.
“Our findings using this protocol suggest that the caudate nucleus, as well as regions in the wider speech and language network, show alterations in myelin in children with DLD,” explained the authors.
“Given myelin’s role in enabling fast and reliable communication in the brain, reduced myelin content may explain why children with DLD struggle with speech and language processing,” they highlighted.
Significant advance in DLD understanding
The study findings established changes in striatal and cortical myelin as a “neural basis for DLD,” explained the journal editor, who highlighted that this was a “significant advance” in the understanding of DLD. “These brain differences may explain the poorer language outcomes in this group,” the authors said.
The findings “strongly point” to a role for the striatum in the development of DLD, and this role is likely to be in the “learning of habits and sequences,” the authors said.
They pointed out, however, that myelin patterns can change over development, and that myelination can be observed after successful training. “It is important to assess whether these differences in myelin persist over development in DLD, and if they can be targeted through training using behavioral interventions,” they emphasized.
Professor Watkins commented: “The findings might help us understand the pathways involved at a biological level and ultimately allow us to explain why children with DLD have problems with language learning.”
A spokesperson for the RADLD (Raising Awareness of Developmental Language Disorder) organization, commented: “Developmental language disorder has long been understood to have a neurological basis; however, these differences in the brain development have received limited attention in research.” It added that utilizing new technology helps to better understand the “potential neurological differences” experienced by people with DLD.
More studies are needed to determine if these brain differences cause language problems and how or if experiencing language difficulties could cause these changes in the brain, explained the authors. They hoped that further research may help scientists find new treatments that target these brain differences.
Funding was provided by UK Research and Innovation, Wellcome Trust. The authors declared no competing interests.
A version of this article first appeared on MedscapeUK.
Developmental language disorder (DLD) is characterized by receptive or expressive language difficulties or both. Children with the neurodevelopmental condition “struggle to comprehend and use their native language for no obvious reason,” said the authors of a new study. This leads to problems with grammar, vocabulary, and holding conversations, and in turn an increased risk of “difficulties when learning to read, underachieving academically, being unemployed, and facing social and mental health challenges.”
The condition is common and estimated to affect 7% of children – approximately two in every classroom – but is “underrecognized” said the authors.
Saloni Krishnan, PhD, reader at Royal Holloway, University of London, who led the study as a research fellow at the University of Oxford, England, explained: “DLD is a relatively unknown and understudied condition, unlike better known neurodevelopmental conditions such as ADHD, dyslexia, or autism.”
It is suspected that children with DLD may have differences in areas of the brain involved with learning habits and rules. “Although we know that DLD does not result from gross neural lesions, we still do not have a clear picture of how brain anatomy differs in children with DLD,” the authors highlighted.
Language learning difficulties linked to brain differences
For their study, published in eLife, researchers used an MRI technique called multiparameter mapping (MPM) to investigate microstructural neural differences in children with DLD. The technique measures the properties of brain tissue and is particularly useful for measuring the amounts of myelin.
“Understanding the neural basis of DLD is particularly challenging given the developmental nature of the disorder, as well as the lack of animal models for understanding language,” explained the authors. However, they pointed out that MPM allows an “unparalleled in vivo method” to investigate microstructural neural changes in children with DLD.
Kate Watkins, PhD, professor of cognitive neuroscience at the University of Oxford and senior author, said: “This type of scan tells us more about the makeup or composition of the brain tissue in different areas.”
As part of the Oxford Brain Organisation in Language Development (OxBOLD) study, the researchers recruited and tested 175 children between the ages of 10 and 15 years. Subsequently, 56 children with typical language development and 33 children with DLD were scanned using MPM.
The researchers compared the two groups and found that children with DLD have less myelin in parts of the brain responsible for speaking, listening, and learning rules and habits.
Specifically, maps of magnetization transfer saturation (MTsat) – which index myelin – in children with DLD showed reductions in MTsat values in the caudate nucleus bilaterally, and in the left ventral sensorimotor cortex and Heschl’s gyrus.
“Our findings using this protocol suggest that the caudate nucleus, as well as regions in the wider speech and language network, show alterations in myelin in children with DLD,” explained the authors.
“Given myelin’s role in enabling fast and reliable communication in the brain, reduced myelin content may explain why children with DLD struggle with speech and language processing,” they highlighted.
Significant advance in DLD understanding
The study findings established changes in striatal and cortical myelin as a “neural basis for DLD,” explained the journal editor, who highlighted that this was a “significant advance” in the understanding of DLD. “These brain differences may explain the poorer language outcomes in this group,” the authors said.
The findings “strongly point” to a role for the striatum in the development of DLD, and this role is likely to be in the “learning of habits and sequences,” the authors said.
They pointed out, however, that myelin patterns can change over development, and that myelination can be observed after successful training. “It is important to assess whether these differences in myelin persist over development in DLD, and if they can be targeted through training using behavioral interventions,” they emphasized.
Professor Watkins commented: “The findings might help us understand the pathways involved at a biological level and ultimately allow us to explain why children with DLD have problems with language learning.”
A spokesperson for the RADLD (Raising Awareness of Developmental Language Disorder) organization, commented: “Developmental language disorder has long been understood to have a neurological basis; however, these differences in the brain development have received limited attention in research.” It added that utilizing new technology helps to better understand the “potential neurological differences” experienced by people with DLD.
More studies are needed to determine if these brain differences cause language problems and how or if experiencing language difficulties could cause these changes in the brain, explained the authors. They hoped that further research may help scientists find new treatments that target these brain differences.
Funding was provided by UK Research and Innovation, Wellcome Trust. The authors declared no competing interests.
A version of this article first appeared on MedscapeUK.
Developmental language disorder (DLD) is characterized by receptive or expressive language difficulties or both. Children with the neurodevelopmental condition “struggle to comprehend and use their native language for no obvious reason,” said the authors of a new study. This leads to problems with grammar, vocabulary, and holding conversations, and in turn an increased risk of “difficulties when learning to read, underachieving academically, being unemployed, and facing social and mental health challenges.”
The condition is common and estimated to affect 7% of children – approximately two in every classroom – but is “underrecognized” said the authors.
Saloni Krishnan, PhD, reader at Royal Holloway, University of London, who led the study as a research fellow at the University of Oxford, England, explained: “DLD is a relatively unknown and understudied condition, unlike better known neurodevelopmental conditions such as ADHD, dyslexia, or autism.”
It is suspected that children with DLD may have differences in areas of the brain involved with learning habits and rules. “Although we know that DLD does not result from gross neural lesions, we still do not have a clear picture of how brain anatomy differs in children with DLD,” the authors highlighted.
Language learning difficulties linked to brain differences
For their study, published in eLife, researchers used an MRI technique called multiparameter mapping (MPM) to investigate microstructural neural differences in children with DLD. The technique measures the properties of brain tissue and is particularly useful for measuring the amounts of myelin.
“Understanding the neural basis of DLD is particularly challenging given the developmental nature of the disorder, as well as the lack of animal models for understanding language,” explained the authors. However, they pointed out that MPM allows an “unparalleled in vivo method” to investigate microstructural neural changes in children with DLD.
Kate Watkins, PhD, professor of cognitive neuroscience at the University of Oxford and senior author, said: “This type of scan tells us more about the makeup or composition of the brain tissue in different areas.”
As part of the Oxford Brain Organisation in Language Development (OxBOLD) study, the researchers recruited and tested 175 children between the ages of 10 and 15 years. Subsequently, 56 children with typical language development and 33 children with DLD were scanned using MPM.
The researchers compared the two groups and found that children with DLD have less myelin in parts of the brain responsible for speaking, listening, and learning rules and habits.
Specifically, maps of magnetization transfer saturation (MTsat) – which index myelin – in children with DLD showed reductions in MTsat values in the caudate nucleus bilaterally, and in the left ventral sensorimotor cortex and Heschl’s gyrus.
“Our findings using this protocol suggest that the caudate nucleus, as well as regions in the wider speech and language network, show alterations in myelin in children with DLD,” explained the authors.
“Given myelin’s role in enabling fast and reliable communication in the brain, reduced myelin content may explain why children with DLD struggle with speech and language processing,” they highlighted.
Significant advance in DLD understanding
The study findings established changes in striatal and cortical myelin as a “neural basis for DLD,” explained the journal editor, who highlighted that this was a “significant advance” in the understanding of DLD. “These brain differences may explain the poorer language outcomes in this group,” the authors said.
The findings “strongly point” to a role for the striatum in the development of DLD, and this role is likely to be in the “learning of habits and sequences,” the authors said.
They pointed out, however, that myelin patterns can change over development, and that myelination can be observed after successful training. “It is important to assess whether these differences in myelin persist over development in DLD, and if they can be targeted through training using behavioral interventions,” they emphasized.
Professor Watkins commented: “The findings might help us understand the pathways involved at a biological level and ultimately allow us to explain why children with DLD have problems with language learning.”
A spokesperson for the RADLD (Raising Awareness of Developmental Language Disorder) organization, commented: “Developmental language disorder has long been understood to have a neurological basis; however, these differences in the brain development have received limited attention in research.” It added that utilizing new technology helps to better understand the “potential neurological differences” experienced by people with DLD.
More studies are needed to determine if these brain differences cause language problems and how or if experiencing language difficulties could cause these changes in the brain, explained the authors. They hoped that further research may help scientists find new treatments that target these brain differences.
Funding was provided by UK Research and Innovation, Wellcome Trust. The authors declared no competing interests.
A version of this article first appeared on MedscapeUK.
Long COVID could cost the economy trillions, experts predict
from restaurants struggling to replace low-wage workers, to airlines scrambling to replace crew, to overwhelmed hospitals, experts are predicting.
“There’s a lot we need to do to understand what it takes to enable disabled people to participate more in the economy,” said Katie Bach, a senior fellow with Brookings Institution and the author of a study looking into long COVID’s impact on the labor market.
Data from June 2022 from the Centers for Disease Control and Prevention shows that, of the 40% of American adults who contracted COVID-19, nearly one in five still have long COVID symptoms. That works out to 1 in 13, or 7.5%, of the overall U.S. adult population.
Drawing from the CDC data, Ms. Bach estimates in her August 2022 report that as many as 4 million working-age Americans are too sick with long COVID to perform their jobs. That works out to as much as $230 billion in lost wages, or almost 1% of the U.S. GDP.
“This is a big deal,” she said. “We’re talking potentially hundreds of billions of dollars a year and that this is big enough to have a measurable impact on the labor market.”
Other sources have suggested lower figures, but the conclusions are the same: Long COVID is an urgent issue that will cost tens of billions of dollars a year in lost wages alone, Ms. Bach said. But it’s not just lost income for workers. There is a cost for businesses and the public.
Throughout the pandemic, COVID-19’s crippling force could be felt across multiple industries. While business has picked up again, staffing shortages remain a challenge. At some airports this summer, air passengers spent hours in security lines; were stranded for days as flights were canceled, rebooked, and canceled again on short notice; and waited weeks for lost luggage. Restaurants have had to cut back their hours. Those seeking medical care had longer than usual wait times in EDs and urgent care clinics. Some EDs temporarily closed.
These challenges have been attributed in part to the “great resignation” and in part because so many infected workers were out, especially during the Omicron waves. But increasingly, economists and health care professionals alike worry about long COVID’s impact on employers and the broader economy.
David Cutler, PhD, a professor of economics at Harvard University, Cambridge, Mass., believes the total economic loss could be as high as $3.7 trillion, when factoring in the lost quality of life, the cost in lost earnings, and the cost of higher spending on medical care. His estimate is more than a trillion dollars higher than a previous projection he and fellow economist Lawrence Summers, PhD, made in 2020. The reason? Long COVID.
“The higher estimate is largely a result of the greater prevalence of long COVID than we had guessed at the time,” Dr. Cutler wrote in a paper released in July.
“There are about 10 times the number of people with long COVID as have died of COVID. Because long COVID is so new, there is uncertainty about all of the numbers involved in the calculations. Still, the costs here are conservative, based on only cases to date.”
In Ms. Bach’s Brookings report, she projected that, if recovery from long COVID does not pick up and the population of Americans with long COVID were to grow by 10% a year, the annual cost of lost wages alone could reach half a trillion dollars in a decade.
Meanwhile, a working paper by the National Bureau of Economic Research found that workers who missed an entire week of work because of probable COVID-19 illnesses were roughly 7 percentage points less likely to be working a year later, compared with those who did not miss work for health reasons.
“It’s not just individuals with long COVID who are suffering from this. It impacts their families, their livelihoods, and the economy on a global scale. So, we have to raise awareness about those ripple effects,” said Linda Geng, MD, a clinical assistant professor of medicine with Stanford (Calif.) University’s Primary Care and Population Health.
“I think it’s hard for the public to grasp ... and understand the scale of this public health crisis.”
Debilitating fatigue
Long COVID is roughly defined; the CDC defines it as symptoms that linger 3 or more months after a patient first catches the virus.
The symptoms vary and include profound fatigue and brain issues.
“It’s a new degree of extreme and debilitating fatigue and exhaustion, to the point where you can’t do your daily tasks,” said Dr. Geng, who is also the codirector of Stanford’s Post-Acute COVID-19 Syndrome Clinic.
“People can be so debilitated, they can’t even do basic things, like the activities of daily living, let alone do their job, particularly if it’s physically or mentally demanding.”
Patients can also have postexertional malaise, where they feel especially bad and symptoms worsen when they exert themselves physically or mentally, Dr. Geng said. Compounding the issue for many long COVID patients is their trouble getting restful sleep. Those with brain fog have issues with memory, processing information, focused concentration, confusion, making mistakes, and multitasking. Pain is another debilitating symptom that can disrupt daily life and ability to work.
Even people with relatively mild infections can end up with long COVID, Dr. Geng said, noting that many of the patients at the Stanford clinic were never hospitalized with their initial infections. While existing research and Dr. Geng’s clinical experience show that long COVID can hit any age, she most commonly sees patients from ages 20 to their 60s, with an average age in the 40s – people in their prime working ages.
Jason Furman, PhD, a former White House economic adviser who is now a professor at Harvard University, noted in August that the labor force participation rate was far below what could be explained by standard demographic changes like an aging population, with the decline evident across all age groups. Dr. Furman does not speculate about why, but others have.
“We are pessimistic: Both the aging of the population and the impact of long COVID imply that the participation rate will be slow to return to its prepandemic level,” Anna Wong, Yelena Shulyatyeva, Andrew Husby, and Eliza Winger, economists with Bloomberg Economics, wrote in a research note.
Supportive policies
There is some evidence that vaccination reduces the risk of long COVID, but not completely, and it is too early to know if repeat infections increase long COVID risks. There is also no definitive data on how fast or how many people are recovering. Economists often assume that those with long COVID will recover at some point, Ms. Bach noted, but she is careful not to make assumptions.
“If people aren’t recovering, then this group keeps getting bigger,” she said. “We’re still adding, and if people aren’t coming out of that group, this becomes a bigger and bigger problem.”
For now, the number of new people being diagnosed with long COVID appears to have slowed, Ms. Bach said, but it remains to be seen whether the trend can be sustained.
“If people are impaired longer than we think and if the impairment turns out to be severe, then we can have a lot of people who need services like disability insurance,” Dr. Cutler said.
“That could put a really big strain on public sector programs and our ability to meet those needs.”
Policies that support the research and clinical work necessary to prevent and treat long COVID are essential, experts say.
“To me, that is the biggest economic imperative, to say nothing of human suffering,” said Ms. Bach.
Employers also have a role, and experts say there are a number of accommodations businesses should consider. What happens when an employee has long COVID? Can accommodations be made that allow them to continue working productively? If they spend a great deal of time commuting, can they work from home? What can employers do so that family members do not have to drop out of the workforce to take care of loved ones with long COVID?
Disability insurance
To be sure, there is one piece of the puzzle that does not quite fit, according to Dr. Cutler and Ms. Bach. There is no sign yet of a large increase in federal disability insurance applications, and no one quite knows why. Publicly available government data shows that online applications actually dipped by about 4% each year between 2019 and 2021. Applications in 2022 appear on track to remain slightly below prepandemic levels.
To qualify for Social Security Disability Insurance (SSDI), people need to have a disability that lasts at least a year.
“If you’re disabled with long COVID, who knows, right? You don’t know,” said Ms. Bach. “Two of the most dominant symptoms of long COVID are fatigue and brain fog. So, I’ve heard from people that the process of going through an SSDI application is really hard.”
Some long COVID patients told Ms. Bach they simply assumed they would not get SSDI and did not even bother applying. She stressed that working Americans with debilitating long COVID should be aware that their condition is protected by the Americans with Disabilities Act. But the challenge, based on guidance issued by the government, is that not all cases of long COVID qualify as a disability and that individual assessments are necessary.
While more long COVID data are needed, Ms. Bach believes there is enough information for decisionmakers to go after the issue more aggressively. She pointed to the $1.15 billion in funding that Congress earmarked for the National Institutes of Health over the course of 4 years in support of research into the long-term health effects of COVID-19.
“Now, $250 million a year sounds like a lot of money until you start talking about the cost of lost wages – just lost wages,” Ms. Bach said. “That’s not lost productivity. That’s not the cost of people whose family members are sick. Who have to reduce their own labor force participation. That’s not medical costs. Suddenly, $250 million doesn’t really sound like that much.”
A version of this article first appeared on WebMD.com.
from restaurants struggling to replace low-wage workers, to airlines scrambling to replace crew, to overwhelmed hospitals, experts are predicting.
“There’s a lot we need to do to understand what it takes to enable disabled people to participate more in the economy,” said Katie Bach, a senior fellow with Brookings Institution and the author of a study looking into long COVID’s impact on the labor market.
Data from June 2022 from the Centers for Disease Control and Prevention shows that, of the 40% of American adults who contracted COVID-19, nearly one in five still have long COVID symptoms. That works out to 1 in 13, or 7.5%, of the overall U.S. adult population.
Drawing from the CDC data, Ms. Bach estimates in her August 2022 report that as many as 4 million working-age Americans are too sick with long COVID to perform their jobs. That works out to as much as $230 billion in lost wages, or almost 1% of the U.S. GDP.
“This is a big deal,” she said. “We’re talking potentially hundreds of billions of dollars a year and that this is big enough to have a measurable impact on the labor market.”
Other sources have suggested lower figures, but the conclusions are the same: Long COVID is an urgent issue that will cost tens of billions of dollars a year in lost wages alone, Ms. Bach said. But it’s not just lost income for workers. There is a cost for businesses and the public.
Throughout the pandemic, COVID-19’s crippling force could be felt across multiple industries. While business has picked up again, staffing shortages remain a challenge. At some airports this summer, air passengers spent hours in security lines; were stranded for days as flights were canceled, rebooked, and canceled again on short notice; and waited weeks for lost luggage. Restaurants have had to cut back their hours. Those seeking medical care had longer than usual wait times in EDs and urgent care clinics. Some EDs temporarily closed.
These challenges have been attributed in part to the “great resignation” and in part because so many infected workers were out, especially during the Omicron waves. But increasingly, economists and health care professionals alike worry about long COVID’s impact on employers and the broader economy.
David Cutler, PhD, a professor of economics at Harvard University, Cambridge, Mass., believes the total economic loss could be as high as $3.7 trillion, when factoring in the lost quality of life, the cost in lost earnings, and the cost of higher spending on medical care. His estimate is more than a trillion dollars higher than a previous projection he and fellow economist Lawrence Summers, PhD, made in 2020. The reason? Long COVID.
“The higher estimate is largely a result of the greater prevalence of long COVID than we had guessed at the time,” Dr. Cutler wrote in a paper released in July.
“There are about 10 times the number of people with long COVID as have died of COVID. Because long COVID is so new, there is uncertainty about all of the numbers involved in the calculations. Still, the costs here are conservative, based on only cases to date.”
In Ms. Bach’s Brookings report, she projected that, if recovery from long COVID does not pick up and the population of Americans with long COVID were to grow by 10% a year, the annual cost of lost wages alone could reach half a trillion dollars in a decade.
Meanwhile, a working paper by the National Bureau of Economic Research found that workers who missed an entire week of work because of probable COVID-19 illnesses were roughly 7 percentage points less likely to be working a year later, compared with those who did not miss work for health reasons.
“It’s not just individuals with long COVID who are suffering from this. It impacts their families, their livelihoods, and the economy on a global scale. So, we have to raise awareness about those ripple effects,” said Linda Geng, MD, a clinical assistant professor of medicine with Stanford (Calif.) University’s Primary Care and Population Health.
“I think it’s hard for the public to grasp ... and understand the scale of this public health crisis.”
Debilitating fatigue
Long COVID is roughly defined; the CDC defines it as symptoms that linger 3 or more months after a patient first catches the virus.
The symptoms vary and include profound fatigue and brain issues.
“It’s a new degree of extreme and debilitating fatigue and exhaustion, to the point where you can’t do your daily tasks,” said Dr. Geng, who is also the codirector of Stanford’s Post-Acute COVID-19 Syndrome Clinic.
“People can be so debilitated, they can’t even do basic things, like the activities of daily living, let alone do their job, particularly if it’s physically or mentally demanding.”
Patients can also have postexertional malaise, where they feel especially bad and symptoms worsen when they exert themselves physically or mentally, Dr. Geng said. Compounding the issue for many long COVID patients is their trouble getting restful sleep. Those with brain fog have issues with memory, processing information, focused concentration, confusion, making mistakes, and multitasking. Pain is another debilitating symptom that can disrupt daily life and ability to work.
Even people with relatively mild infections can end up with long COVID, Dr. Geng said, noting that many of the patients at the Stanford clinic were never hospitalized with their initial infections. While existing research and Dr. Geng’s clinical experience show that long COVID can hit any age, she most commonly sees patients from ages 20 to their 60s, with an average age in the 40s – people in their prime working ages.
Jason Furman, PhD, a former White House economic adviser who is now a professor at Harvard University, noted in August that the labor force participation rate was far below what could be explained by standard demographic changes like an aging population, with the decline evident across all age groups. Dr. Furman does not speculate about why, but others have.
“We are pessimistic: Both the aging of the population and the impact of long COVID imply that the participation rate will be slow to return to its prepandemic level,” Anna Wong, Yelena Shulyatyeva, Andrew Husby, and Eliza Winger, economists with Bloomberg Economics, wrote in a research note.
Supportive policies
There is some evidence that vaccination reduces the risk of long COVID, but not completely, and it is too early to know if repeat infections increase long COVID risks. There is also no definitive data on how fast or how many people are recovering. Economists often assume that those with long COVID will recover at some point, Ms. Bach noted, but she is careful not to make assumptions.
“If people aren’t recovering, then this group keeps getting bigger,” she said. “We’re still adding, and if people aren’t coming out of that group, this becomes a bigger and bigger problem.”
For now, the number of new people being diagnosed with long COVID appears to have slowed, Ms. Bach said, but it remains to be seen whether the trend can be sustained.
“If people are impaired longer than we think and if the impairment turns out to be severe, then we can have a lot of people who need services like disability insurance,” Dr. Cutler said.
“That could put a really big strain on public sector programs and our ability to meet those needs.”
Policies that support the research and clinical work necessary to prevent and treat long COVID are essential, experts say.
“To me, that is the biggest economic imperative, to say nothing of human suffering,” said Ms. Bach.
Employers also have a role, and experts say there are a number of accommodations businesses should consider. What happens when an employee has long COVID? Can accommodations be made that allow them to continue working productively? If they spend a great deal of time commuting, can they work from home? What can employers do so that family members do not have to drop out of the workforce to take care of loved ones with long COVID?
Disability insurance
To be sure, there is one piece of the puzzle that does not quite fit, according to Dr. Cutler and Ms. Bach. There is no sign yet of a large increase in federal disability insurance applications, and no one quite knows why. Publicly available government data shows that online applications actually dipped by about 4% each year between 2019 and 2021. Applications in 2022 appear on track to remain slightly below prepandemic levels.
To qualify for Social Security Disability Insurance (SSDI), people need to have a disability that lasts at least a year.
“If you’re disabled with long COVID, who knows, right? You don’t know,” said Ms. Bach. “Two of the most dominant symptoms of long COVID are fatigue and brain fog. So, I’ve heard from people that the process of going through an SSDI application is really hard.”
Some long COVID patients told Ms. Bach they simply assumed they would not get SSDI and did not even bother applying. She stressed that working Americans with debilitating long COVID should be aware that their condition is protected by the Americans with Disabilities Act. But the challenge, based on guidance issued by the government, is that not all cases of long COVID qualify as a disability and that individual assessments are necessary.
While more long COVID data are needed, Ms. Bach believes there is enough information for decisionmakers to go after the issue more aggressively. She pointed to the $1.15 billion in funding that Congress earmarked for the National Institutes of Health over the course of 4 years in support of research into the long-term health effects of COVID-19.
“Now, $250 million a year sounds like a lot of money until you start talking about the cost of lost wages – just lost wages,” Ms. Bach said. “That’s not lost productivity. That’s not the cost of people whose family members are sick. Who have to reduce their own labor force participation. That’s not medical costs. Suddenly, $250 million doesn’t really sound like that much.”
A version of this article first appeared on WebMD.com.
from restaurants struggling to replace low-wage workers, to airlines scrambling to replace crew, to overwhelmed hospitals, experts are predicting.
“There’s a lot we need to do to understand what it takes to enable disabled people to participate more in the economy,” said Katie Bach, a senior fellow with Brookings Institution and the author of a study looking into long COVID’s impact on the labor market.
Data from June 2022 from the Centers for Disease Control and Prevention shows that, of the 40% of American adults who contracted COVID-19, nearly one in five still have long COVID symptoms. That works out to 1 in 13, or 7.5%, of the overall U.S. adult population.
Drawing from the CDC data, Ms. Bach estimates in her August 2022 report that as many as 4 million working-age Americans are too sick with long COVID to perform their jobs. That works out to as much as $230 billion in lost wages, or almost 1% of the U.S. GDP.
“This is a big deal,” she said. “We’re talking potentially hundreds of billions of dollars a year and that this is big enough to have a measurable impact on the labor market.”
Other sources have suggested lower figures, but the conclusions are the same: Long COVID is an urgent issue that will cost tens of billions of dollars a year in lost wages alone, Ms. Bach said. But it’s not just lost income for workers. There is a cost for businesses and the public.
Throughout the pandemic, COVID-19’s crippling force could be felt across multiple industries. While business has picked up again, staffing shortages remain a challenge. At some airports this summer, air passengers spent hours in security lines; were stranded for days as flights were canceled, rebooked, and canceled again on short notice; and waited weeks for lost luggage. Restaurants have had to cut back their hours. Those seeking medical care had longer than usual wait times in EDs and urgent care clinics. Some EDs temporarily closed.
These challenges have been attributed in part to the “great resignation” and in part because so many infected workers were out, especially during the Omicron waves. But increasingly, economists and health care professionals alike worry about long COVID’s impact on employers and the broader economy.
David Cutler, PhD, a professor of economics at Harvard University, Cambridge, Mass., believes the total economic loss could be as high as $3.7 trillion, when factoring in the lost quality of life, the cost in lost earnings, and the cost of higher spending on medical care. His estimate is more than a trillion dollars higher than a previous projection he and fellow economist Lawrence Summers, PhD, made in 2020. The reason? Long COVID.
“The higher estimate is largely a result of the greater prevalence of long COVID than we had guessed at the time,” Dr. Cutler wrote in a paper released in July.
“There are about 10 times the number of people with long COVID as have died of COVID. Because long COVID is so new, there is uncertainty about all of the numbers involved in the calculations. Still, the costs here are conservative, based on only cases to date.”
In Ms. Bach’s Brookings report, she projected that, if recovery from long COVID does not pick up and the population of Americans with long COVID were to grow by 10% a year, the annual cost of lost wages alone could reach half a trillion dollars in a decade.
Meanwhile, a working paper by the National Bureau of Economic Research found that workers who missed an entire week of work because of probable COVID-19 illnesses were roughly 7 percentage points less likely to be working a year later, compared with those who did not miss work for health reasons.
“It’s not just individuals with long COVID who are suffering from this. It impacts their families, their livelihoods, and the economy on a global scale. So, we have to raise awareness about those ripple effects,” said Linda Geng, MD, a clinical assistant professor of medicine with Stanford (Calif.) University’s Primary Care and Population Health.
“I think it’s hard for the public to grasp ... and understand the scale of this public health crisis.”
Debilitating fatigue
Long COVID is roughly defined; the CDC defines it as symptoms that linger 3 or more months after a patient first catches the virus.
The symptoms vary and include profound fatigue and brain issues.
“It’s a new degree of extreme and debilitating fatigue and exhaustion, to the point where you can’t do your daily tasks,” said Dr. Geng, who is also the codirector of Stanford’s Post-Acute COVID-19 Syndrome Clinic.
“People can be so debilitated, they can’t even do basic things, like the activities of daily living, let alone do their job, particularly if it’s physically or mentally demanding.”
Patients can also have postexertional malaise, where they feel especially bad and symptoms worsen when they exert themselves physically or mentally, Dr. Geng said. Compounding the issue for many long COVID patients is their trouble getting restful sleep. Those with brain fog have issues with memory, processing information, focused concentration, confusion, making mistakes, and multitasking. Pain is another debilitating symptom that can disrupt daily life and ability to work.
Even people with relatively mild infections can end up with long COVID, Dr. Geng said, noting that many of the patients at the Stanford clinic were never hospitalized with their initial infections. While existing research and Dr. Geng’s clinical experience show that long COVID can hit any age, she most commonly sees patients from ages 20 to their 60s, with an average age in the 40s – people in their prime working ages.
Jason Furman, PhD, a former White House economic adviser who is now a professor at Harvard University, noted in August that the labor force participation rate was far below what could be explained by standard demographic changes like an aging population, with the decline evident across all age groups. Dr. Furman does not speculate about why, but others have.
“We are pessimistic: Both the aging of the population and the impact of long COVID imply that the participation rate will be slow to return to its prepandemic level,” Anna Wong, Yelena Shulyatyeva, Andrew Husby, and Eliza Winger, economists with Bloomberg Economics, wrote in a research note.
Supportive policies
There is some evidence that vaccination reduces the risk of long COVID, but not completely, and it is too early to know if repeat infections increase long COVID risks. There is also no definitive data on how fast or how many people are recovering. Economists often assume that those with long COVID will recover at some point, Ms. Bach noted, but she is careful not to make assumptions.
“If people aren’t recovering, then this group keeps getting bigger,” she said. “We’re still adding, and if people aren’t coming out of that group, this becomes a bigger and bigger problem.”
For now, the number of new people being diagnosed with long COVID appears to have slowed, Ms. Bach said, but it remains to be seen whether the trend can be sustained.
“If people are impaired longer than we think and if the impairment turns out to be severe, then we can have a lot of people who need services like disability insurance,” Dr. Cutler said.
“That could put a really big strain on public sector programs and our ability to meet those needs.”
Policies that support the research and clinical work necessary to prevent and treat long COVID are essential, experts say.
“To me, that is the biggest economic imperative, to say nothing of human suffering,” said Ms. Bach.
Employers also have a role, and experts say there are a number of accommodations businesses should consider. What happens when an employee has long COVID? Can accommodations be made that allow them to continue working productively? If they spend a great deal of time commuting, can they work from home? What can employers do so that family members do not have to drop out of the workforce to take care of loved ones with long COVID?
Disability insurance
To be sure, there is one piece of the puzzle that does not quite fit, according to Dr. Cutler and Ms. Bach. There is no sign yet of a large increase in federal disability insurance applications, and no one quite knows why. Publicly available government data shows that online applications actually dipped by about 4% each year between 2019 and 2021. Applications in 2022 appear on track to remain slightly below prepandemic levels.
To qualify for Social Security Disability Insurance (SSDI), people need to have a disability that lasts at least a year.
“If you’re disabled with long COVID, who knows, right? You don’t know,” said Ms. Bach. “Two of the most dominant symptoms of long COVID are fatigue and brain fog. So, I’ve heard from people that the process of going through an SSDI application is really hard.”
Some long COVID patients told Ms. Bach they simply assumed they would not get SSDI and did not even bother applying. She stressed that working Americans with debilitating long COVID should be aware that their condition is protected by the Americans with Disabilities Act. But the challenge, based on guidance issued by the government, is that not all cases of long COVID qualify as a disability and that individual assessments are necessary.
While more long COVID data are needed, Ms. Bach believes there is enough information for decisionmakers to go after the issue more aggressively. She pointed to the $1.15 billion in funding that Congress earmarked for the National Institutes of Health over the course of 4 years in support of research into the long-term health effects of COVID-19.
“Now, $250 million a year sounds like a lot of money until you start talking about the cost of lost wages – just lost wages,” Ms. Bach said. “That’s not lost productivity. That’s not the cost of people whose family members are sick. Who have to reduce their own labor force participation. That’s not medical costs. Suddenly, $250 million doesn’t really sound like that much.”
A version of this article first appeared on WebMD.com.
Meet our newest genetically engineered frenemy, herpes
Herpes to the rescue
Let’s face it: When people hear the word “herpes,” their first thoughts are not positive. But what if herpes could be a hero?
Scientists have found a way to make a strain of herpes that kills cancer because, hey, it’s 2022, and anything is possible. Trials have been going well and this seems like a safe and effective way to fight cancer.
Viruses may be one of our oldest enemies, but it’s also been said that the enemy of my enemy is my friend. So why not make herpes the enemy of cancer, thereby turning it into our friend? The genetically modified herpes virus is injected directly into tumors, where it destroys cancer cells from within. But wait, there’s more! The patient’s immune system also senses the virus and springs into action against it and the cancer in which it is residing.
During the phase 1 trial, three of the nine patients saw tumor reduction and the therapy proved safe as well. Future trials will be able to more specifically target various cancer types and make the treatment better. For once, we are rooting for you, herpes.
A breath of not-so-fresh air
There’s nothing quite like that first real warm day of spring. You can finally open the windows and clear out the old stuffy air that’s been hanging around all winter long. It’s a ritual that’s now backed up with some science in the form of a new study. Turns out that there’s actually a fair amount of smog in the average home. That’s right, smog’s not just for the big city anymore.
As part of the HOMEChem project, a whole host of scientists gathered together under one roof in a typical suburban house and immediately started doing chores. Cooking, cleaning, the works. No, it wasn’t because they had trashed the place the night before. They had set up instrumentation all around the house to measure the chemical makeup of the air inside. A scientist’s idea of a wild party.
The results are perhaps not all that surprising, but interesting nonetheless. Your homemade smog certainly won’t kill you, but there’s both an increased amount and higher concentration of airborne toxins in indoor air, compared with outdoors. Benzene and formaldehyde were common, as were acrolein (a pulmonary toxicant emitted by lumber and burning fats) and isocyanic acid (which can react with proteins in the human body). The researchers noted that most of these chemicals can be removed with proper ventilation.
Although cleaning is certainly responsible for a fair share of the chemicals, cooking generally produced more toxic compounds, similar to what’s found in wildfire smoke. One of the researchers said this makes sense, since a wildfire can be considered an “extreme form of cooking.” Scientists may not know how to party, but their idea of a barbecue sounds … interesting. We’re looking forward to an upcoming study out of California: Can a 1-million acre wildfire adequately cook a ribeye steak?
We’re dying to try composting ... with humans, that is
We here at LOTME are not really fans of politicians, except as objects of ridicule. That is kind of fun. Whether we’re watching Fox News, listening to NPR, or reading Vladimir Putin’s fashion blog, one thing remains clear: If you want actual information, don’t ask a politician.
There are, of course, always exceptions, and we just found one: California state representative Cristina Garcia. Rep. Garcia sponsored a bill just signed into law by Gov. Gavin Newsom that legalizes the practice of human composting, the reduction of remains by “placing bodies in individual vessels and fostering gentle transformation into a nutrient-dense soil.”
Since we’ve written about this sort of thing before – Washington was the first state to legalize the process back in 2019 – we’re more interested now in what Rep. Garcia told NBC News while describing her motivation: “I’ve always wanted to be a tree. The idea of having my family sitting under my shade one day – that brings a lot of joy.” How great is that? Tree-hugging is just not enough. Be the tree.
California is the fifth state to provide its residents with the human composting option, the other three being Colorado, Oregon, and Vermont. The process “typically involves putting a body into a steel vessel, then covering it with organic materials like straw, wood chips and alfalfa. Microbes break down the corpse and the plant matter, transforming the various components into nutrient-rich soil in roughly 30 days,” Smithsonian Magazine explained.
We just happen to have some good news for Rep. Garcia about that wanting-to-be-a-tree business. She’s already pretty close. For more on that, we go to our correspondent from beyond the grave, Carl Sagan, who shares a thought about trees. And no, we couldn’t just write out his quote here. You have to hear it in Dr. Sagan’s own voice.
That’ll be one pandemic with extra distress. Hold the goals
When the COVID-19 pandemic first hit it put a lot of stuff on hold for everyone. Couldn’t eat inside at your favorite restaurant, attend that long-awaited concert, or travel out of the country. Those were all pretty bad, but it was the disruption of pursuing long-term goals that seemed to have the most effect on people’s mental health.
Investigators from the University of Waterloo (Ont.) looked at how putting such goals on hold affected people’s mental well-being. The study’s 226 participants were asked about their “COVID-frozen” goals and the degree to which they were able to actively pursue each goal and how committed they were to achieving it.
What they found was that the participants’ COVID-frozen goals were associated with feelings of psychological distress, such as anxiety, depressive symptoms, stress, and lowered life satisfaction. It was only when participants were able to disengage from goal rumination that well-being was impacted positively.
“Goal rumination is compulsive and can aggravate worries and frustrations while also taking away mental resources from other goals,” Candice Hubley, lead author and a PhD candidate in psychology, said in a written statement. So in short, you’re only stressing yourself out more about something that is far off in the distance when you could be focusing more on short-term, tangible goals instead.
Now, no one is saying to give up on your goals. Just take them one at a time. You’ll have better life satisfaction and your COVID-frozen goals will thaw out before you know it.
Herpes to the rescue
Let’s face it: When people hear the word “herpes,” their first thoughts are not positive. But what if herpes could be a hero?
Scientists have found a way to make a strain of herpes that kills cancer because, hey, it’s 2022, and anything is possible. Trials have been going well and this seems like a safe and effective way to fight cancer.
Viruses may be one of our oldest enemies, but it’s also been said that the enemy of my enemy is my friend. So why not make herpes the enemy of cancer, thereby turning it into our friend? The genetically modified herpes virus is injected directly into tumors, where it destroys cancer cells from within. But wait, there’s more! The patient’s immune system also senses the virus and springs into action against it and the cancer in which it is residing.
During the phase 1 trial, three of the nine patients saw tumor reduction and the therapy proved safe as well. Future trials will be able to more specifically target various cancer types and make the treatment better. For once, we are rooting for you, herpes.
A breath of not-so-fresh air
There’s nothing quite like that first real warm day of spring. You can finally open the windows and clear out the old stuffy air that’s been hanging around all winter long. It’s a ritual that’s now backed up with some science in the form of a new study. Turns out that there’s actually a fair amount of smog in the average home. That’s right, smog’s not just for the big city anymore.
As part of the HOMEChem project, a whole host of scientists gathered together under one roof in a typical suburban house and immediately started doing chores. Cooking, cleaning, the works. No, it wasn’t because they had trashed the place the night before. They had set up instrumentation all around the house to measure the chemical makeup of the air inside. A scientist’s idea of a wild party.
The results are perhaps not all that surprising, but interesting nonetheless. Your homemade smog certainly won’t kill you, but there’s both an increased amount and higher concentration of airborne toxins in indoor air, compared with outdoors. Benzene and formaldehyde were common, as were acrolein (a pulmonary toxicant emitted by lumber and burning fats) and isocyanic acid (which can react with proteins in the human body). The researchers noted that most of these chemicals can be removed with proper ventilation.
Although cleaning is certainly responsible for a fair share of the chemicals, cooking generally produced more toxic compounds, similar to what’s found in wildfire smoke. One of the researchers said this makes sense, since a wildfire can be considered an “extreme form of cooking.” Scientists may not know how to party, but their idea of a barbecue sounds … interesting. We’re looking forward to an upcoming study out of California: Can a 1-million acre wildfire adequately cook a ribeye steak?
We’re dying to try composting ... with humans, that is
We here at LOTME are not really fans of politicians, except as objects of ridicule. That is kind of fun. Whether we’re watching Fox News, listening to NPR, or reading Vladimir Putin’s fashion blog, one thing remains clear: If you want actual information, don’t ask a politician.
There are, of course, always exceptions, and we just found one: California state representative Cristina Garcia. Rep. Garcia sponsored a bill just signed into law by Gov. Gavin Newsom that legalizes the practice of human composting, the reduction of remains by “placing bodies in individual vessels and fostering gentle transformation into a nutrient-dense soil.”
Since we’ve written about this sort of thing before – Washington was the first state to legalize the process back in 2019 – we’re more interested now in what Rep. Garcia told NBC News while describing her motivation: “I’ve always wanted to be a tree. The idea of having my family sitting under my shade one day – that brings a lot of joy.” How great is that? Tree-hugging is just not enough. Be the tree.
California is the fifth state to provide its residents with the human composting option, the other three being Colorado, Oregon, and Vermont. The process “typically involves putting a body into a steel vessel, then covering it with organic materials like straw, wood chips and alfalfa. Microbes break down the corpse and the plant matter, transforming the various components into nutrient-rich soil in roughly 30 days,” Smithsonian Magazine explained.
We just happen to have some good news for Rep. Garcia about that wanting-to-be-a-tree business. She’s already pretty close. For more on that, we go to our correspondent from beyond the grave, Carl Sagan, who shares a thought about trees. And no, we couldn’t just write out his quote here. You have to hear it in Dr. Sagan’s own voice.
That’ll be one pandemic with extra distress. Hold the goals
When the COVID-19 pandemic first hit it put a lot of stuff on hold for everyone. Couldn’t eat inside at your favorite restaurant, attend that long-awaited concert, or travel out of the country. Those were all pretty bad, but it was the disruption of pursuing long-term goals that seemed to have the most effect on people’s mental health.
Investigators from the University of Waterloo (Ont.) looked at how putting such goals on hold affected people’s mental well-being. The study’s 226 participants were asked about their “COVID-frozen” goals and the degree to which they were able to actively pursue each goal and how committed they were to achieving it.
What they found was that the participants’ COVID-frozen goals were associated with feelings of psychological distress, such as anxiety, depressive symptoms, stress, and lowered life satisfaction. It was only when participants were able to disengage from goal rumination that well-being was impacted positively.
“Goal rumination is compulsive and can aggravate worries and frustrations while also taking away mental resources from other goals,” Candice Hubley, lead author and a PhD candidate in psychology, said in a written statement. So in short, you’re only stressing yourself out more about something that is far off in the distance when you could be focusing more on short-term, tangible goals instead.
Now, no one is saying to give up on your goals. Just take them one at a time. You’ll have better life satisfaction and your COVID-frozen goals will thaw out before you know it.
Herpes to the rescue
Let’s face it: When people hear the word “herpes,” their first thoughts are not positive. But what if herpes could be a hero?
Scientists have found a way to make a strain of herpes that kills cancer because, hey, it’s 2022, and anything is possible. Trials have been going well and this seems like a safe and effective way to fight cancer.
Viruses may be one of our oldest enemies, but it’s also been said that the enemy of my enemy is my friend. So why not make herpes the enemy of cancer, thereby turning it into our friend? The genetically modified herpes virus is injected directly into tumors, where it destroys cancer cells from within. But wait, there’s more! The patient’s immune system also senses the virus and springs into action against it and the cancer in which it is residing.
During the phase 1 trial, three of the nine patients saw tumor reduction and the therapy proved safe as well. Future trials will be able to more specifically target various cancer types and make the treatment better. For once, we are rooting for you, herpes.
A breath of not-so-fresh air
There’s nothing quite like that first real warm day of spring. You can finally open the windows and clear out the old stuffy air that’s been hanging around all winter long. It’s a ritual that’s now backed up with some science in the form of a new study. Turns out that there’s actually a fair amount of smog in the average home. That’s right, smog’s not just for the big city anymore.
As part of the HOMEChem project, a whole host of scientists gathered together under one roof in a typical suburban house and immediately started doing chores. Cooking, cleaning, the works. No, it wasn’t because they had trashed the place the night before. They had set up instrumentation all around the house to measure the chemical makeup of the air inside. A scientist’s idea of a wild party.
The results are perhaps not all that surprising, but interesting nonetheless. Your homemade smog certainly won’t kill you, but there’s both an increased amount and higher concentration of airborne toxins in indoor air, compared with outdoors. Benzene and formaldehyde were common, as were acrolein (a pulmonary toxicant emitted by lumber and burning fats) and isocyanic acid (which can react with proteins in the human body). The researchers noted that most of these chemicals can be removed with proper ventilation.
Although cleaning is certainly responsible for a fair share of the chemicals, cooking generally produced more toxic compounds, similar to what’s found in wildfire smoke. One of the researchers said this makes sense, since a wildfire can be considered an “extreme form of cooking.” Scientists may not know how to party, but their idea of a barbecue sounds … interesting. We’re looking forward to an upcoming study out of California: Can a 1-million acre wildfire adequately cook a ribeye steak?
We’re dying to try composting ... with humans, that is
We here at LOTME are not really fans of politicians, except as objects of ridicule. That is kind of fun. Whether we’re watching Fox News, listening to NPR, or reading Vladimir Putin’s fashion blog, one thing remains clear: If you want actual information, don’t ask a politician.
There are, of course, always exceptions, and we just found one: California state representative Cristina Garcia. Rep. Garcia sponsored a bill just signed into law by Gov. Gavin Newsom that legalizes the practice of human composting, the reduction of remains by “placing bodies in individual vessels and fostering gentle transformation into a nutrient-dense soil.”
Since we’ve written about this sort of thing before – Washington was the first state to legalize the process back in 2019 – we’re more interested now in what Rep. Garcia told NBC News while describing her motivation: “I’ve always wanted to be a tree. The idea of having my family sitting under my shade one day – that brings a lot of joy.” How great is that? Tree-hugging is just not enough. Be the tree.
California is the fifth state to provide its residents with the human composting option, the other three being Colorado, Oregon, and Vermont. The process “typically involves putting a body into a steel vessel, then covering it with organic materials like straw, wood chips and alfalfa. Microbes break down the corpse and the plant matter, transforming the various components into nutrient-rich soil in roughly 30 days,” Smithsonian Magazine explained.
We just happen to have some good news for Rep. Garcia about that wanting-to-be-a-tree business. She’s already pretty close. For more on that, we go to our correspondent from beyond the grave, Carl Sagan, who shares a thought about trees. And no, we couldn’t just write out his quote here. You have to hear it in Dr. Sagan’s own voice.
That’ll be one pandemic with extra distress. Hold the goals
When the COVID-19 pandemic first hit it put a lot of stuff on hold for everyone. Couldn’t eat inside at your favorite restaurant, attend that long-awaited concert, or travel out of the country. Those were all pretty bad, but it was the disruption of pursuing long-term goals that seemed to have the most effect on people’s mental health.
Investigators from the University of Waterloo (Ont.) looked at how putting such goals on hold affected people’s mental well-being. The study’s 226 participants were asked about their “COVID-frozen” goals and the degree to which they were able to actively pursue each goal and how committed they were to achieving it.
What they found was that the participants’ COVID-frozen goals were associated with feelings of psychological distress, such as anxiety, depressive symptoms, stress, and lowered life satisfaction. It was only when participants were able to disengage from goal rumination that well-being was impacted positively.
“Goal rumination is compulsive and can aggravate worries and frustrations while also taking away mental resources from other goals,” Candice Hubley, lead author and a PhD candidate in psychology, said in a written statement. So in short, you’re only stressing yourself out more about something that is far off in the distance when you could be focusing more on short-term, tangible goals instead.
Now, no one is saying to give up on your goals. Just take them one at a time. You’ll have better life satisfaction and your COVID-frozen goals will thaw out before you know it.
Safer opioid supply program in Canada helps those who face overdose risks
An analysis indicates that the program is associated with a reduction in emergency department visits, hospitalizations, and overall health care costs. In addition, there were no opioid-related deaths among participants who were at high risk of overdose.
“Not only did hospital engagements decline immediately after starting SOS programs, but also the risk of overdose did not change, and there were no opioid-related deaths in the 1-year follow-up,” study author Tara Gomes, PhD, an assistant professor of health policy, management, and evaluation at the University of Toronto and a scientist at the Li Ka Shing Knowledge Institute of St. Michael’s Hospital in Toronto, said in an interview.
Dr. Gomes is the lead principal investigator of the Ontario Drug Policy Research Network, a collaboration between researchers and drug policy decision-makers in the province.
“These changes were not seen in a group of similar individuals who lived in the same city – so were exposed to the same illicit drug supply – but who were not part of this program, helping to reinforce that these changes are specific to SOS participation,” she said.
The study was published in the Canadian Medical Association Journal.
Hospital admissions declined
More than 29,000 opioid-related toxicity deaths occurred in Canada between 2016 and 2021, often as a result of high levels of fentanyl in the drug supply, according to the investigators. In response, SOS programs have been launched in several provinces, including the first formal SOS program at the London (Ont.) InterCommunity Health Centre. As part of the program, clients are prescribed pharmaceutical opioids as an alternative to the fentanyl-adulterated drug supply and are given health and social supports.
Dr. Gomes and colleagues conducted an interrupted time series analysis of residents in London, Ont., who had received a diagnosis of opioid use disorder and had had a health care encounter related to the diagnosis between January 2016 and March 2019. They followed 82 participants who entered the SOS program, as well as a comparison group of 303 people who were matched on the basis of demographic and clinical characteristics but who did not participate in the program.
The research team focused on the population’s numbers of emergency department visits, hospital admissions, infection rates, and health care costs. They used autoregressive integrated moving average models to evaluate the effect of starting the SOS program and to compare the population’s outcome rates in the year before and after entering the program.
For participants who entered the program, the rate of emergency department visits declined by about 14 visits per 100 people. In addition, hospital admissions declined by about 5 admissions per 100 people. Health care costs that weren’t related to primary care or outpatient medications declined by about $922 per person. The rate of hospital admission for infections remained about the same; the investigators observed a decline of about 1.6 infections per 100 people.
In the year after entry into the program, emergency department visits, hospital admissions, infection-related admissions, and total health care costs declined significantly among SOS clients, compared with the year before.
Conversely, there were no significant changes in any of the measured outcomes among the 303 people who didn’t participate in the program.
Medication costs increased
DR. Gomes and colleagues noted that the findings provide preliminary evidence that SOS programs can play a role in the harm-reduction options available to those who are at high risk of drug poisoning and overdose. At the same time, many questions remain.
For instance, although total health care costs declined among those enrolled in the program, the medication-related costs increased. About 34% of participants had HIV, 69.5% had hepatitis C virus infection, and 28% had infectious complications in the year before entering the program. This finding may indicate that the participants had serious medical complications resulting from their drug use and were able to seek health care services.
“We interpret that to be a positive finding, because of the very high prevalence of HIV and hepatitis C in the SOS clients. Treatments for HIV and hepatitis C are lifesaving but expensive,” said Dr. Gomes. “Therefore, these higher medication costs are likely reflective of improved access to treatments for these infections, which can greatly improve people’s health and quality of life but also save the health care system money over the longer term.”
DR. Gomes and colleagues are now beginning to evaluate other SOS programs across Ontario. They hope to better understand the various approaches that are available and determine which models can best support people who face high risks because of drug use.
A limited solution?
Commenting on the study, Andrew Ivsins, PhD, a postdoctoral fellow in social medicine at the University of British Columbia in Vancouver and a research scientist at the British Columbia Centre on Substance Abuse, said, “This is an important study and one of the first to show how safe supply can help by building connections to the health care system that didn’t exist previously.”
Dr. Ivsins, who wasn’t involved with this study, has researched safe supply programs around Vancouver. He and colleagues found that among participants in these programs, the use of illicit street-purchased drugs decreased, which led to improved health and wellness.
“Safe supply is fundamentally, at the most basic level, a response to the highly toxic drug supply and out-of-control poisoning crisis in North America,” he said. “It’s a contentious issue, but it makes so much sense that, if what’s killing people is highly toxic drugs, we need to find a way to provide an option that doesn’t kill them.”
“Up to now, safer supply has mostly been used to reduce harms, including mortality and morbidity, in persons using illicit opioids. But if we really want to lower the risk linked to heavy contamination of the unregulated drug supply, safer supply programs will have to be extended to all substances potentially sold illegally,” Marie-Eve Goyer, MD, an assistant professor of family medicine at the University of Montreal, said in an interview.
Dr. Goyer, who wasn’t involved with this study, has conducted research about substance replacement therapy in Quebec. She found that many provinces are now reporting on new potent designer benzodiazepines that are being used or that are contaminating fentanyl, which calls for a broader approach to address the drug overdose crisis.
“Let’s realize that safer supply prescription is a very medicalized (and limited) solution to an epidemic that is made of stigma, criminalization, and repressive public policies,” she said. “Without true changes in the law, we will continue to see our people dying every day.”
The study was funded by grants from the Ontario Ministry of Health and the Canadian Institutes of Health Research. Dr. Gomes has received grants to support the research of both groups, and other authors have received support or fees related to the London InterCommunity Health Centre. Dr. Ivsins and Dr. Goyer have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
An analysis indicates that the program is associated with a reduction in emergency department visits, hospitalizations, and overall health care costs. In addition, there were no opioid-related deaths among participants who were at high risk of overdose.
“Not only did hospital engagements decline immediately after starting SOS programs, but also the risk of overdose did not change, and there were no opioid-related deaths in the 1-year follow-up,” study author Tara Gomes, PhD, an assistant professor of health policy, management, and evaluation at the University of Toronto and a scientist at the Li Ka Shing Knowledge Institute of St. Michael’s Hospital in Toronto, said in an interview.
Dr. Gomes is the lead principal investigator of the Ontario Drug Policy Research Network, a collaboration between researchers and drug policy decision-makers in the province.
“These changes were not seen in a group of similar individuals who lived in the same city – so were exposed to the same illicit drug supply – but who were not part of this program, helping to reinforce that these changes are specific to SOS participation,” she said.
The study was published in the Canadian Medical Association Journal.
Hospital admissions declined
More than 29,000 opioid-related toxicity deaths occurred in Canada between 2016 and 2021, often as a result of high levels of fentanyl in the drug supply, according to the investigators. In response, SOS programs have been launched in several provinces, including the first formal SOS program at the London (Ont.) InterCommunity Health Centre. As part of the program, clients are prescribed pharmaceutical opioids as an alternative to the fentanyl-adulterated drug supply and are given health and social supports.
Dr. Gomes and colleagues conducted an interrupted time series analysis of residents in London, Ont., who had received a diagnosis of opioid use disorder and had had a health care encounter related to the diagnosis between January 2016 and March 2019. They followed 82 participants who entered the SOS program, as well as a comparison group of 303 people who were matched on the basis of demographic and clinical characteristics but who did not participate in the program.
The research team focused on the population’s numbers of emergency department visits, hospital admissions, infection rates, and health care costs. They used autoregressive integrated moving average models to evaluate the effect of starting the SOS program and to compare the population’s outcome rates in the year before and after entering the program.
For participants who entered the program, the rate of emergency department visits declined by about 14 visits per 100 people. In addition, hospital admissions declined by about 5 admissions per 100 people. Health care costs that weren’t related to primary care or outpatient medications declined by about $922 per person. The rate of hospital admission for infections remained about the same; the investigators observed a decline of about 1.6 infections per 100 people.
In the year after entry into the program, emergency department visits, hospital admissions, infection-related admissions, and total health care costs declined significantly among SOS clients, compared with the year before.
Conversely, there were no significant changes in any of the measured outcomes among the 303 people who didn’t participate in the program.
Medication costs increased
DR. Gomes and colleagues noted that the findings provide preliminary evidence that SOS programs can play a role in the harm-reduction options available to those who are at high risk of drug poisoning and overdose. At the same time, many questions remain.
For instance, although total health care costs declined among those enrolled in the program, the medication-related costs increased. About 34% of participants had HIV, 69.5% had hepatitis C virus infection, and 28% had infectious complications in the year before entering the program. This finding may indicate that the participants had serious medical complications resulting from their drug use and were able to seek health care services.
“We interpret that to be a positive finding, because of the very high prevalence of HIV and hepatitis C in the SOS clients. Treatments for HIV and hepatitis C are lifesaving but expensive,” said Dr. Gomes. “Therefore, these higher medication costs are likely reflective of improved access to treatments for these infections, which can greatly improve people’s health and quality of life but also save the health care system money over the longer term.”
DR. Gomes and colleagues are now beginning to evaluate other SOS programs across Ontario. They hope to better understand the various approaches that are available and determine which models can best support people who face high risks because of drug use.
A limited solution?
Commenting on the study, Andrew Ivsins, PhD, a postdoctoral fellow in social medicine at the University of British Columbia in Vancouver and a research scientist at the British Columbia Centre on Substance Abuse, said, “This is an important study and one of the first to show how safe supply can help by building connections to the health care system that didn’t exist previously.”
Dr. Ivsins, who wasn’t involved with this study, has researched safe supply programs around Vancouver. He and colleagues found that among participants in these programs, the use of illicit street-purchased drugs decreased, which led to improved health and wellness.
“Safe supply is fundamentally, at the most basic level, a response to the highly toxic drug supply and out-of-control poisoning crisis in North America,” he said. “It’s a contentious issue, but it makes so much sense that, if what’s killing people is highly toxic drugs, we need to find a way to provide an option that doesn’t kill them.”
“Up to now, safer supply has mostly been used to reduce harms, including mortality and morbidity, in persons using illicit opioids. But if we really want to lower the risk linked to heavy contamination of the unregulated drug supply, safer supply programs will have to be extended to all substances potentially sold illegally,” Marie-Eve Goyer, MD, an assistant professor of family medicine at the University of Montreal, said in an interview.
Dr. Goyer, who wasn’t involved with this study, has conducted research about substance replacement therapy in Quebec. She found that many provinces are now reporting on new potent designer benzodiazepines that are being used or that are contaminating fentanyl, which calls for a broader approach to address the drug overdose crisis.
“Let’s realize that safer supply prescription is a very medicalized (and limited) solution to an epidemic that is made of stigma, criminalization, and repressive public policies,” she said. “Without true changes in the law, we will continue to see our people dying every day.”
The study was funded by grants from the Ontario Ministry of Health and the Canadian Institutes of Health Research. Dr. Gomes has received grants to support the research of both groups, and other authors have received support or fees related to the London InterCommunity Health Centre. Dr. Ivsins and Dr. Goyer have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
An analysis indicates that the program is associated with a reduction in emergency department visits, hospitalizations, and overall health care costs. In addition, there were no opioid-related deaths among participants who were at high risk of overdose.
“Not only did hospital engagements decline immediately after starting SOS programs, but also the risk of overdose did not change, and there were no opioid-related deaths in the 1-year follow-up,” study author Tara Gomes, PhD, an assistant professor of health policy, management, and evaluation at the University of Toronto and a scientist at the Li Ka Shing Knowledge Institute of St. Michael’s Hospital in Toronto, said in an interview.
Dr. Gomes is the lead principal investigator of the Ontario Drug Policy Research Network, a collaboration between researchers and drug policy decision-makers in the province.
“These changes were not seen in a group of similar individuals who lived in the same city – so were exposed to the same illicit drug supply – but who were not part of this program, helping to reinforce that these changes are specific to SOS participation,” she said.
The study was published in the Canadian Medical Association Journal.
Hospital admissions declined
More than 29,000 opioid-related toxicity deaths occurred in Canada between 2016 and 2021, often as a result of high levels of fentanyl in the drug supply, according to the investigators. In response, SOS programs have been launched in several provinces, including the first formal SOS program at the London (Ont.) InterCommunity Health Centre. As part of the program, clients are prescribed pharmaceutical opioids as an alternative to the fentanyl-adulterated drug supply and are given health and social supports.
Dr. Gomes and colleagues conducted an interrupted time series analysis of residents in London, Ont., who had received a diagnosis of opioid use disorder and had had a health care encounter related to the diagnosis between January 2016 and March 2019. They followed 82 participants who entered the SOS program, as well as a comparison group of 303 people who were matched on the basis of demographic and clinical characteristics but who did not participate in the program.
The research team focused on the population’s numbers of emergency department visits, hospital admissions, infection rates, and health care costs. They used autoregressive integrated moving average models to evaluate the effect of starting the SOS program and to compare the population’s outcome rates in the year before and after entering the program.
For participants who entered the program, the rate of emergency department visits declined by about 14 visits per 100 people. In addition, hospital admissions declined by about 5 admissions per 100 people. Health care costs that weren’t related to primary care or outpatient medications declined by about $922 per person. The rate of hospital admission for infections remained about the same; the investigators observed a decline of about 1.6 infections per 100 people.
In the year after entry into the program, emergency department visits, hospital admissions, infection-related admissions, and total health care costs declined significantly among SOS clients, compared with the year before.
Conversely, there were no significant changes in any of the measured outcomes among the 303 people who didn’t participate in the program.
Medication costs increased
DR. Gomes and colleagues noted that the findings provide preliminary evidence that SOS programs can play a role in the harm-reduction options available to those who are at high risk of drug poisoning and overdose. At the same time, many questions remain.
For instance, although total health care costs declined among those enrolled in the program, the medication-related costs increased. About 34% of participants had HIV, 69.5% had hepatitis C virus infection, and 28% had infectious complications in the year before entering the program. This finding may indicate that the participants had serious medical complications resulting from their drug use and were able to seek health care services.
“We interpret that to be a positive finding, because of the very high prevalence of HIV and hepatitis C in the SOS clients. Treatments for HIV and hepatitis C are lifesaving but expensive,” said Dr. Gomes. “Therefore, these higher medication costs are likely reflective of improved access to treatments for these infections, which can greatly improve people’s health and quality of life but also save the health care system money over the longer term.”
DR. Gomes and colleagues are now beginning to evaluate other SOS programs across Ontario. They hope to better understand the various approaches that are available and determine which models can best support people who face high risks because of drug use.
A limited solution?
Commenting on the study, Andrew Ivsins, PhD, a postdoctoral fellow in social medicine at the University of British Columbia in Vancouver and a research scientist at the British Columbia Centre on Substance Abuse, said, “This is an important study and one of the first to show how safe supply can help by building connections to the health care system that didn’t exist previously.”
Dr. Ivsins, who wasn’t involved with this study, has researched safe supply programs around Vancouver. He and colleagues found that among participants in these programs, the use of illicit street-purchased drugs decreased, which led to improved health and wellness.
“Safe supply is fundamentally, at the most basic level, a response to the highly toxic drug supply and out-of-control poisoning crisis in North America,” he said. “It’s a contentious issue, but it makes so much sense that, if what’s killing people is highly toxic drugs, we need to find a way to provide an option that doesn’t kill them.”
“Up to now, safer supply has mostly been used to reduce harms, including mortality and morbidity, in persons using illicit opioids. But if we really want to lower the risk linked to heavy contamination of the unregulated drug supply, safer supply programs will have to be extended to all substances potentially sold illegally,” Marie-Eve Goyer, MD, an assistant professor of family medicine at the University of Montreal, said in an interview.
Dr. Goyer, who wasn’t involved with this study, has conducted research about substance replacement therapy in Quebec. She found that many provinces are now reporting on new potent designer benzodiazepines that are being used or that are contaminating fentanyl, which calls for a broader approach to address the drug overdose crisis.
“Let’s realize that safer supply prescription is a very medicalized (and limited) solution to an epidemic that is made of stigma, criminalization, and repressive public policies,” she said. “Without true changes in the law, we will continue to see our people dying every day.”
The study was funded by grants from the Ontario Ministry of Health and the Canadian Institutes of Health Research. Dr. Gomes has received grants to support the research of both groups, and other authors have received support or fees related to the London InterCommunity Health Centre. Dr. Ivsins and Dr. Goyer have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM CANADIAN MEDICAL ASSOCIATION JOURNAL
Could a vaccine (and more) fix the fentanyl crisis?
This discussion was recorded on Aug. 31, 2022. This transcript has been edited for clarity.
Robert Glatter, MD: Welcome. I’m Dr. Robert Glatter, medical advisor for Medscape Emergency Medicine. Today we have Dr. Paul Christo, a pain specialist in the Division of Pain Medicine at Johns Hopkins University School of Medicine in Baltimore, Maryland, and host of the national radio show Aches and Gains on SiriusXM Radio, joining us to discuss the ongoing and worsening fentanyl crisis in the U.S.
Welcome, Dr Christo.
Paul J. Christo, MD, MBA: Thanks so much for having me.
Dr. Glatter: I want to begin with a sobering statistic regarding overdoses. , based on recent data from the CDC.
Let’s start by having you explain how deadly fentanyl is in terms of its potency compared with morphine and heroin.
Dr. Christo: Fentanyl is considered a synthetic opioid. It’s not a naturally occurring opioid like morphine, for example, or codeine. We use this drug, fentanyl, often in the anesthesia well. We’ve used it for many years as an anesthetic for surgery very safely. In the chronic pain world, we’ve used it to help reduce chronic pain in the form of a patch.
What we’re seeing now, though, is something entirely different, which is the use of synthetic fentanyl as a mind- and mood-altering substance for those who don’t have pain, and essentially those who are buying this off the street. Fentanyl is about 80-100 times more potent than morphine, so you can put that in perspective in terms of its danger.
Dr. Glatter: Let me have you take us through an evolution of the opioid crisis from the 1990s, from long-acting opioid OxyContin, which was approved in 1995, to where we are now. There are different phases. If you could, educate our audience on how we got to where fentanyl is now the most common opiate involved in drug overdoses.
Dr. Christo: It really stems from the epidemic related to chronic pain. We have over 100 million people in the United States alone who suffer from chronic pain. Most chronic pain, sadly, is undertreated or untreated. In the ‘90s, in the quest to reduce chronic pain to a better extent, we saw more and more literature and studies related to the use of opioids for noncancer pain (e.g., for lower back pain).
There were many primary care doctors and pain specialists who started using opioids, probably for patients who didn’t really need it. I think it was done out of good conscience in the sense that they were trying to reduce pain. We have other methods of pain relief, but we needed more. At that time, in the ‘90s, we had a greater use of opioids to treat noncancer pain.
Then from that point, we transitioned to the use of heroin. Again, this isn’t among the chronic pain population, but it was the nonchronic pain population that starting using heroin. Today we see synthetic fentanyl.
Addressing the synthetic opioid crisis
Dr. Glatter: With fentanyl being the most common opiate we’re seeing, we’re having problems trying to save patients. We’re trying to use naloxone, but obviously in increasing amounts, and sometimes it’s not adequate and we have to intubate patients.
In terms of addressing this issue of supply, the fentanyl is coming from Mexico, China, and it’s manufactured here in the United States. How do we address this crisis? What are the steps that you would recommend we take?
Dr. Christo: I think that we need to better support law enforcement to crack down on those who are manufacturing fentanyl in the United States, and also to crack down on those who are transporting it from, say, Mexico – I think it’s primarily coming from Mexico – but from outside the United States to the United States. I feel like that’s important to do.
Two, we need to better educate those who are using these mind- and mood-altering substances. We’re seeing more and more that it’s the young-adult population, those between the ages of 13 and 25, who are starting to use these substances, and they’re very dangerous.
Dr. Glatter: Are these teens seeking out heroin and it happens to be laced with fentanyl, or are they actually seeking pure fentanyl? Are they trying to buy the colorful pills that we know about? What’s your experience in terms of the population you’re treating and what you could tell us?
Dr. Christo: I think it’s both. We’re seeing young adults who are interested in the use of fentanyl as a mind- and mood-altering substance. We’re also seeing young and older adults use other drugs, like cocaine and heroin, that are laced with fentanyl, and they don’t know it. That’s exponentially more dangerous.
Fentanyl test strips
Dr. Glatter: People are unaware that there is fentanyl in what they’re using, and it is certainly leading to overdoses and deaths. I think that parents really need to be aware of this.
Dr. Christo: Yes, for sure. I think we need better educational methods in the schools to educate that population that we’re talking about (between the ages of 13 and 25). Let them know the dangers, because I don’t think they’re aware of the danger, and how potent fentanyl is in terms of its lethality, and that you don’t need very much to take in a form of a pill or to inhale or to inject intravenously to kill yourself. That is key – education at that level – and to let those who are going to use these substances (specifically, synthetic fentanyl) know that they should consider the use of fentanyl test strips.
Fentanyl test strips would be primarily used for those who are thinking that they’re using heroin but there may be fentanyl in there, or methamphetamine and there may be fentanyl, and they don’t know. The test strip gives them that knowledge.
The other harm reduction strategies would be the use of naloxone, known as Narcan. That’s a lifesaver. You just have to spritz it into the nostril. You don’t do it yourself if you’re using the substance, but you’ve got others who can do it for you. No question, that’s a lifesaver. We need to make sure that there’s greater availability of that throughout the entire country, and we’re seeing some of that in certain states. In certain states, you don’t need a prescription to get naloxone from the pharmacy.
Dr. Glatter: I think it’s so important that it should be widely available. Certainly, the COVID-19 pandemic exacerbated the number of overdoses we saw. Are overdoses coming down or are we still at a level that’s close to 2020?
Dr. Christo: Unfortunately, we’re still seeing the same level, if not seeing it escalate. Certainly, the pandemic, because of the economic cost associated with the pandemic – loss of employment, underemployment – as well as the emotional stress of the pandemic led many people to use substances on the street in order to cope. They’re coping mechanisms, and we really haven’t seen it abate quite yet.
Dr. Glatter: Do you have a message for the lawmakers on Capitol Hill as to what we can do regarding the illegal manufacturing and distribution, how we can really crack down? Are there other approaches that we could implement that might be more tangible?
Dr. Christo: Yes. No. 1 would be to support law enforcement. No. 2 would be to create and make available more overdose prevention centers. The first was in New York City. If you look at the data on overdose prevention centers, in Canada, for example, they’ve seen a 35% reduction in overdose deaths. These are places where people who are using can go to get clean needles and clean syringes. This is where people basically oversee the use of the drug and intervene if necessary.
It seems sort of antithetical. It seems like, “Boy, why would you fund a center for people to use drugs?” The data from Canada and outside Canada are such that it can be very helpful. That would be one of my messages to lawmakers as well.
Vaccines to combat the synthetic opioid crisis
Dr. Glatter: Do you think that the legislators could approach some of these factories as a way to crack down, and have law enforcement be more aggressive? Is that another possible solution?
Dr. Christo: It is. Law enforcement needs to be supported by the government, by the Biden administration, so that we can prevent the influx of fentanyl and other drugs into the United States, and also to crack down on those in the United States who are manufacturing these drugs – synthetic fentanyl, first and foremost – because we’re seeing a lot of deaths related to synthetic fentanyl.
Also, we’re seeing — and this is pretty intriguing and interesting – the use of vaccines to help prevent overdose. The first human trial is underway right now for a vaccine against oxycodone. Not only that, but there are other vaccines that are in animal trials now against heroin, cocaine, or fentanyl. There’s hope there that we can use vaccines to also help reduce deaths related to overdose from fentanyl and other opioids.
Dr. Glatter: Do you think this would be given widely to the population or only to those at higher risk?
Dr. Christo: It would probably be targeting those who are at higher risk and have a history of drug abuse. I don’t think it would be something that would be given to the entire population, but it certainly could be effective, and we’re seeing encouraging results from the human trial right now.
Dr. Glatter: That’s very intriguing. That’s something that certainly could be quite helpful in the future.
One thing I did want to address is law enforcement and first responders who have been exposed to dust, or inhaled dust possibly, or had fentanyl on their skin. There has been lots of controversy. The recent literature has dispelled the controversy that people who had supposedly passed out and required Narcan after exposure to intact skin, or even compromised skin, had an overdose of fentanyl. Maybe you could speak to that and dispel that myth.
Dr. Christo: Yes, I’ve been asked this question a couple of times in the past. It’s not sufficient just to have contact with fentanyl on the skin to lead to an overdose. You really need to ingest it. That is, take it by mouth in the form of a pill, inhale it, or inject it intravenously. Skin contact is very unlikely going to lead to an overdose and death.
Dr. Glatter: I want to thank you for a very informative interview. Do you have one or two pearls you’d like to give our audience as a takeaway?
Dr. Christo: I would say two things. One is, don’t give up if you have chronic pain because there is hope. We have nonopioid treatments that can be effective. Two, don’t give up if you have a substance use disorder. Talk to your primary care doctor or talk to emergency room physicians if you’re in the emergency room. The Substance Abuse and Mental Health Services Administration is a good resource, too. SAMHSA has an 800 number for support and a website. Take the opportunity to use the resources that are available.
Dr. Glatter is assistant professor of emergency medicine at Lenox Hill Hospital in New York City and at Hofstra University, Hempstead, N.Y. He is an editorial advisor and hosts the Hot Topics in EM series on Medscape. He is also a medical contributor for Forbes.
Dr. Christo is an associate professor and a pain specialist in the department of anesthesiology and critical care medicine at Johns Hopkins University, Baltimore. He also serves as director of the multidisciplinary pain fellowship program at Johns Hopkins Hospital. Christo is the author of Aches and Gains, A Comprehensive Guide to Overcoming Your Pain, and hosts an award-winning, nationally syndicated SiriusXM radio talk show on overcoming pain, called Aches and Gains.
A version of this article first appeared on Medscape.com.
This discussion was recorded on Aug. 31, 2022. This transcript has been edited for clarity.
Robert Glatter, MD: Welcome. I’m Dr. Robert Glatter, medical advisor for Medscape Emergency Medicine. Today we have Dr. Paul Christo, a pain specialist in the Division of Pain Medicine at Johns Hopkins University School of Medicine in Baltimore, Maryland, and host of the national radio show Aches and Gains on SiriusXM Radio, joining us to discuss the ongoing and worsening fentanyl crisis in the U.S.
Welcome, Dr Christo.
Paul J. Christo, MD, MBA: Thanks so much for having me.
Dr. Glatter: I want to begin with a sobering statistic regarding overdoses. , based on recent data from the CDC.
Let’s start by having you explain how deadly fentanyl is in terms of its potency compared with morphine and heroin.
Dr. Christo: Fentanyl is considered a synthetic opioid. It’s not a naturally occurring opioid like morphine, for example, or codeine. We use this drug, fentanyl, often in the anesthesia well. We’ve used it for many years as an anesthetic for surgery very safely. In the chronic pain world, we’ve used it to help reduce chronic pain in the form of a patch.
What we’re seeing now, though, is something entirely different, which is the use of synthetic fentanyl as a mind- and mood-altering substance for those who don’t have pain, and essentially those who are buying this off the street. Fentanyl is about 80-100 times more potent than morphine, so you can put that in perspective in terms of its danger.
Dr. Glatter: Let me have you take us through an evolution of the opioid crisis from the 1990s, from long-acting opioid OxyContin, which was approved in 1995, to where we are now. There are different phases. If you could, educate our audience on how we got to where fentanyl is now the most common opiate involved in drug overdoses.
Dr. Christo: It really stems from the epidemic related to chronic pain. We have over 100 million people in the United States alone who suffer from chronic pain. Most chronic pain, sadly, is undertreated or untreated. In the ‘90s, in the quest to reduce chronic pain to a better extent, we saw more and more literature and studies related to the use of opioids for noncancer pain (e.g., for lower back pain).
There were many primary care doctors and pain specialists who started using opioids, probably for patients who didn’t really need it. I think it was done out of good conscience in the sense that they were trying to reduce pain. We have other methods of pain relief, but we needed more. At that time, in the ‘90s, we had a greater use of opioids to treat noncancer pain.
Then from that point, we transitioned to the use of heroin. Again, this isn’t among the chronic pain population, but it was the nonchronic pain population that starting using heroin. Today we see synthetic fentanyl.
Addressing the synthetic opioid crisis
Dr. Glatter: With fentanyl being the most common opiate we’re seeing, we’re having problems trying to save patients. We’re trying to use naloxone, but obviously in increasing amounts, and sometimes it’s not adequate and we have to intubate patients.
In terms of addressing this issue of supply, the fentanyl is coming from Mexico, China, and it’s manufactured here in the United States. How do we address this crisis? What are the steps that you would recommend we take?
Dr. Christo: I think that we need to better support law enforcement to crack down on those who are manufacturing fentanyl in the United States, and also to crack down on those who are transporting it from, say, Mexico – I think it’s primarily coming from Mexico – but from outside the United States to the United States. I feel like that’s important to do.
Two, we need to better educate those who are using these mind- and mood-altering substances. We’re seeing more and more that it’s the young-adult population, those between the ages of 13 and 25, who are starting to use these substances, and they’re very dangerous.
Dr. Glatter: Are these teens seeking out heroin and it happens to be laced with fentanyl, or are they actually seeking pure fentanyl? Are they trying to buy the colorful pills that we know about? What’s your experience in terms of the population you’re treating and what you could tell us?
Dr. Christo: I think it’s both. We’re seeing young adults who are interested in the use of fentanyl as a mind- and mood-altering substance. We’re also seeing young and older adults use other drugs, like cocaine and heroin, that are laced with fentanyl, and they don’t know it. That’s exponentially more dangerous.
Fentanyl test strips
Dr. Glatter: People are unaware that there is fentanyl in what they’re using, and it is certainly leading to overdoses and deaths. I think that parents really need to be aware of this.
Dr. Christo: Yes, for sure. I think we need better educational methods in the schools to educate that population that we’re talking about (between the ages of 13 and 25). Let them know the dangers, because I don’t think they’re aware of the danger, and how potent fentanyl is in terms of its lethality, and that you don’t need very much to take in a form of a pill or to inhale or to inject intravenously to kill yourself. That is key – education at that level – and to let those who are going to use these substances (specifically, synthetic fentanyl) know that they should consider the use of fentanyl test strips.
Fentanyl test strips would be primarily used for those who are thinking that they’re using heroin but there may be fentanyl in there, or methamphetamine and there may be fentanyl, and they don’t know. The test strip gives them that knowledge.
The other harm reduction strategies would be the use of naloxone, known as Narcan. That’s a lifesaver. You just have to spritz it into the nostril. You don’t do it yourself if you’re using the substance, but you’ve got others who can do it for you. No question, that’s a lifesaver. We need to make sure that there’s greater availability of that throughout the entire country, and we’re seeing some of that in certain states. In certain states, you don’t need a prescription to get naloxone from the pharmacy.
Dr. Glatter: I think it’s so important that it should be widely available. Certainly, the COVID-19 pandemic exacerbated the number of overdoses we saw. Are overdoses coming down or are we still at a level that’s close to 2020?
Dr. Christo: Unfortunately, we’re still seeing the same level, if not seeing it escalate. Certainly, the pandemic, because of the economic cost associated with the pandemic – loss of employment, underemployment – as well as the emotional stress of the pandemic led many people to use substances on the street in order to cope. They’re coping mechanisms, and we really haven’t seen it abate quite yet.
Dr. Glatter: Do you have a message for the lawmakers on Capitol Hill as to what we can do regarding the illegal manufacturing and distribution, how we can really crack down? Are there other approaches that we could implement that might be more tangible?
Dr. Christo: Yes. No. 1 would be to support law enforcement. No. 2 would be to create and make available more overdose prevention centers. The first was in New York City. If you look at the data on overdose prevention centers, in Canada, for example, they’ve seen a 35% reduction in overdose deaths. These are places where people who are using can go to get clean needles and clean syringes. This is where people basically oversee the use of the drug and intervene if necessary.
It seems sort of antithetical. It seems like, “Boy, why would you fund a center for people to use drugs?” The data from Canada and outside Canada are such that it can be very helpful. That would be one of my messages to lawmakers as well.
Vaccines to combat the synthetic opioid crisis
Dr. Glatter: Do you think that the legislators could approach some of these factories as a way to crack down, and have law enforcement be more aggressive? Is that another possible solution?
Dr. Christo: It is. Law enforcement needs to be supported by the government, by the Biden administration, so that we can prevent the influx of fentanyl and other drugs into the United States, and also to crack down on those in the United States who are manufacturing these drugs – synthetic fentanyl, first and foremost – because we’re seeing a lot of deaths related to synthetic fentanyl.
Also, we’re seeing — and this is pretty intriguing and interesting – the use of vaccines to help prevent overdose. The first human trial is underway right now for a vaccine against oxycodone. Not only that, but there are other vaccines that are in animal trials now against heroin, cocaine, or fentanyl. There’s hope there that we can use vaccines to also help reduce deaths related to overdose from fentanyl and other opioids.
Dr. Glatter: Do you think this would be given widely to the population or only to those at higher risk?
Dr. Christo: It would probably be targeting those who are at higher risk and have a history of drug abuse. I don’t think it would be something that would be given to the entire population, but it certainly could be effective, and we’re seeing encouraging results from the human trial right now.
Dr. Glatter: That’s very intriguing. That’s something that certainly could be quite helpful in the future.
One thing I did want to address is law enforcement and first responders who have been exposed to dust, or inhaled dust possibly, or had fentanyl on their skin. There has been lots of controversy. The recent literature has dispelled the controversy that people who had supposedly passed out and required Narcan after exposure to intact skin, or even compromised skin, had an overdose of fentanyl. Maybe you could speak to that and dispel that myth.
Dr. Christo: Yes, I’ve been asked this question a couple of times in the past. It’s not sufficient just to have contact with fentanyl on the skin to lead to an overdose. You really need to ingest it. That is, take it by mouth in the form of a pill, inhale it, or inject it intravenously. Skin contact is very unlikely going to lead to an overdose and death.
Dr. Glatter: I want to thank you for a very informative interview. Do you have one or two pearls you’d like to give our audience as a takeaway?
Dr. Christo: I would say two things. One is, don’t give up if you have chronic pain because there is hope. We have nonopioid treatments that can be effective. Two, don’t give up if you have a substance use disorder. Talk to your primary care doctor or talk to emergency room physicians if you’re in the emergency room. The Substance Abuse and Mental Health Services Administration is a good resource, too. SAMHSA has an 800 number for support and a website. Take the opportunity to use the resources that are available.
Dr. Glatter is assistant professor of emergency medicine at Lenox Hill Hospital in New York City and at Hofstra University, Hempstead, N.Y. He is an editorial advisor and hosts the Hot Topics in EM series on Medscape. He is also a medical contributor for Forbes.
Dr. Christo is an associate professor and a pain specialist in the department of anesthesiology and critical care medicine at Johns Hopkins University, Baltimore. He also serves as director of the multidisciplinary pain fellowship program at Johns Hopkins Hospital. Christo is the author of Aches and Gains, A Comprehensive Guide to Overcoming Your Pain, and hosts an award-winning, nationally syndicated SiriusXM radio talk show on overcoming pain, called Aches and Gains.
A version of this article first appeared on Medscape.com.
This discussion was recorded on Aug. 31, 2022. This transcript has been edited for clarity.
Robert Glatter, MD: Welcome. I’m Dr. Robert Glatter, medical advisor for Medscape Emergency Medicine. Today we have Dr. Paul Christo, a pain specialist in the Division of Pain Medicine at Johns Hopkins University School of Medicine in Baltimore, Maryland, and host of the national radio show Aches and Gains on SiriusXM Radio, joining us to discuss the ongoing and worsening fentanyl crisis in the U.S.
Welcome, Dr Christo.
Paul J. Christo, MD, MBA: Thanks so much for having me.
Dr. Glatter: I want to begin with a sobering statistic regarding overdoses. , based on recent data from the CDC.
Let’s start by having you explain how deadly fentanyl is in terms of its potency compared with morphine and heroin.
Dr. Christo: Fentanyl is considered a synthetic opioid. It’s not a naturally occurring opioid like morphine, for example, or codeine. We use this drug, fentanyl, often in the anesthesia well. We’ve used it for many years as an anesthetic for surgery very safely. In the chronic pain world, we’ve used it to help reduce chronic pain in the form of a patch.
What we’re seeing now, though, is something entirely different, which is the use of synthetic fentanyl as a mind- and mood-altering substance for those who don’t have pain, and essentially those who are buying this off the street. Fentanyl is about 80-100 times more potent than morphine, so you can put that in perspective in terms of its danger.
Dr. Glatter: Let me have you take us through an evolution of the opioid crisis from the 1990s, from long-acting opioid OxyContin, which was approved in 1995, to where we are now. There are different phases. If you could, educate our audience on how we got to where fentanyl is now the most common opiate involved in drug overdoses.
Dr. Christo: It really stems from the epidemic related to chronic pain. We have over 100 million people in the United States alone who suffer from chronic pain. Most chronic pain, sadly, is undertreated or untreated. In the ‘90s, in the quest to reduce chronic pain to a better extent, we saw more and more literature and studies related to the use of opioids for noncancer pain (e.g., for lower back pain).
There were many primary care doctors and pain specialists who started using opioids, probably for patients who didn’t really need it. I think it was done out of good conscience in the sense that they were trying to reduce pain. We have other methods of pain relief, but we needed more. At that time, in the ‘90s, we had a greater use of opioids to treat noncancer pain.
Then from that point, we transitioned to the use of heroin. Again, this isn’t among the chronic pain population, but it was the nonchronic pain population that starting using heroin. Today we see synthetic fentanyl.
Addressing the synthetic opioid crisis
Dr. Glatter: With fentanyl being the most common opiate we’re seeing, we’re having problems trying to save patients. We’re trying to use naloxone, but obviously in increasing amounts, and sometimes it’s not adequate and we have to intubate patients.
In terms of addressing this issue of supply, the fentanyl is coming from Mexico, China, and it’s manufactured here in the United States. How do we address this crisis? What are the steps that you would recommend we take?
Dr. Christo: I think that we need to better support law enforcement to crack down on those who are manufacturing fentanyl in the United States, and also to crack down on those who are transporting it from, say, Mexico – I think it’s primarily coming from Mexico – but from outside the United States to the United States. I feel like that’s important to do.
Two, we need to better educate those who are using these mind- and mood-altering substances. We’re seeing more and more that it’s the young-adult population, those between the ages of 13 and 25, who are starting to use these substances, and they’re very dangerous.
Dr. Glatter: Are these teens seeking out heroin and it happens to be laced with fentanyl, or are they actually seeking pure fentanyl? Are they trying to buy the colorful pills that we know about? What’s your experience in terms of the population you’re treating and what you could tell us?
Dr. Christo: I think it’s both. We’re seeing young adults who are interested in the use of fentanyl as a mind- and mood-altering substance. We’re also seeing young and older adults use other drugs, like cocaine and heroin, that are laced with fentanyl, and they don’t know it. That’s exponentially more dangerous.
Fentanyl test strips
Dr. Glatter: People are unaware that there is fentanyl in what they’re using, and it is certainly leading to overdoses and deaths. I think that parents really need to be aware of this.
Dr. Christo: Yes, for sure. I think we need better educational methods in the schools to educate that population that we’re talking about (between the ages of 13 and 25). Let them know the dangers, because I don’t think they’re aware of the danger, and how potent fentanyl is in terms of its lethality, and that you don’t need very much to take in a form of a pill or to inhale or to inject intravenously to kill yourself. That is key – education at that level – and to let those who are going to use these substances (specifically, synthetic fentanyl) know that they should consider the use of fentanyl test strips.
Fentanyl test strips would be primarily used for those who are thinking that they’re using heroin but there may be fentanyl in there, or methamphetamine and there may be fentanyl, and they don’t know. The test strip gives them that knowledge.
The other harm reduction strategies would be the use of naloxone, known as Narcan. That’s a lifesaver. You just have to spritz it into the nostril. You don’t do it yourself if you’re using the substance, but you’ve got others who can do it for you. No question, that’s a lifesaver. We need to make sure that there’s greater availability of that throughout the entire country, and we’re seeing some of that in certain states. In certain states, you don’t need a prescription to get naloxone from the pharmacy.
Dr. Glatter: I think it’s so important that it should be widely available. Certainly, the COVID-19 pandemic exacerbated the number of overdoses we saw. Are overdoses coming down or are we still at a level that’s close to 2020?
Dr. Christo: Unfortunately, we’re still seeing the same level, if not seeing it escalate. Certainly, the pandemic, because of the economic cost associated with the pandemic – loss of employment, underemployment – as well as the emotional stress of the pandemic led many people to use substances on the street in order to cope. They’re coping mechanisms, and we really haven’t seen it abate quite yet.
Dr. Glatter: Do you have a message for the lawmakers on Capitol Hill as to what we can do regarding the illegal manufacturing and distribution, how we can really crack down? Are there other approaches that we could implement that might be more tangible?
Dr. Christo: Yes. No. 1 would be to support law enforcement. No. 2 would be to create and make available more overdose prevention centers. The first was in New York City. If you look at the data on overdose prevention centers, in Canada, for example, they’ve seen a 35% reduction in overdose deaths. These are places where people who are using can go to get clean needles and clean syringes. This is where people basically oversee the use of the drug and intervene if necessary.
It seems sort of antithetical. It seems like, “Boy, why would you fund a center for people to use drugs?” The data from Canada and outside Canada are such that it can be very helpful. That would be one of my messages to lawmakers as well.
Vaccines to combat the synthetic opioid crisis
Dr. Glatter: Do you think that the legislators could approach some of these factories as a way to crack down, and have law enforcement be more aggressive? Is that another possible solution?
Dr. Christo: It is. Law enforcement needs to be supported by the government, by the Biden administration, so that we can prevent the influx of fentanyl and other drugs into the United States, and also to crack down on those in the United States who are manufacturing these drugs – synthetic fentanyl, first and foremost – because we’re seeing a lot of deaths related to synthetic fentanyl.
Also, we’re seeing — and this is pretty intriguing and interesting – the use of vaccines to help prevent overdose. The first human trial is underway right now for a vaccine against oxycodone. Not only that, but there are other vaccines that are in animal trials now against heroin, cocaine, or fentanyl. There’s hope there that we can use vaccines to also help reduce deaths related to overdose from fentanyl and other opioids.
Dr. Glatter: Do you think this would be given widely to the population or only to those at higher risk?
Dr. Christo: It would probably be targeting those who are at higher risk and have a history of drug abuse. I don’t think it would be something that would be given to the entire population, but it certainly could be effective, and we’re seeing encouraging results from the human trial right now.
Dr. Glatter: That’s very intriguing. That’s something that certainly could be quite helpful in the future.
One thing I did want to address is law enforcement and first responders who have been exposed to dust, or inhaled dust possibly, or had fentanyl on their skin. There has been lots of controversy. The recent literature has dispelled the controversy that people who had supposedly passed out and required Narcan after exposure to intact skin, or even compromised skin, had an overdose of fentanyl. Maybe you could speak to that and dispel that myth.
Dr. Christo: Yes, I’ve been asked this question a couple of times in the past. It’s not sufficient just to have contact with fentanyl on the skin to lead to an overdose. You really need to ingest it. That is, take it by mouth in the form of a pill, inhale it, or inject it intravenously. Skin contact is very unlikely going to lead to an overdose and death.
Dr. Glatter: I want to thank you for a very informative interview. Do you have one or two pearls you’d like to give our audience as a takeaway?
Dr. Christo: I would say two things. One is, don’t give up if you have chronic pain because there is hope. We have nonopioid treatments that can be effective. Two, don’t give up if you have a substance use disorder. Talk to your primary care doctor or talk to emergency room physicians if you’re in the emergency room. The Substance Abuse and Mental Health Services Administration is a good resource, too. SAMHSA has an 800 number for support and a website. Take the opportunity to use the resources that are available.
Dr. Glatter is assistant professor of emergency medicine at Lenox Hill Hospital in New York City and at Hofstra University, Hempstead, N.Y. He is an editorial advisor and hosts the Hot Topics in EM series on Medscape. He is also a medical contributor for Forbes.
Dr. Christo is an associate professor and a pain specialist in the department of anesthesiology and critical care medicine at Johns Hopkins University, Baltimore. He also serves as director of the multidisciplinary pain fellowship program at Johns Hopkins Hospital. Christo is the author of Aches and Gains, A Comprehensive Guide to Overcoming Your Pain, and hosts an award-winning, nationally syndicated SiriusXM radio talk show on overcoming pain, called Aches and Gains.
A version of this article first appeared on Medscape.com.
Out-of-state telehealth visits could help more patients if restrictions eased: Study
About 5% of traditional Medicare patients who had telehealth visits were seen virtually by out-of-state clinicians in the first half of 2021, according to a new study in JAMA Health Forum.
Since then, however, many states have restored restrictions that prevent physicians who are licensed in one state from having telehealth visits with patients unless they’re licensed in the state where the patients live.
This is not fair to many people who live in areas near state borders, the authors argued. For those patients, it is much more convenient to see their primary care physician in a virtual visit from home than to travel to the doctor’s office in another state. This convenience is enjoyed by most patients who reside elsewhere in their state because they’re seeing physicians who are licensed there.
Moreover, the paper said, patients who live in rural areas and in counties with relatively few physicians per capita would also benefit from relaxed telemedicine restrictions.
Using Medicare claims data, the researchers examined the characteristics of out-of-state (OOS) telemedicine visits for the 6 months from January to June 2021. They chose that period for two reasons: by then, health care had stabilized after the chaotic early phase of the pandemic, and in most states, the relaxation of licensing rules for OOS telehealth had not yet lapsed. Earlier periods of time were also used for certain types of comparisons.
Among fee-for-service Medicare beneficiaries, the number of OOS telemedicine visits peaked at 451,086 in April 2020 and slowly fell to 175,545 in June 2021, according to the study. The fraction of OOS telehealth visits among all virtual visits was 4.5% in April 2020 and increased to 5.6% by June 2021.
Staying close to home
Of all beneficiaries with a telemedicine visit in the study period, 33% lived within 15 miles of a state border. That cohort accounted for 57.2% of all OOS telemedicine visits.
The highest rates of OOS telehealth visits were seen in the District of Columbia (38.5%), Wyoming (25.6%), and North Dakota (21.1%). California (1%), Texas (2%), and Massachusetts (2.1%) had the lowest rates.
Though intuitive in retrospect, the correlation of OOS telemedicine use with proximity to state borders was one of the study’s most important findings, lead author Ateev Mehrotra, MD, a professor at Harvard Medical School, Boston, said in an interview. “It makes sense,” he said. “If you’re in D.C. and you need a cardiologist, you don’t think: ‘I’ll stay in D.C.’ No, Maryland is right there, so you might use a Maryland cardiologist. Now you’re out of state, even though that office might be only half a mile away from you.”
Similar dynamics, he noted, are seen in many metropolitan areas that border on other states, such as Cincinnati; Philadelphia; and Portland, Ore.
This finding lines up with another result of the study: The majority of patients who had OOS telemedicine visits had previously seen in person the doctor who conducted the virtual visit.
Across all OOS telemedicine visits in the first half of 2021, the researchers observed a prior in-person visit between March 2019 and the date of the virtual visit with the same patient and the same clinician in 62.8% of those visits. Across all in-state telehealth visits, 75.8% of them were made by patients who had seen the same clinician in person since March 2019. This preponderance of virtual visits to clinicians whom the patients had already seen in person reflects the fact that, during the pandemic, most physicians began conducting telehealth visits with their own patients, Dr. Mehrotra said.
It also lays to rest the concern that some states have had about allowing OOS telemedicine visits to physicians not licensed in those states, he added. “They think that all these docs from far away are going to start taking care of patients they don’t even know. But our study shows that isn’t the case. Most of the time, doctors are seeing a patient who’s switching over from in-person visits to out-of-state telemedicine.”
More specialty care sought
The dominant conditions that patients presented with were the same in OOS telemedicine and within-state virtual visits. However, the use of OOS telemedicine was higher for some types of specialized care.
For example, the rate of OOS telemedicine use, compared with all telemedicine use, was highest for cancer care (9.8%). Drilling down to more specific conditions, the top three in OOS telemedicine visits were assessment of organ transplant (13%); male reproductive cancers, such as prostate cancer (11.3%); and graft-related issues (10.2%).
The specialty trend was also evident in the types of OOS clinicians from whom Medicare patients sought virtual care. The rates of OOS telemedicine use as a percentage of all telemedicine use in particular specialties were highest for uncommon specialties, such as hematology/oncology, rheumatology, urology, medical oncology, and orthopedic surgery (8.5%). There was less use of OOS telemedicine as a percentage of all telemedicine among more common medical specialties (6.4%), mental health specialties (4.4%), and primary care (4.4%).
Despite its relatively low showing in this category, however, behavioral health was the leading condition treated in both within-state and OOS telemedicine visits, accounting for 30.7% and 25.8%, respectively, of those encounters.
States backslide on OOS telehealth
Since the end of the study period, over half of the states have restored some or all of the restrictions on OOS telemedicine that they had lifted during the pandemic.
According to Dr. Mehrotra, 22 states have some kind of regulation in place to allow an OOS clinician to conduct telehealth visits without being licensed in the state. This varies all the way from complete reciprocity with other states’ licenses to “emergency” telemedicine licenses. The other 28 states and Washington, D.C., require an OOS telemedicine practitioner to get a state license.
Various proposals have been floated to ameliorate this situation, the JAMA paper noted. These proposals include an expansion of the Interstate Medical Licensure Compact that the Federation of State Medical Boards organized in 2014. Since the pact became effective in 2014, at least 35 states and the District of Columbia have joined it. Those states have made it simpler for physicians to gain licensure in states other than their original state of licensure. However, Mehrotra said, it’s still not easy, and not many physicians have taken advantage of it.
One new wrinkle has emerged in this policy debate as a result of the Supreme Court decision overturning Roe v. Wade, he noted. Because people are using OOS telemedicine visits to get prescriptions to abort their fetuses, “that has changed the enthusiasm level for it among many states,” he said.
Dr. Mehrotra reported personal fees from the Pew Charitable Trust, Sanofi Pasteur, and Black Opal Ventures outside the submitted work. One coauthor reported receiving grants from Patient-Centered Outcomes Research, National Institute on Aging, Roundtrip, Independence Blue Cross; personal fees or salary from RAND Corporation from Verily Life Sciences; and that the American Telemedicine Association covered a conference fee. No other disclosures were reported.
A version of this article first appeared on Medscape.com.
About 5% of traditional Medicare patients who had telehealth visits were seen virtually by out-of-state clinicians in the first half of 2021, according to a new study in JAMA Health Forum.
Since then, however, many states have restored restrictions that prevent physicians who are licensed in one state from having telehealth visits with patients unless they’re licensed in the state where the patients live.
This is not fair to many people who live in areas near state borders, the authors argued. For those patients, it is much more convenient to see their primary care physician in a virtual visit from home than to travel to the doctor’s office in another state. This convenience is enjoyed by most patients who reside elsewhere in their state because they’re seeing physicians who are licensed there.
Moreover, the paper said, patients who live in rural areas and in counties with relatively few physicians per capita would also benefit from relaxed telemedicine restrictions.
Using Medicare claims data, the researchers examined the characteristics of out-of-state (OOS) telemedicine visits for the 6 months from January to June 2021. They chose that period for two reasons: by then, health care had stabilized after the chaotic early phase of the pandemic, and in most states, the relaxation of licensing rules for OOS telehealth had not yet lapsed. Earlier periods of time were also used for certain types of comparisons.
Among fee-for-service Medicare beneficiaries, the number of OOS telemedicine visits peaked at 451,086 in April 2020 and slowly fell to 175,545 in June 2021, according to the study. The fraction of OOS telehealth visits among all virtual visits was 4.5% in April 2020 and increased to 5.6% by June 2021.
Staying close to home
Of all beneficiaries with a telemedicine visit in the study period, 33% lived within 15 miles of a state border. That cohort accounted for 57.2% of all OOS telemedicine visits.
The highest rates of OOS telehealth visits were seen in the District of Columbia (38.5%), Wyoming (25.6%), and North Dakota (21.1%). California (1%), Texas (2%), and Massachusetts (2.1%) had the lowest rates.
Though intuitive in retrospect, the correlation of OOS telemedicine use with proximity to state borders was one of the study’s most important findings, lead author Ateev Mehrotra, MD, a professor at Harvard Medical School, Boston, said in an interview. “It makes sense,” he said. “If you’re in D.C. and you need a cardiologist, you don’t think: ‘I’ll stay in D.C.’ No, Maryland is right there, so you might use a Maryland cardiologist. Now you’re out of state, even though that office might be only half a mile away from you.”
Similar dynamics, he noted, are seen in many metropolitan areas that border on other states, such as Cincinnati; Philadelphia; and Portland, Ore.
This finding lines up with another result of the study: The majority of patients who had OOS telemedicine visits had previously seen in person the doctor who conducted the virtual visit.
Across all OOS telemedicine visits in the first half of 2021, the researchers observed a prior in-person visit between March 2019 and the date of the virtual visit with the same patient and the same clinician in 62.8% of those visits. Across all in-state telehealth visits, 75.8% of them were made by patients who had seen the same clinician in person since March 2019. This preponderance of virtual visits to clinicians whom the patients had already seen in person reflects the fact that, during the pandemic, most physicians began conducting telehealth visits with their own patients, Dr. Mehrotra said.
It also lays to rest the concern that some states have had about allowing OOS telemedicine visits to physicians not licensed in those states, he added. “They think that all these docs from far away are going to start taking care of patients they don’t even know. But our study shows that isn’t the case. Most of the time, doctors are seeing a patient who’s switching over from in-person visits to out-of-state telemedicine.”
More specialty care sought
The dominant conditions that patients presented with were the same in OOS telemedicine and within-state virtual visits. However, the use of OOS telemedicine was higher for some types of specialized care.
For example, the rate of OOS telemedicine use, compared with all telemedicine use, was highest for cancer care (9.8%). Drilling down to more specific conditions, the top three in OOS telemedicine visits were assessment of organ transplant (13%); male reproductive cancers, such as prostate cancer (11.3%); and graft-related issues (10.2%).
The specialty trend was also evident in the types of OOS clinicians from whom Medicare patients sought virtual care. The rates of OOS telemedicine use as a percentage of all telemedicine use in particular specialties were highest for uncommon specialties, such as hematology/oncology, rheumatology, urology, medical oncology, and orthopedic surgery (8.5%). There was less use of OOS telemedicine as a percentage of all telemedicine among more common medical specialties (6.4%), mental health specialties (4.4%), and primary care (4.4%).
Despite its relatively low showing in this category, however, behavioral health was the leading condition treated in both within-state and OOS telemedicine visits, accounting for 30.7% and 25.8%, respectively, of those encounters.
States backslide on OOS telehealth
Since the end of the study period, over half of the states have restored some or all of the restrictions on OOS telemedicine that they had lifted during the pandemic.
According to Dr. Mehrotra, 22 states have some kind of regulation in place to allow an OOS clinician to conduct telehealth visits without being licensed in the state. This varies all the way from complete reciprocity with other states’ licenses to “emergency” telemedicine licenses. The other 28 states and Washington, D.C., require an OOS telemedicine practitioner to get a state license.
Various proposals have been floated to ameliorate this situation, the JAMA paper noted. These proposals include an expansion of the Interstate Medical Licensure Compact that the Federation of State Medical Boards organized in 2014. Since the pact became effective in 2014, at least 35 states and the District of Columbia have joined it. Those states have made it simpler for physicians to gain licensure in states other than their original state of licensure. However, Mehrotra said, it’s still not easy, and not many physicians have taken advantage of it.
One new wrinkle has emerged in this policy debate as a result of the Supreme Court decision overturning Roe v. Wade, he noted. Because people are using OOS telemedicine visits to get prescriptions to abort their fetuses, “that has changed the enthusiasm level for it among many states,” he said.
Dr. Mehrotra reported personal fees from the Pew Charitable Trust, Sanofi Pasteur, and Black Opal Ventures outside the submitted work. One coauthor reported receiving grants from Patient-Centered Outcomes Research, National Institute on Aging, Roundtrip, Independence Blue Cross; personal fees or salary from RAND Corporation from Verily Life Sciences; and that the American Telemedicine Association covered a conference fee. No other disclosures were reported.
A version of this article first appeared on Medscape.com.
About 5% of traditional Medicare patients who had telehealth visits were seen virtually by out-of-state clinicians in the first half of 2021, according to a new study in JAMA Health Forum.
Since then, however, many states have restored restrictions that prevent physicians who are licensed in one state from having telehealth visits with patients unless they’re licensed in the state where the patients live.
This is not fair to many people who live in areas near state borders, the authors argued. For those patients, it is much more convenient to see their primary care physician in a virtual visit from home than to travel to the doctor’s office in another state. This convenience is enjoyed by most patients who reside elsewhere in their state because they’re seeing physicians who are licensed there.
Moreover, the paper said, patients who live in rural areas and in counties with relatively few physicians per capita would also benefit from relaxed telemedicine restrictions.
Using Medicare claims data, the researchers examined the characteristics of out-of-state (OOS) telemedicine visits for the 6 months from January to June 2021. They chose that period for two reasons: by then, health care had stabilized after the chaotic early phase of the pandemic, and in most states, the relaxation of licensing rules for OOS telehealth had not yet lapsed. Earlier periods of time were also used for certain types of comparisons.
Among fee-for-service Medicare beneficiaries, the number of OOS telemedicine visits peaked at 451,086 in April 2020 and slowly fell to 175,545 in June 2021, according to the study. The fraction of OOS telehealth visits among all virtual visits was 4.5% in April 2020 and increased to 5.6% by June 2021.
Staying close to home
Of all beneficiaries with a telemedicine visit in the study period, 33% lived within 15 miles of a state border. That cohort accounted for 57.2% of all OOS telemedicine visits.
The highest rates of OOS telehealth visits were seen in the District of Columbia (38.5%), Wyoming (25.6%), and North Dakota (21.1%). California (1%), Texas (2%), and Massachusetts (2.1%) had the lowest rates.
Though intuitive in retrospect, the correlation of OOS telemedicine use with proximity to state borders was one of the study’s most important findings, lead author Ateev Mehrotra, MD, a professor at Harvard Medical School, Boston, said in an interview. “It makes sense,” he said. “If you’re in D.C. and you need a cardiologist, you don’t think: ‘I’ll stay in D.C.’ No, Maryland is right there, so you might use a Maryland cardiologist. Now you’re out of state, even though that office might be only half a mile away from you.”
Similar dynamics, he noted, are seen in many metropolitan areas that border on other states, such as Cincinnati; Philadelphia; and Portland, Ore.
This finding lines up with another result of the study: The majority of patients who had OOS telemedicine visits had previously seen in person the doctor who conducted the virtual visit.
Across all OOS telemedicine visits in the first half of 2021, the researchers observed a prior in-person visit between March 2019 and the date of the virtual visit with the same patient and the same clinician in 62.8% of those visits. Across all in-state telehealth visits, 75.8% of them were made by patients who had seen the same clinician in person since March 2019. This preponderance of virtual visits to clinicians whom the patients had already seen in person reflects the fact that, during the pandemic, most physicians began conducting telehealth visits with their own patients, Dr. Mehrotra said.
It also lays to rest the concern that some states have had about allowing OOS telemedicine visits to physicians not licensed in those states, he added. “They think that all these docs from far away are going to start taking care of patients they don’t even know. But our study shows that isn’t the case. Most of the time, doctors are seeing a patient who’s switching over from in-person visits to out-of-state telemedicine.”
More specialty care sought
The dominant conditions that patients presented with were the same in OOS telemedicine and within-state virtual visits. However, the use of OOS telemedicine was higher for some types of specialized care.
For example, the rate of OOS telemedicine use, compared with all telemedicine use, was highest for cancer care (9.8%). Drilling down to more specific conditions, the top three in OOS telemedicine visits were assessment of organ transplant (13%); male reproductive cancers, such as prostate cancer (11.3%); and graft-related issues (10.2%).
The specialty trend was also evident in the types of OOS clinicians from whom Medicare patients sought virtual care. The rates of OOS telemedicine use as a percentage of all telemedicine use in particular specialties were highest for uncommon specialties, such as hematology/oncology, rheumatology, urology, medical oncology, and orthopedic surgery (8.5%). There was less use of OOS telemedicine as a percentage of all telemedicine among more common medical specialties (6.4%), mental health specialties (4.4%), and primary care (4.4%).
Despite its relatively low showing in this category, however, behavioral health was the leading condition treated in both within-state and OOS telemedicine visits, accounting for 30.7% and 25.8%, respectively, of those encounters.
States backslide on OOS telehealth
Since the end of the study period, over half of the states have restored some or all of the restrictions on OOS telemedicine that they had lifted during the pandemic.
According to Dr. Mehrotra, 22 states have some kind of regulation in place to allow an OOS clinician to conduct telehealth visits without being licensed in the state. This varies all the way from complete reciprocity with other states’ licenses to “emergency” telemedicine licenses. The other 28 states and Washington, D.C., require an OOS telemedicine practitioner to get a state license.
Various proposals have been floated to ameliorate this situation, the JAMA paper noted. These proposals include an expansion of the Interstate Medical Licensure Compact that the Federation of State Medical Boards organized in 2014. Since the pact became effective in 2014, at least 35 states and the District of Columbia have joined it. Those states have made it simpler for physicians to gain licensure in states other than their original state of licensure. However, Mehrotra said, it’s still not easy, and not many physicians have taken advantage of it.
One new wrinkle has emerged in this policy debate as a result of the Supreme Court decision overturning Roe v. Wade, he noted. Because people are using OOS telemedicine visits to get prescriptions to abort their fetuses, “that has changed the enthusiasm level for it among many states,” he said.
Dr. Mehrotra reported personal fees from the Pew Charitable Trust, Sanofi Pasteur, and Black Opal Ventures outside the submitted work. One coauthor reported receiving grants from Patient-Centered Outcomes Research, National Institute on Aging, Roundtrip, Independence Blue Cross; personal fees or salary from RAND Corporation from Verily Life Sciences; and that the American Telemedicine Association covered a conference fee. No other disclosures were reported.
A version of this article first appeared on Medscape.com.
FROM JAMA HEALTH FORUM
Heart failure drug a new treatment option for alcoholism?
(AUD), new research suggests.
Researchers at the National Institute on Drug Abuse, the National Institute on Alcohol Abuse and Alcoholism, and Yale University, New Haven, Conn., investigated the impact of spironolactone on AUD.
Initially, they studied rodents and found that spironolactone reduced binge drinking in mice and reduced self-administration of alcohol in rats without adversely affecting food or water intake or causing motor or coordination problems.
They also analyzed electronic health records of patients drawn from the United States Veterans Affairs health care system to explore potential changes in alcohol use after spironolactone treatment was initiated for other conditions and found a significant link between spironolactone treatment and reduction in self-reported alcohol consumption, with the largest effects observed among those who reported hazardous/heavy episodic alcohol use prior to starting spironolactone treatment.
“Combining findings across three species and different types of research studies, and then seeing similarities in these data, gives us confidence that we are onto something potentially important scientifically and clinically,” senior coauthor Lorenzo Leggio, MD, PhD, senior investigator in the Clinical Psychoneuroendocrinology and Neuropsychopharmacology Section, a joint NIDA and NIAAA laboratory, said in a news release.
The study was published online in Molecular Psychiatry.
There is a “critical need to increase the armamentarium of pharmacotherapies to treat individuals with AUD,” the authors note, adding that neuroendocrine systems involved in alcohol craving and drinking “offer promising pharmacologic targets in this regard.”
“Both our team and others have observed that patients with AUD often present with changes in peripheral hormones, including aldosterone, which plays a key role in regulating blood pressure and electrolytes,” Dr. Leggio said in an interview.
Spironolactone is a nonselective mineralocorticoid receptor (MT) antagonist. In studies in animal models, investigators said they found “an inverse correlation between alcohol drinking and the expression of the MR in the amygdala, a key brain region in the development and maintenance of AUD and addiction in general.”
Taken together, this led them to hypothesize that blocking the MR, which is the mechanism of action of spironolactone, “could be a novel pharmacotherapeutic approach for AUD,” he said.
Previous research by the same group of researchers suggested spironolactone “may be a potential new medication to treat patients with AUD.” The present study expanded on those findings and consisted of a three-part investigation.
In the current study, the investigators tested different dosages of spironolactone on binge-like alcohol consumption in male and female mice and assessed food and water intake, blood alcohol levels, motor coordination, and spontaneous locomotion.
They then tested the effects of different dosages of spironolactone injections on operant alcohol self-administration in alcohol-dependent and nondependent male and female rats, also testing blood alcohol levels and motor coordination.
Finally, they analyzed health records of veterans to examine the association between at least 60 continuous days of spironolactone treatment and self-reported alcohol consumption (measured by the Alcohol Use Disorders Identification Test-Consumption [AUDIT-C]).
Each of the spironolactone-exposed patients was matched using propensity scores with up to five unexposed patients who had reported alcohol consumption in the 2 years prior to the index date.
The final analysis included a matched cohort of 10,726 spironolactone-exposed individuals who were matched to 34,461 unexposed individuals.
New targets
Spironolactone reduced alcohol intake in mice drinking a sweetened alcohol solution; a 2-way ANOVA revealed a main effect of dose (F 4,52 = 9.09; P < .0001) and sex, with female mice drinking more alcohol, compared to male mice (F 1,13 = 6.05; P = .02).
Post hoc comparisons showed that spironolactone at doses of 50, 100, and 200 mg/kg significantly reduced alcohol intake (P values = .007, .002, and .0001, respectively).
In mice drinking an unsweetened alcohol solution, the 2-way repeated measures ANOVA similarly found a main effect of dose (F 4,52 = 5.77; P = .0006), but not of sex (F 1,13 = 1.41; P = .25).
Spironolactone had no effect on the mice’s intake of a sweet solution without alcohol and had no impact on the consumption of food and water or on locomotion and coordination.
In rats, a 2-way ANOVA revealed a significant spironolactone effect of dose (F 3,66 = 43.95; P < .001), with a post hoc test indicating that spironolactone at 25, 50, and 75 mg/kg reduced alcohol self-administration in alcohol-dependent and nondependent rats (all P values = .0001).
In humans, among the exposed individuals in the matched cohort, 25%, 57%, and 18% received daily doses of spironolactone of less than 25 mg/day, 25-49 mg/day, and 50 mg/day or higher, respectively, with a median follow-up time of 542 (interquartile range, 337-730) days.
The AUDIT-C scores decreased during the study period in both treatment groups, with a larger decrease in average AUDIT-C scores among the exposed vs. unexposed individuals.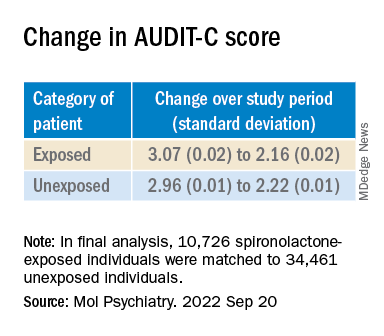
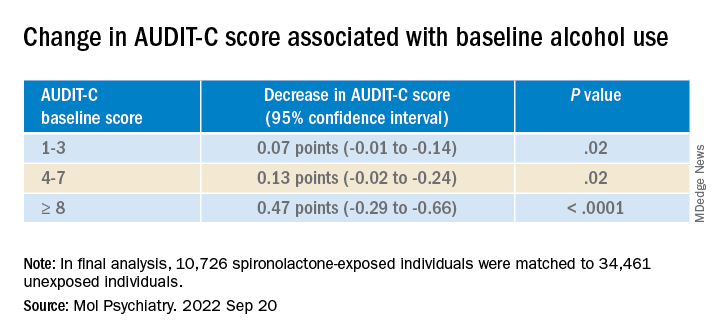
“These are very exciting times because, thanks to the progress in the addiction biomedical research field, we are increasing our understanding of the mechanisms how some people develop AUD; hence we can use this knowledge to identify new targets.” The current study “is an example of these ongoing efforts,” said Dr. Leggio.
“It is important to note that [these results] are important but preliminary.” At this juncture, “it would be too premature to think about prescribing spironolactone to treat AUD,” he added.
Exciting findings
Commenting on the study, Joyce Besheer, PhD, professor, department of psychiatry and Bowles Center for Alcohol Studies, University of North Carolina at Chapel Hill, called the study an “elegant demonstration of translational science.”
“While clinical trials will be needed to determine whether this medication is effective at reducing drinking in patients with AUD, these findings are exciting as they suggest that spironolactone may be a promising compound and new treatment options for AUD are much needed,” said Dr. Besheer, who was not involved with the current study.
Dr. Leggio agreed. “We now need prospective, placebo-controlled studies to assess the potential safety and efficacy of spironolactone in people with AUD,” he said.
This work was supported by the National Institutes of Health and the NIAAA. Dr. Leggio, study coauthors, and Dr. Besheer declare no relevant financial relationships.
A version of this article first appeared on Medscape.com.
(AUD), new research suggests.
Researchers at the National Institute on Drug Abuse, the National Institute on Alcohol Abuse and Alcoholism, and Yale University, New Haven, Conn., investigated the impact of spironolactone on AUD.
Initially, they studied rodents and found that spironolactone reduced binge drinking in mice and reduced self-administration of alcohol in rats without adversely affecting food or water intake or causing motor or coordination problems.
They also analyzed electronic health records of patients drawn from the United States Veterans Affairs health care system to explore potential changes in alcohol use after spironolactone treatment was initiated for other conditions and found a significant link between spironolactone treatment and reduction in self-reported alcohol consumption, with the largest effects observed among those who reported hazardous/heavy episodic alcohol use prior to starting spironolactone treatment.
“Combining findings across three species and different types of research studies, and then seeing similarities in these data, gives us confidence that we are onto something potentially important scientifically and clinically,” senior coauthor Lorenzo Leggio, MD, PhD, senior investigator in the Clinical Psychoneuroendocrinology and Neuropsychopharmacology Section, a joint NIDA and NIAAA laboratory, said in a news release.
The study was published online in Molecular Psychiatry.
There is a “critical need to increase the armamentarium of pharmacotherapies to treat individuals with AUD,” the authors note, adding that neuroendocrine systems involved in alcohol craving and drinking “offer promising pharmacologic targets in this regard.”
“Both our team and others have observed that patients with AUD often present with changes in peripheral hormones, including aldosterone, which plays a key role in regulating blood pressure and electrolytes,” Dr. Leggio said in an interview.
Spironolactone is a nonselective mineralocorticoid receptor (MT) antagonist. In studies in animal models, investigators said they found “an inverse correlation between alcohol drinking and the expression of the MR in the amygdala, a key brain region in the development and maintenance of AUD and addiction in general.”
Taken together, this led them to hypothesize that blocking the MR, which is the mechanism of action of spironolactone, “could be a novel pharmacotherapeutic approach for AUD,” he said.
Previous research by the same group of researchers suggested spironolactone “may be a potential new medication to treat patients with AUD.” The present study expanded on those findings and consisted of a three-part investigation.
In the current study, the investigators tested different dosages of spironolactone on binge-like alcohol consumption in male and female mice and assessed food and water intake, blood alcohol levels, motor coordination, and spontaneous locomotion.
They then tested the effects of different dosages of spironolactone injections on operant alcohol self-administration in alcohol-dependent and nondependent male and female rats, also testing blood alcohol levels and motor coordination.
Finally, they analyzed health records of veterans to examine the association between at least 60 continuous days of spironolactone treatment and self-reported alcohol consumption (measured by the Alcohol Use Disorders Identification Test-Consumption [AUDIT-C]).
Each of the spironolactone-exposed patients was matched using propensity scores with up to five unexposed patients who had reported alcohol consumption in the 2 years prior to the index date.
The final analysis included a matched cohort of 10,726 spironolactone-exposed individuals who were matched to 34,461 unexposed individuals.
New targets
Spironolactone reduced alcohol intake in mice drinking a sweetened alcohol solution; a 2-way ANOVA revealed a main effect of dose (F 4,52 = 9.09; P < .0001) and sex, with female mice drinking more alcohol, compared to male mice (F 1,13 = 6.05; P = .02).
Post hoc comparisons showed that spironolactone at doses of 50, 100, and 200 mg/kg significantly reduced alcohol intake (P values = .007, .002, and .0001, respectively).
In mice drinking an unsweetened alcohol solution, the 2-way repeated measures ANOVA similarly found a main effect of dose (F 4,52 = 5.77; P = .0006), but not of sex (F 1,13 = 1.41; P = .25).
Spironolactone had no effect on the mice’s intake of a sweet solution without alcohol and had no impact on the consumption of food and water or on locomotion and coordination.
In rats, a 2-way ANOVA revealed a significant spironolactone effect of dose (F 3,66 = 43.95; P < .001), with a post hoc test indicating that spironolactone at 25, 50, and 75 mg/kg reduced alcohol self-administration in alcohol-dependent and nondependent rats (all P values = .0001).
In humans, among the exposed individuals in the matched cohort, 25%, 57%, and 18% received daily doses of spironolactone of less than 25 mg/day, 25-49 mg/day, and 50 mg/day or higher, respectively, with a median follow-up time of 542 (interquartile range, 337-730) days.
The AUDIT-C scores decreased during the study period in both treatment groups, with a larger decrease in average AUDIT-C scores among the exposed vs. unexposed individuals.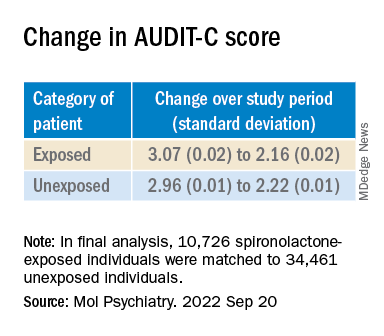
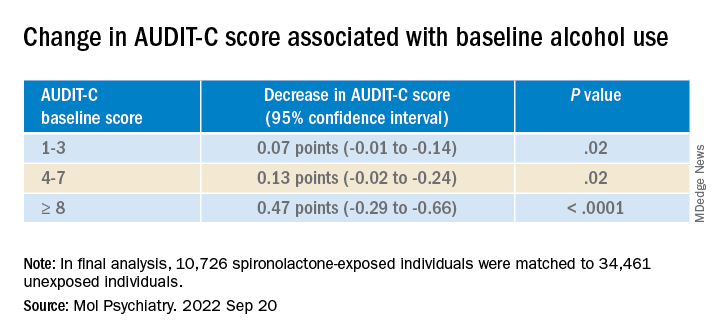
“These are very exciting times because, thanks to the progress in the addiction biomedical research field, we are increasing our understanding of the mechanisms how some people develop AUD; hence we can use this knowledge to identify new targets.” The current study “is an example of these ongoing efforts,” said Dr. Leggio.
“It is important to note that [these results] are important but preliminary.” At this juncture, “it would be too premature to think about prescribing spironolactone to treat AUD,” he added.
Exciting findings
Commenting on the study, Joyce Besheer, PhD, professor, department of psychiatry and Bowles Center for Alcohol Studies, University of North Carolina at Chapel Hill, called the study an “elegant demonstration of translational science.”
“While clinical trials will be needed to determine whether this medication is effective at reducing drinking in patients with AUD, these findings are exciting as they suggest that spironolactone may be a promising compound and new treatment options for AUD are much needed,” said Dr. Besheer, who was not involved with the current study.
Dr. Leggio agreed. “We now need prospective, placebo-controlled studies to assess the potential safety and efficacy of spironolactone in people with AUD,” he said.
This work was supported by the National Institutes of Health and the NIAAA. Dr. Leggio, study coauthors, and Dr. Besheer declare no relevant financial relationships.
A version of this article first appeared on Medscape.com.
(AUD), new research suggests.
Researchers at the National Institute on Drug Abuse, the National Institute on Alcohol Abuse and Alcoholism, and Yale University, New Haven, Conn., investigated the impact of spironolactone on AUD.
Initially, they studied rodents and found that spironolactone reduced binge drinking in mice and reduced self-administration of alcohol in rats without adversely affecting food or water intake or causing motor or coordination problems.
They also analyzed electronic health records of patients drawn from the United States Veterans Affairs health care system to explore potential changes in alcohol use after spironolactone treatment was initiated for other conditions and found a significant link between spironolactone treatment and reduction in self-reported alcohol consumption, with the largest effects observed among those who reported hazardous/heavy episodic alcohol use prior to starting spironolactone treatment.
“Combining findings across three species and different types of research studies, and then seeing similarities in these data, gives us confidence that we are onto something potentially important scientifically and clinically,” senior coauthor Lorenzo Leggio, MD, PhD, senior investigator in the Clinical Psychoneuroendocrinology and Neuropsychopharmacology Section, a joint NIDA and NIAAA laboratory, said in a news release.
The study was published online in Molecular Psychiatry.
There is a “critical need to increase the armamentarium of pharmacotherapies to treat individuals with AUD,” the authors note, adding that neuroendocrine systems involved in alcohol craving and drinking “offer promising pharmacologic targets in this regard.”
“Both our team and others have observed that patients with AUD often present with changes in peripheral hormones, including aldosterone, which plays a key role in regulating blood pressure and electrolytes,” Dr. Leggio said in an interview.
Spironolactone is a nonselective mineralocorticoid receptor (MT) antagonist. In studies in animal models, investigators said they found “an inverse correlation between alcohol drinking and the expression of the MR in the amygdala, a key brain region in the development and maintenance of AUD and addiction in general.”
Taken together, this led them to hypothesize that blocking the MR, which is the mechanism of action of spironolactone, “could be a novel pharmacotherapeutic approach for AUD,” he said.
Previous research by the same group of researchers suggested spironolactone “may be a potential new medication to treat patients with AUD.” The present study expanded on those findings and consisted of a three-part investigation.
In the current study, the investigators tested different dosages of spironolactone on binge-like alcohol consumption in male and female mice and assessed food and water intake, blood alcohol levels, motor coordination, and spontaneous locomotion.
They then tested the effects of different dosages of spironolactone injections on operant alcohol self-administration in alcohol-dependent and nondependent male and female rats, also testing blood alcohol levels and motor coordination.
Finally, they analyzed health records of veterans to examine the association between at least 60 continuous days of spironolactone treatment and self-reported alcohol consumption (measured by the Alcohol Use Disorders Identification Test-Consumption [AUDIT-C]).
Each of the spironolactone-exposed patients was matched using propensity scores with up to five unexposed patients who had reported alcohol consumption in the 2 years prior to the index date.
The final analysis included a matched cohort of 10,726 spironolactone-exposed individuals who were matched to 34,461 unexposed individuals.
New targets
Spironolactone reduced alcohol intake in mice drinking a sweetened alcohol solution; a 2-way ANOVA revealed a main effect of dose (F 4,52 = 9.09; P < .0001) and sex, with female mice drinking more alcohol, compared to male mice (F 1,13 = 6.05; P = .02).
Post hoc comparisons showed that spironolactone at doses of 50, 100, and 200 mg/kg significantly reduced alcohol intake (P values = .007, .002, and .0001, respectively).
In mice drinking an unsweetened alcohol solution, the 2-way repeated measures ANOVA similarly found a main effect of dose (F 4,52 = 5.77; P = .0006), but not of sex (F 1,13 = 1.41; P = .25).
Spironolactone had no effect on the mice’s intake of a sweet solution without alcohol and had no impact on the consumption of food and water or on locomotion and coordination.
In rats, a 2-way ANOVA revealed a significant spironolactone effect of dose (F 3,66 = 43.95; P < .001), with a post hoc test indicating that spironolactone at 25, 50, and 75 mg/kg reduced alcohol self-administration in alcohol-dependent and nondependent rats (all P values = .0001).
In humans, among the exposed individuals in the matched cohort, 25%, 57%, and 18% received daily doses of spironolactone of less than 25 mg/day, 25-49 mg/day, and 50 mg/day or higher, respectively, with a median follow-up time of 542 (interquartile range, 337-730) days.
The AUDIT-C scores decreased during the study period in both treatment groups, with a larger decrease in average AUDIT-C scores among the exposed vs. unexposed individuals.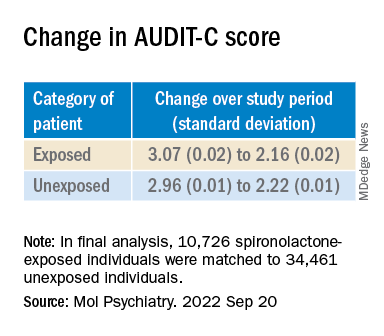
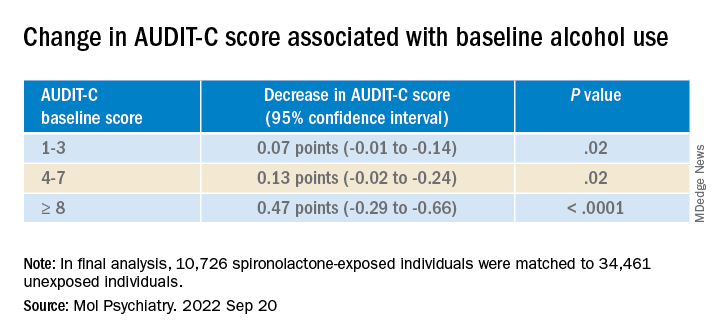
“These are very exciting times because, thanks to the progress in the addiction biomedical research field, we are increasing our understanding of the mechanisms how some people develop AUD; hence we can use this knowledge to identify new targets.” The current study “is an example of these ongoing efforts,” said Dr. Leggio.
“It is important to note that [these results] are important but preliminary.” At this juncture, “it would be too premature to think about prescribing spironolactone to treat AUD,” he added.
Exciting findings
Commenting on the study, Joyce Besheer, PhD, professor, department of psychiatry and Bowles Center for Alcohol Studies, University of North Carolina at Chapel Hill, called the study an “elegant demonstration of translational science.”
“While clinical trials will be needed to determine whether this medication is effective at reducing drinking in patients with AUD, these findings are exciting as they suggest that spironolactone may be a promising compound and new treatment options for AUD are much needed,” said Dr. Besheer, who was not involved with the current study.
Dr. Leggio agreed. “We now need prospective, placebo-controlled studies to assess the potential safety and efficacy of spironolactone in people with AUD,” he said.
This work was supported by the National Institutes of Health and the NIAAA. Dr. Leggio, study coauthors, and Dr. Besheer declare no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM MOLECULAR PSYCHIATRY
Unconventional wisdom: Major depression tied to childhood trauma is treatable
Despite a higher symptom burden, patients with major depressive disorder (MDD) and a history of childhood trauma (CT) can achieve significant recovery following treatment with a combination of pharmacotherapy and psychotherapy, new research suggests.
Results from a meta-analysis of 29 studies from 1966 to 2019, which included almost 7,000 adults with MDD, showed that more than 60% reported a history of CT. But despite having more severe depression at baseline, those with CT benefited from active treatment. Effect sizes were comparable, and dropout rates were similar to those of their counterparts without CT.
“Evidence-based psychotherapy and pharmacotherapy should be offered to depressed patients, regardless of their childhood trauma status,” lead author Erika Kuzminskaite, MSc, a PhD candidate at Amsterdam UMC department of psychiatry, the Netherlands, told this news organization.
“Screening for childhood trauma is important to identify individuals at risk for more severe course of the disorder and post-treatment residual symptoms,” she added.
The study was published online in the Lancet Psychiatry.
Common and potent risk factor
The researchers note that CT is common and is a potent risk factor for depression. Previous studies have “consistently indicated significantly higher severity and persistence of depressive symptoms in adult patients with depression and a history of childhood trauma.”
Previous individual and meta-analytic studies “indicated poorer response to first-line depression treatments in patients with childhood trauma, compared to those without trauma, suggesting the need for new personalized treatments for depressed patients with childhood trauma history,” Ms. Kuzminskaite said.
“However, the evidence on poorer treatment outcomes has not been definitive, and a comprehensive meta-analysis of available findings has been lacking,” she added.
The previous meta-analyses showed high between-study heterogeneity, and some primary studies reported similar or even superior improvement for patients with CT, compared with those without such history, following treatment with evidence-based psychotherapy or pharmacotherapy.
Previous studies also did not investigate the “relative contribution of different childhood trauma types.”
To address this gap, investigators in the Childhood Trauma Meta-Analysis Study Group conducted the “largest and most comprehensive study of available evidence examining the effects of childhood trauma on the efficacy and effectiveness of first-line treatments for adults with MDD.”
To be included, a study had to focus on adults over 18 years old who had received a primary diagnosis of depression. The study had to have included an available assessment of childhood trauma, and patients were required to have undergone psychotherapy and/or pharmacotherapy for depression alone or in combination with other guideline-recommended treatments. Studies were also required to have a comparator group, when applicable, and to have reported depression severity before and after the acute treatment phase.
Of 10,505 publications, 54 trials met inclusion criteria; of these, 29 (20 randomized controlled trials and 9 open trials), encompassing 6,830 participants aged 18-85 years, included data that had been made available by authors of the various studies and were included in the current analysis.
Most studies focused on MDD; 11 trials focused on patients with chronic or treatment-resistant depression.
The primary outcome was “depression severity change from baseline to the end of the acute treatment phase” (expressed as standardized effect size – Hedges’ g).
Greater treatment motivation?
Of the included patients, 62% reported a history of CT. They were found to have more severe depression at baseline, compared with those without CT (g = .202; 95% confidence interval, 0.145-0.258; I² = 0%).
The benefits from active treatment obtained by these patients with CT were similar to the benefits obtained by their counterparts without CT (between-group treatment effect difference: g = .016; 95% CI, –0.094-0.125; I² = 44.3%).
No significant difference in active treatment effects (in comparison with control condition) was found between individuals with and those without CT (g = .605; 95% CI, 0.294-0.916; I² = 58.0%; and g = .178; 95% CI, –0.195-0.552; I² = 67.5%, respectively; between-group difference P = .051).
Dropout rates were similar for the participants with and those without CT (risk ratio, 1.063; 95% CI, 0.945-1.195; I² = 0%).
“Findings did not significantly differ by childhood trauma type, study design, depression diagnosis, assessment method of childhood trauma, study quality, year, or treatment type or length,” the authors report.
The findings did, however, differ by country, with North American studies showing larger treatment effects for patients with CT, compared with studies conducted in Asian-Pacific countries (g = 0.150; 95% CI, 0.030-0.269; vs. g = 0.255; 95% CI, –0.508- –0.002, respectively; corrected false discovery rate, 0.0080). “However, because of limited power, these findings should be interpreted with caution,” the authors warn.
“It could be a chance finding and is certainly not causal,” Ms. Kuzminskaite suggested.
Most studies (21 of the 29) had a “moderate to high risk of bias.” But when the researchers conducted a sensitivity analysis in the low-bias studies, they found that results were similar to those of the primary analysis that included all the studies.
“Treatments were similarly effective for patients with and without childhood trauma, with slightly larger active treatment (vs. control condition – placebo, wait list, care-as-usual) effects for patients with childhood trauma history,” Ms. Kuzminskaite said.
“Some evidence suggests that patients with childhood trauma are characterized by greater treatment motivation,” she noted. Moreover, “they are also more severely depressed prior to treatment [and] thus have more room for improvement.”
‘Hopeful message’
Commenting for this news organization, Yvette Sheline, MD, McLure professor of psychiatry, radiology, and neurology and director of the center for neuromodulation in depression and Stress, University of Pennsylvania, Philadelphia, called it a “well-executed” and “straightforward” study “with clear-cut findings.”
Dr. Sheline, the director of the section on mood, anxiety, and trauma, who was not involved with the study, agrees with the authors’ conclusions – “to use evidence-based treatments for depression in all patients,” with or without a history of CT.
In an accompanying editorial, Antoine Yrondi, MD, PhD, of Université de Toulouse (France), called the findings “important and encouraging” but cautioned that CT could be associated with conditions other than depression, which could make MDD “more difficult to treat.”
Nevertheless, the meta-analysis “delivers a hopeful message to patients with childhood trauma that evidence-based psychotherapy and pharmacotherapy could improve depressive symptoms,” Dr. Yrondi said.
Dr. Yrondi encouraged physicians not to neglect CT in patients with MDD. “For this, it is important that physicians are trained to evaluate childhood trauma and to take it into account in their daily practice.”
No source of funding for the study was listed. The authors and Dr. Sheline have disclosed no relevant financial relationships. Dr. Yrondi has received speaker’s honoraria from AstraZeneca, Janssen, Lundbeck, Otsuka, and Jazz and has carried out clinical studies in relation to the development of a medicine for Janssen and Lundbeck that are unrelated to this work.
A version of this article first appeared on Medscape.com.
Despite a higher symptom burden, patients with major depressive disorder (MDD) and a history of childhood trauma (CT) can achieve significant recovery following treatment with a combination of pharmacotherapy and psychotherapy, new research suggests.
Results from a meta-analysis of 29 studies from 1966 to 2019, which included almost 7,000 adults with MDD, showed that more than 60% reported a history of CT. But despite having more severe depression at baseline, those with CT benefited from active treatment. Effect sizes were comparable, and dropout rates were similar to those of their counterparts without CT.
“Evidence-based psychotherapy and pharmacotherapy should be offered to depressed patients, regardless of their childhood trauma status,” lead author Erika Kuzminskaite, MSc, a PhD candidate at Amsterdam UMC department of psychiatry, the Netherlands, told this news organization.
“Screening for childhood trauma is important to identify individuals at risk for more severe course of the disorder and post-treatment residual symptoms,” she added.
The study was published online in the Lancet Psychiatry.
Common and potent risk factor
The researchers note that CT is common and is a potent risk factor for depression. Previous studies have “consistently indicated significantly higher severity and persistence of depressive symptoms in adult patients with depression and a history of childhood trauma.”
Previous individual and meta-analytic studies “indicated poorer response to first-line depression treatments in patients with childhood trauma, compared to those without trauma, suggesting the need for new personalized treatments for depressed patients with childhood trauma history,” Ms. Kuzminskaite said.
“However, the evidence on poorer treatment outcomes has not been definitive, and a comprehensive meta-analysis of available findings has been lacking,” she added.
The previous meta-analyses showed high between-study heterogeneity, and some primary studies reported similar or even superior improvement for patients with CT, compared with those without such history, following treatment with evidence-based psychotherapy or pharmacotherapy.
Previous studies also did not investigate the “relative contribution of different childhood trauma types.”
To address this gap, investigators in the Childhood Trauma Meta-Analysis Study Group conducted the “largest and most comprehensive study of available evidence examining the effects of childhood trauma on the efficacy and effectiveness of first-line treatments for adults with MDD.”
To be included, a study had to focus on adults over 18 years old who had received a primary diagnosis of depression. The study had to have included an available assessment of childhood trauma, and patients were required to have undergone psychotherapy and/or pharmacotherapy for depression alone or in combination with other guideline-recommended treatments. Studies were also required to have a comparator group, when applicable, and to have reported depression severity before and after the acute treatment phase.
Of 10,505 publications, 54 trials met inclusion criteria; of these, 29 (20 randomized controlled trials and 9 open trials), encompassing 6,830 participants aged 18-85 years, included data that had been made available by authors of the various studies and were included in the current analysis.
Most studies focused on MDD; 11 trials focused on patients with chronic or treatment-resistant depression.
The primary outcome was “depression severity change from baseline to the end of the acute treatment phase” (expressed as standardized effect size – Hedges’ g).
Greater treatment motivation?
Of the included patients, 62% reported a history of CT. They were found to have more severe depression at baseline, compared with those without CT (g = .202; 95% confidence interval, 0.145-0.258; I² = 0%).
The benefits from active treatment obtained by these patients with CT were similar to the benefits obtained by their counterparts without CT (between-group treatment effect difference: g = .016; 95% CI, –0.094-0.125; I² = 44.3%).
No significant difference in active treatment effects (in comparison with control condition) was found between individuals with and those without CT (g = .605; 95% CI, 0.294-0.916; I² = 58.0%; and g = .178; 95% CI, –0.195-0.552; I² = 67.5%, respectively; between-group difference P = .051).
Dropout rates were similar for the participants with and those without CT (risk ratio, 1.063; 95% CI, 0.945-1.195; I² = 0%).
“Findings did not significantly differ by childhood trauma type, study design, depression diagnosis, assessment method of childhood trauma, study quality, year, or treatment type or length,” the authors report.
The findings did, however, differ by country, with North American studies showing larger treatment effects for patients with CT, compared with studies conducted in Asian-Pacific countries (g = 0.150; 95% CI, 0.030-0.269; vs. g = 0.255; 95% CI, –0.508- –0.002, respectively; corrected false discovery rate, 0.0080). “However, because of limited power, these findings should be interpreted with caution,” the authors warn.
“It could be a chance finding and is certainly not causal,” Ms. Kuzminskaite suggested.
Most studies (21 of the 29) had a “moderate to high risk of bias.” But when the researchers conducted a sensitivity analysis in the low-bias studies, they found that results were similar to those of the primary analysis that included all the studies.
“Treatments were similarly effective for patients with and without childhood trauma, with slightly larger active treatment (vs. control condition – placebo, wait list, care-as-usual) effects for patients with childhood trauma history,” Ms. Kuzminskaite said.
“Some evidence suggests that patients with childhood trauma are characterized by greater treatment motivation,” she noted. Moreover, “they are also more severely depressed prior to treatment [and] thus have more room for improvement.”
‘Hopeful message’
Commenting for this news organization, Yvette Sheline, MD, McLure professor of psychiatry, radiology, and neurology and director of the center for neuromodulation in depression and Stress, University of Pennsylvania, Philadelphia, called it a “well-executed” and “straightforward” study “with clear-cut findings.”
Dr. Sheline, the director of the section on mood, anxiety, and trauma, who was not involved with the study, agrees with the authors’ conclusions – “to use evidence-based treatments for depression in all patients,” with or without a history of CT.
In an accompanying editorial, Antoine Yrondi, MD, PhD, of Université de Toulouse (France), called the findings “important and encouraging” but cautioned that CT could be associated with conditions other than depression, which could make MDD “more difficult to treat.”
Nevertheless, the meta-analysis “delivers a hopeful message to patients with childhood trauma that evidence-based psychotherapy and pharmacotherapy could improve depressive symptoms,” Dr. Yrondi said.
Dr. Yrondi encouraged physicians not to neglect CT in patients with MDD. “For this, it is important that physicians are trained to evaluate childhood trauma and to take it into account in their daily practice.”
No source of funding for the study was listed. The authors and Dr. Sheline have disclosed no relevant financial relationships. Dr. Yrondi has received speaker’s honoraria from AstraZeneca, Janssen, Lundbeck, Otsuka, and Jazz and has carried out clinical studies in relation to the development of a medicine for Janssen and Lundbeck that are unrelated to this work.
A version of this article first appeared on Medscape.com.
Despite a higher symptom burden, patients with major depressive disorder (MDD) and a history of childhood trauma (CT) can achieve significant recovery following treatment with a combination of pharmacotherapy and psychotherapy, new research suggests.
Results from a meta-analysis of 29 studies from 1966 to 2019, which included almost 7,000 adults with MDD, showed that more than 60% reported a history of CT. But despite having more severe depression at baseline, those with CT benefited from active treatment. Effect sizes were comparable, and dropout rates were similar to those of their counterparts without CT.
“Evidence-based psychotherapy and pharmacotherapy should be offered to depressed patients, regardless of their childhood trauma status,” lead author Erika Kuzminskaite, MSc, a PhD candidate at Amsterdam UMC department of psychiatry, the Netherlands, told this news organization.
“Screening for childhood trauma is important to identify individuals at risk for more severe course of the disorder and post-treatment residual symptoms,” she added.
The study was published online in the Lancet Psychiatry.
Common and potent risk factor
The researchers note that CT is common and is a potent risk factor for depression. Previous studies have “consistently indicated significantly higher severity and persistence of depressive symptoms in adult patients with depression and a history of childhood trauma.”
Previous individual and meta-analytic studies “indicated poorer response to first-line depression treatments in patients with childhood trauma, compared to those without trauma, suggesting the need for new personalized treatments for depressed patients with childhood trauma history,” Ms. Kuzminskaite said.
“However, the evidence on poorer treatment outcomes has not been definitive, and a comprehensive meta-analysis of available findings has been lacking,” she added.
The previous meta-analyses showed high between-study heterogeneity, and some primary studies reported similar or even superior improvement for patients with CT, compared with those without such history, following treatment with evidence-based psychotherapy or pharmacotherapy.
Previous studies also did not investigate the “relative contribution of different childhood trauma types.”
To address this gap, investigators in the Childhood Trauma Meta-Analysis Study Group conducted the “largest and most comprehensive study of available evidence examining the effects of childhood trauma on the efficacy and effectiveness of first-line treatments for adults with MDD.”
To be included, a study had to focus on adults over 18 years old who had received a primary diagnosis of depression. The study had to have included an available assessment of childhood trauma, and patients were required to have undergone psychotherapy and/or pharmacotherapy for depression alone or in combination with other guideline-recommended treatments. Studies were also required to have a comparator group, when applicable, and to have reported depression severity before and after the acute treatment phase.
Of 10,505 publications, 54 trials met inclusion criteria; of these, 29 (20 randomized controlled trials and 9 open trials), encompassing 6,830 participants aged 18-85 years, included data that had been made available by authors of the various studies and were included in the current analysis.
Most studies focused on MDD; 11 trials focused on patients with chronic or treatment-resistant depression.
The primary outcome was “depression severity change from baseline to the end of the acute treatment phase” (expressed as standardized effect size – Hedges’ g).
Greater treatment motivation?
Of the included patients, 62% reported a history of CT. They were found to have more severe depression at baseline, compared with those without CT (g = .202; 95% confidence interval, 0.145-0.258; I² = 0%).
The benefits from active treatment obtained by these patients with CT were similar to the benefits obtained by their counterparts without CT (between-group treatment effect difference: g = .016; 95% CI, –0.094-0.125; I² = 44.3%).
No significant difference in active treatment effects (in comparison with control condition) was found between individuals with and those without CT (g = .605; 95% CI, 0.294-0.916; I² = 58.0%; and g = .178; 95% CI, –0.195-0.552; I² = 67.5%, respectively; between-group difference P = .051).
Dropout rates were similar for the participants with and those without CT (risk ratio, 1.063; 95% CI, 0.945-1.195; I² = 0%).
“Findings did not significantly differ by childhood trauma type, study design, depression diagnosis, assessment method of childhood trauma, study quality, year, or treatment type or length,” the authors report.
The findings did, however, differ by country, with North American studies showing larger treatment effects for patients with CT, compared with studies conducted in Asian-Pacific countries (g = 0.150; 95% CI, 0.030-0.269; vs. g = 0.255; 95% CI, –0.508- –0.002, respectively; corrected false discovery rate, 0.0080). “However, because of limited power, these findings should be interpreted with caution,” the authors warn.
“It could be a chance finding and is certainly not causal,” Ms. Kuzminskaite suggested.
Most studies (21 of the 29) had a “moderate to high risk of bias.” But when the researchers conducted a sensitivity analysis in the low-bias studies, they found that results were similar to those of the primary analysis that included all the studies.
“Treatments were similarly effective for patients with and without childhood trauma, with slightly larger active treatment (vs. control condition – placebo, wait list, care-as-usual) effects for patients with childhood trauma history,” Ms. Kuzminskaite said.
“Some evidence suggests that patients with childhood trauma are characterized by greater treatment motivation,” she noted. Moreover, “they are also more severely depressed prior to treatment [and] thus have more room for improvement.”
‘Hopeful message’
Commenting for this news organization, Yvette Sheline, MD, McLure professor of psychiatry, radiology, and neurology and director of the center for neuromodulation in depression and Stress, University of Pennsylvania, Philadelphia, called it a “well-executed” and “straightforward” study “with clear-cut findings.”
Dr. Sheline, the director of the section on mood, anxiety, and trauma, who was not involved with the study, agrees with the authors’ conclusions – “to use evidence-based treatments for depression in all patients,” with or without a history of CT.
In an accompanying editorial, Antoine Yrondi, MD, PhD, of Université de Toulouse (France), called the findings “important and encouraging” but cautioned that CT could be associated with conditions other than depression, which could make MDD “more difficult to treat.”
Nevertheless, the meta-analysis “delivers a hopeful message to patients with childhood trauma that evidence-based psychotherapy and pharmacotherapy could improve depressive symptoms,” Dr. Yrondi said.
Dr. Yrondi encouraged physicians not to neglect CT in patients with MDD. “For this, it is important that physicians are trained to evaluate childhood trauma and to take it into account in their daily practice.”
No source of funding for the study was listed. The authors and Dr. Sheline have disclosed no relevant financial relationships. Dr. Yrondi has received speaker’s honoraria from AstraZeneca, Janssen, Lundbeck, Otsuka, and Jazz and has carried out clinical studies in relation to the development of a medicine for Janssen and Lundbeck that are unrelated to this work.
A version of this article first appeared on Medscape.com.
FROM LANCET PSYCHIATRY